Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR128107. The contractual start date was in December 2019. The draft manuscript began editorial review in March 2023 and was accepted for publication in April 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Sheaff et al. This work was produced by Sheaff et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Sheaff et al.
Chapter 1 Policy and research setting
Third sector organisations contribute substantially to the English health and care systems. This study examined how the NHS and local authorities (LAs) have commissioned voluntary, community and social enterprises (VCSEs); some of the outcomes for commissioners, VCSEs and the health and care systems; and which contexts facilitate or impede the production of these outcomes. Our aim was to examine which factors strengthen collaboration between commissioners and VSCEs in commissioning all kinds of health and care activities, as a contribution to making publicly funded services more responsive to patients’ and carers’ needs.
Health and care
Defining the sector and issue
This section summarises some definitional debates about health and care, the healthcare sector and commissioning, and positions the study vis-à-vis earlier studies of commissioning and of VCSEs, and situates its analytic framework against other conceptualisations.
A standard definition takes health as the ‘absence of disease’, as opposed to a ‘complete sense of well-being’, reflecting a tension between medical and social models of health, respectively. This report adopts the social model as it offers a more holistic picture and acknowledges the social determinants of health (SDoH), and therefore enables a broader assessment of agencies’ roles and contributions. For commissioning is concerned not solely with service delivery (‘health care’) but also with health improvement (including addressing health inequalities). 1 Furthermore, the three tracers (concrete examples used to trace causal relationships through a complex system) that we deploy in this study – social prescribing, end-of-life care and learning disability support – span activities which do not fall neatly into the category of healthcare provision. We take ‘health and care’ to include health care and social care. 2
In the UK there is a tendency to conflate healthcare funding and provision with the NHS, but a key purpose of the 1991 reforms was to separate them. While the NHS provides 85% of health spending in the UK,3,4 there is now increasingly diverse provision. The NHS itself continues to provide the bulk of services, but the independent sector plays key roles especially in some specialties, notably mental health and elective surgery. The independent sector includes for-profit businesses (corporations), not-for-profit organisations, social enterprises, and voluntary and community interest companies (CICs). LAs are responsible for the provision of adult and children’s social care (as well as other key public services such as social housing and public health). Social care funding consists of local authority (LA) funding and user payments.
Notwithstanding the NHS England (NHSE) role in commissioning tertiary and national services, LAs also commission services from the statutory and independent sectors, something especially relevant to the tracers that this report follows. Inevitably, there are some inconsistencies whereby commissioning arrangements at different geographical and organisational scales conflict. For example, regarding obesity, weight management services have traditionally been commissioned locally whereas bariatric surgery has been commissioned centrally. The idea of subsidiarity is that ‘a higher authority should not accredit itself with responsibilities which could otherwise be carried out by a lower authority or at a more local level’. 5 Likewise, debates about co-terminosity have assumed that contiguous boundaries of NHS commissioners and LAs foster interorganisational collaboration,6 but such benefits are not always realised.
The 2012 reforms had two impacts relevant for this analysis: increasingly complex accountabilities and greater fragmentation. The increased complexity arose from the dense pattern of accountabilities of Clinical Commissioning Groups (CCGs), which in turn arose from the proliferation of other NHS organisations involved in health system governance at local level. 7–9 This was not simply the tension between accountability upwards to the centre (through performance management) and accountability downwards (to local stakeholders including communities and public), with accountability upwards arguably predominating;8 the commissioning of primary medical care by CCGs created a (potential) conflict of interest, since CCGs were membership bodies whose members were mostly general practitioners (GPs), who would therefore be commissioning themselves to provide a service.
A second impact was greater fragmentation within the statutory sector and among other agencies (including VCSEs). While such fragmentation had been a consequence of the quasi-market since 1991, the 2012 reforms exacerbated it, with consequences for patient outcomes and for workarounds by commissioners to ‘knit back together pre-existing systems of service planning and delivery’. 9,10 The response of NHSE in the Five Year Forward View was therefore that ‘Increasingly we [the NHS] need to manage systems – networks of care – not just organisations’ and that ‘services need to be integrated around the patient’. 11 It proposed five new models of care (oriented towards primary and ‘out of hospital’ care) including multispecialty community providers, primary and acute care systems (vertically integrating hospitals and general practices), and urgent and emergency care networks. These models were intended to contain the growth of demand, and therefore waiting times and costs, in NHS hospitals.
The most recent step in that direction was the introduction of Integrated Care Systems (ICSs). Each ICS will contain an Integrated Care Board (ICB), primarily an NHS body and responsible for planning and delivering NHS services in the ICS area. Alongside, an Integrated Care Partnership – a committee jointly formed between LAs in the ICS, the ICB, and relevant wider partners – is responsible for creating a strategy stating how the health and care needs of the local population will be met by the ICB, LAs and NHSE. 12 The ICSs face the tasks of trying to make progress on local or longer-term priorities such as increasing healthy life expectancy and reducing avoidable ill health while also addressing the national policy focus on shorter-term challenges such as the elective care backlogs and accident and emergency (A&E) waiting times. Another unresolved issue remained ICB relationships with non-NHS providers, both corporate and third sector, which were outside the collaborative commissioning framework. This issue was connected with that of how different strategic, planning and commissioning roles will be allocated between the ICSs and ‘Place’-level entities within them. Initially, at least, VCSEs (among others such as ambulance trusts, education sector, police) appear to be involved for particular projects rather than as core members of the Place-based partnership. 13
Commissioning and the commissioning cycle
In the 1990s the original rationale for commissioning was to separate funding and provision, enabling more diverse provision, and separating the ‘rowing’ (operational) and ‘steering’ (strategic) functions of public agencies. 14–16 Commissioning has thus been applied to health and social care, besides education, social housing, transport and so on. However, there was an apparent asymmetry as originally (in 1991) health authorities were the NHS commissioners, but at the same time GP fundholding offered an alternative form of commissioning. For many years there was limited engagement between these commissioners, or between them and local government, which commissioned social care and many VCSEs. The introduction of primary care groups did secure a LA representative on the boards of these NHS commissioners17 but the multiple commissioners’ objectives and interests rarely aligned because, as Checkland et al. argue, ‘commissioners and providers struggled with the more fundamental ideas underpinning commissioning, suggesting that shared understanding is far from the norm’. 18 Other rationales for commissioning included:
increasing choice, devolving decision-making to local areas, increasing public services efficiency while making them more accountable, transparent and opening services to a wider set of providers… increasing value for money, encouraging increased joint working and information sharing, as well as creating shared and pooled budgets. 19
Across different LAs there developed different combinations of outsourcing services, spinning LA services off into independent but still publicly owned enterprises, and keeping services in-house. Earlier and more widely than the NHS in many cases, LAs also developed commissioning relationships with VCSEs. 20,21 Because VCSEs were somewhat tangential to commissioning activities and budgets focused especially on NHS secondary, curative care, NHS commissioners have had a more partial understanding of VCSEs’ capacities and resources, with less embedded relationality, perhaps displaced or fractured by staff turnover (with loss of organisational memory), and shifting information systems and performance metrics.
Commissioning is a cyclical activity. As Figure 1 shows, the commissioning cycle has resonances with strategic planning tools also employing a somewhat normative model comprising: health and care needs assessment, goal-setting and planning, procurement and contracting, monitoring performance, and revision subject to performance. 22,23 The Cabinet Office defined it as ‘a cycle of assessing the needs of people in an area, designing and then securing an appropriate service’. 24 Figure 1 shows how the commissioning cycle can be implemented through a ‘purchasing/contracting’, that is a procurement, cycle.
FIGURE 1.
Commissioning and procurement cycle. SLA, service level agreement. Source: Blackpool JNSA. 25
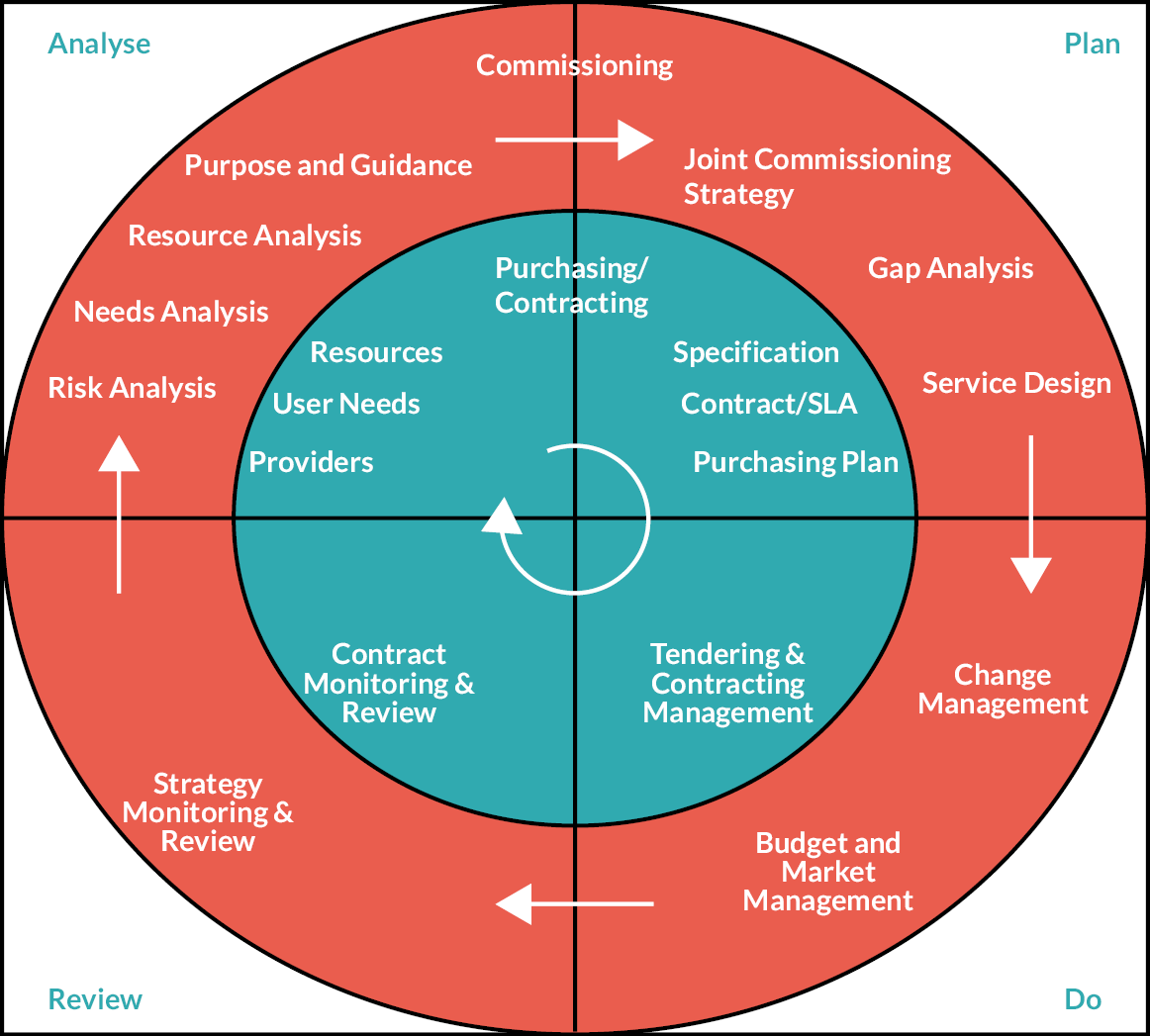
This model is as much normative as descriptive. In practice, commissioning may often be closer to that of managers searching the ‘garbage can’ of already available ideas, methods and resources for any they might apply to their current tasks or problems. 26 The complexity of commissioning is perhaps explained by the relationality (importance of connectedness and relationships) in the quasi-market and the social and institutional embeddedness (persistent multiple connections) of the actors in it. Granovetter argued that ‘[C]ontinuing economic exchanges become overlaid with social content that carries strong expectations of trust’. 27 The result is ‘relational contracting’, in which contractual obligations are heavily supplemented, and attenuated, by non-contractual relationships between the parties. 28–30 Multiple relations – social as much as economic – between commissioners and providers are then likely to develop, especially between those organisations with the most resource dependency on each other. 31,32 (Indeed, one study found up to 85% of commissioner budget was spent with ‘local’ providers. 33) Consequences of this are profound. Commissioners lacking detailed knowledge of providers may rely more on social relations (including trust and reputation33) to influence the providers. They may fear that removal of resource (however small) from one provider may precipitate undermining other services (especially if there is an element of cross-subsidy). Over time, individual commissioners may build strong relationships and develop relational contracts with individual providers, possibly in the VCSE sector.
Co-commissioning
There has been growing interest in the co-production of public services with users and communities;34 that is, in ‘professionals and citizens making better use of each other’s assets, resources and contributions to achieve better outcomes and/or improved efficiency’. 35 Co-production is not simply closer collaboration between agencies but crucially with users, citizens and communities, often undertaken through and with VCSEs36 (Figure 2).
FIGURE 2.
Co-commissioning.
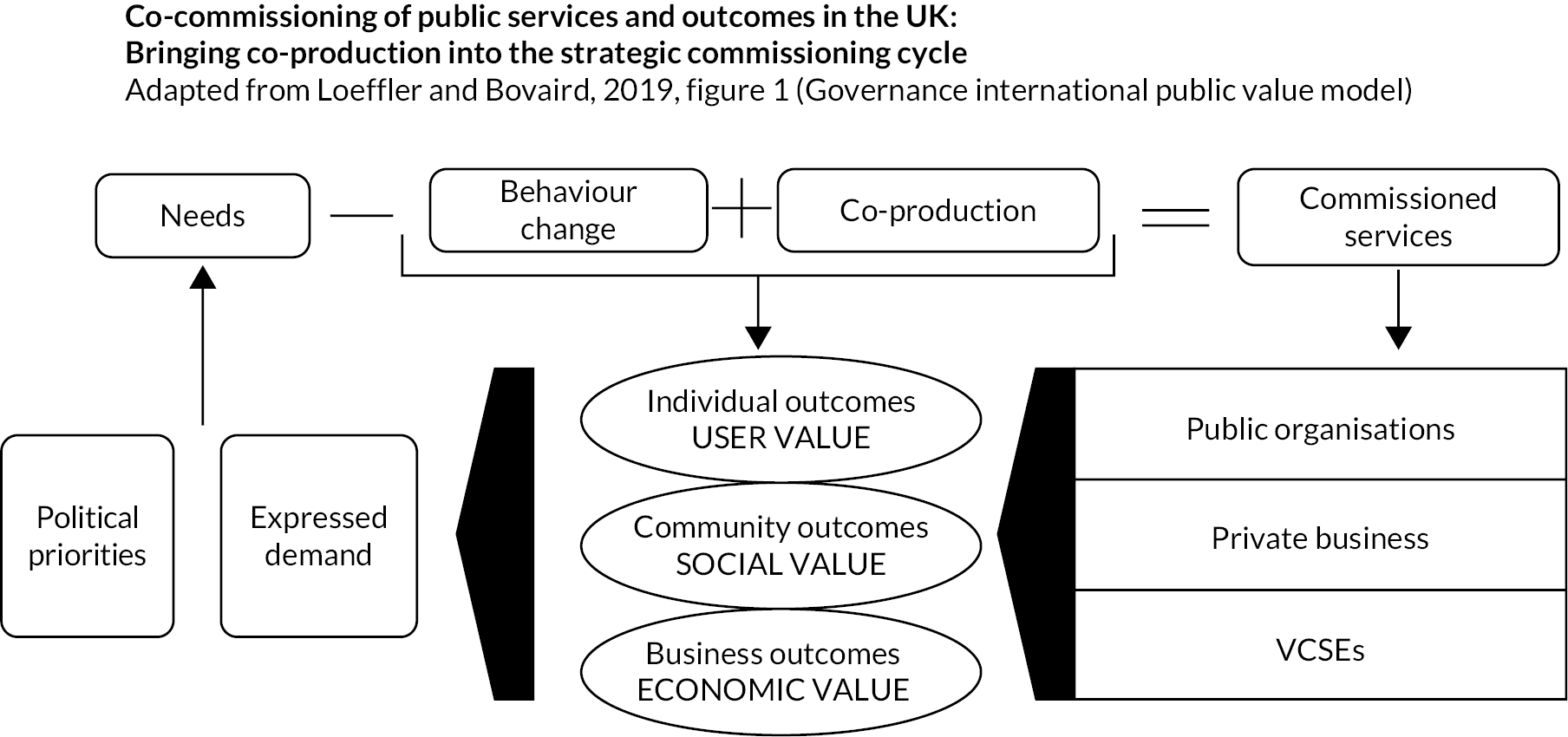
Loeffler and Bovaird distinguish four types of co-production: co-commissioning, co-design, co-delivery and co-assessment. 37 At minimum, commissioning might simply secure services in response to observed need, but through co-production, improved outcomes are likely. However, commissioners have traditionally been weak at co-production and, more specifically, co-commissioning. Through the mechanism of ‘citizen voice’, co-commissioning might comprise:
-
‘service users and community representatives on commissioning boards and procurement panels,
-
participatory budgeting to prioritise public policies or budgets,
-
personalisation – micro-commissioning and
-
crowdfunding’37
Practically, this might entail ‘co-deciding priority outcomes and services’, ‘joint monitoring of in-house services and external contracts’, ‘revising commissioning strategy’, and ‘joint analysis’.
Co-commissioning has been applied somewhat differently in various settings (e.g. mental health). 38 For example, in primary care, where it is relatively new, its first iteration followed the Five Year Forward View11 which announced enhanced powers for CCGs including greater involvement in primary care decision-making, joint commissioning and delegated commissioning arrangements. 39 Petsoulas et al. saw policy documents as making two main arguments for this shift: commissioning could be a ‘sticky plaster or solution to a problem’ or an ‘opportunity to develop place-based commissioning’. 40 Furthermore, co-commissioning can also be applied at an individual level such as through personalised budgets whereby ‘individuals are active participants in the planning and purchasing of their support’. 34 Yet while co-commissioning in this setting is an ‘iterative learning process’, it is also riven with power asymmetries and competing notions of expertise. There has been limited evidence of co-commissioning with VCSEs despite the call in the Civil Society Strategy41 for ‘a renewed focus on collaborative commissioning arrangements’. 19 Empirical studies of the health-related commissioning of VCSEs remain sparse.
Conceptual perspectives: commissioning as governance
Commissioning is among other things a form of governance which applies when, having relinquished line management control over other organisations, governments attempt to ‘steer’ and control in less direct ways the activities and independent organisations that they fund. Thus commissioning ‘remains the dominant process by which England’s state and third sector (and arguably NHS providers) financial relationships are managed’. 19 Governance (control without line management) through commissioning uses six main media of power:23
-
Managerial techniques, including those of the new public management, are extended from use purely within an organisation to the monitoring, and even management, of external organisations. 42–44 One way to do so is through a stable interorganisational network with the commissioner as its coordinating centre:45 a quasi-hierarchy. 42
-
Negotiated order: separate organisations may come to agree (perhaps only implicitly) a division of labour46 through which they coordinate resources in pursuit of shared activities or aims.
-
Discursive control by means of persuasion, whether scientific or ideological. That requires a shared discourse across the separate organisations, hence that each organisation has the ACAP to learn and use the common discourse.
-
Resource dependency and financial incentives: a commissioner stipulates the conditions under which it will purchase services,47 or pay more, thereby setting up financial incentives.
-
Provider competition: a commissioner can threaten to replace a non-compliant provider with another, whether only in principle (‘contestability’: the quasi-market is always open to new entrants48) or in practice if alternate providers already exist. 49–52
-
Juridical control: application of law, regulations or official inspections, or enforcement of the terms of a contract. 31,53
Different selections of media of power come to the fore at different stages in the commissioning cycle (e.g. competition, during provider selection). Similarly, commissioners select and hybridise these media of control according to local history and geography,54 provider ownership (public, corporate, practitioner-owned, third sector, etc.),55 the type of service being commissioned, and of course their own policy aims. 56
Commissioning reforms are seldom implemented entirely as intended. 57,58 As ‘street-level bureaucrats’, local commissioners have a degree of discretion. 59 Irrespective of national directives or guidelines, commissioners usually have some leeway in how they respond to local pressures and opportunities. 19 Commissioners must therefore engage in the ‘communicative and adaptive work’ of ‘street-level diplomacy’. 60 Bossert argued that the impact of decentralisation needed to be viewed in response to three dimensions:
-
‘the amount of choice that is transferred from central institutions to institutions at the periphery of health systems
-
what choices local officials make with their increased discretion (which may entail innovation, no change or directed change) and
-
what effect these choices have on the performance of the health system’. 61
In addition, commissioners are constrained ‘horizontally’ by having to collaborate with other local agencies, including other commissioners. The decision space framework (DSF) represents this intersection between vertical (central–local) and horizontal (local–local) constraints as the space for autonomy or ‘room for manoeuvre’62 that local agents have in making decisions about matters such as finance or human resources; Exworthy distinguished between inputs, process and outcomes. 63 Hence, local agents may have some discretion in certain aspects of their responsibility but not others. This can, of course, create tensions and ambiguities with higher-level agents. Moreover, the DSF highlights commissioners’ interdependencies, crucially, with other local agencies and organisations: for this study, VCSEs and LAs especially.
While the DSF aids understanding in the dimensions of autonomy for a local agency such as a commissioning organisation, it says little about how such autonomy is exercised in practice. Autonomy also needs to be understood in terms of the willingness and ability to exercise such autonomy,64 which a combination of factors might affect, including:
-
ongoing effects of centralisation (through behaviours and actions)
-
risk aversion, especially in financial matters
-
fragile managerial capacity and capability
-
concerns in adverse consequences of decisions for other local organisations.
The combination of willingness and ability to exercise their autonomy creates four possible scenarios for an agency:64
-
able but unwilling: unused or underused powers
-
unable but willing: frustration and disempowerment
-
unable and unwilling: acceptance of centralisation
-
able and willing: genuine local freedom.
Decision space does not remain fixed but is shaped by exigencies such as the dynamics of local politics, local agents’ capacity and capability and the central authorities’ demands, inter alia. Hence, the character of local (social and professional) networks has a strong bearing on how commissioning is conducted. 65,66 Moreover, it is likely that organisations will adopt workarounds to cope with and accommodate any perceived discrepancies between national policy and local networks. 67 These workarounds are likely to reinforce the local social and institutional embeddedness of commissioners and those whom they commission. 7
Voluntary, community and social enterprises in health and care
Defining the third sector
Next arises the question of what the third sector – a contested term – is. Alternatives include ‘voluntary sector’, ‘voluntary and community sector’, ‘social sector’ and ‘voluntary, community and social enterprises’ (VCSEs: the term we standardise on here). The wider concept of ‘civil society’ denotes all the non-state and non-market public spheres where citizens can express their different viewpoints and negotiate a sense of their common interests. 68 At any rate, the third sector is neither the state nor the market nor the family or entire community. Salamon and Anheier defined it as comprising all organisations that have all the following characteristics:69
-
institutionalised to some extent, either by being formally constituted or by having regular meetings, procedures, etc.
-
institutionally separate from government
-
not profit-distributing, reinvesting any profits internally
-
self-governing with their own internal governance procedures without external control
-
resourced to a meaningful degree by voluntary participation,70 whether in their activities or management
Besides noting characteristics which are not unique to VCSEs, such as having multiple stakeholders, revenue sources and activities, and complex accountabilities and tensions between senior staff and boards, many writers add that VCSEs are distinguished by the centrality of such aims (‘values’, ‘mission’) as empowerment and social justice. 71–73 Their functions correspondingly range across service delivery, self-help, mutual aid, capacity-building, campaigning and advocacy. In recent years, the boundaries between VCSEs and the public and private sectors have frequently become blurred and organisational hybrids more common,74 for instance the social enterprises encouraged by successive governments, including some in health and care. 75
Voluntary, community and social enterprises are very diverse, ranging from large household-name charities operating across the country to small organisations with few or no paid staff. VCSEs vary, firstly, in legal terms; contrary to popular belief, a charity is in England a legal status not a kind of organisation. VCSEs also differ by who controls them, having varying degrees of trustee, member and service user involvement in their governance. Some are democratically controlled by their working members (not just the trustees), beneficiaries or users,76 giving these VCSEs correspondingly distinct aims and motivations. 72,73
Voluntary, community and social enterprises and the policy setting
Many VCSEs originated in response to the failure both of markets and of the state to supply specific services or cater for particular care groups,77 although, conversely, much of the state welfare system including the NHS in turn arose in response to failures in VCSE coverage. 78 Governments have fairly consistently expanded the VCSE role of the sector in public service provision since the late 1970s, although their reasons have differed. 79 In the 1990s LAs predominated as the commissioners of VCSEs. Labour’s ‘Third Way’ emphasised partnership between sectors and mainstreaming VCSEs,80 and saw some substantial public investment in that. A ‘compact’81 between the government and VCSEs in England set out commitments for both sides to improve their collaboration. Several large capacity-building programmes were funded, including Futurebuilders which aimed to help VCSEs bid for public sector contracts and ChangeUp, designed to improve the sector’s infrastructure. NHS staff and other employees were encouraged to leave the public sector and create new VCSEs, usually social enterprises or mutuals. 15 Later initiatives paid more attention to the commissioning system itself and to public sector commissioners, in order to address some of the issues and challenges experienced by the third sector when contracting for public services. 20
David Cameron’s ‘Big Society’ agenda in 2010 promoted a changed relationship between citizens and the state, including new opportunities and spaces for voluntary action. One was opening public services to greater competition from charities and social enterprises, moving away from the partnership model of the Labour government. 82 However, the coalition government’s austerity policies radically changed the setting and terms of commissioning. Constrained public spending at both national and local levels put additional pressures on commissioners to procure services that provided value for money, while VCSEs faced growing demand for their services.
In 2018 the government highlighted the need to ‘reform commissioning in favour of charities and social enterprises’ in its Civil Society Strategy,41 supporting alternative commissioning models such as collaborative commissioning, flexible contracting (including Innovation Partnership projects) and Social Impact Bonds83 and, concomitantly, more extensive NHS commissioning of VCSEs. During the COVID-19 pandemic, many commissioners adapted by giving VCSEs unprecedented levels of flexibility in delivering public sector contracts to respond to local needs. Commissioning relationships became viewed as less transactional and more collaborative. 84 Macmillan suggests that in the pre-pandemic decade much of the sector’s infrastructure was dismantled, which fragmented the provider landscape, but also that recent events have stimulated collaboration between national infrastructure bodies, greater recognition of their role, more spaces for dialogue and greater coordination. 85
Commissioning voluntary, community and social enterprises
Voluntary, community and social enterprise commissioning: size and scope
Government funding for VCSEs has largely mirrored wider policy. It grew substantially during 2000–10, fell during the period of public spending austerity, and then plateaued. In 2019–20 VCSEs comprised almost 166,000 organisations with a total income of £58.7B;86 26% of their income (£15.4B) was from government sources. Not all VCSEs were involved in public service delivery or received public funds. Approximately 38,000 VCSEs were active in health and in social services with a combined income of £19.7B (£6.4B and £13.3B, respectively), 34% of it from government sources. More recent Charity Commission (CC) data show a large increase in the percentage of VCSEs receiving government funding in 2020–1 due to the COVID-19 pandemic support packages. However VCSEs’ loss of income because of the pandemic was far bigger than in the 2008–9 recession and the period of austerity which followed. Public sector procurement data show that between March 2016 and April 2020, 3140 VCSEs were named on 7330 published public sector contracts together worth £17B,87 but these were only 5% of the total value and volume of contracts awarded. Local government awarded substantially more contracts to VCSEs by value (£8.9B) and number (4871 distinct contracts) than did central government and the NHS. Nevertheless, the value of NHS contracts awarded to VCSEs increased annually after 2017–8 and in 2018–9 equalled the value of contracts awarded by local government. Of the VCSEs named on a published public sector contract, 56% had only 1 contract, 41% had between 2 and 10 contracts, and 3% had more than 10.
Health and care was by far the largest activity by total value of VCSE contracts, with £11.6B awarded between 2016 and 2020, representing 24% of the total value of contracts awarded in health and care, although other activities saw higher proportions of the total number of contracts awarded to VCSEs, particularly those concerned with domestic violence and sexual abuse (66%) and homelessness (69%).
Kinds of activities and work-processes undertaken by voluntary, community and social enterprises
Voluntary, community and social enterprises’ health and care work is hugely varied, falling into four main categories: service provision; advice to commissioners, planners and funders; medical research; and policy and campaigns. 88 Their services range from specialist clinical provision (e.g. hospices) to community-based support (e.g. day care and home-based support), condition-specific and general wellness support and advocacy; and accommodation services (e.g. residential and nursing care). 88,89 Many VCSEs act as advocates in order to influence and shape practice and policy, including local commissioning priorities and co-design initiatives for specific care groups. Some focus explicitly on prevention and promoting healthy lifestyles, others on social prescribing activities which support the health and well-being of patients with complex health conditions and needs. 90 Some VCSEs, usually the larger ones, co-fund services with public commissioners through contracts for specific care groups and personal budgets or grants for individuals; and some contribute to financing medical research. However, many other VCSEs fund their own evaluations to assess the effectiveness and impact of their services, and so inform their advocacy work. Table 1 distinguishes the level of support that VCSEs provide for local health systems.
| Level of support | Activity | Definition |
|---|---|---|
| Individuals | Direct treatment and support | Health and care treatment/support delivered directly to people (including wider non-medical support) |
| Engaging people in keeping healthy, prevention | Activities designed to reduce the likelihood of people becoming unwell, including behaviour change campaigns, information services, outreach work with specific at-risk communities | |
| Supporting self-management | Activities designed to help manage an existing condition, information services, signposting to available support, health coaching | |
| Involving families and carers | Services providing support and information to families and carers to improve or work towards integration of families and carers into treatment processes and decisions | |
| System | Integrating and coordinating care | Coordinating care through statutory actors and organisations (e.g. relaying information along the patient pathway, research) and through patients (e.g. giving them knowledge and advice about services) |
| System redesign | Activities to inform how services and care pathways are designed and delivered (research, pilots and relaying the views of beneficiaries to commissioners and policy-makers) | |
| Support for health and care professionals | Training health professionals in specific areas, bringing them together with patients and other interested actors, providing relief capacity |
Dayson and Wells suggest that VCSEs’ comparative advantage lies in how VCSEs carry out their work, who they work and engage with, and the role they play within their communities. 92 They are trusted intermediaries and can act as a conduit for people’s views and engagement, and can access and reach communities which statutory providers can find difficult to reach. They also bring additional resources to the health and care system, including charitable funds and volunteers. 91
Who undertakes the activities within voluntary, community and social enterprises?
While charities, community groups, social enterprises, mutuals and cooperatives have all been commissioned by the NHS, there is no comprehensive overview of their level of involvement, by type of VCSE, in health and care. Procurement data for 2020 indicate that two-thirds of the income (£6.2B) from government contracts was secured by VCSEs with incomes above £10M, a group of just over 500 providers. 93 Especially for smaller VCSEs, the hidden transaction costs of contracting – especially those of tendering, process and of fulfilling information and monitoring requirements once the contract is let – can deter involvement. 94 Smaller organisations are often ill-equipped to navigate the complexities of commissioning and procurement systems and compete with better resourced VCSEs and corporations. 95
Voluntary, community and social enterprise services and activities can be undertaken by paid employees or volunteers or a mix. Although not all VCSEs involve them, volunteers are integral to the value of VCSEs because of their proximity to service users and connections within local communities. Volunteer labour can also be seen as a way of saving money. VCSE approaches to involving service users vary greatly according to each VCSE’s organisational form, interests and governance arrangements. 96 With co-production and co-commissioning rising on the commissioners’ agenda, the role of user-led VCSEs has come to the fore. In these organisations the boundaries between staff, users, members and volunteers are often blurred, with people having multiple and overlapping roles. 97
Voluntary, community and social enterprise relationship to public and corporate sectors
Voluntary, community and social enterprises are motivated to engage with commissioners for a range of reasons depending on their purpose and activities. For service delivery organisations, winning a public sector contract gains funding which helps them pursue their mission and goals, and diversifies their income stream in an increasingly challenging environment. As additional motivations, many VCSEs work with commissioners because they believe their experience, expertise and importantly, their relationships with users, members and communities put them in good stead to deliver public services and respond to users’ and communities’ needs. In England the Public Services (Social Value) Act 2012 required commissioners to consider the wider social, economic and environmental benefit of contracting, an attempt to acknowledge the social value that VCSEs generate and so make it easier for them to compete for contracts. However, ongoing debates as to how social value should be defined and measured have made its implementation challenging.
Finally, some VCSEs engage with commissioners as ‘strategic partners’, not to deliver services themselves but at a more strategic level, whether local or national, by seeking to shape public services, influence commissioning priorities, address health inequalities and change the relationship between the commissioners and VCSEs.
Consequences of entering a relationship with commissioners
Some studies have argued that being commissioned has led to the increased professionalisation of VCSE management, but also bureaucratisation98 and loss of internal democracy, even ‘managerial capture’. 99 A ‘degeneration’ theory suggests that a result has been VCSEs becoming assimilated to corporate and public sector organisations, losing the features that make them distinctive. 100 Similarly, the theory of institutional isomorphism101 suggests similar transformations occur as VCSEs mimic private and public sector managerial practices such as audit, performance management and outcomes measurement. 102–104 Other studies report risks to VCSEs’ independence, mission, finances and reputation, and that ‘co-optive’ relationships develop between the VCSEs and the statutory sector. 105 A literature review20 noted such adverse impacts as:
-
compromised independence, challenging VCSE advocacy and campaigning capacity106,107
-
mission drift away from VCSEs’ original core purpose,108 for example as VCSEs seek income to finance service changes that commissioners insist upon109
-
contract requirements diminishing VCSEs’ innovativeness and flexibility to respond to changing user needs
-
insecure employment terms and conditions, creating problems of staff retention and morale; or a shift from volunteer to paid labour110
-
more competitive relationships between VCSEs
-
stratification between VCSEs that deliver public services and those that do not
Yet the evidence is mixed, including VCSEs’ own views about whether their independence has been compromised or whether their mission has drifted. In some VCSEs public commissioning has led to more formalised volunteer management practices, especially the adoption of a work-based model of volunteer management with more developed training opportunities for volunteers and more emphasis on volunteering outcomes for service users and the volunteers themselves, alongside organisational culture changes as VCSEs have become more bureaucratic and business-like, placing additional pressures on volunteers. 111
This pattern of findings suggests that VCSEs’ experiences are context-dependent. While VCSEs are often portrayed as rather passive players in the commissioning landscape and facing multiple challenges, such accounts tend to underestimate how VCSEs’ strategies, practices and experiences vary, and underestimate VCSEs’ own active role. 36
Interfaces and interaction
Publicly funded services are often, even typically, provided under contract by corporatised112 but still publicly owned organisations or completely independent providers, including VCSEs. 113 Commissioning these providers is, among other things, a way for governments to exercise governance over these policy subjects in the absence of direct hierarchical control108,114–116 (see Chapter 1, Health and care). To that extent, commissioning relationships can be conceptualised as the application of different forms and combinations of media of control over the providers,23,117 through which governments attempt to implement their current policies for the sector (see Chapter 1, Health and care). In practice, governance through commissioning has had varying degrees of success. Alongside instances of policy subjects implementing a policy up to118 or even beyond119 policy-makers’ expectations are reports of implementation failures. 120 In other cases, policy subjects have tried to delay the implementation of policies which they expected to harm them,121 or implement them selectively,122 or resist them. 123 Either party may try to influence, even ‘capture’,124 their counterpart organisations, for instance by managing their access to information. 125,126
Realist evaluation,127 an established method for explaining such differences, makes six main assumptions about policy and its implementation:
-
Policy-making is understood agentially as stemming from the intentions and actions of policy-makers in particular, among the many actors involved.
-
Every policy is implicitly a theory:128,129 in the present case, a programme theory that specific ways of commissioning VCSEs will lead them to help produce the policy outcomes which the policy-makers first intended (see Chapter 1, Health and care).
-
To induce the policy subjects to implement a policy, the policy-makers apply or create implementation mechanisms which bring resources,130 persuasion, payment and the possibility of coercion to bear upon the policy subjects.
-
Achieving these outcomes also depends on the contexts in which these ways of commissioning are implemented. 131–133
-
Depending on the contexts, the resulting policy and organisational outcomes may approximate to the policy-makers’ original intentions but may also include perverse, unforeseen and emergent outcomes.
-
The programme theory and its implementation can therefore be evaluated instrumentally, in the policy’s own terms; that is, how far the observed outcomes satisfied the policy intentions which motivated it.
Items 1–5 together constitute a context–mechanism–outcome configuration (CMOC), which is defined relative to a focal agent. When evaluating attempts at policy implementation, the decision- or policy-maker is the focal agent. The policy subjects’ reactions may be a mechanism or outcome, depending on the case. The policy subjects and any other actors involved are parts of the implementation context. The latter influences how far the mechanism had the effects which the focal agent expected, including any intended effects on the policy subjects’ behaviour.
Whether the mechanisms for implementing a policy produce the outcomes that the policy-makers intended therefore depends critically upon how the policy subjects react. As Chapter 4, Voluntary, community and social enterprises aims outlines in respect of VCSEs, the policy subjects also bring their aims, assumptions and resources into the policy implementation mechanisms. Therefore the ways in which VCSEs engage in commissioning, and its consequences for them, can be explained – hence researched – by a reasoning symmetrical to the realist evaluation of the commissioners’ commissioning practice but in reverse, now taking VCSEs rather than commissioners as the focal actor.
The policy outcomes and other consequences of commissioning VCSEs can therefore be understood as resulting from two interacting sets of mechanisms at the interfaces between commissioners and VCSEs: those that the commissioners use in commissioning VCSEs, and those that VCSEs use when engaging with commissioning. In one CMOC, commissioners are the focal actor. In commissioning VCSEs, they apply programme resources (e.g. finance, legitimation, influence) as mechanisms134 which, if VCSEs respond as the commissioners expect, will realise the commissioners’ current commissioning and policy aims. The ways in which VCSEs participate in the workings of those mechanisms by contributing resources and ideas over time are thus contexts133 which affect what outcomes the commissioning mechanisms produce. However, the ways in which the VCSEs engage with commissioning, and the outcomes for them, can be explained in a symmetrical fashion but with the roles reversed. In a second CMOC, VCSEs are conversely the focal actor, commissioning being (also) a mechanism through which they pursue their aims. How commissioners respond to VCSEs’ attempts to become commissioned are for the VCSEs a context which affects what outcomes commissioning mechanisms produce for the VCSEs. NHS commissioning of VCSEs can thus be understood as working of these two CMOCs which intersect where the commissioners and VCSEs interact, each party using the available governance structures as a means through which to secure and negotiate a contract, then letting the contract or making some alternative payment arrangement (e.g. a grant), and finally either ceasing, revising or repeating the experience. Figure 3 shows diagrammatically the two mechanisms and their points of intersection (surrounded by a dotted line). (For clarity,Figure 3 omits the feedback loops from monitoring to the possible revision of the commissioners’ and VCSEs’ respective aims in light of the outcomes achieved.)
FIGURE 3.
Commissioners and VCSEs: dual CMOC, common mechanism.
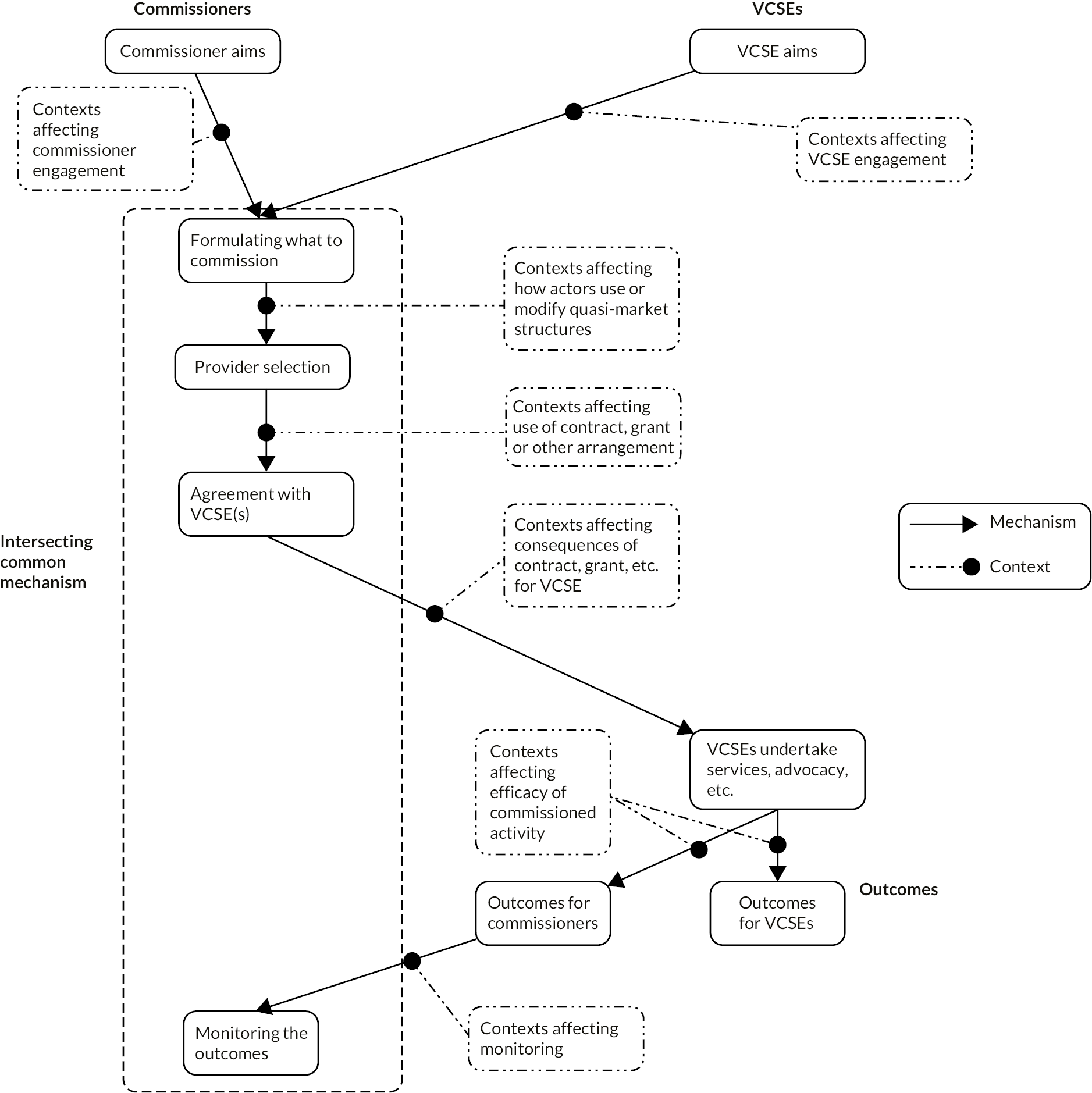
The area of intersection in Figure 3 thus contains the commissioning cycle (see Figure 1).
The outcome of an attempt to implement policy, in this case through commissioning, will therefore depend on what knowledge commissioners and VCSEs absorb about each other’s respective policy objectives or mission, intended mechanisms for achieving these objectives, assumptions about the likely consequences, and any side-effects of doing so (e.g. how their interaction will affect their other concurrent objectives). Such assumptions about mechanisms (the programme theories) underlie their respective ways of practising, or engaging with, commissioning. An important context for the mechanisms shown in Figure 3 would therefore appear to be what commissioners and VCSEs believe about each other’s intentions and likely behaviour, which results from how they learn these things; that is, their respective organisations’ capacity to access and apply knowledge from external sources135–137 – in short, their ACAP. ACAP consists of knowledge acquisition, assimilation, transformation and exploitation in sequence. 138 Of the media of power, ACAP especially potentiates negotiated order (because ACAP both arises from and promotes relationality and organisations’ embeddedness in their local health economy) and discursive control.
By analogy with small and medium enterprises (in existing research, the nearest parallel to VCSEs in terms of organisational size and local embeddedness), one would expect ACAP in the present setting to develop, at least partly, out of networking between the organisations involved,138,139 with networking giving VCSEs a cheap and easy way to expand their knowledge; and in turn, to reinforce such networking138 in a virtuous circle. ACAP thus develops cumulatively in two senses. First, the knowledge acquisition phase is a precondition for assimilation, assimilation for translation, and translation for exploitation. Secondly, ACAP develops by building upon prior knowledge, and hence tends to be more fully developed in older organisations. 138,140
Absorptive capacity development thus has successive phases and multiple dimensions. It requires multiple organisational capabilities. These include combinative capability: the organisation’s socialisation processes141 (organisational eultures,142,143 internal dialogue,144–146 ‘mental models’ receptive to knowledge acquisition), its systems capabilities (formal policies, managerial support, training) and coordination capabilities (internal networking,147 access to expertise). Hence ACAP development is not a unilinear increase in just one characteristic but involves multiple linked changes in the profile of an organisation’s knowledge-absorption activities across the four phases (acquisition, assimilation, translation, exploitation) and in the profile of capabilities noted above. Which capabilities are most relevant to an organisation depends on whether its tasks and environment are stable (systems capability is most relevant), fragmented and diverse (socialisation capability) or dynamic (coordination capability). 139,148
First applied to corporations,135,140,149 then small and medium-sized enterprises (the German Mittelstand),150 and later CCGs,141 the concept of ACAP has yet to be adapted for or applied to the commissioning of VCSEs. A priori, all four phases of knowledge absorption appear likely to assist a more accurate translation of commissioner and VCSE aims and knowledge into needs assessments during co-commissioning, and enable VCSEs as prospective providers to attune their proposals or bids more closely to the needs assessments. Insofar as ACAP did develop among commissioners, among VCSEs and between commissioners and VCSEs, these organisations’ acquisition of knowledge would focus on each other’s aims, resources, and assumptions about the needs of their focal care groups in their localities, and knowledge of technical developments in the field. What matter here are the actors’ actual beliefs, not the a priori normative accounts of ‘rationality’ that microeconomics and game theory start from. Assimilation of this knowledge would involve translation between the different discourses by which commissioners and VCSEs formulate their aims and describe their organisations and activities. 108 Transforming the assimilated knowledge would firstly involve each organisation comparing, even reconciling, the other party’s with their own factual assumptions (e.g. about population needs, what costs are considered). Depending on how fully aligned the different organisations’ aims were, it might secondly involve reframing the acquired knowledge from a focus on the other party’s or parties’ aims (e.g. commissioners’ data structured around performance indicators) towards one’s own practical perspective (e.g. a VCSE demonstrating unmet service needs). Exploitation would consist of finding either new ways of delivering services and other activities, or new ways of performing the commissioning cycle, or both. Assimilation and transformation are more internal activities, although external expertise might contribute (indeed, be sought). Exploitation again involves external networking with commissioners, but also engagement, even co-production, with service users themselves. Greater capacity to acquire, assimilate and transform knowledge together appear likely to make provider selection better informed, help the negotiation of agreements between commissioners and VCSEs contribute to meeting the aims of both, and make the monitoring of VCSEs’ commissioned activity more accurate and informative. However, all these claims require empirical testing. In the NHS, both commissioners141 and VCSEs151 have often lacked sufficient skills and resources.
The preceding two sections suggest where our existing knowledge of the interactions shown in Figure 3 is incomplete, especially in the present changing setting. In summary, previous studies show that commissioners tend to find different combinations of methods (i.e. different ‘modes of commissioning’) effective in influencing different kinds of providers (NHS-owned, corporate, VCSE, etc.), rather than how the effective combinations of methods might differ for VCSEs, or indeed different kinds of VCSE. Neither is it known whether or how commissioning works differently when VSCEs contribute to their local commissioners’ priority-setting (i.e. to co-commissioning) besides, or instead of, as providers. At present (early 2024) there is little published evidence about how VSCEs will engage with the new ICSs. On the VCSE side, existing studies tend to focus on the risks, or potential risks, of commissioning to VCSEs rather than on how VCSEs try to engage with commissioners in pursuit of their own missions. We also lack knowledge of what specifically the contexts are which affect the working of the intersecting mechanisms in Figure 3.
These gaps in existing research, and the two-sided conception of commissioning practice outlined above, motivate our research questions.
Chapter 2 Aims and research questions
Research aims and objectives
This study therefore aimed to produce knowledge about which factors strengthen (or weaken) collaboration between health and care commissioners and VSCEs in commissioning all kinds of health and care providers, and make commissioning relationships between the NHS and VCSEs more productive for both, and so contribute to making publicly funded services more responsive to patients’ and carers’ needs. That is, to:
-
strengthen the evidence base for guidance to commissioners on how:
-
VSCE contributions can strengthen health and care commissioning
-
Commissioners and VCSEs can gain knowledge of each other’s needs
-
VCSEs can use research to inform their activities, to encourage and enable them to produce evidence in their own cause.
-
-
Produce evidence about how, and under what conditions, health and care commissioning of VCSEs and co-commissioning with them tends to produce the consequences which are positive or negative in the above terms: specifically, to evaluate empirically the two-sided programme theory outlined in Chapter 1, Interfaces and interaction and Figure 3.
-
extend the earlier typology of commissioning methods23 to commissioning VCSE providers and co-commissioning with VCSEs.
Additional study aims are to help develop:
-
commissioners’ capacity for co-commissioning with VCSEs, and the training and knowledge mobilisation methods required.
-
practice guides on the commissioning of VCSEs, for both VCSEs and commissioners.
Research questions
The earlier findings, explanations and frameworks which Chapter 1, Health and care and Voluntary, community and social enterprises in health and care summarised suggest making VCSE–commissioner interactions the focus of this research and a route towards mobilising the resulting knowledge. However, many of the relationships and contexts shown in Figure 3 have still to be researched. We therefore addressed four research questions. RQ1 concerns what the organisations commissioning VCSEs bring to, and take from, those interactions; that is, why commissioners try to commission VCSEs and how far the outcomes of that activity satisfy the commissioners’ aims. RQ2 addresses the same issues from the standpoint of the VCSEs who are commissioned, and RQ3 in regard to co-commissioning.
-
RQ1. How do healthcare commissioners address the task of commissioning VCSEs as service providers, and what barriers do they face?
-
RQ2. What are the consequences for VCSEs of the public bodies commissioning services from them?
-
RQ3. How are VCSEs involved in CCG, LA and other (e.g. ICS, NHSE) commissioning decisions?
-
RQ4. What ACAPs do healthcare commissioners and VCSEs, respectively, need for enabling VCSEs to be commissioned and for co-commissioning?
In this report, we conceptualise commissioning as an essentially quasi-market activity, not just as a synonym for planning or paying for health and care, even when quasi-markets are hybridised with other structures. ‘Healthcare commissioners’ are defined as all such publicly funded organisations, taking NHS commissioners and LAs together unless explicitly separated and, unless otherwise stated, as referring to commissioning organisations not individual employees. ‘Co-commissioning’ means the involvement of VCSEs as advisers, advocates or consultees to identify health and care needs and prioritise activities or services to commission. The term ‘media of power’ refers to governance through commissioning (see Chapter 1, Health and care), but on the VCSE side the media of power through which VCSEs pursue their own missions. We define ‘resources’ widely to include real-side inputs (staff, equipment, consumables, energy, help-in-kind, practical collaboration, etc.)152 and information, but also money, legitimation153 and status. Among ‘outcomes’ we include any unintended, unforeseen, emergent or perverse consequences of commissioning VCSEs.
Each research question corresponds to specific elements in the dual CMOC schema (see Figure 3), as Table 2 shows.
| Research question | Dual CMOC element(s) |
|---|---|
| RQ1: How do healthcare commissioners address the task of commissioning VCSEs as service providers, and what barriers do they face? | Commissioners’ and VCSEs’ aims, and their compatibility Intersecting common mechanisms (‘How do… providers’) Missing, ineffectual or conflicting mechanisms or parts of mechanism (‘barriers’) Favourable and unfavourable contexts (‘barriers’) |
| RQ2: What are the consequences for VCSEs of the public bodies commissioning services from them? | VCSE aims Outcomes for VCSEs |
| RQ3: How are VCSEs involved in CCG, LA and other (e.g. ICS, NHSE) commissioning decisions? | Intersecting common mechanisms Missing, ineffectual or conflicting mechanisms or parts thereof Favourable and unfavourable contexts |
| RQ4. What ACAPs do healthcare commissioners and VCSEs, respectively, need for enabling VSCEs to be commissioned and for co-commissioning? | Context: ACAP |
Chapter 3 Methods
Study design and its theoretical framework
Our research design was based on realist evaluation, since the latter has been developed specifically for explaining policy implementation (in this case, commissioning health-related VCSEs), its consequences and facilitating contexts. Whether implementing that policy had the outcomes that the policy-makers intended depends upon how the VCSEs reacted (see Chapter 1, Interfaces and interaction). As the mechanism for achieving their aims, commissioners use some selection and variants of the commissioning methods listed in Chapter 1, Health and care (and see Chapter 4, Commissioner and voluntary, community and social enterprise aims). From the VCSEs’ standpoint, becoming commissioned is a mechanism for achieving the outcomes that they seek (see Chapter 1, Voluntary, community and social enterprises in health and care and Chapter 4, Commissioner and voluntary, community and social enterprise aims), for which VCSEs will use their own distinctive working practices, governance structures, and external relationships. However, these two CMOCs intersect, as Figure 3 shows. Commissioners’ and VCSEs’ interactions during the commissioning cycle constitute a common mechanism that both parties use. We therefore require a study design that will identify separately the respective aims (intended outcomes) of either party; the common, intersecting mechanisms (both intraorganisational and interorganisational) which both parties think will achieve them and therefore use; how each party uses these mechanisms; the actual effects for each party separately; and what contexts these effects depend upon. Similar reasoning applies to co-commissioning. How each organisation acts and reacts depends on its ACAP, so the study design also required methods for describing ACAP, its development and effects. This reasoning implies making the relationship and interactions between VCSE and commissioner the research focus and the unit of analysis or ‘case’ when explaining the commissioning of VCSEs.
Because multiple components and methods were required to research these complex relationships, the study contained five work packages:
-
Preliminary scoping work with national-level NHS and VCSEs to identify important current developments in this domain and likely data sources (late 2019 to mid 2020).
-
A cross-sectional profile of CCG spending on VCSEs, both as a sampling frame for the three following work packages and as a source of data about patterns of VCSE commissioning (late 2019 to mid 2020).
-
Using findings from the preceding work packages, we drew a maximum-variety sample of places primarily in terms of the proportion of CCG spending of VCSEs [secondary sampling criteria are reported below (see Chapter 3, Sampling strategy: site selection criteria and methods)], and systematically compared case studies of VCSE–commissioner collaboration in formulating local commissioning strategies across all providers (‘co-commissioning’) in them (late 2020 to summer 2022). The aims of their commissioning activities, and the corresponding outcomes, were examined separately for the commissioners and the VCSEs. The structures and activities through which they interacted were examined in common.
-
A systematic comparison of case studies of the co-commissioning of VCSEs (late 2020 to summer 2022).
-
A group of action learning interventions (late 2020 to early 2023) and a survey of ACAP.
The third and fourth of these were analytically distinct and addressed different research questions but used the same research design, study sites and methods. Table 3 shows which work packages contributed to answering which research question.
| Research question | Work package(s) |
|---|---|
| RQ1: How do healthcare commissioners address the task of commissioning VCSEs as service providers, and what barriers do they face? |
|
| RQ2: What are the consequences for VCSEs, of the public bodies commissioning services from them? |
|
| RQ3: How are VCSEs involved in CCG, LA and other (e.g. ICS, NHSE) commissioning decisions? |
|
| RQ4. What ACAPs do healthcare commissioners and VCSEs, respectively, need for enabling VSCEs to be commissioned and for co-commissioning? |
|
In combination, these mixed methods were synergistic. Our methods for synthesising them (see Chapter 3, Synthesising the findings) yielded a systematic overview of the commissioning of VCSEs as a whole (see Figure 3).
The sampling method (explained below), the cross-sectional spending profile and the national-level components of the action learning research work package provide means of checking the generalisability of findings. As Figures 9 and 10 in Chapter 5, Fiscal constraints show, these sites were well distributed across the range of levels of CCG funding and across the range of sizes of budget increases.
Preliminary scoping
Scoping work yielded a preliminary classification of the kinds of VCSE commissioning and co-commissioning relationships likely to be found in the wider study. Following Project Oversight Group (POG; see Chapter 3, Patient and public involvement and engagement) advice, we identified and interviewed 16 key informants from VCSEs, VCSE networks and national health and care bodies in late 2019 and early 2020, and consulted published policy statements and guidance, position papers (e.g. Carers Support Centre, NHS Choices provider lists, National Council for Voluntary Organisations), and rapportage (see Table 5). The interviews used a semistructured interview schedule (see Appendix 1) whose open questions included a final question asking what other relevant topics, if any, the interview had not so far covered. We piloted the interview schedule with two VCSE members. The interviews were recorded and professionally transcribed. Later, the transcript contents were coded into the framework described below (see Chapter 3, Synthesising the findings) to enable automated searching in common with the other data sets when we synthesised findings across the work packages. Meantime we analysed the contents thematically (inductively)154 in order to identify the main ways and locations in which commissioners and VCSEs interacted, what objectives each pursued, and what issues and problems arose; and so produce some categorisations and initial middle-range theories about variations in the commissioning of VCSEs.
As explained below, later work packages used the findings to:
-
indicate criteria for selecting a maximum-variety sample of sites for the case studies and action learning
-
contribute to developing the project’s analytic frameworks
-
contribute to the final data synthesis
Cross-sectional profile of Clinical Commissioning Group spending on voluntary, community and social enterprises
Design
This cross-sectional census of CCG spending on VCSEs proceeded in four steps (further details in Appendix 5, data in the project’s GitHub data repository155):
-
Extract data from CCG ‘Expenditure over threshold’ accounts We harvested 689,536 records from 189 of the 195 CCGs extant in 2018–9. Data for four CCGs could not be obtained or made machine-readable. Data for two further CCGs appeared unreliable. Following HM Treasury guidance156 the accounts all included details on: (1) CCG name, (2) expense area, (3) expense type, (4) provider name and (5) amount. Treasury guidance required public bodies to report all transactions over £25k, although many accounts include invoices for smaller amounts. To ensure comparability between CCGs, only invoices ≥ £25k were used.
-
Obtain information about providers The ‘expense type’ field often referred to ‘voluntary’, ‘not-for-profit’ and other categorisations, but this was neither comprehensive nor reliable. For information on providers it was thus necessary to link provider names with Companies House (CH) and CC registers, and search their public-facing websites. Care Quality Commission (CQC) active and inactive registers157 and the NHS Payments to General Practice, England, 2018/19 data set158 were also used to obtain information on care homes and GPs respectively. The search of CH and CC databases was largely automated, using ‘fuzzy matching’ techniques to deal with the variation of names used in the accounts (trading names, acronyms and contractions, misspellings, etc.) but the search for, and of, provider websites was entirely manual.
-
Classify providers as VCSE, NHS/LA organisations or other NHS and LA providers were identified on the basis of name (n = 538 and 212, respectively), as were government and service providers (e.g. police and fire and rescue services). The legal status of providers given in the CH and CC registers was then used to classify non-NHS/LA providers as VCSE or otherwise. Additional information was obtained from providers’ own websites.
-
Quantifying VCSE activity at CCG level VCSE activity can be expressed in a number of ways (VCSEs’ share of invoices, providers or spend, or per capita VCSE spending in different CCGs), although to ensure comparability across all CCGs, all methods must include only spending > £25k. The denominator can most usefully be defined using:
-
all invoices except redacted personal health budgets, or
-
all invoices except personal health budget and NHS/LA spending.
-
The design was limited by difficulties linking providers as named in the accounts with those in the CH/CC registers. It is inevitable that automated fuzzy matching and subsequent manual follow-up will have missed, or indeed misidentified, some providers on the registers. Moreover, the approach cannot capture:
-
VCSE activity subcontracted via other providers (which our fieldwork suggested does occur)
-
NHS money reaching VCSEs via LAs (probably a larger amount).
Data collection
The www.data.gov.uk website and all CCG websites were searched and the relevant accounts were downloaded. Despite the 2013 guidance, freedom of information (FoI) requests then had to be sent to 106 of the 195 CCGs: 12 because no accounts were publicly available, 11 because one or more of the monthly accounts were missing, corrupted or referred to the wrong CCG, and 83 because the data, contrary to the guidance, were in the .pdf (portable document format) file format and could not be reliably converted into machine-readable numeric data. Mostly the FoI process was straightforward, but 17 requests were rejected and a formal follow-up was needed. By March 2020 four CCGs had still not provided useable data. With the arrival of the COVID-19 pandemic, we stopped pursuing our FoI requests, leaving us with data for 191 of the 195 CCGs (see Appendix 5, Table 11).
Preliminary data cleaning resulted in the exclusion of one CCG whose accounts were badly out of line with the most recent available NHSE CCG consolidated accounts,159 respectively, covering only 20.8% and 47.5% of total spending.
Using PowerShell® (Microsoft Corporation, Redmond, WA, USA) and R Statistics (The R Foundation for Statistical Computing, Vienna, Austria), we amalgamated and aggregated the monthly accounts for the final set of 189 CCGs, extracted all invoices > £25k, and identified unique providers. The resulting data set comprised 226,138 invoices capturing £70.525B (representing 97.7% of all spending recorded in the accounts) and listing 10,930 named, and around 10,592 unique, providers.
Providers not categorised as NHS organisations, LAs or government organisations were then used to seed automated ‘fuzzy matching’ algorithms to search the CH register (using its application programming interface) and downloaded CC databases. Any providers not yet identified were then subject to a manual search for public-facing websites. In some cases this revealed CH/CC registration numbers, which were then followed up. In other cases explicit statements were found to the effect that they were ‘not-for-profit’, ‘social enterprise’ or ‘volunteer-led’ organisations. Only 188 (1.8%) providers [receiving just £189.361M (0.3%) of CCG spending] could not be linked to organisational websites or entries in the CC/CH registers. Some 6416 non-NHS/LA organisations could not be found in the CC/CH registers (60.7% of all providers), although these accounted for only 8.6% of total CCG expenditure > £25k.
Data on all invoices and providers, R analytical scripts and outputs are available on our project GitHub,155 with some summary analyses of patterns in Appendix 5, Figures 21–28.
Analysis
From these data we estimated, for each of the 187 CCGs, the proportion of expenditure on contracts worth > £25k on VCSEs during 2018–9. We ranked the CCGs in descending order by this proportion and divided the resulting list into quartiles. This created the sampling frame for study site selection (see Appendix 5, Figures 33 and 34). We also interrogated this list, and the data, to elicit the patterns of CCG use of and spending upon VCSEs, and the patterns of VCSEs contracts reported in Chapter 6, On mission or mission drift?.
