Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/49/70. The contractual start date was in March 2019. The final report began editorial review in November 2021 and was accepted for publication in September 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Gillard et al. This work was produced by Gillard et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Gillard et al.
Chapter 1 Introduction
Mental health crisis care
People living with challenges to their mental health can experience an acute mental health crisis while living in the community. This can include intense feelings of depression, anxiety or paranoia, including feeling suicidal, and can result in the individual and/or their family and loved ones feeling that they are unable to cope without urgent, professional support. In England, people who are already using secondary mental health services in the NHS might be able to contact their care coordinator, an out-of-hours service or mental health crisis line, and be referred directly to crisis care services. For example, they might receive regular visits from a crisis resolution and home treatment (CRHT) team for a short period until the immediate crisis has passed or be admitted to psychiatric inpatient care for a period of assessment and/or treatment. People who are not already in contact with mental health services, or who are unable to wait to be referred to specialist care, will often present at hospital emergency departments (ED). People who self-harm or attempt suicide as a result of their distress can self-present at, or be transported to, an ED by emergency services. In ED, people will first be triaged by a member of the ED team and if a mental health need is identified – and once any immediate medical need (e.g. resulting from self-injury) is resolved – be seen by a member of the liaison psychiatry, assessed, and follow-up care arranged (including, if deemed necessary, a psychiatric inpatient admission).
Mental health crisis care, as described above, is under intense pressure in the UK1 and in equivalent systems internationally. 2–6 Visits to EDs for mental health issues are increasing while the number of available psychiatric inpatient beds is decreasing, resulting in challenges to the ED system7 and lengthy waits in ED for people in mental health crisis. 8 In England, the ED system has been described as near breaking point. 9 Approximately two in three of all people with multiple attendances at ED have been in contact with specialist mental health services or have had a previous acute psychiatric admission,10 with frequent attenders at greater risk of psychiatric inpatient admissions. 11 People presenting with a mental health issue are over six times more likely than people presenting with a physical concern to wait more than 4 hours at the ED12 (in England breaches of a 4-hour wait are a key performance indicator for EDs). Mental disorders are estimated to account for around 5% of ED attendances in the UK and almost 30% of acute inpatient bed occupancy and acute readmissions. 13 Poor experiences and low levels of satisfaction with mental health care all point to the ED as not being a far from ideal environment for support and treatment for mental health crisis. 12,14
Psychiatric inpatient stays can be costly,15 in some cases detrimental to mental health,16 disproportionately harmful to people from some minority ethnic groups,17 and reportedly unnecessary for as many as 17% of referred individuals. 18 Admissions following an acute crisis can be brief (often < 5 days), yet the effectiveness, cost-effectiveness and outcomes of short stays on psychiatric wards followed by early discharge is unclear. 19 Bed occupancy in inpatient psychiatric facilities is well above recommended levels with 91% of wards operating above the recommended occupancy rate. 13
The emergence of liaison psychiatry services has enabled mental health NHS trusts to provide responsive mental health assessment, advice and onward referral within emergency care settings, but wide variations in service provision20 remain and there are ongoing challenges to sustainability. 21 The introduction of CRHT teams22,23 and triage wards24 has offered little benefit in reducing contact with acute services, inpatient admissions or costs across the wider inpatient system compared with standard models of care, with ongoing staff concerns over the accuracy of triage decisions for mental health presentations in ED. 25,26 To address these growing challenges, policy in England has called for the development and evaluation of new, more effective models of crisis care as collaborations between health, mental health, social care, third sector and emergency service providers locally. 27,28 Alongside new street triage services,29 crisis houses30 and crisis cafes,31 some delivered in the third sector,32 psychiatric decision units (PDUs) have emerged as just one of a number of responses.
The psychiatric decision unit
Psychiatric decision units – also known in England as mental health decision units, crisis assessment units or assessment suites, among similar terms – have been set up in response to policy and the need to manage demand, to reduce unhelpful admissions to acute inpatient care, especially avoidable short admissions and expensive out-of-area or private admissions, and reduce mental health presentations at ED. International counterparts to the PDU fulfil a similar function,33 can be known as a psychiatric emergency service (PES), crisis stabilisation units or behavioural assessment units, and have become increasingly critical to the delivery of mental health crisis care. 34–36 This is particularly true for the USA where a third of hospitals are estimated to provide these emergency units,37 but they are also present in, for example, France,38 Singapore39 and Australia. 40
There is no single service specification for PDUs in England but rather a shared set of characteristics. PDU are short-stay facilities, based either on psychiatric or general hospital sites, for people in acute mental health crisis, offering time-limited care (typically up to 24–72 hours) including overnight stay. Units target people who experience repeat, often extended stays in ED, frequent use of other services such as the police and ambulance services, and have complex and frequent crisis-related needs but who might not benefit from a psychiatric inpatient stay. The focus of the units is on providing a comprehensive assessment in a calm, safe environment, offering therapeutic input as appropriate, and onward signposting and referral to a range of community-based care, both within and outside the NHS, hopefully breaking the cycle of repeat ED presentation and/or unhelpful acute admission. PDUs are distinguishable from triage or assessment wards; short-stay wards which typically accept all patients likely to require assessment or treatment in an inpatient setting. 41 Additionally, PDUs typically only accept informal patients (i.e. people not admitted assessment or treatment sections of the Mental Health Act), whereas triage wards will admit people formally under the Mental Health Act. Furthermore, as admission to PDU is not a formal inpatient admission, PDU staff are not required to complete inpatient treatment plans or the clustering tool for admission as they would on a ward, freeing up more time for individual face to face contact. Staff-to-patient ratio – at around 1 : 2 – is also typically higher than in an inpatient ward (typically around 1 : 4). 42 PDUs are often nurse led, supported by healthcare assistants (HCAs), with consulting input from psychiatry and other mental health professionals. PDUs can be co-located and share staffing with a Section 136 Place of Safety. Overnight accommodation is single sex, sometimes with flexible partitioning to enable the unit to respond to different numbers of male and female visitors, generally comprising reclining seating rather than beds. Units tend to be small with a capacity of around six to eight.
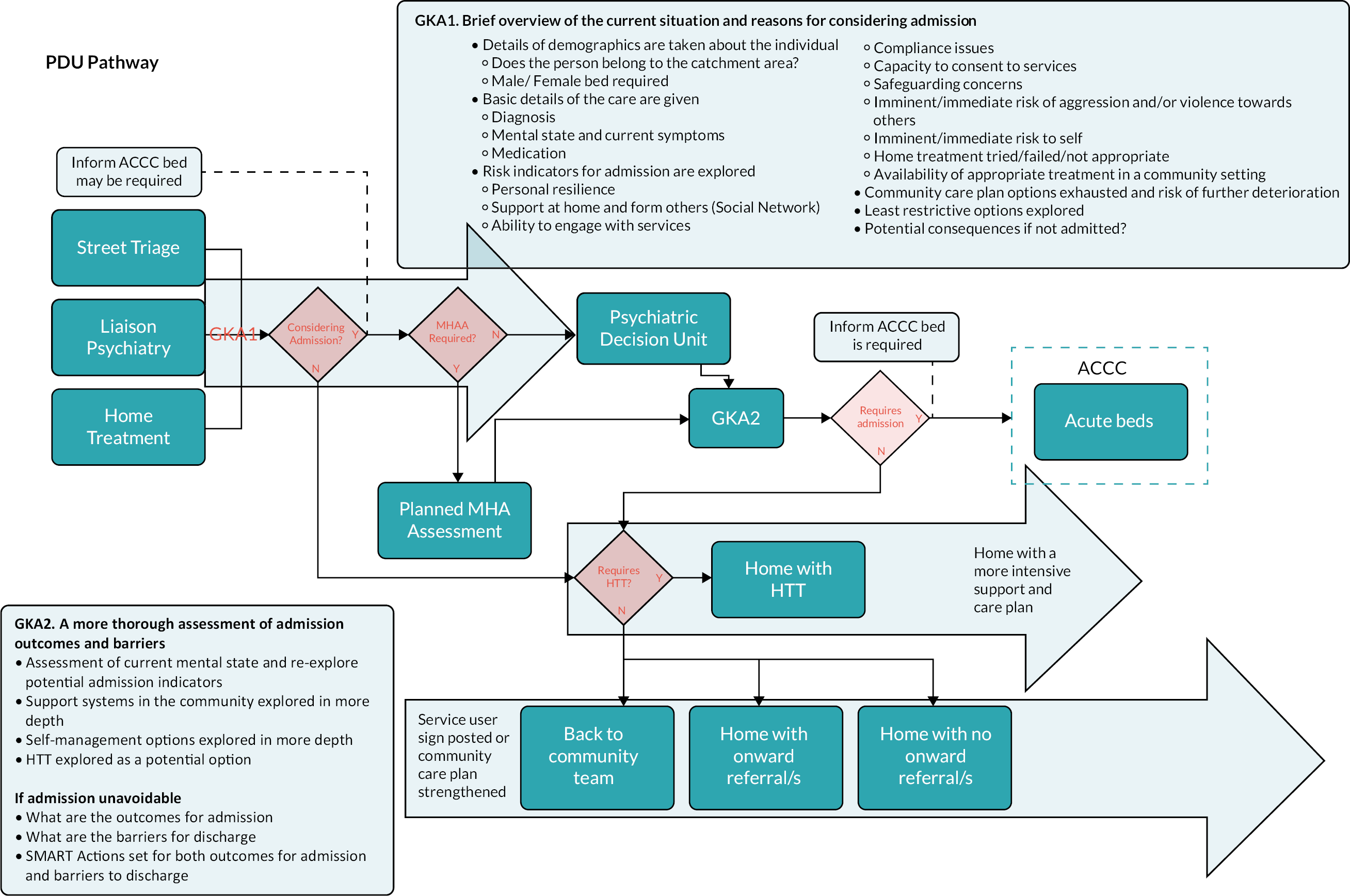
Efforts have been made to establish PDUs as an integrated part of the crisis care pathway. 43 PDUs accept referrals directly from liaison psychiatry teams based in ED, other mental health crisis services (e.g. CRHT and street triage teams), and sometimes community mental health services, primary care or third sector services – but do not generally accept self-referrals – with formal gatekeeping procedures in place. An example of the location of a PDU in the crisis care pathway in one of our sites can be seen in Figure 1, with the PDU playing a gatekeeping (assessment and referral) role for people identified by crisis services as having a higher level of need than might be met by intensive home treatment yet not in need of a Mental Health Act assessment, and from where a decision can be made about either subsequent inpatient admission or a return home with an appropriate support plan.
FIGURE 1.
Crisis care pathway map.
Aims and objectives
Although formal evaluations of recently developed PDUs in the USA and Australia have suggested that PDU-type units might reduce length of stay (LOS) in EDs and inpatient psychiatric admissions among people experiencing mental health crisis,37,40 evidence regarding the characteristics and effectiveness of PDUs in England is restricted to informal local evaluations. 44,45 While these reports suggest PDUs have potential to reduce demand on ED and psychiatric admissions, key data have not been reported (e.g. LOS in the ED) and study designs have not adequately accounted for variables that might confound comparison. In addition, PDUs in England have been developed organically, in response to policy and the pressure on services rather than the evidence base. There is a need for a clear description of the PDU model, including identification of key variables in unit configuration and function, and an understanding of how PDUs fit alongside other services in the crisis care pathway. It is possible PDUs introduce further fragmentation to the system, and, if not effective, may waste critical resources. As such, a formal evaluation of these services is urgently required to describe the model of care and generate much-needed knowledge about impacts, quality, and cost benefits.
The aim of the study is to ascertain the structure and activities of operational PDUs in England and to provide an evidence base for their effectiveness, costs and benefits, and optimal configuration. The study aim is addressed through the following research questions:
-
What is the range of hospital-based, short stay interventions internationally designed to reduce admissions to acute psychiatric inpatient care and what is their effectiveness?
-
What is the scope and prevalence of PDUs nationally and how are they configured?
-
How has the introduction of PDUs impacted on psychiatric inpatient admissions and ED psychiatric episodes/breaches?
-
What are the care pathways before and following an admission to the PDU?
-
What is the impact of the introduction of PDUs on inequalities of access to acute mental health services?
-
How do service users experience PDUs, as well as crisis care pathways before and after admission to PDU?
-
How are decisions made about referral and admission to PDU, and assessment and onward signposting and referral?
-
How do the economic costs and impacts of PDUs compare with areas without PDUs?
-
How do the costs for individual service users post PDU implementation compare with their costs prior to the introduction of PDUs to crisis care pathways?
Chapter 2 Methods
A mixed-methods approach
This is a mixed-methods study in six work packages (WP): WP1 – systematic review and service mapping; WP2 – interrupted time series (ITS) analysis; WP3 – synthetic control study; WP4 – cohort study; WP5 – qualitative interview study; WP6 – health economic analysis. A mixed-methods approach is taken to address the range of research objectives identified in Chapter 1, incorporating a number of different types and sources of data necessary to answer a broad set of research questions. 46 The underlining framework is a multilevel organisational research approach proposing that findings at an individual level cannot be assumed to apply at a higher (e.g. population) level or vice versa, because the ‘nested complexity of organisational life’ impacts on the phenomena we are trying to understand or measure. 47 Drawing on Goffman’s multilevel frame analysis,36 it is necessary to ‘frame’ our enquiry at macro, meso and micro levels ‘to understand the pace, direction and impact of organisational innovation and change’37 as well as the interconnection between levels. This involves specifying, at each level, the construct we wish to test, how we will measure that construct, what our sample or data source will be, and what analytical approaches we will use. Best available data are used from a range of sources at each level to produce utilisable knowledge,35 informing the further development and implementation of PDUs nationally. We conceptualise our levels of enquiry as:
-
Macro – national: how do policy, clinical guidance and other trends at a national level impact on the effectiveness and cost benefits of PDUs?
-
Meso – organisational: how does the configuration of crisis care pathways (including the provision of other crisis care services) and the structure of PDUs at site level impact on the effectiveness and cost benefits of PDUs?
-
Micro – individual: how do individual service user experiences of crisis care (including the PDU) and individual clinical staff decision-making processes along the pathway impact on the effectiveness and cost benefits of PDUs?
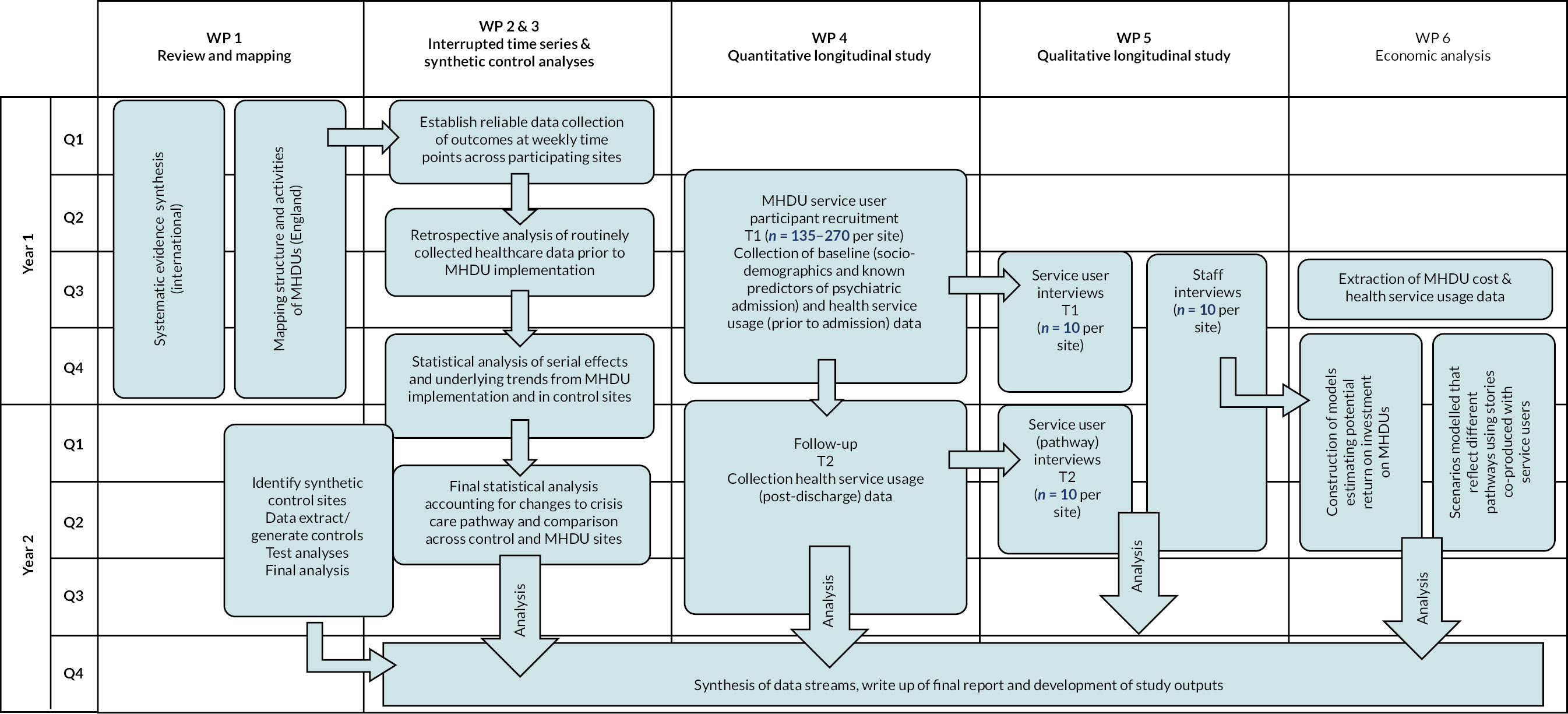
The specific way in which we frame research questions at each level and identify data sources and research methods for each of the six WPs is detailed in Table 1. Note that some questions (3 and 9) are broken down further with subquestions (a and b) and that on question, 3a is addressed in three different WPs (2–4), each using a different data set and, in some cases, covering different time periods. The challenges of this for data synthesis are addressed in Chapter 9. A diagram indicating how WPs are sequenced is given in Figure 2.
| WP | Question | Method | Level | Data source |
|---|---|---|---|---|
| WP 1 – review and mapping | 1) What is the range of hospital-based, short-stay interventions internationally designed to reduce standard admissions to acute psychiatric inpatient care and what is their effectiveness? | Systematic review | Macro | Peer-reviewed literature |
| 2) What is the scope and prevalence of PDUs nationally and how are they configured? | Service mapping | Macro | Telephone interviews, MHT strategic leads | |
| WP 2 – ITS | 3a) How has the introduction of PDUs impacted on psychiatric inpatient admissions and ED psychiatric episodes/breaches? | ITS analysis; qualitative interview study | Meso | Routinely collected, aggregate data from MHTs and EDs at hospital NHS trusts |
| 3b) What is the impact of policy changes at local and national level? | ||||
| Macro | Semistructured interviews with MHT and ED strategic leads and commissioners | |||
| WP 3 – SC study | 3a) How has the introduction of PDUs impacted on psychiatric inpatient admissions and ED psychiatric episodes/breaches? | Synthetic control study | Macro | Comparison of NHS Digital data between study sites and comparator sites |
| WP 4 – cohort study | 3a) How has the introduction of PDUs impacted on psychiatric inpatient admissions and ED psychiatric episodes/breaches? 4) What are the care pathways before and following an admission to the PDU? 5) What is the impact of the introduction of PDUs on inequalities of access to acute mental health services? |
Cohort study | Meso | Routinely collected, individual data of mental health and ED service use (new admissions to PDU) Participant characteristics (sociodemographic, psychiatric history etc.) |
| WP 5 – qualitative study | 6) How do service users experience PDUs, as well as crisis care pathways before and after admission to PDU? | Qualitative interview study | Micro | Semistructured interviews with service users admitted to PDU |
| 7) How are decisions made about referral and admission to PDU, and assessment and onward signposting and referral? | Semistructured interviews with ED, MHT crisis services and PDU staff | |||
| WP 6 – economic analysis | 8) How do the economic costs and impacts of PDUs compare with areas without PDUs? 9a) How do the costs for individual service users post PDU implementation compare with their costs prior to the introduction of PDUs to crisis care pathways, as well as in areas without PDUs? |
ITS; synthetic control study; cohort study | Meso and macro | Economic analysis of aggregate and individual-level MHT and ED service use data Appropriate unit cost data attached to services Liaison with PDU service providers and use of administrative data to determine resources used to deliver PDU services |
| 9b) What are the potential cost impacts of: i) alternative configuration of PDU pathways or access by specific populations, and ii) roll out and scale up of PDUs nationally? | All | Macro | As above, plus qualitative pathway stories, referral source and participant characteristics data |
FIGURE 2.
Sequencing of work programmes.
Patient and public involvement in the project
A co-production approach to research has underpinned this project. The team leading the research has a strong track record in methodological development, support and evaluation of coproduction throughout a research project. In previous National Institute for Health and Care Research (NIHR)-funded research we developed a set of characteristics of co-produced research:
-
High-value research decision-making roles distributed across the research team (including team members with lived experience of using mental health services and/or mental distress, as well as clinical and university researchers).
-
Different interpretations of data within the research team owned and understood in terms of who offered the interpretation.
-
Consideration given to whether all members of the team are involved in the production of knowledge and the impact of this on the knowledge produced.
-
Methodological flexibility in the research process (where the scientific conventions of how research is usually might constrain the input of team members with lived experience).
-
Rigorous and critical reflection on how the research was done and the impact of this on findings.
-
Research outputs that report critically on how knowledge was produced. 48
Lived experience in the research team in this project comprised:
-
co-investigator (KT): a qualitative researcher with many years’ experience of working from a lived experience perspective in mental health research
-
three researchers explicitly employed to work from a lived-experience perspective (KA, LG, JL)
-
Peer Expertise in Education and Research (PEER) group (a lived-experience research reference group at the lead site)
-
Lived Experience Advisory Panel (LEAP): a group of eight people recruited nationally with lived experience of mental health distress, crisis and attending a PDU and or experience as an informal carer of someone with those experiences
-
lived-experience representation on the project steering group.
We used lived experience in developing the project as follows:
-
Two workshops with the PEER group discussing the study as a whole and the importance of employing a non-randomised study design in the context of crisis care, the ethics of use of routinely collected patient data in the cohort study, and identifying specific questions to be explored in qualitative interviews.
-
Co-investigator KT contributed to developing the proposal from a lived-experience perspective, playing a key role in developing the co-produced approach to interpreting qualitative data sets,48 extended here to our data synthesis approach.
Using lived-experience during the research:
-
A third workshop was held with the PEER group to support the application for NHS ethical approval for the study, including development of participant information sheets and informed consent procedures.
-
The two researchers working from lived experience focused on development and delivery of WP5 data collection, analysis and write-up, as well as shaping and carrying out the WP1 mapping exercise and systematic review.
-
The LEAP was facilitated by the two researchers working from lived experience with co-investigator KT’s support; the group met eight times during the study. The LEAP provided input into conduct of the study as it progressed, with input into material and application for ethical approval and the development of qualitative interview schedules.
-
The LEAP also played an active role in the analysis of qualitative research data with members involved in the preliminary coding of interview data and in interpretive workshops.
-
A second interpretive workshop involving the LEAP was held to ensure that lived experience informed the synthesis process bringing together data from all WPs to develop our final report.
-
A final session of the LEAP was held to plan and design an applied output for the study (not reported here) aimed at helping people in crisis better negotiate the crisis care pathway.
-
The lived-experience researchers on the team provided training to LEAP members as necessary, including around data analysis processes.
-
Co-investigator KT oversaw patient and public involvement on the project and provided support to the lived experience researchers on the team, including facilitating a regular lived experience reflective space.
-
There was lived experience on the study’s independent steering committee, brought by two committee members with who had made use of mental health crisis care, one of whom had also worked on a PDU in a support worker capacity.
We reflect on the impacts of patient and public involvement and our approach to coproduction in the study in the section on the Impact of patient and public involvement on the research.
Setting
With the exception of WP1, the study took place in four sites; sites were MHTs that had an operational PDU and the EDs at NHS hospitals in the same locality as the MHT that referred to the PDU. Key characteristics of study sites, including configuration of the PDU and other crisis care services available locally, are given in Table 2. Any changes in PDU or other crisis care provision during the time frame of the research, including those resulting from the COVID-19 pandemic, are indicated in parentheses.
| PDU | Referring ED(s) | Geography | Date opened | Location | Maximum LOS (hours) | Capacity (n) | Referral route | Staffing | Staff : patient ratioa | Other crisis services |
|---|---|---|---|---|---|---|---|---|---|---|
| Lotus Assessment Suite, SWLSTG MHT | SWLSTG; KHFT | Urban | November 2016 | Psychiatric hospital | 48 | 5 (increased to 7 during COVID-19 pandemic) | ED, CRHT, street triage | Mental health nurse, HCA, psychiatrist | 1 : 1 | Crisis house, crisis rather (x 2), (mental health ED opened during COVID-19) |
| Decision Unit, STHFT | STHFT | Urban | March 2019 | Psychiatric unit on a general hospital site | 48 (decreased to 24 during COVID-19 pandemic) | 5 | ED, CRHT, street triage, CMHT | Mental health nurse, support worker, psychiatrist | 4 : 5 | Crisis house |
| Psychiatric Clinical Decisions Unit, LPFT | ULHFT | Rural | January 2018 | Psychiatric hospital | 24 | 6 | ED, CRHT, street triage (16 months after PDU opens), AMHPs | Mental health nurse, HCA, psychiatrist (plus CMHT during COVID-19) | 1 : 2 | Triage ward, crisis house |
| PDU – BSMHFT MHTs | SWBHFT; UHBFT | Urban | November 2014 | Psychiatric hospital | Target 24 (72 maximum, reducing to 12 from 2019) | 8 (decreased to 5 during COVID-19 pandemic) | ED, CRHT, street triage | Mental health nurse, HCA, psychiatrist | 1 : 4 | Triage ward (16 months only), acute day unit, crisis café, crisis house (post-WPs 2 & 3) |
Service mapping
Design
We conducted a survey of PDUs in England, establishing their prevalence, structure and how they complement other NHS crisis care locally. A PDU was defined as a specific location where individuals in mental health crisis and using emergency care may be assessed and treatment plans formulated. The specific location should be distinct from the ED and psychiatric wards. We used a formal freedom of information (FOI) request to reduce nonresponses, as government organisations are legally compelled to answer under UK legislation. 49
Participants
NHS FOI and mental health service staff were the participants. Respondent role was noted.
Measures
An iterative cycle of questionnaire development, considering information about PDUs in study sites, was undertaken to establish how to define PDUs for the survey. A 29-item questionnaire was developed to determine whether mental health NHS trusts had a PDU and the operational structure of PDUs (e.g. capacity, maximum LOS, referral sources, staffing). We also asked about existence of alternative assessment provision (e.g. triage ward) and other crisis care (e.g. street triage team). Short open questions inquired about the purpose of the PDU.
Procedures
We used a publicly available list of mental health NHS trusts’ FOI e-mail addresses49 to send the survey for completion using LimeSurvey (LimeSurvey GmbH, Hamburg, Germany), a secure web survey system; trusts were given the option to complete the survey on paper. Reminders were sent if trusts failed to acknowledge the FOI request within 7 days or respond to the survey within 20 working days. For precision, data were checked against responses from a recent survey of crisis care50 and incomplete or contradictory responses checked using information on trust websites or direct contact by e-mail or telephone. Follow-up questions were asked about PDUs identified in the survey as planned or closed to determine the reasons for launching or discontinuation. The survey ran between September and December 2019.
Analysis
Descriptive statistics were used to present quantitative data. Qualitative data were analysed using narrative synthesis.
Systematic review
Search strategy
We searched EMBASE, MEDLINE, Cumulative Index to Nursing and Allied Health Literature, PsycINFO® (American Psychological Association, Washington, DC, USA) and the Cochrane Central Register of Controlled Trials from inception until 01 March 2021. Reference list and forwards citation checking of included studies was used to identify additional sources.
Eligibility
Inclusion
-
Studies of adults (over 18 years) experiencing a mental health or behavioural crisis.
-
Any mental health assessment intervention that: (1) is hospital-based; (2) permits overnight stay; (3) specifies a maximum LOS < 1 week; (4) has as its primary aim assessment and/or stabilisation, with the purposes of reducing the need or LOS of standard acute care admission, and/or reducing presentation or length of waiting time at an ED.
-
Measurement of standard acute admissions to psychiatric inpatient care (including number, type and duration of admission), and/or mental health presentations at EDs (including number of presentations and length of wait in ED) and other related outcomes.
Exclusion
-
Children; non-human subjects; all individuals detained under Mental Health Act section (or equivalent in country of study); all individuals who are forensic patients.
-
Community (i.e. no overnight stay is possible) or non-hospital, residential-based assessment or crisis units.
-
No measure of psychiatric inpatient service use or ED attendance.
Eligible study designs
Randomised controlled trials (RCTs) or studies incorporating a control or comparison group (e.g. a control group for between group comparisons or a pre-intervention period for a within-group study) including single-, double- or triple-blinded trials, ITS, quasi-experimental, observational, before-and-after or retrospective studies. We excluded studies with no comparison group or that were entirely qualitative.
Selection of studies
Electronic database search results were uploaded to CADIMA (Julius Kühn-Institut Federal Research Centre for Cultivated Plants, Quedlinburg, Germany)51 and duplicates removed using the CADIMA de-duplication process. To identify papers that potentially met eligibility criteria, 20% of abstracts and titles of retrieved studies were screened independently by two researchers (KA, JL). Inter-rater reliability (IRR) scores were recorded and exceeded the target of a moderate level of IRR (0.41). The remaining study titles and abstracts were screened singly by the two researchers.
Full texts of all papers included at the screening stage were reviewed by two researchers (KA, JL) to confirm eligibility. Disagreements, or where both researchers were uncertain of eligibility, were resolved through discussion with a third researcher (SG).
Data extraction
A standardised, pre-piloted form in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) was used to extract data from included studies for quality assessment and evidence synthesis. Key information for extraction included:
-
characteristics of included study (e.g. study design; number and type of groups)
-
participants (e.g. country, eligibility criteria, recruitment method, number of participants in each group, demographics)
-
intervention groups (maximum LOS, purpose of unit, admission criteria, referral pathway and staffing, theoretical basis for the intervention, resource requirements etc.)
-
comparison groups (description, resource requirements, co-interventions)
-
all outcomes with a comparison group and associated statistics
-
data for risk of bias, assessed as described below.
Two researchers (KA and JL) independently extracted data on items 1–4 above from included studies, and two researchers (KA and LG) on items 5 and 6. Data extraction was cross-checked, with discrepancies resolved through discussion with the wider team.
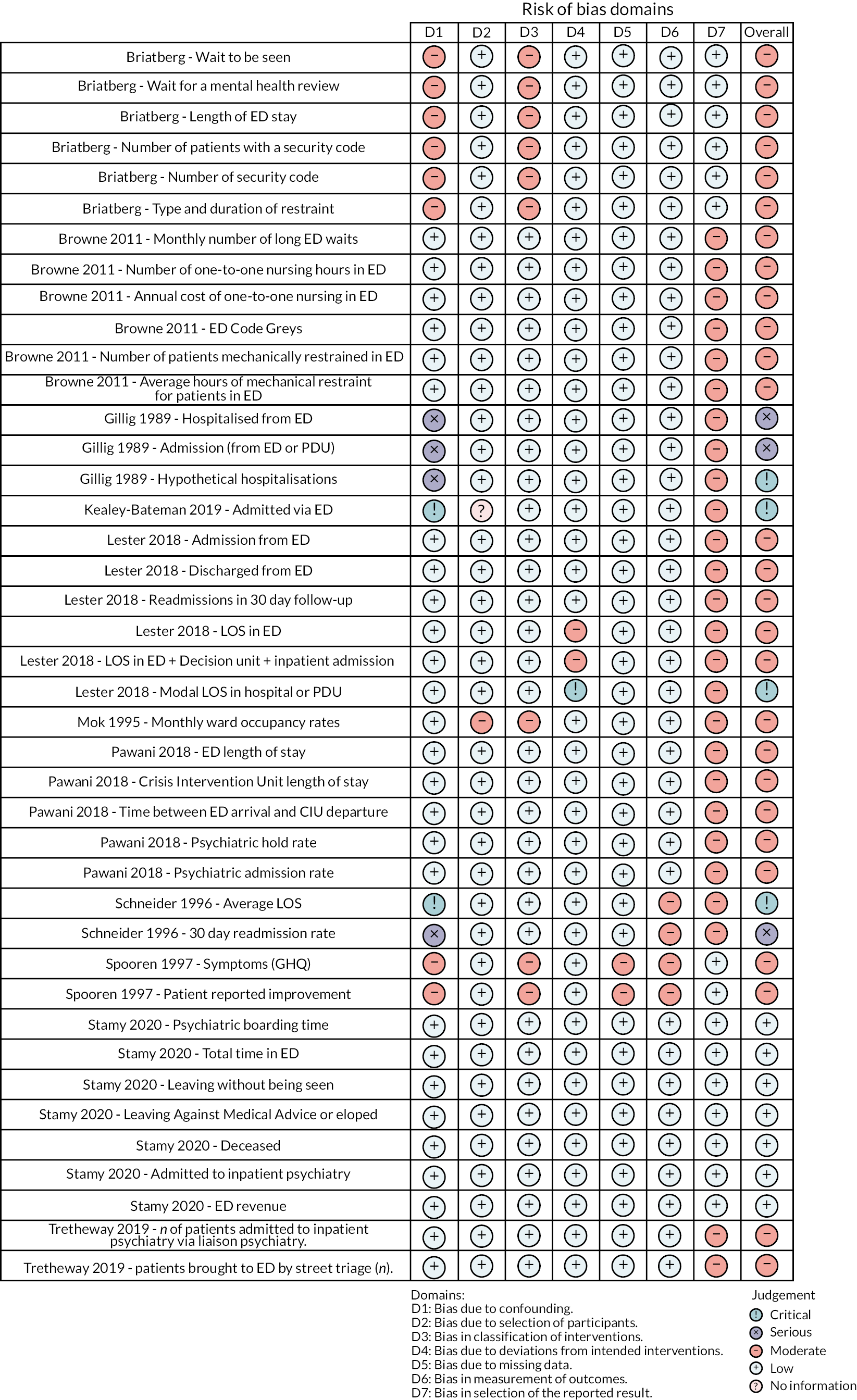
Risk of bias (quality) assessment
For RCTs, the Cochrane Collaboration’s revised risk of bias tool RoB 2 was used. 52 This is a widely used tool to assess bias using a judgement (high, some or low concern) in five domains (randomisation process, deviation from intervention protocol, missing outcome data, measurement of outcome and selection in the reporting of outcomes), as well as overall. For nonrandomised studies, the Risk of Bias in Non-randomised Studies of Interventions (ROBINS-I) tool53 was used. This tool is structured in seven sequential domains (pre intervention, at intervention and post intervention) and the assessment of domain-level and overall risk of bias judgement classified as low, moderate, serious or critical risk of bias. Risk of bias plots were created for all outcomes using the robvis application. 54
Quality was assessed independently by two researchers (KA and LG), with discrepancies resolved through discussion and taken to a third researcher (SG) if unresolved. Studies assessed as being at high risk of bias were included in primary analyses but removed from a secondary, sensitivity analysis (see below). Each meta-analysis was rated for the certainty of the evidence using Cochrane’s Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework. 55 The certainty of the evidence was discussed for all reported outcomes.
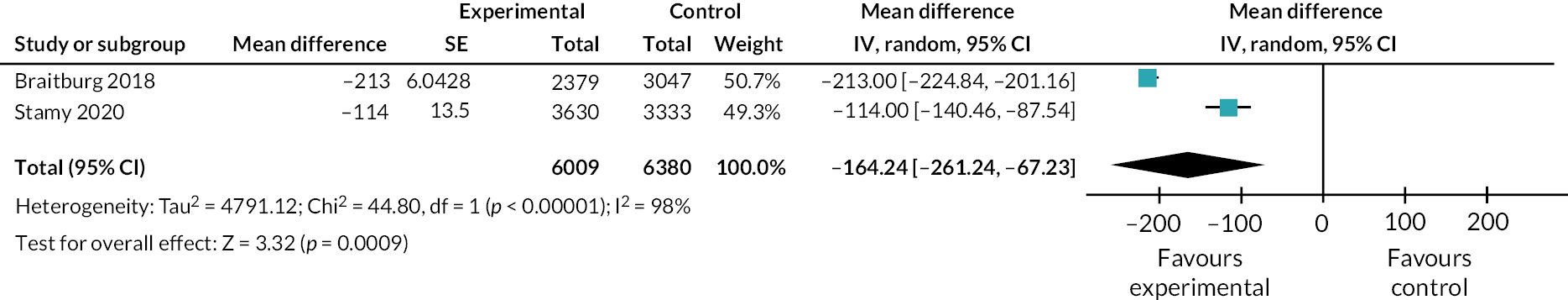
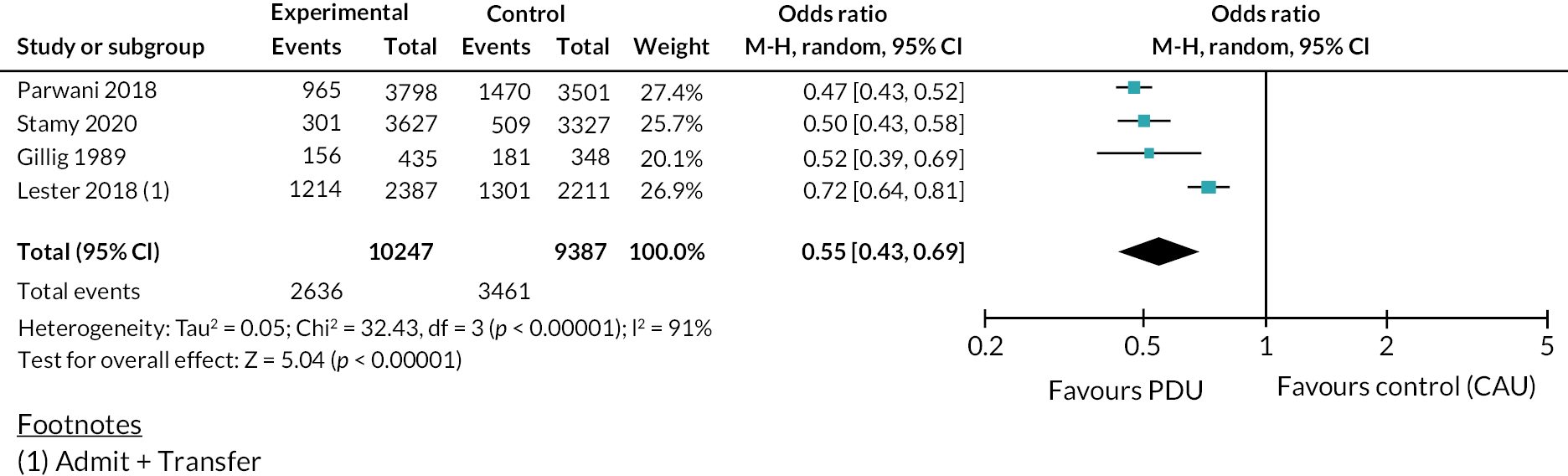
Data synthesis
Narrative synthesis of all included studies was undertaken, including a brief narrative description of risk of bias. Where sufficient studies reporting an outcome of interest were identified for statistical pooling, meta-analyses were performed. We considered standard acute admissions to psychiatric inpatient care (including number, type – formal or informal – and duration of admission), mental health presentations at EDs (including number of presentations and length of wait) and other related outcomes.
For the meta-analyses, we computed relative risk to estimate the effect of interventions on categorical outcomes where events were rare, and random-effects odds ratios (ORs)56 with 95% confidence interval (95% CI) for events that were relatively common (e.g. inpatient admissions) to make the association clearer. We calculated Hedges’ g (an unbiased estimate of the standardised mean difference) for estimates of effect on continuous outcomes (where different ways of measuring the outcome were used). Where the same way of measuring the outcome was used (e.g. minutes), we used a mean difference model. We employed random-effects estimation (which provides estimates of intervention effects assuming heterogeneity) and 95% CIs to calculate the overall effect for interventions.
Analyses were performed using an intention-to-treat approach, with adjustments made for the effect of clustering in relevant trials. 57 Between-study variation in effect sizes was assessed using the I² statistic, a measure that describes the percentage of total variation across studies that is due to heterogeneity rather than chance, with the power to detect heterogeneity even when the number of studies is small. 58
We planned to assess publication bias qualitatively using funnel plots and then statistically, according to study design, by the Egger test, with Harbord modification in the case of categorical outcomes,59 where there were sufficient number of studies for these tests to be meaningful. Subgroup analyses, for example of specific sociodemographic groups, would be carried out, data permitting.
Interrupted times series
Study design
Changes in acute and psychiatric hospital activity following the introduction of PDUs in four sites were assessed via a retrospective, secular trend analysis using an ITS design considering routinely collected healthcare data. The exposure of interest was the implementation of the PDU. Acute adult psychiatric inpatient ward and mental health-related ED attendances in the 24 months prior to PDU implementation were considered unexposed, while those in the 24 months following PDU implementation were exposed. Detailed methodology of the ITS study has previously been described. 60
Setting and data set
Service use data over a 4-year period were directly sourced from MHTs and the EDs (acute hospital trusts) of participating PDU sites. The periods under study therefore differed across participating sites according to the timing of the relevant PDU implementation. The MHTs (and time periods) under study were Birmingham and Solihull Mental Health NHS Foundation Trust (BSMHFT; November 2012 to November 2016), Lincolnshire Partnership NHS Foundation Trust (LPFT; January 2016 to December 2019), Sheffield Health and Social Care NHS Foundation Trust (SHSCFT; March 2017 to March 2021) and South West London and St George’s Mental Health NHS Trust (SWLSTG; November 2014 to November 2018). The acute trusts under study were Sandwell and West Birmingham Hospitals NHS Foundation Trust (SWBHFT; November 2012 to November 2016), Sheffield Teaching Hospital NHS Foundation Trust (STHFT; March 2017 to March 2021), St George’s University Hospitals NHS Foundation Trust (SGUHFT; November 2014 to November 2018) and United Lincolnshire Hospitals NHS Foundation Trust (ULHFT; January 2016 to December 2019).
Interrupted time series outcome measures
Primary and secondary outcome measures concerning mental health crisis care service use in mental health and acute trusts are shown in Table 3. MHT data centred on patterns of activity in acute adult inpatient wards over the relevant period, including admission frequency and type (formal or informal), length of inpatient stay and frequency of ED-referred psychiatric liaison episodes (PLEs). ED-based hospital activity outcomes focused on psychiatric presentation frequency, arrival method (e.g. ambulance) and length of ED stay. Specifically, psychiatric presentations included adult attendances at a hospital ED where the presenting complaint reflected a mental or behavioural health issue and/or the primary diagnostic code was consistent with a diagnosis of either one or more mental and behavioural disorders [F01–F79 of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, (ICD-10)] or self-harm (X60–X84). Count data were adjusted in ITS analyses for size of catchment population. Details of data extraction and considerations are provided in Appendix 2.
| MHT | Acute trust |
|---|---|
| Primary outcome | |
| Voluntary acute adult psychiatric inpatient admissions | ED psychiatric presentations |
| Secondary outcomes | |
| Total acute adult psychiatric inpatient admissions | Proportion of ED psychiatric presentations with 4-hour breach |
| Proportion of acute adult psychiatric inpatient admissions with stay of ≤ 5 days | Average length of psychiatric ED wait |
| Average length of acute adult psychiatric inpatient stay (bed days) | Proportion of ED psychiatric presentations with 12-hour trolley wait |
| Proportion of acute adult psychiatric inpatient admissions that were compulsory | Proportion of ED psychiatric presentations with admission to an acute trust ward bed |
| PLEs referred from ED | Proportion of ED psychiatric presentations with arrival by ambulance/police |
| Mean daily occupied bed-days | |
| Out-of-area admissions (from the site trust to other trust/private provider) | |
Psychiatric decision unit data and pathway reconfiguration/change in model of care
PDU data (e.g. number of visits, LOS) pertaining to the first 2 years of operation for each site was also collected. Additionally, a small number of semistructured interviews were conducted with strategic managers in each site to identify other changes to the crisis care pathway (e.g. introduction or withdrawal of relevant services).
Statistical analyses
Service use parameters, including demographic characteristics of service users, were descriptively summarised for PDUs, psychiatric inpatient and ED mental health attendance activity in each trust. Outcomes were initially assessed for each site via pairwise comparisons of pre and post PDU implementation periods for each variable using chi-squared, t-tests and Mann–Whitney U-tests.
Subsequently, outcome data were collated as time series over a (maximum) 48-month period for each site, aggregated to a single observation at weekly or monthly units depending on the variable under study. Segmented generalised linear model (GLM) regression analyses (with log or identity link) were employed to evaluate whether there was a change in healthcare use outcomes following PDU implementation. This method allowed the calculation of three regression coefficients to quantify the impact of service-level change: underlying trend prior to PDU introduction (b1), level change immediately following PDU introduction (b2) and slope change from pre-to-post PDU introduction (b3). The post PDU implementation trend (b1_b3) was calculated separately in analyses that considered only data from the post PDU period. Subsequently, to estimate overall effects, parameter estimates of PDU effect were pooled across sites in a meta-analytical model.
Additional ITS analyses were conducted for counts of inpatient admissions, ED mental health attendances and PLEs considering only those people who, in the preceding 24 months, had been discharged from psychiatric inpatient services, had attended the ED and been referred to liaison psychiatry, respectively. Secondary analyses of primary outcome measures in ITS were also performed with a view to attempt to account for the impact of any other service reconfigurations relevant to outcome measures by introducing a second break point in ITS models, subject to reconfigurations being sufficiently distant in time from PDU implementation to distinguish any impact.
A p-value of < 0.05 was considered statistically significant in all analyses. Analyses were administered using Stata® 16 (StataCorp LP, College Station, TX, USA) and SPSS (Statistical Product and Service Solutions), version 26 (SPSS Inc., Chicago, IL, USA). A full description of methods of ITS analyses with sample size considerations is provided in Appendix 2.
Synthetic control study
Data sources
Patient-level service use data were obtained from Hospital Episode Statistics admitted patient care (HES-APC) and emergency care datasets61 from November 2011 to December 2020. Data relating to the key characteristics of all NHS hospital trusts for the financial year 2018–19 were obtained from the NHS Trust Peer Finder Tool. 62 Further covariate data relating to the key characteristics of NHS acute hospital trusts from 2011 to 2018 were obtained from Public Health England. 63
Treated and control trusts
The treated trusts comprise the four MHTs with PDUs and their six referring acute trusts (see Table 4). One of the treated MHTs, SHSCFT, was excluded as it did not contribute any data to HES during the study period; 38 other MHTs in England and 136 other adult acute NHS trusts in England that contributed data to HES during our study period were included as potential controls. This was excluding four MHTs (in Coventry, Sussex, Leeds and Lancashire) that have active or decommissioned PDUs and their nine referring acute trusts. See Appendix 2 for full details.
| MHT | NHS trust code | PDU open date | MHT study perioda | Referring acute trust | NHS trust code | Referring acute trust study perioda |
|---|---|---|---|---|---|---|
| SWLSG | RQY | November 2016 | November 2014–October 2018 | SGUHFT | RJ7 | Excluded – sparse data |
| KHFT | RAX | March 2015–October 2018 | ||||
| LPFT | RP7 | January 2018 | January 2016–December 2018 | ULHFT | RWD | January 2016–December 2019 |
| BSMHFT | RXT | November 2014 | November 2012–October 2016 | SWBHFT | RXK | June 2013–October 2016 |
| UHBFT | RRK | November 2012–October 2016 | ||||
| SHSCFT | TAH | March 2019 | Excluded – no data | STHFT | RHQ | March 2017–January 2020* |
Patients
Admissions to a mental health trust adult inpatient ward
HES-APC includes all admissions to an English NHS hospital and English NHS-commissioned admissions in the independent sector. The unit of activity in HES is a finished consultant episode (FCE). Each FCE describes a period of care for a patient under a single consultant at a single hospital. Here, we linked FCEs to describe a continuous spell for a patient in a single hospital. Our analysis is at the spell level, which we hereinafter refer to as an admission. We proxied admissions to a MHT adult inpatient ward using the main specialty of the consultant (= 710, 722 : 726) or treatment function of the episode (= 710, 722–726) or, where these codes were not supplied, using the primary or secondary diagnosis code64 for the patient in the ICD-10 code in F03.0–F69.0, R44.0–R46.9). This approach has been verified for accuracy by comparison with data on NHS beds available and occupied (KH03) returns,65 but in more recent periods HES-APC may understate the true number of admissions to MHT inpatient wards. 1
Emergency department psychiatric attendances
Hospital Episode Statistics emergency care includes all ED attendance at English NHS hospitals. We proxied ED psychiatric attendances using the psychiatric ED diagnosis code (= 35) or patient group (= 30), arrivals by ambulance using the ED arrival mode (= 1), referrals to the ED by police by source of referral (= 6) and admissions to an acute trust inpatient ward at the same healthcare provider by ED attendance disposal (= 1). Referral to liaison psychiatry services could not reliably be determined from HES. 66
Outcomes
Admissions to a mental health trust inpatient ward
The primary outcome for MHTs was the rate of admissions to a MHT inpatient ward per 10,000 patients in the trust catchment population. Secondary outcomes included the proportion of these admissions with a LOS of less than 5 days and the average LOS.
Emergency department psychiatric attendances
The primary outcome for acute trusts was rate of ED psychiatric attendances per 10,000 patients in the trust catchment population. Secondary outcomes included the proportion of these attendances that breached 4/12 hours, where the patient was admitted to an acute bed at the same provider, arrived by ambulance or were referred by police, or were referred to liaison psychiatry; and the average length of wait.
Statistical analysis
Selecting similar controls
To ensure that we compared treated trusts with similar trusts elsewhere in the country, we used data and methods described in the NHS Trust Peer Finder Tool62 to identify each treated trust’s closest peers from the pool of potential controls based on a list of variables capturing key trust patient and operating characteristics. The closest peers are the control trusts with smallest Euclidean distance to the treated trust based upon standardised values of the variables. The closest 10 peers for MHT outcomes and 20 peers for acute trust outcomes, according to annual data available for 2018–19, were used as the control pool for each trust in the main analysis. We used a smaller pool for MHT outcomes as there were only 34 potential control MHTs compared with 127 potential control acute trusts. Chi-square tests for no difference between the distribution of key characteristics in the treated trust and the aggregated pool of controls were performed, allowing for a Bonferroni correction for multiple testing.
The generalised synthetic control
We used the generalised synthetic control (GSC) method67 to estimate the impact of the PDU on each outcome separately at each treated trust. Estimates were risk-adjusted to control for the size of the trust catchment population and other variables that reflect changes over time in the characteristics of the population at risk. Significance was assessed by a parametric bootstrap procedure. 67 Estimated standard errors were used in a random-effects meta-analysis to generate a pooled estimate across studies. Standard diagnostic checks were performed to test the validity of method assumptions. 68
Cohort study
Study design
The cohort study was conducted at all four participating MHTs. Participants were all individuals experiencing their first visit to a PDU over a 5-month period from 1 October 2019. The study was prospective, registered with the International Standard Randomized Controlled Trial Number (53431343) on 11 February 2020, before entry to the cohort closed on 29 February 2020. Routine service use data were analysed for periods of 9 months both preceding and following the first visit to a PDU, extracted from electronic patient records by business intelligence teams at each site, pseudonymised, securely transferred to the study team, cleaned and analysed. The COVID-19 pandemic in the UK and subsequent restrictions to movement and social distancing measures overlapped with the follow-up period for the cohort study. The study was adapted to include a retrospective cohort at each site to identify whether the pandemic created issues for the generalisability of the follow-up period and to check the validity of the results. The retrospective cohort consisted of people who visited a PDU for the first time at one of the four sites during a 5-month period exactly 1 year prior to the prospectively designed cohort.
Measures
As PDUs are designed to ease the pressure on both ED and inpatient psychiatric wards, there were two primary outcomes. For inpatient wards, we examined whether there was a change in informal admissions during the study. For the ED, we examined whether there were changes in mental health presentations at ED, measured as liaison psychiatry episodes (referral to psychiatry within the ED). We examined a range of secondary outcomes that enabled us to identify additional changes to service use. These included total inpatient admissions, short-stay (0- to 5-day) admissions, average length of inpatient stays, compulsory admissions, use of Community Mental Health (CMHT) and CRHT teams and other community-based MHT services.
Statistical analysis
The population was summarised using descriptive statistics to understand who uses PDU services. Pre and post PDU visit periods were compared in the primary cohort to illuminate changes in service use following a service user’s first stay on a PDU. The post-PDU periods in primary and retrospective cohorts at each site were compared to check for changes to service use due to the COVID-19 pandemic. The pre-PDU first visit periods at each site were compared to indicate whether significant differences in the two post periods might be found just through random chance due to repeated testing. We used paired t-tests bootstrapped with 2000 replications for continuous data69 or McNemar’s χ2 tests for binary paired data. 70
For the equalities impact assessment, we compared the demographics of those individuals in the primary cohort accessing the PDU to the general population of service users (calculated over a recent 1-year period) at that site. Z-tests were used to compare the proportions of each demographic where the numbers were sufficient. Z-tests were used as a valid way of comparing a subgroup drawn from a population to a wider population; correction for the overlap was not conducted as each subgroup represented far less than 10% of the whole population. 71
Qualitative interview study
This WP combined a cross-sectional qualitative interview study with PDU staff and crisis care pathway staff referring to PDUs, with a longitudinal interview study with first-time visitors (service user) of PDUs.
Participants
Psychiatric decision unit visitors
Participants were first-time admissions to PDUs, recruited within 1 month of discharge from the PDU, able to give informed consent to participate in research. A sampling framework was considered to ensure that the study included participants with a range of service use histories and sociodemographics, but in practice it was not possible to do so because of challenges in identifying and recruiting sufficient numbers of eligible participants. Our target recruitment was 10 participants at each of three study sites (South West London, Lincolnshire and Sheffield), increased to 12 participants to allow for loss of follow-up and 6 in Birmingham.
Members of the research team or site clinical studies staff visited PDUs in person or made enquiries by telephone on a weekly basis, asking unit staff to identify eligible unit visitors, including any new admissions. Potential participants were given with study information and, if interested, given an opportunity to ask questions about the study, invited to give informed consent to participate and an interview arranged. At the Birmingham site consent could also be taken verbally, by telephone and digitally recorded following ethical approval for amendments to procedures resulting from COVID-19.
Clinical staff
Participants were either working on PDUs or referring to them as part of the crisis care pathway. At each site we aimed to recruit between 10 and 12 staff participants (6 in Birmingham) including 4 members of the PDU team (unit manager, nurse, HCA and psychiatrist consulting to the unit) and 6–8 referring staff (member of the ED-based liaison psychiatry team; ED nurse and/or manager; referring clinicians from CRHT, street triage and other services directly referring to PDU as appropriate locally). A member of the research team contacted the local principal investigator, PDU manager and/or consultant to identify potential participants. Interested individuals were followed up with study information, given an opportunity to ask questions about the study and invited to give informed consent to participate.
Data collection
Psychiatric decision unit visitors
Baseline interviews were conducted either face to face on the unit, at another service, at the participant’s home or by telephone or video-conferencing application and were digitally, audio-recorded. Interviews lasted between 15–98 minutes. At about 8 months post-discharge from the PDU participants in the SWL, Lincolnshire and Sheffield sites were contacted by a member of the research team using their preferred contact details and, if interested, a follow-up interview arranged (between 8 and 10 months post-discharge). Follow-up interviews were conducted by telephone or video-conferencing application and were digitally, audio-recorded.
Interviews were semistructured and at baseline explored participants’ experiences of referral to the PDU, assessment, unit environment and therapeutic input on the PDU, and any immediate referral or signposting to post-discharge care. At follow-up, interviews explored participants’ experience of crisis and community care post-discharge from the unit, any differences in care pathway in the year before and after their stay on the unit, and any impacts of COVID-19 on care received post-discharge. Two workshops with the PEER group identified a number of issues important to explore in interviews. Final interview schedules were coproduced in a workshop conducted by service user researchers and our LEAP (see Appendix 3).
Additional interview questions were developed in collaboration with the health economics team (DMcD, A-LP) to inform economic modelling work in WP6. Participants were asked to complete the EQ5D quality-of-life measure72 at the end of their baseline and follow-up interview.
Clinical staff
Semistructured interviews with crisis care pathway staff explored their experiences and understandings of acute mental health crisis, expectations of the purpose and function of PDUs, the decision-making process and reasons for referral to PDU, who they refer to PDU and why, and their view on the impact PDUs. Interviews with PDU staff explored staff perceptions of the purpose and function of PDUs, appropriateness of referrals from other services, how referrals were assessed and the unit gate kept, experiences of working on the unit, balance of assessment/therapeutic intervention, how supported they felt in their role, decision-making around discharge and onward referral and signposting to other services, and their view on the impact of PDUs. Both clinical and PDU staff were asked about changes to crisis care due to COVID-19. Interview schedules were coproduced in another workshop with service user researchers and the LEAP (see Appendix 3).
Data analysis
Data were analysed thematically73 using a hybrid inductive and deductive approach to integrate both ‘theory-driven’ codes (i.e. a sensitivity to those phenomena that we might expect) and data-driven codes that articulate the idiosyncratic and unexpected in our data). 74 Output from qualitative analyses will be both descriptive, providing a detailed account of the crisis care pathway and PDU, and explanatory, seeking to understand the expectations and experiences of different groups of service users and staff, and the potential impact of differences on the functioning and outcomes of units.
We adopted an approach to coproducing our analysis, developed by the team in previous NIHR-funded research,48 to ensure that service users’ priorities and concerns were integrated alongside those of clinicians and other academic researchers. In the first stage of the process, service-user researchers on the team undertook preliminary thematic analyses of a small number of baseline service user interviews, presenting emerging thematic areas at an interpretive workshop involving the full research team. Emerging themes were discussed and refined by the team and a provisional coding framework produced. A second round took place remotely using virtual meeting software involving members of the LEAP taking a wider participatory approach to interpreting qualitative data, an approach developed by the team in research exploring mental health and experiences of the COVID-19. 75–77 Following training, members of the LEAP undertook preliminary analyses of staff and service-user follow-up interviews, as did service-user researchers and other members of the team. At a second interpretive workshop, including the LEAP, emerging themes from these additional data sets were discussed, expanding and refining the coding framework. Care was taken not to ‘fit’ data from one set of interviews into codes developed from other interviews, and inductive space was retained in the process so that idiosyncratic data were not discounted. The revised coding framework was used to code the entire qualitative data set using NVivo (QSR International, Warrington, UK) qualitative analysis software. In the final, writing stage of the analysis process76,77 themes were amalgamated and refined further through discussion by members of the team (KA, HJ, SG).
Health economic analysis
The potential improved outcomes for mental health service users that may be associated with the creation of PDUs as an alternative option to traditional care pathways also have direct implications for resource use and costs. This is both for service users referred to PDUs, as well as broader impacts on local health economies, if there are spill-over benefits associated with implementation. Some previous analyses have indeed suggested that use of PDUs will lead to a reduction in both the number and length of inpatient admissions, as well as reduced attendance at ED, and therefore lead to a reduction in resource use and costs to healthcare systems. 78–81
The overall objective of the economic analysis was therefore to bring together findings from across WPs to identify potential impacts on the local health economy in each study area following the introduction of PDUs. The analysis draws on both the results of the ITS reported in Chapter 4 and the synthetic control study in Chapter 5 for site-specific decision model parameters on changes in area-level acute hospital ED attendances as well as area-level psychiatric hospital admissions (both informal and informal) at a (clinical) population-level following the introduction of PDUs.
As noted in the section on service mapping (see Chapter 3), the ITS provides data on service use over a 4-year period (spanning 2 years prior to and 2 years post PDU implementation) in MHTs and acute hospital EDs in three of the four sites. The synthetic control study (see the section on the systematic review) sought to match and compare mental health admissions and LOS, as well as ED attendances for the mental health and acute trusts in our four study areas with trusts with similar characteristics in areas of England where PDUs have not been implemented.
In addition to ED attendance and psychiatric inpatient admissions, contact with PDUs might be expected to have an impact on the use of community mental health services. Longitudinal cohort data have been used to explore these impacts. The section on the ITS sets out methods used for the cohort analysis undertaken and Chapter 6 describes how, in each of the four study areas, data have been collected on patterns of service contact and utilisation in the 9 months before and after an initial visit to a PDU. We have then estimated changes in resource use and costs to the NHS in the 9 months following a PDU visit for each of the four sites. To inform scenario modelling, regression analyses have been used to identify potential explanatory factors for differences in levels of cost. Selected service user subgroup analyses for costs also reflect different sociodemographic characteristics or factors associated with the use of mental health services.
The primary function of mental services is to improve health outcomes and not just impact on resource use and costs. Although we did not intend to directly look at changes in clinical outcomes, such as levels of mental distress, it has been possible to collect some self-report data on quality-of-life scores, using the EuroQOL EQ-5D-5L (EuroQol-5 Dimensions, five-level version) quality-of-life instrument for 148 participants referred to PDUs in two of the study areas, Lincoln and Sheffield. These data have been used to inform scenario modelling to help indicate the potential scope for improving quality of life of PDU service users. This can be useful, given that quality of life is the primary outcome measure used in economic analysis to inform decision-making in England, where judgements are typically concerned with assessing whether the additional costs incurred by a service are justified by quality-of-life gains.
Using these different sources of data chapter describes economic impact and the return on investment (RoI), from an NHS perspective, in each of the different study site areas. This compares the costs associated with PDU implementation with any subsequent cost offsets as well as additional costs incurred. Our service mapping review (see Chapter 3), where the resources required to implement PDUs in the different areas have been collected,82 has been used to estimate the costs of providing PDU services in each site; this review can also be used to explore the budgetary cost of expanding provision in England. In addition, we also look at impacts an individual service user level, scenarios that reflect the experiences of service users in qualitative analysis (see Chapter 7) have also been used to describe some potential individual journeys along service use pathways.
For all analyses costs are reported in 2019–20 prices, with costs for acute hospital-based contacts and specialists CMHTs taken from national reference cost. 83 Costs for psychiatric inpatient stays, as well as hourly costs for some additional community and hospital-based staff costs, are taken from the annual Unit Costs of Health and Social Care. 84 These staff costs estimate hourly costs using mean full-time equivalent basic salary for Agenda for Change (AfC) bands 4–9 of the April 2019 to March 2020 NHS staff earnings estimates. These estimates include salary overheads and other oncosts, including training, office, travel/transport, general supplies and utilities such as water, gas and electricity, as well as a share of capital overheads. The costs associated with PDUs have been estimated by applying these national salary costs to information provided by participating site area trust on the configuration of their PDU services, as well as previous publications that have estimated the costs of PDU (or similar) service provision. Discounting is not applied in this analysis, as only costs for up to 12 months are included.
Data synthesis
Synthesis of data from across WPs and across sites was conducted to critically appraise findings from the separate WPs, to provide insight into optimal configuration of PDUs in relation to the wider crisis care pathway and to inform potential future upscale and roll out of PDUs nationally. Data synthesis adopted a critical interpretive synthesis approach, as has been widely applied to the synthesis of quantitative and qualitative evidence in systematic reviews85 and the development of evidence-based practice. 86,87 In this approach, ‘constructs’ are derived from the various analyses (i.e. from descriptive analysis or hypothesis testing of quantitative data and thematic analysis of qualitative data) and mapped to an integrative grid that explores how those analyses interface. This enables the development of ‘synthesising arguments’ (analytical narrative) that offer explanatory insight into findings and inform applied learning from the research. An interpretive workshop involving members of the research team and LEAP was held to ensure that service user views and experiences informed this process alongside clinical and academic perspectives.
Following the workshop, a provisional set of constructs was specified, derived from preliminary findings from WP2–5. These constructs were further refined through discussion in the investigator team as we completed our analyses. The final data synthesis is presented in Chapter 9 and, together with our health economic analysis, provides the basis of our implications for policy and practice.
Changes from the proposal
The impact of COVID-19
As described for the cohort study above, follow-up to the WP4 cohort study began as lockdown measures were introduced, with many mental health services either closed or provided remotely during this period. 88 Recruitment of a retrospective pre-pandemic cohort to enable us to consider the impact of COVID-19 on crisis care is specified above. In addition, we were unable to access data on participant service use for the WP4 cohort study using the clinical record interactive system system at two of our sites, as site business intelligence staff were diverted to COVID-related work and the system was not updated as a result. Instead, we obtained pseudonymised data from all first-time attendees at PDUs directly from patient record at all sites.
Finally, working with our LEAP, we added questions specific to the impact of COVID-19 to WP5 qualitative interview schedules for both service user follow-up and staff interviews. Note that the 2-year period following the opening of the PDU had been completed prior to lockdown beginning in March 2020 for three of our four sites (Sheffield was the exception), so we did not change the design of the WP2 ITS or WP3 synthetic control studies. Amendments to NHS ethical approval were obtained for all changes detailed above.
Qualitative interviews at the Birmingham site
Birmingham was added as a fourth site at the funding stage of the research process in those WPs that involved routinely collected data only so as not to impact on the feasibility of undertaking the research within the proposed cost envelope. As such the original protocol did not include Birmingham in the WP5 qualitative interview study. It became apparent that the Birmingham PDU had a shorter typical LOS than our other sites. As we had identified LOS as a key variable in PDU configuration, we felt that we needed to include Birmingham in WP5 to better understand how the model worked and was experienced. An extension to the study was funded, and amendment of NHS ethical approval obtained that allowed us to collect a data set of staff and service user interviews at one time point.
Access to data
There were a small number of deviations from the methods described in the published protocol,60 primarily arising from the use of reduced datasets where availability was limited in WPs 2 and 3 (ITS and SC study). This resulted in a reduced set of outcomes in some sites in some WPs. Details are given within WPs and limitations on the study as a whole considered in the section on strengths and limitations.
Chapter 3 Service mapping and systematic review
Service mapping
A copy of the survey questionnaire has been published elsewhere. 82 This is an open access article distributed under the Creative Commons Attribution licence 4.0 (CCBY), which permits unrestricted use, distribution and reproduction in any medium, provided that the original work is properly cited. See https://creativecommons.org/licenses/by/4.0. The text and Tables 5 and 6 below include minor additions and formatting changes to the original. Survey responses were obtained from 50 of 53 NHS trusts with a relevant remit (94% response rate). The survey was completed by FOI officers, acute care pathway leads, service directors and lead nurses.
| Theme | PDU characteristic | n/N (%) |
|---|---|---|
| PDU setting | Psychiatric hospital | 6/6 (100) |
| Acute hospital | 1/6 (17)a | |
| Co-located with place of safety (section 136 suite)b | 5/6 (83) | |
| Trust-wide aim of service | Reduce presentations at ED | 4/6 (67) |
| Reduce ED breaches | 3/6 (50) | |
| Reduce inpatient admissions | 3/6 (50) | |
| Reduce out-of-area beds | 1/6 (17) | |
| Improve patient experience | 1/6 (17) | |
| Two or more aims | 5/6 (83) | |
| PDU environment | Overnight stays | 6/6 (100) |
| Recliners rather than beds | 6/6 (100) | |
| Partitioned areas | 6/6 (100) | |
| Maximum hours of stay | 12 hours | 2/6 (33) |
| 23 hours | 1/6 (17) | |
| 2 days | 2/6 (33) | |
| 3 days | 1/6 (17) | |
| Referral/entry to unit | Voluntary admissions only | 6/6 (100) |
| Liaison psychiatry | 6/6 (100) | |
| CRHT team | 5/6 (83) | |
| Street triage | 5/6 (83) | |
| CMHT | 2/6 (33) | |
| GP | 1/6 (17) | |
| Third or voluntary sector services | 1/6 (17) | |
| Police | 1/6 (17) | |
| Self-referral | 0/6 (0) | |
| Self-referral if included in crisis care plan (also known as joint crisis plan), a plan developed between service users and their clinical teams, typically for service users who experience crisis frequently. | 1/6 (17) | |
| Approved mental health professional | 1/6 (17) | |
| Activity on unit | Primarily assessment | 1/6 (17) |
| Primarily therapeutic input | 1/6 (17) | |
| Both assessment and therapeutic input | 4/6 (67) | |
| Capacity and duration of stay | Mean (SD), range (N) | |
| Capacity | 5.6 (1.4), 4–8 (6) | |
| Average LOS on unit (hours) | 25.3 (18.4), 8–48 (6) |
| Role (NHS pay band) | Sites including role in staff team |
|---|---|
| Nurse (band 6), n (%) | 6 (100) |
| Nurse (band 5), n (%) | 1 (17) |
| Healthcare assistant (band 3), n (%) | 4 (67) |
| Healthcare assistant (band 2), n (%) | 1 (17) |
| Administrative support (band 4), n (%) | 3 (50) |
| Administrative support (band 3), n (%) | 1 (17) |
| Psychiatrist; part time, n (%) | 6 (100) |
| Staff on shift; nurses and healthcare assistants: | |
| Day shift, mean (SD), range | 1.7 (0.31), 1–3 |
| Night shift, mean (SD), range | 1.7 (0.31), 1–3 |
| Staff : patient ratio; nurses and healthcare assistants: | |
| Day shift, ratio (SD), range | 1 : 21 (1.2), 1 : 1 to 1 : 4 |
| Night shift, ratio (SD), range | 1 : 2.3 (1.2), 1 : 1 to 1 : 4 |
PDUs were present in a relatively small number of trusts, six (12% of trusts), with a further two planned but yet to open. 82 The locations of the trusts that had a PDU were Sheffield, Lincolnshire, Birmingham, Coventry and Warwickshire, South West London and Sussex. Of the PDUs planned, one would be in Nottinghamshire and one serving Rotherham, Doncaster and South Humber. Four decommissioned PDUs were identified – one in Leeds and three in Lancashire. Of the decommissioned PDUs, the unit in Leeds had operated with ward status and so staff had been unable to refer patients onward for inpatient care. This meant a protracted LOS for some in what was designed to be a short-stay unit with communal sleeping areas. Of the Lancashire units, one received an unfavourable quality report due to lengthy patient stays and dissatisfaction with unit layout and sleeping arrangements. 89 The Lancashire trust repurposed units as crisis assessment spaces without overnight stays.
All six PDUs were located on the mental health NHS trust site (see Table 5), although one of those was in a shared site by the MHT and the acute hospital. In five of six sites, the PDU was co-located with the trust’s place of safety (Section 136 facility). The majority of units were designed to reduce pressure on EDs, and half were designed to reduce inpatient admissions. Two PDUs had addition aims to reduce out-of-area placements and improve the patient experience. All PDUs facilitated overnight stays, with partitioned areas for sleeping in recliners rather than beds, and had a capacity of four to eight service users. All units only accepted voluntary patients. The majority of PDUs aimed to deliver both assessment and therapeutic input (four of six). All PDUs accepted referrals from liaison psychiatry, with the majority accepting referrals from CRHT teams and street triage (an outreach service run by the police and mental health services). However, substantial heterogeneity of pathways was also identified: referrals from third or voluntary sector services, police, general practitioner, approved mental health professional or self-referral when included in crisis care plan, were each only available at one trust. 82
PDUs had a high staff-to-patient ratio. In the day, the mean staff-to-patient ratio for nurses and HCAs combined was 1 : 2.1 [standard deviation (SD = 1.2)], rising at night to a mean of 1 : 2.3 (SD = 1.2). Staffing includes some allocated staff time from psychiatry (see Table 6). Although all units have a high staff-to-patient ratio, a sizeable difference was observed; units ranged from 1 : 1 staffing to 1 : 4 staffing. 83
Survey findings indicate that trusts with a PDU were approximately twice as likely than trusts without a PDU to have several crisis services, including crisis houses, crisis cafes or crisis drop-in services and acute day units (see Table 7). About half of trusts have hospital-based assessment services without overnight stays, and this is the same whether a trust has a PDU or not. The percentage of trusts with short-stay assessment wards was similar across trusts which have and do not have a PDU. 82
| Components of crisis care pathway | Trusts nationally, n/N (%) | Trusts with PDU, n/N (%) |
|---|---|---|
| PDU | 6/50 (12) | – |
| Community-based assessment servicea | 50/50 (100) | 6/6 (100) |
| Hospital-based assessment service without overnight staysb | 23/50 (46) | 3/6 (50) |
| Street triage servicec | 29/50 (58) | 5/6 (83) |
| Sanctuary/crisis caféd/crisis drop-in service | 18/50 (36) | 4/6 (66) |
| Crisis house(s)e | 17/50 (34) | 4/6 (66) |
| Acute day unit | 7/50 (14) | 2/6 (33) |
| Crisis family placements | 1/50 (2) | 0/6 (0) |
| Short-stay assessment wards | ||
| Triage or short-stay assessment ward | 13/50 (26) | 1/6 (17) |
| Maximum length of stay on triage or short-stay assessment ward | ||
| 1–7 days | 4/13 (31) | – |
| > 7 days | 9/13 (69) | – |
| Number of triage/short-stay assessment wards at trust | ||
| 1 | 7/13 (54) | – |
| 2 | 5/13 (38) | – |
| 3 | 1/13 (8) | – |
| Number of triage/short-stay assessment beds at trust | ||
| < 10 | 3/13 (23) | – |
| 10–19 | 5/13 (38) | – |
| ≥ 20 | 5/13 (38) | – |
Systematic review
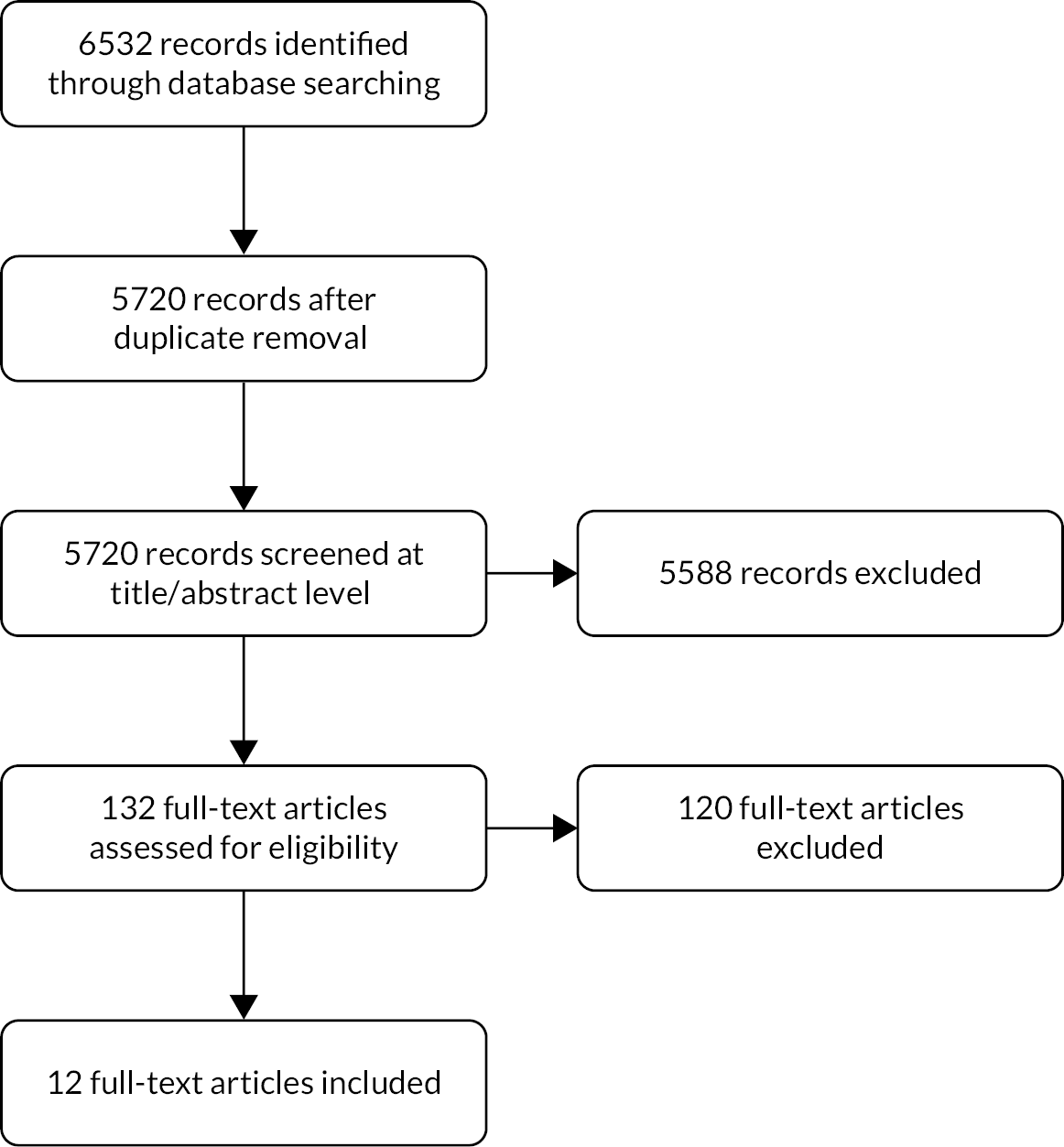
Twelve studies were included in the review. Figure 3 depicts the flow of information through the review. Study characteristics and further information regarding units evaluated in included studies can be seen in Table 8 and in Appendix 1, Table 33.
