Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR131316. The contractual start date was in May 2021. The draft manuscript began editorial review in August 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Slowther et al. This work was produced by Slowther et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Slowther et al.
Chapter 1 Introduction
Background and study rationale
Anticipatory treatment plans
When a person develops a life-threatening condition or has a sudden deterioration in an existing illness, rapid treatment decisions may be needed. Often, the person is unable to be involved in the decision at the time, and there is limited clinical information or information about what their treatment preferences might be in this situation. Anticipatory treatment decisions and recommendations can improve this decision-making process and help to guide healthcare professionals while ensuring the person’s values and preferences are respected in the future. Anticipatory treatment plans can take several forms. A person may decide to make an advance decision to refuse treatment and specify particular treatments that should not be given to them should they be unable to speak for themselves. 1 More commonly an advance care plan (ACP) may be made between a person, their family and those caring them to document their future priorities of care more broadly, including preference for place of death. 2–4 ACP is mainly advocated in the context of end-of-life care, although an international consensus definition of ACP states that: ‘Advance care planning is a process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals and preferences regarding future medical care’. 5
Emergency care treatment plans (ECTPs), sometimes called treatment escalation plans, focus specifically on treatment decisions in emergency or acute illness situations. Their aim is to make treatment recommendations that reflect the person’s preferences and values, and they are reached in discussion with the person or their family. However, the specific recommendations are made by the healthcare professional and are intended to guide future treating clinicians. 6 An important distinction between ACPs and ECTPs is that, whereas the ultimate focus of ACPs is on end-of-life care preferences, ECTPs focus on steps to be taken in the event of an acute pathophysiological deterioration in which recovery is possible, although it may be unlikely. 7 Prior to 2016, stand-alone do not attempt cardiopulmonary resuscitation (DNACPR) recommendations were the most commonly used form of emergency care treatment planning document in acute NHS hospitals (72% of hospitals). 8 However, concerns existed about their use, including lack of discussion with patients and/or their family, failure to consider cardiopulmonary resuscitation (CPR) recommendations before a patient deteriorates, and lack of transferability of forms between primary and secondary care and ambulance services. 9,10 A particular concern was that a focus on CPR leads to lack of consideration of other treatments that may or may not be appropriate. 11–13 Responding to these concerns, some hospitals and health networks developed ECTPs to provide a more holistic approach to anticipatory medical decision-making. 14–16 In 2016, the Resuscitation Council United Kingdom (RCUK) led development of a national standardised approach to support conversations about goals of care and to provide guidance to clinicians about treatments to be recommended in an urgent situation when the patient lacks capacity to decide for themselves: Recommended Summary Plan for Emergency Care and Treatment (ReSPECT). 6
The ReSPECT process
ReSPECT is both a process and a form documenting the process (see Report Supplementary Material 1 for copy of ReSPECT form, versions 2 and 3). As described on the RCUK website, the ReSPECT process creates a summary of personalised recommendations for a person’s clinical care in a future emergency in which they do not have capacity to make or express choices. The process takes into account both patient preferences and clinical judgement and records ‘agreed realistic clinical recommendations’ including a recommendation whether or not CPR should be attempted if the person’s heart or breathing stop. Implementation of ReSPECT in NHS acute trusts began in December 2016 and within 3 years it was used in 22% of trusts. While other forms of ECTPs were used in some trusts, ReSPECT accounted for 60% of the observed move away from stand-alone DNACPR forms to ECTPs during this time. 17 Since its initiation the ReSPECT form has been modified in response to feedback from clinicians and patients (in 2023 both versions 2 and 3 were in use).
Although ReSPECT implementation occurred first in acute trusts, it was always envisaged that this process would cross the primary and secondary care interface. Indeed, it was developed as a patient held form rather than a clinical record. An evaluation of ReSPECT in early-adopter trusts found that many clinicians thought that the ReSPECT conversation and documentation of recommendations fitted better into a primary-care setting. 18 Patients may have an established relationship with their general practitioner (GP), conversations can occur over an extended period, patients are often less sick and more able to engage in discussion, and conversations can be placed in a wider context of ACP. However, there are also potential difficulties in moving ReSPECT conversations to primary care; patients and families may be less ready to think about these things until a crisis emerges, GPs may be uncertain about hospital-based interventions, and both may have concerns about the effect of a conversation on the patient–doctor relationship. Another challenge to the use of ReSPECT across the primary and secondary care interface is that hospital doctors and GPs use the process in different ways and recommendations do not always translate to different settings. 19
Emergency care treatment plans and person-centred care
There is an ethical and professional obligation to balance benefits and burdens of treatment from the patient’s perspective. 20 Current NHS policy and professional guidance emphasises a model of personalised care and shared decision-making. 21 ECTPs can facilitate person-centred shared decision-making in the acute situation by summarising earlier considered assessments of the potential benefits and burdens of a range of future treatments, taking into account what is important to the patient.
People with a learning disability might particularly benefit from emergency care treatment planning as their needs and wishes are often not met in acute situations. 22 Health outcomes are often poor for people with a learning disability because health professionals do not understand their needs. 22–24 Obstacles include lack of education and training among health professionals, communication challenges and/or a perception that individuals lack capacity because of their disability. 25,26 Anticipatory care planning with people with a learning disability is minimal due to a lack of confidence and awareness among medical staff. 27–29 This further disadvantages people with a learning disability by denying them input into decisions about future treatment.
The impact of COVID-19 on emergency care treatment planning
The COVID-19 pandemic generated increased interest in the use of ECTPs in general and ReSPECT in particular. High mortality, particularly among older frail people and those with specific medical conditions, few effective treatments and restrictions on hospital visiting, all had a potential impact on decisions about whether a person would benefit from or would want hospital admission or treatment if they developed COVID-19. GPs and hospital doctors admitting acutely ill patients were encouraged to have these conversations with patients early and to document the resulting treatment recommendations. In a UK teaching hospital, completion of treatment escalation plans more than doubled during COVID-19 from 20% of inpatients to 50%, and the scope of the recommendations was broader than before COVID-19. 30 This renewed emphasis on anticipatory decision-making during COVID-19 was seen as supporting best practice in person-centred care. A paper reporting a retrospective analysis of a multicentre cohort study of patients admitted to hospital with COVID-19 also found more nuanced decision-making around life-sustaining treatments, such as CPR. Participating clinicians explained that the use of the ReSPECT process allowed more nuanced treatment recommendations to be made compared with using DNACPR forms. 31 It was also an opportunity to embed the principles and practice of ACP and emergency care treatment planning into clinical practice more generally. 32 However, there were concerns that the impetus to complete ECTPs early, and the restrictions on communicating with patients and their families in person, might lead to inappropriate use of ECTPs and result in poor patient care, leading to guidance being issued by professional and regulatory organisations. 33,34 The Care Quality Commission’s report into its review of DNACPR recommendations during the COVID-19 pandemic recommended that decisions about DNACPR should be made as part of a wider conversation about ACP, and that people and their representatives should be supported in having these conversations. The report suggested that ReSPECT was a good example of an ACP process that enabled these conversations to occur. 35 The Royal College of General Practitioners and British Medical Association recognised the specific challenges for GPs in having these conversations during a pandemic and provided guidance to its members reiterating the requirement for individualised conversations about future treatment decisions. 36,37 It is not clear to what extent practice around emergency care treatment planning has changed since the pandemic.
Evaluating the use of emergency care treatment plans in the United Kingdom
We identified six UK evaluation studies of locally developed ECTPs published between 2010 and 2017. 14,15,38–41 All reported that the ECTP improved communication and documentation of treatment escalation decisions. Three studies reported perceived improvement in appropriate decision-making around treatment escalation and resuscitation, although appropriate was not defined. ECTPs were positively evaluated by staff. Two studies demonstrated a significant reduction in patient harms associated with the use of the ECTP compared with patients who had a standalone DNACPR form documented in their notes. 40,41 Since the introduction of ReSPECT, the focus of published evaluation studies has been on this model of ECTP. An evaluation of the first ReSPECT pilot in Scotland, which included 200 ReSPECT forms completed in a range of settings (hospital, hospice and community), found that patients with a ReSPECT form were more likely to die in their preferred place of care and had a reduced chance of readmission within 3 months of hospital discharge. Patients and staff were generally positive about the process. Challenges included time pressures, staff reluctance to initiate a conversation or lack of confidence to do so. 42 A multicentre evaluation of the use of ReSPECT in early adopter sites involving six acute NHS trusts in England took place between 2017 and 2019. It found that ReSPECT conversations were mainly initiated with patients nearing the end of their life or at imminent risk of deterioration and focused on CPR decisions. However, a move towards a more holistic approach in terms of treatment recommendations and conversations with patients and their families was observed. 8 Doctors’ uncertainty about a patient’s prognosis, constraints of time and external environment, and the need to minimise patient distress, influenced both the prioritisation and content of conversations. 18 An interview study with GPs and care home staff in the West of England found a generally positive attitude to the use of ReSPECT but noted that its use was complex and there were challenges in incorporating patients’ preferences into decision-making. The authors recommended a multidisciplinary approach that engaged care staff more in the process. 43 There has been no large study of the use of ReSPECT or other ECTP in the community setting.
Chapter 2 Overview of study design
Here, we outline the study aims and objectives, and corresponding work packages (WPs), describe the theoretical approach underpinning the research and the ethical considerations raised by the research. Finally, we explain changes made to the original protocol in response to challenges encountered during the research process.
Study aims and objectives
Our overall aim was to evaluate the ReSPECT process for adults in primary care to determine how, when and why it is used, and what effect it has on patient treatment and care.
Our objectives were:
-
To understand how ReSPECT is currently used in primary care from the perspective of patients, their families, clinicians and care home staff
-
To describe the views of patients, the public, primary and community healthcare professionals, and home care workers on ECTPs in general and ReSPECT in particular
-
To identify enablers and obstacles to embedding ReSPECT in primary care practice
-
To explore the impact of ReSPECT on patient treatment decisions
-
To understand how health and social care professionals can optimally engage people with a learning disability in the ReSPECT process and co-produce relevant support materials
-
To develop a consensus on how ReSPECT should be used in primary care.
Study design
Work package 1
A qualitative study exploring the experience of ReSPECT in primary care and community settings drawing on interviews with GPs, patients and their families/carers and staff in care homes, and conversations with other members of staff in the participating GP practices (see Chapters 4, 5 and 6).
Work package 2
Focus groups and interviews with healthcare professionals, home care workers, members of the public and faith leaders to explore their views on the principles and practice of ReSPECT and other forms of anticipatory decision-making; two national surveys, one of the public’s attitudes to ECTPs and one of GPs’ experiences and views of anticipatory decision-making (see Chapters 3 and 4).
Work package 3
Quality assessment of ReSPECT form completion in the GP practice sites involved in WP1 (see Chapter 4).
Work package 4
Co-production workshops with adults with a learning disability to explore their understanding of and views on emergency care treatment planning and to co-create resources to support the engagement of people with a learning disability with ReSPECT; focus groups and interviews with relatives of people with a learning disability to capture their views and experiences of emergency care treatment planning. This WP was added to the original protocol following a successful application to NIHR for additional funding in response to a call for proposals to be submitted by current NIHR award holders for additional research related to social care, to be completed within their current award time frame (see Chapter 7).
Work package 5
An initial synthesis of findings across the WPs informed the content of a stakeholder meeting with participants from professional and patient organisations and implementers of ReSPECT across the UK; final synthesis of all findings (see Chapter 8).
See Report Supplementary Material 2 for study flow-chart.
Theoretical framework
Our overarching theoretical framework for analysis was normalisation process theory (NPT). 44,45 We wished to investigate to what extent ReSPECT is embedded in routine primary care practice and how it is perceived and enacted by health and care professionals and patients. NPT characterises a set of mechanisms (coherence, cognitive participation, collective action and reflexive monitoring) that influence the embedding of new interventions or processes into clinical practice.
Data from WPs 1, 2 and 3 primarily informed our NPT analysis. In this analysis, we asked how do clinicians, care home staff, patients and their families:
-
conceptualise ReSPECT (coherence)
-
initiate or engage with the process (cognitive participation)
-
use the process and the documentation (collective action)
-
evaluate the impact of ReSPECT and how it changes behaviour (reflexive monitoring).
Data from the focus groups with members of the public and the public attitudes survey (WP2) provided a broader societal perspective to provide context for ReSPECT implementation.
Localities
Three Clinical Research Networks (CRNs) recruited practices across three diverse Clinical Commissioning Group (CCG) areas in England. To maintain participant confidentiality, we are not reporting which CCG areas were involved.
Ethics and regulatory approvals
We gained NHS/Health Research Authority (HRA) ethics approval (21/LO/0455) and Confidentiality Advisory Group (CAG) approvals (21/CAG/0089) for the study. A summary table of the approvals, including amendments, is presented in Report Supplementary Material 3. The sponsor was the University of Warwick.
Ethical considerations
Ethical issues for this study included recruitment and conduct of interviews on a sensitive and emotive topic; responding to distress of participants during interviews and focus groups; verbal consent for conversations with practice staff; responding to concerns raised regarding safeguarding or unprofessional conduct; accessing medical records without explicit consent; and involvement of people with a learning disability in co-production workshops. We describe how we addressed these in Appendix 1. Access to patient records and ReSPECT forms by study researchers was approved by the HRA Confidentiality Advisory Group under Section 251 of the NHS Act. Our justification for CAG approval is in Report Supplementary Material 4.
Changes to the protocol
Changes to recruitment of care homes
In our original protocol, we aimed to recruit two care homes associated with each GP practice site. Planned care home involvement included interviews with senior care home staff, involving care homes in recruitment of patients and their relatives, and identification of ReSPECT forms. Of 23 care homes identified by our GP practices, only 11 agreed to participate and, of those, 8 agreed to take part in the interview element only. Service delivery pressures related to COVID-19 and its consequences and frequent changes in senior staff contributed to the challenge of recruitment. To ensure that we captured the full range of care home experience, we expanded our recruitment through care home networks to include care home staff not linked to our GP sites.
Changes to recruitment approach for patient and relative interviews
Recruitment of patients and relatives of patients who lacked capacity was low. In response, we simplified our recruitment approach by removing the link between interview (WP1) and access to patient records (WP3) in the invitation letter. We also sought to advertise the interview study directly through care home networks.
Decision to stop data collection for congruence
We originally planned a retrospective analysis of patient records and ReSPECT forms to measure congruence between ReSPECT recommendations and clinical decision-making at the time of an acute event for people with a ReSPECT form completed in the previous 6 months. The estimated sample size for this analysis was 413 ReSPECT forms, assuming that the acute clinical event rate within 6 months of a ReSPECT form completion was 70%. Across our first 6 practice sites, we identified 233 patients with a record of a ReSPECT form completed in the previous 12 months, of whom 169 were eligible to participate. Of eligible patients, we were only able to identify and extract data from 65 ReSPECT forms. We had anticipated that GP practices may not always have a copy of a patient’s ReSPECT form as they are designed as patient held forms. However, we had expected that we would be able to identify additional ReSPECT forms through the care homes recruited to the study. As noted above, recruitment of care homes to this element of the study was extremely challenging and so this method of data collection was not possible. Additionally, analysis of the clinical records of patients with a ReSPECT form found an acute event rate of 24%. Following discussion between the study team, the study independent steering committee and the funder, it was agreed that it would not be possible to achieve the required sample size within the parameters of the current study. Therefore, data extraction from clinical records was discontinued for the remaining sites but collection of data from anonymised ReSPECT forms continued to enable a quality analysis of form completion.
We then obtained the relevant approvals to conduct a feasibility study to explore whether a different study design, using care home records only, could answer this research question. We encountered several challenges in recruitment of care homes and recruited two from a target of three homes. We found that 17/75 (22.7%) of residents had both a ReSPECT form and an acute event in a 6-month period. We estimate that we would need to work with 50–60 care homes to complete a congruence analysis (see Appendix 2 for a more detailed report). This finding and our findings on the quality of recorded recommendations in our review of ReSPECT forms in general practices lead us to conclude that at present a congruence analysis as originally conceived is not feasible.
Patient and public involvement
The main aim of ECTPs is to create personalised recommendations for clinical care and treatment in emergency situations where someone cannot make decisions for themselves. Key to this is involving the person, or someone close to them if the person lacks capacity, in conversations about what is important to them so that their preference can inform the clinical recommendations. This aim is set out on the RCUK ReSPECT web pages. As we sought to evaluate how such an explicitly patient-focused process is used in primary care and community settings, we recognised the importance of patient and public involvement (PPI) and engagement at every stage and embedded PPI in our project governance structure.
Scope of patient and public involvement
Project design
Before submission of the application for funding, we held two meetings with the lay advisory group that had contributed to our previous study evaluating ReSPECT in acute NHS trusts. The group was originally recruited through Warwick University’s University/User Teaching and Research Active Partnership and members had lived experience of health conditions or being a carer. During the first meeting, we presented findings from the initial ReSPECT study evaluating its use in secondary care. The group discussed the identified lack of evidence of how the ReSPECT process works in primary care and the difference in how it is viewed between primary and secondary care. We discussed the proposed aim of this research, the suggested research questions and study methods. The group was asked for their views particularly about how to conduct the research in a way that was sensitive to patients and their families, and how to engage with the wider public, including hard to reach groups, to ascertain their opinions on ReSPECT and emergency care treatment planning. At the second meeting, the group considered feedback from our outline application and commented on our proposed responses to reviewers’ comments.
The group agreed that this research was important. They noted that it was crucial for patients and their families to have their preferences about future treatment decisions taken into account and that the process for supporting this needs to be robust and properly evaluated. The group discussed the importance of including the perspectives of marginalised and hard to reach groups and offered suggestions on recruitment from these groups for WP1 and 2. They also gave advice on the approach and conduct of interviews with patients and their families. Our lay advisors also reviewed and contributed to our application for additional funding to include a WP that focused on the experiences and perspectives of people with learning disability with regard to ReSPECT (WP4, see Chapter 7).
Investigator team
The study investigator team included a PPI member (CB) who was involved from inception in the design and development of the project and was also a member of the lay advisory group to support linkage across the project. He provided guidance on the acceptability of proposed methods, attended lay advisory group meetings, commented on all patient and family information materials and contributed to the writing and editing of reports from the different WPs. A PPI lead from the main study team (JH) also ensured linkage, communicated with the advisory group between scheduled meetings regarding project progress and any matters arising.
Advisory group
Our lay advisory group of five members had between them a range of lived experience of health care. The group met at 6-monthly intervals during the project to discuss project progress and develop and review fieldwork instruments and study documentation. They commented on draft questions for the survey of members of the public with their suggestions being incorporated into the final version. They also reviewed and commented on interim analyses of qualitative data to help interpret patient and relative experiences, and the stakeholder meeting report to help shape key messages. The group also advised on approaches and audiences for dissemination of the study findings to the public.
An integral part of WP4 (perspectives of people with a learning disability) was the inclusion of a reference group for this WP. The reference group was recruited through CHANGE (Leeds, UK) a national advocacy group for people with a learning disability, and all members had a lived experience of learning disability. This group worked closely with the study researcher and CHANGE to develop the format and content of the study workshops and pilot activities to be used in the workshops. They also contributed to the development of the resources that were created as part of this WP (see Chapter 7).
Stakeholder meeting
We invited delegates from a range of patient and public support organisations to the stakeholder meeting in addition to our lay advisory group members. Delegates participated in group discussions to develop recommendations on issues to consider in the future development of ReSPECT in community settings. Two members of the learning disability reference group presented findings from their WP at the stakeholder meeting, and examples of the materials produced and used by people with a learning disability during the workshops were displayed for delegates to view throughout the day.
Summary
The importance of PPI was recognised at an early stage of development of the project and was integral to its development, conduct, delivery and successful completion. Embedding the lived experience of people with a learning disability in development and outputs for WP4 was particularly important and enriched the overall study findings. The presence of PPI throughout the project also helped to ensure that the work retained its focus on the person at the heart of the ReSPECT process, and that language and communication was consistently clear and accessible.
Chapter 3 Attitudes and experiences of the public around emergency care treatment planning
Introduction
The development of ReSPECT involved a public consultation but beyond that, there is little information on public perceptions of emergency care treatment planning in the UK. 46 There is some literature on the attitudes and experiences of patients and their families regarding DNACPR decision-making. 10,47 A YouGov survey of the public commissioned by Compassion in Dying in 2020 found that most people did not understand why a DNACPR decision is made, or what treatment and care will be given if a doctor decides they are ‘not for CPR’. 48 Attitudes to ACP, which may include emergency care treatment preferences, have been investigated although, as with DNACPR studies, they have tended to focus on patients rather than the general public. 49–51 A study of public attitudes to ACP in Northern Ireland found that ACP was recognised as important despite limited awareness, lack of knowledge and misperceptions. 52
To situate our qualitative evaluation of ReSPECT in primary care in the wider public context we carried out focus groups and a national survey to answer the research question: What does the wider public think about the concept and use of ECTPs? Additionally, we sought to interview faith leaders to explore how faith perspectives might influence public attitudes to ReSPECT.
Focus groups with members of the public and interviews with faith leaders
Methods
Recruitment
We sought expressions of interest for focus group participation from members of the public with an interest in health through local Health Watch, community and patient organisations and patient groups linked to our participating general practices in each of our three study areas. 53 We asked our PPI advisory group for suggestions of relevant networks to approach and carried out desktop research to identify local patient and carer organisations in each area, including those representing minority groups. We provided a poster about the study, an invitation e-mail and brief information leaflet. Most expressions of interest came from advertising through local Health Watch organisations. Potential participants contacted the study team directly and were provided with further information and offered a range of dates for planned focus groups. If they agreed to participate, they were given details of how to join their focus group. Online participants had unique links to a Zoom™ (Zoom Video Communications, San Jose, CA, USA) meeting. One participant unable to attend a focus group was interviewed separately. Prior to data collection, participants were sent a copy of the ReSPECT form and a consent form. We obtained written consent at the start of the in-person group. Online, we went through the consent form with each participant and recorded their consent.
We advertised the study to faith leaders through community faith groups, local councils, university chaplaincy and NHS trust chaplaincy services in our three study areas and followed up expressions of interest as above.
Data collection
We developed topic guides with input from our lay advisory group. Focus groups were facilitated by researchers JH, SR or CM. Online and face-to-face focus groups and the individual interview followed the same process. After introducing the purpose and format of the discussion, and the ReSPECT process, facilitators used a topic guide to guide the discussion (see Report Supplementary Material 5). They prompted participants to consider potential benefits and disadvantages of emergency care treatment planning for patients, relatives, the health service and wider public, and consider aspects of implementation, including how and when ReSPECT conversations should be initiated, any potential challenges in using the forms, and if, and when ReSPECT forms should be reviewed.
Interviews with faith leaders followed the topic guide for the focus groups with additional prompts on how the values embedded in ReSPECT interact with key values in their faith.
Participants received a shopping voucher as a thank you for participation. We ran four focus groups; one of which was in person. Interviews were online apart from one faith leader interview. Focus groups lasted between 53 and 66 minutes; interviews with faith leaders lasted 56 and 62 minutes, respectively. All focus groups and interviews were recorded with consent, professionally transcribed and checked by the study team.
Analysis
We analysed the data as one data set using framework analysis. 54 Four study team members (FG, AS, JH, SR) initially each read a transcript from study area one, discussed the data and identified potential themes for public survey questions. JH read and coded all transcripts from area one using the topic guide as a framework, identifying themes from which we confirmed topics for the survey questions. Two researchers (CB and CM) then independently coded one focus group transcript to check for consistency and themes were discussed with JH. CM then further developed and refined the coding framework to analyse the remaining focus group and interview transcripts. Finally, AS read all transcripts and confirmed final themes with CM.
Results
We recruited 21 public participants to 4 focus groups, mostly in area one (3 focus groups 16 participants) and 1 individual interview. Recruitment in areas two and three was extremely challenging. We conducted two faith leader interviews; both participants were from Christian faiths. We identified four themes.
ReSPECT could help normalise discussion about emergency care
Participants across the focus groups acknowledged that death and planning for the end of one’s life were sensitive topics, and many people resist having these conversations. They agreed that ReSPECT could offer a way for individuals, families, and clinicians to begin the conversation.
It’s a really helpful tool, a kind of lever to, to have a conversation about end of life and about dying with people, and I think that’s a conversation that people find very hard to have, but it’s a really important conversation to have and I think having a document that acts as a stimulus to a conversation about end of life is really useful and really important and we don’t do enough of it, so I think it’s a good thing to have.
Public focus group 2
Participants initially discussed ReSPECT conversations as important for people approaching the end of life or with a progressive or life-limiting condition. This progressed to a discussion of relevance of ReSPECT for a much wider range of people, as emergencies could occur at any age, and that everyone inevitably would have deteriorating health. Early conversations and records of a person’s wishes could help families make difficult decisions.
I think you’re focusing more, aren’t you, on the elderly people, but you talk, it’s got the word ‘emergency’ in the title, and you could be in a car accident at 25, you know, there’s all sorts of reasons when it could be brought in.
Public focus group 2
I think life is a terminal illness. You know, … we’re all gonna get there. And I think it’s important to think about these things while you’re able to, you know, whatever your circumstances are, because it, it takes so much pressure off your family.
Public focus group 4
Good communication during the ReSPECT conversation between patient, relatives and health professional was seen as important to ensure good understanding of the purpose of the plan and the potential future scenarios and treatments. Participants were clear that the health professional needed to be skilled in having these conversations and thought that conversations would work best when the person had an established relationship with the health professional, although they recognised that this was not always possible: ‘I think it, it’s, it’s the person you have the best relationship with, not everybody has a good relationship with their doctor’ (public focus group 1).
Some participants suggested that increased public awareness of ReSPECT, for example through the media, would encourage more people to have these conversations. They suggested ideally it should become normalised ‘like the organ donor card’ (public focus group 2). The person should be at the centre of the process
A key theme across focus groups was that the ReSPECT process should focus on the individual, recording a plan that reflected their wishes and preferences about their future treatment. Some participants thought the ReSPECT plan was an excellent means for a person to communicate their wishes.
… I think they seem like a very useful tool so that you can, kind of, convey your wishes before being in that situation, if ever. At least you’ve laid out a sort of plan and your, your wishes can be respected.
Public focus group 4
However, some participants expressed concern that the ReSPECT process was insufficiently focused on the person. The form seemed medically orientated rather than person orientated. In one focus group where participants were mainly care home residents’ relatives, several compared the ReSPECT form to an ACP that they had completed for their relative on entering the home. They felt the ReSPECT plan, with its focus on emergency treatments, did not capture their relative’s reality which was more of a slow decline rather than sudden emergencies.
the one we filled in here for when my mother came in, I thought was wonderful, it was about how she wanted to be treated, you know, and it was very reassuring. I look at this and think it’s not really relevant to her, … it’s not really suitable, ’cause it’s so difficult to answer the questions. Whereas the, the form we filled in here was very warm … and personal and this is very bleak.
Public focus group 3
Participants were concerned that the person may not understand what was being discussed in a ReSPECT conversation, particularly if conversations were initiated at a late stage in a person’s illness trajectory. They commented on the potential complexity of treatment options discussed and the uncertainty of prognoses or potential future events. One participant expressed a feeling of disempowerment when considering completing a ReSPECT plan at a time of deteriorating health.
But actually, in a, a real-life scenario I think I would feel quite disempowered, that other people hold the power about things to do with my life. And I really, you know, in my most vulnerable state I don’t even know what my options are.
Public focus group 1
One faith leader suggested that it could be helpful for some people to include a faith leader in their discussions about life-sustaining treatment.
All participants across the focus groups felt strongly that the plan needed to be reviewed regularly to reflect changes in the persons health status and wishes over time.
… your views definitely change … I think it should be re-evaluated, as I say, I think to a certain degree you like to put it in the back of your mind, but sometimes I think when you’ve had more time to think about it, your views might have changed. So, I do think there should be a follow-up on it, definitely.
Public focus group 3
Yeah, that already then is a flaw in the system to me. Because what I might wish to do today may change due to experience, different circumstances. Your health might, you know, you, you, you might think your health is A today, and in two years’ time something else happens.
Public focus group 4
ReSPECT and the patient’s family
There were mixed views across the focus groups about the extent to which families should be involved in the ReSPECT process. Many thought it was important that the person’s family was involved in or aware of the ReSPECT plan to ensure that the person’s wishes were followed and take pressure off the family.
If you’ve got that understanding, there’s no fear …, you’re then at, at, at peace internally, you know, you’re at peace with what is happening to your other, to your other half, rather than not knowing what that person wants.
Faith leader 2
This will help your relatives make a difficult decision in a time when you’re not there to advise.
Faith leader 1
The ReSPECT process could also reduce conflict between family members when decisions needed to be made when the person was very unwell.
I think it helps promote clarity between the, … patient and, and their relatives about what might be wanted … It’s not necessarily going to fix all of the misapprehensions that people have, but it’s, it is a clear way of having that conversation and, and, you know, flushing out whether there are agreements or disagreement, it’s a really important thing.
Public focus group 2
[I]t, it really needs to, to be a, an open discussion which is not just linked to the immediate close person in your life. I think it has to, it has to be wider. And then the, because it’s, it will be for, for everyone it would be a very, very emotional situation to deal with.
Public interview 1
However, other participants noted that not everyone wanted their families to be involved in or know about their healthcare decisions.
And, you know, in, in some cases perhaps somebody doesn’t want this to be discussed with the whole of the family, because it is their treatment, and there are issues about confidentiality, even within the family.
Public focus group 1
Participants recognised that it was often difficult for clinicians when faced with families who wanted them to intervene for their sick relative, even when there was a form specifying that this was not what the patient wanted.
Scepticism about use of the plan in an emergency
While many participants talked about the benefits of having a ReSPECT plan, they were not confident it would be followed in the situations it was designed for.
I’m not entirely confident that having … an emergency care treatment plan will necessarily produce the result that the person was expecting, because I think there are all sorts of things that could get in the way of what somebody wants actually being implemented.
Public focus group 2
Participants identified several obstacles to effective use. They discussed practical problems in ensuring the plan was available when needed. Someone living at home may forget where the form is kept or be too sick to tell the health professional, usually a paramedic, who is attending. A potential solution would be a centrally held form or record of the plan that was accessible to clinicians at the time. Participants were generally sceptical of the ability of current NHS electronic systems to provide reliable access to these plans. Participants were not confident the recommendations on the plan would be followed. Examples were given of paramedics noting plans but then taking a different course of action because of their clinical judgement.
And both of those people had the ambulance service come, both of them showed the ambulance service the documentation, and both of them were told that they would not take that action, they were there to save life. And that upset both families very much.
Public focus group 4
Ambiguity in the plan recommendations could result in actions that were inconsistent with the plan’s intention. For example, a recommendation about not being admitted to hospital without specifying the relevant circumstances may lead to someone being admitted/not admitted inappropriately. Participants recognised that it was impossible to specify every circumstance and provide detailed management recommendations. They recognised that recommendations would need to be read quickly in an emergency so should be quite brief, but that this created a tension with communicating detailed person specific instructions about a person’s care.
You do need something that’s fairly quick to refer to, because you can’t give a, a long kind of detailed set of instructions if it’s going to be read by paramedics and, and that sort of thing in an emergency situation.
Public focus group 2
Some participants commented that it was important to think of the recommendations as guidance but that the attending clinician would need to ultimately make the treatment decision, and people would need to trust that the clinician would act in their best interests.
I’m still convinced that the doctor makes the decision at the end of the day.
For me the form is a way to help people think about these things, express an opinion, but it’s not obligatory, as it says on the form…it’s useful for clinicians who don’t know that patient. To have something there, as guidance, and know that there has been a discussion, particularly in an emergency.
Public focus group 1
Lack of resources could result in recommendations not being fulfilled. For example, if treatment at home rather than hospital was recommended this might require urgent nursing or other support.
Reflecting on these challenges to effective use of ReSPECT plans, some participants questioned how person centred the plan was: ‘it seems to me control is taken away from you and that’s what’s so frustrating and tiring and bureaucratic’ (public focus group 3). However, even if the plan was not available or could not be followed precisely, some participants still regarded the process as helpful to ensure the person’s wishes were taken into account.
I’m a realist though and I perfectly understand that come the day when I get unplanned admission to hospital nobody is actually gonna dig through my file in the GP practice, and dig this out from seven years ago, and respect my wishes. But at least my daughters might remember something that was said.
Public focus group 1
Survey of attitudes of the British public to emergency care treatment plans
Parts of this section are reproduced with permission from Underwood et al. 55 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/. To understand the views and attitudes of the public on the concept and use of emergency care treatment planning, we carried out a national survey. Here, we describe the survey and its findings.
Methods
Questionnaire development
To ensure a high-quality nationally representative population sample, we commissioned the National Centre for Social Research to include our questions in the annual British Social Attitudes (BSA) survey. 56 The BSA is the UK’s longest-running survey of public opinion. It provides a high-quality nationally representative attitudinal survey with a stratified sample based on postcode and includes face-to-face data collection using computer-assisted personal interviewing and self-completion. Question development was a collaborative process between the study team and the BSA team. Firstly, members of the study team (AS, FG, SR, JH) developed a draft set of questions, drawing on data from focus groups. Following feedback from our co-investigators and lay advisory group the questions were further refined. Next, the study team met with the BSA team and, through an iterative process, the final set of questions to be included in the BSA annual survey were agreed. We aimed to determine the willingness of members of the public to complete an ECTP for themselves or someone close to them, under what circumstances they would consider completing one and who they would prefer to complete the plan with. We also sought their views on potential benefits or harms of having an ECTP. A sample of the questions were then tested by the BSA team in cognitive interviews with 10 people, and the full set of finalised questions was piloted with a sample of 56 participants recruited from the BSA panel database and using telephone interviews. Results of the cognitive interviews and pilot were discussed with the study team and minor modifications made to question wording (see Report Supplementary Material 6 for final questions).
Data collection
Data collection was carried out in accordance with the National Centre for Social Research’s protocol for delivery of the BSA survey. Invitations to participate in the survey, with the option of online or telephone interview completion, are sent to a stratified sample of households in the UK identified from the postcode address file with up to two adults in each household able to participate. Two online access codes are provided to each household. If selected households do not wish to complete the survey online, they are able to call a freephone number and arrange to complete the survey by telephone with a specialist telephone interviewer. To maximise response up to three invitation mailings are made. Respondents are offered a conditional £10 incentive to participate. Fieldwork took place between 9 September and 30 October 2022. The target sample for administration of our question set was 1000.
Analysis
In addition to descriptive statistics for each question, we present logistic regression analyses investigating the variables associated with the three dichotomised dependent variables: (1) being in favour of anyone being able to have an ECTP (strongly and somewhat in favour vs. the other categories); (2) whether they would like an emergency care and treatment plan at present (definitely and probably would like vs. the other categories) and (3) (for those who did not already have an a emergency care and treatment plan) how comfortable (very and fairly comfortable vs. the other categories) they would feel about making such a plan for themselves. For each analysis, the independent variables were age, gender, ethnicity, educational level, having an illness lasting more than 12 months, caring for someone ill or with a disability and being close to someone with a condition that could shorten their life. These were chosen after discussion within the study team to identify ‘a priori’ the most important possible independent variables. Using the statistical software R Core Team (2023; R Foundation for Statistical Computing, Vienna, Austria) for each dependent variable, both fully adjusted model and non-adjusted models were fitted at the 5% significance level. With very few missing data, the logistic regression models for binary data fit well.
Results
All data used in these analyses have come from the National Centre for Social Research British Social Attitudes Survey 2023 © National Centre for Social Research September 2023.
Of the 6699 respondents to the BSA survey 1135 completed our module. Overall, they were sociodemographically representative of the UK although minority ethnic groups were slightly under-represented against age standardised values (see Appendix 3, Table 10). Seventeen respondents (1.5%) currently had an ECTP. Among these respondents, the most common trigger for ECTP completion was a diagnosis of a life-threatening illness (7/17) or long-term condition (6/17) (see Appendix 3, Table 11). Eight respondents with a completed ECTP were aged under 45 years and 7 aged 45 years or over. Most plans (10/17, 59%) were completed by the respondent’s GP (6/17) or another doctor who knew them well (4/17; see Appendix 3, Table 12). Of respondents with an ECTP, most were very comfortable (9/17) or comfortable (5/17) with the discussion. However, one respondent was fairly uncomfortable and one very uncomfortable with the discussion.
Attitudes to emergency care treatment plans
A large majority of respondents were in favour of people being able to have an ECTP if they so wished, with 908/1135 (80%) at least somewhat in favour (see Appendix 3, Table 13). Females were slightly more likely to be in favour than males [82% vs. 77%; odds ratio (OR) 1.45; 95% confidence interval (CI) 1.06 to 1.97; p = 0.02]. When compared with those with no qualifications, people with degrees were significantly (p = 0.002) more likely to be in favour (70% vs. 84%; OR 2.68, 95% CI 1.42 to 5.07). However, the absolute difference is modest and there is not a clear trend for more people with a higher educational level to be more in favour of ECTPs. Overall, ethnicity did not appear to affect people’s views, although the numbers in each group were small. However, people of Asian ethnicity might be less likely than those identifying as white British to be in favour of everyone being able to have an ECTP 67% versus 82% (OR 0.45, 95% CI 0.25 to 0.84, p = 0.012) (Table 1).
| Are you in favour or against anyone being able to have an emergency care and treatment plan if they wish?a N = 1135 | ||||
|---|---|---|---|---|
| In favour | p-value | OR (95% CI) | ||
| (n/N) | (%) | |||
| Gender | ||||
| Male | 380/493 | 77 | 1 | |
| Female | 510/619 | 82 | 0.02 | 1.45 (1.06 to 1.97) |
| Other | 7/8 | 88 | 0.382 | 2.62 (0.3 to 22.69) |
| Age (years) | ||||
| 18–24 | 51/66 | 77 | – | 1 |
| 25–34 | 137/173 | 79 | 0.922 | 1.04 (0.51 to 2.11) |
| 35–44 | 138/172 | 80 | 0.748 | 1.12 (0.55 to 2.3) |
| 45–54 | 160/205 | 78 | 0.955 | 1.02 (0.51 to 2.04) |
| 55–59 | 85/99 | 86 | 0.14 | 1.89 (0.81 to 4.4) |
| 60–64 | 86/107 | 80 | 0.598 | 1.24 (0.56 to 2.73) |
| 65–69 | 82/107 | 77 | 0.992 | 1 (0.47 to 2.17) |
| 70 + | 168/205 | 82 | 0.295 | 1.48 (0.71 to 3.07) |
| Ethnicity | ||||
| White | 820/1005 | 82 | – | 1 |
| Black | 10/14 | 71 | 0.285 | 0.52 (0.15 to 1.73) |
| Mixed | 30/44 | 68 | 0.115 | 0.57 (0.29 to 1.15) |
| Asian | 37/55 | 67 | 0.012 | 0.45 (0.25 to 0.84) |
| Qualifications | ||||
| No qualifications | 43/61 | 70 | – | 1 |
| Qualifications less than A level | 138/183 | 75 | 0.358 | 1.37 (0.7 to 2.66) |
| A-levels/SCE Highers | 127/158 | 80 | 0.048 | 2.05 (1.01 to 4.17) |
| Other Higher Education | 129/170 | 76 | 0.346 | 1.38 (0.7 to 2.72) |
| Degree or equivalent | 446/528 | 84 | 0.002 | 2.68 (1.42 to 5.07) |
| Do you have any physical or mental conditions or illnesses lasting or expected to last 12 months or more? | ||||
| No | 624/777 | 80 | – | 1 |
| Yes, but does not reduce activity | 82/99 | 83 | 0.704 | 1.12 (0.63 to 1.98) |
| Yes, and reduces activity | 198/254 | 78 | 0.528 | 0.89 (0.61 to 1.29) |
| Is there anyone who you look after or give special help to, for example, someone who is sick, has a long-term physical or mental disability or is elderly? | ||||
| No | 670/829 | 81 | 1 | |
| Yes | 195/246 | 79 | 0.431 | 0.86 (0.58 to 1.26) |
| Yes, but only in a professional capacity as part of my job | 43/60 | 72 | 0.12 | 0.61 (0.33 to 1.14) |
| Do you or does someone close to you have a condition or illness that you think is likely to shorten life? | ||||
| No | 647/817 | 79 | 1 | |
| Yes | 261/318 | 82 | 0.298 | 1.22 (0.84 to 1.76) |
Of respondents who did not currently have an ECTP, 698/1112 (63%) felt they would be at least fairly comfortable making an ECTP, with only 49/1112 (4%) saying they would be very uncomfortable having an ECTP discussion (see Appendix 3, Table 14). Compared with those with no qualifications, people with degrees were more likely to feel comfortable having an ECTP (70% vs. 49%; OR 2.48, 95% CI 1.40 to 4.39; p = 0.002; Table 2). Comfort with completing an ECTP was not significantly associated with age, gender, or experience of caring for someone with a long-term health condition. Of those respondents who said they would like to have an ECTP for themselves, half (316/618, 51%) would want their GP to complete this with them while one-quarter (161/618, 26%) would want a doctor or nurse who did not know them but was trained in making ECTPs to do this (see Appendix 3, Table 12).
| How comfortable or uncomfortable do you feel about making an emergency care and treatment plan yourself with a doctor or nurse?a (N = 1112)b | ||||
|---|---|---|---|---|
| Comfortable | p-value | OR (95% CI) | ||
| (n/N) | (%) | |||
| Gender | ||||
| Male | 309/482 | 64 | – | 1 |
| Female | 380/609 | 62 | 0.647 | 0.94 (0.72 to 1.22) |
| Other | 2/7 | 29 | 0.118 | 0.25 (0.05 to 1.41) |
| Age (years) | ||||
| 18–24 | 40/62 | 65 | – | 1 |
| 25–34 | 116/168 | 69 | 0.977 | 1.01 (0.53 to 1.92) |
| 35–44 | 100/168 | 60 | 0.197 | 0.66 (0.35 to 1.24) |
| 45–54 | 117/204 | 57 | 0.141 | 0.63 (0.34 to 1.17) |
| 55–59 | 66/98 | 67 | 0.822 | 1.08 (0.53 to 2.21) |
| 60–64 | 73/107 | 68 | 0.885 | 1.05 (0.52 to 2.13) |
| 65–69 | 65/104 | 63 | 0.487 | 0.78 (0.39 to 1.56) |
| 70 + | 121/200 | 61 | 0.359 | 0.74 (0.39 to 1.41) |
| Ethnicity | ||||
| White | 633/987 | 64 | – | 1 |
| Black | 6/13 | 46 | 0.092 | 0.38 (0.12 to 1.17) |
| Mixed | 22/43 | 51 | 0.097 | 0.58 (0.30 to 1.11) |
| Asian | 32/54 | 59 | 0.354 | 0.76 (0.42 to 1.36) |
| Educational level | ||||
| No qualifications | 29/59 | 49 | – | 1 |
| Qualification less than A level | 91/179 | 51 | 0.792 | 1.08 (0.59 to 1.99) |
| A-levels/SCE Highers | 94/153 | 61 | 0.064 | 1.82 (0.97 to 3.44) |
| Other Higher Education | 100/166 | 60 | 0.273 | 1.65 (0.68 to 4.02) |
| Degree or equivalent | 365/521 | 70 | 0.002 | 2.48 (1.4 to 4.40) |
| Do you have any physical or mental conditions or illnesses lasting or expected to last 12 months or more? | ||||
| No | 479/765 | 63 | – | 1 |
| Yes, but does not reduce activity | 74/97 | 59 | 0.013 | 1.91 (1.14 to 3.19) |
| Yes, and reduces activity | 144/245 | 59 | 0.452 | 0.89 (0.65 to 1.21) |
| Is there anyone who you look after or give special help to, for example, someone who is sick, has a long-term physical or mental disability or is elderly? | ||||
| No | 512/816 | 63 | ||
| Yes | 154/238 | 65 | 0.57 | 1.10 (0.79 to 1.53) |
| Yes, but only in a professional capacity as part of my job | 32/58 | 58 | 0.31 | 0.74 (0.42 to 1.32) |
| Do you or does someone close to you have a condition or illness that you think is likely to shorten life? | ||||
| No | 494/805 | 61 | ||
| Yes | 204/307 | 66 | 0.193 | 1.23 (0.90 to 1.67) |
Who would like an emergency care treatment plan for themselves and when would they want to have it in place?