Systematic comparison of case studies of co-commissioning and the commissioning of voluntary, community and social enterprises
These work packages used the same study sites, data and analytic frameworks, so we report their common methods together.
Sampling strategy: site selection criteria and methods
Since the research questions and theoretical framing of the study suggest making the relationship and interactions between VCSE and commissioner the research focus and unit of analysis or ‘case’, our sampling strategy was to select case study sites which, together, seemed likely to provide a maximum variety of commissioner–VCSE relationships. In theoretical terms, such a sample was the most likely to show a range of modes of commissioning VCSEs, commissioning contexts and outcomes.
The scoping work suggested that the dimensions of variation in commissioning relationships included:
-
The proportion of VCSE-provided services in each site. The larger that proportion, the greater the likely extent, complexity, variety and sophistication of commissioning relationships between commissioners and VCSEs.
-
The size of VCSEs involved, ranging through national VCSEs with local branches, large single local VCSEs (e.g. some hospices), and VCSEs which struggle to win contracts at all. One would expect all these VCSEs to differ in bargaining power and resources, especially access to specialised bidding expertise, and ACAP.
-
How long-standing the commissioning relationships are, because mutual trust and working relationships, and the concomitant skills, take time to develop.
-
Which organisations were involved in commissioning, and which ones interacted with which. The scoping work suggested that the main patterns were:
-
One commissioner commissions one VCSE, for example when a CCG or an NHS Trust subcontracts a VCSE: a simple bilateral relationship.
-
Multiple commissioners collaboratively commission a VCSE, for example an NHS body transfers a budget to a LA (perhaps its public health department) which then commissions a VCSE.
-
One commissioner commissions an intermediary which then subcontracts or makes grants to further VCSEs.
-
Multiple commissioners collaboratively commission an intermediary which then coordinates further VCSEs.
-
Key local VCSEs advise or are consulted by one or more commissioners. The VCSEs involved may or may not then be commissioned by the commissioner(s) which consulted them.
-
Our sampling therefore proceeded through three stages. First we selected tracer activities likely to show maximum variety in types of VCSE activity, in case such differences affected how VCSEs were commissioned, and the consequences. Since it was impractical to study the entire range of VCSE activities (see Chapter 1, Voluntary, community and social enterprises in health and care), we took three tracer care groups as a maximum-variety sample of these differences, on the following assumptions:
-
Social prescribing This is a tracer with many fragmented, diverse, often small VCSEs, largely providing preventive activities usually requiring only modest resources and considerable self-help. Only relatively recently (post 2010) has the NHS commissioned such activities on a substantial scale (although many of these VCSEs and their activities pre-dated that). We therefore assumed that these VCSEs may be less accomplished than older, larger VCSEs in commissioning-related monitoring, evaluation and research.
-
End-of-life care, especially hospices This tracer covers larger-scale, more medicalised, intense and often inpatient care, and care provision rather than self-help. Its small range of specialist VCSEs are publicly commissioned, predominantly but not exclusively by the NHS, but have substantial other sources of funding.
-
Services for people with learning disability This tracer contains public, proprietary and corporate providers besides VCSEs. The latter are predominantly but not exclusively LA commissioned, although joint commissioning is also common. They serve a mixture of home, residential care and inpatient care settings.
These tracers thus provided opportunities to contrast VSCEs of different sizes, ages, and health system functions (prevention, self-management, formal care); and different mixes of contracts and funding sources, hence different degrees of dependence on commissioners. Some organisations and services (e.g. for learning disability, hospices) which cater for children and young people among others were likely to be included, but not those which exclusively served children or young people.
Next, as a proxy for how large a proportion of services VCSEs provided in each site, we selected a sample of study sites with maximum variety in size of expenditure on commissioning VCSE activity (see Appendix 5, Figure 7), on the assumption that such a selection was likely to reveal wide variety in commissioner–VCSE relationships and interactions. When this study started, CCGs were the main NHS commissioners of VCSEs. As explained (see Chapter 3, Cross-sectional profile of Clinical Commissioning Group spending on voluntary, community and social enterprises: Analysis), we ranked CCGs by their spending (on invoices > £25k) on voluntary and not-for-profit providers during 2018–9 as a percentage by value of all their spending on transactions of £25k or more (see Appendix 5, Figure 31). We divided the list into quartiles and invited the POG – whose membership consisted of experts in the field, VCSE and NHSE representatives – to produce for each quartile a shortlist of sites most likely to have the variety of commissioning relationships suitable for the study. Table 4 (sites anonymised) shows how, for the shortlist of sites that the POG suggested, this distribution across quartiles was sensitive to how ‘scale of CCG commissioning of VCSEs’ is defined.
| CCG | Total VCSE expenditure | Per transaction VCSE expenditure | % of transactions with VCSEs | % of transaction value (£) with VCSEs | Number of VCSE providers | % of providers that are VCSEs | % of value of transactions > £25k with VCSEs |
|---|---|---|---|---|---|---|---|
| A | 4 | 3 | 3 | 2 | 4 | 2 | 2 |
| B | 2 | 2 | 3 | 2 | 1 | 1 | 2 |
| C | 1 | 1 | 4 | 1 | 4 | 3 | 1 |
| Da | 4 | 4 | 2 | 3 | 1 | 1 | 4a |
| E | 3 | 3 | 1 | 2 | 1 | 2 | 2 |
| Fb | 3 | 3 | 2 | 3 | 1 | 1 | 2b |
| Ga | 2 | 2 | 3 | 1 | 1 | 2 | 1a |
| H | 4 | 4 | 1 | 3 | 1 | 1 | 3 |
| Ia | 1 | 1 | 1 | 1 | 1 | 1 | 1a |
| J | 1 | 1 | 3 | 1 | 3 | 3 | 1 |
| Ka | 2 | 2 | 4 | 3 | 2 | 3 | 3a |
| L | 2 | 2 | 1 | 2 | 2 | 2 | 2 |
| Mb | 1 | 3 | 1 | 2 | 2 | 1 | 3b |
| Na | 3 | 3 | 2 | 3 | 1 | 1 | 2a |
| Oa | 2 | 3 | 3 | 3 | 1 | 4 | 4a |
We selected sites by the criterion of total value of transactions rather than percentage or number of VCSE providers. Most CCGs commissioned many VCSEs but only a few NHS Trusts and, in some cases, corporations, so non-VCSE providers would make up only a small proportion of the number of providers, and one unlikely to vary much across CCGs. Having decided to select by value of activity, not numbers of VCSEs commissioned, we selected by the criterion ‘% of value of transactions > £25k that are VCSEs’ on the assumption that a percentage would differentiate sites where the weight of VCSEs within overall commissioning varied, abstracting from the absolute size of expenditure of VCSEs.
On this basis, we selected two sites (see Table 4) from each quartile, checking the resulting sample with the POG for balance in terms of geographic spread, inner-city, suburban and rural sites, ethnic variation, population size, socioeconomic diversity (characteristics likely to affect the availability, size, range and character of VCSEs160,161), party political control of the LA, and the availability of volunteers. We also checked that the sites covered the range of commissioning relationships found in the preliminary scoping work. For two sites, CCG mergers occurred as we were selecting our sample. There, we continued with the new CCG containing the originally selected site. A final, practical consideration was site access. One site in the second quartile was in London. As other researchers have found, the volume of their day-to-day work and organisational ‘churn’ (reorganisations; staff turnover), and then the COVID-19 pandemic, made it practically impossible during 2020–1 to gain research access there. The other site was a large provincial city which, while its CCGs were being restructured, lacked a working research governance body. This left us with an accessible sample of one site per quartile plus one more in the upper and one more in the lower quartile, making six sites in all.
In each site, we sampled individual informants, and thus their organisations, by starting with a CCG manager responsible for commissioning VCSEs, and on the VCSE side, the coordinator (or equivalent) of the infrastructure body which coordinated the VCSEs’ joint interactions with commissioners (there was at least one such body in every site: see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks). We paid the infrastructure bodies an honorarium in recognition of their help in arranging research access. From these we snowballed to further informants. We attempted to interview one commissioning and one VCSE informant for each tracer in each site. In practice the numbers of interviews and interviewees varied between sites and between tracer groups due to differences in the scale, complexity, and configuration of the tracer services. In each site, far fewer organisations provided end-of-life care than learning disability support or, still more, social prescribing. Learning disability services were in some sites predominantly provided by a small number of organisations but elsewhere more numerous smaller providers. The extent of separate versus collaborative NHS and LA commissioning, and the division of commissioning roles, differed, and commissioners gave us wider access to informants in some sites than others. In CS1b and CS4b we could not access a commissioner of end-of-life care, nor in CS1b a commissioner of learning disability support services (see Table 5).
| Tracer | End of life | Learning disability | Social prescribing | Cross-tracer | Totals | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Site | C | VCSE | C | VCSE | C | VCSE | C | VCSE | C | VCSE | Total |
| 1a | 1 | 4 | 2 | 8 | 3 | 5 | 6 | 5 | 12 | 22 | 34 |
| 1b | 0 | 1 | 0 | 3 | 1 | 2 | 4 | 4 | 5 | 10 | 15 |
| 2b | 1 | 2 | 2 | 3 | 1 | 4 | 8 | 8 | 12 | 17 | 29 |
| 3b | 2 | 1 | 2 | 3 | 3 | 8 | 3 | 3 | 10 | 15 | 25 |
| 4a | 1 | 5 | 1 | 4 | 2 | 5 | 5 | 5 | 11 | 19 | 30 |
| 4b | 0 | 3 | 3 | 2 | 2 | 2 | 1 | 1 | 7 | 8 | 15 |
| National | 0 | 1 | 1 | 2 | 0 | 2 | 8 | 8 | 3 | 13 | 16 |
| Total | 5 | 17 | 11 | 25 | 12 | 28 | 32 | 34 | 60 | 104 | 164 |
A majority of informants were at ‘Place’ (CCG) level, where most of the commissioning of VCSEs, especially for our tracer groups, occurred. However, we also interviewed respondents at ‘system’ (ICS) and ‘neighbourhood’ levels, and reinterviewed nine as their roles changed. The VCSE informants were often either the Chief Executive or a senior management team member, but also included operational managers of a commissioned service within the VCSE. National-level informants on the VCSE side included two academic experts. From commissioning organisations [LAs, CCGs, ICSs, primary care networks (PCNs) and NHS Trusts] we interviewed a mix of strategic and operational commissioners. We found that the people responsible for commissioning the VCSEs for our tracer groups as often had a general management background as one in front-line service provision, and still less a clinical background.
Data collection
We interviewed these informants using a semistructured schedule (see Appendix 2) which we piloted, then modified, with members of the POG. We used it as an omnibus questionnaire, emphasising in each interview the components most relevant to the informant’s role and considering what data we already had, including any ambiguities or apparent contradictions. We included informants’ accounts of how other organisations worked, but only if they were speaking from recent first-hand experience and observation. The interviews varied in duration from 20 to 107 minutes. One was undertaken with a British Sign Language interpreter as the informant was deaf. Four interviews involved two participants, and five were with small groups of respondents. Because of COVID-19 lockdowns, we interviewed informants mostly by videoconference; there seems, however, no a priori reason to expect this to have biased the data collection. Where we could triangulate such data against documents and data collected face to face, we found no evidence that videoconferencing yielded substantively different reports from informants than face-to-face data collection. With consent, all interviews were recorded and professionally transcribed. Participants were asked at interview if they would like to receive a copy of their interview transcript to check for accuracy, but none did. We obtained administrative documents (e.g. the end-of-life commissioning strategy) that these informants described as germane to commissioning in their site. In a similar way, we identified relevant commissioning meetings and observed those whose participants were willing, and took field notes. We observed forums and meetings between commissioners and VCSEs, including learning disability partnership and end-of-life care commissioning board meetings, social prescribing forums, and health and care partnership working meetings. Much of this observational data collection occurred during the development of ICSs and the COVID pandemic. Additional data were obtained both from e-mails and conversations while managing site access, and from subsequent ad hoc enquiries. Further data were collected as a by-product of the action learning (see below). We continued data collection until theoretical saturation; that is, until additional data were no longer yielding any new explanations of how the commissioning of VCSEs worked, its consequences and outcomes. The use of multiple sources enabled not only fuller data collection but also data triangulation when the data were analysed.
Data analysis
For ease of analysis, we did not yet anonymise the data and coded them into a coding frame (see Appendix 3, Table 9) based on the double-CMOC schema in Figure 3. To elaborate that framework, we began with inductive coding. Reusing whenever possible our informants’ terms and language, we developed a list of first-order codes related to commissioners’ and VCSEs’ strategies, actions, resources and ACAPs. When populating the framework with data revealed any gaps or apparent contradictions in the data, we undertook further checking, data collection or triangulation. Applying the methods of Gioia et al.,162 and in light of known health and care system characteristics, purchasers’ strategies and actions, and earlier research (see Chapter 1), we inductively translated the first-order codes into aggregated second-order codes. This resulted in the categorisation which shapes the results sections, and which contained those health and care system characteristics that directly influenced the different purchasing strategies and actions. In terms of purchaser strategies and actions, we also searched for goals, plans, and intended or emergent actions. 163,164 We developed case descriptions for each study site to enhance our understanding of commissioning there. Through this coding process and case analysis, and discussions among the researchers, we linked the different health and care system characteristics with the purchasers’ strategies and actions.
Each major block in the coding frame included an ‘other’ category for data that did not fit into the elaborated framework and hence might suggest findings or patterns which we had not originally anticipated. To pilot the coding frame, the researchers independently coded six transcripts, compared coding, and removed discrepancies by agreeing the definition and interpretation of each initially ambiguous code. Appendix 3, Table 9 is the resulting coding frame. To store the data electronically and populate the coding frame, we used qualitative data management software (NVivo; QSR International Pty Ltd, Warrington, UK).
Using the elaborated framework, we thematically analysed the patterns in the data. First we made a within-case analysis of the findings for each study site, then consulted the respective local project reference group (see Chapter 3, Design) to check the face validity of these findings for each site. Next we systematically compared the sites to find similarities and differences between them. As explained above, we analysed data about commissioners’ aims in commissioning VCSEs (intended outcomes, the nature of what they commissioned, the modes of commissioning and media of power that they used, and their ACAPs or lack of them) separately from the corresponding data about VCSE aims, activities to be commissioned, media of power and ACAPs and their absence. We made a common, single analysis of the intersecting mechanisms (see Figure 3) and any other structures where VCSEs and interacted, and for the contexts which potentiated or weakened their operation. We separately analysed the outcomes for commissioners, VCSEs and any affected third parties. To check the face validity of the findings from this cross-case analysis, we consulted our national action learning workshops and the POG (see Chapter 3, Design).
Action learning and absorptive capacity
Design
Using action learning methods165,166 as a means of organisational learning,145 this work package sought to generate insights on how the commissioning process with VSCEs can be practically improved (RQ4), in particular by increasing VCSEs’ and commissioners’ capacity to use evidence for commissioning purposes and VCSEs’ ability to bid credibly for health and care commissions. This extended case method167 (i.e. extending the two case study work packages during 2020–3) used three action learning methods in parallel:
-
In each site, a local research project reference group was established with the dual aim of shaping the research and learning from the emerging findings. Each group brought together a mix of commissioners (CCG and LA) and VCSEs. It advised the researchers, reviewed emerging project findings, used them to identify implications and areas of developmental activity for their own organisations and networks, and provided a neutral space for strengthening relationships between VCSEs and commissioners. Each group met at least three times. As fieldwork was conducted during the pandemic, all six local project reference groups met online. At the participants’ request, we added to those initially planned a workshop on NHS commissioning practice and structures. To facilitate cross-site networking and learning, we held four national action learning workshops, inviting all participants from all the local project reference groups. Three were held online, focusing on sharing emerging findings from the study, exploring how far they resonated with respondents, what they felt the implications were, and what actions they might take in response. The final, face-to-face, workshop focused on formulating the implications of, and producing practical impacts from, the project findings.
-
Our local project reference groups nominated co-researchers of both genders, with an age range from young adult to retired, and one researcher from a minority ethnic group from local VCSEs in five of our six case study sites (mainly local infrastructure bodies, but also front-line organisations). Each of the 16 co-researchers took part in a series of research development workshops and they were then supported to undertake small-scale research projects aimed at mobilising knowledge and evidence in support of their organisation’s commissioning-related activities. In the event, 9 of the co-researchers completed their projects, and all 16 used their insights to shape the wider study. In mentoring these co-researchers, we emphasised falsificationist methods168 (explicitly checking for evidence against their initial interpretations and conclusions) and fieldwork techniques such as interviewing, and explained cognitive bias (e.g. availability, confirmation and reporting biases). 169
-
Our conceptualisation of VCSE commissioning (see Chapter 1, Interfaces and interaction) suggested how ACAP facilitates the commissioning of VCSEs. We therefore made an initial exploratory survey of commissioners’ and VSCEs’ ACAP; that is, the values, skills, behaviours and knowledge mobilisation practices relevant to bidding, commissioning and co-commissioning. The questions followed the phases of ACAP development (from acquisition to assimilation, transformation) to respondents’ reports of how satisfied they were with the outcomes of their organisation’s activity and with its collaborations. The survey instrument (see Appendix 4) explored the ACAP of individual organisations and of the networks linking commissioners and VCSEs (see Figure 5). It was distributed online. Findings were discussed within the local project reference groups.
In these ways, this work package and the researchers were research intermediaries151 stimulating knowledge mobilisation by certain key evidence users. These activities together suggested some development needs, for evidence use and knowledge mobilisation, in the study site organisations.
Sample
We used the same sample of sites as in the case studies:
-
We invited all interviewees to join their local project reference group (hence also the national action learning workshops). This ensured a mix of VCSEs and commissioners. Excluding researchers, the numbers attending each group varied from 7 to 13.
-
The co-researchers were all from VCSEs. Invitations to become co-researchers were issued to VCSEs via the local project reference groups. We had initially intended to work with one co-researcher from each case study site but given the enthusiastic response to our invitations in all but one of our case study sites, and as all activities had moved online (due to the pandemic), reducing the costs associated with supporting additional participants, we decided to include all who expressed an interest: 16 participants, from 12 VCSEs across five case study sites. Each participating organisation received an honorarium to compensate for their members’ time commitment to the study.
-
The ACAP survey used the same five case study sites as the other action learning activities (in CS1b, site access was granted too late for a scoping survey to be undertaken contemporaneously with the other sites). The local project reference group members and co-researchers were the initial respondents, from whom they then snowballed to others. The recruitment method was intended to achieve a maximum qualitative variation in the ranges of respondents rather than to be a randomised representative sample of the individual commissioners and VCSE members in each study site, but it meant that we could not know how many questionnaires were distributed (the response rate denominator). The 131 responses came more from VCSEs (108 responses, 82% of the responses) than commissioners (23 responses, 18%), across five study sites. The responses covered all the tracers and the infrastructure bodies, and both commissioners and VCSEs, in all the sites surveyed. Of the 18 commissioner respondents who specified what organisation they worked for, most (11) were LA commissioners, 3 each were from CCGs and local care partnerships, and 1 was from a PCN. Apart from the absence of one study site, the intended qualitative variety of respondents was thus achieved.
Data collection
We collected the following data:
-
Because no measure of ACAP for VCSEs existed for the preliminary survey to use, we began by producing such an instrument (see Appendix 4), starting from the work of Currie et al.,141 itself building upon earlier studies of small and medium-sized enterprises, and corporations. 148,150,170 First we combined the items about knowledge acquisition, assimilation, transformation and exploitation from Flatten’s questionnaire150 with those about socialisation, systems and coordination capabilities from Currie’s. 141 We removed duplications and terms only relevant to corporations (e.g. ‘our company’, ‘our business’) or to industrial production (e.g. ‘prototype’, ‘technology’). We paraphrased the remaining items to cover volunteers besides employees and knowledge transfer between organisations. Our co-researchers reviewed and amended successive drafts. The survey instrument combined tick-box lists [respondents could tick any response(s) applicable to them], Likert scales (with a verbal description of what each point on the scale represented) and free-text questions.
-
Participant observations, recorded in field notes, of 18 local research project reference group (6 sites × 3 groups), 4 national action learning events and attendance at numerous forums and meetings between commissioners and VCSE organisations in each case study site.
-
Co-researchers’ enquiries and project outputs, including ad hoc enquires and discussions as each project proceeded.
Together, these methods were intended to collect data from VCSEs about what capacities commissioners require for constructive collaboration with VCSE providers and, reciprocally, what capacities VCSEs require from commissioners and for co-commissioning; and what competences, capacities and other support VCSEs have to acquire, in order to bid more successfully and then evidence their contributions to it.
Data analysis
The survey data were analysed to compare commissioner and VCSE profiles across the four successive ACAP phases (knowledge acquisition, assimilation, transformation, exploitation). The Likert scale responses were scored between 1.0 and 5.0 depending on what verbal response the respondent chose. To summarise the scores, we took the mean for each scale, which thus also had a possible range of 1.0–5.0 with 3.0 as the mid-point. A lower score meant stronger agreement. Because of the exploratory, qualitative sampling strategy, we only made simple descriptive comparisons of the scales. Formal statistical analysis would have overinterpreted the data. We thematically analysed the free-text responses.
Synthesising the findings
Table 6 summarises the combination of component data sets (each more fully reported above) from which answers to the research questions were synthesised.
| Data set | Contents |
|---|---|
| Preliminary scoping | Advisory meeting with POG; 16 interviews; 58 policy and position papers; 37 items of rapportage |
| CCG profile of spending on CCGs | Documents: 692,659 invoices; extracts from CH, CC and CQC databases; 102 FoI requests |
| Co-commissioning and commissioning case studies | 173 interviews, observations at forums/meetings between commissioners and VCSEs (plus the above policy and position papers and rapportage) |
| Action learning and ACAP | 131 exploratory survey responses; 18 local project advisory group meetings; 4 national action learning events; 6 cross-site meetings for co-researchers across all the study sites; 1 stakeholder dissemination event |
| Secondary data | 360 peer-reviewed papers; 36 grey research reports |
The secondary data were used (unevenly) across all four work packages, as were the policy documents and rapportage, both attributed to the scoping study which for most of these data sources saw their first use.
A first stage in synthesising the findings was to analyse and produce intermediate findings from the separated work packages, as reported above. To pool the interview data, we coded those from the preliminary scoping study in the same way as the case study data. We first made within-case analyses and shared each of them with the respective local project reference group for verification before doing the cross-case analysis. The next stage was to combine findings from the work packages. For this we used a framework analysis,171,172 with the dual CMOC schema in Figure 3 as its organising framework. Onto it we mapped the codes of the coding frame first developed for the case studies (see above). In effect, the method for collating the data sets was logically equivalent to a tabulation with one virtual row (and its sub-rows) for each component of Figure 3, and one virtual column for each work package. Mapping the exploratory and case study data onto this virtual table was largely automated. We then manually added the findings from the CCG spending profile and action learning work packages. From each virtual row, we then noted any general patterns found in the collated data, and any exceptions, gaps and ambiguities. Again we retained an ‘other’ category for data that did not fit into the final framework. These supernumerary data were then analysed inductively to reveal additional patterns in them. We then compared all the findings synergistically with the initial programme theory outlined in Figure 3, so as to operationalise empirically the meaning of its broader terms (e.g. ‘contexts affecting how actors use or modify quasi-market structures’) and test empirically whether, how, and under what conditions the generative mechanisms in it worked.
As Table 2 (see Chapter 2, Research questions) shows, each research question corresponded to specific elements in the dual CMOC schema of the commissioning of VCSEs (see Figure 3). This correspondence enabled us to map findings about each element and relationship in the dual CMOC onto the relevant research question, and so answer them. To these answers were added further findings, largely from the ‘other’ data categories mentioned above, which also appeared relevant to the working of the dual CMOC and thus the commissioning of VCSEs and the corresponding two-sided programme theory, but went beyond our original research questions. By these methods, we formulated findings in ways that are generalisable, empirically (with due caution, particularly noting the contexts on which they depend) by means of qualitative generalisation173 and theoretically, in that explanations of mechanisms, contexts and outcomes are middle-range theories that are formulated to apply to qualitatively similar mechanisms and contexts elsewhere. 127
In presenting our findings, we use labels like ‘(CS1a_C5a)’ or ‘(CS4a_V6a)’ to label data extracts. ‘CS’ means ‘case study’; the number 1–4 shows which sampling quartile that site was in, followed by ‘a’ or ‘b’ to identify the site itself; the second ‘C’ in the ‘_C5a’ (or equivalent) shows that this informant was a commissioner, ‘V’ that they were from a VCSE; ‘NSS’ means a national-level stakeholder. Labels such as ‘(ID 13403829701)’ refer to ACAP survey responses. To prevent repetition, we write ‘and CS1b …’ or ‘also CS1b …’ when essentially similar findings recurred across sites.
Patient and public involvement and engagement
Patient and public involvement and engagement (PPIE) occurred through a POG established to oversee the general course of the study and offer advice and guidance, and through the local project reference groups, national action learning workshops, and co-researchers (see Chapter 3, Action learning and absorptive capacity). The POG’s aims were to:
-
help embed patient and public involvement throughout the study
-
check that the research was completed on time and as agreed with the National Institute for Health and Care Research (NIHR)
-
provide advice on all aspects of the project
-
act as advocates for the project
-
help identify and address potential issues for consideration in the research
-
act as a sounding board for emerging research findings
-
contribute to the identification of implications and recommendations
-
advise on outputs, dissemination and impact activities
-
support the research through facilitating access to networks of contacts
Accordingly, the POG comprised representatives from statutory health and care organisations, academia, the VCSE and general public. It had 12 members and was chaired by the CEO of National Voices, a coalition of VCSE health and care organisations working to strengthen the voice of people in health and care. It met six times, five of them online due to the pandemic, and was invited to the final national action learning workshop. Its practical influences on study design and implementation are reported above. The local project reference groups (see Chapter 3, Action learning and absorptive capacity) and co-research activities secured additional public involvement: the participants were from commissioning (NHS and LA) and VCSE organisations (front-line and infrastructure) in each study site. Through these activities, participants both shaped the research at local and national level and were able to verify, comment upon, and learn from its emerging findings. In these extensive PPIE activities, we aimed to ensure diversity of VCSE and commissioning experiences and perspectives (qualitative rather than demographic or statistical representativeness). As outlined above, we worked closely with key stakeholders from national and local NHS, LA and VCSE infrastructure bodies to identify potential participants for each of the groups, from whom we snowballed participants to fill any apparent gaps in the breadth of coverage. The local project reference groups, co-researchers and action learning work were a further important contributor to PPIE for this project. Fuller details are given above (see Chapter 3, Action learning and absorptive capacity).
Chapter 4 Findings: aims, activities, mechanisms
This chapter explains what the parties to the commissioning of VCSEs aimed to achieve by it, then how they used two main mechanisms for those purposes. One was the quasi-market structures, and specifically the commissioning cycle, which together constituted a commodified mode of commissioning. Second, supplementing and modifying them was a set of networks, some recent and others pre-dating the quasi-market, which constituted a collaborative mode of commissioning.
Commissioner and voluntary, community and social enterprise aims
Commissioner aims
National Health Service commissioners’ prime responsibility was to implement national policies and guidance (see Chapter 1, Health and care); that of the LA commissioners was to implement their councils’ decisions and, again, national policies and guidance, albeit a somewhat different set than for the NHS commissioners. Statutes and regulations also mandated certain aims of commissioning, including end-of-life care being provided in conformity with CQC standards, and some learning disability support services (e.g. individual advocacy through the Care Act). Also mandated, although less strictly and narrowly, was the commissioning of further activities (e.g. social prescribing) addressing health inequalities. Commissioning other activities and services was discretionary. Even if these mandates were not aims that they would otherwise have adopted, commissioners nevertheless had to pursue them and, insofar as VCSEs appeared able to contribute, to commission VCSEs. Indeed, increasing VCSE contributions was itself a current policy (see Chapter 1, Health and care). VCSEs’ potential contribution was apparent where:
[T]hey deliver some of the statutory services we’re meant to [commission] around mental health, as well as all those additional things that we don’t necessarily commission but are of high value to their local community
CS1a_C5a
However, commissioners also perceived the limits of VCSEs:
[T]he third sector often and rightly don’t provide the things directly that help us to meet our statutory duties. We can’t just commission the third sector to provide an extra A&E so that we don’t have the waiting times or whatever, or cancer services.
CS1a_C1a
Not only were VCSEs unable to provide such services but NHS commissioners had long-standing, embedded relationships with local NHS Trusts, the greater part of commissioner payments to whom could not be easily or quickly altered, being to that extent also non-discretionary.
Fiscal austerity was a major policy-based aim:
[B]ecause of the financial situation for the NHS over a number of years and local authority, public sector generally, the focus really when you’re making procurement and commissioning decisions, it’s always about the bottom line.
CS4b_C7a
Obviously, austerity constrained commissioners’ decisions about co-commissioning, what to commission and provider selection (see Chapter 4, Deciding what to commission and Provider selection), and motivated commissioners to commission VCSE projects which offered the prospect of reducing, or at least postponing, demand for NHS services.
To these policy aims, commissioners added their own reasons for commissioning VCSEs. VCSEs appeared to have expertise and knowledge about inequalities and the SDoH in local communities:
[T]he third sector have got so much expertise in that area both in terms of knowledge of local populations, but also in many cases being the providers of some of that care and support as well
CS1a_C3a
and to reach into those communities, with:
significant capacity to be able to build trust and work with people long term in a way that statutory organisations don’t.
CS1b_C7a
Consequently, VCSEs could also channel, or proxy, service users’ and communities’ voices:
They give that kind of voice of the people that they work with in all the communities they serve. Especially for those kind of marginalised third sector organisations because again they are all kind of seldom-heard voices and are totally disempowered to feel they’ve got any ability to speak up. I think that’s what the third sector do really well.
CS1a_C11a, also CS1b
Voluntary, community and social enterprises also offered the ability to link and coordinate different parts of the system for both individual service users and organisations, for example to increase the uptake of regular health checks by people with a learning disability (CS1a, CS1b, CS4b).
Commissioners believed that for provided care or those preventive care activities that social prescribing gives access to:
I see the VCSE as being much more flexible. Much more responsive. Creative in their thinking. I’ve commissioned VCSE sector to do a number of things over the last four or five years and they get stuff up and running.
CS4b_C3a
For example, VCSEs lacked the organisational boundaries between, say, learning disability and other mental health teams that some NHS Trusts were reported to have (CS1a). Responsiveness included getting ‘providers to deliver more personalised care’ (CS1a_C3a, also CS2b, CS4b), which was an NHSE policy priority. Some commissioners thought that VCSEs also seemed better adapted to prevention and self-care activity than NHS services were:
the NHS quite often [. . .] we’ll see a need, we’ll go, ‘Oh no, people are really lonely’, so we’ll commission befriending services [. . .] let’s put people back into the community rather than trying to hold them in commissioned health services.
CS4a_C4a
Commissioners also believed that commissioning VCSEs added social value insofar as they employed local people and created opportunities to develop community-based activities. More pragmatically, commissioners saw VCSEs as providing additional capacity, and value for money, both important under austerity conditions:
[M]ore recently with the financial constraints on the local authority obviously there’s a move towards working more closely with the voluntary sector in terms of needing to – well, for two reasons – one is partly the cost-effectiveness of the voluntary sector but the other one is because the formal care sector is just in such a crisis with lack of care, lack of staff.
CS2b_C11a
Voluntary, community and social enterprises were:
more creative, they’re more astute with funds. [. . . than] profit-making organisations, [. . .] And then any surplus that they [VCSEs] have is being reinvested and we can see that. And they can clearly demonstrate and articulate how they do that.
CS1b_C4a
Commissioners’ aims were more often expressed in terms of a generalised dependence on, and support for, the VCSE sector rather than in terms of dependence on any particular VCSE, hospices apart.
Voluntary, community and social enterprises’ aims
Voluntary, community and social enterprises’ aims in being commissioned were to pursue their ‘mission’ to improve provision and outcomes for the patients, carers or other groups. To do so, VCSEs aimed both at influencing local health and care policy and practice and therefore advocacy, and at gaining income that:
improves what they can do with people in their community, then of course they’ll [VCSEs] engage with that. [. . .] it’s not just so I’m making it better for people who I’m working with, but making it better for the system as a whole. [. . .] So if I can get funding through that [commissioning] route, it saves me having to get 50 people to run a half marathon or to do a lottery bid or to do whatever else.
NSS_NS13V
Voluntary, community and social enterprises supporting people with learning disability emphasised cross-sectoral activity:
Mission? It’s all about supporting people with learning disabilities and autism to be independent, to live their best lives.[. . .] We see ourselves as straddling social care, going across into health and well-being, but also going across into education as well.
CS1a_V14; also CS3b
Some of these VCSEs added helping prepare people with learning disability for employment (CS1b) and parenthood, and activities such as art, sport, drama and gardening and other social prescribing (CS1b, CS3b, CS4a). Many added advocacy for individuals (CS1a, CS1b, CS2b, CS4b).
Certain VCSE informants prioritised influence and challenging the system through commissioning relationships above funding:
I think there’s organisations often, and some of the smaller ones, just see it being about money and it being about income. And I don’t think it is; I think it’s about position, and positioning yourselves into those areas where you can influence.
CS4a_V6a
Voluntary, community and social enterprises thus saw influence, advocacy and money together as enabling them to ensure better outcomes for service users, and ultimately contribute to their ability to fulfil their mission. Of these, advocacy was the more fundamental in the sense that VCSEs would continue that activity even if being commissioned failed to give them influence or money.
Quasi-market mechanisms for commissioning voluntary, community and social enterprises
According to the default policy assumptions about how NHS commissioners would commission providers (originally framed with NHS Trusts and later corporations in mind), commissioners and VCSEs would pursue their respective aims through the commissioning cycle with its common, intersecting four-stage commissioning mechanism (see Chapter 1, Health and care and Commissioning voluntary, community and social enterprises and Figure 3). These stages were: needs assessment, the basis for deciding what VCSEs should be commissioned to do; selecting which VCSEs would do so; negotiating an agreement and payment with the VCSE(s) chosen as provider(s); and, afterwards, evaluating what the VCSE(s) did. The last step provided feedback by which either side might re-evaluate their aims, and if both parties wished, the cycle would repeat. The simplest prototype of this cycle was bilateral commissioning between one commissioner and one VCSE, or in some cases (e.g. CS1a, CS3b, CS4a) the commissioner who paid most of the costs on behalf of a second commissioner as well as itself. Within each commissioner, parallel commissioning cycles occurred: ‘There is quite a lot of silos in terms of commissioning and procurement with the voluntary sector’ (CS4a_C1a, and CS1a, CS3b). Even bilateral commissioning was implemented somewhat differently across our study sites. As we shall see (see Chapter 4, Shift to networking and Commissioners and voluntary, community and social enterprises interacting through a network of networks), the default policy assumptions also differed from the practice of commissioning VCSEs.
Deciding what to commission
National policy apart, commissioners’ other priorities and projects for commissioning VCSEs were also ‘very much commissioner-led’ (CS4a_V6a). The opening step in the default policy model of a commissioning cycle was to make a needs assessment and negotiate what kinds and quantities of activity VCSEs might be commissioned to undertake. At this stage, VCSEs gave expert advice about particular care groups, bringing them and commissioners closer towards co-designing (‘co-producing’) services, for example for blind people and deaf people (CS4a), palliative care (CS1a), advocacy (CS2b), mental health (CS1a, CS1b), independent living support (CS1a,CS3b), or learning disability and autism (CS1a). We heard mixed reports about how much influence VCSEs therefore had on what activities were commissioned. One commissioner asserted that:
from a local authority point of view, we’ve always worked really closely with providers of all shapes and sizes from the voluntary sector and from the private sector when we’re designing what services should look like. I wouldn’t go as far as to say it’s always co-production but it’s an attempt.
CS1b_C1a
Collectively, VCSEs did not always speak with one voice and make a ‘coherent offer to the statutory sector’:
There are multiple organisations that are charities or from the voluntary sector and they don’t always talk with one voice. So it’s difficult for commissioners to communicate with the sector and it’s difficult to hear back or engage with the sector and to hear common messages.
CS4b_C2a
Later findings suggest possible reasons. At one pole, VCSE informants made such comments as:
[I]f they [commissioners] are paying for a specific [learning disability support] service, we should try and do that specific service in the way that they’re asking us to do it [. . .] and not just say, ‘Well, this works in this area so we want to do this’.
CS4b_V6a
Against this,
I [VCSE member] don’t have very much to do with the CCG. [. . .] they say things about how important it is to partner with the VCSE and stuff, but I don’t get the sense that on the ground [. . .] that’s lived out. So they might say it but you don’t see it.
CS2b_V14a
Some VCSEs were isolated from networks linking commissioners and VCSEs (see Chapter 4, Networking between voluntary, community and social enterprises). VCSEs sometimes competed (see Chapter 4, Provider selection), and different VCSEs might simply be the voices of different groups, interests and aims (cf. Chapter 1, Voluntary, community and social enterprises in health and care).
Given commissioners’ wide view of VCSEs’ potential, what VCSEs were commissioned to do varied. Most often, VCSEs were commissioned to provide specific services, but both commissioners and VCSEs suggested that the VCSEs’ role should not be reduced to that:
I really want to get away from the idea of if you look at a person, ‘Oh if they’re in supported living they can go to day services five days a week’, and it’s one size fits all, you just look at the person and actually start to look at what services are out there and shoehorn them into whatever’s available.
CS3b_C9a
Those who articulated what VCSEs contributed to health and care frequently said that VCSEs were not ‘replacing hips’ or ‘providing widgets’:
[G]overnment likes buying widgets, because you can point to what you’ve bought and you can say, ‘This is what it did’ [. . .] Whereas what my members are doing is working with communities and saying, ‘What do people need? What’s required here?’ and then they’re doing that bottom up, which is a fundamentally different approach.
NS13V_I; also CS1a
As noted above (see Chapter 4, Voluntary, community and social enterprises aims), VCSEs often sought to be advocates and influencers as much as, and in some cases rather than, service providers.
Attempting to move beyond service-based approaches and reflecting national policy (see Chapter 1, Health and care), commissioners were increasingly looking towards commissioning for outcomes (generally; not only for VCSEs). This change had considerable implications for the role of commissioners:
So my role now is around how do I bring bits of the system together to work collectively for outcomes? And we’re just starting to form what we think those outcomes will be with partners and then the new structure of the boards will want to gain assurance of all the programmes underneath and to check whether we are achieving our outcomes using the metrics.
CS1a_C11a, and CS4b
Designing metrics appeared to increase commissioners’ need to collaborate with, rather than dictate to, VCSEs, albeit for the purpose of ensuring commissioner scrutiny of VCSEs:
[T]hey’re the experts and let them design an intervention or a service or whatever it is the way that they think will get the best outcomes [. . .] just as long as the outcomes are there, I don’t really care.
CS3b_C8a; and CS1a, CS4a
However, many VCSE activities were ‘not transactional type services, they’re messy and woolly, they don’t have clear outcomes, it’s really hard to specify [key performance indicators]’ (NSS_NS10A). Then, a different approach was to commission VCSEs to maintain a certain capacity to provide care or other activities:
[O]ur exec. recently agreed to provide a grant to our local voluntary bodies through the coordinating organisation, to help support them with the cost of living and energy and fuel prices. So I think we’re very keen to retain the voluntary sector as an active part of service delivery, and I think that sends a really strong message to those organisations that we feel they’re a long-term partner and want them to be part of that discussion going forward.
CS1b_C4a, and CS2b, CS3b
This was particularly the case when both parties understood that the commissioner was not paying the full cost of a service (see Chapter 4, Quasi-market mechanisms for commissioning voluntary, community and social enterprises and Chapter 6, Outcomes and consequences for voluntary, community and social enterprises). Finally, some VCSEs were commissioned purely to provide advocacy for local groups of patients, carers or other interest groups, others to provide the network infrastructure described below (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks).
Their experience using performance indicators and targets (and evidence-based medicine, in the NHS) nevertheless predisposed commissioners to seek specific, preferably quantified, activities or outcomes from commissioning a VCSE.
[W]hat we did ensure is that clearly it was outcomes-based, we did need organisations to evidence [. . .] how they would add value and how they would deliver the service and what that service would look like.
CS1a_C10a; and CS4a, CS4b
Some VCSEs valued ‘soft’ local intelligence more:
[T]hey [commissioners] recognise there’s a need based on statistics, rather than people’s stories, thoughts, feelings and what actually matters locally and they go with a top-down method, ‘This is a need, we need to do this, let’s pay someone to do it’.
CS4a_V4a
Voluntary, community and social enterprises also valued flexibility in the plans:
[B]ecause we know things change, I mean God, the last two years [2019–21] has taught us that, hasn’t it, so things that you might need to do to deliver a health outcome or an improvement for someone could shift, could easily shift.
CS1b_v10a, also CS1b
For commissioners, the result of these needs assessment activities was an indicative list or ‘mandate’ of intended activities. In CS3b the components of hospice services were ranked in order of necessity (as the commissioner judged it), starting with those that the NHS would have to commission at full cost if the VCSE did not exist, then its support services such as physiotherapy and social work, and ‘spiritual care’ (CS3b_V11a). Site CS1a commissioners set up an internal bidding system by which to select the VCSE activities to commission. Fiscal austerity always constrained what could be commissioned. Such lists were sometimes adjusted later as opportunities and budgets appeared, but they were the basis of agreements with the VCSE.
Provider selection
A first provider selection decision was whether to commission a VCSE instead of a publicly owned, corporate or proprietary provider. The largest (by value) providers to English CCGs were NHS Trusts and LAs, which undertook the bulk of clinical, mental health and community service activity and accounted for 83.3% of all 2018–9 expenditure by way of invoices over £25k although, as Figure 4 shows, this varied substantially between CCGs: from only 52.7% and 57.3% in two CCGs to over 90% in seven CCGs. In one CCG, for instance, two CICs and a community benefit society accounted for 24.7% of all CCG expenditure. These contracts were largely for community health services, a wide range of activities, unlike the more specific activities of many VCSEs (e.g. supporting domestic violence survivors). In East Staffordshire, meanwhile, Virgin Care Services received 30.9% of CCG spending but that was short-lived as following a contractual dispute the Midlands Partnership NHS Foundation Trust took those services over in 2020. The resulting shifts in provider ownership (from corporate to NHS or vice versa), and the background churn in ownership structures which is common in corporate health care,94 show not only how the commissioning landscape changed after the 2018–9 data (from 195 CCGs to 42 ICSs by July 2022) but how, in some localities, the provider landscape did too.
FIGURE 4.
Distribution of proportions of CCG > £25k spend to LAs and NHS Trusts.
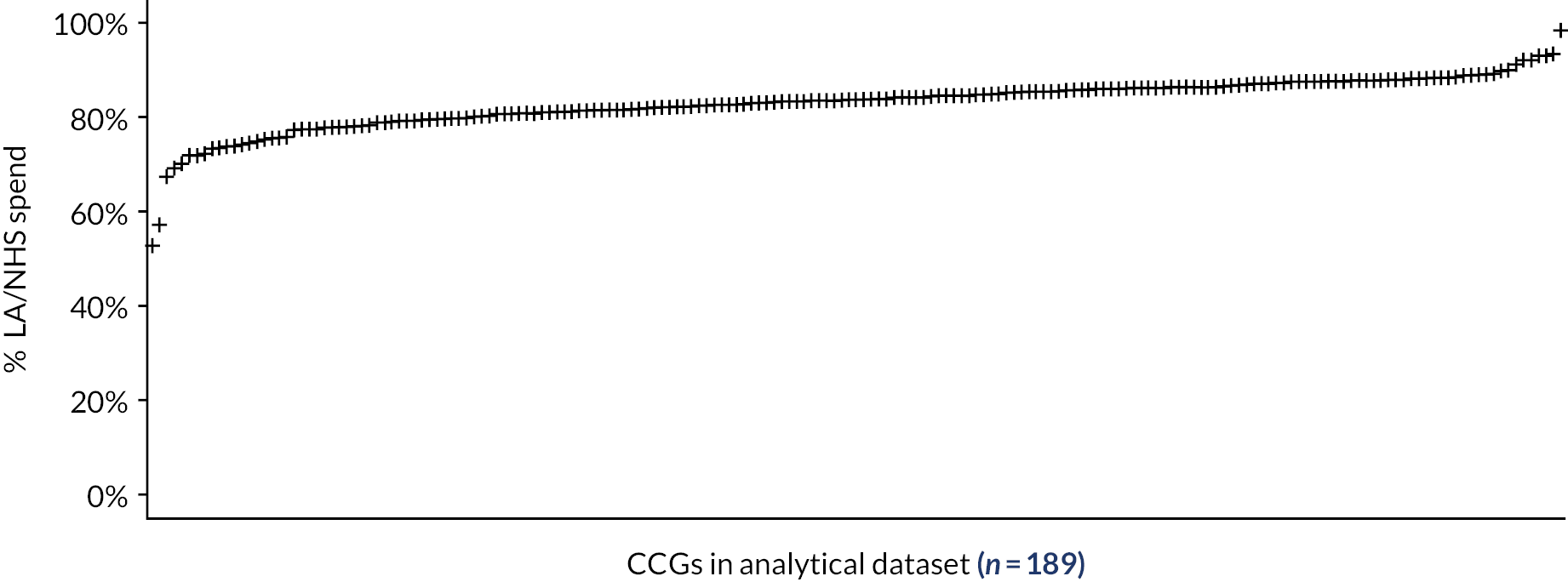
The proportion of non-NHS/LA spending directed to VCSEs also varied hugely between CCGs: from 69.2% and 68.3% in Greater Huddersfield and North East Lincolnshire respectively, to ˂ 1% in three CCGs. Thus selecting VCSE providers was not always a foregone conclusion. To some VCSEs, it seemed that NHS Trusts were the default choice:
The first port of call is NHS, NHS, NHS, and I have to say what about us? We could help you with this [. . .] they’re not used to working that way, they’re not used to us saying what can we do.
CS4a_V15a
Voluntary, community and social enterprises might be commissioned as a complement (not substitute) for NHS providers, for example ‘because we now have that understanding at that kind of granular level of how much more effective it is if district nursing is working in partnership with third sector organisations more’. (CS1a_C4a). Some commissioners regarded VCSEs just as further independent providers, ones who happened to be third sector rather than corporate. As a commissioner of learning disability services put it:
[G]enerally, we’re focused on what outcomes we need to achieve and at what value for money, and I’m not really bothered whether that’s private, voluntary sector or in-house.
CS4b_C2
As noted, even commissioners who clearly distinguished the two often thought more in terms of supporting the VCSE sector as a whole through commissioning than of selecting any particular VCSE (hospices were the exception, there being few or even just one per study site).
As for which VCSEs were commissioned, both commissioners and VCSEs noted competitive tensions and rivalry between VCSEs (e.g. sites CS2b, CS4b), although it varied across sites due to local historical commissioning practices and decision-making. Its main manifestation was that VCSEs became guarded about sharing information or practical ideas immediately before, and at, the bidding stage in the commissioning cycle. Fiscal austerity intensified VCSEs’ competition for funding (reported in CS1b) and made provider selection price-sensitive: ‘Local authorities want to create and design solutions to put them out to the market, and while they say “We’re not just interested in the lowest bidder”, that tends inevitably to be the case’ (CS4b_C6a). At least one commissioner encouraged competition because ‘there are going to be providers out there who will have specialist skills that our current providers don’t necessarily have’ (CS4b_C3a). In learning disability support, there nevertheless was extensive ‘cooperative and partnership-based’ working between VCSEs, attributed partly to historical collaboration and the learning disability partnership boards which brought providers together. Hospices typically worked in their own locality and often collaborated, although they still competed in public fundraising, and there was some competition between local hospices and national providers. With their name recognition, large or confederated VCSEs (e.g. Age UK) often had an advantage over small local VCSEs.
Procurement regulations raised problems for VCSEs. One was exposure to corporate competition. Commissioners often told us the procurement regulations required that
we shouldn’t treat organisations differently based on the fact that they’re from one sector or another. I would say we were probably willing to give third sector organisations more support in terms of managing contracts and that sort of thing. It’s difficult to provide that at the procurement stage because that would be treading on the regulations somewhat.
CS1a_C12a
Indeed, there have been legal disputes about commissioning processes, although none about the chosen type of provider (e.g. VCSE vs. corporate). 53,174 Some commissioner informants said that VCSEs (NSS_NS14V, CS2b) feared that the procurement regulations might enable corporations to displace VCSEs:
[B]ecause we still have regulation requirements to do with value, it’s again whether we could attract larger organisations into the city who might not have the same values as the third sector to come in and take those contracts on.
CS1a_C11a
On a strict interpretation of the regulations, VCSEs could either participate in formulating the service specifications put to bidders, or bid to provide the specified activities, but not both. Then ‘as a direct consequence of that, I am prevented, as being a provider, from being involved in health service development of specifications’ (CS3a_V1a). Commissioners would sometimes issue tenders without prior discussion with VCSEs (CS1b, CS3b) or without much time for bidding. But where there had been discussion, procurement rules could then stop the co-producing VCSEs bidding for the contract. Thus:
if you give your intellectual property freely, in a process of co-design, you then are almost de facto excluded from being able to then participate in that work going forward. [. . .] I’m talking about the system here, steal, they steal their [VCSEs’] ideas, they put them into their contracts and then they screw those whose ideas started there in the first place.
CS2b_V1a
In some but not all study sites, commissioners also reportedly made it difficult for consortia or partnerships of VCSEs to bid for services collaboratively. Apparently these commissioners extended the assumptions that there must be a conflict of interest between commissioners and potentially commissioned providers from the commissioning of corporate providers into the commissioning of VCSEs, although this difficulty was attenuated if providers presented themselves as consortia from the start of the commissioning cycle.
Commissioner informants gave examples of how procurement systems limited their scope to commission small local VCSEs, but also often described workarounds, for example using Section 256 agreements, transferring NHS money to the LA or using open procurement selectively, to ensure local VCSEs were commissioned. For VCSEs that commissioners felt they worked well with, repeated competitive tendering appeared counterproductive:
I have seen things improve, for example [VCSE name], that was a full tender process, we had to do it every year, and now what they’ve done is, actually we don’t want competition. We want to work with partners. So it’s now a grant process, which is very different.
CS3b_V7a; and CS1b, CS4a
Then, a workaround to avoid competition was that ‘after a soft market exercise which nobody else applied for, were given the [advocacy work] contract without having to go through a very rigorous process’ (CS1a_V8a). Another way was to keep contract values below the level that necessitated open competitive tendering. Commissioners could also offer grants rather than contracts. Yet another, in learning disability services, was that ‘the commercial team and the county council also look at the social value in terms of our procurement approaches, etc., and that goes a long way to helping the voluntary sector as well’ (CS4b_C2).
Sudden announcements of short-term funding, especially on the NHS side, created the tight deadlines for the provider selection and agreement and payment stages of the commissioning cycle. For speed, commissioners would often reuse any previous specifications and calls for bids, making only minor adjustments. VCSEs responded in kind by reusing a previous bid with minor changes.
Agreements and payments
Perhaps the most common forms of VCSE contract were fixed-sum block contracts and cost-and-volume contracts which supplemented a block payment with per-patient payments for additional clients over the ‘block’ amount (CS1a, CS1b), because:
blocks give the provider an ability to run the service regardless of the number of patients [. . .] quite often if you said, ‘We’re going to pay you on a price per patient coming through your door’ they would fall over immediately because you cannot sustain staff if you don’t have the income.
CS1b_C3a
A variant was to supplement block contracts with ad hoc spot purchases, which were not prepriced and so were used to increase the average per-client payment to the VCSE (CS1a, CS3b). These payments had the advantage for VCSEs of being quick and flexible, but were also unpredictable, and often came without risk and other assessments for the placement (CS1a, CS2b).
Often, especially for learning disability support, these per-client payments were spot contracts or commissioner-managed personal budget payments because ‘they [commissioners] just haven’t got the money any more, so they’re really looking at [. . .] everybody’s plans of how many hours each person is using [. . .] Each person will just be on an individual level’ (CS1a_V12a, also CS2b). However, parents of children with learning disability did not necessarily want individual budgets:
[W]hen they [commissioner] went to parents and asked them what they wanted, they couldn’t bear the idea because they knew they were going to have to do all the admin. And they’re just too worn out [. . .]. They wanted to just be able to bring the child along and leave them for a few hours and then come and pick them up.
CS3b_V13a
When personalised budgets were agreed in principle, we still found examples of VCSE negotiating about the
transfer of risk in terms of demand risk from the local authority to ourselves and we’re in the process of negotiating that with them to make sure [. . .] Some of the certainties that we had in block contract, we are keen to make sure that we cover those off.
CS1a_V21a
Spot contracts rather than grants were often used when a learning disability client needed additional support urgently. Hospices typically received around 30–40% of their funding from statutory bodies. Grants dominated, although contracts were sometimes used. NHS tariffs [Healthcare Resource Groups (HRGs)] covered few hospice activities and when they did, ‘[T]he tariff structure is risky for a hospice because of our overhead base, and you just need low occupancy for whatever reason’ (CS4b_V2a). Tariffs thus placed the financial risk of low referrals with the VCSE and that of high referrals with the NHS commissioner, but (supposing the tariffs were accurately priced) reduced the scope for commissioners to pay far below the cost of providing those services. Social prescribing had a mix of grants and contracts and made extensive use of competitive tendering. The low levels of mutual resource dependency between commissioners and VCSEs made provider contestability (provider competition and replacement) a theoretically feasible medium of commissioner power, but in practice it did not occur. Neither, beyond the limited extent described above, did payment for performance. 175
Often grants were conditional on the VCSE providing specified activities, making them little different to a block contract. One, for instance, ‘says what we agree to provide for the funding that we receive and that is paid as a lump sum upfront at the start of the financial year’ (CS1a_V17a; and CS4a). Such specifications were recognised as ‘unofficial’ (CS1a_C6a). Other uses of grants were to maintain capacity and continuity to cover unforeseen ad hoc activity, for example in response to COVID-19. Grants were also used (CS1b, CS3b) to pay for activities which were hard to specify in advance, such as representation or advocacy, knowledge, capacity or community development (although not social prescribing), and where patient flow was unpredictable. However, this same indefiniteness made a minority of VCSEs favour contracts instead: ‘our funding should be more commercially based on what we’re delivering, rather than the haggling and negotiations that have gone on over the last 20 years, which is really what it is based on’ (CS1a_V5b). Except for the large payments to hospices, grants were generally small by commissioning standards. Awarding grants for several years gave commissioners more time for needs assessment (see Chapter 4, Deciding what to commission).
Commissioners were tending to issue fewer, larger contracts. ‘[I]n part that’s driven by the commissioners because they can’t deal with the multiplicity of small contracts… smaller organisations find it difficult to be part of that’ (CS1a_V3a; and CS1b_C7a). There were also fiscal and policy reasons:
[C]ommissioners say, ‘but, we’ve only got this much budget to play with. We need to find a system that accommodates the whole county. We need consistency with how it’s monitored and evaluated’ and then they come to the conclusion that then it can only be a county-wide service, rather than a local service.
CS4a_V4a
A consequence was a tendency towards market concentration on the VCSE side, by restricting bidding to the few VCSEs large enough to bid credibly:
[A] contract for eye services was given to [large national VCSE] and then we’re just a little bit tagged on the end because they don’t want to give us our own commissioned contract, they want to do it through a bigger organisation.
CS4a_V18a; also CS1b, CS1a
One way to avoid this scenario while still minimising transaction work was to use a standard ‘framework’ contract with VCSEs:
The framework approach from the county council has developed over the last two or three years and worked quite successfully to encourage the more specialist providers at a local level who really work with those different communities to be able to bid for contracts, not put everything into one big contract.
CS4a_C1a
We thus had conflicting accounts about whether aggregating contracts encouraged VCSEs to bid and work in partnership or instead motivated each VCSE to try bid for, and do, everything itself. An aggregated contract might become large enough to necessitate compulsory competitive procurement, which some commissioners and VCSEs wanted to avoid (see above). Another risk was of particular care groups’ interests becoming submerged within a larger programme:
[T]hey might be a young person’s organisation working in health and it’s been such a battle for them to try and get to be a prime provider [. . .] and part of the reason why they wanted to become a prime organisation is to try and be able to protect the young person’s element of that work.
NSS_NS1V
The same applied to the particular needs of small localities (CS1a, CS1b, CS4a). Learning disability VCSE informants gave conflicting accounts as to whether spot payments or grants gave them greater latitude to innovate.
Monitoring and adjustment
Commissioners’ desires to define commissioned VCSE activity in specific, even quantified, contractual terms or metrics implied equally specific monitoring data and reporting (CS1a, CS2a, CS4b). We found just one instance of a commissioner comparing VCSE activity with its absence:
[W]e had measurable secondary care savings that we had [for] the [VCSE name] cohort of eligible population, but we also had a control group in another part of the city that didn’t have access to the social prescribing intervention at the time.
CS1b_C2a
More usually, monitoring concerned just the focal VCSE and was conducted through regular meetings, informed by routine administrative data [e.g. on occupancy, place of death, falls, etc. for hospices (CS1a, CS4b)], and sometimes supplemented with soft intelligence gained through ad hoc informal discussions (CS1b, CS1a). In the short term at least, these discussions did not seem to affect payment to the VCSE.
Some VCSEs were hardly monitored:
For a lot of them [. . .] no data reporting, very little understanding of the care that’s being provided [. . .] which seems quite strange because the vast majority of hospice care falls under NICE guidelines, it’s regulated by CQC, it’s under the NHS constitution and it’s highly regulated.
NSS_NS2V, and CS4b
Others were only monitored infrequently, one (in CS1b) not for 18 months at the time we interviewed. In the extreme case, ‘we’ve been open seven years and there’s been no official review’ (CS4b_V1a). The requisite data were sometimes lacking. For instance, plotting learning disability referral patterns ‘would require them [commissioner] being able to say how many people with a learning disability had their children taken into care. And I don’t know that they would have that information’ (CS2b_V9). It was questionable how feasible detailed monitoring was at all: ‘the V in voluntary is a big giveaway here that lots of people are not paid. You want us to performance manage that in a spreadsheet?’ (CS3b_C10a). For the less-defined VCSE activities it was ‘difficult to measure impact and outcomes from a small group, you know? And it’s because we want numbers, we want to look at life expectancy or how do we measure? And that’s the great unknown’ (CS3b_C10a). Some VCSE activities had affected other parties besides the VCSEs themselves and commissioners, which posed another complication:
[T]he other thing that we’re working on and haven’t got right yet is [. . .] how we demonstrate the value in a way that we know that it’s not just pounds spent in health [. . .] it might be that the beneficiary is another partner in the system, so we get into all sorts of complexities.
CS4a_C4a
COVID-19 lockdowns of course disrupted face-to-face monitoring meetings.
Yet providing monitoring data could be onerous for VCSEs. For hospices, the NHS monitoring scheme for beds had ‘been quite a lot of work [. . .] hospices had to enter data in a format that the NHS would [put] into a capacity tracker’ (NSS_NS2V) with the opportunity cost, for example, that ‘it’s too much data really, which then reduces the time that they can have with people face to face’ (CS4a_C1a; this was a commissioner’s comment). Commissioners often stated that monitoring should be proportionate: less intensive for a small VCSE than, say, a big hospital. VCSEs interpreted very detailed monitoring as a sign of low trust: ‘[W]e’re more suspicious when we’re asked to provide lots of data’ (CS4b_V2a, and CS4a). So did commissioners:
[R]ather than every six months having to do a review and prove your [VCSE’s] worth, ‘Have you really done what you’d say you’d do?’ [. . .] we just assume that they know what they’re doing. If we’ve commissioned with them and given them a contract, let’s trust that they can do it for more than six months at a time.
CS3b_C8a
Nevertheless, monitoring had practical uses. For one hospice, ‘The NHS needed to know every morning what was the capacity and every evening, what they’d actually delivered [. . .] so GPs could refer into it, so capacity wasn’t wasted’ (NSS_NS2V). In monitoring, too, commissioners could sometimes work around the procurement regulation limitations. For these learning disability support providers, a commissioning manager
wanted to be able to say to some of the residential particularly homes in this area, ‘I think that what you pay people is related to your staff turnover, so tell me what you pay people,’ and his legal team wouldn’t let him do that, but he could [get] publicly available information [. . .]. He started taking that into his monitoring meetings in a kind of, ‘this is all anonymised but let me show you, these people pay 50p an hour more and look at how different they are, talk to me about why you can’t do that because I pay you all the same rates?’
NSS_NS7V
However, monitoring did not always remedy problems:
Another home for people with a learning disability has been closed by CQC, and you just think at what point do commissioners go, ‘No, let’s stop this now’? Because they keep recommissioning, or the company change their name and then come back.
CS2b_V6a
National Health Service commissioners met only about one-third of hospices’ costs and recognised their resource dependency on them, and so might hesitate to change provider (CS1b, NSS_NS14V) even when monitoring exposed problems:
[W]e didn’t want to see the provider fail, we all wanted to see that provider succeed and to address those quality issues [. . .] because we know that people who were in there liked that provider and they wanted to see continuity of the service.
CS1b_C1a
Neither did financial monitoring necessarily bring funding increases:
[P]roviders come to us and they say, we need X to deliver this that we’ve already got a contract for, or it needs to be more. And I think obviously part of the push is to do things within existing resources [. . .]. Especially if we’ve still got high-end spend against particular services and pathways which we know will grow.
CS1a_C11a
Shift to networking
The quasi-market structures (mechanisms) thus embodied a principal–agent relationship,176 with the commissioners paying VCSEs to act as their agents and at their behest:
If you’ve got a piece of work for a group of people with learning disabilities, commissioning used to come to me and say, ‘I’ve got this piece of work, this is how much we’ll pay you, this is what we expect, and go away and do it’.
CS2b_V6a; also CS1a, CS3b
Through the commissioning cycle, commissioner and VCSE use of quasi-market structures varied, firstly, in the degree to which the commissioners unilaterally specified what population needs the commissioned VCSEs should address (see above) or whether VCSE initiatives were also entertained. Some commissioners relied heavily on formal, competitive procurement to select providers; others softened provider competition between VCSEs or worked around it. The ill-defined nature of many VCSE activities and outputs made contracts, in particular the standard NHS contract, often unsuitable for use with VCSEs, so commissioners substituted cost-and-volume or block contracts, or grants. When it occurred, the monitoring of VCSEs relied heavily on dialogue and negotiation but varied in the extent of data-based, standardised comparisons with contract specifications. Often, too, the commissioning cycle was implemented in a messier, patchier way than policy guidance might suggest.
