Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR131606. The contractual start date was in October 2021. The draft manuscript began editorial review in April 2023 and was accepted for publication in December 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Aunger et al. This work was produced by Aunger et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Aunger et al.
Chapter 1 Introduction
Some text in Chapters 1 and 2 has been reproduced with permission from Maben et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In 2019, we sought funding to better understand the unprofessional behaviours (UB) of healthcare staff towards each other; it is important to note the broader context in which this work took place. 1 While we knew there was a problem, the extent was not yet prevalent in public discourse and in the mainstream media. In 2023, as we write, this has significantly changed. Multiple investigations have revealed that UB appears rife in many public-sector workplaces. The Casey report revealed misogyny, racism and homophobia in the Metropolitan Police,2 a parliamentary report in 2021 found that two-thirds of women in the armed forces have experienced bullying, sexual harassment and discrimination during their career,3 and the Fire and Rescue Inspectorate has found that every fire brigade in England is plagued by bullying and harassment claims. 4 During our study, society has also started to pay greater attention to misogyny and racism. The #MeToo and #BLM movements have become global rallying cries to change societies throughout the world.
| Stakeholder feedback summary – capturing wider context |
| Stakeholders highlighted ongoing societal contexts throughout our review, including #BLM, #MeToo and the bullying and harassment scandals occurring at the highest levels of UK government. These can normalise bullying and harassment and fail to set a good example for healthcare organisations implementing initiatives to address UB.5 While identified literature for our review did not refer to these societal shifts, we have sought to place our review within this broader societal and historical context, as noted above. |
| We ran a specific stakeholder spotlight session that helped us hone our language when discussing staff with protected characteristics throughout this review. This session highlighted that different people prefer different terms: there was no single consensus. Some people found the use of the term ethnic minorities problematic, whereas others found the term ‘minoritised groups’ problematic. As a result, we are as specific as possible when we are referring to particular groups throughout this report. |
Healthcare organisations have also been under significant scrutiny during this period: a series of reports have highlighted the prevalence of staff-on-staff UB, creating cultures that do not allow staff to thrive at work. The Ockendon report into maternity services at the Shrewsbury and Telford Hospital NHS Trust6 found a culture of bullying and lack of psychological safety in the workplace. The Kirkup report7 – also into maternity services, this time at East Kent hospitals – found ‘unprofessional behaviours by some consultant obstetricians were not tackled’ and that ‘bullying, harassment, and discrimination were endemic at East Kent’, with the culture described as ‘“horrible” and “sickening”’. The systems that might have supported psychological safety, enabling staff to voice concerns, were weak or absent. Staff feared retaliation yet were ‘perversely blamed for their lack of courage’. 7 In 2023, Professor Bewick’s investigation into the clinical safety at University Hospitals Birmingham NHS Foundation Trust8 ‘heard repeated reports of a longstanding “bullying and toxic” environment’ (p. 10) with negative impacts on patient care.
We have used the term UB to encompass a range of specific behaviours such as incivility, transgressions, disruptive behaviour, physical and verbal aggression and bullying. 9,10 According to one definition, UBs cover a wide spectrum of behaviours that can subtly interfere with team functioning, such as poor communication, passive aggression, lack of responsiveness, public criticism of colleagues and humour at others’ expense. These behaviours can be either casual and generalised or highly targeted with the intention to cause harm. In modern, inclusive healthcare settings, UBs are increasingly recognised as unacceptable because they negatively affect the work and psychological well-being of others. 11
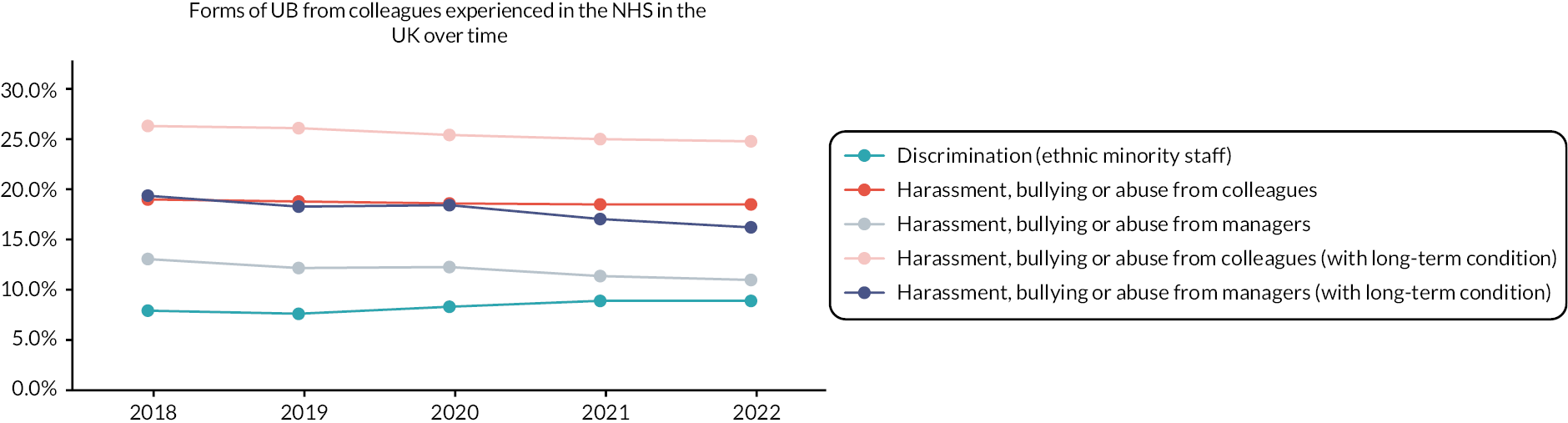
As the reports above suggest, UB – and specifically bullying and harassment – is, unfortunately, still prevalent in the United Kingdom’s (UK) National Health Service (NHS). Figures from the 2022 NHS Staff Survey indicate that 18.7% of staff experienced harassment, bullying or abuse from colleagues that year while 11.1% experienced the same from managers. Additionally, 9% of staff from ethnic minority backgrounds reported experiencing discrimination at work from managers or colleagues. According to Workforce Race Equality Standard data from 2022, the percentage of staff experiencing harassment, bullying or abuse from colleagues in the NHS was 22.5% for white respondents and 27.6% for ethnic minority respondents. The difference was much starker in corresponding groups at management levels, with 6.8% for white staff yet 17.0% for ethnic minority staff. 12 For those with a long-term health condition or illness, data show another significant increase in reports of UB compared to those without (Figure 1).
FIGURE 1.
Forms of UB from colleagues experienced in the NHS in the UK over time. Data adapted from NHS Staff Surveys 2018–22. 16
Unprofessional behaviours are not just present in the UK: they are a widespread problem in healthcare systems around the world and have negative impacts on the psychological well-being of staff, patient safety and organisational costs. 13,14 Data from Australia across seven hospitals indicate that the problem is widespread, with 38.8% of 5178 respondents reporting experiencing UB on a frequent (weekly or more) basis during the past year and with 14.5% even experiencing extreme events such as physical assault. 15 Therefore, this study is unfortunately very timely; there is still much work to be done to mitigate, manage and prevent this global and pressing issue.
Unprofessional behaviour can negatively impact people targeted by it, as well as witnesses, patients, organisations in which it occurs and, by extension, society. 17–19 For targets and witnesses of UB, it can lead to mental problems such as burnout and depression and, in extreme cases, can lead to suicidal ideation. 20 Physical problems such as sleep disturbance, headaches and gastrointestinal symptoms are also common and both these physical and mental consequences can result in staff taking sick leave. 21 This results in organisations experiencing elevated staff turnover, which can have large economic consequences. 22 For patients, studies have shown that the presence of UB can lead to staff being less likely to follow safety procedures23 and more prone to making errors and being distracted. 14,24 Furthermore, patients whose surgeons behave more unprofessionally have been found to have worse outcomes. 25 A conservative estimate of the cost of UB to the NHS (due to sickness absence, employee turnover, reduced productivity, compensation and litigation costs) suggests damages from bullying alone were approximately £2.28 billion per annum or 1.52% of the NHS budget for 2019/20. 1,26 In the United States of America (USA), sources report the cost of replacing each nurse at between $2200 and $64,000 (USD). 27
The global COVID-19 pandemic and resulting healthcare workforce crisis has made the retention of healthcare staff critical in most healthcare systems. Tackling UB – a problem that contributes to staff turnover and losses of organisational reputation – could go some way to helping address workforce recruitment and retention. 7 Bullying and harassment have been cited as one of the primary reasons that NHS staff are quitting for other opportunities, with a recent report suggesting 49% of healthcare staff who have experienced UB are seeking another job as soon as possible. 28,29
Previous studies have sought to collate and understand interventions to reduce UB both within21 and outside of health care. 30 However, either these have focused on bullying alone21 or their applicability to acute healthcare settings may be limited. 31 Existing contributions to the literature have noted that interventions to reduce UB in general ‘are underpinned by the assumption that workplace mistreatment will be lessened if more people know about it, know how to recognise it and be more assertive in their responses to it. This is a flawed assumption’. 31 Whether this ‘flawed’ approach is also dominant in health care is important to investigate, in order to improve future intervention efficacy.
A realist approach is ideal for investigating causes of UB in health care and interventions to reduce them because interventions in this area are heterogeneous, not well articulated, and complex in nature. This study builds directly on previous work, including the 2013 National Institute for Health and Care Research (NIHR) Illing et al. review21 to address the following aims and objectives.
Review aims and objectives
Our focus is on interpersonal (i.e. directed toward others or occurs in the presence of others32) UBs that are intended to cause harm between staff (not staff towards patients or vice versa).
Aim
To improve context-specific understanding of how, why and in what circumstances UBs between staff in acute healthcare settings occur and evidence of strategies implemented to mitigate, manage and prevent them.
Objectives
This review seeks to:
-
conceptualise and refine terminology: by mapping behaviours defined as unprofessional to understand differences and similarities between terms referring to UBs (e.g. incivility, bullying, microaggressions, etc.) and how these terms are used by different professional groups in acute healthcare settings;
-
develop and refine context, mechanism and outcome configurations (CMOCs): to understand the causes and contexts of UBs, the mechanisms that trigger different behaviours, and the outcomes on staff, patients and wider system of health care;
-
identify strategies designed to mitigate, manage and prevent UBs and explore how, why and in what circumstances these work and whom they benefit;
-
produce recommendations and comprehensive resources that support the tailoring, implementation, monitoring and evaluation of contextually sensitive strategies to tackle UBs and their impacts.
Chapter 2 Methodology
Rationale for and use of realist methods
This study uses realist review methodology. Realist reviews are driven by theories that seek to explain how and why certain strategies may or may not work in different contexts. 33 They focus on understanding the mechanisms by which strategies do or do not work, and seek to understand contextual influences on if, why, how and for whom these might work. In a realist framework, contexts can be either observable features that can facilitate or hinder an intervention or they can be dynamic and relational factors that shape the mechanisms through which an intervention operates. 34 Mechanisms, in turn, are seen as changes in participants’ reasoning in response to the resources introduced by the intervention. 35 These contexts, mechanisms and outcomes are combined into programme theories (i.e. a mapping of taken-for-granted assumptions) represented by a heuristic known as a CMOC to depict what is expected to happen when an intervention is delivered in a certain contextual environment. 36 The revised Medical Research Council (MRC) Complex Interventions Framework identified the important role of theory-based research perspectives such as realism within the iterative development, feasibility, evaluation and implementation phases of action-oriented research to address practice and policy issues. 37
Adopting a realist approach enables an examination of the mechanisms underlying both the UBs and the interventions designed to address them, which is particularly useful when context is likely to influence the effectiveness (or otherwise) of an intervention. This allows for the identification of direct links between the interventions and the environmental factors that contribute to, for example, UBs. In realist reviews, included evidence spans beyond academic literature to non-empirical studies, commentaries and grey literature from government and voluntary organisations. This illuminates the topic from multiple viewpoints, making it valuable for studying complex issues such as UBs in that it enables a more comprehensive understanding of the problem and its potential solutions.
The realist approach to data collection and analysis is based on retroduction – a form of logical inference beginning with empirical observations and seeking to explain them by identifying the underlying mechanisms that are capable of producing them. 38 This approach is indispensable when considering UBs within the healthcare workforce as it allows, for example, the examination of differences and similarities between staff groups based on factors such as speciality, professional group, setting and seniority. By examining these contextual factors and working practices using realist review methodology, it is possible to determine how context might influence the presence of UBs among healthcare staff working in acute settings.
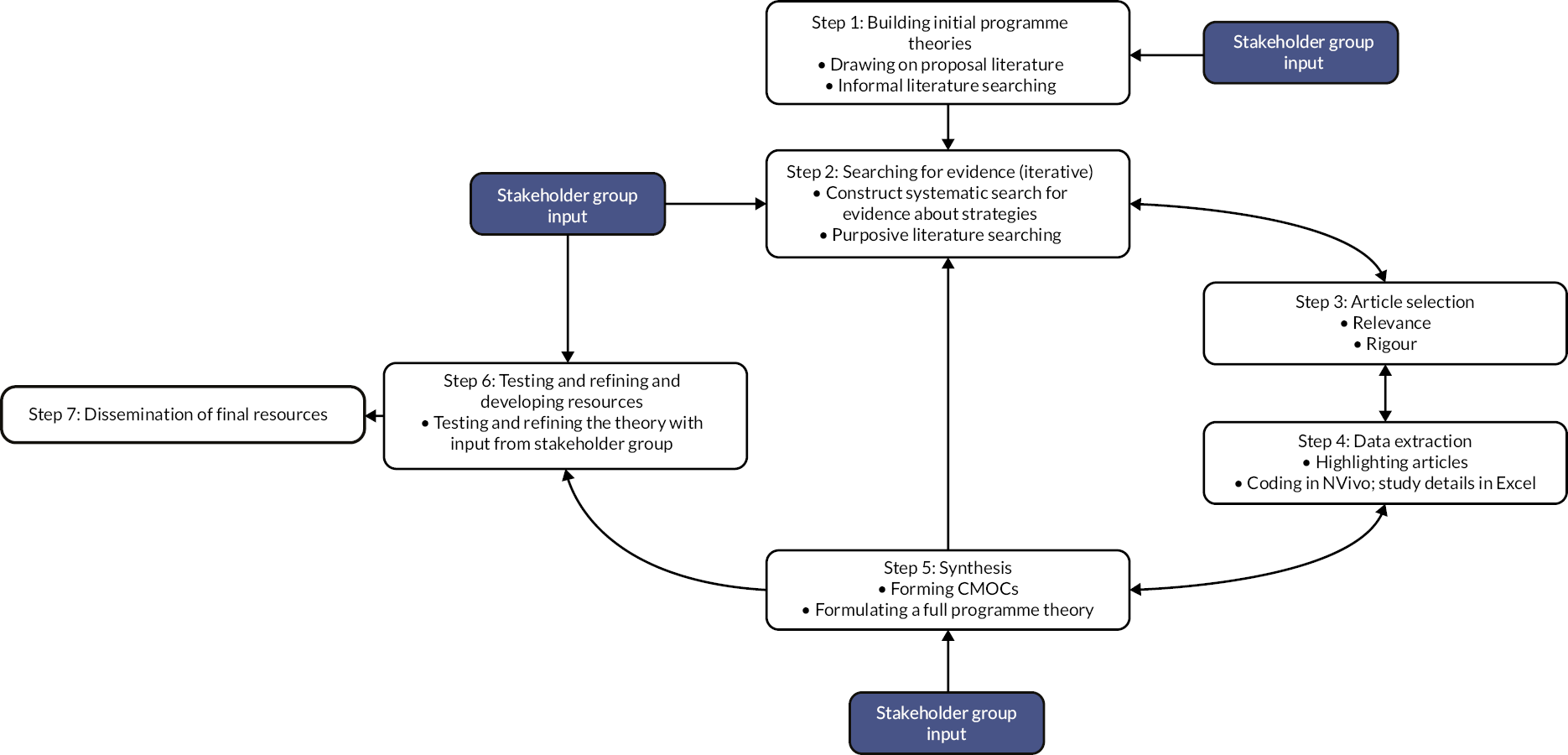
This review and report followed the Realist And MEta-narrative Evidence Syntheses: Evolving Standards (RAMESES) guidelines on quality and reporting. 39 The RAMESES checklist is reported in Report Supplementary Material 1. There have been no further protocol changes since NIHR protocol version 4.0_120822. An overview of the review process is shown in Figure 2, with the steps we took to achieve our objectives explained in the following sections.
FIGURE 2.
Review process flow diagram.
Step 1: Identifying existing theories and scoping the literature
Initial informal screening of the literature sensitised the team to the breadth and depth of published and unpublished literature on UBs within health care. By investigating the theoretical underpinnings of interventions, we mapped the conceptual and theoretical landscapes of UB causes and outcomes, as well as how any identified strategies and interventions are theorised to work in acute healthcare settings. This step helped identify the mechanisms at individual, group and professional levels by which strategies prevent or reduce the impact of these behaviours across and within healthcare staff groups. This process (of identifying existing theories) informed the construction of our initial programme theories. To do this, we iteratively:
-
drew on preliminary discussions within the project team, with the healthcare workforce, patients and the public
-
consulted with our multidisciplinary stakeholder and advisory groups (as outlined above)
-
examined healthcare literature known to the research team (papers, reviews and reports identified in our initial scoping review that informed the funding proposal were independently screened by JAA and RA)
-
sought additional literature to form theories across strategies and causes. Informal searches were conducted on relevant websites [e.g. The King’s Fund, NHS Employers, NHS England, the British Medical Association (BMA) and Health and Care Professions Council (HCPC)] from 19 October 2021 to 11 November 2021; search terms included ‘Bullying’, ‘Unprofessional’, ‘Incivility’, ‘Violence’ and ‘Harassment’, using built-in filters where possible to limit search results to relevant topics such as bullying, gender equality, lesbian, gay, bisexual, transgender, queer, intersex, asexual and more (LGBTQ+) and whistleblowing.
Data from this step were imported and coded into NVivo 12 (QSR International, Warrington, UK). In this early phase, we were interested in identifying how contributing factors lead to UB, as well as how strategies work in different contexts. As part of this process, we developed ‘if, then, because’ statements, as well as a visual map/typology. These documents were then discussed by team members and presented to stakeholders for refinement. This step also helped to identify directions for future analysis, with further literature searches in step 2. Our initial programme theories for different portions of the analysis are presented in Appendix 1, Tables 22–24.
Step 2: Searching for evidence
Of the three realist synthesis search models identified by Booth et al., our approach follows the ‘Exclusive (Realist-only) searches’ model. 40 Therefore, step 2 was the formal stage at which we undertook systematic searches for evidence.
Search strategy
In step 2, we identified studies addressing strategies to reduce UBs among staff in acute healthcare settings by:
-
Systematically searching academic databases Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOhost), EMBASE Classic + EMBASE (Ovid) 1947 to 11 February 2022, and Ovid MEDLINE(R) ALL 1946 to 11 February 2022 on 14 and 15 February 2022. Search strategies comprised search terms, synonyms and index terms for: Acute care AND Healthcare staff AND UBs. Searches from existing similar reviews such as Illing et al. (2013) were consulted to aid identifying relevant search terms. 41 The National Institute for Health and Care Excellence (NICE) OECD geographic search filters were used in MEDLINE and EMBASE to exclude studies based in non-OECD countries since these were deemed not relevant to the UK NHS acute care setting and UK workplace culture. 42 The OECD filter was adapted for use in CINAHL. Limits for language and publication date were not used; however, animal, child and elder abuse studies were removed from the search.
-
Conducting similar searches for trade, policy and grey literature on Google Scholar (via Harzing’s Publish or Perish software), Google, HMIC (Health Management Information Consortium) (Ovid) 1979 to November 2021, NICE Evidence Search (www.evidence.nhs.uk/), Patient Safety Network (https://psnet.ahrq.gov/) and websites, including NHS Employers and NHS Health Education England.
See Report Supplementary Material 2 for the full search strategies used across these databases and grey literature sources. The range of databases and sources was chosen to identify relevant health research and policy reports in peer-reviewed journals, trade journals and organisation reports. For example, we sourced opinion pieces likely to discuss how and why UB interventions work in trade journals (e.g. AACN Bold Voices, Nursing Times, ED Management) via CINAHL and HMIC databases. Search strategies were peer-reviewed using the Peer Review of Electronic Search Strategies method. 43 All search results were saved in EndNote X9 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] software and duplicates removed using University of Leeds Academic Unit of Health Economics (AUHE) guidance. 44
Step 3: Selection and appraisal of documents
Inclusion and exclusion criteria
We included peer-reviewed and grey literature that helped explain how and why strategies to reduce UBs in acute care settings work and whom they benefit. The inclusion criteria shown in Table 1 were used. 1
| Category | Criterion |
|---|---|
| Study design | Any (including non-empirical papers/reports) |
| Study setting | Acute healthcare settings – acute, critical, emergency and, potentially wider (see relevance criteria below) |
| Types of UB | All as exhibited and experienced by healthcare staff (not patients nor patient-to-staff) |
| Types of participants | Employed staff groups including students on placements |
| Types of interventions/strategies | Individual, team, organisational and policy-level interventions. Cyber-bullying and other forms of online staff-to-staff UB |
| Causes of UBs | All |
| Outcomes | Included but not limited to a focus on one or more of: staff well-being (stress, burnout, resilience), staff turnover, absenteeism, malpractice claims, patient complaints, magnet hospital/recruitment, patient safety (avoidable harm, errors, speaking-up rates, safety incidents, improved listening/response), cost |
| Language | English only |
Screening, relevancy and rigour
Screening of search results was primarily undertaken by JAA, but RA independently screened a 10% random sub-sample for quality control at title and abstract, full text and relevancy stages. An additional 50% of November 2021 Google Scholar searches were double-screened. Any disagreements were resolved by discussion between JA, RA and JM (see below). The remaining 90% of decisions at these stages were made by JAA. Title and abstract screening was performed using Rayyan.ai software (www.rayyan.ai/) and full texts were screened using Mendeley (Mendeley Ltd.). 45
Decisions regarding sources were based on the inclusion and exclusion criteria (above) and a combination of relevance (based on both the major/minor criteria below and the ability to inform programme theories, i.e. conceptual richness and depth of sources) and rigour (whether the methods used to generate the relevant data are credible and trustworthy). Assessment of rigour focused on the extent to which sources provided a detailed description of their methods and how generalisable and trustworthy their findings were based on those methods. 36
Our formal criteria for classifying the potential relevancy of sources included assessing for:
-
major contribution for sources that:
-
contributed to the study aims and are conducted in an NHS context in acute care; or
-
contributed to the study aims and are conducted in an NHS context; or
-
contributed to the study aims and are conducted in contexts with similarities to the NHS (e.g. universal, publicly funded healthcare systems); and
-
-
minor contribution for sources that:
-
were conducted in non-UK healthcare systems that are markedly different from the NHS (e.g. fee-for-service, private insurance scheme systems) but where the mechanisms causing or moderating UBs could plausibly operate in the context of those working in the NHS; or
-
contributed to the study aims and can clearly help to identify mechanisms that could plausibly operate in the context of the NHS (e.g. law, police, military).
-
We prioritised the sources of major relevance in relation to the above criteria. The criteria that are italicised reflect those criteria we adopted in our final review. We did not seek studies beyond health care because we reached theoretical saturation. These sources were then sorted into the above categories and assessed for their ability to inform the refinement of programme theories (theoretical relevancy and conceptual richness). Where a scarcity of ‘major contribution’ sources meant that we were unable to develop and refine aspects of the programme theory, we drew on literature from the minor relevancy criteria. In addition, we also classified documents according to their conceptual richness (thickness vs. thinness) using adapted criteria from Pearson et al. 46 These criteria reflected the usefulness of each document to the realist analysis so that we could judiciously draw on a wide range of sources in a timely manner.
The criteria for appraising conceptual richness are defined in Table 2, with examples.
| Element | Conceptually thick | Conceptually thin |
|---|---|---|
| Description | Possessing rich description of how causes of UB may increase UB or how strategies to reduce UB may work | Little or no useful description of how causes of UB or strategies to reduce UB work |
| Context | Consideration of context in which UB develops/intervention is implemented | Little or no description of context |
| Implementation | Description of how implementation of strategies deviated from expectations or presenting multiple theories for how causes may lead to UB | No description of how implementation of strategies deviated from expectations. Limited, single, surface-level explanation for how causes may lead to UB |
| Qualitative vs. quantitative | Exploration of the qualitative aspects of phenomena | Limited description, focus on quantitative aspects, for example associations between variables, prevalence of UB, etc., without further detail on the how or why |
| Example extract and explanation | ‘For example, it is now noted that some methods of delivering interventions to staff may induce feelings of being “targeted”, “at fault” and perhaps being bullied themselves, if content is “aimed” at certain negative behaviours, say “anger management”, or staff groups, say “the doctors”’.47 This example is rich because it provides evidence regarding in what context an intervention may have unintended consequences |
‘The Joint Commission’s Sentinel Event Alert outlined the need for institutions to develop the following educational programme to address bullying in the nursing workforce: (a) skills-based training and coaching; (b) ongoing, nonconfrontational surveillance; (c) a system for assessing staff perceptions of the seriousness and extent of unprofessional behaviors; and (d) policies that support early reporting’.48 This example is thin because it simply lists the content of a proposed intervention without any explanation as to how it may work |
Results of searching and screening
The following results are in chronological order and reflect multiple cycles of searches, screening and relevance/rigour assessments. Figure 3, however, displays the process of searching, screening and inclusion in a non-chronological order, that is, all cycles of search results are incorporated with the initial search results in the diagram. This demonstrates more clearly how many studies were found, included and excluded, at Step 1 versus Step 2 of the review.
FIGURE 3.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) style diagram outlining our search processes and results.
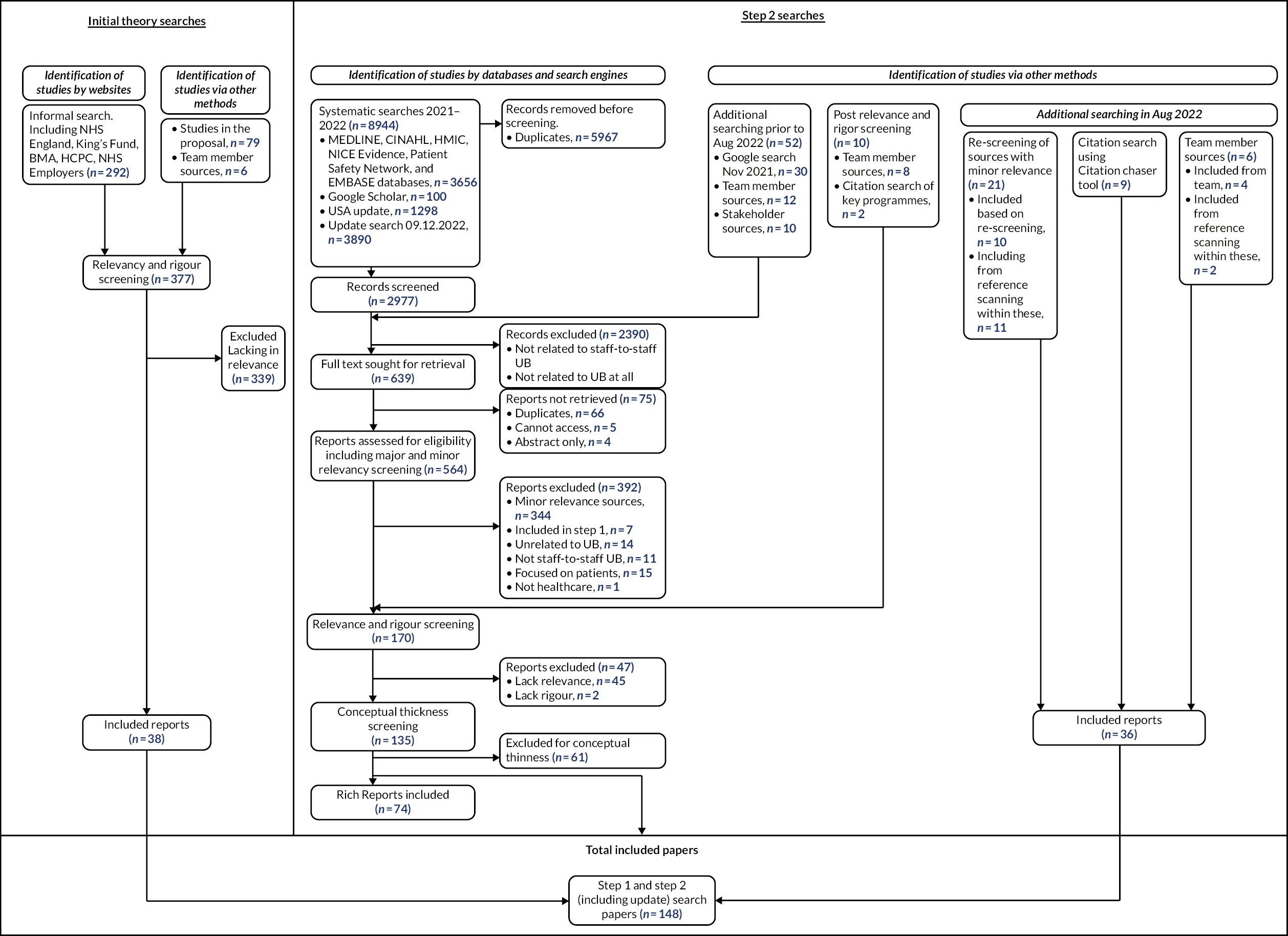
Step 1 (November 2021): Identifying existing theories and scoping the literature
We included 38 documents in the initial theory-generation step, comprising 30 identified from the proposal, five from informal searches and three from the team.
Step 2 (November 2021–February 2022): Searching for evidence
The initial systematic search identified 2629 records after 99 Google Scholar search results after cross-database deduplication. Initial independent pilot screening of 54 (of 2629) records resulted in 16 papers included for full-text screening with 100% agreement. Independent screening by two reviewers (JAA and RA) of 267 (10% of 2629) records led to 72 being included for the next step. Disagreement occurred on 40 items (15%) and was resolved through discussion between JAA and RA. The remaining 2308 papers were screened by JAA against the inclusion/exclusion criteria: of these, 400 papers were selected for full-text screening.
Google and Google Scholar searches (November 2021)
Two searches were performed on Google Scholar via use of Harzing’s Publish or Perish software (each was limited to the 50 most relevant results). This was to ensure we captured relevant grey or academic literature identified by Google’s algorithms. Search strategies are presented in Report Supplementary Material 2. After duplicate removal, 99 papers remained for title and abstract screening. Papers were excluded largely because they were not related to UBs between staff (Figure 4). Sixty-three papers were selected for full-text screening and then combined with the systematic search results at the full-text screening stage. An additional 52 sources were identified through searches on Google (30) in 2021, from the project team (12) and from stakeholders (10) during 2022 (see Additional searching). In total, 603 papers were selected for full-text screening. After cross-deduplication of these various sources of literature, 537 full-text papers were eligible for screening.
FIGURE 4.
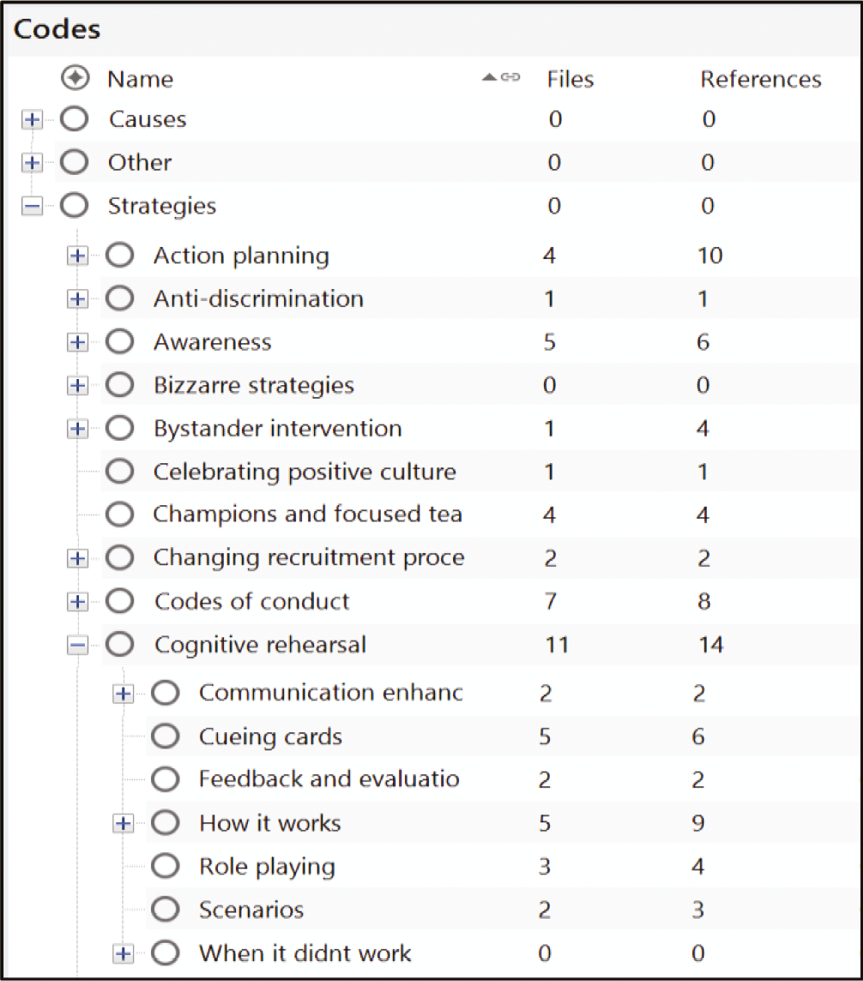
Example NVivo 12 coding structure for strategies.
Full-text screening
Following application of major/minor screening criteria to the 537 potentially relevant papers, 193 papers were determined to have major relevance and 352 were excluded for having minor relevance. In addition, 34 (10%) of those papers excluded at this stage were selected for independent screening (JAA and RA). From these, two decisions were found to be in conflict. These two discrepancies were resolved through discussion and remained excluded. The 193 papers were then screened against inclusion criteria and conceptual richness and 148 papers were included.
Relevance and rigour
The remaining 148 papers were screened for relevance according to the realist method, meaning papers had to include passages suitable for theory gleaning, testing or refining with respect to either causes or strategies. 49 Studies that lacked such passages were, therefore, screened out (n = 45), resulting in 103 papers. An additional six studies from the team and two studies from citation-tracking key intervention papers were added at this stage; thus, 111 documents were included for conceptual-thickness screening.
Conceptual-thickness screening
As a result of conceptual-thickness screening as outlined in Table 2, 47 sources were excluded at this stage for lacking conceptual thickness. This meant that 64 rich sources were included at this stage.
Additional searching and evidence gathering (August–November 2022)
Search update to expand relevancy criteria to US intervention studies (August 2022)
The team decided to include US-based literature because we wanted to include wider interventional literature, and exploratory searches indicated a significant amount of literature available from the USA. We reran the same searches for Step 2 but limited results to the USA (excluding HMIC due to its predominance of UK content, and NHS Evidence, which was withdrawn in April 2022). This identified 1298 records, which reduced to 57 once duplicates and previously screened records were removed. These 57 records were screened but none were included because no interventions were identified. However, we did re-include 10 USA studies from our Step 2 search, which had previously been excluded due to country.
A further nine relevant studies were identified by citation searching (forwards and backwards) from nine key further US studies using the CitationChaser Shiny App. 50 Four studies were identified by the team. Reference scanning of the 10 included US studies and the four identified by the team found a further eleven and two, resulting in a total of 36 additional papers from August 2022 searches. A total of 138 papers were included (Steps 1 and 2) prior to final update searches.
Searches for behavioural and organisational psychology theories (November 2022)
Members of the advisory group indicated that literature from behavioural or organisational psychology may provide useful evidence, so we searched for anti-bullying interventions that use behavioural science theory in ABI/INFORM® Collection (ProQuest, Ann Arbor, MI, USA), Business Source Premier [EBSCOhost (Elton B. Stephens Company)] and Google Scholar. The lack of relevant search results prompted a further search [in ABI/INFORM Collection (ProQuest) and Google Scholar]. Due to low relevance of results during screening, papers found in this search were not utilised.
Search update (December 2022)
The above searches were repeated on 9 December 2022 (except for NICE Evidence, which was withdrawn in April 2022) to ensure our review remained up to date. The search strategies were reviewed before running the final update searches and no changes made. This identified 3890 records, which reduced to 192 records when we removed duplicates and previously identified records. After title and abstract screening, 36 papers were retained for full-text screening. Included from this update were eight papers and an additional two studies from the team (10 in total).
Total included literature (March 2023)
One hundred and forty-eight total papers were included. This included 38 papers from Step 1, 100 papers from Step 2, and 10 from our updated December 2022 search. Full search results are depicted in Figure 3.
Step 4: Data extraction
To aid in data extraction, sources were first categorised in Mendeley according to country and healthcare setting (e.g. acute care) and whether they described an intervention. To further organise our data, relevant sections of texts were coded and organised in NVivo 12 software (QSR International) (see Figure 4). This coding was both inductive (codes created to categorise data reported in included sources) and deductive (codes created in advance of data extraction and analysis as informed by the initial programme theory). Each new element of relevant data was used to test and refine aspects of the programme theory. A realist review aims to reach theoretical saturation in relation to the objectives, rather than to aggregate every relevant study.
Descriptive study information was extracted into an Excel spreadsheet. Sources reporting on interventions were explored in greater depth with samples, duration of interventions, behaviour-change strategies used, study design, theoretical frameworks, outcome measures and findings extracted and tabulated for each study.
Step 5: Synthesising evidence, refining initial theories and drawing conclusions
Realist analysis
During the review, we moved iteratively between analysis of examples from the literature, refinement of programme theory and further iterative searching to test particular programme theories as required (see Figure 2). We also used the strategies listed in Table 3 to make sense of the data. 46,51 This type of analysis enabled us to understand how the most relevant and important mechanisms work in different contexts, allowing us to build more transferable CMOCs.
| Strategies for synthesising evidence |
|---|
| Comparing and contrasting sources of evidence: e.g. where evidence about interventions or its mechanisms in one source allowed insights into evidence about outcomes in another paper |
| Reconciling of sources of evidence: where results differed in apparently similar circumstances, further investigation to find explanations as to why these different results occurred |
| Adjudication of sources of evidence: made the synthesis more manageable, i.e. dividing papers that make ‘major’ or ‘minor’ contributions to our research questions46 |
| Consolidation of sources of evidence: where outcomes differed in particular contexts, an explanation was constructed as to how and why these outcomes occurred differently |
These strategies found in Table 3 were also drawn upon in the theory-refinement process. In this process, we compared initial theories with novel data from Step 2 literature. Novel data were compared with initial theories to see if they affirmed, refuted or altered the existing initial theory and, in these cases, the above comparison strategies were drawn upon to make a decision regarding how theories were to be refined. Where novel data leading to candidate theories were identified that did not match with any initial theory from Step 1, we formulated novel theories and tested them further using literature from within Step 2 onwards.
Descriptive analyses
To ensure that the same information is not referred to in different ways in the report, our categories of contributors and strategies – developed based on underlying common realist mechanism (i.e. how and why they work) – were also used to organise the descriptive analysis. These categories were developed in an inductive way and discussed with the team and stakeholder group to ensure rigour. Additional codes were created in NVivo 12 for data relevant to the descriptive analysis, including the experience of particular professional groups of the contributors of UB (such as nurses and doctors) and for those from minoritised communities. In Chapter 5, we report on some basic statistics, such as mean or median sample sizes for included studies. These statistics were computed in Microsoft Excel using in-built formulae.
Categorising and collapsing contributors and strategies
When developing our programme theories to underpin individual contributors and strategies, the theories became too numerous and complex; we needed to collapse these to be more manageable and reportable. We accomplished this by forming categories according to common mechanisms underpinning how contributors lead to UB, as well as how strategies may mitigate or reduce UB. These categories were initially formed by JAA before refinement through intensive discussion with RA and JM, and input from the wider team and stakeholder groups.
Identification of key dynamics
We operationalised many of the demi-regularities (or ‘semi-predictable patterns or pathways of programme functioning’ across studies) identified across studies as ‘key dynamics’36 and ‘implementation principles’ (see Chapters 7 and 8). Key dynamics were defined as contradictions within, considerations for or frequent unintended consequences of interventions/strategies. These dynamics and principles were iteratively discussed within the team before they were presented to our stakeholders to be sense-checked against their expertise. Our intention was to surface these often-implicit contradictions, which should be actively managed by those involved in implementing interventions in organisational settings.
Formatting of context, mechanism and outcome configuration in this report
Throughout this report, CMOCs are most commonly formatted as ‘if, then, because’ statements for simplicity: meaning ‘if [context], then O [outcome], because [mechanism]’. In Chapter 6, where particular strategies are discussed, we formulated the CMOCs using a method outlined by Dalkin et al. 35 This format is as follows: R (Resources introduced by the intervention) + C (Context) → M (Change in participant reasoning) = O (Outcome).
The purpose of the differing CMOC formulation in Chapter 6 is to make a greater distinction between the resource offered by the intervention (i.e. the strategy) and the context in which that strategy is delivered.
Step 6: Testing, refining and developing resources with stakeholders
Informed by the ‘Evidence Integration Triangle’ (EIT)52 and stakeholder involvement in March 2023, we used our realist review findings to produce actionable evidence to support NHS managers/leaders to better understand how work environments may help or hinder UBs and identify what strategies work where. Further detail on patient and public involvement (PPI) is in Chapter 9, Discussion.
Chapter 3 Characterising unprofessional behaviours
Introduction
This chapter outlines the characteristics of our included sources and explores the terminology used to describe UBs among staff in acute healthcare settings. We also propose a definition of staff-to-staff UB and outline the middle-range theories (MRTs) drawn upon in this report, which added depth to our analysis. Full detail on MRTs is given in Appendix 2.
Document characteristics
Source types
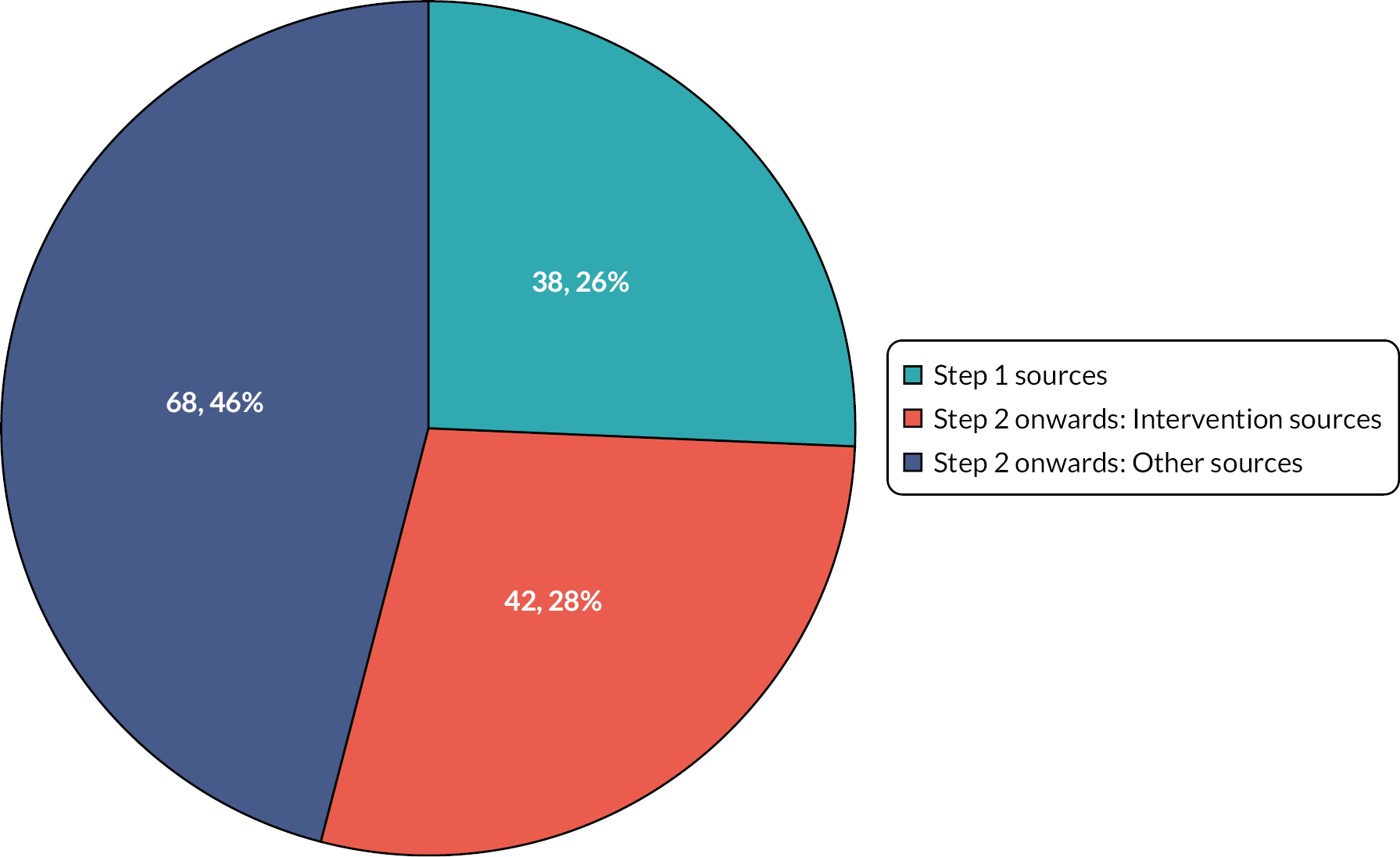
The 148 included sources encompassed 113 empirical and 45 non-empirical sources (Table 4). The largest source type was acute care intervention papers (n = 42) (Figure 5), all identified in Step 2 onwards. These interventions, the characteristics of their evaluations and their components are discussed in Chapter 5. Full details on all 148 included sources – including country, healthcare setting, samples, etc. – can be found in Appendix 3, Table 25.
| Study type | Step 1 | Step 2 and updates | Total (%) |
|---|---|---|---|
| Empirical (total n = 113) | |||
| Systematic review | 8 | 5 | 13 (8.8) |
| Narrative review | 3 | 8 | 11 (7.4) |
| Cross-sectional/case studies | 5 | 17 | 22 (14.9) |
| Intervention | 1 | 42 | 43 (29.1) |
| Report | 6 | 8 | 14 (9.5) |
| Simulation study | 3 | 1 | 4 (2.7) |
| Theoretical/modelling | 1 | 5 | 6 (4.1) |
| Non-empirical (n = 45) | |||
| Web page | 2 | 0 | 2 (1.4) |
| Opinion article | 3 | 0 | 3 (2.0) |
| News article | 1 | 1 | 2 (1.4) |
| Editorial | 5 | 23 | 28 (18.9) |
| Total | 38 | 110 | 148 (100) |
FIGURE 5.
Pie chart depicting distribution of included literature and to which step of the project it corresponds.
Healthcare settings
Included sources focus predominantly on acute healthcare settings, as per our protocol, comprising 37% of included sources (Table 5). We also included ambiguous healthcare settings (e.g. sources that referred to simply ‘bullying in health care’) or sources that encompassed multiple healthcare settings (general healthcare settings, 38.5%). We also included several sources focusing on a setting with medical professionals who were still in education or training. These comprised 5.4% of sources.
| Healthcare setting | Step 1 | Step 2 and updates | Total (%) |
|---|---|---|---|
| Non-specified health care | 28 | 29 | 57 (38.5) |
| Acute healthcare settings | 3 | 52 | 55 (37.2) |
| Speciality care (e.g. surgery, neonatal, obstetrics, military, mental health) | 5 | 9 | 14 (9.5) |
| Emergency | 1 | 12 | 13 (8.8) |
| Medical education | 0 | 8 | 8 (5.4) |
| Non-health care | 1 | 0 | 1 (0.7) |
| Total | 38 | 110 | 148 (100) |
Countries of focus
We collated information regarding the country on which the source content focused, not the country in which the source was published. Our included sources were predominantly focused on the USA or UK, together comprising over 52% of sources. A further 24.3% had a focus in no specific geographical region (Table 6).
| Country | Step 1 | Step 2 and updates | Total (%) |
|---|---|---|---|
| USA | 7 | 32 | 39 (26.4) |
| UK | 16 | 23 | 39 (26.4) |
| Australia and New Zealand | 1 | 14 | 15 (10.1) |
| Canada | 0 | 6 | 6 (4.1) |
| Turkey | 0 | 3 | 3 (2.0) |
| Ireland | 0 | 2 | 2 (1.4) |
| South Korea | 0 | 2 | 2 (1.4) |
| Iran | 1 | 1 | 2 (1.4) |
| Sweden | 0 | 1 | 1 (0.7) |
| Spain | 0 | 1 | 1 (0.7) |
| Jordan | 0 | 1 | 1 (0.7) |
| EU-wide | 1 | 0 | 1 (0.7) |
| No focus | 12 | 24 | 36 (24.3) |
| Total | 38 | 110 | 148 (100) |
Terminology used to understand unprofessional behaviours
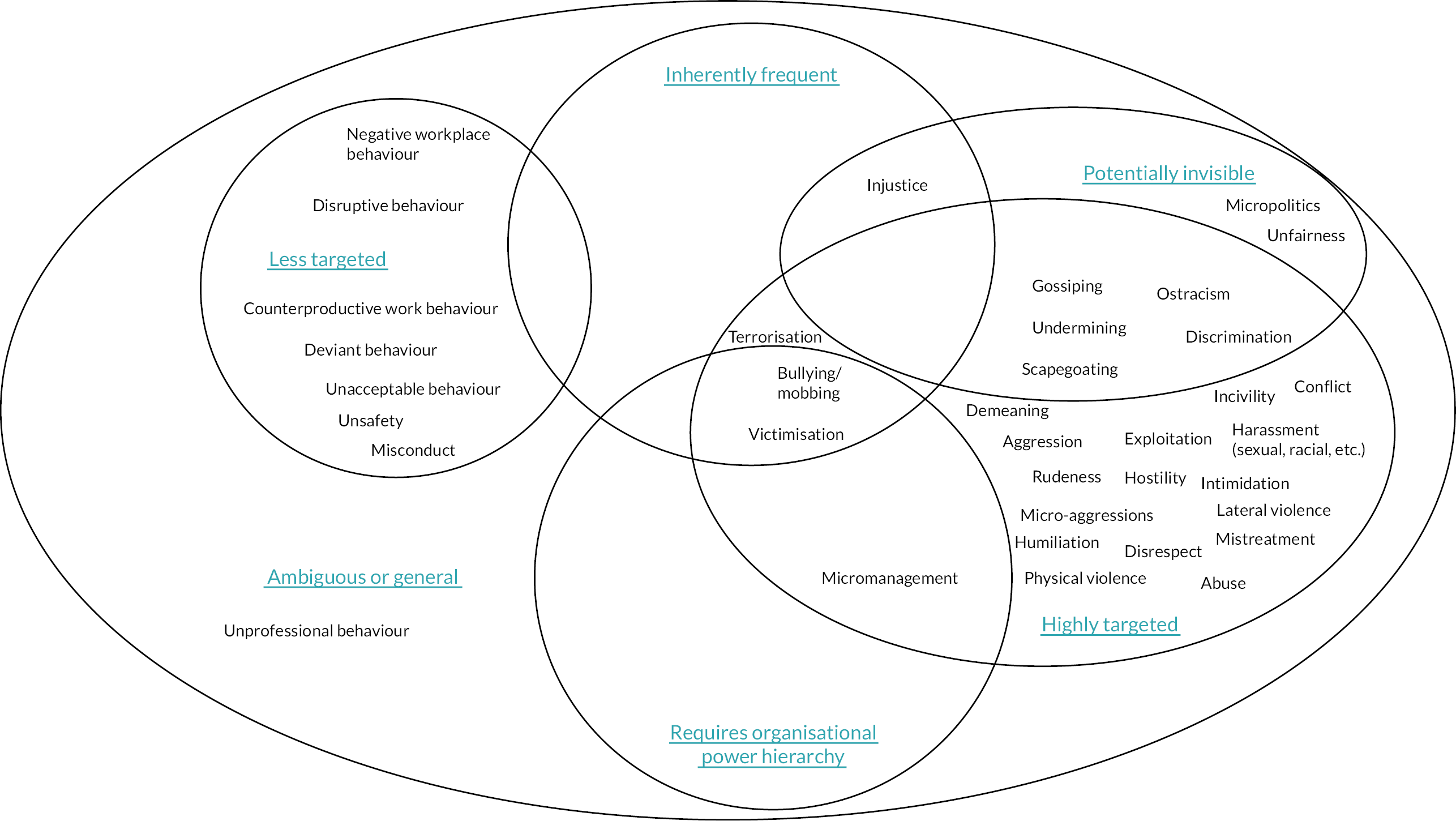
In this review, we focused on interpersonal forms of UB between staff – that is, those who can be targeted – as outlined in Figure 6. We did not examine counterproductive workplace behaviours such as laziness or lateness. UBs have been defined as ‘a wide spectrum that includes conduct that more subtly interferes with team functioning, such as poor or ambiguous communication, passive aggression, lack of responsiveness, public criticism of colleagues and humour at others’ expense’. 1 UBs can, therefore, be casual and generalised or highly targeted with the intention to cause distress or harm. The operational definition for UBs developed by the team, with stakeholder input, for use in this study is: ‘Any interpersonal behaviour by staff that causes distress or harm to other staff in the healthcare workplace’. We also acknowledge that UB can have many dimensions, and so also developed the following ‘extended’ definition: ‘Any interpersonal behaviour by staff that acutely or frequently undermines, humiliates, intimidates, or causes distress or harm to other staff, in the healthcare workplace’.
FIGURE 6.
Typology of UB terms and their dimensions.
| Stakeholder feedback summary – definition of UB |
| At our stakeholder group meeting in March 2023, we presented two definitions to the stakeholders – one simplified and one with more detail. The stakeholders were split as to which definition they preferred. They emphasised the importance of capturing the impact on bystanders of UB, as well as discussing whether ‘harm’ or ‘distress’ was a more appropriate term. Consequently, we made refinements to the definitions and included both. |
While some sources discussed more than one term to describe UBs, we synthesised terms that were used as the primary focus of each study. In so doing, we identified 21 different types of UB across our included documents (Table 7). Results show that over 50% of sources were focused on bullying, incivility and horizontal or lateral violence. Ten sources focused on more specific forms of UB that affect particular groups such as microaggressions, racism or sexual harassment. Twelve sources also focused on an issue adjacent to UB, such as organisational climate or communication issues between staff, and these were included where sufficiently rich to inform our analysis. It is also important to note that these terms are also a product of the focus of our search and may not be representative of proportions of such terms prevalent in the wider literature.
| UB type | Number of sources (%) |
|---|---|
| Bullying | 47 (31.8) |
| Incivility | 18 (12.2) |
| Horizontal/lateral violence | 16 (10.8) |
| Other (e.g. organisational climate, interpersonal collaboration, communication issues, discouraging environment) | 12 (8.1) |
| Unprofessional behaviour | 9 (6.1) |
| Positive environment (e.g. civility, professionalism, respect) | 8 (5.4) |
| Disruptive behaviour | 5 (3.4) |
| Microaggressions | 4 (2.7) |
| Undermining | 4 (2.7) |
| Racism | 3 (2.0) |
| Conflict | 3 (2.0) |
| Negative workplace behaviour | 3 (2.0) |
| Unacceptable behaviour | 2 (1.4) |
| Rudeness | 2 (1.4) |
| Hostility | 2 (1.4) |
| Mobbing | 2 (1.4) |
| Sexual harassment | 2 (1.4) |
| Harassment | 1 (0.7) |
| Misconduct | 1 (0.7) |
| Aggression | 1 (0.7) |
| Disrespect | 1 (0.7) |
| Mistreatment | 1 (0.7) |
| Discrimination | 1 (0.7) |
We also collated and mapped definitions and behaviours inherent to 33 different UB-related terms, including those in Table 7 (see Appendix 4, Table 26). Our findings indicate that literature generally refers to terms that encompass a wide set of behaviours, such as bullying, incivility, harassment and lateral violence.
Dimensions of terminology
Some terms – such as ‘unprofessional behaviour’ – are used in more ambiguous ways and can include ‘poor or disrespectful communication, irresponsible behavior, inappropriate care, and lack of professional integrity’. 53 As such, this term encompasses all behaviours that compromise a professional environment, from more ‘active’ behaviours (e.g. being rude to a co-worker) to those that can be considered more passive (e.g. being late to work). Disruptive behaviour is another similar term that was used by included sources but typically focuses more on those behaviours that compromise patient safety.
As well as terms that encompass more passive types of behaviour, there are also those that are more ‘active’, targeted and intended to cause distress or harm. These include bullying, harassment, disrespect, rudeness, conflict, and those that are actively harmful. Lateral violence is one example; it has been defined as ‘any repetitive behaviour among peers that is considered offensive, abusive, or intimidating by the target’. 54 This suggests that lateral violence typically occurs between individuals in the same group (e.g. frontline nurses) and highlights another dimension of included UB terms: whether or not they are targeted.
While lateral violence involves staff on the same hierarchical level, other forms of UB may require a vertical hierarchy. This is typical for bullying, for example. Included articles suggested that bullying was an interpersonal form of UB that was repeated and often from a person higher in an organisational hierarchy towards a person lower in the hierarchy: ‘bullying encompassed a range of disruptive, repetitive, and ineffective behaviors, such as criticism and humiliation, negative acts perpetrated by an individual in a position of power intended to cause fear in a targeted individual’. 55 This adds two further dimensions to UBs: frequency and requirement of a hierarchy.
Unprofessional behaviours can also be more insidious and invisible. While such behaviours are difficult to target or measure, they can also be highly targeted in nature. Such behaviours can include undermining, which is defined as ‘conduct that subverts, weakens or wears away a person’s confidence, and may occur when one practitioner intentionally or unintentionally erodes another practitioner’s reputation or intentionally seeks to turn others against them’. 56 As such, the behaviour may be invisible from the target’s perspective and can be difficult to identify from an organisation’s perspective. This adds the dimension of visibility to UBs.
Mapping dimensions of unprofessional behaviours
The above results identified that UBs can: be general or more specific in nature, be more or less targeted, require an organisational hierarchy or not, inherently be frequent (i.e. must occur more than once) as per its definition, and be more or less visible to both the organisation and the target. Figure 6 outlines our typology of UB terms and their location within the various dimensions. Terms such as ‘deviant’, ‘disruptive’ and ‘unacceptable behaviour’, which include non-targeted passive behaviours, sit at the top-left of Figure 6 and none are inherently frequent by definition (i.e. they can all be one-off events). Inherently frequent behaviours include bullying/mobbing, terrorisation, victimisation and injustice. Some of these behaviours – such as bullying – also require an organisational power hierarchy (according to most definitions), whereas micromanagement also requires a hierarchy but does not need to be frequent.
Most behaviours on which we focus in this review are targeted interpersonal behaviours, such as incivility, conflict, harassment, aggression, rudeness, microaggressions and disrespect. Some are also specifically targeted towards a person or entire group but are less visible. Such behaviours include discrimination, scapegoating and ostracism (see Figure 6). We considered a dimension of severity but these were fraught with complexity and are likely to be subjective, related to recipients’ perceptions. However, we acknowledge that some types of UB are broadly considered to be more ‘severe’ than others, that is, physical assault is worse than rudeness.
| Stakeholder feedback summary – typology |
| When we presented this typology to our stakeholders in January 2022, they pointed out that some behaviours were not classified correctly, e.g. discrimination is always highly targeted and does not necessarily require a hierarchy. They also provided us with the dimension that some behaviours may be ‘hidden’ or potentially invisible as our final typology reflects. We adjusted our typology accordingly. |
Conflicting definitions
Included sources often used terms in conflicting ways. Bullying, it seems, is often used as a catch-all term for UBs of all kinds – perhaps because it has been in use in the literature for a longer period. However, ‘there is no single, universal definition of workplace bullying either nationally or internationally’. 57 While many definitions suggested a hierarchy or power imbalance was essential for bullying, others did not. One definition stated that ‘[bullying has] been used to explain aggression between colleagues who are on the same level within the organizational hierarchy and who, because of their (supposed) low personal self-esteem and poor group identity, direct abusive behaviour toward each other’. 58 Evidently, this definition does not suggest that a hierarchy must be present. For the purposes of our review – and since most definitions state that bullying occurs within a hierarchy – we have included it in the part of our typology that requires hierarchy. Without the hierarchy component, it is not clear how the definitions of bullying and harassment differ as both are frequent forms of persistent UB.
Similarly, while it might be expected that ‘lateral violence’ occurs at the same level, there was disagreement on this in the literature. One included source suggested that: ‘Terms such as horizontal violence and lateral violence suggest the perpetrator is a nurse colleague of equal status, but this is not always the case. It might be a person in a higher position – or it might not even be a nurse’. 59 Table 8 depicts examples of selected terms where conflicting definitions were identified.
| Term | Definition 1 | Definition 2 | Key discrepancy |
|---|---|---|---|
| Bullying | ‘a form of harassment which involves persistent, intimidating behaviour, usually by a supervisor toward an employee’60 | ‘repeated exposure to person‐, work‐, and intimidation‐related negative acts such as abuse, teasing, ridicule, and social exclusion over a period of time in the workplace’61 | Definition 1 suggests a hierarchy must be present but definition 2 does not |
| Lateral violence | ‘Lateral violence (LV) is described as behavior demonstrated by nurses who overtly or covertly direct dissatisfaction toward those less powerful than themselves and each other’62 | ‘LATERAL VIOLENCE is any repetitive behavior among peers that is considered offensive, abusive, or intimidating by the target’54 | Definition 1 suggests lateral violence can be towards those lower on the hierarchy, whereas hierarchy is not mentioned in definition 2 and suggests incivility must be frequent |
| Incivility | ‘subtle behaviors not intended to harm anyone but contrary to workplace standards’55 | ‘… repeated offensive, abusive, intimidating, or insulting behavior, abuse of power, or unfair sanctions that make recipients upset and feel humiliated, vulnerable, or threatened, creating stress and undermining their self-confidence’63 | Definition 1 suggests that incivility encompasses more subtle behaviours but definition 2 suggests they are not at all subtle |
| Disruptive behaviour | ‘The American Medical Association’s Council on Ethical and Judicial Affairs defines disruptive behavior as behavior that ‘tends to cause distress among other staff and affect overall morale within the work environment, undermining productivity and possibly leading to high staff turnover or even resulting in ineffective or substandard care’64 | ‘… we define disruptive behaviour as constituting the following three criteria: (a) interpersonal (i.e. directed toward others or occurs in the presence of others); (b) results in a perceived threat to victims and/or witnesses; (c) violates a reasonable person’s standard of respectful behaviour’32 | Definition 1 suggests disruptive behaviour includes passive-type behaviours that undermine productivity, whereas definition 2 suggests it must be targeted |
How conflicting terminology impacts staff in practice
Included sources emphasised the importance of terminology and that staff understanding forms of UB such as bullying, microaggressions etc. – including their definitions and appearance – is essential to staff understanding their experience of UB in the workplace and for being able to interpret when it is appropriate to speak up. 65–67 One source stated ‘the absence of a comprehensive descriptive framework capturing and cataloguing those behaviours make identification, seeking assistance and intervention difficult’. 68 Included literature highlighted that the lack of uniform definitions can result in different interpretations of UB by staff members and from different perspectives (e.g. individual vs. organisational), which creates an atmosphere of confusion and inhibits speaking up.
Lack of uniform definitions also impacts the ability to assess prevalence of UB or identify where and how it is occurring, which can make implementing strategies more difficult. For example, differing definitions of what constitutes UB could impact ability to understand its prevalence, reduce the likelihood of speaking up and impact ability to intervene effectively. One study showed a lack of a uniform definition and clarity regarding bullying in the nursing profession meant that: ‘those who are exposed to such behaviour, including new graduate nurses, senior nurses, and nurse unit managers would have reported based upon their own understanding of these behaviours’. 58
Evolution of literature focus
One general trend noted in the literature over time was the articulation of more specific forms of UB, indicating that greater attention was paid to the experiences of minoritised communities – through the study of microaggressions or racism, for instance. All sources (n = 7) discussing microaggressions and racism more broadly were published from 2019 onwards, which is reflective of the more recent societal focus on racism and discrimination. 69–75 The same can also be said for literature relating to sexism (n = 9), which begins in 201362 and is more prevalent from 2016 onwards. 11,32,62,76–80
No such trends were observed for more widespread and generally used terms such as ‘bullying’ or ‘harassment’, as these have always been used frequently. While the greater focus on issues affecting groups with protected characteristics is encouraging, much more needs to be done to help address the greater burden these groups face from the impact of UB in the workplace.
