Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 14/197/44. The contractual start date was in February 2017. The final report began editorial review in March 2021 and was accepted for publication in November 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Butler et al. This work was produced by Butler et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Butler et al.
Chapter 1 Introduction
Context
Hospice and palliative care services in England
The UK is world-leading in hospice and palliative care (H&PC) services, which care for people with life-limiting health conditions and those approaching the end of their lives. 1 These services are small or extremely small players operating in a complex system of health and social care that people approaching the end of life must use and navigate. Hospice services in the UK historically began in the charitable sector, and most of the funding for H&PC services continues to be derived from charitable sources. H&PC organisations are also in receipt of NHS funding (on average, the NHS contributes 32% of total funding to hospices in England2) and are subject to NHS commissioning processes. These factors, together with their small size, provide a range of challenges for H&PC organisations in terms of funding and sustainability.
Individual H&PC services have developed in localities as a result of voluntary activity led by key local people. There is a strong sense of ownership in communities of their ‘local hospice’, which continues to be vital for fundraising activities and generates a large supply of willing volunteers. The reputation of the hospice, both as a worthy, local charity and for excellence in care, is held very dear for all of these reasons . The public’s sense of identification with its local hospice tends to focus on the bricks and mortar building, and there is often less awareness or understanding of palliative care community services, including hospice at home (HAH) services.
National strategic direction
National strategy in England sets further context in terms of the drive towards encouraging choice about where people receive care and increasing the opportunities to be cared for and to die at home (moving away from the acute hospital sector). 3 This would seem to be in step with public preferences; evidence suggests that the majority of people would wish to die at home,4 and also indicates that the number of people expressing this wish is increasing. 5,6 Identifying how care can be delivered and maintained at home was a top research priority in a public consultation by the James Lind Alliance in 2015. 7 However, in 2019, only 24.4% of all deaths in England occurred at home (not including care home deaths)8 and it seems that, overall, health and social care services are not well equipped to meet this demand. 9
Another direction of national strategy that provides context for this study is that towards the integration of health and social care. H&PC services lend themselves naturally to this integration because holistic care, recognising the physical, psychological, social and spiritual aspects of people’s needs, has long been a basic precept of good palliative care. H&PC services routinely employ social care professionals, counsellors and spiritual care staff in addition to health-care professionals (HCPs).
Broader cultural and societal issues
Although H&PC services are prized and respected, as described previously, the reality of talking about and accepting death and dying in contemporary health care is more of a challenge. The public increasingly demands more and better acute, interventional health care into older and older age, staving off the inevitability of the ending of life. In this context, HCPs may lack the skills or confidence to open discussions about curtailing interventional medical care when it can no longer offer benefit and about planning for death and dying. H&PC services, which are so explicitly geared to death and dying, may therefore struggle to be accepted and to attract referrals of people who could benefit from their care. This issue may have even more impact in some cultural or faith communities or among those with diseases other than cancer, which are not as clearly identified with dying.
In addition to these influences, caring for and enabling people to die at home is affected by significant societal changes that have been under way over many decades. It can no longer be assumed that families will live nearby or have the resources to provide unpaid care. Home-based care of any description is heavily dependent on family/informal care, and those without such support have a more limited range of options.
Hospice at home services and the evolution of this project
Hospice at home services sit within this web of factors as a subset of H&PC services, often, but not always, linked to a local hospice organisation and building. Most of these services explicitly aim to support care and dying at home when this is the preferred place of death (PPOD).
In 2007, Pilgrims Hospices in East Kent decided to increase community palliative care provision to enable more patients to die in their own homes. To ensure that these service changes were in line with the best available evidence, a literature review of the evidence for HAH services was commissioned from the University of Kent. The literature review10 indicated that the evidence base for the efficacy of such services was weak, with few controlled studies, although many qualitative studies indicated that such services were appreciated by patients and families. The characteristics of services that appeared to produce the most favourable outcomes included care given by palliative care specialists, out-of-hours (OOH) availability, crisis intervention and rapid-response capability. Based on the findings from the literature review, the hospice designed and implemented a new HAH service.
A successful application to the National Institute for Health and Care Research (NIHR) Research for Patient Benefit funding stream was made to evaluate the impact of the new service. The evaluation used a quasi-experimental cluster design and the results have been published. 11,12 This new service did not improve patients’ chances of dying in their preferred place (> 60% of patients died in their preferred place in both the intervention and the control groups), although patients in areas where the HAH service was operating had a significantly higher rate of a preference to die at home.
From the results of this study, a number of questions remained unanswered:
-
Is there a better service configuration than the one examined here that would allow more patients to die where they prefer and to have a good quality of death?
-
One of the gaps in this service was difficulty accessing medications, which was, in part, due to challenges in working with other community providers – how can we improve this with our partners in the community?
-
What would be the highest level of achievement of PPOD we could hope to reach, that is what is a realistic gold standard and what services are able to deliver this?
Our collaboration with the National Association for Hospice at Home (NAHH) for this current study confirmed that these questions, and the overall question of ‘what does an optimal HAH service look like?’, were commonly debated across the sector.
An updated literature review confirmed that the published evidence for HAH services continued to demonstrate wide variation in HAH service provision and the settings in which such services operated around England. Services that had been evaluated often demonstrated positive benefits for patients, such as increased choice and dying at home. 13,14 However, the published studies reported such a range of different outcome measures that there was no opportunity to synthesise the data or to make useful comparisons. It was also unclear what elements of HAH services delivered which outcomes and to what extent such outcomes were delivered in conjunction with other services that formed part of the whole system of care. This lack of clarity about what aspects of services produce the desired outcomes for patients (and their families/informal carers) makes sharing good practice between HAH services difficult and limits efficient service development.
Aim and objectives
Parts of this section have been reproduced from Butler et al. 15 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The aim of this study was to investigate the impact of the organisation, delivery and settings of different models of HAH on patient and carer outcomes and experiences of end-of-life care (EOLC) in England. Given the complexity of the whole system of care used by patients at the end of life, the range and variation of HAH services themselves, and the many different settings in which they operate, a realist evaluation methodology was chosen. 16,17 This theory-driven methodology uses iterative, qualitative data analysis, supplemented in this study by quantitative data, to identify the underlying generative mechanisms that produce outcomes in complex systems. In addition, the study looked at the financial cost of care in the different services and settings.
The overarching research question that the study addressed was as follows: what are the features of HAH models that work, for whom and in what circumstances?
The detailed study objectives were as follows:
-
phase 1
-
identify the range and variation of HAH services operating across England
-
categorise the HAH services into models according to key features and setting
-
-
phase 215
-
assess the impact of each model on patient and carer outcomes
-
investigate the resource implications and costs of patient care in each model
-
explore the experiences of patients, family carers, and providers and commissioners of the different HAH models
-
identify the enablers of and barriers to embedding HAH models as part of service delivery.
-
Report structure
Chapter 2 describes the published literature about evaluations of HAH services in England. As a spin-off from this study, a realist-informed review of the literature was also undertaken and was utilised in the qualitative analysis. 18 Chapter 3 includes information about realist methods, descriptions of the three-phase study design with diagrammatic illustrations and details about the mixed-methods data analysis. Chapter 4 describes the development, management and contribution of patient and public involvement (PPI) in the study. Chapters 5–7 present the results: Chapter 5 presents the results of the survey undertaken in phase 1, Chapter 6 presents the quantitative data and the health economics results and Chapter 7 presents the results of the qualitative data analysis. The synthesis of the overall mixed-methods data set is addressed in Chapter 8, alongside the discussion. Chapter 9 presents the study conclusions, implications for health care, limitations and recommendations for future research.
Chapter 2 Review of the literature
Parts of this chapter have been reproduced from Butler et al. 15 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
This chapter reports the review of the literature to understand existing models of HAH services in the UK and their evaluation.
Background
Providing patients with choice about where they receive their care at the end of life remains central to UK policy3 and HAH services have been introduced to support patient choice if their wish is to die at home. The number of patients wishing to die at home has been increasing. 5,6 Home palliative care increases the chance of dying at home and reduces patient symptom burden and grief for family carers post death. 19
Stosz10 conducted a literature review in 2008 to establish the evidence base for HAH services. The characteristics identified and the terms describing the services operating included the following: a palliative care service provided in the home environment, OOH, hospital at home, community specialist palliative care, crisis intervention and rapid-response teams. The recommendations from that review were that a successful intervention should include the following:
-
a service operating in addition to existing community services that is available throughout the course of the end stages of illness (particularly in the last few weeks of life when crises may occur)
-
rapid access to specialist input at all hours
-
providing access to medication and equipment
-
viewing the informal carer as integral to the care team and recognising carer burden.
Based on the findings and recommendations of the Stosz10 literature review, Pilgrims Hospices in East Kent developed a new HAH ‘rapid-response’ service caring for adults in the last 72 hours of life. 20 Evaluation of this service was conducted through a pragmatic quasi-controlled trial. 11 Although the new service was cost neutral and enabled more people to die at home, it did not improve hospice patients’ chances of achieving PPOD (primary outcome).
In 2012, the NAHH and Help the Hospices (now Hospice UK; London, UK) collaborated to conduct a multiservice survey (across 76 services in England), which started to describe the landscape of HAH services across the country (Heather Richardson and Andrew Thomson, Hospice UK, 2014, personal communication). The conclusions from this work were that HAH services were not homogeneous and that there were at least two models of care, despite the shared name of HAH. A clear distinction was found between one set of services, delivering high numbers of completed episodes of care (> 50 episodes of care per service per month), and the other set, providing significantly fewer completed episodes of care (< 50 per month). In addition, there were notable differences relating to reasons for referral, episode duration, who was involved in care, and knowledge regarding preferences and PPOD. The recommendations from this survey acknowledged that there was a need to further increase understanding of HAH. There was lack of clarity about what was the best model of care, for example there was uncertainty about skill mix and to what degree teams should incorporate senior staff alongside more junior nurses and social carers (Heather Richardson and Andrew Thomson, personal communication).
The NAHH also published recommendations in the form of national standards for HAH services, which they developed through workshops with HAH service professionals in May 2011, November 2011 and May 2012. These resulted in six agreed core standards, with examples of structural, process and outcome criteria underpinning them:21
-
The HAH service has a workforce management, education and development strategy that ensures the competence and confidence in practice of its employees to deliver and support high-quality clinical services.
-
The HAH service is integrated into the local EOLC service provision and involved in providing co-ordinated care for patients and families.
-
The HAH service clearly defines and communicates referral criteria and pathways to all referrers, key stakeholders and other partners.
-
The HAH service ensures that patients, and their families and carers, receive the service information required to enable them to make informed choices in relation to their preferred place of care and support, including at the end of life.
-
The HAH team’s care and support service, in partnership with other agencies, meets the assessed needs of patients, carers and families.
-
The HAH service has systems and processes to ensure pre-and post-bereavement support for patients (when appropriate), carers and families. 15
The findings from these projects indicated that there was value in HAH as a concept, but led to the broader question of what would be the most successful and cost-effective model of HAH that could improve the outcomes for an even higher proportion of patients whose preference was to die at home, in their area. This prompted a further review of the existing literature, to understand what different HAH models existed in the UK and their value, that is whether or not any comparative data or assessment of optimum HAH service model delivery existed. This review of the literature, initially conducted in 2014, and updated in 2017, 2019 and 2020, is described in the following sections.
Search strategy for hospice at home models, comparators and outcomes
The search sought to identify any type of literature or study that aimed to describe or evaluate a HAH model in the health and social care setting of the UK that was providing care to adults with a life-limiting illness who wished to die at home. The service could be described as a HAH service by name or could potentially be a community service under a different name. Therefore, the search strategy included concepts that could identify these services in the literature. The search concepts were chosen based on the previous literature review. 15
The criteria for selection of articles were as follows:
-
HAH service
-
community service under a different name with clear HAH characteristics:
-
rapid response
-
crisis management
-
24-hour coverage
-
staff in service were palliative care specialists who were hospice trained.
-
-
UK based.
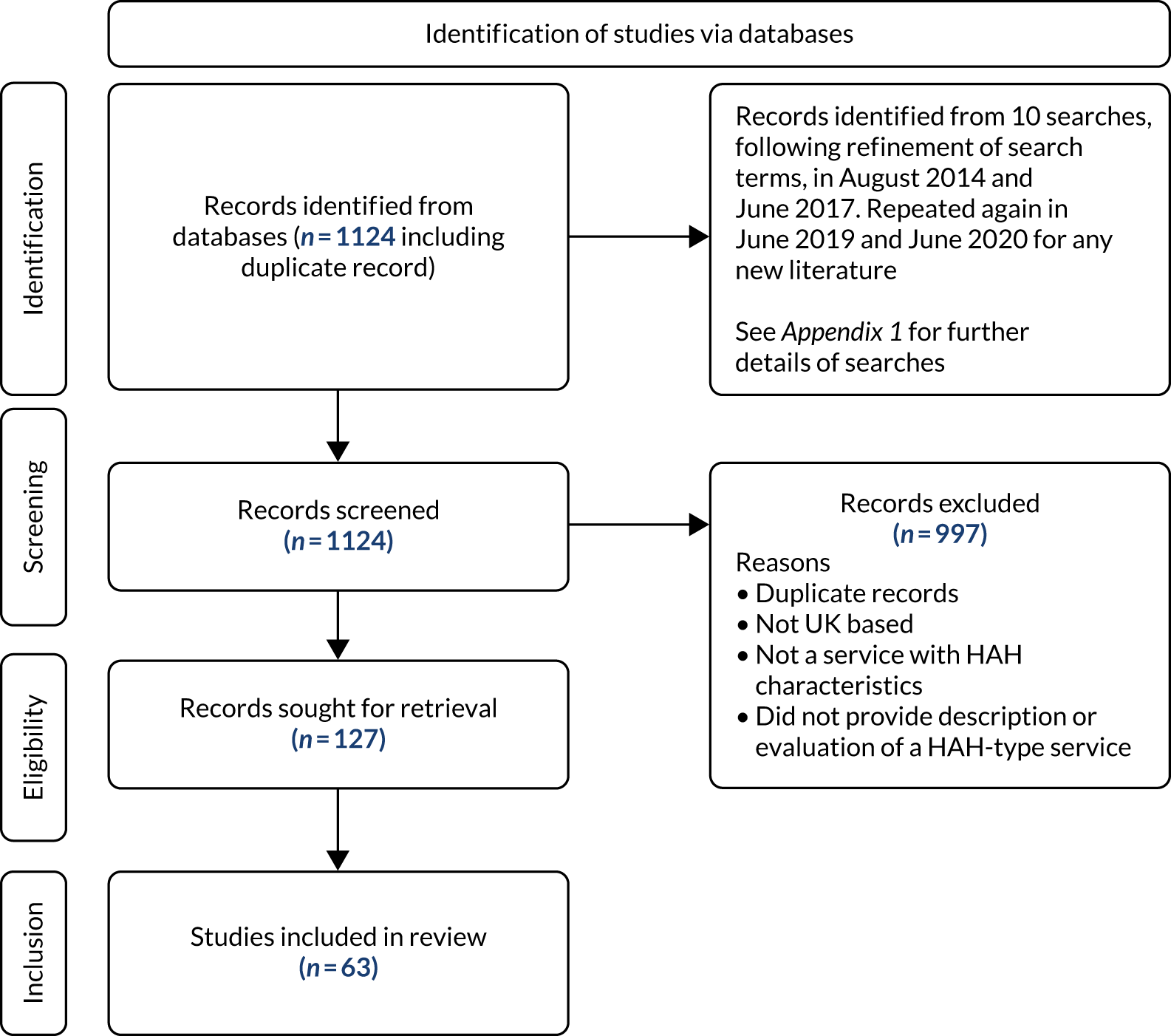
A set of searches was carried out on several databases of academic publications, grey literature and current research (Figure 1; also see Appendix 1, including Tables 19–21, for further details).
FIGURE 1.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 flow diagram.
Scoping the literature on service models and evaluations
Sixty-three papers/grey literature sources were identified from the searches. The articles were analysed by recording key information from each article relating to (1) study design and (2) service description (Table 1). This provided information to scope what types of services existed and what work had been undertaken to evaluate them. Any identified barriers to and facilitators of accessing the service, or the service achieving its aims, were also included.
| 1. Study design | 2. Service description |
|---|---|
| Aim of study | Location |
| Population | Description |
| Methods | Aim of service |
| Primary outcome(s) | Rapid-response service? |
| Cost analysis? | Target group |
| Main findings | Definition of HAH provided? |
| Limitations | Barriers |
| Future research suggestions | Facilitators |
Many articles included were evaluations or descriptions of one service model in one locality. However, 13 articles (involving 11 studies) looked at several models of care. Two of these were multiservice surveys to understand and scope HAH models: the NAHH/Help the Hospices survey mentioned previously (Heather Richardson and Andrew Thomson, personal communication) and the survey conducted as phase 1 of the OPtimum hospice at home services for End of Life care (OPEL) study. 22 Eight were literature reviews or syntheses. 5,10,18,23–27 Hashem et al. 18 applied a realist logic of analysis to their review of HAH. Taylor et al. 23 conducted a literature review of the international evidence for models of care supporting effectiveness in reducing inappropriate/non-beneficial hospital bed-days for people nearing the end of life; they concluded that such evidence was generally limited or absent. HAH was one type of care described in the review. 23
The criteria for ‘home palliative care’ services were much broader than the definition used for HAH in some of the reviews, and looked at literature beyond the UK. 5,24,25 Sarmento et al. 25 undertook a review of qualitative evidence to understand patients’ and family caregivers’ experiences, and the key components of care that shaped the experiences of service users. Shepperd et al. 5 undertook systematic reviews of the trial and controlled study literature on home-based EOLC. Bainbridge et al. 24 identified components of home-based programmes: a total of 30 unique components were identified by a content analysis of the literature. Efficacious programmes included multiple components; the most common were linkage with acute care, multidisciplinary nature, end-of-life expertise and training, holistic care, pain and symptom management, and professional psychosocial support. Luckett et al. 26 looked to understand elements of effective palliative care models in a range of settings, not just home care. They identified essential attributes of effective palliative care models to be communication and co-ordination between providers, rapid response to individuals’ changing needs and preferences over time, skill enhancement and specialist expertise. Another study looking at care models provided a set of criteria to define and compare models of UK specialist palliative care, which distinguished home-based care from other forms of care as one criterion, with several other cross-cutting criteria. 28 Another looked at a number of models of care, but only within a primary care setting. 29,30
A smaller number of articles (seven) identified in the review looked at variations of the same service model: the Midhurst Macmillan Specialist Palliative Care at Home Service31–33 and the Marie Curie Delivering Choice Programme;34–37 realist evaluation principles were used in one evaluation of each service model. 32,37 The Marie Curie programme was implemented across two counties, and included co-ordination centres, a telephone advice line, ‘discharge in reach’ nurses, a specialist community personal care team and nurse educators. The importance of having ‘highly skilled’ palliative professionals with ‘dedicated and sufficient time’ to support informal carers in navigating the system was noted. The whole-system approach of the Delivering Choice Programme underpinned its success, which relied on the collective effort of senior and front-line professionals across hospices, the NHS and social care services. In contrast, Johnston et al. 32 found variation in the implementation of the Macmillan service across its six sites. Overall, they concluded that users of the service were more likely to die at home, and identified the importance of rapid response, early referral, good leadership, flexible working and the added value of health-care assistants (HCAs) and volunteer roles within the service, in particular for psychosocial support. These studies assessing specialist palliative care models highlighted the variation in the components of HAH or home-based palliative care services.
Description of services
The majority of HAH services offered service provision that had long periods of involvement (i.e. not just for the last days or weeks of life) and did not provide a crisis management element or a 24-hours-per-day, 7-days-per-week (24/7), rapid-response service.
Common service characteristics identified in the literature were as follows:
-
enabling patients to be cared for and to die in their place of choice, namely home
-
specialist staff [whether HCA or registered nurse (RN) core staff] with high levels of palliative care expertise
-
ability to provide more staff time with a patient
-
some HAH named services offered ‘sitting’ services or assisted discharge from hospital.
A diverse range of multifaceted services was described in the literature based on locally perceived need, for example population/geography, which tended to complement other existing services. However, some inequality of access was observed, for example:
-
Association between greater deprivation/lower socioeconomic status and lower rates of access to HAH. 38,39
-
Inequality in referral practices in primary care – difficulties in prognosis and identifying terminal phase of non-malignant diseases. The majority of patients seen by HAH were cancer patients. 39,40
Some publications described the process of service development20,41,42 through learning from the evidence base, listening to their local stakeholders and service users or by replicating service models that seemed to work elsewhere. An example of sharing of lessons learned for service development was published by a service in north-west England, which provided its own 10 steps to develop an effective HAH service: preparation, being clear on what it can offer, clinical leadership, staff have community or palliative care experience, comprehensive induction with the hospice, support for staff, good lines of communication with primary care teams, reassurance to other health professionals (e.g. about not ‘taking over’), clear referral criteria agreed by all stakeholders and publicity among the public. 43 The provision of services was often still evolving, and services were being evaluated in the light of the need to secure further funding to continue. 44,45
Evaluations of services
The majority of evaluations of single HAH services were descriptive, capturing views of service users and/or the service staff. 13,14,43,45–47 They did not have a control group and had small sample sizes. Tyrer and Exley40 focused on the demographics of the service users, referrals and service use.
Some evaluations captured the views of bereaved carers. 12,20,48–50 Grande et al. 51 looked at the impact of HAH on carer bereavement. Other studies included views of referrers to the service, such as community nurses/district nurses (DNs) and general practitioners (GPs). 52–56 These descriptive studies tended to use surveys or qualitative methods such as focus groups and interviews.
Buck et al. 39,44 evaluated services by reviewing case notes, and Koffman et al. 47 measured clinical and psychological changes at the time of referral to HAH and after receiving the service, for patients with advanced human immunodeficiency virus/acquired immunodeficiency syndrome using the support team assessment schedule. 47 Others reviewed their current service provision by how well they had met key performance indicators or other objectives of their services, or patient outcomes. 42,57,58
Some evaluations assessed the extension of already established HAH services. These included the introduction of additional OOH support,59,60 a respite service61 and combining existing services to enable cross-working between multidisciplinary teams. 62 Strategic changes played a key part in the success of one service. 60
The difficulty of trial designs in palliative care was acknowledged in the literature, and only two of the evaluations reported were trial designs. One of these was in east Kent, where a pragmatic, quasi-experiential, controlled trial to evaluate a rapid-response HAH service was undertaken. 11,20 The second trial was of a ‘hospital at home’ service in the Cambridgeshire area in the late 1990s. 38,63–65 The latter service was more focused on the provision of respite care, rather than rapid response, and was not a ‘specialist’ service as is characteristic of the more recent HAH services. There were two retrospective cohort studies in which patients were not randomised: one observed outcomes of patients who accessed the service43 and the other compared the outcomes of patients who accessed the service with those of patients who did not. 36 One evaluation did attempt a before-and-after study, but had to abandon it because of small numbers. 41
Only four evaluations included a health economic component to try to assess the cost-effectiveness of their service. 53,66,67 The Spiro et al. 67 pilot study suggested a model that could offer an economic propostion, but concluded that assessing the cost of EOLC was complex. 67 Gage et al. 66 and Addicott and Dewar68 found the services they were evaluating to be cost neutral, but offered an increased likelihood of achieving death at home. Grady and Travers53 were not able to draw firm conclusions because of the limited number of data.
Place of death was a common outcome measure for evaluations to assess what proportion died at home and prevention of admission to hospital/hospice. Otherwise, outcomes were weaker and looked at ‘impact’ or ‘strengths and weaknesses’ in line with the descriptive nature of the majority of studies.
Themes identified in the literature
The following themes were identified as features of HAH services that work well, but there were also challenges:
-
Staff offered specialist knowledge and something over and above other service provision at home. A particular feature was that HAH services were able to spend time with the patient that other services visiting the home could not provide. Good communication was also key.
-
A minority were rapid-response/24-hour services; only seven offered rapid response. 40,42,43,45,48,53,69,70 Services providing rapid response reported effectiveness in enabling patients to remain at home.
-
Eight services in the literature offered 24/7 OOH provision. Some provided full service, whereas others offered a reduced service OOH, for example a telephone advice line or voluntary staff. OOH provision was seen as desirable for many services that were not offering it. However, difficulties continued to be identified, even for those that were offering 24/7 services, for example access to medication, fewer staff and less medical support OOH.
-
Instead of 24/7 rapid response, services tended to offer ‘sitting’ respite, appointment-based services or assisted discharge from inpatient units to allow a patient to be at home.
-
The role of the carer was key: HAH services helped to provide physical, emotional and social support to relieve carer burden, and also provided bereavement support in some cases.
-
Working with primary care teams (GPs and DNs). Patients remained under the care of the primary care teams, so HAH services complemented this. Communication was key to reassure them that the HAH service was not ‘taking over’.
-
Issues of timeliness in receiving equipment into, and removing it from, the home.
Conclusions of the review of the literature
Hospice at home is an umbrella term with no clear service specification. Many hospices have adapted and used elements of what could be described as HAH, resulting in many different models of HAH being implemented in practice.
This literature review set out to identify the literature that described HAH service models in the health and social care setting of the UK, or community models under a different name that had HAH ‘characteristics’ in terms of rapid response, crisis management, 24-hour coverage and palliative care specialist staff who were hospice trained. A limited number of studies of services, described as HAH, met all these characteristics. Most often, HAH services shared the objective of enabling a patient to die at home if that was their place of choice, but they were less likely to provide the service on a 24/7 basis that offered rapid-response crisis management. Other elements that these services did provide were appointment-based services such as ‘sitting’ respite-type services or assisted discharge from inpatient units to allow a patient to be at home. A theme present through all the service models was staff with high levels of palliative care experience. The additional time they were able to spend with patients, which other services visiting the home could not provide, was a highly regarded element of HAH service provision, whether the core staff were RNs or HCAs.
The literature supported the proposition that HAH services at the end of life are valuable and complement existing service provision, but much of the literature was limited and the evidence was relatively weak.
Summary
The literature endorsed the value of HAH services in supporting patients to remain at home to receive their care at the end of life. However, the review of the literature posed important outstanding questions and highlighted continuing gaps in evidence about the most successful and cost-effective service configuration and activity. These questions cover the following topics: staffing profile, working patterns, communication and co-ordination with other local services, and support for carers. The review informed the funding application to Health and Social Care Delivery Research for the development of the OPEL study to identify optimum HAH services at the end of life. 15
Chapter 3 Methodology
Parts of this chapter have been reproduced from Butler et al. 15 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Hospice at home is a complex intervention operating within the wider system of health and social care delivery. Hence, research methods were required that could capture the complexity of the intervention and the impact of the implementation of different HAH models on the organisation, delivery and experience of EOLC from the perspective of service users (patients) and their family carers, and service providers and commissioners.
The research design was informed by realist evaluation,17 a theory-driven methodology increasingly used to evaluate complex interventions,71 including services for EOLC. 37 Realism provides the philosophical foundation for realistic evaluation. At the core of realism is the notion of ‘generative mechanisms’. A generative mechanism is a causal link, the ‘black box’ that leads from A to B and creates an ‘effect’. 72 Realist evaluation attempts to theorise what the mechanisms are, even though they are not necessarily ‘measurable’ in an empirical sense, and it seeks to find evidence of their existence. The relationships between mechanisms, the contexts in which they are operating and the effects they produce are represented through propositions that take on a basic formula: context + mechanism = outcome. Thus, the aim of empirical research is to identify patterns to support an explanatory theory about what mechanisms are working (or not) in a given situation. 73 A pluralist approach to data collection suits a realist evaluation.
Realist evaluation analysis in mixed-methods research
Realist evaluation analysis aims to understand both what is happening and how it is happening in an intervention. Understanding how contextual factors influence health interventions, such as HAH, is central to this methodology. It is acknowledged that an intervention and its outcome are dependent on contextual factors, and understanding how, why, for whom and when an intervention works16 is core to the approach. The context–mechanism–outcome (CMO) configuration is central to the analysis, which is intended to be pragmatic in that findings can be transferable across settings. 74 The idea that it is people and their responses to interventions that create change is also important.
In realist evaluation, data analysis takes a ‘retroductive’ approach. 75 This means that those factors that lie behind observed patterns are identified with the aim of understanding causation. Retroduction is the idea that we can explore the underlying social and psychological drivers that influence intervention outcomes by looking behind observable patterns to understand what produces them. Multiple data sources are typically required for realist evaluation. 75 Both quantitative and qualitative data can be used to generate evidence to support and refine the CMO configurations.
Overall design and development of context–mechanism–outcome configurations
The OPEL HAH study employed a mixed-methods design, using realist evaluation methodology and incorporating an economic analysis. The design of the study comprised three phases, alongside which programme theories and CMO configurations were developed (Figure 2).
FIGURE 2.
Study design, analysis and CMO configuration development. AHCR, Ambulatory and Home Care Record; AKPS, Australia-modified Karnofsky Performance Status; ECOG, Eastern Cooperative Oncology Group; IPOS, Integrated Palliative care Outcome Scale; MRT, middle-range theory; NPT, normalisation process theory; QODD, Quality of Dying and Death questionnaire; VOICES, Views of Informal Carers – Evaluation of Services.
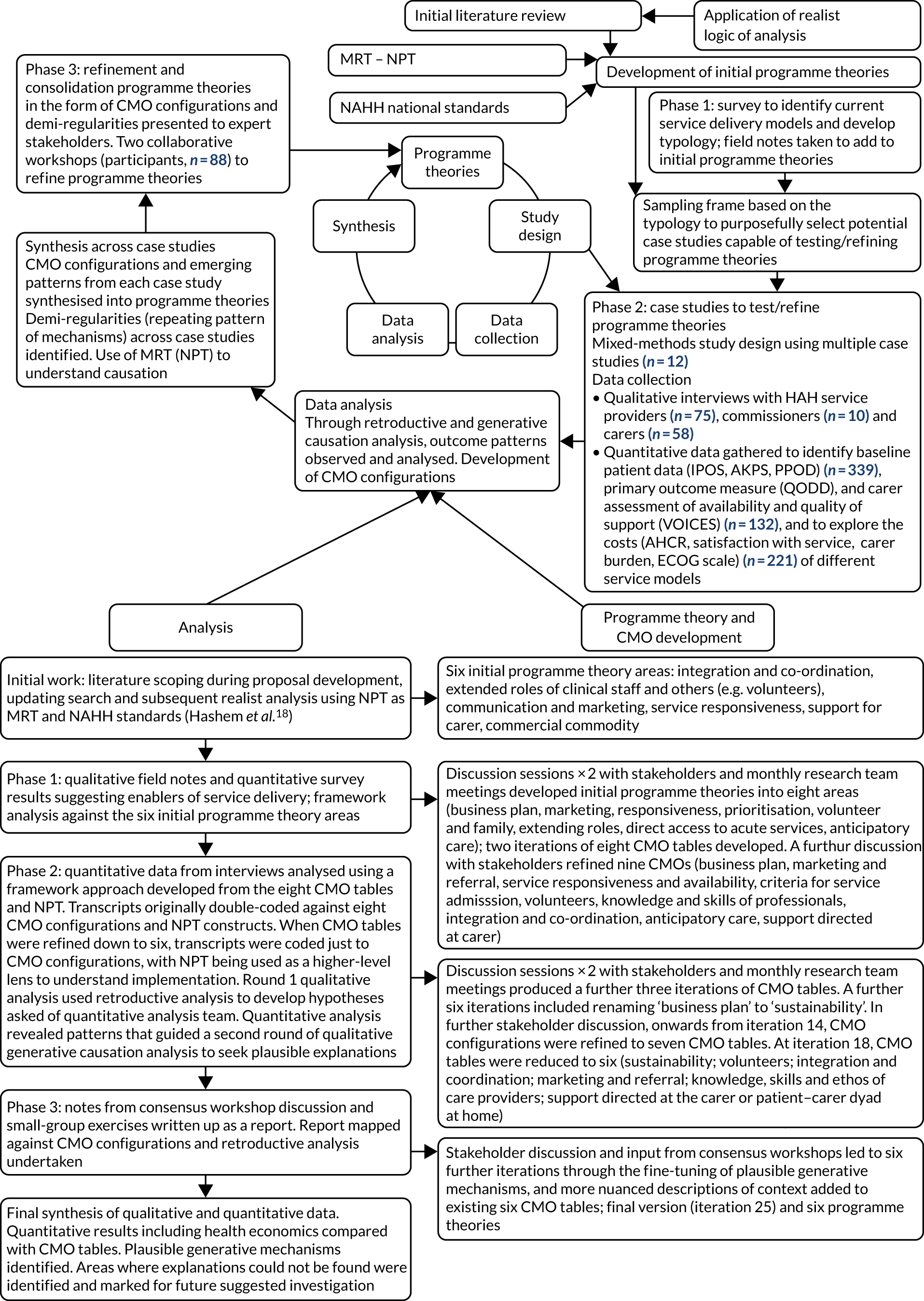
The first stage of a realist evaluation is to develop initial programme theories. These were elicited through a variety of sources. 76 First, the NAHH standards21 were taken as indicative of an overall programme theory (how HAH should work). Second, an initial review of the literature (undertaken during proposal development and subsequently updated) was synthesised through a realist logic of analysis. 18,77 Finally, as a theory-driven methodology, concepts from abstract theories were sought to inform the initial programme theories. Normalisation process theory (NPT)78 was identified as a suitable candidate theory. NPT is increasingly being used in combination with realist evaluation to understand what needs to be in place for the implementation of complex interventions,79 and it was anticipated that it would aid understanding of how HAH may become embedded as part of a local health-care economy. Data collection then occurred, based on these initial theories. CMO configurations emerging from the programme theories were identified and coded within the qualitative data. 80 During analysis, CMO configurations were synthesised in an iterative process to refine and evolve the understanding. Quantitative data were analysed in tandem, with qualitative data reinterrogated to seek plausible explanations of quantitative findings.
Stakeholder involvement is integral to the whole process and is a key feature of realist studies; by engaging lay or content experts, evidence is built to support theories on the basis of coherence and plausibility. 81 Stakeholder involvement was operationalised through PPI activities (see Chapter 4); 6-monthly meetings with the Project Oversight Group, which included lay and content experts; and two national consensus workshops.
Patterns within the data were used to refine and justify the emerging theory. The resulting CMO configurations describe common patterns (‘demi-regularities’)75 that can be applied to different settings and, in particular, the generative mechanisms at work.
Detailed design of each phase
Phase 1: national telephone survey
Hospice at home services serving adult palliative care patients in England were surveyed.
The survey aims were to (1) develop an understanding of the range of services and operations and (2) identify categories (types) of services from the survey information to use as a sampling framework for recruiting case study services in phase 2 of the study.
A total of 128 HAH services in England and the appropriate contact (e.g. service lead) were identified from the NAHH and Hospice UK directories of services and approached to take part in a telephone survey. Each service contact was posted an information letter, a survey and opt-out slip. An interview to collect the data over the telephone was proposed. Contacts were followed up 2 weeks later to arrange the interview if they had not already responded or opted out.
Telephone survey calls were conducted by a nurse with palliative care experience to facilitate understanding of the services. The survey was semistructured, comprising a selection of closed and open questions. Respondents were asked to provide details of the population characteristics in the catchment area; other relevant local services and access to palliative care beds; and HAH activity levels, staffing, facilities, equipment, processes, budget, and barriers to and facilitators of operating (see Report Supplementary Material 1 for the full questionnaire). HAH services were asked to provide supporting documents and to indicate willingness (or not) to consider becoming a case study site in phase 2.
Phase 2: case studies
Case study methods are a well-established approach to conducting research in ‘real-life’ health-care settings. 82 The approach employs mixed methods to gain an in-depth understanding of the impact of service models, resource implications and the experiences of all stakeholders, including service users, providers and commissioners. Yin83 describes case study design as orientated towards a realist perspective The design allows methodological flexibility to generate theoretical insights from the findings,84 which is a key requirement for realist evaluative design. 17 We adopted Yin’s83 approach to defining a case as an individual organisation. Although each case needed to be bounded, there was also some need to maintain flexibility, and each case was defined as what the site described as their HAH service.
Plan of investigation for case study sites
When HAH services had agreed to take part, full training on the study and the informed consent process was provided to site staff (research nurses, clinical staff, managers, etc.) by the members of the research team. The training was delivered in person at site initiation visits and follow-up training was also provided on site and remotely, as needed.
Recruitment and informed consent
Patient and informal carer dyads
Participants at each site were invited to take part in the research at the time they were admitted to the HAH services. A patient-directed flyer was made available at HAH sites to raise awareness about the study (see Report Supplementary Material 2).
The inclusion criteria were as follows:
-
patient admitted to HAH service
-
patient had a lay informal/family carer who also agreed to take part in the study (defined as someone who provided care and support at home on a daily basis)
-
ability to obtain informed consent from patient and carer.
The exclusion criteria were as follows:
-
patients without a suitable informal carer
-
inability to obtain consent from the participants
-
participants unable to complete questionnaires in English
-
patients in a care home at the time of admission to the HAH service.
Hospice at home service staff introduced the study to the patient and their carer. Information sheets (see Report Supplementary Material 3) were given to the participants and they were allowed time to read the information and ask any questions; if needed, the information sheet was read out.
Patients were asked to consent to taking part in data collection at one time point (on admission to the study or as soon as possible thereafter). They were also asked to agree to the collection of information on their use of health and social care services from 2 weeks prior to joining the study until death. The carers were asked for their consent to be contacted to complete a post-bereavement questionnaire, and informed that the option of taking part in an in-depth interview post bereavement would also be offered.
Service staff took consent from the patient and carer, using the study consent forms (see Report Supplementary Material 4), and both were given a copy of their information sheets and consent forms. Copies of the consent forms were filed in the study site file; a copy of the patient consent form was also filed in the patient’s medical notes. The carer was asked to provide contact details and to indicate the best time of day for the research team to call to collect data.
Owing to the nature of the patient population, some of the potential participants lacked capacity and were unable to provide informed consent. For this reason, a variable consenting process, involving consultee assent, was used. The local HAH team made the decision to proceed using one of the following options:
-
If the patient was deemed to have capacity by the local team, then consent was sought from the patient in the normal manner.
-
If the patient was deemed not to have capacity, then a personal consultee (i.e. someone who has a role in caring for the person who lacks capacity or is interested in that person’s welfare but is not doing so for remuneration or acting in a professional capacity) was approached for advice regarding the patient entering the study. The personal consultee could be a relative or friend of the person, in practice often the informal carer. 15
-
If the main carer or personal consultee was not available, a nominated consultee was approached for advice regarding the patient entering the study. The nominated consultee was a clinically qualified member of the patient’s care team who was not involved in patient consent or in study procedures such as data collection.
When a personal or nominated consultee was used, they were given an information sheet (see Report Supplementary Material 3) about being a consultee and the patient information sheet. They were given time to read the information and the opportunity to ask questions about the study and asked if, in their opinion, the patient would object to taking part in the study. The local staff member then gained a declaration from the consultee, using the study consultee declaration form (see Report Supplementary Material 4), as to whether or not they agreed that the patient would be willing to participate in the study.
Service providers and commissioners
The managers of HAH services identified a range of staff from their organisations for interview, to give a detailed picture of each organisation and its operations. These included clinical staff, the HAH service manager, charity trustees, fundraising staff and volunteers. Relevant commissioners from the local area were identified by HAH service providers for interview . Potential participants were invited by e-mail or by telephone by the research team and an information sheet (see Report Supplementary Material 3) and consent form (see Report Supplementary Material 4) were sent by e-mail or post. If they agreed, interviews were arranged (either by telephone or in person) at a time and location convenient for the interviewee. Prior to the interview, the participant was asked to complete a consent form.
Data collection
Baseline patient data
After consent, a member of the participant’s clinical care team assessed the patient using the Integrated Palliative care Outcome Scale (IPOS) (staff version),85,86 the Phase of Illness87,88 and the Australian modified Karnofsky Performance Status. 87,89 These instruments are recommended measures reflecting the key domains of palliative care, and have been validated for use in research. Patients were also asked if they had a PPOD (i.e. home, hospice, hospital).
Service use data
After consent, a member of the research team contacted the carer by telephone as soon as possible to collect health service use data retrospectively for the patient for the 2 weeks prior to recruitment. Data were collected using the Ambulatory and Home Care Record90 (AHCR), an instrument designed for capturing the use of health, social and voluntary services and informal caring for palliative care patients based at home. Items relate to services received both inside and outside the home [e.g. hospital appointments, accident and emergency (A&E) visits, inpatient stays]. The AHCR was customised for use in this study following piloting with a hospice population in England. 91 Carers were sent an optional ‘home care diary’ to assist with tracking service use.
Completion of each AHCR included three additional questions: satisfaction with services (scaled as follows: 1, exceeded expectations; 2, just met expectations; 3, fell short of expectations), carer burden [Short Form Zarit Burden Interview: six items relating to stress, strain, relationships, health, control and time for self, each scored on a 5-point scale, leading to a total score ranging from 0 (best) to 24 (worst)]92 and the patient’s health status [Eastern Cooperative Oncology Group (ECOG) scale, range: 0 (fully active) to 4 (completely disabled)]. 93 The last satisfaction and carer burden responses prior to death were used as measures of the performance of services.
After the collection of retrospective service use data, contact was made with the carer by telephone every 2 weeks to request completion of another AHCR covering the intervening 2-week period. In this way, a continuous record of services used by the patient could be collected. Researchers were assigned to data collection in specific case study sites to enable continuity with carers. Each telephone call lasted approximately 15 minutes.
Post-bereavement data collection from carers
Post bereavement, a follow-up letter was sent to carers to remind them that the research team would be in touch to collect further data. This letter included information sheets about the questionnaire and about the optional in-depth interview. Participants were given a choice about how to complete the questionnaire: by telephone, using an online survey tool or by post. The original protocol stated that the invitation to complete the Quality of Dying and Death questionnaire (QODD) would be offered either when hospice bereavement services made contact with the carer (usually around 6 weeks post death) or at 4 months [replicating the design of the Views of Informal Carers – Evaluation of Services (VOICES) survey94]. The researchers, who were already in contact with the participants to collect AHCR data, found that some participants expressed that they would prefer to compete the QODD earlier; a study amendment was approved to enable this.
The questionnaire contained the primary outcome measure, namely the QODD (English, 7-day recall, version 1), a validated 30-item instrument95–97 (note that we removed a question on euthanasia not relevant for use in the UK). Two short questions about the overall care received were also included in this questionnaire. The first asked if the carer and family had received as much support as they needed when caring for the patient (five-point scale, from ‘as much as needed’ to ‘no help at all’); the second was a rating of the quality of care received (five-point scale, from ‘outstanding’ to ‘poor’). These questions were taken from the VOICES questionnaire, a national survey of bereaved people conducted by the Office for National Statistics and commissioned by NHS England, based on research by Addington-Hall and McCarthy. 94
Three attempts were made to contact carers by telephone; if these were not successful, a paper copy of the QODD and VOICES questions was posted to the carer for completion (on one occasion only). This was accompanied by a cover letter to explain that the research team had been unable to contact them and if they would prefer to self-complete the questionnaire at home they could do so. A stamped addressed envelope was provided for return of the questionnaire.
Optional interview, bereaved carers
An in-depth interview was completed by a subset of participants; we aimed for up to 20 interviews per service model type, with a stopping criterion of three interviews if no new themes were coded, to achieve data saturation. 98 If the QODD was completed by telephone, the researcher asked the participant if they would be willing to participate in an optional in-depth interview by telephone or in person to understand more about the HAH service received. If the QODD was completed in the postal or online formats, carers could indicate at the end of the questionnaire if they would be happy to take part in an optional interview. If the postal or online QODD was not completed within 1–2 months, a final follow-up letter was sent to invite carers to take part in the optional interview only. Interviews were semistructured, following a topic guide (see Report Supplementary Material 5), and explored the experience of the HAH service and the EOLC the patient received.
Interviews with service providers and commissioners
The research team conducted interviews with 5–10 managers, health-care staff and commissioners per case study site. Interview schedules were designed for both staff and commissioners (see Report Supplementary Material 5) and were semistructured; they included questions to explore the service history, logic, rationale, funding, processes and contextual features facilitating or inhibiting service delivery, as well as enablers of and barriers to providing HAH services.
Withdrawal criteria
Participants were free to withdraw from the study at any time. Patients and carers were made aware in the information sheet that withdrawal would not affect the care they would receive. If a participant withdrew from the study, they were asked, if possible, if the data collected to date may still be used in the final analysis. If they did not wish for their data to be used in this way, all data collected from the participant were destroyed. If it was not possible to consult the participant on this, data collected up to the point of withdrawal were utilised according to the original consent.
Distress
A distress protocol was designed and made available to all case study sites (see Report Supplementary Material 6).
Phase 3: stakeholder consensus
Two national consensus workshops, with up to 60 participants each, were held. To maximise potential attendance from stakeholders, one workshop was held in London and one in Leeds. Each event took place over 1 whole day at a conference venue, facilitated by the project research team, including PPI members. HAH services that had participated in the phase 1 survey were offered a £50 bursary to support attendance at a workshop. Additional invitees were identified through the NAHH, study co-applicants’ networks and the Project Steering Group. Other organisations also advertised the events: Clinical Research Networks, Applied Research Collaborations, Clinical Commissioning Groups (CCGs), Healthwatch and other national charities and groups (e.g. Marie Curie). Stakeholders included service providers, commissioners, researchers, members of the public and service users. The purposes of the workshops were to fine-tune the CMO configurations developed in phase 2 of the study and to provide a more nuanced understanding of the features of HAH models that work, for whom and under what circumstances.
Emerging findings and relationships between contexts, mechanisms and outcomes were presented to stakeholders using a mix of formats and approaches, including lecture-style, small-group work and poster presentations (see Report Supplementary Material 7). Consensus workshop methods were used99 to facilitate discussion. Consensus event delegates also contributed to planning the methods of communicating the study findings, in particular advising on the presentation of information relevant and accessible to the public, service providers and commissioners of HAH services. After the events, participants were sent a workshop report.
Analysis
Phase 1
A descriptive analysis of survey responses was undertaken using Statistical Product and Service Solutions (SPSS) software, version 15 (SPSS Inc., Chicago, IL, USA), to gain an understanding of the range of HAH services. The analysis also sought to enable the identification of types of HAH service models for phase 2. Findings were presented in tables. Categorical variables [e.g. urban/rural setting, presence of hospice building(s), yes/no] were cross-tabulated with each other to identify underlying associations. Associations were explored between all variables. These results were used to identify any natural groupings of service features that could be defined as service models or types. Based on prior survey work from the NAHH21/Hospice UK (Heather Richardson and Andrew Thomson, personal communication), it was projected that approximately four high-level types of the model would be distinguished.
Qualitative field notes collected during the survey data collection were typed up and analysed inductively to identify relevant factors for the development of the typology. These were combined with the output from quantitative analysis and discussed at a meeting of the full team, resulting in agreement on a typology that could provide a framework for the recruitment of services as case studies for phase 2 (Figure 3).
FIGURE 3.
Service model typology. a, A 24-hour service provision is defined as two or all of the following: 24-hour hands-on care, 24-hour symptom assessment and management or fast response time (< 4 hours); b, provider size is based on having either more or fewer than 365 referrals per annum (one per day).
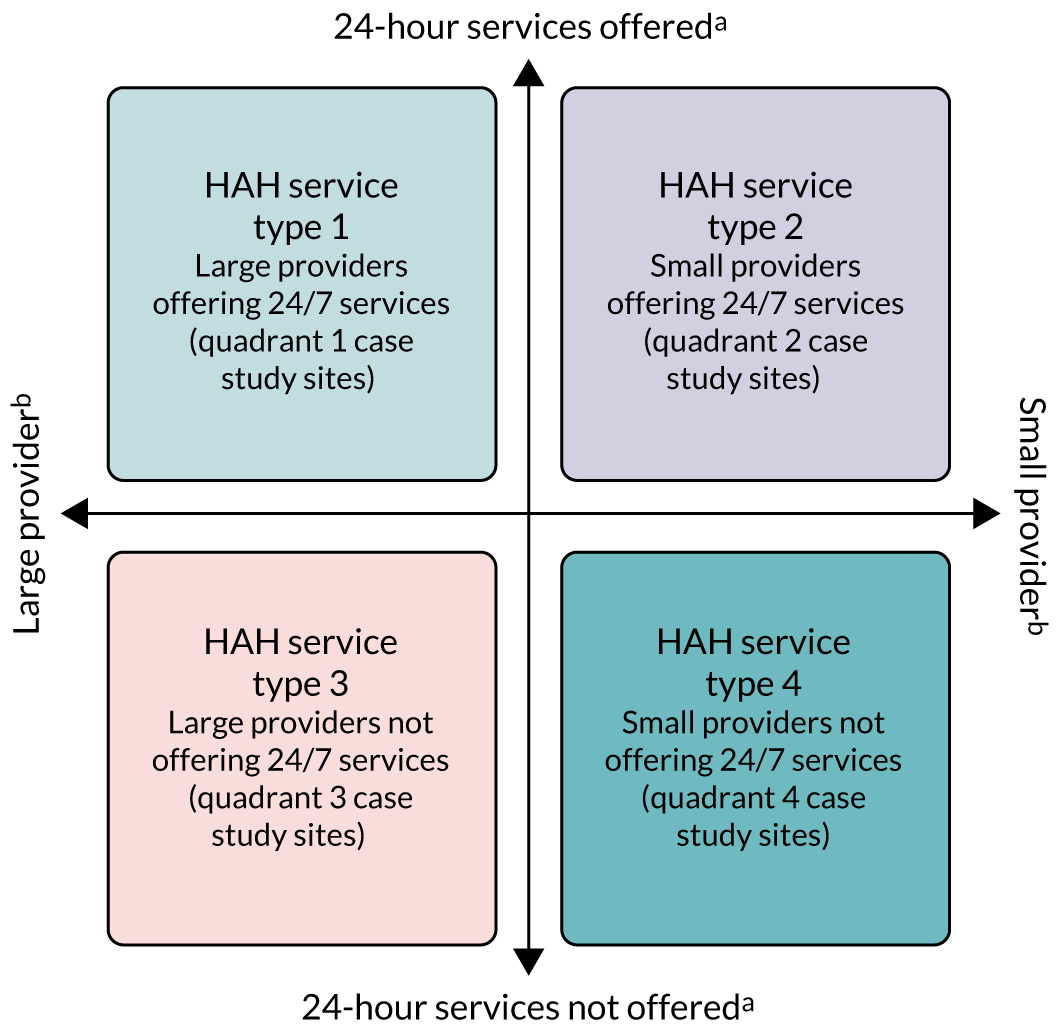
Based on survey responses, hospices that had indicated willingness to consider becoming a case study site were then approached to represent the identified service types as case study sites. We purposively sought diversity in geographical spread, socioeconomic profile, staffing mix and funding sources. Services were approached initially by e-mail; further queries and negotiation were managed by e-mail and telephone follow-up.
Phase 2
Sample size
The total score for the primary outcome measure, the QODD, ranges from 0 to 100 (a higher score indicates better quality). Hales et al. 100 identified scores of 30 and 70 as cut-off points for distinguishing terrible/poor (< 30), intermediate (30–70) and good/almost perfect (> 70) quality of death. 15 Hence, on the basis of a difference of 10 representing a meaningful change, and using a standard deviation (SD) of 16.41,101 at least 44 participants in each model would be required for comparisons between any pair of models. To allow for a participant non-completion rate of 33%, a sample size of 66 patients per model type (up to four models) was proposed. The non-completion rate was based on the 55.4% response rate obtained when the 24-item intensive care unit QODD was mailed to carers 4–6 months post death;102 a higher response rate was expected in this study because telephone interviews were being used.
Based on estimated HAH service size and annual throughput of patients, it was anticipated that recruitment of 66 patients per model type was achievable, for medium and large units in particular. The national minimum data set 2013/14 by the National Council for Palliative Care103 grouped HAH services by size into roughly three equal groups: small, < 191 patients per annum; medium, 191–310 patients per annum; and large, > 310 patients per annum. If small sites were recruited, it was agreed by the steering group to recruit two case study sites of the same model type to reach an overall sample size of 66. In the final regression modelling process (outlined below), a dummy variable would be used to distinguish between providers if comparisons were necessary.
Statistical analysis
Availability of data from the various sources [background/baseline, AHCRs, date of death (DOD) from hospice services or carer, post-bereavement interview for QODD and VOICES] was examined and patient–carer dyads were broken down into four categories according to the data they provided (with categories 3 and 4 merged for analysis purposes because no post-bereavement interview was possible):
-
date of patient death known and occurred before the end of the study period
-
patient/carer withdrew from the study before the end of the study period; data were available for analysis up until withdrawal unless the participant requested otherwise
-
patient still alive at the end of the study period
-
patient died at unknown date after the end of the study period.
The baseline sociodemographic characteristics of patients and carers, and the clinical status of patients in the different service models, were summarised using relevant descriptive statistics (proportions, medians, ranges, means, SDs, 95% confidence intervals, etc.) before being compared on the basis of each patient sociodemographic, clinical and carer feature using the appropriate bivariate test [including one-way analysis of variance (ANOVA), chi-squared tests and Kruskal–Wallis tests, depending on the nature of the variable]. The time between recruitment to the study and death was calculated and compared across models.
A minimum of six responses [from the total of 30 items (20%)] were required for the calculation of the total QODD score (as 10 × mean of all non-missing responses) from each carer. Several questions were not always applicable (e.g. spend time with pets), so a response rate of 100% was unlikely in most instances. The frequency of responses and summary statistics for total QODD score, and for the dichotomised form of the total QODD score (≤ 70 vs. > 70, the latter indicating a good/almost perfect death), were calculated, as recommended by Hales et al. 100
The secondary outcomes VOICES 1 (five-point scale relating to the sufficiency of the help and support from health and social care services that had been received) and VOICES 2 (a five-point quality rating of that help and support) were presented as frequency tables, given their ordinal nature. Achievement of PPOD was calculated for each patient for whom both the preferred and actual places of death were known; these values were presented by place of death as numbers and percentages. Means and SDs were calculated for the final secondary outcomes derived from the AHCRs: carer burden in last 28 days and service satisfaction in last 28 days. For each AHCR, the six-item carer burden (Zarit Burden Interview) total score92 was calculated [sum of six responses, 0 = never to 4 = nearly always, range 0 (best) to 24 (maximum worst burden)]. The mean of non-missing responses was assigned to missing items. For each AHCR, the service satisfaction was coded as ‘exceeded expectations’ = 1 (best outcome), ‘just met expectations’ = 2 and ‘fell short of expectations’ = 3 (worst outcome). A ‘last 28 days’ carer burden or service satisfaction score was included only if the final AHCR was conducted no earlier than 28 days before the patient died; any patient alive at the end of the study period, or with no known DOD, was therefore counted as missing.
All outcomes were compared between models using appropriate statistical tests. Because three of the four models included multiple HAH services, summary statistics were also generated at the HAH service level. Bivariate associations were explored between the QODD primary outcome score (total QODD score) and a set of covariates that were agreed as important by the research team. These included sociodemographic and clinical characteristics of the patient at baseline; place of death; how long before death the patient was aware that they were dying (from the QODD); number of days the carer had seen the patient in the last 7 days before death (from the QODD); how long the patient was in the study, and hence receiving hospice services (between recruitment and death); and time between death and when the carer completed the QODD. Appropriate statistical tests were used, depending on the nature of the variables.
Linear regression was used to model total QODD score, VOICES 1 and 2, carer burden in the last 28 days and service satisfaction in the last 28 days; logistic regression modelling was used for the dichotomised total QODD score and achieved PPOD. All outcomes were modelled (using forward stepwise selection) against predictors agreed on as important by the research team, with results including 95% confidence intervals for fitted parameters and goodness-of-fit statistics for the overall model. Service model was always included as a predictor, such that the fitted parameters in the final models indicate if service type is associated with differences in QODD scores. The characteristics of service types that result in better QODD outcomes were identified from descriptive data collected at each site as part of the realist evaluation.
Economic analysis
The economic analysis was planned at two levels. First, a descriptive analysis of the resources and costs of running each case study HAH service, covering staff; service facilities, inpatient beds, equipment, overheads; transport for home care; and other sundry items associated with care delivery. These data were requested during the interviews with service managers, together with information on activity rates and financing, so that costs per patient receiving the HAH service could be calculated and compared between case studies.
Second, a patient-level analysis was undertaken. Owing to the nature of this study, patients recruited were likely to have short and variable life expectancy, leading to an inconsistent time horizon for the individual patient-level data captured. This lack of a normalised time-integrated measure of health outcome (such as a quality-adjusted life-year) or cost, makes a traditional comparative cost-effectiveness analysis problematic. Hence, the economic analysis was limited to a descriptive analysis of service use and cost for the different HAH models. Whole-system resource use (provided by the hospice; local NHS primary, community and hospital services; and the voluntary sector) in EOLC was captured prospectively from the point of recruitment to the study for each patient. A customised version of the AHCR,91 which included informal care, was used for this purpose, as described in Service use data. At their first interview, participants were asked to report retrospectively, via recall, service use for the 2 weeks prior to recruitment.
Service use data, once captured, were grouped into time periods of approximately equal sample sizes, delimited by survival time following the start of the service use data collection. The cut-off points were determined by the distribution of the data. The methodology explaining how service use data were allocated to time periods, and how missing AHCR data were dealt with, is given in Appendix 2. Resource use was converted to costs [in 2019 Great British pounds (GBP)] using national tariffs. 104 Informal care was valued using replacement cost methods (see Appendix 3).
For each of the models of HAH service provision, an average cost per day of treatment was estimated for each time period. This provided descriptive cost data, independent of expected survival time, that can be compared between HAH models. Costs are presented as means and medians, given the typical skew in the distribution of costs. Comparisons of costs between each pair of HAH models were performed using the Mann–Whitney U-test and are presented as box plots showing medians and interquartile ranges (IQRs). Analysis was also broken down by individual HAH services within models to illustrate variability. Costs were considered in relation to outcomes from different models in a cost–consequences framework.
Qualitative data analysis of phases 2 and 3
A four-stage framework approach98,105 was undertaken, using retroductive analysis of the data. Retroduction demands counterfactual thinking based on knowledge and experience, analysing why expected phenomena anticipated in initial programme theories (such as volunteering) may or may not be present, and identifying what conditions are needed for them to be in place. 106 Consequentially, qualitative data analysis throughout the project was characterised by monthly team meetings to discuss what the data were suggesting could be happening, regular sounding-out with lay and content expert stakeholders and testing out these hypotheses in subsequent batches of data.
Stage 1, familiarisation, involved the research team reading the detailed written field notes taken during the telephone survey in phase 1, alongside phase 1 quantitative results suggestive of enablers of HAH services. In addition to monthly research team meetings, two discussion sessions with project stakeholders were conducted; from these, eight initial CMO configuration tables were developed (see Report Supplementary Material 8). These CMO configuration tables and the four core constructs of NPT78 (i.e. coherence, cognitive participation, collective action and reflexive monitoring) were used in stage 2, constructing an initial thematic framework. This framework was uploaded to qualitative data software (NVivo 12; QSR International, Warrington, UK). Interviews were transcribed verbatim and coded in NVivo. During monthly meetings, the research team reviewed a set of six to eight transcripts that were independently coded and then compared, discussed emerging themes and ensured a shared understanding of the coding framework. Stage 3, reviewing data extracts, was conducted during these regular meetings. Over 18 months, interviews from all participants and sites were reviewed by the research team. This involved organising data into more coherent groupings. 98 CMO configuration tables were refined down to six after further stakeholder discussions and it was noted that coding to CMO configuration tables and to NPT core constructs was not adding to interpretation at this level, but that NPT was useful as a lens for the next stage. Stage 4, mapping and interpretation, involved further refinement of CMO configuration tables before presenting them at phase 3 consensus workshops. Feedback from small-group exercises and group discussions was recorded by facilitators (research team members, including lay co-applicants) and compiled into a detailed report (see Appendix 4, including Table 26, Boxes 9–17 and Figures 18–22). The report was mapped against the CMO configuration tables and further refinements were made. NPT was used as a higher level of interpretation and to check that implementation of HAH could be explained through the generative mechanisms identified. Quantitative questions were derived from qualitative data and used for quantitative analysis (see Appendix 5). One example of this was that carers’ qualitatively described the perception of staff having time to provide extensive hands-on care and develop a relationship with the family. Quantitative data were then tested for staff grade (it being hypothesised that lower bands of staff were more likely to be providing hands-on care), number of visits per day, duration of visits and the relationship with the QODD scores. Once quantitative data analysis was completed, suggested statistical associations were used as a guide to further interrogate the qualitative data for plausible generative mechanisms. For example, quantitative data suggested that smaller service models had more positive outcomes, and the qualitative data were analysed for possible explanations.
In total, 25 iterations of CMO configuration tables were developed. These were based on the qualitative data findings (what was working and why), literature (what, in theory, should be working but is not present, and why) and outcome patterns suggested by quantitative data.
Ethics
Patients approaching the end of their lives are entitled to evidence-based care as much as any other NHS service user, and research is required to develop high-quality palliative care. There are, however, important considerations and vulnerabilities to be taken into account when planning research in this context and safeguards need to be put in place. The family/informal carers of dying patients are also experiencing a key life event and their vulnerability must be taken into account in study design. 107
Key areas of concern were as follows.
-
Emotional distress exacerbated by the demands of the research. A number of strategies were put in place to deal with this concern:
-
A leaflet was made available in all case study sites to advertise the research, so that potential participants might already be prepared to be approached when referred to HAH.
-
The study required written consent from both patient (or consultee) and carer, supported by full information about the study procedures. There was also a strength in the patient–carer dyad recruitment – because study subjects (patients and their carers) were recruited together as a pair, they were mutually supportive of the research and processes.
-
The majority of the data were collected by telephone, with support from researchers [there was a distress protocol for researchers to follow if a carer became distressed during data collection (see Report Supplementary Material 6)].
-
Participants were made aware of their right to withdraw from the study at any time, without providing a reason or jeopardising their clinical care.
-
-
Patients lacking capacity at recruitment or losing capacity as the study proceeded. For this reason, we had a variable consent process (see Patients lacking capacity) and we did not collect data directly from patients; instead, we used staff or carer proxy data collection methods.
-
Gate-keeping by staff as a result of patient vulnerability. We offered training and support to all staff involved in recruitment to address this concern and additional training and support resources were deployed when staff voiced concerns about this issue or when recruitment did not proceed as expected.
Summary
This chapter summarises the methods used in this study, which used mixed methods with an overarching realist evaluation approach. 108 The study was in three phases. Phase 1 was a survey of HAH services in England, to understand the range of contexts and operations and to develop a broad typology of services for further investigation. Literature reviewing, stakeholder insight and phase 1 of the study all contributed to the development of initial programme theories and candidate CMO configurations. Phase 2 involved quantitative, qualitative and health economics data collection from case study sites across England, to assess the impact of each model on patient and carer outcomes; to investigate the resource implications and costs of patient care in each model; to explore the experiences of patients, family carers, providers and commissioners of the different HAH models; and to identify the enablers of and barriers to embedding HAH models as part of service delivery. As the qualitative data were collected, the CMO configurations were iteratively tested and refined. Reciprocal reviews of CMO configurations and qualitative interview data were undertaken with quantitative and health economics data to synthesise the findings. In phase 3, through stakeholder consensus workshops, the data and explanatory CMO configurations were presented, further refined and validated.
Chapter 4 Patient and public involvement
Patients and members of the public whose care is the subject of research are well placed to work with researchers to design and deliver the best possible research. Although PPI is becoming more widely accepted in palliative care research, challenges remain with involvement being sought from a vulnerable population, and a potential lack of confidence among researchers to undertake it. 109,110 However, we integrated PPI in this study from development through to dissemination, incorporating co-production in some elements of the project. This chapter explains the work undertaken and highlights the important role that PPI played in the project.
The aim of patient and public involvement in this study
Parts of this section have been reproduced from Butler et al. 15 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In line with best practice, PPI informed and shaped the development stage, and contributed throughout the project and into dissemination. An advisory group was formed to support the development of the project for the grant application. Members were identified through Pilgrims Hospices and the University of Kent via links with existing PPI groups. The group consisted of four members, including two bereaved carers and two members of the public. The bereaved carers had previously had direct experience of HAH services as carers for patients receiving the service. The public members (one a hospice volunteer) had a keen interest in research and the work of the hospice. 15 The group provided advice on project design, research questions, outcome measures and the lay summary for the funding application. Two PPI representatives became public co-applicants on the project. Involvement from bereaved carers was key, as carers were the main participants in the study, providing proxies for the views and experiences of patients who were at the end of life.
The project’s public co-applicants were active in every part of the research. During the course of the project, the public co-applicants worked in partnership with the research team on the following tasks:
-
Designing the study materials, including information sheets, and study outputs, such as lay summaries, to disseminate the results to study participants and the wider public.
-
Analysing and interpreting study results, including reading and coding qualitative interviews and contributing to the development of CMO configurations. One public co-applicant (GS) also attended quantitative analysis meetings, providing insight on the possible causation of significant results.
In previous experience, we had not found it possible to recruit and retain patient representatives in palliative care research over the course of research projects, owing to their ill-health, but we aimed to consult with palliative care patients during this project. This was possible through links with the local hospice, Pilgrims Hospices; a consultation with patients attending day services was undertaken.
Patient and public involvement methods
The public co-applicants on the project increased the breadth of experience, knowledge and skills within the research team. 111 This added value to the project, particularly as it was a realist evaluation, whereby different perspectives contribute to theory generation and interpretation of the data. More broadly, being integral members of the research team ensured that the project was iteratively informed by the end-beneficiary perspective.
Facilitation of patient and public involvement in the project
All members of the research team worked with the public co-applicants, but a hospice research facilitator (CBr) had a dedicated role on the team to co-ordinate their involvement and provide support. The support was tailored to the individual needs of the public co-applicants, and included the following: partnership approaches to developing roles and expectations within the project; an introduction to understanding the research and governance approaches; and preparation and support for research meetings, for qualitative analysis in the case study phase and for facilitation in the consensus phase.
Charlotte Brigden also provided administration support relating to public co-applicant travel, accommodation, expenses and payments. The public co-applicants were paid for their time on the project and out-of-pocket expenses, in line with guidance from INVOLVE. 112 Honorary researcher contracts with the University of Kent were issued to them. For the ‘one-off’ PPI consultation via the Pilgrims Hospices with service users, carers and volunteers, a £10 voucher was provided as a token of thanks for their time and input, and travel expenses were offered.
Training for the public co-applicants was provided by the Centre for Health Services Studies, University of Kent, which had an existing PPI support programme. This included tailored training to support them with the analysis and interpretation of the qualitative interviews, including coding of these interviews. Additional training was provided on realist evaluation methodology and the concept of CMO configurations by experts on the research team at the beginning of the project and again during the analysis phase. A realist evaluation lay guide was produced for the public co-applicants as an additional support tool (see Appendix 6, including Table 28).
Effect of patient and public involvement on the study
In this section, detailed examples demonstrate how PPI and co-production were incorporated into the project through each phase.
Phase 1: survey of hospice at home services
The public co-applicants were part of the research team, interpreting and discussing the findings from the survey at a consensus meeting. This enabled co-production by a process of joint decision-making, which included the following:
-
The development of the model typologies.
-
The selection of the shortlist of potential case study sites for phase 2 of the study. The public co-applicants encouraged and supported the inclusion of mixed populations in diverse areas (e.g. including services from the north and south of the country, rural and urban areas, and deprived and affluent areas).
Phase 2: in-depth case studies
Patient and public involvement activities included advising on public-facing study documents so that they were ready to submit for Health Research Authority governance and ethics approval, such as participant information sheets and data collection forms. They also provided insight into appropriate processes and procedures for approaching patients and carers.
As patients with capacity were invited to participate, feedback on a patient version of the participant information sheet was also sought from current hospice patients through day-care services, and local HAH service staff were also consulted. This input resulted in the following:
-
Improvement of the language and content of the documents to make them more accessible and understandable to potential participants.
-
Advice about when and how to follow up potential participants.
-
The suggestion that a flyer should be designed to give out to potential participants in advance. The concept was to introduce the research to patients and carers prior to them accessing HAH services. Then, if they became eligible for inclusion, when it may be a more difficult and sensitive time to ask, they would already be aware of the research and more likely to be able to consider participating. The public co-applicants provided further feedback on the detailed content of the flyer when it was produced (see Report Supplementary Material 2).
A co-production approach evolved as the project progressed through each phase. Co-production takes PPI one step further to an approach in which researchers, practitioners and the public work together, sharing power and responsibility, including the generation of new knowledge. 113
One public co-applicant described this process:
At the outset, our role was far less hands-on, but as the project progressed, we wanted, and felt more confident, to be more actively involved. To facilitate this, specific training was arranged to make this possible. The team too had to be very accommodating to our frequent presence at meetings.
Examples of co-production in phase 2 between the researchers and public co-applicants included working on the following:
-
The processes and procedures for data collection from carers using the questionnaire tools (i.e. the QODD and the AHCR).
-
The recruitment procedures for the study, how and when to approach potential participants to complete the questionnaire tools.
-
How to approach the follow-up of carer participants when researchers were having difficulties contacting them (e.g. three attempts was enough).
-
Input on the decision-making on the timing of data collection after a loved one had died (e.g. 4 months seemed too long, 6 weeks about right, or sooner if it was the carer’s wish).
-
Interpretation and discussion of the quantitative data from carers (i.e. the QODD and the AHCR).
-
Development of the qualitative interview topic guide.
-
Feedback on the qualitative interview coding framework.
-
Iteratively analysing and discussing the interview data from service provider, commissioner and carer interviews (public co-applicants helped code carer interviews). This work was used to modify and develop the CMO configurations.
The public co-applicants in particular contributed to the interpretation of:
-
the relationships between carers and HAH service and other care professionals
-
the changing relationship between carer and patient as the illness progressed and needs were greater
-
how the care was negotiated, how much the carer accepted taking on/carrying on versus wanting or seeking outside support
-
models of service support available to the carer and patient, including volunteers
-
the importance of, and threats to, continuity of the care offered
-
the importance of what HAH services offered that was different (e.g. ‘time to care’, not ‘task orientated’, not just the length of time but the ‘pace’, ‘presence in the moment’), while still doing what was needed and filling the gaps in care.
In addition, in phase 2, the public co-applicants recommended that a newsletter be provided for all the participating project sites, ensuring that those services were kept informed of project progress.
Phase 3: consensus meetings
The final phase of work involved stakeholder consensus and feedback on the emerging results. Targeted advertising flyers for the events were designed for professional and public audiences and the public co-applicants advised on content, language and design/layout.
Each of the consensus event workshops focused on an emergent CMO, two of which were ‘support directed at the carer’ and ‘volunteers’. In preparation for these workshops, discussion groups were undertaken with a local group of volunteers and carers identified through Pilgrims Hospices. One public co-applicant (GS) helped to design and facilitate the groups, which took place on 25 November 2019. The groups covered topics on access to services and co-ordination of care, bereavement support and involvement of volunteers. When direct experience was lacking, Graham Silsbury was able to tease out some responses ‘in theory’ on what attendees thought would be good care in relation to the emergent themes of the CMO configurations. Knowing who to call and being responsive when needed, particularly OOH, were the main areas of concern for the carers.
The volunteers’ group generally saw that there could be a role for volunteers in HAH services, but more for befriending-type services, rather than personal care or even bereavement, which they felt should be the domain of the professionals. They felt that having structure and support as a volunteer, with reporting/communication mechanisms in the organisation, was preferable to being more autonomous in their volunteering roles.
Co-production continued in the consensus phase of the project. Examples of co-production in this phase of the project included the following:
-
the most relevant discussion groups for the consensus events were planned and facilitated collaboratively between Charlotte Brigden, Graham Silsbury and Mary Goodwin
-
the planning and organisation of the consensus events were agreed collaboratively between the researchers and the public co-applicants
-
co-facilitation of some of the workshops/sessions at the consensus events (e.g. the ‘supporting carers’ workshop, the speed-dating poster session and the ‘so now you know’ session on ideas for project outputs and dissemination).
The feedback from the consensus events was synthesised by the research team, including the public co-applicants, which validated and provided further support for the CMO configurations.
Project outputs and dissemination
The public co-applicants were consulted during the writing of the lay summary for this report. For broader dissemination, the public co-applicants have helped with ideas to summarise and present the findings of the project in a way that is more easily accessible to service users and members of the public. Further advice on outputs for different audiences was gathered at the consensus events, with significant contributions from the public attendees.
Poster and oral presentations of the co-production work and the roles that the public co-applicants had on the project have been disseminated at regional and national conferences. The public co-applicants helped with the content and design of a poster114 and one public co-applicant co-presented with the research facilitator at a regional London/South East co-production conference, showcasing OPEL as an example of co-production in action in health research. 115 The public co-applicants have also been given opportunities to comment on other outputs from the project, for example a journal article, for which they have been included in the authorship. 22
Assessing impact
To provide feedback to our public co-applicants and assess the impact of PPI in the OPEL study, we used guidance produced in the East of England, led by the University of Hertfordshire. 116,117 An impact form was completed after every activity involving PPI. The information in the feedback forms was collated into flow charts, which were shared with the public co-applicants at the end of each project year (see Appendix 7).
The summary flow charts also acted as prompts for the public co-applicants to provide their own feedback at a dedicated session at the end of each project year. These sessions worked well when run at a time separate to the more formal project meetings at the university; for example, at the end of year 1 of the project, Charlotte Brigden and Claire Butler arranged to meet the public co-applicants in a local pub. This provided a more informal environment that enabled open discussion about how they had found the activities so far and how they would like to be involved in the future. At this meeting, we realised that they would like to be more aware of what was happening with the study day to day, not just those things specifically related to their PPI activities. As a result, they subsequently attended monthly project management meetings. It was also a good time to explain and discuss the case study phase of the research (phase 2) and establish what activities they would be happy to be involved in.
Feedback sessions were also organised so that the wider research team was included, for example a post-meeting afternoon tea at the end of year 2. At this meeting, it emerged that one public co-applicant was finding the coding of the interviews challenging, and we suggested alternative ways to contribute and provide interpretation of the interviews through summarised feedback. They also found that the coding felt quite isolating, as they wanted to be able to cross-check with others. Furthermore, they highlighted the contextual importance of listening to the interview alongside reading the transcript. A session was then arranged for the two public co-applicants to listen to some interviews.
Discussion and conclusions
Patient and public involvement (and co-production) have positively affected each stage of the OPEL study. Having two public representatives as co-applicants on the project, equally and fully part of the research team, as well as having a dedicated PPI facilitator, helped to enable their continuous involvement with the study. One public co-applicant highlighted the importance of the role of a dedicated PPI facilitator:
Although the whole team were welcoming, supportive and valued our input, the facilitator role was pivotal in creating a closer working relationship that was always available. It made it easier to discuss personal concerns about potential limitations on our input or areas of uncertainty.
Other learning from the PPI experiences in this project included the importance of responding to individual PPI preferences and differing degrees of involvement, for example one public co-applicant very much enjoyed detailed coding of transcripts, whereas another preferred to have the audio file of the interview to listen to and to ‘tell the story’. These different approaches added richness to the analysis.
Reflections/critical perspective
The challenges of PPI in the context of palliative care109,110 were arguably easier to overcome in the OPEL study as the main PPI representatives were bereaved carers/those with experience of caring at the end of life, as opposed to patients and carers currently in receipt of services. However, as they were recalling their own experiences as carers, we had to be mindful of any unintended effects and offer and provide support to them as needed.
We felt that our approach was fitting, as bereaved carers were the main participants in the research and we did try to address different perspectives by reaching out to consult with patients and others for elements of the study when appropriate. The absence of views and experiences of ethnic minorities in the research has been a limitation; involving a more diverse population as PPI representatives, as well as research participants, could be considered in future projects.
Recommendations for facilitating PPI in future studies:
-
There is a need to be flexible, responding to and respecting the different needs of the PPI representatives. It should not be assumed that the needs will be the same for all PPI representatives involved for the same activities/tasks. The degree of involvement of each does not have to be identical.
-
Having some informal ‘space’ or time away from the project activities/meetings to discuss how PPI is working with PPI representatives is valuable. This should be conducted alongside regular recording of PPI impact and careful feedback.
-
Having a dedicated PPI facilitator role in the research team enriched and facilitated the PPI contribution throughout the project. It is important that the person in this role has an understanding of the research and is up to date with project activities, particularly if they are not directly involved as a project researcher.
-
Having the PPI representatives as project co-applicants helped to establish them as equal members of the project team. However, this is not enough on its own, and it is important to ensure that they feel included, as other members of the team are, in the day-to-day running of the project.
-
Developing relationships and building the team is work in itself and does not happen automatically. For this project, the realist evaluation method helped to foster the co-production, which evolved over time.
-
There would be benefit in being able to involve patients and the public from ethnic minority groups who are interested in health-care research and would be willing to be PPI representatives. This would help to ensure that their views and experiences are taken into account in future research.
These points are by no means unique to this study; similar findings have been expressed elsewhere. 118
Summary
Patient and public involvement, through a range of different approaches, made important contributions to all elements of the study, and, in some areas, developed into full co-production. PPI input was well suited to realist evaluation, which is interested in engaging the views of a range of stakeholders at each stage, from selection of initial programme theories and the interpretation of the data collected to testing these propositions and their further refinement as CMO configurations.
Chapter 5 National survey results and identification of service models
National survey
The aims of the survey of HAH services were to identify the range and variation in HAH delivery models across England and to categorise the services into models according to key features and settings. The survey findings enabled the identification of services representing each model.
Of the 128 services invited, 113 (88%) were charity-led services and 15 (12%) were NHS-led services. Survey data were collected from 70 HAH services (55% response rate) over a 5-month period (February 2017 to July 2017). Twenty-two services opted out of taking part in the survey and a further 36 services could not be contacted after three attempts. There were no significant differences between responders and non-responders based on urban/rural settings.
Characteristics of hospice at home services
Responding HAH services reported varied numbers of referrals per annum [mean 452 (SD 393.7) referrals, minimum 62, maximum 2222]. Some services covered very large areas (across counties). They served total populations ranging from 5000 to 1.2 million (mean 323,488). On average, 2.5 referrals were received per 1000 of the total population (SD 2.5 referrals) annually.
Key characteristics of responding HAH services are shown in Table 2. Two-thirds of services relied on charitable funds or donations as their main sources of income, one-quarter of services were funded mainly by the NHS and three were fully funded by the NHS or their local authority. Many HAH services (n = 44, 62.9%) received NHS funding as a secondary source, but nine services (12.9%) received no NHS funding at all. When asked if having inadequate funding made it difficult to provide HAH services, 59 (84.3%) indicated that it made service provision somewhat or substantially difficult, whereas nine (12.9%) felt that inadequate funding did not affect service provision.
| Variable | Characteristic | n (%) | Mean (SD) | Minimum, maximum |
|---|---|---|---|---|
| Main funding source (missing 4) | NHS | 17 (25.8) | – | – |
| Charitable/donations | 47 (71.2) | – | – | |
| Other | 2 (3.0) | – | – | |
| Geographical area | Rural | 11 (15.7) | – | – |
| Urban | 7 (10.0) | – | – | |
| Mixed | 52 (74.3) | – | – | |
| Level of deprivation | Predominantly deprived | 5 (7.1) | – | – |
| Mixed | 54 (77.1) | – | – | |
| Predominantly affluent | 11 (15.7) | – | – | |
| Life expectancy referral criteria | Within hours/days | 1 (1.4) | – | – |
| Last 2 weeks of life | 11 (15.7) | – | – | |
| Last month of life | 9 (12.9) | – | – | |
| Last 3 months of life | 7 (10.0) | – | – | |
| Last 6 months of life | 2 (2.9) | – | – | |
| Last year | 12 (17.1) | – | – | |
| Life expectancy > 12 months | 28 (40.0) | – | – | |
| Setting/other services in area | Local district nursing 24/7 | 54 (78.3) | – | – |
| Other HAH services | 18 (25.7) | – | – | |
| Marie Curie services | 49 (70.0) | – | – | |
| Inpatient palliative care beds | 66 (94.4) | – | – | |
| Hospital palliative care beds | 5 (7.6) | – | – | |
| Community hospital beds | 17 (25.8) | – | – | |
| Care/nursing home beds | 3 (4.6) | – | – | |
| Care provided | Hands-on personal care | 68 (97.1) | – | – |
| Of which 24/7 | 35 (52.2) | – | – | |
| Symptoms: assess and manage | 64 (91.4) | – | – | |
| Of which 24/7 | 39 (60.9) | – | – | |
| Psychosocial support | 66 (94.3) | – | – | |
| Of which 24/7 | 40 (60.6) | – | – | |
| Practical support at home | 15 (21.4) | – | – | |
| Of which 24/7 | 2 (2.9) | – | – | |
| Respite care | 52 (74.3) | – | – | |
| Of which 24/7 | 33 (52.2) | – | – | |
| Time that HAH services cared for patients | < 1 week | 9 (15.0) | – | – |
| Between 1 week and 2 months | 36 (60.0) | – | – | |
| > 2 months | 15 (25.0) | – | – | |
| Response rates | Within 4 hours | 44 (65.7) | – | – |
| Within 24 hours | 20 (29.9) | – | – | |
| Next working day | 3 (4.5) | – | – | |
| Number of dedicated staff (missing 2) | HCA | 59 (86.8) | 9.13 (7.68) | 0, 40 |
| RN | 58 (85.3) | 5.55 (4.79) | 0, 22 | |
| Medical consultant/other doctor | 18 (26.5) | 0.36 (0.69) | 0, 3 | |
| Physiotherapist | 17 (25.0) | 0.28 (0.51) | 0, 2 | |
| Occupational therapist | 15 (22.1) | 0.24 (0.46) | 0, 2 | |
| Counsellor | 22 (32.4) | 0.54 (0.97) | 0, 4 | |
| Social worker | 9 (13.2) | 0.15 (0.40) | 0, 2 | |
| Chaplaincy | 15 (22.1) | 0.24 (0.46) | 0, 2 | |
| Volunteers | 26 (38.2) | 8.79 (30.26) | 0, 220 | |
| Administrators | 47 (69.1) | 1.18 (1.24) | 0, 5 | |
| Management (all RNs) | 64 (89.7) | 1.10 (0.69) | 0, 4 | |
| All staff (not including volunteers) | – | 19.0 (10.84) | 1, 51 | |
| RN-to-HCA ratio, FTE (missing 2) | More RNs than HCAs | 24 (35.3) | – | – |
| More HCAs than RNs | 40 (58.8) | – | – | |
| Equal numbers of RNs and HCAs | 4 (5.9) | – | – | |
| Ease to recruit/retain (missing 2) | No difficulty | 38 (55.9) | – | – |
| Somewhat difficult | 28 (41.2) | – | – | |
| Substantially difficult | 2 (2.9) | – | – |
Services operated predominantly in mixed urban and rural settings and across areas with mixed deprivation levels; few services were operating in predominantly deprived areas. When asked whether or not the geography of the area made it difficult to provide services, most responders (97%) thought that this factor made service provision challenging. Most, but not all, services operated alongside 24-hour district nursing NHS services; just over one-quarter were operating alongside other HAH services in the same area.
