Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 15/25/20. The contractual start date was in December 2016. The final report began editorial review in March 2021 and was accepted for publication in September 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Papoutsi et al. This work was produced by Papoutsi et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Papoutsi et al.
Chapter 1 Introduction
Material throughout this report has been reproduced from Papoutsi et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text throughout includes minor additions and formatting changes to the original text.
Background and context
Diabetes represents one of the most significant global public health challenges of our time. 2 The global prevalence of diabetes has nearly doubled since 1980, with an estimated 8.5% of the global adult population living with the condition in 2014. 3 In the UK, recent figures place the number of adults living with diabetes at 3.9 million, of whom approximately 90% have type 2 diabetes (T2D) and 8% have type 1 diabetes (T1D). 4 It has been found5 that the prevalence of T1D and T2D has increased significantly in children and adolescents, and that these increases (particularly relating to early presentation in T2D) disproportionately affect people in ethnic minority groups. In the UK, the rising prevalence of diabetes has raised the cost of diabetes care to 10% of the annual NHS budget and has highlighted an urgent need to investigate different ways of delivering diabetes prevention and care. 6,7
In England and Wales, more than 30,000 children and young people with diabetes receive care in paediatric diabetes units. 8 Young people with diabetes constitute an important group, as the early adoption of good self-management practices at a young age can significantly reduce the risk of lifetime complications, prevent early mortality and lower costs for the health service. 9,10 An estimated 642 million people will be living with diabetes worldwide in 2040. 2 Yet, in 2018/19 only 36% of children and young people with T1D in England and Wales achieved recommended blood glucose control [haemoglobin A1c (HbA1c) levels of < 58 mmol/mol as per the National Diabetes Audit target],11 and a similarly low proportion received all recommended care processes, with high variability between care providers. 8 These audit data are reinforced by research12 showing that mortality among young adults with diabetes in the UK is worse than in other European countries and that it rose significantly between 1990 and 2010. Diabetes is also known to have serious consequences in those diagnosed in childhood: diabetes-related complications (such as kidney and eye disease) were seen in one in three of those with T1D, and in three in four with T2D in their early 20s, within 8 years of diagnosis. 13,14 People diagnosed with T1D before the age of 10 years (compared with those of older ages) have been shown in one study to have a 30-fold greater risk of future cardiovascular disease. 15 In recent years, there has been a considerable increase in young women entering pregnancy with pre-existing diabetes,16 and this is associated with adverse pregnancy outcomes (to mother and child) that are exacerbated by suboptimal glycaemic control and the absence of pregnancy planning.
Barriers to accessing health care for younger people include a lack of equitable access to services, a lack of developmentally appropriate consultations, a fear of being judged and stigmatised, and diabetes-related distress. 17 Young adults report the worst NHS experience of any age group, and their health-care needs and priorities are distinct from those of other age groups. 18,19 This may be even more important for young people from socioeconomically deprived areas, who achieve worse blood glucose control and present with more complications and unplanned pregnancies than those from more affluent areas,20 and for those in ethnic minority groups who are disproportionately affected by T2D. 21
Why is research on group clinics needed?
Current practice of diabetes care and who/what it fails to reach
The research described in this report is important for people who have diabetes and for the NHS for a number of reasons. First, after the transfer (or ‘transition’) of care from paediatric to adult care, young adults (usually defined as people aged 16–25 years) frequently exhibit a deterioration in glycaemic control. Loss to follow-up is common22,23 and attendance rates are low. 24 Many young adults with diabetes report poor experiences of, and dissatisfaction with, the care that they receive and challenges navigating health-care systems. 25 High diabetes distress and poor self-care have also been widely recognised in young people with diabetes. 26 A well-conducted multicentre trial27 found that enhanced transition care, including close support from a transition co-ordinator, had only short-term benefits for young people with T1D, and there is little trial evidence for T2D care during transition and young adulthood. These issues have been recognised internationally in a consensus statement by the American Diabetes Association28 and by the NHS, which has designed service specifications to support transition and young adult care for people with diabetes. 29 As described above, diabetes outcomes are disproportionately poorer among children and young adults from ethnic minority backgrounds and living in deprivation than among those who are not. 21 These findings highlight a need to look beyond traditional models of diabetes care, currently based on one-to-one clinic appointments with health professionals, to try to improve engagement with care, quality and experiences of care, and diabetes-related outcomes.
The focus on young adults living with diabetes reflects a key point in an individual’s life course at which effective intervention has the potential to lead to major improvements in long-term health outcomes and could potentially have an impact on lifelong health behaviours and engagement with care.
Improving care design and delivery through participatory involvement
Recent quality improvement work within the NHS30 has built on accumulating patient experiences that suggest that current care models do not adequately support individuals to take control of their health or work with their care providers to achieve their desired outcomes and experiences. The concept of person-centred care is central to these quality improvement programmes and has been widely adopted by organisations designing, delivering and evaluating complex care models, such as the NHS, The Health Foundation and The King’s Fund. 30 A number of different approaches to developing person-centred care have been proposed, including collaborative care models and experience-based co-design (EBCD). 31 Person-centred approaches have been shown to engage diverse and underserved communities32 and young people,33 particularly in mental health-care settings.
Collaboration and co-design in health care are increasingly built into health services research and intervention development, with a relevant example in T1D structured education. 34 EBCD offers an approach to examine, test, review and refine the new care model it designs in an iterative evaluation process, valuably applied to health-care implementation research.
Could group clinics enhance the care of people with diabetes?
Group clinic-based care (also known as ‘shared medical appointments’) for people with diabetes has been used and evaluated before in specific contexts. 35 Group-based education, in models such as Dose Adjustment For Normal Eating (DAFNE), is already used widely in diabetes treatment, but is typically a single, time-limited intervention based on education to support a limited range of diabetes self-management practices. There is little evidence to support group-based models that incorporate a broader scope of care in health services. A study36 of Italian adults with diabetes who underwent group-based care, which focused on lifestyle interventions, found that those who underwent group-based care maintained better glycaemic control and required less clinician time than those receiving standard one-to-one care. This trial identified that group care requires the ‘reallocation of tasks, roles, and resources and a change in providers’ attitudes from the traditional prescriptive approach to a more empathic role of facilitator’,36 highlighting the need for innovation away from standard models of care in the delivery of such an intervention. Other evidence37 suggests that shared medical appointments can yield measurable improvements in patient trust, patient perception of quality of care and quality of life. Some studies suggest38 that shared medical appointments offer a route to better support and engagement in health care for underserved racial and ethnic minorities. With specific relevance to young adults, recent advances39 in neuroscience and psychology highlight that peer influences are likely to be particularly important for controlling risk behaviour and that this may have a significant impact in adolescence and young adulthood. The development of group clinics has exploited the potential for peer support to improve health-related behaviour, for example in the successful introduction of a group clinic for young adults following renal transplant, which led to a significant reduction in the incidence of graft loss. 40
To our knowledge, no studies have incorporated or evaluated group clinics designed with extensive participation of service users, have been designed to meet a wide range of health and social care needs or have been evaluated extensively in young adults with diabetes. Furthermore, recent systematic reviews have found that group clinics often had a positive effect on clinician- and patient-reported outcomes but have not undertaken detailed work on their mechanisms of action and context in which they work,41 and this is vitally important if group clinics are to be implemented within a health system, such as the NHS.
The National Institute for Health and Care Research (NIHR) identified a need to generate an evidence base for the use of group clinics in chronic conditions, and supported a commissioned systematic review in 2015,41 followed by a commissioned funding call for primary studies, of which this is one. The systematic review identified previously published mixed-methods research, including 22 randomised controlled trials, of group-based clinics, the majority of which had been aimed at delivering care to people with diabetes. Their review concluded that, although group clinics seemed to have consistent and promising evidence of benefit on some biomedical outcomes, there remained significant uncertainty as to their potential benefit within the NHS and whether or not they would meet the needs of people from ethnic minority groups. The review41 also identified the need for greater understanding of the context in which group clinics might offer an appropriate alternative to individual consultations, and the conditions in which they would be less appropriate.
Research objectives
Aims
-
To explore the scope, feasibility, impact and potential scalability of group clinics for young adults with diabetes.
-
To contribute to NHS service redesign and improve care for people from underserved groups with long-term conditions.
Research questions
-
How and to what extent might an innovative, co-designed, group clinic-based care model meet the complex health and social needs of young people with diabetes?
-
Could a group approach help support diabetes self-management? If so, what can the experiences of participants, the functioning of the group and the wider context in which the new model takes place tell us about its mechanisms of action?
-
What is the feasibility, acceptability, cost and impact on outcomes of introducing group clinics for their users and stakeholders? What is the organisational impact of this model to the NHS and other stakeholders?
-
What would be the optimal size and study design of a cluster-randomised controlled study to evaluate the clinical benefit and cost-effectiveness of offering group clinics to young adults with diabetes? What other factors should be considered when planning such a randomised controlled trial (e.g. factors relating to patient characteristics, existing models of service delivery, acceptability and mechanisms of action of group clinics on clinical outcomes)?
Chapter 2 Evidence synthesis (realist review)
Our evidence synthesis of group clinics for young adults with diabetes was underpinned by a theory-driven realist methodology. Realist reviews consider the mechanisms by which a programme (in this case, group clinics) works (or not) and the contexts in which these mechanisms are triggered to produce certain outcomes. Realist reviews (and evaluations) have been extensively applied in health services research.
A realist review was performed to synthesise findings from existing literature to understand how group clinics may work for young adults with diabetes and other complex needs. This detailed evidence synthesis followed the approach and standards of the NIHR-funded Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) project to understand ‘what works, for whom, under what circumstances’ in group clinics for young adults with diabetes. 42,43 The review synthesised existing qualitative, quantitative and mixed-methods studies relevant to this topic area. The findings of this evidence synthesis supported the empirical research undertaken subsequently, including the co-design and context-sensitive development of a group clinic model and its implementation and evaluation within the NHS.
The realist review is presented as a published paper and includes a detailed description of its methodology and results. 44 Its findings highlighted four main principles that should be taken forward in the contextualisation and design of group clinics to support engagement from young people:
-
emphasis on self-management as practical knowledge
-
development of a sense of affinity between patients
-
provision of safe, developmentally appropriate care
-
the need to balance group and individual needs.
The realist review highlighted that the implementation of group clinics within health systems was rarely, if ever, straightforward. Numerous adjustments were needed to existing operational and clinical processes to deliver high-quality care through group clinics, and there was substantial ‘hidden’ work (i.e. work that was not recognised, measured or rewarded, and which was often carried out by relatively low-status staff in their own time) involved in doing so. Finally, it was noted that group clinics worked best alongside individual care and there was no evidence to suggest that they offer a means to replace it.
Chapter 3 Methods
Study design overview
The study, which built on the findings of the realist review described in Chapter 2,44 was conducted in three phases and embedded in a continuous process of participatory and dissemination activities; it is summarised in Figure 1. First, we undertook a scoping exercise, combining questionnaire data with NHS audit data, to generate a descriptive understanding of existing group-based care and the current state of diabetes care for young adults. Second, we carried out in-depth participatory co-design activities to develop a model of group clinic-based care that was then implemented in two NHS diabetes services (‘group clinic sites’). Third, we evaluated this group clinic model using mixed, qualitative and quantitative methods, and a cost analysis, with a further two NHS diabetes services used as ‘control sites’. Our evaluation assessed both the impact of the group clinics on young adults and the potential impact of group clinics within the NHS. Our quantitative evaluation of group clinics was not designed to provide a definitive estimate of differences in outcomes; rather, it was intended to contextualise the qualitative evaluation and, in combination with the cost analysis, to guide the feasibility of a future at-scale evaluation.
FIGURE 1.
Study design overview.

Our study design and methods have been published in a protocol paper. 1
Changes to the original protocol
There were three changes from our original (published) protocol, highlighted below.
Revised aims of National Diabetes Audit analyses
We had intended to perform unit-level (i.e. per clinical service) comparisons of the care delivered to all patients at our group clinic and control sites, using the NHS Digital National Diabetes Audit to provide a descriptive background and a comparison with national data. However, after data access had been granted by NHS Digital, it became apparent that complete unit-level data from our research sites were not available because the required data sets were not complete and, at one research site, could not be disaggregated at unit level from within a larger hospital trust provider. We, therefore, undertook an alternative analysis by using data collected at the individual level from our recruited research participants and comparing this with national-level data from the National Diabetes Audit (NDA). 45
Inclusion of an additional research site for group clinics
During the course of recruitment to our group clinic care model at Newham University Hospital, it became apparent that we would not meet our recruitment target because of a recent reduction in the total clinic population (owing to recent local service changes), as well as incomplete uptake. We, therefore, made a proactive decision to open a new research site at the Central Middlesex Hospital to run the group clinics. Central Middlesex serves a comparable multiethnic, deprived, urban population to Newham University Hospital. The inclusion of this new site had both advantages and disadvantages to the research process. The advantages were that we could evaluate the delivery of group clinics in an NHS setting with different staff, care processes and organisational structures, and we were able to study the group clinic model at a more advanced stage of its development following its co-design and implementation at Newham. This provided new insights and richness to the evaluation of implementation, and contributes to the generalisability of the research findings. There were fewer disadvantages: the variation in delivery of the care model made the direct comparison of quantitative data between Newham and Central Middlesex challenging, and, therefore, data from both sites have not been aggregated.
Comparative quantitative analyses
We had planned to undertake an intention-to-treat analysis, in which we would compare participants at the intervention sites who had been offered and agreed to participate in the group clinics with those who had not been offered group clinics. However, owing to the challenges of recruitment at the group clinic sites, and the variable attendance at group clinics of the recruited participants, we instead offered the group clinic to all young adults at each clinic site and compared those who did with those who did not attend (DNA). As planned, we then compared characteristics and trajectories of all participants at intervention sites with participants at control sites (intention-to-treat analysis).
Theoretical approach
Our work was underpinned by a set of theoretical ideas that influenced intervention development and implementation, and informed qualitative data analysis and interpretation; a more detailed theoretical analysis will be included in upcoming publications. Our approach to intervention development and implementation was underpinned by complexity theory, primarily drawing on an understanding of complex systems as characterised by uncertainty, unpredictability and emergence. 46,47 This means that we treated the introduction of group clinics as a complex change process in which mechanistic replication and standardisation were not sufficient, and attention to the dynamic properties of context and the ongoing tensions raised was necessary. 46,48 Following previous work,46,49 the principles driving our implementation effort can be summarised thus: acknowledging unpredictability, harnessing the capacity of implementation teams to self-organise differently in the different settings, facilitating interdependencies between clinical and operational processes, and encouraging sense-making and experimentation with different group clinic delivery formats. In addition, we focused on developing adaptive capability in staff so that they could make good judgements on how best to introduce this new model of care, attending to human relationships that would make this complex change feasible (e.g. through goodwill and reciprocity), and, finally, harnessing conflict productively to contribute to positive solutions. 46 Following a complexity-informed approach, our evaluation also produced a nuanced account of how change came about by drawing on different data collection methods and through developing close relationships with the field sites.
By drawing on ecological theories,50,51 we viewed patient self-management and self-care not as activities carried out in isolation, but as activities nested in multiple, proximal and distal contexts (e.g. family, education, employment, social life) that afforded particular opportunities and constraints, especially so in the context of socioeconomic deprivation. This was acknowledged not only in terms of how group clinic interactions attempted to influence self-care, but also in terms of how the evaluation elicited an understanding of how group clinics worked (or not) for young people.
The evaluation delved further into social theory to make sense of the way that group clinics worked and theoretically substantiate an understanding of their change mechanisms. We drew from ideas on practices of solidarity as theorised by Prainsack and Buyx,52 who conceptualise solidarity as enacted, embodied and contextual, based on a view of personhood as relational (i.e. in which people are dependent on and open to their environments). Our analysis draws not only on instances of solidarity at an interpersonal level (i.e. manifestations of willingness to carry costs to assist others with whom a person recognises similarity in at least one relevant respect), but also on instances of solidarity at a group level, through shared commitment to engage together with others in diabetes care, including through a sense of a joint purpose. 52
In contrast to individual appointments, group clinics put relational aspects of self-care to the fore, with the focus on interactions between patients rather than just patient–clinician relationships. This introduced new types of ethics relations between patients and projected new ways of enacting patienthood. We explored what it meant for clinical care to be harnessing experiential knowledge directly through active patient participation in service provision. This included an understanding of how a balance was achieved between biomedical knowledge and practical experiential knowledge in group clinics. Following Pols,53 we examined how embodied patient knowledge becomes transferable and useful in the context of group-based care. 54 We asked the following question: what kinds of knowledge are shaped in group clinics and what are the conditions for doing so? This was supplemented by burden of treatment theory, which focuses on how self-management work and responsibility become delegated to patients and the demands that these place on them. 55
Finally, another theoretical perspective that informed our analysis of group clinic implementation related to articulation work as the hidden, invisible adjustments and alignments necessary to successfully carry out tasks in sociocultural settings. 56 We were specifically influenced by the three different types of articulation work proposed by Allen:56 (1) temporal articulation, with health professionals acting proactively to facilitate care processes or reactively to address unexpected developments; (2) material articulation, referring to how tools and other artefacts become mobilised and embedded in care pathways to maintain their stability; and (3) integrative articulation, which covers relational aspects of receiving input and managing co-ordination and coherence in care, including working with contradictions.
National context
Existing use of group clinics in the NHS
To investigate the existing and potential use of group clinics in diabetes management and treatment, a scoping survey was set up for interested health-care professionals in May 2017. An online questionnaire tool was disseminated to clinical networks and professionals via e-mail and social media.
National Diabetes Audit
The NDA is a large audit managed by NHS Digital. It contains individual- and service-level data on diabetes care processes and outcomes from NHS trusts in England, benchmarked against quality standards (e.g. guidance from NICE). 57 We planned to use NDA data to provide a national context to our research and make unit-level comparisons with our research sites. We used the standard NDA audit reporting of eight routine care processes [HbA1c levels, blood pressure (BP), cholesterol, renal function, urinary albumin, foot examination, body mass index (BMI) and smoking review, recorded in the previous year] and three treatment targets (HbA1c levels of ≤ 48 mmol/mol, BP of ≤ 140/80 mmHg and total cholesterol of ≤ 4 mmol/l in the previous year).
As planned, an application was submitted to the NHS Digital Data Access Request service on 22 May 2017 for service-level data on patients aged 16–25 years in the NDA. However, there were a number of changes to the process for accessing NDA data over the study period, which caused a long delay in receiving these data. Our data application (DARS-NIC-228637-P6N0L) was not approved until 14 August 2019, and at this point we were given access to 2016/17 and 2017/18 data.
During the course of this application, a number of unexpected issues arose. First, it became apparent that we would not be able to obtain unit-level data disaggregated by our research sites to compare with data from other units or national-level data. This is because the NDA is designed predominantly for analysis by general practices and Clinical Commissioning Groups (CCGs) rather than hospital services. In addition, data from all patients at Newham University Hospital (NUH) (a group clinic site) and Mile End Hospital (MEH) (a control site) were aggregated and reported by the overseeing NHS trust provider [Barts Health NHS Trust (BH)] in 2017/18. Data were not available from Central Middlesex Hospital (CMH), which is part of the larger London North West University Healthcare NHS Trust. Second, the data extraction process changed to a new system in 2017/18 and we were advised that national comparison would not be possible between 2016/17 and 2017/18. Finally, we were given access only to data with small numbers suppressed. For this reason, statistical analysis of unit-level data was often inappropriate owing to the relatively small sample size.
Within these limitations, we had to change our intended aim of using NDA data to make unit-level comparisons between our group clinic sites and national data, and instead we used the data to make more general descriptive comparisons, as follows:
-
describe sociodemographic and clinical characteristics of young people (aged 16–25 years) under the care of adult diabetes services in England
-
study performance on the three treatment targets and eight care processes for young people (aged 16–25 years) under the care of adult diabetes services in England
-
compare descriptive characteristics of young people (aged 16–25 years) at our research sites with young people and older people (> 26 years) nationally.
We studied NDA data from England cross-sectionally from 2017/18 audit submissions. Data were aggregated by type of diabetes; however, owing to small numbers, rare types of diabetes defined by NDA as ‘other’ (e.g. cystic fibrosis-related diabetes and monogenic diabetes) were included with the T2D data. The aggregation of rare types of diabetes with T2D is unlikely to distort the findings because they are a small fraction of the whole, especially outside tertiary specialist centres (which were not included in our research sites). We obtained national data (from all England sites submitting to the NDA) as well as data from BH (which included our group clinic site NUH and our control site MEH, in addition to two other clinical services). NDA data were not available from CMH. We made descriptive comparisons between young adults (aged 16–25 years) at our research sites and national data on the same age group, as well as people aged ≥ 26 years.
Setting
We included four research sites based at clinical services delivering young adult diabetes care (Table 1). These included two sites (NUH and CMH) that would deliver group clinics, and two sites [MEH and Whittington Hospital (WH)] that would act as comparator (control) sites.
| Characteristic | Group clinic sites | Control sites | ||
|---|---|---|---|---|
| NUH | CMH | MEH | WH | |
| Setting | ||||
| Borough | London Borough of Newham | London Borough of Brent | London Borough of Tower Hamlets | London Boroughs of Islington and Haringey |
| Ethnic minorities (%) | 72 | 65 | 69 | 32 and 38, respectively |
| Childhood poverty rate (%) | 52 | 43 | 57 | 47 and 40, respectively |
| Clinic | ||||
| Approximate size of the young adult clinic | 200 young adults aged 16–25 years | 75 young adults aged 16–25 years | 150 young adults aged 16–25 years | |
| Percentage of young adults with T2D | ≈ 30 | ≈ 15 | ≈ 15 | ≈ 15 |
| Clinic organisation | Monthly multidisciplinary clinic and weekly nurse clinic with virtual option and mobile telephone access | Multidisciplinary clinic twice per month, with daily walk-in clinics and mobile telephone access to a named diabetes specialist nurse | Bimonthly multidisciplinary clinic. Diabetes specialist nurse input offered as required by telephone/e-mail | Multidisciplinary clinic runs twice per month and incorporates transition clinic. Diabetes specialist nurse is available daily |
| Staffing | Consultant diabetologist, diabetes specialist nurse, dietitian, psychologist and youth worker. Close work with the paediatric team post transition | Consultant diabetologist, diabetes specialist nurse, dietitian, with input from a psychologist as required | Consultant diabetologist, diabetes specialist nurse, dietitian, psychologist | Consultant diabetologists from both adult and paediatric services and a diabetes specialist nurse. Dietitians and a psychologist contribute to the clinic when available |
| Other notable features | Recent service improvement work, e.g. offering peer support groups | Recent service improvements including delivery of a new structured education programme (TEAM T1) tailored specifically for young adults | Peer support offered to type 1 patients, but not specific to young adults | |
Research participants
We recruited young adults (aged 16–25 years) living with diabetes (of any type) and receiving care at the four research sites, with the aim of recruiting 80–100 participants across all sites. There were no exclusion criteria. Young adults recruited at the ‘group clinic sites’ were invited to join group clinics co-designed and implemented during the course of this research. Young adults recruited at ‘control sites’ were involved in data collection only.
When the study was designed, we did not anticipate that we would invite all young adults (if eligible) under each service to join the study. However, after observing the high patient turnover in the clinics and low attendance rates, we revised this plan and instead attempted to recruit all young adults under each service.
Potential participants were identified by usual-care teams, and were approached by the research team (which included usual-care team members), and were given invitation letters and patient information sheets. Informed consent was then sought from interested individuals. An example of all patient-facing documents (i.e. invitation letter, patient information sheet and consent form) is given in Report Supplementary Material 1. The research was given a branding and logo and named ‘Together Study’, which was used across all patient-facing documents.
Co-design
Methodological approach
Our research drew on key theoretical and practical approaches to participatory research that allow researchers, practitioners and service users to learn together for the benefit of service redesign. 58,59 The group clinic interventions were co-designed using a participatory approach to ensure cultural, developmental and practical relevance; enhance recruitment and retention; and attempt to instigate system change and support sustainability. 59 Co-design focuses on improving patient and staff experiences, with equal importance being given to each perspective. Participants in co-design, whether patients, staff or other stakeholders,60 are seen as being ‘expert through experience’, and this experience is utilised in co-design to identify opportunities for improvement and adaptations to service design, focused on the functionality (usability) for patients and staff. In co-design approaches, patients and staff work alongside each other to identify problems that can be practically overcome and to develop a jointly negotiated outcome. Co-design with young people may require special facilitation skills and adaptation to be developmentally and age appropriate. The role of the facilitator is key in building trust,61 but there are also considerations around the special challenges of engaging young people to take part and in ensuring informed consent.
We used The King’s Fund Experience-based Co-design Toolkit. 31,61–63 This approach was chosen because research64 suggests that co-designed services can lead to service improvement. The EBCD process provides a template for co-designing service development, drawing on the expertise of patients and staff, with regular review and iteration. EBCD gives a detailed insight into the experiences of all participants, including both patients and staff. When EBCD is conducted, patients and staff work separately at first and are then brought together for joint work. This careful approach supports participation from patients and staff (including wider stakeholders), in prioritising aspects of existing care to build on, as well as areas for improvement and change.
We planned a co-design process that would evolve and adapt as the project developed, and would fit around availability of participants, practical constraints and hospital procedures. Previous work65 indicates that there are particular challenges of engaging young people in co-production work, especially if they are also coping with a long-term condition as well as the day-to-day challenges of education and/or work.
We made adaptations to the full EBCD process, which ordinarily includes the production of a series of films that help to share perspectives between the groups. We omitted this step because it was decided that this aspect would be too time-consuming and might be a disincentive to young adults and staff engaging with the process. Instead of filming, we relied on audio-recording and verbal feedback at meetings. These changes are consistent with reports from other users and researchers of co-design who have also streamlined these EBCD processes. 64
Co-design processes
We undertook co-design in two phases.
Phase 1
In year 1, co-design was used to develop and build the new group clinic-based model of care and involved the following:
-
Group and individual sessions – group co-design sessions were formed for young people and staff/stakeholders separately, and were complemented by additional one-to-one interviews.
-
Analysis of the main themes arising from the interviews.
-
A joint patient and staff/stakeholder event to bring perspectives together.
-
Further analysis of emerging themes.
-
Follow-up interviews with additional participants as necessary.
-
Feedback to participants.
Phase 2
In year 2, the second phase of co-design supported iterative development of the group clinic model, refining its design and delivery after the clinics had already been implemented for 1 year. This involved the following:
-
Group sessions – further group sessions involving both patients and staff took place across both research sites.
-
Individual interviews with both staff and patients at both research sites.
Continuous co-design processes
Ongoing co-design was built in alongside the implementation of the group clinics, using discussion and feedback after each session and facilitated by the clinician and researcher in residence. This supported wider participation from young adults beyond the discrete co-design sessions outlined above, allowing iterative adaptation.
Consent/information procedures
Patient participants for co-design were recruited from the clinical settings in which we planned to deliver group clinics. In addition, staff and stakeholder participants were also selected as representatives from organisations (e.g. CCGs) with responsibility for the care of young adults with diabetes. Formal informed consent procedures were used for all co-design participants.
Conducting the co-design sessions
Co-design workshops took place in community and clinical facilities linked to NUH and CMH. Co-design was led by the Association for Young People’s Health (AYPH) (London, UK), an external and third-sector organisation with particular expertise in participation work with young people and health professionals. The clinical teams delivering diabetes care to young adults at NUH and CMH also contributed to the delivery of the co-design process, as did the research team.
The facilitation of co-design sessions was led by experienced staff from the AYPH. Sessions were audiotaped and transcribed. The following principles and approaches were used:
-
Young people living with diabetes. Each individual was encouraged to tell their own story, recalling their own voice and experiences and communicating their own personal ‘truths’. The facilitator had prepared a workshop of questions and workshop activities to defuse any anxiety or embarrassment and provide a way to encourage sharing. However, the issues raised mainly came from the participants, and discussions followed the line that they wanted to take. Sessions lasted no longer than 2 hours and opened and ended with a ‘check-in’ to raise any emotional anxieties and to ensure that young people left the process in a safe state of mind, feeling supported and listened to. Young people were also given an outline of the next steps in the work and details about how to find further information.
-
Health-care professionals. It was important to allow staff the same freedom as the patients to share their perspective. Participants included a wide range of professionals and stakeholders, including dietitians, specialist nursing staff, a CCG commissioner, representatives from primary care, representatives from the voluntary sector (Diabetes UK, London, UK), consultant diabetologists and reception staff.
-
Joint discussions. To focus and support discussions, all those attending the joint sessions (patients and staff/stakeholders) were asked to prepare in advance three issues to present to the group, instead of collating and sharing issues during the group session. This supported the effective use of the time available and provided a valuable structure for discussions.
Discussion topics introduced in the co-design
We drew on the findings from our realist review to identify the following areas of discussion during co-design:
-
Group composition and continuity. At the time of our study, to our knowledge, there was little certainty in the literature around the ‘ideal’ composition of group clinics, and we considered the possible importance of age-related developmental stages, sex and disease type in the co-design of our group clinic model. We also discussed the possible importance of factors such as independence (e.g. living at home, away at university), time from diagnosis, family circumstances and general life experiences. Our realist review highlighted the importance of continuity within the group (participants and/or staff) to support relationship building, cohesion and the sharing of stories.
-
Role of parents. The realist review identified parents as possible active participants in a group clinic model for young adults, and that their involvement could have both positive and negative effects.
-
Individual versus collective experiences. We identified the need to manage group discussions in such a way that they would support both individual and shared experiences.
-
Content and approach specific to young people. Our review suggested that many young people prioritised fitting in with their peers as more appealing than closely following diabetes self-management advice, and that this challenge was a potentially fruitful area of focus in the group clinics.
-
Logistical considerations. We identified a number of logistical considerations important to the design of group clinics, including the time of day they should be scheduled and the location they should be held in.
-
Clinical aspects. Previous literature44 highlighted a range of strategic considerations relating to the clinical care delivered in group clinics, including whether group clinics should replace existing care appointments or run in parallel to them (i.e. offer additional care), how the group should be led and facilitated and by whom, how frequently they should be held and how the safety of participants could be ensured through setting ground rules.
Evaluation of the group clinic model
Qualitative methods
Embedded research
A ‘researcher in residence’ model was adopted as a practical manifestation of a participatory approach to research and evaluation. The researcher was an integral member of the front-line implementation team, contributed theoretical and practical insights based on research findings, and helped to navigate different bodies of expertise within the study. The embedded researcher worked towards bridging the qualitative and quantitative evaluations, helping to include practitioner and patient views into the design and feeding back early findings to stakeholders. We followed previous experience with how the researcher-in-residence model was applied in a number of different settings. 66
Ethnographic observation
The researcher in residence (CP) worked closely with the clinical teams throughout the project and carried out ethnographic observation in the two hospitals. This primarily included three types of observations, involving different degrees of participation depending on the encounters observed:
-
Group clinics. The researcher was involved in different aspects of the group clinics programme, including planning and setting up, co-ordination between the clinical teams, and de-briefing and discussing ongoing adjustments to the model of care. She carried out ethnographic observation in most group clinics organised in the two hospitals, had informal discussions with patients ahead of the clinic, participated in icebreakers and generally helped with delivery where needed. To support the ongoing co-design of this new model of care, at the end of each clinic the researcher held brief feedback discussions with patients to understand what had worked well and what they thought should change next time (when the researcher was absent this was led by the diabetes specialist nurse or the youth worker). The researcher introduced herself to the group as a researcher from the university interested in finding out how group clinics work for young people, and she worked towards building rapport. Especially with some of the frequent attenders, she managed to build a good relationship and understand people’s experiences not just as a one-off interaction but longitudinally over the course of the group clinics programme. A significant amount of field notes was collected from ethnographic engagement. These notes included information on clinic characteristics, such as session content, context, group dynamics and facilitation style. The majority of group clinics were also audio-recorded with participant consent and transcribed for analysis.
-
Individual appointments. To gain a wider understanding of standard diabetes care and to be able to draw comparisons with group clinics, the researcher also conducted ethnographic observations in 15 individual appointments in young adult clinics. These were sampled to achieve maximum variation between different consultants and nurses in the two hospitals. Some of these appointments were with patients taking part in group clinics, which allowed a broader understanding of their engagement with care as part of different interactions. It was striking how some patients presented themselves differently in the one-to-one appointments and in the group clinics.
-
Other interactions. The qualitative researcher also collected field notes from ethnographic observations in co-ordination meetings; facilitation trainings; and other informal interactions with clinical teams in the context of setting up, managing and delivering group-based care alongside standard clinical practice.