Half of respondents without an ECTP (620/1112; 56%) would want one at present (see Appendix 3, Table 15). Overall, fewer people in older age groups would want an ECTP at present; however, the difference was only statistically significant for one comparison; 63% in those aged 18–24 years compared with 47% for those aged 65–69 years (p = 0.045, OR 0.5, 95% CI 0.26 to 0.98; Table 3). People with a chronic physical or mental health condition that reduces their activity were more likely to want a plan at present compared with those in good health (64% vs. 52%; OR 1.78, 95% CI 1.30 to 2.45; p < 0.001; see Table 3). Knowing or caring for someone with a long-term physical or mental health condition did not affect whether they would want an ECTP for themselves (see Table 3). In answer to a more specific question of when you would want an ECTP in place for yourself, 152/1112 (14%) would want one ‘now’ with just 36/1112 (3%) saying that they would never want one. Developing a long-term condition or becoming disabled would lead 467/1112 (42%) and 481/1112 (43%) respondents respectively to want an ECTP. Even more 534/1112 (57%) would want a plan if they developed a life-threatening condition (see Appendix 3, Table 16). Of the 441 people who said they would want an ECTP when they were older, the peak decades identified were their 60s and 70s with 270/441 (61%) wanting an ECTP in place by the time they were aged 70 years (see Appendix 3, Table 17). When asked if they would like to be involved in completing an ECTP for a close family member if they were not able to do this for themselves, 930/1135 (82%) said that they definitely or probably would (see Appendix 3, Table 14).
| Would you or would you not like to have an emergency care and treatment plan for yourself at present?a (N = 1112)b | ||||
|---|---|---|---|---|
| Willing | p-value | OR (95% CI) | ||
| (n/N) | (%) | |||
| Gender | ||||
| Male | 260/482 | 54 | ||
| Female | 349/609 | 57 | 0.321 | 1.14 (0.88 to 1.46) |
| Other | 2/7 | 29 | 0.18 | 0.3 (0.05 to 1.73) |
| Age (years) | ||||
| 18–24 | 39/62 | 63 | – | 1 |
| 25–34 | 109/168 | 65 | 0.912 | 1.04 (0.55 to 1.94) |
| 35–44 | 90/168 | 54 | 0.164 | 0.64 (0.35 to 1.20) |
| 45–54 | 106/204 | 52 | 0.089 | 0.59 (0.32 to 1.08) |
| 55–59 | 56/98 | 57 | 0.366 | 0.73 (0.37 to 1.44) |
| 60–64 | 61/107 | 57 | 0.275 | 0.69 (0.35 to 1.35) |
| 65–69 | 49/104 | 47 | 0.045 | 0.50 (0.26 to 0.98) |
| 70 + | 108/200 | 54 | 0.195 | 0.66 (0.35 to 1.24) |
| Ethnicity | ||||
| White | 544/987 | 55 | – | 1 |
| Black | 10/13 | 77 | 0.117 | 2.91 (0.76 to 11.06) |
| Mixed | 23/43 | 53 | 0.595 | 0.84 (0.44 to 1.60) |
| Asian | 33/54 | 61 | 0.461 | 1.25 (0.69 to 2.25) |
| Educational level | ||||
| No qualifications | 33/59 | 56 | – | 1 |
| Qualification less than A level | 95/179 | 53 | 0.699 | 0.89 (0.48 to 1.63) |
| A-levels/SCE Highers | 74/153 | 48 | 0.285 | 0.71 (0.38 to 1.33) |
| Other Higher Education | 93/166 | 56 | 0.681 | 1.13 (0.64 to 1.99) |
| Degree or equivalent | 310/521 | 60 | 0.681 | 1.13 (0.64 to 1.99) |
| Do you have any physical or mental conditions or illnesses lasting or expected to last 12 months or more? | ||||
| No | 400/765 | 52 | – | 1 |
| Yes, but does not reduce activity | 56/97 | 58 | 0.159 | 1.37 (0.88 to 2.14) |
| Yes, and reduces activity | 158/245 | 64 | < 0.001 | 1.78 (1.30 to 2.45) |
| Is there anyone who you look after or give special help to, for example, someone who is sick, has a long-term physical or mental disability or is elderly? | ||||
| No | 461/816 | 56 | ||
| Yes | 130/238 | 55 | 0.481 | 0.89 (0.65 to 1.23) |
| Yes, but only in a professional capacity as part of my job | 27/58 | 47 | 0.054 | 0.57 (0.32 to 1.01) |
| Do you or does someone close to you have a condition or illness that you think is likely to shorten life? | ||||
| No | 437/805 | 54 | ||
| Yes | 181/307 | 59 | 0.348 | 1.15 (0.86 to 1.55) |
Perceived potential benefits and harms of emergency care treatment plans
To explore how responders felt about potential benefits and harms of ECTPs, they were asked whether they agreed to a series of statements in relation to ECTPs. Predominately, 938/1135 (83%) respondents agreed or strongly agreed that ECTPs would help avoid their family needing to make difficult decisions on their behalf, and that a plan would ensure doctors and nurses knew their wishes (Table 4). Nevertheless, a small majority 628/1135 (55%) agreed that there is a serious risk that a plan could be out of date and so not reflect their current views or health condition, and a substantial minority 330/1135 (29%) agreed that in having a plan they might not get a treatment that would save their life (see Table 4).
| Please say how much you agree or disagree with the following statements about having an emergency care and treatment plan (N = 1135) | ||||
|---|---|---|---|---|
| I might not get the treatment that could save my life, n (%) | Having a plan can avoid my family having to make difficult decisions for me, n (%) | There is a serious risk that the plan could be out of date and not reflect my current views or my current health condition, n (%) | Having a plan ensures that doctors and nurses know my wishes, n (%) | |
| Strongly agree | 66 (6) | 302 (27) | 90 (8) | 227 (20) |
| Agree | 264 (23) | 636 (56) | 538 (47) | 712 (63) |
| Neither agree nor disagree | 445 (39) | 143 (13) | 346 (30) | 142 (13) |
| Disagree | 256 (23) | 20 (2) | 124 (11) | 29 (3) |
| Strongly disagree | 89 (8) | 22 (2) | 23 (2) | 13 (1) |
| Don’t know/refused | 15 (1) | 12 (1) | 14 (1) | 12 (1) |
For each of our regression models, the results of our univariable analyses were not materially different from our multivariable analyses (see Appendix 3, Tables 18–20).
Summary
Overall, participants in the focus groups and faith leader interviews were supportive of the concept of ReSPECT or emergency care treatment planning. They thought it could be an important tool in precipitating and facilitating important conversations about end-of-life care. However, they thought the process and form needed to be more person centred. They emphasised the importance of in-depth conversations to understand the person’s preferences and to be confident that the person understood the future options being discussed. Involving the family was seen as important but the level of involvement needs to be determined by the person whose plan it is. Several concerns were raised about whether the plans would be available or followed in an emergency.
From our survey, we found that members of the public across the UK are overwhelmingly supportive of anyone being able to have an ECTP if they wished, and half of those without a plan would want one for themselves. However, very few respondents currently have an ECTP in place. Most respondents would also like to be involved in completing a plan for a close family member if the person was unable to do so for themselves. Respondents with a chronic physical or mental condition that reduces daily activity were more likely to want an ECTP than those in good health. Unexpectedly, younger participants, were more likely to want a plan for themselves than older participants. Potential triggers for completing an ECTP were a change in health status with a diagnosis of a chronic disabling or life-threatening condition or increasing age. Respondents recognised benefits of ECTPs including ensuring their wishes about treatment are known and easing decision-making burdens on their family. However, they also recognised potential risks of ECTP recommendation becoming out of date and a potential risk that they may not receive a life-saving treatment. Respondents would prefer to complete an ECTP with their GP or a doctor or nurse trained in ECTP conversations, reflecting views expressed in our qualitative data about the importance of the relationship and quality of the conversation.
Strengths and limitations
To our knowledge, we have completed the first community survey of the UK public’s views and attitudes to the completion of ECTPs. The use of the annual BSA survey to collect these data means that we can be confident that our sample is nationally representative and that the data quality is good. However, this approach will exclude many for whom ECTPs are most relevant, that is frail older people and those with cognitive impairment. The slight under-representation for people from minority ethnic groups is typical of push surveys of this nature but is not large enough to affect our overall conclusions. The rigorous process for developing our questions, including preparatory qualitative work, and their piloting by the BSA survey team minimises question ambiguity. Nevertheless, it is still possible that some respondents misunderstood the purpose of each question. Some caution is needed when interpreting statistical significance because of the large number of analyses done.
Despite contacting a wide range of community and faith groups, several of whom supported advertising the study, we received very few expressions of interest for focus group participation. Feedback suggested that many groups had insufficient resources to support recruitment. GP patient groups had often stopped during the COVID-19 pandemic. We were unable to purposively select participants for demographic variability because of lack of interest in two study areas. The small number of faith leader participants meant that it was not possible to achieve our aim of exploring the impact of different faith values on how people might view or engage with ReSPECT. All participants had a particular interest in, or experience of ReSPECT or ACP so may not have reflected the views of the general public. However, because of their interest and experience, our participants were able to provide in depth reflection on the topic.
Chapter 4 How ReSPECT is used in primary and community care, experiences of health and social care professionals
In this chapter, we focus on how ReSPECT is used and experienced in practice in a community setting. First, we report our survey documenting how GPs from across England view and use ReSPECT. Then using our qualitative data, we explore how GPs and their staff conceptualise ReSPECT, initiate and carry out the ReSPECT conversation and complete the plan. We explore their views and experiences of how they negotiate challenges, what happens after the ReSPECT plan is complete and any monitoring of the ReSPECT process within their practice. Similarly, we report the views and experiences of ReSPECT among senior staff in care homes and other health and social care staff who encounter the ReSPECT process and ReSPECT plans completed in the community. We then report on the content of ReSPECT forms stored in general practice medical records.
General practitioner survey
Parts of this section are reproduced with permission from Underwood et al. 57 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/
Methods
Obtaining good response rates to surveys of GPs’ views is challenging; return rates of ˂ 30% are common. 58–60 There are substantial operational challenges in sourcing up-to date contact details of groups of GPs that can provide national representation, and that include the range of professional roles (partners, salaried non-principals, locums and trainees). For these reasons, we commissioned a market research company, medeConnect, to include our questions in their monthly online survey of 1000, regionally representative, UK GPs (GP Omnibus). 61
Questionnaire development
Drawing on initial analysis of our interviews with GPs, and reflecting the questions in our public attitudes survey, members of the study team (AS, FG, JH, CB) developed a draft set of questions. We aimed to measure experience of using ECTPs compared with standalone DNACPR forms, views on the use of ECTPs in primary care, and how likely they were to complete a plan for their patients. During question development, we identified that knowing which factors might predict how comfortable GPs were at having an emergency care treatment planning consultation with a patient, or family member, as a key questions of interest, and likely to reflect how likely a GP was to complete a plan with their patients. We originally planned to use 11-point numerical rating scales to assess GPs’ attitudes to aspects of emergency care treatment planning. Input from our qualitative work and the work we did refining the questions led us to conclude that five-point Likert scales were more likely to be satisfactorily completed and the findings would be easier to interpret; that is, ‘very comfortable’ to ‘very uncomfortable’ for our main outcomes of interest.
Following feedback from our lay advisory group and GP co-applicants, a revised set of questions was further refined through cognitive, think-aloud interviews with a small number of GPs not involved in the study. The final set of questions were piloted within the format of the online survey (see Report Supplementary Material 6).
Data collection
The market research company, medeConnect, draw their sample from GPs who are registered with Doctors.net.uk and who have been active on this online platform. Opportunity to take part in the monthly survey is posted on the home page of all GPs who have been active on the site within the previous 90 days and an e-mail is sent inviting participation to all GPs who have given consent to be approached to take part in research. Each GP can only participate once. Doctors.net.uk undertakes weekly automated checks of its membership base against the publicly available licensed status of practising doctors in the UK as published and maintained by the General Medical Council. Before a survey starts, the questions are tested by the internal research team, the sponsor (in this case the research team based at Warwick) and a small sample of the target group (Miles N, personal communication, medeConnect, Abingdon, 16 February 2023).
Analysis
For a binary outcome on our key question of interest (very comfortable or comfortable completing a plan vs. all other responses) a sample size of 1000 would, if 50% were ‘comfortable’, provide precision of 6.2%, or if 80% were comfortable a precision of 5%. This is the size of the medeConnect monthly survey and hence our original sample size. However, this includes UK GPs based outside England who were not covered by our research ethics approval. Thus, a smaller number of responses was expected. We present descriptive statistics for each question. For the outcome of how comfortable GPs are in having emergency care and treatment plan discussions, with patients or with someone close to the patient, using the statistical software R Core Team (2023), we first did univariable logistic regression analyses at the 5% significance level with gender, GP role, NHS region, type of area (major conurbation, large town/city, medium town/city, small town/city, hamlet) years since completion of GP training, and use of ReSPECT form versus DNACPR/Other as explanatory variables. We then constructed a fully adjusted logistic regression model. We repeated this using a backward elimination approach to select the most statistically significant variables.
Results
The survey ran from 4 November to 27 November 2022. We received 841 valid responses, all fully completed. Our respondents’ demographic characteristics are largely representative of the whole population of English GPs (see Appendix 4, Table 21). Half (426/841, 51%) of respondents reported that their practice used standalone DNACPR forms. ReSPECT forms were used by 41% (345/842) and 7% (55/841) used other locally developed ECTPs with 2% (15/841 reporting no ECTP or no knowledge of ECTP use) (Table 5). There were substantial regional differences in the forms used; ReSPECT was the predominant form used in the East Midlands (49/62, 79%) and West Midlands (74/92, 80%) whereas a DNACPR form was most commonly used in London (87/114, 76%), the North East (33/44, 75%) and the North West (88/115, 77%) (see Appendix 4, Table 22).
| Totals and percentages for the emergency care and treatment planning form completion | ||
|---|---|---|
| Total, n (N = 841) | % (CI) | |
| What form of emergency care and treatment plans does your practice use? | ||
| ReSPECT | 345 | 41 (0.38 to 0.44) |
| DNACPR | 426 | 51 (0.47 to 0.54) |
| Other ECTP | 55 | 7 (0.05 to 0.08) |
| None/don’t know | 15 | 2 (0.01 to 0129) |
| Who completes emergency care and treatment plans within your practice? | ||
| GP | 780 | 93 (0.91 to 0.94) |
| GP trainee | 0 | – |
| Practice nurse | 79 | 9 (0.07 to 0.11) |
| Advanced nurse practitioner | 234 | 28 (0.25 to 0.31) |
| Specialist nurse practitioner for elderly care | 140 | 17 (0.14 to 0.19) |
| Who do you think should be able to complete ECTPs in a GP practice? | ||
| GP | 797 | 95 (0.93 to 0.96) |
| GP trainee | 522 | 62 (0.59 to 0.65) |
| Practice nurse | 350 | 42 (0.38 to 0.45) |
| Advanced nurse practitioner | 648 | 77 (0.74 to 0.80) |
| Specialist nurse practitioner for elderly care | 663 | 79 (0.76 to 0.82) |
| Emergency care practitioner | 550 | 65 (0.62 to 0.69) |
| Who do you think should be able to complete ECTPs in the community? | ||
| Specialist nurse practitioner for palliative care | 802 | 95 (0.94 to 0.97) |
| Other specialist nurse practitioner | 691 | 82 (0.80 to 0.85) |
| Community matron/senior nurse practitioner for community care | 690 | 82 (0.79 to 0.85) |
| District nurse | 467 | 56 (0.52 to 0.59) |
| Senior care home staff | 207 | 25 (0.22 to 0.28) |
| Senior nurses in nursing home | 430 | 51 (0.48 to 0.55) |
| When would you consider completing an emergency care and treatment plan for a patient? | ||
| When a patient reaches a certain age | 199 | 24 (0.21 to 0.27) |
| When a patient is diagnosed with a life-threatening condition | 722 | 86 (0.83 to 0.88) |
| When a patient is diagnosed with a chronic long-term condition | 509 | 61 (0.57 to 0.64) |
| When a patient is severely disabled | 497 | 59 (0.56 to 0.62) |
| When you think a patient is likely to die within 12 months | 813 | 97 (0.95 to 0.98) |
| When a patient is admitted to a care home | 596 | 71 (0.68 to 0.74) |
| When do you review an emergency care and treatment plan for a patient? | ||
| When a patient requests it | 477 | 57 (0.53 to 0.60) |
| When a patient is discharged from hospital with an ECTP | 389 | 46 (0.43 to 0.50) |
| Annually | 309 | 37 (0.33 to 0.40) |
| 6-monthly | 104 | 12 (0.10 to 0.15) |
| Annually or 6-monthly, or a > 75 years health check | 486 | 58 (0.54 to 061) |
| During or following the annual health check for patients aged 75 years or over | 238 | 28 (0.25 to 0.31) |
| When you think the patient’s health has changed | 595 | 71 (0.68 to 0.74) |
| My practice does not have a system for reviewing ECTP forms | 169 | 20 (0.17 to 0.23) |
Almost all respondents (780/841, 92%) reported that in their practice ECTPs were completed by GPs, with some practices also including advanced nurse practitioners (234/841, 28%) or specialist nurse practitioners in elderly care (140/841, 17%) in this role. No respondents reported GP trainees being involved in completing ECTPs. However, respondents thought a wider range of healthcare professionals should be able to complete these forms, including GP trainees (522/841, 62%), advance nurse practitioners (648/841, 77%) and specialist nurse practitioners in elderly care (663/841, 79%; see Table 5). Similarly, there was broad support for a wide range of community-based health and social care professionals being able to complete ECTPs, with over 80% respondents supporting senior community nurses completing ECTPs (82–95%), half supporting senior nurses in nursing homes completing the forms (430/841, 51%) and 25% (207/841) supporting senior care home staff to do this (see Table 5).
The primary trigger for considering completing an ECTP was a change in the patient’s health state, particularly if the health state was life limiting (diagnosed with a life-threatening condition (722/841, 86%), or likely to die within the next 12 months (813/841, 97%). Plans were less frequently considered for someone living with a long-term condition (509/841, 61%) or who was severely disabled (497/841, 59%). Admission to a care home was a prompt for 71% (596/841) respondents, whereas only 24% (199/841) would consider completing a plan based on the patient’s age alone. Change in health status was the main trigger for a review of an ECTP (595/841, 71%), with only 58% (486/841) of respondents reporting any form of regular review (annual, 6-monthly or at over 75 years health check). Strikingly, only 57% (477/841) of respondents reported reviewing an ECTP in response to a patient request (see Table 5).
Overall, emergency care treatment planning was viewed positively, with 90% (751/841) respondents agreeing that having a plan ensures that treating clinicians know the patient’s wishes and 82% (689/841) agreeing it can avoid patients’ families making difficult decisions. However, 50% (425/841) respondents agreed that a patient’s current health condition may not be reflected in the plan when implemented and 41% (348/841) that there is a serious risk it could be out of date when needed (Table 6). A minority (142/841, 17%) of respondents agreed with the statement that having an ECTP means that the patient might not get a treatment that would save their life (see Table 6).
| Strongly agree, n (%) | Agree, n (%) | Neither agree nor disagree, n (%) | Disagree, n (%) | Strongly agree, n (%) |
|---|---|---|---|---|
| Having a plan means that the patient might not get a treatment that could save their life | ||||
| 14 (2) | 128 (15) | 131 (16) | 375 (45) | 193 (23) |
| Having a plan can avoid the patient’s family having to make difficult decisions for them | ||||
| 200 (24) | 489 (58) | 104 (12) | 38 (5) | 10 (1) |
| There is a serious risk that the plan could be out of date when implemented and not reflect the patient’s current views | ||||
| 33 (4) | 315 (37) | 277 (33) | 200 (24) | 16 (2) |
| The patient’s current health condition may not be reflected in the plan when implemented and there is a serious risk it could be out of date | ||||
| 34 (4) | 391 (46) | 235 (28) | 166 (20) | 15 (2) |
| Having a plan ensures that treating clinicians know the patient’s wishes | ||||
| 224 (27) | 527 (63) | 80 (10) | 9 (1) | 1 (0) |
Seventy-two respondents (9%) reported that a family member or someone close to the patient was not involved in the conversation the last time they had completed an ECTP. The most common reason for not involving the patient’s family was that the patient had capacity (54/72, 75%), although on occasion the family were not available (18/72, 25%) or the patient did not want the family involved (11/72; 15%). On just one occasion, this was because the family did not want to be involved (see Appendix 4, Table 23).
Most responders reported being comfortable having ECTP conversations with both the patient (679/841, 81%) and the patient’s family (668/841, 79%; Table 7). In our univariable analyses, for conversations with patients we found that when compared with London, GPs in five regions were more comfortable in having emergency care planning conversations. GPs working in a larger practice (> 12,500), and those who reported using a ReSPECT form were also more comfortable with emergency care and treatment planning discussions. Those completing their GP training more than 20 years ago were less comfortable, and locum/salaried GPs were also less comfortable with these discussions (see Appendix 4, Table 24). A similar pattern was seen for discussions with the patient’s family or someone important to the patient (see Appendix 4, Table 25).
| How comfortable or uncomfortable do you feel having conversations about an emergency care and treatment plan? (N = 841) | ||||
|---|---|---|---|---|
| Very comfortable, n (%) | Fairly comfortable, n (%) | Neither comfortable nor uncomfortable, n (%) | Fairly uncomfortable, n (%) | Very uncomfortable, n (%) |
| How comfortable or uncomfortable do you feel having conversations about an emergency care and treatment plan with patients? | ||||
| 251 (30) | 428 (51) | 112 (13) | 46 (5) | 4 (0) |
| How comfortable or uncomfortable do you feel having conversations about an emergency care and treatment plan with the patient’s family (or someone important to the patient)? | ||||
| 227 (27) | 441 (52) | 122 (15) | 45 (5) | 6 (1) |
In our adjusted analyses, for conversations with patients, locum and salaried GPs were substantially less likely than GP partners to be comfortable having ECTP conversations (OR 0.51, 95% CI 0.31 to 0.83, and 0.53, 95% CI 0.34 to 0.82, respectively; see Appendix 4, Table 24). For conversations with family members, the difference was only statistically significant for salaried GPs (OR 0.58, 95% CI 0.38 to 0.88; see Appendix 4, Table 25).
General practitioners in the South West and the North East were substantially more likely to be comfortable with emergency care treatment planning conversations with patients than GPs in London (OR 4.30, 95% CI 1.50 to 13.3 and 4.10, 95% CI 1.29 to 15.1, respectively). Considering conversations with family members, GPs from the South-East, East Midlands and Yorkshire and Humber were also more comfortable than GPs from London (OR 3.06, 95% CI 1.24 to 7.59; 4.03, 95% CI 1.23 to 13.2; 3.15, 95% CI 1.21 to 8.25, respectively; see Appendix 4, Tables 24 and 25).
General practitioners whose practices used ReSPECT reported being more comfortable having these conversations with both patients and family members compared with GPs who reported use of DNACPR forms (OR 1.72, 95% CI 1.1 to 2.69 and OR 1.85, 95% CI 1.19 to 2.87, respectively). A broadly similar pattern was seen for conversations with family members or someone important to the patient (see Appendix 4, Tables 24 and 25). Results from our sensitivity analysis using a backwards elimination model were not materially different (see Appendix 4, Table 26).
Primary and community health and social care professionals’ experiences of the ReSPECT process
Parts of this section are Reproduced with permission from Slowther et al. 62 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/
Methods
We visited GP practices and talked to staff to understand their processes related to ReSPECT, interviewed GPs and other practice staff involved in the ReSPECT process, interviewed senior staff from care homes and carried out focus groups with other health and social care professionals. We obtained from participating practices, anonymised demographic data on all patients with a completed ReSPECT form documented in the previous 12 months.
Recruitment
General practices and their staff
Three CRNs recruited practices across three diverse CCG areas in England (Figure 1). During site initiation visits, we obtained consent from the designated principal investigator at each site for their practice to be involved in the study. We arranged a suitable time for the researcher to spend a day at their practice to learn about their ReSPECT procedures from clinical and administrative staff. Each principal investigator was asked to identify two to three GPs and/or specialist nurses who were involved in conducting the ReSPECT process in their practice. Invitations to participate were e-mailed and interviews arranged.
FIGURE 1.
Recruitment flowchart for GP practices.
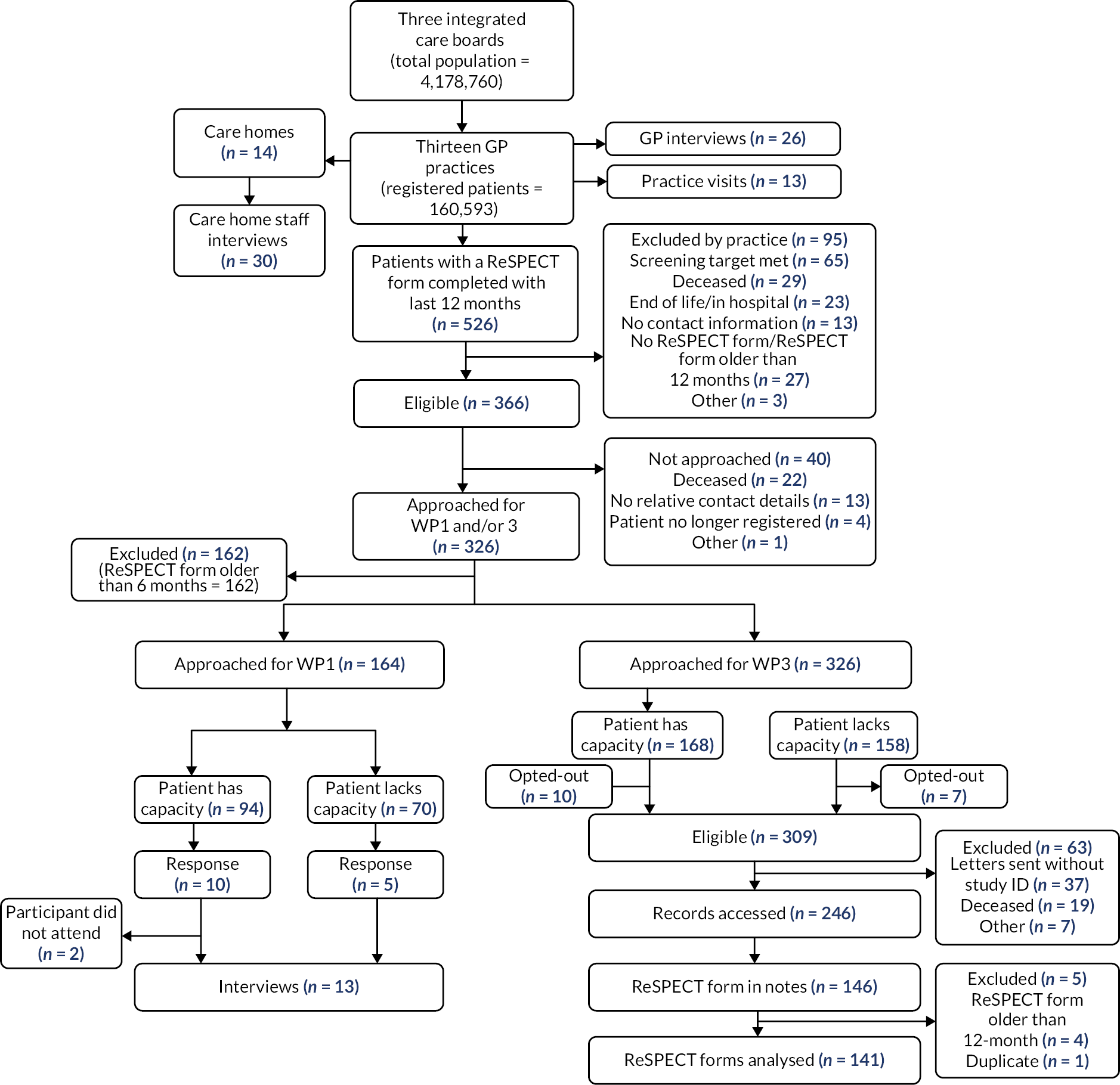
Care homes and care home staff
We recruited care homes through the GP practices participating in the study plus additional care home staff through the local Enabling Research in Care Homes (ENRICH) team. 63 Care homes that expressed interest in participating were contacted by the study team. We contacted interested care homes to provide further information and arrange a meeting (in person or online) with the care home manager to discuss the study and what it would involve for them and their staff if they took part. We purposively sampled care home staff most likely to have engaged with the ReSPECT form or process, guided by the care home manager/senior staff member who had knowledge of the care home and ReSPECT. Care home staff recruited by ENRICH contacted the study team directly.
Other health and care professionals who engage with ReSPECT
We aimed to run focus groups in each of our three study areas, with community-based nurses, allied health professionals working in the community, emergency department staff and social care professionals. We advertised the study through networks and teams of local practitioners and for home care workers, through local private home care organisations. Potential participants contacted the study team directly and were provided with further information and offered a range of dates for planned focus groups. If they were unable to join a focus group a time for an individual interview was agreed.
Data collection
Participating practices identified patients with ReSPECT form completion documented in the previous 12 months and provided anonymised demographic data for these patients to the study team.
During visits to GP practices the researcher aimed to find out about the ReSPECT process from initiation through to form storage. Anonymised field-notes of behaviours, actions and conversations were taken and typed up and expanded after each visit.
All interview and focus group participants were provided with a participant information sheet and blank consent form to read in advance. Focus group participants received a shopping voucher as a thank you for participation. Interviewees were given the choice of remote [telephone, Zoom™ or Microsoft Teams® (Microsoft Corporation, Redmond, WA, USA)] or face-to-face interview. Focus groups were held remotely (using Zoom). For face-to-face data collection, we obtained written consent. For remote data collection, the consent form was read out and consent recorded by the researcher for each item. During practice visits, we obtained and documented verbal consent at the start of each conversation. All interviews were audio and/or video-recorded, apart from one GP interview, one group interview with care home staff and one focus group with paramedics. Consent to audio-record was not given for these interviews; therefore, detailed fieldnotes were made instead.
Our topic guide for the semistructured interviews and focus groups (see Report Supplementary Material 5) was informed by our research questions and developed with input from the co-applicant team and lay advisory group. It covered experiences of initiating, conducting and organising the ReSPECT process in the context of their work, completing forms with patients/residents, managing any challenges or tensions arising from implementing ReSPECT, and how ReSPECT form recommendations were used.
Five researchers (CJB, JH, KE, CM and JW) carried out semistructured interviews with GPs, care home staff and other health and social care professionals. Focus groups were facilitated by one or two researchers (CM, JH, SR and KE). Researchers recorded and shared reflective notes about the data collection process to refine the topic guide to consistently address any new issues or topics emerging during the interviews.
Audio-recorded data were transcribed by a professional transcribing company. We checked and anonymised the interview transcripts and allocated each transcript a study identification number.
Analysis
For GP practices and care homes, we initially grouped the data by practice/care home then read and reread the data before writing a summary of how ReSPECT was approached and managed within each practice or care home. Then for each interview/focus group, we used an a priori coding framework developed using the stages of the ReSPECT process and the main constructs of NPT: coherence building (conceptualisation), cognitive participation (initiation and engagement), collective action (use and documentation) and reflexive monitoring (evaluation). 44,45 The study team (FG, CJH, CJB, JH, CM, AS) made several refinements to the coding framework to increase its relevance to the data set. We used the agreed framework to code in NVivo™ software (NVivo v1.6.1, QSR International, Warrington, UK), a purposive sample of 50% of the interviews with GP and care home staff (sampled across all practices and care homes and types of staff) and all focus groups/interviews with other health and social care professionals. For emergency department staff, we limited our analysis to data about their engagement with community completed ReSPECT plans. During the coding process, we wrote memos of the key messages and themes emerging from the data. CM performed intercoder reliability on four interviews early in the process. The team then read the remaining data, looking for new codes or additional nuances in the data. 64 The ethnographic fieldnotes were used to supplement the clinician interview data. We analysed the coded data in three groups according to the participant’s relationship to the ReSPECT process: GPs and their staff who take responsibility for completing ReSPECT forms in the community, staff of care homes as residents commonly have ReSPECT forms and the staff use them in emergencies, and other staff who engage with community-based ReSPECT processes and forms. Within each data set, we compared data coded for each stage of the ReSPECT process and report our analysis following the ReSPECT process. Finally, we compared findings across the data sets and summarised the results.
In presenting our results, we mostly use the term ‘patient’ as this is the term used by many of our participants. Care home staff use the term ‘resident’, so we use that term in reporting data from these participants. Home care staff use the term ‘client’. As the data from these participants are reported together with health professionals who use the term ‘patient’, we use the word patient in this section to avoid confusion. Unless we specify a clinical role, we use the term ‘clinician’ for registered health professionals.
Results
We recruited 13 general practices across the study sites which were generally representative of England in terms of indices of deprivation (Table 8). 65 We recruited 11 care homes via our participating GP practices of which 3 provided nursing care (see Figure 1). One care home was specifically for younger adults. We recruited two care home staff via ENRICH.
| Thirteen practices, 162,798 people registered | |||
|---|---|---|---|
| Participating practices | England (%) | ||
| (n) | (%) | ||
| Gender | |||
| Male | 50.0 | 50.0 | |
| Female | 81,399 | 50.0 | 50.0 |
| Age (years) | |||
| < 20 | 36,354 | 22.3 | 23.0 |
| 20–59 | 84,592 | 52.0 | 52.6 |
| 60–79 | 33,443 | 20.5 | 19.3 |
| ≥ 80 | 8409 | 5.2 | 5.0 |
| Ethnicity a | |||
| White | 145,387 | 89.3 | 81.7 |
| Asian | 11,645 | 7.2 | – |
| Black | 2430 | 1.5 | – |
| Mixed | 2162 | 1.3 | – |
| Non-white ethnic group | 619 | 0.4 | – |
| Other | 555 | 0.3 | |
| Deprivation b | |||
| Decile | Practices | Practice (%) | People (%) |
| 1 | 1 | 8 | 5 |
| 2 | 2 | 15 | 12 |
| 3 | 1 | 8 | 9 |
| 4 | 2 | 15 | 5 |
| 5 | 2 | 15 | 16 |
| 7 | 2 | 15 | 16 |
| 8 | 2 | 15 | 28 |
| 10 | 1 | 8 | 7 |
Characteristics of patients with a ReSPECT form completion documented in the previous 12 months are presented in Table 9. There was wide variation in proportion of patients with a ReSPECT form recorded across practices. The reasons for this are multifactorial and include variation in patient populations, systems for identifying patients for whom a ReSPECT plan may be indicated, and practice systems for recording ReSPECT plan completion.
| N = 526 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Practice | A | B | C | D | E | F | G | H | I | J | K | L | M | Total | % |
| Indicative list size a | |||||||||||||||
| 12,000 | 11,000 | 9000 | 12,000 | 10,000 | 12,000 | 14,000 | 9000 | 15,000 | > 30,000 | 5000 | 15,000 | 4000 | > 160,000 | ||
| Respect forms per practice | |||||||||||||||
| 27 | 33 | 5 | 56 | 38 | 74 | 45 | 19 | 14 | 124 | 40 | 30 | 21 | 526 | ||
| Respect forms/1000 patients | |||||||||||||||
| 2.25 | 3.00 | 0.56 | 4.67 | 3.80 | 6.17 | 3.21 | 2.11 | 0.93 | 4.13 | 8.00 | 2.00 | 5.25 | 3.29 | ||
| Gender | |||||||||||||||
| Male | 15 | 14 | 1 | 19 | 14 | 29 | 16 | 12 | 3 | 46 | 15 | 15 | 3 | 202 | 38 |
| Female | 12 | 19 | 4 | 37 | 24 | 45 | 29 | 7 | 11 | 78 | 25 | 15 | 18 | 324 | 62 |
| Age band (years) | |||||||||||||||
| 20–59 | 1 | 2 | 0 | 2 | 0 | 1 | 0 | 0 | 1 | 4 | 1 | 2 | 0 | 14 | 3 |
| 60–79 | 5 | 11 | 2 | 4 | 4 | 13 | 12 | 7 | 4 | 25 | 8 | 4 | 4 | 103 | 20 |
| ≥ 80 year | 21 | 20 | 3 | 50 | 34 | 60 | 33 | 12 | 9 | 95 | 31 | 24 | 17 | 409 | 78 |
| Ethnicity | |||||||||||||||
| White | 19 | 12 | 0 | 38 | 25 | 0 | 42 | 19 | 14 | 119 | 40 | 17 | 2 | 347 | 66 |
| Mixed | 5 | 9 | 0 | 10 | 4 | 0 | 3 | 0 | 0 | 3 | 0 | 0 | 0 | 34 | 6 |
| Asian | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | 18 | 33 | 6 |
| Black | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | 1 |
| Unknown | 1 | 11 | 5 | 8 | 7 | 74 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 108 | 21 |
| Care home resident | |||||||||||||||
| Yes | 9 | 2 | 0 | 36 | 4 | 42 | 26 | 12 | 0 | 53 | 20 | 19 | 8 | 230 | 44 |
| No | 18 | 31 | 5 | 20 | 34 | 32 | 19 | 7 | 14 | 71 | 20 | 25 | 4 | 300 | 57 |
| 0 | |||||||||||||||
| e-Frailty score range (where available) | |||||||||||||||
| 0.083, 0.444 | 0.139, 0.528 | 0.139, 0.389 | 0.278, 0.611 | 0.056, 0.500 | – | 0.110, 0.610 | 0.250, 0.500 | 0.139, 0.722 | – | – | 0.170, 0.560 | – | |||
We undertook 1-day fieldwork visits at 11 of the practices (2 were unable to accommodate a visit) involving 124 clarifying conversations with clinical (n = 49) and administrative staff (n = 75) with varying levels of knowledge, experience and involvement in the ReSPECT process. Conversations took place in offices, staffrooms, patient waiting areas, consulting rooms, meeting rooms and/or main reception. Across the practices, we spoke with GPs, nurses working in the GP practices, healthcare assistants, paramedics working in the GP practices, a community pharmacist, a social prescriber, receptionists, medical secretaries, clerks, administrators and managers.
We interviewed 21 GPs, 5 specialist nurses, 12 care home managers, 3 senior care home nurses and 16 senior carers/care co-ordinators. Following their request, 11 care home staff were interviewed in small groups (1 of 6, 1 of 3 and a pair). All interviews were remote except for 1 GP and 18 care home staff interviews. Interviews lasted between 13 and 100 minutes.
We conducted remote focus groups with seven home care workers (in two groups), three community palliative care nurses, two paramedics, six community nurses (across two groups) and interviewed remotely five emergency care doctors and one community nurse. Sessions lasted between 28 and 65 minutes.
The views and experiences of general practitioners and their staff of the ReSPECT process
Conceptualisation of the ReSPECT process
There was broad consensus that ReSPECT plans were more comprehensive than older DNACPR forms and could empower patients to vocalise their wishes and take some control over their care: ‘It allows for a wider discussion than just a DNACPR discussion’ (GP 1, area 2). ‘We see it [ReSPECT] as a way of giving the patients control back about their future care’ (GP 2, area 2).
Clinicians saw the ReSPECT process as something that should not be rushed or viewed as a tick-box exercise but rather, used as a prompt to have nuanced and explorative discussions about patients’ varied needs. This included tailoring the plan to the patient’s lived experience:
You can tailor-make the document depending on what the patient’s views are about a variety of aspects of their future care … It’s important that it’s a holistic conversation rather than a just a tick-box exercise … [that] encompasses all of the aspects of a patient’s care, rather than just that one specific question.
GP 1, area 2
Sometimes clinicians seemed to conflate ReSPECT plans with ACPs, which encompass broader preferences around end-of-life support.
Clinicians saw the ReSPECT process as a way of reassuring patients that they would be able to access the appropriate treatment to protect their quality of life: ‘Because I think it’s reassuring them we’re not abandoning them … it’s just giving them the best treatment in the best place for them’ (GP 3, area 2).
Although many healthcare professionals thought the ReSPECT process could promote patient empowerment there was concern that it could ‘be more harmful [psychologically to the patient] to force a ReSPECT … than not’ (GP 4, area 1).
Clinicians viewed the ReSPECT process as primarily benefiting those who had capacity and could be involved in the discussion. In a staff room, two GPs and a nurse discussed that the patient-centred dimensions of the ReSPECT process could be lost in situations where the patient lacked capacity and could not vocalise their wishes easily, if at all:
it is important that ReSPECT forms are not completed during a crisis when everything is in disarray, the patient has lost capacity and is unable to express their own preferences. The GP felt that this would defeat the point of the form, which is there to document the wishes of patients.
Fieldnote practice A
Two GPs interviewed suggested the ReSPECT form would be improved by having a place for patients to sign to indicate their shared ownership of its content:
The form lacks somewhere for them [patients] to sign … And that often I give it to them to sign anyway because it feels like it’s their form as well.
GP 4, area 1
Patient-shared ownership of the ReSPECT plan content was considered important if relatives have different views. One GP during a visit to his practice was noted to say:
It is crucial for the patient to tell their family what they want before they lose capacity and equally important for clinicians to talk to the family about the patient’s wishes so that everyone is ‘singing from the same hymn sheet’. The GP said, if relatives disagree with the wishes of the patient, the clinician can say that ‘I have on paper what the patient wants’.
Fieldnote practice B
A specialist nurse felt that the ReSPECT form provided patients with the opportunity to confirm in writing their preferences for treatment so the relatives could communicate this in an emergency. The relatives would be able to give ‘this piece of paper’ (specialist nurse 1, area 2) to the paramedics who could read it and know immediately what the patient wanted.
Some clinicians referred to patients’ wishes and ReSPECT form recommendations as decisions to emphasise the conclusive and fixed dimensions of acceptable care. They highlighted the need for these to be respected and upheld in a crisis:
I said [to patient] it’s a document, it tells what action needs to be done if you are not well. What are the actions any healthcare professional needs to take and decide? So your decision is the future if you really become unwell.
GP 5, area 3
Conceptualising it as a final clinical decision particularly applied to the section on DNACPR.
I tried reassuring [the patient that having a DNACPR in place did not mean that active treatment would be withdrawn] but in the end I did have to remove it because she felt so strongly. I am aware it’s a clinical form and it’s a clinical decision, especially do not attempt resuscitation.
GP 2, area 2
Other clinicians considered a ReSPECT form to be a guide to steering the clinician, relative and patient through difficult situations. One GP said that the form was particularly useful for: ‘Agency staff [in care homes] at a weekend who are unfamiliar with the patient [because] it acts as more of a guide for them for what to do with that patient’ (GP 3, area 2).
Initiating the ReSPECT process: general practitioners and their staff
The ReSPECT process was initiated both systematically and opportunistically, with systematic initiation by far the most common. Systematic initiation occurred when patients were added to the palliative care register or admitted to a care home. Sometimes, a hospital discharge letter would suggest initiating the ReSPECT process. At end-of-life care meetings, staff discussed the need to initiate the ReSPECT process or review an existing ReSPECT form and how quickly this was needed.
Clinicians said that most of their patients who had forms were elderly and frail, receiving palliative care or in the advanced stages of their illness. The clinician would ask the administration team to make an appointment for patients they thought would benefit from the ReSPECT process.