Services had highly variable referral criteria with respect to the life expectancy of patients accepted for HAH care. Very few services provided care solely for the actively dying, defined as having hours or days to live; more than half of services accepted patients with a prognosis of up to or > 1 year. When asked if the referrals made to the service were manageable and appropriate, 97% of service managers responded that the referrals received were somewhat or substantially manageable and appropriate for their service.
Most HAH services reported providing personal, hands-on care for patients (such as washing and personal care), symptom assessment and management, psychosocial support and respite care for carers. Approximately half of HAH services were able to provide care 24/7. Fewer services provided practical support (household tasks, e.g. shopping) directly for family members or carers. Most HAH services were able to provide rapid response times (including at weekends) within 4 hours.
On average, services cared for patients for between 1 week and 2 months once referred. Service managers reported that intensity of care data were not routinely collected and were difficult to provide. Nearly half (n = 32), however, stated that they provided intensive care to patients (> 3 hours per day). Almost all services had local access to inpatient palliative care beds, if required, in a hospice, a hospital or a care home setting.
When asked about factors that made it difficult to provide HAH services, two main factors emerged. Delay in being able to administer anticipatory medicines by injection in a timely fashion was cited by 43 (61.4%) HAH services as somewhat or substantially difficult, and an inability to access necessary equipment and anticipatory medicines was problematic for 39 (55.7%). Almost all service managers felt that HAH services received substantial non-monetary support from local commissioners, the hospices themselves, community nurses and GPs (98.1%, 98.6%, 100.0% and 100.0%, respectively).
Staffing
On average, HAH services employed 19 members of staff, but the range was large (see Table 2). More than half (n = 37, 52.6%) of the services had at least three or more different disciplines among their staff. Nearly all services employed RNs and/or HCAs to provide day-to-day care (n = 66, 98.6%). Most services used more HCAs than RNs. Four HAH services were staffed with RNs only, and four with HCAs only. Many services (n = 45, 66.2%) did not employ additional staff solely dedicated to HAH services, instead drawing on clinicians and HCPs working across hospices and/or NHS services. Just over half of the HAH services reported no difficulty recruiting and retaining staff. Detailed staffing data proved difficult to collect and analyse, as many HAH services could not provide accurate data at the time of the survey. Therefore, findings on type of staff employed by HAH services and full-time equivalents should be interpreted with caution.
Views on enablers of hospice at home services
Parts of this section have been reproduced from Butler et al. 15 © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2018. All rights reserved. No commercial use is permitted unless otherwise expressly granted. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The survey asked service managers about elements that supported provision or made it difficult to provide HAH services in their areas (Figure 4). Field notes recorded during survey interviews provided further insight into key contributing features for successful services. First, planning and integration of services locally was a major factor contributing to the provision of HAH services. Having a detailed business plan for commissioning and integration with other local end-of-life services enabled HAH service provision and funding. Furthermore, direct access to NHS trust services or other suppliers of medication and equipment, as well as suitably trained and prepared people to undertake medication administration, were key factors to patient care remaining within the home. The presence of an integrated patient record also allowed better integration and facilitated arrangement of anticipatory prescribing and advance care planning across providers.
FIGURE 4.
Enablers of and barriers to HAH services.
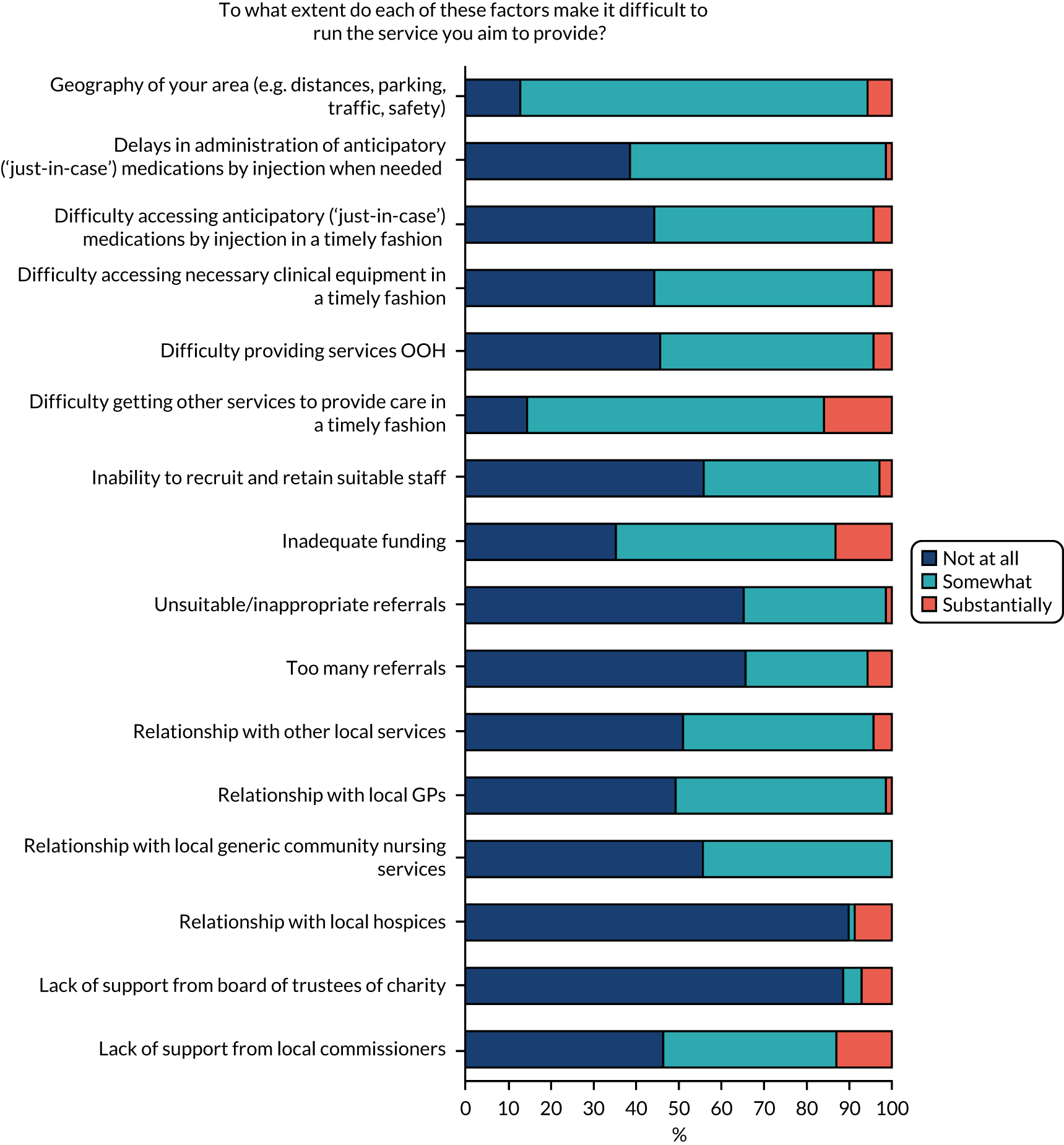
Workforce, staff skills and wider support also emerged as key to supporting HAH services that allowed patients to die at home. Service managers expressed the need to have a service able to respond to changes in demand, as patients could deteriorate at any time in the last hours/days/weeks of life, and their resulting service needs fluctuated accordingly. Using a skilled workforce mix of permanent and flexible staff (under zero-hour contracts) enabled services to adapt to demand. Many service managers also reported that identifying patients requiring rapid response or intensive support using trained triage staff and being able to communicate the support available to patients and families were key features of success. HAH services also benefited from a well-trained and extensive network of third-sector support, volunteers and a responsive family support system. 15
Service models: typology
The goals of the survey were to understand the current national landscape of HAH provision and to identify ‘model types’ of HAH services for further investigation. A typology of services was explored from national survey responses, but the heterogeneity meant that it was difficult to see clear groupings. Hence, a pragmatic approach was taken. The size of a service had been stipulated in the protocol as an important criterion for differentiating services. Following discussion among the full team and with the steering group, whether or not a service provided care 24/7 was selected as a second distinguishing feature. This resulted in four model types (quadrants): large and small services with and without provision of 24/7 care (see Figure 3).
The size of a service was defined in terms of number of referrals, with large services being those reporting > 365 referrals per year (i.e. more than one per day), and small services being those with fewer referrals than this.
Whether or not a service provided care 24/7 was defined according to whether or not a service met two or more of the following conditions (based on the service’s response to the national survey):
-
hands-on care provided 24/7
-
symptom assessment and management provided 24/7
-
able to respond within 4 hours.
Recruitment of hospice at home services
Eight HAH services were originally included in phase 2 of the project. All eight were inducted into the study between November 2017 and February 2018. One service dropped out as a research site owing to workforce changes, having recruited three patient–carer dyads. As recruitment for the study fell behind the projected target, a further five HAH services were recruited to the study between October 2018 and February 2019. Two HAH sites were closed to the study in January 2019, having met recruitment targets, and the remaining nine continued to recruit until close of study recruitment on 30 June 2019. Although no patient–carer dyads were recruited to the study after 30 June 2019, data collection continued until 30 October 2019. In all, data were analysed for 12 HAH services, four in quadrant 1 (Q1) (larger, 24/7 services), four in Q2 (smaller, 24/7 services), one in Q3 (larger, not 24/7 services), three in Q4 (smaller, not 24/7 services).
The characteristics of the HAH services according to eligibility criteria for service models are shown in Appendix 8. The 24/7 availability of NHS district nursing services is also shown.
Among the five HAH services not meeting the criteria for providing 24/7 care (i.e. models in Q3 and Q4), one HAH service reported 24/7 symptom assessment and management and another reported ability to respond within 4 hours; two reported that DNs were available in the area 24/7.
Summary
The survey provided, to our knowledge, the first detailed description of the range of HAH service provision existing in England. Services reported widely varying levels of activity, staffing configurations and referral criteria. The term ‘hospice at home’ does not have consistent meaning. Although almost all of the HAH services provided personal care, psychosocial support and symptom management, not all provided this 24/7. Most services were providing care for, on average, 1 week to 2 months from referral, and most had staffing with a greater proportion of HCAs than of RNs. Two-thirds of services reported charity donations as the main source of funds. The main difficulties faced by HAH services were geography of their area, difficulty getting other services to provide care in a timely fashion and difficulties accessing equipment and medications (both drugs and administration) in the home. A typology of services was explored from national survey responses, but the heterogeneity within the sample meant that it was difficult to see clear groupings. Hence, a pragmatic approach was taken, grouping services depending on their size and on whether or not they provided 24/7 support.
Chapter 6 Case study findings: patient and carer outcomes and costs
Recruitment of participants within hospice at home and service models
A total of 339 dyads were recruited from 12 HAH services. The target sample size of 66 patients was reached in each service model; there were four HAH services in models 1 and 2, three HAH services in model 4 and one in model 3 (Table 3). The number and proportion of dyads by model ranged from 75 (22.1%) in model 4 to 103 (30.4%) in model 1; the number of dyads from individual hospices ranged from three to 81 (see Table 5). Over-recruitment of patient–carer dyads (compared with the original protocol) was undertaken because it became clear as the study progressed that the QODD completion rate was lower than had been predicted; this amendment received ethics approval.
| Model | HAH service | Participants (dyads) | Pie chart: participant numbers by service models | ||
|---|---|---|---|---|---|
| n | % of total | % of service model | |||
| Q1: large, 24/7, N = 103 (30.4%) | Acacia | 3 | 0.9 | 2.9 | |
| Camellia | 12 | 3.5 | 11.7 | ||
| Echinacea | 22 | 6.5 | 21.4 | ||
| Peony | 66 | 19.5 | 64.1 | ||
| Q2: small, 24/7, N = 80 (23.6%) | Dahlia | 21 | 6.2 | 26.2 | |
| Gardenia | 16 | 4.7 | 20.0 | ||
| Lavender | 24 | 7.1 | 30.0 | ||
| Violet | 19 | 5.6 | 23.7 | ||
| Q3: large, not 24/7, N = 81 (23.9%) | Wisteria | 81 | 23.9 | 100.0 | |
| Q4: small, not 24/7, N = 75 (22.1%) | Hyacinth | 31 | 9.1 | 41.3 | |
| Marigold | 34 | 10.0 | 45.3 | ||
| Xyris | 10 | 2.9 | 13.3 | ||
| Total | 339 | 100.0 | |||
Data availability for analysis
Although 339 dyads were recruited, data were not available for all participants for all outcomes. Of the 339 patients recruited, 284 (83.8%) died during the study period. A DOD was established (either reported by carers post bereavement or obtained from the HAH service) so that time in the study from recruitment to death could be calculated.
A post-bereavement interview to collect responses to the QODD was given by 132 carers (46.5%) of the 284 people who died during the study period.
Of the 339 dyads recruited, 221 (65.2%) provided service use data by completing one or more AHCRs. Of these 221, it was possible to include 178 (80.5%) in the analysis of costs because they died during the study period and had a known DOD.
The availability of data on key outcome measures is summarised in Table 4. There were 327 dyads for which different combinations of outcomes were available. Twelve dyads provided no AHCRs (service use information) and no QODD because the patient was still alive at the end of the study. There were 43 dyads that had supplied at least one AHCR but for which the DOD was not known, and there were 67 dyads for which the DOD was known but there were no AHCRs or QODD data.
| Combination | With QODD | With AHCR | n (%) |
|---|---|---|---|
| Did not die during study, no DOD | No | No | 12 (3.5) |
| No | Yes | 43 (12.7) | |
| Died during study and DOD known | No | No | 67 (19.8) |
| No | Yes | 85 (25.1) | |
| Yes | No | 39 (11.5) | |
| Yes | Yes | 93 (27.4) | |
| Total (N) | 339 | ||
Characteristics of participants at recruitment, by service model
There were no differences in background sociodemographic characteristics of participants recruited across the four models, except that carers in models 1 (larger, 24/7 services) and 4 (smaller, not 24/7 services) were more likely to be partners (rather than friends) of patients, and they were significantly older than the carers in the other models (see Appendix 9).
Clinical measures collected by hospice staff at recruitment showed differences between the models, with patients in models 3 (larger, not 24/7 services) and 4 (smaller, not 24/7 services) having worse health status than those in models 1 (larger, 24/7 services) and 2 (smaller, 24/7 services). Scores for the IPOS for each service model are shown in Table 5 and Figure 5, confirming the significantly worse health status of participants in models 3 and 4 at the point when they joined the study. The severity of reported outcomes was also explored. Of the 337 non-empty IPOS forms, 306 (90.8%) had at least one ‘severe’ (score 3) or ‘overwhelming’ (score 4) response [model 1: 88/102 (86.3%); model 2: 70/79 (88.6%); model 3: 79/81 (97.5%); and model 4: 69/75 (92.0%); chi-squared test, p = 0.058]. Individual IPOS items by service model are given in Appendix 10, Tables 31–48.
| Model | Completed IPOS (n) | IPOS score | ANOVA | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | SE | 95% CI for mean | Minimum | Maximum | |||
| 1: Large providers, 24/7 | 102 | 22.36 | 8.20 | 0.81 | 20.75 to 23.97 | 4.25 | 45.90 | p < 0.0005 |
| 2: Small providers, 24/7 | 79 | 24.06 | 9.94 | 1.12 | 21.84 to 26.29 | 2.13 | 49.30 | |
| 3: Large providers, not 24/7 | 81 | 27.62 | 7.46 | 0.83 | 25.97 to 29.27 | 3.92 | 46.36 | |
| 4: Small providers, not 24/7 | 75 | 28.14 | 9.80 | 1.13 | 25.89 to 30.39 | 6.00 | 51.00 | |
| Total | 337 | 25.31 | 9.15 | 0.50 | 24.33 to 26.29 | 2.13 | 51.00 | |
FIGURE 5.
The IPOS score at recruitment: mean with 95% CIs for each service model. CI, confidence interval; Q, quadrant.
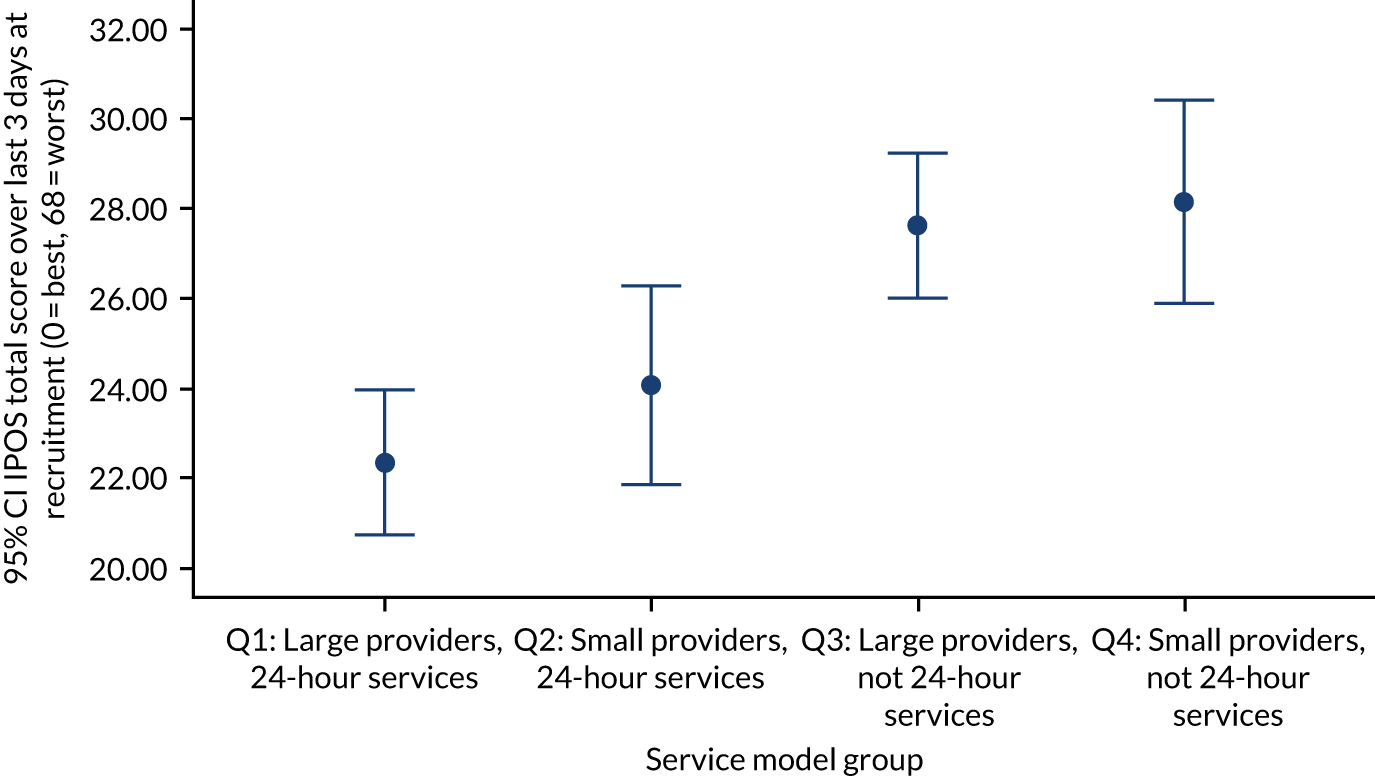
Data at recruitment on functional status (Karnofsky score: 0% = dead . . . 30% = almost completely bedfast . . . 100% = normal) identified patients in models 2, 3 and 4 as being sicker at baseline. The proportions of patients in the ‘deteriorating’ and ‘dying’ categories of the patient Phase of Illness measure were also highest in models 2, 3 and 4 (Table 6).
| Indicator | Service model | Total, N (%) | Difference between models, test (p-value) | |||
|---|---|---|---|---|---|---|
| 1: Large providers, 24/7, n (%) | 2: Small providers, 24/7, n (%) | 3: Large providers, not 24/7, n (%) | 4: Small providers, not 24 /7, n (%) | |||
| Karnofsky score, patient functional status (%) (N = 327), sample mean 42.3% | ||||||
| 10 (worst, 0 = dead) | 0 (0) | 4 (5.6) | 2 (2.5) | 1 (1.4) | 7 (2.1) | ANOVA (< 0.0005) |
| 20 | 12 (11.7) | 30 (41.7) | 19 (24.1) | 18 (24.7) | 79 (24.2) | |
| 30 | 8 (7.8) | 8 (11.1) | 13 (16.5) | 13 (17.8) | 42 (12.8) | |
| 40 | 7 (6.8) | 9 (12.5) | 10 (12.7) | 16 (21.9) | 42 (12.8) | |
| 50 | 14 (13.6) | 12 (16.7) | 27 (34.2) | 17 (23.3) | 70 (21.4) | |
| 60 | 32 (31.1) | 5 (6.9) | 8 (10.1) | 8 (11.0) | 53 (16.2) | |
| 70 | 18 (17.5) | 2 (2.8) | 0 (0) | 0 (0) | 20 (6.1) | |
| 80 | 10 (9.7) | 0 (0) | 0 (0) | 0 (0) | 10 (3.1) | |
| 90 | 2 (1.9) | 1 (1.4) | 0 (0) | 0 (0) | 3 (0.9) | |
| 100 (normal) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (0.3) | |
| Patient Phase of Illness scores (N = 332), median 2 | ||||||
| 1. Stable | 28 (27.2) | 32 (42.1) | 15 (18.8) | 20 (27.4) | 95 (28.6) |
Kruskal–Wallis (0.002) Chi-squared (< 0.0005) |
| 2. Unstable | 39 (37.9) | 6 (7.9) | 8 (10.0) | 22 (30.1) | 75 (22.6) | |
| 3. Deteriorating | 33 (32.0) | 25 (32.9) | 51 (63.7) | 29 (39.7) | 138 (41.6) | |
| 4. Dying | 3 (2.9) | 13 (17.1) | 6 (7.5) | 2 (2.7) | 24 (7.2) | |
There were also differences between models in the time (days) between recruitment to the study and death. Of the 284 patients who died during the study period, those in model 1 were in the study for significantly more days (mean 87 days) than those in the other three service models (overall mean 56.2 days), but there was considerable variability. The 36 patients still alive at the end of the study had been recruited, on average, 267.8 days beforehand (Table 7).
| Number of days from recruitment (patient consent) to death | Service model | Total (N = 320)a | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: Large providers, 24/7 | 2: Small providers, 24/7 | 3: Large providers, not 24/7 | 4: Small providers, not 24/7 | ||||||||||||
| n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | |
| Died during studyb | 78 | 87.0 (84.5) | 60.0 (1–377) | 67 | 32.1 (43.7) | 15.0 (1–181) | 74 | 57.2 (124.2) | 13.0 (0–750) | 65 | 43.0 (56.9) | 17.0 (0–235) | 284 | 56.2 (86.8) | 21.0 (0–750) |
| Still alive at end of study | 19 | 182.3 (131.0) | 131.0 (12–461) | 6 | 190.2 (89.6) | 212.0 (53–302) | 3 | 803.0 (101.9) | 814.0 (696–899) | 8 | 328.4 (192.3) | 326.5 (101–690) | 36 | 267.8 (219.8) | 219.5 (12–899) |
Outcomes
Primary outcome: the Quality of Dying and Death questionnaire
A QODD was returned by the carers of 132 of the 284 patients (46.5%) who died during the study. Four respondents answered fewer than six of the 30 questions from which the total score is derived; they were excluded from the analysis. Response rates by service model and by individual HAH service are shown in Appendix 11. The proportion of carers who returned a QODD was significantly higher in model 1 than in the other service models. The frequency with which each of the 30 QODD questions were answered is shown in Appendix 12. The baseline sociodemographic and health status variables of the 152 carers who did not provide a QODD differed from those of the 132 who did only with respect to the education levels of the carer and the patient, which were higher among those responding than among those not responding (data not shown).
The total mean QODD score [range 0 (terrible) to 100 (almost perfect)] was 66.25 (SD 21.98, median 70.74, range 0–100, IQR 54.1–82.0) (n = 128). The distribution of the total QODD score (Figure 6) is not bell-shaped, with a slightly extended left-hand tail and a right-censored right-hand tail, the latter being caused by 100 being the maximum possible score. The distribution does not preclude the use of parametric techniques to analyse the total QODD score, but renders the median a slightly more appropriate summary statistic to describe the distribution alone. A score of 70 is associated with ‘a good death’. 100
FIGURE 6.
Histogram of total QODD score (with superimposed normal distribution).
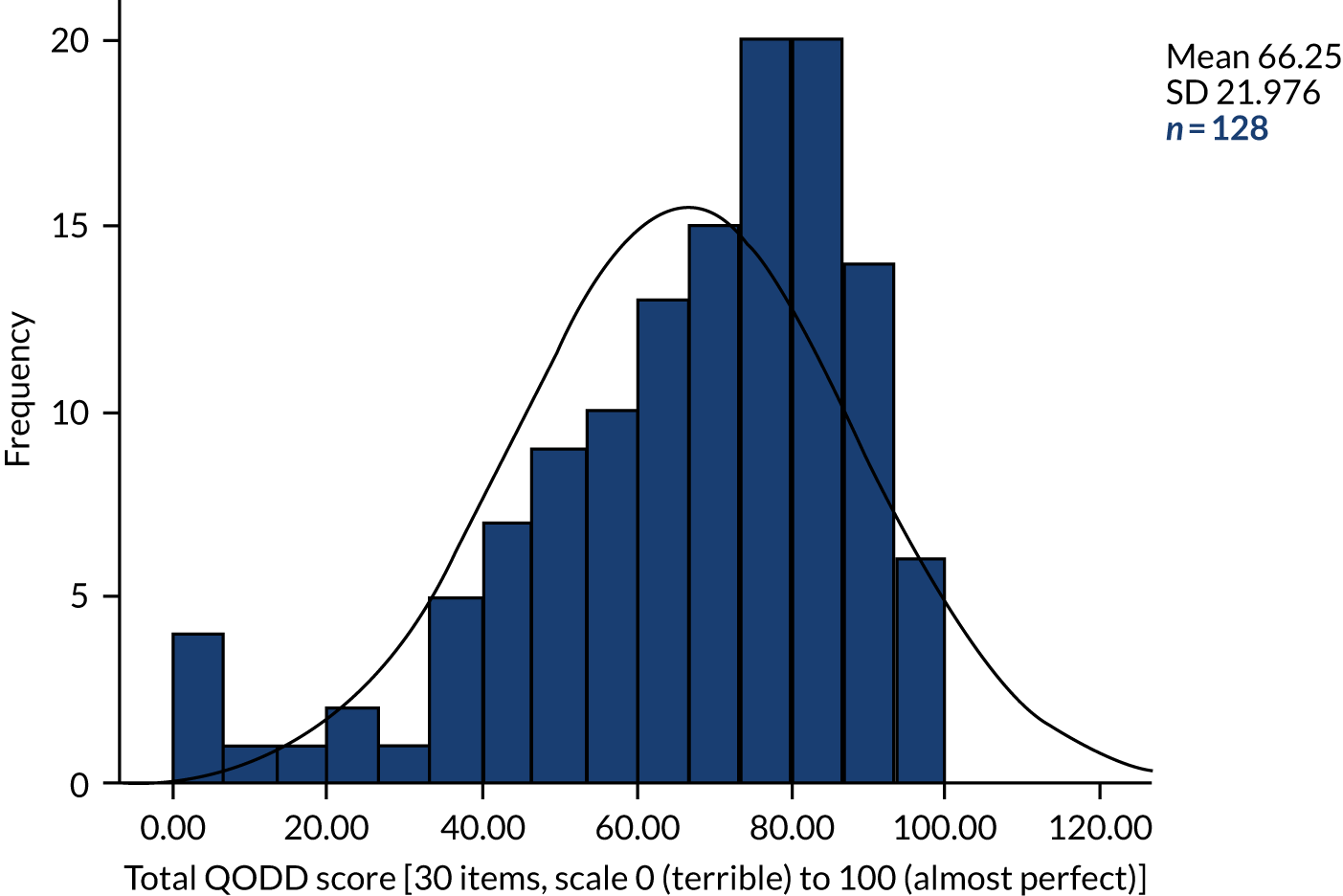
Secondary outcomes
Patient achieved preferred place of death
Of the 284 dyads for which the patient died during the study period, information on both the PPOD and the actual place of death was available for 222 (78.2%); of these, 162 (73.0%) (shaded in Table 8) achieved their PPOD and 60 (27.0%) did not. If care/nursing home is interpreted as the patient’s home (although it was not when the PPOD was collected at recruitment), then the percentage who achieved PPOD rises to 75.7% (168/222) (see Table 8).
| PPOD | Actual place of death | Total, n (%) | |||
|---|---|---|---|---|---|
| Home, n (%) | Hospice, n (%) | Hospital, n (%) | Care/nursing home, n (%) | ||
| Home | 143 (64.4) | 26 (11.7) | 15 (6.8) | 5 (2.3) | 189 (85.1) |
| Hospice | 6 (2.7) | 12 (5.4) | 1 (0.5) | 2 (0.9) | 21 (9.5) |
| Hospital | 1 (0.5) | 0 (0) | 0 (0) | 0 (0) | 1 (0.5) |
| Home or hospice | 2 (0.9) | 4 (1.8) | 3 (1.4) | 1 (0.5) | 10 (4.5) |
| Home or hospital | 0 (0) | 0 (0) | 1 (0.5) | 0 (0) | 1 (0.5) |
| Total | 152 (68.5) | 42 (18.9) | 20 (9.0) | 8 (3.0) | 222 (100.0) |
For the 62 patients who died without having expressed a PPOD, the places of death were distributed as follows: home, n = 29 (46.8%); hospice, n = 17 (27.4%); hospital, n = 8 (12.9%); care/nursing home, n = 4 (6.5%); and unknown, n = 4 (6.5%). Comparing the 58 patients who had a known place of death but an unknown PPOD with the 222 patients with a known place of death and a known PPOD, there was no statistically significant difference in the percentages dying in hospital: 8 out of 58 (13.8%) of the former versus 20 out of 222 (9.0%) of the latter (chi-squared test: p = 0.280).
Post-bereavement carer satisfaction: Views of Informal Carers – Evaluation of Services 1 and 2
Of the 284 eligible dyads, 132 (46.5%) carers returned a completed QODD, of whom 127 (96.2%) completed VOICES 1 and 128 (97.0%) completed VOICES 2. Responses are shown in Table 9. The median response to VOICES 1 was 1 (the best) (i.e. agreement that the carer and family got as much help and support from the health and social care services as they needed); for VOICES 2, it was 2 (i.e. that the carer rated the help and support they had received as excellent). Treating the 1–5 scales as linear, the mean for VOICES 1 was 1.31 (SD 0.64) and the mean for VOICES 2 was 1.98 (SD 1.06).
| Question | Responses, n (%) |
|---|---|
| VOICES 1: overall, did you and your family get as much help and support from health and social care services as you needed when caring for the patient? | |
| 1. Yes, we got as much as we needed | 97 (76.4) |
| 2. Yes, we got some support but not as much as wanted | 22 (17.3) |
| 3. No, although we tried to get more | 6 (4.7) |
| 4. No, but we did not ask for more help | 2 (1.6) |
| 5. We did not get any help at all | 0 (0) |
| Total (missing 5) | 127 (100.0) |
| VOICES 2: overall, how was the help and support you and your family received from health and social care services when caring for the patient? | |
| 1. Outstanding | 50 (39.1) |
| 2. Excellent | 47 (36.7) |
| 3. Good | 19 (14.8) |
| 4. Fairly good | 7 (5.5) |
| 5. Poor | 5 (3.9) |
| Total (missing 4) | 128 (100.0) |
Service satisfaction and carer burden in the last 28 days of life
Completion of each AHCR included a question on satisfaction with services (scaled as follows: 1, exceeded expectations; 2, just met expectations; and 3, fell short of expectations) and a question on carer burden score (range 0 = best to 24 = worst). The last responses prior to the death of the patient (provided it was recorded within 28 days of death) were analysed (i.e. 143 service satisfaction ratings and 149 carer burden scores). The mean satisfaction and carer burden scores were 1.52 (SD 0.66) and 7.78 (SD 6.12), respectively. Histograms are shown in Figures 7 and 8.
FIGURE 7.
Histograms of service satisfaction (with superimposed normal curve). a, Responses for last 28 days of life, for which 1 = exceeded expectations, 2 = just met expectations and 3 = fell short of expectations.
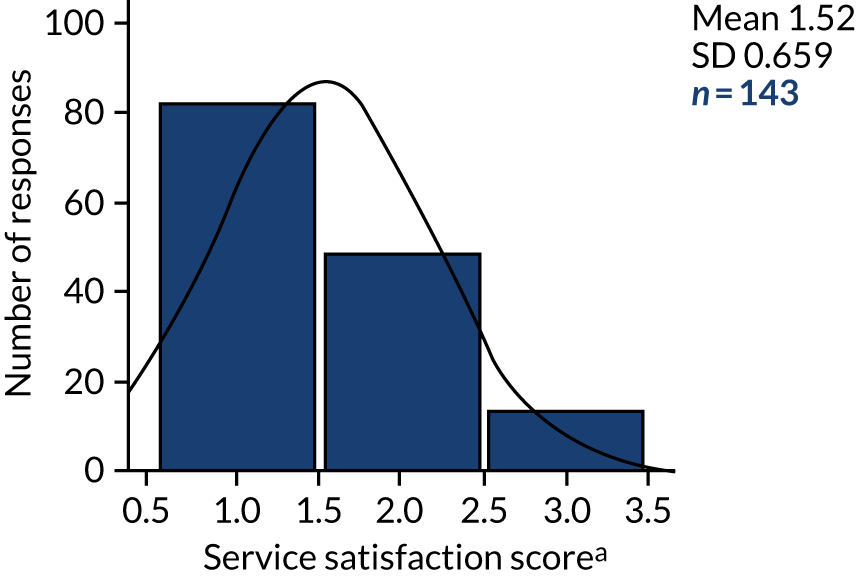
FIGURE 8.
Histograms of carer burden (with superimposed normal curve). a, Responses for last 28 days of life; mean of six questions for which 0 = best and 24 = worst.
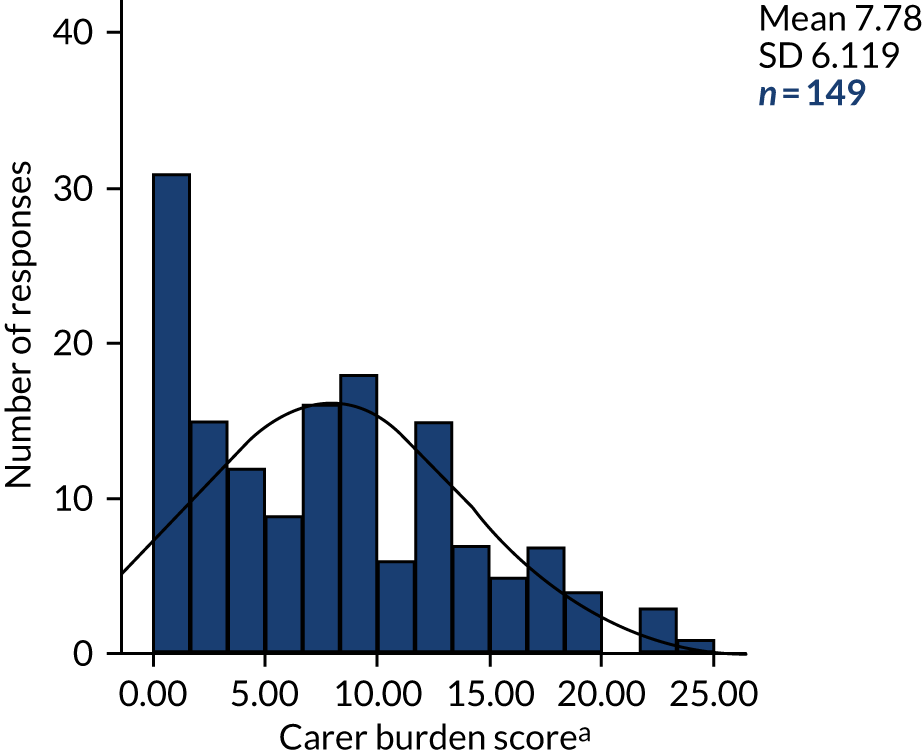
Comparison of outcomes by service model
Outcomes are summarised by service model in Table 10. Outcomes by individual HAH service are shown in Appendix 13. There was a statistically significant difference in the QODD scores between the four service models. Comparison of both mean scores and using the dichotomised scoring [≤ 70 (terrible, poor, intermediate) vs. > 70 (good, almost perfect)] reveals that carers in model 3 reported a significantly worse death than those in models 2 and 4 (Tables 11 and 12). Responses to each item of the QODD by individual HAH service are shown in Appendices 13 and 14 (including Tables 52–81). Significant differences were found between service models on service satisfaction (worst in model 1) and carer burden in last 28 days (least in model 1); model 2 scored marginally better than the other models on VOICES 1 and 2. There was no statistically significant difference between models in achievement of PPOD, although the proportion was higher in model 2.
| Outcome | Service model | Total | Difference between models, test (p-value) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: Large providers, 24/7 | 2: Small providers, 24/7 | 3: Large providers, not 24/7 | 4: Small providers, not 24/7 | |||||||||||||
| n | Mean (SD) | Median, maximum | n | Mean (SD) | Median, maximum | n | Mean (SD) | Median, maximum | n | Mean (SD) | Median, maximum | N | Mean (SD) | Median, maximum | ||
| Total QODD score [30 items, scale 0 (terrible) to 100 (almost perfect)]a | 46 | 62.5 (21.3) | 66.0, 98.6 | 31 | 75.2 (19.4) | 81.7, 98.6 | 30 | 57.0 (23.9) | 59.2, 90.4 | 21 | 74.4 (17.2) | 78.3, 100.0 | 128 | 66.2 (22.0) | 70.7, 100.0 | ANOVA (< 0.0005) |
| QODD: % of patients who achieved good/almost perfect death (i.e. score of > 70)a | 46 | 41.3 | 0, 100.0 | 31 | 67.7 | 100.0, 100.0 | 30 | 36.7 | 0, 100.0 | 21 | 76.2 | 100.0, 100.0 | 128 | 52.3 | 100.0, 100.0 | Chi-squared (0.005) |
| Percentage of patients who achieved PPOD | 51 | 64.7 | 100.0, 100.0 | 62 | 82.3 | 100.0, 100.0 | 57 | 71.9 | 100.0, 100.0 | 52 | 71.2 | 100.0, 100.0 | 222 | 73.0 | 100.0, 100.0 | Chi-squared (0.204) |
| VOICES 1 score: overall, did you and your family get as much help and support from health and social care services as you needed when caring for the patient? (1 = best, 5 = worst)a | 44 | 1.4 | 1.0, 4.0 | 31 | 1.1 | 1.0, 2.0 | 31 | 1.4 | 1.0, 3.0 | 21 | 1.3 | 1.0, 3.0 | 127 | 1.3 | 1.0, 4.0 | Kruskal–Wallis (0.075) |
| VOICES 2 score: overall, how was the help and support you and your family received from health and social care services when caring for the patient? (1 = best, 5 = worst)a | 45 | 2.2 | 2.0, 5.0 | 31 | 1.6 | 1.0, 4.0 | 31 | 2.2 | 2.0, 5.0 | 21 | 1.7 | 2.0, 4.0 | 128 | 2.0 | 2.0, 5.0 | Kruskal–Wallis (0.044) |
| Service satisfaction score, last 28 days/final response (1 = exceeded expectations, 2 = just met expectations, 3 = fell short of expectations)b | 61 | 1.7 | 2.0, 3.0 | 22 | 1.4 | 1.0, 3.0 | 36 | 1.4 | 1.0, 3.0 | 24 | 1.5 | 1.0, 3.0 | 143 | 1.5 | 1.0, 3.0 | Kruskal–Wallis (0.029) |
| Carer burden score, last 28 days/final response. Mean of six items (0 = best, 24 = worst)b | 62 | 5.9 | 4.5, 24.0 | 21 | 8 | 9.0, 20.0 | 37 | 9.6 | 11.0, 22.0 | 29 | 8.6 | 8.0, 22.0 | 149 | 7.8 | 7.0, 24.0 | Kruskal–Wallis (0.010) |
| Service model | n | Mean | SD | SE | 95% CI for mean | Range | Difference between models |
|---|---|---|---|---|---|---|---|
| 1: Large providers, 24/7 services | 46 | 62.45 | 21.31 | 3.14 | 56.13 to 68.78 | 0–98.57 | ANOVA (p = 0.002) |
| 2: Small providers, 24/7 services | 31 | 75.24 | 19.40 | 3.48 | 68.13 to 82.36 | 0–98.62 | |
| 3: Large providers, not 24/7 services | 30 | 57.05 | 23.93 | 4.37 | 48.11 to 65.98 | 0–90.38 | |
| 4: Small providers, not 24/7 services | 21 | 74.44 | 17.18 | 3.75 | 66.62 to 82.26 | 21.33–100 | |
| Total | 128 | 66.25 | 21.97 | 1.94 | 62.41 to 70.09 | 0–100 |
| Service model | HAH services split by QODD score group | Total (N) | Difference between models, test (p-value) | |
|---|---|---|---|---|
| Terrible/poor/intermediate (≤ 70), n (%) | Good/almost perfect (> 70), n (%) | |||
| 1: Large providers, 24/7 services | 27 (58.7) | 19 (41.3) | 46 | Chi-squared (0.005) |
| 2: Small providers, 24/7 services | 10 (32.3) | 21 (67.7) | 31 | |
| 3: Large providers, not 24/7 services | 19 (63.3) | 11 (36.7) | 30 | |
| 4: Small providers, not 24/7 services | 5 (23.8) | 16 (76.2) | 21 | |
| Total | 61 (47.7) | 67 (52.3) | 128 | |
Factors associated with the Quality of Dying and Death questionnaire score (primary outcome)
Bivariate tests were used to explore the association between the QODD scores (available for 128 dyads) and a range of potential influencing factors (listed in Appendix 15): patient and carer characteristics; place of death and achieving PPOD; length of time the patient was involved with the hospice; three items from the QODD reflecting the condition of the patient, communication with the carer during the last 7 days and how prepared the patient was for death; and the number of days between death and completion of the QODD (which could affect carer adjustment to life after the loss of a loved one).
Results revealed that higher total QODD scores (i.e. a better quality of dying and death) were associated with:
-
the carer being educated to university level (n = 40; QODD mean score 74.42, SD 16.95), versus not (n = 74; QODD mean score 64.85, SD 20.72; unpaired t-test: p = 0.014; using highest level of education, Spearman’s rank-order correlation: r = 0.282; p = 0.002)
-
the carer seeing the patient for more days during the last week of life (Spearman’s rank-order correlation: r = 0.194; p = 0.029)
-
death taking place at home (n = 87; QODD mean score 68.74, SD 19.03), in a hospice (n = 27; QODD mean score 67.12, SD 26.02), in hospital (n = 11; QODD mean score 56.27, SD 20.12) or in a care/nursing home (n = 3; QODD mean score 22.93, SD 24.92); ANOVA: p = 0.001.
A lower total QODD score was associated with the patient being in the study for a longer time (days) (Pearson’s correlation r = –0.217; p = 0.014). No other statistically significant associations with the total QODD score were found.
Exploratory regression analysis to investigate the effect of service model on outcomes
Seven outcome variables were modelled using the variables listed in Appendix 16. Four of these outcomes were gathered from the post-bereavement interview [total QODD score, achieved a good death (i.e. QODD score of > 70), VOICES 1 and 2]; two were gathered from the last AHCR completed prior to death, provided it was within 28 days of death (service satisfaction in the last 28 days, carer burden in the last 28 days); and achieving PPOD was gathered from the baseline assessment at recruitment and HAH service records of death.
Associations between the total QODD score (primary outcome) and secondary outcomes indicated positive correlations with VOICES 1 and 2 and service satisfaction in the last 28 days, but not with carer burden in the last 28 days (Table 13). The total QODD scores were available for 77 (47.5%) of the 162 patients who achieved their PPOD and for 25 (41.7%) of the 60 who did not achieve their PPOD. There was no difference in the mean QODD scores between these groups: 70.1 (SD 18.5) in the PPOD achieved group versus 61.2 (SD 20.0) in the PPOD not achieved group; unpaired t-test: p = 0.162. Reducing the QODD score to its dichotomous form, a good/almost perfect death (score of > 70) was reported for 46 out of 77 (59.7%) who achieved their PPOD, compared with 11 out of 25 (44.4%) who did not (chi-squared test: p = 0.168).
| Spearman rank-order correlation | VOICES 1: got as much help as we wanted (1 = best, 5 = worst) | VOICES 2: quality of support received overall (1 = best, 5 = worst) | Last 28 days: carer burden. Overall mean of six questions (0 = best, 24 = worst) | Last 28 days: service satisfaction (range 1–3: exceeded, just met or fell short of expectations) |
|---|---|---|---|---|
| Correlation coefficient | –0.279 | –0.420 | –0.127 | –0.273 |
| Significance (two-tailed) | 0.002 | < 0.0005 | 0.258 | 0.016 |
| n | 125 | 126 | 81 | 77 |
Linear or logistic regression modelling was performed, with service model entered initially (model 3 was withheld as baseline) and additional predictors then determined by forward stepwise selection. Results in the form of fitted parameters for service model and for all other statistically significant predictors are summarised in Table 14, with interpretations provided in Box 1. Results of the logistic regressions are presented as adjusted odds ratios.
| Outcome | Predictor | |||||||
|---|---|---|---|---|---|---|---|---|
| Total QODD score (0 = worst, 100 = best) | Achieved good death – yes (i.e. total QODD score of > 70) | Achieved PPOD – yes | VOICES 1: got as much help as we wanted (yes vs. all lesser responses) | VOICES 2: quality of support received overall (1 = best, 5 = worst) | Last 28 days: carer burden. Overall mean of six questions (0 = best, 24 = worst) | Last 28 days: service satisfaction (1 = best, 3 = worst) | ||
| Model 1: Large providers, 24/7 | 4.171 | AOR = 1.148 | AOR = 0.942 | AOR = 1.070 | –0.071 | –4.547** | 0.251* | |
| Model 2: Small providers, 24/7 | 12.950** | AOR = 3.700** | AOR = 1.351 | AOR = 8.174** | –0.487* | –0.349 | –0.020 | |
| Model 4: Small providers, not 24/7 | 11.371** | AOR = 5.389** | AOR = 0.790 | AOR = 1.003 | –0.461 | –0.916 | 0.027 | |
| Patient: female | AOR = 0.409** | |||||||
| Carer working | –0.326** | |||||||
| Number of days from recruitment to death | AOR = 0.988** | |||||||
| Patient died at home | 24.831** | AOR = 6.825** | –3.592** | |||||
| Patient died in hospital | 0.762** | 0.351** | ||||||
| Carer educated to university level | 8.763** | –0.411** | ||||||
| Carer: female | 11.056** | AOR = 2.938** | ||||||
| Patient died in hospice | 28.143** | AOR = 5.810* | ||||||
| How long before death patient was aware of dying (1 = never aware, 2 = 1 week, 3 = 2–4 weeks, 4 = 2–6 months, 5 = 6–12 months) | 5.885** | AOR = 1.711** | ||||||
| Patient ever talked comprehensibly in last 7 days | 9.643** | |||||||
| Constant | –1.419 | 2.273 | 12.076 | 1.470 | ||||
| Final model diagnostics (n) | 106 | 118 | 215 | 127 | 114 | 148 | 141 | |
| R 2 | 0.399 | 0.149 | 0.153 | 0.140 | ||||
| Cox and Snell’s R2 | 0.250 | 0.138 | 0.091 | |||||
| Nagelkerke’s R2 | 0.333 | 0.199 | 0.137 | |||||
Total QODD score (a higher score indicates a better-quality death) = –1.419 + 11.056 (if carer female) + 8.763 (if carer is university educated) + 24.831 (if died at home) + 28.143 (if died in hospice) + 5.885 × (how long patient knew they were dying: 1 = never aware, 2 = 1 week before death, 3 = 2–4 weeks before death, 4 = 2–6 months before death, 5 = 6–12 months before death) + 9.643 (if patient ever talked in a comprehensible way in last 7 days before death) + 4.171 (if model 1) + 12.950 (if model 2) + 0 (if model 3) + 11.371 (if model 4).
Achieving a good deathFinal model for achieving a good death (i.e. total QODD score of > 70, indicating a good/almost perfect death):
-
A female carer is 2.938 times more likely than a male carer to report a good/almost perfect death.
-
Carers of patients who died at home are 6.825 times more likely to report a good/almost perfect death than those who died in hospital or in a care/nursing home.
-
Carers of patients who died in a hospice are 5.810 times more likely to report a good/almost perfect death than those who died in hospital or in a care/nursing home.
-
For every point moved up the timescale reflecting how long the patient was aware they were dying (never aware/1 week before death/2–4 weeks before death/2–6 months before death/6–12 months before death), the carer is 1.711 times more likely to report a good/almost perfect death experience. For example, a carer whose patient was aware that they were dying 2–6 months before death would be (1.711 × 1.711 = )2.928 times more likely to report a good/almost perfect death than a carer whose patient was aware that they were dying only 1 week before death.
-
Carers under small-provider models 2 and 4 are more likely to report a good/almost perfect death experience: 3.700 times more likely in the case of model 2, and 5.389 times more likely in the case of model 4.
Final model for achieving PPOD:
-
for each additional 10 days the patient was under HAH care, the patient was 0.98810 = 0.886 times less likely achieve their PPOD
-
patients in model 2 were most likely to achieve their PPOD, although there was no statistically significant difference between the four models.
Final model for VOICES 1:
-
when a patient is female, the carer is 0.409 times less likely to report ‘yes, we got as much help and support as we wanted’
-
carers in service model 2 are 8.174 times more likely to report ‘yes, we got as much help and support as we wanted’ than carers in the other three service models, which showed no discernible differences.
VOICES 2 (a lower score indicates a better quality of help and support) = 2.273 – 0.411 (if carer is university educated) + 0.762 (if place of death is hospital) – 0.071 (if model 1) – 0.487 (if model 2) – 0.461 (if model 4).
Service satisfactionService satisfaction last 28 days (a lower score indicates greater satisfaction) = 1.470 – 0.326 (if carer employed full time/part time or self-employed) + 0.351 (if place of death was hospital) + 0.251 (if service model 1) – 0.020 (if model 2) + 0.027 (if model 4).
Carer burdenCarer burden last 28 days (a lower score indicates less burden) = 12.076 – 3.592 (if place of death is home) – 4.547 (if model 1) – 0.349 (if model 2) – 0.916 (if model 4).
Modelling of the two QODD outcomes produced the most robust findings and the highest levels of explanatory power. Both revealed that improved quality of death was associated with small providers (models 2 and 4), dying at home or in a hospice and when the patient was aware for a longer time that they were dying. The QODD total score model also showed that carers who were female and carers who were educated to university level were more likely to report a good death.
Achieving PPOD was less likely when there was a longer time between recruitment to the study and death. This may be because the PPOD was recorded at recruitment and patients can change their minds. This would be consistent with the finding that patients in model 2 were both (on average) in the study for less time and more likely to achieve their PPOD.
Regarding views on help and support received, carers of service model 2 reported more help and support in the post-bereavement interview and that it was of better quality (VOICES 1 and 2). Service model 1 was associated with less satisfaction in the last 28 days. Lower quality of help and support (VOICES 2) and levels of satisfaction in the last 28 days were reported by carers whose patients died in hospital. The carers of female patients reported lower levels of support (VOICES 1) and university-educated carers provided better ratings (VOICES 2).
Carer burden was less in the last 28 days when the patient died at home, and in service model 1 [in which patients (on average) had longer associations with the hospice].
Service-level analysis of resources and costs
Information on the resources involved in running each hospice and costs was sought through interviews with case study site managers during phase 1. Most hospices found it difficult to provide the detailed data on human and other resources that would be needed for a costing analysis. Either the information was not easily available to them or sharing it posed confidentiality issues. In the case of variables such as the ratio of nurses to HCAs, respondents were sometimes unsure of staff grades; they also reported that staffing levels and composition changed frequently, as professionals joined and left the service during the study. Based on interview responses, the home care delivered by each HAH service was designated as led by either RNs or HCAs. Except for the three smaller HAH services in model 1 (Acacia, Camellia and Echinacea) and one HAH service in model 4 (Marigold), all sites were led by HCAs (see Appendix 9).
Patient-level analysis of service use
Data on service use for the patient-level analysis were gathered through the AHCR, which was completed by interview at baseline (with reference to the previous 2 weeks). Telephone interviews (mostly with carers) to collect subsequent service use data were intended to take place every 2 weeks, up to the death of the patient. In some cases, carers were unavailable or busy and interviews could not be undertaken to schedule. When patients were in the study for many weeks or months, administering AHCRs became burdensome and the interval between interviews was extended.
The AHCR requested information on service contacts inside the home (i.e. community nurses/DNs/HCAs, hospice nurses/HCAs, home/personal care workers, GPs, allied health professionals, social workers, representatives of voluntary organisations) and outside the home (outpatient appointments at hospitals/hospices/clinics, visits to A&E, Day care), inpatient stays (hospital, hospice and care/nursing home), telephone calls, medications, supplies and equipment, and informal caring. At the end of the AHCR, there are three items for recording carer burden (six items, each on a five-point scale), the patient’s functional status (ECOG Performance Status Scale, six levels: 0 if fully active, 5 if dead) and satisfaction with services (whether they had exceeded, met or fallen short of expectations) over the period covered by the data collection. 91
Completion of Ambulatory and Home Care Records
Of the 339 patient–carer dyads in the study, 221 (65.2%) provided at least one AHCR, of whom 178 had a known DOD and could be included in the economic analysis (see Table 4). The distribution of the 178 patient–carer dyads was not even across service models: most (n = 68, 66.0%) were in service model 1 and the fewest were in service model 2 (n = 27, 33.8%). The progress of patients through the study and the provision of AHCRs (service use data) by service model and by individual HAH service are shown in Appendix 17, Tables 83 and 84.
In total, 613 AHCRs were returned for the 178 patients who had died and provided at least one AHCR (mean 3.44 per patient, maximum 23). Almost half of the total AHCRs available for analysis were in service model 1 (304/613, 49.6%); only 78 out of 613 (12.7%) related to model 2. As health and social care use changes in the months, weeks and days prior to death, the service use data were broken down initially into seven periods of number of days before death (0–7, 8–14, 15–21, 22–28, 29–92, 93–182 and ≥ 183 days). The dates covered by AHCRs did not coincide with these time periods, so an allocation algorithm was designed and implemented (explained in detail in Appendix 2). The number of AHCRs available by hospice and time period is shown in Appendix 18. The number of patients with AHCR data by service model and time period is shown in Appendix 19. Because an algorithm allocated AHCR data to study time periods, the number of AHCRs and patients in any time period may not be the same; this is explained in the footnote to Table 86 in Appendix 19. The pattern of AHCR completion reflected recruitment to the study, with most AHCRs relating to service model 1, which had recruited the most participants and recruited them furthest from the time of death (see Table 7).
As the availability of AHCR data diminished considerably after the period 29–92 days, subsequent analysis of service use and costs was conducted for three time periods: the last 2 weeks before death (days 0–14), the penultimate 2 weeks before death (days 15–28) and between 4 weeks and 3 months from death. Beyond 92 days from death, the number of AHCRs returned was < 10 in three of the four models; therefore, it was decided that analysis in this time period was not viable.
Service use
Table 15 shows summaries of service use in each of the three time periods: ‘nursing’ (RNs and HCAs) and social care home visits, all formal care contacts (health, social and voluntary sectors, in and out of the home, except for inpatient care), total inpatient nights (hospital, hospice, care/nursing home) and informal care. Informal care was measured in hours per day (rather than visits/contacts). (Full details of service use, broken down into individual items by time period and model, are shown in Appendix 19.) Data are presented as mean, SD, median and maximum number of visits per day (computed as the number of visits in the time period divided by the number of days covered by the AHCR in the period). The number of patient–carer dyads reporting zero contacts is also shown for each item.
| Days before death | All nursing/HCA (district and hospice) and social care contacts (visits per day) | Total formal care visits (health, social, voluntary sector), includes nursing, excludes inpatient stays (contacts per day) | Total inpatient nights (hospital, hospice, care home) | Informal caring (main carer and secondary carers) (hours per day) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | |
| 0–14 | 125 (11) | 1.76, 6.63 | 2.18 (1.90) | 127 (0) | 2.36, 12.86 | 2.85 (2.16) | 133 (74) | 0.00, 1.00 | 0.20 (0.31) | 133 (23) | 20.00, 66.00 | 17.18 (14.46) |
| 15–28 | 112 (10) | 1.14, 10.50 | 2.08 (2.38) | 112 (0) | 1.61, 11.21 | 2.54 (2.42) | 116 (70) | 0.00, 1.00 | 0.15 (0.27) | 116 (14) | 15.50, 48.00 | 15.28 (10.75) |
| 29–92 | 95 (4) | 0.43, 10.50 | 1.46 (1.93) | 95 (0) | 0.93, 11.21 | 1.85 (2.04) | 95 (48) | 0.00, 0.88 | 0.09 (0.17) | 95 (5) | 12.00, 56.00 | 14.40 (11.32) |
The largest item of formal service use for all service models and for all time periods was nursing and social care delivered in the home. Three sources of nursing and other care support were distinguished in the data (community nurses/DNs and HCAs from local NHS services, nursing and HCAs from HAH services, and care workers provided by social services). Because there is substitutability between these three groups, and respondents were not always sure which source a visiting professional had come from, the data are presented with the three groups combined, to provide a measure of the total in-home nursing and social/personal care support received by patient–carer dyads (see Table 15), and separately (see Appendix 20). Very little in-home contact with voluntary services was reported in any site (see Appendix 20).
Across the whole sample, there was a general trend for rates of formal and informal care to be higher in the periods closer to death (see Table 15). The median number of hours of informal care in the last 2 weeks of life was > 20 hours per day (total of main carer and any additional carers). The median number of nursing and personal/social care visits was 1.76 per day; the median number of total health, social and voluntary sector contacts, including nursing but excluding inpatient stays, was 2.36 per day. On average, the number of inpatient nights (hospital, hospice and care home) was low. There was a lot of variability between individuals in all categories of service use (see Table 15).
On average, respondents reported using two items of equipment (e.g. beds, bedding, hoists, commodes, walking frames, shower seats). Many also reported use of continence pads and food supplements (data not shown).
Differences between service models
The main summary measures of service use [in-home nursing/carer visits, total formal care contacts (including nurses, excluding inpatient care), informal caring hours] by model are shown in box plots in Figures 9–11. Box plots for individual HAH services are shown in Appendix 21, Figures 24–26.
FIGURE 9.
Service use by model: total community health and social care visits per day. This includes DNs/community nurses, and HAH staff and personal carers, and includes night sits. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
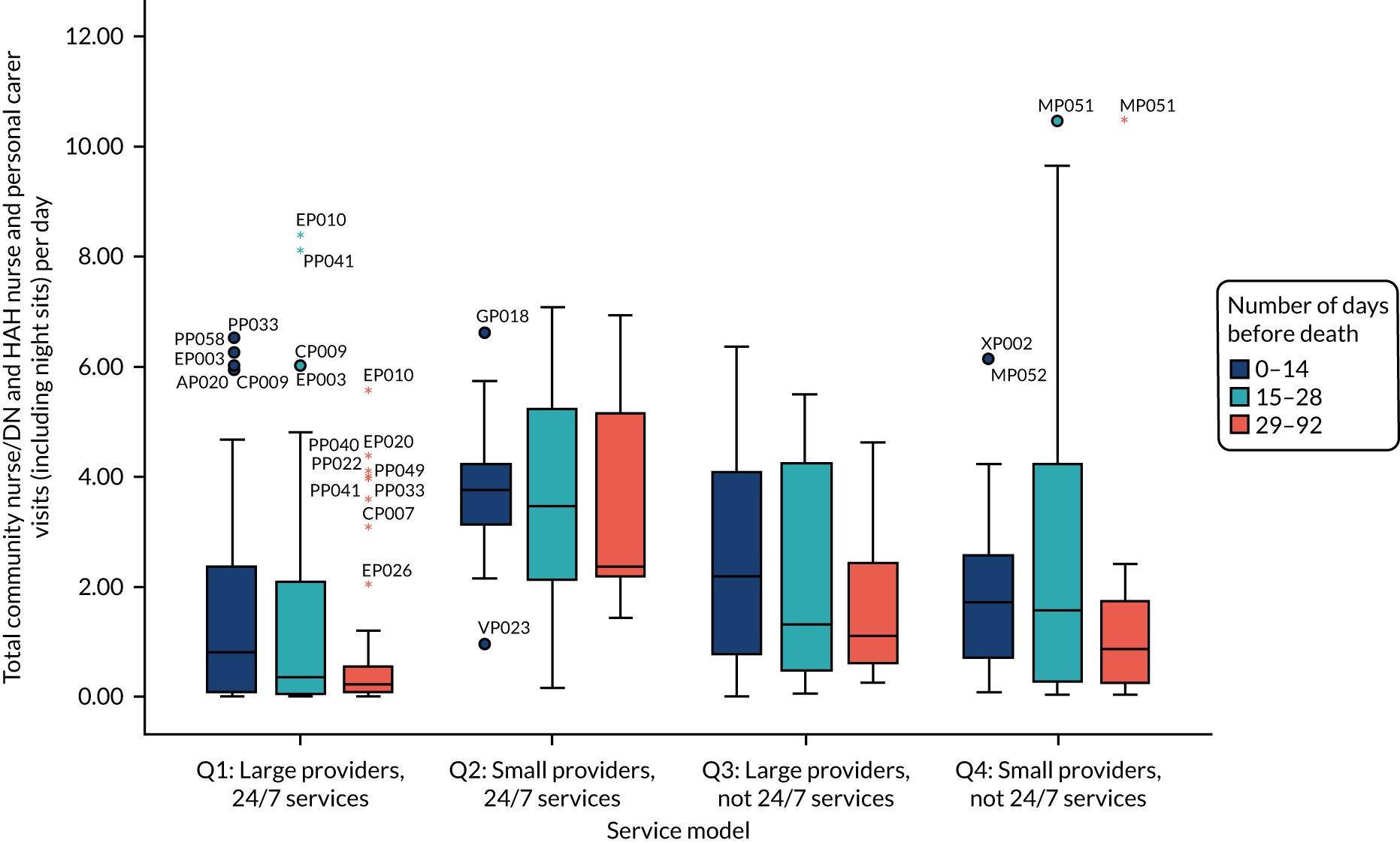
FIGURE 10.
Service use by model: total visits excluding inpatient stays and informal care. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
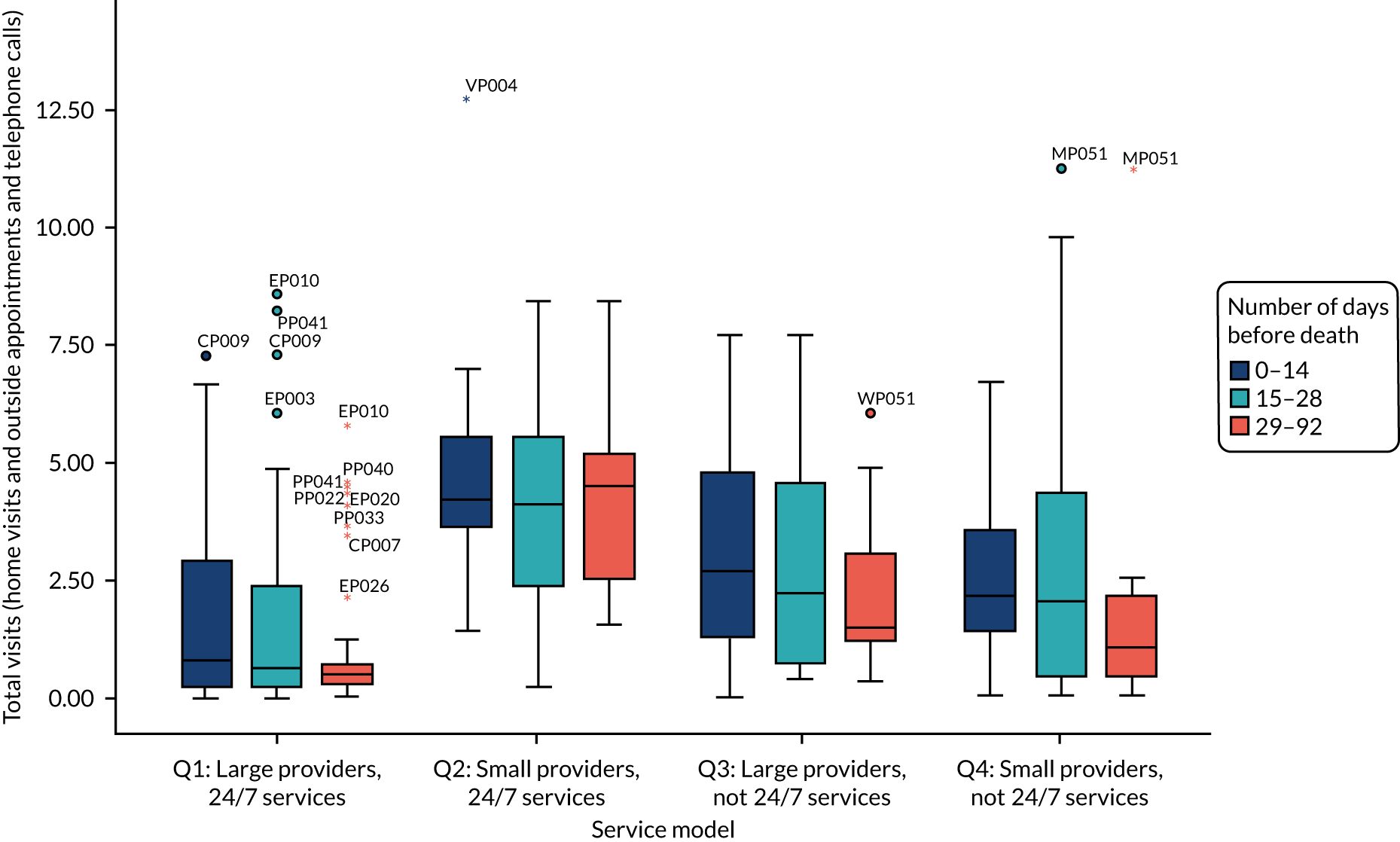
FIGURE 11.
Service use by model: informal caring. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
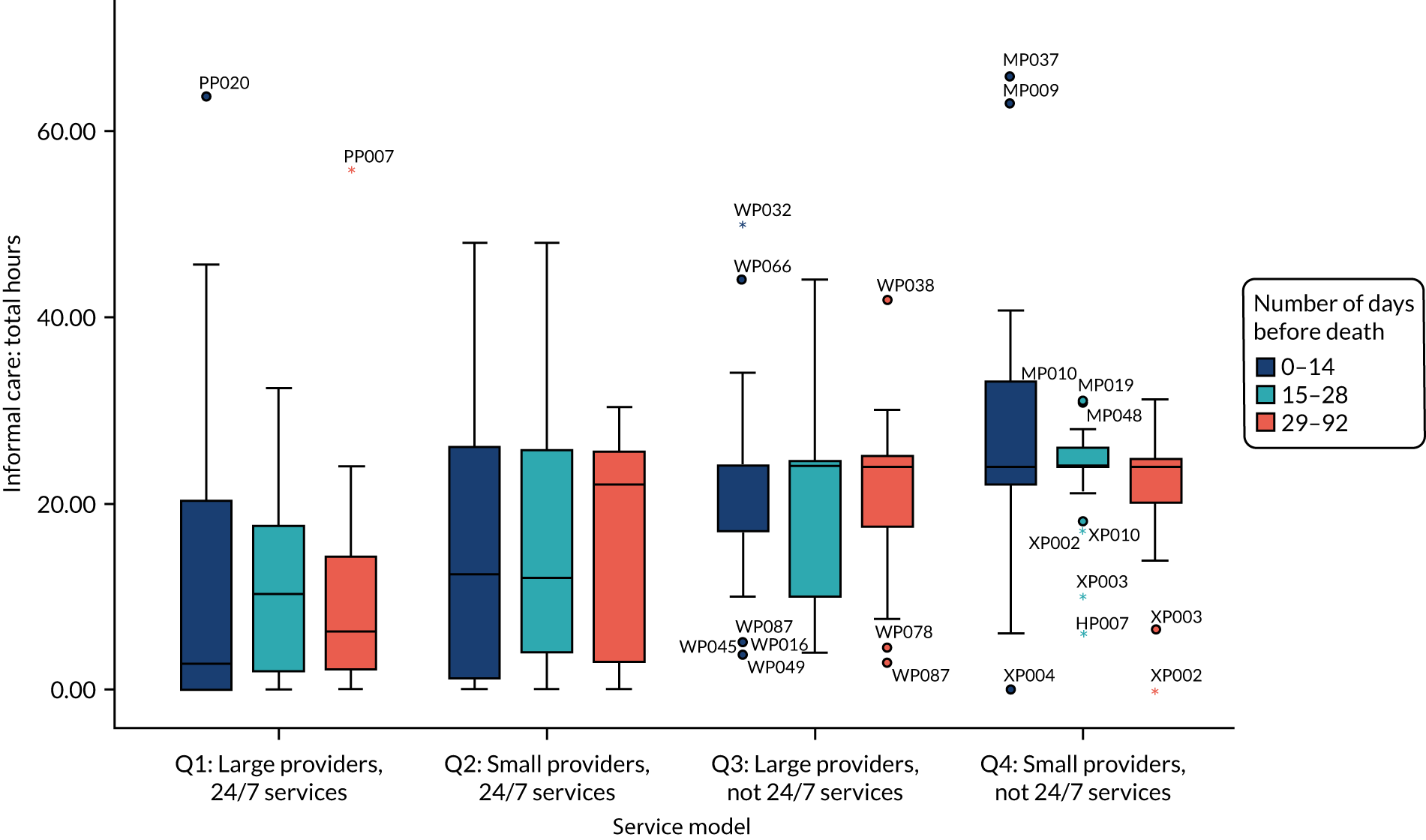
Inspection of the data showed differences in service use between model 1 (larger, 24/7 services) and the other models. In the last month of life (0–14, 15–28 days), larger proportions of dyads in model 1 reported no visits into the home at all; use of out-of-home care was, however, greater than in the other three models. A total of 12% of dyads in model 1 reported no in-home care, no out-of-home care and no telephone calls between 0 and 14 days (7% between 15–28 days). Furthermore, relatively high proportions in model 1 reported no informal care (32% between 0 and 14 days, 18% between 15 and 28 days). Between 29 and 92 days, there continued to be smaller proportions of dyads in model 1 reporting in-home service use and greater proportions reporting out-of-home care than in the other three models, but all dyads reported use of at least one in-home, out-of-home or telephone contact, and all respondents reported informal care. Greater proportions of dyads in model 1 reported overnight stays (hospital, hospice or care home) during days 0–14, but not in the other time periods (see Appendix 20). As comparisons across models were standardised for time from death, a plausible reason for these differences between model 1 and the other models could not be identified.
Provision of nursing and care by hospice at home services
The overall numbers of home visits per day of community nurses/DNs and HCAs, nurses and HCAs from a HAH service and personal carers from social services were highest in model 2 (smaller, 24/7 services) and lowest in model 1 (larger, 24/7 services). There was no difference between the models with respect to the proportion of all nursing and personal caring visits that were made by community nurses/DNs in any of the three time periods (between 30% and 35% of all visits), but differences did exist between models in the proportions of HAH nurses or HCAs and social service personal carer visits. Pairwise comparisons of models showed that greater proportions of visits were from HAH staff in models 2 (smaller, 24/7 services) and 4 (smaller, not 24/7 services) than from HAH staff in models 1 (larger, 24/7 services) and 3 (larger, not 24/7 services); the proportion of visits from social service carers was greater in model 3 (larger, not 24/7 services) than in the other three models (Tables 16 and 17) (see also Appendix 22, Figures 27–29).
| Service item | Number of days before death | Service model | Difference between models (p-value) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: Large providers, 24/7 services | 2: Small providers, 24/7 services | 3: Large providers, not 24/7 services | 4: Small providers, not 24/7 services | Total | |||||||||||||
| Dyads, n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | Dyads, n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | Dyads, n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | Dyads, n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | Dyads, n (dyads reporting zero contacts, n) | Median, maximum | Mean (SD) | |||
| Number of visits per day | |||||||||||||||||
| Total visits per day: NHS community nurse/HCA, HAH nurse/HCA and social services personal caring | 0–14 | 49 (8) | 0.81, 6.50 | 1.58 (1.93) | 17 (0) | 3.76, 6.63 | 3.77 (1.34) | 34 (3) | 2.18, 6.36 | 2.36 (1.80) | 25 (0) | 1.71, 6.14 | 2.02 (1.72) | 125 (11) | 1.76, 6.63 | 2.18 (1.90) | |
| 15–28 | 58 (10) | 0.35, 8.42 | 1.45 (2.09) | 16 (0) | 3.46, 7.07 | 3.70 (2.02) | 16 (0) | 1.31, 5.50 | 2.08 (1.91) | 22 (0) | 1.56, 10.50 | 2.57 (3.02) | 112 (10) | 1.14, 10.50 | 2.08 (2.38) | ||
| 29–92 | 52 (4) | 0.22, 5.59 | 0.88 (1.47) | 11 (0) | 2.37, 6.93 | 3.69 (1.99) | 17 (0) | 1.10, 4.61 | 1.73 (1.42) | 15 (0) | 0.86, 10.50 | 1.53 (2.60) | 95 (4) | 0.43, 10.50 | 1.46 (1.93) | ||
| Proportions of total | p-valuea | ||||||||||||||||
| % of total visits that are NHS community nursing/HCA visitsb | 0–14 | 41 (5) | 22.89, 100 | 41.01 (40.08) | 17 (1) | 18.75, 71.74 | 25.29 (22.42) | 31 (2) | 21.43, 100 | 29.84 (26.11) | 25 (4) | 18.03, 85.50 | 25.27 (23.88) | 114 (12) | 22.00, 100 | 32.17 (31.45) | 0.699 |
| 15–28 | 48 (8) | 18.82, 100 | 36.23 (38.24) | 16 (1) | 26.25, 100 | 29.65 (26.65) | 16 (0) | 21.44, 55.56 | 23.42 (15.50) | 22 (6) | 9.17, 80.95 | 24.33 (28.15) | 102 (15) | 20.56, 100 | 30.62 (31.91) | 0.654 | |
| 29–92 | 48 (5) | 38.11, 100 | 42.79 (34.57) | 11 (0) | 21.13, 41.24 | 19.44 (14.20) | 17 (0) | 11.29, 56.25 | 22.49 (19.00) | 15 (3) | 21.30, 80.95 | 29.75 (28.35) | 91 (8) | 29.50, 100 | 34.03 (30.51) | 0.130 | |
| % of total visits that are HAH nursing/HCA visitsb | 0–14 | 41 (10) | 19.58, 100 | 34.93 (37.40) | 17 (0) | 64.29, 100 | 59.09 (33.09) | 31 (2) | 12.50, 100 | 26.74 (30.45) | 25 (1) | 53.57, 100 | 52.39 (34.44) | 114 (13) | 27.64, 100 | 40.14 (35.98) | 0.004 |
| 15–28 | 48 (10) | 11.15, 100 | 30.30 (36.04) | 16 (2) | 67.82, 100 | 59.12 (34.68) | 16 (1) | 11.26, 80.00 | 21.91 (23.38) | 22 (1) | 52.91, 100 | 52.64 (38.45) | 102 (14) | 28.89, 100 | 38.32 (36.85) | 0.005 | |
| 29–92 | 48 (9) | 21.36, 100 | 29.62 (29.05) | 11 (0) | 76.67, 98.38 | 67.49 (30.35) | 17 (0) | 20.97, 61.62 | 27.52 (19.59) | 15 (12) | 60.19, 100 | 57.07 (35.64) | 91 (11) | 33.33, 100 | 38.33 (32.15) | 0.001 | |
| % of total visits that are social services personal carer visitsc | 0–14 | 41 (27) | 0.00, 98.82 | 24.06 (35.57) | 17 (12) | 0.00, 88.89 | 15.63 (29.50) | 31 (10) | 60.00, 87.50 | 43.43 (35.61) | 25 (15) | 0.00, 94.92 | 22.34 (35.72) | 114 (64) | 0.00, 98.82 | 27.69 (35.77) | 0.027 |
| 15–28 days | 48 (26) | 0.00, 100 | 33.48 (40.27) | 16 (13) | 0.00, 78.43 | 11.23 (24.87) | 16 (3) | 62.71, 90.32 | 54.67 (33.25) | 22 (13) | 0.00, 94.92 | 23.03 (36.30) | 102 (55) | 0.00, 100 | 31.06 (38.10) | 0.007 | |
| 29–92 | 48 (28) | 0.00, 99.59 | 27.59 (36.47) | 11 (8) | 0.00, 95.41 | 13.06 (29.66) | 17 (0) | 67.74, 94.88 | 49.98 (37.20) | 15 (5) | 0.00, 91.67 | 13.18 (31.39) | 91 (53) | 0.00, 99.59 | 27.64 (36.70) | 0.022 | |
| Type of nursing/social care | Number of days before death | Service model | Comparing pairs of models, Mann–Whitney U-test (refer to median for direction of difference) (p-value)a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: Large providers, 24/7 services | 2: Small providers, 24/7 services | 3: Large providers, not 24/7 services | 4: Small providers, not 24/7 services | ||||||||||||
| Dyads, n (dyads reporting zero contacts, n) | Median number of visits | Dyads, n (dyads reporting zero contacts, n) | Median number of visits | Dyads, n (dyads reporting zero contacts, n) | Median number of visits | Dyads, n (dyads reporting zero contacts, n) | Median number of visits | 1 vs. 2 | 1 vs. 3 | 1 vs. 4 | 2 vs. 3 | 2 vs. 4 | 3 vs. 4 | ||
| Hospice nursing visitsb | 0–14 | 41 (10) | 19.58 | 17 (0) | 64.29 | 31 (2) | 12.50 | 25 (1) | 53.57 | 0.021 | 0.793 | 0.040 | 0.002 | 0.564 | 0.004 |
| 15–28 | 48 (10) | 11.15 | 16 (2) | 67.82 | 16 (1) | 11.26 | 22 (1) | 52.91 | 0.018 | 0.907 | 0.010 | 0.007 | 0.849 | 0.011 | |
| 29–92 | 48 (9) | 21.36 | 11 (0) | 76.67 | 17 (0) | 20.97 | 15 (0) | 60.19 | 0.001 | 0.709 | 0.014 | 0.002 | 0.574 | 0.040 | |
| Model 1 > 2 | Model 4 > 1 | Model 2 > 3 | Model 4 > 3 | ||||||||||||
| Personal carer visitsc | 0–14 | 41 (27) | 0.00 | 17 (12) | 0.00 | 31 (10) | 60.00 | 25 (15) | 0.00 | 0.553 | 0.016 | 0.806 | 0.012 | 0.464 | 0.054 |
| 15–28 | 48 (26) | 0.00 | 16 (13) | 0.00 | 16 (3) | 62.71 | 22 (13) | 0.00 | 0.033 | 0.076 | 0.469 | 0.001 | 0.246 | 0.017 | |
| 29–92 | 48 (28) | 0.00 | 11 (8) | 0.00 | 17 (5) | 67.74 | 15 (5) | 0.00 | 0.288 | 0.039 | 0.135 | 0.022 | 0.799 | 0.012 | |
| Model 3 > 1 | Model 3 > 2 | Model 3 > 4 | |||||||||||||
Costs
Costs are presented in GBP, at 2019 values. Full details of daily costs for all items of service use by time period and model are shown in Appendix 23, and for individual HAH services in Appendix 24, Figures 30–33. Summaries of costs by service model and time period for the main cost items (all nursing and personal care; all formal care, including nursing, personal and inpatient; informal care; grand total of formal and informal care) are shown in Figures 12–14 and in Appendix 25.
FIGURE 12.
Costs per service model: all formal care. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.

FIGURE 13.
Costs per service model: informal care. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
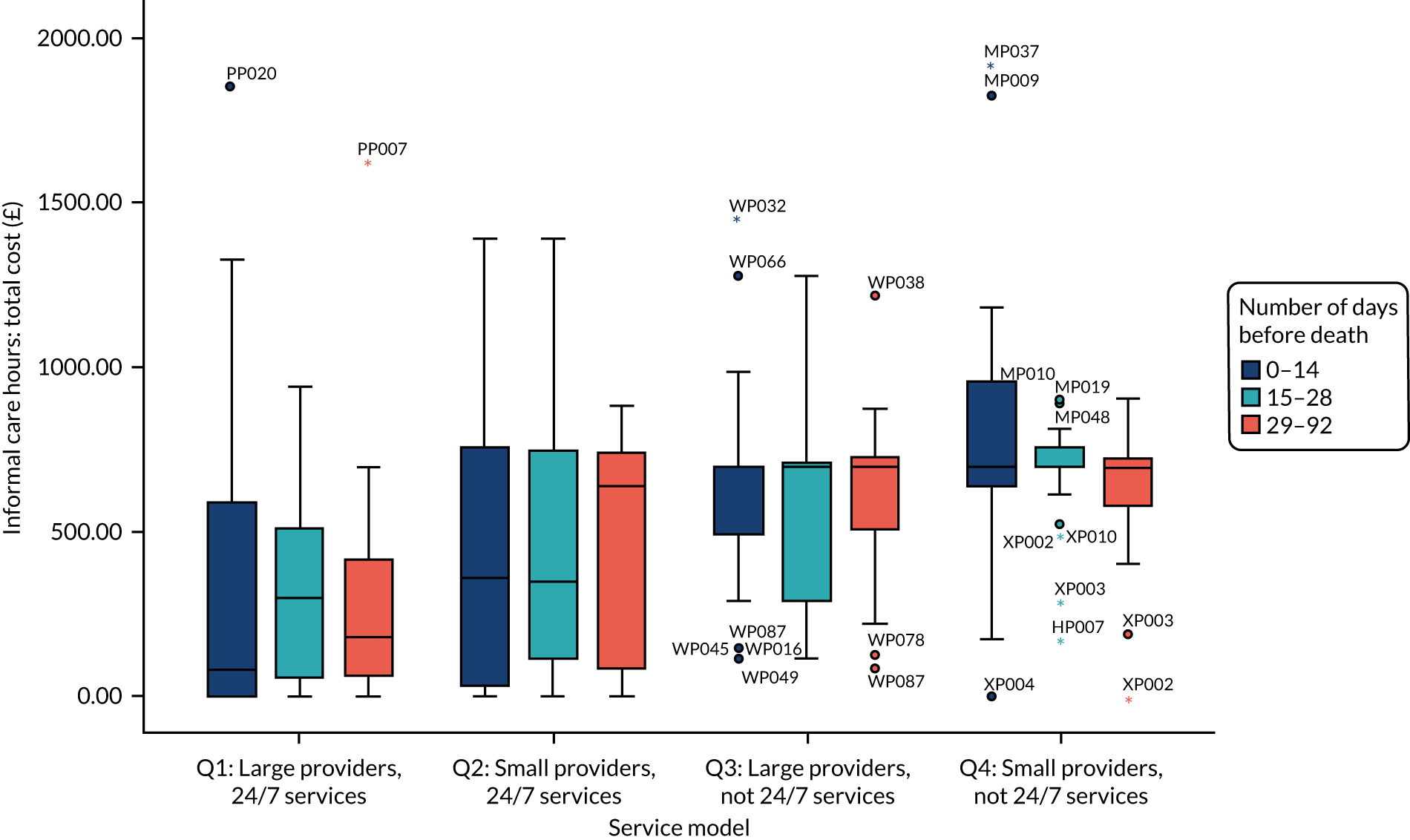
FIGURE 14.