Qualitative interviews
Between February 2018 and October 2019, the researcher in residence carried out 31 semistructured interviews with patients, group facilitators and other clinical and non-clinical staff (see Appendix 1 for further details). Interviews lasted 30–110 minutes and followed a semistructured format (see Appendix 2 for interview guides with indicative questions). One staff participant was interviewed twice to reflect on the development of group-based care over time. Another interview involved two siblings who were interviewed jointly about their experiences living with diabetes and attending group care. Most patient interviews took place in hospital settings or other mutually convenient locations either before or after the group clinics, although five patients preferred to be interviewed on the telephone. Staff interviews were conducted in offices or other hospital settings; two took place on the telephone. Interviews formed only part of the encounters with participants in the context of a broader relationship developed with the qualitative researcher during the project (e.g. through ethnographic observations in clinics or informal discussions during clinic set-up). The purpose of the interviews was, therefore, to continue conversations that had already been taking place over the course of the project and to consolidate some of the learning from patient and staff perspectives. The researcher took contemporaneous field notes to contextualize interactions and encounters with research participants, bringing together data from different formal and informal discussions throughout the 2 years of fieldwork. Most interviews were audio-recorded with consent and professionally transcribed; in two of the telephone interviews it was more practical to keep field notes.
-
Patient interviewees (n = 19). We recruited 19 young people in interviews, nine female and 10 male, who were between 18 and 25 years of age and from a variety of ethnic backgrounds. Four patients had attended 7–10 clinics, nine had attended three to six clinics and six had attended zero to two clinics (one of whom withdrew from the research study after one clinic and another consented but never attended). Most interviewees were living with T1D (of whom two were also using an insulin pump) and two had T2D. This was representative of the broader composition of participants in group clinics, which predominantly included patients with T1D in both hospitals. Interviews addressed experiences of being diagnosed and living with diabetes as a young person; experiences of receiving diabetes care; and experiences of participating in group clinics, including encounters with health professionals and other young people. Guided by clinicians’ knowledge of patients and the relationships with the researcher as part of the ethnographic engagement, we recruited patients with varied clinical background, time since diagnosis and experiences of diabetes care. Despite our efforts, we were only able to recruit one young person who had not attended any of the clinics; most of those who did not engage with group-based care also declined participation in interview.
-
Staff interviewees (n = 11). We recruited three diabetes consultants, three diabetes specialist nurses, one youth worker, one research nurse, one dietitian, one psychologist and one sexual health advisor who delivered sessions and/or supported the group clinic programme. Discussions covered clinicians’ experiences of providing care for young people with diabetes and their views on how diabetes health services could better meet the needs of this population, as well as their experiences of setting up and delivering group-based care in the two hospitals involved. We focused our sampling on clinical and non-clinical staff who had been involved in the group clinic programme (as group facilitators or in other roles) to understand their views and experiences.
Documents
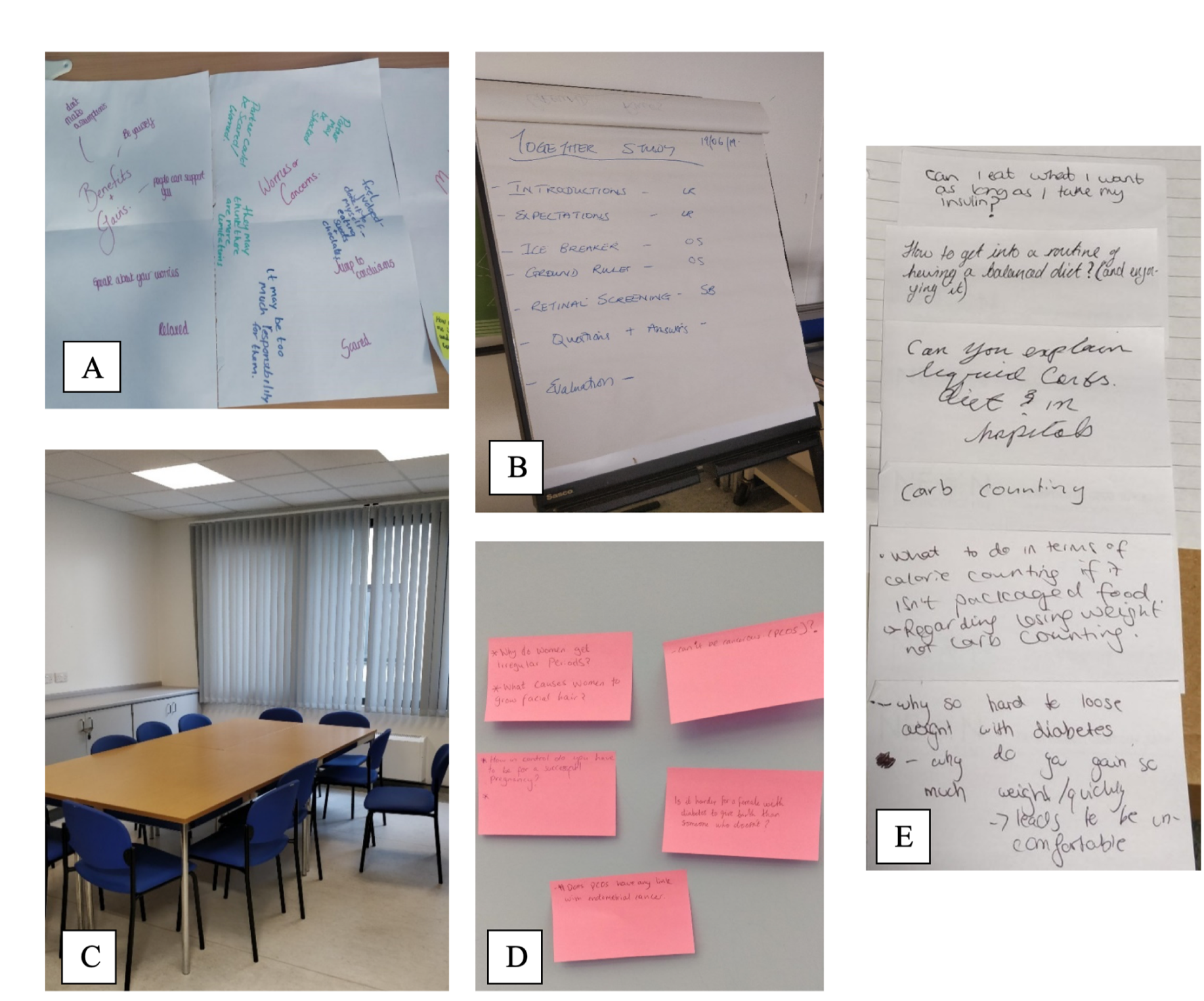
We collected all documentation produced in co-design sessions, project and steering group meetings, facilitation training and other interactions. Other materials collected as part of our ethnographic fieldwork in group clinics included outputs of group activities using flip charts, icebreaker materials, sick-day rules diagrams and other artefacts used in the group context (Figure 2).
FIGURE 2.
Photographs illustrating the group clinic materials and room set-up (photographs A and D from NUH; and B, C and E from CMH).
Qualitative data analysis
Owing to the iterative nature of the research, the researcher in residence carried out analysis in parallel to data collection throughout the project, with emerging findings presented and discussed in team meetings and used to adapt the model of care. The analysis drew on different theoretical lenses (see Theoretical approach), such as complexity approaches in health services research47,49 and frameworks on invisible, hidden work,56,67 as well as burden of treatment and patient work theory,55 solidarity practices52 and critical perspectives on patient expertise. 53 We moved between an inductive and a deductive approach to our analysis, paying attention to emergent themes and using substantive theory as a sensitising device to drive further interrogation of the data. We also drew on the programme theory developed as part of our realist review in earlier stages of the project (see Chapter 2) and refined its different components based on further analysis of our empirical data. We continuously developed the overall narrative emerging from our analysis and iteratively added to the coding framework. A second researcher (AF), with a background in psychology and complex intervention development, was involved in later stages of the analysis of the group clinic transcripts, independently verifying the coding framework and developing consensus on emergent themes. Interim analysis was also driven by pragmatic requirements to inform implementation, as well as to ensure that no safety issues were raised by participants.
NVivo version 12 (QSR International, Warrington, UK) and Microsoft Word (Microsoft Corporation, Redmond, WA, USA) documents were used to support management and analysis of qualitative data, which included anonymised interview and group clinic transcripts, ethnographic field notes, e-mail communications and other documents. An example NVivo analysis is presented in Appendix 3.
Quantitative methods
Data collection
Members of the research team at each site (both group clinic and control sites) collected sociodemographic and questionnaire data through face-to-face or telephone interviews with recruited study participants. We were unable to collect data on participants who did not wish to be recruited, but collated brief information on their reasons behind that decision. Clinical data were accessed through each site’s clinical record system. Data were then collated on a standard template [see the NIHR project web page; URL: www.journalslibrary.nihr.ac.uk/hsdr/NKCR8246) using the study number of each participant as the only unique identifier. No identifiable information was recorded on this template.
Baseline data were collected at entry to the study. Follow-up data were collected approximately 1 year later (a window of 9–15 months was used to allow co-ordination with clinic visits, university holidays and other practical considerations).
The following data were collected at baseline:
-
Sociodemographic characteristics – age, sex, Index of Multiple Deprivation (IMD) quintile, ethnicity, English as first language (yes/no), education and employment status (education/employment, both/neither).
-
Clinical characteristics (including health-care activity) – type of diabetes (1/2/other), most recent HbA1C mmol/mol level, reported frequency of blood glucose monitoring per day, age at diagnosis, use of technology within the last year and previous attendance at any group education for diabetes. In addition, we captured the percentages of planned diabetes appointments, emergency department (ED) attendances (diabetes related), inpatient admissions (diabetes related) and primary care consultations, all within the previous year.
-
Patient-reported instruments – the Problem Areas In Diabetes Score and Patient Enablement Instrument were used. 68,69 Relevant information about these instruments is presented in Table 2; for example questionnaires see the NIHR project web page (URL: www.journalslibrary.nihr.ac.uk/hsdr/NKCR8246).
At the follow-up visit, all of these variables were again collected and recorded in the study template, with the exception of age, sex, IMD quintile, ethnicity, first language being English and type of diabetes, for which duplicate information was not necessary.
Quantitative data analysis
Four main sets of quantitative analyses were performed to compare the following:
-
baseline sociodemographic and clinical characteristics of all participants, with comparisons made among sites, and among those at group clinic sites who did and did not choose to attend group clinics
-
trajectories of participants who did and did not choose to attend group clinics (‘difference in difference’ analysis)
-
differences in trajectories of participants attending group clinics according to the number of group clinics attended (‘dose response’ analysis).
All groups were compared using chi-squared tests for categorical variables and t-tests for continuous variables with normal distribution. Trajectories were analysed by subtracting the follow-up from the baseline values to derive a new set of variables that reflected change over time.
In addition, linear regression models were used to investigate the association between clinic attendance and trajectories among participants at group clinic sites. Initially, the independent variable was entered as a binary variable (attended any vs. attended no group clinics) and each derived trajectory variable was entered in turn as the dependent variable. These models were then repeated, adjusting for the participants’ diabetes type, age, sex, ethnicity, age at diagnosis and deprivation. Unadjusted and adjusted models were then performed in which attendance was entered as a categorical variable (attended zero, one, two or three or more clinics), with zero clinics used as the reference category.
p-values of > 0.05 were not considered to be significant. Values below this level are highlighted but are interpreted with caution. It is recognised that we are making multiple comparisons and some values of < 0.05 owing to chance would be expected.
Quantitative methods: health economics
An NHS perspective was adopted, spanning primary and secondary health-care sectors. Economic evaluation methods followed the Guide to the Methods of Technology Appraisal 2013,70 which provides guidance on how to assess the clinical effectiveness and cost-effectiveness of new and established technologies in the NHS.
Microcosting of the group clinic intervention
Microcosting was used as a means to estimate the economic cost of the group clinic intervention to the health system (the NHS) using Personal Social Services Research Unit (PSSRU) 2018 costs. 71,72 Microcosting is particularly applied to the costing of new interventions; including the large variability across providers of the group clinics for young people with diabetes we also included a bottom-up construction of the costs associated with co-design and delivering the intervention.
The cost of co-design included time spent preparing workshop materials, recruiting participants, running and recording the workshops, transcribing records and analysing transcripts.
The clinic running costs included staff costs of running the clinics, preparing the room and materials, arranging appointments, chasing non-attenders, booking the venue, arranging refreshments and making patient notes. Data on resources associated with designing and delivering clinics were collected prospectively using purposely designed questionnaires; staff completing these questionnaires were encouraged to report all staff work and time commitments, including that of ‘hidden’ work. Staff time was costed using the NHS pay scales 2018–19. 73
Cost of intervention per clinic and per participant
The estimated cost of the intervention was based on the number of clinics and the number of patients who attended the clinics using PSSRU costs. 72 The average cost per participant for each centre was derived by dividing the total cost of running clinics by the number of attenders (per-protocol analysis). Sensitivity analyses were conducted, varying the number of clinics and the number of participants for both CMH and NUH.
Use of health-care resources
Data on the use of primary and secondary health-care services (usual care) for a 12-month pre-intervention period was extracted from clinical records. These data included the number of contacts with a diabetologist, diabetes specialist nurse, dietitian or psychologist (planned and attended); unplanned contacts with a GP, practice nurse or diabetes specialist nurse; accident and emergency (A&E) attendances; and hospital admissions. Individual-level resource use data were combined with unit costs to calculate the total cost of health services use for each participant. Primary care consultations and referrals to community care were costed using the National Schedule of Reference Costs 2017–18. 74 The list of unit costs used for costing health care services are included (see Appendix 4). Data analyses were conducted in Microsoft Excel® 2016.
Summary of data sources
A summary of the data sources used in this project is given in Table 2.
| Characteristic | Scoping | Co-design data | Qualitative data | Quantitative data | Health economic data |
|---|---|---|---|---|---|
| Setting | National | Group clinic sitesa | Group clinic sitesa | Group clinic sitesa and control sitesb | Group clinic sitesa and control sitesb |
| Data source | Survey and NDA (2017–18) | Group co-design session and individual interviews | Individual interviews, ethnographic observation and documentary evidence | Questionnaires (including Patient Enablement Instrument and Problem Areas in Diabetes) and clinical record data | Health economics usual-care costing template completed by usual-care team |
| Purpose | Contextual data on existing use of group clinics and care quality for young adults with diabetes in the NHS | Design and implementation of the group clinic model | Evaluation of the group clinic model. Experience of those engaging with it, and its organisational impact | Descriptive data to inform qualitative analysis and help design of future at-scale research | Estimate use of resources and cost of the group clinics |
| Analysis | Descriptive | Descriptive | Qualitative (thematic) analysis | Quantitative (thematic) analysis | Microcosting |
Project management and governance
The study received ethics approval from the Office for Research Ethics Committees Northern Ireland (ORECNI) on 23 February 2017 (reference 17/NI/0019) and is registered on the UK National Research Register as ISRCTN 27989430.
Standard rules applied for data security, confidentiality and information governance. Informed consent was sought for ethnographic observations during group clinics and interviews, and for accessing routinely collected NHS data on participants. Confidentiality and safety among group clinic participants was a priority, and all participants who attended were asked to agree to a code of conduct and confidentiality to ensure that all clinic discussions were kept within the group.
The study was led by Sarah Finer, with co-leadership from Dougal Hargreaves. Owing to Sarah Finer taking maternity leave, Trish Greenhalgh temporarily led the study, with Dougal Hargreaves, from April 2019 to January 2020. The study was delivered and managed by a core working group (SF, DH, CP, SV, MK, AH and GC) and supported by 6-monthly independent steering group meetings, along with ad hoc communication with steering group members when necessary. Monthly research management meetings were held throughout the lifetime of the project, which focused on progress towards short- and long-term milestones, administrative tasks and general project management. These were attended by the core team identified above and often supported by others, such as clinical teams, depending on the focus of the meeting. Action points and minutes circulated after all meetings enabled team members to keep track of study progress and ensured steady progression towards milestones and early identification of potential challenges.
A routine internal audit was carried out by the study sponsor on 10 September 2018. No critical or major findings were identified, and following action of nine minor findings the audit was closed and a certificate was issued on 5 December 2018.
Project steering group
Project steering group meetings were held every 6 months, starting on 6 November 2017 and finishing with a final wrap-up meeting on 20 April 2020. Group members included representatives from Diabetes UK and their young adult panel, along with expert lay people, clinicians, external academics and team members. Support from this group with a wide range of experiences and perspectives was invaluable to the development of the work, and the external, critical viewpoint has been very helpful in raising and highlighting areas that have benefited from further development. In particular, the group has helped the project to maintain a wide perspective so that findings and dissemination could be accessible to a variety of audiences, including commissioners, stakeholders and service users, as well as an academic audience.
Dissemination and patient and public involvement
Patient and public involvement (PPI), and wider dissemination to the academic and practitioner community, were both built into our research from the outset and followed INVOLVE guidance. 75 We built on research priorities identified through the James Lind Alliance Priority Setting Partnerships for type 1 and 2 diabetes,76,77 which identified the need to research approaches to the patient-centred management and delivery of social support for people living with diabetes. Our PPI approach was also built on the foundations set by the participatory co-design of the group clinic model.
Key patient and public involvement elements
The main planned elements of PPI in our research were led by our voluntary sector partner, the AYPH, in partnership with the main project delivery team and academic partners.
The overall intention of the PPI and dissemination activities was to share learning about the challenges and achievements of the group clinic model as it was implemented across the sites, so that others could understand and, potentially, replicate the model. As the project unfolded, dissemination was focused on sharing the results of the realist review, the co-designed new care model, its evaluation and messages for generalising findings to a wider context. We also focused on disseminating specific outputs related to co-design, so that others could learn from our successes and failures and apply these to their own service improvement work.
Patient and public involvement processes can bring challenges relating to the relationships of power between patients and public services,62 and we were mindful of this in our PPI and dissemination activities, for example involving a young person in the design and delivery of stakeholder events.
Patient and public involvement methodology
The main methods employed for involving patients and the public, local and national stakeholders and the wider dissemination list included the following:
-
Co-design. A co-design approach to developing the group clinic model supported involvement from young people, clinicians, commissioners and others from the outset.
-
Management of the research. An external steering/advisory group was convened and worked alongside the research team throughout the duration of the research, and included a patient representative from Diabetes UK with lived experience of T1D as a young adult.
-
Developing participant information resources. Patient representatives and stakeholders were involved in reviewing all patient-facing documents (e.g. information sheets and consent forms).
-
Dissemination of research findings. We planned to produce a range of events and outputs, including stakeholder engagement events, briefing papers and summaries, and these are discussed in Chapter 9. Our intended target audiences included young adults with diabetes (‘patients’) and stakeholders with roles in service use, service delivery, policy-making and health service design. In addition to this, we used social media engagement though our website and project-specific Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) account.
Dissemination networks
We built wide networks for dissemination, drawing on the contacts of the main project partners. This included the following:
-
local clinical and academic networks –
-
institution based: Queen Mary University of London, University College London, University of East London, BH, Newham CCG and Newham Borough Council
-
Local Transforming Services Together Programme
-
NHS England London Region Children and Young People’s Programme
-
Improvement Science London
-
NIHR Clinical Research Networks North Thames.
-
-
clinical and patient networks –
-
Diabetes UK.
-
-
strategic and national networks –
-
national children and young adult working groups chaired by the national leads for children and teenage and young adults
-
royal colleges, including the Royal Colleges of Physicians, General Practice and Paediatrics and Child Health.
-
-
national policy forums –
Chapter 4 National context
Scoping survey
We had 42 respondents to our survey from across the UK (including Scotland and Northern Ireland); these included hospital diabetologists (56%), dietitians (33%), diabetes specialist nurses (8%) and diabetes educators (3%). There were no respondents from paediatric services.
Although the majority of respondents reported delivering group-based education programmes (e.g. DAFNE), only 16 out of 42 respondents reported that actual group clinics or shared medical appointments were offered in their services, and these were delivered to young adults in only half of these instances. Group clinics were predominantly delivered by specialist nurses and dietitians, rarely doctors, and they were mostly situated in hospital. The content of existing group clinics was predominantly lifestyle management and peer support.
The majority view towards group clinics was positive, and reasons given were that they would offer a means to provide more peer support, be a more efficient use of resources and potentially provide more holistic care. However, 8 out of 42 respondents felt that group clinics were not a good idea, listing lack of proven benefit, lack of suitable staff or environment and potential detriment to patient–professional relationship as reasons.
The sample size of this scoping survey is small and, therefore, its findings are limited. However, the illustrative findings give some indication that adopting group clinics might be acceptable to NHS clinicians, given that the scene for group-based processes is already set by group education.
National Diabetes Audit data
Young people with diabetes at two study sites, Barts Health NHS Trust and the Whittington Health NHS Trusts, were more ethnically diverse (higher proportion of people from ethnic minority groups) than both older patients at the same trust and young people nationally. This was seen particularly in young adults with T2D, with 75.0% at BH and 100% at Whittington Hospital being from ethnic minority groups, compared with 41.4% and 33.3% with T1D, respectively (see Table 3). Nationally, young adults with T2D were predominantly female (males represented 25.8% of the total) and, compared with those with T1D, were more likely to come from an ethnic minority group (20.3% vs. 11.2%; Table 3).
| Data source | Age band (years) | Type of diabetesa | n (%) | Male (%) | Whiteb (%) | Ethnic minority groupb (%) | Ethnicity not knownb (%) |
|---|---|---|---|---|---|---|---|
| BH | 16–25 | T1D | 145 (78) | 41.4 | 55.2 | 41.4 | 3.4 |
| T2_other | 40 (22) | 37.5 | 12.5 | 75.0 | 0.0 | ||
| All, N | 185 | 40.5 | 45.9 | 48.6 | 2.7 | ||
| ≥ 26 | T1D | 625 (49) | 53.6 | 75.2 | 24.8 | 0.8 | |
| T2_other | 640 (51) | 56.3 | 33.6 | 66.4 | 0.8 | ||
| All, N | 1265 | 54.9 | 54.2 | 45.8 | 0.8 | ||
| Whittington Trust | 16–25 | T1D | 90 (86) | 61.1 | 55.6 | 33.3 | 11.1 |
| T2_other | 15 (14) | 33.3 | 33.3 | 100.0 | 33.3 | ||
| All, N | 105 | 57.1 | 52.4 | 42.9 | 14.3 | ||
| ≥ 26 | T1D | 510 (31) | 55.9 | 81.4 | 16.7 | 2.0 | |
| T2_other | 1110 (69) | 54.1 | 44.1 | 55.0 | 1.4 | ||
| All, N | 1620 | 54.6 | 55.9 | 42.9 | 1.5 | ||
| National data | 16–25 | T1D | 14,020 (81) | 52.0 | 84.4 | 11.2 | 4.4 |
| T2_other | 3320 (19) | 25.8 | 65.4 | 20.3 | 14.5 | ||
| All, N | 17,340 | 47.0 | 80.7 | 13.0 | 6.3 | ||
| ≥ 26 | T1D | 67,885 (28) | 53.3 | 89.2 | 7.8 | 3.0 | |
| T2_other | 172,685 (72) | 53.0 | 73.2 | 21.0 | 5.8 | ||
| All, N | 240,570 | 53.1 | 77.7 | 17.3 | 5.0 |
Young adults with diabetes (of all types) were less likely than patients aged ≥ 26 years to receive all eight care process checks (i.e. assessment of HbA1c, blood pressure, cholesterol, serum creatinine, urine albumin, foot surveillance, body mass index and smoking status) at all sites and nationally. These differences were not apparent in the small number of young adults with T2D at Whittington Hospital (Table 4). Nationally, there was a striking age difference in the proportion of people with T2D receiving all eight care processes, with 19.1% of 16- to 25-year-olds versus 52.2% of those aged ≥ 26 years receiving all recommended checks. Irrespective of age, measurement of urinary albumin was the least likely of all of the eight care proceses to be carried out among patients with diabetes, and it has been hypothesised that this is because of the practical difficulties of giving urine samples, as well as the fact that it is not promoted in the NHS Quality and Outcomes Framework. 80
| Data source | Age band (years) | Type of diabetesa | n (%) | All eight care processes received (%) | All three treatment targets met (%) | Structured education offered (%) | Structured education attended (%) |
|---|---|---|---|---|---|---|---|
| BH | 16–25 | T1D | 145 (78) | 31.0 | 22.2 | 58.6 | 13.8 |
| T2_other | 40 (22) | 50.0 | 20.0 | 62.5 | 25.0 | ||
| All, N | 185 | 35.1 | 21.7 | 59.5 | 16.2 | ||
| ≥ 26 | T1D | 625 (49) | 35.2 | 22.2 | 71.2 | 17.6 | |
| T2_other | 640 (51) | 58.6 | 16.1 | 74.2 | 23.4 | ||
| All, N | 1265 | 47.0 | 18.9 | 72.7 | 20.6 | ||
| Whittington Hospital | 16–25 | T1D | 90 (86) | 44.4 | 28.6 | 27.8 | 5.6 |
| T2_other | 15 (14) | 66.7 | 33.3 | 66.7 | 0.0 | ||
| All, N | 105 | 47.6 | 29.4 | 33.3 | 4.8 | ||
| ≥ 26 | T1D | 510 (31) | 46.1 | 27.4 | 24.5 | 2.0 | |
| T2_other | 1110 (69) | 54.5 | 20.6 | 25.2 | 2.7 | ||
| All, N | 1620 | 51.9 | 22.7 | 25.0 | 2.5 | ||
| National data | 16–25 | T1D | 14,020 (81) | 39.1 | 15.8 | 32.5 | 10.1 |
| T2_other | 3320 (19) | 19.1 | 25.1 | 26.5 | 2.7 | ||
| All, N | 17,340 | 35.3 | 16.8 | 31.3 | 8.7 | ||
| ≥ 26 | T1D | 67,885 (28) | 52.9 | 16.5 | 30.4 | 15.1 | |
| T2_other | 172,685 (72) | 52.2 | 27.1 | 34.7 | 7.1 | ||
| All, N | 240,570 | 52.4 | 23.9 | 33.5 | 9.4 |
The proportion of people living with diabetes reaching all three treatment targets (i.e. HbA1c levels of ≤ 48 mmol/mol, blood pressure of < 140/80 mmHg and total cholesterol levels of< 4 mmol/l) was low across all groups: nationally only 16.8% of young adults with diabetes met these targets, compared with 23.9% of people aged ≥ 26 years (see Table 4). Attainment of all three treatment targets was lower for young adults with T2D receiving care at Barts Health Trust than for those receiving care at Whittington Hospital and nationally (20.0%, 33.3% and 25.1%, respectively). Data per individual treatment targets are presented in Appendix 5. In national and local figures, the differences in attainment of treatment targets varied by type of diabetes, with young adults with T2D more likely to attain HbA1c targets than those in any other group, probably because they were early in the course of a progressive disease. Only 6.2% of young adults with T1D in England attained the HbA1c target. Attainment of the total cholesterol target was lower for all young adults in England (16.8%) than for older adults (23.9%), with comparable effects seen in local data.
The proportion of people living with diabetes attending structured education was also low across all groups (see Table 4). Nationally, only 8.7% of 16- to 25-year-olds and 9.4% of those aged ≥ 26 years attended structured education, with rates slightly higher for people with T1D than for people with T2D. This reflects, in part, the fact that structured education is offered to only about one-third of people living with diabetes. Compared with national data, offers of and attendance at structured education was higher at BH for all people with diabetes, irrespective of age and type of diabetes (e.g. 59.5% of young adults had been offered structured education, but only 16.2% of young adults had received it). The low conversion (approximately 30%) from an offer of structured education to uptake of it was seen across all groups; this is an important area to address further.
These data indicate significant areas for improvement in delivering diabetes care, and disproportionately poor uptake of care process checks and attainment of treatment targets in young adults compared with older adults living with diabetes. We also identify variation between two hospitals delivering diabetes care and national data that could result from differences in care quality or patient factors. The low uptake of care process checks and attainment of treatment targets is likely to translate to higher future risk of diabetes complications and poor outcomes.
Chapter 5 The group clinic model: co-design and delivery
Co-design: phase 1
Attendance at phase 1 co-design sessions
The composition of the co-design sessions that took place were as follows:
-
Patient sessions. Six sessions were planned and four took place, and these comprised a single young adult with diabetes with a facilitator. The young adults comprised two females aged 18 years, one female aged 20 years and one male aged 24 years, and between them represented people living with T1D and T2D of varying duration.
-
Staff sessions. Two staff sessions took place at NUH, one with 6 and one with 10 participants. Participants comprised a range of professionals and stakeholders, including dietitians, specialist nursing staff, a CCG commissioner, representatives from primary care, representatives from the voluntary sector (Diabetes UK), consultant diabetologists and reception staff.
-
Joint patient and staff session. For the joint session, the professionals attending one of the group sessions and two of the young people who had been interviewed in patient sessions met together. The service users had separately prepared three issues to present to the other group and wide-ranging discussion ensued.
It proved challenging to engage young people in co-design and, although several expressed an interest in taking part while discussing this informally by telephone/instant message/in person, many lost interest when followed up to confirm dates and details. Many of those who did attend arrived late or had limited time available. Barriers to attendance and participation included educational commitments and caring responsibilities at home.
Major themes arising from the phase 1 co-design
Overall, the co-design process demonstrated that young people and staff shared similar ambitions for the new group clinic model in terms of bringing a more social and participatory approach to a medical issue. Running three types of co-design session, for (1) young adults only, (2) staff only and (3) joint young adult and staff, helped to understand areas of potential difference and to draw together consensus and a working model for the group clinics. There was reassuring consistency across all co-design sessions that the group clinics should address the specific needs of young adults at a challenging life stage, and the sessions reflected a shared understanding that current care models may not currently engage them well or meet their perceived needs. All participants in the co-design sessions felt optimistic that group clinics might be able to play a positive role in delivering better care for young adults with diabetes.
However, there was significant uncertainty as to how the group clinics should be delivered, and it was felt that specific design aspects would need to be developed and tested as they were implemented. Therefore, the co-design had a limited number of ‘hard-and-fast’ recommendations. Further concerns were raised, particularly by staff and commissioners, about how a new model of group clinic-based care would fit into the existing NHS framework, and how this could be resourced and structured appropriately so that it could contribute to existing NHS clinical frameworks. There was tension between this potential organisational constraint and the need for the group clinics to be flexible and adaptive to adequately meet the unpredictable and changing needs of young people.
The outputs and recommendations arising from the phase 1 co-design were as follows:
-
A group clinic is a good idea for supporting diabetes self-management in young people and for reducing feelings of isolation, particularly in local communities. However, it was recognised that attendance at group clinics would be a challenge to young people with diabetes.
-
Group clinics should include young adults with all types of diabetes, irrespective of diabetes type, as this reflects shared experiences and life stages and their displeasure with being defined by their diagnosis.
-
The purpose and benefits of group clinics (for both patients and staff) need to be clear to everyone taking part from the outset. Everyone should be clear what they will get out of the process, and this should be an appealing outcome for them. Young adults expressed a further wish to know what the group clinics would deliver, and to know in advance the content of sessions so that they could decide whether or not to attend.
-
Young people are nervous of being judged for not taking good care of their health. Promoting feelings of safety, security, confidentiality and trust in the group clinics was deemed important. The young adults felt that a group clinic may not help them to discuss very personal and individual issues, but they might help them to address wider (including emotional) challenges in managing their health and look beyond ‘only’ medical issues.
-
The facilitator role is critical to delivering an acceptable model of group-based care and requires skills in youth participation.
-
There was no consensus on the ideal timing of the group clinic. There was a clear recognition that the clinic times should fit around work and educational commitments, but that the model would need to develop flexibility and use ‘trial and error’ to establish what works best. Clinics should have a minimum of two people and a maximum of around six to eight people. Parents were considered to have an important role in supporting young adults with diabetes, but should not be part of the regular groups.
-
Group clinics may not fit easily into the existing NHS structure and constraints, and may need more people/resources than anticipated to keep them going. It may also be necessary to be creative about how to measure successful outcomes and explain the benefits.
-
Groups could potentially be combined with traditional clinic visits and one-to-one time, or there may be other ways of ‘pegging’ groups to existing appointments or schedules. There was uncertainty as to whether young adults and their clinicians would want group clinics to replace some of their routine one-to-one care appointments or run in parallel with them, and it was felt that this should be established during their implementation and evaluation.
The findings of the phase 1 co-design were summarised in a co-design report (see Report Supplementary Material 1).
Delivery of the group clinic model: phase 1
Initial group clinic design
We used findings of our co-design process to implement an initial model of group clinic-based care for young adults aged 16–25 years with all types of diabetes. We used the name ‘Together Study’ to give the research an approachable and descriptive name. We aimed to form groups of 6–10 young adults who would be invited to (and hopefully attend) a facilitator-led group clinic every 3 months, although we noted that the co-design findings indicated that a group clinic could comprise as few as two people. The hope was that groups would build relationships and form their own identity, get to know each other and build rapport. All group clinic sessions started with introductions and icebreakers, followed by setting ground rules within the group to ensure that the young adults felt safe and secure in the session, the importance of which had been highlighted in the co-design.
The co-design findings led us to decide that the group clinics would be led by a diabetes specialist nurse with specific training in facilitation, and who had experience working with young people in a non-judgemental way.