Terms not included: ‘professionalism’, ‘civility’ and ‘other behaviours’
We also wanted to highlight the many adjacent behaviours that are not included in our review. These include those behaviours that may be the ‘inverse’ of UB, including behaviours and terms such as ‘civility’ and ‘professionalism’. It is important to highlight that professionalism may be more than the simple absence of UB, such as maintaining appropriate appearance, upholding patient confidentiality, applying clinical skills according to standards, and interacting honestly with patients. 81 On the other hand, some behaviours may be unprofessional from the perspective of an organisation – but not from that of colleagues. One example is the use of workarounds employed by healthcare staff that may deviate from organisational procedures perceived as barriers (and hence may be unprofessional from the perspective of the organisation) but that can improve patient safety. 82 Such nuanced cases are beyond the remit of this review; only interpersonal forms of UB are included.
Key concepts, middle-range theories and wider context for this review
Throughout this report, we draw on a number of MRTs to better interpret and add depth to various elements of our analysis, outlined in Table 9. Additionally, we want to highlight the influence of wider context on organisations – including societal events and transitions, such as COVID-19, #MeToo and #BLM – that form the wider, cultural and historical backdrop within which our review takes place. A full description of these MRTs can be found in Appendix 2.
| Middle-range theory | Description |
|---|---|
| Psychological safety | Psychological safety refers to staff perceptions of consequences of the risks of speaking up in the workplace83 and is defined as ‘a shared belief held by members of a team that the team is safe for interpersonal risk taking’84 |
| Moral injury | Moral injury in a healthcare context has been defined as ‘perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations’85 which may leave ‘long-lasting emotionally, psychologically, behaviourally and spiritually harmful impacts’86 |
| The JDR | Many included sources drew upon the JDR model as a contributor to bullying, explaining a lack of organisational resources could worsen UB.87 Originally used as a model to better understand burnout, it sets out the range of job demands that can contribute to exhaustion, as well as job resources that, if lacking, can lead to disengagement87 |
| FAE | The FAE is a phenomenon from social psychology whereby people tend to attribute a person’s behaviour solely to their personality – rather than acknowledging that, often, behaviour is a combination of a person’s personality and their environment.88 This applies mostly to other people’s negative actionss89 |
| Trust | Our report frequently discusses trust in management by staff, which is easily lost when UB is not addressed. Trust is defined by Robinson (1996) as ‘one’s expectations, assumptions or beliefs about the likelihood that another’s future actions will be beneficial or at least not detrimental to one’s interests’.90 Inherent to our understanding is the importance of managers’ roles in trust and UB; staff interests lie in managers providing a safe organisational environment free from UB |
Key findings and summary
In total, 148 sources are included in this review. We mapped different types of UB according to several main dimensions, including whether UB is more or less targeted, visible to organisations and their targets, and required an organisational hierarchy. Definitions of UB were found to have little agreement, making synthesis difficult and likely to sow confusion in practice. This review draws on the following MRTs: (1) theory of psychological safety, (2) moral injury, (3) the job demands and resources model (JDR) model to shed light on organisational processes that can contribute to UB, (4) the fundamental attribution error (FAE) and (5) trust, particularly in management. The literature does not yet sufficiently represent these wider societal events such as COVID-19 and movements such as #MeToo or #BLM and resultant changes in societal views.
Chapter 4 Contributors to and outcomes of unprofessional behaviour between staff in acute healthcare settings
Introduction
This chapter identifies and describes the contributors to and contexts of UB. It explains the ways interpersonal UBs are defined, developed and experienced across professional staff groups in acute healthcare settings according to the literature. We use the term ‘contributors’ to reflect the range of antecedents involved in how UBs manifest themselves and are discussed within current literature.
Results
This initial section sets out the lens with which we have viewed contributors to UB, as shaped by our analysis of the literature and discussions with our stakeholder group. Then, we discuss the four identified categories of contributors to UB. These categories include: (1) workplace disempowerment, (2) organisational confusion, uncertainty and stress, (3) job and organisational design that inhibits social connection and (4) harmful work cultures. Within these categories, we also elaborate a range of more specific contributors (e.g. shift working, leadership behaviours, etc.). Use of these categories allowed us to identify similar or shared mechanisms and explore how these categories and sub-contributors broadly work.
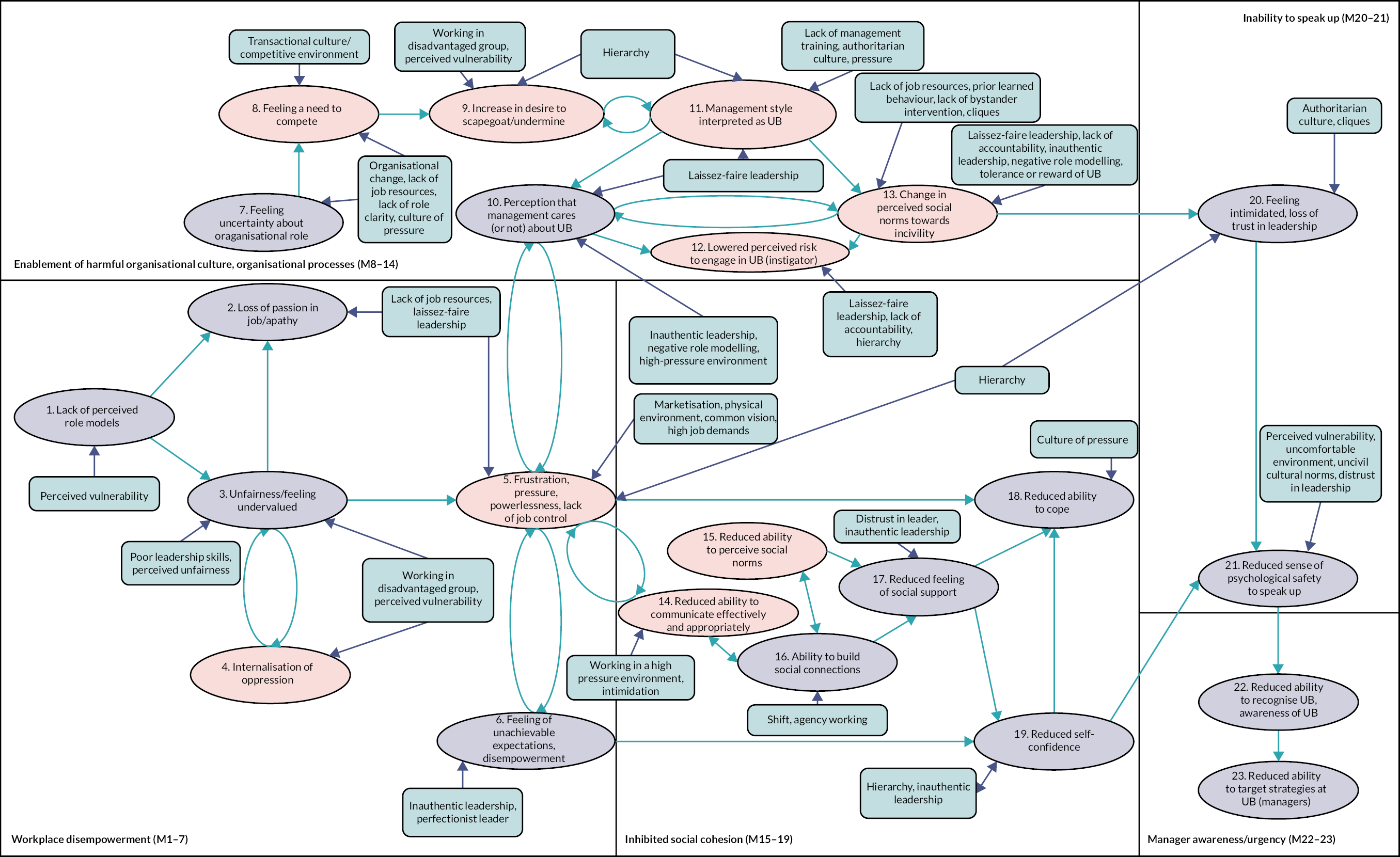
To elucidate how contributors lead to a worsening of UB, throughout this chapter we draw on a selection of CMOCs. In each section, we present a partial programme theory diagram (Figures 7–9). In these diagrams, mechanisms are depicted in ellipses; the contributors are in green boxes. Connections between these are indicated by arrows. Those mechanisms that can directly lead to an increase in UB are depicted by orange ellipses, while the blue ones simply connect to other aspects as indicated in the fully assembled programme theory (Figure 11). When CMOCs are depicted in the text, the mechanisms will be numbered. These numbers will correspond with the numbers in the partial programme theory diagrams to help locate where a CMOC lies in the causal chain. It is important to note that these diagrams may depict more information than there is capacity to discuss in the text because the emerging causal chain became increasingly complex with multiple and overlapping mechanisms and outcomes. The headings in each section explore the main sub-contributors identified in the literature.
FIGURE 7.
How CMOCs underpinning workplace disempowerment interact.

FIGURE 8.
How CMOCs underpinning poor social cohesion interact.

FIGURE 9.
How CMOCs underpinning enablement of harmful cultures, and battling organisational processes, interact.
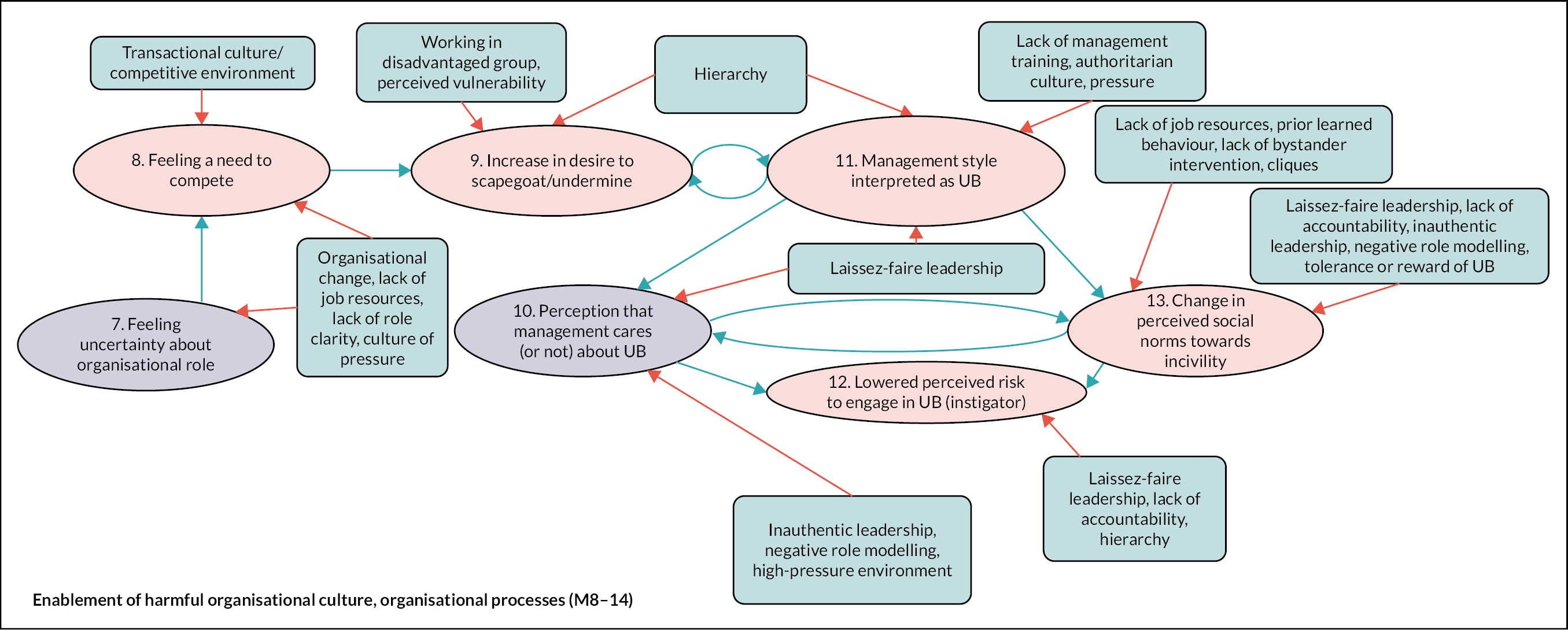
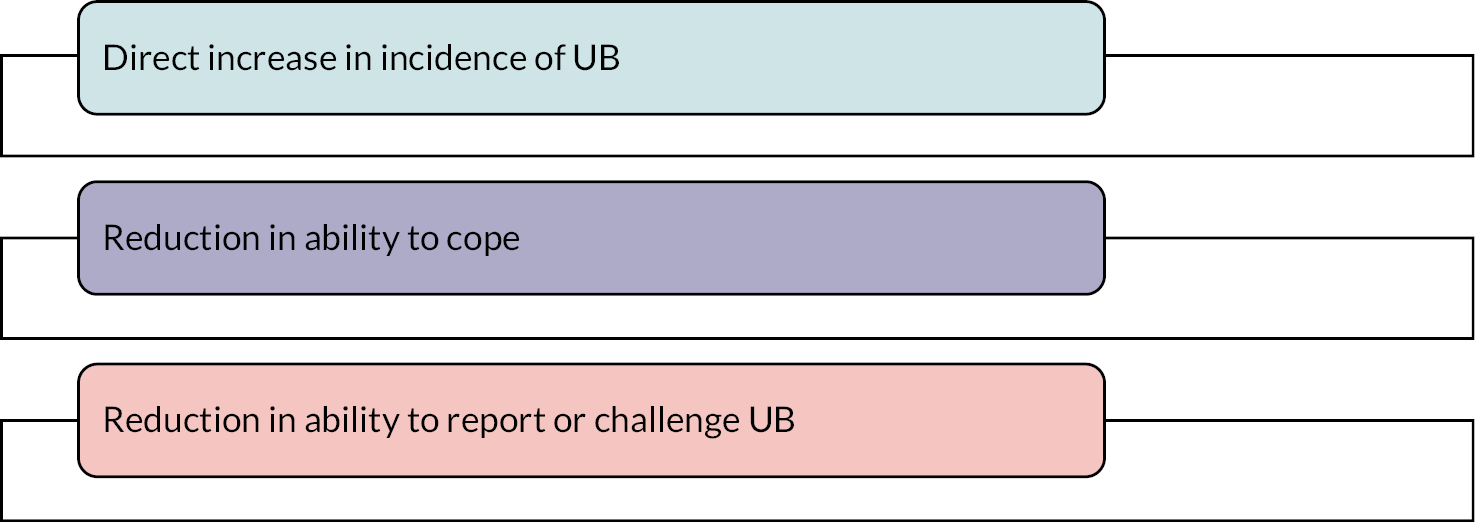
FIGURE 10.
Key outcomes from contributors to UB.
At the end of this section, in Figure 11, we present our fully assembled programme theory to depict the connections between the categories of UB. Consistent numbering of mechanisms across the partial programme and full programme theory diagrams allow the CMOCs to be cross-referenced with the full programme theory diagram. Our CMOCs are further tabulated (see Appendix 5, Table 27) with additional quotes from the literature, further explaining some of the dynamics explored in this chapter. At the end of the chapter, we explore the outcomes of both these contributors and UB, as well as the impact on different groups.
FIGURE 11.
Revised programme theory depicting interactions of different contributors and underlying mechanisms. Green squares are contributors and ellipses are mechanisms. Orange mechanisms are those that can directly increase proclivity to engage in UB.
The ‘bad apple’ approach
We noted a focus in the literature on individual and personal characteristics as contributors to UBs. One source, for example, discussed ‘maladaptive personality traits’ – such as being ‘paranoid, narcissistic, passive-aggressive and borderline types’ – as well as describing instigators of UB as having ‘poorly controlled anger’ and experiencing a ‘spillover of home problems’. 91 These individuals are determined by the literature as having a greater proclivity to engage in UB than others and are often referred to as ‘bad apples’. 92 The organisational response to such individuals is often to weed them out and try to discipline them. Over time, the hope is that this may lead to culture change, as a critical mass of instigators have their behaviour addressed.
However, other literature in our review argued that a focus on individual characteristics is often used by organisations as a ‘get out of jail free’ card that enables abrogation of responsibility and accountability to implement wider cultural change or strategies targeting UB. 61,93,94 Moreover, evidence regarding individual-level contributors – such as personality types, gender or professional group – is often very mixed. For example, in terms of professional group, some sources find surgeons to be more frequent instigators of UB towards nurses because of inherent power dynamics, whereas other sources find nurses more frequently uncivil towards one another as a result of negative self-esteem, competition and fear. 32 Additionally, possessing certain personality traits does not guarantee that someone will behave poorly, which makes the effectiveness of understanding such contributors questionable. 95
Therefore, it may be more productive for organisations to focus on modifiable factors that are targetable by interventions in order to reduce UB. This can include improving working conditions, improving climate and culture, fostering a psychologically safe culture and eliminating barriers to providing high-quality care. 96 In this manner, an organisation can create an environment that is least enabling of UB, regardless of the individual staff working at their organisation. Mannion et al. referred to this as addressing problems at the level of bad cellars (organisations), bad barrels (health systems) and bad orchards (professions), rather than bad apples. 92 Professional accountability programmes such as Ethos in Australia and Vanderbilt in the USA show promise in fostering this kind of culture change. 97,98 As such, this report and chapter will focus on factors that can be modified by interventions and not focus on what makes someone a ‘bad apple’ or a less resilient target.
| Stakeholder feedback summary – contributors |
| We presented an early understanding of contributors to our stakeholders in January and May 2022. We received feedback that some of our understanding was too focused on the individual. This shaped our direction for the refined analysis in Step 2 of the project going forward, in which we focused on aspects that were within an organisation’s control to change. For example, in our initial theory of ‘causes’ of UB, we had many factors considered as individual-level, including professional or personal backgrounds, job demands and ability to cope. However, in our refined understanding, we now acknowledge that many of these factors are a function of the organisational environment rather than resulting from individual differences. |
| The stakeholder group also helped shape our language, moving from an understanding of ‘causes of UB’ – which was too deterministic – to ‘contributors to UB’. |
Category 1: Workplace disempowerment
Workplace disempowerment can be caused by (1) organisational hierarchies, (2) physical environment and (3) unfairness. 70,99–101 How these elements contribute to UB will be explained further, aided by presentation of CMOCs throughout this section.
Organisational hierarchies
The NHS and healthcare systems worldwide are known to be hierarchical; clinical professionals working across different grades and there are a range of disciplines, alongside non-clinical and/or support staff. As identified in the literature, working in a hierarchy was a key structure through which staff were disempowered. These hierarchies can exist both within and between professions and are often exemplified by the relationship between doctors and nurses, whereby doctors are often considered to be in a position of power relative to nurses. 101,102 Hierarchy can either be a result of the design of the system in which organisations operate68 or a result of a socially constructed environment whereby certain groups or individuals are perceived to have more power than others. As such, hierarchies also interact with existing societal power dynamics – with hierarchies having generational, cultural, professional and gender-based roots. 78
Hierarchies can contribute to UB because those lower in the hierarchy have less power – which, as well as making them an easy target, also makes them feel less safe to speak up. One source provides an example of creating an environment in which it is unsafe to speak up in which vertical hierarchies can lead to a culture of blame and intimidation:
There appeared to be a style of management within nursing at this hospital that was based on fear rather than respect. There was an impression that nurses were tolerated rather than valued, that they should keep their heads down and not threaten those above them by disagreeing with them. 103
This is highlighted in CMOC 1.
CMOC 1. If staff work in a disempowered position, such as at the bottom of an organisational or professional hierarchy (C), then this can inhibit willingness to speak up (M21/O1) and reduce ability to communicate (M14/O2) because a sense of intimidation and reduced psychological safety is experienced (M20).
With hierarchy as a ‘direct’ contributor to UB, the following quote from a patient support staff member from a qualitative study in Australia highlights the dynamic whereby a vertical hierarchy combined with a high-pressure environment creates more opportunity for ‘bullying down’:
If the surgeon is really anxious and tense, it flows down … they bully the anaesthetist, they bully the scrub nurse and scout nurses, and the techs cop it from everyone. 93
This dynamic is depicted in CMOC 2.
CMOC 2. If staff work in a disempowered position, such as at the bottom of a hierarchy (C), then this can increase likelihood of experiencing and being impacted by UB (O) because it can make staff an easier target (M12).
Literature also reported that UB may manifest itself within flattened structures or between peer groups where there can be powerlessness. For example:
Frustration with their powerlessness often turns to internal hostility, known as ‘horizontal violence’, because of negative self-esteem and fear of the oppressor. 104
Certain minority or disadvantaged groups can also be negatively affected and feel powerless (CMOC 3).
CMOC 3. If staff work in a disadvantaged group (C), then this can lead to displacement of aggression onto others (O1) and a feeling of being undervalued (O2) because of internalisation of oppression (M4).
Physical environment
Working in a physically uncomfortable environment (which is common in healthcare workplaces), for example where it is too hot or crowded or in close proximity to disease (such as during the COVID-19 pandemic), can increase a sense of pressure and frustration and reduce ability to cope (see Figure 7). 21 Sources highlighted that certain environments could become associated with past traumatic experiences, causing regular and repeated post-traumatic triggers such as flashbacks, which further reduces ability to cope. 77 See CMOC 4 (below).
Unfairness
Working in a lower position in a hierarchy can make staff feel they are disempowered and that organisational processes are unfair or unjust. Unfair processes – such as ‘bestowing apparent favours on some doctors in training by giving them access to resources, such as study leave or training opportunities, while denying these to others’105 and similar treatment – can be considered discrimination, ostracisation or undermining in themselves. Over time, this can lead to a sense of annoyance, frustration or anger that can eventually lead to conflict. 21 This is highlighted in CMOC 4.
CMOC 4. If staff work in a disempowered position where there does not seem to be a level playing field (C1) or work in a physically uncomfortable environment (C2), then this can cause them to externalise these frustrations – increasing proclivity to engage in UB (O2) because staff feel like they are being treated unfairly (M3), experience frustration (M5) and have a reduced ability to cope (M18/O1).
Depicting the processes of disempowerment
Figure 7 depicts how the contributors underpinning workplace disempowerment interact. You will notice that other factors, such as inauthentic leadership, are also depicted in this diagram; these will be discussed in the harmful work cultures section.
Category 2: Organisational confusion, uncertainty and stress
When staff experience organisational confusion, uncertainty and stress, these factors contribute to increased instances and experiences of UB. The following four headings demonstrate how this happens, showing that when staff experience a lack of control in their day-to-day work, they encounter challenges in building relationships that, in turn, increase conflict: (1) organisational change, (2) a lack of resources and high job demands, (3) a culture of pressure and (4) a lack of role clarity.
Organisational change
The literature and stakeholders suggested that whether or not organisational change increases UB often depends on the pre-existing culture and how change is managed. The primary evidence regarding how changes may contribute to UB is through an increase in uncertainty about one’s organisational role and a further increase in workload, as well as potential job insecurity,76 which may result in an increase in competitive attitudes that can set employees against each other. For example:
In competitive environments, organizational re-structure or periods of rapid change may create opportunities for individuals to engage in the misuse of legitimate authority for furthering self-interest or career opportunities. 58
This increase in competitive attitudes can further reduce the ability to engage in teamwork and generate conflict and UB in an organisation. This can also interact with hierarchy, whereby the power dynamic can be enhanced by the threat of organisational change and managers can seek to scapegoat employees beneath them to entrench their position. 21
CMOC 5. If staff experience a period of organisational uncertainty, such as organisational change (C), or they experience a lack of job resources (C2), then this can lead to conflict and UB (O) because staff perceive their job to be at risk; an increase in competitive attitudes ensues (M8).
Demanding work environments and lack of resources
Demanding work environments with high job demands and lack of resources were also identified as contributors to UB through reduced achievements, leading to reduced ability to communicate effectively with colleagues. For example, one source highlighted the ED as a highly demanding work environment, due to:
acuity and complexity of patient presentations, the lack of predictability of workflow and the need to attend to patients in a timely manner. 106
Such demands can impact staff in several ways, including reducing the quality of communication, which may increase the chance of it being perceived as UB. For example, one source highlighted that:
… consultants told us they were more likely to speak sharply to doctors in training when they themselves were stressed. They reported that they were less able to prioritise the training needs of their juniors, and less likely to treat them with respect at all times. 105
This dynamic is explored further in the culture of pressure section (below).
Job demands can also include the complexities of healthcare work, as well as organisational bureaucracy that could theoretically be more streamlined. For example, opaque organisational processes were found to needlessly add to frustration and drive conflict. In other cases, irreconcilable responsibilities lead to conflict between individuals as they attempt to resolve such difficult organisational issues:
When incompatible social structures bear on a situation, the clash creates unresolvable conflicts fuelled by the simultaneous compulsion to fulfill irreconcilably oppositional obligations, creating a downward spiral of communication that circles back to escalate the conflicts. 107
CMOC 6. If high job demands are experienced regularly in the absence of adequate resources (C1), then escalation of conflicts is more likely (O2) because there is both a high-pressure environment (M5) and a reduced ability to communicate effectively (M14/O1).
A lack of job resources can include financial, human and clinical resources, all of which contribute to an inability to adequately perform one’s role. There are known healthcare staff shortages in the UK and worldwide. One paper highlighted the impact of austerity in the UK on reducing job resources, noting that:
… tightening regulation and oversight requires staff to provide efficient, high quality and safe care despite growing material and staff scarcity, increasingly complex workloads, worsening pay, morale and development prospects and a pressurized, high stakes environments. Unsurprisingly, this can undermine cultures of solidarity and respect between frontline professionals. 108
This lack of resources could lead to staff feeling unable to work in a team, due to:
… contexts governed by rising stress, fear and precarity in which fellow health staff can feel in competition with each other, with each cadre of professional all too aware of the need to justify their own position and worth. 108
These dynamics tie in with CMOC 6 (above) but can also lead to a culture of pressure (CMOC 7).
Culture of pressure
Significant job demands or a lack of resources can contribute to a sense of a pervasive culture of pressure which can make it difficult to meet expectations and get work done to a high standard, and can increase stress. This manifests itself in a feeling that one is not in control, which can generate a sense of frustration. In some cases, frustration can be externalised to attempt to relieve stress or regain some element of control. One source highlighted this dynamic:
… nurses commit negative workplace behaviours in order to release the feelings of frustration and regain a sense of control. 68
These dynamics again relate to CMOC 4.
The sense of pressure can also cause stress and result in people being curt in their communications, which can lead to more miscommunication and a lack of empathy between employees. To emphasise this, a review of a culture of bullying at an NHS trust highlighted that:
… ‘often the people doing the bullying are actually stressed’ and ‘under more pressure’, resulting in aggression ‘in how they approach and manage people’. 70
Unfortunately, the inhibition of communication caused by pressure can further increase the pressure due to the impact made when crucial information is not imparted; a vicious circle is created (see Figure 11). One study highlighted the link between pressure and communication, stating that:
… excessive workload, inadequate time for preoperative patient preparation, and unclear job descriptions all resulted in communication to be either disrupted, rushed, or incomplete. 109
This vicious circle is highlighted in CMOC 7.
CMOC 7. If staff experience a lack of resources or high job demands that increase pressure (C), then this may lead to an inability to cope with the impact of UB (M18/O1) because communication with co-workers can be inhibited (M14). This makes it difficult to build relationships (M16), which can reduce feelings of social support (M17).
Lack of role clarity
A lack of role clarity is another contributor that could be considered to be an aspect beyond the control of staff and that can impede their ability to work effectively. This can result in a situation in which the demarcation lines between their responsibilities and those of another are blurred, and staff can find themselves in unnecessary conflicts through no fault of their own (CMOC 8). One study highlighted a dilemma one participant faced:
Lack of clarity in workflow processes and management appeared to contribute to work-related discontent. ‘Roles are blurred. Instructions are unclear and when you try to sort something out you are verbally attacked (or emailed) if something is not done “correctly” even though you tried to seek out the “correct” process …. 77
Quote reproduced in part from BMC Health Services Research (https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-07763-3) in line with the CC-BY 4.0 Licence.
These micro-conflicts resulting from a lack of role clarity, which can be considered forms of UB in themselves, can further impact communication, the ability to build relationships with colleagues and the ability to cope, as depicted by CMOC 8.
CMOC 8. If staff are disadvantaged by organisational processes outside their control – such as a lack of role clarity or high job demands (C) – then this may increase levels of curtness in communication (O2) because they begin to feel pressured and their tasks become rushed (M5), which reduces their ability to communicate effectively (M14/O1).
These relationships are depicted in Figure 9 because the mechanisms underlying organisational confusion, uncertainty and stress are entangled with those that enable harmful cultures.
Category 3: Job and organisation designs that inhibit social connection
When job or organisational designs inhibit the ability of staff to connect with one another, social isolation and siloed working occur. This can increase the likelihood of UB occurring as well as reduce one’s ability to cope with UB, if present, through: (1) a lack of social support, (2) shift or agency working and (3) reduced ability to communicate effectively.
Lack of social support
Experiencing a lack of social support is at the core of this category and predominantly leads to an inability to cope with UB. 80 A lack of social support is generally more distal in the causal chain and can be a result of other contributors outlined throughout this chapter, including – as discussed previously – a culture of pressure undermining the ability to have time to build relationships. One included study stated that when social support exists:
… rallying around a victim in solidarity demonstrates a united front against the bully and is a means of taking power away, thus deflating the perceived outcomes from the bullying. 110
A lack of social support causes a reduced sense of self-confidence. This can inhibit speaking up (see Figure 8). Thus, where social support does not exist, staff can be silenced or dehumanised. For example, one – a woman who had experienced sexual assault by co-workers in a healthcare workplace – was further ostracised by unsupportive co-workers:
Claire commented that even though she was taking calls from lawyers ‘in the middle of operating’, none of her colleagues offered support: ‘they were just pretending nothing was happening’ […]. The silencing and banishment from her workplace ‘reduced me into an enigma, and has depersonalised me’. 80
Shift or agency working
Figure 8 demonstrates that reduced self-confidence can lead to an inability to cope, as well as a reduction in ability to speak up and report or challenge future instances of UB that may be encountered. Use of agency staff rather than permanent NHS staff is increasingly common in the UK; spending on agency workers in Scotland, for example, doubled in 2021. 111 Similarly, a move to shift working in recent decades has made it less likely to see familiar faces or even have consistent managers while working, which ‘can lead to isolation and multiple cultures being developed across the organisation’. 112 A move to shift and agency working can make it more difficult to build social connections with colleagues, which reduces the ability to communicate effectively and makes staff less likely to feel supported. 113 The consequences of this were highlighted by one study, in which a participant reported that shift working was:
… leading to staff being unable to build a sense of team collegiality ‘because I now work with so many different people – no-one has my back any more’. 76
This was highlighted as inhibiting an ability to cope, because: ‘I can’t confide to my manager because I never see them and now I can’t confide with my mate because I don’t know who my mate is’. 76 When staff are unable to cope, this can cause a spillover of frustrations in the form of UB:
… when [staff] themselves might not be coping [they] take out their frustration by lashing out at other staff. Such behaviours reportedly led to conflicts. 106
The dynamics of social support are reflected in CMOC 9.
CMOC 9. If staff work in shifts (C), then this can reduce the ability to cope when experiencing UB or workplace stressors (M18/O1) and reduce self-confidence (M19/O2), which can worsen the impact of UB on health and well-being (O3) because shift work can reduce the ability to build social connections (M16) and lessen feeling that one is socially supported (M17).
Reduced ability to communicate effectively
Connected to social support and many other contributors of UB, the ability to communicate effectively is also crucial. As highlighted earlier, several factors can reduce the ability to communicate effectively, including a culture of pressure or intimidation and high job demands. As such, an inability to communicate effectively can form vicious circles that increase the impact of UB on staff and directly exacerbate conflicts. This is highlighted in the following quote, in which a cycle between communication and frustration is outlined:
a lack of communication between the physician and the nurse can result in stress for the nurse […], and conflict between nurses and physicians and between nurses results in feelings of anger and frustration. 110
This causal chain is depicted in Figure 7, whereby working in a high-pressure environment, for example (C), can lead to a reduced ability to communicate effectively (M4) and, therefore, to greater frustration (O1/M5) – which can directly lead to conflict and escalating UB (O2). One study interviewing hospital staff reported that a high-pressured clinical environment could also become associated with feeling psychologically unsafe:
…I felt unsafe in that environment… In the theatre environment at this hospital, I have been sexually harassed verbally and bullied by senior staff …. 77
Additionally, an inability to communicate begets further UB as it undermines a sense of social support. 109 Sources highlighted that ‘simple gestures such as open, honest, transparent communication go a long way to build rapport with workers’. 114 This is reflected in CMOC 10. Issues with communication quality can also cause clinical information to go uncommunicated and can allow medical mistakes to go unchallenged, affecting patient safety (see Figure 12). 14
FIGURE 12.
Diagram depicting programme theory of the causal chain from UB to reduced patient care quality and safety. ‘M/O’ = mechanism/outcome (depending on component of causal chain which is in focus).

CMOC 10. If staff work in a high-pressure environment or in a culture of intimidation (C), then this can lead to reduced ability to build social connections (M16/O1), a reduced sense of social norms (M15/O2) and a reduced sense of social support (M17/O3) because there is a reduced sense of psychological safety and ability to communicate effectively (M14).
Depicting the process of reduced social cohesion
Figure 8 depicts the core CMOCs underlying the contributors in this section. CMOC 10 is depicted by drawing on M15, 16 and 17. The figure also depicts how these mechanisms – such as M17: Reduced feeling of social support – can impact both self-confidence and ability to cope.
Category 4: Harmful work cultures
Leadership is a key contributor to how harmful work cultures come into being and persist. Behaviours exhibited by those in senior positions enable, model or tacitly permit UB to continue in their organisations. We articulate this in the following ways: (1) complicit and permissive leadership, (2) negative role-modelling and prior learned behaviour, (3) an authoritarian culture, (4) a lack of organisational accountability, (5) organisational deafness and (6) cliques.
Complicit and permissive leadership
Our findings indicate that enablement of harmful work cultures generally requires the permission (active or tacit) of leadership in order to persist – that is, being complicit. One example from the USA is the promotion of ‘high-performers’, even when it is known that they engage in UB. This reflects both a complicit and permissive leadership team:
The work environment is toxic with male surgeons who bring in high revenue streams to the hospital (and) seem to be allowed to treat staff as they please despite the fact that staff have raised concerns. 77
This can result in staff learning that UB is acceptable or even necessary to succeed, causing such behaviours to be replicated (CMOC 11).
Laissez-faire (permissive) leadership can lead to a situation where UB is allowed to persist through avoidance or negligence and can signal that there would not be consequences for potential instigators. 76,101 With respect to UB, if a hands-off leadership team does not address UB, it further reinforces their complicity – a dynamic reflected in CMOC 12. At the other extreme, leaders and managers engaging in micromanagement may also be perceived as bullying. 68
CMOC 11. If a workplace has a prevalence of UB and leaders/managers are not seen to address it by being complicit or laissez-faire (C1), then this can cause staff to engage in UB (O) and reduce trust in leadership (O2), because UB is perceived to be normal (M13).
Negative role-modelling and prior learned behaviour
Negative role-modelling and prior learned behaviour within the workplace – particularly by those more senior – can reinforce negative prevailing social norms within an organisation (in line with CMOC 11) by giving the impression that management tacitly support engaging in UB. 93 This can directly lead to staff replicating these negative behaviours, reducing the sense of social cohesion within an organisation. For example, in some cases, negative role-modelling created learned behaviours, for example where ‘nursing students can be bullied by one another and by faculty in both face-to-face and online learning environments’. 99 This can lead students or staff moving organisations to bring practices with them into the workplace that propagate a bullying culture. 115 See CMOC 12, below, for a depiction of how this contributor works.
CMOC 12. If a workplace has a prevalence of UB and leaders/managers are not seen to address it (C) – or they role-model it themselves (C2) – then there is an increasing likelihood of others engaging in UB (O) and reducing trust in leadership (O2) and little change (O3), because the impression can be given that incivility and other UB is tolerated and normalised (M13), which reduces perceived risk for instigators (M12) and, for victims, ability to speak up (M21).
Authoritarian culture
An authoritarian leadership style was also reported as creating an environment in which UB can thrive. One study cited that this may happen in high-pressure environments, such as operating departments in which ‘professional stressors related to surgical processes and procedures appear to activate or elicit authoritarian and hierarchical modes of interacting between inter-professional groups’. 77 Existence of such a leadership style for a prolonged period can lead to the development of an authoritarian culture, which can also inhibit psychological safety and, consequently, speaking up. Chadwick and Travaglia57 highlight how an authoritarian management style might result in UB: ‘An autocratic manager may engage in workplace bullying simply by exerting their authority over others, making unreasonable demands or excluding staff in decision-making processes which are within their authority’. 57 By excluding staff from processes that should be in their remit, authoritarian management styles can reduce ‘problem-solving efficacy’, which has been put forward as an antecedent to psychological safety and can impact patient safety. 83 It also creates an atmosphere of intimidation in which people do not feel psychologically safe to speak up. This dynamic is reflected in CMOC 13.
Lack of accountability by leadership
A culture of tolerance of UB can also be signalled by a lack of accountability taken by leaders when UB is reported. From interviews with healthcare staff, one included study highlighted the impact this has on healthcare staff directly:
(e.g.) a clinician raising unprofessional behaviour of another clinician from a different discipline, reports up through line manager/stream manager, only for the reporting clinician to be made ‘the problem’… shunt off to EAP (employee assistance services) … unprofessional behaviour continues …. Line manager and line manager’s manager continually demonstrate unprofessional behaviour. 77
Quote reproduced in part from BMC Health Services Research (https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-07763-3) in line with the CC-BY 4.0 Licence.
Such a dynamic and the impact this has on perception of the organisation by staff are reflected in CMOC 13.
CMOC 13. If UB is prevalent in a workplace and managers are seen not to address it – or even negatively role-model such behaviours themselves (C) – then this can reduce psychological safety (M21/O1) and reduce trust in management (O2) because staff sense that the organisation is deaf (i.e. that they do not care about UB) (M10): creates an intimidating culture (M20).
Organisational deafness
The literature reviewed suggests that how organisations visibly respond to UB sends a strong signal indicating cultural direction. Turning a blind eye or the organisation (represented by managers and leaders) not reacting to staff concerns can cause proliferation or at least lack of reduction in UB. When people speak up but do not feel heard and no action is taken, this can be referred to as organisational deafness116 in the literature. Jones and Kelly116 highlight that, in many cases, employees who do try to speak up and indicate that there is a problem receive no acknowledgement or response from their managers or the organisation (a ‘deaf’ effect). The signal this sends to staff cannot be overestimated and the damage to trust between employees and their leaders may be as damaging as the UB itself. This places an onus on organisations to be actively listening and acting on concerns in order to tackle UB issues as they arise.
In some cases, the deafness may be more purposeful, in which case it could be termed a form of organisational tolerance of UB. 117 One example behaviour, as mentioned previously, is promotion of high-performing clinicians who are known by staff to engage in UB. 115 The literature highlighted that active tolerance of UB was noted in some organisations. Additionally, in other situations, organisations and managers may not know that UB is taking place, because a lack of psychological safety means that issues are not reported and hence not known to managers (CMOC 14).
CMOC 14. If a reduced sense of psychological safety leads people to not speak up (C), then strategies to address UB are not implemented (M23/O1), reducing trust in leadership (O2) because managers are not aware that UB is taking place (M22).
Cliques
One paper identified that informal alliances or cliques can create an environment in which UB is tolerated or even encouraged by local line managers, with one included study stating ‘a tolerance of bullying behaviour formed because of the power of these alliances. “They were really a strong force, really opposing anything different. And, they were (...) fairly united and stuck together”’. 118 Included sources suggest that cliques can manifest themselves at any hierarchical level and operate to undermine and minimise challenge and speaking out by weaponising social ostracisation and intimidation tactics. 119 By amplifying a culture of intimidation that can damage psychological safety and inhibit speaking up, the dynamics through which cliques work can reflect CMOC 1 as well as CMOC 14.
Depicting how harmful culture and organisational processes affect UB
Figure 9 depicts how both a harmful organisational culture and organisational processes (as evidenced in a recent report regarding University Hospitals Birmingham8) can drive UB. For example, CMOC 12 is reflected in M12 and M13 in the diagram and a ‘vicious circle’ is depicted between social norms that enables incivility and a reduction in the perception that management cares about UB.
Proximal outcomes
Development of our CMOCs led us to understand that contributors had three main outcomes that worsened UB and its impacts: (1) an increase in proclivity to engage in UB, (2) reduced ability to cope with the effects of UB and (3) reduced ability to report or challenge UB, which allows it to continue as UB is not directly challenged and managers are not aware of where UB is taking place (Figure 10). This is reflected in existing CMOCs throughout this chapter and is also depicted in Figure 11.
Interactions of contributors
This chapter has so far elucidated the core contributors to UB, which include: (1) feelings of workplace disempowerment, (2) organisational confusion, uncertainty and stress, (3) job and organisational designs that inhibit social connection and (4) harmful work cultures as a direct result of poor leadership and management. Within each category, we have discussed and depicted a number of ‘vicious circles’ that impact day-to-day practice in the partial programme theory diagrams. 120 However, there was not space to textually discuss every aspect of the complexity. We have formulated Figure 11 to depict the full scope of relationships between contexts, mechanisms and outcomes. Mechanisms (ellipses) are still numbered and are consistent with other CMOCs and figures throughout this chapter.
The proximal outcomes discussed above are reflected in Figure 11 as a reduced ability to cope in contexts where UB occurs (see Figure 11, mechanism 18), as well as a reduced ability to speak up to address UBs (mechanism 21). As discussed above, some contributors (such as a competitive environment, working in a disadvantaged group or a lack of job resources) also lead to an increased proclivity to engage in UB. The mechanisms (shown as orange ellipses in the figure) that increase proclivity to engage in UB include: feeling the need to compete (M8), scapegoating/undermining (M9), low risk to engage in UB (M12), frustration (M5), reduced ability to communicate effectively (M14), internalisation of oppression and (M4) reduced ability to perceive social norms (M15).
Our overarching programme theory in Figure 11 presents the complexity of the contributors and their interactions to allow us to better understand the underlying contexts, mechanisms and outcomes and how they interconnect. For example, a lack of job resources (C) can lead to frustration and a feeling of powerlessness (M5), which can then lead to reduced ability to cope (O/M18). As another example, permissive leadership (C) can lead to a management style interpreted as UB (M12) increasing incivility among staff (O/M14). This can then form a causal chain: the change in organisational norm towards incivility (C) can create an atmosphere of intimidation (M20), which can reduce sense of psychological safety to speak up (O/M21). These dynamics highlight that mechanisms for one CMOC can form contexts or outcomes for another – meaning that one contributor can have echoes throughout the rest of the system, which can dangerously escalate.
Figure 11 also shows how contributors generally feed into each other from left to right. That is, workplace disempowerment connects to social cohesion, before affecting ability to speak up and manager awareness of UB, whereas battling organisational processes and enablement of a harmful culture more directly connects to reduced ability to speak up. Additionally, social cohesion connects directly to a reduced ability to speak up (M19 to M21). It is important to note that, while the diagram is complex, it is still a simplification of the complexity inherent in understanding UB in healthcare organisations.
Distal outcomes
The outcomes presented below are too distal to connect to any one example or CMOC above. However, any of the reported contributors already mentioned could negatively impact (1) psychological well-being of staff, (2) the organisation in terms of productivity, engagement and motivation and (3) patient safety and care quality.
Impact on psychological well-being
Being exposed to UB can have a negative impact on psychological well-being. 121 A recent realist review of factors impacting psychological ill-health in nurses, midwives and paramedics found that working in an environment in which staff mistreat one another can create moral distress that can lead to stress and burnout. 121 Other impacts on psychological well-being from UB exposure include post-traumatic stress, anxiety, depression and sleep disturbances. 122 Bystanders and those witnessing UB can also experience a corresponding impact on their own psychological well-being or moral injury from not being able to prevent the UB. 21 In some extreme cases, those on the receiving end of UB have resulted in suicide. 123 Other impacts of UB explored in this chapter – such as a loss of confidence – can also reverberate and further reduce staff’s ability to cope with UB. While we have formulated a programme theory for how patient safety is impacted by the presence of UB in Figure 12, we were not able to do so for staff well-being. This is because the impact on well-being from UB is highly variable, dependent on individual and circumstantial factors, and no one type of UB is guaranteed to lead to a particular type of well-being impact (such as anxiety or post-traumatic stress).
Impacts for organisation
As well as affecting staff psychological well-being, impacts of UB on an organisation can include reduced productivity due to time spent tackling UB, low morale, coping strategies such as staff taking time off, increased staff turnover, lack of work engagement and loss of respect for management,124 with significant economic ramifications. Included sources highlighted, for example, that hiring a new nurse can cost twice a nurse’s salary. 54 Likewise, in the USA, one study reported that an average-sized hospital will spend $379,500 per percentage point increase in turnover rates (based on 2011 figures) in recruitment costs, with poorly performing organisations faring worse and paying up to $3.6 million per percentage point increase. 62 Put another way, sources indicated this cost was $30,000–$100,000 per nurse actively experiencing incivility,63 with another study estimating this at $22,000–$64,000 per nurse (figures from 2015). 125 Another study identified that, prior to an intervention in their hospital, costs due to annual staff turnover being 11.5% were $19 million annually. 126 Finally, one study calculated that a ‘conservative estimate’ of the total cost of incivility on a per incident basis was $250,000 even in 2008. 62 These figures, universally high, indicate the considerable financial impact of UB if left unaddressed by organisations, with the US-based literature generally having more focus on the economic impact of UB. However, it is unclear whether these numbers include the hidden clinical cost of reduced performance in terms of care quality, safety and impact on psychological well-being.
Impact on patient safety and care quality
An environment rife with UB can inhibit provision of quality care for patients. 97,127,128 This occurs largely through ineffective communication, which makes it difficult to transmit the accurate information for complex medical procedures. During our analysis, we coded and analysed passages from our sources to understand how and why patient safety might be impacted by UB. Our realist analysis of how this occurs allowed us to form a programme theory that underpins the causal chain from UB to patient safety and care quality (see Figure 12). As Figure 12 shows, the presence of UB has four immediate impacts: (1) a loss of self-worth and confidence, (2) impaired communication, (3) reduced trust in teams and (4) impaired concentration. Intermediary outcomes identified include (1) inhibition of psychological safety, (2) being dishonest to avoid criticism, (3) inability to communicate essential clinical information and (4) working while distracted. Likewise, the presence of UB can cause (1) loss of passion, (2) inability to point out clinical errors and (3) reduced ability to learn. These factors can lead directly to an increase in clinical errors, as well as longer-term impacts – such as staff turnover and entrenched bad practices – ultimately leading to reduced care quality and safety (Figure 12).
Outcomes for different groups
Evidence within included sources was mixed regarding the susceptibility of various professional groups to UB – except for a few cases, which are explored here.
Minoritised groups
Our results indicated that exposure to UB among marginalised groups may be a combination of harmful cultures that reflect wider societal attitudes, that is, issues such as structural racism and patriarchy69 – as well as interactions of other dynamics highlighted here, including hierarchy. As such, societal attitudes provide the wider context in which UBs occur in healthcare organisations. Groups that may be oppressed and/or who experience more UB than others in the healthcare workplace include (but are not limited to) nurses,102 women, members of disadvantaged social groups such as staff from ethnic minority backgrounds70 and people with a disability. 129 Staff from marginalised backgrounds are more likely to work in shifts or as agency staff, which led to 47% of minority staff being in pandemic-specific roles compared to 31% of all staff. 79 However, at the same time, the pandemic and social movements in the early 2020s (such as #BLM and #MeToo) were reported to have increased focus on misogyny, sexism, racism, homophobia, equality issues and UB more generally. 75,79
Staff from abroad were also found to encounter difficulties, even while many health systems (e.g. the NHS) are recruiting internationally and becoming increasingly diverse. Speaking English less well than others or with a strong accent was found to affect peer relationships69 and could cause staff to feel marginalised. The difficulties of coming from a non-white racial background was reflected in included sources, where, for example, ‘… in my earlier job when I was leading the team, people will come … and will meet me sitting down and they will bypass me and go to white staff’. 69
In terms of forms of UB, we did find staff with protected characteristics were more likely to be targets of UB in the form of harassment, discrimination and microaggressions. 74,75 People with protected characteristics can be discriminated against based on age, gender, race, religion, sexual orientation, relationship status, country of origin, disability or pregnancy. Included literature highlighted that LGBTQ+ staff were the second-most likely to experience UB in the healthcare workplace after staff with a disability. Although staff networks were mentioned as a resource LGBTQ+ staff can turn to, no interventions in the literature sought to improve forms of UB such as homophobia or transphobia. 130 Staff with a disability were found to more frequently experience forms of ableism from managers, often stemming from a sense that managers were not sufficiently accommodating of their needs in the workplace. 131
Microaggressions have been defined as ‘stunning and automatic acts of disrespect arising from unconscious attitudes inflicted by the culturally dominant groups’. 69 The impact of microaggressions was found to build up and have a detrimental impact over time, silencing recipients and making them feel disregarded – as well as, for example, reducing their job performance and leading to poor psychological health,132 indicating that microaggressions are no less serious than other forms of UB. 74,75 A review of NHS culture by Kline70 highlighted that microaggressions are an insidious form of racial harassment but that, in their review of culture at an NHS trust, few people could define them or their impact. Additionally, one report on culture in an NHS trust found that the presence of a harmful culture in which senior leaders ‘won’t say anything because they’re afraid of being called racist’70 led to inhibition of strategies being implemented to address the issue. These factors are represented in CMOC 15.
People with protected characteristics (C) are more likely to experience UB from other staff members (O) because they are at higher risk of being in disempowered positions in the workplace (M1), may be less likely to receive social support from colleagues (M2) and because stigma can prevent structural issues (racism, sexism, ableism or transphobia) being acknowledged or addressed (M3).
Students and those new to the profession
One group highlighted within the literature as more susceptible to being on the receiving end of UB were newly qualified staff and students, who are often at the bottom of the workplace hierarchy and are unsure about social norms when entering work. 133 Included sources referred to both medical students and graduate nurses as more prone to impacts of UB. For example, one study reported 31% of newly graduated nursing students indicated they were experiencing bullying. 134 Other sources reported that this could lead to nurses leaving the workforce at an early stage and changing career, particularly those from ethnic minority backgrounds. 32 Many of the UB contributors that impact graduate nurses are the same as those already explored in this chapter but amplified. Sources often reported that graduate nurses experienced UB more frequently – often with exclusionary behaviours such as other staff being dismissive of them. 135
During the early years of their careers, graduate nurses are highly reliant on their relationships with mentors and supervisors, and trust in their supervisor is key. At the same time, for students, this must be balanced with a feeling that they are useful and contributing to their work environment. 101 The impact of high job demands can most negatively impact those new to the profession, reducing time interacting with more experienced colleagues. 136 Seeking interaction with mentors and supervisors generally is analogous to a search for role models. If mentors and supervisors model UB-promoting behaviours, graduate students are more at risk of internalising such negative behaviours and potentially subsequently reproducing them (and perceiving them to be normal). 137
Sources suggested it should be possible to intervene at the junction between studentship and entering the workforce, perhaps with education and awareness or role-playing interventions (e.g. anticipatory socialisation interventions), delivered as they join an organisation. 68,138,139 One intervention with students implemented problem-based learning to prepare them for UB they may face upon graduation and reported success at raising awareness of UB and mechanisms to tackle it139 (see CMOC 16).
Staff such as students and others new to the healthcare profession (C) can experience more UB than other groups (O) because they are seeking to integrate into the social environment and be accepted, which makes them socially vulnerable (M1). They may have less concept of the pervading social norms (M2) and may be perceived by others as less capable (M3).
Surgeons, doctors and nurses
As previously reported, evidence regarding doctor-to-nurse interactions overall was mixed. 95 However, one consistently reported problematic interprofessional interaction was in a surgical context. This perhaps relates both to stricter hierarchy and the high-pressure environment of surgery. 91 The presence of a steep hierarchy was often cited as inhibiting effective communication (reducing psychological safety), which can impact patient safety and care quality. 109 A study across seven Australian hospitals in 2022 highlighted that this is still an ongoing problem, with one participant stating ‘Some (surgical medical staff) in theatres are still very rude to nurses – every week I would witness a surgeon raising his voice, yelling, throwing things out of anger and impatience …’. 77 However, despite the incidence of steep hierarchy leading to increased UB in a surgical setting, nurses reported that UB originating from other nurses was more hurtful than that from other professional groups – indicating that intraprofessional or ‘in-group’ UB may be perceived to be more psychologically damaging110 (see CMOC 17).
If UB is experienced at an intraprofessional level (C), then it can be perceived to be more harmful (O) because it can feel like more of a betrayal (from within one’s own profession) when horizontal violence occurs (M1) and can have a greater impact on interpersonal relationships that are more frequent and meaningful (M2).
Key findings
This chapter focused on the four broad types of contributors to UB: (1) workplace disempowerment, (2) organisational confusion, uncertainty and stress, (3) work and organisation designs that inhibit social connection and (4) harmful workplace cultures that tolerate UB. Our full programme theory has depicted how these categories can also interact with one another to form vicious circles (e.g. frustration limiting ability to communicate thus causing more frustration) (see Figure 11). These contributors can broadly lead to: increased propensity to engage in UB, a reduction in the ability to cope when UB is present, and a decrease in ability to report or challenge UB. In terms of who is most at risk, women and new entrants to the profession, as well as individuals from marginalised groups including black, minority, and disabled staff, are at greater risk of UB. Evidence regarding interprofessional interactions (e.g. doctors and nurses) was mixed in terms of frequency but evidence did suggest that intraprofessional UB was more harmful than interprofessional UB to well-being.
Our findings have identified outcomes at both a distal and a proximal level. Proximal outcomes included impacts to reduced ability to cope, increases in UB and inhibition of ability to speak up. Distal outcomes included directly reducing patient care quality and safety through several mechanisms, including inhibiting ability to report mistakes, reducing ability to learn and impairing concentration and communication. Sources also identified negative impacts on staff psychological well-being from being exposed to UB in the workplace. Sources reporting on the effects of UB on organisations (such as reduced staff engagement and poor retention, leading to economic impact) highlight potential significant cost savings when reducing UB. This chapter and the associated evidence challenges the ‘bad apples’ individual approach and emphasises considering broader and more systemic contributors to UB, such as workplace design.
Chapter 5 Interventions to reduce unprofessional behaviours between staff in acute healthcare settings
Introduction
This chapter describes and explores the 42 interventions identified in the 148 sources included in our review. We categorise interventions in the first instance, before exploring their settings, evaluations and findings within acute healthcare settings. Strategies to change behaviour are outlined in Chapter 6, which discusses how they work. Chapters 7 and 8 explore more contexts in which interventions may or may not work. We conclude this chapter with some summary CMOCs to reflect differences between different identified intervention types.
Interventions versus strategies
In this chapter, we refer to both interventions and strategies. Interventions are defined as ‘co-ordinated sets of activities designed to change specified behaviour patterns’. 140 Interventions are broad, typically comprising (1) the apparatus for delivering strategies, (2) the strategies themselves and (3) the evaluation methods assessing their effectiveness. 140 Strategies, on the other hand, are components of interventions and comprise the specific activities of an intervention. 140 This may include, for example, behaviour-change techniques (BCTs). BCTs and related strategies are defined as the ‘active ingredients’ within interventions that aim to change behaviour in specific ways. 140 Figure 13 provides a visual depiction.
FIGURE 13.
Umbrella diagram depicting components of an intervention.
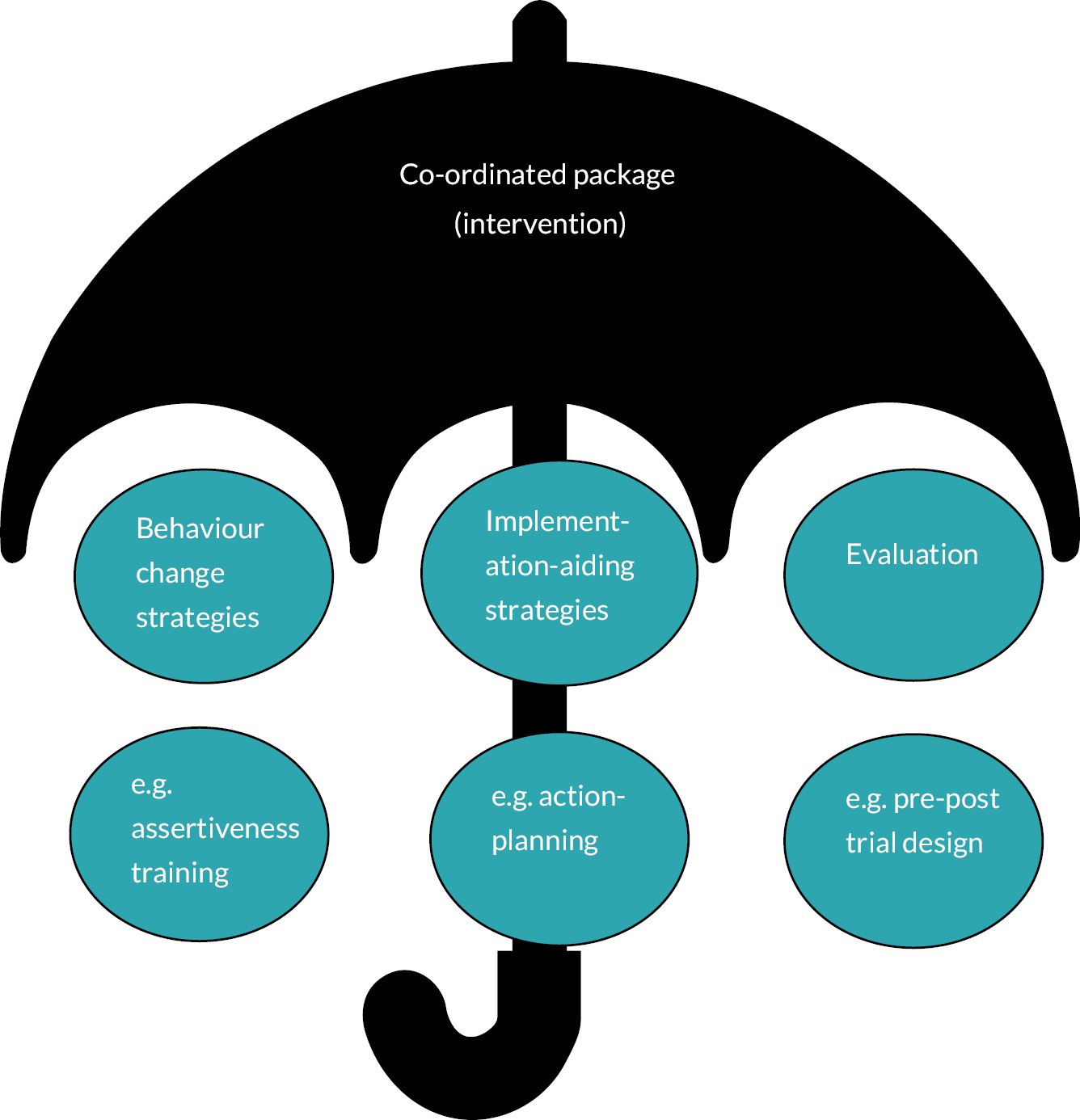
We have fully tabulated details on the 42 included intervention papers in Appendix 6, Table 28. Of the 42 interventions discussed in the first part of this chapter, 30 were conducted in the USA,53,54,62–67,71,72,98,104,107,125,126,134,137–139,141–152 5 in Australia,93,97,103,127,153 2 in Canada154,155 and 2 in South Korea. 61,156 One intervention was delivered in Turkey,157 another in Ireland152 and one final one in Iran. 158 We identified no sources reporting on an intervention that was implemented in the UK. Thus, no interventions have been delivered and reported from a UK context – which is striking, given the high rates of bullying reported in NHS staff surveys. 16 However, we do acknowledge that there are several ‘in-practice’ interventions taking place in the UK and elsewhere; we explore these in Appendix 7.
Intervention design and types
This section explores the characteristics of the 42 papers directly reporting on interventions, including study designs, use of theory, samples, duration, flexibility, effectiveness and use of outcome measures. Where possible, we categorise our analysis by intervention type. We categorised interventions into five types (Figure 14):
FIGURE 14.
Intervention types and quantities.
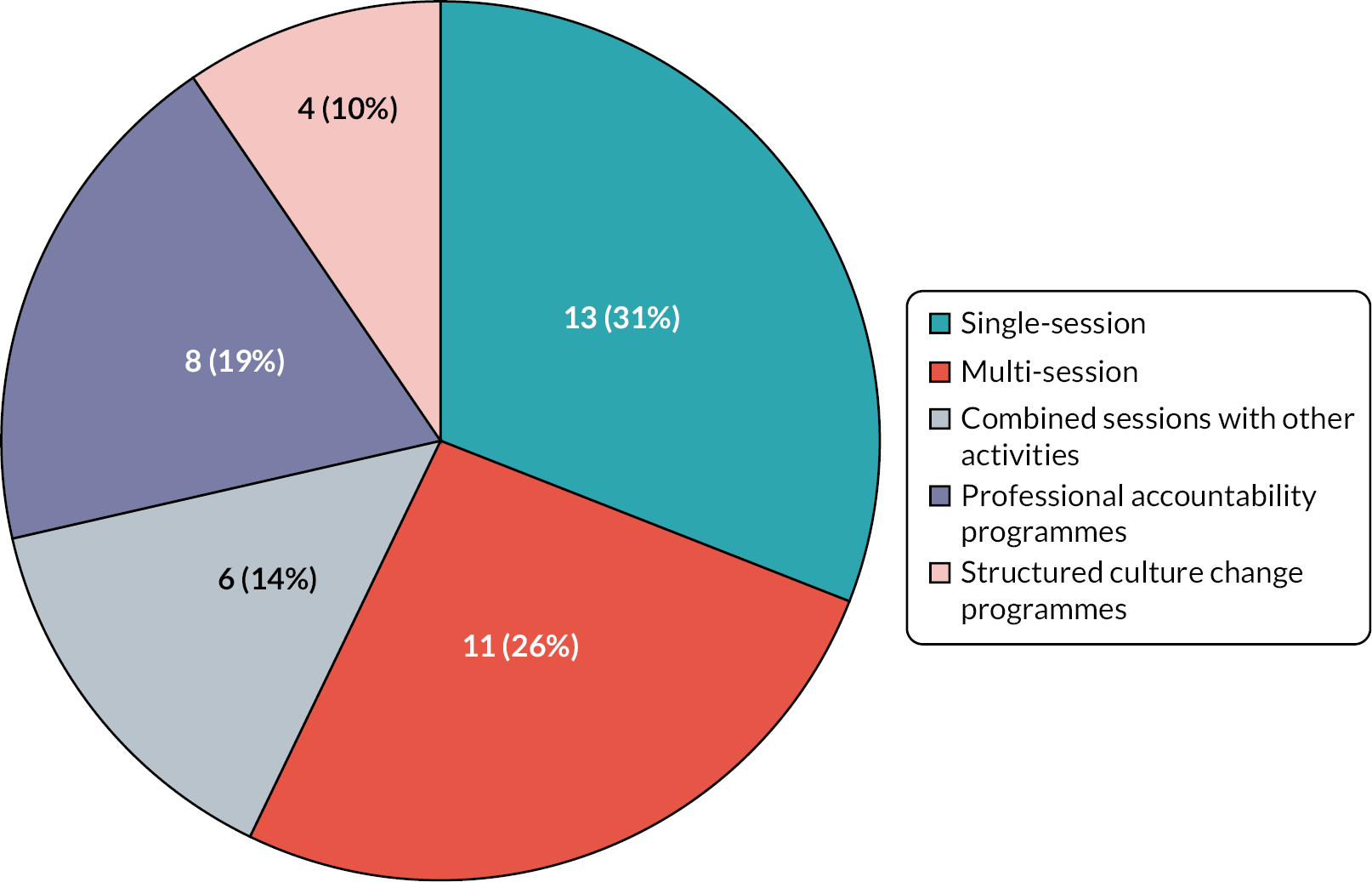
-
Single-session education/training-based interventions (n = 13: Ceravolo et al., 2012; Clark et al., 2013; Dahlby and Herrick, 2014; Embree et al., 2013; Griffin, 2004; Griffith et al., 2019; Hawkins et al., 2022; Kile et al., 2019; Nikstaitis and Simko, 2014; O’Connell et al., 2019; Stagg et al., 2011, 2013; Warrner et al., 2016)
-
Multiple session education/training-based interventions (n = 11: Asi Karakaş and Okanli, 2015; Banerjee et al., 2022; Barrett et al., 2009; Demarco et al., 2005; Jenkins et al., 2011; Kang et al., 2017; Kousha et al., 2022; Lasater et al., 2015; Nicotera et al., 2014; O’Keeffe et al., 2022; Saxton, 2012)
-
Combined intervention sessions with other activities, such as codes of conduct to form one intervention (n = 6: Chipps and McRury, 2012; Dimarino, 2011; Kang and Jeong, 2019; Parker et al., 2016; Stevens, 2002; Thorsness and Sayers, 1995)
-
Professional accountability and reporting interventions, such as Vanderbilt and Ethos (n = 8: Baldwin et al., 2022; Churruca et al., 2022; Dixon-Woods et al., 2019; Hickson et al., 2007; McKenzie et al., 2019; Speck et al., 2014; Webb et al., 2016; J. I. Westbrook et al., unpublished); and
-
Structured culture-change interventions, such as civility, respect and engagement in the workplace (CREW) (n = 4: Armstrong, 2017; Laschinger et al., 2012; Leiter et al., 2011; Osatuke et al., 2009).