Costs per service model: all care (formal and informal). Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.

Costs per day were higher closer to death: the median daily costs for 0–14, 15–28 and 29–92 days before death for all formal care were £104.57, £80.08 and £56.07, respectively. Among these overall costs, the median daily costs for in-home nursing and personal/social care were £40.43, £27.93 and £12.22 for 0–14, 15–28 and 29–92 days before death, respectively. Informal care costs, valued at replacement costs (support worker), exceed formal care costs, with daily medians of £580.00, £449.50 and £348.00 for 0–14, 15–28 and 29–92 days before death, respectively.
Statistically significant differences existed between models in all cost summary items and time periods (Table 18). Pairwise comparisons of models revealed that costs per day were consistently lower in model 1 (larger, 24/7 services) than in the other three models (for both formal and informal care). Daily costs in model 2 (smaller, 24/7 services) were higher than those in model 4 (smaller, not 24/7 services) for in-home nursing and personal/social care (all periods), but only for all formal care for days 29–92. Overall formal care costs were lower in model 4 (smaller, not 24/7 services) than in model 3 (larger, not 24/7 services). There were few differences in costs between model 2 (smaller 24/7 services) and model 3 (larger, not 24/7 services) (see Table 18).
| Service use item | Number of days before death | Service model | Comparing pairs of models, Mann–Whitney U-test (refer to median for direction of difference) (p-value)a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1: Large providers, 24/7 services | 2: Small providers, 24/7 services | 3: Large providers, not 24/7 services | 4: Small providers, not 24/7 services | ||||||||||||
| Participants (n) | Median | Participants (n) | Median | Participants (n) | Median | Participants (n) | Median | 1 vs. 2 | 1 vs. 3 | 1 vs. 4 | 2 vs. 3 | 2 vs. 4 | 3 vs. 4 | ||
| All nursing and personal care | 0–14 | 50 | 17.23 | 17 | 75.21 | 34 | 59.30 | 25 | 32.64 | < 0.0005 | 0.009 | 0.188 | 0.299 | 0.003 | 0.096 |
| 15–28 | 59 | 6.52 | 16 | 61.14 | 16 | 35.75 | 22 | 34.66 | 0.001 | 0.017 | 0.078 | 0.402 | 0.084 | 0.473 | |
| 29–92 | 52 | 4.60 | 11 | 57.54 | 17 | 32.37 | 15 | 18.25 | < 0.0005 | < 0.0005 | 0.201 | 0.134 | 0.003 | 0.037 | |
| Model 2 > 4 | Model 3 > 4 | ||||||||||||||
| All formal health, social and voluntary careb | 0–14 | 50 | 85.80 | 17 | 97.85 | 33 | 169.71 | 25 | 89.86 | 0.471 | 0.010 | 0.937 | 0.091 | 0.547 | 0.033 |
| 15–28 | 58 | 64.55 | 16 | 85.35 | 16 | 167.41 | 22 | 74.36 | 0.834 | 0.017 | 0.813 | 0.003 | 0.849 | 0.021 | |
| 29–92 | 52 | 40.73 | 11 | 102.34 | 17 | 88.69 | 15 | 43.50 | 0.019 | 0.022 | 0.940 | 0.677 | 0.041 | 0.044 | |
| Model 3 > 2 | Model 2 > 4 | Model 3 > 4 | |||||||||||||
| Informal care | 0–14 | 56 | 80.79 | 18 | 359.39 | 34 | 696.00 | 25 | 696.00 | 0.045 | < 0.0005 | < 0.0005 | 0.193 | 0.016 | 0.079 |
| 15–28 | 61 | 298.29 | 17 | 348.00 | 16 | 696.00 | 22 | 696.00 | 0.212 | 0.002 | < 0.0005 | 0.465 | 0.077 | 0.246 | |
| 29–92 | 52 | 180.44 | 11 | 638.00 | 17 | 696.00 | 15 | 696.00 | 0.245 | < 0.0005 | < 0.0005 | 0.430 | 0.259 | 0.628 | |
| Model 4 > 2 | |||||||||||||||
| Total formal and informal care | 0–14 | 50 | 246.54 | 17 | 541.86 | 33 | 840.55 | 25 | 849.25 | 0.042 | < 0.0005 | < 0.0005 | 0.122 | 0.042 | 0.475 |
| 15–28 | 58 | 395.68 | 16 | 458.89 | 16 | 753.89 | 22 | 770.36 | 0.198 | 0.001 | < 0.0005 | 0.305 | 0.078 | 0.404 | |
| 29–92 | 52 | 247.62 | 11 | 728.38 | 17 | 749.71 | 15 | 734.29 | 0.089 | < 0.0005 | < 0.0005 | 0.495 | 0.646 | 10.00 | |
| Model 1 always has lower costs | Model 4 > 2 | ||||||||||||||
Summary and conclusions
Characteristics of participants
Differences existed between service models in the characteristics of patients recruited, with implications for the extent of data collection and interpretation of outcomes. Patients in model 1 (larger, 24/7 services) were in the study for longer (recruited further from death) than those in the other three models and had significantly better Australian modified Karnofsky Performance Status (functional status) scores at recruitment. There were similar differences in Phase of Illness scores at recruitment. The carers in models 1 and 4 were older than those in models 2 and 3.
There were also differences in patient characteristics between HAH services within service models that further impeded the interpretation of findings. In addition, some HAH services recruited small numbers, such that model outcomes reflected the outcomes from one larger service.
Primary outcome
The post-bereavement QODD was completed by 128 carers (response rate of 46.5%). Greater proportions of bereaved carers provided QODD responses in model 1; a higher education level was also associated with completion of the QODD. Across all models, the median QODD score (achieved by 52.3% of respondents) was 70.7, equivalent to a ‘good death’ [QODD scores range from 0 (worst) to 100, with > 70 being deemed ‘a good death’]. Higher QODD scores were elicited from female carers, from university-educated carers, when patients had known for a longer time that they were dying and when patients had died at home or in a hospice. When all items were adjusted for, models 2 and 4 (smaller providers, 24/7 and not 24/7 services, respectively) delivered significantly higher (around 12) QODD scores.
Preferred place of death
Of 222 patients who had expressed a PPOD (at recruitment) and for whom the actual place of death was known, 162 (73.0%) died in their preferred location [168 (75.7%) if care/nursing home deaths are counted as ‘home’]. There was no statistically significant difference between the four service models in achieving PPOD. Overall, 152 (68.5%) participants died at home [160 (71.5%) if deaths in care/nursing homes are included as home deaths]. Being in the study for a longer period of time was associated with a lower likelihood of achieving PPOD, possibly reflecting that preferences were gathered at recruitment and may change closer to death.
Satisfaction with care
Views on satisfaction with care were gathered from carers post bereavement, at the same time as completion of the QODD. Responses to VOICES 1 showed that most (76.4%) respondents thought that they had got as much help and support as they needed in the period before the patient died. The carers of female patients reported lower levels of support than the carers of male patients; carers in model 2 (smaller, 24/7 services) were eight times more likely to report getting all the help and support they needed than carers in the other three models. Most carers (75.8%) rated the help and support they received as excellent or outstanding (VOICES 2). Better ratings were associated with university-educated carers; the patient dying in hospital was associated with worse ratings. There was a trend for carers in model 2 to report better quality of support.
Service use
Rates of formal and informal care tended to increase closer to death, but there was considerable individual-level variation. During the last 2 weeks of life, carers reported medians per day of > 20 hours of informal caring, 1.76 in-home nursing and personal care visits and 2.36 total contacts (health, social and voluntary sectors, including nursing but excluding inpatient stays). Use of inpatient beds (hospital, hospice and care/nursing home) was low.
Role of hospice at home
Local NHS community services, HAH services and social services worked together to provide in-home nursing and care, and this was the most frequently reported item of formal service used. The highest daily average number of visits was reported in model 2 (smaller, 24/7 services) and the lowest in model 1 (larger, 24/7 services). There was no difference between the four models in the proportion of in-home nursing and care provided by local NHS community services (between 30% and 35% of all visits), but HAH and social services support appeared substitutable, with HAH input being greater in models 2 and 4 (smaller services).
Costs
Daily formal and informal care costs increased closer to death. Median daily total formal care costs were £104.57 in the last 2 weeks of life and £56.07 prior to the last month, of which in-home nursing and personal care daily costs were £40.43 and £12.22 in the last 2 weeks and prior to the last month, respectively. In line with reported service use, costs per day were consistently lower in model 1 (for formal and informal care) than in the other three models. Daily in-home nursing and care costs were higher in model 2 (smaller, 24/7 services) than in model 4 (smaller, not 24/7 services); the daily costs of all formal care were higher in model 3 (larger, not 24/7 services) than in model 4 (smaller, not 24/7 services). Informal care costs (which were valued by replacement cost methods) were higher than formal care costs in all models: the median daily costs (using replacement value) were £580.00 in the last 2 weeks of life and £348.00 beyond the last month.
Chapter 7 Qualitative results from the case studies
This chapter presents findings from the qualitative data collected in the case studies. We first describe the sample of interview respondents. Next, we introduce the initial programme theories; revised programme theories are then presented, followed by detailed CMO configurations. The inter-relation between the CMO configurations is illustrated diagrammatically.
Sample
A total of 143 interviews were conducted (see Appendix 26, Tables 90 and 91). Two of these were group interviews with two interviewees at a time, and three individuals were interviewed twice (once at the start of phase 2 data collection and once around the time of the site closing to recruitment to find out about substantial changes). All sites that were in the study for > 1 year had follow-up interviews conducted. Interviews comprised:
-
nine interviews with 10 commissioners (including one interview with a pair)
-
58 interviews with carers (including one in which the carer provided a written response)
-
76 interviews with 75 service providers (three of whom were interviewed twice and four of whom took part in interviews as a pair); this group of interviewees included front-line staff (HCAs, nurses), middle management (e.g. HAH leads, volunteer co-ordinators, fundraising managers), senior managers/executives (e.g. chief executives and trustees) and HAH volunteers.
Full carer interviewee details can be found in Appendix 27. Carer gender proportions were 63.2% female and 36.8% male; the average carer age was 63.4 years, with a minimum of 29 years and a maximum of 88 years (age was unknown for two carers).
Illustrative quotations indicate the site (i.e. A = Acacia, C = Camellia, D = Dahlia, E = Echinacea, G = Gardenia, H = Hyacinth, L = Lavender, M = Marigold, P = Peony, V = Violet, W = Wisteria and X = Xyris), role (C for carer; Comm for commissioner and SP for service provider) and each interviewee’s unique identifier. For example, PC03 refers to the third carer we interviewed in the site Peony; EComm01 refers to the first commissioner interviewed in the site Echinacea. For service providers, their exact role is provided in brackets, for example CSP01 (trustee). Site summaries and patient flow diagrams for each site aided analyses, and can be seen in Appendix 28, Figures 34–45.
Initial programme theories
Our initial programme theories were developed through the literature review18 and the national HAH standards detailed in Chapter 2. We drew on NPT to provide a theoretical understanding of how HAH services might be embedded within a local EOLC economy. Results from the phase 1 survey were also used to shape initial programme theories. With stakeholder input, we developed seven iterations of eight CMO configurations before articulating the final programme theories (see Appendix 29).
As described in Chapter 3, the initial programme theories were tested in the case studies. We used them to guide interview questions and as a basis for monthly qualitative data meetings. These involved field researchers Claire Butler, Patricia Wilson and Charlotte Brigden, and Graham Silsbury and Mary Goodwin as the lay co-applicants. All transcripts were scrutinised to refine the existing CMO configurations, or to suggest further causal mechanisms. The final version of CMO configurations was then presented at two national consensus workshops, for verification and endorsement.
Final programme theories
From the initial eight CMO configurations, the final iteration comprised six CMO configurations (see Appendix 30 for the full CMO configurations, Tables 92–97). From these, we propose the following final programme theories.
Sustainability
Hospice at home services exist in an environment in which there are constantly changing funding arrangements and commissioners, and an increasing requirement for data to provide evidence to support commissioning. There are also local and national shortages of health and social care staff, alongside a national drive towards care at home. For sustainable, longer-term funding within this context, a HAH service needs to proactively seek control over available statutory funding; engage with the wider health and social care environment; and, if a charitable organisation, undertake fundraising and income generation from a range of sources. To recruit and retain staff to deliver the care that patients need, a HAH service requires a reputation for excellence and for investing in staff development, and will need to alter skill-mix profiles in response to local workforce shortages.
Volunteers
Workforce shortages and the willingness of many people in the local community to volunteer makes the volunteer workforce attractive to H&PC organisations. Changing societal norms around family and community structures have affected the social networks of many patients and carers, with demand on carers compounded by HAH services’ limitations in providing longer periods of input. Although a volunteer workforce could result in extending this period of care, HAH services need to effectively recruit, train and manage volunteers, including providing clear responsibilities, support and lines of reporting. However, to reduce the bureaucratic burden, the HAH service may take a different approach to some aspects of volunteering, along the lines of the Compassionate Communities model120 in which volunteers act as good neighbours.
Integration and co-ordination
Services across the whole system commonly act in silos, resulting in both duplication and gaps in services received by patients. This is compounded by a limit to services, funding and workforce. In addition, issues of professional ownership of EOLC are at play, and organisations seek their own branding and distinctiveness for sustainability purposes. Patients in the last phase of life often have unpredictable needs, at times that are difficult to anticipate. Some patients and carers will not know when to ask for help or who to contact. The HAH service needs to work in a co-ordinated and effective way with other service providers. This may be through a blended service without hard boundaries around roles or services, a secondment to a different setting that facilitates integration, or an agreed division of labour between services. If patients and carers are provided and updated with information, including who and how to contact professionals, then the chances of them receiving a seamless service and continuity of care with consistent information increase.
Marketing and referral
There is a complex system of health and social care providing EOLC for patients in the community. Furthermore, hospice services are often thought of as a building, and there is less understanding of HAH services. HAH functions in a society in which there is a fear and stigma around death and dying (particularly in some communities), with potential referrers reluctant to have conversations with the patient regarding prognosis. To increase referrals in general, and in particular of those who are poorly represented in hospice services, HAH needs to actively market its service to professionals and the public through clinical and public engagement. Referral systems need to be as simple as possible and not require complex transfers of information.
Knowledge, skills and ethos of care providers
Although all health and social care workers should have basic knowledge and skills in EOLC, sometimes these are lacking, including a lack of confidence in communicating at the end of life. For some patients, basic skills may not be adequate to meet their difficult or complex needs. Palliative care and EOLC have developed into specialty area of knowledge, skills and ethos, and this distinctiveness is prized by HAH organisations. However, much of this expertise still resides in cancer care, meaning that patients with other illnesses, such as dementia, may present challenges to staff and organisations. Some services (HAH and non-HAH) may also lack the time to offer personalised and patient-led care, and commissioners may prioritise equity of access across the population, rather than time and expertise. To add value to the whole system of care, HAH services need to provide expert knowledge and skills in EOLC with a suitable ethos to support this care. This is enabled by experienced staff who have spent a significant proportion of their time in EOLC so that patients and families trust them. Staff at all levels, including volunteers, are suitably trained, including appropriate communication skills, so that they can create an environment in which patients and carers have confidence and feel that they are in expert hands. HAH services value the time to offer personalised patient-led care, leading to better patient and carer experiences and sense of agency.
Support directed at the carer or patient–carer dyad at home
Unpaid care provided by family and friends is critical to enable patients to remain at home. How the patient and their informal carer, as a unit in the home, feel about dying at home and respond to the challenge of this situation will be key to achieving death at home. The carer may require confidence and new skills to enable them to provide care up to and including the point of death at home. In bereavement, there may be short- or long-term consequences of caring on the carer’s mental and physical health. However, there is a concern about medicalising bereavement, which is a normal process.
A full assessment of care needs including the whole family/care unit is required. The HAH service fully informs the carer about what might happen in terms of the trajectory of illness and the increasing burden of caring over time. Carers will then know what to expect and can rapidly recognise a change in caring situation from control to crisis. If carer and patient choices are affirmed and supported whenever possible, the carer and patient have an increased sense of control. The HAH service should negotiate a partnership with the carer, including clarity about what can and cannot be provided, and recognition of what the patient–carer dyad wants. Pre-and post-bereavement support is based on relationship and understanding of the situation, and a shared story of caring for the patient. In addition, those not experiencing normal bereavement need to be recognised and additional help made available. This should not rely on self-referral and the timing may be many months post bereavement.
The relationship between these six programme theories is illustrated in Figure 15.
FIGURE 15.
Relationship between programme theories.
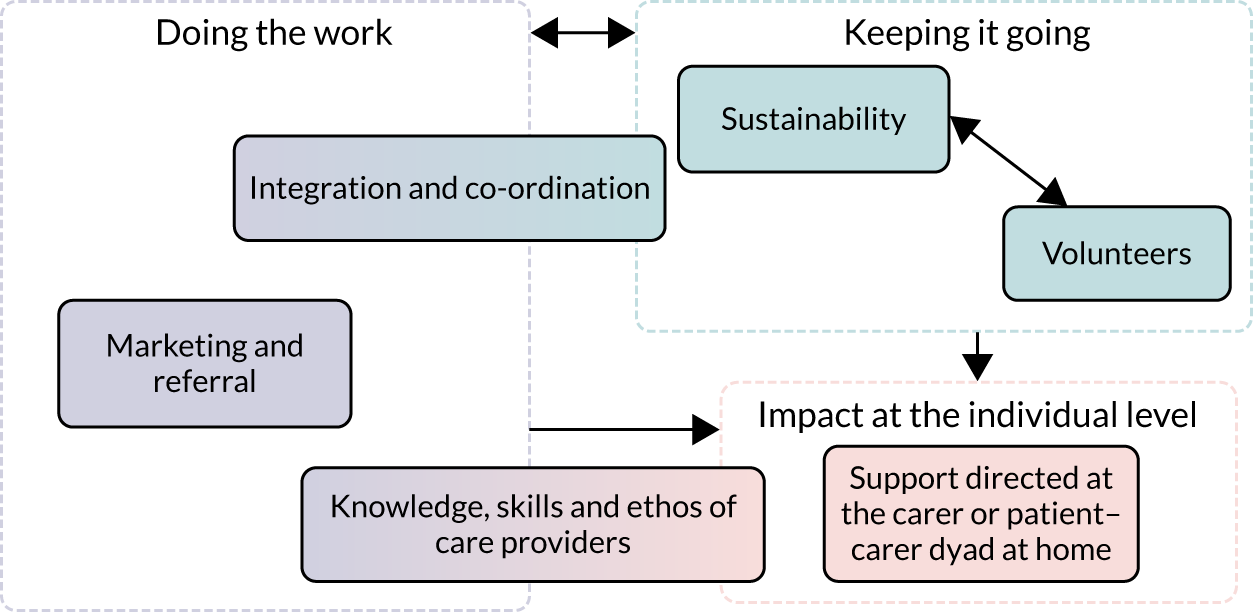
An analysis of the data supporting each CMO configuration will now be presented. Data will be presented from interviews, and feedback from the consensus workshops.
Keeping it going
The first group of CMO configurations is concerned with how services ensure longer-term viability to ‘keep the service going’. The way individual services have developed these functions is often closely related to the history and the setting of the HAH service in its locality.
Sustainability
The CMO for this configuration is shown in Box 2.
-
Statutory funding conditions and arrangements change over time.
-
There is often difficulty establishing consistent relationships with commissioners.
-
Commissioners may not be knowledgeable about palliative care and EOLC.
-
Commissioners may not recognise the full economic cost of what they are commissioning.
-
There is a shortage of staff in health and social care nationally.
-
In response to patient choice and cost savings, there is a national drive towards care at home.
-
Hospice inpatient beds are a relatively scarce resource.
-
NHS commissioners and charity boards require the collection of data to provide ‘evidence’ to support continuing service provision and development.
-
The HAH service actively seeks external engagement with the wider health and social care environment and/or
-
The HAH service proactively seeks control over the available statutory funding and/or
-
If run by an independent charitable organisation, the HAH service undertakes fundraising and income generation from different sources.
-
The HAH service is trusted and respected to know what services are needed, to raise funds to deliver them and to deliver them.
-
The HAH service has a reputation for investing in staff through CPD and/or
-
The service or leader has a reputation for excellence and/or
-
Skill-mix profiles are altered/redeployed in response to staff shortages.
-
Home-based care is supported by local commissioning and funding.
-
Patient/family preferences for place of death are revisited over time.
-
Meaningful data are collected.
-
Sustainable longer-term funding is enabled and patients will continue to receive the HAH service or
-
Access to statutory funds may be compromised, as an assumption is made that they are not needed by charitably funded organisations or
-
Short-term, non-recurring funding may be provided but is not sustainable and
-
Inequities of care may result.
-
Recruitment and retention of staff needed to deliver care but
-
This may deplete workforce in other parts of the wider system and/or
-
Staff take on roles that they lack skills and training for, or that may not be their preferred work.
-
Policy supports provision of home-based care but
-
Patients/carers may feel under an obligation to manage dying at home.
-
Activity data may satisfy some stakeholders but
-
Very little outcome or cost–benefit data are derived.
-
Time is wasted in collecting data that cannot richly inform funding and service decisions.
CPD, continuing professional development.
Funding
Ensuring sustainable funding to enable the long-term viability of the service was a major concern for all the case studies. This challenge was further complicated by frequent changes of commissioners, with very few in post long enough to develop a good understanding of palliative care and EOLC services, including national initiatives. In contrast, having an established relationship with a commissioner was beneficial:
. . . we’ve been quite open and honest with each other and from my point of view I think it’s helped, having me consistently be involved with them. I think if you had a number of commissioners over a number of years, which other CCGs [Clinical Commissioning Groups] have had to contend with, you’ve just got to rebuild relationships every time.
EComm01
One commissioner also highlighted that the relationship was easier with smaller HAH services:
It feels like a particularly open relationship . . . they’re not a big provider for us, . . . so I guess that the risk perhaps isn’t there, so that that relationship can develop in that way for that reason.
VComm01 (local authority commissioner)
For commissioners, the challenge was keeping up with the constant pace of change:
. . . commissioners are permanently chasing their tail doing 100 brand new projects that NHS England have imposed and there’s much less time to actually think about, you know, the next 1/3/5 years of local services because there’s just, you know, there’s so much change all the time.
XComm01
In addition, the landscape of change did not have EOLC as a priority:
. . . it’s just not a priority at the moment with everything else that’s going on, the transitions that’s happening around CCGs merging and things like that.
EComm01
Many of the sites also expressed a concern that commissioners may not recognise the full cost of what they are commissioning, not recognising that charitable funds were significantly supporting the service. Paradoxically, there was also the perception that fundraising was compromised by a public perception that HAH was substantially supported by statutory funding.
Case studies had taken different approaches to ensure sustainable funding. Many proactively presented a business plan, continually selling it to commissioners, or the HAH service simply took the lead and provided services. In all examples, this was facilitated by a board of trustees or an executive leader with a known reputation for excellence, resulting in being trusted by commissioners to use the funding well. Having a trustee who was closely linked with NHS commissioning was particularly beneficial:
. . . hopefully through my influence as clinical chair of the Commissioning Group, is to increase the amount of funding we have provided for hospice at home.
CSP01 (trustee)
This sense of trust was often matched by light-touch scrutiny. However, feedback from the consensus workshops highlighted that, although light-touch scrutiny may be welcomed, reputation and trust were also enhanced if commissioners had a greater understanding through scrutiny of the quality of care the service was delivering.
In the early months of fieldwork, one case study site had taken on a lead provider role, subcontracting work to other providers in the area:
. . . we subcontract some bits to [another charity]. . . . I think there’s certainly efficiencies to be made.
GSP06 (business manager)
Other case studies were also considering this model. The disadvantage of this approach was that there were variations in quality and access from different providers. This, in turn, became a new context whereby the HAH service was forced to set standards and manage contracts, similar to taking on a commissioner role. Feedback from the consensus workshops suggested that there was a possible negative reputational impact of this. In later phases of fieldwork, this approach had been rejected by case studies previously contemplating it because of the possible negative impact on collaborative partnerships with other local providers. Although a shared caseload may allow the most appropriate staff and services to be deployed, and create economies of scale and efficiencies, corporate identity may be diluted, which could have a negative effect when competing for funding (this information was gathered at the consensus workshops).
Accepting a block contract from commissioners to enable predictability of the funding available was another approach used by services. These were seen by commissioners as representing very good value for money:
. . . it was quite clear from all of the information we got back that [hospice name] were by far the best provider, they offered us the best value for money, they had all of the schemes and initiatives already established, they had staff working in the area . . . so on that basis we awarded them a contract.
EComm01
However, these contracts often lasted only 1 year at a time, which was not long enough to adequately sustain services and did not encourage innovation. Capacity, demand and community priorities often outpaced the duration of the contract cycle. An alternative approach used by several case studies was to secure NHS Continuing Healthcare (NHS CHC) funding to provide or part-fund services. However, this may result in inequities, particularly if some NHS CHC packages are topped up, or, conversely, it may result in rigidity of service when providing only what is funded by NHS CHC in terms of amount of service and duration of service:
The difficulty we have with our HAH service and we’ve had twice recently is where people need HAH but they’re not at the stage of their illness where they’re eligible for continuing fast-track funding. Then we have a dilemma because the size of our services versus the need, . . . we would be showing inequality if we were taking on people who were not funded through Continuing Healthcare in place of people who were.
LSP04 (director of clinical services)
It was uncommon to find services accepting funding for elements of service from personal health budgets. Overall, patients and families towards the end of life struggled to manage this process. There was some concern at the consensus workshops that the use of personal health budgets may result in actual or perceived inequities, in which preferential treatment may drift towards those who pay.
There were a few examples of HAH services accepting other NHS funds to support HAH, but this came with a requirement to deliver other non-palliative care roles, such as OOH urinary catheter replacements. Although case studies using this approach justified positive outcomes as building professional credibility and relationships, feedback from the consensus workshops identified concerns around maintaining competencies, the loss of specialist palliative care skills and the potential to squeeze out available resources for EOLC.
One case study had developed income-generating care services, which subsidised elements of HAH service provision:
. . . the care agency is a separate organisation to the hospice, but it’s a sister organisation so it’s very close-working in the sense that it’s a social enterprise, so any profits that the agency make completely come 100% back into the hospice.
HSP01 (lead nurse)
This element of privatisation of care could lead to availability being only for those who can afford to pay and may cause dissonance with the charitable ethos (this information was gathered at the consensus workshops).
Finally, to manage public assumptions that HAH is significantly funded by the NHS, and hence does not require charitable donations, there was some evidence that hospice charities may not be fully transparent about their access to statutory funding, to make their fundraising activities more effective. Although this may simplify information about complex funding and charitable arrangements as a public message, there was the potential risk of harming reputation if transparency was not maintained (this information was gathered at the consensus workshops):
One of the things that we are hoping is that our providers and hospices will get to a point where they’re willing to be more financially transparent with each other about the level of funding that they’re receiving from commissioners and the level that’s coming from charitable donations or other income.
XComm01
Overall, being a smaller provider necessitated working with other local services, although how this linked to sustainability varied. Strategic direction for sustainability was exemplified in one smaller provider by a focus on its relationship with other providers, in particular with the local NHS trust. This had resulted in a meshing of NHS community nursing services with the HAH service in providing a rapid-response team:
We are fortunate that our rapid-response service actually is a combined service with the community health team who also provide the district nurses, so therefore we forged a really strong relationship with the district nursing teams.
VSP03 (chief executive)
Hospice at home staff held honorary NHS contracts, and were able to deliver some elements of care outside the end of life, such as catheterisation. Perceived benefits of this blended model included the upskilling of community nurses (through working with experienced HAH staff) and earlier identification of patients who would need EOLC in due course. In addition, for this HAH service, one of the main anticipated benefits was increased visibility and having a presence on the strategic agenda for local care provision. However, this investment in the outward-facing focus, on external relationships, may have resulted in losing inward focus and investment in the service. For example, staff motivation to strive for self-development was questioned. In contrast, another site worked closely with community nurses at the care level, but there were more concerns about sustainability at this site because of its difficulties in having a ‘seat’ at local provider strategic meetings. Nevertheless, this small provider exhibited several positive benefits of being an inward-facing organisation, including high staff morale and fewer issues in recruitment and retention. This need to have effective outward- and inward-facing investment and relationships for sustainability is explored further in Chapter 8.
Staffing
The need to recruit and retain staff was set against a backdrop of local and national health and social care staff shortages. As mentioned earlier, inward-facing organisations often had a focus on investing in staff through continuing professional development (CPD). They also tended to be organisations that deployed staff in preferred areas of work with the necessary skills training. In contrast, some services needed to adapt their skill-mix profiles in response to local shortages, particularly RNs. In some cases, this led to RNs being solely office based, or non-registered staff taking on roles previously held by RNs:
. . . there’s such a lot of training available now and opportunities for non-registered general nurses, I think we need to think more about that. Not just to be able to give our non-registered nurses the opportunity to develop, but also because the pool of registered general nurses has become so difficult to recruit.
WSP02 (clinical director)
However, this was not without its problems:
. . . I think it’s a bit embarrassing when you’ve got to, you know, wait for a district nurse to come and give medication. But a lot of hospice at home staff are not qualified nurses so I get that.
LSP06 (medical director)
The reputation of a HAH service proved a strong magnet for attracting staff. This pull was created by either the reputation for staff investment or the HAH (or its leader) having a reputation for excellence:
I think it’s a popular service to work in and . . . so certainly in my experience it’s never been a problem with patients accessing the service because of difficulties with recruitment or retention or whatever.
CSP01 (trustee)
Although this success in recruitment and retention was welcomed by the HAH service, there was the potential to have a negative knock-on effect through depleting the workforce in other parts of the local health and social care system.
National policy
There is a national drive towards care at home, which is clearly linked to the discourse of enabling patient choice. However, it was also recognised that care at home offers a potential cost-saving, and the argument for commissioning HAH was underpinned by both rationales:
. . . by far the best value for money because there’s no overheads . . . often the family are the carers as well, which means that you don’t necessarily need to staff them like you would an inpatient bed . . . Hospice at home is probably by far the most effective model.
EComm01
The reality in all the case study sites was that hospice beds were a relatively scarce resource and the provision of HAH was one way of meeting that gap. Commissioning decisions were inevitably influenced by economic factors, alongside a desire to reduce inequalities in EOLC:
. . . there are big gaps all over the place for people who are dying at home . . . you know, when you look at the landscape, there are a lot of incredible Rolls Royce services being delivered in hospices and then there are a lot of very patchy, very much less good services being delivered for people that choose to be at home.
XComm01
For most of our patient and carer participants, HAH brought high-quality care to the place where patients and carers wanted to spend their last days together. However, for some patients and carers, this drive towards care at home led to a sense of obligation to manage dying at home that they found difficult. Preferences can change and there was a need for HAH services to explore and revisit the wishes of patients and carers over time.
Data and evidence
To support decisions about sustained funding, NHS commissioners and charity boards required data to be collected:
. . . it was a matter of persuading the board that it would be cost effective . . . then it was quite a hard sell at commissioner level because the perception was, ‘well we’ve got a service already, we’ve got district nursing, we’ve got primary care, you know, we’ve got a hospice if need be for patients to go in, why would we need hospice at home . . ., what’s the added value of it for the money we’re going to have to put in?’.
CSP01 (trustee)
This resulted in huge numbers of activity data being harvested, but with very little outcome and very few cost–benefit data (such as avoided hospital admissions). Hence, the usefulness of activity data was questioned and the consensus workshop also confirmed the sense of frustration felt by staff, with a consequent resistance to collecting the data. However, larger providers with 24/7 services (model 1) were more orientated to a data collection culture, and had sought to address data utility:
We’ve done a piece of work with the commissioners where . . . we can give NHS numbers to them, so all through the proper data-sharing agreements. They can then do analysis on the admissions to hospital . . . so we can say, ‘yes, we’ve avoided hospital admissions . . .’.
CSP03 (chief executive)
Keeping the work of the HAH service going could also potentially be supported by volunteers.
Volunteers
The CMO for this configuration is shown in Box 3.
-
Societal norms regarding neighbours, community support networks and families living in proximity have changed, resulting in increased burden for carers.
-
Many people in communities offer their time and skills as volunteers to hospices, and hospices rely heavily on the volunteer workforce to support other activities, particularly fundraising (including charity shops, sponsored events, etc.).
-
Using a volunteer workforce may potentially ameliorate national health and social care workforce shortages. However, employers may be concerned about utilising this workforce, particularly in the clinical setting, feeling that it is not as manageable or reliable as the paid workforce, and having concerns about legal liability, health and safety, etc.
-
Hospice at home services commonly offer shorter periods of care, in situations where there is a focus on health-care needs that are significant and rapidly increasing.
-
Limiting the volunteer workforce to focus on non-clinical activities may be more straightforward and easier to manage.
-
The employing organisation has a good understanding of employment law and volunteers are effectively recruited, trained and managed for roles in hospices or HAH; this reassures the employing organisation about working with a volunteer workforce and
-
Volunteers have clear responsibilities and expectations, and have lines of support and reporting but
-
Significant resourcing is required to train and manage volunteers to meet the health-care needs that dominate when a patient is actively dying, or volunteering work at this time may be solely concerned with indirect tasks such as shopping.
-
There is active recruitment of volunteers with particular skills (e.g. retired nurses).
-
Within the paradigm of Compassionate Communities, the employing organisation reframes its approach to volunteering, tolerating a different level of ‘risk’ and allowing volunteers to act more like neighbours, without a great deal of bureaucracy and procedure.
-
Volunteers make a valuable contribution to fundraising, without which services would be more limited.
-
The employing organisation will feel confident to utilise a volunteer workforce and additional resources will be available to provide support to patients and families.
-
More volunteers may be able to get involved with directly supporting people at home.
-
Volunteers feel confident and clear in their roles, volunteer well-being is facilitated and volunteers are retained within the HAH service to provide enhanced support to patients and families.
-
Volunteers can maintain appropriate boundaries that safeguard the patient, their family and the volunteer but
-
Inconsistencies develop when setting multiple ‘rules’ for volunteers who are offering non-professional support and befriending; there is a tension between holding a ‘quasi-professional’ versus a befriending role and
-
Volunteers in general may have a limited role in providing support to patients and family in the last days of life when the focus is on rapidly escalating health-care needs.
Although many carers had friends and family to support them, we found evidence of increased carer burden when little social network support was available. Some carers would have greatly valued more support from someone to provide longer breaks:
. . . the length of time that they said they [HAH paid staff] could do it for was not helpful at all . . . there’s not a lot you can do in 2 hours . . . if I’d had to catch the bus, I would have literally have had enough time to run into the chemist, get the prescription and come home.
WC48
However, because HAH services were predominantly focused on the patient rather than the carer, the rapidly escalating health-care needs of the patient and the requirement for skilled hands-on care to meet these needs, many HAH services did not see a potential role for volunteers to support the patient in their own home. One volunteer organiser was aghast at a potential volunteer role in providing physical care:
. . . I was a bit, um, instantly gut reaction adverse to that idea that they would have health-care assistant roles as well . . . it would be ‘oh somebody might need to be fed or got up in the morning’ and that’s not what the volunteers want to do . . .
XSP02 (volunteer manager)
For volunteers, the length of time to develop a relationship with a patient and family was important, which was unlikely to be available in some of the HAH services when contact was only in the last few weeks of life:
. . . the longer that relationship goes on, then the more that person relies on you . . . it would seem that the patient gets a great deal of benefit out of my visiting.
WSP06 (volunteer)
Nevertheless, although some carer interviews suggested that it was more befriending or ‘errand-running’ that would have helped, one of the case study sites did have volunteers providing hands-on physical care. This site ran an adult care certificate programme for volunteers. Training included personal care and symptoms to look out for, and initial experience was gained in the inpatient unit. A volunteer interviewee described how they were asked to consider providing respite care in a patient’s own home. With no previous experience in health or social care, the volunteer describes how they:
. . . have been trained on how to, if they’ve had a bowel accident or something, I know what I need to do. I’ve also been trained on suction because a couple of patients can’t swallow, can’t do anything, so they’re at risk of choking, so I’ve been trained on how to clear the throat.
ESP05 (volunteer)
The volunteer provided 2 hours of respite care every other week. They described their role as taking a referral with minimal information; preparing for the visit, which included trying to glean knowledge about the patient’s interests; and doing basic care, if necessary. The volunteer was also able to double up with a HCA for HAH visits. The volunteer described their remit as being a friend to the patient and carer, giving the carer a break and freeing up skilled staff.
When interviewing the commissioner for this case study site, they felt that the volunteers were an essential part of the service as it made ‘the money stretch’. However, as the service was contracted by the CCG, they needed to be sure that volunteers were adequately trained and appraised, which led to a cost for the service. Added to this were concerns from the site on the challenges of managing a workforce that was not in an official contract with the organisation:
. . . you are beholden to volunteers that have, you know, they’re not contracted to us, they can go on holiday whenever they please and they can go away for 6 months if they want to . . .
ESP06 (head of well-being)
However, this hands-on volunteering role was often a very positive experience for volunteers and had led some to a career change, as described by a HCA who, from an unrelated work background, had started volunteering in the hospice after experiencing hospice care for a relative, completed the care certificate and eventually became a full-time HCA.
Volunteers who had previously been health or social care professionals were particularly valued. Examples of this role included advance care planning with patients, and being used in bereavement support services:
Fifty-odd volunteers offering bereavement support . . . we have quite a few that have been nurses in the past and things like that . . . you are obviously retired from that role but then come back as volunteers.
VSP03 (chief executive)
Although volunteers were used extensively in bereavement services, we found little evidence that carers found this particularly helpful. What they desired most was to keep some contact with HAH care staff with whom they had developed a close relationship during difficult times (discussed further later in this chapter).
One case study site was notable for the range of community-based volunteer roles provided; these included:
-
hospice neighbours – social support provided early on during the palliative phase
-
carer companion – provided later on during EOLC, with the relationship extending up to 3 months post bereavement
-
bereavement support volunteers – 10-day training provided; volunteers –
-
delivered one-to-one bereavement support for up to 6 weeks; each volunteer has a maximum caseload of three bereaved carers
-
facilitated monthly support groups
-
participated in ‘walk and talk’
-
attended early bereavement cafes.
-
-
discharge buddies – supporting patients discharged from the inpatient hospice
-
CCG/hospice hub volunteer – particular remit to draw up advance care plans with patients not in the EOLC phase
-
compassionate neighbours – facilitating a more natural friendship than the more purposeful hospice neighbours:
. . . compassionate neighbours . . . the expectation is that you visit someone for about an hour a week, that you would spend time with them that way. But the idea of a compassionate neighbour . . . it’s like generating genuine friendships and connections . . .
PSP05 (volunteer manager)
At this site, volunteering was perceived as innovative, was embedded within policies and was facilitated by a volunteer manager. However, there were challenges. In addition to the resource implications of managing and training the volunteer workforce, one of the biggest issues was ensuring that volunteers kept within boundaries:
. . . I think sometimes people feel for themselves as a volunteer that it’s different to a member of staff, which of course it is, but it doesn’t mean that boundaries are different. But I think people think ‘well it’s OK for me to because I’m a volunteer’, well it’s not actually . . . you’re a representative of an organisation.
PSP05 (volunteer manager)
The potential benefits and challenges of volunteers were also expressed by sites considering developing their volunteer workforce. One respondent from a site felt that:
. . . there’s an untapped resource we could use there and so many of our volunteers have the skills that could be developed into the clinical development . . . clinical volunteer role . . . so it is something we would like to develop.
VSP03 (chief executive)
In contrast, another respondent from the same site expressed:
. . . there’s a risk to our reputation that if we put volunteers in doing respite in someone’s house and that patient became soiled, that actually that volunteer can’t deal with that, and then that we’re kind of leaving a patient suffering . . . the boundaries would need to be very, very clear before we introduced volunteers.
VSP04 (director of operations)
This tension between recognising a potential volunteer role in the last days of life and seeing any benefit of this role outweighed by potential risks was amplified in the consensus workshops. Although there was acknowledgement that the volunteer workforce has ‘huge potential’, the risks to the reputation of the employing organisation were frequently mentioned. Concerns centred on governance and health and safety, and maintaining the fine balance in ensuring that boundaries are clear and adhered to, versus allowing natural responses of compassion and empathy that underpin much of the motivation to volunteer. These issues were prevalent in the case studies, illustrated by this caveat on using volunteers to assist physiotherapists:
We’ve already assessed the person at home and they say ‘I would like a Zimmer frame’ [Zimmer Biomet Holdings, Inc., Warsaw, IN, USA], so then the volunteer would go out and give them a Zimmer frame and just check that they’re all right with the height, etc. . . . we’re looking into that, but obviously we’ve got to look at the insurance side of it.
GSP02 (physiotherapist)
Commissioners appeared aware of the potential benefit of volunteers, but cognisant of less formalised approaches to quality monitoring:
. . . we would expect to see certain training needs met, appraisals being done, that sort of thing and that’s not always the case with volunteers, so I think our safety and quality team are working with them to try and come up, like, with a meet-halfway-type scenario. . .
EComm01
This ambiguity and tension within the volunteer role will be explored further in Chapter 8, but realising the potential of a volunteer workforce could, quite clearly, contribute to the sustainability of the HAH services. As shown in Figure 15, it also straddles the next group of CMO configurations, ‘doing the work’, and has the potential to positively affect carer burden.
Doing the work
The second group of CMO configurations is concerned with how services operate on a day-to-day basis to ‘do the work’ of delivering HAH. The ways individual services have developed these functions were linked to how the wider health and social care economy functioned locally, as well as to the history and ethos of the HAH service itself. The first of these CMO configurations, integration and co-ordination, straddles the intersection of the previous group of CMO configurations (keeping it going) as it also contributes towards sustainability.
Integration and co-ordination
The CMO for this configuration is shown in Box 4.
-
Integration of health and social care is a national driver; the boundaries between the two types of care needs are often difficult to define clearly and many years have been spent putting in divides between health and social care for the purposes of previous funding divisions.
-
A range of services needed by people at end of life are operating in the community with different organisational, funding, staffing, IT, etc., arrangements.
-
There is a limit to services, funding and workforce across the system.
-
Services across the system commonly act in silos.
-
Hospice at home organisations seek their own branding and distinctiveness for sustainability purposes.
-
Not all HAH services provide 24/7 care.
-
Issues of professional ‘ownership’ of palliative care and EOLC are at play, whereby designated palliative care services may want to see other services providing high-quality EOLC, but also see this as a threat.
-
Individual professionals seek to differentiate their roles and functions, so they all continue to be ‘needed’, for their own personal and professional requirements.
-
Professional boundaries are shifting across health and social care, including those between doctors, nurses and other professionals (e.g. paramedics, physician associates) and between registered and non-registered workers.
-
Patients in the last phase of life and their family carers require and use services from a wide range of statutory, voluntary, and health and social care providers.
-
Towards the end of life, patients have a constantly changing trajectory of illness and needs that are difficult to anticipate in terms of exactly what will happen and when.
-
Patients and carers may not always know when to ask for help or which service/person to contact; sometimes they are concerned about making too many demands on busy (charitably funded) services.
-
Readiness of HAH providers to participate fully in collaborative commissioning.
-
‘Outward-facing’ work with commissioners and other providers to promote integration.
-
Elements of budgets, workforce and organisational structure are managed in an integrated way across provider organisations.
-
The provision of anticipatory care plans, arrangements and information. This becomes even more critical if elements (e.g. night-time cover) are not provided directly by a HAH service.
-
Regardless of ‘formal’ arrangements for integration and co-ordination, much of this works on the ground, as colleagues get on to work for the patient and are co-dependent.
-
Patients and carers are provided and updated with information, including who and how to contact professionals.
-
Services are able to provide staff to respond rapidly to unpredictable and fluctuating workloads in a cost-effective way.
-
There is reduced tension between provider organisations.
-
There is the professional satisfaction for individuals of providing good-quality care, in collaboration with colleagues, regardless of organisational arrangements; however
-
The multiplicity of organisations and roles may cause confusion and conflict on the ground.
-
Patients and carers receive a seamless service and continuity of care without delay, duplication or gaps.
-
Needs are anticipated as far as possible and patients experience continuity of care when providers change.
-
Patients know who to contact in an emergency and get the response they need.
-
Fewer patients have unwanted emergency admissions to hospital.
-
More patients can potentially have enhanced hospital discharge.
IT, information technology.
National perspective
National policy and strategic direction affected integration and co-ordination, particularly through their influence on commissioners and commissioning practices. One commissioner expressed a view at the consensus meeting that HAH organisations in general were not in a state of readiness to participate fully in collaborative commissioning.
Hospice at home organisations that keep a close eye on national policy could capitalise on or anticipate the impact of this and plan their local strategies for integration, co-ordination and, thereby, sustainability accordingly. Some case studies invested substantial effort in this (see Sustainability above and Chapter 8, Sustainability, which explores outward- vs. inward-facing organisational focus).
Service perspective
Hospice at home services commonly formed part of a hospice organisation, often a charity, which was providing other palliative care and EOLC services. Even the largest hospice organisations were relatively small players in local health and social care economies, but many were small or very small provider organisations, which often triggered a focus on developing partnerships with other providers. Some of these smaller services had worked hard to become involved in commissioning decisions:
. . . we make sure we always inform them what’s going on, we make sure that we write in the notes, we communicate, if we’ve been out to see a patient we would phone the district nursing team and talk to them if we’ve got any concerns . . . then we have the quarterly meetings where we all get together and talk about if we’ve got any issues. And then either, as the lead within the service, would go to the end-of-life community meetings within the trust, so that we’ve got that strategic-level conversation that’s ongoing.
MSP05 (community team leader)
Good-quality integration and co-ordination at the service level were not automatically straightforward and required a considerable investment of time and effort. We found examples of a range of strategies employed by HAH services to enhance integration and co-ordination.
A ‘blending’ approach between services
Different services can provide what is needed by a patient without hard boundaries between services via several strategies, for example:
-
joint posts, for example consultants working across settings/organisations; honorary contracts with the NHS were emblematic and may facilitate this
-
shared clinical records/information technology (IT) systems (this was not common)
-
a whole range of collaborative hub, co-ordinator and single-point-of-access arrangements
-
systems to facilitate communication and reduce bureaucracy between services.
Building relationships
-
Joint clinical visits, regular meetings between clinical colleagues from different services (e.g. primary care end-of-life meetings).
-
A secondment to a different setting (e.g. a health-care worker into social care) may facilitate integration by the ‘learning of another language’ (dependent on workforce availability).
Agreed ‘division of labour’
-
Community nurses provide and administer all anticipatory medications.
-
The HAH service is trusted to make assessments that other professionals will act on; this trust is based on individuals and/or on the reputation of the HAH service.
-
The HAH service has direct access to shared equipment stores or has its own stores.
A number of the smaller HAH services worked alongside other providers, for example through palliative care hub working:
. . . we just refer to each other and talk to each other. You know, there’s no having to refer to a specialist nurse with a particular form, I would actually just speak to them and discuss it and they’ll pick up the referral.
XSP04 (community matron end of life and supportive care)
Secondments to a different setting also helped integration; for example, XSP04, a community matron, had worked in various settings in the area and had strong links with her palliative care colleagues:
I’ve turned to [HAH] for support in complex situations like that, you know. I’ve used their social worker, I’ve used, you know, I know their therapists and I know their senior nurse, I could phone and discuss anything.
XSP04 (NHS community matron)
Good working relations often stemmed from the bottom up, based on pragmatic decisions of ‘finding the best person to do the job at the time’ (XSP04, community matron) and, for the smaller HAH services, agreeing how tasks were divided up, keeping patient need at the forefront:
. . . when the hospice at home service started with the registered nurse part of that service, that involved quite a lot of negotiation with the district nurse about who should actually do what and it’s definitely an ongoing discussion about how things are divided up.
XSP01 [clinical nurse specialist (CNS)]
There was less evidence of effective joint working with social services:
. . . if you’re talking social services, they talk a different language, don’t they, you know, urgent to them means completely something different than urgent to me.
XSP04 (community matron)
There were also examples of silo working, even within the wider hospice organisation, for example between the inpatient unit, day service and HAH, which partly related to capacity, but affected integrated working between staff:
. . . we are trying to break down any barriers between the departments. I’d like to have, for example, the rota-ing . . . is done by each department on their own at the moment and looking at whether or not that should be blended together as one. So that actually staff are much more used to working across departments rather than I’m a ward HCA, or I’m a HAH HCA.
HSP02 (chief executive)
Professional perspective
There were many examples of HAH staff working closely with colleagues in partner organisations, particularly community nursing, to enhance integration and co-ordination, regardless of organisational arrangements or constraints:
. . . he was discharged without a hospital bed without a care package . . . the wife was feeling very anxious, they felt very on their own and so . . . I phoned my colleague at the hospital first of all to find out what was going on. She referred to the district nurses; the district nurses were able to order a hospital bed that actually arrived by that evening. I then came and fast-tracked the patient and care was initiated . . . the carer started the next morning, then they attended regularly . . . so that is a really good example of how myself, the hospital clinical nurse specialist, the district nurses, the team, the carers’ team here were all able to work together to make sure that he actually did die at home.
GSP03 (CNS)
Nevertheless, there were times when HAH staff felt overburdened with attempts to co-ordinate services on behalf of the patient:
. . . different services that are involved, families find it difficult to get their head round sometimes, you’ve got Marie Curie, you’ve got us going in and then sometimes you’ve community carers going in four times a day, they go in just to do the personal care, sometimes they’ll say who are you, where are you from . . . so I do think they find it difficult.
DSP03 (health-care support worker)
And, in some cases, there were ‘ruffled feathers’ as services, individuals or roles came into conflict:
. . . the district nurses get to know the patients . . . and build up relationships with them . . . and then we suddenly go in and they are sort of pushed to the side. I think that’s what they feel, and we can tend to look . . . overzealous . . .
MSP03 (HCA)
Patient and family perspective
Patients and their carers in the home were not overly concerned about which organisation, funding stream or system was providing the care, provided their needs were met as and when they arose. Examples of arrangements that improved ‘right care, right place and right time’ included a single point of access and 24-hour access to advice and support from a readily accessible telephone number or local rapid-response service:
And we’d been looking after mum all those years and struggling to get appropriate help and advice about the dementia, and it had been extremely frustrating at times but at the end of that phone call, the nurse at the end of that phone said to me ‘now you do realise we have a 24-hour helpline at the hospice, if you have any queries, any problems whatsoever just pick up the phone and someone is here’ . . . And I put the phone down and I burst into tears because it was the first time I felt we were being truly supported to care for mum.
DC21
There were many examples of the hospice telephone service being the gateway to solving problems; in this example, the carer was talking about his mother’s poor inpatient experience:
. . . when [hospice] became involved, nothing went amiss . . . I’d ring ’em up and say ‘I’ve got this problem’ and within hours the problem was solved . . . people would be forced to react after the [hospice] had spoken to them.
EC03
The role of individual professionals on the ground was pivotal to the patient/carer experience, particularly ‘just to have a name and know that there was support if we needed it’ (PC12) and if they called, a response would be forthcoming:
I’d always said right from the start I wanted him at home and he’d said, you know, ‘it’s too much and what if we don’t get the support?’ . . . one Sunday night he said ‘I feel really awful . . . can you call the nurses?’ and it suddenly, it’s sort of 9/10 o’clock and I said ‘Why? Why are we calling them?’ And he said ‘I just need them to come here’ . . . they literally come, they reassured him and then they went away and I think it was his sort of test that if we called someone, they would come.
GC04
Regardless of what services or organisational arrangements for integration and co-ordination were in place, carers did not always know who to contact, when or how, and sometimes found themselves in unhappy situations as a result. In this example, the husband explained how they received monthly monitoring calls from the HAH service. However, when his wife deteriorated unexpectedly, they did not know who to call:
During the day, she was in pain a couple of times and wasn’t – I suppose being naive and never being involved in this – wasn’t quite sure who we should call so we phoned the hospice and uh, they said ‘well, I think you better call the doctor or ring’ was it, 111 or something like that? . . . and eventually the ambulance took her to the hospital, and the final time she never came out, so we never used the hospice. Although she did want to go to the hospice but things didn’t turn out that way.
EC05
Despite many examples and evidence of good ideas and areas of good practice, the overall impression from public attendees at the consensus workshops was of a whole health and social care system in chaos. People frequently experienced multiple assessments, conflicting advice and information, and delays to their care and treatment and often found that they (or their carer) were the only source of up-to-date information, in a sense acting as their own care co-ordinator. This was compounded for several carers by scant knowledge of local services and, for some, a lack of prior awareness of their local HAH service. In response to this and other contextual factors, HAH services focused some salient actions around marketing and referral.
Marketing and referral
The CMO for this configuration is shown in Box 5.
Both professionals and the public often think of hospice services as hospice buildings and as being only for patients with cancer.
Fear of death and dying-
Professionals may be reticent to refer patients to HAH services because it means having a conversation about death and dying with the patient, for which they may not feel skilled, or be willing or have enough time to do.
-
The public also find talking about death and dying difficult; this may have more impact in some communities.
-
Many professionals are not aware of HAH services or of the details of patient suitability; therefore, not all patients who could benefit from HAH services are currently referred to or receive such services. Data to show the extent of these unmet needs are not readily available.
-
A number of patient groups are poorly represented in hospice services in general, that is they do not receive an equitable share of available services, for example older-age people (> 85 years), those with a non-cancer diagnosis, those experiencing deprivation.
-
Hospice at home services aim to offer care to patients with ‘complex’ and suitable needs, which may include short prognosis (note significant differences between services).
-
Hospice at home services prefer to avoid discharging patients from services because of the impact on reputation and sustainability and the difficulty of replacing HAH care with other available services.
The term ‘hospice’ encourages expectations of quality and specialism, which HAH services may not be able to replicate at home.
Mechanisms Raising awarenessThe HAH service actively raises the awareness of professionals and the public through clinical and public engagement.
Fear of death and dying-
Hospice at home services offer education and skills training to other professionals about the recognition of end of life, having end-of-life conversations and the use of palliative care registers.
-
A HAH service focuses its message on living well at all stages; this may make the process of referral more palatable for professionals and patients alike.
-
The HAH service proactively seeks suitable referrals through a range of systems or relationships.
-
The HAH service has robust criteria for identifying which referrals are suitable.
-
Clearly bounded funding arrangements (e.g. NHS CHC funding) enable more robust management when accepting or discharging patients from the HAH service.
-
Criteria, explanation of the service and treatment are clearly communicated to patients, informal/family carers, and health and social care professionals.
-
The HAH service is seen as essential by professionals and the public and more patients with suitable needs are referred.
-
These concerns do not impede the referral and care of suitable patients.
-
Suitable referral of patients, who can benefit, and will receive the service in a timely fashion.
-
Patients representing the diagnostic, demographic, cultural and socioeconomic diversity of the area served receive HAH services and services are provided equitably.
-
Professionals, patients and families will be clear about when and what they can expect to receive from the HAH service.
-
Patients make choices based on correct information and understanding and their choices are not over-ridden by professionals.
Raising awareness
Organisations employed a range of strategies to achieve knowledge and understanding of the HAH service and its role, for example:
-
Allowing self-referral and raising awareness among the public directly (via telephone number, website, GP, previous experience of hospice services). At times people who became aware of the service were able to ‘get a foot in the door’, even if they were not able to self-refer directly.
-
The fundraising element of the organisation used events to market the service and educate the public about its role.
-
Clinical staff had an important role in encouraging referral to the service through their day-to-day work and interactions with colleagues and the public.
One site reviewed the demographics of patients coming through the service and acted:
. . . we knew that there were patients in the local community, the Chinese community, not far from us that weren’t accessing any of the services . . . So, a couple of the HAH nurses went there and spoke to the residents . . . we talked specifically to them about HAH and the sorts of things we could offer . . . to try and break down some of the barriers.
MSP04 (head of service improvement and quality)
Fear of death and dying
This context was well recognised as a backdrop in which all the HAH services operated:
. . . you’d be surprised how many local people just don’t know we’re there because people go around quite blinkered you don’t want to be involved with a hospice unless you need it. And we’re trying to dispel those kinds of myths and get people aware of what we do.
GSP07 (fundraiser)
The provision of training for staff outside the HAH service was one response to this, explored further in the next CMO (knowledge, skills and ethos) but also relevant here.
Getting to the right patients and equity
To continue to function effectively and equitably, services had referral criteria and strategies to discharge or transfer care out of the HAH service. Several services, particularly the larger, 24/7 services (model 1) in this study, had patients under their care for longer periods of time (> 6 months) and had patients with varying levels of need over time. Although carers appreciated early support, paradoxically this left carers to proactively contact the HAH service if needed between visits, and many of the carer respondents from these services had less contact with the service:
. . . when they made their appointments said ‘oh we’ll come and see you in such-and-such a . . .’ you know, in a few weeks’ time and in-between we didn’t really need to ring them for anything.
PC30
A range of strategies were employed to manage demand for HAH services, including:
-
admission criteria, which varied between HAH services, in terms duration of service, patient factors and the funding source
-
having trained triage staff to manage service admission
-
the provision of clear information about referral on to other services when the HAH service was not, or no longer, deemed suitable
-
categorising patients’ levels of need and adjusting the service level accordingly and/or
-
the use of other hospice services (e.g. day care).
One site triaged patients into six categories, according to their level of need, from ‘actively dying’ to ‘three monthly monitoring’ (i.e once every 3 months):
. . . we have our ‘blues’ who don’t need a face to face but you need to keep in contact with them because they’re the type that will hit crisis and won’t think about phoning in, so they have like a monthly phone call . . .
ESP01 (deputy director of care)
Another site employed strict criteria in terms of the duration of their input:
We have a 4-week end-of-life criteria, . . . so we will review at 2 weeks and look to see whether or not people have had onward referral to CHC or social services and we will pull out at 4 weeks if appropriate. Now if it’s 4 weeks and somebody’s clearly dying then we would stay, but generally we would, we don’t provide ongoing care . . . We’ve got limited resource.
MSP05 (integrated community team leader)
Another site described criteria as follows:
. . . one is somebody that’s on the end of life, maybe the last week of life, few days, and we will go in as a team and do whatever that patient needs to keep them at home . . . the other one is if somebody’s in their last 12 months of life but has got an acute episode, and that may be uncontrolled pain . . . most of the time it’s carer fatigue, where the carer just can’t do it anymore.
CSP02 (team leader, HAH)
Overall, we found that services were reticent to discharge patients: ‘we’d never leave someone in the lurch’ was a common refrain. Mostly, it seemed preferable for HAH services to control their caseload by managing access at the point of referral. One site took only NHS CHC referrals, but the conflicts remained:
The difficulty we have with our HAH service and we’ve had twice recently is where people need HAH but they’re not at the stage of their illness where they’re eligible for continuing fast-track funding. Then we have a dilemma because the size of our services versus the need, you know, we would be showing inequality if we were taking on people who were not funded through Continuing Healthcare in place of people who were. We wouldn’t really be fulfilling our contractual agreement . . . [however] . . . we would never leave anybody in a true crisis.
LSP04 (hospice director)
It seemed that none of the services had waiting lists as such, but some (re)prioritised in times of high demand according to unofficial criteria, for example:
. . . if it does peak then we’ll look at our bank . . . see if anybody else can do any extra hours . . . If it becomes . . . you know, over a long period of time or a sickness or whatever we’re not able to meet demand, then we have to prioritise . . . although our primary remit is for patients who are in their last days or weeks of life . . . and you know we can’t see those patients if they have low complexity and low need, we go back to the district nurses and say ‘we’re really struggling today; we can’t go’.
MSP04 (head of service improvement and quality)
Managing expectations
Managing patient and family expectations was a process of continuous work over time, involving information provision and negotiation between the HAH service and those in the home (see also the ‘support directed at the carer’ CMO). When this worked well, patients and their carers could make informed decisions and choices at each stage of the care pathway, even adapting their requirements to the availability of the HAH service:
Did you feel there was quite a lot of expectation from you in terms of care provision for your husband?
No. No, I did a lot more than what was expected, you know, because they would always say, ‘oh well we usually do this’ you know, they joked with me because they got to know me, because I liked to do it, you know, that was something I could do for my husband. But no, it wasn’t expected of me to have done any of it.
Some family carers did not feel prepared for the complexity of needs and challenges:
. . . the process of encouraging people to die at home I’m sure is absolutely fine . . . But I’m quite sure there are going to be many, many, many cases . . . where it places an enormous strain on the family . . . We had no preparation . . .
XC01
When expectations were not well managed, disappointment and frustration could result:
I called every day to that last week saying, ‘Any beds, any beds?’ and [nurse] saying ‘Nope, nope, sorry, sorry, sorry’ and on Friday she said ‘we’ll talk on Monday’ and I said, ‘it’s not . . . he’s not going to last that long’ . . . and I was right, he died on the Sunday morning, on his birthday. And at that point I would’ve thought ‘is it worth moving him?’ because he’s not, you know, he’s so unwell and it’s that mad – ‘you have to be sick enough to get in, but not so sick that you’re about to die any second’, so, it’s like the Goldilocks of terminal illness, . . . that makes me sad.
PC12
The need for marketing to increase visibility and referral numbers for sustainability purposes, together with a genuine desire to encourage the identification and referral of the whole range of suitable patients who could benefit from HAH, seemed to conflict with elements of the ‘hospice ethos’ of services: preferring not to discharge patients, not trusting other services to provide adequately, and not wanting to abandon patients and families. As a result, caseload management became a significant challenge (overlapping with the next CMO, ‘knowledge, skills and ethos’).
Knowledge, skills and ethos
The CMO for this configuration is shown in Box 6.
-
There is wide variability in the levels of knowledge, skills and performance, which may vary from GP to GP, from community nurse to community nurse, from carer to carer.
-
Many professionals may lack experience of interaction with dying patients.
-
Palliative care and EOLC have developed into ‘specialty’ areas of knowledge, skills and ethos and this distinctiveness is prized by HAH organisations; however
-
Most of the expertise in palliative care and EOLC still resides in cancer care; patients with other illnesses may present challenges to staff and organisations.
-
Health and social care workers outside HAH services lack time to offer personalised and patient-led care.
-
HAH services are designed to respond to the needs of the patient at a pace that works for patients and carers. As part of this context, HAH services can pick and choose their workload more than services that are statutory or profit-making, and HAH services choose to value time over volume.
-
Commissioners do not always value time and expertise, but prioritise equity of access across the population.
-
All health and social care workers should have training to support and maintain basic knowledge and skills in palliative care and EOLC. However, these are sometimes lacking, resulting in, for example, a lack of confidence in identifying the end of life or a lack of skills in communicating at the end of life.
-
Not all health and social care workers receive adequate support to care for patients at the end of life.
Hospice at home services provide experienced staff, spending a significant proportion of their time in palliative care and EOLC, who are capable and competent in these settings, so patients, families and other HCPs trust them.
TimeHospice at home staff take time to offer personalised, patient-led care, giving the feeling that they have time and that they work at the pace of the patient.
Training-
Hospice at home staff at all levels (including volunteers) are suitably trained, including appropriate communication skills and investment in CPD, so that they can create an environment in which patients and carers feel that they are in expert hands.
-
The HAH service also provides training in palliative care and EOLC to other health and social care professionals.
-
The HAH service retains skilled staff by providing staff support to manage the stress of their work and to develop the necessary emotional resilience.
-
Staff can call for advice and support with their work from expert colleagues who are part of the HAH (or wider) organisation.
-
Patients who receive HAH have a high-quality patient and carer experience and a sense of agency.
-
Patients from groups with which HAH is not so experienced (e.g. dementia) may not get the care they want.
-
Patients who receive HAH receive the care they need at a pace tailored to them.
Health and social care workers outside the HAH service may receive training from the HAH service to increase their skills; others may become deskilled if HAH services take on work they previously covered. If the balance falls towards deskilling, then knowledge, experience and confidence decrease over time, resulting in poorer care for those who do not access specialist services.
Supported staffStaff satisfaction, recruitment and retention are positive and facilitate sustainability.
Know-how, experience and expertise
Hospice at home services identified and prized their specialist status:
. . . we are the only specialist provider and so HAH is the only specialist palliative/end-of-life care service in the area . . .
HSP02 (chief executive)
And the patient and their carer or family were the ultimate beneficiaries of the know-how, experience and expertise of HAH staff:
It’s a skill level, isn’t it, to be able to detect, because I hadn’t detected it and I’m his wife. [HAH staff] had. She said ‘no his breathing’s changed’, and she knew. So I was very grateful that she was there because [. . .] she had had quite a deep nursing background so she had the skill, so I’m very grateful for that.
PC48
Time
The resource of ‘time’ was a context that all HAH services prioritised, but was a particularly strong theme among the smaller providers. It was also a mechanism that achieved high-quality care and confidence in the support that patients and carers received:
I keep coming back to time. I just feel time is such a massive, massive factor. And that just allows people to open up more when we’re there each day. They can see that there’s no rush. . . . It’s priceless isn’t it – time.
MSP01 (RN)
It was very good, very professional. They took me and my husband at our pace.
LC01
This was such a valued resource that patients and carers were prepared to compromise in some respects (e.g. not knowing what HAH care they will receive that day until the morning of the day or accepting a reduced service when they knew that the HAH service was under pressure, provided it was clearly communicated):
[T]hey always let me know what was happening . . . and if they might say ‘oh we’ve got to go to [another area] first, would you like us early or later, I said ‘oh, can you come later now, that settles him down for the night’. They said ‘no that’s fine with us’ and we sort of worked it all between us; it was brilliant.
LC29
Again, time pressures were well managed by HAH organisations through consistent communication with patients and carers (e.g. if they are going to be delayed).
[I]f there was going to be a change [HAH] ring you up and say ‘look we’re running about 20 minutes late, we’ll be with you at such and such a time’. And that even went for the weekend, absolutely brilliant . . ..
MC10
Training
Both the experience in EOLC and the training of HAH staff contributed to making patients and carers feel that they were in expert hands, which inspired trust and confidence:
Even, you know, doctoring dad’s pyjama trousers so they could pass tubes through . . . and things like that, it was . . . again without that knowledge you . . . without their support we wouldn’t have even thought of things like that . . .
MC10
Providing training to upskill staff outside the HAH service was also seen as important.
Supported staff
Policies and processes in some HAH services supported and allowed for extended roles (flexibility of roles) as necessary to meet patient needs. This feature characterised services that prioritised responsiveness to patient need, rather than a more rigid service structure and functioning, and may also be a feature of smaller, potentially nimbler, organisations. For example, one smaller service had set up a new urgent-care service:
. . . the Urgent Response has changed the culture of the HAH team because they recognise that they’ve got the skills to be able to go out and deal with things urgently, so they don’t need to refer on to a CNS to do that, but actually we trust and respect them to go out and do that. It’s changed the culture of the wider team because it’s bridged how they work together and improved the working relationships and it’s changed our culture of care . . . we know that, within the total service, that we can respond much, much more quickly.
MSP005 (community team leader)
Support directed at carers or the patient–carer dyad at home
The CMO for this configuration is shown in Box 7.
-
Unpaid care provided by family and/or friends is critical to enabling patients to remain at home.
-
How the patient and their informal carers as a unit in the home feel about dying at home and respond to the challenge of this situation will be key to achieving death at home.
-
The carer may require confidence and new skills to enable them to provide care up to and including the point of death at home.
-
Caring can have short- or long-term consequences for the mental and physical health of the carer later on, when they are bereaved.
-
There is concern about ‘medicalising’ bereavement, which is a normal process.
-
Hospice at home services cease abruptly when the patient dies.
-
Assessment of the needs of the carer and the whole family unit, including patient–carer dyad preferences (e.g. how much outside intervention is wanted).
-
Multidisciplinary team available to meet the needs.
-
The carer is fully informed, including about what might happen in terms of the trajectory of illness and the increasing burden of caring over time, so that they will know what to expect and can prepare, and will be able to recognise a change in the caring situation from control to crisis.
-
The patient and carer choices are affirmed and supported whenever possible, giving the carer and the patient an increased sense of control.
-
A negotiated partnership between the carer and staff including clarity on what can and what cannot be provided by the HAH service.
-
Negotiations take place with the carer about how much they are happy to take on and the carer receives skills training and
-
The carer is given permission to do caring tasks that are traditionally seen as ‘professional’ tasks and
-
There is regular contact, and an ongoing relationship of feedback, response and adaptation and
-
The carer has timely access to an appropriate point of contact 24/7, thus
-
The carer has trust and confidence in the backup provided by the service and in their caring role.
-
There is support pre and post bereavement, which is based on relationship and a shared story of caring for the patient.
-
There is a process to identify those who are not experiencing ‘normal’ bereavement and may need additional/expert help.
-
Carers can continue to care, enabling more sustainable patient care at home.
-
Carers receive the care and support they need, including sleep, taking a break, reassurance and confidence-building, but
-
Occasionally, carer needs may become the focus at the expense of the patient.
-
Carers have appropriate skills that they find are acceptable but
-
If too much is expected of the carer then this may lead to some tasks they may not be able to manage, or they may not be able to continue to provide care.
-
The carer will have the best chance of a positive outcome following bereavement and recovery from the caring role.
-
Carers may have a negative experience of care and of the burden and difficulties but
-
Some carers may accept this negative experience as a price they wish to pay to allow their loved one to achieve their PPOD.
The impact of all the HAH services (with their various approaches to sustainability; volunteering; integration and co-ordination; marketing and referral; and knowledge, skills and ethos) was ultimately felt in the patient’s home, and this CMO configuration draws together many of the themes from all of the CMO configurations.
During end-of-life care
Hospice at home staff recognised the need to extensively support carers, and some of the case study sites offered specific carer interventions such as support groups and sitting services. Practical carer courses were also found to be useful:
I thought the mobility one was very good, which was teaching us how to use the slidey sheet and how to get people out of a chair . . . all that sort of stuff . . .. There’s one about nutrition, interesting, . . . and then there’s another one . . . about the actual dying process and the symptoms and what to look for and you know, how the process proceeds.
EC06
Communicating with carers was key:
. . . massive part of our job, yeah, talking to families because they feel the responsibility . . . if the agreement has been made that they wish to die at home, most people haven’t done it before . . . we’re there preparing for it so they’re not quite so frightened when it does actually happen. I would do extra visits for that reason, not for symptom management, but just to support the family.
XSP01 (CNS)
Although wishing to support the choice of their loved one, some carers were anxious about whether or not a ‘good death’ would be possible in their own home. For these and many other carers, the arrival of the HAH service brought a huge reduction in their sense of physical and emotional burden:
I felt a great sense of relief from the very first time they came here . . . They’re just so compassionate and they were so wonderful with me as well, it was as if I was a patient as well really, as far as they were concerned . . . she explained to me that he was going downhill . . . And then on the morning that he died, coincidentally, she was meant to come that morning and she just took charge, . . . she just did everything for me.
MC36
When asked what was unique about the care from the HAH service, many carers spoke of the professional, competent, caring and calming nature of the HAH team, in which the family could fully trust, providing the space for them to prepare themselves, and spend quality time with their loved one:
. . . just caring for my dad and I know that’s putting it simply, but because they were, as you might say, experienced, qualified, they could spot any signs, . . . it sort of gave us the peace of mind and confidence that whilst we were there they were more than caring for me dad.
DC11
Although, for many carers, the ‘handing over’ of care to a HAH service felt almost like a rescue, for others this was tinged with a sense of sadness that they were unable to continue caring for their loved one without help:
I felt rather sadder than when I had been able to do something like help. I felt I was more of a spectator, and hopefully a comfort, but was unable to physically do anything, but I felt sad that this was the case she needed and I was pretty happy that they had come and were exceptional . . .
PC58
Nevertheless, for carers wanting a more proactive role in the hands-on care, the HAH service often enhanced their sense of confidence and backed up decisions that they made. Positive experiences of carers also included being able to ‘double up’ with the HAH and undertake care as a partnership, with some HAH services describing how they would teach carers to undertake care activities. Compared with the other services they may have been receiving, HAH was often characterised by a relationship underpinned by continuity and, in most cases, being easy to contact.
For many carers, this relationship was strengthened when extended to the whole family. Indeed, the use of ‘family’ as a metaphor was frequently used by both carers and HAH staff to describe the relationship, particularly among the smaller providers:
. . . I felt comfortable, almost like a family . . . you feel cocooned in this world of they’re there to help you and I felt comfortable . . .
GC18
Although the HAH service was often seen as a temporary extension to the family unit, it was also important to tailor the relationship to the patient–carer dyad, with some couples wanting more marked boundaries to maintain a sense of the home as private.
Most carers highly valued HAH. However, for some, the HAH service did not meet expectations. For a few carers, this was influenced by home not being the PPOD for their loved one, but feeling that there was an inherent pressure in seeing dying at home as the preferred option:
The main thing that I came away from all of this was the concept of, you know, encourage people to do it, have this happen in their home and service results you get asked quite frequently, you know, ‘are you happy to die at home?’ and we get asked ‘are you happy for your mother to die or your wife to die at home?’. And, you know, the natural instinct that question is yes because you feel, you know, you want to be in the body of the family and it’s a nice way for anything to happen . . . It’s very seductive to say to somebody ‘do you want to die at home?’ . . .
XC01
This perceived pressure was extended, in the view of another carer, by expectations that the HAH service would be providing the same level and intensity of care provided in an inpatient hospice, including physiotherapy and 24/7 attention.
Expectations of HAH service delivery were also recognised as a potential issue by HAH providers:
. . . we have had a couple of comments from families, who said, ‘we want more’. But, you know, when you’ve had a good service for a couple of days and you suddenly realised, actually, this is wonderful, but actually the patient stabilises and we have to sort of re-evaluate how much care we’re putting in because this other patients who also need, then they’ll say, ‘oh, please don’t take it away from us’ . . .
DSP02 (director of care)
The majority of the carers we interviewed were realistic about HAH capacity. However, the following quotation also demonstrates that earlier support would have been welcomed, whereas many of the smaller providers provided input only in the last few weeks of life:
. . . if we could’ve had that similar service right from the start, I know that sounds a bit selfish in a way, . . . just that unfortunately a lot of organisations just don’t have the capacity to provide, if you like, the service we got at the very end, or towards the end.
DC11
Nevertheless, there was evidence that information about HAH services was lacking. This fell into two categories. First, some carers commented that they had little awareness in the early days of how to contact palliative care support staff, and what HAH offered, with detail on the latter being seen as important in reducing anxiety when deciding to care for a loved one at home. This was less likely to occur when carers were already well networked and knowledgeable about the whole system of care:
. . . we were very lucky in that our GP is a friend who’s known us for 20 years so, you know, we were very good friends so we did have a lot of support there and also [name]’s oncologist, our daughters went to school together so, again, we had a good solid . . .
GC04
However, for some, even when in the HAH service, they were still not clear on who to contact:
. . . who the hell am I going to turn to? Have I got to phone the ambulance because I can’t get you out of the chair, do I phone the [HAH], the community lifeline? I didn’t know, in that situation [patient stuck in chair], who I was supposed to call . . .
EC14
Overall, most carers felt that the HAH service had more than exceeded their expectation of care and support. In contrast, only a very few carers received the support they wanted post bereavement.
After death
One carer described how she felt supported by the HAH service after bereavement:
. . . the lady that came was here for a couple of hours talking; it’s always nice, when something happens, it’s not just ‘that’s the end, they’ve gone’, there is someone following it up to make sure that things were OK and things are OK.
WC69
Nevertheless, many of the carers we interviewed found it very difficult to move from a relationship with the HAH team as being part of an extended family to a sudden halt in their visits, almost creating a second sense of loss:
. . . the one thing I found hard is [husband] passed away, the girls [HAH team] left and that was it. Now, you’re very busy at first . . . we had the funeral, we did all the form-filling and then suddenly, I’m on my own . . .
LC29
Carers appeared reluctant to proactively seek bereavement support from the HAH service, recognising that the service was already very busy, or not knowing who to contact. Some HAH staff also recognised that, although bereavement support tended to be delivered by a different part of the hospice organisation, there may be times when follow-up by the HAH team may be beneficial:
I think there are certain patients and families that we could probably go in and see once or twice after the patient has died, and I think they would benefit greatly from that, because obviously they have built up a relationship with us . . . it’s kind of cut off from that moment that the patient has died.
ESP04 (HCA)
For those who had proactively sought support from the hospice, there was evidence that the format was not matched to the carer:
I tried last week to go to a bereavement group because they send me mail-outs and things, for walking, in [name of] Park. So I tried to do that, but I took my dog, because I wouldn’t want to go walking in a park without the dog, and nobody – I mean . . . I ended up walking the dog by myself, like . . . [pauses], . . . I dunno, I’m not a joiner-in of groups with people.
PC12
The importance of being supported in bereavement by someone who had shared the EOLC journey was summed up by this carer:
[HAH nurse] came after [husband] died. She came the next day or 2 days later and I think she came once after that, but following that they were telephone calls, yeah . . . It was a huge difference because I think that makes you feel more comfortable, . . . you know, they’re aware of what you’ve been through so it’s easier to talk to somebody that you’ve already . . . that you know that’s empathetic towards the situation that you’re in and that you’ve been through than it is to a complete stranger who you’ve never seen before so, yeah . . . I think it made me aware or feel that, you know, if I did run into a brick wall at any point, you know, that I could pick the phone up and talk to somebody.
VC09
Summary
Six CMO configurations captured the key factors relevant to providing optimum HAH services: sustainability (of the HAH service); volunteers (use of, in the HAH service); integration and co-ordination (with the wider health and social care system, including commissioners); marketing and referral (of the HAH service); knowledge, skills and ethos (of HAH staff); and support directed at the carer or patient–carer dyad at home.
The following chapter draws these findings together, along with the quantitative and health economics results from Chapter 6 and other information in the literature, to explore what conclusions can be drawn from the synthesis of the combined data.
Chapter 8 Discussion
This realist evaluation identified programme theories that explained the contexts and mechanisms leading to optimal outcomes for patients and their carers. Qualitative, quantitative and health economics data were cross-referenced through the analysis to enrich understanding.
This chapter will discuss the salient actions HAH services undertook that appeared to lead to optimal outcomes. The discussion will be structured around three key areas. First, there is the impact that HAH services had on the patient and their carer, with HAH services creating a valued partnership that cared for both the patient and the carer. Impact was enhanced because HAH staff had the time to care, and their expertise and professionalism was a consistent feature of carer feedback. This was particularly notable when the patient–carer dyad was a couple, because care was moulded around both parties, as a unit, to support and meet their needs. Second, we discuss how the model of HAH care influenced this impact and shaped service provision, ‘filling gaps’ in statutory services. There appeared to be a continuum of models, from a predominantly medical model to a largely social model of care, reflected in, for example, staff mix. Third, issues of sustainability reflected the importance of reputation and maintaining influence in the commissioning landscape, branding, finances and fundraising, which had to be balanced against the needs of staff and recruitment/retention issues.
Hospice at home service impact on the patient–family carer dyad
Hospice at home services enabled most patients to achieve their PPOD (73%, 162/222 patients who had a PPOD and known place of death), which is similar to the results of other studies of home-based palliative care programmes. 11,120,121 Ali et al. 122 reviewed the deaths of all patients (n = 2176) known to a specialist palliative care service over a 5-year period (2009–13); 73% of patients who expressed a choice about their PPOD, and 69% who wanted to die at home, were able to achieve their preferences. However, during their illness, 9.5% of patients changed their preference whereas 30% of patients either refused to discuss it or no preference was elicited for place of death. 122 We were unable to ascertain if patients changed their PPOD, but 21.8% (74/339) did not express a PPOD when entering the study, possibly reflecting the large variation in length of time from recruitment to death. Ali et al. 122 found that patients whose PPOD was unknown were more likely to be admitted to hospital for EOLC, but we did not find this association.
Time and expertise
Most striking across all sites was the emphasis on ‘having time to care’, which permeated all aspects of ‘doing the work’, and was strongly embedded in the HAH ethos and was inextricably linked with expertise.
An important example of the interplay between mixed-methods data strengthened the evidence for this theme. The quantitative data found that smaller HAH providers were associated with higher scores for the QODD. Qualitative interview data, revisited when this finding emerged, found that an advantage of smaller providers (models 2 and 4) was that they were particularly agile, providing a rapid response and hands-on care 7 days per week, which appeared to facilitate a trusting relationship with the patient and carer. Furthermore, the service use data showed that patients in model 2 (smaller, 24/7 services) received, on average, more in-home nursing and personal caring visits than those in the other models; in-home visits were fewest in model 1 (larger, 24/7 services). However, some carers commented that it would have been helpful to have received support sooner, with smaller providers tending to provide support only in the last few (or even just 2) weeks of life. Informal carers from a service in model 1 were more likely to report no in-home visits in the last month of life than carers in other models. The reasons for this were unclear, although the qualitative data hint that carers had to proactively approach services in model 1 (which provided less frequent and more hands-off contact over a longer period of time), and this may have acted as a deterrent to accessing services.
We may tentatively assume that the greater intensity of HAH staff visits in the smaller providers might be linked with the more positive QODD scores. The qualitative data suggested that QODD scores were linked to the temporal concept of time, which also incorporated the perception of having time and working at a pace suited to individual need, providing a compassionate experience that helped ease the burden of care (and indirectly boosted the HAH service’s reputation). Carers shared this perception and appreciated that staff also knew when to leave, so that their presence was not overly intrusive, especially in the very end stages, reflecting a need to have time alone with the patient and ‘manage boundaries of home and private space as the dying person’s needs escalated’. 123 This flexibility attracted staff to the service (compared with what was regarded as more task-orientated community nursing), appeared to contribute to retention and was highly valued by families (compared with time-limited and less skilled agency carers). Other literature has explored the provision of EOLC by non-specialist RNs and found a significant gap between patients’ needs and nurses’ capacity, particularly insufficient time to provide comfort to patients/carers and to reflect on the care process. 124 This was largely due to workload and increasing care complexity,125 alongside a lack of knowledge, experience and organisation support. 124
Wye et al. 37 noted the importance of ‘highly skilled’ palliative professionals with ‘dedicated and sufficient time’. We also found that it was the HAH team’s skills and professionalism that differentiated them from other services; this included all staff, not just those professionally trained. This finding held for model 2 services which were HCA-led, albeit by highly skilled HCAs and not agency staff, but other studies have not differentiated. Expertise was strongly associated with trust, in that carers expected any input under the umbrella of the HAH service (or their specific brand) to be of high quality, and when that expectation was not met, satisfaction plummeted. Carvajal et al. ’s124 literature review identified the importance of developing a relationship based on trust, presence and availability, but also on involving reciprocity and shared ‘values, beliefs and expectations’ between nurses, patients and families. In our context, this suggests that if carers trusted HAH staff, who responded rapidly when required, carers were more likely to expect that the service could meet their needs. This was largely true, but there were examples when a HAH service could not provide the perceived or actual intensity of care required, and this may account for carers feeling let down when the anticipated rapid response was lacking, with unmet expectations expressed by a small number of carers who stated that the HAH service could not meet patient needs at home and a hospice bed was unavailable, resulting in a hospital death and significant distress.
