Notes
Article history
The research reported here is the product of an HSDR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HSDR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HSDR journal.
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/05/88. The contractual start date was in September 2018. The final report began editorial review in July 2020 and was accepted for publication in January 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2022. This work was produced by Meader et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2022 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Epidemiology
General health risks associated with multiple risk behaviours
Health risk behaviours (e.g. smoking, physical inactivity, unhealthy diet, excess alcohol consumption and illicit drug use) are common in the UK and internationally. Smoking is the single largest directly avoidable cause of death in the UK, and a major cause of respiratory disease, cancer and cardiovascular disease. 1 Physical inactivity and unhealthy diet are strongly associated with weight gain, obesity, cancer, cardiovascular disease and type 2 diabetes. 2 Excessive alcohol consumption is also associated with greater risk for cancer, liver disease and cardiovascular disease. 3 Drug use is associated with greater risk of developing human immunodeficiency virus, hepatitis C and tuberculosis infections. 4
There is good evidence, both in the UK and internationally, that health risk behaviours cluster. 5 The majority of adults report engaging in two or more risk behaviours, and approximately one-quarter engage in three or more risk behaviours. 6 A 2017 Norwegian population-based cohort study7 of > 30,000 participants found a dose–response relationship between number of risk behaviours and all-cause mortality (i.e. increase in risk of all-cause mortality of 1.55-fold for two behaviours, 2.26-fold for three behaviours and 3.16-fold for four behaviours). There was a similar dose–response effect for risk of stroke in a large UK study of > 20,000 participants: the relative risks for people who engaged in four risk behaviours were 2.31 when compared with people who engaged in no risk behaviours, 2.18 when compared with people who engaged in one risk behaviour, 1.58 when compared with people who engaged in two risk behaviours and 1.15 when compared with people who engaged in three risk behaviours. 8 There is strong evidence that social and health inequalities are associated with engaging in multiple risk behaviours. People in the UK who do not complete secondary school or who have an unskilled occupation are three to five times more likely to engage in multiple risk behaviours. 9
Multiple risk behaviour interventions in general populations were associated with small reductions in smoking, unhealthy diet and physical inactivity, but there is currently insufficient evidence for reductions in alcohol and drug use. 10 In addition, small benefits were found in terms of reductions in weight, blood pressure and total cholesterol in the general population. 10
Health risk and inequalities in severe mental illness populations
Preventing long-term conditions has been a key policy priority for some time, and people with severe mental illness (SMI) constitute a particularly vulnerable subgroup of the population.
Risk of cardiovascular mortality is two to three times higher in people with SMI11 and life expectancy is 15–20 years lower than that of the general population. 12 This substantial risk is probably driven and sustained by complex interactions between social inequalities13, genetics, neurobiology, psychosocial impairment and symptoms associated with SMI,14 side effects of medication15,16 and a lack of access to physical and mental health interventions. 13
Smoking is the largest cause of premature mortality in the UK, and the biggest contributor to health inequalities among people with a mental health condition. 17 Therefore, it is particularly concerning that smoking is up to three times as prevalent in SMI populations than the general population, and even higher in certain subgroups (e.g. mental health inpatients). Although the prevalence of smoking in the general population has reduced by one-quarter in the past 25 years, the change in prevalence for smoking among people with a mental health condition in the same period is negligible. 1 This means that 42% of all cigarettes in the UK are now smoked by people with a mental health condition,1 who have been shown to lose, on average, 17 years of life as a result of tobacco smoking. 18
Similarly, people with schizophrenia are more likely to engage in an unhealthy diet, including lower fibre and fruit intake and higher saturated fat and calorie intake than the general population. 19 A study of people with SMI in psychiatric rehabilitation programmes found that only 4% met physical activity guidelines. 20 People with schizophrenia engaging in multiple risk behaviours are more likely to be overweight, to have high low-density lipoprotein (LDL) cholesterol, to have low high-density lipoprotein (HDL) cholesterol and to have increased fasting glucose levels. 19 Antipsychotic treatment, and other commonly prescribed medications, are associated with increased weight gain, particularly within the first years of psychosis. For example, a systematic review estimated an average 12-kg weight increase in the first 24 months of taking antipsychotics. 21 Similarly, Kahn et al. 22 found that people with first-episode psychosis experienced a 7% increase in body weight during the first year of treatment.
However, it should also be noted that, although antipsychotic use may increase risk of cardiovascular disease, there is also evidence that antipsychotic use overall may be associated with improvements in mortality in people with schizophrenia. 23
People with SMI are also substantially more likely to engage in substance use. A large US study of > 20,000 participants found that people with psychosis were four times more likely to engage in heavy alcohol use, cannabis use and use of other recreational drugs. 24 A UK study found that 30% of people with first-episode psychosis engaged in illicit drug use, 25% engaged in both alcohol misuse and illicit drug use and 10% engaged in excess alcohol consumption. 25
People with SMI are more likely to engage in multiple health risk behaviours. For example, in one study, on average, people with SMI were found to engage in five risk behaviours. 26 Therefore, an important question is whether to target these risk behaviours concurrently (i.e. multiple risk behaviour interventions) or to focus on a particular behaviour alone (i.e. single risk behaviour intervention).
Why this research is needed
Reducing risk behaviours in people with SMI is a clear priority for the NHS. These aims relate to wider initiatives such as the Mental Health Taskforce’s Five Year Forward View for Mental Health,27 which highlights the importance of integrating physical and mental health care. However, there are key evidence gaps that are important in informing practice:
-
Most people with SMI engage in multiple risk behaviours – a key question is whether interventions should target multiple risk behaviours in parallel or target single behaviours.
-
The importance of investigating factors that are likely to influence the clinical effectiveness of risk behaviour interventions in this population (e.g. intervention delivery, frequency) has been recognised.
Multiple compared with single risk behaviour interventions
There are several systematic reviews that have focused on the effectiveness of interventions among people with SMI for particular behaviours: smoking,28 unhealthy diet and/or physical activity. 29–31
Despite a relatively developed literature of primary studies in this area, to our knowledge, there are currently no systematic reviews specifically focused on multiple risk behaviour interventions in people with SMI. It is not possible from current systematic reviews to delineate the benefits of focusing on a particular risk behaviour, compared with targeting multiple behaviours concurrently, in a SMI population. Risk behaviours cluster; therefore, it is important to question whether services should seek to reduce risk behaviours in parallel or to target risk behaviours one at a time, as interventions to promote change in a health risk behaviour have important implications for engaging in other behaviours. For example, our systematic review of multiple risk behaviour interventions in general populations10 found that changes in diet were positively associated with changes in physical activity, and that both, in turn, were associated with increased weight loss. This is consistent with evidence from qualitative studies; for example, people with diabetes reported that improvements in physical activity acted as a ‘gateway’ to changes in diet. 32 Conversely, changing some risk behaviours may have negative consequences for engaging in others.
Identifying ‘active ingredients’ of risk behaviour interventions
Behaviour change interventions are typically complex with multiple interacting components. Therefore, behaviour change technique taxonomies (BCTTs) have been developed to help identify the effective components in these interventions to help inform future research [e.g. which behaviour change techniques (BCTs) should be included in future trials] and implementation in services. 33 We are unaware of any systematic reviews that have investigated the impact of intervention content using these methods in SMI populations.
Qualitative studies on barriers to and facilitators of change and experiences of risk behaviour interventions
There is an important need to synthesise qualitative data on the experiences of people with SMI to inform interpretation of the quantitative data and future trial design. For example, qualitative data are important for identifying barriers to and/or facilitators of behaviour change. This enables us to compare which barriers or facilitators were addressed in trials and to identify intervention content for future trials. Similarly, we can compare the extent to which the reported experiences of people with SMI in the qualitative data reflect findings from the quantitative data. As far as we are aware, this is the first systematic review to have synthesised this literature specifically focused on multiple risk behaviour interventions, especially in a SMI population.
Chapter 2 Methods of effectiveness review, meta-analysis and qualitative review
The systematic review protocol was registered with PROSPERO (CRD42018104724).
Objectives
We aimed to provide a comprehensive and objective summary of available primary research about the clinical effectiveness of health risk behaviour interventions in people with SMI.
More specifically, the objectives of the systematic review were to:
-
provide a descriptive overview of all the evidence for multiple health risk behaviour interventions on behaviour change (e.g. fat intake, smoking abstinence) targeted by the intervention, and change in outcomes affected by these behaviours [e.g. weight, body mass index (BMI), blood pressure]
-
examine the clinical effectiveness of multiple risk behaviour interventions, compared with single risk behaviour interventions, using network meta-analyses (NMAs), in terms of their impact on behavioural outcomes (e.g. smoking abstinence) and outcomes affected by changes in behaviour (e.g. weight, BMI).
-
examine the effect of study-level intervention content (e.g. using BCTTs) and participant characteristics (e.g. targeted by study for physical comorbidities) as moderators of effectiveness of risk behaviour interventions using meta-regression and component NMAs.
-
explore, through qualitative evidence, factors affecting the clinical effectiveness of risk behaviour interventions (including barriers and facilitators) for people with SMI.
Literature searches
Searches were carried out in October 2018 in the Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE™ (Elsevier, Amsterdam, the Netherlands), MEDLINE, PsycInfo® (American Psychological Association, Washington, DC, USA) and Science Citation Index (Clarivate Analytics, Philadelphia, PA, USA). The date range searched was inception to October 2018. The searches identified 27,795 records, which was reduced to 18,513 records after deduplication using EndNote (Clarivate Analytics) bibliographic software.
Updated searches were carried out in March 2020 in EMBASE, MEDLINE, PsycInfo and the Science Citation Index; these identified a further 2822 records, which was reduced to 1433 records after deduplication. It was not possible to download records from CENTRAL owing to issues with the database at the time of the updated search (28 March 2020). We searched Applied Social Sciences Index and Abstracts (ASSIA) (date range inception to September 2020), and conducted an updated CENTRAL search in September 2020. The updated search of CENTRAL identified a further 1843 records, which was reduced to 1579 after deduplication. The search of ASSIA identified 658 records, which was reduced to 151 after deduplication.
The strategies used for both the original and updated searches are reproduced in Appendix 1.
Study selection
Population
Adults (aged ≥ 18 years) diagnosed with SMI (defined as schizophrenia or other psychoses, depression with psychotic features, or bipolar disorder) were included. Interventions aimed at people with SMI who were overweight or obese, had long-term conditions or risk factors for long-term conditions (e.g. high blood pressure, high cholesterol) were also included.
Interventions
Behavioural interventions were included with no restrictions on whether the focus of the intervention content was psychological, educational or environmental, nor were any restrictions applied based on setting.
For some health risk behaviours (e.g. smoking, excess alcohol consumption, opioid use), pharmacological treatment may be a component of standard care. When this was the case, behavioural interventions in combination with standard pharmacological interventions were included. However, studies were excluded if they primarily aimed to evaluate the effectiveness of pharmacological interventions.
Single health risk behaviour interventions were included if they aimed to change one of the following risk behaviours: smoking, unhealthy diet, physical inactivity, excess alcohol consumption or drug use. Multiple health risk behaviour interventions were included if they aimed to change two or more of these behaviours.
Comparators
-
No intervention.
-
Treatment as usual (TAU).
-
Treatment as usual with additional active control elements (e.g. attention control).
Outcomes
For quantitative studies, we included data on the following outcomes:
-
changes in behaviours directly targeted by the intervention (smoking, diet, physical activity, alcohol use, drug use)
-
anthropometric measures [weight (kg), BMI]
-
metabolic outcomes (systolic blood pressure, diastolic blood pressure, HDL cholesterol, LDL cholesterol, total cholesterol)
-
quality of life
-
mental health symptoms.
Study designs
For the clinical effectiveness analyses, we included randomised controlled trials (RCTs).
In addition, we included qualitative studies assessing the experiences of behaviour change in people with SMI (including barriers and facilitators).
Methods of effectiveness review and meta-analysis
Data extraction and screening
Data extraction, screening and risk-of-bias assessment were conducted by one reviewer and checked by a second reviewer. Discrepancies were resolved by discussion, with involvement of a third reviewer if necessary.
The data extraction form was piloted on a selection of studies by three reviewers to ensure consistency. Data from multiple publications of the same study (or data set) were extracted and reported as a single study. When there were data from multiple time points, we grouped these data into the following categories: end point, ≤ 6 months post intervention, 6–12 months post intervention, and ≥ 12 months post intervention.
Two reviewers extracted information about the content of each intervention and control, including which risk behaviours were targeted, whether the choice of risk behaviour was fixed or tailored to the individual, background/expertise of the intervention provider, mode of delivery (e.g. group or individual focused), intensity of intervention (duration of sessions, duration of intervention, etc.), setting (e.g. outpatient, inpatient), and adaptation of content for people with SMI. BCTs were categorised using the Behaviour Change Technique Taxonomy version 1 (BCTT v1). 33
The participant characteristics extracted included mental health diagnoses, whether or not the intervention was given at first initiation of antipsychotics, antipsychotic use (proportion of participants receiving antipsychotics, and which type of antipsychotic), physical health comorbidities, age, sex and ethnicity.
Risk-of-bias assessment
The risk of bias of the individual studies was assessed using the Cochrane Risk of Bias tool version 2 for RCTs. 34 As per recommendations, we conducted separate risk-of-bias assessments for the key outcomes: the most widely reported behavioural outcomes (smoking abstinence) and the most widely reported outcomes affected by behaviour (weight and BMI).
Data analysis
All analyses were performed in a Bayesian framework with a random-effects model using WinBUGS (MRC Biostatistics Unit, Cambridge, UK),35 taking into account the correlation between multiarm trials when appropriate. However, when there were sparse networks (and potentially insufficient data to reliably estimate between-study heterogeneity), we compared the goodness of fit of fixed-effect and random-effects models and used data from the better-fitting model. When both models fitted equally well, we selected the simpler model.
A binomial likelihood was used for dichotomous data and a normal likelihood for continuous data. We assumed a common between-study heterogeneity variance of the relative treatment effects for every treatment comparison. We used vague prior distributions for trial baselines, heterogeneity and relative treatment effects. For WinBUGS code (including prior distributions), see WinBUGS code for models (see the National Institute for Health Research Journals Library projects web page; URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/170588/#/). Network geometry for NMAs was illustrated using network diagrams (see Appendix 7).
We assessed convergence of two chains based on visual inspection of history, Brooks–Gelman–Rubin and autocorrelation plots.
Network meta-analysis enables the estimation of indirect comparisons not addressed in the primary trials. 36 Such analyses assume consistency in the evidence network between indirect and direct evidence. Unfortunately, few trials compared single or multiple risk behaviour interventions directly; therefore, there were insufficient data to assess the consistency of direct and indirect evidence.
Intervention effects were estimated along with 95% credible intervals (CrIs). Continuous outcomes were usually pooled mean differences (MDs) on natural units such as number of cigarettes, weight (kg), BMI (kg/m2) and blood pressure (mmHg). Some outcomes, such as physical activity and alcohol use, were measured in various ways across studies, so we used standardised mean differences (SMDs) to analyse these data.
The analysis proceeded in three stages.
Model 1: intervention effects model
Across studies, interventions targeted a range of single (e.g. unhealthy diet alone, physical inactivity alone) or multiple health risk behaviours (e.g. unhealthy diet and physical inactivity). We used NMAs to assess the effectiveness of targeting these different combinations of risk behaviours.
Studies varied in terms of participant (e.g. targeting people with SMI who also had comorbid physical illness) and intervention characteristics (e.g. whether studies were primarily delivered to groups or individuals). Therefore, we extended the model to include covariates estimating the association between these participant and intervention characteristics and intervention effectiveness.
Model 1a: effectiveness of targeting different combinations of risk behaviours
-
Targeting any risk behaviour.
We used a random-effects NMA model to compare any health risk behaviour intervention with TAU. Studies with TAU with additional active components (hereafter referred to as TAU+) as a comparator were also included in the network to inform estimates.
-
Targeting combinations of risk behaviours. We used a similar random-effects NMA model, as model 1a:1, but, instead of comparing any intervention with TAU, we assessed the impact of targeting different health risk behaviours compared with TAU.
Model 1b: impact of intervention and participant characteristics
Second, we assessed the impact of intervention and participant characteristics on effectiveness estimates by adding the following covariates to model 1a:
-
participants selected for physical comorbidities (yes/no)
-
intervention delivered primarily to individuals (yes/no)
-
intervention setting (inpatient or not inpatient)
-
authors reported tailoring the intervention for people with SMI (yes/no).
We assessed the impact of these intervention and participant characteristics by assessing the magnitude of the covariate estimate, along with its 95% CrI. In addition, we conducted a more global assessment, comparing the goodness of fit of model 1b with covariates and model 1a without covariates in terms of deviance information criterion (DIC), total residual deviance and between-study standard deviation (SD).
Model 2: does targeting multiple risk behaviours lead to positive or negative synergies (interaction model)?
Model 1 gives some insight into the benefits of targeting different combinations of risk behaviours. But it does not directly assess whether or not targeting multiple risk behaviours leads to positive or negative synergies (e.g. does targeting diet and physical activity together result in greater or fewer benefits than expected from the sum of their effects?).
There were sufficient data to conduct interaction models for weight and BMI models only. We used a components NMA approach,37 where µj is the mean weight (kg) or BMI (kg/m2) for the TAU group bi in trial j. θjk is mean weight (kg) or BMI for any risk behaviour intervention k from trial j:
where
δjk represents the MD between TAU and any risk behaviour intervention k, compared with TAU bj, in trial j, with between-study SD τ; dk is the pooled estimate of the MD comparing any risk behaviour intervention with TAU.
Model 2 is an extension of model 1a:1, in which the MD dk was the MD comparing any intervention with TAU, which assumed that:
Model 2 allowed for each component to have its own independent impact on the MD. For example, targeting diet and physical activity together may each have contributed separately to reductions in weight or BMI. The model also allows components to interact with each other. For example, targeting diet and physical activity may lead to greater reductions (positive synergies) in weight or BMI than would be expected by the sum of these components. Model 2 also allowed for lesser reductions in weight or BMI than would be expected if the components were summed (negative synergies). We did not include targeting alcohol or smoking as separate effects as all interventions in the analyses targeting one of these behaviours also targeted diet and physical activity:
where PA = physical activity.
Model 3: effectiveness of behaviour change techniques
Risk behaviour interventions vary not only in terms of which behaviours are targeted, but also in terms of the BCTs included in these interventions.
We therefore fitted models that classified interventions in terms of BCTs (using the BCTT v1). 33 We fitted two models and compared them in terms of goodness of fit (total residual deviance, between-study SD and DIC). As above, there were sufficient data to conduct these analyses for only weight and BMI.
Model 3a: additive model (independent model)
Similar to model 2, we fitted a model that allowed each BCT to have an independent impact on the MD (dk) between any risk behaviour intervention compared with TAU. The BCTs included in the weight and BMI models were largely the same, but with slight variation, depending on what studies reported these outcomes.
For weight, the following BCTs were independent components contributing to the MD between any intervention and TAU:
For BMI, the following BCTs contributed to the MD between any intervention and TAU:
The models included a total of nine BCTs [BCTT v1: 1.1 goal-setting (‘goal’), 1.2 problem-solving (‘prob’), 1.4 action-planning (‘action’), 2.2 feedback on behaviour (‘feedback’), 2.3 self-monitoring of behaviour (‘mon’), 3.1 social support (unspecified) (‘soc_sup’), 4.1 instruction on how to perform a behaviour (‘inst’), 5.1 information about health consequences (‘info’) and 6.1 demonstration of the behaviour (‘demonst’)] that were used in at least five studies.
Model 3b: two-way interaction model (interaction model)
We extended model 3a to allow for pairs of BCTs to interact with one another. There was little overlap between BCTs used across studies, which limited the extent to which we could explore interactions.
For weight, the interaction model included only two further parameters in the model (studies that included BCTT v1 4.1 instruction in how to perform a behaviour and BCTT v1 1.2 problem-solving, and studies that included BCTT v1 4.1 instruction in how to perform a behaviour and BCTT v1 2.3 self-monitoring of outcomes):
For BMI, it was possible to include further interaction parameters in the model:
Methods of the qualitative review
Objective
The objective of the qualitative review was to address the following question (with consideration for methodological quality and certainty of evidence):
What are service user perspectives on the acceptability and feasibility of using risk behaviour interventions to change behaviour and improve physical health-related outcomes, with specific reference to intervention uptake, adherence and service experience?
Quality assessment
Established guidelines by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group [www.gradeworkinggroup.org (accessed 3 February 2020)] and the Cochrane Qualitative and Implementation Methods Group [cqim.cochrane.org (accessed 3 February 2020)] were followed, to implement the Confidence in the Evidence from Reviews of Qualitative research (CERQual)38 approach to assess both the methodological limitations of individual studies and the coherence of our review findings.
The Critical Appraisal Skills Programme (CASP) tool [https://casp-uk.net/casp-tools-checklists/ (accessed 3 February 2020)] was used to assess limitations of the methods used in included studies, per GRADE–CERQual guidance.
The CASP tool is not a rating system, but facilitated transparent assessment across 10 prompts relating to the quality of the design and reporting of studies. Each prompt on the checklist was answered with a ‘no’, ‘yes’, or ‘cannot tell’. ‘Cannot tell’ was allocated when authors’ reporting did not allow reviewers to make a clear decision.
The CERQual approach is similar to GRADE in that both approaches aim to assess the certainty of (or confidence in) the evidence, and both also rate this certainty for each finding across studies, rather than for each individual study. Unlike GRADE, which is only relevant to evaluations of effectiveness, CERQual offered a framework to evaluate the certainty of evidence that addresses questions beyond effectiveness of interventions, such as acceptability. Coherence of the review was assessed by identifying patterns across the data contributed by each of the individual included studies, for example when findings are consistent across multiple settings or different subgroups of people with SMI. The certainty of evidence in each individual study was rated as being high, moderate or low, and ranked according to the methodological limitations and coherence of each finding of our review.
Data analysis
Papers were read in detail to identify core ideas for comparison across studies based on quotations from participants. Interpretations from authors of the included studies were not extracted unless required to contextualise an abbreviated quotation from a participant.
Drawing on guidance for qualitative syntheses to inform policy-making and research prioritisation, a narrative synthesis approach was used. 39 This approach gave a descriptive account that forms the basis of an interpretative synthesis. Published data were analysed using principles of thematic synthesis, as described by Thomas and Harden,40 to facilitate the identification of recurring and emergent themes. Themes within and between transcripts were categorised, with iterative classification, development and refining of categories. 41
Initial line-by-line coding of participant quotations was undertaken in NVivo version 12 (QSR International, Warrington, UK) by one reviewer, and data extraction was a function of coding. The data could be used to support the development of different, but overlapping, themes. Initial coding was descriptive, remaining close to original reports and began without hierarchical structure. Translation of codings was iterative.
Analytical themes were developed through further refinement of coding, comparing primary data with developed themes. This process was repeated within themes to draw out subthemes. A second reviewer helped reduce repetition and overlap, thereby producing more focused themes.
Greater emphasis was placed on studies with in-depth examinations of user experience. Studies that lacked this detail were used to augment and contextualise the findings. The relative contribution of individual studies, the impact of methodological limitations and certainty on the findings were summarised narratively, in line with the CERQual approach.
Methods for integrating quantitative and qualitative data
There remains a lack of consensus on the most appropriate methods for integrating quantitative and qualitative data. Our approach used methods commonly used in systematic reviews that were also appropriate for the nature of our data. 42,43
The overall themes and subthemes identified in the synthesis of qualitative studies were used as the basis for examining whether or not the findings from the quantitative data approximated those found in the qualitative data. For example, when a particular factor was identified as a barrier or facilitator in the qualitative data, we examined whether or not intervention content seeking to address this barrier or facilitator affected the effectiveness estimates using meta-regression analyses (based on the magnitude of the covariate and precision of the 95% CrI). If these meta-regression analyses were unplanned, we conducted these analyses post hoc, when possible.
For each theme, we investigated whether or not we could identify an analogue of this theme in the included quantitative studies. We then categorised the relationship between findings from the qualitative and quantitative data according to four categories adapted from a recent study:44 silence (no overlap between quantitative and qualitative data), dissonance (conflicting findings), partial agreement (complementary findings, but limited overlap) and agreement (convergence in the data). However, when there was overlap in quantitative and qualitative findings, but the data were insufficiently precise to categorise, the finding was labelled inconclusive.
Methods for patient and public involvement
People with lived experience of SMI and carers contributed significantly to all stages of the project. Sophie Corlett (Director of External Relations, Mind) was a member of our advisory group that provided oversight on the progress of the project.
We also formed two patient and public involvement (PPI) groups that met throughout the course of the project. One group began meeting in York and consisted of four members. The group was chaired by a relative of a person with SMI (DS), and also included one peer researcher (CD) and a peer researcher who is also a carer (HK). One further group member (a carer) was no longer able to attend after the first meeting because of other commitments.
We also regularly met with two peer researchers (MS and GJ) who are members of the Lived Experience Research Collective hosted by the Mental Health Foundation.
All the members of our PPI groups were included as authors of the report, reflecting their substantial contribution to the project. The PPI groups decided on the name of the project (HEALTH study), provided extensive comments on the protocol, contributed to interpretations of the study results, played a key role in disseminating the findings of the project, participated in the webinar and provided feedback on an animation summarising the findings of this project. For further details, see Chapter 7.
Chapter 3 Search results
Flow of studies included
The original searches were carried out in October 2018 using CENTRAL, EMBASE, MEDLINE, PsycInfo and the Science Citation Index. The date range searched was inception to October 2018. The searches identified 27,795 records, which reduced to 18,513 records after deduplication using EndNote bibliographic software.
Updated searches were carried out in March 2020 using EMBASE, MEDLINE, PsycInfo and the Science Citation Index; these identified a further 2822 records, which reduced to 1433 after deduplication. An updated search of CENTRAL in September 2020 identified a further 1843 records, reduced to 1579 after deduplication. A search of ASSIA in September 2020 identified 658 records, reduced to 151 after deduplication (the date range searched was inception to September 2020). An additional record was located through reference-checking. Therefore, 21,677 titles and abstracts were screened in total.
Of these, 436 full-text records were then double-screened, and 276 were subsequently excluded, as summarised in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram in Figure 1. A table of excluded studies with rationale for exclusion can be found in Appendix 2.
FIGURE 1.
The PRISMA flow diagram summarising the flow of studies.
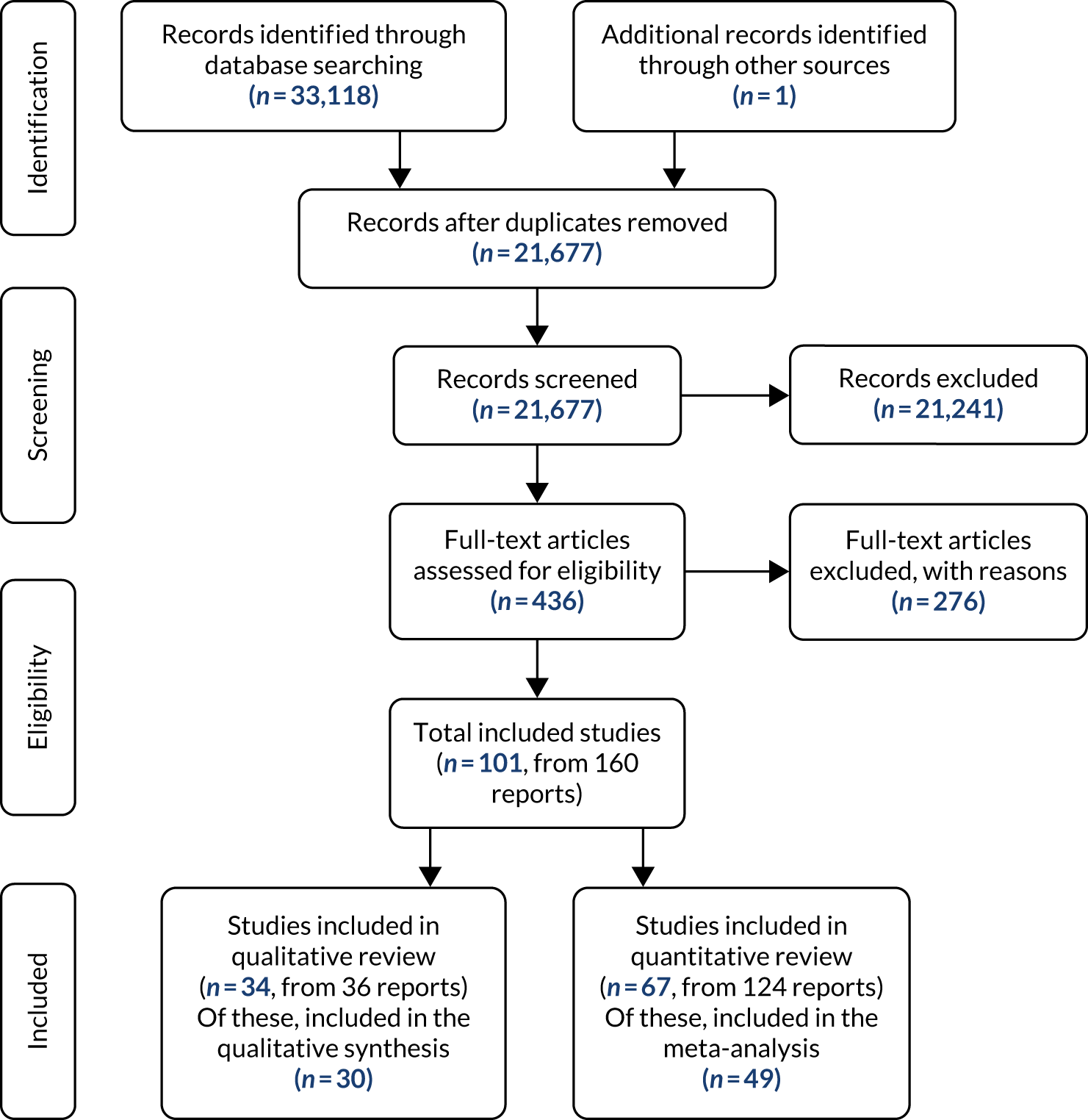
Studies included
Overall, 101 studies were included. Of these, 67 were RCTs included in the effectiveness review,45–111 and 34 studies (reported in 36 records) using a qualitative study design were included in the review of qualitative studies. 112–147
Characteristics of the randomised controlled trials included
For detailed summaries of population characteristics of included RCTs, see Appendix 3; for detailed summaries of intervention characteristics, see Appendix 4. Descriptions of the interventions are provided in Appendix 5. The majority were conducted in the USA (n = 2250,51,54,55,57–59,61,65,68,72,77,81,83,84,89,95,96,103,105,108,111) and the UK (n = 1257,67,69,71,75,76,78,88,93,94,100,109), followed by other European countries [Italy (n = 548,52,87,92,99), Switzerland (n = 353,70,80), Denmark (n = 373,74,102), Spain (n = 263,86), Germany (n = 249,60), Sweden (n = 164), the Netherlands (n = 198), Greece (n = 179) and Croatia (n = 1101)], Asian countries [Thailand (n = 291,106), China (n = 1110), Japan (n = 1104), India (n = 166) and the Republic of Korea (n = 182)], then Australia (n = 446,47,62,107), Canada (n = 285,97), Israel (n = 190) and Brazil (n = 145).
Of the included trials, 43 investigated multiple health risk behaviour interventions, and 24 investigated single health risk behaviour interventions. Risk behaviours were mostly targeted in pairs (n = 33), with few studies targeting three or more risk behaviours (n = 10). The most commonly targeted risk behaviours were physical inactivity (n = 48 studies) and unhealthy diet (n = 41 studies), which were also commonly targeted in combination.
Across included studies, the most commonly reported BCTs were instruction on how to perform behaviours (BCTT v1: 4.1; n = 40), social support (unspecified) (BCTT v1: 3.1; n = 27), self-monitoring of behaviour (BCTT v1: 2.3; n = 23), problem-solving (BCTT v1: 1.2; n = 23), information about health consequences (BCTT v1: 5.1; n = 23), goal-setting (BCTT v1: 1.1; n = 21), action-planning (BCTT v1: 1.4; n = 15), feedback on behaviour (BCTT v1: 2.2; n = 14) and social support (emotional) (BCTT v1: 3.3; n = 10). The totals reported here are much greater than the number of included studies as most interventions used several BCTs. For details of all BCTs reported across studies, see Appendix 4.
Fifty-two RCTs were included in the meta-analysis (see Figure 1). 45–49,54–56,59–64,67–70,72–76,78–87,89–91,93,94,96–99,101,102,104–111
Characteristics of the qualitative studies included
The flow of studies can be seen in the PRISMA diagram in Figure 1. Thirty-four studies (from 36 reports) were included;112–147 three records were based on the same cohort and so represent one study,126–128 and four conference abstracts were also included in the systematic review, but not in the synthesis, owing to limited data. 112–115 Therefore, 30 studies were included in the synthesis. Included studies used qualitative designs such as interviews and focus groups, and applied qualitative data analysis techniques such as the interpretative phenomenological approach and thematic analysis. Further details on population characteristics and study designs can be found in Appendix 6.
Multiple risk behaviours were considered in 18 studies,116,117,121,122,126,132,133,135–137,139–141,143–147 and 12 considered single risk behaviours. 118–120,123–125,129–131,134,138,142 Multiple risk behaviours were most commonly considered in pairs (14/18 studies);116,117,122,126,132,133,135–137,140,141,145–147 the most common combination of risk behaviours was physical activity and diet (11 studies). 116,117,122,126,135,137,140,141,145–147 Two studies139,143 addressed risk behaviour outcomes in a way that did not appropriately fit with the risk behaviour targets of this review and, therefore, were classified as ‘other’. One considered health promotion (classified as a multiple risk intervention)143 and the other considered weight loss (also classified as a multiple risk behaviour intervention). 139 The most commonly addressed single risk behaviour was physical activity (6/11 studies). 118–120,124,125,134 See Appendix 6 for further details.
Chapter 4 Results of effectiveness review
Summary of network meta-analyses results
Model 1: intervention effects models
Network diagrams for all outcomes are provided in Appendix 7. Although most trials aimed to change behaviour, few studies directly reported behavioural data. Weight and BMI were, by far, the most commonly reported outcomes. Smoking-related outcomes (quit rates and number of cigarettes smoked) were the most common behavioural outcomes reported. However, these data were too heterogeneous to combine in NMAs, so we conducted narrative syntheses for smoking outcomes. There were insufficient data to conduct NMAs of multiple and single risk behaviour interventions (i.e. model 1a:2) for diet, physical activity, alcohol use and cannabis use outcomes.
Table 1 summarises the results of the NMAs (model 1a) where it was possible to assess the clinical effectiveness of multiple and single risk behaviour interventions. All models converged after 20,000 iterations. Effect estimates are based on a further 60,000 iterations after discarding earlier iterations.
| Risk behaviours targeted | Outcome, MD (95% CrI) | Quality of life (9 RCTs, n = 1853), SMD (95% CrI) | |||
|---|---|---|---|---|---|
| Weight (kg) (30 RCTs, n = 2614) | BMI (kg/m2) (36 RCTs, n = 3308) | Blood pressure (mmHg) (SBP: 15 RCTs, n = 1790; DBP: 13 RCTs, n = 1489) | Cholesterol (mmol/l) (HDL: 15 RCTs, n = 2121; LDL: 9 RCTs, n = 1071; total cholesterol: 11 RCTs, n = 1727) | ||
| Any risk behaviour | –2.10 (–3.14 to –1.06) | –0.49 (–0.97 to –0.01) |
|
|
|
| Diet alone | –2.27 (–6.22 to 1.60) | –0.04 (–1.72 to 1.65) |
|
|
– |
| Physical activity alone | –1.40 (–6.00 to 2.99) | –1.23 (–2.63 to 0.20) |
|
|
– |
| Smoking alone | – | – | – | – |
|
| Diet + physical activity | –2.12 (–2.94 to –1.34) | –0.53 (–1.07 to 0.04) |
|
|
|
| Diet + physical activity + alcohol misuse + smoking | 1.27 (–1.46 to 3.42) | –0.02 (–1.05 to 0.98) |
|
|
|
Smoking
Smoking abstinence
Eight trials46,47,55,67–69,102,148 were included in the narrative synthesis for smoking abstinence.
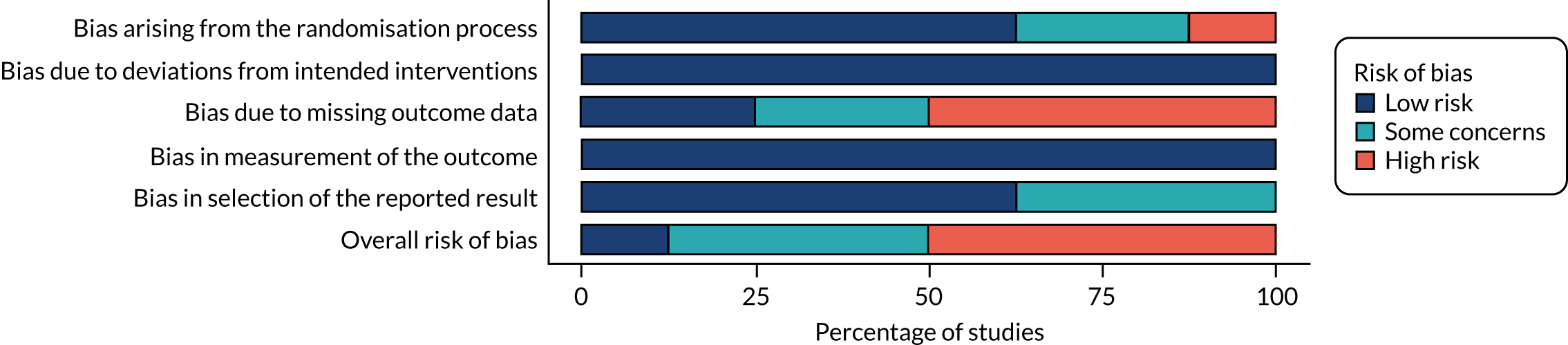
Figure 2 summarises the risk-of-bias judgements across studies measuring smoking abstinence. Just over half of included studies in the NMA were rated as having a high overall risk of bias. The most common reason for studies being judged to have a high risk of bias was missing outcome data (e.g. uncertainty over whether or not missing data depended on the outcome’s true value). Bias arising from the randomisation process was the next most common risk of bias (e.g. allocation concealment not reported and important baseline differences between groups).
FIGURE 2.
Summary of risk of bias across studies measuring smoking abstinence.
Given the diversity of the data, we conducted narrative syntheses rather than NMAs on smoking abstinence. Five trials targeted smoking alone. 46,55,68,69,148 Controls ranged from very low intensity46 and low intensity69,148 to high intensity. 55,68 Interventions in all five trials were high intensity.
Four of these trials found that interventions targeting smoking alone may be more effective than controls (Figure 3) in promoting smoking abstinence. 46,55,69,148 Odds ratios (ORs) for these studies ranged from 1.60 [95% confidence interval (CI) 0.91 to 2.82]69 to 5.99 (95% CI 0.64 to 55.94),55 but effect estimates were imprecise for all studies. One trial68 targeting smoking alone did not favour the intervention over the control, although the CI was very wide (OR 1.02, 95% CI 0.29 to 3.58). This trial included a high-intensity control, which may potentially explain different effects, compared with other included studies.
FIGURE 3.
Forest plot comparing smoking abstinence in interventions targeting smoking either alone or in combination with other behaviours. PA, physical activity.
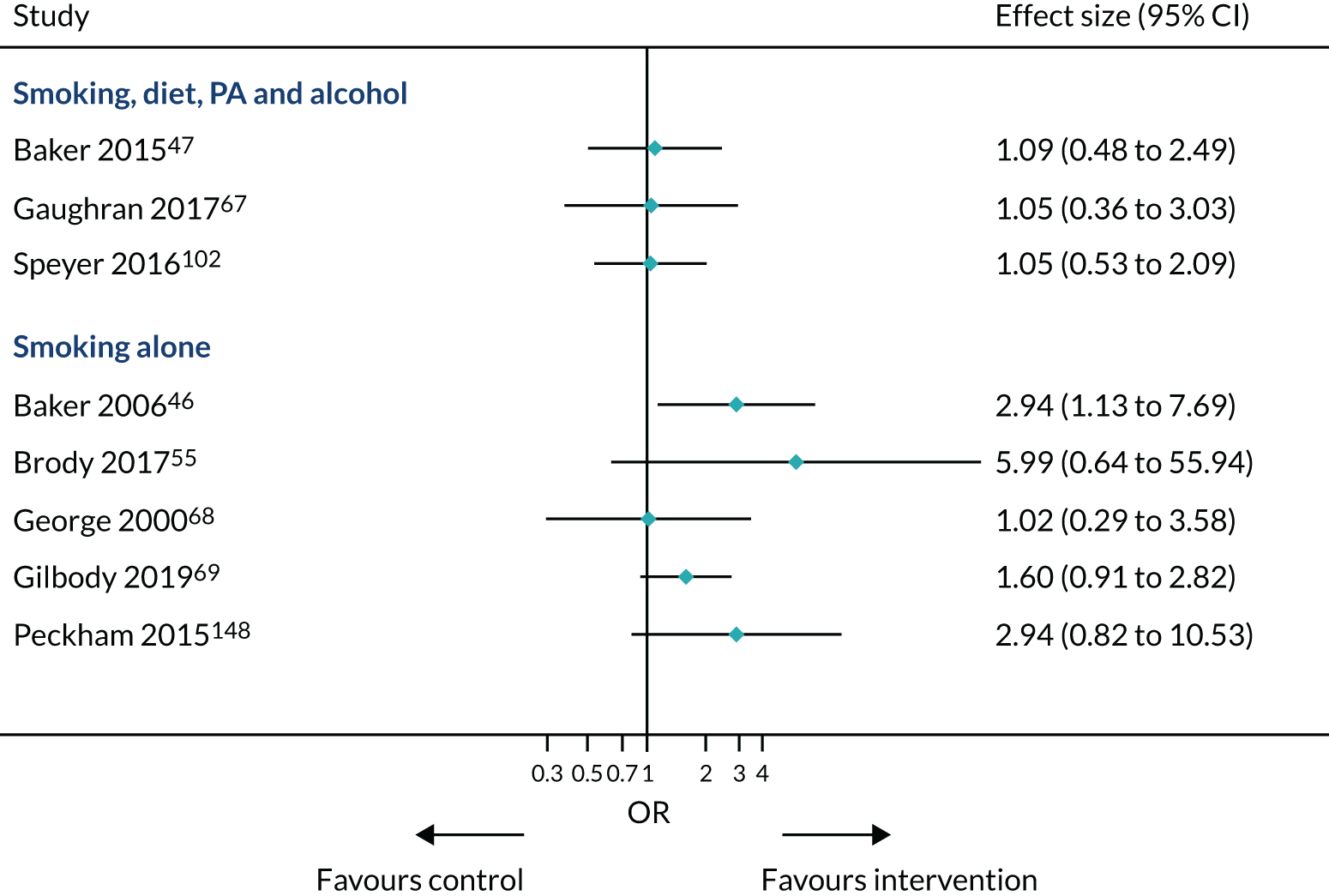
Three trials targeted smoking with other risk behaviours (including unhealthy diet, physical inactivity and excess alcohol consumption). 47,67,102 Controls ranged from very low intensity67,102 to medium intensity. 47 One intervention was of low intensity,67 one was of medium intensity102 and another was of high intensity. 47 The results were very similar in these three trials that targeted smoking in combination with other behaviours such as diet, physical activity and alcohol use. ORs ranged from 1.05 to 1.09, suggesting that there may be no difference between intervention and control in promoting smoking abstinence, although 95% CIs were consistent with both increased and reduced odds.
Number of cigarettes smoked
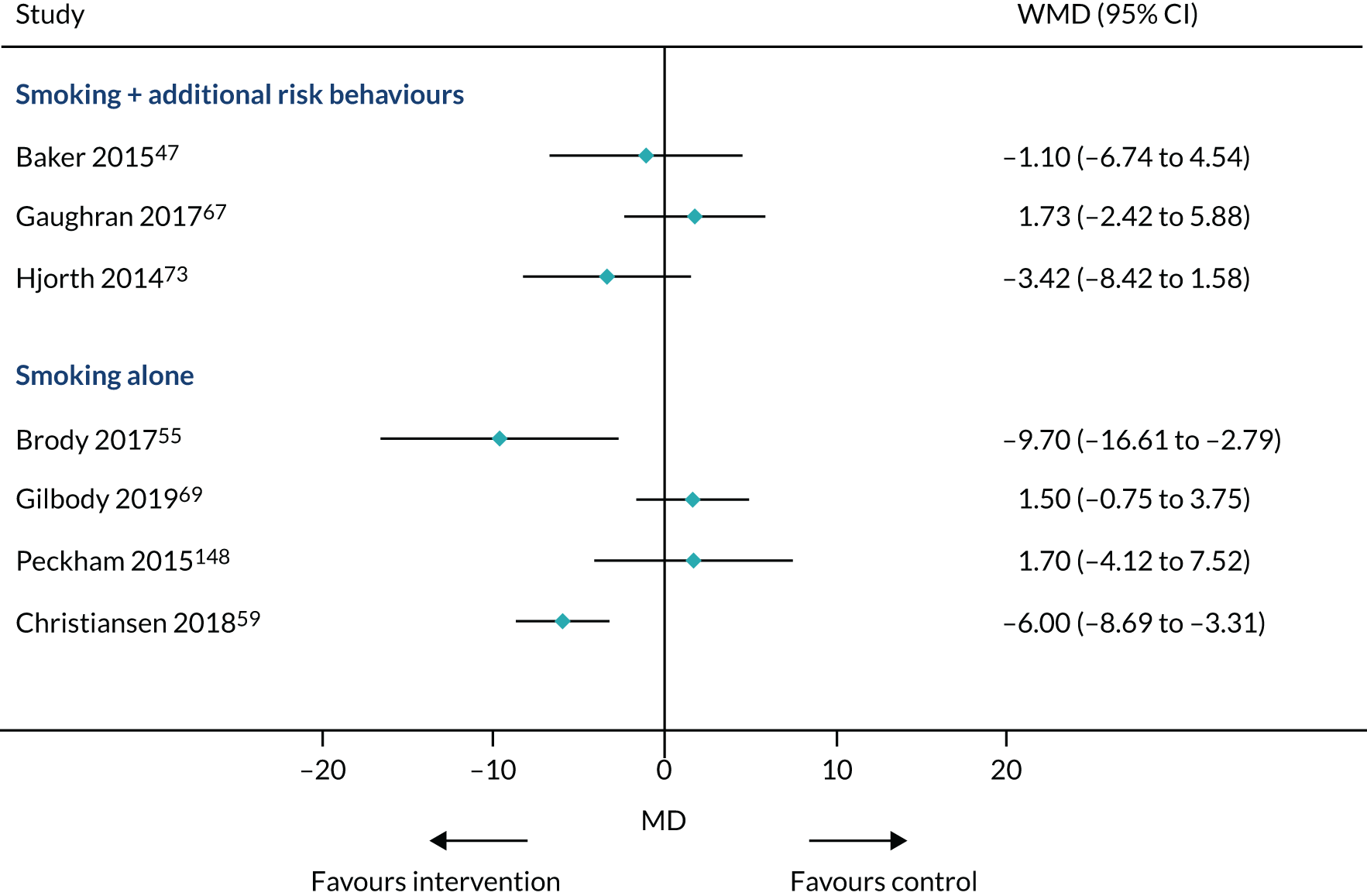
Seven trials47,55,59,67,69,73,148 were included in the narrative synthesis for assessing the number of cigarettes smoked.
There was a high level of variability between studies (Figure 4). Similar to Smoking abstinence, trials focusing on smoking along with other risk behaviours showed limited evidence of effectiveness in reducing the number of cigarettes smoked. Trials focusing on smoking alone found mixed evidence for reducing the number of cigarettes smoked. Two studies found evidence of effectiveness in reducing number of cigarettes,55,59 whereas two other studies did not. 69,148
FIGURE 4.
Summarising effect estimates of the number of cigarettes smoked at the end point for studies targeting smoking alone or with additional risk behaviours. WMD, weighted mean difference.
Cannabis
Four trials, with 716 participants providing data, were included in the NMA on cannabis use. 47,49,67,74
Each trial targeted a different combination of risk behaviours: alcohol, drugs or both;49 diet, physical activity, smoking and alcohol;47 physical activity, smoking and alcohol;73 and smoking, diet, physical activity, alcohol, any drug use. 67
Therefore, there were sufficient data to only compare any intervention with TAU at the end point. Given the sparse nature of the network, we decided to use a fixed-effects model, as there were insufficient data to reliably estimate between-study heterogeneity.
Goodness of fit was acceptable for the model (total residual deviance was 3.14 data points, compared with 4 data points). There was no evidence that interventions reduced cannabis use (SMD –0.05, 95% CrI –0.25 to 0.15). However, CrIs were relatively wide, indicating uncertainty about this effect estimate.
Alcohol misuse
Five trials (731 participants) were included in the NMA on alcohol use. 47,49,67,73,78 Trials targeted a range of combinations of risk behaviours: alcohol alone;78 alcohol, drugs or both;49 diet, physical activity, smoking and alcohol use;47 physical activity, smoking and alcohol use;73 and smoking, diet, physical activity, alcohol use and drug use. 67
There were sufficient data to only compare any intervention with TAU at the end point. Goodness of fit was acceptable for the model (total residual deviance was 5.25 data points, compared with 5 data points) and the between-study SD was 0.36 (95% CrI 0.02 to 2.01, SMD scale). There was no evidence that interventions reduced alcohol misuse (SMD 0.14, 95% CrI –0.71 to 1.00). CrIs were very wide, indicating considerable uncertainty about this effect estimate.
Physical activity
Seven trials45,67,86,89,105,109,149 reported data on physical activity. Most of these trials measured total physical activity (including self-report measures, such as the International Physical Activity Questionnaire, and objective measures, such as an accelerometer).
Five trials45,75,86,89,105 targeted diet and physical activity; one trial targeted physical activity and sedentary behaviour;109 and one trial targeted diet, physical activity, smoking, alcohol misuse and drug misuse. 67
Therefore, there were sufficient data to conduct only meta-analyses of any intervention and TAU. Goodness of fit for this model was acceptable [total residual deviance was 8.51 data points, compared with 7 data points and between-study SD was 0.23 (95% CrI 0.01 to 0.96)]. Evidence was very limited for the effect of any interventions compared with TAU for improving total physical activity (SMD 0.10, 95% CrI –0.25 to 0.49).
Diet
Six trials45,47,67,88,89,93 reported data on diet. Diet was measured using a diverse range of outcomes: calorie intake,89 fat intake45,67,93 and fruit and vegetable intake. 47,88 We considered these outcomes too diverse to combine in meta-analyses. Therefore, despite an unhealthy diet being one of the most commonly targeted health risk behaviours, it is difficult to conclude how effective interventions are at promoting a healthier diet.
Anthropometric outcomes
Weight (kg)
Thirty trials45,47,48,54,56,60–64,76,80,82,84,85,87,89,91,96,97,99,101,102,104,105,107,108,110,149,150 with data from 2614 participants were included in the NMA of weight outcomes at the end point.
Figure 5 summarises the risk-of-bias judgements across studies measuring weight loss. Just over half of the included studies in the NMA were rated as having a high overall risk of bias. The most common reason for studies being judged to have a high risk of bias was missing outcome data. Bias arising from the randomisation process was the next most common.
FIGURE 5.
Summary of risk of bias across studies measuring weight loss.
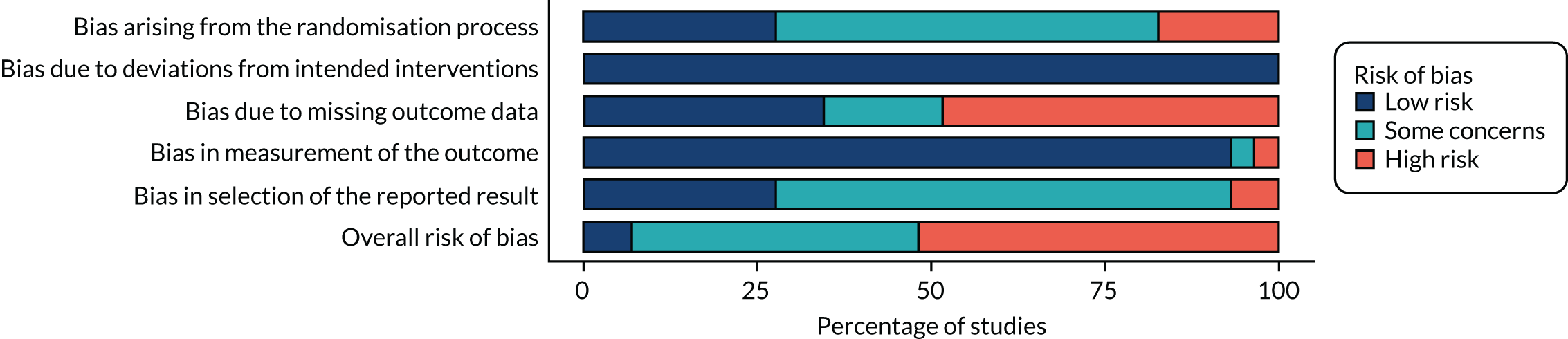
Figure 6 illustrates the different risk behaviours targeted by weight loss interventions and their comparators. By far the most commonly targeted risk behaviours for intervention were diet and physical activity compared with TAU (17 trials)45,54,56,60–62,70,75,76,84,87,91,96,104,105,107,108 or TAU+ (five trials). 64,80,82,89,110 Interventions targeted diet alone and TAU in two trials,99,104 and diet alone and TAU+ in one trial. 101 Three trials targeted physical activity alone and TAU,48,85,97 and none targeted physical activity alone and TAU+. Interventions targeted diet, physical activity, smoking and alcohol use and TAU in two trials,63,102 and diet, physical activity, smoking and alcohol use and TAU+ in one trial. 47
FIGURE 6.