Use of strategies across intervention designs
There were differences between intervention types and the strategies used, outlined as follows:
-
Single-session interventions drew predominantly on awareness-raising strategies such as education about UBs (n = 2). In 11 cases, this was also combined with role-playing and other activities intended to enhance and practise the ability to speak up and challenge UB in the moment.
-
Multisession interventions typically drew on similar strategies but often diversified the approach to include strategies aimed at increasing the ability to speak up or improving the ability to work together, such as assertiveness training (n = 1), problem-based learning (n = 1), conflict-management training (=1) group writing or journalling (n=2), and communication training (n = 1). However, most still drew on a mix of cognitive rehearsal/role-playing and education (n = 4).
-
Combined sessions with other activity interventions often sought to (1) have a training or education session to, for example, improve knowledge and awareness of UB and ability to speak up, alongside (2) non-session activities, such as the addition of a code of conduct (n = 6).
-
Professional accountability interventions often including a reporting and escalation system. These interventions typically combined this with training to enhance speaking up and role-modelling by leadership (in the case of Ethos97,127) or incorporated championing – that is, encouraging individuals to role-model and espouse the benefits of the intervention (in the case of Vanderbilt interventions53,93,98,143,147,151).
-
Structured culture-change interventions tended to utilise a case-by-case or bespoke response to organisational needs, including (1) action-planning to assess which strategies to implement and (2) surveys to understand the initial landscape of UB. Strategies used within these interventions included training on assertiveness, communication and conflict resolution, as well as for leaders and other social support-building strategies.
Intervention evaluation designs
The majority of studies did not use rigorous study designs to evaluate the interventions or assess effectiveness (Figure 15).
FIGURE 15.
Pie chart depicting number of studies using different evaluation types.
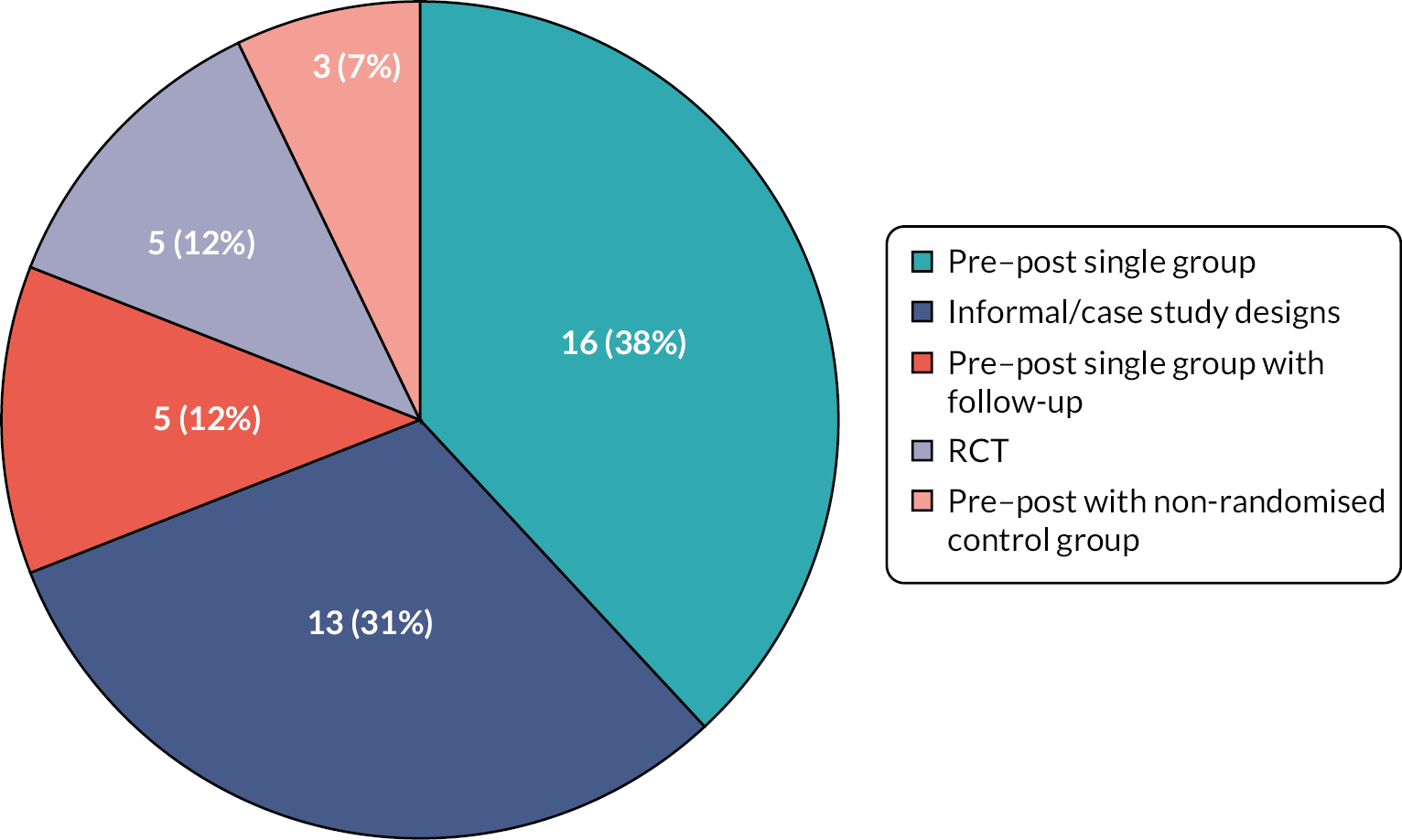
-
Sixteen of the studies used pre–post intervention study designs with very short follow-up periods (e.g. a survey immediately following a training session) and no control group. 54,62,65–67,72,104,126,127,139,141,142,148–150,157
-
Three further studies applied a pre–post design with a non-randomised control group. 107,146,153
-
Five other studies used a pre–post design with no control group but with the addition of follow-up data collection, ranging from 2 weeks to a year post intervention. 63,64,134,137,145
-
Five used a randomised or quasi-randomised controlled trial (RCT) design. 61,154–156,158
-
Thirteen were descriptive case studies or feasibility studies that did not report on effectiveness of the interventions. 53,71,93,97,98,103,125,138,143,144,147,151,152
Table 10 breaks down the intervention design against the evaluation design of included studies.
| Intervention design | Single session | Multiple session | Combined-session interventions | Professional accountability | Structured culture change | Total |
|---|---|---|---|---|---|---|
| Pre–post without control | 10 | 3 | 1 | 1 | 1 | 16 |
| Pre–post without control but with follow-up | 2 | 2 | 1 | 0 | 0 | 5 |
| Pre–post with control | 1 | 1 | 0 | 0 | 1 | 3 |
| RCT | 0 | 2 | 1 | 0 | 2 | 5 |
| Descriptive | 0 | 3 | 3 | 7 | 0 | 13 |
| Total | 13 | 11 | 6 | 8 | 4 | 42 |
Professional accountability interventions may be more difficult to evaluate and, thus far, they have only been reported in descriptive studies – with few data regarding effectiveness. It is also of note that interventions relying on single sessions to deliver their strategies also typically drew on pre–post designs without control groups, despite their lack of complexity – which should theoretically make them easier to evaluate in an RCT. This, perhaps, highlights a general lack of resources devoted to these interventions. CREW interventions originating in the USA seem to have been more well-resourced; as such, they have been assessed with more rigorous study designs, typically drawing on randomisation of entire hospitals or organisational units.
Use of theoretical frameworks and logic models
We extracted information regarding use of theoretical frameworks and logic models where it was explicitly mentioned. Descriptions of each theory are summarised in Table 11.
| Intervention type | Number of studies using theories | Theories used (and frequency) |
|---|---|---|
| Single session (contact time) | 3 out of 13 | Psychological theories:
|
| Multisession (contact time) | 7 out of 11 | Psychological theories:
|
| Sessions combined with other actions | 4 out of 6 | Psychological theories:
|
Organisational theories:
|
||
| Professional accountability | 0 out of 8 | N/A |
| Structured culture change | 4 out of 4 | Psychological theory:
|
Organisational theories:
|
Five interventions used organisational theories, including Model of Improvement by Langley,141 Kanter’s theory of structural power in organisations,155 a National Center for Organisation Development practice model,146 a Three-Level Intervention Model by Longo138 and Kilmann’s Model for transforming organisations. 150
Thirteen interventions drew on psychological theories, including Social Learning Theory by Bandura,137,145,158 Oppressed Group Behaviour,104 ‘Cognitive Learning Theories’,67 a ‘Six-Step approach to curricular development’,72 a theory of Non-Violent Communication,61,156 Einarsen’s predisposing factors for workplace bullying,134 Theory of Social Interactions at Work,154 Structurational Divergence theory107 and Transformative Learning Theory,152 and a final paper incorporated Harmonising Nursing Communication Theory. 64
In terms of intervention types:
-
Three (out of 13) single-session interventions drew on a psychological theory.
-
Seven (out of 11) of the multisession interventions drew on a psychological theory.
-
Four (out of six) of the combined sessions drew on psychological theories (n = 2) and organisational theories (n = 2) (Table 11).
-
All of the professional accountability interventions had entirely unknown theoretical frameworks (n = 8).
-
Four structured culture-change interventions drew on organisational development (OD) and organisational theories, with one drawing on a psychological theory; thus, all of this intervention type drew on some kind of theoretical framework.
As such, these results indicate that use of theoretical frameworks is most common in structured culture-change interventions and multisession interventions.
Use of theory in included studies was either weakly integrated or not adequately reported (Figure 16). In those studies that did draw on a theoretical framework, intervention developers generally used theory to understand only one aspect of the causal chain linking intervention components to a reduction in UB. For example, interventions either had a focus on ‘how people learn’ (e.g. Social Learning Theory) or ‘how conflict arises’ (e.g. Structurational Divergence Theory). No included intervention depicted a comprehensive logic model explaining the entire causal chain from intervention components to a decrease or reduction in impact of UB.
FIGURE 16.
Pie chart depicting use of theory in included interventions.
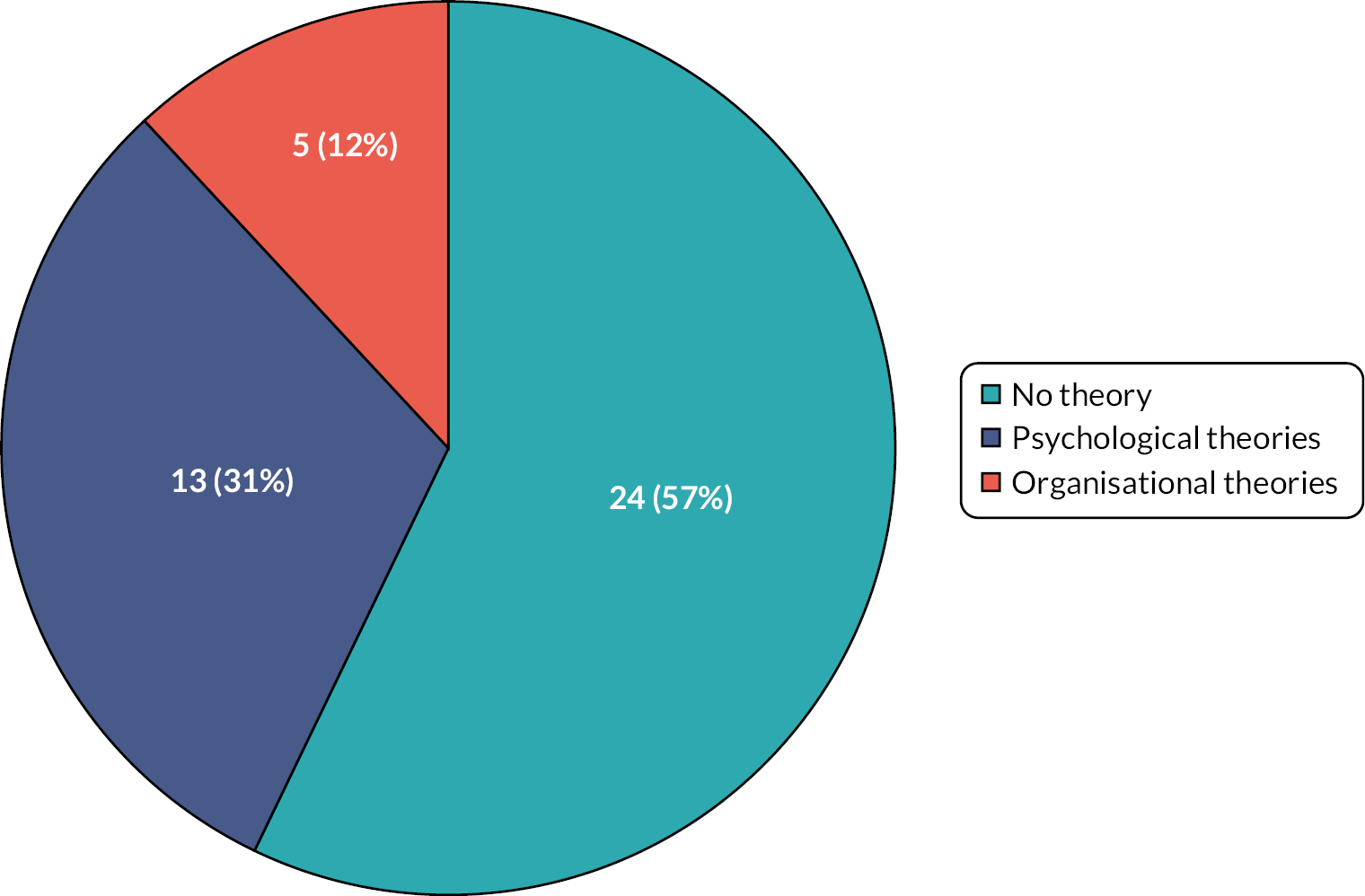
Intervention participant backgrounds
In terms of the professional background of participants, in 12 studies the samples were nurses,61,62,137,141,142,145,148,149,153,156–158 nursing students were sampled in three studies104,139,144 and ‘newly enrolled nurses’ in one further study. 67 One study included only doctors. 71 Another study drew on ‘nurses, students and faculty’. 126 A further 11 studies drew on a range of staff members. 54,64–66,72,93,107,134,146,150,152 Three studies drew on organisational ‘units’,63,154,155 seven on entire hospitals, multiple hospitals or healthcare organisations53,97,127,138,143,147,151 and three were unclear. 98,103,125 Unfortunately, it was not possible to combine and include professional groups for each intervention type in Table 12 due to heterogeneity and some studies including multiple professional groups; however, these data are tabulated for each study in Appendix 6, Table 28.
| Intervention type | Number of study types providing figures | Mean (SD) number of participants | Median number of participants |
|---|---|---|---|
| Single session | 12/13 | 53 (1422) | 26 |
| Multisession | 11/11 | 38 (53) | 45 |
| Combined-session interventions | 2/6 | 34 (28) | 44 |
| Professional accountability interventions | N/A | N/A | N/A |
| Structured culture-change interventions | 3/4 | 241 (588) | 1173 |
Table 12 depicts the average (mean and median) number of participants according to intervention type. Although numbers are limited, it shows that numbers for training interventions were similar, while efforts in structured culture-change interventions were typically broader in scope, reaching much greater numbers of participants. Some studies used an approach of intervening in entire units or sections of hospitals, with limited information provided with respect to the number of employees who received the strategies (n = 9) (Table 12); this may be due to the nature of the intervention (e.g. implementing a reporting system). Other interventions (n = 28) were delivered to a specific number of people, ranging from five participants to 5192. A small number of interventions had no defined number of organisational units or participants (n = 5). Interventions delivered to entire units or organisations may theoretically be more effective due to their breadth of coverage.
Duration of interventions
Many studies reporting durations of sessions gave a range of, for example, 60–90 minutes; this made it difficult to calculate averages. For example, Armstrong141 used a CREW intervention lasting 4 weeks with one 20- to 30-minute meeting per week, and Jenkins et al. 144 drew on a journal club intervention that had monthly 6-hour sessions for 6 months. Nonetheless, we have synthesised intervention durations where possible according to our identified intervention types.
In terms of intervention types, for single and multisession interventions we calculated total ‘contact time’ in minutes, rather than study duration, according to when outcome measures were delivered. This is because study duration according to evaluation timing was too heterogeneous and often not reported. Where possible, we calculated study contact time by multiplying session length by number of sessions (Table 13).
| Intervention type | Number of studies possible to homogenise | Mean (SD) duration | Median duration |
|---|---|---|---|
| Single session (contact time) | 11/13 | 93.14 (27.9) minutes | 120 minutes |
| Multisession (contact time) | 10/11 | 747.91 (520.0) minutes | 750 minutes |
| Sessions combined with other actions | Not possible | N/A | N/A |
| Professional accountability | 7/8 | 2.56 (1.2) years | 2 years |
| Structured culture change | 3/4 | 3.3 (2.36) months | 6 months |
-
Thirteen of the included studies relied on single ‘sessions’ of 2.5-hour duration or less (see Appendix 6, Table 28). Eleven out of 13 single-session interventions reported session duration. The mean contact time of single-session interventions was 93.14 (SD 27.9) minutes with a median of 120.
-
Ten out of 11 multisession interventions reported session duration. For multisession interventions the mean time was 747.91 (SD 520.0) minutes, with a median of 750 minutes. Ten studies relied on use of multiple sessions or sessions lasting longer than 2.5 hours. This shows the substantially greater contact time in multisession interventions, which could have given them greater opportunity to change behaviour. We can speculate that this may be one reason why such interventions report marginally greater effectiveness. The minimum contact time for multisession interventions was 240 minutes; this was greater than the maximum time in single-session interventions, which stood at 120 minutes.
-
The combined-session interventions were too heterogeneous to quantify and four out of six of these did not provide information on duration, while one comprised 8 weeks61 and another 3 weeks. 134
-
For professional accountability interventions and structured culture-change interventions, we were unable to calculate overall duration. Since these do not use ‘sessions’, their components may be engaged in by participants for multiple months or years. For professional accountability interventions, seven out of eight reported length in years. Of these, the mean was 2.56 (SD 1.20) years, with a median of 2.
-
For the structured culture-change interventions, these involved the CREW interventions; two of these were 6 months in duration,154,155 with one being only 1 month (see Appendix 6, Table 28). A final CREW intervention was unclear. 146
Table 13 depicts intervention durations or contact times where we were able to homogenise these.
Effectiveness
Most studies evaluated an intervention and assessed some measures of effectiveness (Table 14). Thirteen of the 42 studies were descriptive or examined only implementation or feasibility issues (see Table 10). Of the 29 studies that assessed intervention effectiveness, the majority (n = 23) reported positive results, while six studies did not report statistically significant results – and three even reported a negative result. 54,62,66,134,153,158 The most common reason for these ‘negative’ results was the use of education strategies, which led people to become more active in reporting UB; this, in turn, led to an increase in reports after the study when compared to baseline. 66,134,158
| Intervention type | Number of studies measuring effectiveness, n = 29 (69%) | Number reporting some positive effects, n = 23 (55%) |
|---|---|---|
| Single session (contact time) | 13 | 9 (69.2%) |
| Multisession (contact time) | 8 | 7 (87.5%) |
| Sessions combined with other actions | 3 | 2 (66.6%) |
| Professional accountability | 1 | 1 (100%) |
| Structured culture change | 4 | 4 (100%) |
In terms of intervention types reporting themselves as effective (where measured):
-
nine out of 13 single-session interventions
-
seven out of eight multisession interventions
-
two out of three combined-session interventions (although one did not report statistical significance150)
-
all (one out of one) professional accountability interventions
-
all (n = 4) structured culture-change interventions.
Figure 17 depicts the number of studies that self-reported effectiveness. However, some, for example, simply did assertiveness training, measured an increase in assertiveness and considered that a success. 157
FIGURE 17.
Pie chart depicting number of studies reporting ‘positive’ vs. ‘negative’ results, as well as those that did not measure effectiveness.
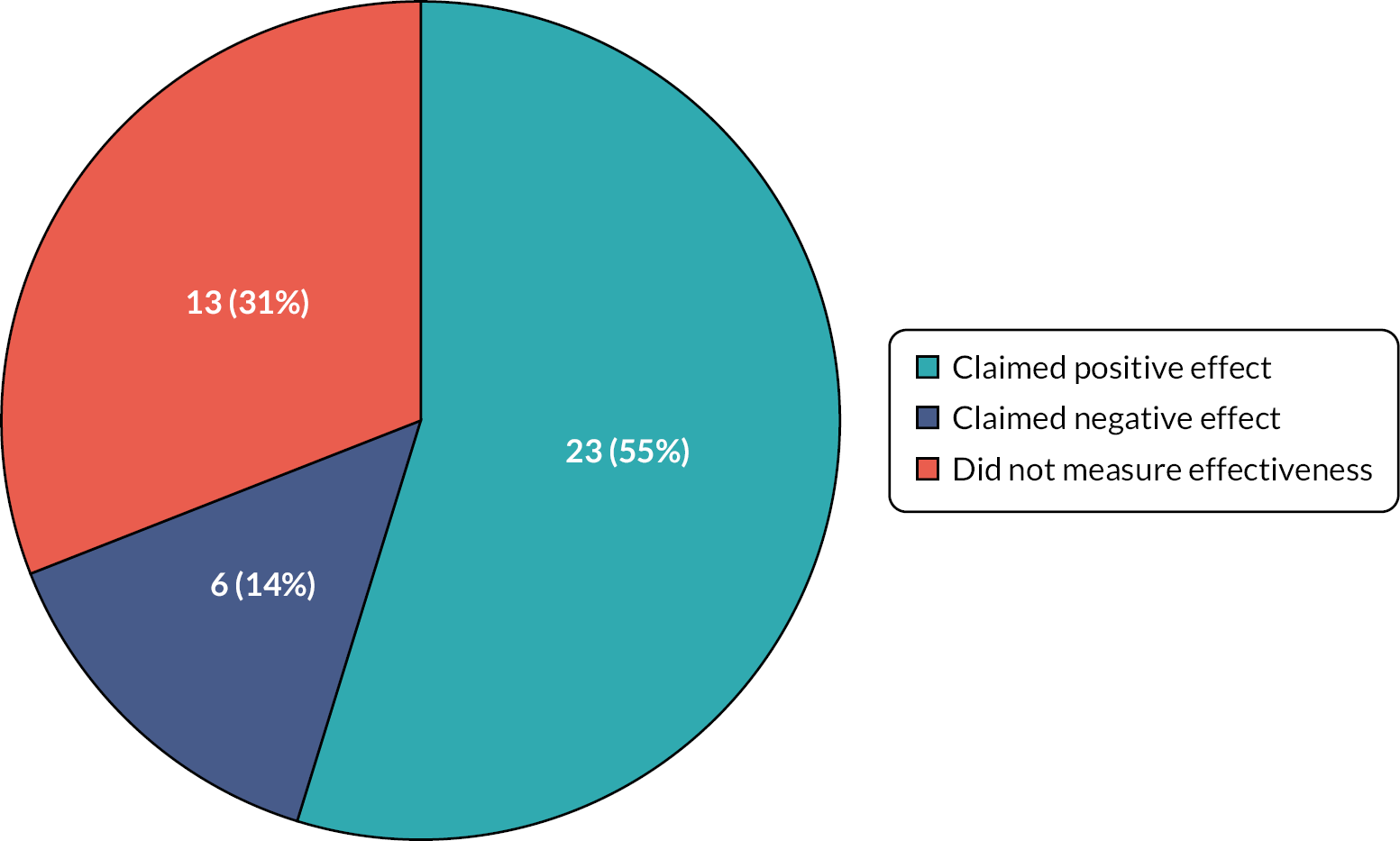
Outcome measures
Studies used a wide range of outcome measures; the most common was change in the prevalence of UB following implementation of the intervention. Overall, 23 studies measured prevalence. Common tools used to measure experience of UB in studies included the Negative Acts Questionnaire – Revised (NAQ-R) (n = 5), the Nursing Incivility Scale (n = 3)159 and the CREW Civility Scale146 (n = 2).
One study evaluating the CREW intervention used a range of measurement tools, including the CREW Civility Scale, Effort-Reward Imbalance Questionnaire, trust in management using an Interpersonal Trust at Work Scale, Turnover Intentions and Professional Effectiveness, among others. 154 Other studies that relied upon, for instance, assertiveness training, measured assertiveness with the Rathus Assertiveness Inventory as their primary outcome. 157 Several studies relied on qualitative measures primarily, such as interviews. 93,104,143 Other studies – primarily ones evaluating the Vanderbilt or Ethos interventions – drew on statistics from their reporting systems to determine its effects. 97,151 Appendix 5, Table 28, outlines the full range of outcome measures in included studies. No studies assessed improvements to patient safety – perhaps due to their limited intervention durations or difficulty in attributing changes in such outcomes to their intervention.
Intervention design responsiveness to context
Interventions may involve single or multiple strategies. For example, most of the classroom/single-session interventions draw upon single strategies. Interventions with multiple sessions may be bundle interventions where all strategies are implemented in every context. Indeed, most interventions drew on pre-planned study designs that were fixed (i.e. their implementation could not adapt or change during the intervention period). While this provided an easier way to evaluate the intervention, the trade-off was adaptability to unforeseen events that may occur during implementation. Those using a more responsive design included structured culture-change interventions and professional accountability interventions. These approaches tended to take an organisation-wide approach, relying on a repertoire of strategies that could be implemented on-demand depending on the type of UB encountered or setting. As such, intervention content could change and flex depending on the situation, which acknowledges that organisations are changing and dynamic systems. 146 Structured culture-change interventions such as CREW,141,146,154,155 for example, scheduled regular meetings to survey the organisational context and deliver different strategies depending on what factors were deemed to be contributing to unprofessionalism at any given time or in certain units. Osatuke et al. 146 set this out in their paper outlining the CREW intervention, stating that ‘for the intervention period, the VHA organizations commit to giving time, attention, and support to having regular (weekly) workgroup-level conversations about civility’. This builds momentum and a scaffolding around which other strategies can be implemented. The intervention can vary according to its context and the authors highlight that ‘across the sites, the specifics of in-group process and follow-ups are allowed to vary greatly, and as a result, the interventions become driven by responsiveness to local needs and local culture-based civility definitions’. 146 Taking this responsive approach – particularly with structured culture-change interventions – is purported to be integral to the success of these interventions.
Professional accountability interventions, such as Ethos and Vanderbilt, rely on a reporting and escalation system at their core. However, they also implement other strategies, including capability training and championing. 97 While professional accountability interventions such as Ethos are not as flexible as CREW, they do enable a variety of different escalating organisational responses depending on specifics of individual cases of UB. 127
Interventions outside the scope of this report
Our review and search strategy focused on identifying interventions specific to UB. We did not intentionally search for those seeking to improve civility and professionalism alone. Additionally, there may be many interventions that occur in practice but are not published in the grey or academic literature. Lastly, we identified some simulation studies investigating cognitive bias modification (CBM), a technique that may limit the impact of UB on ability to report medical errors. These were not included, as simulation studies were not interventions taking place in actual healthcare practice. Full discussion of these three categories of interventions outside the scope of this report is presented in Appendix 7.
Summarising intervention findings with context, mechanism and outcome configuration
In keeping with realist methodology, we present our overall findings with respect to different intervention types with CMOCs in Table 15.
| Intervention type | CMOCs |
|---|---|
| Single session | 19. If an intervention relies solely on single sessions (C) then, while they may raise awareness and knowledge of skills to tackle UB in an organisation in the moment (O1), any planned behaviour change may not be sustained (O2), because they are intended as a one-time hit of information or training and may be forgotten (M). 20. If an intervention relies solely on single sessions (C), then behaviour and sustained culture change may not happen (O), because it relies on individuals changing their behaviour without any systemic organisation-wide approach (M) |
| Multisession | 21. If an organisation seeks to implement a multisession intervention then, compared to single-session interventions (C), a greater transference of intervention content will occur (O), because it is possible to include more material and learning is repeated and reinforced, which facilitates greater retention (M) |
| Sessions combined with other actions | 22. If an organisation implements sessions combined with other strategies (e.g. a code of conduct) (C), then this may increase the spread of knowledge about how to address UB (O), because they are both establishing more systemic change and individual knowledge gain/attitude changes through training or education (M) |
| Professional accountability | 23. If reporting and escalation systems – and education about how to use – them are implemented to address UB (C), then a clear message of no tolerance is sent to employees (O), because a new and structured route for speaking up is created (M) |
| Structured culture change | 24. If organisations have access to financial and material resources that allow them to address UB in a setting-specific manner with a structured culture-change intervention (C), then they will be better able to tailor their response to local UB as it occurs (O), allowing for contributors to be more directly addressed over time (M) |
Chapter 6 Strategies to mitigate, manage and prevent unprofessional behaviours, and how and why they work
Introduction
This chapter focuses on describing behaviour-change strategies that are incorporated into interventions (or are more informal activities) that seek to mitigate, manage or prevent UB, and how and why they may work. In the following section, we first explain what we mean by evaluated versus unevaluated strategies and then present our identified categories of strategy, discussing each with CMOCs to explain how strategies work in specific scenarios. The formulation of CMOCs in this chapter will draw upon the method outlined by Dalkin et al. 35 (further discussed in Chapter 3).
Evaluated versus unevaluated strategies
Throughout this chapter, we have made distinct whether strategies are evaluated or unevaluated, where unevaluated means not yet assessed for feasibility or effectiveness. We have separated discussion of these throughout this chapter to increase our ability to discuss whether evaluated strategies were found to be effective. We have explicitly noted all strategies we identified, as well as those that have been evaluated in some form as part of an intervention in Table 16. Even though some strategies have not been formally evaluated in the academic literature, these strategies may still be widely used in practice and considered to be effective by those implementing or using them.
| Strategy | Description | Publications reporting an intervention using the strategy (evaluated) or example sources that mention the strategy (unevaluated) |
|---|---|---|
| 1. Direct or indirect approach to instigator (victim, bystander or managers) | ||
| Informal resolution | Approaching an instigator individually or their line manager, to have the individual reflect on behaviour or change future behaviour or resolve the situation | 97,98,147,151 |
| Disciplinary action | Process of individual being identified as problematic and disciplinary action taken against them by managers. Usually combined with reporting system of sorts | 93,97,98,143,147,151 |
| Peer messengers | Peer messengers deliver reports about UB to potential instigators, on behalf of other people who have been targeted and submitted a report to a reporting system | 53,97,127,151 |
| Mediation (unevaluated) | Victim and instigator try to resolve their differences with aid of a trained mediator who creates safe environment for discussion | 78,112,124 |
| Changing/ softening language (unevaluated) | Attempts to change or soften language when reporting mistakes made by clinicians | 160 |
| Speaking up (unevaluated) | Going to a person (e.g. Freedom to Speak Up Guardian161) or authority to report the incidence of UB in an organisation – or could be simply to state in the moment that one is uncomfortable with someone’s behaviour. Requires adequate psychological safety | 11,78,103,143 |
| 2. Improving confidence to come forward (victim, bystander) | ||
| Assertiveness training | Training intended to boost self-confidence and increase people’s ability to challenge UB as it happens | 126,157 |
| Role-playing | Similar to cognitive rehearsal, role-playing involves practising resolution behaviours and thoughts with others in group setting. May enhance ability to cope or improve confidence to come forward | 54,107,137–139,141,142,152,156 |
| Cognitive rehearsal | Learning of specific cognitive responses to prepare staff when they encounter UB. Intended to move responses from automatic towards deliberated to enhance coping and reduce escalation67 | 54,61,63,65,67,138,145,148,149,156 |
| Keeping records | Recording incidences of UB and details of the events to provide evidence/improve trustworthiness when coming forward to make a claim against people | 72 |
| 3. Improving ability to cope with UB (victim, bystander) – all unevaluated | ||
| Seeking help externally (unevaluated) | Looking outside one’s organisation for help with UB, e.g. union representative, regulatory body or GP | 69,76,124 |
| Journalling (unevaluated) | Reflective writing about one’s experience of UB in the workplace may help with coping | 55,119 |
| Moving victims (unevaluated) | Moving victims away from instigators in organisation. | 56,118 |
| Individual coping strategies (unevaluated) | Various strategies to help improve coping – e.g. taking sick days, hiding emotions/breathing exercises | 68,135 |
| Reflection (unevaluated) | Engaging in self-reflection or group reflection to enhance ability to cope e.g. Schwartz Rounds | 152,162 |
| 4. Understanding prevalence of UB (managers/leaders) | ||
| Survey | Survey to identify the level of UB occurring within an organisation, which may help to target or design other strategies | 150,154,155 |
| Multisource feedback (unevaluated) | Similar to reporting systems, but identifies/investigates individuals from different perspectives – ‘360-degree’ view of individual’s historical behaviour | 163 |
| 5. Improving teamwork (all) | ||
| Team-building exercises | Generally group sessions that incorporate activities to build a sense of social support and camaraderie | 141,142,152 |
| Conflict-management training | Training to be able to de-escalate situations or avoid escalating them altogether | 107,134,154,155 |
| Communication training | Training to enhance ability to communicate in a way that is less likely to be interpreted as or foster UB. | 64,134,150,154,156,164 |
| Journal club/group writing | Writing as a group, often to reflect on experiences of UB and build a sense of social support | 104,144 |
| Problem-based learning | Group learning, involving identifying with and attempting to tackle real-life problems. It often involves peer-to-peer teaching | 139 |
| Staff networks (unevaluated) | Establishing internal or external networks for staff from specific backgrounds (e.g. minority ethnic or female) to share coping strategies/improve social support | 79 |
| 6. Social norm-setting (all) | ||
| Championing | Encouragement for certain individuals to espouse anti-UB values and behaviours and, sometimes, to act as trusted contacts for reporting UB incidents | 93,138,142,147,151 |
| Code of conduct | Document clarifying organisational policies on acceptable behaviour and processes to report or otherwise tackle UB | 103,125,134,138,150,154,164 |
| Role-modelling | Similar to championing, leaders or managers seeking to espouse the behaviours and values they want to encourage in staff | 97,126,127,138 |
| Environmental modification (unevaluated) | Modifying physical environment can increase awareness of UB (e.g. posters) or reduce discomfort (i.e. more comfortable temperature), which may reduce UB. | 47,93 |
| Allyship (unevaluated) | When an individual from a more privileged background publicly comes out in support of less privileged colleagues and actively furthers their cause | 131 |
| 7. Improving leadership competence and empathy (managers/leaders) | ||
| Leadership training | Training to improve management or communication styles so that they are less likely to be perceived to use bullying as a management tactic | 98,154 |
| Reverse mentoring (unevaluated) | Enables people in senior positions to learn from and understand issues from the perspective of people in less senior roles, often from under-represented groups | 131 |
| 8. External pressure on organisations (managers/leaders) | ||
| Seeking hospital Magnet status | Seeking Magnet status can lead to managers and leaders becoming more focused on addressing a culture of incivility | 138,142 |
| Regulator action (unevaluated) | CQC or regulatory body inspection may identify culture of UB, which can place pressure on managers to tackle UB | 55,124 |
| Laws (unevaluated) | Legislation may place responsibilities on organisations for ensuring equality and employee well-being and safety, which increases urgency to address UB | 136,165,166 |
| 9. Reporting and escalation systems (all) | ||
| Reporting system | System to report incidences of UB in the workplace. Can be web-based, report to a specific person or other way. Can be anonymous or not | 53,93,97,98,127,147,151 |
| 10. Workplace redesign (all) | ||
| Democratisation of workplace | Reorganisation of workplace processes to drive an increased sense of job control, reduce frustration and reduce hierarchy | 103 |
| 11. Improving awareness and knowledge (all) | ||
| Education, awareness and general group discussions | Training to increase knowledge of what UB look like, how to tackle/increase general awareness of it | 54,62,63,65,66,72,93,107,125,126,134,137,138,142,145,148–150,152,154,164 |
| 12. Implementation-aiding strategies (managers/leaders) | ||
| Action-planning or goal setting | Staff come together to plan other strategies to tackle UB. Can foster a sense of co-creation | 72,93,98,103,134,137,150,154,164 |
| Building a repertoire of strategies | Enables flexible intervention delivery, with repertoire of activities to tackle UB enabling targeted responses to different scenarios | 154,155 |
| 13. Changing recruitment processes (all) – all unevaluated | ||
| Changing recruitment criteria (unevaluated) | Recruitment criteria to include personality/emotional intelligence tests to decrease recruitment of people who will not flourish in civil organisational culture | 70,76 |
| Dismissal (unevaluated) | Dismissing instigator known to have UB behaviour from employment | 125 |
Strategies used to tackle unprofessional behaviour between staff, how they work and why
We formed 13 categories of strategy by grouping strategies per common underlying mechanism. For example, social norm-setting strategies work by setting an expectation for normal behaviour in the workplace and include individual strategies such as championing, positive role-modelling and codes of conduct. Table 16 sets out the range of strategies identified in this review, arranged by category, and provides an overview to contextualise our CMOCs to follow. Strategies currently unevaluated in the literature are in italics.
Category 1: Direct or indirect approach to instigator (victim, bystander or managers)
Approaching an instigator of UB can be performed by a target, bystander or manager in the workplace; it can be done at the time at which UB occurs, or later. However, this strategy relies on a great deal of self-confidence and the ability to overcome fear of reprisal in those approaching the instigator. Strategies to improve confidence and ability to do this are discussed in Category 2, which focuses specifically on the act of approaching an instigator (either directly or indirectly).
Approaching an instigator as a victim or bystander directly and telling them how it felt when exposed to their behaviour would be an attempt at informal resolution. A direct approach can also take other forms, such as writing a letter to the instigator or approaching human resources to facilitate a meeting to attempt to resolve differences with the instigator. 124 Disciplinary strategies include a formal investigation of an instigator. This could include reporting an instigator to management and/or writing a formal complaint whereby organisations may investigate patterns of UB and deliver a warning, or other disciplinary strategies or action if required. 97 Often, this is according to legal and investigative requirements.
Disciplinary action, however, also requires receptivity from management to engage with the process. If some organisations do not have a culture that enables resolution of these issues, then individuals can seek help externally – a strategy discussed in Category 3.
Included sources mention informal direct approaches very frequently (see Table 16) but it is difficult to evaluate the success of these strategies as they tend to occur more naturally or as an outcome of other strategies. Only reporting and professional accountability interventions, such as those in Ethos or Vanderbilt, formally include direct approaches to instigators as a strategy and enable both informal resolution via a peer messenger (to encourage reflection) and behaviour change while including an escalation to formal investigation if poor behaviours persist. 97,98 However, other interventions that encourage speaking up or build confidence may also be indirectly attempting to encourage recipients of UB to engage in informal resolution.
Direct or indirect approach to instigator – unevaluated
Mediation was mentioned as a strategy often used ‘in practice’ to deal with UB, generally where it is limited to a single victim and an instigator. Mediation involves the use of a mediator (ideally, trained) who helps conflicting parties resolve differences and continue to work together. As one included source highlights, a mediator ‘is there not to judge right or wrong or take sides but to assist the parties in reaching an agreement to improve the situation and resolve a problem’. 167 The Royal College of Nursing124 mentions mediation being used in cases of bullying and harassment and highlights mediation as a strategy to be performed separately with the target and instigator of UB, as well as with both together. Due to the impartiality of mediators, mediation may not be appropriate when participants are at different levels of seniority, where one party lacks insight into their behaviour or in very serious cases of misconduct. 167 As such, it may be most suitable for lateral violence and forms of UB that do not involve power imbalance.
One informal strategy mentioned infrequently in the literature was simply being more aware of language when reporting incidents such as medical errors (i.e. with nurses and surgeons). We have called this softening language and it may involve modifying language to sound less judgemental or harsh. One study referred to a case in which someone who spoke up avoided blame despite the existence of an interprofessional hierarchy and ‘used neutral language focusing on what happened and how the patient was treated. They focused on the patient and made no reference to “who” was involved in the incident’. 160 This was particularly mentioned in relation to attempts to challenge behaviour in the moment and may, in some cases, reduce conflict and backlash. 160
Speaking up is the action individuals can take to convey concern about incidences of UB, either in the moment or by discussing or reporting after the event to the individual involved, to a supervisor or an organisational reporting system. Speaking up can be an informal resolution approach – discussed earlier – and refers to challenging negative behaviour, which is typically but not necessarily in-person and direct. Speaking up is often what many other strategies in this category are trying to stimulate, enabling identification of problem areas and implementation of other strategies to address UB. It is very closely tied to the concept of psychological safety (see Chapter 3 and Appendix 2). 15,168 In the UK, this can include reporting to a Freedom to Speak Up Guardian. 11
How and why informal or disciplinary strategies may work
Included studies highlighted that it was important to attempt informal approaches before moving onto formal disciplinary procedures. This is because informal approaches were found to generally be sufficient to resolve a situation without making the instigator themselves feel unfairly targeted, which may worsen any conflict. 22,91 This approach works through a couple of mechanisms. Firstly, it may prompt reflection and a change in behaviour by the instigator in the future (CMOC 25): ‘Individually, the programme provides doctors with an opportunity for reflection and to change their behaviour to align with professional standards’. 97 In cases where it does not feel safe to do so, individuals can approach more senior employees or utilise reporting systems, where available, to alert senior employees to serious UB or a pattern of UB. In this case, the second mechanism comes into play. Here, instigators gain knowledge that one has been reported and investigated, which may lead to a perception that it is risky to engage in such behaviour and can enable follow-up strategies to be implemented by managers (CMOC 26).
When feeling psychologically safe (C1), approaching an instigator directly (R) can provide an opportunity for the instigator to reflect (M1), which may cause them to be less likely to engage in UB in the future (O1) and change their behaviours (O2).
CMOC 26. Formal approach.When either an informal approach hasn’t worked (C1) or it feels psychologically unsafe to informally approach (C2), then taking a more formal approach [e.g. using a reporting system (R)] may increase an individual’s or perpetrator’s perception of risk when behaving unprofessionally (M) and reduce their future UB (O).
Category 2: Improving confidence to come forward/speak up
Several strategies seek to improve an individual’s confidence – and thus ability – to come forward to report or challenge someone who is engaging in UB. Examples include assertiveness training, cognitive rehearsal and role-playing; these were all evaluated in the included intervention papers. One study conducted in Turkey sought to assess the impact of assertiveness training to tackle mobbing (defined as ‘unethical communication and antagonistic action directed by one or several people toward a single individual systematically’157). A rationale for including assertiveness training was the claim that when encountering mobbing, the majority of nurses ‘act passively’. 157 The authors found that, according to a self-developed mobbing scale, mobbing decreased after the intervention – decreasing from a score of 226.4±27.7 to 159.6 ± 47.9 – and assertiveness improved from 6.23 ± 15.6 to 17.0 ± 16.06 (measured by the Rathus Assertiveness Inventory). A second study combined assertiveness training with other strategies, such as education, and found an associated decrease in reported verbal abuse rates from 90% to 76%, as well as reduced feelings of powerlessness among nurses. 126
Cognitive rehearsal and role-playing involve practising scenarios to improve mental readiness for when UB is encountered in the workplace. 67,152 Cognitive rehearsal involves practising responses to UB, usually mentally, to change them from automatic towards deliberated, as a means by which to enhance coping and reduce UB escalation. Ten of the included studies used cognitive rehearsal, making it one of the most used strategies. Five studies54,63,65,148,149 attempted to replicate a study by Griffin (2004), undertaken with 26 newly registered nurses, drawing upon cognitive rehearsal as their main behaviour-change strategy. While 62 new nurses received the intervention, only 26 nurses provided outcome data. The intervention drew on both education and presentation of appropriate responses to 10 common UB scenarios – such as staff engaging in broken confidences, scapegoating, backstabbing, undermining and verbal affront. The strategy included the use of cueing cards covering appropriate responses, to which nurses could refer later. The researchers reported that 100% (n = 26) of nurses reported confronting instigators during focus groups that took place 12 months post intervention. The organisational retention rate was reported to have been positively affected but no comparison of pre- to post-retention rates was provided.
All sources drawing on cognitive rehearsal as a strategy reported positive results, except for a study by O’Connell et al.,54 which also drew on the strategy of role-play. Role-playing is similar to cognitive rehearsal but involves practising responses with other people, as opposed to purely mental rehearsal. O’Connell et al.’s54 study was conducted with military nurses in the USA and drew on Griffin’s work, incorporating education, cognitive rehearsal and role-play. 54 The NAQ was administered before and 3 months after their intervention and no statistically significant changes in experience of UB after the intervention were found. This lack of change, they stated, could have been due to senior and junior staff being mixed together, which inhibited engagement in role-playing due to the strict military hierarchy. 54 All other studies drawing on role-playing reported positive results. 107,137–139,141,142,156
One final evaluated confidence-improving strategy is keeping records, which is a strategy that individuals can use to enhance the likelihood they are believed when speaking up, as well as providing evidence about who was involved. This may take the form of notes, journals or screenshots if harassed electronically. One study recommended this as a strategy as a result of a workshop, stating that ‘session participants recommended instructing residents to document very clearly what was said or done, and by whom, in order to equip the institution with the necessary information to make an intervention’. 72 This study reported raising awareness of UB – but it is not clear if or how keeping records had an impact on subsequent behaviours.
How and why improving confidence may work
All the above strategies are focused on improving an underlying mechanism of self-confidence and a feeling that the rewards of speaking up are greater than the risks of doing so. Further to self-confidence-building, sources referred to concepts such as self-efficacy and/or assertiveness as essential to increasing individuals’ abilities to speak up, with these skills being the focus of these strategies. One study drawing on role-playing stated that ‘To immediately challenge the bully with a recommended response, the nurse needed to feel adequately prepared for the task. Practicing the responses before actual use helped to build the nurse’s self-confidence in performing the technique in difficult bullying situations’. 149 Likewise, for keeping records, its contribution to improving confidence through offering evidence was implicit in this quotation:
it is essential to ensure you keep written records of the bullying incidents. This can be a helpful way for you to clarify what is going on and whether the behaviour is occurring on an ongoing and persistent basis, but it will also form essential evidence if you decide to make a formal complaint. 169
This dynamic is reflected in CMOC 27. It is important to note that encouraging speaking up is an individualised approach to tackling UB and, alone, does not necessarily promote a psychologically safe organisational culture or environment.
Use of role-playing, cognitive rehearsal strategies or keeping records as an individual (R) to encourage speaking up about UB (C) can lead to improved self-confidence when coming forward (M), which can lead to the victim speaking up (O1), the instigator reducing their UB (O2) and increased management awareness of UB (O3).
Category 3: Improving ability to cope (victim, bystander)
Some strategies can be a means to improve an individual’s ability to withstand the negative impact of UB, a concept also referred to by some as resilience. 170
Improving ability to cope (victim, bystander) – unevaluated
The strategies designed to improve individuals’ abilities to cope were all unevaluated. These strategies also tend to assume at their core that people are simply not sufficiently resilient to be able to handle UB. This is an individual-focused mindset and can send a signal that UB is inevitable and staff should just learn to ‘live with it’. Journalling can be a reflective exercise said to help improve the ability to cope in the workplace; it can be performed alone rather than in a group (such as with group writing or journal clubs, explored above). Journalling has been found to increase awareness of civility and one’s role in the creation of a civil environment. 55 Journalling may be a form of reflection strategy; however, other sources mentioned group discussions serving to promote reflection – in addition to self-reflection – by filling out self-reflective paper-based tools, for example. 162 Included sources also mentioned other miscellaneous individual coping strategies that individuals can engage in, such as talking with family and friends, ‘positive thinking’, ‘stockpiling human favours’ (such as ‘helping senior nurses with their workload so that the senior nurses would help them in return’)171 and taking sick leave. 68 After an individual speaks up, it is possible that some organisations simply move the victim out of reach of those claimed to be instigators. However, this can inhibit subsequent speaking up, erode psychological safety and typically sends a message that an instigator ‘gets away with it’. 115
Seeking help externally can also help someone experiencing UB to cope. This may include seeking help at a worker’s union or dedicated body to help with such issues. For example, one study mentioned that Canada has a Vancouver Island Health Authority Employee and Family Assistance intervention to support staff with such issues. 119
How and why improving ability to cope may work
Trying to improve ability to cope or improve mood and resilience were commonly reported as ways the above strategies had been intended to work; therefore, this is the main underlying mechanism. Improved ability to cope may occur through coming to terms with things that have happened or building the ability to withstand future episodes of UB in some way (CMOC 28). Some sources call this ‘resilience’ and highlight that, for example, ‘Evidence of resilience was reflected in various comments of study participants, such as, “never have too many negative thoughts, otherwise they will make you unhappy …. So I will think positively and I won’t be too miserable”’. 171 These dynamics are highlighted in CMOC 28. However, it is important to highlight that assuming that people should be able to withstand UB better does not help to address core contributors to UB.
Use of coping strategies – such as seeking help externally, journalling, reflection or other individual actions (such as taking sick days) (R) – in a situation where one is experiencing UB (C) can lead to an increased ability to cope (M), thereby reducing the impact of UB on the victim’s psychological well-being (O).
Category 4: Understanding prevalence of unprofessional behaviour (managers/leaders)
Many studies, prior to an intervention, assessed prevalence of UB in their sample as part of an evaluation. However, few studies drew on prevalence surveys as a strategy to identify where UB was occurring in order to better focus and tailor the intervention. 146,150,154,155 This strategy category involves understanding where and how UB is occurring, to allow contributors to be better targeted by other strategies. Three studies using prevalence surveys drew on the CREW intervention, which incorporated myriad systemic strategies for reducing UB;146,154,155 another non-CREW intervention study also drew on a bespoke and highly systemic approach that included action-planning, communication skills training and workplace rearrangement. 150 The CREW intervention draws on a custom-designed CREW survey called the ‘civility scale’, which assesses a range of civility-related metrics such as respect, cooperation, anti-discrimination and value differences. 146 As such, it does not test for prevalence of particular types of UB.
Use of this strategy only in more intensive interventions demonstrates that the use of surveys to understand prevalence is typically performed either before a larger culture-change effort to identify where ‘problem areas’ are or to identify baseline data against which to compare changes following an intervention. Use of qualitative investigation and interviews with staff may also enhance survey data by identifying specific contributors to UB present in organisations. One study drew on a comprehensive 4-month investigation of workplace culture at a UK ambulance service, using a mixed-methods approach as well as over 120 hours of one-to-one telephone interviews. 76 The study gathered sufficient data to understand how different professional and demographic groups experience UB in unique ways and identified many systemic factors propagating UB. This enabled the proposal of organisational and/or bureaucratic changes that could minimise aspects leading to frustration etc. in the workplace – in addition to individual-level interventions that are so often the focus. 76
Understanding prevalence – unevaluated
Although mentioned in the literature, multisource feedback has not been evaluated in healthcare settings. Similar to reporting systems, multisource feedback (such as 360-degree appraisals) involves use of multiple raters to assess the behaviour of one individual. Unlike reporting systems, however, which are more universal, multisource feedback is a more targeted process that requires seeking opinions about one particular individual. 21
How and why understanding of prevalence of UB may work
Understanding the prevalence of UB is useful to managers and leaders in order to better understand the contributors to and extent of UB in an organisation. This enables implementation of other strategies that can more directly reduce UB. As such, the mechanism underlying this strategy is an increase in understanding for managers or leaders of the places in which UB occurs. This dynamic was highlighted by a study: ‘cultural audits, using measures such as those developed and validated in our study, may enable organizations to learn about the existence and sedimented nature of sub-climates and alliances that perpetuate tolerance of workplace bullying’. 58 CMOC 29 depicts how and why this may work.
Implementing strategies to understand prevalence of UB – such as performing an audit of an organisation’s culture (R) in an organisational environment in which UB is suspected to be prevalent (C) – can give managers a better understanding of contributors and where UB is occurring (M1), increase knowledge about interventions that might help (O2) and provide a sense of urgency to tackle UB (M3). This can lead to improved ability to target strategies towards core contributors to UB (O1), which can improve effectiveness at reducing UB (O2)
Category 5: Improving teamwork (all)
We have collated strategies explicitly attempting to mitigate UB by increasing a sense of camaraderie or improving the ability to work together as those that try to improve teamwork. These include activities such as team-building exercises,141,142 communication training (which may lower the risk of conflict caused by improper or unprofessional communication64,134,150,154,156,164), problem-based learning139 and journal clubs or group writing strategies. 104,144 On team-building exercises, for example, Armstrong141 drew on a modified CREW intervention and included team-building exercises, facilitating discussions about workplace incivility and role-playing. Their examples of team-building exercises included ‘Anything Anytime’, which involved ‘providing a generic subject and discussing how it is viewed differently by different members of the group’, as well as ‘Geometry of Work Styles’, which ‘involves participants selecting from four geometric shapes that relate to a personality type’. 141 The authors found no differences in exposure to incivility post intervention but did find it was able to modify nurses’ self-assessed ability to respond to incivility. Overall, two out of three interventions drawing on team-building were reported to be successful, with the other reporting improvements to group cohesion. 142 One did not assess efficacy. 152
Five studies drew on the strategy of communication training. 64,150,154,156,164 All reported positive results except for Chipps and McRury,134 who reported training on ‘techniques for giving feedback’ and anecdotally reported an increase in a ‘learning community’ after the intervention; however, details were sparse. They found that reported negative acts nearly doubled post intervention, alongside a paradoxical decrease in self-identified engagement in bullying. A more well-defined intervention by Saxton64 involved collaborating with a certified Crucial Conversations trainer – who, over a 2-day intervention, drew on several techniques including videos, role-play and reflection to improve communication abilities. They found an increase in self-effectiveness immediately post and 4 weeks after the intervention and a self-reported increase in ability to address disruptive physician behaviour. 64
Problem-based learning involves identifying with and attempting to tackle real-life problems, often drawing on peer-to-peer teaching and learning. Problem-based learning was only used by one study, which happened to draw on live actors ‘acting out a situation in which one of the staff nurses was extremely uncivil to her two colleagues’ in which students ‘observed the scenario, provided written feedback on the effectiveness of the scenario, and participated in small-group discussions to debrief after observing the scenarios’. 139 Post intervention, the authors reported that participants felt better prepared to address incivility in the workplace.
Two studies drew on journal club/group writing techniques. 104,144 One sought to decrease negative workplace behaviours by enhancing voice and connection among nurses, with music-assisted meditation lasting 15 minutes followed by a 1 hour 45 minutes creative writing exercise. This took place once a week for 6 weeks (although the wording in the study is slightly unclear). The creative writing drew on several steps: ‘(1) an explanation of the writing group method, (2) an introduction to the exercise, (3) 20 minutes of writing, (4) an invitation to read their writing aloud and (5) the group listens and comments on what is liked and remembered’. 104 This study did not assess effectiveness but found participants reported it as a ‘positive experience’. The other study using this strategy involved 6-hour-long monthly meetings over 6 months and drew on article-reading as well as other activities in each session, such as ‘role-play’, ‘breathing techniques’ and ‘stress-ball activities’. The authors did not assess effectiveness. 144
Conflict-management training107,134,154,155 can overlap with communication training and focuses on communication styles, problem-solving methods and conflict-resolution methods that can de-escalate situations to avoid UB issues. 107,134 For example, one included intervention drew on teaching problem-solving methods that ‘transformed from competition to joint problem-solving, which is the hallmark of competent conflict communication’. 107 This study reportedly managed to improve conflict management and communication skills;107 however, another found that UB increased after the intervention but did not assess actual conflict-management abilities. 134 The two other studies using this strategy adopted conflict-management training on a flexible basis as part of the CREW intervention strategy repertoire.
Improving teamwork – unevaluated
Staff networks were mentioned in the literature as having the ability to build social ties between staff such as by offering a ‘safe space’ in which to discuss issues affecting particular professional or demographic groups. 131 These networks can take several forms, such as operating within or between organisations and having different foci. For example, one paper reported that an NHS trust had an ‘LGBT+ network focusing on education raising and “myth-busting”; its Black and minority ethnic network being “issues-led”; [and] its disability network focusing on “small differences” achieving impact’. 79 This paper also warned that setting these networks up correctly can require significant resource,79 and another suggested buy-in can be required from both minority and non-minority staff. 131 This source highlighted that
creating a safe space for ethnic minority staff to talk about race-related issues could inadvertently create new (or exacerbate old) divisions between different groups. And, at worst, ethnic minority staff could find themselves having to justify why this type of recognition of difference is needed. 131
Such dynamics are explored further in Key Dynamic 10 in Chapter 7.
How and why improving teamwork may work
These strategies focused on improving the ability of individuals to work together effectively and without conflict. Increasing empathy via building a sense of team and improving the ability to effectively communicate without miscommunication are core mechanisms by which to reduce likelihood of conflict with colleagues. These strategies also underlie why UB may lead to a reduction in patient safety, providing other benefits beyond directly reducing UB. One included review highlighted the importance of avoiding low-level conflict, for example:
Several papers recommended the use of teambuilding activities to prevent or reduce bullying For example, [one] suggested informal gatherings and regular meetings, as well as interpersonal skills training, to foster positive interpersonal relationships and informally encourage collegial repair attempts for low-level conflict. 21
Staff networks were also highlighted as increasing empathy between different staff groups: ‘In hearing those perceptions and experiences first-hand, staff can have more empathy towards people with different characteristics from their own’. 131 How and why these strategies work is depicted in CMOC 30.
Implementing interventions to improve teamworking (R) in an environment with low levels of social support (C) can increase empathy for one another, improving the sense of being supported by others (M1) and improve ability to communicate (M2), thereby reducing chance of experiencing conflict with colleagues (O1), reducing UB (O2) and increasing ability to cope (O3).
Category 6: Social norm-setting (all)
The strategies in this category revolve around setting new expectations for behaviour in the workplace. Championing was used by five studies93,138,142,147,151 and involves encouraging certain individuals to espouse anti-UB values and behaviours to help drive changes in social norms and, sometimes (as in the case of Freedom to Speak Up Guardians) to act as trusted contacts to whom incidents of UB can be reported. 168 The impact of drawing upon champions is highly difficult to measure, as culture-change may be subtle and champions were always used alongside other strategies, often over a long period of time. For example, three of these studies used the Vanderbilt intervention approach, which draws on many strategies – including a reporting system for identifying problematic individuals. 93,147,151 In this approach, champions were identified from individuals already known to espouse the positive values being sought. 151 These individuals were then used as go-to people to help implement other intervention activities, train peer messengers and disseminate project messages to various staff types.
Other social norm-setting activities include role-modelling, which can be done by champions but is more typically performed by leaders seeking to act as a model for lower-level employees. 126,138 Positive role-modelling as an active choice is a strategy; however, negative role-modelling can be a contributor to UB. One study used workshops on role-modelling, delivered to nurse managers first in order to train them to be role models for other staff. 126 A second tier of workshops were then delivered to 20 regular staff to train them to be trainers to other staff and be role models for those who attend their sessions. All studies using role-modelling reported positive results as per their selected outcome measures. 97,126,127,138
Codes of conduct also seek to set expectations of behaviour in the workplace; seven included studies drew upon implementing new codes of conduct. 103,125,134,138,150,154,164 Codes of conduct often form the backbone of a wider intervention and are not often delivered on their own – rather, they set out policies and practices for the organisation. These can include what UB in the workplace looks like, how to tackle it, what resources are available to employees to address it and resolution pathways, among others. Sometimes, codes of conduct can be enhanced by increasing awareness of the policy or by asking employees to sign a pledge to abide by them during hiring or performance reviews. For example, one study drew on this approach, stating that ‘beginning in 2008, at the time of the annual performance review, each leader commits in writing to consistently holding staff, peers, and leader colleagues accountable to the Highland Promise Standards of behavior’. 138 This demonstrates that annual reviews can also be used as a time point at which to raise awareness of the code of conduct and to re-commit to it.
Social norm setting – unevaluated
Unevaluated social norm-setting strategies included environmental modification and allyship. Environmental modification was only identified as a means of providing awareness of or prompts to staff members and, therefore, can be intended as a means of signalling culture change as well as enhancing knowledge of other strategies to tackle UB being rolled out in an organisation. 172 For example, one study using posters to signpost their intervention’s existence reported enhanced engagement with the intervention. 93 Blakey et al. 47 also highlighted use of posters to signal what was and was not acceptable behaviour – similar to a code of conduct but more constantly visible to employees.
Allyship was also identified as important for indicating that an organisation is not tolerant of discrimination against minority groups. Allyship was not often mentioned in the included sources, with only one discussing it in any real depth. 131 Allyship involves individuals with privileges ‘us[ing] those advantages to further the cause of marginalised groups’. 131 Similar to being a champion or intervening as a bystander, the article highlights the potential risk of reprisal (see also Key Dynamic 5 in the preceeding section) but that being an ally also sends a strong message regarding what is and is not tolerated in an organisation. This can be more effective when more senior employees become allies.
How and why setting social norms may work
Setting social norms is important and often healthcare staff look to leaders for an understanding of what the social norms are. If leaders tolerate or role-model negative behaviours, this sets an expectation that UB is normal. However, inversely, if leaders role-model positive behaviours, enforce rigid behavioural standards and implement genuine culture-change efforts, it can signal strongly that the social norm does not tolerate UB (M1 below, CMOC 31). One included study highlighted this dynamic, stating: ‘Executives and senior leaders enable change when they role model positive behaviours and inhibit change when their own behaviours are inappropriate’. 112 A code of conduct, for example, may set out behavioural expectations in writing but these are only effective if visibly enforced, as indicated in this study:
Demonstrated top management commitment to a policy of zero tolerance is of core importance, with this commitment included in mission/vision statements and embedded in strategic plans. Organisational focus on a regulatory approach of policy and legislation is not effective on its own. 57
Another study highlights that ‘employees closely and carefully monitor leader and manager behaviours. This is often forgotten or misunderstood by leaders and managers’. 76 Negative role-modelling can also undermine otherwise well-designed interventions (see Key Dynamic 7). As such, the core mechanism underlying these strategies setting out social norms is an assessment by employees of the cultural direction. CMOC 31 depicts how and why these social norm-setting strategies may work.
As long as leaders are seen to embody and enforce positive behavioural norms (C), then implementing social norm-setting strategies such as a code of conduct or positive role-modelling (R) can signal culture change towards civility (M1), making it socially unacceptable and, therefore, riskier to engage in UB for instigators (M2) – thus increasing the sense of psychological safety (O1) and reducing the likelihood of UB (O2).
Category 7: Improving leadership competence and empathy (managers/leaders)
UB originating with management is unfortunately common, as statistics from the NHS staff survey and others indicate. 16 Within this category lie strategies that try to improve how leaders and managers interact with their employees and their management styles through leadership training. We did not include conflict-resolution strategies delivered only to management in this category – these are in the conflict-management category. Only one paper drew on some form of leadership or management training and this was using the Vanderbilt programme. 98 This paper drew on an academic leadership programme using role-playing techniques for skill development, as well as a programme called Elevate to promote professionalism in leadership. 98 However, this paper did not assess effectiveness. Despite a lack of management skills being a major cause of UB and UB originating with management being a core statistic within the NHS staff survey, for example, the dearth of papers evaluating this as a strategy was surprising.
Improving leadership competence and empathy – unevaluated strategies
When leaders are paired up with employees in less senior roles to try to understand the issues affecting them and their co-workers, this is termed reverse or reciprocal mentoring. These employees may be of a different gender or from a different minority group to the leader. Kline70 reviewed the use of the programme in a UK university hospital and found they tend to garner support only for the individuals involved in the programme (rather than the group), and that wide-scale change was not likely to be achieved by use of this strategy alone. As such, evidence for this strategy is mixed. Another paper reported senior leaders finding it a useful programme while also emphasising it has not been evaluated, nor demonstrated to have benefits for junior employees. 131
How and why improving leadership competence and empathy may work
Included literature highlighted that a lack of management skills can result in employees feeling bullied or harassed due to poor communication, micromanagement and undermining. As such, the core mechanism by which strategies to improve leadership competence and empathy may work is improvement in day-to-day line management skills by reducing miscommunications that can lead to interpretation of management styles as a form of UB (M1, CMOC 32), and improving empathy for staff (M2, CMOC 32). A lack of empathy by managers towards staff was highlighted as especially important for perceived UB:
Some participants with underlying conditions felt their managers were dismissive of their fears around Covid-19. Some participants talked about coming back off sick leave and being ‘interrogated’ about their time off or feeling the Trust unthinkingly applied its sickness absence policy. 70
Likewise, another included study highlighted the importance of management skills in avoiding UB stemming from management styles:
The most frequently cited perpetrator of bullying by employees is their immediate manager or supervisor […], the ‘people side’ of management is often neglected and nurse managers may not be trained to deal effectively with the behaviours of their team members. 169
These excerpts highlight the importance of underlying empathy and management skill-improving mechanisms (CMOC 32).