We noted the clear suggestion from the co-design that group clinics should support diabetes self-management, so the content of the group clinics was designed with this in mind. Given that young adults and staff expressed a wish for the purpose of the group clinics to be clearly stated, we planned that the content of each session would be predetermined and made apparent to the invitees. A list of potential group clinic topics was drawn up by the clinical team and included (1) self-management-focused subjects, such as carbohydrate counting and sick-day rules; (2) broader lifestyle-related topics, for example psychological health, sexual health or women’s health (covering menstruation, pregnancy and polycystic ovary syndrome); and (3) care process-themed topics, for example initiation of flash glucose monitoring (Freestyle Libre, Abbott Laboratories Limited, Maidenhead, UK) and review, and annual review checks. Sessions were frequently supplemented by experts in specific areas depending on the topic, for example a youth outreach worker from the local sexual health services delivered a session on sex and healthy relationships. The co-design participants highlighted the importance of giving clarity regarding the purpose of the group clinics and, for this reason, we ensured that all notifications and reminders about sessions contained a description of the topic that would be covered using accessible language (e.g. a session on physical activity delivered in January was called ‘New Year, New Me’). Invitations and reminders for the group clinics used standard hospital processes when possible, and were complemented by text messages sent by the facilitator. The majority of group clinic sessions were designed to be open to all young adults, irrespective of type of diabetes, but a few sessions were targeted at specific patient groups (e.g. a women-only session discussing women’s health issues, a Libre start session for eligible young adults with T1D).
The co-design did not lead to concrete views on the location of the clinics, but given the concerns that it would be difficult to integrate them into existing care, it was decided to hold the group clinics in a large room on the hospital site close to where the diabetes clinics are run. After trying out different start times, the group clinics settled on a 16.00 start because this was thought to offer the most flexibility around daytime education or work and evening work and social plans. Sessions were facilitated by an experienced diabetes specialist nurse.
The group clinic model was developed to run alongside routine care initially, offering additional group-based appointments that were mostly scheduled on different days from usual care. The diabetes specialist nurse delivering the group clinics was also ‘additional’ to the existing team, although she had previously been an employee of the wider diabetes service. Our prespecified plan had been that there would then be a transition from a model of ‘additional care’ to one in which some routine one-to-one care would be ‘replaced’ by group clinics. This transition was expected to happen after approximately 12 months, once the research team and steering group were happy with the progress (assessed through monitoring of engagement, attendance and experience) of the group clinics.
Monitoring the roll-out of group clinics
We kept detailed spreadsheets recording numbers of young adults approached and consented at the group clinic sites, as well as the number of successful and unsuccessful contacts with group clinic study participants and their attendance at group clinic sessions. These data were collected by the research team and reviewed jointly by the research and clinical teams to monitor implementation of the group clinics and to allow for responsive adaptation to the care model. This also fed into the second, and iterative, phases of co-design.
Early adaptations to the group clinic model
Low attendance at the group clinics was evident from the early stages of roll-out: this had been anticipated by the young adults at the co-design. This low attendance occurred despite young adults showing their interest in joining the care model by signing up to be participants in the research. We, therefore, changed our invitation approach, and instead offered the group clinic sessions to all consented participants (unless otherwise indicated, e.g. by a women-only session), rather than try to create parallel group clinics, which we had planned to do to try to facilitate group cohesion. This approach provided participants with more flexibility and choice about which clinics they would attend, which had been deemed important in the co-design.
A youth worker joined the team after about 6 months to support engagement with the young adults. The youth worker took over the invitations to group clinics (by telephone and text message) and contributed to the group clinic facilitation with expertise in using a non-judgemental and inclusive approach to engage young adults and make them feel safe sharing personal information in a group setting. This was achieved using initial icebreakers at the start of group clinics, setting boundaries and using a young person-centric, facilitatory approach to delivering the group clinics.
During the initial roll-out, it became apparent that group clinics were unlikely to easily replace routine care, partly because of the low attendance at group clinic sessions and partly because of administrative and information technology (IT) barriers in developing a flexible model of care in which a young adult could easily cross in and out of group and existing one-to-one care appointments. We, therefore, did not proceed with the intended transition from ‘additional’ to ‘replacement’ care.
Involvement of an additional research site
A second site, CMH, was opened 1 year after initial study set-up to expand recruitment and give additional opportunities for study engagement with, and attendance at, group clinics. Having a research site after gaining 1 year of experience running group clinics at NUH also provided a useful contrast to study (1) the delivery of a more ‘finished’ group clinic model that had been developed and improved through iterative co-design, and (2) the implementation in a different clinical service. The group clinics at CMH were also facilitated by a diabetes specialist nurse and youth worker, and were scheduled on the same day as the routine young adult clinic so that people could attend both a one-to-one appointment and a group clinic in one afternoon.
Staff training
Staff who delivered the group clinics were all experienced clinicians with several years’ experience of delivering both individual care and group-based educational sessions (e.g. DAFNE courses) to people living with diabetes. However, staff training needs were identified during the co-design and the development of the group clinics, especially around taking a facilitatory approach to the group clinic delivery. All clinical staff involved in delivering group clinics were offered (and attended) a 1-day facilitation skills workshop. The youth worker, with experience and expertise in facilitation and working with young people, offered informal training for staff involved in the group clinics. Staff involved in delivering group clinics at NUH gave training and mentorship to staff at the CMH, and there was an easy rapport between the two sites so that support was readily available when required.
A training manual was developed by the study team and researcher in residence to support health professionals who facilitate or support group clinics in this study and in future work. The manual covers (1) preparing for group clinic sessions, (2) delivering the group clinic session and (3) useful resources [for the training manual see the NIHR project web page; URL: www.journalslibrary.nihr.ac.uk/hsdr/NKCR8246).
Co-design: phase 2
Phase 2 and iterative co-design
The second round of co-design took place after group clinics had been under way for 9 months at NUH and as CMH started up its own group clinics. The focus of the second round was on suggestions for improving the model. The procedure mirrored the first round by including a session with young people (n = 6; this time these were young people who had experienced a group clinic) and a session with professionals (n = 3) who were involved in running groups. Participants were asked the following key questions:
-
If we wanted to change the model, what would that look like? (e.g. should it be more peer led, and if so, how?)
-
How should we try to enhance engagement with and attendance at group clinics (e.g. change to the role and remit of the youth worker)?
-
Do we need more work before and after groups with young people to prepare/debrief?
-
How is the relationship between the different professional groups working, and does this need improving?
The findings of the phase 2 co-design were summarised in a co-design report (see Report Supplementary Material 1).
Delivery of the group clinic model: phase 2
Improvements to the group clinic model
Overall, the second phase of co-production confirmed the messages that we heard in phase 1, but provided some more detail about how the model could be optimised. The role of the youth worker and other staff who were able to engage with young people effectively was particularly important, and this included a focus on building group relationships, establishing boundaries and confidentiality. Young people liked the youth-focused nature of the groups and the space that they gave them to raise issues about their diabetes that they would not raise elsewhere.
Again, as with the first round of co-design, there was a lot of synergy between the messages from the two groups. Overall, key suggestions for changes to the group model included:
-
experimenting with minor changes to timing, but probably staying within the overall 17.00–20.00 window
-
experimenting with the extent to which the groups were ‘pegged’ to existing appointments and clinics
-
building into the model realistic expectations of attendance and engagement, and understanding that attendance and engagement could take considerable time (beyond the duration of the research) to build up
-
continuing to encourage external contributors to the group clinic themes, but ensuring that they can fit in with the unique delivery model adopted by the group clinics.
Delivery of the group clinic model: overview
As summarised above, the group clinic model evolved and changed during its implementation through a combination of discrete co-design phases (1 and 2) and continuous co-design embedded in the delivery of group clinics, and through regular discussion and feedback to promote iterative adaptations. There were challenges to involving young adults in the discrete co-design sessions that could have under-represented their views and led to staff-centric outcomes; however, it is hoped that the continuous elements of co-design embedded in the group clinic sessions will have mitigated this. The co-design led to a group clinic model that incorporated education on broad topics relevant to living with diabetes, specific aspects of diabetes self-management and diabetes care. There are some commonalities between the educational and the self-management topics and existing group-based education, such as DAFNE. The core aspects of the group clinic sessions are summarised below (Table 5) with illustrative photos of the clinic set-up (see Figure 2).
| Key principles | Inclusion of all young adults with diabetes (irrespective of type) in the care model, and recognition of the difficulties that they will have in attending |
| More than two young adults constitutes a group, but six to eight young people might be desirable | |
| Group clinics should be facilitated by a member of the clinical care team (e.g. DSN) | |
| Group clinics should provide a non-judgemental, confidential, safe space for young adults, and should look beyond purely ‘medical’ issues | |
| Make explicit the content and purpose of the model and individual sessions | |
| Staff delivering group-based care will face challenges from existing NHS structures | |
| Preparing for the group clinic | Invitations to group clinic via usual care processes, with additional telephone/SMS communication from youth worker |
| Topic/theme for the group clinic confirmed and young adults notified in SMS invitation | |
| Invitation sent to all young adults, unless session relevant only to a specific group (e.g. a women-only session) | |
| The group clinic | Scheduled for afternoon/early evening in usual-care setting |
| Delivered by group clinic facilitators (DSN and youth worker) with/without an external ‘expert’ | |
| First 15 minutes: welcome and introductions, icebreaker, setting the scene and ground rules | |
| Next 60 minutes (maximum): topic/themed facilitated session and using interactive resources when possible | |
| Last 15 minutes: wrap-up to reflect and recap, discuss take-home messages and plan the next group clinic | |
| After the group clinic | Follow-up SMS to all invitees (including those who DNA) with take-home points, relevant online resources and plans for the next group clinic |
| Team (staff) debrief to reflect, learn and plan the next group clinic |
At NUH, group clinics primarily took place in a local community health centre that also housed one of the trust’s multidisciplinary diabetes units. This was a familiar place for young people who were attending their one-to-one appointments in the same clinic. Group sessions were held in a large seminar room on the first floor, accessed through a passcode-protected door. This room was a neutral space as it served multiple purposes in the community centre, for example clinical training and team meetings, as well as patient education sessions (such as DAFNE), and could easily fit 20–30 people. Long folding tables in various conditions were stacked against two of the walls. The diabetes specialist nurse facilitating the clinic configured the room differently every time depending on the number of patients expected and the structure of the session. In most cases, she would place one or two tables in the middle, with comfortable visitor office chairs dotted around them, not too far from each other but not too close either to give a sense of personal space. Refreshments and snacks were available on one side of the room. On the tables there were usually Post-It® Notes (3M, Saint Paul, MN, USA), pens, markers or any materials needed for the session.
At CMH, group clinics were also held in the same clinical area as the diabetes unit, this time within the hospital setting. A smaller room was used that could fit up to 10–15 people maximum (see photo B in Figure 2). Patients would sit around the table and clinicians would be standing at the side or at the front of the room. A flip chart was always available and different materials (e.g. leaflets, handouts and presentations) were used, depending on the session. The space was plain and clinical, not customised for the young adult group in any way as this was another multipurpose room, one of the few seminar rooms available to clinical teams.
Chapter 6 Participation in the research and attendance at group clinics
Baseline characteristics of all research participants
We present the baseline characteristics of the young adults (n = 135) recruited to the study, by recruiting site, including both group clinic sites (NUH and CMH) and control sites (WH and MEH) in Tables 6 and 7.
| Site | Number of participants (n) | Mean (SD) age (years) | Mean (SD) age (years) at diagnosis | Characteristic, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Ethnic minority | In education | In employment | Living in highest deprivation quintile | English as first language | T1D | Technology use in the last year | Previous group education | ||||
| NUH (all) | 50 | 21 (2.7) | 14 (6.9) | 24 (48) | 40 (80) | 13 (26) | 15 (30) | 26 (52) | 22 (44) | 40 (80) | 17 (34) | 11 (22) |
| NUH attended | 23 | 21 (2.7) | 11a (6.9) | 11 (48) | 20 (87) | 7 (30) | 9 (39) | 11 (48) | 9 (39) | 20 (87) | 10 (44) | 9 (39)b |
| NUH non-attended | 27 | 21 (2.8) | 16a (6.2) | 13 (48) | 20 (74) | 6 (22) | 6 (22) | 15 (56) | 13 (48) | 20 (74) | 7 (26) | 2 (7)b |
| CMH (all) | 23 | 20 (2.3) | 11 (6.1) | 10 (43) | 18 (78) | 9 (39) | 10 (43) | 4 (17) | 15 (65) | 19 (83) | 5 (22) | 7 (30) |
| CMH attended | 14 | 20 (2.3) | 11 (4.8) | 6 (43) | 10 (71) | 4 (29) | 7 (50) | 3 (21) | 9 (64) | 12 (86) | 3 (21) | 2 (14) |
| CMH non-attended | 9 | 21 (2.1) | 11 (8.1) | 4 (44) | 8 (89) | 5 (56) | 3 (33) | 1 (11) | 6 (67) | 7 (78) | 2 (22) | 5 (56) |
| WH (all) | 30 | 20 (2.5) | 12 (5.6) | 16 (53) | 14 (47) | 6 (20) | 10 (33) | 10 (33) | 23 (77) | 24 (80) | 6 (20) | 10 (33) |
| MEH (all) | 32 | 20 (1.6) | 11 (5.3) | 11 (34) | 17 (53) | 13 (41) | 8 (25) | 17 (53) | 29 (91) | 26 (81) | 18 (56) | 10 (31) |
| Site | Number of participants (n) | HbA1C levels, mean (mmol/mol) | Mean frequency of blood glucose testing per day | Mean PAID score | Mean PEI score | Planned diabetes appointments attended, % | Mean ED attendances (diabetes related) | Mean inpatient diabetes-related admissions | Mean primary care diabetes-related consultations |
|---|---|---|---|---|---|---|---|---|---|
| NUH (all) | 50 | 73 | 2 | 25 | 7 | 70 | 0.3 | 0.2 | 2 |
| NUH attended | 23 | 73 | 3 | 23 | 8 | 70 | 0.2 | 0.1 | 1 |
| NUH non-attended | 27 | 72 | 2 | 27 | 7 | 70 | 0.3 | 0.2 | 2 |
| CMH (all) | 23 | 80 | 3 | 27 | 6 | 70 | 0 | 0 | 0.6 |
| CMH attended | 14 | 68a | 3 | 29 | 6 | 80b | – | – | 0.5 |
| CMH non-attended | 9 | 98a | 3 | 25 | 7 | 50b | – | – | 0.7 |
| WH (all) | 30 | 76 | 4 | 19 | 5 | 80 | 0.2 | 0.1 | 1 |
| MEH (all) | 32 | 71 | 4 | 24 | 5 | 80 | 0.2 | 0.2 | 2 |
Across all sites, we note that the mean age of participants was > 20 years, highlighting the difference between this clinic population and a population that covers paediatric-to-adult transition. The majority of participants had T1D, reflective of the relatively higher prevalence of this condition than T2D in young adults. As expected, a relatively high proportion of ethnic minority participants was found at all study sites (see Table 7), with the highest being 80% at NUH and the lowest 47% at WH. Unfortunately, it is not possible to make direct comparisons with NDA data at NUH, as data from this hospital are aggregated with other BH hospital sites. However, we can see that our 50 young adult recruits at NUH represent a greater ethnic minority population than at the young adult clinics across BH more generally (47% ethnic minority). In contrast, the 30 WH recruits were representative of its young adult clinic population (43%). Both show disproportionately large numbers of ethnic minority recruits and patients compared with participants in the National Diabetes Audit (13% ethnic minority). These proportions reflect the wider clinic populations at these sites [which was above the national average (see Table 3)]. The ratio of males to females and the performance of each site on two key national audit targets (percentage with eight care processes achieved and percentage meeting three treatment targets) were broadly in line with national data. Our study had limited power to detect such difference owing to the relatively small number of participants at each site, especially for participants with T2D or other diabetes. A total of 81% of our research participants across all study sites had T1D, and this reflected the NDA data at local and national level. It is also important to observe the fact that the majority of young adults involved in the research had not previously attended group-based structured education.
We analysed the baseline characteristics of all participants according to the group and control sites that they were recruited to. For group clinic sites, we present characteristics of those who attended and DNA. Non-attendance denotes attendance at no group clinics, and attendance denotes attendance at one or more group clinics.
We compared baseline characteristics and showed expected differences between sites in the proportion of ethnic minority participants, those who did not speak English as a first language and those who lived in the most deprived areas. However, there were no significant differences in the age, age at diagnosis, type of diabetes or the proportion who had experience using technology or attending group education sessions for diabetes (see Table 6). Similarly, there were no significant differences between sites in the clinical measures and questionnaires scores at baseline (see Table 6). Participants had previously positive experiences of care and had attended at least 50% of planned appointments in the year prior to joining the research.
At NUH, comparing participants who did (n = 23) with participants who did not (n = 27) attend any group clinics, there were no significant differences in sex, ethnicity, deprivation, speaking English as a first language, type of diabetes or use of technology within the last year. Those who attended were, on average, diagnosed at a younger age (11 vs. 16 years) and more likely to have attended group education sessions in the past (39% vs. 7%), with borderline statistical significance (p = 0.033 and 0.053, respectively) (see Table 6). No significant differences were seen in these variables when comparing attenders and non-attenders at CMH.
Comparison of attenders with non-attenders at NUH showed no significant differences between these groups when comparing baseline clinical characteristics and questionnaire scores (see Table 7). By contrast, attenders at CMH were more likely to have well-controlled diabetes (mean HbA1C levels of 68 mmol/mol vs. 98 mmol/mol; p = 0.023) and had attended 80% compared with 50%, respectively, of planned appointments within the previous year (p = 0.009).
Group clinic invitations: responses and attendance
Attendance at group clinics is presented in Tables 8 and 9. These data indicate low (mean 32% and 33% at NUH and CMH, respectively) attendance at group clinics. On average, there were four and five young adults present at each group clinic at NUH and CMH, respectively. In the early stages of group clinic delivery, invitations were sent to targeted groups of individuals, hence multiple instances of the same topic theme. Over time, it was decided that the group clinics would be offered to all young adults except when there was a specific reason not to [e.g. offering a women-only session (i.e. periods, pregnancy, polycystic ovary syndrome) or a session targeted at Libre-eligible young adults].
| Date | Topic | Contacted (n) | Attended, n (%) | Response to invitation but DNA, n (%) | No response to invitation and DNA, n (%) | Number of attendees who had attended one or more previous group clinic (n) |
|---|---|---|---|---|---|---|
| Phase 1 co-design | ||||||
| 11 September 2017 | Healthy eating | 8 | 2 (25) | 0 (0) | 6 (75) | |
| 9 October 2017 | Healthy eating | 9 | 5 (56) | 0 (0) | 4 (44) | 0 |
| 8 December 2017 | Physical activity | 8 | 0 (0) | 0 (0) | 8 (100) | 0 |
| 15 December 2017 | Physical activity | 9 | 1 (11) | 5 (56) | 3 (33) | 0 |
| 18 December 2017 | Young mums | 6 | 1 (17) | 5 (83) | 0 (0) | 0 |
| 8 January 2018 | Healthy eating | 8 | 3 (38) | 5 (63) | 0 (0) | 0 |
| 26 February 2018 | Healthy eating | 15 | 4 (27) | 6 (40) | 5 (33) | 0 |
| 12 March 2018 | Healthy eating | 10 | 3 (30) | 2 (20) | 5 (50) | 0 |
| 9 April 2018 | Psychological health | 17 | 2 (12) | 9 (53) | 6 (35) | 2 |
| 16 April 2018 | Psychological health | 22 | 6 (27) | 5 (23) | 11 (50) | 5 |
| 18 June 2018 | Sex and healthy relationships | 34 | 3 (9) | 14 (41) | 17 (50) | 3 |
| Phase 2 co-design | ||||||
| 9 July 2018 | Freestyle Libre start | 15 | 4 (27) | 5 (33) | 6 (40) | 4 |
| 6 August 2018 | Freestyle Libre follow-up | 3 | 3 (100) | 0 (0) | 0 (0) | 3 |
| 30 August 2018 | Freestyle Libre follow-up | 2 | 2 (100) | 0 (0) | 0 (0) | 2 |
| 19 September 2018 | Hypos and blood tests | 7 | 2 (29) | 4 (57) | 1 (14) | 2 |
| 22 October 2018 | Periods, pregnancy, PCOS | 21 | 6 (29) | 8 (38) | 7 (33) | 6 |
| 16 November 2018 | Carbohydrate counting | 33 | 6 (18) | 14 (42) | 13 (39) | 5 |
| 19 December 2018 | Freestyle Libre follow-up | 6 | 5 (83) | 1 (17) | 0 (0) | 5 |
| 16 January 2019 | Diabetes annual review | 22 | 7 (32) | 10 (45) | 5 (23) | 5 |
| 20 February 2019 | Psychological health | 42 | 7 (17) | 24 (57) | 11 (26) | 6 |
| 20 March 2019 | Sexual health | 41 | 4 (10) | 17 (41) | 20 (49) | 1 |
| 15 May 2019 | Sick day rules and diabetes | 32 | 1 (3) | 24 (75) | 7 (22) | 1 |
| Mean of all clinics, n (%) | 17 | 4 (32) | 7 (36) | 6 (33) | 2.4 | |
| Date | Topic | Contacted (n) | Attended, n (%) | Response to invitation but DNA, n (%) | No response to invitation and DNA, n (%) | Number of attendees who had attended one or more previous group clinic (n) |
|---|---|---|---|---|---|---|
| 19 September 2018 | Healthy eating | 15 | 6 (40) | 0 (0) | 9 (60) | |
| 5 December 2019 | Healthy eating | 12 | 5 (42) | 1 (8) | 6 (50) | 0 |
| 23 January 2019 | Physical activity | 5 | 3 (60) | 1 (20) | 1 (20) | 3 |
| 20 March 2019 | Physical activity | 22 | 4 (18) | 3 (14) | 15 (68) | 2 |
| 19 June 2019 | Retinal screening | 24 | 5 (21) | 5 (21) | 14 (58) | 4 |
| 4 September 2019 | Sex and healthy relationships | 24 | 4 (17) | 8 (33) | 12 (50) | 4 |
| Mean of all clinics, n (%) | 17 | 5 (33) | 3 (16) | 10 (51) | 2.6 | |
There was significant variation in attendance between sessions, with the highest attendance at group clinics to which a highly selected group of patients were invited for a specific care-focused intervention (i.e. young adults eligible for, and offered, group clinic-based initiation and follow-up of Freestyle Libre flash glucose monitoring). Lower attendance was observed at sessions themed to broad educational topics (e.g. psychological health and healthy eating) and self-management topics (e.g. sick day rules), but with considerable variation across these themes.
Attendance and response rates were highly consistent between NUH and CMH, despite the clinics being run for longer at NUH. The second phase of co-design does not seem to have had a major impact on subsequent attendance rates. Across all group clinics at NUH that were delivered, an average of one-third (36%) of the young adults invited responded to short message service (SMS) and telephone contact from the group clinic facilitator and youth worker, but then DNA. Overall, the attendance data suggest that group clinics may be of interest in up to two-thirds of young adults in routine care, but that attendance is considerably lower (average attendance across all group clinics was around one-third).
At both sites, as group clinics continued, attendance was mostly from people who had attended previous sessions, suggesting that they appealed to, and continued to attract, a specific group of young adults. We noted that at each site, a core group of young adults attended several of the group clinic sessions on offer. At NUH, 6 out of 26 young adults attended five or more group clinics, and 5 out of 14 young adults attended three or more group clinics.
Chapter 7 Qualitative evaluation of the group clinic model
Description of the data set
Our mixed-methods approach evaluates the impact of the group clinic model on people living with diabetes, primarily using qualitative techniques with patients and health-care professionals. First, we present data analysis based on individual interviews and ethnographic study with patients and health-care professionals. Second, we present data analysis that draws in a wider evaluation of how group clinics could be embedded at an organisational level within the NHS.
The qualitative evaluation included 19 interviews with young people with diabetes who had been recruited to the study and were offered group clinics. The characteristics of these interviewees and their attendance at the group clinics is presented in Appendix 1.
All direct quotations (Qs) from interviewees are included in Appendix 6 and their corresponding numbers are in the text below.
Setting the scene: the experience of being a young adult living with diabetes
The young people interviewed described living with diabetes as ‘an ever-growing curve of learning’ (interview 15, patient 10). Case vignettes from three interviewees are presented in Box 1. Some interviewees were newly diagnosed and were taking their first steps in managing their diabetes. Others, although diagnosed in childhood, were only just starting to learn how to live independently with their condition. Many described feeling demotivated and unable to gain control or look after themselves in the way that they felt was expected. Mental health difficulties, such as anxiety and depression, were commonly mentioned in interviews. These were compounded by challenges with social and individual transitions in young adulthood, including managing and disclosing their condition in the workplace and educational settings. Diabetes was often seen as a burden that young people preferred to forget about, in an attempt to fit in with their wider social circle.
K was a 21-year-old woman who had been living with T1D for 10 years. Her older sister also had T1D, but they rarely talked about their condition. Her family was from Pakistan and they had been very active in helping the two sisters manage their diabetes as they were growing up. K lived with her family in east London while studying computing at a local college. She took metformin tablets and multiple daily-dose insulin, and had completed the DAFNE programme previously. She found it difficult to control her diabetes (HbA1C levels of 90 mmol/mol) even with a Freestyle Libre glucose sensor, which she tried but did not find useful. She had diabetes-related emergency attendances owing to diabetic ketoacidosis and hospital admissions, but suggested that her condition did not worry her. Although she was open about her diabetes, she still felt different from her peers. K thought it was easier for young people with the same condition to understand each other than for clinicians, and would like everyone to be supportive in group clinics. She saw group clinics as an addition to individual appointments, which she attended regularly (more so for consultant appointments than diabetes specialist nurse). When group clinics were held in the evening it was more difficult to attend as she was expected to be home for dinner.
M was an 18-year-old man who was in his last year of school when he joined the group clinics and subsequently started university studies in medicine. He had been recently diagnosed with T1D, following his sister, who was diagnosed 2 years earlier. This meant that he recognised the symptoms and just ‘got on with it’. He kept his HbA1C levels well controlled (at 46 mmol/mol) by monitoring his blood glucose four times per day. He self-administered multiple daily insulin injections via pens, had completed the DAFNE programme and was trying to become eligible for insulin pump therapy. His father had been looking after him and they often did daily carbohydrate counting with his younger sister, although he was trying to become more independent before leaving home. He preferred to keep his diagnosis private, had told only very few people at school and did not inject in public, as he felt uncomfortable in social situations. Group clinics helped him see how others dealt with their diabetes, as he had never met anyone else with the condition apart from his sister. He would have preferred to meet more people in the groups. He also regularly attended his planned individual appointments with the consultant and nurse. At the time of his interview he had no hospital admissions or emergency attendances on record.
C was diagnosed at age 7 and at the start of the study had been living with T1D for 13 years. At baseline, she had HbA1C levels well above target (82 mmol/mol). She had had a poor attendance record (had attended 2/5 planned doctors’ appointments in the previous year) and had a relatively low PEI score of 4 out of 12. One year later, her HbA1C levels had improved significantly to 72 mmol/mol and her PEI score increased to 7 out of 12. There was ongoing relatively poor clinic attendance (2/4) but good attendance at group clinics (attended 8/14 to which she was invited). This young patient engaged well with group sessions, in terms of both attendance and participation in discussions, asking questions and encouraging others to share. She was also one of the patients who started using Libre about 6 months into the programme (which may have also played a role in the improvement in HbA1C levels). She felt that the clinics fulfilled her needs because the group talked about things that mattered to her.
PEI, Patient Enablement Instrument.
Reducing HbA1C levels by 10% is associated with a reduced risk of microvascular complications (e.g. retinopathy, neuropathy, nephropathy) of about 40%.
Health professionals from the two participating hospitals also discussed the specific needs of young patient populations in areas with high levels of social deprivation. Their patients came from a range of ethnic backgrounds, family circumstances and socioeconomic conditions, with a large proportion from low-income backgrounds. Some were looked after by social services, were in secure training facilities or had to provide for their families, which meant that they had little time to take care of themselves or engage with diabetes. There was little stability for some of the young people, who often moved between houses or jobs. Other patients had more support at home, performed well in education and attended top universities. Clinicians recognised that young patients had poor experiences with diabetes care and appeared less engaged than other patient groups, so they tried to organise young adult services flexibly to improve attendance and outcomes. In interviews, they often explained how it takes time and effort to build therapeutic relationships with young people, and how it is necessary to take into account the wider social and developmental issues that the patient may be facing, rather than just their diabetes. It is these experiences that are thought to explain, at least partly, the low uptake of routine diabetes checks and structured education, and low attainment of treatment targets seen in young adults (described in Chapter 4).
Understanding the role of group clinics
Motivations for engaging with group clinics
In interviews with young people, we explored what drove them to consider engaging with a new care model centred on group clinics. Young people explained how they were primarily motivated by the need to meet other people their age and understand how they manage their diabetes. Overall, a minority of young people recruited into the study had previous experience of group-based structured education. The low prior uptake of group-based structured education in this patient group may explain why the co-design process generated a model of care that was heavily focused on educational topics that are ordinarily part of programmes such as DAFNE. At NUH, young people who were recruited into the study and attended group clinics were more likely to have previous experience of group-based education than those who were recruited but DNA, suggesting that prior experience of group education may have been a positive influence and that there may be an appetite to receive more group-based care. Young people were interested in learning from the experiences of their peers, but also to balance this learning against clinical advice from health professionals (Q1 and Q2).
Some suggested that by meeting others with better control they would become more motivated to manage their condition. They expressed a need for emotional support from peers facing the same challenges and suggested that this would make them feel less isolated. For some, the key driver was listening to others, rather than talking about their own difficulties. Young people became interested in group clinics to bring variety to their usual care and to find an opportunity to extend beyond what was normally discussed in individual appointments (Q3).
Low uptake of group clinics and ambivalence around attending
The quantitative data show that, overall, the attendance at group clinics among recruited participants was low (32% and 33% at NUH and CMH, respectively). Not all patients were enthusiastic when group clinics were first introduced to them. Some described feeling ambivalent or in ‘two minds’ about this new service model (interview 12, patient 7). They were reluctant to attend as they did not know what to expect from the group sessions and how it might feel to attend clinics with other people. Some had not disclosed their diabetes in their communities and were worried about meeting people from their social circle. Others, although recognising the value of meeting peers, were worried about whether or not they could forge a connection to allow them to share deeply personal experiences (Q4).
Despite initial ambivalence, some of those who attended group clinics found that their concerns quickly subsided and they became comfortable with the new service model (Q5).
Some patients expressed the opinion that group clinics were not right for them at the time, as they did not feel ready to engage with their condition or place diabetes at the forefront of their interactions with other people their age (Q6).
Other reasons for low attendance included patients finding it difficult to fit group clinics alongside other life commitments and responsibilities (e.g. family, education). Those in fixed or flexible employment were often unable to take extra time off work to attend both group clinics and scheduled one-to-one appointments. These logistical barriers had been discussed at length in the co-design, but with the conclusion that there was no one ideal time for the group clinics to be run given how varied and unpredictable the lives of young adults are. Over the 2 years that group clinics that were running, some patients moved away for work or study and were unable to continue attending. A handful of patients also mentioned how they feared that group clinics would eventually replace individual appointments for reasons of cost efficiency, which made them less willing to attend sessions to avoid showing support for this model of care.
Staff views on attendance
Staff spent time reflecting on best ways to engage young people in this new model of care, given the low attendance: ‘I think attendance is the biggest [barrier] and engagement. How do you get the young adults to actually attend?’ [interview 1, diabetes specialist nurse (DSN)]. Different communication modes were trialled to inform and remind patients about the group clinics. Letters were unsuccessful, therefore clinicians (and later on the youth worker or the research officer) used telephone calls and personalised text messages: ‘I try to keep to their language, even if it means using emojis, I get an emoji back [. . .] I have to break a little bit of a boundary where it’s non-threatening’ (interview, 1 DSN). There were concerns about how many times to contact young people to avoid alienating them: ‘It’s very, very important that we don’t overdo it. One call or one text is more than enough. [. . .] it will just stop them from attending if you start constantly calling them’ (interview 7, youth worker). However, low attendance rates (especially at early stages) made regular communication necessary to sustain the link with young people participating in the study. The fact that approximately one-third of non-attendees did actively respond to communication was widely considered by clinicians to indicate ongoing engagement with the clinical service and potential interest. Barriers with engagement also meant that clinicians were reluctant to introduce direct clinical care with a focus on individuals within the group clinic, and opted for a more indirect approach focusing on educational topics related to lifestyle and self-management with general applicability to all attendees in initial sessions. Over time, staff were happy to allow evolution and adaptation of the topics to incorporate distinct elements of clinical care, such as Libre initiation and review, and annual review checks.
Attempts to communicate with patients about group clinics became one of the ways that the DSN at NUH developed relationships with patients who were new to her. She found it rewarding when young people started being more responsive to the texts, even if they did not end up attending the clinic (Q7). At CMH, a decision was made (based on experience at NUH) to move away from a model of inviting selected patients to each group clinic to contacting everyone who had consented to the study in an attempt to drive up attendance (Q8). Low attendance was not just an issue in group clinics but was also common in standard young adult diabetes care, although the two models were different and direct comparisons are not viable (Q9).
Could group clinics benefit young adults living with diabetes?
What is the experience of care delivered in group clinics?