Resonating with our findings, Jack et al. 126 explored patient/carer experiences of HAH provided by ‘hospice nurses’ who comprised RNs and HCAs, but the findings did not differentiate. However, hospice nurses were perceived as having a level of training and expertise that resulted in ‘the provision of a fundamentally different service to that provided by other health professionals and staff from care agencies’. Patients and carers trusted nurses because they took time to develop a close relationship and were skilled communicators, enabling sensitive discussions around the end of life. Their expertise meant that carers felt reassured and able to take time out from caring,126 in contrast to generic HCAs who were unable to carry out routine tasks, which then became the carer’s responsibility, thereby increasing carer burden. 127
Some of our service providers were focused on sharing their expertise with colleagues, such as district (or community) nurses, which seems appropriate, given that they are ‘generalists’ with limited time so would benefit from the support of palliative specialists. 37 However, this highlights a tension between community nursing, with limited capacity and expertise but providing the majority of EOLC in the community, and time-rich, highly skilled HAH services that only treated a fraction of those requiring input, an inequity our commissioners noted.
The patient–carer dyad
Hospice at home services were skilled at building a valued partnership that acknowledged the needs of, and cared for, both the patient and the carer. Many carers noted that HAH staff were adept at moulding their input to what was needed, spanning personal care, listening, support and even ‘becoming part of the family’. Nearly all HAH services considered carers’ needs, and our evidence suggests that this should be integral to service provision. In services positively evaluated by carers, HAH was moulded around the dyad, supporting both the patient and the carer, and meeting different needs at different times with ‘dedicated and sufficient time to engage in difficult conversations’. 37 Regarding patient and carer as a unit stems from the concept that dyadic coping is a reciprocal process whereby each partner supports the other to manage problems jointly. 128 The importance of treating interdependent couples as a dyad has been identified in other condition-specific literature, including dementia,129 long-term conditions130 and traumatic brain injury,131 with common themes relating to loss of valued roles and autonomy for the patient, and carer burden, affecting quality of life for both.
Holdsworth et al. ’s12 study of bereaved carers who had received HAH found that care providers, especially nurses and HCAs who visited frequently, became part of the patient–carer social network. Holdsworth et al. 12 did not differentiate nurses from HCAs, but commented that ‘some degree of informality’ was appreciated, as carers became familiar with the same faces, as opposed to doctor’s less frequent and more task-orientated visits. However, building informal relationships is not acknowledged in frameworks for professional practice, presumably because professionals have a duty to ‘stay objective and have clear professional boundaries at all times’. 132 Our carer interviews indicated that HAH staff successfully negotiated the balance between moulding into the family’s world versus remaining ‘professional’, but that this tension was less well managed with the sudden cut-off post bereavement.
In qualitative data, our carers identified night-time cover as highly important, as found elsewhere. 54,127 Even if carers did not use it, they needed to know it was available and had concerns around service limitations, especially on weekends and bank holidays, which could be detrimental to the continuity of care. 54 From the quantitative data, there appeared to be a weak association (p = 0.042) between having one or more night visits in the last 7 days (from HAH or district/community nurses) and a better QODD score; however, this must be interpreted with caution and does not specify that night care needs to be provided by a HAH service.
For patients with cancer, there was a statistically significant positive association (Spearman’s rank-order correlation test: n = 95; p = 0.020) between the length of time the patient had known they were dying and the total QODD score, with significantly better QODD scores (Spearman’s rank-order correlation test: n = 21; p = 0.493) for those who were aware for a longer period before death that they were dying. This suggests that having time to prepare enabled couples to adjust, plan and achieve the experience that they wanted, although we were unable to ascertain why this association was not significant for non-cancer patients (p = 0.493). Murray et al. 133 suggested that the illness trajectory for patients with cancer is more predictable than that for patients with long-term conditions. Consequently, palliative services are better matched to the needs of those with cancer, who may regard planning for the end of life as a way of feeling more in control of their situation. This compares with long-term conditions in which the illness trajectory is longer and more unpredictable; Murray et al. 133 suggest that these patients/carers may be reluctant to acknowledge or plan for the end of life, and that clinicians may collude. Holtslander et al. ’s134 meta-summary of the experiences of bereaved carers identified six studies in which ‘saying goodbye’ was identified as a positive factor pre bereavement, but this does not necessarily equate with the length of time pre death nor the extent to which it is influenced by uncertainty, changes in role and relationships. 135
Carer needs were routinely addressed at the micro level, but less consistently at the meso level, for example formal (re)assessment of need. However, larger, 24/7 services (model 1) tended to run a more extensive programme of peer groups and training courses specifically to support carers, which the qualitative data suggest were valued by carers. Although more expensive support partially related to differences in the length of involvement across sites, carer (re)assessment is enshrined in policy136 and tools exist to assess carer burden. For example, the Carer Support Needs Assessment Tool aims to facilitate carer-led assessment and support, specifically identifying potential areas of unmet need and co-producing an action plan. 137
Carers also required consideration at the strategic (macro) level to address needs across the whole system of care, given how reliant it is on the input of informal carers. Carer lobby groups have long argued for formal recognition, including payment, but this was not something our carers suggested, simply that they needed the right support at the right time to successfully assume the ‘mantle of care’, with all that is involved. 123 Wye et al. ,37 commenting on the policy drive for dying at home, noted that the burden of care falls on family members who may have little or no relevant previous experience, and ‘lack of knowledge, skills and support among informal carers’ can be a key barrier to dying at home. 127
Most HAH services signposted patients/carers to relevant services, and detailed informal knowledge of local services can be very helpful. 37 Many of our HAH service providers also fulfilled the role of service co-ordination, but some carers had to bring services together themselves. However, with growing fragmentation of services across health and social care (despite the rhetoric of integrated care), families will ‘have ever greater need of experienced, committed, proactive staff’ who can provide an overview across all sectors to help carers navigate the system. 37
Post-bereavement support
Our qualitative data suggested that carers were least satisfied with bereavement support, commenting on the shock of the HAH team rapidly retreating from being part of the family. Carers understood that the HAH service had to redirect its efforts to others, but this lack of continuity was a common refrain and carers reported significant gaps. Carers wanted to connect with someone, even just briefly, who had been part of the caring process, knew the patient and understood the context. Some HAH services offered universal and generic follow-up to all carers, in the format of, for example, a postal leaflet. Others tried to selectively contact those perceived as likely to need help, based on clinical experience or an assessment, but carer interviews indicated that both approaches had shortcomings.
Post-bereavement activities included formal group or individual counselling and informal activities such as carers’ cuppa, men’s cooking classes and walking groups. For those carers who had investigated available support post bereavement, the format (particularly for those with children/teenagers) and timing of follow-up was not ideal, with only one site meeting carer expectations, although many carers found it difficult to articulate what would have been helpful. However, carers were clear that it related to talking to someone who they regarded as familiar and who knew the patient, and with whom they had a combined background or narrative. This suggests that it was the joint link to the patient that was important, just as its loss was felt strongly when HAH staff withdrew.
As stated, most sites provided counselling and group activities, but evaluation of implementation and outcomes in this setting is limited. 26 In addition, the current (COVID-19) funding crisis is likely to lead to a reduction in the availability of bereavement services. 138 The lack of suitable, or any, follow-up is a common finding in the literature, alongside the importance of providing support that meets individual need, given that everyone’s experience is unique. 134 Although primary care is recognised as a suitable avenue for providing (standard) bereavement support, we found few examples of this. Most GPs have had little training in this area and are not sufficiently familiar with families to make contact in bereavement. 139
The need for standard bereavement follow-up and complex grief follow-up is recognised26,28 but what this should comprise is not well defined. Hudson et al. 140 commented on the ‘dearth of contemporary practice standards that explicitly articulate what resources palliative care services should allocate, when they should allocate them, how, and by whom’. Most literature differentiates between normal grief, whereby intensity subsides over time, and a prolonged grief disorder141 or complicated grief. 142 Some of our case study sites tried to identify those at risk of complex grief reactions, but rarely systematically or supported at the meso level, instead depending on individual clinical decision-making.
The ambitions for palliative and EOLC framework143 endorses bereavement care tailored to individual context, but lacks guidance on how to achieve this. Luckett et al. ’s26 review of models for palliative care found that only Ireland specifically recommended that bereavement support ‘should begin early in the disease process, long before the death of the patient’. 144 The report suggested that palliative services should be able to anticipate severe grief reactions and prepare the family for impending bereavement. 144
Axelsson et al. 145 also acknowledged that pre-and post-death grief are part of the same process, again questioning our sites’ separation of pre- and post-death support when the experiences of caring, grieving and ‘facing life without that person are connected chapters’. 134 This suggests that screening and assessing for emotional distress and risk of complicated grief should be ‘a continuous process’ from referral to many months post bereavement. 146
Follow-up varied among our case study sites, but mostly involved a telephone call at a set interval, for example 6 weeks post bereavement. Aoun et al. ’s147 survey of carers found mixed patterns of follow-up, and although over two-thirds of carers reported that they had received enough support, the dominant view was that support for themselves, as carers, pre and post bereavement was either lacking or too generic. 147 It was recommended that services consider when to contact carers post death, who should do so and how to make the contact focused on the specific needs of the carer. 147
How the model of hospice at home shaped care
Our typology categorised HAH services by size and availability of 24-hour care, but there were significant service variations within each model. Firth et al. 28 acknowledged the diversity of staff configurations, processes and interventions in specialist palliative care and used a mixed-methods approach to derive 20 criteria. An early finding was that stakeholders struggled to define their model, owing to the complexity of providing care across multiple settings and there being multiple services within each setting, often overlapping. Our case studies demonstrated similar organisational complexities, with multiple services not necessarily integrated even within an organisation. For example, one service provider commented on silo working between the day service (social model), inpatient unit (medical model) and HAH service (mixed). However, the different emphasis on social versus medical orientation resonated throughout case study sites, with HAH services often bridging the medical–social continuum of EOLC.
The medical–social continuum of end-of-life care
Figure 16 demonstrates how HAH services were rarely at the extremes of either paradigm, but aligned themselves more closely to one or the other, differentiated by staffing configurations and interventions. Each HAH service has been placed along the continuum, based on phase 2 data. More medically aligned services had a higher proportion of qualified nurses, including CNSs (either alongside or as part of a single point of access to community palliative care), carrying out medical tasks, for example managing syringe drivers. Conversely, social model services provided significantly more hands-on care than ‘medical’ ones and had a higher proportion of (or only) HCAs, but were reliant on district nursing for medical/pain management. However, even services predominantly providing hands-on care did so with a level of expertise that carers consistently rated as higher than that of social services agency staff, linking it also with having time to care and a flexible service.
FIGURE 16.
Hospice at home services bridging the medical–social continuum of palliative care.
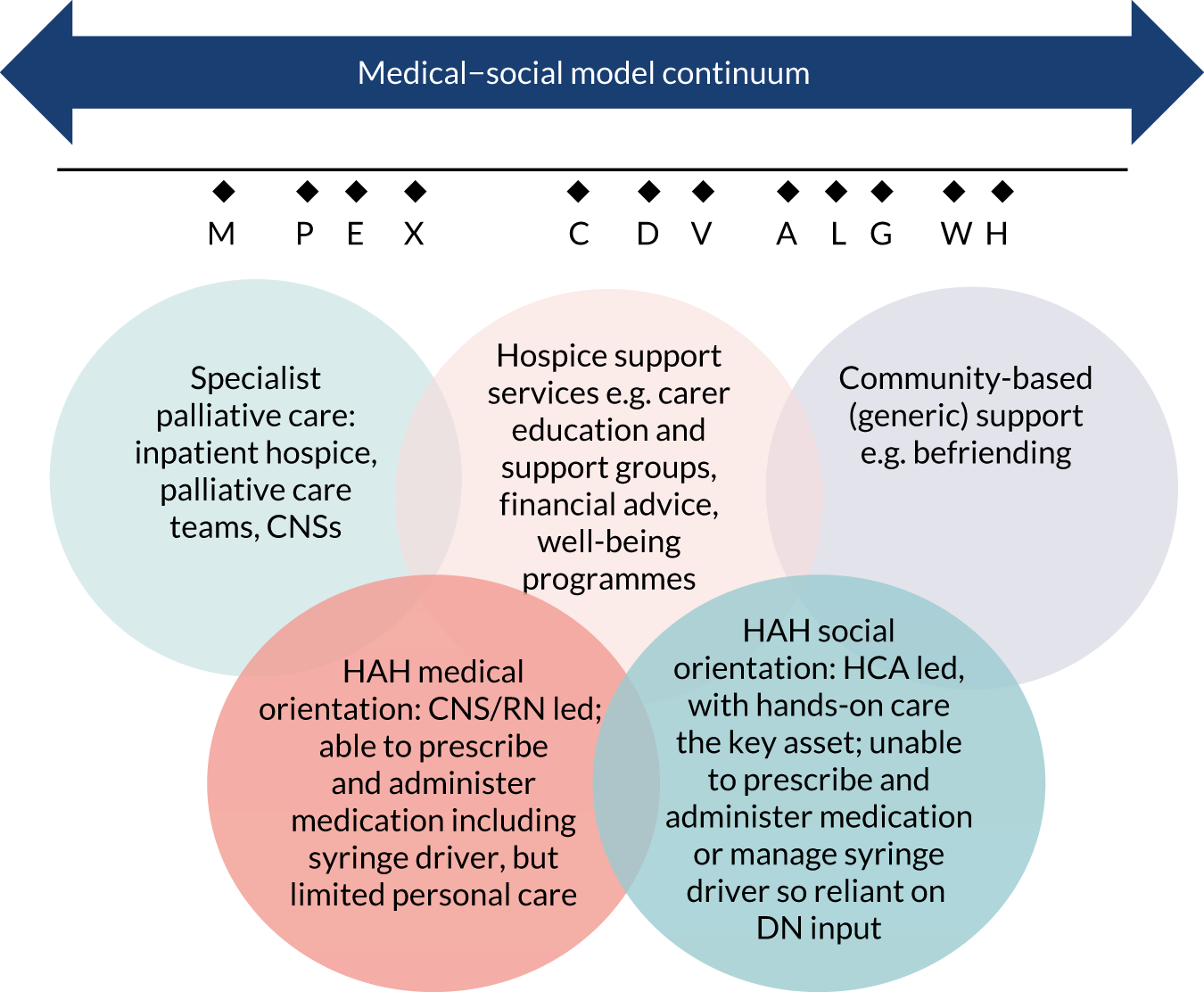
Our typology of HAH services shares components of Firth et al. ’s28 criteria for palliative care, including type of care (e.g. hands on vs. advisory); size (number of referrals annually); OOH care (five criteria); number of disciplines delivering care; and mode of delivery, bereavement follow-up, funding and discharge criteria. However, 20 components do not constitute a model and their different constellations across services reflect the wide variety in hospice (and HAH) provision.
Bainbridge et al. ’s24 review of systematic reviews focused on positive outcomes and identified multiple components of HAH care that were divided into five categories: type of services offered, availability, characteristics of care model, linkages to other resources and process interventions. Most programmes had components from multiple categories and the most common components were associated with positive effects on multiple outcomes. First, linkages across services and settings (formal and informal, as we also found) helped decrease the barriers that silo working creates, increased interagency accountability and information transfer, and facilitated seamless transitions across settings. Bainbridge et al. 24 did not mention a single point of access, but we found that this, combined with an effective triaging system, helped direct patients/carers to the right service(s) with the right information, but did not entirely avoid silo working. Second, care that was multidisciplinary and holistic was more capable of meeting the diverse needs of patients and carers, where holistic was defined as ‘whole-person care that considered physical, emotional, and spiritual needs’. 24 Third, that providers had sufficient end-of-life expertise to know what to expect as an individual deteriorated, how to prevent or manage symptom exacerbations and how to broach sensitive discussions with patients and carers. Neither Bainbridge et al. 24 nor Firth et al. 28 mentioned balancing supply with demand and, although our case study sites had very different lengths of involvement, nearly all had an ethos of not discharging patients. This contrasted with commissioners’ preferences for equity of access across the population above length (and frequency) of involvement. From Firth et al. ’s28 data, programmes found to significantly reduce costs most frequently reported components of on-call, around-the-clock home visits available (not necessarily provided by the HAH service), a customised care plan driven by individual needs and linkage with hospital. However, the lower costs found in our larger, 24/7 services (model 1) were associated with fewer home visits, particularly by HAH staff, with no increased informal caring time.
Front-line co-ordination and communication
Luckett at al. ’s26 rapid review focused on essential attributes of palliative care as a more meaningful unit of analysis than models, and identified case management as a recurring key component to meeting patient/carer needs across the medical–social spectrum. However, case management exists as part of a complex intervention, so it was difficult to claim that ‘positive outcomes have resulted from case management per se’. 26 In addition, other attributes appeared to overlap with case management, including integrated care (e.g. palliative services supporting GPs/nurses in rural areas), managed clinical networks (formal linking of health-care professions across settings and organisational boundaries) and shared care (lead clinician co-ordinating with health professionals across disciplines). We did not find explicit reference to case management, but integration and co-ordination was a key programme theory, with experiences ranging from highly positive, when HAH service providers acted as the go-between with other providers when carers had struggled to ‘make things happen’, to carers stating that they had to take on the role of co-ordination themselves. Taking on the role of co-ordinating care can add to the structural burden for carers, having to navigate service fragmentation, complex bureaucracy, lack of transparency and gatekeeping, albeit this is more marked with generic services for older people. 148 However, our qualitative data indicated that it was front-line staff who worked hard to co-ordinate services, often when meeting each other in the patient’s house (micro level), regardless of their organisations’ formal policies or arrangements (meso level). These front-line co-ordinations and communications were opportunistic and therefore not without limits, but suggest that when staff are allowed to use their initiative, without excess organisational constraints, and even facilitated by structural supports such as shared records, this facilitates a co-ordinated service, possibly reducing carer burden. However, there needs to be a balance between structure/policy (meso level) providing necessary parameters and trusting staff (micro) to use their initiative. Ganann et al. ’s125 review of factors influencing the optimisation of home care nurses in Canada also identified interprofessional and interorganisational collaboration as something that develops at the micro level when staff have ‘opportunities to interact and communicate’, but it must be consolidated by ‘leadership that supports joint collaborations and joint capacity building’. This links with sustainability (next section), in which we found a tension between hospices needing to brand their unique contribution while also seeking to co-ordinate care with other services.
The importance of co-ordination relates to care navigation, discussed earlier, in which the goals are to link patients and families to primary care services, specialist care and community services; provide more holistic patient-centred care; and identify and resolve patient barriers to care. 149 These goals appear to be common sense, but were not always the case, and HAH services appeared to be filling service gaps that shaped the whole system. Our carers consistently expressed the need for continuity in service provision, whoever provided it, indicating the need for a whole-system approach to EOLC, from diagnosis to bereavement. However, HAH input was significantly shaped by historical commissioning decisions and the need to fill service gaps (particularly community nursing) alongside supplementing existing services. It was unclear if the orientation on the medical–social continuum was by choice or necessity, driven by a competitive marketplace where each hospice had to demonstrate its unique contribution to raise funds from commissioners and the public.
A whole-system approach
A whole-system approach is not a new concept, as the first government end-of-life strategy was published in 2008 and ‘strongly recommended’ a whole system with ‘a care pathway approach both for commissioning services and for delivery of integrated care’,3 from the initial identification of those at end of life to post-bereavement support for carers (Contains public sector information licensed under the Open Government Licence v3.0). The intention was that, through enhancing choice, quality, equality and value for money, people would be supported to have a ‘good death’. Subsequent National Institute for Health and Care Excellence quality statements, appertaining to the last 12 months of life,150 and the ambitions for a palliative and EOLC framework,143 also endorse a co-ordinated approach across the care pathway. Care should be ‘coordinated effectively across all relevant settings and services at any time of day or night, and delivered by practitioners who are aware of the person’s current medical condition, care plan and preferences’. 150 However, it is less clear how what amounts to (but is not called) a whole-system approach should be organised and sustained, and the inequity remains between the small proportion of people who receive high-quality EOLC, often those from high socioeconomic status (and more likely to have a cancer diagnosis in our study), and the majority who receive generic care. 151
More recent literature on patient (or carer) navigation programmes suggests that navigators can help address service fragmentation, for example communicating across organisations and facilitating access to care. 152 The original concept was intended as a strategy to improve outcomes in ‘vulnerable populations by eliminating barriers to timely diagnosis and treatment’153 and the literature largely appertains to early diagnosis and treatment. 154 However, there are many models reflecting different orientations (medical, social or combined) and patient groups, but the development of these programmes indicates ‘unmet needs for coordination and facilitation of care, particularly in relation to populations for whom social determinants of health create additional barriers to accessing social and health care services’. 152 This was reflected in our findings, in which university-educated carers rated service quality significantly higher (VOICES 2) than those without a university education. This inequality may reflect demand outstripping supply, as reflected in an evaluation of a HAH service (data collected 2012–13) that found that the most deprived and rural area of the county was poorly served by HAH services. 44 Care inequality between cancer/non-cancer has been found in other literature155,156 and is not a new finding. However, we also found variation by sex: when a patient was female, the carer was 0.409 times less likely to report that they received sufficient care (VOICES 1, predominantly male carers), and female carers were 2.938 times more likely than a male carer to report a good/almost perfect death experience (total QODD score > 70).
Sustainability
Sustainability has been defined as being able to survive, so that the organisation can serve its purpose and fulfil its commitments to its clients and the community in which it operates. 157 Our findings suggested that sustainability related to a hospice’s orientation to strategic and front-line integration, which reflects a classic organisational problem in the private sector between integration (internal facing) and differentiation (external facing),158 or a trade-off between pleasing commissioners and looking after staff.
Internal/external orientation: a trade-off
One approach taken by hospice services to ensure that they had the widest possible coverage was an external-facing orientation whereby managers made every effort to sit at the table with policy-makers and commissioners so that the hospice had a stake in decision-making. It was not only about being on strategic boards, but also related to branding and marketing the hospice to ‘communicate, differentiate, and enhance’159 its unique contribution to EOLC. All sites had active marketing teams, demonstrating the tension between the ethos of altruism and compartmentalised commercialisation. 158 In our consensus workshops, we used the phrase ‘Hospice charities may give the impression to the public that they are fully dependent on charitable funding . . . to make their fundraising activities more effective’, which was clearly contentious, but reflected a tension between public accountability, the constant need to generate funding and the ethos of being a charity. Branding is a necessary tool to compete, but as the pool of resources becomes more limited, competition increases, and highlights a tension between adhering to market forces while trying to stay true to the ethos of an organisation. Branding is particularly challenging for organisations such as HAH services where different stakeholder groups hold strong and personal values, but it is a necessary tool to communicate an organisation’s role. 159 However, some service leads commented that commissioners had varied levels of understanding and experience of EOLC and some appeared to lack the required skills and knowledge, as found elsewhere. 160 Several toolkits are available, including, for example, Commissioning Person Centred End of Life Care,161 which acknowledges the complexity of commissioning, ‘involving a dynamic and continuous process of review and improvement to ensure alignment with changes to national policy, commissioning models, local demand, workforce changes and procurement options’. At the time of interview, commissioners were transitioning from working predominantly at the level of the CCG to commissioning a range of services at larger scale through Sustainability and Transformation Partnerships (STPs). Managing this requires significant competencies, yet these may not be well defined during recruitment; consequently, commissioners may be appointed without the full range of skills,160 although some of our managers suggested that inexperienced commissioners allowed the HAH more leverage. The only formally allocated budget relating to EOLC in the NHS is specialist palliative care and the NHS CHC budget, ‘yet controlling the size of this pot is often something that is said to feel out of the control of CCG commissioners’. 160
Commissioning behaviours may also be influenced by a reported power imbalance between commissioners and service providers, exacerbated by the fast turnover of commissioning staff; the move away from smaller commissioning models (CCG level) towards the larger STP level could help transfer more power and resources back into the hands of commissioners. 160 However, this could be to the detriment of HAH services, and even when sites had an excellent relationship with their commissioner, we did not find evidence that this resulted in securing increased funding. In fact, some commissioners appeared complacent, assuming that if the HAH service was pushed, it would raise further funds (Box 8).
-
Staff focus:
-
manageable caseloads and workloads
-
investing in training and education – all levels, all staff
-
support and mentorship embedded
-
autonomy is valued alongside time to care.
-
-
Outcome: high staff morale; better retention than external-facing organisation; reputation for high-quality care at the micro level, but at the cost of having a low local/national profile and little leverage with other providers/commissioners.
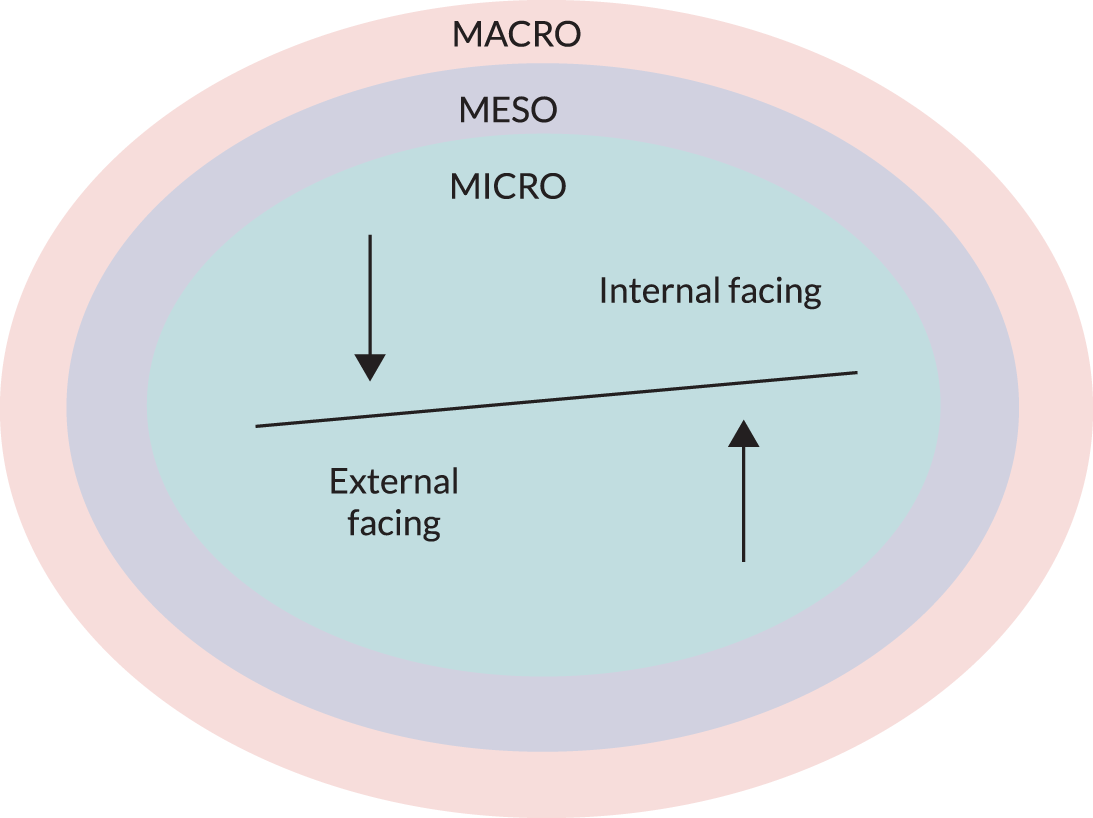
-
Macro:
-
establishing national representation and reputation.
-
-
Meso:
-
building reputation and community awareness
-
influencing local commissioners
-
educating/upskilling other providers.
-
-
Outcome: high profile at meso/macro level, but potentially at the cost of staff morale, with relatively high rates of staff attrition.
In contrast to externally focused HAH services, other sites appeared internally focused, with an emphasis on staff well-being, support, and education and training, and internal service development. Chamanga et al. ’s162 review of factors influencing recruitment and retention of RNs in community nursing identified work pressure (caseload and workload) as an important factor influencing the decision to remain or leave employment. Increased pressure correlated with reduced commitment and ‘subsequent negative job satisfaction, impacting on patient safety and quality of service’,162 alongside emotional exhaustion and depersonalisation. This mirrors our data, in which carers consistently commented that HAH staff had the time and emotional space that non-HAH staff lacked. Chamanga et al. 162 also identified lack of autonomy, lack of educational opportunities, lack of appreciation by managers and salaries as factors hindering retention. Except for salaries (which we did not explore), these factors had all been identified as tools to maximise retention by HAH providers/managers.
Market forces, skills mix and managing demand
Haslam et al. 163 developed a business model for hospices to account for sustainability, based on interviews with key hospice stakeholders. At the centre were hospice staff and volunteers, working for patients/families, and commissioned by the NHS and commissioning bodies within the wider context of government policy, legislative arrangements and regulations. Haslam et al. 163 argued that, as funding sources have widened to include a portfolio of health-care contracts, lottery income, trading profits from shops and earnings from financial investments, these newer funding streams are prone to uncertainty and volatility, particularly in the current financial climate, and hospices must work continually to adjust their approach. 163 These changes have ‘encouraged a shift towards a more administrative and managerial led medicalization of palliative/end of life care’ as hospices have ‘migrated from their initial charitable financing model to one that has become embedded within a wider system of healthcare funding . . . challenging their traditional independence’. 163 The reliance on the NHS for 20–35% of their income has added new risk alongside demands for value for money, specialist care, expecting more year on year and increased bureaucracy. 163 Our data also evidenced commissioner expectations that hospices would provide specialist care and increased capacity while remuneration stayed static. However, we found that not all HAH services accorded with increased medicalisation, such as the socially orientated HAH services (see Figure 16).
Haslam et al. 163 identify three interconnected issues that threaten sustainability. First, having to secure more income in an increasingly fragmented and volatile market, as already discussed. Second, recruitment, retention and skills issues with the expectation that staff will be highly skilled palliative specialists, but also generalists able to manage increasing numbers of chronically ill patients with non-cancer diagnoses, alongside trying to match salaries to NHS and private pay scales. Third, the increasing complexity of chronic illnesses bringing people into the system with longer life expectancies than previously. All of these make it increasingly difficult to maintain a financial buffer to allow for changes in income or expenditure and to plan for service redevelopment or update buildings/facilities. 163 Our sites discussed the need to maintain a financial buffer and were aware of the arguments around accepting more patients with long-term conditions and longer prognoses. Referral criteria varied, but all services were selective and limited intake in ways that were dictated by capacity but meant that services dealt with only a subset of people. How this affected (or influenced) staff mix and skill set was hard to ascertain, but length of involvement, from referral to death, varied widely. Services that were involved for significantly longer (> 3 months) mostly provided initial expertise from qualified staff and telephone monitoring/advice, but limited hands-on care, whereas HCA-led services focused on providing personal care for a much shorter duration. This reflected the more medical paradigm of the former compared with the latter, but there was no obvious association with internal-/external-facing orientation.
Ganann et al. ’s125 review of home care nurses in Canada explored how manageable workloads, funding models and appropriate staff allocation influenced staff mix and staffing levels. The issues are equally applicable in the UK, where home care staff also have to manage heavy workloads and increasingly complex patient needs and the funding model promotes competition, driving down skill levels and ‘the ability to align staffing mixes with client needs’. 125 Our HAH sites guarded against this through maintaining their palliative focus, as a way of managing caseloads, staff mix and skill set.
When comparing internal- and external-facing sites, it was apparent that the latter had a strong focus on educating others, for example GPs and paramedics. Firth et al. 28 regarded the ‘extent of education/training provided to external professionals’ as a defining feature of palliative care models, but this was less apparent with internal-facing sites. The difference between external- and internal-facing organisations was also reflected in service innovation, for example one site had a markedly external focus (at the meso level), but there was a sense in which their own staff did not feel supported or included in decision-making. This contrasted with one site with strong internal integration whereby all staff felt listened to and the service focused on what it could provide that the community needed. Not all sites were one or the other, but those that fell in between appeared to find it difficult to provide both a cohesive service with contented staff and to have a meaningful seat at the table with commissioners. One exception was a site with an internal focus, but not strongly so, because the hospice had the security of taking only patients with NHS CHC funding, so there was less imperative to innovate externally.
Arguably, commitment to marketing and branding the hospice, demonstrating its uniqueness and maintaining a good reputation took priority above almost all else, particularly for externally focused sites, stemming from the need to generate increased funding as NHS monies stayed the same year on year while caseloads increased. Our qualitative data also suggested that the larger, 24/7 services in model 1 had a strong discourse around demonstrating their value for money. However, for all services, this need to define and sustain themselves could lead to inflexibility and conflict with other objectives. For example, integration and co-ordination clashed with being unique and maintaining the brand; at our consensus event, commissioners commented that hospices were not ready for joined-up commissioning. A similar tension centred around OOH services: hospices wanted the contract but did not want to take on any generic community nursing roles. Given the policy drive for integration this suggests that hospices wedded to marketing their uniqueness may not do well, although the qualitative data did suggest that smaller providers were more open to integration.
Volunteers: an underutilised resource
For the majority of HAH services, the hospice building was a visible symbol of the organisation’s function that helped raise awareness, engage volunteers and promote community fundraising. However, this did not necessarily ensure sustainability; for example, one of our sites was situated in a building that was highly valued by all stakeholders, but was ultimately too costly to maintain. Given that hospices depend on their communities for both income and volunteers, linking with the local community is a key factor in hospice sustainability. 164 Volunteers can bridge the gap from hospice to community, ‘both in a philosophical sense and a practical way of giving information and promoting fundraising’,165 and can help to reduce the fear and taboos around hospice care. 164
Our data found that volunteers were integral to sustainability, for example providing transport and volunteering in day and inpatient services, as found elsewhere. 164 However, our quantitative data suggested that patients and carers had very little contact with volunteers; only one site integrated ‘semi-professional’ volunteers into the HAH team, and clinicians had reservations about using them, based around overstepping boundaries at such a sensitive time. Most of the case study sites regarded volunteers as part of a triad (hospice, volunteer and patient/carer), with the hospice monitoring the relationship between patients/carers and volunteers. Volunteer co-ordinators acknowledged potential pitfalls and the need for clear boundaries, but were less risk averse than clinicians, although acknowledging potential risks to reputation. Only one HAH service was part of an organisation with a wider Compassionate Neighbours scheme, based on a community befriending model, in which the relationship was negotiated between volunteer and patient/carer, with minimal hospice oversight.
Aoun et al. 166 argued that professional care can only supplement, not replace, existing social networks, so it is important to support all assets in the community, given that it is the community that supports most people. Our carers wanted continuity post bereavement; with appropriate training and mentoring, volunteers could fill this gap. The public health approach to EOLC has argued for two decades that promoting palliative care has the potential to address inequity of provision, drawing on the wider community to address the continuity between long-term conditions, EOLC and bereavement. 167,168 The compassionate community model of EOLC draws on the patient and carer’s existing social network, including a small, inner network of close family and friends who perform personal tasks; an outer network of family, friends and neighbours who can assist with routine tasks such as shopping, cooking, cleaning, walking the dog and gardening; community members who can assist with routine or other peripheral activities; and health and social care professionals. The focus is on building a resilient network to support both patient and carer, emotionally as well as practically, and encouraging carers to accept support when the default position is often to decline. 169 However, Aoun et al. 166 acknowledge that this support is less effective post bereavement.
Despite the undoubted positives of the volunteer workforce, our volunteer co-ordinators highlighted problems around reliability and lack of flexibility. Scott et al. 164 also issued a note of caution that volunteers may not always be available or willing to meet the increasing demand that is anticipated.
Summary
This chapter explored three key areas: (1) the impact of the HAH model of care on the patient–carer dyad, (2) how the model of HAH shaped care provision and (3) sustainability. HAH enabled most patients to achieve their PPOD with sufficient practical and emotional care to support the patient–carer dyad.
Our study suggested tensions faced by commissioners and organisations when providing HAH services. Larger, 24/7 services were associated with lower costs, but with worse QODD scores, than the smaller HAH services. This appeared to be linked to the higher proportion of HAH visits closer to dying, but also highlighted an inequity between the small proportion who received HAH and the majority of EOLC in the community, constrained by time and lack of expertise.
Our typology categorised HAH services by size and availability of 24-hour care, but also important was how HAH services aligned themselves along the medical–social care continuum, differentiated by staffing configurations and interventions. However, it was unclear if the orientation on the medical–social continuum was by choice or necessity, driven by a competitive marketplace where each HAH service had to demonstrate its unique contribution to be sustainable.
Sustainability was a major tension for all HAH services and appeared to relate to a HAH service’s orientation to strategic and front-line integration, reflecting a classic organisational problem in the private sector between integration (internal facing) and differentiation (external facing).
Only one service incorporated volunteers directly in HAH, with others citing concerns around how appropriate or useful volunteers would be in the last phase of life. However, this appeared to be a missed opportunity that could help bolster sustainability, provide support for patient and carer, and enable continuity of care post bereavement.
Arguably, commitment to marketing and branding the HAH, maintaining a good reputation and ensuring sustainability took priority above almost all else, but there were examples in which this led to inflexibility and conflict with other objectives, for example integration and co-ordination.
Chapter 9 Conclusions
This chapter will present the following:
-
summary of the findings for each research objective
-
synthesis of these findings into a summary of what worked best
-
articulation of the limitations of the study
-
suggested implications for providers and commissioners
-
recommendations for future research.
Summary of the findings for each research objective
Identify the range and variation of hospice at home models operating across England and categorise the models by type, key features and setting
Services calling themselves HAH in England varied in multiple dimensions (i.e. size and setting, patient referral criteria, services provided, staffing, funding). It was not possible to deduce a ‘definition’ of a HAH service, or even to easily allocate them into broad types or categories. In common, they all offered care designed to support patients approaching the end of their lives at home, provided and supported by staff with experience and expertise in palliative care and EOLC. Almost all HAH services provided personal care, psychosocial support and symptom management, but not all provided this 24/7. The majority of services were providing care for, on average, 1 week–2 months from referral, and most had staffing with a greater proportion of HCAs than of RNs. Two-thirds of services reported charitable sources as the main source of funds.
Assess the impact of each model on patient and carer outcomes and explore the experiences of patients, family carers, providers and commissioners of the different hospice at home models
For people approaching the end of their lives who wanted to die at home, HAH services overall provided care that was likely to deliver ‘a good death’ [median QODD score 70.7 (range 0–100, with 70 a ‘good’ death)], was highly valued by its recipients and was recognised by them as special(ist) in comparison with other services. The majority of HAH services overall were being delivered to patients dying of cancer (77%). HAH services also assisted people to achieve their PPOD; 73% of patients achieved their PPOD, with no statistically significant differences between the four service models, although the proportion was higher in model 2 (smaller, 24/7 services) than in the other models.
Higher (i.e. better) QODD scores were associated with patients having died at home or in a hospice; female carers; university-educated carers; and patients having known they were dying for a long longer time. When all items were adjusted for, smaller services (models 2 and 4) attained a significantly higher QODD score. The qualitative analysis suggested that this might be explained by their ability to be more agile, to integrate better with other services and to provide more specialised care.
Carer satisfaction with the help and support received from health and social care services and the quality of those services was high. In terms of the help and support received, female patients reported a lower level of support. Carers in model 2 (smaller, 24/7 services) were eight times more likely than carers in other models to report that they had received all of the support they needed. In terms of the quality of services, university-educated carers were associated with better ratings, and patients dying in hospital were associated with worse ratings. There was a trend for carers in model 2 to report better quality of support. Qualitative data described the difference in care provided by HAH versus other services and focused on the time, person-centredness, expertise and the quality of relationships offered.
Investigate the resource implications and costs of patient care in each model
There tended to be more formal and informal caring closer to death, but there was a lot of individual variation. ‘In-home’ nursing and personal care was the largest item of service use and was delivered collaboratively in all models by local NHS nursing/HCA services (accounting for about one-third of visits), HAH professionals and social services carers. The highest daily average number of in-home visits was in model 2 (smaller, 24/7 services) and the lowest was in model 1 (larger, 24/7 services).
Service use in relation to outcomes
Carers in model 2 reported higher QODD scores and higher levels of satisfaction, which may be associated with the higher number of nursing or caring visits that they received in the pre-death period. Although costs in model 1 in any period were lower than in the other models, and patients received less intensive support, they were in the study longer, and they may therefore have received an overall larger amount of resources. This model of care may be less cost-effective because outcomes in model 1 were generally worse than in model 2, in which support was more intensive.
Identify the enablers of and barriers to embedding hospice at home models as part of service delivery
Hospice at home services reported that the main barriers to providing their services were geography, getting other services to provide care in a timely fashion and inadequate funding. Difficulties accessing equipment and medications (both drugs and administration) in the home were also challenges.
Synthesis of the findings: a summary of what worked best
The staffing and operations of a HAH service were optimum when it was integrated and embedded in its particular locality setting with other relevant services and had a seat at the table with commissioners and other providers. HAH providers benefited from taking a proactive approach to securing the available statutory funding and were trusted to do this on the basis of their reputation. On the ground, HAH and other staff often worked well together regardless of organisational arrangements, with a focus on a patient’s needs, and HAH organisations that allowed their staff flexibility and autonomy enabled this.
Other key features of HAH services that promoted good outcomes for patients and their families were as follows:
-
Having sufficient time and taking the time to provide seemingly unhurried, person-centred care.
-
Developing a supportive relationship with the patient, carer and family (even being perceived as becoming part of the family), which would ideally continue on into bereavement (see below).
-
HAH staff who demonstrated knowledge, skills and experience in dealing with death and dying and thereby gave reassurance and confidence in the home.
-
Internal investment in the training and support of HAH staff.
-
Agility to respond rapidly to changing patient needs, including access to 24/7 advice and support by telephone, and confidence that help would be forthcoming in crises.
-
Support from the service directed at assessing and meeting the informal carers’ needs, as well as those of the patient. Expectations, planning, information and points of contact were particularly important to carers.
-
Smaller services performed better. Their small size necessitated closer working with other local services and smaller HAH services provided a higher proportion of the total care received.
-
However, although the above points had an impact on the last weeks of life, earlier contact (and this was primarily found in the larger services) also positively affected outcomes.
The study also highlighted areas where most HAH services could look to improve their impact:
-
Overall, carers were not being offered the bereavement support they would have preferred. Shortly after bereavement, the clear preference was for support from the HAH staff who had been part of the story of caring, and not for referral to other elements of service.
-
Hospital at home services could capitalise more on the volunteer workforce by considering a wider range of roles for volunteers and/or by relaxing the bureaucracy around some volunteer roles.
Implications for health-care providers and commissioners
For service commissioners, this study demonstrated that HAH care for people who want to die at home, and have a family/informal carer who can support them, mostly supported patients to experience a ‘good death’ at home and left their carers well satisfied with services. People in receipt of HAH services were very likely to die at home and unlikely to die in hospital; indeed, having been accepted into HAH, patients were, on the whole, unlikely to use inpatient services. Commissioners could therefore utilise some of their budget effectively by funding HAH and achieving objectives enabling choice about place of care and reducing acute hospital pressures. Furthermore, as significant funding for HAH across the country comes from charitable sources, commissioners who spend NHS funds on HAH are likely to get good added value. Commissioners should also consider the sustainability of HAH services when determining the amount of funding and the duration of contracts (which were often too short to provide adequate stability).
Commissioners have important responsibilities for the equity of service availability. With the pressure to provide equitable services, however, some of the key features of HAH that drive better outcomes cannot be compromised, in particular the elements of time, expertise and relationship described above. Commissioners may also want to consider how to work with HAH providers to extend their services to more people, and particularly to address the inequities of provision for those with diagnoses other than cancer.
For HAH service providers, this study identified a number areas for consideration about where their organisation sits on a spectrum and how it might reposition itself to optimise its services:
-
Integration–independence. Integration as described above is important, but did provide some challenges, particularly to HAH organisations protective of their ‘branding’, reputation and ‘specialism’. These factors may limit opportunities to participate fully in, for example, collaborative commissioning.
-
Medical/clinical–social care. An element of ‘fit’ into the local service landscape that providers should consider is where to place their HAH service on a spectrum from a ‘medical/clinical’ focus at one end to a more social care model (not omitting the relevant expertise) at the other. The timing and accessibility of different elements of input is key.
-
Outward investment–inward investment. A third area for service providers to consider hinges around investment in the outward-facing feature of successful services, as partners in wider service planning and provision. There is a balance to be struck with internal investment in the training and support of HAH staff.
-
Value for money–quality and intensity. Finally, there is a balance to be struck between providing value for money and providing sufficient expertise and intensity of care to improve patient and carer outcomes.
Study limitations
-
The data collection for the study relied heavily on informal/family carers; therefore, we were unable to recruit patients who did not have such a carer involved on a daily basis.
-
Key outcomes (QODD and VOICES 1 and 2) relied on self-report.
-
We were not able to provide translation services, and therefore could not recruit patients whose informal/family carer was unable to complete questionnaires in English.
-
We omitted to gather data on the ethnicity of patients and carers, which was a significant oversight and one that was highlighted at the consensus meetings.
-
A significant number of patients admitted to HAH services lived for longer than we had anticipated when the study was designed. As a result, not as many patients as we estimated died during the study and thus post-bereavement data were missing.
-
The QODD proved difficult and arduous for carers to complete. This also had an impact on recruitment for post-bereavement interviews, which was lower than expected. The QODD and VOICES response rates were < 50%, and there were many missing items in the QODDs that were returned.
-
Recruitment of dyads to the study was slow, so additional HAH services were included, creating the possibility of heterogeneity within models and difficulties for interpreting the outcomes. The number of patients recruited by some HAH services was small, and individual HAH services dominated the data in some models.
-
The precision of estimates of service model effects was impeded by missing data, notably a failure to obtain the key factor, education level, for 41 carers (> 10%).
-
Collection of the service use data (with the AHCR) every 2 weeks proved burdensome when patients were in the study for a lengthy period of time, so the intervals between collection were extended, creating difficulties for assembling a continuous series. The number of AHCRs per patient was low. Closer to death, the dates of AHCR data collection did not coincide with the time periods from death that were used in the analysis; therefore, an allocation algorithm was devised and applied.
-
Carers may have had difficulty distinguishing whether in-home nurses and carers came from NHS district nursing services, HAH or social care services. Hence the main analysis was conducted by combining these groups and the examination of the distribution of care between the three services may not be fully accurate.
-
Some carers (where more than one informal carer was involved) reported well over 24 hours per day of caring. This, together with use of replacement methods for valuing informal caring costs, may have inflated total informal caring costs.
Recommendations for research
In order of priority:
-
exploration of the scope, training, acceptability and support of volunteers in this specific care setting
-
the timing and personnel involved in bereavement support
-
implications for patients, carers and services of varying the time before death at which HAH care is introduced and the intensity of support that is provided
-
further adaptation and validation of the QODD for UK use, for example 30 QODD questions (sometimes with many non-responses) might be improved via sensitivity analysis.
Summary
This has been the first study, to our knowledge, to attempt to synthesise learning from a range of different HAH services around England, and to report on what features of HAH services, in the local health and social care settings in which they were embedded, gave rise to the best outcomes for patients and their informal carers. This chapter summarises the study’s conclusions and draws out implications for commissioners and health-care service providers. The limitations of the study are articulated, as are recommendations for future research.
Acknowledgements
Sincere thanks and appreciation go to the following people and organisations. First, patients and their informal carers who gave generously of their time and commitment during a critical phase of their lives. Not many years ago, it was believed to be unacceptable to approach dying patients to participate in research. Fortunately, the case has now been made for pursuing such research so that, in death and dying, people can expect the same levels of evidence-based, excellent care as with any other element of health or social care. This succeeds because of the generosity of spirit of people who participate in research, often aware that their own experience of care may not be altered, for the future and greater good.
Patient and public involvement has been a major feature of this study and has made significant contributions to our understanding of the topic. This includes our inspiring and committed co-applicants, Graham Silsbury and Mary Goodwin; other patient, carer, volunteer and public representatives from Pilgrims Hospices in East Kent; public attendees of our consensus workshops; and the PPI representatives (Helen Teresa Edwards and Alan West) on our Project Oversight Group.
Members of the Project Oversight Group, chaired by Professor Fliss Murtagh, for their time given and their experience and wisdom, in support of the project. HAH organisations across England and their staff have given generously of their time and support for each phase of this project, in particular at the 12 case study sites. The NAHH whose board advised us and supported the involvement and recruitment of HAH organisations and provided us with the invaluable Kay Greene as a co-applicant on the study. Dr Ferhana Hashem who worked hard on the project in the first 18 months, before she was promoted on to new responsibilities. Mrs Cathy Hayes who brought her passion for palliative care and her clinical experience to the survey data collection and assisted with interview coding.
Project Oversight Group members
-
Professor Fliss Murtagh (Professor of Palliative Care, Hull York Medical School, Centre for Health and Population Studies, University of Hull) chaired the group.
-
Dr Catherine Evans (Health Education England/NIHR Senior Clinical Lecturer in Palliative Care and Nursing, Research, Development and Innovation Director, and Honorary Nurse Consultant, Sussex Community NHS Foundation Trust and Cicely Saunders Institute).
-
Dr Anna-Marie Jones (NIHR Research Design Service South East Research Adviser, Statistician, University of Brighton) was the statistics expert.
-
Professor Catherine Walshe (Director at International Observatory on End of Life Care, Lancaster University).
-
Ms Lisa Irvine (Senior Research Fellow at the Centre for Research in Public Health and Community Care, University of Hertfordshire) was the health economist.
-
Professor Patricia Wilson (Professor of Primary Care, Centre for Health Services Studies, University of Kent) was the realist evaluation expert.
-
Professor Claire Butler (Clinical Professor of Palliative Medicine, Centre for Health Services Studies, University of Kent) was the chief investigator of the study.
-
Mr Alan West was a public member of the Project Oversight Group.
-
Ms Helen Teresa Edwards was a public member of the Project Oversight Group.
Contributions of authors
Claire Butler (https://orcid.org/0000-0001-9501-2861) (Project Chief Investigator, Clinical Professor of Palliative Medicine, Consultant in Palliative Medicine) wrote the introduction, conclusions and summary sections, and had overall responsibility for the content of the report.
Patricia Wilson (https://orcid.org/0000-0002-5787-9736) (Professor of Primary and Community Care) was the realist evaluation expert on the project, was responsible for the qualitative results chapter (Chapter 7) and provided expert advice for the discussion (Chapter 8). Patricia Wilson also mentored Claire Butler throughout the project and report writing.
Vanessa Abrahamson (https://orcid.org/0000-0002-1169-9457) (Research Associate) was responsible for the drafting of the discussion (Chapter 8), with supervision. Vanessa Abrahamson was also responsible for providing qualitative quotations for Chapter 7 and for site descriptions and flow diagrams in the appendices.
Rasa Mikelyte (https://orcid.org/0000-0002-2772-8240) (Research Associate) is a mixed-methods researcher; she was jointly responsible for writing Chapter 5 and providing qualitative quotations for Chapter 7 and site descriptions and flow diagrams in the appendices. Rasa Mikelyte acted as a key link between qualitative and quantitative data analyses. She was responsible for the formatting and presentation of the report.
Heather Gage (https://orcid.org/0000-0002-2049-9406) (Professor of Health Economics) was the expert health economist, responsible for the health economics analysis and the writing of the quantitative and health economics elements of the methods, results (Chapter 6) and discussion sections.
Peter Williams (https://orcid.org/0000-0001-7885-0564) (Statistics Consultant) was responsible for quantitative data analysis for phases 1 and 2 of the study and relevant tables and figures.
Charlotte Brigden (https://orcid.org/0000-0003-4917-4338) (Hospice Research Facilitator) facilitated the PPI element of the study from the inception of the project proposal through to completion. She wrote the literature review (Chapter 2) and the PPI (Chapter 4) sections.
Brooke Swash (https://orcid.org/0000-0003-2457-954X) (Research Associate) was responsible for the first draft of the methods section (Chapter 3) and for site descriptions and flow diagrams in the appendices.
Melanie Rees-Roberts (https://orcid.org/0000-0002-7121-0414) (Project Manager) participated in the writing of the results of the survey data (Chapter 5). Melanie Rees-Roberts also provided documents for the appendices.
Graham Silsbury (PPI co-applicant) and Mary Goodwin (PPI co-applicant) commented on the final draft of the report.
Kay Greene (Director of Clinical Services at Mary Ann Evans Hospice and Vice-Chair for NAHH), Bee Wee (https://orcid.org/0000-0002-7714-0349) (National Clinical Director for End of Life Care) and Stephen Barclay (https://orcid.org/0000-0002-4505-7743) (University Senior Lecturer, GP and Honorary Consultant Physician in Palliative Care) were study co-applicants and commented on the final draft of the report.
Publications
Butler C, Brigden C, Gage H, Williams P, Holdsworth L, Greene K, et al. Optimum hospice at home services for end-of-life care: protocol of a mixed-methods study employing realist evaluation. BMJ Open 2018;8:e021192.
Hashem F, Brigden C, Wilson P, Butler C. Understanding what works, why and in what circumstances in hospice at home services for end-of-life care: applying a realist logic of analysis to a systematically searched literature review. Palliat Med 2020;34:16–31.
Rees-Roberts M, Williams P, Hashem F, Brigden C, Greene K, Gage H, et al. Hospice at home services in England: a national survey. BMJ Support Palliat Care 2021;11:454–60.
Data-sharing statement
All data requests should be submitted to the corresponding author. Access to data will be granted where possible in line with the principle of open access, but provided that anonymity can be preserved.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Economist Intelligence Unit . The 2015 Quality of Death Index. Ranking Palliative Care Across the World 2015.
- Hospice UK . Facts and Figures about Hospice Care, 2015 n.d. https://professionals.hospiceuk.org/about-hospice-care/media-centre/facts-and-figures (accessed 21 February 2021).
- Department of Health and Social Care . End of Life Care Strategy: Promoting High Quality Care for All Adults at the End of Life 2008.
- Gomes B, Higginson IJ, Calanzani N, Cohen J, Deliens L, Daveson BA, et al. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol 2012;23:2006-15. https://doi.org/10.1093/annonc/mdr602.
- Shepperd S, Gonçalves-Bradley DC, Straus SE, Wee B. Hospital at home: home-based end-of-life care. Cochrane Database Syst Rev 2016;2. https://doi.org/10.1002/14651858.CD009231.pub2.
- Higginson IJ, Sarmento VP, Calanzani N, Benalia H, Gomes B. Dying at home – is it better: a narrative appraisal of the state of the science. Palliat Med 2013;27:918-24. https://doi.org/10.1177/0269216313487940.
- Palliative and end of life care Priority Setting Partnership (PeolcPSP) . Putting Patients, Carers and Clinicians at the Heart of Palliative and End of Life Care Research 2015. www.jla.nihr.ac.uk/priority-setting-partnerships/palliative-and-end-of-life-care/downloads/Palliative-and-end-of-life-care-PSP-final-report.pdf (accessed 1 March 2021).
- Public Health England . Palliative and End of Life Care Profiles 2021.
- Garber J, Leadbeater C. Dying for Change. London: Demos; 2010.
- Stosz L. Literature Review of the Evidence Base for a Hospice at Home Service. Canterbury: Centre for Health Services Studies, University of Kent; 2008.
- Holdsworth LM, Gage H, Coulton S, King A, Butler C. A quasi-experimental controlled evaluation of the impact of a hospice rapid response community service for end-of-life care on achievement of preferred place of death. Palliat Med 2015;29:817-25. https://doi.org/10.1177/0269216315582124.
- Holdsworth LM. Bereaved carers’ accounts of the end of life and the role of care providers in a ‘good death’: a qualitative study. Palliat Med 2015;29:834-41. https://doi.org/10.1177/0269216315584865.
- Jack B, Groves K, Baldry C, Gaunt K, Sephton J, Whelan A, et al. Evaluation of the Queenscourt at Home Pilot Service. Ormskirk: Edge Hill University; 2010.
- King G, Mackenzie J, Smith H, Clark D. Dying at home: evaluation of a hospice rapid-response service. Int J Palliat Nurs 2000;6:280-7. https://doi.org/10.12968/ijpn.2000.6.6.9077.
- Butler C, Brigden C, Gage H, Williams P, Holdsworth L, Greene K, et al. Optimum hospice at home services for end-of-life care: protocol of a mixed-methods study employing realist evaluation. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021192.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 2001.
- Pawson R, Tilley N. Realist Evaluation 2004. www.urban-response.org/system/files/content/resource/files/main/pawson---tilley-%282004%29-realist-evaluation.pdf (accessed 1 July 2022).
- Hashem F, Brigden C, Wilson P, Butler C. Understanding what works, why and in what circumstances in hospice at home services for end-of-life care: applying a realist logic of analysis to a systematically searched literature review. Palliat Med 2020;34:16-31. https://doi.org/10.1177/0269216319867424.
- Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev 2013;6. https://doi.org/10.1002/14651858.CD007760.pub2.
- Butler C, Holdsworth LM, Coulton S, Gage H. Evaluation of a hospice rapid response community service: a controlled evaluation. BMC Palliat Care 2012;11. https://doi.org/10.1186/1472-684X-11-11.
- Bell G, Greene K, Hunt J, Varvel S. Developing national standards for hospice-at-home services. End Life J 2013;3:1-5. https://doi.org/10.1136/eoljnl-03-01.8.
- Rees-Roberts M, Williams P, Hashem F, Brigden C, Greene K, Gage H, et al. Hospice at home services in England: a national survey. BMJ Support Palliat Care 2021;11:454-60. https://doi.org/10.1136/bmjspcare-2019-001818.
- Taylor R, Ellis J, Gao W, Searle L, Heaps K, Davies R, et al. A scoping review of initiatives to reduce inappropriate or non-beneficial hospital admissions and bed days in people nearing the end of their life: much innovation, but limited supporting evidence. BMC Palliat Care 2020;19. https://doi.org/10.1186/s12904-020-0526-2.
- Bainbridge D, Seow H, Sussman J. Common components of efficacious in-home end-of-life care programs: a review of systematic reviews. J Am Geriatr Soc 2016;64:632-9. https://doi.org/10.1111/jgs.14025.
- Sarmento VP, Gysels M, Higginson IJ, Gomes B. Home palliative care works: but how? A meta-ethnography of the experiences of patients and family caregivers. BMJ Support Palliat Care 2017;7. https://doi.org/10.1136/bmjspcare-2016-001141.
- Luckett T, Phillips J, Agar M, Virdun C, Green A, Davidson PM. Elements of effective palliative care models: a rapid review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-136.
- Shepperd S, Wee B, Straus SE. Hospital at home: home-based end of life care. Cochrane Database Syst Rev 2011;7. https://doi.org/10.1002/14651858.CD009231.
- Firth AM, O’Brien SM, Guo P, Seymour J, Richardson H, Bridges C, et al. Establishing key criteria to define and compare models of specialist palliative care: a mixed-methods study using qualitative interviews and Delphi survey. Palliat Med 2019;33:1114-24. https://doi.org/10.1177/0269216319858237.
- Addington-Hall J, Gerard K, Brien S, England H, Salisbury C, Leydon G, et al. Variations in ‘out of hours’ end of life care service provision across primary care organisations in England and Scotland: the case of nursing care (oral presentation). Palliat Med 2012;26:426-7.
- Addington-Hall J, Gerard K, Brien S, Brailsford S, Salisbury C, Heaney D, et al. Variations in Out of Hours End of Life Care Provision Across Primary Care Organisations in England and Scotland. Final Report 2013.
- Waight C, Noble B. Dying at home the Midhurst way. Future Healthc J 2018;5:7-9. https://doi.org/10.7861/futurehosp.5-1-7.
- Johnston B, Patterson A, Bird L, Wilson E, Almack K, Mathews G, et al. Impact of the Macmillan specialist Care at Home service: a mixed methods evaluation across six sites. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0281-9.
- Woodyatt N, Singh S. P-162 Championing specialist care at home in everyday dying. BMJ Support Palliat Care 2016;6. https://doi.org/10.1136/bmjspcare-2016-001245.184.
- Wye L, Lasseter G, Percival J, Simmonds B, Duncan L, Purdy S. Independent Evaluation of the Marie Curie Cancer Care Delivering Choice Programme in Somerset and North Somerset. Bristol: University of Bristol; 2012.
- Payne S. Independent Evaluation of the Marie Curie Cancer Care ‘Delivering Choice Programme’. Lancaster: International Observatory on End of Life Care; 2008.
- Purdy S, Lasseter G, Griffin T, Wye L. Impact of the Marie Curie Cancer Care Delivering Choice Programme in Somerset and North Somerset on place of death and hospital usage: a retrospective cohort study. BMJ Support Palliat Care 2015;5:34-9. https://doi.org/10.1136/bmjspcare-2013-000645.
- Wye L, Lasseter G, Percival J, Duncan L, Simmonds B, Purdy S. What works in ‘real life’ to facilitate home deaths and fewer hospital admissions for those at end of life? Results from a realist evaluation of new palliative care services in two English counties. BMC Palliat Care 2014;13. https://doi.org/10.1186/1472-684X-13-37.
- Grande GE, Todd CJ, Barclay SI, Farquhar MC. Does hospital at home for palliative care facilitate death at home? Randomised controlled trial. BMJ 1999;319:1472-5. https://doi.org/10.1136/bmj.319.7223.1472.
- Buck J, Webb L, Moth L, Morgan L, Barclay S. Persistent inequalities in hospice at home provision. BMJ Support Palliat Care 2020;10. https://doi.org/10.1136/bmjspcare-2017-001367.
- Tyrer F, Exley C. Receiving care at home at end of life: characteristics of patients receiving Hospice at Home care. Fam Pract 2005;22:644-6. https://doi.org/10.1093/fampra/cmi071.
- Travers E, Grady A. Hospice at home 1: the development of a crisis intervention service. Int J Palliat Nurs 2002;8:162-8. https://doi.org/10.12968/ijpn.2002.8.4.10374.
- Spencer L. Hospice to home: a patient-centric multi professional community approach. Int J Palliat Nurs 2015;21:245-50. https://doi.org/10.12968/ijpn.2015.21.5.245.
- Baldry CR, Jack BA, Groves KE, Birch H, Shard A. Establishing a hospice at home service: lessons to share. Int Pract Dev J 2011;1:1-9. https://doi.org/10.1136/bmjspcare-2011-000105.95.
- Buck J, Moth L, Webb L, Morgan L, Morris Z, Lay M, et al. Hospice at home: optimising care and enabling home death. BMJ Support Palliat Care 2014;4:A44.2-A44. https://doi.org/10.1136/bmjspcare-2014-000654.123.
- Davis C. End of life care: a rapid response hospice at home service. Nurs Older People 2010;22:22-4. https://doi.org/10.7748/nop2010.05.22.4.22.c7733.
- Gibson V, McEvilly L, Standfield R. Help the hospices poster presentations: P12 hospice at Home Service Listening, responding, developing. BMJ Support Palliat Care 2013;3:A13-14. https://doi.org/10.1136/bmjspcare-2013-000591.34.
- Koffman J, Higginson I, Naysmith A. Hospice at home – a new service for patients with advanced HIV/AIDS: a pilot evaluation of referrals and outcomes. Br J Gen Pract 1996;46:539-40.
- Exley C, Tyrer F. Bereaved carers’ views of a hospice at home service. Int J Palliat Nurs 2005;11:242-6. https://doi.org/10.12968/ijpn.2005.11.5.242.
- Jack BA, O’Brien MR, Scrutton J, Baldry CR, Groves KE. Supporting family carers providing end-of-life home care: a qualitative study on the impact of a hospice at home service. J Clin Nurs 2015;24:131-40. https://doi.org/10.1111/jocn.12695.
- McLaughlin D, Sullivan K, Hasson F. Hospice at home service: the carer’s perspective. Support Care Cancer 2007;15:163-70. https://doi.org/10.1007/s00520-006-0110-1.
- Grande GE, Farquhar MC, Barclay SI, Todd CJ. Caregiver bereavement outcome: relationship with hospice at home, satisfaction with care, and home death. J Palliat Care 2004;20:69-77. https://doi.org/10.1177/082585970402000202.
- Jack BA, Baldry CR, Groves KE, Whelan A, Sephton J, Gaunt K. Supporting home care for the dying: an evaluation of healthcare professionals’ perspectives of an individually tailored hospice at home service. J Clin Nurs 2013;22:2778-86. https://doi.org/10.1111/j.1365-2702.2012.04301.x.
- Grady A, Travers E. Hospice at home 2: evaluating a crisis intervention service. Int J Palliat Nurs 2003;9:326-35. https://doi.org/10.12968/ijpn.2003.9.8.11522.
- Wilson J, Steers J, Steele K, Turner J, Tinker A. Service evaluation of community-based palliative care and a hospice-at-home service. End Life J 2015;5:1-11.
- Lucas B, Small N, Greasley P, Daley A. A reassuring presence: an evaluation of Bradford District Hospice at Home service. BMC Palliat Care 2008;7. https://doi.org/10.1186/1472-684X-7-9.
- Blanchard H. An evaluation of a hospice at home service: a questionnaire survey of GP & district nurse referrers. BMJ Support Palliat Care 2011;1:264-4. https://doi.org/10.1136/bmjspcare-2011-000105.182.
- Richardson R, Maw K, Willis D. Hospice at home. BMJ Support Palliat Care 2020;10. https://doi.org/10.1136/spcare-2020-PCC.168.
- Taylor K, Ali S, Bunting M. P-163 The palliative care partnership . . . the story so far. BMJ Support Palliat Care 2016;6. https://doi.org/10.1136/bmjspcare-2016-001245.185.
- Morgan L. P-212 The design and implementation of the hospice night support team. BMJ Support Palliat Care 2019;9:A88-9. https://doi.org/10.1136/bmjspcare-2019-HUKNC.234.
- Sevant D. P-201 Strategic success of a whole system approach to end of life care. BMJ Support Palliat Care 2019;9. https://doi.org/10.1136/bmjspcare-2019-HUKNC.223.
- Varnam D. P-214 Hospice at home respite service. BMJ Support Palliat Care 2019;9. https://doi.org/10.1136/bmjspcare-2019-HUKNC.236.
- Connolly A, Meissner J. P-213 Willen at home an integrated community service. BMJ Support Palliat Care 2019;9. https://doi.org/10.1136/bmjspcare-2019-HUKNC.235.
- Grande GE, Todd CJ, Barclay SI, Farquhar MC. A randomized controlled trial of a hospital at home service for the terminally ill. Palliat Med 2000;14:375-85. https://doi.org/10.1191/026921600701536200.
- Grande GE, McKerral A, Todd CJ. Which cancer patients are referred to hospital at home for palliative care?. Palliat Med 2002;16:115-23. https://doi.org/10.1191/0269216302pm519oa.
- Todd CJ, Grande GE, Barclay SI, Farquhar MC. General practitioners’ and district nurses’ views of hospital at home for palliative care. Palliat Med 2002;16:251-4. https://doi.org/10.1191/0269216302pm513oa.
- Gage H, Holdsworth LM, Flannery C, Williams P, Butler C. Impact of a hospice rapid response service on preferred place of death, and costs. BMC Palliat Care 2015;14. https://doi.org/10.1186/s12904-015-0065-4.
- Spiro S, Ward A, Sixsmith J, Graham A, Varvel S. The cost of visit-based home care for up to two weeks in the last three months of life: a pilot study of community care based at a hospice at home service in south east of England. J Community Health Nurs 2020;37:203-13. https://doi.org/10.1080/07370016.2020.1809856.
- Addicott R, Dewar S. Improving Choice at End of Life: A Descriptive Analysis of the Impact and Costs of the Marie Curie Choice Programme in Lincolnshire. London: The King’s Fund; 2008.
- Whitmore S. An innovative approach to creating a hospice at home team. BMJ Support Palliat Care 2011;1:226-6. https://doi.org/10.1136/bmjspcare-2011-000105.65.
- Butler C, Holdsworth L. Setting up a new evidence-based hospice-at-home service in England. Int J Palliat Nurs 2013;19:355-9. https://doi.org/10.12968/ijpn.2013.19.7.355.
- Marchal B, Dedzo M, Kegels G. A realist evaluation of the management of a well-performing regional hospital in Ghana. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-24.
- Bhaskar R. A Realist Theory of Science. London: Routledge; 2013.
- Porter S, Millar R, Brewer J. A to Z of Social Research. London: SAGE Publications Ltd; 2003.
- Fletcher A, Jamal F, Moore G, Evans RE, Murphy S, Bonell C. Realist complex intervention science: applying realist principles across all phases of the Medical Research Council framework for developing and evaluating complex interventions. Evaluation 2016;22:286-303. https://doi.org/10.1177/1356389016652743.
- Gilmore B, McAuliffe E, Power J, Valliéres F. Data analysis and synthesis within a realist evaluation: toward more transparent methodological approaches. Int J Qual Methods 2019;18:1-11. https://doi.org/10.1177/1609406919859754.
- Shearn K, Allmark P, Piercy H, Hirst J. Building realist program theory for large complex and messy interventions. Int J Qual Methods 2017;16:1-11. https://doi.org/10.1177/1609406917741796.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: meta-narrative reviews. J Adv Nurs 2013;69:987-1004. https://doi.org/10.1111/jan.12092.
- May C, Rapley T, Mair FS, Treweek S, Murray E, Ballini L, et al. Normalization Process Theory Online Users’ Manual, Toolkit and NoMAD Instrument n.d. www.normalizationprocess.org/npt-toolkit/ (accessed 28 June 2017).
- Dalkin SM, Hardwick RJL, Haighton CA, Finch TL. Combining realist approaches and normalization process theory to understand implementation: a systematic review. Implement Sci Commun 2021;2. https://doi.org/10.1186/s43058-021-00172-3.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. https://doi.org/10.1111/j.1468-0009.2012.00665.x.
- Wong G, Emmel N, Greenhalgh J, Manzano A, Monaghan M, Dalkin S. Doing Realist Research. London: SAGE Publications Ltd; 2018.
- Exworthy M, Peckham S, Powell M. Shaping Health Policy: Case Study Methods and Analysis. Bristol: Policy Press; 2011.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications Inc.; 2014.
- Marinetto M. Studies of the Policy Process: A Case Analysis. Hoboken, NJ: Prentice Hall Europe; 1998.
- Cicely Saunders Institute . Integrated Palliative Care Outcome Scale (IPOS) n.d. https://pos-pal.org/maix/ipos_in_english.php (accessed 28 June 2021).
- Murtagh FE, Ramsenthaler C, Firth A, Groeneveld EI, Lovell N, Simon ST, et al. A brief, patient- and proxy-reported outcome measure in advanced illness: validity, reliability and responsiveness of the Integrated Palliative care Outcome Scale (IPOS). Palliat Med 2019;33:1045-57. https://doi.org/10.1177/0269216319854264.
- Witt J, Murtagh FEM, de Wolf-Linder S, Higginson IJ, Daveson BA. Introducing the Outcome Assessment and Complexity Collaborative (OACC) Suite of Measures: A Brief Introduction. London: King’s College London; 2014.
- Masso, M, Allingham, SF, Banfield M. Palliative care phase: inter-rater reliability and acceptability in a national study. Palliat Med 2015;29:22-30. https://doi.org/10.1177/0269216314551814.
- Abernethy AP, Shelby-James T, Fazekas BS, Woods D, Currow DC. The Australia-modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice [ISRCTN81117481]. BMC Palliat Care 2005;4. https://doi.org/10.1186/1472-684X-4-7.
- Guerriere DN, Coyte PC. The Ambulatory and Home Care Record: a methodological framework for economic analyses in end-of-life care. J Aging Res 2011;2011. https://doi.org/10.4061/2011/374237.
- Holdsworth LM, Gage H, Williams P, Butler C. Adaptation of the ambulatory and home care record for collecting palliative care service utilisation data from family carers in the UK: a pilot study. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0332-2.
- Higginson IJ, Gao W, Jackson D, Murray J, Harding R. Short-form Zarit Caregiver Burden Interviews were valid in advanced conditions. J Clin Epidemiol 2010;63:535-42. https://doi.org/10.1016/j.jclinepi.2009.06.014.
- Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649-55. https://doi.org/10.1097/00000421-198212000-00014.
- Addington–Hall J, McCarthy M. Regional study of care for the dying: methods and sample characteristics. Palliat Med 1995;9:27-35. https://doi.org/10.1177/026921639500900105.
- Hales S, Zimmermann C, Rodin G. Review: the quality of dying and death: a systematic review of measures. Palliat Med 2010;24:127-44. https://doi.org/10.1177/0269216309351783.
- Curtis JR, Patrick DL, Engelberg RA, Norris K, Asp C, Byock I. A measure of the quality of dying and death. Initial validation using after-death interviews with family members. J Pain Symptom Manage 2002;24:17-31. https://doi.org/10.1016/S0885-3924(02)00419-0.
- End-of-Life Care Research Program at UW School of Medicine . Instruments – Quality of Dying and Death (QODD) n.d. https://depts.washington.edu/eolcare/products/instruments/ (accessed 9 February 2022).
- Ritchie J, Lewis J, McNaughton Nicholls C, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2013.
- Stanfield RB. The Workshop Book: From Individual Creativity to Group Action. Gabriola Island, BC: New Society Publishers; 2013.
- Hales S, Chiu A, Husain A, Braun M, Rydall A, Gagliese L, et al. The quality of dying and death in cancer and its relationship to palliative care and place of death. J Pain Symptom Manage 2014;48:839-51. https://doi.org/10.1016/j.jpainsymman.2013.12.240.
- Clark K, Cain J, Campbell L, Byfieldt N. Caring for people dying in acute hospitals: a mixed-methods study to examine relative’s perceptions of care. Palliat Support Care 2015;13:335-43. https://doi.org/10.1017/S1478951514000066.
- Lewis-Newby M, Curtis JR, Martin DP, Engelberg RA. Measuring family satisfaction with care and quality of dying in the intensive care unit: does patient age matter?. J Palliat Med 2011;14:1284-90. https://doi.org/10.1089/jpm.2011.0138.
- The National Council for Palliative Care . Minimum Data Set for Palliative Care, Individual Reports 2013 14 2014.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: Personal Social Services Research Unit, University of Kent; 2019.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 2002.
- Eastwood JG, Jalaludin BB, Kemp LA. Realist explanatory theory building method for social epidemiology: a protocol for a mixed method multilevel study of neighbourhood context and postnatal depression. Springerplus 2014;3. https://doi.org/10.1186/2193-1801-3-12.
- Gysels M, Evans CJ, Lewis P, Speck P, Benalia H, Preston NJ, et al. MORECare research methods guidance development: recommendations for ethical issues in palliative and end-of-life care research. Palliat Med 2013;27:908-17. https://doi.org/10.1177/0269216313488018.
- Hewitt G, Sims S, Harris R. The realist approach to evaluation research: an introduction. Int J Ther Rehabil 2012;19:250-9. https://doi.org/10.12968/ijtr.2012.19.5.250.
- Chambers E, Gardiner C, Thompson J, Seymour J. Patient and carer involvement in palliative care research: an integrative qualitative evidence synthesis review. Palliat Med 2019;33:969-84. https://doi.org/10.1177/0269216319858247.
- Gott M, Payne S, Seymour J, Ingleton C. Palliative Care Nursing: Principles and Evidence for Practice. Buckingham: Open University Press; 2004.
- Elliot J, Lodemore M, Minogue V, Wellings A. Public Co-applicants in Research: Guidance on Roles and Responsibilities. Southampton: INVOLVE; 2019.
- INVOLVE . Budgeting for Involvement: Practical Advice on Budgeting for Actively Involving the Public in Research Studies 2013.
- Hickey DG. The potential for coproduction to add value to research. Health Expect 2018;21:693-4. https://doi.org/10.1111/hex.12821.
- Brigden CL, Goodwin M, Silsbury G, Rees-Roberts M, Butler C, Greene K, et al. Patient and Public Involvement (PPI) in Hospice Research: An Example of Co-Production in Action n.d.
- Brigden C, Silsbury G. Co-Production in the OPEL Hospice at Home Study n.d.
- Centre for Research in Public Health and Community Care (CRIPACC) . Guidance for Researchers: Feedback. Patient and Public Involvement (PPI): Feedback from Researchers to PPI Contributors 2018.
- Mathie E, Wythe H, Munday D, Millac P, Rhodes G, Roberts N, et al. Reciprocal relationships and the importance of feedback in patient and public involvement: a mixed methods study. Health Expect 2018;21:899-908. https://doi.org/10.1111/hex.12684.
- Howe A, Mathie E, Munday D, Cowe M, Goodman C, Keenan J, et al. Learning to work together – lessons from a reflective analysis of a research project on public involvement. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-016-0051-x.
- Cicely Saunders Institute . How to Score POS n.d. www.pos-pal.org/maix/how-to-score.php (accessed 30 November 2020).
- Aoun SM, Ewing G, Grande G, Toye C, Bear N. The impact of supporting family caregivers before bereavement on outcomes after bereavement: adequacy of end-of-life support and achievement of preferred place of death. J Pain Symptom Manage 2018;55:368-78. https://doi.org/10.1016/j.jpainsymman.2017.09.023.
- Cai J, Zhang L, Guerriere D, Coyte PC. Congruence between preferred and actual place of death for those in receipt of home-based palliative care. J Palliat Med 2020;23:1460-7. https://doi.org/10.1089/jpm.2019.0582.
- Ali M, Capel M, Jones G, Gazi T. The importance of identifying preferred place of death. BMJ Support Palliat Care 2019;9:84-91. https://doi.org/10.1136/bmjspcare-2015-000878.
- Lobb EA, Bindley K, Sanderson C, MacLeod R, Mowll J. Navigating the path to care and death at home – it is not always smooth: a qualitative examination of the experiences of bereaved family caregivers in palliative care. J Psychosoc Oncol Res Pract 2019;1. https://doi.org/10.1097/OR9.0000000000000003.
- Carvajal A, Haraldsdottir E, Kroll T, McCormack B, Errasti-Ibarrondo B, Larkin P. Barriers and facilitators perceived by registered nurses to providing person-centred care at the end of life. A scoping review. Int Pract Dev J 2019;9. https://doi.org/10.19043/ipdj.92.008.
- Ganann R, Weeres A, Lam A, Chung H, Valaitis R. Optimization of home care nurses in Canada: a scoping review. Health Soc Care Community 2019;27:e604-e621. https://doi.org/10.1111/hsc.12797.
- Jack BA, Mitchell TK, Cope LC, O’Brien MR. Supporting older people with cancer and life-limiting conditions dying at home: a qualitative study of patient and family caregiver experiences of Hospice at Home care. J Adv Nurs 2016;72:2162-72. https://doi.org/10.1111/jan.12983.
- Wahid AS, Sayma M, Jamshaid S, Kerwat D, Oyewole F, Saleh D, et al. Barriers and facilitators influencing death at home: a meta-ethnography. Palliat Med 2018;32:314-28. https://doi.org/10.1177/0269216317713427.
- von Heymann-Horan A, Bidstrup PE, Johansen C, Rottmann N, Andersen EAW, Sjøgren P, et al. Dyadic coping in specialized palliative care intervention for patients with advanced cancer and their caregivers: effects and mediation in a randomized controlled trial. Psycho-Oncology 2019;28:264-70. https://doi.org/10.1002/pon.4932.
- Hydén LC, Nilsson E. Couples with dementia: positioning the ‘we’. Dementia 2015;14:716-33. https://doi.org/10.1177/1471301213506923.
- Rand S, Forder J, Malley J. A study of dyadic interdependence of control, social participation and occupation of adults who use long-term care services and their carers. Qual Life Res 2017;26:3307-21. https://doi.org/10.1007/s11136-017-1669-3.
- Abrahamson V, Jensen J, Springett K, Sakel M. Experiences of patients with traumatic brain injury and their carers during transition from in-patient rehabilitation to the community: a qualitative study. Disabil Rehabil 2017;39:1683-94. https://doi.org/10.1080/09638288.2016.1211755.
- Nursing and Midwifery Council . The Code. Professional Standards of Practice and Behaviour for Nurses, Midwives and Nursing Associates 2015.
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ 2005;330:1007-11. https://doi.org/10.1136/bmj.330.7498.1007.
- Holtslander L, Baxter S, Mills K, Bocking S, Dadgostari T, Duggleby W, et al. Honoring the voices of bereaved caregivers: a metasummary of qualitative research. BMC Palliat Care 2017;16. https://doi.org/10.1186/s12904-017-0231-y.
- Duke S. An exploration of anticipatory grief: the lived experience of people during their spouses’ terminal illness and in bereavement. J Adv Nurs 1998;28:829-39. https://doi.org/10.1046/j.1365-2648.1998.00742.x.
- Department of Health and Social Care . Care and Support Statutory Guidance 2016.
- Grande GE, Austin L, Ewing G, O’Leary N, Roberts C. Assessing the impact of a Carer Support Needs Assessment Tool (CSNAT) intervention in palliative home care: a stepped wedge cluster trial. BMJ Support Palliat Care 2017;7:326-34. https://doi.org/10.1136/bmjspcare-2014-000829.
- Hewitt D. Coronavirus: Third of hospices on brink of redundancies and service cuts ahead of ‘surge in demand’. ITV News 2020. www.itv.com/news/2020-09-24/exclusive-third-of-hospices-on-brink-of-redundancies-and-services-cuts-ahead-of-surge-in-demand (accessed 26 January 2022).
- Nagraj S, Barclay S. Bereavement care in primary care: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e42-8. https://doi.org/10.3399/bjgp11X549009.
- Hudson P, Hall C, Boughey A, Roulston A. Bereavement support standards and bereavement care pathway for quality palliative care. Palliat Support Care 2018;16:375-87. https://doi.org/10.1017/S1478951517000451.
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM-V and ICD-11. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000121.
- Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety 2011;28:103-17. https://doi.org/10.1002/da.20780.
- National Palliative and End of Life Care Partnership . Ambitions for Palliative and End of Life Care: A National Framework for Local Action 2015–2020 2015. www.nationalvoices.org.uk/sites/default/files/public/publications/ambitions-for-palliative-and-end-of-life-care.pdf (accessed 26 January 2022).
- Department of Health and Children . Report of the National Advisory Committee on Palliative Care 2001.
- Axelsson L, Alvariza A, Holm M, Årestedt K. Intensity of predeath grief and postdeath grief of family caregivers in palliative care in relation to preparedness for caregiving, caregiver burden, and social support. Palliat Med Rep 2020;1:191-200. https://doi.org/10.1089/pmr.2020.0033.
- Hall C, Hudson P, Boughey A. Bereavement Support Standards for Specialist Palliative Care Services. Melbourne, VIC: Department of Health; 2012.
- Aoun SM, Rumbold B, Howting D, Bolleter A, Breen LJ. Bereavement support for family caregivers: the gap between guidelines and practice in palliative care. PLOS One 2017;12. https://doi.org/10.1371/journal.pone.0184750.
- Funk LM, Dansereau L, Novek S. Carers as system navigators: exploring sources, processes and outcomes of structural burden. Gerontologist 2019;59:426-35. https://doi.org/10.1093/geront/gnx175.
- Valaitis RK, Carter N, Lam A, Nicholl J, Feather J, Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2046-1.
- National Institute for Health and Care Excellence (NICE) . End of Life Care for Adults. Quality Standard [QS13] 2017.
- Stajduhar KI. Provocations on privilege in palliative care: are we meeting our core mandate?. Prog Palliat Care 2020;28:89-93. https://doi.org/10.1080/09699260.2019.1702334.
- Carter N, Valaitis RK, Lam A, Feather J, Nicholl J, Cleghorn L. Navigation delivery models and roles of navigators in primary care: a scoping literature review. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-2889-0.
- Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer 2011;117:3539-42. https://doi.org/10.1002/cncr.26262.