FIGURE 3.
Selection of studies for inclusion in systematic review.
| Study reference | Service description | Study design and duration | Setting | Participants | Outcomesa | ||
|---|---|---|---|---|---|---|---|
| Intervention | Comparison | N (alternative n/comparison n) | |||||
| Braitberg et al.40 | 24-hour BAU | Pre/post study; 2-year comparison period | Australia, Royal Melbourne Hospital; 72,000 ED presentations per annum | Adults admitted to the BAU; no patients with a medical diagnosis | Adults aged 16+ years ED presentations with LOS 3–24 hours, diagnosis coded as MH issue, psychosocial crisis or related to intoxication | n = 5426 (2379/3047) | ED LOS; time to ED clinician; time to EMH clinician; ED security (‘code grey’) rates; ED restrictive intervention rates |
| Browne et al.91 | 48-hour PAPU | Pre/post study; multiple comparison periods | Australia, Royal Melbourne Hospital | All ED patients; no transfers from other EDs or other psychiatric catchment areas | All ED patients; no transfers from other EDs or other psychiatric catchment areas | Not reported | ED LOS Long waits in ED; ED security (‘code grey’) rates; ED mechanical restraint rates; ED 1 : 1 nursing time; ED 1 : 1 nursing cost |
| Gillig et al.92 | 24-hour extended evaluation unit | Comparison study; 2.5-week (intervention)/4-week comparison period; 30-day follow-up for intervention | Louisville, Ohio (intervention); Cincinnati, Ohio (comparison). Ohio Valley urban area, 600 patient visits per month | Adults aged 18+ years attending the PES | Adults aged 18+ years attending the PES | n = 783 (435/348) | Hospitalisation rates from ED; inpatient admissions (from ED & unit); hypothetical hospitalisations |
| Kealey-Bateman et al.93 | 72-hour joint SSU and Missenden assessment | Comparison study; 18-month (intervention)/unknown comparison period | Royal Prince Alfred Hospital, inner-city Sydney | Patients admitted to the SSU via ED | Patients admitted to a PECC | Not reported | Admission to unit via ED |
| Lester et al.94 | 48-hour CALM service | Pre/post study; 1-year comparison period; 30-day follow-up | USA, Ohio; 72,000 annual ED visits, ~7% for behavioural health complaints | ED patients who received a psychiatric consult | ED patients who received a psychiatric consult | n = 4598 (2387/2211) | ED LOS; hospital LOS; psychiatric hospitalisation rate; admission to unit via ED; discharged from ED; 30-day readmission rate; unit LOS |
| Mok and Walker95 | 3-day SSU | Comparison study; 8-month comparison period | Canada, metro Halifax | Patients admitted to the regular-stay unit | Patients admitted to regular-stay unit | n = not reported (124/not reported) | Ward occupancy rates |
| Parwani et al.37 | 24-hour Psychiatric Observation Unit | Pre/post study; ITS for analysis; 18-month comparison period | North Eastern USA; 1541-bed tertiary care academic medical centre | Adult ED patients aged 17+ years evaluated by the acute psychiatry service. No patients who: left ED, diverted elsewhere, never arrived, or discharged to court/law enforcement | Adult ED patients aged 17+ years evaluated by the acute psychiatry service. No patients who: left ED, diverted elsewhere, never arrived, or discharged to court/law enforcement | n = 7299 (3798/3501) | ED LOS; Crisis Intervention Unit LOS; hospital LOS; psychiatric hold rate; inpatient admission rate |
| Schneider and Ross96 | 3-day crisis unit | Comparison study; 2-year comparison period; 30-day follow-up | USA, Connecticut, community hospital | Patients admitted to the crisis unit | Patients admitted to the inpatient service | n = 1370 (590/780) | Average unit LOS; 30-day readmission rate |
| Spooren et al.97 | Three 72-hour psychiatric crisis units | Pre/post study, case–control design; 6-month (pre)/13-month (post) comparison period; 1-month follow-up | Belgium, three urban hospitals (intervention); University of Ghent (comparison) | ED patients referred every third week to the psychiatric crisis units | ED patients referred every third week for short-term psychiatric inpatient treatment | n = 208 (171/37) | Psychological scales: symptoms; patient reported improvement |
| Stamy et al.80 | EmPATH unit | Pre/post economic evaluation; 2-year comparison period | USA, Midwestern academic ED | All ED patients aged 18+ years | All ED patients aged 18+ years | n = 46,567 (23,231/23,336) | ED revenue; psychiatric boarding time (time waiting for a bed or for transfer); ED LOS; leaving ED without being seen; leaving ED against medical advice or eloped; inpatient admissions; fatalities |
| Tretheway et al.45 | Short-term PDU | Comparison study; 1-year comparison period | UK, Birmingham | All patients referred to the PDU, ED presentations via street triage team and patients admitted to an inpatient unit following assessment by rapid assessment interface and discharge | All ED presentations via street triage team and patients admitted to an inpatient unit following assessment by rapid assessment interface and discharge | n = 980 (385/595) | Inpatient admissions via liaison psychiatry; ED presentations via street triage |
| Van der Sande et al.98 | 4-day special care unit for suicide attempters (SOS-afdeling) | RCT, 12-month follow-up | Netherlands, Utrecht University Hospital | Aged 15+ years and attending for somatic treatment of the consequences of a suicide attempt | Aged 15+ years and attending for somatic treatment of the consequences of a suicide attempt | n = 274 (140/134) | Occurrence of subsequent suicide attempts; medical care received in the year subsequent to index suicide attempt; psychological scales: symptoms; psychological scales: hopelessness |
Narrative synthesis
Study characteristics
In the review, 12 studies were included, of which five studies were from the United States,37,79,91,93,95 three from Australia,40,90,92 and one each from the Netherlands,97 Belgium,96 UK45 and Canada. 94 The review comprised four pre/post studies,40,79,90,93 five comparison studies,45,91,92,94,95 one ITS,37 one case–control study96 and one RCT. 97
Pre/post studies took ED or psychiatric patients as their population, except for a study where the 2379 intervention participants of 5426 participants in total were from the short-stay behavioural assessment unit. 40 Browne et al. 90 took ED patients as their population, as did Stamy et al. 79 who included 46,567 patients in total in their study sample. Lester et al.,93 used data from 4598 patients in total, all of whom had received a psychiatric consult in the ED.
From the comparison studies, comparison groups comprised 348 patients accessing PESs;91 psychiatric emergency care centres;92 admitted to the regular-stay units;94 780 patients admitted to the inpatient service;95 and 595 ED presentations via street triage teams and patients admitted to an inpatient unit via liaison psychiatry. 45
In terms of study outcomes, five studies examined ED LOS,37,40,79,90,93 of which three studies had this as a primary outcome. 37,40,93 Four studies had inpatient admissions as an outcome,37,45,91,93 one as a primary outcome. 93 Two studies looked at security code events and the use of restrictive interventions, such as mechanical restraint and sedation,40,90 psychometric outcomes,96,97 and 30-day readmission rates. 93,95 One study assessed rates of admission to the short-stay unit via the ED. 92
Unit characteristics
Units could be designed with multiple purposes in mind. Five units were designed to reduce pressure on ED,37,45,79,90,92 four to provide a more therapeutic environment than the ED,40,45,90,92 three to reduce psychiatric admissions,45,91,94 three to reduce time spent in hospital,95–97 and units to stabilise or improve patient well-being. 95–97 In addition, individual units had specific remits: to reduce the risk of future suicide attempts,97 reconnect with outpatient treatment,95 reduce out-of-area transfers,94 and offer crisis-focused psychotherapy and case management services. 93 Refer to Table 2 for more information regarding individual units.
Admission criteria were variable. Units accepted patients with mental health problems or who required psychiatric care (n = 4),40,90,92,93 who were likely to be discharged within a short time frame or benefit from short-term admission (n = 4),37,40,92,94 under the influence of drugs or alcohol (n = 2),40,92 experiencing an acute behavioural disturbance (n = 1),40 experiencing acute symptoms in relation to specific and short-term stressors (n = 1),95 requiring inpatient admission but there was no available bed (n = 1),37 or receiving medical treatment for a suicide attempt (n = 1). 97
Patients were excluded from admission if they were under the influence of or dependent on drugs or alcohol,90,97 aggressive or displaying non-stable behaviour,79,92,93 had medical issues,79,90,92,93 resided outside of the catchment area,90,97 had a pattern of self-harming97 or required an inpatient admission. 79,97
Units received referrals from the ED,40,45,79,90,92–94,96,97 the PES,91 other assessment and intervention units,37,92,94 outpatient clinics,79,94 other crisis services45,90 and other parts of the hospital. 92 The units were most commonly staffed by psychiatrists,37,40,79,90,93–97 social workers,37,79,93,94,96 nurses,37,40,92,94,96 psychiatric nurses,79,93,96–97 and psychiatric technicians or nursing assistants. 79,95 Units also employed: a psychologist,97 drug and alcohol clinicians,40 and high numbers of staff with knowledge of trauma-informed care. 92 Some units described themselves as hosting a multidisciplinary team90,96 and having a high staff-to-patient ratio. 92
Quality rating of included studies
Quality rating of each outcome of interest, for each study, are given for randomised (see Figure 4) and non-randomised studies (see Figure 5).
FIGURE 4.
Risk of bias ratings for outcomes from randomised studies.
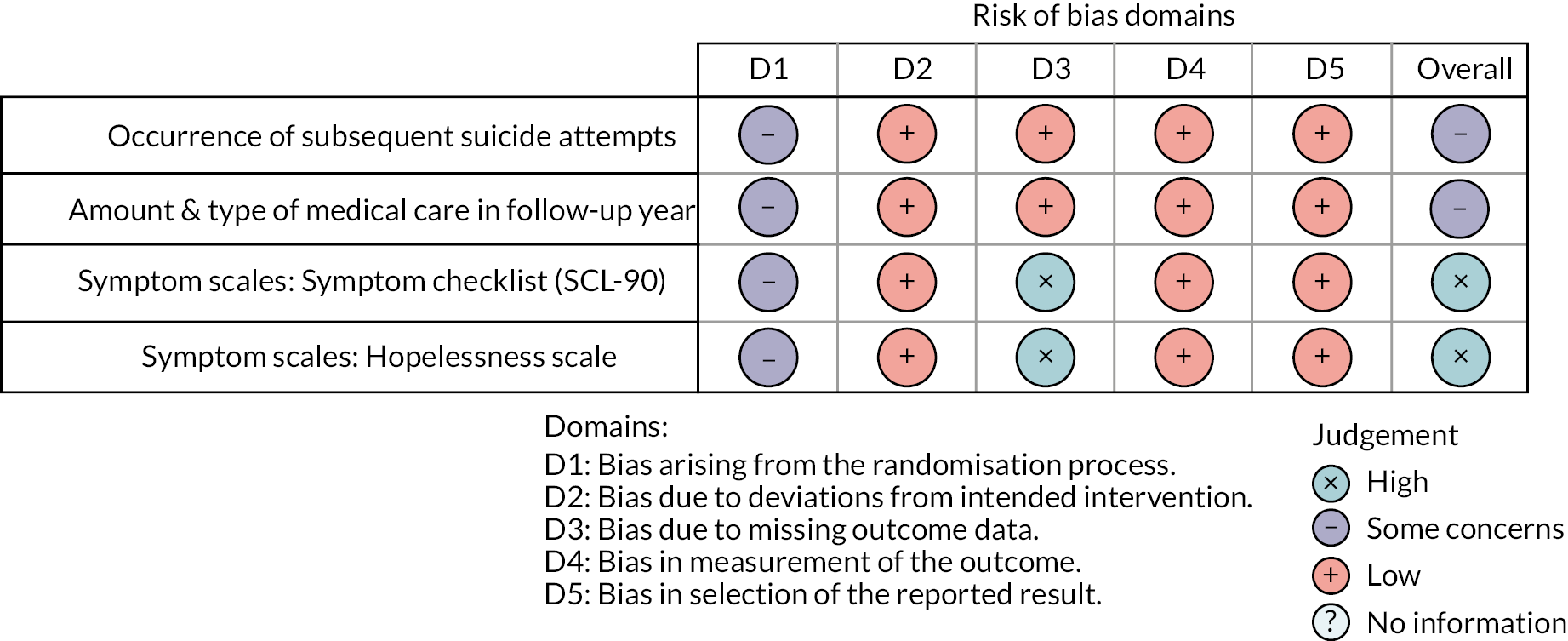
We extracted 41 outcomes from 11 non-randomised studies, and four outcomes from a single RCT. 97 First, looking at the non-randomised studies, as indicated in Figure 5, we assessed there to be moderate risk of bias in a majority of outcomes considered in the review (27/41), from across most included studies (7/12). The most prevalent source of bias was potential bias in selection of reported result (in the absence of published protocols for most studies it was not clear that the full range of outcomes assessed in studies had been analysed and reported). Three outcomes from two studies91,95 were assessed as of serious risk of bias due to the risk of bias from confounding as the comparison groups were considered to be defined in a way which suggests that they are too dissimilar. Three further outcomes were at critical risk of bias because of additional biases identified or the bias due to confounding being rated as critical. Seven outcomes from one study79 were assessed as of low risk of bias. In the single RCT,97 two outcomes were assessed as of some concerns because of potential bias arising from the randomisation process, and two further outcomes of high concern because of, in addition, bias due to missing outcome data.
Synthesis of outcomes
Total emergency department length of stay
All four studies assessing total LOS in ED reported a significant reduction in this outcome. 37,40,80,94 Lester et al. 93 reported a mean decrease from 14.48 to 11.11 hours (p < 0.001), employing mixed model analysis using log-transformed ED lengths of stay. Parwani et al. 37 reported a reduction in median ED LOS from 155 minutes [interquartile range (IQR) 19–346] to 35 minutes (IQR 9–209) with autoregressive integrated moving-average modelling indicating this difference to be highly significant (p < 0.0001). Braitberg et al. 40 reported a reduction in median LOS from 328 minutes (IQR 227–534) in the pre-PDU period to 180 minutes (IQR 101–237; p < 0.001) in the post-PDU period, and Stamy et al. 79 a reduction from 351 minutes (IQR 204–631) to 334 minutes (IQR 212–517); a mean difference of 114 minutes (95% CI 87 to 143).
Where possible, data for ED lengths of stay were combined meta-analytically using mean difference random-effects models, with a pooled estimate for a reduction in total ED LOS of 164.24 minutes (95% CI −261.24 to −67.23 minutes; p < 0.001). The data from two studies could not be combined meta-analytically as one study did not report a measure of variance93 and another reported only reported medians. 37 An I2 of 98% indicated high heterogeneity (see Figure 6). A GRADE starting rating of ‘low certainty, confidence or quality’ for outcomes of meta-analyses of non-randomised studies was upgraded to ‘moderate certainty’ due to the ROBINS-I ratings, indicating that authors believe that the true effect is probably close to the estimated effect.
Emergency department wait time
One study40 reported a reduction in wait to be seen by a clinician in ED from a median of 68 minutes (IQR 24–130) in the control group to 40 minutes (IQR 17–86) in the experimental group (p < 0.001) and a reduction in median wait time for a mental health review from 139 minutes (IQR 57–262) to 117 minutes (IQR 49–224; p = 0.001). In another study,79 psychiatric boarding – time waiting in ED for a bed or transfer – decreased from 212 minutes (SD 119–536) to 152 minutes (SD 86–307) (mean difference 189 minutes; 95% CI 50 to 228). A reduction in long waits in ED was reported by one study,90 down from 12 patients per month who waited in ED for at least 24 hours in the pre-PDU opening period to only six 24-hour waits in the entire post-PDU period.
Emergency department environment: use of security services and restraint
Two studies40,90 assessed changes in adverse violent or threatening events that require a formal response from a security team (code grey events) and restrictive interventions from the pre- to post-PDU periods, although neither study was of high quality. Braitberg et al. 40 reported a reduction in events from 538 to 349 (p = 0.003) and a reduction in number of patients involved from 370 to 259 (p = 0.159). Browne et al. 90 reported a reduction in events in the ED but this was accompanied by an increase in events in the linked unit. Braitberg et al. 40 reported a reduction in number of patients experiencing any restrictive intervention from 338 patients (12.7%) to 255 patients (10.7%; p = 0.02), reduction in number of physical restraints from 339 (11.3%) to 224 (9.4%; p = 0.04), reduction in mechanical restraint from 275 (9.0%) to 156 (6.6%; p < 0.001) and reduction in use of therapeutic sedation from 250 (8.2%) to 156 (6.6%; p < 0.001). Browne et al. 90 reported a reduction in the total number of patients restrained from the pre- to post-PDU period, although size of cohort, total hours of restraint and average hours of restraint per patient were unclear.
Other emergency department outcomes
A single study79 reported no significant difference in the number of patients leaving ED without being seen between pre- and post-PDU opening periods, and similarly no difference in the combined number of patients leaving against medical advice. One study reported a reduction in numbers of patients brought to ED by street triage teams from the pre- to post-PDU opening periods but did not test this for significance. 45
Psychiatric inpatient admissions
A number of studies reported the impact of the PDU on inpatient psychiatric admissions. Parwani et al. 37 reported a significant reduction in the proportion of ED patients who experienced a psychiatric admission after the unit opened, from 42% to 25% (p < 0.001). Stamy et al. 79 reported that 301 (8.3%) patients presenting to ED were admitted to inpatient psychiatry in the ‘post’ period compared to 509 (15.3%) patients in the ‘pre’ period, representing a difference of −7.0 (95% CI −8.5 to −5.5). Lester et al. 93 reported that admissions to wards from ED reduced from 47.9% of presenting psychiatric patients to 38.0%, that discharge from ED rates were reduced by 39.1% to 28.2%, and that the total number of admissions to ward and transfers reduced from 58.8% to 50.9%. Gillig et al. 91 reported that 35% (156/435) of the intervention group were hospitalised from either ED or the PDU compared with 52% (181/348) of the control group, but these outcomes were assessed as being at serious risk of bias due to differences between the sites and populations they served. Tretheway et al. 45 reported that the number of patients admitted to a psychiatric ward by the ED-based liaison psychiatry team reduced from the pre- to post-PDU opening period but did not test for significance.
The data for psychiatric admissions from four studies where data were sufficiently well reported were combined meta-analytically (see Figure 7). As Gillig et al. 91 was assessed to be at critical risk of bias, a sensitivity analysis was conducted excluding the study. The combined OR is 0.55 (95% CI 0.43 to 0.68), with an I2 value of 91%; data from 19,634 patients). The result was effectively unchanged in the sensitivity analysis (combined OR is 0.55; 95% CI 0.42 to 0.73, with I2 of 94%). The GRADE rating for outcomes for meta-analyses of non-randomised studies of ‘low certainty, confidence or quality’ was upgraded to ‘moderate certainty’ due to the ROBINS-I ratings, indicating that we believe that the true effect is probably close to the estimated effect.
Psychiatric ward occupancy rates
Only one study94 reported data for occupancy rates for the ‘regular-stay unit’ as 94%, 98%, 99% and 95% in the pre-PDU period compared with 89%, 91%, 96% and 85% post PDU. The results are difficult to interpret as ‘regular-stay unit’ is not clearly defined, within month variance is not reported and no statistical analysis was conducted.
Length of psychiatric admission
One study93 reported a reduction in total time in hospital following ED presentation from a mean of 100.89 hours (median 46.15) hours to 91.00 hours (median 31.35), a significant reduction (p = 0.03) using log-transformed data in a mixed model. Van der Sande et al. 97 reported no significant difference in total number of inpatient days when time spent on the experimental unit was included; 33 days (SD 73.5) in the active group compared with 37 days (SD 83.0) in the control group. However, when inpatient days were compared excluding time spent on the experimental unit the difference was significant (z = −5.51, p < 0.001).
Hospitalisation in the follow-up period
Lester et al. 93 reported similar rates of hospitalisation across the groups following discharge from the unit (6.9% vs. 6.7%). Van der Sande et al. 97 reported a reduction in the number of patients who had a psychiatric inpatient admission during a 1-year follow-up in the PDU group (24%) compared with 38% in the control group but did not test for significance. Schneider and Ross95 reported a 30-day readmission rate for participants who stayed in the intervention unit similar to other patient samples, but this was deemed to be at serious risk of bias as the comparison groups were not clearly defined.
Psychometric outcomes
No psychometric outcomes (symptom scales or patient-reported outcomes) showed significant difference between the groups. Spooren et al. 96 (a study at moderate risk of bias) found no significant difference in scores on the General Health Questionnaire 2898 between groups at 1-month follow-up (t = –0.37, p = 0.715) or in the proportions of patients in each group who reported improvement in each group (t = 0.42, p = 0.677). Van der Sande et al. 97 reported no significant in any of the general symptom index [F(8,112) < 1, p = 0.72], hopelessness scale [F(1,110) = 2.14, p = 0.15] or Symptom Checklist-90; [F(8,110) = 1.03, p = 0.42].
Suicidality
Only one study, which described an experimental unit designed for those who had attempted suicide, reported data about changes to suicidality. 97 The study found that there was no significant difference in the number of suicide attempts per patient in the follow-up period (Z = 0.49, p = 0.62) and no difference in the probability of repeat suicide attempts in the follow-up period (hazard ratio of repetition for patients in the experimental group compared with the care as usual group was 1.24 (95% CI 0.68 to 2.27). For patients identified as at high risk of a repeat suicide attempt (a score of at least four on the Buglass and Horton scale),99 there was a non-significant difference in repeat attempts between experimental and control groups (log rank 2.69; p = 0.10). However, when gender was controlled for, males in the experimental group were found to be significantly more likely to repeat the suicide attempt (log rank 4.28; p = 0.04). Significantly more patients in the experimental group received outpatient care (including care specifically connected to the PDU) in the first year of follow-up (χ2 = 37.42; df = 1, p < 0.001).
Deaths
Stamy et al. 79 reported a decrease in deaths – in the ‘pre’ sample of 23,336 individuals there was one fatality and in the ‘post’ sample (23,231 patients) there were no fatalities – but a power calculation was not reported and the result is unlikely to have sufficient power for conclusions to be drawn.
Health economic outcomes
Browne et al. 90 reported an annual reduction in the cost of one-to-one nursing in ED for those presenting with psychiatric problems of A$129,000, congruent with a reduction in time spent in ED and a decrease in the number of hours of one-to-one nursing care in the first 3 months after the unit fully opened compared with the same period in the previous year. However, no denominator or significance test was reported for this analysis. In the United States, Stamy et al. 79 reported additional revenue for the ED as a result of the experimental unit opening of US$404,954 in the 6 months and $861,065 annually.
Appraisal of findings
The main source of variation in quality was found in the way in which the control group was defined. There were also differences in populations, including differences in the study setting and surrounding health and social care services; it is worth noting that all studies were conducted in high-income countries. Many studies reported similar types of results, but differences in reporting – especially of events data – limited the number of meta-analyses we could perform. Studies reporting median with IQR (and not mean values) also limited how many studies could be included in meta-analyses. Selective reporting, in which studies have reported only outcomes of particular interest to their unit or only positive outcomes, is possible. Although this review included non-randomised studies, the quality of these was carefully scrutinised using the ROBINS-I tool. Many studies were of moderate quality and only one included study received the highest quality rating; as such we should be cautious about the results.
Chapter 4 Interrupted time series
Psychiatric decision units: structural characteristics and patterns of activity
Activity patterns and attendee characteristics from the first 2 years of PDU operation in each site are shown in Table 9. The number of PDU attendances was highest in BSMHFT, which has the largest capacity (eight) and several referral routes. Attendances were much less frequent in SHSCFT PDU, although the unit was closed for a 10-week period during 2020. Units were attended by a small majority of female service users, except for BSMHFT, where there was an even split between men and women. The distributions of attendees’ ages were comparable across sites, reflecting a tendency for about three-quarters of attendees to be aged 25–64 years. LOS on PDUs was longest for SWLSTG and shortest for LPFT. Precise LOS was not available for BSMHFT, although 43.4% and 39.4% of attendees, respectively, were discharged on the same day as admission or the next day, suggesting a relatively short LOS for most attendees. There were marked differences in the proportion of attendees subsequently admitted to psychiatric inpatient wards, ranging from just under one-third in LPFT to less than one in 10 in SHSCFT.
| Variable and level | BSMHFT | LPFT | SWLSTG | SHSCFT |
|---|---|---|---|---|
| Attendances (service users) | 2506 (1864) | 1793 (1255) | 1429 (1006) | 876 (565) |
| Female gender | 1227 (49.0) | 966 (53.9) | 752 (53.2) | 516 (58.9) |
| Age, mean (SD) | 36.1 (12.8) | 36.3 (13.6) | 37.8 (13.4) | 38.1 (13.2) |
| 18–24 years | 580 (23.1) | 428 (23.9) | 295 (20.9) | 140 (16.0) |
| 25–64 years | 1869 (74.6) | 1326 (74.0) | 1087 (76.9) | 707 (80.7) |
| 65+ years | 57 (2.3) | 39 (2.1) | 31 (2.2) | 29 (3.3) |
| Length of stay | ||||
| Median hours (IQR) | – | 23.0 (10.3–37.7) | 37.0 (21.0–48.0) | 30.5 (16.0–48.8) |
| Discharge to psychiatric hospital | 506 (20.2) | 237 (13.2) | 457 (32.0) | 68 (7.8) |
There were notable differences in the trajectories of attendance frequencies over the initial 24 months in each site (see Appendix 4, Figure 16). The number of attendances grew over the first 3 months post PDU implementation in BSMHFT, LPFT and SWLSTG sites but was steady thereafter for LPFT (70–80/month) and SWLSTG (50–60/month); in contrast, attendance levels in BSMHFT increased markedly from months 11–14 and afterwards the PDU maintained over 100 attendances/month. The frequency of attendances in SHSCFT was low initially, steadily climbing to 40/month by month 8 and largely maintaining that level thereafter aside from the closure period in March to June 2020.
Mental health trust outcomes
The catchment populations, annual rates and user characteristics of adult acute inpatient admissions and PLEs for each participating MHT, stratified by pre and post PDU implementation periods with pairwise comparisons, are described fully in Appendix 4, Table 34. Reliable data on inpatient admission and psychiatric liaison activity could not be sourced from SHSCFT and consequently they are not provided here nor included in subsequent ITS analyses.
In general, inpatient admission and PLE activity levels were considerably greater in BSMHFT (1772/year, 7446/year, respectively) and SWLSTG (1578/year, 4195/year) than LPFT (630/year, 1719/year). The frequency of inpatient admissions was comparable between pre and post PDU periods for BSMHFT and SWLSTG but higher in the latter period for LPFT. Across all trusts, the number of PLEs were significantly higher in the post PDU period. Individuals with previous (in last 24 months) inpatient admissions and PLE activity, respectively, made up a notable proportion of admissions (36.8–44.3%) and PLE (33.8–48.1%) in the study period, with a significant increase from pre to post PDU periods for the latter. There was a high proportion of women admitted to inpatient wards in SWLSTG (almost half) relative to BSFMHT and LPFT (40–45%). The (broad) distributions of age were more comparable, with approximately four of five admissions of service users aged 25–64 years. Overall, informal admissions made up about half of the admissions in BSMHFT and SWLSTG and over 60% in LPFT, although all trusts observed a significant post PDU decrease in the proportion of admissions that were informal. Length of inpatient stay was highest in BSMHFT where only 1 in 10 service users admitted stayed 5 days or less and lowest in SWLSTG where 1 in 5 had short stays. In the post-PDU period, length of inpatient stay increased in SWLSTG and LPFT as indicated by significant changes in median days and/or decreased frequency of 0- to 5-day stays, but there was a small but reliable decrease in LOS in BSMHFT. Daily bed occupancy significantly increased in the post-PDU period for all trusts where data were available. Out-of-area admissions, available for SWLSTG only, showed a marked decrease (from 75.5/ to 47.0/year) following PDU implementation.
Interrupted times series outcomes: psychiatric inpatient admissions and psychiatric liaison episodes
Weekly aggregated data concerning the frequency of informal acute adult inpatient admissions in pre and post PDU periods in participating MHTs are presented graphically in Figures 8–10. Corresponding parameter estimates from ITS analysis and estimates for secondary outcome measures are shown in Tables 10–12 (see Appendix 4, Figures 17–36 for accompanying graphical depictions).
FIGURE 8.
Impact of PDU implementation on informal inpatient admissions in BSMHFT. Note: The black vertical line represents implementation of the PDU.
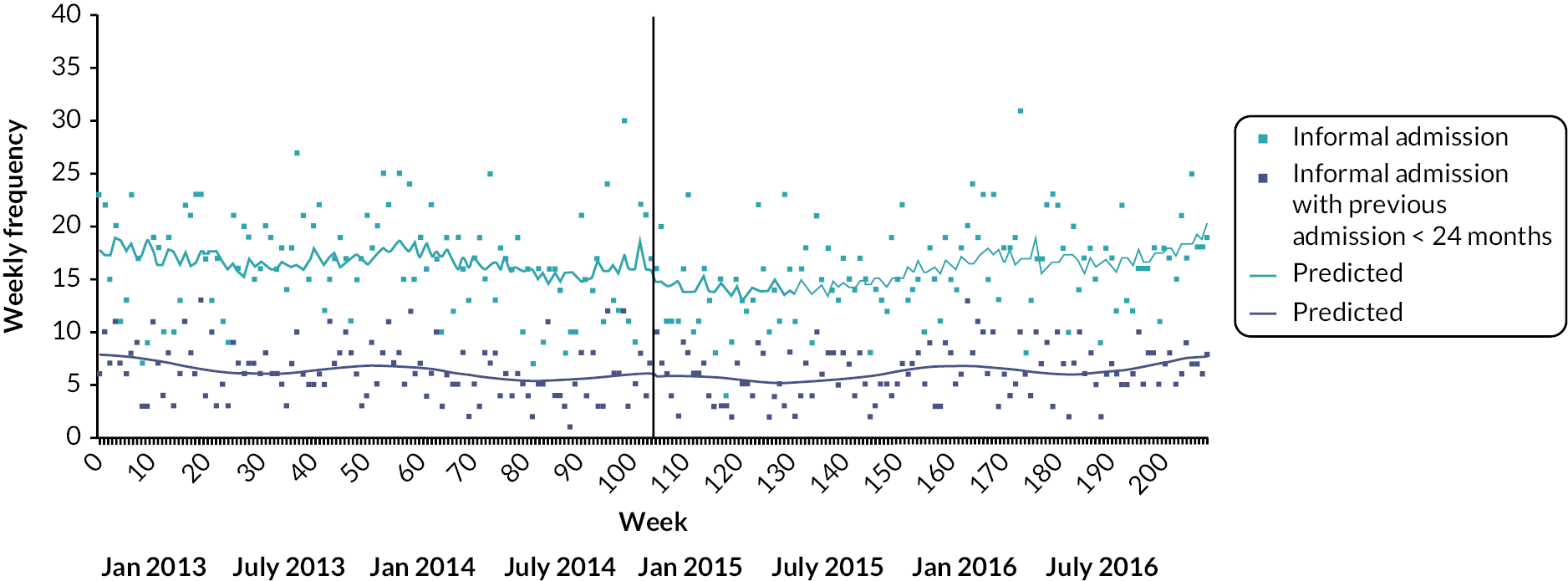
| Initial trend (pre PDU) | Step change (post PDU) | Trend change (post PDU) | Post PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| Results using Poisson GLM | ||||
| Informal inpatient admissions | −0.001 (−0.003 to 0.001) | −0.176 (−0.334 to −0.018)a | 0.003 (0.001 to 0.006) a | 0.003 (0.001 to 0.005) c |
| −0.07% | −16.16% | 0.33% | 0.30% | |
| Informal inpatient admission with previous admission (< 24 months) | −0.003 (−0.005 to 0.0001) | −0.052 (−0.286 to 0.182) | 0.005 (0.002 to 0.009) b | 0.003 (0.0003 to 0.006) a |
| −0.26% | −5.06% | 0.53% | 0.29% | |
| All inpatient admissions | −0.0001 (−0.001 to 0.001) | −0.047 (−0.150 to 0.056) | 0.001 (−0.001 to −0.002) | 0.001 (−0.0004 to 0.002) |
| −0.01% | −4.56% | 0.07% | 0.09% | |
| Results using GLM with identity link | ||||
| Formal inpatient admission (%) | 0.039 (−0.030 to 0.108) | 6.308 (0.813 to 11.803) a | −0.156 (−0.246 to −0.067) c | −0.112 (−0.174 to −0.050) c |
| 0.04% points | 6.31% points | −0.16% points | −0.11% points | |
| Length of inpatient stay | ||||
| Five days or less inpatient admission (%) | 0.003 (−0.030 to 0.036) | −0.924 (−3.729 to 1.881) | 0.020 (−0.028 to 0.069) | 0.028 (−0.012 to 0.069) |
| 0.003% points | −0.92% points | 0.02% points | 0.03% points | |
| Log mean days | 0.002 (−0.0003 to 0.004) | −0.170 (−0.369 to 0.029) | −0.001 (−0.004 to 0.002) | 0.001 (−0.002 to 0.003) |
| 0.21% points | −15.63% points | −0.11% points | 0.07% points | |
| Daily bed occupancy (mean) | 0.147 (0.073 to 0.221) c | −1.248 (−4.049 to 1.554) | −0.171 (−0.252 to −0.090)c | −0.027 (−0.056 to 0.002) |
| 0.15 beds | −1.25 beds | −0.17 beds | −0.03 beds | |
| Results using Poisson GLM | ||||
| PLEs | 0.002 (0.002 to 0.003) c | −0.108 (−0.159 to −0.056) c | −0.0004 (−0.001 to 0.0003) | 0.002 (0.001 to 0.003) c |
| 0.24% | −10.22% | −0.05% | 0.21% | |
| With previous episode (< 24 months) | 0.005 (0.004 to 0.006) c | −0.158 (−0.226 to −0.090) c | −0.003 (−0.004 to −0.002) c | 0.002 (0.001 to 0.003) c |
| 0.48% | −14.58% | −0.28% | 0.20% | |
Inpatient admission and psychiatric liaison episode activity in Birmingham and Solihull Mental Health NHS Foundation Trust
Data indicate a significant decrease in the number of informal admissions immediately following PDU implementation (by 16%) but an increase in informal admission rate in the post PDU period (of 0.33%/week; see Figure 8, Table 10). There was a smaller (non-significant) drop in informal admissions upon implementation of the PDU for those with a recent previous admission, but a similar, reliable post-PDU increase in admission rate. These findings were mirrored by a significant increase in the proportion of formal admissions immediately after PDU implementation (from 52% to 58%) but a steady decrease in the weekly proportion of formal admissions in the 2 years following PDU implementation, reflecting a highly significant change in rate from pre to post PDU.
While there was no effect (either short- or long-term) of the PDU on overall admission rates or on admitted service users’ length of inpatient stay, there was a significant difference in trend of daily bed occupancy between pre and post PDU periods, reflecting a shift from a pre-PDU increase of 0.15 beds/week to a more stable pattern of daily bed occupancy post PDU (decrease of 0.03 beds/week). PLE frequency in the pre-PDU period was significantly increasing, by 0.24%/week, but decreased immediately following PDU implementation (by 10%). There was no significant change in the underlying increasing weekly trend post PDU, however, with PLE frequency continuing to increase (by 0.21%/week) in the post-PDU period. However, there were highly significant short- and long-term decreases in weekly frequency of PLE considering episodes by individuals with a recent previous episode, albeit in the context of an increasing weekly pre-PDU trend in this group of service users.
Inpatient admission and psychiatric liaison episode activity in Lincolnshire Partnership NHS Foundation Trust
The weekly frequency of informal admissions decreased immediately following PDU implementation by more than 10%, although this failed to reach significance (see Figure 9, Table 11). Nevertheless, there was a significant (long-term) change in pre- to post-PDU trend; in the 2-year post-PDU period, the number of informal admissions decreased by almost half a per cent/week. A similar pattern emerged (at a monthly level) considering only those informal admissions by service users with a recent previous admission. Prior to PDU implementation, weekly admission (formal and informal) frequency was increasing by 0.29%/week. This pattern was reversed in the post-PDU period where admissions decreased significantly by 0.18%/week, representing a highly significant change pre- to post-PDU trend (of 0.45%/week). The proportion of admissions that were formal was significantly increasing each week before PDU implementation. There was a further (immediate) increase (from 30% to 40%) on PDU implementation, and the pre-PDU trend continued in the post-PDU period pattern at the same rate (increase of 0.14% points/week). The PDU had less impact on length of inpatient stay, although the proportion of short stays, which was increasing prior to PDU implementation, did stabilise in the post-PDU period. There were significant trends during pre- and post-PDU periods indicating increasing PLE frequency, although when considering only those episodes by individuals with a recent previous episode there was a significant pre- to post-PDU trend decrease in (monthly) episode frequency.
FIGURE 9.
Impact of PDU implementation on informal inpatient admission in LPFT. Note: the black vertical line represents implementation of the PDU.
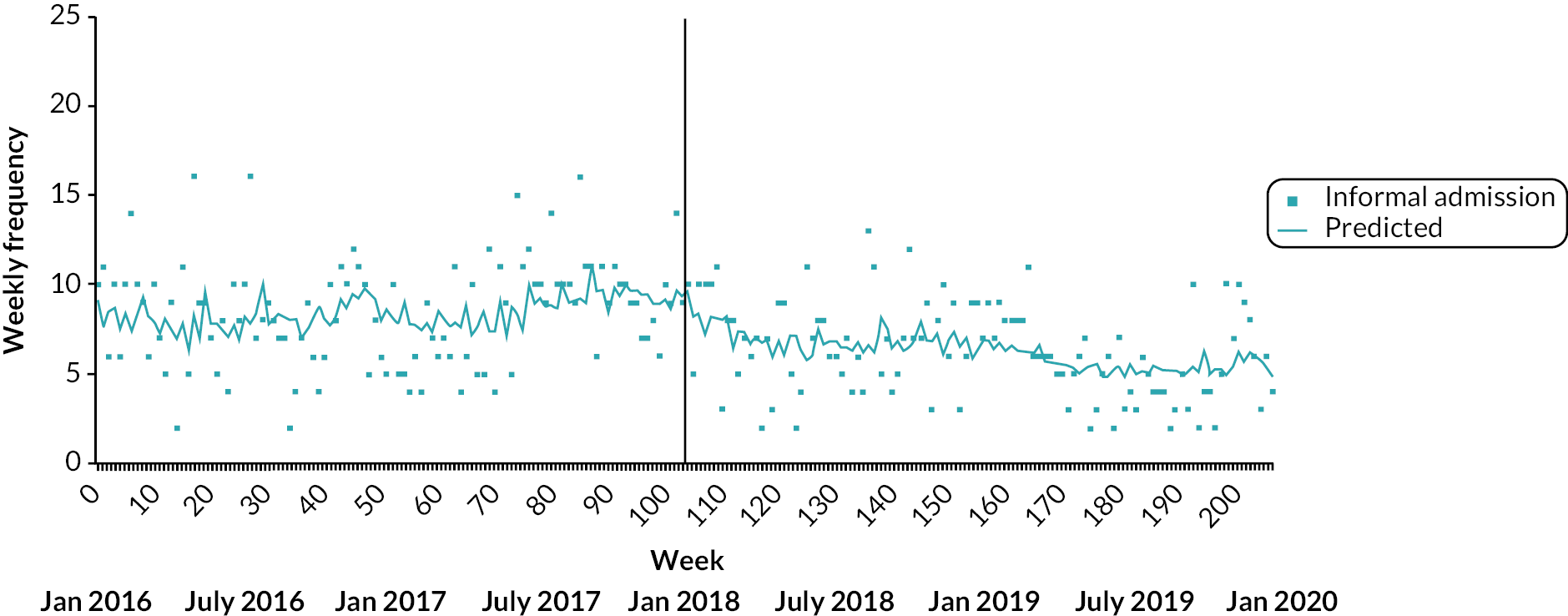
| Initial trend (pre PDU) | Step change (following PDU) | Trend change (following PDU) | Post PDU trend | ||
|---|---|---|---|---|---|
| Results using Poisson GLM | B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| Informal inpatient admissions | 0.001 (−0.001 to 003) | −0.113 (−0.313 to 0.086) | −0.004 (−0.008 to −0.001) b | −0.005 (−0.007 to −0.002) b | |
| 0.09% | −10.72% | −0.45% | −0.45% | ||
| All inpatient admissions | 0.003 (0.001 to 0.005) b | −0.031 (−0.180 to 0.119) | −0.004 (−0.007 to −0.002) c | −0.002 (−0.003 to −0.0001) a | |
| 0.29% | −3.03% | −0.45% | −0.18% | ||
| Monthly change | Step change | Monthly change | Monthly change | ||
| Informal inpatient admission with previous admission (< 24 months) | 0.010 (−0.008 to 0.028) | 0.036 (−0.264 to 0.335) | −0.030 (−0.053 to −0.007) a | −0.017 (−0.034 to −0.001) a | |
| 1.00% | 3.64% | −2.96% | −1.72% | ||
| Results using GLM with identity link | B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| Formal inpatient admission (%) | 0.143 (0.049 to 0.236) b | 10.275 (2.425 to 18.126) a | −0.025 (−0.152 to 0.103) | 0.139 (0.050 to 0.228) b | |
| 0.14% points | 10.28% points | −0.03% points | 0.14% points | ||
| Length of inpatient stay: | |||||
| ≤ 5 days inpatient admission (%) | 0.085 (0.016 to 0.154) a | −2.502 (−8.444 to 3.441) | −0.064 (−0.157 to 0.029) | 0.012 (−0.056 to 0.080) | |
| 0.09% points | −2.50% points | −0.06% points | 0.01% points | ||
| Log mean days | −0.003 (−0.007 to 0.001) | 0.083 (−0.243 to 0.409) | 0.001 (−0.004 to 0.006) | −0.002 (−0.004 to −0.0001) a | |
| −0.27% | 8.64% | 0.12% | −0.21% | ||
| Daily bed occupancy (mean) | 0.007 (−0.007 to 0.018) | 0.938 (−0.252 to 2.13) | −0.014 (−0.031 to 0.004) | −0.009 (−0.023 to 0.005) | |
| 0.01 beds | 0.94 beds | −0.01 beds | −0.01 beds | ||
| Results using Poisson GLM | B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| PLEs | 0.002 (0.0003 to 0.003) a | 0.005 (−0.104 to 0.114) | 0.001 (−0.001 to 0.003) | 0.004 (0.003 to 0.005) c | |
| 0.18% | 0.51% | 0.13% | 0.39% | ||
| Monthly change | Step change | Monthly change | Monthly change | ||
| With previous episode (< 24 months) | 0.039 (0.027 to 0.051) c | −0.002 (−0.187 to 0.183) | −0.028 (−0.043 to −0.014) c | 0.009 (0.0003 to 0.018) a | |
| 3.97% | −0.22% | −2.79% | 0.93% | ||
Inpatient admission and psychiatric liaison episode activity in South West London and St George’s Mental Health NHS Trust
Prior to PDU implementation, there was a significant trend indicating an increase (of 0.27%/week) in informal admission frequency. Informal admissions decreased by almost 20% immediately following implementation of the PDU, and there was a highly significant change in pre- to post-PDU (long-term) trend, reflecting a decrease of 0.5%/week (see Figure 10, Table 12). The effect of the PDU on informal admissions for service users with a recent previous admission was very similar, although the post-PDU trend also indicated a significant weekly decrease. A significant change of weekly trend from pre- to post-PDU periods was also observed when considering all admissions (formal and informal), suggesting that PDU implementation arrested the prior trend of increasing admission frequency. The opening of the PDU in SWLSTG had an immediate impact on the proportion of patients admitted formally (increase by almost 7% points, from approximately 43% to 50%) and there was a significant change (weekly increase) in the pre- to post-PDU trend. There was little indication of an effect of PDU implementation on length of inpatient stay or daily bed occupancy rates over the study period. In a similar manner, there was no significant impact of PDU implementation on PLE frequency, which was increasing over the pre-PDU period (both for all service user episodes and for those by service users with a recent episode).
FIGURE 10.
Impact of PDU implementation on informal inpatient admissions in SWLSTG. Note: the black vertical line represents implementation of the PDU.
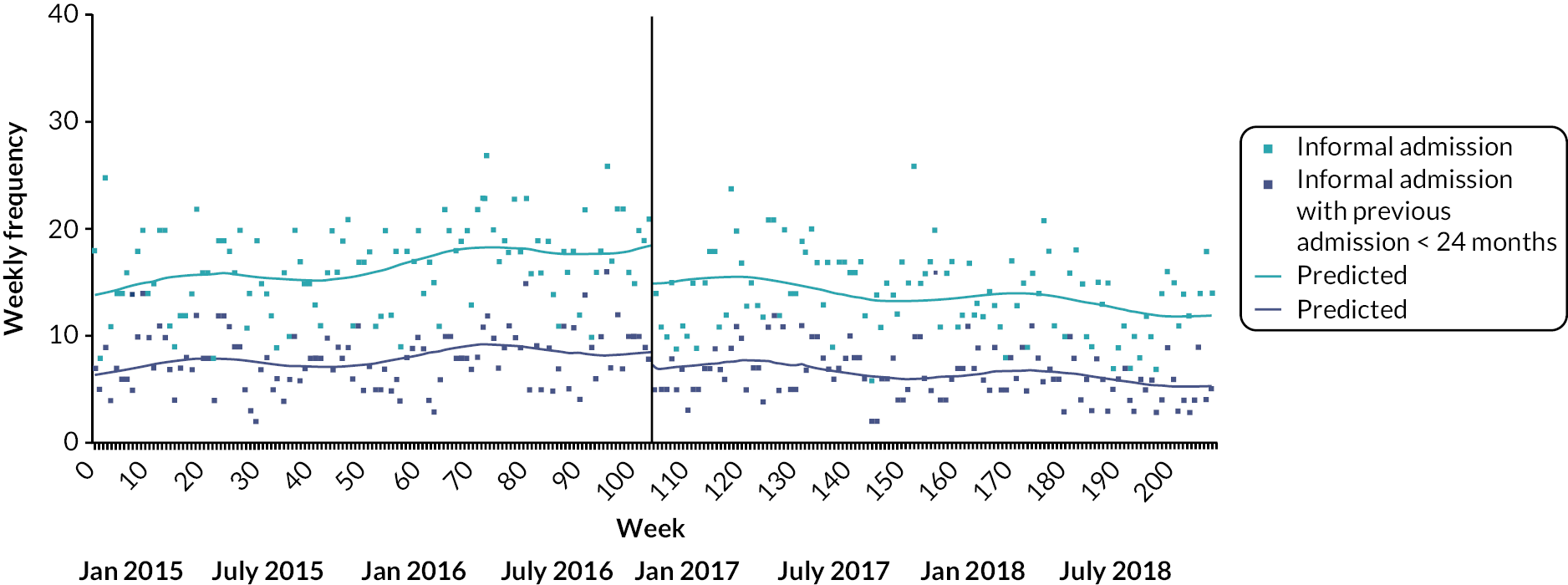
| Initial trend (pre-PDU) | Step change (following PDU) | Trend change (following PDU) | Post PDU trend | |
|---|---|---|---|---|
| B (95% CI) Weekly change | B (95% CI) Step change | B (95% CI) Weekly change | B (95% CI) Weekly change | |
| Results using Poisson GLM | ||||
| Informal inpatient admissions | 0.003 (0.001 to 0.004) b | −0.218 (−0.357 to −0.078) b | −0.005 (−0.007 to −0.003) c | −0.002 (−0.004 to 0.0001) |
| 0.27% | −19.56% | −0.49% | −0.19% | |
| Informal inpatient admission with previous admission (< 24 months) | 0.003 (0.001 to 0.005) a | −0.219 (−0.402 to −0.037) a | −0.005 (−0.008 to −0.002) c | −0.002 (−0.005 to −0.0001) a |
| 0.28% | −19.70% | −0.53% | −0.24% | |
| All inpatient admissions | 0.002 (0.001 to 0.003) c | −0.089 (−0.184 to 0.007) | −0.003 (−0.004 to −0.001) c | −0.001 (−0.002 to 0.0002) |
| 0.22% | −8.50% | −0.28% | −0.09% | |
| Results using GLM with identity link | ||||
| Formal inpatient admission (%) | −0.036 (−0.098 to 0.026) | 6.85 (1.685 to 12.017) b | 0.109 (0.021 to 0.197) a | 0.068 (−0.005 to 0.141) |
| −0.04% points | 6.85% points | 0.11% points | 0.07% points | |
| Length of inpatient stay: | ||||
| ≤ 5 days inpatient admission (%) | −0.044 (−0.093 to 0.005) | 1.110 (−3.478 to 5.697) | −0.005 (−0.076 to 0.065) | −0.044 (−0.097 to 0.010) |
| −0.04% points | 1.11% points | −0.01% points | −0.04% points | |
| Log mean days | −0.002 (−0.005 to 0.0003) | 0.128 (−0.059 to 0.315) | 0.002 (−0.001 to 0.005) | 0.0003 (−0.002 to 0.002) |
| −0.021% | 13.66% | 0.24% | 0.03% | |
| Daily bed occupancy (mean) | 0.035 (0.001 to 0.068) a | −1.234 (−3.492 to 1.024) | −0.029 (−0.069 to 0.010) | 0.014 (−0.009 to 0.037) |
| 0.04 beds | −1.23 beds | −0.03 beds | 0.01 beds | |
| Results using Poisson GLM | ||||
| PLEs | 0.002 (0.001 to 0.003) c | 0.018 (−0.050 to 0.087) | −0.001 (0.002 to 0.0003) | 0.001 (0.001 to 0.002) c |
| 0.23% | 1.86% | −0.07% | 0.14% | |
| PLEs with previous episode (< 24 months) | 0.003 (0.002 to 0.004) c | 0.075 (−0.034 to 0.184) | −0.001 (−0.003 to 0.0003) | 0.001 (−0.0001 to 0.003) |
| 0.30% | 7.79% | −0.15% | 0.13% | |
Acute trust outcomes
The catchment populations, annual rates and user characteristics of ED mental health attendances for each participating acute trust, stratified by pre- and post-PDU implementation periods with pairwise comparisons, are described fully in Appendix 4, Table 35. In general, attendances were more frequent in SWBHFT (2242/year) and STHFT (2200/year) than SGUHFT (1980/year) and ULHFT (1620/year). Annual rates were comparable between pre- and post-PDU periods in SWBHFT and in SGUHFT but higher in the latter period for LPFT and lower post PDU in STHFT. A small majority of attendances in SWBHFT (55.1%), SGUHFT (61.1%) and STHFT (62.9%) were by service users who had previously attended (for any reason) in the last 24 months; there was a marked decreased in STHFT from pre (67.0%) to post PDU (53.8%), however. The overall proportion was much lower in ULHFT (34.4%) most likely because these attendances considered only those individuals with previous attendances involving a mental health presentation.
The sex of attending service users was, overall, evenly split between women and men in STFHT, SGUHFT and ULHFT but women only made up 39.5% of the attendees in SWBHFT over the study period, although this significantly increased post-PDU implementation. Approximately two-thirds of service users were aged 25–64 years in STHFT and ULHFT. This compared with three-quarters of attendees in SGUHFT, although the proportion of younger service users (aged 18–24 years) significantly increased post PDU. In all trusts, more than half of ED mental health attendances were by individuals arriving by ambulance or police. This was particularly apparent at ULHFT (66.8%), although there was a significant reduction in ambulance/police arrivals post PDU. Rate of admissions to an acute trust ward from ED was also higher in ULHFT (19.6%) relative to other trusts (8.6–12.7%) where significant decreases in acute trust ward admissions in the period following PDU implementation were observed. Median LOS for ED mental health attendances varied between 3 and 4 hours, depending on the trust, with 4-hour breach rates ranging from just under one-quarter in SWBHFT (23.8%) to almost 40% (39.2%) in ULHFT. While length of ED stay significantly decreased from pre to post PDU in SWBHFT, STHFT and ULHFT, it increased in SGUHFT. Further, the proportion of 4-hour breaches significantly increased post PDU in SGUHFT (by 2.4% points) and ULHFT (by 5.0% points).
Interrupted times series outcomes: emergency department mental health attendances
Weekly aggregated data concerning the frequency of ED mental health attendances in pre- and post-PDU periods in participating MHTs are presented graphically in Figures 11–14. Corresponding parameter estimates from ITS analysis and estimates for secondary outcome measures are shown in Tables 13 and 14 (see Appendix 4, Figures 37–52 for accompanying graphical depictions).
FIGURE 11.
Impact of PDU implementation on weekly number of ED mental health attendances in SWBHFT. Note: the black vertical line represents implementation of the PDU.

Emergency department mental health attendances in Sandwell and West Birmingham Hospitals NHS Foundation Trust
The data indicate that prior to PDU implementation, there was a highly significant increase in ED mental health presentations in SWBHFT (by approximately 0.5%/week). There was a significant decrease in the number of ED mental health attendances immediately following PDU implementation (by around 20%) but there was little impact on long-term trend, and ED attendance frequency continued to rise in the post-PDU period (by 0.4%/week; see Figure 11, Table 13). The pattern was similar when considering only those attendances by service users with a (recent) previous ED attendance, although the initial period was characterised by a more marked weekly increase in frequency (by approximately 0.8%/week) and there was a significant change (decrease) in trend from pre to post PDU. There was little impact of PDU implementation on the proportion of ED mental health attendances via ambulance or police or rates of 4-hour breaches, although there was a significant drop (> 10%) in length of ED stay immediately following PDU implementation. Curiously, the proportion of ED mental health attendances discharged to an acute trust ward decreased significantly in the period before PDU implementation but increased by about 4% on opening of the PDU, although was still steadily declining in the post-PDU period.
Emergency department mental health attendances in United Lincolnshire Hospitals NHS Foundation Trust
While there was no evidence of an immediate effect of PDU implementation on ED mental health attendances in ULHFT, there was a significant increase (by 0.3%/week) in attendance frequency in the post-PDU period, reflecting a change in pre- to post-PDU trend (see Figure 12, Table 13). PDU implementation had no significant short- or long-term effects on the proportion of ED mental health attendances where individuals arrived by ambulance or police, which was significantly decreasing in the pre-PDU period. There was, however, a significant increase from pre to post-PDU in the proportion of attendances where service users were discharged from ED to an acute trust ward, reversing the decreasing pre-PDU trend. There was evidence for a small but reliable weekly increase in (mean) LOS in ED following PDU implementation but no effect on 4-hour breach rate.
FIGURE 12.
Impact of PDU implementation on weekly number of ED mental health attendances in ULHFT. Note: the black vertical line represents implementation of the PDU.

| Initial trend (pre-PDU) | Step change (following PDU) | Trend change (following PDU) | Post-PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| SWBHFT | ||||
| Number of ED mental health attendances | 0.005 (0.001 to 0.008) a | −0.229 (−0.352 to −0.105) b | −0.001 (−0.004 to 0.002) | 0.004 (0.003 to 0.005) b |
| 0.47% | −20.43% | −0.06% | 0.40% | |
| Number of ED attendances for those with previous attendance (< 24 months) | 0.008 (0.004 to 0.011) b | −0.268 (−0.406 to −0.129) b | −0.004 (−0.007 to −0.0004) c | 0.004 (0.003 to 0.005) b |
| 0.79% | −23.48% | −0.37% | 0.40% | |
| Arrival by ambulance/police (%) | 0.010 (−0.141 to 0.161) | −1.818 (−7.169 to 3.533) | −0.005 (−0.155 to 0.145) | 0.004 (−0.047 to 0.054) |
| 0.01% points | −1.82% points | −0.01% points | 0.004% points | |
| Discharge to acute trust ward (%) | −0.128 (−0.225 to −0.031) a | 4.021 (0.579 to 7.463) c | 0.086 (−0.011 to 0.183) | −0.041 (−0.074 to −0.008) c |
| −0.13% points | 4.02% points | 0.09% points | −0.04% points | |
| Length of stay in ED | ||||
| 4-hour breach (%) | 0.061 (−0.112 to 0.235) | −6.00 (−12.25 to 0.247) | −0.014 (−0.187 to 0.158) | 0.045 (−0.003 to 0.094) |
| 0.06% points | −6.00% points | −0.01% points | 0.05% points | |
| Log mean minutes | 0.0005 (−0.001 to 0.002) | −0.121 (−0.202 to −0.040) a | 0.0001 (−0.002 to 0.002) | 0.001 (−0.0003 to 0.001) |
| 0.05% | −11.43% | 0.01% | 0.06% | |
| ULHFT | ||||
| Number of ED mental health attendances | 0.0001 (−0.001 to 0.001) | 0.047 (−0.066 to 0.161) | 0.003 (0.001 to 0.004) a | 0.003 (0.001 to 0.004) b |
| 0.01% | 4.84% | 0.26% | 0.27% | |
| Number of ED attendances for those with previous attendance (< 24 months) | 0.002 (−0.001 to 0.004) | 0.095 (−0.084 to 0.274) | 0.0005 (−0.003 to 0.004) | 0.002 (0.0003 to 0.004) c |
| 0.18% | 9.98% | 0.05% | 0.24% | |
| Arrival by ambulance/police (%) | −0.074 (−0.132 to −0.016) c | 1.702 (−3.693 to 7.097) | 0.036 (−0.040 to 0.111) | −0.050 (−0.113 to 0.012) |
| −0.07% points | 1.70% points | 0.03% points | −0.05% points | |
| Discharge to acute trust ward (%) | −0.094 (−0.148 to −0.041) a | 3.885 (−0.513 to 8.283) | 0.121 (0.056 to 0.186) b | 0.027 (−0.014 to 0.068) |
| −0.09% points | 3.89% points | 0.12% points | 0.03% points | |
| Length of stay in ED | ||||
| 4-hour breach (%) | 0.005 (−0.052 to 0.063) | 1.38 (−3.87 to 6.63) | 0.032 (−0.045 to 0.110) | 0.032 (−0.031 to 0.096) |
| 0.01% points | 1.38% points | 0.03% points | 0.03% points | |
| Log mean minutes | −0.0001 (−0.001 to 0.001) | 0.029 (−0.043 to 0.100) | 0.001 (0.0002 to 0.002) c | 0.001 (0.0001 to 0.002) c |
| −0.01% | 2.94% | 0.12% | 0.11% | |
Emergency department mental health attendances in Sheffield Teaching Hospital NHS Foundation Trust: interrupted time series outcomes
There was a pre-PDU trend indicating a significant decrease (by 0.16%/week) in ED mental health attendances. There was a non-significant decrease in attendance frequency immediately following PDU implementation but a significant increase in pre- to post-PDU trend over the longer term (a single year post PDU in the case of STHFT), although weekly attendances did not increase in the post-PDU period (see Figure 13, Table 14). These effects were in the same direction, although more marked, when considering only those attendances by individuals with a recent ED attendance. In the pre-PDU period, the proportions of mental health presentations in ED where individuals arrived by ambulance or police and/or were discharged to an acute trust ward were decreasing significantly. However, following PDU implementation, significant short- and long-term increases in the rate of arrivals by ambulance or police and a significant increase in pre to post trend for attendances with discharge to acute trust ward occurred. LOS in ED was also significantly decreasing prior to implementation of the PDU, both with respect to (mean) minutes in ED and proportion of 4-hour breaches, although there was no significant (short- or long-term) impact on this trend following PDU implementation.
FIGURE 13.
Impact of PDU implementation on weekly number of ED mental health attendances in STHFT. Note: the black vertical line represents implementation of the PDU.
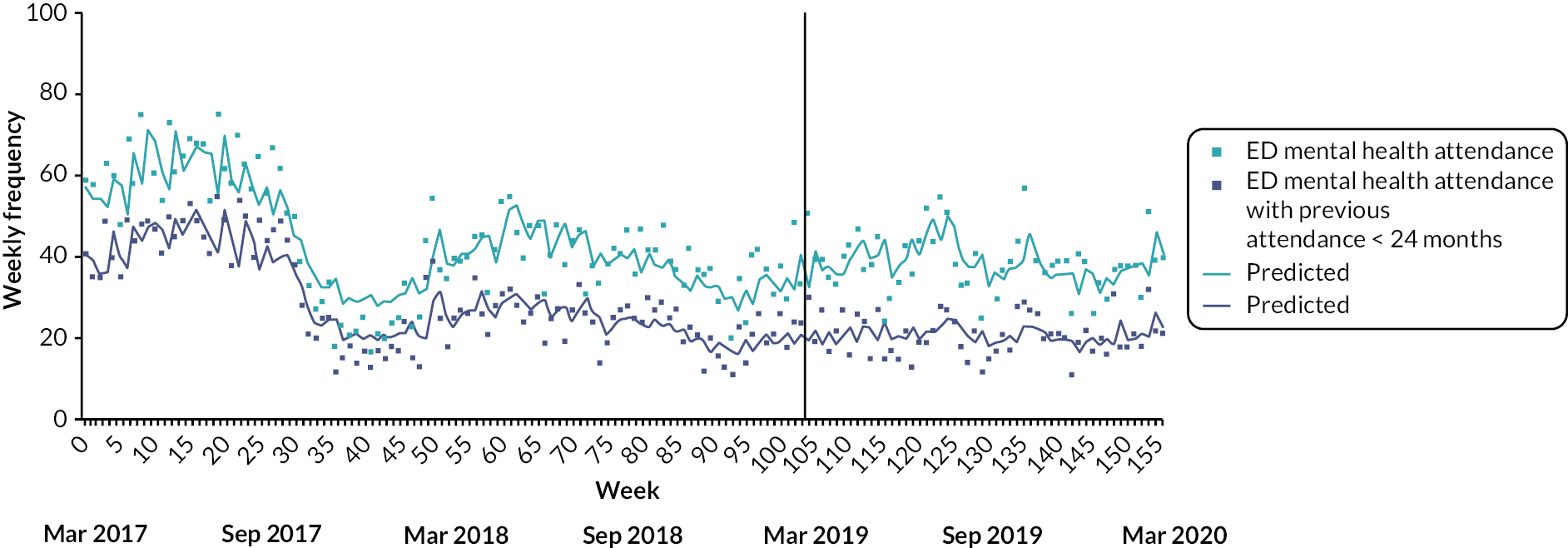
Emergency department mental health attendances in St George’s University Hospital NHS Foundation Trust
There was little evidence for either an immediate or long-term effect of the introduction of the PDU on attendances in SGUHFT. There was a small but reliable decrease (of 0.06% points/week) in the proportion of attendances where individuals arrived via ambulance or police in the post-PDU period (see Figure 14, Table 14). The rate of ED attendances with discharge to an acute trust ward increased significantly following PDU implementation and there was a highly significant change in pre to post PDU trend, although the proportion remained in steady decline in the post-PDU period. Average LOS in SGUHFT ED increased in the post-PDU period (by approximately 0.2%/week), significantly reversing a pattern of decreasing LOS prior to PDU implementation, although there was little evidence for an impact of the PDU on 4-hour breach rate.
FIGURE 14.
Impact of PDU implementation on weekly number of ED mental health attendances in SGUHFT. Note: the black vertical line represents implementation of the PDU.

| Initial trend (pre-PDU) | Step change (following PDU) | Trend change (following PDU) | Post-PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| STHFT | ||||
| Number of ED mental health attendances | −0.002 (−0.003 to −0.00001) a | −0.040 (−0.199 to 0.118) | 0.005 (0.0001 to 0.009) a | −0.001 (−0.006 to 0.005) |
| −0.16% | −3.96% | 0.46% | −0.08% | |
| Number of ED attendances for those with previous attendance (< 24 months) | −0.003 (−0.005 to −0.001) b | −0.085 (−0.288 to 0.117) | 0.007 (0.0004 to 0.013) a | −0.003 (−0.009 to 0.004) |
| −0.32% | −8.19% | 0.68% | −0.25% | |
| Arrival by ambulance/police (%) | −0.288 (−0.446 to −0.129) c | 10.128 (3.279 to 16.976) b | 0.226 (0.034 to 0.418) b | 0.033 (−0.138 to 0.204) |
| −0.29% points | 10.13% points | 0.23% points | 0.03% points | |
| Discharge to acute trust ward (%) | −0.144 (−0.182 to −0.106) c | −0.965 (−4.466 to 2.536) | 0.206 (0.125 to 0.287) c | 0.030 (−0.066 to 0.125) |
| −0.14% points | −0.97% points | 0.21% points | 0.03% points | |
| Length of stay in ED | ||||
| 4-hour breach (%) | −0.102 (−0.161 to −0.043)c | 6.810 (−0.633 to 14.253) | −0.027 (−0.217 to 0.162) | −0.025 (−0.304 to 0.253) |
| −0.10% points | 6.81% points | −0.03% points | −0.03% points | |
| Log mean minutes | −0.002 (−0.003 to −0.001) c | 0.089 (−0.040 to 0.218) | −0.0004 (−0.004 to 0.003) | −0.001 (−0.006 to 0.004) |
| −0.17% | 9.31% | −0.04% | −0.10% | |
| SGUHFT | ||||
| Number of ED mental health attendances | −0.001 (−0.002 to 0.0005) | 0.087 (−0.010 to 0.184) | −0.0001 (−0.002 to 0.001) | −0.001 (−0.002 to 0.0002) |
| −0.0.06% | 9.12% | −0.01% | −0.08% | |
| Number of ED attendances for those with previous attendance (< 24 months) | −0.0003 (−0.002 to 0.001) | 0.062 (−0.051 to 0.175) | −0.0004 (−0.002 to 0.001) | −0.001 (−0.002 to 0.001) |
| −0.02% | 6.43% | −0.04% | −0.09% | |
| Arrival by ambulance/police (%) | 0.014 (−0.042 to 0.070) | −3.215 (−8.000 to 1.570) | −0.067 (−0.140 to 0.006) | −0.059 (−0.116 to −0.003) a |
| 0.01% points | −3.22% points | −0.07% points | −0.06% points | |
| Discharge to acute trust ward (%) | −0.172 (−0.208 to −0.137) c | 5.374 (3.041 to 7.706) c | 0.133 (0.093 to 0.173) c | −0.035 (−0.059 to −0.010) b |
| −0.17% points | 5.37% points | 0.13% points | −0.04% points | |
| Length of stay in ED | ||||
| 4-hour breach (%) | −0.035 (−0.090 to 0.020) | 2.576 (−2.116 to 7.268) | 0.075 (−0.003 to 0.153) | 0.041 (−0.018 to 0.101) |
| −0.04% points | 2.58% points | 0.08% points | 0.04% points | |
| Log mean minutes | −0.001 (−0.002 to −0.0002) a | 0.006 (−0.066 to 0.078) | 0.003 (0.001 to 0.004) c | 0.002 (0.001 to 0.003) c |
| −0.11% | 0.59% | 0.27% | 0.17% | |
Pooled estimates of impact of psychiatric decision unit implementation
Table 15 shows the fixed and random effect pooled estimates for primary ITS outcomes concerning informal inpatient admission and ED mental health attendance activity. Significant heterogeneity in site outcomes were observed for all estimates except informal inpatient admission step change, which suggested a robust decrease (of 16.6%) in informal admission frequency following PDU implementation across participating sites. While fixed effects suggested that, overall, there was a significant decrease in informal admission frequency trend from pre to post PDU (by about 0.2%/week), reversing a steady weekly increase in trend prior to PDU implementation, after adjustment for random effects, the pre-to post-PDU change in weekly trend was not significant. The introduction of PDUs had no overall effect on level or trend in mental health presentations at ED. Although fixed-effects modelling suggested a highly significant weekly increase in ED attendances in the post-PDU period, this was not significant after adjustment for random effects.
| Initial trend (pre PDU) | Step change (following PDU) | Trend change (following PDU) | Post-PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| Informal inpatient admission | ||||
| Fixed | 0.001 (0.0002 to 0.002) a | −0.181 (−0.273 to −0.088) c | −0.002 (−0.003 to −0.0003) a | −0.0002 (−0.001 to 0.001) |
| 0.12% | −16.56% | −0.19% | −0.02% | |
| Random | 0.001 (−0.001 to 0.003) | −0.181 (−0.273 to −0.088) c | −0.002 (−0.007 to 0.003) | −0.001 (−0.005 to 0.003) |
| 0.11% | −16.56% | −0.20% | −0.10% | |
| Mental health ED attendance | ||||
| Fixed | −0.0003 (−0.001 to 0.0004) | −0.012 (−0.071 to 0.047) | 0.001 (−0.00004 to 0.002) | 0.002 (0.001 to 0.003) c |
| −0.03% | −1.22% | 0.10% | 0.19% | |
| Random | 0.0001 (−0.002 to 0.002) | −0.031 (−0.174 to 0.113) | 0.001 (−0.0001 to 0.003) | 0.002 (−0.001 to 0.004) |
| 0.01% | −3.00% | 0.13% | 0.16% | |
Meta-analysis of secondary ITS outcomes indicated that (after adjustment for random effects where appropriate) PDU implementation had significant overall effects on formal inpatient admission percentage (step change increase by 7.3%), PLE frequency in individuals with recent episode activity (pre-to post-PDU trend decrease of 0.25%/week), proportion of ED mental health attendances with discharge to acute trust ward (step change increase of 3.2% points, pre-to post-PDU trend increase of 0.14% points/week) and length of mental health ED stay (pre-to post-PDU trend increase of 0.10%/week). Fixed- and random-effect pooled estimates for secondary ITS outcomes are detailed in Appendix 4, Tables 36–38.
Psychiatric decision unit and pathway reconfiguration
Key changes to the crisis care pathway (other than PDU introduction) within the duration of the study period, elicited through semistructured interviews with strategic managers and contact with trust staff in each site, are presented in (superimposed on) graphs showing ITS analyses of PDU implementation on primary outcomes in Appendix 4, Figures 53–56. Explanation of these changes to the crisis care pathway and a more detailed list including minor changes are provided for each site in Appendix 4, Tables 39–42.
Implementation of the PDU often occurred as part of or concurrently with reconfiguration or expansion of crisis care services at participating sites. The influence of each major service initiative (that occurred sufficiently distant in time from the study period start/end and from PDU implementation) on primary outcomes was (separately) examined in ITS analyses that included each in conjunction with PDU implementation (see Appendix 4, Tables 43–46 for parameter estimates and detailed commentary). These analyses tended to reaffirm the significant decrease in informal inpatient admissions following PDU implementation in BSMHFT, LPFT and SWLSTG. But they also suggested some earlier initiatives significantly affected short-term admission rates, such as the introduction of street triage services in BSMHFT (decrease of 20.5%) and the opening of a psychiatric intensive care unit in LPFT (increase of 34.7%). In addition, the introduction of some services post-PDU implementation were also potentially impactful, particularly in sites where significant long-term post-PDU decreases in admissions were observed (LPFT and SWLSTG). For example, there was an immediate decrease in informal observed admissions after the launch of a crisis vehicular response unit (15 months post PDU) in LPFT (by 40.1%) and long-term changes in trend (decreases) in weekly admission rates in SWLSTG following the introduction of crisis cafe (20 weeks post-PDU) and street triage services (30 weeks post-PDU).