Young people who attended group clinics discussed their experiences as predominantly positive: they felt better understood and supported, learnt new things from peers and clinicians, normalised diabetes self-care and became more motivated. There were a few instances in which peer comparison did not lead to motivation for improved self-care. Although enjoyable, group clinics required a certain level of input and responsibility from patients (especially when the number of young adults in attendance was small), and the internal power dynamics of the group had to be managed carefully.
Feeling understood and supported
The vast majority of group clinic participants ‘enjoyed’ the sessions, as they found that their peers could understand and identify with their experiences, which made them feel less isolated (Q10). Their positive experiences related less to sharing clinical details about their condition and more to exploring their feelings around living with diabetes as young people. Group clinics provided the opportunity to discuss emotions and frustrations with others going through the same challenges (Q11).
This shared understanding meant that young people were able to feel supported without necessarily having to explain themselves, something they found hard with peers outside the group clinic who did not understand their condition or even with their health professionals, whom they perceived as less likely to understand their emotional burden. Being able to explore the emotional challenges of living with diabetes was repeatedly mentioned as a key aspect of positive experiences in group clinics (Q12).
Some people felt understood and cared for, even when they did not always actively participate in sessions. A young girl with badly controlled T1D and recent diabetic ketoacidosis (DKA) admissions attended group clinics regularly, but did not engage fully in icebreakers or group discussions. Her body language often seemed defensive and distant (Q13). As we found out over time, she had always been private about her diabetes because her family had encouraged her to do so to avoid stigma. Despite her passive stance and reluctance to participate in discussions, this young girl still benefited from listening to others.
There was some initial reluctance from a few patients to share details that they considered to be private, such as glucose levels (see, for example, quotations Q106 and 107, mentioned again later), especially in the context of Libre group clinics, at which readings were displayed on the computer screen for discussion. However, this reluctance subsided when patients saw others struggling in the same way as them, as in the example of the young woman in Box 2, who opted for discussing her individual readings outside the group, but then felt more comfortable and ended up sharing openly in one of the following clinics.
What we’re going to do, we’re going to log onto a computer and we’re going to go through some of these Libre sensor readings.
Oh, OK, yeah.
Yeah, that’s all right, yeah.
[. . .] we can all comment and look at it jointly, if that’s OK, because this is like a clinic for everyone together so it’s nice for us all to have a look and, I might see something that, perhaps you will see something different and I might not spot it when we look at other people’s glucose, everybody spots something different in the patterns. So, it’s quite nice if we do it together. So, is that OK with everyone? Yeah?
Yeah.
I don’t know about sharing.
You don’t like to, OK.
Because it’s like up and down and you guys are going to be like, what, this girl’s unconscious [. . .] I don’t really want anybody else to see it with the high blood sugars, anyway.
At the end you can have a one to one if you want. Is that OK?
Yeah, that’d be fine.
You can show it, I don’t care.
But we’re not here to judge, we’re not here to judge each other, that’s one thing we’re definitely not.
Yeah, let’s just do it because then I’ll hear what other people are going to say about it but, yeah.
I’m sure your peers will be very supportive of you, yeah, because that’s what this is about to support each other, isn’t it?
Yeah.
[later discussing what went well during the feedback session at the end of the group clinic].
Listening to everyone’s experience.
Yeah, there’s some interesting ones.
What did you guys think about [F2 patient name] readings, her stats, yeah?
Great, yeah. Now I don’t feel too bad about sharing mine.
How did you feel [F2 patient name]?
I knew they were going to be a bit high but I thought I might as well just, it helped me as well so, good to share it.
[. . .]
How do you feel now that we’ve started looking at someone’s?
Fine. I didn’t really care but I just didn’t want you guys to see my higher readings, but I feel like I’ve got similar readings to [F2], so whatever was told to her, I was just like, OK, I’m going to do that for the next time.
F, female; M, male.
Social and situated learning
Young people perceived group clinics as prioritising their emotional needs rather than the requirements, constraints and targets of the health service. The ability of the group clinics to engage with and deliver emotional care represents an important difference from pre-existing models of group education, such as DAFNE. The environment and structure of the clinics, described in Chapter 5, emphasised peer interaction, triggered discussion and invited patients to open up about things they wanted to know more about. This created a number of practical learning opportunities for patients. Examples included how to manage insulin injections by alternating injection sites, how to avoid hypos when exercising, and how pregnancy and contraception would be managed for women with diabetes. This learning did not just emerge out of conversations between patients: clinical input was also deemed to be important (Q14 and Q15).
Many of the young adults attending group clinics had lived with diabetes for several years already (the mean age at diagnosis of all group clinic attendees was 11 years), and it emerged that the group clinic was a supportive environment for them to learn (or relearn) basic aspects of diabetes care. For example, a young woman diagnosed 13 years ago suggested that she was not aware of ketone testing and was grateful to a newly diagnosed patient for explaining how to test for ketones (Q16). Exchanges such as this (Q16) seemingly happened spontaneously but were also a result of careful facilitation by the DSN (Q17).
Learning also emerged from group discussions when new aspects of patient care were delivered, such as the use of Libre. In the Libre-focused clinics (illustrated in Box 3), individual patient readings and graphs were shared with the group, and the nurse invited everyone to interpret these and discuss the rationale for different management options to improve glycaemic control.
So, always have a look at night time to see are you getting any hypos? Is [patient name] getting any hypos at night time?
She seems safe.
She seems safe, yeah? If anything, she’s a little bit high at night time, so what could we do there, [patient name]?
Increase my basal.
Yeah. Because why basal? Because you’re going to have to explain to people like [patient name] and [patient name] because they have basal and bolus, don’t they, and you have just your one insulin?
Yeah, because that’s the one that acts during the night so that’s the only one that’s giving me insulin.
OK.
So, if I increase that, then during the night my sugar levels will also go low.
[. . .]
So, some days, if you eat late, is your blood glucose is likely to be high when you go to bed?
Yeah.
Definitely.
It is, isn’t it? Yeah, it’s likely to be high. So, would you take any action?
Yeah.
I don’t usually.
I don’t but I know I should because in the morning it will be really high.
Who said yes and who said no? Who said, yes, I will take some action?
I’m just sitting on the fence.
F, female; M, male.
Contrary to what might be expected, many of the young patients had been looked after by their families and were only just beginning to learn how to care for themselves independently. Young patients diagnosed when entering adulthood seemed to have a lot of lessons to share, especially around the practical aspects of managing diabetes (Q18). The group clinics represented young adults with a diverse range of experience of living with diabetes, and this seemed to create further opportunities for learning. Instead of patients assuming that answers to others’ questions may not relate to them, they took the opportunity to learn as much as possible in case they ran into similar problems (Q19 and Q20).
Some patients were too shy to ask questions or questions did not always occur to them at the right time, so they appreciated listening to other patients discussing with each other and with clinicians. This also meant that they did not have to shoulder all the responsibility for gaining information that may be useful to them (although it created a responsibility for those seen as more vocal as a subsequent section suggests) (Q21).
There were few occasions when patients found that the learning gained in group discussions did not apply to them, as in the case of a young person with T2D who could not relate to what others with T1D were talking about (Q22). Another young man suggested that learning from other patients was not a priority for him, but later in the same interview went on to explain how he was asking another participant about Freestyle Libre (Q23), generating a constructive exchange and social learning (see also their exchange at the group clinic in Box 4).
In one of the clinics, a patient demonstrated his Libre blood glucose monitor and others were interested in how it worked and the practical implications of wearing one:Pt1:Pt2:Pt1:Pt2:Facilitator:Pt1:Pt2:
Pt, patient.
Clinicians were sometimes surprised at how patients gained learning from group clinics that they had not already acquired through individual appointments in which similar topics (Q24 and Q25) were covered. One potential explanation could lie in the fact that the co-design of group clinics had led to their being a more supportive environment to learn in, and the sometimes repetitive content across clinics. In addition, some patients seemed more receptive to experiences shared by other patients as they had first-hand knowledge of the emotional and practical impact and how to manage that (Q26 and Q27).
Normalising diabetes through sharing with peers
Young people talked about how group discussions with peers helped them think about their diabetes differently and normalise their experiences through getting to know how others approached their self-care. This even resulted in patients feeling more confident and comfortable with their condition, to the extent that they started disclosing their condition in their workplace and to their friends (Q28 and Q29). Another patient, who had not met others with diabetes before and had thus far felt more comfortable injecting insulin in private, started to reconsider his approach after hearing from another patient who was more open with her self-care (Q30). Some of the emotional support between young people emerged not from sharing things they were doing well, but from admitting what they were doing less well or not at all. They felt better able to engage in such discussions as they gained encouragement from each other when they started to realise many of them were struggling to follow clinical recommendations (Q31 and Q32).
Sharing and normalising diabetes was not always straightforward. Less regular attendees remained concerned about the implications of opening up on deeply personal matters. They were not always prepared to discuss aspects of their self-care that they were struggling with or to manage a group discussion that might lead to sharing beyond what they were comfortable with, so chose to limit their contributions because of fear of embarrassment (Q33). Participants managed what they were sharing carefully depending on who else was in the room and what they knew about them. For example, a long-diagnosed patient did not want to open up about her lack of motivation when talking to a newly diagnosed patient who was still managing well (Q34).
There were instances when patients continued sharing with each other after the group session had finished. One young man advised another patient to do more testing, in what he describes to be a ‘blunt’ way (Q35). It is unclear how this was received by the other patient, who might in fact have found the exchange helpful. What this points to, however, is that facilitating connections between patients could bring unanticipated consequences outside the boundaries of the clinic and it is unclear how these could be managed.
Peer comparison
Patients commonly mentioned benchmarking their own self-care practices to those of their peers to get a sense of how well they were doing. One young girl who had not been managing well thought that she would gain motivation by hearing from others who were doing better than her (Q36). Other patients, some of whom were not controlling their diabetes well, felt reassured in that others in the group seemed to be doing even worse than them and more psychologically affected by their diabetes (Q37).
For newly diagnosed patients, comparison with peers was not always motivating, especially when they were comparing themselves with those who were doing worse. For example, one participant reflected on a Libre group session in which patients were discussing their home blood glucose monitoring results (Box 5). As he was still in a ‘honeymoon’ period, his blood glucose was well controlled, whereas he saw other patients struggling to manage their numbers. He became apprehensive about what the future may hold (Q38).
[Clinician discussing individual Libre readings with patient while others watching]
So which [graph] shall we go into? Got monthly summary, got daily log, which ones do you use?
I think monthly.
[Selecting the right graph on the computer . . .]
It’s like just a bird’s eye view, isn’t it? It’s telling you how many scans you’re doing every day. [Patient name whose readings are being shown] doing quite a few, aren’t you?
Yeah. I know last week I haven’t been doing that many. But before I used to also try and keep 10 days, 10 scans a day.
If this is the last 14 days, then yeah, you have been a little bit on the higher side, isn’t it? If you calculate, look, all your total average, they’ve all been, more or less, above 10, just above 10. So yeah, if you’re going to work out your HbA1c just on that, it probably is going to be a bit higher. But your overall HbA1c for the last three months . . . [looking to find latest blood results]
Yeah.
I hope that’s not at the expense of hypos though. Have you had a lot of hypos or not really?
I have noticed a little bit of increase on hypos, but some of them is based on because when I changed my base rate because –
Changed it too much?
Yeah.
Then you went back to . . .
I went down again to, back to the normal one but then I went up just to see if that would help.
That’s one page, and then you get the, is it the Snapshot? You get the Snapshot which we just went on [other patient name], yeah? So you get your average and then you get low glucose events. [Moving to a different graph]
I see a lot of reds.
Yeah, yeah. Is this where you were getting the hypos then?
I think, yeah.
Then, you made changes to basal rate before?
Yeah. So it’s like around three, it’s sort of around midnight to really early.
Then, that makes sense, isn’t it? So you changed your basal rate before sort of 6 o’clock, so you reduced those hypos, OK. You’ve had nine, now anyone find that the glucose events, when the Libre sensor says you’ve got a low event and then you check your blood glucose and it isn’t low, what difference do you find?
Probably about, maybe by about one that’s different. So it could be –
Lower or higher?
Higher.
M, male.
Patient ‘work’ and responsibility
Attending group clinics was not always straightforward, as outlined in earlier sections (see Motivations for engaging with group clinics). Many patients initially expressed ambivalence about joining the sessions and reflected on the advantages and drawbacks that their involvement would potentially bring. For many, this included negotiating with their employers for extra time off on top of usual diabetes care, which was described as a ‘lot of work’ (Q39). Some patients in more precarious employment felt that they had no option if the group clinic happened to coincide with job responsibilities. Other practical ‘work’ included negotiating with families who were expecting them to be at home in the evenings, managing how to get to and from the clinic, and organising their schoolwork and family responsibilities to be able to attend the sessions. Although clinicians in both sites attempted to organise group clinics on the same day as other appointments to minimise the burden of patients, for logistical and operational reasons, this was not always feasible.
When managing to attend group clinics, young people had to work through not only how to look after and express themselves in this novel group context, but also how to be responsible for the care of others in group clinics of varying sizes. This implied a shift from their normal role as patients coming in to be cared for in usual diabetes clinics. In group-based consultations, they were receiving care together with a group of other patients, each with a different background and experience and each contributing to the care process in different ways. Group care would not be possible unless a critical mass of participants decided to actively share and exchange with others to make the experience successful for everyone and realise the benefits outlined in previous sections. Some patients expressed how this placed a responsibility on them, as they were not just gaining learning from group sessions but felt that they were also expected to ‘deliver’ (Q40 and Q41). Another young patient described how he found it difficult when patients were asked what topics they wanted to cover in group sessions (Q42). Although it is good practice to organise care centred on patient needs and priorities, young people were not always prepared to answer this question or did not see themselves as knowledgeable enough on what they should count as important priorities (Q42).
Patient work and moral judgements were also necessary when deciding the extent to which young people wanted to share personal experiences, either to avoid discouraging others or to protect their own privacy. For example, a girl who had been long diagnosed explained that she did not want to discourage a boy diagnosed only 1 year ago by sharing her motivational difficulties (Q43). In another interview, a young man discussed the emotional work needed to gauge how much others were prepared to open up before sharing his own experiences (Q44).
Conflict and power dynamics
One clinic generated conflict between patients debating their different approaches to living with diabetes. When a young woman admitted that she was not willing to disclose her diabetes at work, she was met with strong criticism by another patient, who saw her behaviour as misguided. The young woman felt threatened and judged, practically disengaging from group discussion (Q45). In the same clinic, another young woman was criticised by other patients when she mentioned going on holiday without taking her medicines and intentionally consuming more carbohydrates than the amount she had calculated in her insulin dose. Patients assumed responsibility for giving advice and guidance about what was right and ‘normal’ (Q46) in a way that the rest of the group did not perceive as productive. This conflict resulted in significant emotional and care work for the DSN facilitating the clinics. To ensure that patients involved were not negatively affected, she followed up with each of them individually to understand how they might be feeling, talk through the incident, reassure everyone and understand implications on their participation in subsequent groups.
During interviews, patients reflected how best to fulfil their role in group clinics, in which they were essentially being asked to care for each other through sharing experiences. They thought that other patients should not approach discussions in a way that makes them personal, trying to role model their own behaviours or convince others about the best ways of managing diabetes. They saw ground rules as key to group clinic facilitation and to sustaining a positive environment (Q47).
However, challenge and conflict also seemed to play a useful role in raising issues that clinicians found more difficult to address (both in group and in individual appointments) as they did not want to alienate patients from the service. With the challenge coming from other patients in the group setting, there was an opportunity to open up discussions that, despite initial difficulty, could result in positive outcomes (Q48–50). In the specific instance described above, and combined with other factors, one of the young women started becoming more open about her diabetes and continued attending clinics. The second young woman did not engage much more with the process, although it is unclear whether or not this was as a result of this incident.
Individual attention and therapeutic relationships
Although group clinics primarily focused on building supportive relationships between peers, clinicians played an equally important role in ensuring that patients continued to engage with this model of care. One way of doing this was by addressing their individual needs. Group logistics meant that patients got in closer contact with the nurse facilitating the clinics than they normally would in the usual diabetes service. At least for part of the sessions, the nurse would directly communicate details of the clinics with patients, receive confirmation of attendance or apologies and would follow up afterwards when necessary to resolve outstanding issues (as described in Chapter 5). The relatively small numbers of attendees per group clinic (four and five young adults, on average, at group clinics run at NUH and CMH, respectively) was likely to have been beneficial because it made individual attention more feasible for the nurse delivering it. The individual attention to group clinic participants also supported routine one-to-one care by offering an additional route to access clinical support. Patients commented on an emotional bond that they developed with the nurse, who had a well-rounded insight on their struggles from reading their clinical history, discussing with usual-care clinicians and observing young people interacting and sharing in group clinics. This allowed the nurse to develop a unique perspective on their needs and on how best to approach them, which contributed to the development of therapeutic relationships (Q51).
How does the way group clinics are designed and delivered support good experiences for young adults with diabetes?
For groups to support a positive experience, critical mass was necessary not only in terms of the number of people participating, but also in terms of the amount of contributions (i.e. more people did not always guarantee a high level of contribution, whereas some smaller groups with four patients were very successful). On average, there were four and five young adults in attendance at each group clinic at NUH and CMH, respectively. Patients had different views on the ‘right’ number of participants (the co-design suggested that the optimal size might be six to eight people, but that even two patients would constitute a group) but strongly suggested that group clinics were successful when they provided the opportunity for mutual sharing between different perspectives, irrespective of the number of attendees. There was no fixed number of participants that would make group clinics work better, as this also largely depended on the focus of the session (e.g. exercise vs. psychology) and the mode of facilitation. A larger number of participants meant that even if a few participants were shy and quiet, or if facilitation was not very successful, there would be enough contributions from everyone else (Q52–55).
Some continuity of membership between group clinics was welcomed, but patients also wanted new perspectives to be included so that the discussion did not dry up because the same people kept attending (Q56 and 57). The age difference between participants was raised by only one interviewee, a 25-year-old patient, who mentioned that she found it difficult to associate with the experiences of 18- to 19-year-olds in the same group session. This did not appear to be a concern for any other patients, however, with age differences presenting few barriers to sharing experiences. Group clinics were predominantly attended by young patients with T1D. In one clinic, the only patient with T2D expressed feeling a bit left out initially, as he thought that he would not be able to identify with T1D patients, but this concern quickly subsided (Q58). Given the mobility of the young adult population, it was difficult to allocate people to groups that would meet consistently and build long-term relationships. Therefore, it became important to quickly build affinity between patients in the moment so that they would open up in their discussions and feel supported.
Patients also considered how they would judge whether or not group clinics continued to provide added value to them so that they would keep attending. Many saw their involvement as time limited, as they assumed a point would come when discussions would start getting repetitive and they would not be gaining any new learning from others. This suggests that some young adults perceived the group clinic model as something that delivered finite education more than a continuous process of care. However, some young adults felt that if they observed others continuing to participate in the clinics then that would also motivate them to continue attending (Q59 and Q60). Other young adults saw group clinics as a free space to provide information, explore patient understanding and prepare to bring more value in one-to-one appointments, but also highlighted the role of the clinician as facilitator rather than expert (Q61 and Q62).
Finding the right balance between being clinically driven and prioritising patient engagement in this patient population was difficult, and this highlights the challenge of developing a group clinical model that contains elements of care in addition to simply education. For example, clinicians considered whether or not to discuss blood glucose profiles with patients from a more clinical perspective, but decided against it to avoid limiting engagement at early stages in the delivery of this new model (Q63).
Delivering group clinic care in the NHS
Setting up a new model of care using group clinics
Clinical and non-clinical staff involved in setting up and delivering group consultations described the process as a slow and steep learning curve, which involved a lot of trial and error. All staff members were new to group consultations and, at the time that the clinics were implemented, there was little previous learning or guidance to draw on. Interviews with DSNs, who had the most responsibility for the organisation and delivery of the group clinics, indicated enthusiasm (‘I want to learn. And this is something completely new’ – interview 1, DSN), but with this came realisation of the challenges and efforts required to deliver benefits for patients (‘I feel it’s definitely beneficial. I’m just trying to think how we can, how I can manage it’ – interview 26, DSN). A successful clinic was hard to achieve but rewarding: ‘when we get a good group it really lifts our spirits up’ (interview 2, DSN).
A significant part of developing and implementing this new model of care involved building trust and relationships among the clinicians involved, as well as with patients invited to take part. One of the DSNs who had not been involved with the young adult clinic previously described how it took time to build these relationships on which group-based care depended (Q64 and Q65). In-depth knowledge and good rapport with young patients and sometimes with their families was needed to support attendance and engagement (Q66).
The process of selecting patients for group clinics was not always straightforward. Health professionals had initially suggested that group clinics would work better for newly diagnosed patients who had more need and motivation to learn about their condition, but that everyone should be invited and allowed to judge whether or not it would be useful for them to attend. During interviews, there seemed to be little difference in motivation to attend between young adults who had had diabetes for many years and young adults with a more recent diagnosis, and there was appetite to learn from each other’s different experiences. Although a clear outcome of the co-design was that young adults with different types of diabetes should be included in the same group clinics when appropriate, there were some instances in which group clinics had to be tailored to the specifics of diabetes type and other factors (e.g. Libre clinics were available only to young adults with T1D meeting nationally agreed criteria for eligibility, or women-only sessions on periods and pregnancy). Bringing together patient groups in purposeful ways created ‘hidden work’ as it required careful deliberation between clinicians to allow learning to emerge (Q67 and Q68).
To communicate with young adults about group sessions, the diabetes nurses trialled different options (e.g. letters, text messages at different frequency and telephone calls) and attempted to move away from formal NHS language (e.g. as used in clinic letters) to engage patients in a more direct, age-appropriate way that would not feel alienating (see Chapter 6, Group clinic invitations: responses and attendance). It became necessary to spend time and effort to sustain communication with patients and ensure that enough people would be attending the clinics to make the effort of organising the sessions worthwhile. Non-clinical staff were also needed to support communication with patients, as explained in Chapter 5, Co-design: phase 2, Phase 2 and iterative co-design, on the role of the youth worker.
In early clinics at our second site, CMH, patients invited to group sessions also had their individual appointments arranged for the same day to provide combined individual and group care, as well as to reduce how often patients were asked to come to clinic. This raised the level of effort for clinicians even further, as the diabetes nurse had to rearrange appointments and communicate with patients about this change (Q69). Eventually, CMH adopted the same recruitment approach as NUH, where all consented patients were invited to attend the same group clinic regardless of when their individual appointments had been scheduled for. Although this meant that less co-ordination was needed, different operational problems emerged (Q70). Trying to keep track of which patients attended each of the sessions and how to set up groups for subsequent clinics was also viewed as messy and cumbersome (Q71).
Other operational challenges ensued, such as booking seminar rooms when there was only one room available for use by several clinical services in each of the two hospitals, and adjusting booking processes to accommodate a group session compared with a standard individual appointment (Q72).
Group clinic delivery was not simply a matter of delivering individual care to multiple people at the same time. It required a different degree and mode of preparation by clinicians delivering the sessions and incorporated aspects of education around broad lifestyle issues, specific diabetes self-management support and delivery of care. At initial stages, there was a lot of uncertainty around what preparation would lead to a successful clinic (Q73 and Q74). Patients also mentioned that group clinics worked less well when clinicians were unprepared to adjust their content or usual individual practices for the group setting (again pointing to additional work needed to make group clinics work: Q75). It took time to build a process from the ground up, as clinicians and patients alike familiarised themselves with this new model of care, and found approaches that worked well and supported interaction in the group setting. This often required group facilitators to work with clinicians in advance of the session to ensure that the content was appropriate, but also following up after the session to address any feedback from patients, record all details as needed and provide individual support (Q76–78).
Although patients provided broad suggestions about the content of group clinics, translating these into sessions that were beneficial and appropriate for everyone required significant work. In-depth knowledge of patients, through either experience or careful review of patient records, guided the decisions of DSNs, including how to focus each of the sessions, what speakers to invite, and how to steer the discussion so that patients would feel supported and gain value (Q79).
Some clinicians found it difficult to address individual problems in the context of group clinics, compared with how these would be managed in a one-to-one consultation (Q80). These difficulties led to some sessions being heavily focused around broad support for education and self-management, without what might be construed as ‘care’ (e.g. review of blood glucoses, starting a new treatment for an individual) being delivered. It was assumed that the ‘anxiety’ to discuss individual diabetes issues would subside once health professionals and patients became more comfortable with the group clinics model (Q81). Indeed, Libre sessions carried out at NUH involved significant clinical discussion on individual results that were downloaded from the Libre device and displayed on a computer screen for everyone to view. By the time that Libre clinics were delivered, young patients had built up enough trust between them and with the clinicians delivering the groups to be comfortable with individual discussions in a group setting (although some preferred to see others’ results first before agreeing to show their own).
A lot of the time, clinicians had to steer discussion in ways that would indirectly open up opportunities for learning and support, rather than themselves directing questions about self-management to individuals, as would have been the case in one-to-one consultations. For example, if clinicians had looked into someone’s record and realised the patient did not understand how to manage insulin-to-carbohydrate ratios, they would bring this up as a topic for general discussion in the group session with the hope that the patient would indirectly gain the knowledge needed. This required a lot of background work and co-ordination, also making sure that the discussion remained relevant for everyone while addressing individual needs (Q82 and Q83).
In group clinic delivery, flexibility and adaptability became important in different ways. First, in many sessions it was difficult to predict who would be attending (and whether or not they would arrive on time); therefore, facilitators had to adopt a flexible plan to address different patient priorities, needs and abilities as they emerged in the moment (Q84–86). Although recognising its importance, some clinicians found it difficult to manage the unpredictability inherent in interactive group discussions compared with more structured or scripted education programmes. The dual pressure of delivering good clinical care and education while facilitating a group of young people who had never met each other (Q87 and Q88) was notable. In some situations, it was important for clinicians to engage proactively in emotional work to support groups in which conflict and competition emerged through interaction (Q89 and Q90).
As a new model of care delivered in the context of a research programme, group clinics were less integrated in the day-to-day planning of the diabetes service, which meant that interdependencies with wider care needed to be actively managed (more prominently at NUH as this work was spread across more health-care staff). For example, co-ordination was needed to ensure that patients understood the different purposes of individual and group appointments, and continued to attend both. Ensuring continuity between what was covered on an individual basis and what was discussed in the context of the group also became a matter of active discovery, to fill gaps and take patient care a step further each time (Q91). Based on their experiences delivering group-based care, clinicians took a pragmatic view on the outcomes that could be achieved with a new group clinics programme. They valued group clinics primarily for their potential to engage young patients who previously were not attending their appointments (Q92 and Q93). They also talked about the outcome of group clinics being to help young people feel more supported and to change the conversations happening on a one-to-one basis with clinicians (Q94 and Q95).
Differences to the delivery of existing one-to-one care
Patients commonly discussed differences between group clinics and individual appointments. Some suggested that group clinics, by opening up discussion on self-care between peers, became more focused on ‘how to live’ with the condition, rather than just seeing diabetes as something young people need to ‘manage’ clinically. They also described feeling better able to contribute their experiences and ask questions in the group clinics, whereas in individual appointments they often found it difficult to voice their difficulties or engage productively in the interaction (Q96 and Q97).
A patient who had recently transitioned to the adult service felt the need to be more frequently monitored and saw group clinics as providing this additional point of contact. Another patient suggested that young people felt less comfortable with individual appointments because they perceived them as ‘professional’, an environment focused around the clinical transaction in a way that felt impersonal, which would also explain low attendance rates (Q98 and Q99). The power difference in individual clinics and the obstacles this posed in the consultation was also recognised by clinicians themselves (Q100–102).
In group clinics, patients saw an opportunity to discuss with peers how to go about making changes, rather than just what changes to make, with others who understood their experiences (Q103 and Q104). Being able to spend more time with patients in group clinics than in individual appointments was also deemed important by some health professionals, such as in the diet sessions (Q105). Patients and health professionals alike saw value in combining individual clinics and group appointments. They found that these two different consultation modes fulfilled different purposes; individual appointments would cover individual management, treatment options and urine or blood test results, whereas group clinics would cover topics of common interest to everyone and sharing experiences (Q106–108). There was a clear feeling that the review of blood glucose readings and/or insulin dose adjustments were more comfortably suited to individual appointments; in some group clinics these were successfully covered, but only with significant hidden work prior to the group clinic to be ready to steer the discussion in a way that could meet individual needs (Q109–111).
Very few patients considered group clinics as something that would substitute for a large number of individual appointments. There was one suggestion for individual appointments to be driven by patients when they felt that there was need, rather having appointments over prespecified periods (Q112). Only one patient, who had been struggling with diabetes and self-care, expressed more confidence in attending group clinics than individual appointments, and a preference for continuing in a group for her diabetes care (Q113). One of the consultants also mentioned an encounter with a patient who attended group clinics but did not want to engage with his usual care (Q114).
Critical staff roles: the youth worker
Our implementation of group clinics involved a highly skilled youth worker in the set-up and delivery of group clinics. He had been working with a youth organisation local to NUH, and had previous experience supporting young people in difficult circumstances, such as in prisons or on probation, as well as those at risk of radicalisation and extremism. The youth worker contributed valuable insights on how best to approach young people, how to build rapport and relationships, how to create a safe and informal environment, and how to approach clinical topics in ways more engaging for this group. At CMH, the youth worker role focused largely on facilitating the group clinics with the DSN, whereas in NUH he also played a significant role in inviting patients to group clinics.
For example, the youth worker introduced icebreakers to the group clinic programme and this made a visible difference in what patients thought about this new model of care. Given that most group clinics involved some new people who had not been introduced to others before, icebreakers served to create a relaxed atmosphere and to get everyone talking in a way that did not immediately focus on their diabetes (Q115–119). It was important to deliver icebreakers in an authentic way that made participants (patients and clinicians) laugh but also start sharing a little bit about themselves (e.g. with the human bingo icebreaker; see Figure 2). Instead of treating icebreakers as a mechanistic activity to go through quickly before starting the ‘real’ business of the group clinic, icebreakers were more effective when seen as an activity that had purpose and meaning in itself (Q120).
Clinicians valued the contribution of the youth worker in group clinics because it allowed them to focus on the clinical interaction and take some pressure off having to juggle multiple roles that (in some cases) they had never been trained for (such as group facilitation with young people) (Q121 and Q122). The role of the youth worker was not just about adding a fun, age-appropriate element to what would otherwise be a more structured, ‘professional’ interaction. The role was primarily about straddling the balance between developing a model of care that would flexibly respond to patient needs without imposing too many boundaries and providing consistency and structure so that young patients would know what to expect from their participation in the sessions (Q123 and Q124).
Finally, there was recognition that the practicalities of finding a suitable youth worker and funding them to support group clinics might not be easily achieved beyond the research project (Q125).
Summary of qualitative findings
Our rich qualitative data indicate that the young adults with diabetes in this study had positive experiences of group clinic care. In particular, the ability to share understanding of diabetes and normalise experiences with other young adults with diabetes led to feelings of being supported. The situated, social learning that came about from the groups and the facilitatory approach used by the health-care professionals delivering them was also favoured. However, both young adults and health-care professionals noted the extra work required in joining a new model of care, including the need to negotiate new roles and relationships, the potential for confrontation and the changed power dynamics within groups. Unexpectedly, the diversity of attendees within the groups (e.g. by duration of diabetes, type of diabetes and age) was mostly seen as a positive to expand the opportunities for learning and sharing experiences. Group clinics incorporated educational content, support for self-management and the delivery of care, but the last topic was seen as more of a challenge as it was felt to require a greater individual focus than could be supported in a group setting (e.g. in supporting insulin dose adjustments or reviewing blood test results). Some group clinics focused heavily on the delivery of care (e.g. a session on annual review diabetes checks), and others incorporating Libre initiation and follow-up, but the majority focused on supporting self-management and education. The ability to receive one-to-one care in addition to group-based care was considered to be important to all those involved, and was perceived as something that could augment individual care and provide flexible, multidimensional care, support and education.
The delivery of group clinics within an existing model of care based around one-to-one appointments was challenging, in part because of the need to recruit individual patients and follow formal research processes, and also because of the amount of hidden work required to deliver group clinics and engage the young adults with them. However, the group clinics were flexible and adaptive, for example supporting the change in home blood glucose testing from capillary testing to Freestyle Libre. What evolved over time was an understanding that group and one-to-one clinical care fulfilled some different purposes but that the two worked synergistically in delivering a model that could better meet the wider needs of young people with diabetes. Existing staff were critical to the delivery of group clinics, and the role of the youth worker was highly supported in engaging young adults and providing a facilitatory and age-appropriate approach.
Chapter 8 Quantitative evaluation of group clinics and costs analysis
Description of the data set
The quantitative evaluation of the group clinic model was designed to contextualise the findings of our primarily qualitative study and to determine the feasibility of collecting outcome data for a future at-scale evaluation. We combined questionnaire data with data from electronic health records from all research participants, including from those at research sites at which group clinics were delivered and from those at sites used as control sites. Our costs analysis provides an early insight into the economics of delivering group-based diabetes care for young adults in the NHS.
Data quality and completeness
Data quality was monitored and assured through site visits by the project team, with reviews and discussions of preliminary findings at project meetings, additional site visits when needed, and e-mail and telephone conversations.