Their attempts to commission VCSEs through quasi-market structures which were originally devised for commissioning NHS Trusts or corporations led many of our commissioner informants to adjust or work around that mechanism. Increasingly, commissioners and VCSEs supplemented and hybridised it with additional commissioning mechanisms based on interorganisational networks, for example to surmount the division between CCGs (who commissioned inpatient care for learning disability) and LAs (community living) (CS3b). Commissioner and VCSE informants each had fairly clear aims (see Chapter 4, Commissioner and voluntary, community and social enterprise aims), but the nearest they came to what realist evaluators would call a programme theory127 of the commissioning of VCSEs was a burgeoning perception that these aims might be more fully served by more collaborative mechanisms,
treating them [VCSEs] as equal players in the system. They are there as a strong alliance which could help us deliver our overall outcomes. We want the people of [place] to live healthier lives and we want to reach the poorest the fastest and improve outcomes. I think by saying that to the sector and saying that you play a crucial role in that, listening to their issues and challenges, and then doing something about it and bringing them onboard alongside, then that’s ultimately how we do it.
CS1a_C11a; also CS4a, CS3b
Additional networked commissioning mechanisms had therefore also developed.
Commissioners and voluntary, community and social enterprises interacting through a network of networks
Although learning disability partnership boards were mandated, these networks had mostly emerged organically for practical reasons [in 1993, for one self-help network for parents of people with learning disability (CS1a)], not from policy mandates, as a negotiated order at the VCSE–commissioner interfaces. Because of their longer involvement with VCSEs, the founding organisation was usually a LA (CS1a, CS3b, CS4a, CS4b, and more erratically CS2b), but CCGs also took an active role (in CS1a, CS4a) including co-funding the network and running subnetworks for specific care groups.
[W]e were talking the other day weren’t we about who gets a seat around the table, I think they were people that we knew in all honesty, to get us started. And organisations where initially they were willing to work with us and one of the reasons [. . .] was [. . .] that increase in referrals would enable them to attract funding from different sources.
CS4a_C6a; also CS1a, CS1b
The networked commissioning mechanisms had three functionally distinct components (Figure 5):
-
horizontal networking through which different commissioners collaborated
-
horizontal networking through which VCSEs who might be commissioned collaborated
-
vertical networking linking groups of commissioners with one or more VCSEs, and vice versa
FIGURE 5.
Three networking patterns.
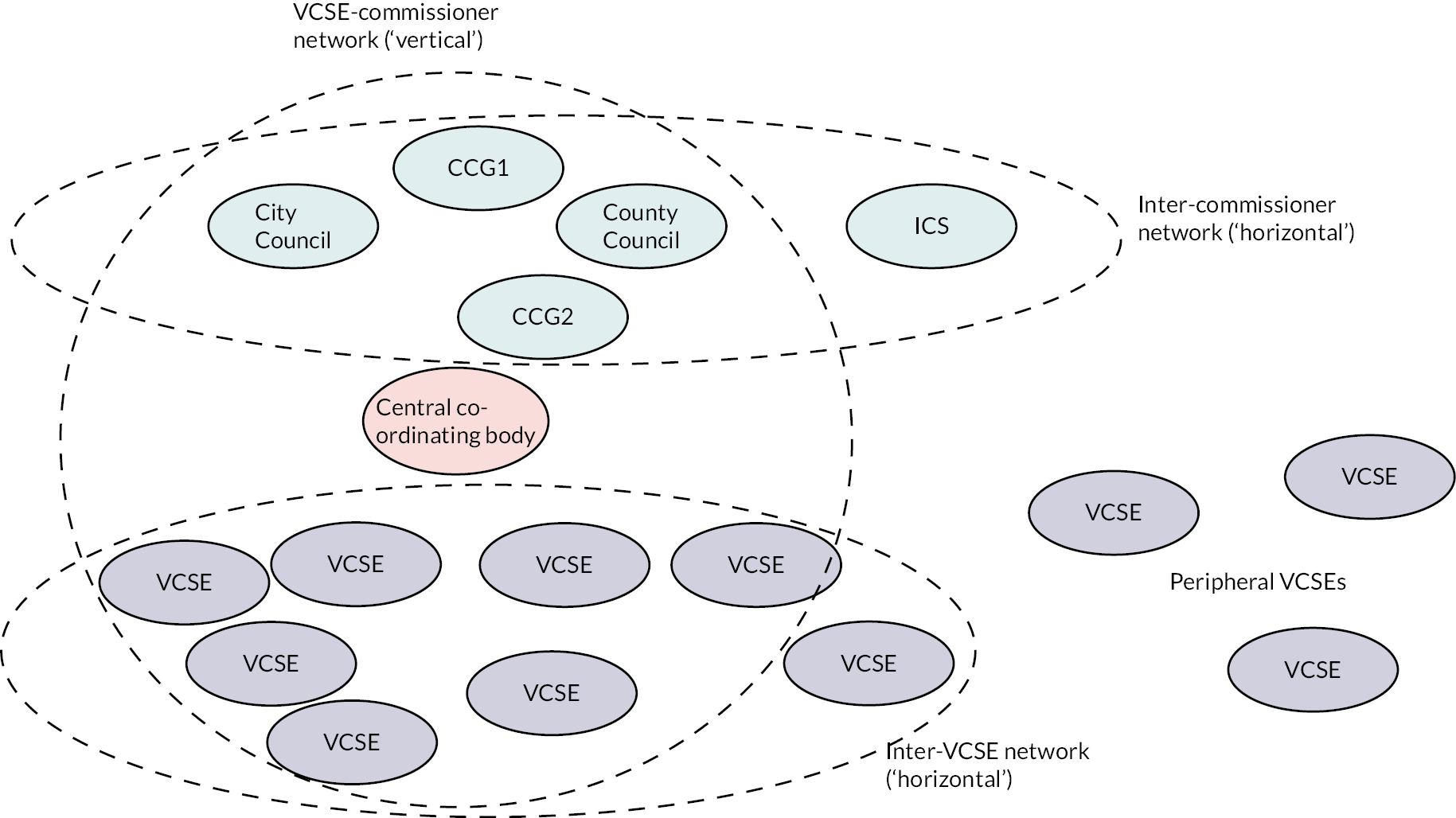
Instead of one commissioner commissioning one VCSE (the classic quasi-market mechanism), a network of commissioners might collaboratively commission one VCSE to provide, say, advocacy (site CS1a), community beds (NSS_NS10A), mental health services (NNS_NS10A), learning disability services (CS3b), or social prescribing (CS4a). Conversely, a single commissioner might commission a network of VCSEs jointly to undertake activities; and finally, a commissioner network might commission a network of VCSEs.
In several sites there was a practical distinction between networking (an interorganisational activity serving one of the functions listed above) and the particular networks (particular coalitions of organisations). In some sites, two or more parallel networks served the same function (e.g. coordinating VCSEs). All had networks which served two or more functions at once (e.g. ‘horizontal’ intercommissioner coordination and ‘vertical’ networked commissioning of VCSEs). In four study sites a single network, centred on one organisation, served all three functions. The other two had several such networks. We therefore describe and analyse the networks in terms of their practical functions: kinds of networking.
Commissioner networking: co-commissioning
A first, ‘horizontal’ type of networking informed and coordinated local commissioners’ commissioning strategy, including shaping the priorities and strategies for commissioning all providers, VCSEs among them. This networking usually involved VCSEs as advisers, consultees, ‘strategic partners’ or indeed advocates for particular care groups, services or activities [e.g. co-production (CS4b), support for young carers (CS3b), deaf people (CS4a), or community hospitals (CS2b)]. For short, we call these activities ‘co-commissioning’.
Many VCSEs had longer-established, denser networking with LA than with NHS commissioners. LA participation involved public health, including health and well-being boards with their own subnetwork of working groups which (e.g. in CS4a) included district councils, the CCG, the police, and NHS Trusts but not, initially, the VCSEs. However, this network (and its equivalents in CS1a and CS3b), did later include VCSE representatives and VCSE service providers. We had mixed reports of how much influence these networks gave VCSEs over local commissioning strategies. In one:
It does feel like the county’s strategy, and it does feel that everyone has contributed. It has been led by the CCG, and they obviously take ownership of it, but it does genuinely feel that we have all contributed to it.
CS4a_V15a
However, national policies governed NHS commissioners’ aims, while councillors sometimes saw their legitimacy as stemming from local democracy:
NHS England can come down with lots of ideas and rules and targets and the council elected members can go, ‘Well we don’t care about that, that’s not what our people in [county] want, so sorry NHS England you have no authority over us, we’re the council’.
CS3b_C8a; and CS2b
In site CS4b
some [elected councillors] members will say ‘you’ve got 70 members, what else do you need? We’ve been elected to give you the answer so why do you need to go and ask all these [VCSE] people?’
CS4b_C5a; also CS1b
During the COVID-19 pandemic, collaboration between the commissioners and VCSEs intensified, with more frequent meetings and other interactions, and faster, more flexible (and larger) allocation of funds (from the commissioners) and resources, especially volunteers, from the VCSEs. After the pandemic, this pattern partly reverted (see Chapter 5, Tracer activity).
Collaboration between the commissioners of VCSEs was effected in many ways: by pooling budgets (although with one commissioner still having lead financial responsibility) (CS1a, CS1b, CS4b), joint posts (CS1a, CS1b, CS2b, NSS_NS10A) [including community nurses (CS3b)], jointly participating in each stage of the commissioning cycle (CS3b), formal agreements between commissioners (CS1b), exchanging guidance documents (CS1b), feeding information into each other’s formal decision-making bodies (CS4b), matched funding [including matching VSCE funding (CS1b)], formulating joint priorities (CS1a, NS_NS10A), informal shared working groups for particular services (CS1a, CS1b, CS2b, CS3b, CS4a), and supporting local forums for discussion with VCSEs and the public (CS2b). We heard one report of pooled budgets money causing disputes between commissioners (in CS3b), but most accounts described constructive, productive collaborations. This variety and distribution of activities indicates that collaboration between commissioners was more than rhetorical.
From 2021 ICSs and PCNs superseded CCGs as the main NHS commissioners. Although national guidance (see Chapter 1, Health and care) mandated ICSs to collaborate with LAs, Healthwatch and VCSEs, many of the latter were initially uncertain how far ICSs would accommodate co-commissioning. ICSs were so large that
the only thing you can commission at that level is probably the ambulance services and tertiary services. The bit in the middle that we do have here, localities, [. . .] those are the geographies you want to commission acute services at.
CS1b_C2
By default, ‘Place’ level was where the commissioning of VCSEs would mainly occur. ICS boards for specific care groups and locality bodies generally included VCSEs, but among many other interested parties. For example, one board for end-of-life care recruited several doctors (including hospital consultants), various NHS and LA managers, the chair of the (pre-existing) palliative care network, a senior nurse and senior VCSE hospice representation. Some of our VCSE informants therefore feared that the ‘statutory-heavy’ (CS2b_V14a) ICSs would marginalise VCSEs, especially if (as in CS4a) the ICB had no VCSE members:
[O]ur whole ICS actually has had very much of an acute trust focus since it set up and, you know, people who are at the influential partnership boards are particularly NHS leaders. And people at the acute and the mental health trust, by and large, not everyone but generally they have worked less with the voluntary and community sector than other people like CCGs.
CS2b_V2a, and CS1a, CS3b
On the VCSE side, too, some bigger VCSEs had from the outset very close relationships with the ICS because they had been able to lobby for that and were able to run services on a larger scale. A VCSE member thought it symptomatic that ‘they’ve [ICS] sent a document with 25 sections in it or whatever, and there are three mentions of VCS, and I don’t quite understand how it’s actually going to happen’ (CS1a_V7a). These uncertainties led at times to ‘tension around the new infrastructure that’s being proposed for this integrated care partnership, because I would have thought that the third sector would prefer this new way… But they do feel hugely threatened’ (NSS_NS10A).
When they did participate in commissioner networks, it was usually unclear whether VCSEs did so as advocates, third sector representatives, or expert advisers. Their potential representative role was widely discussed, but informants were usually sceptical about whether anyone could fulfil it:
I’m a voluntary sector representative but (1) I can’t possibly speak for thousands of voluntary sector organisations and (2) because I am a provider of services, I’ve got a conflict of interest in that as well. [. . .] I do go and try and faithfully represent the sector and report back to sector colleagues about the opportunities and try and create more opportunities for us but inevitably I’ve got half an ear on what the opportunities might be for us as an organisation.
CS3b_V1a, and CS1a, CS2b, CS4a
For example, the absence of minority ethnic organisations was mentioned in CS4a, and that of small VCSEs across study sites. One commissioner response was to consult both the VCSE network coordinating body and, in parallel, individual VCSEs:
VCS infrastructure organisations [. . .] shouldn’t feel that they have to represent the views of the stroke group, or the social prescribing group, or whatever group it is. We would go and then do further work with those groups once we’ve targeted them.
CS4a_C5a
Primary care networks were the other addition to commissioning networks. In CS3b, CS1a, CS4b and CS2b, LAs had already commissioned locality-level bodies [e.g. the Council for Voluntary Service (CVS) in CS2b; in CS4b, two organisations] to coordinate social prescribing activities. On the NHS side, CCGs in CS4b commissioned link workers on behalf of groups of general practices. Sites CS1a, CS1b and CS2b reconfigured the earlier local care partnerships to match the footprint of, and collaborate with, the new PCNs. In CS1a, CS2b, CS3b and CS4a the two kinds of network for commissioning social prescribing therefore coexisted with some linkages between them [e.g. via CVS or practice-level facilitators or link workers (CS4a)]. A partial division of labour developed in CS2b, CS4a and CS4b, with the PCNs concentrating on more directly NHS-related activities. In CS2b and CS4b, some PCNs thought that they should control the social prescribing link workers that they received funding for, since (as they saw it) the NHS was mostly paying for and coordinating those link workers’ activity; in effect, commissioning it.
The shaded area in Figure 6 shows which parts of the common commissioning mechanism the co-commissioning networks affected.
FIGURE 6.
Parts of the common commissioning mechanism affected by co-commissioning networking.
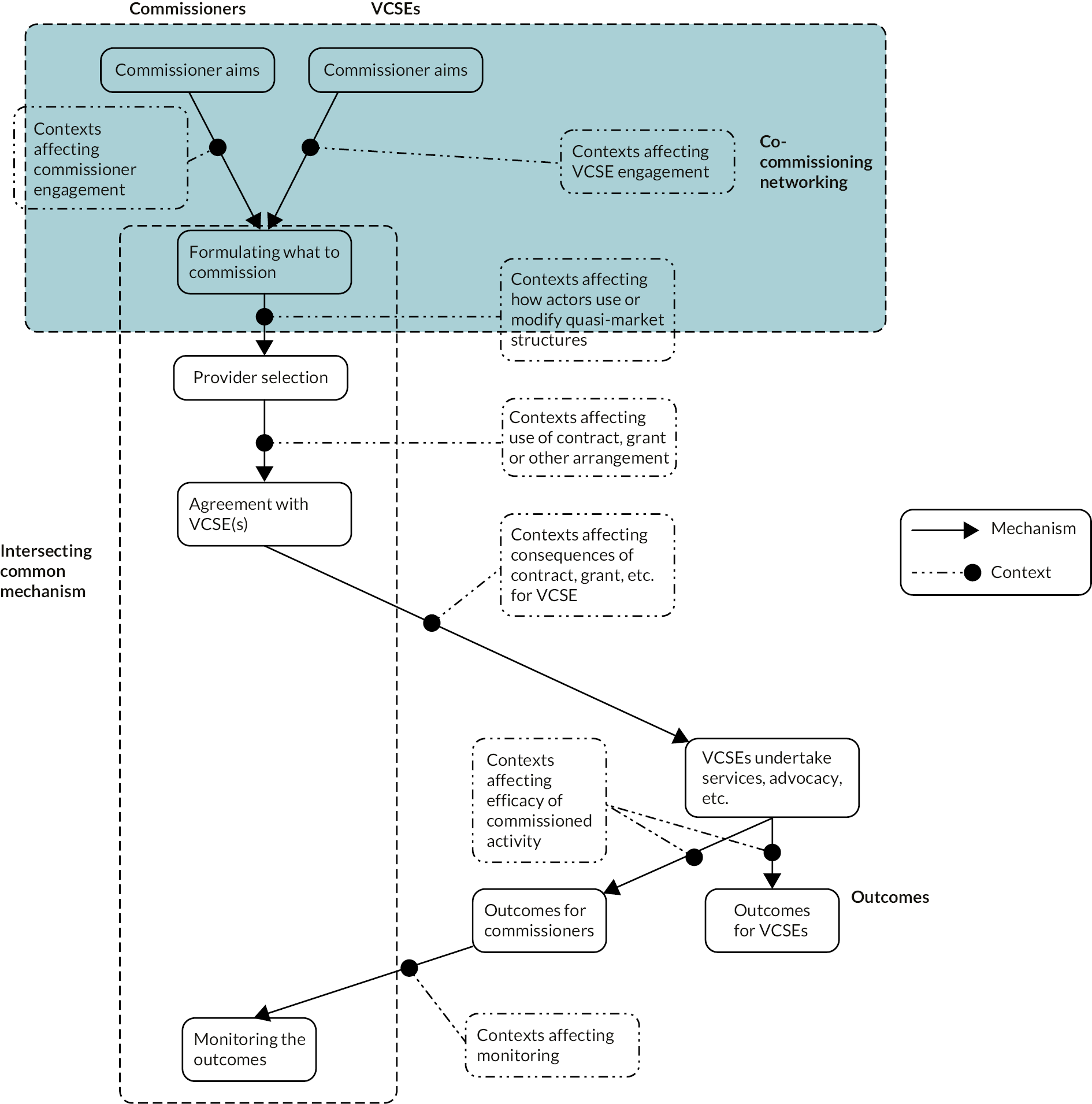
Networking between voluntary, community and social enterprises
Under different names (e.g. ‘infrastructure body’, ‘alliance’, ‘forum’), horizontal networks of VCSEs existed in all sites. Indeed, CS4b had two and CS4a several, including one specifically for small rural VCSEs. This horizontal networking originated among the VCSEs themselves, sometimes developing through multiple changes, but now included LA- and NHS-funded VCSEs.
All sites had a central network coordinating body, itself a VCSE – although one that just coordinated the other VCSEs without providing services itself might lack credibility. While ‘they obviously are in a voluntary and community group [. . .] they don’t deliver services, they’re not on the ground, they’re not embedded in the community’ (CS4a_C2a). One coordinating body (site CS4b) had become a charitable incorporated organisation, as had one for learning disability support in CS1a. These networks and their coordinating bodies were a ready-made route for commissioners to access VCSEs, which was why commissioners in five sites (CS1a, CS1b, CS2b, CS3b, CS4a) helped fund them.
The extent of networking varied from region-wide (CS1b, CS4a) to rural council-wide (CS4a). Some networks focused on a client group or condition [e.g. mental health, unpaid carers (CS2b)], ethnic minority organisations (CS1a, CS3b), religious VCSEs (CS1a), issues such as ‘green social prescribing’ (CS1a) and, everywhere, COVID-19. Indeed, inter-VCSE networking in CS1a arose from the amalgamation of five smaller networks, one of them in turn an amalgamation of smaller mental health and learning disability networks. On occasions a single group acted as a subnetwork of both the VCSE and the commissioner networks. While these inter-VCSE networks were arguably the core of the local third sector, there were also in all sites large peripheries of VCSEs that did not participate – often small VCSEs, including some which were LA- or NHS-commissioned. The periphery often contained many more VCSEs than the active network itself: reportedly 600 versus 30 (CS3b), 400 versus 40 (CS4b). Unlike co-commissioning networking, this networking also involved non-health-related VCSEs. CS4a and CS4b both had participants from other counties.
Network activities included: preparing joint bids to commissioners (CS1a, CS4a); information sharing (CS3b); co-designing activities and holding (CS1a) and administering shared contracts for them (see Chapter 4, Vertical networking between voluntary, community and social enterprises and commissioners) (CS2b, CS3b); capacity-building (CS2b); coordinating joint working across VCSEs (CS4a), such as single points of access to services (CS1a, CS2b); representing VCSEs in the intercommissioner networking described above (see Chapter 4, Commissioner networking: co-commissioning) (CS1a,CS1b), including negotiating the distribution of budget cuts among VCSEs (CS2b, CS3b) and sharing information about learning disability services (CS1a, CS1b). In particular, they tried to reduce bidding competition between VCSEs:
[W]e try and not be too competitive. It tends to be more kind of, ‘Look, we’ve got some funding from funder X; they’re interested in working in these areas. What are our best ideas? What’s our best offer?’ We’ll share them.
CS1a_V9a
This multiplicity of activities was evidence of these horizontal networks playing a substantial practical role in linking VCSEs with commissioners.
Figure 7 shows (shaded) what parts of the common, intersecting commissioning mechanism the inter-VCSE networking affected.
FIGURE 7.
Parts of the common commissioning mechanism affected by networking between VCSEs.
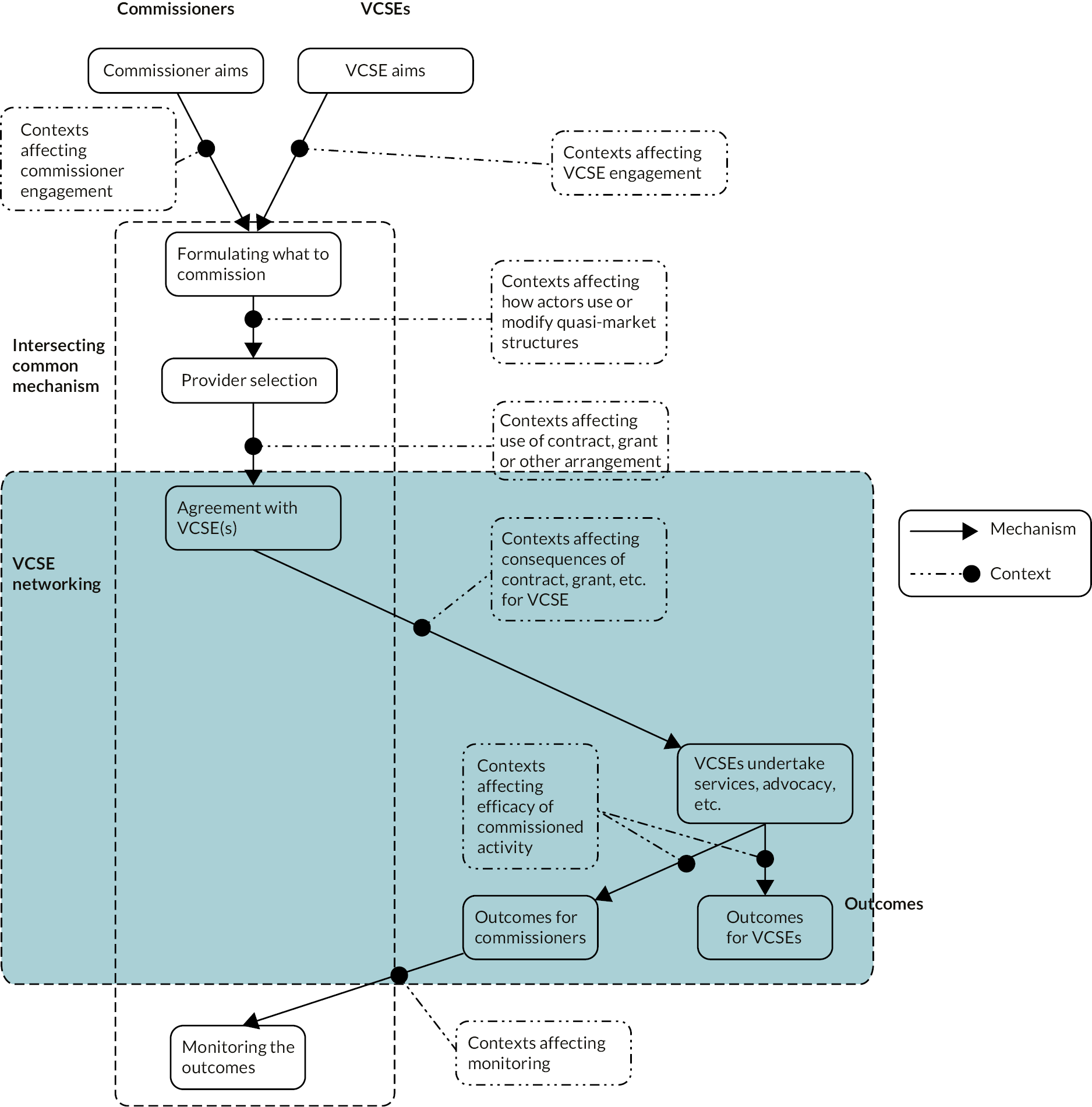
Vertical networking between voluntary, community and social enterprises and commissioners
One activity of these networks was to draw upon VCSEs’ knowledge and experience as input to the co-commissioning networking described above (see Chapter 4, Commissioner networking: co-commissioning and Appendix 6, Tables 24, 27 and 28), especially when the formal information systems seemed not to help that (cf. Appendix 6, Table 25). Another concerned VCSEs as providers. All sites had instances of commissioners commissioning a network or subnetwork of VCSEs jointly to provide services or activities. Another way was to commission one VCSE as ‘lead provider’: ‘we [commissioner] could say, “Well we’ll do one contract for all of these things but one of the providers would then be subcontracting underneath” so there’s that additional layer’ (CS3b_C10a; also CS1a, CS1b, CS2b). For some activities, CS4a was divided into five territories, each with one lead provider. We were also told of similar arrangements, outside our study sites, of instances of ‘alliance commissioning’, and of NHS Trusts acting as lead provider, although outside all these networks in CS2b. Either way, the effect was to reduce competition between VCSEs at the commissioner–provider interface or, more exactly, to make the alliance coordinator or lead provider responsible for managing inter-VCSE relationships, including any rivalries. Some infrastructure bodies and some lead provider VCSEs acted as gateways to commissioning for some smaller VCSEs, but other VCSEs described them as gatekeepers obstructing smaller VCSEs’ access to commissioning networks. In one site, we heard allegations of systemic discrimination against ethnic minority organisations.
Figure 8 shows (shaded) which parts of the common commissioning mechanism this vertical networking affected.
FIGURE 8.
Parts of the common commissioning mechanism affected by ‘vertical’ networking.
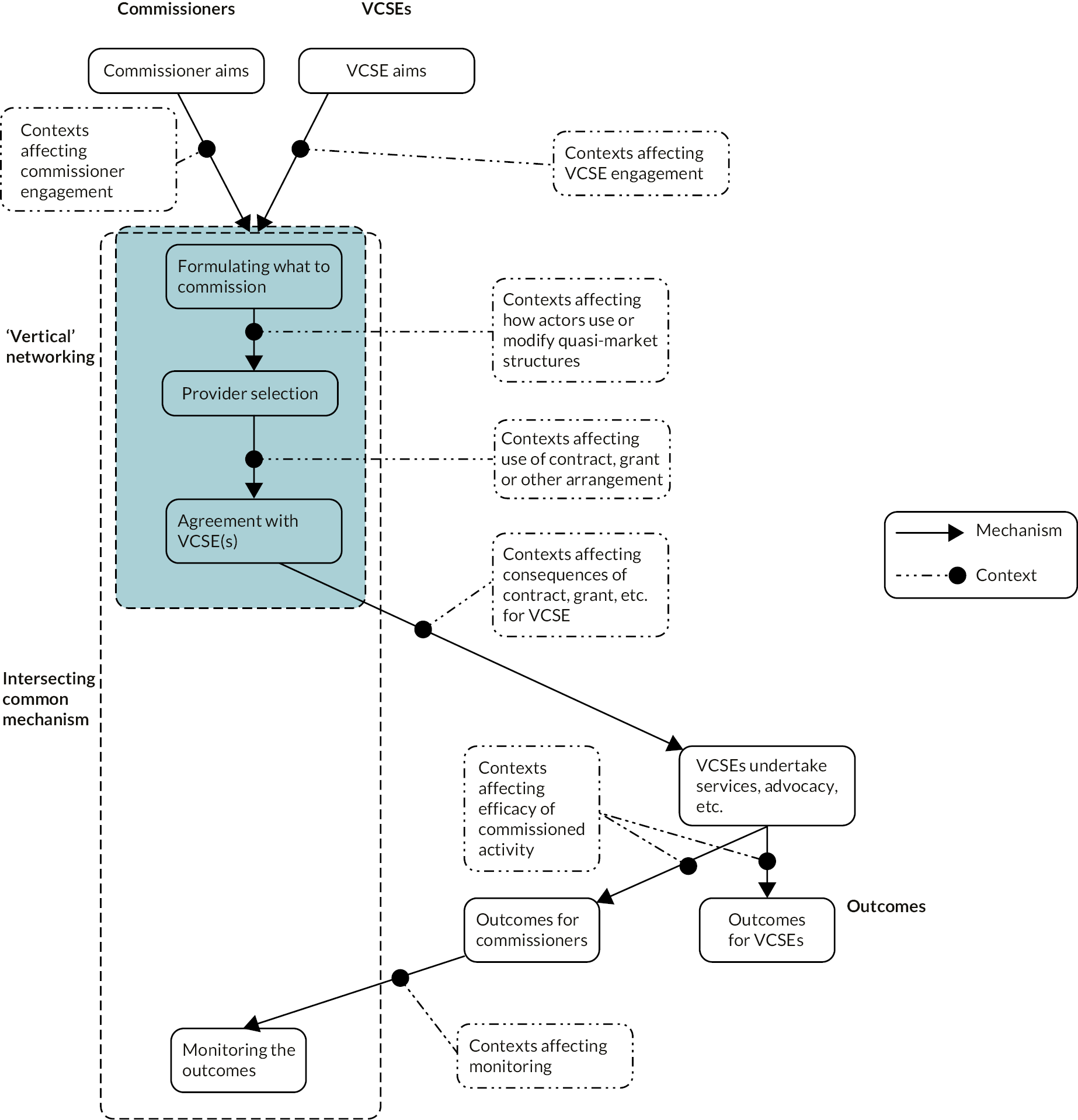
Dual commissioning mechanisms: two modes of commissioning
Commissioners and VCSEs across the study sites thus used hybrid commissioning mechanisms for pursing their respective aims. Interorganisational networking coexisted and interacted with the quasi-market structures which are the essence of commissioning. The findings suggest a distinction between two modes of commissioning – commodified and collaborative – which emphasised correspondingly distinct media of control or of action (see Chapter 1, Health and care).
The commodified, quasi-market mechanisms centred on the commissioning cycle and resource dependencies, formalised procurement (a regulatory practice) and provider competition, with consulted VCSEs often being excluded at the provider selection stage of the cycle. VCSE financial dependency on commissioners was a central medium of power for the commissioners. Insofar as formal contracts were involved, juridical power was in the background but seldom used in practice. Its paradigm form was a direct bilateral principal–agent relationship between one commissioner and one VCSE, in which the latter appeared less powerful.
In the collaborative mode of commissioning, the networking mechanisms supplemented and attenuated the quasi-market mechanisms and media of power, and indeed were partly intended to do so. The networks consisted of negotiated orders among commissioners (see Chapter 4, Commissioner networking: co-commissioning), among VCSEs (see Chapter 4, Networking between voluntary, community and social enterprises) and between commissioners and VCSEs (see Chapter 4, Vertical networking between voluntary, community and social enterprises and commissioners). Persuasion and legitimation were the main, discursive media of power, supplemented by mutual ‘real-side’ (as opposed to financial) resource dependency. The ‘agility’, ‘reach’, ‘expertise’ and ‘responsiveness’ that commissioners attributed to them gave VCSEs legitimation and, to that extent, discursive power. Workarounds such as alliance and lead provider commissioning (see Chapter 4, Vertical networking between voluntary, community and social enterprises and commissioners) were important media of managerial power, adopted in order to diminish the expected, and in some cases observed, adverse consequences of commodified commissioning. Collaborative commissioning (see Chapter 4, Commissioner networking: co-commissioning) relied heavily on dialogue and negotiation between commissioners and VCSEs at each stage in the commissioning cycle. VCSEs’ commissioning and co-commissioning activities overlapped considerably. They were seldom found in observationally distinct, separate network spaces or institutions.
We emphatically do not suggest that where one mechanism or mode of commissioning existed, the other did not. Both modes coexisted and interacted everywhere but the balance between them varied. This brings us to the questions of what contexts affected the balance between these mechanisms and how they worked (see Chapter 5), and what outcomes resulted for whom (see Chapter 6).
Chapter 5 Contexts: variations in the commissioner/voluntary, community and social enterprise relationship
Multiple contexts shaped how the commissioning mechanisms worked in each site. Here, we use the term ‘context’ in the realist sense of the forces which reinforced, restricted or frustrated the operation of the mechanisms explored in Chapter 4. In particular, they affected the balance and interactions between commodified and collaborative commissioning. Furthermore, different contexts affected each other. The main contexts were:
-
local health system characteristics:
-
fiscal constraints
-
the mix of commissioned organisations, including VCSEs
-
-
geographical and historical characteristics:
-
population deprivation
-
spatial dispersion
-
commissioners’ co-terminosity
-
local policies, ethos and history
-
local networking spaces
-
-
organisational characteristics:
-
ACAP
-
organisational systems and bureaucracy, shaping individual role, discretion and influence
-
-
the nature of VCSE activity:
-
statutory or non-statutory status
-
tracer characteristics
-
-
a temporal context: COVID-19
All these contexts took effect within the wider national policy setting (see Chapter 1, Health and care), which often constrained (but sometimes enabled) site-level commissioning and relationships.
Local health and care system characteristics
Fiscal constraints
The local fiscal environment influenced how much activity, including VCSE activity, the commissioners in each site could commission at all. Figure 9 shows CCG per capita allocations in 2020–1, which varied from £1530.42 to £2365.87, and where our study sites fell in the distribution.
FIGURE 9.
Per capita CCG budget allocations 2020–1. For anonymity, the marked points are jittered by up to ±3 places.
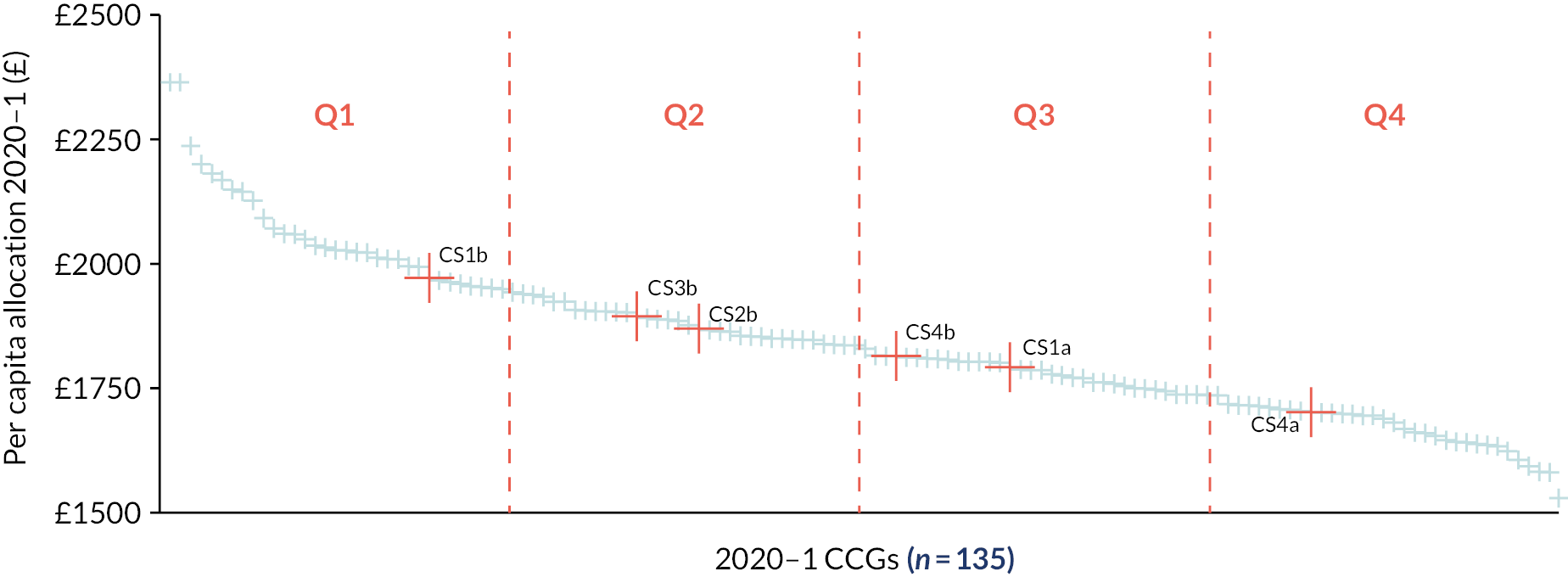
Similarly, our study sites differed in how much their allocations had increased early in the study period as NHSE adjusted them due to reduce each CCG’s distance from targets177 (see Figure 10).
FIGURE 10.
Clinical Commissioning Group financial allocation increases (percentage) from 2018–9 to 2020–1. For anonymity, the marked points are jittered by up to ± 3 places.
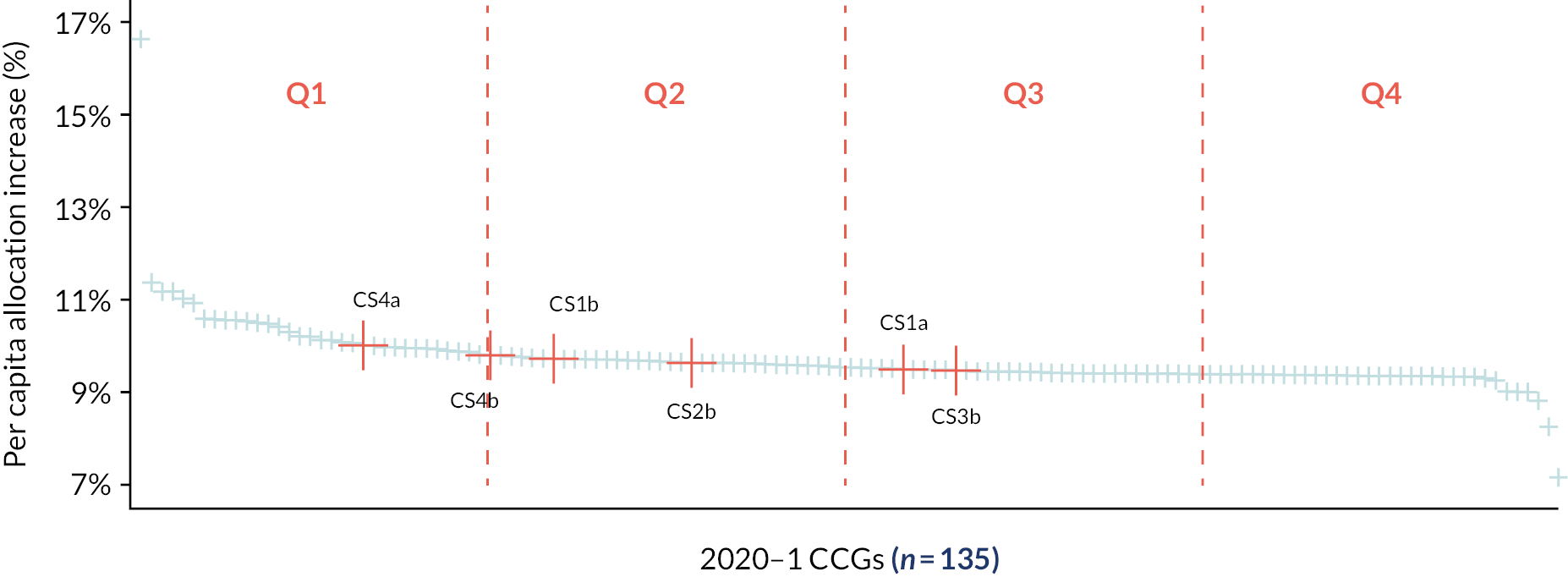
Across the board, LAs’ spending power had declined since 2015–6,178 but some areas experienced smaller funding cuts and budget deficits than others. 179,180 In our study site CCGs, the highest increases in per capita funding over the 2 years were for the two predominately rural sites, and the smallest increases in two of the large cities. Nevertheless, CCG spending on VCSEs remained higher in the other rural site (see Figures 11 and 12).
FIGURE 11.
Clinical Commissioning Group spending on VCSEs, 2018–22: study sites CS1a, CS1b, CS2b.
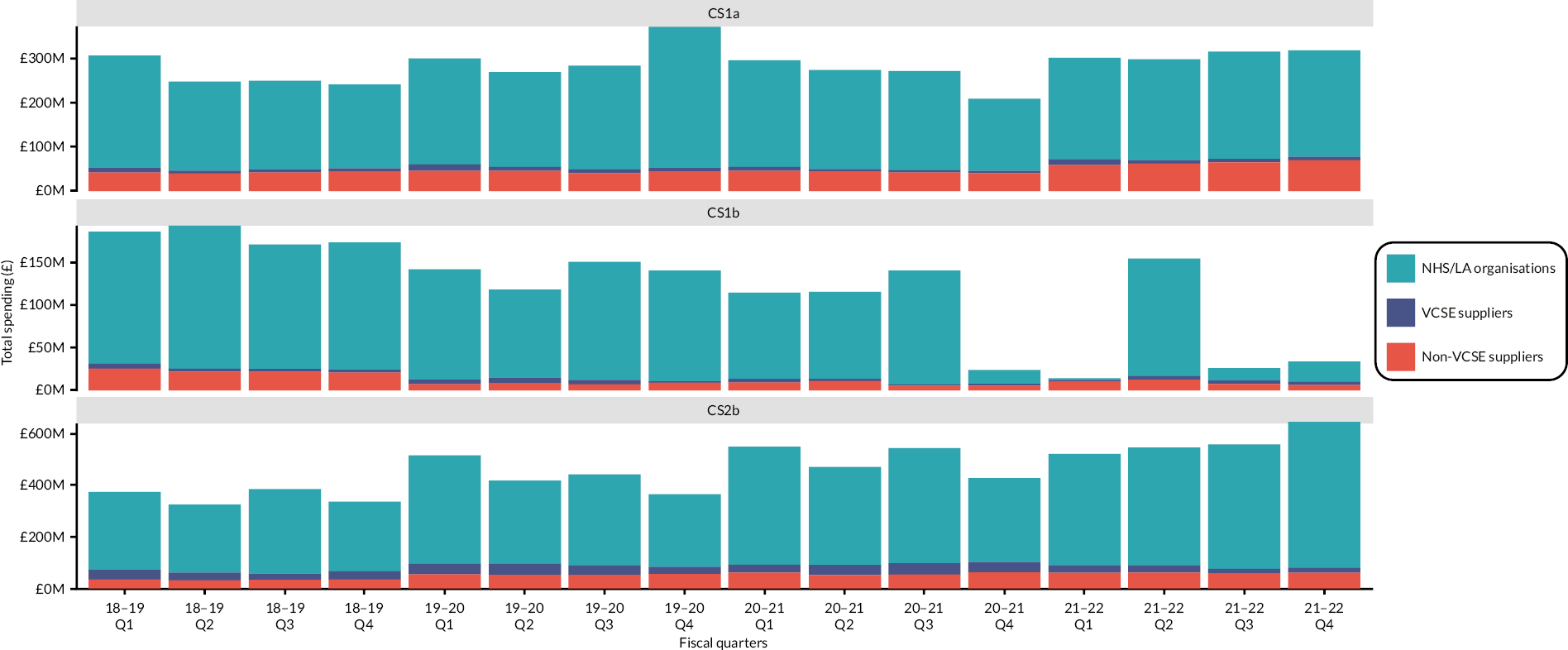
FIGURE 12.
Clinical Commissioning Group spending on VCSEs, 2018–22: study sites CS3b, CS4a, CS4b.

Patterns of CCG spending on VCSEs, and how it compared with the same CCGs’ spending on other kinds of provider, were more stable within than across sites (see Figures 11 and 12). Furthermore, commissioners’ own funding was short term, insecure and conditional.
So we’ve got various pots of funding coming in, but it is really hard work. And it’s unfair on the staff, it causes us acute problems. So we don’t have our funding secured to the end of this year… So at the moment it’s always conditional.
CS2b_C4a, and CS3b
The instability of commissioners’ own funding made the funding of VCSEs also unstable, requiring more frequent changes to contracts (in effect, higher transaction costs for commissioners and VCSEs) and often very short notice to VCSEs of new tendering opportunities.
The smaller the fiscal scope for commissioning VCSEs, the greater the pressure to commission activities that appeared to offer short-term savings:
[I]n the face of deficit in the council and quite obviously deficit in the NHS, it’s an unhappy place whether it’s no investment for something that would have a return on investment or a preventative agenda further down the line. It’s got to be quick wins this year, savings, savings, savings, no investment.
CS4b_C1a
A second consequence was to limit the practical scope for co-commissioning: ‘there’s so little new money to co-design anything around. And when we are co-designing we’re co-designing with a view to cutting costs. So that makes it really difficult to be innovative’ (CS1b_V6a). Indeed, in CS2b and CS3b co-commissioning discussions included the question of where to cut spending on VCSEs.
Decreasing interactions between commissioners and VCSEs reduced opportunities to develop ACAP on either side. VCSEs also perceived financial constraints as barriers to the development of their own ACAP: ‘if you’re talking about data capture and that does cost money and the beauty of smaller organisations is all the funds are used for front-line delivery, there is not that infrastructure money to pay for databases’ (CS2b_VS1).
Narrow though the financial decision spaces might be, the decisions made within them remained important. Commissioners in CS1a and CS3b chose to protect funding to VCSEs and invest resources in building and strengthening relationships with VCSEs, while in other sites investment in VCSEs was not prioritised, a pattern which in part reflected the leadership, policies and historical funding patterns there (see Chapter 5, Local history, policies and ethos).
The mix of commissioned organisations
More diverse ownership of providers – public, corporate, proprietary, VCSE – made commissioners more likely to follow formal procurement rules in order to pre-empt challenges to their provider selection decisions; and with reason, since some corporations had challenged them elsewhere. Then commissioners inclined towards more commodified commissioning (see Chapter 4, Provider selection). This context mainly concerned learning disability support. Commercial providers of hospices and social prescribing were rare if not unknown.
Within the VCSE component, the mix and number of VCSEs varied across case study sites160,181 and the tracers (see Chapter 1, Voluntary, community and social enterprises in health and care). Across our study sites, for example, the number of registered charities ranged from 0.002 to 0.004 per head. The fewer VCSEs were involved in a given activity, the easier it was for collaborative commissioning to develop. The more VCSEs there were, the more important network structures and spaces became, for facilitating co-commissioning and collaborative commissioning. There were only a few hospices – sometimes only one – in each study site, which exposed commissioners’ resource dependency on them. Commissioners stated how this was reflected in the funding mechanisms used and ways of working:
[T]hey provide a huge support to the NHS in terms of facilitating discharge from hospital, which is a huge problem for us nationally at the moment. So I think we are mindful of the contribution that these organisations take, and sort of reflect that in the way that we work with them.
CS1b_C4a
Then, commissioners tended to be flexible in their choice of payment mechanism (see Chapter 4, Agreements and payments) and to prefer the VCSE to ‘learn’, rather than try to replace it with another provider, when monitoring revealed problems (see Chapter 4, Monitoring and adjustment).
End-of-life care was dominated by small numbers of VCSE hospices, partly NHS-funded and each typically working in their own ‘patch’. Hospices typically described their relationships with each other as collegiate, but in some cases there was an element of competition; then the commissioner had to mediate between potentially competing hospices. Where there were many small VCSEs (e.g. in social prescribing), commissioning them one by one would impose a heavy transaction workload on the commissioner, and was one reason for the move towards lead provider, alliance and other ways of combining and delegating contract and grant allocation (see Chapter 4, Vertical networking between voluntary, community and social enterprises and commissioners). The overlaying of new PCNs onto established third sector networks led in CS3b and CS4b to fragmentation and a lack of collaboration:
[Y]ou’ve got so many autonomous players, you’ve got the commissioners, you’ve got the providers who are also autonomous [. . .]. And then you have the PCNs, 30 extra autonomous players in this picture, how do you get one strategy that brings all of that together?
CS3b_C1a
This question remained unresolved at the time of this report (2024). Learning disability services were an intermediate case, with multiple providers of different sizes, including non-VCSE providers, implying greater provider contestability. Furthermore, the extent to which LAs had contracted out these services or retained them in-house varied across sites. Among the VCSEs, however, there was extensive cooperation and partnership working, attributed in part to historical collaboration.
Geography, history, local policy
Population deprivation
Deprivation levels, a key driver of ill health and disease,182 varied across and within our case study sites, as did their influence on commissioning. CS2b and CS4b also included coastal areas which have high concentrations of poor health and low well-being,183 compounded by older age profiles. COVID-19 disproportionately impacted deprived areas,184,185 increasing need and putting further pressure on commissioners and VCSEs and their constrained finances (see Chapter 5, Fiscal constraints). High deprivation levels exposed commissioners’ and VCSEs’ mutual dependency and gave an impetus to collaboration:
Those three districts face a unique set of coastal and rural challenges. [CS4b] deprivation indicators really ramp up across those three areas so there’s [. . .] more of an openness to say these problems are not just things that we can do alone and [. . .] we need those partnerships. There’s a recognition that transactional partnerships are yesterday’s way of working.
CS4b_v4a
How much practical collaboration then resulted was, however, another matter. In another example, deprivation and consequent health inequalities were key drivers for the development of a multisectoral strategic plan for a town in CS2b:
This complete cycle of continued deprivation [. . .] was obviously resulting in inequalities. So social inequalities resulting in health inequalities. We knew that actually there was no way this could be tackled by one organisation or another, it had to come together as a multisector approach so we got the key stakeholders together.
CS2b_C9a
Spatial dispersion
The spatial dispersion of individuals, organisations and services also shaped commissioner–VCSE relationships. Three study sites covered large mixed rural and urban areas where populations and organisations were more dispersed than in the three geographically concentrated urban sites. Dispersion made it more challenging for some VCSEs, particularly in rural areas, to collaborate and for commissioners and VCSEs to physically come together, for co-commissioning among other things. COVID-19 restrictions and lockdowns exacerbated these conditions and complicated the networks described above (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks). Digital working, catalysed by the pandemic, to some extent counteracted this, enabling networks to reach more people and organisations. In dispersed sites the VCSE infrastructure bodies were more fragmented, and there were more charities per head of population and more interfaces between organisations, while the urban sites had fewer charities per head of population and less fragmented inter-VCSE networking and infrastructure bodies.
Co-terminosity and boundaries
In CS1a, CS3b, CS4a and CS4b, the LA and CCG were co-terminous. Local government boundaries in two sites were more complex. In CS2b the ICS covered a mixture of unitary and two-tier LAs. The ICS and (former) CCG were co-terminous in CS2b, CS4a and CS4b but not the other three sites. Some informants noted that a shared footprint reduced complexity and facilitated connectivity across the system, and therefore the networking (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks) which supplemented quasi-markets:
We only have one acute trust, we only have one mental health and community provider, so it’s just the number of stakeholders that you need to engage with as default… so [. . .] how do they get on with each other, who’s got the power, and all of the other dynamics that go on don’t play in. And then maybe there’s more time then to think about who are the other partners around the table.
CS4a_C4a
Co-terminosity reduced the number of interorganisational interfaces, which facilitated co-commissioning and practical collaboration. Co-terminous local government and NHS commissioners were dealing with the same populations of residents and of VCSEs, and the same non-VCSE providers. Some informants highlighted the challenges, including with commissioner networking, where the ‘system doesn’t match the geography’ (CS2b_V8a).
Local history, policies and ethos
Commissioners across the case studies aspired to partnership working and collaborative commissioning, but some had gone further towards them than others. That largely reflected whether commissioners and VCSEs had sustained a long-term commitment to work in that way, hence the extent to which relationships between them had become based on mutual trust. In CS1a especially, informants spoke of developing trust between organisations over long periods of time, a foundation for collaboration and partnership working. Provider continuity was typically more common in end-of-life care than in learning disability or social prescribing, meaning there was greater likelihood of an accumulation of mutual knowledge and trust, and to that extent ACAP, and less risk aversion, hence more collaborative, less commodified commissioning. In CS1b, though, commissioning had a history of strained relationships and lack of partnership working, so that ‘there’s a lot of history as a result of commissioning decisions that impact on trust and relationships and [that] contributes to quite a difficult atmosphere sometimes’ (CS1b_C7a). Discrepant aims and low trust were not favourable conditions for ACAP to develop across organisations.
Variations in local VCSE infrastructure, and therefore interorganisational networking and collaboration, were another consequence of locally different historical patterns of funding and support. While organisations from CS4a, for example, pointed to disinvestment and fragmentation, those from CS1a suggested historical decisions to fund and invest in the sector had strengthened VCSE infrastructure bodies in their area.
When sites already had a strong policy focus on population health and the wider determinants of health, VCSEs were seen as ‘fundamental’ to the policy agenda:
[T]he heart of achieving long-term population outcomes is the acknowledgement that we need to invest in those non-health-care wider determinants of health, and that again the third sector have got so much expertise in that area… also in many cases being the providers of some of that care and support as well. It’s fundamental to the model.
CS1a_C3a
Commissioners there saw VCSEs as having a legitimate, essential place in decision-making, and what we have called collaborative commissioning and an equal place for VCSEs as a ‘prerequisite’ for meeting commissioners’ aims. This view extended to value, place and voice of VCSEs and service users in shaping and delivering services. Some organisations suggested that this ethos had been mainstreamed or that they were working towards ‘hardwiring’ it into commissioning practice. This was most evident in learning disability services, where facilitating the voice of users and carers was more mainstream in commissioning practice, contributing to a greater tendency to engage with VCSEs as a route to co-production. Across the study sites, these characteristics were clearly strongest in CS1a. Elsewhere, local health and care policies aligned less strongly with VCSEs’ interests, restricting VCSEs’ legitimacy and engagement in commissioning, so that ‘there’s still that lack of understanding and [. . .] valuing what the sector does, putting it on an equal footing in terms of being a key player in the health and care system’ (CS4a_C1a).
Some commissioners and VCSEs in CS4a suggested that party political ideology influenced commissioning priorities and ways of working:
We had some seats that got lost from Labour that switched to Conservatives. So we’ve been very much a council that’s led around wanting to build, invest in the economy, building roads, and creating employment and working with businesses, rather than with communities.
CS4a_C1b
To determine whether this was a wider pattern would require an England-wide analysis of spending on VCSEs by party control of LAs. National policies, including NHS priorities (see Chapter 1, Health and care), do not, of course, depend on local party political alignments.
Networking spaces
Multiple commissioners and multiple VSCEs in our study sites collaborated through interorganisational networking (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks), but these networks differed in the availability of ‘spaces’ that brought commissioners and VCSEs together, how these spaces operated, and who controlled them.
The main spaces were the infrastructure bodies described above (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks), health and well-being boards, and latterly ICSs. Commissioners in all sites highlighted local infrastructure bodies’ connecting role, linking commissioners and VCSEs, and connecting VCSEs, often through forums and partnerships. Thus ‘[O]ur [infrastructure body] role is to create partnership opportunities… the more organisations work in partnership, the better positioned they are to take on commissioning opportunities’ (CS4a_V1a). However, the extent, coverage and strength of local infrastructure bodies varied markedly across our study sites. As noted (see Chapter 4, Networking between voluntary, community and social enterprises), commissioners in five sites helped fund these bodies, in particular individual posts to build the networking between VCSEs and between VCSEs and commissioners. Sometimes these posts focused on building networks across health and care as a whole, sometimes on building networks between VCSEs and statutory bodies (including commissioners) for a specific service.
The extent and strength of local infrastructure bodies’ influencing role therefore also varied, affecting VCSEs’ ability to influence commissioning agendas and the commissioning cycle. Commissioners in all study sites viewed infrastructure organisations as their conduit to VCSEs, one on which they were ‘reliant’ because the infrastructure bodies ‘influence the conversations, and they influence how we set our priorities and how we set up groups’ (CS3b_C8a); and the effectiveness of that conduit partly depended on whether (other) VCSEs perceived the infrastructure body as independent, impartial, and able to amplify local people’s voices and bring a collective VCSE voice to the commissioners.
In some sites (e.g. CS1a), our informants largely agreed that commissioners and VCSEs had forums in which to engage with each other and that VCSEs had a place in key decision-making forums. However, despite the policy endorsement of commissioner engagement with VCSEs (see Chapter 1, Health and care and Voluntary, community and social enterprises in health and care), the latter found it challenging to secure representation:
We are involved, we have a place… none of these have come easy, but we’ve got hard-won places at health and well-being board and the partnership executive group that meets, the chief executives and the great and the good [. . .]. We’re having conversations about how we flip the power and bring people’s voices and communities of interest voices into different conversations.
CS1a_ V1a
Other study sites had fewer such spaces, which inhibited networking and collaborative working, especially at a strategic level. In CS4a, ‘VCS doesn’t have a place on the ICS. The VCS still does not have a place on the highest table where they’re equal around the table to be able to contribute. That speaks volumes, doesn’t it’ (CS4a_C1b). Supposing the necessary spaces existed, the next question was whether VCSEs had an equal voice, or which VCSEs did. Across all sites, VCSE informants spoke of equity, namely who is invited to participate in forums and co-commissioning activities:
We describe each one of our local care partnerships as very much having their own personality [. . .] So when we’re talking about things like an equal voice at the table and how that works in practice, the reality is it plays out differently in different areas, and some of them get that much more right maybe than others do.
CS1a_C4a
In another site, VCSEs participated,
but that’s obviously not all of them and it tends to be the, not necessarily the bigger ones actually, but the more established ones that would be invited to take part.
CS1b_C7a
For the VCSEs who were present, a last question was who controlled the agenda, especially whether statutory bodies ‘owned’ the agenda and recognised the value of VCSE participation:
We are very small but it feels for us like it’s always their agenda, as opposed to finding out from us who are working with those people and doing that work or that prevention work [. . .]. Rather than listening to us and trying to work out, it just tends to be it’s an information-giving. [. . .] people from health come, it’s generally ‘I can’t stay long, I’ve just got to deliver all this information to you and then I’m gone’.
CS2b_Vs2_fg
These network spaces were an important venue for the development of organisations’ ACAP.
Organisational characteristics
Size
Larger VCSEs were more likely to have managerial expertise and specialist bid writers, fuller monitoring data, and the ability to cover the transaction costs of commissioning. Similarly, on the commissioning side, some commissioning organisations were able to invest in commissioner skills and expertise. Larger organisational size thus assisted the development of ACAP. Those in two sites were able to employ an expert procurement manager with the skills to work more flexibly and innovatively with VCSEs. Similarly, ‘[Y]ou need a big CCG because running costs are fixed as a percentage of your commissioning budget… you need quite a big CCG that’s got enough running cost budget to afford to get a specialist’ (CS1a_C12a). Conversely, the transaction work (cost) of being commissioned was proportionately greater for small VCSEs.
Absorptive capacity
How commissioners and VCSEs acted towards each other depended partly on their ACAP (cf. Chapter 1, Interfaces and interaction). The exploratory survey showed somewhat different ACAP profiles (which components were more and which were less developed) between commissioners and VCSEs. Fuller details are in Appendix 6, Tables 18–25 but in summary, VCSEs gathered and used primarily experiential and informal knowledge and evidence, acquired from staff and volunteers working with communities and organisations. The networking described above (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks) facilitated the exchange of soft intelligence, but the diversity of network membership, especially in learning disability networks, did the opposite:
[T]here are mechanisms for sharing information [. . .] we try different things in different network meetings. I don’t think there’s ever a perfect answer to it just because of the volume and the number of organisations and the difference, and learning disability being such a broad specialism.
CS1a_V18a
Voluntary, community and social enterprise informants valued commissioners who understood the organisations they worked with, and the challenges faced by communities.
In contrast, commissioners typically relied on more formal knowledge from external sources, including national statistics and professional networks. Nevertheless, some commissioners spoke extensively of partnering with others, including research bodies and networks, while others relied more on service user feedback and engagement (cf. Appendix 6, Table 18). Some commissioners were rather passive; although ‘voluntary organisations have quite a lot of power in being able to contact and connect with councils themselves [. . .] it’s not something that seems to, councils don’t seem to obviously invite that’ (CS1b_C7a). VCSE respondents most often mentioned e-mail messages, meetings and ‘professional’ networks as sources for knowledge acquisition, although some also mentioned networking (infrastructure) bodies. Six mentioned NHS bodies. ACAP involved not only cognitive but also relational skills in communicating with VCSEs, and being able to co-produce with VCSEs and the wider community:
I think there is something to say about individuals. I think, you know, just compatibility in terms of how you like to communicate, what level of detail people like to communicate with [. . .] that’s less about the commissioner themselves, but more about the team around them. And I think, as well, a like-mindedness in terms of where you want the project to go.
CS4a_V6a
For these things to develop, however, required interaction between commissioners and VCSEs – a precondition for ACAP development. Compared to social prescribing and end-of-life care, commissioners within the learning disability tracer more commonly used forums, workshops and co-production to engage those who had experienced the services.
Overall, there was a gap between organisations’ capacity to acquire and assimilate knowledge (‘potential ACAP’) and their capacity to transform and use it (‘realised ACAP’) (see Appendix 6, Tables 19–21). VCSE informants were less confident than commissioners that commissioners applied new knowledge gained from VCSEs (see Appendix 6, Table 31). Only one in four commissioners in the survey reported that their organisation regularly reviewed and adapted how they commissioned VCSEs in light of new knowledge (see Appendix 6, Tables 22 and 23). Some commissioners spoke extensively of the importance of evidence and how they used it in decision-making (cf. Appendix 6, Table 18): ‘[S]o I think you’ve always got to be aware of and ensuring that you are following the evidence and ensuring that you’re working from an evidence-based place’ (CS1a_C10a). Other commissioners attributed their more informal approach to lack of data –
if we don’t have adequate, regular, consistent and trustworthy evidence base to make decisions off, it really gives credence to the fact [sic: idea] that often how decisions are made as to what to spend money on happens on quite a personal, informal level.
CS1b_C7a
– and lack of skills or capacity to transform and exploit data for commissioning purposes (cf. Appendix 6, Table 23). That is, ‘I don’t think we know how yet to use that information and that insight [. . .] what to do with it and how to interpret it and how to use it and how to apply it’ (CS1b_C7a). In ACAP terms, this was a weakness in assimilating, transforming and exploiting external information. Although they seldom used ACAP language to describe it, commissioners and VCSEs often recognised the value of ACAP and knowledge mobilisation, but organisational structures, skills and resources constrained knowledge mobilisation and evidence use to support commissioning.
Organisational systems, bureaucracy and culture
Differences in organisations’ commissioning rules, processes, practices and behaviours also enabled or constrained relationships between commissioners and VCSEs. In some sites, commissioning staff at strategic and operational levels seemed disconnected. Where there were vision, intention and capabilities at a senior level, they did not always get translated into or followed through within the wider commissioning team:
[W]hat I tend to see is good commissioning in the leadership role. A bit wishy-washy down below. I think there are some exceptions but it feels like they’ve got the wrong people in the wrong roles with the wrong skill set.