Network diagram illustrating risk behaviours targeted in weight loss interventions (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
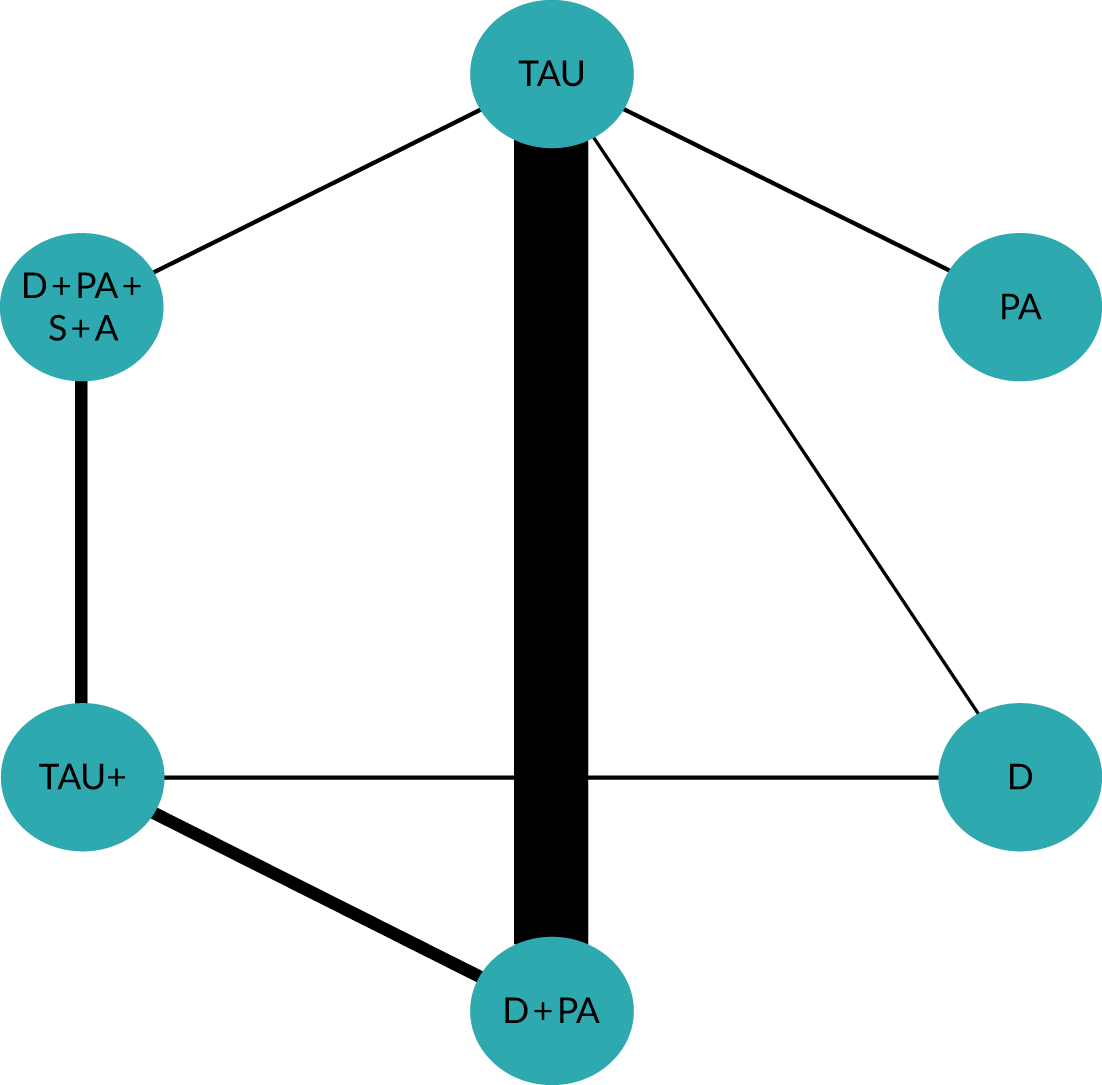
Total residual deviance did not suggest problems with model fit (mean 59.5 data points, compared with 63 data points) and between-study SD was 0.71 [95% CrI 0.04 to 1.89, MD on weight (kg) scale].
Targeting diet alone was the most effective intervention, although it was not possible to rule out a lack of effectiveness or weight gain (MD –2.27 kg, 95% CrI –6.22 to 1.60 kg). Targeting both diet and physical activity was a little less effective at reducing weight than TAU (MD –2.12 kg, 95% CrI –2.94 to –1.34 kg). However, CrIs were narrower, as more studies directly compared these interventions with TAU. Targeting physical activity alone was the next most effective strategy for reducing weight, compared with TAU (MD –1.40 kg, 95% CrI –6.00 to 2.99 kg). Interventions targeting diet, physical activity, smoking and alcohol misuse were unlikely to be effective on weight loss, compared with TAU (MD 1.27 kg, 95% CrI –1.46 to 3.42 kg), and may potentially lead to a mild weight increase.
The effect estimate comparing any risk behaviour intervention with TAU was similar to that found for interventions targeting diet and physical activity (MD –2.10 kg, 95% CrI –3.14 to –1.06 kg). This is probably because interventions targeting these risk behaviours had most weight in the NMA (see Figure 6).
Follow-up data were relatively sparse; there were sufficient data to only assess effectiveness at ≤ 6 months’ follow-up. All six trials targeted diet and physical activity. 60,62,80,84,91,150 Effectiveness at ≤ 6 months post intervention was similar to that found at the end point (MD –2.88 kg, 95% CrI –7.09 to 0.42 kg).
Body mass index
The most common reported outcome in all included studies was BMI. The NMA included data from 36 trials and 3308 participants. 45,47,48,54,60–64,73,75,76,79,80,82–87,89–91,93,97–99,101,102,104,105,107,108,110,111,150
Figure 7 summarises the risk-of-bias judgements across studies measuring BMI. Just under half of the included studies in the NMA were rated as having a high overall risk of bias. The most common reason for studies being judged to have a high risk of bias was missing outcome data. Bias arising from the randomisation process was the next most common reason.
FIGURE 7.
Summary of risk of bias across studies measuring BMI.
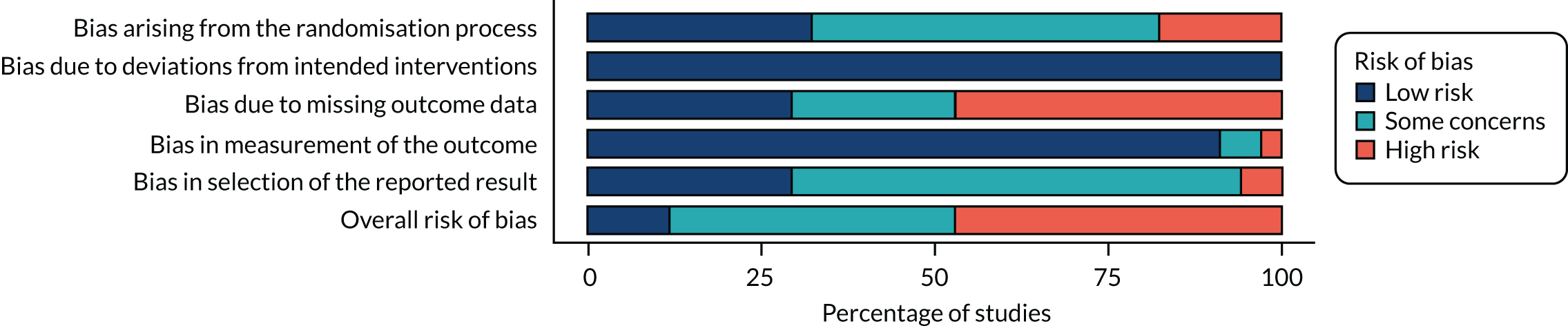
Figure 8 shows that most data were available for the comparison of interventions targeting diet and physical activity (17 trials) with TAU. 45,54,61,62,70,75,76,84,86,87,89,91,104,105,107,108,111 A further five RCTs compared diet and physical activity with TAU+. 64,80,82,90,110 Interventions targeting diet, physical activity, alcohol use and smoking were next most common (four trials compared such interventions with TAU60,63,73,102 and two trials compared them with TAU+47,102).
FIGURE 8.
Network diagram illustrating risk behaviours targeted in interventions to promote reduction in BMI (thickness of edge weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
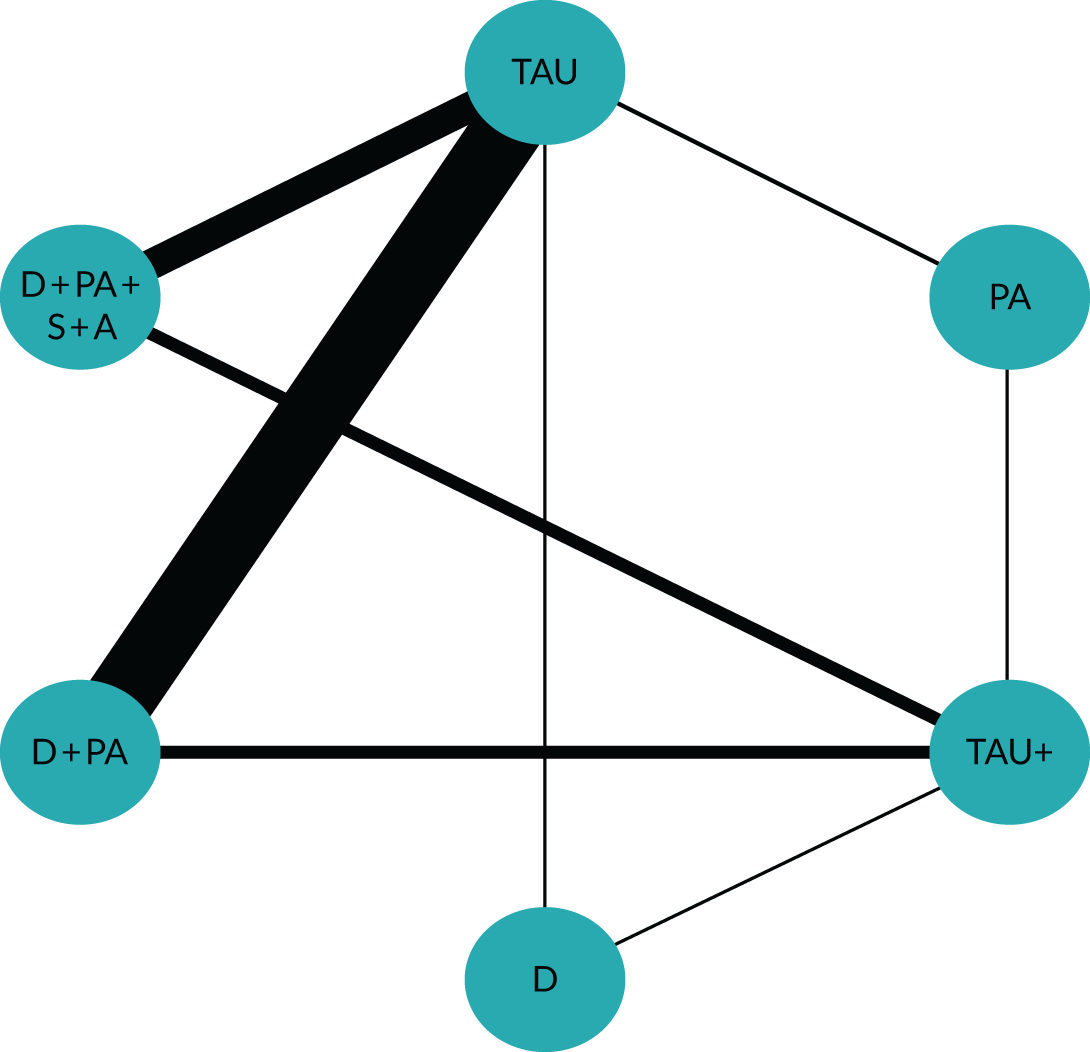
There were very limited data on interventions targeting physical activity alone (five trials48,79,83,85,97 compared such interventions with TAU and one trial101 compared them with TAU+) or diet (two trials99,104 compared such interventions with TAU and one trial101 compared them with TAU+).
The total residual deviance suggested that there were no problems with model fit (mean 71.77 data points, from 75 data points), and between-study SD was 0.89 (95% CrI 0.57 to 1.36; BMI scale).
Interventions targeting physical activity alone were most effective, compared with TAU, in reducing BMI (MD –1.23 kg/m2, 95% CrI –2.63 to 0.20 kg/m2). Interventions targeting diet and physical activity were the next most effective (MD –0.53 kg/m2, 95% CrI –1.07 to 0.04 kg/m2), compared with TAU. There was no evidence that either targeting diet alone (MD –0.04 kg/m2, 95% CrI –1.72 to 1.65 kg/m2) or targeting diet, physical activity, alcohol misuse and drug misuse concurrently (MD –0.02 kg/m2, 95% CrI –1.05 to 0.98 kg/m2) were effective in reducing BMI.
Follow-up data were also scarce for BMI; there were sufficient data to only assess effectiveness at ≤ 6 months’ follow-up. Seven trials targeted diet and physical activity62,70,80,81,84,89,91 and two trials targeted a broader range of behaviours (including diet, physical activity, smoking and alcohol misuse). 60,93 Given the lack of diversity of risk behaviours targeted, we were able to conduct an analysis only on any intervention and TAU. Effectiveness at ≤ 6 months’ follow-up was similar to that found at the end point (MD –1.33 kg/m2, 95% CrI –2.65 to –0.10 kg/m2).
Cardiovascular-related outcomes
Systolic blood pressure
Fifteen trials45,47,54,61,63,64,83,89,93,97,98,101,102,104,150 with 1790 participants were included in the NMA.
Similar to anthropometric outcomes, trials targeting both diet and physical activity compared with TAU were most common (five trials); 45,54,61,70,104 two further trials compared interventions with TAU+. 64,89 Four trials targeted diet, physical activity, smoking and alcohol use compared with TAU. 47,63,93,102 Only one trial targeted diet alone and TAU,104 and one trial targeted diet alone and TAU+. 101 Two trials targeted physical activity alone and TAU,83,97 and one trial targeted physical activity alone and TAU+. 98
Total residual deviance did not identify any problems with model fit (mean 29.54 data points, compared with 32 data points), and between-study SD was 1.45 (95% CrI 0.07 to 3.95; MD scale for systolic blood pressure).
In contrast to the risk behaviours and anthropometric outcomes, studies targeting multiple risk behaviours were more effective in reducing systolic blood pressure than those targeting single behaviours. The most effective interventions targeted diet, physical activity, smoking and alcohol misuse concurrently (MD –2.17 mmHg, 95% CrI –5.46 to 0.87 mmHg), although the CrI did not rule out no benefit. Interventions targeting diet and physical activity were the next most effective (MD –1.56 mmHg, 95% CrI –4.42 to 0.98 mmHg), although the CrI did not rule out no effect. Substantially lower effect estimates and wide CrIs were found for studies targeting diet alone (MD 0.42 mmHg, 95% CrI –4.52 to 5.30 mmHg) or physical activity alone (MD –0.26 mmHg, 95% CrI –5.43 to 4.97 mmHg).
Diastolic blood pressure
Thirteen trials45,47,61,63,64,83,89,93,97,98,101,104,150 were included in the NMA, comprising data on 1489 participants.
Total residual deviance did not identify any problems with model fit (mean 26.78 data points, compared with 27 data points), and between-study SD was 1.78 (95% CrI 0.16 to 4.27; MD scale on diastolic blood pressure).
Credible intervals were wide for all comparisons, indicating uncertainty about their effectiveness. The most effective interventions in reducing diastolic blood pressure targeted diet, physical activity, smoking and alcohol misuse (MD –2.04 mmHg, 95% CrI –5.76 to 1.23 mmHg). The next most effective intervention targeted diet alone (MD –1.60 mmHg, 95% CrI –6.37 to 2.94 mmHg), followed by interventions targeting diet and physical activity (MD –1.06 mmHg, 95% CrI –4.04 to 1.48 mmHg), and, finally, interventions targeting physical activity alone were not associated with any benefit (MD 0.34 mmHg, 95% CrI –3.80 to 4.25 mmHg).
High-density lipoprotein cholesterol
Fifteen trials45,61,63,64,67,83,89,93,97,98,101,102,104,149,150 were included in the NMA, with data from 2121 participants. Total residual deviance did not identify any problems with model fit (mean 33.95 data points, compared with 32 data points), and between-study SD was 1.75 (95% CrI 0.18 to 4.26).
Most trials targeted diet and physical activity together compared with TAU (five trials)45,61,70,75,104 or compared with TAU+ (two trials). 64,89 Four trials targeted diet, physical activity, smoking and alcohol use compared with TAU,63,67,93,102 and one trial targeted diet, physical activity, smoking and alcohol compared with TAU+. 102 Interventions targeted diet alone and TAU in one trial,104 and diet alone and TAU+ in another trial. 101 Interventions targeted physical activity alone and TAU in two trials,83,97 and physical activity alone and TAU+ in one trial. 98
The most effective interventions for increasing HDL cholesterol targeted diet alone (MD 4.88 mg/dl, 95% CrI –0.02 to 9.66 mg/dl), although it was not possible to rule out no benefit. Physical activity alone (MD 2.99 mg/dl, 95% CrI –1.42 to 7.26 mg/dl) was the next most effective intervention, but the 95% CrI was wide. Targeting diet, physical activity, smoking and alcohol misuse was a little less effective (MD 2.59 mg/dl, 95% CrI –0.53 to 5.78 mg/dl). There was limited evidence for the benefits of targeting diet and physical activity (MD 0.15 mg/dl, 95% CrI –2.46 to 2.40 mg/dl).
Low-density lipoprotein cholesterol
Nine trials45,61,67,83,89,93,97,101,150 were included in the NMA, comprising 1071 participants.
Given the sparse nature of the network, and concerns over whether or not there were sufficient data to estimate between-study heterogeneity, we compared the goodness of fit between a random-effects and fixed-effects model. The greater complexity of the random-effects model did not result in a better fit (random-effects model: DIC = 111.65, total residual deviance 17.24 data points; fixed-effects model: DIC = 110.62, total residual deviance 18.00 data points; compared with 18 data points); therefore, we used a fixed-effects model for the analysis of LDL cholesterol.
Data were imprecise for all interventions; therefore, it was not possible to draw conclusions on the effectiveness of reducing LDL cholesterol.
Total cholesterol
Eleven trials,45,61,67,83,86,89,93,97,101,149,150 with 1727 participants, were included in the NMA.
Both the fixed-effects and random-effects models were an acceptable fit (random-effects model: total residual deviance 21.09 data points; fixed-effects model: total residual deviance 22.36 data points; compared with 22 data points). But the greater complexity of the random-effects model meant that the fixed-effects model was preferred (random-effects model DIC = 138.95, fixed-effects model DIC = 137.99).
Data were imprecise for all interventions; therefore, it was not possible to draw conclusions on the effectiveness of reducing total cholesterol.
Quality of life
Quality-of-life data help to assess the overall self-reported benefits of interventions to physical health. In addition, these data help to assess if there are any self-reported benefits or deterioration to mental health-related quality of life.
Physical health
Nine trials,45–47,67,69,81,86,107,148 with 1853 participants, were included in the NMA.
Three trials targeted smoking alone and TAU; intensity of TAU was judged similar enough to be included in the NMA. Interventions targeted diet and physical activity and TAU in three trials, and diet and physical activity TAU+ in one trial. One trial targeted diet, physical activity, smoking and alcohol use and TAU, and a further trial targeted these behaviours and TAU+.
Total residual deviance was low for the random-effects (6.21 data points, compared with 9 data points) and fixed-effects (5.72 data points, compared with 9 data points) models, possibly indicating overfitting. Because of the greater complexity of the random-effects model, we preferred the fixed-effects model, as there was no difference in goodness of fit (random-effects model DIC = –5.68, fixed-effects model DIC = –7.43).
Interventions targeting smoking alone improved physical health-related quality of life (SMD 0.19, 95% CrI 0.05 to 0.34). There appeared to be no difference between interventions targeting diet and physical activity and TAU in physical health-related quality of life (SMD 0.02, 95% CrI –0.14 to 0.18). Interventions targeting diet, physical activity, smoking and alcohol misuse may have led to a small reduction in physical health-related quality of life (SMD –0.21, 95% CrI –0.43 to 0.02).
Mental health
Nine trials45–47,67,69,81,86,107,148 were included in the NMA, with 1853 participants.
Total residual deviance was low for the random-effects (6.09 data points, compared with 9 data points) and fixed-effects (5.31 data points, compared with 9 data points) models, possibly indicating overfitting. Because of the greater complexity of the random-effects model, we preferred the fixed-effects model, as there was no difference in goodness of fit (random-effects model DIC = –5.72, fixed-effects model DIC = –7.74).
Three trials targeted smoking alone and TAU;46,69,148 the intensity of TAU (i.e. low to very low) was judged to be similar enough to be included in the NMA. Interventions targeted diet and physical activity and TAU in three trials,45,86,107 and diet and physical activity TAU+ in one trial. 81 One trial targeted diet, physical activity, smoking and alcohol use and TAU,67 and one trial targeted these behaviours and TAU+. 47
There was no evidence that either single (interventions targeting smoking alone: SMD 0.01, 95% CrI –0.14 to 0.16) or multiple risk behaviour (interventions targeting diet and physical activity: SMD –0.09, 95% CrI –0.25 to 0.07; diet, physical activity, smoking and alcohol misuse: SMD –0.09, 95% CrI –0.32 to 0.14) interventions led to a reduction in mental health-related quality of life. This is an important finding, given concerns that trying to promote physical health may lead to deterioration in mental health.
Positive and Negative Syndrome Scale
The Positive and Negative Syndrome Scale (PANSS) was the most commonly reported mental health outcome measure; it is designed to monitor symptom severity in people with schizophrenia. We used these data to assess whether or not risk behaviour interventions had adverse effects on mental health for people with SMI.
There were insufficient data to assess the impact of which behaviours were targeted; therefore, we assessed differences between any risk behaviour intervention and TAU on the PANSS. As there were only two comparisons in the network, this was equivalent to conducting a pairwise meta-analysis. In addition, only data on the PANSS total score51,54,60,67,79 were sufficiently reported to conduct meta-analyses.
Given that only five trials were included in the analysis, and concerns about whether or not there were sufficient data to estimate between-study heterogeneity, we compared the goodness of fit between a random-effects and a fixed-effects model. The greater complexity of the random-effects model did not result in a better fit with the data (random-effects model DIC = 56.91, total residual deviance = 10.25 data points; fixed-effects model DIC = 56.63, total residual deviance = 11.09 data points, compared with 10 data points); therefore, we used a fixed-effects model for the analysis of the PANSS total score.
There was no evidence on the PANSS total score (MD 0.03, 95% CrI –2.56 to 2.65) that any risk behaviour intervention had a harmful effect on mental health in people with schizophrenia, although the CrI was wide, suggesting uncertainty on estimating the true effect.
Model 1b: meta-regression analyses to investigate the impact of intervention and participants characteristics on effectiveness
There were only sufficient data to conduct meta-regression analyses for weight and BMI outcomes (Table 2).
| Covariate | Beta (95% CrI) | |
|---|---|---|
| Weight (kg) | BMI (kg/m2) | |
| Initiation of antipsychotic treatment | 0.36 (–2.69 to 3.37) | 0.34 (–1.27 to 2.12) |
| Targeting people with comorbid physical conditions | –0.74 (–11.61 to 10.18) | –0.39 (–2.34 to 1.61) |
| Individual-based intervention | –2.70 (–4.69 to –0.75) | –1.11 (–2.15 to –0.01) |
| Inpatient setting | 3.18 (0.21 to 6.12) | 0.45 (–1.29 to 2.23) |
| Tailoring for people with SMI | 1.31 (–0.66 to 3.32) | –0.16 (–1.32 to 0.98) |
Weight
We investigated the impact of including five study characteristic covariates to NMA model 1a: behaviour change intervention at initiation of antipsychotic treatment, if participants were targeted for specific comorbid conditions (e.g. diabetes), if the intervention was delivered to individuals, if the intervention was delivered in an inpatient setting and if the intervention was tailored for people with SMI. We then compared the goodness of fit of this covariate model with model 1 without covariates.
We compared model 1b (covariate model) with model 1a (model without covariates). Total residual deviance showed that goodness of fit was acceptable in both models (model 1b = 55.30 data points, model 1a = 60.00 data points, compared with 63 data points). The DIC did not substantially differ between models (model 1b = 279.52, model 1a = 282.17).
However, the inclusion of covariates in model 1b explained some of the heterogeneity, indicated by a reduction in the between-study SD (model 1b: SD 0.44, 95% CrI 0.02 to 1.54; model 1a: SD 0.69, 95% CrI 0.04 to 1.78).
Interventions delivered to individuals were more effective than those delivered to groups (beta –2.70, 95% CrI –4.69 to –0.75). In addition, interventions delivered in inpatient settings were less effective than interventions delivered in community settings (beta 3.18, 95% CrI 0.21 to 6.12). CrIs were very wide for all other covariates.
Body mass index
Differences in DIC values indicated that the covariate model (model 1b: DIC = 186.91) fitted the data better than the model without covariates (model 1a: DIC = 196.76), although the covariates included in the model reduced the between-study SD only a little (model 1b: SD 0.83, 95% CrI 0.46 to 1.40; model 1a: SD 0.88, 95% CrI 0.56 to 1.35).
Total residual deviance was acceptable for the covariate model (mean 68.53 data points, compared with 70 data points). Similar to weight outcomes, interventions delivered to individuals were more effective than those delivered to groups (beta –1.11, 95% CrI –2.15 to –0.01). All other covariates had very wide CrIs.
Model 2 (interaction model): does targeting multiple risk behaviours lead to positive or negative synergies?
The preceding analyses provide some insight on how targeting particular risk behaviours affects outcomes. A different way of exploring that question is to assess whether or not targeting risk behaviours together results in positive (i.e. larger benefits than would be expected from the sum of their effects alone) or negative synergies (i.e. less benefits than expected from the sum of their effects). There were sufficient data to explore these interactions on weight and BMI only (Table 3).
| Risk behaviours | Outcome (95% CrI) | |
|---|---|---|
| Weight (kg) | BMI (kg/m2) | |
| Diet | MD –2.56 (–6.34 to 1.35) | MD –0.01 (–1.65 to 1.67) |
| Physical activity | MD –1.61 (–6.09 to 2.67) | MD –1.08 (–2.28 to 0.13) |
| Diet and physical activity | MD 1.88 (–4.02 to 7.57) | MD 0.56 (–1.48 to 2.61) |
| Diet, physical activity, smoking, alcohol misuse and drug misuse | MD 2.97 (1.03 to 4.84) | MD 0.66 (–0.43 to 1.68) |
| Total residual deviance | Mean 58.42 | Mean 71.78 |
| Between-study SD | 0.77 (0.05 to 1.73) | 0.86 (0.56 to 1.31) |
Weight
Model fit was acceptable (mean total residual deviance = 58.42 data points, compared with 63 data points). The findings were similar to those of model 1. We did not find evidence of positive interactions. There did not appear to be additional benefits of targeting diet and physical activity concurrently, compared with summing the effects of targeting each of these behaviours alone (MD 1.88 kg, 95% CrI –4.02 to 7.57 kg).
There was evidence of negative synergistic effects when targeting diet, physical activity, smoking, alcohol misuse and drug misuse. Benefits on weight loss were less than would be expected if these behaviours were targeted alone (2.97 kg, 95% CrI 1.03 to 4.84 kg).
Body mass index
Model fit was acceptable (total residual deviance was 71.78 data points, compared with 75 data points). Targeting physical activity was associated with a small reduction in BMI (MD –1.08 kg/m2, 95% CrI –2.28 to 0.13 kg/m2). There was insufficient evidence for the effectiveness of targeting diet alone (MD –0.01 kg/m2, 95% CrI –1.65 to 1.67 kg/m2).
There was no evidence of a positive interaction when targeting diet and physical activity concurrently (0.56 kg/m2, 95% CrI –1.48 to 2.61 kg/m2). There was also no evidence of a positive interaction when targeting diet, physical activity, smoking and alcohol misuse (MD 0.66 kg/m2, 95% CrI –0.43 to 1.68 kg/m2).
Model 3: effectiveness of behaviour change techniques
We fitted component NMA models to evaluate the effectiveness of BCTs in models assuming these BCTs affected outcomes independently of one another (independent model) and in models allowing for interaction effects between these BCTs (interaction model) (Table 4).
| BCTs (BCTT v1) | Model 3a: independent model (95% CrI) | Model 3b: interaction model (95% CrI) | ||
|---|---|---|---|---|
| Weight (kg) | BMI (kg/m2) | Weight (kg) | BMI (kg/m2) | |
| 1.1 Goal-setting (behaviour) | –2.22 (–4.54 to –0.44) | –0.61 (–1.53 to 0.28) | –2.26 (–4.68 to –0.25) | –1.85 (–2.91 to –0.69) |
| 1.2 Problem-solving | 3.61 (1.18 to 5.32) | 1.56 (0.61 to 2.36) | 3.82 (0.36 to 7.03) | 1.46 (0.11 to 2.67) |
| 1.4 Action-planning | – | –0.61 (–1.29 to 0.27) | – | –0.34 (–1.07 to 0.42) |
| 2.2 Feedback on behaviour | –0.83 (–2.70 to 1.77) | –0.58 (–1.43 to 0.28) | –0.67 (–2.73 to 1.97) | 0.02 (–0.78 to 0.84) |
| 2.3 Self-monitoring of behaviour | –0.12 (–1.91 to 1.78) | –0.35 (–0.96 to 0.40) | –0.96 (–3.55 to 1.38) | –0.70 (–1.42 to 0.07) |
| 3.1 Social support (unspecified) | 0.84 (–1.48 to 2.65) | –0.24 (–1.04 to 0.51) | 0.47 (–2.25 to 2.83) | –0.42 (–1.12 to 0.32) |
| 4.1 Instruction on how to perform the behaviour | –2.10 (–3.42 to –0.45) | –0.59 (–1.10 to –0.02) | –2.50 (–4.40 to –0.34) | –1.19 (–1.85 to –0.55) |
| 5.1 Information about health consequences | –0.94 (–2.75 to 1.30) | 0.69 (–0.11 to 1.38) | –0.60 (–2.59 to 1.81) | 0.05 (–1.23 to 1.29) |
| 6.1 Demonstration of the behaviour | –0.94 (–2.75 to 1.30) | – | –0.85 (–3.24 to 1.56) | – |
| 4.1 × 5.1 | – | – | – | 1.71 (0.44 to 3.00) |
| 4.1 × 1.2 | – | – | –1.43 (–5.54 to 2.31) | –0.84 (–2.10 to 0.45) |
| 4.1 × 2.3 | – | – | 2.10 (–1.06 to 5.53) | 0.93 (–0.05 to 1.96) |
| 5.1 × 2.3 | – | – | – | 0.07 (–1.23 to 1.38) |
| 1.1 × 2.3 | – | – | – | 1.11 (–0.54 to 2.51) |
| 1.2 × 2.3 | – | – | 0.75 (–0.52 to 2.12) | |
Weight
Goodness of fit was acceptable for both models (independent model: total residual deviance = 59.42 data points, interaction model: total residual deviance = 58.46 data points, compared with 63 data points).
The DIC values (independent model: DIC = 281.67, interaction model: DIC = 282.37) and between-study SDs were similar (independent model: SD 0.81, 95% CrI 0.03 to 2.22; interaction model: SD 0.91, 95% CrI 0.04 to 2.43). This may reflect that there were sufficient data for only two interactions to be included in the interaction model and that both covariates were very imprecise. Therefore, the summary of results will focus on the simpler independent model.
The strongest evidence was found for goal-setting (behaviour) (MD –2.22 kg, 95% CrI –4.54 to –0.44 kg) and instruction on how to perform the behaviour (MD –2.10 kg, 95% CrI –3.42 to –0.45 kg).
In addition, problem-solving was associated with weight gain (MD 3.61 kg, 95% CrI 1.18 to 5.32 kg).
Body mass index
Goodness of fit was acceptable for both models (independence model: total residual deviance = 77.86, interaction model: total residual deviance = 73.31).
The interaction model (DIC = 192.86) fitted the data better than the independent model (DIC = 198.84) and explained more of the heterogeneity [between-study SD: interaction model, 0.21 (95% CrI 0.01 to 0.74); independence model, 0.55 (95% CrI 0.12 to 1.07)]. Therefore, the summary will focus on results from the interaction model.
Similar to the weight NMA, the strongest evidence was found for goal-setting (behaviour) (MD –1.85 kg/m2, 95% CrI –2.91 to –0.69 kg/m2), instruction on how to perform a behaviour (MD –1.19 kg/m2, 95% CrI –1.85 to –0.55 kg/m2) and self-monitoring of behaviour (MD –0.70 kg/m2, 95% CrI –1.42 to 0.07 kg/m2), although it was not possible to rule out negligible benefits for self-monitoring of behaviour.
As for weight, problem-solving was associated with a worsening of BMI outcomes (MD 1.46 kg/m2, 95% CrI 0.11 to 2.67 kg/m2).
Chapter 5 Results of the qualitative review
Quality of included studies
Methodological limitations of included studies were assessed using the CASP tool. Reporting was generally acceptable across studies, allowing for consideration of most, if not all, prompts in the CASP tool for each study. However, authors’ consideration of the relationship between researcher and participant (question 6) was consistently poorly addressed. Only 4 of the 25 included studies addressed this issue adequately.
One consideration that was addressed well was ethics issues (question 7), which require sufficient detail in gaining ethics approval and informed consent of participants. When this did not score ‘yes’, it was because of an apparent lack of reporting.
Results of the GRADE–CERQual assessment per subtheme can be found in Appendix 8. There was moderate to high confidence in the evidence presented by the subthemes reported here. The four components of CERQual also raised only very minor to moderate concerns. Methodological limitations (as assessed by the CASP tool) were not a general concern: coherence was largely assessed as a minor concern; adequacy was mostly assessed as a very minor to minor concern; and relevance was a slightly larger concern, predominantly assessed as being of minor to moderate concern.
Narrative synthesis
Here we are going to address the question: what are service user perspectives on the acceptability and feasibility of using risk behaviour interventions to change behaviour and improve physical health-related outcomes, with specific reference to intervention uptake, adherence and service user experience?
Data from primary studies organised around four higher-tier themes: interaction of physical and mental health, motivational contexts for change, barriers to behaviour change, and experiences of interventions.
Interaction between physical and mental health
Across the studies, data highlighted the reciprocal nature of physical and mental health. Participants reported the impact of mental health states on their engagement in healthy behaviours, and there was an emerging consensus that physical health risk behaviours had the potential to affect mental health negatively.
Healthy behaviours improving mental health and well-being
People with SMI reported that physical activity was helpful in changing mental health. But, overall, mental health and a sense of well-being were valued more than changes in activity.
When discussing physical activity, data gathered around two core ideas: physical activity to refresh the mind and physical activity for symptomatic relief. Engaging in activity was frequently reported to result in mental clarity:
. . . I’d notice, after I’d done the gym sessions, I felt really fresh. Like, afterwards, like my mind felt kind of washed, if you like.
Firth et al. ,119 single risk behaviour intervention (SRB), physical activity
Healthy behaviours were also used for immediate symptom relief in one study:
. . . when I feel like I’m just so angry, and stuff like that, I’ve gone training, I’ve done press-ups and stuff at home and it’s cleared my head, killed me anger . . .
Firth et al. ,119 SRB, physical activity
An overarching concept from this theme related to participants’ desire to find a suitable space to bring about positive mental change:
[The gym] gives me somewhere to go to vent out stress.
Jimenez et al. ,127 multiple risk behaviour intervention (MRB), physical activity and diet
Similarly, reports of physical activity to relieve mental health symptoms spoke of exercise as a mental release, and relieving SMI symptoms:
Exercise relieves stress, sweat relieves stress; those two things, I really use them. There’s all kinds of ways you can relieve stress. I think exercise helps me to relieve stress.
Jimenez et al. ,127 MRB, physical activity and diet
The voices, I do not hear them as much.
Forsberg et al. ;121 MRB; physical activity, diet, alcohol, drug use, smoking
There was also widespread recognition that exercise could have immediate impact on well-being, as well as physiological benefits:
. . . physical exercise, it lets endorphins off in your brain, doesn’t it. So even if you are a bit depressed, it can, erm, make you not depressed [laughs], or make you slightly more happy.
Firth et al. ,119 SRB, physical activity
Being considered more holistically
One of the core components of participants’ preferences and expectations for engaging with behaviour change revolved around their desire to be treated as a whole person. In studies, participants wanted to be recognised in totality as individuals, rather than as a collection of risk behaviours to be changed. According to authors in one study, participants expressed dislike for the term ‘intervention’, perceiving it as:
Someone else intervening.
Bauer et al. ,117 MRB, physical activity and diet
When trying to improve health risk behaviours, there was a sense that outcomes such as weight loss were secondary to the overarching idea of well-being:
Even if I don’t necessarily lose so much weight, but just living healthier, eating healthier, being healthier is enough.
Yarborough et al. ,147 MRB, physical activity and diet
Mental and physical health were not necessarily viewed as separate, which may be critical to multiple risk behaviour interventions:
[M]y big goal is to be fully recovered from all the physical and psychological problems I’ve got. That’s my goal, to be fully recovered.
Forsberg et al. ;121 MRB; physical activity, diet, alcohol, drug use, smoking
Self-medicating
Smoking, drug use, and/or alcohol use emerged as key behaviours that typified the ways in which participants sought relief from symptoms or were proactive in trying to change unhelpful mental states. Behaviours related to addictive substances were used to cope with, and manage, mental health symptoms. In one study, engaging in a risk behaviour was experienced as taking positive action to change health state:
[Smoking] gives you the feeling that you’re doing something about it.
Thornton et al. ,142 SRB, smoking
Smoking was sometimes interpreted as a coping strategy for mental health symptoms, which can be considered a misattribution of relief from nicotine withdrawal, and viewed as a ‘high[ly] addictive antidepressant’,142 and was perceived to be used to provide immediate relief of depression:
[I]t gives you that instant effect that you’ve had some sort of mood relaxant . . . a bit of a stress relief against depression . . .
Thornton et al. ,142 SRB, smoking
For some participants, addictive behaviours were part and parcel of their existence and biographical memory, and were perceived as reliable, and even comforting, behaviours:
With the bipolar illness, it’s hard for me to remember things, but something that I’ve always done is smoke and that’s something that I’ve, you know, it’s just been there all along.
Heffner et al. ,123 SRB, smoking
Other studies also mirrored this supportive role of risk behaviours; in one study, such behaviours were conceptualised as a companion:
You have nobody to talk to, you have nobody to do things with. All you have is that drug; that drug keeps you company.
Maisto et al. ,133 MRB, alcohol and drug use
The stable support that risk behaviours can offer was exemplified as something to retreat to, when managing schizophrenia and depression:
I find myself escaping back to drugs.
Maisto et al. ,133 MRB, alcohol and drug use
There were also reports that highlighted that, for some participants, their relationship with addictive substances was driven by their mental health:
[T]he stress that I’m under, the anxiety that I’m under all the time just forces me right back to drink again.
Maisto et al. ,133 MRB, alcohol and drug use
Motivational contexts for change
Motivations and motivational contexts for change were broadly grouped into three subthemes: individual factors, social factors and environmental factors.
Individual factors
Various personal motivations to change were reported. Identifying and holding on to a personal motivation was noted as an important guiding light:
I think it’s important to, you know, like, have a, like, a north star like that to look at, like, this is why I’m doing it and this is why it’s important.
Heffner et al. ,123 SRB, smoking
The commitment to succeed, in the face of challenges presented by SMI, was also important:
. . . I felt as though I took it serious and I wanted to do it, and then something would come along and sort of like take my mind off everything.
Knowles et al. ,131 SRB, smoking
Motivation stemming from concerns with physical appearance and weight were reported in some studies: ‘I’m a bit fat and have a big stomach.’ (Forsberg et al. ,121 MRB; physical activity, diet, alcohol, drug use, smoking), and they remember being ‘skinny . . . proportioning’ (Jimenez et al. ,127 MRB, physical activity and diet). Concerns over personal appearance could also affect concerns for romantic lives (related to concepts of confidence and acceptance; see Valued benefits of behaviour change interventions):
I want to get married one day or have a girl and girls don’t like fat guys. I want to be able to have a girl and be confident.
Jimenez et al. ,127 MRB; physical activity and diet
This sense of participants wanting to promote a more positive future version of themselves extended to how they looked to protect themselves from the negative health outcomes associated with long-term conditions and ageing:
I will soon be over 50 years old; you must be aware of the blood sugar and such values . . . It can change. It gives the desire to keep good values and not to get diabetes and other diseases.
Rönngren et al. ,140 MRB, physical activity and diet
For others, motivations to change to healthier patterns of behaviour stemmed from an awareness of familial risks and the impact of witnessing others suffer health consequences of weight gain and smoking:
It seems there’s a lot of health issues with family and that plays a part in wanting to exercise and lose weight because I’m at severe risk of getting all these things.
Jimenez et al. ,126 MRB, physical activity and diet
My dad, as he’s got a diseased lung . . . he smokes a lot and just watching him, cos he’s a pack a day smoker, I don’t want to be that.
Thornton et al. ,142 SRB, smoking
In contrast to these direct health concerns, one study reported motivation stemming from particular scenarios, such as avoiding associated risks of possible surgery for weight loss:
I don’t want to have to go through any weight loss surgery and stuff like that. That’s stuff I worry about.
Yarborough et al. ,147 MRB, physical activity and diet
Social factors
Feedback and reinforcement of positive messaging from family and friends was also critical to some participants’ motivations to engage in more positive health behaviours:
‘Gee, you look better’, so I’m on the right road.
Aschbrenner et al. ,116 MRB, physical activity and diet
My family is starting to notice that I’m losing weight. I like the positive comments.
Yarborough et al. ,147 MRB, physical activity and diet
A sense of belonging could also be found in motivation from peers, and group interventions were reported as a good starting point to engaging in exercise:
Exercise in a group could be a good way to start when it comes to engaging in physical activity.
Rönngren et al. ,141 MRB, physical activity and diet
The presence of help suggested increased engagement with support. Having ‘someone to call and talk things over with . . . 24 hours a day every day’ (Maisto et al. ,133 MRB, alcohol and drug use). The idea of the intervention as a constant to return to was also present:
So maybe if you just keep . . . keep going back to them. You’re saying ‘look, we’re here and we’ll keep letting you know we’re here’.
Knowles et al. ,131 SRB, smoking
However, verbal support alone did not necessarily translate into helpful actions (needing to be seen as credible), as, in one study, someone reported:
My husband verbally supports me but he eats whatever he wants to eat and has it in the house.
Yarborough et al. ,147 MRB, physical activity and diet
The presence of key others could positively support behaviour change, but not always, with some studies reporting that goals to enact behaviour change were viewed with scepticism:
[W]hen I was talking about quitting there was [sic] a couple of people that were like would verbally basically be like, ‘Yeah, right, I’ll believe it when I see it.’.
Heffner et al. ,123 SRB, smoking
Accountability to friends, family and intervention groups was a prominent component of this subtheme. Group interventions offered inherent accountability among peers. Interpersonal relationships with family and friends offered the ability to monitor behaviour, which was supportive of positive efforts made by individuals. 133 In one study, participants arranged accountable relationships between themselves, calling each other. 126
Peer support was important for some participants, who derived a sense of accountability to each other by their membership and participation of intervention groups:
The accountability of being part of the group is very important.
Yarborough et al. ,147 MRB, physical activity and diet
This level of accountability to the group often translated into supporting each other to adhere to positive behaviour change:
He’ll ask, ‘Did you go to the gym?’ If I say no, he’ll say, ‘I’m disappointed at you.’. But you see, that’s all we got, is this friendship. We have nothing, so we make the best of nothing.
Jimenez et al. ,126 MRB, physical activity and diet
In another instance, the support of friends was often experienced in direct and instructional ways:
I have this friend, she has this attitude, if I say that I’m not going somewhere she’s like, ‘You’re so going. Get dressed.’. Then I have to go.
Jimenez et al. ,126 MRB, physical activity and diet
Another component of this subtheme was surveillance and scrutiny from others. Familial involvement or surveillance could stir individuals into action, not necessarily for themselves, but to appeal to the desires and wishes of others and preserve good relations with significant others:
. . . my parents told me that this treatment was a gift – the sort of habits and things that I was getting into wasn’t something that my parents could tolerate forever.
Luciano et al. ,132 MRB, alcohol and drug use
In another study, motivation to change stemmed from a desire to not become stigmatised or attract negative attention:
I don’t want to have to deal with people’s negative comments about me smoking because I already feel that in other areas.
Heffner et al. ,123 SRB, smoking
Environmental factors
Having a safe and stable place might be the foundation for people with SMI to consider the challenges of behaviour change:
Safe environments are the most important thing to people with mental illness.
Huck et al. ,125 SRB, physical activity
Therefore, environmental factors refers to the external context of an individual on a micro level, for example where they live, and structures created by, or imposed on, a person.
Creating schedules was an important means to shape and structure environments for individuals. Scheduling also offered accountability and was interpreted as motivating. This included scheduling intervention meetings or even behaviour change activities. For physical activity, this notion of environmental scheduling related to practical elements such as specific times, locations and goals that could be set objectively. By structuring their environments through scheduling, participants were, in some senses, bound to complete tasks linked to behaviour change:
I guess it’s because it’s a little motivator. It’s like I can’t get away with it [skipping the gym].
Aschbrenner et al. ,116 MRB, physical activity and diet
Pacing the frequency of intervention meetings was an important consideration. Meetings may prompt behaviour change, rather than just acting as check-in points. For one participant, if the meetings were too infrequent, then they would engage in risk behaviours and:
. . . a week later [as the monthly meeting approaches] I’ll try to improve on it.
Yarborough et al. ,147 MRB, physical activity and diet
A feature of environmental factors contributing to motivation to change were interactions with formal health care. Appointments with intervention providers were another form by which environmental scheduling drove engagement with positive health behaviours. Here ‘providers’ refers to those providing, organising and/or delivering the intervention, whether medical professional or community organiser. The authority held by a provider could increase the sense of accountability felt by participants to stick to their schedules. One participant stated:
You see, when I got an appointment or something I’m very faithful to that. Like he tells me, ‘Come tomorrow’, I got it in my mind I gotta come to him tomorrow. So I won’t miss that appointment.
Jimenez et al. ,126 MRB, physical activity and diet
Providers could set the tone and make participants feel welcome and bring a sense of humanity:
I enjoyed the warmth of the welcome I got from the staff and the interest they showed.
Roberts and Bailey,139 MRB, other – weight
My therapist, even though I’m a mentally ill psychiatric patient in a mental institution, she still treats me like everybody else.
Maisto et al. ,133 MRB, alcohol and drug use
In one instance, a provider was described as confrontational, but also as a source of stability to promote change:
She used to confront me on it like that . . . she didn’t push me away . . . it helped me quit.
Maisto et al. ,133 MRB, alcohol and drug use
Positive relationships with providers were interpreted as supportive. Providers could be personal cheerleaders or provide a touchpoint for change:
He was like persuading us on like ‘come on you can do it, you can do it!’ when he says things like that it makes me more activate.
Firth et al. ,119 SRB, physical activity
[O]nce [the exercise physiologist and nursing staff] helped me out I began to get fitter, not a great deal fitter, just enough to get through the day.
Fogarty and Happell,120 SRB, physical activity
A positive relationship could also benefit perceptions of intervention providers, as one participant was unaware of their positive impact:
I didn’t know they could do some good things, some of them, I didn’t really know that.
Forsberg et al. ;121 MRB; physical activity, diet, alcohol, drug use, smoking
Barriers to behaviour change
As with motivations to change, we found that barriers to behaviour change were broadly grouped under three subthemes: individual factors, social factors and environmental factors.
Individual factors
One of the main contributors to individual barriers to change was SMI symptoms. Across studies, SMI symptoms presented challenges to engaging in behaviour change interventions, as exemplified in participants’ accounts about difficulties with concentrating and difficulties accepting information when delusional:
Many of us can get tired and lose concentration . . . When you’ve had a psychosis you work a lot with thoughts darting around inside your head.
Wärdig et al. ,144 MRB; physical activity, diet, alcohol use and smoking
[I] probably just think it’s a load of rubbish or, you know . . . Because like when you’re delusional you don’t, well I know that . . . I don’t believe anything.
Thornton et al. ,142 SRB, smoking
Deteriorations in mental health were often emphasised by participants as their main concern; therefore, enacting positive behaviour change was of secondary importance:
It’s hard to make changes in your diet and follow the routine . . . when you’re at a point where you just don’t care.
Yarborough et al. ,147 MRB, physical activity and diet
Mental health treatments were also identified as restricting the scope to change behaviours through their impact on bodily systems:
When I am feeling down or depressed, I have almost no energy. In these periods, I have to take more psychotropic drugs, resulting in even less energy.
Verhaeghe et al. ,143 MRB, other – health promotion
Poorer mental health on the part of participants had the capacity to magnify barriers that might have ordinarily been surmountable:
My husband drives me there [to the gym] even when I don’t want to be there. I can walk. It’s not that far from my house to the gym [. . .].
Aschbrenner et al. ,116 MRB, physical activity and diet
However, reluctance to engage in physical activity was not always associated with mental health status:
I just get lazy sometimes. I just don’t want to do it, so I sit on the couch and watch TV.
Yarborough et al. ,147 MRB, physical activity and diet
Another feature of individual barriers to behaviour change was derived from participants’ responses about their self-efficacy to enact change. A lack of knowledge or skill affected participants’ capability to carry out healthy behaviours. For example, not understanding how to use exercise equipment as part of a gym routine was cited as a block to effectively engaging in physical activity:
[Knowing] how many repetitions and how to use the handles and set the chair and everything, that would’ve made it a lot more enjoyable for me.
Huck et al. ,125 SRB, physical activity
In the case of taking exercise in public, stigma around body image was prohibitive of activity:
I hate getting into that pool because I think people are staring at me . . . but it’s that whole confidence thing . . . you see those skinny people . . . that’s what helps to put you off . . .
Roberts and Bailey,139 MRB, other – weight
Physiological as well as psychological barriers emerged as common factors in this theme about individual-level barriers to behaviour change. Cravings for addictive substances were commonly reported among participants with histories of addictive behaviours such as smoking, alcohol use and drug use. Cravings appeared to be powerful and intangible, described as ‘screaming’ (Thornton et al. ,142 SRB, smoking) and like a ‘forcefield’ (Maisto et al. ,133 MRB, alcohol and drug use) that could trap people in cycles of negative behaviours.
An element of timing was also present, as cravings were reported at the beginning of a transition:
The first week I felt like every cell in my body wanted a cigarette.
Heffner et al. ,123 SRB, smoking
Distractions were used in response to a craving to engage in a risk behaviour, and building a resilience over time was described:
Maybe call a sponsor, call a friend, go for a walk, and go to the gym. The cravings do pass, and they do pass more easily when you have longer-term sobriety under your belt.
Luciano et al. ,132 MRB, alcohol and drug use
This progression was challenged in one report, as overcoming cravings was described as ‘almost impossible’,142 even when presented with visual consequences of smoking:
[E]ven with those pictures sitting right in front of me because my body is asking me for that.
Thornton et al. ,142 SRB, smoking
Social factors
Influences of the social and cultural contexts were a rich subtheme of data. People with SMI reported the benefits of positive peer support, but also the difficulties with negative peer group pressure.
Participants typically remarked that obligations to family and the cultural significance of dietary behaviours could prevent behaviour change. Eating together was seen as part of their ‘identity’ in a study of a Latino subpopulation:
. . . being together, eating our traditional food with our family, and remembering.
Jimenez et al. ,126 MRB, physical activity and diet
Such family gatherings were an example of social challenges to healthy diet and alcohol consumption:
‘One plate isn’t going to hurt you’, but the plate is like this [gestures] big, and it’s all mounded, it’s huge, and then everyone had to have a drink, and I’m like, ‘I don’t drink anymore’.
Aschbrenner et al. ,116 MRB, physical activity and diet
Engagement in risk behaviours (such as smoking) was often encouraged rather than restrained by others:
People are just like, ‘Dude, if you need to smoke, smoke.’.
Heffner et al. ,123 SRB, smoking
The absence of social support was also detrimental to healthy behaviours. In a few studies, there were reports of the negative impacts of loneliness:
The biggest culprit is loneliness, a terrible problem, I think. Nobody feels good when they’re alone.
Rönngren et al. ,141 MRB, physical activity and diet
Interventions that built in behaviour change activities into people’s schedule interrupted the sense of loneliness felt by some:
[I]t just helps to get me out really, that’s what it does, for people that are isolated like me, that do suffer from mental illness and do find it hard to go out and about.
Hodgson et al. ,124 SRB, physical activity
Environmental factors
The subtheme of environmental barriers to behaviour change emerged from reports about how certain environments induced rather than prevented health risk behaviours.
In some situations, environments were sources of behavioural triggers that were difficult to avoid and promoted engagement in risk behaviours:
You’re sitting there watching it and it’ll come on and triggers cigarette thoughts and . . . instead of putting you off, it would make you want to have a cigarette . . .
Thornton et al. ,142 SRB, smoking
I’d been smoking for so many years that there’s so many situations where it was extremely automatic for me to smoke.