- Bernardo BM, Zhang X, Beverly Hery CM, Meadows RJ, Paskett ED. The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: a systematic review. Cancer 2019;125:2747-61. https://doi.org/10.1002/cncr.32147.
- Bennett MI, Ziegler L, Allsop M, Daniel S, Hurlow A. What determines duration of palliative care before death for patients with advanced disease? A retrospective cohort study of community and hospital palliative care provision in a large UK city. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012576.
- Gadoud A, Kane E, Oliver SE, Johnson MJ, Macleod U, Allgar V. Palliative care for non-cancer conditions in primary care: a time trend analysis in the UK (2009–2014) [published online ahead of print January 13 2020]. BMJ Support Palliat Care 2020. https://doi.org/10.1136/bmjspcare-2019-001833.
- Weerawardena J, McDonald RE, Mort GS. Sustainability of nonprofit organizations: an empirical investigation. J World Bus 2010;45:346-56. https://doi.org/10.1016/j.jwb.2009.08.004.
- Hodgson DE, Bailey S, Exworthy M, Bresnen M, Hassard J, Hyde P. On the character of the new entrepreneurial NHS in England: reforming health care from within? [published online ahead of print November 3 2021]. Public Adm 2021. https://doi.org/10.1111/padm.12797.
- Stuart H. Managing a corporate brand in a challenging stakeholder environment: charity branding. Int Stud Manag Organ 2016;46:228-34. https://doi.org/10.1080/00208825.2016.1140519.
- Barker R. How Does English End of Life Care and the Views of Stakeholders Fit with the Ambitions of National Policy: Insights From a Realist Evaluation. Canterbury: University of Kent; 2020.
- NHS England . Commissioning Person Centred End of Life Care: A Toolkit for Health and Social Care 2016.
- Chamanga E, Dyson J, Loke J, McKeown E. Factors influencing the recruitment and retention of registered nurses in adult community nursing services: an integrative literature review. Prim Health Care Res Dev 2020;21. https://doi.org/10.1017/S1463423620000353.
- Haslam C, Tsitsianis N, Theodosopoulos G, Lee E. Accounting for voluntary hospices in England: a business model perspective. Crit Perspect Account 2018;54:27-40. https://doi.org/10.1016/j.cpa.2017.10.001.
- Scott R, Jindal-Snape D, Manwaring G. Exploring the relationship between volunteering and hospice sustainability in the UK: a theoretical model. Int J Palliat Nurs 2018;24:212-19. https://doi.org/10.12968/ijpn.2018.24.5.212.
- Morris SM, Payne S, Ockenden N, Hill M. Hospice volunteers: bridging the gap to the community?. Health Soc Care Community 2017;25:1704-13. https://doi.org/10.1111/hsc.12232.
- Aoun SM, Keegan O, Roberts A, Breen LJ. The impact of bereavement support on wellbeing: a comparative study between Australia and Ireland. Palliat Care Soc Pract 2020;14. https://doi.org/10.1177/2632352420935132.
- Abel J, Bowra J, Walter T, Howarth G. Compassionate community networks: supporting home dying. BMJ Support Palliat Care 2011;1:129-33. https://doi.org/10.1136/bmjspcare-2011-000068.
- Sallnow L, Richardson H, Murray SA, Kellehear A. The impact of a new public health approach to end-of-life care: a systematic review. Palliat Med 2016;30:200-11. https://doi.org/10.1177/0269216315599869.
- Abel J. Compassionate communities and end-of-life care. Clin Med 2018;18:6-8. https://doi.org/10.7861/clinmedicine.18-1-6.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; n.d.
Appendix 1 Literature search strategy
Databases searched
The following databases were searched: PubMed, ScienceDirect, Allied and Complementary Medicine Database, British Nursing Index, Cumulative Index to Nursing and Allied Health Literature, EMBASE, Health Business Elite, Health Management Information Consortium, MEDLINE, PsycINFO, Scopus and Web of Science. Additional searches were also carried out in the Database of Abstracts of Reviews of Effects (a search database for systematic and Cochrane reviews), Google Scholar (Google Inc., Mountain View, CA, USA), NHS Evidence, NIHR Clinical Research Network Portfolio database and the NIHR Journals Library of funded studies. Searches on websites of relevant professional bodies (e.g. Hospice UK, NAHH) were also conducted.
Search terms
“hospice at home”, “Hospital at home”, “hospices”, “hospice”, “home” “care”, “hospice care”, “community”, “palliative”, “palliative care”, “end of life”, terminal”, “crisis management” “crisis intervention”, “rapid response”, “24 hour”, “twenty-four hour” “UK”, “England “, “Wales”, “Scotland”, “Northern Ireland”.
Original literature search, August 2014
The following set of searches of academic databases was carried out in August 2014.
| Database | Dates covered | Hits (n) |
|---|---|---|
| PubMed | No restriction | 27 |
| ScienceDirect | No restriction | 59 |
| AMED, BNI, CINAHL, EMBASE, Health Business Elite, HMIC, Medline, PsycInfo | No restriction | 67 |
| NHS Evidence | No restriction | 64 |
| Scopus | No restriction | 16 |
| Web of Science | No restriction | 20 |
| Database | Dates covered | Hits (n) |
|---|---|---|
| PubMed | No restriction | 4 |
| ScienceDirect | Palliative care filter applied | 45 |
| AMED, BNI, CINAHL, EMBASE, Health Business Elite, HMIC, MEDLINE, PsycINFO | No restriction | 6 |
| NHS Evidence | No restriction | 427 |
| Scopus | No restriction | 2 |
| Web of Science | No restriction | 1 |
| Database | Dates covered | Hits (n) |
|---|---|---|
| PubMed | No restriction | 13 |
| ScienceDirect | Palliative care filter applied | 126 |
| AMED, BNI, CINAHL, EMBASE, Health Business Elite, HMIC, MEDLINE, PsycINFO | No restriction | 0 |
| NHS Evidence | No restriction | 3726 – abandoned |
| Scopus | No restriction | 15 |
| Web of Science | No restriction | 4 |
NHS Evidence was later abandoned as part of the database inclusion owing to the large volume of hits that were not retrieving relevant records.
Update of the literature search, June 2017
A further search was generated in June 2017, to search for any as yet unidentified literature since August 2014, in preparation for synthesis. This kept within the parameters of the original search, which was description or evaluation of adult services in the UK with HAH characteristics (e.g. rapid response, crisis intervention) for palliative/EOLC at home. There was slight variation in how the search terms were inputted for these later searches and only PubMed was searched.
Search 4
Database searched: PubMed only.
Date searched: 5 June 2017.
(((“hospices”[MeSH Terms] OR “hospices”[All Fields] OR “hospice”[All Fields] OR “hospice care”[MeSH Terms] OR (“hospice”[All Fields] AND “care”[All Fields]) OR “hospice care”[All Fields]) AND home[All Fields]) AND (“UK”[All Fields] OR “England “[All Fields] OR “Wales”[All Fields] OR “Scotland”[All Fields] OR “Northern Ireland”[All Fields]) AND (palliative[All Fields] OR “end of life”[All Fields])) AND (“2014/09/12”[PDAT] : “2017/06/05”[PDAT]).
Number of articles found: 97.
Search 5
Database searched: PubMed only.
Date searched: 8 June 2017.
((“palliative care”[All Fields] OR “Hospice Care”[All Fields] OR “end of life”[All Fields] OR terminal$[All Fields]) AND (“rapid response”[All Fields] OR “crisis intervention”[All Fields] OR “hospice at home”[All Fields])) AND (“2015/07/31”[PDAT] : “2017/06/08”[PDAT]).
Number of articles found: 45.
Nine additional articles were found to be relevant and were added to the total number of articles screened for the systematic literature synthesis (including one article we were made aware of currently in press).
Updated literature search, June 2019
A further search was generated on 25 June 2019, to search for any as yet unidentified literature since 5 June 2017. The search conducted in June 2017 was repeated.
Search 6
Database searched: PubMed only.
Date searched: 25 June 2019.
(((“hospices”[MeSH Terms] OR “hospices”[All Fields] OR “hospice”[All Fields] OR “hospice care”[MeSH Terms] OR (“hospice”[All Fields] AND “care”[All Fields]) OR “hospice care”[All Fields]) AND home[All Fields]) AND (“UK”[All Fields] OR “England “[All Fields] OR “Wales”[All Fields] OR “Scotland”[All Fields] OR “Northern Ireland”[All Fields]) AND (palliative[All Fields] OR “end of life”[All Fields])) AND (“2017/06/05”[PDAT] : “2019/06/25”[PDAT]).
Number of articles found: 75.
Search 7
Database searched: PubMed only.
Date searched: 25 June 2019.
((“palliative care”[All Fields] OR “Hospice Care”[All Fields] OR “end of life”[All Fields] OR terminal$[All Fields]) AND (“rapid response”[All Fields] OR “crisis intervention”[All Fields] OR “hospice at home”[All Fields])) AND (“2017/06/08”[PDAT] : “2019/06/25”[PDAT]).
Number of articles found: 44.
Three additional articles found to be relevant in these two searches. These included the article identified in 2017 that was in print and the OPEL study protocol paper.
Updated literature search, June 2020
A further search was generated on 25 June 2020, to search for any literature published in the preceding year.
Search 8
Database searched: PubMed only.
Date searched: 25 June 2020.
(((“hospices”[MeSH Terms] OR “hospices”[All Fields] OR “hospice”[All Fields] OR “hospice care”[MeSH Terms] OR (“hospice”[All Fields] AND “care”[All Fields]) OR “hospice care”[All Fields]) AND home[All Fields]) AND (“UK”[All Fields] OR “England “[All Fields] OR “Wales”[All Fields] OR “Scotland”[All Fields] OR “Northern Ireland”[All Fields]) AND (palliative[All Fields] OR “end of life”[All Fields])) AND (“2019/06/25”[PDAT] : “2020/06/25”[PDAT]).
Number of articles found: 278.
Search 9
Database searched: PubMed only.
Date searched: 25 June 2020.
(((((“palliative care” OR “hospice care” OR “end of life” OR terminal$)) AND (“rapid response” OR “crisis intervention” OR “hospice at home”)) AND “last 1 years”[PDat])) AND (UK OR England OR Wales OR Scotland OR “Northern Ireland”).
Number of articles found: 169.
Search 10
Database searched: Google Scholar.
Date searched: 25 June 2020.
“Hospice at home” in the last year.
Number of articles found: 11.
Results
Eleven of the articles in searches 8–10 were relevant. Two related to the OPEL study.
Appendix 2 Service use data manipulation
Allocation of Ambulatory and Home Care Record data to time periods
All AHCR data for which a patient’s DOD was known were used in the analysis of service use. Patients were in the study for variable numbers of days before they died. Time periods were defined for the purposes of analysis and comparison across models. For each patient, daily service usages were initially calculated within the following seven specified time periods (counting up all days from day of death = 0 going backwards, i.e. day 3 = third day before day of death): days 0–7, 8–14, 15–21, 22–28, 29–92 (1–3 months), 93–182 (3–6 months), ≥ 183 (> 6 months). However, time periods were subsequently amalgamated.
The periods covered by AHCRs did not perfectly coincide with the study time periods. The following rules were applied for allocating data to time periods.
For each patient’s first AHCR, collected at recruitment and intended to cover the previous 2 weeks, each recorded service use for the patient (number of visits, number of nights, number of telephone calls or number of caring hours per day) was divided by 14 and then assigned equally to the AHCR interview day and each of the 13 previous days, irrespective of whether or not the patient had been recruited to the study during the entirety of this period. If the first AHCR interview took place on a day following the death of the patient, each service use record was divided by 14 and assigned equally to the day of death and each of the 13 previous days, irrespective of whether or not the patient had been recruited to the study during the entirety of this period.
For each subsequent AHCR, each service use record was divided by the number of days since the previous AHCR had been administered and assigned equally to each day from the day after the previous AHCR to the current AHCR interview day. If an AHCR interview took place on a day following the death of the patient and the previous AHCR had taken place on a day prior to the patient’s death, each service use record was divided by the number of days from the day after the previous AHCR up to and including the day of death and assigned equally to each day in this time period.
Note that for all AHCRs, service use is deemed to have been recorded for the day of interview in addition to all relevant previous days, irrespective of the time at which the AHCR was performed (times ranged from 09.00 to 19.45). Thus, in subsequent summation calculations across specific time periods, ‘days 0–7’ refers to the day of patient death and the 7 previous days.
If AHCRs were discontinued prior to a patient’s death and no service use record was available for any day in one or more of the above time periods, all service use was recorded as missing for each day of the time period for this patient. If AHCR data were available for ≥ 1 days (but not all) in any of the above time periods, the daily service use was extrapolated across the whole time period.
When calculating the service use for any of the seven specified time periods above, any missing observations were estimated using the mean of non-missing values within the time period. If all observations were missing for any service use item, then the participant did not contribute to service use summary statistics for the relevant item, as usage was unknown.
Where service use was recorded for at least 1 day in a time period, the mean daily service use for the item was calculated within the time period.
Imputing of missing ‘double-hander’ visits
Attendance of two nurses/carers together was not consistently collected in all sites at the start of the study (November 2017), but was introduced in August 2018. The proportion of ‘double handers’ within each service model (for day and night visits) was calculated when available, and multiple imputation was used to estimate the number of ‘double handers’ when this was not recorded. It was assumed that no night sits were ‘double handers’.
Appendix 3 Unit costs used in the economic analysis
| Section/item in AHCR | Details (from Curtis and Burns 2019104) | Cost (£, 2019) |
|---|---|---|
| Inside the home | ||
| Nurse, HCA – district, community, other (NHS) | p. 117, section 10.1, band 6 for NHS nurses/HCAs and band 4 for hospice nurses/HCAs (on advice of research team). Cost per working hour – used for day, twilight (18.00–21.00) and night (20.00–06.00) visits. Assumed 30 minutes per visit, or actual time when specified. When time of day not specified, assumed day. Double-hander visits counted as two separate nurses. Night sits – assumed £15 per hour and 8 hours = £120, based on average of home care agency costs from the internet, or applied exact time when provided | Band 6: 46 per hour |
| Nurse, HCA – hospice | Band 4: 27 per hour | |
| GP, other doctor | p. 120, section 10.36. Surgery consultation for direct patient care, £39, was doubled because this is a home visit (£78 is equivalent to 30 minutes of General Medical Services activity) | 78 |
| Other health professional (includes physiotherapist, occupational therapist, speech therapist, dietitian, chiropodist, others) | p. 111, section 9, scientific and professional staff, band 6. Cost per working hour, used for day and night visits. Assumed 1 hour per visit | 45 |
| Social worker | p. 130, section 11.1, social worker (adult services), cost per hour. Assumed 1 hour per visit (also used for care agency manager) | 51 |
| Charity, voluntary sector visitors, includes chaplain | p. 136, section 11.7, support/outreach worker. Cost per hour used for day and night visits. Assumed 1 hour per visit | 24 |
| Visiting carer | p. 134, section 11.5, home care worker. Cost per hour, used for day and night visits. Used number of minutes pro rata when provided or assumed 1 hour per visit if length of visit not stated. Double-hander visits counted as two separate carers. Night sits – assumed £15 per hour and 8 hours = £120, based on average of home care agency costs from the internet, or applied exact time when provided | 29 |
| Outside the home | ||
| At GP practice | p. 120, section 10.36. Surgery consultation for direct patient care | 39 |
| Doctor/clinic at hospital, hospice | p. 82, section 7.1. NHS reference costs for hospital services. Weighted average of outpatient attendances | 135 |
| Hospital for test | ||
| Hospital, hospice for treatment | ||
| A&E visit | p. 82, section 7.1. NHS reference costs for hospital services (2017/18) | 135 |
| Use of ambulance | p. 82, section 7.1. NHS reference costs for hospital services. Weighted average of all ambulance attendances | 125 |
| Complementary therapist | pp. 119–22, scientific and professional staff, aromatherapy/massage. Band 6. Cost for 30-minute session | 28 |
| Other: hospice classes | Cost per class attendance (expert professional opinion) | 10 |
| Other: day care | p. 31, section 1.4, £60 per attendance, £13 per hour, £45 for 3.5-hour session | 60/13/45 |
| Other: allied health professionals (physiotherapists, dietitian, chiropodist, counselling, etc.) | p. 111, section 9, scientific and professional staff, band 6. £45 per hour. Assumed 30 minutes per consultation | 23 |
| Inpatient | ||
| Hospital | p. 82, section 7.1. NHS reference costs for hospital services. Non-elective average cost. Short stay (1 or 2 nights) £631; excess bed-days rate (2017/18) £337; long stay ≥ 3 nights £631 + £337 per night | 631 (+ 337) |
| Hospice | ||
| Care home | p. 28. Private-sector nursing home per day: £119; private-sector residential home per day: £99 | 119/99 |
| Telephone calls | ||
| Doctor | p. 123, section 10.5. Per call | 15 |
| Nurse/other | p. 123, section 10.5. Per call | 8 |
| Informal care | ||
| Main carer and other carers | p. 134, section 11.5. Home care worker. Hours per day providing personal care. Social service rate, face to face. Cost per working hour, used for day, twilight (18.00–21.00) and night (20.00–06.00) visits. Assumed 30 minutes per visit, or actual time when specified. Where time of day not specified, assumed day. Double-hander visits counted as two. Night sits – assumed £15 per hour and 8 hours = £120, based on average of home care agency costs from the internet, or applied exact time when provided | 29 per hour |
Appendix 4 Phase 3 report
Event attendance
| Participant group | Location (n) | Total (N) | |
|---|---|---|---|
| London | Leeds | ||
| Service provider (hospice) | 22 | 22 | 44 |
| Service provider (other) | 6 | 5 | 11 |
| Commissioner | 1 | 2 | 3 |
| Member of public | 17 | 5 | 22 |
| Other (e.g. researcher) | 3 | 5 | 8 |
FIGURE 17.
Proportional event attendance by location and participant group.
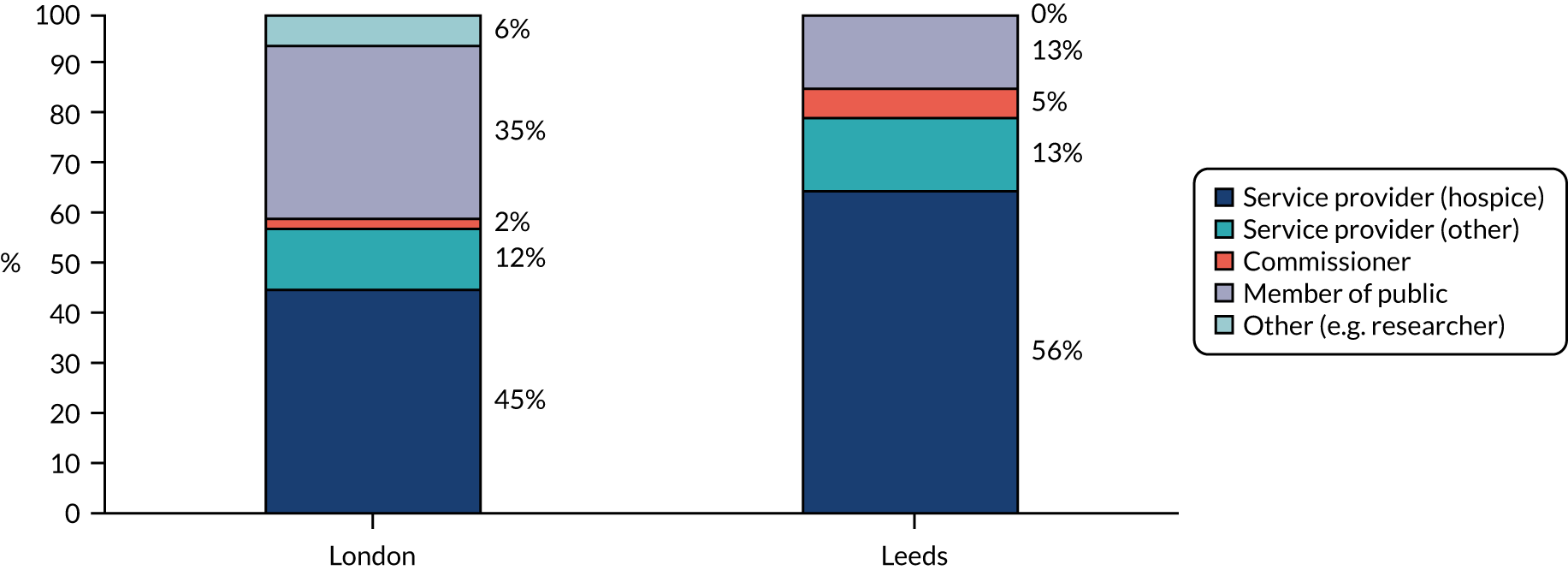
Sustainability workshop
Quantitative summary
| Location | Participant group (n) | Total (N) | ||||
|---|---|---|---|---|---|---|
| Service provider | Provider (non-HAH) | Commissioner | Member of the public | Undeclared | ||
| London | 17 | 1 | 1 | 8 | 3 | 30 |
| Leeds | 18 | 1 | 1 | 3 | 0 | 23 |
| Total | 35 | 2 | 2 | 11 | 3 | 53 |
-
Mechanism (M).01: proposing a business plan and ‘selling it’ to commissioners.
-
M.02: providers take the lead and provide services without a great deal of scrutiny, trust.
-
M.03: board of trustees or executive leader develop a reputation for excellence, meaning they are trusted to use funding well.
-
M.04: taking on a lead provider role and subcontracting with other providers in the area.
-
M.05: provider partnerships may enable small organisations to maintain their responsiveness and alacrity.
-
M.06: accepting a block contract from commissioners to enable predictability to the funding available.
-
M.07: securing NHS CHC funding to provide or part-fund services.
-
M.08: accept NHS funding that will support the HAH service and requires it to deliver other (‘non-palliative care’) roles, such as OOH catheter replacement, general rapid response.
-
M.09: accept funding for elements of service from personal health budgets.
-
M.10: develop a ‘profit-making’ element of the service that charges and subsidises other elements of service provision.
-
M.11: hospice charities may give the impression to the public that they are fully dependent on charitable funding (i.e. they do not overtly advertise their access to statutory funding), to make their fundraising activities more effective.
FIGURE 18.
Mechanism importance versus application for service providers only. M.01: one service provider said this was done at their HAH service, but they did not see it as important; M.02: one service provider said this was done at their HAH service, but they did not see it as important; M.03: one service provider said this was done at their HAH, but they did not see it as important; M.05: one service provider said this was done at their HAH, but they did not see it as important; M.08: one service provider said this was done at their HAH, but they did not see it as important.
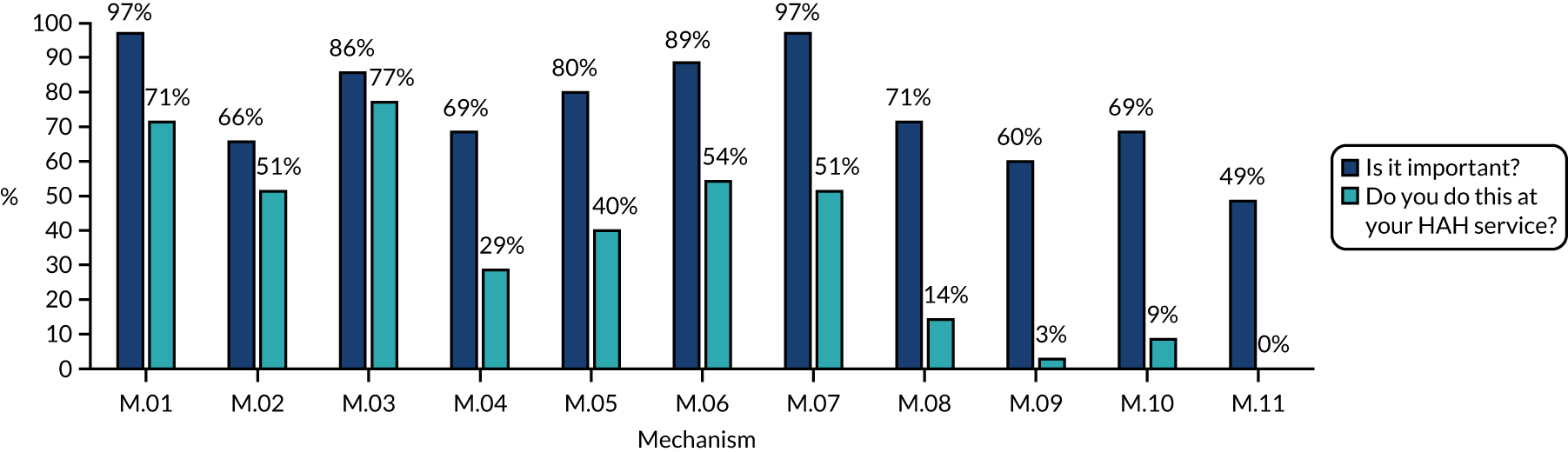
FIGURE 19.
Ranking of mechanism importance (Leeds only, sheet for professionals only). Response rates: M.01 – 95%; M.02 – 100%; M.03 – 100%; M.04 – 95%; M.05 – 95%; M.06 – 85%; M.07 – 90%; M.08 – 90%; M.09 – 95%; M.10 – 95%; M.11 – 80%.
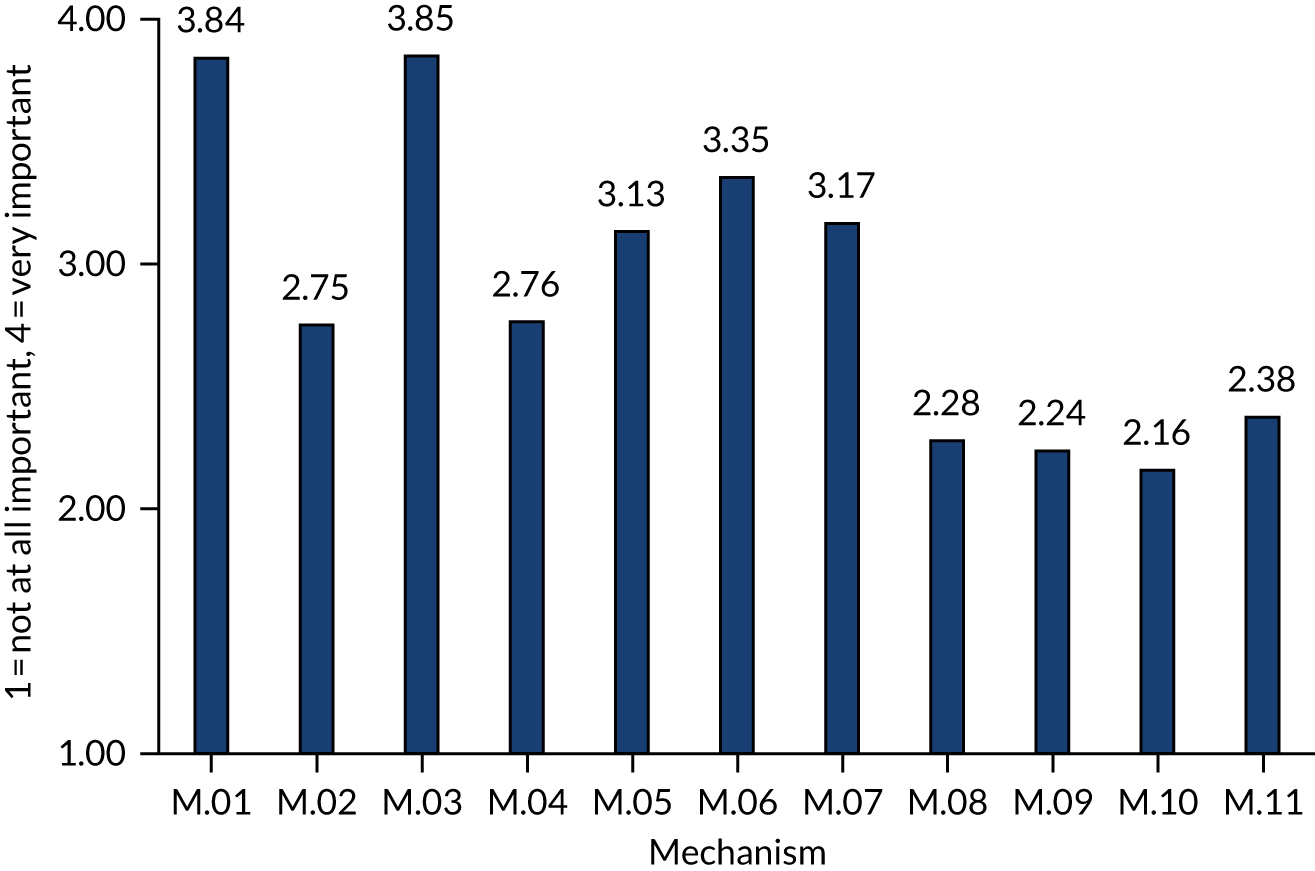
Member of the public responses
Mechanisms presented to members of the public
-
M.01: proposing a business plan and ‘selling it’ to commissioners.
-
M.02: board of trustees or executive leader develop a reputation for excellence, meaning they are trusted to use funding well, and provide services without a great deal of scrutiny.
-
M.03: taking on a lead provider role and subcontracting with other providers in the area.
-
M.04: provider partnerships may enable small organisations to maintain timely responsiveness.
-
M.05: accepting a block contract from commissioners to enable predictability to the funding available.
-
M.06: securing NHS CHC funding to provide or part-fund services.
-
M.07: accept NHS funding that will support the HAH service and requires it to deliver other (‘non-palliative care’) roles, such as OOH catheter replacement, general rapid response.
-
M.08: accept funding for elements of service from personal health budgets.
-
M.09: develop a ‘profit-making’ element of the service that charges and subsidises other elements of service provision.
-
M.10: hospice charities may give the impression to the public that they are fully dependent on charitable funding (i.e. they do not overtly advertise their access to statutory funding), to make their fundraising activities more effective.
FIGURE 20.
Member of public ratings of mechanism importance.
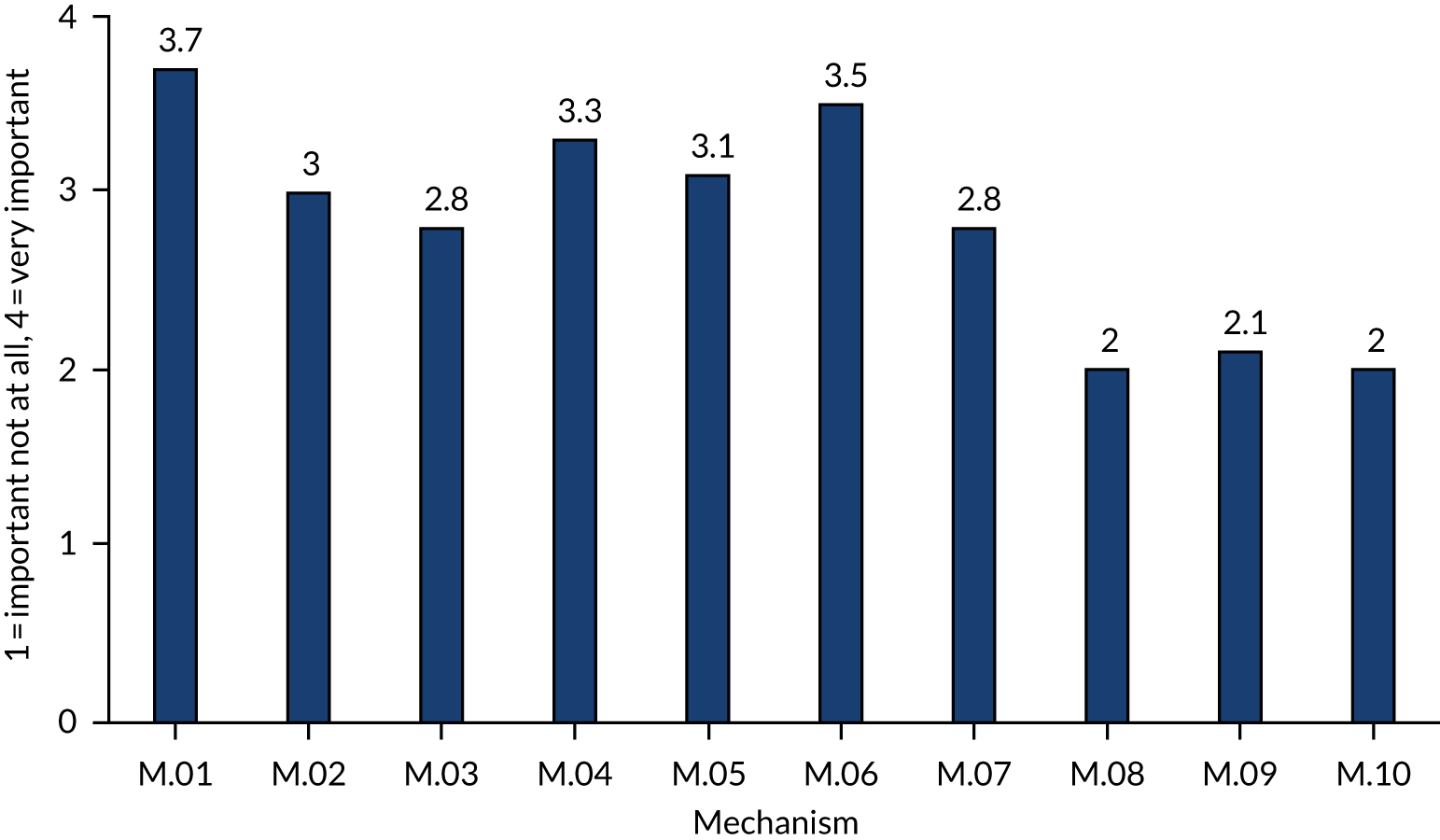
Integration and co-ordination workshop
Quantitative summary: integration mechanisms
| Location | Participant group (n) | Total (N) | ||||
|---|---|---|---|---|---|---|
| Service provider | Provider (non-HAH) | Commissioner | Member of the public | Undeclared | ||
| London | 15 | 4 | 2 | 15 | 1 | 37 |
| Leeds | 14 | 1 | 2 | 5 | 3 | 25 |
| Total | 29 | 5 | 4 | 20 | 4 | 62 |
-
M.01: a blended service is provided whereby different services can provide what is needed by the patient without hard boundaries around particular roles; honorary contracts with NHS may facilitate this.
-
M.02: budgets and workforce and organisational structures are managed in an integrated way across provider organisations.
-
M.03: a secondment into a different setting (e.g. a health-care worker into social care) may facilitate integration by the ‘learning of another language’.
-
M.04: other providers trust the HAH service to make assessments and will act on its recommendations.
-
M.05: an element of flexible workforce is employed (by the HAH service or others) or staff are flexibly deployed from other areas (e.g. inpatient unit).
-
M.06: clinical records are shared with other organisations.
-
M.07: DNs provide and administer all anticipatory medications (agreed division of labour).
-
M.08: advance plans are made and the need for medications and equipment are anticipated and provided on time.
-
M.09: the HAH service may have medical or non-medical prescribers available within its service.
-
M.10: the HAH service has direct access to shared equipment stores or has its own stores.
FIGURE 21.
Approaches used in the respondent’s local HAH service (represented by respondent’s professional group).
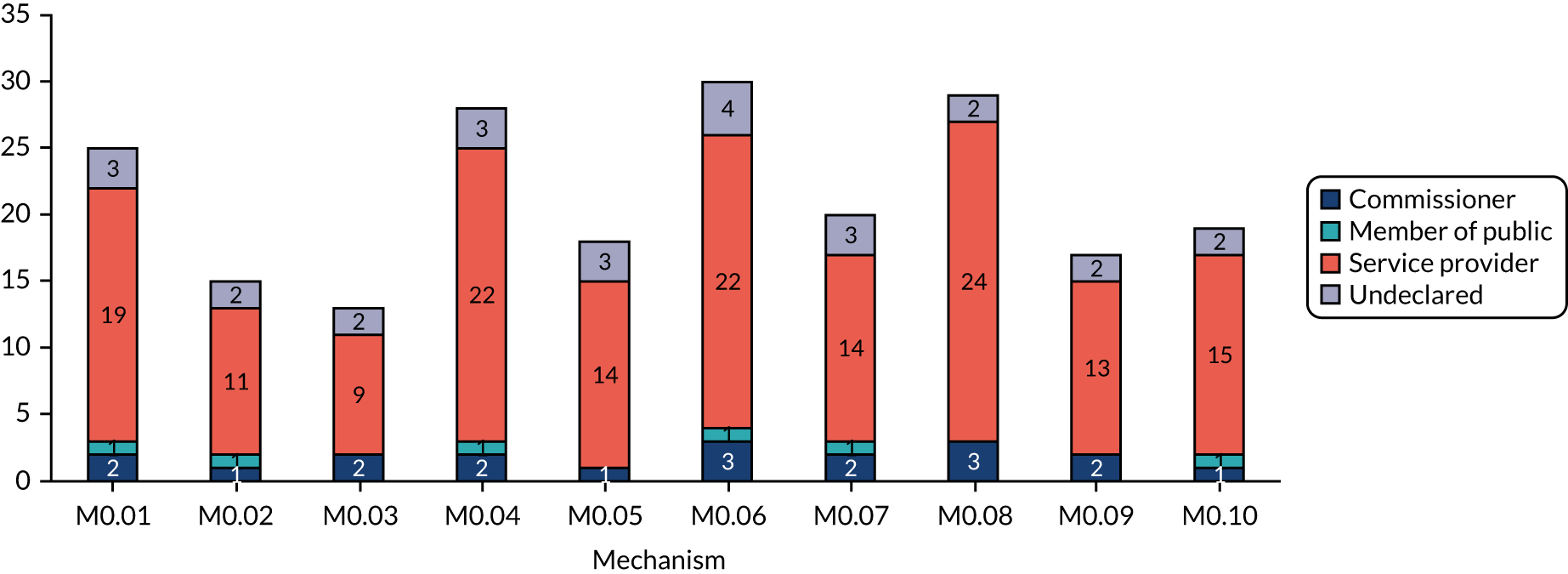
Quantitative summary: integration with hospice at home
FIGURE 22.
Number of respondents (out of 46) reporting integration between HAH service and these organisations in their area. IPU, inpatient unit; OT, occupational therapy; SPDN, specialist practitioner district nurse.
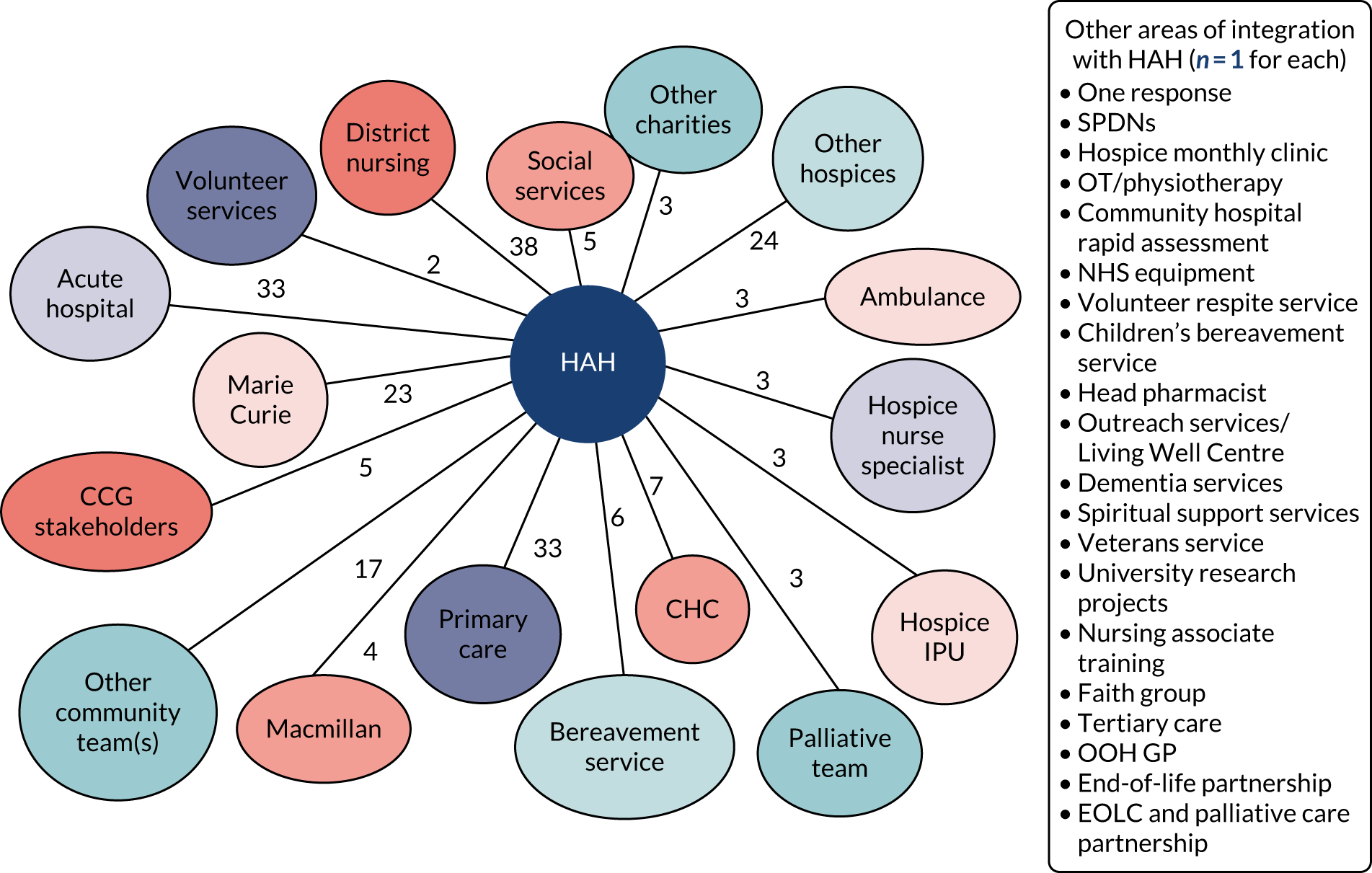
| Acute integrated with | Primary care integrated with | Other Community Teams integrated with | DNs integrated with | Marie Cure integrated with | Other Hospices integrated with | Other integrated services |
|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
Qualitative feedback summary: member of the public sheet
-
Single person to contact – who can help us or point us in the right direction.
-
All service providers talk to each other.
-
We receive the help we need when we need it.
-
Being kept informed of services available – because needs change.
-
Kept updated with any changes to services.
-
Being allowed to select the level of support needed – keeping it fluid.
-
One hub where one number and all services are connected.
-
Shared IT/record system.
-
Having flexibility to provide care.
-
Joined-up care and connection.
-
Co-ordination in timely manner.
-
Provided all contact details and information in patient house.
-
Everyone who walks through the door knows about the status of the patient and what care they have had.
-
Access to medical reviews to make alterations to med[ication]s, e.g. pain relief quickly. May have to wait a long time for the DN to arrive and there are not many.
-
Social care automatically arriving as per pre-agreed plan.
-
Many HAH team members used to be local community nurses so have good local connections and relationships.
-
Good evaluation from local stakeholders/partners.
-
HAH able to plug the gaps left by community nursing.
-
HAH hands over and gives good support to agency carers, when needed.
-
Marie Curie services TUPE’d to HAH team, which has led to a seamless service.
-
Seamless handover to next link in chain and ‘person in charge’, e.g. consultant – hospice who told GP what to do!
-
Integrated services – person in charge can access all sectors, e.g. tell DNs to visit.
-
Integrated information folder of notes and information for all parties to update on kitchen table.
-
Carer/patient input to decisions, e.g. I arranged to call DNs as req[uired], not the set 3 or 4 times per day.
-
Professionals’ knowledge of different services available.
-
Local authority to provide integrated blue badge, carer support, local parking permit for carers.
-
Listen to carers/patients – improved services.
-
Access to services when needed and a response.
-
Joint MDT/referrals meeting.
-
Eye test and dental test organisation.
-
Now able to see DN and hospital record with updated IT system.
-
HAH offering support to DNs as required. Happy to let DNs run with patient if they wish to.
-
Support to care homes and nursing homes with little palliative care/end-of-life knowledge.
-
Shared electronic recorder view only of systems.
-
Referrals direct from community teams by telephone.
-
I am currently being treated for a low immunity after chemotherapy! Have found that this team explained the reasons why therapy and tests were essential. Very supportive group – communicative consultant, e.g. when GP would or could not do the requested blood test, they solved the issue!
-
Linked CNS in hospitals and teams, communication between hospice and hospital. Frimley [Park] Hospital have pall[iative] CNS in A&E and this has significant impact on admissions and length of stay.
-
Echo (end of life care) hub in Coastal West Sussex with hospice, hospital, ambulance, OOH GPs, shared records.
-
Well-joined-up nurses and doctors.
-
Able to administer analgesics if already available.
-
Early MDT meeting and care planning very helpful.
-
Anyone who visits can access records and knows who else has been and what they did.
-
Care is spaced out across the day and week according to my preferences.
-
HAH staff have access to advice and support if they need it.
-
HAH can get medication when I need it and administer it.
-
There is a plan for my care and emergency services can see it.
-
Handover from HAH practical care team to agency carers support with joint shadow visit/handover.
-
Regular HAH attendance at hospital MDT palliative care meeting and similar multi-agency meetings.
-
FP10s (prescription forms) allowing prescribing in community, GP records informed/updated.
-
Interoperable electronic records; access for health care providing including OOHs.
-
We have a partnership agreement with the DN team so that we can use their notes to provide seamless care to patients.
-
We can highlight needs to DN teams who will arrange equipment/medication.
-
Support and advice from the ONS team of local hospice.
-
Gold-standards meetings.
-
ILT meetings.
-
SS and CCG funding would be able to help make end of life a better service if money was pooled and shared with HAH.
-
Palliative nurses could be more proactive in linking with HAH and medical teams including with GP, CCG and DN.
-
Service users and carers could be trained about how things should work with the help of volunteers.
-
Care providers could remain with service users regardless of funding stream.
-
Hospice providers should be invited to attend team meetings to train staff in SS and CCG.
-
Marketing and education could link to raise the profile of HAH – a list of top 10 tips to be accessible to ALL.
-
Good communication between hospital discharge team and rapid-response team at HAH.
-
Small team of community nurses and carers so feels more friendly and personal.
-
Good working with OOH hospice.
-
Good working with GP for patient visits and prescriptions.
ILT, integrated locality team; MDT, multidisciplinary team; TUPE, Transfer of Undertakings (Protection of Employment) Regulations 2006.
-
Not knowing who to contact.
-
Having to keep repeating the story.
-
No communication between service providers.
-
Being kept waiting too long for help.
-
Not knowing what help is available.
-
Different stream of funding.
-
Different roles from one patient.
-
Fragmented care.
-
Carers’ needs not met.
-
Being asked the same questions every time meet someone new.
-
Slow response time on receiving needed equipment.
-
Social care seeming distant – lack of empathy. Having to chase up care provision that has not arrived.
-
No urgency.
-
Multiple agencies all doing their own assessments.
-
Multiple sets of independent records.
-
Unable to contact other teams – community nurses not answering phones.
-
Community nurses only doing ‘tasks’ – not holistic care.
-
Neighbouring hospices not respecting boundaries and trying to ‘invade’ your patch.
-
Carer contacting each sector for their input.
-
Separate carer/provider contact for each service needed.
-
No one knows what anyone else is doing.
-
None. Miserable, waste of time, energy and resources.
-
No access to services that are needed.
-
Nil offered. Requests non-actioned – carer left ‘banging head against wall’.
-
Carer/patient needs not met and both suffer as a result.
-
NB LA provided 0.
-
Some carers work during office hours.
-
Conflicting information from different organisations.
-
Each organisation wishing to undertake their own assessment – no ‘trust’ when professionals to accept what is required.
-
At times there is now less communication between DN teams and HAH due to constant change within/across teams.
-
Too many individuals; who do I ask.
-
Would have appreciated a single person to oversee all our needs or for us to contact for any query.
-
[NHS] CHC funding assessed by strangers rather than palliative nurse and GP – waste of resources using different people who do not know patient.
-
Having to explain to an admin[istrative] person at single point of contact what the issue is rather than someone clinically trained.
-
Being told you need rapid-response team to come out to you. Then having to wait 11 hrs for them to turn up.
-
Coming empty handed because they cannot access dressings, etc. because colleagues gone home with key!
-
Rapid-response team saying they will not come out because it’s during DNs working hours.
-
Even more DNs very busy so help delayed.
-
GPs not issuing administrative paperwork in line with end-of-life drugs prescribed by GP.
-
Rang GP to help with pain relief – told to ring for ambulance. Going through two layers of questions before ambulance dispatches (taking a total of 5 hrs!). To A&E. Admitted to hospital palliative care department. Consultant telling us off for coming into hospital. Explained current pain relief not sufficient, we have mothing else to administer and GP won’t help and suggest ringing 999. Consultant took 9 days to sort out correct pain relief.
-
No visibility to OOH doctor, GP, ambulance service.
-
Updating GP on medication changes, deterioration, syringe drives, etc.
-
Appear to be minimal links within social care. This may mean care does not follow or flex with the patient needs.
-
Variable systems across CCGs can lead to confusion of who does what in each area.
-
Variable services across the CCGs – i.e. HF nurses in one area but not another.
-
Poor communication between carers or hospice and hospital for specific tests or treatment.
-
Unresponsive hospital transport requested for specific tests of medication.
-
Indifferent communication between hospital trusts causes poor care.
-
Local authority involved for assessment but not communicated with accurately with the hospice.
-
Why are ‘hospices’ being closed down.
-
Lack of information-sharing. Fear of information governance law. Poor communication.
-
Lack of commissioning/funding leads to a closure of hospice beds/IPU.
-
Where hospices will accept referrals from, some only from GPs.
-
Availability of 24-hr HAH services or for telephone advice. Leads to admissions.
-
Lack of advance care planning.
-
Prescription medication not available OOH.
-
I am responsible for telling professionals who else is involved when they visit and what they do.
-
No one visits or too many people turn up on one day.
-
I have to call the GP or tell staff what needs to be done.
-
I have to wait for a doctor to receive pain relief.
-
I have to explain my preferences every time or my carer has to guess.
-
Poor communications re patient needs – not updating timely.
-
Fail to act on information give re patient’s medication needs.
-
Not visit in a timely manner when requested.
-
Poor communication between health and social care.
HF, heart failure; IPU, inpatient unit; LA, local authority.
Context–mechanism–outcome configuration speed-dating session
-
Trust between HAH providers and commissioners is key to sustainable funding. Both sides need to be as open and honest as possible about what is and isn’t possible.
-
Funding at every level is needed to ensure services in place meet the needs of the local population, it should come from one big pot and not little amounts as this does not allow for robust planning. Health and social care need to join their budgets and see EoL as a priority as this will provide the support to patient/family and community.
-
Communication between all services and service users so everyone is aware of what is expected and by whom. Working together to provide best care.
-
Recognise standard pay scales.
-
Community stakeholders – who will this benefit? Asking them to speak up.
-
Agreed standards and KPIs.
-
Competency-based training passport.
-
Attracting staff: working conditions offered need to be attractive to NHS/other staff.
-
Higher wages or low-cost housing for local health and social care providers are needed in areas where cost of housing is too great to attract staff.
-
Staff shortages and lack of inpatient hospice beds will both lead to reduced patient choice in the future.
-
Looking at jointly commissioned service, e.g. specialist rotational paramedics between hospice, GP, ambulance.
-
Hospices and organisations using data more effectively to support the approach for increased statutory funding.
-
Recruit young volunteers with a view to have ‘work experience’ in a care setting – may encourage future career choice.
-
Uncertainty of ongoing NHS funding – on fixed-term contract – difficulties of recruiting staff on fixed-term contract.
-
Consider voluntary charging for hospice services – Cruse [Bereavement Care] accept donations in exchange for service.
-
Funding limits HAH. Data on hospital avoidance would help prove our worth.
-
If service is commissioned to respond to meeting patient choice, then the methods of evaluating success must reflect this.
-
Too much focus on ACP versus evolving picture – wishes and needs change.
Inpatient beds are still required – there are too few in my area.
Comments from researchers-
Worse for some hospices who don’t pay NHS salary scales.
-
HAH is working in integrated way with services like GPs, MDTs [multidisciplinary teams].
-
Patient then carer is at the centre of all thinking/planning provision, otherwise it fails.
-
Funding is key to help all but to reason why seems long and drawn out so many lose out so maybe a better process needed.
-
What will happen if it becomes apparent that dying at home so not the dominant preferred choice and choice is limited by the reduction/absence of hospice beds based on a false premise.
-
Collect data from carer and/or patient their view of success/failure may be radically different to [that of] providers and commissioners.
-
Carers (paid) are often perceived as the lowest common denominator, which affects skills and service! How do you ensure they are skilled and appreciated?
-
Funds are not effectively used and quality of care is compromised so long as private entities (e.g. care agencies) are involved.
ACP, advanced care planning; EoL, end of life; KPI, key performance indicator; MDT, multidisciplinary team.
Lots of commissioning focus at the moment on population health management. Volunteers and volunteering have a role in this, e.g. social prescribing recommends volunteers.
Comments from service providers-
Safeguarding volunteers, giving/allowing access to services, which paid staff have access to, e.g. reflective sessions after deaths with patients they have been involved with. Look after each other!
-
GDPR [General Data Protection Regulation] re patients’ information – volunteers have access to patients’ information. Do patients want volunteers providing care for them?
-
Hospices could produce bespoke training packages for volunteers who wish to work in the community – specific needs of service.
-
Trust the skills of the carer.
-
Think about using a different term to volunteer – it can carry wrong impression, i.e. do-gooder. Think about ‘champion’ ‘mentor’ etc.
-
Volunteers could provide a lot of practical and carer support. Investment in training and support needed to keep them and work well.
-
Hospices role in compassionate communities – signposting? Linking?
-
Need to understand what is preventing volunteers from delivering personal care and overcome it? Start with joint visits with HCAs?
-
Clear boundaries – link to integration across services, not just HAH.
-
Provide post-bereavement groups with trained volunteers that are accessible to carers of people who didn’t have access to HAH/hospice, i.e. outreach work.
-
Clear boundaries and regular meetings.
-
Explore what volunteers expect from the role.
-
Support, debriefing, closure, satisfaction for volunteers if involved in EoL.
-
I’m taking this back to my hospice and respectfully challenge the HAH team as to why they don’t use volunteers!
-
Provide volunteer supervision.
-
The time it takes to recruit and (effectively) train volunteers and then provide ongoing support is very time-consuming if done well.
-
Bring Compassionate Communities to the heart of all we do – less paternalistic, more empowering.
-
Volunteers need training e.g. confidentiality.
-
I volunteer at a football club, I have had training to do this role. So makes sense if someone has a role then they get the right training.
-
Volunteers help promote feeling of well-being within wider community, which supports people to be cared for and die at home.
-
Clear boundaries, active supervision structure (not just peer), well-being checking, emotional safety maintained.
-
HR [human resources] and legal perspective of volunteerism.
-
Be less risk averse to use of properly trained volunteers.
-
Volunteers can make more contribution if their ‘needs’ are recognised?
-
Possible for selected volunteers (by self and co-ordinator) to have a powerful role in the last weeks (days) of patient’s life – both carer and patient support.
-
Consistency and familiarity in volunteering to providing care for dementia patients is a must.
EoL, end of life.
-
Need to increase uptake and access for non-cancer patients.
-
If patient/family can self-refer how do we ensure equitable access? e.g. those in deprived areas.
-
Different criteria for services provided by one hospice can be confusing. Fundamental decision about whether HAH is for all or is a specialist palliative care service.
-
Information to social care providers or other voluntary agencies for homeless/traveller community.
-
Earlier referral to improve outcomes.
-
HAH team visited local DNs – outreach – implications is increased referrals and two-way working.
-
Much greater understanding of all hospice services, not just HAH, to public, a wider service.
-
Time to spend with other professionals to improve their understanding of what HAH does.
-
If HAH is marketed to public, they should be able to self-refer and personalise the service they receive.
-
Public engagement projects and increase awareness, e.g. Dying Matters and similar initiatives.
-
GP education is key to establishing appropriate referrals but also management in primary care.
-
The HAH and inpatient unit have identical criteria to minimise confusion. Likewise the referral process.
-
Clear guidelines and indicators essential to ensure equity of care for all.
-
One contact number or front door to palliative advice and support.
-
How can HAH integrate with ambulance service to empower, educate, support ambulance staff to identify appropriate referrals? Biannual training?
-
Culture of hospice can sometimes mean hospice staff cannot/do not say ‘no’ or discharge. This can be a challenge re referrals and discharges sometimes.
-
Can HAH open referrals to differing professionals (e.g. paramedic) to allow open access to services.
-
Manage expectations of service users.
-
Patient/family expectations are very different and variable, which can’t always be sustained.
-
‘Essential’ where does this fit in with NHS responsibilities duty of care?
-
Educating public – open days so public can see and be informed what HAH are about. School projects.
-
How can local public access HAH as fast-track funding needs the paperwork?
-
Ensure HAH services are seen as generalist with access to specialist knowledge:
-
use of websites/IT
-
primary care networks
-
palliative care register MDT meetings
-
clear referral criteria – feedback/involvement of referrers
-
know your stakeholders
-
patient information literature
-
publicise/share feedback on the service
-
local media, radio.
-
-
Joined up IT/patient records will make referrals easier.
-
Need ability to step down from care if patient stabilises.
-
Lack of understanding by general public of services provided by charities.
-
Funding equity required.
-
Self-referral to be encouraged.
-
Clear explanation of what’s excluded from the service and why and signposting to who can help.
-
A clear feedback loop form HAH back to referrers on outcomes experienced by patient/carer – help make it not one-way and demonstrate impact.
-
Has the HAH service got capacity to look after all patients requiring this ‘specialist care’?
-
How are all patients, especially hard to reach, going to be informed about the service?
-
Actively promote ACP [advance care planning] much earlier e.g. 50+.
-
Volunteers also provide ‘honest’ views on marketing, to family, friends and neighbours.
-
Link with other charities, e.g. Healthwatch.
-
Should HAH have a main base – say in a hospice? How are potential patients’ families informed?
-
Since NHS funds 20% of HAH, I would recommend the information provided today be available to NHS staff and updated annually.
-
Equity of access to specialist hospices versus generalist services.
-
Are hospices willing to lose their status as specialists in return for increased reach and integration?
MDT, multidisciplinary team.
-
A top 10 tips of the benefits would give reassurance and clarity to those needing services and carers.
-
A seamless service will go a long way to help those in need to not have to deal with the bureaucracy and hoop-jumping they have to do at the moment.
-
Brand and fundraising can be carriers to deeper integration for charities.
-
Palliative care experts need to be involved in training for other services and building on what we have rather than adding new stand-alone services.
-
Giving the patient choice. Allowing them to have some control over a situation they feel powerless in. EoL is situation you can’t control.
-
Person-centred care.
-
Improving information-sharing and removing boundaries of CCG/STPs to allow information-sharing across wider areas, e.g. hospital, ambulance service.
-
HAH to support national ambulance services to co-design ease of referral pathways and escalation strategies.
-
Openness and collaborative working, care packages would go some way in preventing declining care packages when no availability. We can’t be precious about who we accept.
-
Lead provider model – overview so can subcontract to right service with right skills for whatever aspect of palliative care. Lead to:
-
good co-ordination and use of skills
-
not taking work away from local providers
-
gets round tribalism.
-
-
I appreciate that some organisations are stand alone, some part of a hospice; more working together with those independent ones needs to happen.
-
Care should follow the patient regardless of funding stream and be flexible according to need.
-
IT services are different and not visible to other services.
-
Difficulties in ‘claiming’ ownership.
-
Redefinition of hospice care in line with modern health services.
-
EoL care co-ordination centres.
-
With different organisations – issues such as sharing information.
-
Need to consider legal aspects when referring for medications and equipment provision; all services bidding for the same funding and in competition.
-
Consider approaching retired HCPs – see if they want to continue profession on voluntary basis.
-
Time is like gold dust so this seems so important to get the small things right then the bigger stuff becomes so easy.
-
Better integration and co-ordination between social care – paid into by patient and seamless transfer and a joint approach regarding planning – person centred, e.g. applying for CHC funding.
-
Communication and listening.
-
Leadership – a group of partners who have a shared agenda and willing to engage in partnership without fear of losing their own funding.
-
Integration is a constant struggle – other services have a tendency to discharge patients once palliative care services involved.
-
Contracting supports integration – use multiple providers and one commissioner.
-
Shared records – co-ordination of care.
-
How much should HAH integrate with other services that provide EoL care?
-
Positive: more equity, better care for those who don’t access HAH, e.g. elderly/LTCs.
-
Neg[ative]: dilute our focus, territorial.
-
-
HAH need to integrate with all services including voluntary and frailty-based services.
-
Use professionals more flexibly at local level, be less risk averse. Buurtzorg model?
-
Devolve resources to local MDTs [multidisciplinary teams] based around primary care networks.
-
The multiplicity of organisations causes confusion and wasted resources. E.g. why is CHC assessment carried out by a strange[r]? GP and palliative nurses best placed for assessment.
EoL, end of life; LTC, long-term condition; MDT, multidisciplinary team.
-
Could education and training be co-ordinated and delivered at a wider level.
-
In social care there is a lack of creativity and services are regimented. This needs to change to be more responsive to EoL.
-
Commissioners want to make care more equal, not put more services in place for the minority who already access high-quality hospice/specialist palliative care.
-
HAH services providing CHC etc. statutory-funded packages of care increases the risk of a two-tier system unless a mechanism is found for them to see more non-cancer patient etc. equity of access is key.
-
Danger if specialist providers take generalist roles others are deskilled – less available care (??).
-
More funding for training should be available.
-
Make care more patient centred. Encourage independence where possible, respecting dignity and wishes at all times.
-
Accredited training that is transferable across providers. Competency based.
-
Public still under misconception that we only provide care for cancer patients.
-
Lots of misunderstanding among HCPs about the role of hospices.
-
If the HAH team can support and influence other agencies involved in EoL to ensure consistency and adequate care delivery.
-
How do we measure effectiveness?
-
More joint working across health and social care – allowing hospice ‘specialists’ to teach domiciliary care agency.
-
Overlap in role of staff – need to agree and acknowledge each other’s roles and skills.
-
Not only more teaching but also in the variety of ways teaching takes place – situated learning.
-
Some GPs disengage at EoL and refer to palliative care if they feel lack of knowledge.
-
Ongoing training and development of all staff for generalist EoL care.
-
Integration of NHS education, university education and hospice education.
-
Time is a resource that is not valued by commissioners/budgets.
-
Skills escalator – expectation for training defined at each level – generalists and specialists delivered by specialist palliative care team.
-
HAH in-reach into hospitals, nursing homes etc. in order to share models of care.
-
Palliative care needs to be on the pre- and post- registration skills/education frameworks. Including all professionals e.g. paramedics who currently have minimal learning on the topic.
-
Identifying how HAH can monitor and support these patients in their environment e.g. care/nursing homes, GP, specialist CNS services, ambulances.
-
Local projects between specialist palliative care and heart/renal/respiratory teams incorporating shared learning as project outcomes have worked to varying degrees for our service.
-
Extending role of HCA.
-
High turnover of untrained staff makes training a challenge; conversely good training retains staff.
-
As HAH work a lot with other specialties joint education sessions, steering groups.
-
Importance of remembering the roles and values of social workers having knowledge to engage in early conversations.
-
Encouraging organisations to promote principles of palliative care in policy.
-
Communication skills underpin all.
-
Prospects available; multi-agency training; competency framework.
-
More training and education required as increasing numbers of non-malignant patients requiring EoL care.
-
Improving training for non-hospice professionals in recognising last year of life and services to refer to.
-
Allowing non-hospice care providers and professionals to come on observation shifts at the hospice would improve knowledge but also cross-disciplinary understanding and networking.
-
Is it our responsibility to upskill workforce – I’d say yes it is. Just because it is should be that HCPs have knowledge, doesn’t mean that’s the case.
-
End of life is for all.
-
Preference of place to die is dependent on that being available, not always related to skills and knowledge but money and will to provide.
-
Skilled carers need to be recognised – with such low pay, what’s the encouragement?
-
Generalist not specialist – not complex elitist; HAH care is not specialist/complex – they specialise in EoL care. Don’t assume that the ethos of non-specialist services is ‘lesser’.
-
Focus on frailty and LTCs [long-term conditions].
-
Define specialist and complex.
-
Increase in teaching/sharing knowledge with other health professionals.
-
Increase in specialist palliative care in community is leading to deskilling and reduced confidence for DNs.
EoL, end of life; LTC, long-term condition.
-
After death – are there alternative bereavement services available? Are there enough resources for a specific HAH service?
-
Local authorities would benefit from inviting HAH to team meetings to tell their staff what they do and how they do it and we can work collaboratively to support carers.
-
There is a real need to find a way to evidence outcomes for carers and bereaved people otherwise this will be ignored when making commissioning decisions.
-
Exploring basics of EoL care for carers – training.
-
Not all carers have the same level of basic understanding of services.
-
24-hour cover often not available. Increased anxiety for carers feeling unsupported overnight.
-
Is bereavement support appropriate for HAH?
-
What do the carer and patient need to make the situation a little better/easier to manage or cope with?
-
Easier to offer an inpatient bed in a crisis – needs more network locally to give alternatives.
-
Assuming carers can manage EoL care at home is dangerous.
-
Consider that carer may be new to caring and from diagnosis to death maybe a few weeks.
-
Carers need a single point of access.
-
Automatic assessment of carers’ need[s] as standard.
-
Grief may hit hardest some time on. Having support/information available when this happens.
-
It is always a struggle to balance carer/patient needs. Part of role of palliative care specialists to assist with this.
-
If the HAH staff and carer have the opportunity to ‘debrief’ post bereavement and offer services that can support in bereavement.
-
Awareness of anticipatory grief/early intervention.
-
Access to chaplaincy, psychology and counselling – different level of intervention as appropriate.
-
HAH involvement means families/carers have full access to bereavement follow-up after – 1 : 1, group sessions, social sessions, drop-in facilities of the hospice.
-
Big need for signposting and co-ordination of services – too much for many carers to take in – creates extra stress.
-
Proactive planning rather than reactive – what skills will the carer need? Are they well enough themselves?
-
Anticipation of the care needs and role of the carer in order to have meaningful/realistic planning.
-
Recognising those families who want to be part of care rather than those who feel obliged to care. Need to support both in their decision-making.
-
Upskilling carers to administer subcutaneous medication etc. in order to be sustainable at home.
-
Ensuring national ambulance services know that they can refer patients/next of kin etc. for bereavement support or services. (Paramedics are used to referral pathways.)
-
Out of hours support – lots of overlap between services in the working week and minimal out-of-hours support available.
-
Having access 24/7 is usually unavailable?? – Mechanisms – outcomes difficult to achieve.
-
I’m not sure where children fit in with this flow chart.
-
How do you manage people from minority groups and issues with language and faith?
EoL, end of life.
-
Happy, caring, competent, knowledgeable staff.
-
Being honest, if you don’t know the answers tell the patient and carer but help them find out what they need to know.
-
Being human.
(CMO 5, knowledge and skills.)
Comments from service providers-
Retail shops provide community presence and connection.
(CMO 1, marketing.)
Appendix 5 Hypotheses for quantitative analysis generated from qualitative data
| CMO | Context | Mechanism | Outcome | Research question for quantitative analysis |
|---|---|---|---|---|
| Sustainability |
|
|
|
|
| Volunteers |
|
|
|
Does having visits from volunteers (recorded on AHCRs) relate to better patient and carer outcomes? |
| Raising awareness, service profile, criteria and referral |
|
|
|
|
|
|
More patients with suitable needs receive timely HAH care, including non-cancer patients (e.g. those with dementia, frailty) |
|
|
| A number of patient groups are poorly represented in hospice services in general, that is do not receive an equitable share of available services [e.g. older age (> 85 years), non-cancer diagnosis, deprivation] |
|
Caseload reflects suitable diagnostic, demographic, cultural and socioeconomic diversity of the area served and services are provided equitably |
|
|
| Integration and co-ordination | Service perspective
|
|
|
|
|
This specific example may result in unnecessary duplication when a qualified member of staff who is in the home cannot perform a task because it has been allocated to another service and requires a separate visit |
|
||
Patient and family, needs ‘at the front door’
|
|
|
|
|
In-hours vs. OOH services
|
Anticipatory care and information become yet more critical, and, in particular, if night-time cover is not provided by the HAH service, a well-advertised 24-hour contact number is crucial | Needs are anticipated as far as possible and patients experience continuity of care when providers change |
|
|
| Knowledge, skills and ethos of care providers |
|
HAH services provide expert knowledge and skills in palliative care and EOLC and have a suitable ethos to support this care through:
|
|
|
| Most of the expertise in palliative care and EOLC still resides in cancer care; patients with other illnesses (e.g. dementia) may present particular challenges to staff and organisations | Accessing other elements of hospice services because prognosis is longer than HAH can provide for may support some of these patients | Inequity and mismatch in care provided, patient/carer feel patronised and not understood |
|
|
| Support directed at the carer or patient–carer dyad |
|
|
|
|
Appendix 6 Lay guide to realist evaluation
Optimum hospice at home services for end-of-life care
Background
Offering people a choice about where they receive their care at the end of life is central to UK policy, and the number of people wishing to die at home is increasing. We know from work undertaken with the general public that care at home is an important concern for many people. Much effort has been invested in health services to support care at home, including services called HAH that aim to offer hospice care in an individual’s home. The aim of hospice care is to improve the quality of life of people who have an incurable illness up to the point of death. This includes medical, emotional, social, practical, psychological and spiritual care, and, in addition, addressing the needs of the person’s family and carers. Currently a range of different HAH services exist across England and it is unclear which features of these services enable better care and outcomes at the end of life for patients and families.
Research question
The research question we asked was ‘What are the features of HAH services that work, for whom and under what circumstances?’.
Study design
The study started with a national telephone survey of all HAH services to find out about the services they provide. We sent surveys to all HAH services recorded on the NAHH and the Hospice UK directories; a total of 132 were listed. We collected information on how these services are funded, which HCPs work for them and what kind of roles they have, and whether or not they provide care overnight and at weekends.
Using this survey data, we categorised the HAH services into different ‘model’ types, called a typology. From this typology, we selected four to six case study sites (one or two case studies per model) for in-depth investigation. To do this, we used a method called ‘realist evaluation’. This method allowed us to gain an understanding of how the services were delivered within the different models, the impact on patients and carers, and whether or not patients and carers are supported and cared for as well as possible. We also compared the costs of delivering services in the different models, and talked to providers of services about local issues that help or hinder the delivery of a good service.
How did we make sure the research was on the right track for patients and families?
We were aware that this needed to be done sensitively, and we are experienced in undertaking research with bereaved people. The team included two lay co-applicants who had experienced bereavement as carers; they had a key role in the team to ensure a thoughtful and ethically sound approach. In addition, we worked closely with members of the Project Oversight Group, which advised us on the most sensitive approaches.
How did we make the research findings available?
The findings were presented at two national workshops. At these workshops, we sought feedback from the audiences on the application and implications of the findings. The audience included HAH providers, carers, members of the public, local health service planners and service user representatives. By combining all this information, we assessed which models are likely to lead to the best outcomes and represent the best value for money.
A project report and summaries for lay audiences will be produced. Guidelines will be developed and made freely available for use in planning HAH services in the future. We will reach professional audiences through articles in peer-reviewed journals and through presentations. The people who will benefit will be NHS patients at the end of life and their families and carers.
Introduction to realist evaluation as a research method
What is realist evaluation?
Realist evaluation is a form of theory-driven evaluation. Pawson and Tilley170 developed the first realist evaluation approach, although other interpretations have been developed since. Pawson and Tilley argued that, to be useful for decision-makers, evaluations need to identify ‘what works in which circumstances and for whom?’, rather than merely ‘does it work?’.
To answer that question, realist evaluators aim to identify the underlying mechanisms that explain ‘how’ the outcomes were caused and the influence of context.
Why have we chosen this approach?
A realist evaluation design is well suited to assess how interventions in complex situations work because it allows the evaluator to deconstruct the causal web of conditions underlying such interventions and the resulting outcomes. A realist evaluation yields information that indicates how the intervention works (the mechanism) and the conditions that are needed for a particular mechanism to work (context); thus, it is likely to be more useful to policy-makers than other types of evaluation.
How does a realist evaluation work?
Realist evaluation considers that an intervention works (or not) because actors make particular decisions in response to the intervention (or not). The ‘reasoning’ of the actors in response to the resources or opportunities provided is what causes the outcomes.
Realist evaluation starts with a programme theory. The programme theory describes how the intervention is expected to lead to its effects and in which conditions it should do so. The initial theory may be based on previous research, knowledge, experience and the assumptions of the intervention designers about how the intervention will work.
This programme theory is laid out at the study design stage as CMO configurations. What mechanisms will generate the outcomes and what context will affect whether or not those mechanisms operate.
-
Context: the conditions or circumstances in which the service is operated that affect how it works.
-
Mechanism: the particular drivers that ‘cause’ the delivery of the intervention.
-
Outcome: the desired or undesired outcome.
A realist evaluation design does not need to construct comparison groups. We are using the case study design, whereby data will be collected from HAH services to enable ‘testing’ of the initial theory (or CMO configurations) in all its dimensions. Data collected in the case studies will then determine which CMO configuration(s) offer the most robust and plausible explanation of the observed successful or unsuccessful service outcomes. The data analysis will produce a final set of CMO statements. CMO statements explain how contexts and mechanisms lead to outcomes (i.e. ‘In this context, that particular mechanism fired for these actors, generating those outcomes; in that context, this other mechanism fired, generating these different outcomes’).
| Context | Mechanisms | Outcomes |
|---|---|---|
| For example, ‘if’ the service has this . . . | For example, ‘then’ the service will . . . |
|
| Because patients could deteriorate at any time in the last hours/days/weeks of life, service needs fluctuate significantly. If the HAH service has a mix of permanent and flexi staff (zero hours) . . . | Then the service is able to respond rapidly to unpredictable and heavily fluctuating workloads in an affordable way |
|
Use of findings from a realist evaluation
This approach is specific enough to generate particular features to test, but also general enough to apply across different situations. Because realist evaluation uses the idea of generative causality (i.e. mechanisms fire only when the context is conducive), realists are modest in their claims, stating that an evaluation cannot produce universally applicable findings. At best, this evaluation can make sense of the complex processes underlying HAH services by formulating plausible explanations. It can indicate the conditions in which the interventions work (or not) and how they do so. This realistic specification allows decision-makers to assess whether or not interventions that proved successful in one setting may be so in another setting, and assists HAH service planners in adapting interventions to suit specific contexts.
Useful links if you want further information
Video introductions
Note that the four parts to the introduction largely repeat the ‘short overview’ video, with additional detail, argument and examples. Part 4 also includes some additional material on the scientific method.
-
‘Realist Evaluation Short Overview’ (14 minutes). Ray Pawson introduces the basics of realist evaluation (https://vimeo.com/84215487).
-
‘Realist Evaluation – Introduction Part 1’ (7 minutes) introduces the key elements of realist evaluation (https://vimeo.com/84216696).
-
‘Realist Evaluation – Introduction Part 2’ (9 minutes) looks at how realist evaluation helps to address complexity in social programmes (https://vimeo.com/84386879).
-
‘Realist Evaluation – Introduction Part 3’ (8 minutes) looks at how the method makes use of evidence and the value of a multimethod approach (https://vimeo.com/84227829).
-
‘Realist Evaluation – Introduction Part 4’ (7.5 minutes) looks at how evaluation can better contribute to cumulative learning and employ the scientific method (https://vimeo.com/84228311).
-
Pawson R, Tilley N. Realist Evaluation. 2004. URL: www.urban-response.org/system/files/content/resource/files/main/pawson---tilley-%282004%29-realist-evaluation.pdf (accessed 1 July 2022).
FIGURE 23.
Study overview.