The impact of additional crisis care pathway changes on ED mental health attendances was more mixed. A Secure Quality Involvement initiative specifically intended to reduce repeat ED mental health attendances in STHFT introduced at the start of the time series is likely relevant to the highly significant decreases in attendances observed prior to PDU implementation, although expansion of the liaison psychiatry service (step decrease of 26.3%) and closure of assertive outreach and intensive rehabilitation teams (increase of 1.0%/week) in this period also significantly influenced short- and long-term ED activity. Also, there were immediate decreases in ED mental health attendances in SGUHFT following introduction of a street triage service (by 16.7%/week) and subsequent development/expansion of the PDU service (by 26.6%/week). But changes in crisis care pathway appeared to have less impact in SWBHFT and ULHFT.
Chapter 5 Synthetic control study
Data cleaning and selection of control trusts
After all exclusions 38 (3 treated and 35 controls) MHTs and 133 (6 treated and 127 controls) acute NHS trusts were included. The data set for the 37 MHTs extracted from HES-APC to proxy admissions to a mental health inpatient ward included 549,343 admissions for patients aged between 18 and 75 years from December 2012 to January 2021. The data set for the 133 acute trusts extracted from HES-ED data set to proxy mental health attendances at ED contained 1,775,237 attendances for patients aged between 18 and 75 years from December 2012 to January 2021. Patient-level data were aggregated to trust level to create 24-month data series pre and post implementation at each trust.
For each of the treated and control trusts, we plotted the primary outcomes during the 24 months before and 24 months after the opening of the PDU. SGUHFT was excluded due to low data counts, indicating that not all data were submitted to HES. Selected months for the study periods for the treated trusts also had to be excluded from the analysis due to data recording and quality issues. See Table 4 for updated pre and post intervention study periods for each of the treated studies. Three control MHTs and 12 control acute trusts that had clearly irregular patterns of the outcome as a result of reporting errors, or non-submission of data to HES, were also excluded. The 20 and 10 closest peers for each of the 5 remaining treated acute trusts and the 3 remaining treated MHTs, respectively, were identified from the remaining pool of 115 control acute trusts and 32 control MHTs as described in the methods (see Appendix 5, Table 47).
Characteristics of patients
Control trusts were carefully selected based on their similarity to the treated trusts across a range of variables. These variables, which include data on capacity, workforce availability, patient characteristics, management structures, regional characteristics (including index of multiple deprivation and rurality), target similarity across the trust and catchment population as a whole, rather than across mental health services and patients presenting with mental health issues. This process thus aims to ensure that treated and control trusts are similar in their potential capacity to deal with patients presenting with mental health issues, rather than the actual capacity, but should account for a wide variety of unobserved variables that impact on the outcomes studied here. We further control for the specific characteristics of patients at risk of the outcomes studied here in the synthetic control method.
To assess whether the controls trusts were similar to the treated trusts in terms of key patient characteristics of patients with a mental health admission or ED psychiatric attendance, we compared the average distribution of key patient characteristics across the treated trusts to the average distribution across the pool of 20 selected control trusts, and across the excluded control trusts, in the 24 months prior to the opening of the PDU (see Appendix 5, Tables 48 and 49).
Psychiatric admissions
In the 24-month periods before each PDU opened, patients admitted to an MHT inpatient ward in each treated trust and their corresponding pool of control trusts were broadly similar with the following exceptions (see Appendix 5, Table 48):
-
At SWLSG there were significant differences in the ethnicity and the method of admission. SWLSG had a smaller proportion of patients with white ethnicity (66.1% vs. 77.9% in the controls). SWLSG had a greater proportion of booked and planned admissions (14.7% booked and 22.1% planned vs. 6.2% and 17.5%, respectively, in the controls), admissions from mental health crisis resolution teams (29.2% vs. 15.3% in the controls) and fewer emergency admissions (< 1% vs. 4.6%).
-
At LPFT, there were significant differences in the method of admission and multimorbidity. A much higher proportion of admissions came via mental health crisis resolution teams (65.2% vs. 23.7% In the controls) and there was a greater proportion of patients with two or more Elixhauser comorbidities (44.5% vs. 25.2% in the controls).
-
At BSMHFT, there were significant differences in the ethnicity, source and method of admission. BSMHFT had a greater proportion of black, Asian and minority ethnicities (17.7% Asian and 16.2% black ethnicity vs. 5.6% and 4%, respectively, in the controls), fewer patients admitted from their usual place of residence (47.1% vs. 66.6%) and more admitted from penal establishments (16.1% vs. 4.3%). There were no admissions from mental health crisis resolution teams in BSMHFT (0% vs. 5% in controls) and fewer ED or emergency admission transfers from another provider (6.5% vs. 37.3%).
The majority of patients had a primary ICD-10 diagnosis code F20–29 indicating schizophrenia, schizotypal and delusional disorders (ranging from 26% to 40.2% in the treated trusts and from 23.8% to 24.5% in the aggregated control trusts).
Mental health attendances at emergency department
There were no significant differences in sex, age or ED arrival mode of patients of patients with an mental health ED attendance in the 24-month periods before each PDU opened between each treated trust and their pool of control trusts (see Appendix 5, Table 49).
There were no significant differences in ethnicity between each treated trust and their control trusts except in SWBHFT where there were greater proportions of black, Asian and mixed populations. The distribution of ED diagnosis codes and patient groups were significantly difference in all the acute treated trusts compared with their control trusts, except for ULHFT. There was no difference in the pattern of referral source between SWBHFT and their control trusts, but significantly fewer patients were referred by emergency services in Kingston Hospital NHS Foundation Trust (KHFT), ULHFT and UHBFT, and significantly more patients were referred by emergency services in STHFT, in comparison to their respective control trusts. There were significant differences in the distribution of discharge methods between each treated trust and their control trusts.
In summary, the comparisons across each treated trust and their respective pools of control trusts reveal some significant differences in the different trust catchment populations, perhaps reflecting differences in the disease burden, socioeconomic and other patient characteristics, or differences in the trust or local healthcare infrastructure, workforce or ways in which healthcare use is coded. It is not possible using these data to accurately determine the causes of these differences but since we are comparing the relative differences across the treated and control trusts, as long as these differences do not vary over time, the analysis should be unaffected. However, these differences highlight the difficulty of aggregating findings across multiple treated trusts.
Outcomes analysed
The GSC method was unable to provide adequate estimates for some of the outcomes in particular trusts due to a lack of fit in the pre-intervention period, or evidence that the result was obtained by extrapolation. These issues can arise either as a result of variability in the outcome in the treated trust that is not matched by any of the control trusts, often occurring because of data sparsity in the treated trust (e.g. KHFT had < 1000 mental health admissions in both the pre- and post-intervention periods), or evidence that the result was obtained by extrapolation.
The following outcomes related to admissions to a MHT inpatient ward failed:
-
Mental health admissions and average LOS on a mental health inpatient adult ward: LPFT (lack of pre-intervention fit).
The following outcomes related to ED psychiatric attendance failed:
-
ED psychiatric attendances: KHFT (lack of pre-intervention fit)
-
percentage ED psychiatric attendances less than 4 hours: UHBFT (lack of pre-intervention fit)
-
percentage ED psychiatric attendances less than 12 hours: all trusts except UHBFT and STHFT (lack of pre-intervention fit)
-
percentage ED attendances admitted: KHFT and ULHFT (evidence of extrapolation).
Estimated trends in hospital use
Tables 16 and 17 summarise the estimated impact of the opening of the PDU on each of the outcomes during the study period after the opening of the PDU at each treated trust and in a meta-analysis at the MHTs and acute trusts, respectively. Hospital use can vary over time even without changes to the way that care is delivered and it would be misleading to attribute normal variation in hospital use to the opening of the PDU. To check this, we report the p-value, which is the probability that that an effect of at least the magnitude of that observed could have arisen by chance. If this probability is low (here we assume that a low p-value is one that is < 5%), the estimate is considered to represent a significant difference between the hospital use in the treated trust compared with the control trusts.
| MH admissions (per 10,000 trust catchment patients per month) | Length of stay (days) | Percentage of MH admissions with length of stay < 5 days | ||||||
|---|---|---|---|---|---|---|---|---|
| Trust | Diff. (RD%) | p-value | Trust | Diff. (RD%) | p-value | Trust | Diff. (RD%) | p-value |
| SWLSTG (November 2016 to October 2018) | ||||||||
| 13.8 | −0.4 (−2.5) | 0.310 | 57.3 | 2.6 (4.7) | 0.331 | 11.0 | −6.5 (−36.9) | < 0.001 |
| LPFT (January 2018 to December 2018)a | ||||||||
| 32.4 | – | – | 37.6 | – | – | 16.4 | 0.8 (5.4) | 0.578 |
| BSMHFT (November 2014 to October 2016) | ||||||||
| 17.3 | −0.5 (−2.8) | 0.749 | 73.7 | −15.5 (−17.3) | < 0.001 | 12.6 | 4.6 (58.3) | 0.044 |
| Meta-analysis (24 months after the PDU opened) | ||||||||
| - | −0.4 | 0.310 | – | −6.4 | < 0.001 | – | −0.5 | 0.688 |
| Attendance (per 10,000 trust catchment patients per month) | Wait | Admissions an acute bed at same provider | Arrival by ambulance or police | Length of wait (minutes) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 4 hours | < 12 hours | ||||||||||||||||
| Trust | Diff. (RD%) | p-value | Trust | Diff. (RD%) | p-value | Trust | Diff. (RD%) |
p-value | Trust | Diff. (RD%) | p-value | Trust | Diff. (RD%) | p-value | Trust | Diff. (RD%) | p-value |
| KHFT (November 2016 to October 2018) | |||||||||||||||||
| 8.6 | – | – | 99.6 | 4.0 (4.2) | 0.012 | 99.9 | – | – | 11.5 | – | – | 46.7 | −3.3 (−6.6) | 0.957 | 26.2 | −24.6 (−48.5) | 0.034 |
| ULHFT (January 2018 to December 2019) | |||||||||||||||||
| 7.0 | 0.5 (7.2) | 0.510 | 90.1 | −2.4 (−2.6) | 0.114 | 100.0 | – | – | 7.1 | – | – | 35.8 | −9.1 (−20.4) | 0.003 | 121.8 | 23.6 (24.0) | 0.328 |
| SWBHFT (November 2014 to October 2016) | |||||||||||||||||
| 9.9 | 2.0 (25.3) | 0.146 | 99.2 | 0.2 (0.2) | 0.307 | 100.0 | – | – | 13.1 | −1.1 (−8.0) | 0.877 | 58.9 | 0.4 (0.7) | 0.869 | 82.1 | −4.7 −5.4) | 0.360 |
| UHBFT (November 2012–October 2016) | |||||||||||||||||
| 3.1 | −0.1 (−2.3) | 0.904 | 99.5 | – | – | 100.0 | 0.3 (0.3) | 0.715 | 12.9 | 6.7 (106.2) | 0.159 | 57.3 | 1.8 (3.3) | 0.994 | 71.5 | −2.9 (−3.9) | 0.970 |
| STHFT (March 2019 to January 2020)a | |||||||||||||||||
| 4.7 | −1.5 (−24.9) | 0.034 | 88.2 | −1.8 (−2.0) | 0.437 | 99.9 | −0.1 (−0.1) | 0.843 | 7.9 | −3.6 (−31.3) | 0.451 | 48.8 | 5.3 (12.3) | 0.062 | 141.7 | 35.0 (32.9) | 0.550 |
| Meta-analysis (24 monthsa after the PDU opened) | |||||||||||||||||
| – | −0.2 | 0.774 | – | 0.2 | 0.907 | – | 0.1 | 0.580 | – | 0.0 | 0.989 | – | −1.0 | 0.723 | – | 1.1 | 0.902 |
As an alternative approach to presenting these data, Appendix 5, Figures 57 and 58 show the trends in each of the outcomes for the treated trusts (red lines) and the counterfactual trend estimated by the GSC method (blue line) using a pool of 10 control trusts at the MHTs and 20 at the acute trusts, respectively. The blue line is our estimate of the trend in the treated trust if the PDU had not been implemented. Note that the two lines are similar, by design, in the period prior to the opening of the PDU (i.e. to the left of the first grey dashed line), as we aimed to find a counterfactual that tracked the outcome in the treated trust over this period. The difference between the two lines in the study period after the opening of the PDU (i.e. to the right of the grey dashed line) provides an estimate of the impact of the PDU on that outcome.
Psychiatric admissions
We found no significant impact of the opening of the PDU on admissions to mental health inpatient wards at any of the treated trusts or in a meta-analysis. Although there was a consistent trend towards fewer admissions per 10,000 people per month in SWLSG (RD −2.5%, p = 0.310), and in BSMHFT (RD −2.8%, p = 0.749) for the first 24 months after the PDU opened, compared with the counterfactual, these results were not significant (see Appendix 5, Figure 57a and b).
Length of stay on mental health inpatient wards
The average LOS for patients admitted to an MHT inpatient ward was 15.5 days lower (RD −17.3%, p < 0.001) in BSMHFT (see Appendix 5, Figure 57d) compared with the counterfactual in the 24 months after the PDU opened in November 2014 (averaging 89.2 days in the counterfactual and 73.7 days in BSMHFT during this period). This trend was evident in the first 12 months after the PDU opened in November 2014 (RD −15.5%, p < 0.001), and from November 2015 to the end of the study period in October 2016 (RD −19.3%, p < 0.001). There was no significant impact of the opening of the PDU on average LOS for patients admitted to an MHT inpatient ward in SWLSG. In a meta-analysis including both trusts, there was a significant reduction of 6.4 days (p < 0.001).
Length of stay in mental health inpatient wards less than 5 days
The average proportion of patients admitted to an MHT inpatient ward for less than 5 days in SWLSG in the first 12 months after the PDU was opened was 11%. This was 6.5% lower than the counterfactual during this period (RD −36.9%, p < 0.001). Conversely, LPFT had an increase in the proportions of patients with a LOS less than 5 days of 4.6 days compared with their counterfactual (RD 58.3, p = 0.044). There was no significant impact of the opening of the PDU on LOS less than 5 days in Birmingham and Solihull. A meta-analysis across the three sites indicated no evidence of any impact (see Appendix 5, Figure 57e–g).
Emergency department mental health attendances
Between March 2019 and January 2020, during the first year after the opening of the PDU, STHFT had 1.5 fewer ED attendances per 10,000 trust population per month than the counterfactual. This represented approximately one-quarter fewer ED attendances (RD −24.9%, p = 0.034; Figure 58b, A.4). There was no significant impact of the opening of the PDU on ED attendances at any of the other treated trusts (see Appendix 5, Figure 58a–c) nor any impact after meta-analysis.
Proportion of psychiatric patients waiting at emergency departments less than 4 hours
The proportion of ED psychiatric attendances waiting to be seen, transferred or discharged in less than 4 hours stayed fairly constant after the opening of the PDU in KHFT in November 2016 compared with a sharp decline in the counterfactual from March 2017 onwards (see Appendix 5, Figure 58e). Compared with the counterfactual, the percentage was 4.0% higher in KHFT between November 2016 and October 2018 (RD 4.2%, p = 0.012). There was no significant opening of the PDU on the proportion of psychiatric ED attendances at any of the other treated trusts (see Appendix 5, Figure 58f–h) individually or in the meta-analysis.
Psychiatric waits at emergency departments less than 12 hours
All treated trusts had close to 100% of ED psychiatric waits of < 12 hours. However, no significant effects of the opening of the PDU were seen in either of the two treated trusts, UHBFT and STHFT, for which the GSC was able to produce a satisfactory counterfactual (see Appendix 5, Figure 58i and j), or in the meta-analysis.
Proportion of psychiatric admissions to an emergency department
We found no significant impact of the opening of the PDU on the proportion of ED psychiatric admissions to an acute bed at any of the treated trusts or in a meta-analysis. Although there was a consistent trend towards a greater proportion of admissions in UHBFT after the opening of the PDU (see Appendix 5, Figure 58l), and a smaller proportion in STHFT, in the months studied after the opening of the PDU (see Appendix 5, Figure 58m) compared with the counterfactual, these results were not significant.
Psychiatric arrivals at emergency departments by ambulance or police
The proportion of psychiatric patients arriving at the ED either by ambulance or police in the months studied after the opening of the PDU ranged from 35.8% in ULHFT up to 58.9% in SWBHFT. We only found a significant impact of the opening of the PDU on these proportions in ULHFT, where the rate was 9.1% lower than the rate that would have been expected if the PDU had not opened (RD −20.4%, p = 0.003; see Appendix 5, Figure 58o). Given an estimated trust catchment population size of 354,756 for patients aged between 18 and 74 years in 2018, and a rate of ED psychiatric attendances of 7.0/10,000 in this catchment population, this represents approximately 23 fewer ED psychiatric arrivals by ambulance or police each month in ULHFT. There was no significant impact of the opening of the PDU on the proportion of psychiatric arrivals by ambulance or police in the meta-analysis.
Emergency department psychiatric length of wait
Consistent with the lower proportion of patients seen within 4 hours compared with the counterfactual, the average length of ED psychiatric wait for ED psychiatric attendances in KHFT was 24.6 minutes lower. This represented an almost 50% reduction in the expected wait time if the PDU had not opened (RD −24.6%, p = 0.034; see Appendix 5, Figure 58s). At the other trusts, our estimates of impact ranged from a lower average wait time of 4.7 minutes to a higher average wait time of 35.0 minutes compared with the counterfactual, but these estimates were not significant. There was no significant impact of the opening of the PDU on ED psychiatric length of wait in the meta-analysis.
Sensitivity analysis
In sensitivity analyses – including just the nearest 10, rather than the nearest 20, control trusts in the control pool for the acute trust outcomes and vice versa for MHT outcomes – all significant results were replicated either as a significant result with a similar effect size, or with a similar effect size but not significant. As results are robust to choice of controls, we are reasonably confident that the results we are seeing are not just by chance alone.
Chapter 6 Cohort study
Sample characteristics
Primary cohort
A total of 1176 eligible people (i.e. first-time referees to PDUs during the recruitment period) were included in the analysis, 277 (23.55%) from SWLSTG, 308 (26.19%) from LPFT, 387 (32.91%) from BSMHFT and 204 (17.35%) from SHSCFT. A total of 609 participants (51.79%) were female, with only BSMHFT having a majority of male participants (216; 55.81%). Mean age of participants across sites was 36.38, while 821 (69.81%) of all participants were White British and missing data on sexuality were high (for 842, 71.60%, of participants there were no recorded data). A total of 871 participants (74.06%) had no recorded mental health diagnosis. Many people on first visit to PDU were also relatively new to mental health services, with 372 (38.27%) having had first contact with mental health services in the 9 months preceding their first PDU visit (based on data from 972 participants only, excluding participants from SHSCFT, where these data were not available). The largest single source of referrals to the PDU, across sites, was directly from the ED (488; 41.50%), with crisis and home treatment teams providing the second highest number of referrals (246; 20.92%), although these data are somewhat obscured as 157 (76.96%) of participants in SHSCFT were referred to the PDU via a single point of access to adult mental health crisis care.
In the 9-month period following discharge from the PDU, participants were most often discharged back to their usual place of residence (404, 41.56%, of 972 participants, with data on discharge destination missing from the SHSCFT site), followed by crisis and home treatment team (156; 16.05%) and acute psychiatric hospital admission (124; 12.76%). For participants across all four sites, on average, just over 50% of the follow-up period was spent while social distancing measures as a result of the COVID-19 pandemic were in place. Comprehensive data on participant characteristics by site are given in Appendix 6, Table 50.
Pre-pandemic cohort
Data on a pre-pandemic cohort of first-time referrals to PDUs in a similar period 12 months prior to our primary cohort was only available from three of the four sites as the SHSCFT PDU had yet to be opened at that point in time. A total of 934 people from the three sites were included in the pre-pandemic cohort, compared with 972 in the primary cohort, with fewer people included from SWLSTG (218 compared with 277) and LPFT (289 compared with 308) and more from BSMHFT (427 compared with 387). Characteristics of cohorts are broadly similar across all sites. Notably, the SWLSTG site accepted a much higher percentage of referrals to the PDU from CMHTs in the pre-pandemic cohort (35.3%) compared with the primary cohort (11.2%) and a correspondingly lower percentage of referrals from crisis and home treatment teams (17.9% compared with 38.6%).
Data on discharge destination were only available for the SWLSTG and LPFT sites. In SWLSTG, a slightly higher percentage of people were discharged to usual place of residence and lower to crisis and home treatment team in the pre-pandemic cohort (67.4% and 8.3%, respectively) compared with the primary cohort (51.3% and 17.0%). The discharge data from LPFT are hard to compare between cohorts, given that missing data are higher in the pre-pandemic data (24.57% compared with 9.42%), with no participants reported as discharged to usual place of residence in the pre-pandemic cohort. This may be due in part to changes in the way data are recorded. A full set of participant characteristics in the pre-pandemic cohort can been seen in Appendix 6, Table 51.
Pre and post first psychiatric decision unit visit findings by site (primary cohort)
South West London and St George’s Mental Health NHS Trust
The general picture presented by the SWLSTG data is of a marked increase in most mental health service use in the 9 months following first admission to the PDU compared with the 9 months preceding admission (see Table 18). For our primary MHT outcome, numbers of informal psychiatric admission increased highly significantly from two in the pre-admission period to 54 post admissions (χ2 = 48.29, p < 0.001). However, mental health presentations at ED, our primary ED outcome (as measured by liaison psychiatry episodes in the ED) decreased highly significantly from a mean of 1.33 per participant pre admission to 0.67 post admission (t = 5.98, p < 0.001).
| Outcomes | SWLSTG | LPFT | BSMHFT | SHSCFT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre–post comparison | Pre | Post | Pre–post comparison | Pre | Post | Pre–post comparison | Pre | Post | Pre–post comparison | |
| Primary | ||||||||||||
| Mental health: n experiencing an informal admission | 2 | 54 | χ2 = 48.29, p < 0.001 | 17 | 78 | χ2 = 52.41, p < 0.001 | 13 | 64 | χ2 = 36.63, p < 0.001 | 9 | 15 | χ2 = 1.5, p = 0.31 |
| Acute trust: ED presentations (total) | 1.33 (1.30) | 0.67 (1.86) | t = 5.98, p < 0.001 | 0.68 (0.85) | 0.45 (1.00) | t = 3.30, p < 0.001 | 1.64 (1.45) | 1.73 (2.20) | t = 0.98, p = 0.33 | 1.82 (2.11) | 1.70 (5.42) | t = 0.32, p = 0.40 |
| Secondary: binary events data (number experiencing one or more) | ||||||||||||
| Inpatient admissions | 6 | 64 | χ2 = 49.47, p < 0.001 | 11 | 51 | χ2 = 30.77, p < 0.001 | 26 | 95 | χ2 = 50.12, p < 0.001 | 24 | 41 | χ2 = 6.42, p = 0.01 |
| 0–5 days’ inpatient admissions | 1 | 26 | χ2 = 23.15, p < 0.001 | 4 | 11 | χ2 = 3.77, p = 0.05 | 3 | 11 | χ2 = 4.57, p = 0.06 | 8 | 4 | χ2 = 1.33, p = 0.39 |
| Compulsory admissions | 4 | 21 | χ2 = 11.56, p < 0.001 | 8 | 31 | χ2 = 19.59, p < 0.001 | 13 | 37 | χ2 = 15.16, p < 0.001 | 20 | 37 | χ2 = 7.41, p < 0.01 |
| Continuous, n (SD) | ||||||||||||
| Average length of inpatient stay, for those with a stay, mean (SD), n | 15.00 (16.10), 6 | 23.35 (26.71), 64 | t = 0.75, p = 0.46 | 26.11 (21.65), 17 | 35.77 (41.31), 78 | t = −0.93, p = 0.35 | 30.04 (39.96), 26 | 41.75 (60.88), 95 | t = 0.93, p = 0.36 | 19.63 (14.11), 24 | 54.61 (57.73), 41 | t = 4.03, p < 0.001 |
| Use of CMHT and other trust services | ||||||||||||
| Community contacts with services (mean, SD) | 12.47 (19.75) | 23.31 (27.42) | t = 7.78, p < 0.001 | 12.03 (18.29) | 27.38 (31.37) | t = 9.76, p < 0.001 | 3.09 (7.51) | 5.52 (11.82) | t = 5.38, p < 0.001 | 25.45 (38.28) | 36.60 (48.38) | t = 3.71, p < 0.001 |
| Contact type: face to face (mean, SD) | 8.79 (13.42) | 13.62 (16.61) | t = 5.27, p < 0.001 | 7.71 (12.25) | 12.07 (12.45) | t = 5.98, p < 0.001 | 2.58 (6.64) | 2.45 (6.91) | t = 0.39, p = 0.70 | 16.37 (26.06) | 19.43 (25.46) | t = 1.59, p = 0.11 |
| Contact type: telephone/video (mean, SD) | 3.69 (8.10) | 9.69 (13.68) | t = 9.23, p < 0.001 | 4.32 (8.46) | 15.31 (22.49) | t = 9.77, p < 0.001 | 0.51 (1.63) | 3.06 (7.91) | t = 6.90, p < 0.001 | 9.08 (15.05) | 17.17 (26.71) | t = 5.16, p < 0.001 |
| Use of CMHT and other trust services by category: continuous data; mean (SD) | ||||||||||||
| CMHT | 3.21 (8.58) | 7.50 (13.30) | t = 6.36, p < 0.001 | 4.52 (13.12) | 9.75 (22.91) | t = 5.41, p < 0.001 | 3.16 (7.72) | 5.76 (12.29) | t = 5.70, p < 0.001 | 15.65 (29.50) | 21.00 (36.97) | t = 2.56, p < 0.01 |
| Crisis resolution or home treatment team | 4.34 (9.82) | 9.18 (12.44) | t = 5.74, p < 0.001 | 5.13 (8.75) | 13.84 (17.64) | t = 8.29, p < 0.001 | 5.22 (14.79) | 8.64 (18.38) | t = 5.51, p < 0.005 | 8.62 (18.87) | 13.73 (23.17) | t = 2.62, p < 0.01 |
| Mental health support line | 0.42 (3.35) | 0.72 (5.90) | t = 1.78, p = 0.76 | – | – | – | – | – | – | – | – | – |
| Single point of access | 1.18 (2.78) | 1.88 (5.83) | t = 1.98, p < 0.05 | |||||||||
| Number of contacts (for small numbers); n | ||||||||||||
| Mental health support line (also summarised above) | 117 | 199 | – | – | – | – | – | – | ||||
| DBT service | 0 | 52 | – | – | 4 | 4 | 78 | 32 | ||||
| Service contracted by trust | 32 | 80 | – | – | 0 | 0 | ||||||
| Art therapies | 8 | 52 | – | – | 0 | 40 | 4 | 79 | ||||
| Other | 71 | 97 | 4 | 26 | – | – | 35 | 47 | ||||
| Outpatient ED service | 67 | 54 | 81 | 72 | 6 | 3 | – | – | ||||
| Exercise therapy team | 11 | 59 | – | – | – | – | – | – | ||||
| PD team/PD intensive team | 0 | 8 | – | – | – | – | 462 | 789 | ||||
| Complex needs service | 221 | 258 | 0 | 1 | 109 | 91 | – | – | ||||
| Family therapy | 7 | 21 | – | – | – | – | – | – | ||||
| EI team | 153 | 407 | 168 | 369 | 93 | 41 | 311 | 754 | ||||
| Learning disabilities service | 2 | 80 | 3 | 14 | – | – | 0 | 0 | ||||
| Perinatal community team | 9 | 35 | 61 | 108 | 252 | 166 | 29 | 0 | ||||
| Traumatic stress service | 45 | 63 | – | - | – | – | 0 | 0 | ||||
| Older peoples service (including but not limited to dementia services) | 3 | 44 | 55 | 245 | – | – | 122 | 316 | ||||
| Forensic/criminal justice liaison service | – | – | 53 | 3 | 142 | 85 | – | – | ||||
| CAMHS | – | – | 16 | 0 | – | – | – | – | ||||
| Individual placement and support (for work) | – | – | 38 | 57 | – | – | – | – | ||||
| SARC | – | – | 10 | 38 | – | – | – | – | ||||
| PDU visits (people experiencing one or more), n | 0 | 31 | – | 54 | – | 54 | – | 20 | ||||
Most MHT secondary outcomes also demonstrated significant increases, including highly significant increases in numbers of compulsory admissions, total admissions and 0- to 5-day (short) admissions, and highly significant increases in mean number of contacts with community mental health services, including CMHTs and CRHTs. Of those community mental health service contacts, there were highly significant increases in both face-to-face and remote contacts (which nearly tripled). Increases in average length of inpatient stay (for those who had an admissions) and in mental health support line use was non-significant. There were increases in use of many other mental health service types (numbers of outpatient ED contacts fell slightly), noting also that 31 of the SWLSTG cohort had one or more subsequent additional admissions to the PDU in the 9 months following their first admission.
Lincolnshire Partnership NHS Foundation Trust
Results from LPFT reflected SWLSTG findings very closely (see Table 18). In terms of primary outcomes, there was a highly significant increase in numbers of informal psychiatric admissions from 17 in the 9 months prior to first admission to the PDU compared with 78 in the post-admission period (χ2 = 52.41, p < 0.001), while there was a highly significant decrease in mental health presentations at ED from a mean of 0.68 per participant pre admission to 0.45 post admission (t = 3.30, p < 0.001).
Again, there were highly significant increases in numbers of compulsory admissions and total admissions, and significant increases in 0- to 5-day admissions from the pre to post period. There were highly significant increases in mean number of contacts with community mental health services, including CMHTs and CRHTs and, again, of those community mental health service contacts, there were highly significant increases in both face to face and remote contacts (which nearly quadrupled). There was a non-significant increase in length of inpatient stay. As with SWLSTG, there were increases in many other service use types (with a slight drop in ED outpatient appointments), and 54 people experienced one or more subsequent PDU admissions in the 9 months post first admission.
Birmingham
The picture for BSMHFT was slightly different (see Table 18). We did see a highly significant increase in informal inpatient admissions from pre to post first PDU admission – from 13 to 64 (χ2 = 36.63, p < 0.001) – but no change in mean number of mental health presentations at ED (1.64 to 1.73; t = 0.98, p = 0.33). There were highly significant increases in compulsory and total inpatient admissions but no significant change in short, 0- to 5-day admissions and no significant change in average length of inpatient stay. There were highly significant increases in community mental health service use including contacts with CMHTs, and significant increases in contacts with CRHT teams. There was no change in mean numbers of face-to-face contacts but a six-fold increase in remote contacts. Atypically, numbers of contacts with a wide range of other mental health services dropped from the pre to post first PDU admission periods, and 54 people had one or more subsequent PDU admissions.
Sheffield Teaching Hospital NHS Foundation Trust
SHSCFT saw no change in either primary outcome – informal psychiatric admissions or mental health presentations at ED – from the pre-PDU first visit to post-PDU visit periods (see Table 18). There was, however, an increase in overall admissions (from 24 to 41; χ2 = 6.42, p = 0.01), compulsory admissions (from 20 to 37; χ2 = 7.41, p < 0.01) and a highly significant increase in average length of inpatient stay (from 19.63 to 54.61 minutes; t = 4.03, p < 0.001). Mean number of contacts with community services was significantly higher (increasing from 25.45 to 36.6; t = 3.71, p < 0.001) and there were more remote contacts (up from a mean of 9.08 to 17.17; t = 5.16, p < 0.001) while numbers of face to face contacts remained unchanged. There were more mean contacts with CMHTs (15.65–21; t = 2.56, p < 0.01), CRHT teams (8.62–13.73; t = 2.62, p < 0.01) and with the trust’s single point of access (1.18–1.88; t = 1.98, p < 0.05). As with SWLSTG and LPFT, numbers of contacts with a wide range of other community-based services increased from the pre- to post-first PDU visit periods. There were 20 subsequent PDU visits in the post first-visit period.
Pre-pandemic comparisons by site
As described in Chapter 2 for the cohort study, the same set of pre- and post-first PDU visit comparisons were made for our additional, pre-COVID cohort (see Appendix 6, Table 51), and then service use for the pre-COVID cohort, in both pre- and post-PDU visit period (see Appendix 6, Table 52), compared with our primary cohort (see Appendix 6, Table 53). These are presented below for all sites except SHSCFT, where the PDU had yet to be opened in the pre-COVID period.
South West London and St George’s Mental Health NHS Trust
There were few differences observed in either the pre- or post-PDU visit periods between the pre-pandemic and primary cohorts in SWLSTG (see Appendix 6, Tables 52 and 53). In the pre-PDU visit period there was a higher proportion of informal (8/218 people who had an informal admission vs. 2/277; OR 5.36, p < 0.05), total (14/218 with 6/277; OR 3.10, p < 0.05) and 0- to 5-day (7/218 vs. 1/277; OR 9.16, p < 0.05) admissions in the pre-pandemic cohort compared with the primary cohort, although these analyses are based on very low numbers of admissions. In the post-PDU visit period there were no differences in admissions of any kind or in average length of inpatient stay for those with an admission or in numbers of ED mental health presentations. While there was no change in mean number of community mental health service contacts from pre-pandemic to primary cohort (during the pandemic), mean numbers of face to face contacts with community services were significantly lower (13.62 vs. 17.6; t = 2.51, p = 0.01). There were also fewer CRHT team contacts in the primary cohort compared with pre-pandemic cohort (a mean of 9.18 vs. 14.83), a difference that was highly significant (t = 4.15, p < 0.001).
We also note that patterns in changes in service use from pre- to post-first PDU visit were similar across pre-pandemic and primary cohorts. In general, service use increased in both cohorts, although in the pre-pandemic period there was no increase in mean number of remote contacts with community mental health services (as was observed in the primary cohort, during the pandemic) and no increase in mean CMHT contacts.
Lincolnshire Partnership NHS Foundation Trust
Similarly, there were few differences between pre-pandemic and primary cohort in LPFT (see Appendix 6, Tables 52 and 53), including in either primary outcome (informal admissions or ED mental health presentations). In the pre-PDU visit period, there were proportionally more total admissions in the pre-pandemic cohort compared with primary cohort (24/289 people experienced one or more admissions vs. 11/309; OR 2.45, p = 0.01) and while mean numbers of face to face contacts with community services were lower (5.89 vs. 7.71; t = 2.10, p = 0.04), remote contacts higher (7.08 vs. 4.32; t = 3.21, p < 0.01). In the post-PDU visit period, there were again proportionally more total admissions in the pre-pandemic cohort compared to primary cohort (97/289 vs. 51/309) and this finding was highly significant (OR 2.55, p < 0.001). There were more contacts with community mental health services post-PDU visit in the primary cohort compared with the pre-pandemic cohort (a mean of 27.38 vs. 21.94; t = 2.36, p < 0.05) and more of those contacts were remote (a mean of 15.31 compared to 7.96), this finding being highly significant (t = 4.97, p < 0.001).
As observed in SWLSTG, patterns in pre- to post-first PDU visit changes in service use were highly similar across pre-pandemic and primary cohorts in LPFT, with significant increases in both inpatient and community service use varying only in magnitude between cohorts. The only difference observed was the significant increase in remote community contacts in the primary cohort (during the pandemic), not seen in the pre-pandemic cohort.
Birmingham and Solihull Mental Health NHS Foundation Trust
BSMHFT demonstrated even fewer differences between pre-pandemic and primary cohorts (see Appendix 6, Tables 52 and 53), with only a higher mean number of CRHT team contacts in the primary cohort (5.22 vs. 4.9; t = 6.48, p < 0.001) being different in the pre-PDU first visit period. In the post-PDU first visit period, there were no differences in inpatient service use between cohorts, while there were highly significant findings showing fewer mean face to face community contacts in the primary cohort (2.45 vs. 4.28; t = 3.62, p < 0.001), more mean remote contacts (3.06 vs. 0.69; t = 6.00, p < 0.001), and fewer mean CRHT team contacts during the pandemic (8.64 vs. 12.31; t = 50.03, p < 0.001).
Again, patterns in increased pre-post PDU visit service use were highly similar in both cohorts in BSMHFT, the only difference being an increase in face to face community contacts observed in the pre-pandemic cohort not being replicated in the primary cohort (during the pandemic).
Equalities impact assessment
There were a small number of differences in sociodemographics observed between samples in our primary cohort and a recent sample of all people using mental health services in each site (see Table 19). In all sites, the PDU sample was significantly younger that the population of people using each trust’s services as a whole. There were no other differences between groups in SWLSTG and LPFT. In BSMHFT, first-time visitors to the PDU were also less likely to be female (171/387; 44.19%) compared with the trust-wide population (37,669/69,513; 54.19%; z = 2.62, p < 0.01) and less likely to be White British (257; 66.41% vs. 41,019; 59.01%; z = 2.41, p = 0.02). In STHFT, the PDU sample was more likely to be black than the trust population (11/204, 5.39% vs. 828/31, 190 2.65%; z = 2.06, p = 0.04), although numbers were low in the PDU sample.
| Characteristic | SWLSTG | LPFT | BSMHFT | Sheffield | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary cohort | Trust population | Comparison | Primary cohort | Trust population | Comparison | Primary cohort | Trust population | Comparison | Primary cohort | Trust population | Comparison | |
| Population (N) | 277 | 17,982 | 308 | 59,824 | 387 | 69,513 | 204 | 31,190 | ||||
| Female, n (%) | 162 (58.48) | 10,362 (57.62) | z = 0.22, p = 0.84 | 167 (54.25) | 36,150 (60.49) | z = 1.65, p = 0.10 | 171 (44.19) | 37,669 (54.19) | z = 2.62, p < 0.01 | 109 (54.43) | 15,978 (51.23) | z = 0.67, p = 0.50 |
| Age (years) mean (SD) | 36.74 (13.77) | 48.12 (21.53) | t = 13.75, p < 0.001 | 37.43 (15.22) | 43.75 (24.65) | t = 7.29, p < 0.001 | 34.64 (13.53) | 47.66 (21.71) | t = 19.17, p < 0.001 | 37.63 (13.46) | 48.29 | t = 11.31, p < 0.001 |
| Asian/British Asian, n (%) | 19 (6.86) | 1452 (8.07) | z = 0.19, p = 0.85 | 0 (0.0) | 270 (0.45) | – | 36 (9.30) | 9572 (13.77)) | z = 0.78, p = 0.44 | 10 (4.90) | 913 (2.93) | z = 0.37, p = 0.71 |
| Black/Black British, n (%) | 24 (8.66) | 1895 (10.54) | z = 0.23, p = 0.76 | 3 (0.97) | 171 (0.29) | z = 0.219, p = 0.83 | 27 (6.98) | 4284 (6.16) | z = 0.18, p = 0.86 | 11 (5.39) | 828 (2.65) | z = 2.06, p = 0.04 |
| White British, n (%) | 163 (58.84) | 9603 (53.40) | z = 1.39, p = 0.16 | 265 (86.04) | 51,338 (85.82) | z = 0.10, p = 0.92 | 257 (66.41) | 41,019 (59.01) | z = 2.41, p = 0.02 | 136 (66.67) | 18,574 (59.55) | z = 1.67, p = 0.10 |
| White Irish/white other, n (%) | 40 (14.44) | 2306 (12.82) | z = 0.31, p = 0.76 | 9 (2.92) | 1853 (3.10) | z = 0.03, p = 0.98 | 15 (3.88) | 2551 (3.67) | z = 0.045, p = 0.96 | 5 (2.45) | 554 (1.78) | z = 0.11, p = 0.91 |
| Other, n (%) | 26 (9.39) | 1458 (8.11) | z = 0.24, p = 0.81 | 0 | 147 (0.25) | – | 8 (2.07) | 1876 (2.70) | z = 0.11, p = 0.91 | 7 (3.43) | 519 (1.66) | z = 0.37, p = 0.71 |
| Mixed, n (%) | 1 (0.36) | 755 (4.31) | – | 1 (0.32) | 612 (1.02) | – | 18 (4.65) | 2347 (3.38) | z = 0.30, p = 0.77 | 2 (0.98) | 582 (1.87) | z = 0.09, p = 0.93 |
| Missing, n (%) | 4 (1.44) | 493 (2.74) | z = 0.16, p = 0.87 | 30 (9.74) | 5433 (9.08) | z = 0.13, p = 0.90 | 26 (6.72) | 7864 (11.31) | z = 0.74, p = 0.46 | 33 (16.18) | 9220 (29.56) | z = 1.68, p = 0.09 |
Chapter 7 Qualitative interview study
Characteristics of the sample
Service users (first-time visitors to PDU) and PDU and referral pathway staff were recruited at all four study sites. Recruitment took place between 4 November 2019 and 27 February 2020 at the SWLSTG, LPFT and SHSCFT sites – roughly coincident with the recruitment period for the WP4 cohort study – and between 17 May 2021 and 1 September 2021 at the BSMHFT site. Follow-up interviews of service users (at all sites except BSMHFT) were conducted between 8 and 10 months post discharge, with the final follow-up interview taking place on 12 November 2020.
Service users
In total, 39 service user participants were recruited across the four sites (see Table 20), 18 of whom were followed up approximately 9 months later (six in each of sites 1–3). Given the low numbers of participants at each site, we identify site by number here and in the analysis that follows to reduce the risk of identifying participants.
| Site 1 | Site 2 | Site 3 | Site 4 | All sites | |
|---|---|---|---|---|---|
| Service users | |||||
| Sex | |||||
| Male | 4 | 4 | 7 | 1 | 16 |
| Female | 8 | 7 | 4 | 4 | 23 |
| Ethnicity | |||||
| Asian | |||||
| Black | |||||
| Mixed race | 1 | 1 | |||
| White British | 10 | 11 | 11 | 4 | 36 |
| White other | 1 | 1 | 2 | ||
| Age (years) | |||||
| 18–24 | 3 | 2 | 1 | 6 | |
| 25–34 | 5 | 3 | 1 | 9 | |
| 35–44 | 1 | 1 | 1 | 1 | 4 |
| 45–54 | 3 | 4 | 5 | 1 | 13 |
| 55–64 | 2 | 3 | 1 | 6 | |
| 65+ | 1 | 1 | |||
| Total service users | 12 | 11 | 11 | 5 | 39 |
| PDU staff | |||||
| HCA/support worker | 1 | 1 | 1 | 3 | |
| Nurse | 1 | 1 | 1 | 1 | 4 |
| Psychiatrist | 1 | 1 | 1 | 1 | 4 |
| Unit manager | 1 | 1 | 1 | 1 | 4 |
| Total PDU staff | 4 | 4 | 4 | 3 | 15 |
| Referral pathway staff | |||||
| Liaison psychiatry | 1 | 2 | 2 | 1 | 6 |
| ED nurse | 1 | 1 | 2 | ||
| ED manager | 1 | 1 | 2 | ||
| CMHT | 2 | 1 | 3 | ||
| CRHT team | 1 | 1 | 2 | ||
| Street triage | 1 | 1 | 2 | ||
| Social worker | 1 | 1 | |||
| Other referral pathway staff | 1 | 1 | |||
| Total referral pathway staff | 7 | 3 | 7 | 2 | 19 |
Staff
Interviews with a PDU nurse, psychiatrist and unit manager were completed at every site, with an interview with a PDU HCA/support worker at three of the four sites. Interviews with liaison psychiatry staff took place at all sites, with other members of the ED team at two sites. Interviews with other referral pathway staff reflected referral pathways locally. In total, 34 staff participants were recruited (see Table 20).
Thematic analysis
The final coding framework, as applied to the whole qualitative data set, can be found in Appendix 7, Table 54. Thematic analysis of both service user and staff interviews was produced and is presented below, organised by themes and subthemes. For service user interviews, themes follow a roughly chronological journey from ‘arrival’ to ‘discharge, signposting and onward referral’. Themes for staff interviews begin by considering ‘clarity’ around different staff perspectives on the function of PDUs and who the units might work best for, the referral pathway to the PDU, and then the PDU environment and experience of working on the units.
In quotation of data from verbatim transcripts of interviews, single speech marks are used for reported speech or thought and ellipsis for any truncation of data. Where names of people, places or services are anonymised, general terms are given in square brackets. Square brackets are also used for other insertions for clarity. No other annotation is used. Participant identification numbers following quotes indicate site number (as above), role (S = service user; P = PDU staff, R=pathway staff) and identification number and, for service user interviews only, indication of whether the data were collected in the baseline or follow-up interview (B = baseline; F = follow-up). To note, most interviewees, where relevant, used the term accident & emergency (A&E) to refer to the ED. We have not amended this usage in the data.
Service user interviews
Arrival
Being in crisis
Service users entered the PDU disorientated or suicidal. Their crises had often been precipitated by relationship breakdown, family stressors, bereavement, or living in extreme isolation. Often, crises had been exacerbated by self-harm or substance use. Some service users found accessing the PDU straightforward:
I rang the crisis team, told them that I was going to take all my tablets. Then they came and saw me and then took me to the unit.
(2S09B)
Most, however, had found asking for and accessing help difficult:
… [the paramedic] said ‘well we’ve been on to the crisis team’ and they basically blanked them. They said ‘well we might get somebody out today’ and they might not. They said ‘well we just can’t leave you at home … the only thing we could do is take you to ED’.
(2S04B)
Being sent to the psychiatric decision unit
Most service users were admitted to the PDU through the ED, although a minority arrived directly by ambulance. Experiences of EDs were primarily determined by the quality of communication and levels of connectedness between triage staff, mental health crisis teams and the PDU. At best, service users had been transferred smoothly and directly to the PDU:
Mental health team came down and had a word with me. They spoke to me and they made a decision saying that I wasn’t right and then they said ‘would you come to our decisions unit?’ I said ‘yes, fine’ and I just went along.
(3S08B)
However, service users had sometimes been told conflictual or contradictory things, had been passed between several teams or professionals, or had waited for many hours. This had sometimes left them unsure what was happening, struggling to manage the uncertainty, or feeling as though they were a nuisance or a burden on services. On one occasion, this led to inappropriate treatment:
… the nurse in A&E … instructed them to turn me over so they could inject me in the backside but they did it so violently I hit the side rail and that’s how I got bruises on my breast and down my arm.
(4S01B)
Impressions
Atmosphere
Many service users described their initial impression of the PDU as of a quiet, calming, soporific place. For those who had previously been treated on noisy and chaotic psychiatric wards, this atmosphere was a pleasant surprise:
It was warm and it was thoughtful, do you want a bit of toast, with no stress. You could lay your head down and there was nobody coming wake you for anything.
(2S08B)
For some whose mental health crisis had been precipitated by trauma, this sudden calm could, however, trigger further anxiety:
… when I got there everybody was asleep, so I was like thinking ‘oh God’, creeping about really quietly and then when you got in the chair the chair started creaking and I was like ‘oh God I’m going to wake people up’. So, I didn’t know who the people were, I didn’t know what sort of mood they’d be in.
(2S06B)
Service users were particularly struck by the reclining chairs in place of beds. For many, sleeping problems had precipitated their mental health crisis, and for some, being able to catch up on sleep at the PDU proved the most valuable part of their stay. The flexibility which the chairs enabled promoted an atmosphere conducive to sleep:
If you had one of the ordinary beds there it wouldn’t feel comfortable going to sleep in the daytime, you’d feel wrong. They there … you can sleep when you want, it’s … as though they take you out of the real world … all the fear is left on the outside.
(2S07B)
It was fine. I think having recliner chairs is probably nicer in a way than having a bed … I feel like if they’d put me in a bed I’d have been like ‘this is an admission’ but having a recliner chair was like ‘OK this is fine’.
(4S05B)
However, some service users disliked the chairs:
They need to go … They’re weird. Also, or don’t get rid of them but just put something on top of it when it’s a bed because otherwise you stick to it. The sheets do not stay on the things.
(3S11B)
Staff
Service users generally spoke appreciatively of PDU staff, describing them as calm and non-judgemental, and treating them with care and compassion:
She didn’t just say words but she spoke to me in a way that I know without a doubt that she believes that I can move forward, get better and work one day. She’s so kind and loving.
(1S06B)
Service users particularly liked the way that staff responded to their distress in very humanising ways, helping them to feel worthwhile and not ‘mad’ or ‘crazy’:
They’re not frightened of anything you tell them. I didn’t see one of them look one bit concerned. They made you feel normal.
(2S07B)
Well I think the staff were amazing … It felt like a safe place without and it didn’t stigmatised like oh no what’s wrong with me, am I a crazy person.
(3S05F)
Some of the service users had been told that staff were using the CCTV cameras to observe them continually and some had worked this out themselves. Generally, they valued this as an unintrusive way that staff provided them with personal space, especially if they had experienced close observations on psychiatric wards in the past. For some, however, this more ‘hands off’ approach compounded feelings of isolation, hopelessness, or confusion:
Not just leave you in a room and just sit in the office … how does that help? They are sitting in the office and you are like the guinea pig in a cage.
(4S05B)
Safety
Feeling safe, feeling unsafe
Most service users reported feeling safe on the PDU. Service users described how the calm and calming atmosphere of the PDU provided them with a sense of containment and security:
I felt safe there [because] I knew I had someone there to talk to in case I got distressed or didn’t feel safe or something, I knew someone was there to speak to. I couldn’t try harming myself there, I couldn’t do it there so I just felt safe.
(3S02F)
Sometimes, however, this sense of safety was tempered by service users’ experience of a lack of visible staff presence:
I mean I suppose in a sense I was at least safe in quotes, that I was supposedly being monitored but I was not conscious that an eye was being kept on me in any way. Occasionally but very occasionally, I think like once an hour, someone would just stick their head around the door.
(3S03F)
Service users were aware that the safety the PDU offered was limited by the time limits placed on admissions. Those who were feeling suicidal worried that the PDU would not prevent their deaths:
I didn’t feel very safe there as I was suicidal. One chap said to me there, ‘I said I’m going to leave and they [a staff member] said “well leave and just get on with it then”.’.
(2S09B)
Several female service users felt unsafe with the presence of male staff and service users in proximity to the female sleeping area:
I suffer with really bad anxiety as well and you’ve got all these people, you don’t know what they’re capable of … you are supposed to feel safe, there’s no privacy at all. I know they’ve got the wall but there’s no privacy.
(1S12B)
One male service user affirmed this concern, echoing the women’s requests for more explicitly segregated sleeping facilities:
I think there could have done with some more privacy because the room was off a corridor and there was a glass partition running down the side and there were no curtains up or blinds … they gave me some pyjamas to put on for bedtime and I just got changed in the room and anyone could have been walking past and I’m half undressed.
(3S04B)
One woman felt particularly unsafe:
I don’t know what his role was, he was just a staff member maybe a nurse or something, but he just stood there watching Love Island drooling over all these ladies … Having been sexually abused and raped and all kinds of things in my life I’ve got a very strong, very sensitivity to and … it just felt horrible in that room.
(1S06F)
Negotiating the balance between freedom and support
Striking the right balance between feeling supported and enjoying daily freedoms could be important to service users’ experience of the unit. This balance seemed to be expressed by both the physical environment and the way the staff ran the unit. Being able to go outside and smoke by themselves could become a welcome symbol of everyday life, in contrast to more traditional experiences of psychiatric care:
[I liked] the fact that I can go out without having a nurse with me. Just go outside and have a fag … I need my freedom. I don’t like having someone around me all the time because it makes me feel trapped, which I can’t really do nothing.
(1S11B)
Similarly, service users appreciated the opportunity to take responsibility for their own care, such as preparing food or taking medications while also being checked on by staff:
[Staff member] just meets you where you are at and if you want to go further down the runway, she gently just keeps you where you are now and gives you little nudges forward … OK the first night you are there, ‘yes, I’m going to bring you a glass of water and a tablet. Tomorrow I’m going to say right pop and get yourself some water and I‘ve got your tablets here when you want it’… [Service users] need to be empowered to take the tiniest steps that they can and move forward otherwise you are paralysed, mentally paralysed again.
(1S06B)
For those struggling with intense and difficult thoughts, staff awareness and protection was particularly welcome:
We were allowed to go and smoke, we had to give our lighters in and stuff like that. You were monitored and checked on. It wasn’t people in and out, in and out, in and out all the time.
(1S10B)
However, some service users found the levels of restriction disempowering:
I didn’t like the fact that you couldn’t just get out whenever you wanted. You had to ask staff. I didn’t like that, I felt as though I was locked in because there were locks on all the doors so you couldn’t get out … I vape and I wanted to go outside to vape and so I had to ask every time I wanted to go outside and then just felt like I was being a nuisance. I mean they didn’t make me feel like that but I didn’t like that aspect about it.
(3S04F)
Talking
I could talk to the staff at a deeper level
Service users described the PDU staff as easily approachable and calm, empathic listeners, never shocked or frightened by anything they heard. This meant that many were able to talk to staff at a deeper level than they could with family, friends, or other mental health professionals:
[It was] absolutely fantastic [talking to them]. Just having somebody to listen to you who is not going to judge and understands.
(3S03F)
They’re not frightened of anything you tell them. I didn’t see one of them look one bit concerned. They made you feel normal.
(2S07B)
I didn’t manage to talk to the staff
Although service users concurred that staff were kind and non-judgemental, they did not necessarily feel able to talk to them:
The staff were lovely, they weren’t nasty or anything. I know one of them just came and asked me you know ‘there’s drinks there if you want a drink or something or you want to eat something there’s biscuits there’. But that’s it. There wasn’t anything like have a conversation.
(4S04B)
Some service users found the staff difficult to talk to. In many cases, staff had waited for service users to approach them, and service users had not felt confident in initiating conversation:
it just didn’t seem appropriate, like it didn’t seem like I would say to them this is what’s going on in my head, this is why I’m here … I suppose because they didn’t open that conversation … Like ask me and I will tell you but I’m not just going to sit here and openly say this, this, this and this.
(3S11B)
Service users from PDUs with a shorter maximum LOS reported that there was not enough time to enable talking at any depth:
There was an assessment but it was just like they didn’t want to hear anything else they just wanted to hear what happened that day. But it wasn’t only that day that brought me to that situation. It wasn’t just that day it was the whole month … they just cut me off, they just cut me off and just asked what happened that day.
(4S04B)
Decisions
It was about more than just the decision-making
Many service users also derived significant benefit simply from the PDU’s calming environment and caring staff. This sometimes became particularly apparent in retrospect, and they used follow-up interviews to identify their PDU as a turning point in their crises:
it gave you a bit of time to just, you felt yourself, you didn’t feel pressured if that makes sense. You didn’t feel you had to be someone else, if that makes sense.
(2S10F)
For service users who had previously been treated badly by psychiatric services, the calm, compassion and respect they received at the PDU proved uplifting:
I went in with no expectations but they probably exceeded that by not being horrible to me.
(4S05B)
It was the first time I ever received the help I needed
Several service users described having spent many years, and often many decades, making unsuccessful attempts to seek help for their mental health. For some, being offered by the PDU the time and space to explain their needs to staff led to decisions being made which provided them with support they had never previously received:
Well basically [I’d] been neglected [by mental health services] for 20 years… [and the PDU was a] new thing. It’s like doctors, trainee doctors I say that to them and they look more space cadet than me. I don’t know if I‘m mad or is it everybody else that’s mad.
(2S04B)
They made their decision without involving me
Service users could describe a very professionalised, staff-led model of decision-making within which they were informed rather than consulted about what would happen to them.
I don’t know, that was just their, what they decided to do … They didn’t give me any options what I wanted to do, I think they just decided [that an inpatient admission] was the best place.
(2S05B)
Some struggled with this dearth of participation or involvement in the decision-making process. Whenever they felt as though staff were not listening to or considering the views or needs they expressed, service users could find this undermined their ability to talk in depth with staff:
I was expecting more. I was expecting a proper assessment of what brought you here, what happened, what’s going on, what meds are you on … A) make sure that I am safe, B) ensuring surely the idea of those things is to avoid people coming back into them, right? … Not one person asked me … what can be done to help you not get back there.
(3S11B)
Discharge, signposting and onward referral
Discharge went smoothly
For some service users, the discharge process went smoothly:
I think I’m getting all the support I need. I get those two people and as I say hopefully when this lockdown eases my [community psychiatric nurse] will be able to come and see me.
(3S04F)
One man, whose precarious living conditions had led to his crisis, described how the PDU had organised him an appointment with emergency housing services and had booked him a hotel to stay in until this appointment. When service users had been able to communicate such detailed challenges and concerns, the PDU could respond with flexibility and creativity.
Discharge overshadowed by lack of connectedness between mental health services
However, the PDU did not always work in such synchrony with the services to which it made referrals. Some service users, though broadly complimentary of the discharge process, were left not understanding what future care they might receive, or from whom:
[The crisis team] came to see me for a bit. There was no, I can’t remember if there was a plan put in place, I can’t remember.
(2S10F)
Some service users reported that the PDU had not adequately explained what was happening with their discharge, making it difficult for them to engage with other services:
But on the Monday morning they sort of just put me in a car and said ‘we’re taking you to a local council building’ with a piece of paper and said ‘just go in there’. I wasn’t ready for that … [but] they said they can’t do everything for me and I had to do things myself.
(3S10B)
The service user quoted felt so distressed by his confusion and the lack of explanation or support that he subsequently attempted suicide and was then detained under the Mental Health Act.
They discharged me too quickly
Some service users reported that they had not felt safe returning home, with service users sent home from PDUs with a shorter maximum LOS frequently reporting feeling that they their discharges had been overly hasty and insufficiently attentive to their needs, and that they still felt overwhelmed by voice-hearing or suicidal thoughts:
In the morning when they let me go I felt as if they just kicked me out the door … They gave me a leaflet, well a booklet with a few numbers on that I could call which I already knew about. It was ‘OK we’ve done our job now go’ … It wasn’t a nice way of leaving the place.
(4S02B)
Some service users at PDUs with a longer maximum LOS also reported this sense of hurriedness. This was particularly problematic for those living alone who were being sent back to a home where equipment that might be used for self-harm or suicide was still spread around. For some, the haste of discharge appeared more about staff attitudes towards them than the duration of their PDU admission:
every time I go in there [to the PDU] I’m left several days before they do anything … they come to me and they go ‘right what would you like us to do, you’ve come to the end of your two days’? I don’t know, that’s why I’m here.
(2S07F)
What next?
Most service users had been referred or signposted to the local crisis team or similar community-based services on discharge. Some service users spoke appreciatively of this transition. Nevertheless, many described less satisfactory experiences:
I know when you come out of it there’s hardly any help. So actually you can have the night off being safe and resting but knowing when you come out of it you are back to square one again which is where I am, which is what I did.
(2S10B)
Whereas most service users were sent either home or to a crisis house, a minority were transferred to an acute psychiatric ward. These individuals described a diversity of experiences of this. Some felt reassured by the bed and the privacy but others felt unsettled by the abrupt changes to their surroundings:
I don’t know if, I hope I haven’t been sectioned because I don’t know what’s happened with me. I don’t know I think I’m still voluntary or something. But all my body is aching and everything.
(2S02B)
In his initial interview (cited above), one service user described his PDU stay as the first mental health support he had been able to access in 20 years. At his follow-up interview several months later, he reported that he still had no consistent or satisfactory care:
No, I’ve got nothing. They [mental health team] came in my house … I said ‘what about [sickness benefits having been stopped due to admin error]’, ‘no, we can’t help you, that’s the dole’. Crisis team don’t know you well enough, that’s it … absolute disaster.
(2S04F)
There isn’t the capacity within mental health services
Despite the problematic post-discharge experiences they reported, service users remained largely complimentary about the PDU. Service users attributed the lack of longer-term mental health support the PDU could access for them and the lack of connectedness between services to wider structural, cultural and systemic problems with the mental health system:
I think when you can go somewhere like that I think you are really looked after and they obviously know what they’re doing. I think when you come out of it I think the help and the services are actually shit to be honest.
(2S10B)
Signposting and onward referral from the PDU rarely led to service users receiving the longer-term help they needed. For many, the value and effectiveness of the PDU lay not in their referrals or signposting to other services, but in their short-term crisis support. As one service user concluded:
the DU is great but it’s like a sticking plaster on a broken bone.
(3S11B)
Staff interviews
Clarity around psychiatric decision unit service
Psychiatric decision unit as a more therapeutic space
All staff agreed that the PDU provided a therapeutic space for service users, perceived as preferable to the busy, chaotic environment of ED:
somewhere to go that isn’t A&E which I’m all for because I hate telling people to go to ED … it’s not a therapeutic environment. So [the PDU is] a therapeutic environment for people with mental health needs in crisis to go somewhere safe away from A&E.
(3R04)
Although there were different understandings of the PDU’s purpose, it was also primarily seen as a space for further assessment and crisis containment which could potentially prevent inpatient admission or further escalation of a crisis:
If they feel after that [ED] assessment that they need a little bit of further assessment because they might not be sure or they might feel that their risk at the moment is still too high to go home they would then refer to PDU.
(4R01)
it’s having people around and having a bit of containment and feeling as if there is somewhere safe to go with people to talk to, they can sit and play cards. It’s that kind of breathing space.
(3R01)
Appreciating the service
On the whole, staff appreciated the role the PDU performed within the crisis pathway. They valued being able to refer into a crisis service where service users could access much-needed care from mental health staff, and where further support in the community could be set up, avoiding risky discharges:
For me … [PDU] assessments are a really valuable service because sometimes patients don’t feel safe to stay at home for various reasons .. the person may need further support and may not need a long-term admission.
(1R02)
Unmet expectations
However, staff did want more functionality from the PDU service. The functionality desired seemed to depend on which service the staff member was located within, as each service had its own priorities and problems. For example, the liaison psychiatry team wanted service users awaiting their Mental Health Act assessment in ED to be able to wait in the calmer PDU environment, although this was outside of the unit’s remit:
it’s about best interests isn’t it, it’s a nicer place and a much calmer place to wait for your Mental Health Act assessment than it is waiting in a busy A&E department.
(3R03)
The psychiatric decision unit cohort
Staff reported that two primary groups of service users seemed to be attending the PDU; service users who had been diagnosed with (or who were likely to meet the criteria for diagnosis of) a personality disorder, and those who had self-harmed, often with the intention of taking their own life:
a lot of the referrals that we do get are people that potentially suffer with personality disorder.
(4P02)
Staff explained that these service users came to the PDU due to the ‘in-between’ nature of the unit. The PDU seemed to provide for a cohort where a hospital admission would be considered too lengthy or restrictive and for whom home discharge was considered too risky:
sometimes people would self-harm or personality disorder, they come very distressed so we offer them, they are not really for admission in a hospital bed … we don’t feel that they are really fit to go home so something in between is the [PDU].
(2R01)
However, there was a query from one staff member over the efficacy of the PDU for service users with personality disorders, suggesting that perhaps this group of service could benefit from a slightly increased LOS:
Sometimes our service users with personality disorders don’t necessarily need an acute inpatient admission and the [PDU] maybe doesn’t provide a lengthy enough time that sometimes meets that individual’s needs … maybe that person needs 72 hours or a little bit longer in hospital than the [PDU] can provide.
(4R02)
In addition, a variety of other crisis triggers were identified which might lead someone to come onto the PDU, such as housing and employment issues, bereavement, difficult family dynamics, and other relationship stressors. More complex cases could involve several precipitating issues and perhaps a mental health diagnosis as well. Other problems could be less predictable, such as people presenting with psychosis presentations, or anxiety practical stressors in response to the COVID-19 pandemic.
Pathway and capacity
Pressure in the pathway
There were multiple pressures on the crisis pathway and a lack of capacity felt throughout the mental health system, in both crisis and community care. While for referral pathway staff the PDU could be perceived as positively easing this pressure, PDU staff discussed the impact of pressure being passed down to the unit, particularly from ED and inpatient wards:
sometimes we’re just forced to take them to be honest . . we don’t actually think this person is suitable but they seem to be pushing it on us quite a lot and I think it’s simply because they’re under pressure as well to get people out of A&E.
(1P03)
It was not always possible to push back on ‘unsuitable’ referrals. These inappropriate referrals could also be seen as linked to the proximity of other services like the 136 suite and, at one site during the pandemic, a temporary mental health ED unit. However, co-location of services could also have the benefit of increasing communication between teams as they spoke face to face more frequently.
The lack of service capacity could be also witnessed in community services. Community teams could have high caseloads, where it was difficult to spend significant one-to-one time with service users, and there was a lack of community resources at one site. Not receiving the right service clearly has a negative impact on service users yet it also detrimentally affects staff working with them, as they described the toll of not providing a good service:
It’s just really shit because you are left either having to … discharge people home or to a family member when people are already highly stressed and unwell. It just doesn’t feel nice, you are not giving a good service, patients are not getting what you think they need.
(3R03)
Communication
Communication was seen as key to the operation of both the PDU and the pathway; for example, being able to communicate the referral criteria of the PDU. However, referral staff sometimes reported the criteria of the PDU as unclear and inconsistent:
I’ve no idea what the criteria is at the moment because whenever we try and agree something, something different comes up.
(4R02)
There were other referral staff who saw the criteria as flexible, and responsive to individual need:
it’s all just case by case … you can be flexible and use it to your patient’s advantage.
(3R03)
Within the PDU, staff largely described open channels of communication. If there were staff disagreements (and these seemed to occur rarely), these were discussed before they escalated. There were also examples of healthy communication between different services. At most sites, staff within liaison psychiatry and the PDU described positive working relationships which were reflected in the ease of referral and ultimately how useful they felt the service was:
I think we tend to have quite a decent relationship with the decisions unit staff … I can’t really say that I’ve had anybody refused that I’ve referred in because … I think that we’ve come to understand what their purpose is a little bit and I’m sure that will change, it’s an evolving service.
(3R06)
Greater communication between services seemed to enable better communication with service users. When staff were more aware of what different parts of the pathway, include the PDU, could do and what they were like, they could then pass this information along to service users.
‘Us versus them’ split between services
An ‘us versus them’ dynamic could emerge between the PDU and other services, as well as a break between other crisis services. At one site, liaison psychiatry felt it was very hard to refer into the PDU but, equally, staff at the PDU felt referrals weren’t always well-considered:
I know that someone had complained to me that they had tried to send someone over to PDU at around 4am a couple of months ago and PDU declined because the person was tired because it was 4am … So, it’s at the point where it’s quite petty and quite difficult.
(4R02)
Sometimes [they] are not [appropriate] … because we have had patients who have been sent to us without telling us that patient is actively withdrawing from alcohol. They came and had a fit on the unit … It’s not fair for the patient either is it.
(4P03)
There was also a perceived split between physical and mental healthcare staff at one ED:
We do work quite closely with them but sometimes it feels like them and us.
(3R07)
This split could have real consequences in terms of service users and staff safety. One PDU staff member spoke about service users who had come to them without their physical needs being met, while another staff member’s own safety had been compromised when information around a service user’s risk profile had not been passed on and they had spent extended time alone with that service user.
Unmet expectations (see Clarity around psychiatric decision unit service) of the unit could feed into this dynamic, as other crisis services perceived the PDU as not addressing their primary concerns. This might be a gap in service provision they thought the PDU should address or feel that the unit had originally been (mis)sold to them. For example, ED staff had been expecting the PDU to take pressure off ED but felt that this had not transpired:
I think sometimes the unit was sold as ‘imagine it’s like an emergency department for patients with mental health’ … But actually . there’s very much of a gatekeeping role that they have about deciding what they will and won’t take.
(1R06)
Responsibility and reward
PDU staff reported that the nurse-led PDU provided them with more responsibility than other roles and this enabled them to develop their skills:
on [PDU] it’s nurse led so you are making that decision about that person’s life, that person’s risk. So, it’s enabled me to build confidence, being able to look at the patient as a whole.
(2P05)
Staff appreciated the holistic approach favoured on the unit where they were interested in ‘the patient as a whole’. This allowed them to address the causes of crisis, such as housing, relationship, or drug and alcohol issues. They were also able to spend long periods of time with each person, which was highly valued, and felt as though they were able to reduce that person’s distress. These ways of working within the unit added to a sense of satisfaction and accomplishment:
I just absolutely love working with patients and one-to-one and … what I quite like about the unit is we give them quite a lot of practical help as well as just talking to them.
(1P03)
However, it was emotionally demanding working with service users in crisis, both due to the acuity of their distress and the lack of formal detaining powers. The latter could leave staff worrying about service user safety. The unit was described by several staff members as a very busy place to work and could be ‘pretty relentless’ (2P01). The difficulty and responsibility of the role could therefore be seen as a double-edged sword; boosting career trajectory but also linked to a high staff turnover at one of the sites:
I think the unit has always had a very high turnover, part of that is due to .. [the PDU] really builds up your skills very quickly and because of that people get into more senior roles very quickly and .. because of the stress and the decision making. I think some people they just find that too much.
(1P04)
Supportive working environment on the psychiatric decision unit
Despite challenges of working on the PDU, such as the emotional demands described above, the overall experience for PDU staff seemed to be that units provided a supportive working environment. The helpful atmosphere on the unit seemed to manifest for staff in two main ways: informal and formal means of accessing support and feeling able to make and challenge decisions. Staff described good working relationships with colleagues and felt able to ask for and offer support on an informal basis:
It’s quite a tight team because we all do this together day in and day out and we are almost each other’s clinical supervisors. We get each other through it. You get a terrible sense of humour because that’s the only way you can make each other laugh sometimes. I feel like we support each other.
(2P02)
There were also a variety of formal support systems in place, such as supervision and reflective spaces.
I have individual clinical supervision usually with one of my seniors from bed management team so somebody at a high level who is much more experienced in this environment.
(4P02)
However, due to the nuances of how reflective spaces were run (with team members of all seniority levels present), staff could feel constrained about how they used those spaces:
I go to reflective practice but I’m trying not to make use of it in a way, I’m trying to be someone who is supporting other people in it.
(1P02)
Staff also felt able to challenge decisions being made, such as whether to accept a referral or the discharge destination of a service user. Even if a decision still stood, the freedom to challenge authority in and of itself was seen as valuable:
when I read through the referral and had my reservations first thing I did was pick up the phone and call the manager and aired my grievances in terms of being made to take this referral. Not thinking it would change anything but just as an opportunity to vent off if you like. But I guess that’s an example of where I feel able … to challenge decisions.
(2P01)
Tensions
Tensions were perceived between the service staff wanted to offer and the service they were required or able to offer. These tensions were often related to time and capacity. The pressure to move service users through ED increased during the COVID-19 pandemic, and units sometimes brought in new measures to assist with this, such as admitting people despite already being at maximum capacity. However, this adaptive response could bring its own issues of feeling ‘almost like a conveyor belt, which is awful to describe it like that’ (SWMDU1, PDU manager). An increase in number of service users on the unit could compromise standards of care, with service users undergoing lengthy waits to be spoken to. Subjecting service users to long wait times or depriving them of adequate time and engagement with staff was experienced as particularly difficult where staff prioritised these elements of their care:
the number one thing that helps is the time and the space. It’s an opportunity to slow things down a bit for them and to help get to a position where they can consider their circumstances with the guidance of staff.
(2P01)
If you can sit down with someone and listen to everything that’s happened and then just go you know what that sounds really shit, I can really get why you are here … I think for a lot of people that’s the first step for them getting better.
(1P04)
Impact of COVID-19
The impact of the COVID-19 pandemic was wide-ranging, for staff, service users and the crisis pathway. Almost all staff agreed that there was an initial lull in presentations and referrals at the start of the first lockdown. This was countered by higher numbers accessing services later on during the pandemic:
So, after the first few weeks that were very, very quiet we then saw a huge influx of much more unwell people than I’ve been used to seeing.
(1R06)
The issues with which service users presented and the cohort of people accessing services also changed. For example, staff reported increased cases of self-harm, domestic abuse, psychosis, the effects of isolation, drug and alcohol issues, loss of employment, and anxiety and depression. Some staff also described seeing more young people and people who were new to mental health services. One staff member summed up the variety in presentations:
There were a lot of issues regarding mental health patients who had been stable up until the lockdown and then that had intensified symptoms that they were dealing with naturally. So everything from people who were well treated and their anxiety and the lockdown and people cooped up in their house had triggered off a response to people who were drinking more heavily with lots of time on their hands, to people losing jobs or relationships.
(1R02)
There were two key changes staff saw as impacting service users. First, a lack of face to face contact (both in terms of service delivery and regular social contact) particularly for service users and people already feeling isolated. Second, the closure of certain services, particularly support groups in the community, although some new services were also developed specifically to address concerns around COVID-19. The crisis pathway was modified in response to the pandemic. Some services were temporarily suspended, and new services were opened, as well as the composition of teams and the way existing services were used both changed. For example, at one site the capacity of the PDU was increased, while at another the PDU closed temporarily and staff were reassigned to other services. In another site a new mental health ED unit was opened which impacted on referrals to the PDU:
It just feels that we are constantly taking referrals from them and constantly having pressure from the bed manager to take people as well. Just quite a lot of pressure at the moment.
(1P03)
For staff themselves, if they had been reassigned to another service this could be experienced as unsettling and high numbers of staff sickness, shielding or isolation could increase staffing pressures:
we couldn’t do the things that we normally do for our well-being so all that it was for us was work and home.
(3R06)
Chapter 8 Economic analysis
Overall approach and aims
The objective of the health economic analysis is to bring together findings from earlier chapters to identify potential impacts on the local health economy in each study area following the introduction of PDUs. The analysis makes use of the findings of all earlier chapters in this report. Using these different types of information, the chapter describes the economic impact and the RoI, from an NHS perspective, in each of the different study site areas. This compares the costs associated with PDU implementation with subsequent cost offsets as well as additional costs incurred. In addition, we also look at some impacts at an individual service user level; individual service scenarios provide illustrative estimates of changes in quality of life that would be needed for PDUs to be considered cost-effective from an NHS perspective.
All costs are reported in 2019–20 prices, with costs for acute hospital-based contacts and specialists community mental health teams taken from national reference costs. 83 Costs for some psychiatric inpatient stays, as well as hourly costs for some additional community and hospital-based staff costs, are taken from the annual Unit Costs of Health and Social Care. 84 These staff costs, estimate hourly costs, using mean full-time equivalent basic salary for AfC bands 4–9 of the April 2019/March 2020 NHS staff earnings estimates and include salary overheads and other oncosts. Further information on unit costs used in this chapter and their sources are reported in Appendix 8, Table 55.