Heffner et al. ,123 SRB, smoking
In one study, there were reports of individuals seeking new residences to change environmental triggers around them. However, group homes could also be a trigger, as occupants’ shared experiences made for talking points with unintended side effects:
[A]ll those war stories used to get me excited about [using alcohol and drugs].
Maisto et al. ,133 MRB, alcohol and drug use
Another component of environmental barriers to behaviour change was the interface with formal health care. Intervention providers and prescribers are gatekeepers for interventions, with the power to bestow decisions on who gets access to opportunities and support to promote positive behaviour change. This was illustrated through reports of the difficulties participants faced in being prescribed antismoking treatment, as well as in collecting prescriptions:
‘We’re not putting you on the Champix’ [Champix®; Pfizer Inc., New York, NY, USA] and the other one as well, ‘Not putting you on them’. And that was it. I was out the door, gone.
Knowles et al. ,131 SRB, smoking
Providers may be considered a natural authority in an intervention, which lends their advice legitimacy, as providing advice suggests that there is improvement to be made:
When she [nurse] gives me advice how to cook using healthy ingredients or to go to the fitness, I would follow this advice. The fact that she mentions it means for me that here is a problem.
Verhaeghe et al. ,143 MRB, other – health promotion
However, the naturally authoritative role of providers was sometimes perceived by participants as obstructive. This was especially true when participants perceived that providers lacked knowledge about their lived experience and were guilty of poorly expressing instructions:
How do they know it does that? You ever took drugs?
Maisto et al. ,133 MRB, alcohol and drug use
[H]e [therapist] says ‘that’s because you eat too much and don’t get enough exercise’. That’s pretty blunt, isn’t it? If you’re overweight, the last thing you want someone to tell you is that you’re fat.
Roberts and Bailey,139 MRB, other – weight
Support from health-care providers could also be construed as too sparse and restricted to addressing risk behaviours in isolation from other issues, thereby limiting the relevance of advice:
[O]nly really advice they give is, one time they said, ‘Now really try this time, [patient name]. Really try’. And I was like ‘alright’. They just signed the prescription and I take it away and try, so that was that.
Knowles et al. ,131 SRB, smoking
In a rehabilitation centre, a typically intense setting, care was not perceived as being supportive enough:
All they did was throw books and papers at you and told you to do this and talk about health, health food, and nothing about yourself.
Maisto et al. ,133 MRB, alcohol and drug use
Access to appropriate resources and practical barriers were other features of environmental barriers. The cost of healthy food was raised as a barrier to changing dietary behaviours. This may be common among a SMI population on a fixed income:
If you buy fresh, raw vegetables, they’re expensive. And I’m on a fixed income.
Jimenez et al. ,126 MRB, physical activity and diet
Locating suitable spaces for physical activity was also a common problem that affected participants’ ability to regularly and effectively take part in physical activity:
When we’re at [nursing facility], you could go on a long walk, but it’s all the way around the building and then you can’t really stop anywhere to rest.
Huck et al. ,125 SRB, physical activity
Barriers can mount up and environmental constraints can be multiplicative, such as when bad weather impeded taking outdoor exercise among those with a relatively low tolerance for exercise:
. . . I was out walking and focusing on my diet. And then I got sloppy with that. I don’t like to walk in the mall, and I don’t like to walk in the cold, the rain.
Yarborough et al. ,147 MRB, physical activity and diet
Experiences of behaviour change interventions and success
This theme draws together data on participants’ experiences of behaviour change interventions. In addition, more general benefits beyond the duration of a behaviour change intervention are also incorporated.
Tailoring interventions to severe mental illness populations
The most prominent intervention consideration reported by people with SMI was the role of mental health and SMI symptoms in behaviour change, as described in the subtheme of individual barriers to behaviour change. Symptoms of paranoia and delusion were highlighted as challenging for receiving information in one study that investigated perceptions of a population health intervention, for antismoking, in people with SMI. 142 This was the only study to consider the impacts of a population health intervention in this group. People with mental health problems are just as willing to bring about positive behaviour change as the general population. However, for some people with SMI, assistance in organising and structuring their lives to help them engage in positive behaviour change was seen as a vital first step:
[Talking in third person] because it’s not that they can’t think for themselves in the same way as other people, but it’s more a case of they can’t organise themselves or their thoughts in the same way as other people.
Knowles et al. ,131 SRB, smoking
In this sense, the structure and organisation of interventions themselves were positively associated with a greater sense of order and regularity on the part of participants. Engaging with an intervention created a basic schedule for participants:
[G]roups run regularly . . . there’s a schedule every week.
Maisto et al. ,133 MRB, alcohol and drug use
The structure provided by this was touched on in different ways, and described as helping to provide order to life more generally:
It means, how shall I say it? Maybe a bit more order in my life. You see, I have Tuesday and Thursday and I know that time I will . . . That will be, yes . . .
Forsberg et al. ;121 MRB; physical activity, diet, alcohol, drug use, smoking
A feature of structure that was present in some interventions was record keeping, particularly for diet and physical activity, but also applied to other behaviours. Having this organisational reference point seemed to link with self-education about personal health:
Well, it wasn’t until I started writing things down that I realized my intake was terrible.
Yarborough et al. ,147 MRB, physical activity and diet
Participants suggested that the routine and structure gained from interventions were important to continuing progress beyond the intervention:
Some of the most helpful things, it’s a combo, the structure and the day-to-day routine that I developed there. It has helped me for when I’m on my own.
Luciano et al. ,132 MRB, alcohol and drug use
Such organisation was also interpreted as applicable to participants’ cognitive approach:
[B]y maintaining an active, healthy lifestyle, helps me take the reins of my life [. . .].
Jimenez et al. ,127 MRB, physical activity and diet
Knowledge and skills to enact behaviour change
Psychoeducation and knowledge provision components were common among interventions. In studies, individuals reported awareness of the consequences of risk behaviours:
As [service provider] has told me, if I don’t start [exercising], COPD [chronic obstructive pulmonary disease], and that’s all I got to say.
Huck et al. ,125 SRB, physical activity
However, people with SMI may be less informed about behaviour change strategies and healthy choices. Some participants found education necessary, and being taught skills to practice healthy behaviours was enabling and enhanced their self-efficacy. While in a physical activity intervention, fear of incorrectly implementing change as a result of a lack of knowledge was prohibitive to taking action:
SMART [self-management and recovery training] gave me the information I needed no matter what I did.
Penn et al. ,138 SRB, alcohol
There are different ways to walk. It was a big step because I have a lack of knowledge of what is good.
Rönngren et al. ,140 MRB, physical activity and diet
The way in which knowledge was imparted by providers was also crucial to how participants responded to advice and encouragement. Non-tailored communication was especially obstructive and led to disengagement from positive behaviour change:
Sometimes I don’t understand [my therapist]. I let her say what she’s got to say, and I just stay quiet.
Maisto et al. ,133 MRB, alcohol and drug use
In other instances, participants recalled that providers had withheld information and not prepared them for what was to come, leading to only partial engagement in activities that they would have preferred to excel at:
I wish I had been pushed more, it would have been good if I could have been on Survivor on TV.
Wärdig et al. ,144 MRB; physical activity, diet, alcohol use and smoking
Physical activity was often referred to as a work in progress, that led to incremental change over time:
We did some small things and then we built up . . . we just walked around the back alley way quite a few times . . . flat ground so we didn’t have to walk up hills . . .
Fogarty and Happell,120 SRB, physical activity
Being prepared to experience physical exertion was cited as a necessary precursor to taking exercise, as individuals who were not comfortable might disengage before starting. Other paths to exercise were reliant on taking personal responsibility for following advice:
The program works if you follow the steps and the things you do. You get what you put into it I guess.
Luciano et al. ,132 MRB, alcohol and drug use
Intentions to enact behaviour change were also prompted in response to receipt of educational interventions that focused on the poor health consequences of negative health behaviours:
I learned a lot of stuff from the group . . . like how . . . beer and alcohol . . . [do] to your body . . . I’m going to be more careful . . .
Maisto et al. ,133 MRB, alcohol and drug use
Finding out that I’m a borderline diabetic . . . about six months ago . . . was also a push too.
Yarborough et al. ,147 MRB, physical activity and diet
A counterpoint to this sense of personal responsibility to change was noted in responses to public health antismoking campaigns, whereby shocking facts and imagery did not prohibit smoking; instead, people interpreted the risks as possible outcomes that were unlikely to affect them:
One’s [antismoking campaign] sitting right in front of me and I’m still smoking a cigarette, but yeah there is a lot of campaigns to scare people from smoking.
Thornton et al. ,142 SRB, smoking
For others, the risk of poorer health outcomes was divorced from a sense of responsibility for their own health; instead, they perceived the likelihood of being unwell as being inevitable:
[S]ometimes I think it’s in my DNA that . . . everything has been harder for me.
Heffner et al. ,123 SRB, smoking
Group delivery formats
A subtheme emerged about the merits of group delivery of interventions, and is related to broader themes about social motivations for behaviour change. This subtheme particularly highlighted the importance of how group formats fostered peer support and engendered a sense of togetherness:
I think a big part, if you’re going to deal with this, is to have people in the same boat with you. That helped – I didn’t know anyone else that would have been a dual diagnosis.
Luciano et al. ,132 MRB, alcohol and drug use
From bonding and togetherness came trust and understanding among participants and signalled how group delivery could also facilitate more tailored delivery to meet the needs of people with SMI. For example, in one study, it was reported that one individual experienced panic attacks during sessions. Peers understood their reactions and knew ‘to leave me alone in that situation or come over and have a quick word or maybe give me a quick nudge to get back on the pitch, and I just think it’s cus they know [pause] about your needs’ (Hodgson et al. ,124 SRB, physical activity). Put simply, peers ‘know where you’re coming from’ (Maisto et al. ,133 MRB, alcohol and drug use).
Another feature of group-based interventions was the point of comparison they provided. Within a group of peers experiencing the same intervention, there is an inherent comparison:
[M]eeting once a week and comparing notes with people, and knowing that I’m not alone with all these obstacles, and that there are people that care.
Yarborough et al. ,147 MRB, physical activity and diet
This could be a negative, as peers may also police engagement in interventions, as reported in a lifestyle intervention:
Half of them don’t listen. Many of them didn’t even wear that pedometer, and I always wore mine. Even when I slept I wore it. I think I was the most diligent one of us all.
Wärdig et al. ,144 MRB; physical activity, diet, alcohol use and smoking
Choices and adapting interventions to suit the individual
In the context of group interventions, it was apparent that, for some participants, the chance to draw up personalised approaches to behaviour change was an important driver for success. This was especially apparent among those taking part in physical activity interventions:
It was good that we got to choose something out of like a list. We could have done all different things . . . I thought the options were quite good. But I would have like to have done boxercise as well.
Firth et al. ,119 SRB, physical activity
Forewarning about the nature of interventions was also highlighted as critical to making informed choices about taking part in interventions:
[P]eople turn up and then it’s not right for them . . . if they’d had the information . . . they wouldn’t have come, well waste their time really . . .
Roberts and Bailey,139 MRB, other – weight
Because individuals favoured interventions that offered choice, they adapted activities to suit their needs and capabilities, for example incorporating physical activity into their daily routine:
This [exercise] is a really challenging thing for me. What I do is doing errands. I walk from place to place rather than take the bus and the train.
Jimenez et al. ,126 MRB, physical activity and diet
Providers can help facilitate the tailoring of activities so that they are suitable for each individual:
The health co-ordinators were great people who made everything feel spontaneous. They were good at finding the right level for each and every one.
Wärdig et al. ,144 MRB; physical activity, diet, alcohol use and smoking
There were instances, however, when interventions had competing priorities owing to the focus on multiple risk behaviours; the delivery of such interventions did not always map to individual needs and preferences:
[T]he walking [is helpful]. The exercise portion of the group, that can get set on the back burner. And I don’t think it should be.
Yarborough et al. ,147 MRB, physical activity and diet
Purpose to activity
Among studies, a subtheme on intervention activities providing a sense of purpose emerged:
It’s just that I’ve got an activity for the afternoon that I’m not sat watching TV, something like that.
Carless and Douglas,118 SRB, physical activity
Similarly, in two studies, interventions were seen as providing something to look forward to:
[G]roup gives you a place to be, a reason to be there.
Maisto et al. ,133 MRB, alcohol and drug use
It’s a routine you get used to I think. It’s like football, I get excited about football on a Monday.
Carless and Douglas,118 SRB, physical activity
More broadly, the purpose of activity also related to the concepts of loneliness (see Barriers to behaviour change, Social factors). Purposeful activity could help resolve loneliness.
Valued benefits of behaviour change interventions
Across studies, the benefits of behaviour change interventions extended beyond health outcomes, with participants reporting improvements in well-being and ability to navigate day-to-day life. Interventions featuring physical activity were particularly prominent in this subtheme.
Cognitive benefits of behaviour change interventions included memory and decision-making:
My memory has returned.
Rönngren et al. ,140 MRB, physical activity and diet
I wouldn’t make any decisions, I was too worried about making the wrong one. I was very scared [pause] of stepping on people’s feet and just everything like that, . . . now I just get on with it.
Hodgson et al. ,124 SRB, physical activity
Valued benefits of intervention experiences also included opening doors for individuals’ everyday functioning and socialising, with greater control over their lives. As interventions were structured, this, in turn, gave individuals a sense of order over their lives. It can be through simple routine to daily life, or returning to education, work and hobbies:
I’m going to school, I’m looking for work, I go home every other week to see my family. I run, I’ve really gotten into that. I have friends now, I go fishing twice a week . . .
Luciano et al. ,132 MRB, alcohol and drug use
[B]y maintaining an active, healthy lifestyle, helps me take the reins of my life and have a connection with the outside and inside world.
Jimenez et al. ,127 MRB, physical activity and diet
Some of the most generally affecting and prevalent benefits reported in the data were improved confidence, self-esteem and optimism. Confidence was described as part of a package of cognitive and emotional changes:
I think I’m in a much better mood . . . I am up, I’m confident, I’m sleeping well, my appetite is good, my self-esteem is healthy . . . I have a brighter outlook, you know.
Heffner et al. ,123 SRB, smoking
SMART [self-management and recovery training – the intervention] gave me pride. It showed me how to get self-worth. It was basically building me up in order to be receptive to everything else. It started with me.
Penn et al. ,138 SRB, alcohol
Participants’ expressions of excitement and fulfilment in achieving change could bring about greater confidence that, in turn, acted as a spur to continue to engage with interventions:
I love it. It’s just like, thinking yeah, I couldn’t do this 4 months ago, now look at me doing it comfortably. Let’s throw it up a gear!
Firth et al. ,119 SRB, physical activity
This positive change, was summed up in feeling the beginning of a fresh start:
I feel like this program has benefited me and I feel like I’ve got my second wind out of this program.
Fogarty and Happell,120 SRB, physical activity
Chapter 6 Integration of quantitative and qualitative findings
Table 5 presents a matrix comparing the findings of the qualitative and quantitative studies included in our systematic review. We investigated whether or not overall themes and subthemes from the synthesis of qualitative studies were investigated in the quantitative data. We noted narratively if there was any overlap and investigated whether or not it was possible to conduct meta-regression analyses, component NMAs or multivariate meta-analyses related to these themes. When qualitative and quantitative data overlapped, we assessed the relationship according to four categories: silence (no overlap), partial agreement (complementary findings), agreement (coherence between quantitative and qualitative data) and dissonance (conflicting findings from quantitative and qualitative data). When there was overlap in quantitative and qualitative data but the relationship between the findings was unclear, we categorised this as inconclusive.
| Themes from qualitative studies | Were the themes from the qualitative studies addressed in the quantitative studies? | Comparing quantitative and qualitative data |
|---|---|---|
| Interaction of mental and physical health | ||
| Health behaviours improving mental health and well-being: engaging in healthy behaviours was reported to improve mental health. In addition, mental health symptoms were reported as a barrier to engaging with behaviour change | Partially, although trials focusing on improving physical health outcomes also measured mental health outcomes. However, interactions between these outcomes were not assessed | Partial agreement: NMAs of mental health-related quality of life included nine trials that targeted smoking alone; diet and physical activity; or diet, physical activity, alcohol and smoking. These studies show that there is currently no evidence that trying to improve physical health worsens mental health |
| Being considered holistically: participants reported that interventions were sometimes experienced as impersonal and not taking into account the needs of the person as a whole | No – we did not identify intervention content that specifically reported emphasising the importance of considering people holistically | N/A |
| Self-medicating: participants reported using smoking, alcohol and cannabis as a way of managing their mental health | No – we did not identify intervention content that specifically reported targeting self-medicating | N/A |
| Motivational contexts and barriers to change | ||
Individual: importance of personal motivations for change. These included managing health, improving physical appearance and working to a positive future
|
Partially – several studies included BCTs related to identifying individual motivations or barriers. However, the focus of the qualitative studies and quantitative studies was quite different | Inconclusive – there were insufficient data to explore this further in component NMAs |
Social: feedback and reinforcement from family and friends was often motivating, group interventions sometimes led to a sense of belonging with peers
|
BCTs related to social support were common in quantitative studies | Inconclusive – it was inconclusive whether or not social support improved effectiveness based on component NMAs |
Environmental: some reported the importance of a safe and stable place as a foundation for change, an intervention could also provide a schedule and structure that helped facilitate change
|
Not specifically addressed in quantitative studies | N/A |
| Experiences of behaviour change interventions | ||
| Tailoring interventions to SMI: some mentioned the need for extra help with providing structure and organisation as a platform for change | Several studies reported tailoring interventions for the benefit of people with SMI. Although tailoring was mentioned in some quantitative studies, authors generally did not report the tailoring process with much detail | Inconclusive: it was inconclusive whether or not tailoring interventions to SMI improved effectiveness based on component NMAs |
| Knowledge and skills to enact behaviour change: education and skills training was reported as important for motivating and equipping people to change | Several studies included BCTs related to knowledge and skills |
|
| Group delivery formats: some reported that group-based interventions promoted peer support, a feeling of belongingness and togetherness, and a useful point of comparison | Several quantitative studies were group focused and others were largely individual focused, providing opportunities to compare the impact on effectiveness of these delivery methods |
|
| Choices and adapting the intervention to suit the individual: the importance of adapting interventions for the needs and preferences of those participating | Partially: a small number of interventions sought to tailor intervention content and risk behaviour targets to the individual | Silence: there were insufficient studies to explore the impact of such approaches on effectiveness |
| Purpose to activity: some reported that interventions provided an overall sense of purpose beyond changing specific targeted behaviours | Not specifically addressed | Silence: no overlap between quantitative and qualitative studies |
| Valued benefits of behaviour change interventions: some reported experiencing additional benefits beyond the interventions, including greater confidence and wanting to build on what they’d already achieved | Not specifically addressed | Silence: minimal overlap between quantitative and qualitative studies |
Interaction of mental and physical health
Health behaviours improving mental health and well-being
There were insufficient quantitative data to explore whether or not engaging in healthy behaviours (e.g. physical activity) contributed to mental well-being as characterised in the synthesis of qualitative studies. Trials did not directly assess the impact of improved physical health on mental health outcomes.
Another way of looking at this relationship between physical and mental health is to assess whether or not engaging in a behaviour change intervention is associated with a deterioration of mental health outcomes. Importantly, neither the quality of life nor PANSS outcomes found evidence that interventions targeting smoking; diet and physical activity; or diet, physical activity, alcohol and smoking led to deterioration of mental health symptoms or quality of life. However, as acknowledged previously, the data are currently limited and future research could change these conclusions.
Being considered holistically
The primary outcome in most intervention studies was either behavioural (e.g. smoking) or primarily related to markers of physical health (e.g. weight, BMI, blood pressure). This focus reflects the importance that researchers have placed on tackling the public health challenge of improving the physical health of people with SMI.
However, this subtheme from the synthesis of qualitative studies highlights that people with SMI may value responses to this public health challenge differently. Many people with SMI reported more holistic goals for well-being encompassing both physical and mental health. Attempts to change risk behaviours sit in a complex context of mental health, lifestyle and environment that interact with behaviours and affect the individual experience of change.
This difference in emphasis in the quantitative studies is reflected in the focus on outcomes related to those behaviours targeted in interventions. For example, quality of life was rarely a primary outcome (Gaughran et al. 67 was an exception). Mental health outcomes were even less often reported in health risk behaviour intervention studies, once more reflecting a slightly different focus in these interventions than that reported in the qualitative data.
The lack of overlap between the experiences of people with SMI and intervention design suggests that future intervention trials may benefit from greater input from people with SMI in both designing and delivering interventions.
Self-medicating
Another subtheme from the qualitative studies was the perception among participants that smoking, alcohol use and drug use played a role in managing their mental health symptoms (i.e. ‘self-medicating’). This was indirectly targeted in some studies (e.g. by including BCTs related to mental health symptoms such as reducing negative emotions) or assessing whether or not participants increased cannabis use after quitting smoking. 69 However, interventions rarely reported strategies for tackling the problem of self-medicating directly.
Motivational contexts and barriers to change
For the sake of brevity, we considered motivational contexts and barriers to change in combination in this analysis, as there was a large overlap in content between the quantitative and qualitative findings.
Individual motivations and barriers to change
Evidence from the synthesis of qualitative studies identified a range of individual factors that acted as motivations or barriers to change. Several trials sought to address these factors using BCTs such as problem-solving, and pros and cons.
We investigated the impact of BCTs on outcomes using component NMAs. There were sufficient data for only weight and BMI outcomes. The component NMAs were inconclusive in terms of whether or not including these BCTs was associated with effective reduction of weight or BMI.
Social motivations and barriers to change
Evidence from the synthesis of qualitative studies identified a range of social factors that acted as motivations or barriers to change. Family and friends, as well as fellow participants in interventions, were often identified as sources of motivation to engage in behaviour change. However, these same people could also be unsupportive and overly critical, and their presence could act as barriers to change.
Several quantitative studies sought to use social support as a positive factor for encouraging behaviour change. These interventions included BCTs such as social support (unspecified), social support (practical) and social support (emotional).
There were sufficient data to explore the impact only of social support (unspecified) in component NMAs of weight and BMI. However, these analyses were inconclusive on the benefits of this BCT.
Environmental motivations and barriers to change
Qualitative studies reported the importance of environmental factors acting as barriers to change (e.g. participants sharing ‘war stories’ about previous use of alcohol and other drugs). We did not identify any quantitative studies that specifically addressed these barriers. In addition, it was not possible to assess if such barriers lead to unintentional adverse effects in interventions.
Participants also reported interventions as providing a helpful structure and accountability that helped them to engage in healthier behaviours. Although this was not specifically assessed in quantitative studies, the qualitative data provide further insights into contextual factors associated with intervention delivery that may have an impact on effectiveness. This further highlights the importance of including process measures in assessments of the delivery of BCT interventions.
Experiences of behaviour change interventions
Tailoring interventions to people with severe mental illness
One of the subthemes from qualitative studies was the need to tailor interventions for people with SMI. Various aspects of tailoring were discussed, including additional help to organise thoughts. Some reported difficulty with concentrating and also the challenge of accepting information when experiencing delusions. Others reported that interventions provided structure, routine and accountability that helped them to put into practice what they had learnt.
Although some quantitative studies reported tailoring interventions for people with SMI, often, little detail was reported. Therefore, although we could assess the impact of tailoring of interventions in the meta-regression analyses, it was difficult to tell the extent to which types of tailoring reported in qualitative studies mapped onto those reported in quantitative studies.
The meta-regression analyses found that there was insufficient evidence from quantitative studies to confirm that studies reporting tailoring of interventions for people with SMI were more effective in reducing weight or BMI.
Knowledge and skills to enact behaviour change
There was clearer agreement between the quantitative and qualitative evidence on the need for knowledge and skills acquisition as part of a behaviour change intervention. Qualitative studies found that people with SMI valued learning how to engage in more healthy behaviours and how to build on incremental changes.
This was confirmed in the component NMAs in which the BCT instruction on how to perform a behaviour was associated with effectiveness in reducing weight and BMI. However, the impact of the BCTs ‘information about health consequences’ and ‘demonstration of the behaviour’ were inconclusive in the component NMAs.
Group delivery formats
Data from qualitative studies identified several benefits of group interventions, including fostering peer support and providing a point of comparison to assess progress in changing a behaviour. However, a disproportionate number of included studies in the synthesis of qualitative studies were focused on experiences of group interventions. Therefore, the reported benefits of these interventions may have been over-represented in the review.
The meta-regression analyses that focused on delivering interventions to individuals were found to be more effective than interventions that focused on group delivery to reduce weight and BMI. This does not necessarily rule out the benefits of group interventions, but it may suggest that the benefits of group interventions (in terms of outcome) are different from those of individual interventions. Therefore, it may be important for interventions to build on the different strengths of group-delivered and individually delivered approaches.
Choices and adapting the intervention to suit the individual
The value of adapting interventions to the needs and abilities of the person was commonly reported in qualitative studies.
However, there were insufficient studies that reported choice of which behaviours/activities to focus on, or adaptation of intervention content, to assess their impact on outcomes. Qualitative studies may have identified subtle distinctions in delivery between individuals that are not straightforward to quantify, but that may still be important when supporting people with SMI to change their behaviour.
Purpose to activity
Another subtheme from qualitative studies was that interventions provided a sense of purpose and routine to life. These wider benefits of interventions are difficult to quantify and, therefore, tend not to be addressed in quantitative research, although literature on the importance of purpose and its association with health outcomes is beginning to emerge. 151
Valued benefits of behaviour change interventions
Other wider benefits of behaviour change (e.g. improvement in memory and cognition, self-esteem) were reported in qualitative studies. These broader outcomes were not commonly measured as part of quantitative studies, so we know little about these broader impacts in controlled studies.
Chapter 7 Patient and public involvement and dissemination of findings
Patient and public involvement
People with lived experience of SMI and carers significantly contributed to every stage of the project. Sophie Corlett (Director of External Relations, Mind) provided oversight on the progress of the project as a member of our multidisciplinary advisory group (including Dr Ian Kellar, health psychologist, University of Leeds; Dr Peter Coventry, health services researcher, University of York; Dr Stephen Wright, psychiatrist, Tees, Esk and Wear Valleys NHS Foundation Trust; and Professor Paul French, psychiatrist, Manchester Metropolitan University).
In January 2019, we presented the aims of the project and received feedback on the protocol from the York Service User Network (a PPI group connected to Tees, Esk and Wear Valleys NHS Foundation Trust).
We also formed two PPI groups that met throughout the course of the project. One group began meeting in York and consisted of four members, chaired by a carer for a relative with SMI (DS), one peer researcher (CD) and a peer researcher who is also a carer (HK). One further group member (a carer) was no longer able to attend after the first meeting because of other commitments.
We also regularly met with two peer researchers (MS and GJ) who are members of the Lived Experience Research Collective hosted by the Mental Health Foundation.
All the members of our PPI groups were included as authors of the report, reflecting their substantial contribution to the project. The PPI groups decided on the name of the project (HEALTH study), provided extensive comments on the protocol, contributed to interpretations of the study results, played a key role in disseminating the findings of the project, participated in the webinar and provided feedback on an animation summarising the findings of this project.
Dissemination activities
A study-specific Twitter account (@UoY_HEALTH_SMI, run by HM) (www.twitter.com; Twitter, Inc., San Francisco, CA, USA) was created and has developed a presence over the course of the study, engaging in promotion and dissemination activities, which are reported below.
On 2 March 2020, we published an article in The Conversation on the mortality gap in people with SMI. 152 At the time of writing (June 2020), the article had been read 14,742 times, with an audience mainly from the UK (1205 reads), USA (6785 reads) and India (2512 reads). The article was also widely shared on social media such as Twitter (14 times) and Facebook (737 times) (www.facebook.com; Facebook, Inc., Menlo Park, CA, USA).
We organised a webinar to communicate the findings of the study to people with SMI, carers, health and social care professionals, and researchers. To promote the webinar, peer researchers Gordon Johnston and Michel Syrett published a blog article in June 2020 on physical activity among people with SMI for the Mental Elf website. 153
In addition, peer researcher Ceri Dare (see Patient and public involvement) was interviewed by Andre Tomlin for the Mental Elf website on 23 June 2020. 154
On 24 June 2020, we live-streamed a webinar on Zoom (www.zoom.us; Zoom Video Communications, Inc., San Jose, CA, USA) and YouTube (www.youtube.com; YouTube, LLC, San Bruno, CA, USA). 155
We received 128 registrations for the webinar, which included a combination of health professionals (n = 56), researchers (n = 32), people with lived experience (n = 17), family/carers (n = 2) and other (n = 11). Most were from the UK (n = 116). We posted the recorded webinar on YouTube155 and received a further 100 views, at the time of writing.
We registered a hashtag (#HealthSMI) to monitor engagement with the webinar on Twitter. More than 100 people participated in the Twitter conversation. The webinar generated > 200 tweets and > 3,500,000 impressions.
The event was chaired by Andre Tomlin (the founder of the Mental Elf website) and included presentations from the research team (NM and HM), including a peer researcher (MS). There was a panel discussion with a carer, former general practitioner and researcher (DS); peer researcher (GJ); and a physiotherapist and researcher (Brendon Stubbs).
Audience members were also assigned to one of nine ‘breakout rooms’ for small group discussions on the implications for practice and research, facilitated by members of the research team (NM, HM, PC, ER, DS, SD and RC) and peer researchers (GJ and MS). Summaries and feedback from each small group were used to inform conclusions of the study. The webinar concluded with two Zoom polls (audience members rated their key implications for practice and further research) and a reflection from peer researchers (MS and GJ). Equal access for people with SMI to health risk behaviour interventions was, by far, the most popular implication for practice. Identifying how best to adapt health-promoting interventions for people with SMI was the most popular research recommendation.
We commissioned a production company to develop an animation summarising the findings of the study; this was disseminated through YouTube and Twitter from 7 July 2020. 156
Through links with the UK Research and Innovation Closing the Gap Network, we have written an article summarising the findings from the synthesis of qualitative studies for the Equally Well blog, published on 11 August 2020. 157
We also plan to continue disseminating the findings of the study in peer-reviewed publications in 2022.
Chapter 8 Discussion
Summary of findings
Summary of synthesis of quantitative studies
We identified a growing literature on smoking (eight trials were included in the narrative synthesis of smoking abstinence and seven trials were included in the narrative synthesis for number of cigarettes smoked). Interventions focusing on smoking alone were generally more effective than controls at increasing the odds of abstinence, whereas studies targeting smoking in addition to other risk behaviours (such as unhealthy diet, physical inactivity, alcohol misuse) did not find evidence of increased odds of abstinence. However, there was a great deal of conceptual heterogeneity, including the intensity of control groups and smoking interventions across trials.
Data on reducing the number of cigarettes smoked varied widely between studies. This made it difficult to draw conclusions on the clinical effectiveness of risk behaviour interventions for this outcome. For all other behavioural outcomes, data were limited.
By far the most commonly reported outcomes were weight (30 trials included in the NMA) and BMI (36 trials included in the NMA). Interventions targeting diet alone, physical activity alone or diet and physical activity concurrently all appeared to be effective in improving weight loss (e.g. any intervention vs. TAU: –2.10 kg, 95% CrI –3.14 to –1.06 kg) and BMI reduction (e.g. any intervention vs. TAU: –0.49 kg/m2, 95% CrI –0.97 to –0.01 kg/m2). The magnitude of weight loss and reduction in BMI did not appear to differ substantially between studies targeting diet or physical activity alone and studies targeting diet and physical activity concurrently. We also did not find evidence of positive synergies in targeting diet and physical activity to promote weight loss or reduction in BMI.
Improvements in blood pressure and cholesterol outcomes as a whole were modest (e.g. systolic blood pressure, any intervention vs. TAU: –1.23 mmHg, 95% CrI –3.34 to 0.68 mmHg). However, in contrast to the other outcomes, targeting multiple behaviours appeared to result in greater improvements. Targeting diet (e.g. systolic blood pressure: 0.42 mmHg, 95% CrI –4.52 to 5.30 mmHg) or physical activity alone (e.g. systolic blood pressure: –0.26 mmHg, 95% CrI –5.43 to 4.97 mmHg) led to modest improvements, whereas effect estimates were higher in trials targeting diet and physical activity (e.g. systolic blood pressure: –1.56 mmHg, 95% CrI –4.42 to 0.98 mmHg) and also in trials targeting diet, physical activity, alcohol use and smoking (e.g. systolic blood pressure: –2.17 mmHg, 95% CrI –5.46 to 0.59 mmHg). This potentially reflects synergies in targeting multiple health behaviours in reducing systolic and diastolic blood pressure.
Fewer data were reported on quality of life and mental health outcomes. We found no evidence that interventions aiming to reduce physical health risk behaviours in people with SMI led to negative impacts on mental health (PANSS total score: 0.03, 95% CrI –2.56 to 2.65) or mental health-related quality of life (SMD –0.04, 95% CrI –0.14 to 0.06). However, there was also no evidence that interventions promoted physical health-related quality of life (SMD 0.06, 95% CrI –0.04 to 0.16).
There was limited overlap of BCTs in included studies, which reduced our ability to assess the impact on effectiveness and how BCTs interacted with one another. Goal-setting was associated with weight loss (–2.22 kg, 95% CrI –4.54 to –0.44 kg) and reduction in BMI (–1.85 kg/m2, 95% CrI –2.91 to –0.69 kg/m2). Instruction on how to perform the behaviour was also associated with weight loss (–2.10 kg, 95% CrI –3.42 to –0.45 kg) and reduction in BMI (–1.19 kg/m2, 95% CrI –1.85 to –0.55 kg/m2). Self-monitoring of behaviour was associated with reduction in BMI (–0.70 kg/m2, 95% CrI –1.42 to 0.07 kg/m2), although it was not possible to rule out no benefit.
For BMI, we were able to include more interaction parameters in the model, and the interaction model appeared to fit the data better than the model that assumed BCTs acted independently of one another. However, all estimates of interactions were very imprecise, so we could not draw any conclusions on how the effects of specific BCTs interacted with each other.
Similarly, lack of reporting of data limited our abilities to explore the impact of other intervention and participant characteristics. However, we found that interventions focusing on delivery to individuals were more effective on weight loss than group-delivered interventions (–2.70 kg, 95% CrI –4.69 to –0.75 kg) and reduction in BMI (–1.11 kg/m2, 95% CrI –2.15 to –0.01 kg/m2).
Summary of synthesis of qualitative studies
We used the CERQual approach to rate the certainty of the evidence. All themes were rated to be of moderate certainty.
Interaction of mental and physical health
Participants reported that engaging in health behaviours improved their mental health and well-being, and mental health changes affected their engagement with healthy behaviours. Participants in the included studies wanted to be treated holistically, and sometimes felt that interventions had an impersonal focus on behaviours rather than people. There were also data reporting the use of smoking, alcohol use and drug use to help manage mental health symptoms.
Motivational contexts for behaviour change
A range of individual factors were reported to be personally motivating. These included managing health, improving physical appearance and working towards a positive future. Family and friends were also an important source of motivation, providing feedback and reinforcement of positive change. However, others could also be discouraging when they were careless with their words or actions. Interventions were interpreted as a safe and stable place to work on changing their unhealthy behaviours, also providing a schedule and accountability, which helped to make changes.
Barriers to behaviour change
Mental health symptoms affected individuals’ ability to change. For example, it can be difficult to engage in physical activity when feeling a lack of motivation and low mood related to mental health state, likewise with difficulty concentrating when receiving information related to health. However, mental health symptoms were not the only factors affecting motivations. A general lack of motivation to change unhealthy behaviours was also unrelated to mental health for some. Stigma about body image was another factor considered to act as a barrier to change. Social support from family and friends, although often a positive influence, could also act as a barrier. For example, some family members encouraged unhealthy behaviours. Alternatively, a lack of social support was a barrier for persevering with behaviour change. Environmental factors could act as triggers for unhealthy behaviours (e.g. advertisements on television), as could living in group homes where peers shared their experiences of engaging in risk behaviours.
Experiences of behaviour change interventions
It was suggested that people with SMI needed additional help providing structure and assistance in organising their lives. This was considered an important aspect of tailoring interventions for people with SMI. Interventions providing education and imparting skills to promote healthy behaviours were also considered beneficial. Group interventions were helpful for building peer support and also as a point of comparison with others, which could be double-edged if used to police behaviour. Interventions that took into account the needs, abilities and preferences of participants were felt to be beneficial. A wealth of data reported that interventions had an impact on individuals’ lives beyond just improving their health-related behaviours. For example, interventions sometimes provided a structure and purpose to everyday life. Interventions also helped to build confidence: if positive changes were made in one area of their lives, then it was thought possible in other aspects of life.
Integrative synthesis of quantitative and qualitative studies
The integrative synthesis generally showed limited overlap between quantitative and qualitative studies. Many of the themes in qualitative studies, such as importance of interventions benefiting the person as a whole rather than just specific health-related outcomes, were not directly addressed in quantitative studies. Similarly, qualitative studies reported that people with SMI engaging in physical activity interventions experienced wider benefits than simply improving their physical activity. Interventions often provided purpose and organisation to people’s lives that affected their overall well-being. Although this was captured by trials measuring broader outcomes (such as quality of life) to some extent, interventions were rarely designed to take advantage of these benefits valued by many people with SMI. The lack of overlap between the quantitative and qualitative evidence may suggest the importance of people with SMI contributing to the design and delivery of interventions. Such interventions may go some way to addressing the needs and preferences of people with SMI, especially in relation to addressing both physical and mental health together.
Quantitative and qualitative studies agreed on the importance of gaining knowledge and skills to live healthier lives. This theme from the qualitative literature was backed up by the component NMAs that found that the BCT instruction to perform behaviour was associated with weight loss and reduction in BMI.
Strengths and limitations of the review
Strengths
This systematic review had a number of strengths. As far as we are aware, this is the first systematic review comparing the clinical effectiveness of multiple and single health risk behaviour interventions among people with SMI using NMAs. This is also, to our knowledge, the first systematic review to examine the effectiveness of BCTs using component NMA in people with SMI.
In addition, as far as we are aware, this is the first systematic review of qualitative studies on experiences of a broad range of multiple risk behaviour interventions in people with SMI. This is also the first systematic review, to our knowledge, to have integrated quantitative and qualitative studies on this range of health risk behaviours in people with SMI.
Limitations
As noted previously, there were very limited data for most behavioural outcomes [diet, physical activity, alcohol use and drug use (e.g. cannabis use)]. This is surprising, given that these interventions are designed to change behaviour. Even if the primary outcomes of most trials were weight, BMI or clinically related outcomes (e.g. blood pressure, cholesterol), the mechanism by which interventions aimed to affect these outcomes was mainly through behaviour.
Most studies targeted diet and physical activity; therefore, we have limited data on studies targeting a single risk behaviour (e.g. unhealthy diet, physical inactivity, excessive alcohol consumption or drug use). Similarly, we have limited data on studies investigating the effects of interventions targeting a more extensive combination of risk behaviours. This limits our ability to draw conclusions on the comparative benefits of targeting risk behaviours in isolation or in combination.
There were sufficient data to compare any risk behaviour intervention with TAU for quality-of-life outcomes. However, the more complex models, with separate nodes for interventions targeting different BCTs, lacked data.
Similarly, there was limited overlap in the BCTs targeted between studies. This limited our conclusions on what BCTs were more effective and the extent to which their effects on outcomes interact.
No studies specifically focused on interventions for people from minority ethnic groups or assessed the impact of ethnicity on outcomes. Therefore, it is unclear whether or not ethnicity has an impact on the effectiveness of interventions.
There was a lack of overlap between quantitative and qualitative evidence. Therefore, it was difficult to assess the relationship between these sources of data.
A further limitation is that we did not search specifically for grey literature (other than conference abstracts indexed in electronic databases), and we were only able to assess studies in languages understood by the project team (i.e. English, French, German, Dutch, Spanish, Portuguese, Russian and Japanese).
Comparison with previous systematic reviews
One way to compare our findings is with systematic reviews of multiple risk behaviour interventions in the general population. A 2017 systematic review10 in the general population found a more developed literature on behavioural outcomes. Multiple risk behaviour interventions were associated with improvements in fruit and vegetable intake, fat intake, total physical activity and moderate/vigorous physical activity. However, the current review found very limited reporting of behavioural outcomes.
In both reviews, comparable data were available on weight and BMI. However, the method of analysing multiple risk behaviour interventions differed a little. The general population review combined all interventions targeting weight (–0.59 kg, 95% CI –1.02 to –0.16 kg) and BMI (–0.27 kg/m2, 95% CI –0.46 to –0.07 kg/m2). In this current review, among people with SMI, we assessed the effectiveness of interventions targeting diet and physical activity for weight (–2.12 kg, 95% CrI –2.94 to –1.34 kg) and BMI (–0.53 kg/m2, 95% CrI –1.07 to 0.04 kg/m2), which suggested a slightly larger improvement in both than was observed by combining all interventions targeting these outcomes in the general population. We also assessed the effectiveness of interventions targeting diet, physical activity, alcohol misuse and smoking concurrently. This review found that these sorts of interventions resulted in a smaller reduction in weight (1.27 kg, 95% CrI –1.46 to 3.42 kg) and BMI (–0.02 kg/m2, 95% CrI –1.05 to 0.98 kg/m2) than was observed in the general population. Taken together, interventions among people with SMI appear at least as effective on weight loss and reducing their BMI as those among the general population.
It is also important to compare our findings with systematic reviews specifically on trials of people with SMI. A 2019 review158 focusing on weight management in people with SMI found similar results to our current study. As above, methods of pooling data were a little different. Speyer et al. 158 conducted an analysis combining all interventions with all controls. They also found similar modest benefits on weight (–2.25 kg, 95% CI –3.01 to –1.42 kg) and BMI (–0.63 kg/m2, 95% CI –1.02 to –0.23 kg/m2).
There is a much wider literature on pharmacological interventions for promoting smoking cessation among people with SMI. 28 Although many of these trials provide additional behaviour change interventions (along with pharmacological interventions), the content is usually the same for both intervention and control groups; therefore, it is not possible to draw conclusions about the effectiveness of behaviour change interventions in this context. However, our findings are consistent with broader reviews of pharmacological and/or behavioural interventions28 of smoking cessation, which also found that smoking cessation interventions were of similar effectiveness to those found in general population samples.
Systematic reviews of qualitative studies in this area on people with SMI have mainly focused on smoking cessation. 159 Despite the wider range of risk behaviours included in our review, there were many overlapping themes such as the importance of tailoring interventions, addressing the common perception that smoking helps manage mental health symptoms (when the relief experienced is likely attributable to relieving symptoms of nicotine withdrawal: the ‘misattribution hypothesis’) and the importance of social support.
Chapter 9 Conclusions
Implications for practice
This review found preliminary support for focusing on smoking alone rather than targeting smoking in combination with other behaviours. For weight loss and reduction in BMI, there did not appear to be evidence of synergies when targeting more than one health behaviour at a time, although targeting multiple health risk behaviours appeared to be more beneficial in reducing blood pressure. These findings are consistent with group discussions in our webinar on the importance of setting realistic targets for behaviour change. Targeting multiple risk behaviours may have the potential to make some feel overwhelmed.
This systematic review found no evidence that interventions promoting health behaviours were associated with deterioration in mental health symptoms or mental health-related quality of life. Group discussions and polls from our webinar suggested that this was a key finding. This was rated as the key implication for practice and was a common theme across our discussion groups. Many webinar participants noted that this evidence challenged the tendency towards a risk-averse approach that had low expectations of people with SMI making positive changes to health risk behaviours.
Another key implication from the systematic review was the need for communication between staff and people with SMI on the goals of health risk behaviour interventions. Qualitative data found that people with SMI favoured holistic approaches to well-being that integrated the promotion of physical and mental health, whereas the quantitative data, mainly led by researchers and health-care professionals, consisted of trials focused on smoking cessation and weight loss. This may reflect important differences in the aims of such interventions between people with SMI and professionals delivering interventions. Our webinar group discussion also provided important context to these challenges. Several webinar participants pointed out potential barriers to a more holistic approach. Mental and physical health care in many services are often provided separately, which makes it difficult to deliver holistic approaches, because of a lack of multidisciplinary teams. In addition, some staff spoke of the training needs of delivering integrated interventions that aimed to promote both mental and physical health.
Providing choice and adapting interventions for the needs of the individual were key implications from the qualitative data. These included taking into account the preferences and capabilities of each individual and taking into account the challenges of managing a mental health condition. Webinar group discussions emphasised the importance that ‘one size does not fit all’ and the importance of adapting interventions to best reflect the person.
Suggestions for further research
Identifying how best to adapt interventions for the needs of people with SMI was the key research recommendation identified in our webinar poll. Although qualitative data showed that people with SMI valued the adaptation of interventions, the trial data rarely investigated how best to tailor interventions (particularly in trials aiming to promote weight loss). A recent trial has shown the benefits of adapting smoking cessation interventions for people with SMI. 69 The many gaps between findings from the qualitative literature and the quantitative literature suggests the importance of future research being co-produced by people with SMI.
Future quantitative research should take advantage of qualitative evidence to inform future trials, as well as how to develop these. Elements of co-production were missing from the evidence base, and discussion with our PPI group highlighted the importance of stakeholder engagement from the beginning.
Another important suggestion for further research that emerged from group discussions and interactions during the webinar was the need for trials specifically targeting people with SMI who have recently received a diagnosis. Epidemiological evidence shows that weight gain increases exponentially in the first year after diagnosis. However, few trials in this review targeted participants at this stage in their lives. Future trials are needed to assess the clinical effectiveness of health risk behaviour interventions among people with SMI who have recently received a mental health diagnosis.
We also identified a lack of studies with follow-up data of at least 12 months post intervention, although current data suggests that, at ≤ 6 months’ follow-up, BMI and weight loss are maintained. These findings need to be confirmed in future research to assess the long-term benefits of health risk behaviour interventions, as well as potential barriers such as the impact of episodic depression and anxiety or periods spent as an inpatient in a psychiatric facility.
We found few trials that directly compared interventions targeting multiple health risk behaviours with interventions targeting single health risk behaviours. As seen previously, targeting smoking alone may be more effective than targeting smoking in combination with other behaviours. Future research is needed to clarify which combinations of behaviours to target for interventions.
Acknowledgements
We would like to express our gratitude to the members of our advisory group for their support and contribution to the review: Dr Ian Kellar (University of Leeds), Dr Peter Coventry (University of York), Sophie Corlett (Mind), Dr Stephen Wright (Tees, Esk and Wear Valleys NHS Foundation Trust) and Professor Paul French (Manchester Metropolitan University). Any errors or omissions in the review are the responsibility of the review team and not of the Study Advisory Group.
We thank York Service User Network for its comments on the protocol at the beginning of the project.
We thank André Tomlin (Minervation Ltd, Oxford, UK) for facilitating, organising and promoting the webinar. We also thank all the participants who attended the webinar, and those who took part in small group discussions and/or in the Zoom chat during the webinar. We thank Digifish Ltd (York, UK) for producing an animation summarising the project and Dr Jessica Hendon for feedback on a draft version of the animation.
Contributions of authors
Nick Meader (https://orcid.org/0000-0001-9332-6605) (Research Fellow, Evidence Synthesis and Statistics) had overall responsibility for the project, led on the systematic review (screening, data extraction, risk-of-bias assessment, conducted the NMA and integrative synthesis of quantitative and qualitative studies), led on the writing of the report and participated in the webinar.
Hollie Melton (https://orcid.org/0000-0003-3837-510X) (Research Fellow, Evidence Synthesis) conducted the systematic review (screening; data extraction; risk-of-bias assessment; led on the synthesis of qualitative studies and the CASP and CERQual assessments); led the write-up of the synthesis of qualitative studies, the description of included studies and the compilation of the final report; participated in the webinar; and ran the HEALTH study Twitter account.
Connor Evans (https://orcid.org/0000-0002-4525-2100) (Research Support Officer, Evidence Synthesis) conducted the systematic review (screening, data extraction, risk-of-bias assessment), revised the report and attended the webinar.
Kath Wright (https://orcid.org/0000-0002-9020-1572) (Information Service Manager, Information Specialist) was principally responsible for compiling and running database searches, and building and maintaining the EndNote libraries.
David Shiers (https://orcid.org/0000-0003-2531-5837) (retired general practitioner, carer of daughter with schizophrenia) chaired the PPI group; contributed to the protocol, interpretation of the analysis and write-up; and participated in the webinar.
Elena Ratschen (https://orcid.org/0000-0003-4128-9608) (Senior Lecturer, Health Services Research) contributed to the protocol, interpretation of analysis and write-up; and participated in the webinar.
Sofia Dias (https://orcid.org/0000-0002-2172-0221) (Professor in Health Technology Assessment) contributed to the protocol, interpretation of analysis and write-up; supervised the statistical analysis; and participated in the webinar.
Ceri Dare (https://orcid.org/0000-0002-6762-506X) (Peer Researcher), Gordon Johnston (https://orcid.org/0000-0003-4483-8932) (Peer Researcher), Harminder Kaur (https://orcid.org/0000-0002-3377-9511) (Peer Researcher) and Michel Syrett (https://orcid.org/0000-0002-8919-7318) (Peer Researcher) contributed to PPI group meetings; contributed to the protocol, interpretation of the analysis and write-up; and participated in the webinar.
Christopher J Armitage (https://orcid.org/0000-0003-2365-1765) (Professor of Health Psychology) contributed to the protocol, interpretation of the analysis and write-up.
Rachel Churchill (https://orcid.org/0000-0002-1751-0512) (Professor of Evidence Synthesis) contributed to the protocol, interpretation of the analysis and write-up; and participated in the webinar.
Simon Gilbody (https://orcid.org/0000-0002-8236-6983) (Professor of Health Services Research, Psychological Medicine) contributed to the protocol and participated in the webinar.
Peter Coventry (https://orcid.org/0000-0003-0625-3829) (Senior Lecturer, Health Services Research) was an advisory group member; contributed to the protocol, interpretation of the analysis and write-up; provided oversight of the synthesis of qualitative studies; and participated in the webinar.
All authors contributed to the report and approved the final version.
Publications
Meader N, Melton HA. People with severe mental illness live shorter lives – but the solution isn’t simple. The Conversation, 2 March 2020. URL: https://theconversation.com/people-with-severe-mental-illness-live-shorter-lives-but-the-solution-isnt-simple-127397 (accessed 3 June 2021).
Melton H, Meader N. Healthy Living: Adapting Physical Health Programmes to the Needs of People with Severe Mental Illness. URL: https://equallywell.co.uk/2020/07/28/healthy-living-adapting-physical-health-programmes-to-the-needs-of-people-with-severe-mental-illness/ (accessed 3 June 2021).
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HSDR programme or the Department of Health and Social Care.
References
- Royal College of Psychiatrists . Improving the Physical Health of Adults With Severe Mental Illness: Essential Actions n.d. www.aomrc.org.uk/reports-guidance/improving-physical-health-adults-severe-mental-illness-essential-actions/ (accessed 7 October 2020).
- Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save?. Lancet 2005;366:1578-82. https://doi.org/10.1016/S0140-6736(05)67341-2.
- Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis 2014;11. https://doi.org/10.5888/pcd11.130293.
- Belani H, Chorba T, Fletcher F, Hennessey K, Kroeger K, Lansky A, et al. Integrated prevention services for HIV Infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: summary guidance from CDC and the U.S. Department of Health and Human Services. Morb Mortal Wkly Rep 2012;61:1-40.
- Noble N, Paul C, Turon H, Oldmeadow C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev Med 2015;81:16-41. https://doi.org/10.1016/j.ypmed.2015.07.003.
- Chou CP, Montgomery S, Pentz MA, Rohrbach LA, Johnson CA, Flay BR, et al. Effects of a community-based prevention program on decreasing drug use in high-risk adolescents. Am J Public Health 1998;88:944-8. https://doi.org/10.2105/AJPH.88.6.944.
- Krokstad S, Ding D, Grunseit AC, Sund ER, Holmen TL, Rangul V, et al. Multiple lifestyle behaviours and mortality, findings from a large population-based Norwegian cohort study – the HUNT study. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-016-3993-x.
- Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years’ follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. BMJ 2009;338. https://doi.org/10.1136/bmj.b349.
- Meader N, King K, Moe-Byrne T, Wright K, Graham H, Petticrew M, et al. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 2016;16. https://doi.org/10.1186/s12889-016-3373-6.
- Meader N, King K, Wright K, Graham HM, Petticrew M, Power C, et al. Multiple risk behavior interventions: meta-analyses of RCTs. Am J Prev Med 2017;53:e19-e30. https://doi.org/10.1016/j.amepre.2017.01.032.
- Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiat 2007;64:242-9. https://doi.org/10.1001/archpsyc.64.2.242.
- Davies S. Annual Report of the Chief Medical Officer 2013. Public Mental Health Priorities: Investing in the Evidence n.d. https://mrc.ukri.org/documents/pdf/chief-medical-officer-annual-report-2013/ (accessed 7 October 2020).
- Shiers D, Bradshaw T, Campion J. Health inequalities and psychosis: time for action. Br J Psychiatry 2015;207:471-3. https://doi.org/10.1192/bjp.bp.114.152595.
- Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med 2016;46:2869-81. https://doi.org/10.1017/S0033291716001732.
- Treuer T, Hoffmann VP, Chen AK, Irimia V, Ocampo M, Wang G, et al. Factors associated with weight gain during olanzapine treatment in patients with schizophrenia or bipolar disorder: results from a six-month prospective, multinational, observational study. World J Biol Psychiatry 2009;10:729-40. https://doi.org/10.1080/15622970903079507.
- Blouin M, Tremblay A, Jalbert ME, Venables H, Bouchard RH, Roy MA, et al. Adiposity and eating behaviors in patients under second generation antipsychotics. Obesity 2008;16:1780-7. https://doi.org/10.1038/oby.2008.277.