In an organisation in which there is substantial pressure on organisational leaders (C1) or situations in which leaders have been perceived to engage in bullying-type management practices (C2), implementing training to improve management skills (R) can enhance ability to communicate with employees (M1), enhance empathy for less senior colleagues and report supporting ability to manage compassionately (M2), which reduces the likelihood of leadership directly contributing to UB (O).
Category 8: External pressure on organisations (managers/leaders)
External pressure on organisations can come in several forms, typically leading to managers or leaders gaining an increased sense of urgency to tackle the issue. Seeking hospital Magnet status for being a positive place to work can drive motivation for leadership when tackling UB and can indicate a path to achieve it. Two studies mentioned seeking Magnet status, which is a certification indicating a high-quality place to work – currently in use most frequently in the USA. 138,142 Achieving Magnet status requires exemplary performance in terms of transformational leadership, structural empowerment, professional practice, new knowledge generation and empirical outcomes;173 as such, reducing unprofessionalism is key to achieving this status. Magnet was the only such programme we identified in the literature, although other such ‘awards’ for hospital culture may also exist. Included interventions mentioned that Magnet was a motivating force for implementing interventions; however, Magnet was not an intervention in itself. Since the status is mostly a motivating force for managers and leaders, one critique of seeking an accreditation is that it may only change behaviour of managers and leaders. This is a feature of all the strategies that place external pressure on organisations within this category.
External scrutiny and pressure on organisations – unevaluated strategies
Events such as public failures that reach the media (e.g. bullying cultures) exposed as a result of external inspections [e.g. care quality commission (CQC)] are examples of public pressure leading to actions being taken by management. For example, one included media article outlined the unearthing of a bullying culture resulting from a CQC inspection in the UK. It led to leaders needing to make a public commitment to addressing UB in the organisation. 174 Thus, a renewed focus on UB may require actions and interventions and strategies to be implemented to address it.
Legislation can also be a form of pressure impacting organisation leaders to provide a safe work environment. For example, one included source highlighted how occupational health and safety legislation in Australia provides an obligation for healthcare employers to provide a workplace free from horizontal violence. 166
How and why external pressure on organisations may work
The external factors discussed here can all act on managers and leaders to foster a sense of urgency to address UB in their organisation. For example, in order to attain Magnet status, an organisation cannot have a culture rife with UB and should drive managers to implement strategies to address UB. This was reflected in a study that suggested achieving this status as a motivator for their intervention: ‘applying the CORS process to nursing should support an organization’s pursuit of Magnet, high reliability, and quality nursing outcomes while promoting self-governance, self-evaluation, and a culture of safety and respect’. 53 This highlights the primary mechanism of increasing pressure on managers (as a result of external pressures), as reflected in CMOC 33.
If there is societal pressure or organisational reputational risk placed on an organisation (R) due to findings of an unsafe culture or prevalence of UB (C), then this can lead to pressure on management to resolve the problem – often speedily (M) – which can increase the likelihood of other strategies to address UB being designed, resourced and implemented (O).
Category 9: Reporting and escalation systems (all)
Reporting systems involve implementing a process by which co-workers can document instances of UB (often online). These reports or messages are then reviewed by dedicated personnel to tackle the issues raised, usually in a graduated manner (which may then be escalated). Although it is possible to implement a more basic reporting system without a graduated component, we did not encounter this in the literature. Both the Ethos97 and Vanderbilt93,98,147,151 systems pair the reporting system with a means by which to escalate the approach taken to the instigator over time, typically starting with a message delivered informally by a peer messenger. If UB continues, then a more formal investigation process or management plan is initiated. The reported messages can be anonymous, which can increase willingness to speak up. 97 Vanderbilt has seen significant proliferation in the USA93,151 but included papers did not report on effectiveness of the intervention. One paper assessing Ethos found it to be associated with a reduction in the prevalence of UB. 127 We provide more details of Vanderbilt in the section below on the flexibility of interventions.
How and why reporting and escalation systems may work
Such systems can enable staff to speak up about events even when there may be a low level of psychological safety, and enable poor behaviour to be identified early – facilitating reflection. As such, this type of strategy is largely individual-focused and presents its own issues (see Key Dynamics 1, 2 and 4). The ability to increase ease of speaking up is highlighted in an included study, which suggests the Ethos system is intended for use ‘when staff do not feel safe or able to address behaviour with the person in the moment’. 97 Receipt of messages in the reporting system then enables others to address issues on a case-by-case basis, such as facilitating reflection, escalating to a formal investigation or implementing other strategies. This case-by-case follow-up is also reflected in the CORS system, which is part of the Vanderbilt programme: ‘The CORS [Coworker Observation Reporting System] process offers an approach to identifying and addressing professionals who resist adoption and inhibit sustainability of safety initiatives’. 151 As mentioned earlier, if this results in an informal approach by a peer messenger, for example, it can allow recipients to reflect on their behaviour and change it:
Delivering reflective feedback involves the peer messenger having an informal conversation with the message recipient, providing them with insight into how their behaviour was perceived by another staff member (whose identity is not revealed) and an opportunity to reflect upon this. 97
This is highlighted in CMOC 34.
In an organisation where people may not feel psychologically safe (C), implementing a reporting system such as Ethos or Vanderbilt (R) can provide an alternative means to speak up – one that feels safer (M1), enabling instigators to be approached to cause them to reflect on their behaviour (M2), which can lead to a reduction in UB (O).
Category 10: Workplace redesign (all)
As mentioned in Chapter 3, when a workplace reduces job control and worker participation in decision-making, this can increase worker frustration, which is a contributing factor to UB. As such, redesigning the workplace can be considered to be addressing systemic contributors to UB. Despite this, only one included study sought to redesign work processes to facilitate worker involvement and increase job control. This study did not specifically refer to their strategy as democratisation – but in response to findings of a culture of intimidation, it did seek to include less senior employees more in decision-making processes around how to address this culture. 103 This, they reported, may have contributed to a reduction in staff turnover rate from 28.4% in the preceding 3 years to an average of 21.9% in the 3 years thereafter. Unfortunately, we were not able to find larger-scale workplace democratisation efforts in the UB literature in health care.
How and why workplace redesign may work
Redesigning the way in which the workplace functions – whether through democratisation efforts or by increasing role clarity to reduce organisational frustrations – may go a long way to reducing UB by addressing core organisational contributors. However, it is difficult to address such systemic issues, given workplace design is traditionally considered somewhat disconnected from UBs themselves. One recommendation from a study that modelled bullying in the nursing workplace was that ‘organizations must provide more democratic and less hierarchical workplaces’ to address key antecedents. 58 This is reflected in a study which stated that horizontal violence would be reduced if ‘nurse managers were given authentic authority and decision-making abilities to break down hierarchies and power imbalances that sustain RNs in an oppressed position within organisations’. 175 Breaking down hierarchies and increasing democratisation in the workplace could also enable staff to feel greater ownership and passion for their work and increase psychological safety by reducing the perceived risk of reprisal from more senior colleagues. Existence of a hierarchy also often inhibits effective communication. CMOC 35 shows how making these workplace adjustments may reduce some of the mechanisms that contribute to UB in the first place, such as a sense of unfairness, poor psychological safety and poor communication.
Adjusting the workplace to give more decision-making power to employees or increasing role clarity (R) in an environment in which workplace factors inhibit ability to do one’s work (C) can increase a sense of fairness in the workplace (M1), improve psychological safety (M2), improve communication within teams (M3), and improve work engagement and motivation (M4) – which can reduce proclivity to engage in UB (O1), increase ability to speak up (O2) and improve psychological well-being (O3).
Category 11: Improving awareness and knowledge (all)
Education was the most common strategy employed by included interventions (see Table 16). It is also a strategy relatively easy to deliver, typically in a lecture-type format or ‘session’, or with use of simple leaflets. 65,72,145 However, the content of the educational sessions varied substantially. Most interventions provided educational content about what UB is, ways to cope or how to address it in the moment. Generally, information covered a wide range of UB types; however, some interventions mentioned including specific behaviours such as education about microaggressions. 72 Others drew on education about specific ways in which UB might arise; for example, one study drew on Structurational Divergence Theory (a theory suggesting UB arises due to inherently conflicting and opaque organisational structures)176 to teach participants that an underlying source of their workplace frustration might be a ‘treacherous institutional landscape’, which can sometimes be unnavigable. 107 This, they hoped, would change the way staff perceived UB and its origins; the authors reported reduced negative conflict attitudes and behaviours and greater empowerment to manage workplace conflicts among participants. 103 Most commonly, studies simply drew on education regarding UB and its effects, and some simple strategies for attempting to address it. 54,125 The use of education alone was not always successful in changing behaviour and, although such strategies often resulted in greater awareness of UB (which was perhaps the aim in many cases), this came with the unintended side effect of simply leading to more reports of UB. 66,134
How and why improving awareness and knowledge may work
As mentioned above, providing education was intended to improve awareness of UB and provide knowledge of basic coping or ‘speaking up’ strategies staff can apply in the workplace. This may be important to ‘fill the gaps’ in terms of what people understand UB to be. For example, many may not understand that certain communication styles are more likely to be construed as UB and, therefore, education may be able to address such issues rapidly. The increase in reports of UB seen after educational or awareness-raising interventions are delivered suggests such interventions can successfully impart increased awareness of and knowledge about what UB looks like. This was as highlighted by Nikstaitis and Simko:66
Another important indication seen in the results of this study is that the nurse’s perception of incivility after education was higher. In other words, nurses were unfamiliar with the concept of incivility, and once they were made aware, it was perceived more, and now it can be rectified. 66
Similarly, for people who may have been inadvertently engaging in behaviour that could be construed as UB, education can provide a ‘clear understanding of what bullying and harassment are, so they can prevent their own behaviour from crossing the line and identify when others might be being bullied or harassed and need support’. 167 Education can also avoid any misunderstandings because it ‘eliminates differing opinions about what lateral violence is. For example, one nurse may attribute another nurse’s incivility to being stressed out, while a second nurse may define that same behavior as lateral violence’. 125 CMOC 36 depicts how education may work.
If employees are engaging in UB inadvertently (C1) or are working in an environment where UB is not obvious (C), then interventions to increase knowledge and improve awareness (R) can lead to an improved ability to recognise UB (M1) and can lead to reflection about past behaviour (M2), stimulating behaviour change away from UB (O1), as well as likelihood of addressing UB in the moment (O2) while reducing likelihood of UB occurring in the future (O3).
Category 12: Implementation-aiding strategies (managers/leaders)
This category of strategies includes activities that may help sustain engagement or plan other behaviour-change strategies within a larger intervention, such as ongoing co-creation efforts. This can range from simple one-off exercises, such as where ‘full-day workshops were attended by more than 90% of nursing supervisors to receive feedback on the research and to develop compatible strategies for their areas’103 to large 6-month efforts in which action-planning is a constant feature, such as in the CREW programme. 154,155 The CREW programme offers a selection of activities from a repertoire that can be chosen for implementation depending on the situation. Indeed, development of such a repertoire of strategies or activities that can be implemented on demand can itself be considered an implementation-aiding strategy. While many of these strategies are formulated in advance and are part of the repertoire, others are developed as required for circumstances that may arise during implementation. 146 To facilitate this, meetings are scheduled to provide dedicated time every week for 6 months, to provide space and time for planning or implementing anti-incivility activities in addition to larger meetings at the beginning and the 3-month midpoint. This ensures there are no excuses relating to capacity for delivering programme activities. To facilitate these meetings, facilitators are chosen and trained to ensure that activities can be delivered in a high-quality and consistent manner by those passionate about tackling UB. The existence of dedicated time enables action-planning to occur, whereby the plans to address cases or contributors to UB are formulated. Many included interventions drew on action-planning. 93,98,103,134,137,154,164 Another implementation-aiding strategy can be the provision of dedicated personnel whose role it is to have dedicated time and space for helping deliver the programmes and initiatives. As such, all these activities serve to generate momentum. However, building in more implementation-aiding techniques is likely to require increasing organisational resource.
How and why implementation-aiding strategies may help interventions
Strategies that aid implementation do so by providing spaces and capacity for delivering other essential behaviour-change intervention components. As mentioned above, the CREW intervention schedules meetings far in advance in order to provide such space ‘in which employees work with a trained facilitator to establish goals and develop ways to improve how they work together in the unit’. 155 One study drawing on action-planning found that drawing employees into the process fostered a sense of empowerment and engagement with the process, and helped hold managers to account:
… others felt empowered to promote a different way of doing things in their own spheres of control and to remind more senior management of their commitment to change. They subsequently began to implement some of the strategies produced at the workshop. 103
Additionally, these sessions were found to increase motivation for leaders to implement changes; this was recognised by other staff attending the session, which suggests that these strategies can help further the aim of reducing UB while building trust in management: ‘this leader appeared in a new light as someone willing and able to acknowledge shortcomings in the profession and in this specific organization’. 103 These dynamics are reflected in CMOC 37.
When delivering a complex intervention to reduce UB (R) that must be sustained over a longer period (C), providing time and resource to implement momentum-building strategies can enable greater belief that the programme is an authentic effort to reduce UB, thereby increasing engagement (M1), increasing commitment to the intervention by key actors (M2) and increasing motivation for leaders and managers to implement further strategies to reduce UB (M3) – which can increase effectiveness of other strategies to reduce UB (O).
Category 13. Changing recruitment processes (all)
These strategies relate to changes that can be made to hiring, firing and recruitment processes, to try to remove or avoid hiring ‘bad apples’. As such, this is also a category of individual-focused efforts.
Changing recruitment processes (all) – unevaluated
Changing recruitment criteria to include personality or emotional intelligence tests was an example given as to how organisations could seek to hire people who better match the culture the organisation seeks to cultivate. 76 However, these were not mentioned frequently in the literature and have not been evaluated. In severe cases of UB – such as repeated engagement in UB which informal and other graduated approaches have not been able to resolve – employees with a pattern of behaviour could be subject to dismissal. 122 This was not formally evaluated as a strategy, however. Some interventions mentioned earlier in this chapter (such as the Vanderbilt programme) could potentially escalate formal investigations until dismissal was necessary – but Webb et al.,151 for instance, reported not doing so.
How and why changing recruitment processes may work
Changing the criteria for recruitment processes is not likely to have an immediate impact; nor is it likely to work well alone. One included study highlighted that
Change via selection requires bullies to leave or be dismissed before new personnel can be hired using the new selection process. Culture change using selection may require a ‘critical mass’ of staff to have been recruited using the new system. 21
Since these strategies rely on sufficient individuals leaving and then joining an organisation, it is important to note that managers or leaders and other high-performing individuals who help set the organisational culture may still be part of the problem, and that such individuals are unlikely to leave because of such changes. CMOC 38 reflects this.
Implementing strategies to reduce UB, for example novel selection methods (R) at the point of recruitment (C), can slowly change the perception of social norm towards civility (M) if the individuals behaving badly leave (C2), which can reduce likelihood of staff engaging in UB (O).
Summary
Table 17 summarises the strategies identified in this chapter.
| Overall strategy categories (whom it impacts) | All strategies within category |
|---|---|
|
Informal resolution, disciplinary action, peer messengers, mediation, changing/softening language, speaking up |
|
Assertiveness training, role-playing, cognitive rehearsal, keeping records |
|
Seeking help externally, journalling, moving victims, individual coping strategies (e.g. taking sick leave), reflection |
|
Survey, multisource feedback |
|
‘Team-building activities’, conflict-management training, communication training, group writing, problem-based learning, staff networks |
|
Championing, codes of conduct, role-modelling, environmental modification, allyship |
|
Leadership and management training, reverse mentoring |
|
Seeking hospital Magnet status, government and regulator action, laws |
|
Reporting systems, e.g. Ethos or Vanderbilt programme reporting methods |
|
Democratisation of workplace |
|
Education, awareness and group discussions |
|
Action-planning, building a repertoire of strategies |
|
Changing recruitment criteria, dismissal |
Chapter 7 Key dynamics shaping intervention delivery: when and why strategies to address unprofessional behaviours do or do not work
In addition to our findings regarding how and why certain strategies work (see Chapter 6), we also identified patterns in the literature that we have formulated into 12 key dynamics. These key dynamics explore common issues, contradictions, tensions or considerations identified as important as they may inadvertently undermine intervention success, even if other aspects are well-designed.
Key Dynamic 1: Interventions should address systemic factors that contribute to unprofessional behaviour, not only individual factors
As highlighted earlier in this report, many interventions ultimately assume that individual failings primarily cause UB. For example, interventions and associated strategies to improve awareness and knowledge assume that people do not know what UB is or how to address it. Likewise, strategies that improve confidence to come forward assume that people simply need to have more confidence to be able to speak up and address an incident of UB in the moment. This may be assumed to be easier to address than fostering a psychologically safe environment. As highlighted in Chapter 4, many contributors are organisational or systemic and are not likely to be solved with a solely individual focus. Our MRT of fundamental attribution error (FAE) (see Appendix 2 for more details) occurring in the minds of key leaders and intervention architects may explain how organisations inadvertently slip into the mindset of considering UB an individual-level issue while downplaying the role of systemic factors. 94 However, a focus on identifying and resolving individual attitudes and issues can, in many cases, lead to larger systemic issues remaining unaddressed. When these systemic factors are unaddressed, they can continue to lead people to behave poorly.
| Stakeholder feedback summary – understanding what works |
| Our stakeholders acknowledged a lack of understanding of what works exists within practice. One stakeholder mentioned that when they ask NHS boards why their action plan to address UB is expected to work, they are met with ‘blank looks’. They highlighted that often the onus is placed on individuals, rather than organisations, to do better. |
It is important to note that systemic issues are, of course, often more difficult to tackle. This is evidenced by the lack of workplace redesign efforts in included studies. One study highlighted a quote from a participant regarding efforts to reduce UB that their organisation was employing:
NGN1 explained: ‘I honestly think if we just had more staff and more resources, if we reduced the stress levels, that in itself would reduce incivility and bullying drastically. Because if you do that, people are less stressed and people are respecting each other more’. 177
This dynamic is highlighted in CMOC 39.
If systemic issues such as understaffing, stress and lack of resources are addressed at the same time as implementing an intervention (C), then interventions to address UB will have greater success (O), because staff feel better supported and psychological distress levels are reduced (M).
Key Dynamic 2: Focusing on individual staff can have unintended consequences for psychological safety
This dynamic builds upon dynamic 1 (above) and concentrates on the unintended consequences of focusing on individual staff members. Like Ethos or Vanderbilt, several programmes – while incorporating other strategies – have at their core the notion of ‘professional accountability’, that is, that it is an individual problem if staff are not behaving professionally. One reported side effect of interventions focused on reporting badly behaving individuals is that they create the conditions in which the default behaviour is to report colleagues when they are behaving badly, rather than seeking to resolve issues face-to-face as they happen. This also furthers the perception that the root cause of UB is problematic individuals, which can further absolve an organisation of responsibility or blame. The ability to report colleagues easily can inadvertently make it appear less necessary to tackle those conditions that make poor behaviour more likely (addressing other, more difficult-to-tackle, contributors).
Top-down interventions that focus on identifying problematic individuals (C) can lead to other/wider contributors of UB remaining unaddressed (O) and have a negative effect on team cohesion (O2) because they can inhibit the development of an open culture that promotes psychological safety (M1) and increase retaliatory reporting (M2).
vs.
CMOC 41: Enhancing psychological safety.In an environment dominated by hierarchy and power dynamics, interventions addressing systemic contributors to UB (e.g. by reorganising the workplace, increasing role clarity and improving worker decision-making) (C) can reduce UB more effectively (O) because an open culture and psychological safety are fostered (M).
One included study using the Vanderbilt approach highlighted such unexpected consequences, stating that ‘introducing feedback about co-worker concerns may have unintended consequences ranging from increases in unprofessional conduct and retaliatory reporting to negative effects on team cohesion and a culture that emphasises reporting over colleague-to-colleague conversations about concerns’. 151 The same study highlighted that recipients of negative messages generally did not take them well, demonstrating that it can be a somewhat traumatic experience to receive such reports: ‘recipients’ responses included blaming systems and other people, asserting inaccurate reporting, minimizing their behavior’s impact, expressing disbelief that three reports over three years constituted a pattern, focusing on who might have reported, and offering to “apologize”’. 151 Another study went further, to suggest that preventing an accused from resolving an issue with an accuser can be a form of marginalisation in itself:
an accused is ‘isolated’ from communicating about a complaint with other staff [...]. While a laudable goal, such an act can be experienced as kind of marginalisation, in itself a harmful practice which is understood by some to indicate management’s complicity with bullying acts. 47
Based on this excerpt, it is unlikely that this fosters a psychologically safe environment in which trust between colleagues is maximised (see CMOC 41). Indeed, one can argue that creating an anonymous reporting system simply allows psychological safety to be bypassed and, instead, seeks to maximise ease of ‘speaking up’ (Figure 18).
FIGURE 18.
Locating bad apples is not the same as enhancing psychological safety.
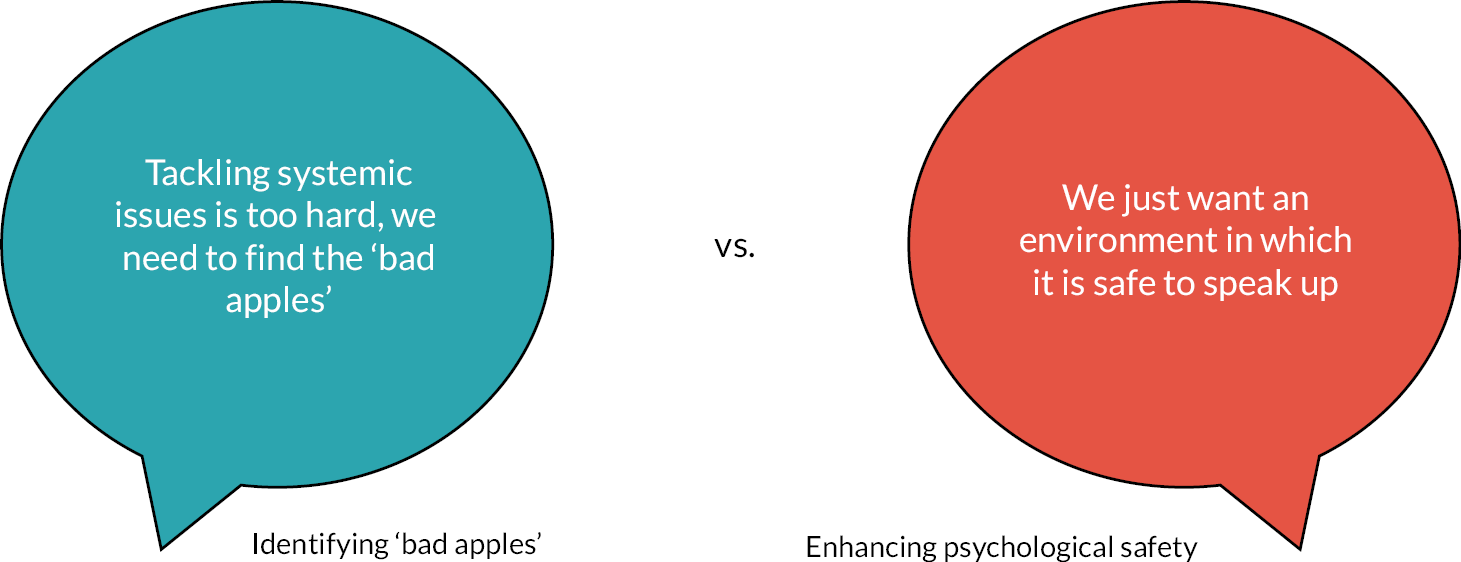
It is important to note that the literature suggests that identifying problematic individuals may be very effective at reducing incidence of UB, despite the risk that such systems may also be used to undermine others. Individuals may have lesser or greater proclivity to engage in UB due to their personalities or susceptibility to systemic issues such as pressure or lack of job resources etc. As such, reporting systems may eventually ‘weed out’ people from the environment; this may have the effect of changing the culture towards one in which UB is not tolerated.
Addressing this dynamic
While we emphasised that anonymising speaking up using online systems can effectively sidestep psychological safety and might not develop the intended culture change, it is possible to combine a reporting system with strategies that address other, more fundamental, contributors to UBs. For example, the Ethos programme also includes educational materials, appointment of intervention champions to help normalise speaking up and the ability to report positive ‘feedback for recognition’, which has actually comprised the majority of reports submitted to date. 97 Addressing other systemic contributors may further help to foster psychological safety in key moments and might be more effective than a reporting system alone. However, the cultural impact of mixing a reporting system with other strategies is, as yet, unclear.
Key Dynamic 3: How and why an intervention is expected to work must be clear; otherwise, evaluations of interventions can be misleading
Many of the included studies used intermediate outcome indicators – such as ‘assertiveness’ or ‘communication quality’ – as a measure of overall success. However, these are not sufficient to determine whether UB has been addressed. This issue may partially be due to underuse of theory and logic models when designing these interventions. One pertinent example of this is use of ‘awareness’ to assess intervention success.
Reliance on measures of awareness or prevalence of UB to gauge the success of an intervention is problematic. For example, four included interventions that relied on reports of UB as their primary outcome measure were reported by their authors as being ‘unsuccessful’. This was due to an increase in reports of UB seen in the intervention groups post intervention. 66,134,153,158 As the authors state, an increased number of reports of UB means that awareness was increased, which these authors consider in the ‘limitations’ sections of their studies. These authors also consider it to mean that their interventions are unsuccessful; however, this may be an erroneous judgement. If interventions were more robustly designed with a logic model that took intermediary concepts such as ‘awareness of UB’ into consideration, then improved awareness that led to staff increasing their reports of UB could be considered a successful example of behaviour change. This could then lead to more incidences of UB being addressed in the moment.
It is also important to note that while there are strategies that specifically seek to raise awareness of UB, many strategies do not. However, many strategies that do not aim specifically to raise awareness of UB are likely to do so as the intervention will raise the presence of UB as an issue in participants’ minds. As such, relying on decreased awareness or reports of UB to indicate intervention success may be problematic. To properly assess intervention effectiveness, the use of a wide range of outcome measures is required that enables an understanding of how and why awareness is key to reducing UB and improving patient safety (Figure 19). CMOC 42 highlights the risk intervention architects may encounter if they do not rely on robust logic models.
FIGURE 19.
Figure demonstrating that much of how interventions are intended to benefit UB or patient safety is left unclear.
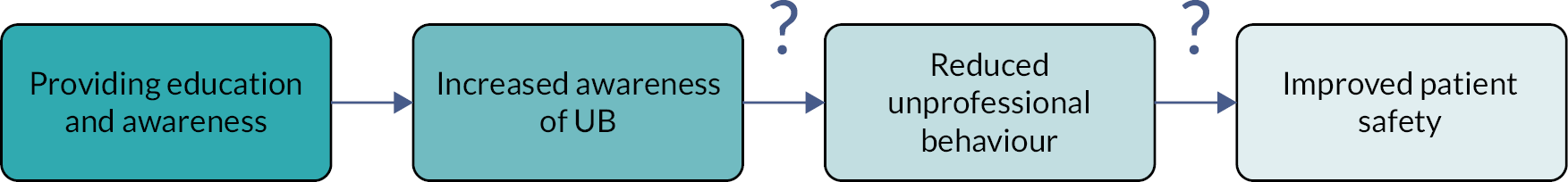
If those responsible for developing and implementing a UB intervention clearly map out how it could work, draw on theory and invest in sufficient evaluation (C), then how it impacts patient safety, staff psychological well-being and marginalised staff groups can be determined (O), because greater nuance regarding success can be determined (M).
Key Dynamic 4: Maintaining a focus on why it is important to reduce unprofessional behaviour (e.g. to improve patient safety) is key when designing an intervention to reduce unprofessional behaviour
We identified a dynamic whereby interventions may seek to reduce UB for the sake of reducing UB – but do so without enhancing ability to speak up in the moment and/or without improving staff conditions or patient safety. While reducing UB is the main goal of such interventions, it is important to remember that the primary reason to reduce UB should be to improve the psychological well-being of staff, and improve patient safety and quality of care. Improving ability to speak up in the moment can often be essential to improving patient safety14,24 (Figure 20); thus, interventions should seek to improve psychological safety. Included studies highlighted in some scenarios that, despite a programme being implemented to reduce UB, managers were still dismissive of patient safety concerns: for example
FIGURE 20.
Highlighting the juxtaposition between enabling speaking up in a way that enhances patient safety vs. a way that is less impactful to patient safety.
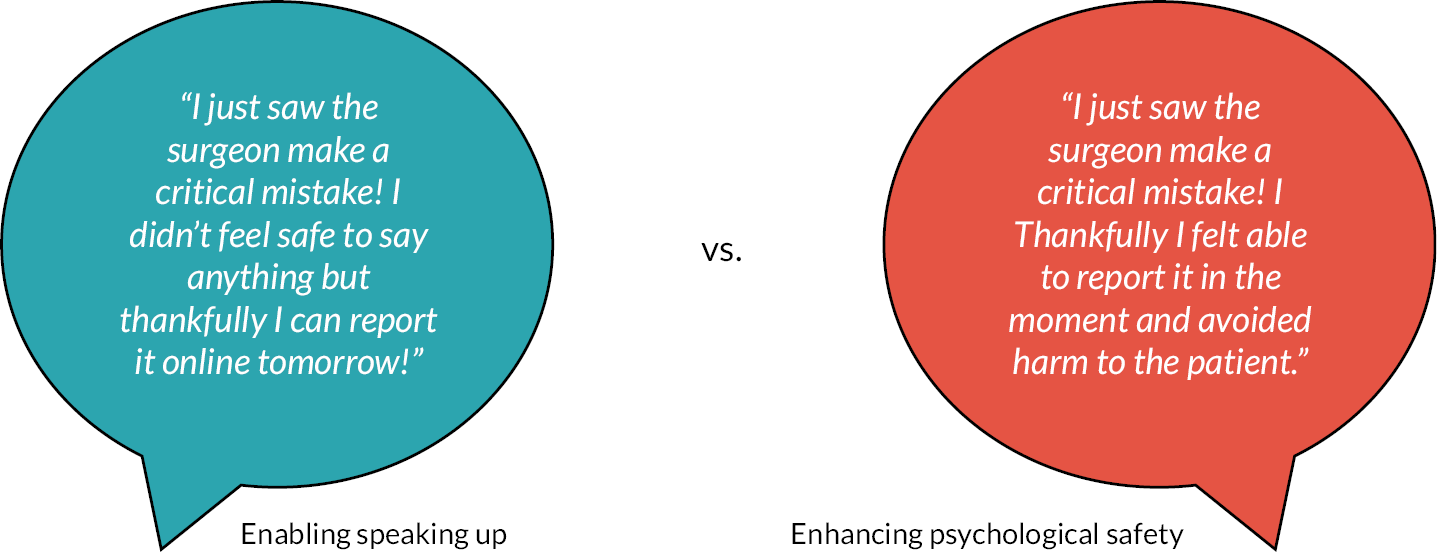
On multiple occasions over the past six months, [managers] have been disrespectful and dismissive of staff when patient management and safety issues have been raised …. Whilst I applaud the new safety system … the cultural change looks like it will take much longer. 93
However, such concerns should be an impetus for attempting to reduce UB in the first place.
Since many interventions discussed in this report involve rather distal aspects to improving patient safety – such as trying to increase staff assertiveness, for example – it is theoretically possible that novel methods such as CBM (discussed in full in Appendix 7) may have a greater direct impact on patient safety. CBM might be a valuable addition as it focuses on improving information-sharing, which is essential to maintaining safe patient care. 14
Included studies were not able to demonstrate that reducing UB improved patient safety or staff psychological well-being and that doing so is quite difficult since patient safety and well-being are a result of many factors. Despite the recognised importance of a patient safety basis for reducing UB, studies rarely attempt to measure improvements on patient safety metrics. Likewise, evidence that attempting to improve the ability for staff to cope with UB has an impact on the organisational culture or workplace design is absent. Very few interventions attempted to measure worker psychological well-being, while some drew on turnover rate as a proxy for worker satisfaction. While turnover rate may give some indication of staff satisfaction with their workplace, it is likely to also be a result of myriad other factors.
When interventions to reduce UB maintain a focus on improving patient safety (C), then challenging UB in the moment and speaking up about medical mistakes is more likely to be improved (O), because staff may feel more psychologically safe (M1); a greater focus on patient safety may enhance engagement (M2) and improve culture change (M3).
Key Dynamic 5: Encouraging bystanders to intervene is important for culture change but can lead to moral injury
Encouraging bystander intervention was a common strategy in the direct approach to instigator category in Chapter 6. Encouraging bystanders to intervene can send an important message that UB is no longer tolerated in an organisation and can lead to UB being addressed in the moment. However, encouraging bystanders to intervene can create a sense of moral imperative and may lead to moral injury (a MRT we outline in Chapter 3 and Appendix 2) if bystanders do not then have the courage or skills to intervene the moment UB is occurring. Alternatively, they may intervene and experience reprisal – or inadvertently escalate the conflict. A debate between demanding bystander intervention and being wary of it was frequently present in the literature. On the one hand, sources stated ‘We believe health professionals have a moral duty to practice ‘upstanding’ — intervening as bystanders’178 and on the other, ‘We thus find some of the advice offered rather out of place, e.g. for a bystander to confront a bully, given that the main remit of any bullying intervention should be to encourage harmony, not discord, in a workplace’. 47 This debate is reflected in CMOCs 44 and 45.
Encouraging bystander intervention (C) can lead to UB being addressed in the moment (O+) and drive social norms moving towards civility (O2+), because bystanders feel protected and able to act on their sense of moral duty to intervene (M2).
CMOC 45. Encouraging bystander intervention may lead to moral injury or reprisal.Encouraging bystander intervention (C) can cause moral injury if the bystander does not feel confident intervening (O−) or can lead to reprisal if intervening when it was not safe to do so (O2−), because they may feel that they have failed in their moral duty to intervene (M1).
Resolution
This dynamic suggests that care is needed when suggesting that staff intervene as it puts the onus on individuals to solve potentially systemic issues – at risk to themselves. There is also a risk it can lead to further conflict. As such, organisations should emphasise that it is not a moral duty to intervene and bystanders should only do so when they are certain they are not at risk of reprisal. Organisations should focus on creating psychologically safe conditions in which the risk of reprisal is low and there is safety for individuals when speaking up.
Key Dynamic 6: Identifying unintended consequences of anonymous reporting systems is essential
While allowing anonymous submissions about UB may increase speaking up behaviour, it may also increase the chance that systems may be misused. Systems that enable other people to be easily reported – especially anonymously – sidestep direct person-to-person resolution and may be used for purposes of undermining and scapegoating (CMOC 46). Sources highlighted the potential misuse of reporting systems: for example, one reporting system used within an adapted Vanderbilt approach identified how ‘a few staff described feeling distressed after receiving weCare feedback based on what they deemed vexatious and fictitious content’. 93 Another example arose from the Ethos intervention, which itself was ‘reported’ to the media for, among other issues, fostering alleged ‘implicit sexism’. In this case, ‘Ethos data from St Vincent’s public hospital for the 12 months to this month, seen by The Age, shows female medical staff were the subject of about 30 per cent more complaints than male medical staff’. However, it is also possible that going to the media regarding the intervention was itself an attempt by entrenched cliques to avoid a problematic culture from being addressed. Undermining of intervention measures seeking to address UB by cliques is a common theme, as this example demonstrates:
The continued emphasis upon in-house reporting schemes as a central plank to address workplace bullying inadvertently risks the protection of perpetrators, as it is possible that actors in alliances m0ay work together to subvert organizational reporting processes to protect their own interests. 117
Similar unintended consequences have been identified with the UK Datix electronic incident-reporting system; an incident-reporting system intended to aid patient safety used within NHS organisations. 179 Although primarily focused on patient safety, Datix is also known to be used to report UB between healthcare staff. For example, a recent publication highlights that ‘several high-risk events, including the assault of my team member by another staff member within a forensic unit, mandated the completion of an online Datix form’. 180 Informal accounts via social media provide some examples in which staff (Figure 21) report the weaponisation of the Datix system to the point where ‘Datixing’ has become a verb and is used as a threat. 180
FIGURE 21.
Tweet depicting the Datix system being used intentionally or unintentionally to undermine a doctor in practice in the NHS.
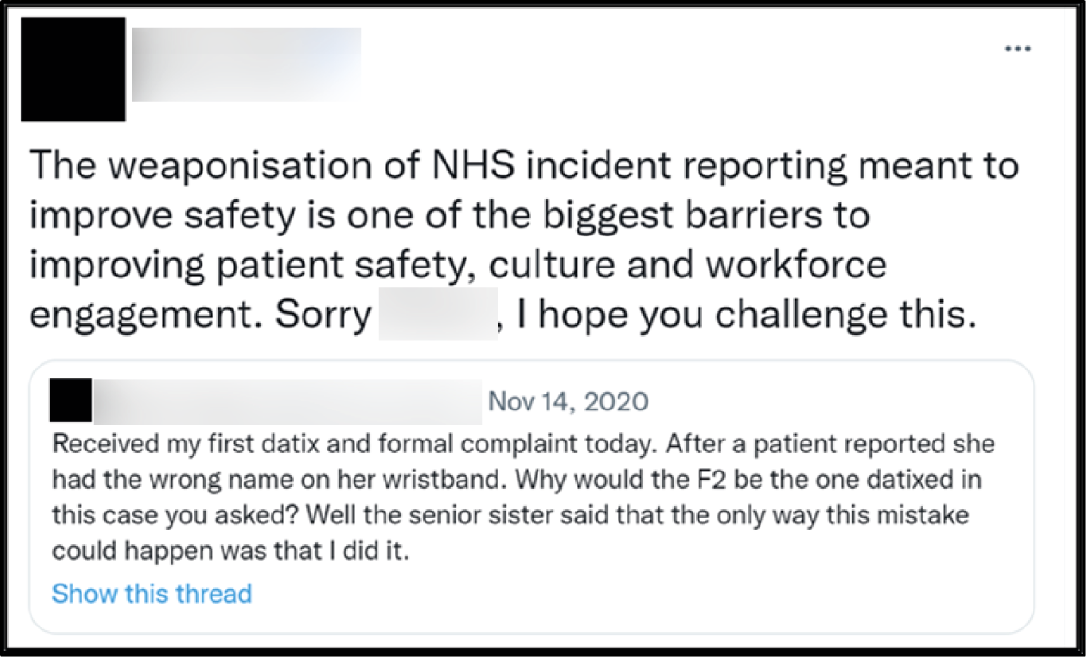
Bal et al. 180 highlight the weaponisation of Datix, stating that
45% of reports attributed blame to an individual, potentially reflecting an organizational culture in health which leads to retribution, rather than one of learning, along with ‘a failure to appreciate the contribution of system factors’, undermining the original purpose of the incident reporting system. 180
These dynamics are reflected in CMOCs 46 and 47.
Enabling anonymous reporting of colleagues (C) can mean instigators are approached by messengers or line managers, directly reducing UB (O) because recipients or witnesses of UB have been able to speak up where there are low levels of psychological safety (M1).
and
CMOC 47: Misuse.Enabling anonymous reporting of colleagues (C) can lead to an increase in UB in the form of undermining and scapegoating (O) because informal alliances and nefarious individuals can co-opt the reporting system to target specific individuals with false reports (M1).
Addressing this dynamic
Although misuse and unintended consequences of some reporting systems are quite commonly mentioned – as with the given Datix example – evidence from formal evaluations such as that of the Ethos intervention suggests that false complaints are not very common. They report that ‘there have been < 10 vexatious complaints in over 2000 submissions, and the triage process aims to identify such reports’. This triage process involves ensuring reports submitted are consistent with the purpose of the system and that reports ‘(1) should relate to a specific event, (2) the event was recent and (3) the feedback is likely to be useful’. 97 As such, it is currently not clear whether there is genuine abuse of these systems or simply a fear of abuse of such systems: this may have a negative impact on adoption. Either way, careful triage of messages is essential to avoiding unintended consequences of such methods that increase ease of speaking up. Use of ‘natural language processing software’, such as in the Coworker Observation System53 or use of even more novel artificial intelligence methods, to identify language indicative of a false or inflammatory report may also be a means to solving the issue. 53 Additionally, the use of a database to store reports and actions taken can also help to identify problematic messaging patterns.
Key Dynamic 7: Interventions must be perceived as authentic to foster trust in management
Many of the key dynamics we identified relate to building trust in management, which is often undermined when staff see UB occurring around them, unaddressed.
| Stakeholder feedback summary – rebuilding trust in management |
| Our spotlight session highlighted that trust in management is often particularly low among people from minoritised backgrounds. Often, there is a passing of the torch when it comes to accountability and often management do not want to acknowledge racism or sexism within their organisations. This lowers trust in management. |
| Stakeholders also helped us to make clearer the distinction between manager intentions behind interventions, how they are perceived by recipients and that there may often be a large gap between positive intentions of managers and poor receipt of the intervention. This helped us to refine Key Dynamic 7. |
Staff make a constant assessment of the culture of an organisation, particularly in terms of UB. Staff will notice behaviours by managers and take these as a signal for what is tolerated and acceptable. In organisations that have historically had an issue with UB, it is likely that staff strongly desire change towards a civil environment and seek signs that this is the direction of travel. This ties in with trust in management (a MRT outlined in Chapter 3 and Appendix 2), because staff who experience unaddressed UB for a prolonged period of time will lose trust in management. 48,143,155 To assess whether it is worth trusting management to provide a safe working environment, healthcare staff will assess the authenticity of efforts that management make to reduce UB. By authenticity (and genuineness) of the intervention in this section, we mean the perception of ‘whether there is a collective change in management intention to properly address UB and regain employee trust’. This notion of a ‘changing wind’ was highlighted by another included study: ‘The commissioning of the interview study and the wide public sharing of the findings functioned as an intervention in its own right, demonstrating to sceptical colleagues a new appetite for learning in the organization’. 143
An assessment of authenticity may involve looking at the intervention itself and assessing whether its components are likely to have the desired effect (i.e. is it a ‘tick box’ or a real attempt at changing culture?) (Figure 22). For example, one included study found that
FIGURE 22.
Perception of programme intervention authenticity.
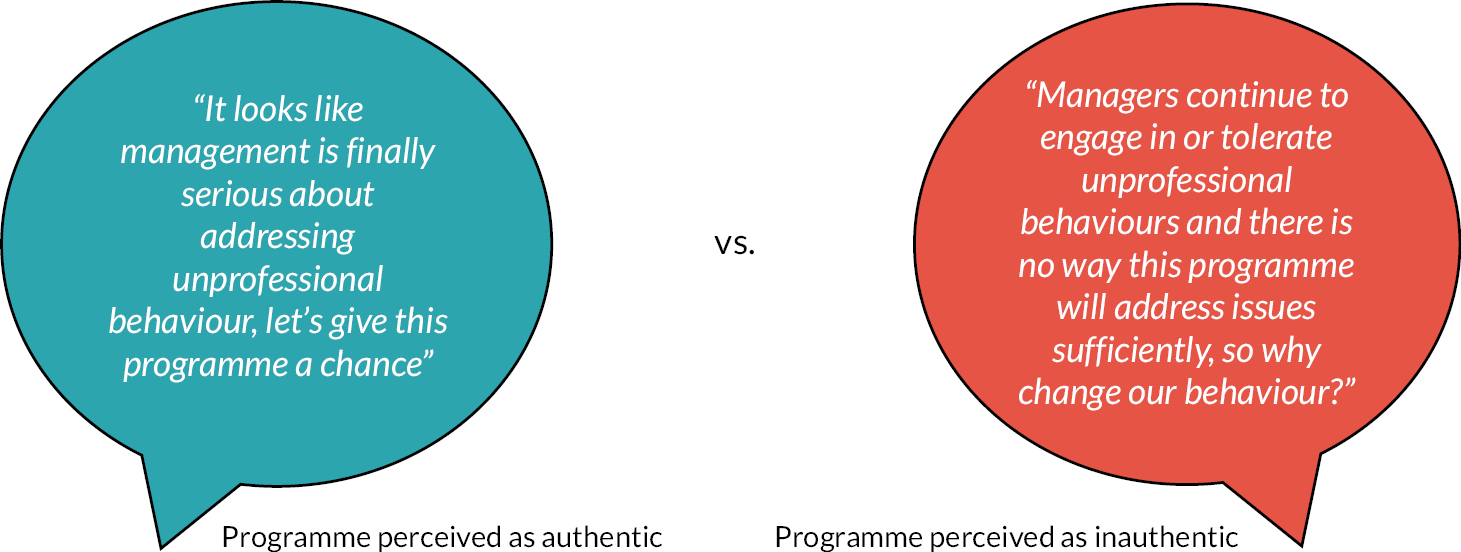
employees’ attributions and perceptions of the organisation’s intention to prevent negative employee behaviours (bullying) only have their desired effect when policies are perceived to be implemented effectively. Effective implementation appears to signal to employees that bullying behaviours will not be regarded as acceptable behaviours within the organisation. 181
Staff will also look to managers to ensure they are not continuing to role-model negative behaviours themselves. One included intervention was undermined in this way: ‘at mid-intervention several participants had observed leaders behaving in an unprofessional manner which was sending inconsistent messages and perceived as impeding implementation’. 93 Likewise, another study reported interventions to be less successful if an organisation was known to be poor at following up and sustaining initiatives. 21 As such, the sense that interventions are genuine must be fostered, otherwise healthcare staff will not properly engage with interventions because they will not trust management and not trust that it is worth their time. This will undermine the intervention’s effectiveness.
Manager intentions
It is important to highlight that managers may have very positive intentions when it comes to changing the organisational culture but that the perception by healthcare staff can differ. This may particularly be the case with well-meaning interventions that are simply not sufficiently wide-ranging to be effective – perhaps due to resource constraints. One included paper highlighted this dynamic: ‘it is also possible that a type of intervention is selected for perceived value-for-money rather than quality, relevance or efficacy, such as that required for staff to genuinely change or develop their values’. 47 Similarly, ‘“good” initiatives, once out of the spotlight, can be quickly forgotten, especially if there is high turnover of staff. This can make well-intentioned activities feel tokenistic, regardless of the actual commitment of those instigating them’. 131 In other cases, managers and leaders may want to be seen to be addressing UB while knowing that the interventions they are implementing are not going to be sufficient to address the problem. This situation risks being perceived as ‘virtue-signalling’ (a public expression of opinions or sentiments intended to demonstrate one’s good character or social conscience), ‘box-ticking’ or tokenistic. Frustrations with efforts that were clearly inadequate and not going to work were highlighted by one study:
Informants suggested that senior management had very little accountability, took little action and instead gave token rewards to staff to improve culture, such as barbeques, pizza days and bacon and egg rolls. Informants described those actions as ‘insulting’ (CNE1) and ‘having little effect upon culture’ (CNE2). 177
Another paper highlighted some strategies leaders could use to avoid their interventions seeming to be ‘tokenistic’: ‘Emphasising the judgements that leaders at all levels make as to what to do, modelling curiosity, admitting mistakes, encouraging participation and showing genuine commitment seem to be important so that interventions do not come across as tokenistic or inauthentic’. 131 Authentic interventions will see greater engagement, greater cultural impact and an improved sense of psychological safety (CMOC 48). However, if staff do not see interventions as genuine, engagement and effectiveness will be reduced (CMOC 49).
When interventions are seen to be authentic and senior staff role-model professional behaviour (C), then staff feel more able to buy into the intervention (O) because it is perceived to be a legitimate attempt at reducing UB (M).
vs.
CMOC 49. Intervention perceived as inauthentic.If managers implement an intervention to address UB but continue to role-model or tolerate negative behaviours (C1) or the intervention content is perceived as unlikely to have any effect (C2), then staff will disengage from the intervention (O−) because staff dismiss it as inauthentic (M).
Solving this dynamic
Resolving this dynamic requires building a sense of intervention authenticity and building trust in management (and thus interventions and strategies they introduce) by increasing engagement with interventions and avoiding negative leadership behaviours. Key to building a sense of authenticity and trust in management are activities whereby major organisational contributors to UB are identified and targeted, always ensuring leaders role-model positive intervention-coherent behaviour, ensuring managers are targetable/included in the intervention, using co-creation to build engagement, and ensuring the intervention is widely advertised and that it has the staying power and resource backing that gives people confidence it will deliver (see Chapter 8). Lastly, interventions need to pass a ‘common sense’ inspection by those participating to ensure its strategies might be able to have the stated impact.
Key Dynamic 8: One size does not fit all – tackling unprofessional behaviour generally requires multiple and sustained interventions to address underlying contributors
Related to Key Dynamic 7, we also identified that doing something to tackle UB is not the same as doing enough. Interventions will likely require many strategies, sustained over a long period of time and with genuine systemic changes to address contributors leading to UB. One study, for example, identified that their one-off educational intervention was insufficient to address UB in their organisation, stating ‘a one size fits all approach is not sufficient to mitigate negative workplace behaviour and that using education as a “tick box approach” is unlikely to be effective in developing sustainable cultural changes in organizations’. 177 This, however, relies on sufficient resource being available to implement follow-up action that draws on more strategies. Organisations also run the risk of becoming complacent because they are already doing ‘something’ to address UB, which can lead to other contributors remaining unaddressed. In these cases, for example, ineffective policies or procedures are seen as adequate and can lead to situations in which ‘workplaces with prominently posted policies that mandate respect or decry bullying often fail to address actual complaints’. 114 One study also demonstrated this, stating that a bullying intervention was ‘management’s “one hit wonder”’ but that it ‘would require concurrent and similarly successful initiatives to raise their level of trust in management’. 122 This dynamic is highlighted in CMOC 50.
If an intervention does not address all UB contributors (C), this can allow UB to continue (O−) and inhibit trust in management (O2−) because contributors remain unaddressed and more comprehensive interventions to reduce UB are ignored (M).
It is also important to note that failing to tackle systemic issues, such as unfairness in the workplace, can disproportionately impact those individuals with protected characteristics who suffer from systemic or less visible forms of UB, such as discrimination. One included study highlighted this, stating that
race equality and inclusion may be unamenable to simple applications to evidence-based interventions that do not take into account the subtleties of local context and history. A ‘do-once’ attitude, or well-intended processes that do not model the spirit of the outcome, may even be harmful. 131
Key Dynamic 9: Addressing manager behaviour is essential for building trust in management
Interventions work best when they are seen to include management; it is essential for trust in management to be (re)built (Figure 23 and CMOC 51). If an intervention involves ‘targeting’ individuals – such as with a reporting system – then it must include the ability for managers to be targeted, too. If it delivers training, this is less important but still helpful when it comes to demonstrating that management is involved in moving the culture in a positive direction in some way. The importance of this is explained in one study:
FIGURE 23.
Managers must implement programme interventions that include themselves.
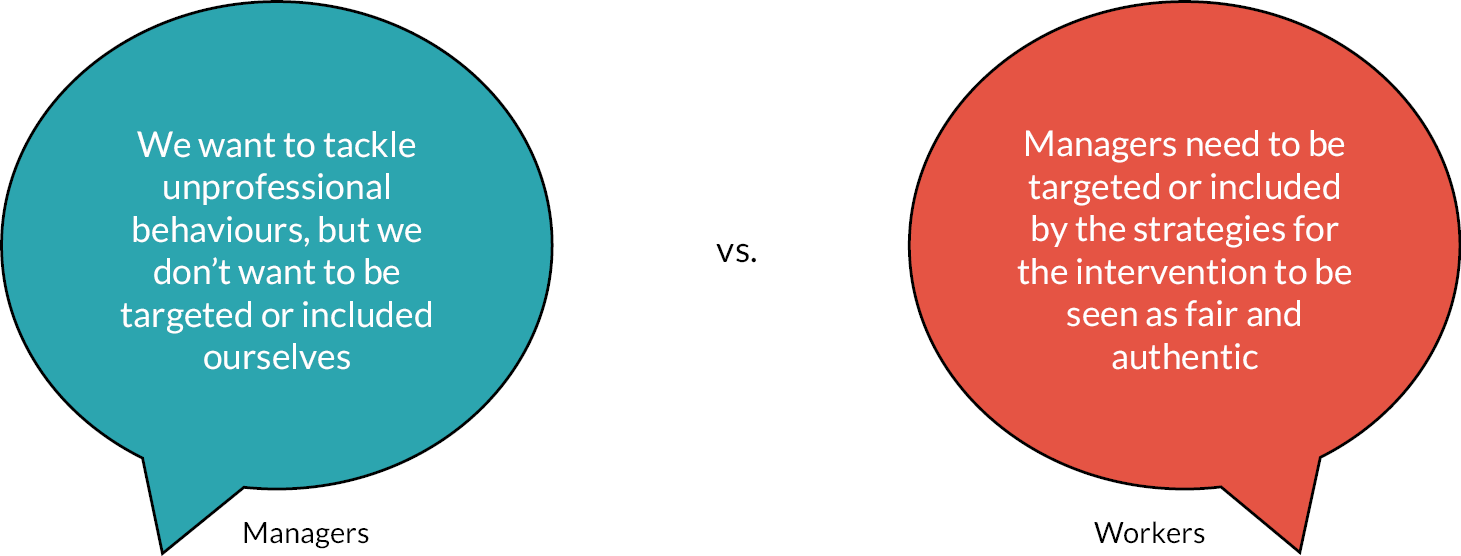
Management participation is also important because these staff are not immune to bullying behaviours, and in some cases are central protagonists. Either way, ‘what management do’ (role modelling and showing they are learning and supporting other staff) has been shown to vastly influence workplace culture and any intervention. 22
However, managers or leaders are usually the ones who implement any intervention to reduce UB (CMOC 52). Thus, from the outset, there’s already a potential incentive to exclude themselves being targeted or involved in the intervention, creating a dilemma that organisations need to address. This will be especially important for those organisations in which managers have been seen to engage or tolerate UB themselves, with subsequent low levels of trust in management. In cases in which managers do not want to be targeted by the interventions they implement, interventions may not be successful; in such cases, the only resolution may be external pressure from regulatory bodies or enforced leadership changes.
If managers include themselves as a recipient or target of an intervention (C), this can show that UB is no longer tolerated (O+) and can build trust in management (O2+) because it signals to other employees that the intervention is genuine (M1) and suggests there is a real cultural shift taking place (M2).
vs.
CMOC 52: No participation.If managers do not include themselves as recipient or target of the intervention (C), this can allow UB to continue (O−) and reduces trust in management (O2−), because it signals to other employees that the intervention is unfair and/or managers that are not taking it seriously (M1) and suggests there is no real cultural shift taking place (M2).
Key Dynamic 10: Interventions that are both inclusive and equitable are critical to ensure effectiveness and sustainability and for addressing inequalities
Interventions should be seen as both inclusive and equitable. However, we identified that it was rarely possible to achieve both, particularly when it came to creating equitable solutions across different groups. As discussed earlier in this report, certain groups with protected characteristics experience more UB in the workplace. Yet these groups are currently rarely catered for in existing interventions to tackle UB. One could argue that this reduces fairness and equity of access. For example, the following excerpt from one study notes: ‘despite their selflessness and arduous work, Black African nurses face structural and institutionalised discrimination within the NHS. Employers must challenge the dominance and hegemony that exists within the NHS to ensure greater equality of all employees’. 69 Interventions could – and arguably should – be more accessible and designed and specifically focused on reducing UB for these groups. One way to do this could be to deliver an intervention to improve opportunities for these staff with protected characteristics or to deliver an intervention specific to racism.
However, at the same time, included sources have highlighted that being inclusive is also important. While equity is essential to the success of interventions, it is also important to include as many people as possible in an intervention and not target one group over another. This is because targeting interventions at specific groups could alienate certain groups or imply they are at fault. Examples could include targeting doctors with an anti-bullying intervention because they are perceived to be bullies more often than nurses. One study highlighted that
it is now noted that some methods of delivering interventions to staff may induce feelings of being ‘targeted’, ‘at fault’ and perhaps being bullied themselves, if content is ‘aimed’ at certain negative behaviours, say ‘anger management’, or staff groups, say ‘the doctors’. 47
This highlights that this dynamic can apply to professional – as well as demographic – groups (e.g. gender).
One included study highlighted a participant reacting to the existence of a leadership programme open only to staff from an ethnic minority background:
For the [ethnic minority] leadership programme, it’s well, ‘What [have you] been taught which I couldn’t be taught?’ What is actually being said [to programme participants]? Is it, this sounds really bad and really racist, but is it, ‘Don’t listen to the white man’?. 131
In addition to the perception that such interventions are unfair, sources also reported that deficit-led interventions may have unfortunate connotations as ‘development programmes aimed at ethnic minority staff might create a sense that they somehow need to be “brought up” to the same level or standard as white people’131 (see Stakeholder feedback summary – inclusion and equity). As such, these dynamics highlighted a tension between inclusion and fairness, and that picking one or the other may result in negative consequences (Figure 24). These dynamics are also reflected in CMOCs 53 and 54.
| Stakeholder feedback summary – inclusion and equity |
| When we presented this dynamic to our stakeholder group, we received feedback that ‘deficit-led’ interventions (those that try to ‘bring up’ one group to the level of another) can be problematic for both those receiving the intervention (due to the implications of this) and for those who are not (due to feeling of unfairness). This suggests that policies that are deficit-led may inadvertently increase UB towards certain groups; however, this has not yet been tested. |
FIGURE 24.
Interventions that are both inclusive and fair are difficult to achieve.
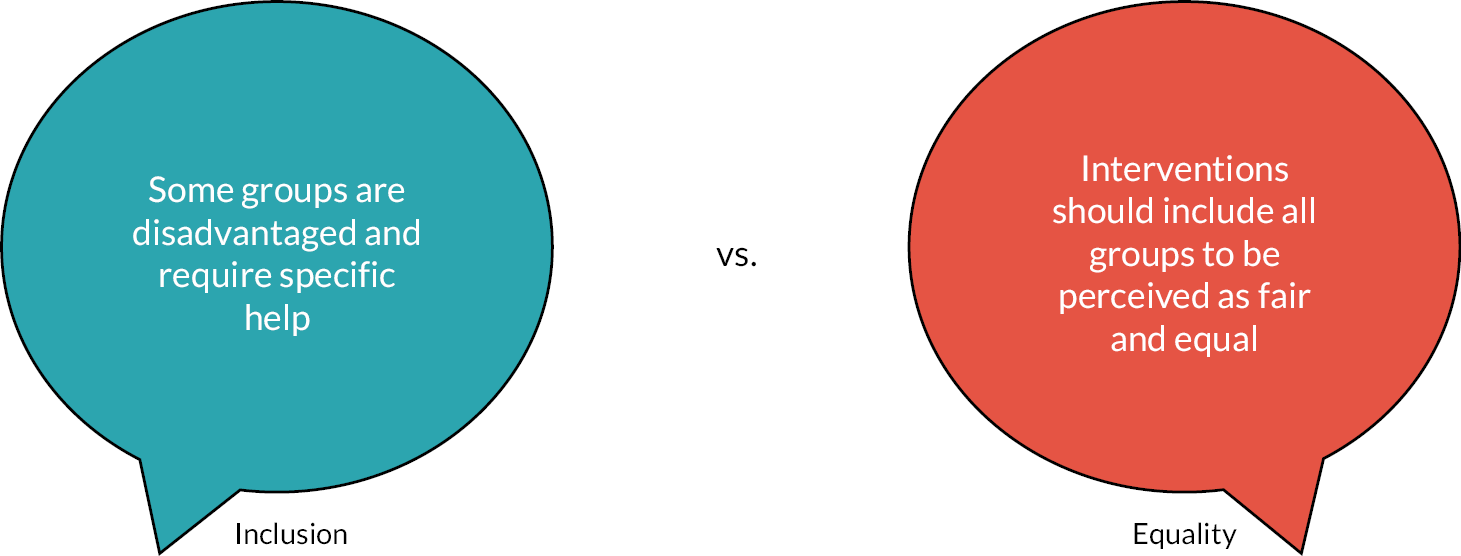
A further risk is that delivering interventions for only one marginalised group may inadvertently also exclude those from other disadvantaged backgrounds, such as those from an economically deprived background, LGBTQ+ people or people with a disability. It also shows that interventions to enhance fairness at the cost of inclusion may generate unnecessary conflict. Simply ensuring all employees have equal access to opportunities (equity) may be the less risky option for organisations. It is not clear whether a lack of interventions seeking to address UB towards marginalised groups is due to leaders wrestling with this key dynamic or simply due to underinvestment and lack of prioritisation of this issue.
When UB interventions cater to the specific needs of groups that experience systematic inequalities (C), then they will feel better supported in their workplace (O), because they feel heard, seen and validated where previously they felt ignored (M).
vs.
CMOC 54: Inclusion.If UB interventions seek to include all staff, including minoritised staff, and recognise differences in experiences such as higher rates of bullying directed at minoritised groups (C), then interprofessional conflict may be reduced (O), because staff feel included and their differences acknowledged (M).
Solving this dynamic
This dynamic reflects a situation in which both sides have negative outcomes and only one can be chosen. Theoretically, it is possible to design an intervention that has both inclusive components open to all, as well as elements that can boost opportunities for specific groups. This may lessen the backlash to group-specific elements but, since it has not been tested, it is not clear by how much.
Addressing these issues and overcoming this dynamic may again require better data to enhance understanding of the contributors to UB that impact these groups. For example, one included source surveyed the culture in their organisation and performed a demographic analysis. They found that people with a disability experienced undermining- and scapegoating-type behaviours more than others and this was found to stem from management. They found that in their organisation
people with disabilities and chronic health conditions are often poorly managed in terms of workloads and deadlines and procedures around making reasonable adjustments are often seriously misunderstood by managers […]. The data here is very clear – disability is correlated with several unreasonable management behaviours. 76
As such, performing a root-cause analysis was able to identify that management style was the source of the greater experience of UB by this group and that management training could be a solution. As such, better data may enable more simple solutions to problems facing specific groups in cases such as these, avoiding this dynamic.
Key Dynamic 11: There are trade-offs between fixed interventions and flexibility
As discussed in Chapter 5, we identified that some interventions were adaptable to the situation and organisational context. This meant that certain strategies might be used in some contexts but not in others. Theoretically, this adaptability can enable enhanced efficacy, because drawing on a repertoire of strategies can mean strategies can be chosen that better fit the context (CMOC 55). For example, Laschinger et al. 155 set out how certain strategies can be used to tackle certain goals in the CREW intervention. In CREW, weekly meetings enable identification of the challenges ahead and strategies can be either drawn from a repertoire or created on demand, to be implemented on a case-by-case basis. An example they provide is one in which junior managers identified that a lack of conflict-management skills in their unit may have been leading to UB. As such, discussion in a weekly meeting led to implementation of role-playing scenarios to build the missing conflict-management skills. 155
This trade-off between flexibility and fidelity necessarily means that it is more complex and difficult to be able to assess why the intervention worked since the intervention will not be the same when delivered in different contexts. For example, was success due to implementing this conflict-management strategy or was it due to another strategy targeting another situation – or did it work despite implementing these strategies? As such, when implementing CREW in one organisation versus another, the actual implementation may comprise entirely different delivered components and thus be similar to comparing two totally different interventions in behavioural terms. This difficulty of evaluation is reflected in CMOC 56.
When implementing an intervention to address UB that draws on flexible implementation (C), this can enhance efficacy of the intervention to reduce UB (O) because it may enable better adaptability of strategies to specific scenarios (M).
and
CMOC 56. Fidelity.When implementing an intervention to address UB that draws on flexible implementation (C), this can reduce the ability to identify how to change the intervention to improve future efficacy (O) because variability in implementation delivery across organisations can make it difficult to identify which components work (M).
Key Dynamic 12: There are trade-offs between a theory-first and practice-first intervention design
In Chapter 5, we identified that many interventions lack a strong theoretical framework and logic model, and that many interventions are being conducted in practice and are not reported in the academic literature. Key Dynamic 12 refers to two main ways we identified to design an intervention: (1) top-down (i.e. drawing on robust theory, logic models, modelling the assumptions and components behind how UB may occur, developing an intervention that targets the antecedents of the behaviours) or (2) bottom-up (i.e. identifying a problem on the ground, searching for an applicable solution and implementing it to prevent UB as quickly as possible). Academics may use the former top-down strategy, while many working in practice in the NHS often use the latter strategy.
A top-down approach may have more ability to test what works and why, whereas the bottom-up approach may provide adequate results more rapidly. One limitation of a top-down approach could be that it does not properly target the contributors ‘on the ground’, as highlighted by one study:
The Program’s implementation was commonly viewed as being ‘top-down’ and not adequately reflecting the unique needs of unit-level sub-cultures: ‘I feel that the staff aren’t really connected with the organisational programme because it kind of sits up here and it’s very disconnected from what goes on at grassroots level’. 93
While we are portraying this as a key dynamic, we do believe it is possible for a theory-based, well-articulated and practical intervention to be constructed. However, this will require suitable guidance to be in place that would enable practitioners on the ground to easily access information required for tackling UB in the workplace (see draft manager’s guide, Appendix 8). This includes which strategies target which contributors and a basic introduction to changing behaviour, as well as factors that can inadvertently affect intervention implementation such as these key dynamics. CMOCs 57 and 58 highlight the key trade-offs.