Clinicians reported that the COVID-19 pandemic prompted many care home staff to request that practices complete ReSPECT forms for all residents upon their admission to the home. However, clinicians noted that there were several negative media reports claiming that clinicians were completing ReSPECT forms to ‘write off their relatives because they lived in a care home or they’re elderly’ (specialist nurse 2, area 1). In some practices, training was provided for relevant clinical staff during the pandemic to: ‘ensure that the ReSPECT forms were fairly done for those who needed them … especially with the care home patients’ (specialist nurse 3, area 1).
Clinicians felt that care homes’ requests to ask GPs to complete ReSPECT forms for all new admissions was sometimes to reassure care home staff particularly regarding resuscitation, rather than to benefit the patient or their relatives:
The patient didn’t ask for a ReSPECT form; the family didn’t ask for a ReSPECT form. It’s their care home that had flagged that they don’t have a ReSPECT form, and yes, it would be appropriate for them not to be resuscitated, but often they, they are still for treatment, they are for admission … it just felt like I was doing that more for the care home than for the patients.
GP 2, area 2
General practitioners reported requests from patients for ReSPECT plans including older people who were fit and well and patients who had advanced illness. However, these requests were uncommon. Clinicians suggested the lack of public awareness around ReSPECT may have precluded more people from asking for one. ‘I wish patients understood what ReSPECT was … more information, more awareness among the general public would be really helpful’ (GP 7, area 1). Our researcher noted there was no information about ReSPECT in waiting areas.
Occasionally, a GP would initiate the ReSPECT process at the time of a treatment decision:
If the patient at the time needs an admission and they don’t want to go in, we say, ‘Okay, well, actually they don’t have a ReSPECT form, this is an opportunity to take time to talk about it’.
GP 8, area 3
Deciding when to initiate the ReSPECT process was a challenge for the clinicians – not too early and not too late.
There have been a few situations where we’ve spoken to patients who have had bad news that their cancer has progressed … I have sort of tested the water and said, ‘It, it’s important that whilst you’re still relatively well that we have a discussion about future care … and it’s been quite clear they have not felt ready, so you just leave it and revisit it’.
GP 2, area 2
When the patients are very angry about diagnosis, then it’s not always appropriate to discuss [ReSPECT] with them.
Specialist nurse 4, area 1
Some clinicians thought that building relationships and getting to know the person first would enable them to gain insight into when ‘the right time to discuss’ ReSPECT would be (GP 6, area 2).
However, one clinician was concerned that waiting could lead to poor clinical outcomes for the patient if they were taken to hospital against their wishes simply because a form hadn’t been completed in time:
Sometimes it will be said in a meeting, ‘Oh, the, the patient’s not ready to have that discussion yet’. I think really that’s a bit of a code for, ‘I felt uncomfortable bringing this up as a clinician because the patient was upset’, which is something slightly different … because I think the worst-case scenario is a patient who deteriorates quickly who doesn’t have any opportunity to discuss their wishes … and therefore defaults to full escalation in hospital. It might not be what they want, you know.
GP 1, area 2
Another clinician felt that sometimes the best course of action was not to initiate the ReSPECT process. The example given was when likely length of life was uncertain, and the patient had fluctuating capacity:
And if you are looking at a very elderly dementia patient … they could pass away either tomorrow or they could pass away in weeks and months … to make a judgment on … not for resuscitation and the patient doesn’t really understand it, who has fluctuating capacity, that’s a very difficult … I have refused to do a ReSPECT form in those situations.
GP 7, area 1
Some clinicians did not want to invest time starting a conversation that was unlikely to be successful because the patient and/or family were unsure about it:
Occasionally you do think, I’ve not got the time to go into ... whys or wherefores when you’ve made it quite clear already that this isn’t something you’re going to even consider.
GP 9, area 3
However, clinicians said that they often took time to prepare patients and/or family before having the formal ReSPECT conversation. One said that she would refer the patient to the palliative care nursing team for emotional support before initiating a ReSPECT conversation, if she felt the patient was distressed by the news of their terminal diagnosis: ‘The palliative care nurses … probably have to go and visit them [patient] a few times before they did it [ReSPECT] if they are really angry’ (specialist nurse 4, area 1).
An advantage of delaying initiation of the ReSPECT process until late in a patient’s illness trajectory was that there was more certainty about the trajectory and so the views of the patient and their family were more likely to align with those of the clinician. One GP described her experiences of starting a ReSPECT conversation in a care home setting as ‘easy’ given that residents ‘haven’t got a great quality of life and they’ve got lots of advanced health problems’ (GP 15, area 1). A similar view was also expressed for patients with capacity who were coming towards the end of their life ‘and [were] really quite unwell … focused and knew what they want[ed] to do’ (GP 4, area 1). These patients felt ‘relieved’ that ‘somebody [was] taking notice’ of their situation and listening to their concerns (specialist nurse 3, area 1).
Having the ReSPECT conversation and completing the form
Clinicians recognised the need to take time for most ReSPECT conversations unless a patient was very clear what they wanted. Although many used a normal appointment slot, some scheduled ReSPECT appointments as a last appointment of the session when the clinician might have more time or they allocated ‘dedicated time’ (specialist nurse 3, area 1) to conduct the conversation with housebound patients. Some combined it with the completion of other care plans to maximise time efficiency. Some conversations were completed as a one off, but others were conducted over several consultations according to patient need:
I guess it makes it nice and straight forward if you’re able to have that one conversation … [it] makes it easier if the family are on board and they understand the whole process. So, it’s whatever’s easier for the patient and their family. If they need that extra time or they’re not ready, then that’s fine.
GP 3, area 2
One clinician described how a care home resident became very agitated when she tried to talk about a ReSPECT plan with them. They dealt with the situation by asking one of the care home staff to lead the conversation with the clinician present as the patient trusted the care home staff member:
This lady had capacity and we had a discussion about end-of-life care and the ReSPECT form. But it is a bit odd because the consultation was led by the carer rather than myself … So the carer said, ‘Because you got quite agitated at the doctor’s last time’, She said, ‘Oh, it’s better if I talk about it’.
GP 10, area 3
If a patient was rapidly nearing end-of-life clinicians said that they tended to discuss with the patient broad issues of prognosis, future care and treatment. Where there was more uncertainty about end of life and the focus was on resuscitation status and ceilings of care, they asked more in-depth questions about patient wishes about treatment, hospital admission and CPR. Clinicians said that they explained to patients/families the differences between treating reversible health problems and offering comfort care to manage the symptoms associated with an illness:
After review of care plan, medication, and medical conditions, we discuss with the patient and if they’ve got any dementia, then the family members who have got a power of attorney … what is best way forward if their condition deteriorates…whether they want admissions during acute illnesses, or they want treatment at home. Do they treat illnesses if condition progresses, what are the options? Will the patient or the family want CPR for the patient or not.
GP 5, area 3
Clinicians said the ReSPECT form gave them a structure for carefully exploring and listening to the patient’s views and wishes:
I think that’s what the ReSPECT form does it helps you to know these patients well … that’s really valuable because other people speak over you [the patient] or talk around you [the patient] it’s nice for somebody to listen to actually what you [the patient] would like.
Specialist nurse 2, area 1
Clinicians thought that the ReSPECT form questions worked well and: ‘allow[ed] a degree of tailor-made … approach to the patient, rather than just a one-size-fits-all approach’ (GP 1, area 2). A few clinicians found the personal preferences scale not always useful. For example, one GP mentioned: ‘A drawback of the ReSPECT plan is the personal preferences scale and how to interpret it when patients want to prioritise comfort care and life sustaining treatment’ (fieldnote, practice C). This GP suggested tick boxes regarding whether the patient or family wished (or not) to have hospital treatment in the event of different scenarios might be more helpful than text as paramedics could read it quickly (fieldnote, practice C).
Families were viewed as important contributors to the ReSPECT conversation. They were relied upon to give their perspectives when the patient had impaired mental capacity. For patients with capacity, it was still considered important for families to be involved in the discussion, so they understood, valued and supported the use of the completed ReSPECT form in an emergency. Clinicians had to manage differing views and allow families time to process the information about their loved one’s situation:
Unless the immediate carers or family are on board then you run the risk of the ReSPECT form being a bit useless because it’s not abided by … the family needed a bit of time to take on board what was being said and have that conversation between themselves, making sure that they were happy with everything. They really needed time to absorb … the diagnosis and prognosis.
GP 3, area 2
Clinicians said that they had to carefully balance the wishes of patients and/or family with their own clinical judgement to avoid conflict during the ReSPECT conversation. Most talked about the difficulty of negotiating with patients and family who wanted resuscitation to prolong life when the clinician believed this was unlikely to be successful:
It’s more of a difficulty when you clearly see it’s futile, for example resuscitation, but the family members say, ‘But I want that’, [you] try to give scenarios why perhaps it wouldn’t work out as they would expect. Sometimes people have a slightly glorified view of resuscitation from TV and the reality is quite different, certainly in the sort of patients that we’re mostly dealing with.
GP 9, area 3
Sometimes a clinician would attempt to dissuade patients and families from agreeing to CPR by speaking candidly about the potentially harmful consequences of undergoing the procedure. With some patients, they repeated this annually:
If you’ve got a healthy heart … you should go for it [CPR], but you’ve got a heart which is hardly functioning … CPR may help or you might survive an episode if you’re lucky, if you’re unlucky you might have a heart rhythm which goes irregular, and it might go into stroke. Or you might have more physical problems, so you’ve got to decide…we have a patient we feel they shouldn’t be for CPR, but they want to be for CPR, so every year we tell them.
GP 5, area 3
To avoid patient distress, a clinician would leave the CPR recommendation box blank although in their clinical judgement CPR was unlikely to be successful:
I’d been there three or four times to discuss it [CPR] over a period with them and didn’t seem to get anywhere at all and I thought I’d feel like I’m just going to make them distressed if I pursue this any further.
Specialist nurse 2, area 1
Clinicians described the challenge of writing clinical recommendations in sufficient detail and clarity to be useful in a future emergency scenario. The form did not provide enough space or prompts for them to write about every eventuality that could befall the patient. One commented that even if there was enough room on the form to write down everything that might happen to the patient, it would still be impractical. Clinicians described how they attempted to provide recommendations that were broad enough to cover a range of scenarios for paramedics and care home staff to follow and specific enough to provide guidance on the patient’s unique situation:
I guess really what needs to happen is a much more consistent way [of writing clinical recommendations], a little bit more guidance regarding phraseology … rather than it being too vague, making it with a bit of sensible vagueness rather than – don’t send into hospital unless they need to be sent into hospital … which doesn’t really say very much.
GP 12, area 2
One clinician completed the ReSPECT form by referring to the recommendations on the more detailed care plan: ‘In a ReSPECT form I try to mention the important things. The rest … I just write there, “Please follow the care plan”’ (GP 5, area 3). Some clinicians filled in the ReSPECT form after the conversation with the patient/family. Others completed it during the conversation for transparency: ‘I will write the ReSPECT form in front of them, so they can see what we’re doing, why we’re doing it, explain each section of the ReSPECT form’ (GP 6, area 2).
Once the conversation had been completed, a few clinicians said that they checked that the patient or family had understood what had been written on the form:
I’ve done the ReSPECT Form and the care plan, have you had a chance to look at it and check it over … if there’s anything you want to discuss then just feel free to give our receptionist a call and book in to have a chat with me and … any questions you’ve got about it.
GP 10, area 3
Lack of time for ReSPECT conversations and ReSPECT training was commonly mentioned. Clinicians would be: ‘rushing from one thing to another and … could never [give] things quite the time that [they] would … want, because just sheer amount of numbers’ (GP 9, area 3). Clinicians were concerned that lack of training continued to feed into a cycle of avoidance because clinicians felt too uncomfortable with the emotional issues that ReSPECT raised and did not have the experience to know what treatments were likely to be successful on a particular patient.
You want to have that empathetic conversation with the patient in the end-of-life … How do you know … that point in life … [when] this patient is not fit for further treatment? It’s experience, it comes … But if you ask a junior doctor [to do this], you are talking about missed opportunities.
GP 7, area 1
Since the ReSPECT conversation required clinicians to draw on their expertise, experience, and empathy rather than the interpretation of quantifiable medical data, it was described as ‘worse than breaking news’ that relied on ‘a histology … something that you could tell [and show] that to the patient’ (GP 7, area 1).
Storing and sharing completed ReSPECT forms
Eight practices had policies on completed ReSPECT form storage and sharing. All practices said they entered a code in the electronic medical record when a ReSPECT form was completed, but how completed ReSPECT forms were stored and shared varied. In practices using paper forms, administrative staff scanned signed forms onto the medical record and stored the original in reception until the patient, family or care home collected it. Clinicians sometimes took completed ReSPECT forms to care homes on their regular visits. In three practices, forms were left with the patients during home visits and a note made in the clinical notes that the conversation had been completed or a photograph of the completed form was uploaded. One practice stored the unsigned and signed copies of digital forms on their electronic medical record so if the patient or family lost their ReSPECT form, the signed form could be reprinted and given to them. Other practices using digital forms stored the unsigned copy in the electronic medical record and then printed and signed in wet ink and/or stamped a hard copy for the patient/relative.
Patients/families or care home staff were contacted to ask them to collect completed forms. Occasionally forms were posted to patients. Forms that had not been collected within a certain time frame would be followed up with a phone call. One receptionist thought that ReSPECT forms were more likely to be left at the practice if patients had changed their minds about their wishes since having a ReSPECT plan completed. However, how long ReSPECT forms remained uncollected varied and there were no standardised procedures to manage this, which meant that administrative members of staff often felt uncertain about what to do with them. There was also variation in how, if at all, reception or administrative staff formally documented in the medical record when a completed ReSPECT form had been collected and who had collected it. Some practices shared or sent completed ReSPECT forms to community nurses, paramedic staff and out-of-hours GPs.
Hospital discharge summaries usually contained brief details about what had been recorded on the ReSPECT form, often only the patient’s resuscitation status. One GP suggested it would be helpful for the GP to have a copy of the hospital completed ReSPECT form:
I think it would be very useful if the information from the original discussion could be [reported in the discharge summary] in more detail … exactly what discussion took place [with] who … an electronic copy to us, apart from just a patient copy, that would also be very useful … that would clear a lot of miscommunications … sometimes they [ReSPECT forms] just get lost because they will go through so many hands from the time they leave hospital to the time they come to their own house … And, we struggle to put in an emergency package in place if they [patient] lose any of that vital paperwork.
GP 13, area 3
When clinicians managed to obtain the hospital completed ReSPECT form, they often found it was incompletely filled out with information that was incomprehensible ‘half things scribbled here and there’ (GP 5, area 3) or irrelevant to a community context: ‘ReSPECT forms completed in hospitals aren’t as useful as those completed at the practice because details are often limited to “ward-based care”, which becomes less meaningful when patients are returned home to the community’ (fieldnote, practice A). Clinicians felt obliged to review the patient’s situation and complete the form again to ‘see if it was still valid’ (GP 13, area 3).
Concern was expressed that ReSPECT forms held by the patient and practice might not be synchronised: ‘The actual paper copy might not get updated as much as the actual clinical system notes get updated’ (GP 3, area 2). This could potentially create confusion for paramedics and other clinicians. Paper-based plans could get lost, which could slow up care planning or prevent it altogether if the patient rapidly deteriorated. One GP reported that care home residents had been wrongly taken to hospital when their care home had misplaced their form but storage of forms at the care home had now improved. Many GPs and their staff said that practice-issued forms were printed in colour or stamped to verify their originality for paramedics. One GP thought that ‘now anything is accepted [by ambulance crews]’ (GP 5, area 3), including black and white forms.
Reviewing completed ReSPECT forms
None of the practices had a system for regularly reviewing all patients’ ReSPECT plans. One practice said they reviewed annually the care plans and accompanying ReSPECT plans of patients with dementia. In some practices, ReSPECT plans for patients nearing end of life were reviewed every 3 months or more. Other practices only reviewed a plan if a concern was raised during a palliative care meeting, a clinician thought to review it when a patient deteriorated, or a patient asked it to be updated:
Interviewer: Is there a formal process in place for reviewing the ReSPECT forms?
Respondent: They get reviewed at palliative care meetings … they tend to be reviewed if people have got concerns rather than there being an automatic process.
GP 4, area 1
Paramedics triggered a review opportunistically if they noticed that the patient’s plan was outdated while treating them.
High workload volume was a reason cited why plans were not reviewed systematically:
When I asked the GP whether the practice reviews forms … she said bluntly that the practice can’t do this because they are already swamped and ‘I want a life’. She works 15 hours a day and is under a lot of pressure at work. She said that there is already too much bureaucracy to do. In an ‘ideal world’, she would review forms, but this isn’t currently practical.
Fieldnote, general practice D
Use of completed ReSPECT plans in medical emergencies
A clinician reflected on whether they could have made a ReSPECT plan clearer after a patient had died and the recommendations in their plan had not been followed:
We could have got a palliative care team in there within two hours, but instead she [patient] was admitted [to hospital] … what could I have put on there [ReSPECT plan] that makes any difference? I’ll tell you what I put … prioritise comfort, not for admission to hospital unless in the event of severe infection … [Patient Name] would not tolerate a hospital environment well. I’m now thinking, what else? Do I need to be more explicit? and it’s difficult because the form doesn’t lend itself to giving you plenty of room to be able to … put that information in.
Specialist nurse 3, area 1
This participant felt upset that she had subjected the patient to numerous ReSPECT conversations when it had no ‘bearing at all on her outcomes’. She recognised how little control she had over what happened to the patient.
Most clinicians considered the ReSPECT clinical recommendations to be for guidance only:
I think it’s there to give the person who’s making a decision in an emergency situation some guidance and, and that’s how I view it … I think a ReSPECT form is, this is what’s been discussed, this is what their wishes are. But you can certainly override a ReSPECT form if you felt it was appropriate.
GP 2, area 2
Clinicians acknowledged that not all healthcare professionals would know the patient and therefore, be as confident in making the clinical judgement to follow a ReSPECT plan recommendation to avoid hospital admission, as the clinicians who did know them:
There’s always that risk of out of hours that, somebody with heart failure they deteriorate you know, we’ll ship them off to hospital. It’s quite explicit on the ReSPECT form what the patient’s wishes are, but I know that these aren’t always carried out … within normal working hours and it was one of the GP’s who know her then … following the ReSPECT form is much more likely to occur … out of hours is a slightly different scenario … I think that just comes down to not knowing patients and the risk profile slightly changes when you’re dealing with patients you don’t know.
GP 9, area 3
This same GP felt frustrated that out of hours services seemed to ignore what had been agreed in the plan: ‘Out of hours are called and they ship them off to hospital and never bother looking at the ReSPECT form’ (GP 9, area 3).
Many clinicians had little confidence in paramedics following the clinical guidance recorded on the form because they were perceived to lack ReSPECT experience. One GP reported an account of a paramedic misunderstanding the form:
The paramedics came, saw the ReSPECT form … phoned the relative and said, ‘She’s end of life’, but she wasn’t end of life, it was just because she had a ReSPECT form saying, ‘Not for admission for hospital unless discussed with relatives’. … I don’t know if it was a junior paramedic.
GP 6, area 2
A minority of clinicians said it would be acceptable for non-GP healthcare professionals to reject ReSPECT plan recommendations particularly if patients/family have changed their minds:
The ambulance and people like that, I think it [the completed ReSPECT plan] is taken into account, but then people [patients and/or relatives] change their mind and so they [paramedics] go by the acute situation, and I think that’s the right way to do it.
GP 4, area 1
Patient safety was suggested by one clinician as a reason for overriding ReSPECT recommendations for home-based care if support at home was unavailable:
We have frailty consultants sitting in A&E … actually trying to very much follow what’s on the ReSPECT form … One recently that I’ve had is a gentleman who’s got quite severe postural hypotension. Didn’t have any carers at home, so he wasn’t safe to be discharged, but it’s, ‘Well, you know, you’ve got a ReSPECT form. You shouldn’t be here’. … I still believe that every clinician has got their own responsibility of what they need to do in that circumstance, regardless of what’s written down on a piece of paper … I wouldn’t want them … doing anything really invasive with him. But please keep him safe.
Specialist nurse 1, area 2
Reflecting on the ReSPECT process
Our interview data suggest that GPs and their staff informally reflected on how they initiated and undertook ReSPECT conversations. In contrast, there were sparse data on formal types of reflexivity, such as audits. GP 7, area 1, mentioned that their practice conducted death reviews every two years which included whether ReSPECT wishes were met: ‘we do this death audit … to see whether the criteria for deaths at home, whether the patient’s ReSPECT have been met, whether they died at home or in hospital or at a care home’ (GP 7, area 1).
The views and experiences of care home staff of the ReSPECT process
Conceptualisation of the ReSPECT process
Care home staff understood ReSPECT as part of providing person-centred care for residents. ‘I think it’s a tool to make their care more person-centred … it allows us to do exactly what they want’ (care home manager/deputy manager 1). ReSPECT was viewed as a means for residents to express and have documented their personal preferences and wishes for care and treatment in a clinical emergency and was therefore understood as empowering the resident: ‘The power is in their hands, rather than our hands and the medical professionals’ hands’ (care home manager/deputy manager 3).
In the context of the care home, ReSPECT was seen as enabling the enactment of residents’ wishes to die within the care home, rather than in hospital: ‘Certainly, in this setting, to be able to say if they would prefer to stay here for treatment rather than go to hospital’ (care home manager/deputy manager 1).
Several care home staff contrasted ReSPECT plans positively to DNACPR forms in terms of promoting more choice and ‘options’ (care home manager/deputy manager 3). ReSPECT plans were seen as facilitating a more holistic and person-centred conversation for residents that went beyond resuscitation whereas DNACPR was about what not to do for residents. For these staff, ReSPECT plans represented a shift in values of how to engage with people who were approaching the end-of-life, and facilitated more active and nuanced discussions with residents about their future:
I think the ReSPECT process has opened the door to have a freer conversation with people … With the ReSPECT now it can say, ‘Well actually, I don’t want to be resuscitated but if I did get an infection that, that could be treated then I would want to be treated for that’. So, it, it’s, it’s broadened the horizons and it’s given us the opportunity to have a more meaningful conversation with people really and say to them, ‘Well, you know, you actually can tailor what you want to happen to you’ … Whereas before I think peoples fear was that it was just, they were signing up to say, ‘I don’t want you to do anything to me’. You know, which is quite a significant difference really isn’t it?
Care home manager/deputy manager 1
However, two staff stressed that ReSPECT recommendations were ‘in practice’ (senior nurse/nursing lead 1) about determining resuscitation decisions for residents and they referred to ReSPECT and DNACPR interchangeably during interviews: ‘Ultimately, whether it’s a DNAR, it’s a ReSPECT, they all boil down to the same thing that this person doesn’t want to be resuscitated, or does, and then we have to act on that accordingly’ (senior nurse/nursing lead 1).
While a ReSPECT plan was understood by care home staff to primarily inform, and be used by, medical professionals, it provided important guidance for care home staff and reassurance they were acting in alignment with residents’ and their family’s wishes, particularly in clinical emergencies. For some, the plan was interpreted as a way to ensure resident wishes were upheld in situations where alternative decisions might otherwise be made. They made sense of their role as advocating for and promoting resident wishes:
Whereas before, our hands would be tied. We would always have to go with what the medical professional advised. If somebody didn’t have the ReSPECT form and they said that they needed to go into hospital even though that resident didn’t want to, the resident would still have to go into hospital. And we would be pushing for that resident to go into hospital. Whereas with the ReSPECT form, we can respect their wishes. And we’ve got that document to reassure us that we’re doing the right thing.
Care home manager/deputy manager 3
Initiating the ReSPECT process
The ReSPECT plans were typically completed with residents who were anticipated to be permanent or long term, at or nearing end of life, and/or who were seen as frail. ReSPECT plans were not typically completed with residents who were anticipated to be short-term stays (e.g. for respite care), who had moved into the care home to avoid social isolation or who were perceived as having a ‘good quality of life’ (care co-ordinator/senior carer 1).
Most residents who moved into the care home from hospital had hospital-completed ReSPECT plans. Few residents arrived with a community-completed ReSPECT plan. For new residents without a ReSPECT plan, where appropriate, ReSPECT conversations would be arranged as soon as possible after their arrival, usually within 6 weeks:
Having the ReSPECT form now is a part of our admission … rather than waiting until somebody’s unwell … if somebody’s moving in we wouldn’t scare them straight away and be like, ‘Right, we need, we now need to talk about your, the end of life and your ReSPECT and what your wishes are’. But very quickly into their stay here we will start that process and start talking about the ReSPECT form and what the nurses are here to do and their choices.
Care home manager/deputy manager 3
For new residents arriving with a ReSPECT plan, a GP review of the plan was requested and promptly carried out to ensure recommendations were ‘valid’ (care home manager/deputy manager 5). For residents who did not have a ReSPECT plan completed on admission, they were completed in response to changes in their health. The COVID-19 pandemic in 2020 had prompted the completion and/or review of ReSPECT plans within most care homes. In many cases, staff reported this had been initiated by local GP practices. However, a small number of care homes reported they liaised with GP practices themselves so that they were clear about resident wishes during COVID-19.
Care home staff were often the first to raise the issue of a ReSPECT plan with residents/families. Care staff would ‘mention’ (care home manager/deputy manager 7) ReSPECT plans with residents and/or families before the formal conversation. This included providing general information about ReSPECT and what it was about, prompting consideration of what resident wishes might be, and giving general reassurances about the process. This preparatory work was considered important for encouraging residents and/or their family to engage with the process, have conversations among themselves and to minimise distress.
Being able to explain to them how the ReSPECT process works has definitely helped to open the door for that conversation … So, I can sit down long before the doctor has that conversation and introduce … the ReSPECT process [so resident/relative can] digest it themselves ... that’s an important part of what we do, to take away the stigma … that then in turn makes the job a lot easier for the doctor.
Care home manager/deputy manager 1
However, care home staff asked clinicians to approach the family themselves if the family expressed reluctance to engage or did not understand the ReSPECT process:
[F]amily didn’t want the ReSPECT form or didn’t understand what the ReSPECT form was. So, we asked the GP to speak with the family member and just explain a little bit more in, the statistics of people being resuscitated at over 65 and, and all the important facts to consider when signing the ReSPECT form.
Care home manager/deputy manager 3
Having the ReSPECT conversation and completing the plan
General practitioners completed ReSPECT plans for residents in seven of the study homes; in four they were completed by specialist nurses. Care homes typically had weekly clinician visits or telephone meetings, during which new residents or changes in residents’ health could be discussed. Care staff would also telephone the GP practice to request ReSPECT plan completion or review if it was considered urgent.
Residents with capacity were often seen face to face, with family members present if appropriate/desired. Where residents lacked capacity families were consulted. If they were not local, conversations between the clinician and family were generally held by telephone.
Staff emphasised the importance of involving families as in emergency situations the care home staff would need to inform the family. Having common understanding about the ReSPECT plan with the family enabled the staff to ‘get it right’ (care home manager/deputy manager 7) for a resident in an emergency.
In four care homes, a care home staff member would sometimes ‘sit in’ (care home manager/deputy manager 3) during ReSPECT conversations to ‘support’ (care co-ordinator/senior carer 1) residents, ‘backing up’ (care home manager/deputy manager 3) the GP during difficult questions, and so that staff were aware of what had been discussed. One participant said that holding the conversation ‘together’ produced a ‘nicer outcome on the form’ (care home manager/deputy manager 2). Staff presence was seen as particularly helpful for conversations with residents who had communication difficulties. Staff presence was described as resident choice in the care home for younger adults.
Several care staff explained that they had trusting relationships with the residents which enabled them to support and reassure the resident during what was a sensitive and stressful time:
It’s a very delicate matter … when a resident’s here for quite a long while, you know, they gain trust … I think it is important, because they may want somebody with them just to sit with them for reassurance.
Care home manager/deputy manager 7
Care staff emphasised that responsibility for making clinical recommendations should lie firmly with the clinician, in discussion with the resident/family. One senior nurse commented that being able to write a plan themselves would be beneficial because they would include ‘more information’ (senior nurse/nursing lead 2).
Care staff generally felt that conversations held by specialist nurses were particularly person centred, as they knew the residents well and had more dedicated time to conduct conversations:
[The specialist nurses have] great relationships with the residents and their families. And they know them, which I think is really important … It’s not somebody who has no empathy with you as an individual. They have the detail … it’s a delicate conversation … has to be approached with empathy. If you know those residents … it makes it a lot easier for [the residents].
Care home manager/deputy manager 6
When asked about residents’ views of ReSPECT, care staff reported that most residents (with capacity) were generally ‘happy’ (care co-ordinator/senior carer 13) and receptive to conversations about ReSPECT, provided they were handled with sensitivity. Some referred to ‘the odd case’ (care home manager/deputy manager 3) where residents had surprised staff by expressing alternative wishes to GP recommendations (typically that they wanted to be resuscitated and/or receive further interventions). However, they felt that many residents did not think about their ReSPECT plan once it had been completed. One participant explained that they would not refer to the plan as ReSPECT per se but talked about it to residents in terms of ‘making choices’ about future care/treatment and end-of -life (care home manager/deputy manager 4).
Storing and sharing completed ReSPECT forms
Once ReSPECT conversations had been held with residents/families, plans were typically finalised and signed-off by the clinician at the GP practice who would then notify the care home when the completed form was ready for collection. Alternatively, the clinician would bring completed forms to the home on their weekly visit.
Most care homes also uploaded scanned copies of ReSPECT forms into an electronic system for managing resident data. In some homes, this could be accessed on staff devices. Care homes flagged ReSPECT resuscitation recommendations within these electronic systems. Three care homes stored only hard copies of forms. Four care homes also used a ‘grab pack’ (care home manager/deputy manager 6) or ‘grab sheet’ (care co-ordinator/senior carer 15) for ambulance call-outs that contained a residents’ relevant documentation (ReSPECT form, medication list; ACP).
ReSPECT form storage was planned for quick retrieval in an emergency. Original forms were either stored in residents’ individual care file or in one folder/cabinet accessible to staff, with a prompt in residents’ individual files/records to indicate ReSPECT form for retrieval. Some care homes also used a purple wallet or purple file tab within resident files for quick identification of forms.
Visual symbols were used including a ‘red sticker’ (care home manager/deputy manager 8) or ‘butterfly sticker’ (senior nurse/nursing lead 1) in the front and sometimes spine of resident files/folders to signify do not resuscitate. Another care home used a ‘love heart’ (care co-ordinator/senior carer 10) on residents’ rooms’ doors to signify for resuscitation.
A challenge faced by staff was the inability to share paper-based plans when reporting an emergency. In one case, care home staff reported they had been asked to begin CPR for a resident by the emergency call handler who had insisted staff had a duty of care to do this until the paramedics arrived, although the resident’s ReSPECT form recorded not for CPR. They were then questioned by paramedic staff about why they had attempted CPR.
Staff pointed out that paramedic staff had no formal way of checking whether a ReSPECT plan was up to date. A strongly held view among the majority of staff was that as well as the paper copy (and scanned upload to the care home system), it would be beneficial to have a centralised system which could be accessed by all health and care professionals involved in treatment decisions for a resident, so that everybody was following ‘the same information’ (care home manager/deputy manager 7).
Several care staff reported paper forms could ‘get lost’ (care home manager/deputy manager 6) in transit or do to not ‘come back’ (care home manager/deputy manager 6) from hospital with residents. Staff were unclear how GPs stored completed ReSPECT forms and were unclear if paramedics had access to them.
Many of the homes used ACPs or integrated care plans for residents, which expand on ReSPECT recommendations and address different types of clinical scenarios. These plans were completed by the clinician and provided medical history for residents, details regarding conversations held with residents/family and greater depth regarding agreed treatment in different situations. Care homes that used these plans found they provided greater clarity and ‘detail’ (care home manager/deputy manager 8) to follow in an emergency. These plans were shared with paramedic staff who used them alongside ReSPECT forms to decide on treatment. Some participants suggested that where ACPs or integrated care plans were available the ReSPECT form tended to be used just to guide them regarding resuscitation decisions. ACPs would be kept for residents in their personal files/with their care plan.
Reviewing completed ReSPECT plans
Care home staff emphasised that a ReSPECT plan could be updated to reflect changes in resident wishes or circumstances. However, only half described a clear or routinised process with GP practices for reviewing completed plans. In the others, reviews were mostly ad hoc and arose ‘naturally’ (care home manager/deputy manager 2) in response to changes in a resident’s health or condition:
We don’t touch them really once they’re in place … the doctor reviews them when they first come in, if there’s any clinical changes then she would review them again whenever we ask her to. Obviously if she’s seen somebody that’s become end of life or something like that, she would review it, that’s the only input we have with them, they’re not taken in and out of the file.
Senior nurse/nursing lead 1
In care homes that undertook regular review, these were part of overall care plan reviews for residents. These occurred at different intervals – monthly, 6-monthly, annually. Staff at one home described using a checklist during their care plan review which included question prompts to check the ReSPECT form was still on file, up to date (in terms of personal details and resident’s health/condition) and reflected the resident’s wishes. Where reviews occurred at regular intervals, they were typically carried out by specialist nurses rather than GPs.
Most interviewees did not express strong views about a routinised review process. One senior care home nurse suggested that it should involve more in-depth discussions with residents than was experienced currently:
I think that it should be a discussion again because things might have changed within a year, and a resident may have forgotten what they said a year ago. I think that rather than just, ‘Do you feel the same?’ ‘Yes’. ‘Okay, we’ll sign you off’, kind of thing, it should, should be a whole discussion again.
Care co-ordinator/senior carer 1
By contrast, one staff member considered that reviewing ReSPECT plans regularly was burdensome for residents:
If they’ve got capacity at that time to make that decision, why is this then being questioned repeatedly, again and again and again. Because asking somebody every six months if they want to be resuscitated or not and talking about death and dying with them every six months, is quite harsh on somebody that’s approaching that stage of their life and having memory problems. They don’t really know what’s what.
Care co-ordinator/senior carer 11
Use of completed ReSPECT plans in medical emergencies
Care home staff stressed the importance of making all staff aware of the presence of a ReSPECT form so that a resident’s wishes could be upheld, and the right treatment given:
making sure all the staff are aware … if somebody doesn’t want to be resuscitated or if somebody does want to be resuscitated, if they don’t want to have hospital treatment, or if there’s specific scenarios where they would want to go to hospital.
Care home manager/deputy manager 1
However, a common practice was that a senior staff member would be called upon to manage and provide leadership in emergency situations and to liaise with healthcare professionals attending the emergency. Several participants reflected that understanding regarding ReSPECT plans and their use varied among staff, and in some cases was more limited among junior frontline staff. One participant found it confusing that ReSPECT forms could state not for resuscitation alongside active treatment recommendations: ‘I don’t understand it … they’re not for CPR, but they’re for hospital. That’s what is not clear’ (senior nurse/nursing lead 3).
Another respondent recounted how resuscitation had been delayed for a resident as staff interpreted the presence of a ReSPECT form for a resident as equivalent to a DNACPR recommendation, leading to feelings of guilt and remorse among staff. A small number of staff therefore expressed a preference for ‘the old DNAPCR form’ (senior nurse/nursing lead 3) because it signified clearly and immediately that someone was not for resuscitation:
I liked them because you knew they were just not for resus. You just knew … with these new ReSPECT forms, you’ve got two boxes, and I’m not sure if these carers, or seniors, actually know that you need to see which one is ticked.
Senior nurse/nursing lead 3
A few other staff also reported frustration that staff needed to check which resuscitation recommendation had been made.
Some staff were uncertain as to whether recommendations could be overridden and in what circumstances:
Sometimes, if you feel that the resident needs to go to hospital, we sometimes talk to the family and then ask them if we could ... because, in case, you never know, they might get better or not … I’m not sure if we can override their [the resident’s ReSPECT] decision … without talking to them [relatives]
Care co-ordinator/senior carer 9
Some staff reported struggling to interpret recommendations. Recommendations such as ‘for ward-based care’ or ‘not for admission’ were considered unhelpful and ‘vague’ (care home co-ordinator/senior carer 8). ReSPECT forms that had been completed in hospital for residents were described as especially ‘basic’ (senior nurse/nursing lead 2), ‘sketchy’ (care home manager/deputy manager 4) and lacking personalised information. For example, one form was described to stipulate: ‘Very frail. Not for resuscitation’, which was felt by care staff to be ‘not person-centred at all’ (care home manager/deputy manager 7). Such recommendations lacked a plan for ‘treatment escalation’ (care home manager/deputy manager 4) and active directives that staff could follow. Where ReSPECT recommendations were vague or ambiguous, some staff used the ReSPECT form only for resuscitation decisions.
Staff suggested that ReSPECT recommendations did not always neatly reflect scenarios encountered within the care home, leading to uncertainty for staff over the right course of action.
Interpreting ReSPECT recommendations in emergency situations was ‘difficult’ (care home manager/deputy manager 7) for some care home staff as they were ‘not nurses … not doctors’ (care co-ordinator/senior carer 12) and struggled to assess the precise condition of residents:
What are we to do if somebody’s unresponsive, and it’s unusual for them? We’re not just going say, ‘Oh, well, they’ve got a DNR in place, it’s normal’, because it’s not normal … I know they’re not for resuscitation, but if somebody’s got palpitations or problems with their heart, and they’re not having a heart attack, they still need looking at …They still may need medication or treatment that can be sorted rather than leaving it and having a full-blown heart attack when it’s something that can be controlled.
Care co-ordinator/senior carer 12
Uncertainty among staff was particularly pronounced in incidents where ‘it’s something that could be treatable’ (care home manager/deputy manager 7) and/or where they had a resident that ‘clearly needs some medical help’ (care home manager/deputy manager 8). Staff often felt compelled to seek further medical assistance.
Some care home staff expressed difficulty with conveying to emergency services their need for additional medical interpretation and/or enactment of ReSPECT recommendations. In some cases, emergency call handlers and/or paramedic staff had questioned why they had been called when a ReSPECT form was in place, particularly where ReSPECT recommendations were not for resuscitation, or not for admission to hospital.
Once that ReSPECT form is in place, and we then need to call an ambulance for some reason, it’s like, ‘Well, why have you called them? They’ve got a ReSPECT form in place. It says not for hospital admission’, … but sometimes, there are reasons that we do need to call them.
Care co-ordinator/senior carer 12
One care home manager recounted how clinical recommendations such as ‘not for admission’ had, in their view, prevented any treatment for a resident because they felt the paramedics had interpreted it as meaning no treatment at all could be given:
Sometimes it will say, ‘Not for admission. Prioritise care and comfort’. … they [paramedics] are interpreting that [as] maybe they can’t give treatment because it says, ‘Not for admission’. You know, if it said, ‘Prescribe within the community’, … [there] needs to be more in it.
Care home manager/deputy manager 5
Care home staff described tensions both with and between healthcare professionals about care and treatment decisions. One resident was taken to hospital contrary to their ReSPECT recommendation, as paramedic staff had called relatives who requested that the resident was taken. Staff reported feeling frustrated that they later needed to explain the chain of events to the resident’s GP, who challenged the decision to admit the resident to hospital. Another resident with a ‘not for hospital admission’ recommendation had been transported to hospital by paramedic staff. The ambulance staff had explained that they ‘need to make the decision based on what I find here’ (care home manager/deputy manager 5), and they were not happy for the resident to remain untreated within the care home. The decision-making process was not clear to the care home manager, but she had felt unable to argue. Later, when discussing the incident with the resident’s GP, the care home manager recalled that the GP had expressed their frustration that ‘a different health care [professional] would make a different decision’. The care home manager described such incidents as ‘confusing’ and ‘demoralising’ and had resulted in a ‘lack of confidence in the ReSPECT system now’ (care home manager/deputy manager 5).
Reflecting on the ReSPECT process
Our interview data suggests that care home staff informally reflect on the ReSPECT process. Established processes for reviewing care plans for residents were used in half the care homes to check on residents’ ReSPECT plans. Several homes reported they had reviewed their ReSPECT plans and were planning to review them at least ‘annually’ (care co-ordinator/senior carer 8) prompted by this study.
The views and experiences of the ReSPECT process among other health and care professionals who engage with community-based ReSPECT process and resulting completed forms
Conceptualisation of the ReSPECT process
Participants in all focus groups agreed ReSPECT should be a person-centred process. Nurses and an emergency department clinician talked about the ReSPECT process as empowering for patients.
Sometimes when you do talk to your patients who are elderly with multiple long-term conditions, when you explain it to them, and you have that time … they’re quite thankful. And [say things] like, ‘No, I wouldn’t want to be, have CPR’, or ‘I wouldn’t want to be going to hospital’, or ‘I’m always worried that somebody’s going take me from my home’. And maybe when you get to a certain age in life some, not all, are, are okay at discussing their death and dying.
Nurse, focus group 3
I think it’s a brilliant form … gives the patient a voice … out of habit with the NHS and the healthcare system, I think we steal peoples’ voices quite a lot, and make decisions on their behalf, so I think it’s really important from that point of view, because it gives them their voice back.
Emergency department clinician interview 1
Another focus group with nurses discussed ReSPECT as a conversation people do not want to have when they are living well, so it must take place around a deterioration in health.
Home care workers emphasised that ReSPECT was an important mechanism for their clients to document and record their wishes for emergency treatment: ‘It’s getting your wishes … across isn’t it?’ (home care worker, focus group 2). ‘It’s a good way to have something in writing, that the person has a choice in what happens to them when they are in a state where they’re not able to make decisions’ (home care worker, focus group 1).
Many nurse participants discussed how the ReSPECT plan is considered the same as DNACPR. One nurse commented that if a healthcare professional asks if a patient has a ReSPECT plan, they might be asking if the patient is for CPR.
People [healthcare professionals] say, ‘Oh, have you got a ReSPECT form?’ Well, that doesn’t mean they’re not [for CPR] you need to know what it says on the ReSPECT form … not just that they’ve got a ReSPECT form … are you asking have they got a DNACPR? Or are you asking if they’ve got a ReSPECT form? Because it might not be the same.
Nurse interview 4
Some home care workers expressed a similar interpretation of ReSPECT plans as being predominantly about resuscitation decisions. Some emergency department staff talked about a tendency in hospital to treat the document as mainly about DNACPR.
One emergency department clinician had only seen two ReSPECT forms which said ‘for resuscitation’ and one nurse had only ever seen one example of this, which runs the risk of creating assumptions and that ‘the purple plan’ becomes associated with the DNACPR concept.
Initiating the ReSPECT process
Nurses discussed initiating ReSPECT conversations as part of their normal duties when interacting with very ill patients. Home care workers ask patients if they have a ReSPECT plan when they first assess them: ‘We … document what … the information is, so that we know the wishes of that person … how their care needs to be’ (home care worker, focus group 2). However, a few home care workers said they would make patients aware of ReSPECT plans if the patient didn’t not know about them.
Sometimes you ask people have they got a ReSPECT form, and they look at you blank, so you completely know that they have no idea what you’re talking about … that always leads me into a conversation about what it is.
Home care worker, focus group 2
I think we may make people aware that they’re available to people if they … want [to] consider them, but we don’t ever give people options in terms of that.
Home care worker, focus group 1
Nurses agreed that timing for the conversation works best when it fits with the developing relationship between the nurse and patient. They prefer not to complete a ReSPECT plan on a first visit when they are still building a relationship with the patient; however, sometimes patients begin expressing these wishes in a first visit and it can be a good opportunity to start completing a plan. It was agreed that the conversation evolves as relationships build. ‘So, you want to have those conversations at a time that feels right for the patient. You don’t want to lose that relationship by, by taking them there too soon’ (nurse, focus group 2).