Estimating the costs of psychiatric decision units
Our service mapping review (see Chapter 3), where the resources required to implement PDUs in the different areas have been collected,82 has been used to estimate the costs of providing PDU services in each site. An online survey completed by senior staff within PDUs included basic features on the structure of each unit, capacity, average and maximum LOS. The survey also collected information on staffing levels for both the day and night shifts in each PDU. This included type and number of staff members as well as their NHS AfC pay bands. We used these data to estimate the annual costs of running each PDU service. We assumed that there were two shifts, each of 12 hours in length and that the service operated 365 days per year.
The cost per PDU visit varies considerably from £741 in BSMHFT to £4800 in SHSCFT, with cost per PDU service user also ranging between £996 and £7442 (see Table 21). This is partly due to the considerable variation in staff ratios across the four MHTs, as well as differences in the level of throughput. BSMHFT, which has very short average stays of 12 hours, has an average of 1253 PDU visits for 932 service users per annum, compared with 438 visits by 283 service users in STHFT.
| BSMHFT | LPFT | SWLSTG | SHSCFT | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n) | Band | Annual cost (£) | (n) | Band | Annual cost (£) | (n) | Band | Annual cost (£) | (n) | Band | Annual cost (£) | |
| Day shift | ||||||||||||
| Nurses | 1 | 6 | 219,000 | 1 | 6 | 219,000 | 1 | 5–7 | 657,000 | 2 | 6 | 438,000 |
| HCAs | 1 | 3 | 118,260 | 2 | 3 | 236,520 | 2 | 2–4 | 236,520 | 1 | 3 | 118,260 |
| Psychiatrist | 0.5 | Consa | 254,040 | 0.5 | Consa | 254,040 | 0.5 | Consa | 254,040 | 0.5 | Consa | 254,040 |
| Support workers | 2 | 2 | 210,240 | |||||||||
| Service manager | 1 | 4 | 131,400 | 1 | 8a | 302,220 | ||||||
| Administrator | 1 | 4 | 131,400 | 1 | 4 | 131,400 | ||||||
| Total day shift | 591,300 | 840,960 | 1,278,960 | 1,454,160 | ||||||||
| Night shift | ||||||||||||
| Nurses | 1 | 6 | 219,000 | 1 | 6 | 219,000 | 1 | 5–6 | 394,200 | 2 | 6 | 438,000 |
| HCAs | 1 | 3 | 118,260 | 2 | 3 | 236,520 | 2 | 2–4 | 236,520 | 0 | ||
| Psychiatrist | ||||||||||||
| Support workers | 2 | 2 | 210,240 | |||||||||
| Total night shift | 337,260 | 455,520 | 630,720 | 648,240 | ||||||||
| Total cost | 928,560 | 1,296,480 | 1,909,680 | 2,102,400 | ||||||||
| Cost per PDU visit | 741 | 1446 | 2673 | 4800 | ||||||||
| Cost per service user | 996 | 2066 | 3797 | 7442 | ||||||||
Area-level economic impact
The ITS reported in Chapter 4 and the synthetic control study in Chapter 5 have examined the impact of PDUs on area-level acute hospital ED attendances, as well as area-level psychiatric hospital admissions (both informal and informal) at a (clinical) population-level. In this section, using the results of these analyses we estimate economic impacts from an NHS perspective that may be associated with the implementation of PDUs at an area level. Chapters 4 and 5 set out in detail the methods used and results of the two approaches. As noted in Chapter 4, the ITS provides data on service use over a 4-year period (spanning 2 years prior to and 2 years post PDU implementation) in MHTs and acute hospital EDs in three of the four sites. The synthetic control study (described in Chapter 5) sought to match and compare mental health admissions and LOS, as well as ED attendances, for the mental health and acute trusts in our four study areas with trusts with similar characteristics in areas of England where PDUs have not been implemented.
While there are some similarities in the conclusions reached from each method there are also differences in findings. In this section, we look at potential impacts of using both of these approaches independently.
Interrupted time series analysis
For the ITS, we only considered changes in the pre- to post-PDU long-term trend rather than short-term step change impacts or just post-PDU impacts. Conservatively, in our analyses we also only assumed that there may be an economic impact where statistically significant changes in service use were seen; we did not look at the economic impacts of consistent but not significant trends. As noted in Chapter 4, insufficient data were available from SHSCFT to conduct an ITS, so ITS impacts on MHTs was restricted to three areas: BSMHFT, LPFT and SWLSTG.
Impacts on mental health trusts: interrupted time series analysis
We start by looking at the impacts on overall inpatient admissions, both informal and formal, into study MHTs. All these impacts were calculated from a segmented Poisson regression (GLM with log link) and therefore can be interpreted as a percentage change in admission/attendance frequency on PDU implementation per week (trend change). The ITS revealed that there was no significant impact on admissions at BSMHFT, but there was a highly significant change in the pre- to post-PDU (long-term) trend for all inpatient admissions at SWLSTG, with a decrease of 0.28%/week over the 2 years post PDU. A highly significant change in the pre-to post-PDU (long-term) trend of 0.45%/week for all inpatient admissions was also seen at LPFT. These modest impacts on inpatient admissions would equate to annual costs averted of £32,405 for LPFT and £47,919 at SWLSTG. We assumed that the LOS for each averted inpatient admission would be the median LOS, given that there were no significant changes in lengths of stay in any of the three sites.
Data were also available on liaison psychiatry contacts. For all service users no significant changes in pre-to post-PDU (long-term) trends were observed, but when focused solely on service users who had a previous episode in the last 24 months the ITS indicated a highly significant 2.79% monthly reduction in contacts in LPFT and a smaller but still highly significant reduction of 0.28% contacts in BSMHFT. This would be equivalent to small annual costs averted of £4739 and £2630 in the two areas, respectively. Overall, at site level the ITS suggests that all MHTs (BSMHFT, LPFT and SWLSTG) averted some costs following PDU implementation of £2630, £37,144 and £47,919, respectively.
However, these estimates of averted costs would almost entirely be no longer be seen if data across all three sites were pooled. As reported in Chapter 4, after adjustment for random effects, this meta-analysis indicated no significant impacts on inpatient admissions or LOS and hence no impact on costs. The meta-analysis did, though, find a highly significant but modest reduction of 0.24% weekly contacts with psychiatric liaison services for service users who had experienced a prior episode for poor mental health in the previous 24 months. This would be equivalent to a small annual saving across all three sites of £3765.
Impacts on acute trusts: interrupted time series analysis
For pre-to post-PDU (long-term) trends, the ITS analysis reported significant increases in weekly accident and ED attendance at ULHFT and STHFT of 0.26% and 0.46%, respectively. This is equivalent to an additional 4.67 and 9.32 attendances at accident and EDs per annum at a total cost of £880 and £1755, respectively. There was no significant change at SGUHFT, while at SWBHFT there was a significant fall in ED attendances for service users who had a previous admission in the previous 24 months. This was equivalent to an annual reduction of 4.75 in accident and ED presentations, with total costs averted of £895. Only one of the trusts, STHFT, saw a significant change in arrivals by ambulance or police; this increased by 0.23% points per week. This is equivalent to 4.66 additional ambulance visits per annum at a cost of £1362.
At ULHFT, SGUHFT and STHFT, there were highly significant increases from pre-to post-PDU in the proportion of attendances where service users were admitted from the accident and ED to an inpatient ward at the acute trust of 0.12% points, 0.13% points and 0.21% points per week, respectively. This leads to an additional 2.15, 2.64 and 4.26 inpatient admissions per annum at a total cost of £1598, £1962 and £3161, respectively, using the assumption that a typical inpatient stay is related to the weighted average of all NHS tariffs for short-stay non-elective treatment for the most common form of deliberate self-harm, poisoning.
Meta-analysis, pooling data across all four site areas, after adjustment for random effects, did not reveal any significant long-term change in accident and emergency mental health related attendances. It did, however, report a highly significant but small increase of 0.14% points per week increase in discharge to acute hospital trust wards. This would imply an additional 9.03 acute hospital admissions per annum at a cost of £6700.
Table 22 summarises changes in NHS impacts following the introduction of the PDUs. Overall, at an area level, the ITS analyses, because of the limited number of significant effects observed and the small magnitude of these effects, suggests only very modest impacts on NHS costs at an area level. For the three areas, BSMHFT, LPFT and SWLSTG, where data on both MHT and acute trust activity were available, there would be an annual net reduction in total NHS costs of £3525, £34,666 and £45,957, respectively. For STHFT, only acute hospital trust impacts could be measured, with annual increased costs of just £6278. When looking at the results of meta-analysis alone, there are even fewer significant effects, with a net overall increase in costs of just £2935.
| MHTs | BSMHFT | LPFT | SWLSTG | SHSCFT | Meta-analysis |
|---|---|---|---|---|---|
| Inpatient admissions | 0.00 | −2.92 | −4.41 | 0.00 | 0.00 |
| Liaison psychiatry contacts | −11.02 | −19.85 | 0.00 | 0.00 | −15.77 |
| Inpatient costs | 0.00 | −32,405.44 | −47,919.15 | 0.00 | 0.00 |
| Liaison psychiatry costs | −2630.22 | −4738.79 | 0.00 | 0.00 | −3765.00 |
| Total MHT costs | −2630.22 | −37,144.23 | −47,919.15 | 0.00 | −3765.00 |
| Acute hospital/ambulance trusts | SWBHFT | ULHFT | SGUHFT | STHFT | Meta |
| ED mental health attendancesa | −4.75 | 4.67 | 0.00 | 9.32 | 0.00 |
| Ambulance/police conveyance | 0.00 | 0.00 | 0.00 | 4.66 | 0.00 |
| Acute inpatient admissions | 0.00 | 2.15 | 2.64 | 4.26 | 9.03 |
| ED mental health attendance costsa | −894.69 | 880.03 | 0.00 | 1755.28 | 0.00 |
| Ambulance/police conveyance costs | 0.00 | 0.00 | 0.00 | 1361.63 | 0.00 |
| Acute inpatient admission costs | 0.00 | 1598.46 | 1962.14 | 3161.30 | 6700.39 |
| Total acute hospital/ambulance trusts | −894.69 | 2478.49 | 1962.14 | 6278.22 | 6700.39 |
| Overall impact on local area costs | −3524.90 | −34,665.74 | −45,957.01 | 6278.22 | 2935.39 |
Synthetic control analysis
The synthetic control study (see Chapter 5) matched and compared mental health admissions and lengths of stay, as well as ED attendances, for the mental health and acute trusts in our study areas with trusts with similar characteristics in areas of England where PDUs have not been implemented. The analysis did not however include data from SHSCFT as this site did not contribute any data to HES during the study period.
Impacts on mental health trusts: synthetic control analysis
For the remaining three MHTs, the synthetic control study did not identify any significant impact of the opening of the PDU on admissions to inpatient wards at any of the MHTs. However, a highly significant lower average LOS of 1.5 days for service users admitted to mental health inpatient wards at BSMHFT compared with control trusts was observed. There was no significant difference in LOS in the other two MHTs. Meta-analysis pooling data from all three trusts suggested a significantly lower average LOS of 6.4 days compared with the control areas. These data should, however, be treated cautiously, as the diagnostic codes in HES data for acute mental health admissions may include some specialist admissions or non-hospital acute admissions, such as diversions to home treatment teams.
Despite these uncertainties the synthetic cohort study implies potential economic benefit for all three MHTs following implementation of PDUs relative to control trusts. If average lengths of stay were lower by 15.5 days per 10,000 trust catchment population per month in BSMHDT compared with control MHTs, this could imply economic costs avoided in the area of £1.27 million per annum. This does not necessarily mean that costs have reduced since the PDU was introduced, it could also mean that there has been a lower rate of increase in LOS in comparison with control areas.
Similarly, if lengths of stay across all three MHTs were on average lower than the control areas by 6.4 days per 10,000 trust catchment population per month, as shown in the meta-analysis, the total in costs averted for all three MHTs compared with control trusts could be up to £1.16 million.
Impacts on acute trusts: synthetic control analysis
The synthetic control study revealed that there were no impacts of PDU opening on acute hospital trusts in BSMHDT. There were no significant differences in ED attendances between acute trusts and their comparators, with one exception. For STHFT, the study reported a significant reduction of 1.5 mental health-related ED attendances per 10,000 trust population per month compared with the control areas. This would equate to 87 ED visits averted per month, with total costs averted of £196,620 per annum. There were no significant differences in ambulance and policy conveyance to hospital between acute trusts and their comparators, with one exception: ULHFT reported a significant 9.1% reduction per 10,000 trust catchment population compared with control areas. This would mean 23 fewer ambulance/police conveyances each month compared with the counterfactual areas, potentially avoiding costs of £80,617 per annum. No significant differences in acute inpatient admissions to the same provider were reported for any of the acute trusts. There were also no significant differences in any category of resource use when data were pooled across all acute trusts in meta-analysis.
Return on investment
An objective of this chapter was to draw on findings of earlier chapters to identify potential impacts on the local health economy in each study area following the introduction of PDUs. One element of this is a RoI, from an NHS perspective, in each of the different study site areas. Essentially this compares the costs associated with PDU implementation with observed changes in costs of health services.
Table 23 summarises the RoI for each of the four sites. Here we have assumed that all the impacts on costs from the ITS and synthetic cohort studies are independent and cumulative. Even with this assumption, the limited impacts of PDU implementation on resource use reported by the analyses in Chapters 4 and 5, means that the level of direct annual RoI for most areas is low, being just 2.41% of PDU annual costs in SWLSTG, 8.89% in LPFT and 9.05% of PDU annual costs in STHFT. The exception is BSMHFT, which because of the highly significant reduction in average length of inpatient stay of 15.5 days, has an annual return of 1868% compared with the costs of PDU investment. Our survey in Chapter 3 indicates that the four PDU services were operating between 63% and 83% of full capacity; if services were operating at full capacity and assuming a proportionate change in cost impacts would have a negligible impact on the RoI in three areas but would increase to a maximum of 2990% in BSMHFT (see Appendix 8, Table 56 for full results).
| Costs | BSMHFT | LPFT | SWLSTG | STHFTa |
|---|---|---|---|---|
| PDU (£) | 928,560 | 1,296,480 | 1,909,680 | 2,102,400 |
| ITS impacts (£) | ||||
| Inpatient | 0 | −32,405 | −47,919 | 0 |
| Liaison psychiatry | −2630 | −4739 | 0 | 0 |
| Acute hospital ED visits | −895 | 880 | 0 | 1755 |
| Ambulance/police conveyance | 0 | 0 | 0 | 1362 |
| Acute hospital inpatient admissions | 0 | 1598 | 1962 | 3161 |
| Total impacts | −3525 | −34,666 | −45,957 | 6278 |
| Synthetic control impacts (£) | ||||
| Inpatient | −17,347,601 | 0 | 0 | 0 |
| Acute hospital ED visits | 0 | 0 | 0 | −196,620 |
| Ambulance/police conveyance | 0 | −80,617 | 0 | 0 |
| Acute hospital inpatient admissions | 0 | 0 | 0 | 0 |
| Total impacts | −17,347,601 | −80,617 | 0 | −196,620 |
| Overall averted (£) | −17,351,126 | −115,283 | −45,957 | −190,342 |
| Return on investment (%) | 1868.61 | 8.89 | 2.41 | 9.05 |
Our original intention was to use the results of the RoI analysis to look at the potential costs and benefits of scaling up access to services across England, but this is not appropriate given the uncertainty around the levels of return, which are low with the clear exception of BSMHFT. While the synthetic control method indicates that the difference in mental health inpatient LOS following the introduction of the PDU in BSMHFTis highly significant, this method does not allow us to isolate the effects of the PDU from other factors that could contribute to difference in LOS. The introduction of the PDU would not be expected to have such a major effort on LOS, given its focus on reducing the number of short (< 5 days) rather than long hospital stays; the relative contribution to average LOS of other innovative services introduced in the same time frame in BSMHFT, including the more intensive use of liaison psychiatry, using the rapid assessment, interface and discharge service needs to be explored. The limited change on resource use seen in both the ITS and synthetic cohort studies in the other areas should also not be interpreted as indicating that there is no economic case for investing in PDUs, but it does indicate that they may be unlikely to offset a substantial proportion of their cost to the NHS.
That said, there are additional resources saved on which we have not placed an economic value; these include any reductions in waiting time in ED. The synthetic cohort study in Chapter 5 pointed to significantly lower waiting times in the ED at KHFT in comparison with control sites. While we have valued contacts with EDs using tariffs that do not vary by time spent waiting, reducing waiting times potentially frees up time of ED staff to see and treat other patients. Furthermore, evidence from previous analysis suggests that individuals detained under section 136 of the Mental Health Act may wait in EDs on average up to 12 hours compared with a general population average of 2.5 hours, owing to the complexity of their needs. This, it has been suggested, is the equivalent of being able to treat 10 other patients in the same time period. 100 Our study also does not look at whether PDUs services have displaced existing local mental health services (e.g. have replaced triage wards or other community-based assessment services) or are instead an addition to existing services. There may also be impacts on the use of specialist CMHTs that we do not know about. The costs of providing PDUs will be lower and the RoI greater if they have substituted for some existing services.
It should also be stressed that the time period for this analysis is still relatively short; if individuals benefit from contact with PDUs then their long-term mental health service use costs may be considerably lower, but our analysis at most only covers a 2-year post-PDU implementation period. Untreated poor mental health can have consequences that last for many years or even decades, so a longer time frame may also be needed to fully capture these consequences. Our return on analysis has been conducted from an NHS perspective, but there may be other impacts on other agencies, such as the police and local authorities arising from any improvement in mental health outcomes for service users.
Critically, the most fundamental impacts of all are the short-, mid- and long-term outcomes on PDU service users. Longitudinal analyses are still needed at an individual service user level that compare the long-term costs and outcomes of PDU service users directly with those of individuals that have not used these services. If PDUs help improve levels of recovery from poor mental health as well as social inclusion, this will also have economic benefits for these individuals such as economic independence and wider society (higher levels of productivity from participation in education, paid employment, family caring and volunteering). These could not be included in our RoI analysis. PDUs will also have impacts on quality of life. Another fundamental question is whether contact with PDUs leads to incremental gains in quality of life compared with care as usual.
The remaining sections of this chapter look at some of these missing potential individual-level impacts of PDUs, by drawing on analysis of service use and pathways of care observed in cohort study in Chapter 6, as well as the qualitative analysis in Chapter 7. We also examine the quality of life of individuals attending PDUs and therefore there is scope for substantial improvements in quality of life following PDU contact.
Changes in cost of mental health services following psychiatric decision unit assessment
In addition to ED attendance and psychiatric inpatient admissions, contact with PDUs might be expected to have an impact on the use of community mental health services. Longitudinal cohort data collected as part of decision have been used to explore these impacts. Chapter 6 describes how in each of the four study areas data have been collected on patterns of service contact and utilisation in the 9 months prior to and following an initial visit to a PDU. We have then examined differences in resource use and costs to the NHS in the 9 months after a PDU visit for each of the four sites. Unit costs are drawn from NHS national reference costs and the Personal Social Services Research Unit’s Unit Costs of Health and Social Care used in estimating these costs. Specific sources are reported in Appendix 8, Table 55.
Table 24 shows summary results of pairwise comparisons on per-PDU and post-PDU costs, using 2000 bootstraps, bias corrected and accelerated to account for the non-normal distribution of costs (full results for each site are given in Appendix 8, Tables 57–60). Overall increased contacts with services and inpatient hospitalisations meant that post-PDU costs are significantly greater than pre-PDU costs in all four areas (p = 0.000). Mean total costs post PDU were £6945 greater in BSMHFT £8446 in LPFT, £5803 in SWLSTG and £7908 in SHSCFT. Similarly, the mean costs of inpatient stays were significantly greater in all four sites: £4696 greater in BSMHFT £5059 in LPFT, £3671 in SWLSTG and £5179 in SHSCFT. The cost of liaison psychiatry costs was significantly lower in the post-PDU in LPFT (p = 0.001) and SWLSTG (p = 0.000) although the absolute level of costs was low. Use of both CMHTs, as well as crisis/home treatment teams, were also significantly greater in all four sites. Potentially PDU visits may have led to different patterns of onward referral and signposting to community-based services.
| BSMHFT | LPFT | SWLSTG | SHSCFT | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre (£) | Post (£) | p-value | Pre (£) | Post (£) | p-value | Pre (£) | Post (£) | p-value | Pre (£) | Post (£) | p-value | |
| Inpatient stays | 1021 | 5718 | 0.000 | 922 | 5981 | 0.001 | 160 | 3832 | 0.001 | 1455 | 6634 | 0.004 |
| Liaison psychiatry | 328 | 347 | 0.333 | 135 | 90 | 0.001 | 266 | 134 | 0.000 | 364 | 340 | 0.753 |
| CMHT | 779 | 1423 | 0.000 | 1115 | 2406 | 0.001 | 791 | 1851 | 0.000 | 3863 | 5181 | 0.008 |
| Crisis teams | 1888 | 3383 | 0.000 | 1265 | 2417 | 0.000 | 1071 | 2267 | 0.000 | 2128 | 3389 | 0.011 |
| Nurses | 5 | 9 | 0.303 | 21 | 26 | 0.328 | 63 | 50 | 0.255 | – | – | – |
| Psychologist | 4 | 18 | 0.010 | 4 | 4 | 0.969 | – | – | – | – | – | – |
| Social workers | 0 | 0 | 0.135 | 3 | 1 | 0.101 | 7 | 10 | 0.609 | – | – | – |
| Perinatal team | 43 | 96 | 0.208 | 41 | 73 | 0.481 | 7 | 26 | 0.178 | – | – | – |
| Criminal diversion | 41 | 61 | 0.215 | 48 | 3 | 0.315 | – | – | – | – | – | – |
| All non-inpatient | 3089 | 5337 | 0.000 | 2632 | 6019 | 0.000 | 2206 | 4338 | 0.000 | 6645 | 9374 | 0.000 |
| Total | 4110 | 11,055 | 0.000 | 3554 | 12,000 | 0.000 | 2367 | 8170 | 0.000 | 8100 | 16,008 | 0.000 |
Regression analyses
Multiple statistical analyses were performed to explore the extent to which individual characteristics and pre-PDU costs were associated with costs of service use for the 9-month period following initial visit to the PDU at each of the four PDU study areas. Having determined that there was no statistical difference in costs between the pre COVID-19 cohorts and the primary cohorts where service access may have been affected by COVID-19, we used data from both time periods in three cohorts (BSMHFT, LPFT and SWLSTG) in regression analysis, to increase available cases. There were no pre-pandemic cohort data available for SHSCFT.
In these analyses, the dependent variables were total costs after visiting PDU over the 9-month period in each of the four sites. GLM was used for these analyses to allow flexibility to deal with skewness in the dependent variables and we tested for the best-fitting distributional forms in the regression equations. All pre-PDU baseline variables for the individual characteristics were tested for statistical significance using a significance level of 0.05 and were explored for potential inclusion in the cost models. They were added one at a time to the cost model, given statistical significance and theoretical importance. Variables considered for potential inclusion were: age, sex, ethnicity (White British vs. all other), marital status, employment status (working vs. all other), accommodation (mainstream housing vs. insecure housing, supported housing, health facility, unknown), and primary diagnosis using ICD-10 subcategories (psychoactive substance use, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, disorders of psych development, behavioural and emotional disorders, other). Stata 15 and SPSS version 24 were used for these analyses.
Tables 25–28 provide summary results for all four areas. For all models a gamma log function model was best fitting. In summary, female sex is an explanatory factor for higher costs in three of the four sites and increased age is associated with higher costs in all four sites. Not being White British was associated with higher post-PDU costs in one area but did not feature in best-fitting models for the other three areas. Insecure or unknown housing status relative to being in mainstream housing was associated with lower costs in both BSMHFT and SHSCFT. Associations between different primary mental disorder diagnoses and post-PDU costs varied across sites.
In the case of BSMHFT, total costs for the 9 months prior to PDU visit were highly significantly associated with post-PDU costs, although their impact on costs was minimal, with a one-unit increase associated with a 0.004% increase in post-PDU costs (p = 0.000). Sex and ethnicity were also significant and had substantial associations with post-PDU costs. Being a woman was associated with 43.15% higher total post-PDU costs than being a man (p = 0.033), while not being White British was associated with 55.28 % higher total post-PDU costs (p = 0.012). Age was also a potential explanatory factor for higher costs; for an increase of age by 1 year, there was a significant increase (2.07%) in the post-PDU total costs (p = 0.004). Relative to a primary diagnosis of a mood disorder (ICD-10 codes F30–F39), diagnosis was not associated with post-PDU costs; this lack of association may be due to the high level of missing data for diagnosis (82%).
In the case of LPFT, total costs for the 9 months prior to PDU visit were highly significantly associated with post PDU costs, although again their impact on costs was minimal, with a one-unit increase associated with a 0.003% increase in post PDU costs (p = 0.004). Sex and ethnicity were also significant and had substantial associations with post-PDU costs. Being a woman was associated with 37.15% higher total post-PDU costs than being a man (p = 0.027). Age was also a potential explanatory factor for higher costs; for an increase of age by 1 year, there was a significant increase (1.55%) in the post-PDU total costs (p = 0.003). Living in insecure housing was associated with 48.8% lower post-PDU costs than those in mainstream housing (p = 0.010); this might be because they are more difficult to reach that people with a fixed address; similarly having an unknown housing status was associated with 56.6% lower post-PDU costs than those in mainstream housing (p = 0.010).
Relative to individuals with a primary diagnosis of mood disorder, having a psychoactive substance use (F10–F19) was associated with 148% higher costs (p = 0.013). Similarly, a diagnosis of schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders (F20–F29) was associated with 406% higher post-PDU costs than for those with mood disorders (p = 0.000). Anxiety, dissociative, stress-related, somatoform and other non-psychotic mental disorders (F40–F48) were associated with 209% higher post-PDU costs (p = 0.000) and personality disorders (F60–F69) with 504% higher post-PDU costs (p = 0.000).
For SWLSTG, being a woman was associated with 45.1% higher total post-PDU costs than being a man (p = 0.013). Age was also a potential explanatory factor for higher costs; for an increase in age by 1 year, there was a significant increase (1.4%) in the post-PDU total costs (p = 0.012). Relative to individuals with a primary diagnosis of mood disorder, many other diagnostic conditions were associated with lower post-PDU costs in contrast to the other study areas. Having a psychoactive substance use (F10–F19) was associated with 79.1% lower post-PDU costs (p = 0.000). Anxiety, dissociative, stress-related, somatoform and other non-psychotic mental disorders (F40–F48) were also associated with 70.4% lower post-PDU costs (p = 0.000). Although primary diagnoses of pervasive and specific development disorders (F80–F89) and behavioural and emotional disorders with onset usually occurring in childhood and adolescence (F90–F98) were also significantly associated with lower PDU costs, only 5 of 494 individuals in the SWL data set had these diagnoses. Ethnicity was not selected for the best-fitting model.
For SHSCFT, which only had 204 individuals in the primary cohort, few significant associations were found between individual characteristics and post-PDU costs. Total costs for the 9 months prior to PDU visit were highly significantly associated with post-PDU costs, although their impact on costs was minimal, with a one-unit increase associated with a 0.004% increase in post-PDU costs (p = 0.001). Age was also a potential explanatory factor for higher costs; for an increase of age by 1 year, there was a significant increase (1.6%) in the post-PDU total costs (p = 0.03). Different diagnostic categories were not associated with post-PDU costs, with the exception of behavioural and emotional disorders with onset usually occurring in childhood and adolescence (F90–F98), but this was based on the costs solely of one individual. Ethnicity was not selected for the best-fitting model.
| Covariates | E(Beta) | Std. error | z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Total costs for 9-month pre-PDU visit | 1.000 | 0.000 | 4.630 | 0.000 | 0.000 | 0.000 |
| Age | 1.021 | 0.007 | 2.910 | 0.004 | 0.007 | 0.034 |
| Female sex (ref: male) | 1.431 | 0.169 | 2.130 | 0.033 | 0.028 | 0.689 |
| Ethnicity: non-White British (ref White British) | 1.553 | 0.176 | 2.500 | 0.012 | 0.095 | 0.785 |
| Not employed (ref: employed) | 1.175 | 0.187 | 0.860 | 0.387 | −0.205 | 0.528 |
| F10–F19a | 1.078 | 0.522 | 0.140 | 0.886 | −0.948 | 1.097 |
| F20–F29a | 1.197 | 0.286 | 0.630 | 0.530 | −0.381 | 0.740 |
| F40–F48a | 1.074 | 0.478 | 0.150 | 0.882 | −0.866 | 1.008 |
| F50–F59a | 0.684 | 1.049 | −0.360 | 0.718 | −2.437 | 1.677 |
| F60–F69a | 0.717 | 0.430 | −0.770 | 0.439 | −1.176 | 0.510 |
| F90–98a | 2.054 | 0.733 | 0.980 | 0.326 | −0.716 | 2.156 |
| Other diagnosisa | 1.097 | 0.602 | 0.150 | 0.878 | −1.087 | 1.273 |
| Constant | 1784.701 | 0.515 | 14.540 | 0.000 | 6.478 | 8.496 |
| Covariates | E (beta) | Std. error | z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Total costs for 9-month pre-PDU visit | 1.000 | 0.000 | 2.840 | 0.004 | 0.000 | 0.000 |
| Age | 1.015 | 0.005 | 2.970 | 0.003 | 0.005 | 0.025 |
| Female sex (ref: male) | 1.376 | 0.144 | 2.210 | 0.027 | 0.036 | 0.602 |
| Insecure housinga | 0.512 | 0.260 | −2.580 | 0.010 | −1.180 | −0.160 |
| Supported housinga | 1.114 | 0.392 | 0.280 | 0.783 | −0.660 | 0.876 |
| Health facilitya | 0.858 | 1.556 | −0.100 | 0.922 | −3.202 | 2.896 |
| Unknown accommodationa | 0.434 | 0.324 | −2.580 | 0.010 | −1.468 | −0.200 |
| Not employed (ref: employed) | 0.978 | 0.147 | −0.150 | 0.880 | −0.310 | 0.266 |
| F10–F19b | 2.482 | 0.367 | 2.480 | 0.013 | 0.189 | 1.629 |
| F20–F29b | 5.056 | 0.289 | 5.600 | 0.000 | 1.054 | 2.188 |
| F40–F48b | 3.091 | 0.315 | 3.580 | 0.000 | 0.511 | 1.746 |
| F60–F69b | 6.406 | 0.278 | 6.690 | 0.000 | 1.313 | 2.402 |
| Other diagnosisb | 2.738 | 0.443 | 2.270 | 0.023 | 0.139 | 1.876 |
| Constant | 2592.949 | 0.371 | 21.190 | 0.000 | 7.133 | 8.588 |
| Covariates | E (beta) | Std. error | z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Total costs for 9-month pre-PDU visit | 1.000 | 0.000 | 2.460 | 0.014 | 0.000 | 0.000 |
| Age | 1.014 | 0.006 | 2.500 | 0.012 | 0.003 | 0.025 |
| Female sex (ref: male) | 1.451 | 0.149 | 2.490 | 0.013 | 0.079 | 0.665 |
| Insecure housinga | 1.707 | 0.304 | 1.760 | 0.079 | −0.061 | 1.131 |
| Supported housinga | 1.935 | 0.371 | 1.780 | 0.075 | −0.067 | 1.388 |
| Unknown accommodationa | 1.999 | 0.817 | 0.850 | 0.397 | −0.909 | 2.294 |
| Not employed (ref: employed) | 1.226 | 0.163 | 1.250 | 0.211 | −0.115 | 0.523 |
| F10–F19b | 0.209 | 0.448 | −3.490 | 0.000 | −2.442 | −0.686 |
| F20–F29b | 1.306 | 0.426 | 0.630 | 0.531 | −0.569 | 1.103 |
| F40–F48b | 0.296 | 0.275 | −4.430 | 0.000 | −1.755 | −0.679 |
| F60–F69b | 0.283 | 0.266 | −4.740 | 0.000 | −1.785 | −0.741 |
| F80–89b | 0.098 | 0.983 | −2.370 | 0.018 | −4.255 | −0.400 |
| F90–98b | 0.253 | 0.984 | −1.400 | 0.163 | −3.303 | 0.555 |
| Other diagnosisb | 0.293 | 0.397 | −3.090 | 0.002 | −2.005 | −0.448 |
| Constant | 2289.794 | 0.401 | 19.290 | 0.000 | 6.950 | 8.522 |
| Covariates | E (beta) | Std. error | Z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Total costs for 9 months pre-PDU visit | 1.000 | 0.000 | 3.260 | 0.001 | 0.000 | 0.000 |
| Age | 1.016 | 0.008 | 2.170 | 0.030 | 0.002 | 0.031 |
| Female sex (ref: male) | 0.973 | 0.227 | −0.120 | 0.906 | −0.473 | 0.419 |
| Insecure housinga | 1.342 | 0.524 | 0.560 | 0.574 | −0.733 | 1.322 |
| Supported housinga | 1.562 | 0.587 | 0.760 | 0.447 | −0.704 | 1.596 |
| Health facilitya | 2.086 | 1.378 | 0.530 | 0.594 | −1.965 | 3.435 |
| Unknown accommodationa | 0.187 | 0.232 | −7.200 | 0.000 | −2.130 | −1.219 |
| F10–F19b | 0.469 | 0.795 | −0.950 | 0.340 | −2.316 | 0.800 |
| F20–F29b | 1.668 | 0.295 | 1.730 | 0.083 | −0.067 | 1.091 |
| F40–F48b | 0.769 | 0.434 | −0.600 | 0.546 | −1.112 | 0.588 |
| F60–F69b | 0.570 | 1.450 | −0.390 | 0.698 | −3.403 | 2.279 |
| F80–89b | 1.399 | 0.323 | 1.040 | 0.300 | −0.298 | 0.969 |
| F90–98b | 0.043 | 1.108 | −2.830 | 0.005 | −5.308 | −0.966 |
| Other diagnosisb | 0.708 | 1.377 | −0.250 | 0.802 | −3.044 | 2.354 |
| F10–F19b | 0.062 | 1.441 | −1.930 | 0.054 | −5.602 | 0.049 |
| Constant | 5882.793 | 0.523 | 16.600 | 0.000 | 7.655 | 9.705 |
Insights into the quality of life of psychiatric decision unit service users
The primary function of mental health services is to improve health outcomes and not just impact on resource use and costs. Although the study did not intend to directly look at changes in clinical outcomes, such as levels of mental distress, it has been possible in the study to collect some self-report data on quality-of-life scores, using the EuroQOL EQ-5D-5L quality-of-life instrument. 101 The instrument has five domains: mobility, self-care, ability to perform usual activities, pain and depression/anxiety levels, with a score of 1 indicating perfect quality life and a score of 0 being equivalent to death. The five response levels for each domain are: no problems, slight problems, moderate problems, severe problems and extreme problems. The instrument is widely used to generate estimates of quality adjusted life-years used to help assess the cost-effectiveness of health system interventions.
In our analysis quality-of-life data can inform scenario modelling to help indicate the potential plausibility for improving quality of life of PDU service users. This can be useful given that quality of life is the primary outcome measure used in economic analysis to inform decision-making in England, where judgements are typically concerned with assessing whether the additional costs incurred by a service are justified by the quality-of-life gains made.
PDU service users in the cohort study in two of the study areas, LPFT and STHFT were invited to complete the EQ-5D-5L at baseline and at 9-month follow-up. Individuals were able to post their completed instruments back to the PDU and these questionnaires could then be linked to individual service user identifiers. Complete responses were received from 148 participants, 107 from LPFT and 41 from STHFT.
Currently there is no accepted value set in England for the five-level version of EQ-5D, so in line with current recommendations from the National Institute for Health and Care Excellence,102 we have used the crosswalk mapping function developed to map five-level values to the existing English three-level value set103 to generate utility scores. Figure 15 shows the distribution of EQ-5D-5L scores at baseline. The average utility score of just 0.14 is extremely low, being for example, much lower than average values reported for young people in England who have self-harmed of 0.68. 104 41% of these scores were less than zero, indicating that these individuals had utility scores that could be viewed as worse than death; these very low values in a high proportion of individuals might be expected, given that many individuals attending PDUs may have been experiencing suicidal thoughts.
FIGURE 15.
Distribution of EQ-5D-5L scores in reporting participants at baseline in LPFT and SHSCFT.
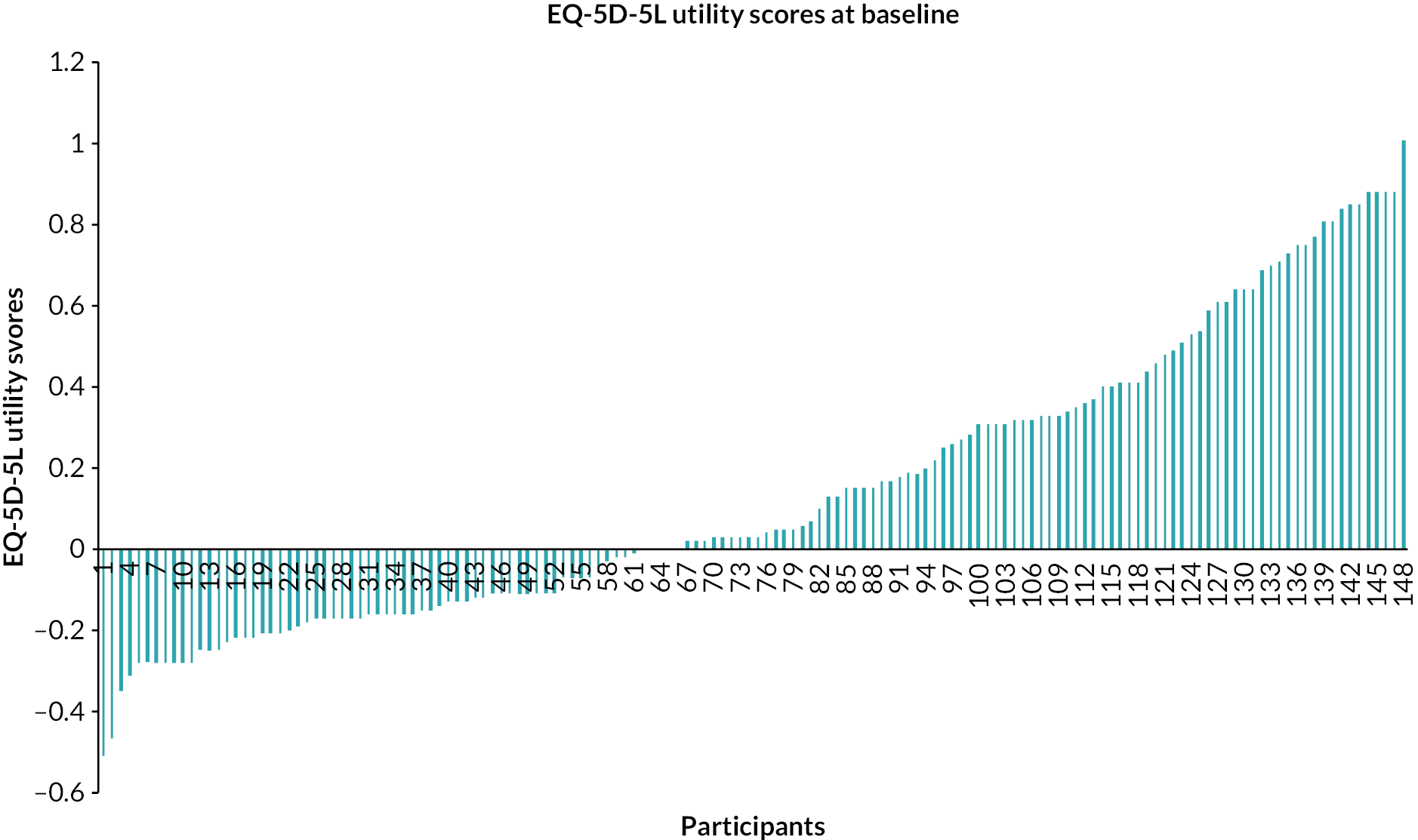
While this sample is small, the data suggest that there is potential for substantial changes in utility values with appropriate treatment; if PDUs do lead to such improvements then the economic case for investment will be strengthened. Although only 28 follow-up responses at 9 months on utility scores were returned to the study team, average utility scores in these 28 individuals were much greater at 0.41, compared with 0.10 for the 28 at baseline. While too small to have clinical meaning, nonetheless pairwise analysis indicated that this 0.30 improvement in utility scores was significant (p = 0.002).
Regression analysis
The association of quality-of-life scores pre-PDU visit, individual characteristics and total costs were also explored by using multiple regression analyses. GLM was used, testing for the distributional forms for the best-fitting models. All individual characteristics, pre-PDU quality-of-life scores and pre-PDU total costs were tested for inclusion in the models, using a p-value of 0.05.
A gamma log function model was best fitting. Better quality of life was associated with less use of services. As Table 29 shows the ED-5D-5L utility scores at baseline were significantly associated with total post-PDU costs (p = 0.041). For each one-unit increase in utility scores, there was a 15% decrease in total costs. Being a woman was associated with 13% higher costs than being a man (p = 0.000). Having an unknown housing situation was also associated with 76% lower post-PDU costs than those in mainstream housing (p = 0.000). Living in a health facility at baseline was associated with 71% higher post-PDU costs but this only concerned two individuals. Relative to a primary diagnosis of a mood disorder (ICD-10 codes F30–F39), being diagnosed with psychoactive substance use was associated with 43% higher post-PDU costs (p = 0.027). Similarly, a diagnosis of schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders (F20–F29) was associated with 201% higher costs (p = 0.000), while anxiety, dissociative, stress-related, somatoform and other non-psychotic mental disorders (F40–F48) were associated with 134% higher costs than those with mood disorders (p = 0.007).
| Covariates | E (beta) | Std. Error | Z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Utility score at baseline | 0.849 | 0.080 | −2.040 | 0.041 | −0.322 | −0.006 |
| Total costs for 9 months pre-PDU visit | 1.000 | 0.000 | 7.940 | 0.000 | 0.000 | 0.000 |
| Age | 0.998 | 0.002 | −1.600 | 0.109 | −0.005 | 0.001 |
| Female sex (ref: male) | 1.133 | 0.013 | 9.890 | 0.000 | 0.100 | 0.150 |
| Insecure housinga | 1.412 | 0.262 | 1.320 | 0.187 | −0.168 | 0.858 |
| Supported housinga | 1.016 | 0.142 | 0.110 | 0.911 | −0.262 | 0.294 |
| Health facilitya | 1.710 | 0.073 | 7.380 | 0.000 | 0.394 | 0.679 |
| Unknown accommodationa | 0.237 | 0.328 | −4.400 | 0.000 | −2.083 | −0.799 |
| F10–F19b | 1.434 | 0.164 | 2.200 | 0.027 | 0.040 | 0.682 |
| F20–F29b | 3.012 | 0.042 | 26.450 | 0.000 | 1.021 | 1.184 |
| F40–F48b | 2.339 | 0.315 | 2.690 | 0.007 | 0.232 | 1.468 |
| F60–F69b | 1.700 | 0.276 | 1.930 | 0.054 | −0.009 | 1.071 |
| Other diagnosisb | 2.786 | 0.050 | 20.300 | 0.000 | 0.926 | 1.123 |
| Constant | 9659.614 | 0.218 | 42.000 | 0.000 | 8.747 | 9.604 |
Individual service user scenarios
Decision has shown that PDUs support individuals with a wide range of differing personal and social circumstances, as well as differing mental health problems. Our analysis of service use in the 9 months after initial visit to the PDU for the longitudinal cohorts in all four sites indicates this is associated with significantly greater levels of both community and inpatient mental health service utilisation than received in the 9 months pre-PDU visit.
A key question is whether service pathways followed after PDU visits are more appropriate to service user needs and lead to better outcomes than would otherwise be the case. The time that PDU staff have to influence service pathways is very limited, usually no more than 48 hours per stay, at which point a decision must be made as to whether a service user is simply discharged home, referred or signposted to a local crisis team or other community mental health service, or transferred to an acute psychiatric ward.
Ideally, this question is best addressed through longitudinal analyses comparing the experiences of individual service users who come into contact with mental health services as a result of crises and are referred to PDUs, with those service users who do not have this option. While we do not have such data, we can illustratively look at the level of impact that a PDU would potentially have to have to be considered cost-effective. This can be done by creating simple scenarios looking at potential experiences and outcomes for hypothetical individual service users.
We can construct some scenarios drawing on information on the cost of PDU service provision, together with observed patterns of short-term service use drawn from the cohort analysis, as well as quality-of-life utility scores we have collated from 148 PDU service users. In addition, we also refer to qualitative research in Chapter 7 on whether PDUs are perceived as helpful in recovery.
We have illustrated the potential economic case for 16 hypothetical PDU service users, 4 in each of our PDU sites. Sex in the cohort analysis was associated with increased service use costs in the 9 months post PDU use, so our scenarios include two men and two women from each site. Our cohort analyses also indicate that costs are highly skewed, with a small number of individuals having substantial inpatient mental health stays in each area, while the majority of individuals only use community services post PDU visit. To reflect this cost variation simply, four of the scenarios look at median incremental costs post PDU visit compared with pre-PDU service use, as there was no use of inpatient services (‘low cost’), while the other four scenarios apply mean costs identified in each of the cohort sites which do account for inpatient costs (‘high cost’).
We do not know what impacts PDUs have on quality of life, but we can estimate the minimum level of quality adjusted life-year (QALY) gain that would be needed for the PDU intervention to have a cost per QALY below the accepted cost-effectiveness threshold of £30,000 for each of the 16 scenarios. Some service users in qualitative interviews also pointed to the role that PDUs can play in signposting towards support to help stay or return to employment, for instance signposting to recovery colleges and employment service-related information. One individual also expressed an interest in getting a job in future in a PDU. Equally, some service users did not have good experiences in post-PDU support to obtain employment and also mentioned the practical difficulties sometimes faced when wanting to return to an existing job, particularly after a long period of absences. The desire to maintain or return to employment was an issue raised in interviews so we also considered how varying the proportion of individuals who are in employment at 9 months post PDU might also impact on cost per QALY gained from a societal perspective.
As Table 30 indicates for the low-cost scenarios where service users do not spend time in inpatient care, then the QALY gains over 9 months required to produce a cost per QALY below £30,000, range from 0.06 for a woman or man in Birmingham to 0.19 for a woman in Sheffield. If on average over 9 months an additional 30 days were spent in work, valued conservatively at the minimum wage rate in 2020 for the over 25s, then the cost per QALY would fall further, in the case of Birmingham almost being cost neutral.
| Low service use scenarios | BSMHFT | LPFT | SWLSTG | SHSC |
|---|---|---|---|---|
| Woman | ||||
| Cost PDU visit | 741 | 1446 | 2673 | 4800 |
| Community service use | 987 | 1593 | 1669 | 940 |
| Inpatient stays | 0 | 0 | 0 | 0 |
| Total costs | 1728 | 3039 | 4342 | 5740 |
| QALY gains required | 0.06 | 0.10 | 0.14 | 0.19 |
| Cost per QALY gained (NHS perspective) | 29,923 | 29,796 | 29,995 | 29,896 |
| Productivity gains | −1724 | −1724 | −1724 | −1724 |
| Total costs including productivity gains | 4 | 1315 | 2618 | 4016 |
| Cost per QALY gained (including productivity gains) | 69 | 12,893 | 18,084 | 20,916 |
| Man | ||||
| Cost PDU visit | 741 | 1446 | 2673 | 4800 |
| Community service use | 1017 | 1034 | 1185 | 494 |
| Inpatient stays | 0 | 0 | 0 | 0 |
| Total costs | 1758 | 2480 | 3858 | 5294 |
| QALY gains required | 0.06 | 0.08 | 0.13 | 0.18 |
| Cost per QALY gained (NHS perspective) | 29,672 | 29,792 | 29,905 | 29,910 |
| Productivity gains | −1724 | −1724 | −1724 | −1724 |
| Total costs including productivity gains | 34 | 756 | 2134 | 3570 |
| Cost per QALY gained (including productivity gains) | 573 | 9082 | 16,540 | 20,169 |
For the high-cost scenarios in Table 31 when service users do spend time in inpatient care, then the QALY gains required to produce a cost per QALY below £30,000 range from 0.25 for a man in SWL to 0.42 for a man in Sheffield. If on average individuals spend an extra 15 days in work over 9 months then the cost per QALY gained could range between £25,000 and £27,000.
| High service use scenario | BSMHFT | LPFT | SWLSTG | SHSCFT |
|---|---|---|---|---|
| Woman | ||||
| Cost PDU visit | 741 | 1446 | 2673 | 4800 |
| Community service use | 2554 | 3303 | 2794 | 3276 |
| Inpatient stays | 6228 | 7974 | 5092 | 4604 |
| Total costs | 9523 | 12,723 | 10,559 | 12,680 |
| QALY gains required | 0.32 | 0.42 | 0.35 | 0.42 |
| Cost per QALY gained (NHS perspective) | 29,947 | 29,972 | 29,954 | 29,976 |
| Productivity gains | −1264 | −1264 | −1264 | −1264 |
| Total costs including productivity gains | 8259 | 11,459 | 9294 | 11,416 |
| Cost per QALY gained (including productivity gains) | 25,971 | 26,994 | 26,367 | 26,987 |
| Man | ||||
| Cost PDU visit | 741 | 1446 | 2673 | 4800 |
| Community service use | 2515 | 2100 | 2045 | 2101 |
| Inpatient stays | 4448 | 4966 | 2782 | 5839 |
| Total costs | 7704 | 8512 | 7500 | 12,740 |
| QALY gains required | 0.26 | 0.28 | 0.25 | 0.43 |
| Cost per QALY gained (NHS perspective) | 29,948 | 29,946 | 29,939 | 29,959 |
| Productivity gains | −1264 | −1264 | −1264 | −1264 |
| Total costs including productivity gains | 6440 | 7248 | 6235 | 11,476 |
| Cost per QALY gained (including productivity gains) | 25,033 | 25,498 | 24,892 | 26,986 |
These estimates are purely illustrative, but they do indicate, particularly for service users who do not need to make use of inpatient care, that only very modest improvement in quality of life might be required for the PDU intervention to be considered cost-effective. For high service uses the picture is more complex, with a much higher level of improvement in quality of life needed for the PDU to be considered cost-effective. Our earlier collection of data on quality of life, did however indicate that mean changes in quality-of-life utility values of 0.3 were seen in the very small number of individuals who provided these utility values at 9 months post PDU. These scenarios are also potentially conservative as they assume that there would be no increase in use of services for individuals who do not make use of PDUs; there will also be impacts on the use of acute hospital services that were not included in service use data in the cohort analyses. The scenarios only cover a 9-month period, if any quality of life and productivity benefits are sustained beyond this time period then the case for investment would be strengthened.
Chapter 9 Discussion
Data synthesis
We saw evidence of some effect of the introduction of PDUs on our primary outcomes of informal acute psychiatric admissions and mental health presentations at ED but, given the complexity of the study, have an opportunity to use the full range of data we collected to better understand those findings. Synthesis of data from across WPs, developed through our synthesis workshop and subsequent discussion in the research team (as described in Chapter 2) produced the following set of ‘synthesising arguments’ that are indicative of our overall findings from the research (the analyses that support each argument are presented in Table 32). Note that these propositions are data-driven and as such do not always correspond directly to our initial research questions:
-
PDUs reduce overall levels of informal acute psychiatric admissions, but there is no clear trend in informal admissions after units open.
-
First time PDU visitors (about 40% of whom are relatively new to mental health services) experience increases in admissions of all types and community mental health service use in the months following their first PDU visit as they are connected with care and support (some service users report being able to access the care they need for the first time after their first PDU visit).
-
Following PDUs opening there is an increase in formal admissions (but with no clear trend in formal admissions after units opening).
-
There is little overall change in inpatient psychiatric service use as a whole after PDUs open, with no clear evidence of an effect on numbers of overall admissions, no evidence of change in bed occupancy or proportion of 0- to 5-day admissions (there is some evidence of reduction in average LOS), suggesting that PDUs might have a general impact on the balance of admissions away from informal and towards formal admissions.
-
There is little evidence of additional benefits of PDUs for people at high risk of psychiatric admission (i.e. people with previous admissions/diagnoses of psychosis), but there is evidence to suggest that PDUs provide a safe, calming environment) for people with a high level of acute need who might be too at risk for immediate discharge from ED but who are unlikely to benefit from an admission (PDU population is most likely to comprise this group, including people with diagnoses of mood or personality disorders).
-
PDUs can provide improved quality of care for this group of people (e.g. people with complex emotional needs) who might benefit from a PDU where there is a longer LOS with substantial opportunity for in-depth therapeutic input (including psychosocial interventions and higher staff-to-patient ratio) and onward referral/signposting to a wide range of community support.
-
PDUs have no overall effect on level or trend in mental health presentations at ED, but do have the potential to reduce presentations at ED where they are specifically set up to do so (i.e. higher capacity, shorter maximum LOS).
-
PDUs have no overall effect on liaison psychiatry episodes in ED, mental health presentations of people at risk of attending (people with previous attendances) or on 4-hour breaches or average length of wait except, potentially, where the PDU is specifically set up to impact mental health presentations in ED.
-
Conversely, while larger units with a shorter maximum LOS might be more likely to reduce pressure on ED, PDU staff can feel pressurised to admit inappropriate referrals and discharge service users while still feeling suicidal; referral and signposting to appropriate aftercare might also suffer where LOS on the PDU is shorter (i.e. configuring PDUs in this way, primarily to reduce pressure on ED, is unlikely to improve quality of care).
-
The effectiveness of PDUs in impacting either informal psychiatric admissions or mental health presentations at ED is associated with the aims of units and the way in which units are configured; in practice priorities for PDUs reflect trends in outcomes prior to PDU opening and the existence of other initiatives to address either psychiatric admissions or mental health presentations at ED.
-
A lack of clarity of function, differences in expectation and poor communication between PDU team and referral pathway staff, and inappropriate referrals mitigate the potential effectiveness of units; this reflects systematic review of the literature on similar units internationally which indicates that units with a clear purpose and configuration to impact ED wait times are effective in doing so, and units that primarily aim and are configured to reduce psychiatric admissions are effective in doing so (service users’ experiences of the crisis care pathway and of PDUs negatively impacted by a lack of clarity in unit function).
-
The impact of PDUs on cost to trusts of psychiatric admissions and ED attendances are marginal at most sites, resulting in only small savings; potential savings result from shorter length of psychiatric inpatient stay, and some site level savings relate to ED presentations and arrivals by ambulance compared to control but these do not offset cost of running PDUs (except at the BSMHFT site, where a substantial reduction in psychiatric inpatient LOS was observed in one analysis).
-
PDUs with a short LOS and low staff to patient ratio have considerably lower cost per visit (and can impact mental health ED presentations) than PDUs with longer LOS and higher staff to patient ratio (which can impact informal psychiatric admission and improve quality of care for people in crisis).
-
Significant additional costs of both inpatient and community mental health services are incurred by first time visitors to PDU as they are connected to care post first visit.
-
PDUs generally do not offer a simple financial return on investment in the short term, but the potential for reducing longer term costs of care as people access more appropriate community care (and less emergency care) and experience improved quality of life as a result indicate that PDUs may be cost-effective in at least some scenarios.
-
Changes in wider configuration of the crisis care pathway (e.g. introduction of street triage services) can support and reinforce the effects of introducing PDUs on both psychiatric admissions and ED mental health presentations (this was especially the case at BSMHFT, where a substantial reduction in length of psychiatric inpatient stay might be attributable to the introduction of an enhanced psychiatric liaison service).
-
Impact of changes in crisis care pathway on mental health presentations at ED are less clear (introduction of street triage and expansion of PDU provision to include psychosocial intervention reduced ED presentations in SWLSTG).
-
No overall evidence that PDUs might reduce inpatient admissions for sociodemographic groups over-represented in acute mental health care (although in one site, BSMHFT, indicated that, potentially, younger, male, non-White British service users might benefit from the introduction of PDUs); noting the exploratory nature of the analyses, costs of post-PDU care were generally higher for women and older people (i.e. people who already have better access) although cost of care was higher for non-White British service users in BSMHFT (people with insecure housing appeared to access less care post-PDU visit).
-
While working on the PDU can be rewarding and supportive for staff, the high-pressure nature of the role is also demanding and might mitigate the extent to which PDUs can provide higher quality of care.
-
Sustained benefits of PDUs (including where PDU visits are experienced positively) are likely to be mitigated by the capacity of crisis and community mental health services as a whole; where there are not sufficient appropriate options to refer or signpost for people (within mental health services and the wider community sector) or where the experience of discharge is hurried, then the potential longer-term effects of PDUs on ED presentations and psychiatric admissions might be diluted.
-
The pandemic did not have a major impact on the overall level of service use for people post first visit to the PDU, although there were often fewer face to face and more remote community contacts (compared with a similar pre-pandemic cohort), some reduction in CRHT team contacts and fewer inpatient admissions in rural areas (offset by increase in remote contacts).
-
The pandemic increased pressure on PDUs, even where there was an increase in capacity in the unit or other elements of the crisis pathway (e.g. the introduction of psychiatric ED provision), exacerbating many of the issues impacting quality of care described above.
| Proposition | WP1 | WP2 | WP3 | WP4 | WP5 | WP6 |
|---|---|---|---|---|---|---|
| SR & mapping exercise | ITSa | SCb | Cohort studyc | Qualitative study | Economic evaluation | |
| PDUs have the potential to reduce informal acute psychiatric admissions (but individual visitors can experience an immediate increase in admissions – informal and formal –after first visit) | Meta-analysis in SR indicated reduced psychiatric admission post-PDU (note: not clear that this refers to informal admissions but review excluded units that only accepted formal patients) | Reduction on opening SWLSTG, BSMHFT. Continued reduction in SWLSTG, LPFT (reversing upward trend in SWLSTG). Upward trend post opening in BSMHFT. MA indicates overall immediate reduction on opening but no change in trend due to heterogeneity | No data | At an individual level, informal admissions significantly higher in period post first PDU visit at all sites except STHFT | Service users: safe, therapeutic space away from stressors, calm atmosphere someone to talk to, feeling supported, talking on a deeper level, balance between freedom and support (staff are kind, gentle, non-judgemental, humanising) | ITS: marginal reduction in cost to MHT at site level (mostly from reductions in admissions at SWLSTG and LPFT). Cohort study: increased individual costs of informal admissions (and community) mental health care post first visit to PDU. As above, increased costs of formal admissions post first visit to PDU |
| The effect of PDUs appears to be an immediate increase in level of formal psychiatric admissions with a mixed picture on trend post opening (again immediate increased individual need) | SWLSTG, BSMHFT and LPFT increase in formal admissions on opening; downward trend thereafter in BSMHFT, upward in LPFT, reverse from down to up in SWLSTG. MA confirms immediate increase, no change in trend due to heterogeneity | No data | Significantly more formal admissions post-discharge from first PDU visit at all sites | Staff: units have an effective purpose and provide a better environment than ED, offering containment and opportunity for proper assessment (ED staff; more appropriate place to send people), provides for a cohort who would not; benefit from admission but too risky to send home (PD or self-harm). Not enough time on unit or too much time waiting results in lack of opportunity to talk on a deeper level, not feeling supported, and leaving while still feeling suicidal (some staff felt LOS on PDU not long enough). Some issues reported regarding gender and safety in sleeping area or when others very disturbed | ||
| There is little overall change in total admissions post opening of PDUs | Change in trend from upward to downward post opening in SWLSTG and LPFT. MA shows no change | Lower in SWLSGT and BSMHFT and overall, but not significant | Significant increase in total admissions post first visit to PDU | As above, increased costs of total admissions post first visit to PDU | ||
| No evidence of change in bed occupancy rates as a result of PDUs opening | No effect | Change in trend from upward to downward post opening in Birm No other or overall change |
No data | No data | ||
| Some evidence of reduction in LOS No evidence of effect on 0–5 days’ admissions post opening of PDUs |
No effect; no data | Downward trend in LOS in LPFT post opening; no change in SWLSTG and BSMHFT. No impact on 0- to 5-day stays. MA shows no change in either outcome | Shorter LOS in BSMHFT and trend to longer LOS in SWLSTG. Smaller prop of 0.5-day stays in SWLSTG and greater in BSMHFT. MA indicates shorter LOS | More 0–5 days’ admissions SWLSTG and LPFT; LOS longer in STHFT | SC: potential cost saving at site level and overall resulting from shorter LOS | |
| Limited evidence of additional impact on admissions for people at high risk of admission (more likely to be people with psychosis diagnosis). Some evidence to suggest that PDUs can provide a helpful and cost-effective model for people with high level of acute need but unlikely to benefit from admission (e.g. complex emotional needs, depression and anxiety) | Mapping study indicative of contrasting configurations of units including LOS, capacity and staffing levels | SWL, greater immediate reduction and steeper rate of decrease, BSMHFT rate of increase higher in this group. MA shows (smaller reduction than whole sample). Enhancement of PDU in SWLSTG to include psychosocial interventions = significant reduction in informal admissions and mental health presentations at ED (not in expansion of PDU capacity) | No data | Of participants with a recorded diagnosis, low numbers with psychosis (5–10%; i.e. most likely to be admitted), mood disorders and PDs 10–30%. Increased use of CMHT and CRHT teams post-visit all sites. SWLSTG, LPFT and STHFT increased number of contacts in range of community-based services; fall in number of contacts in BSMHFT (e.g. CEN/PD, EIS, forensics, perinatal) | Increased costs of community mental health care post first visit to PDU reflect increased access to community care for people at risk of admission. Costs of care post first PDU visit show a mix of relationship to diagnostic group at different sites, perhaps reflecting high levels of missing data for diagnosis. Extremely low QoL scores for many first-time visitors at baseline; significant improvement at follow-up. QoL gains needed to indicate that PDUs might be cost-effective in some scenarios within range of observed QoL improvement | |
| Little evidence that PDUs are likely to provide an alternative to psychiatric admission for over-represented demographic groups | No data | No data | No data | PDU sample younger than trust-wide sample across sites, less likely to be White British in BSMHFT and more likely to be black in STHFT, more likely to be male in BSMHFT | Insufficient data | Costs of care post first visit to PDU higher for older people at all sites, women in most sites and for non-White British people in one site; costs lower for people in insecure housing in two sites |
| PDUs have little impact on increasing liaison psychiatry episodes | No data | Immediate reduction in BSMHFT but upward trend thereafter (greater immediate reduction for at risk group and reduction in upward trend); upward trend continues in LPFT (reduction in upward trend for at-risk group) Meta-analysis – significant upward trend continues post-PDU. In at-risk group there is a reduction in upward trend (but continues to increase significantly) |
No data | Reduction in ED liaison episodes in SWLSTG and LPFT, no change in BSMHFT and STHFT (these individuals are accessing more community mental health care and therefore might not need ED) | ITS: marginal reduction in liaison psychiatry costs at some sites and overall | |
| PDUs potentially have some impact on mental health presentations at ED | No effect | BSMHFT drop on opening and slight reduction in rate of increase thereafter. Increased rate of increase in LPFT. MA shows no overall effect or change in trend | Lower rate of ED mental health attends at STHFT; no impact elsewhere or in MA | No data | Differing expectations of PDU/referral criteria. ‘Us vs. them’ especially PDU and ED teams compounded by poor communication. Linked to pressure on services (lack of capacity) Pressure to move people out of ED (< 4 hours) contributes to tensions |
ITS: mixed, very marginal impact on costs at site level, no overall impact. SC: site-level saving resulting from lower rate of mental health attendances |
| PDUs have no effect on 4-hour breaches in ED which continue to increase post PDU opening | No data | No effect in BSMHFT, Lincs or SWLSTG. MS shows upward trend post opening | Lower proportion of waits 4 hour+ in Kingston (SWL) (no effect on 12-hour waits); no effect in MA | No data | ||
| Little impact of PDUs on increasing length of wait in ED | Individual studies in the systematic review reported reductions in waits to be seen by a clinician, to be transferred and long waits. MA suggests that PDUs reduce overall wait time | Immediate reduction in BSMHFT but no change in upward trend, change to upward trend in SWLSTG and LPFT. MA shows change in direction of trend from decrease to significant increase | Shorter length of wait in Kingston (SWL) – no effect in MA | No data | ||
| Limited effect on mental health presentations at ED for high-risk population | No data | Larger drop and greater reduction rate of increase in Birm; reduction in rate of decrease in Sheff Meta-analysis – no overall effect |
No data | No data | ||
| Evidence of increase in acute admissions from ED | No data | Increase in admissions in BSMHFT and SWLSTG, continued downward trend in BSMHFT, reduction in downward trend in SWLSTG; change from downward to no trend in LPFT. MA shows sig increase in admissions and change in direction of trend from decrease to increase | No change within sites or overall | No data | ITS: marginal site level and overall increase in costs of acute admissions from PDU | |
| No or small effect on arrivals to ED by ambulance or police | No data | Increase and change to upward trend in STHFT. MA shows no change | Decrease in LPFT compared with control. MA shows no change | ITS: small site-level increase in costs SC: site-level savings resulting from fewer conveyances to ED by emergency services |
||
| Primary aim and configuration of PDU associated with effect on either psychiatric admissions or ED mental health presentations | Review indicates that studies that report significant impact on psychiatric admissions have this as their primary objective (similarly re mental health attendance at ED) Mapping differentiates units in terms of LOS and staffing levels |
Data from across WPs are indicative of the idea of distinctive PDU models that relate to aim: e.g. reduction in informal attendances, sustained decrease at some sites, and increased community service use where LOS on PDU was longer and staff-to-patient ratio higher; effects least strong in BSMHFT, where most issues reported with short LOS, but where there was some impact on mental health presentations at ED, number of LP contacts and length of wait at ED Note: effects (and aim) of PDU relate to trends in outcome in the pre-PDU period (WP2); e.g. where informal psychiatric admissions were increasing prior to implementation and a higher proportion of referrals from community-based CRHT teams PDUs appeared to impact admissions, but where ED presentations where increasing prior to implementation and the highest proportion of referrals to PDU came from ED-based Psychiatric Liaison teams mental health presentations at ED reduced (no impact on ED presentations where a SeQuIn had been associated with reducing ED presentations prior to the PDU opening) |
Large differential in annual PDU costs linked to staffing levels; large differential in per PDU visit cost linked to staffing and LOS Costs of units NOT offset by potential cost savings indicated above (max. RoI approx. 10%) |
|||
| Impact of PDUs moderated by capacity and quality of crisis care pathway | Secondary analysis of ITS data | Qualitative interview data | ||||
| Configuration of crisis care pathway reinforces effects of introducing PDUs on psychiatric admissions (e.g. introduction of street triage in SWLSTG and LPFT (crisis vehicular response) and opening of crisis cafes in SWLSTG contributed to long-term significant decrease in informal psychiatric admission at those sites, as did introduction of street triage in BSMHFT prior to PDU opening); opening of a psychiatric ICU in LPFT resulted in increased psychiatric admissions prior to PDU opening; expansion of liaison psychiatry in STHFT had already reduced ED mental health presentations prior to the PDU opening; introduction of street triage in SWLSTG reduced ED mental health attendances in a way the PDU had not managed to do | Effectiveness of units linked to quality, capacity and appropriateness of post-PDU support in the community (service users and staff); existing crisis care worked for some people but not for others who felt they were being discharged to the same services that did not work for them | |||||
| Qualitative data only | ||||||
| Pros and cons to co-location of PDU with other services | Co-location/proximity to 136 suite or ED could increase inappropriate referrals but also provide opportunity for improved communication between teams | |||||
| Referral and arrival at the PDU | Range of experiences from smooth to very elongated process being passed thorough many different teams. Staff appreciated having somewhere to refer people to, avoided risky discharges; liaison team expectation not met if referral was not possible. PDU team under pressure to take inappropriate referrals to remove pressure from elsewhere. Poor communication and unclear criteria not helpful (ED/LP expecting PDU to take the pressure off them, PDU receiving inappropriate referrals). Negative emotional impact on staff not being able to provide good service (conveyor belt) | |||||
| Working on the PDU | Nursing staff welcomed the additional responsibility and felt that they learnt and gained new skills quickly. Additional responsibility brought pressure, including emotional strain and could result in burnout and high staff turnover. Support within the PDU team was often good but the additional demands of the role not always well supported | |||||
Results in context
It is helpful to consider the implications of our findings in terms of the multilevel approach to addressing organisational research questions we proposed in Chapter 1,47 discussing the wider relevance of our findings at micro (individual), meso (service and organisational) and macro (policy) levels.
The psychiatric decision unit and individual experiences of crisis care
At the micro (individual) level, many people’s experiences of the PDU were positive, with the PDU described as a warm, caring, safe space offering time away from the stressors of everyday life, offering a considerably more supportive environment than the ED. 12,14,27 Service users found staff kind and supportive, and appreciated opportunities to talk in depth in a way that had not often experienced in mental health services more generally. 16 For many, PDUs offered a good balance between a safe, contained space, and a sense of freedom and being in control. However, both feelings of safety and of being supported were compromised where it was felt that staff were too busy or there was a lack of time to talk,16 or where people were discharged while still feeling suicidal or in distress. 19 Staff also felt that the group of people for whom the PDU worked best – typically people who might receive a diagnosis of personality disorder – would benefit from a longer LOS, and at times they were discharging people too early. Mixed-sex spaces sometimes made women feel unsafe or anxious, and the presence of others in distress was could also be anxiety provoking. 16
Many first-time PDU visitors were relatively new to mental health services and as such PDUs provided an entry point to care. Use of inpatient and community mental health care increased substantially for these people in the months following their first PDU visit, with some individuals reporting that it was only following their stay at the PDU that they received meaningful support for their mental health. While we were unable to follow-up these individuals for an extended period of time, being linked in to appropriate mental health care potentially reduces the need for crisis care and we saw liaison psychiatry episodes in the ED drop-in sites where there were the biggest increases in community mental health care use post-PDU visit.
The psychiatric decision unit environment, staffing and crisis care pathway
The way in which PDUs were configured and their place in the crisis care pathway at each site offered a meso-level perspective on the context of implementing PDUs into practice. Staff echoed service users’ experiences of the PDU as a calm, containing space that was preferable to the busy, chaotic environment of the ED. The use of recliners rather than beds met with a mixed response from service users, some people appreciating the fact that the unit did not feel like a ward, while others found them uncomfortable and disconcerting.
The journey to the PDU was experienced as straightforward for some, but challenging for others, involving uncertainty, waiting for transfer to the ED before eventually arriving at the PDU. As noted above, for some people the PDU worked well in linking them into appropriate care, but others, perhaps who had been using mental health services for some time, could find themselves discharged back to a level of care that had not hitherto worked to help address crisis, the PDU offering only a brief respite with no sustainable change to the way in which they were supported during a crisis.
PDU staff echoed these concerns, reporting pressure to take referrals of people who they felt were unsuitable to reduce pressure elsewhere on the pathway and having to discharge people home without the options or resources in the community to signpost them. Staff on the referral pathway could also express frustration related to a lack of clarity around who to refer or a feeling that expectation of the unit – to take pressure off the ED – had not been met. Co-location of the PDU with other services, typically the Section 136 place of safety could exacerbate these challenges. It is possible that these tensions and the resulting communication issues between staff teams contributed to a lack of clarity of function of the PDU.
On the whole, PDU staff teams enjoyed working on the units, reporting that the additional responsibility of working on a nurse-led unit and being able to take and challenge decisions enabled them to develop new skills. The additional time they had to spend with service users allowed them to work in more depth with people’s experiences of distress and to provide wider, social support. However, working continually with high levels of distress was emotionally very demanding and could lead to burnout and high staff turnover. The PDU staff team was experienced as highly supportive although team members did not always feel able to take advantage of the support available.
The psychiatric decision unit and mental health crisis care in England
Our findings have implications for policy-making in mental health crisis care in England, the macro-level, and therefore decision-making by commissioners and NHS trusts. PDUs, or their equivalents internationally, are not a new phenomenon, with units from North America94,95 and Europe96,97 dating from the mid-1990s. However, as noted in our mapping study, PDUs are far from ubiquitous in England with some MHTs decommissioning or repurposing PDUs (as wards) while other trusts initiate new units. 82 As such, the jury is very much still out on whether or when PDUs offer a viable complement to the mental health crisis care pathway. Taken as a whole (and reflecting the international literature), our analyses suggest that PDUs can, and perhaps should, be clearly configured in such a way as to address, specifically, the primary crisis care need locally (in terms of our primary outcomes); that is, to reduce either unhelpful or avoidable informal psychiatric admissions,37,79,91,93 or impact mental health presentations at ED. 40,79 The lack of clarity resulting from unit function sitting somewhere between the two objectives probably mitigates beneficial effect.
PDUs that successfully reduce informal psychiatric admissions have longer average lengths of stay (up to 40 hours), higher staff–patient ratio (approximately 1 : 2) and have a focus on therapeutic input, including delivery of psychosocial interventions and effective signposting to community resources. These units improve the experience and quality of crisis care, especially for people with a high acute level of need but who might not benefit from an inpatient admission,18 and reflect findings from the United States indicating the potential for PESs there to improve patient experience of crisis care. 105,106 However, they are expensive to run and this cost is largely not offset by savings accrued from reduced admissions and shorter lengths of stay. It should be noted that resulting reductions in informal inpatient admissions were counterbalanced by increased formal admissions, with limited net change in inpatient service use. As such, the benefits of delivering PDUs in this way are largely associated with quality of care for a particular population that generally falls into a gap between the ED and psychiatric ward (typically people with diagnoses of personality disorders or complex emotional needs and/or people who had self-harmed who might not be best served by existing crisis and home treatment services). 15 While in the short term this led to increased service use (and increased associated costs) for first-time PDU visitors, the PDU potentially acts as a gateway to more appropriate care for this population and, in the longer term, less costly use of crisis and acute care. In addition, we note that we did not assess reduction in non-healthcare costs that might accrue following PDU attendance, wider social benefits such as increased employment or improvement in mental health outcomes. Nor did we compare the effect of PDUs with that of triage wards,24,41 noting in our mapping survey that MHTs with PDUs were no less likely to have one or more triage wards than trust without PDUs. Our study did provide tentative evidence of significantly increased quality of life for people in the months following their first visit to PDU. If realised more widely, for the group of people for whom PDUs seem most suited – those with a high level of crisis need but who might not benefit from extensive inpatient and home treatment care – PDUs may well be cost-effective. As such, wider clinical and cost benefits are potentially understated here.