- Royal College of Physicians, Royal College of Psychiatrists . Smoking and Mental Health: A Joint Report by the Royal College of Physicians and the Royal College of Psychiatrists n.d. www.rcplondon.ac.uk/projects/outputs/smoking-and-mental-health (accessed 7 October 2020).
- Action on Smoking and Health (ASH) . The Stolen Years: The Mental Health and Smoking Action Report n.d. https://ash.org.uk/information-and-resources/reports-submissions/reports/the-stolen-years/ (accessed 7 October 2020).
- Dipasquale S, Pariante CM, Dazzan P, Aguglia E, McGuire P, Mondelli V. The dietary pattern of patients with schizophrenia: a systematic review. J Psychiatr Res 2013;47:197-20. https://doi.org/10.1016/j.jpsychires.2012.10.005.
- Jerome GJ, Young DR, Dalcin A, Charleston J, Anthony C, Hayes J, et al. Physical activity levels of persons with mental illness attending psychiatric rehabilitation programs. Schizophr Res 2009;108:252-7. https://doi.org/10.1016/j.schres.2008.12.006.
- Alvarez-Jiménez M, González-Blanch C, Crespo-Facorro B, Hetrick S, Rodríguez-Sánchez JM, Pérez-Iglesias R, et al. Antipsychotic-induced weight gain in chronic and first-episode psychotic disorders: a systematic critical reappraisal. CNS Drugs 2008;22:547-62. https://doi.org/10.2165/00023210-200822070-00002.
- Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet 2008;371:1085-97. https://doi.org/10.1016/S0140-6736(08)60486-9.
- Tiihonen J, Lönnqvist J, Wahlbeck K, Klaukka T, Niskanen L, Tanskanen A, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet 2009;374:620-7. https://doi.org/10.1016/S0140-6736(09)60742-X.
- Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiatry 2014;71:248-54. https://doi.org/10.1001/jamapsychiatry.2013.3726.
- Crebbin K, Mitford E, Paxton R, Turkington D. Drug and alcohol misuse in first episode psychosis: an observational study. Neuropsychiatr Dis Treat 2008;4:417-23. https://doi.org/10.2147/NDT.S2178.
- Prochaska JJ, Fromont SC, Delucchi K, Young-Wolff KC, Benowitz NL, Hall S, et al. Multiple risk-behavior profiles of smokers with serious mental illness and motivation for change. Health Psychol 2014;33:1518-29. https://doi.org/10.1037/a0035164.
- Mental Health Taskforce . The Five Year Forward View for Mental Health 2016. www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf (accessed 7 October 2020).
- Peckham E, Brabyn S, Cook L, Tew G, Gilbody S. Smoking cessation in severe mental ill health: what works? an updated systematic review and meta-analysis. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1419-7.
- Cabassa LJ, Ezell JM, Lewis-Fernández R. Lifestyle interventions for adults with serious mental illness: a systematic literature review. Psychiatr Serv 2010;61:774-82. https://doi.org/10.1176/ps.2010.61.8.774.
- Bonfioli E, Berti L, Goss C, Muraro F, Burti L. Health promotion lifestyle interventions for weight management in psychosis: a systematic review and meta-analysis of randomised controlled trials. BMC Psychiatry 2012;12. https://doi.org/10.1186/1471-244X-12-78.
- Teasdale SB, Ward PB, Rosenbaum S, Samaras K, Stubbs B. Solving a weighty problem: systematic review and meta-analysis of nutrition interventions in severe mental illness. Br J Psychiatry 2017;210:110-18. https://doi.org/10.1192/bjp.bp.115.177139.
- Malpass A, Andrews R, Turner KM. Patients with type 2 diabetes experiences of making multiple lifestyle changes: a qualitative study. Patient Educ Couns 2009;74:258-63. https://doi.org/10.1016/j.pec.2008.08.018.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019 n.d. www.training.cochrane.org/handbook (accessed 7 October 2020).
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS: a Bayesian modelling framework: concepts, structure and extensibility. Stat Comput 2000;10:325-37. https://doi.org/10.1023/A:1008929526011.
- Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 2004;23:3105-24. https://doi.org/10.1002/sim.1875.
- Welton NJ, Caldwell DM, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol 2009;169:1158-65. https://doi.org/10.1093/aje/kwp014.
- Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE–CERQual to qualitative evidence synthesis findings-paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0689-2.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20. https://doi.org/10.1258/1355819054308576.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Whitley R, Crawford M. Qualitative research in psychiatry. Can J Psychiatry 2005;50:108-14. https://doi.org/10.1177/070674370505000206.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- Petticrew M, Rehfuess E, Noyes J, Higgins JP, Mayhew A, Pantoja T, et al. Synthesizing evidence on complex interventions: how meta-analytical, qualitative, and mixed-method approaches can contribute. J Clin Epidemiol 2013;66:1230-43. https://doi.org/10.1016/j.jclinepi.2013.06.005.
- Tonkin-Crine S, Anthierens S, Hood K, Yardley L, Cals JW, Francis NA, et al. Discrepancies between qualitative and quantitative evaluation of randomised controlled trial results: achieving clarity through mixed methods triangulation. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0436-0.
- Attux C, Martini LC, Elkis H, Tamai S, Freirias A, Camargo Md, et al. A 6-month randomized controlled trial to test the efficacy of a lifestyle intervention for weight gain management in schizophrenia. BMC Psychiatry 2013;13. https://doi.org/10.1186/1471-244X-13-60.
- Baker A, Richmond R, Haile M, Lewin TJ, Carr VJ, Taylor RL, et al. A randomized controlled trial of a smoking cessation intervention among people with a psychotic disorder. Am J Psychiatry 2006;163:1934-42. https://doi.org/10.1176/ajp.2006.163.11.1934.
- Baker AL, Richmond R, Kay-Lambkin FJ, Filia SL, Castle D, Williams JM, et al. Randomized controlled trial of a healthy lifestyle intervention among smokers with psychotic disorders. Nicotine Tob Res 2015;17:946-54. https://doi.org/10.1093/ntr/ntv039.
- Battaglia G, Alesi M, Inguglia M, Roccella M, Caramazza G, Bellafiore M, et al. Soccer practice as an add-on treatment in the management of individuals with a diagnosis of schizophrenia. Neuropsychiatr Dis Treat 2013;9:595-603. https://doi.org/10.2147/NDT.S44066.
- Bechdolf A, Pohlmann B, Güttgemanns J, Geyer C, Lindner K, Ferber C, et al. State-dependent motivational interviewing for people with schizophrenia and substance use: results of a randomised controlled trial. Nervenarzt 2012;83:888-96. https://doi.org/10.1007/s00115-011-3331-6.
- Beebe LH, Smith K, Burk R, McIntyre K, Dessieux O, Tavakoli A, et al. Effect of a motivational intervention on exercise behavior in persons with schizophrenia spectrum disorders. Community Ment Health J 2011;47:628-36. https://doi.org/10.1007/s10597-010-9363-8.
- Beebe LH, Tian L, Morris N, Goodwin A, Allen SS, Kuldau J. Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues Ment Health Nurs 2005;26:661-76. https://doi.org/10.1080/01612840590959551.
- Bonfioli E, Mazzi MA, Berti L, Burti L. Physical health promotion in patients with functional psychoses receiving community psychiatric services: results of the PHYSICO-DSM-VR study. Schizophr Res 2018;193:406-11. https://doi.org/10.1016/j.schres.2017.06.017.
- Bonsack C, Gibellini Manetti S, Favrod J, Montagrin Y, Besson J, Bovet P, et al. Motivational intervention to reduce cannabis use in young people with psychosis: a randomized controlled trial. Psychother Psychosom 2011;80:287-97. https://doi.org/10.1159/000323466.
- Brar JS, Ganguli R, Pandina G, Turkoz I, Berry S, Mahmoud R. Effects of behavioral therapy on weight loss in overweight and obese patients with schizophrenia or schizoaffective disorder. J Clin Psychiatry 2005;66:205-12. https://doi.org/10.4088/jcp.v66n0208.
- Brody AL, Zorick T, Hubert R, Hellemann GS, Balali S, Kawasaki SS, et al. Combination extended smoking cessation treatment plus home visits for smokers with schizophrenia: a randomized controlled trial. Nicotine Tob Res 2017;19:68-76. https://doi.org/10.1093/ntr/ntw190.
- Brown C, Goetz J, Hamera E. Weight loss intervention for people with serious mental illness: a randomized controlled trial of the RENEW program. Psychiatr Serv 2011;62:800-2. https://doi.org/10.1176/ps.62.7.pss6207_0800.
- Brown S, Chan K. A randomized controlled trial of a brief health promotion intervention in a population with serious mental illness. J Ment Health 2006;15:543-9. https://doi.org/10.1080/09638230600902609.
- Brunette MF, Ferron JC, McGurk SR, Williams JM, Harrington A, Devitt T, et al. Brief, web-based interventions to motivate smokers with schizophrenia: randomized trial. JMIR Ment Health 2020;7. https://doi.org/10.2196/16524.
- Christiansen BA, Carbin J, TerBeek E, Fiore MC. Helping smokers with severe mental illness who do not want to quit. Subst Use Misuse 2018;53:949-62. https://doi.org/10.1080/10826084.2017.1385635.
- Cordes J, Thünker J, Regenbrecht G, Zielasek J, Correll CU, Schmidt-Kraepelin C, et al. Can an early weight management program (WMP) prevent olanzapine (OLZ)-induced disturbances in body weight, blood glucose and lipid metabolism? Twenty-four- and 48-week results from a 6-month randomized trial. World J Biol Psychiatry 2011;15:229-41. https://doi.org/10.3109/15622975.2011.592546.
- Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med 2013;368:1594-602. https://doi.org/10.1056/NEJMoa1214530.
- Evans S, Newton R, Higgins S. Nutritional intervention to prevent weight gain in patients commenced on olanzapine: a randomized controlled trial. Aust N Z J Psychiatry 2005;39:479-86. https://doi.org/10.1111/j.1440-1614.2005.01607.x.
- Fernández Guijarro S, Pomarol-Clotet E, Rubio Muñoz MC, Miguel García C, Egea López E, Fernández Guijarro R, et al. Effectiveness of a community-based nurse-led lifestyle-modification intervention for people with serious mental illness and metabolic syndrome. Int J Ment Health Nurs 2019;28:1328-37. https://doi.org/10.1111/inm.12644.
- Forsberg KA, Björkman T, Sandman PO, Sandlund M. Physical health – a cluster randomized controlled lifestyle intervention among persons with a psychiatric disability and their staff. Nord J Psychiatry 2008;62:486-95. https://doi.org/10.1080/08039480801985179.
- Frank E, Wallace ML, Hall M, Hasler B, Levenson JC, Janney CA, et al. An integrated risk reduction intervention can reduce body mass index in individuals being treated for bipolar I disorder: results from a randomized trial. Bipolar Disord 2015;17:424-37. https://doi.org/10.1111/bdi.12283.
- Ganguli R, Brar JS. Behavioural intervention for weight loss in schizophrenia: an RCT with active controls. Indian J Psychiatry 2011;53.
- Gaughran F, Stahl D, Ismail K, Greenwood K, Atakan Z, Gardner-Sood P, et al. Randomised control trial of the effectiveness of an integrated psychosocial health promotion intervention aimed at improving health and reducing substance use in established psychosis (IMPaCT). BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1571-0.
- George TP, Ziedonis DM, Feingold A, Pepper WT, Satterburg CA, Winkel J, et al. Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. Am J Psychiatry 2000;157:1835-42. https://doi.org/10.1176/appi.ajp.157.11.1835.
- Gilbody S, Peckham E, Bailey D, Arundel C, Heron P, Crosland S, et al. Smoking cessation for people with severe mental illness (SCIMITAR+): a pragmatic randomised controlled trial. Lancet Psychiatry 2019;6:379-90. https://doi.org/10.1016/S2215-0366(19)30047-1.
- Gillhoff K, Gaab J, Emini L, Maroni C, Tholuck J, Greil W. Effects of a multimodal lifestyle intervention on body mass index in patients with bipolar disorder: a randomized controlled trial. Prim Care Companion J Clin Psychiatry 2010;12:e1-e8. https://doi.org/10.4088/PCC.09m00906yel.
- Graham HL, Copello A, Griffith E, Freemantle N, McCrone P, Clarke L, et al. Pilot randomised trial of a brief intervention for comorbid substance misuse in psychiatric in-patient settings. Acta Psychiatr Scand 2016;133:298-309. https://doi.org/10.1111/acps.12530.
- Green CA, Yarborough BJ, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, et al. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: a randomized trial. Am J Psychiatry 2015;172:71-8. https://doi.org/10.1176/appi.ajp.2014.14020173.
- Hjorth P, Davidsen AS, Kilian R, Pilgaard Eriksen S, Jensen SO, Sørensen HØ, et al. Improving the physical health of long-term psychiatric inpatients. Aust N Z J Psychiatry 2014;48:861-70. https://doi.org/10.1177/0004867414533011.
- Hjorthøj CR, Fohlmann A, Larsen AM, Gluud C, Arendt M, Nordentoft M. Specialized psychosocial treatment plus treatment as usual (TAU) versus TAU for patients with cannabis use disorder and psychosis: the CapOpus randomized trial. Psychol Med 2013;43:1499-510. https://doi.org/10.1017/S0033291712002255.
- Holt RIG, Gossage-Worrall R, Hind D, Bradburn MJ, McCrone P, Morris T, et al. Structured lifestyle education for people with schizophrenia, schizoaffective disorder and first-episode psychosis (STEPWISE): randomised controlled trial. Br J Psychiatry 2019;214:63-7. https://doi.org/10.1192/bjp.2018.167.
- Iglesias-García C, Toimil-Iglesias A, Alonso-Villa MJ. Pilot study of the efficacy of an educational programme to reduce weight, on overweight and obese patients with chronic stable schizophrenia. J Psychiatr Ment Health Nurs 2010;17:849-51. https://doi.org/10.1111/j.1365-2850.2010.01590.x.
- Jean-Baptiste M, Tek C, Liskov E, Chakunta UR, Nicholls S, Hassan AQ, et al. A pilot study of a weight management program with food provision in schizophrenia. Schizophr Res 2007;96:198-205. https://doi.org/10.1016/j.schres.2007.05.022.
- Jones SH, Riste L, Robinson H, Holland F, Peters S, Hartwell R, et al. Feasibility and acceptability of integrated psychological therapy versus treatment as usual for people with bipolar disorder and co-morbid alcohol use: a single blind randomised controlled trial. J Affect Disord 2019;256:86-95. https://doi.org/10.1016/j.jad.2019.05.038.
- Kaltsatou A, Kouidi E, Fountoulakis K, Sipka C, Theochari V, Kandylis D, et al. Effects of exercise training with traditional dancing on functional capacity and quality of life in patients with schizophrenia: a randomized controlled study. Clin Rehabil 2015;29:882-91. https://doi.org/10.1177/0269215514564085.
- Khazaal Y, Fresard E, Rabia S, Chatton A, Rothen S, Pomini V, et al. Cognitive behavioural therapy for weight gain associated with antipsychotic drugs. Schizophr Res 2007;91:169-77. https://doi.org/10.1016/j.schres.2006.12.025.
- Kilbourne AM, Goodrich DE, Lai Z, Clogston J, Waxmonsky J, Bauer MS. Life goals collaborative care for patients with bipolar disorder and cardiovascular disease risk. Psychiatr Serv 2012;63:1234-8. https://doi.org/10.1176/appi.ps.201100528.
- Kwon JS, Choi JS, Bahk WM, Yoon Kim C, Hyung Kim C, Chul Shin Y, et al. Weight management program for treatment-emergent weight gain in olanzapine-treated patients with schizophrenia or schizoaffective disorder: a 12-week randomized controlled clinical trial. J Clin Psychiatry 2006;67:547-53. https://doi.org/10.4088/jcp.v67n0405.
- Lee H, Kane I, Brar J, Sereika S. Telephone-delivered physical activity intervention for individuals with serious mental illness: a feasibility study. J Am Psychiatr Nurses Assoc 2014;20:389-97. https://doi.org/10.1177/1078390314561497.
- Littrell KH, Hilligoss NM, Kirshner CD, Petty RG, Johnson CG. The effects of an educational intervention on antipsychotic-induced weight gain. J Nurs Scholarsh 2003;35:237-41. https://doi.org/10.1111/j.1547-5069.2003.00237.x.
- Marzolini S, Jensen B, Melville P. Feasibility and effects of a group-based resistance and aerobic exercise program for individuals with severe schizophrenia: a multidisciplinary approach. Ment Health Phys Act 2009;2:2-36. https://doi.org/10.1016/j.mhpa.2008.11.001.
- Masa-Font R, Fernández-San-Martín MI, Martín López LM, Alba Muñoz AM, Oller Canet S, Martín Royo J, et al. The effectiveness of a program of physical activity and diet to modify cardiovascular risk factors in patients with severe mental illness after 3-month follow-up: CAPiCOR randomized clinical trial. Eur Psychiatry 2015;30:1028-36. https://doi.org/10.1016/j.eurpsy.2015.09.006.
- Mauri M, Simoncini M, Castrogiovanni S, Iovieno N, Cecconi D, Dell’Agnello G, et al. A psychoeducational program for weight loss in patients who have experienced weight gain during antipsychotic treatment with olanzapine. Pharmacopsychiatry 2008;41:17-23. https://doi.org/10.1055/s-2007-992148.
- McCreadie RG, Kelly C, Connolly M, Williams S, Baxter G, Lean M, et al. Dietary improvement in people with schizophrenia: randomised controlled trial. Br J Psychiatry 2005;187:346-51. https://doi.org/10.1192/bjp.187.4.346.
- McKibbin CL, Patterson TL, Norman G, Patrick K, Jin H, Roesch S, et al. A lifestyle intervention for older schizophrenia patients with diabetes mellitus: a randomized controlled trial. Schizophr Res 2006;86:36-44. https://doi.org/10.1016/j.schres.2006.05.010.
- Melamed Y, Stein-Reisner O, Gelkopf M, Levi G, Sivan T, Ilievici G, et al. Multi-modal weight control intervention for people with persistent mental disorders. Psychiatr Rehabil J 2008;31:194-200. https://doi.org/10.2975/31.3.2008.194.200.
- Methapatara W, Srisurapanont M. Pedometer walking plus motivational interviewing program for Thai schizophrenic patients with obesity or overweight: a 12-week, randomized, controlled trial. Psychiatry Clin Neurosci 2011;65:374-80. https://doi.org/10.1111/j.1440-1819.2011.02225.x.
- Milano W, Grillo F, Del Mastro A, De Rosa M, Sanseverino B, Petrella C, et al. Appropriate intervention strategies for weight gain induced by olanzapine: a randomized controlled study. Adv Ther 2007;24:123-34. https://doi.org/10.1007/BF02850000.
- Osborn D, Burton A, Hunter R, Marston L, Atkins L, Barnes T, et al. Clinical and cost-effectiveness of an intervention for reducing cholesterol and cardiovascular risk for people with severe mental illness in English primary care: a cluster randomised controlled trial. Lancet Psychiatry 2018;5:145-54. https://doi.org/10.1016/S2215-0366(18)30007-5.
- Peckham E, Arundel C, Bailey D, Brownings S, Fairhurst C, Heron P, et al. Smoking Cessation Intervention for Severe Mental Ill Health Trial (SCIMITAR+): study protocol for a randomised controlled trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-1789-7.
- Penn PE, Brooks AJ. Five years, twelve steps, and REBT in the treatment of dual diagnosis. J Ration Emot Cogn Behav Ther 2000;18:197-208. https://doi.org/10.1023/A:1007883021936.
- Ratliff JC, Palmese LB, Tonizzo KM, Chwastiak L, Tek C. Contingency management for the treatment of antipsychotic-induced weight gain: a randomized controlled pilot study. Obes Facts 2012;5:919-27. https://doi.org/10.1159/000345975.
- Romain AJ, Fankam C, Karelis AD, Letendre E, Mikolajczak G, Stip E, et al. Effects of high intensity interval training among overweight individuals with psychotic disorders: a randomized controlled trial. Schizophr Res 2019;210:278-86. https://doi.org/10.1016/j.schres.2018.12.021.
- Scheewe TW, Backx FJ, Takken T, Jörg F, van Strater AC, Kroes AG, et al. Exercise therapy improves mental and physical health in schizophrenia: a randomised controlled trial. Acta Psychiatr Scand 2013;127:464-73. https://doi.org/10.1111/acps.12029.
- Scocco P, Longo R, Caon F. Weight change in treatment with olanzapine and a psychoeducational approach. Eat Behav 2006;7:115-24. https://doi.org/10.1016/j.eatbeh.2005.08.003.
- Sheridan Rains L, Marston L, Hinton M, Marwaha S, Craig T, Fowler D, et al. Clinical and cost-effectiveness of contingency management for cannabis use in early psychosis: the CIRCLE randomised clinical trial. BMC Med 2019;17. https://doi.org/10.1186/s12916-019-1395-5.
- Sorić T, Mavar M, Rumbak I. The effects of the Dietary Approaches to Stop Hypertension (DASH) diet on metabolic syndrome in hospitalized schizophrenic patients: a randomized controlled trial. Nutrients 2019;11. https://doi.org/10.3390/nu11122950.
- Speyer H, Christian Brix Nørgaard H, Birk M, Karlsen M, Storch Jakobsen A, Pedersen K, et al. The CHANGE trial: no superiority of lifestyle coaching plus care coordination plus treatment as usual compared to treatment as usual alone in reducing risk of cardiovascular disease in adults with schizophrenia spectrum disorders and abdominal obesity. World Psychiatry 2016;15:155-65. https://doi.org/10.1002/wps.20318.
- Steinberg ML, Williams JM, Stahl NF, Budsock PD, Cooperman NA. An adaptation of motivational interviewing increases quit attempts in smokers with serious mental illness. Nicotine Tob Res 2016;18:243-50. https://doi.org/10.1093/ntr/ntv043.
- Sugawara N, Sagae T, Yasui-Furukori N, Yamazaki M, Shimoda K, Mori T, et al. Effects of nutritional education on weight change and metabolic abnormalities among patients with schizophrenia in Japan: a randomized controlled trial. J Psychiatr Res 2018;97:77-83. https://doi.org/10.1016/j.jpsychires.2017.12.002.
- Sylvia LG, Pegg SL, Dufour SC, Janos JA, Bernstein EE, Chang WC, et al. Pilot study of a lifestyle intervention for bipolar disorder: Nutrition Exercise Wellness Treatment (NEW Tx). J Affect Disord 2019;250:278-83. https://doi.org/10.1016/j.jad.2019.03.033.
- Tantirangsee N, Assanangkornchai S, Marsden J. Effects of a brief intervention for substance use on tobacco smoking and family relationship functioning in schizophrenia and related psychoses: a randomised controlled trial. J Subst Abuse Treat 2015;51:30-7. https://doi.org/10.1016/j.jsat.2014.10.011.
- Usher K, Park T, Foster K, Buettner P. A randomized controlled trial undertaken to test a nurse-led weight management and exercise intervention designed for people with serious mental illness who take second generation antipsychotics. J Adv Nurs 2013;69:1539-48. https://doi.org/10.1111/jan.12012.
- Weber M, Wyne K. A cognitive/behavioral group intervention for weight loss in patients treated with atypical antipsychotics. Schizophr Res 2006;83:95-101. https://doi.org/10.1016/j.schres.2006.01.008.
- Williams J, Stubbs B, Richardson S, Flower C, Barr-Hamilton L, Grey B, et al. ‘Walk this way’: results from a pilot randomised controlled trial of a health coaching intervention to reduce sedentary behaviour and increase physical activity in people with serious mental illness. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2274-5.
- Wu RR, Zhao JP, Jin H, Shao P, Fang MS, Guo XF, et al. Lifestyle intervention and metformin for treatment of antipsychotic-induced weight gain: a randomized controlled trial. JAMA 2008;299:185-93. https://doi.org/10.1001/jama.2007.56-b.
- Young AS, Cohen AN, Goldberg R, Hellemann G, Kreyenbuhl J, Niv N, et al. Improving weight in people with serious mental illness: the effectiveness of computerized services with peer coaches. J Gen Intern Med 2017;32:48-55. https://doi.org/10.1007/s11606-016-3963-0.
- Alba A, Weich S, Griffiths FE. Service users’ experiences of a physical activity and lifestyle intervention for people with severe mental illness: a longitudinal qualitative study. J Epidemiol Community Health 2011;65. https://doi.org/10.1136/jech.2011.143586.42.
- Hoffmann KD. A participatory approach to physical activity among people with severe and persistent mental illness. Diss Abstr Int B Sci Eng 2014;75.
- McDonell MG, Skalisky J, Leickly E, Oluwoye O. Perspectives of individuals with serious mental illness on contingency management for alcohol use. Alcohol Clin Exp Res 2018;42:19A-270A. https://doi.org/10.1111/acer.13747.
- Moltke A, Kampmann J, Nordentoft M. Habits of physical activity in everyday life among individuals suffering from schizophrenia – a qualitative research project based on participant observations. Early Interv Psychiatry 2014;8.
- Aschbrenner K, Carpenter-Song E, Mueser K, Kinney A, Pratt S, Bartels S. A qualitative study of social facilitators and barriers to health behavior change among persons with serious mental illness. Community Ment Health J 2013;49:207-12. https://doi.org/10.1007/s10597-012-9552-8.
- Bauer IE, Kiropoulos LA, Crist NP, Hamilton JE, Soares JC, Meyer TD. A qualitative study investigating bipolar patients’ expectations of a lifestyle intervention: a self-management program. Arch Psychiatr Nurs 2018;32:555-60. https://doi.org/10.1016/j.apnu.2018.03.002.
- Carless D, Douglas K. Narrative, identity and mental health: how men with serious mental illness re-story their lives through sport and exercise. Psychol Sport Exerc 2008;9:576-94. https://doi.org/10.1016/j.psychsport.2007.08.002.
- Firth J, Carney R, Jerome L, Elliott R, French P, Yung AR. The effects and determinants of exercise participation in first-episode psychosis: a qualitative study. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0751-7.
- Fogarty M, Happell B. Exploring the benefits of an exercise program for people with schizophrenia: a qualitative study. Issues Ment Health Nurs 2005;26:341-51. https://doi.org/10.1080/01612840590915711.
- Forsberg KA, Lindqvist O, Bjorkman TN, Sandlund M, Sandman PO. Meanings of participating in a lifestyle programme for persons with psychiatric disabilities. Scand J Caring Sci 2011;25:357-64. https://doi.org/10.1111/j.1471-6712.2010.00834.x.
- Gossage-Worrall R, Hind D, Barnard-Kelly KD, Shiers D, Etherington A, Swaby L, et al. STEPWISE Research Group . STructured lifestyle education for people WIth SchizophrEnia (STEPWISE): mixed methods process evaluation of a group-based lifestyle education programme to support weight loss in people with schizophrenia. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2282-5.
- Heffner JL, Watson NL, McClure JB, Anthenelli RM, Hohl S, Bricker JB. ‘I smoke like this to suppress these issues that are flaws of my character’: challenges and facilitators of cessation among smokers with bipolar disorder. J Dual Diagn 2018;14:32-9. https://doi.org/10.1080/15504263.2017.1390278.
- Hodgson MH, McCulloch HP, Fox KR. The experiences of people with severe and enduring mental illness engaged in a physical activity programme integrated into the mental health service. Ment Health Phys Act 2011;4:23-9. https://doi.org/10.1016/j.mhpa.2011.01.002.
- Huck GE, Finnicum C, Morrison B, Kaseroff A, Umucu E. Consumer perspectives on physical activity interventions within assertive community treatment programs. Psychiatr Rehabil J 2018;41:312-18. https://doi.org/10.1037/prj0000311.
- Jimenez DE, Aschbrenner K, Burrows K, Pratt SI, Alegría M, Bartels SJ. Perspectives of overweight Latinos with serious mental illness on barriers and facilitators to health behavior change. J Lat Psychol 2015;3:11-22. https://doi.org/10.1037/lat0000020.
- Jimenez DE, Burrows K, Aschbrenner K, Barre LK, Pratt SI, Alegría M, et al. Health behavior change benefits: perspectives of Latinos with serious mental illness. Transcult Psychiatry 2016;53:313-29. https://doi.org/10.1177/1363461516632388.
- Jimenez DE, Thomas L, Bartels SJ. The role of serious mental illness in motivation, participation and adoption of health behavior change among obese/sedentary Latino adults. Ethn Health 2019;24:889-96. https://doi.org/10.1080/13557858.2017.1390552.
- Keller-Hamilton B, Moe AM, Breitborde NJK, Lee A, Ferketich AK. Reasons for smoking and barriers to cessation among adults with serious mental illness: a qualitative study. J Community Psychol 2019;47:1462-75. https://doi.org/10.1002/jcop.22197.
- Klein P, Lawn S, Tsourtos G, van Agteren J. Tailoring of a smartphone smoking cessation app (Kick.it) for serious mental illness populations: qualitative study. JMIR Hum Factors 2019;6. https://doi.org/10.2196/14023.
- Knowles S, Planner C, Bradshaw T, Peckham E, Man MS, Gilbody S. Making the journey with me: a qualitative study of experiences of a bespoke mental health smoking cessation intervention for service users with serious mental illness. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0901-y.
- Luciano A, Bryan EL, Carpenter-Song EA, Woods M, Armstrong K, Drake RE. Long-term sobriety strategies for men with co-occurring disorders. J Dual Diagn 2014;10:212-19. https://doi.org/10.1080/15504263.2014.961884.
- Maisto SA, Carey KB, Carey MP, Purnine DM, Barnes KL. Methods of changing patterns of substance use among individuals with co-occurring schizophrenia and substance use disorder. J Subst Abuse Treat 1999;17:221-7. https://doi.org/10.1016/S0740-5472(99)00005-7.
- Mason OJ, Holt R. A role for football in mental health: the Coping Through Football project. Psychiatrist 2012;36:290-3. https://doi.org/10.1192/pb.bp.111.036269.
- O’Hara K, Stefancic A, Cabassa LJ. Developing a peer-based healthy lifestyle program for people with serious mental illness in supportive housing. Transl Behav Med 2017;7:793-80. https://doi.org/10.1007/s13142-016-0457-x.
- Oddie S, Davies J. A multi-method evaluation of a substance misuse program in a medium secure forensic mental health unit. J Addict Nurs 2009;20:132-41. https://doi.org/10.1080/10884600903078944.
- Olmos-Ochoa TT, Niv N, Hellemann G, Cohen AN, Oberman R, Goldberg R, et al. Barriers to participation in web-based and in-person weight management interventions for serious mental illness. Psychiatr Rehabil J 2019;42:220-8. https://doi.org/10.1037/prj0000363.
- Penn PE, Brooke D, Brooks AJ, Gallagher SM, Barnard AD. Co-occurring conditions clients and counselors compare 12-step and smart recovery mutual help. J Groups Addict Recover 2016;11:76-92. https://doi.org/10.1080/1556035X.2015.1104643.
- Roberts SH, Bailey JE. An ethnographic study of the incentives and barriers to lifestyle interventions for people with severe mental illness. J Adv Nurs 2013;69:2514-24. https://doi.org/10.1111/jan.12136.
- Rönngren Y, Björk A, Haage D, Audulv Å, Kristiansen L. Perspectives of a tailored lifestyle program for people with severe mental illness receiving housing support. Perspect Psychiatr Care 2018;54:309-16. https://doi.org/10.1111/ppc.12239.
- Rönngren YM, Bjork A, Haage D, Kristiansen L. LIFEHOPE.EU: lifestyle and healthy outcome in physical education. J Psychiatr Ment Health Nurs 2014;21:924-30. https://doi.org/10.1111/jpm.12175.
- Thornton LK, Baker AL, Johnson MP, Kay-Lambkin FJ. Perceptions of anti-smoking public health campaigns among people with psychotic disorders. Ment Health Subst Use 2011;4:110-5. https://doi.org/10.1080/17523281.2011.555066.
- Verhaeghe N, De Maeseneer J, Maes L, Van Heeringen C, Annemans L. Health promotion in mental health care: perceptions from patients and mental health nurses. J Clin Nurs 2013;22:1569-78. https://doi.org/10.1111/jocn.12076.
- Wärdig R, Bachrach-Lindström M, Hultsjö S, Lindström T, Foldemo A. Persons with psychosis perceptions of participating in a lifestyle intervention. J Clin Nurs 2015;24:1815-24. https://doi.org/10.1111/jocn.12782.
- Watkins A, Denney-Wilson E, Curtis J, Teasdale S, Rosenbaum S, Ward PB, et al. Keeping the body in mind: a qualitative analysis of the experiences of people experiencing first-episode psychosis participating in a lifestyle intervention programme. Int J Ment Health Nurs 2020;29:278-89. https://doi.org/10.1111/inm.12683.
- Weinstein LC, Chilton M, Turchi R, Klassen A, LaNoue M, Lamar S, et al. Reaching for a healthier lifestyle: a photovoice investigation of healthy living in people with serious mental illness. Prog Community Health Partnersh 2019;13:371-83. https://doi.org/10.1353/cpr.2019.0061.
- Yarborough BJ, Stumbo SP, Yarborough MT, Young TJ, Green CA. Improving lifestyle interventions for people with serious mental illnesses: qualitative results from the STRIDE study. Psychiatr Rehabil J 2016;39:33-41. https://doi.org/10.1037/prj0000151.
- Peckham E, Man MS, Mitchell N, Li J, Becque T, Knowles S, et al. Smoking Cessation Intervention for severe Mental Ill Health Trial (SCIMITAR): a pilot randomised control trial of the clinical effectiveness and cost-effectiveness of a bespoke smoking cessation service. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19250.
- Holt RI, Hind D, Gossage-Worrall R, Bradburn MJ, Saxon D, McCrone P, et al. Structured lifestyle education to support weight loss for people with schizophrenia, schizoaffective disorder and first episode psychosis: the STEPWISE RCT. Health Technol Assess 2018;22. https://doi.org/10.3310/hta22650.
- Greil W, Gillhoff K, Emini L, Maroni C, Tholuck J, Gaab J. Effects of a multimodal lifestyle intervention on body mass index in patients with bipolar disorder – a randomized controlled trial. Int Clin Psychopharmacol 2011;26. https://doi.org/10.1097/01.yic.0000405617.57707.3a.
- Kim ES, Kawachi I, Chen Y, Kubzansky LD. Association between purpose in life and objective measures of physical function in older adults. JAMA Psychiatry 2017;74:1039-45. https://doi.org/10.1001/jamapsychiatry.2017.2145.
- Meader N, Melton HA. People with severe mental illness live shorter lives – but the solution isn’t simple. The Conversation 2020. https://theconversation.com/people-with-severe-mental-illness-live-shorter-lives-but-the-solution-isnt-simple-127397 (accessed 30 April 2021).
- Johnston G, Syrett M. Walk This Way: Can a Health Coaching Intervention Increase Physical Activity in People With Severe Mental Illness? n.d. www.nationalelfservice.net/treatment/exercise/walk-this-way-can-a-health-coaching-intervention-increase-physical-activity-in-people-with-severe-mental-illness/ (accessed 30 April 2021).
- National Elf Service . Ceri #HealthSMI n.d. https://soundcloud.com/national-elf-service/ceri-healthsmi (accessed 30 April 2021).
- Mental Elf . Improving Physical Health in People With Severe Mental Illness #HealthSMI n.d. www.youtube.com/watch?v=reEGLYTUlwY (accessed 30 April 2021).
- Centre for Reviews and Dissemination . Improving Physical Health in Severe Mental Illness (SMI) – Focus on One Risk at a Time? n.d. https://youtu.be/dGaTNmYjGOI (accessed 30 April 2021).
- Melton H, Meader N. Healthy Living: Adapting Physical Health Programmes to the Needs of People With Severe Mental Illness n.d. https://equallywell.co.uk/wp-content/uploads/2020/07/Equally-Well_Banner-Healthy-living-adapting-physical-health-programmes-to-the-needs-of-people-w-severe-mental-illness (accessed 30 April 2021).
- Speyer H, Jakobsen AS, Westergaard C, Nørgaard HCB, Jørgensen KB, Pisinger C, et al. Lifestyle interventions for weight management in people with serious mental illness: a systematic review with meta-analysis, trial sequential analysis, and meta-regression analysis exploring the mediators and moderators of treatment effects. Psychother Psychosom 2019;88:350-62. https://doi.org/10.1159/000502293.
- Trainor K, Leavey G. Barriers and facilitators to smoking cessation among people with severe mental illness: a critical appraisal of qualitative studies. Nicotine Tob Res 2017;19:14-23. https://doi.org/10.1093/ntr/ntw183.
- Sagae T. NNP project. Nutrition Needs in Psychiatry 2007;2:15-7.
- Goldberg RW, Reeves G, Tapscott S, Medoff D, Dickerson F, Goldberg AP, et al. ‘MOVE!’: outcomes of a weight loss program modified for veterans with serious mental illness. Psychiatr Serv 2013;64:737-44. https://doi.org/10.1176/appi.ps.201200314.
Appendix 1 Search strategies
Serious mental illness and multiple risk behaviours: literature searching 4 March 2020
The original searches were carried out in October 2018 using CENTRAL, EMBASE, MEDLINE, PsycInfo and the Science Citation Index. The searches identified 27,795 records, reduced to 18,513 records after deduplication using EndNote bibliographic software.
Updated searches were carried out in March 2020 using EMBASE, MEDLINE, PsycInfo and the Science Citation Index; these identified a further 2822 records, reducing to 1433 after deduplication. It was not possible to download records from CENTRAL because of issues with the database at the time of the updated searches (28 March 2020).
The strategies used for both the original and updated searches are reproduced here.
Cochrane Central Register of Controlled Trials via the Cochrane Library
Date range searched: from inception to 24 October 2018.
Date searched: 24 October 2018.
Records identified: 3370.
Search strategy
#1 MeSH descriptor: [Schizophrenia] explode all trees
#2 MeSH descriptor: [Bipolar Disorder] explode all trees
#3 MeSH descriptor: [Psychotic Disorders] explode all trees
#4 MeSH descriptor: [Affective Disorders, Psychotic] explode all trees
#5 ((acute or chronic* or persistent* or serious* or severe*) NEAR/2 (mental* or psych*) NEAR/2 (disease* or disorder* or disturbanc* or ill*)):ti,ab,kw (Word variations have been searched)
#6 (SMI NEAR/3 (individual* or inpatient* or in-patient* or outpatient* or out-patient* or patient* or people or person* or population*)):ti,ab,kw (Word variations have been searched)
#7 ((mental health or psychiatric) NEAR/2 (inpatient* or in-patient*)):ti,ab,kw (Word variations have been searched)
#8 (schizophren*):ti,ab,kw (Word variations have been searched)
#9 (psychotic or psychosis or psychoses):ti,ab,kw (Word variations have been searched)
#10 (bipolar):ti,ab,kw (Word variations have been searched)
#11 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10
#12 (healthy NEAR/2 (diet* or eating)):ti,ab,kw OR (fruit* NEAR/2 (intake or consum* or increase or portion* or serving* or frequenc* or number* or preference* or choice*)):ti,ab,kw OR (vegetablet* NEAR/2 (intake or consum* or increase or portion* or serving* or frequenc* or number* or preference* or choice*)):ti,ab,kw OR (“5 a day”):ti,ab,kw OR (“five a day”):ti,ab,kw (Word variations have been searched)
#13 MeSH descriptor: [Feeding Behavior] explode all trees
#14 MeSH descriptor: [Food Preferences] explode all trees
#15 MeSH descriptor: [Nutrition Therapy] explode all trees
#16 MeSH descriptor: [Diet Therapy] explode all trees
#17 MeSH descriptor: [Diet] explode all trees
#18 MeSH descriptor: [Obesity] explode all trees
#19 MeSH descriptor: [Overweight] explode all trees
#20 #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19
#21 #11 and #20
#22 (physical NEAR/3 (fit* or train* or activ* or endur*)):ti,ab,kw OR (exercis* NEAR/3 (fit* or train* or activ* or endur*)):ti,ab,kw OR ((promot* or uptak* or encourag* or increas* or start* or adher*) NEAR/3 (exercis* or gym* or sport* or fitness)):ti,ab,kw OR ((decreas* or reduc* or discourag*) NEAR/3 (sedentary or deskbound)):ti,ab,kw OR (sport* or walk* or running or jogging or bicycling or biking or swimming):ti,ab,kw (Word variations have been searched)
#23 (active NEAR/1 (travel* or transport* or commut*)):ti,ab,kw (Word variations have been searched)
#24 MeSH descriptor: [Physical Fitness] explode all trees
#25 MeSH descriptor: [Recreation] explode all trees
#26 MeSH descriptor: [Exercise Therapy] explode all trees
#27 MeSH descriptor: [Exercise] explode all trees
#28 MeSH descriptor: [Running] explode all trees
#29 MeSH descriptor: [Jogging] explode all trees
#30 MeSH descriptor: [Swimming] explode all trees
#31 MeSH descriptor: [Walking] explode all trees
#32 #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31
#33 #11 and #32
#34 MeSH descriptor: [Smoke] explode all trees
#35 MeSH descriptor: [Smoking Cessation] explode all trees
#36 MeSH descriptor: [Smoking Reduction] explode all trees
#37 MeSH descriptor: [Nicotine] explode all trees
#38 MeSH descriptor: [Tobacco] explode all trees
#39 MeSH descriptor: [Tobacco Smoking] explode all trees
#40 MeSH descriptor: [Tobacco Use Disorder] explode all trees
#41 MeSH descriptor: [Tobacco Use Cessation] explode all trees
#42 MeSH descriptor: [Tobacco, Smokeless] explode all trees
#43 MeSH descriptor: [Tobacco Smoke Pollution] explode all trees
#44 MeSH descriptor: [Electronic Nicotine Delivery Systems] explode all trees
#45 (smoking or antismoking or anti-smoking):ti,ab,kw OR (smoker or smokers):ti,ab,kw OR (“electronic cigarette*” or e-cigarette* or e-cig or e-cigs):ti,ab,kw OR (vape or vapes or vaper or vapers or vaping):ti,ab,kw (Word variations have been searched)
#46 #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45
#47 #11 and #46
#48 MeSH descriptor: [Alcohol Drinking] explode all trees
#49 MeSH descriptor: [Alcoholic Intoxication] explode all trees
#50 MeSH descriptor: [Alcoholic Beverages] explode all trees
#51 MeSH descriptor: [Drinking Behavior] explode all trees
#52 (beer* or wine* or cider* or alcopop* or spirit or spirits):ti,ab,kw OR (alcohol*):ti,ab,kw OR (drink* NEAR/2 (binge or excessive* or harm* or heavily or heavy or misus* or abus* or consum*)):ti,ab,kw OR (intoxicat* or inebriat* or drunk*):ti,ab,kw (Word variations have been searched)
#53 #48 or #49 or #50 or #51 or #52
#54 #11 and #53
#55 MeSH descriptor: [Substance-Related Disorders] explode all trees
#56 MeSH descriptor: [Inhalant Abuse] explode all trees
#57 MeSH descriptor: [Marijuana Abuse] explode all trees
#58 MeSH descriptor: [Substance Abuse, Intravenous] explode all trees
#59 MeSH descriptor: [Drug Users] explode all trees
#60 ((drug* or substance*) NEAR/2 (use* or using or abuse* or abusing or misuse* or misusing)):ti,ab,kw OR ((heroin or opiate* or cocaine or crack) NEAR/2 (use* or using or abuse* or abusing or misuse* or misusing)):ti,ab,kw OR ((cannabis or marijuana) NEAR/2 (use* or using or abuse* or abusing or misuse* or misusing)):ti,ab,kw OR ((benzodiazepine* or amphetamine* or methamphetamine* or MDMA or ecstasy) NEAR/2 (use* or using or abuse* or abusing or misuse* or misusing)):ti,ab,kw OR (solvent* NEAR/2 (use* or using or abuse* or abusing or misuse* or misusing)):ti,ab,kw (Word variations have been searched)
#61 (“street drug*” or “recreational drug*” or “illicit drug*”):ti,ab,kw OR ((“prescri* drug*”) NEAR/2 (use* or using or abuse* or abusing or misuse* or misusing)):ti,ab,kw OR (“polydrug use*”):ti,ab,kw OR (“inject* drug use*”):ti,ab,kw OR ((needle* OR syringe*) NEAR/3 shar*):ti,ab,kw (Word variations have been searched)
#62 #55 or #56 or #57 or #58 or #59 or #60 or #61
#63 #11 and #62
#64 #21 or #33 or #47 or #54 or #63
#65 (lifestyle NEAR/2 (intervention* or program*)):ti,ab,kw OR (“life style” NEAR/2 (intervention* or program*)):ti,ab,kw OR (“behavior* change” NEAR/1 (intervention* or program*)):ti,ab,kw OR (“behaviour* change” NEAR/1 (intervention* or program*)):ti,ab,kw OR (“risk factor*” NEAR/2 (program* or intervention*)):ti,ab,kw (Word variations have been searched)
#66 (“multifactorial lifestyle” NEAR/1 (intervention* or program*)):ti,ab,kw OR (“health behavior*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“health behaviour*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“health risk behavior*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“health risk behaviour*” NEAR/1 (program* or intervention*)):ti,ab,kw (Word variations have been searched)
#67 (“risk behavior*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“risk behaviour*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“health behavior* change intervention*”):ti,ab,kw OR (“health behaviour* change intervention*”):ti,ab,kw OR (“behavior* risk factor* intervention*”):ti,ab,kw (Word variations have been searched)
#68 (“risk behavior*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“risk behaviour*” NEAR/1 (program* or intervention*)):ti,ab,kw OR (“health behavior* change intervention*”):ti,ab,kw OR (“health behaviour* change intervention*”):ti,ab,kw OR (“behavior* risk factor* intervention*”):ti,ab,kw (Word variations have been searched)
#69 (“behaviour* risk factor* intervention*”):ti,ab,kw OR (“behavior* risk factor* program*”):ti,ab,kw OR (“behaviour* risk factor* program*”):ti,ab,kw OR (“risk behaviour* intervention*”):ti,ab,kw OR (“risk behavior* intervention*”):ti,ab,kw (Word variations have been searched)
#70 (“risk behaviour* program*”):ti,ab,kw OR (“risk behavior* program*”):ti,ab,kw (Word variations have been searched)
#71 #65 or #66 or #67 or #68 or #69 or #70
#72 #11 AND #71
#73 #64 OR #72.
EMBASE via Ovid® (Wolters Kluwer, Alphen aan den Rijn, the Netherlands)
Date range searched: 1974 to 19 October 2018.
Date searched: 22 October 2020.
Records identified: 6199.
Search strategy
-
exp schizophrenia/ (165,050)
-
exp bipolar disorder/ (55,219)
-
exp psychosis/ (253,831)
-
((acute or chronic$ or persistent$ or serious$ or severe$) adj2 (mental$ or psych$) adj2 (disease$ or disorder$ or disturbanc$ or ill$)).ti,ab,kw. (18,709)
-
(SMI adj3 (individual$ or inpatient$ or in-patient$ or outpatient$ or out-patient$ or patient$ or people or person$ or population$)).ti,ab,kw. (1481)
-
((mental health or psychiatric) adj2 (inpatient$ or in-patient$)).ti,ab,kw. (12,391)
-
schizophren$.ti,ab,kw. (151,316)
-
(psychotic or psychosis or psychoses).ti,ab,kw. (86,293)
-
bipolar.ti,ab,kw. (82,270)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 (373,041)
-
(healthy adj2 (diet$ or eating)).ti,ab,kw. (15,028)
-
(fruit$ adj2 (intake or consum$ or increase or portion$ or serving$ or frequenc$ or number$ or preference$ or choice$)).ti,ab,kw. (10,978)
-
(vegetable$ adj2 (intake or consum$ or increase or portion$ or serving$ or frequenc$ or number$ or preference$ or choice$)).ti,ab,kw. (11,216)
-
“5 a day”.ti,ab,kw. (220)
-
“five a day”.ti,ab,kw. (61)
-
((food or diet$) adj (choice$ or frequenc$ or intake)).ti,ab,kw. (96,918)
-
Feeding behavior/ (74,811)
-
Food preferences/ (10,664)
-
exp diet/ (282,043)
-
obesity/ (370,339)
-
11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (728,864)
-
(editorial or letter).pt. (1,616,116)
-
21 not 22 (698,752)
-
(physical adj3 (fit$ or train$ or activ$ or endur$)).ti,ab,kw. (153,242)
-
(exercis$ adj3 (fit$ or train$ or activ$ or endur$)).ti,ab,kw. (47,156)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$) adj3 (exercis$ or gym$ or sport$ or fitness)).ti,ab,kw. (39,955)
-
((decreas$ or reduc$ or discourag$) adj3 (sedentary or deskbound)).ti,ab,kw. (1664)
-
(sport$ or walk$ or running or jogging or bicycling or biking or swimming).ti,ab,kw. (311,717)
-
(active adj (travel$ or transport$ or commut$)).ti,ab,kw. (9344)
-
exp fitness/ (34,746)
-
exp recreation/ (61,858)
-
running/ (24,432)
-
jogging/ (1834)
-
swimming/ (19,775)
-
exp walking/ (101,072)
-
24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 (597,469)
-
(editorial or letter).pt. (1,616,116)
-
36 not 37 (585,776)
-
exp smoking/ (343,129)
-
smoking cessation/ (52,639)
-
smoking reduction/ (65)
-
(smoking or antismoking or anti-smoking).ti,ab,kw. (283,613)
-
(smoker or smokers).ti,ab,kw. (116,016)
-
nicotine/ (41,696)
-
tobacco/ (41,521)
-
“tobacco use”/ (7462)
-
tobacco smoke/ (12,136)
-
electronic cigarette/ (3860)
-
(electronic cigarette$ or e-cigarette$ or e-cig or e-cigs).ti,ab,kw. (3825)
-
(vape or vapes or vaper or vapers or vaping).ti,ab,kw. (625)
-
39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 (486,274)
-
(editorial or letter).pt. (1,616,116)
-
51 not 52 (462,985)
-
drinking behavior/ (44,511)
-
alcohol intoxication/ (11,353)
-
exp alcoholic beverage/ (25,943)
-
drinking behavior/ (44,511)
-
(beer$ or wine$ or cider$ or alcopop$ or spirit or spirits).ti,ab,kw. (42,083)
-
(alcohol$ adj2 (binge or excessive$ or harm$ or heavily or heavy or misus$ or abus$ or consum$)).ti,ab,kw. (90,980)
-
(drink$ adj2 (binge or excessive$ or harm$ or heavily or heavy or misus$ or abus$ or consum$)).ti,ab,kw. (23,956)
-
(intoxicat$ or inebriat$ or drunk$).ti,ab,kw. (60,002)
-
54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 (229,090)
-
(editorial or letter).pt. (1,616,116)
-
62 not 63 (223,747)
-
exp drug dependence/ (210,017)
-
inhalant abuse/ (504)
-
cannabis addiction/ (8769)
-
((drug$ or substance$) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (264,725)
-
((heroin or opiate$ or cocaine or crack) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (21,470)
-
((cannabis or marijuana) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (15,565)
-
((benzodiazepine$ or amphetamine$ or methamphetamine$ or MDMA or ecstasy) adj2 (use$ or using or abuse$ or abusing or misuse$ or misuising)).ti,ab,kw. (11,819)
-
(solvent$ adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (12,664)
-
(street drug$ or recreational drug$ or illicit drug$).ti,ab,kw. (17,283)
-
(prescri$ drug$ adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (3309)
-
polydrug use$.ti,ab,kw. (1032)
-
inject$ drug use$.ti,ab,kw. (12,111)
-
(needle adj3 shar$).ti,ab,kw. (1633)
-
(syringe$ adj3 shar$).ti,ab,kw. (877)
-
65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 (464,270)
-
(editorial or letter).pt. (1,616,116)
-
79 not 80 (449,328)
-
23 or 38 or 53 or 64 or 81 (2,132,733)
-
10 and 82 (49,143)
-
clinical trial/ (950,305)
-
randomized controlled trial/ (517,116)
-
randomization/ (79,616)
-
single blind procedure/ (32,661)
-
double blind procedure/ (153,895)
-
crossover procedure/ (56,850)
-
placebo/ (324,536)
-
randomi?ed controlled trial$.tw. (187,656)
-
rct.tw. (29,684)
-
random allocation.tw. (1857)
-
randomly allocated.tw. (30,836)
-
allocated randomly.tw. (2373)
-
(allocated adj2 random).tw. (875)
-
single blind$.tw. (21,697)
-
double blind$.tw. (191,182)
-
((treble or triple) adj blind$).tw. (846)
-
placebo$.tw. (278,797)
-
prospective study/ (475,629)
-
or/84-101 (1,953,083)
-
case study/ (56,829)
-
case report.tw. (364,419)
-
abstract report/or letter/ (1,074,387)
-
or/103-105 (1,486,683)
-
102 not 106 (1,903,347)
-
83 and 107 (6687)
-
(animal/or animal experiment/or animal model/or animal tissue/or nonhuman/) not exp human/(5,563,208)
-
(rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys).ti. (1,984,529)
-
editorial.pt. or case report.ti. (838,717)
-
109 or 110 or 111 (6,771,530)
-
108 not 112 (6650)
-
(lifestyle adj2 (intervention$ or program$)).ti,ab,kw. (10,866)
-
(life style adj2 (intervention$ or program$)).ti,ab,kw. (523)
-
(behavior$ change adj (intervention$ or program$)).ti,ab,kw. (931)
-
(behaviour$ change adj (intervention$ or program$)).ti,ab,kw. (727)
-
(risk factor adj2 (program$ or intervention$)).ti,ab,kw. (1267)
-
(single risk factor adj2 (program$ or intervention$)).ti,ab,kw. (13)
-
(multifactorial lifestyle adj (intervention$ or program$)).ti,ab,kw. (22)
-
(health behavior$ adj (program$ or intervention$)).ti,ab,kw. (239)
-
(health behaviour$ adj (program$ or intervention$)).ti,ab,kw. (87)
-
(health risk behavior$ adj (program$ or intervention$)).ti,ab,kw. (5)
-
(health risk behaviour$ adj (program$ or intervention$)).ti,ab,kw. (0)
-
(risk behavior$ adj (program$ or intervention$)).ti,ab,kw. (70)
-
(risk behaviour$ adj (program$ or intervention$)).ti,ab,kw. (11)
-
health behavior$ change intervention$.ti,ab,kw. (108)
-
health behaviour$ change intervention$.ti,ab,kw. (52)
-
behavior$ risk factor$ intervention$.ti,ab,kw. (4)
-
behaviour$ risk factor$ intervention$.ti,ab,kw. (0)
-
behavior$ risk factor$ program$.ti,ab,kw. (0)
-
behaviour$ risk factor$ program$.ti,ab,kw. (0)
-
risk behaviour$ intervention$.ti,ab,kw. (9)
-
risk behavior$ intervention$.ti,ab,kw. (60)
-
risk behaviour$ program$.ti,ab,kw. (2)
-
risk behavior$ program$.ti,ab,kw. (10)
-
114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 (14,472)
-
83 and 137 (222)
-
(animal/or animal experiment/or animal model/or animal tissue/or nonhuman/) not exp human/ (5,563,208)
-
(rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys).ti. (1,984,529)
-
editorial.pt. or case report.ti. (838,717)
-
139 or 140 or 141 (6,771,530)
-
138 not 142 (222)
-
qualitative research/ (56,931)
-
qualitative.ti,ab. (231,093)
-
patient attitude/ (61,649)
-
feasibility study/ (98,850)
-
(accept$ or attitude$ or barrier$ or belief$ or believ$ or consider$ or experienc$ or facilitat$ or feasib$ or implement$ or option$ or preference$ or promot$ or view or views or viewpoint$).ti. (949,167)
-
144 or 145 or 146 or 147 or 148 (1,269,494)
-
83 and 149 (2676)
-
(animal/or animal experiment/or animal model/or animal tissue/or nonhuman/) not exp human/ (5,563,208)
-
(rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys).ti. (1,984,529)
-
editorial.pt. or case report.ti. (838,717)
-
151 or 152 or 153 (6,771,530)
-
150 not 154 (2590)
-
113 or 143 or 155 (8976)
-
limit 156 to yr=“1990 -Current” (8722)
-
limit 157 to embase (6199).