Appendix 7 Patient and public involvement feedback documents
Appendix 8 Characteristics of hospice at home services
| Model | HAH service/case study | Deprivation | Urban/rural | RN or HCA led | Referral criteriaa | Visit intensityb | Inpatient beds (n) | Referrals per year (n) | Hands-on care 24/7 | Symptom care 24/7 | Respond in 4 hours | Local DN 24/7 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Criteria 1: size (≤/> 365 referrals per year) | Criteria 2: care available 24/7 or not (any two of three) | |||||||||||
| Q1: large, 24/7 | Acacia | Mixed | Mixed | RN | Short | Low | 24 | 600 | – | ✓ | ✓ | ✓ |
| Camellia | Mixed | Mixed | RN | Short | High | 18 | 442 | ✓ | ✓ | ✓ | – | |
| Echinacea | Deprived | Mixed | RN | Long | Low | 15 | 1173 | – | ✓ | ✓ | ✓ | |
| Peony | Affluent | Mixed | HCA | Long | Mixed | 24 | 2222 | – | ✓ | ✓ | ✓ | |
| Q2: small, 24/7 | Dahlia | Mixed | Mixed | HCA | Medium | High | 30 | 360 | ✓ | ✓ | ✓ | ✓ |
| Gardenia | Mixed | Urban | HCA | Medium | High | 17 | 323 | – | ✓ | ✓ | – | |
| Lavender | Mixed | Mixed | HCA | Long | Mixed | 16 | 100 | ✓ | – | ✓ | ✓ | |
| Violet | Deprived | Mixed | HCA | Long | High | 0 | 240 | ✓ | ✓ | – (Next day) | – | |
| Q3: large, not 24/7 | Wisteria | Deprived | Urban | HCA | Medium | High | 14 | 425 | – | – | – (Next day) | ✓ |
| Q4: small, not 24/7 | Hyacinth | Affluent | Rural | HCA | Long | Mixed | 8 | 200 | – | – | – (Next day) | – |
| Marigold | Mixed | Urban | RN | Long | High | 16 | 200 | – | ✓ | – (Next day) | ✓ | |
| Xyris | Affluent | Mixed | HCA | Medium | Low | 12 | 342 | – | – | ✓ | – | |
Appendix 9 Characteristics of participants at recruitment
| Characteristic | Service model | Total (N = 339) | Difference between models, test (p-value)a | |||
|---|---|---|---|---|---|---|
| Q1: Large providers, 24-hour services | Q2: Small providers, 24-hour services | Q3: Large providers, not 24-hour services | Q4: Small providers, not 24-hour services | |||
| Patient gender, n (%) | ||||||
| Male | 55 (53.4) | 35 (43.8) | 47 (58.0) | 46 (61.3) | 183 (54.0) | Chi-squared (0.136) |
| Female | 48 (46.6) | 45 (56.3) | 34 (42.0) | 29 (38.7) | 156 (46.0) | |
| Patient’s education level, n (%) | ||||||
| GCSE or less | 44 (46.3) | 36 (58.1) | 20 (51.3) | 40 (61.5) | 140 (53.6) | Kruskal–Wallis (0.329) |
| A Levels | 4 (4.2) | 2 (3.2) | 1 (2.6) | 3 (4.6) | 10 (3.8) | |
| Any vocation or college | 27 (28.4) | 14 (22.6) | 12 (30.8) | 11 (16.9) | 64 (24.5) | |
| Any undergraduate | 10 (10.5) | 2 (3.2) | 3 (7.7) | 5 (7.7) | 20 (7.7) | |
| Postgraduate | 10 (10.5) | 8 (12.9) | 3 (7.7) | 6 (9.2) | 27 (10.3) | |
| Patient’s marital status, n (%) | ||||||
| Single | 6 (5.9) | 6 (7.7) | 3 (3.9) | 6 (8.0) | 21 (6.3) | Chi-squared (0.198) |
| In a relationship | 6 (5.9) | 6 (7.7) | 5 (6.5) | 2 (2.7) | 19 (5.7) | |
| Married | 70 (69.3) | 42 (53.8) | 54 (70.1) | 57 (76.0) | 223 (67.4) | |
| Widowed | 19 (18.8) | 24 (30.8) | 15 (19.5) | 10 (13.3) | 68 (20.5) | |
| Patient’s living arrangements, n (%) | ||||||
| Lives alone | 11 (10.7) | 14 (17.5) | 12 (15.4) | 7 (9.3) | 44 (13.1) | Chi-squared (0.137) |
| Lives with spouse | 68 (66.0) | 45 (56.3) | 58 (74.4) | 57 (76.0) | 228 (67.9) | |
| Lives with child(ren) | 16 (15.5) | 16 (20.0) | 6 (7.7) | 7 (9.3) | 45 (13.4) | |
| Lives with others | 8 (7.8) | 5 (6.3) | 2 (2.6) | 4 (5.3) | 19 (5.7) | |
| Patient had cancer, n (%) | ||||||
| No | 24 (23.8) | 21 (26.9) | 14 (17.7) | 17 (24.6) | 76 (23.2) | Chi-squared (0.566) |
| Yes | 77 (76.2) | 57 (73.1) | 65 (82.3) | 52 (75.4) | 251 (76.8) | |
| Carer gender, n (%) | ||||||
| Male | 31 (30.1) | 28 (35.0) | 20 (24.7) | 22 (29.3) | 101 (29.8) | Chi-squared (0.561) |
| Female | 72 (69.9) | 52 (65.0) | 61 (75.3) | 53 (70.7) | 238 (70.2) | |
| Carer: partner of patient, n (%) | ||||||
| No | 32 (31.4) | 40 (50.6) | 34 (44.2) | 26 (34.7) | 132 (39.6) | Chi-squared (0.040) |
| Yes | 70 (68.6) | 39 (49.4) | 43 (55.8) | 49 (65.3) | 201 (60.4) | |
| Carer’s education level, n (%) | ||||||
| GCSE or less | 38 (38.0) | 30 (41.1) | 28 (50.0) | 33 (47.8) | 129 (43.3) | Kruskal–Wallis (0.209) |
| A Levels | 2 (2.0) | 4 (5.5) | 4 (7.1) | 4 (5.8) | 14 (4.7) | |
| Any vocation or college | 28 (28.0) | 17 (23.3) | 12 (21.4) | 14 (20.3) | 71 (23.8) | |
| Any undergraduate | 14 (14.0) | 7 (9.6) | 8 (14.3) | 8 (11.6) | 37 (12.4) | |
| Postgraduate | 18 (18.0) | 15 (20.5) | 4 (7.1) | 10 (14.5) | 47 (15.8) | |
| Carer’s employment status, n (%) | ||||||
| Employed full time | 11 (10.9) | 20 (25.3) | 21 (27.3) | 7 (9.3) | 59 (17.8) | Chi-squared (0.085) |
| Employed part time | 11 (10.9) | 9 (11.4) | 7 (9.1) | 8 (10.7) | 35 (10.5) | |
| Self-employed | 9 (8.9) | 7 (8.9) | 4 (5.2) | 5 (6.7) | 25 (7.5) | |
| Unemployed | 11 (10.9) | 9 (11.4) | 7 (9.1) | 5 (6.7) | 32 (9.6) | |
| Retired | 59 (58.4) | 34 (43.0) | 38 (49.4) | 50 (66.7) | 181 (54.5) | |
| Age (years) | ||||||
| Patient, mean (SD) | 75.0 (12.5) (n = 120) | 75.6 (13.5) (n = 80) | 75.3 (10.1) (n = 79) | 77.5 (10.4) (n = 75) | 75.8 (11.8) (N = 336) | ANOVA (0.537) |
| Median (range) | 76.5 (32–96) | 77.0 (37–101) | 77.0 (44–97) | 79.0 (45–98) | 77.0 (32–101) | |
| Carer, mean (SD) | 65.9 (13.6) (n = 97) | 60.7 (12.3) (n = 78) | 61.8 (13.1) (n = 75) | 67.8 (13.1) (n = 73) | 64.1 (13.3) (N = 323) | ANOVA (0.002) |
| Median (range) | 66.0 (29–93) | 61.0 (31–89) | 60.0 (33–89) | 68.0 (32–92) | 63.0 (29–93) | |
Appendix 10 Summary statistics for Integrated Palliative care Outcome Scale variables for all 339 patients recruited
| Summary statistic | n | Mean | Median | SD | Minimum, maximum |
|---|---|---|---|---|---|
| Current pain | 335 | 1.34 | 1.00 | 1.06 | 0, 4 |
| Current shortness of breath | 332 | 1.31 | 1.00 | 1.24 | 0, 4 |
| Current weakness or lack of energy | 326 | 2.80 | 3.00 | 0.97 | 0, 4 |
| Current nausea | 326 | 0.58 | 0.00 | 0.88 | 0, 4 |
| Current vomiting | 332 | 0.25 | 0.00 | 0.67 | 0, 4 |
| Current appetite | 329 | 1.89 | 2.00 | 1.35 | 0, 4 |
| Current constipation | 327 | 1.05 | 1.00 | 1.20 | 0, 4 |
| Current sore or dry mouth | 328 | 1.17 | 1.00 | 1.22 | 0, 4 |
| Current drowsiness | 329 | 1.87 | 2.00 | 1.26 | 0, 4 |
| Current mobility | 325 | 2.67 | 3.00 | 1.13 | 0, 4 |
| Over the last 3 days (at recruitment) | |||||
| Has the patient felt worried or anxious about their illness? | 291 | 1.57 | 2.00 | 1.28 | 0, 4 |
| Have friends and family felt worried or anxious about their illness? | 320 | 2.59 | 3.00 | 1.19 | 0, 4 |
| Has patient felt depressed? | 281 | 1.08 | 1.00 | 1.19 | 0, 4 |
| Has patient been at peace? | 284 | 1.72 | 1.00 | 1.21 | 0, 4 |
| Has patient been able to share how they are feeling with friends and family? | 290 | 1.57 | 1.00 | 1.40 | 0, 4 |
| Has patient received as much information as they have wanted? | 270 | 0.53 | 0.00 | 0.90 | 0, 4 |
| Have any practical matters resulting from their illness been addressed? | 301 | 0.95 | 1.00 | 0.95 | 0, 4 |
| IPOS total score (0 = best, 68 = worst) | 337 | 25.31 | 25.5 | 9.14 | 2.13, 51.00 |
| Current paina | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 33 | 26 | 18 | 10 | 87 |
| % within model | 32.4 | 33.3 | 22.2 | 13.5 | 26.0 |
| Slightly | |||||
| Count | 32 | 21 | 24 | 24 | 101 |
| % within model | 31.4 | 26.9 | 29.6 | 32.4 | 30.1 |
| Moderately | |||||
| Count | 25 | 19 | 29 | 27 | 100 |
| % within model | 24.5 | 24.4 | 35.8 | 36.5 | 29.9 |
| Severely | |||||
| Count | 10 | 10 | 9 | 10 | 39 |
| % within model | 9.8 | 12.8 | 11.1 | 13.5 | 11.6 |
| Overwhelmingly | |||||
| Count | 2 | 2 | 1 | 3 | 8 |
| % within model | 2.0 | 2.6 | 1.2 | 4.1 | 2.4 |
| Total | |||||
| Count | 102 | 78 | 81 | 74 | 335 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current shortness of breatha | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 32 | 25 | 29 | 29 | 115 |
| % within model | 32.0 | 32.5 | 36.3 | 38.7 | 34.6 |
| Slightly | |||||
| Count | 24 | 24 | 16 | 16 | 80 |
| % within model | 24.0 | 31.2 | 20.0 | 21.3 | 24.1 |
| Moderately | |||||
| Count | 25 | 18 | 22 | 13 | 78 |
| % within model | 25.0 | 23.4 | 27.5 | 17.3 | 23.5 |
| Severely | |||||
| Count | 15 | 5 | 7 | 9 | 36 |
| % within model | 15.0 | 6.5 | 8.8 | 12.0 | 10.8 |
| Overwhelmingly | |||||
| Count | 4 | 5 | 6 | 8 | 23 |
| % within model | 4.0 | 6.5 | 7.5 | 10.7 | 6.9 |
| Total | |||||
| Count | 100 | 77 | 80 | 75 | 332 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current weakness or lack of energya | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 5 | 1 | 1 | 1 | 8 |
| % within model | 5.1 | 1.3 | 1.3 | 1.4 | 2.5 |
| Slightly | |||||
| Count | 10 | 4 | 3 | 1 | 18 |
| % within model | 10.1 | 5.3 | 3.8 | 1.4 | 5.5 |
| Moderately | |||||
| Count | 34 | 14 | 18 | 22 | 88 |
| % within model | 34.3 | 18.7 | 23.1 | 29.7 | 27.0 |
| Severely | |||||
| Count | 39 | 29 | 34 | 26 | 128 |
| % within model | 39.4 | 38.7 | 43.6 | 35.1 | 39.3 |
| Overwhelmingly | |||||
| Count | 11 | 27 | 22 | 24 | 84 |
| % within model | 11.1 | 36.0 | 28.2 | 32.4 | 25.8 |
| Total | |||||
| Count | 99 | 75 | 78 | 74 | 326 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current nauseaa | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 63 | 50 | 54 | 39 | 206 |
| % within model | 64.9 | 66.7 | 68.4 | 52.0 | 63.2 |
| Slightly | |||||
| Count | 15 | 12 | 16 | 21 | 64 |
| % within model | 15.5 | 16.0 | 20.3 | 28.0 | 19.6 |
| Moderately | |||||
| Count | 16 | 9 | 6 | 12 | 43 |
| % within model | 16.5 | 12.0 | 7.6 | 16.0 | 13.2 |
| Severely | |||||
| Count | 3 | 4 | 3 | 2 | 12 |
| % within model | 3.1 | 5.3 | 3.8 | 2.7 | 3.7 |
| Overwhelmingly | |||||
| Count | 0 | 0 | 0 | 1 | 1 |
| % within model | 0.0 | 0.0 | 0.0 | 1.3 | 0.3 |
| Total | |||||
| Count | 97 | 75 | 79 | 75 | 326 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current vomitinga | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 82 | 66 | 70 | 61 | 279 |
| % within model | 81.2 | 84.6 | 89.7 | 81.3 | 84.0 |
| Slightly | |||||
| Count | 12 | 4 | 6 | 10 | 32 |
| % within model | 11.9 | 5.1 | 7.7 | 13.3 | 9.6 |
| Moderately | |||||
| Count | 4 | 4 | 1 | 4 | 13 |
| % within model | 4.0 | 5.1 | 1.3 | 5.3 | 3.9 |
| Severely | |||||
| Count | 3 | 2 | 1 | 0 | 6 |
| % within model | 3.0 | 2.6 | 1.3 | 0.0 | 1.8 |
| Overwhelmingly | |||||
| Count | 0 | 2 | 0 | 0 | 2 |
| % within model | 0.0 | 2.6 | 0.0 | 0.0 | 0.6 |
| Total | |||||
| Count | 101 | 78 | 78 | 75 | 332 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current appetitea | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 28 | 15 | 15 | 12 | 70 |
| % within model | 27.7 | 19.7 | 19.0 | 16.4 | 21.3 |
| Slightly | |||||
| Count | 18 | 16 | 18 | 13 | 65 |
| % within model | 17.8 | 21.1 | 22.8 | 17.8 | 19.8 |
| Moderately | |||||
| Count | 28 | 14 | 16 | 13 | 71 |
| % within model | 27.7 | 18.4 | 20.3 | 17.8 | 21.6 |
| Severely | |||||
| Count | 18 | 16 | 25 | 19 | 78 |
| % within model | 17.8 | 21.1 | 31.6 | 26.0 | 23.7 |
| Overwhelmingly | |||||
| Count | 9 | 15 | 5 | 16 | 45 |
| % within model | 8.9 | 19.7 | 6.3 | 21.9 | 13.7 |
| Total | |||||
| Count | 101 | 76 | 79 | 73 | 329 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current constipationa | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 43 | 45 | 36 | 26 | 150 |
| % within model | 43.4 | 60.0 | 45.6 | 35.1 | 45.9 |
| Slightly | |||||
| Count | 26 | 11 | 19 | 17 | 73 |
| % within model | 26.3 | 14.7 | 24.1 | 23.0 | 22.3 |
| Moderately | |||||
| Count | 14 | 10 | 17 | 15 | 56 |
| % within model | 14.1 | 13.3 | 21.5 | 20.3 | 17.1 |
| Severely | |||||
| Count | 12 | 4 | 7 | 10 | 33 |
| % within model | 12.1 | 5.3 | 8.9 | 13.5 | 10.1 |
| Overwhelmingly | |||||
| Count | 4 | 5 | 0 | 6 | 15 |
| % within model | 4.0 | 6.7 | 0.0 | 8.1 | 4.6 |
| Total | |||||
| Count | 99 | 75 | 79 | 74 | 327 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current sore or dry moutha | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 44 | 30 | 42 | 23 | 139 |
| % within model | 44.9 | 39.5 | 52.5 | 31.1 | 42.4 |
| Slightly | |||||
| Count | 18 | 21 | 10 | 10 | 59 |
| % within model | 18.4 | 27.6 | 12.5 | 13.5 | 18.0 |
| Moderately | |||||
| Count | 24 | 16 | 16 | 23 | 79 |
| % within model | 24.5 | 21.1 | 20.0 | 31.1 | 24.1 |
| Severely | |||||
| Count | 10 | 7 | 9 | 10 | 36 |
| % within model | 10.2 | 9.2 | 11.3 | 13.5 | 11.0 |
| Overwhelmingly | |||||
| Count | 2 | 2 | 3 | 8 | 15 |
| % within model | 2.0 | 2.6 | 3.8 | 10.8 | 4.6 |
| Total | |||||
| Count | 98 | 76 | 80 | 74 | 328 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current drowsinessa | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 21 | 12 | 16 | 13 | 62 |
| % within model | 21.2 | 15.6 | 20.5 | 17.3 | 18.8 |
| Slightly | |||||
| Count | 21 | 14 | 13 | 14 | 62 |
| % within model | 21.2 | 18.2 | 16.7 | 18.7 | 18.8 |
| Moderately | |||||
| Count | 37 | 23 | 22 | 17 | 99 |
| % within model | 37.4 | 29.9 | 28.2 | 22.7 | 30.1 |
| Severely | |||||
| Count | 15 | 16 | 15 | 23 | 69 |
| % within model | 15.2 | 20.8 | 19.2 | 30.7 | 21.0 |
| Overwhelmingly | |||||
| Count | 5 | 12 | 12 | 8 | 37 |
| % within model | 5.1 | 15.6 | 15.4 | 10.7 | 11.2 |
| Total | |||||
| Count | 99 | 77 | 78 | 75 | 329 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Current mobilitya | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Not at all | |||||
| Count | 12 | 1 | 1 | 0 | 14 |
| % within model | 12.1 | 1.3 | 1.3 | 0.0 | 4.3 |
| Slightly | |||||
| Count | 17 | 5 | 5 | 9 | 36 |
| % within model | 17.2 | 6.7 | 6.3 | 12.5 | 11.1 |
| Moderately | |||||
| Count | 35 | 14 | 21 | 16 | 86 |
| % within model | 35.4 | 18.7 | 26.6 | 22.2 | 26.5 |
| Severely | |||||
| Count | 23 | 20 | 31 | 22 | 96 |
| % within model | 23.2 | 26.7 | 39.2 | 30.6 | 29.5 |
| Overwhelmingly | |||||
| Count | 12 | 35 | 21 | 25 | 93 |
| % within model | 12.1 | 46.7 | 26.6 | 34.7 | 28.6 |
| Total | |||||
| Count | 99 | 75 | 79 | 72 | 325 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days, has patient felt anxious or worried about their illness?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| No, not at all | |||||
| Count | 32 | 28 | 3 | 20 | 83 |
| % within model | 35.2 | 43.1 | 4.5 | 29.0 | 28.5 |
| Occasionally | |||||
| Count | 24 | 12 | 14 | 8 | 58 |
| % within model | 26.4 | 18.5 | 21.2 | 11.6 | 19.9 |
| Sometimes | |||||
| Count | 24 | 16 | 19 | 13 | 72 |
| % within model | 26.4 | 24.6 | 28.8 | 18.8 | 24.7 |
| Most of the time | |||||
| Count | 8 | 7 | 27 | 16 | 58 |
| % within model | 8.8 | 10.8 | 40.9 | 23.2 | 19.9 |
| Yes, always | |||||
| Count | 3 | 2 | 3 | 12 | 20 |
| % within model | 3.3 | 3.1 | 4.5 | 17.4 | 6.9 |
| Total | |||||
| Count | 91 | 65 | 66 | 69 | 291 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days, have friends and family felt anxious or worried about their illness?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| No, not at all | |||||
| Count | 7 | 14 | 0 | 5 | 26 |
| % within model | 7.3 | 18.7 | 0.0 | 6.8 | 8.1 |
| Occasionally | |||||
| Count | 12 | 7 | 3 | 8 | 30 |
| % within model | 12.5 | 9.3 | 3.9 | 11.0 | 9.4 |
| Sometimes | |||||
| Count | 26 | 27 | 8 | 13 | 74 |
| % within model | 27.1 | 36.0 | 10.5 | 17.8 | 23.1 |
| Most of the time | |||||
| Count | 34 | 17 | 35 | 24 | 110 |
| % within model | 35.4 | 22.7 | 46.1 | 32.9 | 34.4 |
| Yes, always | |||||
| Count | 17 | 10 | 30 | 23 | 80 |
| % within model | 17.7 | 13.3 | 39.5 | 31.5 | 25.0 |
| Total | |||||
| Count | 96 | 75 | 76 | 73 | 320 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days, has the patient felt depressed?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| No, not at all | |||||
| Count | 44 | 40 | 15 | 24 | 123 |
| % within model | 51.2 | 59.7 | 23.4 | 37.5 | 43.8 |
| Occasionally | |||||
| Count | 21 | 11 | 19 | 13 | 64 |
| % within model | 24.4 | 16.4 | 29.7 | 20.3 | 22.8 |
| Sometimes | |||||
| Count | 10 | 11 | 20 | 12 | 53 |
| % within model | 11.6 | 16.4 | 31.3 | 18.8 | 18.9 |
| Most of the time | |||||
| Count | 8 | 5 | 10 | 7 | 30 |
| % within model | 9.3 | 7.5 | 15.6 | 10.9 | 10.7 |
| Yes, always | |||||
| Count | 3 | 0 | 0 | 8 | 11 |
| % within model | 3.5 | 0.0 | 0.0 | 12.5 | 3.9 |
| Total | |||||
| Count | 86 | 67 | 64 | 64 | 281 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days, has the patient been at peace?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Yes, all the time | |||||
| Count | 17 | 13 | 0 | 11 | 41 |
| % within model | 21.3 | 19.7 | 0.0 | 15.7 | 14.4 |
| Most of the time | |||||
| Count | 33 | 26 | 19 | 24 | 102 |
| % within model | 41.3 | 39.4 | 27.9 | 34.3 | 35.9 |
| Sometimes | |||||
| Count | 15 | 17 | 22 | 15 | 69 |
| % within model | 18.8 | 25.8 | 32.4 | 21.4 | 24.3 |
| Occasionally | |||||
| Count | 9 | 2 | 20 | 8 | 39 |
| % within model | 11.3 | 3.0 | 29.4 | 11.4 | 13.7 |
| No, not at all | |||||
| Count | 6 | 8 | 7 | 12 | 33 |
| % within model | 7.5 | 12.1 | 10.3 | 17.1 | 11.6 |
| Total | |||||
| Count | 80 | 66 | 68 | 70 | 284 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days, has the patient been able to share how they are feeling with friends and family?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Yes, as much as wanted | |||||
| Count | 34 | 22 | 13 | 20 | 89 |
| % within model | 38.2 | 32.8 | 18.6 | 31.3 | 30.7 |
| Most of the time | |||||
| Count | 27 | 12 | 15 | 13 | 67 |
| % within model | 30.3 | 17.9 | 21.4 | 20.3 | 23.1 |
| Sometimes | |||||
| Count | 10 | 13 | 20 | 8 | 51 |
| % within model | 11.2 | 19.4 | 28.6 | 12.5 | 17.6 |
| Occasionally | |||||
| Count | 7 | 11 | 16 | 12 | 46 |
| % within model | 7.9 | 16.4 | 22.9 | 18.8 | 15.9 |
| No, not at all with anyone | |||||
| Count | 11 | 9 | 6 | 11 | 37 |
| % within model | 12.4 | 13.4 | 8.6 | 17.2 | 12.8 |
| Total | |||||
| Count | 89 | 67 | 70 | 64 | 290 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days has the patient received as much information as they have wanted?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| Enough | |||||
| Count | 59 | 45 | 33 | 45 | 182 |
| % within model | 78.7 | 69.2 | 48.5 | 72.6 | 67.4 |
| Received but hard to understand | |||||
| Count | 4 | 13 | 25 | 8 | 50 |
| % within model | 5.3 | 20.0 | 36.8 | 12.9 | 18.5 |
| Received but would like more | |||||
| Count | 8 | 5 | 8 | 6 | 27 |
| % within model | 10.7 | 7.7 | 11.8 | 9.7 | 10.0 |
| Very little and would like more | |||||
| Count | 1 | 1 | 2 | 2 | 6 |
| % within model | 1.3 | 1.5 | 2.9 | 3.2 | 2.2 |
| None received and would like | |||||
| Count | 3 | 1 | 0 | 1 | 5 |
| % within model | 4.0 | 1.5 | 0.0 | 1.6 | 1.9 |
| Total | |||||
| Count | 75 | 65 | 68 | 62 | 270 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Over the last 3 days, have any practical matters resulting from their illness been addressed?a | Service model | Total | |||
|---|---|---|---|---|---|
| Q1: Large providers, 24/7 services | Q2: Small providers, 24/7 services | Q3: Large providers, not 24/7 services | Q4: Small providers, not 24/7 services | ||
| No problems/problems addressed | |||||
| Count | 42 | 41 | 4 | 22 | 109 |
| % within model | 49.4 | 57.7 | 5.2 | 32.4 | 36.2 |
| Problems being addressed | |||||
| Count | 24 | 22 | 47 | 33 | 126 |
| % within model | 28.2 | 31.0 | 61.0 | 48.5 | 41.9 |
| Problems partly addressed | |||||
| Count | 9 | 5 | 24 | 10 | 48 |
| % within model | 10.6 | 7.0 | 31.2 | 14.7 | 15.9 |
| Most problems not addressed | |||||
| Count | 4 | 2 | 1 | 2 | 9 |
| % within model | 4.7 | 2.8 | 1.3 | 2.9 | 3.0 |
| Problems not addressed at all | |||||
| Count | 6 | 1 | 1 | 1 | 9 |
| % within model | 7.1 | 1.4 | 1.3 | 1.5 | 3.0 |
| Total | |||||
| Count | 85 | 71 | 77 | 68 | 301 |
| % within model | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Appendix 11 Number and percentage of Quality of Dying and Death questionnaires returned, by hospice and by model
| Service model | Hospice | QODD data collected, n (%) | Total number of patients who died during study | Total QODDs returned by service model, N (%) | Difference between service models, test (p-value) | |
|---|---|---|---|---|---|---|
| Did not return QODD | QODD returned | |||||
| Q1: Large providers, 24-hour services | Acacia | 2 (100.0) | 0 (0) | 2 | 48 (61.5) | Chi-squared (0.008) |
| Camellia | 8 (66.7) | 4 (33.3) | 12 | |||
| Echinacea | 4 (26.7) | 11 (73.3) | 15 | |||
| Peony | 16 (32.7) | 33 (67.3) | 49 | |||
| Q2: Small providers, 24-hour services | Dahlia | 10 (50.0) | 10 (50.0) | 20 | 31 (46.3) | |
| Gardenia | 8 (66.7) | 4 (33.3) | 12 | |||
| Lavender | 8 (44.4) | 10 (55.6) | 18 | |||
| Violet | 10 (58.8) | 7 (41.2) | 17 | |||
| Q3: Large providers, not 24-hour services | Wisteria | 43 (58.1) | 31 (41.9) | 74 | 31 (41.9) | |
| Q4: Small providers, not 24-hour services | Hyacinth | 17 (58.6) | 12 (41.4) | 29 | 22 (33.8) | |
| Marigold | 20 (71.4) | 8 (28.6) | 28 | |||
| Xyris | 6 (75.0) | 2 (25.0) | 8 | |||
| Total | 152 (53.5) | 132 (46.5) | 284 | 132 (46.5) | ||
Appendix 12 Frequency of responses to individual Quality of Dying and Death questionnaire questions
| Number of QODD questions answered | Frequency | % | Valid % | Cumulative % |
|---|---|---|---|---|
| 0 | 1 | 0.4 | 0.8 | 0.8 |
| 1 | 1 | 0.4 | 0.8 | 1.5 |
| 2 | 1 | 0.4 | 0.8 | 2.3 |
| 4 | 1 | 0.4 | 0.8 | 3.0 |
| 7 | 1 | 0.4 | 0.8 | 3.8 |
| 9 | 1 | 0.4 | 0.8 | 4.5 |
| 10 | 1 | 0.4 | 0.8 | 5.3 |
| 12 | 1 | 0.4 | 0.8 | 6.1 |
| 13 | 1 | 0.4 | 0.8 | 6.8 |
| 14 | 2 | 0.7 | 1.5 | 8.3 |
| 15 | 4 | 1.4 | 3.0 | 11.4 |
| 16 | 5 | 1.8 | 3.8 | 15.2 |
| 17 | 4 | 1.4 | 3.0 | 18.2 |
| 18 | 4 | 1.4 | 3.0 | 21.2 |
| 19 | 4 | 1.4 | 3.0 | 24.2 |
| 20 | 3 | 1.1 | 2.3 | 26.5 |
| 21 | 8 | 2.8 | 6.1 | 32.6 |
| 22 | 4 | 1.4 | 3.0 | 35.6 |
| 23 | 8 | 2.8 | 6.1 | 41.7 |
| 24 | 2 | 0.7 | 1.5 | 43.2 |
| 25 | 9 | 3.2 | 6.8 | 50.0 |
| 26 | 10 | 3.5 | 7.6 | 57.6 |
| 27 | 12 | 4.2 | 9.1 | 66.7 |
| 28 | 16 | 5.6 | 12.1 | 78.8 |
| 29 | 20 | 7.0 | 15.2 | 93.9 |
| 30 | 8 | 2.8 | 6.1 | 100.0 |
| Total | 132 | 46.5 | 100.0 | |
| Missing | 152 | 53.5 | ||
| Total | 284 | 100.0 |
Appendix 13 Summary statistics for each outcome, by hospice at home service
| Outcome | Site (service model) | Total | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acacia (Q1) | Camellia (Q1) | Echinacea (Q1) | Peony (Q1) | Dahlia (Q2) | Gardenia (Q2) | Lavender (Q2) | Violet (Q2) | Wisteria (Q3) | Hyacinth (Q4) | Marigold (Q4) | Xyris (Q4) | |||||||||||||||
| n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | n | Mean (median) | |
| Number of days from recruitment (patient consent) to death | 2 | 6.0 (6.0) | 12 | 26.2 (16.0) | 15 | 125.1 (112.0) | 49 | 93.5 (77.0) | 20 | 24.7 (8.5) | 12 | 28.6 (15.0) | 18 | 43.1 (29.5) | 17 | 31.8 (8.0) | 74 | 57.2 (13.0) | 29 | 45.1 (17.0) | 28 | 32.9 (15.0) | 8 | 70.8 (54.5) | 284 | 56.2 (21.0) |
| Total QODD score [30 items, scale 0 (terrible) to 100 (almost perfect)]a | 0 | – | 4 | 57.6 (67.4) | 11 | 47.7 (50.4) | 31 | 68.3 (70.0) | 10 | 77.0 (81.3) | 4 | 70.3 (72.2) | 10 | 73.0 (82.2) | 7 | 78.7 (81.7) | 30 | 57.0 (59.2) | 11 | 81.9 (81.3) | 8 | 65.4 (72.9) | 2 | 69.1 (69.1) | 128 | 66.2 (70.7) |
| QODD: % who achieved good/almost perfect death (score of ≥ 70)a | 0 | – | 4 | 50.0 (50.0) | 11 | 18.2 (0) | 31 | 48.4 (0) | 10 | 70.0 (100.0) | 4 | 50.0 (50.0) | 10 | 70.0 (100.0) | 7 | 71.4 (100.0) | 30 | 36.7 (0) | 11 | 90.9 (100.0) | 8 | 62.5 (100.0) | 2 | 50.0 (50.0) | 128 | 52.3 (100.0) |
| Percentage of patients who achieved PPOD | 1 | 0.0 (0) | 11 | 90.9 (100.0) | 12 | 66.7 (100.0) | 27 | 55.6 (100.0) | 20 | 85.0 (100.0) | 11 | 81.8 (100.0) | 16 | 81.3 (100.0) | 15 | 80.0 (100.0) | 57 | 71.9 (100.0) | 24 | 58.3 (100.0) | 26 | 80.8 (100.0) | 2 | 100.0 (100.0) | 222 | 73.0 (100.0) |
| VOICES 1. Overall, did you and your family get as much help and support from health and social care services as you needed when caring for the patient? (1 = best, 5 = worst)a | 0 | – | 3 | 1.3 (1.0) | 11 | 1.8 (2.0) | 30 | 1.3 (1.0) | 10 | 1.1 (1.0) | 4 | 1.3 (1.0) | 10 | 1.0 (1.0) | 7 | 1.0 (1.0) | 31 | 1.4 (1.0) | 12 | 1.4 (1.0) | 7 | 1.3 (1.0) | 2 | 1.0 (1.0) | 127 | 1.3 (1.0) |
| VOICES 2. Overall, how was the help and support you and your family received from health and social care services when caring for the patient? (1 = best, 5 = worst]a | 0 | – | 4 | 2.0 (2.0) | 11 | 2.5 (2.0) | 30 | 2.1 (2.0) | 10 | 1.7 (1.0) | 4 | 1.8 (1.5) | 10 | 1.4 (1.0) | 7 | 1.9 (2.0) | 31 | 2.2 (2.0) | 12 | 1.7 (2.0) | 7 | 1.9 (1.0) | 2 | 1.0 (1.0) | 128 | 2.0 (2.0) |
| Service satisfaction: last 28 days/final response. (1 = exceeded expectations, 2 = just met expectations, 3 = fell short of expectations)b | 2 | 1.5 (1.5) | 2 | 2.0 (2.0) | 13 | 2.1 (2.0) | 44 | 1.5 (1.5) | 2 | 1.5 (1.5) | 8 | 1.6 (1.0) | 8 | 1.1 (1.0) | 4 | 1.3 (1.0) | 36 | 1.4 (1.0) | 10 | 1.3 (1.0) | 8 | 1.6 (1.5) | 6 | 1.5 (1.5) | 143 | 1.5 (1.0) |
| Carer burden: last 28 days/final response. Mean of six items (0 = best, 24 = worst)b | 2 | 10.5 (10.5) | 3 | 2.7 (4.0) | 14 | 4.1 (3.5) | 43 | 6.6 (6.0) | 2 | 14.5 (14.5) | 7 | 8.0 (8.0) | 8 | 7.3 (8.0) | 4 | 10.5 (10.0) | 37 | 9.6 (11.0) | 11 | 11.2 (12.0) | 11 | 9.1 (6.0) | 7 | 3.6 (2.0) | 149 | 7.8 (7.0) |
Appendix 14 Responses to Quality of Dying and Death questionnaire questions, part A, by service model
| Service model | How often did patient appear to have his/her pain under control? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 2 | 3 | 7 | 7 | 17 | 9 | 45 |
| % within model | 4.4 | 6.7 | 15.6 | 15.6 | 37.8 | 20.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 2 | 0 | 4 | 3 | 15 | 7 | 31 |
| % within model | 6.5 | 0.0 | 12.9 | 9.7 | 48.4 | 22.6 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 0 | 4 | 5 | 3 | 11 | 7 | 30 |
| % within model | 0.0 | 13.3 | 16.7 | 10.0 | 36.7 | 23.3 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 0 | 2 | 1 | 3 | 7 | 9 | 22 |
| % within model | 0.0 | 9.1 | 4.5 | 13.6 | 31.8 | 40.9 | 100.0 |
| Total | |||||||
| Count | 4 | 9 | 17 | 16 | 50 | 32 | 128 |
| % within model | 3.1 | 7.0 | 13.3 | 12.5 | 39.1 | 25.0 | 100.0 |
| Service model | How often did patient appear to have control over what was going on around them? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 6 | 9 | 5 | 6 | 14 | 7 | 47 |
| % within model | 12.8 | 19.1 | 10.6 | 12.8 | 29.8 | 14.9 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 6 | 5 | 5 | 4 | 7 | 4 | 31 |
| % within model | 19.4 | 16.1 | 16.1 | 12.9 | 22.6 | 12.9 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 5 | 4 | 4 | 5 | 7 | 6 | 31 |
| % within model | 16.1 | 12.9 | 12.9 | 16.1 | 22.6 | 19.4 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 2 | 4 | 5 | 4 | 3 | 4 | 22 |
| % within model | 9.1 | 18.2 | 22.7 | 18.2 | 13.6 | 18.2 | 100.0 |
| Total | |||||||
| Count | 19 | 22 | 19 | 19 | 31 | 21 | 131 |
| % within model | 14.5 | 16.8 | 14.5 | 14.5 | 23.7 | 16.0 | 100.0 |
| Service model | How often was patient able to feed themselves? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 15 | 8 | 8 | 2 | 7 | 6 | 46 |
| % within model | 32.6 | 17.4 | 17.4 | 4.3 | 15.2 | 13.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 16 | 5 | 1 | 1 | 6 | 2 | 31 |
| % within model | 51.6 | 16.1 | 3.2 | 3.2 | 19.4 | 6.5 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 15 | 8 | 1 | 4 | 1 | 2 | 31 |
| % within model | 48.4 | 25.8 | 3.2 | 12.9 | 3.2 | 6.5 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 9 | 3 | 1 | 0 | 7 | 2 | 22 |
| % within model | 40.9 | 13.6 | 4.5 | 0.0 | 31.8 | 9.1 | 100.0 |
| Total | |||||||
| Count | 55 | 24 | 11 | 7 | 21 | 12 | 130 |
| % within model | 42.3 | 18.5 | 8.5 | 5.4 | 16.2 | 9.2 | 100.0 |
| Service model | How often patient had bladder/bowel control | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 17 | 9 | 3 | 2 | 7 | 6 | 44 |
| % within model | 38.6 | 20.5 | 6.8 | 4.5 | 15.9 | 13.6 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 17 | 2 | 3 | 1 | 5 | 3 | 31 |
| % within model | 54.8 | 6.5 | 9.7 | 3.2 | 16.1 | 9.7 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 13 | 5 | 3 | 1 | 4 | 4 | 30 |
| % within model | 43.3 | 16.7 | 10.0 | 3.3 | 13.3 | 13.3 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 8 | 4 | 3 | 2 | 2 | 3 | 22 |
| % within model | 36.4 | 18.2 | 13.6 | 9.1 | 9.1 | 13.6 | 100.0 |
| Total | |||||||
| Count | 55 | 20 | 12 | 6 | 18 | 16 | 127 |
| % within model | 43.3 | 15.7 | 9.4 | 4.7 | 14.2 | 12.6 | 100.0 |
| Service model | How often did the patient breathe comfortably? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 3 | 6 | 5 | 7 | 18 | 7 | 46 |
| % within model | 6.5 | 13.0 | 10.9 | 15.2 | 39.1 | 15.2 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 1 | 2 | 2 | 4 | 16 | 6 | 31 |
| % within model | 3.2 | 6.5 | 6.5 | 12.9 | 51.6 | 19.4 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 2 | 7 | 7 | 3 | 9 | 3 | 31 |
| % within model | 6.5 | 22.6 | 22.6 | 9.7 | 29.0 | 9.7 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 1 | 2 | 1 | 1 | 11 | 6 | 22 |
| % within model | 4.5 | 9.1 | 4.5 | 4.5 | 50.0 | 27.3 | 100.0 |
| Total | |||||||
| Count | 7 | 17 | 15 | 15 | 54 | 22 | 130 |
| % within model | 5.4 | 13.1 | 11.5 | 11.5 | 41.5 | 16.9 | 100.0 |
| Service model | How often did patient appear to feel at peace with dying? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 7 | 4 | 7 | 1 | 12 | 7 | 38 |
| % within model | 18.4 | 10.5 | 18.4 | 2.6 | 31.6 | 18.4 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 3 | 3 | 3 | 3 | 7 | 7 | 26 |
| % within model | 11.5 | 11.5 | 11.5 | 11.5 | 26.9 | 26.9 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 3 | 5 | 3 | 3 | 3 | 4 | 21 |
| % within model | 14.3 | 23.8 | 14.3 | 14.3 | 14.3 | 19.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 1 | 1 | 3 | 3 | 4 | 3 | 15 |
| % within model | 6.7 | 6.7 | 20.0 | 20.0 | 26.7 | 20.0 | 100.0 |
| Total | |||||||
| Count | 14 | 13 | 16 | 10 | 26 | 21 | 100 |
| % within model | 14.0 | 13.0 | 16.0 | 10.0 | 26.0 | 21.0 | 100.0 |
| Service model | How often did the patient appear to be unafraid of dying? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 4 | 5 | 7 | 2 | 9 | 11 | 38 |
| % within model | 10.5 | 13.2 | 18.4 | 5.3 | 23.7 | 28.9 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 5 | 6 | 1 | 3 | 7 | 4 | 26 |
| % within model | 19.2 | 23.1 | 3.8 | 11.5 | 26.9 | 15.4 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 4 | 2 | 3 | 3 | 3 | 7 | 22 |
| % within model | 18.2 | 9.1 | 13.6 | 13.6 | 13.6 | 31.8 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 0 | 2 | 2 | 2 | 5 | 8 | 19 |
| % within model | 0.0 | 10.5 | 10.5 | 10.5 | 26.3 | 42.1 | 100.0 |
| Total | |||||||
| Count | 13 | 15 | 13 | 10 | 24 | 30 | 105 |
| % within model | 12.4 | 14.3 | 12.4 | 9.5 | 22.9 | 28.6 | 100.0 |
| Service model | How often did the patient laugh and smile? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 8 | 14 | 7 | 11 | 6 | 0 | 46 |
| % within model | 17.4 | 30.4 | 15.2 | 23.9 | 13.0 | 0.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 2 | 7 | 8 | 6 | 7 | 0 | 30 |
| % within model | 6.7 | 23.3 | 26.7 | 20.0 | 23.3 | 0.0 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 5 | 7 | 6 | 5 | 2 | 4 | 29 |
| % within model | 17.2 | 24.1 | 20.7 | 17.2 | 6.9 | 13.8 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 4 | 6 | 6 | 3 | 2 | 0 | 21 |
| % within model | 19.0 | 28.6 | 28.6 | 14.3 | 9.5 | 0.0 | 100.0 |
| Total | |||||||
| Count | 19 | 34 | 27 | 25 | 17 | 4 | 126 |
| % within model | 15.1 | 27.0 | 21.4 | 19.8 | 13.5 | 3.2 | 100.0 |
| Service model | How often did patient have enough energy? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 21 | 16 | 4 | 3 | 2 | 0 | 46 |
| % within model | 45.7 | 34.8 | 8.7 | 6.5 | 4.3 | 0.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 17 | 11 | 1 | 0 | 2 | 0 | 31 |
| % within model | 54.8 | 35.5 | 3.2 | 0.0 | 6.5 | 0.0 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 21 | 8 | 1 | 0 | 0 | 0 | 30 |
| % within model | 70.0 | 26.7 | 3.3 | 0.0 | 0.0 | 0.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 15 | 1 | 3 | 2 | 0 | 0 | 21 |
| % within model | 71.4 | 4.8 | 14.3 | 9.5 | 0.0 | 0.0 | 100.0 |
| Total | |||||||
| Count | 74 | 36 | 9 | 5 | 4 | 0 | 128 |
| % within model | 57.8 | 28.1 | 7.0 | 3.9 | 3.1 | 0.0 | 100.0 |
| Service model | How often did the patient appear worried about strain on loved ones? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 3 | 10 | 12 | 6 | 7 | 4 | 42 |
| % within model | 7.1 | 23.8 | 28.6 | 14.3 | 16.7 | 9.5 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 4 | 2 | 5 | 5 | 7 | 3 | 26 |
| % within model | 15.4 | 7.7 | 19.2 | 19.2 | 26.9 | 11.5 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 1 | 4 | 3 | 5 | 7 | 4 | 24 |
| % within model | 4.2 | 16.7 | 12.5 | 20.8 | 29.2 | 16.7 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 5 | 2 | 6 | 2 | 3 | 3 | 21 |
| % within model | 23.8 | 9.5 | 28.6 | 9.5 | 14.3 | 14.3 | 100.0 |
| Total | |||||||
| Count | 13 | 18 | 26 | 18 | 24 | 14 | 113 |
| % within model | 11.5 | 15.9 | 23.0 | 15.9 | 21.2 | 12.4 | 100.0 |
| Service model | How often did the patient appear to keep dignity and self-respect? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 3 | 6 | 8 | 9 | 12 | 8 | 46 |
| % within model | 6.5 | 13.0 | 17.4 | 19.6 | 26.1 | 17.4 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 1 | 1 | 2 | 5 | 13 | 8 | 30 |
| % within model | 3.3 | 3.3 | 6.7 | 16.7 | 43.3 | 26.7 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 4 | 2 | 4 | 2 | 8 | 8 | 28 |
| % within model | 14.3 | 7.1 | 14.3 | 7.1 | 28.6 | 28.6 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 3 | 2 | 0 | 2 | 9 | 5 | 21 |
| % within model | 14.3 | 9.5 | 0.0 | 9.5 | 42.9 | 23.8 | 100.0 |
| Total | |||||||
| Count | 11 | 11 | 14 | 18 | 42 | 29 | 125 |
| % within model | 8.8 | 8.8 | 11.2 | 14.4 | 33.6 | 23.2 | 100.0 |
| Service model | How often did the patient spend time with their spouse/partner? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 0 | 0 | 2 | 4 | 12 | 16 | 34 |
| % within model | 0.0 | 0.0 | 5.9 | 11.8 | 35.3 | 47.1 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 0 | 0 | 1 | 0 | 4 | 10 | 15 |
| % within model | 0.0 | 0.0 | 6.7 | 0.0 | 26.7 | 66.7 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 0 | 0 | 0 | 2 | 9 | 15 | 26 |
| % within model | 0.0 | 0.0 | 0.0 | 7.7 | 34.6 | 57.7 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 1 | 0 | 0 | 0 | 7 | 7 | 15 |
| % within model | 6.7 | 0.0 | 0.0 | 0.0 | 46.7 | 46.7 | 100.0 |
| Total | |||||||
| Count | 1 | 0 | 0 | 6 | 32 | 48 | 90 |
| % within model | 1.1 | 0.0 | 0.0 | 6.7 | 35.6 | 53.3 | 100.0 |
| Service model | How often did the patient spend time with children? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 1 | 3 | 2 | 12 | 14 | 7 | 39 |
| % within model | 2.6 | 7.7 | 5.1 | 30.8 | 35.9 | 17.9 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 1 | 1 | 3 | 5 | 6 | 10 | 26 |
| % within model | 3.8 | 3.8 | 11.5 | 19.2 | 23.1 | 38.5 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 1 | 1 | 0 | 7 | 8 | 10 | 27 |
| % within model | 3.7 | 3.7 | 0.0 | 25.9 | 29.6 | 37.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 0 | 1 | 0 | 6 | 6 | 7 | 20 |
| % within model | 0.0 | 5.0 | 0.0 | 30.0 | 30.0 | 35.0 | 100.0 |
| Total | |||||||
| Count | 3 | 6 | 5 | 30 | 34 | 34 | 112 |
| % within model | 2.7 | 5.4 | 4.5 | 26.8 | 30.4 | 30.4 | 100.0 |
| Service model | How often did the patient spend time with other family/friends? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 8 | 7 | 13 | 10 | 6 | 1 | 45 |
| % within model | 17.8 | 15.6 | 28.9 | 22.2 | 13.3 | 2.2 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 1 | 4 | 6 | 10 | 8 | 2 | 31 |
| % within model | 3.2 | 12.9 | 19.4 | 32.3 | 25.8 | 6.5 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 2 | 8 | 4 | 9 | 5 | 3 | 31 |
| % within model | 6.5 | 25.8 | 12.9 | 29.0 | 16.1 | 9.7 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 2 | 6 | 4 | 4 | 5 | 0 | 21 |
| % within model | 9.5 | 28.6 | 19.0 | 19.0 | 23.8 | 0.0 | 100.0 |
| Total | |||||||
| Count | 13 | 25 | 27 | 33 | 24 | 6 | 128 |
| % within model | 10.2 | 19.5 | 21.1 | 25.8 | 18.8 | 4.7 | 100.0 |
| Service model | How often did the patient spend time alone? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 16 | 18 | 7 | 3 | 2 | 0 | 46 |
| % within model | 34.8 | 39.1 | 15.2 | 6.5 | 4.3 | 0.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 15 | 12 | 3 | 0 | 0 | 0 | 30 |
| % within model | 50.0 | 40.0 | 10.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 15 | 13 | 3 | 0 | 0 | 0 | 31 |
| % within model | 48.4 | 41.9 | 9.7 | 0.0 | 0.0 | 0.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 11 | 7 | 3 | 1 | 0 | 0 | 22 |
| % within model | 50.0 | 31.8 | 13.6 | 4.5 | 0.0 | 0.0 | 100.0 |
| Total | |||||||
| Count | 57 | 50 | 16 | 4 | 2 | 0 | 129 |
| % within model | 44.2 | 38.8 | 12.4 | 3.1 | 1.6 | 0.0 | 100.0 |
| Service model | How often did the patient spend time with pets? | Total | |||||
|---|---|---|---|---|---|---|---|
| None of the time | A little bit of the time | Some of the time | A good bit of the time | Most of the time | All of the time | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 5 | 3 | 3 | 3 | 3 | 1 | 18 |
| % within model | 27.8 | 16.7 | 16.7 | 16.7 | 16.7 | 5.6 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 2 | 2 | 2 | 1 | 4 | 3 | 14 |
| % within model | 14.3 | 14.3 | 14.3 | 7.1 | 28.6 | 21.4 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 1 | 2 | 1 | 1 | 1 | 2 | 8 |
| % within model | 12.5 | 25.0 | 12.5 | 12.5 | 12.5 | 25.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 1 | 1 | 0 | 2 | 1 | 2 | 7 |
| % within model | 14.3 | 14.3 | 0.0 | 28.6 | 14.3 | 28.6 | 100.0 |
| Total | |||||||
| Count | 9 | 8 | 6 | 7 | 9 | 8 | 47 |
| % within model | 19.1 | 17.0 | 12.8 | 14.9 | 19.1 | 17.0 | 100.0 |
| Service model | Did patient appear to find meaning and purpose in life? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 28 | 3 | 31 |
| % within model | 90.3 | 9.7 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 20 | 2 | 22 |
| % within model | 90.9 | 9.1 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 15 | 9 | 24 |
| % within model | 62.5 | 37.5 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 8 | 7 | 15 |
| % within model | 53.3 | 46.7 | 100.0 |
| Total | |||
| Count | 71 | 21 | 92 |
| % within model | 77.2 | 22.8 | 100.0 |
| Service model | Was the patient touched/hugged by loved ones? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 45 | 1 | 46 |
| % within model | 97.8 | 2.2 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 29 | 1 | 30 |
| % within model | 96.7 | 3.3 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 27 | 2 | 29 |
| % within model | 93.1 | 6.9 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 21 | 0 | 21 |
| % within model | 100.0 | 0.0 | 100.0 |
| Total | |||
| Count | 122 | 4 | 126 |
| % within model | 96.8 | 3.2 | 100.0 |
| Service model | Did the patient attend any important events? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 6 | 40 | 46 |
| % within model | 13.0 | 87.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 3 | 28 | 31 |
| % within model | 9.7 | 90.3 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 4 | 23 | 27 |
| % within model | 14.8 | 85.2 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 0 | 21 | 21 |
| % within model | 0.0 | 100.0 | 100.0 |
| Total | |||
| Count | 13 | 112 | 125 |
| % within model | 10.4 | 89.6 | 100.0 |
| Service model | Were all of the patient’s health-care costs taken care of? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 44 | 2 | 46 |
| % within model | 95.7 | 4.3 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 27 | 4 | 31 |
| % within model | 87.1 | 12.9 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 28 | 2 | 30 |
| % within model | 93.3 | 6.7 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 20 | 1 | 21 |
| % within model | 95.2 | 4.8 | 100.0 |
| Total | |||
| Count | 119 | 9 | 128 |
| % within model | 93.0 | 7.0 | 100.0 |
| Service model | Did the patient say goodbye to loved ones? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 20 | 24 | 44 |
| % within model | 45.5 | 54.5 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 17 | 14 | 31 |
| % within model | 54.8 | 45.2 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 14 | 14 | 28 |
| % within model | 50.0 | 50.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 12 | 8 | 20 |
| % within model | 60.0 | 40.0 | 100.0 |
| Total | |||
| Count | 63 | 60 | 123 |
| % within model | 51.2 | 48.8 | 100.0 |
| Service model | Patient visited by religious/spiritual advisor | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 14 | 32 | 46 |
| % within model | 30.4 | 69.6 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 7 | 23 | 30 |
| % within model | 23.3 | 76.7 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 9 | 21 | 30 |
| % within model | 30.0 | 70.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 6 | 15 | 21 |
| % within model | 28.6 | 71.4 | 100.0 |
| Total | |||
| Count | 36 | 91 | 127 |
| % within model | 28.3 | 71.7 | 100.0 |
| Service model | Did the patient have a spiritual service/ceremony before death? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 6 | 40 | 46 |
| % within model | 13.0 | 87.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 1 | 29 | 30 |
| % within model | 3.3 | 96.7 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 7 | 23 | 30 |
| % within model | 23.3 | 76.7 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 5 | 16 | 21 |
| % within model | 23.8 | 76.2 | 100.0 |
| Total | |||
| Count | 19 | 108 | 127 |
| % within model | 15.0 | 85.0 | 100.0 |
| Service model | Ventilator or dialysis used to prolong patient’s life | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 3 | 43 | 46 |
| % within model | 6.5 | 93.5 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 0 | 29 | 29 |
| % within model | 0.0 | 100.0 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 2 | 28 | 30 |
| % within model | 6.7 | 93.3 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 1 | 20 | 21 |
| % within model | 4.8 | 95.2 | 100.0 |
| Total | |||
| Count | 6 | 120 | 126 |
| % within model | 4.8 | 95.2 | 100.0 |
| Service model | Did the patient clear up any bad feelings with others? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 6 | 20 | 26 |
| % within model | 23.1 | 76.9 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 9 | 14 | 23 |
| % within model | 39.1 | 60.9 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 6 | 13 | 19 |
| % within model | 31.6 | 68.4 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 4 | 14 | 18 |
| % within model | 22.2 | 77.8 | 100.0 |
| Total | |||
| Count | 25 | 61 | 86 |
| % within model | 29.1 | 70.9 | 100.0 |
| Service model | Funeral arrangements in order prior to death | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 23 | 23 | 46 |
| % within model | 50.0 | 50.0 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 17 | 14 | 31 |
| % within model | 54.8 | 45.2 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 12 | 18 | 30 |
| % within model | 40.0 | 60.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 10 | 11 | 21 |
| % within model | 47.6 | 52.4 | 100.0 |
| Total | |||
| Count | 62 | 66 | 128 |
| % within model | 48.4 | 51.6 | 100.0 |
| Service model | Did the patient discuss wishes for EOLC with his/her doctor? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 34 | 12 | 46 |
| % within model | 73.9 | 26.1 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 23 | 7 | 30 |
| % within model | 76.7 | 23.3 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 17 | 12 | 29 |
| % within model | 58.6 | 41.4 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 14 | 6 | 20 |
| % within model | 70.0 | 30.0 | 100.0 |
| Total | |||
| Count | 88 | 37 | 125 |
| % within model | 70.4 | 29.6 | 100.0 |
| Service model | Where did the patient die? | Total | |||||
|---|---|---|---|---|---|---|---|
| Patient’s own home | Surrogate’s home | Other home | Hospital | Inpatient hospice | Nursing home | ||
| Q1: Large providers, 24-hour services | |||||||
| Count | 24 | 0 | 0 | 9 | 10 | 3 | 46 |
| % within model | 52.2 | 0.0 | 0.0 | 19.6 | 21.7 | 6.5 | 100.0 |
| Q2: Small providers, 24-hour services | |||||||
| Count | 23 | 1 | 2 | 1 | 4 | 0 | 31 |
| % within model | 74.2 | 3.2 | 6.5 | 3.2 | 12.9 | 0.0 | 100.0 |
| Q3: Large providers, not 24-hour services | |||||||
| Count | 21 | 0 | 1 | 1 | 7 | 0 | 30 |
| % within model | 70.0 | 0.0 | 3.3 | 3.3 | 23.3 | 0.0 | 100.0 |
| Q4: Small providers, not 24-hour services | |||||||
| Count | 14 | 0 | 1 | 0 | 7 | 0 | 22 |
| % within model | 63.6 | 0.0 | 4.5 | 0.0 | 31.8 | 0.0 | 100.0 |
| Total | |||||||
| Count | 82 | 1 | 4 | 11 | 28 | 3 | 129 |
| % within model | 63.6 | 0.8 | 3.1 | 8.5 | 21.7 | 2.3 | 100.0 |
| Service model | Was anyone present at the moment of death? | Total | |
|---|---|---|---|
| Yes | No | ||
| Q1: Large providers, 24-hour services | |||
| Count | 42 | 3 | 45 |
| % within model | 93.3 | 6.7 | 100.0 |
| Q2: Small providers, 24-hour services | |||
| Count | 28 | 1 | 29 |
| % within model | 96.6 | 3.4 | 100.0 |
| Q3: Large providers, not 24-hour services | |||
| Count | 29 | 1 | 30 |
| % within model | 96.7 | 3.3 | 100.0 |
| Q4: Small providers, not 24-hour services | |||
| Count | 17 | 3 | 20 |
| % within model | 85.0 | 15.0 | 100.0 |
| Total | |||
| Count | 116 | 8 | 124 |
| % within model | 93.5 | 6.5 | 100.0 |
| Service model | Patient’s status at moment before death | Total | ||
|---|---|---|---|---|
| Awake | Asleep | In a coma/unconscious | ||
| Q1: Large providers, 24-hour services | ||||
| Count | 7 | 14 | 20 | 41 |
| % within model | 17.1 | 34.1 | 48.8 | 100.0 |
| Q2: Small providers, 24-hour services | ||||
| Count | 4 | 13 | 11 | 28 |
| % within model | 14.3 | 46.4 | 39.3 | 100.0 |
| Q3: Large providers, not 24-hour services | ||||
| Count | 7 | 9 | 13 | 29 |
| % within model | 24.1 | 31.0 | 44.8 | 100.0 |
| Q4: Small providers, not 24-hour services | ||||
| Count | 3 | 7 | 10 | 20 |
| % within model | 15.0 | 35.0 | 50.0 | 100.0 |
| Total | ||||
| Count | 21 | 43 | 54 | 118 |
| % within model | 17.8 | 36.4 | 45.8 | 100.0 |
Appendix 15 Responses to Quality of Dying and Death questionnaire questions, part B, by service model
| QODD question (0 = terrible, 10 = almost perfect) | Service model | Total | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1: Large providers, 24-hour services | Q2: Small providers, 24-hour services | Q3: Large providers, not 24-hour services | Q4: Small providers, not 24-hour services | ||||||||||||
| n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | n | Mean (SD) | Median (range) | |
| Pain | 44 | 6.0 (3.4) | 7.0 (0–10) | 30 | 7.7 (3.0) | 8.5 (0–10) | 31 | 5.5 (3.4) | 6.0 (0–10) | 21 | 7.8 (2.3) | 8.0 (1–10) | 126 | 6.6 (3.3) | 8.0 (0–10) |
| Control | 44 | 5.8 (3.2) | 6.0 (0–10) | 29 | 7.0 (3.3) | 8.0 (0–10) | 28 | 4.8 (3.2) | 5.0 (0–10) | 20 | 6.9 (2.7) | 7.5 (1–10) | 121 | 6.0 (3.2) | 7.0 (0–10) |
| Self-feeding | 41 | 5.0 (3.4) | 5.0 (0–10) | 26 | 6.2 (3.1) | 6.5 (0–10) | 27 | 3.1 (3.2) | 2.0 (0–10) | 20 | 5.8 (3.1) | 6.5 (0–10) | 114 | 5.0 (3.4) | 5.0 (0–10) |
| Bladder/bowel control | 41 | 4.1 (3.3) | 4.0 (0–10) | 30 | 5.7 (3.6) | 6.5 (0–10) | 28 | 3.4 (3.6) | 2.0 (0–10) | 19 | 5.3 (3.3) | 6.0 (0–10) | 118 | 4.5 (3.5) | 5.0 (0–10) |
| Breathing | 45 | 5.5 (3.2) | 6.0 (0–10) | 31 | 7.2 (2.9) | 8.0 (0–10) | 30 | 3.8 (3.3) | 3.5 (0–10) | 19 | 7.4 (2.9) | 8.0 (0–10) | 125 | 5.8 (3.4) | 7.0 (0–10) |
| At peace with dying | 35 | 5.2 (3.7) | 6.0 (0–10) | 26 | 6.2 (3.9) | 8.0 (0–10) | 20 | 5.5 (3.5) | 6.0 (0–10) | 16 | 6.8 (2.9) | 7.5 (1–10) | 97 | 5.8 (3.6) | 7.0 (0–10) |
| Unafraid of dying | 32 | 5.9 (3.3) | 6.5 (0–10) | 25 | 5.9 (3.7) | 8.0 (0–10) | 22 | 5.3 (3.9) | 6.0 (0–10) | 18 | 7.2 (2.8) | 8.0 (1–10) | 97 | 6.0 (3.5) | 7.0 (0–10) |
| Laugh and smile | 39 | 5.2 (3.2) | 5.0 (0–10) | 29 | 6.4 (2.9) | 7.0 (0–10) | 28 | 5.4 (3.4) | 5.0 (0–10) | 18 | 6.6 (1.9) | 7.0 (2–10) | 114 | 5.8 (3.0) | 6.0 (0–10) |
| Energy | 43 | 3.1 (2.7) | 2.0 (0–10) | 29 | 3.6 (3.3) | 3.0 (0–10) | 28 | 2.0 (2.2) | 1.0 (0–8) | 20 | 2.6 (2.9) | 2.0 (0–10) | 120 | 2.9 (2.8) | 2.0 (0–10) |
| Worried about strain on loved ones | 34 | 4.7 (2.9) | 5.0 (0–10) | 25 | 5.0 (3.0) | 5.0 (0–10) | 23 | 4.1 (3.5) | 3.0 (0–10) | 17 | 5.2 (2.9) | 5.0 (1–10) | 99 | 4.7 (3.0) | 5.0 (0–10) |
| Dignity and self-respect | 41 | 5.2 (3.1) | 5.0 (0–10) | 30 | 7.4 (2.8) | 8.0 (0–10) | 27 | 4.9 (3.9) | 6.0 (0–10) | 21 | 6.3 (3.5) | 8.0 (0–10) | 119 | 5.9 (3.4) | 7.0 (0–10) |
| Time with spouse/partner | 31 | 7.7 (2.8) | 8.0 (0–10) | 15 | 8.9 (2.6) | 10.0 (0–10) | 25 | 7.9 (3.0) | 9.0 (0–10) | 13 | 8.8 (1.0) | 9.0 (7–10) | 84 | 8.2 (2.7) | 9.0 (0–10) |
| Time with children | 32 | 7.4 (2.9) | 8.0 (0–10) | 25 | 8.4 (2.1) | 9.0 (0–10) | 26 | 7.1 (3.8) | 9.0 (0–10) | 19 | 8.5 (2.3) | 9.0 (1–10) | 102 | 7.8 (2.9) | 9.0 (0–10) |
| Time with other family/friends | 40 | 6.7 (3.1) | 8.0 (0–10) | 30 | 8.1 (1.9) | 8.0 (2–10) | 29 | 6.7 (3.4) | 8.0 (0–10) | 19 | 7.8 (2.0) | 8.0 (3–10) | 118 | 7.2 (2.8) | 8.0 (0–10) |
| Time alone | 39 | 6.7 (2.9) | 8.0 (0–10) | 29 | 8.3 (2.4) | 9.0 (0–10) | 27 | 6.6 (3.6) | 7.0 (0–10) | 19 | 7.6 (3.0) | 9.0 (2–10) | 114 | 7.2 (3.0) | 8.0 (0–10) |
| Time with pets | 16 | 6.0 (3.4) | 8.0 (0–10) | 14 | 7.7 (2.4) | 8.0 (2–10) | 7 | 5.3 (3.3) | 5.0 (0–10) | 7 | 8.3 (2.1) | 8.0 (4–10) | 44 | 6.8 (3.0) | 8.0 (0–10) |
| Meaning and purpose in life | 25 | 7.4 (2.4) | 8.0 (2–10) | 21 | 8.3 (2.3) | 9.0 (0–10) | 22 | 6.0 (3.6) | 7.5 (0–10) | 13 | 6.8 (2.7) | 8.0 (2–10) | 81 | 7.2 (2.9) | 8.0 (0–10) |
| Touched/hugged by loved ones | 39 | 8.0 (2.4) | 9.0 (0–10) | 30 | 9.0 (2.0) | 10.0 (0–10) | 28 | 7.7 (3.3) | 9.0 (0–10) | 19 | 9.3 (1.4) | 10.0 (4–10) | 116 | 8.4 (2.5) | 9.0 (0–10) |
| Attended important events | 25 | 6.2 (3.3) | 6.0 (0–10) | 22 | 5.9 (3.5) | 6.0 (0–10) | 20 | 4.5 (3.3) | 5.0 (0–10) | 13 | 6.8 (3.5) | 8.0 (0–10) | 80 | 5.8 (3.4) | 5.0 (0–10) |
| Health-care costs taken care of | 40 | 8.7 (2.4) | 10.0 (0–10) | 31 | 8.4 (2.6) | 10.0 (0–10) | 29 | 7.6 (3.5) | 9.0 (0–10) | 16 | 9.1 (1.3) | 10.0 (6–10) | 116 | 8.4 (2.7) | 10.0 (0–10) |
| Said goodbye to loved ones | 31 | 6.4 (3.4) | 8.0 (0–10) | 28 | 7.6 (3.3) | 8.5 (0–10) | 24 | 4.6 (4.3) | 4.5 (0–10) | 17 | 7.5 (2.9) | 8.0 (2–10) | 100 | 6.5 (3.7) | 8.0 (0–10) |
| Visit(s) from religious/spiritual advisors | 26 | 7.7 (2.9) | 9.0 (0–10) | 25 | 8.7 (2.2) | 10.0 (0–10) | 25 | 7.3 (3.3) | 9.0 (0–10) | 16 | 8.5 (2.0) | 9.0 (3–10) | 92 | 8.0 (2.7) | 9.0 (0–10) |
| Spiritual service/ceremony | 24 | 7.2 (3.0) | 8.0 (0–10) | 24 | 8.6 (2.4) | 10.0 (0–10) | 25 | 7.2 (3.4) | 9.0 (0–10) | 17 | 8.5 (1.8) | 9.0 (4–10) | 90 | 7.8 (2.8) | 9.0 (0–10) |
| Ventilator or dialysis used | 15 | 7.9 (3.3) | 10.0 (0–10) | 22 | 8.1 (2.9) | 9.0 (0–10) | 18 | 6.1 (4.0) | 7.5 (0–10) | 12 | 8.8 (1.7) | 9.0 (4–10) | 67 | 7.7 (3.2) | 9.0 (0–10) |
| Cleared up bad feelings with others | 22 | 6.6 (3.5) | 8.5 (0–10) | 21 | 8.3 (2.6) | 10.0 (0–10) | 14 | 7.2 (3.6) | 9.0 (0–10) | 13 | 8.9 (1.7) | 10.0 (5–10) | 70 | 7.7 (3.1) | 9.0 (0–10) |
| Funeral arrangements in order | 32 | 7.3 (2.7) | 8.0 (0–10) | 27 | 8.2 (2.8) | 9.0 (0–10) | 25 | 6.9 (3.2) | 8.0 (0–10) | 17 | 9.0 (1.4) | 10.0 (5–10) | 101 | 7.7 (2.7) | 9.0 (0–10) |
| EOLC wishes | 34 | 8.1 (2.4) | 9.0 (0–10) | 27 | 8.7 (1.8) | 10.0 (4–10) | 26 | 6.2 (3.6) | 6.5 (0–10) | 20 | 8.4 (2.3) | 9.0 (1–10) | 107 | 7.9 (2.8) | 9.0 (0–10) |
| Place of death | 45 | 7.9 (3.1) | 9.0 (0–10) | 31 | 9.5 (1.9) | 10.0 (0–10) | 27 | 7.8 (3.6) | 10.0 (0–10) | 20 | 9.6 (1.2) | 10.0 (5–10) | 123 | 8.5 (2.8) | 10.0 (0–10) |
| Presence of anyone at moment of death | 36 | 7.9 (3.2) | 9.0 (0–10) | 30 | 9.7 (0.6) | 10.0 (8–10) | 25 | 7.8 (3.0) | 9.0 (0–10) | 20 | 9.5 (1.1) | 10.0 (6–10) | 111 | 8.7 (2.5) | 10.0 (0–10) |
| Status at moment before death | 29 | 6.7 (3.5) | 8.0 (0–10) | 29 | 9.1 (1.6) | 10.0 (3–10) | 25 | 6.2 (3.8) | 8.0 (0–10) | 18 | 9.1 (1.3) | 10.0 (6–10) | 101 | 7.7 (3.1) | 9.0 (0–10) |
| Quality of patient’s life during last 7 days of life | 42 | 3.9 (3.6) | 3.0 (0–10) | 30 | 6.1 (3.5) | 7.0 (0–10) | 30 | 4.4 (3.8) | 4.5 (0–10) | 19 | 4.5 (3.4) | 5.0 (0–10) | 121 | 4.7 (3.7) | 5.0 (0–10) |
| Quality of patient’s moment of death | 36 | 6.9 (3.3) | 8.0 (0–10) | 31 | 8.3 (2.7) | 10.0 (0–10) | 28 | 6.2 (4.0) | 8.0 (0–10) | 18 | 8.9 (1.5) | 9.5 (4–10) | 113 | 7.4 (3.3) | 9.0 (0–10) |
Appendix 16 Variables used in the analysis of the Quality of Dying and Death questionnaire scores and number of observations
Patient sociodemographic and clinical characteristics (gathered at recruitment):
-
gender (dichotomous; n = 128)
-
age in years at recruitment (continuous; n = 127)
-
single (dichotomous; n = 126)
-
in relationship/married (dichotomous; n = 126)
-
living alone (dichotomous; n = 128)
-
highest education level (ordinal; n = 104)
-
educated to university level (dichotomous; n = 104)
-
had cancer (dichotomous; n = 125).
Carer sociodemographic characteristics (gathered at recruitment):
-
gender (dichotomous; n = 128)
-
age in years at recruitment (continuous; n = 121)
-
is patient’s partner (dichotomous; n = 127)
-
living with patient (dichotomous; n = 128)
-
working (dichotomous; n = 123)
-
highest education level (ordinal; n = 114)
-
educated to university level (dichotomous; n = 114).
Place of death:
-
patient died at home (dichotomous; n = 128)
-
patient died in hospice (dichotomous; n = 128)
-
patient died in hospital (dichotomous; n = 128)
-
patient achieved PPOD (dichotomous; n = 102).
Features around death (from QODD):
-
How long before death was patient aware of dying (ordinal; n = 119) (1 = never, 2 = 1 week, 3 = 2–4 weeks, 4 = 2–6 months, 5 = 6–12 months)?
-
Patient ever talked comprehensibly in last 7 days (dichotomous; n = 128).
-
Number of days carer saw patient in last 7 days (continuous; n = 127).
Temporal:
-
number of days from patient recruitment to death (i.e. length of hospice involvement with patient) (continuous; n = 128)
-
number of days from patient’s death to date that carer responded to QODD (continuous; n = 127).
Appendix 17 Progress of patients through the study and provision of Ambulatory and Home Care Records (service use data), by model and hospice at home
| Service model | Patient/AHCR status, n (%) | Total, N (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Alive, no AHCRs | Alive with AHCR(s) | Died at known date, no AHCRs | Died at known date with AHCR(s) | Died at unknown date, no AHCRs | Died at unknown date with AHCR(s) | Withdrew, no AHCRs | Withdrew with AHCR(s) | ||
| Q1: Large providers, 24-hour services | 1 (1.0) | 18 (17.5) | 10 (9.7) | 68 (66.0) | 1 (1.0) | 0 (0.0) | 1 (1.0) | 4 (3.9) | 103 (100) |
| Q2: Small providers, 24-hour services | 0 (0.0) | 6 (7.5) | 40 (50.0) | 27 (33.8) | 3 (3.8) | 2 (2.5) | 0 (0.0) | 2 (2.5) | 80 (100) |
| Q3: Large providers, not 24-hour services | 1 (1.2) | 2 (2.5) | 27 (33.3) | 47 (58.9) | 1 (1.2) | 3 (3.7) | 0 (0.0) | 0 (0.0) | 81 (100) |
| Q4: Small providers, not 24-hour services | 3 (4.0) | 5 (6.7) | 29 (38.7) | 36 (48.0) | 0 (0.0) | 1 (1.3) | 1 (1.3) | 0 (0.0) | 75 (100) |
| Total | 5 (1.5) | 31 (9.1) | 106 (31.3) | 178 (52.5) | 5 (1.5) | 6 (1.6) | 2 (0.6) | 6 (1.8) | 339 (100) |
| HAH | Patient/AHCR status, n (%) | Total, N (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Alive, no AHCRs | Alive with AHCR(s) | Died at known date, no AHCRs | Died at known date with AHCR(s) | Died at unknown date, no AHCRs | Died at unknown date with AHCR(s) | Withdrew, no AHCRs | Withdrew with AHCR(s) | ||
| Model 1: Large providers, 24-hour services | |||||||||
| Acacia | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (66.7) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (100.0) |
| Camellia | 0 (0.0) | 0 (0.0) | 6 (50.0) | 6 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 12 (100.0) |
| Echinacea | 0 (0.0) | 5 (22.7) | 1 (4.5) | 14 (63.6) | 0 (0.0) | 0 (0.0) | 1 (4.5) | 1 (4.5) | 22 (100.0) |
| Peony | 1 (1.5) | 13 (19.7) | 3 (4.5) | 46 (69.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (4.5) | 66 (100.0) |
| Model 2: Small providers, 24-hour services | |||||||||
| Dahlia | 0 (0.0) | 0 (0.0) | 17 (81.0) | 3 (14.3) | 1 (4.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 21 (100.0) |
| Gardenia | 0 (0.0) | 1 (6.3) | 4 (25.0) | 8 (50.0) | 0 (0.0) | 1 (6.3) | 0 (0.0) | 2 (12.5) | 16 (100.0) |
| Lavender | 0 (0.0) | 3 (12.5) | 8 (33.3) | 10 (41.7) | 2 (8.3) | 1 (4.2) | 0 (0.0) | 0 (0.0) | 24 (100.0) |
| Violet | 0 (0.0) | 2 (10.5) | 11 (57.9) | 6 (31.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 19 (100.0) |
| Model 3: Large providers, not 24-hour services | |||||||||
| Wisteria | 1 (1.2) | 2 (2.5) | 27 (33.3) | 47 (58.0) | 1 (1.2) | 3 (3.7) | 0 (0.0) | 0 (0.0) | 81 (100.0) |
| Model 4: Small providers, not 24-hour services | |||||||||
| Hyacinth | 1 (3.2) | 1 (3.2) | 16 (51.6) | 13 (41.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 31 (100.0) |
| Marigold | 2 (5.9) | 2 (5.9) | 12 (35.3) | 16 (47.1) | 0 (0.0) | 1 (2.9) | 1 (2.9) | 0 (0.0) | 34 (100.0) |
| Xyris | 0 (0.0) | 2 (20.0) | 1 (10.0) | 7 (70.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (100.0) |
| Total | 5 (1.5) | 31 (9.1) | 106 (31.3) | 178 (52.5) | 5 (1.5) | 6 (1.8) | 2 (0.6) | 6 (1.8) | 339 (100.0) |
Appendix 18 Number of patients for whom there was Ambulatory and Home Care Record availability, by hospice at home service and days before death
| Service model | Number of patients recruited | Number (%) who died during study with known DOD and at least one AHCR | Number of days before death | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–7 | 8–14 | 15–21 | 22–28 | 29–92 | 93–182 | ≥ 183 | |||
| Q1: Large providers, 24-hour services | |||||||||
| Acacia | 3 | 2 (66.7) | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| Camellia | 12 | 6 (50.0) | 2 | 5 | 4 | 4 | 2 | 1 | 0 |
| Echinacea | 22 | 14 (63.6) | 8 | 11 | 13 | 13 | 12 | 8 | 3 |
| Peony | 66 | 46 (69.7) | 32 | 37 | 39 | 40 | 39 | 22 | 5 |
| Total | 103 | 68 (66.0) | 44 | 55 | 56 | 57 | 53 | 31 | 8 |
| Q2: Small providers, 24-hour services | |||||||||
| Dahlia | 21 | 3 (14.3) | 3 | 3 | 2 | 0 | 0 | 0 | 0 |
| Gardenia | 16 | 8 (50.0) | 7 | 7 | 6 | 6 | 4 | 2 | 0 |
| Lavender | 24 | 10 (41.7) | 5 | 5 | 6 | 4 | 5 | 3 | 0 |
| Violet | 19 | 6 (31.6) | 3 | 3 | 1 | 2 | 2 | 1 | 0 |
| Total | 80 | 27 (33.8) | 18 | 18 | 15 | 12 | 11 | 6 | 0 |
| Q3: Large providers, not 24-hour services | |||||||||
| Wisteria | 81 | 47 (58.0) | 32 | 35 | 16 | 15 | 17 | 6 | 5 |
| Total | 81 | 47 (58.0) | 32 | 35 | 16 | 15 | 17 | 6 | 5 |
| Q4: Small providers, not 24-hour services | |||||||||
| Hyacinth | 31 | 13 (41.9) | 10 | 11 | 6 | 4 | 4 | 1 | 1 |
| Marigold | 34 | 16 (47.1) | 9 | 10 | 8 | 6 | 6 | 2 | 0 |
| Xyris | 10 | 7 (70.0) | 4 | 5 | 6 | 6 | 5 | 3 | 0 |
| Total | 75 | 36 (48.0) | 23 | 26 | 20 | 16 | 15 | 6 | 1 |
| Total | 339 | 178 (52.5) | 117 | 134 | 107 | 100 | 96 | 49 | 14 |
Appendix 19 Ambulatory and Home Care Record service use data available, by service model and days before death
| Service model | Number of patients recruited | Number (% of all recruited) who died during study with a known DOD and at least one AHCR | Number of days before death | Total, N (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0–7 | 8–14 | 15–21 | 22–28 | 29–92 | 93–182 | ≥ 183 | ||||
| Q1: Large providers, 24-hour services | 108 | 68 (66.0) | 46 | 56 | 55 | 56 | 52 | 31 | 8 | 304 (49.6) |
| Q2: Small providers, 24-hour services | 80 | 27 (33.8) | 17 | 18 | 15 | 11 | 11 | 6 | 0 | 78 (12.7) |
| Q3: Large providers, not 24-hour services | 81 | 47 (58.0) | 32 | 34 | 16 | 15 | 17 | 6 | 5 | 125 (20.4) |
| Q4: Small providers, not 24-hour services | 75 | 36 (48.0) | 23 | 25 | 20 | 16 | 15 | 6 | 1 | 106 (17.3) |
| Total | 339 | 178 (52.5) | 118 | 133 | 106 | 98 | 95 | 49 | 14 | 613 |
Appendix 20 Use per day of services by three time periods (0–14, 15–28, > 28 days) and service model
| Service use item, utilisation per day | Number of days before death | Service model | Total | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1: Large providers, 24-hour services | Q2: Small providers, 24-hour services | Q3: Large providers, not 24-hour services | Q4: Small providers, not 24-hour services | |||||||||||||
| n (n with zero) | Median, maximum | Mean (SD) | n (n with zero) | Median, maximum | Mean (SD) | n (n with zero) | Median, maximum | Mean (SD) | n (n with zero) | Median, maximum | Mean (SD) | N (N with zero) | Median, maximum | Mean (SD) | ||
| In home | ||||||||||||||||
| Community nursing visitsa | 0–14 | 50 (14) | 0.14, 2.00 | 0.38 (0.53) | 17 (1) | 0.71, 2.69 | 0.81 (0.67) | 34 (5) | 0.39, 1.86 | 0.53 (0.47) | 25 (4) | 0.29, 4.14 | 0.53 (0.84) | 126 (24) | 0.29, 4.14 | 0.51 (0.62) |
| 15–28 | 59 (19) | 0.07, 2.00 | 0.24 (0.42) | 16 (1) | 0.69, 2.86 | 0.83 (0.76) | 16 (0) | 0.20, 1.21 | 0.38 (0.40) | 22 (6) | 0.19, 8.50 | 0.86 (1.93) | 113 (26) | 0.17, 8.50 | 0.46 (0.98) | |
| 29–92 | 52 (9) | 0.07, 1.00 | 0.16 (0.24) | 11 (0) | 0.43, 2.86 | 0.77 (0.85) | 17 (0) | 0.15, 0.42 | 0.19 (0.09) | 15 (3) | 0.07, 8.50 | 0.82 (2.16) | 95 (12) | 0.13, 8.50 | 0.34 (0.94) | |
| Hospice nursing visitsa | 0–14 | 52 (19) | 0.07, 6.33 | 0.45 (1.00) | 17 (0) | 2.64, 5.80 | 2.36 (1.74) | 34 (5) | 0.25, 6.29 | 0.60 (1.19) | 25 (1) | 0.50, 6.00 | 0.87 (1.24) | 128 (25) | 0.29, 6.33 | 0.83 (1.35) |
| 15–28 | 59 (21) | 0.03, 4.59 | 0.29 (0.85) | 16 (2) | 2.36, 6.43 | 2.51 (2.06) | 16 (1) | 0.14, 0.71 | 0.18 (0.18) | 22 (1) | 0.36, 3.86 | 0.75 (0.97) | 113 (25) | 0.13, 6.43 | 0.68 (1.31) | |
| 29–92 | 52 (13) | 0.05, 2.10 | 0.16 (0.45) | 11 (0) | 1.86, 6.12 | 2.33 (1.73) | 17 (0) | 0.29, 0.57 | 0.27 (0.14) | 15 (2) | 0.29, 2.11 | 0.56 (0.71) | 95 (15) | 0.08, 6.12 | 0.49 (0.99) | |
| Personal carer visitsb | 0–14 | 52 (38) | 0.00, 5.51 | 0.71 (1.40) | 17 (12) | 0.00, 4.00 | 0.60 (1.20) | 34 (13) | 0.57, 4.00 | 1.22 (1.41) | 25 (15) | 0.00, 4.00 | 0.62 (1.17) | 128 (78) | 0.00, 5.51 | 0.81 (1.35) |
| 15–28 | 59 (37) | 0.00, 7.69 | 0.89 (1.60) | 16 (13) | 0.00, 2.86 | 0.36 (0.85) | 16 (3) | 1.02, 4.00 | 1.52 (1.53) | 22 (13) | 0.00, 8.00 | 0.95 (2.02) | 113 (66) | 0.00, 8.00 | 0.92 (1.61) | |
| 29–92 | 52 (32) | 0.00, 4.26 | 0.55 (1.23) | 11 (8) | 0.00, 4.30 | 0.59 (1.37) | 17 (5) | 0.67, 4.00 | 1.26 (1.41) | 15 (12) | 0.00, 1.00 | 0.15 (0.33) | 95 (57) | 0.00, 4.30 | 0.62 (1.22) | |
| Total community and hospice nursing and personal caring visits | 0–14 | 49 (8) | 0.81, 6.50 | 1.58 (1.93) | 17 (0) | 3.76, 6.63 | 3.77 (1.34) | 34 (3) | 2.18, 6.36 | 2.36 (1.80) | 25 (0) | 1.71, 6.14 | 2.02 (1.72) | 125 (11) | 1.76, 6.63 | 2.18 (1.90) |
| 15–28 | 58 (10) | 0.35, 8.42 | 1.45 (2.09) | 16 (0) | 3.46, 7.07 | 3.70 (2.02) | 16 (0) | 1.31, 5.50 | 2.08 (1.91) | 22 (0) | 1.56, 10.50 | 2.57 (3.02) | 112 (10) | 1.14, 10.50 | 2.08 (2.38) | |
| 29–92 | 52 (4) | 0.22, 5.59 | 0.88 (1.47) | 11 (0) | 2.37, 6.93 | 3.69 (1.99) | 17 (0) | 1.10, 4.61 | 1.73 (1.42) | 15 (0) | 0.86, 10.50 | 1.53 (2.60) | 95 (4) | 0.43, 10.50 | 1.46 (1.93) | |
| GP home visits | 0–14 | 52 (25) | 0.01, 0.79 | 0.07 (0.13) | 17 (3) | 0.07, 0.29 | 0.11 (0.09) | 34 (10) | 0.07, 0.71 | 0.10 (0.13) | 25 (7) | 0.07, 0.29 | 0.08 (0.08) | 128 (45) | 0.07, 0.79 | 0.08 (0.11) |
| 15–28 | 59 (26) | 0.03, 0.21 | 0.04 (0.06) | 16 (6) | 0.04, 0.21 | 0.05 (0.06) | 16 (2) | 0.04, 0.12 | 0.05 (0.04) | 22 (11) | 0.01, 0.14 | 0.04 (0.05) | 113 (45) | 0.03, 0.21 | 0.05 (0.05) | |
| 29–92 | 52 (22) | 0.00, 0.20 | 0.02 (0.04) | 11 (3) | 0.05, 0.07 | 0.04 (0.03) | 17 (5) | 0.03, 0.09 | 0.03 (0.03) | 15 (7) | 0.01, 0.14 | 0.03 (0.04) | 95 (37) | 0.01, 0.20 | 0.03 (0.04) | |
| Other health/social care professional visits | 0–14 | 53 (43) | 0.00, 0.16 | 0.01 (0.03) | 17 (14) | 0.00, 0.21 | 0.03 (0.06) | 34 (24) | 0.00, 0.29 | 0.04 (0.08) | 25 (20) | 0.00, 0.07 | 0.01 (0.03) | 129 (101) | 0.00, 0.29 | 0.02 (0.05) |
| 15–28 | 59 (47) | 0.00, 0.13 | 0.01 (0.03) | 16 (15) | 0.00, 0.21 | 0.01 (0.06) | 16 (8) | 0.01, 0.29 | 0.04 (0.08) | 22 (15) | 0.00, 0.15 | 0.02 (0.04) | 113 (85) | 0.00, 0.29 | 0.02 (0.05) | |
| 29–92 | 52 (34) | 0.00, 0.08 | 0.01 (0.02) | 11 (10) | 0.00, 0.05 | 0.00 (0.01) | 17 (4) | 0.03, 0.25 | 0.06 (0.07) | 15 (6) | 0.02, 0.07 | 0.02 (0.03) | 95 (54) | 0.00, 0.25 | 0.02 (0.04) | |
| Charity/voluntary visits | 0–14 | 54 (53) | 0.00, 0.05 | 0.00 (0.01) | 17 (16) | 0.00, 0.07 | 0.00 (0.02) | 34 (32) | 0.00, 0.29 | 0.01 (0.05) | 25 (20) | 0.00, 0.07 | 0.01 (0.03) | 130 (121) | 0.00, 0.29 | 0.01 (0.03) |
| 15–28 | 60 (59) | 0.00, 0.02 | 0.00 (0.00) | 16 (16) | 0.00, 0.00 | 0.00 (0.00) | 16 (15) | 0.00, 0.15 | 0.01 (0.04) | 22 (20) | 0.00, 0.07 | 0.01 (0.02) | 114 (110) | 0.00, 0.15 | 0.00 (0.02) | |
| 29–92 | 52 (50) | 0.00, 0.16 | 0.00 (0.02) | 11 (10) | 0.00, 0.21 | 0.02 (0.06) | 17 (16) | 0.00, 0.09 | 0.01 (0.03) | 15 (15) | 0.00, 0.00 | 0.00 (0.00) | 95 (91) | 0.00, 0.21 | 0.01 (0.03) | |
| Total inside-home visits | 0–14 | 51 (8) | 0.81, 6.67 | 1.61 (1.96) | 17 (0) | 3.97, 6.77 | 3.91 (1.33) | 34 (3) | 2.25, 6.43 | 2.51 (1.87) | 25 (0) | 1.86 6.21 | 2.13 (1.73) | 127 (11) | 1.86, 6.77 | 2.26 (1.95) |
| 15–28 | 58 (7) | 0.40, 8.49 | 1.51 (2.10 | 16 (0) | 3.50, 7.14 | 3.76 (2.04) | 16 (0) | 1.40, 5.57 | 2.19 (1.94) | 22 (0) | 1.64, 10.64 | 2.64 (3.04) | 112 (7) | 1.29, 10.64 | 2.15 (2.39) | |
| 29–92 | 52 (3) | 0.26, 5.63 | 0.91 (1.48) | 11 (0) | 2.50, 7.00 | 3.75 (1.99) | 17 (0) | 1.31, 4.63 | 1.82 (1.43) | 15 (0) | 0.93, 10.64 | 1.58 (2.63) | 95 (3) | 0.50, 10.64 | 1.51 (1.96) | |
| Outside home | ||||||||||||||||
| Total outside-home visitsc | 0–14 | 56 (32) | 0.00, 0.06 | 0.04 (0.21) | 18 (18) | 0.00, 0.00 | 0.00 (0.00) | 34 (27) | 0.00, 0.26 | 0.02 (0.06) | 25 (19) | 0.00, 0.29 | 0.02 (0.06) | 133 (96) | 0.00, 0.29 | 0.03 (0.06) |
| 15–28 | 61 (33) | 0.00, 0.06 | 0.04 (0.21) | 17 (15) | 0.00, 0.12 | 0.01 (0.03) | 16 (12) | 0.00, 0.36 | 0.05 (0.11) | 22 (16) | 0.00, 0.07 | 0.01 (0.02) | 116 (76) | 0.00, 0.36 | 0.03 (0.06) | |
| 29–92 | 52 (11) | 0.07, 0.07 | 0.07 (0.30) | 11 (8) | 0.00, 0.16 | 0.02 (0.05) | 17 (9) | 0.00, 0.43 | 0.10 (0.14) | 15 (6) | 0.02, 0.14 | 0.04 (0.05) | 95 (34) | 0.03, 0.43 | 0.07 (0.09) | |
| Overnight stays | ||||||||||||||||
| Inpatient hospital nights | 0–14 | 56 (41) | 0.00, 1.00 | 0.09 (0.21) | 18 (15) | 0.00, 0.58 | 0.09 (0.21) | 34 (26) | 0.00, 0.93 | 0.13 (0.26) | 25 (22) | 0.00, 0.63 | 0.06 (0.18) | 133 (104 | 0.00, 1.00 | 0.09 (0.22) |
| 15–28 | 61 (45) | 0.00, 1.00 | 0.08 (0.20) | 17 (16) | 0.00, 0.47 | 0.03 (0.11) | 16 (12) | 0.00, 0.47 | 0.07 (0.15) | 22 (19) | 0.00, 0.36 | (0.03 (0.09) | 116 (92) | 0.00, 1.00 | 0.06 (0.16) | |
| 29–92 | 52 (31) | 0.00, 0.80 | 0.06 (0.15) | 11 (10) | 0.00, 0.09 | 0.01 (0.03) | 17 (14) | 0.00, 0.16 | 0.02 (0.05) | 15 (11) | 0.00, 0.57 | 0.06 (0.15) | 95 (66) | 0.00, 0.80 | 0.05 (0.13) | |
| Inpatient hospice nights | 0–14 | 56 (44) | 0.00, 1.00 | 0.10 (0.26) | 18 (17) | 0.00, 0.14 | 0.01 (0.03) | 34 (26) | 0.00, 1.00 | 0.12 (0.27) | 25 (19) | 0.00, 0.93 | 0.11 (0.25) | 133 (106) | 0.00, 1.00 | 0.10 (0.24) |
| 15–28 | 61 (51) | 0.00, 1.0 | 0.08 (0.24) | 17 (16) | 0.00, 0.21 | 0.01 (0.05) | 16 (11) | 0.00, 0.79 | 0.14 (0.26) | 22 (18) | 0.00, 0.93 | (0.07 (0.21) | 116 (96) | 0.00, 1.00 | 0.08 (0.22) | |
| 29–92 | 52 (43) | 0.00, 0.45 | 0.02 (0.07) | 11 (8) | 0.00, 0.50 | 0.05 (0.15) | 17 (13) | 0.00, 0.33 | 0.03 (0.09) | 15 (12) | 0.00, 0.18 | (0.02 (0.05) | 95 (76) | 0.00, 0.50 | 0.03 (0.08) | |
| Inpatient care/nursing home nights | 0–14 | 56 (51) | 0.00, 0.66 | 0.03 (0.12) | 18 (18) | 0.00, 0.00 | 0.00 (0.00) | 34 (33) | 0.00, 0.34 | 0.01 (0.06) | 25 (25) | 0.00, 0.00 | 0.00 (0.00) | 133 (127) | 0.00, 0.66 | 0.02 (0.08) |
| 15–28 | 61 (56) | 0.00, 0.37 | 0.02 (0.07) | 17 (17) | 0.00, 0.00 | 0.00 (0.00) | 16 (15) | 0.00, 0.59 | 0.04 (0.15) | 22 (22) | 0.00, 0.00 | 0.00 (0.00) | 116 (110) | 0.00, 0.59 | 0.01 (0.07) | |
| 29–92 | 52 (49) | 0.00, 0.11 | 0.00 (0.02) | 11 (11) | 0.00, 0.00 | 0.00 (0.00) | 17 (16) | 0.00, 0.85 | 0.05 (0.21) | 15 (15) | 0.00, 0.00 | 0.00 (0.00) | 95 (91) | 0.00, 0.85 | 0.01 (0.09) | |
| Total inpatient nights | 0–14 | 56 (26) | 0.05, 1.00 | 0.22 (0.32) | 18 (14) | 0.00, 0.58 | 0.10 (0.21) | 34 (18) | 0.00, 1.00 | 0.26 (0.34) | 25 (16) | 0.00, 0.93 | 0.18 (0.28) | 133 (74) | 0.00, 1.00 | 0.20 (0.31) |
| 15–28 | 61 (33) | 0.00, 1.00 | 0.18 (0.30) | 17 (15) | 0.00, 0.47 | 0.04 (0.12) | 16 (7) | 0.05, 1.00 | 0.24 (0.32) | 22 (15) | 0.00, 0.93 | 0.10 (0.22) | 116 (70) | 0.00, 1.00 | 0.15 (0.27) | |
| 29–92 | 52 (24) | 0.01, 0.88 | 0.09 (0.16) | 11 (7) | 0.00, 0.50 | 0.06 (0.15) | 17 (9) | 0.00, 0.85 | 0.10 (0.21) | 15 (8) | 0.00, 0.57 | 0.08 (0.15) | 95 (48) | 0.00, 0.88 | 0.09 (0.17) | |
| Telephone calls | ||||||||||||||||
| Telephone calls with doctor | 0–14 | 56 (39) | 0.00, 0.24 | 0.02 (0.06) | 18 (7) | 0.07, 0.50 | 0.12 (0.16) | 33 (24) | 0.00, 0.29 | 0.05 (0.08) | 25 (10) | 0.07, 0.50 | 0.08 (0.11) | 132 (80) | 0.00, 0.50 | 0.05 (0.10) |
| 15–28 | 61 (40) | 0.00, 0.21 | 0.02 (0.04) | 17 (7) | 0.05, 0.29 | 0.06 (0.08) | 16 (9) | 0.00, 0.27 | 0.04 (0.08) | 22 (10) | 0.01, 0.29 | 0.05 (0.08) | 116 (66) | 0.00, 0.29 | 0.04 (0.06) | |
| 29–92 | 52 (22) | 0.01, 0.14 | 0.03 (0.04) | 11 (4) | 0.03, 0.29 | 0.07 (0.09 | 17 (7) | 0.03, 0.21 | 0.03 (0.05) | 15 (5) | 0.04, 0.29 | 0.05 (0.07) | 95 (38) | 0.02, 0.29 | 0.04 (0.05) | |
| Total telephone calls (doctors and other) | 0–14 | 56 (25) | 0.03, 1.36 | 0.13 (0.25) | 18 (3) | 0.31, 9.00 | 0.85 (2.06) | 34 (8) | 0.21, 2.14 | 0.46 (0.61) | 25 (5) | 0.24, 1.43 | 0.34 (0.34) | 133 (41) | 0.14, 9.00 | 0.35 (0.86) |
| 15–28 | 61 (19) | 0.06, 1.36 | 0.12 (0.24) | 17 (3) | 0.08, 1.43 | 0.27 (0.40) | 16 (4) | 0.18, 2.14 | 0.43 (0.65) | 22 (5) | 0.14, 0.86 | 0.22 (0.26) | 116 (31) | 0.07, 2.14 | 0.20 (0.36) | |
| 29–92 | 52 (3) | 0.07, 0.31 | 0.09 (0.07) | 11 (2) | 0.07, 2.00 | 0.46 (0.69) | 17 (0) | 0.20, 1.97 | 0.32 (0.45) | 15 (1) | 0.11, 0.57 | 0.18 (0.18) | 95 (6) | 0.08, 2.00 | 0.19 (0.33) | |
| Grand total formal care | ||||||||||||||||
| Total events (in home, out of home, nights, telephone calls) | 0–14 | 51 (0) | 1.09, 7.43 | 2.00 (1.93) | 17 (0) | 4.31, 12.86 | 4.88 (2.44) | 34 (0) | 2.71, 7.71 | 3.25 (1.94) | 25 (0) | 2.21, 6.71 | 2.68 (1.71) | 127 (0) | 2.36, 12.86 | 2.85 (2.16) |
| 15–28 | 58 (0) | 1.00, 8.58 | 1.85 (2.09) | 16 (0) | 4.13, 8.43 | 4.08 (2.20) | 16 (0) | 2.54, 7.71 | 2.91 (1.96) | 22 (0) | 2.04, 11.21 | 2.98 (3.06) | 112 (0) | 1.61, 11.21 | 2.54 (2.42) | |
| 29–92 | 52 (0) | 0.62, 5.77 | 1.16 (1.45) | 11 (0) | 4.50, 8.43 | 4.30 (2.08) | 17 (0) | 1.50, 6.22 | 2.35 (1.58) | 15 (0) | 1.07, 11.21 | 1.88 (2.72) | 95 (0) | 0.93, 11.21 | 1.85 (2.04) | |
| Informal care | ||||||||||||||||
| Informal care: total hours | 0–14 | 56 (18) | 2.79, 63.71 | 9.87 (13.30) | 18 (4) | 12.39, 48.00 | 16.16 (13.38) | 34 (0) | 24.00, 50.00 | 21.97 (9.78) | 25 (1) | 24.00, 66.00 | 27.79 (14.50) | 133 (23) | 20.00, 66.00 | 17.18 (14.46) |
| 15–28 | 61 (11) | 10.29, 32.43 | 11.06 (9.29) | 17 (3) | 12.00, 48.00 | 15.87 (13.60) | 16 (0) | 24.00, 44.00 | 19.96 (10.28) | 22 (0) | 24.00, 31.00 | 23.14 (6.02) | 116 (14) | 15.50, 48.00 | 15.28 (10.75) | |
| 29–92 | 52 (3) | 6.22, 56.00 | 10.05 (10.39) | 11 (1) | 22.00, 30.41 | 15.42 (12.41) | 11 (0) | 24.00, 42.00 | 20.82 (9.64) | 15 (1) | 24.00, 31.13 | 21.47 (8.78) | 95 (5) | 12.00, 56.00 | 14.40 (11.32) | |
Appendix 21 Box plots for hospice service use by individual hospice at home services
FIGURE 24.