If an intervention to reduce UB is being implemented drawing on theories about how UB may arise (C), then an intervention may take longer to design and implement (O), because it is facilitating a more robust evaluation process (M).
vs.
CMOC 58. Practice-led.If an intervention to reduce UB is implemented rapidly (C), then understanding its effectiveness will be compromised (O), because due consideration of the evaluation process has not been factored in (M).
| Stakeholder feedback summary – key dynamics |
| We presented a selection of these findings to the stakeholder group in November 2022 and March 2023. The group helped us to ensure we name these as ‘dynamics’; previously we had referred to them as ‘tensions’, which was not reflective of all findings. |
| The meetings also helped us to surface other dynamics. For example, in the November 2022 meeting, one stakeholder asked: ‘How many organisations ask what evidence there is that what they plan to do might do what it aims to do’. This was a pertinent point to raise and helped us formulate Key Dynamic 3. |
Summary
We identified 12 key dynamics across the literature, which are essential considerations for understanding when strategies to address UB work (Table 18).
| Key dynamics |
|---|
| Key Dynamic 1. Interventions should address systemic factors that contribute to UB – not only individual factors. Individual factors were overestimated as contributors to UB, which leaves systemic contributors unaddressed and can lead to implementation of interventions that do not tackle root causes of UB |
| Key Dynamic 2. Focusing on individual staff can have unintended consequences for psychological safety. When systems are implemented that seek to weed out the bad apples, this has implications for psychological safety because staff do not feel protected and systemic issues (see Key Dynamic 1) remain unaddressed |
| Key Dynamic 3. How and why an intervention is expected to work must be clear; otherwise, intervention evaluation can be misleading. Existing studies have claimed success or failure based on intermediate outcomes such as ‘level of awareness’ of UB or adjacent outcomes e.g. ‘assertiveness’. Use of logic models is essential to improve fidelity of such evaluations and get closer to measuring actual improvements in UB |
| Key Dynamic 4. Maintaining a focus on why it is important to reduce UB (e.g. to improve patient safety) is key when designing an intervention to reduce UB. For example, increasing the ease and normality of speaking up in the moment will have a greater, more positive impact on patient safety than facilitating it later on |
| Key Dynamic 5. Encouraging bystanders to intervene is important for culture change but can lead to moral injury. Encouraging bystanders to intervene sends signals regarding unacceptability of UB. However, creating an imperative to intervene can also lead to moral injury if staff subsequently do not intervene and can place staff at risk of reprisal |
| Key Dynamic 6. Identifying unintended consequences of anonymous reporting systems is essential. Systems that enable anonymously speaking up also enable subversion of these systems to drive behaviours such as scapegoating by filing false reports. This can be avoided with triage systems or databases |
| Key Dynamic 7. Interventions must be perceived to be authentic to foster trust in management. Authenticity can be lost if managers are simultaneously engaging in negative behaviours and sending mixed messages or if the intervention itself is clearly inadequate for its intended purpose |
| Key Dynamic 8. One size does not fit all: tackling UB generally requires multiple and sustained interventions to address underlying contributors. Many interventions do not address systemic contributors; rather, only a small number of them for a certain duration. Existence of an inadequate intervention may inhibit more adequate interventions from being developed and put into place |
| Key Dynamic 9. Addressing manager behaviour is essential for building trust in management. To be seen as genuine, interventions need to include managers and senior employees at all levels. This is especially important for those organisations in which managers have been seen to engage in or tolerate UB themselves, with subsequent low levels of trust in management |
| Key Dynamic 10. Interventions that are both inclusive and equitable are critical to ensure effectiveness and sustainability and for addressing inequalities. Gaining a greater understanding of the differences in experience of UB by different groups and the root causes for these may help drive greater understanding of how to address UB in a fair and inclusive manner for people with protected characteristics |
| Key Dynamic 11. There are trade-offs between fixed interventions and flexibility. Some interventions are inherently flexible, enabling use of a repertoire of strategies that may be more effective in different contexts. However, different components in different contexts make it difficult to evaluate what was effective |
| Key Dynamic 12. There are trade-offs between a theory-first and a practice-first intervention design. A theory-first design risks being distant from what occurs in practice whereas a practice-first design risks lacking articulation of how and why it is supposed to work. As the study of such interventions progresses, provision of materials for those embedded in practice may help bring these two approaches closer together |
Chapter 8 Implementation principles to optimise future interventions to reduce unprofessional behaviours
Introduction
This chapter presents both general implementation principles that span interventions and specific recommendations for organisations. We have begun to translate the intervention guidance in this chapter into practical resources for managers to fully address this objective. We have done this in collaboration with our stakeholders and advisory group members; indicative content can be found in Appendix 8. The guidance will be finalised with stakeholders and published as an output of this study.
What follows is an exploration of 15 implementation principles applicable to a range of UB interventions and organisational scenarios. These have been developed within the context of the preceding chapters (particularly Chapters 6 and 7). Their development was based on our realist understanding of the mechanisms by which interventions seek to reduce UB or mitigate the effects, as identified in the categories and key dynamics. As such, we refer to the key dynamics from Chapter 7 throughout this chapter. For each principle, we have developed CMOCs to help explain the mechanisms of action, the contexts that are conducive (or otherwise) and the outcomes that may be expected.
Implementation principles to optimise unprofessional behaviour intervention effectiveness
This section will explore the key implementation principles identified through our analysis that apply across a wide range of interventions seeking to tackle UB. These CMOCs are formulated as ‘action statements’ – that is, if (context), then (outcome), because (mechanism) – for simplicity.
Implementation Principle 1: Reach
It is important that interventions seeking to address UB have broad reach. This means including all staff groups, including management and senior leaders, to demonstrate a serious effort by the organisation. 151 Evidence suggests that including as wide a range of staff as possible could also provide additional benefits, such as improving interprofessional interactions22 and reducing ostracisation of certain groups, as discussed in Key Dynamic 9. However, consideration must be given to how different groups are brought together to promote psychological safety; particularly if hierarchies are mixed (see Implementation Principle 15).
| CMOC 59. If an intervention is delivered to as many staff as possible (C), then it may be more effective at reducing UB (O), because it can improve engagement and interprofessional interactions, reduce ostracisation and demonstrate that management is serious about tackling UB (M). | ‘… a relatively “broad” approach, including all staff, can also optimise engagement particularly where positive relationships begin to be reinforced or forged between professional groups. For example, an approach which crosses disciplines and groups of people, and aims to include everyone’.22 |
Implementation Principle 2: Co-creation
Including staff in the design and delivery of intervention content can be a practical way to increase a sense of ownership among staff. 119 Engaging staff in this way can also help to empower them (by making them feel involved in doing something to tackle the issue),138 as well as ensuring that intervention content is tailored appropriately to ensure uptake. 138 Examples in the literature indicated that staff can both help plan the intervention and become agents of change during intervention implementation. 126,138 Similarly, co-creation can help increase a sense that managers are now serious about addressing UB and that they are making an authentic effort to design a proper intervention. This can help to resolve Key Dynamic 5 and can help sustain engagement with the intervention for longer.
| CMOC 60. If UB interventions are designed and implemented with staff at the helm (i.e. co-created) (C), then staff feel a sense of ownership (O), because they have been engaged with the process and perceive it to be authentic (M). | ‘Involving nurses in policy development gives them the opportunity to take ownership and responsibility for the environment in which they work. Enabling nurses themselves to develop a policy addressing workplace bullying is one strategy to decrease bullying’. 119 |
Implementation Principle 3: Assess before implementation
Identifying organisational antecedents is an important initial step. Surveying organisational culture and identifying the contributors to UB within an organisation can enable better tailoring of strategies to an organisational context. Assessing organisational context before implementing any interventions or strategies can be useful in multiple ways: it can identify pockets of UB that may require more targeted approaches, enable an understanding of how the existing culture is contributing to UB, and identify specific UB that require specific tailored interventions or strategies. In the CREW intervention, for example, the pre survey determines how a site can best implement the intervention. Conversely, one included study highlighted that ‘failure to identify and address catalysts could itself be understood as a way to “facilitate” or perpetuate bullying’. 22
| CMOC 61. If delivering an intervention to reduce UB (C), then assessing the organisational landscape in terms of culture, presence and types of UB before the intervention is implemented can improve effectiveness (O), because it enables the specific targeting of appropriate strategies at contributors (M). | ‘… analysis of risks or of potential organisational antecedents of bullying can be conducted through the application of particular instruments, pre-intervention surveys, interviews, focus groups, introductory meetings, and joint discussions’. 21 |
Implementation Principle 4: Dedicated staff to lead work to tackle unprofessional behaviour
Identifying dedicated staff to tackle UB can facilitate intervention sustainability and provide a single point of contact for organisational expertise and knowledge, thereby enhancing its success. One study referred to drawing on an ‘interventionist’ to ‘develop a knowledge and understanding of what exactly staff do and a department’s clinical function within the health system’ to ‘offer appropriate, applicable content’ for an intervention, as well as to ‘ensure the offering is accessible’. 22 Use of dedicated staff can increase the perception that management is engaging in a genuine effort to address UB (Key Dynamic 5).
| CMOC 62. If delivering an intervention to reduce UB (C), then having dedicated staff in place to tackle UB can improve intervention momentum and sustainability (O), because staff can collate relevant information for implementing the intervention, which may enhance applicability of content, increase perception that management is serious about addressing UB and increase staff engagement (M). | ‘An interventionist taking time to acquire such knowledge, and to develop an intervention around it, can help staff to engage in learning as it indicates a degree of respect for those taking part and understanding of their personal situation’. 22 |
Implementation Principle 5: Skilled facilitation
Many types of intervention require a facilitator to deliver content. This can include the use of training strategies, such as conflict-management training, educational activities or the training of essential staff members as mentioned above (e.g. peer messengers97). Comprehensive training enables foresight of any issues that may crop up during intervention delivery, avoiding unintended consequences before they happen.
| CMOC 63. If an intervention to reduce UB relies on facilitation (C), then the facilitator must have adequate training and be skilled at delivering intervention content to be successful (O), because a facilitator with the ‘right’ skills will be capable of building an alliance between themselves and participants, keeping discussion on track and engaging participants, which can lead to better intervention outcomes (M). | ‘… an interventionist’s process and content might be appropriate, but their lack of skill can mean participants side-track discussion away from a central remit’. 22 |
Implementation Principle 6: Multiple simultaneous strategies
Use of many simultaneous strategies (as opposed to only one or two) in an intervention was often cited as a major factor in success. 68,93,138,141 Purported reasons indicate that use of many strategies ‘link together to form social systems that promote changes in behaviour norms’172 and that strategies ‘must be multidimensional in order to reach all constituents in an organization’. 138 It is thought that the use of multiple strategies may be more effective at changing culture and practice. 68,141 This works best when there is a full understanding of both what strategies are appropriate for the type of UB (see Implementation Principle 3) and why and how those strategies may interact and complement each other. Evidence for this is currently lacking. Additionally, inclusion of a greater number of strategies will incur a resource cost. Nonetheless, drawing on multiple strategies can help to improve intervention authenticity (Key Dynamic 5) and address a greater number of contributors to UB (Key Dynamic 6).
| CMOC 64. If an intervention draws on a greater number of simultaneous strategies (C), then it may have a greater culture-change impact (O), because they create social systems that promote behaviour change, reach more people, increase uptake, address multiple contributors and send a signal that management is serious about addressing UB (M). | ‘Our approach also suggests why bundles of interventions packaged together seem more effective than single interventions. This is not because they have an aggregate or cumulative effect, but because they link together to form social systems that promote changes in behaviour norms’. 172 |
Implementation Principle 7: Maximise visibility
Interventions must be highly visible. Maximising visibility of activities or interventions to address UB sends a strong signal about leadership and culture change and can improve effectiveness. During the project lifecycle, advertising successes of the intervention can also be extremely important: for example, in organisation-wide e-mails from leadership or organisational newsletters. This can help sustain momentum and build trust in the intervention, which can help build a sense of authenticity essential to Key Dynamic 5. For example: ‘The Programme is well advertised, information about it is everywhere – posters, intranet page, computer screen savers. I think this helps provide a strong stance that this programme and changing our culture is a priority’. 93
| CMOC 65. If delivering an intervention to reduce UB (C), then ensuring it is highly visible through advertising improves its momentum and effectiveness (O), because it helps engage staff, sends a signal that culture change is happening and increases participation (M). | ‘Participants noted mid-intervention that formal communications promoting the Programme were important in engaging staff in cultural change and demonstrating organisational commitment’. 93 |
Implementation Principle 8: Early intervention
Intervening early – as soon as any negative patterns of behaviour are identified – was often recommended as the best approach to send a signal that UB is not tolerated. Yet, implementing an extremely well-designed intervention, drawing on many of the principles laid out in this section, can also be in competition with intervening quickly (see Key Dynamic 12). Nonetheless, intervening quickly is important because any delay can unintentionally give the impression that management tacitly tolerates or has a hands-off approach towards UB. Additionally, any potential impact on patient safety and care quality must also be addressed rapidly. It may be possible to implement interim measures in an organisation while a more robust and complex intervention is developed.
| CMOC 66. If a pattern of UB is identified in an organisation (C), then it is important to demonstrate that something is being done to address it rapidly (even if working on implementing a more complex intervention alongside a smaller rapid action) to ensure it does not take hold (O), because doing so indicates that management will not tolerate any UB and mitigates loss of trust in management (M). | ‘Early identification and intervention are essential when it comes to managing disruptive behaviours. Ignoring inappropriate conduct will result in the problem persisting and becoming entrenched. Disruptive behaviour needs to be confronted and addressed before it takes hold’. 91 |
Implementation Principle 9: Manager and leader engagement
The engagement of managers and leaders with the intervention is essential both to ensure the content of the intervention is properly delivered and to ensure staff see that reducing UB in the organisation is a priority of senior staff. This relates to Key Dynamic 5 (enhancing authenticity) and Key Dynamic 7 (engaging managers). For example:
… If senior personnel … promote and encourage [a programme to address UB], that will certainly have a positive impact … and vice versa, if there’s not a lot of interest shown … then people under them are less likely to be engaged and see it as a valued program. 93
| CMOC 67. If implementing an intervention to reduce UB (C), then ensuring senior staff (i.e. managers and leaders) are engaged (e.g. role model behaviour, provide resources and focus) is crucial to maintaining engagement and effectiveness (O), because this transmits the message that UB is not tolerated and fosters psychological safety (M). | ‘leaders regularly connecting with frontline staff [is important…]. Firstly, it shows leaders are prioritising the removal of barriers to safe care. Secondly, staff who observe leaders improving safety may be encouraged to follow suit. Finally, these interactions provide an opportunity to build respect across hierarchical levels and promote psychological safety’. 93 |
Implementation Principle 10: Intervention perceived as just and not punitive
It is important that interventions are perceived to be justified and not overly punitive or staff may become apathetic and disengage from the intervention and its content. For example, ‘Just culture is also supported by sharing and addressing behaviors that undermine teamwork by promoting collaboration, accountability, self-evaluation, and decency to help solve system issues and create a blame-free error reporting system that supports peer feedback without punitive measures’. 53 It is also important to avoid an intervention undermining psychological safety, which links to Key Dynamic 2. Natural justice – the notion of ‘innocent until proven guilty’ and the ‘right of reply’ – is also essential in specific strategy types, such as with reporting systems. In these, there are graduated systems depending on whether there is a one-off negative behaviour or a pattern of UB. It is important that the perception of justice in the system is maintained to ensure that one-off or less severe events are not treated the same way as patterns of behaviour or severe forms of UB. For example, ‘anonymity has led to frivolous complaints and some staff feel a divide growing between the messengers and ordinary staff. Ethos is providing a system of no accountability for complainants, no just hearing and no records for due process’. 182
| CMOC 68. If seeking to implement an intervention to address UB (C), then ensuring the intervention is just and not punitive is essential to ensuring effectiveness of the intervention and avoiding backlash (O), because a sense of injustice can lead to disengagement with the intervention and generate a sense of outrage or discontent (M). | ‘A positive focus is engaging and empowering for participants, and important to the eventual creation of a blame-free environment, again, similar to that described in the field of clinical error prevention’. 22 |
Implementation Principle 11: Maximising existing opportunities
Existing organisational processes such as onboarding processes, appraisals or development reviews can be used to reduce UB. Although we did not identify any interventions doing so in the literature, some sources did mention the possibility of using existing organisational processes. For example, ‘the use of a pre-existing educational conference block to ensure protected time for fellows was helpful in seamlessly integrating the curriculum into a busy academic fellowship programme and division’. 71 Our stakeholder group also highlighted the importance of tying in with ongoing efforts that are related to addressing UB in organisations, such as the Freedom To Speak Up Guardians. 168 Since these events and activities are already taking place, it can be low cost and low risk to use them to help drive behaviour change. Included studies cited drawing on onboarding processes, for example, to introduce the signing of ‘conduct pledges’, which can ensure awareness of the behavioural policy and make it easier to discipline those who behave badly in the future.
| CMOC 69. If an organisation is seeking to reduce UB (C), then using existing organisational processes such as reviewing or appraising staff to discuss UB can build momentum (O), because using existing processes may enable other strategies to be more easily rolled out (M). | ‘SWAST should consider establishing a contract of respectful behaviour to enable managers to brief employees during induction, at appraisals and in team meetings as to what the expectations of the Trust are. This should explicitly make clear issues of equality, diversity and inclusion as well as fair and respectful behaviour’. 76 |
Implementation Principle 12: Organisational turnover and change
Staff and leaders who were championing an intervention and then leave an organisation can take much experience and momentum with them. The same can be said for processes of organisational change, whether that is changes in leadership or organisational mergers, which can serve as a distraction from efforts to reduce UB. It is important for those implementing UB interventions to plan for succession, intervention continuation and sustainability in cases of disruption to processes or staff.
| CMOC 70. If implementing a longer-term intervention to reduce UB (C), then organisational change and turnover can disrupt intervention momentum (O), because there can be a loss in staff, expertise, resource and engagement (M). | ‘… participants from both units were not confident in their collective ability to sustain the impact of the intervention over time, given staff and leadership changes’.137 ‘Challenges to programme adoption […] were retirement or departure of faculty members invested in the programme’.183 |
Implementation Principle 13: Tackle the instigator of unprofessional behaviour
Literature reported that in cases where conflict was occurring between two people, some organisations simply moved the instigator or the target of UB to another department. This enables the instigator to continue his or her behaviour, either in the same or in another setting, and sends the signal that the organisation is tolerant of UB. This was cited in the literature as occurring most frequently when an instigator is a high-performing doctor or surgeon.
| CMOC 71. If an individual is frequently engaging in UB, then moving the victim or instigator out of the situation (C) can lead to a worsening of social norms about UB (O), because it sends a signal that an organisation is tolerant of UB (M). | ‘Perpetrators of bullying often have a history of this type of behaviour and instead of dealing with it, managers may transfer the bully to other areas within the organisation where the same behaviours continue’. 115 |
Implementation Principle 14: Incorporate ongoing evaluation
Incorporating ongoing evaluation into an intervention may increase resource costs but it can also enable greater adaptability that can enhance efficacy either while the intervention is running or when implementing new versions of an intervention (Plan, Do, Study, Act cycles). It can potentially save costs in the longer term because an evaluation can identify contextual factors that may have undermined its success. An evaluation can help with understanding the setting in which an intervention is implemented and improving understanding of contexts that influence its success, as well as proximal (i.e. psychological safety), intermediate (i.e. reports of UB) and distal outcomes (i.e. patient safety metrics) (Key Dynamic 11). Evaluation results can also demonstrate to staff that interventions are effective and thereby enhance both trust in the organisation and support for the intervention.
| CMOC 72. If implementing an intervention to tackle UB (C), then embedding an ongoing evaluation can enable strategies to be adjusted and adapted (O), because there can be a greater understanding of the organisational and implementation context (M). | ‘As with all interventions, the applicability of these resources to local contexts will vary, and there has been no attempt at formal evaluation that would help to establish the contexts in which they may be more or less helpful’. 131 |
Implementation Principle 15: Do not mix hierarchies
While managers should be involved in interventions, it is important to also highlight that hierarchies have a large impact on ability to speak up (as outlined in Chapter 4, Category 1). As such, mixing of hierarchies can inhibit psychological safety in group-based interventions, undermining the ability of lower-level staff to engage with the intervention. This is purportedly a reason why one included intervention did not meet its objectives (see quotation, below). This principle is reflected in CMOC 73.
| CMOC 73. Seeking to include employees at all levels of an organisation with managers and lower-level staff present when implementing interventions that rely on group sessions (C) can cause disengagement with the intervention (O−), because speaking up can be inhibited due to mixing of hierarchies reducing psychological safety for lower-level staff (M). | ‘… staff did not appear to fully engage in the role play when the management staff was present. For future studies, the research team decided to either restrict the participants in the intervention to clinical staff only or to have two intervention groups, one for management and one for clinical staff’. 54 |
This principle could be resolved by designing an intervention that is seen to include managers in another way without mixing hierarchies, thereby avoiding this pitfall.
Table 19 provides an overview of our key implementation principles, mapped on to the consolidated framework for implementation research (CFIR), to facilitate stronger links to implementation theory.
| CFIR domain | Key considerations | Application to developing UB resources |
|---|---|---|
| Outer setting | (Wider NHS/governmental and societal context) What is there in the wider NHS to support the systemic change required? e.g. patient needs/priorities, peer pressure, external policies/incentives |
|
|
||
| Inner setting | (organisational context) What are the barriers/facilitators from within Trusts/organisations and how can these be mitigated/capitalised upon? e.g. networks/communications, culture, tension for change, compatibility, relative priority, organisational incentives/rewards, learning climate, readiness for implementation, leadership engagement, available resources |
|
| Characteristics of individuals | (individual context) e.g. knowledge/beliefs about the interventions and resources among healthcare staff and managers/leaders; self-efficacy |
|
|
||
| Intervention characteristics (s) – the resources | (mechanisms) e.g. evidence strength/quality, relative advantage compared to other things, adaptability, complexity, cost, stakeholders’ perceptions of the potential benefits |
|
|
||
| Process of implementing | (context + mechanism) What is the strategy for implementing, sustaining and evaluating? e.g. planning, engaging, opinion leaders, implementation leaders, champions, reflecting/evaluating |
|
|
||
|
Chapter 9 Discussion
This chapter integrates our review findings firstly by situating and summarising them within wider societal and NHS organisational contexts. We provide the reader with a final orientation to our findings by mapping them to our objectives, follow this with recommendations for various stakeholders, detail the strengths and limitations of this research, and, finally, identify directions for future research.
Contextualising and summarising our findings
Over the past 5 years, we have seen a significant shift in discourse relating to sexual harassment, with the #MeToo movement raising awareness about whether and how women are believed when they experience sexual harassment and abuse – particularly in the workplace. 17 We have also seen a shift in awareness relating to race and racism, with the black lives matter (#BLM) movement shining a spotlight on the poor treatment of black communities by societal institutions – such as the police and health service – with reported institutionalised racism. 69
These movements and important societal shifts in consciousness have implications as to how organisations respond and uphold recognition of any wrongdoing. In healthcare settings, we have seen a plethora of reports with claims of bullying, harassment and abuse, which have led to dire consequences for patients and staff. 3,6–8 The findings from our report may go some way to changing the downward spiral of these events and contribute to a broader societal narrative about how we can all do better.
Our overall aim in this study was to improve context-specific understanding of how, why and in what circumstances UBs between staff in acute healthcare settings occur, and evidence of strategies implemented to mitigate, manage and prevent them. Through our analysis (see Chapters 3–8) and discussions with our stakeholder and advisory groups, we surfaced several issues previously unaddressed by prior research. Our overall review findings are summarised in Boxes 1–4 and are organised in relation to our four study objectives.
Our first objective was to ‘Conceptualise and refine terminology: to understand differences and similarities between terms referring to unprofessional behaviours (e.g. incivility, bullying, microaggressions)’. Chapter 3 addresses this by exploring the use of UB-related terminology in the literature (see also Appendix 3, Table 26). Findings allowed us to conceptualise UBs on a spectrum according to their inherent dimensions, such as how specific they were, whether visible to the organisation or their targets and whether they required a hierarchical structure to occur (see Figure 6). However, we found little agreement across organisations or professional groups regarding what constitutes UB, which can cause confusion and make it challenging to synthesise the literature on this topic. In practice, the lack of a shared definition or understanding of UB could lead to difficulties in understanding its prevalence, reduce the likelihood of individuals reporting it and hinder the effectiveness of interventions to address it. We present a shorter and longer definition of UB in Chapter 3, refined with our stakeholders, as operationalised in this project. This provides a definition that can help bring clarity both in practice and in understanding the academic literature.
Our second objective was to ‘Develop CMOCs to understand the causes, contexts, mechanisms, and outcomes of unprofessional behaviours on staff, patients and wider healthcare system’. Chapter 4 explored the contributors to UB among staff in acute healthcare settings and its outcomes. Our analysis produced 17 CMOCs and a comprehensive programme theory, which categorised contributors of UB (see Figure 11 and Box 1). This level of analysis demonstrated the overlapping nature of many mechanisms and outcomes, emphasising the complexity of the emergence of UB. In terms of who and how UB is experienced, we found that UB is experienced more by people from a minoritised background (including ethnic minority staff, LGBTQ+ staff and staff with disabilities) and those new to the profession. Lastly, we created an overarching programme theory regarding how the presence of UB can impact staff and patient safety through various mechanisms, such as inability to effectively communicate and loss of learning.
Workplace disempowerment:
-
Factors such as organisational and professional hierarchies can lead to staff becoming an easier target for instigators, foster a sense of unfairness and cause a reduction in psychological safety, which can all encourage UB.
Organisational uncertainty, confusion and stress:
-
When staff experience organisational confusion, uncertainty and stress due to factors such as organisational change or a lack of resources, this also contributes to increased instances and experiences of UB. When staff experience a lack of control in their day-to-day work, they encounter challenges in building relationships which can, in turn, worsen conflict.
Social cohesion:
-
A lack of social support from colleagues, shift or agency working and reduced ability to communicate effectively (e.g. due to stress and pressure as outlined above) can all lead to undermining of social relationships between staff. These would otherwise enable a greater ability to cope with UB, understand norms of the workplace and help to avoid forms of UB, such as feeling ostracised.
Enablement of harmful cultures that tolerate UB:
-
Leadership and the culture that is created within an organisation can enable, model or tacitly permit UB to continue in their organisations. This can create an environment where UB is part of the social norm. Factors such as permissive, complicit toxic and dysfunctional leadership, negative role-modelling and cliques come into play here.
Our third objective sought to ‘Identify strategies designed to mitigate, manage and prevent unprofessional behaviours, how, why, and in what circumstances these work and whom they benefit’. This is answered in Chapters 5 and 6, wherein we explored interventions intended to address UB (see Chapter 5), alongside strategies they incorporated (see Chapter 6). We made a distinction between interventions (a bundle of strategies and evaluation methods delivered in a particular context) and strategies (BCTs used to drive reductions in UB), to aid our analysis and to be more applicable to modern behavioural science. Our investigation of interventions allowed us to report on which interventions are effective according to their outcome measures. We identified 13 categories of strategies (see Box 2), which we explored according to whether they had been evaluated in an intervention or only used in practice.
-
Informal or disciplinary strategies to address UB (e.g. by a victim, bystander, manager or peer) and speaking up. This included approaching an instigator or their line manager, which could prompt reflection and a change in behaviour. It also included more formal disciplinary procedures if a serious pattern is identified.
-
Improving confidence to come forward (victim, bystander). Strategies such as assertiveness training could seek to boost an individual’s ability to report instances of UB.
-
Improving ability to cope (victim, bystander). Strategies to improve ability to cope could reduce the impact of UB on workers’ well-being, for example.
-
Understanding prevalence of UB (managers/leaders). Delivering surveys or qualitative interviews with staff members to identify how prevalent UB is and where it is occurring can enable better targeting of other strategies at the issue.
-
Improving teamwork (all staff). Improving ability to communicate through communication training or doing team-building activities may increase a sense of social support and rapport, which can decrease UB.
-
Social norm-setting (all). Strategies such as role-modelling by leaders and incorporating a code of conduct can signal a new cultural direction and set new social norms with an organisation.
-
Improving leadership competence and empathy (managers/leaders). Delivering management training, for example, can reduce the likelihood of managers engaging in behaviours that could be considered bullying or micromanagement, etc.
-
External pressure on organisations (managers/leaders) (e.g. regulatory inspections, laws). These stimulated managers or leaders to increase focus on reducing UB.
-
Reporting and escalation systems (all staff). These were able to identify where UB was taking place and enabled approaches to instigators to be made (strategy group 1).
-
Workplace redesign (all staff). These included efforts to redesign the work environment to reduce pressure and frustration experienced by staff. These approaches were discussed frequently but rarely implemented through an intervention.
-
Improving awareness and knowledge (all staff). These included training or education workshops; for example, to improve ability to recognise UB.
-
Strategies to aid implementation (managers/leaders). These included strategies that could help implement other behaviour-change strategies (e.g. action-planning).
-
Changing recruitment, promotion and dismissal processes (all staff). These included attempts to screen out people who may not fit with an organisational culture during recruitment, in order to slowly change social norms. These were not often used, however.
Chapter 7 presented 12 key dynamics highlighting common issues, contradictions, tensions or considerations that may inadvertently undermine intervention success, even if otherwise well-designed (see Box 3 for summary).
Key Dynamic 1: Interventions should focus on systemic issues (e.g. workplace designs that promote frustration) as a priority rather than focusing on problematic individuals; otherwise, systemic contributors can continue to undermine a programme.
Key Dynamic 2: Enhancing a culture of psychological safety and openness should take priority if intending to improve staff well-being.
Key Dynamic 3: A comprehensive evaluation relying on greater number of outcome measures at multiple points in the causal chain will give greater insight into what works, how and why.
Key Dynamic 4: Maintaining a focus on why it is important to reduce UB (e.g. to improve patient safety) is key when designing an intervention to reduce UB.
Key Dynamic 5: Encouraging bystanders to intervene is important for culture change but can lead to moral injury if people do not feel capable of intervening.
Key Dynamic 6: Triage of messages in systems that enable anonymously speaking up is essential to ensure messages are not used to undermine others.
Key Dynamic 7: Programmes must be perceived as authentic to foster trust in management. Authenticity can be lacking due to either negative role-modelling by leaders or a programme that can be easily seen as inadequate by staff.
Key Dynamic 8: One size does not fit all – tackling UB generally requires multiple and sustained programmes to address underlying contributors.
Key Dynamic 9: Addressing manager behaviour is essential for building trust in management.
Key Dynamic 10: Interventions that are both inclusive and fair are critical to ensure effectiveness and sustainability, and for addressing inequalities.
Key Dynamic 11: There are trade-offs between intervention flexibility (i.e. adaptability to circumstances) and rigidity (i.e. fixed intervention content and design). Enabling flexibility may enhance effectiveness – but at the cost of ability to determine what worked and why.
Key Dynamic 12: There are trade-offs between a theory-first and a practice-first intervention design.
A programme theory highlighting which strategies address which contributors to unprofessional behaviour
Our realist analysis was able to give us a sense for which strategies address which mechanisms that underlie contributors to UB and which may not. It was able to indicate where there may be contributors that are currently not addressed by existing strategies. Figure 25 depicts the result of this mapping exercise.
FIGURE 25.
Final programme theory: contributors and strategies, and which mechanisms they target. Black squares are strategies, and orange and blue ellipses are mechanisms underlying how various contributors work.
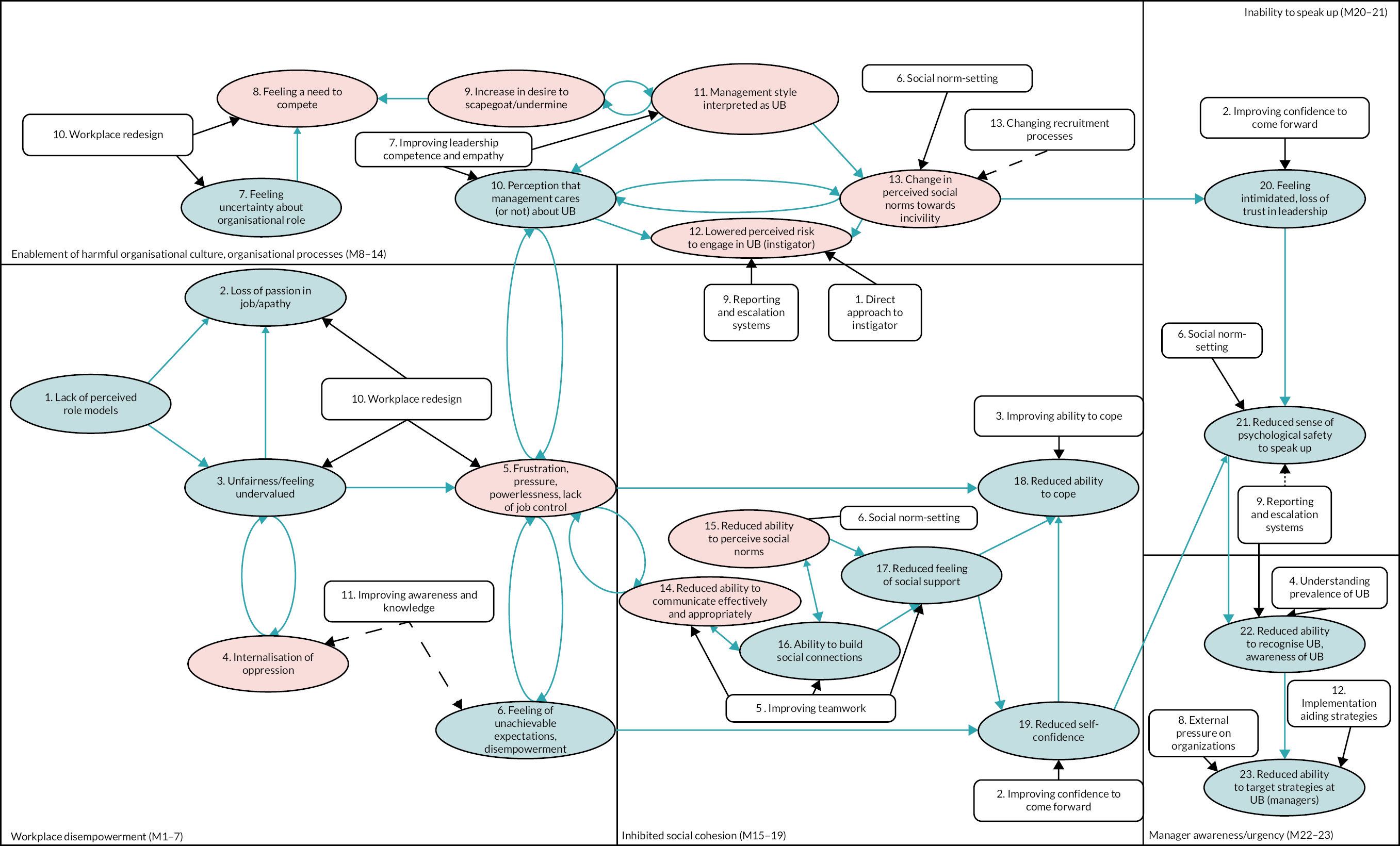
It is evident from this mapping exercise that the systemic contributors (left of the diagram) contributing to a sense of unfairness, frustration and powerlessness, role uncertainty, feeling a need to compete and loss of motivation or passion are only really addressed by workplace redesign efforts. However, such efforts were only incorporated by a single evaluated intervention to a very limited extent. 103 This further emphasises the findings of Key Dynamic 1, whereby systemic contributors can continue to undermine an intervention that is focused on individual behaviour. Examples of this include the use of social norm-setting strategies or those that improve ability to cope rather than a more holistic approach to addressing UB.
Figure 25 presents our final programme theory. Building upon this, Figure 26 highlights strategies according to the level at which they are implemented: whether at individual, team, organisational, health system or societal levels. Some strategy categories (understanding prevalence of UB, workplace redesign, reporting and escalation systems, changing recruitment processes and social norm setting) are highlighted here multiple times since they can operate at multiple levels (e.g. setting social norms can occur at both team and organisational levels). Figure 26 also identifies the number of evaluated intervention papers we identified that tested interventions at each level and the total for each level itself, in brackets (e.g. 57 individual-level strategies were tested across the intervention papers, with 21 of these attempting to improve awareness and knowledge of UB). This analysis shows that most strategies are implemented at the individual level (i.e. with sessions or workshops) and few strategies try to alter organisational culture, health systems or societal dynamics.
FIGURE 26.
Interventions mapped according to their level of implementation. Numbers indicate how many strategies were evaluated within each category. Strategy categories mentioned more than once are reflected in different colours for ease of identification.

Recommendations
Our fourth objective was to ‘produce recommendations and comprehensive resources to tailor, implement, monitor, and evaluate strategies to tackle UB and their impacts’. Our results enabled us to create guidance for healthcare managers and leaders seeking to address UB in their organisations (see Appendix 8 for indicative content). It may also provide insight for researchers who want to identify and implement novel strategies to address contributors that are, as yet, unaddressed by existing strategies.
The evidence and analyses presented in this review have been translated through an iterative process with the stakeholder and advisory groups and policy-makers (as outlined in our protocol – see also Chapter 2), to produce 10 overarching recommendations (see Box 4). These are targeted at national and local Freedom to Speak Up Guardians and executive boards, those responsible for leading teams, and/or those designing or refining interventional strategies to tackle interpersonal UB between healthcare staff. We have also begun to translate these recommendations for different audiences (noting that these recommendations are interdependent) (Table 20).
| Audience | Recommendations |
|---|---|
| Individuals |
|
|
|
| Teams |
|
| Organisations |
|
|
|
| Broader healthcare systems |
|
|
|
| Society and service users |
|
| Regulators |
|
| Policy |
|
| Researchers |
|
-
The default position statement of the employer (NHS), leaders and managers needs to be ‘we do not tolerate unprofessional behaviour of any kind’. Doing something to address UB is better than doing nothing, maximises visibility to engagement and signals seriousness about addressing UB.
-
Assess organisational landscape (understand organisational contributors to UB), then invest in implementation of multiple interventions and strategies (cover as broad a section of the organisation as possible to avoid perceptions of singling out specific groups and foster culture change), design a model outlining how and why the intervention should work and plan both ongoing formative and summative evaluations.
-
Implement multiple strategies: using a greater number of (aligned) strategies can increase uptake and spread.
-
Intervene early when UB is first detected – important to reinforce the message that UB is not tolerated and maintain trust in management, but make sure the intervention is seen as just and not overly punitive (e.g. relatively minor instances of UB are addressed informally).
-
Plan and implement a UB strategy to address organisational need, use societal shifts and changes in discourses relating to bullying, harassment and racism.
-
Shift the balance towards organisational as well as individual-level responsibility by encouraging allyship and workplace redesigns that minimise frustration, and foster social support and the ability to speak up.
-
Identify and nurture leaders capable of modelling ‘good’ behaviours and encourage their visibility so they can lead by example, avoid simply moving the instigator or recipient of UB (sends negative signals regarding tolerance of UB).
-
Harness existing organisational processes to emphasise organisational commitment to reducing UB (repurpose existing meetings or build into professional development reviews and appraisals).
-
Co-create interventions with staff (to foster intervention authenticity and increase engagement), including those more at risk (e.g. minority group members or those lower in organisational hierarchies), and senior groups to ensure buy-in, authenticity and reach.
-
Appoint dedicated staff to lead work to tackle UB (intervention implementation and monitoring to improve design, enhance intervention implementation and sustainability) and maximise manager engagement.
What our review adds
This research had several strengths. We included a significant number of sources (148) for a realist review, and the realist methodology enabled us to build a greater understanding of this area than previously articulated. Although a realist synthesis by Illing et al. 21 had been performed in this area a decade ago in 2013, the vast majority of the literature we included was published after 2013, including 27 out of 42 intervention studies. 21 Additionally, Illing et al. 21 did not include behaviours beyond bullying, whereas we sought to include all forms of staff-to-staff UB. A more modern and developed realist methodology informed by the RAMESES standards39 enabled us to open up the black box of included interventions, understand the range of strategies at use in this area and articulate how and why they were intended to work. The methods used for the project and its results are reported clearly and in great detail (e.g. incorporating stakeholder engagement methods, iterative screening and searches described in the Preferred Reporting Items for Systematic reviews and Meta-Analyses diagram), enabling researchers to understand how the results have been reached and offer a template of methods for future realist reviews. The review searches are a strength; we drew on a range of published and grey literature sources, multiple searches ensured we were drawing on literature likely to be relevant at different stages of the review, and searches were updated throughout the project until December 2022 – ensuring the team was up-to-date with the latest and emerging research.
Combined with our analysis of contributors to UB, we were able to create a complex and coherent programme theory. This will enable those studying UB to understand the available options to address UB while navigating the key dynamics and implementation guidance we identified. Incorporation of stakeholder and advisory group feedback at multiple timepoints throughout our analysis applied a ‘reality check’ to our findings. Since we expanded the international breadth of our included sources to capture more intervention literature, the applicability of our findings to multiple healthcare system types is also a strength.
Limitations of this research
The focus of our review was specifically on UB between staff in acute healthcare settings. We sought to define UB and identify contributors and strategies to reduce it. However, in having UB as our focal point, we did not seek detailed investigation of the opposite, that is, civility and professionalism. This means we did not, for instance, include analysis of interventions to improve civility but rather only to reduce incivility. Therefore, we may have excluded interventions capable of addressing UB, simply because of the way in which they were presented. We searched a range of academic databases but our search may have been enhanced further if we had included databases such as PsycINFO. Nonetheless, we drew on Google and Google Scholar searches to overcome these limitations and are confident our programme theories are fully representative of the range of strategies, interventions and contributors present in the literature. We are also aware that there may be practice-based interventions not captured by our review methods. For example, while we have sought and identified grey literature, there may still be live interventions not yet documented in the literature that we did not identify.
While our initial relevance criteria enabled us to go wider and include sources from outside health care if necessary, due to the volume of literature identified within health care we did not require additional literature. As such, there may be opportunity to learn from other sectors but this was beyond the scope of our review. Likewise, we did not expand to areas such as primary or community care, deeming these fundamentally different in their working environments. When analysing contributors to UB, we also did not include sources reporting from countries beyond the UK, as we found sufficient depth and breadth without this.
Lastly, while in line with RAMESES guidelines, our search relied upon independent screening by two people for only 10% of total titles, abstracts and full texts at each relevant stage, rather than full independent screening, which may have increased the chance of human error in the screening process. Additionally, we did not employ independent data extraction – but this is not typical in a realist review.
Public, patient and stakeholder involvement
Stakeholders and advisors informed our review throughout the project lifecycle. Those involved came from relevant backgrounds, including patients and the public, heads of professional standards bodies, members of regulatory bodies and unions in the UK, influential theorists in the field, healthcare professionals with experience of UBs and minority ethnic perspectives. The review included four points at which stakeholder and advisory group feedback was incorporated (Table 21). This feedback was used to sense-check our initial programme theories, identify the most relevant evidence, ensure that our CMOCs reflect lived experience, and refine the final programme theories. Our methodology is aligned with the ACTIVE (Authors and Consumers Together Impacting on eVidencE) framework for stakeholder involvement in systematic reviews, which advocates a continuous, multiple-time closed-event approach in which stakeholders are able to influence the results of the review. 185 We also used the three components of the EIT52 to inform the structure and conduct of our stakeholder meetings; namely (1) practical evidence-based strategies, (2) pragmatic, longitudinal measures of progress and (3) participatory implementation processes – particularly in the development and shaping of our resources.
| Date | Group | Meeting purpose/focus |
|---|---|---|
| 18 January 2022 | Stakeholder | Introductions, refining initial theories of strategies to reduce UB and typology of UB types |
| 26 April 2022 | Advisory | Keeping to timeline, assessing methodology used to refine initial theories of strategies to reduce UB and typology of UB types |
| 23 May 2022 | Stakeholder | Refining initial theories of contributors to UB |
| 10 November 2022 | Stakeholder | Presenting and refining tensions (became dynamics/considerations) |
| 1 December 2022 | Advisory | Keeping to timeline, presenting tensions methodology (became dynamics/considerations) |
| 16 January 2023 | Stakeholder | Spotlight session: how to mitigate UB towards disadvantaged groups |
| 28 March 2023 | Stakeholder | Refining manager materials and terminology |
During the project, we held a total of five stakeholder group sessions and two advisory group meetings (see Table 21).
We incorporated stakeholder and advisory group feedback into our processes to ensure rigour and relevance by recording: (1) what aspects of the developing theory were presented to stakeholders for refinement and how they were presented, (2) any suggested alterations, (3) additional searches undertaken to sense-check recommendations, (4) how as a team we came to a consensus and (5) changes made in response to feedback and presenting this back for sense-checking. 186 To facilitate this process, we took detailed notes of the meetings with the help of a project administrator and followed up with stakeholders and advisors individually to address specific points that were raised. To highlight stakeholder contributions to our project, we have added ‘stakeholder feedback summary’ boxes (no direct quotations) in each of our results chapters to reflect contributions.
Equality, diversity and inclusion
When envisioning this project, we were aware of the greater burden of UB experienced by people with protected characteristics or from minoritised backgrounds. To ensure we incorporated an understanding of how different groups are impacted by UB, we sought evidence regarding specific types of UB affecting these groups – such as racism, ableism, sexism, discrimination and microaggressions – and included these as terms in our search strategy from the outset to capture all relevant literature. Additionally, in line with the NIHR-INCLUDE framework,187,188 we sought to ensure representation in our stakeholder group by including people from many backgrounds, areas of expertise and perspectives, and geographical locations throughout the country. However, we may not have captured viewpoints from all types of sociodemographic groups (such as social class or breadth of generational views).
As mentioned above, during our theory-refinement phase, we also held a ‘spotlight session’ with a focus on the experience of marginalised groups and people with protected characteristics of UB in health care. The agenda for this session explored what our findings were with respect to these groups, an exploration of potential reasons why there is a paucity of interventions in this area (including the relevant key dynamics) and in what directions research must go to address this issue. Additionally, it helped us to refine the language we use in this report to refer to such issues.
What is missing in the literature
In terms of different staff groups (the ‘who’), the literature we reviewed did not include much work on understanding intersectionality, and the experiences of women in the healthcare workplace or LGBTQ+, minority ethnic or staff with a disability. We found only one intervention that sought to reduce racism towards minority groups. 71 We were not able to locate research that seeks to address homophobia, transphobia or ableism, despite disabled and LGBTQ+ people experiencing UB to a greater degree than other groups. While we have situated our review societally and historically, we cannot say that much included literature did the same. This has limited us in our provision of recommendations in this area, other than to indicate that further research is needed with these specific groups. Notably missing were interventions in a UK context, which was a surprising finding. We also found a dearth of logic models and theoretical underpinnings in the interventions reviewed and, overall, a lack of robust evaluations. Interventions did not adequately report implementation issues and contextual factors; this would have enabled us to better understand why they did or did not work, which made comparing contexts difficult. This may have been easier if included papers outlining intervention results had reported their findings in a standardised and best-practice way, such as by using the ‘template for intervention description and replication (TIDieR)’189 method.
Recommendations for future research
Terminology
As highlighted in Chapter 3, terminology used to refer to UB is highly inconsistent and can present issues in practice, as well as when attempting to synthesise literature in this area. Definitions should be provided when seeking to assess the incidence of certain forms of UB or when referring to UB in a study. The academic and practitioner space would greatly benefit from a more uniform and clear understanding of the range of UB terms to help avoid such issues, as would staff in NHS organisations seeking to address UB. Drawing upon an understanding of the differences in dimensions of UB types may help shed some light on essential differences between them. To this end, we hope our typology outlining the dimensions and breadth of UB-related terms in the healthcare space will be an important first step towards the goal of mapping UB terms. Although it is not possible or advisable to dictate how UB should be defined, future studies should work on compiling a compendium of terms: perhaps through use of the Delphi method, for example. We believe our initial definition or understanding of UB, presented in Chapter 3 and refined with our stakeholder group, will help serve as a basis for future efforts in this area.
Behavioural science
More robust logic models (and indeed, programme theories) may also include depiction of how various intervention strategies are anticipated to interact and may even pre-empt implementation challenges and assumptions, and how to overcome them. No studies drew on modern theories originating in behaviour-change psychology, such as the COM-B approach (capability, opportunity and motivation for changing behaviour)190 or implementation science frameworks or theories [e.g. CFIR, i-PARIHS (Integrated Promoting Action on Research Implementation in Health Services),191,192 normalisation process theory193]. Future studies must fully explicate how and why they think the intervention components will lead to the outcomes they intend, including how implementation challenges in diverse contexts will be addressed. Future research may need to draw on multiple theories to explain how and why their intervention is intended to drive the desired effects. As our review indicates, mechanisms and outcomes are often overlapping.
Enhancing ability to synthesise findings
In addition to not adequately explaining how and why interventions are intended to work, reports of evaluations of interventions should give greater priority to reporting implementation context and how it could impact effectiveness. This will enable future evidence syntheses to gain a greater understanding of why a particular strategy may work in one context but not another.
Need for tools to assess UB prior to intervention
For interventions to address the actual contributors to UB, they need to first understand what they are. Our review identified that this was a limitation with existing interventions, yet few tools and instruments exist that are adequate for determining anything more specific than the prevalence of UB prior to intervening. 146 Tools should be formulated that provide greater insight into what is contributing to UB in an organisation and where it is taking place. Such tools may need to be mixed methods in nature, to capture both the prevalence quantitatively and ‘how or why’ it is occurring qualitatively.
Other healthcare settings
While our research sought to identify work around UB in acute care, we believe our findings should be contrasted and understood against other healthcare settings, such as private health care or primary care, too. This will enhance applicability of our findings while supporting research in other areas.
Conclusion
UB is a pervasive issue that is currently incompletely addressed by existing interventions. We identified many contributors to UB, most of which relate to worker disempowerment and organisational barriers to being able to carry out work effectively. Most existing interventions do not address these systemic contributors to UB and largely rely on education or training workshops to boost individual knowledge or awareness, as well as identifying problematic individuals or improving ability for staff to speak up. Such approaches may reduce prevalence of UB but it is unclear whether this has a positive impact on staff well-being or patient safety. In addition to the individual focus, issues such as lack of trust in management caused by pervasive, unaddressed UB present significant barriers to enabling staff to engage with interventions. Interventions that focus on both individual and systemic contributors are required to change culture and, at the same time, address the UB of instigators quickly, support staff who report and are on the receiving end of UB and signal that UB is not tolerated. We identified no interventions to reduce UB evaluated in a UK context; the majority were USA-based. Future interventions would benefit from being designed and tested in UK settings, drawing on modern behavioural science principles and focusing on systemic issues that produce UB.
Additional information
Acknowledgements
We would like to sincerely thank all those who supported this study: specifically, members of our stakeholder and advisory groups, who so generously gave their time and expertise, even when talking about difficult subject matter. These Stakeholder Group members included (alphabetically by first name) Alice Hartley, Anna Conolly, Anna Rowland, Anna Van der Gaag, Bob McAlister, Cydavia Patterson, Diana Bass, Emily Williams, Fiona Kilpatrick, Gail Adams, Gemma Clay, Helen Stanley, Heather Caudle, Janet Holah, Jessie Cunnett, Joy Warmington, Karen Pudge, Katherine Timms, Mary Lawson, Narinder Kapur, Paul Jebb and Roger Kline. Their invaluable contributions are presented throughout our report.
We would also like to thank the members of our Study Advisory Group (alphabetically by first name): Chris Woodrow, David Naylor, Ewen Speed, Graham Martin, Jean McHale, Joanne Greenhalgh, Karen Mattick, Lilith Whiley, Manjit Darby, Ruth Riley, Sarah Peddle and Vinice Thomas. These advisory group members helped keep us on track and provided valuable input.
Finally, we would like to thank Elizabeth Campbell for her administrative support throughout the project.
Contributions of authors
Justin A Aunger (https://orcid.org/0000-0001-6975-4570) (Research Fellow) carried out the exploratory literature searches, contributed to the formal search strategies, screened and analysed the resulting references, applied a realist logic of analysis to the data, developed and refined the CMOCs and programme theories, contributed theoretical ideas underpinning this analysis and led the drafting and revisions of the final report.
Ruth Abrams (https://orcid.org/0000-0002-2974-7859) (Lecturer: Workforce, Organisation and Wellbeing Research) developed the research project, contributed to the formal search strategies, screened and analysed the resulting references, applied a realist logic of analysis to the data, developed and refined the CMOCs and programme theories, contributed theoretical ideas underpinning this analysis and drafted and revised the final report.
Johanna I Westbrook (https://orcid.org/0000-0003-1083-8192) supported development of the research project, contributed to the analysis through subject expertise, contributed theoretical ideas underpinning this analysis and revised the final report.
Judy M Wright (https://orcid.org/0000-0002-5239-0173) (Senior Information Specialist) supported development of the research project, developed and conducted the main and additional search strategies, supported screening of the resulting references and contributed to drafting and revising the methods chapter and strengths and limitations sections for the final report.
Mark Pearson (https://orcid.org/0000-0001-7628-7421) (Reader in Implementation Science) supported development of the research project, provided realist methodology expertise on the study design and conduct, supported application of realist logic of analysis and revised the final report.
Aled Jones (https://orcid.org/0000-0002-2921-8236) supported development of the research project, contributed to the analysis through subject expertise, contributed theoretical ideas underpinning this analysis and revised the final report.
Russell Mannion (https://orcid.org/0000-0002-0680-8049) supported development of the research project, contributed to the analysis through subject expertise, contributed theoretical ideas underpinning this analysis and revised the final report.
Jill Maben (https://orcid.org/0000-0002-6168-0455) developed and led the research project, contributed to the analysis through the development and refinement of programme theory and CMOCs and programme theories, provided realist methodological support and input, contributed theoretical ideas underpinning this analysis, facilitated patient and public involvement in the stakeholder group and drafted and revised the final report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/PAMV3758.
Primary conflicts of interest: Jill Maben was a member of NIHR, Health Services and Delivery Research Funding Committee (2019–22). Mark Pearson was a member of the Health Services and Delivery Research Funding Committee from 1 January 2019 to 31 January 2022.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Ethics statement
This study did not require ethical approval as it was a secondary analysis of published papers. Contributions from our stakeholder groups were managed with care and adherence to ethical principles but, as these contributions do not constitute data, no ethical approval was required.
Information governance statement
This project did not handle or store personal data as part of its research processes.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Maben J, Aunger JA, Abrams R, Pearson M, Wright JM, Westbrook J, et al. Protocol: why do acute healthcare staff engage in unprofessional behaviours towards each other and how can these behaviours be reduced? A realist review protocol. BMJ Open 2022;12(7).
Aunger J, Maben J, Abrams R, Wright J, Mannion R, Pearson M, et al. Drivers of unprofessional behaviour between staff in acute care hospitals: a realist review. BMC Health Serv Res 2023;23. https://doi.org/10.1186/s12913-023-10291-3
Maben J, Aunger JA, Abrams R, Mannion R, Pearson M, Wright J, et al. Addressing unprofessional behaviours between healthcare staff: a guide. 2023:1–38. URL: https://workforceresearchsurrey.health/projects-resources/addressing-unprofessional-behaviours-between-healthcare-staff/ (accessed 22 April 2024).
Maben J, Aunger JA, Abrams R, Wright JM, Pearson M, Westbrook JI, et al. Interventions to address unprofessional behaviours between staff in acute care: what works for whom and why? A realist review. BMC Med 2023;21. https://doi.org/10.1186/s12916-023-03102-3
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Maben J, Aunger JA, Abrams R, Pearson M, Wright JM, Westbrook J, et al. Why do acute healthcare staff engage in unprofessional behaviours towards each other and how can these behaviours be reduced? A realist review protocol. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2022-061771.
- Casey L. An Independent Review into the Standards of Behaviour and Internal culture of the Metropolitan Police Service. Baroness Casey Review: Metropolitan Police; 2023.
- Atherton S. Protecting Those Who Protect Us: Women in the Armed Forces from Recruitment to Civilian Life. The Defence Sub-Committee on Women in the Armed Forces; 2021.
- Wilsher R. Values and Culture in Fire and Rescue Services. HMICFRS; 2023.
- Hasan M. Keep calm and carry on – there is nothing to see here: a study of organisational response towards racist bullying and harassment of BAME women in policing. Soc Sci 2021;10:269-78. https://doi.org/10.11648/j.ss.20211006.13.
- Ockenden D. Final Report of the Ockenden Review: Findings, Conclusions and Essential Actions from the Independent Review of Maternity Services at the Shrewsbury and Telford Hospital NHS Trust. Department of Health and Social Care; 2022.
- Dixon-Woods M. Learning from maternity service failures at East Kent Hospitals. BMJ 2022;379. https://doi.org/10.1136/bmj.o2755.
- Improving Quality in all Sectors . University Hospitals Birmingham NHS FT (UHB). Phase 1 Review by IQ4U. Clinical Safety 2023. www.birminghamsolihull.icb.nhs.uk/application/files/5316/7994/0284/Phase_1_Review.pdf (accessed 1 December 2021).
- Felblinger DM. Bullying, incivility, and disruptive behaviors in the healthcare setting: identification, impact, and intervention. Front Health Serv Manage 2009;25:13-2. https://doi.org/10.1097/01974520-200904000-00003.
- Westbrook J, Sunderland N, Atkinson V, Jones C, Braithwaite J. Endemic unprofessional behaviour in health care: the mandate for a change in approach. Med J Aust 2018;209:380-1. https://doi.org/10.5694/mja17.01261.
- National Freedom to Speak Up Guardian . Bullying Behaviour Is Unacceptable. It Is Unprofessional and Unnecessary. It Affects the Wellbeing of Individuals and the Teams Within Which They Work 2018. https://resolution.nhs.uk/wp-content/uploads/2020/01/BullyingA4-final-Dec-2019-002.pdf (accessed 1 December 2021).
- Wilkinson-Brice E, Evans N. NHS Workforce Race Equality Standard (WRES) 2022 Data Analysis Report for NHS Trusts. NHS Workforce Race Equality Standard (WRES) 2022. www.england.nhs.uk/long-read/nhs-workforce-race-equality-standard-wres2022-data-analysis-report-for-nhs-trusts/ (accessed 1 December 2021).
- Katz D, Blasius K, Isaak R, Lipps J, Kushelev M, Goldberg A, et al. Exposure to incivility hinders clinical performance in a simulated operative crisis. BMJ Qual Saf 2019;28:750-7. https://doi.org/10.1136/bmjqs-2019-009598.
- Riskin A, Erez A, Foulk TA, Riskin-Geuz KS, Ziv A, Sela R, et al. Rudeness and medical team performance. Pediatrics 2017;139. https://doi.org/10.1542/peds.2016-2305.
- Westbrook J, Sunderland N, Li L, Koyama A, McMullan R, Urwin R, et al. The prevalence and impact of unprofessional behaviour among hospital workers: a survey in seven Australian hospitals. Med J Aust 2021;214:31-7. https://doi.org/10.5694/mja2.50849.
- NHS England . NHS Staff Survey 2022 National Results Briefing 2023.
- Kline R. Racism Which Impacts Healthcare Staff Endangers Patient Care. Middlesex University London; 2021.
- BBC News . NHS Highland Pays Out Millions to Bullied Staff 2021.
- Pisklakov S, Tilak V, Patel A, Xiong M. Bullying and aggressive behavior among health care providers: literature review. Adv Anthropol 2013;03:179-82. https://doi.org/10.4236/aa.2013.34024.
- Lever I, Dyball D, Greenberg N, Stevelink SAM. Health consequences of bullying in the healthcare workplace: A systematic review. J Adv Nurs 2019;75:3195-209. https://doi.org/10.1111/jan.13986.
- Illing J, Carter M, Thompson NJ, Crampton PES, Morrow GM, Howse JH, et al. Evidence Synthesis on the Occurrence, Causes, Management of Bullying and Harassing Behaviours to Inform Decision Making in the NHS. NIHR Service Delivery and Organisation; 2013.
- Gamble Blakey A, Smith-Han K, Anderson L, Collins E, Berryman E, Wilkinson TJ. Interventions addressing student bullying in the clinical workplace: a narrative review. BMC Med Educ 2019;19:1-13. https://doi.org/10.1186/s12909-019-1578-y.
- Livshiz-Riven I, Hurvitz N, Grinberg K, Halperin O, Spitz A, Itzhaki M, et al. Nursing students’ experiences of unprofessional behaviours and associations with guideline compliance: a multicenter survey. Nurse Educ Pract 2023;71. https://doi.org/10.1016/j.nepr.2023.103739.
- Riskin A, Erez A, Foulk TA, Kugelman A, Gover A, Shoris I, et al. The impact of rudeness on medical team performance: a randomized trial. Pediatrics 2015;136:487-95. https://doi.org/10.1542/peds.2015-1385.
- Cooper WO, Spain DA, Guillamondegui O, Kelz RR, Domenico HJ, Hopkins J, et al. Association of reports about unprofessional behavior by surgeons with surgical complications in their patients. JAMA Surg 2019;154:828-34. https://doi.org/10.1001/jamasurg.2019.1738.
- Kline R, Lewis D. The price of fear: estimating the financial cost of bullying and harassment to the NHS in England. Public Money Manag 2018;39:166-74. https://doi.org/10.1080/09540962.2018.1535044.
- Jones CB, Michael Gates RN. The costs and benefits of nurse turnover: a business case for nurse retention. OJIN 2007;12:1-12. https://doi.org/10.3912/OJIN.Vol12No03Man04.
- Culture Shift . Protecting Your People: The Importance of Adopting a People-Centric Workplace Culture 2021.
- Campbell D. NHS staff quitting due to burnout and bullying, report says. Guardian 2019. https://www.theguardian.com/society/2019/jun/03/nhs-staff-quitting-due-to-burnout-and-bullying-report-says (accessed 1 December 2021).
- Gillen PA, Sinclair M, Kernohan WG, Begley CM, Luyben AG. Interventions for prevention of bullying in the workplace. Cochrane Database Syst Rev 2017;12:1-67. https://doi.org/10.1002/14651858.CD009778.pub2.
- Hodgins M, MacCurtain S, Mannix-McNamara P. Workplace bullying and incivility: a systematic review of interventions. Int J Work Health Manag 2014;7:54-72. https://doi.org/10.1108/IJWHM-08-2013-0030.
- Villafranca A, Hamlin C, Enns S, Jacobsohn E. Disruptive behaviour in the perioperative setting: a contemporary review. Can J Anesth 2017;64:128-40. https://doi.org/10.1007/s12630-016-0784-x.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Greenhalgh J, Manzano A. Understanding ‘context’ in realist evaluation and synthesis. Int J Soc Res Methodol 2022;25:1-13. https://doi.org/10.1080/13645579.2021.1918484.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist synthesis: RAMESES training materials. RAMESES Proj 2013;55:1-54.
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374. https://doi.org/10.1136/bmj.n2061.
- Sayer RA. Method in Social Science: A Realist Approach. London: Routledge; 1992.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11:1-14. https://doi.org/10.1186/1741-7015-11-21.
- Booth A, Briscoe S, Wright JM. The ‘realist search’: a systematic scoping review of current practice and reporting. Res Synth Methods 2020;11:14-35. https://doi.org/10.1002/jrsm.1386.
- Illing J, Carter M, Thompson NJ, Crampton PES, Morrow GM, Howse JH, et al. Evidence Synthesis on the Occurrence, Causes, Management of Bullying and Harassing Behaviours to Inform Decision Making in the NHS. NIHR Service Delivery and Organisation; 2013.
- Ayiku L, Levay P, Hudson T. The NICE OECD countries’ geographic search filters: Part 1 – methodology for developing the draft MEDLINE and EMBASE (Ovid) filters. JMLA 2021;109:258-66. https://doi.org/10.5195/jmla.2021.978.
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016;75:40-6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
- AUHE Information Specialists . AUHE Information Specialists, University of Leeds: Checking for Duplicates Guidance 2016.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Rev 2016;5:1-10. https://doi.org/10.1186/s13643-016-0384-4.
- Pearson M, Chilton R, Wyatt K, Abraham C, Ford T, Woods HB, et al. Implementing health promotion programmes in schools: a realist systematic review of research and experience in the United Kingdom. Implement Sci 2015;10:1-20. https://doi.org/10.1186/s13012-015-0338-6.
- Blakey AG, Anderson L, Smith-Han K, Wilkinson T, Collins E, Berryman E. Time to stop making things worse: an imperative focus for healthcare student bullying research. N Z Med J 2018;131:81-5.
- Lee YJ, Bernstein K, Lee M, Nokes KM. Bullying in the nursing workplace: applying evidence using a conceptual framework. Nurs Econ 2014;32:255-67.
- Dada S, Dalkin S, Mukumbang FC, Gilmore B, Hunter R. Applying and reporting relevance, richness and rigour in realist evidence appraisals: advancing key concepts in realist reviews. Res Synth Methods 2023;14:1-11. https://doi.org/10.1002/jrsm.1630.
- Haddaway NR, Grainger MJ, Gray CT. Citationchaser: An R Package and Shiny App for Forward and Backward Citations Chasing in Academic Searching. Zenodo; 2021.