MEDLINE via Ovid
Ovid MEDLINE® and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily.
Date range searched: 1946 to 18 October 2018.
Date searched: 19 October 2018.
Records identified: 3450.
Search strategy
-
exp Schizophrenia/ (98,539)
-
Bipolar Disorder/ (37,622)
-
exp Psychotic Disorders/ (48,550)
-
exp Affective Disorders, Psychotic/ (2210)
-
((acute or chronic$ or persistent$ or serious$ or severe$) adj2 (mental$ or psych$) adj2 (disease$ or disorder$ or disturbanc$ or ill$)).ti,ab,kw. (13,950)
-
(SMI adj3 (individual$ or inpatient$ or in-patient$ or outpatient$ or out-patient$ or patient$ or people or person$ or population$)).ti,ab,kw. (1040)
-
((mental health or psychiatric) adj2 (inpatient$ or in-patient$)).ti,ab,kw. (9545)
-
schizophren$.ti,ab,kw. (117,306)
-
(psychotic or psychosis or psychoses).ti,ab,kw. (61,647)
-
bipolar.ti,ab,kw. (56,740)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 (259,622)
-
(healthy adj2 (diet$ or eating)).ti,ab,kw. (10,696)
-
(fruit$ adj2 (intake or consum$ or increase or portion$ or serving$ or frequenc$ or number$ or preference$ or choice$)).ti,ab,kw. (8756)
-
(vegetable$ adj2 (intake or consum$ or increase or portion$ or serving$ or frequenc$ or number$ or preference$ or choice$)).ti,ab,kw. (8962)
-
“5 a day”.ti,ab,kw. (167)
-
“five a day”.ti,ab,kw. (44)
-
((food or diet$) adj (choice$ or frequenc$ or intake)).ti,ab,kw. (73,165)
-
Feeding Behavior/ (75,218)
-
Food preferences/ (13,009)
-
nutrition therapy/or exp diet therapy/or exp diet/ (264,431)
-
obesity/or overweight/ (172,728)
-
12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 (506,530)
-
(comment or editorial or letter).pt. (1,663,957)
-
22 not 23 (485,772)
-
(physical adj3 (fit$ or train$ or activ$ or endur$)).ti,ab,kw. (110,746)
-
(exercis$ adj3 (fit$ or train$ or activ$ or endur$)).ti,ab,kw. (34,892)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$) adj3 (exercis$ or gym$ or sport$ or fitness)).ti,ab,kw. (31,395)
-
((decreas$ or reduc$ or discourag$) adj3 (sedentary or deskbound)).ti,ab,kw. (1308)
-
(sport$ or walk$ or running or jogging or bicycling or biking or swimming).ti,ab,kw. (239,832)
-
(active adj (travel$ or transport$ or commut$)).ti,ab,kw. (8634)
-
physical fitness/ (25,838)
-
exp Recreation/ (189,425)
-
exp Exercise Therapy/or exp exercise/ (199,415)
-
running/or jogging/or swimming/or walking/ (61,927)
-
25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 (540,109)
-
(letter or editorial or comment).pt. (1,663,957)
-
35 not 36 (521,636)
-
exp smoking/ (137,824)
-
Smoking Cessation/or Smoking Reduction/ (26,021)
-
(smoking or antismoking or anti-smoking).ti,ab,kw. (201,198)
-
(smoker or smokers).ti,ab,kw. (78,963)
-
exp Nicotine/ (24,185)
-
exp Tobacco/ (28,846)
-
exp Tobacco Smoking/ (878)
-
“Tobacco Use Disorder”/ (10,429)
-
“Tobacco Use Cessation”/ (1034)
-
Tobacco, Smokeless/ (3414)
-
Tobacco Smoke Pollution/ (12,348)
-
Electronic Nicotine Delivery Systems/ (2007)
-
(electronic cigarette$ or e-cigarette$ or e-cig or e-cigs).ti,ab,kw. (3440)
-
(vape or vapes or vaper or vapers or vaping).ti,ab,kw. (594)
-
38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 (314,465)
-
(letter or editorial or comment).pt. (1,663,957)
-
52 not 53 (301,222)
-
exp Alcohol Drinking/ (63,656)
-
exp Alcoholic Intoxication/ (12,115)
-
exp Alcoholic Beverages/ (18,386)
-
exp Drinking Behavior/ (69,908)
-
(beer$ or wine$ or cider$ or alcopop$ or spirit or spirits).ti,ab,kw. (33,610)
-
alcohol$.ti,ab,kw. (305,539)
-
(drink$ adj2 (binge or excessive$ or harm$ or heavily or heavy or misus$ or abus$ or consum$)).ti,ab,kw. (17,180)
-
(intoxicat$ or inebriat$ or drunk$).ti,ab,kw. (47,727)
-
55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 (395,310)
-
(comment or editorial or letter).pt. (1,663,957)
-
63 not 64 (384,701)
-
substance-related disorders/or inhalant abuse/or marijuana abuse/or substance abuse, intravenous/ (107,638)
-
Drug Users/ (2555)
-
((drug$ or substance$) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (191,716)
-
((heroin or opiate$ or cocaine or crack) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (16,274)
-
((cannabis or marijuana) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (11,836)
-
((benzodiazepine$ or amphetamine$ or methamphetamine$ or MDMA or ecstasy) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (8864)
-
(solvent$ adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (9608)
-
(street drug$ or recreational drug$ or illicit drug$).ti,ab,kw. (12,452)
-
(prescri$ drug$ adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (2241)
-
polydrug use$.ti,ab,kw. (849)
-
inject$ drug use$.ti,ab,kw. (9504)
-
(needle adj3 shar$).ti,ab,kw. (1311)
-
(syringe$ adj3 shar$).ti,ab,kw. (726)
-
or/66-78 (272,714)
-
(letter or editorial or comment).pt. (1,663,957)
-
79 not 80 (262,481)
-
24 or 37 or 54 or 65 or 81 (1,748,549)
-
11 and 82 (27,989)
-
randomized controlled trial.pt. (469,898)
-
controlled clinical trial.pt. (92,702)
-
randomized.ab. (424,124)
-
placebo.ab. (192,498)
-
clinical trials as topic.sh. (185,008)
-
randomly.ab. (298,839)
-
trial.ti. (188,739)
-
84 or 85 or 86 or 87 or 88 or 89 or 90 (1,177,116)
-
exp animals/not humans.sh. (4,506,067)
-
91 not 92 (1,083,038)
-
83 and 93 (2417)
-
(lifestyle adj2 (intervention$ or program$)).ti,ab,kw. (7301)
-
(life style adj2 (intervention$ or program$)).ti,ab,kw. (266)
-
(behavior$ change adj (intervention$ or program$)).ti,ab,kw. (897)
-
(behaviour$ change adj (intervention$ or program$)).ti,ab,kw. (629)
-
(risk factor adj2 (program$ or intervention$)).ti,ab,kw. (1029)
-
(single risk factor adj2 (program$ or intervention$)).ti,ab,kw. (12)
-
(multifactorial lifestyle adj (intervention$ or program$)).ti,ab,kw. (14)
-
(health behavior$ adj (program$ or intervention$)).ti,ab,kw. (278)
-
(health behaviour$ adj (program$ or intervention$)).ti,ab,kw. (87)
-
(health risk behavior$ adj (program$ or intervention$)).ti,ab,kw. (6)
-
(health risk behaviour$ adj (program$ or intervention$)).ti,ab,kw. (0)
-
(risk behavior$ adj (program$ or intervention$)).ti,ab,kw. (98)
-
(risk behaviour$ adj (program$ or intervention$)).ti,ab,kw. (15)
-
health behavior$ change intervention$.ti,ab,kw. (105)
-
health behaviour$ change intervention$.ti,ab,kw. (45)
-
behavior$ risk factor$ intervention$.ti,ab,kw. (2)
-
behaviour$ risk factor$ intervention$.ti,ab,kw. (0)
-
behavior$ risk factor$ program$.ti,ab,kw. (0)
-
behaviour$ risk factor$ program$.ti,ab,kw. (0)
-
risk behaviour$ intervention$.ti,ab,kw. (11)
-
risk behavior$ intervention$.ti,ab,kw. (47)
-
risk behaviour$ program$.ti,ab,kw. (2)
-
risk behavior$ program$.ti,ab,kw. (9)
-
95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 (10,433)
-
11 and 82 and 118 (137)
-
94 or 119 (2513)
-
limit 120 to yr=“1990 -Current” (2312)
-
qualitative research/ (41,870)
-
qualitative.ti,ab. (190,253)
-
“Patient Acceptance of Health Care”/ (40,335)
-
Feasibility Studies/ (59,810)
-
(accept$ or attitude$ or barrier$ or belief$ or believ$ or consider$ or experienc$ or facilitat$ or feasib$ or implement$ or option$ or preference$ or promot$ or view or views or viewpoint$).ti. (817,156)
-
122 or 123 or 124 or 125 or 126 (1,056,514)
-
83 and 127 (1538)
-
exp animals/not humans.sh. (4,506,067)
-
128 not 129 (1491)
-
limit 130 to yr=“1990 -Current” (1331)
-
121 or 131 (3450).
PsycInfo via Ovid
Date range searched: 1806 to week 4 October 2018.
Date searched: 25 October 2020.
Records identified: 10,354.
Search strategy
-
exp Schizophrenia/ (85,600)
-
Bipolar Disorder/ (25,219)
-
exp Psychosis/ (109,658)
-
((acute or chronic$ or persistent$ or serious$ or severe$) adj2 (mental$ or psych$) adj2 (disease$ or disorder$ or disturbanc$ or ill$)).ti,ab,kw. (16,838)
-
(SMI adj3 (individual$ or inpatient$ or in-patient$ or outpatient$ or out-patient$ or patient$ or people or person$ or population$)).ti,ab,kw. (931)
-
((mental health or psychiatric) adj2 (inpatient$ or in-patient$)).ti,ab,kw. (11,386)
-
schizophren$.ti,ab,kw. (113,900)
-
(psychotic or psychosis or psychoses).ti,ab,kw. (68,011)
-
bipolar.ti,ab,kw. (36,173)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 (209,491)
-
(healthy adj2 (diet$ or eating)).ti,ab,kw. (3697)
-
(fruit$ adj2 (intake or consum$ or increase or portion$ or serving$ or frequenc$ or number$ or preference$ or choice$)).ti,ab,kw. (1871)
-
(vegetable$ adj2 (intake or consum$ or increase or portion$ or serving$ or frequenc$ or number$ or preference$ or choice$)).ti,ab,kw. (2298)
-
“5 a day”.ti,ab,kw. (82)
-
“five a day”.ti,ab,kw. (12)
-
((food or diet$) adj (choice$ or frequenc$ or intake)).ti,ab,kw. (14,493)
-
Eating Attitudes/ (1530)
-
Food preferences/ (4452)
-
Diets/or Food Intake/ (24,024)
-
obesity/or overweight/ (23,672)
-
11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (56,824)
-
10 and 21 (1093)
-
(physical adj3 (fit$ or train$ or activ$ or endur$)).ti,ab,kw. (34,827)
-
(exercis$ adj3 (fit$ or train$ or activ$ or endur$)).ti,ab,kw. (5926)
-
((promot$ or uptak$ or encourag$ or increas$ or start$ or adher$) adj3 (exercis$ or gym$ or sport$ or fitness)).ti,ab,kw. (5944)
-
((decreas$ or reduc$ or discourag$) adj3 (sedentary or deskbound)).ti,ab,kw. (438)
-
(sport$ or walk$ or running or jogging or bicycling or biking or swimming).ti,ab,kw. (72,925)
-
(active adj (travel$ or transport$ or commut$)).ti,ab,kw. (646)
-
physical fitness/ (4026)
-
exp Recreation/ (33,080)
-
exp Exercise Therapy/or exp exercise/ (24,104)
-
Physical Activity/ (17,162)
-
23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 (144,672)
-
10 and 33 (2237)
-
exp Tobacco Smoking/ (29,372)
-
Smoking Cessation/ (12,191)
-
(smoking or antismoking or anti-smoking).ti,ab,kw. (44,133)
-
(smoker or smokers).ti,ab,kw. (20,066)
-
Nicotine/ (10,413)
-
Smokeless Tobacco/ (773)
-
Passive Smoking/ (776)
-
Electronic Cigarettes/ (730)
-
Tobacco, Smokeless/ (773)
-
(electronic cigarette$ or e-cigarette$ or e-cig or e-cigs).ti,ab,kw. (1138)
-
(vape or vapes or vaper or vapers or vaping).ti,ab,kw. (175)
-
35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 (55,798)
-
10 and 46 (2676)
-
exp Alcohol Abuse/ (46,611)
-
exp Alcohol Drinking Patterns/ (63,984)
-
exp Alcohol Intoxication/ (3029)
-
(beer$ or wine$ or cider$ or alcopop$ or spirit or spirits).ti,ab,kw. (16,133)
-
(alcohol$ adj2 (binge or excessive$ or harm$ or heavily or heavy or misus$ or abus$ or consum$)).ti,ab,kw. (34,787)
-
(drink$ adj2 (binge or excessive$ or harm$ or heavily or heavy or misus$ or abus$ or consum$)).ti,ab,kw. (12,209)
-
(intoxicat$ or inebriat$ or drunk$).ti,ab,kw. (11,855)
-
48 or 49 or 50 or 51 or 52 or 53 or 54 (99,930)
-
10 and 55 (5834)
-
exp Drug Abuse/ (105,866)
-
exp Drug Addiction/ (13,397)
-
Heroin Addiction/ (2508)
-
((drug$ or substance$) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (108,973)
-
((heroin or opiate$ or cocaine or crack) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (10,568)
-
((cannabis or marijuana) adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (10,161)
-
((benzodiazepine$ or amphetamine$ or methamphetamine$ or MDMA or ecstasy) adj2 (use$ or using or abuse$ or abusing or misuse$ or misuising)).ti,ab,kw. (5549)
-
(solvent$ adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (270)
-
(street drug$ or recreational drug$ or illicit drug$).ti,ab,kw. (7932)
-
(prescri$ drug$ adj2 (use$ or using or abuse$ or abusing or misuse$ or misusing)).ti,ab,kw. (1169)
-
polydrug use$.ti,ab,kw. (834)
-
inject$ drug use$.ti,ab,kw. (4229)
-
(needle adj3 shar$).ti,ab,kw. (584)
-
(syringe$ adj3 shar$).ti,ab,kw. (387)
-
57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 (175,902)
-
10 and 71 (16,517)
-
22 or 34 or 47 or 56 or 72 (22,832)
-
clinical trials/ (11,117)
-
clinical trial.md. (21,833)
-
placebo/ (5150)
-
control$.ti,ab. (635,515)
-
random$.ti,ab. (181,628)
-
exp treatment/ (720,498)
-
74 or 75 or 76 or 77 or 78 or 79 (1,330,498)
-
73 and 80 (11,362)
-
(lifestyle adj2 (intervention$ or program$)).ti,ab,kw. (1742)
-
(life style adj2 (intervention$ or program$)).ti,ab,kw. (40)
-
(behavior$ change adj (intervention$ or program$)).ti,ab,kw. (702)
-
(behaviour$ change adj (intervention$ or program$)).ti,ab,kw. (217)
-
(risk factor adj2 (program$ or intervention$)).ti,ab,kw. (126)
-
(single risk factor adj2 (program$ or intervention$)).ti,ab,kw. (3)
-
(multifactorial lifestyle adj (intervention$ or program$)).ti,ab,kw. (3)
-
(health behavior$ adj (program$ or intervention$)).ti,ab,kw. (182)
-
(health behaviour$ adj (program$ or intervention$)).ti,ab,kw. (26)
-
(health risk behavior$ adj (program$ or intervention$)).ti,ab,kw. (2)
-
(health risk behaviour$ adj (program$ or intervention$)).ti,ab,kw. (0)
-
(risk behavior$ adj (program$ or intervention$)).ti,ab,kw. (47)
-
(risk behaviour$ adj (program$ or intervention$)).ti,ab,kw. (4)
-
health behavior$ change intervention$.ti,ab,kw. (101)
-
health behaviour$ change intervention$.ti,ab,kw. (25)
-
behavior$ risk factor$ intervention$.ti,ab,kw. (2)
-
behaviour$ risk factor$ intervention$.ti,ab,kw. (0)
-
behavior$ risk factor$ program$.ti,ab,kw. (0)
-
behaviour$ risk factor$ program$.ti,ab,kw. (0)
-
risk behaviour$ intervention$.ti,ab,kw. (3)
-
risk behavior$ intervention$.ti,ab,kw. (43)
-
risk behaviour$ program$.ti,ab,kw. (1)
-
risk behavior$ program$.ti,ab,kw. (4)
-
82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 (3008)
-
10 and 105 (179)
-
81 or 106 (11,482)
-
qualitative research/ (7974)
-
qualitative.ti,ab. (143,449)
-
(accept$ or attitude$ or barrier$ or belief$ or believ$ or consider$ or experienc$ or facilitat$ or feasib$ or implement$ or option$ or preference$ or promot$ or view or views or viewpoint$).ti. (298,416)
-
108 or 109 or 110 (416,644)
-
73 and 111 (1132)
-
107 or 112 (12,057)
-
animal models/ (30,681)
-
(animal not (animal and human)).po. (346,436)
-
(rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys).ti. (143,111)
-
114 or 115 or 116 (366,257)
-
113 not 117 (11,736)
-
limit 118 to yr=“1990 -Current” (10,354).
Science Citation Index via Web of Science
Date range searched: 1990 to 25 October 2018.
Date searched: 25 October 2018.
Indexes = SCI-EXPANDED.
A series of five separate searches were carried out to identify specific risk factors in relation to low levels of physical activity, alcohol use, drug use, poor diet and smoking. Each of these is reproduced here.
Records identified for each search:
-
search 1, physical activity – 506
-
search 2, alcohol use – 283
-
search 3, drug use – 2154
-
search 4, diet – 603
-
search 5, smoking – 732.
Search strategies
Search 1: physical activity search history
# 1 TS=(schizophren*) (142,689).
# 2 TOPIC: (“psychotic disorder*”) (7659)
# 3 TOPIC: (“bipolar disorder*”) (39,462)
# 4 TOPIC: ((acute or chronic* or persistent* or serious* or severe*) NEAR/2 (mental* or psych*) NEAR/2 (disease* or disorder* or disturbanc* or ill*)) (12,675)
# 5 TOPIC: (SMI NEAR/3 (individual* or inpatient* or in-patient* or outpatient* or out-patient* or patient* or people or person* or population*)) (697)
# 6 TOPIC: ((“mental health” or psychiatric) NEAR/2 (inpatient* or in-patient*)) (7262)
# 7 TOPIC: (psychotic or psychosis or psychoses) (57,961)
# 8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 (204,357)
# 9 TOPIC: (“clinical trial”) (160,171)
# 10 TOPIC: (randomized NEAR/2 trial) (491,946)
# 11 TOPIC: (randomised NEAR/2 trial) (491,946)
# 12 TOPIC: (randomisation or randomization or randomly) (317,197)
# 13 TOPIC: (“single blind*” or “double blind*”) (228,207)
# 14 TOPIC: (placebo) (223,067)
# 15 TOPIC: (RCT) (15,997)
# 16 #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 (1,044,182)
# 17 #16 AND #8 (21,145)
# 18 TOPIC: (physical NEAR/3 (fit* or train* or activ* or endur*)) OR TOPIC: (exercis* NEAR/3 (fit* or train* or activ* or endur*)) (165,537)
# 19 TOPIC: ((promot* or uptak* or encourag* or increas* or start* or adher*) NEAR/3 (exercis* or gym* or sport* or fitness)) (32,224)
# 20 TOPIC: ((decreas* or reduc* or discourag*) NEAR/3 (sedentary or deskbound)) (1231)
# 21 TOPIC: (recreation or sport* or walk* or running or jogging or bicycling or biking or swimming) (555,309)
# 22 TOPIC: (active NEAR/1 (travel* or transport* or commut*)) (9768)
# 23 #22 OR #21 OR #20 OR #19 OR #18 (709,486)
# 24 #23 AND #17 (506)
Search 2: alcohol search history
# 1 TS=(schizophren*) (142,689).
# 2 TOPIC: (“psychotic disorder*”) (7659)
# 3 TOPIC: (“bipolar disorder*”) (39,462)
# 4 TOPIC: ((acute or chronic* or persistent* or serious* or severe*) NEAR/2 (mental* or psych*) NEAR/2 (disease* or disorder* or disturbanc* or ill*)) (12,675)
# 5 TOPIC: (SMI NEAR/3 (individual* or inpatient* or in-patient* or outpatient* or out-patient* or patient* or people or person* or population*)) (697)
# 6 TOPIC: ((“mental health” or psychiatric) NEAR/2 (inpatient* or in-patient*)) (7262)
# 7 TOPIC: (psychotic or psychosis or psychoses) (57,961)
# 8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 (204,357)
# 9 TS=(“clinical trial”) (160,171)
# 10 TOPIC: (randomized NEAR/2 trial) (491,946)
# 11 TOPIC: (randomised NEAR/2 trial) (491,946)
# 12 TS=(randomisation or randomization or randomly) (317,197)
# 13 TOPIC: (“single blind*” or “double blind*”) (228,207)
# 14 TOPIC: (placebo) (223,067)
# 15 TOPIC: (RCT) (15,997)
# 16 #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 (1,044,182)
# 17 #16 AND #8 (21,145)
# 18 TOPIC: (drink* NEAR/2 (binge or excessive* or harm* or heavily or heavy or misus* or abus* or consum*)) OR TOPIC: (alcohol* NEAR/2 (binge or excessive* or harm* or heavily or heavy or misus* or abus* or consum*)) OR TOPIC: (alcohol* NEAR/2 (intoxicat* or inebriat* or drink* or drunk*)) OR TOPIC: (“drinking behaviour” or “drinking behavior”) (76,396)
# 19 #18 AND #17 (283)
Search 3: drug use search history
# 1 TS=(schizophren*) (142,689).
# 2 TOPIC: (“psychotic disorder*”) (7659)
# 3 TOPIC: (“bipolar disorder*”) (39,462)
# 4 TOPIC: ((acute or chronic* or persistent* or serious* or severe*) NEAR/2 (mental* or psych*) NEAR/2 (disease* or disorder* or disturbanc* or ill*)) (12,675)
# 5 TOPIC: (SMI NEAR/3 (individual* or inpatient* or in-patient* or outpatient* or out-patient* or patient* or people or person* or population*)) (697)
# 6 TOPIC: ((“mental health” or psychiatric) NEAR/2 (inpatient* or in-patient*)) (7262)
# 7 TOPIC: (psychotic or psychosis or psychoses) (57,961)
# 8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 (204,357)
# 9 TS=(“clinical trial”) (160,171)
# 10 TOPIC: (randomized NEAR/2 trial) (491,946)
# 11 TOPIC: (randomised NEAR/2 trial) (491,946)
# 12 TS=(randomisation or randomly) (317,197)
# 13 TOPIC: (“single blind*” or “double blind*”) (228,207)
# 14 TOPIC: (placebo) (223,067)
# 15 TOPIC: (RCT) (15,997)
# 16 #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 (1,044,182)
# 17 #16 AND #8 (21,145)
# 18 TS=(drug* NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (164,816)
# 19 TS=(substance* NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (56,008)
# 20 TS=((heroin or opiate* or cocaine or crack) NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (26,814)
# 21 TS=((cannabis or marijuana) NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (11,144)
# 22 TS=((benzodiazepine* or amphetamine* or methamphetamine* or MDMA or ecstasy) NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (9994)
# 23 TS=(solvent* NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (44,507)
# 24 TS=((“prescri* drug*”) NEAR/2 (use* or using or abuse* or abusing or dependen* or misuse* or misusing)) (2120)
# 25 TOPIC: (“street drug*” or “recreational drug*” or “illicit drug*” or “polydrug use”) OR TOPIC: (“inject* drug use*”) OR TOPIC: ((needle* or syringe*) NEAR/3 shar*) (21,063)
# 26 #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 (279,350)
# 27 #26 AND #17 (2154)
Search 4: diet search history
# 1 TS=(schizophren*) (142,689).
# 2 TOPIC: (“psychotic disorder*”) (7659)
# 3 TOPIC: (“bipolar disorder*”) (39,462)
#4 TOPIC: ((acute or chronic* or persistent* or serious* or severe*) NEAR/2 (mental* or psych*) NEAR/2 (disease* or disorder* or disturbanc* or ill*)) (12,675)
# 5 TOPIC: (SMI NEAR/3 (individual* or inpatient* or in-patient* or outpatient* or out-patient* or patient* or people or person* or population*)) (697)
# 6 TOPIC: ((“mental health” or psychiatric) NEAR/2 (inpatient* or in-patient*)) (7262)
# 7 TOPIC: (psychotic or psychosis or psychoses) (57,961)
# 8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 (204,357)
# 9 TOPIC: (healthy NEAR/2 (diet* or eating)) (11,006)
# 10 TOPIC: (fruit* NEAR/2 (intake or consum* or increase or portion* or serving* or frequenc* or number* or preference* or choice*)) (21,834)
# 11 TOPIC: (vegetable* NEAR/2 (intake or consum* or increase or portion* or serving* or frequenc* or number* or preference* or choice*)) (13,776)
# 12 TOPIC: (“5 a day”) (211)
# 13 TOPIC: (“five a day”) (42)
# 14 TOPIC: ((food or diet*) NEAR/1 (choice* or frequenc* or habit* or intake or preference*)) (123,099)
# 15 TOPIC: (obesity) (255,034)
# 16 TOPIC: (overweight) (68,056)
# 17 #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 (397,907)
# 18 #17 AND #8 (2955)
# 19 TS=(“clinical trial”) (160,171)
# 20 TOPIC: (randomized NEAR/2 trial) (491,946)
# 21 TOPIC: (randomised NEAR/2 trial) (491,946)
# 22 TS=(randomisation or randomly) (317,197)
# 23 TOPIC: (“single blind*” or “double blind*”) (228,207)
# 24 TOPIC: (placebo) (223,067)
# 25 TOPIC: (RCT) (15,997)
# 26 #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 (1,044,182)
# 27 #26 AND #18 (603)
Search 5: smoking search history
# 1 TS=(schizophren*) (142,689).
# 2 TOPIC: (“psychotic disorder*”) (7659)
# 3 TOPIC: (“bipolar disorder*”) (39,462)
# 4 TOPIC: ((acute or chronic* or persistent* or serious* or severe*) NEAR/2 (mental* or psych*) NEAR/2 (disease* or disorder* or disturbanc* or ill*)) (12,675)
# 5 TOPIC: (SMI NEAR/3 (individual* or inpatient* or in-patient* or outpatient* or out-patient* or patient* or people or person* or population*)) (697)
# 6 TOPIC: ((“mental health” or psychiatric) NEAR/2 (inpatient* or in-patient*)) (7262)
# 7 TOPIC: (psychotic or psychosis or psychoses) (57,961)
# 8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 (204,357)
# 9 TS=(“clinical trial”) (160,171)
# 10 TOPIC: (randomized NEAR/2 trial) (491,946)
# 11 TOPIC: (randomised NEAR/2 trial) (491,946)
# 12 TS=(randomisation or randomly) (317,197)
# 13 TOPIC: (“single blind*” or “double blind*”) (228,207)
# 14 TOPIC: (placebo) (223,067)
# 15 TOPIC: (RCT) (15,997)
# 16 #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 (1,044,182)
# 17 #16 AND #8 (21,145)
# 18 TOPIC: (smoking) OR TOPIC: (“smoking cessation”) OR TOPIC: (“smoking reduction”) OR TOPIC: (smoker or smokers) OR TOPIC: ((stop* or ceas* or give or gave or prevent*) NEAR/2 smok*) (241,392)
# 19 TOPIC: ((stop* or ceas* or give or gave or prevent*) NEAR/2 tobacco*) OR TOPIC: (“tobacco use”) (13,340)
# 20 TOPIC: (“passive smoking”) OR TOPIC: (“tobbaco smok*”) (4960)
# 21 TOPIC: (“electronic cigarette*” or e-cigarette* or e-cig or e-cigs) (3312)
# 22 TOPIC: (vape or vapes or vaper or vapers or vaping) (511)
# 23 #22 OR #21 OR #20 OR #19 OR #18 (246,692)
# 24 #23 AND #17 (732)
Applied Social Sciences Index and Abstracts via ProQuest® (ProQuest LLC, Ann Arbor, MI, USA)
Date searched: 2 September 2020.
Six separate searches were conducted.
Serious mental illness and risk behaviours and poor diet
Records identified: 48.
Search strategy
((((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses))) AND ((noft(healthy NEAR/2 (diet* OR eating)) OR noft(fruit* NEAR/2 (intake OR consum* OR increase OR portion* OR serving* OR frequenc* OR number* OR preference* OR choice*)) OR noft((vegetable* NEAR/2 (intake OR consum* OR increase OR portion* OR serving* OR frequenc* OR number* OR preference* OR choice*)))) OR noft(“five a day” OR “five a day”) OR noft((food OR diet*) NEAR/1 (choice* OR frequenc* OR intake)) OR (MAINSUBJECT.EXACT(“Diet”) OR (MAINSUBJECT.EXACT(“Healthy food”) OR MAINSUBJECT.EXACT(“Food”) OR MAINSUBJECT.EXACT(“Food consumption”) OR MAINSUBJECT.EXACT(“Food habits”) OR MAINSUBJECT.EXACT(“Takeaway food”)) OR (MAINSUBJECT.EXACT(“Nutritional therapy”) OR MAINSUBJECT.EXACT(“Nutrition programmes”) OR MAINSUBJECT.EXACT(“Nutrition”)) OR MAINSUBJECT.EXACT(“obesity”)))) AND MAINSUBJECT.EXACT(“randomized controlled trials”)) OR ((((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses))) AND ((noft(healthy NEAR/2 (diet* OR eating)) OR noft(fruit* NEAR/2 (intake OR consum* OR increase OR portion* OR serving* OR frequenc* OR number* OR preference* OR choice*)) OR noft((vegetable* NEAR/2 (intake OR consum* OR increase OR portion* OR serving* OR frequenc* OR number* OR preference* OR choice*)))) OR noft(“five a day” OR “five a day”) OR noft((food OR diet*) NEAR/1 (choice* OR frequenc* OR intake)) OR (MAINSUBJECT.EXACT(“Diet”) OR (MAINSUBJECT.EXACT(“Healthy food”) OR MAINSUBJECT.EXACT(“Food”) OR MAINSUBJECT.EXACT(“Food consumption”) OR MAINSUBJECT.EXACT(“Food habits”) OR MAINSUBJECT.EXACT(“Takeaway food”)) OR (MAINSUBJECT.EXACT(“Nutritional therapy”) OR MAINSUBJECT.EXACT(“Nutrition programmes”) OR MAINSUBJECT.EXACT(“Nutrition”)) OR MAINSUBJECT.EXACT(“obesity”)))) AND (MAINSUBJECT.EXACT(“Qualitative research”) OR noft(qualitative*) OR ti((accept* OR attitude* OR barrier* OR belief* OR believ* OR consider* OR experienc* OR facilitat* OR feasib* OR implement* OR option* OR preference* OR promot* OR view OR views OR viewpoint*)))).
Serious mental illness and risk behaviours and lack of physical activity
Records identified: 127.
Search strategy
(((noft((physical OR exercise*) NEAR/3 (fit* OR train* OR activ* OR endur*)) OR noft((promot* OR uptak* OR encourag* OR increas* OR start* OR adher*) NEAR/3 (exercis* OR gym* OR sport* OR fitness)) OR noft((decreas* OR reduc* OR discourag*) NEAR/3 (sedentary OR deskbound)) OR noft(sport* OR walk* OR running OR jogging OR bicycling OR biking OR swimming) OR noft(active NEAR/1 (travel* OR transport* OR commut*))) OR (MAINSUBJECT.EXACT(“Physical fitness”) OR (MAINSUBJECT.EXACT(“Aerobic fitness”) OR MAINSUBJECT.EXACT(“Fitness”))) OR MAINSUBJECT.EXACT.EXPLODE(“Sports”)) AND ((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses)))) AND (MAINSUBJECT.EXACT(“randomized controlled trials”) OR (MAINSUBJECT.EXACT(“Qualitative research”) OR noft(qualitative*) OR ti((accept* OR attitude* OR barrier* OR belief* OR believ* OR consider* OR experienc* OR facilitat* OR feasib* OR implement* OR option* OR preference* OR promot* OR view OR views OR viewpoint*)))).
Serious mental illness and risk behaviours and smoking
Records identified: 68.
Search strategy
MAINSUBJECT.EXACT(“randomized controlled trials”) OR (MAINSUBJECT.EXACT(“Qualitative research”) OR noft(qualitative*) OR ti((accept* OR attitude* OR barrier* OR belief* OR believ* OR consider* OR experienc* OR facilitat* OR feasib* OR implement* OR option* OR preference* OR promot* OR view OR views OR viewpoint*)))) AND (((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses))) AND ((noft(smoking OR antismoking OR anti-smoking) OR noft(smoker OR smokers) OR noft(electronic cigarette* OR e-cigarette* OR e-cig OR e-cigs) OR noft(vape OR vapes OR vaper OR vapers OR vaping) OR noft(tobacco)) OR (MAINSUBJECT.EXACT.EXPLODE(“Smoking”) OR MAINSUBJECT.EXACT.EXPLODE(“Tobacco”) OR MAINSUBJECT.EXACT.EXPLODE(“Nicotine”)))).
Serious mental illness and risk behaviours and alcohol use
Records identified: 141.
Search strategy
(MAINSUBJECT.EXACT(“randomized controlled trials”) OR (MAINSUBJECT.EXACT(“Qualitative research”) OR noft(qualitative*) OR ti((accept* OR attitude* OR barrier* OR belief* OR believ* OR consider* OR experienc* OR facilitat* OR feasib* OR implement* OR option* OR preference* OR promot* OR view OR views OR viewpoint*)))) AND (((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses))) AND ((noft(beer* OR wine* OR cider* OR alcopop* OR spirit OR spirits) OR noft(alcohol*) OR noft(drink* NEAR/2 (binge OR excessive* OR harm* OR heavily OR heavy OR misus* OR abus* OR consum*)) OR noft(intoxicat* OR inebriat* OR drunk*)) OR (MAINSUBJECT.EXACT.EXPLODE(“Alcohol abuse”) OR MAINSUBJECT.EXACT.EXPLODE(“Alcohol intoxication”) OR MAINSUBJECT.EXACT(“Alcohol consumption”) OR MAINSUBJECT.EXACT.EXPLODE(“Alcoholic beverages”) OR MAINSUBJECT.EXACT(“Alcoholics”) OR MAINSUBJECT.EXACT(“Alcohol related problems”) OR MAINSUBJECT.EXACT.EXPLODE(“Alcoholism”) OR MAINSUBJECT.EXACT.EXPLODE(“Alcohol dependence”)))).
Serious mental illness and risk behaviours and drug misuse
Records identified: 257.
Search strategy
((MAINSUBJECT.EXACT(“Qualitative research”) OR noft(qualitative*) OR ti((accept* OR attitude* OR barrier* OR belief* OR believ* OR consider* OR experienc* OR facilitat* OR feasib* OR implement* OR option* OR preference* OR promot* OR view OR views OR viewpoint*))) OR MAINSUBJECT.EXACT(“randomized controlled trials”)) AND (((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses))) AND ((noft((drug* OR substance*) NEAR/2 (use* OR using OR abuse* OR abusing OR misuse* OR misusing)) OR noft((heroin OR opiate* OR cocaine OR crack) NEAR/2 (use* OR using OR abuse* OR abusing OR misuse* OR misusing)) OR noft((cannabis OR marijuana) NEAR/2 (use* OR using OR abuse* OR abusing OR misuse* OR misusing)) OR noft((benzodiazepine* OR amphetamine* OR methamphetamine* OR MDMA OR ecstasy) NEAR/2 (use* OR using OR abuse* OR abusing OR misuse* OR misusing)) OR noft(solvent* NEAR/2 (use* OR using OR abuse* OR abusing OR misuse* OR misusing)) OR noft(“street drug*” OR “recreational drug*” OR “illicit drug*”) OR noft(“polydrug use*”) OR noft(“inject* drug use*”) OR noft(needle NEAR/3 shar*) OR noft(syringe* NEAR/3 shar)) OR ((MAINSUBJECT.EXACT(“Drug abuse”) OR MAINSUBJECT.EXACT(“Drug abusers”)) OR MAINSUBJECT.EXACT.EXPLODE(“Heroin”) OR MAINSUBJECT.EXACT(“Cocaine”) OR MAINSUBJECT.EXACT.EXPLODE(“Cannabis”)))).
Serious mental illness and lifestyle interventions
Records identified: 17.