CS1b_V3a
However, some commissioners had established specifically boundary-spanning roles with the aim of developing more collaborative relationships between VCSEs and statutory bodies, either cross-cutting or for a tracer (e.g. end-of-life care in CS1a, social prescribing in CS3b).
How much decision space individual commissioning staff had reflected different degrees of bureaucratisation and hierarchy within their commissioning organisations, and differences in organisational cultures. Both commissioners and VCSEs often perceived bureaucratisation and procurement structures as barriers to commissioning VCSEs, especially collaborative commissioning:
[S]ome of our commissioning experience would be ‘computer says X + Y = Z’ which means either you get it or you don’t and all of that great work around building relationships and understanding and shared visions, goals, shared challenges. Space to fail and learn. All of that stuff goes out the window as soon as it hits procurement.
CS1b_V3a
The organisational positioning and integration of commissioning and procurement influenced the severity of these effects. In some commissioning organisations (e.g. CS1b), commissioning and procurement were in one department, but in others (e.g. CS3b) they were separated, making it more challenging to navigate the commissioning systems and work flexibly:
[S]ome commissioning teams and procurement teams operate almost as two separate entities so the commissioners do their bit and then when it moves into procurement, almost a different group of people [. . .]. In some authorities which are particularly risk adverse there’s a strong personality drive in their approach to procurement and they take that kind of risk adverse interpretation of legislation.
CS1b_V3a
Closer intraorganisational working and integration, for example, between commissioners’ procurement and commissioning teams strengthened the mobility of knowledge within commissioning organisations. However, the procurement teams sometimes gainsaid other (more collaborative) commissioning teams, so knowledge mobilisation did not necessarily produce agreement about how commissioning should be done.
The greater a commissioner’s reliance on narrowly implemented procurement systems, the harder it became at the provider selection and agreement stages of the commissioning cycle to maintain collaborative, negotiative relationships with VCSEs. Commissioners in different organisations had varying levels of discretion. Its main uses were to develop workarounds and stretch procurement rules and procedures so as to widen the scope for collaboration between commissioners and VCSEs, making commissioning less commodified and more collaborative (see Chapter 4, Shift to networking).
Individual roles, background, discretion and influence
Symmetrically in both commissioning organisations and VCSEs, leading figures assisted the commissioning of VCSEs by, firstly, promoting and legitimating it. Then commissioning was likely to become more relational and collaborative. In some sites, especially CS1a, key individuals in LAs and CCGs played a large role in facilitating VCSE engagement and a more collaborative mode of commissioning and co-commissioning. When they ‘championed’ VCSEs’ role and value, partnership working and co-commissioning, ‘the third sector does tend to get included. That’s driven very much because of the leadership of the both the leader and the chief officer of the local authority [who] are very outward-looking people’ (CS1a_V3a). In some sites ‘leadership’ referred not just to one person but to shared, ‘distributed’ leadership. Leadership in other sites was weaker and more fragmented, although some commissioners recognised that as a key issue and expected ICSs would accelerate ‘systems’ leadership.
The presence of boundary-spanning individuals working across the boundaries between VCSEs and commissioners, or across clinical and managerial roles in commissioning, or across both, facilitated collaboration between commissioners of VCSEs, and information and knowledge transfer (contributing to ACAP). Some of these individuals had also crossed those boundaries during their careers, for example moving from front-line service delivery into commissioning roles. They seemed to be more prolific in some sites than in others, and more in end-of-life care and learning disability than social prescribing. Boundary-spanners played an important role bringing and translating new knowledge into commissioning and VCSEs:
My role is really to act as an interface between the VCS and the statutory health and care system [. . .] supporting the development and understanding an intelligence base that connects community needs and the insights of organisations and the people those organisations support with the decision-making process in the statutory health and care system.
CS3b_V5a
From the VCSE perspective, individuals who had crossed from the statutory sector brought with them knowledge and understanding of commissioning processes and ways of working, and useful networks:
I worked in local government before. So in my head I’ve got a bit of an understanding… that political understanding of a local authority, the slowness of the wheels turning… They’ve got that layer of politics that goes on and sometimes their hands are tied but also things like the hoops they might have [to] jump through, the evidence they have to gather to be able to persuade or influence on a political side.
CS4b_V5a
Equally, commissioners spoke of how they drew on their experiences from working in the third sector or other front-line roles when interacting with VCSEs. They were able to use and extend their discursive control by using third sector language and communicating how they shared their values. Commissioners felt that they were able to ‘speak authentically’ from a position of knowledge and gave the sector someone to relate to, particularly if they had experience of front-line delivery. They spoke of how they better understood the sector, how it operates and its challenges as well as, in some cases, the needs of communities:
I’m blessed a little bit with having experience being operational and a commissioner, I’ve worked in the voluntary sector so I can sort of see the landscapes through different lenses to start with, which is a string to my bow, probably a benefit there. But for me it’s sometimes actually how am I going to help this organisation.
CS3b_C7a
The more bureaucratised organisations were, the less decision space their individual members had. In several sites, commissioners and VCSEs highlighted the important role of ‘maverick’ commissioners who took risks ‘in spite of the system’, facilitating more flexibility in working with VCSEs and through co-commissioning. Such individuals pushed the boundaries of the procurement system:
[S]ome people have more rebelliousness than others, naturally, but also it’s about longevity, so say for example in the NHS, someone who’s been there for a long time will have more confidence that they could try something a bit unusual. I think there’s also something about what sort of theories you subscribe to about ways of working.
CS1b_V10a
These were often the people who instigated the more collaborative commissioning methods and workarounds described in Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks. However, in commissioning organisations where relationships and ways of working were less well embedded and more fragile, the turnover of such people was a concern:
The challenge is how we ingrain it so that everyone does it and it’s normal… I suppose you need one person to be the one that’s maybe innovating and trying to push the boundaries… how do you move people into that space behind me?… You can’t have it all dependent on that person, because if that person goes, the relationships and things like that go.
CS3b_C7a
When individuals with these characteristics could be influential, relational and collaborative commissioning was more likely to develop.
The nature of voluntary, community and social enterprise activity
Statutory status
Legislation and statutory frameworks shaped how commissioners worked with the VCSEs that delivered statutory services. End-of-life services were statutorily required and predominately provided by VCSEs. Typically, that exposed commissioners’ resource dependency on VCSEs, reduced provider contestability and motivated commissioners to apply contractual terms and monitoring flexibly, although statutory regulation also confronted commissioners and VCSEs with prescriptive external monitoring (e.g. by the CQC). These circumstances gave hospices a strong negotiating position, for example, when resisting a move from grants to contracts or when negotiating funding uplifts:
So we went to commissioners and said we have this huge black hole. You’re statutory obligated to do this service. You’ve just done a soft tender exercise which has demonstrated to you that nobody else can do this within 200 miles… you’re over a barrel… so we renegotiated those costs.
CS1b_V2a
In learning disabilities the position was more mixed, with different responsibilities for health and care, although heavily dominated in our study sites by LAs. In the statutory learning disability services:
There’s the statutory obligations from central government to deliver on certain promises [. . .] But there’s all these different pressures that are always ongoing, so the space left for commissioning in an innovative way is really small and I guess just contributes to another feeling of, ‘Oh, well, we haven’t been able to do that and now we’re just taking the easy route’.
CS1b_C7a
Some VCSEs felt that the positioning of some learning disability services as non-statutory made these services a lower priority for commissioners, making it challenging for VCSEs to engage with commissioners ‘to make things happen’: ‘[F]or both local authorities and health, in a way we’re small fry and the service we deliver is not their statutory duty that they’ve got to deliver… we’re not the most urgent thing they’ve got to deliver’ (CS1b_ V8a). The effects of small size here reinforced those of non-statutory status.
Social prescribing was another non-statutory service with VCSEs sitting between health and care organisations. Social prescribing was being commissioned and delivered in different ways across the case study areas, with commissioners operating under fewer constraints than in end-of-life care and, to a lesser extent, learning disabilities. They were therefore also less salient in commissioners’ monitoring of VCSE activity. A mixture of formal and less formal relationships had developed in our study sites between commissioners (recently also including PCNs) and VCSEs, with in some cases fewer monitoring and performance measures such that, for example, the commissioners were
saying within certain parameters they’re happy that I go ahead with this, and we just keep an eye on it. And social prescribing is one of those. So that’s one illustration of how the commissioning process has felt very fuzzy, and that we entered into a contract two years ago that had some hard deliverables against it, but nobody’s ever gone back to those deliverables.
CS4b_V4a
Statutory status gave both commissioners and VCSEs an opportunity to use juridical methods (regulation, law) to influence each other, but in practice that seldom if ever occurred in our study sites.
As noted, commissioners in some sites spoke of how national regulations ‘tied people’s hands’ (CS1a_C10a) and reduced flexibility:
I would say one of the significant barriers of the process is the NHS have to use a national contract. We have a lot more flexibility within the county council in terms of I only give out a lot of grants [and] don’t have to go through the procurement process.
CS4a_C1a
National Health Service regulations appeared to limit the discretion commissioners had to move away from commodified approaches and pursue co-commissioning.
Tracer activity
Differences in tracer characteristics also contributed to variations in commissioning practice. The aforementioned contexts of provider ownership mix (see Chapter 5, The mix of commissioned organisations), VCSE size and number (see Chapter 5, Size), and statutory status (see Chapter 5, Statutory status) applied differentially to each group (see Appendix 7 summaries).
To those must be added variations in the outcome specificity of tracer activities. Outcome specificity was comparatively high (although still not as high as for some kinds of acute secondary care) in end-of-life care, intermediate for learning disabilities, and low for social prescribing. Where outcome specificity was lower, contracts often specified case numbers or activity rather than outcomes, typically resulting in less specific monitoring for VCSEs. Where activity was more medicalised, for example in end-of-life care, commissioners were more likely to require specific outcomes (or at least activity) measures and monitoring. Lower specificity also meant that commissioning was more likely to span CCGs and LAs, hence there was a greater role for horizontal co-commissioning networking, for example in learning disabilities compared to end-of-life care.
High specialisation (e.g. hospice care) was a barrier to new provider entry, tending to reduce the number of providers (here, compared to social prescribing) and hence provider contestability, and to that extent commodified commissioning. Then:
We do direct awards without competition… with a lot of voluntary sector, that is relevant and applicable because a lot of, particularly like the small ones are very, very specialist and they are the only people operating in that area.
CS1a_C12a
In some case study sites a lack of ‘suitable’ providers propelled a shift towards more collaborative approaches, although in the example below this remained more an aspiration than a reality:
[W]ithin some of these sectors we haven’t got lots of providers [. . .]. So actually how do we solve that problem? And do we have the skills as a single organisation to be able to do that? And I don’t think we do. So therefore we have to take a different approach. That approach could be collaboration or co-production/co-design to solve a problem. But I don’t think that’s been fully explored.
CS4b_C5a
In short, VCSE specialisation tended to make commissioning more collaborative.
Stability of demand for a service or activity also affected commissioning practices and relationships. Where it was less predictable, for example in social prescribing compared to end-of-life care, risk-averse behaviour among commissioners was more probable (and for them, rational), leading to more commodified commissioning and more standardised contracts (as in the learning disability example described in Chapter 4, Agreements and payments). Thus the stability of demand affected the choice of pricing and payment mechanism that either party preferred.
The characteristics of learning disability also modified how VCSEs and commissioners used quasi-market structures, reinforcing the tendency to supplement commodified with more collaborative modes of commissioning. Because learning disability is lifelong, the support that people with learning disability needed changed as they moved into adulthood, parenthood and old age, between different housing arrangements, and into and out of education, employment, illness and short-term crises:
anything from supporting people with advice around neighbour relations, diet, managing your money, managing relationships etc, etc right through to people who’ve got 24/7 physical care and support needs [. . .] that whole gamut.
CS1a_V21a
People with learning disability were not always well equipped to access the health-related activities (e.g. social contact, access to physical activity) and formal health care that they needed. Consequences included mental health problems, increased risks to health (e.g. weight gain during COVID lockdowns) and increased prevalence of preventable illness (e.g. diabetes), leading to lower life expectancy and greater use of A&E services than the rest of the population. 186 People with learning disability varied considerably in these respects and in their capacity for self-management and self-advocacy, with informal carers (or in their absence, VCSEs) providing much support. One commissioning priority was to get people onto the learning disability register (CS4b) and so increase their access to GP services [e.g. cervical cancer screening (CS1b), social prescribing (CS1b)] and, during the pandemics, increase their COVID vaccination uptake (CS1a, CS4b).
Occasionally, commissioning one VCSE could meet several needs at once – for example, a cookery group provided dietary advice, food, self-help and social contact (CS1a, CS1b) – but many informants noted that supporting people with learning disability involved commissioning, and hence coordinating, multiple organisations in and beyond the health sector (education, housing, etc.), hence collaboration between providers rather than a competitive ‘race to the bottom’ (CS4b_C2). Consequently:
the learning disability sector is very collaborative and cooperative and partnership based. [. . .] it’s just interesting to see the politics and then the competition in tenders that come out [for sensory disability support] and that kind of thing compared to learning disability.
CS1a_V18a
Therefore:
I see the role of the commissioner as almost there to be the facilitator between different partners and actually the commissioner, yes they need to drive and work through some of that cycle, but it’s not something that’s done dry.
CS3b_C7a
Many VCSE informants thought that personal budgets stimulated provider competition, but some nevertheless welcomed them for people with learning disability:
[P]eople have got choice over what they do, they’ve got control over their lives that they never had before. They can walk away tomorrow if they don’t like the service we provide. [. . .] And that’s wonderful, isn’t it?
CS3b_V13a
Even they, however, acknowledged that personal budgets might increase informal carers’ burden. Because learning disability support often extended into activities of daily living, some VCSEs volunteered to be commissioned to complement, supplement and extend professionals’ roles [e.g. supplementing dietitians’ work with cooking clubs (CS1b)]. CS3b set up a direct referral path from one of its commissioned VCSEs into the NHS community learning disability team. All sites commissioned individual advocacy support for people with learning disability. Especially in CS1a, CS3b and CS4b, commissioners systematically consulted people with learning disability about services, finding oral communication preferable even to easy-read materials for that purpose.
A temporal context: the COVID-19 pandemic
COVID-19 substantially disrupted health and care commissioning and was a catalyst for different ways of commissioning VCSEs. Across all the study sites, commissioners and VCSEs described how the pandemic had substantially strengthened or deepened relationships between commissioners and VCSEs.
The fuel and the energy came from trying to find a good response in terms of the pandemic, the crisis was driving the innovation and the desire to work together, but what people got out of it, I think, was closer working relationships that they’d not experienced for some time I think.
CS2b_C5
The pandemic heightened commissioners’ recognition of VCSEs’ role and value, and exposed their mutual dependency, particularly regarding end-of-life care. Commissioners relied on VCSE infrastructure bodies and learning disability services to help meet increased local healthcare needs, while hospices depended on additional public funding to compensate for decreases in their own fundraising. COVID-19 thus helped to strengthen the co-commissioning voice and position of VCSEs. Many VCSEs reported how they had a seat at the table, how they were ‘listened to’ and how partnerships felt more equal. Commissioners spoke of how COVID-19 ‘turbo-charged’ more ‘systems’ thinking and co-commissioning, often in relation to the vaccination programme (CS1b, CS2b, CS4a). Joint decision-making and co-production of health and care (CS1a, CS4a) represented a fundamental shift in VCSEs’ engagement in commissioning. The peaks in CCG spending on VCSEs in Figure 13 correspond to COVID-19 pandemic peaks, especially the 2020 peak.
FIGURE 13.
Total CCG spending on VCSEs per study site, 2018–22.
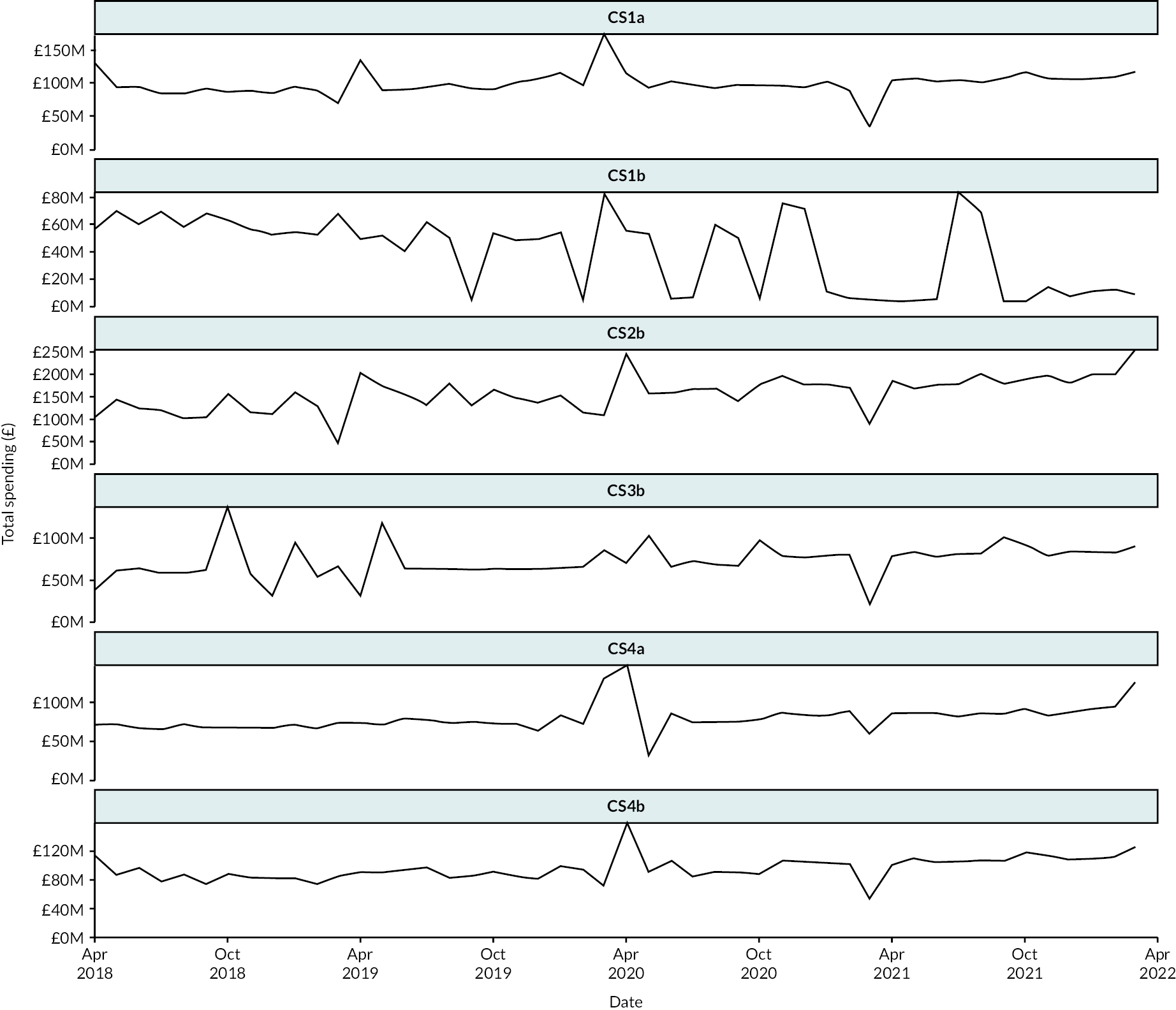
Also, the pandemic necessitated greater flexibility in how VCSEs were commissioned (CS2b, CS4a, CS4b), although this varied across case study organisations. Typically, this meant less bureaucracy, increased tolerance of risk and more discretionary space for commissioners. Commissioners’ relaxation of this decision space was mutually beneficial when commissioners and VCSEs had to respond to new needs quickly:
Actually, your appetite for risk rockets, that’s what happened during COVID… I have never, ever heard in my entire career as many people going, ‘Just do it’… actually a whole load of barriers and walls and things fell down and there was a spirit of collective action that I think everybody found immensely freeing.
CS2b_V1a
Commissioners and VCSEs across case study sites felt that these changes represented a higher level of trust in terms of commissioners giving VCSEs more freedom and flexibility to ‘just get on with it’. ‘[T]here has been a change of attitude in the local authority at commissioner level in terms of trusting external organisations to deliver on work and really trusting us’ (CS1a_V17a). These changes, however, seemed to be less durable in sites with less history of pre-pandemic collaboration and partnership working.
The intercalation of contexts
The contexts that shaped commissioner–VCSE relationships interacted in complex ways. While some factors seemed to facilitate more collaborative commissioning, other elements might offset them. For example, some areas had higher levels of CCG spending power which could facilitate collaborative approaches, but also in some cases had more fragmented local VCSE infrastructure which acted to constrain it.
Table 7 summarises what consequences these contexts had for commissioning VCSEs (see Appendix 7, Table 35 for further details).
| Contexts which tended to promote collaborative commissioning | Contexts which tended to promote commodified commissioning | |
|---|---|---|
| Local health and care system |
|
|
| Geography, history, local policies |
|
|
| Organisational characteristics |
|
|
This brings us to the question of what outcomes, qualified by all these contexts, the commissioning of VCSEs produced for commissioners and VCSEs.
Chapter 6 Commissioning consequences and outcomes
Commissioning outcomes include those that commissioners and VCSEs sought (see Chapter 4, Commissioner and voluntary, community and social enterprise aims) but also any emergent, unforeseen, unintended or perverse effects of commissioning VCSEs. We consider these outcomes for the commissioners (CCG and LA), then VCSEs, and lastly the wider health and care system. The outcomes for commissioners and VCSEs included the introduction of new activities, which were also an outcome for patients themselves. Our six case studies were chosen for variation in their CCGs’ spending on VCSEs, not any apparent success or prowess in commissioning or engagement with VCSEs.
Outcomes for commissioners
Awareness and engagement
Many commissioners described how collaboration with VCSEs had heightened their awareness of the framing of spending decisions; issues concerning the patterns of service delivery; and awareness of, sensitivity to, and practical engagement with communities. This collaboration provided commissioners with expertise and knowledge that they would otherwise have overlooked: ‘Having a third sector representative round the table, as well as public health colleagues as well, really pushed my thinking in terms of what would make a difference’ (CS1a_C1a and CS3b). In these ways the experience of collaborating with VCSEs helped commissioners’ ACAP to develop. Many commissioners recognised that the organisational setting in which commissioning was implemented was not (or had not been) conducive to collaborative behaviour towards VCSEs:
So my reflections after having spent 30 years working in this system, or more than that, is the interface that was created with the Community Care Act is dysfunctional. So the attempt to create a market has not succeeded. I see behaviours in providers and in commissioners that are unhelpful towards an effective system.
CS4b_C6a; also CS2b, CS3b
Commissioners thus attributed this outcome to commissioning system characteristics.
Some respondents highlighted the different purposes and objectives of commissioners and VCSEs. ‘They [VCSEs] were created and set up for a very clear purpose. They emerged not to provide services, but they emerged in response to the demands of people in neighbourhoods and communities’ (CS4b_C6a). While commissioners’ aims also differed, at times, from those of public and corporate providers,23 the difference in aims was important for VCSEs given their avowed social ‘mission’.
Outcomes from the commissioned activities
Reducing demand pressures on NHS services was an important practical outcome which commissioners had aimed at in commissioning VCSEs. It was not, perhaps, surprising that VCSE informants claimed that their commissioned activities helped meet that aim:
[I]f we stopped delivering [service] the amount of children going into care would be a significant percentage increase in [city], and that is quite significant. If we stopped becoming the [. . .] service that supports people that use A&E and other services on a frequent basis, the cost to the health economy of [city] will increase by £1 million, and also A&E get inundated again at a time where it can’t afford to be.
CS1a_V19a
In CS3b:
we’ve sat down and we’ve shown the data, we’ve shown the improvements in health and well-being, we’ve shown GP reductions, we’ve shown secondary care reductions, we’ve shown 999 call reductions.
CS3b_V3a
However, some of their commissioners agreed, in respect of hospitals:
[W]ithout the […] hospices that we have in [city] we wouldn’t be delivering the level of end-of-life care, the quality of end-of-life care that we’re delivering. We would have significantly more pressures on our beds in hospital.
CS1a_C8a; also CS4a
general practice:
Some GPs I understand have really got on board once they’ve actually seen and felt the benefits of social prescribing, they’ve seen the difference in who’s not coming back to them continually in GP practice and that’s helped influence their thinking.
CS3b_C1a
and preventive care in the community:
The VCSE demonstrated that those patients who have not had [VCSE name] input were costing more and then having more attendance in secondary care before their long-term condition is even on the map.
CS1b_C3a; and CS1a, CS3b
and
from a different project that the council were running, but a tower block and a residents’ association within the tower block, and nobody knew each other. All they ever asked for was some money to buy some saucepans, plates, cups, knives and forks so that they could have a fish and chip supper together once a week. So it might be just really small things that just start bringing people together and building those communities. The idea being that this will have a positive effect on health and equality, but also reduce demand for statutory services as well.
CS1a_C1a
Without such activities ‘[W]e would have significantly more pressures on our beds in hospital, so they [VCSEs] play a really important role’ (CS1a_C8a). Commissioners’ perception of generally positive practical outcomes led them in one site to commission more VCSE activity:
An example probably of where it’s changed in practice was December last year we had some, as all CCGs, health organisations get, Winter Pressures Funding comes through. Our CCG said, ‘Oh, can we put some money into the voluntary sector?’
CS3b_C7a
Nevertheless, some commissioners also highlighted failures. For example, one spoke about ways in which social prescribing targets had been missed:
[W]e haven’t hit the target in any one of our PCNs this year because of the scenario, they didn’t connect into the [shared database], so we’re trying to fight our corner for that but I think we’ve lost the funding for it. So, actually, that’s another nail in the coffin, so to speak.
CS4b_C1a
For learning disability, one outcome was to link the provision of accommodation with access to social activities (CS1a, CS4b) and support healthy living activities such as cooking clubs, physical activity and drama (CS1a, CS3b, CS4a). Another was to extend the reach of clinical services:
[W]e go to our local dietitians in the learning disability trust and say ‘[. . .] you do need a specialist if you’ve got somebody who’s choking on food and is at risk of asphyxiation, but you don’t need a specialist to teach someone what a healthy plate of food looks like. And if you allow the voluntary sector and trust us to do it, then not only do you get people talking about healthy eating but they get a community that they’re joining [. . .]. You don’t have all the time to do that if you’re the dietitian’.
CS1b_V8a
In CS4b, VCSEs helped develop services which enabled ‘repatriation’ of out-of-county placements. VCSEs also worked to increase access to health checks (CS1a, CS1b, CS4b).
Commissioners’ critiques of commissioning outcomes often focused on small VCSEs, which were less financially and organisationally resilient to external forces, including commissioning changes:
Small [VCSE] organisations, how do they get their piece of that funding that they may require to continue that piece of work, that’s probably hugely beneficial to a small population in a local area, versus some of the bigger organisations that are winning contracts across [CS1a] to deliver possibly health and well-being type projects, that sort of thing.
CS1a_C10a; and CS1b, CS4a
This statement draws attention to the differences in scale and reach between social prescribing and some other kinds of public health activity (see Chapter 7, Additional findings). It was not always clear whether the positive and negative aspects cited here were necessarily due to commissioning per se, although our informants did usually assume a connection between commissioning and the observed outcomes and consequences, intended or otherwise.
Relieving cost pressures
Fiscal austerity often meant that VCSEs were commissioned to implement low-cost (or lowest-cost) activities (see Chapter 4, Provider selection), which might not necessarily have been the most cost-effective or offer value for money. Moving residential care for people with learning disability, and moving from block to spot contracts shifted the risks and costs of vacant capacity to the VCSE:
[I]t’s a block contract, effectively we’ve never priced in for voids, for example. Whereas once we go to a personalised budget, the concept of voids will be a new thing for us. [. . .] Whether you’ve got three people or four people in a property, you still need the same level of staffing [. . .] if you just divided what it cost for our supported living [. . .] by the 325 [places] and we only had 315 [filled], we’d still have all our liabilities but we wouldn’t have enough income coming in.
CS1a_V21a
Cost minimisation was apparent not only in NHS settings but also in LAs, especially post-2010. Nevertheless, commissioning VCSEs was alleged to give commissioners high value for money compared to public or corporate providers:
[A] key lesson for me, particularly becoming a trustee of a charity, was what a charity can do for £1 compared to the services I was commissioning from NHS and independent private for-profit sector was phenomenal. I just couldn’t get over how much better value for money I get from charities, on the whole.
NSS_NS9C
What complicated this picture, though, was when VCSE activity, especially social prescribing, exposed unmet patient needs.
Demonstrating the outcomes
Besides obtaining the practical benefits themselves, commissioners sought evidence of VCSE performance, most often of activity (outputs) but sometimes in terms of outcomes. A first complication was how long the above outcomes would take to appear. There was an active ‘conversation’ between commissioners and VCSEs about the uncertainty of evidence about cause, effect and attribution, and how long securing the right data would take.
[I]f we want to shift the money and we want to shift the emphasis and we want to change people’s relationship with their health, then you’ve got to have that little bit of time where it’s changing before you see the impact. It doesn’t happen tomorrow, it’s in a year or two years. I think that’s quite a challenge there.
CS1a_C2a
This especially applied to the connection between commissioning VCSEs to undertake social prescribing and any ensuing changes in population health. According to this VCSE respondent:
Those [housing] estates have had investment, investment, investment over the years and they’re still on the lists as the top most deprived, so because we keep saying, ‘Oh yeah, it’s great, the policeman goes in and the health visitor goes in and we invest all this money in those areas’, those estates wouldn’t be there if that worked.
CS2b_V10a
Reducing health inequalities was often cited as an objective for commissioners, but the commissioners’ ability to address them was limited.
We weren’t coming up with anything new, and we knew we had to come up with something new because we actually hadn’t made any difference [to health inequalities] over the past. You track the data back as long as we’ve got, it goes back to 2007 I think, and the gap’s widening in terms of differences in life expectancy and things like that.
CS1a_C1a
The tension between hard and soft information187 was apparent, with the former being routine administrative data while the latter (stories, narratives) were powerful but less transferable. On the one hand, in CS4b ‘There’s quantifiable targets through the income and investment fund, one of those indicators is social prescribing’ (CS4b_C1a), but some aspects of VCSE activity were less easily measurable than traditional healthcare services. In another instance:
that was just softer feedback. We have a full evaluation going on of that first pathfinder so that we have something in a more concrete report. Because that was verbal, it was some photos, it was we want to get you on board, we want you to know how well this is going.
CS1a_C2a
The reliance on hard measures to ‘prove’ effectiveness was problematic for some. ‘I think we’ve lost the Impact and Investment Fund money that will come from the national team back to PCNs for the social prescribing indicator, because we haven’t been seen to have done enough referrals’ (CS4b_C1a). Costs were sometimes mentioned but were not as salient as might have been expected, a pattern which tended to favour long-standing and larger VCSEs.
Reflecting their partly different aims, VCSEs did not always accept commissioners’ views about what outcomes should be monitored:
[T]hey [VCSE] kind of basically turned round and said to me, ‘[name], we’ve had that conversation and we’ve decided that we’re measuring our success by the number of people that we serve and the amount of money that goes through our books, and that’s what we’re focused on as a leadership team’, which is the point at which I said, ‘Okay, we’ll probably not bother coming back. We’re not on the same wavelength’.
CS4b_C6a, and CS1b
This prompted new discussions between commissioners and VCSEs as to how they might rectify the situation.
I [commissioner] said I’m not providing you with metrics that make no sense and they don’t sum up what we do because that’s just a waste of my time and everyone else’s time. So why don’t we think about how we can do this and it means something and it tells the story. Why don’t we challenge this? Isn’t it time?
CS1a_C2a
Patchy monitoring and review systems (see Chapter 4, Monitoring and adjustment) meant claims about the outcomes at which the commissioners aimed were rarely quantified, measured, or even observational, but usually qualitative assertions (and counter-assertions) (and cf. Appendix 6, Tables 32 and 34). For example:
how much money are we saving the CCGs by giving people an experience of a good death with no complaints? I know for a fact having worked in the NHS and I read papers and things, the extortionate amount of millions of pounds that is paid out to families who have complaints around end-of-life care in the hospitals.
CS4a_V15a
One informant also conceded that although in essence such claims might be valid, the attempt to quantify them might be somewhat arbitrary:
I was with a GP and he said, ‘I think we can assume that each interaction you have had, you have saved half a day of hospital admission’ and I remember challenging him saying, ‘Following the conversation we’ve just had, I think it could be more reasonable to think it was a three-quarters, 0.75 instead of 0.5’, or maybe I even went as far as one. […] And I was aware that in that 30-second exchange, I had doubled the value of the impact of our project.
CS2b_VS1
Given our findings about the unevenness of monitoring and data collection (see Chapter 4, Monitoring and adjustment), it is perhaps not surprising that these claims were more often qualitative than estimates of impact size. Formalised and prescriptive monitoring was more emphasised in a commodified mode of commissioning, while collaborative commissioning tended to involve monitoring more through discussion, negotiation and VCSE ‘learning’.
Prospective innovations: scaling up small pilot projects
Many commissioners had commissioned VCSEs to undertake small pilot projects, often in limited time. Thus: ‘[W]e’re particularly looking to pilot a number of potential solutions. We don’t know whether they’re going to work. They’ve been developed by [local VCSE], not by commissioners’ (CS4a_C9a). In this case, the problem needing a solution was that of increasing the number of people with learning disability getting an annual health check (an NHSE target), and raising the quality of those checks. Other pilot schemes in learning disability included learning disability digital inclusion networks (CS1a, CS1b), a scheme for reviewing the lives and deaths of people with learning disability (CS1b), mindfulness training (CS1b), fitness training (CS1b), support for high users of A&E services (CS4a), and a scheme for supporting people with learning disability with multiple problems whom few providers would accept (CS4a).
If the potential solutions appeared promising, then:
As a result of that thinking, and after many conversations, the CCG have made a piece of resource available. It’s reasonably significant. We want to try and make it available over the next… we don’t just want it to be a year or two years, we want it to be a five-year thing.
CS1a_C1a
While this is common elsewhere in the health and care sector,188 it seems to contrast with some large-scale funding decisions elsewhere which had not required the same conditionality, for example decisions regarding the secondary care contracts with NHS Trusts which account for over half of an NHS commissioner’s budget. 189 The pilot projects clearly pursued the aim of finding out ‘what works’,190 and therefore what would count as confirming (or disconfirming) evidence, the criteria for impact or effectiveness, and whether the project might be more widely generalisable.
The problem with [VCSE project] is it has always been measured against a cohort group. If you expand [VCSE project] and now deliver it for the whole of [locality], you’ve lost your measure, and this is a problem with the outcome.
CS1b_C3a
Irrespective of any evaluation, commissioners did not always fund these pilot projects for long enough to expect any impacts, which frustrated the intended outcome of discovering ‘what works’.
Outcomes and consequences for voluntary, community and social enterprises
Receiving funding through being commissioned contributed to VCSEs delivering services that met their mission, but VCSEs also experienced some unintended, even perverse, outcomes.
On mission or mission drift?
Mission drift has long been highlighted as a potential outcome of commissioning for VCSEs (see Chapter 1, Consequences of entering a relationship with commissioners). A minority of informants presented some evidence, or perhaps claims, about it. Thus, in learning disability services:
lots of small organisations [. . .] need grant funding in order to survive, and so they don’t have the luxury of being able to… And this is where our self-generated income really comes in handy. Where they don’t have the luxury to say, ‘Does this department have the same priorities that we do? Do we actually get on with the commissioning team? Do we have the same vision?’
CS4a_V6a
Another minority described VCSEs sacrificing commissions to mission. Most described marginal adjustments to VCSE mission and aims in response to becoming commissioned.
Commissioners mentioned mission drift more often than VCSEs themselves did. One commissioner commented on how the VCSE sector had prioritised the financial needs of organisations, which had resulted in them losing their distinctiveness:
So I think what I’ve seen is the voluntary sector’s [. . .] been forced to chase resource so it’s had to morph itself into a money chasing machine, as opposed to delivering what it could do really, really well and it’s distorted the role of the voluntary sector, I think, which is a real shame because when they’re given free rein to do what they know works well, they’re brilliant and highly effective. When they’re doing what they think the system wants it to do just so that they can get a bit of funding, it doesn’t really fit.
CS3b_C3a
This was a commissioner commenting, but a VCSE informant also noted the challenges of staying on mission, having ‘strategic coherence’ when delivering a multitude of services, and the need to have clear boundaries to guide decision-making processes (CS1a).
At the opposite pole, organisational values and ethos were identified as guiding principles that helped VCSEs maintain integrity and stay on mission:
It’s those principles and our charitable objectives of making a difference, improving lives, enabling choices, enabling change. That’s everything that we do but it’s about using that to focus the mind when you’re looking at change or decision or commissioning opportunity, can we make a difference, will it help change lives and if the answer is no, then the answer is no.
NSS_NS12V
In CS2b a VCSE decided to end a contract, having reviewed progress after 2 years and concluded that it was not leading to the social change that was core to their mission and values.
More often, we were told of examples of VCSEs’ mission being expanded and pursued in different ways. For some VCSEs, having a broad mission allowed them to be flexible and experiment with different activities and initiatives including through commissioning, and ‘tweak’ their mission by framing and describing activities in a way that mirrored the commissioners’ language and funding requirements. What then happened at the implementation stage could differ, which was referred to as ‘mission re-manipulation’ (CS2b). For instance, in CS3b a VCSE whose mission focused on young people developed new health and well-being services partly through their involvement in social prescribing. Some VCSEs and commissioners spoke of the pressures on VCSEs to expand their scope or geographical remit because of increasing demand for their activities (CS1a). Perhaps inevitably, though, VCSEs’ reach into communities remained incomplete:
There are still lots of people who don’t interact with these organisations or can’t interact with the organisations. We have to be mindful of [. . .] how else we can communicate or give people that opportunity to feed into the work that we do.
CS1b_C6a
Another learning disability organisation explicitly stated, but also restricted, its own financial aims:
[I]t’s not sensible for us to be at risk financially, but neither do we want to make an undue amount of surplus. [. . .] we try to keep our surplus to around between 0.5% and 2% a year. Because we’ve got that public service ethos that we’re not here to strip money out of the sector but we’d need enough financial resilience in the event of risk being transferred to us.
CS1a_V21
Other VCSEs, however, described a narrowing mission, related to the NHS focus on achieving health outcomes for individuals through the delivery of services, without comprehending the wider social aims of these VCSEs’ work, in particular wider societal change brought about through advocacy and campaigning. These cases illustrated how, even with the broad compatibility of aims described in Chapter 4, Commissioner and voluntary, community and social enterprise aims, VCSE and commissioner goals and agendas could diverge. However, interviewees also provided examples of VCSEs and commissioners having or working towards shared goals and agendas (CS1a, CS3b).
Commissioners’ and hospices’ mutual dependency meant that while hospices partially relied on statutory bodies for funding, there was a limit to what commissioners could ask them to do. Commissioners therefore took a more flexible, collaborative approach to working with hospices, weakening commissioners’ managerial control:
[A]s a commissioner we would like to move to NHS contracts, but it works, it suits the hospices to be under grant agreements. They get paid all the money upfront [. . .] there’s the reporting, it’s not particularly onerous for them, it all works nicely for them, so they’re not sort of falling over themselves to go onto an NHS contract.
CS1a_C8a
Hospices were aware of an organisational outcome of this payment mechanism (see Chapter 4, Agreements and payments):
Most clinical services are all paid on activity [. . .] We’re not [. . .] The one advantage for us is that we keep our independence, [. . .] we’re able to respond and react very quickly, we don’t have all the bureaucracy of the NHS. We don’t have all the reporting that we need to do in the NHS as well [. . .] The disadvantage of course is that finances are always going to be an issue.
CS2b_V11a
Nevertheless, the hospices were insulated from commissioning-induced changes of mission, with the outcome of preserving these VCSEs’ autonomy and discretion.
On balance, VCSEs mostly alluded to mission drift as something that was only minor and which they had learned from. It was part of their commissioning journey and it had allowed them to refocus, backtrack and ultimately reinforce their original mission (CS2b).
Competition, integration and collaboration
Voluntary, community and social enterprises engaged in commissioning partly in order to sustain and develop their services and other activities (see Chapter 4, Voluntary, community and social enterprises aims). Commissioners engaged with VCSEs of sizes ranging from large national charities to local grassroots organisations. Variations of scale in commissioning opened or closed opportunities for different types of VCSEs. Larger contracts and grants (see Chapter 4, Agreements and payments) favoured larger, more formally organised VCSEs that were able to work with the demands and complexities of the system and offered economies of scale, squeezing small organisations out of the market (CS1a, CS3b, CS4a). Several VCSEs and commissioners highlighted how the increased competition for contracts as well as grants had generated rivalries and tensions among VCSEs (CS1a, CS1b, CS3b, CS4a). They thought this had damaged and reduced VCSEs’ capacity to collaborate (CS1a, CS1b). Some informants suggested that certain VCSEs could become ‘favoured’ organisations dominating the local commissioning landscape, leaving little space for other (often smaller) VCSEs. In those circumstances, commissioners could, at least in theory, encourage provider competition as a mechanism to help new VCSEs become commissioned.
A commissioner in CS1a added that they felt that NHSE supported a lead provider model with subcontractors rather than an alliance model of equal partners which was more conducive to collaboration. In CS4b a VCSE expressed concerns that commissioners wanted to achieve service ‘integration’ by seeking a single VCSE provider to address issues of fragmentation and duplication within the VCSE sector, but were failing to recognise and value the diversity of providers and services. Another VCSE described how they had been asked to sign a contract stipulating identical service developments across VCSEs in the area.
I said, ‘Well I’d rather not have the £250,000, because it ties our hands so much’, because [. . .] It was almost as [. . .] though they were trying to make the [. . .] hospices behave as one hospice, and I said, ‘If you really only want one hospice, we need to have that conversation, which is a different conversation from the one that we’re having’.
CS1a_V5b
However, there were counter-examples. Some commissioners had tried to use, for example, Section 256 agreements to work around the procurement system so as to include VCSEs that might otherwise be excluded. Some VCSEs set up consortia and alliances of smaller VCSEs (NSS_NS1V). The co-design and co-production of services and activities also addressed some of these issues, for example:
a project where it seems that the commissioners or the project leads there are very trusting in us and bringing in our real lived experience in what we’re trying to deliver and how that’s going to be delivered on a county-wide and how they’re entrusting us to work with smaller organisations to create that feedback loop into them around the decision-making. And to me I think that’s real true co-production.
CS4a_V18a
Commissioning changed services and activities in a number of ways. At times they were extended with the development of new services and activities, or reduced when existing contracts came to an end.
These changes happened sometimes because of changes within commissioning bodies such as restructuring and budget restrictions, or in response to policy agendas or changed funding mechanism such as a shift to personalised budgets. But sometimes the changes arose from VCSEs having to conform to commissioning and particularly procurement requirements.
[O]ne of the difficulties is that it starts as a commission because there is an understanding and an admiration of the way that the service is done. But the rules of commissioning often dictate that that service actually changes to meet the need of the [commissioning] organisation, not the existing [VCSE] organisation who has set up deliberately to provide something that might be slightly different or delivered in a different way. So I think that there is sort of a slight pressure for the commissioned organisation to change its practice in order to be able to fit the targets of the commissioning organisation.
CS4a_V17a
The case study sites illustrated generally how commissioning had affected the VCSE sector and relationships among VCSEs depending on whether it tended towards a more commodified mode of commissioning or a more collaborative mode that was more compatible with the involvement of a wider range of providers, and how this in turn had shaped the services and activities that were being delivered.
Income and financial precarity
A recurrent VCSE motive for being commissioned was to obtain income to support their activities and mission (see Chapter 4, Voluntary, community and social enterprises aims). Table 8 summarises the proportion of CCG spending on VCSEs compared with other kinds of provider in 2018–9.
| Type | Number | Total spending (£m) |
|---|---|---|
| VCSE | 1051 | 1912.409 |
| Non-VCSE | 9511 | 68,583.872 |
| All providers | 10,562 | 70,496.281 |
Whether measured by number of providers or income, VCSEs’ market share of CCG spending was still modest (10% and 3%, respectively). Figure 14 shows the variation and skew across CCGs within these totals. Appendix 5, Table 15 shows the distribution between types of VCSE.
FIGURE 14.
National (189 CCGs) expenditure on individual VCSEs, 2018–9.
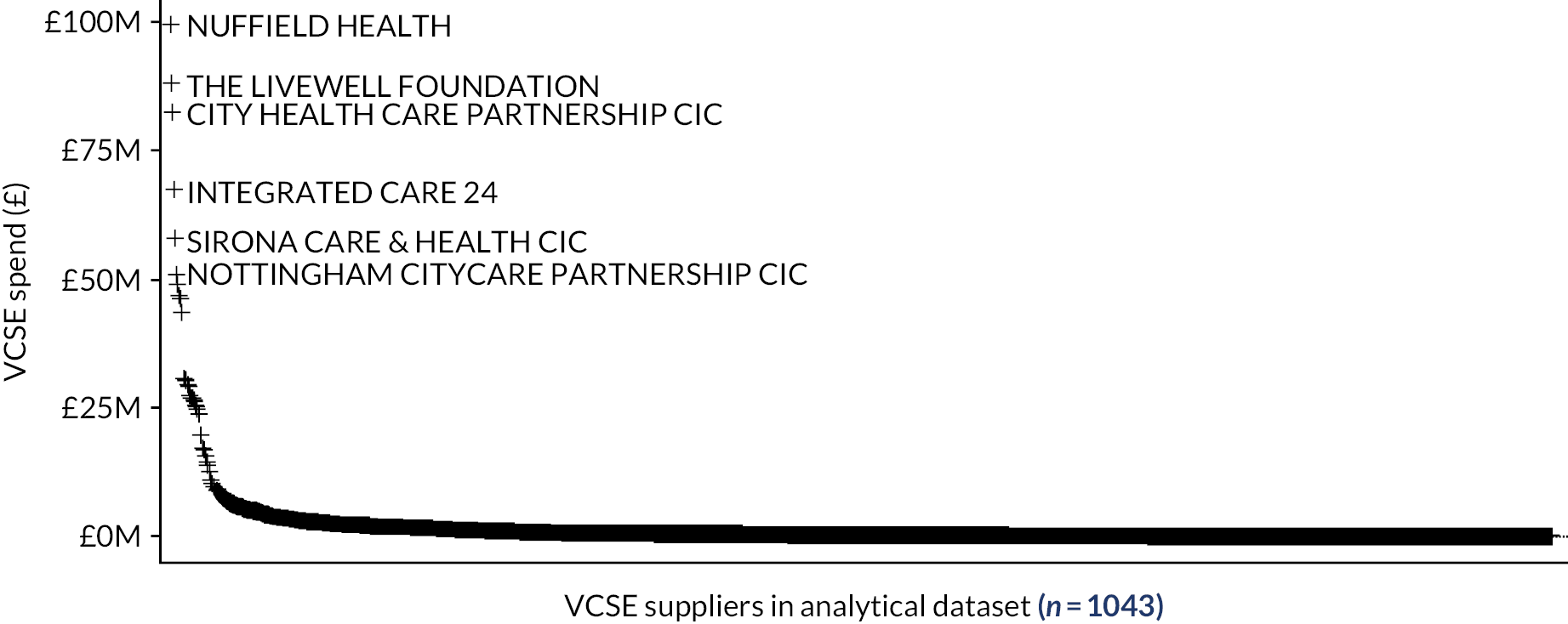
Within CCG spending on VCSEs the distribution was also highly skewed, with a few VCSEs receiving substantial funding and a very long tail of minor providers (see Figure 14). This tail would have been far more pronounced had we been able to include invoices of ˂ £25k.
In 2018–9 just six VCSEs (see Figure 14) received more than £50M from the 189 CCGs for which there are reliable data, together 23.5% of the total national CCG spend on VCSEs. Some 34 providers received more than £10M (totalling 60.6% of total VCSE spend), and 242 providers more than £1M (91.1% of total VCSE spend). Figure 15 highlights the major VCSEs in terms of either total income from CCGs or the number of CCGs in which they have at least some presence. In contrast, the bulk of VCSEs receive relatively little and from only a few CCGs.
FIGURE 15.
Total CCG spending on VCSEs against number of CCGs served.
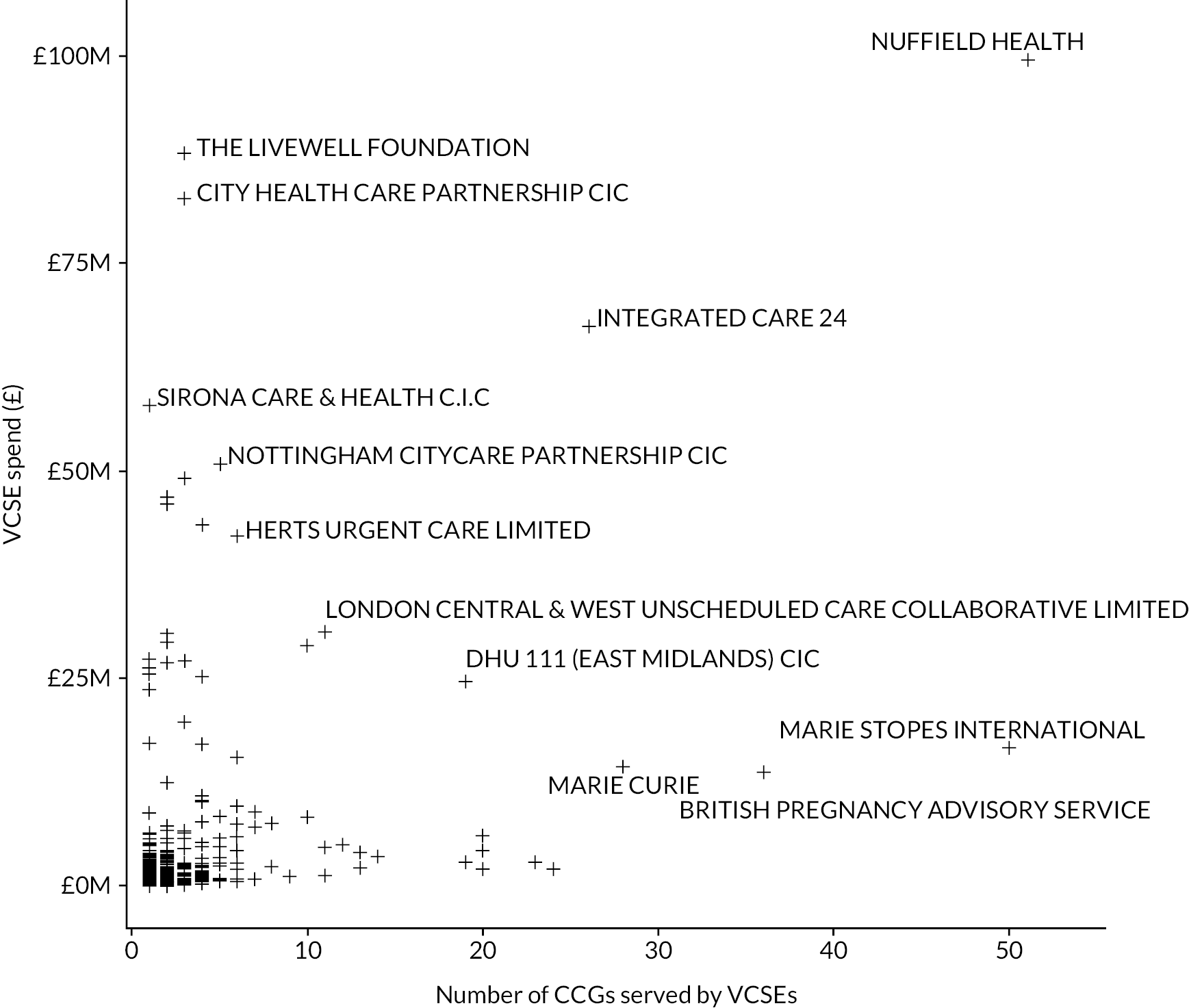
For our study sites specifically,Figures 16 and 17 respectively show for each site the quarterly number of unique commissioned VCSEs and total spending on them during the study period (note that the y-axis scales vary as this is the best way to highlight the changes over time in each CCG, although that tends to obscure the fact that the CCGs exhibited quite different levels of VCSE activity).
FIGURE 16.
Number of VCSEs commissioned by each study site CCG, longitudinal profile.

FIGURE 17.
Value of VCSE commissioning by CCG per study site, longitudinal profile.
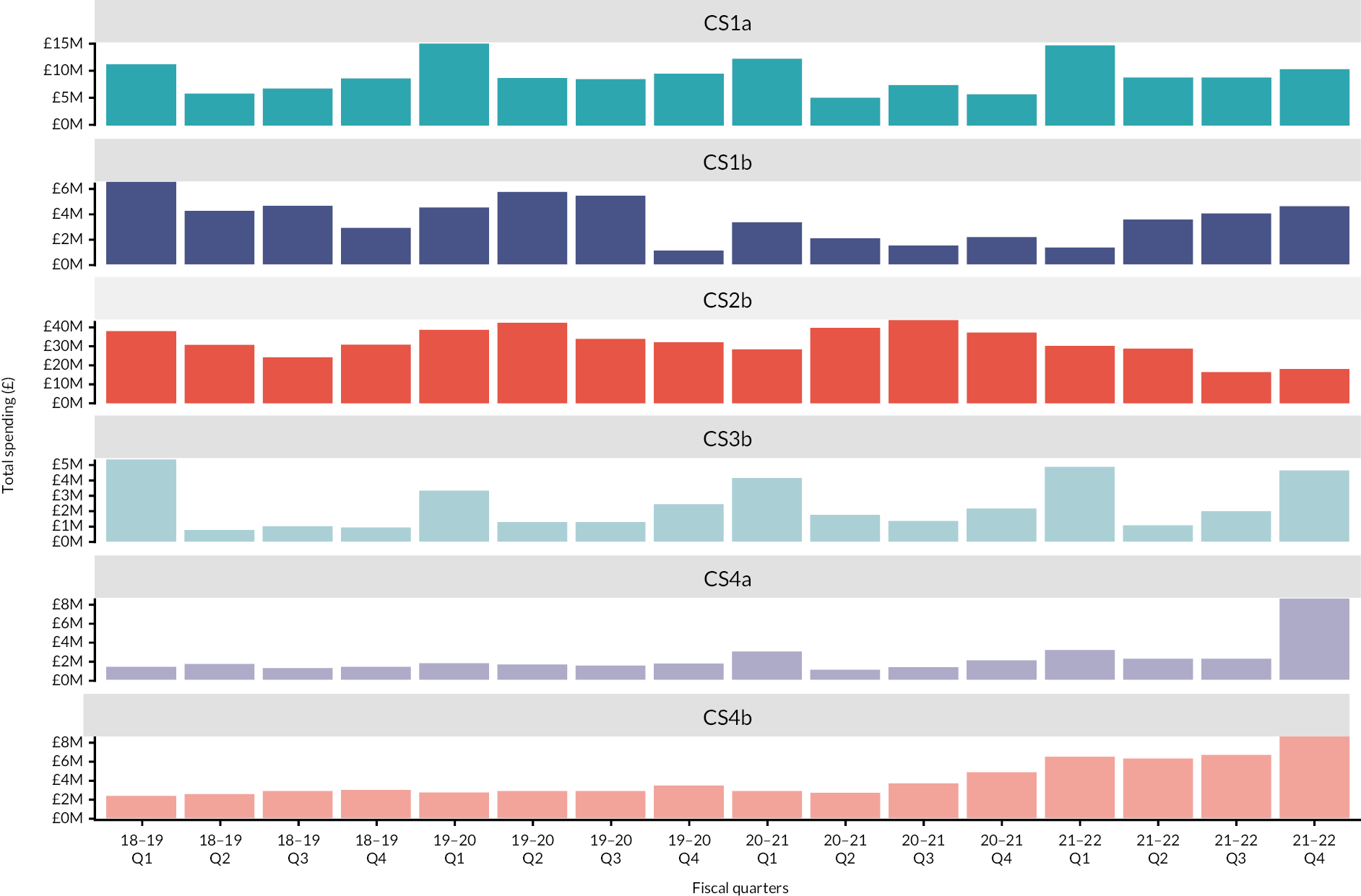
Clinical Commissioning Group spending on VCSEs in CS1a and CS3b was somewhat erratic. The apparent fluctuation in CS1b was apparently due to data quality, not necessarily actual spending changes. These were city sites. The trend in the three more rural sites was more interesting. In CS2b the numbers of unique VCSE providers were fairly stable but the amount spent on them fell away in 2021–2. It remains to be seen whether that will be a permanent post-COVID-19 shift. In CS4a and CS4b spending increased slightly, though from a low base. The highest increases in per capita funding among our case study CCGs were also in these two sites.
Figures 18 and 19, respectively, focus on the study site CCGs’ percentage of total spending on VCSEs and the per capita spend (again, note that the y-axis scales vary).
FIGURE 18.
Study site CCGs’ percentage spending on VCSEs, longitudinal profile.
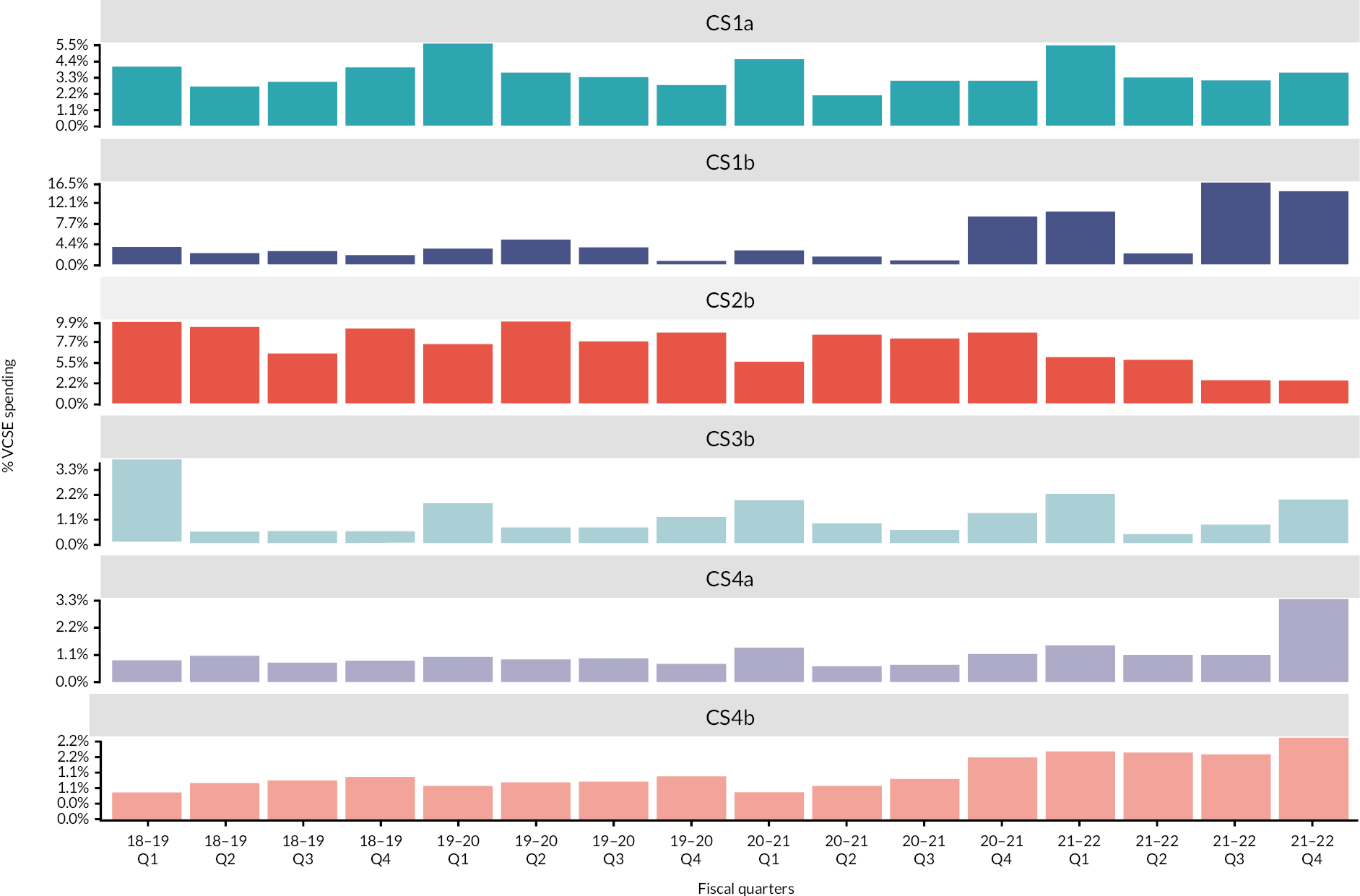
FIGURE 19.
Study site CCG spending on VCSEs per capita of population, longitudinal profile.