Patients may initiate the conversation, often through a casual comment about their wishes, which can be used to trigger plan completion. If someone was very unwell, imminently dying and the process had not been completed, a nurse would start the ReSPECT process but, ideally, the conversation would happen before a medical emergency arose.
If patients are not ready to talk or feel disempowered by a previous negative conversation, starting a conversation about ReSPECT can be difficult. Nurses talked about the need to avoid damaging their relationship with the patient through starting the conversation at the wrong time for the patient. They felt it is better to wait until the patient expresses that they are ready.
One group of nurses talked about patients being reluctant to engage with the ReSPECT process if they perceive it to be only DNACPR and that patients need to be made aware the process gives many choices beyond DNACPR. One participant suggested that some patients and families are scared to discuss the topic due to their fear of an implied ceiling of care.
Some people are quite open and they’re happy to talk about it and, they’re open with their wishes. Some people have said ... straight away, ‘No, I don’t want to be resuscitated’. And others … they’re quite reluctant to speak about death and whether they would want CPR if their heart was to stop. Because sometimes they take it as, ‘They’re not gonna do anything for me, they’re not going to treat me anymore’.
Nurse, focus group 3
Home care workers explained that asking patients whether they had a plan in place during their initial support assessment required sensitivity:
It’s not nice to think about. Whenever we ask at assessments … we’re like, we’re, we’re really sorry to ask you these questions, but what are your funeral plans, and things like that. But they’ve got to be asked.
Home care worker, focus group 2
Undertaking the ReSPECT conversation and completing the plan
There was broad agreement that in the community, the ReSPECT conversation should be held by the clinician with the closest relationship to the patient, who has time available and can meet the patient and relatives in the patient’s home. This is usually the GP or palliative care nurse.
It’s a big part of our [palliative care nurse] role is trying to plan for what somebody wants as they enter the last months or weeks or days of life.
Nurses’ focus group 1
[The GP] is kind of the linchpin of all that … medical lead for their care in the community.
Nurses’ focus group 1
Several focus groups discussed how high staff turnover and high rates of agency and junior staff limited expertise within community nursing teams for undertaking ReSPECT conversations. The loss of GP–patient familiarity was mentioned by several groups as patients see a range of GPs and have other people involved in their care including pharmacists and other allied health professionals. Having a range of healthcare professionals trained and able to undertake ReSPECT conversations and completing plans would be helpful.
Palliative care nurses noted that other healthcare professionals might record having a ReSPECT conversation with a patient but would leave it to them to complete the plan:
I see it documented a lot of the time: ‘had ReSPECT conversation, they [patient] will discuss with palliative care nurse when they go’ or things like that. So, it might be that they’ve initiated a conversation but not necessarily gone through with the whole conversation and the document and completing it. And a lot of it is left for us.
Nurses’ focus group 1
In several focus groups of nurses, there was discussion of the need for communication training for ReSPECT conversations with patients. Participants who had received this training talked about the confidence it had given them.
There was broad agreement of the importance of involving families in ReSPECT conversations but that this can be complex. ‘Some people don’t want to have the discussions with the family members there and some people clearly don’t want to have the discussion until their family members are there’ (nurses’ focus group 1).
Involving families was considered an opportunity to get them to talk about what might happen and what was important to the patient:
It gives less responsibility … to the family members because you’ve already made those choices for yourself when you’re capable of doing so. People aren’t having … guesswork and fight amongst themselves because it’s already been discussed and written up.
Home care worker, focus group 2
As for the family, it can give them a little foresight … they will know ahead of time that their relative has already said ‘I don’t want to do this when it hits this point’. The family can kind of prepare themselves that this could be that point … rather than us just having to tell them there and then in that minute, and then them going through all the emotions in that second.
Emergency department clinician interview 5
However, participants also talked about families who have been upset when they have not been involved:
I had a conversation the other day with somebody who really didn’t understand what the form was all about. It was the daughter of a relative [who had been involved with ReSPECT conversation], and their concern was that the DNACPR box was ticked, and they didn’t think that was fair.
Emergency department clinician interview 1
Several participants commented that the level of literacy and health literacy of patients/families can make involvement in ReSPECT conversations difficult.
Storing and sharing completed ReSPECT forms
Community nurses talked about patients who took a paper ReSPECT form into hospital with them but it did not come home with them. Paramedics suggest that some patients can be reluctant to take the form with them to the hospital for fear it will be lost. Emergency department staff are frustrated that more long-term ill patients do not arrive with forms. In one focus group of nurses, there was uncertainty about knowing you have the most recent copy of the form. Several focus groups with nurses discussed the need for a shared electronic version of the form but expressed despondency about this coming about.
Home care workers explained that ReSPECT forms were stored in patients’ care files, within their home, and were slightly oversized compared with other documentation so that they were visible and quickly retrievable in an emergency. ReSPECT recommendations were also written and highlighted in red at the front of care plans and were recorded electronically so that they could be accessed by all home care staff.
Participants talked about the content of ReSPECT forms they had read. They commented that when doctors complete a ReSPECT form the resuscitation section is always completed but the patient preference section might not be. They suggested that the plan is only useful to patients when their wishes are accurately considered and recorded. ‘The forms are only as good as the information that’s on there and the detail that’s on them’ (nurses focus group 1).
Home care workers found handwritten forms difficult to read and they struggled to understand clinical shorthand:
The only thing that I think is wrong with them is you can’t read the writing on them sometimes when the doctor writes on them … it can be hard … you can’t quite understand what those conditions are that they’ve noted on there.
Home care worker, focus group 2
Can’t understand it … It’s like hieroglyphics.
Home care worker, focus group 2
It was generally agreed that there can be great variety in the content of the form depending on who has undertaken the conversation with the patient.
Reviewing completed ReSPECT plans
Nurses working in the community acknowledged there was no formal system for reviewing ReSPECT plans but that they should be reviewed. Some reviewed ReSPECT plans during routine annual reviews with their patients. Others talked about initiating a review when the patient expressed wishes about treatment during a conversation. The nurses agree that ensuring that the plan is up to date could help improve the quality of the recommendations.
Use of completed ReSPECT plans in medical emergencies
Many participants thought a completed ReSPECT form was very helpful for clinicians: ‘Having a clear documentation that a patient has had the opportunity to make their wishes known, makes everybody’s life easier’ (emergency department clinician interview 3).
There was agreement across the data that the absence of a ReSPECT form can be very distressing for healthcare professionals attending an emergency, especially if the decision is whether to perform CPR. Nurses, home care workers and paramedics talked about how paramedics now usually ask for the ReSPECT form as soon as they arrive, and always in a care home. Paramedics report that ReSPECT forms are sometimes not kept physically close to the patient which can cause delay and impact treatment. ‘If staff walk all the way to the office where the form is located it can take 10 minutes, but this may be too late, and you have already started CPR’ (paramedics focus group). Paramedics found some patients have multiple forms; in which case they use the most recent.
Nurses gave positive examples of where ReSPECT plans worked well in practice – many of these examples referred to patients who did not wish to go to hospital. ‘Some patients, it is that plan in place, you know, “I don’t want to be put in hospital”, or, you know, it’s only for reversible things, infections or broken bones’ (nurses focus group 3).
One participant of this group explained how this decision to not go to hospital can be empowering for patients. Another talked about the benefits, not only for patients but also for carers including care home staff who need to decide what action to take in a medical emergency. A ReSPECT form might give them confidence to call the GP service rather than an ambulance. ‘May go right down the route of a GP as opposed to a 999 call or 111 services’ (nurses focus group 3).
However, nurses and home care workers reported that patient wishes were not always recorded in the plan in a way that is helpful to determine actions. Emergency incidents requiring home care workers to use the form were described as rare, but home care workers stressed that they did not feel the form provided sufficient information to guide them in an emergency:
I think it could be clearer whether we’re supposed to take action or not take action on, on the wishes that are on there. Naturally you want to help someone when they’re in that state … and it would be good maybe if there was an outline of what we’re expected to do.
Home care worker, focus group 1
In emergency situations, home care workers therefore always called an ambulance or phoned NHS 111 for medical assistance and emphasised their role in informing emergency health professionals of the presence of a ReSPECT plan.
Emergency department staff and paramedics indicated that ReSPECT forms completed well give them confidence to act in an emergency and feel that they are respecting the patient wishes. ‘We are probably the most dependent on them from a perspective of urgency. And I think what is very difficult to get across to anybody else is how vitally important they are at that time-critical moment’ (emergency department clinician interview 3). However, they found that patient wishes are not always clearly recorded in a way that is helpful to emergency decision-making. Paramedics said that sometimes there is not enough information recorded on the ReSPECT form to defend a decision not to take a patient into hospital even when you know it is what would be best for them. They mentioned that the paramedic workforce is generally young and inexperienced, and it is hard to make challenging decisions on the spot, so paramedics need clear and easy guidelines to follow that they can defend.
A nurse focus group and most of the emergency department participants discussed how disagreement between the wishes of families and patients can complicate access to or use of ReSPECT forms in emergency scenarios. One nurse gave an example of a couple where the husband had a form marked ‘not for resuscitation’, which his wife conveniently forgot to find each time he had to go into hospital as she felt that the paramedics treated him differently and more slowly if they knew he had a ReSPECT form. An emergency clinician had also encountered the situation where families do not want to bring the form because of a perceived ceiling of care. ‘I get the impression that, sometimes, families won’t bring in a ReSPECT form for fear that we will discount their relative as being unsavable, in inverted commas’ (emergency department clinician interview 2).
Reflecting on the ReSPECT process
There was no mention of any formal reviews of the ReSPECT process by any of our participants. However, our data indicate that participants informally reflected on the ReSPECT process and how they engaged with it. Some reflected on its impact within the NHS more generally.
Several participants remarked on the allocation of NHS resources to end-of-life care and suggested that enabling patient choice could also have significant cost-saving benefits. Paramedics and emergency department staff also suggested facilitating patient choice can improve the patient relationship with the NHS. ‘I think people would feel more empowered and supported if, if, yeah, if they had more choice about their treatment rather than just becoming part of the sausage factory’ (emergency department clinician interview 1).
One emergency department doctor suggested as well as empowering patients to make choices about their care there is a wider benefit for society in managing expectations.
I think that one of the things the NHS has done since its advent is assumed the responsibility for peoples’ life decisions and care decisions. People have become used to doing what the doctor tells them to do … But I think what it’s done, it’s distanced everybody from their own mortality, the end-of-life process and from their own death. So, between that and media coverage and [tv] dramas, everybody expects that every illness and disease is reversible. So, there is a huge disconnect between the reality of being a human being and what people expect.
Emergency department clinician interview 1
The content of ReSPECT forms stored in general practice medical records
Methods
To evaluate the content of ReSPECT plans we reviewed ReSPECT plans stored in the medical records of the general practices who participated in our qualitative study.
Evaluation framework for completed ReSPECT forms
We used a modified version of a tool developed during our previous study of ReSPECT in secondary care. 66 This was based on the ethical framework of accountability for reasonableness, which focuses on fair decision-making processes rather than on specific ethical principles. 67 The framework stipulates that decision-making should be transparent, based on reasons agreed as justifiable by the relevant stakeholders and open to review. 67 The process should be consistently applied to justify the ethical principle of equity. The evaluation tool is structured to answer the following questions:
-
Consistency: what is the variation in content in terms of the detail requested on the ReSPECT form and associated guidelines?68
-
Transparency: how complete is the information about the patient’s preferences, diagnoses, reasons for treatment recommendations and who participated in the ReSPECT discussion?
-
Ethical justifiability: do the reasons for treatment recommendations indicate that clinicians considered the patient’s preferences and clinical conditions, as well as the benefits and burdens of specific treatments? How complete is the documentation of patient capacity and who provided input to completion of the ReSPECT form?
The tool provides a structure for evaluating each ReSPECT form and providing counts of how many ReSPECT forms in the survey meet quality criteria.
Team members CJH, KE, CAH, AS and FG modified the existing tool and associated guidance to take account of changes to the ReSPECT form since our previous study (introduction of version 3). We each independently used the tool to evaluate three completed ReSPECT forms, using a total of eight forms, so several team members evaluated each form. We met to discuss adaptations needed and repeated the process again to ensure each version of our tool provided consistent evaluation of each domain (see Report Supplementary Material 7). The relevant version of the tool was then used to assess each completed ReSPECT form (version 2 or version 3).
Sampling and recruitment
The 13 GP practices identified adults registered with the practice recorded as having a ReSPECT form completed within the previous 12 months. Following eligibility screening, patients or their next of kin if it was known to the GP practice that they lacked capacity, were sent information about the study, that the study involved accessing their medical records and what to do if they did not wish to participate.
Data collection
A study researcher or member of practice staff accessed the records of all eligible patients who did not opt out of the study and identified whether they contained a ReSPECT form. Identified ReSPECT forms were scanned (hard copies) or electronically copied. Data collection took place from February 2021 to January 2023.
Data extraction and evaluation of each ReSPECT form
CJH extracted data and evaluated content of all forms. KE, CAH, AS and FG extracted data and evaluated 25% of the total. To ensure consistency, the team met to compare findings, discuss and resolve discrepancies after evaluating half of the forms and again after evaluating the remaining forms.
Ethics considerations
Data were collected with approval from the CAG (reference 21/CAG/0089). Personal identifiers were redacted prior to transfer to the study team using NHS encrypted e-mail or an encrypted NHS platform. Data were stored in password-protected files on a secure University of Warwick server.
Results
Practices identified 526 patients with a ReSPECT form completed in the past 12 months. Practices excluded 200 patients prior to invitation (see Figure 1) and 17 patients opted out of the study. One practice did not hold any completed ReSPECT forms in patient records. We were unable to retrieve forms from one practice because, in error, 63 recruitment letters were sent without study identification numbers, so it was not possible to accurately record opt-outs. Of the remaining 246 participants, we retrieved 146 (60%) ReSPECT forms. Four forms were excluded because they were completed over 12 months prior to data collection, and one was a duplicate. This left 141 forms for analysis (see Figure 1). Of these forms, 55 (39%) were handwritten and 86 (61%) electronic; 102 (72%) were version 2 and 39 (27%) version 3. Three (version 2) forms were incomplete, with the second page missing. Completion rates for different sections of the form varied (see Appendix 5).
Consistency of recorded decision-making processes
Of the 141 forms, 64 (45%) had a mark on the scale for patient preference [Balance of priorities (version 2)/What matters to me (version 3)]. Over half (81/142, 57%) of the forms recorded free-text personal preferences (54%, 37/68). For people with capacity, this increased to 69% (47/68).
Fifty-three forms (37%) had a clinician signature in one of the CPR recommendation boxes (42/55, 76%) for handwritten forms and (11/86, 13%) for electronic forms). Of the electronic forms, 54/86 (63%) had the CPR recommendation typed in place of a signature.
Most forms recorded free-text recommendations for treatments other than CPR (87%, 122/141) but the focus of the clinical recommendations (extending life/prioritising comfort) was less well recorded (52/141, 35%).
Most forms recorded that the patient or (if the patient lacked capacity) someone close to them was involved in discussing the ReSPECT form content (133/141, 94%).
Most forms (108/141, 77%) recorded the clinician’s role or registration number but less than half (64/141, 45%) included a signature. The senior clinician signature was only present on 14/141 (10%) forms. This may be because of confusion about where the clinician completing the form should sign if they are also the senior responsible clinician (usually the GP).
Confirmation of validity of the form was completed in 11 forms (8%).
Transparency
Nearly all forms (129/1411 92%) recorded the person’s health conditions. Some provided a detailed list of diagnoses; while others used terms, such as ‘frailty’ and ‘decreasing health’ without clarification, or used abbreviations (e.g. ‘AF, CKD, IHD, OA’). Only 27/141 (19.0%) forms documented reasons underpinning the clinical recommendations.
Where free-text personal preferences were recorded, text was often brief and usually referred to a preference for being kept comfortable or remaining at home. More detailed explanations were noted in version 3 forms where the clinician is prompted to record what the person most values and what they most fear/wish to avoid for example:
Values; ‘Being kept comfortable, familiar surroundings, husband and daughter present’. Fears; ‘Hospital admission, uncertainty’.
Most forms recorded free-text recommendations for treatments other than CPR (122/141, 87%). Most (94/122, 76%) provided detailed recommendations on what treatment should be provided in a range of situations, for example: ‘Not for resuscitation. Not for admission under any circumstances, apart for suspected fracture or head injury that requires A&E assessment’, while 28 (23%) gave general instructions, such as ‘Not for hospital admission’. The focus of the clinical recommendations (extending life/prioritising comfort) was less well recorded (52/141, 35%).
Ethical justifiability of recorded decision-making processes
Of the 26 forms where reasons for clinical recommendations were provided, 22 (85%) included a reference to the patient’s wishes. Of these, 6 (27%) did not complete any part of the personal preference section.
Only five forms included a reference in the recommendations to the patient’s condition and ability to benefit from future interventions. We found only one form which explicitly referred to the patient’s preferences and considered the benefits and burdens of treatment.
In 131/141 forms (93%), the person’s capacity was recorded. Version 3 requires clinicians to say in what way the person lacks capacity. Of the 23 relevant forms analysed, 17 (73%) provide a reason which includes in some cases reference to capacity ‘unable to process or retain information’ or a more general reference to the person’s cognitive status ‘dementia’ or ‘cognitive impairment’.
Among the people who lacked capacity, the involvement of someone close to them (relative or friend) was recorded on 39/59 (66%) forms and this person’s name and role was recorded on 25/59 (42%). Whether the person who lacked capacity had a legal proxy was recorded on 45/5 forms (76%).
Summary
Our survey of GPs in England showed that ECTPs are a standard part of GP practice, with 98% (828/841) of respondents using some form of ECTP. GPs overall are supportive of their use, agreeing that they help to ensure that patients’ wishes are known and support patients’ families. However, just over half of survey respondents reported using DNACPR forms rather than a more holistic ECTP that includes other treatment recommendations and specifically acknowledges patient’s preferences and values. Most respondents using a broader ECTP used ReSPECT.
The main trigger for initiating an ECTP conversation is a diagnosis of a life-limiting or life-threatening condition, suggesting that they are considered primarily as anticipating end-of-life events.
While completion of an ECTP in primary care is currently carried out mainly by GPs, respondents thought that a much broader range of health and social care professionals could complete these plans, with a substantial minority of respondents including senior care home staff. GPs who used ReSPECT were more likely to feel comfortable in having these conversations with patients and their relatives.
Only half of GPs reported that their practice had a regular system for reviewing ECTPs despite a similar proportion agreeing that the plan could be out of date at the time it is needed.
Our qualitative exploration of health and social care professionals’ experiences of using ReSPECT showed that ReSPECT is conceptualised as a patient-centred process, allowing patients to have a nuanced discussion about future medical care and treatment decisions and take some control over these decisions, particularly when nearing the end of life. However, it is also clear that a ReSPECT plan is often seen as mainly about CPR, and sometimes interpreted as simply a DNACPR form. Clinicians see ReSPECT recommendation as a guide to decision-making in an emergency, while care home staff see them as a record of a residents wishes, enabling them to advocate on their behalf.
Generally, the ReSPECT process is initiated when a patient changes care context, such as moving to a care home, starts to receive palliative care or a relevant health condition becomes worse. Care home staff want early completion of ReSPECT forms after admission for almost all residents. Careful timing and preparation for a ReSPECT conversation is important to minimise any distress for patients and their families particularly as many see initiation of ReSPECT conversations as acknowledgement of a terminal illness. Care home staff can have an important role in preparing residents and their families for the ReSPECT conversation.
Completion of a ReSPECT plan needs time, sometimes involving several conversations, and should be led by a clinician trusted by the patient. The involvement of families in the conversation, including when the patient has capacity, is seen as important to ensure that families understand the patient’s wishes and to reduce conflict during decision-making in an emergency. The level of uncertainty about a patient’s illness trajectory and future treatment options can affect the type of conversation held and the confidence with which clinicians are prepared to make recommendations.
Processes for storing and sharing completed ReSPECT plans vary across GP practices. There is concern about lack of synchronisation between paper and electronic versions, and forms do not always follow the patient between hospital and home. Paramedics sometimes encounter more than one version of a plan when attending in an emergency.
Participants across the data sets describe challenges in interpreting ReSPECT recommendations in an emergency. This can be because recommendations are poorly written, vague, or not applicable to the situation. Even when recommendations are more detailed there may be differences in interpretation with decisions not always appearing to fit with the recommendations. Clinicians need to make judgements in relation to patient safety guided by, but not constrained by, the recommendations.
The approach to reviewing completed ReSPECT plans varies from no systematic process to routine review as part of an annual review or more frequent review for a few patients.
Our evaluation of completed ReSPECT forms found that most forms contained text about treatment recommendations other than resuscitation, with text about patient preferences recorded on just over half of the completed forms. CPR recommendations were recorded on around two-thirds of forms, but this figure may have been higher if we had been able to see the patient held form. Clinicians rarely recorded their reasons for treatment recommendations on the form. Where reasons were given, these usually referred to the patient’s wishes about hospital admission.
Most completed ReSPECT forms recorded that the patient or someone close to them was involved in the ReSPECT conversation. However, where a patient lacked capacity and so the involvement of a relative/lasting power of attorney holder is expected, only two-thirds of these forms indicated they were involved and fewer than half named the person.
Strengths and limitations
To our knowledge, this is the first survey of GPs’ use of ECTP. We obtained a high-quality data set with no missing data. Although we did not achieve our original target of 1000 respondents, this is still much larger than most GP surveys. 69,70 We have sufficient data to produce a precise estimate for all our outcomes of interest and a robust statistical model exploring factors influencing how comfortable GPs are having emergency care and treatment planning discussions. Our respondents were representative in terms of region, age, practice size, years since qualification and region. Nevertheless, using a market research company working through a commercially funded, free to use website for data collection may have introduced bias into the sample selection.
Our qualitative data provide us with evidence of how a wide range of clinicians and carers conceptualise ReSPECT and an in-depth account of how the ReSPECT process is operationalised in general practice and care homes. Recruiting clinicians and carers working in other community/care services and emergency departments was challenging; recruiting more participants may have provided further and different accounts of ReSPECT. We used NPT as a framework for our analysis but to gain traction on the bulk of the data which related to the ‘cognitive participation’ and ‘collective action’, we used the ReSPECT process itself as an analysis framework.
A strength of our evaluation of completed ReSPECT forms is that it evaluates the actual content of ReSPECT forms. However, ReSPECT forms are designed to be held by the patient, we were limited to copies of ReSPECT forms which GP practices had chosen to store in the patient’s clinical notes. Some practices stored electronic copies that did not include signatures, so we do not know what signatures were on the copy held by the patient.
Chapter 5 How do patients and families experience the ReSPECT process?
Parts of this chapter are reproduced with permission from Eli et al. 71 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/
Introduction
At the heart of the ReSPECT process is a conversation between a clinician and a patient, a patient and relative(s) or a relative of a patient who lacks capacity. The conversation aims to facilitate shared decision-making about planning for treatments wanted and unwanted in a future emergency. 72 Yet, despite the centrality of patients and relatives, little is known about how they experience ReSPECT. Only one previous study has examined patient and relative experiences of ReSPECT conversations. 8 The study, in hospitals in England, found that during an acute admission, patients and relatives often felt unprepared for ReSPECT conversations, were confused about what the conversation meant, and were unsure about how ReSPECT would influence their future care. 8 No research has explored how patients and relatives experience ReSPECT in community contexts.
In this chapter, we report on interviews with patients, the relatives of patients without capacity, and patient and relative pairs to explore how they experienced the ReSPECT process, and what enablers and obstacles to the implementation of ReSPECT in primary care were revealed in these experiences.
Methods
Participant recruitment
Patients who had a ReSPECT plan completed in the previous 12 months were identified by the 13 GP practices who participated in the study (see Figure 1). Eligible patients and the next of kin of patients without capacity were sent information letters. Interested patients and relatives sent expressions of interest, which we followed up with an introductory phone call and a detailed information sheet and consent form (by e-mail and/or post); patient participants were told they could invite a relative to accompany them during the interview. Consent was taken before each interview, either written (in-person interviews) or verbal (telephone interviews). For verbal consent, the researcher went through the consent form with the participant, documenting their consent for each item. A copy of the completed consent form signed by the researcher was sent to each participant following the interview.
Data collection
We developed semistructured interview topic guides (see Report Supplementary Material 5). The questions were designed with reference to the NPT framework and focused on understandings of the ReSPECT process and form (coherence), narratives of the process from first consideration to completion and updating (collective action), views of the process (cognitive participation), experiences of the ReSPECT conversation and expectations as to how ReSPECT might be used (reflexive monitoring).
Participants were interviewed either in person or by telephone, depending on their preference. The interviews were conducted by one of three researchers (JH, CJH, KE) and were audio-recorded and professionally transcribed.
During the consent process, participants were asked if they could be contacted for a follow-up interview. If participants agreed, we checked with their GP surgery, at least 6 months after the first interview, if they could be approached. We then contacted eligible participants to ask if they would agree to an interview. Follow-up interviews were semistructured and were conducted by JH, KE and CJH by telephone. These interviews explored whether there had been changes in the patient’s health, whether the ReSPECT form had been used or reviewed, and whether the participant’s views of ReSPECT had changed.
Analysis
We initially intended to use framework analysis. The smaller than expected sample size meant inductive thematic analysis was more appropriate. KE coded the first interview transcripts using a semantic and latent approach to capture both direct and implied meanings. 73 Providing intercoder reliability, JH and CJH analysed between them eight interviews. After abstracting from initial to higher order codes, KE drafted candidate themes and met with CJH and JH to discuss these. Following their discussion, the themes were refined and critically reviewed and approved by the research team.
KE read through the follow-up interview transcripts, to ascertain whether participants reported any changes and whether ReSPECT had been used, either of which prompted further analysis.
Findings
Descriptive findings
Study sample
We identified 461 people who had a ReSPECT plan completed in the past 12 months. After excluding those no longer registered with the practice, for whom there were no relative contact details, or who had died 366 were eligible (see Figure 1).
For the interviews, we included people who had a ReSPECT plan completed in the previous 6 months (N = 164). Invitation letters were sent to 94 patients and 70 relatives of people lacking capacity. A total of 15 responses were received (10 patients and 5 relatives), of which 13 led to an interview; 1 person did not remember they had a ReSPECT form, and one could not be contacted (see Appendix 6 for interviews by study area).
We included six patients, four relatives and three patient and relative pairs, where the patient had capacity and chose to be accompanied by a relative who also participated; eight women and five men, 53–93 years (median = 83); nine resided at home and four in a care home.
Four patient participants said they had initiated the ReSPECT discussion with a healthcare professional; in eight cases, a health or social care professional initiated the discussion with the patient or their relative due to a change in health or care circumstances; in one case it was unclear who initiated. Nine participants or participant pairs said they had a ReSPECT conversation with a healthcare professional (five GPs, three nurses, one physiotherapist), whereas four said they did not. This included one participant whose ReSPECT form was completed in hospital, one participant pair who recalled their treatment preferences but not a discussion, and two relatives of patients without capacity who said they had not been included in ReSPECT conversations held with these patients.
Follow-up interviews
Six follow-up interviews took place: four with patients and two with relatives. Seven participants did not take part in a follow-up interview: four died (two had not consented for us to contact their next of kin, one had died recently so we did not contact their relative, and we could not locate contact information for the fourth participant’s next of kin); one did not consent to a follow-up interview; one declined; and one participant’s GP advised against contacting them.
In the six follow-up interviews, four participants said they did not experience a major change in health and their ReSPECT form had not been used in the intervening months. One patient participant said he had been attended by ambulance staff; he recalled they asked about his ReSPECT form and thought they took photographs of it but was unsure whether his ReSPECT form had travelled to hospital with him or been used (patient 11). One relative participant said that ambulance staff had attended her mother several times, in which they either asked about ReSPECT or she mentioned her mother had a ReSPECT form; she said the ambulance staff looked at the form only once, because she described the recorded recommendations to them in all other instances (relative 9). One patient participant said she would like to change her ReSPECT form to indicate her preference for dying in a hospice rather than at home (patient 4). No participant reported changes in their views of ReSPECT.
Feedback on improving the ReSPECT process
In both the first and the follow-up interviews, participants were asked how the ReSPECT process could be improved. Their recommendations included making patients/relatives aware of ReSPECT earlier in the disease process; timing the ReSPECT conversation sensitively; ensuring that the ReSPECT conversation has nuance and that decisions are not presented as binary; reviewing the form regularly and making sure people understand the use and limitations of ReSPECT.
Thematic findings
Patients and their relatives perceive ReSPECT as an end-of-life or do not attempt cardiopulmonary resuscitation form
While most participants knew that ReSPECT included information about treatment options beyond CPR, such as future hospital admission, they spoke of ReSPECT as a DNACPR or end-of-life form. This reflected the timing of ReSPECT conversations for these participants: some initiated the conversation to record their wishes for palliative care or not to have CPR, while others had the ReSPECT conversation initiated by healthcare professionals upon receiving a life-limiting diagnosis or moving to a care home.
This perception of ReSPECT could be both an enabler and an obstacle. Some participants felt positively about this framing, saying they found it reassuring to have their preferences for DNACPR or end-of-life care recorded. One patient characterised ReSPECT as an ‘upgraded DNR’, and spoke about proactively seeking to record their preferences on the ReSPECT form: ‘I don’t want my body to be resuscitated and I believe that if my heart stops that’s the Lord’s time, he knows the number of my days and I don’t want to be brought back to life’ (patient 8).
Another completed the ReSPECT form with their palliative care nurse, with a focus on comfort care:
[M]y view was that I didn’t want any intervention at end of life. So, when end of life arrived … that process would broadly be allowed to happen without any attempt to slow it down at all. All focus being on comfort rather than on, on time to slow that process down. And that was my desire at the start of the form and remained my desire at the end of the form.
Patient 3
Most patient participants spoke of ReSPECT as allowing them to maintain their quality of life and die naturally. However, for one patient framing the ReSPECT form as an end-of-life document meant coming to terms with their prognosis. They described being approached by healthcare professionals multiple times before agreeing to have a ReSPECT conversation:
At first, you know, when she [the GP] was saying about filling it in, I said, ‘Oh, I don’t feel I’ve got to that stage yet’. And she said, ‘Well, the thing is, if you fill it in before you get to that stage, it takes some of the pain out of it, as it were, the emotional pain’.
Patient 12
Some patients and relatives know how to use the ReSPECT form, while others do not
Although the ReSPECT form is patient held, not all participants knew how it would be used in an emergency – a key obstacle to ReSPECT implementation. Some participants kept the form at home but were not aware they had to store it in an easily available location; this dovetailed with misunderstandings of how ReSPECT would be used. The interview with one patient and relative began with the patient participant rummaging through a drawer to find the form. Later in the interview, when asked how ReSPECT would be used, the patient participant said, ‘He didn’t tell me anything. I mean I, I don’t know whether the, the hospital knows or what, I don’t, I don’t know’ (patient 11). Another patient and relative interview began with the patient participant looking for the form and mistaking other forms for ReSPECT. Later in the interview, it transpired that both the patient participant and his wife did not know how ReSPECT would be used; indeed, they turned the question back to the researcher, asking her, ‘What would happen with the form?’ (relative 13). When the researcher asked them ‘did they [healthcare professionals] explain that to you?’, the patient participant said, ‘No, they didn’t, no’.
Other participants kept the form in an easily accessible place, having been told to do so by healthcare professionals, as one patient explained: ‘they [healthcare professionals] said if, if anyone was called to the house, 999 or something, to keep this form in a place where we could show it to them’ (patient 4). Another participant provided a detailed description of how she stored the form to maximise accessibility:
I’ve got one copy in my purse that I take with me everywhere I go and I’ve got this other copy in the fridge in the Lions emergency green ... are you familiar with those green boxes and that you put in the fridge? And there’s a sticker on the front door of the flat so if the paramedics come they, they recognise that and they go look in the fridge.
Patient 8
Patients trust and value the ReSPECT process and recognise that it implicates their family’s well-being
The patient participants expressed trust that the ReSPECT form recommendations would be followed. For example, when one patient was asked if she thought healthcare professionals would follow the recommendations in her daughter’s absence, she said: ‘Well, they’ve got the form to read, haven’t they? (Researcher: yeah.) And I think … they would carry out what it says’ (patient 5). Participants also valued the opportunity to express their wishes and have these recorded. ‘I’m happy about it because … it was my, my decision and I thought about it, in fact, I’d been thinking about for, oh, quite a while’ (patient 5). However, participants described a ReSPECT plan as helpful not only to patients but also to families. Some said it allowed them to relieve their relatives’ future decision-making burden. For patient 12 ReSPECT was about having things ‘in writing [so] that people know my wishes’ but also about ‘[t]aking a bit of the responsibility away from my daughters’. Patient participants also said that ReSPECT provided clarity and would help their relatives advocate for them in an emergency: ‘she [daughter] knows exactly what has been wrong with me and what my wishes are if anything happens to me. And I think it puts her mind at rest’ (patient 5).
Other patient participants said that having their treatment preferences recorded on a ReSPECT form would reduce their family’s future caring responsibilities: ‘if my heart stops I don’t want to be resuscitated and I don’t want to be a burden on my family and surrounding family members’ (patient 5).
While patients considered their relatives’ emotional well-being, they did not backtrack if their relatives disagreed with their preferences. In some cases, participants negotiated with relatives while asserting their own decision-making agency. For example, when the relatives of one patient opposed her preference, she held several conversations with them: ‘as we’ve talked about it two or three times, they, I think, have understood why I’ve, I did it, why I did have a ReSPECT and put “DNR”. So we’re not in conflict’ (patient 4).
The ReSPECT conversation shapes patients’ and relatives’ experiences
The quality of the ReSPECT conversation was pivotal to participants’ experiences and understandings of the ReSPECT plan and thereby to enabling its implementation. The participants who described positive experiences had an open discussion with a healthcare professional, where the ReSPECT plan was clearly explained, and where they felt listened to and able to express their wishes. For example, patient 5 characterised her ReSPECT discussion as ‘a proper two-way conversation’.
Participants who described negative experiences of the ReSPECT process said that they either felt unprepared for the conversation or did not have a conversation. One participant, whose ReSPECT form was completed in hospital while they were acutely unwell, recalled the doctors speaking about her, but not to her, and positioned ReSPECT within a wider story of being treated in hospital as if she did not have capacity: ‘they were having conversations with the, there was a student there, and a nurse and they were talking to themselves, they weren’t talking to me’ (patient 7).
In two other examples, relatives of patients who did not have capacity said that ReSPECT conversations were held with the patients at their new care homes without involving them. Both said they were surprised to discover a ReSPECT form had been completed. One described ReSPECT as, ‘something I felt I had to, sort of, piece together for myself’ (relative 10), saying that the care home staff did not explain ReSPECT to her formally until the later stages of her mother’s illness. The other felt that, ‘I should have been there, and I should have been told about it before’ (relative 6). This permeated their perceptions and experiences of ReSPECT. Although both agreed with the recorded recommendations, they felt negatively about the process and equated having a ReSPECT form to the patient being labelled ‘end of life’ or no longer wishing to live.
Participants who had a positive conversation experience expressed a good understanding of the ReSPECT review process. For example, patient 4 described being ‘very impressed’ by healthcare professionals’ responsiveness to her expressed wish for palliation. She also said that her healthcare team clarified the form could be changed – an option she was actively considering at the time of interview, noting that ‘they’ve put a phone number on it’, which she could call to communicate a change in her preferences. By contrast, relative 1, who described feeling ‘thrown’ by the ReSPECT conversation, said she was unaware the form could be changed and first learnt about the possibility of review during the interview.
Summary
Patients’ and relatives’ experiences of the ReSPECT process were shaped by the ReSPECT conversations they had with healthcare professionals. Participants who had an open discussion with a healthcare professional, where they felt listened to and received clear explanations, spoke about ReSPECT positively. This influenced participants’ understandings of ReSPECT, which in turn either enabled or constrained implementation: those who had positive conversation experiences showed a good understanding of ReSPECT and of how the form may be stored, used and reviewed, while those who did not tended to have a poorer understanding of the process.
Across the sample, patients and relatives associated ReSPECT conversations with DNACPR and end-of-life planning, but this did not necessarily present an obstacle to implementation. The participants expressed trust that, in an emergency, healthcare professionals would follow the recommendations recorded on the ReSPECT form, a key enabler of ReSPECT implementation.
Although participants valued patients’ decision-making autonomy, they conceptualised ReSPECT as affecting family members’ well-being, with patients trying to reduce their relatives’ decision-making burden, help relatives advocate for the patient and decrease future caregiving responsibilities. This underscored the importance of family considerations in enabling ReSPECT implementation in primary care.
Strengths and limitations
A strength of this study is that it includes the voices of patients and their relatives who have had a ReSPECT plan completed in the recent past mitigating problems with recall. The patient voice adds richness to the overall qualitative analysis of how ReSPECT is used and experienced in primary care. However, the small number of participants recruited means that their views and experiences may not be a reflection of the wider patient population with a ReSPECT plan in place.
Chapter 6 Ethical values and dilemmas in the ReSPECT process
Introduction
In this chapter, we consider the ethical values that inform how ReSPECT is conceptualised and enacted, and the ethical issues and questions that arise from its use. The ReSPECT process is designed to facilitate meaningful discussions between healthcare professionals, patients and their families about preferences for treatment in future emergencies, promote shared understandings and treatment recommendations, prevent patient harm and facilitate beneficial treatment provision. 46 Built into the ReSPECT process are healthcare values of patient autonomy, person-centred care and acting in the patient’s best interests. Drawing on interviews with GPs and nurses, patients and relatives, and care home managers and staff, we explore to what extent ReSPECT as used in primary care upholds these values, and what other values may also be at stake.
Methods
Participant recruitment and data collection
Interviews were conducted with GPs and nurses, care home managers and staff, and patients and relatives (refer to Chapters 2 and 4 for participant recruitment and data collection procedures).
Analysis
Interview data were analysed using a modified framework approach and the empirical ethics model of grounded moral analysis. 54,74 Six co-authors (AS, CB, CJH, FG, JH, KE) coded 12 interview transcripts (4 GP, 3 care home and 5 patient/relative interviews), with 11 transcripts intercoded. This initial coding identified semantic (explicit) and latent (implicit) references to ethics. 73 Using these initial codes and the group discussions that followed, AS developed a draft coding framework, including inductive and deductive codes. Topic guides for future interviews were refined to explore the ethical issues and concepts identified.
Interviews were summarised in individual pen portraits by KE (GPs and nurses, care home managers and staff, and patients and relatives) and CJH (GPs). 75 We created 37 pen portraits, capturing all patient and relative interviews (n = 13) and half of the GP/nurse (n = 13) and care home (n = 11) interviews. GP/nurse and care home interviews were purposively sampled to include data from all sites and different types of staff. These sample sizes allowed us to reach code saturation. 64 KE coded each pen portrait using the draft coding framework. AS intercoded 16 pen portraits (7 GP, 5 care home and 4 patient and relative interviews); comparisons showed a high level of consistency. During coding, KE and AS added new codes to the draft framework. To ensure meaning saturation, AS reviewed the interviews not summarised in pen portraits (13 GP and nurse and 11 care home interviews) to check for new codes (none identified) and extract illustrative quotes.
Using the pen portraits, KE outlined the ReSPECT process timeline as described by the participants, from preconversation to the enactment of recommendations, identifying ethical dilemmas at each stage and abstracting candidate themes from the codes to capture the salient ethical values for each dilemma. These themes were further refined and finalised in discussion with AS.
Findings
Participants described the ReSPECT conversation and plan as empowering patients, respecting their wishes and engaging them in decision-making. As such, ReSPECT was seen as honouring patient autonomy and aligned with the professional obligation to provide person-centred care. Participants also emphasised the duty to protect patients from harm and act in their best interests. Additionally, two other ethical values – the moral importance of the family, and the interests of health and social care professionals – were frequently mentioned. Threading through was the importance of trust and relationships between patients, relatives, and health and social care professionals. Ethical tensions between and within these values manifested at different stages in the ReSPECT process, as described below.
When is the right time to have the ReSPECT conversation? Respecting autonomy and protecting from harm
When deciding when to initiate the conversation, GPs and nurses weighed the risk of physical or moral harm, wherein a patient may be subjected to invasive and distressing interventions without their wishes being considered, alongside the risk of emotional harm caused by having the conversation before the patient and/or their relatives were ready. These competing risks posed a dilemma:
Sometimes if you go in too early with the [conversation], and not approach it in the right way … they can sometimes step back … but we don’t want them so unwell that they’re not able to be involved as part of that decision-making and really don’t want them to be going into hospital and just having them made.
GP 18, area 2
In working through this dilemma, unless the patient was imminently approaching death, GPs and nurses tended to favour preventing emotional harm. This was linked to GPs’ and nurses’ perceived need to maintain trust and rapport. GP and nurse participants spoke of postponing conversations if they felt the patient was not emotionally ready or had more pressing needs, and of introducing ReSPECT gently and gradually before discussing the ReSPECT form in detail. One nurse explained this approach led to better patient experiences and higher quality outcomes:
[I]t just feels like it’s a bolt out of the blue, you know, all of a sudden somebody’s talking to you about end of life, it might not be the right time for them and actually if you can invest a bit of time, you get the better quality ReSPECT Form or care plan than if you, you try and force something on to somebody.
Specialist nurse 5, area 3
Trusting and having good rapport with the healthcare professional who facilitated the ReSPECT conversation was important to patients and relatives. As explained by relative 9, although ReSPECT ‘was totally new’ to them,
Because I know the doctors well, I think the process was good. I, I trusted the doctor and we, we know, I know that she knows Mum well, I know her quite well, so we were able to do it on the phone. I think if, if it had been a doctor I didn’t know very well then it would have been much more difficult.
Relative 9
While deferring, waiting with, or gently introducing ReSPECT conversations was a preferred approach among the GP and nurse participants, care home staff favoured early completion to prevent physical/moral harm to residents in an emergency. Not having a ReSPECT form during an emergency could substantially harm patients. A harrowing example was narrated by a carer who, in her previous assignment as a home care worker, witnessed CPR being performed on the frail, elderly woman for whom she had cared – an event which both harmed the patient and traumatised the participant: ‘She was really, really fragile. Really fragile. And because she didn’t have the ReSPECT form, they had to resuscitate her. And I can hear the “crack” sounds’ (care co-ordinator/senior carer 14).
As several participants explained, not having a clinical background or decision-making authority, but still being held responsible by residents’ relatives, carers depended on the ReSPECT form for critical guidance:
Whenever we have a new admission … straight away [Name] will put them on a GP round next day … I can’t imagine how difficult it would be to look after someone if this was not in place … being a care home there’s only so much care and treatment you can provide.
Care home manager/deputy manager 11
Thus, folded into carers’ concern with preventing harm to residents was a concern with protecting care home staff, whose timing may not match that of the resident or their GP/nurse.
The conversation: balancing patients’ wishes, families’ wishes and what is clinically possible
ReSPECT is not a direct record of a person’s wishes, but rather of a shared decision-making conversation. However, when asked what ReSPECT meant to them, most patient participants said it was about their wishes; as patient 12 explained, ReSPECT ensured her wishes were recorded ‘in black and white’. Patient participants also described recording their wishes to reduce their family’s future caregiving and decision-making responsibilities (see Chapter 5).
General practitioners, while emphasising that ReSPECT focused on the patient, viewed family involvement in the ReSPECT process as crucial. When patients lacked capacity, families were essential in representing their wishes. But even when patients had capacity, GPs involved families in ReSPECT conversations to ensure that patients’ wishes, reflected in the recommendations, would be followed. For example, one GP explained that a patient’s ReSPECT form.
needed to be redone so that the family were on board with it really and so that they understood the process and so that they were happy to follow through with the ReSPECT form and not call an ambulance if she deteriorated.