Search strategy
(((noft(lifestyle NEAR/2 (intervention* OR program*)) OR noft(“life style” NEAR/2 (intervention* OR program*)) OR noft(“behavior* change” NEAR/1 (intervention* OR program*)) OR noft(“risk factor” NEAR/2 (program* OR intervention*)) OR noft(“multifactorial lifestyle” NEAR/1 (intervention* OR program*)) OR noft(“health behavior*” NEAR/1 (program* OR intervention*)) OR noft(“health behaviour*” NEAR/1 (program* OR intervention*)) OR noft(“health risk behavior*” NEAR/1 (program* OR intervention*)) OR noft(“health risk behaviour*” NEAR/1 (program* OR intervention*)) OR noft(“risk behavior*” NEAR/1 (program* OR intervention*))) OR (noft(“risk behaviour*” NEAR/1 (program* OR intervention*)) OR noft(“health behavior* change intervention* “) OR noft(“health behaviour* change intervention*”) OR noft(“behavior* risk factor* intervention* “) OR noft(“behaviour* risk factor* intervention*”) OR noft(“behavior* risk factor* program*”) OR noft(“behaviour* risk factor* program* “) OR noft(“risk behaviour* intervention* “) OR noft(“risk behavior* intervention* “) OR noft(“risk behavio* program*”))) AND (MAINSUBJECT.EXACT(“randomized controlled trials”) OR (MAINSUBJECT.EXACT(“Qualitative research”) OR noft(qualitative*) OR ti((accept* OR attitude* OR barrier* OR belief* OR believ* OR consider* OR experienc* OR facilitat* OR feasib* OR implement* OR option* OR preference* OR promot* OR view OR views OR viewpoint*))))) AND (((MAINSUBJECT.EXACT(“Schizophrenia”) OR MAINSUBJECT.EXACT(“Bipolar affective disorder”) OR MAINSUBJECT.EXACT(“Psychotic mood disorders”) OR MAINSUBJECT.EXACT(“Affective disorders”)) OR noft(((acute OR chronic* OR persistent* OR serious* OR severe*) NEAR/2 (mental* OR psych*) NEAR/2 (disease* OR disorder* OR disturbanc* OR ill*))) OR noft((SMI NEAR/3 (individual* OR inpatient* OR in-patient* OR outpatient* OR out-patient* OR patient* OR people OR person* OR population*))) OR noft((psychiatric) NEAR/2 (inpatient* OR in-patient*)) OR noft((mental) NEAR/3 (inpatient* OR in-patient*)) OR (noft(schizophren* OR bipolar) OR noft(psychotic OR psychosis OR psychoses))
Appendix 2 Excluded studies with reasons for exclusion
| Full reference | Reason for exclusion |
|---|---|
| Abed H. What factors affect the lifestyle choices of people with schizophrenia? Ment Health Rev J 2010;15:21–7 | Intervention did not meet criteria |
| Acil AA, Dogan S, Dogan O. The effects of physical exercises to mental state and quality of life in patients with schizophrenia. J Psychiatr Ment Health Nurs 2008;15:808–15 | Study design did not meet criteria |
| Aguiar-Bloemer AC, Agliussi RG, Pinho TMP, Furtado EF, Diez-Garcia RW. Eating behavior of schizophrenic patients. Rev de Nutr 2018;31:13–24 | Study design did not meet criteria |
| Alvarez-Jiménez M, González-Blanch C, Vázquez-Barquero JL, Pérez-Iglesias R, Martínez-García O, Pérez-Pardal T, et al. Attenuation of antipsychotic-induced weight gain with early behavioral intervention in drug-naive first-episode psychosis patients: a randomized controlled trial. J Clin Psychiatry 2006;67:1253–60 | Population did not meet criteria |
| Alvidrez J, Kaiser D, Havassy BE. Severely mentally ill consumers’ perspectives on drug use. J Psychoactive Drugs 2004;36:347–55 | Intervention did not meet criteria |
| Arbour-Nicitopoulos KP, Faulkner GE, Hsin A, Selby P. A pilot study examining the acute effects of exercise on cigarette cravings and affect among individuals with serious mental illness. Ment Health Phys Act 2011;4:89–94 | Outcomes did not meet criteria |
| Archie S, Wilson JH, Osborne S, Hobbs H, McNiven J. Pilot study: access to fitness facility and exercise levels in olanzapine-treated patients. Can J Psychiatry 2003;48:628–32 | Study design did not meet criteria |
| Aschbrenner KA, Pepin R, Mueser KT, Naslund JA, Rolin SA, Faber MJ, Bartels SJ. A mixed methods exploration of family involvement in medical care for older adults with serious mental illness. Int J Psychiatry Med 2014;48:121–33 | Intervention did not meet criteria |
| Aschbrenner K, Mueser K, Bartels S, Carpenter-Song E, Pratt S, Barre L, et al. The other 23 hours: a qualitative study of fitness provider perspectives on social support for health promotion for adults with mental illness. Health Soc Work 2015;40:91–9 | Population did not meet criteria |
| Aschbrenner KA, Naslund JA, Barre LK, Mueser KT, Kinney A, Bartels SJ. Peer health coaching for overweight and obese individuals with serious mental illness: intervention development and initial feasibility study. Transl Behav Med 2015;5:277–84 | Outcomes did not meet criteria |
| Aschbrenner KA, Naslund JA, Bartels SJ. A mixed methods study of peer-to-peer support in a group-based lifestyle intervention for adults with serious mental illness. Psychiatr Rehabil J 2016;39:328–34 | Population did not meet criteria |
| Aschbrenner KA, Naslund JA, Gill L, Hughes T, O’Malley AJ, Bartels SJ,Brunette MF. Qualitative analysis of social network influences on quitting smoking among individuals with serious mental illness. J Ment Health 2019;28:475–81 | Population did not meet criteria |
| Aschbrenner KA, Naslund JA, Gill L, Bartels SJ, O’Malley AJ, Brunette MF. Preferences for smoking cessation support from family and friends among adults with serious mental illness. Psychiatr Q 2017;88:701–10 | Population did not meet criteria |
| Aschbrenner KA, Naslund JA, Gorin AA, Mueser KT, Scherer EA, Viron M, et al. Peer support and mobile health technology targeting obesity-related cardiovascular risk in young adults with serious mental illness: protocol for a randomized controlled trial. Contemp Clin Trials 2018;74:97–106 | Record was a protocol or registry entry |
| Asher CJ, Gask L. Reasons for illicit drug use in people with schizophrenia: qualitative study. BMC Psychiatry 2010;10:94 | Intervention did not meet criteria |
| Bagøien G, Bjørngaard JH, Østensen C, Reitan SK, Romundstad P, Morken G. The effects of motivational interviewing on patients with comorbid substance use admitted to a psychiatric emergency unit – a randomised controlled trial with two year follow-up. BMC Psychiatry 2013;13:93 | Population did not meet criteria |
| Bailey JM, Hansen V, Wye PM, Wiggers JH, Bartlem KM, Bowman JA. Supporting change in chronic disease risk behaviours for people with a mental illness: a qualitative study of the experiences of family carers. BMC Public Health 2018;18:416 | Population did not meet criteria |
| Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, et al. Evaluation of a motivational interview for substance use within psychiatric in-patient services. Addiction 2002;97:1329–37 | Population did not meet criteria |
| Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, et al. Motivational interviewing among psychiatric in-patients with substance use disorders. Acta Psychiatr Scand 2002;106:233–40 | Population did not meet criteria |
| Baker A, Borland R, Bonevski B, Castle DJ, Williams J, Segan C, et al. Quitlink: accessible smoking cessation support for people living with severe and enduring mental illness. Schizophr Bull 2018;44(Suppl. 1):S151 | Record was a protocol or registry entry |
| Barre LK, Ferron JC, Davis KE, Whitley R. Healthy eating in persons with serious mental illnesses: understanding and barriers. Psychiatr Rehabil J 2011;34:304–10 | Population did not meet criteria |
| Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O’Brien R, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psychiatry 2001;158:1706–13 | Intervention did not meet criteria |
| Barrowclough C, Lobbanl F, Warburton J, Choudhry I, Gregg L, Wood H, et al. HELPER ReCAP: Rethinking Choices after Psychosis – a phase-specific psychological therapy for people with problematic cannabis use following a first episode of psychosis. Early Interv Psychiatry 2010;4:161 | Population did not meet criteria |
| Barrowclough C, Haddock G, Wykes T, Beardmore R, Conrod P, Craig T, et al. Integrated motivational interviewing and cognitive behavioural therapy for people with psychosis and comorbid substance misuse: randomised controlled trial. BMJ 2010;341:c6325 | Population did not meet criteria |
| Barrowclough C, Marshall M, Gregg L, Fitzsimmons M, Tomenson B, Warburton J, Lobban F. A phase-specific psychological therapy for people with problematic cannabis use following a first episode of psychosis: a randomized controlled trial. Psychol Med 2014;44:2749–61 | Population did not meet criteria |
| Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, et al. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatr Serv 2013;64:729–36 | Population did not meet criteria |
| Bartels SJ, Aschbrenner KA, Pratt SI, Naslund JA, Scherer EA, Zubkoff L, et al. Implementation of a lifestyle intervention for people with serious mental illness in state-funded mental health centers. Psychiatr Serv 2018;69:664–70 | Study design did not meet criteria |
| Battersby M, Kidd MR, Licinio J, Aylward P, Baker A, Ratcliffe J, et al. Improving cardiovascular health and quality of life in people with severe mental illness: study protocol for a randomised controlled trial. Trials 2018;19:366 | Record was a protocol or registry entry |
| Beebe LH, Smith KD, Roman MW, Burk RC, McIntyre K, Dessieux OL, et al. A pilot study describing physical activity in persons with schizophrenia spectrum disorders (SSDS) after an exercise program. Issues Ment Health Nurs 2013;34:214–19 | Study design did not meet criteria |
| Bellack AS, Bennett ME, Gearon JS, Brown CH, Yang Y. A randomized clinical trial of a new behavioral treatment for drug abuse in people with severe and persistent mental illness. Arch Gen Psychiatry 2006;63:426–32 | Population did not meet criteria |
| Bennett ME, Bellack AS, Gearon JS. Treating substance abuse in schizophrenia: preliminary analysis of data from a randomized treatment trial. Schizophr Res 2003;60:319 | Trial was incomplete |
| Bennett ME, Brown CH, Li L, Himelhoch S, Bellack A, Dixon L. Smoking cessation in individuals with serious mental illness: a randomized controlled trial of two psychosocial interventions. J Dual Diagn 2015;11:161–73 | Population did not meet criteria |
| Bergqvist A, Karlsson M, Foldemo A, Wärdig R, Hultsjö S. Preventing the development of metabolic syndrome in people with psychotic disorders – difficult, but possible: experiences of staff working in psychosis outpatient care in Sweden. Issues Ment Health Nurs 2013;34:350–8 | Population did not meet criteria |
| Bersani FS, Biondi M, Coviello M, Fagiolini A, Majorana M, Minichino A, et al. Psychoeducational intervention focused on healthy living improves psychopathological severity and lifestyle quality in psychiatric patients: preliminary findings from a controlled study. J Ment Health 2017;26:271–5 | Population did not meet criteria |
| Beyraghi N, Mazaheri Meybodi A, Jafarian Bahri RS. Smoking ban in psychiatric inpatient unit: an Iranian study on the views and attitudes of the mental health staff and psychiatric patients. Psychiatry J 2018;2018:2450939 | Population did not meet criteria |
| Biseul I, Icick R, Seguin P, Bellivier F, Scott J. Feasibility and acceptability of the ‘HABIT’ group programme for comorbid bipolar and alcohol and substance use disorders. Clin Psychol Psychother 2017;24:887–98 | Study design did not meet criteria |
| Blanner Kristiansen C, Juel A, Vinther Hansen M, Hansen AM, Kilian R, Hjorth P. Promoting physical health in severe mental illness: patient and staff perspective. Acta Psychiatr Scand 2015;132:470–8 | Population did not meet criteria |
| Bogenschutz MP, Rice SL, Tonigan JS, Vogel HS, Nowinski J, Hume D, Arenella PB. 12-step facilitation for the dually diagnosed: a randomized clinical trial. J Subst Abuse Treat 2014;46:403–11 | Population did not meet criteria |
| Bogomolova S, Zarnowiecki D, Wilson A, Fielder A, Procter N, Itsiopoulos C, et al. Dietary intervention for people with mental illness in South Australia. Health Promot Int 2018;33:71–83 | Population did not meet criteria |
| Bradizza CM, Stasiewicz PR. Qualitative analysis of high-risk drug and alcohol use situations among severely mentally ill substance abusers. Addict Behav 2003;28:157–69 | Intervention did not meet criteria |
| Bradshaw T, Lovell K, Bee P, Campbell M. The development and evaluation of a complex health education intervention for adults with a diagnosis of schizophrenia. J Psychiatr Ment Health Nurs 2010;17:473–86 | Study design did not meet criteria |
| Bradshaw T, Wearden A, Marshall M, Warburton J, Husain N, Pedley R, et al. Developing a healthy living intervention for people with early psychosis using the Medical Research Council’s guidelines on complex interventions: phase 1 of the HELPER – InterACT programme. Int J Nurs Stud 2012;49:398–406 | Outcomes did not meet criteria |
| Broderick J, Knowles A, Chadwick J, Vancampfort D. Yoga vs. standard care for schizophrenia. Schizophr Bull 2016;42:15–17 | Study design did not meet criteria |
| Brooke L, Gucciardi D, Lin A, Ntoumanis N. A qualitative investigation of perceived barriers to and enablers of sport participation for young people with first episode psychosis. Early Interv Psychiatry 2018;12:56 | Population did not meet criteria |
| Brunette MF, Asher D, Whitley R, Lutz WJ, Wieder BL, Jones AM, McHugo GJ. Implementation of integrated dual disorders treatment: a qualitative analysis of facilitators and barriers. Psychiatr Serv 2008;59:989–95 | Outcomes did not meet criteria |
| Brunette MF, Ferron JC, Drake RE, Devitt TS, Geiger PT, McHugo GJ, et al. Carbon monoxide feedback in a motivational decision support system for nicotine dependence among smokers with severe mental illnesses. J Subst Abuse Treat 2013;45:319–24 | Outcomes did not meet criteria |
| Brunette MF, Ferron JC, Robinson D, Coletti D, Geiger P, Devitt T, et al. Brief web-based interventions for young adult smokers with severe mental illnesses: a randomized, controlled pilot study. Nicotine Tob Res 2018;20:1206–14 | Population did not meet criteria |
| Cabassa LJ, Siantz E, Nicasio A, Guarnaccia P, Lewis-Fernández R. contextual factors in the health of people with serious mental illness. Qual Health Res 2014;24:1126–37 | Intervention did not meet criteria |
| Cabassa LJ, Stefancic A, O’Hara K, El-Bassel N, Lewis-Fernández R, Luchsinger JA, et al. Peer-led healthy lifestyle program in supportive housing: study protocol for a randomized controlled trial. Trials 2015;16:388 | Record was a protocol or registry entry |
| Carson NE. Influences on the food choice behavior of adults with severe mental illness. Diss Abstr Int B Sci Eng 2012;72:6678 | Intervention did not meet criteria |
| Castle H, Prestwich A, Gupta A. Effects of a control theory based dietary intervention to promote fruit and vegetable consumption in young people experiencing a first episode of psychosis. Early Interv Psychiatry 2012;6:71 | Population did not meet criteria |
| Chen MD, Yeh YC, Tsai YJ, Chang YC, Yu JW, Hsu CH. Efficacy of baduanjin exercise and feasibility of mobile text reminders on follow-up participation in people with severe mental illness: an exploratory study. J Psychiatr Pract 2016;22:241–9 | Study design did not meet criteria |
| Chen MD, Chang JJ, Kuo CC, Yu JW, Huang MF, Marks B, et al. A pilot comparative study of one-way versus two-way text message program to promote physical activity among people with severe mental illness. Ment Health Phys Act 2017;13:143–51 | Study design did not meet criteria |
| Chen MD, I JH, Pellegrini CA, Tang TC, Kuo CC. A qualitative exploration of facilitators and barriers to physical activity participation in people with severe mental illness in Taiwan. Ment Health Phys Act 2017;13:100–7 | Intervention did not meet criteria |
| Chengappa KN, Perkins KA, Brar JS, Schlicht PJ, Turkin SR, Hetrick ML, et al. Varenicline for smoking cessation in bipolar disorder: a randomized, double-blind, placebo-controlled study. J Clin Psychiatry 2014;75:765–72 | Intervention did not meet criteria |
| Childs HE, McCarthy-Jones S, Rowse G, Turpin G. The journey through cannabis use: a qualitative study of the experiences of young adults with psychosis. J Nerv Ment Dis 2011;199:703–8 | Population did not meet criteria |
| Cole J. The Effects of an Exercise Program on Chronically Mentally Ill Outpatients; A Study of Symptom Reduction, Physical Fitness, and Stress. PhD thesis. Chicago, IL: Illinois Institute of Technology; 1997 | Outcomes did not meet criteria |
| Connolly M, Floyd S, Forrest R, Marshall B. Mental health nurses’ beliefs about smoking by mental health facility inpatients. Int J Ment Health Nurs 2013;22:288–93 | Study design did not meet criteria |
| Curcic D, Stojmenovic T, Djukic-Dejanovic S, Dikic N, Vesic-Vukasinovic M, Radivojevic N, et al. Positive impact of prescribed physical activity on symptoms of schizophrenia: randomized clinical trial. Psychiatr Danub 2017;29:459–65 | Outcomes did not meet criteria |
| Daumit G, Appel L, Leatherman E, Latkin C, Dalcin A, Goggins B, et al. Randomized trial of peer-supported physical activity for persons with severe mental illness in community psychiatry. J Gen Intern Med 2010;25:S378–S9 | Population did not meet criteria |
| Davis KE, O’Neill SJ. A focus group analysis of relapse prevention strategies for persons with substance use and mental disorders. Psychiatr Serv 2005;56:1288–91 | Population did not meet criteria |
| Davis K, Brunette M, Vorhies V, Ferron J, Whitley R. A qualitative study of how individuals with severe mental illness assess smoking risks. Ment Health Subst Use 2010;3:110–23 | Intervention did not meet criteria |
| Dickerson F, Bennett M, Dixon L, Burke E, Vaughan C, Delahanty J, Diclemente C. Smoking cessation in persons with serious mental illnesses: the experience of successful quitters. Psychiatr Rehabil J 2011;34:311–16 | Study design did not meet criteria |
| Dixon LB, Potts W. Smoking Cessation for Veterans with Severe and Persistent Mental Illness. URL: www.clinicaltrials.gov/ct2/show/nct00960375 (accessed 30 April 2021) | Record was a protocol or registry entry |
| Dlack GW, Meador-Woodruff JH. Nicotine replacement and smoking reduction in smokers with schizophrenia conference abstract. Schizophr Res 1999;36:1–382 | Conference abstract only |
| Druss BG, Zhao L, von Esenwein SA, Bona JR, Fricks L, Jenkins-Tucker S, et al. The Health and Recovery Peer (HARP) program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr Res 2010;118:264–70 | Population did not meet criteria |
| Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia – a randomized controlled trial. Acta Psychiatr Scand 2007;116:226–32 | Outcomes did not meet criteria |
| Edwards J, Elkins KS, Hinton MF, Harrigan SM, Donovan KD, Athanasopoulos O. Randomized controlled trial of a cannabis-focused intervention versus psychoeducation for young people continuing to use cannabis in the 12 months following entry to treatment for first-episode psychosis. Schizophr Res 2004;70:61 | Population did not meet criteria |
| Edwards J, Elkins K, Hinton M, Harrigan SM, Donovan K, Athanasopoulos O, McGorry PD. Randomized controlled trial of a cannabis-focused intervention for young people with first-episode psychosis. Acta Psychiatr Scand 2006;114:109–17 | Population did not meet criteria |
| Engh JA, Andersen E, Holmen TL, Martinsen EW, Mordal J, Morken G, Egeland J. Effects of high-intensity aerobic exercise on psychotic symptoms and neurocognition in outpatients with schizophrenia: study protocol for a randomized controlled trial. Trials 2015;16:557 | Record was a protocol or registry entry |
| Esterberg ML, Compton MT. Smoking behavior in persons with a schizophrenia-spectrum disorder: a qualitative investigation of the transtheoretical model. Soc Sci Med 2005;61:293–303 | Intervention did not meet criteria |
| Evins AE. Smoking Relapse Prevention in Schizophrenia. URL: https://clinicaltrials.gov/ct2/show/NCT00320697 (accessed 30 April 2021) | Record was a protocol or registry entry |
| Evins AE, Cather C, Rigotti NA, Freudenreich O, Henderson DC, Olm-Shipman CM, Goff DC. Two-year follow-up of a smoking cessation trial in patients with schizophrenia: increased rates of smoking cessation and reduction. J Clin Psychiatry 2004;65:307–11 | Intervention did not meet criteria |
| Evins AE, Cather C, Deckersbach T, Freudenreich O, Culhane MA, Olm-Shipman CM, et al. A double-blind placebo-controlled trial of bupropion sustained-release for smoking cessation in schizophrenia. J Clin Psychopharmacol 2005;25:218–25 | Intervention did not meet criteria |
| Evins AE, Cather C, Culhane MA, Birnbaum A, Horowitz J, Hsieh E, et al. A 12-week double-blind, placebo-controlled study of bupropion SR added to high-dose dual nicotine replacement therapy for smoking cessation or reduction in schizophrenia. J Clin Psychopharmacol 2007;27:380–6 | Intervention did not meet criteria |
| Faber G, Smid HG, Van Gool AR, Wunderink L, van den Bosch RJ, Wiersma D. Continued cannabis use and outcome in first-episode psychosis: data from a randomized, open-label, controlled trial. J Clin Psychiatry 2012;73:632–8 | Outcomes did not meet criteria |
| Fatemi SH, Yousefi MK, Kneeland RE, Liesch SB, Folsom TD, Thuras PD. Antismoking and potential antipsychotic effects of varenicline in subjects with schizophrenia or schizoaffective disorder: a double-blind placebo and bupropion-controlled study. Schizophr Res 2013;146:376–8 | Intervention did not meet criteria |
| Faurholt-Jepsen M. The effect of smartphone-based treatment interventions in bipolar disorder. Eur Psychiatry 2018;48:S42–3 | Outcomes did not meet criteria |
| Firth J, Carney R, Elliott R, French P, Parker S, McIntyre R, et al. Exercise as an intervention for first-episode psychosis: a feasibility study. Early Interv Psychiatry 2018;12:307–15 | Study design did not meet criteria |
| Forchuk C, Norman R, Malla A, Martin ML, McLean T, Cheng S, et al. Schizophrenia and the motivation for smoking. Perspect Psychiatr Care 2002;38:41–9 | Study design did not meet criteria |
| Forsell Y, Hallgren M, Mattson M, Ekblom O, Lavebratt C. FitForLife: study protocol for a randomized controlled trial. Trials 2015;16:553 | Record was a protocol or registry entry |
| Furness T, Hewavasam J, Barnfield J, McKenna B, Joseph C. Adding an accredited exercise physiologist role to a new model of care at a secure extended care mental health service: a qualitative study. J Ment Health 2018;27:120–6 | Intervention did not meet criteria |
| Ganguli R, Jenkins T, McKinnon K. Weight loss in individuals with diabetes and psychosis: an intervention for community residential settings. Biol Psychiatry 2013;73:319S | Study design did not meet criteria |
| Garcia-Portilla MP, Garcia-Alvarez L, Saiz PA, Diaz-Mesa E, Galvan G, Sarramea F, et al. Effectiveness of a multi-component Smoking Cessation Support Programme (McSCSP) for patients with severe mental disorders: study design. Int J Environ Res Public Health 2013;11:373–89 | Record was a protocol or registry entry |
| George TP, Vessicchio JC, Sacco KA, Weinberger AH, Dudas MM, Allen TM, et al. A placebo-controlled trial of bupropion combined with nicotine patch for smoking cessation in schizophrenia. Biol Psychiatry 2008;63:1092–6 | Intervention did not meet criteria |
| George TP, Vessicchio JC, Termine A, Bregartner TA, Feingold A, Rounsaville BJ, Kosten TR. A placebo controlled trial of bupropion for smoking cessation in schizophrenia. Biol Psychiatry 2002;52:53–61 | Intervention did not meet criteria |
| Glover CM, Ferron JC, Whitley R. Barriers to exercise among people with severe mental illnesses. Psychiatr Rehabil J 2013;36:45–7 | Population did not meet criteria |
| Goldberg RW, Reeves G, Tapscott S, Medoff D, Dickerson F, Goldberg AP, et al. ‘MOVE!’ Outcomes of a weight loss program modified for veterans with serious mental illness. Psychiatr Serv 2013;64:737–44 | Population did not meet criteria |
| Goldberg RW, Dickerson F, Lucksted A, Brown CH, Weber E, Tenhula WN, et al. Living well: an intervention to improve self-management of medical illness for individuals with serious mental illness. Psychiatr Serv 2013;64:51–7 | Outcomes did not meet criteria |
| Gomes E, Bastos T, Probst M, Ribeiro JC, Silva G, Corredeira R. Effects of a group physical activity program on physical fitness and quality of life in individuals with schizophrenia. Ment Health Phys Act 2014;7:155–62 | Study design did not meet criteria |
| Goodrich DE, Kilbourne AM, Lai Z, Post EP, Bowersox NW, Mezuk B, et al. Design and rationale of a randomized controlled trial to reduce cardiovascular disease risk for patients with bipolar disorder. Contemp Clin Trials 2012;33:666–78 | Record was a protocol or registry entry |
| Graeber DA, Moyers TB, Griffith G, Guajardo E, Tonigan S. A pilot study comparing motivational interviewing and an educational intervention in patients with schizophrenia and alcohol use disorders. Community Ment Health J 2003;39:189–202 | Study design did not meet criteria |
| Graham C, Rollings C, de Leeuw S, Anderson L, Griffiths B, Long N. A qualitative study exploring facilitators for improved health behaviors and health behavior programs: mental health service users’ perspectives. Sci World J 2014;2014:870497 | Population did not meet criteria |
| Graham CR, Larstone R, Griffiths B, de Leeuw S, Anderson L, Powell-Hellyer S, Long N. Development and evaluation of innovative peer-led physical activity programs for mental health service users. J Nerv Ment Dis 2017;205:840–7 | Population did not meet criteria |
| Gray R, Brown E. What does mental health nursing contribute to improving the physical health of service users with severe mental illness? A thematic analysis. Int J Ment Health Nurs 2017;26:32–40 | Intervention did not meet criteria |
| Gyllensten AL, Forsberg KA. Computerized physical activity training for persons with severe mental illness – experiences from a communal supported housing project. Disabil Rehabil Assist Technol 2017;12:780–8 | Population did not meet criteria |
| Haddock G, Barrowclough C, Tarrier N, Moring J, O’Brien R, Schofield N, et al. Cognitive-behavioural therapy and motivational intervention for schizophrenia and substance misuse. 18-month outcomes of a randomised controlled trial. Br J Psychiatry 2003;183:418–26 | Intervention did not meet criteria |
| Happell B, Scott D, Platania-Phung C, Nankivell J. Nurses’ views on physical activity for people with serious mental illness. Ment Health Phys Act 2012;5:4–12 | Population did not meet criteria |
| Happell B, Stanton R, Hoey W, Scott D. Cardiometabolic health nursing to improve health and primary care access in community mental health consumers: baseline physical health outcomes from a randomised controlled trial. Issues Ment Health Nurs 2014;35:114–21 | Intervention did not meet criteria |
| Happell B, Stanton R, Hoey W, Scott D. Cardiometabolic health nursing to improve health and primary care access in community mental health consumers: protocol for a randomised controlled trial. Int J Nurs Stud 2014;51:236–42 | Intervention did not meet criteria |
| Hargreaves J, Lucock M, Rodriguez A. From inactivity to becoming physically active: the experiences of behaviour change in people with serious mental illness. Ment Health Phys Act 2017;13:83–93 | Intervention did not meet criteria |
| Hasson-Ohayon I, Kravetz S, Roe D, Rozencwaig S, Weiser M. Qualitative assessment of verbal and non-verbal psychosocial interventions for people with severe mental illness. J Ment Health 2006;15:343–53 | Outcomes did not meet criteria |
| Healey C, Peters S, Kinderman P, McCracken C, Morriss R. Reasons for substance use in dual diagnosis bipolar disorder and substance use disorders: a qualitative study. J Affect Disord 2009;113:118–26 | Intervention did not meet criteria |
| Hearon BA, Beard C, Kopeski LM, Smits JAJ, Otto MW, Björgvinsson T. Attending to timely contingencies: promoting physical activity uptake among adults with serious mental illness with an exercise-for-mood vs. an exercise-for-fitness prescription. Behav Med 2018;44:108–15 | Population did not meet criteria |
| Heffner JL, Kelly MM, Waxmonsky J, Mattocks K, Serfozo E, Bricker JB, et al. Pilot randomized controlled trial of web-delivered acceptance and commitment therapy versus smokefree.gov for smokers with bipolar disorder. Nicotine Tob Res 2019;26:26 | Study design did not meet criteria |
| Heggelund J, Nilsberg GE, Hoff J, Morken G, Helgerud J. Effects of high aerobic intensity training in patients with schizophrenia: a controlled trial. Nord J Psychiatry 2011;65:269–75 | Study design did not meet criteria |
| Hickman NJ, Delucchi KL, Prochaska JJ. Treating Tobacco dependence at the intersection of diversity, poverty, and mental illness: a randomized feasibility and replication trial. Nicotine Tob Res 2015;17:1012–21 | Population did not meet criteria |
| Ho RT, Fong TC, Wan AH, Au-Yeung FS, Wong CP, Ng WY, et al. A randomized controlled trial on the psychophysiological effects of physical exercise and Tai-chi in patients with chronic schizophrenia. Schizophr Res 2016;171:42–9 | Outcomes did not meet criteria |
| Hulse GK, Tait RJ. Six-month outcomes associated with a brief alcohol intervention for adult in-patients with psychiatric disorders. Drug Alcohol Rev 2002;21:105–12 | Population did not meet criteria |
| Hultsjo S. Mental healthcare staff’s knowledge and experiences of diabetes care for persons with psychosis – a qualitative interview study. Prim Health Care Res Dev 2013;14:281–92 | Population did not meet criteria |
| Hultsjo S, Hjelm K. Community health-care staff’s experiences of support to prevent type 2 diabetes among people with psychosis: an interview study with health staff. Int J Ment Health Nurs 2012;21:480–9 | Population did not meet criteria |
| Ikai S, Uchida H, Mizuno Y, Tani H, Nagaoka M, Tsunoda K, et al. Effects of chair yoga therapy on physical fitness in patients with psychiatric disorders: a 12-week single-blind randomized controlled trial. J Psychiatr Res 2017;94:194–201 | Outcomes did not meet criteria |
| James W, Preston NJ, Koh G, Spencer C, Kisely SR, Castle DJ. A group intervention which assists patients with dual diagnosis reduce their drug use: a randomized controlled trial. Psychol Med 2004;34:983–90 | Study design did not meet criteria |
| Jerome GJ, Dalcin AT, Young DR, Stewart KJ, Crum RM, Latkin C, et al. Rationale, design and baseline data for the Activating Consumers to Exercise through Peer Support (ACE trial): a randomized controlled trial to increase fitness among adults with mental illness. Ment Health Phys Act 2012;5:166–74 | Record was a protocol or registry entry |
| Jerome GJ, Young DR, Dalcin AT, Gennusa JV, Oefinger M, Yu A, et al. Association between weight loss program attendance and weight loss among adults with serious mental illness. Circulation 2014;129 | Population did not meet criteria |
| Johnson JL, Malchy LA, Ratner PA, Hossain S, Procyshyn RM, Bottorff JL, et al. Community mental healthcare providers’ attitudes and practices related to smoking cessation interventions for people living with severe mental illness. Patient Educ Couns 2009;77:289–95 | Study design did not meet criteria |
| Johnstone R, Nicol K, Donaghy M, Lawrie S. Barriers to uptake of physical activity in community-based patients with schizophrenia. J Ment Health 2009;18:523–32 | Intervention did not meet criteria |
| Kavanagh DJ, Young R, White A, Saunders JB, Wallis J, Shockley N, et al. A brief motivational intervention for substance misuse in recent-onset psychosis. Drug Alcohol Rev 2004;23:151–5 | Population did not meet criteria |
| Kikkert M, Goudriaan A, de Waal M, Peen J, Dekker J. Effectiveness of Integrated Dual Diagnosis Treatment (IDDT) in severe mental illness outpatients with a co-occurring substance use disorder. J Subst Abuse Treat 2018;95:35–42 | Intervention did not meet criteria |
| Kilbourne AM, Bramlet M, Barbaresso MM, Nord KM, Goodrich DE, Lai Z, et al. SMI life goals: description of a randomized trial of a collaborative care model to improve outcomes for persons with serious mental illness. Contemp Clin Trials 2014;39:74–85 | Population did not meet criteria |
| Kilbourne AM, Barbaresso MM, Lai Z, Nord KM, Bramlet M, Goodrich DE, et al. Improving physical health in patients with chronic mental disorders: twelve-month results from a randomized controlled collaborative care trial. J Clin Psychiatry 2017;78:129–37 | Population did not meet criteria |
| Kinnafick FE, Papathomas A, Regoczi D. Promoting exercise behaviour in a secure mental health setting: healthcare assistant perspectives. Int J Ment Health Nurs 2018;27:1776–83 | Population did not meet criteria |
| Lamont E, Harris J, McDonald G, Kerin T, Dickens GL. Qualitative investigation of the role of collaborative football and walking football groups in mental health recovery. Ment Health Phys Act 2017;12:116–23 | Population did not meet criteria |
| Landi S, Palumbo D, Margolies P, Salerno AJ, Cleek A, Castaldo E, et al. Implementation trial of a wellness self-management program for individuals with severe mental illness in an Italian day hospital setting: a pilot study. J Psychopathol 2018;24:3–9 | Outcomes did not meet criteria |
| Lawn SJ, Pols RG, Barber JG. Smoking and quitting: a qualitative study with community-living psychiatric clients. Soc Sci Med 2002;54:93–104 | Population did not meet criteria |
| Lawn S, Van Agteren J, Zabeen S, Bertossa S, Barton C, Stewart J. Adapting, pilot testing and evaluating the Kick.it app to support smoking cessation for smokers with severe mental illness: a study protocol. Int J Environ Res Public Health 2018;15:E254 | Record was a protocol or registry entry |
| Lee JG, Ranney LM, Goldstein AO, McCullough A, Fulton-Smith SM, Collins NO. Successful implementation of a wellness and tobacco cessation curriculum in psychosocial rehabilitation clubhouses. BMC Public Health 2011;11:702 | Population did not meet criteria |
| Leutwyler H, Hubbard EM, Jeste DV, Vinogradov S. ‘We’re not just sitting on the periphery’: a staff perspective of physical activity in older adults with schizophrenia. Gerontologist 2013;53:474–83 | Population did not meet criteria |
| Leutwyler H, Hubbard EM, Slater M, Jeste DV. ‘It’s good for me’: physical activity in older adults with schizophrenia. Community Ment Health J 2014;50:75–80 | Intervention did not meet criteria |
| Leutwyler H, Hubbard E, Cooper BA, Dowling G. Impact of a pilot videogame-based physical activity program on walking speed in adults with schizophrenia. Community Ment Health J 2018;54:735–9 | Outcomes did not meet criteria |
| Leyland SD, Currie A, Anderson SD, Bradley E, Ling J. Offering physical activity advice to people with serious mental illness: the beliefs of mental health professionals. Ment Health Phys Act 2018;15:1–6 | Population did not meet criteria |
| Lin JJ, Lee HM, Chan KW, Chang WC, Su W, Honer WG, et al. The impacts of aerobic exercise and mind–body exercise (yoga) on neuro-cognition and clinical symptoms in early psychosis a single-blind radomized controlled clinical trial. Schizophr Res 2014;153:S260 | Outcomes did not meet criteria |
| Lin SS, Sheu SJ, Lee YC, Chiang HH. [The physical activity and life healing in psychiatric patients: taijiguan as an example.] Hu Li Za Zhi 2014;61:46–55 | Intervention did not meet criteria |
| Lin JJX, Lee EHM, Chang WC, Chan SKW, Tse M, Phong PL, et al. Aerobic exercise and yoga hold promises for improving neuro-cognition and symptom in early psychosis. Schizophr Bull 2015;41:S320 | Outcomes did not meet criteria |
| Linhardt A, Krger C, Pogarell O, Weltzer V, Wenig J, Rther T. Implementation and evaluation of the smoking cessation programme ‘the smokers’ group’ in psychiatric inpatients. Eur Psychiatry 2014;29 | Study design did not meet criteria |
| Liu NH, Spaulding WD. Pilot study of a health-focused day program on improving health behaviors, clinical functioning, and perceived wellness in individuals with severe mental illness. Psychol Serv 2010;7:233–41 | Study design did not meet criteria |
| Loh SY, Abdullah A, Abu Bakar AK, Thambu M, Nik Jaafar NR. Structured walking and chronic institutionalized schizophrenia inmates: a pilot RCT study on quality of life. Glob J Health Sci 2015;8:238–48 | Outcomes did not meet criteria |
| Looijmans A, Stiekema A, Bruggeman R, Van DML, Stolk RP, Schoevers RA, et al. Improving cardiometabolic health by adjusting the obesogenic environment in severe mentally ill residential patients: a randomised controlled trial. Eur J Epidemiol 2015;30:796 | Study design did not meet criteria |
| Looijmans A, Stiekema A, Bruggeman R, Van DML, Stolk R, Schoevers R, et al. Improving cardiometabolic health by adjusting the obesogenic environment in severe mentally ill inpatients: a randomised controlled trial. Obes Facts 2016;9:74–5 | Study design did not meet criteria |
| Looijmans A, Stiekema APM, Bruggeman R, van der Meer L, Stolk RP, Schoevers RA, et al. Changing the obesogenic environment to improve cardiometabolic health in residential patients with a severe mental illness: cluster randomised controlled trial. Br J Psychiatry 2017;211:296–303 | Population did not meet criteria |
| Looijmans A, Jörg F, Bruggeman R, Schoevers R, Corpeleijn E. Design of the Lifestyle Interventions for severe mentally ill Outpatients in the Netherlands (LION) trial; a cluster randomised controlled study of a multidimensional web tool intervention to improve cardiometabolic health in patients with severe mental illness. BMC Psychiatry 2017;17:107 | Record was a protocol or registry entry |
| Looijmans A, Jörg F, Bruggeman R, Schoevers RA, Corpeleijn E. Multimodal lifestyle intervention using a web-based tool to improve cardiometabolic health in patients with serious mental illness: results of a cluster randomized controlled trial (LION). BMC Psychiatry 2019;19:339 | Population did not meet criteria |
| Lopez-Jaramillo C, Palacio JD, Vargas C. Effects of a multimodal intervention program in patients with bipolar disorder and schizophrenia. Bipolar Disord 2015;17:130 | Outcomes did not meet criteria |
| Lovell K, Wearden A, Bradshaw T, Tomenson B, Pedley R, Davies LM, et al. An exploratory randomized controlled study of a healthy living intervention in early intervention services for psychosis: the INTERvention to encourage ACTivity, improve diet, and reduce weight gain (INTERACT) study. J Clin Psychiatry 2014;75:498–505 | Population did not meet criteria |
| Lutgens D, Iyer S, Joober R, Brown TG, Norman R, Latimer E, et al. A five-year randomized parallel and blinded clinical trial of an extended specialized early intervention vs. regular care in the early phase of psychotic disorders: study protocol. BMC Psychiatry 2015;15:22 | Intervention did not meet criteria |
| Madigan K, Lawlor E, Brennan D, Turner N, Kinsella A, O’Connor J, et al. A multi-centre, randomised controlled trial of a group psychological intervention for psychosiswith comorbid cannabis dependence over the early course of illness. Schizophr Res 2012;136:S371 | Insufficient data to assess eligibility |
| Madigan K, Brennan D, Lawlor E, Turner N, Kinsella A, O’Connor JJ, et al. A multi-center, randomized controlled trial of a group psychological intervention for psychosis with comorbid cannabis dependence over the early course of illness. Schizophr Res 2013;143:138–42 | Population did not meet criteria |
| Maggouritsa G, Kokaridas D, Theodorakis I, Patsiaouras A, Mouzas O, Dimitrakopoulos S, et al. The effect of a physical activity programme on improving mood profile of patients with schizophrenia. Int J Sport Exerc Psychol 2014;12:273–84 | Outcomes did not meet criteria |
| Magni LR, Ferrari C, Rossi G, Staffieri E, Uberti A, Lamonaca D, et al. Superwellness Program: a cognitive–behavioral therapy-based group intervention to reduce weight gain in patients treated with antipsychotic drugs. Braz J Psychiatry 2017;39:244–51 | Study design did not meet criteria |
| Mahony G, Haracz K, Williams LT. How mental health occupational therapists address issues of diet with their clients: a qualitative study. Aust Occup Ther J 2012;59:294–301 | Population did not meet criteria |
| Mangrum LF, Spence RT, Lopez M. Integrated versus parallel treatment of co-occurring psychiatric and substance use disorders. J Subst Abuse Treat 2006;30:79–84 | Outcomes did not meet criteria |
| Martino S, Carroll KM, Nich C, Rounsaville BJ. A randomized controlled pilot study of motivational interviewing for patients with psychotic and drug use disorders. Addiction 2006;101:1479–92 | Intervention did not meet criteria |
| McDevitt J, Snyder M, Miller A, Wilbur J. Perceptions of barriers and benefits to physical activity among outpatients in psychiatric rehabilitation. J Nurs Scholarsh 2006;38:50–5 | Population did not meet criteria |
| McCann TV, Renzaho A, Mugavin J, Lubman DI. Stigma of mental illness and substance misuse in sub-Saharan African migrants: a qualitative study. Int J Ment Health Nurs 2018;27:956–65 | Population did not meet criteria |
| McDonell MG, Srebnik D, Angelo F, McPherson S, Lowe JM, Sugar A, et al. Randomized controlled trial of contingency management for stimulant use in community mental health patients with serious mental illness. Am J Psychiatry 2013;170:94–101 | Population did not meet criteria |
| McDonell MG, Leickly E, McPherson S, Skalisky J, Nepom JR, Srebnik D, et al. Ethylglucuronide based continency management for alcohol in seriously mentally ill outpatients. Alcohol Clin Exp Res 2016;40(Suppl. 1):188A. | Population did not meet criteria |
| McDonell MG, Leickly E, McPherson S, Srebnik D, Roll JM, Ries R, et al. Treatment for alcohol use disorders in seriously mentally ill adults using the ethyl glucuronide biomarker. Drug Alcohol Depend 2017;171:e137–8 | Population did not meet criteria |
| McDonell MG, Leickly E, McPherson S, Skalisky J, Srebnik D, Angelo F, et al. A randomized controlled trial of ethyl glucuronide-based contingency management for outpatients with co-occurring alcohol use disorders and serious mental illness. Am J Psychiatry 2017;174:370–7 | Population did not meet criteria |
| McKibbin CL, Kitchen KA, Wykes TL, Lee AA. Barriers and facilitators of a healthy lifestyle among persons with serious and persistent mental illness: perspectives of community mental health providers. Community Ment Health J 2014;50:566–76 | Population did not meet criteria |
| Melau M, Jeppesen P, Thorup A, Bertelsen M, Petersen L, Gluud C, et al. The effect of five years versus two years of specialised assertive intervention for first episode psychosis – OPUS II: study protocol for a randomized controlled trial. Trials 2011;12:72 | Intervention did not meet criteria |
| Mericle AA, Alvidrez J, Havassy BE. Mental health provider perspectives on co-occurring substance use among severely mentally ill clients. J Psychoactive Drugs 2007;39:173–81 | Population did not meet criteria |
| Metse AP, Bowman JA, Wye P, Stockings E, Adams M, Clancy R, et al. Evaluating the efficacy of an integrated smoking cessation intervention for mental health patients: study protocol for a randomised controlled trial. Trials 2014;15:266 | Population did not meet criteria |
| Metse AP, Wiggers J, Wye P, Wolfenden L, Freund M, Clancy R, et al. Efficacy of a universal smoking cessation intervention initiated in inpatient psychiatry and continued post-discharge: a randomised controlled trial. Aust N Z J Psychiatry 2017;51:366–81 | Population did not meet criteria |
| Morrens M, Dewilde B, Sabbe B, Dom G, De Cuyper R, Moggi F. Treatment outcomes of an integrated residential programme for patients with schizophrenia and substance use disorder. Eur Addict Res 2011;17:154–63 | Study design did not meet criteria |
| Mueser KT, Glynn SM, Cather C, Xie H, Zarate R, Smith LF, et al. A randomized controlled trial of family intervention for co-occurring substance use and severe psychiatric disorders. Schizophr Bull 2013;39:658–72 | Intervention did not meet criteria |
| Muralidharan A, Niv N, Brown CH, Olmos-Ochoa TT, Fang LJ, Cohen AN, et al. Impact of online weight management with peer coaching on physical activity levels of adults with serious mental illness. Psychiatr Serv 2018;69:1062–8 | Study design did not meet criteria |
| Naeem F, Kingdon D, Turkington D. Cognitive behavior therapy for schizophrenia in patients with mild to moderate substance misuse problems. Cogn Behav Ther 2005;34:207–15 | Study design did not meet criteria |
| Naslund JA. Digital technology for health promotion among individuals with serious mental illness. Diss Abstr Int B Sci Eng 2018;79 | Study design did not meet criteria |
| Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemed J E Health 2015;21:213–16 | Population did not meet criteria |
| Naslund JA, Aschbrenner KA, Bartels SJ. Wearable devices and smartphones for activity tracking among people with serious mental illness. Ment Health Phys Act 2016;10:10–17 | Population did not meet criteria |
| Naslund JA, Aschbrenner KA, Scherer EA, Pratt SI, Wolfe RS, Bartels SJ. Lifestyle intervention for people with severe obesity and serious mental illness. Am J Prev Med 2016;50:145–53 | Population did not meet criteria |
| Naslund JA, Aschbrenner KA, Scherer EA, Pratt SI, Bartels SJ. Health promotion for young adults with serious mental illness. Psychiatr Serv 2017;68:137–43 | Population did not meet criteria |
| Nawaz S, Frounfelker R, Ferron JC, Carpenter-Song EA, Davis K, Brunette MF. Smoking and quitting beliefs, attitudes, and behaviors among smokers with severe mental illness from three race/ethnicity groups. J Dual Diagn 2012;8:180–7 | Population did not meet criteria |
| Nehlin C, Fredriksson A, Oster C. Young female psychiatric patients’ reasons for excessive alcohol use: a qualitative interview study. Ment Health Subst Use 2013;6:315–24 | Population did not meet criteria |
| Noordsy DL, Schwab B, Fox L, Drake RE. The role of self-help programs in the rehabilitation of persons with severe mental illness and substance use disorders. Community Ment Health J 1996;32:71–81 | Study design did not meet criteria |
| O’Connell MJ, Sledge WH, Staeheli M, Sells D, Costa M, Wieland M, Davidson L. Outcomes of a peer mentor intervention for persons with recurrent psychiatric hospitalization. Psychiatr Serv 2018;69:760–7 | Population did not meet criteria |
| Oertel-Knöchel V, Mehler P, Thiel C, Steinbrecher K, Malchow B, Tesky V, et al. Effects of aerobic exercise on cognitive performance and individual psychopathology in depressive and schizophrenia patients. Eur Arch Psychiatry Clin Neurosci 2014;264:589–604 | Outcomes did not meet criteria |
| Oluwoye O, Leickly E, Skalisky J, McPherson S, Hirchak K, Srebnik D, et al. Serious mental illness in heavy drinkers is associated with poor treatment outcomes in outpatients with co-occurring disorders. Int J Ment Health Addict 2018;16:672–9 | Population did not meet criteria |
| Oluwoye O, Skalisky J, Burduli E, Chaytor NS, McPherson S, Murphy SM, et al. Using a randomized controlled trial to test whether modifications to contingency management improve outcomes for heavy drinkers with serious mental illness. Contemp Clin Trials 2018;69:92–8 | Record was a protocol or registry entry |
| Owen RR, Drummond KL, Viverito KM, Marchant K, Pope SK, Smith JL, Landes RD. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci 2013;8:120 | Record was a protocol or registry entry |
| Peckham E, Bradshaw TJ, Brabyn S, Knowles S, Gilbody S. Exploring why people with SMI smoke and why they may want to quit: baseline data from the SCIMITAR RCT. J Psychiatr Ment Health Nurs 2016;23:282–9 | Study design did not meet criteria |
| Pedley R, Lovell K, Bee P, Bradshaw T, Gellatly J, Ward K, et al. Collaborative, individualised lifestyle interventions are acceptable to people with first episode psychosis; a qualitative study. BMC Psychiatry 2018;18:111 | Population did not meet criteria |
| Pelham TW, Campagna PD, Ritvo PG, Birnie WA. The effects of exercise therapy on clients in a psychiatric rehabilitation program. Psychosoc Rehabil J 1993;16:75–84 | Outcomes did not meet criteria |
| Pelletier JR, Nguyen M, Bradley K, Johnsen M, McKay C. A study of a structured exercise program with members of an ICCD Certified Clubhouse: program design, benefits, and implications for feasibility. Psychiatr Rehabil J 2005;29:89–96 | Study design did not meet criteria |
| Petersen L, Jeppesen P, Thorup A, Ohlenschlaeger J, Krarup G, Ostergård T, et al. Substance abuse and first-episode schizophrenia-spectrum disorders. The Danish OPUS trial. Early Interv Psychiatry 2007;1:88–96 | Intervention did not meet criteria |
| Petry NM, Alessi SM, Rash CJ. A randomized study of contingency management in cocaine-dependent patients with severe and persistent mental health disorders. Drug Alcohol Depend 2013;130:234–7 | Population did not meet criteria |
| Pettersen H, Ruud T, Ravndal E, Landheim A. Walking the fine line: self-reported reasons for substance use in persons with severe mental illness. Int J Qual Stud Health Well-being 2013;8:21968 | Outcomes did not meet criteria |
| Pettersen H, Ruud T, Ravndal E, Havnes I, Landheim A. Engagement in assertive community treatment as experienced by recovering clients with severe mental illness and concurrent substance use. Int J Ment Health Syst 2014;8:40 | Intervention did not meet criteria |
| Prochaska JJ, Hall SE, Delucchi K, Hall SM. Efficacy of initiating tobacco dependence treatment in inpatient psychiatry: a randomized controlled trial. Am J Public Health 2014;104:1557–65 | Population did not meet criteria |