- Pawson R. Evidence-based Policy: A Realist Perspective. London: SAGE; 2006.
- Glasgow RE, Green LW, Taylor MV, Stange KC. An Evidence Integration Triangle for aligning science with policy and practice. Am J Prev Med 2012;42:646-54. https://doi.org/10.1016/j.amepre.2012.02.016.
- Baldwin CA, Hanrahan K, Edmonds SW, Krumm AM, Sy A, Jones A, et al. CORS Professionalism Collaboratory . Implementation of peer messengers to deliver feedback: an observational study to promote professionalism in nursing. Jt Comm J Qual Patient Saf 2023;49:14-25. https://doi.org/10.1016/j.jcjq.2022.10.001.
- O’Connell KM, Garbark RL, Nader KC. Cognitive rehearsal training to prevent lateral violence in a military medical facility. J Perianesth Nurs 2019;34:645-653.e1. https://doi.org/10.1016/j.jopan.2018.07.003.
- Rutherford DE, Gillespie GL, Smith CR. Interventions against bullying of prelicensure students and nursing professionals: an integrative review. Nurs Forum 2019;54:84-90. https://doi.org/10.1111/nuf.12301.
- Wild JRL, Ferguson HJM, McDermott FD, Hornby ST, Gokani VJ. Council of the Association of Surgeons in Training . Undermining and bullying in surgical training: a review and recommendations by the Association of Surgeons in Training. Int J Surg 2015;23:S5-9. https://doi.org/10.1016/j.ijsu.2015.09.017.
- Chadwick S, Travaglia J. Workplace bullying in the Australian health context: a systematic review. J Health Organ Manag 2017;31:286-301. https://doi.org/10.1108/JHOM-09-2016-0166.
- Hutchinson M, Jackson D, Wilkes L, Vickers MH. A new model of bullying in the nursing workplace organizational characteristics as critical antecedents. Adv Nurs Sci 2008;31:E60-71. https://doi.org/10.1097/01.ANS.0000319572.37373.0c.
- Manton AP. Bullying: a pebble in the pond. J Emerg Nurs 2017;43:389-90. https://doi.org/10.1016/j.jen.2017.07.006.
- Edwards SL, O’Connell CF. Exploring bullying: implications for nurse educators. Nurse Educ Pract 2007;7:26-35. https://doi.org/10.1016/j.nepr.2006.03.004.
- Kang J, Jeong YJ. Effects of a smartphone application for cognitive rehearsal intervention on workplace bullying and turnover intention among nurses. Int J Nurs Pract 2019;25:1-10. https://doi.org/10.1111/ijn.12786.
- Embree JL, Bruner DA, White A. Raising the level of awareness of nurse-to-nurse lateral violence in a critical access hospital. Nurs Res Pract 2013;2013:1-7. https://doi.org/10.1155/2013/207306.
- Warrner J, Sommers K, Zappa M, Thornlow DK. Decreasing workplace incivility. Nurs Manage 2016;47:22-30. https://doi.org/10.1097/01.NUMA.0000475622.91398.c3.
- Saxton R. Communication skills training to address disruptive physician behavior. AORN J 2012;95:602-11. https://doi.org/10.1016/j.aorn.2011.06.011.
- Dahlby MA, Herrick LM. Evaluating an educational intervention on lateral violence. J Contin Educ Nurs 2014;45:344-50. https://doi.org/10.3928/00220124-20140724-15.
- Nikstaitis T, Simko LC. Incivility among intensive care nurses: the effects of an educational intervention. Dimens Crit Care Nurs 2014;33:293-301. https://doi.org/10.1097/DCC.0000000000000061.
- Griffin M. Teaching cognitive rehearsal as a shield for lateral violence: an intervention for newly licensed nurses. J Contin Educ Nurs 2004;35:257-63. https://doi.org/10.3928/0022-0124-20041101-07.
- Hawkins N, Jeong S, Smith T. New graduate registered nurses’ exposure to negative workplace behaviour in the acute care setting: an integrative review. Int J Nurs Stud 2019;93:41-54. https://doi.org/10.1016/j.ijnurstu.2018.09.020.
- Tuffour I. It is like ‘judging a book by its cover’: an exploration of the lived experiences of Black African mental health nurses in England. Nurs Inq 2022;29. https://doi.org/10.1111/nin.12436.
- Kline R. A Review into Culture and Bullying at University Hospitals of North Midlands NHS Trust 2022.
- Banerjee D, Nassikas NJ, Singh P, Andrea SB, Zhang AY, Aswad Y, et al. Feasibility of an antiracism curriculum in an academic pulmonary, critical care, and sleep medicine division. Ats Sch 2022;3:433-48. https://doi.org/10.34197/ats-scholar.2022-0015OC.
- Griffith M, Clery MJ, Humbert B, Joyce JM, Perry M, Hemphill RR, et al. Exploring action items to address resident mistreatment through an educational workshop. West J Emerg Med 2019;21:42-6. https://doi.org/10.5811/westjem.2019.9.44253.
- Chary AN, Molina MF, Dadabhoy FZ, Manchanda EC. Addressing racism in medicine through a resident-led health equity retreat. West J Emerg Med 2021;22:41-4. https://doi.org/10.5811/WESTJEM.2020.10.48697.
- Babla K, Lau S, Akindolie O, Radia T, Modi N, Kingdon C, et al. Racial microaggressions within respiratory and critical care medicine. Lancet Respir Med 2021;9:e27-8. https://doi.org/10.1016/S2213-2600(21)00001-1.
- Miller DT, Chen EH. Helping the learner to deal with microaggressions in the workplace: individual, programmatic, and institutional-level responses. AEM Educ Train 2021;5:S140-3. https://doi.org/10.1002/aet2.10663.
- Lewis D. Workplace Culture at Southwestern Ambulance NHS Foundation Trust. An Independent Report Commissioned by South Western Ambulance services in partnership with Unison. Plymouth University Business School; 2018.
- Pavithra A, Sunderland N, Callen J, Westbrook J. Unprofessional behaviours experienced by hospital staff: qualitative analysis of narrative comments in a longitudinal survey across seven hospitals in Australia. BMC Health Serv Res 2022;22:1-15. https://doi.org/10.1186/s12913-022-07763-3.
- Academy of Medical Royal Colleges . Creating Supportive Environments: Tackling Behaviours That Undermine a Culture of Safety 2016.
- Hemmings N, Buckingham H, Oung C, Palmer W. Attracting, Supporting and Retaining a Diverse NHS Workforce 2021.
- Stone L, Phillips C, Douglas KA. Sexual assault and harassment of doctors, by doctors: a qualitative study. Med Educ 2019;53:833-43. https://doi.org/10.1111/medu.13912.
- Fong W, Kwan YH, Yoon S, Phang JK, Thumboo J, Leung YY, et al. Assessment of medical professionalism using the Professionalism Mini Evaluation Exercise (P-MEX) in a multi-ethnic society: a Delphi study. BMC Med Educ 2020;20:1-9. https://doi.org/10.1186/s12909-020-02147-9.
- Debono DS, Greenfield D, Travaglia JF, Long JC, Black D, Johnson J, et al. Nurses’ workarounds in acute healthcare settings: a scoping review. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-175.
- Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav 2014;1:23-4. https://doi.org/10.1146/annurev-orgpsych-031413-091305.
- Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q 1999;44:350-83. https://doi.org/10.2307/2666999.
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev 2009;29:695-706. https://doi.org/10.1016/j.cpr.2009.07.003.
- Čartolovni A, Stolt M, Scott PA, Suhonen R. Moral injury in healthcare professionals: a scoping review and discussion. Nurs Ethics 2021;28:590-602. https://doi.org/10.1177/0969733020966776.
- Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol 2001;86:499-512. https://doi.org/10.1037/0021-9010.86.3.499.
- Ross L. The intuitive psychologist and his shortcomings: distortions in the attribution process. Adv Exp Soc Psychol 1977;10:173-220. https://doi.org/10.1016/S0065-2601(08)60357-3.
- Ross L. From the fundamental attribution error to the truly fundamental attribution error and beyond: my research journey. Perspect Psychol Sci 2018;13:750-69. https://doi.org/10.1177/1745691618769855.
- Robinson SL. Trust and breach of the psychological contract. Adm Sci Q 1996;41:574-99. https://doi.org/10.2307/2393868.
- Royal College of Surgeons of England . Managing Disruptive Behaviours in Surgery: A Guide to Good Practice 2021.
- Mannion R, Davies H, Powell M, Blenkinsopp J, Millar R, McHale J, et al. Healthcare scandals and the failings of doctors: do official inquiries hold the profession to account?. J Health Organ Manag 2019;33:221-40. https://doi.org/10.1108/JHOM-04-2018-0126.
- McKenzie LN, Shaw L, Jordan JE, Alexander M, O’Brien M, Singer SJ, et al. Factors influencing the implementation of a hospitalwide intervention to promote professionalism and build a safety culture: a qualitative study. Jt Comm J Qual Patient Saf 2019;45:694-705. https://doi.org/10.1016/j.jcjq.2019.07.005.
- Taylor RA, Taylor SS. Reframing and addressing horizontal violence as a workplace quality improvement concern. Nurs Forum 2018;53:459-65. https://doi.org/10.1111/nuf.12273.
- Keller S, Yule S, Zagarese V, Parker SH. Predictors and triggers of incivility within healthcare teams: a systematic review of the literature. BMJ Open 2020;10:1-15. https://doi.org/10.1136/bmjopen-2019-035471.
- Aunger J, Abrams R, Westbrook J, Wright J, Pearson M, Jones A, et al. Why do acute healthcare staff behave unprofessionally towards each other and how can these behaviours be reduced? A realist review (under review). Health Soc Care Deliv Res 2022;12. https://doi.org/10.1136/bmjopen-2022-061771.
- Churruca K, Pavithra A, McMullan R, Urwin R, Tippett S, Cunningham N, et al. Creating a culture of safety and respect through professional accountability: case study of the Ethos program across eight Australian hospitals. Aust Health Rev 2022;46:319-24. https://doi.org/10.1071/ah21308.
- Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med 2007;82:1040-8. https://doi.org/10.1097/ACM.0b013e31815761ee.
- Phillips JM, Stalter AM, Winegardner S, Wiggs C, Jauch A. Systems thinking and incivility in nursing practice: an integrative review. Nurs Forum 2018;53:286-98. https://doi.org/10.1111/nuf.12250.
- Credland NJ, Whitfield C. Incidence and impact of incivility in paramedicine: a qualitative study. Emerg Med J 2021;39:52-6. https://doi.org/10.1136/emermed-2020-209961.
- Blackstock S, Cummings G, Glanfield F, Yonge O. A review: developing an ecological model approach to co‐worker incivility experiences of new graduate nurses. J Adv Nurs 2022;78:1535-50. https://doi.org/10.1111/jan.15190.
- Churchman JJ, Doherty C. Nurses’ views on challenging doctors’ practice in an acute hospital. Nurs Stand 2010;24:42-7. https://doi.org/10.7748/ns2010.06.24.40.42.c7830.
- Stevens S. Nursing workforce retention: challenging a bullying culture. Health Aff 2002;21:189-93. https://doi.org/10.1377/hlthaff.21.5.189.
- Demarco RF, Roberts SJ, Chandler GE. The use of a writing group to enhance voice and connection among staff nurses. J Nurses Staff Dev 2005;21:85-90. http://doi.org/10.1097/00124645-200505000-00001.
- General Medical Council . Building a Supportive Environment: A Review to Tackle Undermining and Bullying in Medical Education and Training 2015. https://heeoe.hee.nhs.uk/sites/default/files/docustore/gmc_bullying_undermining_building_a_supportive_environment_150305.pdf (accessed 1 December 2021).
- Parizad N, Hassankhani H, Rahmani A, Mohammadi E, Lopez V, Cleary M. Nurses’ experiences of unprofessional behaviors in the emergency department: a qualitative study. Nurs Health Sci 2018;20:54-9. https://doi.org/10.1111/nhs.12386.
- Nicotera AM, Mahon MM, Wright KB. Communication that builds teams: assessing a nursing conflict intervention. Nurs Adm Q 2014;38:248-60. https://doi.org/10.1097/NAQ.0000000000000033.
- Owens J, Singh G, Cribb A. Austerity and professionalism: being a good healthcare professional in bad conditions. Health Care Anal 2019;27:157-70. https://doi.org/10.1007/s10728-019-00372-y.
- Işık I, Gümüşkaya O, Şen S, Arslan Özkan H. The elephant in the room: nurses’ views of communication failure and recommendations for improvement in perioperative care. AORN J 2020;111:e1-e15. https://doi.org/10.1002/aorn.12899.
- Longo J, Hain D. Bullying: a hidden threat to patient safety. Nephrol Nurs J 2014;41:193-99.
- Waters A. High spending on agency staff by NHS is a ‘completely false economy’, warns BMA. BMJ 2022;379. https://doi.org/10.1136/bmj.o2749.
- NHS Employers . Tackling Bullying in Ambulance Trusts: A Guide for Action 2016.
- Ariza-Montes A, Muniz NM, Montero-Simó MJ, Araque-Padilla RA. Workplace bullying among healthcare workers. Int J Environ Res Public Health 2013;10:3121-39. https://doi.org/10.3390/ijerph10083121.
- Adams L, Bryan V. Workplace harassment: the leadership factor. Healthc Manag Forum 2021;34:81-6. https://doi.org/10.1177/0840470420978573.
- Wilson JL. An exploration of bullying behaviours in nursing: a review of the literature. Br J Nurs 2016;25:303-6. https://doi.org/10.12968/bjon.2016.25.6.303.
- Jones A, Kelly D. Deafening silence? Time to reconsider whether organisations are silent or deaf when things go wrong. BMJ Qual Saf 2014;23:709-13. https://doi.org/10.1136/bmjqs-2013-002718.
- Hutchinson M, Wilkes L, Jackson D, Vickers MH. Integrating individual, work group and organizational factors: testing a multidimensional model of bullying in the nursing workplace. J Nurs Manag 2010;18:173-81. https://doi.org/10.1111/j.1365-2834.2009.01035.x.
- Rogers-Clark C, Pearce S, Cameron M. Management of disruptive behaviour within nursing work environments: a comprehensive systematic review of the evidence. JBI Libr Syst Rev 2009;7:615-78. https://doi.org/10.11124/jbisrir-2009-196.
- Rocker CF. Addressing nurse-to-nurse bullying to promote nurse retention. Online J Issues Nurs 2008;13:1-10. https://doi.org/10.3912/ojin.vol13no03ppt05.
- Jagosh J, Bush PL, Salsberg J, Macaulay AC, Greenhalgh T, Wong G, et al. A realist evaluation of community-based participatory research: partnership synergy, trust building and related ripple effects. BMC Public Health 2015;15:1-11. https://doi.org/10.1186/s12889-015-1949-1.
- Maben J, Taylor C, Jagosh J, Carrieri D, Briscoe S, Klepacz N, et al. Care Under Pressure 2: Caring for the Carers – A Realist Review of Interventions to Minimise the Incidence of Mental Ill-health in Nurses, Midwives and Paramedics. NIHR HS&DR; 2023.
- Quinlan E, Robertson S, Miller N, Robertson-Boersma D. Interventions to reduce bullying in health care organizations: a scoping review. Health Serv Manag Res 2014;27:33-44. https://doi.org/10.1177/0951484814547236.
- Bambi S, Guazzini A, de Felippis C, Lucchini A, Rasero L. Preventing workplace incivility, lateral violence and bullying between nurses. A narrative literature review. Acta Biomed 2017;88:39-47. www.ncbi.nlm.nih.gov/pmc/articles/PMC6357576/ (accessed 1 December 2021).
- Royal College of Nursing . Bullying and Harassment: Good Practice Guidance for Preventing and Addressing Bullying and Harassment in Health and Social Care Organisations 2015.
- Dimarino TJ. Eliminating lateral violence in the ambulatory setting: one center’s strategies. AORN J 2011;93:583-8. https://doi.org/10.1016/j.aorn.2010.10.019.
- Ceravolo DJ, Schwartz DG, Foltz-Ramos KM, Castner J. Strengthening communication to overcome lateral violence. J Nurs Manag 2012;20:599-606. https://doi.org/10.1111/j.1365-2834.2012.01402.x.
- Westbrook JI, Urwin R, McMullan R, Badgery-Parker T, Pavithra A, Churruca K, et al. Changes in the Prevalence of Unprofessional Behaviours by Co-workers Following a 2 Professional Accountability Culture Change Program Across Five Australian Hospitals. n.d.
- Guo L, Ryan B, Leditschke IA, Haines KJ, Cook K, Eriksson L, et al. Impact of unacceptable behaviour between healthcare workers on clinical performance and patient outcomes: a systematic review. BMJ Qual Saf 2022;31:679-87. https://doi.org/10.1136/bmjqs-2021-013955.
- NHS England . 2020 National NHS Staff Survey n.d.
- British Medical Association . Workplace Bullying and Harassment of Doctors. A Review of Recent Research 2017.
- Ross S, Jabbal J, Chauhan K, Maguire D, Randhawa M, Dahir S. Workforce Race Inequalities and Inclusion in NHS Providers. The King’s Fund; 2020.
- Cruz D, Rodriguez Y, Mastropaolo C. Perceived microaggressions in health care: a measurement study. PLOS ONE 2019;14:e0211620-11. https://doi.org/10.1371/journal.pone.0211620.
- Charette M, Goudreau J, Bourbonnais A. Factors influencing the practice of new graduate nurses: a focused ethnography of acute care settings. J Clin Nurs 2019;28:3618-31. https://doi.org/10.1111/jocn.14959.
- Chipps EM, McRury M. The development of an educational intervention to address workplace bullying: a pilot study. J Nurses Staff Dev 2012;28:94-8. https://doi.org/10.1097/NND.0b013e31825514bb.
- Babenko-Mould Y, Laschinger HKS. Effects of incivility in clinical practice settings on nursing student burnout. Int J Nurs Educ Scholarsh 2014;11:145-54. https://doi.org/10.1515/ijnes-2014-0023.
- Weaver KB. The effects of horizontal violence and bullying on new nurse retention. J Nurses Prof Dev 2013;29:138-42. https://doi.org/10.1097/NND.0b013e318291c453.
- Lasater K, Mood L, Buchwach D, Dieckmann NF. Reducing incivility in the workplace: results of a three-part educational intervention. J Contin Educ Nurs 2015;46:15-24; quiz 25. https://doi.org/10.3928/00220124-20141224-01.
- Parker KM, Harrington A, Smith CM, Sellers KF, Millenbach L. Creating a nurse-led culture to minimize horizontal violence in the acute care setting: a multi-interventional approach. J Nurses Prof Dev 2016;32:56-63. https://doi.org/10.1097/NND.0000000000000224.
- Clark CM, Ahten SM, Macy R. Using problem-based learning scenarios to prepare nursing students to address incivility. Clin Simul Nurs 2013;9:e75-83. https://doi.org/10.1016/j.ecns.2011.10.003.
- Michie S, Wood CE, Johnston M, Abraham C, Francis JJ, Hardeman W. Behaviour change techniques: the development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol Assess (Rockv) 2015;19:1-188. https://doi.org/10.3310/hta19990.
- Armstrong NE. A quality improvement project measuring the effect of an evidence-based civility training program on nursing workplace incivility in a rural hospital using quantitative methods. Online J Rural Nurs Health Care 2017;17:100-37. https://doi.org/10.14574/ojrnhc.v17i1.438.
- Barrett A, Piatek C, Korber S, Padula C. Lessons learned from a lateral violence and team-building intervention. Nurs Adm Q 2009;33:342-51. https://doi.org/10.1097/NAQ.0b013e3181b9de0b.
- Dixon-Woods M, Campbell A, Martin G, Willars J, Tarrant C, Aveling EL, et al. Improving employee voice about transgressive or disruptive behavior: a case study. Acad Med 2019;94:579-85. https://doi.org/10.1097/ACM.0000000000002447.
- Jenkins S, Woith W, Kerber C, Stenger D. Why can’t we all just get along? A civility journal club intervention. Nurse Educ 2011;36:140-1. https://doi.org/10.1097/NNE.0b013e31821fd9b8.
- Kile D, Eaton M, DeValpine M, Gilbert R. The effectiveness of education and cognitive rehearsal in managing nurse-to-nurse incivility: a pilot study. J Nurs Manag 2019;27:543-52. https://doi.org/10.1111/jonm.12709.
- Osatuke K, Moore SC, Ward C, Dyrenforth SR, Belton L. Civility, respect, engagement in the workforce (CREW). J Appl Behav Sci 2009;45:384-410. https://doi.org/10.1177/0021886309335067.
- Speck RM, Foster JJ, Mulhern VA, Burke SV, Sullivan PG, Fleisher LA. Development of a professionalism committee approach to address unprofessional medical staff behavior at an academic medical center. Jt Comm J Qual Patient Saf 2014;40:161-7. https://doi.org/10.1016/S1553-7250(14)40021-7.
- Stagg SJ, Sheridan DJ, Jones RA, Speroni KG. Workplace bullying: the effectiveness of a workplace program. Workplace Health Saf 2013;61:333-8. https://doi.org/10.1177/216507991306100803.
- Stagg SJ, Sheridan D, Jones RA, Speroni KG. Evaluation of a workplace bullying cognitive rehearsal program in a hospital setting. J Contin Educ Nurs 2011;42:395-401; quiz 402. https://doi.org/10.3928/00220124-20110823-45.
- Thorsness R, Sayers B. Systems approach to resolving conduct issues among staff members. AORN J 1995;61:197-202. https://doi.org/10.1016/S0001-2092(06)63859-3.
- Webb LE, Dmochowski RR, Moore IN, Pichert JW, Catron TF, Troyer M, et al. Using coworker observations to promote accountability for disrespectful and unsafe behaviors by physicians and advanced practice professionals. Jt Comm J Qual Patient Saf 2016;42:149-64. https://doi.org/10.1016/s1553-7250(16)42019-2.
- O’Keeffe DA, Brennan SR, Doherty EM. Resident training for successful professional interactions. J Surg Educ 2022;79:107-11. https://doi.org/10.1016/j.jsurg.2021.08.017.
- Hawkins N, Jeong SYS, Smith T, Sim J, Clapham M. Creating respectful workplaces for nurses in regional acute care settings: a quasi-experimental design. Nurs Open 2022;10:78-89. https://doi.org/10.1002/nop2.1280.
- Leiter MP, Laschinger HKS, Day A, Oore DG. The impact of civility interventions on employee social behavior, distress, and attitudes. J Appl Psychol 2011;96:1258-74. https://doi.org/10.1037/a0024442.
- Laschinger HKS, Leiter MP, Day A, Gilin-Oore D, MacKinnon SP. Building empowering work environments that foster civility and organizational trust: testing an intervention. Nurs Res 2012;61:316-25. https://doi.org/10.1097/NNR.0b013e318265a58d.
- Kang J, Kim JI, Yun S. Effects of a cognitive rehearsal program on interpersonal relationships, workplace bullying, symptom experience, and turnover intention among nurses: a randomized controlled trial. J Korean Acad Nurs 2017;47:689-99. https://doi.org/10.4040/jkan.2017.47.5.689.
- Asi Karakaş S, Okanli AE. The effect of assertiveness training on the mobbing that nurses experience. Work Health Saf 2015;63:446-51. https://doi.org/10.1177/2165079915591708.
- Kousha S, Shahrami A, Forouzanfar MM, Sanaie N, Atashzadeh-Shoorideh F, Skerrett V. Effectiveness of educational intervention and cognitive rehearsal on perceived incivility among emergency nurses: a randomized controlled trial. BMC Nurs 2022;21. https://doi.org/10.1186/s12912-022-00930-1.
- Guidroz AM, Burnfield-Geimer JL, Clark O, Schwetschenau HM, Jex SM. The nursing incivility scale: development and validation of an occupation-specific measure. J Nurs Meas 2010;18:176-200. https://doi.org/10.1891/1061-3749.18.3.176.
- Walton MM. Hierarchies: the Berlin wall of patient safety. Qual Saf Health Care 2006;15:229-30. https://doi.org/10.1136/qshc.2006.019240.
- Jones A, Maben J, Adams M, Mannion R, Banks C, Blake J, et al. Implementation of ‘Freedom to speak up guardians’ in NHS acute and mental health trusts in England: the FTSUG mixed-methods study. Health Soc Care Deliv Res 2022;10:1-124. https://doi.org/10.3310/GUWS9067.
- Beale D, Leather P. Working with Care – Improving Working Relationships in Health and Social Care: Self-assessment Tools for Health. Royal College of Nursing – RCN; 2005.
- Markwell A, Smith S, Michalski M, Conroy S, Bell A. Performance management versus bullying and harassment: an educator perspective. Emerg Med Australas 2015;27:468-72. https://doi.org/10.1111/1742-6723.12466.
- Spence Laschinger HK, Wong CA, Grau AL. The influence of authentic leadership on newly graduated nurses’ experiences of workplace bullying, burnout and retention outcomes: a cross-sectional study. Int J Nurs Stud 2012;49:1266-76. https://doi.org/10.1016/j.ijnurstu.2012.05.012.
- Venkatesh B, Corke C, Raper R, Pinder M, Stephens D, Joynt G, et al. Findings of the bullying, discrimination and sexual harassment survey: response of the college of intensive care medicine. Crit Care Resusc 2016;18:228-9.
- Anderson K. Workplace aggression and violence: nurses and midwives say NO. Aust Nurs J 2011;19:26-9. https://pubmed.ncbi.nlm.nih.gov/21853685/ (accessed 9 December 2022).
- British Medical Association . Bullying and Harassment: How to Address It and Create a Supportive and Inclusive Culture 2018.
- National Guardian’s Office . Speaking up in the NHS in England: A Summary of Speaking up to Freedom to Speak up Guardians in NHS Trusts and Foundation Trusts 2018.
- Allen B. Understanding bullying in healthcare organisations. RCN Nurs Stand 2015;30:50-6. https://doi.org/10.7748/ns.30.14.50.s46.
- Yu F, Raphael D, Mackay L, Smith M, King A. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud 2019;93:129-40. https://doi.org/10.1016/j.ijnurstu.2019.02.014.
- Laschinger HKS, Grau AL, Finegan J, Wilk P. New graduate nurses’ experiences of bullying and burnout in hospital settings. J Adv Nurs 2010;66:2732-42. https://doi.org/10.1111/j.1365-2648.2010.05420.x.
- Johnson MJ, May CR. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008592.
- Kelly LA, McHugh MD, Aiken LH. Nurse outcomes in Magnet® and non-Magnet hospitals. J Nurs Adm 2011;41:428-33. https://doi.org/10.1097/NNA.0b013e31822eddbc.
- Mitchell G. Bullying and inadequate leadership found at flagship nursing trust. Nurs Times 2021.
- Blackstock S, Salami B, Cummings GG. Organisational antecedents, policy and horizontal violence among nurses: an integrative review. J Nurs Manag 2018;26:972-91. https://doi.org/10.1111/jonm.12623.
- Nicotera AM, Mahon MM, Zhao X. Conceptualization and measurement of structurational divergence in the healthcare setting. J Appl Commun Res 2010;38:362-85. https://doi.org/10.1080/00909882.2010.514001.
- Hawkins N, Jeong SYS, Smith T, Sim J. A conflicted tribe under pressure: a qualitative study of negative workplace behaviour in nursing. J Adv Nurs 2023;79:711-26. https://doi.org/10.1111/jan.15491.
- Mello MM, Jagsi R. Standing up against gender bias and harassment – a matter of professional ethics. N Engl J Med 2020;382:1385-7. https://doi.org/10.1056/NEJMp1915351.
- RLDatix . Making Healthcare Safer 2023. https://rldatix.com/en-uke/ (accessed 9 December 2022).
- Bal M, Brookes A, Kordowicz M, Mendy J. The Absurd Workplace. How Absurdity Is Normalized in Contemporary Society and the Workplace. Cham: Palgrave Macmillan; 2022.
- Sheehan M, McCabe TJ, Garavan TN. Workplace bullying and employee outcomes: a moderated mediated model. Int J Hum Resour Manag 2020;31:1379-416. https://doi.org/10.1080/09585192.2017.1406390.
- Colangelo A. St Vincent’s reviews anti-bullying program amid staff backlash. The Age 2019. www.theage.com.au/national/victoria/st-vincent-s-reviews-anti-bullying-program-amid-staff-backlash-20190223-p50zri.html (accessed 9 December 2022).
- Gillespie GL, Grubb PL, Brown K, Boesch MC, Ulrich DL. Nurses eat their young’: a novel bullying educational program for student nurses. J Nurs Educ Pract 2017;7:11-2. https://doi.org/10.5430/jnep.v7n7p11.
- Damschroder L, Aron D, Keith R, Kirsh S, Jeff A, Alexander J. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Development of the ACTIVE framework to describe stakeholder involvement in systematic reviews. J Health Serv Res Policy 2019;24:245-55. https://doi.org/10.1177/1355819619841647.
- Abrams R, Park S, Wong G, Rastogi J, Boylan AM, Tierney S, et al. Lost in reviews: looking for the involvement of stakeholders, patients, public and other non-researcher contributors in realist reviews. Res Synth Methods 2021;12:239-47. https://doi.org/10.1002/jrsm.1459.
- National Institute for Health and Care Research . Improving Inclusion in Under-Served Groups in Health and Care Research: Guidance from the NIHR-INCLUDE Project 2017. https://sites.google.com/nihr.ac.uk/include/home/guidance (accessed 9 December 2022).
- Witham MD, Anderson E, Carroll C, Dark PM, Down K, Hall AS, et al. INCLUDE writing group . Developing a roadmap to improve trial delivery for under-served groups: results from a UK multi-stakeholder process. Trials 2020;21. https://doi.org/10.1186/s13063-020-04613-7.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:1-11. https://doi.org/10.1186/1748-5908-6-42.
- Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci 2015;11:1-13. https://doi.org/10.1186/s13012-016-0398-2.
- Harvey SB, Laird B, Henderson M, Hotopf M. The Mental Health of Health Care Professionals. Department of Health; 2009.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- Edmondson A . Psychological Safety 2022. https://amycedmondson.com/psychological-safety (accessed 9 February 2023).
- Anderson MA, MFTC JB. Clash of values: workplace bullying and moral injury. Coun Fam Ther Scholarsh Rev 2021;3. https://doi.org/10.53309/PWEX4999.
- Van den Broek A, Baillien E, De Witte H. Workplace bullying: a perspective from the job demands-resources model: original research. SA J Ind Psychol 2011;37:1-12. http://doi.org/10.4102/sajip.v37i2.879.
- Armstrong N. Management of nursing workplace incivility in the health care settings: a systematic review. Work Health Saf 2018;66:403-10. https://doi.org/10.1177/2165079918771106.
- Barzallo Salazar MJ, Minkoff H, Bayya J, Gillett B, Onoriode H, Weedon J, et al. Influence of surgeon behavior on trainee willingness to speak up: a randomized controlled trial. J Am Coll Surg 2014;219:1001-7. https://doi.org/10.1016/j.jamcollsurg.2014.07.933.
- Benjamin A. British Medical Association; 2021.
- British Medical Association . Promoting a positive working environment BMA 2021.
- Cooper K. Ending the Silence. BMA 2018. www.bma.org.uk/news-and-opinion/ending-the-silence (accessed 9 December 2022).
- Illing J, Thompson N, Crampton P, Rothwell C, Kehoe A, Carter M. Workplace bullying: measurements and metrics to use in the NHS Final Report for NHS Employers. Northumbria University Research Portal 2016:1-58.
- Kaiser JA. The relationship between leadership style and nurse-to-nurse incivility: turning the lens inward. J Nurs Manag 2017;25:110-8. https://doi.org/10.1111/jonm.12447.
- Maben J, Adams M, Peccei R, Murrells T, Robert G. ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples’ experience of hospital care. Int J Older People Nurs 2012;7:83-94. https://doi.org/10.1111/j.1748-3743.2012.00326.x.
- Nursing and Midwifery Council . The NMC Register 2021. www.nmc.org.uk/globalassets/sitedocuments/data-reports/annual-2021/0005b-nmc-register-2021-web.pdf (accessed 9 December 2022).
- Salin D. Ways of explaining workplace bullying: a review of enabling, motivating and precipitating structures and processes in the work environment. Hum Relations 2003;56:1213-32. https://doi.org/10.1177/00187267035610003.
- Al-Ghabeesh SH, Qattom H. Workplace bullying and its preventive measures and productivity among emergency department nurses. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4268-x.
- Al-Rais A. Why we should avoid handover hostility. BMJ 2017;356. https://doi.org/10.1136/bmj.j1272.
- Almost J, Doran DM, Mcgillis Hall L, Spence Laschinger HK. Antecedents and consequences of intra-group conflict among nurses. J Nurs Manag 2010;18:981-92. https://doi.org/10.1111/j.1365-2834.2010.01154.x.
- Alspach G. Critical care nurses as coworkers: are our interactions nice or nasty?. Crit Care Nurse 2007;27:10, 12-4.
- Anonymous . When bullying affects patient safety. AORN J 2018;108:78-80. https://doi.org/10.1002/aorn.12294.
- Carter M, Thompson N, Crampton P, Morrow G, Burford B, Gray C, et al. Workplace bullying in the UK NHS: a questionnaire and interview study on prevalence, impact and barriers to reporting. BMJ Open 2013;3:1-12. https://doi.org/10.1136/bmjopen-2013-002628.
- Efe SY, Ayaz S. Mobbing against nurses in the workplace in Turkey. Int Nurs Rev 2010;57:328-34. https://doi.org/10.1111/j.1466-7657.2010.00815.x.
- Hughes A. Being bullied what an insight. Br J Perioper Nurs 2003;13:166-72. https://doi.org/10.1177/175045890301300403.
- Johnson SL, Haerling KA, Yuwen W, Huynh V, Le C. Incivility and clinical performance, teamwork, and emotions: a randomized controlled trial. J Nurs Care Qual 2020;35:70-6. https://doi.org/10.1097/NCQ.0000000000000407.
- Lovejoy-Bluem A. News of the academy of neonatal nursing. Acad Neonatal Nurs 2016;35:173-80. https://doi.org/10.1891/0730-0832.35.3.173.
- Purpora C, Blegen MA. Horizontal violence and the quality and safety of patient care: a conceptual model. Nurs Res Pract 2012;306948:1-5. https://doi.org/10.1155/2012/306948.
- Shuttleworth A. Can Arrowe Park show other trusts how to beat the bullies?. Nurs Times 2018;114.
- Sillero AS, Buil N. Enhancing interprofessional collaboration in perioperative setting from the qualitative perspectives of physicians and nurses. Int J Environ Res Public Health 2021;18:1-11. https://doi.org/10.3390/ijerph182010775.
- Solheim J. Caring for each other while we care for others. J Emerg Nurs 2018;44:319-20. https://doi.org/10.1016/j.jen.2018.05.001.
- Tame S. The relationship between continuing professional education and horizontal violence in perioperative practice. J Perioper Pract 2012;22:220-5. https://doi.org/10.1177/175045891202200702.
- Tran V. Dealing with bullying and harassment: a practical guide for Australasian emergency medicine trainees. Emerg Med Australas 2015;27:473-7. https://doi.org/10.1111/1742-6723.12467.
- Zhang X, Xiong L. Impact of nurse horizontal violence and coping strategies: a review. Yangtze Med 2019;03:289-300. https://doi.org/10.4236/ym.2019.34028.
- Bamberger E, Bamberger P. Unacceptable behaviours between healthcare workers: just the tip of the patient safety iceberg. BMJ Qual Saf 2022;31:638-41. http://doi.org/10.1136/bmjqs-2021-014157.
- Bry A, Wigert H. Organizational climate and interpersonal interactions among registered nurses in a neonatal intensive care unit: a qualitative study. J Nurs Manag 2022;30:2031-8. https://doi.org/10.1111/jonm.13650.
- Naylor MJ, Boyes C, Killingback C. ‘You’ve broken the patient’: physiotherapists’ lived experience of incivility within the healthcare team – an interpretative phenomenological analysis. Physiotherapy 2022;117:89-96. https://doi.org/10.1016/j.physio.2022.09.001.
- NHS England . The NHS England Civility and Respect Programme 2021. https://restorativejustculture.org/civility-and-respect-nhs/ (accessed 9 December 2022).
- NHS England . Supporting Our Staff: A Toolkit to Promote Cultures of Civility and Respect 2021. www.socialpartnershipforum.org/system/files/2021-10/NHSi-Civility-and-Respect-Toolkit-v9.pdf (accessed 9 December 2022).
- Kilpatrick F. Improving Staff Wellbeing: Using the ‘Your Voice’ Digital Reporting Tool 2022. https://q.health.org.uk/idea/2022/improving-staff-wellbeing-using-the-your-voice-digital-reporting-tool/ (accessed 9 December 2022).
- Garcia MG, Allen S, Griffis L, Tidwell J, Watt J. Incorporating a civility program into a healthcare system: journey or expedition?. Clin Nurse Spec 2021;35:171-9. https://doi.org/10.1097/NUR.0000000000000603.
- Clark CM. Fostering a culture of civility and respect in nursing. J Nurs Regul 2019;10:44-52. https://doi.org/10.1016/S2155-8256(19)30082-1.
Appendix 1 Development of initial programme theories
This appendix lays out our initial programme theories across areas of terminology, contributors to UB (referred to as ‘causes’ here) and strategies to mitigate and reduce UB. These will be explored in the following sections.
Initial mapping of UB terminology
Our initial mapping of types of UB identified that there was a targeted and less targeted dimension, frequency, and power hierarchy. However, this is less developed because it does not include visibility of behaviours, for example, and contains fewer terms than our final version does (see Figure 27).
FIGURE 27.
Dimensions of UBs: initial mapping of terminology.
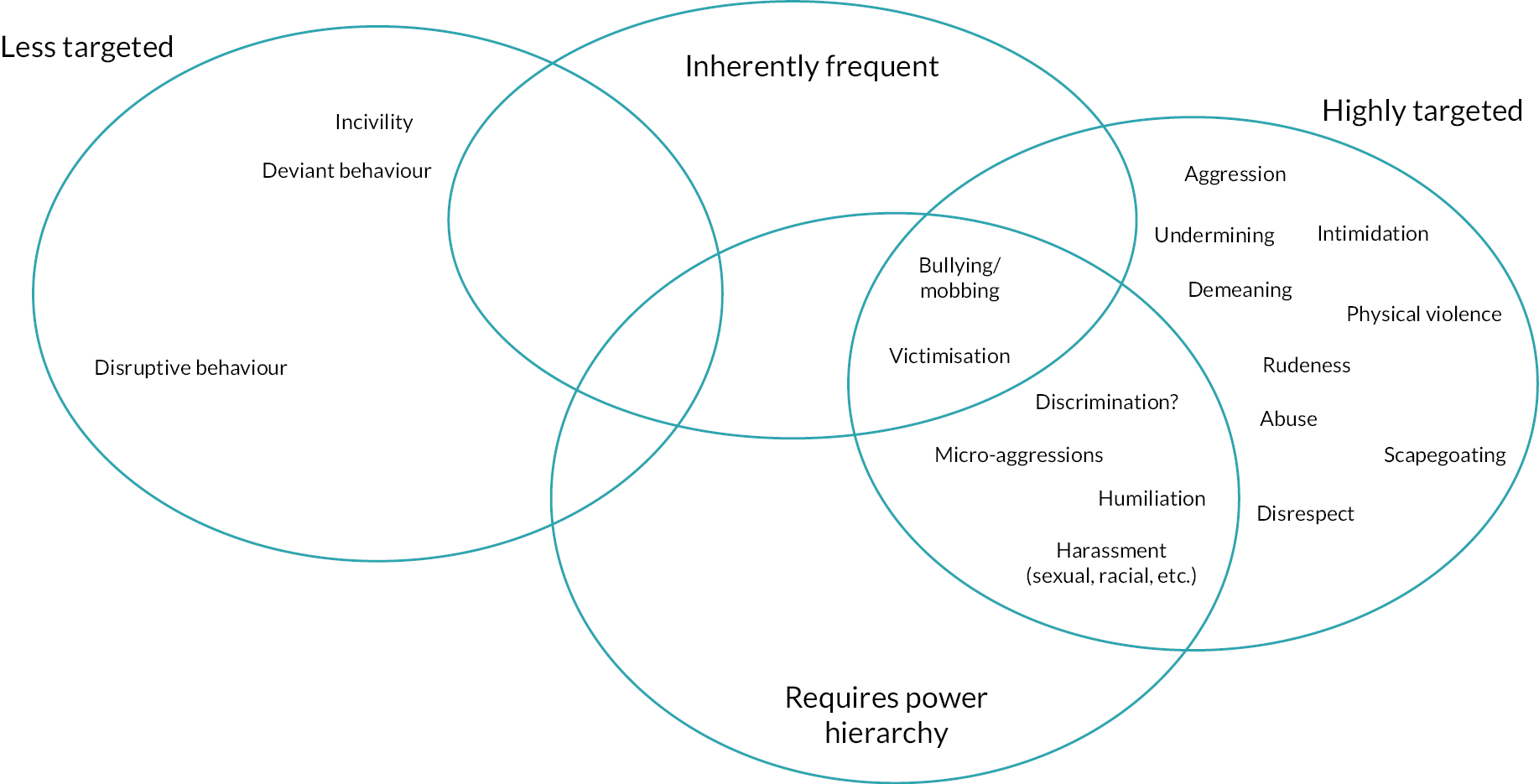
Initial theories around causes
Early on in our review process we surfaced our initial assumptions relating to the possible causes of UB. Our initial programme theory for causes is depicted in Figure 28. We determined a cause as:
Cause (i.e. environmental factor that can cause a change in reasoning) → Mechanism (change in reasoning) which increases proclivity to engage in UB → Outcome (usually increased UB)
At the time, we allocated numbers to reflect how well they were based on data, which is indicated after each CMOC from 1 to 3: (1) indicated the CMOC was based on few data, (2) indicated partial data and (3) meant that every aspect of the CMOC was supported by data. We did not retain this system in our final programme theory because we had more data (110 more studies) to rely on; however, understanding which theories were less supported by the literature helped us to direct our efforts during the refinement stage.
| Causes | CMOCs |
|---|---|
| Individual factors | |
| 1. Perceived unfairness | A consistent sense of perceived unfairness in the workplace (e.g. a feeling that one is being wrongfully passed over for promotion) (C) leads to a feeling of anger and resentment (M) which increases chance of a negative response/becoming an instigator of UB (O) – 3 |
| 2. Personality disorders (instigator) | (Included but CMOC not formulated) |
| 3. Risk/reward analysis of the environment (instigator) | An environment that is not likely to punish an instigator, or otherwise rewards engaging in UB (e.g. a ‘bro’ culture), (C) makes workers perceive the environment as less risky for engaging in UB (M1) or that it may even be socially beneficial to engage in UB (M2) leading to increased proclivity to engage in UB (O) – 3 |
| 4. Interpretation of situation (victim) | If a victim has different expectations of social norms in their workplace (C) then they may interpret more forms of behaviour (i.e. criticism, feedback) as UB (M), therefore this may increase desire to reciprocate by engaging in UB, creating conflict (O1) or lead to more reports of UB (O2) – 3 |
| 5. Job demands (stress, pressure) vs. Job resources (sufficient time, autonomy, lack of organisational constraints) | Perpetual and unsustainable workplace pressure or a decrease in work resources (C) can lead to ineffective ability to communicate (e.g. due to time pressures) (M) which can lead to an increase in conflict (O) – 3 Perpetual and unsustainable workplace pressure or a decrease in work resources (C) can lead to reduced ability to cope (e.g. due to lack of time to break) (M) and therefore increase chance of inappropriate or unprofessional responses (O) – 3 |
| 6. Social support from colleagues | When social support is offered by colleagues (C) it can lead to an improved ability to cope (M1) and improved feeling of respect and belonging from colleagues (M2) which can reduce desire to reciprocate UB (O1) and mitigate impact of UB on mental health/well-being (O2) – 3 |
| 7. Role ambiguity (instigator) | Lack of clarity, control, or clear goals in job role (C) can lead to irritation and frustration (M1), and boredom (M2) which increases search for stimulating behaviours and likelihood to engage in conflict and UB (O) – 3 |
| 8. Physical discomfort | Physical discomfort due to conditions in the workplace (e.g. temperature, crowding) (C) can lead to increased lashing out (O) due to irritation and frustration (M) – 2 |
| 9. Role-modelling, social learning of UB norms, and the cycle of abuse (instigator) | Having a senior role model who frequently engages in UB with no consequence (C) could lead to social learning of inappropriate behavioural norms (M) and therefore increased desire to imitate/model the UB themselves (O) – 3 |
| Organisational factors | |
| 10. Hierarchies | Perceiving oneself to be in a low position in an organisational power hierarchy (C) reduces ability to communicate vertically within the hierarchy (M) and reduces psychological safety (M2) leading to inability to report mistakes by superiors (O) and increase chance of being a target for UB (O2) – 3 Perceiving oneself to be in a low position in an organisational power hierarchy (C) can lead to a reduced perception of respect for one’s role (M). This can increase anger/resentment leading to increased likelihood of engaging in UB (O1) – 3 Perceiving another person to be lower in the hierarchy as an instigator (C) makes the victim a perceptually less risky target than the instigator (M) leading to a higher chance of them becoming a victim (O) – 3 |
| 11. Leadership styles (destructive – autocratic) | Working under a leader using an autocratic leadership style (C) can lead to increased role-modelling of UB by employees (M1), and normalisation of UB in organisational culture (M2) which can lead to increased UB (O) – 3 Working under a leader using an autocratic leadership style (C) can lead to reduced sense of psychological safety (M3) which can lead to inability to speak up about UB (O2) – 3 |
| 12. Leadership styles (destructive – laissez-faire) | Working under leaders who are laissez-faire or ‘hands-off’ (C) can lead to the perception by instigators that there is low risk to engage in UB, as there’s little chance of punishment (M1), leading to increased proclivity to engage in UB (O) – 3 Working under leaders who are laissez-faire or ‘hands-off’ (C) can lead to increased role ambiguity (M1) leading to increased boredom (O1) and frustration (O2) – 3 |
| 13. Leadership styles (destructive – transactional) | Working under a transactional leader (C) can lead to a culture of tolerance of mistreatment (M1) and reduction in risk for instigators to engage in UB (M2) leading to increased proclivity to engage in UB and to become an instigator (O) – 3 |
| 14. Leadership styles (destructive – tyrannical) | Working under a tyrannical leader (C) can lead to a reduction in feeling of social support (M1) and a reduction in psychological safety (M2) leading to an increased chance of becoming a victim of UB (O) and increased personal impact of being exposed to UB (O2) – 2 |
| 15. Leadership styles (constructive – transformational, democratic, or compassionate) | Working under a constructive leader (C) can lead to an increased sense of psychological safety (M) and increased ability to speak up (O) – 3 Working under a constructive leader (C) can lead to an increased perception of risk for potential instigators (M) and reduction in desire to engage in UB (O) – 3 Working under a constructive leader (C) can lead to a reduction in role ambiguity (M) and therefore a reduction in boredom and frustration (O) – 3 Working under a democratic leader (C) can lead to an increased sense of social support from colleagues (M) and therefore improved ability to cope (O1) and improved sense of respect (O2) – 3 |
| 16. Organisational change | Working amidst significant organisational reorganisation or turnover (C) reduces feelings of psychological safety (M1) and can increase uncertainty about one’s organisational role (M2), leading to greater competition, bullying, and incivility between staff (O) – 3 Change in organisational leadership (C) can enlarge the power gap between employees and leaders (M), leading to a reduction in psychological safety (O) – 3 |
| 17. Organisational culture (tolerance of UBs) | A perceived tolerance of UB in the organisation or team (C) can lead to a lowering of risk to engage in UB by instigators (M) leading to increased proclivity to engage in UB (O) – 3 A perceived tolerance of UB in the organisation or team (C) can lead to an increase in perceived role-modelling of UB (M) leading to increased proclivity to engage in UB (O) – 3 A perceived tolerance of UB in the organisation or team (C) can lead to ridiculing of professional behaviours such as acting compassionate (M), leading to reduced desire to act against the social norm where UB is prevalent (O) – 3 Witnessing UB occur without negative consequence in the organisational environment (C) can lead to increased perception that UB is acceptable (M1) and reduce perception of risk to engage in UB (M2) leading to increased proclivity to engage in UB (O) – 3 |
| 18. Organisational culture – (belonging to an ‘outgroup’ or workplace minority in intolerant work environment) | Being a member of a minority group in a workplace that is intolerant towards minorities (C) can lead to a reduced perception by minority members that they have social support (M1) and may appear as being in lower perceived position in the power hierarchy to potential instigators (M2) which may make such minority members more susceptible to experiencing UB (O1) and make victims less likely to speak up (O2) – 3 |
| 19. Organisational culture (oppression of certain workers) | Workers from professional groups that have a lack of power in their organisational structure (C) may engage in greater UBs (O) because they can internalise the oppression and lash out due to frustration (M) – 2 Being a member of an oppressed professional group in an organisation (C) can make you more likely to be a target of UB (O) due to being seen as a less risky target for instigators of UB (M) – 2 |
| 20. Organisational culture (integrity and fairness) | When staff members feel undervalued, underappreciated and oppressed within their workplaces (C), they may internalise the oppression (M1), causing a decrease in empathy for one another (M2), and in turn become bullies of those below or equal to themselves (O) – 3 |
| 21. Organisational culture (social norm of prolonged and unnecessary high stress) | In cultures of high stress and high stakes for patient safety (C), staff may experience anger, frustration and fear (M) making them more likely to lash out and produce an environment rife with conflict (O) – 3 |
| Team factors | |
| 22.Collaboration across departments | If there is significant collaboration across departments when teamworking (C) then there may be an increased chance of being exposed to a perceived interprofessional power hierarchy (M) which can increase chance of conflict (O1) and reduce effective communication (O2) – 2 |
| 23. Team leaders having unreasonable expectations | When senior members of staff have high expectations that feel unreasonable to junior staff members (e.g. a culture of perfectionism) (C), working relationships become tense and unpleasant (M), which creates an environment for bullying to occur (O) – 3 |
| 24. Team – lacking a common vision/direction | If the team lacks a common vision (C) then this may increase sense of frustration (M) which can lead to an increase in conflict and UB between team members (O) – 2 When a team lacks common direction or purpose (C) then boredom/frustration can lead to selection of scapegoats within the team (M) which can lead to targeted forms of UB (O) – 2 |
| 25. Team leadership | A more democratic team leadership style (C) can lead to an improved sense of social support (M1) and psychological safety (M2) which can therefore reduce the impact of UB (O) – 3 |
| 26. Shift working | If team members are working in shifts (C) then they may not be able to build interpersonal relationships with their co-workers (M), leading to an absence of social support (O) – 3 |
| Societal factors | |
| 27. Public pressure | If the public becomes aware through media (or other) reports about high prevalence of UB in an organisation (C) then this can lead to a sense of pressure on management to resolve the problem (M), which can reduce UB (O) – 3 |
| 28. Regulation | If there is regulation in place to reduce UB or punish it, and this is implemented by organisations (C) then this may increase perception of risk for the instigator due to fear of breaking organisational policies and the law (M), leading to a reduction in desire to engage in UB (O) – 2 |
FIGURE 28.
Initial programme theory for causes.

Initial theories regarding strategies to reduce unprofessional behaviour
We also identified and coded excerpts relating to strategies in NVivo and initially classified them as either ‘preventative’ (i.e. intended to prevent UB) or ‘reactive’, that is try to mitigate the impact of UB; however, in the refined version, we did not retain these categories as the distinction between these was not always clear. Our initial CMOCs are presented in Table 23.
| Strategy | Type of behaviours | CMOC |
|---|---|---|
| 1. Education, training of workforce about identifying UBs | UBs (general) | When staff think UBs are necessary (e.g. bullying as part of training ‘to build resilience’) (C) then education regarding the effects of UBs may not lead to reflection on one’s behaviour (M – Instigator) therefore leading to no decrease in UBs (O) – 3 If the intervention is of too short duration (C), then it is unlikely to reduce prevalence of UBs (O), because uptake of the intervention content will not be sufficient across the workforce (M) – 2 If the facilitators have the skills to properly implement the intervention (C), then UBs may become reduced (O), because they will improve collective awareness of UB (M1) and teach attendees how to identify UB (M2) – 1 |
| If the education does not reach a critical mass of key actors in the workforce (e.g. management, bystanders, instigators) (C), then the intervention may not reduce UBs (O), because the intervention may not be taken up by those most proximal to the UBs (M) – 2 If the intervention does not have management support (C), then it is unlikely to be delivered for sufficiently long enough to achieve critical mass (M), because employee commitment will be lacking (O) – 2 If the intervention cannot be delivered in a flexible manner for employees around their other commitments (C) then it may not reduce UBs (O) as it is less likely to be taken up by people most proximal to the UBs (M) – 1 |
||
| If the intervention is delivered to a high-quality standard, i.e. is of sufficient duration (C1), is delivered flexibly around other commitment (C2), has support of management (C3), is delivered skilfully (C4) and reaches a critical mass of key actors (C5), then it may reduce UBs (O) because it can improve awareness of UB (M1), improve identification of UB (M2), enable instigators to reflect on their own behaviour (M3) and empowers victims and bystanders to come forward (M4) – 2 Piloting the educational/training materials with stakeholders (C) can lead to improved ability to reduce UB (O) because it enables facilitators to improve intervention materials for greater efficacy (M) – 3 |
||
| 2. Team-building, Schwartz Rounds | UBs (general) | If the intervention is of too short a duration of implementation (C), then it is unlikely to reduce prevalence of UBs (O), because the workforce will not sense that they are supported by others (M1), and sense of collective empathy/ mutual understanding has not been improved (M2) – 2 If the Schwartz rounds/team-building exercises are not delivered to a critical mass of the workforce (C) or the intervention does not have sufficient management support (C2), then it may not reduce UBs (O), as uptake will not be high enough to improve enough people’s collective sense of social support and empathy (M) – 2 |
| If the intervention resource is of sufficient duration of implementation (C1) and is delivered to enough people (C2) then the intervention might reduce UBs (O), because it can improve sense of social support, making people more likely to come forward to report UBs (M1), can improve sense of empathy which reduces the likelihood of UBs occurring (M2), and can improve empowered decision-making processes in a team setting (M3) – 3 | ||
| 3. Coaching and mentoring | UBs (general) | If the intervention is not visible or accessible to the workforce (C) then it may not reduce UBs (O), as workforce uptake will be low (M) – 2 If the mentor is skilled at mentorship (C1) and if enough of the workforce is mentored (C2) then mentorship may reduce UBs (O), as it would effectively improve perception of social support (M1), understanding of victimhood (M2), and improve victim self-confidence (M3) and individuals will feel in a stronger position to challenge negative behaviours (M4) – 2 |
| 4. Reverse mentoring (when lower-level employee mentors management) | UBs (general), might work better on behaviours which require hierarchy | If managers have prior knowledge/training of the interventions to reduce UBs (C), then reverse mentoring may reduce UBs (O), as managers might gain knowledge, skills and motivation to tackle such behaviours (M) – 2 If managers do have knowledge and skills for how to effectively tackle UBs with follow-up interventions (C), then reverse mentoring may reduce UBs (O), as managers are more likely to accept there is a problem (M1), are more likely to better understand and have empathy for lower-level employees experiences (M2), and trust in management to tackle the problem will be increased (M3) – 3 |
| 5. Code of conduct (organisational) | UBs (general) | If the code of conduct does not apply to all staff equally (C), then UBs may not be reduced (O), as instigators will not have their perception of risk increased (M1), and there will be no greater sense of empathy between staff members (M2) – 3 If the code of conduct does not have visible enforcement (C), then UBs may not be reduced (O), as there is no increase to perceived risk for instigators (M) – 3 |
| If the code of conduct does reward positive behaviours (C), then UBs may be reduced (O), as there may be a greater sense of empathy between staff (M1), and perception of reward for instigators is reduced (M2) – 3 If the code of conduct is not visible and known to all employees (C), then it will not reduce UBs (O), as it will not increase awareness (or knowledge about how to tackle?) of UBs (M1), not increase perception of risk/reward for instigators (M2) nor improve sense of collegiality (M3) – 3 |
||
| If employees sign a pledge to abide by the code of conduct (C1), then the code of conduct may further reduce UBs (O), because it will increase commitment to the code of conduct (M1), further increase awareness of UB (M2) and increase risk for an instigator (M3) – 3 | ||
| 6. Conflict management training | Bullying, harassment, undermining (targeted behaviours) | If there is a lack of follow-up (C1) or short period in which the intervention is offered (C2) then conflict management training might not reduce UBs (O), because collective uptake is not sufficient in the population (M) – 2 If management does not support the intervention (C), then UBs may not be reduced (O), as the workforce would not be committed to the training (M) – 3 If the workforce does not know that they can access and take part in the training (C), then UBs may not be reduced (O), as uptake would not be sufficient in the population (M) – 3 |
| If the organisation has a high prevalence of targeted behaviours such as harassment and bullying (C), then conflict management training might reduce conflict (O), because it may improve sense of collegiality and empathy (M) – 2 If conflict management training is skilfully delivered (e.g. with use of active learning techniques, reframing, role-play or ‘I messages’) (C), then conflict-management training may reduce UBs (O), because the intervention increases awareness of UBs (M1), provides an opportunity to practice new skills (M2); reduces escalation and reciprocity in situations involving conflict (M3), and improves sense of collegiality and empathy (M4) – 3 |
||
| 7. Environmental modification (cues) | UBs (general) | If there are environmental prompts to remind staff of UBs (C) then it may reduce UBs (O) because there will be an increased awareness of UBs (M) and there will be an increased perception of risk to engage in UB (M2 – Instigators) – 2 |
| 8. Flattening hierarchies and training managers | Targeted behaviours that rely on hierarchy | If time and resources are not provided for the training (C), then UBs may not be reduced (O), as collective uptake of the intervention may not be sufficient (M) – 3 If facilitators do not have the requisite skills and knowledge to implement the intervention (C) then UBs may not be reduced (O) because managers will not uptake the required skills properly (M) – 2 If the training does not properly target a critical mass of managers (C) then UBs may not be reduced (O), as the perception of power gradient for victims will not be changed (M) – 3 |
| If time and resources are provided for the training, facilitators have requisite skills to deliver the training, and training is delivered to a critical mass of managers (C1,2,3) then UBs may be reduced (O), as the perception of the power gradient may be changed for victims/bystanders (M1) leading to an increase in psychological safety (M2), there may be a reduced perception of reward for instigators (M3), managers may have a greater sense of empathy for those working under them (M4), and there may be improved team communication (M5) – 2 If there is a prevalence of targeted UBs that rely on hierarchy (e.g. bullying) in the organisation (C), then training to reduce hierarchy may be more effective (O), as it more explicitly targets the causes of these behaviours (M) – 2 |
||
| 9. Improving inclusion (e.g. staff networks, improving representation, unconscious bias training, allyship) | Racism, sexism, behaviours targeted at minority members of workforce | If the intervention is not sustained continuously (C), then UBs against minorities may not be reduced (O), because the intervention would not have reached enough people (low uptake) (M) – 3 Having allies who are not from ethnic minority backgrounds championing an intervention to improve inclusion (C) can improve efficacy of the intervention (O) because it can shine a light on assumptions underpinning structural biases by the challenge coming from less expected sources (M) – 3 |
| If there are not multiple implementers to champion the intervention(s) (C1) or the champions do not have sufficient resource to maintain resilience (C2) then they may not effectively reduce UBs towards minorities (O) because there may not be sufficient uptake of the intervention (M) – 2 If the facilitators are not sufficiently skilled in the delivery of the training (C) then UBs towards minority members may not be reduced (O), because there might be improper uptake of the training by participants (M) – 2 |
||
| If improvements are not able to be measured in response to these interventions (C), then UBs may not be reduced (O), because people will lose commitment to the intervention because they do not see change (M) – 2 If some staff who are not minority members are excluded from the interventions (C) then conflict may occur (O), as resentment could be increased in those who are excluded (M) – 3 If the intervention does not reach a critical mass of the workforce (C), then UBs towards minorities may not be reduced (O), because uptake will not be sufficiently high (M) – 2 |
||
| If you see people of a similar background to yourself represented in senior management in the organisation (C) you are more likely to be committed to your organisation (O) because you will feel more empowered by working there (M) – 2 If the intervention has peer support (C1) and reaches a critical mass of the workforce (C2) then interventions focused on inclusion may reduce UBs towards minorities (O), as they can improve sense of fairness (M1), thereby reducing stress in victims/bystanders (M2), they can reduce the sense of a power gradient (M3), improve empathy towards colleagues from different backgrounds (M4), improve communication within teams (M5), help instigators understand differences in perception of their actions (M6), and provide positive role models for minority members (M–) – 2 |
||
| 10. Monitoring prevalence of UBs | UBs (general) | If the monitoring of UBs is continuous (C) then it may reduce the impact of UBs (O), as it enables other strategies/interventions to be put in place to deal with UB earlier (M) – 3 If staff are made aware of the results of the monitoring (i.e. the prevalence) (C) then UBs may be reduced (O) because staff will gain trust in management (M1) If actions are not taken when data about high prevalence of UB is made available (C) then UBs can be increased (O) because staff will lose morale (M1) and trust in management (M2) – 3 |
| If monitoring is continuous (C1), UBs are seen as a problem (C2), and staff are more widely made aware of the prevalence of UB (C3), then UBs may be reduced (O), because there will be an enhanced awareness of UBs that can lead to further action (M1), it can improve collective trust in management to reduce these behaviours (M2) and knowledge that UB is being monitored can lead to improved psychological safety (M3) – 2 | ||
| 11. Positive role-modelling/championing | UBs (general) | If there are positive role models in place (C1) then UBs may be reduced (O), because victims and instigators can learn how to behave in a positive manner through social learning (M1) thereby collectively changing social norms/culture (M2) – 2 |
| 12. Visible commitment to reducing UBs by managers and gaining of trust from employees Commitment must be followed up by action or risk large decrease in trust | UBs (general) – strategy might be less effective with bullying or harassment | If managers visibly commit to reducing UBs in front of the workforce (C), then UBs may be reduced (O), because victims and bystanders may perceive that management is serious (M1), leading to a greater willingness to come forward (M2). Additionally, instigators may perceive there to be a greater risk to engaging in UBs (M3), and managers may be more likely to acquire more skills to deal with UBs (M4). – 3 If the commitment is not followed up by action by managers (C), then UBs may worsen (O), because staff will lose significant trust in management (M) – 3 |
| 13. Encouraging bystander intervention (once environment is relatively free of risk of reprisal) | UBs (general) | If a bystander speaks up in a situation when they are lower in a power hierarchy than an instigator(C1), or where bullying is prevalent (C2), then they may face reprisal in the form of more UBs (O), because the instigator may perceive this action as an attack (M1) – 3 If bystanders are in a situation without power hierarchy (C1), then being encouraged to speak up may help reduce UBs (O), because it may identify instigators as unprofessional both to themselves and to others (M1), leading instigators to reflect upon their actions (M2). Additionally, training may improve self-confidence of bystanders (M3), improve bystanders’ abilities to correctly identify UBs (M4) can change social norms in the organisation to make UB less acceptable (M5) and can provide a sense of personal responsibility to employees to reduce and call out UB (M6) – 2 |
| 14. More stringent staff-selection processes | UBs (general) | If there is long-term commitment to changing staff-selection processes (C) that results in a change in critical mass of the type of staff working in the organisation with positive values that militate against UB (R), then more stringent staff-selection processes may reduce UB (O), as it will reduce perceived exposure to UB (M1), thereby reducing prevalence of negative role models and reducing social learning of negative behaviours (M2) and desire to reciprocate (M3). Additionally, it may increase the perception of fairness in the workplace (M4) – 1 |
| 15. Improvements to work design | UBs (general) Might be useful with hierarchy where anonymous feedback is provided regarding manager behaviour |
If work processes can be changed to reduce job demands (C), then conflict between staff may be reduced (O), because staff may have reduced stress (M) – 1 |
| 16. Multisource feedback | Bullying/harassment (targeted behaviours) | If 360-degree appraisal raters are able to provide anonymous feedback regarding the behaviour of a specific person (R), then, where there is a hierarchy in place (C), it may be particularly effective in tackling UBs (O) because it can help identify UB and who instigators are (M1) with low risk of reprisal to the reporter (M2). – 2 Additionally, existence of such an intervention (C) may increase collective perception that management is serious about addressing behaviours (O) because it requires managers to be put at risk of appraisal themselves (M) – 2 |
| 17. Training for workforce (assertiveness, resilience, cognitive rehearsal) | More targeted behaviours but also improving ability to speak up | If a critical mass of employees is not trained (C), then these types of training intervention may not be successful at reducing UBs (O), because collective uptake is not sufficient (M) – 2 If the intervention is not visible and accessible (C), then these types of training intervention may not be successful at reducing UBs (O), because the training does not reach a critical mass of staff (M) – 2 |
| If such interventions are not delivered competently by a trained facilitator (C), then UBs may not be reduced (O), because recipients will not have learned greater assertiveness (M) – 2 If a critical mass of employees is trained (C1), and the training is delivered competently (C2), then UBs may be reduced (O), because victims/bystanders may have improved confidence leading to an improved sense of psychological safety (M1), an increased understanding of their victimhood (M2), a reduced desire to escalate or respond (breaking the cycle) (M3), and improved teamworking/communication (M4) – 2 If delivered in a context of prevalent targeted forms of UB (C), then these interventions may be particularly effective (O), because they can enhance resilience of victims (M1) and improve likelihood of bystanders speaking up (M2) – 2 |
Reactive strategies
| Intervention | Type of behaviours | CMOCs |
|---|---|---|
| 1. Acknowledgement of UB problem by management to the workforce | UBs (general) | If staff think UBs are necessary to be able to do their jobs (C) (i.e. when training trainees), then acknowledgement by managers alone will not reduce UBs without further follow-up action (O), because there will be no commitment by employees to any strategies to reduce UB (M) – 2 If managers have the skills, knowledge and capability to follow up on the acknowledgement that there is a problem (C), then psychological safety of employees may be improved (O), because there can be an increased perception of risk to the instigator (M1), improved trust in management by victims/bystanders (M2), and improved perception of social support and self-efficacy (M3) – 2 Acknowledgement of the problem by management (C) may lead to identification and revealing of instigators by the workforce (M) which can lead to their dismissal (O1), lowering prevalence of UBs (O2) – 2 |
| 2. Changing language around reporting incidents | Reduce potential for backlash in situation with hierarchy | If there are situations with a strict hierarchy, such as with surgeons and their trainees (C), then changing language to neutral non-blaming language when reporting errors can lower incidence of UBs (O), as it reduces the desire for senior staff to escalate or respond to critiques, which would generate conflict (M) – 3 |
| 3. Being inspected by regulatory body | Likely to only detect UBs that are having a more severe impact on care quality (e.g. patterns of bullying) | If actions are taken by management in response (C) to inspections by a regulatory body which finds a high prevalence of UB (R), then this may lead to a reduction in UBs (O), because it can increase awareness of UBs in the organisation (M1), leading to acceptance that there is a problem by managers (M2) – 1 |
| 4. Dismissal of offending staff | UBs (general) | If instigators are dismissed and replaced with more appropriately behaving staff (C), then unprofessional behaviours may be reduced (O), because there will be a greater sense of risk to other instigators (M1), reduced frequency of negative role-modelling in the workplace (M2), and a perception that management is serious about addressing these negative behaviours and that there are consequences for perpetrators, thus encouraging others to report (M3) – 2 |
| 5. Warning offending staff, removing key organisational roles from them | Unprofessional behaviours (general) | If removing perpetrators from their roles is considered by instigators to be a sufficient punishment (C), then warning offending staff and removing their roles may reduce UBs (O), because it will increase their perception of risk and serious consequences if they continue negative behaviour (M1), and may cause them to reflect on their actions (M2) – 1 If removing roles from an instigator is implemented (C) then an instigator may have an increased perception of risk when engaging in UB (O) because they will have been identified as an instigator to others (M) – 1 |
| 6. Educating instigators about their impact | UBs (general) | Educating instigators about the impact of their actions (C) may reduce the chance of them engaging in further UB (O), because it may cause reflection upon their actions (M1), help them see the perspective of others (empathy/being in other’s shoes) (M2) and may increase their sense of risk in engaging in such behaviours (M3) – 2 |
| 7. Individual – gathering evidence about UBs (e.g. diaries, e-mails) | Likely to work on targeted behaviours | If an individual is planning to report another for targeted forms of UB towards them or others (C), then collating evidence of these UBs can increase effectiveness of reporting to reduce these behaviours (R), because it can improve confidence and self-efficacy when coming forward (M1) and increase how seriously management takes such claims (M2) – 2 |
| 8. Mediation | Likely to work only with targeted behaviours where there is no hierarchy (e.g. rudeness) | If there is a power gradient between two individuals in mediation (C), then mediation can increase UBs (O), because it gives the instigator further opportunity to engage in such behaviour (M1) and does not reduce the underlying perception of risk in engaging in UB (M2) – 3 If in a case of UBs between two or more individuals with little hierarchy (C1), and a skilled mediator (C2), then mediation may be effective to reduce UBs (O), because it can cause an understanding in differences in perception between the victim and instigator (M1) which can lead to improved mutual understanding and empathy for each other (M2) – 3 |
| If mediation is not known about, visible or trusted by employees (C) then participants may not engage with mediation (M) which will not reduce UB (O) – 3 Use of mediators external to an organisation (C) may be less effective at reducing UB than using internal ones (O) because the targets of mediators may perceive them as less familiar with their situation (M) – 1 |
||
| 9. Rewarding whistle-blowers, presence of ‘speak up guardians’ etc. | More pervasive cultures of UBs | If there is an onus on the victim to report UBs (C), then UBs may not be reduced (O), as there can be significant fear of reprisal from the victim (M1) – 2 If whistle-blowers are rewarded in a manner visible to other employees (C) then this can increase speaking up about UB (O1) and thereby reduce likelihood of UBs (O2), as it can improve perception of social support for victims/bystanders (M1) and improve self-confidence/self-efficacy (M2) thereby increasing sense of psychological safety (M3). Additionally, it can improve trust in management that they will take any claims seriously (M4) – 2 |
| 10. Creating ‘safe space’ and opportunities to speak up anonymously | More effective in situations where there is risk of reprisal (e.g. very prevalent negative cultures, much hierarchy) | If there are opportunities for victims or bystanders to speak up completely anonymously (C) then this can reduce UBs (O) because instigators might have a greater sense of risk from knowing they can be anonymously reported (M1) Additionally, the reduced chance of identification significantly lowers fear of reprisal for the reporter and massively increases sense of psychological safety when doing so (M2) – 2 |
| 11. Increasing safe space to speak up (non-anonymously), e.g. ensuring clear rules are in place and alleviating concerns that individuals may have regarding repercussions, etc. | UBs (general) | If there are significant power differentials in place in the organisation (C1) or high prevalence of UB (C2), then opportunities to speak up non-anonymously can be ineffective (O), because victims and bystanders feel a lack of psychological safety (M) – 2 If there are clear and trusted routes for reporting UBs in an organisation (C), then UBs may be reduced (O), because it can lower perception of risk when speaking up for victims and bystanders (M1), and improve confidence/self-efficacy (M2) – 2 |
| 12. Removing victims from problematic environment | Bullying, harassment, undermining – targeted behaviours | If victims are removed from a problematic environment (R) but the instigators are not removed, or not punished in some way (C1), this may not be effective in reducing UBs towards others (O), because there will be no consequences observed by others for the instigators, who may feel free to continue engaging in UB (less sense of risk for the instigators) (M1) and no change in social norms (M2) – 2 If in an environment rife with targeted UB such as bullying and harassment (C), removing victims from the reach of the instigator within an organisation may reduce their experience of the UBs (O), because they will have less perceived exposure to the instigator (M) – 3 |
| 13. Seeking help at a professional body | Targeted UBs | If the intervention is visible and accessible to victims/bystanders (C1), then seeking help at a professional body (R) can help reduce the impact of UBs (O), because it improves self-efficacy to come forward for victims (M1) and improves sense of social support (M2), thus increasing psychological safety and resilience (M3) – 2 |
| If help is sought at a professional body (R) at the first sign of being exposed to targeted and frequent forms of UB (C) then the impact of UB on the victim may be reduced (O) because the victim may have increased sense of social support and improved ability to cope (M1) – 2 If help is sought at HR of an organisation before seeking help at a professional body (C) then it may avoid further backlash on the reporter (O) because others will perceive them as having done what they could before involving external actors (M) |
||
| 14. Therapeutic/coping strategies | Targeted UBs | If the intervention is visible and accessible (C1), and has sufficient follow-up and duration (C2), then therapeutic strategies may work to reduce targeted UBs (O) because they can increase understanding of victimhood by victims/bystanders to increase sense of empowerment (M1), increase sense of social support (M2) and thus sense of psychological safety (M3), and reduce stress (M4) – 2 |
Appendix 2 Full description of middle-range theories utilised in this review
This appendix discusses MRTs drawn upon in this review in more detail.