GP 3, area 2
Despite the weight given to relatives’ views, patient participants were clear that their wishes should prevail over those of their family. For example, one patient described negotiating with his children, who disagreed with his treatment preferences: ‘I did explain to them that I didn’t want to be brought back if I was going to be like a cabbage … and they sort of thought about it and then they agreed’ (patient 11).
In most cases described by the GP and nurse participants, patients’ and relatives’ wishes matched what was clinically possible; for example, terminally ill patients asked not to be admitted to hospital or receive CPR. However, when patients’ expressed wishes opposed clinical judgement, this presented an ethical dilemma. If patients requested treatment likely to be unavailable, not beneficial or even harmful, GPs and nurses had to consider what counted as an ethically justifiable constraint on patient autonomy. Faced with this dilemma, some GPs and nurses explained to patients that their wishes may have limited impact on future decisions:
[S]ome people are still very much, like, ‘No, I want all treatment to be offered’, and I say, ‘Well, it’s kind of up to the clinician at the time and I can make your views clear in the form, but I also have a responsibility to make the clinical judgment of what your other comorbidities are and what your baseline is in order for that decision to be made’.
GP 9, area 3
Other GPs and nurses preferred to defer or avoid recording specific patient wishes, often suggesting they revisit the conversation. One GP describing this approach explained they tried to respect patient autonomy while being honest about what was possible:
If a person were telling me that they wanted to be resuscitated and I knew it wasn’t physically possible or it [would be] detrimental, I might, although I might not make the DNAR decision, I might make it clear that it’s something that we might have to come back to or it might be a decision that’s made medically if they were to be unwell.
Specialist nurse 5, area 3
Another GP described recording a ‘for CPR’ recommendation to establish trust and open possibilities for a future conversation and reversal of decision:
But again, sometimes it’s helpful to do the form, put the [for] resuscitation, get their trust, get them to know that you’re not trying to force that on them, and then as, once you have got that trust and as you have further conversations and you can slip that in, they will then listen to those things.
GP 19, area 2
Some participants, however, described deferring to the patient even if their wishes opposed clinical recommendations, citing patient autonomy. For example, one GP did not record a ‘not for CPR’ recommendation for a patient who had terminal cancer because the patient had capacity: ‘It felt like it was a bad decision, but he was, had the capacity to make that bad decision at the moment’ (GP 11, area 2).
In another example, a GP described deferring to the wishes of the family of a patient lacking capacity, despite their own clinical judgement:
[I]t seems crazy to do lots of tests and investigations and charging around for this sort of very elderly patient who’s really who is really like quite frail and demented, who wouldn’t really probably want this and there wouldn’t be any benefit anyway. But the, the relative wants that and so therefore it just has to be put down. I mean I guess the patient, the, the patient or the relative can, you know, they have their own autonomy.
GP 12, area 2
In an emergency: how should recommendations be interpreted? The challenge of acting in the patient’s best interests
In an emergency, if a person lacks capacity to contribute to a decision, healthcare professionals have an ethical and legal obligation to make a decision in the person’s best interests; ReSPECT recommendations inform this best-interests decision. Our data show that ReSPECT recommendations can help determine what is best for the patient and ensure a decision is person centred. However, uncertainties inherent in anticipatory recommendations, ambiguities in how recommendations are articulated and conflicting views over interpretation can lead to patient harm.
Among the patient and relative participants, there was near consensus that ReSPECT form recommendations would be followed in an emergency. For example, one patient said that while his preference for comfort care may not be followed immediately, it will be followed eventually: ‘there might be a delay agreeing what I want … which would then change as the message leads the acute medical team knowing this person has a ReSPECT form in place’ (patient 3). In practice, however, care home managers and GP and nurse participants said that recommendations recorded on ReSPECT forms were not always followed. GP and nurse participants explained that ReSPECT recommendations left space for clinical decision-making in the patient’s best interests on a case-by-case basis. They conceptualised ReSPECT recommendations as guidance and acknowledged that, as the recommendations could not encompass every clinical scenario, there needed to be some flexibility in interpreting these recommendations, either implicitly or explicitly: ‘I’ve put that care plan into place with the proviso of that’s, if in the event of a fall or a head injury if the clinician at the time can assess if he does need to be admitted’ (GP 8, area 3).
General practitioner and nurse participants said that, at times, interpretive flexibility was stretched too far, with recommendations not being followed and thereby causing harm to patients, through either not respecting their wishes or providing inappropriate treatment. One nurse described feeling disempowered after a patient died in hospital, having been admitted contrary to carefully worded, detailed recommendations: ‘She didn’t actually receive anything in hospital that we couldn’t have done at home … So it’s left me sort of like thinking, “Well, what could I have put on there that makes any difference?”’ (specialist nurse 3, area 1).
Many care home staff participants perceived ReSPECT recommendations as prescriptive, feeling that deviations could potentially harm patients. This could lead to conflict with the healthcare professionals who had decision-making authority in emergency situations. As one care home manager described: ‘We do tend to speak up and try and fight for the residents and say, “No, this is what it states, this is what should be happening”’ (care home manager/deputy manager 10).
When ambulance staff did not follow ReSPECT recommendations, some carers felt this compromised person-centred care:
[O]ften we find that if the ReSPECT form says ‘not for admission to hospital’, that the healthcare professional will make their own decision based on their assessment at that time. And then the, that person could end up going to hospital … And I find that confusing and a bit demoralising at times.
Care home manager/deputy manager 5
Care home staff also felt that healthcare professionals’ insistence on following ReSPECT recommendations despite their apparent inappropriateness could cause patient harm:
And we have had a bit of resistance from paramedics saying no, their form says not for hospital admission. But if that person needs to go into hospital to be hydrated because they’re dehydrated, or to have intravenous antibiotics, that’s where we get a little bit of resistance.
Care home manager/deputy manager 2
[T]he amount of times we’ve had paramedics come in and refuse to take someone in for sepsis because their [form] says, ‘Not for treatment’, is ridiculous … We, we waste hours and hours of management time trying to get another ambulance out … they don’t understand, because documentation is not clear enough, and the guidelines are not clear enough.
Care home manager/deputy manager 9
When conflict arose in emergency situations, carers sometimes called on family members to influence the decision. One staff member described how they would ‘ring the families then, and then the families are, like, “Yes, but they can go for this”, so then they’re going’ (care home manager/deputy manager 11) – an example that captures the family’s central role in enacting ReSPECT recommendations.
At its extreme, underinterpretation (or misinterpretation) of the ReSPECT form could lead to patient harm through equating the form with DNACPR. This worried several GP and nurse participants:
My biggest worry is that when somebody says, ‘Have they got a ReSPECT Form?’ they’re meaning, ‘Have they got a DNAR decision?’ … And to be fair, I tend to not fill in a ReSPECT Form if I’m not doing a DNAR decision as well for that reason.
Specialist nurse 5, area 3
Another type of conflict was described by a GP whose palliative patients asked to die in hospital: ‘they are scared of dying and their family are scared of dying and they don’t want to see that’ (GP 19, area 2). Despite recording a ‘for admission’ recommendation, hospital clinicians refused to comply, raising questions about how the person’s best interests were understood: ‘I definitely had experience with patients who have wanted to die in hospital, and you ring and try and admit them and they’re like, “What? They, they’re palliative. What, what are we going to do for them?” ’ (GP 19, area 2).
Summary
The ReSPECT process encapsulates a range of ethical principles and values, aiming to provide optimum person-centred in an emergency. Enacting the ReSPECT process in community settings can shape how these values are understood, interpreted and weighed. While the ReSPECT conversation takes place between a clinician and a patient or relative, the ReSPECT process is networked within wider relationships, which can include the patient’s family and professional care staff. Families, clinicians and carers may have differing perspectives on how to respect the patient’s wishes and best interests. Uncertainty about illness trajectory, potential clinical scenarios and treatment options can add to the challenge of balancing respect for patients’ wishes and protecting patients from harm. Conflicting perspectives emerge at the multiple interfaces of health and social care services and may influence how ReSPECT recommendations are followed. The ethical challenges of interpreting ReSPECT recommendations reflect wider challenges inherent in best interests decision-making.
Chapter 7 What do people with a learning disability and their carers want from ReSPECT?
Parts of this chapter are reproduced with permission from Russell et al. 76 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/
Introduction
People living with a learning disability in the UK are underserved in access to health care. 77 They die on average 15–20 years earlier than the general population, have higher rates of long-term health conditions and are more likely to be admitted to hospital as an emergency. 78 During COVID-19, the rate of excess deaths for people with a learning disability was more than two times higher than the general population. 78,79
More people with a learning disability are developing age-related illnesses, such as dementia and cancer, with a corresponding increase in the need for palliative and end-of-life care. 28 This, together with higher rates of emergency hospital admissions, exemplifies why emergency care treatment planning for people with a learning disability is important.
Many adults with a learning disability rely on care from a family carer, often an older parent. Both the person with a learning disability and the parent-carer may make ACPs, including ECTPs, in the context of their caring relationship. While studies have highlighted concerns over proxy decision-making by families, evidence suggests family members can be called upon to make tough decisions if ACPs are not in place. 29,80,81
At an early stage of the project, it became clear that we were unlikely to capture the specific experiences or views of people with a learning disability and their families, from our general study population. We secured additional funding to explore views of people with a learning disability and their families about emergency care treatment planning, and to work with people with a learning disability to co-produce resources to support them in engaging with the ReSPECT process.
We partnered with CHANGE a human rights charity based in Leeds and part of the Advonet Group. Advonet is an independent advocacy charity in Leeds within which multiple services run, including CHANGE. CHANGE operates a co-working model, employing people with learning disabilities to co-run projects, co-deliver training and co-create accessible information. 82 Two CHANGE members worked with the study team to develop the WP design and participant facing documentation. A clinical specialist lead for learning disabilities joined the independent study steering committee. A member of CHANGE staff with lived experience of a learning disability was part of the interview panel for recruiting the research fellow for this WP.
Aim
To understand how health and social care professionals can optimally engage people with a learning disability in the ReSPECT process and to co-produce relevant support materials.
Research questions
-
What are the views of people with a learning disability about ECTPs in general and the ReSPECT process in particular?
-
What are the views of carers of people with a learning disability about emergency care treatment plans in general and the ReSPECT process in particular? What might be the challenges for people with a learning disability and those working with them to access and engage with emergency care treatment planning?
-
What kind of information, processes and support around emergency care treatment planning and ReSPECT would be useful for people with a learning disability and those caring for or supporting them?
Methods
-
A series of workshops with people with a learning disability to explore their views on ReSPECT and emergency care treatment planning and to work with them to coproduce resources to support health and social care professionals to engage with people with a learning disability in the ReSPECT process. We convened a reference group of people with a learning disability to co-design the workshops, contribute to analysis of the workshop findings and review the co-produced resources.
-
Focus groups with family carers of people with a learning disability to explore their experiences of and views on emergency care treatment planning in general and ReSPECT in particular.
Workshops for people with a learning disability
CHANGE allocated two members of staff, one of whom had lived experience of a learning disability, to recruit to the project, support the reference group and facilitate the workshops.
Sampling and recruitment
Reference group
An e-mail describing the study and including contact details for the CHANGE project lead was circulated to learning disability organisations and networks for dissemination. Anyone expressing an interest contacted CHANGE. The CHANGE project lead responded to explain more about the study, check that the person was 18 years or over, had capacity to participate in the reference group, and that they were able to attend meetings at CHANGE.
If the person was still interested in taking part, an easy-read participant information sheet with attached consent form (see Report Supplementary Material 8) was provided via e-mail or post (according to the person’s preference) and a second contact arranged to confirm if the person was willing to participate as a reference group member, and to record their consent. Verbal consent was taken with the CHANGE project lead going through the consent form with the person and recording their response on a copy of the consent form which the CHANGE project lead then signed.
Five adults with a learning disability consented to take part. Four of the five people recruited were unable to attend any of the first three meetings. Thus, the initial preparatory meetings for workshop one were held with the remaining participant and the facilitators from CHANGE, including one with lived experience of learning disability.
Three additional reference group members were then recruited by CHANGE. The four reference group members attended all remaining reference group meetings.
Workshops
Workshops were held online to enable as wide a representation as possible within England. CHANGE disseminated relevant study information to national networks of learning disability carer and self-advocacy organisations. Individuals interested in participating or learning more about the study contacted the project lead at CHANGE by telephone or e-mail. The CHANGE project lead responded to check eligibility (aged 18 years or over, capacity to consent to participate in co-production workshops, resident in England, internet access and able to use online platforms either themselves or with a supporter).
If eligible, the CHANGE project lead explained more about the project and answered any questions. Further written information was provided (see Report Supplementary Material 8) and a second contact arranged to seek consent to participate in the co-production workshop series. Prior to obtaining consent the CHANGE project lead checked that the person had read the information sheet, that any questions had been answered, and the person understood what was involved in workshop participation. Verbal consent was then obtained and documented. The CHANGE project lead had experience of taking informed consent and assessing capacity to participate in research. At the start of each workshop, the CHANGE project lead rechecked consent to participate and to record the meeting with all participants. Workshop participants received a shopping voucher for their time after they attended each workshop.
Workshop development
The reference group met before the workshops began to familiarise themselves with the research and to plan the first workshop, then met in between workshops to receive feedback from the previous workshop(s) and plan the next (see Report Supplementary Material 9 for flowchart of meeting activity).
The researcher (JL), who was embedded in both the reference group and workshop process, linked issues raised from the workshops and drew on findings from other areas of the wider study to sustain critical reflection with reference group members. Worksheets and materials co-produced by reference group members and the CHANGE team were also included in the iterative development of the workshops content (see Report Supplementary Material 10). With consent, meetings were audio-recorded to supplement fieldnotes made by the researcher.
Outline of reference group meetings
Meeting 1
Meeting 1 involved the facilitators, researcher and group member getting to know each other; introducing the concept of research, setting ground rules for meetings and explaining the project and specific goals of this WP. The two people with lived experience of learning disability (participant and facilitator) shared their experience of accessing primary care. This set the context and informed the co-development of a roleplay activity to be used in the first workshop.
Meeting 2
The group discussed the ReSPECT process, what it is, its aims and planned outcomes. The ReSPECT form was reviewed and comments on the accessibility or otherwise of the form noted for use as prompts in the workshops. The roleplay for use in workshop 1 was presented and comments/suggestions noted. The group also trialled a story sheet to be used to explore what would support or hinder an imagined character (animal, mineral or vegetable) in completing their ReSPECT planning process. This co-developed story-sheet was used in workshop 1.
Meeting 3
Extracts from data analysis in other areas of the wider study (interviews with patients, relatives, GPs, care home staff and focus groups with the public) were presented and discussed. These extracts were used to develop a ‘jam board’ game designed to elicit perceptions of the different roles and perspectives of patients and professionals in primary care (see Report Supplementary Material 10). The group tested the jam board game as a proposed activity for workshop 2.
Meeting 4
Additional members were welcomed to the group and the introductory elements of meeting 1 revisited. The group then received feedback from workshop 2 from the researcher and CHANGE team. Members then discussed the ReSPECT process more widely including planning ReSPECT conversations. Worksheets to support someone with a learning disability to think through what they would need to support them before, during and after a planned ReSPECT conversation were co-developed and refined for use in workshop 3 (see Report Supplementary Material 10).
Meeting 5
Members received feedback from workshop 3 and examples of completed worksheets. They then considered additional suggested questions from the research team who had also reviewed the summaries of the first three workshops. These questions were included in the planning for workshop 4. The group also contributed to initial planning of a presentation for the main study stakeholder meeting (see Chapter 8).
Meeting 6
Members discussed feedback from workshop 4. The group then contributed to the development of a body mapping activity for workshop 5. The body-mapping activity was co-developed following feedback from workshop participants, that the full depth and breadth of their activities in daily life were not always recognised by services in any planning process involving them. The body-mapping process enabled participants to illustrate themselves holistically and represent their past, present and ‘hoped for’ future. 83
Meeting 7
Meeting 7 focused on preparation for the stakeholder meeting. Members agreed what they wanted to say about the co-production process and the activities and resources that were co-developed. They also discussed how to present this work, who would be involved in the presentation and the support needs that they anticipated during the planned stakeholder meeting.
Meeting 8
Members reviewed the existing resources available for people with a learning disability on the RCUK ReSPECT web pages and considered how any resources co-developed in this project could complement or add to these resources. The group also celebrated the successful completion of their work and reflected on the stakeholder meeting.
Workshops
Five workshops were held with each of two groups, each with six participants. We began working with group one for the first three workshops. Following reference group review of workshop three, we began the workshop series with group two. Any additional insights or suggestions from group two workshops were included in feedback to subsequent reference group meetings.
Workshop 1 involved the facilitators, researcher and group members getting to know each other, introducing the workshop format and ground rules, the concept of research and co-production, and explaining the specific goals of the workshops. Emergency care treatment planning was introduced and discussed using ReSPECT as an example. The group went through each section of the ReSPECT form to check for accessibility from the perspective of someone with a learning disability. The CHANGE team and the researcher performed a roleplay to demonstrate both negative and positive experiences of accessing primary care from the perspective of people with a learning disability. The story sheets developed in the reference group were introduced and completed by participants who then shared them with each other, describing their chosen story character and their journey through the ReSPECT process.
Workshop 2 began by exploring the ReSPECT process, who can initiate a conversation, when is it usually done, and what might be the benefits or concerns for people with a learning disability. The group then played the jam board game. The results were shared to understand how easy or difficult it was for people with a learning disability to see the viewpoints of other people involved in the ReSPECT planning process. This led to a discussion of what was important for people with a learning disability in preparing and planning for a ReSPECT planning conversation.
In workshop 3, the group reprised what they knew about the ReSPECT process and then used the worksheets developed and tested by the reference group to document (through words and/or pictures) their anticipated needs before, during and after a ReSPECT planning process. The information and suggestions from the completed worksheets were used to inform the co-development of resources for health and social care staff working with people with a learning disability to support them in thinking about and completing a ReSPECT plan.
In workshop 4, a series of additional suggested questions from the research team, who had reviewed the summaries of the first three workshops, were asked of participants. These questions focused on the timing and content of ReSPECT plans and when they should be used; and how do people with a learning disability think about and understand the concept of future planning.
In workshop 5, participants repeated the story sheet exercise to seek suggestions for improvement in developing it as a resource given their increased knowledge of ReSPECT and emergency care treatment planning. The researcher also explained about the wider research project stakeholder meeting and sought their permission to show examples of their work at the meeting. The group celebrated successful workshop completion and their involvement in the co-production process.
With consent, the workshops were video-recorded to supplement researcher fieldnotes. A summary of the meeting was drafted by the researcher based on the recording and their reflections of the meeting. These were used to provide feedback to the reference group meetings which in turn informed their reflections and suggestions for the next workshops.
Co-production of workshop outputs
Researchers (JL and AR) reviewed all workshop summaries to identify key messages and suggestions around information, process, and support for engaging with the ReSPECT process. The researcher (JL) then presented these to the reference group, with a simplified summary of the report and recommendations from the stakeholder meeting. Two reference group members, one workshop participant who had experience of work on ACP, together with JL and the CHANGE team, used this information to establish the content and format of the recommended outputs. These were drafted by JL, reviewed by AR and AS, and then submitted to CHANGE to convert into easy-read format. The full reference group reviewed the draft versions and recommended minor modifications. Additional comments were sought from a further two workshop group members with a specific interest in supporting end of life decision-making for people with a learning disability.
Reflecting on the process: collaborative autoethnography
Following completion of the workshops, a separate meeting was held in which reference group members evaluated their experiences of working on the project. This was facilitated by JL using a series of questions to aid reflection on the reference group process from the personal perspectives of the people with a learning disability who took part.
The researcher (JL) began by asking the question; ‘What do we think and feel about what we did?’ with the following prompts:
-
What meant the most to you?
-
Why did this mean the most to you?
-
Has listening to other people’s stories affected you?
-
In what way?
The reflective process drew on the model of collaborative autoethnography. Collaborative autoethnography extends the idea of autoethnography by involving multiple participants in the process, encouraging the collaboration of multiple voices and perspectives to create a multifaceted account that reflects the complexity and diversity of the shared experiences. 84 The researcher (JL) who led the reference group participated in the collaborative autoethnography.
Analysis
Workshops
Workshop summaries were analysed using thematic analysis. 73 JL developed summaries based on the workshop recordings and her reflections and notes from each workshop. JL and AR read a sample of summaries and identified codes: (1) related to information, process, and support for engaging with the ReSPECT process (which fed into development of resources) and (2) reflecting the meaning of emergency care treatment planning for people with a learning disability. JL coded all summaries and drafted candidate themes which were then discussed and refined with AR.
Collaborative autoethnography
With consent the reflective discussion was recorded. The recording was transcribed by JL and coded by AR. JL reviewed the coding and any disagreements were discussed and resolved. AR then re-read the coded transcript and identified key themes following Braun and Clark. 85
Findings
Workshops
Analysis of the workshop summaries identified three themes: autonomy, trust and process.
Autonomy
Workshop participants in general thought that having a ReSPECT plan was a good idea and could envisage future emergency situations where it would be helpful. ‘If there was an emergency like I said I thought this was a serious emergency, like I was in a car accident or something It’s good to do a ReSPECT form’ (workshop group 1).
Participants felt strongly that ReSPECT plans should reflect their wishes and what was important to them. They were not put off by the emotionally difficult nature of thinking about future illness and life sustaining treatment. ‘I’m in my right mind to make sure what I want is in place. I have a disability but know what I want yeah’ (workshop group 1). ‘I wanna, I wanna put down what I want to happen, how I want people to treat me or speak to me’ (workshop group 2).
Lack of trust in healthcare professionals
Workshop participants expressed doubt about the form itself being found and followed. Many described feeling that they were not seen as a whole person in healthcare appointments and their learning disability overshadowed a clinician’s view of their preferences. They thought this might also be the case with ReSPECT plans with their wishes being disregarded either in completing the plan or in using it in an emergency. ‘I wouldn’t, I won’t be sure if they’re really listening to me or be able to carry out all my preferences’ (workshop group 1). ‘If the ReSPECT form was with you, would they [clinical staff] actually know that you had one. How would they know that you had one?’ (workshop group 1).
Participants also expressed concerns about the capacity assessment documentation on the ReSPECT form and wanted reassurance as to how the capacity assessment was carried out and the justification for a decision of lack of capacity. This mistrust of the process was informed by their experience of healthcare professionals making assumptions about their (lack of) capacity in other clinical situations.
Process
To fully engage someone in the process of completing a ReSPECT plan, and to enable them to make an autonomous decision, they need to understand the process and the content of the plan that is being discussed. Ensuring that the process and form was understandable was a key theme across the workshops. Suggestions to improve this included better information and preparation before a ReSPECT planning conversation occurred, and an opportunity to go over the plan with a trusted supporter after it had been completed. ‘I think things what would help would be having the answers in advance, so you know what you’re going to be asked before you go to the appointment’ (workshop group 2). ‘After the appointment, I’d like to go over everything [with a supporter] and make sure I’ve got it all straight and asked everything I wanted to’ (workshop group 1).
Many of the discussions in the workshops focused on improving the accessibility of the ReSPECT process for people with a learning disability including the need for more time for appointments for a ReSPECT conversation and the presence of a trusted person to support them during the conversation. ‘I would like a friend to come if I could have one for the appointment’ (workshop group 1); ‘and I did a picture of a hand but you’ve gotta have the right support, like people or person to support you. So basically, it’s like you’ve gotta have the right hand’ (workshop group 2).
Group members felt that the language of the form needed to be more accessible, with explanation of terminology on the form itself and not in a separate guidance document. ‘When you’re seeing the DNACPR, someone says, what does that mean?’ (workshop group 1).
Once a ReSPECT plan has been made, it needs to be accessible to the person whose plan it is. Workshop participants noted that a written paper copy was not necessarily accessible for many people with a learning disability. An electronic version may be helpful. Some participants suggested that a recording of the conversation, or of the plan itself, would ensure that the person could have access to it in a format that was useful to them.
Development of resources to support health and social care professionals to engage with people with a learning disability about the ReSPECT process
The development of materials was a staged process to evaluate the explanation of what ReSPECT was, the setting, the preferred format of any resources, key information to be included and suitable terminology to use when explaining ReSPECT and health emergencies. In the workshops, multiple methods were used to support the participants to evidence their thoughts and feelings about the ReSPECT process and to highlight what they felt should be the key elements of any discussion of ReSPECT.
We found that the six-part story method was a popular way to think about the ReSPECT conversation and enabled workshop members to articulate their needs and concerns before, during and after a ReSPECT conversation. 86 This format was then used in the final materials. The concerns and needs of people with a learning disability expressed in the workshops fed into the development of a set of questions or prompts for professionals to discuss with a person with a learning disability to ensure all reasonable adjustments needs are considered and all concerns would be addressed during the process of the ReSPECT conversation.
Reference group reflections on the co-production process (autoethnography)
Analysis of the recording of the reference group reflections identified four themes.
Markers of value
Markers of value spoke to the ways in which the reference group members inferred the perceived value of their contribution to the research. Reference group members articulated a tension inherent in the status of the group as more than PPI members but less than employed research team members. While they felt they were an integral part of their WP a lack of social integration with the wider project team left them feeling less valued: ‘it’s important for us to be represented and to be sort of letting other people know that, that there is a space for us within these spaces’ (reference group member 2).
The spaces used to host the reference group were selected to be community spaces hosted by CHANGE but were sometimes read by the reference group as substandard spaces, inferring a sense of second-class status to the group. However, the arts-based methods used to engage with the group were valued as inclusive activities that took into account what worked for them: ‘that little bit of effort was made to speak to the people that it was both like “that worked”. Yeah, in a way that works with them’ (reference group member 2).
Self and others
The reference group valued their ability to make their own contribution but also hearing the contributions of others. They derived reward from being introduced to alternative perspectives during the stakeholder meeting. ‘I liked listening to the people who were coming, and talking about their experiences I liked listening to them’ (reference group member 3).
The process of participation also created changes in the way the reference group viewed themselves.
[Y]ou give up on yourself and you accept that things are just crap and that you’re not gonna be listened to you. But when you’re in a space, it’s like oh actually they’ve been listened to maybe I’ll be listened to as well.
Reference group member 2
Co-production is not an emotionally neutral process especially when the topic of discussion can resonate with participants’ own experiences and feelings of grief. The immediate effects of this emotional labour are handled by the researcher but we often, wrongly, assume that family or friends will also support the person to debrief: ‘I felt like upset like, sometimes like, like I said to my (family members) … this is how I feel; they don’t even listen’ (reference group member 4).
Tangible rewards
While other studies have reported that PPI participants fear the effect of payments on their benefits, our reference group valued payment as a clear form of recognition of their contribution. 87 Non-financial rewards were also valued. Group members expressed feeling positive reinforcement when they understood that their contribution caused changes in others; that their voice was heard: ‘Makes me feel happy, that I can speak now where we speak that thing, and that some people need to listen to it’ (reference group member 4).
Mirror and bridge: the role of the researcher
The researcher played an important facilitative role for the reference group, supporting the group to see the changes they were creating, reflecting back to the group the value of their contribution and what they have achieved. This was evident in the group’s comments on their experience of the stakeholder meeting. ‘We put all the work that people did around the, the, the room in the conference’ (researcher); ‘yes we did’ (reference group member 3); ‘Yeah that was pretty cool’ (reference group member 2).
The researcher also acted as a bridge for feedback to the research team. The researcher’s ability to explain or ‘come clean’ about the limitations of the project as well as giving confidence to the group that their feedback was valued by the team, appeared to create a bond between the group and the researcher.
The reflections of the group and the researcher illuminated the emotional labour of the researcher in this process, which was freely given, to bond with, and relate to, the reference group members. ‘Now I know (participant) needs this [reassurance] and then (participant) will be alright … I have learned you; you have taught me well’ (researcher).
Focus groups and interviews with carers of people with a learning disability
Methods
In these focus groups, we aimed to capture the experiences of carers of people with a learning disability, some of whom may care for people who would not be able to participate in the study directly. If someone expressed an interest in participating but could not join one of the focus groups, we arranged an individual interview with that person.
Recruitment
We sought expressions of interest for focus group participation from carers of people with a learning disability through CHANGE’s national networks of learning disability and learning disability carers’ support organisations, and through online carers support forums and carers groups identified through social media platforms. We provided an invitation e-mail describing the study for circulation through these groups. Potential participants contacted the study team directly and were provided with further information and offered a range of dates for planned focus groups. If they were unable to join a planned focus group, they were offered an individual interview. Participants were given a unique link to a Zoom meeting for the relevant focus group or interview. Prior to the focus group or interview, participants were sent a copy of the ReSPECT form (see Report Supplementary Material 1) and consent form. Initially, consent was taken at the start of each focus group with each participant in turn. However, this process proved challenging and time consuming online so for focus group 3 onwards a separate online/telephone discussion was arranged between the researcher and participant to obtain consent. Consent for individual interviews was taken prior to the interview. Demographic questionnaires were either returned by focus group participants by e-mail to the study team, completed on the telephone or were completed during individual interviews. Participants received a shopping voucher as a thank you for participation.
Data collection
Focus groups were facilitated by up to three researchers (JL, AR, JH). All individual interviews were carried out by JL. At the beginning of the focus group/interview the researcher briefly described the purpose and format for the discussion and the ReSPECT process. A topic guide was developed by AR and JH and refined by a family carer and chief executive officer of a charity supporting people with learning disabilities: Special Needs Outreach Project (SNOOP). 88 The topic guide was used to structure and facilitate the discussion (see Report Supplementary Material 5). The topic guide prompted participants to consider potential benefits and disadvantages of emergency care treatment planning for people with learning disability and their carers; how an emergency care treatment planning process could be implemented with people with learning disability, the role of carers in the process; and potential benefits for the wider health service.
Focus groups lasted between 38 and 76 minutes and interviews between 45 and 62 minutes. All focus group and interviews were recorded and transcribed.
Problems with online connections and participant engagement meant that no reliable data was obtained from one of the focus groups (four participants) so this was excluded from analysis.
Analysis
Jacqui Lovell and Amy Russell coded focus group transcripts and the joint interview transcript using the topic guide areas as a framework and then met to compare and refine codes. Following agreement of codes, JL developed a coding framework and coded all remaining interview transcripts against this framework. Reading across the coded data, themes were identified which were discussed and refined by JL, AR and AS.
Findings
Twelve participants were included (five from two focus groups, one joint interview with both parents of a person with learning disability, and five individual interviews). Most participants were aged over 60 years (8 participants) and female (10 participants). All identified themselves as carers for someone with a profound learning disability.
Three themes were identified: process, lack of trust in the system and carers as advocates.
Process: (the process should acknowledge the complexity of care and caring for someone with a learning disability)
In general, carers were supportive of ReSPECT planning as a way of providing clear guidance to clinicians in an emergency when the carer may not be there to support the person with a learning disability. They also saw it as a means of helping healthcare professionals in an emergency when they don’t know the patient.
So yes, in that regard erm it could say all the things that you, you want it to say and you could put your numbers down, your involvement down, you could put a second number down if you weren’t available and all that.
Parent-carer interview 4
And also with [person with a learning disability’s name] you can’t learn anything straightaway because he might start gabbling and you think, ‘Oh, he’s just ... is he ...’ you don’t expect him to be, have the, the disabilities that he does have, you know, so ... yeah, it’s got to be a help. It’s got to be a help, having some more information.
Parent-carer interview 6
Carers’ views on the process of ReSPECT planning reflected their role in understanding and advocating for the person with a learning disability and the complexity of care needs to be considered. Carers were clear that they should lead the ReSPECT process including deciding which clinicians should be involved.
Our loved ones are known to a multidisciplinary team and I think we knowing our young people as we do should be the ones to decide who we elect to be that clinician who knows them best rather than one-size-fits-all GP.
Parent-carer interview 4
They emphasised that the ReSPECT conversations needed to be collaborative, possibly involving several family members, and that they required sufficient time to do this properly citing the need for a number of ReSPECT meetings before the completed form is signed. One participant suggested that ReSPECT conversations should follow the format of a best-interest meeting for a person who lacked capacity.
It would actually be it would have to be, it’s got to be over a certain amount of time. It’s not something that can be just, just done in one appointment … and I want to rip it apart so that I know I’m understanding absolutely everything that’s on there so that there’s no regrets.
Parent-carer focus group 2
Different people have different views on what is a meaningful life, and they make decisions based on that … and therefore the best interest meeting, who attended, what was discussed and what were the conclusions is essential in order to make sure that there is no cause for concern.
Sibling-carer focus group 1
All carers felt that it was important to do this process early and review regularly.
Lack of trust in the system
While carers were generally supportive of the ReSPECT process, they expressed doubt about how the process would work in practice. Their past experiences of direct discrimination toward themselves as carers who were not trusted to know and understand the needs of the person in their care, and a general disregard of the quality of life that people with a learning disability may have, influenced carers’ lack of trust in the system. A recurring concern for carers was whether ReSPECT recommendations would be acted on in an emergency. They lacked confidence in the efficiency with which ReSPECT plans would be available when needed.
but sometimes you go to A&E and they or you go to, you know, and they can’t even access a doctor’s letter, can’t you bring your records up. So, God only knows if they’reable to, to, to find this ReSPECT form.
Parent-carer interview 3
Would they ask? Would they ask whether there’s one in existence or not? Would they ask that question?
Parent-carer interview 2
Even if the plan was available, carers expressed fear that recommendations may not be followed unless they were present to reinforce them: ‘I’m, I’m not so sure it would be followed. I would like to feel it would be followed but what, what proof have I got that it’s ever going to be followed’ (parent-carer interview 5). Indeed, one person expressed surprise that the ReSPECT plan was not legally binding.
I think it’s appalling that it’s not a legally binding contract. It needs to be because that security needs to be given in a really difficult time to them families … that you know, yes, we will do what you’ve asked for.
Parent-carer, focus group 2
However, some carers felt that if they had good a relationship with their doctor, they would be confident in trusting that the plan would be followed.
I, I think if my doctor was proving to me that he was being a very good GP and this was going for a couple of years, I’d have no reason to mistrust him. I would then assume that if he’s involved with this plan that he was going to stick by his word and do what he needed to do.
Parent-carer interview 4
Carers as advocates
Carers saw value in the ReSPECT process, but primarily as a secondary enforcement of their own advocacy role and to counter clinician stigma around learning disability. They felt it could be used to indicate their support network and care needs, so the person was not hospitalized without an advocate who knew them: ‘I do have an inherent fear of [son’s name] just being admitted to A&E, somebody forgetting to tell me and then doing whatever they want to him’ (parent-carer interview 4).
For some carers, their role as advocate negated the need for a ReSPECT plan.
So I don’t see the need for one for my family … in the sense that if, if there is an emergency then you know I’m going to be there, I’m going to be talking to them … you know you will have to deal with the emergency incident on its merits at the time and that piece of paper that ReSPECT is almost historical.
Parent-carer interview 3
This carer’s strong sense of advocacy for the person in their care also influenced how they perceived completing a ReSPECT plan for themselves.
I think I would not want anything that is going to make my family’s life more difficult. And for me, [son’s name] is the priority. Therefore, I don’t want anything for me that’s going to make her [daughter] feel, ‘oh Lord, now I’ve got to look after mum too’, so I’m not entirely sure I would want something that’s enabled me to survive but disabled me entirely.
Parent-carer interview 3
Summary
Workshop attendees expressed a desire to engage in the ReSPECT process and to be supported in that process. They made multiple suggestions to enhance the planning of ReSPECT conversations and emphasised the need for preparation before the conversation.
Overall, carers were cautiously supportive of ReSPECT plans but saw them in the context of their lived experience of advocating for a person with learning disability in the healthcare system. Where ReSPECT plans supported this advocacy role, it was welcomed but they did not trust that it would be followed without their input. Developing a ReSPECT plan for a person with a learning disability requires time and understanding of their complex needs.
Overall, the reference group’s experience of the process was positive, particularly when they were able to experience the contribution they were making. Both financial and non-financial benefits of the experience were identified
Strengths and limitations
This WP has embedded the voices of people with a learning disability and their carers in an evaluation of the use ReSPECT in primary and community care, ensuring that their perspectives and experiences inform future developments. Collaboration with CHANGE strengthened the project, providing expertise in working with people with learning disability and production of easy-read resources and information.
The reference group initially struggled to retain members due to their own personal circumstances and had to enter a second round of recruitment. This meant the group had less time to work together and bond which may have impacted on their effectiveness and their experience of participation. Recruitment to carer focus groups was challenging and technical issues meant that online engagement was intermittent for some participants.
Chapter 8 Synthesis of findings and stakeholder meeting
Synthesis of findings
For this synthesis, we started with the analysis framework used for the qualitative data in Chapter 4 and added to it findings from the other chapters. We then identified the consistent messages from across our results and grouped them into themes.
The consistent messages from across our results
The public survey indicates overwhelming support in Great Britain for people being able to have an ECTP. 55 Our qualitative results indicate similar support from all participant groups. 89 There was consistency in the results related to key issues from across our participant groups. All agreed that ReSPECT provides a valued opportunity for patients to express their wishes to the clinicians making treatment decisions, with parent/carers of people with a learning disability seeing it as a means of reinforcing their voice as an advocate for the person they care for. The qualitative data indicate ReSPECT is commonly understood as primarily about resuscitation, including among patients and their relatives. Its role for providing other clinical guidance particularly for patients nearing end of life is also recognised. Across all data, there was agreement about when to initiate an ECTP such as ReSPECT: when there was worsening health especially if the person had a life threatening or life limiting condition. Family members are willing to be involved in completing ECTPs such as ReSPECT and their involvement is considered important to prepare them for potential medical emergencies, recognising that not everyone wants to involve their family in healthcare decisions. For people with a learning disability the involvement of a family member or carer was seen as essential to advocate for or to support the person in the planning process. The range of health and social care professionals who could lead ReSPECT conversations could be broader than at present, if skilled in communication and trained in the ReSPECT process.
There was concern among the public and all those working in health and social care in the community that ECTPs such as ReSPECT could be out of date. On the use of ECTPs such as ReSPECT in an emergency, the consistent message from the qualitative results was that it was problematic. The public and GP survey both asked about the possibility that having an ECTP might result in someone not receiving lifesaving treatment and substantial minorities agreed. Our qualitative results from GPs and their staff and other participant groups working in community health and social care indicate that completed ReSPECT plans are not always perceived as an important influence on treatment decisions in a medical emergency in the community. This perception has potential to undermine the ReSPECT process in the community.
The role of the ReSPECT form in a medical emergency
The ReSPECT form is designed to assist with decision-making across the whole range of potential medical emergencies that can occur in the community. We first consider the role of ReSPECT in the community when a patient appears to have collapsed.
Our home-based care workers and care home staff provide insight into the experience of staff who are not clinically trained when a person they care for appears to be unresponsive. They know the first decision is whether to start CPR and, here, the recommendation recorded in the ReSPECT form is useful. However, they also need help from a clinician as they do not know the cause of the unresponsiveness and whether it can be treated. A call to the emergency services may elicit the request to start CPR, which creates for them a dilemma if the ReSPECT recommendation is not for CPR. If the patient has become severely ill, care staff need help from a clinician to work out what the problem is before the clinical recommendations on the ReSPECT form become useful. Care home staff experiences of a lack of understanding of their dilemma from GPs and paramedics caused them distress. There was no mention on any of the ReSPECT plans we examined of information about which service care staff, or family, should call in a medical emergency.
Paramedics and emergency department doctors attending patients who have apparently collapsed or become severely ill make their assessment and treat following established clinical pathways taking account of patient safety. ReSPECT plan content rarely provided sufficient justification for deviating from these pathways. Although there was recognition among clinicians and care staff that it is the attending clinician’s responsibility to make the clinical decisions, the perception that the attending clinicians ignored ReSPECT recommendations was a source of frustration for care home staff. However, those who completed ReSPECT plans struggled with what to write in the plan that might help the decision-making of the clinicians attending their patient in an emergency. For the attending clinicians knowing patient preferences was valued.
For the ReSPECT process to continue with support from the public, patients, families, clinicians and care staff, we need to find out if it is possible to ensure the content of a completed ReSPECT plan is useful in medical emergencies in the community, and if so, how.
Control of the sharing of ReSPECT forms
The ReSPECT form was designed to be patient held. Our survey results suggest widespread understanding of the role of the ReSPECT plan in ensuring clinicians know the patient wishes. For this to happen, the patient must share the ReSPECT plan with the relevant clinician. There are patients and families who understand this, perceive the plan as having considerable power to influence treatment decisions and actively control access to their patient-held ReSPECT plan, making it accessible or inaccessible to other people. Patients and families active in managing their ReSPECT plan are likely to ensure that it is up to date. Our results indicate that some patients do ask for the plan to be updated. Some patients and families appear not to be active in controlling the sharing of the ReSPECT plans. There is some evidence that they forget about them. Clinicians and care home staff expressed concern that repeated reference to emergency care treatment planning through regular review could cause distress for patients and families who prefer not to think about their plan.
Based on their experience of lost, out of date or inaccessible forms clinicians and care staff felt an electronic form available to all relevant health and care staff would solve the problem of form accessibility and validity. However, this would affect patient control of the form. Our qualitative results include concern that people can change their mind as their circumstances, including their health status, changes. Both surveys identified the risk of the form being out of date.
The tension between patients/families maintaining control of their completed ReSPECT plans and the need for clinicians and care staff to access the plan when needed is a challenge for the current ReSPECT process.
Patient preferences recorded on ReSPECT form
There was agreement on the value of patient preferences recorded in the ReSPECT plan and the importance of clinicians knowing the patient’s wishes when making treatment decisions. People with a learning disability emphasised not only patient wishes but also clinicians knowing what was important to and about the person to minimise clinician bias when making emergency treatment decisions. However, among completed ReSPECT forms we evaluated, we found completion rates of the patient preference scale were under half, and completion of free text preferences only just over half. When text was recorded it usually referred to being kept comfortable and place of death. Our qualitative results suggest the preference scale was not always useful. The public focus groups drew out the tension between the need for text to be brief to be read in an emergency, and the need to communicate details about preferences. Care home staff and GPs talked about ACPs or other care plans holding more detailed information about patient preferences.
Together, these results suggest that, apart from patients on a relatively clear trajectory towards death when options are limited, expressing preferences about medical treatment is not straightforward, which may in part be because the options are not clear. This is a challenge for the ReSPECT process in the community. However, version 3 of the ReSPECT form, which prompts clinicians to record what the patient most values and what they most fear/wish to avoid may have gone some way to meeting this challenge as clinicians had recorded more detail on these forms than on version 2. However, our sample included few version 3 forms and our other data did not distinguish versions of the form.
Clinical recommendations and reasoning recorded on the ReSPECT form
Most of the ReSPECT forms we evaluated contained some detail in the clinical recommendations text box and recorded whether the patient was recommended for CPR. However, clinicians who wrote clinical recommendations talked about their struggle with this, in part because of the wide range of possible medical emergencies that could arise in the community.
The prospect of writing clinical recommendation text influenced the timing of some ReSPECT conversations, as over time as a patient’s health deteriorated, treatment options reduced, and patients and families came to terms with the patient’s condition. However, not having a ReSPECT plan risks patients having difficult treatment experiences including CPR.
Very few ReSPECT forms we reviewed included explicit reasons for the treatment recommendations made with reference to the patient’s condition and ability to benefit from future interventions. Only one included patient preference in their reasoning about benefits and burdens of treatment. Our qualitative data suggest that the ReSPECT process is challenging, and clinicians need training to do it well. In the public survey, one-quarter of respondents wanted a clinician who did not know them but was trained in making ECTPs to complete the plan with them. This minority view suggests a dilemma about whether a clinician who knows the patient well, or one that is highly trained in ReSPECT, is best placed to undertake the ReSPECT process.