Visits per day: nursing and social care. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
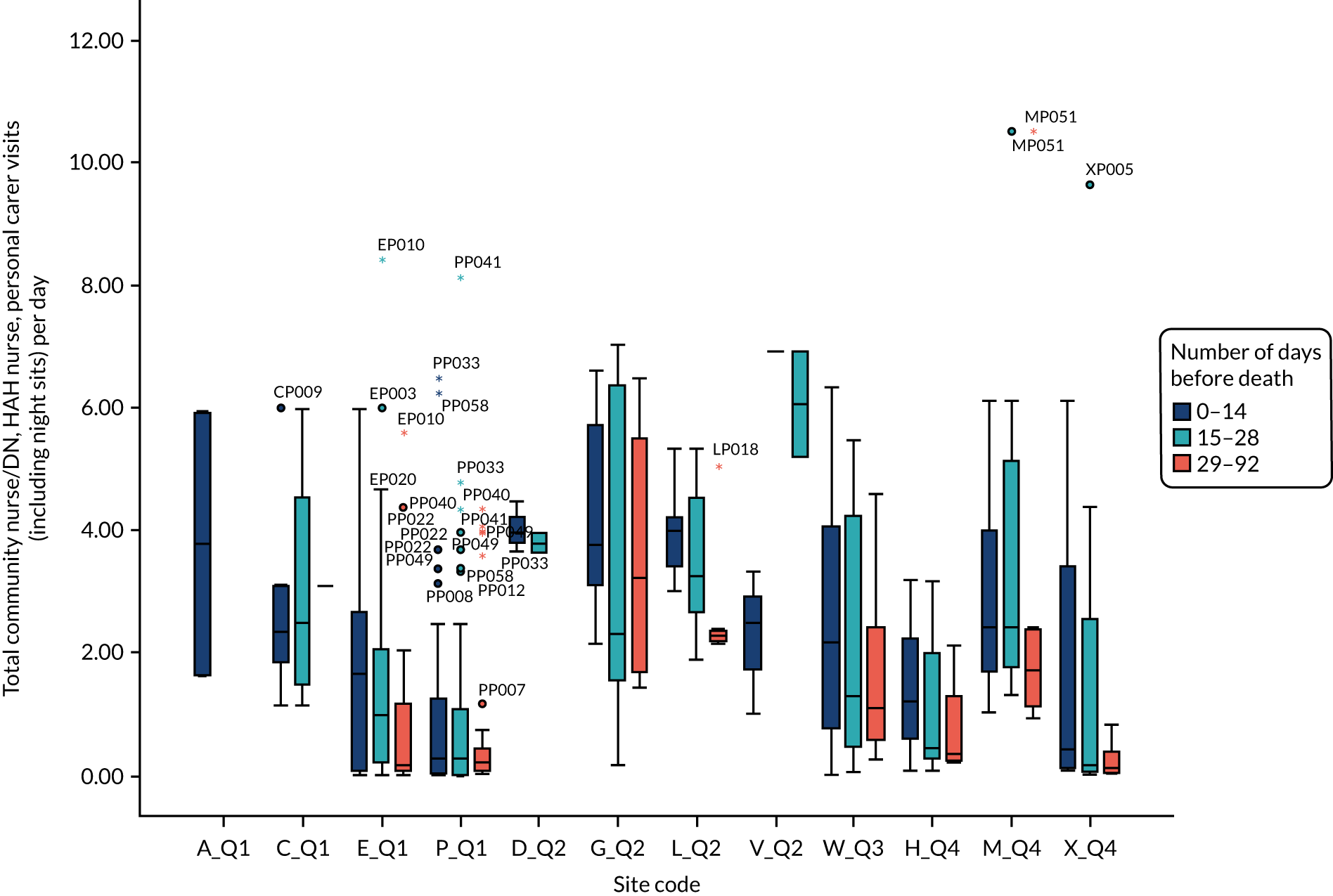
FIGURE 25.
Visits per day: excluding inpatient stays and informal care. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
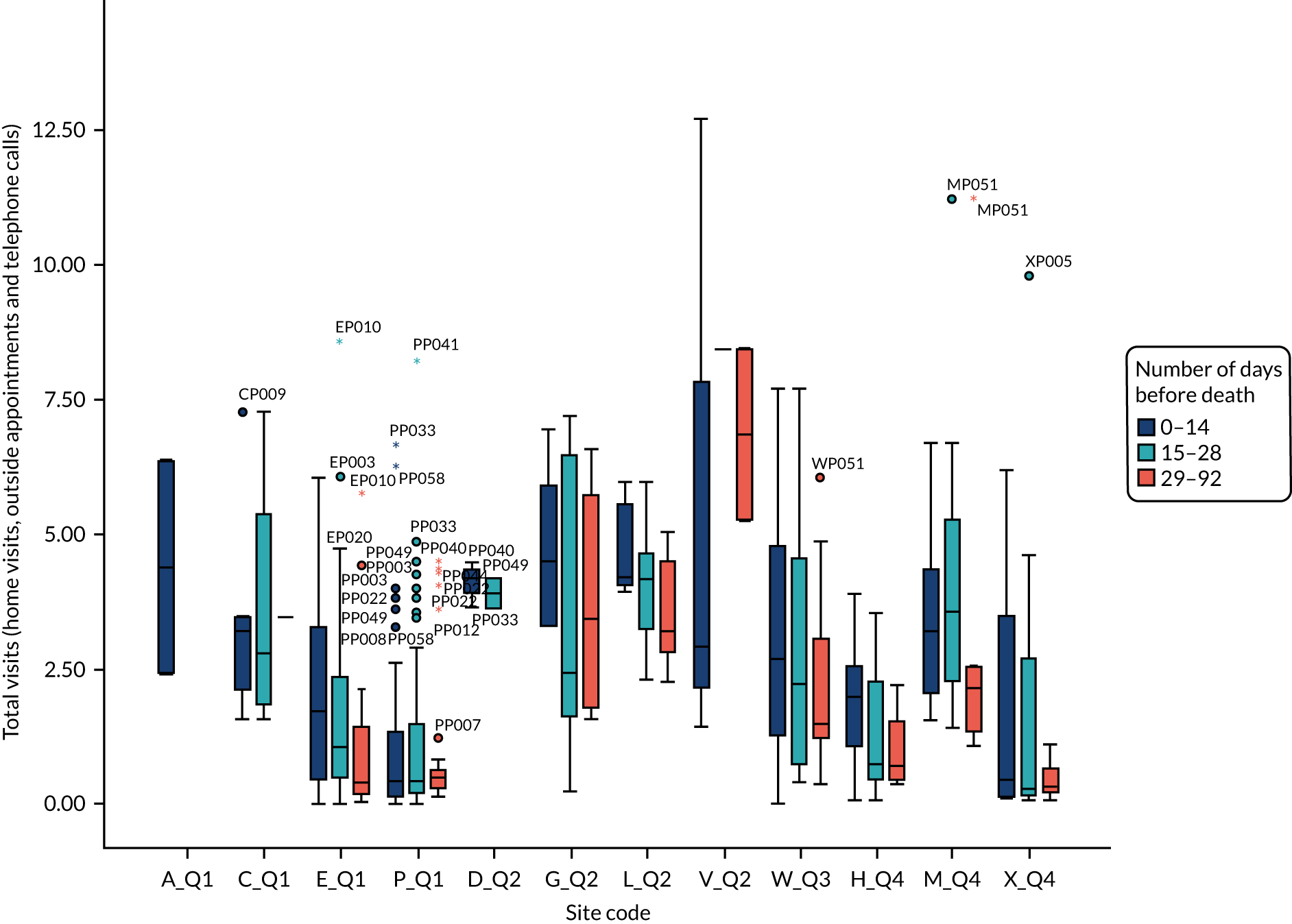
FIGURE 26.
Visits per day: informal caring. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
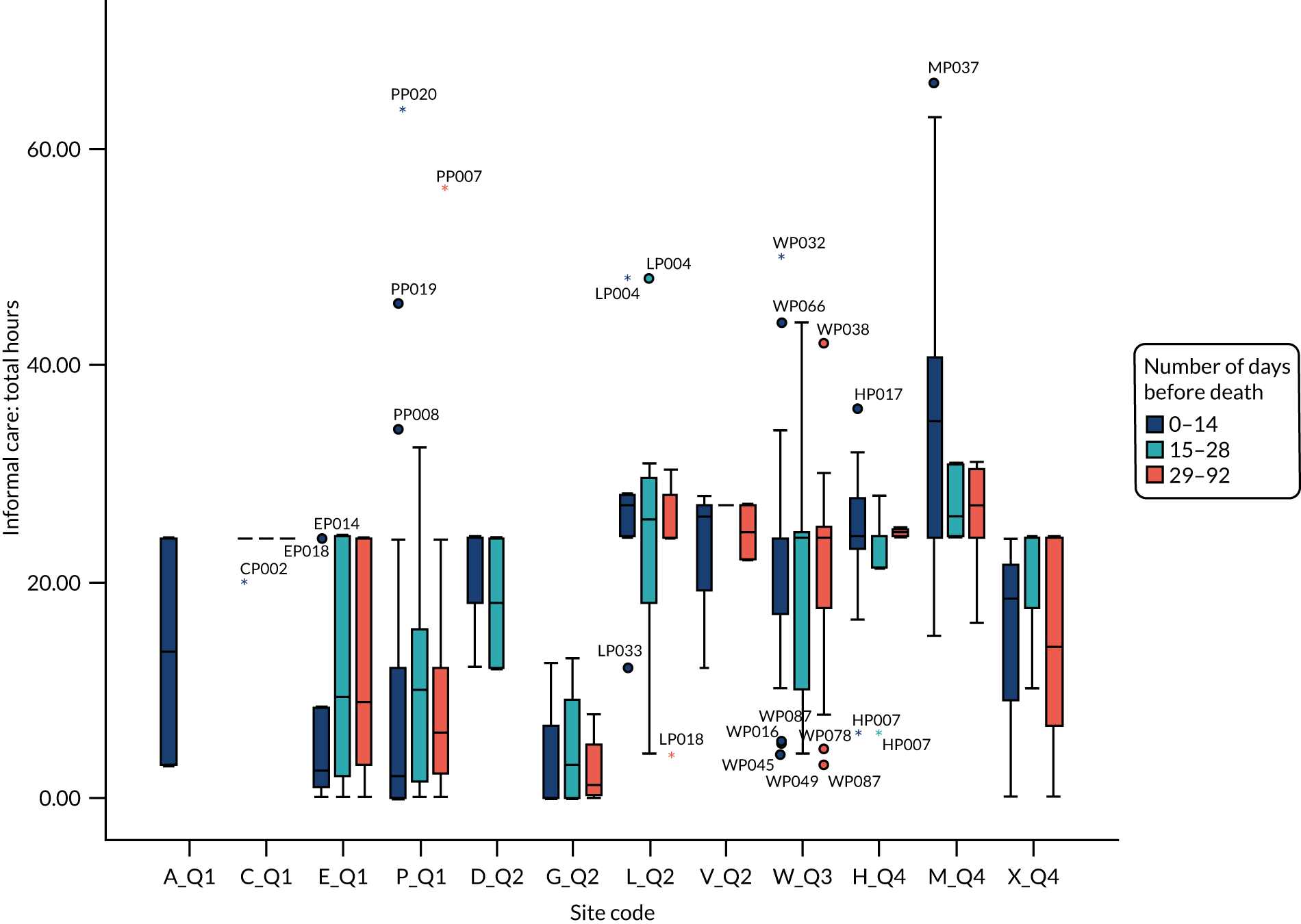
Appendix 22 Box plots for hospice service use by hospice at home model
FIGURE 27.
Proportions of in-home care that are provided by community/district nursing teams. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
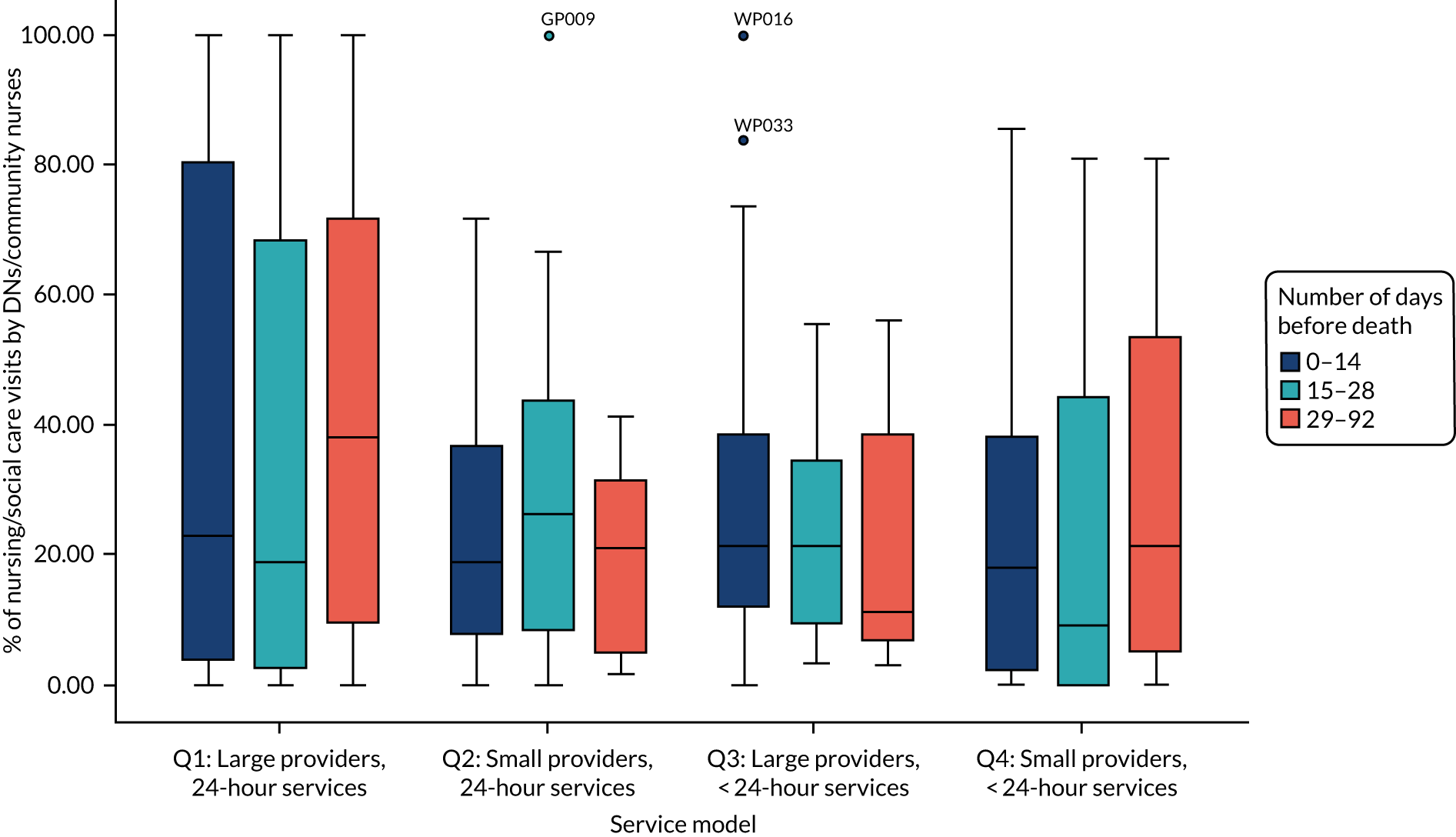
FIGURE 28.
Proportions of in-home care that are provided by HAH teams. Boxes are IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
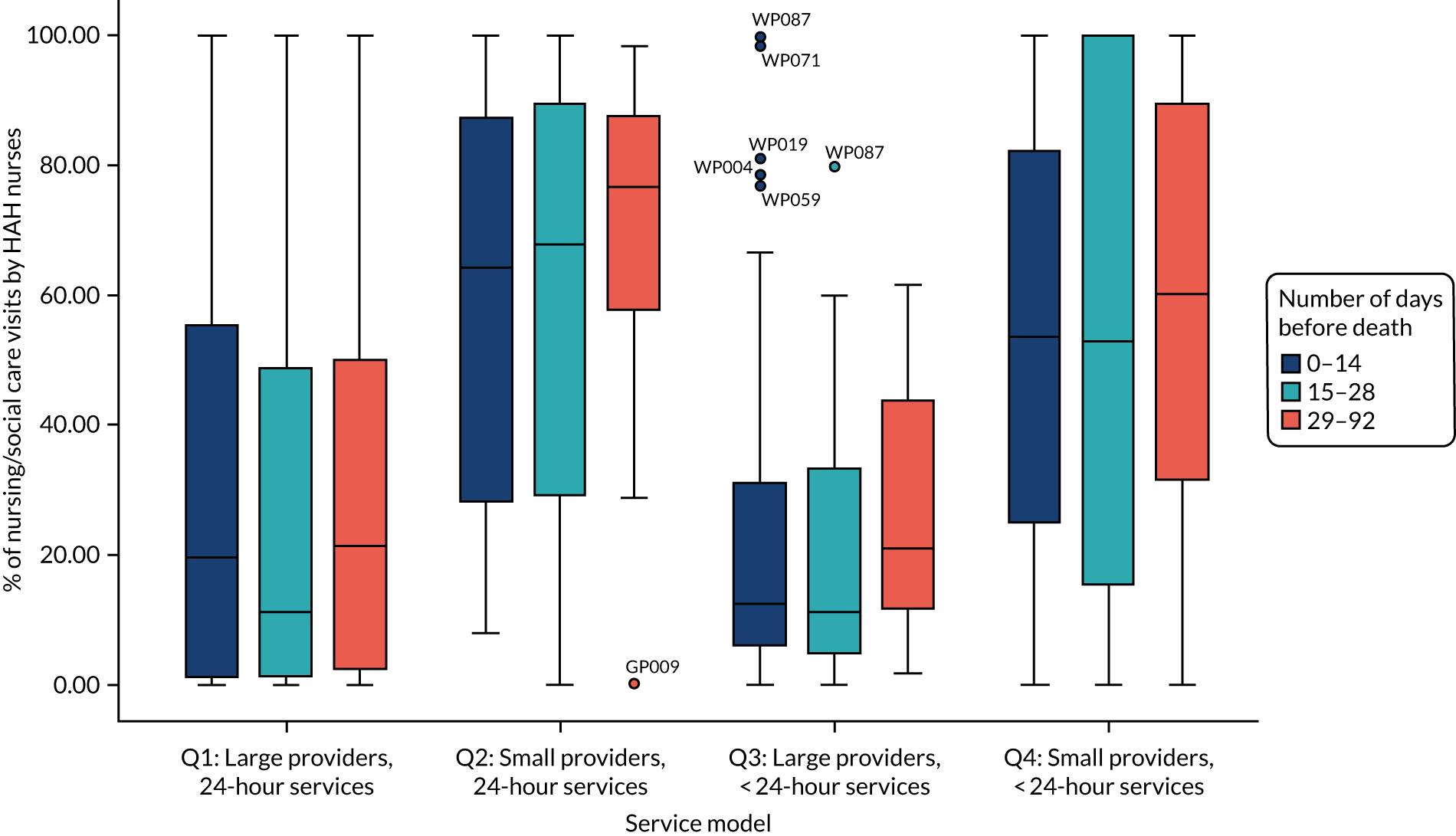
FIGURE 29.
Proportions of in-home care that are provided by social service personal caring teams. Boxes are IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
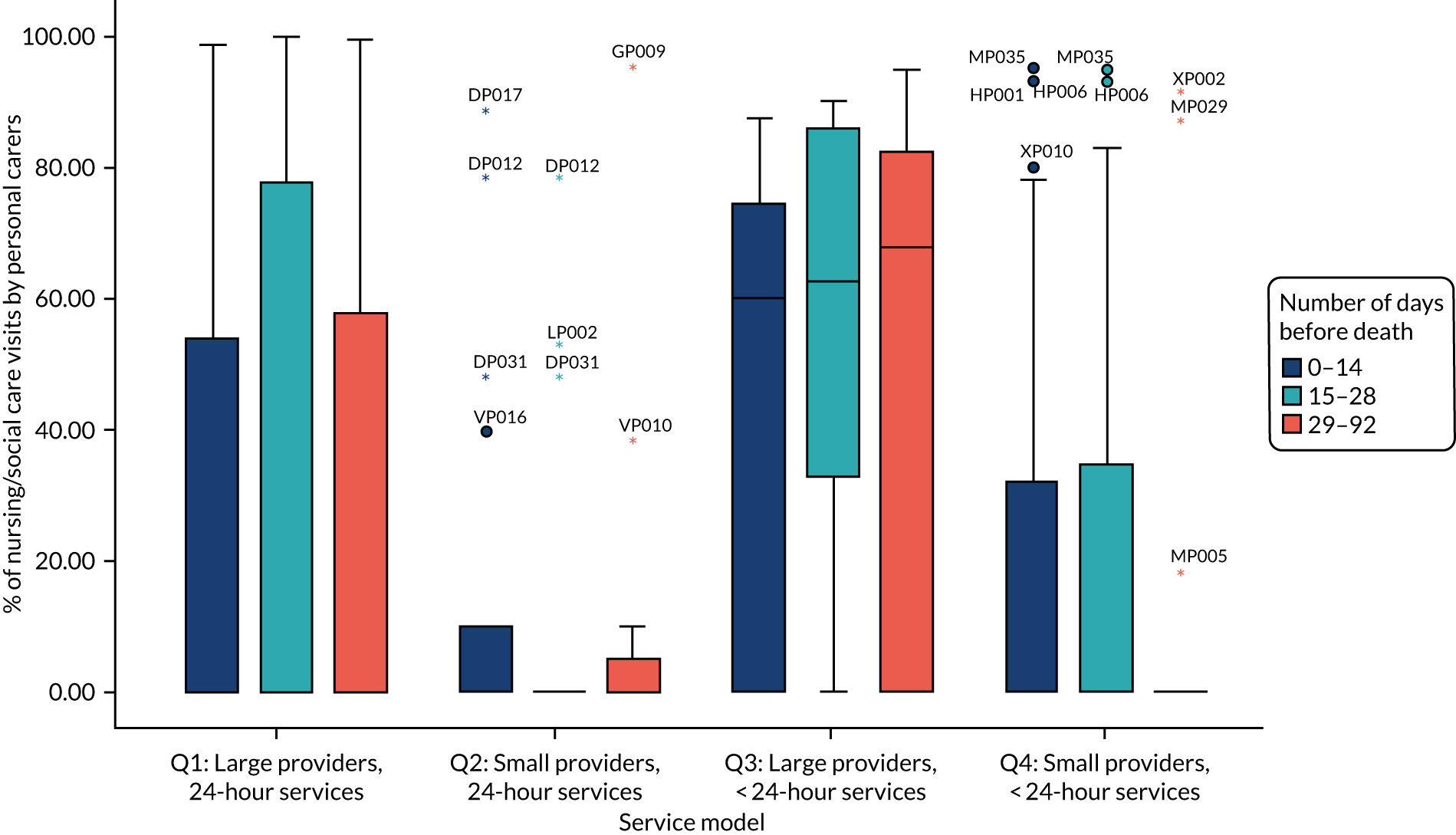
Appendix 23 Cost per day for each service use item by three time periods and service model
| Service use item | Number of days before death | Cost (£) per day | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Service model | Total | |||||||||||||||
| Q1: Large providers, 24-hour services | Q2: Small providers, 24-hour services | Q3: Large providers, not 24-hour services | Q4: Small providers, not 24-hour services | |||||||||||||
| n | Median | Mean (SD) | n | Median | Mean (SD) | n | Median | Mean (SD) | n | Median | Mean (SD) | N | Median | Mean (SD) | ||
| In home | ||||||||||||||||
| Community nursing visitsa | 0–14 | 50 | 3.41 | 9.81 (13.89) | 17 | 18.07 | 23.88 (20.76) | 34 | 9.86 | 14.37 (14.32) | 25 | 8.21 | 12.60 (19.25) | 126 | 6.86 | 13.49 (16.63) |
| 15–28 | 59 | 1.64 | 6.02 (11.07) | 16 | 19.98 | 24.98 (21.41) | 16 | 5.31 | 12.52 (16.34) | 22 | 4.45 | 20.45 (45.97) | 113 | 4.00 | 12.43 (24.77) | |
| 29–92 | 52 | 1.66 | 3.74 (5.41) | 11 | 9.86 | 18.66 (19.98) | 17 | 3.83 | 5.07 (2.66) | 15 | 1.72 | 19.57 (51.70) | 95 | 2.94 | 8.20 (22.45) | |
| Hospice nursing visitsa | 0–14 | 52 | 0.90 | 7.87 (18.89) | 17 | 40.50 | 37.37 (24.98) | 34 | 9.11 | 18.87 (24.31) | 25 | 6.75 | 11.77 (16.85) | 128 | 4.82 | 15.47 (22.89) |
| 15–28 | 59 | 0.55 | 4.28 (12.79) | 16 | 35.80 | 37.50 (30.92) | 16 | 2.94 | 6.30 (8.11) | 22 | 4.81 | 10.17 (13.11) | 113 | 1.93 | 10.42 (19.51) | |
| 29–92 | 52 | 0.67 | 2.41 (6.43) | 11 | 26.02 | 35.82 (27.65) | 17 | 6.18 | 7.60 (6.69) | 15 | 3.86 | 7.57 (9.63) | 95 | 1.29 | 8.02 (15.27) | |
| Personal carer visitsb | 0–14 | 56 | 0.00 | 22.75 (49.89) | 18 | 0.00 | 18.49 (34.75) | 34 | 16.57 | 35.45 (41.02) | 25 | 0.00 | 17.99 (33.98) | 133 | 0.00 | 24.52 (43.22) |
| 15–28 | 61 | 0.00 | 28.90 (55.66) | 17 | 0.00 | 9.83 (23.87) | 16 | 29.71 | 44.18 (44.47) | 22 | 0.00 | 27.65 (58.67) | 116 | 0.00 | 27.97 (51.65) | |
| 29–92 | 52 | 0.00 | 16.59 (37.25) | 11 | 0.00 | 30.81 (82.53) | 17 | 19.33 | 36.67 (40.87) | 15 | 0.00 | 4.31 (9.44) | 95 | 0.00 | 19.89 (43.41) | |
| Total community and hospice nursing and personal caring visits | 0–14 | 50 | 17.23 | 42.98 (61.15) | 17 | 75.21 | 80.83 (36.26) | 34 | 59.30 | 68.69 (55.44) | 25 | 32.64 | 42.36 (37.66) | 126 | 40.43 | 54.90 (54.31) |
| 15–28 | 59 | 6.52 | 40.17 (62.83) | 16 | 61.14 | 72.92 (40.43) | 16 | 35.75 | 63.00 (58.91) | 22 | 34.66 | 58.27 (73.44) | 113 | 27.93 | 51.56 (62.45) | |
| 29–92 | 52 | 4.60 | 22.74 (40.21) | 11 | 57.54 | 85.29 (74.91) | 17 | 32.37 | 49.34 (39.84) | 15 | 18.25 | 31.45 (57.11) | 95 | 12.22 | 36.12 (51.45) | |
| GP home visits | 0–14 | 52 | 0.60 | 5.53 (9.79) | 17 | 5.57 | 8.30 (6.79) | 34 | 5.57 | 7.50 (9.95) | 25 | 5.57 | 6.58 (5.97) | 128 | 5.57 | 6.63 (8.82) |
| 15–28 | 59 | 2.39 | 3.47 (4.39) | 16 | 3.16 | 3.70 (4.36) | 16 | 3.48 | 3.87 (3.13) | 22 | 0.40 | 3.27 (4.10) | 113 | 2.39 | 3.52 (4.12) | |
| 29–92 | 52 | 0.38 | 1.75 (2.95) | 11 | 3.66 | 3.03 (2.50) | 17 | 2.60 | 2.56 (2.38) | 15 | 1.00 | 2.13 (3.16) | 95 | 1.00 | 2.10 (2.84) | |
| Other health-/social care professional visits | 0–14 | 53 | 0.00 | 0.58 (1.51) | 17 | 0.00 | 1.13 (2.77) | 34 | 0.00 | 2.02 (3.94) | 25 | 0.00 | 0.60 (1.28) | 129 | 0.00 | 1.04 (2.57) |
| 15–28 | 59 | 0.00 | 0.59 (1.42) | 16 | 0.00 | 0.60 (2.41) | 16 | 0.23 | 2.18 (3.83) | 22 | 0.00 | 1.17 (2.09) | 113 | 0.00 | 0.93 (2.22) | |
| 29–92 | 52 | 0.00 | 0.58 (1.02) | 11 | 0.00 | 0.19 (0.64) | 17 | 1.43 | 2.63 (3.19) | 15 | 0.70 | 1.01 (1.22) | 95 | 0.00 | 0.97 (1.79) | |
| Charity/voluntary visits | 0–14 | 54 | 0.00 | 0.02 (0.16) | 17 | 0.00 | 0.10 (0.42) | 34 | 0.00 | 0.10 (0.59) | 25 | 0.00 | 0.29 (0.64) | 130 | 0.00 | 0.10 (0.45) |
| 15–28 | 60 | 0.00 | 0.01 (0.07) | 16 | 0.00 | 0.00 (0.00) | 16 | 0.00 | 0.22 (0.89) | 22 | 0.00 | 0.14 (0.45) | 114 | 0.00 | 0.06 (0.39) | |
| 29–92 | 52 | 0.00 | 0.10 (0.56) | 11 | 0.00 | 0.47 (1.55) | 17 | 0.00 | 0.12 (0.49) | 15 | 0.00 | 0.00 (0.00) | 95 | 0.00 | 0.13 (0.70) | |
| Total inside-home visits | 0–14 | 50 | 23.76 | 49.38 (63.95) | 17 | 82.07 | 90.36 (34.16) | 34 | 69.56 | 78.42 (61.17) | 25 | 41.61 | 49.82 (38.46) | 126 | 53.54 | 62.83 (57.44) |
| 15–28 | 58 | 11.08 | 45.01 (64.61) | 16 | 67.60 | 77.22 (41.26) | 16 | 40.45 | 69.27 (60.89) | 22 | 40.24 | 62.85 (74.67) | 112 | 33.48 | 56.58 (63.97) | |
| 29–92 | 52 | 7.85 | 25.16 (40.86) | 11 | 59.28 | 88.98 (75.77) | 17 | 39.61 | 54.65 (40.33) | 15 | 18.25 | 34.59 (59.34) | 95 | 14.71 | 39.32 (52.57) | |
| Outside home | ||||||||||||||||
| Total outside-home visitsc | 0–14 | 56 | 0.00 | 5.06 (8.23) | 18 | 0.00 | 0.00 (0.00) | 34 | 0.00 | 2.88 (6.66) | 25 | 0.00 | 3.16 (8.46) | 133 | 0.00 | 3.46 (7.43) |
| 15–28 | 61 | 0.00 | 5.17 (7.83) | 17 | 0.00 | 0.72 (2.05) | 16 | 0.00 | 6.18 (11.53) | 22 | 0.00 | 1.32 (2.79) | 116 | 0.00 | 3.93 (7.46) | |
| 29–92 | 52 | 7.56 | 7.90 (8.08) | 11 | 0.00 | 2.32 (4.76) | 17 | 0.00 | 10.28 (14.40) | 15 | 0.87 | 3.98 (5.66) | 95 | 3.60 | 7.06 (9.18) | |
| Overnight stays | ||||||||||||||||
| Inpatient hospital nights | 0–14 | 56 | 0.00 | 28.32 (60.43) | 18 | 0.00 | 27.93 (64.80) | 34 | 0.00 | 42.37 (86.54) | 25 | 0.00 | 20.6 (58.62) | 133 | 0.00 | 30.41 (67.95) |
| 15–28 | 61 | 0.00 | 26.82 (60.65) | 17 | 0.00 | 9.20 (37.95) | 16 | 0.00 | 24.06 (50.01) | 22 | 0.00 | 9.08 (27.00) | 116 | 0.00 | 20.49 (51.43) | |
| 29–92 | 52 | 0.00 | 22.67 (46.44) | 11 | 0.00 | 2.68 (8.88) | 17 | 0.00 | 7.22 (19.01) | 15 | 0.00 | 21.57 (50.98) | 95 | 0.00 | 17.42 (41.10) | |
| Inpatient hospice nights | 0–14 | 56 | 0.00 | 31.94 (77.56) | 18 | 0.00 | 2.50 (10.62) | 34 | 0.00 | 42.05 (88.21) | 25 | 0.00 | 37.98 (82.47) | 133 | 0.00 | 31.68 (76.51) |
| 15–28 | 61 | 0.00 | 25.49 (72.58) | 17 | 0.00 | 4.17 (17.20) | 16 | 0.00 | 46.50 (85.07) | 22 | 0.00 | 24.24 (69.07) | 116 | 0.00 | 25.03 (68.80) | |
| 29–92 | 52 | 0.00 | 7.66 (22.62) | 11 | 0.00 | 20.03 (50.08) | 17 | 0.00 | 11.38 (29.08) | 15 | 0.00 | 5.81 (15.52) | 95 | 0.00 | 9.47 (27.24) | |
| Inpatient care/nursing home nights | 0–14 | 56 | 0.00 | 3.29 (12.55) | 18 | 0.00 | 0.00 (0.00) | 34 | 0.00 | 1.18 (6.87) | 25 | 0.00 | 0.00 (0.00) | 133 | 0.00 | 1.69 (8.92) |
| 15–28 | 61 | 0.00 | 1.79 (7.42) | 17 | 0.00 | 0.00 (0.00) | 16 | 0.00 | 4.40 (17.61) | 22 | 0.00 | 0.00 (0.00) | 116 | 0.00 | 1.55 (8.44) | |
| 29–92 | 52 | 0.00 | 0.22 (1.50) | 11 | 0.00 | 0.00 (0.00) | 17 | 0.00 | 5.92 (24.42) | 15 | 0.00 | 0.00 (0.00) | 95 | 0.00 | 1.18 (10.38) | |
| Total inpatient nights | 0–14 | 56 | 27.84 | 63.56 (90.32) | 18 | 0.00 | 30.43 (64.52) | 34 | 0.00 | 85.60 (109.42) | 25 | 0.00 | 58.59 (92.77) | 133 | 0.00 | 63.78 (93.66) |
| 15–28 | 61 | 0.00 | 54.10 (89.00) | 17 | 0.00 | 13.37 (40.67) | 16 | 28.05 | 74.97 (90.95) | 22 | 0.00 | 33.33 (70.99) | 116 | 0.00 | 47.07 (81.85) | |
| 29–92 | 52 | 2.89 | 30.55 (51.64) | 11 | 0.00 | 22.71 (49.69) | 17 | 0.00 | 24.52 (37.34) | 15 | 0.00 | 27.38 (50.71) | 95 | 0.00 | 28.06 (46.36) | |
| Telephone calls | ||||||||||||||||
| Telephone calls with doctor | 0–14 | 56 | 0.00 | 0.36 (0.78) | 18 | 1.07 | 1.86 (2.36) | 33 | 0.00 | 0.68 (1.25) | 25 | 1.07 | 1.22 (1.64) | 132 | 0.00 | 0.81 (1.46) |
| 15–28 | 61 | 0.00 | 0.37 (0.65) | 17 | 0.71 | 0.89 (1.14) | 16 | 0.00 | 0.66 (1.14) | 22 | 0.16 | 0.81 (1.18) | 116 | 0.00 | 0.57 (0.94) | |
| 29–92 | 52 | 0.20 | 0.38 (0.54) | 11 | 0.41 | 1.03 (1.33) | 17 | 0.44 | 0.52 (0.78) | 15 | 0.62 | 0.79 (1.08) | 95 | 0.23 | 0.54 (0.82) | |
| Total telephone calls (doctors and other) | 0–14 | 56 | 0.26 | 1.20 (2.25) | 18 | 3.39 | 7.64 (17.28) | 33 | 1.71 | 4.00 (5.35) | 25 | 2.71 | 3.33 (3.43) | 132 | 1.18 | 3.18 (7.39) |
| 15–28 | 61 | 0.50 | 1.12 (2.13) | 17 | 1.07 | 2.61 (3.65) | 16 | 1.76 | 3.74 (5.62) | 22 | 1.37 | 2.15 (2.55) | 116 | 0.73 | 1.90 (3.23) | |
| 29–92 | 52 | 0.59 | 0.86 (0.78) | 11 | 1.07 | 4.19 (5.83) | 17 | 1.86 | 2.81 (3.63) | 15 | 1.14 | 1.80 (1.85) | 95 | 0.78 | 1.74 (2.84) | |
| Grand total formal care | ||||||||||||||||
| Total events (in home, out of home, nights, telephone calls) | 0–14 | 50 | 85.80 | 114.94 (88.75) | 17 | 97.85 | 119.32 (70.49) | 33 | 169.71 | 170.61 (97.53) | 25 | 89.86 | 114.90 (88.95) | 125 | 104.57 | 130.22 (91.28) |
| 15–28 | 58 | 64.55 | 103.12 (94.20) | 16 | 85.35 | 84.86 (45.29) | 16 | 167.41 | 154.15 (74.18) | 22 | 74.36 | 99.65 (85.26) | 112 | 80.08 | 107.12 (85.81) | |
| 29–92 | 52 | 40.73 | 64.47 (62.29) | 11 | 102.34 | 118.20 (83.96) | 17 | 88.69 | 92.27 (50.79) | 15 | 43.50 | 67.75 (77.75) | 95 | 56.07 | 76.18 (67.34) | |
| Informal care | ||||||||||||||||
| Informal care | 0–14 | 56 | 80.79 | 286.33 (385.84) | 18 | 359.39 | 468.72 (388.02) | 34 | 696.00 | 637.03 (283.50) | 25 | 696.00 | 805.95 (420.64) | 133 | 580.00 | 498.34 (419.22) |
| 15–28 | 61 | 298.29 | 320.66 (269.51) | 17 | 348.00 | 460.10 (394.31) | 16 | 696.00 | 578.83 (298.15) | 22 | 696.00 | 671.14 (174.70) | 116 | 449.50 | 443.18 (311.77) | |
| 29–92 | 52 | 180.44 | 291.47 (301.17) | 11 | 638.00 | 447.19 (359.77) | 17 | 696.00 | 603.92 (279.65) | 15 | 696.00 | 622.68 (254.68) | 95 | 348.00 | 417.71 (328.40) | |
| Total formal and informal care | ||||||||||||||||
| Total cost (formal and informal care) | 0–14 | 50 | 246.54 | 424.02 (399.82) | 17 | 541.86 | 615.61 (392.51) | 33 | 840.55 | 804.97 (294.05) | 25 | 849.25 | 920.85 (412.74) | 125 | 738.46 | 650.02 (424.58) |
| 15–28 | 58 | 395.68 | 434.09 (266.32) | 16 | 458.89 | 573.71 (393.07) | 16 | 753.89 | 732.99 (286.92) | 22 | 770.36 | 770.79 (173.12) | 112 | 584.16 | 562.87 (309.06) | |
| 29–92 | 52 | 247.62 | 355.94 (309.34) | 11 | 728.38 | 565.39 (379.91) | 17 | 749.71 | 696.19 (259.86) | 15 | 734.29 | 690.43 (245.28) | 95 | 511.36 | 493.89 (335.29) | |
Appendix 24 Box plots for hospices’ summary costs by three time periods
FIGURE 30.
Costs: all nursing, including night shifts. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
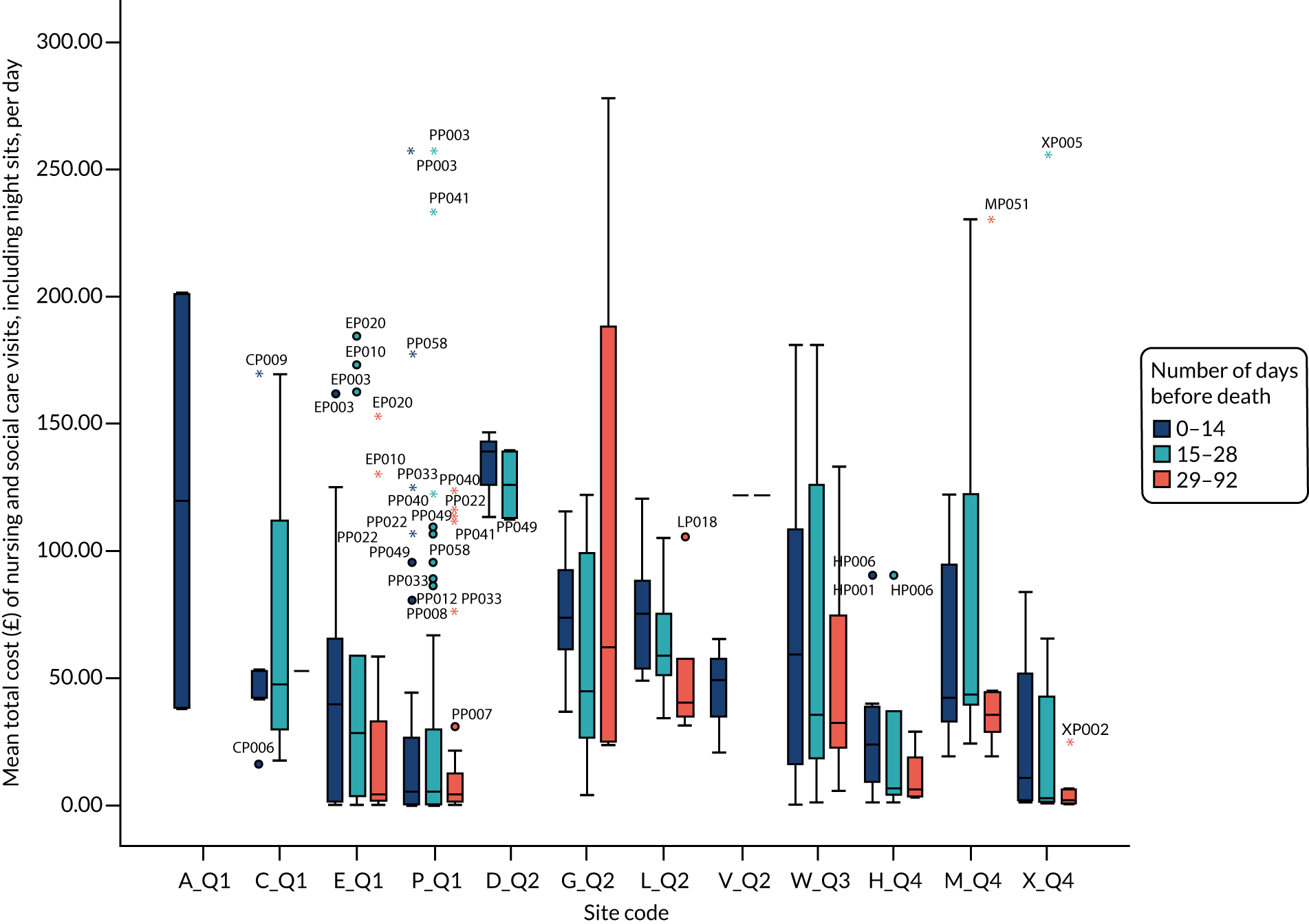
FIGURE 31.
Costs: all formal care, including inpatient care. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
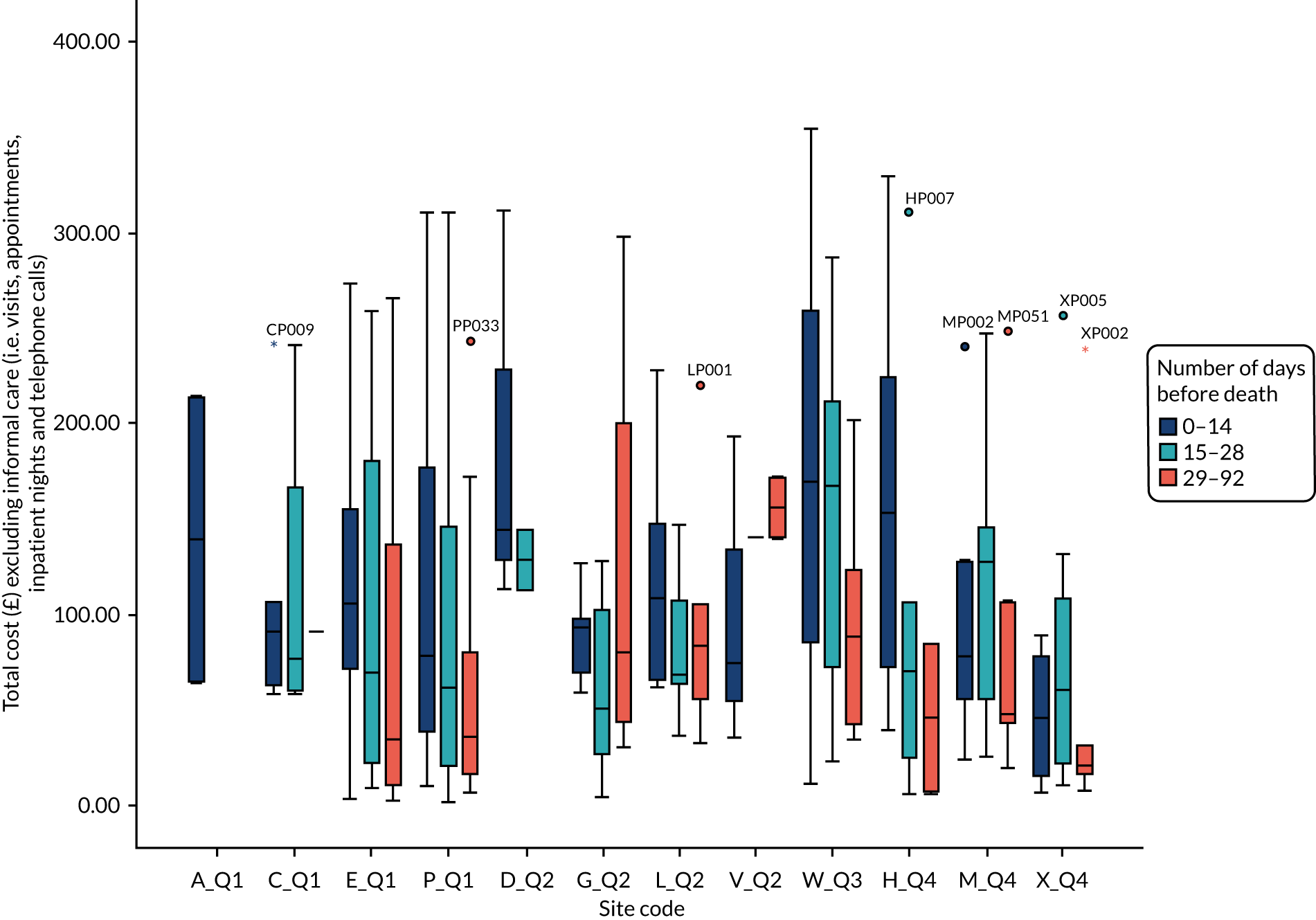
FIGURE 32.
Costs: informal caring. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
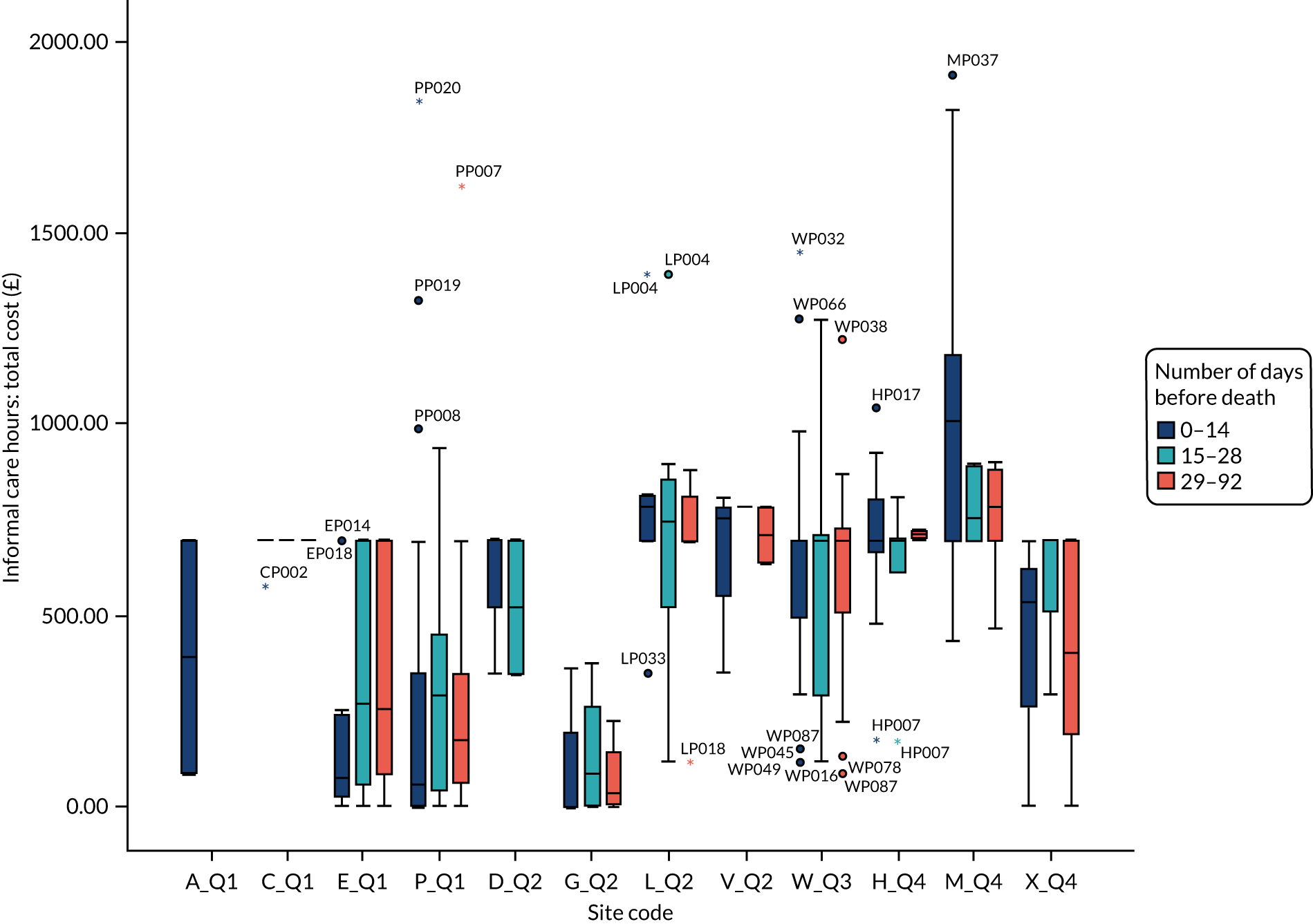
FIGURE 33.
Total costs per day. Boxes show IQR with median bar inside. Whiskers are minimum to maximum, after excluding all outliers. Outliers (small circles) are 1.5–3 IQRs from the end of the box; extreme outliers (asterisks) are > 3 IQRs from the end of the box. Q, quadrant. Patient identifiers are attached to outliers to enable identification of repeat outliers over time.
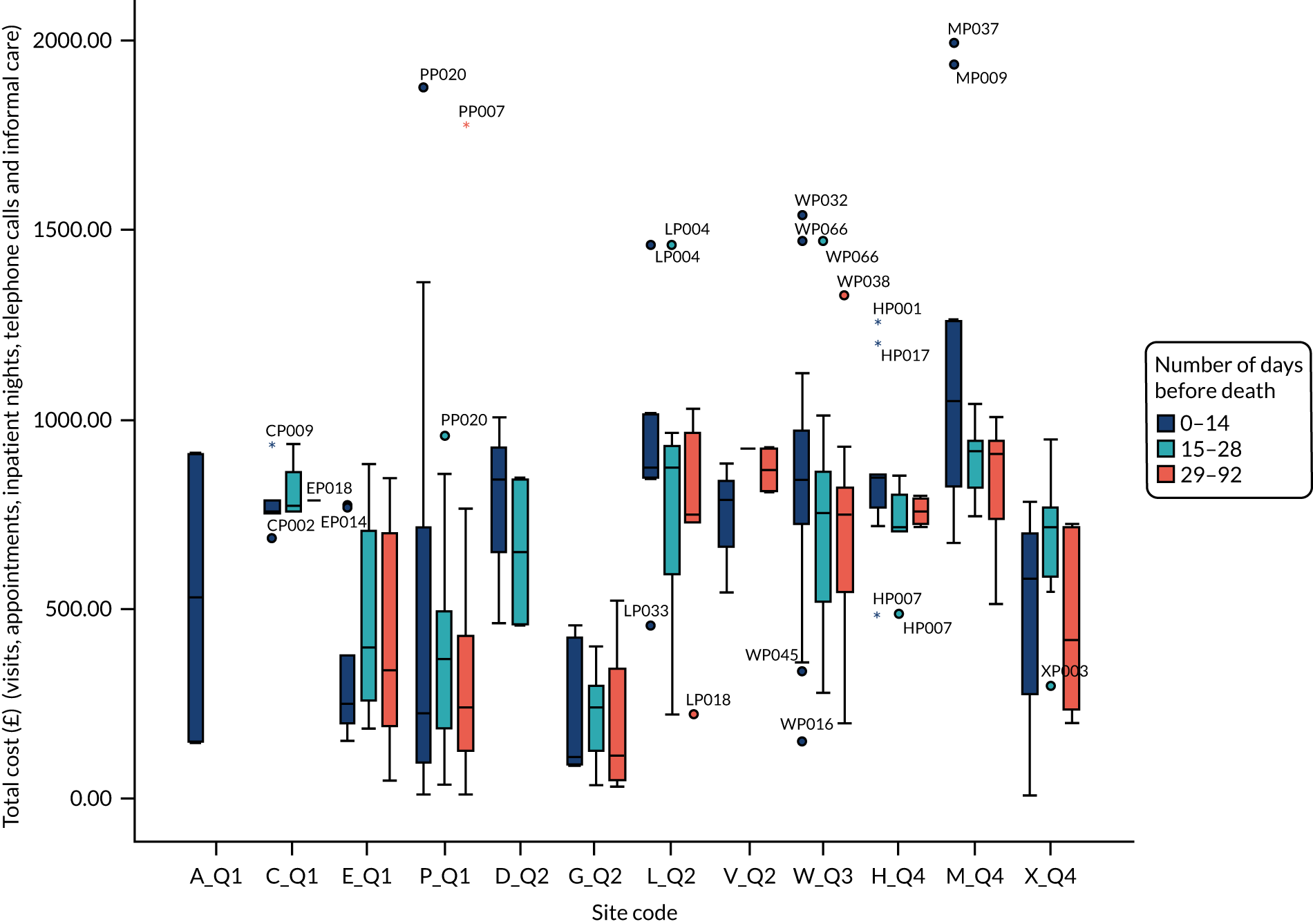
Appendix 25 Costs per day of main items of service use by time period and service model
| Items of service use | Days before death | Model 1: Large providers, 24-hour services | Model 2: Small providers, 24-hour services | Model 3: Large providers, not 24-hour services | Model 4: Small providers, not 24-hour services | p-valuea | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Median | Mean | SD | n | Median | Mean | SD | n | Median | Mean | SD | n | Median | Mean | SD | |||
| All nursing and personal care | 0–14 | 50 | 17.23 | 42.98 | 61.15 | 17 | 75.21 | 80.83 | 36.26 | 34 | 59.30 | 68.69 | 55.44 | 25 | 32.64 | 42.36 | 37.66 | 0.001 |
| 15–28 | 59 | 6.52 | 40.17 | 62.83 | 16 | 61.14 | 72.92 | 40.43 | 16 | 35.75 | 63.00 | 58.91 | 22 | 34.66 | 58.27 | 73.44 | 0.002 | |
| 29–92 | 52 | 4.60 | 22.74 | 40.21 | 11 | 57.54 | 85.29 | 74.91 | 17 | 32.37 | 49.34 | 39.84 | 15 | 18.25 | 31.45 | 57.11 | < 0.0005 | |
| All formal health, social, voluntary careb | 0–14 | 50 | 85.80 | 114.94 | 88.75 | 17 | 97.85 | 119.32 | 70.49 | 33 | 169.71 | 170.61 | 97.53 | 25 | 89.86 | 114.90 | 88.95 | 0.044 |
| 15–28 | 58 | 64.55 | 103.12 | 94.20 | 16 | 85.35 | 84.86 | 45.29 | 16 | 167.41 | 154.15 | 74.18 | 22 | 74.36 | 99.65 | 85.26 | 0.050 | |
| 29–92 | 52 | 40.73 | 64.47 | 62.29 | 11 | 102.34 | 118.20 | 83.96 | 17 | 88.69 | 92.27 | 50.79 | 15 | 43.50 | 67.75 | 77.75 | 0.017 | |
| Informal care | 0–14 | 56 | 80.79 | 286.33 | 385.84 | 18 | 359.39 | 468.72 | 388.02 | 34 | 696.00 | 637.03 | 283.50 | 25 | 696.00 | 805.95 | 420.64 | < 0.0005 |
| 15–28 | 61 | 298.29 | 320.66 | 269.51 | 17 | 348.00 | 460.10 | 394.31 | 16 | 696.00 | 578.83 | 298.15 | 22 | 696.00 | 671.14 | 174.70 | < 0.0005 | |
| 29–92 | 52 | 180.44 | 291.47 | 301.17 | 11 | 638.00 | 447.19 | 359.77 | 17 | 696.00 | 603.92 | 279.65 | 15 | 696.00 | 622.68 | 254.68 | < 0.0005 | |
| Total formal and informal care | 0–14 | 50 | 246.54 | 424.02 | 399.82 | 17 | 541.86 | 615.61 | 392.51 | 33 | 840.55 | 804.97 | 294.05 | 25 | 849.25 | 920.85 | 412.74 | < 0.0005 |
| 15–28 | 58 | 395.68 | 434.09 | 266.32 | 16 | 458.89 | 573.71 | 393.07 | 16 | 753.89 | 732.99 | 286.92 | 22 | 770.36 | 770.79 | 173.12 | < 0.0005 | |
| 29–92 | 52 | 247.62 | 355.94 | 309.34 | 11 | 728.38 | 565.39 | 379.91 | 17 | 749.71 | 696.19 | 259.86 | 15 | 734.29 | 690.43 | 245.28 | < 0.0005 | |
Appendix 26 Interview breakdown by quadrant and site
| Interviewee group | Service model | |||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| Carer | 28 | 17 | 4 | 9 |
| Service provider | 20 | 29 | 8 | 19 |
| Commissioner | 4 | 2 | 0 | 3 |
| Interviewee group | Site | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acacia | Camellia | Dahlia | Echinacea | Gardenia | Hyacinth | Lavender | Marigold | Peony | Violet | Wisteria | Xyris | |
| Carer | 0 | 1 | 7 | 7 | 3 | 2 | 3 | 5 | 20 | 4 | 4 | 2 |
| Service provider | 5 | 4 | 6 | 6 | 9 | 4 | 8 | 7 | 5 | 6 | 8 | 8 |
| Commissioner | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 2 | 1 | 0 | 1 |
Appendix 27 Carer interviewee characteristics
Characteristics of the interviewed carers
-
Carer relationship to patient: 33.3% wives to patient, 19.3% husbands, 1.8% partners, 14.0% daughters, 14.0% sons, 5.3% daughters-in-law, 1.8% sons-in-law, 5.3% friends, 3.5% sisters and 1.8% with status unknown.
-
Carer living situation: 75.4% lived with the patient, 24.6% did not.
-
Carer marital status: 3.5% were in a relationship, 80.7% were married, 10.5% were single and 5.3% were widowed.
-
Carer education: 33.3% were educated to General Certificate of Secondary Education (GCSE) level or less, 1.8% had completed Advanced Levels (A Levels), 26.3% had completed vocation or college, 12.3% were educated to undergraduate level and 26.3% were educated to postgraduate level.
Characteristics of the patients interviewed carers looked after
-
Patient gender: 52.6% female, 47.4% male.
-
Patient age: average age was 75.5 years, with a minimum of 42 and a maximum of 98 years.
-
Patient marital status: 1.8% were in a relationship, 63.2% were married, 12.3% were single, 21.1% were widowed, 1.8% had unknown status.
-
Patients had diverse life-limiting conditions (51 different conditions across 58 patients discussed in interviews): 71.9% had cancer (highly diverse types), 7.1% had dementia (various types), 1.8% had cirrhosis of the liver, 3.5% had chronic obstructive pulmonary disease, 5.3% had heart failure, 3.5% had liver failure, 1.8% had Parkinson’s disease, 1.8% had other diagnoses and 3.5% had no data on life-limiting conditions.
-
Patient education: 36.8% were educated to GCSE level or less, 3.5% were educated to A Levels, 31.6% had completed vocation or college, 7.0% were educated to undergraduate level, 10.5% were educated to postgraduate level and 10.5% had no data on educational level.
-
Patient living arrangements: 15.8% lived alone, 19.3% lived with a child/children, 57.9% lived with a spouse or partner and 7% lived with others.
-
Preferred place of death: 63.2% wanted to die at home, 10.5% at a hospice, 3.5% either at home or at a hospice, and PPOD was not known for 21.1%.
Appendix 28 Site descriptions and patient flows
Acacia (quadrant 1)
Overview
The Acacia HAH site was a large, 24-hour service. It served a mixed population of 940,000 people, covering both urban and rural areas.
Funding
Forty-four per cent of funding for the service was charitable. There was some CCG funding for one specific geographical area covered.
Use of volunteers
The wider hospice had volunteers, but they were not, at the time, used within the HAH service.
Wider hospice organisation structure and where hospice at home fitted
The hospice organisation offered community care, specialist palliative care home care, an inpatient unit, a day centre, counselling services, patient and family care, a lymphoedema service and 24/7 telephone support. The inpatient unit had 23 beds (12 commissioned by the CCG).
Hospice at home service operations
Staffing
The service employed a mix of qualified nurses (n = 12 at the beginning of the study) and HCAs (n = 15 at the beginning of the study).
Eligibility
Patients deemed to be in the last 2–3 weeks of life were eligible for the HAH service. Before referral, patients must have a ‘do not attempt cardiopulmonary resuscitation’ decision in place, have had end-of-life discussions and ‘just-in-case medications’ (anticipatory medications for EOLC) and community prescription chart completed. The service accepted patients who had not had an application for NHS CHC funding completed, although the preference was that DNs would have completed it prior to referral.
The service received 739 referrals in 2018/19. Any HCP could make referrals, but patient self-referrals were also accepted. The service aimed to respond to a new referral within 4 hours.
Care
The service provided a night-sitting service for families, with the staff member remaining in the home overnight. No equivalent daytime care service was provided; RNs worked during the day to co-ordinate with other services and to liaise with families. Assessments were made during the day, but personal care was not undertaken. At night, there were typically five or six HCAs providing care to families, with one nurse covering the shift who was mobile and responded as needed. Hands-on care was provided between 22.00 and 07.00. Access to psychosocial support and respite care was also available.
FIGURE 34.
Patient flow at the Acacia site.
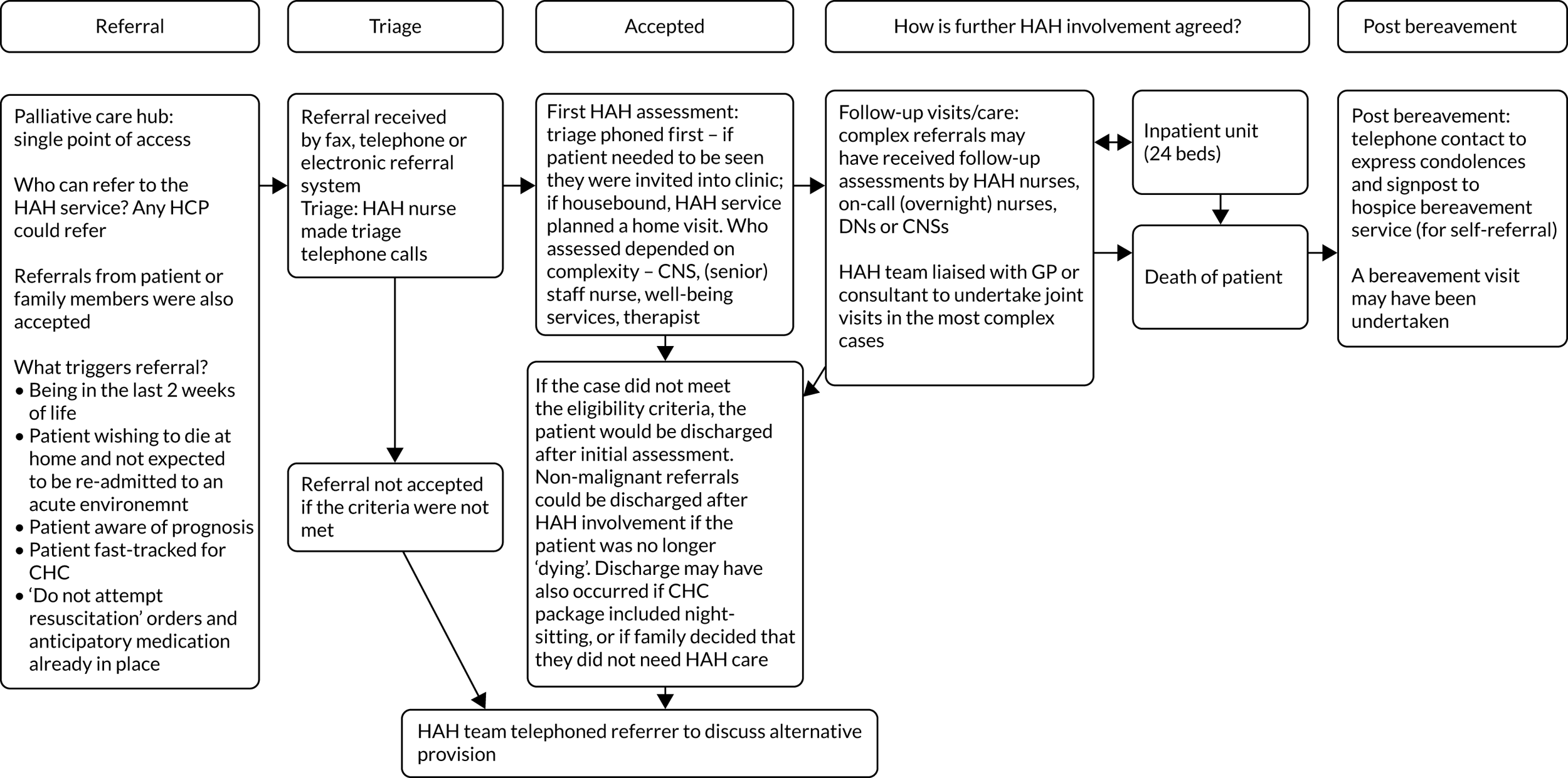
Camellia (quadrant 1)
Overview
The Camellia site was a large, 24-hour service. This service served a mixed population of 162,000 people, covering both urban and rural areas.
Other services in the area
The HAH service had a formal partnership with a national charity that delivered HAH care between the hours of 16.00 and 23.00. The local district nursing service was not a 24-hour service.
Funding
The main source of funding for the service was charitable, with 36% of hospice funding coming from the CCG. The service was part commissioned by the CCG to deliver HAH services to patients registered with local GPs. The service was, at the time of the study, funded to cover only part of the whole CCG area.
Use of volunteers
The hospice had volunteers, but they were not, at the time, used within the HAH service.
Wider hospice organisation structure and where hospice at home fitted
The HAH team sat alongside other hospice community nursing teams, for example its community-based palliative care specialist nurses. The service manager was line managed by the clinical director of services (as were the other community nursing team leaders). There was an inpatient unit with 18 beds.
Hospice at home service operations
The service was intended to provide short-term input only, serving families for around 1 week, either at the very end of life or to provide support through a care crisis. The aim was to provide a comprehensive assessment of need and to make the appropriate referrals to get care in place for the longer term.
Staffing
Staffing was provided by qualified nursing staff (n = 9) and HCAs (n = 8). The HAH service was also staffed by the national charity nursing staff (n = 1) who covered the evening shift.
Eligibility
The service accepted referrals for patients in two main groupings:
-
the last week of life
-
the last 12 months of life to support an acute episode (e.g. pain, carer fatigue).
A total of 442 referrals were received per year. Referrals came from other HCPs, including GPs, DNs, the wider hospice and community health services. Referrals were categorised according to clinical need and response time: a response within 4 hours, within 24 hours or within 2 days. The service reported a 100% success rate in meeting these wait times.
Care
The first visit comprised a comprehensive community assessment and was always conducted by a nurse. The inclusion of nurse prescribers on the team meant that the service was able to respond to medication requests, to administer medication and to set up syringe drivers. The HCAs delivered personal care. Hands-on care was provided 24/7. Hands-on care, psychosocial support and respite care were provided.
The hospice bereavement team made contact after the death. This was a hospice-wide service, rather than a HAH-specific service.
FIGURE 35.
Patient flow at the Camellia site. NVQ, National Vocational Qualification.
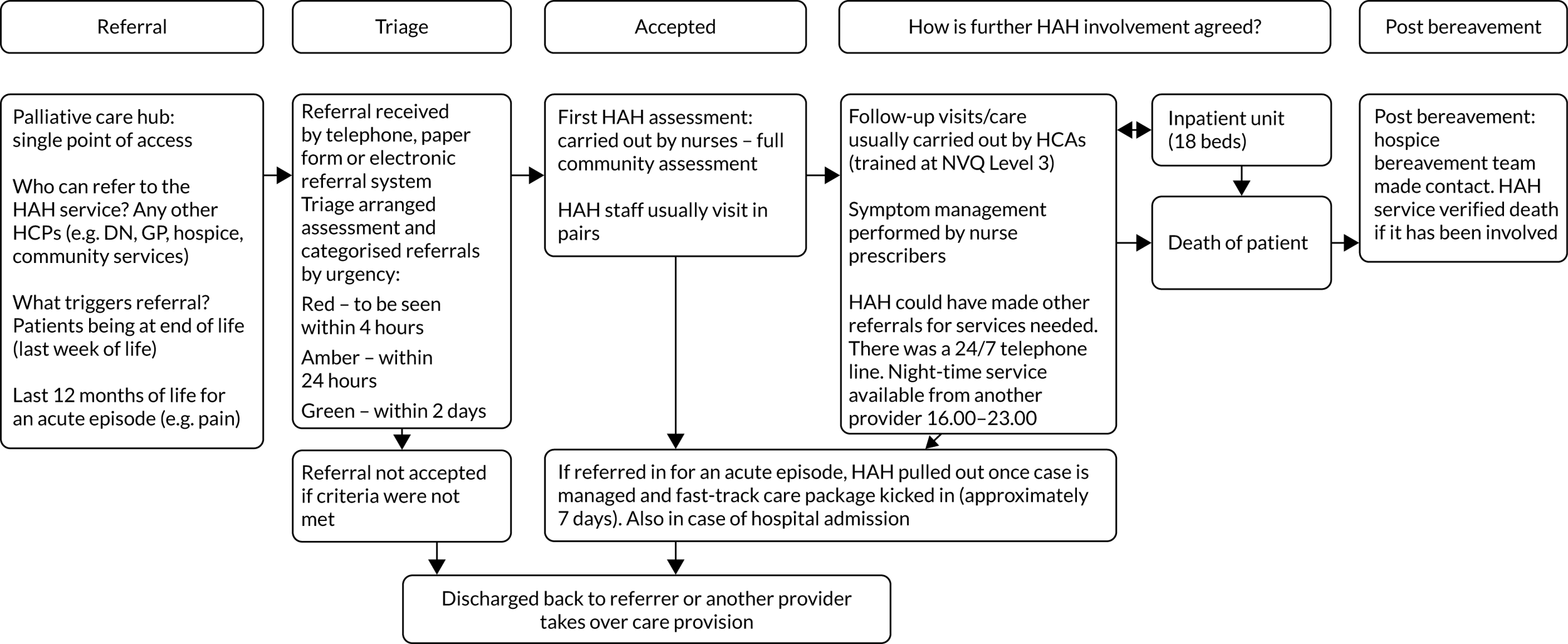
Echinacea (quadrant 1)
Overview
The Echinacea site was based in an independent hospice. It provided care to a population of just over 270,000 people in a mainly urban area. The population was mostly white British; 18% were aged > 65 years; and there were mixed levels of deprivation, albeit more well-off than deprived people.
Other services in the area
The area had a 24-hour community nursing service, rapid-response service and community neurological service. Two inpatient facilities for non-palliative patients were run by the community provider.
Funding
The hospice raised 74% of its total income from voluntary activities and trading; 26% came from NHS funding. The local CCG commissioned seven hospice beds.
Use of volunteers
The hospice used volunteers across all services and was the only site that employed a small number of care volunteers as part of HAH. Befrienders visited the home but did not carry out any hands-on care, whereas care volunteers had a care certificate of basic HCA competencies and could do hands-on tasks, but always visited with another staff member.
Wider hospice organisation structure and where hospice at home fitted
The purpose-built inpatient unit had 7–12 beds, depending on demand. The service provided day therapy, outpatient services, well-being services (including a Living Well programme, volunteer befrienders and complementary therapies), support for carers and spiritual care. Occupational therapy and physiotherapy were available across all services and the therapists could visit patients at home. The service had access to an external speech and language therapist. The well-being service also provided bereavement support.
Patients/carers could access (by telephone) a duty nurse 7 days per week, 09.00–17.00; from 17.00 to 08.00, calls were diverted to the ward and dealt with by an inpatient unit nurse.
Hospice at home service operations
Staffing
The HAH service was originally staffed solely by CNSs, but had evolved into four geographical teams consisting of a CNS, RNs and HCAs, although staff worked across geographical boundaries when necessary. More than 2000 patients were cared for in their own homes in 2018/19. At the start of the study, the service was staffed by approximately 4.6 CNSs, 4 RNs, 5 HCAs and 2 or 3 care volunteers.