(i) Psychological safety
One theory that helps explain and provides a way of understanding the issues outlined above in terms of speaking up or raising concerns about UB is psychological safety, a MRT we drew upon throughout the report to aid our understanding of how various contributors could inhibit willingness to speak up. 84 Psychological safety refers to workers’ perceptions of consequences of the risks of speaking up in the workplace83 and is defined as ‘a shared belief held by members of a team that the team is safe for interpersonal risk-taking’. 84 Edmondson further elaborates that a ‘leader’s job—whether at the top of an organisation or somewhere in the middle—is to create a safe space for people to speak up, make mistakes, and bring their full selves to work’. 194 Essentially, psychological safety means that people won’t be punished or humiliated for speaking up about work challenges, with questions, concerns, or mistakes, and won’t be embarrassed, rejected, or punished by teammates for sharing ideas, taking risks, or asking for feedback. As such, a psychologically safe environment, that is, one in which staff feel safe to report mistakes and medical errors, is a key part of the causal chain in terms of why UB can lead to impacts on staff and ultimately on patient safety. Staff need to feel able to speak up in critical moments to prevent medical errors. A harmful culture where UB thrives is the antithesis of a psychologically safe work environment where leaders want to hear difficult truths to change culture and become a learning organisation. Many of the aspects outlined in the following sections, such as a culture of tolerance of UB in organisations, and hierarchy, can impact psychological safety.
(ii) Moral injury
We draw upon the MRT of moral injury in Chapter 7 to highlight the impact that not intervening can have on healthcare staff, when they witness UB or a medical error or are affected by bullying. Moral injury in a healthcare context has been defined as ‘perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations’85 which may leave ‘long-lasting emotionally, psychologically, behaviourally and spiritually harmful impacts’. 86 This has been used to understand the experience of healthcare professionals, for example, being unable to deliver the quality of care they would like due to resource constraints and the resulting psychological impact this has on them. 89 In terms of UB, moral injury can be a result of workplace bullying, for example, because it is transgressive, asymmetric, and livelihood and identity are at risk. 195
(iii) Job demands and resources
Many included studies drew upon the JDR model as a contributor to bullying, explaining organisational processes that could worsen UB. 87 Originally used as a model to better understand burnout, it sets out the range of job demands which can contribute to exhaustion, as well as the job resources that, if lacking, can lead to disengagement. 87 For example, studies have determined that ‘better job design’ which limits job demands and favours job resources, such as increasing social support and cohesion, can minimise bullying. 196 In our report, in Chapter 4, we outline that job demands can be increased by many factors, such as not being given enough time to complete tasks and due to shift working. On the other hand, job resources include factors such as supervisor support, job security, rewards and job control. Chapter 4 explores in detail how lack of job resources contributes to UB.
(iv) Fundamental attribution error
FAE is a phenomenon from social psychology, in which people tend to solely attribute a person’s behaviour to their personality rather than acknowledging that often behaviour is a combination of a person’s behaviour and their environment. 88 This applies mostly to other people’s negative actions, but when it comes to themselves, negative actions are more likely to be attributed to environmental factors. 89 Taylor and Taylor (2018) highlighted that ‘interventions to address horizontal violence and other disruptive behaviors have focused on identifying “the bad apple”, the problem individual that can be blamed and weeded out’, and that this is akin to an ‘organizational-level fundamental attribution error and ignores the importance of context’. 94 It is likely that many architects of interventions included in this literature are drawing on what we suggest is an individual focus whereby a flawed human perspective influenced by the FAE and we use it in this report to help understand the significant focus by organisations and individuals on ‘bad apples’ as opposed to more systemic contributors that organisations also have power to address.
(v) Trust
Trust is a significant concept in this field, between staff, and trust in management is also specifically a common theme throughout this report. Trust is evident in many parts of the causal chain, such as the effects of trust (or lack of it) on contributors, as an outcome of strategies, as an outcome measure used by included interventions, and as an important dynamic that affects engagement with interventions. We are drawing upon Robinson’s (1996) definition of trust: ‘one’s expectations, assumptions or beliefs about the likelihood that another’s future actions will be beneficial or at least not detrimental to one’s interests’. 90 Inherent to our understanding is the importance of managers’ role in trust and UB; staff’s interests lie in managers providing an organisational environment that is free of UB, because UB will negatively impact their ability to fulfil their job role (i.e. to deliver patient care) and negatively impact their individual well-being. Trust is often easy to lose but hard to regain, and so manager behaviour and actions and the impact of these on trust underpin much of this report.
Appendix 3 Characteristics of all included literature sources (n = 148)
Table 25 sets out all the relevant characteristics of included literature.
| Document | Source type/study design | Country of conduct or focus | Sample | Healthcare type | Area of UB | Key findings and relevancy |
|---|---|---|---|---|---|---|
| Step 1 – Initial theories | ||||||
| Ariza-Montes et al. (2013)113 | Survey | EU member states | Sub-sample of 284 health professionals | General health care | Bullying | Draws on data from the 5th European Working Conditions Survey to identify predictors of bullying in the healthcare workplace. Predictors included shift working, monotonous tasks, stress, and few promotion opportunities |
| Armstrong (2018)197 | Systematic review | N/A | Nurses, 10 studies | General health care | Incivility | A systematic review of strategies used to address incivility in the nursing workplace. It found that some strategies such as communication training and education may have some promise for managing incivility. But studies were low quality |
| Bambi et al. (2017)123 | Systematic review | N/A | Nurses, 7 studies | General health care | Incivility, lateral violence, and bullying | Assesses strategies to prevent incivility between nurses. Limited numbers of studies were available, so it was not possible to assess effectiveness of existing programmes. More innovative interventions are needed. |
| Barzallo Salazar et al. (2014)198 | Simulation study/RCT design | USA | 55 trainees, encouraged (n = 28) and discouraged (n = 27) groups | Surgery | ‘Discouraging environment’ | This study isa RCT that explores how surgeon behaviour affects trainee willingness to speak up during surgeries. Positive surgeon behaviour leads to increased trainee speaking up and improved patient safety |
| BBC News (2021)18 | News article | UK | N/A | General health care | Bullying | News article reporting on a £3.4 million settlement to current and former staff at NHS Highland |
| Benjamin (2021)199 | Opinion article | UK | N/A | General health care | Microaggressions | Opinion article summarising what microaggressions are and how they are experienced in the healthcare workplace. Offers also some accounts from those who have experienced them |
| Blackstock et al. (2018)175 | Integrative review | N/A | Nurses, 22 studies | General health care | Horizontal violence | An integrative review exploring the organisational antecedents of horizontal violence among nurses. Working conditions, organisational culture, and leadership roles were all found to be key themes |
| British Medical Association (2017)130 | Narrative review | UK | Doctors, unclear number of studies | General health care | Bullying and harassment | A review of research by the BMA assessing prevalence of bullying and harassment affecting doctors, as well as antecedents and solutions |
| British Medical Association (2018)167 | Report | UK | N/A | General health care | Bullying and harassment | Report by the BMA about how to address bullying and harassment in the healthcare workplace, including suggestions such as intervening early |
| British Medical Association (2021)200 | Web page | UK | N/A | General health care | Unacceptable behaviour | Web page defining what unacceptable behaviours are in the healthcare workplace, and setting out some informal resolution options |
| Cooper (2018)201 | Opinion piece | UK | N/A | General health care | Bullying | Highlights experience of bullying by different people in the NHS with quotes. Highlights some strategies people can take to address it, such as documenting incidences |
| Cruz et al. (2019)132 | Cross-sectional study | USA | 296 African American and Latino participants | General health care | Microaggressions | Study seeking to provide psychometric evidence for the Microaggressions in Health Care Scale. Provides significant background information regarding microaggressions. Microaggressions were found to correlate with mental health symptoms |
| Felblinger (2009)9 | Editorial paper | N/A | N/A | General health care | Bullying, incivility, and disruptive behaviours | An editorial that assesses how to identify bullying, incivility and disruptive behaviours, as well as how to mitigate their impact. Factors such as changing hierarchies, conflicting loyalties, and stress were stated to increase risk of such behaviour |
| General Medical Council (2015)105 | Report drawing on interviews | N/A | 12 sites | Surgery and obstetrics and gynaecology | Undermining and bullying | A report and review of bullying and undermining behaviours in medical education and training. Explores the groups that experience such behaviours more, factors contributing to them, and wider context for such behaviours |
| Gillespie et al. (2017)183 | Intervention | USA | Five academic campuses, nursing students | General health care | Bullying | Article describing the development process and utility of an educational intervention for use by nursing faculty with nursing students performed in a university context |
| Illing et al. (2013)21 | Evidence synthesis | N/A | 160 papers, 55 described in detail | General health care | Bullying and harassment | An evidence synthesis exploring occurrence, causes, and management of bullying and harassment behaviours in health care |
| Illing et al. (2016)202 | Report | UK | N/A | General health care | Bullying | A review of measures that are appropriate for measuring change in bullying over time in healthcare organisations |
| Jones and Kelly (2014)116 | Editorial paper | UK | N/A | General health care | Organisational deafness | An editorial exploring organisational deafness and highlighting how people often do speak up but that their concerns fall on deaf ears. Suggests some means to attempt to resolve this |
| Kaiser (2017)203 | Survey | USA | 237 staff nurses | General health care | Incivility | Exploration of leadership style and the relationship to nurse-to-nurse incivility. Transformational leadership was found to correlate with lower levels of incivility. However, leadership style was not a very strong factor affecting incivility incidence |
| Keller et al. (2020)95 | Systematic review | N/A | 53 included papers | General health care | Incivility | Systematic review identifying predictors of incivility within healthcare teams. It found conceptualisation of incivility was subjective and varied, and quality of studies low. Results were inconsistent regarding individual characteristics but situational and cultural predictors were identified |
| Kline (2021)17 | Opinion piece/online blog | UK | N/A | General health care | Racism | Explores the risks associated with not tackling racism in the NHS. These include depriving patients of the best talent, blame culture affecting patient safety, impact to staff health, loss of patient benefit attained by greater representation |
| Maben et al. (2012)204 | Mixed-methods case study | UK | 66 survey respondents, 18 staff interviews | Acute care | Incivility and bullying | Explores the link between staff experience of work and care received by acutely ill older people. Finds that incivility and bullying led to worsened patient care experience |
| Mannion et al. (2019)92 | Literature review and textual analysis | UK | Unclear number of documents, 7 in textual analysis | General health care | Misconduct | Examines how doctor misconduct can be understood using metaphors of bad apples, barrels, or orchards |
| Mitchell (2021)174 | Editorial | UK | N/A | Acute care | Bullying | An editorial exploring findings of bullying and racial discrimination at an NHS trust as a result of an inspection |
| National Guardian’s Office (2018)168 | Report | UK | Data from 7087 cases | General health care | Bullying and harassment | An overview of cases of speaking up to Freedom To Speak Up guardians in the NHS between April 2017 and April 2018. Shows that 45% of cases included an element of harassment and bullying |
| Nursing and Midwifery Council (2021)205 | Report | UK | N/A | General health care | Bullying | Report on the register of nurses from April 2020 to 2021 during the COVID-19 pandemic. Reports on instance of bullying in this time |
| Parizad et al. (2018)106 | Qualitative study | Iran | 15 registered nurses | ED | UBs | Explores Iranian nurses’ experiences of unprofessionalism in the ED. Explores contributors to these behaviours as well as prevalence |
| Pislakov et al. (2013)19 | Literature review | USA | Unclear number of sources | Health care in general | Bullying and aggressive behaviour | An informal literature review that explores what types of people engage in bullying, how it is defined, and its causes |
| Quinlan et al. (2014)122 | Scoping review | N/A | 8 sources | Health care in general | Bullying | A scoping review exploring interventions to reduce bullying in healthcare organisations. It revealed eight articles that included education, championing, and zero-tolerance policies |
| Riskin et al. (2015)24 | Simulation study RCT | USA | 24 neonatal intensive care unit teams | Neonatal intensive care unit | Rudeness | A simulation RCT with exposure to rudeness or control conditions. It found that rudeness had adverse consequences on information-sharing and help-seeking behaviours with implications for patient safety |
| Riskin et al. (2017)14 | Simulation study RCT | USA | 39 neonatal intensive care unit teams | Neonatal intensive care unit | Rudeness | A simulation RCT with exposure to rudeness or control, as well as rudeness with and without a preventative or therapeutic intervention. It was found that CBM was able to mitigate adverse effects of rudeness |
| Rogers-Clark et al. (2009)118 | Systematic review | N/A | 24 papers | General health care | Disruptive behaviour | A systematic review of interventions to manage disruptive clinician behaviour in the nursing work environment. It found few sources evaluating effectiveness of interventions |
| Ross et al. (2020)131 | Report drawing on interviews | UK | 12 NHS staff and three case studies of NHS Providers | Acute care | Racism | A report investigating workforce race inequalities and inclusion in NHS Providers. Assesses lived experience of a number of NHS staff as well as interventions used to address these race inequalities in NHS Provider case studies |
| Salin (2003)206 | Review | N/A | Non-health care, bullying in general | Non-health care | Bullying | A review assessing ways of understanding workplace bullying in general and the factors that precipitate it. Such factors include antecedents including power imbalances, low perceived costs, and motivating structures such as reward systems |
| Walton (2006)160 | Editorial | N/A | N/A | Health care in general | Hierarchy and power | Explores the impact of hierarchy on the ability to speak up from a patient safety perspective |
| Westbrook et al. (2018a)10 | Editorial | Australia | N/A | Health care in general | UB | Highlights the impact of UB in the Australian healthcare system, as well as the limited intervention evidence base, while calling for greater culture-change efforts |
| Wild et al. (2015)56 | Editorial | UK | N/A | Surgery | Undermining and bullying | Recommendations by the Association of Surgeons in Training to help create a positive learning environment free of undermining and bullying |
| Yu et al. (2019)170 | Systematic review with narrative synthesis | N/A | 38 articles | General health care | Resilience | This systematic review aimed to identify the personal and work-related factors associated with nurse resilience. The study concluded that understanding nurse resilience can help promote personal and professional growth and reduce the effects of job demands |
| Step 2 – Exhaustive search | ||||||
| Academy of Medical Royal Colleges (2016)78 | Report | UK | N/A | Trainees (general) | Undermining and bullying | Explores causes of UB based on findings of a 1-day seminar and proposes strategies |
| Al-Ghabeesh and Qattom (2019)207 | Survey | Jordan | 120 ED nurses | ED | Bullying | Explores quantitatively the antecedents of bullying in a sample of ED nurses and proposes in limited form some measures to mitigate it |
| Al-Rias (2017)208 | Editorial | UK | N/A | ED | ‘Handover hostility’ | Describes a scenario of handover hostility in the English NHS and explores reasons for it |
| Allen (2015)169 | Narrative review | UK | N/A | General health care | Bullying | Narrative review of bullying with a focus on the English NHS. Presents causes of bullying and preventative measures one can take |
| Almost et al. (2010)209 | Testing theoretical model | Canada | 277 acute care nurses | Acute care | Conflict | Quantitatively testing a theoretical model of causes of intragroup conflict among nurses with a non-experimental design. Explores how factors like self-evaluation, complexity of nursing care, and interactional justice affect incidence of conflict |
| Alspach (2007)210 | Editorial | No specific country | N/A | General health care | Lateral hostility | Explores causes, impacts, and prevention of lateral hostility between critical care nurses |
| Anderson (2011)166 | Editorial | Australia | N/A | ED | Workplace aggression and horizontal violence | Explores violence from patients but also horizontal violence, its causes, the harm it causes, and how legislation may reduce it |
| Anonymous (2018)211 | Case study | No specific country | N/A | Acute care | Bullying | Exploration of how a single event of bullying in the operating room led to an impact on patient safety |
| Armstrong (2017)141 | Intervention | USA | 9 nurses | Acute care | Incivility | Quantitative investigation of an intervention in a rural hospital to reduce nursing workplace incivility. Findings indicated no change in experience of incivility but a greater ability to respond to incivility |
| Asi Karakaş and Okanli (2015)157 | Intervention | Turkey | 30 nurses | Acute care | Mobbing | This study reported an evaluation of an assertiveness training intervention in 30 nurses who experienced a high level of mobbing. Results indicated a statistically significant fall in mobbing after the intervention and an increase in assertiveness |
| Babenko-Mould and Laschinger (2014)135 | Survey | Canada | 126 year-4 nursing students | Acute care | Incivility | Focuses on effect on incivility on nurse burnout and talks about strategies to mitigate this impact. It finds that incivility is strongly related to burnout |
| Babla et al. (2021)74 | Letter | UK | N/A | Critical care | Microaggressions | Focuses on racial microaggressions and what they are, how they manifest themselves in the healthcare workplace, and how they should be addressed |
| Barrett et al. (2009)142 | Intervention | USA | 59 pre-intervention and 45 post-intervention nurses | Critical care | Lateral violence | The study assessed a team-building intervention to reduce lateral violence, using mixed methods. The intervention was found to improve group cohesion |
| Beale and Leather (2005)162 | Report | UK | N/A | General health care | ‘Working relationships’ | Guide by the Royal College of Nursing to help improve collegiality and avoid UBs in the nursing workplace. Presents team and individual assessment tools to improve team and individual behaviours. Also explores what behaviour may or may not be bullying |
| Blackstock et al. (2022)101 | Review | N/A | 15 resources | General health care | Incivility | A review which develops an ecological model to understanding co-worker incivility experiences of new graduate nurses |
| Blakey et al. (2018)47 | Editorial | Australia | N/A | Trainees (general) | Bullying | Explores in in-depth manner the reasons why bullying interventions may and may not be effective, or even counterproductive, with trainees |
| Carter et al. (2013)212 | Mixed-methods survey + interview | UK | Seven NHS trusts in NE England, comprising 2950 NHS staff and 43 in qualitative telephone interviews | General health care (acute, primary and mental) | Bullying | Survey with qualitative elements also which explores prevalence and impact of bullying in the NHS. Largely focuses on prevalence but also has rich description from qualitative findings of impacts of bullying. They find bullying is prevalent in the NHS with 20% of staff reporting being bullied |
| Ceravolo et al. (2012)126 | Intervention | USA | 4032 practising nurses, 1160 students and faculty | Acute care | Lateral violence | This intervention used culture-change and communication-enhancing workshops to decrease lateral violence in a five-hospital integrated health and care system |
| Chadwick and Travaglia (2017)57 | Systematic review | Australia | 62 studies | General health care | Bullying | Explores what types of behaviour comprise bullying, the contributing factors, and factors that can help address it too |
| Chipps and McRury (2012)134 | Intervention | USA | 16 staff members | Rehabilitation | Bullying | This quasi-experimental study assessed pre test and post test an educational intervention to address workplace bullying. They noted an increase in bullying reports as a result (from < 1 act weekly/daily to 1.6 acts weekly/daily), but it did help develop a learning community |
| Churchman and Doherty (2010)102 | Qualitative interviews | UK | 12 nurses | Acute care | ‘Challenging doctors’ practice’ | Unpacks when nurses would be willing to challenge doctors’ practice without fear of reprisal or conflict and the interprofessional status of nurses vs. doctors |
| Churruca et al. (2022)97 | Intervention | Australia | Eight hospitals | Acute care | Respect | Reports on a case study of the Ethos messaging system implemented across eight hospitals in Australia |
| Clark et al. (2013)139 | Intervention | USA | 25 nurses on two units | General health care | Lateral violence | Study of an intervention which used PBL to address incivility. It was found to heighten awareness of incivility, improve favourable reaction to PBL, and give increased confidence |
| Colangelo (2019)182 | Editorial | N/A | N/A | Acute care | Bullying | Reports on the ETHOS programme and how some staff feel that the intervention is unfairly applied |
| Credland and Whitfield (2022)100 | Qualitative study | UK | 14 interviews | Paramedics | Incivility | A qualitative study of the experience of paramedics with incivility in the UK. It highlights the impact on clinical decision-making and well-being |
| Dahlby and Herrick (2014)65 | Intervention | USA | 29 nurses pre test, 29 post test | Acute care | Lateral violence | A study examining the effects of a 1.5-hour educational intervention on lateral violence |
| Demarco et al. (2005)104 | Intervention | USA | 5 graduate nursing students | Acute care | Group cohesion | Pilot study investigating a writing group’s ability to build group cohesion. The group writing drew on the ‘Amherst Writers and Artists’ method which did not focus on UB but nonetheless was intended to help cope with it |
| Dimarino (2011)125 | Intervention | USA | Unclear | Ambulatory setting | Lateral violence | Reporting of one ambulatory surgery centre’s approach to reducing lateral violence through education about lateral violence, and zero-tolerance policies. Did not test effectiveness |
| Dixon-Woods et al. (2019)143 | Intervention | USA | 67 employees (20 senior, 47 frontline) | Acute care | Disruptive behaviour | This study sought to improve employees’ ability to speak up about transgressive and disruptive behaviour at a Johns Hopkins Medicine hospital |
| Edwards and O’Connell (2007)60 | Narrative review | UK | N/A | Nurse education | Bullying | Delves deeply into bullying and its aetiology and presents recommendations for practice to help tackle it |
| Efe and Ayaz (2010)213 | Mixed-methods survey + focus groups | Turkey | 206 nurses in one hospital and four focus groups with 16 total participants | Acute care | Mobbing | Primarily investigated the prevalence of mobbing but also presents rich qualitative data regarding the causes of mobbing and what might be done about it. Suggests assertiveness training and need to solve communication issues |
| Embree et al. (2013)62 | Intervention | USA | 143 nurses | Acute care | Lateral violence | Investigates effectiveness of a cognitive rehearsal education intervention on nurse-to-nurse lateral violence |
| Gamble Blakey et al. (2019)22 | Narrative review | No specific country | 38 articles | General health care | Bullying | Explores interventions to help students with bullying and explores catalysts for bullying, how policies may affect bullying, how targeting of specific groups affects interventions, framing to improve effectiveness, and skills of facilitators |
| Griffin (2004)67 | Intervention | USA | 26 newly licensed nurses | Acute care | Lateral violence | Reporting an intervention assessing use of cognitive rehearsal techniques to reduce lateral violence between newly licensed nurses |
| Griffith et al. (2019)72 | Intervention | USA | 25 clinical staff | ED | Mistreatment | The authors developed an educational advance programme to aid residents and faculty in understanding and improving their learning environment. Attendees proposed coaching, signage, zero-tolerance policies, and more, to tackle mistreatment |
| Hawkins et al. (2019)68 | Integrative review | No specific country | 16 papers included | Acute care | Negative workplace behaviour | Delves into the conceptual differences in terms dealing with negative workplace behaviour, precipitating factors, and interventions to reduce such behaviour |
| Hemmings et al. (2021)79 | Report | UK | N/A | General health care | Non-inclusive culture | Report by NHS Employers and the Nuffield trust focused on means of attracting and keeping a diverse NHS workforce. Explores a number of case studies in rich detail as well as interventions used to improve diversity and why they may have failed |
| Hickson et al. (2007)98 | Intervention | USA | Unknown | Acute care | UBs | Outlines and reviews the Vanderbilt approach to identifying, measuring, and addressing UB using four graduated interventions. |
| Hughes (2003)214 | Editorial | UK | N/A | Acute care | Bullying | Looks at strategies at both an individual and organisational level to reduce bullying and its impact in health care |
| Hutchinson et al. (2008)58 | Outlining theoretical model | No specific country | N/A | General health care | Bullying | Investigates a novel model of bullying in the nursing workplace which includes organisational antecedents and consequences of such behaviour. Goes into detail about the organisational climate that enables bullying |
| Hutchinson et al. (2010)117 | Testing theoretical model | Australia | 370 nurses | General health care | Bullying | Confirms the strengths of the relationships outlined in the model above – as such, explores several causes of bullying and how these may work |
| Işik et al. (2020)109 | Qualitative interviews | Turkey | Two hospitals with 14 interviews with perioperative nurses | Acute care | Communication failure | Qualitatively investigates reasons for communication failures in perioperative environment, and as part of this looks at intrateam violence and other causes of communicative failures that might lead to negative behaviour |
| Jenkins et al. (2011)144 | Intervention | USA | Unknown | General health care | Civility | Explores how 6-monthly hour-long journal club meetings may increase civility. Also incorporated journalling |
| Johnson and May (2015)172 | Systematic review | No specific country | 67 articles | General health care | Professionalism | A systematic overview of systematic reviews using NPT to interpret the results. It found that interventions using normative restructuring of practice, modifying peer group norms, and emphasising expectations of external groups, had the most success |
| Johnson et al. (2020)215 | Simulation | USA | 58 students | General health care (students) | Incivility | An RCT simulation investigating the impact of an occurrence of incivility on clinical performance, teamwork and emotions. It found that 66% of the experimental group made a major error in their cardiopulmonary resuscitation performance |
| Kang and Jeong (2019)61 | Intervention | South Korea | 72 hospital nurses | Acute care | Bullying | Investigates a cognitive rehearsal smartphone-based intervention’s impact on bullying using a cluster quasi-randomised trial |
| Kang et al. (2017)156 | Intervention | South Korea | 40 nurses | Acute care | Bullying | An RCT to investigate a cognitive rehearsal programme on workplace bullying. |
| Kile et al. (2019)145 | Intervention | USA | 19 nurses | Community | Incivility | Investigated with a mixed-methods pilot study the impact of incivility and cognitive rehearsal education on nurse-to-nurse incivility |
| Kline (2022)70 | Case study | UK | 34 interviews and survey of 3506 people at one NHS Trust | Acute care | Bullying | A review of bullying and harassing behaviours at one NHS Trust, using mixed methods. It found significant evidence of negative culture at the Trust and proposes several strategies to implement to tackle this |
| Lasater et al. (2015)137 | Intervention | USA | 94 nursing staff | Acute care | Incivility | Study of a three-part educational intervention to see if it reduced incivility in two units of a hospital |
| Laschinger et al. (2012)155 | Intervention | Canada | 8 units with 33 controls | Acute care | Civility | Investigates the impact of the CREW intervention over 6 months with 8 intervention units and 33 control units |
| Leiter et al. (2011)154 | Intervention | Canada | 1173 workers across 41 units | Acute care | Civility | Assesses the effect of 6 months of the CREW intervention and found that greater group × time interactions were found in the intervention group for civility, supervisor incivility, respect, cynicism, job satisfaction, and management trust, and absences |
| Lewis (2018)76 | Report (mixed methods) | UK | 110+ employees interviewed, 1488+ surveyed (1100 full responses) | ED | UBs | Report on grievances about staff behaviour at an NHS Ambulance Trust. Explores unreasonable management behaviours and their causes, incivility and disrespect, rudeness, and threatening behaviour. Delves deeply into the qualitative data |
| Longo and Hain (2014)110 | Editorial | No specific country | N/A | Nephrology | Bullying | With a focus on dialysis centres, talks about healthy work environments that can counteract inappropriate work behaviours, including collaboration, effective decision-making, authentic leadership, etc. |
| Lovejoy-Bluem (2016)216 | Editorial | No specific country | N/A | Neonatal | Incivility | Discusses incivility in the neonatal ICU, and spends most of its words on discussing strategies to reduce incivility. Also walks through an example of how small incivility can lead to large clinical impact |
| Manton (2017)59 | Editorial | No specific country | N/A | Emergency | Bullying | An editorial exploring bullying, its effect on the work environment, and strategies to reduce it |
| Markwell et al. (2015)163 | Editorial | Australia | N/A | Students (general health care) | Performance management vs. bullying and harassment | Breaks down performance management and how in some cases it may be considered bullying while in other cases it might not be. Presents briefly some strategies to tackle this issue. Also presents a couple ‘vignettes’ as illustrative examples |
| McKenzie et al. (2019)93 | Intervention | Australia | 21 healthcare staff pre-to-post | Acute care | UB | Investigated factors affecting implementation of a multistrategy intervention using education, reporting systems with graduated intervention processes, safety champions, and action plans, to tackle UB |
| Mello and Jagsi (2020)178 | Editorial | No specific country | N/A | General health care | Sexual harassment | Delves into the details of how to respond to sexual harassment, but mostly in an informal manner |
| Miller and Chen (2021)75 | Editorial | No specific country | N/A | Students (general health care) | Microaggressions | Tackles strategies to address microaggressions at a programmatic and institutional level, as well as informally as an individual |
| National Freedom to Speak Up Guardian (2018)11 | Report | UK | N/A | General health care | Bullying | Presents some examples of how various NHS trusts have sought to tackle bullying at their organisations |
| Nicotera et al. (2014)107 | Intervention | USA | 36 working nurses | Acute care | Conflict | Assesses a nursing conflict intervention using mixed pre- and post-test methods with a control sample, which sought to reduce structurational divergence by raising awareness of it and teaching skills to manage it |
| NHS Employers (2016)112 | Report | UK | N/A | Paramedics | Bullying | Explores many real-world strategies implemented by NHS ambulance trusts and how these strategies have been received |
| Nikstatis and Simko (2014)66 | Intervention | USA | 21 nurses | Acute care | Incivility | A quantitative pilot study using a 1-group pre and post intervention test design to assess a 60-minute educational programme |
| O’Connell et al. (2019)54 | Intervention | USA | 76 participants | Military | Lateral violence | A quantitative exploration of nurses’ perceptions of lateral violence within a military setting and the impact of an education, cognitive rehearsal, and role-play intervention |
| O’Keefe et al. (2022)152 | Description of an intervention | Ireland | 203 course participants | General health care | Conflict | Describes an intervention, an instructional course, designed to improve professionalism, and how it is implemented. Course content focuses on conflict management |
| Osatuke et al. (2009)146 | Intervention | USA | 647 post-intervention CREW participants and 680 comparison (total 34 workgroups) | Acute care | Civility | Preliminary evaluation of a nationwide Veterans Health Administration intervention called CREW across 23 sites |
| Owens et al. (2019)108 | Editorial | UK | N/A | General health care | Professionalism | Explores the impact of austerity on professional working environments in health care in the UK context. Suggests mechanisms for how austerity signals to workers and organisations the degree to which professionalism is valued |
| Pavithra et al. (2022)77 | Qualitative study | Australia | 1636 survey respondents (various healthcare staff) | Acute care | UB | Explores qualitative responses to two open-ended survey questions delivered to seven hospitals in Australia. It found that a perceived lack of organisational action erodes confidence in hospital leaders and ability to address and mitigate UB effectively |
| Parker et al. (2016)138 | Intervention | USA | Unclear/organisation-wide | Acute care | Horizontal violence | Explores how nurses at an acute care hospital were able to implement multiple interventions to reduce horizontal violence prevalence in the organisation. These included 13 total organisational, leadership, and individual-level strategies |
| Phillips et al. (2018)99 | Integrative review | No specific country | 38 studies | General health care | Incivility | Explores quite deeply the different antecedents for incivility in health care. It also delves into preventative strategies and leadership behaviours, education, and systems thinking |
| Purpora and Blegen (2012)217 | Theoretical model | No specific country | N/A | General health care | Horizontal violence | Describes a theoretical model of how horizontal violence comes to impact the quality and safety of patient care. Model includes oppression and explores the concept in relation to oppression, as well as how this leads to internalisation and affects communication etc. |
| Rocker (2008)119 | Narrative review | Canada | N/A | General health care | Bullying | A narrative review which explores strategies to prevent nurse-to-nurse bullying, mitigate its effects, legal responses in Canada, and its origins |
| Royal College of Nursing (2014)124 | Report | UK | N/A | General health care | Bullying and harassment | Guidance materials from the RCN oriented towards organisations for preventing bullying and harassment in health care. Provides information about the law, the impact of bullying, prevention and reactive strategies and sample policies and recommendations for investigating incidents |
| Royal College of Surgeons of England (2021)91 | Report | UK | N/A | Acute care | Disruptive behaviour | Guide from the RCSE for surgeons delving deeply into how to tackle disruptive behaviour, as well as what causes it |
| Rutherford et al. (2019)55 | Integrative review | No specific country | 22 articles | Trainees (general health care) | Bullying | Integrative review which focuses on interventions against bullying of pre-licensure students specifically. Explores policy-level interventions, as well as those at individual or organisational levels |
| Saxton (2012)64 | Intervention | USA | 17 perioperative nurses | Surgery | Disruptive behaviour | Development and evaluation of a communication skills intervention to improve perceived self-effectiveness of perioperative nurses using a pre–post design |
| Sheehan et al. (2020)181 | Testing a theoretical model | Ireland | 1507 employees from 47 hospitals | Acute care | Bullying | A study testing a moderated mediated model of workplace bullying and employee outcomes. Explores the mediating influence of well-implemented anti-bullying HR practices and what well-implemented looks like. Delves into factors which comprise good implementation in the model |
| Shuttleworth (2018)218 | News article | UK | N/A | ED | Bullying | News article highlighting how an NHS trust has tried to tackle its culture of bullying after a whistleblower came forward |
| Sillero and Buil (2021)219 | Qualitative interviews | Spain | 16 healthcare professionals | Acute care | Interprofessional collaboration | Examines the interactions between doctors and nurses and how they can be kept civil. Hence it sheds light on how interprofessional collaboration as a cause can lead to incivility |
| Solheim (2018)220 | Editorial | No specific country | N/A | ED | Lateral violence | Discusses lateral violence in nursing and how it is much too prevalent. Mentions some informal means to tackle poor behaviour |
| Speck et al. (2014)147 | Intervention | USA | Three hospitals | Acute care | UB | Assessment of a professionalism committee approach to tackling UB across three large teaching hospitals |
| Stagg et al. (2013)148 | Intervention | USA | 10 nurses | Acute care | Bullying | Assessed the effectiveness of a 2-hour cognitive rehearsal programme, 6 months after completion |
| Stagg et al. (2011)149 | Intervention | USA | 20 nurses | Acute care | Bullying | Evaluated a workplace bullying cognitive rehearsal programme |
| Stevens (2002)103 | Intervention | USA | Unclear | Acute care | Bullying | Informally explores the impact of a multistrategy anti-bullying intervention in a large teaching hospital, delivered mostly through workshops for education, policies, supervisor training, and more |
| Stone et al. (2019)80 | Qualitative interviews | Australia | Six female doctors who were in training when abused | General health care | Sexual harassment and assault | Discusses in depth the assaults that happened to several female doctors in the workplace by other doctors and how they tried to address what happened |
| Tame (2012)221 | Qualitative interviews | UK | 23 perioperative nurses at one NHS Trust | Acute care | Horizontal violence | Qualitative study investigating experience of horizontal violence at an NHS Trust and the causes of it, the personal impacts, and touches upon strategies to resolve it |
| Taylor and Taylor (2018)94 | Editorial | No specific country | N/A | General health care | Horizontal violence | A discussion paper based on a prior review and experience of the authors which argues that horizontal violence is a quality improvement concern. As part of this, it explores strategies such as codes of conduct and how these should be implemented across different contexts |
| Thorsness and Sayors (1995)150 | Intervention | USA | Approximately 100 surgical staff | Acute care | Conduct issues | Evaluation of a programme adopting a systems approach to cultivating a positive work environment for perioperative staff members |
| Tran (2015)222 | Editorial | Australasia | N/A | ED | Bullying and harassment | A practical guide for how trainees should deal with bullying and harassment. Presents a flowchart for decision-making for how to approach the situation in the Australasian context with legal routes if necessary |
| Tuffour (2022)69 | Qualitative interviews | UK | Five nurses from sub-Saharan Africa | Mental health | Discrimination | Goes into depth on the experience of nurses from Africa working in the UK NHS Context. As part of this it explores their experience of discrimination and marginalisation and the ‘snowy peak’ syndrome. Paper makes recommendations for how to decrease discrimination in the NHS |
| Venkatesh et al. (2016)165 | Communication | Australasia | Unclear | Acute care | Bullying, discrimination and sexual assault | Response of College of Intensive Care Medicine of Australia and New Zealand to survey showing high prevalence of bullying, discrimination and sexual assault in their workplace. Outlines actions and longer-term strategies they will be implementing in response |
| Villafranca et al. (2017)32 | Narrative review | No specific country | N/A | Acute care | Disruptive behaviour | Explores the antecedents of disruptive behaviour at intrapersonal, organisational, and interpersonal levels. It also discusses the prevention and management options to tackle it |
| Warrner et al. (2016)63 | Intervention | USA | 60-bed orthopaedic inpatient unit incl. management | Acute care | Incivility | Evaluates an intervention comprising awareness education and cognitive rehearsal, and which included management |
| Weaver (2013)136 | Editorial | No specific country | N/A | General health care (graduates) | Horizontal violence and bullying | Tackles the chain of violence in nursing from one generation to another and seeks to understand how to reduce it from individual, school, and organisational levels |
| Westbrook et al. (2018b)10 | Editorial | No specific country | N/A | General health care | UB | Article discussing need to change approach to tackling UB in health care. Explores the impact, and emphasises the limited evidence base for interventions to tackle UB. However, it does present organisational professional accountability and culture-change programmes as promising avenues |
| Webb et al. (2016)151 | Intervention | USA | Three hospitals | Acute care | Disrespectful and unsafe behaviours | Presents a feasibility study of the Co-Worker Observation Reporting System implemented by Vanderbilt University Medical Centre to reduce disrespectful and unsafe behaviours |
| Wild et al. (2015)56 | Editorial | UK | N/A | Acute health care (trainees) | Undermining and bullying | Editorial which looks at the definitions of undermining and bullying, implications of such behaviours towards trainees, and how such behaviours can be tackled. Towards the end it presents specific recommendations |
| Wilson (2016)115 | Narrative review | No specific country | N/A | General health care | Bullying | Narrative review that explores the root causes, types of perpetrators, behaviours of bullying, and interventions to combat it |
| Zhang and Xiong (2019)223 | Review | No specific country | 44 articles | General health care | Horizontal violence | Review focused on the impact of nursing and coping strategies that help tackle the effects of bullying as well as reduce it. These include educational interventions, leadership styles and enlightenment |
| Step 2 – Search update | ||||||
| Adams and Bryan (2021)114 | Editorial | Canada | N/A | General health care | Harassment | Examines the role of leadership as the ones in a strategic position to address harassment and bullying |
| Baldwin et al. (2022)53 | Intervention | USA | Three academic medical centres | Acute care | Professionalism | Descriptive study analysing the types of reports received during the intervention to promote professionalism with nurse. |
| Bamberger and Bamberger (2022)224 | Editorial | N/A | N/A | General health care | Unacceptable behaviours | Editorial exploring the impact of unacceptable behaviours between healthcare workers on patient safety |
| Banerjee et al. (2022)71 | Intervention | USA | Division faculty members (n = 41) and pulmonary and critical care fellows (n = 12) | Acute care | Racism | Assessed the feasibility of a year-long antiracism educational study. As it was mostly a feasibility study, post-intervention surveying indicated a 15% increase in self-directed learning on related topics |
| Bry and Wigert (2022)225 | Qualitative study | Sweden | 13 neonatal nurses | Neonatal intensive care | Organisational climate and interpersonal interactions | Explores the organisational climate and type of interpersonal interactions experienced by registered nurses in the neonatal unit. As part of this it explores the impact of incivility |
| Hawkins et al. (2022b)153 | Intervention | Australia | 230 nurses from 12 units in four hospitals | Acute care | Negative workplace behaviour | Examined experiences of negative workplace behaviour and ways of coping with nursing staff before and after educational workshops. They did not find statistically significant results |
| Hawkins et al. (2022a)177 | Qualitative study | Australia | 13 nurses | Acute care | Negative workplace behaviour | A qualitative study exploring negative workplace behaviour with nurses and why it occurs. It finds that while some individuals can be more inclined than others to do so, it is facilitated by organisational influences |
| Kousha et al. (2022)158 | Intervention | Iran | 80 emergency nurses | Emergency care | Incivility | Examines the effectiveness of an educational and cognitive rehearsal programme among emergency nurses |
| Naylor et al. (2022)226 | Qualitative study | UK | 6 physiotherapists | Acute care | Incivility | Investigates the impact of incivility on physiotherapists working in the acute hospital setting using Interpretative Phenomenological Analysis |
| Westbrook et al. (2013)127 | Intervention | Australia | Staff across five hospitals | Acute care | UBs | Investigates changes in prevalence of UBs following a professional accountability programme called Ethos being implemented |
Appendix 4 Definitions of UB-related terms and their underlying behaviours identified in the literature
This appendix outlines our mapping of definitions identified in the literature for various UB-related terms.