In the community, the completion of medical recommendations in ReSPECT plans is challenging because of the level of medical uncertainty around future clinical events and treatment options. This uncertainty reduces as someone’s disease trajectory progresses or they near the end of their life, but waiting to complete a ReSPECT plan until this medical uncertainty is reduced risks increased treatment burdens for patients. A further challenge is to bring together medical uncertainty and patient preferences for weighing of benefits and burdens to make clinical recommendations.
Patient trust and ReSPECT
Across our data there was agreement that the person holding a ReSPECT conversation with a patient needed good communication skills and to establish a trusting relationship. Although half of the members of the public surveyed indicated they would want their GP to complete an ECTP with them, other results suggest a wide range of types of professionals who could hold ReSPECT conversations. What was important was a trusting relationship between the professional and the patient.
Qualitative results from our patients/relatives’ interview data indicate they trust that the recommendations on the ReSPECT form would be followed which other results suggests is not necessarily the case. Parent-carers of people with learning disabilities were less trusting that preferences would be followed based on their past experiences of clinical decision-making in an emergency. The public focus group results remind us that patients have little choice but to trust the clinician in a medical emergency and the health service to provide the most appropriate care.
The ReSPECT process requires trust between patients, their families and clinicians but also trust between different healthcare professionals. Engendering patient trust in the ReSPECT process depends on patients and public trusting the health system more generally.
Stakeholder meeting
In March 2023, we held a stakeholder meeting to present key issues arising from our preliminary analysis and seek input from a wider group of stakeholders on how ReSPECT should be used in primary care and the community. 90
Methods
We invited to the meeting representatives of patient and carer support organisations, community and faith groups, relevant professional organisations, clinical leads for end-of-life care, commissioners and policy-makers, practitioners implementing ReSPECT in the community and members of the national ReSPECT working group. There were 47 attendees, including 29 external delegates, 12 members of the study team, 3 members of our lay advisory group and 3 members of our learning disability reference group (see Appendix 7)
Prior to the meeting, the research team reviewed initial study findings, identified key issues to present at the workshop and wrote formal presentations. We identified audio data excerpts from interviews/focus groups that were emotionally significant and edited them together into an audio file to play during the meeting.
Meeting participants were sent introductory material about the project (see Report Supplementary Material 11) and questions that we planned to pose during small group sessions to be held in the meeting (see Report Supplementary Material 12). Members of the research team acted as facilitators and scribes during the small group sessions. We held a training session to ensure all team members were familiar with small group processes including facilitating contributions from all attendees.
The meeting began with formal presentations of the key issues from the study data analysis. We then held a mix of plenary and small group discussions (see Report Supplementary Material 13). Small groups were preplanned to ensure a mix of backgrounds of group members, gender balance and at least two PPI contributors in any one group. The small groups were asked to tackle the questions posed for the meeting in a preplanned order to ensure that there was time for in depth discussion of all questions across the groups. Groups were able to view examples of anonymised text from actual ReSPECT forms to inform their discussion. Small groups reported back to the plenary session focusing on: (1) key points arising from discussion of the questions posed and (2) suggested recommendations for the ReSPECT process.
Scribes took notes of the discussions and the key points and recommendations agreed by the group were recorded on flip charts to present in the plenary sessions. Following the meeting the scribes’ notes and the flip chart content were collated and analysed to identify key messages. A summary of the meeting’s findings was drafted and sent to all attendees who were able to provide comments after which the report was finalised.
Outcomes of meeting
We present here a brief synopsis of key messages; the full report is available in Appendix 8.
Stakeholders reflected on the broad question of whose interests are being served during the ReSPECT process. The consensus across all groups was that the ReSPECT process should serve the interests of the person whose plan it is first and foremost. However, they acknowledged a tension between a process that is person centred and a set of recommendations that are intended to guide or direct clinicians. They also noted that the process could be in the interests of the person’s family, reducing the burden for them at the time of decision-making.
Initiating the conversation
Stakeholders thought it was important that ReSPECT planning should not only be considered in the context of end of life or palliative care. They suggested other potential triggers for initiating a ReSPECT conversation, for example, when a person has specific risk factors for severe acute illness, or during regular reviews of someone with a chronic disease. They distinguished between conversations to prepare someone for discussion of a plan and the planning conversation itself, suggesting that preparation conversations can be initiated by a wide range of people, with appropriate training and support.
Having and recording the conversation
Stakeholders identified several challenges that could occur in the process of the ReSPECT conversation, including lack of time to have what is a difficult and complex conversation. A strong message from the meeting was that ReSPECT conversations needed to be open and honest, and that the healthcare professional should take time to understand what was important to the person and what their preferences were. For good conversations to occur, communication challenges needed to be considered, such as language barriers, and alternative formats for the form. There was a consensus that a digital version of the form was the preferred option to ensure accessibility.
Articulating and interpreting recommendations
Stakeholders agreed it was important that recommendations, including the reasons for them, were understandable to the person and their family and to the health and social care professionals who interpret them in the emergency situation. As it is not possible to cover all potential scenarios, emphasis was placed on the need to carefully document the person’s values and preferences and for healthcare professionals to take account of these when interpreting recommendations. Stakeholders noted the difference between hospital completed recommendations, which were specific to hospital-based scenarios, and primary care-based recommendations, highlighting the need for review as a person moves between healthcare settings.
Training and raising awareness of ReSPECT
Stakeholders agreed that there is a need for training around the whole ReSPECT process from preparatory discussions through to use of the form in an emergency, with training content and format being tailored to the needs of the different groups of health and social care professionals who may be involved in the ReSPECT process. They highlighted the importance of training in interpreting ReSPECT recommendations in an emergency. Examples of training content and format were provided. There was consensus in the meeting of the need to raise awareness of ECTPs including ReSPECT within the general population.
Chapter 9 Discussion
Some parts of this chapter reflect discussion in Slowther et al. 63 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/
Benefits of completing a ReSPECT plan in primary care
There are several reasons why it may be desirable for ReSPECT plans to be completed in a primary or community setting rather than in hospital. When arriving at hospital, people may be too unwell and their family too distressed to engage in a potentially complex conversation about future deterioration and treatment options. Providing sufficient time and a supporting environment for such a conversation may be difficult. 8 Thus, many clinicians suggest that these conversations would be better initiated by a primary care clinician, who may also have an established relationship with the patient. Our participants reflected this view. GPs, nurses and care home staff emphasised the benefit of completing a plan when the person was still able to engage in the discussion and express their wishes. Care home staff also noted the benefit to carers of having a clear plan for the person in their care. Some GPs had incorporated ReSPECT plan completion into wider care planning particularly for patients who were residents in care homes. Care home staff also talked about the benefit of having focussed ReSPECT plans for emergencies but emphasised the need for a more comprehensive care planning document where personal preferences and values could be expanded on. However, GPs also reported lack of time to have these conversations and some patients and families described conversations that were rushed with little preparation.
Providing clear recommendations for use in the event of a clinical emergency or acute deterioration
A major challenge for completion of ReSPECT plans in primary care is the level of uncertainty inherent in anticipating for an individual person their illness trajectory, potential acute clinical scenarios and the range of treatments or interventions that need to be considered. Clinical uncertainty influences secondary care clinicians’ decision to initiate or complete a ReSPECT plan with a patient in their care. 18 However, the scope of uncertainty in the acute care setting is less than in primary care where the range of potential future clinical events and relevant interventions is not constrained by the nature of an admitting event. Drawing on the taxonomy of uncertainty in medicine suggested by Han et al.,91 we can interpret the uncertainty reported by the clinicians in this study as clinical (uncertainty of prognosis or potential future acute events), practical (uncertainty of what might be possible for delivery of care in the future) and personal/ethical (uncertainty over what will be in the person’s best interests at a future date, or how the person’s views and wishes may change over time). As the level of uncertainty increases for each or any of these elements, the level of confidence in the recommendations made in the ReSPECT plan will diminish. In practice, GPs’ implicit response to this uncertainty challenge is to initiate ReSPECT conversations in situations where there may be less uncertainty about illness trajectory, for example, when patients are nearing the end of their life.
This is a challenge for both clinicians completing the plan and for health and social care professionals interpreting the recommendations in different situations. Recommendations may not be relevant to the emergency situation, may not be achievable, or may no longer be consistent with the patient’s wishes. This can result in recommendations being misinterpreted or not followed. This risk was recognised by respondents in both our public and GP surveys and clearly articulated in the experiences of care home staff, who sometimes struggled to translate recommendations into guidance about what they should do in an emergency. They also expressed frustration when ambulance staff acted in a way that they perceived as inconsistent with either the recommendations or patient’s current best interests. The difficulty of translating ReSPECT recommendations during an emergency in a care home setting has been reported elsewhere. 43 There is limited literature on how ECTPs are used by healthcare professionals in an emergency. Evidence is predominantly from the United States where physician orders for life-sustaining treatment (POLST) are extensively used across healthcare settings. A systematic review of 20 observational studies of the influence of POLST on treatment intensity among patients with serious illness and/or frailty concluded that while there was some evidence that treatment limitation recommendations on POLST may reduce treatment intensity among seriously ill patients, there were concerns that a substantial number of patients received POLST discordant care. 92 Two studies investigating understanding of POLST recommendations in the prehospital and emergency department setting found significant confusion in interpretation of the recommendations. 93–95
Considering ACP more widely, there is mixed evidence on their influence on treatment and care decisions. A meta-analysis of 21 studies (N = 33,541) of ACP in cancer care found that the communication element of ACP was more important in influencing outcomes than the documents themselves. 96 Physicians value ACPs as part of their decision-making process but other factors also influence the decision including, prognosis, reversibility of condition and family views. 97 There is a major question for the use of ECTPs, including ReSPECT, as to whether recommendations facilitate, impede or make no difference to provision of care in medical emergencies that is concordant with the patient’s values and wishes.
Person-centred care
In UK law, someone making a decision for a person who lacks capacity must make a decision based on an assessment of that person’s best interests (in Scotland it is the benefit to the person). 98,99 The General Medical Council in its guidance for doctors, refers to overall benefit. 20 Legal and professional guidance for healthcare professionals makes it clear that an assessment of best interests should focus on the patient’s needs, preferences, and values so that any decision is person centred. The decision-maker in the emergency situation must take account of the current clinical needs of the patient, including the risks and benefits of treatment options available at that time. Recommendations on a ReSPECT plan may not anticipate the current clinical situation.
However, the ReSPECT plan is also a record of the patient’s values and preferences, what is important to them and what would be their goals of care in future emergency situations. As such, the ReSPECT plan has the potential to make a strong positive contribution to the assessment of what will be of overall benefit to this patient. It is this element of ReSPECT that is seen as paramount by all our participants and by participants at the stakeholder meeting; ensuring that the patient’s values and preferences are foregrounded in any decision-making if they cannot participate themselves. However, in our review of completed ReSPECT forms, just over half had a completed patient preferences section, although in some the recommendations were framed as patient preferences. Whatever the quality of the conversation, if patient preferences and values are not recorded in the plan, the role of the plan in the decision-making process is diminished.
Whether ECTPs result in, or are associated, with treatment congruent with patients’ preferences and values has been the subject of investigation elsewhere. Studies have found that POLST orders can often be inaccurate, undisclosed, and discordant with patient wishes for medical care. 100 Reasons identified for discordance between POLST and patient preferences include lack of discussion or support during completion of POLST; incomplete documentation; influence of family on preferences or decisions; and changes in patient preferences over time. 101
In over half the ReSPECT forms evaluated, the patient lacked capacity at the time of completion of the plan. Thus, to understand and accurately record the patient’s preferences and values, the GP or nurse completing the plan needs to have the ReSPECT conversation with someone close to the patient who knows them well, usually a member of their family. The requirement to consult with someone close to the patient when making a best interest decision is specified in the relevant mental capacity legislation. There was substantial concern during the COVID-19 pandemic that anticipatory decisions about CPR and other emergency treatments were being documented in DNACPR orders or ReSPECT plans without involving the patient or someone close to them, leading to a review by the Care Quality Commission. 35 Their report emphasised the need for healthcare providers to ensure that people and/or their representatives are included in these conversations, in a way that meets their needs and protects their human rights. We found that, for people who lacked capacity, the name of the person close to them with whom the ReSPECT conversation had taken place was not recorded in 43% of the forms we reviewed. This is similar to the findings in our previous study of ReSPECT in secondary care. This does not necessarily mean that conversations did not take place, but the lack of documentation both reduces transparency of decision-making and makes it more difficult to involve the relevant person in decision-making at the time of an emergency.
Placing more emphasis on the importance of accurate recording of the patient’s preferences and values, and the identity of the person who should be involved in decisions if the patient lacks capacity, would enhance the impact of ReSPECT plans and contribute to treatment decisions likely to be congruent with the patient’s goals of care.
Relationships and trust
A consistent message from the study participants across all WPs was the importance of a trusting relationship between the patient, or the family member if the patient lacked capacity, and the person completing the plan. For many this person was likely to be the patient’s GP, but the important criterion was that they understood the patient’s clinical condition and what was important to them. GPs and specialist nurses were often able to establish a relevant trusting relationship in a short period of time but might require several visits and conversations to do so. For patients or carers of people with complex health conditions, a longer-lasting relationship with an expert in the clinical conditions is important, as described by carers of people with a learning disability. Many people with long-term health conditions or with increased vulnerability to risk of acute illness may have trusted relationships with staff other than doctors and specialist nurses. These may include care home staff, home care workers and support workers for people with a learning disability. Involving these people in conversations about ReSPECT may increase trust in the process for the patient and potentially facilitate a richer discussion of what is important to them. In our interviews with care home staff, some described either having preparatory conversations with a resident or being present during the planning conversation to support and reassure the resident. A willingness by care home staff to take on this facilitative role in ReSPECT conversations has been reported elsewhere. 43 Further exploration is needed of the potential for expanding the range of health and social care professionals who can be involved in ReSPECT conversations, the ways in which they can be involved and the skills training required.
Making ReSPECT work within the complexity of health and social care
The concept of ReSPECT is that it is a single, patient-held plan enabling information about patient preferences and treatment recommendations to be transferred across healthcare settings to facilitate seamless and consistent decision-making for an individual patient. As described by May et al.,7 clinicians see ReSPECT as a means of making possible two desirable goals:
-
the translation of individual patient preferences to mitigate clinical decision-making in an emergency
-
the transportation of agreed actions (recommendations) around organisations and across organisational boundaries to mitigate risks resulting from informational and relational fragmentation.
We found that there are substantial challenges to realising these aims when considering the use of ReSPECT in a community setting. As described above, the interpretation of recommendations in an emergency can be problematic, if they are not clearly articulated and relevant to the situation at hand. From our data, we found that different clinicians may interpret recommendations differently, and that non-clinicians such as care home or home care workers face considerable uncertainty in knowing how to interpret a ReSPECT plan when responding to the collapse or sudden deterioration of a person in their care. The challenge is greatest for plans completed in hospital and not reviewed on discharge where the recommendations relevant for an acute inpatient admission do not translate into a community setting. The difficulties experienced by social care staff are likely to be even greater for family members who may be asked to communicate details of ReSPECT recommendations to a healthcare professional or ambulance responder over the telephone. Problems in sharing decisions and preferences within and between healthcare organisations has also been identified as a barrier to successful implementation of ACP more generally. 102
A more practical challenge in achieving the desired transportation of recommendations across health organisation boundaries is the potential for loss or misplacement of the form documenting the plan, and uncertainty about its validity as the most recent version. Ideally, the plan should remain with the patient but, as we found, patients or their relatives do not necessarily know where their plan is or understand that they are its custodians. Copies are not consistently held in general practice record systems and not all practices have policies or processes to ensure that the most recent version is identifiable. Care homes are more likely to have access to the ReSPECT plans of their residents, but care home staff describe ReSPECT plans being lost when residents attend hospital. All health and social care professionals in our qualitative study and delegates at our stakeholder meeting agreed that an electronic version that was accessible to all people who had a need and authority to access it was the preferred solution for the issue of access and version control.
Shared electronic healthcare records as a means of sharing information to improve patient care is widely supported and many healthcare organisations are investing in these systems. However, studies have identified a need for caution particularly in the context of ACP and emergency treatment. Data, whether electronic or hard copy, need to be accurate, comprehensive and easily retrieved. Studies in the United States have found that ACP documentation in electronic healthcare records may be incorrect and identified challenges in the interoperability of systems between primary and secondary care. 103,104
There are several examples of electronic palliative care co-ordinating systems in the UK. 105–107 While the potential benefit of these systems is recognised, health and social care professionals also express concerns including impact on GP workload, quality of completion of records, and data protection issues. 108 Making decisions about treatment in an emergency brings additional problems for paramedics because of practical issues, such as connectivity and time, as well as ongoing concerns about the quality of the information recorded. 109
Current evidence suggests the use of a shared electronic healthcare record system as a vehicle for delivering information about ECTPs has potential but still requires good documentation of relevant information and issues of accessibility, including accessibility for patients and their families, and data protection must be addressed. These issues were all identified by attendees at our stakeholder meeting.
Implications for decision-makers
The findings of this study have important implications for practitioners, healthcare systems and policy-makers who are involved in providing person-centred emergency care and treatment. A ReSPECT plan, or similar ECTP, has the potential to support clinical decision-making in an emergency that is grounded in the preferences, values, and prior knowledge of that person. However, there are several challenges that need to be considered for ECTPs to achieve their aims.
-
Our findings reveal a gap between the expectation that ReSPECT will translate patients’ values and preferences into recommendations and action in a clinical emergency in the community setting and what happens in practice. Understanding a patient’s values and preferences to inform a best interest decision is often more important to decision-makers than specific clinical recommendations, with the exception of the recommendation on CPR. Care home staff want clearer guidance on how to translate recommendations into their own decision-making for a resident who has become acutely unwell. These findings suggest that:
-
Healthcare professionals should place more emphasis on the importance of accurate recording of the patient’s preferences and values and integration of these into their justification for clinical recommendations in existing plans.
-
There is a need for education and training around the interpretation and implementation of ReSPECT recommendations in an emergency context. Specific consideration should be given to the needs of care home and home care staff in this context.
-
-
Our findings suggest that ReSPECT planning requires time and preparation and works best when there is a trusting relationship between the patient and the healthcare professional participating in the conversation. However, increasing pressure on GPs’ time and the changing nature of the patient doctor relationship in primary care, can create challenges for achieving high quality ReSPECT planning conversations. Our findings suggest that there is support for:
-
widening the pool of healthcare professionals who undertake ReSPECT planning conversations.
-
involving social care staff and patient support workers who may have a more established relationship with a patient in facilitating initial discussions to raise awareness of emergency care treatment planning. Appropriate training would be required to support this development.
-
-
People with a learning disability want to be able to have their wishes and preferences about care and treatment in future emergencies recorded, and to be part of a ReSPECT conversation. Family carers of people with a learning disability emphasise their role as advocate for the person with a learning disability. A key message from our findings was the importance of careful preparation and appropriate support to enable people with a learning disability to take part in ReSPECT conversations. This includes:
-
identifying the right person or people to support the person with a learning disability.
-
time and resources to explain what ReSPECT is and support the person to think about and communicate their preferences.
As part of this study, we have developed resources to support people with a learning disability and their families to prepare for a ReSPECT conversation (https://warwick.ac.uk/fac/sci/med/research/hscience/sssh/research/respect/resources/).
-
-
We identified significant challenges in accessibility and sharing of ReSPECT plans across health and social care systems in this study. As electronic healthcare records become more common, policy-makers and commissioners will need to consider how ECTPs such as ReSPECT are integrated effectively into these systems.
Strengths and limitations of the study
This study provides an overview of the use, experience and perception of emergency care treatment planning in a primary and community care setting. A major strength is its mixed-methods approach and the range of different lenses through which the issue is explored. Our public and GP surveys provide insight into how emergency care treatment planning is conceptualised. Interviews with patients, families, clinicians and care home staff provide a rich understanding of its reality and to what extent the concept and aims of emergency care treatment planning is realised in practice. Including a specific WP that engages with people with a learning disability and their carers provides an important but often missed perspective.
For both our public and GP surveys, we obtained high-quality data sets with sufficiently large samples to produce precise estimates for all our outcomes of interest. Our samples were nationally representative. However, recruitment methods for the public survey may have excluded people for whom ECTPs may be particularly relevant, for example the frail elderly. Using a market research company working through a commercially funded, free to use, website for data collection may have introduced bias into the sample selection for the GP survey. Recruitment to focus groups across the study was challenging and we had particular difficulty in recruiting faith leaders for both interview and stakeholder meeting attendance. Recruiting more participants may have provided further and different accounts of emergency care treatment planning.
Recruitment of GP practices and associated care homes across three CCG areas allowed us to explore a wide range of experiences of the ReSPECT process in different primary care contexts. The conversations with practice administrative and support staff provided additional important insights into how ReSPECT is embedded or not in GP practices. Participating practices and individual interview participants may have a particular interest or strong views about ReSPECT which may not be reflective of health and social care professionals’ views more broadly. However, our qualitative findings were supported by attendees at the stakeholder meeting. A key limitation is the small number of patient and families who agreed to be interviewed about their experience of ReSPECT. This may be reflective of the focus of the study. ReSPECT plans are predominantly completed with people who are frail, nearing the end of their life or in a care home. Completion of a ReSPECT plan is not a live issue and many people with a plan may not recall the conversation or feel it is not currently relevant to them. Those who chose to participate may have been more comfortable with discussing ReSPECT and as such, their experiences and views might not be representative. In both the public survey and qualitative data collection with patients, families and the public, there is under-representation of minority ethnic groups.
Patient and public involvement
We have embedded PPI throughout this project (see Chapter 2). Our lay advisory group contributed to all stages from informing our initial funding application, commenting on patient and public facing materials, advising on recruitment strategies and reviewing initial analyses of data. Members also attended the stakeholder meeting and commented on the overall findings. Feedback from the group at the end of the study was positive, with members expressing that they felt that their contribution had made a difference. Meetings were mainly held online to facilitate access and attendance with an option for two face-to-face/hybrid meetings. Some members felt that further face-to-face meetings would have enabled more social interaction and may have been preferable. A combination of online and face-to-face meetings is probably ideal.
The WP focusing on the experience of people with a learning disability in relation to ECTPs included a reference group who were actively involved in planning study workshops and presenting to the stakeholder meeting. They also had a major contribution to the development of resources that informed the output of this WP. Their involvement, including their combined reflections on their experience of involvement in the study is reported in Chapter 8. Overall, they enjoyed their participation in the project and valued the feedback on how their input shaped the project but felt more could have been done to integrate them into the wider project team.
Equality, diversity and inclusion
Emergency care treatment plans can be relevant for anyone, although previous evidence, confirmed in this study, shows that they are used more often with someone who is nearing the end of their life, resident in a care home, and the frail elderly. In this study, we aimed to capture the views of the whole population using a public survey, as well as exploring the experiences of people who had been involved in the ReSPECT process. We anticipated that cultural values and faith may influence people’s views on ReSPECT and therefore sought to recruit from community faith groups for our focus groups and to interview faith leaders. Where a GP practice had a high population of non-English speakers, we provided invitation letters and information sheets to patients and their families in both English and the relevant language. To capture the needs and perspectives of people with a learning disability we worked with an advocacy organisation and participants with a learning disability in a series of co-production workshops. Easy-read versions of all participant documentation and materials were used in the workshops for people with a learning disability.
The sample for the public survey was generally representative, although minority ethnic groups were slightly underrepresented against age standardised values.
Recruitment of participants from minority ethnic groups and faith leaders was challenging. While the aim of this study was to capture as broad a perspective as possible with multiple methods and data sources, further research is needed that is specifically designed to work with and capture the perspectives of minority ethnic and faith-based populations on the concept and use of ECTPs.
Chapter 10 Conclusion and recommendations for future research
Conclusion
The concept and aims of ECTPs in general, and the ReSPECT process in particular, are widely supported by health and social care professionals, patients and the public. For patients, their families and care home staff, the primary benefit was seen as enabling the patient’s wishes, preferences and values to be recorded to inform future decision-making. Eliciting, understanding and documenting what is important to the patient can take time and multiple conversations, and works best when the patient has a trusted relationship with the healthcare professional. Preparatory conversations, before a plan is introduced, are seen as useful and care home staff sometimes take on this role. Preparation for a ReSPECT planning conversation is seen as particularly important for people with a learning disability. However, despite the consensus that ReSPECT plans should be a means of communicating a patient’s preferences and values, there is wide variation in whether and to what extent the patient preferences section of a ReSPECT plan is completed in practice, and it is not always clear who has been involved in the conversation when a patient lacks capacity.
There is a lack of consensus on the purpose and authority of the recommendations recorded in a ReSPECT plan, with patients, families, care home staff, and some clinicians seeing them as determinative while most clinicians consider them to be guidance. This lack of consensus is compounded in practice by a lack of clarity or detail in many recorded recommendations. The level of uncertainty around potential future clinical events and treatment options for a patient in a community setting cannot be easily translated into specific recommendations, and recommendations recorded in a hospital setting are seen as unhelpful in the community. This can create confusion and conflict in an emergency and consequent risk of harm to patients.
There are major challenges to ensuring timely access to ECTPs by the health and social care professionals who are making treatment decisions. We found significant variation in whether ReSPECT plans were held electronically or in hard copy, confusion by patients about who holds the plan, and unreliable methods of transfer of plans between secondary and primary care.
Recommendations for future research
We have identified four areas where the study findings have implications for practice. Linked to these areas, we have identified three questions for future research. In addition, we have identified a need for further research to specifically engage with and explore the views and experiences of groups with diverse cultural or faith perspectives. In view of the challenge in recruiting paramedics to this study, and given the important role they play in implementing ReSPECT recommendations in practice, further research is needed on the experiences and views of paramedics relating to ECTPs. We have therefore identified the following priority research questions.
-
What are the experiences and perspectives of people from minority ethnic and faith-based communities on the concept and use of ECTPs including ReSPECT?
-
What are the experiences and perspectives of paramedics on the use of ECTPs in general and ReSPECT in particular?
-
How can we improve the integration of ReSPECT recommendations and patient preferences into treatment decision-making in an emergency in a way that is consistent, transparent and ethically justifiable?
-
What interventions are effective for increasing awareness of and preparation for emergency care treatment planning in the general population and in specific at-risk groups?
-
What are the benefits and challenges of a shared electronic record system for storing and accessing ECTPs?
Additional information
Acknowledgements
We would like to thank the staff at CHANGE for their support with this project; Carol Beardmore of SNOOP for her comments on the family carers interview topic guide, and Christopher Porter from North Yorkshire Health Task Group for reviewing the easy-read resources. Members of the project lay advisory group and members of the learning disability reference group for their invaluable contribution throughout the study. The study steering committee who provided oversight of the project. Victoria Tortziou-Brown OBE, Senior Clinical Lecturer in Primary Care, Queen Mary University London (Chair). Juliet Spiller, Consultant in Palliative Medicine, Marie Curie Hospice, Edinburgh. Nick Darlington, PPI member. Paula DuRand, Manager, Kineton Care Home. Victoria Donnelly, Strategic Health Facilitator, Learning Disabilities Health Support Team, Bradford District Care NHS Foundation Trust. James Cant, Chief Executive Officer, RCUK. Sara Shaw, Associate Professor, Nuffield Department of Primary Care Health Sciences, University of Oxford. The West Midlands, East Midlands and Yorkshire and Humber NIHR Clinical Research Networks. NIHR ENRICH teams in the West Midlands, East Midlands and Yorkshire and Humber. Finally, we would like to thank all general practices and care homes that took part in the study and the individual participants across all work packages for sharing their time and experiences.
CRediT contribution statement
Anne-Marie Slowther (https://orcid.org/0000-0002-3338-8457): Conceptualisation (lead), Formal analysis, Funding acquisition (lead), Investigation, Supervision (lead), Writing – original draft (lead), Writing – reviewing and editing (lead).
Jenny Harlock (https://orcid.org/0000-0002-2300-750X): Conceptualisation, Formal analysis, Funding acquisition, Investigation, Supervision (PPI lead), Writing – original draft, Writing – reviewing and editing.
Celia J Bernstein (https://orcid.org/0000-0001-5854-7306): Formal analysis, Investigation, Writing – original draft, Writing – reviewing and editing.
Katie Bruce (https://orcid.org/0009-0007-1460-0057): Data curation, Investigation, Project administration, Writing – reviewing and editing.
Karin Eli (https://orcid.org/0000-0001-9132-8404): Formal analysis, Investigation, Writing – original draft, Writing – reviewing and editing.
Caroline J Huxley (https://orcid.org/0000-0001-9755-6096): Formal analysis, Investigation, Writing – original draft, Writing – reviewing and editing.
Jacqui Lovell (https://orcid.org/0000-0001-8884-1995): Formal analysis, Writing – reviewing and editing, Investigation.
Claire Mann (https://orcid.org/0000-0003-2281-7970): Formal analysis, Investigation, Writing – original draft, Writing – reviewing and editing.
Angela Noufaily (https://orcid.org/0000-0001-8522-6591): Conceptualisation, Formal analysis, Funding acquisition, Writing – reviewing and editing.
Sophie Rees (https://orcid.org/0000-0003-4399-2049): Investigation, Writing – reviewing and editing.
Julia Walsh (https://orcid.org/0000-0002-9787-0349): Investigation, Writing – reviewing and editing.
Chris Bain (https://orcid.org/0009-0001-1786-2956): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Hazel Blanchard (https://orcid.org/0009-0006-4958-6059): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Jeremy Dale (https://orcid.org/0000-0001-9256-3553): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Paramjit Gill (https://orcid.org/0000-0001-8756-6813): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Claire A Hawkes (https://orcid.org/0000-0001-8236-3558): Conceptualisation, Formal analysis, Funding acquisition, Writing – reviewing and editing.
Gavin D Perkins (https://orcid.org/0000-0003-3027-7548): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Rachel Spencer (https://orcid.org/0000-0003-2578-6954): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Chris Turner (https://orcid.org/0000-0002-5150-8109): Conceptualisation, Funding acquisition, Writing – reviewing and editing.
Amy M Russell (https://orcid.org/0000-0002-8891-9059): Conceptualisation, Formal analysis, Funding acquisition, Supervision, Writing – original draft, Writing – reviewing and editing.
Martin Underwood (https://orcid.org/0000-0002-0309-1708): Conceptualisation, Formal analysis, Funding acquisition, Supervision (quantitative lead), Writing – original draft, Writing – reviewing and editing.
Frances Griffiths (https://orcid.org/0000-0002-4173-1438): Conceptualisation, Formal analysis, Funding acquisition, Investigation, Supervision (qualitative lead), Writing – original draft, Writing – reviewing and editing.
Beth Weston: Project administration. Stephanie Selwood: Learning disability work package, Funding acquisition and Easy read document preparation. Dominique Burley: Learning disability work package, Funding acquisition and Easy read document preparation. Imogen Day: Other contributions (recruitment and facilitation, learning disability workshops). Shaun Webster MBE: Other contributions (recruitment and facilitation, learning disability workshops). Tauseef Akram: Other contributions: Learning disability reference group. Kenneth Fletcher: Other contributions: Learning disability reference group. Ray Hurst: Other contributions: Learning disability reference group. Jamie Leigh-Marshall: Other contributions: Learning disability reference group. Jacky Anne Billings: Other contributions: Project PPI oversight; lay advisory group. Deb Smith: Other contributions: Project PPI oversight; lay advisory group. Elyas Khalifa: Other contributions: Project PPI oversight; lay advisory group. Susan Jenkins: Other contributions: Project PPI oversight; lay advisory group. Graham Howkins: Other contributions: Project PPI oversight; lay advisory group.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/NVTF7521.
Primary conflicts of interest: Anne-Marie Slowther: Received grants from the National Institute of Health and Care Research (NIHR) for the conduct of the study and grants from Health and Social Care Delivery Research programme (17/99/34; 15/15/09) and NIHR Health Technology Assessment programme (NIHR131105; NIHR127489) outside the submitted work and was co-author on an evidence synthesis of the do not attempt cardiopulmonary resuscitation decision-making that informed the development of the ReSPECT process. She was a member of the Advisory Board for the Wellcome-funded research programme ‘Balancing Best Interests in Healthcare, Ethics and Law’ and until 2023 was a member of the Board of Trustees, UK Clinical Ethics Network, and member of the Board of Trustees, Institute of Medical Ethics. Since March 2024 she is a member of the RCUK ReSPECT wider stakeholder group.
Jenny Harlock: Received grants from NIHR for the conduct of the study, and grants from Health and Social Care Delivery Research programme (18/02/27) and NIHR Health Technology Assessment programme (13/15/93) outside the submitted work.
Celia Bernstein: No conflict of interest declared.
Katie Bruce: No conflict of interest declared.
Karin Eli: No conflict of interest declared.
Caroline J Huxley: No conflict of interest declared.
Jacqui Lovell: No conflict of interest declared.
Claire Mann: No conflict of interest declared.
Angela Noufaily: Received grants from NIHR for the conduct of the study.
Sophie Rees: No conflict of interest declared.
Julia Walsh: No conflict of interest declared.
Chris Bain: Received grants from NIHR for the conduct of the study and he is Chief Executive of Health Watch Warwickshire.
Hazel Blanchard: Received grants from NIHR for the conduct of the study.
Jeremy Dale: Received grants from NIHR for the conduct of the study, and grants from NIHR Research for Patient Benefit programme (20/00/78), NIHR Health and Social Care Delivery programme (15/32/31, 20/43/54, 20,07,78, PB-PG-1217-20033, 15/145/04), NIHR Health Technology Assessment programme (01/14/10) outside the submitted work.
Paramjit Gill: Received grants from NIHR for the conduct of the study, and grants from NIHR Health and Social Care Delivery Research (13/48/66), NIHR Research for Patient Benefit programme (PB-PG-1217-20038), NIHR Health Technology Assessment programme (15/06/87), NIHR Policy Research programme (20/26/70, 20/09/37), NIHR Programme grants for applied research (RP-PG-0614-20004) and grants from NIHR Applied Research Collaboration West Midlands outside the submitted work. He is a NIHR Senior Investigator.
Claire M Hawkes: Received grants from NIHR for the conduct of the study and grants from NIHR Health and Social Care Delivery Research programme (references 13/16/23; 15/15/09) and NIHR Research for Patient Benefit programme (NIHR20/43/60) and NIHR Health Technology Assessment programme (13/42/57) outside the submitted work.
Gavin D Perkins: Received grants from MIHR for the conduct of the current study and grants from NIHR Health Technology Assessment programme (12/127/126, 14/152/14, NIHR128086, NIHR131105, NIHR131430, 14/150/85, NIHR154501, NIHR154798, 15/08/40, 17/147/33, NIHR156500, NIHR130454, NIHR132871, NIHR154796 NIHR128374, NIHR150027, NIHR155119, NIHR131533, 17/16/04, 17/136/10, 15/116/03, 13/143/02, 15/99/02, 16/93/01), Health and Social Care Delivery Programme (15/15/09, 17/99/34, NIHR127368, NIHR131623, NIHR153264, 14/156/23), ad hoc research grants (COVID-19-RSC) outside the submitted work.
Rachel Spencer: Received grants from NIHR for the conduct of the study, and a personal NIHR Advanced Fellowship award (12/73/68, 30/13/28). She is a member of the Executive Board of the Society for Academic Primary Care.
Chris Turner: Received grants from NIHR for the conduct of the study. He has received fees for multiple lectures in NHS Trusts and professional organisations on the importance of behaviour at individual and organisational team level. He has received a grant from the University of Warwick to undertake simulation studies on communication in resuscitation while wearing FFP3 personal protective equipment.
Amy M Russell: Received grants from NIHR for the conduct of the study and grants from the Wellcome Trust (personal fellowship), the Arts and Humanities Research Council, and the British Medical Association outside the submitted work. She was a Health and Social Care Delivery Research programme Associate Board member.
Martin Underwood: Received grants from NIHR for the conduct of the study and grants from NIHR Health Technology Assessment programme (13/28/03, 12/87/68, 16/77/02, 16/167/56, 13/20/46, 13/28/71, 16/61/18, 13/43/98, 13/31/629, 13/146/02, 17/129/02, 14/224/04), Programme Development Grants programme (20/26/14), Programme grants for applied research (RP-PG-2012-2018) and Health and Social Care Delivery programme (15/15/09), outside the submitted work; grants from the Australian National Health and Medical Research Council, the Norwegian Medical research council, Versus Arthritis, Stryker Ltd and Serco Group plc. He also reports personal fees from Clinvivo Ltd (Tenterden, UK), for which he is also a director and shareholder. Until March 2020, he was an editor of the NIHR journal series and a member of the NIHR Journals Library Editors Group, for which he received a fee. Until March 2021, he was an NIHR Senior Investigator.
Frances Griffiths: Reports grants from NIHR for the conduct of the study and grants from NIHR Health and Social Care Delivery Research programme, Health Technology Assessment programme (15/15/19), Programme grants for applied research (RP-PG-2012-2018, PTC-RP-PG-0213-20002), Artificial Intelligence for long-term conditions (20/39/86) Research and Innovation for global health transformation (20/01/32) outside the submitted work.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used #datasaveslives. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. The data used in the public survey analyses are from the NatCEN social research’s British Social Attitudes Survey © National Centre for Social Research 2023. Archived data are available at ukdataservice.ac.uk. For archive or dataset requests, please email BSA@natcen.ac.uk
Ethics statement
This research received ethics approval from the London South East Research Ethics Committee (REC reference 21/LO/0455; date of approval 17 June 2021) and HRA approval 27 July 2021. The research also received approval from HRA Confidentiality Advisory Group under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (‘section 251 support’) (CAG reference 21/CAG/0089 Provisional approval 21 July 2021, final approval 10 August 2021. Copies of the relevant approvals and table of amendments is included in Report Supplementary Materials 3 and 4).
Information governance statement
The University of Warwick is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation the University of Warwick is the Data Controller for this study. You can find out more about how the University handles personal data, including how to exercise your individual rights and the contact details for the University Data Protection Officer here https://warwick.ac.uk/services/legalandcomplianceservices/dataprotection/ Contact the data protection officer at DPO@warwick.ac.uk. The University also acted as Data Processor for all study research data collected. Data was processed under the University policy and processes for handling personal data, and research related data. Participating GP practices acted as data processors for patient data for the purposes of recruitment of participants. All participating practices were certified as compliant with NHS Digital Data Security and Protection Toolkit. CHANGE acted as the data controller and processor for personal data relating to recruitment of participants for the workshops and reference group members in work package four (co-production of materials with people with a learning disability). The Advonet group is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulations (EU GDPR 2016/670). For more information, please see our policy. https://advonet.org.uk/wp-content/uploads/2021/11/Data_Protection_policy_and_procedures.pdf or speak to a member of our team (01132440606).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Underwood M, Noufaily A, Blanchard H, Dale J, Harlock J, Gill P, et al. GPs views on emergency care treatment plans: an online survey. BJGP Open 2024;2023:0192. https://doi.org/10.3399/BJGPO.2023.0192
Eli K, Harlock J, Huxley CJ, Bernstein C, Mann C, Spencer R, et al. Patient and relative experiences of the ReSPECT process in the community: an interview-based study. BMC Prim Care 2024;25:115. https://doi.org/10.1186/s12875-024-02283-x
Russell AM, Lovell JM, Harlock J, Griffiths F, Slowther A. Autonomy and advocacy in planning for a medical emergency: Adults with a learning disability and family carers experiences and perceptions of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) process. version 2; peer review: 1 approved, 2 approved with reservation NIHR Open Res 2024;4:8. https://doi.org/10.3310/nihropenres.13555.2
Underwood M, Noufaily A, Bain C, Harlock J, Griffiths F, Huxley C, et al. Public attitudes to emergency care treatment plans: a population survey of Great Britain. BMJ Open 2024; 2024 Sep 3;14:e080162. https://doi.org/10.1136/bmjopen-2023-080162. PMID: 39313284; PMCID: PMC11429361.
Slowther AM, Bernstein CJ, Huxley C, Harlock J, Eli K, Mann C, et al. Using the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) in UK general practice: a qualitative exploration of the experiences of general practitioners, community-based nurses, care home staff, patients and their relatives. Br J Gen Pract 2024 Sep 20:BJGP.2024.0248. https://doi.org/10.3399/BJGP.2024.0248; Epub ahead of print. PMID: 39304311.
Huxley CJ, Eli K, Hawkes CA, Griffiths F, Underwood M, Perkins GD, et al. Are completed ReSPECT plans facilitating person-centred care? An evaluation of completed plans in UK general practice. Resusc Plus 2024 Sep 21;20:100780. https://doi.org/10.1016/j.resplu.2024.100780; PMID: 39364226; PMCID: PMC11447405.
Eli K, Bernstein C, Harlock J, Huxley C, Walsh J, Blanchard H, et al. Using the Recommended Summary Plan for Emergency Care and Treatment in a community setting: does it facilitate best interests decision-making? J Med Ethics 2024 In press.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- National Council for Palliative Care; National End of Life Care Programme . Advance Decisions to Refuse Treatment. A Guide for Health and Social Care Professionals 2013.
- Hayhoe B, Howe A. Advance care planning under the Mental Capacity Act 2005 in primary care. Br J Gen Pract 2011;61:e537-41. https://doi.org/10.3399/bjgp11X588592.
- National Institute of Health and Care Excellence . Chapter 15: Advance Care Planning: Emergency and Acute Medical Care in Over 16s Service Delivery and Organisation 2018.
- Gold Standards Framework . Advance Care Planning Online 2018. www.goldstandardsframework.org.uk/advance-care-planning (accessed 26 April 2023).
- Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage 2017;53:821-32.e1. https://doi.org/10.1016/j.jpainsymman.2016.12.331.
- Fritz Z, Slowther AM, Perkins GD. Resuscitation policy should focus on the patient, not the decision. BMJ 2017;356. https://doi.org/10.1136/bmj.j813.
- May C, Myall M, Lund S, Campling N, Bogle S, Dace S, et al. Managing patient preferences and clinical responses in acute pathophysiological deterioration: what do clinicians think treatment escalation plans do?. Soc Sci Med 2020;258. https://doi.org/10.1016/j.socscimed.2020.113143.
- Perkins GD, Hawkes CA, Eli K, Griffin J, Jacques C, Huxley CJ, et al. Recommended summary plan for emergency care and treatment: ReSPECT a mixed-methods study. Health Soc Care Deliv Res 2022;10:1-139. https://doi.org/10.3310/LFPE3627.
- Findlay G, Shotton H, Kelly K, Mason M. Time to Intervene? A Review of Patients Who Underwent Cardiopulmonary Resuscitation as a Result of an In-hospital Cardiorespiratory Arrest: A Report by the National Confidential Enquiry into Patient Outcome and Death. London: University College London; 2012.
- Perkins GD, Griffiths F, Slowther AM, George R, Fritz Z, Sathrley P, et al. Do-Not-Attempt-Cardiopulmonary-Resuscitation Decisions: An Evidence Synthesis. Southampton: NIHR; 2016.
- Beach MC, Morrison RS. The effect of do-not-resuscitate orders on physician decision-making. J Am Geriatr Soc 2002;50:2057-61. https://doi.org/10.1046/j.1532-5415.2002.50620.x.
- Henneman EA, Baird B, Bellamy PE, Faber LL, Oye RK. Effect of do-not-resuscitate orders on the nursing care of critically ill patients. Am J Crit Care 1994;3:467-72.
- Chen JL, Sosnov J, Lessard D, Goldberg RJ. Impact of do-not-resuscitation orders on quality of care performance measures in patients hospitalized with acute heart failure. Am Heart J 2008;156:78-84. https://doi.org/10.1016/j.ahj.2008.01.030.