At baseline, we noted data missingness of 7–14% across some variables, with the greatest missingness in self-report questionnaires [Problem Areas In Diabetes (PAID) and Patient Enablement Instrument (PEI)] and clinical measures. Missingness in self-report questionnaires indicates a lack of acceptability of research processes, and was noted to occur particular when non-face-to-face recruitment took place and participants were asked to complete paperwork and return it by post or e-mail. Missingness in clinical measurement data reflects both under-measurement of clinical variables (e.g. no HbA1c levels measured in the previous year) and the challenge to the research team staff accessing the result across multiple clinical systems.
The greater challenge was in obtaining data at the 1-year follow-up, and there were very high levels of missingness (36–50%) across all variables. This missingness was greatest where self-report questionnaires were applied and reflects the high turnover of our patient population, difficulties in making contact by telephone/e-mail and infrequent clinical contact (owing to non-attendance at group clinics and/or routine care). This data missingness occurred despite major efforts from a research team, most of whom were experienced working with young adults, who took a creative and opportunistic approach to contacting them and obtaining data. Missing data at follow-up was also a major issue for variables recorded on clinical systems, and this was considerably higher at follow-up than at baseline because of patient turnover (e.g. patients moving and no longer receiving care at that clinic); turnover of research staff, with incoming staff having less experience and training working with young adults; and inability to access the multiple clinical systems and databases the research staff needed to acquire routine data. At follow-up, no participants asked to withdraw from the study and for their data not to be included in our study, suggesting that the research process was acceptable in principle but needed to be considerably more accessible and feasible.
After data collection was complete, anonymised, password-protected data sets from each site were sent by secure e-mail connection to the secure server at Imperial College London. Data cleaning was performed to standardise all variables, check for accuracy and consistency of information (e.g. whether or not changes in HbA1C were biologically plausible, or whether or not clinical data were consistent with the diagnosis), and prepare for statistical analysis. Definitive data sets from all sites were submitted by 20 November 2019 and the final, cleaned, data set was locked on 31 December 2019.
Details of data completeness are presented in Table 10.
| Data type | Variables | Data points missing at baseline, n (%) | Data points missing at follow-up, n (%) |
|---|---|---|---|
| Sociodemographic characteristics | Age, sex, deprivation decile, ethnicity, first language and employment status | 55 (7) | NAa |
| Clinical measures (from health records) | Eight care processes: HbA1c levels, blood pressure, cholesterol, BMI, serum creatinine, urine albumin : creatinine ratio, foot check, smoking status | 170 (14) | 494 (40) |
| Self-reported diabetes self-management | Frequency of blood glucose testing per day, technology use in the last year, previous attendance at structured education | 32 (8) | 203 (50) |
| Patient-reported instruments | PAID score and PEI | 39 (14) | 126 (46) |
| Health-care utilisation | Planned diabetes appointments attended, ED attendances (diabetes related), inpatient diabetes-related admissions, primary care appointments (diabetes related) | 61 (11) | 198 (36) |
We proceeded to analyse our quantitative data, despite high levels of missing data at follow-up, in keeping with our aim to explore the feasibility of a future at-scale evaluation. Our findings are, therefore, limited but provide some insight into how future evaluations could be undertaken.
Outcomes for participants at baseline and year 1: ‘difference in difference’ analysis
We analysed trajectories of clinical and questionnaire measures at baseline and 1 year in control sites and group clinic sites, with comparison between attenders and non-attenders at the group clinic sites (Table 11). Trajectory values were calculated by subtracting follow-up data from baseline data, that is a negative value for HbA1c levels indicates that this value has decreased during the course of the study. Analysing trajectories by site, mean PEI scores for CMH patients improved by 2.4 points (95% CI 0.4 to 4.3 points) during the year of the study, a statistically significant increase suggesting an increase in patient enablement. These results were accompanied by a not statistically significant but consistent direction of change in the mean PAID score of –9.9 points (95% CI –24.2 to 4.5 points), suggesting a reduction in symptoms of diabetes distress. No statistically significant changes were seen in these measures at other sites.
| Site | Number of participants (n) | Mean change (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HbA1C levels (mmol/mol) | Frequency of blood glucose testing per day | PAID score (points) | PEI score (points) | Planned diabetes appointments attended | ED attendances (diabetes related) | Inpatient admissions (diabetes related) | Primary care appointments (diabetes related) | ||
| NUH | |||||||||
| All | 50 | –0.02 (–0.11 to 0.07) | 1.77 (–0.10 to 3.64) | 3.06 (–3.43 to 9.54) | 0.63 (–0.85 to 2.11) | –0.02 (–0.14 to 0.09) | –0.06 (–0.27 to 0.14) | 0.04 (–0.20 to 0.12) | –0.02 (–0.77 to 0.72) |
| Attended | 23 | –0.04 (–0.16 to 0.07) | 2.33 (–1.16 to 5.82) | 1.77 (–6.72 to 10.25) | 0.89 (–1.07 to 2.85) | 0.08 (–0.06 to 0.21) | 0.14 (–0.14 to 0.43) | –0.14 (–0.07 to 0.36) | 0.24 (–0.92 to 1.22) |
| Non-attended | 27 | 0.01 (–0.14 to 0.15) | 1.16 (–0.52 to 2.85) | 5.25 (–6.79 to 17.29) | 0.11 (–2.54 to 2.76) | –0.13 (–0.32 to 0.06) | –0.23 (–0.52 to 0.06) | –0.19 (–0.42 to 0.04) | –0.24 (–1.31 to 0.84) |
| CMH | |||||||||
| All | 23 | 0.0005 (–0.09 to 0.09) | 0.37 (–1.32 to 2.06) | –9.88 (–24.24 to 4.49) | 2.38 (0.43 to 4.32)a | 0.04 (–0.19 to 0.12) | – | 0.16 (–0.26 to 0.59) | 0.1 (–0.24 to 0.44) |
| Attended | 14 | 0.05 (–0.04 to 0.14) | 0.37 (–1.32 to 2.06) | –9.88 (–24.24 to 4.49) | 2.38 (0.43 to 4.32)a | 0.02 (–0.16 to 0.19) | – | 0.14 (–0.07 to 0.35) | 0.14 (–0.24 to 0.53) |
| Non-attended | 9 | –0.14 (–0.35 to 0.06) | – | – | – | –0.16 (–0.53 to 0.21) | – | 0.17 (–0.42 to 0.46) | 0.00 (–0.94 to 0.94) |
| WH (all) | 30 | –0.03 (–0.25 to 0.19) | 0.14 (–0.22 to 0.51) | 0.54 (–7.82 to 8.89) | 2.44 (–0.99 to 5.88) | – | – | – | – |
| MEH (all) | 33 | –0.03 (–0.11 to 0.05) | 0.46 (–0.08 to 0.99) | –0.06 (–7.58 to 7.47) | –1.94 (–3.92 to 0.04) | –0.10 (–0.28 to 0.07) | 0.06 (–0.33 to 0.44) | – | –0.41 (–1.67 to 0.85) |
Regression models using unadjusted and adjusted (e.g. type of diabetes, age, sex, ethnicity, age at diagnosis and deprivation) data also showed no difference in trajectories between attenders and non-attenders at either site (Table 12). The only possible exceptions were a small increase in diabetes-related ED attendances and diabetes-related inpatient admissions among group clinic attenders at NUH. However, these were based on a very small number of attendances/admissions (< 10 of each) and were, therefore, of negligible statistical significance. Participants at CMH had no emergency admissions for diabetes at baseline or 1 year, and there were only two inpatient admissions for participants at MEH; therefore, analyses are not presented for either. There was a marginal increase (beta coefficient 0.19, 95% CI 0.02 to 0.37) in HbA1c levels in group clinic attendees at CMH that did not hold up to adjustment.
| Change in diabetes control measures | NUH | CMH | ||
|---|---|---|---|---|
| Beta coefficient (unadjusted) 95% CI | Beta coefficient (adjusted)a 95% CI | Beta coefficient (unadjusted) 95% CI | Beta coefficient (adjusted)a 95% CI | |
| HbA1c levels (mmol/mol) | –0.05 (–0.12 to 0.14) | –0.08 (–0.29 to 0.12) | 0.19b (0.02 to 0.37) | 0.15 (–0.07 to 0.36) |
| Frequency of blood glucose testing per day | 1.17 (–2.62 to 4.96) | 0.68 (–3.74 to 5.09) | ||
| PAID score | –3.49 (–17.13 to 10.16) | –3.31 (–18.77 to 12.16) | ||
| PEI score | 0.78 (–2.41 to 3.96) | 0.68 (–3.02 to 4.38) | ||
| Number of planned diabetes appointments attended | 0.21 (–0.01 to 0.42) | 0.15 (–0.09 to 0.39) | 0.18 (–0.15 to 0.50) | 0.19 (–0.17 to 0.56) |
| Number of ED attendances (diabetes related) | 0.37 (–0.03 to 0.77) | 0.52b (0.08 to 0.96) | ||
| Number of inpatient admissions (diabetes related) | 0.34b (0.02 to 0.65) | 0.31 (–0.08 to 0.68) | –0.02 (–0.41 to 0.36) | –0.05 (–0.64 to 0.54) |
| Number of primary care appointments (diabetes related) | 0.39 (–1.08 to 1.85) | 0.83 (–0.98 to 2.64) | 0.14 (–0.61 to 0.89) | 0.26 (–0.66 to 1.18) |
We looked for evidence of a ‘dose–response’ association between the number of group clinics attended at NUH (chosen because of the bigger sample size and lower rates of missing data), and change in diabetes control measures (Table 13), to further investigate potentially causal associations. We continued to see marginal differences in inpatient admissions and emergency attendances in group clinic attendees, but there was no strong evidence of a dose–response relationship, and this was not unexpected given the small sample size, high rates of data missingness and low recorded event rate (six inpatient admissions and eight emergency attendances).
| Change in diabetes control measures | Number of group clinics attended, beta coefficients (95% CI) compared with participants who DNA any clinics | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | ≥ 3 | 1 (adjusteda) | 2 (adjusteda) | ≥ 3 (adjusteda) | |
| HbA1c levels (mmol/mol) | –0.002 (–0.23 to 0.23) | –0.13 (–0.39 to 0.13) | –0.03 (–0.31 to 0.25) | –0.05 (–0.35 to 0.26) | –0.15 (–0.48 to 0.18) | –0.08 (–0.45 to 0.29) |
| Frequency of blood glucose testing per day | 3.16 (–1.59 to 3.91) | –0.54 (–6.21 to 5.13) | –0.09 (–5.77 to 5.57) | 0.50 (–6.57 to 7.59) | 0.44 (–6.40 to 7.27) | 1.14 (–6.72 to 8.99) |
| PAID score | –8.11 (–24.31 to 8.09) | 7.25 (–9.73 to 24.23) | –11.5 (–30.95 to 7.95) | –2.85 (–32.29 to 26.6) | 5.71 (–16.5 to 27.97) | –11.91 (–37.29 to 13.5) |
| PEI Score | 0.46 (–3.53 to 4.45) | –0.51 (–4.93 to 3.91) | 2.22 (–1.95 to 6.39) | 1.99 (–4.91 to 8.90) | –0.44 (–6.42 to 5.54) | 0.44 (–5.22 to 6.11) |
| Number of planned diabetes appointments attended | 0.24 (–0.04 to 0.51) | 0.18 (–0.17 to 0.53) | 0.17 (–0.18 to 0.52) | –0.03 (–0.34 to 0.29) | 0.43 (0.05 to 0.80) | 0.17 (–0.21 to 0.55) |
| Number of ED attendances (diabetes related) | 0.43 (–0.08 to 0.95) | 0.63 (–0.05 to 1.31) | 0.06 (–0.56 to 0.69) | 0.35 (0.28 to 0.98) | 0.81b (0.12 to 1.49) | 0.45 (–0.25 to 1.16) |
| Number of inpatient admissions (diabetes related) | 0.19 (–0.21 to 0.59) | 0.59b (0.07 to 1.11) | 0.36 (–0.13 to 0.84) | –0.03 (–0.57 to 0.50) | 0.64b (0.54 to 1.22) | 0.43 (–0.18 to 1.03) |
| Number of primary care appointments (diabetes related) | –0.32 (–2.20 to 1.57) | 1.24 (–1.12 to 3.59) | 0.74 (–1.45 to 2.93) | –0.25 (–2.96 to 2.47) | 1.39 (–1.43 to 4.21) | 1.56 (1.27 to 4.38) |
Summary of quantitative analysis
Our quantitative data analysis revealed significant challenges in obtaining data in this study, despite significant efforts to do so, and this has major relevance to the design of a future clinical trial of the care model. At baseline, we observed missing data in up to 14% of our data fields, with considerably higher rates of missingness (up to 50%) at the 1-year follow-up point. These challenges were multifactorial and represent the complexity of working within a clinical environment with high turnover of patients and non-attendance, and the likely unacceptability of research process in this patient group. We also observed the challenge of research process across multiple clinical sites with varied research support infrastructure and experience.
The high rates of data missingness give a clear indication that our quantitative data collection approach was unfeasible and provide important insights into how a future at-scale evaluation of a group clinic care model for young adults should approach quantitative data collection. Instruments such as PAID and PEI are important measures of patient-reported outcomes and could still be an important part of future evaluations, but it may be more acceptable to research participants to complete these if these are designed as electronic forms in a cloud-based research data platform such as REDCap (REDCap®, Nashville, TN). Some diabetes services use patient-reported outcome measures in routine care, and it may be helpful to learn from them about how these can be embedded into practice in a way that is more acceptable to patients. Other non-validated patient-report instruments should be kept to a minimum in future evaluations to improve the acceptability of research processes. Quantitative data collected from health records should be streamlined and simplified in future evaluations to minimise the challenges of multisite research conduct, especially given that future evaluations would be at a much larger scale. It would be pragmatic to consider using the NHS Digital NDA as a means to assess patient-level and service-level outcomes in a future evaluation as this already synthesises the most important clinical outcomes. However, it is important to consider the timescale involved in getting an approval from NHS Digital, which in this research was considerably longer than anticipated, and which would be a more complex process if it was linked at an individual level to research participants. Other potential issues with using NDA data are that some hospitals submit incomplete/no NDA data, which could introduce selection bias, and there are (as was the case in our research) issues around disaggregating individual clinical services within one large overarching NHS trust provider.
Where we did perform analysis of our quantitative data, we found no major effects (positive or negative) between young adults who attended and young adults who did not attend DNA group clinics at the group clinic sites, except for some marginal improvement in a marker of patient enablement at the CMH after 1 year of group clinic attendances. Other differences, including changes in ED attendance, were marginal because of the small sample size and event rate.
Costs of delivering group clinics
Intervention costs
Our microcosting of the group clinic intervention included both the co-design process (at NUH and CMH) and the delivery of the group clinics. The summary of co-design costs is shown in Table 14. This includes costs associated with designing and running the workshops, and costs of recruiting workshop participants. Staff salaries (across all professional groups) were the main expense, amounting to £8175. The total cost of designing the clinics was £8806.
| Expenditure type | Pay band | Time (hours) | Hourly rate (£) | Total cost (£) |
|---|---|---|---|---|
| Designing the intervention | ||||
| Salaries | ||||
| Research lead | 8a | 15 | 66.00 | 990.00 |
| Chief executive | 8c | 2 | 91.00 | 182.00 |
| Project manager | 7 | 7.5 | 55.00 | 412.50 |
| Subtotal | 1584.50 | |||
| Recruiting participants | ||||
| Salaries | ||||
| Project manager | 7 | 3 | 55.00 | 165.00 |
| Research lead | 8a | 3 | 66.00 | 198.00 |
| Chief executive | 8c | 2 | 91.00 | 182.00 |
| Research nurse (NUH) | 7 | 6 | 54.00 | 324.00 |
| Research nurse (CMH) | 7 | 6 | 54.00 | 324.00 |
| Other expenses | ||||
| Printed materials | 7.00 | |||
| Subtotal | 1200.00 | |||
| Workshops | ||||
| Salaries | ||||
| Project manager | 7 | 42 | 55.00 | 2310.00 |
| Research lead | 8a | 13 | 66.00 | 858.00 |
| Chief executive | 8c | 15 | 91.00 | 1365.00 |
| Research nurse (NUH) | 7 | 8 | 54.00 | 432.00 |
| Research nurse (CMH) | 7 | 8 | 54.00 | 432.00 |
| Other workshops costs | ||||
| Facility | N/A | |||
| Travel and subsistence | N/A | |||
| Printed materials | 10.00 | |||
| Dictaphones (×2) | 100.00 | |||
| Workshop transcripts | 484.00 | |||
| Refreshments | 30.00 | |||
| Subtotal | 6021.00 | |||
| Total costs | ||||
| Total salaries | 8174.50 | |||
| Total other costs | 631.00 | |||
| Total co-design | 8805.50 | |||
The costs of delivering group clinics were estimated separately for NUH and CMH (Tables 15 and 16). These included costs of staff running the clinics, arranging appointments and chasing non-attendees, booking rooms and refreshments, and making patient notes. Owing to the different number of clinics at each site (22 and 6 at NUH and CMH, respectively) there was a substantial difference in the total cost of delivering the intervention (£11,992 for NUH and £3432 for CMH). However, the average cost per clinic was very close for two centres (£545 and £572 for NUH and CMH, respectively). The average cost per participant was higher at NUH (£158) than at CMH (£127) because of poorer attendance at NUH (average number of participants was 3.7 for NUH vs. 4.5 for CMH) (see Tables 15 and 16).
| Resource | n (average) | Range | Total cost (£) |
|---|---|---|---|
| Total number of clinics | 22 | ||
| Number of participants invited | 17 | 2–42 | |
| Number of participants attended | 3.7 | 0–7 | |
| Number of staff delivering the clinics | 2–3 | ||
| Time of running the clinics (minutes) | 135 | 120–180 | 8939.16 |
| Time of preparing room and materials (minutes) | 16 | 575.00 | |
| Time of arranging appointments and chasing non-attenders (minutes) | 71 | 1292.00 | |
| Time of making patient notes (minutes) | 35 | 715.00 | |
| Time of other activities (minutes) | 12 | 202.50 | |
| Lunch | 78.00 | ||
| Other expenses | 190.00 | ||
| Total cost of group clinics | 11,991.66 | ||
| Average cost per clinic | 545.08 | ||
| Average cost per participant (one clinic) | 157.79 | ||
| Resource | n (average) | Range | Total cost (£) |
|---|---|---|---|
| Total number of clinics | 6 | ||
| Number of participants invited | 26 | 24–7 | |
| Number of participants attended | 4.5 | 3–6 | |
| Number of staff delivering the clinics | 3–4 | ||
| Time of running the clinics (minutes) | 67 | 30–95 | 1590.09 |
| Time of preparing room and materials (minutes) | 13 | 5–15 | 56.25 |
| Time of arranging appointments and chasing non-attenders (minutes) | 260 | 240–70 | 1170.00 |
| Time of booking room and confirmation (minutes) | 17.5 | 5–30 | 78.75 |
| Time of making patient notes (minutes) | 84 | 50–137 | 309.38 |
| Time of other activities (minutes) | 51 | 30–82 | 227.81 |
| Other expenses (e.g. travel, room hire, printed materials) | 0.00 | ||
| Total cost of group clinics | 3432.28 | ||
| Average cost per clinic | 572.05 | ||
| Average cost per participant (one clinic) | 127.12 | ||
Sensitivity analyses were conducted to allow for different attendance rates and number of clinics (see Appendix 7). The number of clinics varied from 4 to 22 and the number of participants varied from 2 to 10, to reflect observed differences between two centres. Results demonstrate intervention cost per participant to be similar for each site when adjusted for both the number of clinics and the number of attendees (see Appendix 7).
Cost of usual care
The cost of usual care was estimated for scheduled and unscheduled use of health-care services (Tables 17 and 18) using the National Schedule of Reference Costs 2017–1874 (see Appendix 4). The cost of scheduled care (i.e. appointments with diabetologist, diabetes nurse, dietitian and psychologist) was £723 per patient per year. The number of missed appointments accounted for 39% (115/293) of scheduled appointments (see Table 17). The annual cost of missed appointments was £256 per patient, amounting to 26% (£256/£979) of the total annual cost of scheduled care.
| Contact | Number of patients with contacts | Number of contacts | Total cost (£) | Average cost per patient (£) |
|---|---|---|---|---|
| Endocrinologist (planned) | 38 | 101 | 15,554 | 409 |
| Endocrinologist (attended) | 31 | 55 | 8470 | 273 |
| DSN (planned) | 41 | 152 | 10,184 | 248 |
| DSN (attended) | 39 | 101 | 6767 | 174 |
| Dietitian (planned) | 25 | 34 | 2924 | 117 |
| Dietitian (attended) | 17 | 21 | 1806 | 106 |
| Psychologist (planned) | 5 | 6 | 1020 | 204 |
| Psychologist (attended) | 1 | 1 | 170 | 170 |
| Total planned appointments | 293 | 29,682 | 979 | |
| Total attended appointments | 178 | 17,213 | 723 | |
| Total missed appointments | 115 | 12,469 | 256 | |
| Contact | Number of patients with contacts | Number of contacts | Total cost (£) | Average cost per patient (£) |
|---|---|---|---|---|
| A&E | 8 | 13 | 1899 | 237 |
| Hospitalisation | 6 | 8 | 9118 | 1520 |
| Diabetes specialist nurse (face to face) | 7 | 19 | 1273 | 182 |
| Diabetes specialist nurse (non-face to face) | 28 | 76 | 1938 | 69 |
| GP (face to face) | 22 | 44 | 7524 | 342 |
| GP (non-face to face) | 2 | 6 | 294 | 147 |
| Practice nurse (face to face) | 16 | 29 | 1102 | 69 |
| Total unscheduled contacts | 89 | 195 | 23,149 | 2566 |
Unscheduled care (i.e. GP and specialist and practice nurse contacts, A&E attendance and hospital admissions due to hypo- and hyperglycaemia) amounted to £2566 per patient per year (see Table 18). The cost of unscheduled care was 2.6 (£2566/£979) times higher than the cost of scheduled care, indicating that the management of diabetes complications in young people is costly.
Summary of costs analysis
The co-design of the group clinic model cost £8806 and this represented a one-off cost to develop the new care model and, therefore, is not included in the group clinic delivery costs. Should group clinics be implemented or evaluated more widely or at scale, it is likely that some new co-design would be needed but that a shortened process could be followed. The average cost of delivering each clinic was very similar across the two sites at which they were delivered (£545 and £572 for CMH and NUH, respectively), despite differences in their implementation. The average cost of group clinics per participant was £158 for NUH and £127 for CMH, which is equivalent to the national cost of a one-to-one consultation with a diabetes specialist (£144) or A&E attendance (£137). 74 On average, study participants had 3.5 unscheduled contacts per year with health-care specialists (i.e. DSN, GP or practice nurse), with an average cost of £243.
A potential limitation of our health economic analysis is that our estimations of group clinic costs (see Tables 14–17) were based on PSSRU costing, which includes, for example, capital overheads, management, administration and estates costs. Given that the group clinics were delivered by the existing NHS staff, there might be an element of double-counting. At the same time, applying salary-based unit costs (see Appendix 4) would underestimate the cost of group clinics. Another limitation of the health economic analysis was that it was unable to separate research costs from the costs associated with delivering the clinics and, for this reason, the latter may be overestimated.
The costs of delivering the group clinics are unlikely ever to replace existing routine care costs, given that evaluation indicated that the former would be an addition to routine care. However, future evaluations should address whether or not routine care is used differently (e.g. less frequent routine care appointments or a change in the staff delivering them) and include this in health economic analyses.
Our study suggests that group clinics would be good value for money if they prevent at least one unscheduled consultation per year. This observation could be taken forward in future randomised controlled trials in this area, with consideration of the use of unscheduled health care as an outcome measure, and with an appropriate power calculation to determine sample size.
Chapter 9 Dissemination and public patient involvement
Introduction
Dissemination and PPI activities were central to our research and we embedded participatory approaches throughout our work. The methodology of this work is described in Chapters 3 and 4. In this chapter, we provide an overview of how the results of our research study were shared with wider groups of stakeholders, including co-design and research participants, user groups, practitioners interested in group clinics, designers of innovation in health services, the academic community, policy-makers, strategic decision-makers and funders.
The aims of the project dissemination activities were to:
-
share information about ongoing project activities to keep interested parties (including participants) informed
-
share the findings from our study design and evidence synthesis
-
describe the co-designed new care model and share findings and learning from its implementation journey.
Dissemination activities were arranged at regular time points throughout the project, with the aim of keeping a steady flow of outputs throughout. The focus at the outset was raising awareness of the project, which evolved into activities during the mid-point of the project to keep interest engaged and to feed back to participants, culminating at the end with more widespread sharing of findings and main messages. Dissemination activities were guided throughout by the project steering committee and PPI groups.
The three aims resulted in different kinds of dissemination outputs, each of which are described below.
Sharing information about ongoing project activities
Early in the project, we established a ‘branding’ for the work, including a name (Together), logo and website. The website is hosted by our voluntary sector partner, the AYPH, as this offered maximum flexibility and ease of access for anyone looking for information about the project. We also established a Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) account (@TogetherProjec2) and gained followers to broadcast announcements about new outputs and events, and to build interest in the project.
These channels provided us with platforms for circulating regular user-friendly brief outputs to help us spread the word about the project and achievements as they unfolded. These brief outputs are included in supplementary material [see the NIHR project web page; URL: www.journalslibrary.nihr.ac.uk/hsdr/NKCR8246) and included:
-
an initial one-page project summary at the outset of the work
-
a leaflet prepared for young people taking part in the clinics
-
a short report on the activities during the first year of the project, as at September 2018, describing the key elements of the project (i.e. review, clinic design and implementation, and evaluation), information on ‘next steps’ and ‘outputs to date’, and project contact details
-
a professionally printed (trifold A4) study feedback leaflet for participants, produced as the group clinics came to an end (April 2020), to summarise what had been achieved and to thank people who had taken part.
In addition, the AYPH also published two co-design reports. 81,82
We also provided links to academic papers and conference abstracts on our website and Twitter account.
Sharing the findings of our study design and evidence synthesis
We disseminated findings of our study design and protocol1 and our evidence synthesis (realist review) was published in Diabetes Care. 44
Dissemination of the new care model and its evaluation
At the time of writing this report, a manuscript presenting the results of our evaluation has been submitted for publication. These papers include a main evaluation paper and an additional manuscript with an in-depth qualitative analysis on the experience of young adults in group-based care. The main evaluation paper will describe the process of co-designing and implementing group clinics for young adults with diabetes, present our findings on the experience of care, and discuss the potential for group clinics to improve clinical outcomes and patient engagement and/or reduce costs, including in wider settings. In the meantime, a series of conference presentations have begun the process of disseminating the new care model and its evaluation. 83–88
Stakeholder engagement
The research team brought together a wide range of stakeholders through their pre-existing individual and institutional affiliations and networks. These stakeholders included strategic, national and local representatives. Formal engagement took place at two stakeholder engagement activities, aimed a sharing our learning and findings with people potentially interested in implementing similar innovative service models. Details of our stakeholder meetings were as follows:
-
First stakeholder event, November 2018 (‘Together Study: developing new models of care for young adults living with diabetes’, London, 13.30 to 17.00). Half-day event for whole team, patient, stakeholder and other interested participants to share emerging findings, discuss challenges and plan next steps. The event doubled as a ‘celebration event’ for this part of the project. The number of presentations from the different workstreams brought everyone up to speed with the progress of the project as a whole.
-
Second stakeholder event, April 2020. Because of the COVID-19 pandemic and the start of the first national lockdown in the spring, this event had to be cancelled at the last minute, but as an alternative we distributed the published briefing paper summarising the emerging findings of the project and initial thoughts about barriers and enabling factors.
Steering group
A steering group was set up for the duration of the project; in addition to supporting and guiding the research project, they supported dissemination activities. The steering group and its activities are detailed in Chapter 3. Particular steering group members had notable roles in supporting dissemination (e.g. via their longstanding expert and patient networks, e.g. a policy representative from Diabetes UK on the steering group and a patient representative, supported involvement with and dissemination to the Diabetes UK Young Adult Engagement Group).
Chapter 10 Discussion
Summary of main findings
We identified a clear need to improve the care for young adults living with diabetes, based on national audit data. 45 Our evidence synthesis, a realist review, captured a broad range of literature on relevant group clinics and identified critical ingredients for their delivery in a health-care context. We delivered a co-designed model of group clinic-based care to young adults living with T1D and T2D in two clinical settings based in multiethnic, socially deprived populations. The group clinic model was developed and improved over time using continuous and iterative co-design. The care model was flexible and incorporated elements of care, education and peer support, changing over time to incorporate wider service developments. Despite extensive efforts to reach and engage young people with the new care model, the group clinics were attended by only one-third of those invited. Invitations to group clinics led to active responses and communication with the care team by another one-third of young adults (approximately) but without resulting in attendance. For those young adults who did attend group clinics, their primary motivation was to meet other young people with diabetes, and their experiences of the group clinics was largely positive. A notable finding in the experiences of young adults attending group clinics was the ability of the clinics to deliver emotional support and to help them to better navigate what they needed from their one-to-one care. In addition, the young adults attending group clinics found them beneficial with regard to acquiring and reinforcing diabetes self-management techniques through benchmarking with peers and acquiring practical skills. Our qualitative interviews with staff delivering group clinics focused on the new ways of working that they encountered. Staff had to build trust and relationships with clinical colleagues and patients in novel ways, and the facilitatory approach to delivering care was different from traditional one-to-one care and necessitated specific training. Flexibility and adaptation to suit the new context of care delivery was critical, and included a shift in power dynamics and boundaries in the group setting and managing unpredictability. Some staff found these changes challenging, but the youth worker role emerged as a critical support for delivering care in this new way. Future at-scale implementation and evaluation may need to focus on the generalisability of such roles to other settings and outside a research context. Despite the high organisational burden of delivering group care within existing services, and the need for its iterative co-design, the costs of the intervention were modest (up to £158 per participant per group) and reduced with the number of participants, in contrast to a one-to-one appointment with a diabetes consultant (£144).
Our evaluation does not provide evidence for replacing existing one-to-one clinic appointments with group clinics, but indicates that group clinics may augment them through providing an additional means to support young adults in their diabetes care, particularly focusing on emotional needs and self-management skills. Further research is needed, at scale, to evaluate a combined model of individual and group clinic care against clinical outcomes and cost-effectiveness. More work is also needed to better understand how to combine models, such as one-to-one diabetes care, structured education and group clinics, to respond to emergent clinical and self-care needs for different patients at different points in time.
Themes for discussion
Our analysis of national data shows that there is significant need to better engage and support young people with diabetes to receive adequate health checks and reach treatment targets. Strikingly, data from the NDA show that fewer than one in five young adults with diabetes meet the three national treatment targets (i.e. achievement of adequate glycaemic control, blood pressure and cholesterol). Notably, national data also show that ≈ 10% of 16- to 25-year-olds with diabetes have attended structured education.
Our research aimed to explore how group clinics for young adults with diabetes might be designed and used in the NHS, and how they could improve care for people with complex health-care and social care needs who are not well reached by existing care. We identified the following themes.
Relationships as the foundation to improving care
The primary motivation for the young adults in our research to engage in group clinics was to meet other young people living through similar experiences to their own. Despite structured education being one of the cornerstones of good-quality diabetes care, the majority of young adults (nationally and at our research sites) had not previously attended this nor had had the opportunity to engage in tailored education programmes for young people. The opportunity for young adults to build relationships with each other in a group context, delivered regularly and as part of routine care, is significant and novel, and our empirical research suggested that this was beneficial. The young adults who attended the group clinics felt understood and supported, and that the care delivered in them, through the interactions with other young adults and with health-care professionals, prioritised their emotional needs. They found that the social environment was also conducive to their learning (and relearning) diabetes self-management. These experiences coincided with a life stage at which the young adults were negotiating their own independence and control of diabetes and, although this process and its timing varied considerably between young people, group clinics seemed to support this challenging process. Peer support was a component of the emotional care delivered in group clinics, and its role was identified as being that could helpfully normalise the experience of having diabetes and set benchmarked goals and improve self-efficacy. However, some of our group clinic attendees found that the social environment with peers could be demotivating when there were significant differences in group clinic attendees and their diabetes (e.g. in time since diagnosis).
These empirical research findings are consistent with one of the main themes identified in our realist review:44 that the practical sharing of experience, contextualisation of (abstract) medical advice, and exchange of tacit practical knowledge and skills are key elements of successful group-based care. The review also highlighted these as important ways for young adults to gain confidence and motivation from each other and to reduce diabetes distress.
The realist review also highlighted the importance of instilling a connection and sense of affinity between group clinic members, as well as building on pre-existing patient–clinician relationships. However, to achieve this, it was important to recognise that actual and perceived similarities between young adults are not always aligned and to have a broad perspective on what similarities are (e.g. common experience and developmental stage, rather than simply type of diabetes or age). In our empirical research, we had anticipated that young adults would attend group clinics repeatedly and that cohesion would form between repeat attenders; however, low attendance meant that this rarely happened. Instead, group clinics became dynamic and flexible with respect to attendees, content and interaction with existing one-to-one care. This flexibility suited the young adults, but placed greater responsibility on the staff delivering them to create affinity within the groups. The DSN and youth worker had critical roles in forming cohesive groups, and an environment to support them, through facilitation and relationship building. The emotional bond that young adults developed with the DSN was notable and a key factor to the success of the clinics.