| UB types identified and coded according to definitions or features | Example definitions (where available) or behaviours | Number of definitions coded (if 0, then behaviours were not explicitly defined in the included literature) |
|---|---|---|
| Behaviours explicitly defined in the literature | ||
| Bullying | ‘Bullying is defined by Rodwell and Demir (2012) as a situation that occurs over a period of time where individuals perceive themselves to experience negative actions and behaviours from others. This can be carried out by one individual or several and the person being bullied has difficulty defending himself or herself from the abuse being experienced’115 ‘Bullying is the misuse of power or position that undermines a person’s ability, or leaves them feeling hurt, frightened, angry or powerless’124 ‘Bullying is behaviour that hurts or frightens someone who is less powerful, often forcing them to do something they do not want to do’78 ‘repeated exposure to person, work‐, and intimidation‐related negative acts such as abuse, teasing, ridicule, and social exclusion over a period of time in the workplace’61 |
31 |
| Incivility | ‘low-intensity, deviant behaviors that are intended to harm the victim and demonstrate a lack of mutual respect’141 ‘repeated offensive, abusive, intimidating, or insulting behavior, abuse of power, or unfair sanctions that make recipients upset and feel humiliated, vulnerable, or threatened, creating stress and undermining their self-confidence’63 ‘rude or disruptive behaviors that violate workplace norms’215 |
14 |
| Horizontal violence | ‘When behaviors are displayed among workers in the same rank, such as staff nurses, rather than across power gradients, it is referred to as horizontal or lateral violence’110 ‘a variety of unkind, discourteous, antagonistic interactions that occur between persons at the same organizational hierarchy level and are commonly described as divisive, infighting, backbiting, and off-putting’210 ‘Horizontal violence is behavior that is directed by one peer toward another that harms, disrespects, and devalues the worth of the recipient while denying them their basic human rights’217 |
9 |
| Harassment | Legal UK definition: ‘unwanted conduct related to a relevant protected characteristic, which has the purpose or effect of violating an individual’s dignity or creating of intimidating, hostile, degrading, humiliating or offensive environment for that individual124 ‘improper conduct by an individual, that is directed at and offensive to another individual in the workplace, including any event/location related to work, and that the individual knew or ought reasonably to have known would cause offence or harm’114 |
8 |
| Lateral violence | ‘any repetitive behavior among peers that is considered offensive, abusive, or intimidating by the target’54 | 6 |
| Disruptive behaviour | Behaviour that ‘tends to cause distress among other staff and affect overall morale within the work environment, undermining productivity and possibly leading to high staff turnover or even resulting in ineffective or substandard care’64 ‘we define disruptive behaviour as constituting the following three criteria: (a) interpersonal (i.e. directed toward others or occurs in the presence of others); (b) results in a perceived threat to victims and/or witnesses; (c) violates a reasonable person’s standard of respectful behaviour, as defined in the Universal Declaration of Human Rights’32 |
5 |
| Microaggressions | ‘Racial microaggressions are actions, words, or behaviours that undermine or insult a person’s character, abilities, or perceptions based on their ethnicity. Racial microaggressions have been classified into three major types: microassaults, microinsults, and microinvalidations’74 ‘stunning and automatic acts of disrespect arising from unconscious attitudes inflicted by the culturally dominant groups’69 |
3 |
| UBs | ‘Unprofessional behaviour encompasses a spectrum, from overtly hostile, bullying and inappropriate behaviours such as physical and verbal abuse, to more subtle behaviours such as lack of responsiveness, passive aggression, rudeness and incivility’127 ‘behavior that undermines a culture of safety’147 |
3 |
| Mobbing | ‘Mobbing is the activity of a person to force someone out of the workplace through rumour, innuendo, intimidation, humiliation, discrediting and isolation’213 ‘unethical communication and antagonistic action directed by one or several people toward a single individual systematically’157 |
3 |
| Verbal abuse | ‘Communication perceived by a person to be a harsh, condemnatory attack, either professional or personal. Language intended to cause distress to a target’210 | 3 |
| Negative workplace behaviour | ‘repeated, offensive, abusive, intimidating or insulting behaviour, abuse of power, or unfair sanctions that make recipients upset and feel humiliated, vulnerable, or threatened, creating stress and undermining their self-confidence’68 | 2 |
| Undermining | ‘Undermining is conduct that subverts, weakens or wears away a person’s confidence, and may occur when one practitioner intentionally or unintentionally erodes another practitioner’s reputation or intentionally seeks to turn others against them’56 | 2 |
| Violence | ‘the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community that either results in or has a high likelihood of resulting in injury, death, psychological harm, mal-development or deprivation’137 | 2 |
| Mistreatment | ‘when behaviour shows disrespect for the dignity of others and unreasonably interferes with the learning process’22,47 | 2 |
| Sexual harassment | ‘any improper and unwelcome conduct that might reasonably be expected or be perceived to cause offence or humiliation to another person’80 | 1 |
| Gender bias | Gender bias (manifested in discriminatory behaviour that, though not necessarily consciously recognised by the perpetrator, is sexist). | |
| Offensive displays | Displays of offensive material (e.g. flags)60 | 1 |
| Sexual assault and violence | ‘an act of a sexual nature carried out against a person’s will or without their consent, through the use of physical force, intimidation or coercion and/or involving physical contact’80 | 1 |
| Unethical behaviours | ‘negative or exclusionary interpretation and enactment of organisational values that are at odds with patient or staff identity and dignity’77 | 1 |
| Victimisation | ‘Victimisation: is the unfair treatment of an employee as a direct consequence of raising or supporting a complaint of bullying and harassment’112 | 1 |
| Behaviours discussed but not defined in the literature | ||
| Minimisation | ‘having accomplishments and contributions disregarded’149 | 0 |
| Humiliation | Being ‘publicly ridiculed (15%, n = 3), observed and followed (15%, n = 3), disgraced in front of co-workers (10%, n = 2), secluded by work organization (10%, n = 2), and intimidated (5%, n = 1)’149 | 0 |
| Physical abuse | ‘Unwanted physical contact, explicit physical threats or attacks, suggestive gestures (such as mimicking the effects of a disability), unnecessary touching or assault, stalking which occurs at work or outside of work, but is related to work’60 | 0 |
| Racism | ‘its definition including colourism, anti-Blackness in the Asian communities, and more recently, anti-Chinese sentiments in the wake of the COVID-19 pandemic’74 | 0 |
| Aggression | ‘throwing things, hitting, slapping, breaking things, slamming doors, pushing, intimidating, stalking’77 | 0 |
| Disrespect | ‘Participants reported different ways this “disrespect” was expressed, both verbally and non- verbally. You’ll get a sort of derogatory look, you can see their eyes roll when you walk in with a patient, a bit of a tut and a bit of huffing and puffing’100 | 0 |
| Ostracising | ‘The consultant has given me strange looks in the department and tried not to make eye contact with me for over 3 months. This made me feel uncomfortable in the department and led to me avoiding them’78 | 0 |
| Rudeness | ‘When discussing an example of rudeness from a colleague you feel belittled and embarrassed … you feel worthless, you feel completely worthless’100 | 0 |
| Scapegoating | ‘Bully: “Have you noticed that whenever there is a code, Andy is usually working?”’149 | 0 |
| Sexism | ‘Sexism was also used against women to give unfair workloads compared to men and to be used as mechanisms of control’76 | 0 |
| Intimidation | ‘Conduct that belittles in some way, such as being shouted at, Intrusion by pestering, spying, following, Unnecessary closeness, Apportioning blame wrongly’60 | 0 |
| Unacceptable behaviours | ‘using patronising and demeaning language; • shouting or talking aggressively to people; • unacceptable demeanour in meetings – actively looking disengaged and dismissive; • being overly critical of work, often in front of other colleagues; • not being listened to; • being rude and abrupt when direct reports ask questions: some participants talked about managers rolling their eyes when they asked a question’70 | 0 |
| Unreasonable management | ‘“Having your views and opinions ignored”, “Being given unmanageable workloads or impossible deadlines”, “Someone withholding information which affects your performance”, “Your employer not following proper procedures”, “Someone continually checking up on you or your work when it is not necessary”’76 | 0 |
Appendix 5 Summary table of CMOCs and supportive quotes for contributors to UB
| Overarching contributor | Sub-contributors | CMOCs | Primary outcomes | Example supportive quote |
| Workplace disempowerment |
|
1. If staff work in a disempowered position such as at the bottom of an organisational or professional hierarchy (C) then this can inhibit willingness to speak up (M21/O1) and reduce ability to communicate (M14/O2) because a sense of intimidation and reduced psychological safety is experienced (M20) 2. If staff work in a disempowered position, such as at the bottom of a hierarchy (C), then this can increase likelihood of experiencing and being impacted by UB (O) because it can make staff an easier target (M12) |
|
1. ‘Steep hierarchies can give rise to feelings of intimidation which can impair communication, especially on difficult matters, such as raising concerns about patient safety. It was acknowledged that most behaviours that made people feel undermined were unintentional. Marked hierarchies may magnify the impact of relatively slight behaviours or comments if those affected are less able to voice how it made them feel’78 ‘The presence or absence of these variables could influence bullying ratios, i.e. when bullies weigh the potential costs and personal benefits of their actions based on the particular characteristics of their victims. In this sense, certain groups are considered more vulnerable than others (e.g. women or junior employees)’113 |
| 3. If staff work in a disadvantaged group (C) then this can lead to displacement of aggression onto others (O1) and a feeling of being undervalued (O2) because of internalisation of oppression (M4) 4. If staff work in a disempowered position where there does not seem to be a level playing field (C1) or work in a physically uncomfortable environment (C2), then this can cause people to externalise these frustrations increasing proclivity to engage in UB (O2) because staff feel like they are being treated unfairly (M3) experience frustration (M5) and have a reduced ability to cope (M18/O1) |
3. ‘…UBs appear to be tolerated and internalised as normalised behaviour, creating a self- perpetuating cycle of negative behaviours, negative sub- cultures, and self-isolation among victims’77 4. ‘In the model, horizontal violence represents the harmful behaviour oppressed nurses are at risk for engaging in to relieve mounting frustration from working in hierarchical hospitals where they have great responsibility but little power’217 |
|||
| Organisational confusion, uncertainty and stress |
|
5. If staff experience a period of organisational uncertainty, such as organisational change (C) or they experience a lack of job resources (C2), then this can lead to conflict and UB (O) because staff perceive their job is at risk and an increase in competitive attitudes ensues (M8) 6. If high job demands are experienced regularly in the absence of adequate resources (C1) then escalation of conflicts are more likely (O2), because there is both a high-pressure environment (M5) and reduced ability to communicate effectively (M14/O1) |
|
5. ‘In competitive environments, organizational restructure or periods of rapid change may create opportunities for individuals to engage in the misuse of legitimate authority for furthering self-interest or career opportunities’58 6. ‘… some behavioural interactions associated with bullying are because of excessive job demands. What is well-defined is that ‘friction or anger’ between colleagues is widely reported as high across SWAST and extremely high by 111 staff’76 |
| 7. If staff experience a lack of resources, or high job demands that increase pressure (C) then this may lead to an inability to cope with the impact of UB, (M18/O1), because communication with co-workers can be inhibited (M14) meaning it is difficult to build relationships with colleagues (M16) which can reduce feeling of social support (M17) 8. If staff are disadvantaged by organisational processes outside of their control, such as a lack of role clarity or high job demands (C) then this may increase levels of curtness in communication (O2) because they begin to feel pressured and their tasks become rushed (M5), reducing ability to communicate effectively (M14/O1) |
7. ‘The stress caused by the accelerated pace and pressure to complete the activity can decrease communication quality, as explained by the following participants: Surgeon 3: “I cannot work on the patient the way I want, and it affects my work”. Anaesthesiologist 2: “Of course, sometimes you feel understaffed”. Surgeon 1: “The operating room is like this... everything goes fast, practically every-thing must be done immediately, without waiting, with tension”’219 8. ‘Stress and pressures of the ED can cause inappropriate or unprofessional responses that could trigger behaviours affecting colleagues’ relationships and task responsibilities’106 |
|||
| Inhibited social cohesion and support |
|
9. If staff work in shifts (C), then this can reduce the ability to cope when experiencing UB or workplace stressors (M18/O1) and reduce self-confidence (M19/O2) which can worsen the impact of UB on health and well-being (O3) because shift work can reduce ability to build social connections (M16) and lessen feeling that one is socially supported (M17) 10. If staff work in a high-pressure environment or in a culture of intimidation (C) then this can lead to reduced ability to build social connections (M16/O1), a reduced sense of social norms (M15/O2), and a reduced sense of social support (M17/O3) because there is a reduced sense of psychological safety and ability to communicate effectively (M14) |
|
9. ‘Some staff cannot build relationships with their line manager because of rotas and might have very infrequent encounters with them’76 10. ‘Firstly, many participants relayed being subject to one-off experiences, such as being spoken to rudely in meetings or being shouted at for not having completed a task. When context was provided, most people attributed this to managers being “stressed” or “pressured” due to excessive workloads generated by COVID-19 or winter crises’17 |
| Enablement of harmful cultures that tolerate UB |
|
11. If a workplace has a prevalence of UB and leaders/ managers are not seen to address it by being complicit or laissez-faire (C1), then this can cause staff to engage in UB (O) and reduce trust in leadership (O2), because UB is perceived as normal (M13) 12. If a workplace has a prevalence of UB and leaders/ managers are not seen to address it (C) or role model it themselves (C2) then there is an increasing likelihood of others engaging in UB (O) and reducing trust in leadership (O2) and little change (O3), because the impression can be given that incivility and other UBs is tolerated and normalised (M13) which reduces perceived risk for instigators (M12), and ability to speak up for victims (M21) |
|
11. ‘Organisations in which managers do not act on bullying complaints and where co-staff do not act when they witness bullying can create a social climate in which bullying is tolerated and even seen as the norm (Hutchinson et al. 2008). As a result, bullying can become the accepted “way we do things around here”, with some staff adopting the attitude “It was done to me, so I’ll do it to others”’169 12. “Staff raised numerous examples of manager behaviour that they deemed unreasonable. Issues such as being treated differently compared to colleagues such as 'some staff get pulled up, others don’t' was a frequent occurrence while Serious Investigations (SI) were believed by some staff to be seemingly deployed inappropriately”76 |
| 13. If UB is prevalent in a workplace and managers are not seen to address it or even negatively role model such behaviours themselves (C) then this can reduce psychological safety (M21/O1) and reduce trust in management (O2) because staff sense that the organisation is deaf (i.e. that they do not care about UB) (M10) and creates an intimidating culture (M20) 14. If a reduced sense of psychological safety leads people to not speak up (C) then strategies to address UB are not implemented (M23/O1), reducing trust in leadership (O2) because managers are not aware that UB is taking place (M22) |
13. ‘Many at the sharp end expressed frustration that although the organization invited staff and faculty to speak about concerns, it appeared to lack an authentic capacity for listening or a full commitment to address concerns: “[There are] pockets of historically weak leadership where we learn that there have been ongoing issues for years that people [managers] have been either unwilling or uncomfortable addressing. So after a while you just stop talking about it’”143 14. ‘Furthermore, “bad news” is rarely passed upwards by front-line managers who feel it is better that senior managers do not “hear bad news”. This often means senior managers/executives are unaware of what is happening at the front line. Subsequently this can result in “why bother” attitudes from staff – a form of confirmation bias – because some staff perceive action plans will be largely ineffective as senior managers are too detached from employees’ everyday lives’76 |
Appendix 6 Characteristics and findings of the included 42 sources reporting an intervention
| Study | Samplea | Duration | Design and data collection timepoints | Theoretical framework | Strategies | Measures | Findings | Reported effective by study authors (Y, N or N/A) |
|---|---|---|---|---|---|---|---|---|
| Single-session education/training | ||||||||
| Ceravolo et al. (2012)126 | 4032 practising nurses, 1160 students and faculty | 60- to 90-minute workshops over 3 years | Quasi-experimental pre–post design without control. Pre (2007) and post 3-year data collection via survey (2011) | None | Education/awareness (assertiveness training), role-modelling | Verbal Abuse Survey | This intervention used culture-change and communication-enhancing workshops to decrease lateral violence in a five-hospital integrated health and care system. Nursing turnover and vacancy rates decreased but it was not clear if that was due to the intervention | Y |
| Clark et al. (2013)139 | 65 senior nursing students | 70-minute session | Pre–post design without control. Only post measures were delivered, immediately post session |
Unknown | Problem-based learning, role-playing | Custom feasibility questionnaire | Study of an intervention which used PBL to address incivility. It was found to heighten awareness of incivility, improve favourable reaction to PBL, and give increased confidence | Y |
| Dahlby and Herrick (2014)65 | 25 nurses on two nursing units | 1.5-hour session | Pre–post design without control. Post-test timing is unclear | None | Education, cognitive rehearsal | Lateral and Vertical Violence in Nursing Survey | A study examining the effects of a 1.5-hour educational intervention on lateral violence. They found participants were better able to identify causes of lateral violence and it perhaps contributed to reducing frequency too. However, no statistically significant results were noted other than for lateral violence becoming less serious post intervention | Y |
| Embree, et al. (2013)62 | 143 nurses | 2-hour session | Quasi-experimental pre–post design without control. Some post measures were immediate and others such as internalised sexism were 1 year later | None | Education, cognitive rehearsal | Internalised Sexism, Minimisation of Self, Total Nurse Workplace Behavior Scale, and Silencing the Self-Work Scale, RN voluntary turnover | Investigates effectiveness of a cognitive rehearsal education intervention on nurse-to-nurse lateral violence. It found that there was a trend towards increased awareness of lateral violence but no statistically significant results were identified | N |
| Griffin (2004)67 | 26 newly enrolled nurses | 2-hour session | Quasi-experimental pre–post design without control. Data were collected post only, occurring 1 year post intervention | Cognitive learning theories | Cognitive rehearsal | Focus groups | Investigates a cognitive rehearsal intervention as a shield for lateral violence in newly licensed nurses. It finds that knowledge of lateral violence enabled greater coping and confronting skills. Retention rate improved | Y |
| Griffith et al. (2019)72 | 25 participants | One session of unknown length | Quasi-experimental post-only design without control. Data collection was only post intervention via survey over an unclear timeline | Six-step approach to curricular development by Kern et al. | Education, action-planning, keeping records | Custom electronic evaluation of effectiveness | The authors developed an educational advance programme to aid residents and faculty in understanding and improving their learning environment. Attendees proposed coaching, signage, zero-tolerance policies, and more, to tackle mistreatment. There was some evidence it increased awareness | Y |
| Hawkins et al. (2022)153 | 111 nurses across 12 units in four acute care hospitals | One session | Quasi-experimental pre–post design with control group (non-randomised). Baseline data collection occurred over the month prior to the intervention and post data collection occurred over 6 months | None | Education | NAQ-R, Ways of Coping Questionnaire | The intervention group experienced less of a reduction in bullying and negative behaviours than the control group. But no results were statistically significant. Authors recommended against single-session attempts to reduce UB | N |
| Kile et al. (2019)145 | 19 nurses | 2-hour training session | Pilot study with no control group with pre, post (immediate), and 6 week follow-up | Bandura’s social learning theory (1977) | Education, cognitive rehearsal | Adapted versions of the nursing Incivility Survey (NIS), the Nurse Interaction subscale of the National Database of Nursing Quality Indicators (NDNQI), and a questionnaire with two open‐ended questions | Investigated with a mixed-methods pilot study the impact of incivility and cognitive rehearsal education on nurse-to-nurse incivility. They found that it was effective at increasing recognition and confronting of incivility due to movement in means on the NIS subscales, and reduced perceived incivility | Y |
| Nikstatis and Simko (2014)66 | 21 nurses | 1-hour session | Pilot study pre–post design without control group. Both pre and post data collection occurred over a 3-week timeframe | None | Education, group discussion | Nursing incivility scale | A quantitative pilot study using a one-group pre-and post-intervention test design to assess a 60-minute educational programme. They found that it increased perceived incivility. However, this was not statistically significant | N |
| O’Connell et al. (2019)54 | 76 participants | 2-hour session | A pre–post study design with no control group | None | Education, cognitive rehearsal, role-play | NAQ-R | A quantitative exploration of nurses’ perceptions of lateral violence within a military setting and the impact of an education, cognitive rehearsal, and role-play intervention. Six negative acts occurred daily or weekly pre-intervention and nine occurred post-intervention. Putting together staff on different hierarchy levels into one session may have undermined results | N |
| Stagg et al. (2013)148 | 10 nurses | 2-hour session | Pilot study with post-only testing (6-months after the intervention over a 6-week period) without control | None – based on Griffin (2004) | Education, cognitive rehearsal | Workplace Bullying Follow-Up Survey | Assessed the effectiveness of a 2-hour cognitive rehearsal programme, 6 months after completion; 70% of nurses reported changing behaviours, and 40% reported a decrease in bullying behaviours | Y |
| Stagg et al. (2011)149 | 20 nurses | 2-hour session | Pre–post quasi-experimental design with no control group. Unclear when post test was delivered | None – based on Griffin (2004) | Education, cognitive rehearsal | Adapted Workplace Bullying Inventory | Evaluated a workplace bullying cognitive rehearsal programme. Significant differences were found in the results between pre test and post test for observed bullying (Z = −2.636, p< 0.01), bullying of others (Z = −2.449, p < 0.05), and sufficiency of the training on management of bullying (Z = −3.358, p < 0.01) | Y |
| Warrner et al. (2016)63 | 60-bed orthopaedic inpatient unit incl. management | 45-minute session | Pre–post design without control group, with follow-up at 2-months post intervention. | None | Education, cognitive rehearsal, environmental modification | Nursing Incivility Scale (NIS) | Evaluates an intervention comprising awareness education, cognitive rehearsal, and which included management. None of the scores for the five subscales of sources of incivility were statistically significant. Two out of five subscales showed a statistically significant decrease in instances of perceived incivility: general incivility (2.75 to 2.24, p = 0.00) and physician incivility (2.79 to 2.43, p = 0.04), and the others decreased but not significantly | Y |
| Multiple-session education/training | ||||||||
| Asi Karakaş and Okanli (2015)157 | 30 nurses | Eight 2- to 2.5-hour sessions | Quasi-experimental pre–post design without control. Assessment was 6 months post intervention | None | Assertiveness training | Mobbing Scale, Rathus Assertiveness Inventory | This study reported an evaluation of an assertiveness training intervention in 30 nurses who experienced a high level of mobbing. Results indicated a statistically significant fall in mobbing after the intervention from 226.4 ± 27.7 to 159.6 ± 47.9 on the mobbing scale and an increase in assertiveness from 6.23 ± 15.6 to 17.0 ± 16.06 | Y |
| Banerjee et al. (2022)71 | Division faculty members (n = 41) and pulmonary and critical care fellows (n = 12) | 13 × 1-hour sessions over 1 year | Pre–post feasibility study. Time of post assessment is unclear but probably immediately post intervention | None | Education, positive role-modelling | Surveys assessed knowledge on racism in medicine; opinions, understanding, and comfort surrounding race and racism in medicine; as well as additional questions to solicit feedback on the curriculum itself | Assessed the feasibility of a year-long antiracism educational study. As it was mostly a feasibility study, post intervention surveying indicated a 15% increase in self-directed learning on related topics. However, interest in the curriculum actually decreased post intervention by 14%, perhaps since participants now felt they had learned what they needed to | N/A |
| Barrett et al. (2009)142 | An inpatient unit, critical care unit, ED, and inpatient operating room 59 pre-intervention and 45 post-intervention nurses |
Two 2-hour group sessions | Quasi-experimental pre–post design without control. Pre-intervention measures were 2 weeks prior to intervention and post measures were 3 months after intervention | None | Education and role playing, encouragement to become champions, team-building, seeking hospital accreditation | National Database of Nursing Quality Indicators (NDNQI) RN-RN interaction subscale, Group Cohesion Scale | The study assessed a team-building intervention to reduce lateral violence, using mixed methods. The intervention was found to improve group cohesion from 540 pts to 612 pts (p = 0.037) | Y |
| Demarco et al. (2005)104 | Five graduate nursing student participants | 2 hours per week for 6 weeks | Pilot pre–post design without control. Interviews were as soon as possible post intervention | Oppressed group behaviour (Freire, 1990) | Group writing | Interview | Pilot study investigating a writing group’s ability to build group cohesion. The group writing drew on the ‘Amherst Writers and Artists’ method which did not focus on UB but nonetheless was intended to help cope with it. It explored participants’ responses qualitatively, finding it helped build a sense of social support, and recommended potential changes. No quantitative effectiveness testing | Y |
| Jenkins et al. (2011)144 | 10 student leaders | 6-hour-long sessions, monthly, for 6 months | Case study design | Unknown | Journal club/group writing | Weekly journal comments | Explores how 6-hour-long monthly journal club meetings may increase civility. Also incorporated journalling. Anecdotally, it found that participants became more aware and sought to become role models of civility | N/A |
| Kang et al. (2017)156 | 40 hospital nurses | 20 hours over 10 sessions | RCT | 4 stages of cognitive rehearsal by Smith and non-violence communication (Rosenberg and Chopra, 2015) | Cognitive rehearsal, role-playing, and communication training | Relationship Change Scale, NAQ-R, Brief Symptom Inventory-18, Yun’s nurse turnover intention tool | A RCT to investigate a cognitive rehearsal programme on workplace bullying. Post intervention, there were significant differences in interpersonal relationships (F = 6.21, p = 0.022) and turnover intention (F = 5.55, p = 0.024) between groups, but not for workplace bullying | Y |
| Kousha et al. (2022)158 | 80 emergency nurses | Five 2-hour sessions over 3 weeks | Single-blinded RCT with two hospitals as groups (education-only vs. education and cognitive rehearsal). Post collection of data was 1 month after training sessions | Bandura’s social learning theory (1977) | Cognitive rehearsal, education, role-play | The Incivility Scale | The study, focused on incivility between emergency nurses, found that ANOVA and repeated-measures ANOVA indicated overall incivility and supervisor incivility increased in the intervention group but decreased in the control group. There were no notable differences in instances of nurse-to-nurse incivility and physician incivility | N |
| Lasater et al. (2015)137 | 94 nursing staff | One 1-hour session comprising presentation and discussion on incivility, a 4-hour session on norm-setting and action-planning, and a 2-hour simulation role-playing session | Quasi-experimental study with no control group. Data collection occurred pre, post session 1, post session 2, post session 3, > 1 month post session 3, 5 months after the last session, and 24 months after the last session | Bandura’s social learning theory (1977) | Education, action-planning, role-playing | Nurse Incivility Scale (NIS) New General Self-Effectiveness Scale (NGSE), Workplace Collective Effectiveness Scale (WCES), National Database for Nursing Quality Indicators (NDNQI) |
Study of a three-part educational intervention to see if it reduced incivility in two units of a hospital. It was effective in decreasing incidences of perceived incivility across all NIS subscales and self-effectiveness increased significantly | Y |
| Nicotera, Magon and Wright (2014)107 | 19 participants with 47 comparison samples | Six 90-minute sessions | Pilot quasi-experimental pre–post design with comparison group. No randomisation. Post data collection was unclear | Structurational divergence | Education, conflict management, role-playing | Structurational divergence, role conflict, burnout, depression, bullying, beliefs about arguing, verbal aggressiveness, taking conflict personally (TCP, a set of attitudes predisposing one to internalise conflict), ambiguity intolerance, and conflict-management styles (collaborative, avoidant, and aggressive), general conflict orientations, scales for direct constructive discussion and direct destructive discussion | Assesses a nursing conflict intervention using mixed pre- and post-test methods with a control sample, which sought to reduce structurational divergence by raising awareness of it and teaching skills to manage it. They found that participants experienced better understanding of conflicts and how to sustain healthier relationships. The course significantly reduced destructive communication and improved constructive communication skills | Y |
| O’Keefe et al. (2022)152 | 203 participants in surgery | 1-day session with a 1-hour follow-up e-learning course | Case study | Transformative learning theory conceptual framework | Role-playing, team-building, education, reflection | Online qualitative survey | Outlines an intervention based on a Transformative Learning Theory conceptual framework that draws upon role-playing, simulations, case studies, reflection exercises, and peer-peer learning. Anecdotally, 85% of participants reported a perceived improvement in conflict-management skills but effectiveness was not formally tested | N/A |
| Saxton (2012)64 | 17 participants | 2-day programme | Pre–post study design without control group. Post-intervention data were collected immediately. Data collection also at 4-week follow-up | Humanising Nursing Communication Theory and Social Cognitive Theory | Communication training | Self-Effectiveness to Address Disruptive Behavior Scale | Development and evaluation of a communication skills intervention to improve perceived self-effectiveness of perioperative nurses using a pre–post design. Results suggested an improvement in self-effectiveness scores and participants reported the ability to address disruptive physician behaviour 71% of the time 4 weeks after the study intervention | Y |
| Training and/or further actions (e.g. codes of conduct) | ||||||||
| Chipps and McRury (2012)134 | 16 staff members | 3 month | Quasi-experimental pre–post design without control with 4-month follow-up. Post test given immediately post intervention | Einarsen’s (2000) theoretical framework on predisposing factors for workplace bullying | Education, peer learning, action-planning, conflict-management training, code of conduct, communication training | NAQ-R. Log books given for daily documenting of bullying experiences | This quasi-experimental study assessed pre test and post test an educational intervention to address workplace bullying. They noted an increase in bullying reports as a result (from < 1 act weekly/daily to 1.6 acts weekly/daily), but it did help develop a learning community | N |
| Dimarino (2011)125 | Unknown | Unknown – ‘on demand’ sessions and code of conduct | Case study | None | Code of conduct, education | Reports anecdotally on organisational turnover and reports of violence | Reporting of one ambulatory surgery centre’s approach to reducing lateral violence through education about lateral violence, and zero-tolerance policies. Did not test effectiveness | N/A |
| Kang and Jeong (2019)61 | 72 hospital nurses | 2-hour familiarity session followed by 8 weeks on-demand usage (smartphone-based) | Cluster quasi-randomised design with control group with pre, post (4-week post), and 8-week follow-up measurement | Non‐violent communication (Rosenberg and Chopra, 2015) | Cognitive rehearsal (smartphone-based) | NAQ-R, turnover intentions were measured using a modified version of ‘intent to quit’ | Investigates a cognitive rehearsal smartphone-based intervention’s impact on bullying using a cluster quasi-randomised trial. It found that use of the app reduced nurses’ person‐related (21.07 ± 8.38 to 15.41 ± 4.03 at 8 weeks, ICU staff) and work‐related bullying experiences (11.19± 5.02 to 7.81 ± 3.20 at weeks, ICU staff) and turnover intentions (3.52 ± 0.8 to 3.21 ± 0.71 at 8 weeks, ICU staff) between groups, but did not reduce intimidation‐related bullying experiences | Y |
| Parker et al. (2016)138 | Unclear/organisation-wide | One away day and subsequent ongoing efforts of unclear overall duration | Case study design | Longo’s (2010) three-level intervention model: organisation, leadership, and individual | Education, conflict management, leadership training, role-modelling, cognitive rehearsal, code of conduct, championing/becoming agents of change, seeking Magnet status | Briles’s Sabotage Savvy Questionnaire | Explores how nurses at an acute care hospital were able to implement multiple interventions to reduce horizontal violence prevalence in the organisation. These included 13 total organisational, leadership, and individual-level strategies | N/A |
| Stevens (2002)103 | Unclear | Unclear | Case study design | None | Action-planning, code of conduct, democratisation | Turnover rate | Informally explores the impact of a multistrategy anti-bullying intervention in a large teaching hospital, delivered mostly through workshops for education, policies, supervisor training, and more. They anecdotally found a decrease in nursing turnover rate after 1 year but it could have been also a result of other factors and programmes | N/A |
| Thorsness and Sayers (1995)150 | Approximately 100 surgical staff | Unclear | Pre–post design without control group. Survey was conducted before and 2.5 years after intervention | Kilmann model for transforming organisations (1974) | Survey, code of conduct, action-planning, communication skills training, workplace rearrangement, education | Kilmann-Saxton Culture-Gap Survey | Evaluation of a programme adopting a systems approach to cultivating a positive work environment for perioperative staff members. Intervention comprised making action plans for different staff groups, code of conduct, and cultural-change efforts. Post survey showed improvements in culture but statistical significance was not tested | Y |
| Professional accountability and reporting | ||||||||
| Baldwin et al. (2022)53 | Three academic medical centres | Sept 2019 to Aug 2021 (2 years) | Descriptive study assessing feasibility of implementation | None | Vanderbilt intervention (reporting and escalation system, informal and formal resolution, championing, peer messengers, seeking Magnet accreditation) | Statistics from message database | Descriptive study analysing the types of reports received during the intervention to promote professionalism with nurses. 590 reports were received, of which most included more than one problematic behaviour; 76.5% of these messages were shared and completed | N/A |
| Churruca et al. (2022)97 | Eight hospitals | 5 years | Case study/descriptive design. Reported data are from between July 2017 and July 2021 | Unknown | Ethos reporting system with peer messengers, informal resolution, formal investigation, training to enhance speaking up and role-modelling | Reported statistics from reporting system such as percentage of positive vs. negative reports | Reports on a case study of the Ethos messaging system implemented across eight hospitals in Australia to address a culture of respect. The Messaging System had 2497 submissions with approximately 1600 reflection conversations delivered; 54% submissions were about positive behaviours. Peer messengers faced some difficulties when delivering messages | N/A |
| Dixon-Woods et al. (2019)143 | Organisation-wide at Johns Hopkins Medicine | 2-year period, 2014–2016 | ‘Case study’ approach | None | Reporting system and formal investigation | Interviews | This study sought to improve employees’ ability to speak up about transgressive and disruptive behaviour at a Johns Hopkins Medicine hospital. It uses largely qualitative exploration of the results and highlights importance of leader commitment and intolerant culture. Makes suggestions for a testable approach to encouraging voice. Did not test effectiveness | N/A |
| Hickson et al. (2007)98 | Unknown | Variable, depends on requirements | Case study design | Unknown | Vanderbilt approach for graduated intervention (reporting system, informal conversation, awareness, leader-led action-planning, formal investigation) and other variable strategies as required (e.g. communication training, leadership programmes, use of messengers) | Reports statistics on reporting system use and types of complaint | Outlines and reviews the Vanderbilt approach to identifying, measuring, and addressing UB using four graduated interventions. Did not assess effectiveness | N/A |
| McKenzie et al. (2019)93 | 21 healthcare staff pre-to-post | 18 months into a 3-year intervention | ‘Case study’ design | Unknown | Vanderbilt approach (education, reporting system, champions, action plans, graduated informal to formal resolution) | Interviews and Safety Attitudes Questionnaire (SAQ) | Investigated factors affecting implementation of a multistrategy intervention using education, reporting systems with graduated intervention processes, safety champions, and action plans, to tackle UB. They found that leader role-modelling, work condition modification, confidence in accountability systems, and responsiveness enhanced the intervention implementation | N/A |
| Speck et al. (2014)147 | Three teaching hospitals | 4+ years | Case study design | Unknown | Variation on the Vanderbilt reporting system with graduated escalation from informal resolution (peer, then manager) to formal investigation, championing | Reports on professionalism committee statistics and vignettes | Assessment of a professionalism committee approach to tackling UB across three large teaching hospitals. In this variation, department chairs were able to report individuals to the committee rather than any staff member. It found that it was able to identify early specific behavioural issues and refer them appropriately | N/A |
| Webb et al. (2016)151 | Three hospitals | 2 years for study data (but programme running for 9 years) | Case study/evaluation | Unknown | Vanderbilt reporting system with graduated escalation from informal resolution (peer, then manager) to formal investigation, championing | Reports on statistics from the reporting system such as number of reports and escalations | Presents a feasibility study of the Co-Worker Observation Reporting System implemented by Vanderbilt University Medical Center to reduce disrespectful and unsafe behaviours. They found that it was feasible, requiring organisation-wide implementation, and found that most workers self-regulate after being informed a report was received about them | N/A |
| Westbrook et al. (unpublished)127 | Staff across five hospitals | 2.5–3 years after Ethos implementation | Pre–post cross-sectional study. Hospitals were surveyed at baseline, between July and November 2018, prior to programme introduction and repeated between October 2021 and February 2022 (post) | Unknown | Ethos reporting system, training for leaders and staff to support speaking up and to role-model, tiered accountability pathway | Longitudinal Investigation Of Negative behaviour (LION) survey, follow-up survey including questions about the perpetrators of UBs, knowledge and views of the Ethos programme, and the impact of COVID-19 on UBs | There was an overall reduction in the odds of staff experiencing incivility/bullying behaviours by 24%, and a 32% reduction in odds of experiencing extreme UBs in the previous 12 months | Y |
| Structured and structured culture-change interventions | ||||||||
| Armstrong (2017)141 | 9 nurses | Two 8-hour sessions to train facilitators 4 weeks total with one meeting per week. Sessions lasted 20–30 minutes | Pre–post design without control. Assessment 2 weeks post intervention | Model for Improvement by Langley (1996) | CREW (education, team-building exercises, role-playing) | Workplace Incivility Scale, Confidence Scale | Quantitative investigation of an intervention in a rural hospital to reduce nursing workplace incivility. Findings indicated no change in experience of incivility but a greater ability to respond to incivility. There was a statistically significant improvement in the post-test mean score (M = 85.56, SD = 20.07, t (8) = −4.667, p = 0.002), when compared to the pre-test mean score (M = 62.22, SD = 18.56) | Y |
| Laschinger et al. (2012)155 | 8 units with 33 controls | 6 months, selecting strategies from the CREW toolkit as appropriate | Quasi-experimental design using randomised units. Pre and post assessment. Post-assessment timing is unclear | Kanter’s (1977, 1993) Theory of Structural Power in Organizations | CREW intervention (espousing values by leadership/role-modelling, education, signing code of conduct pledge, surveying civility, action-planning, role-playing, training on assertiveness, communication, conflict resolution) | Structural empowerment was measured using four subscales of the Conditions for Work Effectiveness Questionnaire-II, five items from the Workplace Incivility Scale, six items from Cook and Wall’s (1980) Interpersonal Trust at Work Scale | Investigates the impact of the CREW intervention over 6 months with 8 intervention units and 33 control units. A significant interaction of time by intervention was found for the access to support and resources empowerment structures, total empowerment, supervisor incivility, and trust in management | Y |
| Leiter et al. (2011)154 | 1173 workers across 41 units | 6 months | Quasi-experimental design using randomised units. Pre and post assessment. Post-assessment timing is unclear | Social interactions at work | CREW intervention (espousing values by leadership/role modelling, education, signing code of conduct pledge, surveying civility, action-planning, role-playing, training on assertiveness, communication, conflict resolution, leadership) | CREW Civility Scale, the 10-item Workplace Incivility Scale and an additional dimension of instigated workplace incivility was included, Blau and Andersson (2005), respect was measured using two items from the Esteem Reward section of the Effort-Reward Imbalance Questionnaire, trust in management was measured by six items from Cook and Wall’s (1980) Interpersonal Trust at Work Scale, Emotional Exhaustion and Cynicism subscales of the Maslach Burnout Inventory-General Survey, three items were modified from the Turnover Intentions measure developed by Kelloway et al. (1999), Professional Effectiveness was measured using the Professional Effectiveness scale of the MBI-GS, two items from the Affective Commitment Scale (Allen and Meyer, 1990), job satisfaction (Hackman and Oldham, 1975; Tsui, Egan and O’Reilly, 1992), absenteeism from institutional data | Assesses the effect of 6 months of the CREW intervention and found that greater group × time interactions were found in the intervention group for civility, supervisor incivility, respect, cynicism, job satisfaction, and management trust, and absences | Y |
| Osatuke et al. (2009)146 | 647 post-intervention CREW participants and 680 comparisons (total 34 workgroups) | Flexible/various | Quasi-experimental pre–post design with control group but no randomisation. The Civility scale for CREW was administered at CREW-1 sites in September 2005 and July 2006, and at CREW-2 sites in February 2006 and March 2007. Comparison site data were retrospectively matched to intervention sites for respective years | National Center for Organization Development (NCOD) practice model. Prototype approach. | CREW intervention (survey, action-planning, various training, e.g. on communication, education) | CREW civility scale | Preliminary evaluation of a nationwide Veterans Health Administration intervention called CREW across 23 sites. It found significant pre- to post-intervention changes in civility compared to none at comparison sites | Y |
Appendix 7 Interventions outside the scope of this report
This appendix outlines interventions we became aware of during our review but which do not formally meet our inclusion criteria. This included practice-based interventions which were not formally reported in the literature but were mentioned by our stakeholders, for example, as well as interventions to improve civility which may inadvertently reduce UB but are not focused on doing so. Lastly, this includes CBM, which may mitigate the impact of UB on patient safety and ability to speak up; however, this was not formally included because it is currently based on simulation studies.
Practice-led interventions
An example of a practice-based intervention which has not received evaluation is the NHS England Civility and Respect Programme,227 which is a toolkit available for organisations to implement across the UK’s NHS. Formed due to the ongoing concerning results of the NHS staff survey regarding a high prevalence of bullying and unprofessionalism,129 this intervention draws on an Analysis, Intervene, Measure approach organised across four themes. These themes are (1) data and analysis, which suggests to organisations that they should first use a survey to help understand the prevalence of UB in their organisation; (2) policy and process, which highlights the importance of culture and a restorative approach to tackling UB and leadership behaviours as key to working for or against culture-change efforts; (3) staff and management support including providing a structure for staff to speak up against UB in the workplace and leadership training, and strategies for ‘health and well-being’ such as resilience training and counselling; and(4) a just and restorative culture, drawing on leadership role-modelling to drive development of a compassionate, restorative, and learning culture. Interestingly, this intervention also draws on a tiered escalation process to addressing individual conduct which exactly replicates the Vanderbilt escalation model. 151 This escalates from a level 1 awareness intervention (informal resolution) to a level 2 guided intervention by authority (attempt at informal resolution by line manager) and finally a level 3 disciplinary intervention (formal investigation).
This intervention offers a wide range of other strategies, mostly in the form of presentation slides (i.e. ‘sessions’) which can be implemented on a case-by-case basis in their 249-page toolkit including education, leadership training, team-building exercises, assertiveness training and communication training, among others. 228
There are also examples of other organisational approaches to tackling UB in the workplace being developed. One such example is an intervention called the ‘Improving Staff Wellbeing: Using the “Your Voice” Digital Reporting Tool’. 229 This was intended to have been a web-based reporting system for incidents of bullying and harassment across the Leicester, Leicestershire and Rutland Health and Care System but it is unclear whether this intervention received funding to be implemented. As such, there is evidence for uptake of many ideas in the academic literature in practice, but there needs to be greater focus on evaluation and the reporting and sharing of results of such interventions with others to generate knowledge regarding what works, where, and for whom.
Positive, civility-first interventions
We identified some interventions that we may not have included because they focus on driving ‘positive behaviours’ or a culture of civility and do not mention UB-related terms in the title or abstract. One example paper drew on several strategies to try to improve a culture of civility. 230 This included an education session, a computer-based cognitive rehearsal intervention, role-playing and peer-to-peer learning and reflection. After the intervention, they realised more must be done so implemented an action-planning session with leaders, which also led to people becoming champions for the intervention. Evaluation found that behaviours such as being ignored or excluded daily, weekly, or monthly, reported initially as occurring 28.23% of the time, improved to 15.25%. Four other types of negative acts also reduced in prevalence.
Another civility intervention is set out by Clark,231 termed ‘Pathway for Fostering Organisational Civility’ (PFOC). This intervention relies heavily on implementation-aiding strategies, similar to CREW with flexibility. The author states ‘Any model or pathway to foster civility must be considered within the context of the organization’s unique culture and climate and must be nimble and flexible to use in a variety of work environments’. 231 Its first step is to raise awareness of civility through education, then assemble a work team, survey incivility in the organisation at all levels, action-planning, then implementing the action plan drawing on co-creating, and building effective communication and conflict-management skills. The final steps involve evaluation, rewarding civility, and expanding the civility initiative. They also draw on a reporting system for positive and negative behaviours as well as tracking and evaluating progress. This programme has many overlaps with CREW, but demonstrates that some strategies to enhance civility may not have featured in our review (e.g. rewarding positive behaviours).
Overall, the design of these programmes and their findings demonstrate that the types of strategies used to enhance civility or reduce incivility are similar.
| Stakeholder feedback summary – strategies |
| Our stakeholder group meeting in November 2022 focused on our findings around strategies and initial versions of our Key Dynamics presented in this chapter. The stakeholder group helped to make us aware of the substantial amount of work going on ‘in practice’ to address UB in various organisations in the UK and provided us with examples such as the ‘Using Your Voice Digital Reporting Tool’. However, this work does not always get evaluated properly nor does it end up in the academic or grey literature. |
Cognitive bias modification to mitigate impact of UB on patient safety
We identified several interventions that sought to mitigate the impact of UB occurring in the clinical environment on patient safety more directly. Typically, this was done using CBM. CBM involves training (in this case computerised) designed to alter threat-oriented biases in interpretation of rudeness towards a more positive and benign interpretation. For example, one study drawing on a simulation study design randomised 39 neonatal intensive care unit teams to four conditions. These were rudeness or control conditions, as well as rudeness with CBM or therapeutic (narrative) interventions. Judges assessed team performance in medical treatment in each condition. In line with other simulation studies, they found that rudeness inhibited ability to share information and helping behaviours. However, in the CBM condition, effect on information-sharing and helping was reduced. Therefore, the authors report that ‘the CBM intervention succeeded in “immunising” participants from the effects of rudeness’. 14
Due to difficulties with testing CBM with ‘real-world’ UB exposure it is difficult to say how effective it may be or how long such training may last. However, it could be argued that CBM modifications, since they seek to modify the impact of UB on information-sharing and decision-making, may more directly impact on patient safety than other interventions that seek to reduce UB. A final concern with these interventions is that use of such mitigation techniques may tacitly send the message, if used alone without other strategies to reduce UB itself, that UB is going to occur and that the issue is staff’s response to it rather than the culture that enables UB itself. As such, CBM may be best used as a co-ordinated package of measures to avoid inadvertently sending such a message.
Appendix 8 Draft recommendations for stakeholders working in the NHS
Introduction to appendix
This document is a draft version of guidance for stakeholders working in the NHS who are seeking to address UB. We have included this in the appendix of this report to provide a sense of the practical recommendations emerging from our findings. An earlier version of this document was presented to our stakeholders for refinement on 28 March 2023 and feedback has been integrated. Our stakeholders suggested the audience for this guidance may include: people working in areas of OD, and equality, diversity and inclusion (EDI), non-executive directors and NHS managers or leaders.
This document contains (1) a summary of the findings of our review; (2) suggestions for how those seeking to address UB in various ways should approach it; and (3) an overview of what people have done in the past to tackle UB (still in development). A glossary of terms is at the bottom of this document.
After report submission, we will continue to develop this document as a resource for stakeholders, and will also translate information contained here into infographics, a short film and other easily accessed communications forms. We intend to provide more information regarding which strategies help address particular instances of UB, and we will also seek to reach policy-makers, regulators and others, through other means such as policy briefs.
Introduction to guide
This guidance focuses on healthcare staff interpersonal UBs towards each other, not behaviours towards patients or patients towards staff. Following a comprehensive review of the literature, this guidance has been co-produced with NHS staff, managers and leaders, as well as academics, patients and the public. This guidance can be useful to managers and leaders in two ways by specifically helping to consider:
-
what to think about and do when confronted by UB (retrospective intervention)
-
what to hold in mind about work culture as it unfolds in the daily conversations, given the likelihood of UB (prospective interventions).
Context for this review
Tackling unprofessional behaviour matters because
-
18.7% of staff experienced harassment, bullying or abuse from colleagues in 2021/22, while 11.1% experienced the same from managers (NHS staff survey 2022)
-
9% of staff from ethnic minority backgrounds reported experiencing discrimination at work from managers or colleagues (NHS staff survey 2022)
-
22.5% of white respondents and 27.6% of ethnic minority respondents experienced harassment, bullying or abuse from colleagues in the NHS (Workforce Race Equality Standard data from 2022)
-
Unprofessional behaviour can negatively impact:
-
(i) NHS staff (people targeted by it and witnesses) resulting in psychological and physical ill-health
-
(ii) patients, affecting reporting of clinical errors, patient experiences, care quality and outcomes
-
(iii) organisations, who can incur substantial costs from loss of staff, any patient safety issues, and loss of reputation.
-
Findings of this review
Definitions
Unprofessional behaviour is an umbrella term that includes bullying, incivility, harassment, microaggressions and discrimination. We found this term useful, yet across the literature there was no consensus about what constituted UB or other more common terms, such as bullying. This can pose problems for academic work but also for identifying UB and addressing UB in practice. We proposed a short and longer working definition for UB, as used in our review:
Short:‘Any interpersonal behaviour by staff that causes distress or harm to other staff in the healthcare workplace’.
Longer:‘Any interpersonal behaviour by staff that acutely or frequently undermines, humiliates, intimidates, or causes distress or harm to other staff, in the healthcare workplace’.
Contributors
The literature pays significant attention to how individual and personal characteristics contribute to UB (aka ‘bad apples’). We identified how a range of organisational and systemic issues contribute to UB including:
-
workplace disempowerment (includes organisational hierarchies, a physically uncomfortable environment and unfair processes)
-
organisational confusion, uncertainty and stress (includes high job demands and lack of resources, pervasive culture of pressure and lack of role clarity)
-
job and organisational design that inhibits social connection (includes lack of social support which leads to an inability to cope with UB, an (in)ability to communicate effectively)
-
harmful work cultures (includes permissive and complicit leadership, negative role-modelling and prior learned behaviour, authoritarian leadership style, organisational deafness, cliques and lack of accountability by leadership).
These contributors can be targeted by strategies as part of well-designed interventions.
Who is most affected?
-
Women, individuals from black, minority and marginalised groups, LGBTQ+ staff, and new entrants to the profession are at greater risk of UB. Evidence regarding interprofessional interactions (e.g. doctors and nurses) was mixed in terms of frequency but did suggest that intraprofessional UB was more harmful to well-being than interprofessional UB.
Strategies to address unprofessional behaviour
We identified 13 types of activity that seek to address UB in different ways. Strategies we identified in the literature are outlined in Table 29. We will continue to develop this section to be more applicable and specific to various contexts after report submission.
| Activity (and whom it impacts) | Types of strategies |
|---|---|
| 1. Informal or disciplinary strategies to address UB and speaking up (e.g. by a victim, bystander, manager or peer) | Informal resolution, formal investigation, bystander intervention, softening language, mediation, speaking up, use of peer messengers |
| 2. Improving confidence to come forward (victim, bystander) | Assertiveness training, role-playing, cognitive rehearsal |
| 3. Improving ability to cope (victim, bystander) | Seeking help externally, journalling, moving victims, individual coping strategies (e.g. taking sick leave), reflection |
| 4. Understanding prevalence of UB (managers/leaders) | Surveys, multisource feedback, reporting systems; FTSUG reports |
| 5. Improving teamwork (all staff) | ‘Team-building activities’ staff networks, conflict-management training, communication training, problem-based learning, group writing |
| 6. Social norm setting (all) | Anti-discrimination policies, codes of conduct, role-modelling, championing, environmental modification, allyship |
| 7. Improving leadership competence and empathy (managers/leaders) | Leadership and management training |
| 8. External pressure on organisations (managers/leaders) | Public pressure (from social trends (e.g. #BLM) or public knowledge of failings), government and regulator action, legislation, seeking Magnet status |
| 9. Reporting and escalation systems (all staff) | Reporting systems, e.g. Ethos or Vanderbilt programme reporting methods |
| 10. Workplace redesign (all staff) | Democratisation of workplace, new patient pathways, change management |
| 11. Improving awareness and knowledge (all staff) | Education (e.g. about what UB looks like, how to speak up about it) |
| 12. Strategies to aid Implementation (managers/leaders) | Action-planning, scheduling workshops, appointing dedicated personnel to lead programme |
| 13. Changing recruitment, induction and dismissal processes (all staff) | Pledges during hiring, focus on UB in induction, changing recruitment criteria, dismissal, referral to regulators |
What you can do to mitigate, manage and prevent unprofessional behaviour in your organisation
It is important to recognise the problem and DO SOMETHING and not ignore the prevalence and nature of UB, which can have deleterious effects on staff morale and well-being and on patient care quality and outcomes. Interventions can feel like ‘fixes’ but often they are not. The conversational culture (who can talk about what, to whom, with what tone etc.) needs constant attention. To support a turn towards a conversational culture, we suggest the following 10 recommendations:
-
The default position statement of the employer (NHS), leaders and managers needs to be ‘we do not tolerate unprofessional behaviour of any kind’. Doing something to address UB is better than doing nothing; maximise visibility to engage and signal seriousness about addressing UB
-
Assess organisational landscape (understand organisational contributors to UB) then invest in implementation of multiple interventions and strategies (cover as broad a section of the organisation as possible to avoid perceptions of singling out specific groups, and foster culture change) and plan both ongoing formative and summative evaluations
-
Implement multiple strategies: using a greater number of (aligned) strategies can increase uptake and spread
-
Intervening early when UB is first detected is important to reinforce message that UB is not tolerated and maintain trust in management; but make sure the intervention is seen as just and not overly punitive (e.g. relatively minor instances of UB are tackled/ addressed informally)
-
Plan and implement a UB strategy to address organisational need; use societal shifts and changes in discourses relating to bullying, harassment and racism
-
Shift the balance towards organisational as well as individual-level responsibility by encouraging allyship and workplace redesigns that foster social support and the ability to speak up
-
Identify and nurture leaders capable of modelling ‘good’ behaviours and encourage their visibility so they can lead by example; avoid simply moving the instigator or recipient of UB – sends negative signals regarding tolerance of UB
-
Harness existing organisational processes to emphasise organisational commitment to reducing UB (repurpose existing meetings, or build into professional development reviews and appraisals)
-
Co-create interventions with staff (to foster intervention authenticity and increase engagement) including those more at risk (e.g. minority group members; those lower in organisational hierarchies) and senior groups to ensure buy-in, authenticity and reach
-
Appoint dedicated staff to lead work to tackle UB (intervention implementation and monitoring to improve design, enhance intervention implementation and sustainability) and maximise manager engagement.
To aid in translating action into practice we identified seven common factors across the literature which are essential considerations when designing interventions or activities to address UB. These include:
-
Interventions should address systemic factors that contribute to UB, not only individual factors.
Overestimating individual factors as contributing to UB may leave systemic contributors (such as a work environment that promotes frustration) unaddressed. A focus on individual factors has led to a prevalence of interventions which do not tackle systemic root causes and instead have, for example, focused on boosting individual resilience or identifying people who behave badly (‘bad apples’). Recommendations to address this dynamic include:
-
Encouraging those who create and implement programmes to reduce UB to adopt a mindset that explores UB as an organisational, not just an individual, problem.
-
Assessing and understanding potential systemic contributors to UB in an organisation prior to intervening.
-
For example: using Trust-wide OD support; better use of NHS annual staff surveys to understand where any hot spots may be and using NHS staff survey open comments to understand issues and contributors and therefore where and how to intervene
-
-
Identifying nature and extent of UB by providing a system that empowers staff to report/speak up can be beneficial.
-
Important elements to ensure that the system works well include: an anonymous reporting system that facilitates feedback (allowing acknowledgement that reports are delivered; the use of a triage process and database where reports are reviewed and verified) to help avoid ‘weaponisation’ of such systems (e.g. use of system to scapegoat others).
-
-
Multiple strategies – using a greater number of strategies can enable increased uptake and effectiveness as some individuals may respond better to some certain strategies than others. Likewise, use of more strategies can help address a greater number of contributors to UB but this may come at additional resource cost.
-
Including and planning to undertake well-designed evaluations alongside interventions to assess intervention and implementation effectiveness over time are important. Use of ongoing evaluation can help assess how effective an intervention is during implementation and help drive real-time changes to make it more effective.
-
However, caution is required – It is important to keep data in mind as a means to an end rather than an end in itself. Collecting lots of data can be a form of resistance or a defence against anxiety. The data can become the task rather than addressing challenging questions such as ‘why are we like we are’ and ‘what will make UB/ us better?’
-

-
Encouraging bystanders to intervene can help drive culture change but may also lead to moral injury.
Encouraging bystanders to intervene is important to send positive signals regarding culture change and the unacceptability of UB. However, creating an imperative to intervene can also lead to moral injury (failing to prevent acts that transgress deeply held moral beliefs and expectation leading to loss of psychological well-being) if staff subsequently do not intervene. Intervening can also place staff at risk of reprisal, which has its own risks.
Recommendations to address this factor include:
-
The importance of allyship (when the more privileged use those advantages to further the cause of marginalised group): communicate to employees (via comms channels such as posters, intranet, e-mail) that intervening when UBs are witnessed is preferred, but that intervening should only be done when it feels safe to do so.
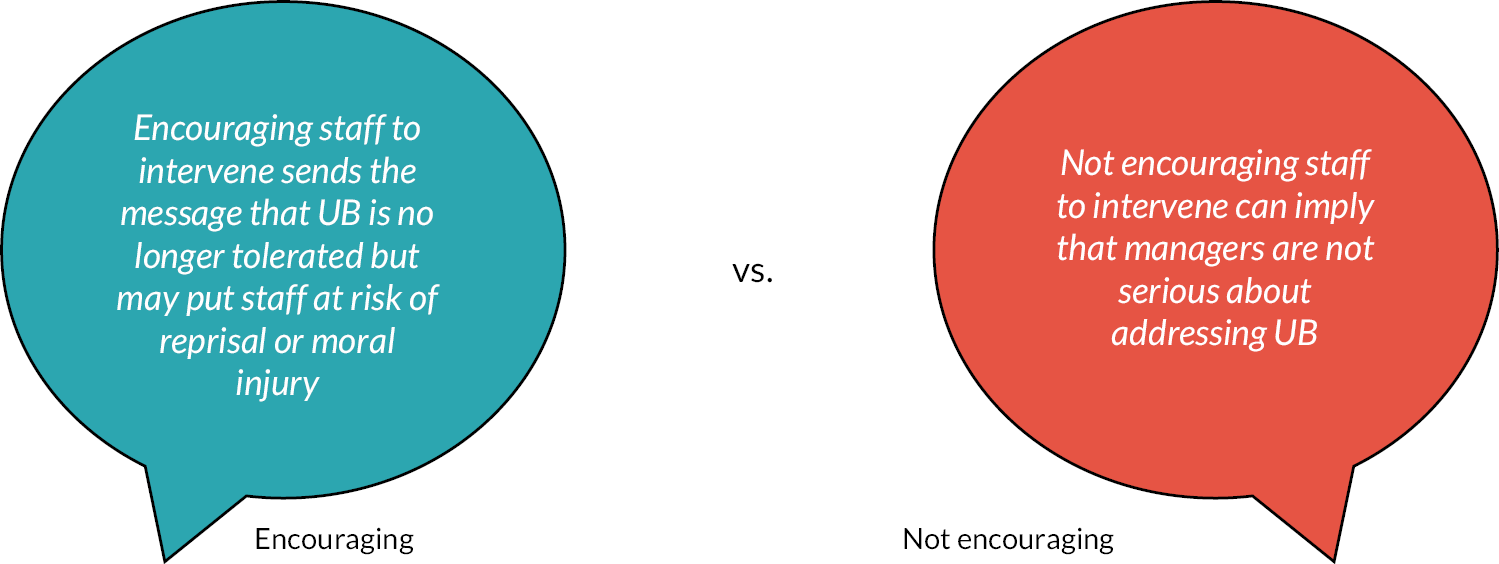
-
Ensuring authenticity of interventions can help build trust in management and leadership.
Staff need to feel that any intervention is genuine. Authenticity can be lost if:
-
managers are seen to engage in negative behaviours themselves during programme
-
an organisation is sending mixed signals about what it will or won’t tolerate; or
-
if the intervention is perceived as a ‘tick-box exercise’. Recommendations to address this factor include:
-
Chief executives are key to driving culture change and ensuring programmes to address UB are sufficiently supported.
-
Providing managers and senior staff with supportive training to better understand and address UB (e.g. communication training, management training).
-
Recognising the importance of role-modelling positive behaviours by leaders and managers and celebrating success and highlighting positive behaviours.
-
Organisations clearly communicating values and standards of behaviour they do and don’t tolerate through for example demonstrable leadership (e.g. CEO attending all inductions and communicating values).
-
Co-creation of interventions or co-decisions regarding intervention implementation (avoiding ‘top down’ ‘done to’ staff programmes) with staff to increase buy-in, engagement and uptake.
-
Breadth – interventions must cover a range of staff groups within the organisation so that everyone benefits equally and a culture change is fostered.
-
Organisational turnover and change – intervention sustainability is key, despite organisational turnover and change processes. If not properly managed, key architects can shift roles and intervention momentum can be lost. Programme leadership must not fall on the shoulders of one or two people – must be the responsibility of all. Loss of momentum or responsibility of a few can tacitly send the impression that there is organisational tolerance of UB if not the responsibility of all. However, this must be balanced with accountability and accountability for intervention success must be maintained (i.e. someone must be responsible).
-
Perception that the intervention is fair – an intervention must be seen as just and not overly punitive for it to be properly engaged with. For example this may mean that one-off relatively minor instances of UB are addressed informally, rather than being immediately escalated into formal proceedings.
-
Dedicated staff to lead work to tackle UB – having dedicated staff in place to manage programme implementation and monitoring can improve design by providing centralised people to collate necessary knowledge, and enhance sustainability of a programme, but, as above, care to be taken that responsibility for engaging is responsibility of all.
-
Skilled facilitation – interventions drawing on the use of a facilitator to impart key messages must ensure they are well trained to avoid unintended consequences (e.g. incorrect information being imparted, groups feeling inadvertently singled out).
-
Maximising existing opportunities – making use of existing organisational processes to emphasise organisational commitment to reducing UB can enhance effectiveness of programmes. This can include regularly scheduled existing meetings that can be repurposed, or use of professional development reviews and appraisals or tying in new activities with existing initiatives such as the Freedom to Speak Up Guardians programme, for example.
-
Maximise visibility – visibility of interventions in an organisation should be maximised through strong communications strategy and advertisement. This can enhance engagement as well as signal that management is serious about addressing UB.
-
Signalling serious commitment rather than quick fix: for example, it may be unwise to simply move the target of UB or even the instigator – moving a target or instigator of UB to another role within an organisation can send negative signals regarding tolerance of UB in an organisation.
-

-
Addressing senior staff behaviour in specific ways.
It is important to include leaders, managers and senior staff in interventions. However, it may not always be advisable to include senior staff in interventions with other employees in group sessions. Doing so can inhibit staff speaking up and engaging fully with intervention development. Recommendations to address this factor include:
-
Those designing and implementing interventions should be aware that seniority and hierarchy can suppress group engagement and learning.
-
Consider delivering group training to staff at the same hierarchy level (such as the same grade or ‘band’ in the NHS).
-
Leader and manager engagement – keeping managers interested and engaged in the intervention is essential to ensuring its sustainability and essential for an intervention’s perception as a genuine effort to reduce UB.
-
Advocate that activity around addressing UB becomes part of the core competencies of managers – featuring in job description/appraisal/promotion assessment processes.
-
Recognise that hearing staff concerns can be difficult (‘deaf effect’). One reason not to like people speaking up is that they will say things we do not want to hear, including wanting to say something about our behaviour as a leader. Providing support to those hearing may over time give them the courage to act and better support their staff.
-
Asking managers and leaders to think about their own behaviour provides an opportunity to stay in role and repair things. The leadership task is to be cognisant of their behaviour and think reflexively – why now? Why am I shutting this person down – what is the issue that must be silenced?
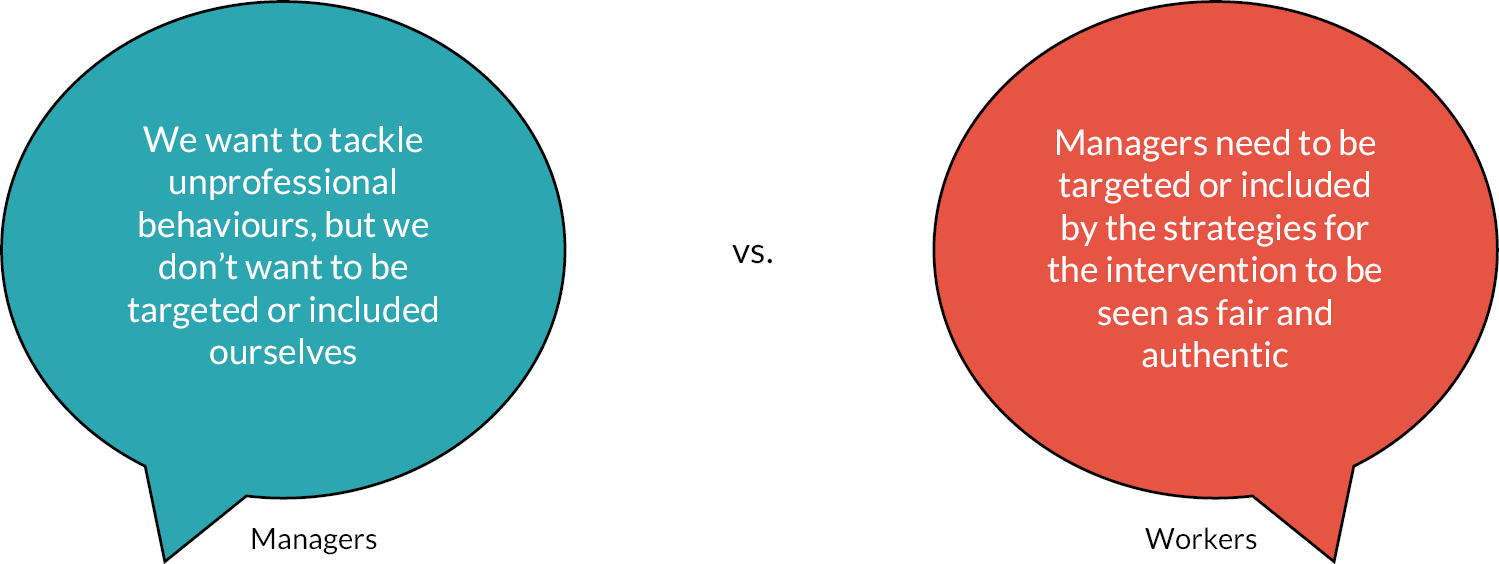
-
Interventions that are both inclusive and fair are essential to ensuring effectiveness and sustainability and for delivering benefits to different groups.
The shared task is to keep people safer, meaning everyone has a duty to help, and being offered the role of ‘victim’, ‘perpetrator’ or ‘bystander’ may abandon people to these roles, which isn’t productive or conducive to behaviour change. Key questions here include:
-
How are different groups of people silenced in our organisation?
-
Who and what tend to get heard and who and what are at risk of being silenced?
Interventions need to be inclusive and cover all individuals to be seen as fair and to avoid resentment in any particular groups. However, at the same time, certain groups do experience a greater impact and incidence of UBs. Gaining a greater understanding of the differences in the experience of UB by different groups and the root causes of these may help drive greater understanding of how to address UB in a fair and inclusive manner for people, for example, women and minority groups. Recommendations to address this factor include:
-
Focusing on getting better organisational data to help identify and thus try and solve the root cause. Better data can help in decision-making and identifying the behaviour to be addressed, with policies changed appropriately in response. This can help avoid situations where one group feels another is being unfairly targeted or is receiving benefits that another group is not receiving.

-
The design of an intervention and its flexibility have implications for how best to evaluate the effectiveness of the intervention to bring about change.
Some interventions are designed to be inherently flexible, including a repertoire of strategies that can be drawn upon in each situation. This can enhance applicability and adaptability of the programme to different scenarios that may occur during programme implementation. However, using different strategies in different contexts can make it more difficult to assess the effectiveness of an intervention (where individual strategies may be effective or ineffective depending upon the context in which they are used). Recommendations to address this factor include:
-
where resources allow, build in an evaluation to identify and evaluate the different strategies of the intervention alongside implementation to monitor any changes to UB and contributors
-
consider, where possible, the use of mixed methods (surveys and interviews, for example) at different timepoints (including baseline before the start of the intervention, mid and end point and follow-up). This will increase understanding of what is working in a given context, particularly with a more responsive, flexible intervention
-
aim to include a range of outcomes both proximal (e.g. impact on frequency and type of UB experiences) versus distal (e.g. impact on staff well-being, retention or patient safety).
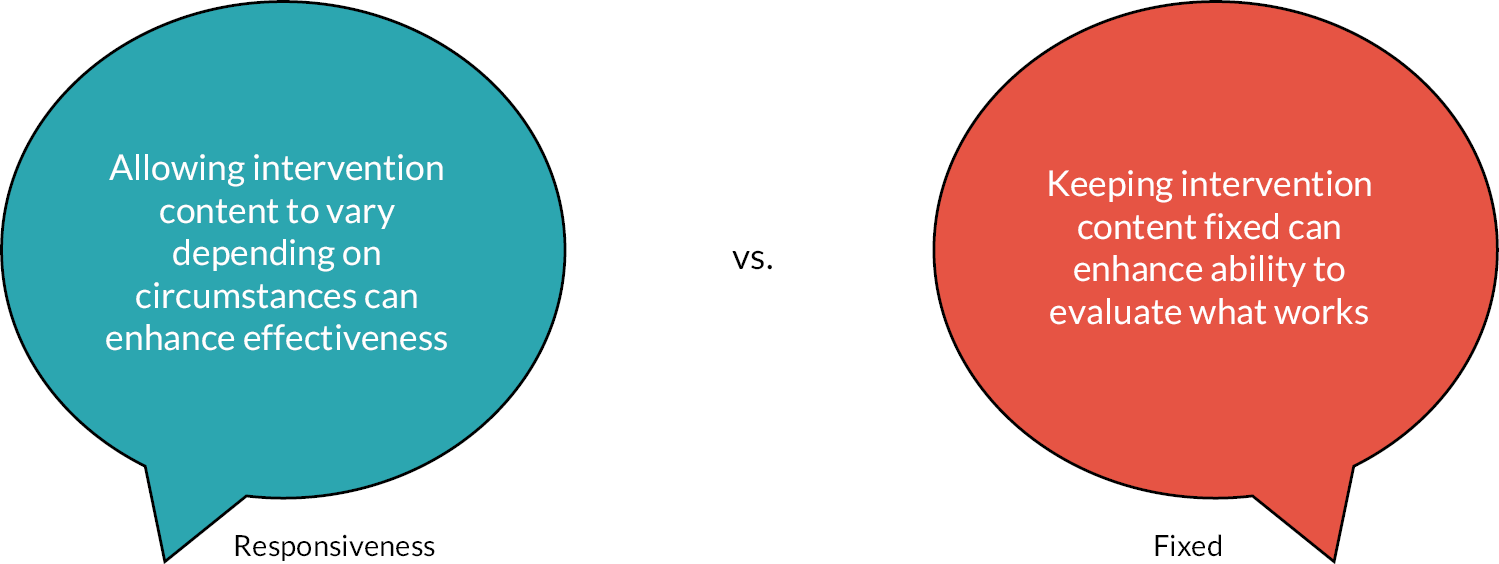
-
Interventions to reduce UB can also enhance patient safety if well considered.
If interventions to reduce UB want to also have a significant impact on improving patient safety, they need to improve the ability to speak up in critical moments when it is important, for example, when medical errors are occurring, and the ability of managers to act on these concerns. Addressing UB is key to keeping people safer. While speaking up retrospectively is important, caution is required to avoid a focus on hindsight only (e.g. Francis report). The use of informal systems may be a useful safety value and syphon of data about how things ‘really work around here’, providing data about the conversational culture (e.g. What would need to be different to make it more likely we can say it in the moment?).
We identified that some interventions may incentivise speaking up later, for example with an online reporting system, which may reduce UB but not help improve patient safety. To address this factor, leaders and managers may wish to:
-
seek to understand the likely impacts of the strategies selected in their intervention, including whether they foster a culture that enables people to speak up ‘in the moment’ or not and consider the consequences of these for patient safety
-
maintain a focus on outcomes further down the causal chain, such as improving patient safety, rather than simply reducing UB – as these may not always be the accomplished through the same means.
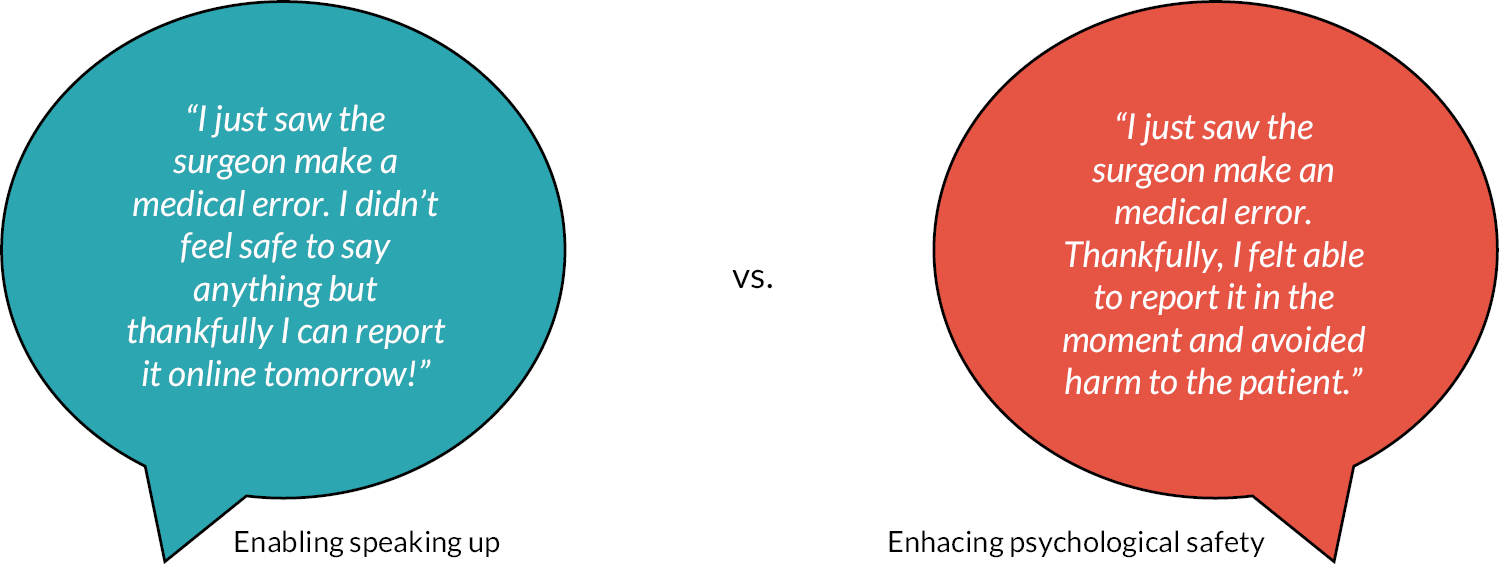
Glossary of terms
| Term | Definition |
|---|---|
| Allyship | When an individual from a more privileged background publicly comes out in support of less privileged colleagues and actively furthers their cause |
| Datix | Datix is a Risk Management Information System to collect and manage data on adverse events (as well as data on complaints, claims and risk) which is currently in use in the UK’s NHS179 |
| Ethos | A professional accountability intervention being tested in Australia. ‘Ethos aims to “redefine normal” and tackle the problem of unprofessional behaviour across all staff groups. The program uses trained peer envoys who provide feedback about reported behaviour to colleagues in an informal, non-punitive manner. The program includes organisation-wide training of staff to increase their skills in identifying and dealing with unprofessional behaviour’10 |
| People with ‘protected characteristics’ | A term originating in the UK, it refers to characteristics which it is against the law to discriminate upon. These include age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation |
| UB (as used in this document) | Any interpersonal behaviour by staff that causes distress or harm to other staff in the healthcare workplace |
| Vanderbilt | A large university medical centre in the USA, Vanderbilt have developed a professional accountability intervention upon which Ethos is also based. Vanderbilt has at its core ‘four graduated interventions: informal conversations for single incidents, nonpunitive “awareness” interventions when data reveal patterns, leader-developed action plans if patterns persist, and imposition of disciplinary processes if the plans fail’98 |
Glossary
Allyship When an individual from a more privileged background publicly comes out in support of less privileged colleagues and actively furthers their cause.
Context Aspects of the setting in which a programme is implemented which affect how mechanisms are triggered. This can include geographical, social, resource, participant or other features (Greenhalgh J, Manzano A. Understanding ‘context’ in realist evaluation and synthesis. Int J Soc Res Methodol 2022;25:1–13. https://doi.org/10.1080/13645579.2021.1918484; Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist synthesis: RAMESES training materials. RAMESES Proj 2013;55:1–54).
Context–mechanism–outcome configurations A realist heuristic that enables an understanding of generative causation. This is typically constructed as ‘an outcome (O) of interest was generated by relevant mechanism(s) (M) being triggered in specific context(s) (C)’ (Wong G et al., 2013).
Datix Datix is a risk management information system to collect and manage data on adverse events (as well as on complaints, claims and risk), which is currently in use in the United Kingdom’s National Health Service (RLDatix, Making Healthcare Safer 2023. https://rldatix.com/en-uke/).
Ethos A professional accountability intervention being tested in Australia. ‘Ethos aims to “redefine normal” and tackle the problem of unprofessional behaviour across all staff groups. The programme uses trained peer envoys who provide feedback about reported behaviour to colleagues in an informal, nonpunitive manner. The programme includes organisation-wide training of staff to increase their skills in identifying and dealing with unprofessional behaviour’ (Westbrook JI, Urwin R, McMullan R, Badgery-Parker T, Pavithra A, Churruca K, et al. Changes in the prevalence of unprofessional behaviours by co-workers following a 2 professional accountability culture-change program across five Australian hospitals. Unpublished).
Mechanisms ‘… mechanisms are a combination of resources offered by the social programme under study and stakeholders’ reasoning in response’. (Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10:49. https://doi.org/10.1186/s13012-015-0237-x).
Outcomes ‘Outcomes are any intended or unintended changes in individuals, teams or organisational culture generated by context-mechanism interactions’ (Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E, Ross S, Shuldham C, Bennett L, Foot C. A realist informed mixed-methods evaluation of Schwartz Center Rounds® in England. Health Serv Deliv Res 2018;6(37):1–260).
People with ‘protected characteristics’ A term originating in the United Kingdom, referring to characteristics against which it is against the law to discriminate. These include age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex and sexual orientation.
Programme theory ‘A set of theoretical explanations or assumptions about how a particular programme, process or interventions is expected to work’ (Maben J, Taylor C, Jagosh J, Carrieri D, Briscoe S, Klepacz N, et al. Care under pressure 2: caring for the carers – a realist review of interventions to minimise the incidence of mental ill-health in nurses, midwives and paramedics. NIHR HS&DR; 2023. https://sites.exeter.ac.uk/careunderpressure/care-under-pressure-2/).
Retroduction ‘Identification of hidden causal forces that lie behind identified patterns or changes in those patterns’ (Maben et al., 2023).
Unprofessional behaviour (as used in this report) Any interpersonal behaviour by staff that causes distress or harm to other staff in the healthcare workplace.
Vanderbilt A large University Medical centre in the United States of America, Vanderbilt have developed a professional accountability intervention upon which Ethos is also based. Vanderbilt has at its core ‘four graduated interventions: informal conversations for single incidents, nonpunitive “awareness” interventions when data reveal patterns, leader-developed action plans if patterns persist, and imposition of disciplinary processes if the plans fail’ (Hawkins N, Jeong S, Smith T. New graduate registered nurses’ exposure to negative workplace behaviour in the acute care setting: an integrative review. Int J Nurs Stud 2019;93:41–54. https://doi.org/10.1016/j.ijnurstu.2018.09.020).
WeCare A professional accountability intervention similar to Ethos that enables users to ‘report unprofessional behaviours or recognise staff who demonstrate the organisation’s values. Reporters can choose to remain anonymous’ (McKenzie LN, Shaw L, Jordan JE, Alexander M, O’Brien M, Singer SJ, Manias E. Factors influencing the implementation of a hospitalwide intervention to promote professionalism and build a safety culture: a qualitative study. Jt Comm J Qual Patient Saf 2019;45:694–705. https://doi.org/10.1016/j.jcjq.2019.07.005).
List of abbreviations
- BCT
- behaviour-change technique
- BLM
- black lives matter
- BMA
- British Medical Association
- CBM
- Cognitive Bias Modification
- CCF
- Central Commissioning Facility
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CFIR
- consolidated framework for implementation research
- CMOC
- context, mechanism and outcome configuration
- COM-B
- capability, opportunity and motivation for changing behaviour (model of behaviour)
- CQC
- care quality commission
- CREW
- civility, respect and engagement in the workforce
- CUP2
- Care Under Pressure 2 (research project)
- ED
- emergency department
- EDI
- equality, diversity and inclusion
- EIT
- evidence integration triangle
- FAE
- fundamental attribution error
- HCPC
- Health and Care Professions Council
- HMIC
- Health Management Information Consortium
- i-PARIHS
- Integrated Promoting Action on Research Implementation in Health Services
- JDR
- job demands and resources model
- LGBTQ+
- lesbian, gay, bisexual, transgender, queer, intersex, asexual and more
- MEDLINE
- Medical Literature Analysis and Retrieval System Online
- MRC
- Medical Research Council
- MRT
- middle-range theory
- NAQ-R
- Negative Acts Questionnaire ‐ Revised
- NETSCC
- NIHR Evaluation, Trials and Studies Coordinating Centre
- NHS
- National Health Service
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OD
- organisational development
- PPI
- patient and public involvement
- RAMESES
- Realist And MEta-narrative Evidence Syntheses: Evolving Standards
- RCT
- randomised controlled trial
- UB
- unprofessional behaviour
Notes
-
RAMESES checklist
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/PAMV3758).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