- Shermon E, Munglani L, Oram S, William L, Abel J. Reducing DNACPR complaints to zero: designing and implementing a treatment escalation plan using quality improvement methodology. BMJ Open Qual 2017;6. https://doi.org/10.1136/bmjoq-2017-000011.
- Stockdale C, Trivedi B, Jerome E, Salih S, Huntley C, Cooke E, et al. Implementation of a combined Cardiopulmonary Resuscitation and Treatment Escalation Plan document in a District General Hospital. BMJ Qual Improv Rep 2014;2. https://doi.org/10.1136/bmjquality.u202653.w1236.
- Northern Cancer Alliance . Deciding Right Regional Forms n.d. https://northerncanceralliance.nhs.uk/deciding-right/deciding-right-regional-forms (accessed 26 April 2023).
- Hawkes CA, Griffin J, Eli K, Griffiths F, Slowther AM, Fritz Z, et al. Implementation of ReSPECT in acute hospitals: a retrospective observational study. Resuscitation 2022;178:26-35. https://doi.org/10.1016/j.resuscitation.2022.06.020.
- Eli K, Ochieng C, Hawkes C, Perkins GD, Couper K, Griffiths F, et al. Secondary care consultant clinicians’ experiences of conducting emergency care and treatment planning conversations in England: an interview-based analysis. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-031633.
- Huxley CJ, Eli K, Hawkes CA, Perkins GD, George R, Griffiths F, et al. General practitioners’ experiences of emergency care and treatment planning in England: a focus group study. BMC Fam Pract 2021;22. https://doi.org/10.1186/s12875-021-01486-w.
- General Medical Council . Guidance for Doctors: Decision Making and Consent n.d. www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/decision-making-and-consent/circumstances-that-affect-the-decision-making-process-continued-3 (accessed 26 April 2023).
- NHS England . Universal Pesonalised Care: Implementing the Comprehensive Model 2019.
- Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889-95. https://doi.org/10.1016/S0140-6736(13)62026-7.
- van Schrojenstein Lantman-de Valk HMJ, Walsh PN. Managing health problems in people with intellectual disabilities. BMJ 2008;337. https://doi.org/10.1136/bmj.a2507.
- House A, Bryant L, Russell AM, Wright-Hughes A, Graham L, Walwyn R, et al. Managing with learning disability and diabetes: OK-diabetes – a case-finding study and feasibility randomised controlled trial. Health Technol Assess 2018;22:1-328. https://doi.org/10.3310/hta22260.
- Kirkendall A, Linton K, Farris S. Intellectual disabilities and decision making at end of life: a literature review. J Appl Res Intellect Disabil 2017;30:982-94. https://doi.org/10.1111/jar.12270.
- Tuffrey-Wijne I, Bernal J, Jones A, Butler G, Hollins S. People with intellectual disabilities and their need for cancer information. Eur J Oncol Nurs 2006;10:106-16. https://doi.org/10.1016/j.ejon.2005.05.005.
- Voss H, Vogel A, Wagemans AMA, Francke AL, Metsemakers JFM, Courtens AM, et al. Advance care planning in palliative care for people with intellectual disabilities: a systematic review. J Pain Symptom Manage 2017;54:938-60.e1. https://doi.org/10.1016/j.jpainsymman.2017.04.016.
- Adam E, Sleeman KE, Brearley S, Hunt K, Tuffrey-Wijne I. The palliative care needs of adults with intellectual disabilities and their access to palliative care services: a systematic review. Palliat Med 2020;34:1006-18. https://doi.org/10.1177/0269216320932774.
- Wagemans A, van Schrojenstein Lantman-de-Valk H, Tuffrey-Wijne I, Widdershoven G, Curfs L. End-of-life decisions: an important theme in the care for people with intellectual disabilities. J Intellect Disabil Res 2010;54:516-24. https://doi.org/10.1111/j.1365-2788.2010.01276.x.
- Coleman JJ, Botkai A, Marson EJ, Evison F, Atia J, Wang J, et al. Bringing into focus treatment limitation and DNACPR decisions: how COVID-19 has changed practice. Resuscitation 2020;155:172-9. https://doi.org/10.1016/j.resuscitation.2020.08.006.
- Sutton L, Goodacre S, Thomas B, Connelly S. Do not attempt cardiopulmonary resuscitation (DNACPR) decisions in people admitted with suspected COVID-19: secondary analysis of the PRIEST observational cohort study. Resuscitation 2021;164:130-8. https://doi.org/10.1016/j.resuscitation.2021.04.028.
- Cooke R. Is there a better way to die?. The Guardian 2020. www.theguardian.com/society/2020/jul/05/is-there-a-better-way-to-die (accessed 4 May 2023).
- Nursing and Midwifery Council . Statement on Advance Care Planning During the COVID-19 Pandemic, Including Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) 2020.
- British Medical Association, Care Provider Alliance, Care Quality Commission, Royal College of General Practitioners . Joint Statement on Advance Care Planning 2020. www.cqc.org.uk/news/stories/joint-statement-advance-care-planning (accessed 4 May 2023).
- Care Quality Commission . Protect, Respect, Connect: Decisions about Living and Dying Well During COVID-19 2021.
- Royal College of General Practice . Ethical Guidance on COVID-19 and Primary Care n.d. https://elearning.rcgp.org.uk/mod/page/view.php?id=10557 (accessed 6 May 2023).
- British Medical Association . COVID-19 Toolkit for GPs and GP Practices n.d. www.bma.org.uk/advice-and-support/covid-19/gp-practices/covid-19-toolkit-for-gps-and-gp-practices (accessed 4 May 2023).
- Fadel MG, Parekh K, Hayden P, Krishnan P. Improving resuscitation decisions: a trust-wide initiative. BMJ Open Qual 2018;7. https://doi.org/10.1136/bmjoq-2017-000268.
- Johnson M, Whyte M, Loveridge R, Yorke R, Naleem S. A unified electronic tool for CPR and emergency treatment escalation plans improves communication and early collaborative decision making for acute hospital admissions. BMJ Qual Improv Rep 2017;6. https://doi.org/10.1136/bmjquality.u213254.w6626.
- Fritz Z, Malyon A, Frankau JM, Parker RA, Cohn S, Laroche CM, et al. The universal form of treatment options (UFTO) as an alternative to do not attempt cardiopulmonary resuscitation (DNACPR) orders: a mixed methods evaluation of the effects on clinical practice and patient care. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070977.
- Lightbody CJ, Campbell JN, Herbison GP, Osborne HK, Radley A, Taylor DR. Impact of a treatment escalation/limitation plan on non-beneficial interventions and harms in patients during their last admission before in-hospital death, using the Structured Judgment Review Method. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-024264.
- Fielden L, Lynch D, Petrie K. A Quantitative and Qualitative Evaluation of the ReSPECT Process in Forth Valley: Scotland’s First ReSPECT Pilot. Edinburgh: NHS Forth Valley; 2019.
- Kesten JM, Redwood S, Pullyblank A, Tavare A, Pocock L, Brant H, et al. Using the recommended summary plan for emergency care and treatment (ReSPECT) in care homes: a qualitative interview study. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afac226.
- May C. Towards a general theory of implementation. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-18.
- Gallacher K, May CR, Montori VM, Mair FS. Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory. Ann Fam Med 2011;9:235-43. https://doi.org/10.1370/afm.1249.
- Hawkes CA, Fritz Z, Deas G, Ahmedzai SH, Richardson A, Pitcher D, et al. ReSPECT Working Group Collaborators . Development of the Recommended Summary Plan for eEmergency Care and Treatment (ReSPECT). Resuscitation 2020;148:98-107. https://doi.org/10.1016/j.resuscitation.2020.01.003.
- Hall CC, Lugton J, Spiller JA, Carduff E. CPR decision-making conversations in the UK: an integrative review. BMJ Support Palliat Care 2019;9:1-11. https://doi.org/10.1136/bmjspcare-2018-001526.
- Compassion in Dying . Better Understanding, Better Outcomes: What We’ve Learned About DNACPR Decisions Before and During the Coronavirus Pandemic 2021 2021.
- Reich AJ, Perez S, Gazarian P, D’Arcangelo N, Gonzales K, Rodgers P, et al. Is this ACP? A focus group study of patient experiences of advance care planning. J Gen Intern Med 2022;37:1484-93. https://doi.org/10.1007/s11606-021-07208-3.
- Tuesen LD, Agard AS, Bulow HH, Fromme EK, Jensen HI. Decision-making conversations for life-sustaining treatment with seriously ill patients using a Danish version of the US POLST: a qualitative study of patient and physician experiences. Scand J Prim Health Care 2022;40:57-66. https://doi.org/10.1080/02813432.2022.2036481.
- Miller H, Tan J, Clayton JM, Meller A, Hermiz O, Zwar N, et al. Patient experiences of nurse-facilitated advance care planning in a general practice setting: a qualitative study. BMC Palliat Care 2019;18. https://doi.org/10.1186/s12904-019-0411-z.
- McIlfatrick S, Slater P, Bamidele O, Muldrew D, Beck E, Hasson F. ‘It’s almost superstition: If I don’t think about it, it won’t happen’. Public knowledge and attitudes towards advance care planning: a sequential mixed methods study. Palliat Med 2021;35:1356-65. https://doi.org/10.1177/02692163211015838.
- Healthwatch . #ShareForBetterCare 2023. www.healthwatch.co.uk/ (accessed 8 August 2023).
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Underwood M, Noufaily A, Bain C, Harlock J, Griffiths F, Huxley C, et al. Public attitudes to emergency care treatment plans: a population survey of Great Britain. BMJ Open 2024. https://dx.doi.org/10.1136/bmjopen-2023-080162.
- National Centre for Social Research . British Social Attitudes n.d. www.bsa.natcen.ac.uk/about/about.aspx (accessed 26 May 2023).
- Underwood M, Noufaily A, Blanchard H, Dale J, Harlock J, Gill P, et al. GPs views on emergency care treatment plans: an online survey. BJGP Open 2024;2023. https://doi.org/10.3399/BJGPO.2023.0192.
- VanGeest JB, Johnson TP, Welch VL. Methodologies for improving response rates in surveys of physicians: a systematic review. Eval Health Prof 2007;30:303-21. https://doi.org/10.1177/0163278707307899.
- Pit SW, Vo T, Pyakurel S. The effectiveness of recruitment strategies on general practitioner’s survey response rates: a systematic review. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-76.
- Bonevski B, Magin P, Horton G, Foster M, Girgis A. Response rates in GP surveys: trialling two recruitment strategies. Aust Fam Physician 2011;40:427-30.
- medeConnect . Solutions 2023. www.medeconnect.net/gp-omnibus.html (accessed 8 August 2023).
- Slowther AM, Bernstein CJ, Huxley C, Harlock J, Eli K, Mann C, et al. Using the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) in UK general practice: a qualitative exploration of the experiences of general practitioners, community-based nurses, care home staff, patients and their relatives. Br J Gen Pract 2024. https://doi.org/10.3399/BJGP.2024.0248.
- National Institute for Health and Care Research . ENRICH n.d. https://enrich.nihr.ac.uk (accessed 8 August 2023).
- Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough?. Qual Health Res 2017;27:591-608. https://doi.org/10.1177/1049732316665344.
- Office for Health Improvement and Disparities . National General Practice Profiles 2023. https://fingertips.phe.org.uk/profile/general-practice/data (accessed 8 August 2023).
- Eli K, Hawkes CA, Fritz Z, Griffin J, Huxley CJ, Perkins GD, et al. Assessing the quality of ReSPECT documentation using an accountability for reasonableness framework. Resusc Plus 2021;7. https://doi.org/10.1016/j.resplu.2021.100145.
- Martin DK, Giacomini M, Singer PA. Fairness, accountability for reasonableness, and the views of priority setting decision-makers. Health Policy 2002;61:279-90. https://doi.org/10.1016/s0168-8510(01)00237-8.
- Resuscitation Council UK . The ReSPECT Process: A Guide for Clinicians Completing the Plan 2023. www.resus.org.uk/sites/default/files/2023-02/ReSPECT%20Guide%20for%20Clinicians_FINAL.pdf (accessed 8 August 2023).
- Schellekens JE, Houtvast CS, Leusink P, Kleiverda G, Gomperts R. Dutch GPs’ views on prescribing mifepristone and misoprostol: a mixed-methods study. Br J Gen Pract 2022;72:e677-83. https://doi.org/10.3399/BJGP.2021.0704.
- Carmody K, Rouse M, Nolan D, Quinlan D. GPs’ practice and attitudes to initiating isotretinoin for acne vulgaris in Ireland: a cross-sectional questionnaire survey in primary care. Br J Gen Pract 2020;70:e651-6. https://doi.org/10.3399/bjgp20X712337.
- Eli K, Harlock J, Huxley CJ, Bernstein C, Mann C, Spencer R, et al. Patient and relative experiences of the ReSPECT process in the community: an interview-based study. BMC Prim Care 2024;25. https://doi.org/10.1186/s12875-024-02283-x.
- Resuscitation Council UK . ReSPECT n.d. www.resus.org.uk/respect (accessed 25 June 2023).
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Davies R, Ives J, Dunn M. A systematic review of empirical bioethics methodologies. BMC Med Ethics 2015;16. https://doi.org/10.1186/s12910-015-0010-3.
- Spiers G, Beresford B. ‘It goes against the grain’: a qualitative study of the experiences of parents’ administering distressing health-care procedures for their child at home. Health Expect 2017;20:920-8. https://doi.org/10.1111/hex.12532.
- Russell AM, Lovell JM, Harlock J, Griffiths F, Slowther A. Autonomy and advocacy in planning for a medical emergency: Adults with a learning disability and family carers experiences and perceptions of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) process. version 2; peer review: 1 approved, 2 approved with reservation. NIHR Open Res 2024;4. https://doi.org/10.3310/nihropenres.13555.2.
- National Institute for Health and Care Excellence . Impact: People With a Learning Disability 2021.
- University of Bristol . The Learning Disability Mortality Review (LeDeR) Programme Annual Report: Norah Fry Centre for Disabilities Studies 2018.
- Henderson A, Fleming M, Cooper SA, Pell JP, Melville C, Mackay DF, et al. COVID-19 infection and outcomes in a population-based cohort of 17 203 adults with intellectual disabilities compared with the general population. J Epidemiol Community Health 2022;76:550-5. https://doi.org/10.1136/jech-2021-218192.
- McNamara B, Same A, Rosenwax L. Creating person-centred support for people with intellectual disabilities at the end of life: an Australian qualitative study of unmet needs and strategies. J Intellect Disabil 2020;24:543-58. https://doi.org/10.1177/1744629518823887.
- Tuffrey-Wijne I, McEnhill L, Curfs L, Hollins S. Palliative care provision for people with intellectual disabilities: interviews with specialist palliative care professionals in London. Palliat Med 2007;21:493-9. https://doi.org/10.1177/0269216307082019.
- CHANGE . Our Services 2023. www.changepeople.org (accessed 25 June 2023).
- Jager A, Tewson A, Ludlow B, Boydell K. Embodied ways of storying the self: a systematic review of body-mapping. Forum Qual Soc Res 2016;17. https://doi.org/10.17169/fqs-17.2.2526.
- Carnemolla P, Kelly J, Donnelley C, Healy A. Reflections on working together in an inclusive research team. Soc Sci 2022;11. https://doi.org/10.3390/socsci11050182.
- Braun V, Clarke V, Hayfield N, Terry G. Handbook of Research Methods in Health Social Sciences. Singapore: Springer; 2019.
- Dent-Brown K, Wang M. The mechanism of storymaking: a grounded theory study of the 6-part story method. Arts Psychother 2006;33:316-30. https://doi.org/10.1016/j.aip.2006.04.002.
- Happell B, Byrne L, McAllister M, Lampshire D, Roper C, Gaskin CJ, et al. Consumer involvement in the tertiary-level education of mental health professionals: a systematic review. Int J Ment Health Nurs 2014;23:3-16. https://doi.org/10.1111/inm.12021.
- SNOOP . Project SNO 2023. www.snoopcharity.org (accessed 8 August 2023).
- Slowther A, Bernstein C, Huxley C, Harlock J, Eli K, . Using the Recommended Plan for Emergency Care and Treatment (ReSPECT) in UK general practice: a qualitative exploration of the experiences of general practitioners, community-based nurses, care home staff, patients and their relatives. Br J Gen Pract 2024.
- Robert GB. Participatory Action Research: Using Experience-Based Co-Design to Improve the Quality of Healthcare Services: Understanding and Using Health Experiences – Improving Patient Care. Oxford: Oxford University Press; 2013.
- Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making 2011;31:828-38. https://doi.org/10.1177/0272989x11393976.
- Vranas KC, Plinke W, Bourne D, Kansagara D, Lee RY, Kross EK, et al. The influence of POLST on treatment intensity at the end of life: a systematic review. J Am Geriatr Soc 2021;69:3661-74. https://doi.org/10.1111/jgs.17447.
- Mirarchi FL, Doshi AA, Zerkle SW, Cooney TE. TRIAD VI: how well do emergency physicians understand Physicians Orders for Life Sustaining Treatment (POLST) forms?. J Patient Saf 2015;11:1-8. https://doi.org/10.1097/PTS.0000000000000165.
- Mirarchi FL, Cammarata C, Zerkle SW, Cooney TE, Chenault J, Basnak D. TRIAD VII: do prehospital providers understand Physician Orders for Life-Sustaining Treatment documents?. J Patient Saf 2015;11:9-17. https://doi.org/10.1097/PTS.0000000000000164.
- Breyre AM, Sporer KA, Davenport G, Isaacs E, Glomb NW. Paramedic use of the Physician Order for Life-Sustaining Treatment (POLST) for medical intervention and transportation decisions. BMC Emerg Med 2022;22. https://doi.org/10.1186/s12873-022-00697-3.
- Levoy K, Sullivan SS, Chittams J, Myers RL, Hickman SE, Meghani SH. Don’t throw the baby out with the bathwater: meta-analysis of advance care planning and end-of-life cancer care. J Pain Symptom Manage 2023;65:e715-43. https://doi.org/10.1016/j.jpainsymman.2023.02.003.
- Arruda LM, Abreu KPB, Santana LBC, Sales Manuela Vasconcelos de Castro. Variables that influence the medical decision regarding advance directives and their impact on end-of-life care. Einstein (Sao Paulo) 2020;18. https://doi.org/10.31744/einstein_journal/2020RW4852.
- Mental Capacity Act 2005 n.d. www.legislation.gov.uk/ukpga/2005/9/contents (accessed 8 August 2023).
- Adults With Incapacity (Scotland) Act 2000 n.d. www.legislation.gov.uk/asp/2000/4/contents (accessed 8 August 2023).
- Mirarchi FL, Juhasz K, Cooney TE, Puller J, Kordes T, Weissert L, et al. TRIAD XII: are patients aware of and agree with DNR or POLST orders in their medical records. J Patient Saf 2019;15:230-7. https://doi.org/10.1097/PTS.0000000000000631.
- Hickman SE, Torke AM, Heim Smith N, Myers AL, Sudore RL, Hammes BJ, et al. Reasons for discordance and concordance between POLST orders and current treatment preferences. J Am Geriatr Soc 2021;69:1933-40. https://doi.org/10.1111/jgs.17097.
- Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0116629.
- Lakin JR, Gundersen DA, Lindvall C, Paasche-Orlow MK, Tulsky JA, Brannen EN, et al. ACP-PEACE Investigators . A yet unrealized promise: structured advance care planning elements in the electronic health record. J Palliat Med 2021;24:1221-5. https://doi.org/10.1089/jpm.2020.0774.
- Dillon E, Chuang J, Gupta A, Tapper S, Lai S, Yu P, et al. Provider perspectives on advance care planning documentation in the electronic health record: the experience of primary care providers and specialists using advance health-care directives and physician orders for life-sustaining treatment. Am J Hosp Palliat Care 2017;34:918-24. https://doi.org/10.1177/1049909117693578.
- Millington-Sanders C, Nadicksbernd JJ, O’Sullivan C, Morgan T, Raleigh A, Yeun P, et al. Electronic palliative care co-ordination system: an electronic record that supports communication for end-of-life care – a pilot in Richmond, UK. London J Prim Care (Abingdon) 2013;5:106-10.
- Finucane AM, Davydaitis D, Horseman Z, Carduff E, Baughan P, Tapsfield J, et al. Electronic care coordination systems for people with advanced progressive illness: a mixed-methods evaluation in Scottish primary care. Br J Gen Pract 2020;70:e20-8. https://doi.org/10.3399/bjgp19X707117.
- Wye L, Lasseter G, Simmonds B, Duncan L, Percival J, Purdy S. Electronic palliative care coordinating systems (EPaCCS) may not facilitate home deaths: a mixed methods evaluation of end of life care in two English counties. J Res Nurs 2016;21:96-107. https://doi.org/10.1177/1744987116628922.
- Standing H, Patterson R, Lee M, Dalkin SM, Lhussier M, Bate A, et al. Information sharing challenges in end-of-life care: a qualitative study of patient, family and professional perspectives on the potential of an Electronic Palliative Care Co-ordination System. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-037483.
- Patterson R, Standing H, Lee M, Dalkin S, Lhussier M, Exley C, et al. Paramedic information needs in end-of-life care: a qualitative interview study exploring access to a shared electronic record as a potential solution. BMC Palliat Care 2019;18. https://doi.org/10.1186/s12904-019-0498-2.
- Health and Social Care Act 2012 n.d. www.legislation.gov.uk/ukpga/2012/7/section/261 (accessed 28 April 2024).
- NHS England . Digital Data Security and Protection Toolkit n.d. www.dsptoolkit.nhs.uk (accessed 28 April 2024).
- Tark A, Song J, Parajuli J, Chae S, Stone PW. Are we getting what we really want? A systematic review of concordance between physician orders for life-sustaining treatment (POLST) documentation and subsequent care delivered at end-of-life. Am J Hosp Palliat Care 2021;38:1142-58. https://doi.org/10.1177/1049909120976319.
- Johnson SB, Butow PN, Kerridge I, Bell ML, Tattersall MHN. How well do current measures assess the impact of advance care planning on concordance between patient preferences for end-of-life care and the care received: a methodological review. J Pain Symptom Manage 2018;55:480-95. https://doi.org/10.1016/j.jpainsymman.2017.09.008.
Appendix 1 Ethical considerations arising from the study and approaches to addressing them
Recruitment and conduct of Interviews with patients and family members
Recommended summary plan for emergency care and treatment discussions are inherently sensitive and emotive conversations. People who have a ReSPECT form completed may often be coming towards the end of their life and any ReSPECT conversation will be precipitated by an acknowledgement that an acute deterioration in health from which recovery may be unlikely is anticipated. We identified processes to avoid approaching a patient who is in the last stages of life and to identify if a relative is bereaved prior to a follow up interview. When a patient lacked capacity to consent to access to their ReSPECT form and medical records, we sought personal consultee agreement from their next of kin.
Responding to distress of participants during interviews and focus groups
Researchers conducting the interviews and focus groups all had experience of conducting sensitive interviews with patients and families. We provided contact details for local support services following the interviews with patients and families and the public focus groups. Warwick Medical School standard operating procedure for researcher response to a concern about risk of serious harm to a patient were in place.
Concerns about unprofessional practice or safeguarding arising in the interview
A study-specific process was developed for researcher response to a concern about unethical or unsafe clinical practice. If any disclosures of data were to be made during this process, the participant involved in the relevant interview would be informed. The need for a researcher to disclose any evidence of serious professional misconduct or safeguarding concern was made clear in the relevant participant information sheets.
Verbal consent for informal conversations with practice staff (work package 1)
When the researcher initiated informal conversations with practice staff members, they obtained verbal consent from the participating staff members to write up these conversations as field notes, to be used in data analysis. To ensure that participants could easily contact the researcher to withdraw their consent, the researcher gave their University of Warwick business card with contact information to each staff member who participated.
Accessing medical records and ReSPECT forms (work packages 1 and 3)
The study required the research team to access relevant information from the patients’ GP records and copies of ReSPECT forms. Our approach sought to balance: (1) respect for the patient’s right to information in their medical record being treated confidentially; (2) the risk to the validity and public interest in the research being harmed by a biased sample; and (3) consideration of practicable alternatives to obtaining consent.
This part of the data collection was the subject of our CAG approvals. CAG approvals allowed us to collect pseudoanonymised data on all eligible patients in participating GP practices without the patient’s consent. We provided study information leaflets that detailed how patients or the relative of someone who lacked capacity could inform study staff that they did not want their data collected. The rationale for CAG approvals is outlined in Report Supplementary Material 4.
Involvement of people with learning disability in co-production workshops
In recruiting and working with people with a learning disability as part of the study, we aimed to balance being as inclusive as possible while ensuring that potential participants were making a free and informed choice to participate. For this WP, we worked closely with CHANGE, a leading learning disability rights charity, who were responsible for recruiting all participants for this WP. CHANGE also worked with the study team to produce easy-read participant information leaflets and consent documentation to facilitate participation. The study team followed CHANGE’s protocols for safeguarding and supporting people who may become distressed during the workshops.
Appendix 2 Feasibility study report
Background
During data collection for WP3 of the main study (review and analysis of ReSPECT forms and GP clinical records) it became clear that we would not achieve the sample size required to measure congruence between ReSPECT recommendations and clinical decisions. We describe the reasons for this in Chapter 2 of the main report. At the request of the funder, alternative approaches to obtaining sufficient data for a congruence analysis were considered by the project management team. They concluded that the most feasible approach would be to conduct a prospective study of the congruence of care and treatment decision-making with ReSPECT recommendations using care home records. This approach would require a different study design with primary recruitment of care homes. To inform a potential future study recruiting care homes we conducted a feasibility study within the current project.
Aim
To assess the feasibility of conducting a national study of care home records to analyse congruence of ReSPECT recommendations and subsequent treatment and care decisions for residents.
Objectives
-
To estimate the percentage of care home residents with a completed ReSPECT form.
-
To identify the frequency of acute medical events or clinical deterioration recorded within 6 months of a ReSPECT form completion.
-
To assess the quality-of-care home records description of treatment and care decisions made for acute medical events or deterioration.
-
To identify the process of retaining and accessing records of residents who have died for retrospective review of treatment decisions.
Methods
Recruitment
We worked with the ENRICH team in West Midlands to recruit three care homes not involved in the main study. Initial information about the feasibility study was provided through ENRICH to research active care homes in the area. Care homes expressing an interest were put in touch with the study team by ENRICH. The study team provided a detailed information sheet and arranged an online meeting between a senior member of the study team and the manager of the care home to discuss the study and answer questions. We received approval from the HRA Confidentiality Advisory Group for an extension of our existing permission under section 261 of the Health and Social Care Act 2012110 to access records without consent. For care homes who agreed to participate, a check was made by the care home to identify if any residents had registered under the national data opt out to ensure their records were not accessed during the study. The study team provided participating care homes with information letters about the study for all residents, and for the designated next of kin of those residents who lacked capacity. Letters were either given to residents or posted to their designated next of kin. The information described the purpose of the study, that the researcher would have access to their care record, and the ways in which the person could let the study team know that they do not want their care home records to be used in the study. No data collection occurred until 4 weeks had elapsed to allow a resident or their next of kin on their behalf to opt out of the study. Opt-outs were recorded in the study screening log kept by the care home and no identifiable data was accessible to the study team.
Data collection
Four weeks after delivery of the information, letters two senior study researchers (FG and AS) with a clinical background in general practice each visited one of the care homes and identified the records of all residents who had not opted out of the study. For each resident, the researcher checked the care home record and noted in a field spreadsheet the following:
-
Presence of a completed ReSPECT form.
-
Any record of acute medical event or significant deterioration in clinical condition within 6 months of ReSPECT form completion (or within the last 6 months if no ReSPECT form or ReSPECT completed more than 12 months previously and number of events if ˃ 1).
-
If the record of decisions for each event sufficiently detailed to enable an analysis of congruence with a ReSPECT recommendation; that is, does the decision specify any treatment given or reasons for decision not to escalate treatment.
We did not review recommendations in ReSPECT forms as part of the feasibility study as a review of ReSPECT forms had been undertaken as part of the main study.
No personal identifying information or specific information about treatment decisions was recorded.
The researcher also identified with the care home manager the process for archiving and retrieval of care home records of deceased residents.
Following the data collection visits, the two researchers compared their findings and discussed the level of detail provided in the clinical records to agree if this was sufficient to perform a congruence analysis against a completed ReSPECT recommendation.
Findings
Recruitment challenges
Despite circulation of information from the ENRICH team, including personal approaches to research active homes, we received very few expressions of interest. Six sites expressed interest, of which two chose not to proceed after receiving further information and one withdrew because of manager turnover. To comply with the CAG requirements, all three recruited sites needed to obtain confirmation of compliance with NHS Digital Data Security and Protection (DSPT) Toolkit. 111 Navigating this process with NHS Digital proved challenging and one home withdrew at this stage. The remaining two participating homes were then required to check eligible residents against the national data opt-out records. This process involved several stages and was highly technical. The two recruited homes were part of a larger organisation with a dedicated data protection officer and information technology support, but even with this specialist support the process was time consuming and complicated. Overall, the time from initial recruitment to confirmation of data opt out compliance was 3 months. No opt-outs were recorded on the national data opt-out system for residents in the participating homes and no opt outs were received in response to the information letters.
Examination of records
Total number of residents in the participating homes was 75. Of these residents, 45 (60%) had a completed ReSPECT form in their care record. For those residents with a ReSPECT form, 17 (38%) had at least one acute event recorded in a 6-month period. For these events the detail provided in the care home record was assessed as sufficient to enable an evaluation of congruence with a relevant ReSPECT form recommendation.
Systems for archiving and retrieval of records of residents who have died
The research team confirmed with each care home manager that the home had a policy and system for archiving the records of residents who have died, and a system for retrieving the record if required for future review. Length of archive period varied but was at least 6 years. Therefore, it would be possible to access these records to compare clinical decisions around end of life with ReSPECT recommendations for residents who had died for a congruence analysis study.
Implications for a future study of congruence between ReSPECT recommendations and clinical decisions using care home records
Recruitment of care homes
Recruitment of care homes for this study, and the main study was challenging. In both studies, we found staff turnover to be a major obstacle to establishing a relationship between the home, ENRICH and the study team. Care homes are under immense workload pressure at present and any additional work may be too much for them to consider, particularly for small independent homes. Studies that involve accessing records without consent under a Section 251 of the NHS Act 2006 approval from HRA CAG add an additional onerous layer of work for care homes to obtain confirmation of DSPT compliance by NHS Digital and to navigate the complex technical system for identifying membership of the national data opt-out for eligible residents. For a future study, it may be advisable to recruit care homes within large national care organisations where there is likely to be central data protection and information technology support. Study teams should allow a long set-up period to ensure all homes can demonstrate compliance with the relevant data protection and data opt out requirements. However, exclusion of smaller independently run homes may bias study findings. Sufficient resources for dedicated and specific research support for care homes may lead to increased recruitment and retention of study sites.
Sample size requirements for a large congruence analysis study
In our feasibility study, homes 17/75 (22.7%) residents had a completed ReSPECT form and an identifiable acute event in the preceding 6 months. In our original sample size calculation for congruence, assuming congruence of around 75%, we needed data on 289 people with an acute event. On a simple calculation, this would mean that we needed to work with homes to recruit 1275 residents. However, the two study homes may not be representative of homes overall. To allow for this uncertainty in our calculations, we have used the lower limit of the 60% CI for events (i.e. 18.6%). This means that we would need to examine the records of at least 1554 residents to ensure that we identified 289 acute events. The mean capacity (number of beds) of all care homes involved in the ReSPECT study (main and feasibility studies) was 49.7, meaning we would need to work with 32 homes. Allowing for some uncertainty about the actual congruence rate level we anticipated that we needed to work with around 40–50 homes to complete this study.
Clarity of ReSPECT recommendations to enable congruence to be assessed (findings from main study)
To enable an accurate assessment of congruence between clinical decision-making and ReSPECT recommendations, there needs to be a clear record of the clinical decision-making in the patient record, and also clear and specific recommendations on the ReSPECT form. Our findings from review of completed ReSPECT forms and qualitative data from interviews with clinicians and care home staff in the main study suggest that recommendations are often not sufficiently specific to inform action in an emergency. The challenge of interpreting recommendations in the context of an emergency or acute clinical episode may also be encountered in evaluating the congruence of decisions with recommendations. Studies of congruence between anticipatory treatment recommendations in the POLST and clinical decisions have been carried out. 112 However, POLST recommendation forms are more structured and do not use free text recommendations which may facilitate the assessment of congruence. A review of methods to evaluate the impact of ACP on concordance between patient preferences for end-of-life care and the care they received identified several challenges. These included a lack of clarity over what is being measured, the use of medical documentation to assess patient preference, and failure to adequately deal with the complexity of the constructs being measured. 113 Based on our main study findings, we anticipate similar challenges in any congruence analysis to assess the impact of ReSPECT plans on patient treatment and care.
In summary, our feasibility study has demonstrated that the substantial logistical challenges in recruiting care homes to a study of this nature, and the large sample size that would be needed, mitigate against embarking on a large-scale study. Additionally, the conceptual challenges identified by Johnson et al. 113 in similar studies of ACP interventions suggest further research is needed to inform the development of an appropriate assessment tool.
Appendix 3 Public survey additional tables
All data used in these analyses have come from the National Centre for Social Research British Social Attitudes Survey 2023 © National Centre for Social Research September 2023.