PDUs that successfully reduce mental health presentations at ED have shorter average LOS (around 12 hours), lower staff–patient ratio more akin to acute ward levels (approximately 1 : 4)42 and primarily address demand management issues on the ED when it is not safe enough to discharge someone to their home. Quality of care was not experienced as being as good on PDUs where people felt they were hurried to discharge before they were ready or were without sufficient opportunity to talk to staff in depth and where onward signposting was limited. However, given that numbers of mental health presentations at ED are high and continue to grow, PDUs that provided the high level of input described above would need to be extremely large and costly. This configuration is cheaper to run but again the cost is not offset by the savings resulting from reduced ED presentations (and do not reflect the more substantial savings estimated in studies internationally). 90,97 The benefits are largely to the ED environment – reduced pressure on ED staff teams whose time would be freed up to attend to non-mental health patients104 – at sites where there was a reduction in mental health presentations or where wait times reduced. 7,8,11,12 There is an inherent challenge for commissioners here in that these costs are met by the MHT in managing demand in the acute trust. In addition, it should be noted that the gains observed here often took place against a backdrop of increasing presentations or length of wait in the ED in England that have continued unabated since earlier reports were produced,9,10 and so were mitigating further increases in demand at best. It remains possible that alternative models, such as mental health assessment spaces directly attached to ED departments, offer a more effective and cost-effective approach to tackling ED wait times and in particular breaches of 4-hour wait targets in England. 107
We have shown how impacts on both psychiatric admissions and ED presentations are best realised, and sustained, where the PDU complements other effective inputs into the crisis care pathway, including street triage,29 crisis cafes,31 crisis houses30 and enhanced psychiatric liaison services, whether as sources of referral to the PDU, alternative support or signposting options. The implications for policy and commissioning are that an interlinked network of crisis supports is necessary, reflecting local priorities and need,27,28 that over time might have a cumulative effect on demand on the ED and psychiatric inpatient care.
Equalities impact assessment
There is an established literature that indicates that people of black ethnicity, especially younger men, are over-represented in acute mental health care and under-represented in mental health services more generally,17,108 and we wondered whether PDUs might contribute to addressing these inequities by providing a pathway away from acute care and towards community-based support. We found some evidence that people referred to a PDU for the first time were younger than the MHT population as a whole, and limited evidence that they were less likely to be White British and more likely to be male. Analysis of increased cost of care post first PDU visit indicates that non-White British people were only accessing increased levels of care at one site (homeless people were failing to access increased levels of care post first PDU visit). While these findings were far from conclusive, they are perhaps indicative of some potential for PDUs and other crisis services, where they function as entry points to mental health care, to begin to address persistent inequalities if they are developed with that purpose in mind.
Impact of COVID-19
The beginning of ‘lockdown’ association with the COVID-19 pandemic coinciding with the follow-up period in our WP4 cohort study and WP5 qualitative interviews provided an opportunity to explore the impact of lockdown on mental health service use and experiences of crisis care. 88 We observed very few differences between our pre-pandemic and primary cohorts (both were admitted to PDUs prior to lockdown) and perhaps surprisingly few differences in service use post-discharge from the PDU. There were no impacts on inpatient care and minimal impacts on the level of community mental health care, although the balance of community contacts shifted significantly from face to face to remote contacts. At some sites there was a reduction in contacts with CRHT teams. The pandemic did not impact on cost of care for people using PDUs.
In qualitative interview, staff reported an initial lull in referrals to PDU as the pandemic broke, but then an increase in demand, and range and severity of presenting issues, attributed in part to isolation and closure of community-based support groups. Some efforts were made to increase capacity of PDUs at some sites, although at one site the PDU was temporarily suspended as staff were assigned elsewhere. The temporary addition of a new mental health ED in one site led to pressure to constantly take new referrals. The combination of increased demand and changes to the crisis care pathway led to additional pressure on staff teams and higher levels of staff sickness.
Strengths and limitations
This was a quasi-experimental study, and as such individual workstreams are reporting using the Transparent Reporting of Evaluations with Nonrandomised Designs for non-randomised/quasi-experimental studies. 109 We identified a range of limitations in the research, within and across WPs. Individual WPs analysed data from different time periods and different samples, and so not all of the comparisons we make in our data synthesis are direct triangulation between data sets. For example, because PDUs opened on different dates, WPs 2 and 3 are not synchronous across sites (interrupted time series and synthetic control studies cover the same time periods within each site). The WP4 cohort study and WP5 interview study were synchronous across sites, but as a result did not take place at the same time as ITS and synthetic control studies. In addition, because of availability of data, while the ITS analysed ED data from SGUHFT in SWLSTG and from SWBHFT, the synthetic control study used ED data from KHFT and UHBFT, respectively.
In our ITS study, we spent considerable time working with business intelligence staff within trusts to collect relatively precise data on both psychiatric admissions and mental health presentations at ED. However, data based on diagnostic coding, such as ED mental health attendances, may be more vulnerable to error, and mental health coding has been shown to be problematic in data sets derived from routine hospital data. 110 In our synthetic control study, classification of ED data was determined by diagnostic coding or a ‘mental health reason for visit’ entry applied by staff in the ED. Admissions to mental health acute inpatient wards are also not explicitly coded as such in HES-APC and we proxied these admissions using the main specialty of the consultant or the treatment function of the episode (and might have included admissions to eating disorders or other specialist wards, or acute admissions to community-based crisis and home treatment teams, for example). Incidence of both our ED and MHT outcomes was substantially higher in the synthetic control study than the ITS as a result, potentially diluting or confounding effects and going some way to explaining differences in effects observed in the two studies.
However, within-site comparisons within each WP are all methodologically appropriate and clearly defined. While it is possible that effects observed in WPs 2 and 3 are at least in part explained by differences between comparators, conditions outside of trusts or by other changes in the delivery of care (indeed we explore this to some extent in secondary analyses in the ITS; see Chapter 4), creation of both the counterfactual in the synthetic control study and the extended time series in WP2 are methodologically robust and were risk-adjusted and included sensitivity analyses where possible.
There were some issues with data within WPs. In WP2, MHT data from Sheffield included a number of missing variables and there were missing data from large numbers of admissions during the times series period. As a result, psychiatric admission data from Sheffield were omitted from the interrupted times series analysis. In the WP3 synthetic control study, reporting requirements of MHT data to NHS Digital did not distinguish psychiatric admissions as formal or informal, capture liaison psychiatry episodes in ED or allow us to specifically identify outcomes for a population with previous admissions; hence we have a slightly smaller set of outcomes for the synthetic control study (compared with the ITS), without informal psychiatric admissions as a comparable primary outcome. Further, there were likely changes in mental health coding practice over the 4-year study period in participating sites, complicating interpretation of trends over time, and for a small number of variables in some trusts, data sets did not cover the entire 4-year period of interest; this decreased the power of corresponding WP2 ITS analyses and their impact in pooled analyses of outcomes.
The late addition of BSMSTG as a site to WP5 meant that we had no follow-up interview data for service users in BSMSTG and could not explore the post-discharge pathway there. We did collect sufficient baseline data from service users, as well as a range of PDU and pathway staff data, to sufficiently explore the model of care in BSMSTG. We were unsuccessful in recruiting a diverse service user sample to WP5; as a result, we did not systematically capture the experiences for black, Asian and minority ethnic visitors to the PDU and were unable to further elucidate findings from our equalities impact analysis in WP5. In WP6, because we relied on patient record data and did not directly recruit and follow-up a cohort of PDU visitors, we did not have sufficient structured quality-of-life data to formally assess cost benefit in terms of quality of life-years (although data we collected from WP5 participants did enable us to include quality of life in our modelling work). Our whole study design was predicated on a synthesis of routinely collected service use data and experiential insight from qualitative interview. This offers an extremely cost-efficient approach to research but as a result we missed out on participant reported outcomes (including quality of life) that are collected through (costly) one-to-one interview.
Nonetheless, our mixed-methods approach46 was a strength of the study as a whole. Given that an experimental study design was not practical, employing two robust quasi-experimental methods offered both within-site and externally controlled estimates of effect enhancing confidence in our findings. The critical synthesis method made systematic use of data from across WPs to generate and explore potential explanatory arguments that might usefully inform research, policy and practice, rather than prioritise and discount analyses solely on the basis of reliability. The inclusion of a cohort study enabled us to explore the impact of PDUs on service use at an individual level while qualitative research, with staff and service users, was indicative of the complex relationship between experience (quality) of care and clarity of purpose of PDUs, and the potential effectiveness of different configuration units. As a result, we were able to give carefully consider if and how different configurations of PDU, in the context of the crisis care pathway as a whole, impact outcomes in different ways, providing us with opportunity to draw nuanced conclusions on PDU configuration in relation to policy and efforts to manage demand on services across acute and mental health NHS trusts that would not have been possible without our mixed method and critical synthesis approach.
Impact of patient and public involvement on the research
There were a number of important impacts of patient and public involvement and of our coproduced approach to research on the study and findings:
-
First, and importantly, in a study where most WPs were quantitative in nature, reducing research questions to measures of service activity, the qualitative WP – where the was most patient and public involvement input – was essential to the interpretation of data.
-
Researchers working from lived experience on the team and through the LEAP ensured that the experiential perspective on PDUs remained front and foremost throughout the study, and particular as we began to analyse and make sense of all of our data.
-
This insight, together with that of the PEER group who helped develop the study and the lived experience researchers on the team, ensured that our qualitative interview questions were very specifically focused on key aspects of the experience of mental health crisis and of staying on a PDU.
-
The lived experience researchers, with input from the LEAP at our interpretive and synthesis workshops,48 also emphasised key aspects of the data that play a crucial role in shaping our data synthesis and overall conclusions. This work underscored:
-
the high levels of suicidality among visitors to the units
-
the importance of both unit environment and the depth of talking and listening required of unit staff to impact such levels of distress
-
the crucial importance of having sufficient time on the unit to begin to address issues for people
-
the sense that the impact of the unit was wholly mediated by the capacity of the crisis pathway to continue to support people post-discharge.
-
These understandings provided a lens through which to make better sense of the balance of impact, cost and benefit of introducing PDUs.
After discussion the lived experience team decided on overt disclosure of their lived experience to people they were interviewing in WP5, both in participant information sheets and in introduction to the qualitative interview. At the end of the interview two questions were asked about what it had been like talking with a researcher with lived experience and whether the interviewee thought this had made any difference. An in-depth analysis of these responses will be the subject of future publications, but a preliminary analysis suggests a marked impact in terms of ease of talking, ability to share difficult experiences, and feelings of being listened to, heard and believed from service user participants.
The co-investigator responsible for supporting the patient and public involvement in the project facilitated regular reflective sessions for the researchers with lived experience. This gave the team an opportunity to openly reflect and gain support in a safe environment about the experience of using their lived experience in the project and of the impacts it had had on them. This was particularly important as many of the interviews including accounts of distressing experiences and feelings of suicidality. It was also an opportunity to continuously reflect and monitor on how patient and public involvement was being used in the study and what was working well and what could be done differently.
Recommendations for future research
Recommendations for future research are both methodological and substantive in nature. While our study benefited from employing a number of different approaches to estimating the impact of introducing a new service model on mental health and ED service use, there is need for research to better understand how the way in which data are coded in national data sets impact the specificity and precision of estimates, especially with MHT data, and how to best interpret differences in estimates obtained from proxies for specific populations derived national data sets and directly from electronic patient record. This understanding would help in the efficient design of studies of service-level/pathway change in the future where a quasi-experimental approach is most appropriate.
In our study we relied on a combination of service use and qualitative, experiential data. We did not assess individual-level clinical or psychosocial outcomes, in part because recruiting a large cohort to do so adds considerable cost to the research and a clear rationale is needed for doing so. However, as a result we struggled to obtain sufficient quality-of-life data and potentially missed out on outcomes that would have shed more light on quality of care (which emerged as important in our qualitative analysis) and provide more conclusive evidence on the potential cost-effectiveness of PDUs. Future research might usefully build on our study to target a group or groups of people who might reasonably be expected to benefit from PDUs and evaluate the impact on a wider range of mental health and psychosocial outcomes, either using an experimental or quasi-experimental design. Alternatively, more attention might be paid to the use of routinely collected patient reported outcome and experiences measures, such as, for example, DIALOG+,111 to enrich our understanding of the impact of service-level change. Further research might also usefully refine, methodologically, a longitudinal approach to qualitative enquiry about experiences of care pathways.
While we were able, in our equalities impact work, to demonstrate some potential for PDUs to impact access to care for underrepresented groups, we did not manage to systematically integrate this work across workstream. Future research might develop, a priori, analysis plans that better explore associations between demographics and outcomes as we did in our cohort study and health economic analyses, while sampling for qualitative research needs a more proactive approach in order to obtain meaningfully diverse samples.
Our study revealed the challenges around evaluating the impact of the introduction of a new service model in the context of an evolving care pathway where other service-level initiatives are also likely bring about change. While we demonstrated some success both in isolating effects and identifying complementary effects, there is a need for a systems-level approach to investigating mental health crisis care building on similar studies elsewhere,50,112,113 including the role that the third and voluntary sector might best play in providing an effective network of crisis support. 32 As designed, our study also lacked an economic perspective on the commissioning and decommissioning of other crisis care services alongside our PDUs. Such an approach might usefully be applied to similar policy driven initiatives that seek to change the wider landscape of health and social care.
We did find evidence that suggested that PDUs might be an appropriate approach to crisis care for a particular group of people (those likely to receive a diagnosis of personality disorder or be identified as having complex emotional needs and/or who experience self-harm) whose needs fall between existing types of acute and community care. This group of people often have underlying experiences of complex trauma that are unmet by mental health services,114 and there is an opportunity for the PDU to identify need and signpost people to more appropriate therapeutic as well as crisis care. Further research would usefully explore in depth the relationship between experiences of trauma and access to appropriate mental health care for this group.
Implications for policy and practice
Our research implies that PDUs make a potential contribution to the mental health crisis care pathway when integrated alongside other service options in order to address specific local need. PDUs should be appropriately commissioned and configured with clear objectives of either: alleviating increasing demand in the ED; or improving the quality of crisis care for people with high levels of acute need who are unlikely to benefit from an inpatient admission. In the case of PDUs designed to support the ED, while these are likely to have higher capacity and higher turnover, more needs to be done to ensure that units do offer a better environment and better quality of care that the ED, with sufficient levels of staffing to ensure that people are not discharged while still feeling suicidal. In the case of units designed to provide an alternative to inpatient admission, LOS needs to be long enough to support the client group with training provided to staff to provide effective psychosocial input. PDUs might also improve access for people who experience inequalities of access to care, although this should not be assumed, with more needed to be done to develop PDUs and care pathways with this in mind. While PDUs have the potential to reduce costs associated with ED mental health attendances and psychiatric admissions these are unlikely to offset the cost of operating the units, and so commissioning should not be primarily financially driven. However, where PDUs are successful in improving access to appropriate care (where there is an effective range of community resources to which to signpost people on discharge), over the longer term it is possible that demand on crisis and acute care, and associated costs, are further reduced.
Acknowledgements
We would like to acknowledge our service user and staff participants at all our sites who gave up their time to contribute their invaluable insight to the study.
Members of our LEAP and the independent project steering committee also gave generously of their experiences, expertise and wisdom to improve the quality of our research, in particular the members of the LEAP who contributed directly to the interpretation of study data through their hands-on involvement in analysis and synthesis workshops.
We would like to thank the principal investigators and management, clinical, and research and development teams at each of our study sites who regularly took time out of their incredibly busy days to support and facilitate the research.
We would also like to express our gratitude to the business intelligence teams and data officers within each trust who patiently and professionally responded to our never-ending demands for more data, different data and even more data, without who the study would not have been possible.
Contributions of authors
Steve Gillard (https://orcid.org/0000-0002-9686-2232) (Professor, Health Services Research) conducted the data synthesis and prepared the report for publication.
Katie Anderson (https://orcid.org/0000-0002-3156-7427) (Lecturer, Psychology) conducted the service mapping and systematic review, analysed qualitative interview data and contributed to preparing the report for publication.
Geraldine Clarke (https://orcid.org/0000-0001-7249-0289) (Senior data analyst) analysed the synthetic control data and contributed to preparing the report for publication.
Chloe Crowe (https://orcid.org/0000-0003-4807-6883) (Mental Health Nurse) contributed to preparing the report for publication.
Lucy Goldsmith (https://orcid.org/0000-0002-6934-1925) (Research Fellow) conducted the service mapping and systematic review, analysed qualitative interview data and cohort study data, and contributed to preparing the report for publication.
Heather Jarman (https://orcid.org/0000-0002-4820-3291) (Professor, Emergency Care Nursing) contributed to preparing the report for publication.
Sonia Johnson (https://orcid.org/0000-0002-2219-1384) (Professor, Social Psychiatry) contributed to preparing the report for publication.
Jo Lomani (https://orcid.org/0000-0001-9243-9229) (Survivor Researcher, mental health) conducted the service mapping and systematic review, analysed qualitative interview data and contributed to preparing the report for publication.
David McDaid (https://orcid.org/0000-0003-0744-2664) (Associate Professor, Health Economics) analysed health economic data and contributed to preparing the report for publication.
Paris Pariza (https://orcid.org/0000-0002-2772-8048) (Senior Data Analyst) analysed the synthetic control data and contributed to preparing the report for publication.
A-La Park (https://orcid.org/0000-0002-4704-4874) (Research Fellow, Health Economics) analysed health economic data and contributed to preparing the report for publication.
Jared Smith (https://orcid.org/0000-0001-6138-136X) (Senior Research Fellow, Psychology) analysed interrupted time series data and contributed to preparing the report for publication.
Kati Turner (https://orcid.org/0000-0002-3271-6826) (Survivor Researcher, mental health) contributed to preparing the report for publication.
Heather Yoeli (https://orcid.org/0000-0001-5505-9366) (Research Fellow) analysed qualitative interview data and contributed to preparing the report for publication.
Ethics statement
The project was given ethical approval from the East Midlands Leicester South Research Ethics Committee (19/EM/0226) on 12 August 2019.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Strategy Unit . Exploring Mental Health Inpatient Capacity across Sustainability and Transformation Partnerships in England 2019.
- Anderson EL, Nordstrom K, Wilson MP, Peltzer-Jones JM, Zun L, Ng A, et al. American Association for Emergency Psychiatry Task Force on medical clearance of adults part I: introduction, review and evidence-based guidelines. West J Emerg Med 2017;18:235-42.
- Schmidt M. Frequent visitors at the psychiatric emergency room – a literature review. Psychiat Quart 2018;89:11-32.
- Shiraishi M, Ishii T, Kigawa Y, Tayama M, Inoue K, Narita K, et al. Psychiatric consultations at an emergency department in a Metropolitan University Hospital in Northern Japan. Psychiat Invest 2018;15:739-42.
- Larkin GL, Beautrais AL, Spirito A, Kirrane BM, Lippmann MJ, Milzman DP. Mental health and emergency medicine: a research agenda. Acad Emerg Med 2009;16:1110-9.
- Wilson MP, Shenvi C, Rives L, Nordstrom K, Schneider S, Gerardi M. Opportunities for research in mental health emergencies: executive summary and methodology. West J Emerg Med 2019;20:380-5.
- Fleury MJ, Grenier G, Farand L, Ferland F. Use of emergency rooms for mental health reasons in Quebec: barriers and facilitators. Admin Policy Ment Health 2019;46:18-33.
- Nicks BA, Manthey DM. The impact of psychiatric patient boarding in emergency departments. Emerg Med Int 2012;2012.
- Blunt I, Edwards N, Merry L. What’s Behind the ED Crisis. London: Nuffield Trust; 2015.
- Care Quality Commission . Right Here, Right Now: People’s Experiences of Help, Care and Support During a Mental Health Crisis 2015.
- Okorie EF, McDonald C, Dineen B. Patients repeatedly attending accident and emergency departments seeking psychiatric care. BJ Psych Bull 2011;35:60-2.
- Care Quality Commission . Key Findings for the National Accident and Emergency Patient Survey 2014 2014.
- Crisp N, Smith G, Nicholson K. Old Problems, New Solutions – Improving Acute Psychiatric Care for Adults in England. London: Commission on Acute Adult Psychiatric Care; 2016.
- Gilburt H. Mental Health under Pressure. London: King’s Fund; 2015.
- McCrone P, Johnson S, Nolan F, Pilling S, Sandor A, Hoult J, et al. Economic evaluation of a crisis resolution service: a randomised controlled trial. Epidemiol Psychiatr Soc 2009;18:54-8.
- Thibaut B, Dewa LH, Ramtale SC, D’Lima D, Adam S, Ashrafian H, et al. Patient safety in inpatient mental health settings: a systematic review. BMJ Open 2019;9.
- Morgan C, Mallett R, Hutchinson G, Leff J. Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Soc Sci Med 2004;58:739-52.
- Stulz N, Nevely A, Hilpert M, Bielinski D, Spisla C, Maeck L, et al. Referral to inpatient treatment does not necessarily imply a need for inpatient treatment. Adm Policy Ment Health 2015;42:474-83.
- Clibbens N, Harrop D, Blackett S. Early discharge in acute mental health: a rapid literature review. Int J Ment Health Nurs 2018;27:1305-25.
- Naidu S, Bolton J, Smith J. London’s liaison psychiatry services: survey of service provision. BJPsych Bull 2015;39:65-9.
- Udo I, Odeyale F, Gash A, Fossey M. The rise of liaison psychiatry: challenges and implications for sustainability. Brit J Hosp Med 2016;77:523-8.
- Glover G, Arts G, Babu KS. Crisis resolution/home treatment teams and psychiatric admission rates in England. Br J Psychiatry 2006;189:441-5.
- Jacobs R, Barrenho E. Impact of crisis resolution and home treatment teams on psychiatric admissions in England. Br J Psychiatry 2011;199:71-6.
- Williams P, Csipke E, Rose D, Koeser L, McCrone P, Tulloch AD, et al. Efficacy of a triage system to reduce length of hospital stay. Br J Psychiatry 2014;204:480-5.
- Gerdtz MF, Weiland TJ, Jelinek GA, Mackinlay C, Hill N. Perspectives of emergency department staff on the triage of mental health-related presentations: implications for education, policy and practice. Emerg Med Australas 2012;24:492-500.
- Innes K, Morphet J, O’Brien AP, Munro I. Caring for the mental illness patient in emergency departments – an exploration of the issues from a healthcare provider perspective. J Clin Nurs 2014;23:2003-11.
- NHS England, Care Quality Commission, Public Health England, Health Education England, Monitor, Care Quality Commission, NHS Trust Development Authority . Five Year Forward View 2014. www.england.nhs.uk/five-year-forward-view (accessed 15 May 2023).
- Department of Health and Concordat Signatories . Mental Health Crisis Care Concordat – Improving Outcomes for People Experiencing Mental Health Crisis 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/281242/36353_Mental_Health_Crisis_accessible.pdf (accessed 21 June 2022).
- Puntis S, Perfect D, Kirubarajan A, Bolton S, Davies F, Hayes A, et al. A systematic review of co-responder models of police mental health ‘street’ triage. BMC Psychiatry 2018;18.
- Johnson S, Gilburt H, Lloyd-Evans B, Osborn DPJ, Boardman J, Leese M, et al. In-patient and residential alternatives to standard acute psychiatric wards in England. Br J Psychiatry 2009;194:456-63.
- North East Hampshire and Farnham Clinical Commissioning Group . ‘The Safe Haven’ Aldershot: Evaluation Report 2014.
- Newbigging K, Rees J, Ince R, Mohan J, Joseph D, Ashman M, et al. The contribution of the voluntary sector to mental health crisis care: a mixed-methods study. Health Serv Deliv Res 2020;8. https://doi.org/10.3310/hsdr08290.
- Zeller SL, Calma NM, Stone A. Effect of a regional dedicated psychiatric emergency service on boarding and hospitalization of psychiatric patients in area emergency departments. West J Emerg Med 2014;15:1-6.
- Allen MH. Definitive treatment in the psychiatric emergency service. Psychiatry Q 1996;67:247-62.
- Wiler JL, Ross MA, Ginde AA. National study of emergency department observation services. Acad Emerg Med 2011;18:959-65.
- Ross MA, Aurora T, Graff L, Suri P, O’Malley R, Ojo A, et al. State of the art: emergency department observation units. Crit Pathw Cardiol 2012;11:128-38.
- Parwani V, Tinloy B, Ulrich A, D’Onofrio G, Goldenberg M, Rothenberg C, et al. Opening of psychiatric observation unit eases boarding crisis. Acad Emerg Med 2018;25:456-60.
- Norotte C, Omnes C, Crozier C, Verlyck C, Romanos M. Facteurs prédictifs d’hospitalisation à partir des lits de crise des urgences d’un hôpital général. L’Encéphale 2017;43:444-50.
- San Thinn DS, Kuswanto CN, Sum MY, Chai SB, Doris Sok HK, Xu C, et al. The 23-hour observation unit admissions within the emergency service at a national tertiary psychiatric hospital: clarifying clinical profiles, outcomes, and predictors of subsequent hospitalization. Prim Care Companion CNS Disord 2015;17. https://doi.org/10.4088/PCC.15m01789.
- Braitberg G, Gerdtz M, Harding S, Pincus S, Thompson M, Knott J. Behavioural assessment unit improves outcomes for patients with complex psychosocial needs. Emerg Med Australas 2018;30:353-8.
- Creswell J, Beavan M. Accreditation for Inpatient Mental Health Services (AIMS) Standards for Assessment/Triage Wards. London: Royal College of Psychiatrists; 2010.
- Care Quality Commission . Brief Guide: Staffing Levels of Mental Health Wards 2015.
- Medway Health and Adult Social Care . Mental Health Decisions Unit Briefing Paper – Medway HASC 2015.
- Perkins C. Lotus Assessment Suite (Psychiatric Decision Unit) Report: Springfield University Hospital 2017.
- Tretheway S, Deepak S, Saad S, Hughes E, Tadros G. Evaluation of the psychiatric decisions unit (PDU): effect on emergency department presentations and psychiatric inpatient admissions. Postgrad Med J 2019;95:6-11.
- Creswell JW, Clark VL. Designing and Conducting Mixed Methods Research. London: SAGE Publications; 2017.
- Klein KJ, Kozlowski SW. From micro to meso: critical steps in conceptualizing and conducting multilevel research. Org Res Methods 2000;3:211-36.
- Gillard S, Simons L, Turner K, Lucock M, Edwards C. Patient and public involvement in the coproduction of knowledge: reflection on the analysis of qualitative data in a mental health study. Qual Health Res 2012;22:1126-37.
- Burgess M. FOI Emails for NHS Mental Health Trusts NHS Mental Health Trusts – Freedom of Information: Sheet 1 2019. www.foi.directory/nhs-mental-health-trusts-2/ (accessed 21 June 2022).
- University College London . Crisis and Acute Care Projects n.d. www.ucl.ac.uk/psychiatry/research/nihr-mental-health-policy-research-unit/projects/acute-care-systems (accessed 21 June 2022).
- Kohl C, McIntosh EJ, Unger S, Haddaway NR, Kecke S, Schiemann J, et al. Online tools supporting the conduct and reporting of systematic reviews and systematic maps: a case study on CADIMA and review of existing tools. Environ Evid 2018;7.
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355.
- McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 2020;12:55-61.
- Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2. London: Cochrane Collaboration; 2021.
- Ranganathan P, Aggarwal R, Pramesh CS. Common pitfalls in statistical analysis: odds versus risk. Perspect Clin Res 2015;6:222-4.
- Deeks JJ, Higgins JP, Altman DG, Green SJ. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0. London: Cochrane Collaboration; 2011.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60.
- Harbord RM, Harris RJ, Sterne JA. Updated tests for small-study effects in meta-analyses. Stata J 2009;9:197-210.
- Goldsmith LP, Smith JG, Clarke G, Anderson K, Lomani J, Turner K, et al. What is the impact of psychiatric decision units on mental health crisis care pathways? Protocol for an interrupted time series analysis with a synthetic control study. BMC Psychiatry 2020;20:1-9.
- NHS Digital . Hospital Episode Statistics (HES) 2019. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed 15 May 2023).
- NHS Digital . NHS Trust Peer Finder Tool 2020. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/innovative-uses-of-data/multi-dataset-analysis/nhs-trust-peer-finder-tool (accessed 21 June 2022).
- Public Health England . NHS Acute (Hospital) Trust Catchment Populations. 2020 Rebase Experimental Statistics 2020.
- World Health Organization . International Statistical Classification of Diseases and Related Health Problems, 10th Revision 2019. https://icd.who.int/browse10/2019/en#/ (accessed 21 June 2022).
- NHS Digital . KH03 Bed Availability and Occupancy 2021. www.england.nhs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy (accessed 15 May 2023).
- Smith C, Hewison J, West RM, Guthrie E, Trigwell P, Crawford MJ, et al. Liaison psychiatry – measurement and evaluation of service types, referral patterns and outcomes (LP-MAESTRO): a protocol. BMJ Open 2019;9.
- Xu Y. Generalized Synthetic Control Method: causal inference with interactive fixed effects models. Polit Anal 2017;25:57-76.
- Samartsidis P, Seaman SR, Presanis AM, Hickman M, De Angelis D. Assessing the causal effect of binary interventions from observational panel data with few treated units. Stat Sci 2019;34:486-503.
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Boca Raton, FL: CRC Press; 1994.
- Fagerland MW, Lydersen S, Laake P. The McNemar test for binary matched-pairs data: mid-p and asymptotic are better than exact conditional. BMC Med Res Methodol 2013;13.
- Hayes LJ, Berry G. Comparing the part with the whole: should overlap be ignored in public health measures?. J Public Health 2006;28:278-82.
- EuroQoL G. EuroQoL: a new facility for the measurement of heath-related quality of life. Health Policy 1990;16:199-208.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92.
- Gillard S, Dare C, Hardy J, Nyikavaranda P, Rowan Olive R, Shah P, et al. NIHR Mental Health Policy Research Unit Covid Coproduction Research Group . Experiences of living with mental health problems during the COVID-19 pandemic in the UK: a coproduced, participatory qualitative interview study. Soc Psychiatry Psychiatr Epidemiol 2021;56:1447-57.
- Richardson L. Handbook of Qualitative Research. London: SAGE Publications Ltd; 2000.
- Simons L, Lathlean J, Squire C. Shifting the focus: sequential methods of analysis with qualitative data. Qual Health Res 2008;18:120-32.
- Kim AK, Vakkalanka JP, Van Heukelom P, Tate J, Lee S. Emergency psychiatric assessment, treatment, and healing (EmPATH) unit decreases hospital admission for patients presenting with suicidal ideation in rural America. Acad Emerg Med 2021;29:142-9.
- Stamy C, Shane DM, Kannedy L, Van Heukelom P, Mohr NM, Tate J, et al. Economic evaluation of the emergency department after implementation of an emergency psychiatric assessment, treatment, and healing unit. Acad Emerg Med 2021;28:82-91.
- Tadros G, Salama RA, Kingston P, Mustafa N, Johnson E, Pannell R, et al. Impact of an integrated rapid response psychiatric liaison team on quality improvement and cost savings: the Birmingham RAID model. Psychiatrist 2013;37:4-10.
- Becker L, Saunders R, Hardy R, Pilling S. London: UCL Partners; 2016.
- Goldsmith LP, Anderson K, Clarke G, Crowe C, Jarman H, Johnson S, et al. The psychiatric decision unit as an emerging model in mental health crisis care: a national survey in England. Int J Ment Health Nurs 2021;30:955-62.
- NHS England . National Schedule of Unit Costs 2021.
- Curtis LA, Burns A. Unit Costs of Health & Social Care 2020. Canterbury: PSSRU, University of Kent; 2020.
- Dixon-Woods M, Bonas S, Booth A, Jones DR, Miller T, Sutton AJ, et al. How can systematic reviews incorporate qualitative research? A critical perspective. Qual Res 2006;6:27-44.
- Lucas PJ, Ingram J, Redmond NM, Cabral C, Turnbull S, Hay AD. Development of an intervention to reduce antibiotic use for childhood coughs in UK primary care using critical synthesis of multi-method research. BMC Med Res Methodol 2017;17.
- Flemming K. The use of morphine to treat cancer-related pain: a synthesis of quantitative and qualitative research. J Pain Symptom Manage 2010;39:139-54.
- Johnson S, Dalton-Locke C, San Juan NV, Foye U, Oram S, Papamichail A, et al. Impact on mental health care and on mental health service users of the COVID-19 pandemic: a mixed methods survey of UK mental health care staff. Soc Psychiatry Psychiatr Epidemiol 2021;56:25-37.
- Care Quality Commission . Lancashire Care NHS Trust: Evidence Appendix 2019.
- Browne V, Knott J, Dakis J, Fielding J, Lyle D, Daniel C, et al. Improving the care of mentally ill patients in a tertiary emergency department: development of a psychiatric assessment and planning unit. Australas Psychiatry 2011;19:350-3.
- Gillig PM, Hillard JR, Bell J, Combs HE, Martin C, Deddens JA. The psychiatric emergency service holding area: effect on utilization of inpatient resources. Am J Psychiatry 1989;146:369-72.
- Kealy-Bateman W, McDonald A, Haber PS, Green T, White B, Sundakov V, et al. Development of a joint mental-health and drug health assessment unit and short-stay unit. Australas Psychiatry 2019;27:374-7.
- Lester NA, Thompson LR, Herget K, Stephens JA, Campo JV, Adkins EJ, et al. CALM interventions: behavioral health crisis assessment, linkage, and management improve patient care. Am J Med Qual 2018;33:65-71.
- Mok H, Walker C. Brief psychiatric hospitalization: preliminary experience with an urban short-stay unit. Can J Psychiatry 1995;40:45-7.
- Schneider SE, Ross IM. Ultra-short hospitalization for severely mentally ill patients. Psychiat Serv 1996;47:137-8.
- Spooren D, van Heeringen K, Jannes C. Short-term outcome following referral to a psychiatric emergency service. Crisis 1997;18:80-5.
- Van Der Sande R, Van Rooijen L, Buskens E, Allart E, Hawton K, Van Der Graaf Y, et al. Intensive in-patient and community intervention versus routine care after attempted suicide. Br J Psychiatry 1997;171:35-41.
- Goldberg D. The Detection of Psychiatric Illness by Questionnaire. Oxford: Oxford University Press; 1972.
- Buglass D, Horton J. A scale for predicting subsequent suicidal behaviour. Br J Psychiatry 1974;124:573-8.
- Healthy London Partnership . Health Based Place of Safety: Business Case 2018.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36.
- National Institute for Health and Care Excellence . Position Statement on Use of the EQ-5D-5L Value Set for England 2019. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 22 August 2022).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15.
- Tubeuf S, Saloniki E-C, Cottrell D. Parental health spillover in cost-effectiveness analysis: evidence from self-harming adolescents in England. PharmacoEconomics 2019;37:513-30.
- Zeller S. Psychiatric boarding: averting long waits in emergency rooms. Psychiatric Times 2013;30.
- Ledet L, Chatmon BN. Treatment and outcomes in adult designated psychiatric emergency service units. Crit Care Nurs Clin North Am 2019;31:225-36.
- Bobrovitz N, Lasserson DS, Briggs AD. Who breaches the four-hour emergency department wait time target? A retrospective analysis of 374,000 emergency department attendances between 2008 and 2013 at a type 1 emergency department in England. BMC Emerg Med 2017;17.
- Bhui K, Halvorsrud K, Nazroo J. Making a difference: ethnic inequality and severe mental illness. Br J Psychiatry 2018;213:574-8.
- Haynes AB, Haukoos JS, Dimick JB. TREND reporting guidelines for nonrandomized/quasi-experimental study designs. JAMA Surg 2021;156:879-80.
- Davis KA, Sudlow CL, Hotopf M. Can mental health diagnoses in administrative data be used for research? A systematic review of the accuracy of routinely collected diagnoses. BMC Psychiatry 2016;16:1-.
- Priebe S, Kelley L, Omer S, Golden E, Walsh S, Khanom H, et al. The effectiveness of a patient-centred assessment with a solution-focused approach (DIALOG+) for patients with psychosis: a pragmatic cluster-randomised controlled trial in community care. Psychother Psychosom 2015;84:304-13.
- Lloyd-Evans B, Paterson B, Onyett S, Brown E, Istead H, Gray R, et al. National implementation of a mental health service model: A survey of Crisis Resolution Teams in England. Int J Ment Health Nurs 2017;27:214-26.
- Lamb D, Lloyd-Evans B, Fullarton K, Kelly K, Goater N, Mason O, et al. Crisis resolution and home treatment in the UK: a survey of model fidelity using a novel review methodology. Int J Ment Health Nurs 2019;29:187-201.
- Sweeney A, Filson B, Kennedy A, Collinson L, Gillard S. A paradigm shift: relationships in trauma-informed mental health services. BJ Psych Adv 2018;24:319-33.
- Digital N . Mental Health Services Data Set 2020. https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-sets/mental-health-services-data-set (accessed 21 June 2022).
- Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci 2010;25:1-21. http://projecteuclid.org/euclid.ss/1280841730 (accessed 22 August 2022).
- NHS England . National Schedule of Unit Costs: Year 2019–2020. NHS Trusts and Foundation Trusts 2021.
- NHS Employers, Pay Journey Tool (England) . Tool Showing Individual Staff Pay Journeys through the Three Years of the Pay Deal 2021. www.nhsemployers.org/articles/pay-journey-tool-england (accessed 5 September 2022).
Appendix 1 Characteristics of psychiatric decision units evaluated in studies included in the systematic review
| Study reference | Unit | Max. length of stay | Capacity and location | Unit purpose | Further service details | Admission criteria | Referral pathway | Staffing |
|---|---|---|---|---|---|---|---|---|
| Braitberg et al.40 | BAU | 24 hours | 6-bedded unit | Move patients from the ED to a dedicated, well-resourced, low-stimulus environment | Fast-track assessment and management of behaviourally disturbed patients presenting to the ED in an environment designed to be safe and secure, allow close observation and provide timely access to specialist expertise and facilities for the appropriate use of sedation and restraint when required, irrespective of the patient’s primary diagnosis40 | Patients with acute behavioural disturbance, specifically behaviour influenced by drugs and alcohol, drug intoxication, mental illness and social crisis. Expected home discharge within 24 hours | ED | EMH and drug and alcohol clinicians. 2–3 nurses always staffed the unit. A psychiatrist and/or psychiatry registrar every morning |
| Browne et al.90 | PAPU | 48 hours | Four-bedded unit. Co-located within an expanded high dependency unit in the Royal Melbourne Hospital adult acute inpatient unit | Reduce ED mental health presentations and wait time for inpatient admissions. Improve care in a more appropriate, less restrictive environment | Intense management in the first 48 hours of admission, including review of all new admissions by a Consultant Psychiatrist within 24 hours to commence a clear management plan, then daily reviews by a consultant psychiatrist or psychiatry registrar thereafter, to ensure this plan is carried through | Patients from ED or within the catchment area requiring an admission for psychiatric evaluation and treatment. No transfers from other EDs or other psychiatric catchment areas Patients intoxicated, sedated or requiring immediate medical attention were excluded | ED or via local crisis assessment and treatment teams | Multidisciplinary team and allows patients and families to have access to psychiatric medical staff earlier in their episode of care than previously occurred, due to long lengths of stay in ED waiting for admission previously |
| Gillig et al.91 | Extended evaluation unit | 24 hours | Not reported | Extended evaluation unit, or holding area, allowing up to 24 hours of evaluation before making a referral. Purpose of which is to reduce hospitalisation rates | No further information | Not reported | PES | Not reported |
| Kealey-Bateman et al.92 | Joint SSU and Missenden assessment unit | 72 hours | 6-bedded unit. Located 300 m from the ED (SSU). Located adjacent to the SSU | Appropriate and efficient care of patients who require brief admission and active therapeutic intervention prior to their return to community-based care (SSU). Attending to patients with a more specific health focus and in a timely manner, relieving pressure on the ED |
Developed in partnership with MH and drug health services and the ED. Physically remote from the ED (approximately 300 m diagonally opposite) and able to provide some medical interventions, including intravenous therapy, because of staff with a mix of competencies | Patients with mental health problems likely to benefit from therapeutic intervention within 72 hours, and patients with comorbid mental health, drug health or toxicology problems deemed suitable. No aggression, acute medical or surgical problems, assessed as having chronic brain syndrome and who present with chronic behavioural or accommodation issues, and more than two SSU admissions in 3 months | ED, MAU, other parts of the hospital system (SSU). ED or self-referral (MAU) | Initially a high proportion of ED staff with resuscitation skills but this then reduced. nursing-to-patient ratio of 1 : 2 and high levels of staff trained in trauma-informed care (SSU). Not reported (MAU) |
| Lester et al.93 | CALM service | 48 hours | 8-bedded unit | Providing patients who would have boarded in the ED active behavioural treatment (e.g. crisis intervention focused psychotherapy, pharmacotherapy, and case management services) | Offers crisis intervention care delivered in a designated behavioural health unit located within the medical centre | ED patients with psychiatric complaints and stable behaviour No medical complaint. Other patients can be referred to CALM for observation care following initial psychiatric assessment in the ED |
ED | Psychiatric nurses and psychiatric care technicians in a 4 : 1 patient-to-staff ratio. Weekday coverage is provided by one independently licensed social worker and one nurse practitioner working in collaboration with a supervising psychiatrist. Weekend coverage is provided by on-call psychiatry faculty |
| Mok and Walker94 | SSU | 3 days | 5-bedded unit | Address decreasing inpatient beds and out-of-area transfers. Provide an integrated assessment, treatment, and follow-up service facilitating discharge within 3 working days | All patients are advised about the brevity of admission and are encouraged to participate in treatment discharge planning. On discharge, patients have access to prompt follow-up through the outpatient department’s rapid response clinic which holds outpatient clinics three times per week | Patients where discharge is likely within 3 working days, according to judgement of the assessing physician(s) | Any source e.g. emergency assessment unit, staff psychiatrist, outpatient clinic, ED. Primary referral route emergency physician | A psychiatrist, a psychiatry resident, staff nurse and a medical social worker. After-hours nursing coverage is provided by staff from the regular-stay unit |
| Parwani et al.37 | Psychiatric observation unit | 24 hours | 12-bedded, locked unit | To reduce boarding and improve ED throughput of psychiatric patients in the ED | No further information | Any patient evaluated in the CIU, at the discretion of the CIU psychiatrist. Patients admitted tended to be considered amenable to an observation stay < 48 hours or likely to require inpatient psychiatric admission but no bed available | Via CIU, after psychiatric evaluation | Two nurses continuously as well as social workers and advanced practice providers during all days. Except for attending physician oversight often provided by the psychiatrist in the CIU, all staff are dedicated to the psychiatric observation unit |
| Schneider and Ross95 | Crisis unit | Three days | Four-bedded unit | Reduce time in hospital without reducing quality of care. Reduce acute symptoms, stabilise precipitating factors, and reconnect with outpatient treatment | Treatment emphasises concrete problem-solving, education and medication stabilisation and compliance. Family therapy or other therapies are added only if relevant to specific precipitating issues. Patients continually reminded that the treatment is focused on crisis resolution and primary treatment site is the outpatient setting | Patients with acute symptoms attributable to specific and short-lived precipitants such as medication non-compliance, disruption of important relationships and interruption of living arrangements | Not reported | 0.25 FTE psychiatrist, 2.5 FTE registered nurses, one FTE psychiatric technician, one FTE crisis worker. Crisis unit and the traditional inpatient service shared some minor responsibilities. The two services share clerical and administrative staff |
| Spooren et al.96 | Three psychiatric crisis units | 72 hours | Not reported | Stabilise condition of the patient. Improve well-being within a shorter time frame | Crisis management, consultations with partners and families, social interventions, short problem-focused therapy, and motivational counselling towards further treatment. Most interventions occurred at the time of the referral. Some patients were invited to return to the unit for a limited follow-up to prepare them for further outpatient treatment | Not reported | ED | Senior psychiatrist supported by psychiatric trainees and a multidisciplinary team of psychiatric and community nurses, social workers and a psychologist |
| Stamy et al.79 | Emergency psychiatric assessment, treatment, and healing (EmPATH) unit | Not reported | 12-person unit, recliners | Outpatient hospital- based programme that accepts ED patients in a psychiatric crisis. These units proclaim to decrease psychiatric boarding time and LOS at reduced costs compared to traditional psychiatric care | No further information | Patients in the ED considered appropriate. Must be non-violent, not requiring inpatient psychiatry and medically cleared | ED or via outpatient psychiatric clinic after consultation with an EmPATH psychiatrist | Psychiatrists, psychiatric nurses, nursing assistants, social workers and providers |
| Tretheway et al.45 | PDU | Not reported | 8-person unit, non-bedded | Primary objective is to provide a safe and calm environment for enhanced assessment and short-term support to more complex patients in mental health crisis. Further aims are to relieve pressure on ED and avoid unnecessary inpatient admissions | No further information | Patients may be referred to the PDU following an initial assessment by rapid assessment interface and discharge or street triage 24 hours a day, 7 days a week | Multiple: street triage team, rapid assessment interface and discharge teams | Not reported |
| Van der Sande et al.97 | Special care unit for suicide attempters (SOS-Afdeling) | 4 days | 4-bedded unit | Reduce the risk of further suicide attempts. Improve well-being | Brief inpatient treatment in a small, specialised psychiatric unit with subsequent 24-hour emergency access to the unit, problem-solving outpatient treatment by a community nurse, and home visits when necessary | Aged 15+ and attending for somatic treatment of the consequences of a suicide attempt. Exclusions: patients displaying habitual self-mutilation, excessive quantities of alcohol/drugs consumed habitually, accidental overdoses, inability to understand and write Dutch, residing outside the catchment area, psychiatric hospitalisation, imprisonment, acute psychosis, and recurrent consultations with a liaison psychiatrist during a prolonged stay (> 2 days) on a somatic ward | ED | One psychiatrist, 2 community psychiatric nurses, 9 psychiatric nurses |
Appendix 2 Detailed interrupted time series and synthetic control study method
Interrupted time series data collection
The study tested the impact of a service-level change at a secular level, namely the implementation of the PDU, within the context of an ITS analysis design. Information management services personnel within eight participating NHS trusts provided relevant (trust-wide) service use data. Data did not include personally identifiable information and was handled in accordance with the UK Data Protection Act 2018 (incorporating the EU20 General Data Protection Regulation).
Mental health trust
MHT data centred on patterns of activity in acute adult inpatient wards over the relevant period, including the admission frequency and type (formal or informal), length of inpatient stay and acute adult ward bed occupancy (for the full list, see Table 3 in main text). Recorded inpatient admissions where discharge and subsequent admission were on the same or consecutive days were considered as a single admission. Where an individual was an inpatient on an acute adult psychiatric ward at the time of data extraction, their continuous data on LOS were excluded from analyses (LPFT; n = 11), although categorical data concerning stay of 5 or fewer days/more than 5 days was recorded (in all cases stay was longer than 5 days).
The frequency of PLE where an individual was referred from an ED was also calculated; referrals included those service users referred to liaison psychiatry irrespective of whether an assessment by liaison psychiatry Services was subsequently carried out. To avoid duplicate admissions for the same event, liaison psychiatry referrals separated by less than 12 hours were considered as a single episode (where subsequent referral occurred < 12 hours after previous referral only the first episode of the two was considered). The number of informal (voluntary) and total acute adult admissions, acute adult ward bed occupancy and frequency of liaison psychiatry episodes were considered against the catchment population of the relevant MHT in each week under study, calculated by linearly interpolating mid-year (adult) population estimates of boroughs served by the trust, or, where appropriate, from mid-year population estimates for clinical commissioning groups in England, both provided by the UK’s Office for National Statistics (ONS). ONS population estimates were available through to 2020.
Acute trust
For each (participating) acute trust, psychiatric presentations in ED over the relevant period were extracted from ‘Presenting Complaint’/‘Reason for Visit’ and ‘Diagnosis’/‘ED Coding’ entries in trust ED data. Specifically, psychiatric presentations included adult attendances to a hospital ED where the presenting complaint reflected a mental or behavioural health issue and/or the primary diagnostic code was consistent with a diagnosis of either one of more mental and behavioural disorders (F01–F79 of ICD-10) or self-harm (X60–X84). The specific terms used to search to initially screen for psychiatric presentations in ‘Presenting Complaint’/‘Reason for Visit’ and ‘Diagnosis’/‘ED Coding’ entries were %MENTAL%, ‘PSYC&’, ‘SUIC&’, ‘SELF&’, and ‘OVERDOSE’. Where an attending individual was recorded as presenting with alcohol intoxication without any accompanying mental health issue or diagnostic code consistent with a diagnosis of one or more mental and behavioural disorders (excluding uncomplicated alcohol abuse with intoxication), the attendance was excluded. Where the presenting complaint was listed as an ‘overdose’, in the absence of a diagnostic code consistent with a diagnosis of self-harm or one or mental and behavioural disorders, only instances where the overdose was stated as ‘deliberate’ or ‘intentional’ were included. For one participating trust (SWBHFT), only the presenting complaint/reason for visit was available and as such considered for including attendances.
ED hospital activity outcomes focused on psychiatric presentation frequency, arrival method (e.g. ambulance) and length of ED stay (see Table 3 in the main text). To avoid duplicate admissions for the same event, recorded ED visits separated by less than 12 hours were considered as a single episode (where subsequent visit was < 12 hours after discharge only the first episode of the two was considered). For one ED site (STHFT), only the frequency of (psychiatric) attendances, and not the number of individuals attending nor the frequency with which each individual attended in the study period was available. In this case, repeat visits within 12 hours were assumed to occur when an individual’s specific age, sex and diagnostic coding were identical to that of a (previous) visit within a 12-hour period; this occurred in 366 cases (4.2%) which was comparable to that observed across the other ED sites. The frequency of ED psychiatric presentations was considered relative to the corresponding hospital catchment population (HCP), calculated for each week under study by linearly interpolating (assuming a mid-year point) yearly (adult) population estimates derived for each site from proportionate flow methods adopted by Public Health England. HCP information was available through to 2018; for two sites where data extended beyond this year, HCPs in subsequent years were estimated via linear extrapolations for the population trend in the prior 3 years (2016–18).
Psychiatric decision unit and service reconfiguration/change in model of care data
PDU data (e.g. number of visits, LOS, destination upon discharge) pertaining to the first 2 years of operation for each site was also collected (to provide context to any observed changes in outcomes post-PDU implementation). Additionally, a small number of semistructured interviews were conducted with strategic managers in each site (e.g. PDU manager, acute care pathway lead, mental health lead commissioner (or their equivalent locally), ED manager, and/or ED clinical director) to identify any changes to the crisis care pathway (e.g. introduction or withdrawal of relevant services, amendments to policy or protocol that target the assessment and/or management of psychiatric presentations in ED). Where possible, these data were accounted for in secondary analyses of primary outcome measures in additional ITS analyses with the intention of controlling for any potentially confounding changes to models of care (e.g. service reconfiguration) that occurred with the time series period of interest.
Interrupted time series design and statistical analyses
Interrupted time series design
Changes in acute and psychiatric hospital activity following the introduction of PDUs in four sites were assessed via a retrospective, secular trend analysis using an ITS design considering routinely collected healthcare data. ITS are robust quasi-experimental designs that are increasingly being used to evaluate the impact of changes to health care or organisational interventions implemented in healthcare settings where randomisation of the intervention is impractical or unethical. Typically, they concern outcomes relevant to service delivery and/or health outcomes at a (clinical) population-level, with the intention to examine whether the data pattern observed post-intervention differs from that observed pre-intervention independent of any secular trends. The methodology of the present ITS study has previously been described in detail. 60 The exposure of interest in this study was the implementation of the PDU. Acute adult psychiatric inpatient ward and mental health-related ED attendances in the 24 months prior to PDU implementation were considered unexposed, while those in the 24 months following PDU implementation were exposed.
Interrupted time series statistical analysis
Descriptive statistics of key service use parameters, including demographic characteristics of service users, were used to describe PDUs, psychiatric inpatient and ED mental health attendance activity in each trust. Outcomes in both mental health and acute trust settings were initially assessed for each site via pairwise comparisons of pre- and post-PDU implementation periods for each variable using chi-squared, t-tests and Mann–Whitney U-tests.
Subsequently, outcome data were collated as time series over a (maximum) 48-month period for each site, aggregated to a single observation at weekly or monthly units depending on the variable under study. Segmented regression analyses were employed to evaluate whether there was a change in health-care utilisation outcomes following the implementation of the PDU. This method allowed the calculation of three regression coefficients that can quantify the impact of a service-level change: the underlying trend prior to PDU introduction (b1), the level change immediately following PDU introduction (b2) and the slope change from pre- to post-PDU introduction (b3). The calculation of the trend post PDU implementation (b1_b3) was calculated separately in analyses that considered only the period after the introduction of the PDU.
Outcomes based on count data (e.g. inpatient admissions, ED mental health attendances) followed a Poisson distribution and segmented GLM using log-transformed rates for outcomes to stabilise variances were fit to perform the statistical analyses. The natural logarithm of population estimates for the catchment area were included in these models as an offset variable (i.e. a predictor variable with a regression coefficient fixed at 1). Where models aggregated data in weekly units, the 52nd, 104th, 156th and 208th weeks of the time series included an additional day (or additional 2 days in the case of a leap year); the corresponding frequency values were adjusted to account for the additional day(s) before inclusion in models. Similarly, where models aggregated data in monthly units, frequency values were adjusted to account for the number of days in each month. Additional ITS analyses were conducted for counts of inpatient admissions, ED mental health attendances and liaison psychiatry episodes considering only those people most likely to be repeat users of these services (i.e. only individuals who, in the preceding 24 months, had been admitted to psychiatric inpatient services, attended the ED and been referred to liaison psychiatry, respectively). Segmented linear regression (GLM with identity link) was used to evaluate outcomes based on proportions (e.g. proportion of compulsory inpatient admissions, proportion of 4-hour breaches at ED), mean length of inpatient/ED stay (log-transformed due to marked skew in data distribution) and mean daily bed occupancy.
In all segmented GLM models, robust (sandwich) variance estimators were applied to account for possible multiple admissions per patient. The presence of autocorrelation was evaluated by reviewing the (residual) autocorrelation and partial autocorrelation functions and the Durbin–Watson test statistic and accounted for by fitting one or more lagged variables as required (first-order, second-order and/or third-order autoregressive lag variables). Since mental healthcare service use is known to follow a seasonal pattern), terms based on (trigonometric) sine and cosine functions with a period of 1 year were included also. Residual analyses of the final models showed no significant deviations from model assumptions. Models based on weekly aggregated data were preferred in the first instance and constituted the majority of segmented regression (ITS) models in reported analyses. Refitting a subsample of these models (across different outcome variables) did not provide proportionately better model fits (according to Akaike’s and Schwarz’s Bayesian information criteria). In a limited number of cases, however, typically where weekly frequencies were very low, models based on monthly aggregated data were preferred.
ITS parameter estimates were presented in the form of beta values with 95% CIs for all outcome variables, with percentage change values for count/log-transformed data [representing (predicted) percentage change in frequency/LOS on PDU implementation (step change) or per week/month (trend change)] and percentage point change values for proportion data [representing increase/decrease in the (predicted) percentage of that variable as a result of PDU implementation (step change) or per week/month (trend change)].
Subsequently, to estimate overall effects, individual site estimates of PDU implementation impact (short- and long-term) were pooled in a meta-analytical model. To minimise imprecision of pooled effect estimates, the inverse variance approach was adopted, whereby the weight assigned to each site was the inverse of the variance of the step and trend change estimates from fitted models (obtained by squaring the standard errors of parameter estimates). Fixed- and random-effect estimates were provided for all outcomes. Where the chi-square statistic (Cochran’s Q) and associated p-value indicated heterogeneity of PDU effects across sites (variation in effect estimates beyond chance), estimates from random-effects model were preferred to interpret overall effects.
Finally, secondary analyses of primary outcome measures in ITS were also performed with a view to attempt to account for the impact of any other crisis care service reconfigurations that may have been relevant to outcome measures by introducing a second break-point in the ITS models, subject to reconfigurations being sufficiently distant in time from the start/end points of the time series and the PDU implementation to distinguish any impact. Specifically, segmented regression models with multiple interventions were fitted. These used a similar structure to the segmented regression models described earlier, but also included a separate term for an additional service change (to describe any immediate effect of the change) and an additional time term to account for time since that service change (to describe a difference between the slopes of the time before and after the service change). Models were administered separately to assess the impact of each additional service change with PDU implementation.
A p-value of < 0.05 was considered statistically significant in all analyses. Analyses were administered using Stata 16 (StataCorp., College Station, Texas) and SPSS.
Interrupted time series sample size
Aggregating psychiatric admission and ED service use data over the relevant period (24 months pre- and post-implementation of PDUs) yielded 208 weekly or 48 monthly time points depending on (baseline) frequency of events. This is more than the 40 data points (20 pre- and 20 post-change) typically considered as adequate for valid ITS model analysis and provided sufficient power to detect any existing medium effects. For instance, assuming five (or less) factors entered in a model testing a single parameter, to detect a time*slope interaction with medium effect size on an outcome, a sample of 208 time points has greater than 99% power (calculated using G-Power, ‘linear multiple regression: fixed model, r2 increase’ module).
Interrupted time series deviations from protocol
There were a limited number of deviations from the methods described in the published protocol. 60 Reliable data concerning acute adult inpatient and PLE activity could not be sourced from one MHT restricting (pooled) analysis of relevant outcomes to three sites only. Further, although the intention was to include ED-based activity data from all acute trust sites that referred a substantial proportion (≥ 25%) of PDU service users, this was not possible for two acute trusts linked with PDUs at BSMHFT and SWLSTG, respectively. Additionally, the COVID-19 crisis led to the PDU in SHSCFT closing for a 10-week period beginning March 2020, precluding ITS analyses of trust activity thereafter (i.e. only post-PDU data in the 12-month period following PDU implementation was considered). Data availability was also limited for some specific variables in some study sites, precluding analyses of weekly or monthly patterns of activity in the entire 4-year study period. Specifically, SWBHFT ED attendance data was only available in the 12-month period prior to and 24 months post-PDU implementation, PLE data were not available in the first 6 months of the time series in LPFT and ED attendance by ambulance or police data were not available in the first 12 months of the time series in STHFT. More generally, across sites, data pertaining to ethnicity and diagnoses of service users visiting the PDU, admitted to a psychiatric inpatient ward and attending ED for a mental health reason was not sufficiently complete to consider in descriptive analyses.
With respect to the plan of statistical analyses detailed in the protocol, ITS analyses concerning the weekly/monthly numbers of inpatient admissions, ED mental health attendances and liaison psychiatry episodes considered raw frequencies rather than estimates per 1000 trust catchment population (as stated). This was primarily because the observed event frequencies were typically low (e.g. < 100) relative to the size of the catchment populations for mental health (700,000–1,000,000) and acute trusts (340,000–640,000) resulting in potential rates that are difficult to interpret unless the adopted denominator is very large (e.g. 100,000) which in most cases would be more than the catchment population served by the trust. Differences in the size of trust catchment populations over the 4-year study period were controlled for in segmented regression models (for count data) by inclusion of the catchment population estimates across the study period as an offset variable. Although cross-site comparisons are more challenging using raw frequencies, three of the four MHT sites and three of the four acute trust sites shared similar catchment populations suggesting broad comparability with respect to the size of the population served by participating sites.
Synthetic control data sources
Hospital Episode Statistics
Aggregated service use data from December 2012 to latest available was collected for the treated trusts and all other trusts in England from HES. 61 HES collect data on all admissions, outpatient appointments and A&E attendances at NHS hospitals in England. Data include information on a range of clinical, demographic, administrative and geographical variables, but no patient identifiable information. Data on admissions to MHT inpatient wards were available from two sources: HES-APC and the Mental Health Services data set (MHSDS). 115 Here, we used HES-APC as it was expected to be more complete, consistent and accurate. 1 Data on ED attendance was obtained from HES-A&E activity.
Covariate data
We also obtained data relating to the key characteristics of all NHS hospital trusts for the financial year 2018–19 from the NHS Trust Peer Finder Tool. 62 We used this tool to identify each treated trust’s 10 closest peers based on a list of variables such as attendances, deprivation, patient profile and location profile and to provide covariate data for acute and MHTs. Further covariate data relating to the key characteristics of NHS acute hospital trusts from 2011 to 2018 were obtained from Public Health England. 63
Treated and control trusts
The treated trusts comprise the four MHTs in Sheffield, Lincolnshire, Birmingham and South West London, where the PDUs are located, and six acute trusts which are main referral sites for one of the MHTs (see Table 1 in the main text). No data for SHSCFT were submitted to HES for the duration of the study so this treated trust was excluded from the analysis. The three remaining MHTs and their six referring acute NHS trusts are our treated trusts. We identified 38 other MHTs in England contributing data to HES-APC and 136 other adult acute NHS trusts in England contributing data to HES-A&E. These trusts were included as potential controls with the following exclusions: four MHTs (in Coventry, Sussex, Leeds and Lancashire) which either have active or decommissioned PDUs and nine acute trusts which make referrals into any of the excluded MHTs were excluded:
-
Active PDUs: Coventry and Warwickshire Partnership NHS Trust, Sussex Partnership NHS Foundation Trust.
-
Decommissioned PDU: Leeds and York Partnership NHS Foundation Trust, Lancashire and South Cumbria NHS Foundation Trust (previously Lancashire Care NHS Foundation Trust).
-
Referring: University Hospitals Coventry and Warwickshire NHS Trust, South Warwickshire NHS Foundation Trust, Surrey and Sussex Healthcare NHS Trust, East Sussex Healthcare NHS Trust, Brighton and Sussex University Hospitals NHS Trust, Western Sussex Hospitals NHS Foundation Trust, Leeds Teaching Hospitals NHS Trust, Lancashire Teaching Hospitals NHS Foundation Trust and East Lancashire Hospitals NHS Foundation Trust.
Patients
We included all patients aged between 18 and 75 years with a record of a hospital admission to a mental health NHS trust adult inpatient ward, or a psychiatric attendance at an acute NHS trust ED, in England between December 2012 and January 2021.
Admissions to a mental health trust adult inpatient ward
Admissions to MHT inpatient wards are not explicitly defined as such in HES-APC. Instead, we proxied these admissions using the main specialty of the consultant (710, 722 : 726) or treatment function of the episode (710, 722–726) or where these codes were not supplied, using the primary diagnosis code64 for the patient (ICD-10 code in F03.0–F69.0, R44.0–R46.9). This approach has been verified elsewhere for accuracy by comparison with data on NHS beds available and occupied (KH03) returns,65 but, in more recent periods HES-APC may understate the true number of admissions to MHT inpatient wards. 1
Emergency department psychiatric attendances
We proxied psychiatric attendances at ED using the ED diagnosis or patient group, arrivals by ambulance using the ED arrival mode, referrals to ED by police by source of referral and admissions to an acute trust inpatient ward at the same healthcare provider by ED attendance disposal. Referral to liaison psychiatry services could not reliably be determined from HES. 66 Instead, it requires access to clinical databases controlled by the MHTs that provide liaison psychiatry services. Since it was infeasible to extract this information for all treated and control trusts, this outcome was excluded from our analysis.
Synthetic control outcomes
Admissions to a mental health trust inpatient ward
Our outcomes for the MHTs were the rate of admissions to a MHT inpatient ward per 10,000 patients in the trust catchment population; the proportion of these admissions with a LOS < 5 days; and the average LOS.
Emergency department psychiatric attendances
Our outcomes for the acute trusts were rate of ED psychiatric attendances per 10,000 patients in the trust catchment population; the proportion of these that breached 4/12 hours, where the patient was admitted to an acute bed at the same provider, that arrived by ambulance or were referred by police, or were referred to liaison psychiatry; and the average length of wait.
Synthetic control statistical approach
Data
The final HES-APC and HES-A&E extracted data sets each comprised all records for patients with a mental health admission at any of the 34 included MHTs or an ED psychiatric attendance at any of the 133 included acute NHS trusts in England between December 2012 and January 2021. To capture patients most likely to have been referred to a PDU, we excluded all patients younger than 18 years or over 75 years. Patient-level data were aggregated to create a monthly series for 24 months pre and 24 months post implementation of the PDU at each treated trust.
Selecting similar controls
In order to make sure that we compared treated trusts to similar trusts elsewhere in the country, we used data and methods described in the NHS Trust Peer Finder Tool62 to identify each treated trust’s closest peers from the pool of potential controls based on a list of variables including, but not limited to, attendances, deprivation, patient profile and location profile. The closest peers are those with the smallest Euclidean distance to the treated trust based upon standardised values of the variables. The closest 20 peers according to annual data available for 2018/19 data were used as the control pool for each trust in the main analysis.
The generalised synthetic control
We used the GSC method67 to estimate the impact of the PDU on each outcome separately at each treated trust. GSC uses a three-step estimation procedure to create a counterfactual – aka synthetic control – using control group data and pre-intervention data from the treated trust. The counterfactual aims to track the outcome of the treated trust in the pre-implementation period. The rationale is then that the model predictions in the post-implementation period will reflect the outcomes that would have occurred in the treated trusts if the PDU had not opened. By comparing these predictions to the actual outcomes in the treated trusts after the PDU opens we can get an estimate of the net effect on outcomes attributable to the PDU. The significance of each estimate was assessed by a parametric bootstrap procedure. 69 Estimated standard errors were used in a random-effects meta-analysis to generate a pooled estimate across studies.
Risk-adjustment
For each outcome, we controlled for the size of the trust catchment population and other variables that reflect changes over time in the characteristics of the population at risk of that outcome. For psychiatric ED attendances and admissions to MHT inpatient ward, the population at risk is the trust catchment population, so we controlled for the monthly proportions of this population by sex and age groups. For all other outcomes, the population at risk is either the subset of patients attending ED or those admitted to a MHT inpatient ward. Here, we controlled for the size of the population at risk, the proportion of that population by sex, age and ethnicity groups, and with two or more comorbidities according to their inpatient admissions in the preceding 24 months.
Assumptions and diagnostic tests
Modelling assumptions play an important role in the GSC method. Firstly, the quality of the synthetic control is measured by how closely its outcomes match those in the treated trust in the pre-implementation period. To check this, we performed a statistical test for no difference between the average outcomes in the synthetic control and treated trust in the pre-implementation period. It is further assumed that if they do track well, then the outcomes in the synthetic control during the post-implementation period will reflect the outcomes that would have occurred in the treated trust in the absence of the PDU. However, this might not be the case if there are ‘dormant’ factors which are not active in the pre-implementation period and which impact the treated or control trusts differently in the post-intervention period. Matching treated and control trusts according to characteristics we can observe may provide indirect matching on a wider set of correlated characteristics,68 including some which may govern post-implementation differences and so reducing the risk of bias associated with dormant factors. Additional diagnostic checks to ensure that the synthetic control was not obtained by extrapolation were also performed. 116
Sensitivity analyses
We performed sensitivity analyses to test the robustness of estimates to changes in the number of controls in the control group by repeating all analyses using control groups comprising the nearest 10 and the nearest 20 peers.
Appendix 3 Qualitative interview schedules
DECISION project: service user qualitative interview T1
Initial questions – a bit about you
First of all, I’d like to ask a few questions about how things are going generally at the moment and ideas for the future, if that’s ok? [This is to get a better sense of how people are doing overall after being on the unit]
-
How are you feeling now?
-
What might you like to do in the future? Suggested prompts: Plans for education, work or volunteering? Moving somewhere new/relationships etc.?
If appropriate, follow-up with housing situation, employment status.
Experiences of referral to the unit
-
What happened when you knew you were in crisis? What steps did you take to access help? What sort of crisis support have you had from mental health services in the past, before the [name of unit] opened?
-
How were you referred to the unit and what that was like? Suggested prompts: Did you go via A&E, street triage, the 136 suite etc.
During your stay
-
How was it on the decision unit [or name of unit]?
Suggested prompts: how was it for you? How helpful was it? (e.g. talking to staff, planning how to get out of the crisis and cope in the future) Were you at ease? How safe did you feel?
Cover: assessment, stabilisation, therapeutic input and signposting
-
Did you have someone you know visit you on the unit?
-
If so, did you want that person there? If not, would you have liked anyone there? Suggested prompts: If helpful, how did them visiting help?
-
What were the least helpful things about the unit?
-
What were the staff on the unit like?
Suggested prompts: Are there any particular interactions that stood out to you?
-
Did you feel able to discuss what you wanted to with staff?
Suggested prompts: If you didn’t feel able to, was there anything that was making you feel reluctant? Was there anything that you felt you couldn’t talk about (What made you feel that way)?
-
Did the staff talk about how to manage your thoughts or emotions? Signpost to other services?
-
How do the Lotus staff compare with mental health staff that have worked with you in the past? Suggested prompt: for example, on a standard mental health ward
-
Have you ever been admitted to a mental health ward? A mental health ward is somewhere you would tend to stay for longer, for example from a few days to several weeks, or perhaps even months, and the focus is more on treating you while you’re there, whereas Lotus has a much shorter stay and is thinking about what treatment or services might be best for you going forward. If so, how did the unit compare to staying on a mental health ward?
Suggested prompts: what was similar? What was different? What would you prefer? Are there any advantages of one over the other? Are there any disadvantages of one over the other?
-
Have you had other experiences of accessing mental health support while in crisis (e.g. going to A&E, help from voluntary services in your local community, like mind, crisis cafes, crisis houses)? If so, how does your experience of the decision unit compare?
-
How long did you stay on the unit and where were you discharged to? What role did you have in deciding what happened when you were discharged? (If still on unit, do you know if any plans have been made for your discharge? What about referral to other services? How connected did you feel to your usual support network while on the unit?)
-
What else could the unit have done for you while you were there?
-
Had you heard about the unit before you went there for the first time? (How did the unit compare in reality)?
After your stay
If discharged to a ward:
-
How did it feel going via the decision unit to the ward?
Suggested prompts: How did the decision unit change your feelings about your journey through mental health crisis care? Would you have preferred to go straight to a ward? Do you think the decision unit meant that you spent less time in A&E?
If discharged home:
-
Was there any follow-up from services when you were discharged?
Suggested prompts: If yes, how did you find this follow-up? Was there any other follow-up you would have found helpful?
-
How connected did you feel to your usual support network while on the unit?
Suggested prompts: [If been on a ward before] How does that compare to when you were on a ward? How are things with people in your support network now?
-
Did the decision unit signpost you to other support services (e.g. from voluntary services in your local community like mind, crisis cafes or crisis houses)? How have you felt about that support? Were there any other services that you might have liked to be referred to?
-
What contact, if any, have you had with mental health services since your stay on the decision unit? (e.g. NHS/voluntary in your local community/crisis services) Suggested prompts: What has your experience of using these services been like?
For both ward or home discharge:
-
Has your stay on the mental health decision unit changed what you think about mental health services and how you might use them if you experienced a crisis in the future?
-
Would going to the decision unit be your preferred crisis care route in future, or would you prefer a different route? Why?
-
Did the decision unit change the way you think about things, or make any other change to yourself in any ways we haven’t talked about yet?
-
What are the most important things about the PDU for it to work well do you think?
-
Is there anything else you want to tell us which we haven’t already covered?
Lived experience evaluation
-
As I mentioned at the beginning of the interview, I have lived experience of mental health issues and of using services. How did it feel being interviewed by someone who has this experience?
-
Do you think that you would have answered differently if interviewed by someone who didn’t have this experience? Prompt: In what way? Why do you think this might be?
DECISION project: service user qualitative interview two
Quality of life
I’d like to ask you a few questions now about how things are going generally, I hope that’s ok.
-
How are you feeling at the moment?
Prompt: what is your current living situation? For example, shielding, home alone, carer? Has COVID-19 and the lockdown affected your mental health and well-being? In a negative way? In a positive way? What’s been happening for you in relation to COVID-19 or lockdown? Any significant losses? Recent death? Bereavement? Do you have access to the internet? Confidence with technology? There’s been a lot of social unrest recently including COVID-19, economic uncertainty, and now protesting police violence. How are you feeling in response to what’s happening?’
-
Do you feel settled and secure?
Suggested prompts: what would you say are the reasons you feel that way? Disruption to benefits, housing, job loss? [If appropriate: what might help you to feel more settled and secure?] Impact of media?
-
Do you feel supported?
Suggested prompts: by family, friends, other people in your life, mental health services? Do you live with anyone? [If so, what is your relationship like with them? Has that been affected by COVID-19 and the lockdown?] Is there any support you’d like to have? How has access to your support network change since the pandemic? Access to solicitors? People to help with benefits? [If so, what kind? From who?]
-
Are you able to lead an independent life at the moment?
Suggested prompts: in what ways are you more independent? In what ways are you less independent? For example, daily activities/getting around/accommodation/how has the pandemic impacted this?
-
Are you able to plan ahead? Manage short-term goals?
Suggested prompts: why do you think that might be? How has that changed over the last 9 months?
-
How satisfied with things are you right now?
Suggested prompts: what things are you enjoying? What are you enjoying less? How has that changed over the last 9 months? Are you doing things that you want to do in your life? Are you able to see your friends? What gives you pleasure?
-
What has changed in your life since you went to the decision unit?
-
How is your physical health? – are there any concerns relating to access to physical health care at the moment? (COVID-19)
About the unit
-
How long did you stay on the unit and where were you discharged to?
-
Has staying on the PDU had any impact on your life
-
Have you had any further experiences of crisis since you went to the decision unit?
Suggested prompts: what services did you use, how did you cope with it? How does your experience of the decision unit compare? How has lockdown impacted on you being able to access crisis services? Any inpatient admissions? Any admissions to new MH ED units?
-
We’re interested in how the decision unit compares to other services. Have you had any other experiences with mental health services since your stay on the decision unit? (NHS/charity/other, including inpatient; ask about planned/compulsory admissions as appropriate; emergency/crisis services.) What has your experience of using these services been like?
Suggested prompts: Has there been any change in how you have used these services compared to how you’ve used them in the past?