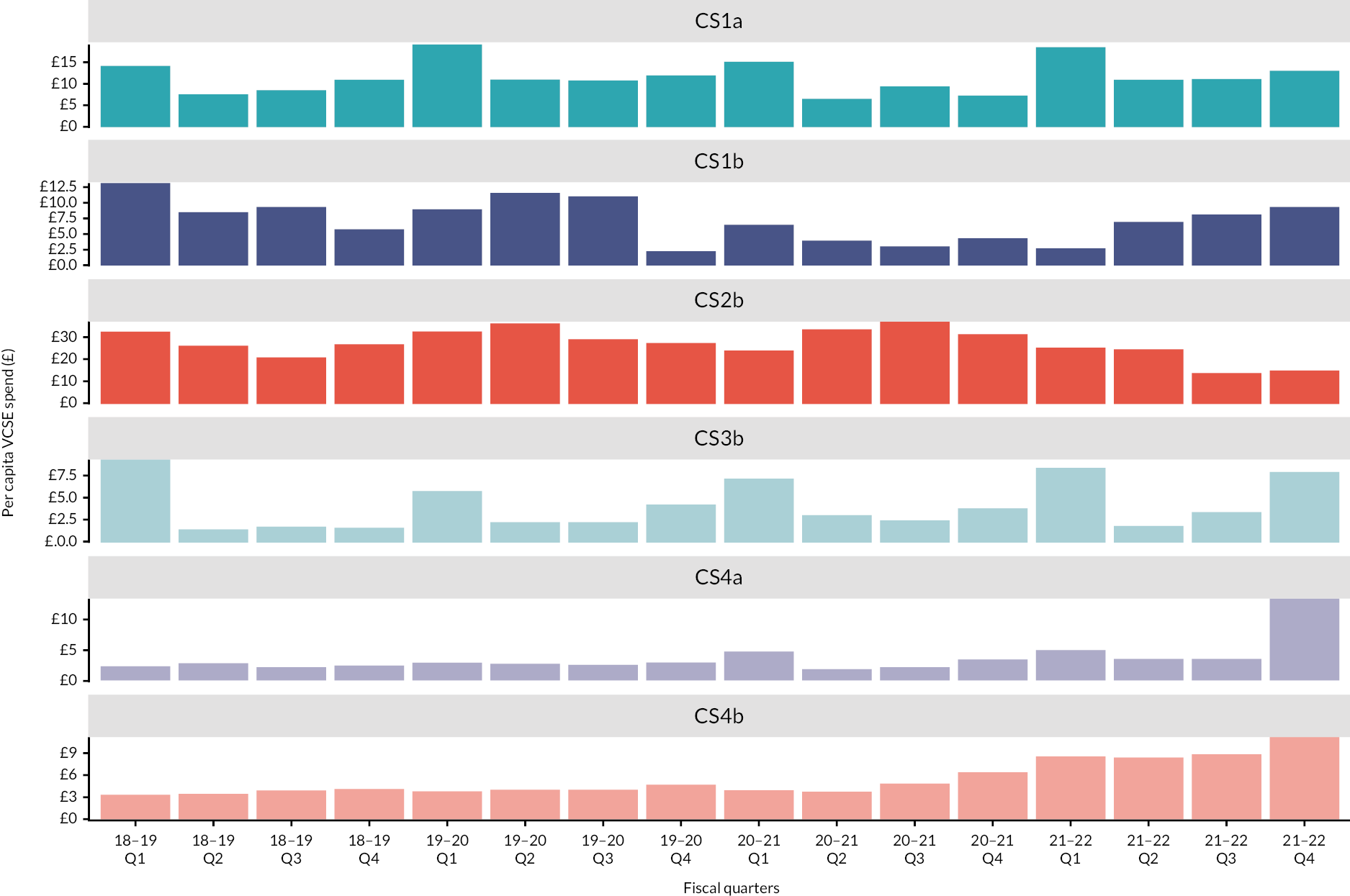
The fall in spending on VCSEs in CS2b, and the increase from a low base in CS4a and CS4b again appear. Although there were minor shifts in activity, study site CCGs’ spending on VCSEs stayed much the same through the study period. The fluctuations in the data for CS1b appear to reflect uncertain data quality as much as real changes. The last vertical bar in each row in Figures 16–19 coincides with the peak in COVID-19 cases. 191
In part, the fiscal pressures on commissioners (see Chapter 5, Fiscal constraints) were passed on to the commissioned VCSEs:
[W]e’re an £11M organisation and literally seven million of that is coming from the community through various different means [. . .] you’re always battling with the money, you’re always battling to, how do I bridge that gap between the service users, what the NHS give us versus what we want to deliver as a service.
CS2b_V11a
The instability of commissioners’ own funding also meant that the funding of VCSEs also became more precarious and required more frequent changes to contracts (in effect, higher transaction costs for commissioners and VCSEs).
Cuts in public spending and the tendency among commissioners to create larger contracts rather than multiple smaller contracts have led to greater competition among VCSEs, often to the detriment of smaller organisations (see Chapter 4, Agreements and payments and Chapter 6, Competition, integration and collaboration). The underfunding of VCSEs was another reported outcome of commissioning them. VCSEs had difficulties in obtaining full cost recovery (CS1a, CS2b, CS3b), whereby a contract or grant covered the total cost of delivering a service or an activity, including proportionate overhead costs and invisible costs such as those of administering volunteer labour (e.g. training, insurance). This was mostly when commissioners failed to recognise the true cost of a service or activity, but in some instances it was because VCSEs wanted to make their pricing more competitive by omitting overheads or indirect costs. Underfunding also happened when the fee uplifts automatically awarded to other providers (e.g. NHS Trusts) were refused or when commissioners did not reimburse VCSE costs such as backfill for VCSE members attending co-commissioning and other meetings. There was also a concealed financial dependence of NHS commissioners on VCSE activities when the latter were provided below their cost of production by means of volunteer labour and, in the case of large VCSEs such as hospices, cross-subsidy from other income sources such as charitable donations. Where informants in learning disability organisations knew the ratio of employees to volunteers, it varied from 1 : 1.5 to 1 : 5.
Given fiscal austerity and wider economic pressures, VCSEs continued trying to diversify income streams in order to spread risk. VCSEs fundraised to remain independent and flexible, obtaining where they could grants from trusts and foundations, charitable donations from the general public, and fees from trading (CS1a, CS2b, CS4a). However, they also used these wider financial resources to supplement the cost of providing commissioned services that were underfunded. For many VCSEs the impact of losing funds and the need for additional funds were constant preoccupations, as were short timescales for preparing bids and then short contract periods. Dealing with those external pressures had led to internal tensions or challenges within VCSEs. In CS2b, for instance, trustees of a VCSE had resisted going public about the financial difficulties of their organisation for fear funders would withdraw their support, and had been nervous about spending any of the organisation’s reserves. In CS1a, a VCSE’s board members with conflicting attitudes towards risk disagreed about whether NHS funding should become more than half of the organisation’s total income. Tensions also surfaced in national charities between head office and branches (CS3b).
Workforce precarity
Among the consequences of these financial outcomes, VCSEs in the case study sites described staffing impacts and workforce insecurity. They mentioned the rise in fixed-term and casual contracts, the inability to compete with public and private sector providers who offered higher salaries and clearer career progression, and the imbalance of workforce composition in organisations with a small core permanent team and a large number of sessional workers. This led to low staff retention which caused a loss of skills, expertise and knowledge, and institutional memory, and negatively affected the VCSEs’ capacity to deliver services and to campaign and influence.
But that’s brought with it its own challenges because we only ever have one year of funding, so we’ve lost brilliant staff who’ve said, ‘I love working here but I’ve got a mortgage to pay, and it’s January, February and I don’t know what’s happening from April’, or, even worse, the funding has been cut and they’ve been made redundant.
CS4a_V2a
Voluntary, community and social enterprises whose work in learning disability support was financed by spot contracts especially felt this insecurity. High demands were placed on staff time for those delivering services and for those in leadership positions to meet targets. Substantial transaction costs were associated with bidding, managing and maintaining relationships with commissioners, and holding representative roles on boards and forums. So:
if there is commissioning for a [learning disability] service and there’s only an expectation that one provider will win the tender, we don’t apply. [. . .] Because the processes and the effort involved are too resource-intensive to make it worthwhile.
CS1a_V14a
There were concerns about employee overwork, well-being and stress due to reduced budgets, staff departures and shortages, but a recognition that this was also the case with commissioners. COVID-19 had exacerbated the problems.
Whether you’re a social worker or whether you’re a nurse or whoever you are, everyone’s feeling pressures because it’s less people doing more work than ever before. There’s less commissioners who then don’t have time to do things. [. . .] if you’ve got a commissioner who’s been covering the whole of learning disability and mental health, that’s quite a job.
CS2b_V4a
Accessing funds through commissioning had contributed to a more diversified funding mix and growth for some VCSEs. However, the underfunding of VCSEs and the short-term nature of many commissioned contracts and grants had increased VCSEs’ financial precarity and workforce insecurity.
Voluntary, community and social enterprises’ experiences across the case study sites highlighted how they routinely faced situations where managing financial complexity and uncertainty was key. This included understanding and dealing with multiple payment mechanisms, for example block contracts and grants. Beyond the money awarded, VCSEs had to consider the implications of the terms and conditions of these different arrangements. Some VCSEs highlighted how they did not always have access to the necessary information in good time, especially when a contract was coming to an end (CS1a, CS3b). Adapting to uncertain time frames and managing the vicissitudes of funding starting and stopping was particularly challenging.
Voice and influence
Although uneven across the study sites, the broad picture was one of relationships between VCSEs and commissioners strengthening over time, particularly through co-commissioning and trust developing (see Appendix 6, Table 26).
Many VCSE interviewees thought they had a ‘seat at the table’ and could challenge and influence commissioners and statutory decision-makers more widely (CS1a, CS2b, CS4b). They spoke of their organisations having numerous conversations with commissioners, walking away from contracts if dialogue had not been possible, and some successes where they had found solutions to problems (CS2b) or made the case to shape or improve services in a way they felt was more adapted to user needs (CS1a; see Appendix 6, Tables 29–31 and 33). They expressed their commitment to seeing the bigger, sectoral picture, thinking beyond their individual organisations, to enhance commissioners’ understanding of VCSEs’ contribution and to engage collectively to effect change and address unmet needs. Staff turnover in commissioning organisations and constant changes and restructuring were perceived as barriers to these activities. Nevertheless, VCSEs felt their capacity to challenge and influence had increased due to an improvement in their relationships with commissioners and greater mutual trust. There remained disparities in commissioning practices and commissioners’ level of skill and competence, but VCSE informants mostly considered that things had changed for the better and that commissioners could be supportive in a pressurised environment and willing to pursue shared goals collaboratively. Chapter 4, Commissioner networking: co-commissioning and Chapter 6, System-wide, emergent and perverse outcomes, respectively, describe more fully the role of networking in collaborative commissioning and the system outcomes of commissioning VCSEs.
Across the ICB we’ve worked with the community voluntary sector to set up our objectives, our vision. So hopefully that has that collective view across all the organisations. So if you’ve got that shared vision, hopefully you’re all moving in the same direction and that makes it easier because when pieces of work come up, that you feel are important, that they are equally important to those people who you’re potentially going to be asking to deliver.
CS1b_C6a
Voluntary, community and social enterprises sometimes succeeded in getting commissioners to change their own working practices:
Just before lockdown, we did a deputation to the council to say that they needed to put their money where their mouth is, really, and employ people with learning disabilities within the council and lead by example. So there’s been a huge change since that deputation and they’re really working, it seems to be that that is one of their number [one] priorities, is to get more people employed within [CS1a] with learning disabilities. So they do listen in that respect.
CS1a_V12a
Nevertheless, both VCSEs and commissioners recognised that in some instances commissioners had excluded VCSEs from decision-making spheres: ‘There’s a group called [name] which is all of the [CS4a] district councils, the CCG, the police, the LEP [Local Enterprise Partnership] and health. VCS doesn’t have a place on that’ (CS4a_C1a). Some interviewees alluded to VCSE capture by commissioners, with integration policies providing platforms for VCSE voice, but failing to address imbalances of power within those platforms, where non-VCSE players (e.g. NHS Trusts) had more power than VCSEs, and power imbalances among the VCSEs. Both VCSEs and commissioners questioned who was at the decision-making table and who was excluded. Collaborative commissioning, including co-commissioning, was demanding for VCSEs because it required them to manage numerous multilateral relationships and partnerships, diverted some of their service delivery capacity, and put smaller VCSEs and/or VCSEs that were less financially secure at a disadvantage.
I think I can see that is so important that you can have a voice. You can only really be sitting on these meetings and doing these things if you’re not worrying about where the money is going to come from.
CS1a_V11a
Voluntary, community and social enterprises were also sometimes excluded at points in the commissioning cycle, for example at the tender formulation phase, when VCSE input would have helped the commissioner to respond to unmet needs, improve outcomes for service users or guide the implementation of local strategies (CS4a, CS2b).
While VCSEs’ capacity to influence commissioners and commissioners’ capacity to listen to VCSEs seemed to have increased, there remained scope to increase it further. In all case study sites, there was a move towards co-commissioning, but many felt it was still at an early stage: the aforementioned power dynamics and barriers to engagement and power dynamics persisted. This move was an important part of the development of collaborative commissioning.
Internal transformation
Some previous studies describe the impact of commissioning on VCSEs’ internal regime in predominantly negative terms (see Chapter 1, Voluntary, community and social enterprise relationship to public and corporate sectors), but our study sites provided a more nuanced picture. There had been moves towards more bureaucratic systems within VCSEs, partly because they increasingly had to manage multiple funding streams with different performance and quality monitoring requirements. The need for robust, sophisticated systems to deal with commissioners’ growing demands for data put considerable pressure on VCSEs, not all of which had the resources and skills to adapt (CS1a, CS4a). Some sought external advice but at great expense (CS4b).
[O]ne of the things I’m really struggling with at the moment is the amount of data they’re asking us for, given that we have quite naive data collection systems, unlike NHS partners who have vast, complicated, very easily interrogated data systems. We have an extremely simple one, and we can’t extract the data, so we’re having to spend hours and hours doing manual counts.
CS4a_V10a
Data management was a good example of commissioning contributing to the professionalisation of VCSEs’ internal organisation with the development of new systems and specialist skills including bid-writing, financial management and partnership working, and the creation of new roles [including safeguarding roles (CS1a)], new career paths to attract new recruits in a competitive labour market (CS4b) and, in some VCSEs, move away from volunteer labour (CS3b). These tendencies were particularly strong among VCSEs that had grown substantially because of being commissioned.
We now send out 200 invoices every month, so our whole back office has had to change. We’ve had to become far more professional in our approach. We are a business – there’s no way around it. We are a business; we are not run by volunteers any more; we are run by a very professional staff who are developed and motivated in a much more business-like way than before.
CS3b_V13a
As a result of winning a large contract or several contracts, some VCSEs had been internally transformed, and the transition had not always been straightforward (CS2b). The impact of contracts coming to an end was also something that leaders had needed to consider and respond to. VCSEs across the study sites painted a picture of constant movement which commissioning contributed to. The way they worked with commissioners showed a high level of adaptability and resilience, especially during the pandemic.
Some informants saw these internal transformations as diluting VCSEs’ identity and distinctiveness:
Despite being part of the VCSE I would say, quite harshly, [that they] have lost sight of the common good in favour of their own good. That depresses me profoundly and I don’t know what we do about that really, I really don’t know what we do about that, because you can’t force – because the joy of the VCSE is what it is, and it’s messy and does its thing and all of the rest of it.
CS2b_V1a
On balance, however, we found more examples of how VCSEs in the case study sites consciously endeavoured to keep their original missions and values while being flexible and responsive to their users’ needs.
System-wide, emergent and perverse outcomes
From commodified to collaborative modes of commissioning
Chapter 4 explained that we found two modes of commissioning VCSEs coexisted in parallel while also partly conflicting, especially at provider selection stage in the commissioning cycle. Commissioners’ rationale for excluding VCSEs involved in co-commissioning from competing as providers appeared partly to be regulatory but there was also a taken-for-granted assumption that there exists a conflict of interest between commissioner and provider, an assumption copied more from the commissioning of corporations (where it is often warranted) than from general practice (where a similar putative conflict of interest recently existed when CCG structures made GPs both commissioners and commissioned; see Chapter 1, Health and care). Collaborative commissioning rested upon a negotiated development strategy for that local health economy (including VCSE roles in it), planned rather than competitive provider selection, and a negotiated division of labour among providers.
In our study sites we found a tendency to move from commodified commissioning towards collaborative commissioning, especially when commissioning relationships developed over time: ‘I suppose the VCSE work that we did with procurement was it’s been a bit of a springboard catalyst into wider opportunities’ (CS3b_C7a). The shift was also a cumulative effect of the multiple workarounds of commodified commissioning, especially the procurement systems (see Chapter 4, Shift to networking). In ascending order of transition towards a collaborative mode of commissioning, the workarounds were, first, making as flexible use of the existing procurement system as possible. For example:
[Name] legal experts in procurement with the voluntary sector and they very much promote this approach that [. . .] as long as you’re transparent about what you’re doing and you do things fairly, you can almost do anything really.
CS2b_C11
Next, one could follow the formal procurement system but implement it as ‘softly’ as possible, both at provider selection (see Chapter 5, Size) and monitoring (see Chapter 4, Monitoring and adjustment) stages. A third step was to limit the procurement system to the very minimum so that in practice most VCSEs were commissioned through alliance, lead provider or similar networking structures (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks). Finally, many commissioners and VCSEs dispensed with formal, competitive procurement altogether by using grants, subsidies (e.g. to sustain VCSEs through the COVID-19 pandemic in CS4a) or other payment mechanisms instead, and by keeping payment sizes below the amount which triggered competitive formal procurement (see Chapter 4, Agreements and payments). These arrangements were instances of commissioners and VCSEs ‘voting with their feet’ (so to speak) in respect of commodified commissioning and supplanting it with more negotiative, collaborative mechanisms. Many of our informants (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks) perceived the creation of ICSs as a more formal move in the same direction, although at the time of this study it was still too early to say how far that belief was warranted.
Commissioning, governance, power
Commissioning can be understood as, among other things, a means for the state to exercise governance over the providers of publicly funded services (see Chapter 1, Health and care). As media of control over VCSEs, commissioners used primarily resource, specifically financial, dependence; and discursive control (developing ACAP on both sides), thereby facilitating managerial controls (monitoring). In some instances commissioners also used competition (provider replacement) and – although it was rare in practice – could invoke regulatory (juridical) controls.
First, VCSEs were aware of their financial dependence on commissioners, and that financial support was conditional on the VCSEs supplying the agreed services or other activities (see Chapter 4, Agreements and payments). A VCSE member commented that ‘[W]hat we are arguing against is the wielding of power through money, but [. . .] the VCSE will always make pot shots at the statutory services if they wield power through money’ (CS2b_V1a, also CS4b). As Chapter 4 reports, both VCSEs and commissioners took steps to attenuate the use of provider competition, thereby attenuating that medium of commissioner control over VCSEs. However, a more pressing motive on the VCSE side was to prevent a ‘race to the bottom’ in cost-cutting (CS4b_C6a).
Intrinsic to co-commissioning and collaborative commissioning was the transmission of ideas and evidence, including the data required at the needs assessment and monitoring stages of the commissioning cycle, and for negotiation at the provider selection and agreement stages. A corollary was the development of ACAP at the interfaces between the organisations involved. In particular this involved the VCSEs familiarising themselves with how to specify services, other activities and outcomes for the purposes of formulating contract (and indeed grant; see Chapter 4, Agreements and payments) specifications, and how to mobilise knowledge, use evidence and conduct research for these purposes. Additionally, ‘there’s a real OD [organisational development] leadership development element to all of this stuff which is, it’s about behaviour and stuff as much as it’s about structures and processes for commissioning’ (NSS_NS10A).
In order to facilitate access to it, ‘within [site], you know, we redefined health and social care workers to include those people in the third sector that provide health and social care services. So we stretched the national definition’ (CS1a_C5a).
Commissioning appeared to involve VCSEs learning commissioners’ discourses and ways of thinking. At the time of this study, however, the development of ACAP at the interfaces between commissioners and VCSEs was still a work in progress, as Chapter 5, The intercalation of contexts reports.
We heard reports of instances where commissioners had replaced providers (the essence of competition as a means of governance over VCSE activities), but less often than reports of commissioners and VCSEs taking steps to attenuate provider competition as far as VCSEs were concerned. One reason for reluctance to change provider was the resulting collateral damage to patients or clients:
[W]e’ve got a lady that we’re going to have to give notice on because we can’t, they [commissioners] owe us [VCSE] £20,000 at this precise moment. We cannot sustain £20,000 because we’re only a small organisation. [. . .] Now this lady we’ve cared for the last, well before I was here, five years, so she knows our staff in and out, we know her, we know what her needs are. So what’s going to happen when she goes to another organisation that’s going to do it for a lot cheaper, what’s going to happen to this lady?
CS4a_V18a
Similarly, regulative control over VCSEs (e.g. CQC reports and decisions) was occasionally reported, but not as the main means by which commissioners exercise power over VCSEs: at most, a commissioner might use a CQC report to justify a subsequent attempt to negotiate changed working practices in a VCSE-provided service.
As Chapter 1, Commissioning voluntary, community and social enterprises explained, in commissioning relationships power and influence are exercised, perhaps unequally, in both directions, not just one. For VCSEs, the main media of power over commissioners were resource dependency (this time, on real-side resources); discursive, in helping legitimate for commissioners’ decisions and activities; and VCSEs attenuating commissioners’ use of provider competition as a means of commissioner control.
Regarding resource dependency, we have already reported how NHS commissioners acknowledged NHS dependence on the real-side resources which VCSEs provided. As Chapter 6, Outcomes for commissioners and Outcomes and consequences for voluntary, community and social enterprises explain, there was also a concealed financial dependence of NHS commissioners on VCSE activities when the latter were provided below their cost of production. NHS commissioners thus had reason to be flexible, on occasion, in their funding methods, monitoring and their responses to adverse monitoring reports; Chapter 4, Monitoring and adjustment describes such instances. Often, too, the resource dependence favoured the power of the VCSE rather than the commissioner:
[O]ne of the questions was, from our commissioner at that time was, ‘What will you do if somebody else gets this contract?’ So, I turned around and said, ‘What are you going to do? Because your funding is 25% of our work, we’ve still got 75% of work, we’re going to carry on doing, so what are you buying with your 25%?’ and they didn’t have an answer because for them they were just seeing themselves as buying a [name] service [. . .] very much stuck to what they’ve got to commission and not seeing the whole picture.
CS3b_V9a
Absorptive capacity and discursive disjunctions at system level
At system level, ACAP is stronger to the extent that organisations can acquire, assimilate, transform and exploit information and knowledge from each other. In our exploratory survey (see Appendix 6) and interviews, commissioners and VCSEs reported that either party tended to know and value the information and knowledge which the other held, but not that good information-sharing systems existed (see Appendix 6, Table 24). As one survey response noted, ‘regular’ contact does not mean ‘frequent’. Commissioners self-reported greater use of national statistics, seminars, databases and (management) consultants than did VCSEs. Trust was reportedly higher among commissioners and among VCSEs than between commissioners and VCSEs. On balance the commissioner respondents neither strongly agreed nor disagreed with the statement ‘Leaders across the local health and care system give relevant stakeholders the opportunity to voice their opinion’, but VCSE respondents clearly disagreed (see Appendix 6, Table 29). Both commissioner and VCSE respondents were uncertain that commissioners and VCSEs used the information they got from each other. Nevertheless, respondents tended to be broadly satisfied with both their own organisation’s performance and the contribution of interorganisational collaboration to it (see Appendix 6, Tables 33 and 34).
In the action learning activities and other fieldwork, the discursive gap between commissioners (latterly including ICSs) and VCSEs was a recurrent theme, especially from the VCSE side. The gap was partly terminological (e.g. what commissioners called ‘social prescribing’ many VCSE informants called ‘community well-being’). Partly it was a difference in concepts (e.g. commissioners understanding VCSEs as being essentially service providers, while VCSEs often saw themselves as promoting and advocating their beneficiaries’ interests). Partly, too, it was a difference in assumptions about what assertions were important and persuasive (e.g. what balance between advocacy and evidence), and about what counted as good evidence in support of the claims, proposals or requests that either party wanted to make. One commissioner, more forthright than most, said:
I am wary of using voluntary sector information as it is often emotive and frankly biased as they want to get their own agenda across. Therefore it’s not necessarily reliable in terms of evidence-based. There are some exceptions but not many.
ID 13403829701
An equally forthright VSCE respondent contrasted the normative assumptions on either side:
Part of the role of [VSCE] sector is not simply to follow national policy objectives, but to reflect what it funds on the ground. For example, the nonsense that is ‘British Values’, against what communities are facing, their identity needs and beliefs, and voice and empowerment to challenge systems.
ID 13395144712
Despite that, VCSEs also had a degree of discursively based power, insofar as NHS commissioners relied on VCSE input to, and endorsement of, their plans for the strategic development of services in their ICS or Place. For the commissioners, VCSEs provided a ready-made, accessible proxy for user voice, which central guidance obliged commissioners to consult. Because of the size of an ICS compared with most VCSEs, the VCSE voice within an ICS (or part of an ICS, such as an ICB) would either be that of an arbitrarily selected VCSE [probably one already known to commissioners, or a large VCSE to the exclusion of smaller VCSEs (CS4a_V18a; and see Chapter 4, Commissioner networking: co-commissioning)] or a collective voice:
[Dealing with commissioners] also made me appreciate that a collective voice was very important, rather than individual organisations, either because the larger organisations could shout loudest, and so were heard, or I suppose also it’s harder to ignore a collective voice and dismiss that as, ‘Well that’s not really the case’. Whereas if it’s just one or two organisations you might be seen as agitators.
CS1a_V13a
Finding out what this collective voice wanted to say might require new communicational (knowledge acquisition) techniques. ‘[O]ur traditional engagement is very much through the patient participation groups, PPGs. Which tend not to be accessible for people with learning disabilities, it’s off-putting for them’ (CS4a_C9a). Co-commissioning, however, could give such a voice a route to influence what was eventually commissioned:
[W]e ended up with a completely different service to anything that existed before, which basically was these 23, let’s call them volunteers, older people, hosted by a range of smaller groups in different neighbourhoods, and one was actually [VCSE name], so it was a community of interest as well as a geographical, the other ones were all neighbourhoods. We didn’t have enough money to do all the neighbourhoods, so it was targeted to certain areas.
CS2b_V3a
While only a minority of VCSEs in any locality may have direct relevance to health and care, it remained unclear how many health-related VCSEs still remained peripheral to the inter-VCSE networks through which VCSEs’ collective voice is often expressed (cf. Chapter 4, Networking between voluntary, community and social enterprises). One problem, however, was the duplication of mechanisms for hearing and transmitting what the VCSE voices said:
[T]he whole point of our [VCSE] contract was to make everything more collaborative so everything was joined up, [. . .] and they [commissioner] just appointed I think it was a £37,000 a year person to do engagement work. What would that have done in the voluntary sector? I’ve got two engagement leads who are on £25,000 who are brilliant, and they’ve just appointed a £37,000 person to do exactly the same job.
CS2b_V2a
Extending preventive care
Many activities (see Chapter 6, Outcomes and consequences for voluntary, community and social enterprises) which VCSEs were commissioned to undertake extended the reach of NHS prevention into personal preventive care, by setting up or coordinating small local self-help or self-care groups. Some VCSE informants thought this approach seemed alien to some in the NHS:
[T]here is very little willingness or capability within the health sector to accept a solution that is anything other than clinical. They really struggle with that. And yet there are huge numbers of people coming through their doors with social issues. [. . . we lack…] voluntary sector organisations in A&E, a rough sleeping organisation, a drug and alcohol organisation, a mental health organisation, a citizens advice organisation that can wrap around a person that comes in [. . . but…] what we get is somebody like that turning up in A&E.
CS1b_V3a; also CS2b
One attempted solution was to train NHS senior clinicians, middle and senior ‘leadership’ together with LA, primary care, GP and VCSE members, with the aim of encouraging clinicians and their managers to make fuller use of link worker and social prescribing (CS1b), and to promote more integrated ‘systems thinking’.
Commissioned VCSEs’ health-maintaining activities were extensive and varied, especially in CS1a (a large city), where their practical foci included sewing (providing activity and social contact for people with mental health problems); reducing alcohol consumption among over-fifties; support for refugees and asylum-seekers, homeless people, the Gypsy and Traveller community and people leaving prison; women’s counselling and therapy services; and employing people with learning disabilities within the council. Another idea there was to support a residents’ association within the tower block (CS1a; see above). VCSEs elsewhere were involved in a range of activities contributing to preventive care, among them befriending, exercise classes, environmental projects, gardening projects, awareness and training for people with a recent diagnosis of diabetes, piloting a well-being service, a bespoke holistic trauma informed service for vulnerable women with highly complex needs; and of course ‘emergency response and stabilising where organisations are dealing with COVID response and supporting vaccinations’ (CS3b_V5a).
There remained parallel structures for coordinating social prescribing, with LAs tending to support (or continue supporting) community asset-focused approaches, GPs and PCNs a more medicalised approach. ‘That is probably the biggest challenge we have, is trying to get them [GPs] to understand how the work that we do is best done out in the community, not in a primary care setting’ (CS4b_V8a; also CS3b). At the time of this study, this dilemma was not yet resolved. NHS commissioners tended to focus on bodies that would coordinate (e.g. refer people to) social prescribing activities rather than undertake these activities themselves, although some also did that. To help coordinate social prescribing activities, one VCSE invented
what we call community well-being agent. So, the way that we worked was that the social prescribers would work very closely with the GP surgeries, with Adult Social Care, with the local hospital, with the physiotherapist, occupational therapist, all those health professionals, and the community well-being agents would be the people within the PCN that would do the mapping, they would know exactly if somebody wanted an art project in [town], they would know exactly where that project was in [town].
CS4a_V16a
These approaches focused on enabling people to maintain their health and self-care within their existing conditions of life, and within the existing policy regime. They were narrower, more immediate interventions than the new public health focus on changing national policies on food production, housing, employment, transport and the other large-scale environmental determinants of health. 2
Emergent outcomes
We define an emergent outcome as one that only becomes visible when one considers the whole system of relationships between VCSEs and commissioners rather than the outcomes for single organisations. Such outcomes were the consequence of case-finding, care integration, and the concentration of the commissioning of VCSE providers.
One outcome of VCSE activity (especially in social prescribing) was to expose a hitherto unrevealed scale and type of need in the community, not previously apparent because of how needs were assessed and measured:
We’ve [VCSE] shown some things that they [commissioner] weren’t expecting, we cost the system lots when people come into our well-being programme because we advocate for them, the cost goes up, but then it goes off. And everyone was going, ‘Hang on, you’re costing us more’, and we were going, ‘No, watch it, it will come down and go away’, so there’s some interesting things we’ve learnt.
CS2b_V10a; and CS1
For one such VCSE:
we then have 350 people, but a sizeable amount of people who are not known to Adult Social Care who we do support who we know do have definite support needs, have quite complex lives are part of our community and we can’t just say, ‘No, sorry, you’re no longer eligible to come to this group’. So we’ve needed to then refer people into social work teams to ask for assessments.
CS1a_V13a
Here ‘eligible’ means ‘whose needs have been assessed as exceeding the current threshold for receiving social care’. Whether non-eligible people would also have their health and care needs or demands reduced by VCSE activities is another matter. When an outcome of commissioned VCSE activity was more case-finding, exposing previously unmet need, the likely short-term consequence would seem to be more demand for NHS services even if in the longer term there would be (as it was too soon to ascertain) a greater fall.
A recent NHS policy priority has been service ‘integration’, in the sense of closer coordination between secondary and primary care, and among primary and social care providers catering for patients whose needs are complex enough to require support from multiple services. By increasing the range of services and providers, commissioning VCSEs increases the complexity of this coordination. One VCSE
went out and spoke to over 400 people that were using services [. . .] from a commissioning point of view, which we loved as providers, we were saying, ‘Yeah! It’s all your bloody fault’, but actually then people who were using services would point their finger at us as service providers saying, ‘And you lot, you’re rubbish as well because you just bounce us around the system and don’t speak to each other!’
CS2b_V7a
Collaboration between commissioners also addressed ‘integration’; the ‘areas where that feels quite integrated with local authority spend is where we’ve perhaps done some of the more exciting [i.e. innovative] work. In other areas that’s felt a bit more challenging’ (CS1b_V3a). In general, though, this was not a focus of what VCSEs and commissioners told us about the commissioning of VCSEs.
A trend towards provider concentration on the VCSE side of the quasi-market was another emergent outcome. Our local informants described it (see Chapter 4, Agreements and payments), but policy statements had not foreseen it. It emerged from the trend towards larger contracts (see Chapter 4, Quasi-market mechanisms for commissioning voluntary, community and social enterprises), and that of commissioning networks of VCSEs (‘alliance’ and ‘lead provider’ contracts; see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks) instead of the more classic quasi-market arrangement of commissioning just one VCSE at a time. It could also happen where ‘we’ve had a few [learning disability] services where other small providers have given notice to the local authority and the local authority have then come to us and asked us to effectively take over the management of those services’ (CS1a_V21a).
The concentration of VCSE providers proceeded somewhat differently to provider competition in a conventional market. Provider competition, collapse (bankruptcy) or merger was not the mechanism of VCSE concentration. Not customers or clients but commissioners tended to stimulate provider concentration, especially under pressure of austerity, in order to contain the commissioners’ own transaction workload and costs (see Chapter 4, Agreements and payments). In one study site, local government devolution motivated VCSEs to merge for both political and economic reasons:
You’ve got [town 1], [town 2], [town 3] from a political point of view wanting to join together I think anticipating devolution. From a practical point of view by saying, ‘We need to save some money here’. From a strategic partnership point of view saying, ‘Maybe we need to do some more enabling and if we’re going to do that, that relationship they want it to be’.
CS4b_V4a
As for perverse (self-defeating) outcomes, the most apparent at system level was the disruption of existing relationships and collaborations between VCSEs and commissioners, and the increase of commissioner workload:
[C]ommissioners are feeling battered and stressed that they’ve been through multiple reorganisations [. . .] you get to know one person and then they move, the job moves because there’s so much reorganisation in the commissioning field [. . .] and we’ve seen huge cuts in commissioning-type jobs because I think, so I think they’re feeling hard done by if I’m honest, so sometimes you’re just trying to get through.
NSS_NS10A
These were side-effects (possibly short term, although it is too early to tell) of restructuring NHS commissioning. The move from CCGs to ICSs as the main commissioning organisation was intended (among other things) to increase VCSE engagement in co-commissioning.
Chapter 7 Discussion and conclusions
Limitations
Our cross-sectional profile of CCG spending on VCSEs was mainly limited by data quality. The raw data classified VCSEs inconsistently, with some CCGs including some general practices. We cleaned these data but, because of the CCGs’ erratic recording and coding, may not have removed all double-counting. Besides contracts below £25k, our data omit VCSEs not registered with the CC or CH, or without high internet visibility. There were, for instance, 9624 voluntary organisations in Greater Manchester172 (not a study site), of which only 4968 had been registered, and only 167 were recorded in the published data (and therefore our data set) as having received payments of above £25k from their CCG. Many small ‘below-the-radar’ VCSEs probably lay hidden within the ‘other providers’ category. The profile also omits NHS spending which reaches VCSEs via LAs and, above all, LA spending on health-related VCSEs. Nevertheless, it approximately doubles the coverage of the only other attempt of this kind known to us. 153
The ACAP survey was designed to (and did) achieve high qualitative variation in the range of respondents but was not a randomised representative sample of commissioners and VCSE members. More VCSE members than commissioners responded.
The size and complexity of the London health system and VCSE sector suggest that if the lack of a London case study biased our findings, it might be towards understating the scale and complexity of networking involved in commissioning VCSEs and understating the contrasts between core and peripheral VCSEs. Local case studies cannot cover the commissioning of national VCSEs. Our observations of commissioning meetings did not include one-to-one commissioner–VCSE interactions, although participants from both sides did describe such meetings. Snowballing from informants who commissioned VCSEs might be expected to yield sanguine rather than sceptical accounts of what the commissioning of VCSEs contributed to health and care. Few data, and then only qualitative, were available on the distal outcomes (e.g. quality of care, health maintenance, prevention of hospital admissions) of commissioning VCSEs. The time required for changes in VCSE commissioning to change these outcomes, especially preventive ones, almost certainly exceeds the time limits on this study. The study was limited to the English health system during a singular period in its history.
Because of the COVID-19 pandemics, nearly all fieldwork had to be conducted by videoconference. The pandemic may have exacerbated the difficulty in accessing research sites in London, and did curtail some FoI requests (see Chapter 3, Analysis), but it also yielded some additional findings (see Chapter 5, A temporal context: the COVID-19 pandemic). That the commissioner informants were mostly managers or experienced service providers but not clinicians might seem a limitation, but it appears to reflect the usual occupational backgrounds of commissioner staff in the study sites. The means of checking the generalisability of the case study and action learning findings were limited (partly by the study resources, partly by the lack of national-level data). The same applies to evidence about the outcomes.
The VCSEs that we investigated were at the core of the networking described in Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks, rather than peripheral or excluded VCSEs. If any bias resulted, it might be towards overstating the connectedness of VCSEs. Our VCSE informants tended to occupy leading roles and be in VCSEs that engaged with commissioners. Their managerial skills, and their organisations’ ACAPs, may therefore have been somewhat greater than among VCSEs generally. A more subtle problem was that while the scale and pattern of commissioner spending on VCSEs is an organisational outcome of that commissioning activity (see Chapter 6, Income and financial precarity), it is also likely to be path-dependent. Current spending partly depends in part on earlier spending patterns (see Chapter 5, Fiscal constraints). To investigate those relationships requires longitudinal data which, as Chapter 3, Cross-sectional profile of Clinical Commissioning Group spending on voluntary, community and social enterprises explained, are not easily available.
What this study adds
Nevertheless, this study extends our knowledge of commissioning, particularly NHS commissioning, into the field of the commissioning of VCSEs.
Among its methodological strengths, our profile of VCSE spending was a census with only a small proportion of incomplete data and so had no substantial selection bias. We ensured that our sample of study sites fell widely across the distribution of CCG spending on VCSEs (see Figures 9 and 10). To the extent that those spending patterns are associated with other aspects of the commissioning of VCSEs, we avoided gross bias in selecting case studies, and our empirical findings appear generalisable. The available study sites included areas of socioeconomic deprivation, areas with ethnic minority groups, rural and city settings, and a geographical spread across England. The COVID-19 pandemic was at once ‘a blight and a revelation’. 173 As Chapter 5, A temporal context: the COVID-19 pandemic explained, it extended and intensified the networking among and between commissioners and VCSEs, moving them further towards collaborative modes of commissioning (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks and Chapter 5, Statutory status). Although that networking decreased in some sites when the pandemic ended, a net increase remained. This enabled us to observe developments in the commissioning of VCSEs which otherwise would have taken much longer to emerge, if ever they did. The replacement of CCGs with ICSs tended to disrupt previous commissioning relationships. That involved both sides rethinking these relationships, which exposed the rationales for them more clearly than might be usual. Our mixed methods enabled us to triangulate findings across interview, documentary, survey and action learning sources. In any event, our findings are empirical generalisations, so we have taken care to report (see Chapters 4–6) the main exceptions and counter-examples to them.
Realist study design enables a theoretical generalisation of findings: a corrigible prima facie assumption that explanations of the commissioning mechanisms and contexts in the study sites will also apply in other places and health systems that use qualitatively similar mechanisms. As such an explanation, our findings enabled us to operationalise, test and empirically revise the initial, two-sided programme theory for the commissioning of VCSEs (see Chapter 1, Interfaces and interaction and Figure 3). It shows more fully than before what is distinctive about commissioning of VCSEs compared with commissioning other providers, and the heavily collaborative character of commissioning of VCSEs compared with commissioning corporate providers and even, in some health systems, publicly owned providers. 67 We show how this collaboration is partly institutionalised but also has emergent, informal elements, thereby extending accounts of informal management and managerial workarounds192–194 into this domain. Combining and supplementing previously separate research, our findings present workarounds as a way in which street-level bureaucrats and diplomats60,195 (commissioners, in this case) unofficially expand their decision space62 when (for instance) procurement regulations put them in the ‘willing but unable’ category in Exworthy’s schema. 64 Our findings expand existing taxonomies of health and care networks45,65,196,197 and describe a specific hybridisation of health system governance structures (the dual commissioning mechanism and structure Chapters 4 and 5) that appear when VCSEs are commissioned. We show that commissioners and VCSEs seldom found principal–agent relationships practically useful or, in that sense, ‘rational’,176 yet regulatory constraints often brought them to the fore (commodified commissioning). Also we show that, as in other settings,27 economic relationships, in this case between commissioners (especially staff who had worked in VCSEs before) and VCSEs, are heavily socially and institutionally embedded. Commissioning staff are often managerial ‘hybrids’, those in learning disability especially having moved into management from service delivery worker or volunteer roles, a partial parallel with the manager–clinician hybridisation found in more clinical services198 (including end-of-life care).
We also corroborate that certain previous empirical findings about commissioning in other parts of the NHS also apply to health-related VCSEs in England. Others have described how NHS commissioners applied procurement regulations in ways that combined competitive and collaborative approaches to commissioning199 and found the VCSEs and commissioners worked more closely and intensively together in the presence of necessity and when they shared goals, particularly during the COVID-19 pandemic. 200 NHS participants in ICS formation also found collaborative, informal relationships with non-NHS organisations important in what they too called ‘horizontal’ coordination and accountability of the ICS. 13 Our findings about how NHS commissioning works in practice under the more stringent application of pro-competition regulations confirms earlier findings75,174 and extends them to the case of VCSEs. Insecure employment terms and conditions did indeed create problems of staff retention and morale for VCSEs, as Davis has suggested for a different setting,110 but they were in the present case effects of unstable, short-term ad hoc commissioning (short-term contracts or grants), not necessarily effects of commissioning per se. We found reports of competition between VCSEs,20 but the networking activities which supplemented commodified with collaborative commissioning more often contributed to restraining competition. Currie et al. also found that commissioners found data exploitation and use more of a challenge than acquiring data. 141 As in other types of commissioning, commissioners and providers (in this case VCSEs) relied on a combination of ‘hard’ and ‘soft’ information. 187 We corroborate Baylis’s finding that commissioners’ monitoring of the quality of end-of-life care was not always thorough nor did it make good use of available data. 201
Turning to VCSEs themselves, we supplement and qualify the literature which reported VCSE ‘degeneration’, in terms of their original mission and their voluntary, democratic internal organisation. In the VCSEs that we studied, we found more complex, partly opposing tendencies. As others100,102–104 have also found, involvement in commissioning impelled VCSEs to develop their management competencies, which did indeed involve a certain formalisation, even bureaucratisation, of VCSE management,111 including attempts to meet commissioners’ need for outcome measurement and monitoring (to that extent, audit). To that modest extent, our findings confirm that in these respects commissioned VCSEs mimicked, when they could, some aspects of public sector management,98 but it would be an exaggeration to say that by itself that behaviour precipitated managerial ‘capture’ of these VCSEs, for these changes concerned the forms, not the contents, of management activity. Becoming commissioned was reportedly associated with a stronger income-seeking motivation in a few VCSEs, to that extent corroborating the findings of Skelcher and Smith108 and Fox. 109 As counter-evidence, however, we also found VCSEs which expressly rejected funding opportunities which they thought inconsistent with their original aims (see Chapter 4, Commissioner and voluntary, community and social enterprise aims and Chapter 6, Outcomes and consequences for voluntary, community and social enterprises). Neither pattern predominated; more usually, our study VCSEs marginally extended or retracted their founding ‘mission’, or translated it into formulations that commissioners could engage with (see Chapter 6, Outcomes and consequences for voluntary, community and social enterprises). If that was mission drift, it was so only insofar as any change would be ‘drift’. Indeed, commissioners engaged with VCSEs partly because they perceived VCSEs as a voice of, and way to engage with, local communities, as advocates for particular subpopulations and care groups, including more marginalised ones, and as adding social value to their communities (see Chapter 4, Provider selection). If anything, that would appear to legitimate, reinforce and indeed fund the kinds of founding ‘missions’ which typify VCSEs (social justice, social change, community well-being, service access and provision for marginal groups, reducing health inequalities and the like; see Chapter 1, Voluntary, community and social enterprises in health and care). In terms of their internal organisation, becoming commissioned produced more a regeneration than a degeneration for the VCSEs, albeit a modest regeneration. One interpretation of this difference between our findings and those of ‘degeneration’ in some earlier studies (see Chapter 1, Consequences of entering a relationship with commissioners) might be that VCSEs themselves now adapt to commissioning in different ways than when the earlier studies were made. Another is that the differences arose from the character of the tracers that we focused on.
Realist evaluation has usually been applied to one specific form of organisational agency: that of state organisations implementing a policy initiative. So far as we are aware, this study is the first to develop and apply this agential perspective symmetrically to other kinds of organisational agency involved in policy implementation, the policy subjects. This two-sided analysis enabled us to analyse, in a realist way, how and where different organisations’ aims and programme theories interacted, with what consequences, what contexts affected that, and why. This study is therefore not only a realist evaluation in the sense of evaluating the policy-makers’ programme theories and the success or failure, in the policy-makers’ terms, of implementing them; it also advances realist methods by incorporating the policy subjects’ agency too, symmetrically to that of the policy-makers and implementers, and evaluating the effects of their agency in their own terms. During co-commissioning, for example, commissioners influenced and informed VCSEs, but the reverse also occurred. We also explore how governance structures can serve as mechanisms, in a realist sense, of policy implementation.
This project included practical interventions to assist the development of ACAP in commissioners and VCSEs. This is not the first research into either commissioning or ACAP (see Chapter 1, Conceptual perspectives: commissioning as governance), but we are aware of only one other study into how the two intersect141 and none in respect of VCSEs.
In summary, this study adds an empirical understanding of the dual CMOC (see Figure 3) from which we began. Figure 20 shows the expanded CMOC resulting from the evidence reported above.
FIGURE 20.
Commissioning VCSEs: evidence-based dual CMOC.
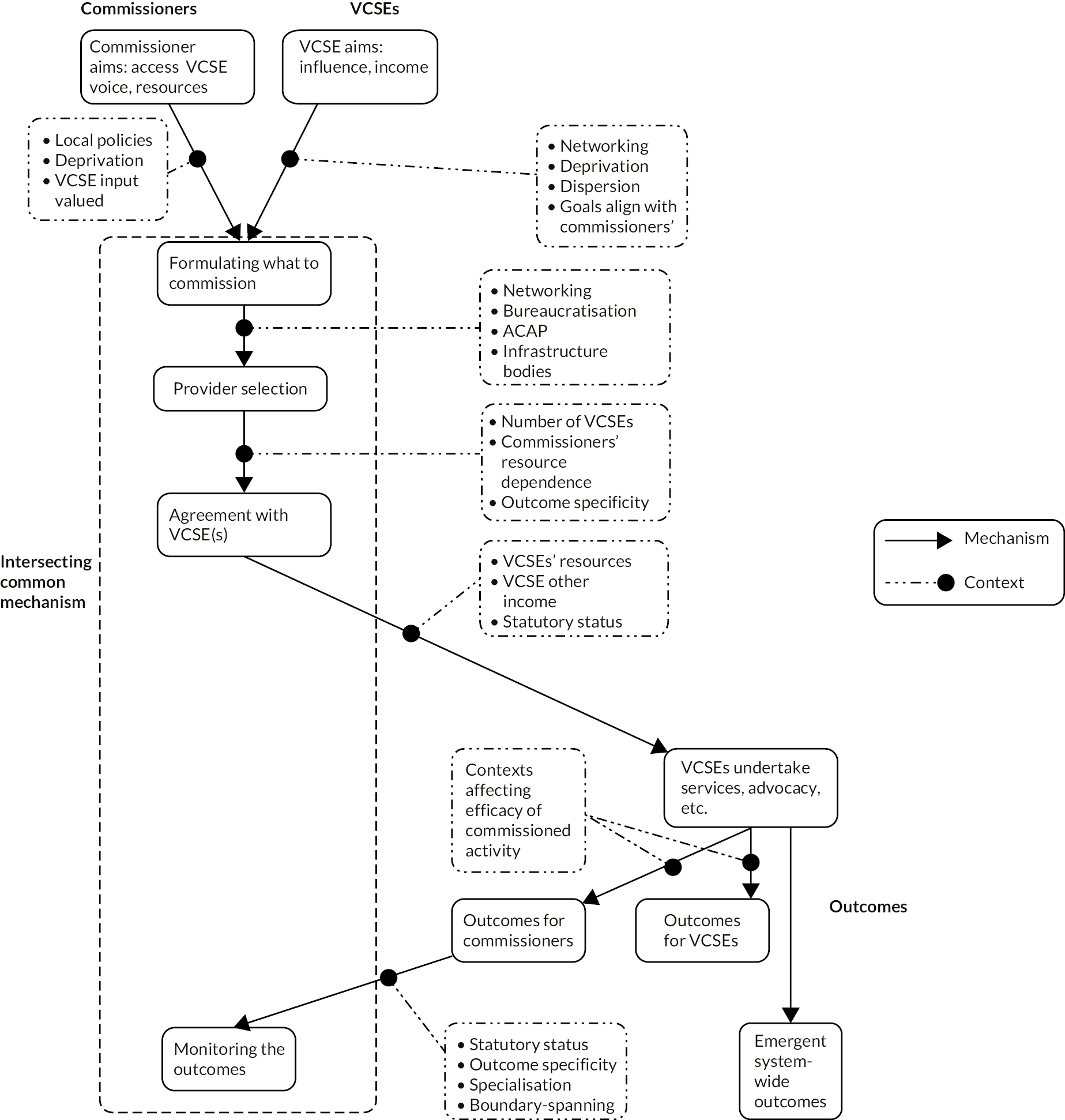
Future research
Our findings revealed several gaps in this research field, hence empirical topics for future research. Closest to NHS commissioning, research is still needed to quantify the impacts that VCSE hospice, social prescribing, mental health services and learning disability support had upon demand on NHS services (cf. Chapter 1, Health and care). The NHS commissioning landscape is still evolving and appears likely to remain complex in future, so the present study is likely to need updating in the medium term (say, the late 2020s). As ICSs develop, it will become possible to research the extent and nature of any influence which VCSEs have within them, compared with other actors (NHS Trusts, corporations, etc.), and the consequences of ICS development for the commissioning of VCSEs more generally. The same applies to PCNs. Taking a wider view, Bismarckian health systems, particularly in Germany, have national and regional-level institutions which formulate health policy and regulation in collaboration with mutualised, social enterprise sick-funds and networks of (among others) third sector care providers. This raises the question of whether there are lessons from such systems for NHS commissioning with, and of, VCSEs. The extent and potential value of the more isolated, peripheral VCSEs’ contributions to the local health sector remain unresearched. Our profiles of NHS commissioner spending on health-related VCSE activity could be developed by adding profiles of such LA spending, a bigger task than profiling CCG spending. Except for our study sites, we also lack longitudinal studies of NHS spending on VCSEs, including how it compared with spending on non-VCSE providers. Although our profiles of CCG spending on VCSEs drew upon published NHS data, they came as new information to our informants, including NHS commissioners, some of whom subsequently requested (and were supplied with) the data set extracts relevant to them. There remains a lack of studies of the commissioning of large (cross-England) VCSEs engaged in health-related activity, which fell beyond the purview of our local case studies, and the extent and character of VCSE commissioning in London, to discover whether it differs from the patterns elsewhere reported in this study. There are few studies, if any, of whether or how commissioning systems systematically discriminate against ethnic minority organisations. Both commissioners and VCSEs might benefit from more detailed research into the costing and pricing of VCSE activities, and how being commissioned affects VCSE staff turnover. The nature, effects and development of ACAP in both commissioners and the VCSEs they commission also merit fuller research, including by means of the survey instrument developed for this study. To research the outcomes of collaborative commissioning would require a combination of social network analysis, quantification of the outcomes, a qualitative account of the mechanisms and contexts linking collaboration with outcomes, and triangulating across the findings.
Methodological research questions arising from this study begin with the task of developing outcome and impact indicators for the commissioning of VCSEs: a considerable project. Use of an ACAP survey in this setting was also an innovation. Next, the Currie et al. 141 survey instrument for assessing commissioners’ internal ACAP required adaptation for application to the external interface between commissioners and VCSEs. As Flatten remarks,
[B]efore the quantitative analysis, extensive qualitative pre-tests, such as team discussion or interviews with practitioners, should be conducted in order to understand the activities that form the ACAP dimensions in these specific contexts… [and] the relative importance of the four ACAP dimensions in different settings. 150
Our existing survey nevertheless enabled a more systematic comparison of VCSEs and commissioners, albeit on more narrowly specified topics, than qualitative systematic comparison readily can. To varying extents across questions, the survey discriminated VCSE and commissioner responses (see Appendix 6 for details). The main difficulty was to define who counted as a VCSE member, and therefore what the survey population and response rate were. We conclude that the survey instrument merits further development and use.
Should later researchers also employ action learning, this study forewarns them how demanding action learning through co-research is of project time and researcher input. Against that, there are considerable rewards in terms of snowballing to new data sources, data enrichment, and verification of findings. The co-researchers, local project reference groups and national learning set participants gained by extending their own networks and acquiring new knowledge and exposure to research expertise. Assuming that the shift towards online data collection during the COVID-19 pandemic will not completely reverse, there is now a stronger case for researching the implications of videoconference rather than face-to-face qualitative data collection in organisational and service delivery research.
Further theoretical frameworks could be used to analyse the present data, with the probable consequence of having to adapt those theories to fit. Transaction cost theory202–204 might be one. Unlike many a priori models, the present study includes direct empirical observation (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks) of how transaction cost considerations helped shaped interorganisational relationships. In becoming commissioned, VCSEs had, we found, wider aims (see Chapter 4, Voluntary, community and social enterprises aims) than those which much policy and research assume, including those drawing upon transaction cost theory. Another candidate theory is that of ‘cooptition’,205 since competition and collaboration among VCSEs appear to differ from that between corporations. The importance of negotiation, and therefore discourse, in collaborative commissioning suggests, also, that theories of organisational discourse206,207 might be an informative way to exploit our data further. We have already noted (see Chapter 1, Voluntary, community and social enterprises in health and care) the possible application, which implies development, of the theory of institutional isomorphism101,208 and that of decision spaces. 62 Theories of political economy209 might offer further explanations of our data about organisational and workforce changes. The theory of the embeddedness27,210 of economic relations might help explain further our findings about co-commissioning and collaborative modes of commissioning.
Conclusions
We present our main conclusions by research question, then some additional findings.
How do healthcare commissioners address the task of commissioning voluntary, community and social enterprises as service providers, and what barriers do they face? (RQ1)
They did so using two commissioning mechanisms, utilising two kinds of governance structure, in parallel. Each mechanism implemented different modes of commissioning; that is, different combinations of media of control (see Chapter 1, Health and care). Centred on the commissioning cycle, and especially the procurement system, the quasi-market mechanisms implemented a heavily commodified211 mode of commissioning whose paradigm was a principal–agent relationship between commissioner and VCSE. Then commissioners’ predominant media of control over VCSE providers were:
-
VCSEs’ resource, or rather financial, dependence on commissioners
-
provider competition, minimising provider collaboration
-
managerial practices, especially system-level needs assessments and provider monitoring
-
juridical controls, above all the procurement regulations; for contract enforcement, juridical power was in the background but seldom used in practice.
Not that these were the sole media of power: commissioners also exercised discursive power and negotiated with VCSEs, but these media of power tended to be less prominent than, and were subordinated to, the four listed above in this mode of commissioning. Then, commissioners treated VCSEs more as service providers and as takers than the initiators of proposals for VCSE activities (see Chapter 4, Quasi-market mechanisms for commissioning voluntary, community and social enterprises). NHS commodified commissioning structures and managerial practices first developed (in the early 1990s) for commissioning of NHS Trusts and corporate providers, then (since c.2000) were more fully extended to VCSEs, aided by the longevity (by NHS reform standards) of CCGs (2013–22). VCSEs’ main media of power were discursive and the use of resource dependencies (they could withdraw from contracts).
The collaborative mode of commissioning mechanism rested on a triple negotiated order: networking among commissioners, networking among VCSEs, and networking between commissioners and VCSEs. The main media of power were:
-
Discursive: persuasion and legitimation. The dominant discourses differed on either side: commissioners used policy and managerial discourse predominantly, VCSEs more normative discourses with strong elements of advocacy.
-
Resource dependency was more balanced, with commissioners acknowledging their own dependency on ‘real-side’ VCSE resources.
-
Formation of a negotiated order between commissioners and VCSEs at each stage in the commissioning cycle was therefore an important way for each party to influence, rather than control, the other.
-
Managerial practices took the forms partly of negotiation and consultation, partly workarounds to the quasi-market, especially procurement, mechanisms.
Commissioners and VCSEs developed this mode of commissioning to alleviate the expected, and in some cases experienced, adverse consequences of commodified commissioning, including the exclusion from bidding of VCSEs whom commissioners judged to be worth consulting. Power was more evenly distributed, and VCSEs could act more as strategic partners, not only service providers.
To repeat, it is not that where one mechanism or mode of commissioning existed, the other did not: everywhere, a hybrid of both existed and the two interacted, but the balance between them varied.
Barriers to using this hybrid mechanism arose from fiscal constraints, tight procurement regulations, and the centralised control over NHS commissioners. At certain points in the commissioning cycle, especially the specification of what to commission and provider selection, the two mechanisms conflicted. When it came to provider selection, many commissioning staff assumed that VCSEs that were involved in co-commissioning (see below) were thereby disqualified from bidding as providers, and vice versa. Even if the procurement regulations bear such a narrow, risk-averse interpretation, this managerial practice interrupted the collaboration that commissioners found useful for other parts of the commissioning cycle. Many commissioners therefore worked around these procurement mechanisms. In ascending order of departure from a narrow interpretation of the regulations, they were:
-
Less narrow, more inventive interpretation and implementation of the regulations, for instance by specifying activities or provider characteristics in terms that favoured small local VCSEs.
-
‘Soft’ implementation, for instance by not trying hard to find competitors for incumbent VCSEs.
-
Procuring the services of an infrastructure body, a lead provider (in some cases an NHS Trust), or VCSE alliance to distribute commissioners’ funds to other VCSEs. In effect, this workaround delegated the provider selection, agreement and payments parts of the commissioning cycle to organisations where the procurement regulations did not apply.
-
Replacing competitive tendering with awarding grants or similar subsidies.
Remaining barriers were some of the contexts affecting the balance between the above two main commissioning mechanisms, how the mechanisms operated, and to what outcomes. More specialised activities, and larger contracts, reduced the number of VCSEs capable of offering to undertake them. Against this, smaller VCSEs were less likely to have managerial capacity to engage with commissioner managers, for instance by writing acceptable bids and supplying monitoring data. Ethnic minority VCSEs were affected in this way in addition, allegedly, to discrimination. A diverse third sector with its many small organisations increased the amount, complexity and cost of commissioning VCSEs, and reduced VCSEs’ negotiative power, although strong coordination could mitigate this problem. Collaborative commissioning was more fragile, to the extent that it depended on a few leaders and boundary-spanning individuals, on the commissioners’ side as much as among VCSEs. The absence of co-terminosity between commissioners increased the number of interorganisational interfaces, which complicated intercommissioner networking (co-commissioning) and the vertical networking between VCSEs and commissioners (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks), all exacerbated in the short term by the instabilities and structural ‘churn’ of replacing CCGs with ICSs (and the earlier reorganisations of NHS commissioner boundaries), but also mitigated by national NHS guidance on VCSE involvement. For social prescribing specifically, commissioning structures were partly duplicated between the NHS and LAs. Either way, what they commissioned was usually an infrastructure body which then coordinated, and in particular signposted people to, but did not necessarily pay, the VCSEs that actually undertook the activities to which social prescribing was intended to give access. Fiscal austerity constrained what could be commissioned from VCSEs. The possibility of competition from corporate and public providers made commissioners commission in more risk-averse ways because they thought that their decisions were more likely to be challenged. To that extent, commissioning practice then inclined towards commodified rather than collaborative commissioning. Fiscal austerity also increased the pressure on VCSEs to compete with each other. A dispersed rural population and high levels of socioeconomic deprivation meant that commissioners (and VCSEs) faced higher demands, and not necessarily with proportionately greater resources given the patterns of budgetary allocations to commissioners. It was technically difficult to specify and quantify, hence monitor, VCSE performance of certain commissioned activities (e.g. advocacy, social prescribing activities such as befriending).
What are the consequences for voluntary, community and social enterprises of the public bodies commissioning services from them? (RQ2)
Immediate outcomes for VCSEs were additional funding and some extension of VCSE activities, including advocacy; and marginal adjustments in mission (with a more financialised mission drift in a minority of VCSEs, and no mission shift at all in another minority). However, the funding was often below the cost of these activities, even ignoring volunteer labour and other free inputs. Commissioners’ funding and payments for some activities, especially recently added ones, were often unstable, short term and ad hoc. In effect, VCSEs then made a hidden subsidy to their commissioners. Closer engagement with health and care commissioning, and the financial pressures on VCSEs, contributed to VCSEs losing staff to other employers who offered better pay and conditions. There was a tendency towards larger contracts, and hence larger contractors, on the VCSE side. This indicates a move towards concentration on the VCSE provider side of the quasi-market.
The commissioned VCSEs adjusted rather than drifted far from their aims (‘mission’) and founding principles. VCSEs’ scope to advocate their aims and principles, and promote the interests of the care groups or populations they represented, increased as their role in co-commissioning extended, especially during the COVID-19 pandemic. VCSEs attempted to develop their ACAPs to manage and specify (e.g. measure) the activities which the VCSEs were commissioned for, and for engaging and negotiating with commissioners. On balance, being commissioned appeared to make VCSEs experience more of an organisational regeneration than a degeneration, and both to a more modest extent than we would perhaps have observed had we done this research in, say, 2010–20, or included large national VCSEs and large national contracts.
How are voluntary, community and social enterprises involved in Clinical Commissioning Group, local authority and other commissioning decisions? (RQ3)
Voluntary, community and social enterprises’ involvement in co-commissioning occurred through networking rather than quasi-market mechanisms. It occurred through VCSE participation, along a spectrum from invited consultee to adviser to ‘strategic partner’, in the co-commissioning (intercommissioner) component of the networking mechanisms. VCSEs with long-established working relationships (‘embeddedness’) with commissioners were often the ones invited, for that very reason, to participate in co-commissioning activities, including those which ICSs were now initiating. For the same reason, larger VCSEs were more often included than smaller local ones. The latter were also involved vicariously, although not to the extent of being systematically ‘represented’ (see Chapter 4, Commissioner and voluntary, community and social enterprise aims), through the VCSE infrastructure bodies which in turn participated in – or nominated other VCSEs or individual VCSE members to participate in – co-commissioning. In theory, VCSEs that were indirectly commissioned through alliance or lead provider arrangements might then be able to influence those bodies, and through those intermediaries gain a voice in co-commissioning bodies and debates, but we found little evidence of that. Each study site also had a large periphery of small VCSEs outside these networks. For some small VCSEs the infrastructure bodies described in Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks acted as a gateway to commissioning, for others as a gatekeeper (barrier).
Even if they had wanted to (and not all did), those VCSEs had no obvious way of becoming involved in commissioning decisions unless, by chance, they already had established (embedded) a working relationship and influence with a commissioner, or were part of a network of VCSEs which was strong enough to ensure that its members’ voices were heard during co-commissioning.
What absorptive capacities do healthcare commissioners and voluntary, community and social enterprises, respectively, need for enabling voluntary, community and social enterprises to be commissioned, and for co-commissioning? (RQ4)
Our findings on ACAP drew on evidence from survey and interview data, and co-research activities. They included statements from VCSEs about ACAPs that, in their view, commissioners ought to have; and conversely, from commissioners about those they thought VCSEs ought to have.