| Provencher MD, Bélanger MÈ, Shriqui C, Lachance I, Bonneville S. [Psychoeducation for overweight patients with psychiatric disorders: the Wellness program developed in Quebec.] Encephale 2016;42:201–7 | Population did not meet criteria |
| Ragaisis KM. Psychiatric Inpatient Nurses’ Perceptions of Using Motivational Interviewing. Issues Ment Health Nurs 2017;38:945–55 | Population did not meet criteria |
| Ratschen E, Britton J, Doody GA, McNeill A. Smoke-free policy in acute mental health wards: avoiding the pitfalls. Gen Hosp Psychiatry 2009;31:131–6 | Population did not meet criteria |
| Ratschen E, Britton J, Doody G, McNeill A. Smoking attitudes, behaviour and nicotine dependence among mental health acute inpatients: an exploratory study. Int J Soc Psychiatry 2010;56:107–18 | Population did not meet criteria |
| Rebgetz S, Hides L, Kavanagh DJ, Choudhary A. Natural recovery from cannabis use in people with psychosis: a qualitative study. J Dual Diagn 2015;11:179–83 | Intervention did not meet criteria |
| Rezaie L, Shafaroodi N, Philips D. The barriers to participation in leisure time physical activities among Iranian women with severe mental illness: a qualitative study. Ment Health Phys Act 2017;13:171–7 | Intervention did not meet criteria |
| Ridgely MS, Jerrell JM. Analysis of three interventions for substance abuse treatment of severely mentally ill people. Community Ment Health J 1996;32:561–72 | Study design did not meet criteria |
| Roberts SH, Bailey JE. Incentives and barriers to lifestyle interventions for people with severe mental illness: a narrative synthesis of quantitative, qualitative and mixed methods studies. J Adv Nurs 2011;67:690–708 | Study design did not meet criteria |
| Romain AJ, Longpre-Poirier C, Tannous M, Abdel-Baki A. Preferences of physical activity and perception of health behaviour in early psychosis individuals. Early Interv Psychiatry 2016;10:193 | Study design did not meet criteria |
| Romain AJ, Fankam C, Karelis A, Letendre E, Mikolajacks G, Stip E, et al. Effect of interval training on metabolic risk factors in overweight individuals with psychosis: a randomized controlled trial. Schizophr Bull 2018;44(Suppl. 1):S17 | Study design did not meet criteria |
| Rosen MI, Rounsaville BJ, Ablondi K, Black AC, Rosenheck RA. Advisor-Teller Money Manager (ATM) therapy for substance use disorders. Psychiatr Serv 2010;61:707–13 | Population did not meet criteria |
| Rosenbaum S, Ward PB. ‘At least 50% of young people experiencing a first episode psychosis should be engaged in age-appropriate physical activity’. Achieving a healthy active lives target for physical activity participation. Early Interv Psychiatry 2014;8:91 | Study design did not meet criteria |
| Rowe M, Bellamy C, Baranoski M, Wieland M, O’Connell MJ, Benedict P, et al. A peer-support, group intervention to reduce substance use and criminality among persons with severe mental illness. Psychiatr Serv 2007;58:955–61 | Population did not meet criteria |
| Sampogna G, Fiorillo A, Luciano M, Del Vecchio V, Steardo L, Pocai B, et al. A randomized controlled trial on the efficacy of a psychosocial behavioral intervention to improve the lifestyle of patients with severe mental disorders: study protocol. Front Psychiatry 2018;9:235 | Record was a protocol or registry entry |
| Shiner B, Whitley R, Van Citters AD, Pratt SI, Bartels SJ. Learning what matters for patients: qualitative evaluation of a health promotion program for those with serious mental illness. Health Promot Int 2008;23:275–82 | Population did not meet criteria |
| Shor R, Shalev A. Identifying barriers to improving the wellness of persons with severe mental illness in community residential mental health facilities. Soc Work Ment Health 2013;11:334–48 | Intervention did not meet criteria |
| Shor R, Shalev A. Barriers to involvement in physical activities of persons with mental illness. Health Promot Int 2016;31:116–23 | Study design did not meet criteria |
| Silva BA, Cassilhas RC, Attux C, Cordeiro Q, Gadelha AL, Telles BA, et al. A 20-week program of resistance or concurrent exercise improves symptoms of schizophrenia: results of a blind, randomized controlled trial. Braz J Psychiatry 2015;37:271–9 | Intervention did not meet criteria |
| Skrinar GS, Huxley NA, Hutchinson DS, Menninger E, Glew P. The role of a fitness intervention on people with serious psychiatric disabilities. Psychiatr Rehabil J 2005;29:122–7 | Intervention did not meet criteria |
| Smeerdijk M, Keet R, Dekker N, van Raaij B, Krikke M, Koeter M, et al. Motivational interviewing and interaction skills training for parents to change cannabis use in young adults with recent-onset schizophrenia: a randomized controlled trial. Psychol Med 2012;42:1627–36 | Population did not meet criteria |
| Smeerdijk M, Keet R, van Raaij B, Koeter M, Linszen D, de Haan L, Schippers G. Motivational interviewing and interaction skills training for parents of young adults with recent-onset schizophrenia and co-occurring cannabis use: 15-month follow-up. Psychol Med 2015;45:2839–48 | Population did not meet criteria |
| Smelson D, Kalman D, Losonczy MF, Kline A, Sambamoorthi U, Hill LS, et al. A brief treatment engagement intervention for individuals with co-occurring mental illness and substance use disorders: results of a randomized clinical trial. Community Ment Health J 2012;48:127–32 | Intervention did not meet criteria |
| Smith J, Williams B, Band M, Hickman D, Bradley E, Richardson J, et al. SHAPE (Supporting Health And Promoting Exercise) project for young people with psychosis. Early Interv Psychiatry 2014;8:122 | Study design did not meet criteria |
| Smith RC, Amiaz R, Si TM, Maayan L, Jin H, Boules S, et al. Varenicline effects on smoking, cognition, and psychiatric symptoms in schizophrenia: a double-blind randomized trial. PLOS ONE 2016;11:e0143490 | Intervention did not meet criteria |
| Snyder M, McDevitt J, Painter S. Smoking cessation and serious mental illness. Arch Psychiatr Nurs 2008;22:297–304 | Intervention did not meet criteria |
| Stasiewicz PR, Bradizza CM, Maisto SA. Alcohol problem resolution in the severely mentally ill: a preliminary investigation. J Subst Abuse 1997;9:209–22 | Population did not meet criteria |
| Steinberg ML, Ziedonis DM, Krejci JA, Brandon TH. Motivational interviewing with personalized feedback: a brief intervention for motivating smokers with schizophrenia to seek treatment for tobacco dependence. J Consult Clin Psychol 2004;72:723–8 | Intervention did not meet criteria |
| Stiekema APM, Looijmans A, van der Meer L, Bruggeman R, Schoevers RA, Corpeleijn E, Jörg F. Effects of a lifestyle intervention on psychosocial well-being of severe mentally ill residential patients: ELIPS, a cluster randomized controlled pragmatic trial. Schizophr Res 2018;199:407–13 | Outcomes did not meet criteria |
| Stockings EA, Bowman JA, Wiggers J, Baker AL, Terry M, Clancy R, et al. A randomised controlled trial linking mental health inpatients to community smoking cessation supports: a study protocol. BMC Public Health 2011;11:570 | Population did not meet criteria |
| Stockings EA, Bowman JA, Baker AL, Terry M, Clancy R, Wye PM, et al. Impact of a postdischarge smoking cessation intervention for smokers admitted to an inpatient psychiatric facility: a randomized controlled trial. Nicotine Tob Res 2014;16:1417–28 | Population did not meet criteria |
| Stockings EA, Bowman JA, Bartlem KM, McElwaine KM, Baker AL, Terry M, et al. Quality of implementation of a smoke-free policy in an inpatient psychiatric facility: association with patient acceptability. Asia Pac J Clin Oncol 2014;10:166–7 | Study design did not meet criteria |
| Stockings EA, Bowman JA, Bartlem KM, McElwaine KM, Baker AL, Terry M, et al. Implementation of a smoke-free policy in an inpatient psychiatric facility: patient-reported adherence, support, and receipt of nicotine-dependence treatment. Int J Ment Health Nurs 2015;24:342–9 | Study design did not meet criteria |
| Strong JR, Lemaire GS, Murphy LS. Assessment of a chronic disease self-management program to increase physical activity of adults with severe mental illness. Arch Psychiatr Nurs 2017;31:137–40 | Study design did not meet criteria |
| Strong Kinnaman JE, Slade E, Bennett ME, Bellack AS. Examination of contingency payments to dually-diagnosed patients in a multi-faceted behavioral treatment. Addict Behav 2007;32:1480–5 | Population did not meet criteria |
| Su CY, Wang PW, Lin YJ, Tang TC, Liu MF, Chen MD. The effects of aerobic exercise on cognition in schizophrenia: a 3-month follow-up study. Psychiatry Res 2016;244:394–402 | Outcomes did not meet criteria |
| Sundgren E, Hallqvist J, Fredriksson L. Health for smokers with schizophrenia – a struggle to maintain a dignified life. Disabil Rehabil 2016;38:416–22 | Intervention did not meet criteria |
| Svatkova A, Mandl RC, Scheewe TW, Cahn W, Kahn RS, Hulshoff Pol HE. Physical exercise keeps the brain connected: biking increases white matter integrity in patients with schizophrenia and healthy controls. Schizophr Bull 2015;41:869–78 | Population did not meet criteria |
| Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. J Nerv Ment Dis 1999;187:630–5 | Population did not meet criteria |
| Teasdale S, Harris S, Rosenbaum S, Watkins A, Samaras K, Curtis J, Ward PB. Individual dietetic consultations in first episode psychosis: a novel intervention to reduce cardiometabolic risk. Community Ment Health J 2015;51:211–14 | Study design did not meet criteria |
| Teasdale SB, Ward PB, Rosenbaum S, Watkins A, Curtis J, Kalucy M, Samaras K. A nutrition intervention is effective in improving dietary components linked to cardiometabolic risk in youth with first-episode psychosis. Br J Nutr 2016;115:1987–93 | Study design did not meet criteria |
| Teferra S, Hanlon C, Alem A, Jacobsson L, Shibre T. Khat chewing in persons with severe mental illness in Ethiopia: a qualitative study exploring perspectives of patients and caregivers. Transcult Psychiatry 2011;48:455–72 | Intervention did not meet criteria |
| Teferra S, Shibre T. Perceived causes of severe mental disturbance and preferred interventions by the Borana semi-nomadic population in southern Ethiopia: a qualitative study. BMC Psychiatry 2012;12:79 | Population did not meet criteria |
| Tidey JW, O’Neill SC, Higgins ST. Contingent monetary reinforcement of smoking reductions, with and without transdermal nicotine, in outpatients with schizophrenia. Exp Clin Psychopharmacol 2002;10:241–7 | Study design did not meet criteria |
| Trainor K, Leavey G. Barriers and facilitators to smoking cessation among people with severe mental illness: a critical appraisal of qualitative studies. Nicotine Tob Res 2017;19:14–23 | Study design did not meet criteria |
| Ursuliak Z, Milliken H, Morgan N. Wellness program for people with early psychosis: promoting skills and attitudes for recovery. Psychiatr Serv 2015;66:105 | Study design did not meet criteria |
| Ussher M, Stanbury L, Cheeseman V, Faulkner G. Physical activity preferences and perceived barriers to activity among persons with severe mental illness in the United Kingdom. Psychiatr Serv 2007;58:405–8 | Study design did not meet criteria |
| Vandyk AD, Baker C. Qualitative descriptive study exploring schizophrenia and the everyday effect of medication-induced weight gain. Int J Ment Health Nurs 2012;21:349–57 | Intervention did not meet criteria |
| Vaughan K, McConaghy N. Megavitamin and dietary treatment in schizophrenia: a randomised, controlled trial. Aust N Z J Psychiatry 1999;33:84–8 | Outcomes did not meet criteria |
| Verhaeghe N, Clays E, Vereecken C, De Maeseneer J, Maes L, Van Heeringen C, et al. Health promotion in individuals with mental disorders: a cluster preference randomized controlled trial. BMC Public Health 2013;13:657 | Population did not meet criteria |
| Vessichio JC, George TP. Treating Nicotine Dependence in Schizophrenic Individuals: Effectiveness of Bupropion – 1. URL: https://clinicaltrials.gov/ct2/show/NCT00124683 (accessed 30 April 2021) | Record was a protocol or registry entry |
| Vilardaga R, Rizo J, Palenski P, Mannelli P, Oliver JA, McClernon FJ. Pilot randomized controlled trial of a novel smoking cessation app designed for individuals with co-occurring tobacco dependence and serious mental illness. Nicotine Tob Res 2019;31:31 | Population did not meet criteria |
| Ward TD. The lived experience of adults with bipolar disorder and comorbid substance use disorder. Issues Ment Health Nurs 2011;32:20–7 | Intervention did not meet criteria |
| Wärdig RE, Bachrach-Lindström M, Foldemo A, Lindström T, Hultsjö S. Prerequisites for a healthy lifestyle-experiences of persons with psychosis. Issues Ment Health Nurs 2013;34:602–10 | Intervention did not meet criteria |
| Weinberger AH, Vessicchio JC, Sacco KA, Creeden CL, Chengappa KN, George TP. A preliminary study of sustained-release bupropion for smoking cessation in bipolar disorder. J Clin Psychopharmacol 2008;28:584–7 | Intervention did not meet criteria |
| Weiner E, Buchholz A, Coffay A, Liu F, McMahon RP, Buchanan RW, Kelly DL. Varenicline for smoking cessation in people with schizophrenia: a double blind randomized pilot study. Schizophr Res 2011;129:94–5 | Intervention did not meet criteria |
| Weiner E, Ball MP, Buchholz AS, Gold JM, Evins AE, McMahon RP, Buchanan RW. Bupropion sustained release added to group support for smoking cessation in schizophrenia: a new randomized trial and a meta-analysis. J Clin Psychiatry 2012;73:95–102 | Intervention did not meet criteria |
| Weinstein LC. Beyond lifestyle factors: Exploring the role of the social determinants of health in weight loss attempts in people with serious mental illness living in supportive housings settings. Diss Abstr Int B Sci Eng 2018;79 | Could not obtain dissertation |
| Weiss RD, Griffin ML, Greenfield SF, Najavits LM, Wyner D, Soto JA, Hennen JA. Group therapy for patients with bipolar disorder and substance dependence: results of a pilot study. J Clin Psychiatry 2000;61:361–7 | Study design did not meet criteria |
| Weiss RD, Griffin ML, Kolodziej ME, Janis IB, Hennen J. A randomized controlled trial of integrated group therapy for patients with bipolar disorder & substance dependence. Alcohol Clin Exp Res 2005;29:158A | Intervention did not meet criteria |
| Weiss RD, Griffin ML, Kolodziej ME, Greenfield SF, Najavits LM, Daley DC, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry 2007;164:100–7 | Intervention did not meet criteria |
| Weiss RD, Griffin ML, Jaffee WB, Bender RE, Graff FS, Gallop RJ, Fitzmaurice GM. A ‘community-friendly’ version of integrated group therapy for patients with bipolar disorder and substance dependence: a randomized controlled trial. Drug Alcohol Depend 2009;104:212–19 | Intervention did not meet criteria |
| Weissman EM, Moot DM, Essock SM. What do people with schizophrenia think about weight management? Psychiatr Serv 2006;57:724–5 | Study design did not meet criteria |
| Wells ME. Increasing motivation to stop smoking among persons with schizophrenia and other chronic mental illnesses. Diss Abstr Int B Sci Eng 2003;63:3946 | Could not obtain dissertation |
| Westman J, Eberhard J, Gaughran FP, Lundin L, Stenmark R, Edman G, et al. Outcome of a psychosocial health promotion intervention aimed at improving physical health and reducing alcohol use in patients with schizophrenia and psychotic disorders (MINT). Schizophr Res 2019;208:138–44 | Study design did not meet criteria |
| Williams JM, Steinberg ML, Zimmermann MH, Gandhi KK, Stipelman B, Budsock PD, Ziedonis DM. Comparison of two intensities of tobacco dependence counseling in schizophrenia and schizoaffective disorder. J Subst Abuse Treat 2010;38:384–93 | Intervention did not meet criteria |
| Williams JM, Anthenelli RM, Morris CD, Treadow J, Thompson JR, Yunis C, George TP. A randomized, double-blind, placebo-controlled study evaluating the safety and efficacy of varenicline for smoking cessation in patients with schizophrenia or schizoaffective disorder. J Clin Psychiatry 2012;73:654–60 | Intervention did not meet criteria |
| Williams J, Stubbs B, Gaughran F, Craig T. ‘Walk This Way’ - a pilot of a health coaching intervention to reduce sedentary behaviour and increase low intensity exercise in people with serious mental illness: study protocol for a randomised controlled trial. Trials 2016;17:594 | Study design did not meet criteria |
| Wilson SM, Thompson AC, Currence ED, Thomas SP, Dedert EA, Kirby AC, et al. Patient-informed treatment development of behavioral smoking cessation for people with schizophrenia. Behav Ther 2019;50:395–409 | Study design did not meet criteria |
| Wright K, Armstrong T, Taylor A, Dean S. ‘It’s a double edged sword’: a qualitative analysis of the experiences of exercise amongst people with bipolar disorder. J Affect Disord 2012;136:634–42 | Intervention did not meet criteria |
| Wu BS, Weinberger AH, Mancuso E, Wing VC, Haji-Khamneh B, Levinson AJ, George TP. A Preliminary feasibility study of varenicline for smoking cessation in bipolar disorder. J Dual Diagn 2012;8:131–2 | Intervention did not meet criteria |
| Wye P, Bowman J, Wiggers J, Baker A, Carr V, Terry M, et al. Providing nicotine dependence treatment to psychiatric inpatients: the views of Australian nurse managers. J Psychiatr Ment Health Nurs 2010;17:319–27 | Population did not meet criteria |
| Xiao S, Baker C, Oyewumi LK. Psychosocial processes influencing weight management among persons newly prescribed atypical antipsychotic medications. J Psychiatr Ment Health Nurs 2012;19:241–7 | Intervention did not meet criteria |
| Xiong G, Ziegahn L, Schuyler B, Rowlett A, Cassady D. Improving dietary and physical activity practices in group homes serving residents with severe mental illness. Prog Community Health Partnersh 2010;4:279–88 | Intervention did not meet criteria |
| Yarborough BJ, Leo MC, Yarborough MT, Stumbo S, Janoff SL, Perrin NA, Green CA. Improvement in body image, perceived health, and health-related self-efficacy among people with serious mental illness: the STRIDE study. Psychiatr Serv 2016;67:296–301 | Outcomes did not meet criteria |
| Zhu Y, Jiang H, Su H, Zhong N, Li R, Li X, et al. A newly designed mobile-based computerized cognitive addiction therapy app for the improvement of cognition impairments and risk decision making in methamphetamine use disorder: randomized controlled trial. JMIR Mhealth Uhealth 2018;6:e10292 | Population did not meet criteria |
Appendix 3 Population characteristics of included randomised controlled trials
| Study (first author, year of publication, country) | Sample size (n) | Age (years) (range, or mean and SD) | Female (%) | Ethnicity | Antipsychotic use | Mental health diagnoses (%) |
|---|---|---|---|---|---|---|
| Attux 2013,45 Brazil | Intervention, 60; control, 66 | Intervention: 36.2 (9.9); control: 38.3 (10.7) | Intervention: 38; control: 42 |
|
|
|
| Baker 2006,46 Australia | Intervention, 147; control, 151 | 37.24 (11.09) | 48 | NR, 84.9% Australian born | 82.9% on antipsychotic medication | 56.7% schizophrenia or schizoaffective disorder; 6.4% severe depression with psychosis; 9.1% bipolar disorder, mania; 27.95% other psychoses |
| Baker 2015,47 Australia | Intervention, 122; control, 113 | 41.6 (11.1) | 41 | NR, 84% Australian born | NR | 59% schizophrenia spectrum disorders, 22% bipolar disorder, 19% non-organic psychotic syndrome |
| Battaglia 2013,48 Italy | Intervention, 10; control, 8 | Intervention: 36.00 (5.00); control: 35.00 (4.00) | 0 | NR | 100% | Schizophrenia or schizoaffective disorder (100%) |
| Bechdolf 2012,49 Germany | Intervention, 30; control, 30 | Intervention: 31.53 (8.9); control: 31.60 (10.2) | 28 | NR | Intervention: 83.3%; control: 93.3% | Schizophrenia or schizoaffective disorder (83.33%), substance-induced psychosis (16.67%) |
| Beebe 2005,51 USA | Intervention, 4; control, 6 | 52 (range 40–63) | 20 | White (80%), African American (20%) | > 90% | Schizophrenia or any subtype (100%) |
| Beebe 2011,50 USA | Intervention, 48; control, 49 | 46.9 (2) | 47.40 | White (54.6%), African American (44.4%), Asian (1%) | NR | Schizophrenia (28.9%), schizoaffective (71.1%) |
| Bonfioli 2018,52 Italy | Intervention, 169; control, 156 | Intervention: 44.6 (10.3); control: 47.5 (10.8) | Intervention: 46.7; control: 46.8 | NR | NR | Schizophrenia and functional psychoses (intervention, 69.8%; control, 66%), affective psychoses (intervention, 30.2%; control, 34%) |
| Bonsack 2011,53 Switzerland | Intervention, 30; control, 32 | 25 (17) | 13 | NR | NR | 100% psychoses (59.4% schizophrenia, 15.6% schizotypal disorder, 12.5% schizoaffective disorder, 4% other) |
| Brar 2005,54 USA | Intervention, 34; control, 37 | Intervention: 40.0 (10.1); control: 40.5 (10.6) | Intervention: 52.9; control: 64.9 | White (intervention, 52.9%; control, 45.9%), Hispanic (intervention, 2.9%; control, 13.5%), black (intervention, 38.2%; control, 32.4%), Asian (intervention, 5.9%; control 5.4%), other (intervention, 0%; control, 2.7%) | 100% risperidone | Schizophrenia (intervention, 61.8%; control, 45.9%), schizoaffective disorder (intervention, 38.2%; control, 54.1%) |
| Brody 2017,55 USA | Intervention, 14; control, 14 | Combination extended treatment: 56.3 (10.6); control: 57.5 (7.6) | 0 |
|
100%; atypical, 79% | Schizophrenia (100%) |
| Brown 2006,57 UK | Intervention, 15; control, 13 | Intervention: 45.1; control: 41.7 | Intervention: 100; control: 69 | NR | NR | Psychosis/major affective illness/severe personality disorder (100%) |
| Brown 2011,56 USA | Intervention, 47; control, 42 | 44.6 (10.9) | 61 (completers, 39%) | Completers: 60% white, 34% African American, 6% other | 100% | NR |
| Brunette 2020,58 USA | Smoking intervention, 78; computerised education, 84 | 45.91 (11.32) | 33.30 | 53% black | NR | 100% schizophrenia |
| Christiansen 2018,59 USA | Intervention, 118; control, 104 | Intervention: 43.8 (9.9); control: 43.6 (10.0) | Intervention: 49.0; control: 46.7 | Black (intervention, 20.8%; control, 32.9%), Hispanic (intervention, 8.4%; control, 5.8%) | NR | Schizophrenia (intervention, 51.4%; control, 46.8%), bipolar disorder (intervention, 51.4%; control, 60.6%), major affective disorder (intervention, 50.5%; control, 48.9%), anxiety disorder (intervention, 39.4%; control, 50.0%), alcoholism (intervention, 12.8%; control, 11.7%), other drug abuse disorder (intervention, 9.2%; control, 8.5%) |
| Cordes 2011,60 Germany | Intervention, 36; control, 38 | Intervention: 38.2 (11.2); control: 35.8 (10.9) | Intervention: 58.3; control: 28.9 | NR | 100% | Schizophrenia or schizoaffective disorder (100%) |
| Daumit 2013,61 USA | Intervention, 144; control, 147 | Intervention: 46.6 (11.5); control: 44.1 (11.0) | Intervention: 48.6; control: 51.0 | 56% white, 38.1% black, 5.8% other | 89.7% any antipsychotic; 82.8% atypicals, 22.3% clozapine or olanzapine | Schizophrenia (intervention, 30.6%; control, 27.9%), schizoaffective disorder (intervention, 28.5%; control, 29.3%), bipolar disorder (intervention, 19.4%; control, 24.5%), major depression (intervention, 12.5%; control, 11.6%), other (intervention, 9.0%; control, 6.8%) |
| Evans 2005,62 Australia | Intervention, 29; control, 22 | Intervention: 34.6 (9.6); control: 33.6 (11.6) | Intervention: 62; control: 50 | NR | 100% olanzapine | Schizophrenia (intervention, 34%; control, 27%), schizoaffective (intervention, 32%; control, 14%), schizophreniform psychosis (intervention, 14%; control, 27%), bipolar (intervention, 14%; control, 18%), depression (intervention, 6%; control, 14%) |
| Fernández Guijarro 2019,63 Spain | Intervention, 21; control, 20 | 46.98 (9.18) | 32.80 | NR | 9.8% first-generation antipsychotics, 90.2% second-generation antipsychotics | 67.2% schizophrenia, 16.4% schizoaffective disorder, 8.2% bipolar disorder, 4.9% delusional disorder, 3.3% major depression |
| Forsberg 2008,64 Sweden | Intervention, 23; control, 14 | 41 | 39 | NR | 73% | Schizophrenia 56%, bipolar disorder 7%, other psychotic diseases 17%, other psychiatric diagnosis 20% |
| Frank 2015,65 USA | Intervention, 61; control, 61 | Intervention: 41.8 (9.5); control: 41.4 (9.7) | NR | NR | NR | Bipolar disorder I (100%) |
| Ganguli 2011,66 India | 260 | NR | NR | NR | NR | 100% schizophrenia |
| Gaughran 2017,67 UK | Intervention, 213; control, 193 | Intervention: 43.76 (10.09); control: 44.65 (10.17) | Intervention: 45.1; control: 39.4 | 55% white, 34% black, 7% mixed and other, 4% Asian | NR | 100% with a diagnosis of a psychotic disorder (ICD-10 codes F20-F29, F31.2, F31.5) |
| George 2000,68 USA | Intervention, 28; control, 17 | Intervention: 41.6 (7.9); control: 36.6 (9.5) | Intervention: 35.7; control: 29.4 | 62% white, 29% black, 9% Hispanic | 60% typical antipsychotics, 40% atypical antipsychotics | 42% schizophrenia, 58% schizoaffective disorder |
| Gilbody 2019,69 UK | Intervention, 265; control, 261 | Intervention: 46.5 (12.5); control: 45.5 (11.7) | Intervention: 40; control: 43 | NR | NR | Bipolar disorder (intervention, 22%; control, 21%), schizoaffective disorder (intervention, 10%; control, 16%), schizophrenia (intervention, 52%; control, 48%), other psychotic disorder (intervention, 16%; control, 15%) |
| Gillhoff 2010,70 Switzerland | Intervention, 26; control, 24 | Intervention: 48.1 (11.5); control: 48.9 (12.0) | Intervention: 41.7; control: 50 | NR | 50% antipsychotics, 100% weight-increasing drugs | 100% bipolar disorder |
| Graham 2016,71 UK | Intervention, 18; control, 18 | Intervention: 39.5 (11.12); control: 37.69 (11.11) | Intervention: 16.7; control: 13.8 | 47% white, 25% black, 10% mixed, 17% Asian | NR | 61% schizophrenia, 8.5% schizoaffective disorder, 1.7% other psychosis, 28.8% bipolar disorder |
| Green 2015,72 USA | Intervention, 104; control, 96 | Intervention: 46.2 (11.4); control: 48.3 (9.7) | Intervention: 72.1; control: 71.9 | 88% white, 12% non-white | 91% atypical antipsychotics | Schizophrenia spectrum disorder (intervention, 31%; control, 27%), bipolar disorder or affective psychosis (intervention, 71%; control, 67%), PTSD (intervention, 2%; control, 2%) |
| Hjorth 2014,73 Denmark | Intervention, 77; control, 97 | Intervention:
|
Intervention: 41.2; control: 49.5 | All but three were white (two Innuits and one Indian) | N/A |
|
Control:
|
||||||
| Hjorthøj 2013,74 Denmark | Intervention, 52; control, 51 | Intervention: 26.6 (6.3); control: 27.1 (6.3) | Intervention: 26.9; control: 21.6 | NR, intervention: 82.7% were born in Denmark; control: 78.4% were born in Denmark | N/A |
|
| Holt 2019,75 UK | Intervention, 207; control, 205 | Intervention: 40 (11.3); control: 40.1 (11.5) | Intervention: 44.4; control: 53.7 |
|
|
Intervention: schizophrenia – ICD-10 = F20, 70%; ICD-10 = F25, 14.5%; first-episode psychosis – 15.5% Control: schizophrenia – ICD-10 = F20, 67.3%; ICD-10 = F25, 17.6%; first-episode psychosis – 15.1% |
| Iglesias-García 2010,76 UK | Intervention, 7; control, 7 | 39.9 (11.3) | 21.4 | N/A | Whole study: 28.6% clozapine, 21.4% olanzapine, 21.4% aripiprazole, 21.4% fluphenazine decanoate, 7.1% risperidone | Schizophrenia (100%) |
| Jean-Baptiste 2007,77 USA | Intervention, 9; control, 9 | Intervention: 52.37; control: 40.73 | Intervention: 77.8; control: 22.2 |
|
Across whole study: clozapine, 38.9%; olanzapine, 38.9%; risperidone, 22.2%; haloperidol, 11.1%; perphenazine, 11.1%; thiothixene, 5.6%; fluphenazine, 5.6%; quetiapine, 5.6%; ziprasidone, 5.6% |
|
| Jones 2019,78 UK | Intervention, 24; control, 20 | 40 | 48 | 91% white | NR | 100% bipolar disorder
|
| Kaltsatou 2015,79 Greece | Intervention, 16; control, 15 | Intervention: 59.5 (19.6); control: 60.4 (8.6) | Intervention: 12.5; control: 26.7 | N/A | Just says that medication included haloperidol, fluphenazine decanoate, risperidone, olanzapine, quetiapine | Schizophrenia (100%) |
| Khazaal 2007,80 Switzerland | Intervention, 31; control, 30 | Intervention: 43 (9.8); control: 38.3 (10.4) | Intervention: 58; control: 50 | N/A |
|
|
| Kilbourne 2012,81 USA | Intervention, 32; control, 33 | Intervention: 47.2 (11.8); control: 43.4 (13.6) | Intervention: 56; control: 66 |
|
|
Bipolar disorder (type 1 or 2 or not otherwise specified) (100%) |
| Kwon 2006,82 the Republic of Korea | Intervention, 33; control, 15 | Intervention: 32 (9.22); control: 29.8 (6.07) | Intervention: 23/33 (70%); control: 10/15 (67%) | N/A | Olanzapine (100%) | Schizophrenia or schizoaffective disorder (100%) |
| Lee 2014,83 USA | Intervention, 8; control, 8 | 44.09 (7.6) | 45.5 | 64% white | N/A | N/A |
| Littrell 2003,84 USA | Intervention, 35; control, 35 | Intervention: 33.66 (9.23); control: 34.51 (9.99) | Intervention: 37; control: 40 |
|
|
|
| Marzolini 2009,85 Canada | Intervention, 7; control, 6 | Intervention: 43 (SEM = 3); control: 46.7 (SEM = 5) | Intervention: 43; control: 33 | NR |
|
Schizophrenia or schizoaffective disorder (100%) |
| Masa-Font 2015,86 Spain | Intervention, 169; control, 163 | Intervention: 46.3 (8.9); control: 47.1 (9.9) | Intervention: 45; control: 45.4 | NR | NR |
|
| Mauri 2008,87 Italy | Intervention, 15; control, 18 | 38.9 (range 19–60) | Intervention: 53.3; control: 62.1 | NR | 100% | Bipolar I disorder (83.6%), bipolar II disorders (4.1%), schizoaffective disorders (10.2%), psychotic depression (2%) |
| McCreadie 2005,88 Scotland | Fruit and vegetable with instruction, 32; fruit and vegetable, 37; control, 33 | 45 (13) | 29 | NR | NR | Schizophrenia (100%) |
| McKibbin 2006,89 USA | Intervention, 28; control, 29 | Control: 54.8 (8.2); intervention: 53.1 (10.4) | Control: 37.9; intervention: 32.1 |
|
NR |
|
| Melamed 2008,90 Israel | Intervention, 28; control, 31 | 46.18 (11.93) | 27 | NR | 91.50% | Schizophrenia or schizoaffective disorder (100%) |
| Methapatara 2011,91 Thailand | Intervention, 32; control, 32 | Intervention: 43.16 (9.27); control: 37.59 (10.83) | Intervention: 28.12; control: 43.75 | NR | Intervention: 43.8%; control: 43.8% | Schizophrenia (100%) |
| Milano 2007,92 Italy | Intervention, 22; control, 14 | Intervention: 46; control: 45 | Intervention: 54.5; control: 57.1 | NR | 100% | Schizophrenia or maniacal episodes in bipolar disease (100%) |
| Osborn 2018,93 UK | Intervention, 155; control, 172 | 51 (10) | Intervention: 57; control: 49 |
|
|
|
| Peckham 2017,94 UK | Intervention, 46; control, 51 | Intervention: 47.8 (12.4); control: 45.9 (12.8) | Intervention: 30.4; control: 49.0 | White British (intervention, 93.3%; control, 80.4%), white Irish (intervention, 0.0%; control, 2.0%), any other white background (intervention, 2.2%; control, 3.9%), mixed white and black Caribbean (intervention, 0.0%; control, 2.0%), any other mixed background (intervention, 0.0%; control, 2.0%), Asian or Asian British Pakistani (intervention, 0.0%; control, 2.0%), black or black British Caribbean (intervention, 2.2%; control, 7.8%), black or black British African (intervention, 2.2%; control, 0%) | NR | Schizophrenia or other psychotic illness (59%), schizoaffective disorder (10%), bipolar disorder (31%) |
| Penn 2000,95 USA | 112 | 34 (range 19–59) | 42 | White (70%), Hispanic (13%) | NR | NR |
| Ratliff 2012,96 USA | CM (weight), 10; CM (attendance), 10; control, 10 | CM (weight): 50.1 (10.6), CM (attendance): 49.0 (8.1), control: 47.3 (8.0) | CM (weight): 60, CM (attendance): 70, control: 70 |
|
100% | 60% schizophrenia or schizoaffective disorder, remainder NR |
| Romain 2019,97 Canada | Intervention, 38; control, 28 | 30.73 (7.23) | 37.90 | White, 65.2%; black, 12.1%; other, 22.7% | Quetiapine 36.4%, risperidone 31.8%, paliperidone 22.7%, clozapine 22.7%, olanzapine 27.3% | Psychosis (100%) |
| Scheewe 2013,98 the Netherlands | Intervention, 29; control, 25 | Intervention: 29.2 (7.2); control: 30.1 (7.7) | Intervention: 25.8; control: 28.1 |
|
100% |
|
| Scocco 2006,99 Italy | Intervention, 10; control, 10 | Intervention: 51.7 (12.4); control: 39.2 (9.9) | Intervention: 70; control: 20 | NR | 100% medium-/long-term medication, 0% atypical antipsychotics | Schizophrenic disorder (intervention, 80%; control, 70%), schizoaffective disorder (intervention, 20%; control, 30%) |
| Sheridan Rains 2019,100 UK | Intervention, 278; control, 273 | 25 (4) | 13 | 53% white, 23% black, 11% Asian, 14% other | NR |
|
| Sorić 2019,101 Croatia | Intervention, 38; control, 41 | Intervention: 53.2 (8.9); control: 50.7 (8.0) | 15 | NR | Atypicals, 60.6%; typicals, 3%; both, 36.4% | 100% schizophrenia |
| Speyer 2016,102 Denmark | CHANGE, 138; care co-ordination, 142; TAU, 148 | CHANGE: 37.8 (12.6); care co-ordinator: 39.5 (12.8); TAU: 38.5 (11.8) | CHANGE: 55.1; care co-ordinator: 57.7; TAU: 54.7 | NR | NR | Schizophrenia (CHANGE, 90.6%; care co-ordinator, 91.5%; TAU, 83.1%) or schizoaffective disorder/persistent delusional disorder |
| Steinberg 2016,103 USA | Intervention, 51; control, 50 | Intervention: 42.61 (11.06); control: 43.49 (9.49) | Intervention: 44.90; control: 42.86 | Black (intervention, 28.57%; control, 26.53%), white (intervention, 59.18%; control, 63.27%), Latino (intervention, 2.04%; control, 8.16%), Asian (intervention, 2.04%; control, 0%), Native American (intervention, 2.04%; control, 0%), other (intervention, 6.12%; control, 2.04%) | NR | Schizophrenia (intervention, 28.6%; control, 34.7%), schizoaffective (intervention, 30.6%; control, 18.4%), bipolar (intervention, 40.8%; control, 46.9%) |
| Sugawara 2018,104 Japan | Advice alone, 67; education group, 61; standard care, 61 | Advice alone (group B): 47.6 (9.6); education group (group C): 46.6 (10.9); standard care (group A): 44.0 (10.3) | Advice (group B): 53.7; education (group C): 47.5; standard care (group A): 42.6 | NR | 100% | Schizophrenia (100%) |
| Sylvia 2019,105 USA | Intervention, 19; control, 19 | 42 (12.3) | 65.80 | 84.2% white, 2.6% black, 2.6% Asian | 66% | 100% bipolar disorder:
|
| Tantirangsee 2015,106 Thailand | BI, 53; BI-FS, 58; control, 55 | BI: 35.52 (10.1); BI-FS: 34.98 (11.0); control: 35.49 (7.0) | BI: 3.7; BI-FS: 1.7; control: 0 | NR | 42% | Schizophrenia (control, 85%; BI, 83.3%; BI-FS, 72.4%), transient psychotic disorder (control, 7%; BI, 9.3%; BI-FS, 15.5%), unspecified non-organic psychosis (control, 7%; BI, 7.4%; BI-FS, 12.1%) |
| Usher 2013,107 Australia | Intervention, 51; control, 50 | NR | 46.50 | White Australian (71.3%), Aboriginal or Torres Strait Islander (13.9%), other (14.9%) | 100%: [olanzapine, 36.6%; clozapine, 18.8%; risperidone, 23.8%; Seroquel® (quetiapine; AstraZeneca plc, Cambridge, UK), 14.9%; amisulpride, 2%; abilify, 3%; avanza, 1%] | Schizophrenia (84.2%), bipolar disorder (6.9%), depression or anxiety (15.8%) |
| Weber 2006,108 USA | Intervention, 15; control, 15 | NR | Intervention: 62.5; control: 77.8 | African American (intervention, 62.5%; control, 44.4%), white (intervention, 25.0%; control, 33.3%), Hispanic (intervention, 12.5%; control, 22.2%) | NR | Schizophrenia or schizoaffective disorder (100%) |
| Williams 2019,109 UK | Intervention, 20; control, 20 | 43 (range 20–56) | 45 | 27.5% white, 50% black, 7.5% Asian, 12.5% mixed | NR | 55% schizophrenia, 12.5% bipolar disorder, 7.5% psychosis, 25% other |
| Wu 2008,110 China | Intervention, 32; control, 32 | Intervention: 26.4 (24.8–28.1); control: 25.8 (24.1–27.6) | Intervention: 46.9; control: 50.0 | NR | 100% | Schizophrenia (100%) |
| Young 2017,111 USA | WebMOVE, 71; MOVE SMI, 78; TAU, 88 | WebMOVE: 55.5 (9.2); MOVE SMI: 53.8 (10.1); TAU: 54.2 (9.9) | WebMOVE: 4.2; MOVE SMI: 7.7; TAU: 2.3 | White (web, 43.7%; MOVE, 38.5%; TAU, 37.5%), African American (web, 42.3%; MOVE, 41.0%; TAU, 51.1%), American Indian (web, 5.6%; MOVE, 1.3%; TAU, 1.1%), Asian (web, 0%; MOVE, 6.8%; TAU, 2.3%), Pacific Islander (web, 0%; MOVE, 0%; TAU, 2.3%), multiple races (web, 4.2%; MOVE, 6.4%; TAU, 3.4%), Hispanic (web, 11.3%; MOVE, 18%; TAU, 10.2%), not given (web, 4.2%; MOVE, 9%; TAU, 2.3%) | 100% | Schizophrenia, schizoaffective disorder, bipolar disorder, PTSD and major depressive disorder |
Appendix 4 Characteristics of interventions of included randomised controlled trials
| Study (first author, year of publication) | BCTs (BCTT v1) | Targeted risk behaviour(s) | Intervention | Intensity (duration, frequency and length of sessions) | Delivery (method, setting and professional) | Control |
|---|---|---|---|---|---|---|
| Attux 201345 |
|
Diet, physical activity | Weight management intervention |
|
|
TAU |
| Baker 201547 |
|
Diet, smoking, physical activity | Healthy Lifestyles intervention – motivational interviewing/CBT + nicotine replacement therapy |
|
|
TAU+ |
| Baker 200646 |
|
Smoking | Motivational interviewing/CBT + nicotine replacement therapy |
|
|
TAU+ |
| Battaglia 201348 |
|
Physical activity | Soccer therapy |
|
|
TAU |
| Bechdolf 201249 |
|
Alcohol, other (cannabis) | Motivational interviewing |
|
|
TAU+ |
| Beebe 200551 |
|
Physical activity | Treadmill walking |
|
|
Wait list |
| Beebe 201150 |
|
Physical activity | Walking programme (WALC-S) |
|
|
Attention control |
| Bonfioli 2018,52 education intervention |
|
Diet, physical activity | Education |
|
|
TAU |
| Bonfioli 2018,52 health promotion |
|
Diet, physical activity | Health promotion |
|
|
TAU |
| Bonsack 201153 |
|
Drug use | Motivational interviewing |
|
|
TAU |
| Brar 200554 |
|
Diet, physical activity | Behaviour weight loss programme |
|
|
TAU |
| Brody 201755 |
|
Smoking | Combination extended treatment |
|
|
TAU |
| Brown 200657 |
|
Diet, smoking, physical activity, alcohol use, drug use | Lilly ‘Meaningful Day’ manual |
|
|
TAU |
| Brown 201156 |
|
Diet, physical activity | RENEW weight loss programme |
|
|
TAU |
| Brunette 202058 |
|
Smoking | Web-based motivational intervention |
|
|
TAU |
| Christiansen 201859 |
|
Smoking | motivational intervention |
|
|
TAU+ |
| Cordes 201160 |
|
Diet, physical activity | Weight management programme |
|
|
TAU |
| Daumit 201361 |
|
Diet, physical activity | Weight loss programme |
|
|
TAU |
| Evans 200562 |
|
Diet, physical activity | Nutrition intervention |
|
|
TAU |
| Fernández Guijarro 201963 |
|
Diet, physical activity | Nurse-led lifestyle intervention |
|
|
TAU |
| Forsberg 200864 |
|
Diet, physical activity | Diet and physical activity intervention |
|
|
TAU+ |
| Frank 201565 |
|
Diet, smoking, physical activity, alcohol use, drug use, other (sleep) | Integrated risk reduction intervention |
|
|
TAU |
| Ganguli 201166 | NR | Diet, physical activity | Behaviour therapy for weight loss |
|
|
TAU |
| Gaughran 201767 |
|
Diet, smoking, physical activity, alcohol use, drug use | IMPaCT intervention |
|
|
TAU |
| George 200068 |
|
Smoking | Smoking cessation |
|
|
TAU |
| Gilbody 201969 |
|
Smoking | SCIMITAR+ |
|
|
TAU |
| Gillhoff 201070 |
|
Diet, physical activity | Multimodal lifestyle intervention |
|
|
TAU |
| Graham 201671 |
|
Alcohol use, drug use | Brief integrated motivational intervention |
|
|
TAU |
| Green 201572 |
|
Diet, physical activity | STRIDE intervention |
|
|
TAU |
| Hjorth 201473 |
|
Smoking, physical activity, alcohol use | Active awareness and motivational interviewing |
|
|
TAU |
| Hjorthøj 201374 |
|
Drug use | CapOpus – motivational interviewing/CBT + TAU |
|
|
TAU |
| Holt 201975 |
|
Diet, physical activity | STEPWISE – weight management |
|
|
TAU |
| Iglesias-García 201076 |
|
Diet, physical activity | Weight management intervention |
|
|
TAU |
| Jean-Baptiste 200777 |
|
Diet, physical activity | Weight management intervention |
|
|
TAU |
| Jones 201978 |
|
Alcohol use | Motivational interviewing and CBT |
|
|
TAU |
| Kaltsatou 201579 |
|
Physical activity | Exercise training with Greek traditional dancing |
|
|
TAU |
| Khazaal 200780 |
|
Diet, physical activity | CBT |
|
|
TAU+ |
| Kilbourne 201281 |
|
Diet, physical activity | Life Goals Collaborative Care (LGCC) – mix of motivational interviewing and CBT |
|
|
TAU+ |
| Kwon 200682 |
|
Diet, physical activity | Weight management intervention |
|
|
TAU+ |
| Lee 201483 |
|
Physical activity | Telephone-delivered physical activity intervention |
|
|
TAU |
| Littrell 200384 |
|
Diet, physical activity | Weight management intervention |
|
|
TAU |
| Marzolini 200985 |
|
Physical activity | Exercise training |
|
|
TAU |
| Masa-Font 201586 |
|
Diet, physical activity | Physical activity and diet programme (CAPiCOR trial) |
|
|
TAU |
| Mauri 200887 |
|
Diet, physical activity | Psychoeducation for weight loss |
|
|
TAU |
| McCreadie 2005,88 free fruit, vegetables and meal planning |
|
Diet | Free fruit, vegetables and meal planning |
|
|
TAU |
| McCreadie 2005,88 free fruit and vegetables | 12.5 Adding objects to the environment ++ | Diet | Free fruit and vegetables |
|
|
TAU |
| McKibbin 200689 |
|
Diet, physical activity, other (diabetes) | Diabetes awareness and rehabilitation training |
|
|
TAU+ |
| Melamed 200890 |
|
Diet, physical activity | Group nutrition counselling and behaviour therapy |
|
|
TAU+ |
| Methapatara 201191 |
|
Diet, physical activity | Pedometer walking and motivational interviewing |
|
|
TAU |
| Milano 200792 |
|
Diet, physical activity | Physical activity, diet and olanzapine |
|
|
TAU |
| Osborn 201893 |
|
Diet, smoking, physical activity, alcohol use | Primrose lifestyle intervention |
|
|
TAU |
| Peckham 201794 |
|
Smoking | Bespoke smoking intervention |
|
|
TAU |
| Penn 200095 |
|
Smoking, alcohol use, drug use | 12-step REBT or SMART |
|
|
Head to head |
| Ratliff 201296 |
|
Diet, physical activity | Lifestyle modification with contingency management for attendance |
|
|
TAU |
|
Lifestyle modification with contingency management for attendance | |||||
| Romain 201997 |
|
Physical activity | Interval training |
|
|
TAU |
| Scheewe 201398 |
|
Physical activity | Exercise therapy |
|
|
TAU |
| Scocco 200699 |
|
Diet | Nutritional programme |
|
|
TAU |
| Sheridan Rains 2019100 |
|
Drug use | Contingency management |
|
|
TAU+ |
| Sorić 2019101 |
|
Diet | DASH diet |
|
|
TAU+ |
| Speyer 2016,102 care co-ordination | 2.7 Feedback on outcome(s) of behaviour ++ | Diet, smoking, physical activity, alcohol use, other (diabetes, cardiovascular disease, obstructive pulmonary disease) | Care co-ordination |
|
|
TAU |
| Speyer 2016,102 CHANGE intervention |
|
Diet, smoking, physical activity, alcohol use, other (diabetes, cardiovascular disease, obstructive pulmonary disease) | Lifestyle intervention CHANGE |
|
|
TAU |
| Steinberg 2016103 |
|
Smoking, other (personal medical conditions, finance) | Motivational interviewing with personalised feedback |
|
|
TAU+ |
| Sugawara 2018,104 nutritional education |
|
Diet | Nutritional education |
|
|
TAU |
| Sugawara 2018,104 weight loss advice |
|
Diet | Weight loss advice |
|
|
TAU |
| Sylvia 2019105 |
|
Diet, physical activity | Nutrition and exercise intervention |
|
|
TAU |
| Tantirangsee 2015,106 brief session |
|
Smoking, alcohol use, drug use | Single-session brief intervention |
|
|
TAU |
| Tantirangsee 2015,106 brief session with family support |
|
Physical activity, alcohol use, drug use | Single-session brief intervention with family support |
|
|
TAU |
| Usher 2013107 |
|
Diet, physical activity | Weight management and exercise intervention |
|
|
TAU |
| Weber 2006108 |
|
Diet, physical activity | Cognitive behavioural group |
|
|
TAU |
| Williams 2019109 |
|
Physical activity |
|
|
TAU | |
| Wu 2008110 |
|
Diet, physical activity | Lifestyle intervention with placebo |
|
|
Other |
| Young 2017,111 MOVE SMI |
|
Diet, physical activity | MOVE SMI |
|
|
TAU |
| Young 2017,111 webMOVE |
|
Diet, physical activity | WebMOVE |
|
|
TAU |
Appendix 5 Descriptions of interventions of included randomised controlled trials
| Study (first author, year of publication) | Intervention | Description of intervention | Control type | Description of control |
|---|---|---|---|---|
| Attux 201345 | Weight management intervention | The Lifestyle Wellness Program is a 12-week weight management intervention aimed to control weight gain in schizophrenic patients who are taking antipsychotics. The programme involves weekly group sessions focusing on dietary choices, physical activity and self-esteem, to modify patients’ lifestyles | TAU | Standard care: use of antipsychotics, regular visits to psychiatrist and attended regular sessions from psychosocial interventions offered by the programme they were already in |
| Baker 200646 | Motivational interviewing | Motivational interviewing. Sessions focused on reviewing personal triggers, strategies to cope with urges, and managing withdrawal, while supplying nicotine patches to enhance abstinence | TAU+ | TAU+: had access to GPs and publicly funded community mental health teams, as well as access to SANE self-help books also given to intervention group |
| CBT + NRT | CBT intervention focused on smoking cessation. Sessions focused on reviewing personal triggers, strategies to cope with urges, and managing withdrawal, while supplying nicotine patches to enhance abstinence | TAU+ | TAU+: had access to GPs and publicly funded community mental health teams, as well as access to SANE self-help books also given to intervention group | |
| Baker 201547 | Healthy lifestyles intervention – motivational interviewing | Motivational interviewing. Designed to encourage smoking cessation and improvements in diet and physical activity. Particular focus on CVD risk factors tailored towards the participant | TAU+ | Telephone-based intervention. Participants had to take part in brief (10-minute) manualised telephone calls conducted to control for number of therapist contacts. Delivered once per week for 8 weeks, followed by three fortnightly sessions, followed by six monthly sessions. At weeks 4 and 8, no telephone call but 30-minute face-to-face session during which NRT is dispensed |
| CBT + NRT | CBT-based intervention focusing on healthy lifestyle choices. Designed to encourage smoking cessation and improvements in diet and physical activity. Particular focus on CVD risk factors tailored towards the participant | TAU+ | Telephone-based intervention. Participants had to take part in brief (10-minute) manualised telephone calls conducted to control for number of therapist contacts. Delivered once per week for 8 weeks, followed by three fortnightly sessions, followed by six monthly sessions. At weeks 4 and 8, no telephone call but 30-minute face-to-face session during which NRT is dispensed | |
| Battaglia 201348 | Soccer therapy | Soccer therapy: every training session lasted about 100–120 minutes and included the following:
|
TAU | No intervention |
| Bechdolf 201249 | Motivational interviewing | Motivational interviewing: four sessions received during inpatient treatment. Session 1: feedback about behaviour, and informed about motivational interviewing. Session 2: negative consequences of substances emphasised. Session 3: participants are asked about their personal goals and the importance of those goals. In addition, attempts are made to resolve ambivalence about abstinence. Session 4: participants set realistic goals for substance use and plans to prevent relapse | TAU+ | Four non-specific support sessions. Focus of sessions was on emotional support, therapeutic attention, empathic listening, bringing in therapeutic optimism, warmth, openness and co-operation |
| Beebe 200551 | Treadmill walking | Warm-up stretches, followed by treadmill walking at target heart rate and then cool-down stretches. Walking duration increased over course of intervention | TAU | No intervention |
| Beebe 201150 | Walking programme (WALC-S) | Walking information (walking not included in intervention, up to individuals): basic safety, walking for exercise, warm-up and cool-down, individualised walking or attendance goals. Address sensations: participants queried about discomforts in exercise, observed for signs of discomfort in warm-up and cool-down. Written materials provided suggestions on reducing discomfort. Learn about exercise: information provided about benefit of exercise, overcoming barriers to exercise and assisted in making solutions to overcome barriers (when necessary). Cue exercise: calendars with walking days and times marked on were provided to cue attendance. Reminder calls made before group | TAU+ | Time and attention control. Focus on health behaviours such as medication adherence, humour and progressive muscle relaxation, smoking cessation, but did not include exercise or motivational content. Reminder calls made before each group |
| Bonfioli 201852 | Health promotion | Health education group sessions: two physical activity, five nutrition. Delivered by trainers and dietitians, over 6 months. Weekly walking sessions, guided by trainer. Prompting by telephone or in person to promote adherence | TAU | Routine care in community psychiatric services |
| Bonsack 201153 | Motivational interviewing | In addition to TAU. Four to six sessions conducted individually. First session lasted 1 hour, followed by feedback session of 45 minutes to 1 hour a week later. Two to four booster sessions for next 6 months. Participants were also offered three optional 1-hour group sessions | TAU | Psychiatric management by a team of at least one psychiatrist, psychiatric nurse or clinical psychologist. Antipsychotic medication, regular treatment monitoring, access to community-based rehabilitation activities |
| Brar 200554 | Behaviour weight loss programme | Manual-driven, didactic programme structured in an incremental and stepwise manner. Two therapy sessions per week for 6 weeks, followed by once per week for 8 weeks. Participants trained in a range of cognitive and behavioural techniques, such as self-monitoring and cognitive restructuring, and educated about healthy eating and burning calories through exercise | TAU | Encouraged to lose weight on their own with no instructions from investigators. Monthly anthropometric assessments |