If has had (an)other stay(s) on the PDU:
-
How have your later stays on the PDU compared to your first?
-
How many stays have you had?
-
What has changed about the unit? (different staff, any other changes, impact of PPE, social distancing measures, COVID-19?)
-
Is it helpful to go back? Why?
-
Has your stay on the PDU affected what happens when you are in mental health crisis? (e.g. what you prefer, your ideas about how long the crisis will last)
For all participants
-
If you could have any kind of help in crisis, what might that look like? (e.g. go to PDU, go directly to a ward, day hospital, crisis café etc.)
-
Are these services available in your area? (How has COVID-19 impacted on these local services in your area? Has the pandemic impacted on whether you feel you can approach services for help?)
-
Has there been any long-term effects of you staying on the PDU? (e.g. any signposting that’s been useful, follow-up services, changes due to therapeutic care there, etc.)
-
Could you describe what might happen if you are in crisis again? (what services might you approach, what services are likely to approach you? what do you typically do when you are really struggling, who do you tell, where do you go for support, what services you go to and where you might be get sent? What impact has your stay on the PDU had on this experience?
-
Would you recommend the PDU to other service users? [if so, why?]
-
Reflecting back, can you think of any good things about the PDU?
-
Can you tell me about anything that might put you off going to the PDU again?
-
Did the decision unit change the way you think about things, or make any other change to yourself in any ways we haven’t talked about yet?
-
Do you know of any recent changes in community services or support?
-
Is there anything else you want to tell us which we haven’t already covered?
Lived experience evaluation
-
As I mentioned at the beginning of the interview, I have lived experience of mental health issues and of using crisis services. How did it feel being interviewed by someone who has this experience?
-
Do you think that you would have answered differently if interviewed by someone who didn’t have this experience? In what way? Why do you think this might be?
DECISION project: PDU staff qualitative interview
(Unit manager, nurse, HCA and psychiatrist consulting to the unit)
A bit about you – a typical working day
-
What made you decide to work on the unit?
-
How long have you worked on the unit? Where did you work before coming to the PDU [substitute name of unit]? What are your career plans/goals? Has working on the unit enabled/prevented you from achieving your career goals? What might the reasons be for you or other staff members to move on from the unit?
-
Can you talk me through what a typical working day might look like for you?
-
How much time do you spend doing paperwork? What kind of paperwork? How much time do you spend with service users? What do you do when you spend time with service users? What other sorts of things do you do as part of your working day (and how much time does that take)?
Prompt: assessment, stabilisation, signposting and therapeutic support and how much time you spend on them
-
What are the rewards and challenges of working on the unit?
-
Has your typical working day changed since COVID-19? In what ways?
-
How has the pandemic impacted on you? Have you remained working on the unit? Where else have you worked? Have you noticed any impact on staffing? NHS being seen as heroes? How safe have you felt? Impact on family members? Appropriate child care?
-
[If relevant] What impact has the creation of the new mental health ED had?
-
Your role? Impact on patients? Impact on the role of the PDU generally?
Staff support and team working
-
How supported do you feel in your role? What support do you currently receive? What support would you like?
-
What might prevent you from getting support? Emotional, occupational, training? Do you feel supported to make assessments and important decisions about service users in crisis? Do you have reflective spaces? Can you describe the supervision you receive? How do you make use of supervision?
-
Do you feel that what you do is valued?
-
Who is it valued/not valued by? Why do you think this is? How are important decisions made on the unit? Are your opinions valued? Who would you say has the most say in terms of how the unit is run? Who makes decisions about assessment and discharge of patients?
-
What roles make up the PDU team currently? Who would you like to see working on the unit?
Prompt: what kinds of staff would you like to work on the unit? Activity workers? Other types of staff? Why?
-
What does it feel like to work in your current team?
-
How are staff disagreements resolved? What impact does having agency/bank staff have on the unit? Staff sickness/absence?
-
Has COVID-19 had any impact on how supported you feel or what it is like to work in your current team? How so? Do you feel that you have been provided with adequate PPE? Did you feel able to take time off?
Unit efficacy
-
How would you describe the main purpose of the unit?
-
How does working on this type of unit compare to working on other types mental health units? Do you think the PDU makes a difference? If so, in what ways? Is there anything else you would like the PDU to do?
-
Can you tell me about your experiences of people in acute mental health crisis?
-
What do you think are the important things for their care at the time of crisis?
-
How would you best describe the work that you do with service users on the unit? Is it therapeutic, or focused on assessment, or onward referral? Do you feel that is the best use of your time and expertise, or are there other things you feel that you might do better? What kind of therapeutic work might you do with service users?
-
What is the typical type of service user who goes to the PDU? [Why?] What role do you have in deciding if an individual is appropriate? What sorts of discussions do you have with referring/gatekeeping staff? Who do you think the unit works well for? Who does the unit not work so well for?
-
Do you feel that the service users referred to the unit are appropriate?
-
What happens if you think a referral isn’t appropriate? Why do you think the wrong people might be referred sometimes? Pressures that influence these decisions? What happens to homeless service users? What about service users who have issues with alcohol/substance misuse? How do you feel about service users with these kinds of problems?
-
How much do referred service users tend to know about the unit when they arrive?
-
What are their expectations of the unit? Are these manageable? What kind of information would you usually give to a service user about the unit when they arrive?
-
What might help to resolve people’s mental health crisis while they are on the unit?
-
What might exacerbate people’s mental health difficulties while on the unit?
-
What are the benefits/disadvantages of having the PDU linked to 136 suite?
-
What are the benefits/disadvantages of being located in the acute hospital/near the ED/at the psychiatric hospital?
-
How often do service users breach the maximum stay allowance? If so, why does this happen?
-
Do you think service users are always ready to be moved on from the unit? If so, why? Are there other pressures here? If so, how do you feel about that? What prevents service users moving on from the unit? What helps service users to move on from the unit?
-
How do you support service users who attend the unit more than once?
-
Is that type of support different to the support you might offer a first attender? How do you feel about these service users?
-
Do unit staff engage with family members and/or carers? If so, how?
-
How do family members feel about the unit?
-
Do you think there have been any changes to the PDU’s effectiveness as a result of COVID-19? How about any impact on how service users in crisis present to the unit?
-
Are you seeing an increase in service users experiencing domestic violence? Increase in specific kinds of distress? Impact of shielding versus standard social distancing measures for service users?
Impact on crisis care pathway
-
Why do you think some people are referred to the mental health decision unit and not others?
-
What is different about these people? What is the criteria? Is the criteria always kept to? What else can affect the pathway – for example, no space at the unit, no beds on wards?
-
Could you tell me a bit about referring people on from the unit?
-
Where do they go? What influences your decisions around this? Are you able to signpost to other services? What helps/hinders this? What do you think of these services and what they can provide? Who do they work well for? Who do they not work as well for?
-
Do you think the PDU helps reduce unnecessary admissions to mental health wards? What about mental health presentations at ED or wait time at ED? If so, how?
-
How has the PDU affected the crisis care pathway as a whole?
-
What are the advantages/disadvantages of having an PDU? Are there any ways in which you think the PDU might work better?
-
Has COVID-19 had any impact on the referral process, either to or from the unit? How about the crisis care pathway as a whole, and the PDU’s role in the pathway?
-
Has there been changes to services you can signpost to due to COVID-19? If so, how do you think this affects service users?
-
Is there anything else you want to tell us about that we haven’t already covered?
Lived experience evaluation
-
As I mentioned at the beginning of the interview, I have lived experience of mental health issues and of using crisis services. How did it feel being interviewed by someone who has this experience?
-
Do you think that you would have answered differently if interviewed by someone who didn’t have this experience? In what way? Why do you think this might be?
DECISION project: referral pathway staff qualitative interview 2
(CRHT staff, liaison psychiatry, mental health nurse, approved mental health professional)
A bit about you
-
Can you tell me a bit about your role?
-
How long have you been in your current role? What did you do before this role?
-
Could you talk me through what a ‘typical’ day might look like for you with regards to working with mental health patients?
-
What did you do during your last shift for example?
-
Why do you think people need crisis mental health services?
-
What are the kinds of difficulties you see in your day to day work? Are there any kinds of issues that take up more/less time?
-
Has your role or typical working day changed at all since COVID-19? In what ways?
-
Any increase/decrease in specific kinds of distress?
Crisis pathways
-
How do people in mental health crisis come to be seen/assessed by you?
-
Who is initiating contact with services? Can you give a few examples of a patient’s journey to see you and what might happen? How much does the family/living/social situation influence this?
-
Who decides where a patient goes in the MH crisis pathway?
-
Is the decision a joint one? What is your role in this process? What can go wrong in terms of referrals to different parts of the pathway? Why? How might this be resolved?
-
How are the needs of people in acute mental health crisis assessed in your experience?
-
Who carries out these assessments? What are the different ways assessment can happen? What about formal and informal assessment?
-
Could you tell me a bit about patient risk?
-
How is this assessed? Are there any issues around more ‘risky’ patients? What options do you have in terms of reducing patient risk?
-
Are there any other schemes/services in place that can support patients in crisis?
-
How do these differ from PDU? Do you have CQIIN for example?
-
Has COVID-19 had any impact on the crisis pathway? For example, how decisions are made about patient care or other services which support patients in crisis?
-
[If relevant] Can you tell me a bit about the new MH ED unit/space and how it came to be?
-
How is it working? Any issues? Do you think it will stay after the pandemic?
PDU – referrals
-
How would you describe the main purpose of the PDU [name of unit]?
-
Have you been involved in any referrals to the mental health decision unit?
-
Could you talk me through that process and what it was like? Why are you referring these particular patients to the PDU? Who makes the final decision? Are there ever disagreements about this? How are they resolved? How much information would you usually give to a service user about the unit when you refer them there?
-
What types of problems/distress do people have in order for you to refer them on to the PDU?
-
Are there any issues that people might have which would exclude them from referral to the PDU? What might prevent you from referring a patient to the PDU? What happens to people if the referral isn’t accepted? What happens if people are homeless?
-
Why are some people referred to the mental health decision unit and others not?
-
Why are some people referred and others not? What are the criteria? How clear is it? Are the criteria always kept to? Are people referred for the reasons the unit was set up for? If not, why not? What are the pressures that influence these decisions? What else can affect the pathway – for example, no space at the unit, no beds on wards?
-
What other services can you refer/transport patients to if they are experiencing a mental health crisis?
-
Crisis houses? Crisis cafes? What exists locally? Are there any problems/restrictions with using these services? What do you think about these services? Who do they work well for? Who do they not work so well for?
-
How much time do you spend on referrals?
-
Which aspects are the most time consuming?
-
Has COVID-19 had any impact on the PDU or the referral process? What about available services to refer on to?
PDU – efficacy
-
What were your ideas about the function of the unit before it was established? (How did the unit compare in reality)?
-
Do you think the PDU addresses the reasons that patients are in mental health crisis?
-
Can you give an example? If not, why do you think this is?
-
What impact does the PDU have on the perceived risk level of patients?
-
Does it feel less risky to refer to the PDU? Why might this be? Which patients might this apply to?
-
Do you think the PDU helps reduce unnecessary admissions to mental health wards? What about mental health presentations or wait time at ED? If so how? If not, why might do you think this?
-
What impact (if any) has the unit had on out-of-area placements (psychiatric inpatient admission sent to other trusts)? Why?
-
Some people might be described as ‘frequent attenders’ at ED or inpatient wards, who are these people? Do you feel that the PDU has had any impact in terms of the ‘most problematic patients’/frequent attenders? If so, how? If not, why not?
-
What are the PDU services strengths and key challenges?
-
How has the PDU affected the crisis care pathway as a whole?
-
What are the advantages, if any, of having an PDU to the crisis care pathway?
-
What are the disadvantages, if any, of having an PDU to the crisis care pathway?
-
Are there any ways in which you think the PDU might work better?
-
Do you think there have been any changes to the PDU’s effectiveness as a result of COVID-19?
-
Do you have any concerns about how things will be after the pandemic?
-
Impact on crisis pathway? Resources? Staffing levels? Impact on how staff feel?
-
Is there anything else you want to tell us about which we haven’t already covered?
Lived experience evaluation
-
As I mentioned at the beginning of the interview, I have lived experience of mental health issues and of using services. How did it feel being interviewed by someone who has this experience?
-
Do you think that you would have answered differently if interviewed by someone who didn’t have this experience? In what way? Why do you think this might be?
DECISION project: non-direct-referral pathway staff qualitative interview 1
(Paramedic staff, police, ED nurse, ED manager, street triage, crisis vehicular response)
A bit about you
-
Can you tell me about your current role?
-
How long have you been in this role? Where were you based before?
-
What is your role in relation to patients experiencing a mental health crisis?
-
For example, do you wait with them in A&E, once seen by psychiatry, do you wait with them to be referred to mental health units, do you accompany service users when they are being transferred from A&E to mental health units. If not admitted, do you drive service users home/somewhere else? Do you feel that your role overlaps with any other staff members?
-
How much time do you spend dealing with people in mental health crisis in contrast to physical health?
-
What is the most time-consuming aspect? How do you think this might be improved? Has the pandemic impacted this at all?
-
How does your role fit alongside what mental health staff do? What are your experiences like of working with mental health staff?
-
Has COVID-19 had any impact on your role with patients in mental health crisis, the amount of time you spend with these patients or how mental health staff work in patients in crisis?
People in mental health crisis
-
What kind of problems do people in mental health crisis present with?
-
Are there any differences in how you work with people with different types of problems? How do you feel about service users who are sometimes defined as ‘frequent attenders’?
-
How do people in mental health crisis come in contact with you?
-
Who is initiating contact with services? How much does the family/living/social situation influence this?
-
What do you do when you think a person in crisis needs to be admitted?
-
Where do you send/take the person? Why? What is the fastest way to get a patient seen?
-
How are the needs of people in acute mental health crisis assessed in your experience?
-
What are the different ways assessment can happen? What about formal and informal assessment?
-
Could you tell me a bit about what it feels like to work with people experiencing a mental health crisis?
-
Do you feel supported? Emotional support? Training?
-
Has COVID-19 had any impact on people in mental health crisis and how you work with them?
-
Are there any new services since the pandemic that you now work with?
Transfers and pathways
-
Can you tell me a bit about what happens when people have to be transferred?
-
Where might they be transferred? Do they have to wait? Are there delays? If so why? What is the impact of waiting/delays on a patient’s mental health?
-
Some people experiencing mental health crisis go to ED or come into contact with services multiple times; what do you think services might do better to support these people?
-
Can you tell me a bit more about the mental health crisis pathway?
-
What do different parts of the pathway do?
-
Do you have opportunities to communicate with other staff who work in different parts of the crisis pathway?
-
What kinds of things can impact on patients getting the help they need?
-
What else can affect the pathway – For example, no space at the unit, no beds on wards?
-
What other services can you refer/transport patients to if they are experiencing a mental health crisis?
-
Crisis houses? Crisis cafes? What exists locally? Are there any problems/restrictions with using these services? What do you think about these services? Who do they work well for? Who do they not work so well for?
-
Has COVID-19 made any changes to transfers to other services or the mental health crisis care pathway?
-
[If relevant] How has the creation of the new mental health ED space impacted on the referral process?
PDUs
-
Can you describe what a [PDU] is? Do you know about [name of unit]?
-
What is your understanding of the role of the PDU?
-
Where did you first hear about it? What function does it serve? Who is it designed for? Where is the unit located? How do you refer into the unit if you need to?
-
Do you think the PDU/PDU in your service is effective?
-
In what way? How does it meet the needs of people experiencing mental health crisis that you come into contact with? If not, what are the barriers to it working well? Does it (how does it) prevent people from coming back into ED?
-
Have you been involved in any referrals to the mental health decision unit?
-
Can you describe what this was like? What worked well and what might have been done differently?
-
What were your ideas about the unit before you went there (or supported people to transfer there) for the first time? (How did the unit compare in reality)?
-
Is there anything else you would like the PDU to do?
-
Has COVID-19 impacted on the PDU and its effectiveness in any way?
-
Is there anything else you want to tell us about which we haven’t already covered?
Lived experience evaluation
-
As I mentioned at the beginning of the interview, I have lived experience of mental health issues and of using services. How did it feel being interviewed by someone who has this experience?
-
Do you think that you would have answered differently if interviewed by someone who didn’t have this experience? In what way? Why do you think this might be?
Appendix 4 Additional interrupted time series data and seconday outcomes
FIGURE 16.
Monthly number of PDU attendances according to MHT site.
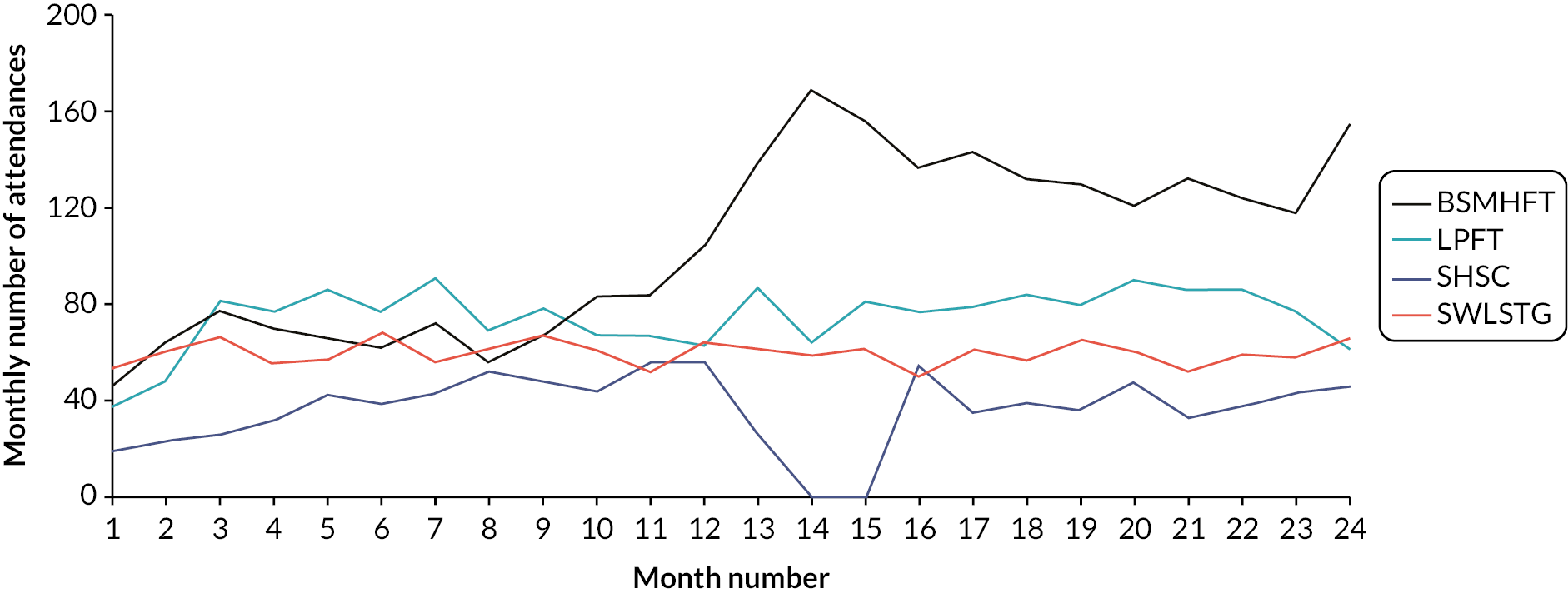
FIGURE 17.
Impact of PDU implementation on total acute adult psychiatric admissions in BSMHFT.

| Service users | BSMHFT (n/year) | LPFT (n/year) | SWLSTG (n/year) | |||
|---|---|---|---|---|---|---|
| Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | |
| Inpatient admission | 1775.0 (1339.5) | 1767.5 (1317.5) | 611.5 (470.0) | 648.0 (479.5) | 1580.0 (1122.5) | 1575.0 (1112.5) |
| Previous admission < 24 months | 1392 (39.2) | 695.5 (39.2) | 214.5 (35.1) | 249.5 (38.5) | 704.5 (44.6) | 692.5 (44.0) |
| Female sex | 703.0 (39.6) | 785.0 (44.4) c | 254.0 (41.5) | 249.5 (38.5) | 805.5 (51.0) | 748.5 (47.5) b |
| Age, years (mean, SD) | 39.0 (13.1) | 38.4 (12.3) | 38.7 (13.1) | 38.5 (13.1) | 40.4 (14.1) | 40.3 (14.1) |
| 18–24 years | 287.0 (16.2) | 242.0 (13.7) | 110.0 (18.0) | 110.5 (17.1) | 244.5 (15.5) | 240.0 (15.2) |
| 25–64 years | 1439.5 (81.1) | 1497.5 (84.7) | 495.0 (80.9) | 526.5 (81.3) | 1243.0 (78.7) | 1241.0 (78.8) |
| 65+ years | 49.0 (2.8) | 28.0 (1.6) c | 6.5 (1.1) | 11 (1.7) | 92.5 (5.9) | 94.0 (6.0) |
| Legal status of admission | ||||||
| Informal acute adult | 871.5 (49.1) | 825.0 (46.7) | 440.0 (72.5) | 327.5 (51.1) | 866.0 (54.8) | 722.5 (45.9) |
| Formal acute adult | 904.0 (50.9) | 942.5 (53.3) a | 166.5 (27.5) | 314.0 (48.9) c | 714.0 (45.2) | 852.5 (54.1) c |
| Length of inpatient stay | ||||||
| Five days or less | 187.5 (10.6) | 196.5 (11.1) | 85.5 (14.0) | 112.5 (17.4) a | 336.0 (21.3) | 275.5 (17.5) c |
| Median days (IQR) | 27.1 (12.2–64.8) | 26.0a (11.0–62.0) | 22.5 (9.2–48.8) | 21.1 (8.7–44.8) | 18.0 (6.0–48.8) | 22.0c (8.0–53.0) |
| Daily bed occupancy (mean, SD) | 628.8 (21.0) | 650.6 (11.1) c | 64.4 (3.9) | 68.6 (3.8) c | 152.0 (11.7) | 158.9 (5.2) c |
| Out-of-area admissions | – | – | – | – | 75.5 (4.8) | 47.0 (3.0) c |
| Liaison psychiatry | ||||||
| Episodes from ED (service users) | 6924.5 (4553.5) | 7967.5 (5092.0) | 1486.0 (1182.7) | 1893.5 (1028.0) | 3590.0 (2575.0) | 4800.5 (3336.0) |
| Previous episode < 24 months | 3225.5 (46.6) | 3935.0 (49.4) c | 451.3 (30.4) | 711.5 (37.6) c | 1835.3 (38.3) | 1925.0 (40.1) a |
FIGURE 18.
Impact of PDU implementation on percentage of compulsory acute adult psychiatric admissions in BSMHFT.
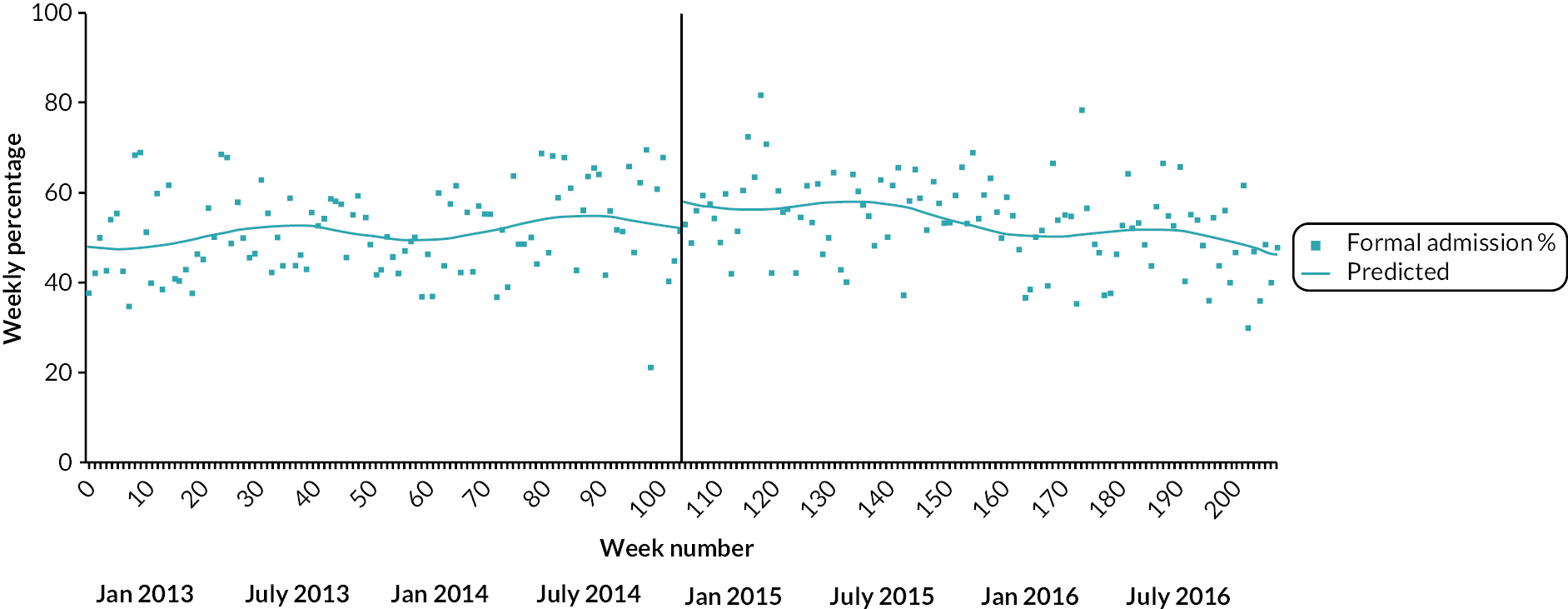
FIGURE 19.
Impact of PDU implementation on percentage of acute adult inpatient stays of 0–5 days in BSMHFT.
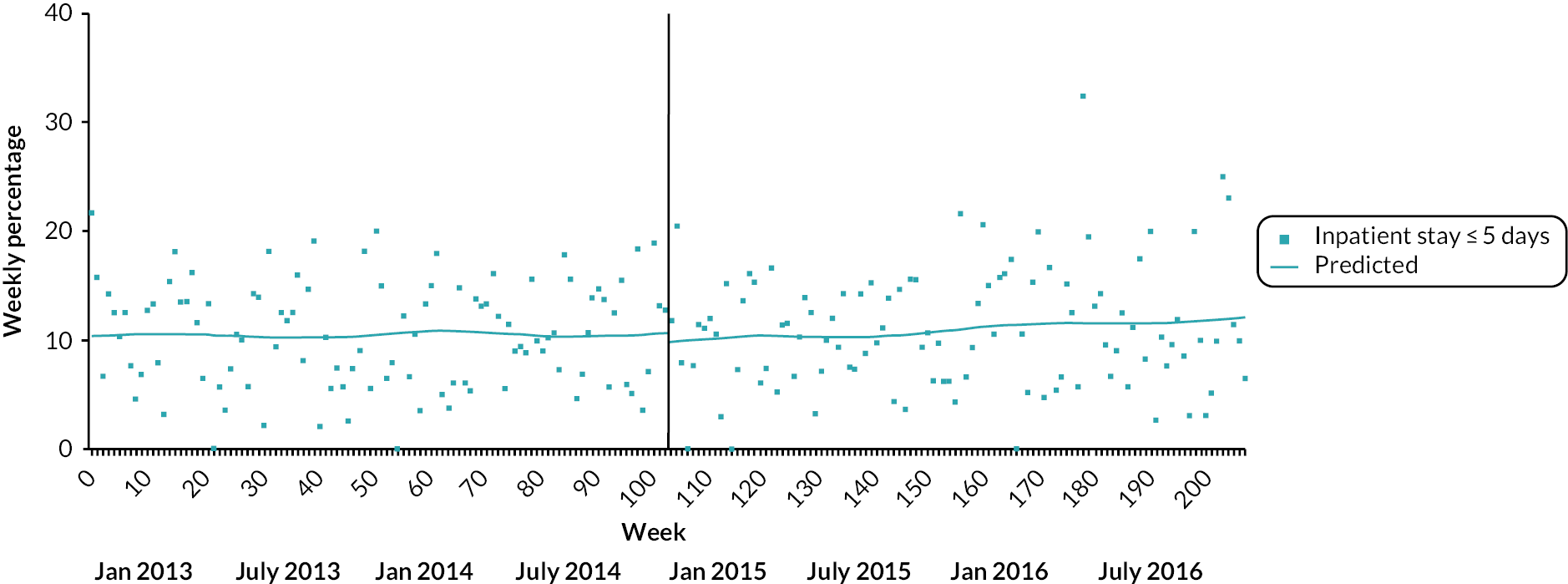
FIGURE 20.
Impact of PDU implementation on (log) mean length of acute adult inpatient stays in BSMHFT.
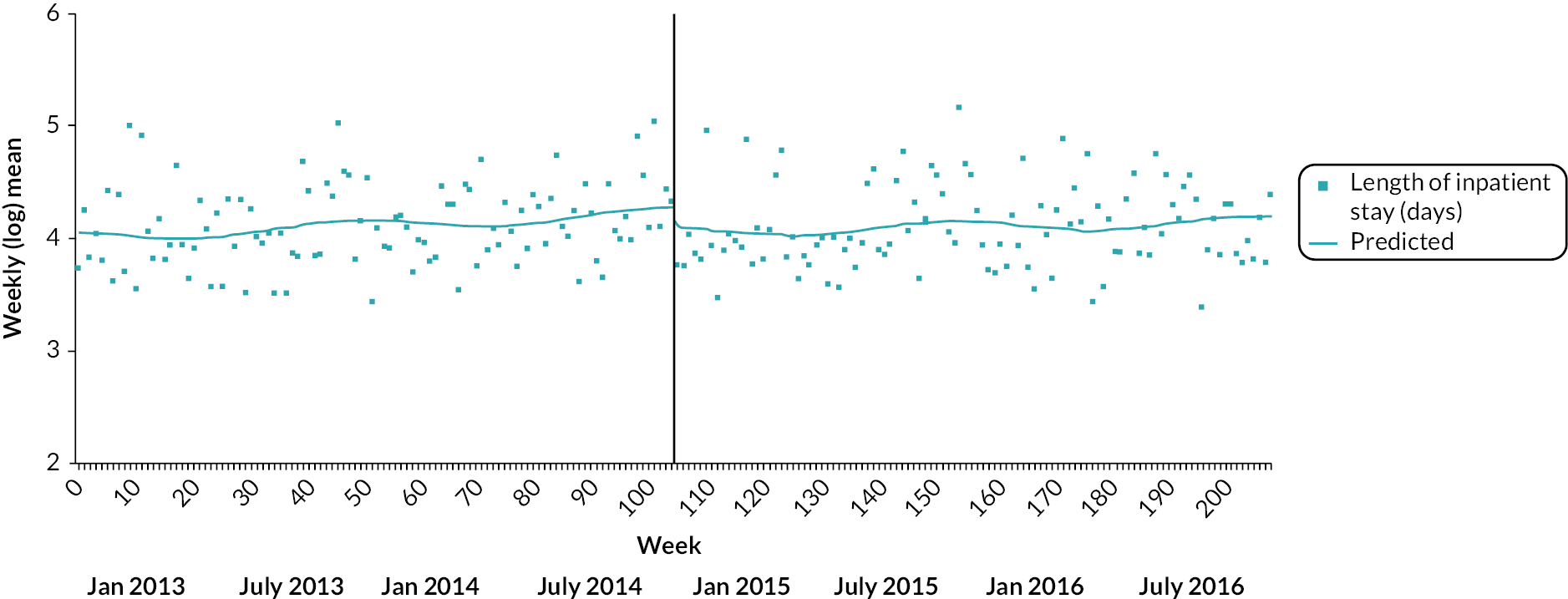
FIGURE 21.
Impact of PDU implementation on mean daily bed occupancy in BSMHFT acute adult inpatient wards.
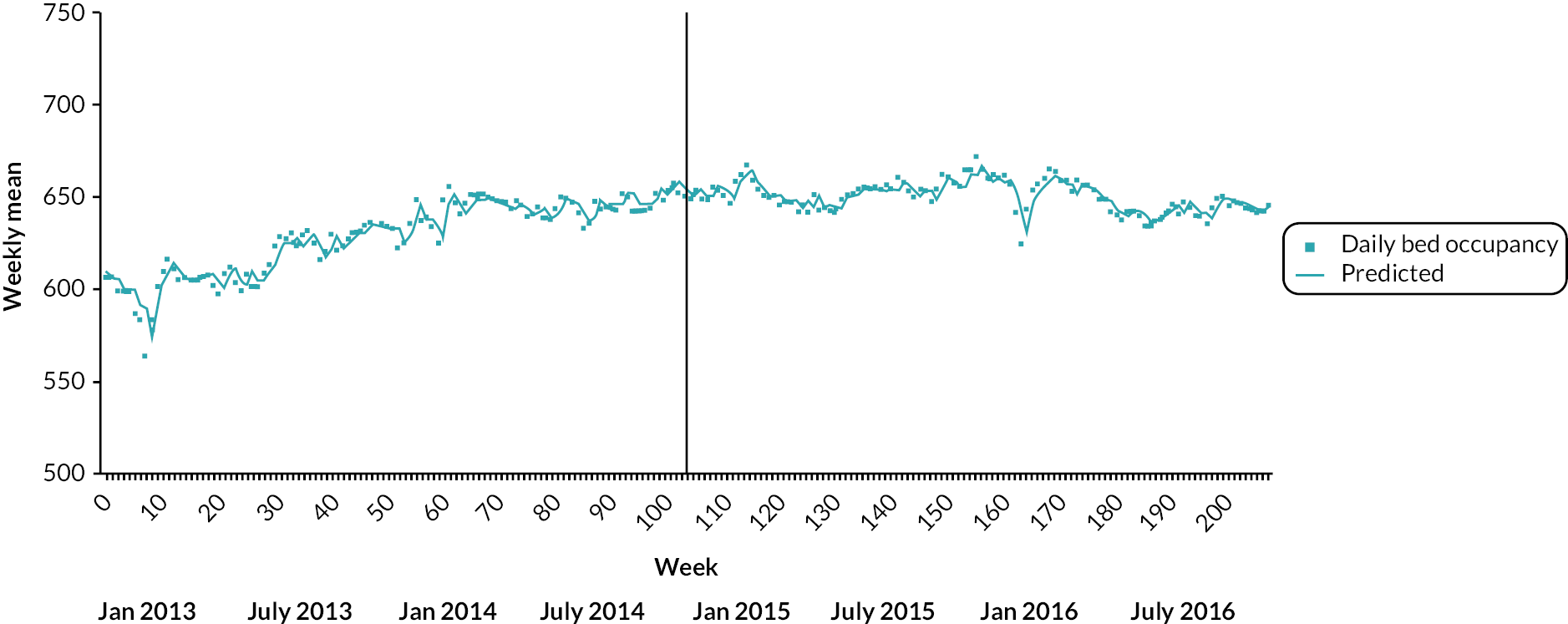
FIGURE 22.
Impact of PDU implementation on ED-referred PLEs in BSMHFT.
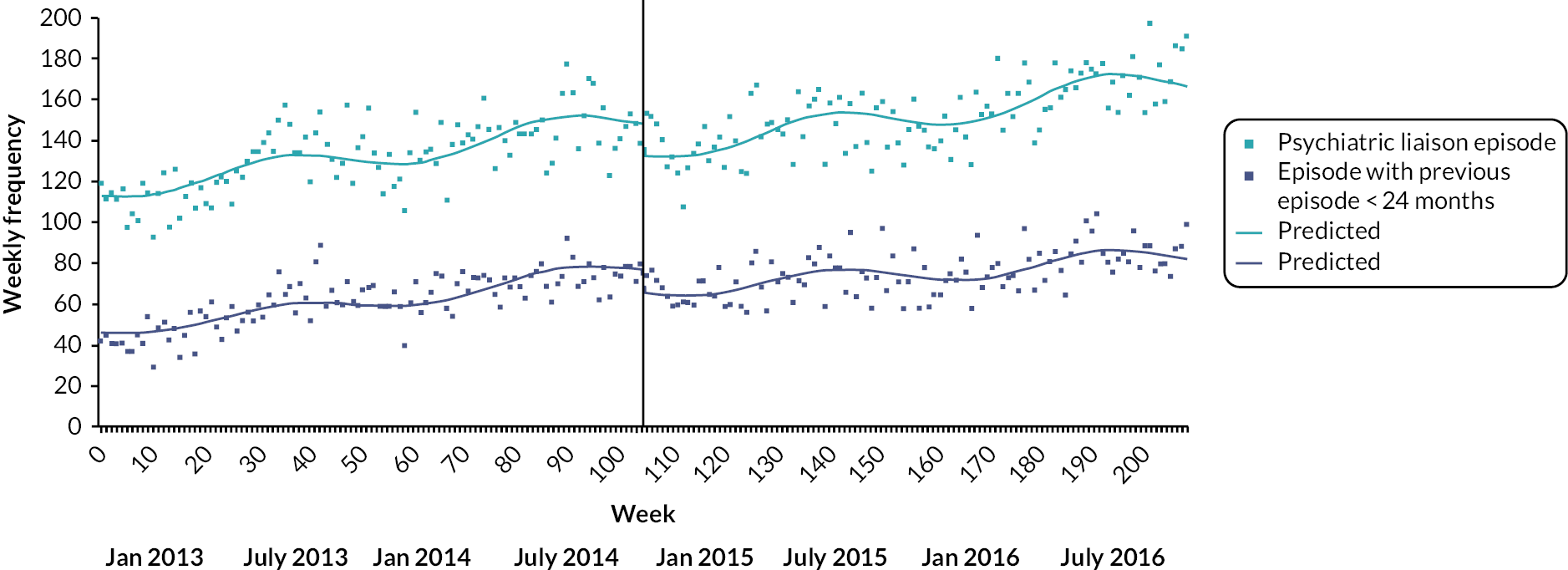
FIGURE 23.
Impact of PDU implementation on informal acute adult psychiatric admissions in LPFT for service users with a previous admission in the last 24 months.
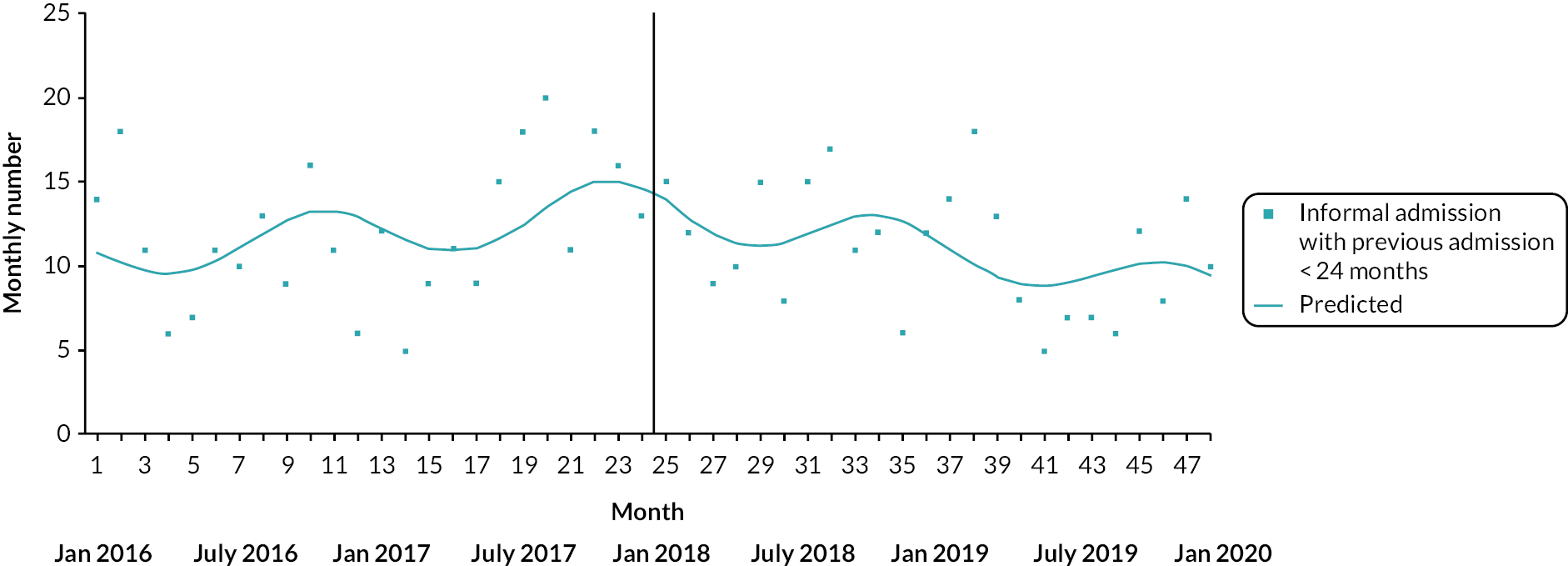
FIGURE 24.
Impact of PDU implementation on total acute adult psychiatric admissions in LPFT.
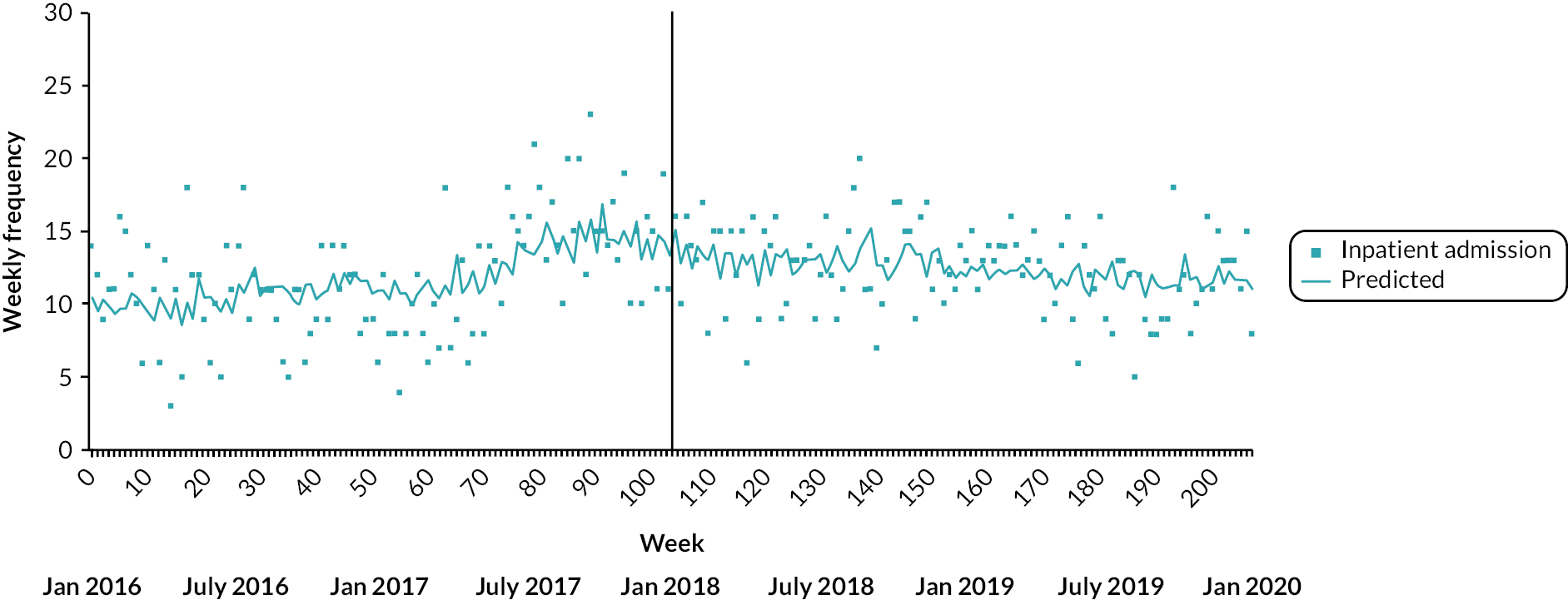
FIGURE 25.
Impact of PDU implementation on percentage of compulsory acute adult psychiatric admissions in LPFT.

FIGURE 26.
Impact of PDU implementation on percentage of acute adult inpatient stays of 0–5 days in LPFT.
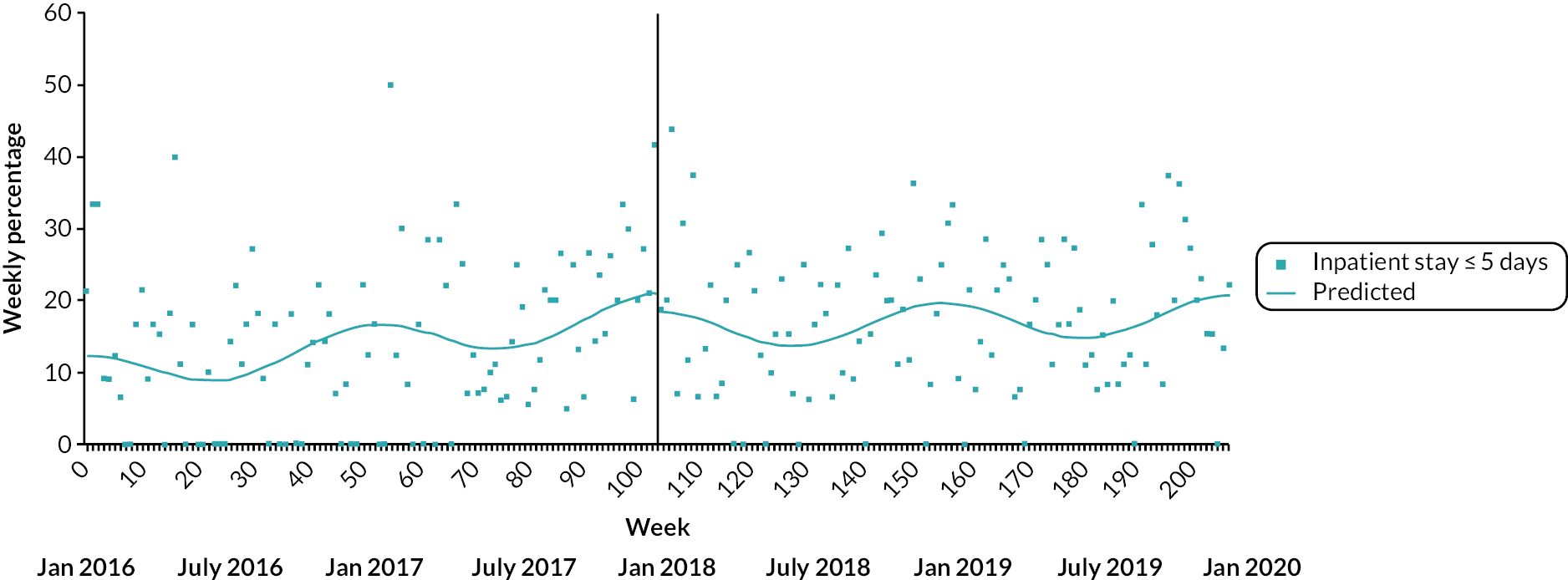
FIGURE 27.
Impact of PDU implementation on (log) mean length of acute adult inpatient stays in LPFT.
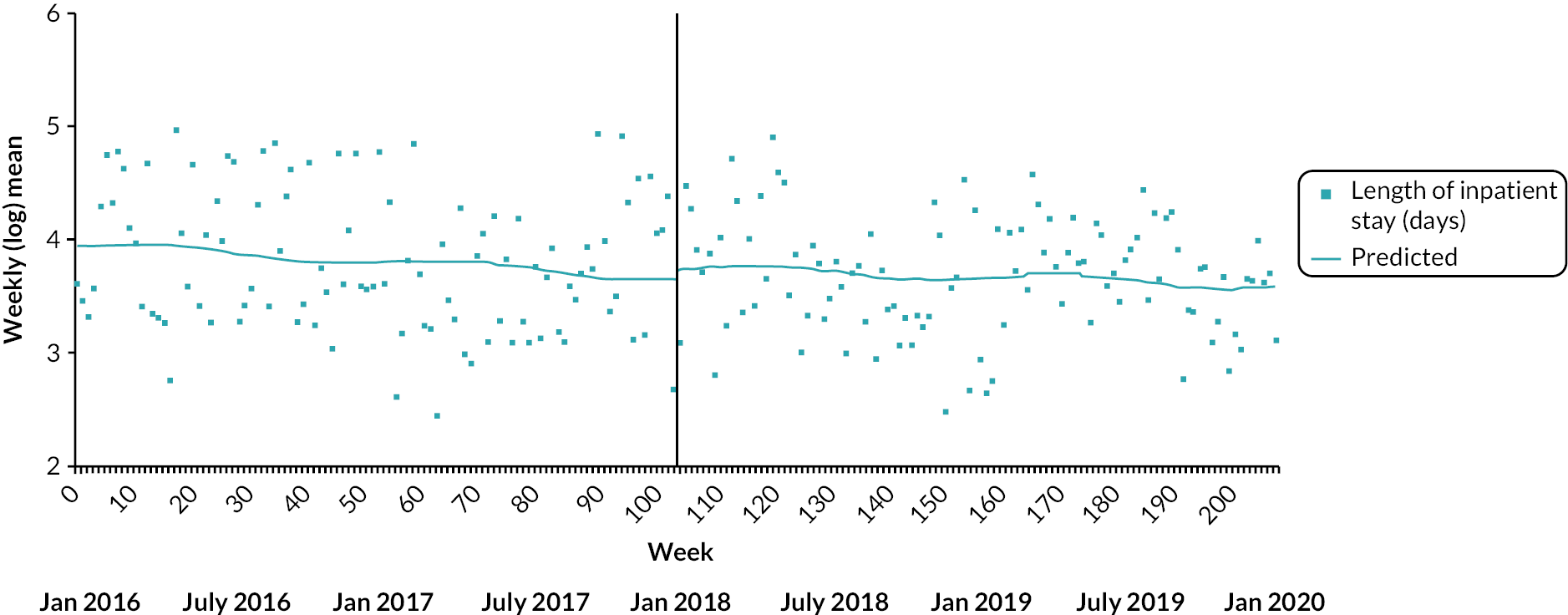
FIGURE 28.
Impact of PDU implementation on meant daily bed occupancy in LPFT acute adult inpatient wards.

FIGURE 29.
Impact of PDU implementation on ED-referred PLEs in LPFT.
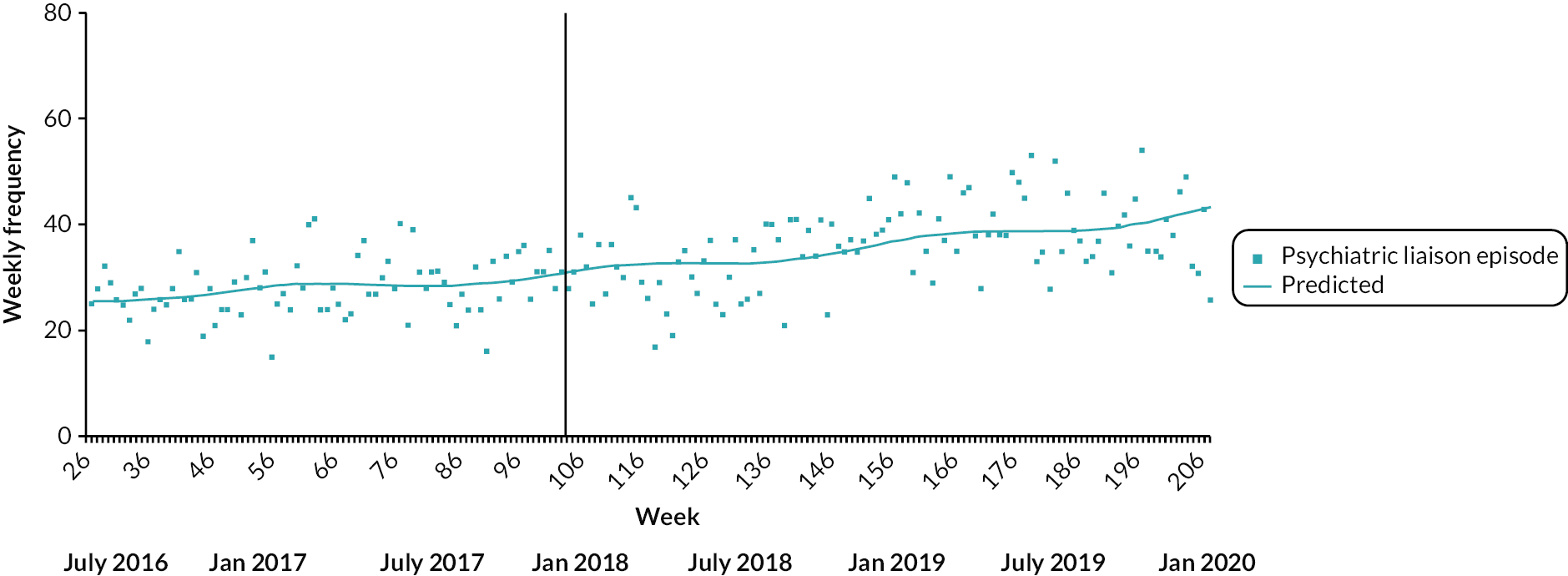
FIGURE 30.
Impact of PDU implementation on ED-referred PLEs in LPFT for service users with a previous episode in the last 24 months.
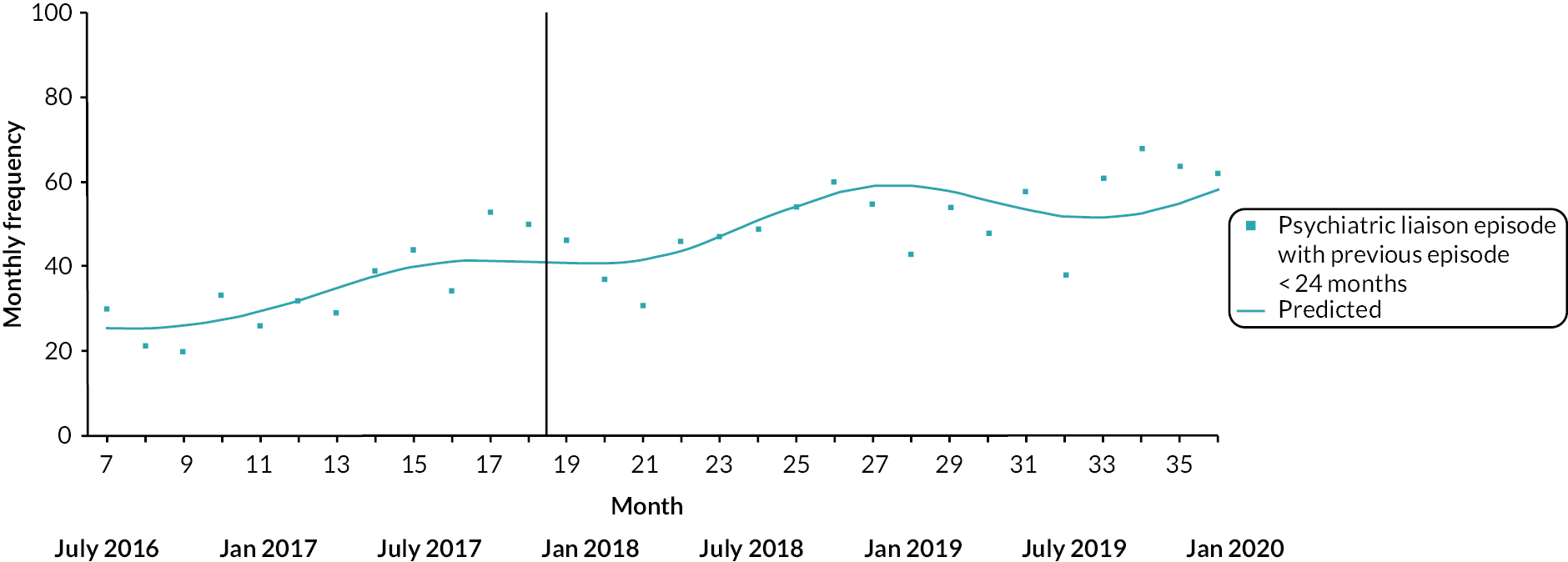
FIGURE 31.
Impact of PDU implementation on total acute adult psychiatric admissions in SWLSTG.
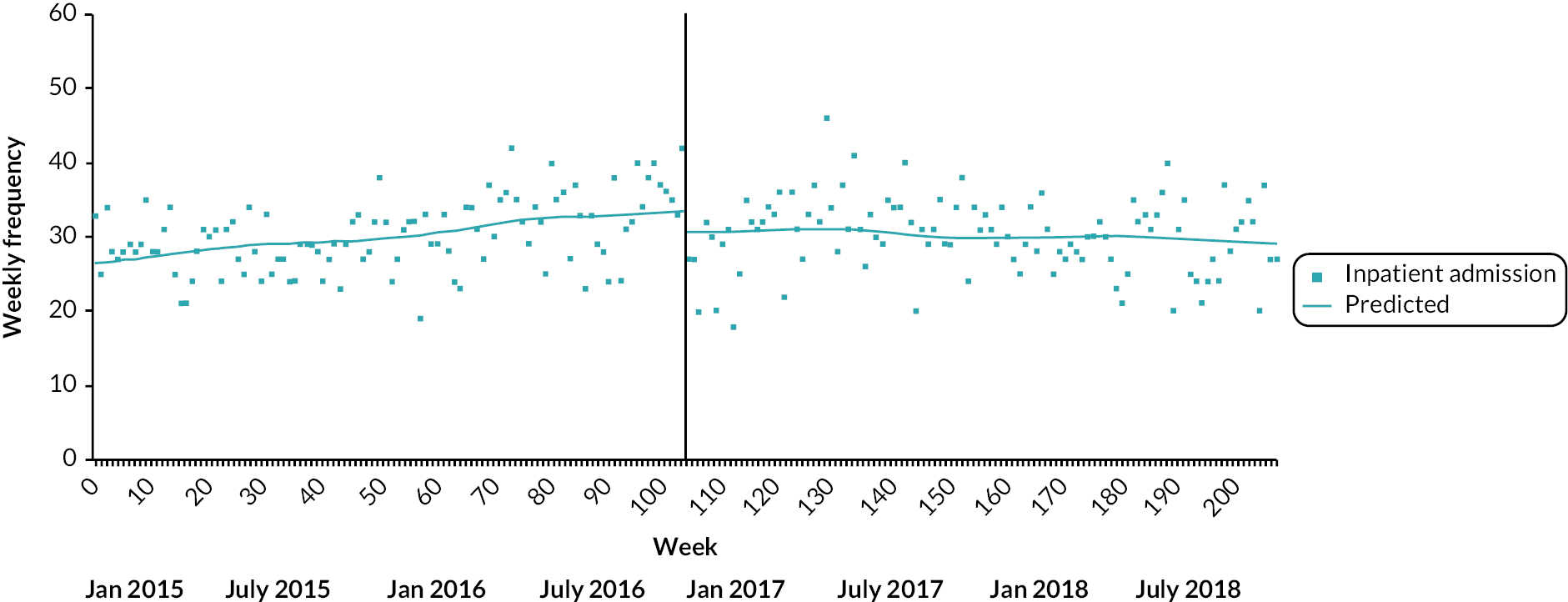
FIGURE 32.
Impact of PDU implementation on percentage of compulsory acute adult psychiatric admissions in SWLSTG.
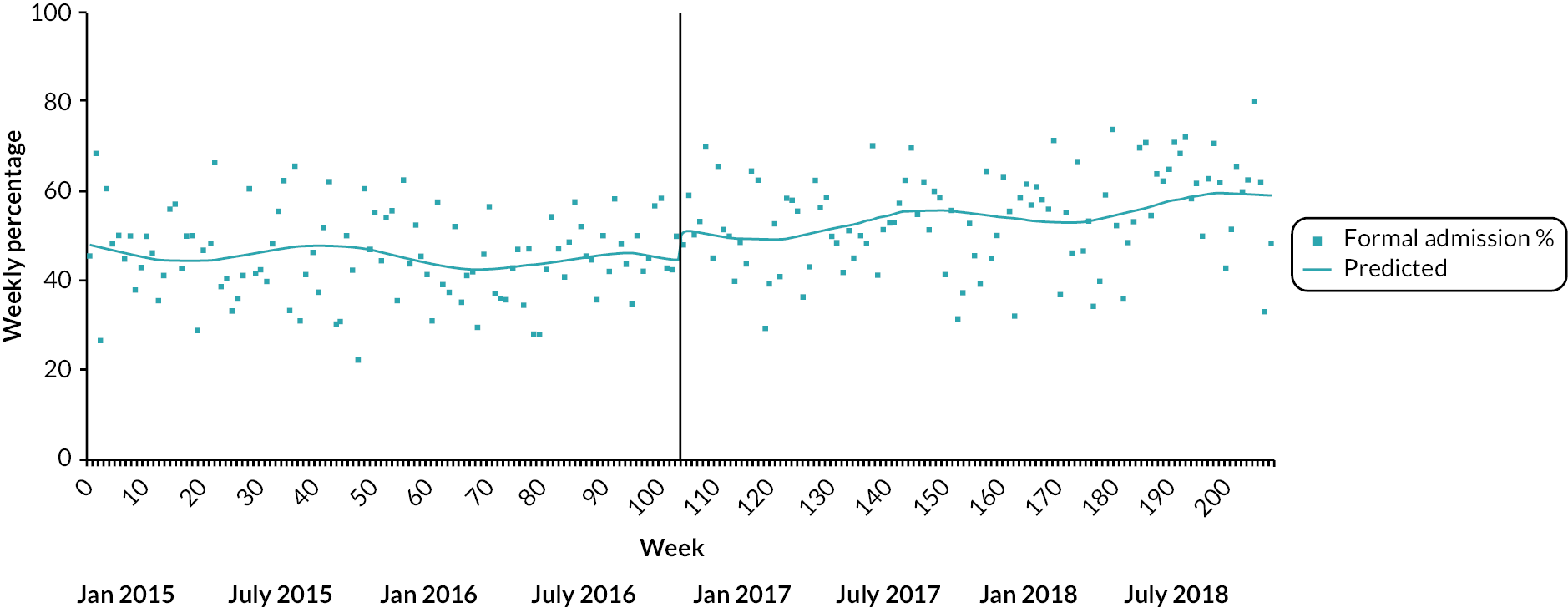
FIGURE 33.
Impact of PDU implementation on percentage of acute adult inpatient stays of 0–5 days in SWLSTG.
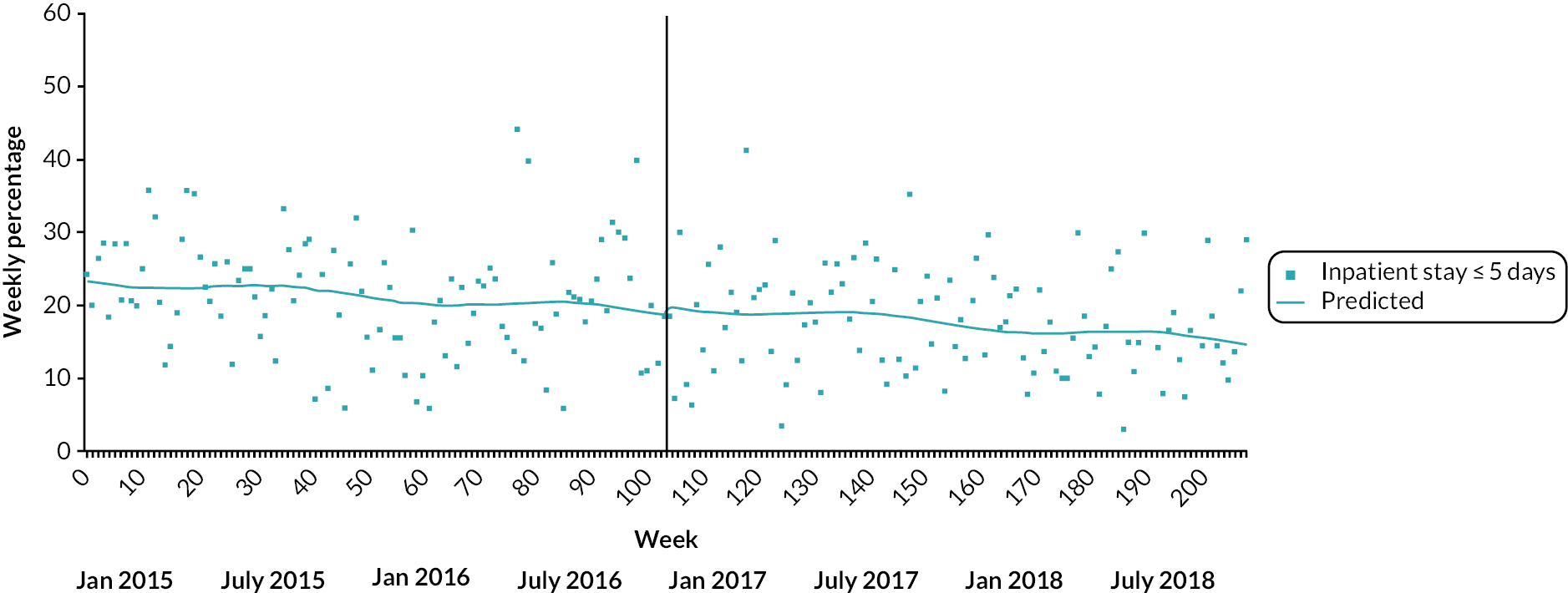
FIGURE 34.
Impact of PDU implementation on (log) mean length of acute adult inpatient stays in SWLSTG.
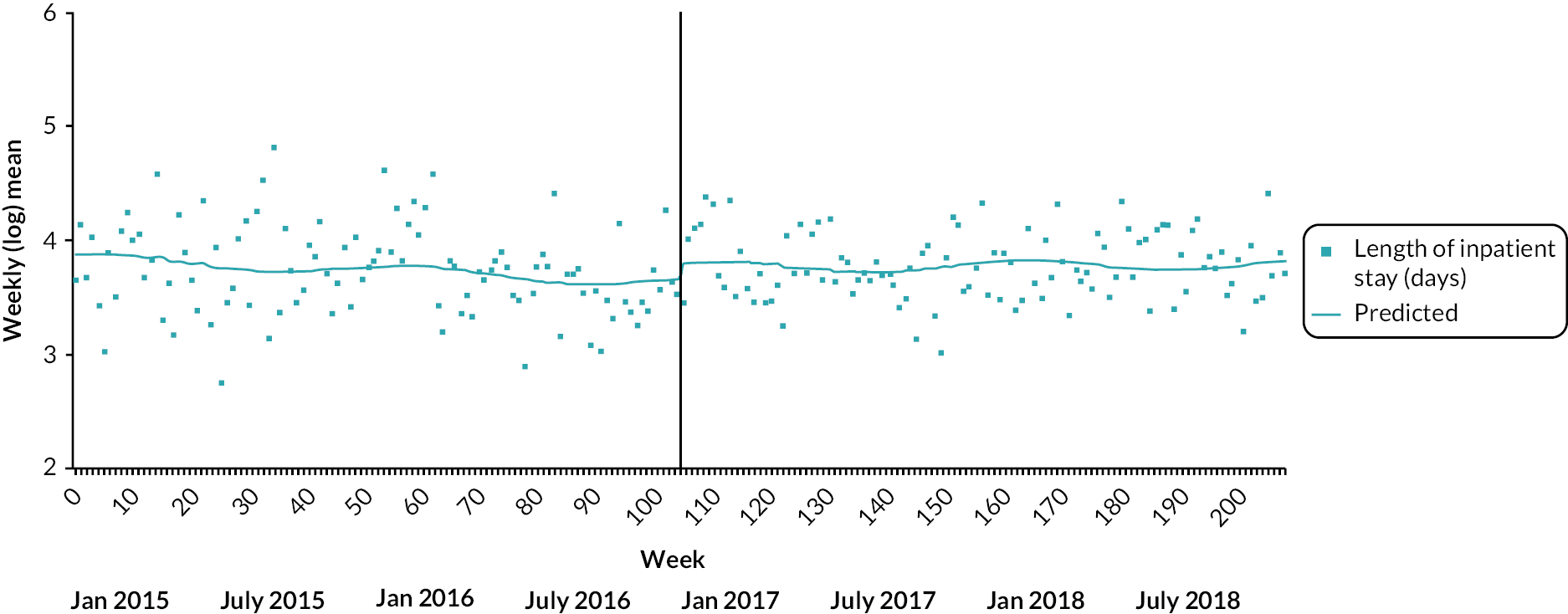
FIGURE 35.
Impact of PDU implementation on mean daily bed occupancy in SWLSTG acute adult inpatient wards.

FIGURE 36.
Impact of PDU implementation of ED-referred PLEs in SWLSTG.
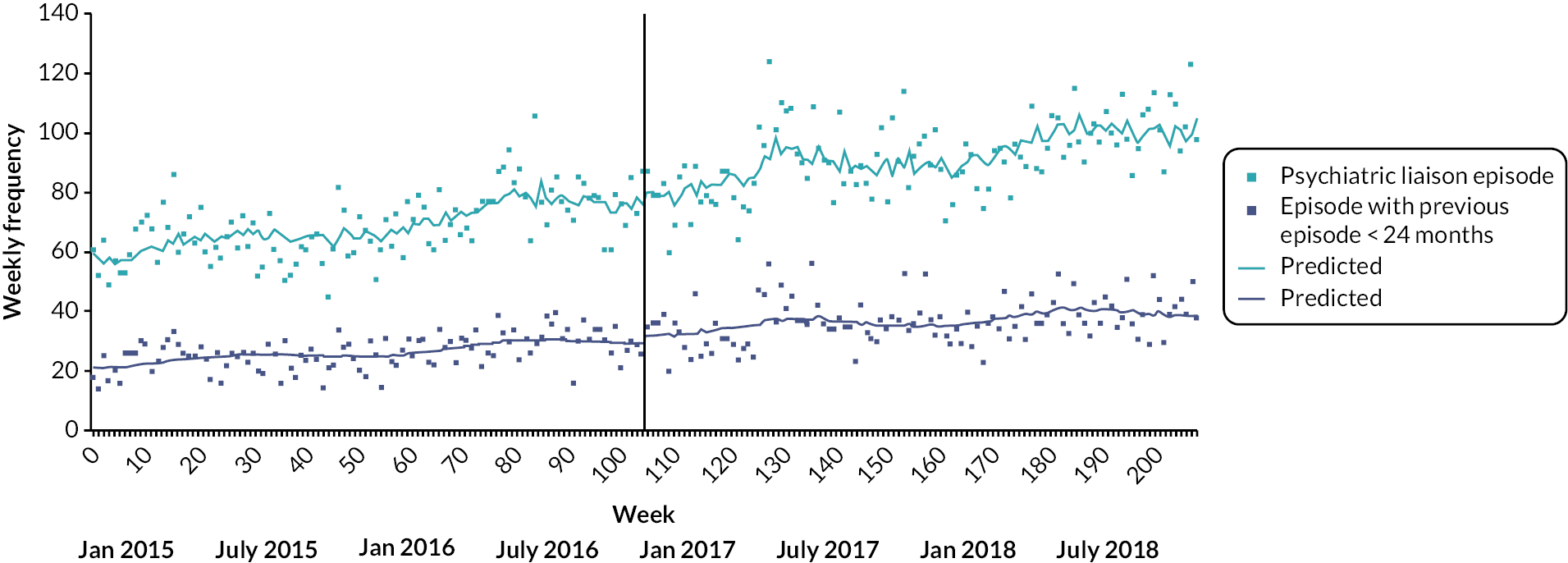
FIGURE 37.
Impact of PDU implementation on weekly numbers of ED mental health attendances with arrival by ambulance or police in SWBHFT.
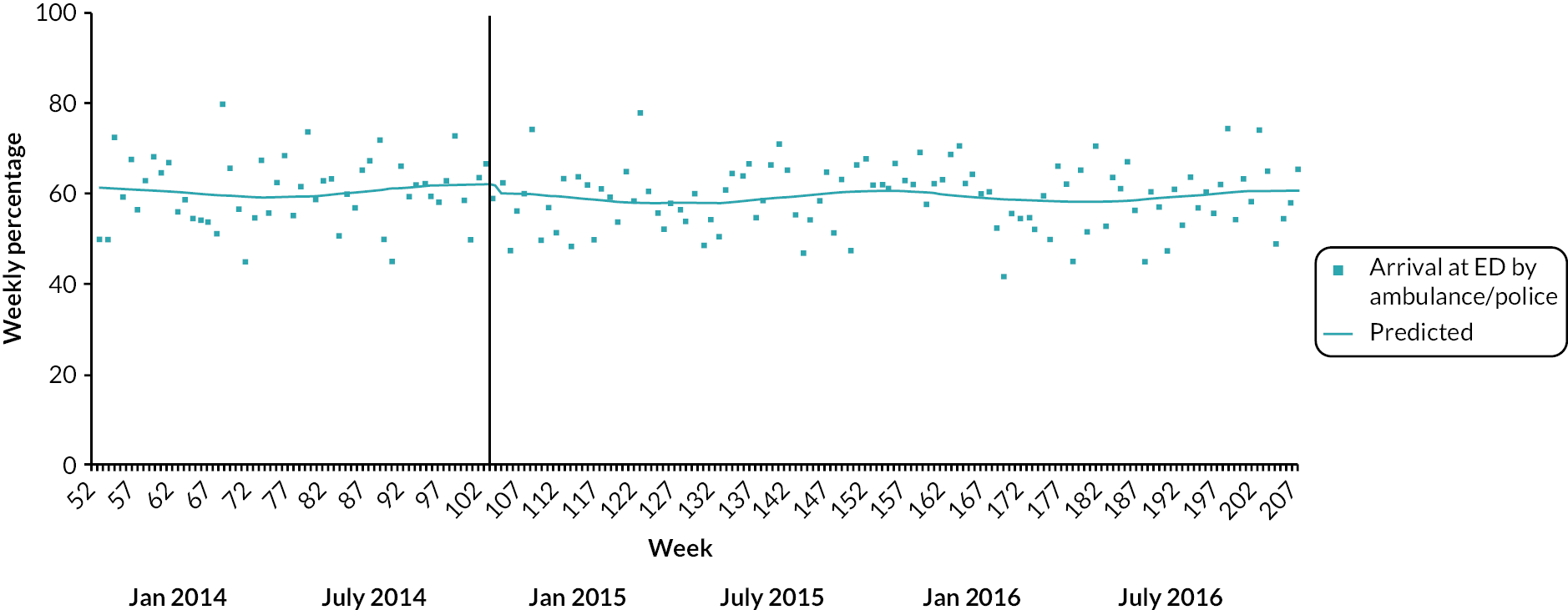
FIGURE 38.