| Responders N = 1135 | National dataa (%) | |||
|---|---|---|---|---|
| (n) | (%) | |||
| Gender | ||||
| Male | 497 | 44 | 49 | |
| Female | 638 | 56 | 51 | |
| Age (years) | ||||
| 18–24 | 66 | 6 | 11 | |
| 25–34 | 173 | 15 | 17 | |
| 35–44 | 172 | 15 | 16 | |
| 45–54 | 205 | 18 | 17 | |
| 55–59 | 99 | 9 | 9 | |
| 60–64 | 107 | 9 | 7 | |
| 65–69 | 107 | 9 | 6 | |
| 70 or over | 205 | 18 | 17 | |
| Missing | 1 | |||
| Location | ||||
| South East | 166 | 15 | 14 | |
| South West | 126 | 11 | 9 | |
| North West | 114 | 10 | 11 | |
| East of England | 107 | 9 | 10 | |
| Yorkshire and Humber | 107 | 9 | 8 | |
| London | 106 | 9 | 14 | |
| Scotland | 105 | 9 | 9 | |
| West Midlands | 100 | 9 | 9 | |
| East Midlands | 96 | 8 | 8 | |
| North East | 59 | 5 | 4 | |
| Wales | 49 | 4 | 5 | |
| Ethnicity | ||||
| White origin | 1005 | 89 | 87 | |
| Asian origin | 55 | 5 | 7 | |
| Mixed origin | 44 | 4 | 1 | |
| Black origin | 14 | 1 | 3 | |
| Don’t know | 7 | 1 | Other + missing 2 | |
| Missing | 10 | 1 | ||
| Highest educational level | Studyb (%) | National (%) | ||
| No qualifications | 61 | 5 | 3 | 6 |
| Below A levelc | 183 | 16 | 13 | 14 |
| A-levels/SCE Highersd | 158 | 14 | 13 | 19 |
| Other Higher Educationd | 170 | 15 | 12 | 6 |
| Degree | 528 | 47 | 40 | 30 |
| Other | 21 | 2 | 1 | 6 |
| Missing | 14 | 1 | 1 | 3 |
| > 70 yearse | – | – | 18 | 16 |
| When did you have your emergency care and treatment plan completed? (N = 17) | |||
|---|---|---|---|
| Yes, n (%) | No, n (%) | Refused, n (%) | |
| When I reached a certain age | 3 (18) | 13 (76) | 1 (6) |
| After I was diagnosed with a life-threatening condition | 7 (41) | 9 (53) | 1 (6) |
| After I was told I had a long-term condition | 6 (35) | 10 (59) | 1 (6) |
| After I became severely disabled | 4 (24) | 12 (71) | 1 (6) |
| Other | 1 (6) | 15 (88) | 1 (6) |
| Who made your ECTP with you? (N = 17) (%) | If you were to have an emergency care and treatment plan completed tomorrow, who would you prefer to discuss it with?a (N = 618) (%) | |
|---|---|---|
| My GP | 6 (35) | 316 (51) |
| Another doctor who knows me well | 4 (24) | 59 (10) |
| A nurse at my GP surgery | 2 (12) | 46 (7) |
| A doctor or nurse who does not know me but is trained in making emergency care and treatment plans | 2 (12) | 161 (26) |
| Family member | – | 18 (3) |
| Other | 3 (18) | 5 (1) |
| Don’t know/ prefer not to answer | – | 6 (1) |
| Are you in favour or against anyone being able to have an emergency care and treatment plan if they wish? (N = 1135), n (%) | |
|---|---|
| Strongly in favour | 513 (45) |
| Somewhat in favour | 395 (35) |
| Neither in favour nor against | 189 (17) |
| Somewhat against | 20 (2) |
| Strongly against | 11 (1) |
| Don’t know/refused | 7 (1) |
| How comfortable or uncomfortable do you feel about making an emergency care and treatment plan yourself with a doctor or nurse? (N = 1112),a n (%) | |
|---|---|
| Very comfortable | 260 (23) |
| Fairly comfortable | 438 (39) |
| Neither comfortable nor uncomfortable | 233 (21) |
| Fairly uncomfortable | 123 (11) |
| Very uncomfortable | 49 (4) |
| Don’t know/refused | 9 (1) |
| Attitudes to emergency care and treatment plan completion | ||
|---|---|---|
| Would you or would you not like to have an emergency care and treatment plan for yourself at present? (N = 1112),a n (%) | Would you or would you not like to be involved in having an emergency care and treatment plan completed for a close family member, if they were not able to do so themselves? (N = 1135), n (%) | |
| Definitely would | 128 (12) | 302 (27) |
| Probably would | 490 (44) | 628 (55) |
| Probably would not | 369 (33) | 138 (12) |
| Definitely would not | 102 (9) | 41 (4) |
| Don’t know/refused | 23 (2) | 26 (2) |
| When, if ever, do you think you would like to have an emergency care and treatment plan in place for yourself? (N = 1112)a | |||
|---|---|---|---|
| Yes, n (%) | No, n (%) | Don’t know/refused, n (%) | |
| Now | 152 (14) | 940 (85) | 20 (2) |
| Never | 36 (3) | 1056 (95) | 20 (2) |
| When I am older | 441 (40) | 651 (59) | 20 (2) |
| If I get diagnosed with a life-threatening condition | 634 (57) | 458 (41) | 20 (2) |
| If I had a chronic long-term condition | 481 (43) | 611 (55) | 20 (2) |
| If I were to become severely disabled | 467 (42) | 625 (56) | 20 (2) |
| Other | 12 (1) | 1080 (97) | 20 (2) |
| You said you would like to have an emergency care and treatment (plan) when you are older. At what age? (N = 441)a | ||
|---|---|---|
| Age (years) | n (%) | Cumulative (%) |
| 18–30 | 4 (10) | 1 |
| 31–40 | 17 (4) | 5 |
| 41–50 | 39 (9) | 14 |
| 51–60 | 65 (15) | 28 |
| 61–70 | 145 (33) | 61 |
| 71–80 | 119 (27) | 88 |
| 81–90 | 40 (9) | 97 |
| Over 90 | 0 (0) | 97 |
| Don’t know/refused | 12 (3) | 100 |
| Are you in favour or against anyone being able to have an emergency care and treatment plan if they wish? Non-adjusted model (N = 1135) | ||||
|---|---|---|---|---|
| Characteristic | Respondents (n/N) | (%) | p-value | OR (95% CI) |
| Gender | ||||
| Male | 380/493 | 77 | 1 | |
| Female | 510/619 | 82 | 0.02 | 1.39 (1.04 to 1.87) |
| Other | 7/8 | 88 | 0.495 | 2.08 (0.2 to 17.1) |
| Age (years | ||||
| 18–24 | 51/66 | 77 | – | 1 |
| 25–34 | 137/173 | 79 | 0.746 | 1.12 (0.57 to 2.22) |
| 35–44 | 138/172 | 80 | 0.613 | 1.19 (0.6 to 2.37) |
| 45–54 | 160/205 | 78 | 0.895 | 1.05 (0.54 to 2.03) |
| 55–59 | 85/99 | 86 | 0.159 | 1.79 (0.8 to 4.00) |
| 60–64 | 86/107 | 80 | 0.626 | 1.2 (0.57 to 2.54) |
| 65–69 | 82/107 | 77 | 0.923 | 0.96 (0.47 to 2) |
| 70 + | 168/205 | 82 | 0.402 | 1.34 (0.68 to 2.63) |
| Ethnicity | ||||
| White | 820/1005 | 82 | – | 1 |
| Black | 10/14 | 71 | 0.338 | 0.56 (0.17 to 1.82) |
| Mixed | 30/44 | 68 | 0.029 | 0.48 (0.25 to 0.93) |
| Asian | 37/55 | 67 | 0.01 | 0.46 (0.26 to 0.83) |
| Qualifications | ||||
| No qualifications | 43/61 | 70 | – | 1 |
| Qualifications less than A level | 138/183 | 75 | 0.448 | 1.28 (0.67 to 2.45) |
| A-levels/SCE Highers | 127/158 | 80 | 0.118 | 1.71 (0.87 to 3.37) |
| Other Higher Education | 129/170 | 76 | 0.408 | 1.32 (0.69 to 2.53) |
| Degree or equivalent | 446/528 | 84 | 0.007 | 2.28 (1.25 to 4.14) |
| Do you have any physical or mental conditions or illnesses lasting or expected to last 12 months or more? | ||||
| No | 624/777 | 80 | – | 1 |
| Yes, but does not reduce activity | 82/99 | 83 | 0.551 | 1.18 (0.68 to 2.05) |
| Yes, and reduces activity | 198/254 | 78 | 0.418 | 0.87 (0.61 to 1.22) |
| Is there anyone who you look after or give special help to, for example, someone who is sick, has a long-term physical or mental disability or is elderly? | ||||
| No | 670/829 | 81 | 1 | |
| Yes | 195/246 | 79 | 0.089 | 0.6 (0.33 to 1.08) |
| Yes, but only in a professional capacity as part of my job | 43/60 | 72 | 0.276 | 1.2 (0.86 to 1.68) |
| Do you or does someone close to you have a condition or illness that you think is likely to shorten life? | ||||
| No | 647/817 | 79 | 1 | |
| Yes | 261/318 | 82 | 0.276 | 1.2 (0.86 to 1.68) |
| Would you or would you not like to have an Emergency Care and Treatment Plan for yourself at present? Non-adjusted model N = 1112a | ||||
|---|---|---|---|---|
| % | p-value | OR (95% CI) | ||
| Gender | ||||
| Male | 260/482 | 54 | ||
| Female | 349/609 | 57 | 0.266 | 1.15 (0.90 to 1.46) |
| Other | 2/7 | 29 | 0.202 | 0.34 (0.07 to 1.78) |
| Age | ||||
| 18–24 | 39/62 | 63 | – | 1 |
| 25–34 | 109/168 | 65 | 0.781 | 1.09 (0.60 to 1.99) |
| 35–44 | 90/168 | 54 | 0.207 | 0.68 (0.37 to 1.24) |
| 45–54 | 106/204 | 52 | 0.131 | 0.64 (0.36 to 1.14) |
| 55–59 | 56/98 | 57 | 0.47 | 0.79 (0.41 to 1.51) |
| 60–64 | 61/107 | 57 | 0.453 | 0.78 (0.41 to 1.49) |
| 65–69 | 49/104 | 47 | 0.05 | 0.53 (0.28 to 1.00) |
| 70 + | 108/200 | 54 | 0.218 | 0.69 (0.39 to 1.24) |
| Ethnicity | ||||
| White | 544/987 | 55 | – | 1 |
| Black | 10/13 | 77 | 0.131 | 2.71 (0.74 to 9.92) |
| Mixed | 23/43 | 53 | 0.834 | 0.94 (0.51 to 1.73) |
| Asian | 33/54 | 61 | 0.389 | 1.28 (0.73 to 2.24) |
| Educational level | ||||
| No qualifications | 33/59 | 56 | – | 1 |
| Qualification less than A level | 95/179 | 53 | 0.702 | 0.89 (0.49 to 1.61) |
| A-levels/SCE Highers | 74/153 | 48 | 0.324 | 0.74 (0.4 to 1.35) |
| Other Higher Education | 93/166 | 56 | 0.99 | 1.00 (0.55 to 1.83) |
| Degree or equivalent | 310/521 | 60 | 0.597 | 1.16 (0.67 to 1.99) |
| Do you have any physical or mental conditions or illnesses lasting or expected to last 12 months or more? | ||||
| No | 400/765 | 52 | – | 1 |
| Yes, but does not reduce activity | 56/97 | 58 | 0.312 | 1.25 (0.81 to 1.91) |
| Yes, and reduces activity | 158/245 | 64 | 0.001 | 1.66 (1.23 to 2.23) |
| Is there anyone who you look after or give special help to, for example, someone who is sick, has a long-term physical or mental disability or is elderly? | ||||
| No | 461/816 | 56 | ||
| Yes | 130/238 | 55 | 0.608 | 0.93 (0.69 to 1.24) |
| Yes, but only in a professional capacity as part of my job | 27/58 | 47 | 0.143 | 0.67 (0.39 to 1.14) |
| Do you or does someone close to you have a condition or illness that you think is likely to shorten life? | ||||
| No | 437/805 | 54 | ||
| Yes | 181/307 | 59 | 0.161 | 1.21 (0.93 to 1.58) |
| How comfortable or uncomfortable do you feel about making an Emergency Care and Treatment Plan yourself with a doctor or nurse?a Non-adjusted model N = 1112a | ||||
|---|---|---|---|---|
| % | p-value | OR (95% CI) | ||
| Gender | ||||
| Male | 309/482 | 54 | ||
| Female | 380/609 | 57 | 0.561 | 0.93 (0.72 to 1.19) |
| Other | 2/7 | 29 | 0.076 | 0.22 (0.04 to 1.17) |
| Age | ||||
| 18–24 | 40/62 | 65 | – | 1 |
| 25–34 | 116/168 | 69 | 0.514 | 1.23 (0.66 to 2.27) |
| 35–44 | 100/168 | 60 | 0.492 | 0.81 (0.44 to 1.48) |
| 45–54 | 117/204 | 57 | 0.316 | 0.74 (0.41 to 1.33) |
| 55–59 | 66/98 | 67 | 0.712 | 1.13 (0.58 to 2.22) |
| 60–64 | 73/107 | 68 | 0.622 | 1.18 (0.61 to 2.29) |
| 65–69 | 65/104 | 63 | 0.794 | 0.92 (0.48 to 1.76) |
| 70 + | 121/200 | 61 | 0.57 | 0.84 (0.47 to 1.52) |
| Ethnicity | ||||
| White | 633/987 | 64 | – | 1 |
| Black | 6/13 | 46 | 0.189 | 0.48 (0.16 to 1.44) |
| Mixed | 22/43 | 51 | 0.087 | 0.59 (0.32 to 1.08) |
| Asian | 32/54 | 59 | 0.468 | 0.81 (0.47 to 1.42) |
| Educational level | ||||
| No qualifications | 29/59 | 49 | – | 1 |
| Qualification less than A level | 91/179 | 51 | 0.822 | 1.07 (0.59 to 1.93) |
| A-levels/SCE Highers | 94/153 | 61 | 0.106 | 1.65 (0.90, 3.02) |
| Other Higher Education | 100/166 | 60 | 0.14 | 1.57 (0.86 to 2.85) |
| Degree or equivalent | 365/521 | 70 | 0.001 | 2.42 (1.41 to 4.17) |
| Do you have any physical or mental conditions or illnesses lasting or expected to last 12 months or more? | ||||
| No | 479/765 | 63 | – | 1 |
| Yes, but does not reduce activity | 74/97 | 59 | 0.009 | 1.92 (1.18 to 3.14) |
| Yes, and reduces activity | 144/245 | 59 | 0.282 | 0.85 (0.63 to 1.14) |
| Is there anyone who you look after or give special help to, for example, someone who is sick, has a long-term physical or mental disability or is elderly? | ||||
| No | 512/816 | 63 | ||
| Yes | 154/238 | 65 | 0.581 | 1.09 (0.81 to 1.47) |
| Yes, but only in a professional capacity as part of my job | 32/58 | 58 | 0.252 | 0.73 (0.43 to 1.25) |
| Do you or does someone close to you have a condition or illness that you think is likely to shorten life? | ||||
| No | 494/805 | 61 | ||
| Yes | 204/307 | 66 | 0.117 | 1.25 (0.95 to 1.64) |
Appendix 4 General practitioner survey additional tables
| Total (N = 841) | % | National data, % | |
|---|---|---|---|
| Age | |||
| 35 or under | 39 | 5 | 11a |
| 36–45 | 319 | 38 | 36 |
| 46–55 | 318 | 38 | 30 |
| 56 or over | 165 | 20 | 22 |
| Gender | |||
| Male | 446 | 53 | 42b |
| Female | 385 | 46 | 57 |
| Other | 1 | 0 | 1 |
| Prefer not to say | 9 | 1 | – |
| Current role | |||
| GP partner/principal | 419 | 50 | 42c |
| Salaried GP | 255 | 30 | 27 |
| Locum GP | 156 | 19 | – |
| GP registrar | 11 | 1 | – |
| English NHS region | |||
| London | 114 | 14 | 16d |
| South West | 85 | 10 | 11 |
| South East | 142 | 17 | 15 |
| West Midlands | 92 | 11 | 19 |
| East Midlands | 62 | 7 | |
| East of England | 93 | 11 | 11 |
| Yorkshire and Humber | 94 | 11 | 15 |
| North East | 44 | 5 | |
| North West | 115 | 14 | 13 |
| Type of area | |||
| Major conurbation | 157 | 19 | 39e |
| Large town/city | 124 | 15 | |
| Medium town/city | 207 | 25 | 52 |
| Small town/city | 254 | 30 | |
| Hamlet | 94 | 11 | 8 |
| Other | 5 | 1 | – |
| Practice size | |||
| Up to 5000 | 89 | 11 | 8f |
| 5001–7500 | 129 | 15 | 14 |
| 7501–10,000 | 181 | 22 | 18 |
| 10,001–12,500 | 147 | 17 | 17 |
| 12,501 or more | 295 | 35 | 44 |
| Time since completing GP training | |||
| 0–5 years ago | 51 | 6 | –g |
| 6–10 years ago | 140 | 17 | – |
| 11–15 years ago | 225 | 27 | – |
| 16–20 years ago | 160 | 19 | – |
| Over 20 years ago | 265 | 32 | – |
| N = 841 | |||
|---|---|---|---|
| Region (n) | ReSPECT, n (%) | DNACPR, n (%) | Other, n (%) |
| London (114) | 10 (9) | 87 (76) | 17 (15) |
| South West (85) | 37 (45) | 29 (34) | 18 (21) |
| South East (142) | 67 (47) | 66 (46) | 18 (21) |
| West Midlands (92) | 74 (80) | 16 (17) | 2 (2) |
| East Midlands (62) | 49 (79) | 12 (19) | 1 (2) |
| East of England (93) | 48 (52) | 43 (46) | 2 (2) |
| Yorkshire and Humber (94) | 40 (43) | 52 (55) | 2 (2) |
| North East (44) | 3 (7) | 33 (75) | 8 (18) |
| North West (115) | 16 (14) | 88 (77) | 11 (10) |
| Total (841) | 345 (41) | 426 (51) | 70 (8) |
| Reason for non-involvement (N = 72) | |
|---|---|
| n (%) | |
| Patient had capacity | 54 (75) |
| Family were unavailable | 18 (25) |
| Patient’s family declined to be involved in conversation | 1 (1) |
| Didn’t consider it at the time | 6 (8) |
| Patient didn’t want family involved | 11 (15) |
| OR, 95% CIs and p-values of the predictors for being comfortable having emergency care and treatment planning conversations with patients (N = 841) | |||||
|---|---|---|---|---|---|
| Comfortable, % (n) | Unadjusted analysis | Adjusted analysis | |||
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| Gender | |||||
| Female | 81 (385) | 1 | 1 | ||
| Male | 81 (446) | 0.98 (0.69 to 1.39) | 0.906 | 0.85 (0.59 to 1.24) | 0.407 |
| Other | 100 (1) | – | 0.982 | – | 0.995 |
| Prefer not to say | 67 (9) | 0.47 (0.11 to 1.92) | 0.291 | 0.36 (0.08 to 1.53) | 0.166 |
| Current role | |||||
| GP partner/principal | 85 (419) | 1 | |||
| GP registrar | 100 (11) | – | 0.975 | – | 0.984 |
| Locum GP | 73 (156) | 0.47 (0.30 to 0.74) | < 0.001 | 0.51 (0.31 to 0.82) | 0.006 |
| Salaried GP | 77 (255) | 0.59 (0.40 to 0.88) | 0.009 | 0.53 (0.34 to 0.82) | 0.004 |
| NHS region | |||||
| London | 69 (114) | 1 | |||
| East of England | 77 (93) | 1.52 (0.81 to 2.85) | 0.192 | 1.24 (0.49 to 3.15) | 0.655 |
| West Midlands | 78 (92) | 1.59 (0.84 to 3.01) | 0.150 | 1.29 (0.53 to 3.16) | 0.577 |
| North West | 77 (115) | 1.52 (0.84 to 2.74) | 0.167 | 1.54 (0.68 to 3.49) | 0.297 |
| Yorkshire and Humber | 83 (94) | 2.16 (1.11 to 4.22) | 0.024 | 1.80 (0.70 to 4.63) | 0.222 |
| South East | 83 (142) | 2.18 (1.20 to 3.94) | 0.010 | 2.08 (0.84 to 5.17) | 0.115 |
| East Midlands | 89 (62) | 3.48 (1.44 to 8.40) | 0.006 | 2.47 (0.78 to 7.86) | 0.124 |
| North East | 89 (44) | 3.46 (1.26 to 9.51) | 0.016 | 4.10 (1.22 to 13.8) | 0.023 |
| South West | 91 (85) | 4.26 (1.86 to 9.78) | < 0.001 | 4.30 (1.45 to 12.7) | 0.008 |
| Type of area | |||||
| Large town/city | 84 (124) | 1 | |||
| Major conurbation | 74 (157) | 0.54 (0.30 to 0.99) | 0.046 | 1.01 (0.43 to 2.35) | 0.987 |
| Medium town/city | 80 (207) | 0.78 (0.43 to 1.40) | 0.404 | 0.75 (0.40 to 1.40) | 0.361 |
| Small town/city | 83 (254) | 0.92 (0.51 to 1.64) | 0.771 | 0.76 (0.41 to 1.41) | 0.391 |
| Village/hamlet | 85 (94) | 1.10 (0.52 to 2.31) | 0.803 | 1.16 (0.53 to 2.54) | 0.714 |
| Other | 60 (5) | 0.29 (0.05 to 2.31) | 0.188 | 0.30 (0.04 to 2.22) | 0.237 |
| Practice size (number of patients) | |||||
| Up to 5000 | 75 (89) | 1 | 1 | 0 | |
| 5001–7500 | 78 (129) | 1.13 (0.60 to 2.14) | 0.701 | 0.98 (0.49 to 1.96) | 0.961 |
| 7501–10,000 | 76 (181) | 1.05 (0.58 to 1.90) | 0.862 | 0.85 (0.44 to 1.62) | 0.614 |
| 10,001–12,500 | 83 (147) | 1.60 (0.84 to 3.06) | 0.152 | 1.40 (0.68 to 2.86) | 0.360 |
| 12,501 or more | 85 (295) | 1.92 (1.08 to 3.44) | 0.027 | 1.60 (0.83 to 3.11) | 0.161 |
| Time since completion of GP training | |||||
| 0–5 years ago | 90 (51) | 1 | 1 | ||
| 6–10 years ago | 83 (140) | 0.53 (0.19 to 1.46) | 0.701 | 0.62 (0.21 to 1.82) | 0.388 |
| 11–15 years ago | 81 (225) | 0.46 (0.17 to 1.23) | 0.862 | 0.54 (0.19 to 1.52) | 0.246 |
| 16–20 years ago | 80 (160) | 0.43 (0.16 to 1.18) | 0.152 | 0.46 (0.16 to 1.35) | 0.158 |
| Over 20 years ago | 78 (265) | 0.39 (0.15 to 1.02) | 0.027 | 0.43 (0.15 to 1.19) | 0.105 |
| Emergency care and treatment form used | |||||
| DNACPR | 77 (426) | 1 | 1 | ||
| ReSPECT | 86 (345) | 1.83 (1.25 to 2.67) | 0.002 | 1.72 (1.10 to 2.69) | 0.017 |
| Other/none/don’t know | 80 (70) | 1.21 (0.65 to 2.67) | 0.550 | 1.00 (0.51 to 1.95) | 0.998 |
| OR (95% CIs) and p-values of the predictors for being comfortable having emergency care and treatment planning conversations with patients’ families (N = 841) | |||||
|---|---|---|---|---|---|
| Comfortable (%) | Unadjusted analysis, OR | Adjusted analysis, OR (95% CI) | |||
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| Gender | |||||
| Female | 80 (385) | 1 | 1 | ||
| Male | 79 (446) | 0.98 (0.70 to 1.37) | 0.896 | 0.86 (0.60 to 1.24) | 0.415 |
| Other | 100 (1) | – | 0.982 | – | 0.992 |
| Prefer not to say | 67 (9) | 0.51 (0.12 to 2.08) | 0.346 | 0.37 (0.09 to 1.64) | 0.193 |
| Current role | |||||
| GP partner/principal | 83 (419) | 1 | 1 | ||
| GP registrar | 100 (11) | – | 0.975 | – | 0.974 |
| Locum GP | 77 (156) | 0.70 (0.45 to 1.10) | 0.125 | 0.75 (0.46 to 1.22) | 0.248 |
| Salaried GP | 75 (255) | 0.63 (0.43 to 0.92) | 0.017 | 0.58 (0.38 to 0.88) | 0.010 |
| NHS region | |||||
| London | 91 (114) | 1 | |||
| East of England | 72 (93) | 1.24 (0.68 to 2.25) | 0.484 | 1.38 (0.55 to 3.44) | 0.491 |
| West Midlands | 73 (92) | 1.29 (0.70 to 2.36) | 0.412 | 1.20 (0.50 to 2.88) | 0.69 |
| North West | 77 (115) | 1.57 (0.87 to 2.81) | 0.131 | 2.05 (0.90 to 4.66) | 0.086 |
| Yorkshire and Humber | 85 (94) | 2.75 (1.38 to 5.47) | 0.004 | 3.15 (1.21 to 8.25) | 0.019 |
| South East | 83 (142) | 2.36 (1.31 to 4.26) | 0.004 | 3.06 (1.24 to 7.59) | 0.016 |
| East Midlands | 90 (62) | 4.48 (1.77 to 11.4) | 0.002 | 4.03 (1.23 to 13.2) | 0.022 |
| North East | 86 (44) | 3.04 (1.18 to 7.83) | 0.021 | 4.65 (1.46 to 14.9) | 0.009 |
| South West | 91 (85) | 4.63 (2.02 to 10.6) | < 0.001 | 6.05 (2.06 to 17.8) | 0.001 |
| Type of area | |||||
| Large town/city | 85 (124) | 1 | 1 | ||
| Major conurbation | 73 (157) | 0.50 (0.27 to 0.91) | 0.023 | 1.27 (0.54 to 2.98) | 0.589 |
| Medium town/city | 78 (207) | 0.65 (0.36 to 1.17) | 0.168 | 0.67 (0.36 to 1.26) | 0.243 |
| Small town/city | 81 (254) | 0.76 (0.42 to 1.35) | 0.347 | 0.69 (0.38 to 1.28) | 0.789 |
| Village/hamlet | 83 (94) | 0.88 (0.43 to 1.82) | 0.735 | 0.90 (0.42 to 1.94) | 0.199 |
| Other | 60 (5) | 0.27 (0.04 to 1.73) | 0.023 | 0.27 (0.04 to 1.99) | 0.589 |
| Practice size (number of patients) | |||||
| Up to 5000 | 78 (89) | 1 | 1 | ||
| 5001–7500 | 78 (129) | 1.05 (0.55 to 2.00) | 0.893 | 0.92 (0.46 to 1.87) | 0.825 |
| 7501–10,000 | 76 (181) | 0.90 (0.49 to 1.65) | 0.739 | 0.74 (0.38 to 1.44) | 0.383 |
| 10,001–12,500 | 82 (147) | 1.29 (0.67 to 2.47) | 0.445 | 1.16 (0.56 to 2.38) | 0.688 |
| 12,501 or more | 82 (295) | 1.29 (0.73 to 2.31) | 0.383 | 1.14 (0.59 to 2.20) | 0.704 |
| Time since completion of GP training | |||||
| 0–5 years ago | 86 (51) | 1 | 1 | ||
| 6–10 years ago | 79 (140) | 0.58 (0.24 to 1.43) | 0.237 | 0.81 (0.31 to 2.08) | 0.658 |
| 11–15 years ago | 79 (225) | 0.60 (0.25 to 1.42) | 0.248 | 0.83 (0.33 to 2.07) | 0.691 |
| 16–20 years ago | 78 (160) | 0.55 (0.23 to 1.32) | 0.180 | 0.73 (0.28 to 1.87) | 0.510 |
| Over 20 years ago | 80 (265) | 0.64 (0.27 to 1.49) | 0.299 | 0.81 (0.32 to 2.02) | 0.653 |
| Emergency care and treatment form used | |||||
| DNACPR | 75 (426) | 1 | 1 | ||
| ReSPECT | 85 (345) | 1.80 (1.25 to 2.60) | 0.002 | 1.85 (1.19 to 2.87) | 0.006 |
| Other | 79 (70) | 1.20 (0.65 to 2.21) | 0.560 | 1.01 (0.53 to 2.87) | 0.965 |
| Statistically significant covariates from the backwards elimination with dependent variable being ‘comfortable having ECTP conversations with patients’ | |||
|---|---|---|---|
| Covariates | Group | p-value | OR (95% CI) |
| GP Role | GP partner/principal | ||
| GP registrar | 0.975 | N/A | |
| Locum GP | 0.003 | 0.50 (0.32 to 0.79) | |
| Salaried GP | 0.014 | 0.60 (0.40 to 0.90) | |
| Area | London | ||
| South West | 0.005 | 3.35 (1.50 to 8.31) | |
| South East | 0.124 | 1.62 (8.79 to 3.02) | |
| West Midlands | 0.915 | 0.96 (0.47 to 1.97) | |
| East Midlands | 0.170 | 1.93 (0.79 to 5.27) | |
| East of England | 0.904 | 1.04 (0.54 to 2.05) | |
| Yorkshire and Humber | 0.217 | 1.55 (0.78 to 3.15) | |
| North East | 0.032 | 3.05 (1.18 to 9.50) | |
| North West | 0.434 | 1.27 (0.70 to 2.34) | |
| ECT form | DNACPR | ||
| ReSPECT | 0.013 | 1.75 (1.13 to 2.72) | |
| Other | 0.963 | 1.02 (0.54 to 2.02) | |
Appendix 5 ReSPECT form section completion rates
| ReSPECT form sectionsa and itemsb | Number completed (n = 142) (%) | Version 2 (n = 103) (%) | Version 3 (n = 39) (%) |
|---|---|---|---|
| Section 1 Personal details/this plan belongs to | |||
| Date | 140 (99) | – | – |
| Section 2 Summary of relevant information for this plan/shared understanding of my health and current condition | |||
| Previous and present conditions/medical conditions | 130 (92) | – | – |
| Reasons for the recommendations (section 4 in version 3) | 27 (19) | 20/103 (19) | 7/39 (18) |
| Other planning documents | 42 (30) | – | – |
| Communications needs | – | 26/103 (25) | – |
| Wishes about organ donation | – | 0/103 (0) | – |
| Personal circumstances | – | – | 7/39 (18) |
| Section 3 Personal preferences to guide this plan (when the person has capacity)/what matters to me in decisions about my treatment and care in an emergency | |||
| Balance of priorities/what matters to me (preference scale) | 64 (45) | – | – |
| What is most important to you/what I most value and fear (preference free text) | 81 (57) | – | – |
| Section 4 Clinical recommendations for emergency care and treatment | |||
| Focus of clinical recommendations | 52 (35) | – | – |
| Details about specific interventions | 123 (87) | – | – |
| Signed CPR recommendation | 53 (37) | – | – |
| Section 5 Capacity and representation at the time of completion/capacity for involvement in making this plan | |||
| Person’s capacity | 132 (93) | – | – |
| Number of people who lacked capacity | 60 (45) | ||
| Legal proxy (section 2 in version 3) | 43 (30) | 21/103 (20) | 22/39 (56) |
| Explanation as to how to person lacks capacity | – | – | 17/22 (77) |
| Section 6 Involvement in making this plan | |||
| Confirmation that the person, or someone close to them, was involved in the ReSPECT discussion | 134 (94) | – | – |
| Names and roles of those involved in ReSPECT discussion | – | 40/103 (39) | – |
| Location of records of discussion | – | 16/103 (16) | – |
| Section 7 Clinicians’ signatures | |||
| Clinicians’ signature | 64 (45) | – | – |
| Clinician’s grade/speciality and registration number | 109 (77) | – | – |
| Senior clinician’s signature | 14 (10) | – | – |
| Senior clinician’s grade/speciality and registration number | 18 (13) | – | – |
| Section 8 Emergency contacts/emergency contacts and those involved in discussing this plan’ | |||
| Emergency contacts | 108 (79) | – | – |
| Names, roles and relationships recorded | – | – | 27/39 (69) |
| Optional primary emergency contact signature | – | – | 3/39 (8) |
| Section 9 Confirmation of validity (e.g. for change of condition)/plan reviewed (e.g. for change of care setting) and remains relevant | |||
| Form review | 11 (8) | – | – |
Appendix 6 Patient/relative interviews by study area
| Area 1 | Area 2 | Area 3 | |
|---|---|---|---|
| First interviews | |||
| Patient | 5 | 1 | |
| Relative | 3 | 1 | |
| Patient/relative pair | 1 | 2 | |
| Follow-up interviews | |||
| Patient second interview | 2 | 1 | |
| Relative second interview | 1 | 1 | |
| Patient/relative pair second interview | 1 | ||
Appendix 7 List of external delegates at stakeholder meeting
| Name | Organisation | Position |
|---|---|---|
| Caitlyn Adkins | NHS Herefordshire and Worcestershire ICB | Palliative and End of Life Care Senior Manager |
| Dr Archana Anandaram | NW Leicestershire CCG | GP and LLR ICB Transformation Clinical Lead for Learning Disabilities |
| Dr Kate Day | Forrest Medical Centre | GP, Forrest Medical Centre |
| Dr Ian Black | Cwm Taf University Health Board NHS Wales | Consultant in Palliative Care |
| Upeka De Silva | Compassion in Dying | Senior Policy Officer |
| Chris Dodds | NHS Tayside | ReSPECT Project Manager, NHS Tayside |
| Dr Zoe Fritz | Cambridge University | Wellcome Fellow in ethics and Society |
| Dr Gregory Gardner | Christian Medical Fellowship | Christian Medical Fellowship |
| Suman Ghaiwal | NHS Coventry and Warwickshire Integrated Care Board | Communications and Involvement Manager |
| Dr Karen Harrison-Dening | Dementia UK | Head of Research and Publications, Dementia UK |
| Michelle Hartanto | University Hospitals Coventry and Warwickshire NHS Trust | Resuscitation Practitioner |
| Louise Holland | NHS England | Senior Programme Manager (LeDeR Action from Learning) |
| Melanie Humphreys | The Dudley Group NHS Foundation Trust | ReSPECT Project Lead |
| Dr Zoebia Islam | LOROS | Deputy Research Lead/Hon. Lecturer University of Leicester |
| Andy Knee | St Mungos Charity (Homelessness) | Palliative Care Co-ordinator |
| Nanette Mellor | The Brain Charity | CEO |
| Karen Morrow | NHS Lanarkshire | Programme Manager in Realistic Medicine, NHS Lanarkshire |
| Dr Sarah Onions | NHS Herefordshire and Worcestershire ICB | Herefordshire & Worcestershire ICS Clinical End of Life Lead |
| Rev Rosemary Pantling | South Warwickshire NHS Foundation Trust | Healthcare Chaplain, South Warwickshire University NHS Foundation Trust |
| Catherine Baldock | RCUK | Clinical Lead for ReSPECT |
| Karita Razzell | St Mungos Charity (Homelessness) | Care Manager |
| Osman Sheikh | Kettering General Hospital | Chaplain |
| Steve Thomson | Age UK Birmingham and Sandwell | CEO |
| Professor Irene Tuffrey | Kingston University | Professor of Intellectual Disability and Palliative Care |
| MBE Jo-Anne Wilson | Royal British Legion | Registered Manager Galanos House |
Appendix 8 Evaluating the use of ReSPECT in primary care: report of the stakeholder conference for conference delegates, 29 March 2023
This report is a summary of the small group discussions at the stakeholder conference on the 29 March 2023 at the Scarman centre at Warwick University. The stakeholders participating in the conference represented a wide range of perspectives and experiences of emergency care treatment planning and advance decision-making. They had a range of backgrounds including health and social care professionals, patient organisations and researchers. This report is a summary of the notes taken in each of the small groups, which have been analysed to extract the key messages and recommendations for how ECTPs in general and the ReSPECT process specifically can be improved for the benefit of patient care. The report begins with a summary of stakeholders’ reflections on the broad question of whose interests are being served during the ReSPECT process. It is then divided into the following sections:
-
initiating the conversation
-
having and recording the conversation
-
articulating and interpreting the recommendations
-
managing the plan
-
training
-
awareness raising and preparation.
Each section ends with key messages and/or recommendations for practice, policy, or training.
Whose interests are being served during the ReSPECT process?
The consensus across all groups was that the ReSPECT process should serve the interests of the person whose plan it is first and foremost. Stakeholders felt that the aim of ReSPECT should be to provide recommendations for future treatment and care that reflect the person’s values and wishes and are consistent with their interests. However, the groups also reflected on the tension between a process that is person centred and a set of recommendations that are intended to guide or direct clinicians: are the recommendations statements of what the person wants to happen or are they clinical recommendations as indicated on the form?
This tension reflects that the process, or at least the recommendations recorded on the form, also serve the interests of healthcare professionals who will be making treatment and care decisions for the person at a time of acute deterioration or in an emergency. Several groups noted that the healthcare professional making these decisions is unlikely to know the person and therefore, having clear recommendations to guide them can reassure the clinician that they are acting in the person’s best interests. Similarly, the form can provide clarity and reassurance for care home staff when communicating with healthcare professionals when a resident is unwell. Some groups also noted that the process, particularly the conversation, could be in the interests of the person’s family, helping them to understand the person’s wishes and to reduce the burden for them at the time of decision-making. Finally, groups also noted that documented ECTPs could benefit the healthcare system by facilitating effective decision-making at times of crises. However, there was also a concern that this could lead patients and their relatives to see ECTPs as a ‘tick box exercise’, causing them to mistrust the process.
In summary, the groups agreed that the process should be person centred foremost, but that healthcare professionals and the person’s family would also benefit. The challenge is to formulate recommendations that serve the interests of both the person and those who use the form as guidance when the person is acutely unwell.
Initiating the conversation
Discussion around the conversation itself focused first on initiating the conversation and then on the content and process of the conversation. In general, there appears to be a (mis)perception that ReSPECT (both the process and the form) is necessarily linked to or embedded in end-of-life discussions and end-of-life treatment and care decisions. This perception has implications for when a ReSPECT conversation might be initiated. For example, triggers for ReSPECT initiation might focus on patients who are receiving palliative care or for whom a life-threatening or life-limiting diagnosis has been made, or whose life expectancy is thought to be short. Stakeholders reflected that this approach limits the population for whom ReSPECT becomes available and could exclude people who might want or benefit from having a ReSPECT conversation and their wishes formally recorded.
While stakeholders recognised the importance of ReSPECT conversations as part of a wider ACP discussion around end of life, they also suggested other potential triggers for initiating a ReSPECT conversation. These included when a person has specific risk factors for severe acute illness or during regular reviews of someone with a chronic disease or disability. One suggestion was that for people with a learning disability, their annual health check could be an opportunity to initiate a conversation (a similar argument could be used for using routine elderly health-check appointments in this way). However, there was also concern that this could be misinterpreted by the person, particularly if ReSPECT is seen as associated with end-of-life care. Also, repeated reference to emergency care treatment planning could be frustrating or distressing for some people who may see it as focusing on their deteriorating health or limited life expectancy, rather than improving their current health. Some stakeholders felt that the driver for the conversation should be the person’s health condition and their risk of requiring emergency treatment and care.
There was clear consensus across the groups that whatever the trigger for initiating a ReSPECT conversation, it should occur early in any disease or illness trajectory, or even before someone became unwell. This would empower people to be involved in the conversation when they had capacity and were not too sick to engage in a conversation. However, delegates also noted that a person’s health changed over time, as did their wishes and preferences regarding treatment. Therefore, ReSPECT was seen as a series of conversations rather than one definitive conversation. Delegates also thought that anyone should be able to initiate a ReSPECT conversation for themselves.
A further discussion point was who should be able to initiate and carry out a ReSPECT conversation. There was agreement that the conversation should ideally occur with a healthcare professional who knows the person and with whom the person has a trusted relationship. The discussions revealed that there were different levels of initiation and involvement in ReSPECT conversations: (1) raising awareness of ReSPECT and preparing a person for a ReSPECT conversation; and (2) the more structured ReSPECT conversation leading to the ReSPECT plan that is then recorded on the ReSPECT form. Stakeholders thought that the raising awareness and preparation conversations could be led by a wide range of different people involved with someone’s care, for example care home staff or support workers but that training and support would be needed that was tailored to specific groups for having these conversations.
Key messages/recommendations
-
ReSPECT should not only be considered in the context of end of life or palliative care.
-
ReSPECT conversations should begin early and not left until emergency or end-of-life situations.
-
There is a distinction between conversations to prepare someone for discussion of a plan and the planning conversations and these preparation conversations can be initiated by a wide range of people, with appropriate training and support.
-
As people’s situation and perspectives change, ReSPECT must be reviewed when this happens.
-
In considering how these conversations are carried out and by whom, the current time pressures on GPs and care home staff need to be taken into account (i.e. balancing the desirable with the possible).
Having and recording the conversation
Stakeholders noted that ReSPECT planning conversations were rarely single conversations but occurred over time, often with several preparatory conversations where the idea of ReSPECT was introduced. They identified several challenges that could occur in the process of the ReSPECT conversation. These included practical challenges such as having enough time to have what is a difficult and complex conversation. It was seen as especially important to ensure that enough time was given for these conversations with a person with a learning disability, in addition to ensuring they had the right support person with them. They also identified challenges in communicating the purpose of the plan, including what it can and cannot do. For example, helping the person to understand the range of situations and treatment options that might be covered in a plan and the uncertainty of predicting future situations. Stakeholders also noted that it was important to talk about what was possible and not possible in relation to recommendations, and what alternative options would be available if there was a recommendation to limit some treatments. A strong message from the meeting was that ReSPECT conversations needed to be open and honest, and that the healthcare professional should take time to understand what was important to the person and what their preferences were. For good conversations to occur, other communication challenges needed to be considered such as language barriers, alternative formats for the form and supporting information, and the environment in which the conversation takes place. A key issue in terms of recording the conversation and the recommendations on the form is how to ensure that these are valid and accessible when needed. There was general consensus that a digital version of the form was the preferred option to ensure accessibility but there is a risk that this could disempower patients who would have less access to or control over their plan than with a patient-held paper copy. Concerns about version control were also raised.
Key messages/recommendations
-
Planning conversations need to be open and honest, person centred and realistic.
-
There needs to be sufficient time to have the conversation(s).
-
Good conversations require effective communication, including appropriate language and alternative formats to written documentation. Use of videos could be considered for recording conversations for people with learning disabilities.
-
Digital records of plans can increase access to the plan when needed but people may feel less in control of their plan if it is in a digital format. Problems with version control need to be addressed.
Articulating and interpreting recommendations
The main purpose of ReSPECT is to provide clear recommendations about emergency treatment and care in a situation where the person is unable to engage in the decision-making process at the time. Stakeholders agreed that it was crucially important that these recommendations were understandable to the person and their family, and to the health and social care professionals who would need to interpret them in the emergency or acute situation. Commonly used phrases such as ‘forward-based care’ or ‘not for hospital admission’ were regarded as too vague and unhelpful. However, there was general agreement that it was challenging to articulate recommendations that capture all likely scenarios. Instead, flexibility should be allowed to encompass other scenarios, and should include options for treatment as well as the limitations of those treatments, and to make it personal to that patient but sufficiently succinct to be read and understood in an emergency. Delegates talked about the need for nuance in recommendations as it is not possible to cover every scenario. This places greater emphasis on the need to carefully and accurately document the person’s values and preferences and for healthcare professionals to take account of these when interpreting recommendations or making a decision. The groups thought that the recommendations section must include a justification or rationale for the recommendations that was linked to the person’s values and preferences. This was seen as necessary to help healthcare professionals interpret the recommendations in a particular situation, but also to enable a person or their family to understand and if necessary, challenge the recommendations if they disagreed with them. Stakeholders noted the difference between hospital completed recommendations, which were specific to hospital-based scenarios, and primary care-based recommendations, highlighting the need for review of recommendations as a person moves from one environment to another. They emphasised the importance of clear communication between primary and secondary care in relation to ReSPECT recommendations. The space allocated to recommendations on the form was considered too little for the level of detail that may be required, which supported stakeholders’ views on the advantage of a digital form that could allow for expansion of sections as required. While they emphasised the need for sufficient detail on the form, they also noted that these recommendations related specifically to emergency care and treatment. Broader recommendations about the person’s treatment and care could be documented in an ACP or personal health plan where appropriate.
Linked to challenges in communicating recommendations in the ReSPECT plan is the challenge of using these recommendations in an acute or emergency situation. Stakeholders emphasised that ReSPECT recommendations are not legally binding and are there to guide healthcare professionals who make a decision in a specific situation. They emphasised that it was important that care home staff and healthcare professionals were made aware of this during training. However, ReSPECT recommendations appear to face two contrasting challenges in their use. In an emergency, relatives, care home staff and healthcare professionals may revert to the instinct to do something and may make a decision that is inconsistent with a ReSPECT recommendation; for example, to send a person to hospital when the recommendation is to be managed at home. Alternatively, delegates described the risk of a ReSPECT recommendation being followed without considering the nuance of the situation; for example, not conveying a patient to hospital because the recommendation not for admission does not specify in what circumstances admission might be appropriate. They expressed concern that having a ReSPECT plan might result in the person being seen as lower priority for a visit from a doctor or paramedic because the assumption is that they do not need an urgent decision about treatment.
Key messages/recommendations
-
There is misunderstanding about the nature and authority of ReSPECT recommendations. Public and patient information and health and social care professional training need to emphasise that they are guidance for decision-makers and are not legally binding.
-
Recommendations should be clear and use language that the person, their family and treating clinicians can understand.
-
Recommendations should be specific to anticipated situations but allow flexibility to encompass other scenarios and include options for treatment as well as the limitations of treatment.
-
Justification for the recommendations should be clearly documented in the plan to support decision-makers and to enable patients and their family to understand and challenge where necessary.
Managing the plan
Delegates identified issues regarding management of the ReSPECT plan once it had been completed. A key concern was related to validity and control of the form itself. The general view was that ideally the form should be in electronic format within a digitised system where it would be accessible to anyone who needed to see it, including the patient (or the patient’s next of kin if the patient lacked capacity), health and social care staff involved in the person’s routine care and emergency care staff. Identified disadvantages of a paper copy were that it might not be accessible or known about in an emergency. Similarly, if the paper version was thought to be a copy and not the original form (because, e.g. it had been printed in the wrong colour), it would not be considered valid. There was also a concern that if the original form was completed electronically and stored in the GP record and a paper copy was given to the person, there was a risk of multiple versions existing, which again could raise questions about a form’s validity. However, some delegates questioned how people who did not have access to digital technology would be able to have control over, or knowledge of, their plan. Thus, the tension between benefit to the health system of a digitised system and the autonomy of individuals who have a plan needs to be considered in developing such a system. There was strong agreement among delegates that ReSPECT plans should be reviewed as a person’s health status changed, noting that a person’s preferences, and the treatment options available to them, may change over time or because of a new diagnosis. Some people suggested a regular review for example at an annual health check might be helpful. Noting the difference in recommendations on a ReSPECT plan completed in hospital during an acute illness episode and one completed in primary care, it was seen as essential that plans were reviewed prior to hospital discharge.
Key messages/recommendations
-
An electronic record held within a digitised system accessible by relevant health and social care professionals and the person or their next of kin should be the preferred model to ensure validity and appropriate use of the plan.
-
However, it is necessary to consider how people who cannot access digital technology will have access to and control of their ReSPECT plan.
-
A robust system of ReSPECT Plan review should be in place that is responsive to changes in a person’s clinical need and preferences.
-
In the absence of a central digitised system for managing forms, a process for ensuring form validity (version control) needs to be put in place.
Training
Stakeholders discussed a wide range of training needs for different groups. Acknowledging that many different people could have preliminary conversations about the ReSPECT process and the idea of an ECTP with someone, it was widely agreed that some training was required for any health and social care professional, and support workers, to give them the knowledge and confidence to initiate a discussion or respond to questions about ReSPECT. More specific training needs were identified for healthcare professionals involved in completing ReSPECT plans with people and the conversation that accompanies this process. A further area of training need related to the use of ReSPECT plans and interpretation of their recommendations. Education in the use of ReSPECT plans may be relevant for healthcare professionals but also for social care staff (care home and home care).
Key elements of training identified include the following (although not all will be relevant for everyone involved in the process, and the detail of the training content will vary between groups):
-
Understanding how ReSPECT fits with ACP, advance decisions to refuse treatment, and lasting power of attorney.
-
Understanding the purpose of ReSPECT recommendations and their legal status.
-
Assessment of capacity, how to accommodate fluctuating capacity, and how to include a person who lacks capacity in the conversation.
-
Training in having these conversations, which are different from other types of conversation that a healthcare professional may be more familiar with. Specific focus on having conversations with people with a learning disability.
-
Training in interpreting recommendations including assessment of their relevance to the situation (e.g. a plan completed in hospital when the person is acutely sick may not be relevant when they have recovered and returned home).
Delegates also discussed how training might be delivered, and again noted that a range of approaches might be required to reflect the needs of different groups. Suggestions included:
-
E-learning module for healthcare professionals with continuing professional development accreditation.
-
Integrating training on ReSPECT into RCUK’s advanced life support training sessions.
-
Identification of champions in GP practices/care homes who can support and advise other members of staff to embed the process into day-to-day practice.
-
Using Extension for Community Health Outcomes communities of practice to share education and practice across different groups for example care homes and other social care organisations, learning disability liaison nurses.
-
Link ReSPECT training to other training resources for example Daffodil Standards training for end-of-life care.
-
Make use of available training resources such as those provided on the RCUK website. It was noted that these are infrequently used so we need to explore the barriers to their use.
Key messages/recommendations
-
There is a need for training around the whole ReSPECT process from preparatory discussions through to use of the form in an emergency.
-
Training content and format should be tailored to the needs of the different groups who may be involved in the ReSPECT process.
-
Better use should be made of existing information resources.
Raising awareness and preparing for conversations
There was general consensus that there should be initiatives to raise public awareness of ReSPECT and ECTPs more widely. Stakeholders thought this would prompt some people to initiate a conversation about their own ReSPECT plan but could also prepare people for the conversation if initiated by a healthcare professional. A range of suggestions were made on how to do this, including enlisting the support of voluntary organisations to communicate to their members; including it in information about other end of life planning such as making a will, developing video narratives that include ReSPECT and including it in popular media programmes.
However, there were also several concerns raised about the potential risks of a strategy to raise public awareness. There was a concern that increased awareness might lead to increased pressure on GPs, as people sought more information or requested a consultation to make a ReSPECT plan. Suggestions to mitigate this included directing people to an online information resource as part of the public awareness campaign. Perhaps a greater challenge that delegates identified was the risk of ReSPECT or ECTPs in general being conflated with ACPs and therefore associated specifically with end-of-life diagnoses and care. Stakeholders noted the opportunities for including ReSPECT awareness raising in public awareness campaigns and conversations about ACP. They saw these opportunities as positive, but also emphasised that it was important to raise awareness of emergency care treatment planning in situations distinct from ACP. Given the challenges, they suggested that any public messaging should be managed by a national ReSPECT lead while being delivered at a grass roots level.
Stakeholders also emphasised the importance of developing trust among the general population as a prerequisite to engaging people in a dialogue about ReSPECT and emergency care treatment planning. Some noted that trust in the NHS generally had been eroded in recent years, and particularly in relation to emergency care treatment decisions during the COVID-19 pandemic. This was particularly relevant for certain groups, for example people with a learning disability, and other underserved populations. One way to improve trust in the process of emergency care treatment planning would be to spend time working with people to introduce them to the concept of ReSPECT, taking care to use language and resources that are tailored to their needs, experiences, and culture. Examples were suggested of using videos to explain and inform people about ReSPECT but also as an option for them to record their values and preferences prior to the ReSPECT-focused conversation with a healthcare professional. Stakeholders with experience of working with people with learning disabilities commented that this approach worked well in other situations where it was important for people to communicate their wishes and life experiences to healthcare professionals, for example, hospital passports for people with a learning disability. Engaging voluntary sector organisations in having these conversations with people in the community prior to any formal ReSPECT conversation was seen as important for facilitating trust and understanding. Stakeholders, however, also noted that these initiatives require resources (both financial and in terms of people) and we have to be realistic about what is achievable in the current resource constrained environment.
Key messages/recommendations
-
People need time, information and support to be able to think about emergency care treatment planning in advance of creating the plan.
-
Public awareness campaigns can be helpful but there are risks that there may be misunderstanding particularly around how ECTPs fit with wider ACP conversations.
-
The impact of a public awareness campaign on increased demand for GPs to have ReSPECT conversations needs to be considered.
-
Supported conversations in the community can help to prepare people for emergency care treatment planning and alternative formats for communication need to be available.
-
Any initiative needs to be achievable within the available resources.
List of abbreviations
- ACP
- advance care plan
- BSA
- British Social Attitudes
- CAG
- Confidentiality Advisory Group
- CCG
- Clinical Commissioning Group
- CPR
- cardiopulmonary resuscitation
- CRN
- Clinical Research Network
- DNACPR
- do not attempt cardiopulmonary resuscitation
- DSPT
- Digital Data Security and Protection
- ECTP
- emergency care treatment plan
- ENRICH
- Enabling Research in Care Homes
- GP
- general practitioner
- HRA
- Health Research Authority
- NPT
- normalisation process theory
- POLST
- physician orders for life-sustaining treatment
- PPI
- patient and public involvement
- RCUK
- Resuscitation Council United Kingdom
- ReSPECT
- Recommended Summary Plan for Emergency Care and Treatment
- SNOOP
- Special Needs Outreach Project
- WP
- work package
Notes
-
Health Research Authority application for Research Ethics and Confidentiality Group Approvals, with amendment table
-
Easy read information sheets and consent forms, learning disability work package
-
Flowchart of reference group and workshop meetings, learning disability work package
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/NVTF7521).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