An unintended, but predictable, consequence of group dynamics was the occasional occurrence of confrontation and conflict. This was managed by clearly setting boundaries and undertaking specific staff training on facilitation.
On balance, the qualitative analysis of our empirical research and realist review suggest that group clinics do provide valuable support for the emotional and practical needs of young adults with diabetes, via hands-on experience with, and modelling against, other young adults with diabetes. However, future research will be required to understand whether or not these positive experiences translate to improvements in clinical (including psychological) outcomes related to diabetes.
The challenges of delivering care differently
Prior to our undertaking this research, others had highlighted that there is no compelling evidence that delivering group clinics within a health service offers efficiencies over the usual care system. 41 Our own realist review concurred with this conclusion, highlighting that, although group-based care may lead to increased satisfaction, it also leads to a reassessment of individualised care needs, resulting in additional and dynamic demands on routine care. Furthermore, we found little evidence that group clinics could work solely as ‘replacement’ care and instead worked primarily in combination with one-to-one care.
Our empirical research confirmed findings from our evidence synthesis: we identified that group clinics did not replace routine care, instead becoming part of a broader and synergistic package of care. Our qualitative interviews with young people suggested that attending group clinics may have offered a means for young adults to use one-to-one care better and more flexibly. Health professionals also commented on how they were able to learn more about their young patients when observing conversations they were having with their peers, which helped to shift patient–clinician interaction and consultation focus in one-to-one appointments as well.
It is important to consider the scope of the ‘care’ delivered in our group clinics. Broadly, diabetes best practice care incorporates education on self-management and lifestyle; glucose-lowering treatment; glucose monitoring; and identification, prevention and treatment of diabetes complications, with gold standard practice set out in NICE guidelines,89 among others. There is little specific national guidance on the care of young adults (after paediatric transition) with diabetes. One of the main elements of the group clinic model that was developed in our empirical research was education and support of diabetes self-management, and it could be argued that this is already delivered in a group context via structured education programmes, such as DAFNE, although less broad in scope, particularly in relation to emotional and psychological health. It is notable that only a small minority of young adults participating in the group clinics had previously attended structured education, so it is perhaps understandable that the co-design of the group clinics led to this overlap. The group clinics covered care relating to diabetes treatments and identification of complications less frequently, and when they did this was predominantly in general discussions rather than tailored care delivered to individuals within the groups. This finding is not unexpected, and represents the boundary between what can be appropriately tailored to individuals within a group setting and what needs to be delivered in a one-to-one appointment. Overall, the delivery of care in our group clinics was nuanced and had significant inbuilt flexibility to be able to adapt to changing needs and context, and rapidly incorporate changes in service delivery and treatment, such as the NHS roll-out of Freestyle Libre blood glucose monitoring. The strength of the ability of our group clinics to deliver care beyond biomedical approaches and comfortably address emotional care needs was evident in the qualitative interviews with young adults. The group care seemed to open a new path for young adults to navigate their emotional needs both with each other and via a therapeutic relationship with the DSN facilitating the group clinics. This also led to conflict when a need emerged for participants to care for each other, but the conflict was managed well through facilitation and with appropriate staff training. It is hoped that future implementation and evaluation of group clinics may identify benefits in outcomes related to emotional health, such as a reduction in diabetes distress and improvement in quality of life. In turn, this could lead to more distal benefits in biomedical outcomes, such as glycaemic control, reduced progression to complications and reduced use of unscheduled care.
Attendance was low at the group clinics we offered, despite iteration and improvement of the design. The main reasons for non-attendance included other commitments (e.g. family, education, employment); uncertainty on what participation in group clinics might entail from a practical and emotional perspective; patient reluctance to engage with their diabetes, especially with other people their age; and fear of stigmatisation in their communities.
Low attendance may indicate a failure of the model or that the offer was not appealing; however, it is well known that non-attendance at outpatient clinics is common. 90 Low attendance may, in part, reflect the additional burden or anxiety of being a ‘research participant’ that would be ‘studied’ in the group clinics; however, as the young adults had been recruited and consented prior to their being invited to a group clinic session, it is unlikely that this is a major reason for non-attendance. Perhaps, more importantly, the offer of group clinics was an additional element of care, and young adults were notified of the topics/themes of the group clinics in advance, allowing them to make proactive decisions about whether or not they wanted to attend. We found that, although only one-third of those invited to group clinics attended, another one-third actively engaged with the clinical team by responding to the invitation and notifying them that they would not attend. This engagement without attendance suggests some commitment to the group clinic model, and indicates that young adults were engaging with it flexibly according to their interests and logistical constraints, and that those who did attend were likely to be particularly interested in and committed to the session. Despite the fact that group clinics comprised, on average, four or five young adults per session (lower than the target of six to eight set out in the co-design), it was possible to deliver a consistent and predictable clinical session that was favoured by the young adults, and this facilitated a ‘dipping in and out’ approach to attendance. Some young adults found the group clinics particularly appealing, attending multiple times. Our attendance findings contribute to further discussion of whether our group clinic care model is a new intervention or whether it represents an enhanced care model that systematises and joins up existing group education and peer support with individual clinician input and makes it more acceptable and appropriate to young adults: our research clearly suggests the latter.
From a staff perspective, delivering group clinics required different group facilitation skills than delivering one-to-one care that were not routinely part of clinical training. We also identified considerable implementation challenges and ‘hidden work’: building good working relationships with other clinicians and external speakers, including to co-ordinate on topics to be covered in clinics and style of engagement; gaining in-depth knowledge of patients and how to manage their unique needs in a group setting; operational work such as booking seminar rooms, sending invitations, managing attendance and scheduling follow-up; adjusting booking processes to accommodate group sessions rather than one-to-one appointments; and managing interdependencies with wider care given less integration with day-to-day planning of the diabetes service.
Some of this hidden work may be reduced without the requirement for research processes (e.g. consent) to run in parallel, and possibly with standardisation of administrative processes to embed group clinics within existing operational and record-keeping infrastructures. The critical nature of the DSN (facilitator) and youth worker have already been discussed in relation to their role in forming relationships within the groups, but their role extended beyond this, and they were central to the delivery and implementation of the clinics, including the flexible interaction with pre-existing one-to-one care.
The complexity of delivering group-based clinics within the NHS
The development of group clinics reflected the uncertainty, unpredictability and emergence that is well-characterised within complex systems, such as the NHS. 46 Complexity science provides a helpful dimension with which to consider our research findings. Our group clinics required continuous adaptation to be implemented and this was supported by our co-design process, which was iterative and continuous throughout the implementation of group clinics. In particular, co-design allowed self-organisation and sense-making across two NHS sites, and in a context that was frequently challenged by uncertainty, unpredictability and complex interdependencies. The ability for our group clinics to be dynamic and responsive to these challenges, and maintain their patient-centred approach, was a strength and could support larger-scale implementation in the future; however, future up-scaling would need further evaluation of effectiveness and cost. However, there were considerable challenges to involving young adults in discrete co-design events, and this may have resulted in a staff-centric approach to adaptation of the group clinics.
Our finding that group clinics offer young adults care that complements and potentially augments their existing one-to-one care, rather than replacing it, is important with regard to further scaling up. The inter-relationship between group-based and one-to-one care is likely to be dynamic and complex, and may necessitate continual adaptation of both. A blended care model that incorporates both one-to-one and group-based care could be an important area of future study, with regard to health service impact and cost.
Our costs analysis identified that, as expected, the per-participant cost of our group clinics were equivalent to a one-to-one diabetes appointment in existing care (£158 vs. £144), but future evaluation will be needed to explore how the costs of routine care would change with the addition of group clinics and if, together, they would be cost-effective by reducing diabetes complications, use of unscheduled care or missed appointments.
Strengths and limitations of the study
Our research investigated whether or not group clinics can meet the needs of young adults with diabetes, and whether or not they can be delivered within the NHS. This work was funded through an NIHR commissioned call that had already determined the high need (and expressed need) for research on group clinics. Our study also addresses a gap identified in a recent NIHR Health and Social Care Delivery Research (HSDR)-funded review41 that suggested that previous studies on group consultations lacked attention to ethnic minorities. A major strength of this research was the application of multiple and in-depth methods to its study, including a rigorous evidence synthesis using a realist review. The methods that were used complemented the area of study, integrating participatory approaches throughout the research process that are integral to developing, and evaluating, a patient-centred group clinic model.
Our realist review was a comprehensive literature synthesis that fulfilled a specific need in generating actionable evidence on how and why group clinics may work for young people living with diabetes. It significantly expanded the evidence base on group clinics, but was mostly based on interpretations deriving from literature on group-based education. Previous research on group clinic interventions has under-reported aspects of content and delivery, and so this has hindered a more detailed analysis of this literature. The evaluation of the group clinics used a predominantly qualitative approach, consistent with the aims of this project to understand how group clinics can influence the experience of care and meet the complex needs of young people living with diabetes. Our theory-driven approach also allowed us to generate a detailed picture of the contextual and organisation factors involved in the implementation of group clinics in the NHS. A major strength of our qualitative methodology was the use of multiple data sources (e.g. interviews, observation, documentary analysis) undertaken by an ‘embedded researcher’ who was involved in the entire project from its inception, underpinning evidence synthesis, co-design and implementation. This qualitative work has generated an understanding of how and why group clinics might work for young adults with diabetes, but with considerable transferability to other conditions and contexts.
The use of co-design harnessed a participatory approach that engaged young adults and clinicians in the new model of group clinic-based care from its inception. However, engaging young people in the co-design process was challenging because it was perceived by some young adults as a non-essential activity, and it was challenging to involve young adults who were not well engaged with the existing clinical service. The total numbers of young adults involved in discrete co-design events were relatively small and may have led to staff-centric outcomes and lack of representation of the needs of people affected by both T1D and T2D. However, by adapting the EBCD co-design process to something shorter and more pragmatic, and ensuring continual and iterative co-design as well as a formal second phase, we were able to gain sufficient contributions throughout the design and implementation of the group clinics. A weakness of this approach was that we did not formally assess the fidelity of the modified co-design methodology in our adaptation of it,91 notably the fact that we had already pre-empted a large part of the design element by specifying that we were going to build a group clinic model.
Recruitment to the study and attendance at group clinics delivered at the intervention sites (CMH and NUH) was challenging. Although this in some way reflects the existing landscape and need for the research, it does also highlight whether or not we would have had better results with an alternative approach. Recruitment might have benefited from using a hybrid of both in-person and online approaches, a model that has been shown to be beneficial in studies with young people in transition care. 92 Studies of young adults living with T2D indicate that long-term retention in research is supported by good relationships with staff, overcoming logistical barriers to retention and inducements. 93 In this referenced study,93 however, the inducements were large (free medication) and being a participant did not require active participation in a new model of care. We decided not to recruit in primary care for this study as young adult diabetes care is delivered by secondary care, and the majority of clinics do not discharge their patients, irrespective of non-attendance, and, therefore, there was a large group of young adults identifiable through the secondary care clinic who could be identified as ‘non-engagers’. However, recruitment to the group clinics might have benefited from a combined approach with invitations from both primary and secondary care, and this could be considered in the future.
The research process itself was a significant barrier to recruitment and engagement in the group clinics model. The requirement for individual consent procedures suggested to some that we were undertaking something risky, when the actual research itself conferred very minimal risk to participants. The reduction in data completeness at the 1-year follow-up point suggests non-acceptability of these research procedures and could have been a barrier to ongoing attendance in group clinics. Unfortunately, it was difficult to explore these issues further as we were unable to interview the young adults who did not wish to participate in the research, or those that consented but DNA.
We made a conscious decision at the start of this research not to deliver social media-platformed or virtual group clinics as we felt that this would be too complex, lacked any supportive evidence base in group clinics and was not prioritised by potential participants in the co-design. However, given that our co-design did not reach a large number of young adults, we should perhaps have been more confident about applying existing evidence that supports the use of video consultations in one-to-one care of young adults with diabetes, and the new online platforms that are now established in routine clinical care of children and young adults with diabetes. 94 This is a fast-changing area of health service delivery, and there has been rapid transition to virtual care during the COVID-19 pandemic, supported by improvements in technology (e.g. cloud-based systems for sharing blood glucose monitoring results) and remote-delivered group-based structured education, offering opportunities to evaluate it further. Since our research started, video group consultations have been gaining significant traction;94 however, further work would be needed to either embed existing resources such as this or build new ones into a group clinic model for young adults with both T1D and T2D. In addition, current evidence suggests that the implementation and uptake of diabetes technology may be inequitable, and further research would need to address the fact that a digital offer could exacerbate health inequalities. 95,96
Our quantitative data collection was limited by major problems with the availability of participant-level clinical data at group clinic and control sites, and we were over-ambitious with the range of participant-level data we planned to collect. Barriers to obtaining data included the high turnover of patients within the clinics studied, but also difficulties encountered by the research support teams in accessing multiple clinical systems that contained the necessary data, which are compounded by a high turnover of research support staff allocated to the project by the Clinical Research Network who had no pre-existing relationship with local clinical staff. As a result, we had considerable variation in data completeness across sites, and this renders our analysis of outcomes highly speculative. However, the evaluation of our group clinics was not designed to be powered to quantitative outcomes, and indeed the methodology was developed as a feasibility test to help the future design of an at-scale trial. Therefore, our quantitative methodology has served a useful purpose: to highlight that future research should use a considerably simpler approach to data collection, perhaps using a minimum data set required from local clinical services, and then linking (via pseudonymisation) to national data sets, such as the NDA and Hospital Episode Statistics. Our brief costs analysis provided a valuable early insight into the health economic implications of delivering group-based care within the NHS, and could help guide future evaluations at scale.
We recognise the broad scope of our group clinics and that they were more suited to delivering support of self-management, education and psychological health than focusing on treatment and individual monitoring of glycaemic outcomes and complications. This broad scope represents a challenge to future, definitive, evaluation, which will be required to guide policy-makers and commissioners. We learnt during the research process that our initial plan to offer group clinics as a ‘replacement’ model of care was not feasible or acceptable, so the clinics became additional to existing care, and this ‘blended’ model of care may be difficult to evaluate. The design of the group clinics was developmental and adaptive, and, therefore, it was challenging to define and formalise, as would be required to deliver an intervention with fidelity in future at-scale evaluation. We also note from our analysis of NDA data the finding that only 39% of young adults with T1D and 19% of those with T2D/other diabetes receive all eight care process checks. There was a missed opportunity to build formal care process checks into the group clinics. Informal signposting towards care processes by the health-care professionals delivering the clinics did take place (e.g. encouraging attendance at retinal screening and for blood tests), but future implementation and evaluations of the group clinic model should consider incorporating this aspect of diabetes care more formally in their design.
Our research took place in ethnically diverse populations affected by high levels of socioeconomic deprivation. We did not explore whether or not the engagement and impact of group clinics would have been different in more affluent and/or less diverse populations and so our findings are not necessarily generalisable.
Transferable lessons from our research relevant to wider practice and policy
There are important transferable lessons from our research that could be used to improve health care delivered to young adults with diabetes, and also more widely to those with other chronic health conditions. First, in a complex health system, such as the NHS, in which innovation in care needs to be adaptive and work interdependently with existing care, we found a continuous process of participatory involvement through co-design to be helpful. This finding could be applied to strengthen the work of existing PPI groups within the NHS, who already contribute to care improvement.
Second, we found that group and one-to-one care are complementary but do not replace each other in diabetes care for young adults; this finding is important particularly when group care might be seen as an opportunity to reduce costs. Development of care models with blended one-to-one and group-based care should be explored further in clinical practice.
Third, we found that our group clinics were critically dependent on key staff roles (i.e. a youth worker and a DSN) who developed non-traditional skills in group facilitation and delivering flexible, developmentally appropriate care, and who contributed emotional labour and supported challenging adaptation and non-attendance. These roles and skills should be recognised in similar models, but may also require further study with regard to their sustainability and feasibility outside a research context.
Our research findings may be generalisable to other chronic health conditions that affect young people (e.g. epilepsy, asthma and sickle cell disease) and where similar challenges exist. In addition, there is also emerging evidence that group-based diabetes care can be helpful for older adults with diabetes97 and in resource-poor settings. 38 The overarching principles arising from our evidence synthesis and qualitative analyses could provide a theoretical framework to be tested more widely in these contexts, and could guide clinicians and health service providers to tailor and operationalise their application in existing services.
Recommendations for further research
One of our main study objectives was to underpin future research on group clinics for young adults with diabetes. We propose that a cluster-randomised controlled study would be the next appropriate step to evaluate the clinical benefit and cost-effectiveness of offering group clinics to young adults with diabetes. However, there remain several challenges to the design of such a trial, and we make the following recommendations to advance this, and other research more generally in the future:
-
Refine the theoretical ‘core’ that constitutes a group clinic model.
Further theoretical research is required to better understand what actually constitutes a group clinic model, especially in the light of low attendance and small group sizes, as well as their potential overlap with other group-based care processes, such as structured education. Future research will need to strike a careful balance between the need to conduct an at-scale trial powered to outcomes that could guide commissioning and policy decisions and the need to further understand the mechanism of action of group clinics on individuals living with diabetes.
-
Strengthening co-design and participatory processes.
Strengthening embedded co-design in future studies could lead to greater engagement with group clinic models, and could also contribute to a better understanding of the theoretical core of group clinics. Our research confirms that embedding participatory techniques, such as co-design, in applied health services research can bring important insights to the implementation and evaluation of a complex new model of care. Ongoing co-design allowed us to retain the interest of those who were attending regularly; however, future research will need to explore how it can help meet the needs of a wider group of service users, staff and stakeholders. This finding is particularly relevant when working in a context of low engagement with existing routine care and we, therefore, strongly recommend that future research in similar contexts incorporates aspects of participatory research. We would especially highlight the importance of reaching out to seldom-heard groups and those who engage less with their care to understand how combinations of one-to-one and group-based care may better serve their needs (or not) to avoid increasing inequalities. Furthermore, we found that having an embedded researcher who led a continuous process of evaluation throughout the development and implementation of the new care model was a major strength in delivering findings with clear contextual and organisational relevance.
-
Consider additional research settings and digital approaches to support engagement.
Future research design should incorporate a new focus on digital and online approaches to engagement and delivery and the involvement of community groups and primary care teams, and should minimise research process as much as possible. Such approaches are also likely to support retention in the research, and be a platform for more effective data collection.
-
Examine blended models of care.
We welcome future research on the use of group clinics for young adults with diabetes and note that other research projects are developing in this area. 98 Most notably, we show the potential value of group clinics as an additional component to existing care models and suggest that future evaluations need to encompass a blended approach to care delivery, incorporating one-to-one and group-based clinics. Evaluation of such blended models of care will be complex and it may be challenging to deliver this in a trial context with sufficient fidelity and replicability. There is also a need to take into account the sustainability of group clinics in the long term, including long-term staff training needs and funding for youth worker roles. It may also be valuable to evaluate how health professionals change their own behaviour when delivering one-to-one consultations or when interacting with patients in group clinics in which listening and participation are emphasised.
Health economic analyses will be key to evaluating such blended models of care, and future research should embed a conceptual model in its health economic analyses to build a decision tree that can compare a new pathway with usual practice and the points of cost and value and a deeper understanding of the costs involved in ‘hidden work’.
-
Develop a pragmatic approach to measuring clinical outcomes at scale.
Clinical outcomes should be streamlined when possible, using quantitative metrics established in the NDA that could, with appropriate approvals, be accessed at a participant level through NHS Digital, avoiding the need for complex data extractions at individual research sites. The more efficient use of routine data at scale could also support a more detailed analysis of the impact of group-based care on health inequalities. In addition, our finding that group clinics met the emotional needs of attendees should be studied further, with full consideration given to the potential inclusion of different psychometric instruments to evaluate psychological outcomes.
Concluding remarks
Our study suggests that the need to improve the experience and quality of care for young adults living with diabetes is unequivocal. Our research aimed to explore the scope, feasibility and impact of group clinics for this patient group in the NHS. We used participatory techniques to engage with young adults and stakeholders and design a new group clinic-based model of care, in response to expressed need for research in this area. We then developed and implemented our co-designed model of group clinic care in two clinical services delivering care to young adults with T1D and T2D in ethnically diverse and socioeconomically deprived populations. Through our evidence synthesis and empirical research, we identified that group clinics were a possible foundation on which to improve care through the support of lasting and constructive relationships among young adults with diabetes, and between them and the clinical staff delivering care. Attendees at group clinics found that they met their emotional care needs in a way that existing one-to-one care did not, and that the social learning was helpful for them to learn or relearn practical self-management. Group clinics appealed to only a minority of young adults and attendance at group clinics was low. However, when young adults did attend, they found them helpful as a means to augment their existing care. Delivering care in group clinics offered both opportunities and challenges to staff, but with appropriate training and support staff were able to respond well to the needs of group clinic participants. The economic costs of delivering group clinics were equivalent to one-to-one care, but should be subject to future evaluation based on a conceptual framework that also reflects the hidden costs involved in their delivery.
In the future, we anticipate that group clinics have the potential become an integral part of a blended model of care for young adults in the NHS that incorporates both one-to-one care and group care. However, further theory-informed iteration and development of this care model is still required, and future evaluation of it will need to be pragmatic and at scale to determine the impact of group clinics on clinical and cost outcomes relevant to NHS in a varied landscape of existing service delivery.
Acknowledgements
Our thanks go to all young people living with diabetes who participated in our research. We also thank the clinical and research teams at BH (Jwali Kanadia, Omar Siddik, Desiree Campbell-Richards, Anne Worthington and Rita Sudra), CMH (Latchmie Ramsammy and Gbadebo Adewetan), WH (Yuva Moyo and Maria Barnard) and the AYPH (Emma Rigby and Jeremy Sachs), without whom this research would not have been possible. Professor Martin Marshall was a key member of the research team until his promotion to become chairperson of Royal College of General Practitioners, and we are grateful to him for his guidance and input during this time. Thanks goes also to Anne Ferrey and Shona Mackinnon who contributed to the analysis of data. We are also grateful to the NIHR HSDR team for their funding and huge support throughout this project, and to the NIHR reviewers for their detailed and expert feedback, which has helped the report considerably.
We are grateful to our steering group members, led by Dr Graham Toms and including Dr Jackie Elliott and representatives from Diabetes UK. Lynsey Choules provided invaluable input to the steering group from the perspective of a young person living with diabetes, as did the Diabetes UK Young Adults Panel.
Contributions of authors
Chrysanthi Papoutsi (https://orcid.org/0000-0003-1189-7100) (Senior Researcher, Health Services Research) was involved in the project design and was the ‘researcher-in-residence’ throughout the entire project. She led the realist review and its publication. She was involved in co-design and development of the group clinic model, and led the qualitative work and analysis. She contributed to project dissemination and contributed significantly to the report writing.
Dougal Hargreaves (https://orcid.org/0000-0003-0722-9847) (Senior Lecturer, Paediatrics) co-led the project. He co-led the funding application and project design, and led the scoping (NDA) data collection and analysis, the quantitative data collection (and monitoring at research sites) and quantitative data analysis. He was involved in dissemination, publication and report-writing.
Ann Hagell (https://orcid.org/0000-0002-3690-1674) (Research Lead, AYPH) was involved in the funding application, project design and conduct and overall analysis, and she led the co-design work. She contributed significantly to project dissemination and report writing.
Natalia Hounsome (https://orcid.org/0000-0003-4460-2495) (Senior Lecturer, Health Economics) led the health economic design and analysis and contributed to the report writing.
Helen Skirrow (https://orcid.org/0000-0002-4383-0616) (Clinical Research Fellow, Public Health) collated and cleaned the quantitative data, and undertook the quantitative data analysis.
Koteshwara Muralidhara (https://orcid.org/0000-0002-0041-7813) (Consultant, Diabetes) led the set-up and conduct of the research at CMH, including facilitating data collection, and contributed to the development of the group clinics model.
Grainne Colligan (https://orcid.org/0000-0001-7357-2390) (Project Manager) managed the entire project, contributing to ethics and governance, supporting research delivery (and monitoring) at all sites and supporting the research team to work effectively and integrate with the clinical teams. She managed the study steering group and dissemination activities.
Shanti Vijayaraghavan (https://orcid.org/0000-0003-0614-9933) (Consultant, Diabetes) was involved in the funding application, project design and group clinic model co-design and development. She led the set-up and conduct of the research at NUH, including facilitating data collection. She contributed to writing publications.
Trish Greenhalgh (https://orcid.org/0000-0003-2369-8088) (Professor, Primary Care) was involved in the funding application, project design and group clinic model development and evaluation. She provided oversight of the project and contributed to data analysis, publications and report writing. She stood in as co-lead of the project during the chief investigator’s maternity leave.
Sarah Finer (https://orcid.org/0000-0002-2684-4653) (Clinical Senior Lecturer, Diabetes) was the chief investigator of the study. She co-led the funding application and research design, led the ethics application, and was responsible for the overall project co-ordination and management, project design and supervision of the research team and administrative staff. She was also involved in data collection and led analysis and dissemination events. She oversaw the study steering group, writing and publications. She led the writing of the final report.
Publications
Papoutsi C, Hargreaves D, Colligan G, Hagell A, Patel A, Campbell-Richards D, et al. Group clinics for young adults with diabetes in an ethnically diverse, socioeconomically deprived setting (TOGETHER study): protocol for a realist review, co-design and mixed methods, participatory evaluation of a new care model. BMJ Open 2017;7:e017363.
Papoutsi C, Colligan G, Hagell A, Hargreaves D, Marshall M, Vijayaraghavan S, et al. Promises and perils of group clinics for young people living with diabetes: a realist review Diabetes Care 2019;42:705–12.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data are vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that data are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration in the first instance. Access to anonymised data drawn from consultations, interviews and questionnaires may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Papoutsi C, Hargreaves D, Colligan G, Hagell A, Patel A, Campbell-Richards D, et al. Group clinics for young adults with diabetes in an ethnically diverse, socioeconomically deprived setting (TOGETHER study): protocol for a realist review, co-design and mixed methods, participatory evaluation of a new care model. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017363.
- International Diabetes Foundation (IDF) . IDF Diabetes Atlas 9th Edition 2019 n.d. https://diabetesatlas.org/en/ (accessed 15 March 2021).
- World Health Organization . Global Report on Diabetes n.d. www.who.int/publications/i/item/9789241565257 (accessed 15 March 2021).
- Diabetes UK. Diabetes Prevalence 2019 n.d. www.diabetes.org.uk/professionals/position-statements-reports/statistics/diabetes-prevalence-2019 (accessed 15 March 2021).
- Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778-86. https://doi.org/10.1001/jama.2014.3201.
- NHS England . NHS Diabetes Prevention Programme (NHS DPP) n.d. www.england.nhs.uk/diabetes/diabetes-prevention/ (accessed 15 March 2021).
- Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012;29:855-62. https://doi.org/10.1111/j.1464-5491.2012.03698.x.
- Royal College of Paediatrics and Child Health . National Paediatric Diabetes Audit (NPDA) Annual Reports n.d. www.rcpch.ac.uk/resources/npda-annual-reports (accessed 15 March 2021).
- Anderson BJ, Wolpert HA. A developmental perspective on the challenges of diabetes education and care during the young adult period. Patient Educ Couns 2004;53:347-52. https://doi.org/10.1016/j.pec.2003.03.001.
- Northam EA, Todd S, Cameron FJ. Interventions to promote optimal health outcomes in children with Type 1 diabetes – are they effective?. Diabet Med 2006;23:113-21. https://doi.org/10.1111/j.1464-5491.2005.01678.x.
- NHS Digital . National Diabetes Audit – Report 1 Care Processes and Treatment Targets 2018–19, Full Report 2020. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/report-1-care-processes-and-treatment-targets-2018-19-full-report (accessed June 2022).
- Viner RM, Hargreaves DS, Coffey C, Patton GC, Wolfe I. Deaths in young people aged 0-24 years in the UK compared with the EU15+ countries, 1970–2008: analysis of the WHO Mortality Database. Lancet 2014;384:880-92. https://doi.org/10.1016/S0140-6736(14)60485-2.
- Viner R, White B, Christie D. Type 2 diabetes in adolescents: a severe phenotype posing major clinical challenges and public health burden. Lancet 2017;389:2252-60. https://doi.org/10.1016/S0140-6736(17)31371-5.
- Nanayakkara N, Curtis AJ, Heritier S, Gadowski AM, Pavkov ME, Kenealy T, et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia 2021;64:275-87. https://doi.org/10.1007/s00125-020-05319-w.
- Rawshani A, Sattar N, Franzén S, Rawshani A, Hattersley AT, Svensson AM, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet 2018;392:477-86. https://doi.org/10.1016/S0140-6736(18)31506-X.
- Chivese T, Hoegfeldt CA, Werfalli M, Yuen L, Sun H, Karuranga S, et al. IDF Diabetes Atlas: the prevalence of pre-existing diabetes in pregnancy – a systematic review and meta-analysis of studies published during 2010–2020. Diabetes Res Clin Pract 2022;183. https://doi.org/10.1016/j.diabres.2021.109049.
- Kibbey KJ, Speight J, Wong JL, Smith LA, Teede HJ. Diabetes care provision: barriers, enablers and service needs of young adults with Type 1 diabetes from a region of social disadvantage. Diabet Med 2013;30:878-84. https://doi.org/10.1111/dme.12227.
- Hargreaves DS, Viner RM. Children’s and young people’s experience of the National Health Service in England: a review of national surveys 2001–2011. Arch Dis Child 2012;97:661-6. https://doi.org/10.1136/archdischild-2011-300603.
- Hargreaves DS, Sizmur S, Viner RM. Do young and older adults have different health care priorities? Evidence from a national survey of English inpatients. J Adolesc Health 2012;51:528-32. https://doi.org/10.1016/j.jadohealth.2012.05.016.
- Bell R, Bailey K, Cresswell T, Hawthorne G, Critchley J, Lewis-Barned N, et al. Trends in prevalence and outcomes of pregnancy in women with pre-existing type I and type II diabetes. BJOG 2008;115:445-52. https://doi.org/10.1111/j.1471-0528.2007.01644.x.
- Khanolkar A, Amin R, Taylor-Robinson D, Viner R, Warner J, Stephenson T. Ethnic minorities are at greater risk for childhood-onset type 2 diabetes and poorer glycemic control in England and Wales. J Adolesc Health 2016;59:354-61. https://doi.org/10.1016/j.jadohealth.2016.05.012.
- Agarwal S, Raymond JK, Isom S, Lawrence JM, Klingensmith G, Pihoker C, et al. Transfer from paediatric to adult care for young adults with type 2 diabetes: the SEARCH for Diabetes in Youth Study. Diabet Med 2018;35:504-12. https://doi.org/10.1111/dme.13589.
- Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 2015;38:971-8. https://doi.org/10.2337/dc15-0078.
- Brewster S, Bartholomew J, Holt RIG, Price H. Non-attendance at diabetes outpatient appointments: a systematic review. Diabet Med 2020;37:1427-42. https://doi.org/10.1111/dme.14241.
- McDowell ME, Litchman ML, Guo JW. The transition experiences of adolescents with type 1 diabetes from paediatric to adult care providers. Child Care Health Dev 2020;46:692-70. https://doi.org/10.1111/cch.12798.
- Vallis M, Willaing I, Holt RIG. Emerging adulthood and type 1 diabetes: insights from the DAWN2 Study. Diabet Med 2018;35:203-13. https://doi.org/10.1111/dme.13554.
- Spaic T, Robinson T, Goldbloom E, Gallego P, Hramiak I, Lawson ML, et al. Closing the gap: results of the multicenter Canadian randomized controlled trial of structured transition in young adults with type 1 diabetes. Diabetes Care 2019;42:1018-26. https://doi.org/10.2337/dc18-2187.
- Peters A, Laffel L. American Diabetes Association Transitions Working Group . Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care 2011;34:2477-85. https://doi.org/10.2337/dc11-1723.
- NHS England . Diabetes Transition Service Specification (January 2016) n.d. www.england.nhs.uk/publication/diabetes-transition-service-specification-january-2016/ (accessed 16 March 2021).
- National Institute for Health and Care Excellence (NICE) . Patient Experience in Adult NHS Services: Improving the Experience of Care for People Using Adult NHS Services n.d. www.nice.org.uk/guidance/cg138 (accessed 16 March 2021).
- Point of Care Foundation . EBCD: Experience-Based Co-Design Toolkit n.d. www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit/ (accessed 16 March 2021).
- O’Brien J, Fossey E, Palmer VJ. A scoping review of the use of co-design methods with culturally and linguistically diverse communities to improve or adapt mental health services. Health Soc Care Community 2021;29:1-17. https://doi.org/10.1111/hsc.13105.
- Hackett CL, Mulvale G, Miatello A. Co-designing for quality: creating a user-driven tool to improve quality in youth mental health services. Health Expect 2018;21:1013-23. https://doi.org/10.1111/hex.12694.