Impact of PDU implementation on weekly numbers of ED mental health attendances with discharge to an acute trust ward in SWBHFT.
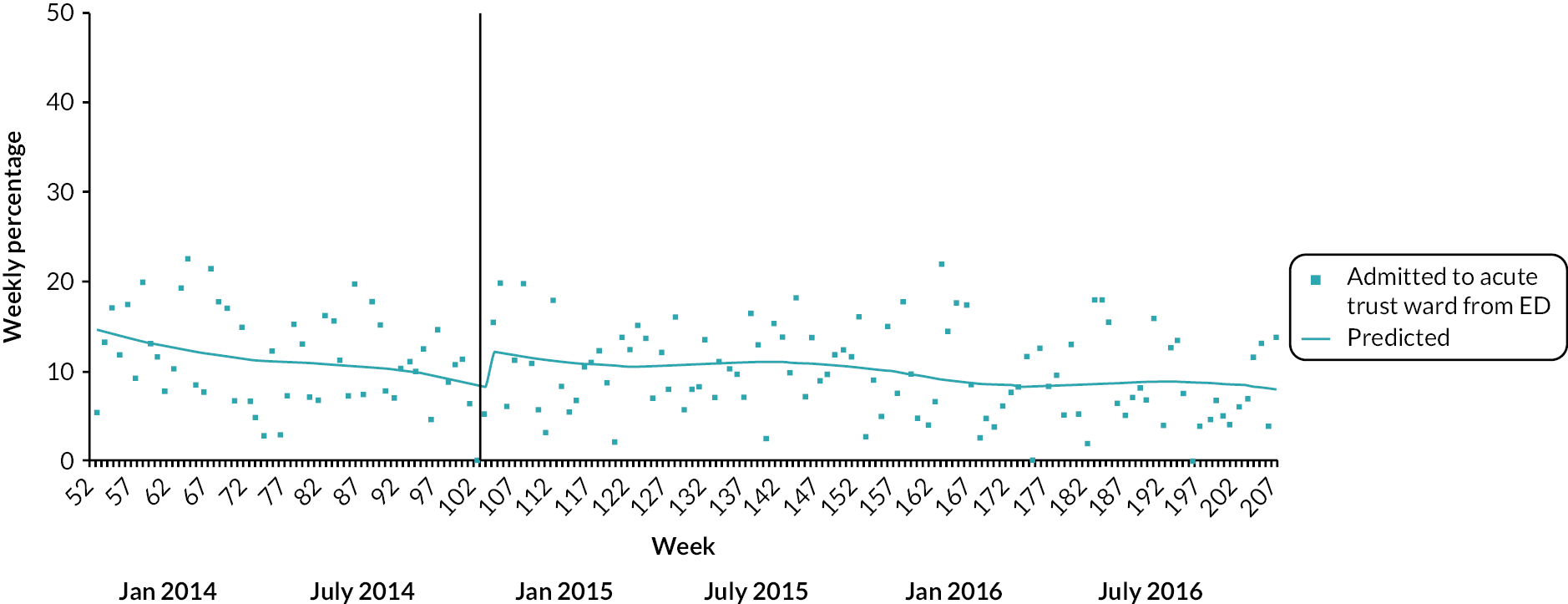
| Service users (variable and level) | SWBHFT (n/year) | ULHFT (n/year) | STHFT (n/year) | SGUHFT (n/year) | ||||
|---|---|---|---|---|---|---|---|---|
| Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | |
| ED mental health attendances | 2159.0 (1577.0) | 2298.5 (1599.5) | 1441.0 (1097.5) | 1798.0 (1274.0) | 2286.5 | 2027.0 | 1916.5 (1383.0) | 2042.5 (1458.5) |
| Previous ED attendance (< 24 months) | 1137 (53.4) | 1284.5 (55.9) | 463.0 (32.1) | 651.0 (36.2) c | 1531.0 (67.0) | 1091 (53.8) c | 1173.5 (61.2) | 1245.0 (61.0) |
| Female sex | 798.0 (37.5) | 929.5 (40.4) a | 738.5 (51.3) | 881.5 (49.1) | 1181.5 (51.7) | 1059.0 (52.2) | 839.0 (48.9) | 968.5 (47.7) |
| Age (mean years, SD) | – | – | 38.7 (16.8) | 38.6 (16.5) | 36.4 (15.4) | 35.9 (14.9) | 39.4 (15.0) | 38.1 (15.0) c |
| 18–24 years | – | – | 368.0 (25.5) | 457.5 (25.5) | 623.0 (27.3) | 580.0 (28.7) | 318.5 (16.6) | 449.5 (22.0) |
| 25–64 years | – | – | 944.5 (65.6) | 1200.5 (66.8) | 1530.0 (67.0) | 1352.0 (66.8) | 1467.0 (76.5) | 1483.5 (72.6) |
| 65+ years | – | – | 128.0 (8.9) | 139.5 (7.8) | 132.0 (5.8) | 92.0 (4.5) | 131.0 (6.8) | 109.5 (5.4) c |
| Arrival by ambulance/police | 1209.0 (56.8) | 1290.5 (56.1) | 1001.5 (69.5) | 1162.0 (64.6) c | 1049.0 (51.2) | 1058.0 (52.2) | 1137.0 (59.3%) | 1103.0 (54.0) c |
| Discharge to acute trust ward | 240.0 (11.3) | 223.0 (9.7) a | 276.5 (19.2) | 359.0 (20.0) | 348.0 (15.2) | 142.0 (7.0) c | 221.5 (11.6) | 120 (5.9) c |
| Length of stay in ED | ||||||||
| 4-hour breach | 537.0 (25.2) | 530.5 (23.1) | 524.4 (36.4) | 744.5 (41.4) c | 800.0 (35.0) | 663.0 (32.7) | 642.5 (33.7) | 718.5 (36.1) a |
| Length of stay (median minutes, IQR) | 186.0 (118.0, 240.0) | 175.0c (111.0, 238.0) | 222.9 (144.9, 319.9) | 221.9a (143.9, 359.9) | 180.0 (60.0, 240.0) | 120.0c (60.0, 240.0) | 225.0 (150.0, 334.0) | 227.0b (161.0, 352.0) |
| 12-hour trolley breach | 28.0 (1.3) | 14.0 (0.6) b | 22.5 (1.6%) | 92.0 (5.1%) c | 1 (0.04) | 0 (0.0) | 90.5 (4.7) | 95.5 (4.8) |
FIGURE 39.
Impact of PDU implementation on proportion of ED mental health attendances with 4-hour breach in SWBHFT.
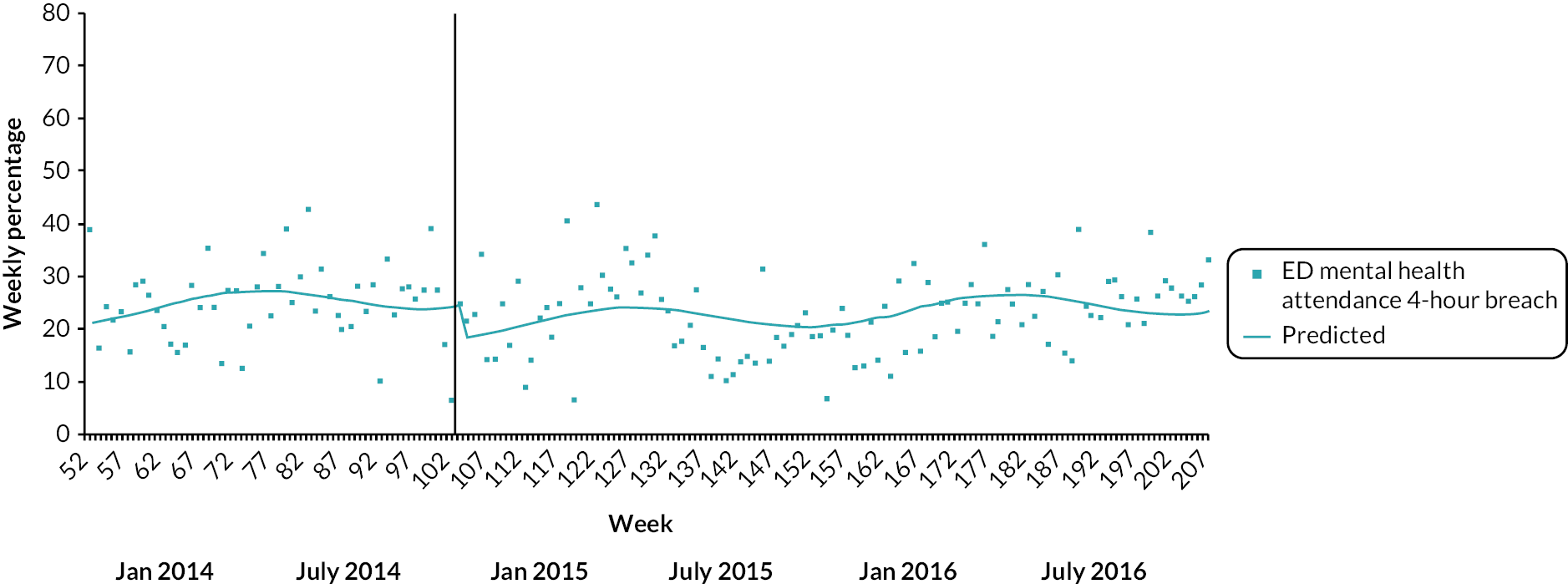
FIGURE 40.
Impact of PDU implementation on mean LOS of ED mental health attendances in SWBHFT.

FIGURE 41.
Impact of PDU implementation on weekly number of ED mental health attendances with arrival by ambulance or police in ULHFT.
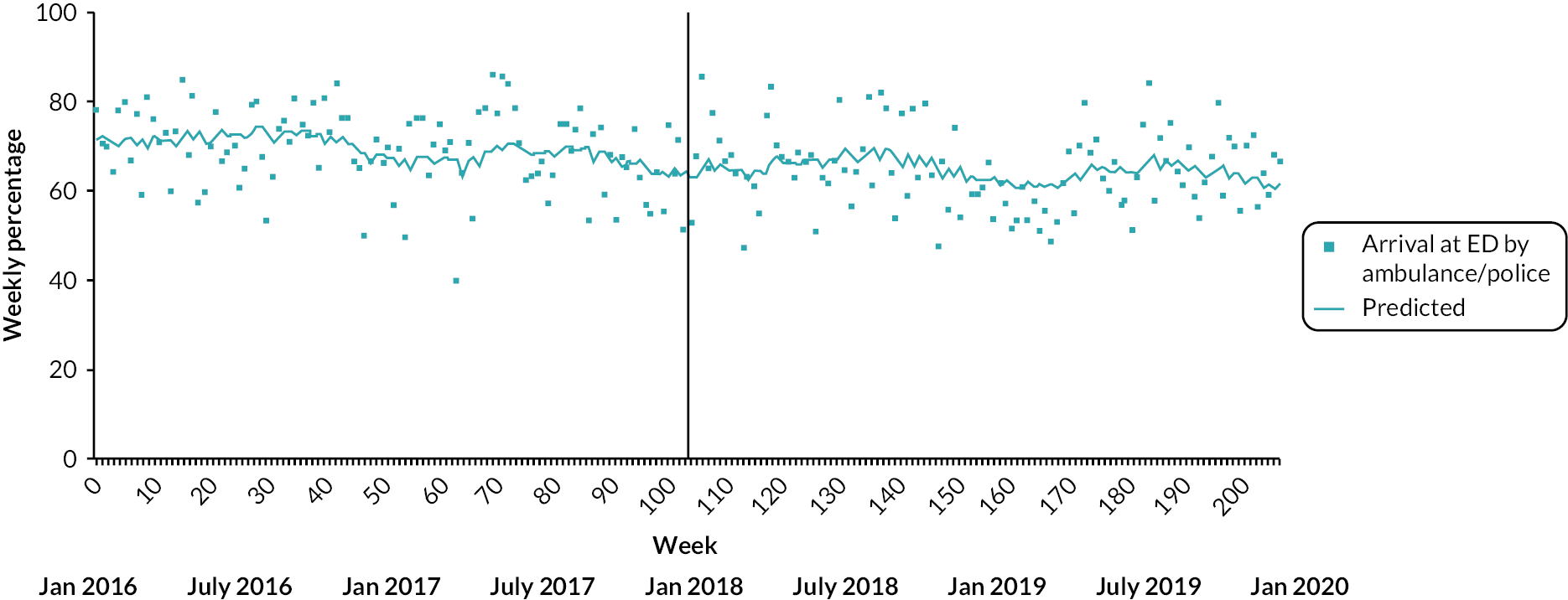
FIGURE 42.
Impact of PDU implementation on weekly number of ED mental health attendances with discharge to an acute trust ward in ULHFT.
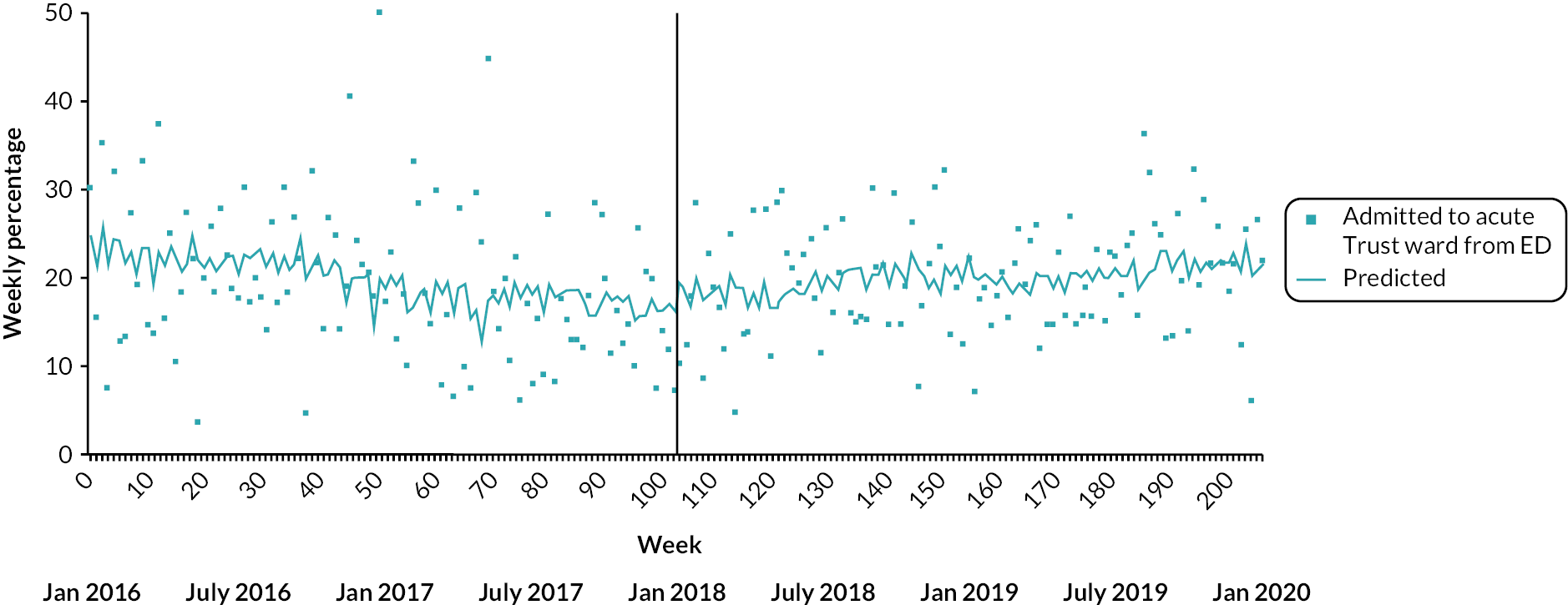
FIGURE 43.
Impact of PDU implementation on the proportion of ED mental health attendances with 4-hour breach in ULHFT.

FIGURE 44.
Impact of PDU implementation on mean LOS of ED mental health attendances in ULHFT.
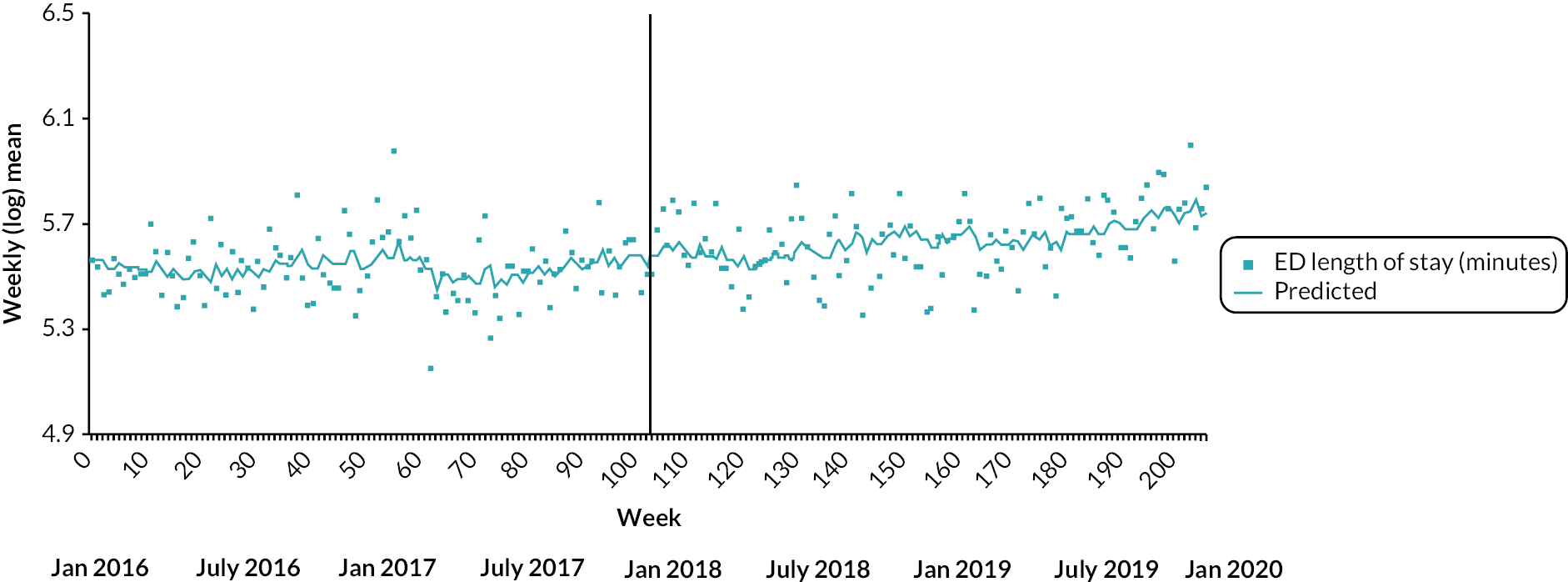
FIGURE 45.
Impact of PDU implementation on weekly number of ED mental health attendances with arrival by ambulance or police in STHFT.

FIGURE 46.
Impact of PDU implementation on weekly number of ED mental health attendances with discharge to an acute trust ward in STHFT.
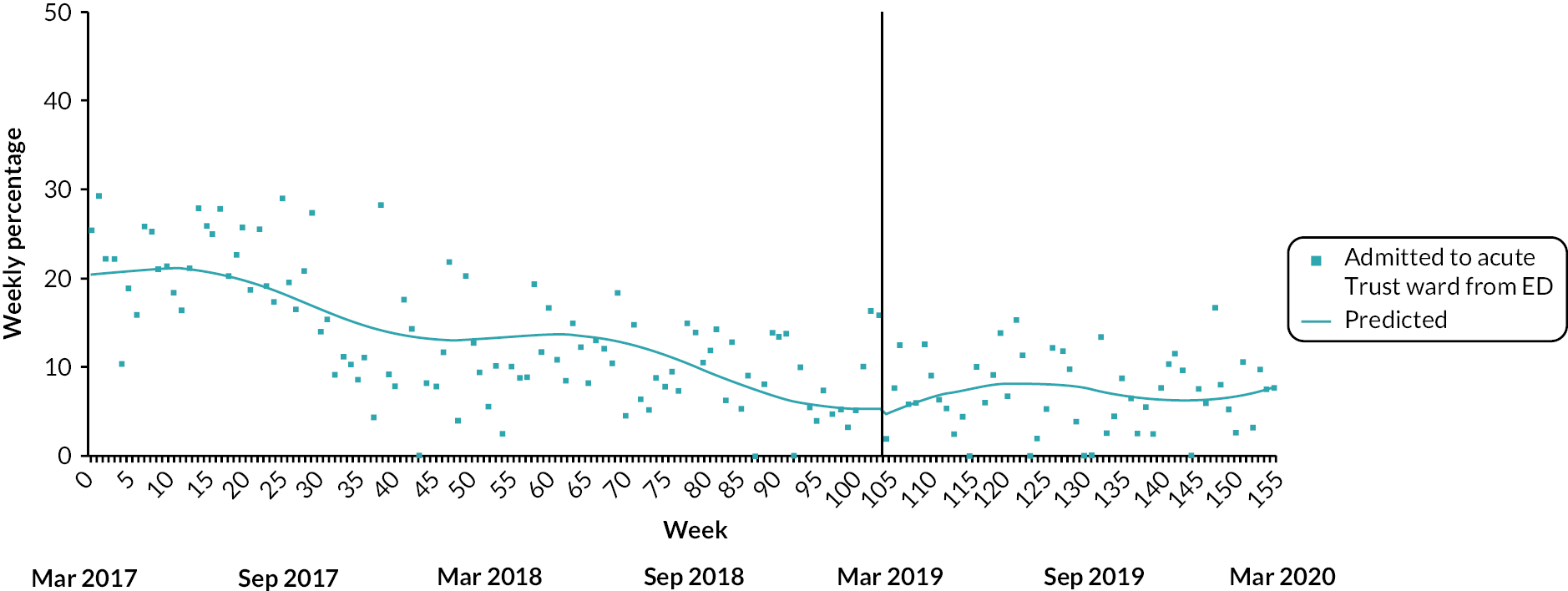
FIGURE 47.
Impact of PDU implementation on the proportion of ED mental health attendances with 4-hour breach in STHFT.
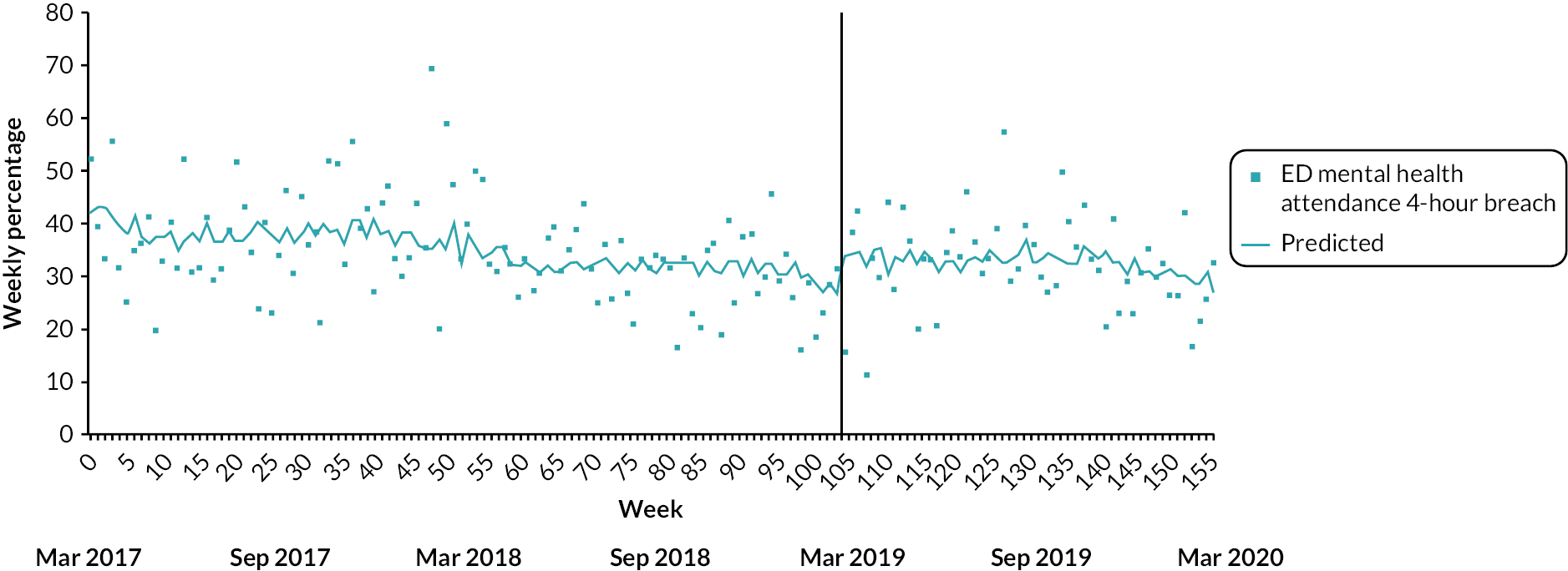
FIGURE 48.
Impact of PDU implementation on mean LOS of ED mental health attendances in STHFT.
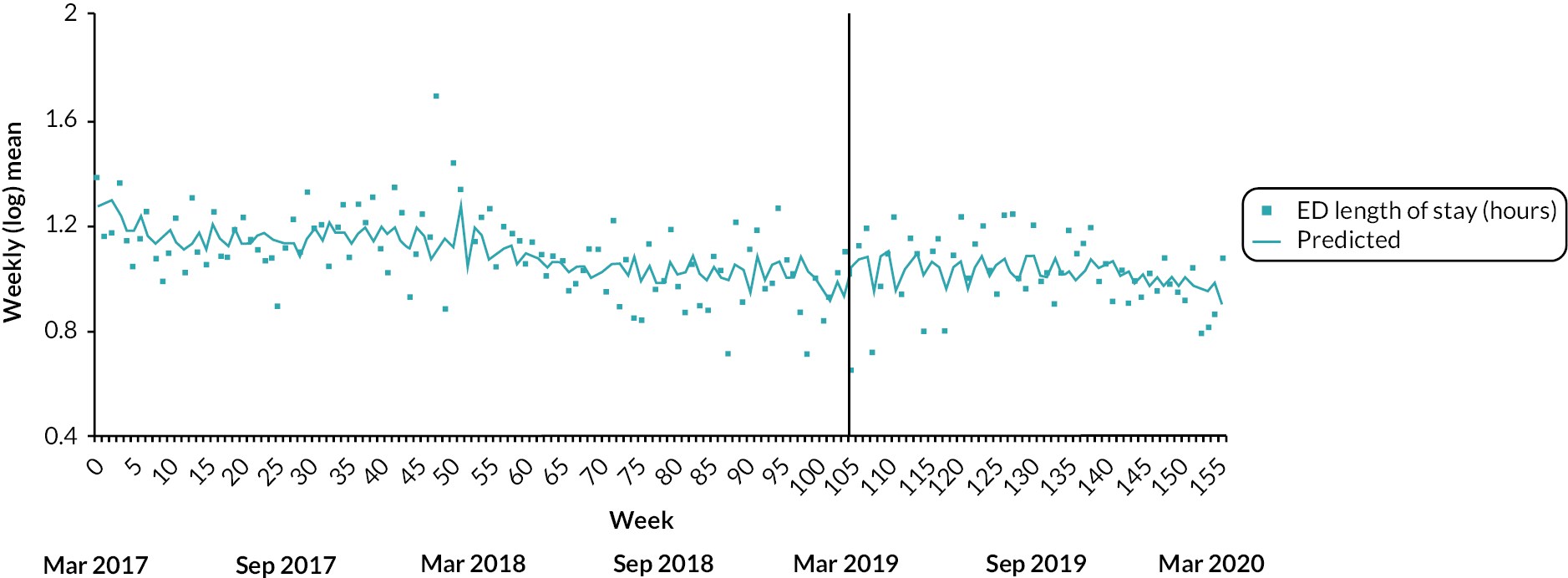
FIGURE 49.
Impact of PDU implementation on weekly number of ED mental health attendances with arrival by ambulance or police in SGUHFT.
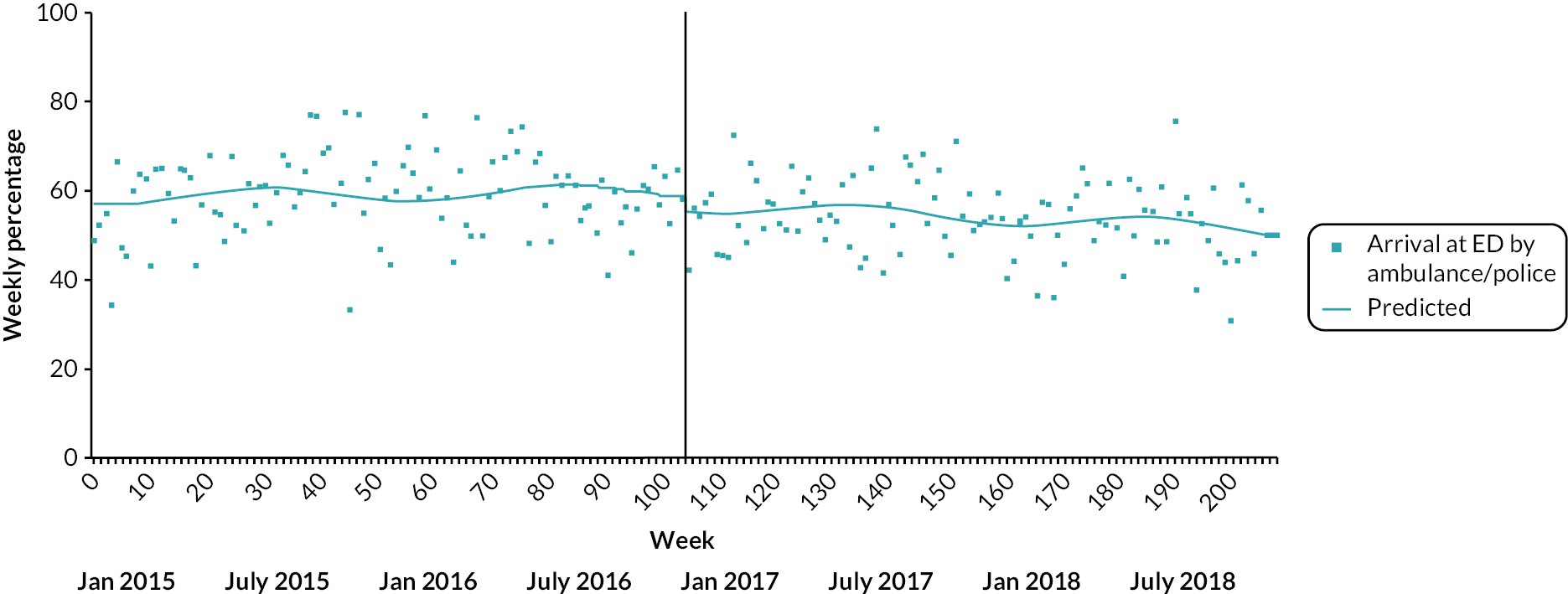
FIGURE 50.
Impact of PDU implementation on weekly number of ED mental health attendances with discharge to an acute trust ward in SGUHFT.

FIGURE 51.
Impact of PDU implementation on the proportion of ED mental health attendances with 4-hour breach in SGUHFT.
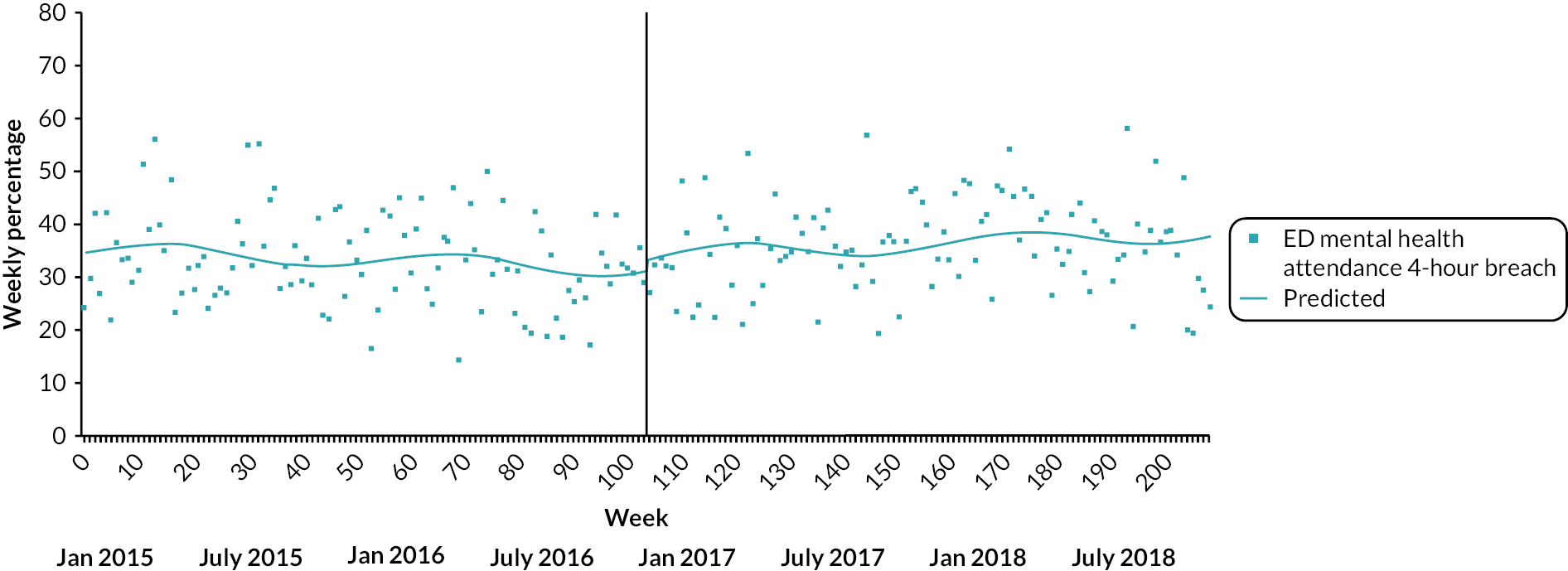
FIGURE 52.
Impact of PDU implementation on mean LOS of ED mental health attendances in SGUHFT.
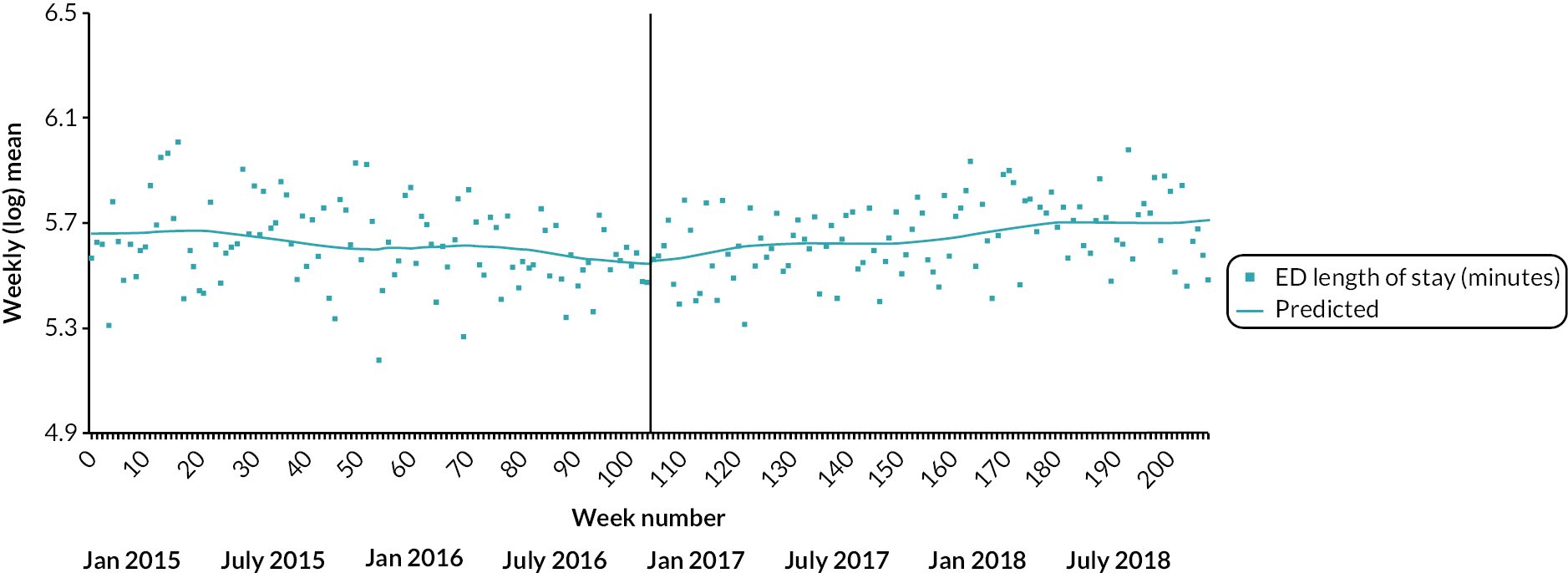
FIGURE 53.
Changes to the crisis care pathway and weekly number of informal psychiatric admissions and ED mental health attendances in BSMHFT/SWBHFT during the study period. The red vertical line represents PDU implementation. MH, mental health.
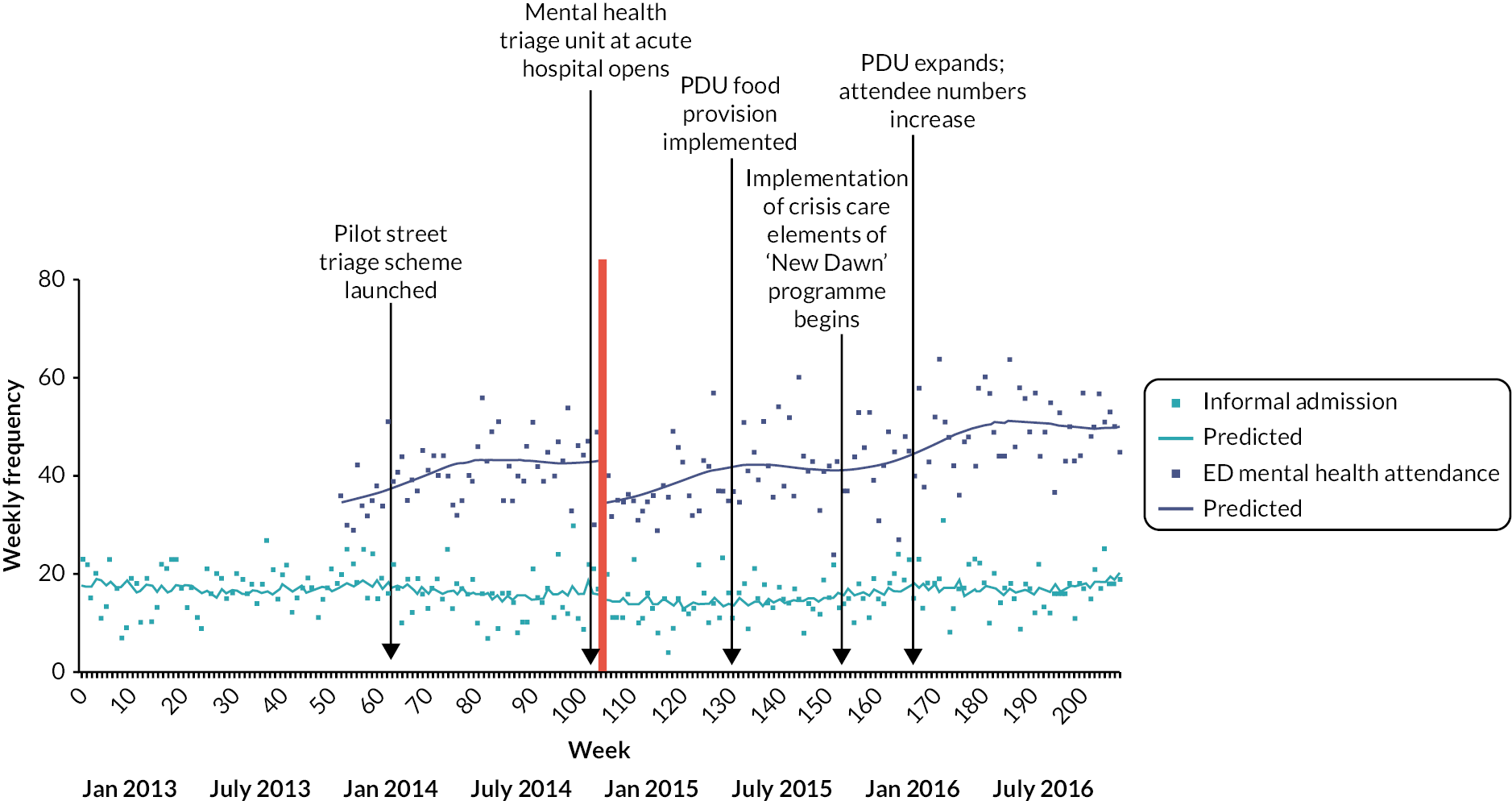
| Initial trend (pre-PDU) | Step change (following PDU) | Trend change (following PDU) | Post-PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| Informal inpatient admission with admission in last 24 months | ||||
| Fixed | 0.001 (−0.001 to 0.002) | −0.156 (−0.300 to −0.012) a | −0.001 (−0.003 to 0.002) | −0.0001 (−0.002 to 0.002) |
| 0.06% | −14.44% | −0.07% | −0.01% | |
| Random | 0.0002 (−0.005 to 0.005) | −0.152 (−0.313 to 0.009) | −0.0001 (−0.010 to 0.010) | 0.0002 (−0.005 to 0.005) |
| 0.02% | −14.10% | −0.01% | 0.02% | |
| Inpatient admission (formal and informal) | ||||
| Fixed | 0.001 (0.001 to 0.002) c | −0.062 (−0.126 to 0.001) | −0.002 (−0.003 to −0.001) c | −0.0004 (−0.001 to 0.0003) |
| 0.14% | −6.05% | −0.17% | −0.04% | |
| Random | 0.002 (0.0002 to 0.003) | −0.062 (−0.126 to 0.001) | −0.002 (−0.005 to 0.001) | −0.001 (−0.002 to 0.001) |
| 0.16% | −6.05% | −0.21% | −0.06% | |
| Formal inpatient admission (%) | ||||
| Fixed | 0.026 (−0.015 to 0.067) | 7.284 (3.889 to 10.679) c | −0.022 (−0.079 to 0.034) | 0.003 (−0.039 to 0.045) |
| 0.03% points | 7.28% points | −0.02% points | 0.003% points | |
| Random | 0.043 (−0.052 to 0.138) | 7.284 (3.889 to 10.679) c | −0.024 (−0.193 to 0.145) | 0.030 (−0.122 to 0.181) |
| 0.04% points | 7.28% points | −0.02% points | 0.03% points | |
| Five days or less inpatient admission (%) | ||||
| Fixed | 0.001 (−0.023 to 0.027) | −0.668 (−2.889 to 1.553) | 0.0003 (−0.036 to 0.037) | 0.004 (−0.025 to 0.033) |
| 0.001% points | −0.67% points | 0.0003% points | 0.004% points | |
| Random | 0.009 (−0.050 to 0.069) | −0.668 (−2.889 to 1.553) | −0.003 (−0.046 to 0.040) | 0.0003 (−0.046 to 0.046) |
| 0.01% points | −0.67% points | −0.003% points | 0.0003% points | |
| Length of inpatient stay (log mean) | ||||
| Fixed | −0.0004 (−0.002 to 0.001) | 0.003 (−0.122 to 0.129) | 0.001 (−0.001 to 0.003) | −0.001 (−0.002 to 0.001) |
| −0.04% | 0.34% | 0.08% | −0.05% | |
| Random | −0.001 (−0.003 to 0.002) | 0.006 (−0.200 to 0.212) | 0.001 (−0.001 to 0.003) | −0.0004 (−0.002 to 0.001) |
| −0.07% | 0.62% | 0.08% | −0.04% | |
| Daily bed occupancy (mean) | ||||
| Fixed | 0.013 (0.002 to 0.025) a | 0.254 (−0.732 to 1.240) | −0.022 (−0.038 to −0.006) b | −0.006 (−0.017 to 0.005) |
| 0.01 beds | 0.25 beds | −0.02% beds | −0.01 beds | |
| Random | 0.049 (−0.005 to 0.103) | −0.186 (−1.827 to 1.454) | −0.057 (−0.119 to 0.004) | −0.006 (−0.017 to 0.005) |
| 0.05 beds | −0.19 beds | −0.06% beds | −0.01 beds | |
| Initial trend (pre-PDU) | Step change (following PDU) | Trend change (following PDU) | Post-PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| PLE | ||||
| Fixed | 0.002 (0.002 to 0.003) c | −0.054 (−0.092 to −0.015) b | −0.0004 (−0.001 to 0.0002) | 0.002 (0.002 to 0.003) c |
| 0.24% | −5.23% | −0.04% | 0.24% | |
| Random | 0.002 (0.002 to 0.003) c | −0.033 (−0.126 to 0.059) | −0.0003 (−0.001 to 0.0005) | 0.002 (0.001 to 0.003) c |
| 0.24% | −3.27% | −0.03% | 0.25% | |
| PLE with episode in previous 24 months | ||||
| Fixed | 0.004 (0.004 to 0.005) c | −0.092 (−0.150 to −0.034) b | −0.002 (−0.003 to −0.002) c | 0.002 (0.001 to 0.002) c |
| 0.42% | −8.79% | −0.25% | 0.18% | |
| Random | 0.004 (0.002 to 0.006) c | −0.045 (−0.273 to 0.182) | −0.002 (−0.004 to −0.001) c | 0.002 (0.001 to 0.002) c |
| 0.40% | −4.43% | −0.24% | 0.18% | |
| Initial trend (pre-PDU) | Step change (following PDU) | Trend change (following PDU) | Post-PDU trend | |
|---|---|---|---|---|
| B (95% CI) weekly change | B (95% CI) step change | B (95% CI) weekly change | B (95% CI) weekly change | |
| ED mental health attendance with attendance in last 24 months | ||||
| Fixed | −0.00002 (−0.001 to 0.001) | −0.044 (−0.118 to 0.029) | −0.0005 (−0.002 to 0.001) | 0.002 (0.001 to 0.003) c |
| −0.002% | −4.33% | −0.05% | 0.18% | |
| Random | 0.001 (−0.002 to 0.005) | −0.050 (−0.226 to 0.127) | −0.0001 (−0.003 to 0.003) | 0.001 (−0.002 to 0.004) |
| 0.13% | −4.83% | −0.01% | 0.13% | |
| Arrival by ambulance/police (%) | ||||
| Fixed | −0.041 (−0.079 to −0.003) a | 0.525 (−2.203 to 3.253) | −0.001 (−0.049 to 0.047) | −0.029 (−0.061 to 0.003) |
| −0.04% points | 0.53% points | −0.001% points | −0.03% points | |
| Random | −0.069 (−0.168 to 0.029) | 1.316 (−3.937 to 6.569) | 0.024 (−0.073 to 0.120) | −0.029 (−0.066 to 0.007) |
| −0.07% points | 1.32% points | 0.02% points | −0.03% points | |
| Discharge to acute Trust ward (%) | ||||
| Fixed | −0.146 (−0.169 to −0.123) c | 3.610 (2.032 to 5.188) c | 0.136 (0.106 to 0.166) c | −0.023 (−0.041 to −0.006) b |
| −0.15% points | 3.61% points | 0.14% points | −0.02% points | |
| Random | −0.141 (−0.175 to −0.107) c | 3.191 (0.337 to 6.045) a | 0.137 (0.099 to 0.175) c | −0.014 (−0.048 to 0.020) |
| −0.14% points | 3.19% points | 0.14% points | −0.01% points. | |
| 4-hour breach (%) | ||||
| Fixed | −0.039 (−0.072 to −0.007) a | 1.088 (−1.736 to 3.912) | 0.042 (−0.008 to 0.092) | 0.040 (0.008 to 0.072) a |
| −0.04% points | 1.09% points | 0.04% points | 0.04% points | |
| Random | −0.035 (−0.092 to 0.023) | 1.069 (−3.545 to 5.683) | 0.042 (−0.008 to 0.092) | 0.040 (0.008 to 0.072) a |
| −0.04% points | 1.07% points | 0.04% points | 0.04% points | |
| Length of ED stay (log mean) | ||||
| Fixed | −0.001 (−0.001 to −0.0002) b | −0.011 (−0.051 to 0.030) | 0.001 (0.0001 to 0.002) c | 0.001 (0.001 to 0.002) c |
| −0.07% | −1.04% | 0.14% | 0.10% | |
| Random | −0.001 (−0.002 to 0.0002) | −0.006 (−0.086 to 0.075) | 0.001 (0.00001 to 0.002) a | 0.001 (0.0004 to 0.002) b |
| −0.07% | −0.55% | 0.12% | 0.10% | |
FIGURE 54.
Changes to the crisis care pathway and weekly number of informal psychiatric admissions and ED mental health attendances in LPFT/ULHFT during the study period. The red vertical line represents PDU implementation. LP, liaison psychiatry.
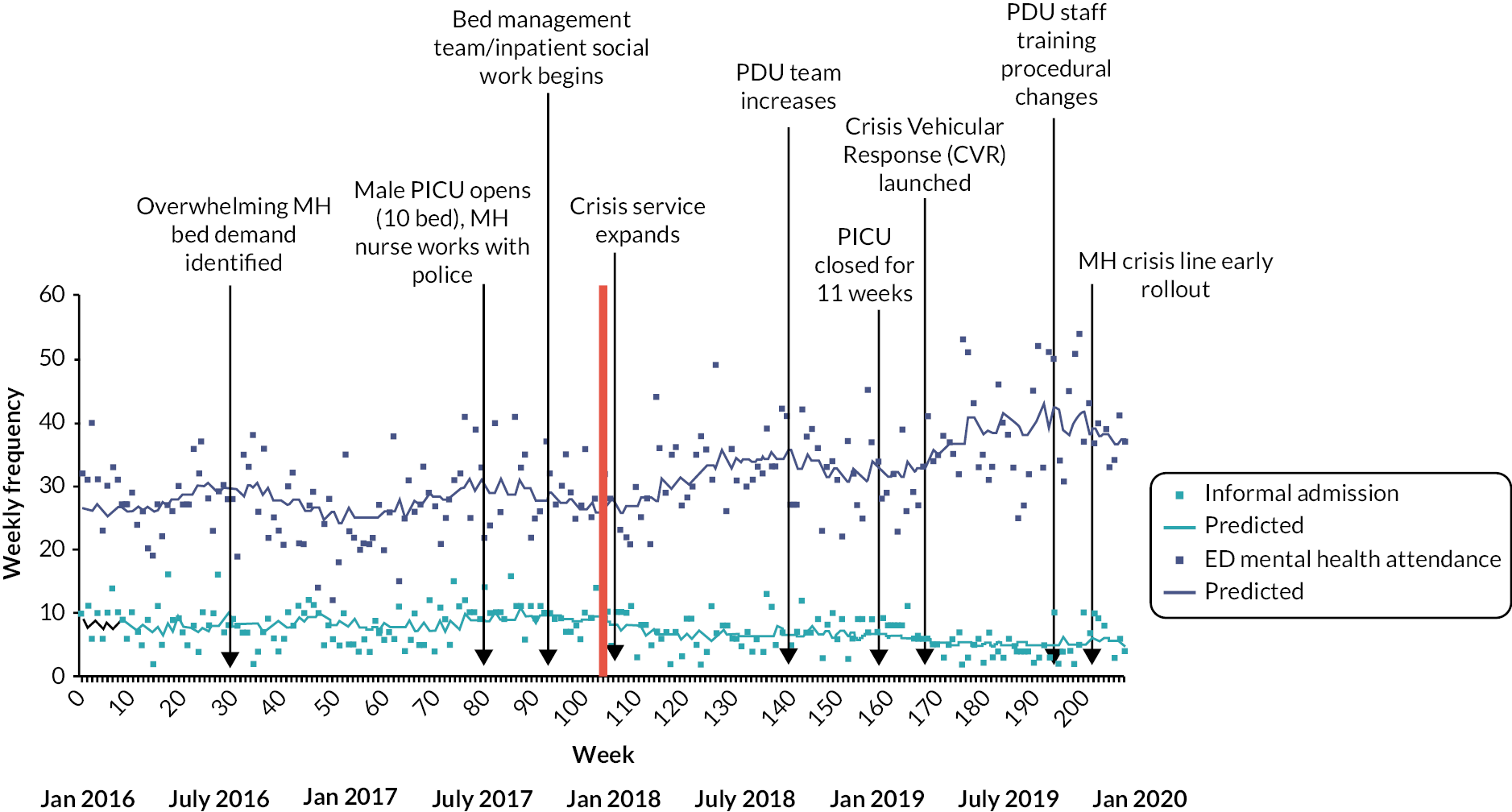
FIGURE 55.
Changes to the crisis care pathway and weekly number of ED mental health attendances in STHFT during the study period. The blue vertical line represents PDU implementation.

FIGURE 56.
Changes to the crisis care pathway and weekly number of informal psychiatric admissions and ED mental health attendances in SWLSTG/SGUHFT during the study period. The red vertical line represents PDU implementation.