| Brody 201755 | Combination extended treatment | Standard doses were used for buproprion and nicotine patches. Weekly medication management visits with a study physician. A 1-hour group CBT treatment each week | TAU | Standard doses were used for buproprion and nicotine patches. Weekly 15-minute medication management visits with a study physician. A 1-hour group CBT treatment each week |
| Combination extended treatment + home visits | Standard doses were used for buproprion and nicotine patches. Weekly medication management visits with a study physician. A 1-hour group CBT treatment each week | TAU | Standard doses were used for buproprion and nicotine patches. Weekly 15-minute medication management visits with a study physician. A 1-hour group CBT treatment each week | |
| Brown 200657 | Lilly ‘Meaningful Day’ manual | Six weekly 50-minute health promotion sessions. Largely focused on weight reduction but tailored to the needs of individuals | TAU | TAU: no further details |
| Brown 201156 | RENEW weight loss programme | Weekly 3-hour session, with information on nutrition and physical activity, setting individualised goals, eating a meal together. Duration: 12 months – 3 months intensive, 3 months maintenance, 6 months intermittent support. Participants receive two meal replacements daily for the first 3 months | TAU | TAU: typical treatment included medication and case management and the opportunity for voluntary participation in day programming |
| Brunette 202058 | Web-based motivational intervention | One-session linear, modularised and interactive programme taking 30–90 minutes to complete. Three modules:
|
TAU | Computerised version of the National Cancer Institute’s Patient Education Publications. Risk and protective factors for cancer and other smoking-related diseases |
| Christiansen 201859 | Motivational intervention | Four sessions motivating participants and helping prepare for a quit attempt. Included reviewing past quit attempts, building self-efficacy, setting goals to reduce smoking and plan quit attempt. All participants received nicotine patches | TAU+ | Attentional control: same number of sessions as intervention, but reviewed booklets about effect of smoking on body; also received nicotine patch |
| Cordes 201160 | Weight management programme | Twelve biweekly weight management sessions. Four modules covering: assessment of eating and exercise behaviour, recommendations for a healthy isocaloric diet, recommendations for regular moderate physical activity, behavioural management strategies | TAU | Control: no further details |
| Daumit 201361 | Weight loss programme | Eighteen-month tailored behavioural weight loss intervention. Included individual and group weight management and exercise sessions. Goals to reduce calorie intake, healthy eating and moderate–intense aerobic exercise | TAU | Control: standard nutrition and physical activity information. Health classes offered quarterly unrelated to weight loss (e.g. cancer screening) |
| Evans 200562 | Nutrition intervention | Six one-to-one sessions. Discussion on healthy eating, exercise, label-reading, high-fibre diets | TAU | Control: standard nutrition and physical activity information |
| Fernández Guijarro 201963 | Nurse-led lifestyle intervention | This programme consisted of 24 weekly group sessions led by mental health nurses. Each session began with 20 minutes of educational material on diet, physical activity, stress, alcohol misuse, smoking, etc., followed by 60 minutes of physical activity (e.g. walking, stretching) led by a nurse | TAU | Usual nurse care |
| Forsberg 200864 | Diet and physical activity intervention | Each group met twice per week for 2 hours over 12 months. Half of the sessions were teaching nutrition and the other half physical activity. Nutrition sessions included theoretical training, buying ingredients and preparing a meal. Physical activity sessions included fitness training, team games, bowling, swimming, etc. | TAU+ | Control: met for a 2-hour session once per week for 40–48 weeks. Had the opportunity to learn and practise various artistic techniques, for example sketching, pencil drawing, oils |
| Frank 201565 | Integrated risk reduction intervention | Intervention included three sessions of bipolar disorder psychoeducation, four sessions of education on healthy sleep, four sessions on nutrition, four sessions on physical activity and two sessions on smoking cessation (if required). Consists of three components: psychiatric treatment by psychiatrist; assessment, referral, monitoring and co-ordination by nurse; and healthy lifestyle behaviours programme by a lifestyle coach | TAU | Psychiatric care with medical monitoring |
| Ganguli 201166 | Behaviour therapy for weight loss | Manualised 20-session behavioural weight loss intervention delivered over 14 weeks by mental health clinicians | TAU | TAU: no further details |
| Gaughran 201767 | IMPaCT intervention | Target one or more health behaviours from list of cannabis, alcohol, other substances, cigarettes, exercise, diet, etc. Prioritised behaviours considered problematic by patient. Intervention used a motivational interviewing and CBT approach supported by manual, reference book and service user handbook | TAU | Control: received training in best practice for physical health awareness to ensure more standardised TAU |
| George 200068 | Smoking cessation | Adapted for schizophrenia patients. Ten weekly sessions: 3 weeks of motivational enhancement therapy; 7 weeks of psychoeducation, social skills training and relapse prevention techniques. After 3 weeks, participants tried to quit and also received nicotine transdermal patches for 6 weeks | TAU | Control: 7-week American Lung Association Freedom from Smoking® group programme, and 3 weeks of supportive group counselling |
| Gilbody 201969 | SCIMITAR+ | Bespoke smoking intervention. Mental health nurses working in conjunction with primary care physician/mental health specialist to provide tailored service. Delivered according to the Manual of Smoking Cessation, with adaptations for persons with SMI. These included several assessments before setting quit date, offering nicotine replacement before setting quit date, recognising purpose of smoking in context of mental illness, providing home visits, providing face-to-face support, support after unsuccessful quit attempt or relapse, informing primary care physician and psychiatrist of successful quit attempt (to review doses of antipsychotic medication if metabolism changes) | TAU | Usual care |
| Gillhoff 201070 | Multimodal lifestyle intervention | Eleven group sessions over 5 months and weekly fitness training. Sessions divided into three modules: lifestyle (including psychoeducation about bipolar disorder), nutrition and physical activity | TAU | Control: TAU; no further information provided |
| Graham 201671 | Brief integrated motivational intervention | Four to six sessions (lasting 15–30 minutes each) over a 2-week period. Three-step approach combining cognitive–behavioural and motivational approaches. First step provides personalised feedback on substance use. Second step aimed to help participants make decisions based on benefits and costs of misuse. Third step encouraged development of a change plan | TAU | TAU: assessment and monitoring of mental state, provision of medication and stabilisation of mental state |
| Green 201572 | STRIDE intervention | Weekly group meetings over 6 months in intensive phase. Based on the DASH diet, aimed to reduce obesity and diabetes risk. Aimed to lose 4.5–6.8 kg over 6 months. Then monthly group meetings to maintain weight loss over 6 months | TAU | TAU: no further details |
| Hjorth 201473 | Active awareness and motivational interviewing | The intervention is an active awareness and motivational interviewing intervention that aims to increase knowledge and improve physical health among people with long-term psychiatric illnesses. Includes individual and group sessions focusing on physical health, smoking, antipsychotic medication and healthy food consumption | TAU | TAU: antipsychotic use and offered individual sessions |
| Hjorthøj 201374 | CapOpus – motivational interviewing/CBT + TAU | Six-month manual-based intervention using motivational interviewing to enhance alliance and motivation, supported by CBT sessions focused on changing cannabis use | TAU | TAU: antipsychotic use and offered sessions using methods such as CBT (not specific to cannabis use) |
| Holt 201975 | STEPWISE: weight management | The STEPWISE weight management intervention is designed for people with mental health issues and schizophrenia to encourage them to change their behaviour in relation to eating and exercise. It also focuses on the psychological processes underlying weight management, and the challenges psychosis has on eating and weight | TAU | TAU: antipsychotic use; advice on lifestyle and risks of weight gain freely available |
| Iglesias-García 201076 | Weight management intervention | An education programme providing information and counselling on nutrition, exercise and health habits, and self-esteem, aiming to reduce weight in schizophrenic population, based on the idea that lifestyle therapies are more effective than pharmacological treatments for weight management in schizophrenic populations | TAU | TAU: weekly visits to clinic to assess anthropometric measures |
| Jean-Baptiste 200777 | Weight management intervention | Weight management intervention based on the principles of the Lifestyle, Exercise, Attitudes, Relationships and Nutrition (LEARN) programme to minimise weight gain and produce weight loss in SMI patients. The intervention encompasses behavioural modification techniques, exercise enhancement, food provision and tailored nutritional support to motivate weight loss in schizophrenia | TAU | Waiting list control: after a 16-week period, they received the intervention |
| Jones 201978 | Motivational interviewing–CBT | Combination of motivational interviewing and CBT elements adapted from an approach designed for people with substance abuse disorder and psychosis. Offered up to 20 sessions in their preferred location, usually at home, typically for 45–60 minutes | TAU | Determined by each participant’s responsible clinician, primarily medication and community mental health team support |
| Kaltsatou 201579 | Exercise training with Greek traditional dancing | Exercise training classes combined with Greek traditional dancing aimed at promoting physical activity based on the theory that social dance interventions increase social support and motivation in individuals with SMI. Each session is designed to promote physical activity, as intensity increases over time. Each session included 10-minute warm-up and cool-down sessions at the start and end, respectively; as well as 40 minutes of dancing | TAU | TAU: antipsychotic medication and some psychotherapy sessions |
| Khazaal 200780 | CBT | The ‘apple-pie’ group CBT intervention focuses on promoting positive eating behaviours, cognitive restructuring for thoughts relating to weight and eating behaviour and behaviour adaptation through monitoring weekly food intake | TAU+ | TAU+: received brief nutritional education and nutritional recommendations to maintain effort to lose weight |
| Kilbourne 201281 | Life Goals Collaborative Care (LGCC): mix of motivational interviewing and CBT | The LGCC intervention was designed to help participants set personal self-management goals based on social cognitive theory to cope with chronic health conditions such as bipolar disorder and cardiometabolic risk factors. Sessions focused on diet, psychiatric symptoms, stigma issues and collaborative care | TAU+ | TAU+: monthly receipt of information on wellness topics, in addition to mental health care and referral to off-site primary care services |
| Kwon 200682 | Weight management intervention | Weight management intervention using a CBT approach to promote weight loss among people with schizophrenia. The intervention incorporated a diet management programme as well as an exercise management programme to educate patients on using food and exercise diaries, eating behaviour improvement and lifestyle modification for weight control | TAU+ | TAU+: antipsychotics plus monthly sessions providing advice on physical activity and eating behaviour, as well as food and exercise diaries |
| Lee 201483 | Telephone-delivered physical activity intervention | Telephone-based physical activity intervention aimed at promoting physical activity among people with SMI. Guided by social cognitive theory, this intervention emphasises the importance of an interplay between personal, behavioural and environmental factors in human behaviours. Through social support, the intervention aims to improve individuals’ self-efficacy, which, in turn, improves health-promoting behaviour (physical activity) | TAU | TAU: antipsychotics and written advice on physical activity |
| Littrell 200384 | Weight management intervention | Weekly psychoeducation classes using the ‘solutions of wellness’ modules to promote healthy eating, and fitness and exercise, specific to people with schizophrenia | TAU | Standard care |
| Marzolini 200985 | Exercise training | Weekly exercise sessions incorporating aerobic training and resistance (weight) training based on the notion that resistance training and aerobic training is more effective than aerobic training on its own. Emphasis on training heart rate during the exercises | TAU | TAU |
| Masa-Font 201586 | Physical activity and diet programme (CAPiCOR trial) | Physical activity and dietary intervention aimed at modifying CVD risk factors for SMD. Included physical activity sessions aimed to promote walking and safe practices, alongside dietary advice sessions providing knowledge on healthy dietary habits. Based on the notion that a collaborative programme is more beneficial | TAU | TAU: antipsychotics and regular psychiatry check-ups |
| Mauri 200887 | Psychoeducation for weight loss |
|
TAU | Olanzapine only |
| McCreadie 200588 | Free fruit, vegetables and meal planning | Provision of fruit and vegetables with food preparation instructions | TAU | No intervention |
| Free fruit and vegetables | Provision of fruit and vegetables | TAU | No intervention | |
| McKibbin 200689 | Diabetes Awareness and Rehabilitation Training (DART) | DART: social cognitive theory provided theoretical foundation and is often used in diabetes education. Basic education (sessions 1–4, repeated sessions 13–16): introduction, understanding motivation, review of blood sugar, symptoms of high and low blood sugar, complications, how to best use glucose meter, doctor visits. Nutrition (sessions 5–8, repeated sessions 17–20): food groups, portion sizes, healthy meals and reading labels, replace sugar with fat and fibre. Exercise (sessions 9–12, repeated sessions 21–24): types of exercise, blood sugar and exercise, tracking exercise/introduction of pedometers, foot care during exercise. Weekly weigh-ins, pedometers, healthy food sampling and reinforcements (such as raffle tickets for small health-related prizes) for attendance and behavioural change | TAU+ | Usual care plus information |
| Melamed 200890 | Group nutrition counselling and behaviour therapy | Education sessions on topics: getting to know the food groups, importance of drinking water, calcium, vitamins, nutritious fibres, weight gain and physical illness, suggestions for menus for home-cooked food, reading food labels in the supermarket, group visits to the cafeteria, exercise, lipids. Weigh-ins, affirmation of successful weight loss, group support, points awarded for behavioural changes and weight loss. Methods for coping with temptation, problem-solving, self-monitoring of eating, and stress management. Healthy nutrition buffet tables were placed alongside standard buffet tables at meal times and participants sat at these with nutrition supervisors. Family visitors were encouraged not to bring sweets or sweetened drinks, and the cafeteria offered reduced price options. Exercise: 30-minute walks five times per week, with warm-up and cool-down. Aerobics guided by cassette tape were delivered when weather prevented walking | TAU+ | Inpatient usual care |
| Methapatara 201191 | Pedometer walking and motivational interviewing (PWMI) | All participants given leaflet called ‘What is a healthy lifestyle?’. PWMI:
|
TAU | TAU and leaflet titled ‘What is a healthy lifestyle?’ |
| Milano 200792 | Physical activity, diet and olanzapine | All participants given olanzapine. Intervention group: followed diet with 500 kcal per day reduction, with nutritional balance, and nutritional advice. Physical activity plan for three times per week. Weeks 1 and 2: 5 minutes of fast step walking alternated with 3 minutes of slow running, for a total of 30 minutes. Weeks 3–5: 5 minutes of fast step walking alternated with 5 minutes of slow running, for a total of 30 minutes. Weeks 6–8: four cycles of 4 minutes of fast step walking alternated with 6 minutes of slow running, for a total of 40 minutes. Weeks 9–12: four cycles of 4 minutes of fast step walking alternated with 8 minutes of slow running, for a total of 48 minutes. Stretching at beginning and end of activity | TAU | No intervention |
| Osborn 201893 | Primrose intervention | This intervention is based on challenging eight key behaviour change strategies used to reduce CVD risk. Incorporates weekly/fortnightly sessions up to 6 months, during which nurse and participants agree on goals to lowering CVD risk | TAU | Feedback of screening results |
| Peckham 201794 | Bespoke smoking intervention | SCIMITAR: trained mental health and smoking cessation specialist works with GP or mental health specialist to provide cessation service tailored to each participant. Delivered in accordance with Smoking Cessation Manual. Includes support sessions specifically adapted for SMI, GP-prescribed pharmacotherapies (NRT, buproprion or varenicline), and regular follow-up. Example adaptations:
|
TAU | TAU |
| Penn 200095 | 12-step REBT | Intensive outpatient treatment/partial hospitalisation up to 5 hours per day, 5 days per week. Weekly activities and topics: relapse prevention, SMI management, daily living skills, goal-setting, mental health and substance abuse education, lunch (including shopping and preparation), healthful recreation (including weekly outing), in-house and community 12-step meetings, written assignments, and individual sessions as needed. Case management and permission to complete the programme in multiple segments if needed. REBT: no ideological position on abstinence, strives to operate within goals and values of individual clients | Head to head | None |
| SMART | Intensive outpatient treatment/partial hospitalisation up to 5 hours per day, 5 days per week. Weekly activities and topics: relapse prevention, SMI management, daily living skills, goal-setting, mental health and substance abuse education, lunch (including shopping and preparation), healthful recreation (including weekly outing), in-house and community SMART meetings, written assignments, and individual sessions as needed. Case management and permission to complete the programme in multiple segments if needed. SMART: abstinence based and aim to serve people who desire to completely stop addictive behaviour | Head to head | None | |
| Ratliff 201296 | Lifestyle modification with contingency management for weight | Lifestyle modification for all participants: Simplified Intervention to Modify Physical Activity and Eating Behaviour (SIMPLE). Standardised lifestyle programme based on social cognitive theory, designed to be used with SMI populations; all concepts presented in basic terms with cultural sensitivity. Weekly group sessions of 8–10 individuals. Topics broadly focus on nutrition and physical activity and include changing attitudes to support weight loss, and implementing social support to aid weight loss. Contingencies for weight: US$20 for each baseline and week-8 assessment; maximum amount possibly earned from contingencies: US$140. Weight: US$5 for initial weight loss of at least 1 lb, US$10 for next weigh-in with weight loss of at least 1 lb, with subsequent weigh-ins escalating by US$5 increments. If no weight lost, payments reset at US$5 | TAU | TAU |
| Lifestyle modification with contingency management attendance | Lifestyle modification for all participants: Simplified Intervention to Modify Physical Activity and Eating Behaviour (SIMPLE). Standardised lifestyle programme based on social cognitive theory, designed to be used with SMI populations; all concepts presented in basic terms with cultural sensitivity. Weekly group sessions of 8–10 individuals. Topics broadly focus on nutrition and physical activity and include changing attitudes to support weight loss, and implementing social support to aid weight loss. Contingencies for attendance: US$20 for each baseline and week-8 assessment; maximum amount possibly earned from contingencies: US$140. Attendance: US$17.50 for each weight loss group attendance | TAU | TAU | |
| Romain 201997 | Interval training | Supervised interval training: 6 months of HIIT on a treadmill twice per week. Each exercise session lasted for 30 minutes. The sessions included a 5-minute low-intensity warm-up (walking), 10 intervals of 2 minutes’ duration each, and a 5-minute cool-down (walking). Each interval was composed of a 30-second sprint followed by an active recovery of 90 seconds | TAU | TAU |
| Scheewe 201398 | Exercise therapy | Designed to improve cardiorespiratory fitness and primarily incorporates cardiovascular exercises. Strength exercises: six exercises a week, 3 × 10–15 repetitions for biceps, triceps, abdominal, quadriceps, pectoral, deltoid muscles. Programme followed recommendations of American College of Sports Medicine. Information on amount of training and compliance registered in logbook | TAU | Occupational therapy |
| Scocco 200699 | Nutritional programme | Personal and dietary detailed notes, emphasis on energy intake and energy expenditure. A nutritional programme and food diary are drawn up. At check-ups, any difficulties are addressed and food diary is discussed | TAU | Olanzapine only |
| Sheridan Rains 2019100 | Contingency management | The voucher value rose by £5 with every two clean samples and the bonuses were removed. In total, participants could receive £240 | TAU+ | Psychoeducation: standard psychoeducation delivered in six modules of 30 minutes’ duration each. Presents information regarding the effects of cannabis; motivational materials; and strategies for coping, minimising potential harms and abstaining from cannabis |
| Sorić 2019101 | DASH diet | Participants were asked to follow the DASH diet. The caloric intake of the prescribed diet was reduced by approximately 1673.6 kJ per day (400 kcal per day) when compared with the standard hospital diet. They also received a standard nutrition counselling programme | TAU+ | Four group sessions of nutritional counselling: dietary guidelines, reading food labels, diet and chronic disease |
| Speyer 2016102 | Lifestyle coaching | Lifestyle coaching: defined as affiliation to a CHANGE team member, offering tailored, manual-based intervention targeting physical inactivity, unhealthy dietary habits and smoking, and facilitating contact to participants’ GPs for medical treatment of somatic comorbidities. Based on theory of stages of change, motivational interviewing and assertive approach adapted from assertive community treatment. Four manuals were created based on this to deal with four tracks: care co-ordination, smoking cessation, healthy diet and physical activity. Coach offered home visits with systematic exploration of possibilities for physical activity in daily life, dietary changes based on dietary exploration, food purchases and cooking habits. Personal and professional networks were included in plans, when possible. Affiliation with team member was for 1 year with at least one weekly meeting, variable duration, further support by text, telephone call, and e-mail. Participants encouraged to select if focus should be one or more of four tracks; coach supports participants in individual goals | TAU | GP consults as needed, annual metabolic testing, no formalised extra effort regarding lifestyle counselling or treatment of physical disorders |
| Care co-ordination | Care co-ordination: incorporated into the CHANGE group, implemented as add-on to TAU. Manual based, co-ordinator was trained psychiatric nurse, facilitated contact to primary care to ensure optimal treatment of physical health problems. Co-ordinator contact comprised meetings, telephone calls and text messages. Frequency adjusted to individual need. First meeting consisted of general health talk about physical well-being and an evaluation of test results from physical exam; special attention paid to symptoms of obstructive pulmonary disease, diabetes and CVD. A decision tree used to plan the further course | TAU | GP consults as needed, annual metabolic testing, no formalised extra effort regarding lifestyle counselling or treatment of physical disorders | |
| Steinberg 2016103 | Motivational interviewing with personalised feedback | Personalised feedback regarding carbon monoxide reading, financial expenditures and information about medical conditions that participants endorsed as personally relevant. Feedback delivered in style consistent with motivational interviewing. Information on carbon monoxide and medical conditions was delivered using ‘elicit–provide–elicit’ strategy; financial expenditures were discussed in manner designed to develop discrepancy between how they were spending money and how they would prefer to be spending money. A modified importance–confidence–readiness ruler exercise focusing on self-reported importance for quitting and confidence in ability to quit was delivered. On conclusion, a referral to a local tobacco dependence treatment clinic was given | TAU+ | Interactive education |
| Sugawara 2018104 | Weight loss advice | Weight loss advice from attending psychiatrist, record weight in notebook to create shared understanding between patient and psychiatrist. Participants given target body weight at baseline. At visits, their body weight is measured and brief advice focused on numeric increase or decrease is given | TAU | Standard care for residual and breakthrough symptoms of schizophrenia |
| Nutritional education | In addition to the above. Individual nutrition education sessions over 1 year. Conducted by dietitians and based on Nutrition Needs in Psychiatry project (Sagae160). Four phases, with learning objectives as follows: understanding the composition of a balanced meal, understanding appropriate food requirements, reducing the consumption of snacks and reviewing the sessions. Each phase comprised three sessions. Dietary energy goals were based on calculating a participant’s ideal body weight (kg) multiplied by 25 kcal. Participants kept daily food records, which dietitians reviewed and discussed with each patient and practised selecting foods using full-sized sample dish cards. First 3 months, participants advised to eat three regular balanced meals: staple food, main dish, side dish including vegetables or dairy. Second phase establishes participants consumption of staple foods (rice, wheat, etc.). Third phase educated about relation between weight gain and snacks. Final phase reinforced the learning by reviewing content | TAU | Standard care for residual and breakthrough symptoms of schizophrenia | |
| Sylvia 2019105 | Nutrition and exercise intervention | CBT-based intervention focusing on nutrition (sessions 1–6: psychoeducation and skills training to make better food choices), exercise (sessions 7–12: focusing on goal of moderate–intensive exercise 5 days per week for 30 minutes) and wellness (importance of healthy choices and how to problem-solve barriers to reducing risk behaviours) | TAU | Wait list |
| Tantirangsee 2015106 | Single-session brief intervention | Single session by nurse giving personalised feedback from the ASSIST and motivating change using motivational interviewing techniques for brief interventions adapted by the WHO ASSIST group. Included following elements: discussion of substance use patterns and motives; education on intoxication, tolerance and withdrawal symptoms; how physical and mental health problems can be caused or exacerbated by substance use; behaviour change options designed to build motivation, intentions and goals; cognitive and spiritual strategies to identify high-risk situations and cope with cravings; and information on changing substance use, and accessing local services and supports | TAU | Risk screened with the ASSIST and advised to stop using all substances, 5-minute appointment |
| Single-session brief intervention with family support | Same as single session without family attendance. Nominated key relative in attendance, session covers same areas as other, supplemented with following: importance and methods of good communication between family members; general problem-solving techniques that the family can use to help members who face personal difficulties; and specific methods the family can use to help the participant stop or reduce their use of the substances declared during the ASSIST | TAU | Risk screened with ASSIST and advised to stop using all substances, 5-minute appointment | |
| Usher 2013107 | Weight management and exercise intervention | Sessions included education and discussion on health lifestyle topic of the week, and participants’ progress with implementation of the healthy lifestyle components of the programme into their lives. Twelve topics:
|
TAU | Healthy lifestyle booklet |
| Weber 2006108 | Cognitive behavioural group | Content of groups based on strategies to promote risk reduction. Sessions included role plays, goal-setting, motivational scaling, problem-solving, risk vs. benefits comparisons, discussions on barriers to change, presentations on low-fat diets, and plans to increase activities such as walking. Participants keep food and activity diaries, which are checked each session | TAU | TAU |
| Williams 2019109 | Walk this way intervention | Intervention aimed to address capability, opportunity and motivational barriers to reducing sedentary behaviour and increasing physical activity. Used a combination of group education, meeting regularly with a health coach to address any barriers to reducing sedentary behaviour and engaging in physical activity. Also had an optional weekly walking group | TAU | Care co-ordination plus written information on the benefits of increasing activity levels |
| Wu 2008110 | Lifestyle intervention with placebo | Daily placebo (for metformin). Psychoeducational, dietary and exercise programs. Psychoeducational: roles of eating and activity in weight management. Topics included healthful weight management, benefits of nutrition, physical fitness, available behavioural techniques. Delivered in groups at baseline, every 4 weeks. Dietary: American Heart Association step 2 diet prescribed. Less than 30% calories from fat, 55% from carbohydrates, and > 15% protein, increase in fibre intake to a minimum of 15 g per 1000 kcal. Three-day food diary analysed to provide feedback on diet, no changes to caloric intake, but adjusted to fit plan. Three-day diary kept before each visit for comparison with plan, and discussions about adherence. Exercise: week 1 directed by exercise physiologist. Endurance exercise on treadmill seven times per week for 30 minutes, to attain 70% of heart rate reserve. After this, exercise was homebased without supervision, using collaboratively developed programmes. Range of exercise and intensity offered for 30 minutes per day. Branch treadmill tests performed at each visit. Participants keep record of exercise activity and heart rate | TAU+ | Placebo |
| Young 2017111 | WebMOVE | WebMOVE: includes (1) internet browser-based provision of 30 interactive educational modules, tracking of activity and weight, and individualised homework, plus (2) weekly telephonic peer coaching. Computer program based on MOVE SMI (Goldberg et al.161). Participants given pedometer. Two online modules per week, each completed in 30 minutes. Tailored for cognitive deficits in SMI: minimal text, all read aloud, fifth-grade reading level, explicit navigational aids, simple presentation of information. Use of goal-setting, homework, automated diet plans and quizzes. System accessible from kiosks at VA clinics, or anywhere with internet access. Weekly manualised peer coaching by telephone with motivational interviewing | TAU | Usual care |
| MOVE SMI | MOVE SMI: in-person management programme, uses handouts, motivational techniques, visual learning aids, behavioural rehearsal, repetition, goal-setting, homework and diet plans. Tailored for cognitive deficits in SMI: minimal text, all read aloud, fifth-grade reading level, explicit navigational aids, simple presentation of information. Use of goal-setting, homework, automated diet plans and quizzes. System accessible from kiosks at VA clinics, or anywhere with internet access. Weekly manualised peer coaching by telephone with motivational interviewing | TAU | Usual care |
Appendix 6 Characteristics of included qualitative studies
| Study (first author, year of publication, country) | Aim | Intervention | Targeted risk behaviour(s) | Population (sample size) | Qualitative approach and data collection |
|---|---|---|---|---|---|
| Aschbrenner116 2013, USA | To explore social facilitators of and barriers to health behaviour change among participants engaged in a healthy lifestyle programme for persons with serious mental illness (In SHAPE) embedded in community-based mental health settings | In SHAPE integrated health promotion programme | Physical activity, diet | Schizophrenia or schizoaffective disorder (73%) (n = 30) |
|
| Bauer117 2018, USA | To understand the needs of individuals with bipolar disorder with regard to lifestyle interventions targeting nutrition and physical activity | Lifestyle intervention | Physical activity, diet | Bipolar disorder (100%) (n = 10) |
|
| Carless118 2008, UK | To explore the ways in which narrative, identity and mental health relate to one another within the specific context of sport, exercise and serious mental illness | Experiences of sport and exercise interventions | Physical activity | Men with SMI (n = 11) |
|
| Firth119 2016, UK | To explore the perceived benefits of exercise as experienced by people with first-episode psychosis, and to establish the barriers to and facilitators of increasing physical activity in this patient group | Individualised exercise programme | Physical activity | First-episode psychosis (100%) (n = 13) |
|
| Fogarty120 2005, Australia | To determine the impact of a structured exercise programme on the physical and psychological well-being of people with a long-term diagnosis of schizophrenia or related psychosis | Exercise intervention | Physical activity | Schizophrenia (100%) (n = 6) |
|
| Forsberg121 2011, Sweden | To illuminate meanings of participating in a lifestyle programme as experienced by persons with psychiatric disabilities | Lifestyle programme | Physical activity, diet, alcohol, drug use, smoking | Schizophrenia (90.1%) (n = 11) |
|
| Gossage-Worrall122 2019, UK | To assess fidelity and quality of implementation. To clarify causal mechanisms and identify contextual factors associated with variation in outcomes | STEPWISE | Physical activity, diet | Schizophrenia (100%) (n = 24) |
|
| Heffner123 2018, USA | Qualitative exploration of challenges and facilitators of quitting in an intervention study for smokers with bipolar disorder to facilitate development of more effective interventions | ACT and NRT | Smoking | Bipolar disorder (100%) (n = 10) |
|
| Hodgson124 2011, UK | (1) To determine the perceived effects of physical activity participation on mental well-being, social well-being and physical well-being; (2) to identify the barriers to physical activity adoption and adherence; and (3) to identify enabling factors influencing adherence to the activity programme | Exercise-based interventions (football and activity programmes) | Physical activity | Severe and enduring mental illness (100%). (n = 17) |
|
| Huck125 2018, USA | (1) To explore the nature of physical activity-related programming within one ACT setting and (2) to gain consumer perspectives related to interventions that would be likely to facilitate greater levels of participation. In addition, the research team hoped to consider how, (3) existing health behaviour theory might relate to these findings in order to offer a better understanding of how existing health behaviour theory applies to this group | ACT physical activity intervention | Physical activity | Schizophrenia (90%) (n = 18) |
|
| Jimenez126–128 2015, 2016, 2019, USA | (1) Identify facilitators of and barriers to engaging in health behaviour change; (2) identify exercise preferences among Latino adults with SMI participating in a health promotion intervention; and (3) identify the role of SMI in motivation, participation and adoption of health behaviour change among overweight Latino adults | In SHAPE integrated health promotion programme | Physical activity, diet | SMI (100%) (n = 20) |
|
| Keller-Hamilton129 2020, USA | (1) A more complete picture of the reasons why people with schizophrenia or bipolar disorder smoke and (2) information for clinicians and public health practitioners to better tailor smoking cessation services to adults with SMI | None – considering barriers to smoking cessation | Smoking | SMI (100%) (n = 24) |
|
| Klein130 2019, Australia | To address these important issues of acceptability, feasibility and usefulness in an Australian context, in relation to tailoring the Kick.it app for SMI populations | Kick.it smoking cessation app | Smoking | Paranoid schizophrenia (75%) (n = 12) |
|
| Knowles131 2016, UK | To qualitatively explore the experiences of service users who received the bespoke smoking cessation intervention, particularly in comparison to their experience of standard stop-smoking services and in the light of their mental health difficulties | Bespoke mental health smoking cessation | Smoking | SMI (100%) (n = 13) |
|
| Luciano132 2014, USA | (1) What is the subjective experience of maintaining sobriety for people with cooccurring psychosis and substance use disorder? (2) What behavioural strategies supported continued lifestyle change from these participants’ points of view? | Residential co-occurring treatment disorder clinic | Alcohol, drug use | Schizoaffective disorder (33%), schizophrenia (17%), bipolar disorder (33%), generalised anxiety disorder (17%) (n = 12) |
|
| Maisto133 1999, USA | To discover what experiences individuals with co-occurring SMI and substance use disorder perceive as more and less beneficial in changing their substance use patterns | Outpatient psychiatric clinic | Alcohol, drug use | Schizophrenia (100%) (n = 21) |
|
| Mason134 2012, UK | To understand service users’, referrers’ and professional coaches’ views of the project’s positive and negative implications for mental and physical health, quality of life and social and community relationships | Coping through Football | Physical activity | Psychotic and/or depressive disorders (n = 12) |
|
| O’Hara135 2017, USA | To describe how ‘group lifestyle balance’ was adapted to fit the needs of people with SMI living in supportive housing | Peer-based group lifestyle balance | Physical activity, diet | Schizophrenia or schizoaffective disorder (50%), major depression (57%), bipolar disorder (57%) (n = 14) |
|
| Oddie136 2009, UK | To gain a deeper understanding of participants’ expectations, and of the acceptability and perceived benefits of the programme | Substance misuse programme | Alcohol, drug use | Predominantly paranoid schizophrenia, patients at medium-secure forensic mental health unit (n = 23) |
|
| Olmos-Ochoa137 2019, USA | (1) To examine the effect of treatment condition (web or in person) on barriers to healthy eating and physical activity over time, (2) to examine the association between anticipated baseline barriers and patient engagement in their respective interventions, and (3) to determine whether or not patient engagement in treatment affected perceived barriers over the course of treatment | Web-based/in-person weight management | Physical activity, diet | Schizophrenia, schizoaffective disorder, bipolar disorder, recurrent major depressive disorder with psychosis, or chronic post-traumatic stress disorder (n = 48) |
|
| Penn138 2016, USA | To uncover themes that are important to the clients and counsellors, including ideas and concerns that we had not considered or been aware of | 12-step recovery/SMART recovery programme | Alcohol | Serious mental illness (n = 12) |
|
| Roberts139 2013, UK | To explore incentives and barriers to engaging people with SMI in an educational lifestyle programme to gain important insights into the ways service users experience these interventions | Lifestyle intervention | Other: weight | Schizophrenia (86%), personality disorder (14%) (n = 8) |
|
| Rönngren141 2014, Sweden | (1) To explore the experiences of physical activity and eating habits of psychiatric clients by interviewing the Local Reference Group, community mental health-care users and community mental health-care workers. (2) To describe the development of a lifestyle programme for people with SMI based on information obtained from the interviews | LIFEHOPE.EU | Physical activity, diet | SMI (n = NR) |
|
| Rönngren140 2018, Sweden | To describe the acceptability of the lifestyle programme at a community mental health service group and to get information about the tools used for assessment of functional exercise capacity, cognitive performance, and self-reported health-related quality of life | Lifestyle programme | Physical activity, diet | SMI (n = 13) |
|
| Thornton142 2011, Australia | To fill gaps in our knowledge by examining exposure, acceptability and attitudes regarding antismoking campaigns and tobacco knowledge among people with psychotic disorders | Public health antismoking campaigns | Smoking | Psychotic disorders (n = 8) |
|
| Verhaeghe143 2013, Belgium | To examine the factors influencing the integration of physical activity and healthy eating into the daily care of individuals with mental disorders living in sheltered housing and to gain insight into the relationships and complexities of these factors | Health promotion | Other: health promotion | Schizophrenia, schizoaffective disorders, bipolar and depressive disorders in sheltered housing (n = 15) |
|
| Wärdig144 2015, Sweden | To describe how persons with psychosis perceive participation in a lifestyle intervention and to use these perceptions to present factors for consideration in future interventions | Lifestyle intervention | Physical activity, diet, alcohol, smoking | Psychosis (100%) in psychiatric outpatient care (n = 40) |
|
| Watkins145 2020, Australia | To explore the personal experiences of the Keeping the Body in Mind programme participants, in particular the aspects of the programme that they perceived to be helpful in achieving physical health and other improvements | Keeping the Body in Mind lifestyle intervention | Physical activity, diet | First-episode psychosis (100%) (n = 16) |
|
| Weinstein146 2019, USA | To investigate social and structural factors that affect weight loss in partnership with community co-researchers enrolled in a group lifestyle programme for overweight/obese people with serious mental illness living in supportive housing settings | Group lifestyle programme | Physical activity, diet | SMI in supportive housing (n = 8) |
|
| Yarborough147 2016, USA | To identify modifiable factors associated with making and maintaining healthy lifestyle changes in order to inform clinicians and improve the development of future interventions for individuals with serious mental illnesses | STRIDE lifestyle intervention | Physical activity, diet | Schizophrenia or schizoaffective disorder (41%), bipolar disorder (20%), affective psychosis (37%), post-traumatic stress disorder (2%) (n = 84) |
|
Appendix 7 Network diagrams
Total physical activity
FIGURE 9.
Network diagram illustrating risk behaviours targeted in studies reporting total PA (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking; SB, sedentary behaviour.

Alcohol use
FIGURE 10.
Network diagram illustrating risk behaviours targeted in studies reporting alcohol use (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
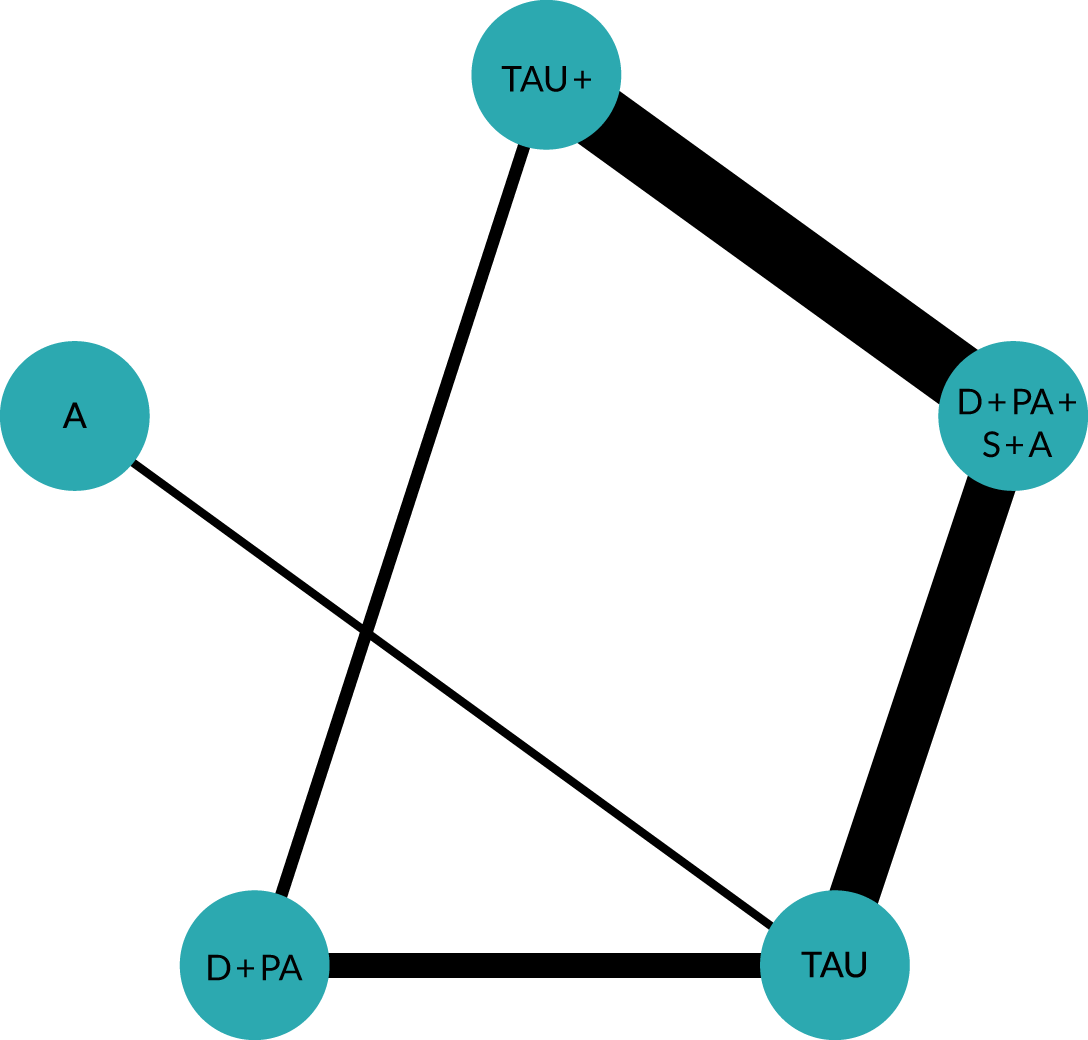
Cannabis use
FIGURE 11.
Network diagram illustrating risk behaviours targeted in studies reporting cannabis use (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.

Weight
FIGURE 12.
Network diagram illustrating risk behaviours targeted in studies reporting weight loss (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
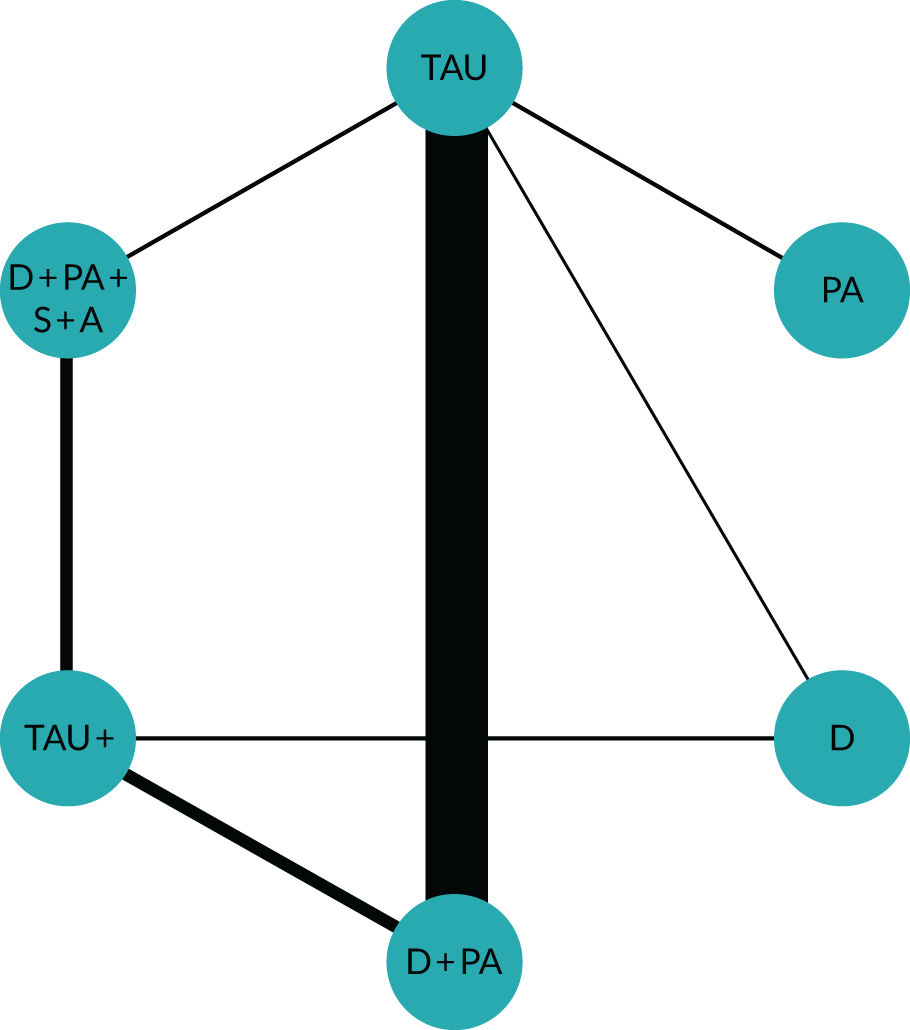
Body mass index
FIGURE 13.
Network diagram illustrating risk behaviours targeted in targeted in studies reporting BMI (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
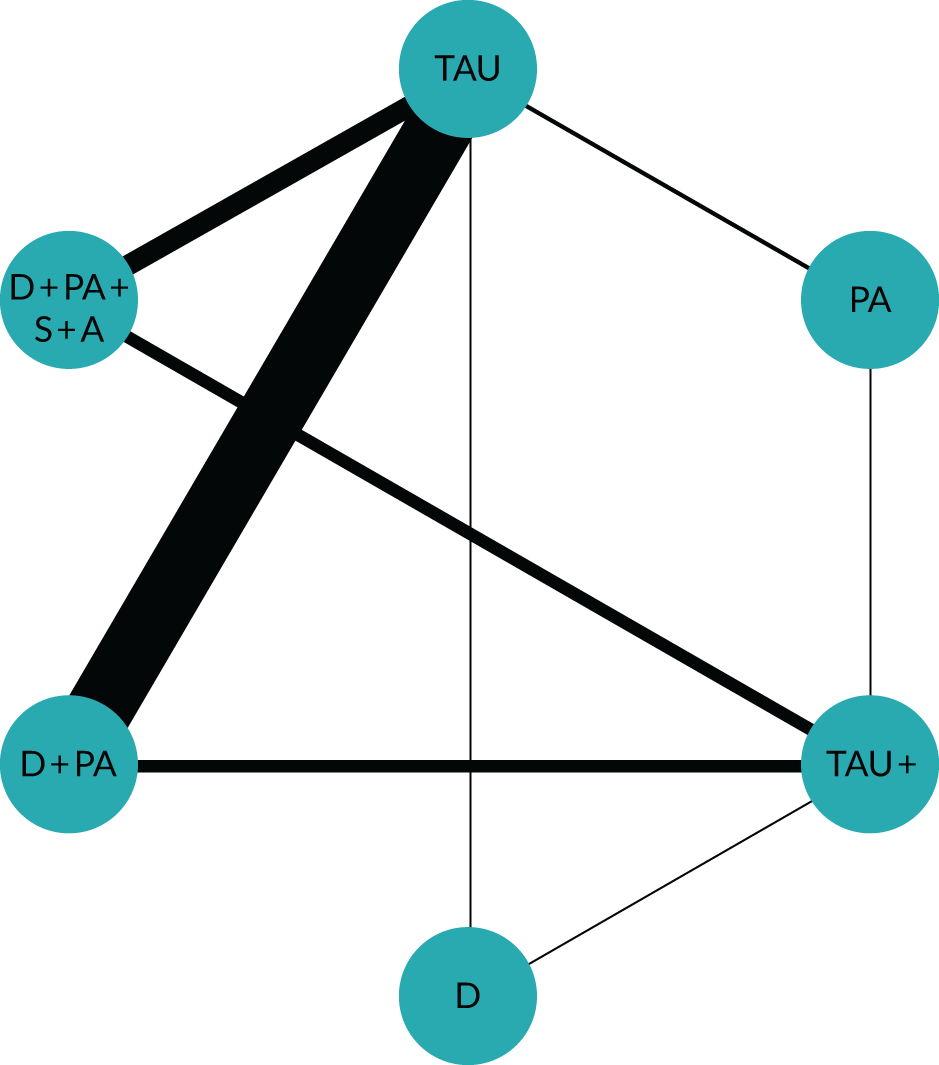
Systolic blood pressure
FIGURE 14.
Network diagram illustrating risk behaviours targeted in studies reporting systolic blood pressure (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
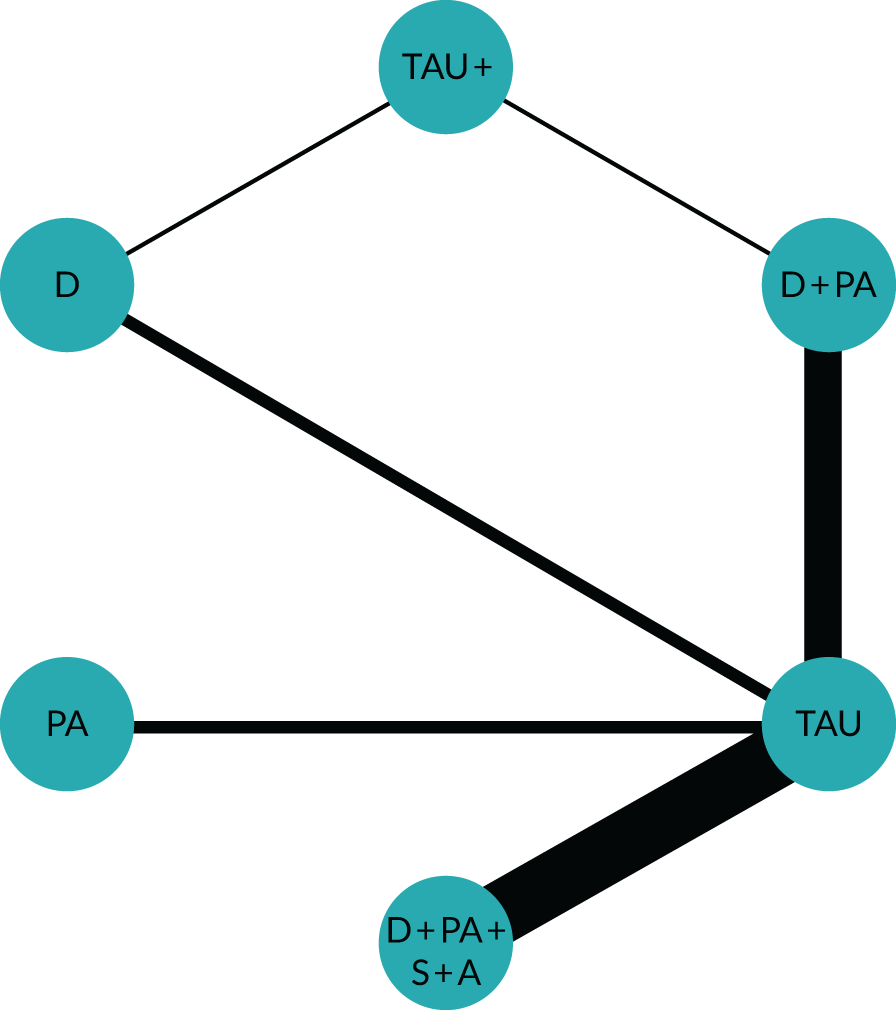
Diastolic blood pressure
FIGURE 15.
Network diagram illustrating risk behaviours targeted in studies reporting diastolic blood pressure (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
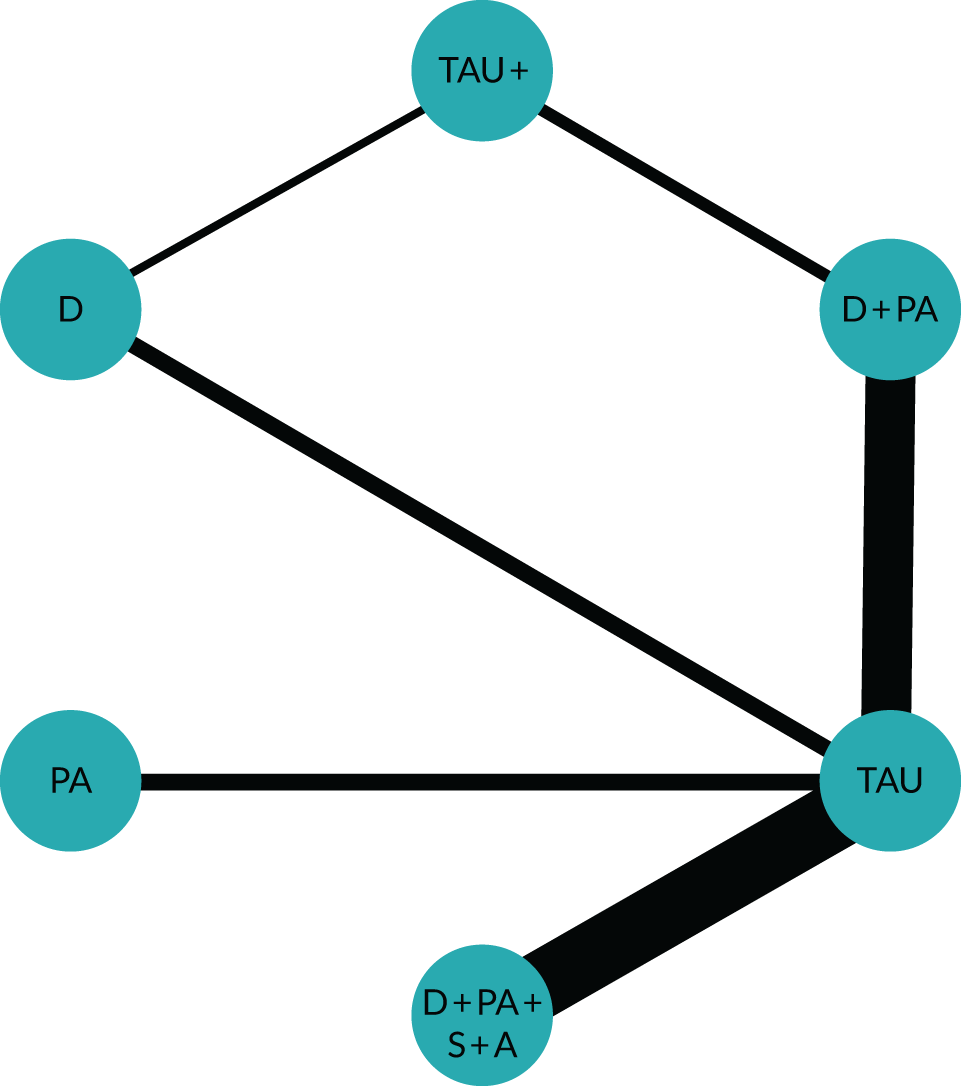
High-density lipoprotein cholesterol
FIGURE 16.
Network diagram illustrating risk behaviours targeted in studies reporting HDL cholesterol (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
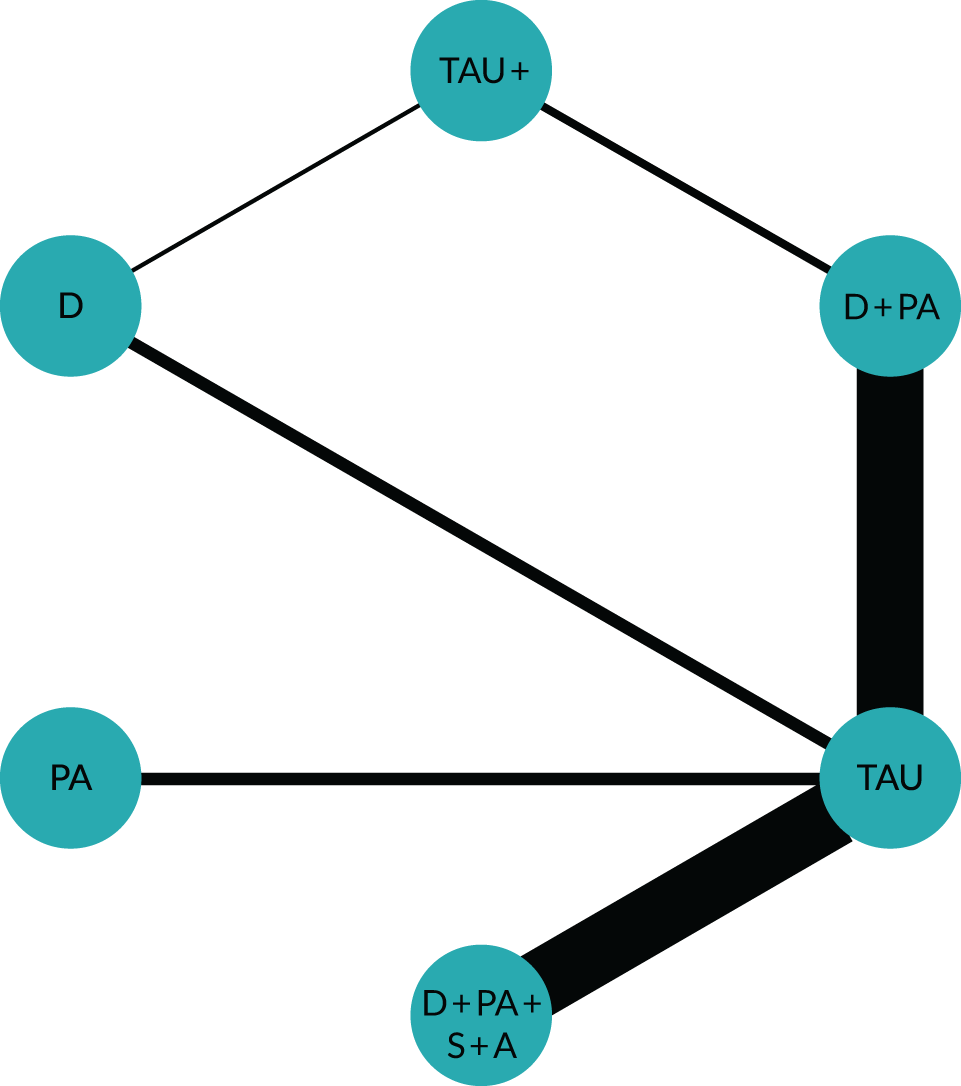
Low-density lipoprotein cholesterol
FIGURE 17.
Network diagram illustrating risk behaviours targeted in studies reporting LDL cholesterol (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
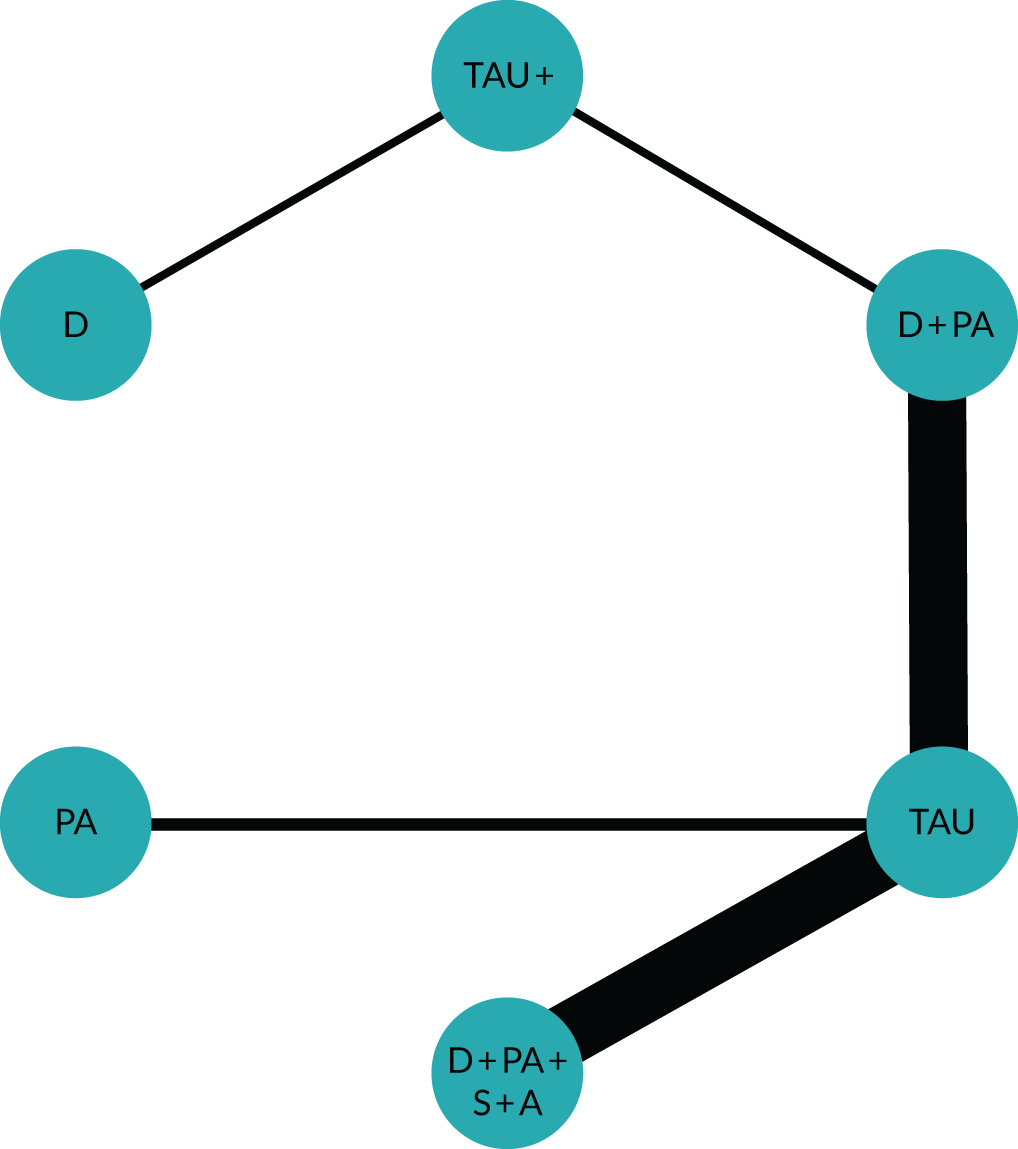
Total cholesterol
FIGURE 18.
Network diagram illustrating risk behaviours targeted in studies reporting total cholesterol (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
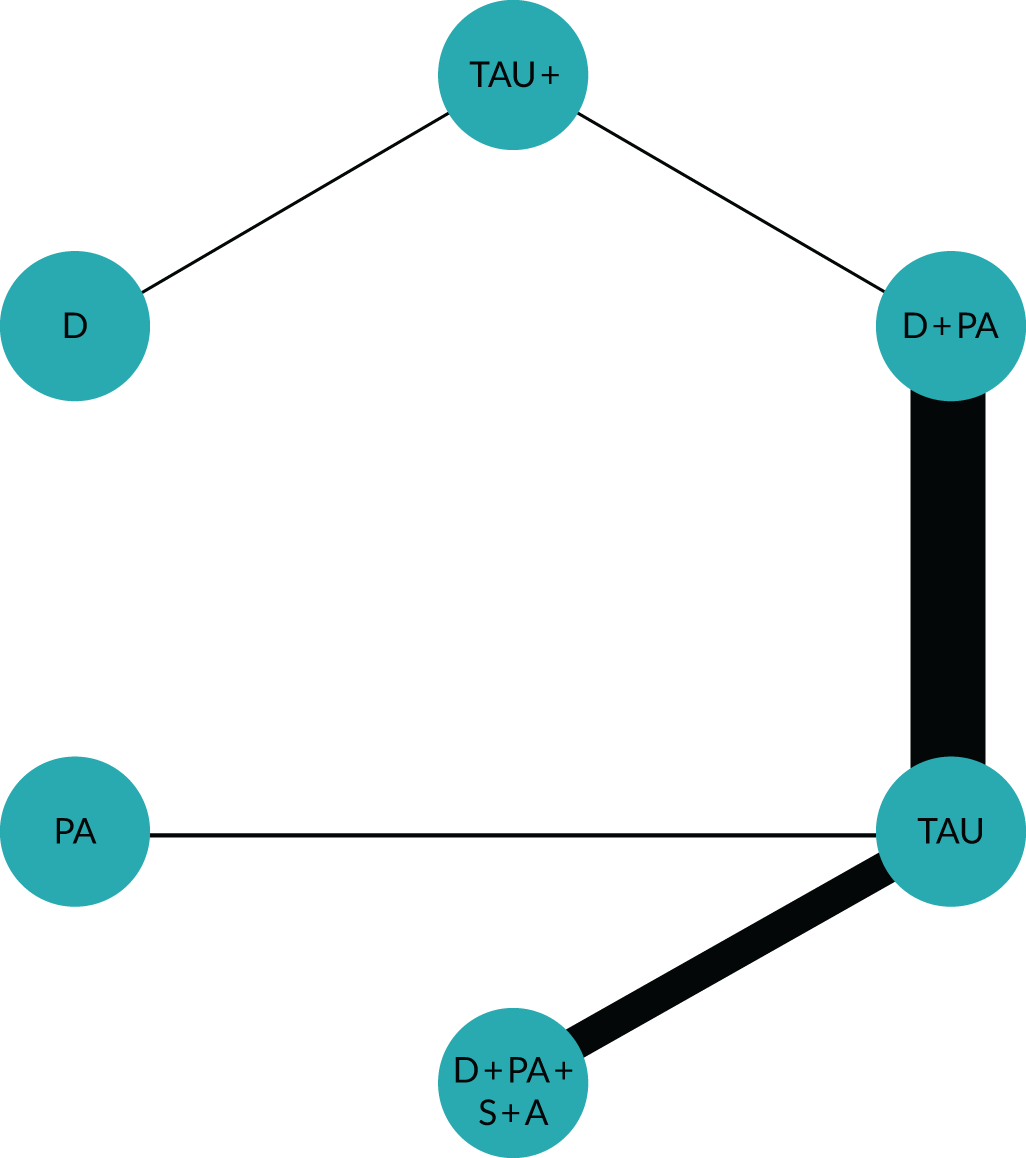
Quality of life: mental health
FIGURE 19.
Network diagram illustrating risk behaviours targeted in studies reporting mental health-related quality of life (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.
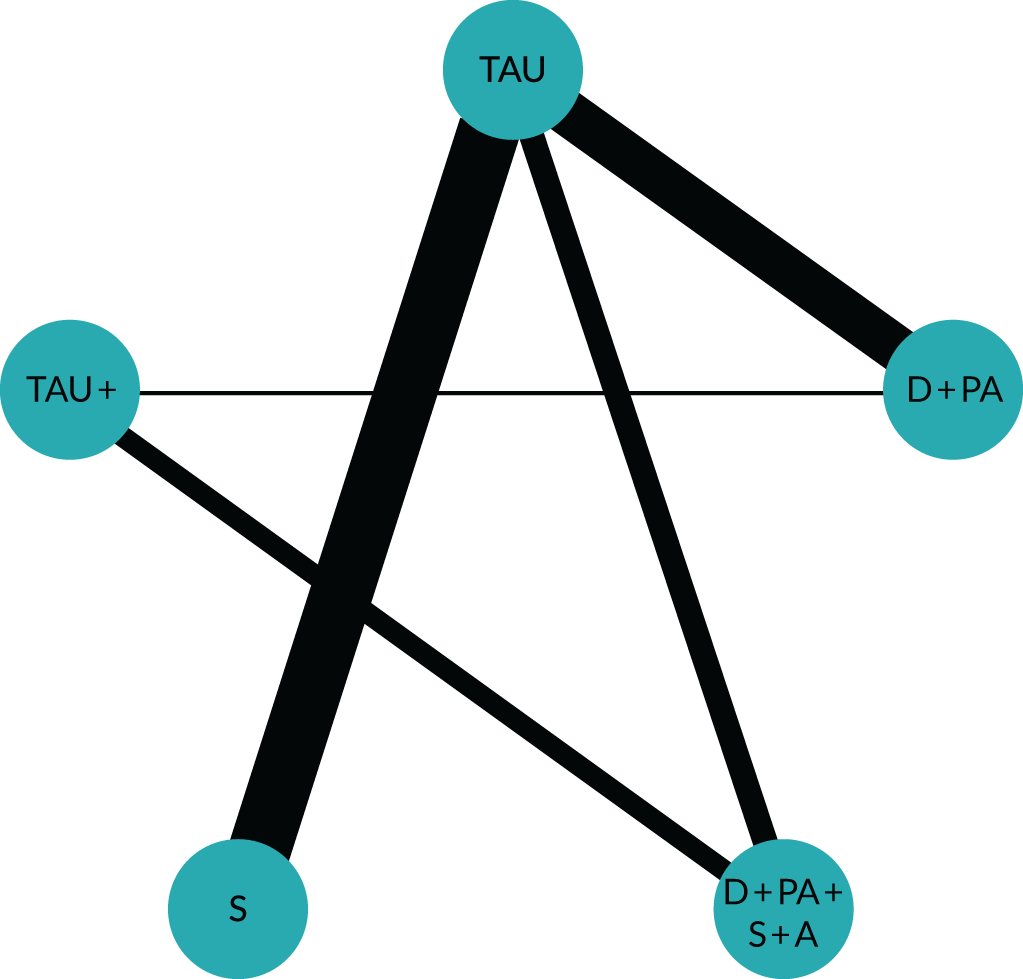
Quality of life: physical health
FIGURE 20.
Network diagram illustrating risk behaviours targeted in studies reporting physical health-related quality of life (thickness of edge is weighted by sample size). A, alcohol use; D, diet; PA, physical activity; S, smoking.

Appendix 8 The GRADE–CERQual evidence profiles
| Summary of review finding | Studies contributing to the review finding | Confidence in evidence based on CERQual assessment | Explanation of CERQual assessment |
|---|---|---|---|
| Interaction between physical and mental health | |||
| Healthy behaviours improving mental health and well-being | High confidence |
|
|
| Being considered more holistically | Moderate confidence |
|
|
| Self-medicating | High confidence |
|
|
| Motivational contexts for change | |||
| Individual factors | Moderate confidence |
|
|
| Social factors |
|
High confidence |
|
| Environmental factors | Moderate confidence |
|
|
| Barriers to behaviour change | |||
| Individual factors |
|
High confidence |
|
| Social factors | Moderate confidence |
|
|
| Environmental factors |
|
||
| Experiences of behaviour change interventions and success | |||
| Tailoring interventions to SMI populations | Moderate confidence |
|
|
| Knowledge and skills to enact behaviour change | Moderate confidence |
|
|
| Group delivery formats | Moderate confidence |
|
|
| Choices and adapting interventions to suit the individual | Moderate confidence |
|
|
| Purpose to activity | Moderate confidence |
|
|
| Valued benefits of behaviour change interventions | Moderate confidence |
|
|
List of abbreviations
- ASSIA
- Applied Social Sciences Index and Abstracts
- BCT
- behaviour change technique
- BCTT
- behaviour change technique taxonomy
- BCTT v1
- Behaviour Change Technique Taxonomy version 1
- BMI
- body mass index
- CASP
- Critical Appraisal Skills Programme
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- CI
- confidence interval
- CrI
- credible interval
- DIC
- deviance information criterion
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HDL
- high-density lipoprotein
- LDL
- low-density lipoprotein
- MD
- mean difference
- MRB
- multiple risk behaviour intervention
- NMA
- network meta-analysis
- OR
- odds ratio
- PANSS
- Positive and Negative Syndrome Scale
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
- randomised controlled trial
- SBP
- systolic blood pressure
- SD
- standard deviation
- SMD
- standardised mean difference
- SMI
- severe mental illness
- SRB
- single risk behaviour intervention
- TAU
- treatment as usual