- Breckenridge JP, Gianfrancesco C, de Zoysa N, Lawton J, Rankin D, Coates E. Mobilising knowledge between practitioners and researchers to iteratively refine a complex intervention (DAFNEplus) pre-trial: protocol for a structured, collaborative working group process. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0314-4.
- Hayhoe B, Verma A, Kumar S. Shared medical appointments. BMJ 2017;358. https://doi.org/10.1136/bmj.j4034.
- Trento M, Passera P, Tomalino M, Bajardi M, Pomero F, Allione A, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care 2001;24:995-1000. https://doi.org/10.2337/diacare.24.6.995.
- Wadsworth KH, Archibald TG, Payne AE, Cleary AK, Haney BL, Hoverman AS. Shared medical appointments and patient-centered experience: a mixed-methods systematic review. BMC Fam Pract 2019;20. https://doi.org/10.1186/s12875-019-0972-1.
- Ganetsky VS, Long JA, Mitra N, Chaiyachati KH, Kaufman ST. Impact of a multidisciplinary, endocrinologist-led shared medical appointment model on diabetes-related outcomes in an underserved population. Diabetes Spectr 2020;33:74-81. https://doi.org/10.2337/ds19-0026.
- Blakemore SJ. The social brain in adolescence. Nat Rev Neurosci 2008;9:267-77. https://doi.org/10.1038/nrn2353.
- Harden PN, Walsh G, Bandler N, Bradley S, Lonsdale D, Taylor J, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ 2012;344. https://doi.org/10.1136/bmj.e3718.
- Booth A, Cantrell A, Preston L, Chambers D, Goyder E. What is the evidence for the effectiveness, appropriateness and feasibility of group clinics for patients with chronic conditions? A systematic review. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03460.
- Wong G, Greenhalgh T, Westhrop G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: The RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) project. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02300.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Papoutsi C, Colligan G, Hagell A, Hargreaves D, Marshall M, Vijayaraghavan S, et al. Promises and perils of group clinics for young people living with diabetes: a realist review. Diabetes Care 2019;42:705-12. https://doi.org/10.2337/dc18-2005.
- NHS Digital . National Diabetes Audit – Report 1 Care Processes and Treatment Targets 2017–18, Full Report n.d. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/report-1-care-processes-and-treatment-targets-2017-18-full-report (accessed April 2022).
- Greenhalgh T, Papoutsi C. Spreading and scaling up innovation and improvement. BMJ 2019;365. https://doi.org/10.1136/bmj.l2068.
- Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1089-4.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol 2009;43:267-76. https://doi.org/10.1007/s10464-009-9229-9.
- Lanham HJ, Leykum LK, Taylor BS, McCannon CJ, Lindberg C, Lester RT. How complexity science can inform scale-up and spread in health care: understanding the role of self-organization in variation across local contexts. Soc Sci Med 2013;93:194-202. https://doi.org/10.1016/j.socscimed.2012.05.040.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991.
- Greenhalgh T. Patient and public involvement in chronic illness: beyond the expert patient. BMJ 2009;338. https://doi.org/10.1136/bmj.b49.
- Prainsack B, Buyx A. Solidarity in Biomedicine and Beyond. Cambridge: Cambridge University Press; 2017.
- Pols J. Knowing patients: turning patient knowledge into science. Sci Technol Hum Values 2014;39:73-97. https://doi.org/10.1177/0162243913504306.
- Mol A, Moser I, Pols J. Care in Practice: On Tinkering in Clinics, Homes and Farms. Bielefeld: transcript Verlag; 2010.
- May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, et al. Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-281.
- Allen D. The Invisible Work of Nurses: Hospitals, Organisation and Healthcare. London: Routledge & CRC Press; 2016.
- NHS Digital . National Diabetes Audit n.d. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit (accessed June 2022).
- Cornwall A, Jewkes R. What is participatory research?. Soc Sci Med 1995;41:1667-76. https://doi.org/10.1016/0277-9536(95)00127-S.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. https://doi.org/10.1111/j.1468-0009.2012.00665.x.
- Jones M, Pietilä I. Personal perspectives on patient and public involvement – stories about becoming and being an expert by experience. Sociol Health Illn 2020;42:809-24. https://doi.org/10.1111/1467-9566.13064.
- Donetto S, Tsianakas V, Robert G. Using Experience-based Co-design (EBCD) to Improve the Quality of Healthcare: Mapping Where We Are Now and Establishing Future Directions. London: King’s College London; 2014.
- Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Des J 2015;18:227-48. https://doi.org/10.2752/175630615X14212498964312.
- Bowen S, McSeveny K, Lockley E, Wolstenholme D, Cobb M, Dearden A. How was it for you? Experiences of participatory design in the UK health service. CoDesign 2013;9:230-46. https://doi.org/10.1080/15710882.2013.846384.
- Locock L, Robert G, Boaz A, Vougioukalou S, Shuldham C, Fielden J, et al. Testing accelerated experience-based co-design: a qualitative study of using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02040.
- Starbuck L, Walker K, Welch J, Rigby E, Hagell A, Brady L. Embedding Young People’s Participation in Health Services: New Approaches. Bristol: Policy Press; 2020.
- Marshall M, Pagel C, French C, Utley M, Allwood D, Fulop N, et al. Moving improvement research closer to practice: the Researcher-in-Residence model. BMJ Qual Saf 2014;23:801-5. https://doi.org/10.1136/bmjqs-2013-002779.
- Star SL, Strauss A. Layers of silence, arenas of voice: the ecology of visible and invisible work. Comput Support Coop Work 1999;8:9-30. https://doi.org/10.1023/A:1008651105359.
- Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care 1997;20:760-6. https://doi.org/10.2337/diacare.20.5.760.
- Wan EY, Fung CS, Wong CK, Choi EP, Jiao FF, Chan AK, et al. Effectiveness of a multidisciplinary risk assessment and management programme-diabetes mellitus (RAMP-DM) on patient-reported outcomes. Endocrine 2017;55:416-26. https://doi.org/10.1007/s12020-016-1124-1.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013: Foreword n.d. www.nice.org.uk/process/pmg9/chapter/foreword (accessed 16 March 2021).
- Xu X, Grossetta Nardini HK, Ruger JP. Micro-costing studies in the health and medical literature: protocol for a systematic review. Syst Rev 2014;3. https://doi.org/10.1186/2046-4053-3-47.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- Royal College of Nursing . NHS Pay Scales 2018–19 n.d. www.rcn.org.uk/employment-and-pay/nhs-pay-2018-19 (accessed 16 March 2021).
- NHS Improvement . Archived Reference Costs n.d. https://webarchive.nationalarchives.gov.uk/ukgwa/20200501111106/https://improvement.nhs.uk/resources/reference-costs/ (accessed 23 June 2022).
- Steel R. Involving the public in NHS, public health, and social care research: briefing notes for researchers (2nd edition). Health Expect 2005;8:91-2. https://doi.org/10.1111/j.1369-7625.2004.00301.x.
- Finer S, Robb P, Cowan K, Daly A, Shah K, Farmer A. Setting the top 10 research priorities to improve the health of people with Type 2 diabetes: a Diabetes UK-James Lind Alliance Priority Setting Partnership. Diabet Med 2018;35:862-70. https://doi.org/10.1111/dme.13613.
- Gadsby R, Snow R, Daly AC, Crowe S, Matyka K, Hall B, et al. Setting research priorities for Type 1 diabetes. Diabet Med 2012;29:1321-6. https://doi.org/10.1111/j.1464-5491.2012.03755.x.
- NHS England . Voluntary, Community and Social Enterprise (VCSE) Health and Wellbeing Alliance n.d. www.england.nhs.uk/hwalliance (accessed June 2022).
- Chimat . Welcome to Chimat 2021. www.chimat.org.uk (accessed June 2022).
- NHS Digital . Quality and Outcomes Framework (QOF) 2022. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/general-practice-data-hub/quality-outcomes-framework-qof (accessed June 2022).
- Hagell A, Sachs J. Together Study: Co-designing Group Clinics for Young Adults with Diabetes. London: Association for Young People’s Health; 2018.
- Hagell A, Rigby E, Sachs J. Together Study: Co-Designing Group Clinics for Young Adults With Diabetes, Year 2 Report 2019.
- Papoutsi C, Greenhalgh T, Hargreaves D, Kanadia J, Colligan G, Hagell A, et al. Solidarity and Contestation in Group Clinics for Young People With Diabetes in Socioeconomically Deprived Settings: Patient and Professional Experiences n.d.
- Papoutsi C, Hargreaves D, Colligan G, Hagell A, Marshall M, Vijayaraghavan S, et al. Towards a More Pragmatic Vision for Group Consultations: Participatory, ‘Researcher-In-Residence’ Evaluation of Group-Based Care for Young People With Diabetes in Ethnically Diverse, Socioeconomically Deprived Settings (TOGETHER Study). n.d.
- Papoutsi C. Group Clinics for Young Adults With Diabetes in an Ethnically Diverse, Socioeconomically Deprived Setting (TOGETHER Study): Participatory, Mixed Methods Evaluation n.d.
- Papoutsi C, Hargreaves D, Colligan G, Hagell A, MacKinnon S, Vijayaraghavan S, et al. G416 Sociodemographic and clinical predictors of attendance at group clinics for young adults with diabetes (together study). Arch Dis Child 2020;105.
- Campbell-Richards D, Kanadia J, Papoutsi C, Hargreaves D, Colligan G, Hagell A, et al. Sociodemographic and clinical predictors of attendance at group clinics for young adults with diabetes (Together study). Diabet Med 2020;37.
- Papoutsi C, Campbell-Richards D, Kanadia J, Hargreaves D, Colligan G, Hagell A, et al. Group clinics for young adults with diabetes in ethnically diverse, socioeconomically deprived settings (Together study): qualitative ethnographic evaluation. Diabet Med 2020;37.
- National Institute for Health and Care Excellence . Type 2 Diabetes in Adults: Management n.d. www.nice.org.uk/guidance/ng28 (accessed 16 March 2021).
- Wolff DL, Waldorff FB, von Plessen C, Mogensen CB, Sørensen TL, Houlind KC, et al. Rate and predictors for non-attendance of patients undergoing hospital outpatient treatment for chronic diseases: a register-based cohort study. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4208-9.
- Green T, Bonner A, Teleni L, Bradford N, Purtell L, Douglas C, et al. Use and reporting of experience-based codesign studies in the healthcare setting: a systematic review. BMJ Qual Saf 2020;29:64-76. https://doi.org/10.1136/bmjqs-2019-009570.
- Salvy SJ, Carandang K, Vigen CL, Concha-Chavez A, Sequeira PA, Blanchard J, et al. Effectiveness of social media (Facebook), targeted mailing, and in-person solicitation for the recruitment of young adult in a diabetes self-management clinical trial. Clin Trials 2020;17:664-74. https://doi.org/10.1177/1740774520933362.
- Walders-Abramson N, Anderson B, Larkin ME, Chang N, Venditti E, Bzdick S, et al. Benefits and barriers to participating in longitudinal research of youth-onset type 2 diabetes: results from the TODAY retention survey. Clin Trials 2016;13:240-3. https://doi.org/10.1177/1740774515613949.
- Shaw S, Wherton J, Vijayaraghavan S, Morris J, Bhattacharya S, Hanson P, et al. Advantages and limitations of virtual online consultations in a NHS acute trust: the VOCAL mixed-methods study. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06210.
- Wilmot E, Crabtree T, Choudhary P, Deshmukh H, Barnes D, Gregory R, et al. Age, Gender and Ethnicity As Potential Barriers to FreeStyle Libre (FSL) Access in the United Kingdom: Analysis from the Association of British Clinical Diabetologists (ABCD) Audit Programme n.d.
- Barnard-Kelly KD, Cherñavvsky D. Social inequality and diabetes: a commentary. Diabetes Ther 2020;11:803-11. https://doi.org/10.1007/s13300-020-00791-4.
- Harris MD, Kirsh S, Higgins PA. Shared medical appointments: impact on clinical and quality outcomes in veterans with diabetes. Qual Manag Health Care 2016;25:176-80. https://doi.org/10.1097/QMH.0000000000000098.
- Salvy SJ, Ruelas V, Majidi S, Thomas A, Ashwal G, Reid M, et al. Team clinic: expansion of a multidisciplinary care model for adolescents with type 1 diabetes. Contemp Clin Trials 2020;95. https://doi.org/10.1016/j.cct.2020.106079.
Appendix 1 Qualitative interviewees
Young adults living with diabetes
| Patient | Diabetes type | Age at time of interview (years) | Ethnic background | Sex | Number of clinics attended |
|---|---|---|---|---|---|
| 1 | 1 | 21 | Asian | Female | 3 |
| 2 | 1 | 19 | Asian | Female | 2 |
| 3 | 1 | 18 | Asian | Male | 2 |
| 4 | 1 | 21 | Black | Female | 8 |
| 5 | 1 (on pump) | 19 | Asian | Female | 8 |
| 6 | 1 | 19 | Asian | Male | 1 (subsequently opted out of group clinics) |
| 7 | 1 | 25 | Asian | Female | 0 |
| 8 | 1 | 22 | Black | Female | 7 |
| 9 | 1 | 25 | Black | Male | 10 |
| 10 | 1 | 23 | White | Male | 3 |
| 11 | 1 | 19 | White | Male | 4 |
| 12 | 1 | 20 | Asian | Male | 3 |
| 13 | 1 (on pump) | 25 | Black | Male | 4 |
| 14 | 2 | 25 | Black | Female | 3 |
| 15 | 2 | 24 | Asian | Male | 4 |
| 16 | 1 | 19 | Black | Female | 3 |
| 17 | 1 | 20 | Arab | Female | 2 |
| 18 | 1 | 21 | Asian | Male | 1 |
| 19 | 1 | 22 | Black | Male | 3 |
Health-care professionals
| Health-care professional | Number interviewed |
|---|---|
| Diabetes consultant | 3 |
| DSN | 3 |
| Youth worker | 1 |
| Clinical research nurse | 1 |
| Dietitian | 1 |
| Psychologist | 1 |
| Sexual health advisor | 1 |
Appendix 2 Qualitative interview guides
Topic guide for group clinic facilitators
Tell me about your role/professional background.
How did you get involved in the project? How did you get involved in group clinics?
Tell me about how your session unfolded. What went well? What went less well/what would you change?
Did anything happen that surprised you?
Did you face any difficulties in preparing for or delivering the session? How did you overcome them, if so?
What would you advise someone starting a similar process now/what would you do differently if you started again?
What makes a good/successful group clinic?
What did you fear would go wrong?
What are your fears now compared with when you first started?
What skills/training do you think are needed to successfully deliver group clinics? What else needs to be in place to facilitate success?
How do you think group clinics are different from one-to-one consultations?
What would you change going forward?
Topic guide for patient interviews
Tell me a bit about you.
When you think about living with diabetes, what are the things that matter most to you? What are your hopes and worries?
What motivated you to attend the group clinic(s)? How was your experience attending the group clinic(s)?
Did you have any problems attending the clinic(s)? Why did you decide not to attend?
Did people talk about things that interested you? Did you feel the group clinics addressed your needs? Was there anything you thought was not particularly relevant to you?
How did it feel being part of that group?
Was it useful to meet other young people living with diabetes? Did you know other young people with diabetes before attending the clinics?
What else did you gain from attending the group clinic(s)? Is this what you expected to gain or were your expectations different?
Do you feel you learned anything you did not know before? Have you used any of the learning you gained in the group clinic and, if so, how?
How was this different from just visiting the doctor on your own? How would you compare group clinics to traditional one-to-one appointments with your doctor?
Do you think there are any negative aspects to attending group clinics? Did anything happen that made you feel uncomfortable?
Was there anything you wanted to ask about but did not get the chance? Why?
What do you think could be improved about the way groups clinics are run so they appeal more to you? What would you change?
Anything else that we have not talked about?
Appendix 3 NVivo Capture example
Appendix 4 Unit costs used in economic analysis
| Code | Currency | Cost (£) |
|---|---|---|
| N15AF | Other currencies data. Specialist nursing, diabetic nursing/liaison. Adult. Face to face | 67 |
| N15AN | Other currencies data. Specialist nursing, diabetic nursing/liaison. Adult. Non-face to face | 34 |
| WF01 A (302) | Consultant-led. Endocrinology. Non-admitted. Face to face attendance. Follow-up | 154 |
| WF01C (302) | Consultant-led. Endocrinology. Non-admitted. Non-face to face attendance. Follow-up | 117 |
| A03 | Other currencies data. Dietitian | 86 |
| 656 | Other currencies data. Clinical psychology | 170 |
| WF01 A (300) | Consultant-led. General medicine. Non-admitted. Face to face attendance. Follow-up | 171 |
| WF01C (300) | Consultant-led. General medicine. Non-admitted. Non-face to face attendance, Follow-up | 49 |
| N02AF | Other currencies data. District nurse, Adult, Face to face | 38 |
| N02AN | Other currencies data. District nurse, Adult, Non-face to face | 19 |
| VB09Z | Emergency medicine, Admitted. Category 1 investigation with category 1–2 treatment | 153 |
| VB09Z | Emergency medicine. Non-admitted. Category 1 investigation with category 1–2 treatment | 130 |
| KB02K | Total HRG activity. Diabetes with hyperglycaemic disorders, with CC score 0–1 | 1140 |
| KB01F | Total HRG activity. Diabetes with hypoglycaemic disorders, with CC score 0–2 | 541 |
Appendix 5 National Diabetes Audit data tables
Care process checks in the 2017–18 NDA, by age band and diabetes type. 45
| Location | Age band (years) | Type of diabetes | Process checks (%) | All eight checks | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI | Blood pressure | HbA1C levels | Creatinine | Urinary albumin | Cholesterol | Foot check | Smoking status | Percentage | Total | |||
| BH | 16–25 | T1 | 82.8 | 93.1 | 79.3 | 69.0 | 37.9 | 69.0 | 79.3 | 89.7 | 31.0 | 145 |
| T2_other | 87.5 | 87.5 | 87.5 | 75.0 | 50.0 | 75.0 | 87.5 | 87.5 | 50.0 | 40 | ||
| All | 83.8 | 91.9 | 81.1 | 70.3 | 40.5 | 70.3 | 81.1 | 89.2 | 35.1 | 185 | ||
| ≥ 26 | T1 | 83.2 | 96.0 | 88.8 | 80.8 | 41.6 | 80.8 | 84.0 | 92.8 | 35.2 | 625 | |
| T2_other | 93.0 | 97.7 | 95.3 | 94.5 | 61.7 | 94.5 | 89.1 | 95.3 | 58.6 | 640 | ||
| All | 88.1 | 96.8 | 92.1 | 87.7 | 51.8 | 87.7 | 86.6 | 94.1 | 47.0 | 1265 | ||
| WH | 16–25 | T1 | 77.8 | 83.3 | 83.3 | 66.7 | 55.6 | 77.8 | 77.8 | 88.9 | 44.4 | 90 |
| T2_other | 100.0 | 100.0 | 100.0 | 66.7 | 66.7 | 100.0 | 66.7 | 66.7 | 66.7 | 15 | ||
| All | 81.0 | 85.7 | 85.7 | 66.7 | 57.1 | 81.0 | 76.2 | 85.7 | 47.6 | 105 | ||
| ≥ 26 | T1 | 74.5 | 90.2 | 86.3 | 77.5 | 53.9 | 85.3 | 83.3 | 87.3 | 46.1 | 510 | |
| T2_other | 79.7 | 91.0 | 88.3 | 85.6 | 60.8 | 87.4 | 86.9 | 88.7 | 54.5 | 1110 | ||
| All | 78.1 | 90.7 | 87.7 | 83.0 | 58.6 | 86.7 | 85.8 | 88.3 | 51.9 | 1620 | ||
| National data | 16–25 | T1 | 86.1 | 91.2 | 87.9 | 81.2 | 52.7 | 76.4 | 70.2 | 89.5 | 39.1 | 14,020 |
| T2_other | 50.0 | 50.9 | 54.4 | 52.9 | 25.8 | 42.8 | 34.9 | 50.8 | 19.1 | 3320 | ||
| All | 79.2 | 83.4 | 81.5 | 75.8 | 47.5 | 70.0 | 63.4 | 82.1 | 35.3 | 17,340 | ||
| ≥ 26 | T1 | 88.0 | 93.7 | 92.9 | 90.7 | 64.2 | 88.2 | 79.6 | 93.0 | 52.9 | 67,885 | |
| T2_other | 78.6 | 83.8 | 85.2 | 85.1 | 59.9 | 81.5 | 74.2 | 82.4 | 52.2 | 172,685 | ||
| All | 81.2 | 86.6 | 87.4 | 86.7 | 61.1 | 83.3 | 75.7 | 85.4 | 52.4 | 240,570 | ||
Diabetes outcomes and structured education in the 2017/18 National Diabetes Audit, by age band and diabetes type.
| Location | Age band (years) | Type of diabetes | Outcomes (%) | All three treatment targets met (%) | Structured education (%) | |||
|---|---|---|---|---|---|---|---|---|
| HBA1C levels of < 48 mmol/mol | Blood pressure of < 140/80 mmHg | Total cholesterol of < 4 mmol/l | Offered | Attended | ||||
| BH | 16–25 | T1 | 9.1 | 74.1 | 30.0 | 22.2 | 58.6 | 13.8 |
| T2_other | 14.3 | 71.4 | 40.0 | 20.0 | 62.5 | 25.0 | ||
| All | 10.3 | 73.5 | 32.0 | 21.7 | 59.5 | 16.2 | ||
| ≥ 26 | T1 | 12.6 | 69.2 | 32.0 | 22.2 | 71.2 | 17.6 | |
| T2_other | 11.5 | 61.6 | 51.2 | 16.1 | 74.2 | 23.4 | ||
| All | 12.0 | 65.3 | 42.5 | 18.9 | 72.7 | 20.6 | ||
| WH | 16–25 | T1 | 6.7 | 86.7 | 35.7 | 28.6 | 27.8 | 5.6 |
| T2_other | 33.3 | 66.7 | 33.3 | 33.3 | 66.7 | 0.0 | ||
| All | 11.1 | 83.3 | 35.3 | 29.4 | 33.3 | 4.8 | ||
| ≥ 26 | T1 | 6.8 | 82.6 | 36.0 | 27.4 | 24.5 | 2.0 | |
| T2_other | 7.7 | 72.3 | 58.3 | 20.6 | 25.2 | 2.7 | ||
| All | 7.4 | 75.5 | 51.4 | 22.7 | 25.0 | 2.5 | ||
| National data | 16–25 | T1 | 6.2 | 76.5 | 28.1 | 15.8 | 32.5 | 10.1 |
| T2_other | 36.7 | 66.9 | 27.0 | 25.1 | 26.5 | 2.7 | ||
| All | 10.1 | 75.4 | 28.0 | 16.8 | 31.3 | 8.7 | ||
| ≥ 26 | T1 | 7.4 | 69.2 | 30.2 | 16.5 | 30.4 | 15.1 | |
| T2_other | 19.3 | 69.1 | 45.4 | 27.1 | 34.7 | 7.1 | ||
| All | 15.8 | 69.1 | 40.8 | 23.9 | 33.5 | 9.4 | ||
Appendix 6 Qualitative quotations
Motivations for engaging with group clinics
Quotation 1:
I don’t personally know any of my friends who have diabetes. So I thought why not? Get to meet other people, see how they manage their diabetes. You know, learn new things from them. [. . .] I learn from their experience. And also the advice from the doctors.
Interview 16, patient 11
Quotation 2:
I wanted to see what their [other young people] feelings and thoughts were about it. Because I – like for the past year, few years, I’ve been feeling alone with it, there’s no one that I know who’s got diabetes.
Interview 13, patient 8
Quotation 3:
I thought maybe a group environment would be better than just like every 3 months seeing a doctor, and just talking about the same things over and over again.
Interview 27, patient 16
Low uptake of group clinics and ambivalence around attending
Quotation 4:
But yeah, it’s like having a group clinic is so much nicer, in order to meet people. But then on the other hand, I think because you don’t really know them, you don’t have that personal connection with them, you don’t really want to voice out everything that you’re going through. Do you get that? I’m a quiet person, like I wouldn’t tell people what I’m going through if I don’t really know them. So it’s kind of like I was in like two minds, so.
Interview 12, patient 7 – never attended
Quotation 5:
If I’m being honest, at the beginning, I didn’t want to come. I did, but I didn’t. I just like – oh, when is it going to be, is it going to be really long, I might not like it. So, but I still came. And, I liked it. I was like ‘OK, this isn’t what I was expecting’. I was not expecting it to be so laid back. I don’t know. It was really comfortable, the setting.
Interview 10, patient 5 – regular attendee
Quotation 6:
[. . .] I didn’t really want to think about it. And like I didn’t want people to know [. . .] I don’t want people to like see me differently, or like less, like always concerned, and stuff like that. I just want to feel normal.
Interview 11, patient 6 – attended only once
Staff views on attendance
Quotation 7:
The good thing was that the ones that didn’t attend did actually make contact, responded on the text. This is what the relationship takes time to build. So for me the fact that I’ve had a response is a win as well.
Interview 1, DSN
Quotation 8:
[. . .] it seemed to be around sort of three, four, five we were getting [to attend], even though you know, we invited more than 20 patients, within a good amount of time. So I think just trying to make sure a lot of people, or as many people as possible would attend, was the biggest challenge. To make sure that the clinics were as full as possible.
Interview 29, research nurse
Quotation 9:
[. . .] from doing my clinics I have really, really bad attendance levels, the ones that I’ve never met they would not come for a few clinics and then they might come to one and they wouldn’t come back, and I had more than 50% DNA rate with my young adults.
Interview 3, dietitian
What is the experience of care delivered in group clinics?
Quotation 10:
[. . .] anyone could just literally talk about their experience, especially at the start when they were getting to know each other. But I do remember feeling a number of times like, it’s nice to see someone like going through the – it’s nice to know that I’m not alone out there. That other people do go through what I’m going through. And it was, it was comforting.
Interview 24, patient 15
Feeling understood and supported
Quotation 11:
[. . .] you know it is not only the doctor there to listen to you, you know that there’s people that will understand your feelings and maybe feel the same way as you do so I think it was really good, I enjoyed that.
Interview 4, patient 1
Quotation 12:
Because when you’re explaining stuff that happens to you, for example when you get a low sugar level or high, it’s hard to explain it to a person who’s not diabetic. Even to the doctor, it’s hard to explain to them. They know what happens, but it’s like, feeling it is a different thing.
Interview 10, patient 5
Quotation 13:
I remember her [patient 13] saying to me, ‘I like listening to people so it’s like I’m here to listen to everyone’. But she didn’t like to be put on the spot to share her experiences. And that’s just where she was, even, I don’t know if you had noticed in the group clinic but her body language was quite [defensive].
Interview 20, DSN
Social and situated learning
Quotation 14:
I think with the [group clinic] with Dr [consultant name], I think that one was very, very important for me as well. Because I learned a lot as well. Because I’m used to jabbing, taking injections in my arms and stuff. And that’s something that I’ve been doing for a very long time. And I don’t really – and I’ve got lumps and stuff in my arms, and I don’t realise that the insulin doesn’t go through there.
Interview 13, patient 8
Quotation 15:
Can you tell me more maybe about what you enjoyed as part of the group clinics?
Conversations. And just getting like professional responses. Just knowing what’s right for diabetics and stuff, it’s very important I think [. . .] also the questions from everyone else, they gave me an insight into people’s lives about diabetes.
Interview 28, patient 17
Quotation 16:
It was just the ketone thing, I never knew that, and then when you said it I was thinking the last couple of days I’ve been having really, though I haven’t checked but I know that I’ve been having high blood sugars, even now my blood sugar’s high. [. . .] So I’ll check my ketones, thank you.
NUH, clinic 9, female patient diagnosed 13 years ago
Quotation 17:
And it was good that I passed it [to the newly diagnosed patient] to explain simply because I wanted him to get involved, he’s just completed one of the very good programmes, DAFNE, and his control is very good and he does do ketone monitoring.
(Interview 2, DSN)
Quotation 18:
I like it how we shared our experiences, what we went through and how, the symptoms of how we knew how to get it. And then we just give each other advice of how to control it or what to do. So, with the air bubble I know that now I can do the air shots and look really, make sure that it’s not blocked or bent.
Clinic 6, male patient
Quotation 19:
So it’s very insightful to know how other people are dealing with their own unique circumstances, and if I ever run into those circumstances, how I could apply it to myself.
Interview 14, patient 9
Quotation 20:
It’s very important to listen to how people manage their diabetes. [. . .] It’s always good to have someone with different experiences. Because that way, you know more about your diabetes. You know generally how to manage it well. And I think having only one way to manage your diabetes is not good. You need to always have a plan A, plan B, plan C. Just to make sure that you’re on the safe side of things.
Interview 16, patient 11
Quotation 21:
When you’re in a group environment you can – you don’t have to – like other people get to ask the questions that you wouldn’t ask, for you. And then you just get that insight. And it, it helps. And it’s just a more comfortable, relaxed setting. So you’re just – and you can gain a lot more information than you could with like 10 minutes with your doctor, so.
Interview 27, patient 16
Quotation 22:
I do remember thinking to myself ‘ah, I’m pretty sure this doesn’t really apply to me, because I don’t – I don’t take insulin injection’ [. . .] I felt like I couldn’t relate to a lot of the stuff they were talking about.
Interview 24, patient 15 with T2D
Quotation 23:
It’s not that I’m stubborn, but I don’t feel like I can learn something from them. It was just to socialise with them, and meet other people, and be like ‘ah, you’re suffering from the same thing I am, nice to meet you’. And when I found out about [the Freestyle Libre], I was like ‘oh my God, do you mind if I ask you some questions, because I’m really intrigued and I really want this’. And then he was showing me, saying ‘yeah man, it’s really easy, look you can scan it’.
Interview 15, patient 10
Quotation 24:
[. . .] despite the fact that I’ve said to them all those things individually they just said, ‘Oh I didn’t know’ and it was quite surprising because every time I examine their feet I tell them, I’m examining your feet for this. But somehow they had not made the connection.
Interview 18, diabetes consultant
Quotation 25:
Which you would think that, they probably would have known having diabetes for a certain amount of time, but it sort of just highlighted, I’d not say limitations, but how far their general knowledge when it comes to their disease area, how much they had, basically.
Interview 29, research nurse
Quotation 26:
[. . .] someone who’s been there and done that, they know, OK, you know what, if you do this, you’ll feel better, but if you did this you’ll feel worse. So people are talking from experiences in the group clinic which is actually a lot of help.
Interview 4, patient 1
Quotation 27:
You’re meeting people who have the same issues as you, who suffer from the same thing as you. Whereas the nurses, yeah they can help you, but, it’s wrong to say this, but like you’re not suffering with this condition – you can give advice and stuff like that, but until you’re dealing with it yourself you don’t really know about it.
Interview 13, patient 8
Normalising diabetes through sharing with peers
Quotation 28:
So you get to just have discussions, even before the group starts. About what people are doing to manage their diabetes. So that helps quite a lot. I think it’s helped me, for the most part overall, it’s helped sort of like normalise things. And if I do have issues, I’ve always got somebody to talk to, or communicate with.
Interview 14, patient 9
Quotation 29:
I remember I was saying that like within the workplace I would never tell people that I’ve got diabetes, and stuff like that. Now, the other day I was speaking to my friend about where I should be injecting, where I shouldn’t be injecting. Feel like now I’m a bit more confident and comfortable with it. And, and they know I need to jab. They’re even helping me to look after my diabetes, to do better control. So yeah, I think with telling people has definitely made a big difference.
Interview 13, patient 8
Quotation 30:
She [other patient] was explaining how she doesn’t mind injecting insulin in front of other people and stuff. I don’t do that, I like to just either go to the toilet or go somewhere, do it and come back, but obviously hearing other people might consider other approaches and stuff, because I’ve not, obviously I’ve not really known anyone with diabetes other than my sister before that.
Interview 5, patient 3
Quotation 31:
How, I just want to ask generally, how are you guys, like those on type 1, how are you guys finding carb counting? How do you get round it, how do you start all up?
I’m not going to lie I haven’t been really carb counting.
OK I’m glad to [have asked], I mean it’s a bad thing but it’s like I’ve been struggling so much I’m just like I’ve given up with it totally. Are you the same like?
[indicates agreement].
NUH, clinic 2
Quotation 32:
When someone else is talking, you know, give you the courage to talk as well. Give you the confidence. It’s good.
Interview 28, patient 17
Quotation 33:
These are other people who you’re with, and you know, diabetes is a very personal thing. And sharing that with other people can be a bit scary.
In what way?
I guess just talking about, I don’t know. Maybe not scary, but maybe more – it can be a bit embarrassing. Especially if you’re not looking after it well. Because then you have to talk about like what you’re doing with it, and how like if – how, how well you’re handling it, I guess. That might come up in conversation.
Interview 24, patient 15
Quotation 34:
I just felt like ‘oh my God’. He’s doing so well now. Because he’s like just recently diagnosed, and I’ve had it for so long, so. It must look like I’m not on top of it, he probably thinks ‘cor, she’s just doing what she wants, it’s not – she’s not like managing her diabetes’. But he doesn’t know, when he probably gets to 14 years, [laugh] he’ll probably be a bit lazy here and there.