For the commissioners’ part, these capacities were, according to the ACAP survey data and our interviews, implicitly a combination of managerial and communication skills. So far as managerial practices are concerned, commissioners needed firstly to routinise seeking (‘acquiring’) and hearing (‘assimilating’) information, opinions and suggestions from VCSEs (see Chapter 5, Spatial dispersion). This included knowing how to discover whether relevant VCSEs, including peripheral ones, had been omitted from co-commissioning networks, including the ICS (see Chapter 4, Agreements and payments). Commissioners needed the capacity for specifying calls for practical proposals or bids from VCSEs in such a way as to elicit the kind of applicant (e.g. small local VCSEs) that the commissioner aimed to commission. Having elicited such proposals and applicants, the commissioner needed to be able to apply (‘exploit’) information and ideas from VCSEs in ways that did not then penalise the VCSEs providing them (e.g. by excluding those VCSEs from tendering) (see Chapter 4, Agreements and payments). Commissioners needed to focus monitoring or reporting on what VCSEs, especially very small ones, could feasibly supply, and avoid overmonitoring; that is, demanding too much data too often (which might be thought of as ‘over-acquisition’) (see Chapter 4, Quasi-market mechanisms for commissioning voluntary, community and social enterprises). As for communicational and discursive capabilities, a first need was that of using dialogue with VCSEs as a means to acquire information and VCSE views, not only downloading the commissioners’ opinions or decisions (see Chapter 5, The mix of commissioned organisations); that is, to assimilate and understand (which does not necessarily mean agree with) VCSEs’ views about local services and how they should be developed. These things required the capacity to translate between VCSE and commissioner discourses (see Chapter 5, The mix of commissioned organisations), and at face-to-face meetings with VCSEs the capacity to adapt networking and consultation activities to make the participation of VCSE service users (e.g. people with learning disability) feasible and productive (see Chapter 4, Agreements and payments and Chapter 5, The mix of commissioned organisations) (we were told of obvious failures). Sustaining long-term, continued interactions with VCSEs demanded of commissioners the capacity to demonstrate trust in, and earn trust by, the other party (see Chapter 5, The mix of commissioned organisations and Chapter 5, Tracer activity), for instance by championing the VCSE role within the co-commissioning networks (see Chapter 5, The mix of commissioned organisations).
Conversely, commissioners suggested that VCSEs needed to develop the capacities to supply evidence, both hard and soft intelligence, about why they prioritised particular community health and care needs or why they wished to supplement or amend commissioners’ assumptions and proposals (see Chapter 4, Deciding what to commission). In proposing activities to be commissioned, the VCSEs needed the capacity to express what outcomes their proposals would offer, what needs they would meet, if possible what metrics the commissioner could use to verify that, and more generally how the VCSE’s proposals would add social value (see Chapter 4, Deciding what to commission). The next stage in the commissioning cycle then required VCSE capacity to make a bid in obvious conformity to the tender or other commissioner requirements, and present it as such (see Chapter 4, Deciding what to commission). VCSEs also needed to acquire the capacity to show what unique selling points their proposals or bids have, compared with these from corporations and NHS Trusts (e.g. that the VCSE has, say, unique specialist skills) (see Chapter 4, Deciding what to commission), which would make the option of commissioning a VCSE more visible and attractive to commissioners (see Chapter 4, Deciding what to commission). Then, VCSEs needed to learn how procurement systems work and why, and develop the capacity to use routine administrative data for monitoring (‘metric’) purposes (see Chapter 4, Agreements and payments). Like commissioners, VCSEs needed the capacity to translate between VCSE and commissioner discourses (see Chapter 5, The mix of commissioned organisations), to sustain long-term, continued collaborations that demonstrate trust in, and reinforce trust by, the other party (see Chapter 5, Geography, history, local policy and Tracer activity). In an organisationally fragmented setting, VCSEs also needed the boundary-spanning capacity to link and deal with fragmented, distributed leaderships (see Chapter 5, The mix of commissioned organisations) on both the VCSE and the commissioner side (see Chapter 5, Organisational characteristics).
The researchers add that it would appear useful to VCSEs to discover the criteria, methods and data by which commissioners internally rank and select VCSE projects (see Chapter 4, Deciding what to commission). A VCSE infrastructure body may be more credible as the collective voice of VCSEs if it appears to be, and is, independent of commissioner control (see Chapter 5, Organisational characteristics). In ACAP terms, the commissioners appear to need to develop their knowledge acquisition and exploitation capacities especially, and the VCSEs their knowledge acquisition and transformation capacities. In our action learning activities, commissioners and VCSEs seemed to benefit from meeting on neutral ground to share experiences and knowledge, and learn about each other. Such networking helped mutual trust to develop, helped the participants identify shared agendas and identities, and so helped strengthen ACAP at a network (system) level, as did the participation of boundary-spanning individuals (whether boundary-spanning in their current roles, or across their career).
Additional findings
Beyond the research questions, some further conclusions emerge from this study.
Tracer characteristics were an important commissioning context. The larger a VCSE was, the more likely it could sustain a managerial infrastructure. The latter therefore differed in sophistication between hospices (mostly large), social prescribing VCSEs (mostly small) and learning disability support (mostly intermediate). How specifically VCSE activity and outcome could be defined constrained the scope for complete (fully specified) contracts. The extent to which VCSE activity was medicalised influenced how specifically it could be defined. Undertaking highly specialised activities (e.g. hospices, in contrast to social prescribing activities) tended to reduce the number of providers in a locality, and hence the scope for provider competition. Diverse ownership of providers (high in learning disability services where VCSE, corporate, proprietary and public providers are all found; low in social prescribing and hospices) promoted more risk-averse commissioning. When VCSEs provided a statutorily mandated activity (e.g. hospices, some learning disability services), commissioners’ resource dependency on VCSEs was more apparent and commissioners were more willing, if problems arose, to encourage providers to ‘learn’ than to replace providers. The same applied where VCSEs obtained only a small proportion of their income from public sector commissioning (as hospices did). With hindsight we might also have adjusted our initial research questions (see Chapter 2, Research questions) to make clearer that in England the commissioning of healthcare-relevant VCSEs is not only, or even mainly, undertaken by NHS organisations but also by local government.
The COVID-19 pandemic stimulated the development of collaborative commissioning mechanisms (more networked and flexible commissioning of VCSEs). After the pandemic, there was a partial but far from complete reversion to previous commodified commissioning practices. An after-effect of increased mutual knowledge and understanding between the commissioners and VCSEs remained, and a widened perception, on the commissioners’ part, of what VCSEs might contribute to the local health system (see Chapter 5, Tracer activity). During the study the development of ICSs progressed and was beginning to influence VCSE–commissioner relationships, especially co-commissioning relations, although it was far from complete when this study ended.
Commissioning VCSEs also extended the reach of NHS-funded preventive activity into community activities aimed at changing personal lifestyles and supporting people with long-term health problems, including long waits for treatment. This contrasts with two other concepts of preventive care: a clinical concept (vaccination, contraception, etc.) and the new public health argument that the most effective forms of prevention occur at SDoH level (food policy, housing policy, female literacy, etc.). 212
Implications
While they arise from our findings (see Chapters 4–6), the predicted implications are inevitably more speculative.
Commissioners funded some VCSE activities (e.g. some hospices, parts of learning disability support) at a level below the VCSEs’ cost of producing them (see Chapter 4, Agreements and payments and Chapter 6, Outcomes and consequences for voluntary, community and social enterprises). In effect those VCSEs then made a hidden subsidy to their commissioner. Insofar as VCSE activity depends on volunteer labour and help-in-kind, that position may appear sustainable (at least, while volunteers still come forward), but it is not necessarily sustainable insofar as VCSE activities also require paid-for inputs, which even volunteer labour often does (coordinators, consumables, etc.). This became particularly (though temporarily) evident when the COVID-19 pandemic restricted VCSEs’ fundraising. However, long periods of economic recession and fiscal austerity appear likely to have similar consequences, and contribute to the pressures on staff retention in VCSEs.
Financial pressures and the instability of their income from commissioning made it difficult for VCSEs to retain paid staff (see Chapter 6, Workforce precarity). Closer engagement with commissioners gave VCSE staff or volunteers experience and expertise in health and care-related activities, which appeared to help them transfer to other employers, not least the NHS and LA, who offered better pay, conditions and continuity of employment. VCSEs cannot necessarily sustain this situation either in the long term.
Commissioners were tending to favour larger contracts and hence larger contractors: larger VCSEs or networks of smaller VCSEs (see Chapter 4, Agreements and payments and Vertical networking between voluntary, community and social enterprises and commissioners). It remains to be seen whether a longer-term consequence may be concentration of the VCSE side of the quasi-market, analogous to market concentration in conventional markets. Then, VCSEs might start to stratify into: a stratum of large VCSEs, including lead providers, alliances and other networks of VCSEs, commissioned by the NHS or LAs; a stratum with some NHS or LA income, but more from other sources; and a large periphery of VCSEs more isolated from the commissioning system. Some VCSEs would then become increasingly involved with ICSs and NHS commissioners than they now are, others less. That, however, might be expected to weaken the local knowledge and reach which commissioners valued in the VCSEs.
The formation of ICSs destabilised (at least, temporarily) NHS commissioners’ existing collaborations with VCSEs. Like previous NHS reorganisations, it reconfigured staff deployment, organisational boundaries and policies, and so disrupted interorganisational relationships. Nevertheless, the formation of ICSs also created new co-commissioning networks, which accommodated a greater advocacy role for VCSEs to influence commissioning. However, non-VCSE providers, especially NHS Trusts, appeared to play a larger and more influential role (see Chapter 4, Commissioner networking: co-commissioning), with the implication that the non-VCSE providers might capture the ICS co-commissioning systems, crowding out VCSE input.
These implications suggest corresponding recommendations about how the commissioners and VCSEs might attain greater mutual benefit during co-commissioning with, and the commissioning of, VCSEs (we also discussed and verified these at the final national action learning event). When VCSE activity provides commissioners with an unsustainable hidden subsidy, the remedy would be for commissioners to increase their payments to VCSEs, although insofar as VCSEs rely on voluntary labour this would still be unlikely to raise VCSE costs to the levels of public, proprietary or corporate providers. Commissioners should ensure contract prices reflect full cost recovery for VCSEs, including the hidden financial costs of volunteer labour (administration, materials, etc.) and backfill for VCSE attenders at meetings, and resist the temptation of cheaper contracts which are not financially sustainable for VCSEs. The same recommendation follows from the instability of VCSE staffing, with a further recommendation that commissioners make longer-term, more stable contracts or grants with VCSEs. This in turn requires a stabilisation of Department of Health and Social Care (DHSC) and NHSE mechanisms for allocating and paying budgets to commissioners, and enabling VCSEs to carry unspent grant income into the following financial year. Longer deadlines should be built into the commissioning cycle to enable more considered responses than a quick recycling of previous specifications and bids. For the same reason, and to enable VCSE input to inform the specifications, commissioners should put contract specifications out to consultation before finalising them and calling for bids. Our attempt to profile CCG spending on VCSEs also generated detailed recommendations for improving the expenditure accounts for health service research purposes (see Appendix 5). Reducing NHS staff turnover (increasing NHS staff retention) might also be expected to reduce staff flows from VCSEs into NHS posts. The commissioning of VCSEs relied heavily on certain key individuals (see Chapter 5, Organisational characteristics), which suggests that succession planning for those roles would be prudent.
In the short term it is not obvious whether recommendations follow from the concentration of provision on the VCSE side of the quasi-market, beyond the general point that such a change would make the collaborative commissioning of VCSEs somewhat more, and commodified commissioning somewhat less, practically relevant to both parties. The capture of ICSs by larger, non-VCSE providers may be practically almost inevitable, but a crowding-out of VCSE voice and influence could be mitigated by ICSs guaranteeing that VCSE members participate at all levels, including the top ICS board itself. Closing the discursive gap between the languages and terminologies of commissioners and VCSEs appears one way to increase the ACAP of both.
We detected a large periphery of VCSEs which were not closely involved in NHS and LA commissioning. Many of these VCSEs will not be relevant to health or care, but there nevertheless appears to be scope for commissioners to increase the number and variety of VCSEs that they co-commission with, and commission. One way would be to establish support networks for small and medium-sized charities, including ethnic minority and other VCSEs disadvantaged by the commissioning system or even by systemic discrimination. For commissioners and the public, and of course VCSEs, commissioning VCSEs may be a more acceptable form of provider diversification than privatisation or the commissioning of corporations.
More generally, our findings support the recommendation213 that commissioners use modes of commissioning which are adapted to the nature of the services and their benefits to the user. For commissioning VCSEs, that means leaning towards a collaborative rather than a commodified mode of commissioning, including using non-financial (‘real-side’) criteria for selecting providers without making lowest cost the sole criterion, using the workarounds listed above and, when commissioning VCSEs, discouraging the more perversely narrow interpretations and use of the procurement regulations until the latter can be revised or repealed.
Additional information
Acknowledgements
We gratefully acknowledge the assistance, support and generous allocation of time to this project by our many informants in the study sites and in national organisations, and by our study site co-researchers, all of whom must remain anonymous under the terms of ethical approval for this project. Similarly, we acknowledge the work of the Project Oversight Group. In addition, Dr Rebecca Hardwick contributed to data collection and the action learning. Dr Chris Q. Smith contributed to data collection and analysis, and the action learning.
Research governance
We obtained research governance approval for each NHS organisation studied. The absence (in one prospective study site), and in CS1b the slow working, of the research governance system, at least during the transition from CCG to ICS responsibility, thus impeded our access to study sites. An independent Project Oversight Group, described above (see Chapter 3, Patient and public involvement and engagement), oversaw and guided the conduct of the study. In reporting this study we conform to the Standards for Reporting Qualitative Research214 and the Consolidated Criteria for Reporting Qualitative research (COREQ). 215 Appendix 8 states how the study complies with the RAMESES II standards for reporting evaluations. 173
Equality, diversity and inclusion
To optimise the inclusion of relevant participants, we consulted national VCSEs and local VCSE infrastructure (network) bodies in each study site. The resulting participant population was inclusive in that the individual participants included people from ethnic minority and some religious groups, both sexes, and ages ranging from young adults to retired. The study sites included areas of high deprivation, both rural and urban. They were widely dispersed across England. We found that studies of the commissioning of ethnic minority group VCSEs, and studies of systematic discrimination against them in commissioning systems, are lacking. We include this point in our recommendations for future research. In presenting materials to our learning group participants, and in disseminating project findings, we have used graphic as well as written materials.
The research team included both sexes, a range of expertise in both subjects and methods, and a mixture of early-career and experienced researchers. The Project Oversight Group included members of the public from groups that are generally under-represented, for example VCSE members who included members of patient self-help groups. They, and the research team members, were widely dispersed across England. Earlier-career members of the research team were encouraged to (and did) present at academic conferences. The local project reference groups consisted predominantly of members of the public active in the voluntary sector. Their roles were to advise the researchers on local commissioning issues and informants, to check the emerging findings for accuracy and balance, and to share experience and knowledge with their counterparts in other study sites. They benefited from the project in that way and by receiving mentorship and assistance with their own local research projects.
Contributions of authors
Rod Sheaff (https://orcid.org/0000-0002-7984-2627) Professor, Health Services Research. Produced the original research proposal and design, coordinated the study and contributed to the acquisition, analysis and interpretation of data for the work and synthesised the data-stream findings.
Angela Ellis Paine (https://orcid.org/0000-0002-4385-5098) Lecturer, Voluntary Sector Management. Designed the action learning component and contributed to the acquisition, analysis and interpretation of data.
Mark Exworthy (https://orcid.org/0000-0003-4791-7513) Professor, Health Policy and Management. Contributed to the original research proposal and design, the acquisition, analysis and interpretation of data.
Alex Gibson (https://orcid.org/0000-0003-2761-2819) Senior Research Fellow, Health Services Research. Designed the cross-sectional analysis of CCG spending on CCGs and contributed to the acquisition, analysis and interpretation of data.
Joanna Stuart (https://orcid.org/0000-0002-2316-6180) Independent researcher, voluntary sector management. Contributed to the acquisition, analysis and interpretation of data.
Véronique Jochum (https://orcid.org/0009-0006-8805-9761) Independent researcher, voluntary sector management. Contributed to the acquisition, analysis and interpretation of data.
Pauline Allen (https://orcid.org/0000-0001-5598-1684) Professor, Health Services Organisation. Contributed to the original research proposal and design and the analysis and interpretation of data.
Jonathan Clark (https://orcid.org/0000-0002-8385-7223) Lecturer, Sociology. Contributed to the original research proposal and design, the analysis and interpretation of data, and supported the Project Oversight Group.
Russell Mannion (https://orcid.org/0000-0002-0680-8049) Professor, Health Systems. Contributed to the original research proposal and design and to the analysis and interpretation of data on absorptive capacity.
Sheena Asthana (https://orcid.org/0000-0002-1483-2719) Professor, Health Policy. Contributed to the original research proposal and design, and the analysis and interpretation of data.
All authors contributed to drafting the work, reviewing it critically, and approving the version to be published. They agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure of interest
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/NTDT7965.
Primary conflicts of interest: Mark Exworthy was an HS&DR Funding Committee Member 2016–9. All other authors report they neither have, nor appear to have, any conflict of interest in the study.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
This study had NHS research ethics approval (IRAS reference 270268, 14 May 2020) on condition of maintaining anonymity of the informants, organisations and study sites involved.
Information governance statement
The University of Plymouth is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679.
Under the Data Protection legislation, the University of Plymouth is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here www.plymouth.ac.uk/students-and-family/governance/information-governance/your-information-rights.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publication
Sheaff R, Ellis-Paine A, Exworthy M, Hardwick R, Smith CQ. (2023). Commodification and healthcare in the third sector in England: from gift to commodity—and back? Public Money Manag 2023;44:298–307. https://doi.org/10.1080/09540962.2023.2244350
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Gadsby EW, Peckham S, Coleman A, Bramwell D, Perkins N, Jenkins LM. Commissioning for health improvement following the 2012 health and social care reforms in England: what has changed?. BMC Publ Health 2017;17:1-11.
- World Health Organization . Health for All by the Year 2000 1985.
- Organisation for Economic Co-operation and Development . Health at a Glance: Europe 2022: State of Health in the EU Cycle 2022.
- Office for National Statistics . Healthcare Expenditure, UK Health Accounts Provisional Estimates: 2021 2022.
- Exworthy M. A review of recent structural changes to District Health Authorities as purchasing organisations. Environ Planning C: Govt Pol 1993;11:279-89.
- Exworthy M, Peckham S. The contribution of coterminosity to joint purchasing in health and social care. Health Place 1998;4:233-43.
- Allen P, Osipovič D, Shepherd E, Coleman A, Perkins N, Garnett E, et al. Commissioning through competition and cooperation in the English NHS under the Health and Social Care Act 2012: evidence from a qualitative study of four clinical commissioning groups. BMJ Open 2017;7.
- Checkland K, Allen P, Coleman A, Segar J, McDermott I, Harrison S, et al. Accountable to whom, for what? An exploration of the early development of Clinical Commissioning Groups in the English NHS. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003769.
- McDermott I, Allen P, Moran V, Coleman A, Checkland K, Peckham S. Commissioning Healthcare in England. Bristol: Policy Press; 2020.
- Allen P, Checkland K, Moran V, Peckham S. Commissioning Healthcare in England Evidence. Bristol: Policy and Practice Policy Press; 2020.
- NHS England . Five Year Forward View 2014.
- House of Commons Committee of Public Accounts . Introducing Integrated Care Systems 2023.
- Sanderson M, Allen P, Osipvic D, Petsoulas C, Lau Y-S, Boiko O, et al. The Developing Architecture of System Management: Integrated Care Systems and Sustainability and Transformation Partnerships 2022. https://prucomm.ac.uk/integrated-care-systems-final-report-published.html (accessed 27 February 2023).
- Ferlie E, Lynn LE, Pollitt C. The Oxford Handbook of Public Management. Oxford: Oxford University Press; 2005.
- Miller R, Rees J. Mental health commissioning: master or subject of change?. Ment Health Rev J 2014;19:145-55.
- Osborne DE, Gaebler T. Reinventing Government: How the Entrepreneurial Spirit Is Transforming the Public Sector. Wokingham: Addison-Wesley; 1992.
- Callaghan G, Exworthy M, Hudson B, Powell M. Prospects for collaboration in primary care: relationships between social services and the new PCGs. J Interprof Care 2000;14:19-26.
- Checkland K, Harrison S, Snow S, Mcdermott I, Coleman A. Commissioning in the English National Health Service: what’s the problem?. J Soc Pol 2012;41:533-50.
- Body A. The commissioner’s perspective: The lived realities of commissioning children’s preventative services in England and the role of discretion. Volunt Sect Rev 2019;10:253-71.
- Macmillan R. The Third Sector Delivering Public Services: An Evidence Review. Birmingham: Third Sector Research Centre; 2010.
- Martikke S, Moxham C. Public sector commissioning: experiences of voluntary organizations delivering health and social services. Int J Publ Admin 2010;33:790-9.
- Bovaird T, Dickinson H, Allen K. Commissioning across Government: Review of Evidence. Birmingham: Third Sector Research Centre; 2012.
- Sheaff R, Charles N, Mahon A, Chambers N, Morando V, Exworthy M, et al. NHS commissioning practice and health system governance: a mixed-methods realistic evaluation. Health Serv Deliv Res 2015;3:1-184. https://doi.org/10.3310/hsdr03100.
- The Cabinet Office . Partnerships in Public Services: An Action Plan for Third Sector Involvement 2006.
- JSNA Blackpool . SNA Blackpool Joint Strategic Needs Assessment 2021.
- Cohen MD, March JG, Olsen JP. A garbage can model of organizational choice. Admin Sci Quart 1972;17:1-25.
- Granovetter M. Economic action and social structure: the problem of embeddedness. AJS 1983;41:481-510.
- Baker G, Gibbons R, Murphy KJ. Relational contracts and the theory of the firm. Quart J Econ 2002;117:39-84.
- Gibbons R, Henderson R. Relational contracts and organizational capabilities. Organ Sci 2012;23:1350-64.
- Macneil IR. Contracts: adjustment of long-term relations under classical, neo-classical and relational contract law. Northw Univ Law Rev 1978;72:854-905.
- Allen P. A socio-legal and economic analysis of contracting in the NHS internal market using a case study of contracting for district nursing. Soc Sci Med (1982) 2002;54:255-66.
- Porter A, Mays N, Shaw S, Rosen R, Smith J. Commissioning healthcare for people with long term conditions: the persistence of relational contracting in England’s NHS quasi-market. BMC Health Serv Res 2013;13.
- Mannion R, Smith P. Changes in Health Care: Reflections on the NHS Internal Market. London: Palgrave Macmillan; 1997.
- Musekiwa E, Needham C. The Palgrave Handbook of Co-Production of Public Services and Outcomes. Berlin: Springer; 2021.
- Bovaird T, Loeffler E. We’re All in This Together: Harnessing User and Community Co-production of Public Outcomes. Birmingham: Institute of Local Government Studies, University of Birmingham; 2013.
- Macmillan R, Paine AE. The third sector in a strategically selective landscape – the case of commissioning public services. J Soc Pol 2021;50:606-26.
- Loeffler E, Bovaird T. Co-commissioning of public services and outcomes in the UK: bringing co-production into the strategic commissioning cycle. Publ Money Manag 2019;39:241-52.
- Newbigging K, Mohan J, Rees J, Harlock J, Davis A. Contribution of the voluntary sector to mental health crisis care in England: protocol for a multimethod study. BMJ Open 2020;7.
- NHS England . Next Steps Towards Primary Care Co-Commissioning 2014.
- Petsoulas C, Allen P, Checkland K, Coleman A, Segar J, Peckham S, et al. Views of NHS commissioners on commissioning support provision: evidence from a qualitative study examining the early development of clinical commissioning groups in England. BMJ Open 2014;4.
- HM Government . Civil Society Strategy: Building a Future That Works for Everyone 2018.
- Exworthy M, Powell M, Mohan J. The NHS: quasi-market, quasi-hierarchy and quasi-network?. Publ Money Manag 1999;19:15-22.
- Petsoulas C, Allen P, Hughes D, Vincent-Jones P, Roberts J. The use of standard contracts in the English National Health Service: a case study analysis. Soc Sci Med (1982) 2011;73:185-92. https://doi.org/10.1016/j.socscimed.2011.05.021.
- Vincent-Jones P. The new public contracting: public versus private ordering?. Indiana J Glob Legal Stud 2007;14:259-78.
- Sheaff R, Schofield J. Oxford Handbook of Health Care Management. Oxford: Oxford University Press; 2016.
- Bishop S, Waring J. Becoming hybrid: The negotiated order on the front line of public–private partnerships. Hum Relat 2016;69:1937-58. https://doi.org/10.1177/0018726716630389.
- Coupet J, McWilliams A. Integrating organizational economics and resource dependence theory to explain the persistence of quasi markets. Admin Sci 2017;7.
- Baumol WJ. Contestable markets: an uprising in the theory of industry structure. Am Econ Rev 1982;72:1-15.
- Krajewski M. Karl Polanyi, Globalisation and the Potential of Law in Transnational Markets. 2010.
- Mazanderani F, Locock L, Powell J. Biographical value: towards a conceptualisation of the commodification of illness narratives in contemporary healthcare. Soc Health Illness 2013;35:891-905. https://doi.org/10.1111/1467-9566.12001.
- McClean S, Moore R. Money, commodification and complementary health care: theorising personalised medicine within depersonalised systems of exchange. Soc Theory Health 2013;11:194-21.
- Stoeckle JD. From service to commodity: corporization, competition, commodification, and customer culture transforms health care. Croat Med J 2000;41:141-3.
- Osipovič D, Allen P, Sanderson M, Moran V, Checkland K. The regulation of competition and procurement in the National Health Service 2015–2018: enduring hierarchical control and the limits of juridification. Health Econ Policy Law 2020;15:308-24. https://doi.org/10.1017/S1744133119000240.
- Noort BAC, Ahaus K, van der Vaart T, Chambers N, Sheaff R. How healthcare systems shape a purchaser’s strategies and actions when managing chronic care. Health Policy 2020;124:628-38. https://doi.org/10.1016/j.healthpol.2020.03.009.
- Chambers N, Sheaff R, Mahon A, Byng R, Mannion R, Charles N, et al. The practice of commissioning healthcare from a private provider: learning from an in-depth case study. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-S1-S4.
- Albalate D, Bel G, Reeves E. Government choice between contract termination and contract expiration in re-municipalization: a case of historical recurrence?. Int Rev Admin Sci 2021;87:461-79.
- Checkland K, Coleman A, Mcdermott I, Peckham S. Dismantling the NHS?. London: Policy Press; 2016.
- Sheaff R, Marshall M, Rogers A, Roland M, Sibbald B, Pickard S. Governmentality by network in English primary healthcare. Soc Policy Admin 2004;38:89-103. https://doi.org/10.1111/j.1467-9515.2004.00378.x.
- Lipsky M. Street-Level Bureaucracy. New York: Russell Sage Foundation; 2010.
- Gale N, Dowswell G, Greenfield S, Marshall T. Street-level diplomacy? Communicative and adaptive work at the front line of implementing public health policies in primary care. Soc Sci Med (1982) 2017;177:9-18.
- Bossert T. Analyzing the decentralization of health systems in developing countries: decision space, innovation and performance. Soc Sci Med (1982) 1998;47:1513-27. https://doi.org/10.1016/S0277-9536(98)00234-2.
- Exworthy M, Frosini F. Room for manoeuvre?: Explaining local autonomy in the English National Health Service. Health Policy 2008;86:204-12. https://doi.org/10.1016/j.healthpol.2007.10.008.
- Exworthy M, Frosini F, Jones L, Peckam S, Powell M, Greener I, et al. Decentralisation and Performance: Autonomy and Incentives in Local Health Economies. Southampton: NCCSDO; 2010.
- Exworthy M, Frosini F, Jones L. Are NHS foundation trusts able and willing to exercise autonomy? ‘You can take a horse to water…’. J Health Serv Res Policy 2011;16:232-7. https://doi.org/10.1258/jhsrp.2011.010077.
- Ferlie E, Addicott R, Exworthy M, Fitzgerald L. Networks in Health Care: A Comparative Study of Their Management Impact and Performance. London: HSDR; 2010.
- Flynn R, Pickard S, Williams G. Contracts and the quasi-market in community health services. J Soc Policy 1995;24:529-50. https://doi.org/10.1017/S0047279400025423.
- Sheaff R, Morando V, Chambers N, Exworthy M, Mahon A, Byng R, et al. Managerial workarounds in three European DRG systems. J Health Organ Manag 2020;34:295-311. https://doi.org/10.1108/JHOM-10-2019-0295.
- Egholm L, Kaspersen LB. Civil Society: Between Concepts and Empirical Grounds. New York: Routledge; 2020.
- Salamon LM, Anheier HK. Defining the Nonprofit Sector: A Cross-National Analysis. Manchester: Manchester University Press; 1997.
- Hall MH, Reed PB. Shifting the burden: how much can government download to the non-profit sector?. Can Publ Admin 1998;41:1-20.
- Baines S, Bull M, Woolrych R. A more entrepreneurial mindset? Engaging third sector suppliers to the NHS. Soc Enterpr J 2010;6:49-58.
- Birchall J, Simmons R. What motivates members to participate in co-operative and mutual businesses?. Ann Publ Cooper Econ 2004;75:465-95. https://doi.org/10.1111/j.1467-8292.2004.00259.x.
- Rose-Ackerman S. Altruism, ideological entrepreneurs and the non-profit firm. VOLUNTAS: Int J Volunt Nonprof Organ 1997;8:120-34. https://doi.org/10.1007/BF02354190.
- Billis D. Hybrid Organizations and the Third Sector: Challenges for Practice, Theory and Policy. Basingstoke: Palgrave Macmillan; 2010.
- Allen P, Bartlett W, Zamora B, Turner S. New forms of provider in the English National Health Service. Ann Public Coop Econ 2011;82:77-95.
- Gintis H, Bowles S. Democracy and Efficiency in the Economic Enterprise. New York: Routledge; 2002.
- Alcock P. A strategic unity: defining the third sector in the UK. Voluntary Sector Review 2010;1:5-24.
- Gorsky M, Mohan J, Willis T. Mutualism and Health Care. Manchester: Manchester University Press; 2006.
- Rees J, Miller R, Buckingham H. Commission incomplete: exploring the new model for purchasing public services from the third sector. J Soc Pol 2017;46:175-94.
- Kendall J. The mainstreaming of the third sector into public policy in England in the late 1990s: whys and wherefores. Policy Pol 2000;28:541-62.
- The Home Office . On Relations Between Government and the Voluntary and Community Sector in England 1998.
- Macmillan R. Decoupling the State and the Third Sector? The ‘Big Society’ as a Spontaneous Order. Birmingham: Third Sector Research Centre; 2013.
- Cabinet Office . Civil Society Strategy: Building a Future That Works for Everyone 2018.
- Baker L, Jochum V, Garforth H, Usher R. Big Local Relationships and Public Agencies. London: Local Trust; 2022.
- Macmillan R. Sheffield Hallam University . A surprising turn of events: episodes towards a renaissance of civil society infrastructure in England. People Place Policy Online 2021;15:57-71.
- National Council for Voluntary Organisations . UK Civil Society Almanac 2022.
- Tussell . UK Public Procurement through VCSEs, 2016–2020 2021.
- Curry N, Mundle C, Sheil F, Weaks L. The Voluntary and Community Sector in Health Implications of the Proposed NHS Reforms. London: Kings Fund; 2011.
- Miller R. Third sector organisations: unique or simply other qualified providers?. J Publ Ment Health 2013;12:103-13.
- Dayson C. Social prescribing ‘plus’: a model of asset-based collaborative innovation?. People Place Policy 2017;11:90-104.
- Bull D, Bagwell S, Weston A, Joy I. Untapped Potential: Bringing the Voluntary Sector Strengths to Health and Care Transformation. Report commissioned by the Richmond Group of Charities and its partners for the Doing the Right Thing project. London: NPC; 2016.
- Dayson C, Wells P. Voluntary and community sector policy under the coalition government. People Place Policy Online 2013;7:91-9.
- Perspective Economics . The Role of Voluntary, Community, and Social Enterprise (VCSE) Organisations in Public Procurement 2022.
- Sheaff R, Halliday J, Exworthy M, Gibson A, Clark J, Asthana S, et al. Diverse Healthcare Providers: Behaviour in Response to Commissioners, Patients and Innovations. London: Department of Health and Social Care; 2018.
- National Audit Office . Developing New Care Models Through NHS Vanguards 2018.
- Mazzei M, Teasdale S, Calò F, Roy MJ. Co-production and the third sector: conceptualising different approaches to service user involvement. Publ Manag Rev 2020;22:1265-83.
- Arvidson M, Kara H. The Third Sector Delivering Public Services: Developments, Innovations and Challenges. Bristol: Policy Press; 2016.
- Garnett E, Baeza J, Trenholm S, Gulliford M, Green J. Social enterprises and public health improvement in England: a qualitative case study. Public Health 2018;161:99-105. https://doi.org/10.1016/j.puhe.2018.04.019.
- Courpasson D, Clegg S. Dissolving the iron cages? Tocqueville, Michels, bureaucracy and the perpetuation of elite power. Organization 2006;13:319-43.
- Storey J, Basterretxea I, Salaman G. Managing and resisting ‘degeneration’ in employee-owned businesses: a comparative study of two large retailers in Spain and the United Kingdom. Organization 2014;21:626-44.
- DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Soc Rev 1983;48:147-60.
- Milbourne L, Cushman M. Complying, transforming or resisting in the new austerity? Realigning social welfare and independent action among English voluntary organisations. J Soc Policy 2015;44:463-85.
- Rees J, Taylor R, Damm C. Opening the ‘black box’: organisational adaptation and resistance to institutional isomorphism in a prime-led employment services programme. Public Policy Admin 2022;39:106-24.
- Shore C, Wright S. Governing by numbers: audit culture, rankings and the new world order. Soc Anthropol 2015;23:22-8.
- Benson A. ‘The Devil That Has Come amongst Us’: The Impact of Commissioning and Procurement Practices NCIA Inquiry into the Future of Voluntary Services. London: NCIA; 2014.
- Carmel E, Harlock J. Instituting the ’third sector’as a governable terrain: partnership, procurement and performance in the UK. Policy Politics 2008;36:155-71.
- Evans B, Richmond T, Shields J. Structuring neoliberal governance: the nonprofit sector, emerging new modes of control and the marketisation of service delivery. Policy Soc 2005;24:73-97.
- Skelcher C, Smith SR. Theorizing hybridity: institutional logics, complex organizations, and actor identities: the case of nonprofits. Public Admin 2015;93:433-48.
- Fox D. Policy commercializing nonprofits in health: the history of a paradox from the 19th century to the ACA. Milbank Q 2015;93:179-210. https://doi.org/10.1111/1468-0009.12109.
- Davis K. Credit union governance and survival of the cooperative form. J Finan Services Res 2001;19.
- Paine AE, Hill M. The Third Sector Delivering Public Services. Bristol: Policy Press; 2016.
- Veronesi G, Kirkpatrick I, Altanlar A, Sarto F. Corporatization, administrative intensity, and the performance of public sector organizations. J Public Adm Res Theory 2022;33:701-15.
- Bevir M, Waring J. Decentring Health Policy: Learning from British Experiences in Healthcare Governance. London: Routledge; 2017.
- Klijn E-H. Governing networks in the hollow state contracting out, process management or a combination of the two?. Public Manag Rev 2002;4:149-65.
- Koppenjan J, Mandell M, Keast R, Brown K. The Role of Context in Hybrid Governance Arrangements n.d.
- Rhodes RAW. The new governance: governing without government. Pol Stud 1996;44:652-67. https://doi.org/10.1111/j.1467-9248.1996.tb01747.x.
- Sheaff R, Chambers N, Charles N, Exworthy M, Mahon A, Byng R, et al. How managed a market? Modes of commissioning in England and Germany. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-S1-S8.
- Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review. BMJ Qual Saf 2018;27:226-40.
- Sheaff R. Healthcare access and mobility between the UK and other European Union stat. Health Policy 1997;42:239-53.
- Herepath A, Kitchener M, Waring J. A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study. Health Serv Deliv Res 2015;3:1-242.
- Feng W, Fox AM. What’s the hold up? The FDA’s delayed implementation of menu-labeling policy. Admin Soc 2022;54:1045-88.
- Checkland K. National service frameworks and UK general practitioners: street-level bureaucrats at work?. Soc Health Illness 2004;26:951-75. https://doi.org/10.1111/j.0141-9889.2004.00424.x.
- Kim AY, Choi WS. Considerations on the implementation of the telemedicine system encountered with stakeholders’ resistance in COVID-19 pandemic. Telemed J E-Health 2021;27:475-80.
- Owen DL, Swift TA, Humphrey C, Bowerman M. The new social audits: accountability, managerial capture or the agenda of social champions?. Eur Account Rev 2010;9:81-98.
- Touati N, Roberge D, Denis JL, Cazale L, Pineault R, Tremblay D. Clinical leaders at the forefront of change in health-care systems: advantages and issues: lessons learned from the evaluation of an integrated oncological services network. Health Serv Manage Res 2006;19:105-22.
- Wagner WE. Administrative law, filter failure, and information capture. Duke LJ 2009;59.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Sayer A. Method in Social Science: A Realist Approach. London: Psychology Press; 1992.
- Wildavsky AB. Speaking Truth to Power. Piscataway, NJ: Transaction Publishers; 1989.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Greenhalgh J, Manzano A. Understanding ‘context’ in realist evaluation and synthesis. Int J Soc Res Methodol 2021;25:583-95.
- Sheaff R, Doran N, Harris M, Lang I, Medina-Lara A, Fornasiero M, et al. Categories of context in realist evaluation. Evaluation 2021;27:184-209.
- The RAMESES II Project . What Realists Mean by Context; Or, Why Nothing Works Everywhere or for Everyone 2017. https://www.ramesesproject.org/media/RAMESES_II_Context.pdf (accessed 27 February 2023).
- The RAMESES II Project . What Is a Mechanism? What Is a Programme Mechanism? 2017. http://ramesesproject.org/media/RAMESES_II_What_is_a_mechanism.pdf (accessed 27 February 2023).
- Lane PJ, Lubatkin M. Relative absorptive capacity and interorganizational learning. Strateg Manage J 1998;19:461-77.
- Newton J, Graham J, McLoughlin K, Moore A. Receptivity to change in a general medical practice. Br J Manage 2003;14:143-53.
- Van Den Bosch FA, Volberda HW, De Boer M. Coevolution of firm absorptive capacity and knowledge environment: organizational forms and combinative capabilities. Organ Sci 1999;10:551-68.
- Flatten TC, Greve GI, Brettel M. Absorptive capacity and firm performance in SMEs: the mediating influence of strategic alliances. Eur Manag Rev 2011;8:137-52.
- Harvey G, Skelcher C, Spencer E, Jas P, Walshe K. Absorptive capacity in a non-market environment. Public Manag Rev 2010;12:77-9. https://doi.org/10.1080/14719030902817923.
- Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Admin Sci Quart 1990;35:128-52.
- Currie G, Croft C, Chen Y, Kiefer T, Staniszewska S, Lilford R. The capacity of health service commissioners to use evidence: a case study. Health Serv Deliv Res 2018;6:1-158.
- Moynihan DP, Hawes DP. Responsiveness to reform values: the influence of the environment on performance information use. Public Admin Rev 2012;72:S95-10.
- Van den Hooff B, Huysman M. Managing knowledge sharing: emergent and engineering approaches. Inform Manag 2009;46:1-8.
- Finkelstein S, Mooney AC. Not the usual suspects: how to use board process to make boards better. Acad Manag Persp 2003;17:101-13.
- Moynihan DP, Landuyt N. How do public organizations learn? Bridging cultural and structural perspectives. Public Admin Rev 2009;69:1097-105.
- Van Ees H, van der Laan G, Postma TJ. Effective board behavior in the Netherlands. Eur Manag J 2008;26:84-93.
- Jansen JJ, Van Den Bosch FA, Volberda HW. Managing potential and realized absorptive capacity: how do organizational antecedents matter?. Acad Manage J 2005;48:999-1015.
- Faraj S, Sproull L. Coordinating expertise in software development teams. Manage Sci 2000;46:1554-68.
- Lane PJ, Salk JE, Lyles MA. Absorptive capacity, learning, and performance in international joint ventures. Strateg Manage J 2001;22:1139-61.
- Flatten TC, Engelen A, Zahra SA, Brettel M. A measure of absorptive capacity: scale development and validation. Eur Manag J 2011;29:98-116. https://doi.org/10.1016/j.emj.2010.11.002.
- Hardwick R, Anderson R, Cooper C. How do third sector organisations use research and other knowledge? A systematic scoping review. Implement Sci 2015;10.
- Pfeffer J, Salancik GR. The External Control of Organizations: A Resource Dependence Perspective. Stanford, CA: Stanford University Press; 2003.
- Hillman AJ, Shropshire C, Cannella Jr AA. Organizational predictors of women on corporate boards. Acad Manage J 2007;50:941-52.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Gibson A. CCG Spend on VCSEs, 2018/19: Data and Analysis. GitHub; 2023.
- HM Treasury . Guidance for Publishing Spend over £25,000 2013.
- Care Quality Commission . Using CQC Data (with Links to the CQC Active and Deactivated Locations Directories) 2022.
- NHS Digital . NHS Payments to General Practice: England, 2018 19 2019.
- NHS England . Clinical Commissioning Groups’ Accounts (2016–17) 2018.
- Clifford D. Voluntary sector organisations working at the neighbourhood level in England: patterns by local area deprivation. Environ Plan A: Econ Space 2012;44:1148-64.
- Halliday J, Asthana S, Hewson P, Gibson A. Playing with fire: limitations of the big society for an emergency service. Publ Policy Admin 2013;28:290-305.
- Gioia DA, Corley KG, Hamilton AL. Seeking qualitative rigor in inductive research: notes on the Gioia methodology. Organ Res Method 2013;16:15-31.
- Mintzberg H. Power in and around Organizations. Englewood Cliffs, NJ: Prentice Hall; 1983.
- Mintzberg H. Power and organization life cycles. Acad Manag Rev 1984;9:207-24.
- Revans RW. What is action learning?. J Manage Dev 1982;1:64-75.
- Revans R. ABC of Action Learning. London: Routledge; 2017.
- Burawoy M. The extended case method. Soc Theory 1998;16:4-33.
- Popper KR. Conjectures and Refutations. London: Routledge Kegan Paul; 1963.
- Rasmussen J. Human error and the problem of causality in analysis of accidents. Philos Trans R Soc London Ser B 1990;327:449-60; discussion 460.
- De Jong BA, Elfring T. How does trust affect the performance of ongoing teams? The mediating role of reflexivity, monitoring, and effort. Acad Manage J 2010;53:535-49.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. J Admin Govern 2009;4:72-9.
- Payne G, Williams M. Generalization in qualitative research. Sociology 2005;39:295-314.
- Sanderson M, Allen P, Osipovič D. The regulation of competition in the National Health Service (NHS): what difference has the Health and Social Care Act 2012 made?. Health Econ Policy Law 2016;12:1-19.
- Mannion R, Davies HTO. Payment for performance in health care. BMJ 2008;336:306-8. https://doi.org/10.1136/bmj.39463.454815.94.
- Bergman M, Lane J-E. Public policy in a principal–agent framework. J Theor Pol 1990;2:339-52.
- Harker R. NHS Funding Allocations: Clinical Commissioning Groups. London: House of Commons; 2019.
- Brien P. Local Government Finances. London: House of Commons; 2022.
- Department for Levelling Up, Housing and Communities . Revenue Outturn (RO) 2020–21 Final: Social Care and Public Health (RO3) Data 2021.
- National Audit Office . Financial Sustainability of Local Authorities Visualisation: Update 2021.
- Corry D. Where Are England’s Charities. London: Think NPC; 2020.
- Marmot M. Health equity in England: the Marmot review 10 years on. BMJ 2020;368.
- Whitty C. Health in Coastal Communities. London: Department of Health and Social Care; 2021.
- Marmot M, Allen J. COVID-19: exposing and amplifying inequalities. J Epidemiol Community Health 2020;74:681-2.
- Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Commun Health 2020;74:964-8.
- The Strategy Unit . Making the Case for Integrating Physical and Mental Health Services in England 2018.
- Goddard M, Mannion R, Smith PC. Assessing the performance of NHS Hospital Trusts: the role of ‘hard’ and ‘soft’ information. Health Policy 1999;48:119-34.
- Ettelt S, Mays N, Allen P. The multiple purposes of policy piloting and their consequences: three examples from national health and social care policy in England. J Soc Pol 2015;44:319-37.
- Exworthy M. Localism in the NHS quasi-market. Environ Planning C: Govt Pol 1998;16:449-62. https://doi.org/10.1068/c160449.
- Davies HT, Nutley SM. What Works? Evidence-Based Policy and Practice in Public Services. London: Policy Press; 2000.
- GOV.UK . Cases in the UK. Coronavirus in the UK 2023. https://coronavirus.data.gov.uk/details/cases (accessed 13 March 2023).
- De Bono DS, Greenfield D, Travaglia JF, Long JC, Black D, Johnson J, et al. Nurses’ workarounds in acute healthcare settings: a scoping review. BMC Health Serv Res 2013;13.
- Halbesleben JRB, Wakefield DS, Wakefield BJ. Work-arounds in health care settings: literature review and research agenda. Health Care Manage Rev 2008;33:2-12. https://doi.org/10.1097/01.HMR.0000304495.95522.ca.
- Lalley C, Malloch K. Workarounds: the hidden pathway to excellence. Nurse Leader 2010;8:29-32. https://doi.org/10.1016/j.mnl.2010.05.009.
- Tummers L, Bekkers V. Policy implementation, street-level bureaucracy, and the importance of discretion. Public Manag Rev 2014;16:527-47.
- Ferlie E, Addicott R. Determinants of Performance in Cancer Networks: A Process Evaluation. London: NCCSDO; 2004.
- Provan K, Kenis P. Modes of network governance: structure, management, and effectiveness. J Public Adm Res Theory 2008;18:229-52.
- Kirkpatrick I, Altanlar A, Veronesi G. Hybrid professional managers in healthcare: an expanding or thwarted occupational interest?. Public Manag Rev 2022;25:859-78. https://doi.org/10.1080/14719037.2021.1996777.
- Allen P, Osipovič D, Shepherd E, Coleman A, Perkins N, Garnett E. Commissioning through Competition and Cooperation. Manchester: Policy Research Unit on Commissioning and the Healthcare System; 2016.
- King D, Chan O, Coule T, Dahill D, Mainard-Sardon J, Martin A, et al. Respond, Recover, Reset: Two Years On. Nottingham: Nottingham Trent University, Centre for People, Work and Organisational Practice; 2022.
- Baylis A, Chikwira L, Robertson R, Tiratelli L. Dying Well at Home: Commissioning Quality End-of-Life Care. London: Kings Fund; 2023.
- North DC. Institutions, transaction costs and economic growth. Econ Inquiry 1987;25:419-28.
- North DC. Institutions, transaction costs and productivity in the long run. Econ History 1993;1993.
- Valentinov V. The transaction cost theory of the nonprofit firm: beyond opportunism. Nonprofit Volunt Sector Quart 2008;37:5-18.
- Gnyawali DR, Ryan-Charleton T. Nuances in the interplay of competition and cooperation: towards a theory of coopetition. J Manage 2018;44:2511-34. https://doi.org/10.1177/0149206318788945.
- Chiapello E, Fairclough N. Understanding the new management ideology: a transdisciplinary contribution from critical discourse analysis and new sociology of capitalism. Discourse Soc 2002;13:185-208.
- Fairclough N. Discourse analysis in organization studies: the case for critical realism. Organ Stud 2005;26:915-39. https://doi.org/10.1177/0170840605054610.
- Frumkin P, Galaskiewicz J. Institutional isomorphism and public sector organizations. J Public Adm Res Theory 2004;14:283-307. https://doi.org/10.1093/jopart/muh028.
- Paton C. The changing political economy of the NHS. Public Finan Manag 2006;6.
- DiMaggio PJ, Anheier HK. The sociology of nonprofit organizations and sectors. Ann Rev Soc 1990;16:137-59. https://doi.org/10.1146/annurev.so.16.080190.001033.
- Sheaff R, Ellis-Paine A, Exworthy M, Hardwick R, Smith CQ. Commodification and healthcare in the third sector in England: from gift to commodity – and back?. Public Money Manag 2023;44:298-307. https://doi.org/10.1080/09540962.2023.2244350.
- World Health Organization . Declaration of Alma-Ata n.d.
- Murphy M, Irwin A, Maher M. Winners and Losers? The Social Marketisation of Civil Society. Maynooth: Maynooth University & Community Work Ireland; 2020.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57. https://doi.org/10.1093/intqhc/mzm042.
- Rahal C. The keys to unlocking public payments data. Kyklos 2018;71:310-37. https://doi.org/10.1111/kykl.12171.
- Rahal C, Mohan J. The role of the third sector in public health service provision: evidence from 25,338 heterogeneous procurement datasets. SocArXiv 2022. https://doi.org/10.31235/osf.io/t4x52.
- Goodair B, Reeves A. Outsourcing health-care services to the private sector and treatable mortality rates in England, 2013–20: an observational study of NHS privatisation. Lancet Public Health 2022;7:e638-46. https://doi.org/10.1016/S2468-2667(22)00133-5.
- Virgin . Introducing HCRG Care Group 2021. www.virgin.com/about-virgin/virgin-group/news/introducing-hcrg-care-group (accessed 24 June 2024).
- Twenty20Capital . How We Work 2021.
- Dayson C, Eadson W, Sanderson E, Wilson I. Greater Manchester State of the Voluntary Sector 013. Sheffield: Centre for Regional Economic and Social Research Hallam University; 2013.
- City Health Care Partnership . Accounts for City Health Care Partnership, Year Ending 31 March 2019 2019.
- Marie Stopes International . Accounts for Marie Stopes International, Year Ending 31 December 2018 2019.
- Mannion R, Smith P. Changing Health Care, Reflections on the NHS Internal Market. Basingstoke: Macmillan; 2007.
- Plickert G, Cote RR, Wellman B. It’s not who you know, it’s how you know them: who exchanges what with whom?. Soc Netw 2007;29:405-29. https://doi.org/10.1016/j.socnet.2007.01.007.
- Thomson AM, Perry JL. Collaboration processes: inside the black box. Public Admin Rev 2006;66:20-32.
Appendix 1 Stakeholder interview topic guide: scoping questionnaire
Reminder: These are TOPIC GUIDES, to guide the interviews rather than to be read as exact questions to be asked. Further they are TEMPLATES, to be adapted and developed for each participant.
Introduction
-
Introduce self and research study.
-
Discuss interview process, recording, confidentiality and consent. CONSENT FORM.
-
Turn recorder on.
About you
-
Can you tell us a bit about your role – what do you do? What does it involve?
-
What is your background? How did you come to be here?
Organisational positioning
PLEASE NOTE – these questions are only relevant for stakeholders from VCSE organisations
-
How would you describe your organisations – its purpose and activities – to someone who knew nothing about it?
-
What are your direct experiences of healthcare commissioning? Are you/have you been commissioned to deliver healthcare services?
-
How would you describe your relationship with commissioners? What makes for a good relationship? And a bad relationship?
-
How has being commissioned to deliver healthcare services affected your organisation, the services it delivers, and/or the way it delivers them? How does this vary?
Wider perspectives – commissioning
-
In a few sentences, what do you think have been the key developments in healthcare commissioning over the past few years?
-
Where has the third sector fitted within this?
-
How has this been affected by COVID-19?
-
In your experience, what are the different ways in which the third sector is involved in healthcare commissioning? Is this changing?
-
Why do you think the third sector is involved in healthcare commissioning?
-
What do you think is distinctive about the third sector and what it contributes to health care? Do you think this informs commissioning decisions?
-
-
In general, how would you describe the nature and quality of relationships between healthcare commissioners (CCGs, local authority, PCC, others) and third sector organisations?
-
Is there anything that particularly that tends to helps or hinders relationships?
-
We’ve been told that both trust and longevity of relationships between commissioners and providers is important for good commissioning relationships: would you agree, or are there other factors which you think are more important?
-
-
How does this vary between groups of commissioners – for example CCGs versus LA?
-
How does it vary between areas (geographic)?
-
And for different third sector organisations?
Co-commissioning
-
There is a lot of talk about co-commissioning and collaborative commissioning – what do you understand co-commissioning, and collaborative commissioning, to mean?
-
And what are your reflections on how this is playing out within health care, particularly in terms of third sector involvement?
-
Can you think of any particular examples where this is working particularly well? Why do you think that was? What happened that made it work that way?
Absorptive capacity
We are particularly interested in how healthcare commissioners and third sector organisations learn about each other, and the type of evidence they draw upon to inform their thinking and to evidence their work.
-
Do you have any reflections on how third sector organisations learn about commissioning processes and/or commissioners?
-
And what about how healthcare commissioners learn about the third sector?
-
What kinds of evidence do healthcare commissioners tend to require of third sector organisations? Can you think of an example? Do you know why they want this kind of evidence/why do they want this kind of evidence?
-
And what kinds of evidence do third sector organisations tend to use when relating to commissioners? Can you think of an example? Why might that be?
-
Apart from routine evaluation and monitoring data and reports, in your experience what other kinds of knowledge or evidence do VCS organisations use in commissioning? How? Why is this?
-
Closing
-
Anything else you would like to add?
-
Happy to be re-contacted?
-
Other people you would recommend we speak to?
Appendix 2 Case study interview schedule
The University of Plymouth, The University of Birmingham, and The London School of Hygiene and Tropical Medicine.
Commissioning, Co-commissioning and Being Commissioned; the NHS and Third Sector
Instructions to interviewers are in italics
These are TOPIC GUIDES, to guide the interviews, to be adapted and developed for each participant.
Before starting interview:
-
Check interviewee has seen PIS/research proposal.
-
Invite interviewee to ask any questions about the research and what is expected of him/her.
-
Ask interviewee to sign consent form (two copies: one for interviewee, one for researchers).
-
Ask permission to audio-record.
-
Offer interviewee opportunity to see and correct transcript.
In our research, we are interested in the commissioning/co-commissioning relationship between the NHS and third sector organisations, many of which are VCSEs (defined as ‘formally organised; non-profit-distributing; constitutionally independent from the state; self-governing and benefiting from some form of voluntarism’.). The key Research Questions are:
-
RQ1. How do NHS commissioners address the task of commissioning VCSEs as service providers, and what barriers do they face?
-
RQ2. What are the consequences for VCSEs, of the NHS commissioning services from them?
-
RQ3. How are VCSEs involved in CCG, local authority and other (e.g. ICS, STP) commissioning decisions?
-
RQ4. What absorptive capacities do commissioners and VCSEs respectively need for enabling VSCEs to be commissioned, and for co-commissioning?
Focal care groups: social prescribing for older people; hospices; people with a learning disability and complex behavioural needs.
Interviewee
-
Please tell us about your role in your organisation and your history as to how/when you came to your current position.
-
How has this role changed (if it has) while you have been involved with NHS commissioning?
-
What services does the NHS commission from your organisation?
-
[Check for focal groups: social prescribing for older people; hospices; People with a learning disability and complex behavioural needs.]
-
What organisations have you commissioned and currently commission?
-
For whom (care groups) are these NHS-commissioned services provided?
-
Have you undertaken or been part of co-commissioning jointly with NHS commissioners?
Commissioning
For the focal care group (social prescribing: learning disability; hospices):
-
What care groups specifically does the NHS commission your organisation(s) to provide?
-
What outcomes were you seeking, from being commissioned by the NHS?
-
What proportion of your VCSE’s income comes from NHS commissioners?
-
-
What kinds of evidence or information did the NHS want from your organisation before deciding whether to commission it as a provider?
-
What kind of evidence or information was your organisation in fact able to supply?
-
What (other) barriers do you face, when trying to get commissioned by the NHS?
-
Do you take a specific, distinct approach when seeking contracts from the NHS (in contrast to, say, a charity or another public body), and if so what is that approach? [Probe:] Any special ways of:
-
Negotiating the contract, for example co-designing services?
-
Formulating or interpreting the contract?
-
Payment and/or non-financial benefits?
-
Supporting or helping the commissioner(s) in other ways?
-
Defining and monitoring satisfactory completion of the contract?
-
Dealing with queries or disputes?
-
-
How (if at all) does your VCSE’s role as patient and/or carer and/or public and/or interest-group advocate affect the way you engage with commissioners?
-
How (if at all) does your VCSE’s reliance on volunteers affect the way you relate to NHS commissioners?
-
Which if any NHS commissioners would you say you had a particularly good (e.g. easy, productive, mutually collaborative) commissioning relationship with?
[Probe:] Reasons for making that judgement?
-
Thinking of the NHS commissioner with which you had the best (e.g. easy, productive, mutually collaborative) commissioning relationship:
-
How did that commissioning relationship change the nature of the services which your VCSE provides? [Prompt:] For example
-
service developments or innovations?
-
implications for long-term overall costs for commissioners (e.g. compared with non-VCSE services)?
-
-
How did that commissioning relationship change the nature of your VCSE itself? For example [Prompts:]
-
signs your VCSE became more ‘managerial’ in their culture?
-
attempts to make NHS/LA income bigger or longer-term?
-
made them less (or more) prone to criticise NHS bodies?
-
-
So far as you can tell, did that commissioning relationship have any other consequences for your VCSE?
-
-
Which if any NHS commissioners would you say you had a particularly difficult (e.g. effortful, unproductive, precarious, antagonistic) commissioning relationship with?
[Probe:] Reasons for making that judgement?
-
Now thinking of the NHS commissioner with which you had the worst (e.g. effortful, unproductive, antagonistic) commissioning relationship:
-
How did that commissioning relationship change the nature of the services which your VCSE provides? [Prompt:] For example
-
service developments or innovations?
-
implications for long-term overall costs for commissioners (e.g. compared with non-VCSE services)?
-
-
How did that commissioning relationship change the nature of the VCSE itself? For example [Prompts:]
-
signs your VCSE became more ‘managerial’ in their culture?
-
attempts to make NHS/LA income bigger or longer-term?
-
made your VCSE less (or more) prone to criticise NHS bodies?
-
-
Did that commissioning relationship have any other consequences for your VCSE?
-
Co-commissioning
By ‘co-commissioning’ we mean VCSEs collaborating with local commissioning bodies (CCG, local authority, ICS, STP or any combination) in the work of commissioning health and social care providers, of any kinds.
-
Has your VCSE been involved in co-commissioning? If so, with which commissioners?
[Probe:]
-
What variations among the commissioners your VCSE co-commissioned with?
-
-
How did your VCSE participate in (co-)commissioning decisions? What did it add or contribute?
-
Specifically, in what ways did this involve co-design of services. What differences, in any, in these commissioners’ approaches to co-commissioning?
-
Is there any evidence that co-commissioning made the commissioned services more (or indeed less):
-
acceptable to service users
-
costly overall to commissioners.
-
-
How, if at all, does user and/or volunteer and/or advocates involvement in VCSEs appear to affect they way that your VCSE engaged in co-commissioning?
-
How, if at all, do your VCSE’s ties with particular localities or care groups appear to affect the way that your VCSE engages in co-commissioning?
Absorptive capacity
-
13. Can you identify what further skills, knowledge, training and perhaps other support both the NHS bodies and the third sector organisations working with the NHS need, in order to more fully:
-
commission VCSEs in collaborative, mutually productive ways?
-
co-commission with VCSEs in collaborative, mutually productive ways?
-
[if applicable:] overcome the barriers that you previously mentioned?
-
-
14. Returning to the commissioner with which your VCSE had the best (e.g. easy, productive, mutually collaborative) commissioning relationship, were there any particular behaviours, skills, or resources that this commissioner had, which made them productive for your VCSE to deal with?
-
15. Returning to the commissioner with which your VCSE had the worst (e.g. effortful, unproductive, antagonistic) commissioning relationship, were there any particular behaviours, skills, or resources that this commissioner lacked, which made them hard for your VCSE to deal with?
Closing
-
Is there any other important aspect of these topics which we have not yet asked about?
-
Are there any VSCE organisations/individuals that you think we should contact to find out more?
-
Are there any further questions you would like to ask us about this research or advice/suggestions that you would like to offer to further this research?
-
Thank you for your participation in this research. Would you be willing to be contacted again should we wish to follow up anything further from this interview?