Care
The HAH service provided short-term support with personal care while awaiting NHS CHC funding. Once NHS CHC funding was agreed, patient care was passed on to its long-term care provider; patients could receive up to four visits per day and two night sits per week. The HAH service also provided a crisis support service whereby respite and night sits were provided.
Bereavement care
Post bereavement, carers were telephoned by the bereavement team and offered follow-up.
FIGURE 36.
Patient flow at the Echinacea site.
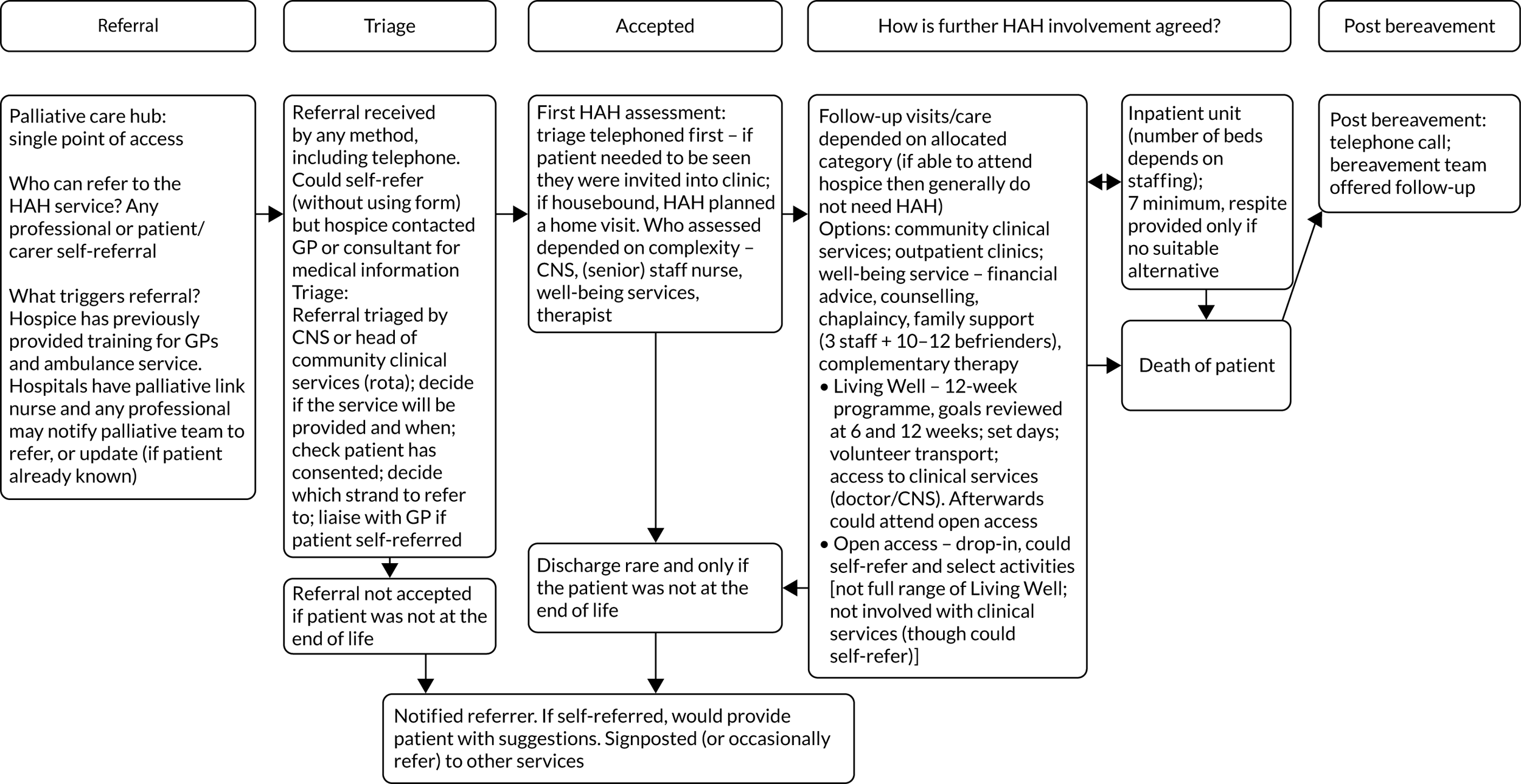
Peony (quadrant 1)
Overview
The Peony site was based at a purpose-built hospice. It provided care to a population of > 1 million people living in largely urban areas. The area had a high proportion of people aged > 65 years (18%); most identified as white British and had mixed levels of deprivation, albeit there were more well-off than deprived people.
Other services in the area
There was some variation between localities in terms of district nursing and hospice night-time cover. The night response service was partly commissioned by the CCGs (22.00–07.00) and covered two localities (as the other two localities had night district nursing services); it was staffed by one band 5 or 6 specialist nurse with a HCA and included a night-sit service in one of the localities. The HAH service provided cover when the DN service did not, and this involved seeing non-hospice patients to avoid hospital admission.
Funding
The NHS contributed 22% in 2018/19, with the hospice having raised the remaining 78% of their income. Of the total budget, 37% provided care in the home.
Use of volunteers
Volunteers were employed across most services, including a Compassionate Neighbours scheme, but do not come under the remit of HAH.
Wider hospice organisation structure and where hospice at home fitted
The term HAH referred to the whole community service, rather than specifically to HAH activities as defined by other case study sites. There was some variation in service provision between localities in order to mesh with other services. The organisation had a 20-bed inpatient unit (none of the beds was CCG funded). Staff included medical consultants, specialist palliative nurses, occupational therapists, physiotherapists, social workers, chaplains and carer companions. There was a well-being centre providing day services and a bereavement team.
Hospice at home service operations
Staffing
Each of the four localities (reflecting CCG boundaries) had an integrated team led by a CNS and comprising nursing staff (band 6 or 7), a physiotherapist, an occupational therapist, a social worker and a social work assistant. In 2018/19, 2165 referrals for HAH were received.
The staffing varied across localities but, collectively, the four localities were staffed by approximately:
-
fourteen full-time equivalent (FTE) CNSs
-
seven FTE specialist nurses
-
two band-5 nurses
-
four FTE HCAs
-
three social workers
-
one or two FTE physiotherapists and occupational therapists.
Care
The HAH team provided CNS advice at home, provided personal care via HCAs and liaised with other services (including DNs and other community nursing teams). The specialist nurses were able to manage syringe drivers. When eligible, patients usually received one or two calls per day from a HCA. Patients did not need to have NHS CHC funding and could be seen in a crisis by the enhanced support service, which bridged the gap while awaiting NHS CHC or social services carers to start. This service provided complex support and short-term support, and aimed to avoid hospital admission.
Bereavement care
Post bereavement, the CNS telephoned carers and offered a visit. All carers were sent a post-bereavement pack. Based on clinical experience, the CNS could refer for bereavement support sooner than the standard 6 months. The bereavement team offered follow-up support including a bereavement café and other activities.
FIGURE 37.
Patient flow at the Peony site.
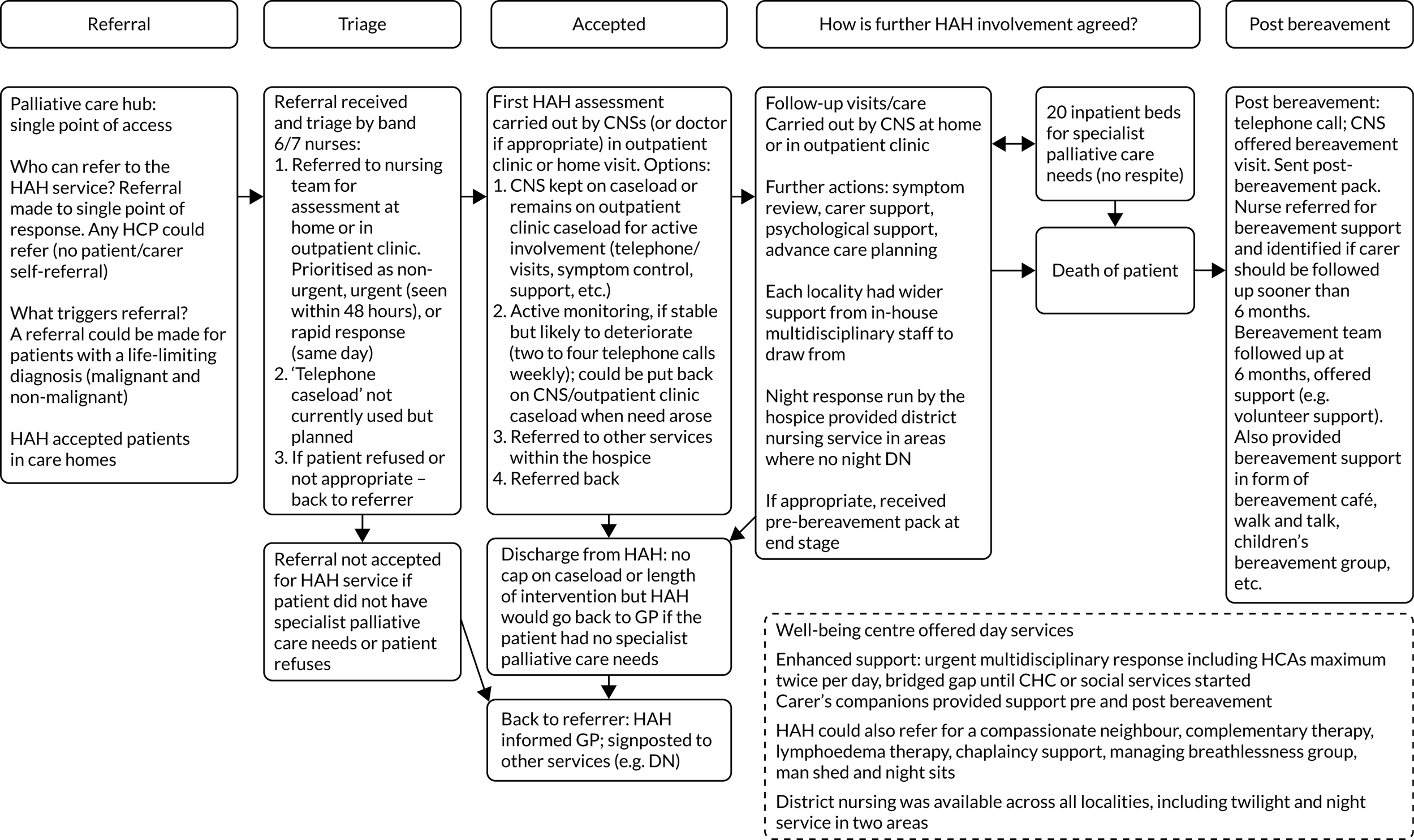
Dahlia (quadrant 2)
Overview
The Dahlia HAH site was a small, 24-hour service.
This service served a mixed population of 470,000 people, covering both urban and rural areas, and received 360 referrals per year.
Other services in the area
The service was part of a local hub, which also included a national charity; the hub was NHS led.
Funding
The main source of funding for the service was charitable. At hospice level, a portion of funding was provided by the CCG (approximately 21%), but the majority was from hospice funds. The CCG funding was not ring-fenced for a specific purpose; no specific element of hospice provision was commissioned by the CCG.
Use of volunteers
The hospice had volunteers, but they were not, at the time, used within the HAH service.
Wider hospice organisation structure and where hospice at home fitted
The hospice offered community care, an inpatient unit, a day centre, counselling services and 24/7 telephone support. The inpatient unit had 33 beds. The hospice had two Admiral Nurses, and offered social work support.
The staff working for the HAH service worked remotely, coming into the main hospice building rarely (e.g. for training or monthly supervision). The team leader communicated handovers and instructions for each shift via telephone.
Hospice at home service operations
The HAH team worked closely with the local palliative care co-ordination hub (see above) to provide services dependent on service availability and patient need.
Staffing
The service was predominantly HCA led, with qualified nursing staff conducting the initial assessments when a patient was referred to the service. During the study, there were two qualified nurses, two band-4 administrators/HCAs and 21 HCAs.
Eligibility
The service accepted patients in three categories:
-
terminal = the last week of life
-
pre terminal = the last 2 weeks of life
-
carer crisis = typically the last 2–6 weeks of life, although there is some flexibility (e.g. awaiting a hospice bed).
It was a requirement that the hospice palliative care specialist nurses had assessed all patients referred to the service; as a result, many referrals were made by the palliative care specialist nurse. If a referral came from another HCP (e.g. a GP, a hospital doctor or the Admiral Nurse), then the palliative care specialist nurse was asked to assess the patient. The service aimed to respond to a new referral within 4 hours.
Care
There was an early shift, a late shift and a night shift. A single member of staff attended for each shift. Each shift was allocated on the same day, according to patient need. Families were notified of care provision on that same day.
Staff members provided physical care for patients and support for the family. The service would cover nursing homes if needed. Hands-on care was provided 24/7.
Bereavement care
Families were sent a letter at 6 weeks. Those deemed high risk could be contacted earlier. This was a central hospice bereavement service, rather than HAH specific.
FIGURE 38.
Patient flow at the Dahlia site.
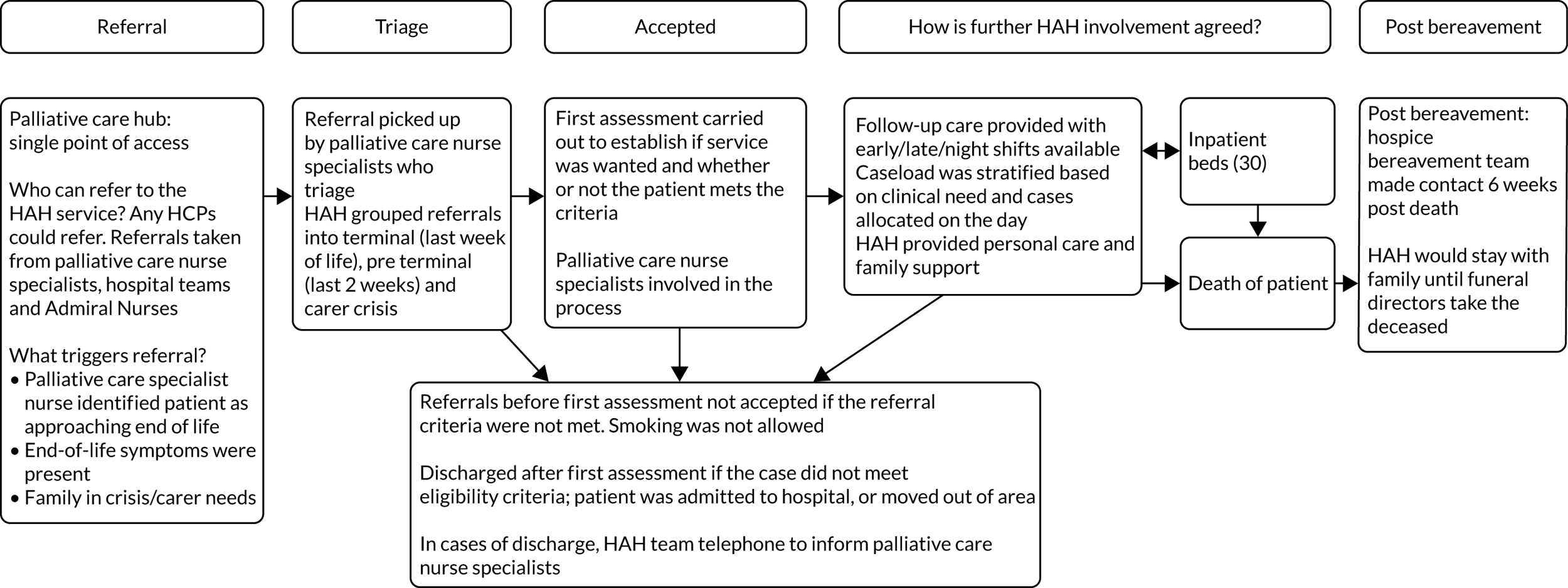
Gardenia (quadrant 2)
Overview
The Gardenia site was in an independent hospice in an urban area with mixed levels of deprivation. It was part of a care partnership with a national charity and a local NHS foundation trust. It covered two boroughs, with a population of > 0.5 million people, and provided services to about 2500 adults each year. The service received about 320 referrals per year. The population was ethnically diverse; of those receiving any hospice input in 2017/18, one-third were from ethnic minority groups.
Other services in the area
Out-of-hours cover was provided by a district nursing telephone line (20.00–22.00), a twilight service that provided cover from 17.30 to 22.30, national charity night sitters funded by the care partnership and based in the hospice 22.00–08.00 and an overnight rapid-response service.
Of note, the two boroughs had different provision of district nursing: one borough had no night service, whereas the other borough did have a night service.
Funding
The hospice was funded by the CCG to provide rapid response, but outsourced it to the local NHS trust; it was managed by a band-6 nurse, with a band 4 and HCAs.
The hospice received nearly 40% of its funding from the NHS and the remainder was generated through fundraising, charity shops and other non-NHS income generation. All HAH patients were NHS CHC funded.
Use of volunteers
Volunteers were not used in HAH but there was an active community of about 450 volunteers involved in all aspects of hospice service delivery. A Compassionate Neighbours scheme was supported by several hospices in the area.
Wider hospice organisation structure and where hospice at home fitted
The purpose-built hospice had an inpatient unit of up to 19 beds, a day centre, a lymphoedema service (provided in one borough only), counselling, a drop-in service, chaplaincy and 24-hour telephone cover. Respite was offered in the day hospice, or occasionally at home or in the inpatient unit. The hospice provided occupational therapy, physiotherapy, social work, a drop-in cafe and a day centre 3 days per week.
The HAH team was a small 24-hour service funded in one of the two boroughs served by the wider hospice organisation. Both boroughs had access to specialist palliative care at home, provided by the CNS team (six in one borough, eight in the other), which was co-located with HAH. CNSs usually reviewed patients at about 4 weeks, 3 months and 6 months after the initial assessment.
Hospice at home service operations
Staffing
The service was staffed predominantly by HCAs. At the time of the phase 1 survey, it was staffed by eight HCAs (bands 2 and 3) and two RNs; during data collection, this changed to seven staff (bands 2–4) and bank staff from the ward.
Care
The HAH service provided personal care for up to 12 weeks, in line with NHS CHC funding. HCAs visited up to three times per day; for patients with a syringe driver, this was managed by the HAH nurses, district nursing or rapid-response unit.
Bereavement care
Post bereavement, carers were not routinely telephoned, but carers could be referred to in-house counsellors (including volunteers) and/or the hospice’s bereavement support group.
FIGURE 39.
Patient flow at the Gardenia site.
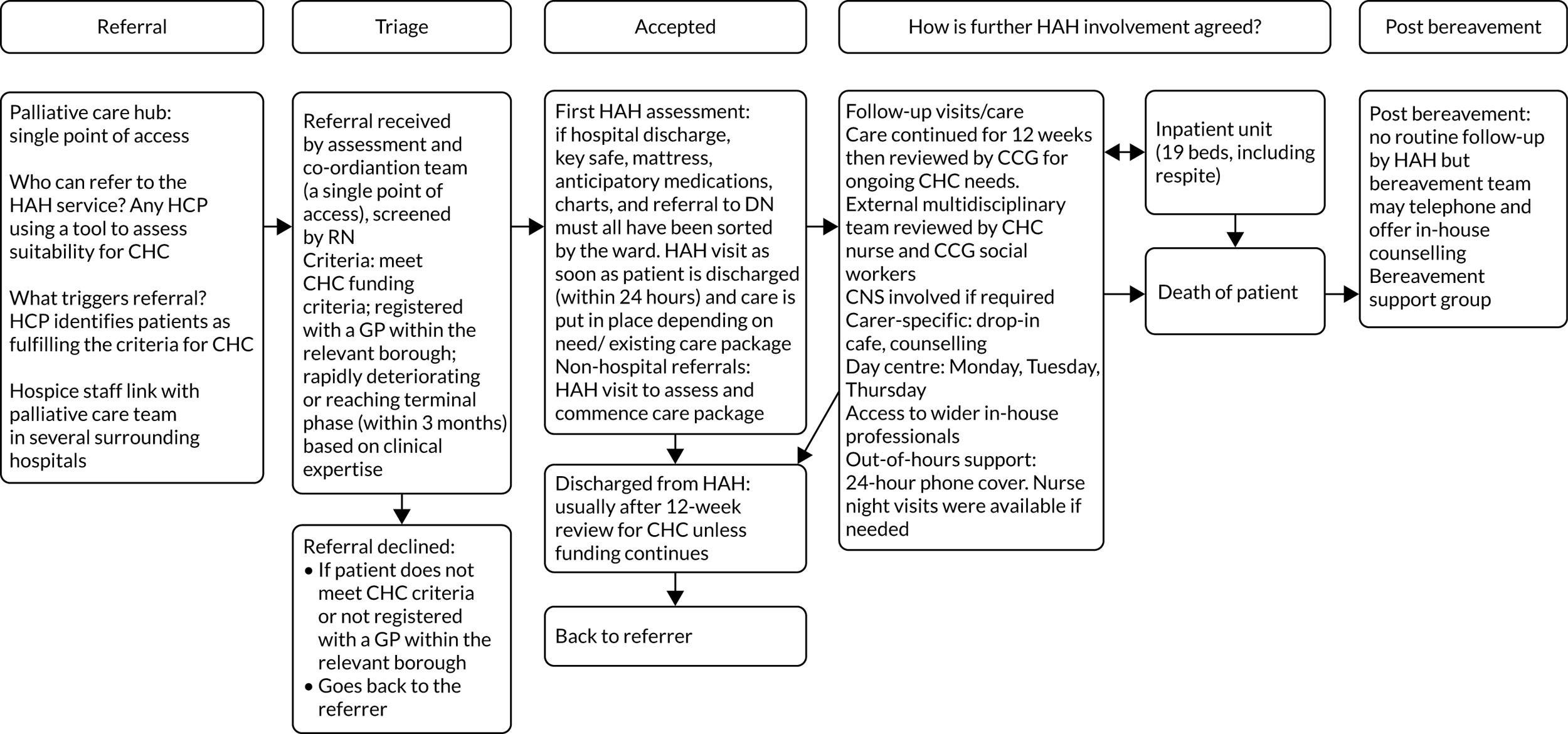
Lavender (quadrant 2)
Overview
The Lavender site was a HAH service with inpatient hospice beds within the organisation, in a mixed-affluence area (with substantial differences in least and most deprived wards within it), covering both rural and urban areas. The HAH services were categorised as ‘small’, with 100 referrals taken on per year, serving a population of 248,000. The service provided 24/7 support.
The entire caseload was made up of NHS CHC with statutory funding. It provided highly intensive service provision (up to four visits per day).
Other services in the area
Seven HAH services were operating in the same area/county. District nursing services were available 24/7 in the area. The HAH service had a strong relationship with commissioners.
Funding
As the HAH service was made up of NHS CHC referrals, the NHS contributed nearly 100% of HAH funding, but there was supplementation from the wider hospice organisation in order to deliver a high-quality service.
Use of volunteers
Volunteers worked across most services at the hospice, but not HAH. Volunteers also provided emotional and practical support to informal carers after bereavement. Volunteer co-ordination was far removed from HAH in terms of organisational structure.
Wider hospice organisation structure and where hospice at home fitted
The hospice organisation offered HAH, inpatient care, a day hospice, family support and spiritual care, education and staff support. The service also ran a 24/7 patient line for advice and other emergencies.
Hospice at home service operations
Staffing
The HAH service was led by HCAs, who provided hands-on care, with nursing staff co-ordinating input and performing assessments only. HCAs were highly trained, and this was reflected in pay bands. At entry to phase 2 of the study, the service had nine HCAs (8.2 FTE cumulatively) and three RNs (2.4 FTE), operating as two geographically defined teams. Towards the end of phase 2, a third team became operational. HCA recruitment and retention was adequate, with some issues around RN retention.
Care
The HAH team provided 24/7 hands-on care, and was able to assess symptoms and offer fast (< 4 hours) response in the day. High-intensity visits were provided up to four times per day, with the ability to respond quickly to changes in need. Operating multiple concurrent teams allowed staff to extend visits in cases of emergency without failing to visit other patients. The caseload was made up mostly of patients in the last 3 months of life (in line with NHS CHC funding criteria).
Bereavement care
The HAH service sometimes visited carers post bereavement (often for the primary purpose of collecting patient notes). Condolence calls were also commonplace, but the HAH service did not offer formal bereavement support. Bereavement services (including professional individual counselling) were provided by the hospice.
FIGURE 40.
Patient flow at the Lavender site.
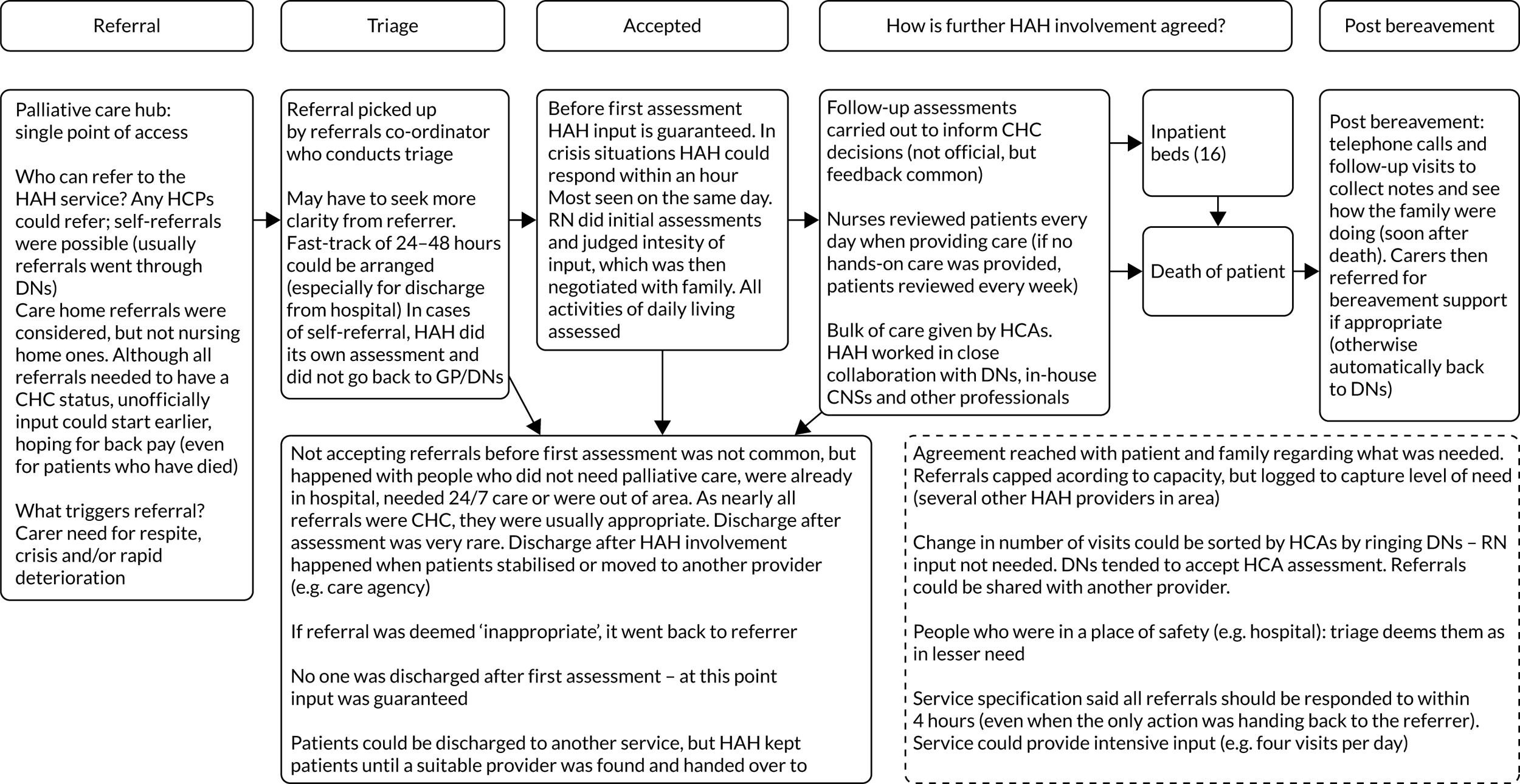
Violet (quadrant 2)
Overview
The Violet site was a HAH service in a predominantly deprived area with both urban and rural populations. The HAH services were categorised as ‘small’, with 240 referrals taken on per year, serving a population of 190,000 people. The service provided 24/7 support.
This service stood out, compared with other case study sites in the following ways. There were no inpatient beds on the hospice site, which required close relationships with other hospices in the area that did have inpatient provision. The HAH service ran a joint night-time rapid-response service with NHS trust staff nurses. Post-bereavement visits by the HAH team were provided for many carers.
Other services in the area
There were other HAH services operating in neighbouring areas. District nursing services were not available 24/7 in the area. HAH was strongly integrated with other palliative care providers (both statutory and third sector) in the area.
Funding
NHS funding made up 28% of all hospice income in 2018/19.
Use of volunteers
Volunteers worked across most services at the hospice, but not HAH. There was no befriending (or similar) volunteer programme.
Wider hospice organisation structure and where hospice at home fitted
The hospice organisation offered HAH, day hospice, a lymphoedema care service, a multitude of family and bereavement support services (including specialist support for complex issues, pre-bereavement support, chaplaincy/spiritual support, one-to-one support and group support for adults, and for children and young people). The hospice did not have inpatient beds.
Hospice at home service operations
Staffing
The HAH service was led by HCAs. At entry to phase 2 of the study, the service had nine HCAs (eight FTE cumulatively) and one RN (one FTE). HCAs had opportunities to develop skills. RN recruitment and retention were suboptimal, with vacancies present during most of the phase 2 period, whereas many of the HCAs had been with the service for > 5 years, with no issues around retention and recruitment noted.
Care
The HAH team provided hands-on nearly 24/7 care (with a gap in the evening, 16.30–20.00, when the DNs ran a late service) and were able to respond within 6 hours (all referrals were seen within 1 week). Night-time service was a rapid-response one, run jointly with a NHS community trust. In terms of general HAH support, there were (1) intensive hands-on visits (up to three times per day, usually by two HCAs) and (2) respite sits (by one HCA).
Eligibility
The HAH service took on referrals under two sets of criteria: patients in the last year of life (who receive respite support rather than personal care; these are often internal referrals from the day hospice) and patients in the last couple of weeks to days of life (for hands-on care). The service aimed not to reject any referrals; increased demand was dealt with by longer working hours, additional staff, negotiating quicker visits across the caseload and fewer respite sits.
Bereavement care
The HAH service often referred carers to pre-bereavement services at the first assessment, ensuring continuity of care for the carer. The HAH service also offered a 6-week post-bereavement visit. Other post-bereavement services were available, but not offered automatically; the 6-week visit was likely to involve a discussion of post-bereavement services.
FIGURE 41.
Patient flow at the Violet site.
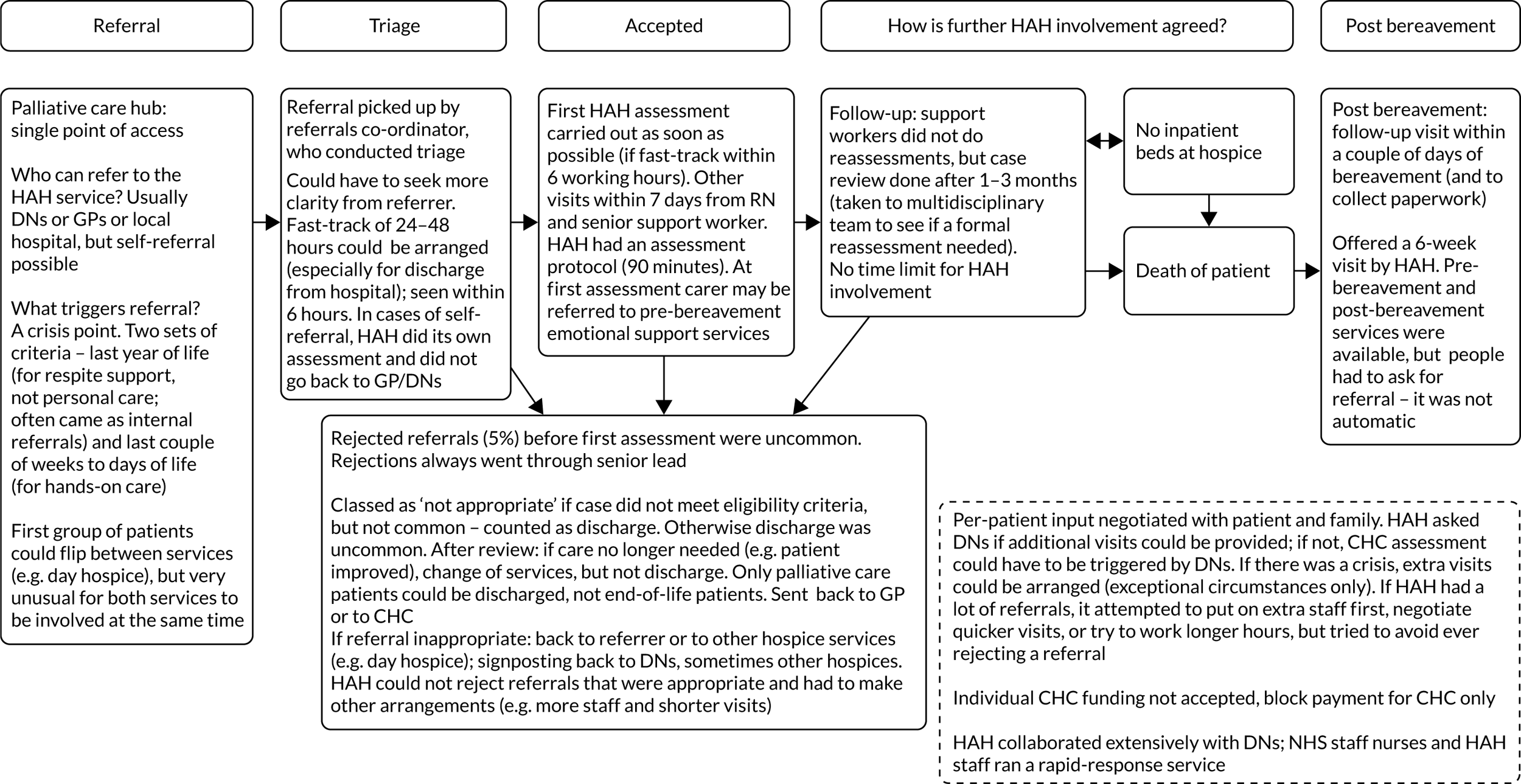
Wisteria (quadrant 3)
Overview
The Wisteria site was large and did not provide 24-hour service. This service served a predominantly deprived, urban area with a population of 320,000. A total of 425 referrals were received per year.
Other services in the area
Hospice at home identified local district nursing teams as the service they had the best relationship with and came in contact with the most (e.g. for access to medication). Other community-based palliative care services also operated in the area.
Funding
The main source of funding for the HAH service is charitable. The service was originally statutory funded by the primary care trust, but has since been internally funded by the hospice.
Use of volunteers
The hospice utilised volunteers across each of its services. A smaller pool of volunteers (n = 9 at the time of the study) acted as befrienders where there was a need, supporting the work of the HAH.
Wider hospice organisation structure and where hospice at home fits
The HAH team sat within the community services team. This was one of five units within the hospice, each with its own manager. There was an inpatient unit with 14 beds. There was also a well-being centre that ran day services, counselling and complementary therapies. The service utilised volunteers across each of the sections.
Hospice at home service operations
Staffing
Staffing is provided by qualified nursing staff (n = 4) and health-care assistants (n = 10), with some input from volunteers. HCAs provide hands-on care, with two qualified nurses who lead the team and carry out assessments. Volunteers (n = 9) act as befrienders where there is a need, supporting the work of the service.
Registered nurse cover was provided during the day only, with HCA staff providing night shifts alongside an advice line. There were two shifts during the day, an early shift (08.30–16.30) and a late shift (13.00–21.00), and there was a night shift (21.30–08.00). Hands-on care was provided 7 days per week, between 08.00 and 20.00. Patients had access to a 24-hour district nursing service during the night. There was a range in the intensity of care provided, from occasional or weekly visits to multiple hours of care per day.
Eligibility
Patients identified as being in the last 2 weeks of life were considered to be eligible for the service. Other criteria included the carer needing extra support at home as the patient is approaching end of life, the patient needing assistance with personal care (has been referred for a care package, but needs interim help), the patient being socially isolated and needing support at home (i.e. befriending) and/or the patient was being ‘fast tracked’ home from hospital.
Care
The HAH service was primarily a sitting service to provide expertise, reassurance and respite for the family. The HAH team did provide ‘hands-on’ care, but this was limited. The team did not administer medications or syringe drivers; these services were provided by the community nursing team.
Bereavement care
The HAH team sent out condolence cards to bereaved families. The hospice-level bereavement team then made contact.
FIGURE 42.
Patient flow at the Wisteria site.
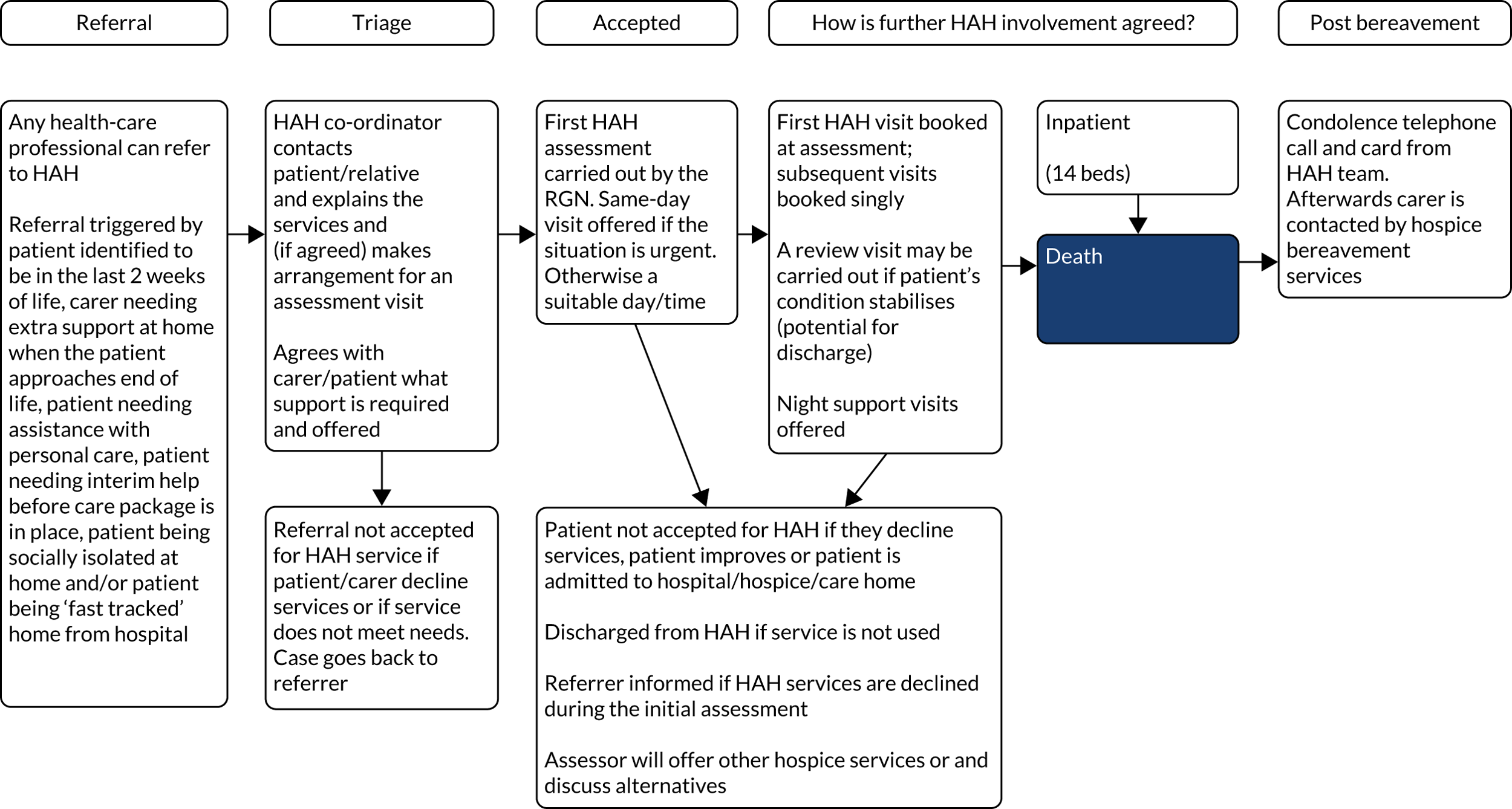
Hyacinth (quadrant 4)
Overview
The Hyacinth site was a hospice with inpatient provision in a predominantly affluent, rural area. The HAH services were categorised as ‘small’, with 200 referrals taken on per year, serving a population of 130,000 people. The service did not provide 24/7 services. Although night services were available, these were sporadic. This service stood out, compared with other case study sites, in a number of ways. By the end of phase 2 of this study, the HAH service no longer operated. Staffing the service proved a persistent difficulty. The service covered a large geographical area, with long travel times between patients.
Other services in the area
No other HAH services were available in the area. The area did not have 24/7 accesses to DNs.
Funding
The NHS contributed 12.58% of hospice funding in 2018/19. At the start of phase 2, the HAH service newly took on NHS CHC referrals as part of its caseload, but continued to see patients whose care was not funded by the statutory sector.
Use of volunteers
Volunteers worked across most services at the hospice. Initially, administrative support for HAH was provided by a volunteer, who left during phase 2 and was not replaced. Volunteers were not part of HAH care delivery for patients. A volunteer-led scheme provided companionship and assistance with everyday tasks for patients in the community; this service was very small for the duration of phase 2 of the study.
Wider hospice organisation structure and where hospice at home fitted
The hospice organisation offered HAH, specialist community nurses, inpatient care, a day hospice, several support groups for patients and informal carers, spiritual support and complementary therapies.
Hospice at home service operations
Staffing
At the start of phase 2, the HAH service had a small team of three HCAs (0.6 FTE) and two RNs (1.13 FTE). A HAH sister (RN) led the team. Staffing remained an issue throughout. A CNS team worked in the same building as the HAH service, but was not part of HAH. Bank staff services were available.
Care
The HAH team provided care for patients with predicted life expectancy of up to 1 year. Visits were not intensive (usually several times a week, rather than daily or several times a day). Per-patient capacity was capped. When need fluctuated, the HAH service drew on bank and inpatient staff when able. A RN in the team provided occasional night care to patients on the caseload.
Although per-patient visits were capped, the HAH service did not cap referrals.
Bereavement care
The HAH service formally referred to in-house bereavement services, most of which were provided in a group format.
FIGURE 43.
Patient flow at the Hyacinth site.
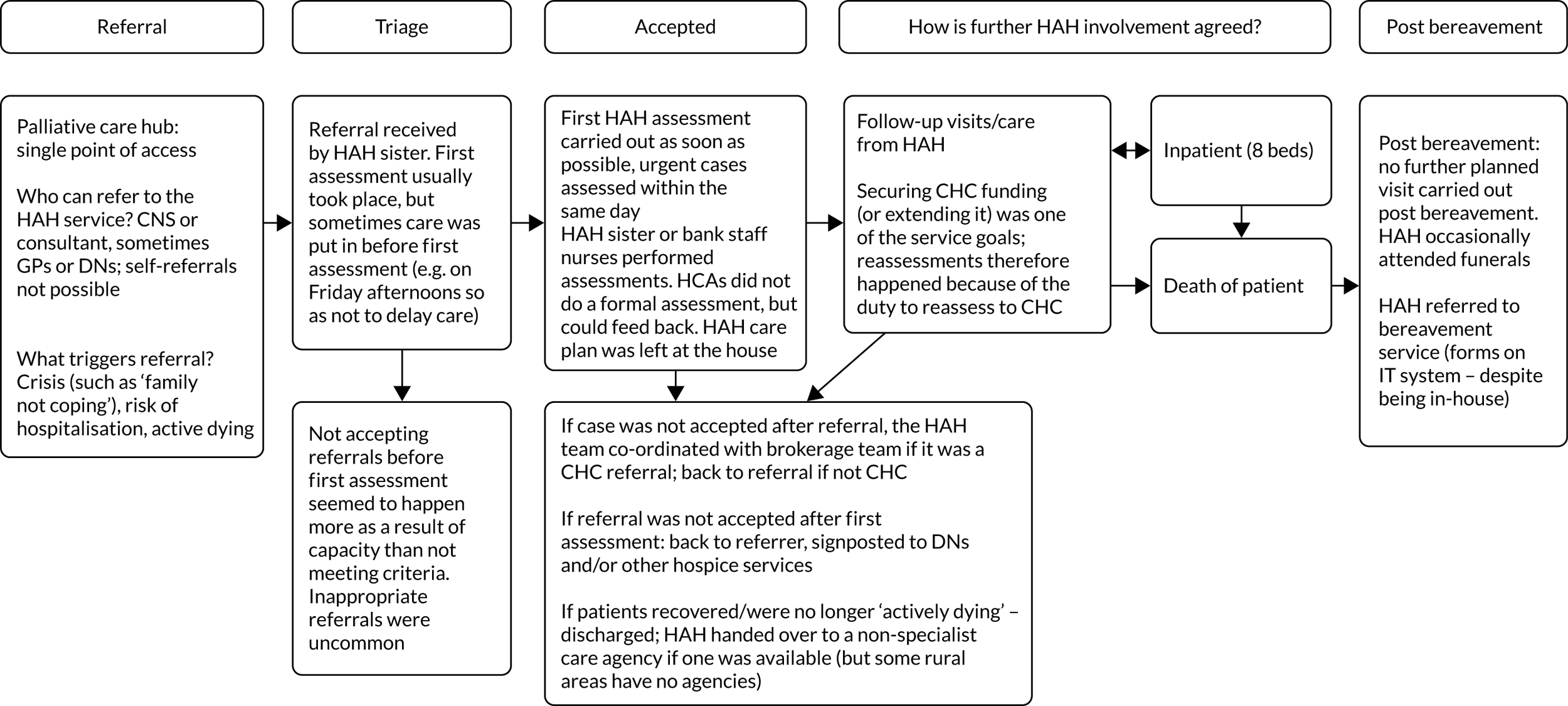
Marigold (quadrant 4)
Overview
The Marigold site was a HAH with inpatient provision available in the wider hospice organisation, in an urban area of mixed affluence. The HAH services were categorised as ‘small’, with 200 referrals taken on per year, serving a population of 500,000 people. The service did not provide 24/7 support.
This service stood out, compared with other case study sites, in that it provided a bridging service for patients waiting to receive NHS CHC funding. As such, none of the HAH caseload involved NHS CHC referrals; if NHS CHC funding was granted, another service would take over patient care. It was customary for double-up visits to be carried out with one RN and one HCA.
Other services in the area
There were other HAH services operating in the same city and wider area. District nursing services were available 24/7 in the area and the HAH service had a strong relationship with district nursing, sometimes co-ordinating visits to take place at the same time.
Funding
NHS funding made up 36% of all hospice income in 2018/19.
Use of volunteers
Volunteers worked across most services at the hospice, but not HAH. The hospice did not have a dedicated befriending service.
Wider hospice organisation structure and where hospice at home fitted
The hospice organisation offered HAH, a community palliative care team staffed by CNSs, outpatient clinics at medical centres with palliative medical consultants and CNSs, inpatient care, a day hospice, family/carer support (both bereavement support and practical support, e.g. funeral planning and financial advice), a patient peer support group, educational courses (e.g. to manage breathlessness) and bereavement support (including a service designed specifically for children).
The HAH service was managed jointly and shared offices with other community services provided at the hospice.
Hospice at home service operations
Staffing
The HAH service was a RN-led service. At entry to phase 2 of the study, the service had three HCAs (3 FTE cumulatively) and five RNs (3.6 FTE). Both RNs and HCAs were highly skilled; this was reflected in pay bands. Staff recruitment and retention were good.
Care
The HAH team provided hands-on care, 09.00–18.00, 7 days per week, and was able to respond rapidly (in < 4 hours). Other hospice community services provided symptom assessment outside HAH working hours. Most visits were carried out by a dyad of a RN and a HCA. In principle, the service aimed to admit patients requiring palliative care who did not (yet) have NHS CHC funding, but as phase 2 progressed, an increasing number of patients were seen within days of/< 1 week to death. The service did not cap referrals, but managed capacity by adjusting provision across the caseload and discharging after 6 weeks of care (in exceptional cases this period could be extended).
Bereavement care
The HAH service often expressed condolences over the telephone, but no post-bereavement visits took place. Carers were referred to hospice bereavement services.
FIGURE 44.
Patient flow at the Marigold site. MDT, multidisciplinary team.
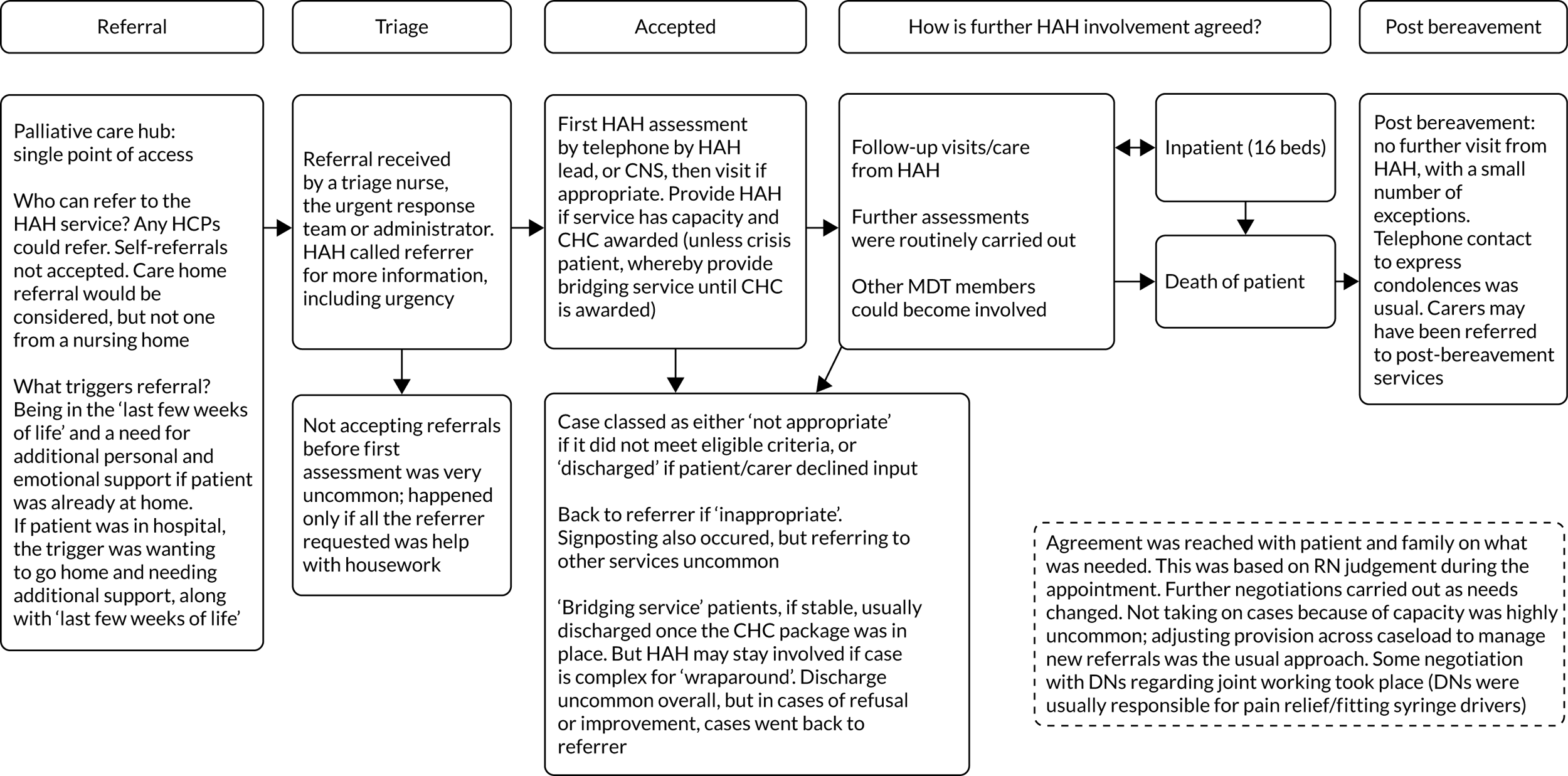
Xyris (quadrant 4)
Overview
The Xyris site was part of a hospice that was based in a listed building, and was part of a national network. The area served by the hospice had a population of 0.75 million people in a predominantly rural and affluent area with a largely white population. The HAH team received 155 referrals from April 2018 to June 2019, with 146 accepted.
Other services in the area
There were several EOLC providers in the area. Other services included district nursing (08.30–18.30); community matrons (7 days per week, 09.00–17.00); and hospital at home (24/7), which had a more acute remit in the day but covered for HAH at night, running parallel with OOH GP services.
Funding
Across all services nationally, NHS and local authority funding amounted to just over half (54%) of the charity’s income. Donations from the public, charitable trusts and corporate partners alongside retail activities made up the rest of the income. However, this specific HAH service was initiated and entirely funded by the hospice.
Use of volunteers
The service utilised volunteers but not specifically in HAH.
Wider hospice organisation structure and where hospice at home fitted
During data collection, the inpatient unit had 12 beds at the start of study, later reduced to six and then to zero (none was CCG funded). There was a well-being team based in the hospice, which ran group activities and provided access to CNSs (six on site), physiotherapy, occupational therapy, social work, family and bereavement support, spiritual support and complementary therapy.
The HAH team sat within a single-point-of-access palliative care hub (7 days per week, 08.00–20.00).
Hospice at home service operations
Staffing
The HAH service was staffed by RNs (n = 5) and nursing assistants (n = 6, and bank staff). The HAH service provided up to three visits per day and had about 15 patients on its caseload.
Care
The HAH service operated between 08.00 and 20.00, 7 days per week, and worked closely with the CNS team, which also worked 08.00–20.00 and was co-located. The HAH service provided a limited twilight service (Friday–Sunday, 20.00–02.00 initially, later reduced to 20.00–22.00).
The HAH service provided a 72-hour crisis service to provide care for patients while applying for and awaiting NHS CHC funding. From Friday afternoon to Monday morning, NHS CHC applications could not be processed, so the HAH service often covered a crisis over the weekend. However, if NHS CHC funding was not forthcoming or approval was delayed, then the HAH continued to provide care until alternatives were secured (e.g. via a social services crisis team, which usually had a waiting list). The crisis care provided by the HAH service was not reimbursed by NHS CHC.
The HAH staff provided help with pain management, alleviating symptoms and personal care, working closely with DNs, community matrons and CNSs. Prescribers in the HAH team or CNSs were able to prescribe pain relief, and it was the DNs’ role to operationalise syringe drivers.
Bereavement care
Post bereavement, the HAH service telephoned (or, if possible, visited) carers and sent a card. The HAH service completed a form (its own) to gauge level of risk post bereavement. Bereavement services were provided by a separate team.
FIGURE 45.
Patient flow at the Xyris site. SW, social work.
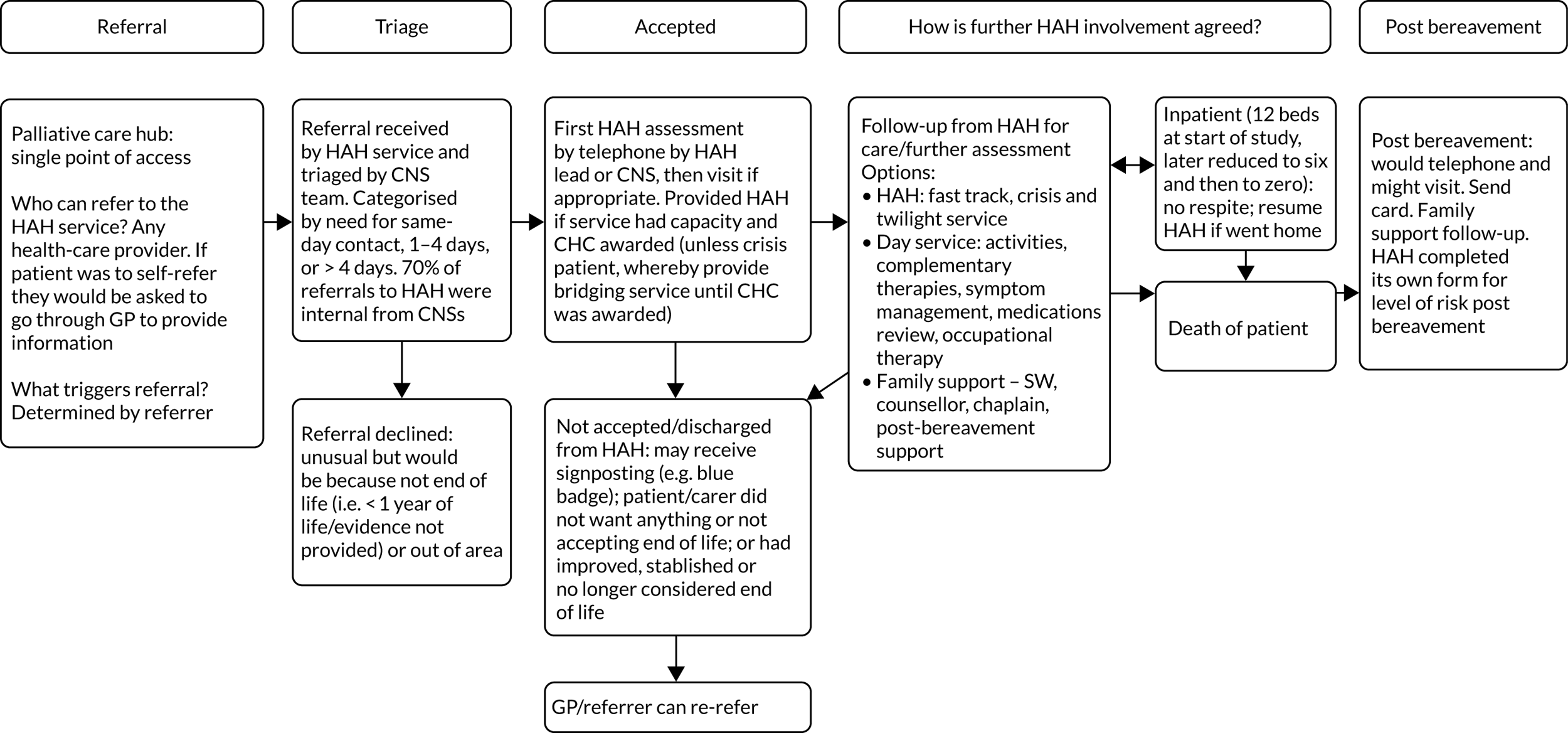
Appendix 29 Initial programme theories
Initial programme theories suggest that the following features of HAH models enable a service to provide optimal EOLC.
For more patients to receive timely HAH services, proactive marketing, engagement with HCPs and the public, and referral strategies are needed to raise awareness and visibility of the HAH service.
Sustainable funding modelFor a HAH service to be able to provide a sustainable service, despite local and national policies and funding changes, collaboration and partnership-working with commissioners and stakeholders promotes an integrated and agile service.
Service responsiveness and availabilityFor fewer patients to require emergency hospital admissions and for more to have enhanced discharge from hospital, suitable arrangements are needed for accessing medications and trained staff, underpinned by a whole package of care, including rapid response, enabling the HAH service to be responsive to patient choice and needs.
Criteria for service admissionFor patients and carers to continue engaging with and using the HAH service, robust referral criteria for identifying suitable patients, and clear explanation to patients and carers of the length of time it would take for a referral to be dealt with, are needed for patients and carers to know what to expect in terms of care input.
Knowledge and skills of care providersFor patients and carers to receive both the quality of care and the respect to uphold patient choice, palliative care training should be available for all HAH (and non-HAH) staff, including further training to support extended role activities, facilitating a recognition by GPs and others of the value of HAH staff having specialist palliative care knowledge and skills to navigate the complex health system.
Integration and co-ordinationFor continuity of care, timely and appropriate HAH provision and fewer emergency hospital admissions, substantial multiagency collaboration is needed between different NHS partners and the HAH, which leads to greater service co-ordination between the HAH service and relevant agencies and helps overcome issues around access and administration of medicines, underpinned by the use of shared electronic records.
Anticipatory careFor patients to receive the care they need in their preferred place of care, and to reduce unplanned hospital admissions, agreements need to be in place for anticipatory prescribing, equipment and care planning, underpinned by good 24-hour communication between HCPs and shared IT systems.
Support directed at the carerFor carers to be able to continue to provide sustainable care at home to partners or family, and for services to understand what carers themselves may need to sustain them, a holistic understanding of a carer’s needs, including an assessment by a multidisciplinary team involving the carer and HAH staff, is needed for carers to receive the practical and emotional support, to be mentored to use equipment, undertake key tasks and receive support through a crisis.
Appendix 30 Full context–mechanism–outcome configuration tables
| Context (the backdrop; this may vary in different case study sites allowing mechanisms to trigger or not) | Mechanism [the causal action(s) and responses to those actions that achieve the outcome in the context] | Outcome (these will be desirable but there may also be undesirable outcomes produced by the same contexts and mechanisms) |
|---|---|---|
|
Funding Statutory funding conditions and arrangements change over time, that is the constantly changing landscape of commissioning structures and provider organisations’ arrangements |
The HAH service needs to ‘be on the front foot’, that is if the HAH service proactively seeks visibility, a seat at the table and control over the available statutory funding by one or more approaches and/or The HAH organisation actively seeks external engagement with the wider health and social care environment Mechanism response The HAH service is trusted and respected (based on its reputation) to know what services are needed, to raise funds to deliver them and then to deliver them and/or If the HAH service is run by an independent organisation that undertakes charitable fundraising from different sources |
Sustainable, longer-term funding is enabled and patients will continue to receive the HAH service |
|
Commissioning There is often difficulty establishing consistent relationships with commissioners Commissioners may not be knowledgeable about palliative care and EOLC (Commissioners change frequently and very few are in post long enough to develop a good understanding of palliative care and EOLC services, including national initiatives) Commissioners may not recognise the full ‘cost’ of what they are commissioning as significant charitable funds are supporting the HAH service |
Commissioners new to EOLC with little history of a relationship with the HAH service may not be aware of the service or have had time to develop trust in the service | Access to statutory funds may be compromised |
|
Staffing There is a shortage of staff in health and social care nationally Some HAH services do not pay salaries compatible with statutory NHS/social care rates Some affluent areas may be too expensive for lower-paid staff to afford to live there Some rural areas may have even more limited workforce availability |
The reputation of the HAH organisation for excellence and investment in staff through CPD and the hospice/charity ethos attract staff, and even outweigh considerations of lower pay |
The HAH service is able to recruit the staff it needs to deliver the care that patients need The HAH service may attract and retain staff from other services, depleting the workforce in other parts of the system |
| Skill-mix profiles may be altered in response to RN shortages and registered staff deployed differently (e.g. office-based, dealing with triaging and work allocation) |
Staff take on roles they are not able to manage (in terms of skills and training) Staff may not be doing their preferred work |
|
|
National policy Commissioning has responsibility for whole population needs and care There is a national drive towards care at home, ostensibly in response to patient ‘choice’, but also with a view to cost savings and reducing pressure on hospital beds There are also societal and family pressures suggesting that ‘home is best’ and Hospice inpatient beds are a relatively scarce commodity |
Home-based care is supported by local health and social care commissioning and funding |
Rolls Royce service for some, none for others Policy supports the provision of home-based care, which suits those who want to die at home |
| If HAH services are available in the area and offered to patients and families and their wishes and preferences are not fully explored and revisited over time | Patients may feel that they have limited options and dying at home is what is expected | |
|
Data and ‘evidence’ NHS commissioners and charity boards require the collection of data to provide ‘evidence’ to support continuing service provision and development |
Enormous volumes of activity data are collected. Very little outcome data or cost–benefit data are collected or derived (e.g. about avoided hospital admissions) |
Activity data may satisfy some stakeholders Time is wasted in data collection that cannot richly inform funding and service decisions May lead to staff frustration and resistance |
| Context | Mechanism | Outcome |
|---|---|---|
|
There are national workforce shortages in health and social care, meaning that the paid workforce is in short supply and Societal norms regarding neighbours, community behaviour, families living in close proximity, etc., have changed and Many people in communities offer their time and skills as volunteers to hospices and other organisations, and recruiting, training and managing volunteers takes considerable time and Some of these people may have relevant health and social care professional skills therefore The volunteer workforce is attractive to employers, but hospices may be concerned about utilising a volunteer workforce, particularly in the clinical setting, feeling that it is not as manageable or reliable as the paid workforce, and may have concerns about legal liability, health and safety, etc. |
If HAH organisations invest in people and systems to recruit and manage volunteers, thereby reassuring the hospice organisation about working with a volunteer workforce If volunteers with existing, relevant skills are identified and they are prepared to use them in the HAH service and If volunteers have roles, remit, boundaries and expectations that are clear If volunteers are well supported by the organisation in their roles or If the organisation or locality takes a different approach to volunteering (e.g. Compassionate Communities), tolerating a different level of ‘risk’ and allowing volunteers to act more like neighbours without a great deal of bureaucracy and procedure |
Then the hospice will feel confident to utilise a volunteer workforce and additional resources will be available to provide care and support to patients and families Volunteers feel confident and clear in their roles, volunteer well-being is facilitated and volunteers are retained within the HAH to provide enhanced care to patients and families Then volunteers will be able to maintain appropriate boundaries that safeguard the patient, their family and the volunteer. More volunteers may be able to get involved with caring and supporting people at home However Volunteers may find the structure and expectations too demanding and inflexible and choose to volunteer elsewhere Inconsistencies, paradoxes and tensions develop when setting multiple ‘rules’ for volunteers who are offering non-professional support and befriending. They cannot, in reality, hold both a ‘semi-professional’ and a befriending role |
| HAH services offer shorter periods of care, in situations where the physical care needs are significant and rapidly increasing |
Volunteers cannot normally be trained and managed to meet the predominant health-care needs when the patient is actively dying There may be exceptions here in terms of volunteers with particular skills (e.g. retired nurses) Volunteers could be utilised specifically to support the carer, thus enabling the whole home situation to be sustained (e.g. doing the laundry, collecting prescriptions) |
Volunteers in general may have a limited role in this element of hospice volunteering |
| Hospices rely heavily on the volunteer workforce to support fundraising activities, including charity shops and sponsored events | The arrangements for volunteers may be more straightforward and easier to manage in this context | Volunteers make a valuable contribution to fundraising, without which services would be more limited |
| Context | Mechanism | Outcome |
|---|---|---|
|
Raising awareness There is a complex system of health and social care providing services for patients in the community at the end of life, and many professionals are not aware of all the possible services or of details of patient suitability In particular, hospice services are often thought of as hospice buildings; there is less understanding of hospice community services |
The HAH actively raises awareness among professionals and the public through clinical and public engagement:
|
The HAH will be seen as an essential service by professionals and the public and more patients with suitable needs receive timely referral and care Raising awareness directly to the public overcomes some of the professional barriers to referral and improves access |
|
Getting to the right patients, and equity Not all patients who could benefit from HAH services are currently referred HAH services aim to offer care to patients with ‘complex’ and suitable needs HAH services prefer to avoid discharging patients from services because of the impact on reputation and the difficulty of replacing HAH care: ‘we’d never leave someone in the lurch’ |
The HAH service proactively seeks suitable referrals through a range of systems or relationships (e.g. NHS CHC pathways, hospital palliative care team relationships) If the HAH has robust criteria for identifying which referrals are suitable, which may include trained triage staff to manage service admission Clearly boundaried funding arrangements (e.g. NHS CHC funding) enable more robust management of accepting or discharging patients from the HAH service If criteria, explanation of the service and treatment are clearly communicated to patients, families, and health and social care professionals |
Suitable patient referrals who can benefit most will receive the service |
|
If there is clear information about referral on to other services when the HAH service is not deemed suitable or Patients and carers accept reduced care at times when HAH resources are stretched. This is based on the quality of care received (they believe that other agencies will not match it) and on the ‘charitable’ ethos that pervades the services |
Professionals, patients and families will be clear about when and what they can expect to receive from the HAH service, leading to better managed expectations of the HAH service | |
|
Professionals may be reticent to refer patients to HAH services because it means having a conversation about death and dying with the patient, which they may not feel skilled or willing or have enough time to do Referrers may think the service is only for cancer patients The public have negative perceptions of the hospice involving the fear and stigma of death and dying (may have more impact in some communities in particular) |
If the HAH focuses its message of living well at all stages, this may make the process of referral more palatable for professionals and patients alike HAH services offer education and skills training about recognition of end of life, having end-of-life conversations and the use of the palliative care register |
More patients with suitable needs receive timely HAH care, including non-cancer patients (e.g. those with dementia, frailty) |
| A number of patient groups are poorly represented in hospice services in general, that is they do not receive an equitable share of available services, for example older age (> 85 years), non-cancer diagnosis, deprivation |
The HAH raises awareness about its service to professionals and the public through clinical and public engagement (see detail above) and/or If the service includes a proactive element to draw in suitable patients (e.g. could specifically target those groups locally known not to access the service by tailoring or directing marketing to those under-represented groups) |
Caseload reflects suitable diagnostic, demographic, cultural and socioeconomic diversity of the area served and services are provided equitably |
| Referrals to the HAH service require transfer of information, which may be time-consuming and require duplication of records and also effort finding the correct format and processes | If referral to the HAH service is easy for clinicians to do; long and formal referral processes are a deterrent | More patients with suitable needs receive timely HAH care |
|
Managing expectations The term ‘hospice’ encourages expectations of quality and specialism, which HAH services may not be able to replicate at home There are limits, including workforce shortages, to what can be provided in the home setting, which cannot mirror exactly the provisions of an inpatient setting |
Patient and carer preferences are explored and Criteria, explanation of the service and treatment are clearly communicated to patients, families, and health and social care professionals |
Professionals, patients and families will be clear about when and what they can expect to receive from the HAH service and Patients make choices based on correct information and understanding, and their choices are not over-ridden by professionals |
| Context | Mechanism | Outcome |
|---|---|---|
|
Service perspective A range of services needed by people at the end of life are operating in the community, with different organisational, funding, staffing, IT, etc. arrangements and Services across the whole system commonly act in silos, resulting in both duplication and gaps in services received by patients and There is a limit to services, funding and workforce across the whole system and Issues of professional ‘ownership’ of palliative care and EOLC are at play whereby designated palliative care services may both wish to see other services providing EOLC, but also see this as a threat and Professional boundaries are shifting across health and social care, including those between doctors, nurses and other professionals (paramedics, physician associates) and between registered and non-registered workers and Integration of health and social care is a national driver; the boundaries between the two in terms of care needs are often difficult to define clearly and many years have been spent creating/putting in divides between them for the purposes of previous funding divisions and Organisations seek their own branding and distinctiveness for sustainability purposes and Individual professionals seek to differentiate their roles and functions so they all continue to be ‘needed’, for their own personal sustainability and Services will be covering a variety of urban and rural areas (majority mixed) and travelling time will be a significant factor in service delivery responsiveness and resources |
The HAH service is working effectively with other service providers internally, externally and on the ground Co-ordination between workers on the ground is pivotal Communication is a key mechanism here, for example: |
Patients and carers receive a seamless service and continuity of care without delay, duplication or gaps, for example care, interventions, equipment and drugs that are needed by the patient will be available in a timely fashion More cost-effective services are delivered to patients and families Less burden on HAH staff trying to ensure co-ordination and reduced tension between care providers but The multiplicity of organisations and roles may cause confusion and conflict (‘ruffled feathers’) |
Examples: medication and equipment
|
This specific example may result in unnecessary duplication when a qualified member of staff who is in the home cannot perform a task because it has been allocated to another service and requires a separate visit | |
|
Patient and family needs ‘at the front door’ Patients in the last phase of life and their family carers require and use services from a wide range of statutory, voluntary, and health and social care providers and Palliative care and EOLC patients have a constantly changing trajectory of illness and a high risk of unexpected and unpredictable needs that are difficult to anticipate Some patients and carers will not know when to ask for help or who to contact Patients are not always clear about when and what they need that should trigger them making contact to request services. They prefer not to feel that they need hospice care (implies their situation is extremely serious). They do not want to make too many demands on busy and charitably funded services |
Regardless of ‘formal’ arrangements for integration and co-ordination, much of this works on the ground as colleagues get on to work for the patient and are co-dependent If patients and carers are provided and updated with information including who and how to contact professionals (within HAH and with other organisations in the locality) If budgets and workforce and organisational structure are managed in an integrated way across provider organisations, for example |
Patients receive a seamless service and continuity of care with consistent information, without delay, duplication or gaps (they really do not care who is providing it) Services are able to provide staff to respond rapidly to unpredictable and fluctuating workloads in a cost-effective way Patients know who to contact in an emergency and get the response they need Fewer patients have unwanted emergency admissions More patients have enhanced hospital discharge |
|
In hours vs. OOH services Not all HAH services provide 24/7 care |
Anticipatory care and information become yet more critical; in particular, if night-time cover is not provided by the HAH service, a well-advertised 24-hour contact number is crucial | Needs are anticipated as far as possible and patients experience continuity of care when providers change |
| Context | Mechanism | Outcome |
|---|---|---|
|
All health and social care workers should have basic knowledge and skills in palliative care and EOLC. However, these are sometimes lacking, for example lack of confidence in identifying the end of life, lack of skills in communicating at the end of life and lack of time to offer personalised and patient-led care Time The provision of time is a context that HAH services aim to offer, to add value to the whole system of care They can pick and choose their workload more than services that are statutory or profit-making Commissioners do not always value time and expertise, but prioritise equity of access across the population There is wide variability within localities in the levels of skills, knowledge and performance of community-based staff, which may vary from GP to GP, community nurse to community nurse and practice to practice Palliative care and EOLC has developed into a ‘specialty’ area of knowledge, skills and ethos, and this distinctiveness is prized by HAH organisations There is a range of other ‘specialists’ also working in the community, who will vary from one locality to the next. This may include other palliative care staff, Admiral Nurses, respiratory teams and heart failure services. They will also have varying levels of skills, knowledge and confidence in dealing with palliative care and EOLC For some patients, basic skills may not be adequate to meet their difficult or complex needs |
HAH services provide expert knowledge and skills in palliative care and EOLC and have a suitable ethos to support this care by: Experience Experienced staff, spending a significant proportion of their time in palliative care and EOLC, who are capable and competent in this setting (mechanism response) so patients, families and other HCPs trust them Time Taking time to offer personalised, patient-led care, not having to rush (pacing) Time pressures are well managed by HAH organisations through sensitive communication with patients and carers (e.g. if they are going to be delayed) |
Better patient and carer experience and sense of agency More patients receive the care they need when they need it and where they prefer to be |
|
Training Staff at all levels (including volunteers) are suitably trained, including appropriate communication skills and investment in CPD, so that they can create an environment (mechanism response) that makes patients and carers feel that they are in expert hands The HAH service also provides training to other health-care and social care professionals Supported staff The HAH retains skilled staff by providing staff support to manage the stress of their work and to develop the necessary emotional resilience Staff can call for advice and support with their work from expert colleagues who are part of the HAH service and Policies and processes allow for extended roles as necessary and staff know who to collaborate with if work is outside their competencies |
Other health and social care workers may be upskilled in some instances or deskilled in others. If the balance falls in terms of deskilling, then knowledge and confidence decrease over time, resulting in poorer care for those who do not access specialist services and increasing demand for specialist services | |
| Most of the expertise in palliative care and EOLC still resides in cancer care; patients with other illnesses (e.g. dementia) may present particular challenges to staff and organisations | Accessing other elements of hospice services because prognosis is longer than HAH can provide for may support some of these patients | Inequity and mismatch in care provided, patient/carer feel patronised and not understood |
| Context | Mechanism | Outcome |
|---|---|---|
|
There is a societal expectation that ‘family’ will support dying at home and services are configured on this basis. Unpaid care provided by family and/or friends is critical to enabling patients to remain at home Informal carers and the home circumstances vary in the extent to which they can or wish to support care at home. This will include cultural differences and preferences. The home ‘unit’ needs to make a decision to aim to support death at home There will be a spectrum of needs and wishes of patients and carers and how they align with each other The carer requires continuing confidence, wellness (physical and emotional) and new skills to enable them to provide care up to and including the point of death at home. The task of caring at home is constantly changing over time People have different views on their home and their willingness to admit outsiders; these views may differ between patient and carer |
If there is an assessment and continuous review of carer needs including the whole family and care unit and if there is a multidisciplinary team available to meet the needs How the patient and their informal carers as a unit in the home feel about caring at home and respond to the challenge of this situation will be key to sustaining the care If carer is informed as early as is appropriate about what HAH can/cannot offer and how it fits in with other services If carer is informed about and signposted to other services and community support (including services specifically directed at carers) If HAH services are able to ‘co-ordinate’ with other services and advocate for the patient if the carer unable If carer is informed about funding options and available financial support is accessed (e.g. carers’ allowance) If cultural preferences are respected |
Carers will be able to continue to care, enabling more sustainable patient care at home Carers will receive the care and support they need, including sleep, taking a break, reassurance and confidence-building Carer is not isolated Occasionally, carer needs may become the main focus at the expense of the patient |
|
If the carer is fully informed, including what might happen in terms of the trajectory of illness and the increasing burden of caring over time, they will know what to expect and prepare and they can rapidly recognise a change in caring situation from control to crisis If carer and patient choices are encouraged, affirmed and supported wherever possible If carer is offered respite services If self-referral/referral by informal carer to HAH is made available and easy to follow |
If too much is expected of the carer (e.g. administering medication injections when they prefer not to), then there are some tasks they may not be able to manage or they may not be able to continue to provide care or they may have a negative or distressing experience The carer and patient feel supported and encouraged |
|
|
Carer sets the pace. If there is a negotiated partnership between the carer and staff and recognition of what the individual patient–carer dyad want (i.e. some may not want a lot of intrusion into their home) and This is followed by an ongoing relationship of feedback, response and adaptation If the carer has (quick) access to an appropriate point of contact 24/7 If there is regular contact with the carer If carer is offered training/information on practical aspects of care (same moving and handling, medication administration, mouth care, preventing pressure sores) If the procedures after death meet cultural needs and preferences (e.g. burial within 24 hours) Mechanism response will be trust and confidence in the backup provided by the service and in their caring role Negotiations take place with the carer about how much they are happy to take on and the carer receives skills training so they will have appropriate skills that they find are acceptable Carer is recognised for their knowledge and given permission to do caring tasks that are increasingly seen as ‘professional’ tasks Carer and patient are supported to make advance care plans and post-death preferences |
There is respect for the relationship between patient and carer, who get the chance to spend quality time together | |
|
After death There may be short- or long-term consequences of caring to the carer’s mental and physical health, in bereavement HAH services usually come to an abrupt halt when the patient dies The existing social networks that carers have vary considerably There is a concern about ‘medicalising’ bereavement, which is a normal process |
There is support pre and post bereavement that is based on relationship and understanding of the situation and also a shared story of caring for the patient There is flexible and varied post-bereavement support (e.g. support groups and one-to-one support) at the hospice and wider community and a way to keep in touch with the hospice (e.g. events) There is carer-centred guidance available on practical tasks after death (e.g. death certification, funerals, legal advice and dealing with leftover equipment/medication/records) There is a mechanism to identify those who are not experiencing ‘normal’ bereavement and may need additional/expert help. Routine bereavement letters and memorial events may provide opportunities for this |
The carer will have the best chance of a positive outcome following bereavement and recovery from the caring role The carer feels that they have done their best for their loved one Carers may have a negative experience of care, and the associated burdens and difficulties and Some carers may accept this negative experience as a price they wish to pay to allow their loved one to achieve their PPOD |
Glossary
- Ambulatory and Home Care Record
- A service use data collection tool.
- Analysis of variance
- A technique used to test the difference between two or more mean values.
- Australian modified Karnofsky Performance Status
- A measure of functional status adapted for palliative care.
- Compassionate communities
- Networks of people (‘neighbours’) supporting each other, often particularly focused on preparing and enabling a good end of life whenever possible. Sometimes referred to as ‘compassionate neighbours’.
- Context–mechanism–outcome configuration
- A heuristic used to generate causative explanations relating to outcomes. The process explores the relationship between an outcome of interest in a particular context and the underlying mechanism.
- Generative mechanism
- The generative force that leads to an outcome of interest, usually hidden and context sensitive. Mechanisms consist of intervention resources and how people respond to them.
- Integrated Palliative care Outcome Scale
- A clinical measure used to assess the palliative care needs of a patient.
- James Lind Alliance
- A non-profit initiative that brings patients, carers and clinicians together in Priority Setting Partnerships.
- NHS Continuing Healthcare
- A package of care for adults aged ≥ 18 years that is arranged and funded solely by the NHS. To receive NHS Continuing Healthcare funding, individuals have to be assessed in accordance with a legally prescribed decision-making process to determine whether or not the individual has a ‘primary health need’. In particular circumstances, this funding can be ‘fast tracked’ to speed up the assessment process.
- NVivo (QSR International, Warrington, UK)
- A qualitative data analysis software package.
- Phase of illness
- A patient assessment measure designed for use in palliative care.
- Programme theory
- The overarching theory of how a particular complex intervention may work; it draws on evidence, data and creative (retroductive) thinking to seek explanations of how, why and in what contexts an intervention works.
- Quality-adjusted life-year
- A generic measure of disease burden that takes into account both the quality and the quantity of life lived.
- Quality of Dying and Death questionnaire 7-day recall, version 1
- A validated instrument measuring quality of care and death in the last 7 days of life.
List of abbreviations
- 24/7
- 24 hours per day, 7 days per week
- A&E
- accident and emergency
- AHCR
- Ambulatory and Home Care Record
- ANOVA
- analysis of variance
- C
- carer
- CCG
- Clinical Commissioning Group
- CMO
- context–mechanism–outcome
- CNS
- clinical nurse specialist
- Comm
- service commissioner
- CPD
- continuing professional development
- DN
- district nurse
- DOD
- date of death
- ECOG
- Eastern Cooperative Oncology Group
- EOLC
- end-of-life care
- FTE
- full-time equivalent
- GBP
- Great British pounds
- GP
- general practitioner
- H&PC
- hospice and palliative care
- HAH
- hospice at home
- HCA
- health-care assistant
- HCP
- health-care professional
- IPOS
- Integrated Palliative care Outcome Scale
- IQR
- interquartile range
- IT
- information technology
- M
- mechanism
- NAHH
- National Association for Hospice at Home
- NHS CHC
- NHS Continuing Healthcare
- NIHR
- National Institute for Health and Care Research
- NPT
- normalisation process theory
- OOH
- out of hours
- OPEL
- OPtimum hospice at home services for End of Life care
- PPI
- patient and public involvement
- PPOD
- preferred place of death
- QODD
- Quality of Dying and Death questionnaire
- RN
- registered nurse
- SD
- standard deviation
- SP
- service provider
- STP
- Sustainability and Transformation Partnership
- VOICES
- Views of Informal Carers – Evaluation of Services
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/MSAY4464).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