Interview 9, patient 4
Quotation 35:
I was like ‘dude, you should test yourself’, and I just left him. But I get – I’m really blunt, like ‘you need to test yourself’. Just some people, it’s not worth arguing with. But, yeah. And it was funny, that was even outside of the clinic. Outside of the group clinic, he then decided to open up to two of us. It was just like ‘whatever, man’.
Interview 15, patient 10
Peer comparison
Quotation 36:
I feel like being around people who probably have good sugars will make me feel like ‘wow, oh my gosh, like I need to do something’. Because how is everybody else around me managing to control theirs, but I can’t manage to control mine?
Interview 13, patient 8
Quotation 37:
I sometimes I feel like, what the hell, why me? I’ve had it all my life. But then looking at how people react to it, I felt like, OK, thank God, I feel way better about myself, I don’t feel like that.
Interview 4, patient 1
Quotation 38:
And so what I was thinking is that would it get to a stage where it’s going to be hard for me to manage my diabetes. Yeah, it definitely did freak me out a bit, yeah.
Interview 14, patient 9
Patient ‘work’ and responsibility
Quotation 39:
Yeah and I had to get a blood test and a urine test and then I was waiting for ages, all in the space of 2 weeks. And then I’m constantly telling work, oh I’ve got an appointment for this. I first said, ‘oh I’ve got a diabetic appointment with my, with my nurse’. And she was like, ‘oh OK, that’s fine’, she’s changed my shift. And then next week I’m like, ‘I’ve got a diabetic appointment’. ‘I thought you had one last week, you didn’t tell me it was every 3 month’. ‘It is because this one is a group clinic so it’s a new thing’. And she doesn’t believe me so I have to bring it up, she doesn’t ask me but I bring it up just so she knows that I’m not messing her about. And I’m like, honestly, it’s a lot of work.
NUH, clinic 9
Quotation 40:
So, I know I attended one group clinic where – I forgot what the topic or subject was. But I didn’t know too much about it, so I didn’t speak as much. And I thought I didn’t engage a lot in the session.
But did you feel that you’ve gained from what other people might have been saying?
I have gained. Yes, I have definitely gained. But I didn’t deliver.
Interview 16, patient 11
Quotation 41:
Because I remember in school, the teacher used to like, encourage the students to respond. Here, it’s the same thing. I feel like the professional should encourage the patient to respond. And also, the patient should do their behalf, as well. Just like in school. Because if the student doesn’t respond, then there’s no point.
Interview 28, patient 17
Quotation 42:
One of the hardest things with the group session I would say is – I always get asked what exactly do you want next? Now I’m never too sure about what I want next, or what is going to happen in the next group session.
Interview 14, patient 9
Quotation 43:
Because he’s just recently diagnosed, so he’s still got a lot to learn. [. . .] I don’t want to throw him off, and he should just continue like to make sure that he doesn’t stop his checking, because once you stop it becomes a habit.
Interview 9, patient 4
Quotation 44:
And that was one problem that we had, where I got a bit emotional about it. Because it’s like I don’t want to open myself up to a room that doesn’t want to open themselves up. Because then I feel a bit of a flake. I look a little bit silly.
Interview 15, patient 10
Conflict and power dynamics
Quotation 45:
I felt like I was being judged [. . .] like he was trying to be the teacher [. . .] like his opinion was the right opinion [. . .] And I just felt like I was being targeted that day by him. And I had to calm myself down, because, I can be an angry person at times.
Interview 13, patient 8
Quotation 46:
But then there was one girl, and she was in self-denial [. . .] she went on holiday but didn’t even have to take her insulin [. . .] she would inject for only one plate of spaghetti, but have another plate. It was almost like she was admitting to her mistakes. But in a way that she was proud of it [. . .] If it wasn’t thanks to us making her realise that she shouldn’t have done that, then she wouldn’t have admitted it and then realised that she did wrong. So in some sense, it worked out well. [. . .] Because they may think it was normal. And then we tell them it’s not normal.
Interview 15, patient 10
Quotation 47:
I think sometimes within the sessions, we did forget to mention like the [ground] rules. Or I don’t know whether it’s [mentioned] because I’m coming in halfway through. Or maybe having the rules in the middle of the table, or somewhere where everybody can see it.
Interview 13, patient 8
Quotation 48:
I bite my tongue, because in a normal situation you’d tackle it totally different, in a group setting you don’t show them up [. . .] you’re just hoping that others come up with the answers [. . .] So the [patient] went to Switzerland and did not take her insulin with her. That was very dangerous yeah? The good thing is that the boys came up and, you know, kind of set her straight [. . .] I am sure she would never go back anywhere, even Birmingham, without making sure she carries it with her.
Interview 20, DSN
Quotation 49:
[. . .] one has to see every individual with an open mind, and then spend a lot of time listening to them. So, rather than giving them straight forward advice. Because, there are so many variables that is influencing that individual’s care, and then whatever we say in terms of their lab numbers, or from their glucose monitors or the sensor, gives us very little information, about the factors that is impacting on their overall control.
Interview 25, diabetes consultant
Quotation 50:
So there was a lot of discussion, you know, a lot of questions around you know, well what do you do if a young person isn’t managing their diabetes, or they’re going into hospital? [. . .] what’s the role of professionals, and how far can they go, how forceful can we be?
Interview 17, psychologist
Individual attention and therapeutic relationships
Quotation 51:
I felt comfortable in talking to [the nurse], a lot. I would go back and forth if I had any problems, I would communicate it to her. Even though she wasn’t my nurse, she was always there, helpful. When I had problems, she was the first person I contacted. So I think having someone there that kind of knows about diabetes and can guide me in the right way kind of helped as well. But I would definitely say that yeah, [the nurse] like filled in that connection, and that bond definitely helped me.
Interview 13, patient 8
How does the way group clinics are designed and delivered support good experiences for young adults with diabetes?
Quotation 52:
[. . .] sometimes there’ll be like five or six people, and then sometimes there’ll be one other person, or two other people. I’ll still talk, regardless. But if they’re shy, they’re going to be a bit more uncomfortable.
Interview 9, patient 4
Quotation 53:
[in a good clinic] you’d have more group involvement, instead of only one person talking, or individuals asking when they felt like they wanted to know things. Because then it just felt like a one-on-one session, with other people listening in. Which at the time, it was a bit weird.
Interview 14, patient 9
Quotation 54:
[group clinics] are amazing in their own way. And everyone can get a benefit out of them, if that person is willing to listen but also speak. Sometimes you won’t learn anything if you don’t decide to open up, and reveal your inner mistakes.
Interview 15, patient 10
Quotation 55:
But what I could say I could improve is, obviously I know some people are very busy, we understand that, but I think if we have the group clinics with more people in there, it will be more interactive. More people to socialise with. You know, experience more ideas, more support. I think that’s the only problem I could say, should be I think more people involved.
Interview 16, patient 11
Quotation 56:
I’m happy to see more people. Like we had a girl that wasn’t here today, we had her the other day, so. She was nice.
Interview 28, patient 17
Quotation 57:
[the last group clinic] went a little bit flat because, we had only two people and you can only do so much and [patient name] is quiet anyway. I knew, I could read [patient 2] thoughts anyway straight away that she wasn’t happy, that’s why I said to her, ‘sorry the two girls [didn’t come]’, because she was looking forward to seeing them.
Interview 2, DSN
Quotation 58:
At times, I was a bit worried, being the only one having type two. But, generally, it was very welcome [environment]. So, feelings of being left out didn’t last too long, to be honest.
Interview 24, patient 15 with T2D
Quotation 59:
I would continue coming. But I, I wouldn’t want it to go on forever. Like, but like for another like couple of months I wouldn’t mind coming at all.
And how would you make that judgement, to say you know, that’s been enough?
If things start repeating themselves. Like things I’ve already heard, and things I already know. Then I guess I’d just be like yeah, that it’s – I don’t need it any more.
Interview 27, patient 16
Quotation 60:
It’s not as fun when there’s not that many people, because it makes me feel like ‘oh, no one else is coming anymore, so I’m not going to go to the next session’.
Interview 9, patient 4
Quotation 61:
[. . .] no finger pointing or no blame zones. So, where the focus is to disseminate information, and to collect the thoughts of the individuals, and then to clarify those thoughts so that would have a better value for one-to-one discussion.
Interview 25, diabetes consultant
Quotation 62:
[. . .] particularly the two young women were starting to talk quite a lot and that was about them sharing, they were educating each other in those moments weren’t they? Because actually, they’re the experts on diabetes, not me [. . .] what I hoped would happen is that I direct it but learn something from them and they would learn from each other.
Interview 6, sexual health advisor
Quotation 63:
So I’ve been thinking about how to address that issue because I know if I ask them to bring their diaries they’ll never bring it. Again, it’s the personal thing. In DAFNE they have to, very strict. DAFNE doesn’t look at all those things that we’re looking at, how they’re going to feel and all of it, no, you commit you come, very regimental.’
Interview 2, DSN
Delivering group clinic care in the NHS
Setting up a new model of care using group clinics
Quotation 64:
[. . .] relationships take time to build, specially trusting relationships. [. . .] And it’s not just me building relationships with the young adults, it’s me building relationships with the clinicians. So I haven’t worked with [name of clinician] before. So it’s, all these things take time, and I only work 2 days a week.
Interview 1, DSN
Quotation 65:
They don’t know me, young adults operate on building relationships which is the proof it’s taken so long to do that, you know, with the ones that are engaging, you know. [. . .] Today I feel very comfortable sitting with them and I can have a conversation not troubled by their diabetes but talk about everything else, you know, that I’m aware that is happening in their life.
Interview 20, DSN
Quotation 66:
You need to have an idea about the patients you’re inviting. You need to have a rapport with them, you need to have some contact with them. So for instance, if I didn’t get through to the patient themselves, I always have their parents – their mum’s number, ‘can you make sure they know that they have an appointment’. So, it’s just not the patient only, but their family is also involved.
Interview 26, DSN
Quotation 67:
I might’ve had consultant send to me such and such person [. . .] but when I’ve spoken to the DSN, who sees the patient far more frequently and spends a longer time, has said to me, ‘no, no, no, she’s very unstable, she’s having suicidal thoughts, she’s not going to be appropriate’. [. . .] There’s a lot of, it’s like a hidden work that’s happening that is not being captured.
Interview 1, DSN
Quotation 68:
So, there’s a lot that goes on in the background before, to try and understand who is going to be able to make use of this group, who is going to fit best with, who actually really needs individual work? Or who needs individual work first, and then they’ll be more ready for a group? And part of it is about the individual – you know, this complex mix between the individual’s preference, the clinical need, and risk level.
Interview 17, psychologist
Quotation 69:
I would try to bring them in to the TOGETHER study, and also see them as a clinic appointment. So, in that way it was quite challenging for me, rearranging the clinics. Doing some research, you know, following up, and having some time like 2 weeks before, to really sort of organise everything and change appointments. And ring them, and trying to get in touch with them, so ‘would you prefer to come to this, and we’ll see you at the same time when you come to TOGETHER study’. [. . .] So, contacting them. Just getting in touch with them. Leaving messages. And getting them to attend. [. . .] But obviously you need the manpower to do all of that. You needed the time, you needed at least 2 weeks to prepare.
Interview 26, DSN
Quotation 70:
[. . .] in a way it was easier, I didn’t have to organise the clinic. But then I would find that if someone came today for the TOGETHER study, they wouldn’t attend the appointment the next time.
Interview 26, DSN
Quotation 71:
[. . .] people from first group couldn’t make it that, you know, particular session they wanted to join the second or third and then, you know, keeping the register going and keeping a tab on who went and when, you know, that was quite messy.
Interview 2, DSN
Quotation 72:
[. . .] just the booking process has created such a problem and how we created the list [for group clinics] because, you know, there’s just no infrastructure within the trust to do group clinics so we need to do some work around how we set up a group clinic, how the patient’s informed, how is the data captured.
Interview 18, diabetes consultant
Quotation 73:
[. . .] for the first session I did I wasn’t quite sure how much to prepare, so whether to keep it just completely blank and do questions and answers or come with something already done and some activities.
Interview 3, dietitian
Quotation 74:
I think because it was the first time I’d done anything like it and I was a bit, I felt quite worried about not really understanding, not really knowing because I was new to it and I didn’t want to say anything that seemed judgemental or, where I seem like I was making an assumption about what people would do.
Interview 6, sexual health advisor
Quotation 75:
[. . .] there wasn’t any relation to diabetes that would sort of help, or what you could do about it. So unfortunately I didn’t find that really helpful [. . .] It wasn’t sort of like well thought out.
Interview 14, patient 9
Quotation 76:
[. . .] it was the third session that I did that worked really well where we had the girls and they split up into separate groups and they planned their meals so they spoke about what they, within themselves, spoke about what they currently eat and then came up with ways that they can make it a bit better.
Interview 3, dietitian
Quotation 77:
[. . .] if they’re doing like a presentation, I would ask them to send the presentation to me and I will look through it and make sure it’s something that would benefit the participants [. . .] you don’t want to get them sort of bored by anything, you want to keep them sort of alive and asking questions.
Interview 26, DSN
Quotation 78:
At the end getting feedback, deciding on the next topic, what they would like and then coming to the office and entering all the details on the database [. . .] if there was an issue raised it would be liaising with the relevant clinician.
Interview 2, DSN
Quotation 79:
[. . .] you really need to understand what are their interests, what are their troubles, you know, to actually win their confidence [. . .] in the beginning I spent a lot of time going through learning about each one of them, their history.
Interview 20, DSN
Quotation 80:
My challenge has been that I know a lot more about them but not knowing how to, I don’t want to challenge them in a group because I want them to come back. Because with the young adults, it’s bad enough with the adults but with the young adults the moment you say something that’s it they don’t want to know you.
Interview 1, DSN
Quotation 81:
[. . .] anxiety is probably there both for the people who are delivering it, and the people who are participating in it. As these programmes mature, and then there are more people convertible with the idea of learning as a group [. . .] they may be able to discuss more issues in the open. And they may be able to say ‘my HbA1c is 100’, so with the same tone as somebody saying ‘my HbA1c is 48’.
Interview 25, diabetes consultant
Quotation 82:
So, you don’t want to embarrass them if they’ve said that they eat something, or they do something and they’re with a group, you don’t want to embarrass them in front of the people they’re with, but you still have to give the information. So maybe like offering advice and asking about if they want certain advice rather than just going out there and giving it.
Interview 3, dietitian
Quotation 83:
I focused on two main activities, but they had kind of little mini steps within them. And one was very much based on scenarios. So, scenario enables people to talk about difficult things, difficult content, without having to expose a lot of their [um], their emotional needs or their difficulties directly [. . .] I didn’t come out saying ‘right, denial is very important for you to know about’, it came naturally through the scenario. But I was well aware that that was something that they had talked about before, and it had been quite a contentious issue.
Interview 17, psychologist
Quotation 84:
But we gave them space to open up because we also realised that they are new, all three of them. We need to give them time to get to know each other.
Interview 2, DSN
Quotation 85:
I think when the one young adult’s mum came, I found that quite difficult to manage. I’ve met her before, so I did know her, and I don’t know if, if we hadn’t met before she would have spoken less or if she’d have spoken more, I don’t know. But that was quite difficult to manage from a group perspective, in she was taking the lead and she was asking because she had diabetes in pregnancy herself, so she had a lot of diabetes-related questions.
Interview 3, dietitian
Quotation 86:
I do think actually the delivery of a group where six or eight people turn up is actually very different to a group where two people turn up. You know? You have to do very different things. And so I think it does definitely present challenges to us.
Interview 8, diabetes consultant/project principal investigator
Quotation 87:
[. . .] it has been a quite rewarding and challenging experience for me, as well. So, every time whenever I say something, I’m questioning myself again internally. So, is that too much for them? Is that too little for them? Or is it reaching everyone? And if somebody’s not asking questions, how should I prompt them to ask questions? Or would that make them more anxious? Or should I kind of take a step back, and? So, how should I kind of interact with them?
Interview 25, diabetes consultant
Quotation 88:
[. . .] the mood, the kind of dynamics, is something that you are attuned to, and you need to be working with within the session. So, how you include people, when they can be splitting, when it can be one person speaking or – and it’s a very dynamic process.
Interview 17, psychologist
Quotation 89:
I’ve only had one young adult, ‘Why should I be sitting listening to other people, I’ve got my issues I need help with’, there’s that element of competition, ‘I have left work I have come here I’ve only got an hour in the car’.
Interview 20, DSN
Quotation 90:
[. . .] in some of the sessions there’s been a bit of a conflict, and conflict management can be quite tricky. And I certainly know that the nurse was quite upset about it after that and so that needs a little bit of help.
Interview 18, diabetes consultant
Quotation 91:
So they finished their session and then they said they were all heading home and then my clinic nurse stopped a lot of them and said you have another appointment and then they said ‘Oh but we’ve already done this’. So they attended my appointment but when they’re attending my appointment I found that in that group session they hadn’t, nobody had looked at their Libre readings and actually highlighted the problems, talked about what changes they needed to make to their insulin on the pump. Looked at why the sugar was high or low, so that session was more about their using the sensors and setting up the system to download the results but not much time had been spent individually for each patient.
Interview 18, diabetes consultant
Quotation 92:
[. . .] just the fact that the study itself has engaged with you know, a few of these young adults who weren’t well engaged before, or you know, were having poor experiences of care before – you know, the fact that we’ve done something a bit different with them and they’ve got on well with it, is a real positive.
Interview 8, diabetes consultant/project principal investigator
Quotation 93:
There’s lots of battles it’s not just HbA1C we’re looking at, you know, whether [um] they, there’s an education component to it [. . .] the fact that they’re engaging, they’ve had a flavour of, you know [um] being amongst, you know, what it is [um] amongst their peers, you know, to be discussing about their diabetes [um] it’s a different way of looking at things other than the one to one.
Interview 20, DSN
Quotation 94:
If anything comes out of the TOGETHER study I’m hoping that they realise that, you know what I was giving myself such a hard time.
Interview 19, DSN
Quotation 95:
[. . .] all they know was – their parents telling them that ‘you’re not doing it the right way’, their doctor’s telling them the same [. . .] When they know that other people are also going through the same problems, then it starts making them feel less guilty. And then that [er] in turn will facilitate how they have the conversation with their clinicians. And they kind of open up. And they may [er] for the first time accept that they’ve not been taking insulin as recommended, or as advised.
Interview 25, diabetes consultant
Differences to the delivery of existing one-to-one care
Quotation 96:
The one to one is more – personalised, like scientific. [. . .] Where [the group clinic] is more like lifestyle based. Like it’s more about how to live with your diabetes, rather than just manage it [. . .] With the doctor, I kind of want to just get it over and done with really quickly, and then just go. So I wouldn’t, I don’t try to ask as many questions or I just forget.
Interview 27, patient 16
Quotation 97:
[In individual appointments] I just personally feel that I’m being judged. Or I feel like I’m a kid, and I’m getting told off again. And I just – me personally, I don’t like that feeling.
Interview 13, patient 8
Quotation 98:
So, with the one to one appointments, it’s – I would say it’s more of a professional atmosphere. And as a young person, you might not be I guess used to that environment very well. And the group clinic is quite a more comfortable atmosphere. More informal. And just I guess a bit more relaxing. It helps, just I guess, talking more. [. . .] I like to imagine that it makes it easier for us to, to turn up to the meetings, I guess. Because I know the individual ones, I know a lot of people haven’t turned up to those as well.
Interview 24, patient 15
Quotation 99:
Yeah I think they’ve got, I feel pretty comfortable because there’s more of us and so I had the cramp problem and then she said she also gets it and she told me about these tablets so I’m going to get.
Water.
Yeah, it’s good because I, when you’re one to one with the doctor it’s only you and what the doctor knows, because there’s so many of us now we can share our experience and hear other peoples’ experiences.
[some agreement].
I feel like the doctor doesn’t understand.
[some agreement].
Clinic 7
Quotation 100:
[. . .] also then the knowledge starts to come from a clinician, it starts sounding like a sermon. And they may forget it as soon as they leave the room. [in group clinics] that knowledge comes in an environment where they don’t perceive the pressure where they have to listen and nod their head. So it might kind of open out, and then they ask the right questions [in group clinics and in individual consultations].
Interview 25, diabetes consultant
Quotation 101:
I think one of the issues with our current clinical model for young adults is about expecting them to behave in a certain way, and conform, and be patients. And probably that encourages them not to tell us about you know, big issues that are affecting them [. . .] we’ve all experienced that when we’ve gone to the doctor. You know, where you feel, I don’t know, a bit patronised or a bit too scared to say something. Or [um] you know, that – inhibited in some way.
Interview 8, diabetes consultant/project principal investigator
Quotation 102:
[. . .] it’s far more likely that a group is going to respond to you to say ‘hang on, that’s rubbish, we’re never going to be able to do that’ than somebody is if they’re sitting opposite you one to one.
Interview 8, diabetes consultant/project principal investigator
Quotation 103:
So the group clinic I think – I feel like it’s more free [. . .] when I go to my doctor’s appointment, I sit there, they have a look at my sugar levels, they’ll tell me ‘OK, you need to improve on this’. I know I need to improve on it. But it’s, it’s very hard to. You know? And you say one thing, but actually doing it is completely different. And we try, I try to get it better. But it’s just sometimes it’s really hard. Things get in the way.
Interview 10, patient 5
Quotation 104:
So it’s easier than talking to your diabetic nurse who’s telling you what to do. But they will never actually know what you’re going through. Like, or how it is. Or, you know, if the insulin’s really working. Even though that insulin’s good, but it might not be working for me. Whereas somebody that’s also on it, she knows that they will – so the boy or the girl would know exactly how it is.
Interview 9, patient 4
Quotation 105:
So, at my clinic appointments, I would say maximum half an hour, sometimes I do run over, but in the group session, because everyone has different questions and it’s a lot longer as well. So, I think he got more out of the group session than he would do in an individual appointment.
Interview 3, dietitian
Quotation 106:
[. . .] some people might not manage their blood levels, the right way. So they might feel a bit inconvenient, or embarrassed about that. So I don’t think they want to present themselves to other people. If that makes sense.
Interview 16, patient 11
Quotation 107:
So results of your tests would probably be the only thing where I would have said – probably want some more privacy.
Interview 14, patient 9
Quotation 108:
I don’t know whether there are certain topics that lend themselves more easily to groups so like with the paediatric group we are told we’re going to be talking about, the psychologist wants to do a session on just wellbeing and [um] just mental and psychical wellbeing.
Interview 18, diabetes consultant
Quotation 109:
you’re looking at blood glucose profiles each visit, each visit. Now, you can’t do that in a group clinic, look at individual ones, it’s just not going to work. You’re looking at the blood biochemistry, you know exactly who’s had what done. And you’re looking at the kidney function, liver function and whether they’ve had their urine done for [inaudible] ratio what their last HbA1c was. I do look at those kind of things to know, understand where they are at the time of consenting. But these are the limiting traits.
Interview 1, DSN
Quotation 110:
[. . .] if they were, in the group clinic if there was eight people there and the nurses had to adjust the insulin for each person and spend time explaining. Then one of two things could have happened, either everybody around would have found the readings interesting could have learned from that experience or they would have got completely bored, saying it doesn’t matter to me why am I sitting here, so we don’t know what, what would happen.
Interview 18, diabetes consultant
Quotation 111:
[. . .] when you have a one to one with your nurse, she can analyse your readings, have a look at them, explain to her what this jump might have been or why you got this hypo. You know, ask any questions that you might have. She can suggest correction doses, or anything else. The problem with that is, that if you were to do that in a group clinic, you’re kind of wasting everyone else’s time.
Interview 15, patient 10
Quotation 112:
But if they’re having more group clinics, then there should be less doctor’s [appointments]. For example, like I could be the one calling them up, saying you know, ‘I need to talk to you about something, can we have a one to one’.
Interview 10, patient 5
Quotation 113:
But I feel like I’m more able to come to the group clinics. I feel more confident and comfortable coming to the group clinics than going to the one to one sessions with my nurses [. . .] I personally don’t know what I’ll do if it stops. I just feel like I would be completely shut off with the whole diabetes thing again. Honestly.
Interview 13, patient 8
Quotation 114:
I asked him if he would come back and keep an appointment and he said no, and he said ‘no I know how to get hold of you if I enter problems but I don’t want to keep coming to see you in clinic regularly’, which is very odd.
Interview 18, diabetes consultant
Critical staff roles: the youth worker
Quotation 115:
What I’d like you guys to do, and I know we haven’t had the chance to say our names, so if you just say your name, and what I’d like you to do is think of a unicorn, everyone know what a unicorn is? I want you guys to think of a unicorn and design it, so if you had a green unicorn how would you have it, what would you want it to do, what superpowers would it have? Use all your imagination, think of something. I’ll give you guys about 30 seconds.
Clinic 1, CMH
Quotation 116:
[The youth worker] was really, really good when it came to ice breaking. We had two different activities, one of them was the fruit and the lion, the other one was chair, we actually were physically swapping chairs. I can’t remember what it was called but yeah. That did take quite a bit of time, but we didn’t finish until 6.50 pm. And the boys they were very happy.
Interview 2, DSN
Quotation 117:
[The icebreakers and youth worker] relaxes the setting a bit more, it’s less formalised [. . .] You get to have like a fun activity, or do something in a group together before we start off, so you get introduced to each other [. . .] you get to do things that you don’t have to think about diabetes.
Interview 14, patient 9
Quotation 118:
[The youth worker] is absolutely amazing. And everyone gets on with him. You can’t fault him at all. So, when he brings up these icebreakers, kind of gives the group an opportunity to get to know each other a little bit and start talking. I don’t have that problem, because I can talk to anyone, to some extent. But there are some people that obviously can’t. And so it’s good for them.
Interview 15, patient 10
Quotation 119:
I think, he’s been fantastic because when we start out it’s not about diabetes, and he’s brought that outside elements of, he admits that he doesn’t know anything about diabetes so he’s just one of them almost [. . .] in the one-to-one sessions when we do clinics, we all have, we all just get straight into the diabetes whereas with the youth worker he just relaxes things and make, takes that step back so that they know it’s a bit different to what they’ve done before.
Interview 3, dietitian
Quotation 120:
I started off with truth or false, I find that, initially it’d be a very, very good game because you get to know something about each other, that’s true, and it’s usually do something fun or something interesting. So, it already sets a fun, energetic mark and I think an icebreaker should always have a couple of getting to know something a bit more about that other person, because you’re starting to now break boundaries and you’re going to start trusting each other and talking.
Interview 7, youth worker
Quotation 121:
So, I think our team never worked with a youth worker, is number one. And having a youth worker just setting the agenda. So our nurses and dietitian – it took the pressure off them, and helped them to focus just on the topics that they had to discuss. And then it made the whole atmosphere very lively, and interactive, even the clinicians were feeling as part of the team, contributing to it [. . .] if you have a youth worker as a facilitator, that changes the role of the person. But if you don’t have, then you need to integrate both the roles, and then that role needs some training.
Interview 25, diabetes consultant
Quotation 122:
So, for me, having [the youth worker] there was a little bit of release. So, someone else can take – you know, I’ve done all the preparation, I’ve organised everything. And during that session, I can just sit down, I can listen, I can look at all the participants, I can see what sort of triggers them, what got them excited, I can observe what’s actually going on a bit.
Interview 26, DSN
Quotation 123:
What I’d like, you guys, to do is, let’s do some ground rules for us, if that’s OK, just while we’re here. Everyone seems really sensible, I’m sure we’re going to have no issues, but just as part of our group I think we should have some rules for each other, just so we can respect each other’s wishes, or whatever they are. We’ll put a few up, if everyone gives one or two each, and I’m sure that will probably be the last we see of the ground rules, but as long as everyone respects them. Superb, anyone want to shout out any to me?
Clinic 1, CMH
Quotation 124:
[young people will think] ‘if these guys don’t finish on time, I’m going to be late, so I’m not going to these guys because my other things is more important’. So, I think finishing on time, not matter how exciting the conversation, let the rest of the group go. [. . .] They might have parents waiting outside, their phone’s ringing but they don’t want to say in front of their peers that they’re getting picked up at this age by a parent. So much goes in play here, so much.
Interview 7, youth worker
Quotation 125:
. . . the funding for a youth worker, and finding a youth worker to run the service throughout, and everywhere – it is an aspirational thing. But I don’t think it will happen everywhere.
Interview 25, diabetes consultant
Appendix 7 Health economic analyses
Results of bivariate sensitivity analyses: cost of the intervention per participant for different number of clinics and people attending (CMH) £
| Number of clinics | Number of participants per clinic | ||||
|---|---|---|---|---|---|
| 2 | 4 | 6 | 8 | 10 | |
| 4 | 1144 | 572 | 381 | 286 | 229 |
| 6 | 1716 | 858 | 572 | 429 | 343 |
| 8 | 2288 | 1144 | 763 | 572 | 458 |
| 10 | 2860 | 1430 | 953 | 715 | 572 |
| 12 | 3432 | 1716 | 1144 | 858 | 686 |
| 22 | 6293 | 3146 | 2098 | 1573 | 1259 |
Results of bivariate sensitivity analyses: cost of the intervention per participant for different number of clinics and people attending (NUH, £).
| Number of clinics | Number of participants per clinic | ||||
|---|---|---|---|---|---|
| 2 | 4 | 6 | 8 | 10 | |
| 4 | 1090 | 545 | 363 | 273 | 218 |
| 6 | 1635 | 818 | 545 | 409 | 327 |
| 8 | 2180 | 1090 | 727 | 545 | 436 |
| 10 | 2725 | 1363 | 908 | 681 | 545 |
| 12 | 3270 | 1635 | 1090 | 818 | 654 |
| 22 | 5996 | 2998 | 1999 | 1499 | 1199 |
Unit costs used in economic analysis (National Schedule of Reference Costs 2017–18). 74
| Code | Currency | Cost (£) |
|---|---|---|
| N15AF | Other currencies data. Specialist nursing, diabetic nursing/liaison. Adult. Face to face | 67 |
| N15AN | Other currencies data. Specialist nursing, diabetic nursing/liaison. Adult. Non-face to face | 34 |
| WF01 A (302) | Consultant-led. Endocrinology. Non-admitted. Face-to-face attendance. Follow-up | 154 |
| WF01C (302) | Consultant-led. Endocrinology. Non-admitted. Non-face-to-face attendance. Follow-up | 117 |
| A03 | Other currencies data. Dietitian | 86 |
| 656 | Other currencies data. Clinical psychology | 170 |
| WF01 A (300) | Consultant-led. General medicine. Non-admitted. Face-to-face attendance. Follow-up | 171 |
| WF01C (300) | Consultant-led. General medicine. Non-admitted. Non-face-to-face attendance. Follow-up | 49 |
| N02AF | Other currencies data. District nurse. Adult. Face to face | 38 |
| N02AN | Other currencies data. District nurse. Adult. Non-face to face | 19 |
| VB09Z | Emergency medicine. Admitted. Category 1 investigation with category 1–2 treatment | 153 |
| VB09Z | Emergency medicine. Non-admitted. Category 1 investigation with category 1–2 treatment | 130 |
| KB02K | Total HRG activity. Diabetes with hyperglycaemic disorders, with a CC score of 0–1 | 1140 |
| KB01F | Total HRG activity. Diabetes with hypoglycaemic disorders, with a CC score of 0–2 | 541 |
Unit costs of health social care used in economic analysis (PSSRU Unit Costs of Health and Social Care 2018). IV Hospital-based health-care staff. 72
| Pay band | Currency | Hourly rate (£) |
|---|---|---|
| 5 | Hospital-based scientific and professional staff | 34 |
| 6 | Hospital-based scientific and professional staff | 45 |
| 7 | Hospital-based scientific and professional staff | 55 |
| 7 | Hospital-based nurses | 54 |
| 8a | Hospital-based scientific and professional staff | 66 |
| 8c | Hospital-based scientific and professional staff | 91 |
| Consultant (medical) | Hospital-based doctors | 108 |
List of abbreviations
- A&E
- accident and emergency
- AYPH
- Association for Young People’s Health
- BH
- Barts Health NHS Trust
- BMI
- body mass index
- BP
- blood pressure
- CCG
- Clinical Commissioning Group
- CMH
- Central Middlesex Hospital
- DAFNE
- Dose Adjustment For Normal Eating
- DNA
- did not attend
- DSN
- diabetes specialist nurse
- EBCD
- experience based co-design
- ED
- emergency department
- HbA1c
- haemoglobin A1c
- HSDR
- Health and Social Care Delivery Research
- IMD
- Index of Multiple Deprivation
- MEH
- Mile End Hospital
- NDA
- National Diabetes Audit
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NPDA
- National Paediatric Diabetes Audit
- NUH
- Newham University Hospital
- PAID
- Problem Areas In Diabetes
- PEI
- patient enablement instrument
- PPI
- patient and public involvement
- PSSRU
- Personal Social Services Research Unit
- T1D
- type 1 diabetes
- T2D
- type 2 diabetes
- WH
- Whittington Hospital
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/NKCR8246).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