Appendix 3 Coding frame
| Name | Description |
|---|---|
| 01. What is being commissioned | Bucket code for all discussions of what is being commissioned – for example a service, an outcome, capacity, learning – and/or why what is being commissioned matters for the nature of commissioning relationships. |
| 02. Who is being commissioned | Bucket code for any descriptions of who is being commissioned, and the implications of this – for example, discussions of single organisations being commissioned, consortia, sub- and prime models and alliances. |
| 03. Who is commissioning | Bucket code for discussions of who is involved in commissioning VCSE organisations – for example, is it a single CCG/LA/Trust, or joint/collaborative commissioning? |
| 04. How are they commissioning | Bucket code for discussion of how VCSE organisations are commissioned by statutory health and care organisations – that is, the commissioning processes, approaches and techniques, and funding mechanisms. |
| 05. Funding mechanism | Discussion relating to funding mechanisms, such as grants, contracts, spot purchases, why and when the different mechanisms are used, with what implications. |
| 06. Co-commissioning or VCSE engagement structures | Discussions relating to the groups, forums, structures and processes which bring commissioners and VCSE organisations together to develop strategies, identify needs and assets, plan and review services, etc. |
| 07. Why get involved in the commissioning relationship | Parent node for bringing together all codes with discussion of the reasons why people/organisations enter into these commissioning relationships. |
| Other reasons | |
| Outcomes | Discussions relating to the desire to meet certain/mutual outcomes as a reason for entering into commissioning relationships, for example addressing inequalities. |
| Resource | Reflections relating to the gaining of financial or human resources being the reason for entering into commissioning relationships. |
| VCSE distinctiveness | Characteristics of VCSE organisations that are identified as distinctive and attractive to commissioning organisations, for example agility, knowledge, expertise, reach. |
| 08. Why not – barriers to commissioning | Bucket code for direct discussions of the barriers to getting involved in commissioning relationships, for VCSE and commissioning organisations. |
| 09. Role – commissioners | Bucket code for discussions about the roles that commissioners play, for example whether they are network facilitators, relationship managers, contract managers, etc. |
| 10. Roles – VCSE | Bucket code for discussions about the roles that VCSE organisations play with commissioning relationships for example provider, partner, strategic partner, advocate, campaigner, challenger. |
| 11. Relationships | Parent node bringing together all codes with discussions about the nature/quality of relationships between VCSE and commissioning organisations and how this is changing [this parent not to be coded to, only child nodes]. |
| Assessments or judgements | General discussions relating to how people feel about commissioning relationships/their assessments or judgements of them, for example whether they are good, bad or variable, etc. |
| Change COVID | Discussions relating to how COVID-19 has impacted upon commissioning relationships. |
| Change other | Discussions relating to non-COVID-related changes in commissioning relationships. |
| 12. Results (impact on VCSE) | |
| Bureaucratisation or professionalisation | |
| Finance | Income levels and security of funding base/financial vulnerability. |
| Mission | |
| Other | |
| Performance or outcomes | |
| Position or influence | |
| Workforce | |
| 13. Results – everyone else | Discussions relating to the impact on VCSE and health and care commissioning on commissioning/statutory organisations, systems, and users. |
| 14. Variations contexts | Parent node bringing together all codes with discussion regarding how different contextual aspects affect commissioning relationships, for example how they enable or constrain commissioning relationships. |
| Fiscal environment | Discussions about financial constraints and/or opportunities and how these influence commissioning relationships. |
| Geography | Characteristics of the area, including demographics, rurality, co-terminosity, etc. |
| Health and social care integration | Discussions relating to how past and existing integration between health and social care has shaped commissioning relationships – horizontal integration between commissioners. |
| History | Discussions regarding how history has shaped commissioning relationships (see also relationships/change in COVID code). |
| ICS structures | |
| Market or field dynamics | Discussions relating to the mix of providers and their relationships with each other within a particular area of commissioning. Also includes discussions relating to the strength of relationships between VCSE organisations (e.g. competition, collaboration, etc.), and how this might affect commissioning relationships. |
| Policy and strategy | Discussions about local and national policy context and how these influence commissioning relationships. |
| Representative structures | Descriptions of the existence of structures that bring together commissioners and VCSE organisations, and how effectively these work. |
| VCSE infrastructure | Descriptions of how VCSE infrastructure (or lack of VCSE infrastructures) influences commissioning relationships. |
| 15. Variations – conduct | Parent node bringing together all codes with discussion regarding how different aspects of people’s conduct (agency) affect commissioning relationships. |
| Attitudes to risk | |
| Autonomy | |
| Capabilities | |
| Knowledge and expertise | |
| Leadership | |
| Other(s) | |
| 16. Boundary objects | Bucket code for discussions regarding the type, nature, form and effect of boundary objects such as key boundary-spanning individuals, forums, organisations, strategy documents, etc. |
| 17. Media of control | |
| Competition | Discussion relating to how competition – or collaboration (among different groupings e.g. within voluntary sector, between VCSE and private) – is used, explicitly or implicitly, to govern relationships. |
| Discursive | Normative, scientific, other – sense of talking different languages and what those languages are – whose discourse has to be used, and what counts as a persuasive argument for doing something. |
| Juridical | Discussion relating to how law, regulation/regulators (CQC, Ofsted, etc.), contracts, etc. are used – explicitly or implicitly – to govern relationships between VCSE and health and care commissioners. |
| Managerial | Discussion of how managerial techniques – e.g. new public management – are used, explicitly or implicitly, to govern relationships. |
| Negotiated | Scale (regional/city or district/neighbour or local); centred (who coordinates, funds the network) vs. uncentred. |
| Other(s) | |
| Resource dependency | Discussion of how money, real resources (help-in-kind) and other incentives (e.g. recognition, legitimation, status) are used, explicitly or implicitly, to govern relationships. |
| 18. Absorptive capacity within organisations | Bucket code for anything relating to the acquisition, assimilation, transformation and exploitation of knowledge and the capabilities that lie behind this for individual organisations. |
| 19. Absorptive capacity across organisations | Parent node bringing together all child nodes relating to knowledge mobilisation, sharing, and use across organisations. |
| Coordination | Discussions relating coordination capabilities – such as spaces that bring organisations together – and how these either facilitate or block the sharing of knowledge across organisations. |
| General knowledge mobilisation, use and sharing | Discussions relating to whether and how knowledge is acquired, assimilated, transformed, and exploited across VCSE and commissioning organisations and the implications of this. |
| Socialisation | Discussions relating socialisation capabilities – such as sense of identity within or beyond individual organisations – and how these either facilitate or block the sharing of knowledge across organisations. |
| Systems | Discussions relating to systems capabilities – such as IT, information governance rules, etc. – and how these either facilitate or block the sharing of knowledge across organisations. |
| 20. Respondent details | Bucket code for general discussions about respondents’ background (ensure other codes used first wherever relevant). |
| 21. Annotations | |
| 22. Other | For data that seems important but does not seem to fit into any existing codes/nodes. |
Appendix 4 Absorptive capacity survey instrument
Assessing the absorptive capacity of VCSEs and health and care commissioning organisations
This survey asks about the mobilisation and use of knowledge within and between voluntary, community and social enterprise (VCSE) and health and care commissioning organisations. It is split into four sections:
-
About your organisation: a few basic questions about your organisation, so we understand who is replying to the survey.
-
Knowledge mobilisation in your organisation: a set of questions about how knowledge in acquired and used specifically within your own organisation.
-
Learning about VCSE and health and care commissioning: a set of questions about how VCSE organisations learn about commissioning, and how commissioners learn about VCSE organisations.
-
Factors that influence knowledge mobilisation: a set of questions based on factors that have been shown to influence knowledge mobilisation. These ask about these factors in relation to your own organisation, other organisations like you, and across VCSE and commissioning organisations.
-
The effects of absorptive capacity: a set of questions about your organisation’s performance and about the effectiveness of collaborations you are involved in between VCSE organisations and health and care commissioners.
The survey should take approximately 10 minutes to complete. By completing the first question you are giving your consent to take part in the research. All responses will be anonymous. Results of the survey will be shared locally and nationally.
Please note, throughout the survey when we talk about ‘staff’, we are referring to both paid staff and/or volunteers, as applicable to your organisation.
Routing question:
-
Please select which of the following categories you most closely fit within:
-
commissioner
-
voluntary, community, social enterprise and faith sector practitioner
-
Section one: about your organisation
For VCSE respondents
First we want to ask a few key questions about your organisation. This will help our analysis. We are interested, for example, in whether the size of your organisation, its sources of income, or its field of activity makes a difference to its absorptive capacity.
-
Please indicate below your organisation’s approximate annual total turnover or income from all sources for the last financial year. Please provide your best estimate, even if you do not have an exact figure available. Please write in (write ‘0’ if none)
£0 (None)
£1–10,000
£10,000–100,000
£100,000–1M
£1M–10M
£10–100M
More than £100M
-
Over the last financial year, has your organisation received income from any of the sources listed below? Please put a cross in all boxes that apply in the first column.
-
Which one of these is the most important for your organisation’s success? Please put a cross in one box only in the second column.
| Some funding received (tick all that apply) | Main source (cross one) | |
|---|---|---|
| Donations and fundraising activities | ||
| Membership fees/subscriptions | ||
| Grants from non-statutory bodies (e.g. trusts and foundations) | ||
| National Lottery (e.g. the National Lottery Community Fund) | ||
| Grants or core funding (including service level agreements) from statutory bodes | ||
| Earned income from contracts | ||
| Earned income from trading including retail | ||
| Income from investments | ||
| Other (please put a cross in the box and write in below) |
-
4. From which, if any, of these local statutory bodies does your organisation currently receive funding or income? By currently we mean received wholly or partly – or due – in this financial year.
| Grant | Contract | |
|---|---|---|
| Local authority (e.g. borough, district or county council) | ||
| Local NHS body e.g. CCG | ||
| Police and Crime Commissioner/local police/fire authority | ||
| Other statutory bodies – please specify | ||
| Does not receive state funding | ||
| Don’t know |
-
5. From which, if any, of these national statutory bodies does your organisation currently receive funding or income? By currently we mean received wholly or partly – or due – in this financial year. Please put a cross in all the boxes that apply.
| Grant | Contract | |
|---|---|---|
| Central government department (e.g. DHSC, Home Office, MHCLG) | ||
| Non-departmental public body (e.g. Arts Council, Sport England, the National Lottery Community Fund) | ||
| Other national statutory funding (please put a cross in the box and specify) | ||
| None of these | ||
| Don’t know |
-
6. Please tell us the approximate number of full-time equivalent (paid) employees currently in your organisation.
-
< 10
-
10–20
-
20–50
-
51 and more
-
-
7. Please tell us the approximate total number of volunteers, including committee/board members, that your organisation currently involves.
-
< 10
-
10–20
-
20–50
-
51 and more
-
-
8. Which one is the main geographic area in which your organisation carries out its activities? (please tick one only)
-
Internationally
-
Nationally
-
Regionally
-
Your local authority area
-
Your neighbourhood
-
Cannot say
-
-
9. How long ago was your organisation established?
-
˂ 8 years ago
-
8–20 years
-
20 years and more
-
-
10. Which of the following areas of activity does your organisation work within? Please tick all that apply
Out of these options, which is its main focus?
| Does some work | Main focus | |
|---|---|---|
| Learning disability | ||
| End-of-life care | ||
| Social prescribing | ||
| VCSE infrastructure/support |
For commissioners
-
Which of the following best describes your organisation?
-
Clinical Commissioning Group
-
Local authority
-
NHS Trust or Foundation Trust
-
Integrated care system
-
Local care partnership
-
Other commissioning body, please specify:
-
-
Please tell us the approximate number of full-time equivalent employees currently in your organisation.
-
< 10
-
10–20
-
20–50
-
51 or more
-
-
Please tell us the annual budget that your organisation has for commissioning VCSEs?
-
£0 (None)
-
£1–10,000
-
£10,000–100,000
-
£100,000–1M
-
£1M–10M
-
£10–100M
-
More than £100M
-
Section two: knowledge mobilisation in your organisation
Section to be answered by all respondents – VCSE and commissioners. Where there are small differences in wording (VCSE wording is within rounded brackets) while [commissioner wording is in square brackets]
The questions in this section ask about your organisation’s ability to acquire, assimilate, transform and exploit knowledge and information. These questions are key for how we measure an organisation’s ‘absorptive capacity’. We will ask later for your more specific reflections on how this applies to commissioning.
-
What are the key sources of information and knowledge that your organisation routinely draws upon? Please tick all that apply, and then rank the top three.
| Tick all that apply | Rank top three | |
|---|---|---|
| Personal networks | ||
| Consultants | ||
| Seminars | ||
| Internet | ||
| Databases | ||
| National statistics | ||
| Trade press | ||
| Professional journals | ||
| Academic publications | ||
| Market research | ||
| Service user consultation/feedback | ||
| Community consultation/feedback | ||
| Staff experience and knowledge | ||
| Conversations with other, related/similar, organisations |
-
2. Thinking about the acquisition of information in your organisation, and particularly the use of external resources (e.g. personal networks, consultants, academic publications, market research, consultation with community members) to obtain information, please rate your agreement with each of the following statements:
(Here and in similar-format questions below, SA = ‘Strongly Agree’; A = ‘Agree’; MA = ‘Mildly Agree’; NA nor DA = ‘Neither Agree nor Disagree’; MD = ‘Mildly Disagree’; D = ‘Disagree’; SD = ‘Strongly Disagree’.)
| SA | A | MA | NA nor DA | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| The search for relevant information concerning our objectives is every day activity in our organisation | |||||||
| Leaders within our organisation motivate our staff to use information sources from within our sector (e.g. from other, similar, organisations) | |||||||
| Leaders within our organisation expect that our staff deal with information from beyond our sector (e.g. national statistics) |
-
3. Thinking about the communication and assimilation of information within your organisation, please rate your agreement with each of the following statements:
| SA | A | MA | NA nor DA | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| Ideas and concepts are communicated across teams | |||||||
| Our organisation emphasises cross-team support to solve problems | |||||||
| There is a quick information flow e.g. if one team obtains important information we communicate this information promptly to other teams | |||||||
| There are periodic cross-team meetings to interchange information about new developments, problems and achievements |
-
4. Please rate how far each of the following statements fit the processing and transformation of information and knowledge within your organisation.
| SA | A | MA | NA nor DA | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| Staff have the ability to structure and use collected knowledge | |||||||
| Staff are used to absorbing new knowledge as well as preparing it for further purposes to make it available | |||||||
| Staff successfully link existing knowledge with new insights | |||||||
| Staff are able to apply new knowledge in their practical work |
-
5. Please rate how far each of the following statements fit the use and exploitation of new knowledge within your organisation
| SA | A | MA | NA nor DA | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| Our leaders support the development of new working practices, activities and technologies | |||||||
| Our organisation regularly reconsiders its working practices, activities and technologies and adapts them accordant to new knowledge | |||||||
| Our organisation has the ability to work more effectively by adopting new working practices, activities and technologies |
Section three: learning about (health and care commissioning) [VCSE organisations]
Section to be answered by all respondents – VCSE and commissioners. Where there are small differences in wording (VCSE wording is within rounded brackets) while [commissioner wording is in square brackets]
The next part of the survey asks specifically about how information and knowledge is used within VCSE and health and care commissioning processes. In particular, we are interested in how VCSE organisations learn about commissioning, and how commissioners learn about the VCSE.
-
Please describe in brief the main sources of knowledge your organisation draws upon to find out about (health and care commissioning) [VCSE organisations] ……………………
-
Thinking about how you acquire and use knowledge in your (health and care commissioning processes) [work with VCSE organisations], please rate how far each of the following statements fits your organisation.
| SA | A | MA | NA nor DA | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| The search for information on (health and care commissioning) (VCSE organisations) is an everyday activity within this organisation | |||||||
| In our organisation, information and knowledge about (health and commissioning) (VCSE organisations) is communicated across teams | |||||||
| Our staff are able to apply new knowledge in (their commissioned services) (the commissioning of VCSE organisations) | |||||||
| In light of new knowledge, our organisation regularly reviews and adapts (how we work with health and care commissioners) (the ways in which we commission VCSE organisations) |
-
3. Thinking generally about the transfer of knowledge between VCSE organisations and health and care commissioning in this area, please rate your agreement with the following statements.
| SA | A | MA | NA nor DA | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| Commissioners are aware of the types of information and knowledge that VCSE organisations hold | |||||||
| VCSE organisations are aware of the types of information and knowledge that health and care commissioners hold | |||||||
| Commissioners value the information and knowledge that VCSE organisations hold | |||||||
| VCSE organisations value the information and knowledge that commissioners hold | |||||||
| Systems and structures are in place to allow for the transfer of information and knowledge from VCSE organisations to commissioners | |||||||
| Systems and structures are in place to allow for the transfer of information and knowledge from commissioners to VCSE organisations | |||||||
| Information and knowledge from VCSE organisations has been used by commissioners to make changes to how they commission services | |||||||
| Information and knowledge from commissioners has been used by VCSE organisations to make changes to how they deliver services |
Please add any comments on the sharing of information and knowledge between VCSE organisations and health and care commissioners and vice versa.
Section four: factors which influence knowledge mobilisation and use
Section to be answered by all respondents – VCSE and commissioners. Where there are small differences in wording (VCSE wording is within rounded brackets) while [commissioner wording is in square brackets]
In the next set of questions, we are interested in some of the different factors that have been found to influence whether/how knowledge is mobilised and used. Each asks you to reflect on how this works within your own organisation, among other organisations like yours (e.g. among VCSE organisations, or among commissioning organisations), and then between VCSE organisations and commissioning organisations. We are asking you to reflect on how these processes work in general, even though we realise that your experiences are likely to vary. There is space to tell us about these variations or specific examples in the comments boxes.
-
Thinking generally about knowledge sharing within and between organisations in this area, please rate your agreement with the following statements.
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| People within my organisation share relevant knowledge with each other | |||||
| (VCSE organisations) [commissioning organisations] share relevant knowledge with each other | |||||
| VCSE organisations and commissioning organisations share relevant knowledge with each other |
Please share any comments on knowledge sharing.
-
2. Thinking about trust within and between organisations in this area, please rate your agreement with the following statements.
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| People within my organisation trust each other | |||||
| (VCSE organisations) [commissioning organisations] trust each other | |||||
| VCSE organisations and commissioning organisations trust each other |
Please share any comments on trust.
-
3. Thinking about engagement with the general public and service users, please rate your agreement with the following statements.
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| My organisation participates in meetings where community members and/or service users are involved | |||||
| (VCSE organisations) [commissioning organisations] participate in meetings where community members and/or service users are involved | |||||
| VCSE organisations and commissioning organisations participate together in meetings where community members and/or service users are involved |
-
4. Thinking about the involvement of service users in decision-making, please rate your agreement with the following statements.
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| My organisation involves service users in its decision-making | |||||
| In general, (VCSE organisations) [commissioning organisations] involve service users in decision-making | |||||
| VCSE organisations and commissioners work collaboratively to involve service users in joint decision-making |
Please add any comments regarding service user involvement.
-
5. Thinking about IT systems, please rate your agreement with the following statements.
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| My organisation has an efficient IT system which helps our decision-making | |||||
| In general, (VCSE organisations) [commissioning organisations] in this area have efficient IT systems in place to help cross-organisational decision-making | |||||
| Across the health and care system, there are efficient IT systems in place to help joint decision-making between VCSE organisations and commissioning organisations |
Please add any comments on IT.
-
6. Thinking about interactions within and between organisations in this area, please rate your agreement with the following statements.
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| There are regular interactions between colleagues within my organisation | |||||
| There are regular interactions among colleagues from across different (VCSE organisations) [commissioning organisations] | |||||
| There are regular interactions among VCSE organisations and commissioning organisations |
Please add any comments on the level of interactions between organisations in this area.
-
7. Thinking about familiarity within and across organisations in this area, please rate your agreement with the following statements:
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| People in my organisation know each other’s job functions | |||||
| People from across different (VCSE organisations) [commissioning organisations] know each other’s job functions | |||||
| People from across VCSE organisations and commissioning organisations know each other’s job functions |
Please add any comments on levels of familiarity in this area.
-
8. Thinking about opportunities for different stakeholders to voice their opinions within this area, please rate your agreement with the following statements:
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| Leaders within my organisations give relevant stakeholders the opportunity to voice their opinion | |||||
| Leaders within the local (VCSE sector) [commissioning community] give relevant stakeholders the opportunity to voice their opinion | |||||
| Leaders across the health and care system give relevant stakeholders the opportunity to voice their opinion |
-
9. Thinking about how health and care leaders within this area make decisions, please rate your agreement with the following statements:
| SA | A | NA nor DA | D | SD | |
|---|---|---|---|---|---|
| Leaders within my organisations make decisions based only on their own ideas | |||||
| Leaders within the local (VCSE sector) [commissioning community] make decisions based only on their own ideas | |||||
| Leaders across the health and care system make decisions based only on their own ideas |
Section five: the effect of absorptive capacity on performance and collaboration
Section to be answered by all respondents – VCSE and commissioners. Where there are small differences in wording (VCSE wording is within rounded brackets) while [commissioner wording is in square brackets]
In this section we are interested in how ‘absorptive capacity’ (or the mobilisation and use of knowledge) affects performance. The first question focuses on the performance of your organisation. The second question focuses on collaborations that your organisation has been involved in that bring VCSE organisations and commissioners together.
-
Thinking about your own organisation’s performance over the past year, please rate your satisfaction along the following dimensions
(VS = ‘Very Satisfied’; S = ‘Satisfied’; MS = ‘Mildly Satisfied’; Neither S nor D = ‘Neither Satisfied nor Dissatisfied’; MD = ‘Mildly Dissatisfied’; D = ‘Dissatisfied’; SD = ‘Strongly Dissatisfied’).
| VS | S | MS | Neither S nor D | MD | D | SD | |
|---|---|---|---|---|---|---|---|
| Quality of decision-making | |||||||
| Level of innovation | |||||||
| Meeting your organisation’s objectives | |||||||
| Meeting service user/community needs | |||||||
| Meeting financial objectives | |||||||
| Delivering on national policy priorities |
Please add any comments on your organisation’s performance over the past year.
-
2. Now thinking about the performance of collaborations that your organisation has been involved in over the past year, which bring VCSE and health and care commissioning organisations together, please rate your satisfaction along the following dimensions
Any other comments about the performance of collaborations?
Finally, please add any other comments on aspects of knowledge mobilisation and use within (VSCE) [commissioning] organisations and between the VCSE sector and health and care commissioners
Thank you for completing this survey.
Appendix 5 Clinical Commissioning Group spend on voluntary, community and social enterprises, 2018–9
Contact: Alex Gibson@plymouth.ac.uk
GitHub: https://github.com/AlexGibsonPlymouth/3SC.git
Introduction
As part of a drive to improve public expenditure transparency, HM Treasury issued guidance in 2013 requiring all government bodies to publish, with few exceptions, ‘all individual invoices, grant payments, expense payments or other such transactions that are over £25,000’. 156
To be published in *.csv format on the www.data.gov.uk website as well as locally (e.g. on individual CCG websites), the following was to be reported for each item of expenditure:
-
Department family (e.g. DHSC) and entity (e.g. NHS Barnet CCG)
-
Expense type (the general nature of the expenditure, e.g. ‘mental health – adults’)
-
Expense area (the part of the entity that has spent the money, e.g. ‘out of hours’)
-
Supplier name and supplier postcode
-
Narrative description of the transaction
-
Date and the amount in GBP.
In theory, therefore, a rich and comprehensive data set should now cover all ‘over-threshold’ expenditure made by all public bodies from 2014 to 2015 onwards. An enormous amount of data has indeed been made publicly available, and this has triggered some innovative analyses of NHS spending. 216–218 Nevertheless, for reasons that will become apparent, the wealth of data has not received the level of attention that might have been expected.
In the context of the present study (Commissioning, Co-commissioning and Being Commissioned; the NHS and Third Sector Organisations – also known as the Third Sector Commissioning or 3SC project), the aim was to use these data to quantify how different CCGs commission VCSEs as opposed to other kinds of providers (NHS-owned, corporate, etc.). As detailed in the research protocol, the resulting insights were to:
-
guide the initial ‘maximum-variety sample of study sites’
-
detail the nature of VCSE engagement in the selected study sites
-
offer a broader cross-sectional and longitudinal perspective on patterns of VCSE commissioning across the country as a whole
As described below, the first two objectives were met and, with some limitations, the ‘over-threshold’ expenditure data proved invaluable. It was also possible to construct a nearly complete cross-sectional analysis of commissioning patterns in 2018–9. Intractable obstacles caused by the ongoing reorganisation of CCGs, and their eventual replacement by ICSs, meant it was not possible to undertake a longitudinal analysis of the data other than for the six study sites. This analysis is not reported here to ensure anonymity of the case study sites, a consideration which restricts the level of detail that can be provided in later sections of this report.
Clinical Commissioning Group reorganisation/replacement also meant that it was impossible to provide a full ‘reproducible analytical pipeline’ (RAP) capturing data acquisition, cleaning and analysis. RAPs are automated statistical and analytical processes which aim to ensure that research is reproducible, auditable, efficient, and of high quality. Considered best practice, they depend on the availability of permanent open-source data (https://tinyurl.com/ycy5b7d4). A RAP requires persistent open-source data, and all CCG websites from which data were retrieved have now disappeared. Moreover: (1) many CCG data sets were in practice only available via FoI requests and (2) establishing the VCSE status of suppliers involved significant manual searching of the internet.
In place of a full RAP, all ‘raw’ 2018–9 CCG ‘over-threshold’ expenditure data sets used in the project have been made available via the project’s GitHub website155 along with a detailed description of the data cleaning and supplier categorisation workflow (below). The resulting analytical data set is included on the project’s GitHub website, along with all non-disclosive R scripts and outputs used to analyse patterns of CCG commissioning (as reported below).
Data collection and cleaning
The most recent accounts available when the data were required (in late 2019) were for 2018–9. These referred to the 195 CCGs then extant, although the number had already dropped to 191. We were, in other words, already dependent on historical data and, as detailed in Chapter 1, Health and care, the reorganisation of commissioning bodies gathered pace during the study period (Table 10).
This reorganisation has posed significant problems. Many newly created CCGs/ICSs incorporate expenditure data relating to their precursors into their websites, but this was, and remains, far from universal. Extensive use of FoI requests may have retrieved this data, but experience with the FoI process, and of the time it takes to identify VCSE suppliers, meant undertaking a longitudinal analysis was not a reasonable proposition and this objective was not pursued.
The focus was thus on the ‘over-threshold’ accounts for the 195 CCGs operating in 2018–9. The www.data.gov.uk website and all CCG websites were searched and, if found, the relevant accounts were downloaded. Disappointingly, given the intention of the 2013 guidance, FoI requests then had to be sent to 106 of the 195 CCGs. Of these, 12 requests were made because no accounts were publicly available, 11 because one or more of the monthly accounts were missing, corrupted or referred to the wrong CCG, and 83 because the data, contrary to the guidance, were provided in PDF format and could not be reliably converted into machine-readable numeric data.
In most cases the FoI process was quick and straightforward, but 17 requests were rejected and a formal follow-up was needed. By March 2020 there remained four CCGs which had yet to provide useable data. With the arrival and obvious impact of the COVID-19 pandemic, we stopped pursuing our FoI requests, leaving us with data for 191 of the 195 CCGs.
| Date | Count | Date | Count | Date | Count |
|---|---|---|---|---|---|
| April 2014 | 211 CCGs | April 2017 | 207 CCGs | April 2020 | 135 CCGs |
| April 2015 | 210 CCGs | April 2018 | 195 CCGs | April 2021 | 106 CCGs |
| April 2016 | 209 CCGs | April 2019 | 191 CCGs | July 2022 | 42 ICSs |
Preliminary evaluation of Clinical Commissioning Group accounts
To test their likely veracity, all CCG expenditure accounts were compared against the most recent available NHSE CCG consolidated accounts (for 2016–7). 159 Given the time lag, some variation was expected, but two CCGs’ accounts were badly out of line: Airedale, Wharfedale and Craven CCG captured 47.5% of the NHSE-reported spend, and Eastern Cheshire CCG just 20.8%. It was clear that these accounts could not be relied upon.
We were thus left with accounts for 189 of the 195 CCGs extant in 2018–9 (Table 11). From these were extracted: (1) CCG name, (2) expense area, (3) expense type, (4) supplier and (5) amount. Only 1287 records (0.19%) had a blank, ‘unknown’, ‘redacted’ or uninformative (e.g. ‘payroll payovers’ or ‘programme projects’) supplier name, although 4.0% and 4.7% of entries for ‘expense area’ and ‘expense type’ respectively were missing, the vast majority in just 14 CCGs. In fact, although these fields initially appeared useful as they occasionally state whether a supplier was ‘independent’, ‘commercial’, ‘not-for-profit’, ‘voluntary’, or ‘public sector’, cross-referencing against the status of named suppliers shows that these statements cannot be used to determine whether suppliers are VCSEs. Our categorisation of suppliers thus rests entirely on linking supplier names given in the accounts with organisations listed in the CC and CH registers, along with information found on organisations’ websites.
Focusing on invoices > £25k
An important difference between CCG accounts was the extent to which they observed the recommended > £25k threshold. This varied hugely, from the 21 CCGs which only contained invoices over £25k through to Merton, Gloucestershire and Wandsworth CCGs where more than 90% of invoices were for sums ˂ £25k (see Figure 24). This undoubtedly reflects variations in recording practice rather than actual expenditure.
To ensure like-for-like CCG comparisons, all invoices of ˂ £25k have been stripped from the working data set. This reduced the number of uniquely named suppliers from 13,455 to 10,930 although, reflecting a frustrating level of imprecision in the use of supplier names, this represents around 10,562 unique suppliers. This can only be a ‘best estimate’ as algorithmic fuzzy matching and manual interrogation of supplier names cannot capture all instances where different names were used to describe the same company. For instance, the company called ‘ACCI’ in one place is (almost certainly) what is elsewhere known as the ‘African Caribbean Community Initiative’. Innumerable such instances have been found, but, inevitably, many will have been missed.
| No data available online or via FoI request |
|
| No machine-readable data available (badly formatted PDF files online with no alternative made available following FoI request) |
|
| Demonstrably unreliable data (serious mismatch with NHSE’s 2016–7 CCG consolidated accounts) |
|
| Working data set |
|
FIGURE 21.
Percentage of invoices > £25k by CCG.
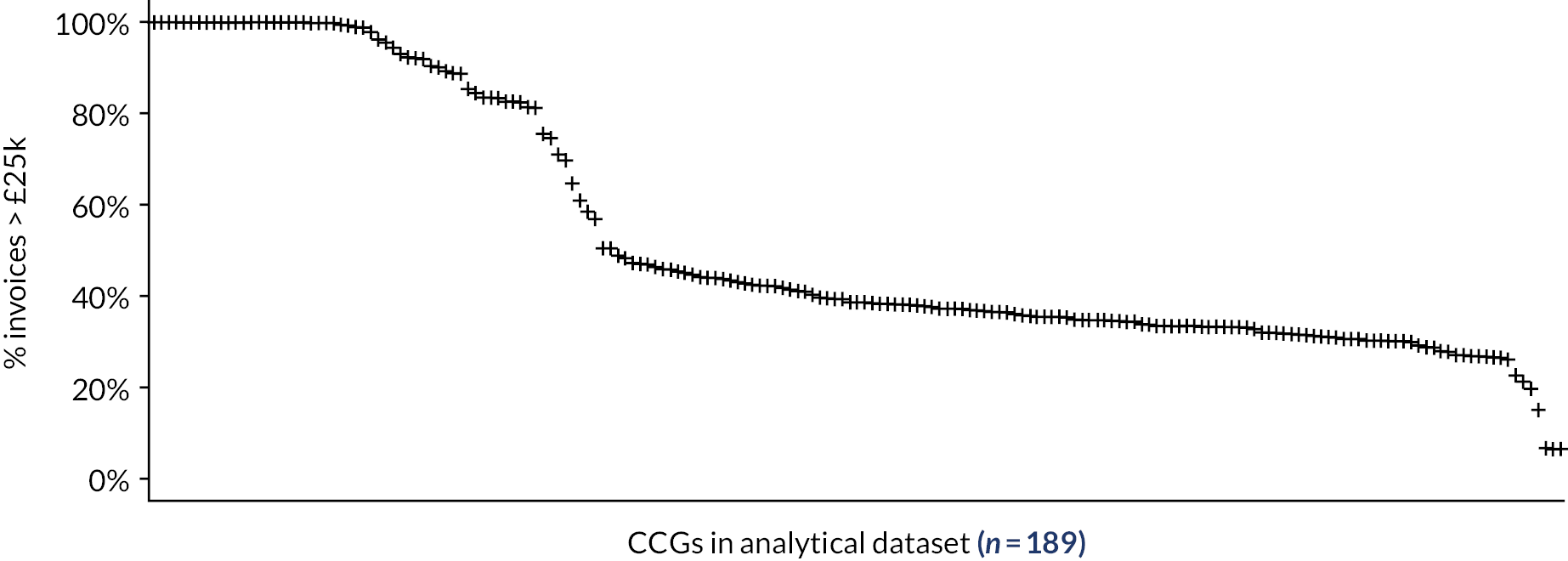
Generic ‘suppliers’ and ad hoc exclusions
There is a small but significant number of suppliers named ‘GP’, ‘Primary Care’ and ‘Prescribing Support Services’. CH includes ‘GP Ltd’, ‘Primary Care Limited’ and ‘Prescribing Support Services Limited’, but it seems highly likely that these names were being used generically. These supplier ‘names’ have been retained in the analytical data set (and the first two categorised as ‘GP Services’), but they will clearly refer to an unknown number of individual suppliers. There are also a number of personal health budget and continuing healthcare payments made to individuals – identified by name, anonymised coded name (e.g. ‘02EKS2540’) or, most commonly, as ‘REDACTED’. All payments to individuals have been excluded from the analytical data set.
Recognising such limitations, the analytical data set (available on GitHub) includes 225,889 invoices of £25k or more across 189 CCGs and refers to 10,478 unique suppliers. These transactions account for £70.496 billion, which is 97.7% of total CCG expenditure.
Recognising the potential impact of using data for 2018–9
The largest suppliers to CCGs were the NHS Trusts and LAs which undertook the vast bulk of clinical, mental health and community service activity. Thus, nationally, LAs and NHS Trusts account for 83.3% of all 2018–9 expenditure by way of invoices over £25k although, as indicated in Figure 22, this varied significantly between CCGs: from only 52.7% and 57.3% in East Staffordshire and North East Lincolnshire, respectively, to over 90% in seven CCGs (Wirral, South Sefton, Thurrock, Manchester, South Devon and Torbay, Morecambe Bay, and Crawley).
This reflects the extent to which different CCGs were, at that time, commissioning independent service providers, whether corporate or VCSE (see Chapter 1, Health and care). In North East Lincolnshire, for instance, two CICs (Navigo and Focus Independent Social Work CIC) and a community benefit society [Care Plus Group (North East Lincolnshire) Ltd] accounted for 24.7% of all CCG expenditure. In East Staffordshire, meanwhile, 30.9% of CCG spend was received by Virgin Care Services. Its involvement was, however, short-lived as, following a contractual dispute, on 1 April 2020 the Midlands Partnership NHS Foundation Trust took over services previously provided by Virgin Care. At the time part of the Virgin Group, in December 2021 Virgin Care was rebranded as the HCRG Care Group and acquired by Twenty20 Capital,219 a venture capital investment company which claims that it looks ‘for significant returns in 2–5 years’. 220 The change in supplier and resulting shift in supplier status (from corporate to NHS), along with the background churn in ownership structures (albeit subsequent to Virgin pulling out of the East Staffordshire contract), illustrates a key problem with the analysis: it is based on 2018–9 data, and not only has the commissioning landscape since transformed (from 195 CCGs to 42 ICSs by July 2022) but, in some localities, so too has the provider landscape.
FIGURE 22.
Proportion > £25k spend to LAs and NHS Trusts.
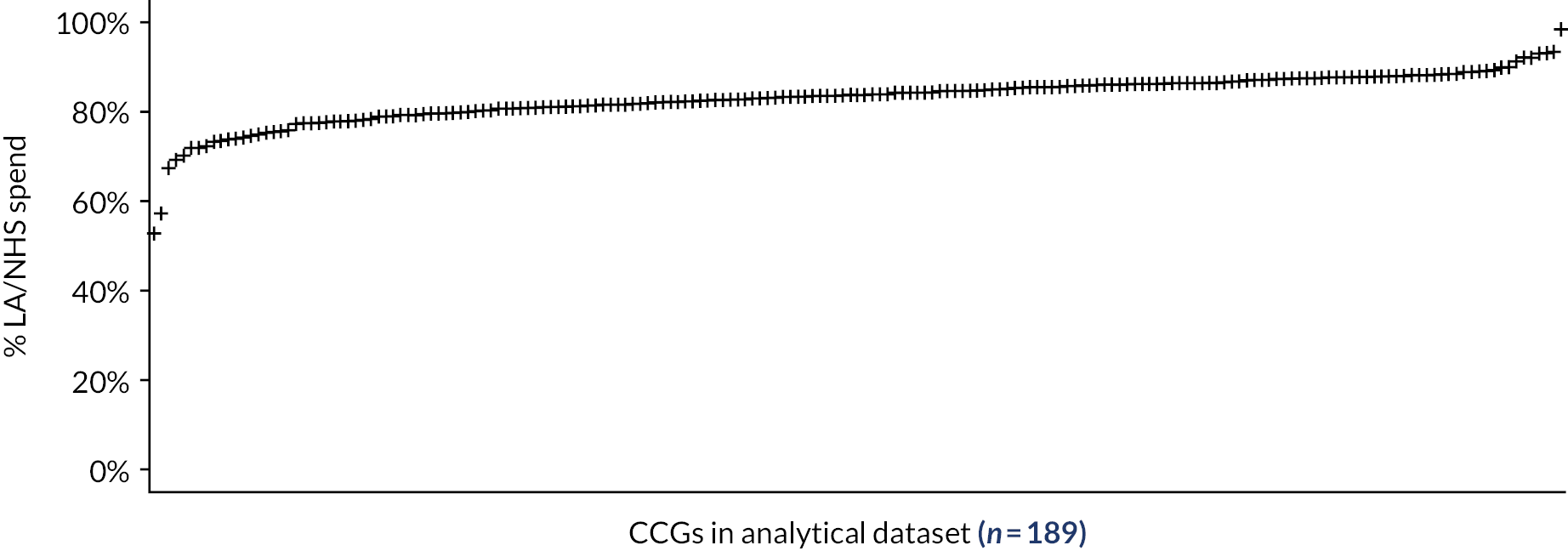
Recognising potential variation in the comprehensiveness of the Clinical Commissioning Group accounts
The occasionally very high proportion of CCG expenditure accounted for by LAs and NHS Trusts points towards a further possible limitation with the data. Nationally, 8.9% of CCG expenditure is directed towards organisations identified as suppliers of primary care services, largely GPs. Yet, as illustrated in Figure 23, this varies from ˂ 0.1% (for Greater Huddersfield and Crawley) to > 20% (for West Norfolk, the East Riding of Yorkshire and Hull). This partly reflects difficulties identifying GPs in the accounts (although 6288 primary care organisations have been identified) and the fact that some primary care activity will be missed because it was being undertaken by organisations with a much wider remit. But the variation also seems to reflect differences in the comprehensiveness of the CCG accounts.
A list of all GPs receiving payments from the NHS in 2018–9158 reveals that the proportion of GPs included in the ‘over-threshold’ accounts varies hugely. In Greater Huddersfield, payments to only 2 of 38 known GPs are recorded. They received just 2.47% of the total NHS payment to Huddersfield GPs. Similarly, the Crawley CCG accounts include only 1 of 12 known GPs (receiving 9.2% of total payments).
FIGURE 23.
Proportion > £25k spend on GP services.
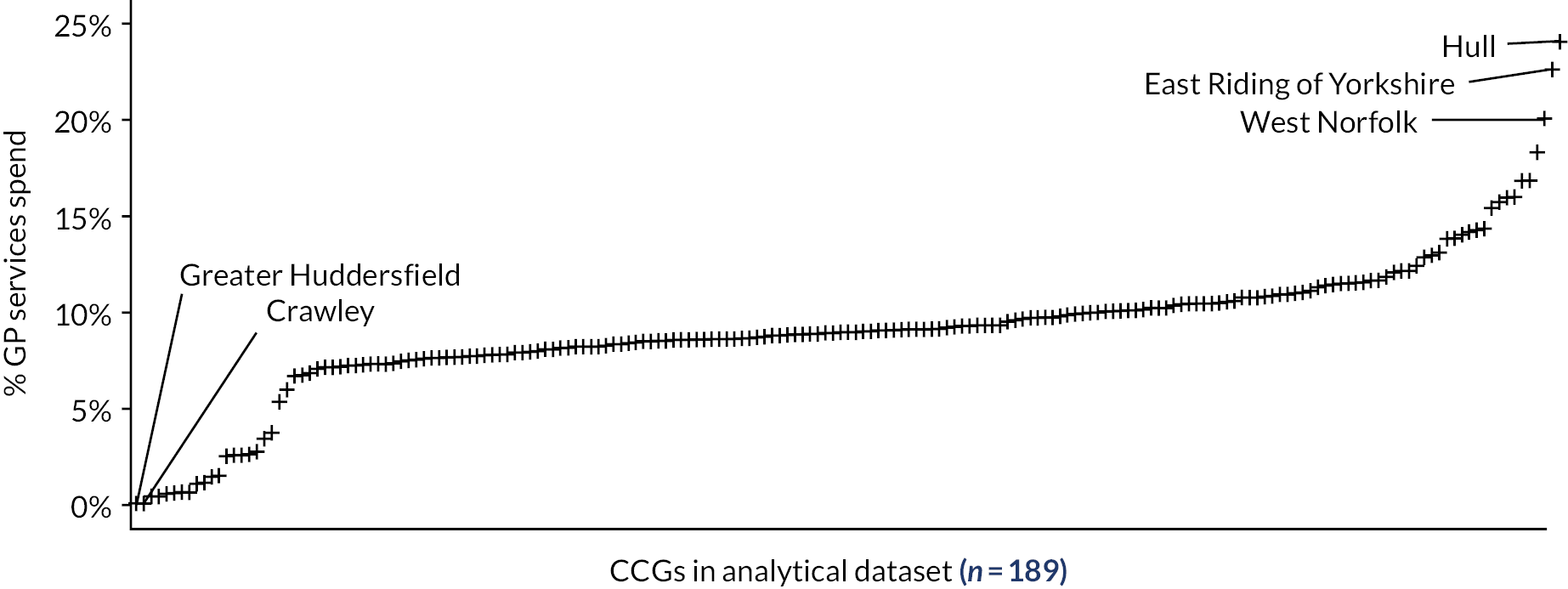
In contrast, in West Norfolk 17 of 21 known GPs (receiving 70.5% of total GP payments) are to be found in the ‘over-threshold’ accounts; in the East Riding of Yorkshire the figure is 23 of 33 GPs (79.9% of payments); and in Hull it is 33 of 41 GPs (85.6% of total GP payments).
Such disparities may stem from local differences in how, since 2015, NHSE has been delegating full or partial responsibility for commissioning primary care services to CCGs. If so, accounting for expenditure on primary care may be uniquely problematic, but it must be accepted that, in a large-scale national overview of spending patterns, unknown CCG-level differences may exist regarding what is considered within the remit of the ‘over-threshold’ accounts.
Identifying suppliers: the workflow
As noted above, determining the VCSE status of individual suppliers depends entirely on linking names in the accounts to various public registers and/or their public-facing websites. The workflow was iterative, but was broadly as follows:
-
From all valid invoices > £25k (n = 225,889/£70.496B), use fuzzy matching algorithms (R Statistics fuzzyjoin package) and manual name comparisons to determine, so far as possible, the actual unique suppliers (n = 10,562) behind the named suppliers (n = 10,929).
-
Manually identify all NHS Trusts, Health Boards, CCGs and Commissioning Support Units (plus miscellaneous NHS organisations such as NHS Property Services, NHS Pensions Agency, etc.): 538 unique suppliers (5.1% of all suppliers), 71,424 invoices (31.6% of all invoices) and £54.263B (77.0% of all expenditure). This excludes non-NHS organisations ‘branded’ as NHS organisations (e.g. various ‘NHS Treatment Centres’).
-
Manually identify all local councils (county, metropolitan, borough, etc.): 212 unique suppliers (2.0%), 11,540 invoices (5.1%) and £4.458B (6.3%).
-
Search the CQC active and inactive provider registers157 for supplier names, using fuzzy matching algorithms followed by manual checking of apparent matches (to address the large number of false positives). The CQC registers provide information on each supplier’s ‘sector’ (e.g. ‘primary medical services’ or ‘social care organisation’), whether a care home and, where appropriate, its CC and CH registration numbers.
-
Use fuzzy matching and manual checking (as above) to search the list of practices in NHS Payments to General Practice, England, 2018/9 to determine whether non-NHS/LA suppliers are GPs, adding to those identified at step 4 and those with keywords ‘Dr’, ‘Drs’, ‘Medical Centre’, ‘Medical Practice’, ‘Surgery’ and similar. Putative practices are confirmed by searching for a corresponding website. Ownership status (including CH registration number) is noted if clearly stated on the website, though this is rare.
-
Use fuzzy matching and manual checking (as above) to search CC and CH registers for (a) all non-NHS/LA supplier names found in the ‘over-threshold’ accounts and (b) CC/CH registration numbers found at steps 4 and 5.
-
For those suppliers not yet identified as NHS or LA organisations, or already found in the CC/CH registers, manually search the internet for supplier websites. The flexible use of supplier names in the accounts makes this somewhat hit-or-miss but, if found, the supplier’s website is searched for CC/CH registration numbers (a legal obligation, albeit clearly not always observed) – in which case details are extracted from CC/CH registers as above – and for explicit statements that they are ‘not-for-profit’, ‘social enterprise’ or ‘volunteer-led’ organisations. Evidence from websites is also used to place suppliers into a number of general ‘supplier sector’ categories.
-
Finally, as the focus is on finding all VCSE organisations, further, more intensive, internet searches were undertaken for suppliers tagged in the ‘expense type’ and ‘expense sector’ entries as being ‘not-for-profit’ or ‘voluntary’.
The process is far from perfect, and misidentification and non-identification remain significant issues. As others have noted,216 although the legislation driving transparency is ambitious, there is no requirement or guarantee that the data are accurate!
Nevertheless, as detailed inTables 12 and13, the vast bulk of CCG expenditure in the ‘over-threshold’ accounts has been accounted for. Idiosyncratic use of names and acronyms means 188 (1.8%) suppliers, receiving just £189.361M (0.3%) of CCG spending, could not be linked to organisational websites or entries in the CC/CH registers.
Of course, some uncertainty also surrounds the status of the 6416 non-NHS/LA organisations that cannot be found in the CC/CH registers (60.7% of all suppliers). However, these suppliers account for only 8.6% of CCG expenditure > £25k and, as registered companies (including CICs) and charities with an annual income over £10,000 are legally required to publish their registration number and name on online publications, it seems reasonable to assume that the vast majority of ‘significant’ VCSEs would be identifiable as such.
| Category | Found in: | Total suppliers | |||
|---|---|---|---|---|---|
| CC and CH | CC not CH | CH not CC | Neither | ||
| NHS a | 0 | 0 | 2 | 536 | 538 |
| LA | 0 | 0 | 0 | 212 | 212 |
| GP services | 3 | 3 | 321 | 5961 | 6288 |
| Care home | 67 | 7 | 547 | 154 | 775 |
| Hospice | 128 | 1 | 0 | 0 | 129 |
| Categorised other b | 3 | 3 | 44 | 113 | 163 |
| Other | 535 | 67 | 1667 | 188 | 2457 |
| 736 | 81 | 2581 | 7164 | 10,562 | |
| Category | Found in: | Total expenditure (£M) | |||
|---|---|---|---|---|---|
| CC and CH (£M) | CC not CH (£M) | CH not CC (£M) | Neither (£M) | ||
| NHS | 0.000 | 0.000 | 113.805 | 54,148.588 | 54,262.880 |
| LA | 0.000 | 0.000 | 0.000 | 4457.706 | 4457.706 |
| GP services | 5.078 | 3.444 | 721.666 | 5,541.260 | 6271.449 |
| Care home | 65.652 | 1.032 | 257.759 | 45.289 | 369.732 |
| Hospice | 201.115 | 0.639 | 0.000 | 0.000 | 201.754 |
| Categorised other | 0.453 | 1.833 | 13.509 | 252.879 | 268.674 |
| Other | 463.166 | 13.501 | 3998.057 | 189.361 | 4664.086 |
| 735.463 | 20.450 | 5104.796 | 64,635.572 | 70,496.281 | |
Evaluation of manual interrogation/extraction of expenditure data
The > £25k CCG accounts provide a reasonable basis for analysing expenditure patterns, though they do require significant FoI effort and an enormous amount of time to manually interrogate the data. The importance of this intensive approach is demonstrated by comparing the resulting data set with expenditure data collected as part of the NHS Spend project. This used fully automated data-scraping methods to interrogate NHS Trust and CCG accounts between 2010 and 2020. For 2018–9, spending data were obtained for only 129 CCGs, with 117,933 invoices > £25k (totalling £37.528B) referring to 13,090 named suppliers. As detailed inTable 14, this is substantially less than has been achieved in the current project – largely through persistent FoI requests. A detailed review of the collated accounts soon reveals, moreover, that the automated data-scraping process resulted in a number of significant errors [an initial review shows that the data for South West Lincolnshire have been duplicated and entered under ‘NHS_SWOR_CCG’ (an acronym which does not appear to match any CCG); data for Crawley CCG appear to include invoices from Horsham & Mid Sussex CCG; and the Surrey Downs data have been corrupted, seemingly by the inclusion of subtotals. Other problems may exist].
As with the current project, the NHS Spend project sought to match suppliers with organisations listed in the CC and CH registers. Once again, being largely dependent on automated pattern-matching techniques, even for those CCG accounts that were retrieved, a smaller number of suppliers could be matched with organisations in the CC and CH registers. Thus, with respect to CCGs covered by both data sets: the NHS Spend project identifies 504 charities rather than 623 in the present study (81%) and 1980 companies rather than 2550 (78%). With a rapid audit of putative links revealing a number of doubtful matches having been made in the NHS Spend project, there are strong reasons to argue that, at least at present, > £25k expenditure data can only be used if subject to intensive manual scrutiny. Of particular concern is the extent to which the effectiveness of pattern matching varies between CCGs, with 17 and 19 CCGs returning ˂ 50% of known charities and companies, respectively. A fully automated identification of suppliers clearly risks seriously biasing the analysis.
Identifying suppliers: establishing voluntary, community and social enterprise status
Returning to our 3SC project, any supplier found in the CC register (n = 817) has been classified as a VCSE. Of these, the vast majority (n = 736) were also found in the CH register, most (n = 691) being listed as ‘private limited companies by guarantee’ (Table 15). Relatively few registered charities were not also found in the CH register (n = 81), possibly because of name variation.
| Invoices > £25k | |||
|---|---|---|---|
| NHS Spend project | 3SC project | % captured by NHS Spend project | |
| CCGs | 129 | 189 | 68.3 |
| Invoices | 117,933 | 225,889 | 52.2 |
| Expenditure | £37.528B | £70.496B | 53.2 |
| Named suppliers | 7651 | 10,929 | 70.0 |
| Suppliers | Spending (£M) | Status | |
|---|---|---|---|
| In CC register and CH register | |||
| Charitable incorporated organisation | 36 | £6.557 | VCSE |
| Private limited companies by guarantee | 691 | £724.221 | VCSE |
| Other company typesa | 9 | £4.685 | VCSE |
| In CC register but not CH register | |||
| Named charities | 81 | £20.450 | VCSE |
| In CH register but not CC register | |||
| CIC | 127 | £801.862 | VCSE |
| Industrial and provident society | 4 | £9.944 | VCSE |
| Registered society | 62 | £177.226 | VCSE |
| Social enterprise company | 1 | £0.048 | VCSE |
| Private limited companies by guarantee | 35 | £161.333 | VCSE |
| Private limited company | 1 | £2.965 | VCSE |
| Private limited companies by guarantee | 68 | £26.149 | Not VCSE |
| Other CH company typesa | 113 | £146.280 | Not VCSE |
| Private limited company | 2168 | £3665.184 | Not VCSE |
| Identified as NHS, LA or government organisations | |||
| NHS organisation | 538 | £54,262.880 | Not VCSE |
| LAs | 212 | £4457.706 | Not VCSE |
| Government bodies | 8 | £220.807 | Not VCSE |
| Other suppliers not in CC or CH registers | |||
| Other suppliers | 4 | £3.118 | VCSE |
| Other suppliers | 6404 | £5804.865 | Not VCSE |
| VCSE suppliers | 1051 | £1912.409 | |
| Not VCSE suppliers | 9511 | £68,583.872 | |
| Total all suppliers | 10,562 | £70,496.281 | |
Also categorised as VCSE is any company listed in the CH register as a CIC (n = 127), industrial and provident society (n = 4), registered society (n = 62), or a social enterprise company (n = 1). A less clear-cut category concerns suppliers registered as ‘private limited companies by guarantee’ but which are not also found in the CC register. This legal form is commonly used by not-for-profit organisations and social enterprises but is also used, for instance, by GP federations, local medical committees, academic health science networks and other similar membership organisations. Our approach has been to search these organisations’ public-facing websites for explicit statements that they are not-for-profit, social enterprise or ‘volunteer-led’. If found, they are classed as VCSE (n = 35). Otherwise, even though we may suspect them to be VCSEs, they have been classified as ‘not VCSE’.
Much less commonly, private limited companies (i.e. limited liability by shares rather than by guarantee) can be set up as VCSEs. Once again, if a supplier’s website explicitly claims it is, for instance, a social enterprise, then it has been classed here as a VCSE. Only one such instance has been found, although we did not systematically search all 2160 private limited company websites.
The 6341 ‘other suppliers’ that were not found in either the CC or CH registers were also left as ‘not VCSE’ unless their websites were found and contained explicit claims that they were VCSEs. Only four such suppliers were identified, though there is little doubt that a significant proportion will, in fact, be VCSEs. The 2013 Greater Manchester State of the Voluntary Sector report221 estimated, for instance, that there were 9624 voluntary organisations in Greater Manchester, of which only 4968 had been registered. It is highly likely that many small ‘below-the-radar’ VCSE organisations lie hidden within the ‘other suppliers’ category.
The overall national picture, therefore, is that 1051 (10.0%) of the 10,562 unique suppliers receiving > £25k in the CCG accounts have been identified as VCSEs. They received just £1912.409M (2.7%) of the total £70496.281M spent by CCGs.
National overview of Clinical Commissioning Group spending on voluntary, community and social enterprise suppliers
Clinical Commissioning Group spending on VCSEs is highly skewed, with relatively few receiving substantial funding and a very long tail of more minor suppliers (Figure 24). This tail would have been far more pronounced had it been possible to include invoices of ˂ £25k.
In 2018/9 just 6 VCSEs (named in Figure 24) received more than £50M, from across all 189 CCGs for which there are reliable data, and together they received 23.5% of the total national CCG spend on VCSEs. Some 34 suppliers received more than £10M (totalling 60.6% of total VCSE spend), and 242 suppliers more than £1M (91.1% of total VCSE spend). Figure 25 highlights the major VCSEs in terms of either total income from CCGs or the number of CCGs in which they have at least some presence. These organisations contrast markedly with the vast bulk of VCSEs which receive relatively little from only a small number of CCGs.
The dependency of VCSEs, however large, on just a few CCGs (e.g. The Livewell Foundation, City Health Care Partnership and Sirona Care & Health) is likely to affect how they engage in the commissioning process and will likely contrast with VCSEs with multiple commissioning relationships (such as Marie Curie, Marie Stopes International, Integrated Care 24, BPAS and Nuffield Health). Commissioning relationships will, of course, also reflect the extent to which individual VCSEs are dependent on CCG income within their overall portfolio of activity – but this cannot be captured through an analysis of CCG accounts alone.
FIGURE 24.
National (189 CCGs) expenditure on individual VCSEs, 2018–9.
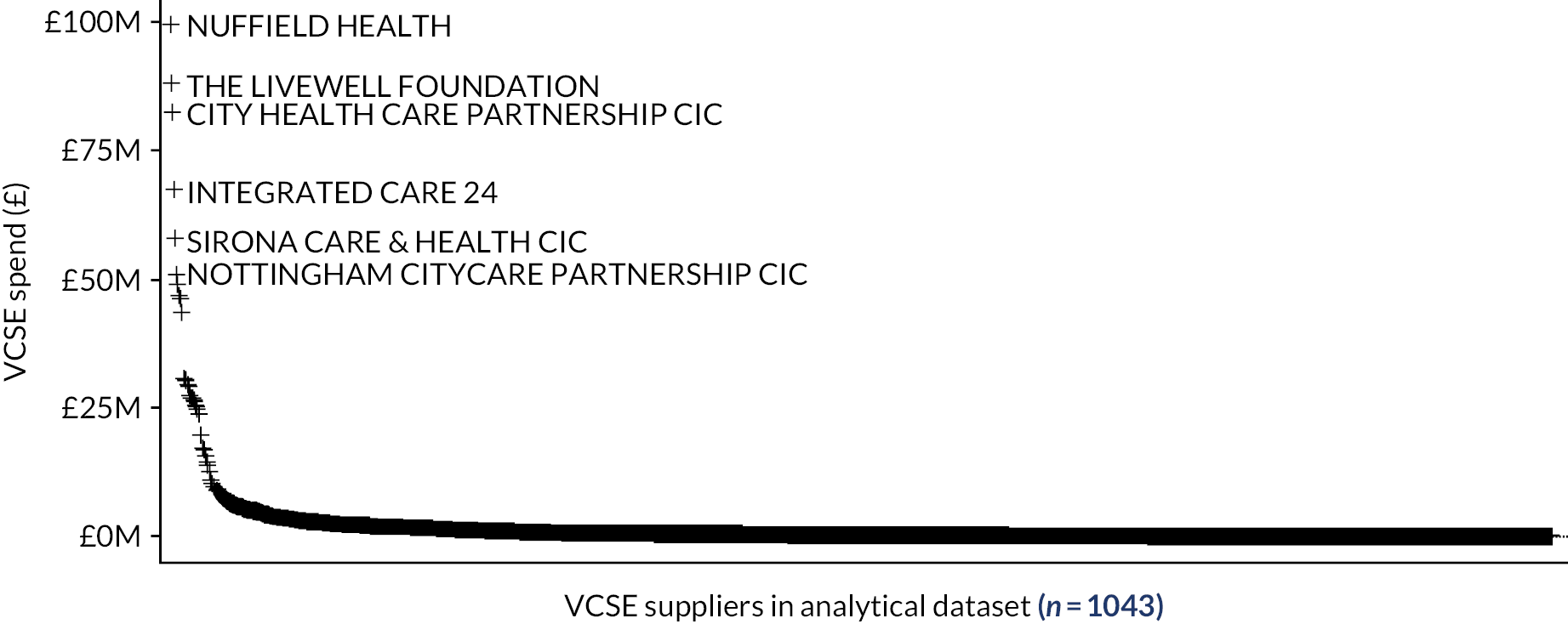
FIGURE 25.
Total CCG spending on VCSEs against number of CCGs served.
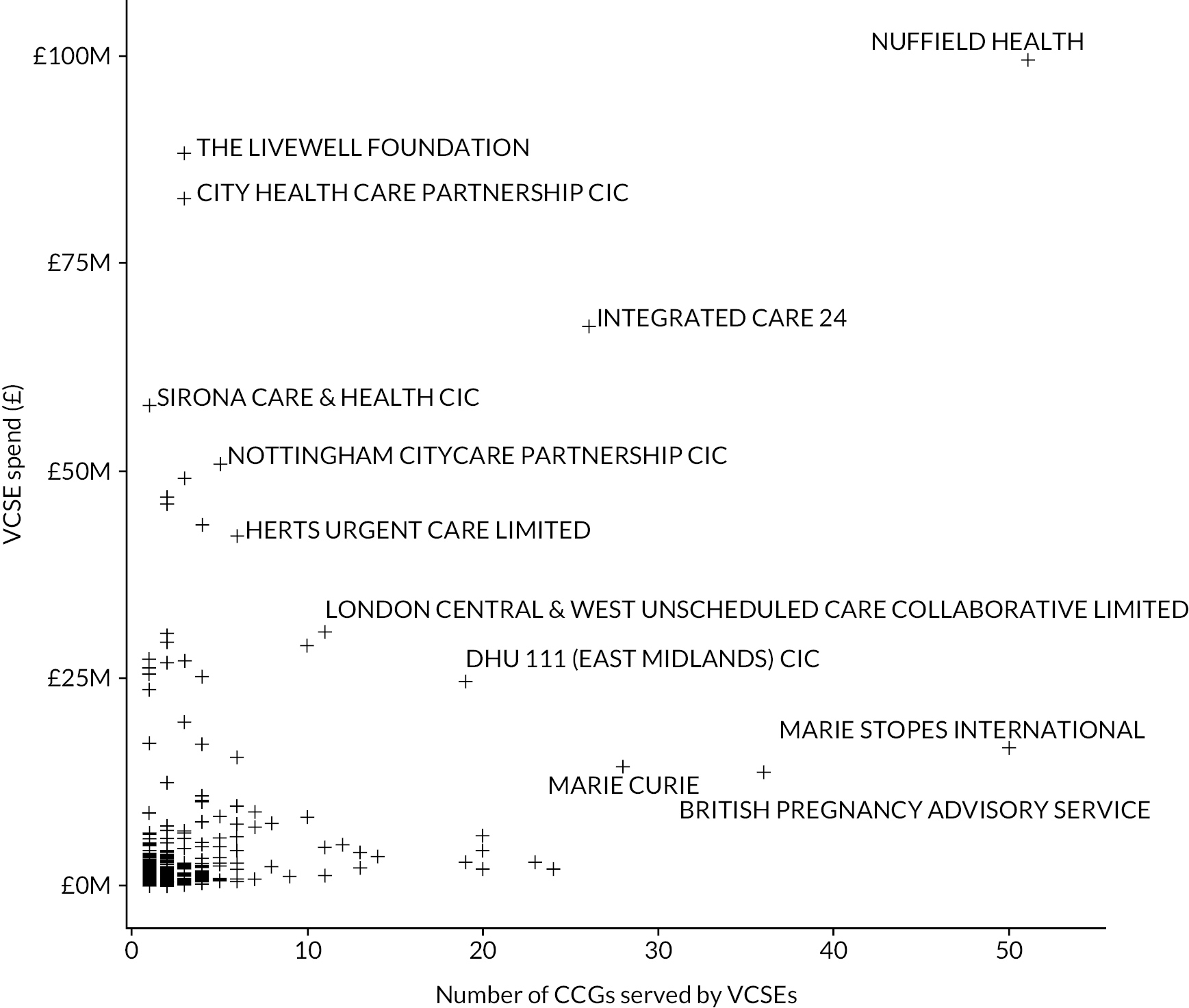
The City Health Care Partnership,222 for instance, had annual revenue of £122.81M in 2018–9, meaning that just two CCGs (Hull and the East Riding of Yorkshire) constituted over 67% of its total income. In contrast, Marie Stopes International received over £296M from across multiple countries,223 meaning that even the largest of its CCG funders (Greenwich) only contributed 0.25% towards its overall income.
The CCG accounts can provide a valuable starting point for understanding the context within which individual VCSEs operate. An analysis of overall patterns of VCSE dependency lay well beyond the scope of the 3SC project, although such information has informed our investigation of commissioning relationships within the six case study sites selected for detailed investigation.
Clinical Commissioning Group variation in spending on voluntary, community and social enterprise suppliers
The selection of the study sites aimed to capture a ‘maximum variety’ of CCGs in terms of their engagement with VCSEs, although secondary criteria included capturing, as far as possible, a range of CCG budget sizes, urban/rural contrasts, diversity in terms of ethnic composition and deprivation, as well as commissioning arrangements (i.e. the different ways in which CCGs coordinated with other NHS bodies and LAs).
Understanding how expenditure on VCSEs varies between CCGs is thus crucial, and this reflects what may constitute two quite separate processes: first, the extent to which different CCGs were willing to commission non-NHS/LA organisations (whether corporate or VCSE), and second, having ‘contracted out’ certain health and care activities, the extent to which CCGs then chose to commission VCSEs.
With regard to the former there was, as Figure 26 illustrates, huge variation in the proportion of CCG spending on non-NHS/LA suppliers; from 47.3% (East Staffordshire) to just 1.4% (Crawley). There may, as illustrated by Figure 27, be some geographical concentration in the use of non-NHS/LA suppliers in Eastern England north and south of The Wash as well as in the North West Midlands. The regional tendency is not, however, pronounced and, with CCGs exhibiting high and low contracting-out rates often being co-terminous, the use of non-NHS/LA suppliers does appear to be a local CCG decision.
The extent to which CCGs then direct any non-NHS/LA expenditure towards VCSEs also varies hugely, as illustrated by Figure 28 (which shows VCSE spend relative to both NHS/LA and non-NHS/LA non-VCSE spend) and Figure 29 (which focuses on the split of non-NHS/LA spend between VCSE and non-VCSE suppliers).
The proportion of non-NHS/LA CCG expenditure directed to VCSEs thus varies from 69.2% to 68.3% in Greater Huddersfield and North East Lincolnshire respectively, to ˂ 1% in Portsmouth, Wyre Forest, and Fareham and Gosport CCGs. Full details are available on the project GitHub site (see CCGSpendingSplit.csv).
As illustrated by Figure 30, there is some suggestion of a regional pattern in VCSE commissioning although, as CCGs exhibiting high and low VCSE engagement are often co-terminous, the use of VCSEs by different CCGs most likely reflects predominately local rather than regional factors.
This split between VCSE and non-VCSE suppliers could have been used as the basis for identifying a ‘maximum-diversity’ selection of case studies, but the relative split does not say anything about the absolute level of VCSE engagement in different CCGs. For this, the two obvious criteria are (1) the percentage of overall CCG spending on VCSE suppliers (Figure 31) or (2) per capita CCG spending on VCSE suppliers (Figure 32). The two are highly correlated but, as per capita spend provides the more explicit measure of the importance of VCSE suppliers to local health economies and the populations they serve, this was used to identify suitable case study sites for the 3SC project.
Shortlisting potential study sites for the 3SC project
Study site selection was thus based on ranking 2018–9 CCGs in terms of per capita VCSE spend and then, using data on the secondary selection criteria (budget size, urban/rural, ethnic composition, deprivation and broad commissioning arrangements), aiming for a short list of two preferred and one reserve CCG from each quartile. The 3SC project team then sought to recruit up to eight CCGs as case study sites.
FIGURE 26.
Relative split of CCG spending on NHS/LA and other suppliers.
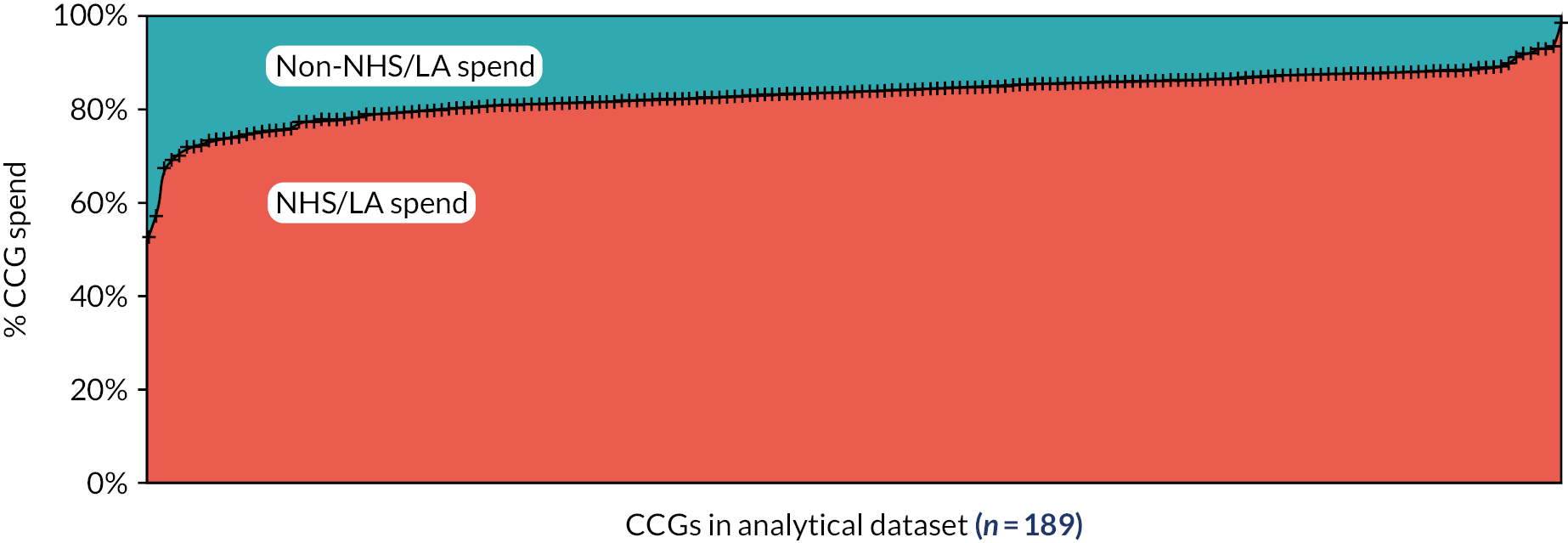
FIGURE 27.
Map of relative split of CCG spending on NHS/LA and other suppliers.
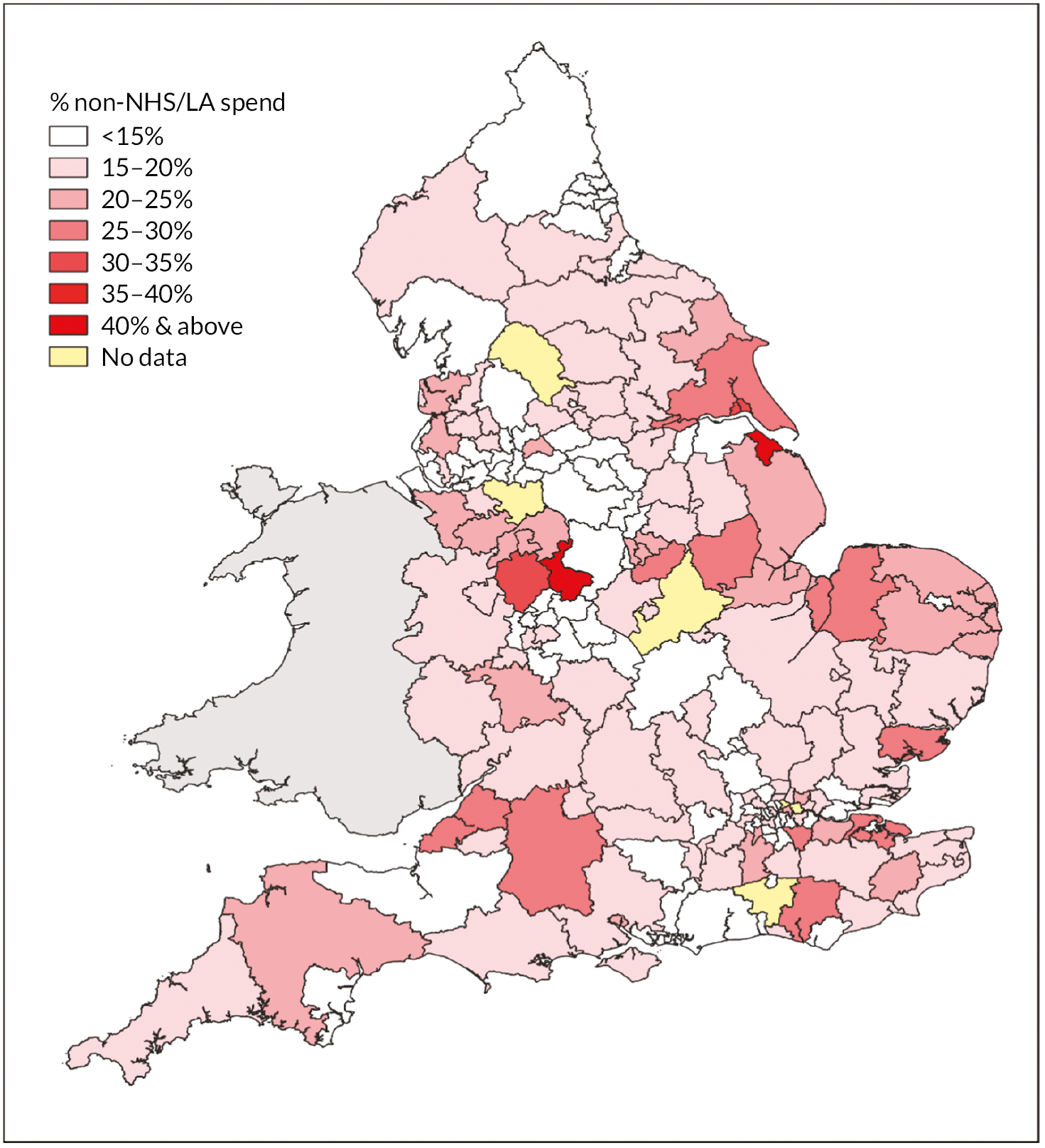
FIGURE 28.
Relative split between NHS/LA, VCSE and other suppliers.
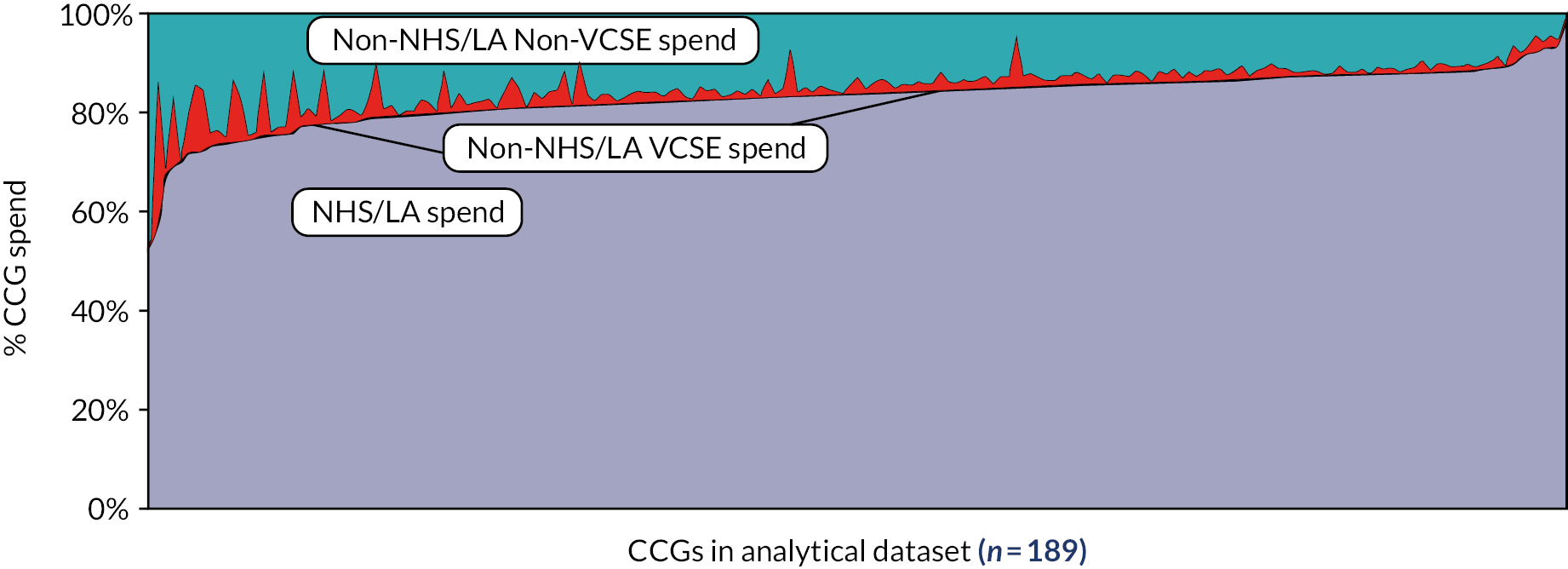
FIGURE 29.
Relative split of non-NHS/LA spend between VCSE and non-VCSE suppliers.
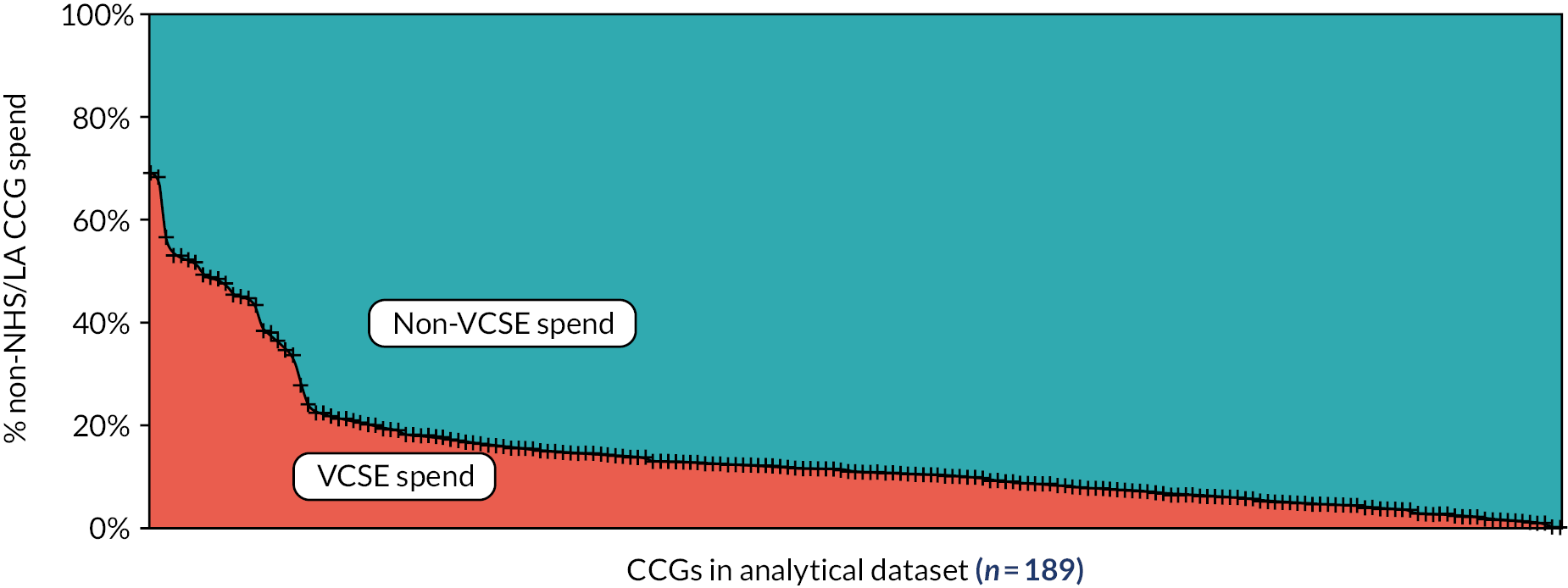
FIGURE 30.
Map of relative split of non-NHS/LA spend between VCSE and non-VCSE suppliers.
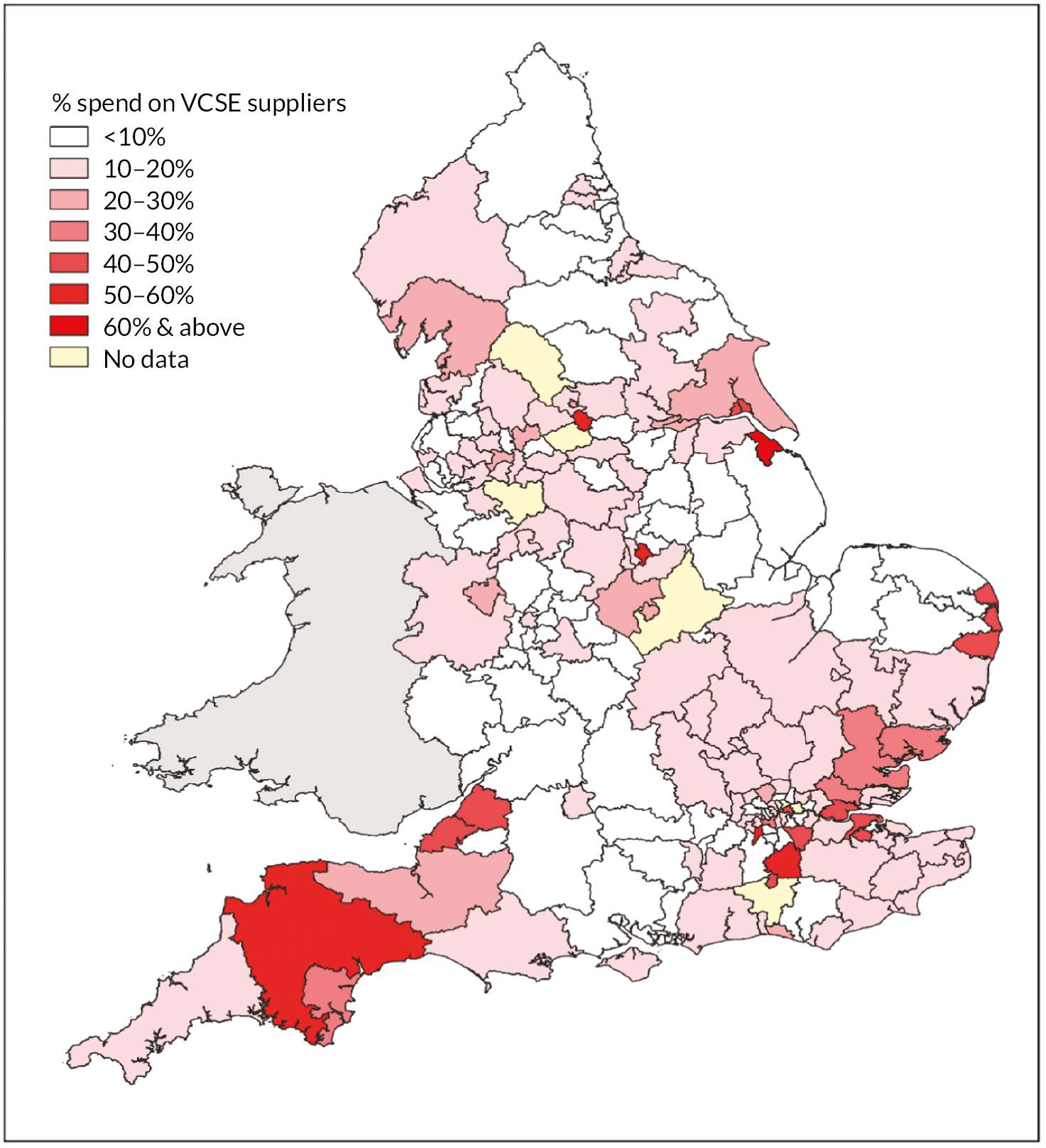
The overall distribution of shortlisted CCGs is indicated in Figure 33 (where, to maintain study site anonymity, rank order position has been randomly ‘jittered’ by between + 3 and −3).
FIGURE 31.
Percentage overall CCG spending of VCSE suppliers.
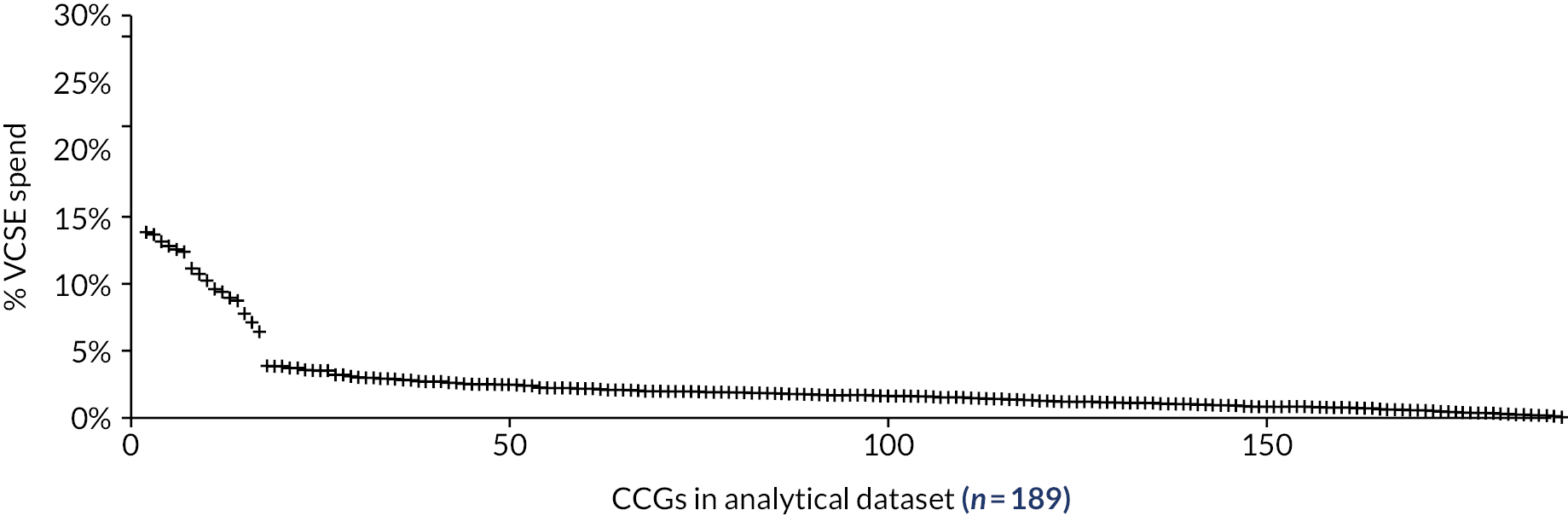
FIGURE 32.
Per capita CCG spending on VCSE suppliers.
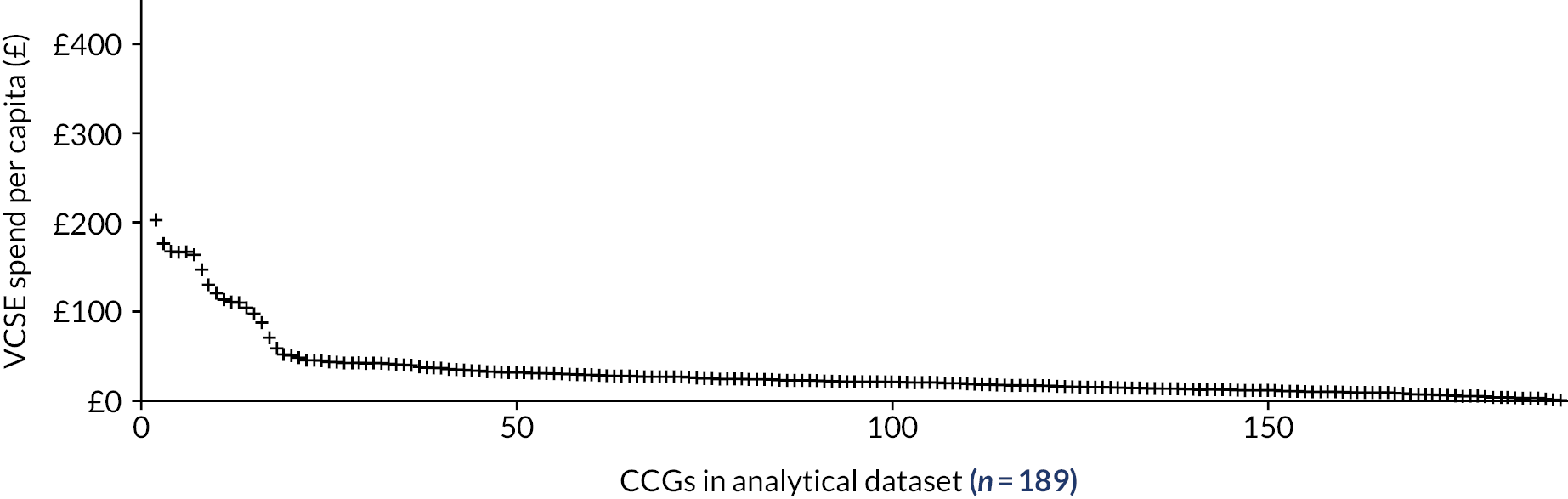
FIGURE 33.
Shortlist of potential case study CCGs (points jittered to preserve anonymity).
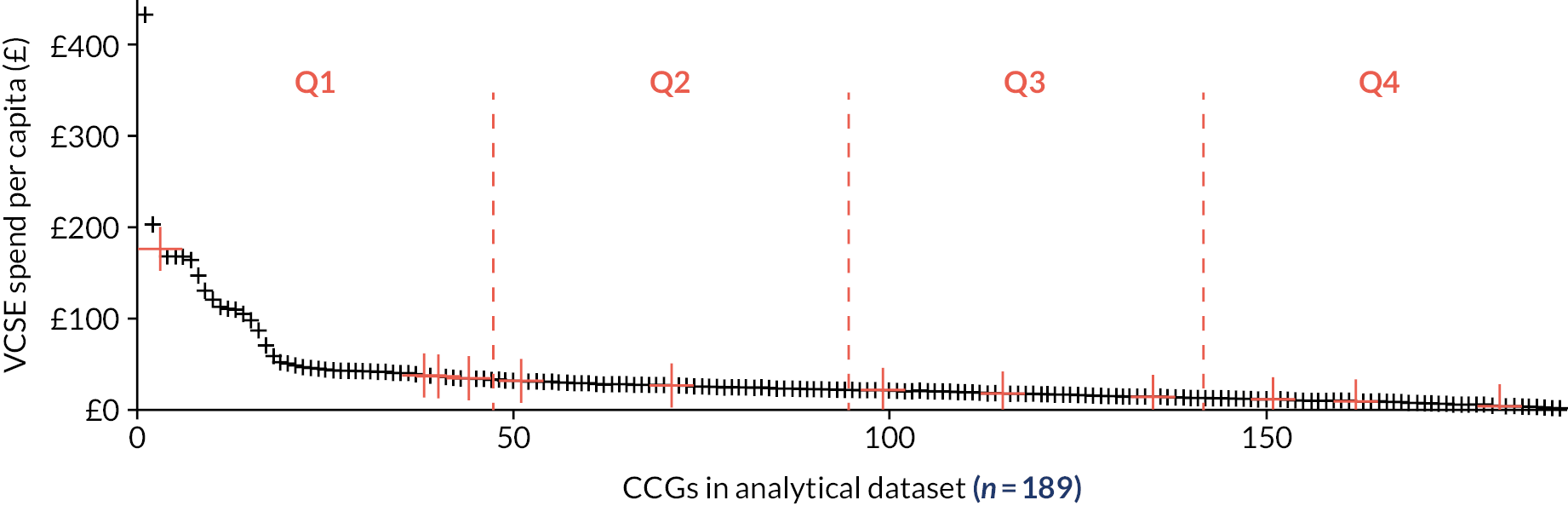
The final distribution of case study sites depended partly on which CCGs were willing to collaborate, but also on the ongoing reorganisation of CCGs. An important practical difficulty was that by the time CCGs were approached (in 2020), the number of CCGs had fallen from the 195 extant in 2018–9 to just 135 – and many of those on the shortlist had amalgamated with neighbouring CCGs. As a result, the final selection of CCGs is somewhat less evenly distributed than intended, as illustrated in Figure 34. The final selection nevertheless includes a wide variety of CCGs, from those likely to have complex, extensive and diverse commissioning relationships between healthcare commissioners and VCSEs through to those which make relatively scant use of VCSE suppliers.
FIGURE 34.
Distribution of study sites by per capita VCSE spend.
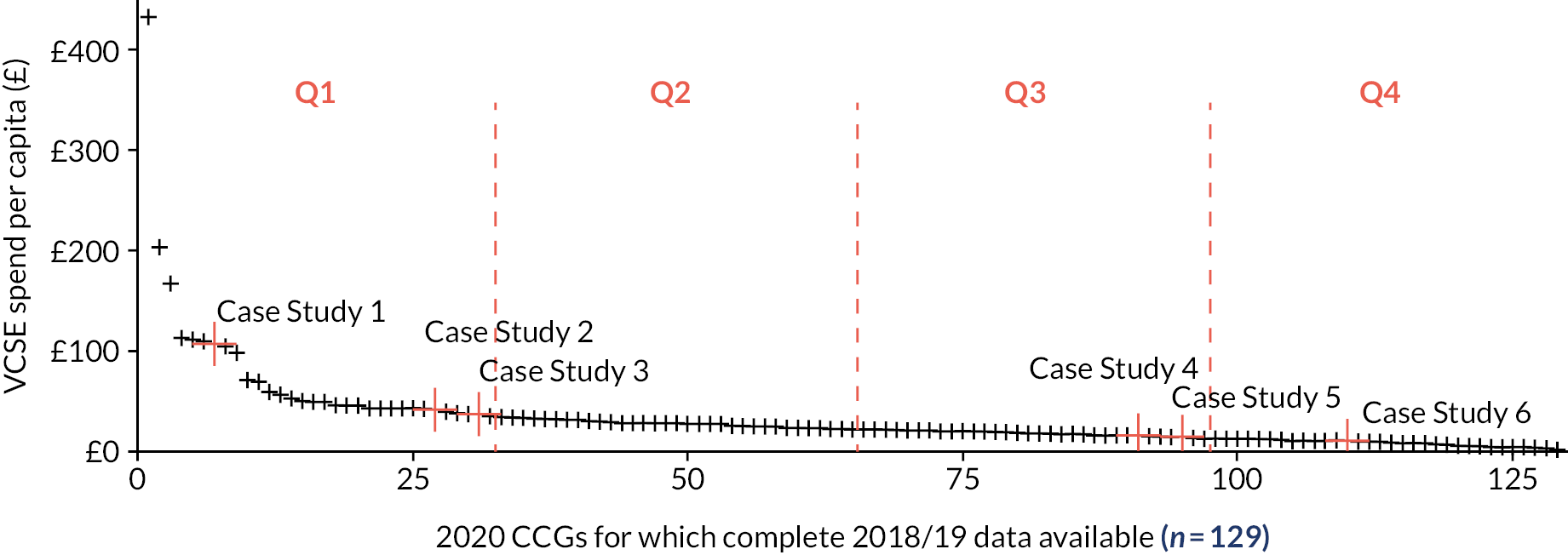
Bespoke reports detailing what could be extracted from the 2018–9 CCG accounts were provided to, and discussed with, panels from each of the study sites. Although these provided a useful point around which to discuss the volume and nature of VCSE commissioning in each CCG, they cannot be shared here as they would compromise the anonymity of the CCGs.
Improving the ‘over-threshold’ expenditure accounts for health service research
As noted in the Introduction, despite its obvious potential, relatively little health service research has sought to utilise the ‘over-threshold’ expenditure data collected by CCGs and NHS Trusts since 2013. The NHS Spend project discussed in Chapter 6, Outcomes and consequences for voluntary, community and social enterprises stands as a notable exception but, depending as it did almost entirely on automated data-scraping and name-matching algorithms, it arguably serves to demonstrate that the expenditure data, at present, cannot adequately support such methods. This represents a missed opportunity, not least because the problems largely lie with the implementation, rather than the ambition, of HM Treasury’s guidelines. 156 We draw particular attention to the need to rigorously enforce the following:
-
The ‘over-threshold’ accounts must be published in *.csv format. The common practice of making files available in pdf format makes the accounts extremely difficult to use.
-
The accounts must be made available using permanent URL addresses to support the use of RAPs and ensure future availability. With the reorganisation of commissioners and ongoing churn of health providers – and resulting loss of both institutional memory and data – this requires that all accounts are submitted to www.data.gov.uk or similar permanent central depository.
-
Greater attention needs to be paid to data entry and quality control. Organisations should not use generic terms (e.g. ‘GP’, ‘Primary Care’ or ‘Prescribing Support Services’) rather than actual supplier names, and our experience points towards an unacceptable number of non-standard, misnamed and misdated accounts – indicative, we suspect, of organisations seeking to meet their quasi-legal responsibilities rather than aiming to provide useful data.
-
All organisations are required to make the monthly ‘over-threshold’ accounts available in *.csv format and, where there are problems, their response to requests for accounts should be quick and effective. This was not always the case and, even after formal FoI requests, we were unable to obtain 2018–9 data for four CCGs.
HM Treasury’s guidance is now somewhat dated, and certainly pre-dates the widespread adoption of data-scraping and other automated techniques used to process large and complex data sets. The following would greatly enhance the value of the ‘over-threshold’ accounts to health services research:
-
Local variation in how suppliers are named poses significant problems. Where organisations are registered companies or charities, the inclusion of CH and/or CC registration numbers would be invaluable.
-
With the huge reduction in the number of commissioners (down to the current 42 ICSs) there has been a concomitant loss of information on how spending varies geographically. The use of supplier postcode, which is currently rare even though HM Treasury’s guidance states that this should be published if available, would help. It would also greatly help in developing an understanding of spending patterns if ICS ‘over-threshold’ accounts state whether particular invoices referred to pan-ICS activity or were focused on one or more of the ‘Places’ or ‘neighbourhoods’ into which ICSs are now divided.
Appendix 6 Preliminary survey of absorptive capacity
Our conceptual model of VCSE commissioning (Figure 3) suggested why and how an increased ACAP facilitates the commissioning of VCSEs (see Chapter 1, Interfaces and interaction). We therefore made an initial exploratory survey of commissioners and VSCEs’ ACAP; that is, values, skills, behaviours and knowledge mobilisation practices relevant to bidding, commissioning and co-commissioning. The questions followed the stages of ACAP (through the acquisition, assimilation, transformation and exploitation of externally sourced information and knowledge) to respondents’ reports of how satisfied they were with the outcomes of their organisation’s activity and with its collaborations.
Sampling
The survey used five of the case study sites. In them, individual respondents were initially the local project reference group members and the co-researchers, from whom they snowballed to further respondents. The survey was intended to achieve a maximum qualitative variation in the ranges of respondents rather than be a randomised representative sample of the individual commissioners and VCSE members in each study site, which the snowballing method achieved, but at the price of making it impossible to know how many people were eventually invited to complete the survey (the response rate denominator). The 131 responses to our exploratory survey came more from VCSEs (108 responses; 82% of the responses) than commissioners (23 responses; 18%), across five of the study sites. (In the sixth site, CS1b, research governance permission for site access was granted too late for a scoping survey to be undertaken contemporaneously with the other sites.) However, the responses covered all the tracer groups and the infrastructure bodies, and came from both commissioners and VCSEs, in all five sites surveyed. Of the 16 commissioner respondents who specified what organisation they worked for, most (11/23) were from LA commissioners, 3 each from CCGs and local care partnerships, and 1 from a PCN. Apart from the absence of one study site, the intended qualitative variety of respondents was thus achieved.
Analysis
The survey data were analysed to compare commissioner and VCSE profiles across the four main stages of knowledge mobilisation, according to ACAP theory: knowledge acquisition, assimilation, transformation, and exploitation. We also compared these four across the three main tracer groups. The Likert scale responses were scored between 1.0 and 5.0 depending on what verbal response the respondent chose. To summarise the scores we took the mean for each scale, which thus also had a possible range of 1.0–5.0 with 3.0 as mid-point. A lower score meant greater agreement with the statement. Because of the exploratory, qualitative sampling strategy these were simple descriptive comparisons; more statistical analyses would have overinterpreted the data. We thematically analysed the free-text responses to the scoping survey.
Findings
Active boundary-spanning (see Chapter 5, Tracer activity) and cross-boundary individual careers (see Chapter 5, Organisational characteristics) appeared to enhance commissioners’ and VCSEs’ ACAP. In presenting the findings, we follow the successive knowledge mobilisation stages, according to recent ACAP research (see Chapter 1, Commissioning voluntary, community and social enterprises), of knowledge acquisition, assimilation, transformation and exploitation. Reflecting the overall response pattern, free-text comments came more from VCSE than commissioner respondents.
To repeat, a lower score means greater agreement with the statement.
Absorptive capacity in general
Comparing ACAP in commissioners and VCSEs,Table 16 ranks the sources from which they and VCSEs routinely obtained information and knowledge in descending order of frequency of mention by commissioners.
The greatest differences were commissioners’ greater use of national statistics, seminars, databases and (management) consultants. Table 17 shows responses about how actively commissioners and VCSEs sought external information. Possible scores range between 5.0 and 1.0 (making 3.0 the mid-point).
The balance of responses thus suggested that these organisations do encourage information-seeking from external sources. Questions about assimilation queried the circulation and discussion of information within the respondent’s organisation (Table 18).
Again, scores in the lower half of the range of possible scores indicated a general pattern of agreement with the statements. When it came to transforming new information and knowledge into forms that the receiving organisation can use, and combining it with existing information and knowledge,Table 19 shows that there was a similar pattern.
| Q3. What are the key sources of information and knowledge that your organisation routinely draws upon? | ||||
|---|---|---|---|---|
| Commissioners | VCSEs | |||
| % of responses mentioning | N | % of responses mentioning | N | |
| Professional networks | 94.74 | 18 | 83.56 | 61 |
| National statistics | 89.47 | 17 | 49.32 | 36 |
| Service user consultation/feedback | 89.47 | 17 | 75.34 | 55 |
| Internet | 84.21 | 16 | 82.19 | 60 |
| Community consultation/feedback | 78.95 | 15 | 69.86 | 51 |
| Staff experience and knowledge | 78.95 | 15 | 89.04 | 65 |
| Membership bodies (e.g. NHS Confederation; Local Government Association) | 78.95 | 15 | 68.49 | 50 |
| Conversations with other related/similar organisations | 78.95 | 15 | 79.45 | 58 |
| Seminars | 57.89 | 11 | 35.62 | 26 |
| Databases | 52.63 | 10 | 42.47 | 31 |
| Professional journals | 36.84 | 7 | 24.66 | 18 |
| Academic publications | 36.84 | 7 | 30.14 | 22 |
| Consultants | 31.58 | 6 | 19.18 | 14 |
| Market research | 21.05 | 4 | 13.7 | 10 |
| Trade press | 15.79 | 3 | 10.96 | 8 |
| Other (please specify) | 5.26 | 1 | 12.33 | 9 |
| QQ4,31 Thinking about the acquisition of information in your organisation, and particularly the use of external resources (e.g. personal networks, consultants, academic publications, market research, consultation with community members) to obtain information, please rate your agreement or disagreement with each of the following statements: | ||
|---|---|---|
| Commissioners weighted average | VCSEs weighted average | |
| The search for relevant information concerning our objectives is everyday activity in our organisation | 1.89 | 2.15 |
| Leaders within our organisation motivate our staff to use information sources from within our sector (e.g. from other, similar, organisations) | 2 | 1.96 |
| Leaders within our organisation expect that our staff deal with information from beyond our sector (e.g. national statistics) | 2 | 2.44 |
| QQ5,32. Thinking about the communication and assimilation of information within your organisation, please rate your agreement or disagreement with each of the following statements: | ||
|---|---|---|
| Commissioners weighted average | VCSEs weighted average | |
| Ideas and concepts are communicated across teams | 2.67 | 1.8 |
| Our organisation emphasises cross-team support to solve problems | 2.21 | 1.81 |
| There is a quick information flow e.g. if one team obtains important information we communicate this information promptly to other teams | 2.74 | 2.14 |
| There are periodic cross-team meetings to interchange information about new developments, problems and achievements | 2.42 | 1.92 |
| QQ6,33. Please rate your agreement or disagreement with each of the following statements concerning the processing and transformation of information and knowledge within your organisation: | ||
|---|---|---|
| Commissioners weighted average | VCSEs weighted average | |
| Staff have the ability to structure and use collected knowledge | 2.26 | 2.15 |
| Staff are used to absorbing new knowledge as well as preparing it to make it available for further purposes | 2.16 | 2.14 |
| Staff successfully link existing knowledge with new insights | 2.32 | 2.18 |
| Staff are able to apply new knowledge in their practical work | 2.26 | 1.83 |
The same applied to the respondents’ responses about how their own organisations exploited (practically applied) new knowledge and information (Table 20).
The responses from informants describing their own organisations might be expected to have a socially expected response bias. Commissioners’ and VCSE respondents’ verbal comments most often mentioned e-mail messages, meetings and ‘professional’ networks as the means of obtaining ideas. VCSE respondents also mentioned networking (infrastructure) bodies, and six mentioned NHS bodies.
| QQ7,34. Please rate your agreement or disagreement with each of the following statements regarding the use and exploitation of new knowledge within your organisation | ||
|---|---|---|
| Commissioners weighted average | VCSEs weighted average | |
| Our leaders support the development of new working practices, activities and technologies | 2.05 | 1.73 |
| Our organisation regularly reconsiders its working practices, activities and technologies and adapts them accordant to new knowledge | 2.58 | 1.96 |
| Our organisation has the ability to work more effectively by adopting new working practices, activities and technologies | 2.16 | 1.89 |
Absorptive capacity in the commissioning of voluntary, community and social enterprises
The above responses concerned ACAP in general. When questions focused specifically on the commissioning of VCSEs, a somewhat different picture emerged, beginning with how actively commissioners acquired knowledge about VCSEs and vice versa (Table 21).
These weighted scores were mostly still below, but now nearer to, the mid-point of the scale; that is, the respondents were on balance weakly inclined to agree with the statements. Table 22 reports responses on whether commissioners and VCSEs knew about what information and knowledge the other held and had systems to obtain it (acquisition); and how they valued and used it to adapt how they engaged in commissioning (exploitation).
| QQ9,36. Thinking about how your commissioning (VCSE) organisation acquires and uses knowledge regarding its work with VCSE (commissioner) organisations, please rate your agreement or disagreement which the following statements: | ||
|---|---|---|
| Commissioner acquiring information and knowledge about VCSEs: weighted average | VCSE acquiring information and knowledge about commissioners: weighted average | |
| The search for information on VCSE (commissioner) organisations is an everyday activity within this organisation | 2.88 | 3.25 |
| In our organisation, information and knowledge about VCSE (commissioner) organisations is communicated across teams | 2.56 | 2.8 |
| Our staff are able to apply new knowledge in the commissioning of (in being commissioned) VCSE organisations | 2.69 | 2.7 |
| In light of new knowledge, our organisation regularly reviews and adapts the ways in which we commission VCSE organisations (become commissioned) | 3.06 | 2.64 |
| QQ10,37 (first six items). Thinking generally about the transfer of knowledge between VCSE organisations and health and care commissioning organisations in this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| Commissioning organisations are aware of the types of information and knowledge that VCSE organisations hold | 3.2 | 3.67 |
| VCSE organisations are aware of the types of information and knowledge that commissioning organisations hold | 3.47 | 3.48 |
| Commissioning organisations value the information and knowledge that VCSE organisations hold | 2.47 | 3.51 |
| VCSE organisations value the information and knowledge that commissioning organisations hold | 3.27 | 2.8 |
| Systems and structures are in place to allow for the transfer of information and knowledge from VCSE to commissioning organisations | 3.07 | 3.79 |
| Systems and structures are in place to allow for the transfer of information and knowledge from commissioning to VCSE organisations | 2.73 | 3.72 |
More obviously than inTable 21, the scores inTable 22 cluster around the scale mid-point; that is, the respondents, on balance, neither clearly agreed or disagreed with the statements. Both commissioner and VCSE respondents mentioned the unevenness of these relationships. Two VCSE respondents emphasised that commissioners appear to underestimate VCSEs’ roles, while one LA commissioner wrote:
I am wary of using voluntary sector information as it is often emotive and frankly biased as they want to get their own agenda across. Therefore it’s not necessarily reliable in terms of evidence based. There are some exceptions but not many.
ID 13403829701
Next (seeTable 23) we compared information sharing (assimilation, in the sense of onward transmission for further use of information or knowledge) within commissioners and within VCSEs, among commissioners, among VCSEs, and between commissioners and VCSEs. The sharing among commissioners, among VCSEs and between commissioners and VCSEs corresponds to the three types of networking described earlier (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks). Table 23 suggests that this information sharing was slightly stronger in the horizontal than the vertical networks described earlier (see Chapter 4, Commissioners and voluntary, community and social enterprises interacting through a network of networks and Figure 5).
| QQ11,38. Thinking generally about knowledge sharing within and between organisations in this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| People within my organisation share relevant knowledge with each other | 2.13 | 1.64 |
| Commissioning organisations in this area share relevant knowledge with each other | 3.07 | 2.29 |
| VCSEs and commissioning organisations in this area share relevant knowledge with each other | 3.27 | 3.18 |
It is unsurprising that respondents tended to think there was more information sharing within their own organisation than with other organisations. The only substantial discrepancy between the commissioner and VCSE responses was that VCSEs thought commissioners shared information more than the commissioners themselves did. VCSE respondents’ comments noted the unevenness of knowledge sharing and its dependence on good relationships between individuals. One added: ‘Friendly on the surface until a contract is up for tender’ (ID 13388193573).
Suitable IT systems assist both information acquisition and its assimilation, but our respondents mostly did not think that such IT systems existed locally (Table 24).
A commissioner (ID 13395895002) and a VCSE respondent (ID 13398168209) both commented that it was difficult for VCSEs to afford such systems. VCSE respondents also remarked on ‘locked down’ and ‘clunky’ NHS systems.
Trust (compatibility of interests and aims) is often considered197,224–226 a condition of interorganisational collaboration, in particular the assimilation and exploitation of externally acquired knowledge and information. Table 25 shows that our respondents tended to think that there was trust within their own organisation, and between it and other organisations of the same kind (commissioner or VCSE), but were less certain whether commissioners and VCSEs trusted each other.
Interorganisational interactions are a means of information and knowledge acquisition, interactions within one’s own organisation a means for information and knowledge transmission. Table 26 shows respondents’ reports about such interactions. On balance the responses did suggest that organisations interacted regularly, even commissioners with VCSEs (and, not surprisingly, that there was more interaction within organisations). Two VCSE respondents (IDs 13388193573, 13385016916) noted that competition for contracts tended to undermine collaboration.
Nevertheless, and as might be expected, respondents claimed they were more familiar with other people in their own organisation, less familiar with other organisations of the same kind (commissioner or VCSE), and less familiar again with organisations on the other side of the commissioning relationship (Table 27). One VCSE respondent pointed out that ‘regular does not imply frequent. We meet twice a year with other vol[untary] sector groups brought together in forums and we also meet with our peer organisations ever[y] 4 months’ (ID 13401603162).
Public and patient participation in co-commissioning is a means of exploiting externally acquired knowledge and information. Such participation requires activities to engage with the public and service users. Respondents rather strongly asserted that their own organisation involved service users and the public (nowadays this is a socially expected response), but less strongly that other organisations of their own kind (commissioner or VCSE) did so, whether alone or with organisations on the other side of the commissioning relationship (Table 28).
| QQ15,42. Thinking about IT systems, please rate your agreement or disagreement with the following statement: | ||
|---|---|---|
| Answer choices | Commissioner weighted average | VCSE weighted average |
| My organisation has an efficient IT system which helps our decision-making | 2.6 | 2.74 |
| In general, commissioning organisations in this area have efficient IT systems in place to help cross-organisational decision-making | 3.73 | 3.72 |
| Across the local health and care system, there are efficient IT systems in place to help joint decision-making between VCFSE and commissioning organisations | 4.13 | 4.36 |
| QQ12,39. Thinking about trust within and between organisations in this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| People within my organisation trust each other | 2.13 | 1.53 |
| Commissioning (VCSE) organisations in this area trust each other | 2.47 | 2.44 |
| VCSE and commissioning organisations in this area trust each other | 2.93 | 3.28 |
| QQ16,43. Thinking about interactions within and between organisations in this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| There are regular interactions between colleagues within my organisation | 1.53 | 1.48 |
| There are regular interactions among colleagues from across different commissioning (VCSE) organisations in this area | 2.6 | 2.3 |
| There are regular interactions among VCSE and commissioning organisations in this area | 2.73 | 3.2 |
| QQ17,44. Thinking about familiarity within and across organisations in this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| People in my organisation know each other’s job functions | 2.53 | 1.65 |
| People from across different commissioning organisations in this area know each other’s job functions | 3.6 | 2.98 |
| People from across VCSE organisations and commissioning organisations in this area know each other’s job functions | 3.47 | 3.65 |
Two VCSE respondents (IDs 13395144712, 13385016916) stated that NHS bodies had gone further than LAs towards such engagement.
A more general means of exploiting external information and knowledge is to create opportunities for stakeholders more generally to express their opinions about services, other practical activities, and commissioning. On that point, the most noticeable difference between commissioner and VCSE respondents was that the latter had a lower estimation of local leaders’ tendency to create such opportunities (Table 29).
| QQ13,40. Thinking about engagement with the general public and service users, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| My organisation participates in meetings where community members and/or service users are involved | 1.6 | 1.75 |
| Commissioning (VCSE) organisations participate together in meetings where community members and/or service users are involved | 2.67 | 2.16 |
| VCSE and commissioning organisations participate together in meetings where community members and/or service users are involved | 2.4 | 3.04 |
| QQ18,45. Thinking about opportunities for different stakeholders to voice their opinions within this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| Leaders within my organisation give relevant stakeholders the opportunity to voice their opinion | 2.07 | 1.79 |
| Leaders across commissioning organisations in this area give relevant stakeholders the opportunity to voice their opinion | 2.67 | 2.7 |
| Leaders across the local health and care system give relevant stakeholders the opportunity to voice their opinion | 2.6 | 3.54 |
The exploitation of these opportunities depends, however, on managers’ and VCSE leaders’ decision-making practices, beginning with the use of others’ information, knowledge and ideas generally (Table 30).
A VCSE respondent, however, stated that the decisions themselves could still be questionable:
rough ideas appear to be frequently turned into funded projects, bearing little relationship to what is needed on the ground, e.g. that many people coming out of hospital need support on returning home ‘to buy bread milk and check the heating is working’. This is frequently not the case but a whole post is funded to find out if this is needed, in a time-consuming, inefficient way.
ID 13401603162
| QQ19,46. Thinking about how leaders within this area make decisions, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| Leaders within my organisation make decisions based only on their own ideas | 4 | 4.14 |
| Leaders across commissioning organisations in this area make decisions based only on their own ideas | 4.6 | 4.29 |
| Leaders across the local health and care system make decisions based only on their own ideas | 4 | 4.11 |
However, respondents were a little less confident about whether this general claim, about managers and leaders not using just their own ideas, applied to commissioning practice specifically (Tables 31 and32).
A VCSE respondent mentioned ‘barriers from NHS England-driven deadlines meaning co-design (which is time-consuming) can often not be of the standard everyone would like’ (ID 13454221090). Table 30 suggests that commissioner and VCSE respondents alike rather strongly agreed that their decision-makers did heed others’ information, knowledge or ideas (scores above 3.0 indicate disagreement with the statement).
Previous studies have assumed (see Chapter 1, Commissioning voluntary, community and social enterprises) that increased ACAP helps produce improved organisational outcomes. Table 33 shows our respondents’ satisfaction with some general outcomes.
One VCSE response contrasted meeting community needs with meeting national policy priorities:
Part of the role of VCSFE sector is not simply to follow national policy objectives, but to reflect what it funds on the ground. For example, the nonsense that is ‘British Values’, against what communities are facing, their identity needs and beliefs, and voice and empowerment to challenge systems.
ID 13395144712
Table 34 reports their satisfaction specifically with interorganisational collaboration in the sphere of commissioning.
| QQ10,37 (last two items). Thinking generally about the transfer of knowledge between VCSE organisations and health and care commissioning organisations in this area, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| Information and knowledge from VCSE organisations has been used by commissioning organisations to make changes to how they commission services | 2.33 | 3.49 |
| Information and knowledge from commissioning organisations has been used by VCSE organisations to make changes to how they deliver services | 3.2 | 3.05 |
| QQ14,41. Thinking about the involvement of service users in decision-making, please rate your agreement or disagreement with the following statements: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| My organisation involves service users in its decision-making | 1.93 | 2.09 |
| In general, commissioning organisations (VCSEs) in this area involve service users in decision-making | 3.2 | 2.75 |
| VCSEs and commissioning organisations work collaboratively in this area to involve service users in joint decision-making | 2.73 | 3.45 |
| QQ20,47. Thinking about your own organisation’s performance over the past year, please say how satisfied or dissatisfied you are along the following dimensions: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| Quality of decision-making | 2.44 | 1.87 |
| Level of innovation | 2.22 | 2.08 |
| Meeting your organisation’s objectives | 2.11 | 1.82 |
| Meeting service user/community needs | 2.44 | 1.95 |
| Meeting financial objectives | 2 | 2.12 |
| Delivering on national policy priorities | 1.89 | 2.17 |
| QQ21,48. Now thinking about the performance of collaborations that your organisation has been involved in over the past year, which bring VCSE and health and care commissioning organisations together, please say how satisfied or dissatisfied you are along the following dimensions: | ||
|---|---|---|
| Commissioner weighted average | VCSE weighted average | |
| Overall success of the collaboration(s) | 2.33 | 2.27 |
| Mutual respect between commissioning and VCSE organisations within the collaboration(s) | 2.33 | 2.27 |
| Quality of the decision-making within the collaboration(s) | 2.67 | 2.44 |
| Level of innovation within/through the collaboration(s) | 3 | 2.45 |
| Outcomes for service users through the collaboration(s) | 2.44 | 2.41 |
| Tackling health inequalities through the collaboration(s) | 2.67 | 2.61 |
General patterns
Well-developed ACAP is a context likely (as Chapter 1, Commissioning voluntary, community and social enterprises explained) to increase commissioners’ adaptation of their commissioning activities to match what VCSEs seek from, and the resources VCSEs bring to, the commissioning cycle, and vice versa. Commissioner and VCSE respondents alike were moderately confident that in general their own organisations undertook all four stages of ACAP use: acquisition, assimilation, transformation, and exploitation of externally sourced information and knowledge. When it came to commissioning specifically, their responses were slightly less confident, more often tending to cluster around than below the mid-point of the response scales. Commissioner respondents indicated a markedly greater tendency towards acquiring evidence from national statistics, databases and academic publications than did the VCSE responses. Commissioners and VCSE responses were more confident that interactions between organisations occurred than they were about being familiar with the other organisations. Commissioner responses expressed greater trust in other commissioning organisations than in VCSEs, and vice versa for VCSE responses. The responses suggested, weakly, that both kinds of organisation transformed their externally sourced information and knowledge. Respondents replied that both kinds of organisation met and consulted patients, public and ‘stakeholders’, and that managers’ or leaders’ decisions exploited externally sourced information and knowledge. Externally sourced information and knowledge appeared to be slightly more influential within organisations of the same kinds as the respondent’s own than across the local health system more widely. Finally, respondents tended to be satisfied with both their own organisation’s performance and the contribution of interorganisational collaboration to it. Apart from their external sources of information and knowledge, the above patterns were similar in commissioners and VCSEs. However, many respondents emphasised that the four main activities that comprise ACAP (information and knowledge acquisition, assimilation, transformation and exploitation) occurred unevenly within their study sites. The reported differences were more apparent between organisations within a study site than between study sites.
Limitations
This was an exploratory survey, not a statistically representative random sample of the individuals involved in commissioning within the study sites (let alone more widely), nor a census of them. The above analysis takes commissioners and VCSEs as homogenous groups (rather than by organisation or even case study, which would require a larger number of respondents). We only have respondents’ word for their answers, and would ideally triangulate them using a larger sample and ethnographic research. The survey elicited respondents’ reports of how satisfied they were with the outcomes of their organisation’s activity and with its collaborations, but that is not the same as measuring collaboration and then its outcomes, which would require a combination of social network analysis, quantification of the outcomes, a qualitative account of the mechanisms and contexts linking collaboration with outcomes, and triangulating the findings of these methods.
Appendix 7 Tracer characteristics as commissioning contexts
Rows marked * in middle column are explained in Chapter 5.
| Causes of commissioning-relevant differences between tracers | Commissioning-relevant differences (contexts) | Effects on commissioning mechanisms |
|---|---|---|
| Technical character | ||
| Size: VCSE requires a minimum membership and other physical resources to be able to carry out its activity | * Generally (but with exceptions) high for hospices, intermediate for learning disability, small for social prescribing |
|
| Number and density of VCSEs | * Ratio of number of VCSEs to population size (small for hospices, intermediate for learning disability, high for social prescribing) |
|
| Technical character of output | * Outcome specificity (high for hospices, mixed for learning disability, low for social prescribing) |
|
| Medicalisation of activity | High for hospices, middling for learning disability, low for social prescribing |
|
| Technical specialisation of care process. Not necessarily associated with outcome specificity; for example, some learning disability providers have high specialisation with low outcome specificity (‘quality of life’ etc.). | Specialisation of activity (high for hospices, mixed for learning disability, low for social prescribing) |
|
| Stability of the kinds and volume of clients’ support needs. | * Uncertainty of demand (high for social prescribing, lower for learning disability and hospices) |
|
| Provider continuity and stability. High for hospices, less for learning disability, social prescribing. | * Local history |
|
| Politico-economic character | ||
| Statutory status. Commissioners have stronger motivation to commission statutorily required activities; less for policy-mandated activities; least for optional activities. | * Statutorily required service or not (yes for hospice and some learning disability, no for other learning disability and social prescribing): policy-mandated or not (yes for social prescribing). |
|
| Provider ownership mix | * Provider mix (learning disability high variation), social prescribing low variation for activity providers, but coordinating of VCSE, LA and NHS ownership. |
|
| Varied sources all make large contribution to VCSE income (hospices high, social prescribing often low) | Multiple sources of substantial income reduce VCSE resource dependence on commissioners |
|
Appendix 8 Compliance with RAMESES II reporting standards
| 1 | In the title, identify the document as a realist evaluation | Title does not, but introductory section and Methods sections (see Chapter 3, Study design and its theoretical framework) discuss explicitly. | |
| Summary or abstract | |||
| 2 | Journal articles will usually require an abstract, while reports and other forms of publication will usually benefit from a short summary. The abstract or summary should include brief details on: the policy, programme or initiative under evaluation; programme setting; purpose of the evaluation; evaluation question(s) and/or objective(s); evaluation strategy; data collection, documentation and analysis methods; key findings and conclusions Where journals require it and the nature of the study is appropriate, brief details of respondents to the evaluation and recruitment and sampling processes may also be included Sufficient detail should be provided to identify that a realist approach was used and that realist programme theory was developed and/or refined |
Abstract; Chapter 3, Study design and its theoretical framework; Preliminary scoping; Cross-sectional profile of Clinical Commissioning Group spending on voluntary, community and social enterprises; Systematic comparison of case studies of co-commissioning and the commissioning of voluntary, community and social enterprises; and Action learning and absorptive capacity | |
| Introduction | |||
| 3 | Rationale for evaluation | Explain the purpose of the evaluation and the implications for its focus and design | Chapter 2, Research aims and objectives and Chapter 3, Study design and its theoretical framework |
| 4 | Programme theory | Describe the initial programme theory (or theories) that underpin the programme, policy or initiative | Chapter 1, Interfaces and interaction |
| 5 | Evaluation questions, objectives and focus | State the evaluation question(s) and specify the objectives for the evaluation. Describe whether and how the programme theory was used to define the scope and focus of the evaluation | Chapter 2, Research questions |
| 6 | Ethical approval | State whether the realist evaluation required and has gained ethical approval from the relevant authorities, providing details as appropriate. If ethical approval was deemed unnecessary, explain why | Additional information, Research governance |
| Methods | |||
| 7 | Rationale for using realist evaluation | Explain why a realist evaluation approach was chosen and (if relevant) adapted | Chapter 3, Study design and its theoretical framework |
| 8 | Environment surrounding the evaluation | Describe the environment in which the evaluation took place | Chapter 3, Sampling strategy: site selection criteria and methods |
| 9 | Describe the programme policy, initiative or product evaluated | Provide relevant details on the programme, policy or initiative evaluated | Chapter 1, Health and care; Voluntary, community and social enterprises in health and care; and Commissioning voluntary, community and social enterprises |
| 10 | Describe and justify the evaluation design | A description and justification of the evaluation design (i.e. the account of what was planned, done and why) should be included, at least in summary form or as an appendix, in the document which presents the main findings. If this is not done, the omission should be justified and a reference or link to the evaluation design given. It may also be useful to publish or make freely available (e.g. online on a website) any original evaluation design document or protocol, where they exist | Chapter 3, Study design and its theoretical framework |
| 11 | Data collection methods | Describe and justify the data collection methods – which ones were used, why and how they fed into developing, supporting, refuting or refining programme theory Provide details of the steps taken to enhance the trustworthiness of data collection and documentation |
Chapter 3, Preliminary scoping; Cross-sectional profile of Clinical Commissioning Group spending on voluntary, community and social enterprises; Systematic comparison of case studies of co-commissioning and the commissioning of voluntary, community and social enterprises; and Action learning and absorptive capacity |
| 12 | Recruitment process and sampling strategy | Describe how respondents to the evaluation were recruited or engaged and how the sample contributed to the development, support, refutation or refinement of programme theory | Chapter 3, Preliminary scoping, Systematic comparison of case studies of co-commissioning and the commissioning of voluntary, community and social enterprises, Action learning and absorptive capacity; Chapter 7, Additional findings |
| 13 | Data analysis | Describe in detail how data were analysed. This section should include information on the constructs that were identified, the process of analysis, how the programme theory was further developed, supported, refuted and refined, and (where relevant) how analysis changed as the evaluation unfolded | Chapter 3, Synthesising the findings; Chapter 7, What this study adds |
| Results | |||
| 14 | Details of participants | Report (if applicable) who took part in the evaluation, the details of the data they provided and how the data was used to develop, support, refute or refine programme theory | Chapter 3, Sampling strategy: site selection criteria and methods, Action learning and absorptive capacity; Chapter 4, Dual commissioning mechanisms, two modes of commissioning; Chapter 7, What this study adds, Additional findings |
| 15 | Main findings | Present the key findings, linking them to contexts, mechanisms and outcome configurations. Show how they were used to further develop, test or refine the programme theory | Chapters 4–6 |
| Discussion | |||
| 16 | Summary of findings | Summarise the main findings with attention to the evaluation questions, purpose of the evaluation, programme theory and intended audience | Chapter 7, Conclusions |
| 17 | Strengths, limitations and future directions | Discuss both the strengths of the evaluation and its limitations. These should include (but need not be limited to): (1) consideration of all the steps in the evaluation processes; and (2) comment on the adequacy, trustworthiness and value of the explanatory insights which emerged In many evaluations, there will be an expectation to provide guidance on future directions for the programme, policy or initiative, its implementation and/or design. The particular implications arising from the realist nature of the findings should be reflected in these discussions |
Chapter 7, Limitations , Future research |
| 18 | Comparison with existing literature | Where appropriate, compare and contrast the evaluation’s findings with the existing literature on similar programmes, policies or initiatives | Chapters 4–6; Chapter 7, What this study adds |
| 19 | Conclusion and recommendations | List the main conclusions that are justified by the analyses of the data. If appropriate, offer recommendations consistent with a realist approach | Chapter 7, Conclusions |
| 20 | Funding and conflict of interest | State the funding source (if any) for the evaluation, the role played by the funder (if any) and any conflicts of interests of the evaluators | Title page, Additional information. |
List of abbreviations
- A&E
- accident and emergency
- ACAP
- absorptive capacity
- CC
- Charity Commission
- CCG
- Clinical Commissioning Group
- CH
- Companies House
- CIC
- community interest company
- CMOC
- context–mechanism–outcome configuration
- CQC
- Care Quality Commission
- CVS
- Council for Voluntary Service
- DHSC
- Department of Health and Social Care
- DSF
- decision space framework
- FoI
- freedom of information
- GP
- general practitioner
- HRG
- Healthcare Resource Group [tariff payment]
- ICB
- Integrated Care Board
- ICS
- Integrated Care System
- LA
- local authority
- NHSE
- NHS England
- PCN
- primary care network
- POG
- Project Oversight Group
- PPIE
- patient and public involvement and engagement
- RAP
- reproducible analytical pipeline
- SDoH
- social determinants of health
- VCSE
- voluntary, community and social enterprise