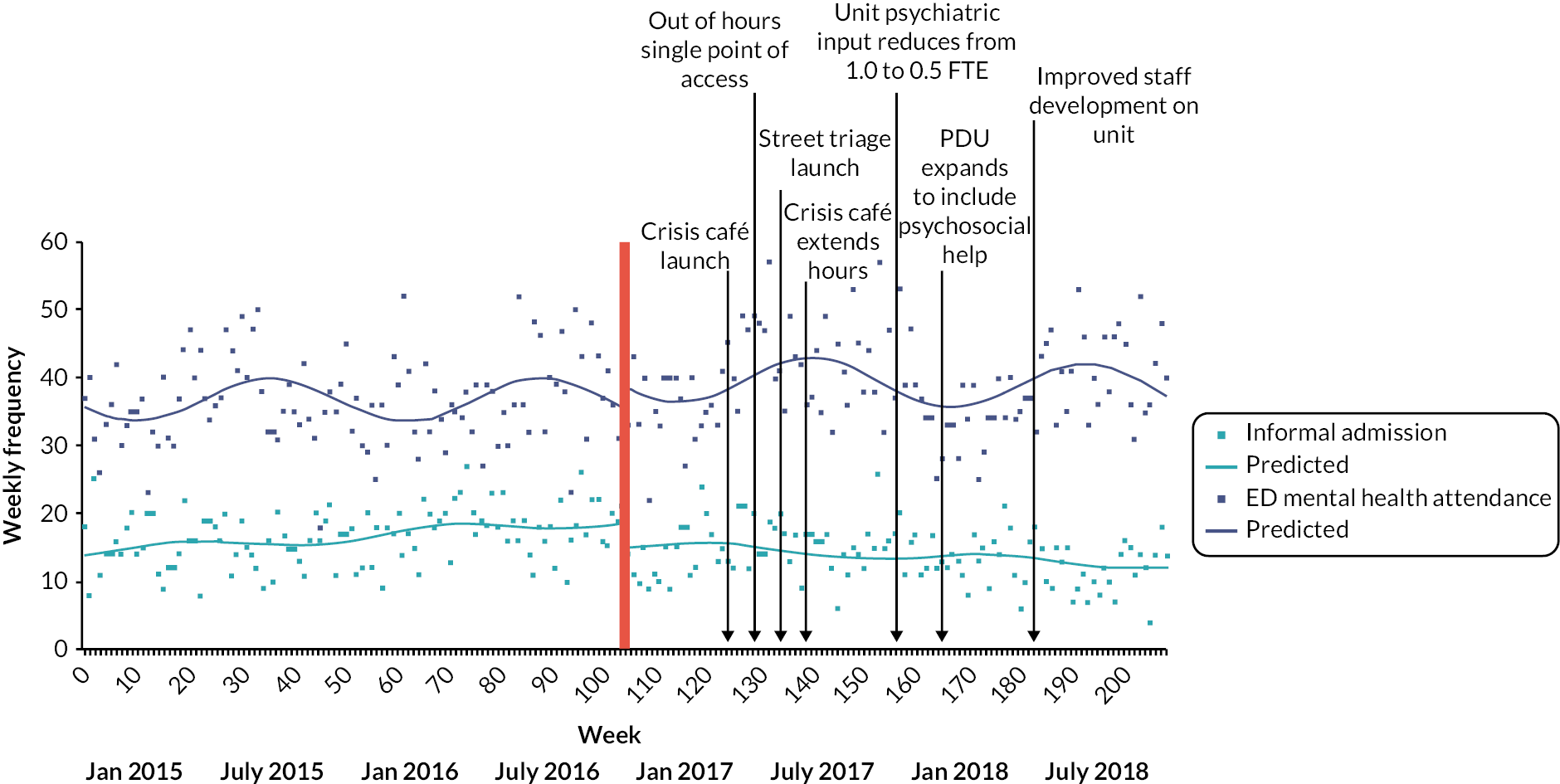
| Date | Change |
|---|---|
| November 2012 | Start of BSMHFT/SWBHFT timeline |
| 2012–13 | ‘New Dawn’ initiative to reorganise community care is proposed. Service users had been dissatisfied with the CRHT response so more service users started attending ED. From the CRHT, the only step-up in care was an inpatient admission |
| January 2014 | BSMHFT joined forces with West Midlands Police and West Midlands Ambulance Service to launch a pilot street triage scheme. This sees a mental health nurse, paramedic and police officer together in one vehicle responding to 999 calls, where it is believed people need immediate mental health support (see Street triage BSMHFT) |
| November 2014 | PDU opened: at the start it was a quiet corner with four couches (not beds) and one nurse; this was open 24 hours/day |
| November 2014 | At the same time as the opening of the PDU, a parallel mental health triage unit at the acute hospital opened. The care here was one-to-one as the MHT staff did not have back-up when incidents occurred. Service users entering the mental health triage unit at the acute hospital went ‘off the clock’. This unit closed in 2016 |
| May 2015 | The staff had realised shortly after the PDU opened that they would need to provide service users with food. At this point the food supply was properly implemented, with the supply of food tagged to a ward and a fridge to store the food in |
| October 2015 | Dedicated ‘innovation and change team’ start implementation of New Dawn initiative/services |
| 2016 (month unknown) | Mental health triage unit located in the acute hospital closes |
| 2016–17 | PDU expands to being close to the current set-up: a unit with eight recliner chairs with a dedicated team. At this point, people visited from other trusts to investigate the unit with a view to opening their own PDU |
| November 2016 | End of BSMHFT/SWBHFT timeline |
| Date unknown | |
| Local area beds – in the West Midlands, there are a number of MHTs who have an agreement to use each other’s beds (the MERIT scheme). These are used in preference to beds further away, and do not count as ‘out of area’ beds | |
| National changes over the entire timeline | |
| Media | The media tackle stigma about mental health more; this means that individuals are more likely to seek help from crisis care services |
| Date | Change |
|---|---|
| January 2016 | Start of LPFT/ULHFT timeline |
| Summer 2016 | A pre-existing problem with the trust relying on out-of-area beds reached its climax, with 60 people simultaneously staying out of area. The trust examined what could be done to address this issue. Demand for beds had increased significantly; unknown reason for this |
| July 2017 | 10-bed male psychiatric ICU opens |
| July 2017 pilot then fully funded from April 2019 | Introduction of a nurse working in the control room with the police about calls coming through (working 2 p.m. to 8 p.m.). Often advises to not take service users to the Section 136 suite (as this was overused), but to take the service users home and that mental health services will visit them at home, or if agreeable to assessment by mental health services, divert to an appropriate base for assessment. Expected reduction in use of Section 136 suite follows |
| October 2017 | Bed management team introduced. This team keeps track of people who are in out-of-area beds (including privately commissioned and block contract out-of-area beds). They visit the private providers and keep up to date with the admission to avoid delays to discharge. The also keep track of the trust’s stock of beds. This service is expanded in February 2020 |
| October/November 2017 | Inpatient social work introduced. This team sits outside Section 75; they are allocated to wards, cover rehabilitation and acute care, and try to unlock social issues including housing |
| January 2018 | Extra funding for crisis teams was made available |
| January 2018 | Collaborative work between the trust and the Richmond Fellowship to increase the capacity and uses for the crisis houses. Following this work, the crisis houses now take more challenging service users as they know they will be supported by the Trust’s crisis teams |
| January 2018 | PDU opened |
| July 2018 | In the first 6 months, there were more people being referred to the PDU without capacity to agree to assessment; referrals reduced as the unit staff worked with other teams to establish a more robust referral procedure. By July 2018, this teething problem had been solved |
| September 2018 | PDU team expanded from the initial staffing level at opening to 11 qualified nurses; (11 HCAs remain the same) |
| April 2019 | Crisis vehicular response (CVR) launched; this was the second adaptation for the trust of the street triage model. The CVR unit consists of a nurse, who is sometimes accompanied by a nursing assistant and/or the police. The vehicle is a van, with a seating area at the back. They will go to visit anyone in mental health crisis in the community, in response to, for example, suicidal thoughts and feelings, a call from the service user’s family, etc. A nurse attends alongside paramedics and police. There are two teams; one in Lincoln, one in Boston |
| April–November 2019 | There was a particular rise in demand for crisis care in this period |
| September 2019 | Expansion of Lincolnshire University to include a medical school (intake = 80 students/year) |
| October 2019 | The PDU became more able to discharge to inpatient beds. The staff team became more experienced, more confident in their approach and felt more able to take positive risks |
| October 2019 | Increase in staff training due to more courses being made available. These include, initially: |
|
|
| Additional courses: | |
|
|
|
|
| October 2019 | Referrals from the 136 suite are now accepted for the PDU |
| November 2019 | One PDU staff member promoted to deputy team co-ordinator; this has helped to increase management supervision rates and provide further clinical support and managerial support for the PDU |
| November 2019 | Helpline for mental health crisis undergoes soft rollout; full rollout across Lincolnshire is now ongoing. Received 300 calls in the first month with a small amount of advertising |
| January 2020 | End of LPFT/ULHFT timeline |
| Date unknown | |
| Mental health triage service (similar to a street triage model, nurses attend alongside paramedics and police). Pilot trial began in June 2014 but official opening date unclear. This was open for 2 years. Over time, the number of referrals reduced, possibly as it was taking too long to travel across the trust area (it can be 2 hours travel time). A similar service (the CVR response – see above) was launched following the closure of this service | |
| National changes over the entire timeline | |
| Social media | More awareness about mental health problems. Young adults possibly seeking a diagnosis; ‘emo’ trend |
| Media | The media tackle stigma about mental health more; this means that individuals are more likely to seek help from crisis care services |
| Street triage | The street triage model becomes more popular with trusts and many of these services are launched |
| April 2016 | Clinical commissioning groups (CCG) were asked to ensure that agreed and funded plans are in place to aim for a ‘core 24’ (24 hours, 7 days a week) service in liaison mental health provision by 2020/21. CCG Improvement and Assessment Framework 2016–17 |
| November 2016 | Achieving Better Access to 24/7 Urgent and Emergency Mental Health Care – Part 2: Implementing the Evidence-based Treatment Pathway for Urgent and Emergency Liaison Mental Health Services for Adults and Older Adults – Guidance: NHS England, the National Collaborating Centre for Mental Health and the National Institute for Health and Care |
| Date | Change |
|---|---|
| March 2017 | Start of SHSCFT/STHFT timeline |
| March 2017 | The Commissioning for Quality and Innovation (CQUIN) initiative launches. This is to become a highly successful 2-year initiative. The target is to reduce the cohort of repeat attenders at ED by 20% in Year 1 and maintain this reduction throughout the year. In Year 2, a new cohort of repeat attenders is added to the project and the target is to reduce the number of repeat attenders by 20% (while maintaining the 20% reduction in the first cohort). This is achieved |
| May 2017 | Liaison Psychiatry CQUIN: police officers were trained in understanding mental health conditions |
| November 2017 | Liaison Psychiatry; service expanded its staffing numbers significantly as part of becoming ‘core 24’ (24 hours, 7 days a week service in liaison mental health provision) |
| April 2018 | Suicide and self-harm presentation signposting for all general practitioners in the CCG |
| May 2018 | Liaison Psychiatry; CQUIN: facilitated a Schwartz round. A Schwartz round is a group reflective practice forum which provides an opportunity for staff from all disciplines to reflect on the emotional aspects of their work. This was inclusive of staff at the teaching hospital |
| Summer 2018 | Intensive rehabilitation community team closed. This team are mentioned earlier in the timeline and specialised in supporting the people who needed a very high level of ongoing support in the community to stay out of crisis services. The team did not tend to discharge service users, and as such, was closed |
| Summer 2018 | Assertive outreach team closed |
| Jan 2019 | Liaison Psychiatry; CQUIN: a new information leaflet was introduced which is about consent for a psychiatric assessment. It explains what Liaison Psychiatry do and why. There are accompanying leaflets about what will happen after the consultation |
| March 2019 | PDU opened. Initial hours: Monday 9 a.m.–Friday 5 p.m. (closed at weekends) |
| February/March 2019 | The teaching hospital introduces a front door response scheme for older people |
| March 2019 | The CQUIN initiative concerning repeat attenders at ED (see March 2017) comes to a close |
| March 2019 | PDU referrals are slow and the PDU team gives presentations to teams, explaining the referral pathways into and out of the PDU |
| March 2019 | ‘The hub’ launches. This is a single point of access. Community teams are re-configured. Single point of access as ‘flow co-ordinators’ who make decisions about service users’ route through services when they area in psychiatric crisis. The teams have good morale, and are strongly interconnected, being in the same physical location. Staff assist each other across teams very reflexively when additional support is needed. In the central hub: |
|
|
| April 2019 | An allocated medic is now attached to the PDU |
| May 2019 | Liaison Psychiatry; CQUIN: security staff at the local general hospital were trained in understanding aggressive behaviour and the relevant legal frameworks. This is because when they are called to incidents involving a patient, often the patient also suffers from mental health problems. The training enables improvements in care for these service users |
| July 2019 | The PDU begins to be used as expected; initially use of the decision unit was lower than expected. This is because it took time for other services to understand what the service is about and feel confident referring service users. The unit is still only open Monday–Friday at this point. Staff have been recruited from inpatient services (as these staff are used to and are willing to do shift work) |
| Summer 2019 | Service reconfiguration. The reconfiguration covers the pathways through the service for staff and the management structure of the service. This defined how recruitment, support and supervision happen |
| October 2019 | Liaison Psychiatry; CQUIN: facilitated a Schwartz round. A Schwartz round is a group reflective practice forum which provides an opportunity for staff from all disciplines to reflect on the emotional aspects of their work. This was inclusive of staff at the teaching hospital |
| November 2019 | The PDU becomes a 24/7 service |
| 2019 (month unknown) | The criteria for the minimum age for service users staying at the PDU is changed to be only 18+. Previously, this had been more flexible, especially for people under Trust services (e.g. the EIP service sees service users aged 14+ years, and service users under the EIP team could also be under the CRHT). When service users under 18 were being considered for a stay on the unit, the environment and other service users were assessed to ensure safety |
| February 2020 | Number of commissioned beds in Sheffield: 3 acute wards: (18 + 2 surge beds); (17 + 2 surge beds); (16 mental health + 5 detox beds) Psychiatric ICU (10 beds) |
| March 2020 | End of SHSCFT/STHFT timeline |
| National changes over the entire timeline | |
| Social media | More awareness about mental health problems. Young adults possibly seeking a diagnosis; ‘emo’ trend |
| Media | The media tackle stigma about mental health more; this means that individuals are more likely to seek help from crisis care services |
| Date (s) | Change |
|---|---|
| November 2014 | Start of SWLSTG/SGUHFT timeline |
| No changes to crisis care pathway in the 2-year period pre-PDU. A revamp of the pathway is planned but opening the PDU is the first planned change to the pathway | |
| November 2016 | PDU (Lotus Assessment Suite) opened |
| April 2017 | Hestia recovery cafe (Tooting) and CDARS recovery Cafe (Wimbledon Chase) launched (365 days a year, between 6 p.m. and 11 p.m. on weekday evenings, and from 12 noon to 11 p.m. at weekends and on bank holidays). Reported effects: small trickle of referrals from the cafes; the cafes are understood to make a reduction to the people presenting at ED in mental health crisis. The bedding in period is understood to be 6 months. ED report that they became a useful place to refer service users to (from ED) |
| May 2017 | Implemented plans to modernise and enhance its urgent care pathway through creating a flexible out of hours crisis service that works across geographic and functional home treatment/street triage boundaries to enable to better response to crisis (within the five boroughs) through: |
|
|
| Through its internal modernisation, the trust has extended some services outside of normal working hours designed to create an out-of-hour hub to ensure co-ordination and consistent response within the urgent care pathway: | |
|
|
| June 2017 | Street triage service launched; street triage operates from 10 p.m. to 6 a.m. This does not involve any change in the resource, it is a more effective and efficient service which is more active. The service aims: – to reduce the overall number of people arrested under Section 136 by providing a more informed assessment that can ensure that the person receives the appropriate mental health/criminal justice intervention. – to increase the proportion of people who receive an inpatient intervention following a Section 136 assessment, thereby evidencing the appropriateness of the initial Section 136 arrest |
| July 2017 | Crisis cafes extend hours to 365 days, from 6 p.m.–11p.m. (Monday–Friday) and 12 noon – 11 p.m. (Saturday/Sunday & bank holidays) |
| August 2017 | Change in gatekeeping practice to out-of-hours contacts. A gatekeeping form being introduced onto the clinical record and gatekeeping policy was amended for liaison services, street triage and Lotus Assessment Suite. Gatekeeping location recording had fallen by 71.8% in 17/18. At the inception of integrated out of hours, home treatment team (HTT) staff were instructed not to record assessment activity on Rio diaries when they carried out joint work with the ED liaison team. This had the obvious result of under-reporting HTT activity at night |
| November 2017 | The consultant psychiatrist for the PDU changes hours from 1*full-time equivalent (FTE) to 0.5*FTE. This change reflects the success of the extra work initially put in to launch, support, embed the service and upskill staff; appropriate to starting a nurse-led unit. Additional support with inappropriate referrals was also helpful towards the start. The consultant psychiatrist now only provides medication reviews and mental health act assessments |
| November 2017 | Professionals from other services show good understanding of the service and want to engage with the PDU. Challenges of establishing the unit included inappropriate referrals and lack of understanding about the aim of the unit from referring services |
| January–May 2018 | Shift in the service offered by the unit – from being purely assessment and discharge plan focused to also providing psychosocial help (e.g. identifying social stressors, low level – short – psychological interventions, creating community links, providing help with homelessness) |
| May 2018 | Changes to PDU introduced by new manager. Changes to professional development for staff on Lotus: (1) bimonthly teaching sessions about risk management (particularly positive risk taking), to support staff to feel confident to reinforce discharge plans; (2) regular reflective practice introduced; (3) arranged professionals’ meetings (i.e. virtual risk meetings in which a range of services work together and have an aligned approach, reinforcing risk management strategies). The unit became more established and skilled up in this area; it’s a short-term service but has a role as a long-term service for some service users in that the involvement in care can stretch over a long period. Many staff study for a master’s in psychosocial interventions (DBT skills). Bimonthly training from the complex needs team (e.g. mentalisation-based treatment specialist (MBT), bespoke training for the needs identified by the staff) |
| Monthly training (between 1 hour and half a day); this could be any topic (e.g. distinguishing between hallucinations and pseudo-hallucinations, diabetes management). Topics suggested by staff on the team; all staff typically attend (an extra HCA may be booked to cover, the unit manager may cover, or staff may be pulled from wards) | |
|
|
| November 2018 | End of SWLSTG/SGUHFT timeline |
| National changes over the timeline | |
| Media – the media tackles stigma more; this means that individuals are more likely to go into crisis care services | |
| April 2016 | CCGs were asked to ensure that agreed and funded plans are in place to aim for a ‘core 24’ (24 hours, 7 days a week) service in liaison mental health provision by 2020–21. CCG Improvement and Assessment Framework 2016–17 |
| November 2016 | Achieving Better Access to 24/7 Urgent and Emergency Mental Health Care – Part 2: Implementing the Evidence-based Treatment Pathway for Urgent and Emergency Liaison Mental Health Services for Adults and Older Adults – Guidance: NHS England, the National Collaborating Centre for Mental Health and the National Institute for Health and Care |
| B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change | B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change |
|---|---|---|---|---|---|
| Informal inpatient admissions | |||||
| Initial trend (pre-street triage) | Step change (post-street triage) | Trend change (post-street triage) | Step change (post-PDU) | Trend change (post-PDU) | Post-PDU trend |
| 0.003 (−0.001 to 0.007) | −0.229 (−0.449 to −0.009) a | −0.001 (−0.010 to 0.008) | −0.208 (−0.453 to 0.037) | 0.001 (−0.007 to 0.009) | 0.003 (0.001 to 0.005) c |
| 0.31% | −20.50% | −0.12% | −18.77% | 0.09% | 0.30% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-New Dawn) | Trend change (post-New Dawn) | Post-New Dawn trend |
| −0.001 (−0.003 to 0.001) | −0.234 (−0.457 to −0.012) a | 0.005 (−0.001 to 0.012) | −0.023 (−0.230 to 0.184) | −0.003 (−0.010 to 0.003) | 0.006 (0.002 to 0.010) b |
| −0.06% | −20.89% | 0.55% | −2.28% | −0.33% | 0.63% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-PDU expand) | Trend change (post-PDU expand) | Post-PDU expand trend |
| −0.001 (−0.003 to 0.001) | −0.206 (−0.397 to −0.015) a | 0.004 (0.0001 to 0.009) a | 0.065 (−0.164 to 0.293) | −0.005 (−0.012 to 0.002) | 0.006 (−0.006 to 0.018) |
| −0.08% | −18.61% | 0.44% | 6.68% | −0.52% | 0.61% |
| ED mental health attendances | |||||
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-New Dawn) | Trend change (post-New Dawn) | Post-New Dawn trend |
| 0.005 (0.001 to 0.008) a | −0.234 (−0.391 to −0.076) b | −0.0002 (−0.005 to 0.004) | 0.021 (−0.140 to 0.181) | −0.001 (−0.005 to 0.003) | 0.004 (0.001 to 0.006) b |
| 0.45% | −20.84% | −0.02% | 2.12% | −0.10% | 0.36% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-PDU expand) | Trend change (post-PDU expand) | Post-PDU expand trend |
| 0.004 (0.001 to 0.008) a | −0.224 (−0.362 to −0.087) b | −0.0002 (−0.004 to 0.003) | 0.032 (−0.124 to 0.189) | −0.002 (−0.006 to 0.003) | 0.004 (−0.003 to 0.012) |
| 0.44% | −20.09% | −0.02% | 3.29% | −0.15% | 0.44% |
| B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change | B (95% CI) weekly % change |
|---|---|---|---|---|---|
| Informal inpatient admissions | |||||
| Initial trend (pre-PICU open) | Step change (post-PICU open) | Trend change (post-PICU open) | Step change (post-PDU) | Trend change (post-PDU) | Post-PDU trend |
| −0.0004 (−0.004 to 0.003) | 0.297 (0.007 to 0.588) a | −0.011 (−0.027 to 0.005) | −0.035 (−0.307 to 0.237) | 0.008 (−0.008 to 0.024) | −0.005 (−0.007 to −0.002)b |
| −0.04% | 34.65% | −1.10% | −3.44% | 0.80% | −0.45% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-PDU staff change) | Trend change (post-PDU staff change) | Post-PDU staff change trend |
| 0.001 (−0.001 to 0.003) | −0.182 (−0.479 to 0.115) | −0.002 (−0.017 to 0.013) | 0.047 (−0.329 to 0.424) | −0.004 (−0.020 to 0.011) | −0.002 (−0.005 to 0.001) |
| 0.10% | −16.66% | −0.21% | 4.84% | −0.43% | −0.22% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-CVR launch) | Trend change (post-CVR launch) | Post-CVR launch trend |
| 0.001 (−0.001 to 0.003) | −0.231 (−0.451 to −0.010)a | −0.0004 (−0.005 to 0.004) | −0.513 (−0.821 to −0.204)b | 0.007 (−0.005 and 0.020) | −0.001 (−0.024 to 0.021) |
| 0.11% | −20.60% | −0.04% | −40.10% | 0.75% | −0.13% |
| ED mental health attendances | |||||
| Initial trend (pre-PICU open) | Step change (post-PICU open) | Trend change (post-PICU open) | Step change (post-PDU) | Trend change (post-PDU) | Post-PDU trend |
| −0.001 (−0.003 to 0.001) | 0.007 (−0.208 to 0.222) | 0.008 (−0.003 to 0.001) | −0.070 (−0.224 to 0.085) | −0.004 (−0.015 to 0.007) | 0.003 (0.001 to 0.004) c |
| −0.11% | 0.70% | 0.78% | −6.73% | −0.38% | 0.27% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-PDU staff change) | Trend change (post-PDU staff change) | Post-PDU staff change trend |
| 0.0001 (−0.001 to 0.001) | 0.033 (−0.154 to 0.220) | 0.004 (−0.003 to 0.010) | −0.022 (−0.159 to 0.115) | −0.001 (−0.008 to 0.006) | 0.003 (0.001 to 0.005) a |
| 0.01% | 3.33% | 0.35% | −2.20% | −0.08% | 0.27% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-CVR launch) | Trend change (post-CVR launch) | Post-CVR launch trend |
| 0.0001 (−0.001 to 0.001) | 0.057 (−0.081 to 0.195) | 0.002 (−0.001 to 0.005) | −0.007 (−0.164 to 0.150) | 0.001 (−0.004 to 0.007) | −0.005 (−0.017 to 0.007) |
| 0.01% | 5.84% | 0.23% | −0.69% | 0.14% | −0.48% |
| B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change | B (95% CI) weekly % change |
|---|---|---|---|---|---|
| ED mental health attendances | |||||
| Initial trend (pre-LP expand) | Step change (post-LP expand) | Trend change (post-LP expand) | Step change (post-PDU) | Trend change (post-PDU) | Post-PDU trend |
| −0.004 (−0.010 to 0.003) | −0.305 (−0.515 to −0.094)b | 0.007 (0.0004 to 0.013) a | −0.194 (−0.364 to −0.023)a | 0.0005 (−0.004 to 0.005) | −0.001 (−0.006 to 0.005) |
| −0.35% | −26.25% | 0.68% | −17.60% | 0.05% | −0.08% |
| Initial trend (pre-IR/AO closure) | Step change (post-IR/AO closure) | Trend change (post-IR/AO closure) | Step change (post-PDU) | Trend change (post-PDU) | Post-PDU trend |
| −0.005 (−0.007 to −0.002)c | 0.022 (−0.133 to 0.177) | 0.010 (0.001 to 0.019) a | −0.240 (−0.497 to 0.017) | −0.001 (−0.008 to 0.007) | −0.001 (−0.006 to 0.005) |
| −0.46% | 2.22% | 0.99% | −21.36% | −0.07% | −0.08% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-PDU upscale) | Trend change (post-PDU upscale) | Post-PDU upscale |
| −0.002 (−0.003 to −0.00005)a | 0.039 (−0.184 to 0.262) | −0.001 (−0.016 to 0.014) | −0.040 (−0.244 to 0.163) | 0.011 (−0.008 to 0.029) | 0.038 (0.006 to 0.070) a |
| −0.17% | 3.98% | −0.12% | −3.96% | 1.09% | 3.86% |
| B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change | B (95% CI) weekly % change | B (95% CI) step % change | B (95% CI) weekly % change |
|---|---|---|---|---|---|
| Informal inpatient admissions | |||||
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-CC launch) | Trend change (post-CC launch) | Post-CC launch |
| 0.003 (0.001 to 0.004) c | −0.589 (−0.809 to −0.368) c | 0.020 (0.001 to 0.039) a | 0.010 (−0.226 to 0.246) | −0.027 (−0.046 to −0.008) b | −0.005 (−0.007 to −0.002) c |
| 0.28% | −44.49% | 2.03% | 1.03% | −2.70% | −0.50% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-street triage launch) | Trend change (post-street triage launch) | Post-street triage launch |
| 0.003 (0.001 to 0.004) c | −0.552 (−0.742 to −0.363) c | 0.014 (0.005 to 0.023) b | −0.162 (−0.346 to 0.022) | −0.021 (−0.030 to −0.012) c | −0.004 (−0.007 to −0.001) b |
| 0.29% | −42.44% | 1.43% | −14.95% | −2.11% | −0.42% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-PDU expands) | Trend change (post-PDU expands) | Post-PDU expands |
| 0.003 (0.001 to 0.005) c | −0.386 (−0.542 to −0.229) c | 0.001 (−0.003 to 0.005) | −0.357 (−0.562 to −0.152) c | −0.002 (−0.010 to 0.005) | 0.012 (0.001 to 0.023) a |
| 0.31% | −31.99% | 0.10% | −30.03% | −0.24% | 0.12% |
| ED mental health attendances | |||||
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-CC launch) | Trend change (post-CC launch) | Post-CC launch |
| −0.001 (−0.002 to 0.001) | 0.006 (−0.166 to 0.179) | 0.002 (−0.010 to 0.013) | 0.088 (−0.033 to 0.210) | −0.003 (−0.014 to 0.009) | −0.002 (−0.003 to −0.0001) a |
| −0.05% | 0.65% | 0.18% | 9.25% | −0.29% | −0.15% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (post-PDU) | Step change (post-street triage launch) | Trend change (post-street triage launch) | Post-street triage launch |
| −0.001 (−0.002 to 0.0005) | −0.050 (−0.203 to 0.104) | 0.010 (0.003 to 0.017) b | −0.182 (−0.312 to −0.052) b | −0.010 (−0.017 to −0.002) a | −0.0004 (−0.002 to 0.001) |
| −0.06% | −4.85% | 0.99% | −16.65% | −0.96% | −0.04% |
| Initial trend (pre-PDU) | Step change (post-PDU) | Trend change (Post-PDU) | Step change (post-PDU expands) | Trend change (post-PDU expands) | Post-PDU expands |
| −0.0003 (−0.001 to 0.001) | 0.002 (−0.111 to 0.116) | 0.003 (−0.0002 to 0.005) | −0.309 (−0.444 to −0.175) c | 0.004 (0.0001 to 0.008) a | 0.004 (−0.001 to 0.009) |
| −0.03% | 0.23% | 0.25% | −26.61% | 0.42% | 0.41% |
Appendix 5 Additional synthetic control study data and figures
| Treated trust code | Peer order | Peer trust code | Peer name |
|---|---|---|---|
| KHFT | |||
| RAX | 1 | R1K | London North West Healthcare NHS Trust |
| RAX | 2 | RAJ | Southend University Hospital NHS Foundation Trust |
| RAX | 3 | RD1 | Royal United Hospital Bath NHS Trust |
| RAX | 4 | RD3 | Poole Hospital NHS Foundation Trust |
| RAX | 5 | RD8 | Milton Keynes Hospital NHS Foundation Trust |
| RAX | 6 | RDD | Basildon and Thurrock University Hospitals NHS Foundation Trust |
| RAX | 7 | RDU | Frimley Park Hospital NHS Foundation Trust |
| RAX | 8 | RHW | Royal Berkshire NHS Foundation Trust |
| RAX | 9 | RJ1 | Guy’s and St Thomas’ NHS Foundation Trust |
| RAX | 10 | RJR | Countess of Chester Hospital NHS Foundation Trust |
| RAX | 11 | RN3 | Great Western Hospitals NHS Foundation Trust |
| RAX | 12 | RN7 | Dartford and Gravesham NHS Trust |
| RAX | 13 | RPA | Medway NHS Foundation Trust |
| RAX | 14 | RQ8 | Mid Essex Hospital Services NHS Trust |
| RAX | 15 | RRV | University College London Hospitals NHS Foundation Trust |
| RAX | 16 | RTK | Ashford and St Peter’s Hospitals NHS Foundation Trust |
| RAX | 17 | RVR | Epsom and St Helier University Hospitals NHS Trust |
| RAX | 18 | RWF | Maidstone and Tunbridge Wells NHS Trust |
| RAX | 19 | RWJ | Stockport NHS Foundation Trust |
| RAX | 20 | RXQ | Buckinghamshire Healthcare NHS Trust |
| ULHFT | |||
| RWD | 1 | RCB | York Teaching Hospital NHS Foundation Trust |
| RWD | 2 | RD1 | Royal United Hospital Bath NHS Trust |
| RWD | 3 | RDE | Colchester Hospital University NHS Foundation Trust |
| RWD | 4 | RGN | Peterborough and Stamford Hospitals NHS Foundation Trust |
| RWD | 5 | RGR | West Suffolk NHS Foundation Trust |
| RWD | 6 | RH8 | Royal Devon and Exeter NHS Foundation Trust |
| RWD | 7 | RJL | Northern Lincolnshire and Goole Hospitals NHS Foundation Trust |
| RWD | 8 | RJR | Countess of Chester Hospital NHS Foundation Trust |
| RWD | 9 | RK5 | Sherwood Forest Hospitals NHS Foundation Trust |
| RWD | 10 | RLQ | Wye Valley NHS Trust |
| RWD | 11 | RN3 | Great Western Hospitals NHS Foundation Trust |
| RWD | 12 | RN5 | Hampshire Hospitals NHS Foundation Trust |
| RWD | 13 | RNS | Northampton General Hospital NHS Trust |
| RWD | 14 | RP5 | Doncaster and Bassetlaw Hospitals NHS Foundation Trust |
| RWD | 15 | RQ8 | Mid Essex Hospital Services NHS Trust |
| RWD | 16 | RWA | Hull and East Yorkshire Hospitals NHS Trust |
| RWD | 17 | RX1 | Nottingham University Hospitals NHS Trust |
| RWD | 18 | RXF | Mid Yorkshire Hospitals NHS Trust |
| RWD | 19 | RXP | County Durham and Darlington NHS Foundation Trust |
| RWD | 20 | RXW | Shrewsbury and Telford Hospital NHS Trust |
| SWBHFT | |||
| RXK | 1 | RBK | Walsall Healthcare NHS Trust |
| RXK | 2 | RBL | Wirral University Teaching Hospital NHS Foundation Trust |
| RXK | 3 | REM | Aintree University Hospital NHS Foundation Trust |
| RXK | 4 | RFR | The Rotherham NHS Foundation Trust |
| RXK | 5 | RJ2 | Lewisham Healthcare NHS Trust |
| RXK | 6 | RK5 | Sherwood Forest Hospitals NHS Foundation Trust |
| RXK | 7 | RL4 | The Royal Wolverhampton NHS Trust |
| RXK | 8 | RLN | City Hospitals Sunderland NHS Foundation Trust |
| RXK | 9 | RMC | Bolton NHS Foundation Trust |
| RXK | 10 | RMP | Tameside Hospital NHS Foundation Trust |
| RXK | 11 | RNA | The Dudley Group NHS Foundation Trust |
| RXK | 12 | RNQ | Kettering General Hospital NHS Foundation Trust |
| RXK | 13 | RP5 | Doncaster and Bassetlaw Hospitals NHS Foundation Trust |
| RXK | 14 | RQ6 | Royal Liverpool and Broadgreen University Hospitals NHS Trust |
| RXK | 15 | RRF | Wrightington, Wigan and Leigh NHS Foundation Trust |
| RXK | 16 | RWW | Warrington and Halton Hospitals NHS Foundation Trust |
| RXK | 17 | RWY | Calderdale and Huddersfield NHS Foundation Trust |
| RXK | 18 | RX1 | Nottingham University Hospitals NHS Trust |
| RXK | 19 | RXF | Mid Yorkshire Hospitals NHS Trust |
| RXK | 20 | RXP | County Durham and Darlington NHS Foundation Trust |
| UHBFT | |||
| RRK | 1 | R1H | Barts Health NHS Trust |
| RRK | 2 | RCB | York Teaching Hospital NHS Foundation Trust |
| RRK | 3 | RDE | Colchester Hospital University NHS Foundation Trust |
| RRK | 4 | RDU | Frimley Park Hospital NHS Foundation Trust |
| RRK | 5 | REF | Royal Cornwall Hospitals NHS Trust |
| RRK | 6 | RGN | Peterborough and Stamford Hospitals NHS Foundation Trust |
| RRK | 7 | RH8 | Royal Devon and Exeter NHS Foundation Trust |
| RRK | 8 | RHM | University Hospital Southampton NHS Foundation Trust |
| RRK | 9 | RHU | Portsmouth Hospitals NHS Trust |
| RRK | 10 | RJE | University Hospital of North Staffordshire NHS Trust |
| RRK | 11 | RL4 | The Royal Wolverhampton NHS Trust |
| RRK | 12 | RN5 | Hampshire Hospitals NHS Foundation Trust |
| RRK | 13 | RTD | The Newcastle Upon Tyne Hospitals NHS Foundation Trust |
| RRK | 14 | RTG | Derby Hospitals NHS Foundation Trust |
| RRK | 15 | RTH | Oxford University Hospitals NHS Trust |
| RRK | 16 | RTR | South Tees Hospitals NHS Foundation Trust |
| RRK | 17 | RVJ | North Bristol NHS Trust |
| RRK | 18 | RWE | University Hospitals of Leicester NHS Trust |
| RRK | 19 | RX1 | Nottingham University Hospitals NHS Trust |
| RRK | 20 | RXF | Mid Yorkshire Hospitals NHS Trust |
| STHFT | |||
| RHQ | 1 | R1H | Barts Health NHS Trust |
| RHQ | 2 | RBN | St Helens and Knowsley Hospitals NHS Trust |
| RHQ | 3 | RCB | York Teaching Hospital NHS Foundation Trust |
| RHQ | 4 | RDE | Colchester Hospital University NHS Foundation Trust |
| RHQ | 5 | RGN | Peterborough and Stamford Hospitals NHS Foundation Trust |
| RHQ | 6 | RGT | Cambridge University Hospitals NHS Foundation Trust |
| RHQ | 7 | RHU | Portsmouth Hospitals NHS Trust |
| RHQ | 8 | RJE | University Hospital of North Staffordshire NHS Trust |
| RHQ | 9 | RK5 | Sherwood Forest Hospitals NHS Foundation Trust |
| RHQ | 10 | RL4 | The Royal Wolverhampton NHS Trust |
| RHQ | 11 | RN5 | Hampshire Hospitals NHS Foundation Trust |
| RHQ | 12 | RNS | Northampton General Hospital NHS Trust |
| RHQ | 13 | RP5 | Doncaster and Bassetlaw Hospitals NHS Foundation Trust |
| RHQ | 14 | RRF | Wrightington, Wigan and Leigh NHS Foundation Trust |
| RHQ | 15 | RTG | Derby Hospitals NHS Foundation Trust |
| RHQ | 16 | RVJ | North Bristol NHS Trust |
| RHQ | 17 | RWA | Hull and East Yorkshire Hospitals NHS Trust |
| RHQ | 18 | RWJ | Stockport NHS Foundation Trust |
| RHQ | 19 | RX1 | Nottingham University Hospitals NHS Trust |
| RHQ | 20 | RXF | Mid Yorkshire Hospitals NHS Trust |
| SWLSTG | |||
| RQY | 1 | RDY | Dorset Healthcare University NHS Foundation Trust |
| RQY | 2 | RH5 | Somerset Partnership NHS Foundation Trust |
| RQY | 3 | RJ8 | Cornwall Partnership NHS Foundation Trust |
| RQY | 4 | RRE | South Staffordshire and Shropshire Healthcare NHS Foundation Trust |
| RQY | 5 | RT5 | Leicestershire Partnership NHS Trust |
| RQY | 6 | RTV | 5 Boroughs Partnership NHS Foundation Trust |
| RQY | 7 | RV3 | Central and North West London NHS Foundation Trust |
| RQY | 8 | RW1 | Southern Health NHS Foundation Trust |
| RQY | 9 | RW4 | Mersey Care NHS Trust |
| RQY | 10 | RXG | South West Yorkshire Partnership NHS Foundation Trust |
| LPFT | |||
| RP7 | 1 | RLY | North Staffordshire Combined Healthcare NHS Trust |
| RP7 | 2 | RMY | Norfolk and Suffolk NHS Foundation Trust |
| RP7 | 3 | RNN | Cumbria Partnership NHS Foundation Trust |
| RP7 | 4 | RNU | Oxford Health NHS Foundation Trust |
| RP7 | 5 | RTQ | 2Gether NHS Foundation Trust |
| RP7 | 6 | RV9 | Humber NHS Foundation Trust |
| RP7 | 7 | RVN | Avon and Wiltshire Mental Health Partnership NHS Trust |
| RP7 | 8 | RXA | Cheshire and Wirral Partnership NHS Foundation Trust |
| RP7 | 9 | RXE | Rotherham Doncaster and South Humber NHS Foundation Trust |
| RP7 | 10 | RXM | Derbyshire Healthcare NHS Foundation Trust |
| BSMHFT | |||
| RXT | 1 | RAT | North East London NHS Foundation Trust |
| RXT | 2 | RH5 | Somerset Partnership NHS Foundation Trust |
| RXT | 3 | RHA | Nottinghamshire Healthcare NHS Trust |
| RXT | 4 | RJ8 | Cornwall Partnership NHS Foundation Trust |
| RXT | 5 | RNN | Cumbria Partnership NHS Foundation Trust |
| RXT | 6 | RT5 | Leicestershire Partnership NHS Trust |
| RXT | 7 | RTV | 5 Boroughs Partnership NHS Foundation Trust |
| RXT | 8 | RXA | Cheshire and Wirral Partnership NHS Foundation Trust |
| RXT | 9 | RXG | South West Yorkshire Partnership NHS Foundation Trust |
| RXT | 10 | RXM | Derbyshire Healthcare NHS Foundation Trust |
| SWLSTG (%) | LPFT (%) | BSMHFT (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | |||||||
| Jan 16–Dec 17 | Jan 18–Dec 18 | Jan 16–Dec 17 | Jan 18–Dec 18 | Nov 12–Oct 14 | Nov 14–Oct 16 | |||||||
| Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | |
| Characteristic (N) | 3864 | 39,007 | 3692 | 37,557 | 1532 | 29,500 | 994 | 30,037 | 4602 | 33,370 | 4532 | 30,919 |
| Sex | ||||||||||||
| Male | 48.9 | 53 | 53.2 | 52.6 | 56.7 | 51.7 | 55.6 | 51.2 | 58.9 | 54.6 | 54.7 | 53.8 |
| Female | 51.1 | 47 | 46.8 | 47.4 | 43.3 | 48.3 | 44.4 | 48.8 | 41.1 | 45.4 | 45.3 | 46.2 |
| Age (years) | ||||||||||||
| 18–24 | 16 | 14.3 | 15.9 | 15 | 14.8 | 14 | 14.9 | 14.7 | 14.9 | 13.1 | 12.6 | 14.3 |
| 25–64 | 76.4 | 76.3 | 77 | 75.5 | 69.5 | 75.1 | 71.2 | 74.7 | 77.5 | 76.5 | 79.3 | 74.9 |
| 65–74 | 7.6 | 9.4 | 7.1 | 9.5 | 15.7 | 10.9 | 13.9 | 10.6 | 7.6 | 10.5 | 8.1 | 10.8 |
| Ethnicity | ||||||||||||
| Asian | 8.4 | 5.1a | 9.4 | 4.7 | < 1 | 1.9 | < 1.5 | 2.3 | 17.7 | 5.6a | 16.3 | 5.7 |
| Black | 16.1 | 4.6 | 16.1 | 5.1 | < 1 | 2.5 | < 1.5 | 2.4 | 16.2 | 4 | 15.5 | 4.6 |
| White | 66.1 | 77.9 | 63 | 75.7 | 90.2 | 85.3 | 86.8 | 84.8 | 54.5 | 85.4 | 56.8 | 82.5 |
| Mixed | 3.3 | 2.1 | 4 | 2.3 | 1.6 | 1.9 | 1.4 | 2 | 4.8 | 1.8 | 4.9 | 1.9 |
| Other | 6.1 | 10.3 | 7.5 | 12.2 | 7 | 8.4 | 10.2 | 8.5 | 6.8 | 3.2 | 6.5 | 5.3 |
| ICD-10 primary diagnosis code | ||||||||||||
| F10–F19: Mental & behavioural psychoactive substance abuse | 7.7 | 12.2a | 6.4 | 9.4 | 8.9 | 8.9 | 8.5 | 7.9 | 5.7 | 12.5 | 5.8 | 12.9 |
| F20–F29: Schizophrenia, schizotypal and delusional disorders | 38.3 | 24.5 | 41.5 | 24.7 | 26 | 23.8 | 17.1 | 22.7 | 40.2 | 24.1 | 36.3 | 25.1 |
| F30–F39: Mood (affective) disorders | 21.4 | 19.3 | 23.7 | 19.5 | 23.4 | 19.3 | 15.3 | 18.5 | 24.6 | 22.3 | 25.6 | 22.3 |
| F40–F48: Neurotic, stress-related and somatoform disorders | 7.1 | 6.5 | 6 | 6.7 | 11.9 | 7.3 | 6.8 | 7.8 | 4.8 | 7.8 | 6.7 | 8.1 |
| F60–F69: Disorders of adult personality and behaviour | 14.6 | 10.7 | 15.2 | 12 | 16.3 | 13.2 | 11.8 | 13.9 | 8.3 | 10.4 | 11.1 | 12.2 |
| Other | 10.9 | 26.8 | 7.2 | 27.7 | 13.4 | 27.5 | 40.5 | 29.2 | 16.5 | 23 | 14.6 | 19.4 |
| Source of admission | ||||||||||||
| Usual place of residence | 44.5 | 61.3 | 41.9 | 56.2 | 66.4 | 56.4 | 56.7 | 56.2 | 47.1 | 66.6a | 40.6 | 64 |
| Temporary place of residence | 3.5 | 2.9 | 4.4 | 3 | < 1 | 3.3 | 2.3 | 2.9 | 2.9 | 2.1 | 2.8 | 2.6 |
| Penal establishment | 7 | 5.5 | 6.1 | 4.9 | < 1 | 5.1 | 3.6 | 4.2 | 16.1 | 4.3 | 27.8 | 4.2 |
| NHS other hospital – general ward or ED | 20.7 | 16.7 | 25.8 | 20 | 12.3 | 15.6 | 10.2 | 15.8 | 22.6 | 15.9 | 20.5 | 13.3 |
| NHS other hospital – mental health ward | 15.3 | 8.1 | 13.4 | 8.2 | 5.5 | 7.3 | 13.8 | 8 | 6.2 | 6.2 | 4.3 | 6.9 |
| Other | 9 | 5.5 | 8.3 | 7.7 | 14.3 | 12.3 | 13.4 | 12.9 | 5.2 | 4.8 | 3.9 | 8.8 |
| Method of admission | ||||||||||||
| Booked | 14.7 | 6.2a | 9.5 | 5.5 | < 1 | 6.4a | < 1 | 8.6 | 7.5 | 7a | 0 | 7.8 |
| Planned | 22.1 | 17.5 | 23.7 | 19.3 | 5.9 | 12.7 | 2.3 | 10.4 | 24.8 | 19.7 | 2.4 | 15.9 |
| ED | < 1 | 4.6 | 33.3 | 5.8 | < 1 | 3.4 | 0 | 5.4 | 0 | 2.3 | 0 | 3.9 |
| Consultant clinic | 6.8 | 6.8 | < 1 | 3.1 | 1.6 | 8.9 | 1.5 | 7.9 | 1.1 | 13 | 11 | 6.4 |
| Mental health crisis resolution team | 29.2 | 15.3 | 17.5 | 25.9 | 65.2 | 23.7 | 59.8 | 25 | 0 | 5 | 0 | 16.9 |
| ED admission transfer from another provider | < 1 | 15.7 | < 1 | 14.1 | 0 | 8.8 | < 1 | 5.4 | 6.5 | 37.3 | 0 | 18.3 |
| Other | 26.9 | 34 | 15.9 | 26.4 | 27 | 36.1 | 36.2 | 37.3 | 60.1 | 15.7 | 86.6 | 30.8 |
| Length of stay | ||||||||||||
| < 5 days | 15.8 | 20.3 | 11.1 | 19.5 | 10.9 | 16.9 | 16.9 | 24.9 | 12.4 | 18.1 | 12.6 | 16 |
| 5 days or longer | 84.2 | 79.7 | 88.9 | 80.5 | 89.1 | 83.1 | 83.1 | 75.1 | 87.6 | 81.9 | 87.4 | 84 |
| No discharge date | 3.4 | 0.7 | 0.8 | 1.1 | 1.5 | 1.7 | 4.9 | 2.2 | 1.3 | 3.8 | 1.5 | 1.8 |
| Number of Elixhauser comorbidities | ||||||||||||
| < 2 | 61.5 | 64.2 | 48.6 | 66.2 | 55.5 | 74.8a | 67.3 | 72.4 | 74.2 | 70.8 | 75.8 | 63.1 |
| ≥ 2 | 38.5 | 35.8 | 51.4 | 33.8 | 44.5 | 25.2 | 32.7 | 27.6 | 25.8 | 29.2 | 24.2 | 36.9 |
| KHFT (%) | ULHFT (%) | SWBHFT (%) | KHFT (%) | ULHFT (%) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | Pre-PDU | Post-PDU | |||||||||||
| Mar 15–Oct 16 | Nov 16–Oct 18 | Jan 16–Dec 17 | Jan 18–Dec 18 | Nov 12–Oct 14 | Nov 14–Oct 16 | Mar 15–Oct 16 | Nov 16–Oct 18 | Jan 16–Dec 17 | Jan 18–Dec 18 | |||||||||||
| Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | Treated | Control | |
| Characteristic (N) | 2245 | 66,743 | 4417 | 69,023 | 6106 | 83,538 | 5983 | 93,641 | 5331 | 78,498 | 7583 | 79,586 | 5788 | 73,338 | 6349 | 78,531 | 6486 | 98,596 | 2928 | 53,085 |
| Sex | ||||||||||||||||||||
| Male | 40.8 | 48.7 | 45.0 | 48.4 | 51.9 | 47.5 | 49.2 | 48.6 | 59.6 | 52.6 | 58.4 | 50.9 | 51.0 | 48.4 | 47.1 | 47.2 | 46.9 | 48.5 | 47.3 | 48.8 |
| Female | 59.2 | 51.3 | 55.0 | 51.6 | 48.1 | 52.5 | 50.8 | 51.4 | 40.4 | 47.4 | 41.6 | 49.1 | 49.0 | 51.6 | 52.9 | 52.8 | 53.1 | 51.5 | 52.7 | 51.2 |
| Age (years) | ||||||||||||||||||||
| 18–24 | 28.9 | 24.4 | 26.4 | 24.7 | 28.6 | 26.4 | 24.9 | 25.7 | 19.4 | 23.5 | 20.2 | 24.8 | 25.0 | 25.7 | 28.0 | 26.6 | 25.2 | 26.3 | 26.1 | 25.0 |
| 25–64 | 64.5 | 71.9 | 67.5 | 70.9 | 67.1 | 69.0 | 66.5 | 67.2 | 78.8 | 73.3 | 77.6 | 71.4 | 71.9 | 70.3 | 68.5 | 69.1 | < 70 | 68.0 | 68.8 | 68.0 |
| 65–74 | 6.6 | 3.7 | 6.1 | 4.4 | 4.3 | 4.6 | 8.6 | 7.1 | 1.8 | 3.2 | 2.2 | 3.8 | 3.2 | 4.1 | 3.5 | 4.3 | < 6 | 5.8 | 5.1 | 7.0 |
| Ethnicity | ||||||||||||||||||||
| Asian | 7.1 | 5.4 | 7.0 | 5.0 | < 1 | 1.5 | < 1 | 1.7 | 17.0 | 3.0a | 15.6 | 2.7 | 8.0 | 3.0 | 7.9 | 2.4 | < 5 | 3.5 | < 5 | 3.5 |
| Black | 2.5 | 4.1 | 3.3 | 4.0 | < 1 | 0.7 | < 1 | 1.1 | 10.8 | 1.3 | 11.8 | 1.1 | 4.0 | 1.1 | 3.8 | 0.8 | < 4 | 1.8 | < 4 | 2.0 |
| White | 77.7 | 74.8 | 73.5 | 73.4 | 83.8 | 85.5 | 82.4 | 81.3 | 56.4 | 80.6 | 57.8 | 83.7 | 70.7 | 85.4 | 69.9 | 85.0 | 76.7 | 78.0 | 78.8 | 74.5 |
| Mixed | 1.8 | 1.1 | 2.1 | 1.2 | 0.8 | 0.9 | 1.2 | 1.0 | 2.6 | 1.0 | 2.2 | 1.1 | 2.4 | 0.9 | 3.2 | 0.9 | 2.0 | 1.2 | 1.5 | 1.2 |
| Other | 10.9 | 14.5 | 14.1 | 16.4 | 14.9 | 11.4 | 15.6 | 14.9 | 13.2 | 14.1 | 12.6 | 11.5 | 14.9 | 9.7 | 15.1 | 10.8 | 13.0 | 15.5 | 12.1 | 18.8 |
| ED diagnosis code | ||||||||||||||||||||
| 01: Laceration (01) | < 1 | 1.7a | 2.8 | 2.2 | 5.2 | 4.6 | 1.4 | 5.2 | 1.1 | 2.7a | 1.2 | 3.0 | 3.4 | 4.0a | 2.7 | 4.5 | < 3 | 4.4a | 1.3 | 4.4 |
| 02: Contusion/abrasion | < 1 | < 1 | 1.1 | 0.6 | 0.9 | 0.7 | < 1 | 2.1 | < 0.5 | 0.5 | < 0.5 | 0.4 | < 0.5 | 0.5 | < 1 | 0.5 | < 2 | 1.3 | < 1 | 1.9 |
| 05: Dislocation/fracture/joint injury/amputation | < 1 | < 1 | 1.3 | 0.6 | 1.2 | 0.6 | < 1 | 1.9 | < 0.5 | 0.4 | < 0.5 | 0.3 | 0.5 | 0.3 | 1.0 | 0.4 | < 2 | 1.3 | < 0.5 | 1.8 |
| 14: Poisoning (incl. overdose) | < 5 | 8.9 | 4.8 | 7.3 | 21.5 | 19.2 | 2.7 | 14.6 | 7.4 | 13.9 | 5.1 | 16.1 | 15.3 | 19.6 | < 15 | 18.0 | < 10 | 13.5 | 5.1 | 12.5 |
| 35: Psychiatric conditions | 74.7 | 69.7 | 65.1 | 73.9 | 52.0 | 54.6 | 90.6 | 65.0 | 81.8 | 49.9 | 87.8 | 50.9 | 73.8 | 41.1 | 75.2 | 48.1 | 79.5 | 65.3 | 87.4 | 67.2 |
| 38: Diagnosis not classifiable | 17.4 | 3.5 | 6.8 | 1.7 | 6.7 | 3.9 | < 1 | 0.9 | 1.6 | 5.8 | < 2 | 9.8 | < 1 | 6.1 | 0.8 | 8.5 | < 5 | 2.1 | 0.6 | 0.6 |
| Other | 4.3 | 15.8 | 18.1 | 13.7 | 12.4 | 16.4 | 4.1 | 10.4 | 7.8 | 26.8 | 4.0 | 19.6 | 6.2 | 28.4 | 5.6 | 20.0 | 4.9 | 12.1 | 4.7 | 11.5 |
| Patient group | ||||||||||||||||||||
| Deliberate self-harm | 19.9 | 29.5a | 36.1 | 23.7 | 45.5 | 45.2 | 3.0 | 31.5 | 15.4 | 48.7a | <8 | 43.7 | 31.6 | 61.0a | 29.3 | 53.9 | 4.3 | 32.3a | 0.0 | 28.5 |
| Other accident | 12.3 | 1.1 | 4.2 | 2.6 | 2.0 | 2.3 | 9.8 | 7.3 | 0.7 | 5.8 | <2 | 5.0 | 0.7 | 1.8 | 0.7 | 1.3 | 11.1 | 5.3 | 15.3 | 7.6 |
| Other | 67.8 | 69.4 | 59.7 | 73.7 | 52.5 | 52.6 | 87.2 | 61.2 | 83.9 | 45.5 | 91.0 | 51.3 | 67.7 | 37.2 | 70.0 | 44.8 | 84.7 | 62.3 | 84.7 | 63.8 |
| Arrival mode | ||||||||||||||||||||
| Ambulance | 48.6 | 50.4 | 40.1 | 46.2 | 48.0 | 52.4 | 35.9 | 46.7 | 60.1 | 56.4 | 56.2 | 54.3 | 58.4 | 60.0 | 55.3 | 59.4 | 48.0 | 48.0 | 48.7 | 46.6 |
| Other | 51.4 | 49.5 | 59.9 | 51.8 | 52.0 | 47.5 | 62.9 | 52.7 | 39.9 | 42.4 | 43.8 | 41.9 | 41.6 | 39.9 | 44.7 | 40.6 | 52.0 | 51.6 | 51.3 | 52.7 |
| Unknown | 0.0 | 0.1 | 0.0 | 2.0 | 0.0 | 0.1 | 1.2 | 0.6 | 0.0 | 1.3 | 0.0 | 3.8 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.7 |
| Referral source | ||||||||||||||||||||
| Self-referral | 62.9 | 53.7a | 73.9 | 56.0 | 63.2 | 45.2a | 75.2 | 53.1 | 59.1 | 52.5 | 55.6 | 54.1 | 83.7 | 40.5a | 81.7 | 39.7 | 69.8 | 51.4a | 89.2 | 54.3 |
| Emergency services | 6.1 | 19.2 | 2.4 | 14.1 | < 5 | 32.8 | 0.0 | 1.0 | 26.3 | 26.4 | 33.2 | 29.4 | 0.0 | 34.5 | < 5 | 37.3 | 17.8 | 12.6 | < 0.5 | 0.3 |
| Police | 4.0 | 5.5 | 6.0 | 5.5 | 8.9 | 6.6 | 0.0 | 5.0 | 3.8 | 6.1 | 3.7 | 5.2 | 5.6 | 6.1 | < 5 | 5.9 | 1.4 | 5.5 | < 0.5 | 4.1 |
| Healthcare provider | 3.1 | 2.7 | 5.8 | 9.5 | < 2 | 7.5 | 5.2 | 32.6 | 1.4 | 2.0 | 1.1 | 2.6 | 1.1 | 4.1 | 0.9 | 5.8 | 4.8 | 21.6 | 4.9 | 33.4 |
| Other | 24.0 | 19.1 | 11.9 | 15.0 | 22.6 | 7.9 | 19.7 | 8.3 | 9.5 | 13.0 | 6.4 | 8.7 | 9.6 | 14.8 | 12.4 | 11.3 | 6.1 | 8.9 | 5.6 | 7.9 |
| Discharge method | ||||||||||||||||||||
| Admitted same provider | < 10 | 22.6a | 9.3 | 19.4 | 15.3 | 21.5a | 7.1 | 16.1 | 17.5 | 23.4a | 13.1 | 21.9 | 13.4 | 36.3a | 12.8 | 32.5 | < 10 | 19.0a | 8.0 | 14.7 |
| Referred other healthcare professional | < 1 | 9.8 | 10.5 | 6.9 | 0.8 | 8.0 | 12.7 | 3.9 | 0.4 | 8.3 | < 0.5 | 8.3 | 9.7 | 4.1 | 16.3 | 5.3 | < 6 | 3.9 | < 5 | 4.0 |
| Discharged to GP | 42.7 | 25.5 | 30.2 | 21.8 | 4.3 | 20.9 | 10.4 | 10.8 | 38.3 | 20.4 | 34.1 | 21.5 | 54.5 | 17.5 | 48.7 | 20.4 | 17.8 | 16.5 | 8.3 | 12.8 |
| Discharged no follow-up | 27.4 | 22.4 | 33.5 | 28.9 | 64.8 | 32.3 | 58.4 | 47.8 | 17.9 | 29.6 | 19.5 | 31.0 | 11.7 | 24.7 | 13.3 | 25.2 | 55.9 | 37.0 | 71.3 | 47.5 |
| Transferred other provider | 13.6 | 6.3 | 12.1 | 9.4 | 1.9 | 4.6 | 9.1 | 2.9 | 17.1 | 4.1 | 28.7 | 4.4 | 0.0 | 2.9 | 0.0 | 3.4 | 4.6 | 5.6 | 4.3 | 6.8 |
| Other | 6.5 | 13.4 | 4.5 | 13.7 | 12.8 | 12.7 | 2.3 | 18.5 | 8.9 | 14.2 | < 5 | 12.8 | 10.7 | 14.4 | 8.9 | 13.2 | 6.5 | 18.0 | < 5 | 14.1 |
FIGURE 57.
Synthetic control MHT outcomes.
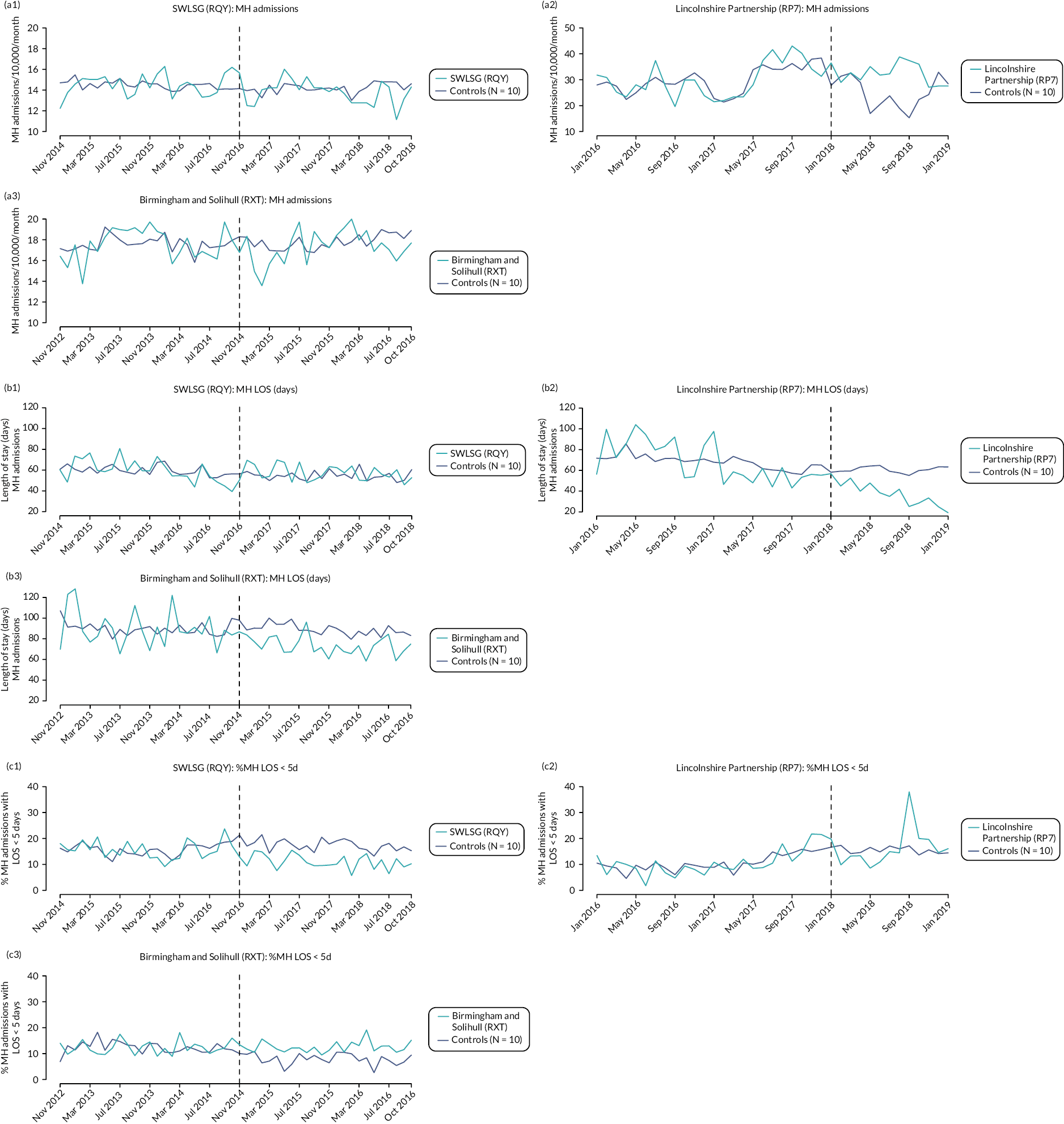
FIGURE 58.
Synthetic control acute trust outcomes.
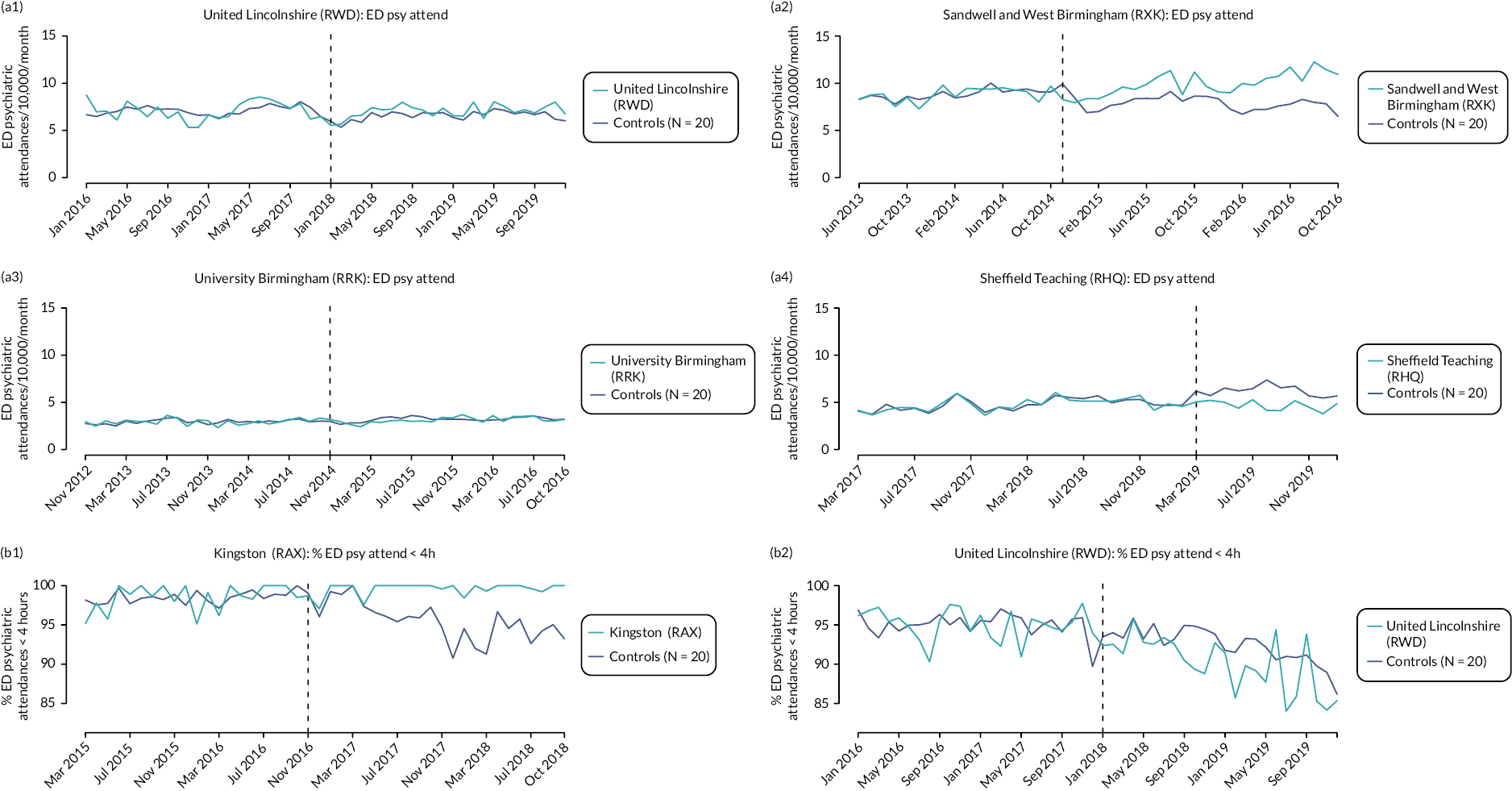
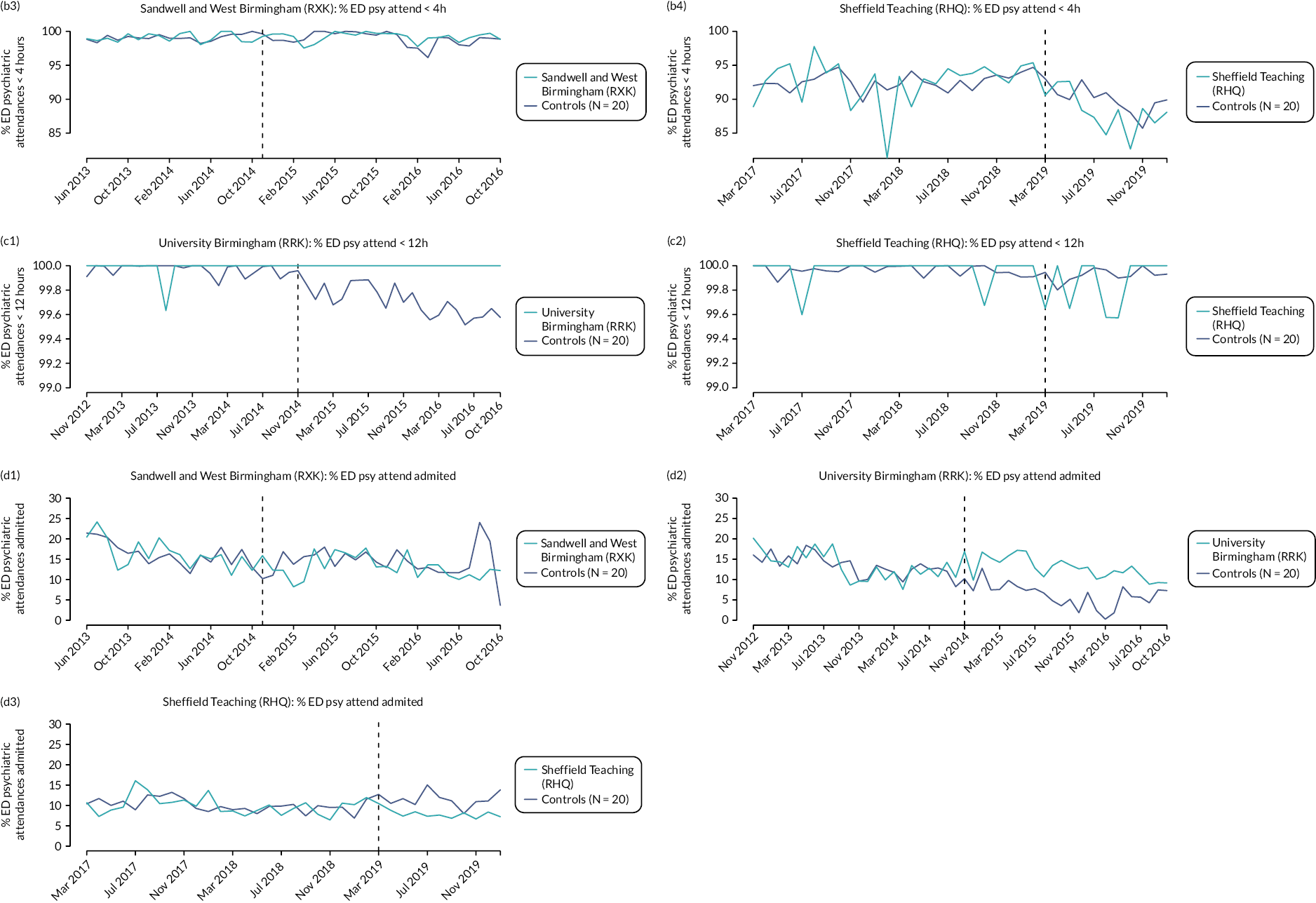
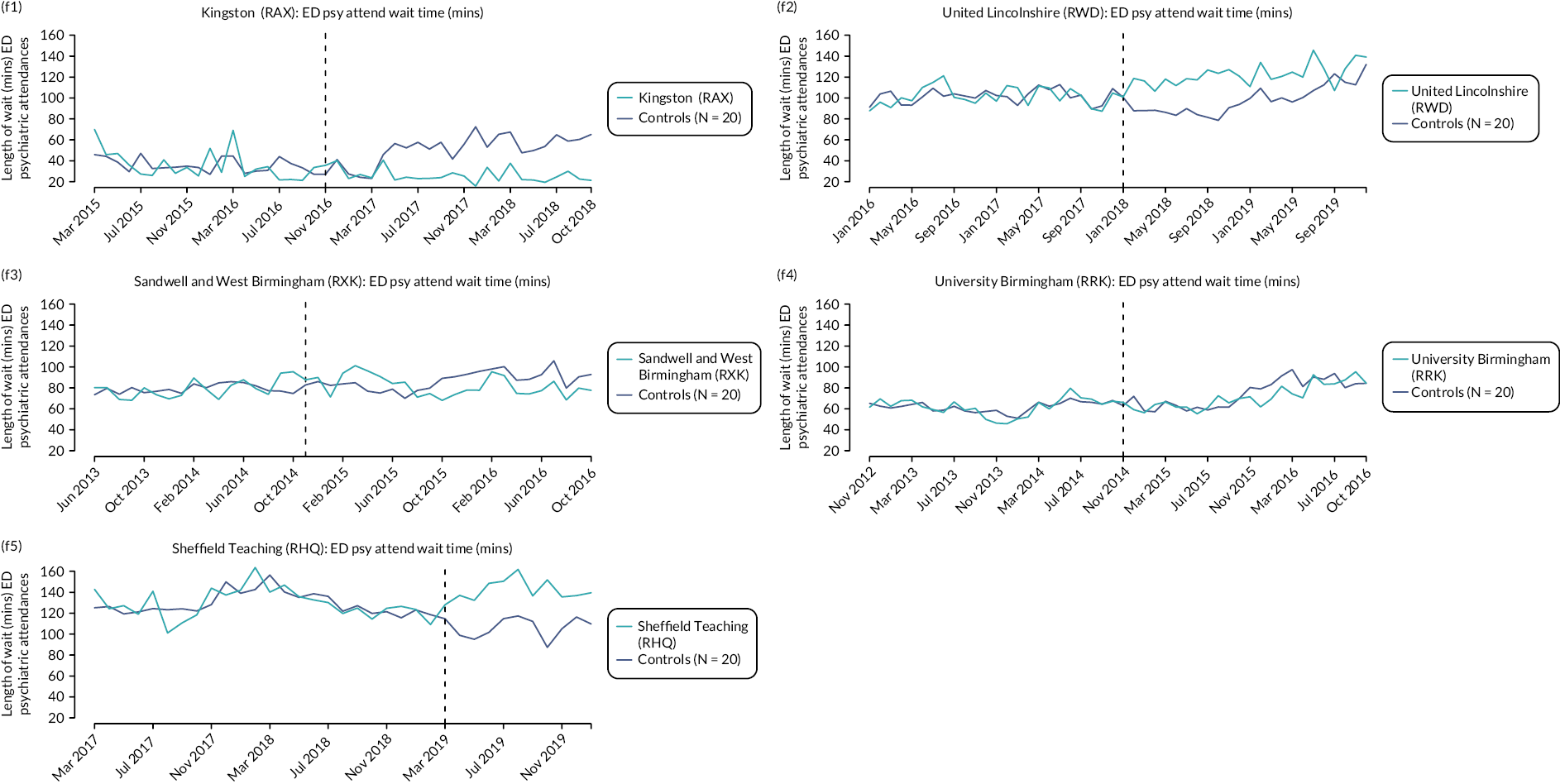
Appendix 6 Additional cohort study data
| SWLSTG | LPFT | BSMHFT | STHFT | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Sample size | 277 | 308 | 387 | 204 |
| N female (%) | 162 (58.48) | 167 (54.25) | 171 (44.19) | 109 (54.43) |
| Age (SD) | 36.74 (13.77) | 37.43 (15.22) | 34.64 (13.53) | 37.63 (13.46) |
| Ethnicity | ||||
| Asian/British Asian | 19 (6.86) | 0 | 36 (9.30) | 10 (4.90) |
| Black/Black British | 24 (8.66) | 3 (0.97) | 27 (6.98) | 11 (5.39) |
| White British | 163 (58.84) | 265 (86.04) | 257 (66.41) | 136 (66.67) |
| White Irish/white other | 40 (14.44) | 9 (2.92) | 15 (3.88) | 5 (2.45) |
| Other | 26 (9.39) | 0 | 8 (2.07) | 7 (3.43) |
| Mixed | 1 (0.36) | 1 (0.32) | 18 (4.65) | 2 (0.98) |
| Missing | 4 (1.44) | 30 (9.74) | 26 (6.72) | 33 (16.18) |
| Primary diagnosis | ||||
| F1 – Psychoactive substance use | 12 (4.33) | 10 (3.25) | 4 (1.04) | 0 |
| F2 – Schizophrenia | 8 (2.89) | 16 (5.19) | 14 (3.62) | 15 (7.35) |
| F3 – Mood disorders | 39 (14.08) | 13 (4.22) | 21 (5.43) | 2 (0.98) |
| F4 – Neurotic disorders | 22 (7.94) | 13 (4.22) | 11 (2.84) | 1 (0.49) |
| F6 – Personality disorders | 21 (7.58) | 14 (4.55) | 10 (2.58) | 15 (7.35) |
| F8 – Disorders of psych development | 3 (1.08) | 0 | 0 | 0 |
| F9 – Behav and emot disorders | 1 (0.36) | 0 | 3 (0.78) | 0 |
| Other | 19 (6.86) | 10 (3.25) | 5 (1.29) | 3 (1.47) |
| Not stated/no diagnosis | 152 (54.87) | 232 (75.32) | 319 (82.43) | 168 (82.35) |
| Secondary diagnosis | ||||
| Mental health | 81 (29.24) | – | 11 (2.84) | – |
| Alcohol or substance abuse | 17 (6.14) | – | 8 (2.07) | – |
| Physical health | 7 (2.53) | – | 4 (1.03) | – |
| Other | 12 (4.33) | – | 1 (0.26) | – |
| No secondary diagnosis | 160 (57.76) | – | 363 (93.80) | – |
| Marital status | ||||
| Single/separated/divorced/widowed | 224 (80.9) | 163 (52.92) | 143 (36.96) | 116 (56.86) |
| Married/civil partnership/cohabiting | 39 (14.1) | 39 (12.66) | 26 (6.72) | 36 (17.65) |
| Missing | 14 (5.1) | 106 (42) | 218 (56.33) | 52 (25.49) |
| Employment status | ||||
| Working/student/volunteer/homemaker | 90 (32.5) | 92 (29.87) | 32 (8.27) | 65 (31.86) |
| Unemployed | 114 (41.2) | 133 (43.18) | 60 (15.50) | 85 (41.67) |
| Retired | 5 (1.8) | 9 (2.92) | 1 (0.26) | 5 (2.45) |
| Missing | 68 (24.6) | 74 (24.03) | 294 (75.97) | 49 (24.02) |
| Housing | ||||
| Mainstream housing | 192 (69.3) | 200 (64.94) | 74 (19.12) | 130 (63.73) |
| Supported housing | 6 (2.2) | 12 (3.90) | 9 (2.33) | 8 (3.92) |
| Insecure housing/homeless | 12 (4.3) | 23 (7.47) | 8 (2.07) | 9 (4.41) |
| Missing | 67 (24.2) | 73 (23.70) | 296 (76.49) | 57 (27.94) |
| Sexual orientation | ||||
| Gay/lesbian/bisexual | 4 (1.4) | 13 (4.22) | 3 (0.78) | 11 (5.39) |
| Heterosexual | 39 (14.1) | 143 (46.43) | 58 (14.99) | 63 (30.88) |
| Missing | 234 (84.5) | 152 (49.35) | 326 (84.24) | 130 (63.73) |
| Referral source | ||||
| ED | 123 (44.4) | 113 (36.69) | 237 (61.24) | 15 (7.35) |
| CMHT | 31 (11.2) | 27 (8.77) | 0 | – |
| Home treatment team | 107 (38.6) | 135 (43.83) | 4 (1.03) | – |
| Local authority and other provider | – | 8 (2.60) | 0 | – |
| Primary care & other medical | 12 (4.3) | 6 (1.95) | 137 (35.40) | 30 (14.71) |
| Section 136 & police | 4 (1.4) | 19 (6.17) | 6 (1.55) | 1 (0.49) |
| Other source within the trust | 0 | 0 | 0 | 157 (76.96) |
| Missing | 0 | 0 | 3 (0.78) | 1 (0.49) |
| Admission to PDU within 7 days of first contact with trust | 63 (22.74) | 62 (20.13) | 110 (28.42) | – |
| First contact with trust during the ‘pre’ period | 114 (41.16) | 97 (31.49) | 161 (41.60) | – |
| English index of social deprivation 2019 mean (SD) score | 18,360 (7282) | 12,990 (8475) | 7240 (7679) | 10,245 (8450) |
| Category of social deprivation mean (SD) | 5.78 (2.34) | 4.40 (2.60) | 2.65 (2.34) | 3.45 (2.58) |
| Category of social deprivation range | 2–10 | 1–10 | 1–10 | 1–10 |
| Supplement: summary of immediate post-discharge data | ||||
| Discharge destination | ||||
| Inpatient – at trust or out of area | 7 (2.5) | – | – | 28 (13.73) |
| Inpatient at trust | – | 31 (10.06) | 53 (13.70) | – |
| Inpatient out of area/non-NHS | – | 19 (6.17) | 14 (3.62) | – |
| Home treatment team | 47 (17.0) | 109 (35.59) | – | – |
| CMHT | 9 (3.3) | 1 (0.32) | – | – |
| Primary care | 23 (8.3) | 0 | – | – |
| Temporary place of residence | 36 (13.0) | 0 | 31 (8.01) | 28 (13.73) |
| Usual place of residence | 142 (51.3) | 34 (11.04) | 228 (58.91) | 136 (66.67) |
| Other | – | 28 (9.09) | 20 (5.17) | 4 (1.96) |
| Continuing care – not specified | – | 57 (18.51) | 29 (7.42) | – |
| Missing | 13 (4.7) | 29 (9.42) | 12 (3.10) | 8 (3.92) |
| Days in the pandemic | 163.15 (54.60) | 157.25 (53.92) | 170.99 (52.72) | 158.62 (52.48) |
| Characteristic | SWLSTG | LPFT | STHFT |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sample size | 218 | 289 | 427 |
| Female | 115 (52.75) | 159 (55.02) | 217 (50.82) |
| Age, years (SD) | 37.94 (14.32) | 38.16 (14.77) | 35.46 (13.79) |
| Ethnicity | |||
| Asian/British Asian | 14 (6.42) | 1 (0.35) | 41 (9.60) |
| Black/Black British | 9 (4.13) | 4 (1.38) | 37 (8.67) |
| White British | 147 (67.43) | 248 (85.81) | 287 (67.21) |
| White Irish/white other | 33 (15.14) | 7 (2.42) | 15 (3.51) |
| Other | 12 (5.50) | 1 (0.35) | 8 (1.87) |
| Mixed | 0 | 1 (0.35) | 17 (3.98) |
| Missing | 3 (1.38) | 27 (9.34) | 22 (5.15) |
| Primary diagnosis | |||
| F1 – Psychoactive substance use | 7 (3.21) | 8 (2.77) | 5 (1.17) |
| F2 – Schizophrenia | 7 (3.21) | 18 (6.23) | 24 (6.62) |
| F3 – Mood disorders | 27 (12.39) | 23 (7.96) | 20 (4.68) |
| F4 – Neurotic disorders | 17 (7.80) | 16 (5.54) | 9 (2.11) |
| F6 – Personality disorders | 14 (6.42) | 0 (0) | 13 (3.04) |
| F8 – Disorders of psych development | 0 | 0 | 0 |
| F9 – Behav and emot disorders | 1 (0.46) | 0 | 1. (0.23) |
| Other | 10 (4.59) | 6 (2.08) | 7 (1.64) |
| Not stated/no diagnosis | 135 (61.93) | 218 (75.43) | 384 (81.50) |
| Secondary diagnosis | |||
| Mental health | 55 (25.23) | 9 (2.11) | |
| Alcohol or substance abuse | 11 (5.05) | NR | 14 (3.28) |
| Physical health | 4 (1.83) | 4 (0.94) | |
| Other | 10 (4.59) | 3 (0.70) | |
| No secondary diagnosis | 138 (63.30) | 397 (92.97) | |
| Marital status | |||
| Single/separated/divorced/widowed | 176 (80.7) | 152 (52.60) | 182 (42.67) |
| Married/civil partnership/cohabiting | 34 (15.6) | 41 (14.19) | 37 (8.67) |
| Missing | 8 (3.7) | 96 (33.22) | 208 (48.71) |
| Employment status | |||
| Working/student/volunteer/homemaker | 77 (35.3) | 94 (32.53) | 29 (6.79) |
| Unemployed | 93 (42.7) | 123 (42.56) | 84 (19.67) |
| Retired | 10 (4.6) | 8 (2.77) | 4 (0.94) |
| Missing | 38 (17.4) | 64 (22.15) | 310 (72.60) |
| Housing | |||
| Mainstream housing | 156 (71.6) | 206 (71.28) | 97 (22.72) |
| Supported housing | 9 (4.1) | 10 (3.46) | 13 (3.04) |
| Insecure housing/homeless | 13 (6.0) | 16 (5.54) | 10 (2.34) |
| Missing | 40 (18.4) | 57 (19.72) | 307 (71.90) |
| Sexual orientation | 156 (71.6) | 206 (71.28) | 97 (22.72) |
| Gay/lesbian/bisexual | 0 (0) | 17 (5.88) | 4 (0.94) |
| Heterosexual | 7 (3.2) | 128 (44.29) | 64 (14.99) |
| Missing | 211 (96.8) | 144 (49.83) | 359 (84.07) |
| Referral source | |||
| ED | 93 (42.7) | 113 (39.10) | 229 (56.63) |
| CMHT | 77 (35.3) | 1 (0.35) | 1 (0.23) |
| Home treatment team | 39 (17.9) | 148 (51.21) | 14 (3.28) |
| Local authority and other provider | – | 2 (0.69) | 0 |
| Primary care and other medical | 8 (3.7) | 6 (2.08) | 166 (38.88) |
| Section 136 and police | 1 (0.5) | 19 (6.57) | 9 (2.11) |
| Other source within the trust | 0 | 0 | 0 |
| Missing | 0 | 0 | 8 (1.87) |
| Admission to PDU within 7 days of first contact with trust | 55 (25.23) | 40 (13.84) | 110 (25.76) |
| First contact with trust during the ‘pre’ period | 93 (42.86) | 69 (23.88) | 172 (40.28) |
| English index of social deprivation 2019 mean (SD) score | 19,762 (7725) | 13,271 (8871) | 7141 (7612) |
| Category of social deprivation mean (SD) | 6.47 (2.33) | 4.42 (2.68) | 2.63 (2.33) |
| Category of social deprivation range | 2–10 | 1–10 | 1–10 |
| Supplement: summary of immediate post-discharge data | |||
| Discharge destination | |||
| Inpatient – at trust or out of area | 7 (3.2) | – | NR |
| Inpatient at trust | – | 21 (7.27) | |
| Inpatient out of area/non-NHS | – | 12 (4.15) | |
| Home treatment team | 18 (8.3) | 80 (27.68) | |
| CMHT | 0 (0) | 1 (0.35) | |
| Primary care | 1 (0.5) | 3 (1.04) | |
| Temporary place of residence | 38 (17.4) | 18 (6.23) | |
| Usual place of residence | 147 (67.4) | – | |
| Other | – | 17 (5.88) | |
| Continuing care – not specified | – | 66 (22.84) | |
| Missing | 7 (3.2) | 71 (24.57) | |
| Days in the pandemic | N/A | N/A | N/A |
| SWLSTG (n = 218) | LPFT (n = 427) | STHFT (n = 427) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre–post comparison | Pre | Post | Pre–post comparison | Pre | Post | Pre–post comparison | |
| Primary outcomes | |||||||||
| MHT: number experiencing an informal admission | 8 | 57 | χ2 = 40.67, p < 0.001 | 16 | 75 | χ2 = 49.03, p < 0.001 | 18 | 81 | χ2 = 47.82, p < 0.001 |
| Acute trust: ED presentations (total) | 1.31 (1.22) | 0.80 (1.55) | t = −4.98, p < 0.001 | 0.61 (0.87) | 0.43 (0.93) | t = 2.78, p < 0.001 | 1.74 (1.60) | 1.83 (2.45) | t = 0.82, p = 0.41 |
| Secondary outcomes: binary events data (number experiencing one or more) | |||||||||
| Inpatient admissions | 14 | 63 | χ2 = 40.69, p < 0.001 | 24 | 97 | χ2 = 59.88, p < 0.001 | 35 | 110 | χ2 = 52.57, p < 0.001 |
| 0–5 days’ inpatient admissions | 7 | 14 | χ2 = 1.00, p = 0.63 | 5 | 17 | χ2 = 10.29, p < 0.001 | 4 | 8 | χ2 = 1.60, p < 0.34 |
| Compulsory admissions | 9 | 12 | χ2 = 0.47, p = 0.65 | 11 | 31 | χ2 = 11.76, p < 0.001 | 19 | 36 | χ2 = 6.42, p = 0.02 |
| Continuous outcomes, n (SD) | |||||||||
| Average length of inpatient stay, for those with a stay, mean (SD), n | 31.37 (40.04), 14 | 30.49 (42.35), 63 | t = 0.07, p = 0.94 | 28.23 (24.74), 24 | 46.44 (61.92), 97 | t = 1.41, p = 0.16 | 24.53 (30.84), 35 | 49.82 (79.73), 110 | t = 1.83, p = 0.07 |
| Use of CMHT and other trust services | |||||||||
| Community contacts with services (mean, SD) | 12.92 (19.26) | 26.98 (30.38) | t = 7.34, p < 0.001 | 12.97 (18.23) | 21.94 (24.33) | t = 6.63, p < 0.001 | 3.06 (8.10) | 4.98 (8.38) | t = 4.58, p < 0.001 |
| Contact type: face to face (mean, SD) | 8.90 (13.96) | 17.60 (18.67) | t = 7.12, p < 0.001 | 5.89 (8.48) | 13.98 (15.68) | t = 9.84, p < 0.001 | 2.65 (7.52) | 4.28 (7.43) | t = 4.23, p < 0.001 |
| Contact type: telephone/video (mean, SD) | 4.02 (6.57) | 9.38 (14.37) | t = 5.81, p < 0.001 | 7.08 (12.28) | 7.96 (11.59) | t = 1.07, p = 0.29 | 0.40 (1.44) | 0.69 (1.94) | t = 3.19, p < 0.05 |
| Use of CMHT and other trust services by category: continuous outcomes; mean (SD) | |||||||||
| CMHT | 3.26 (6.93) | 6.28 (10.27) | t = 5.62, p < 0.001 | 5.40 (12.46) | 7.01 (13.79) | t = 2.31, p = 0.02 | 3.13 (8.33) | 5.30 (8.84) | t = 5.23, p < 0.001 |
| Crisis resolution or home treatment team | 5.92 (14.37) | 14.83 (17.74) | t = 7.05, p < 0.001 | 5.33 (8.21) | 12.42 (14.83) | t = 8.47, p < 0.001 | 4.90 (13.90) | 12.31 (23.46) | t = 6.11, p < 0.001 |
| Mental health support line | 0.19 (0.56) | 0.71 (5.11) | t = 1.58, p = 0.12 | – | – | – | – | – | – |
| Number of contacts (for small numbers); n | |||||||||
| Mental health support line (also summarised above) | 41 | 155 | – | – | – | – | |||
| DBT service | 0 | 12 | – | – | 11 | 11 | |||
| Service contracted by trust | 5 | 26 | – | – | 3 | 0 | |||
| Art therapies | 23 | 18 | – | – | 6 | 6 | |||
| Other | 44 | 88 | 38 | 26 | – | – | |||
| Outpatient ED service | 0 | 5 | 16 | 0 | 55 | 45 | |||
| Exercise therapy team | 19 | 121 | – | – | – | – | |||
| PD intensive team | 116 | 139 | – | – | – | – | |||
| Complex needs service | 63 | 155 | 0 | 0 | 114 | 81 | |||
| Family therapy | 20 | 34 | – | – | – | – | |||
| Early intervention team | 98 | 181 | 65 | 312 | 145 | 145 | |||
| Learning disability service | – | – | 11 | 4 | – | – | |||
| Perinatal community team | 4 | 43 | 29 | 50 | 124 | 122 | |||
| Traumatic stress service | – | – | – | – | – | – | |||
| Older peoples service (including but not limited to dementia services) | – | – | 56 | 82 | – | – | |||
| Forensic/criminal justice liaison service | – | – | 47 | 32 | 207 | 155 | |||
| CAMHS | – | – | 25 | 0 | – | – | |||
| Individual placement and support (for work) | – | – | 25 | 47 | – | – | |||
| SARC | – | – | 17 | 19 | – | – | |||
| PDU visits (people experiencing one or more); n | 0 | 39 | – | 49 | – | 49 | |||
| Primary outcomes | SWLSTG | LPFT | STHFT | |||
|---|---|---|---|---|---|---|
| Pre-periods | Post-periods | Pre-periods | Post-periods | Pre-periods | Post-periods | |
| MHT: number experiencing an informal admission | OR = 5.36, p < 0.05 | OR = 1.46, p = 0.08 | OR = 1.01, p = 0.99 | OR = 1.04, p = 0.84 | OR = 1.27, p = 0.52 | OR = 1.18, p = 0.37 |
| Acute trust: ED presentations (total) | t = 0.22, p = 0.83 | t = 0.81, p = 0.42 | t = 0.90, p = 0.37 | t = 0.24, p = 0.81 | t = 0.97, p = 0.33 | t = 0.57, p = 0.57 |
| Secondary outcomes: binary events data (number experiencing one or more) | ||||||
| Inpatient admissions | OR = 3.10, p < 0.05 | OR = 1.35, p = 0.14 | OR = 2.45, p = 0.01 | OR = 2.55, p < 0.001 | OR = 1.24, p = 0.42 | OR = 1.07, p = 0.69 |
| 0–5 days’ inpatient admissions | OR = 9.16, p < 0.05 | OR = 0.66, p = 0.23 | OR = 1.34, p = 0.66 | OR = 1.69, p = 0.19 | OR = 1.21, p = 0.80 | OR = 0.65, p = 0.36 |
| Compulsory admissions | OR = 3.44, p = 0.06 | OR = 0.71, p = 0.36 | OR = 1.49, p = 0.40 | OR = 1.08, p = 0.78 | OR = 1.34, p = 0.42 | OR = 0.87, p = 0.57 |
| Secondary outcomes: continuous data, n (SD) | ||||||
| Average length of inpatient stay, for those with a stay, mean (SD), n | t = 0.96, p = 0.35 | t = 1.14, p = 0.26 | t = 0.28, p = 0.78 | t = 1.31, p = 0.19 | t = 1.10, p = 0.28 | t = 0.85, p = 0.40 |
| Secondary outcomes: use of CMHT and other trust services | ||||||
| Community contacts with services (mean, SD) | t = 0.25, p = 0.80 | t = 1.41, p = 0.16 | t = 0.62, p = 0.53 | t = 2.36, p < 0.05 | t = 0.06, p = 0.9 | t = 0.76, p = 0.4 |
| Contact type: face to face (mean, SD) | t = 0.09, p = 0.93 | t = 2.51, p = 0.01 | t = 2.10, p = 0.04 | t = 1.65, p = 0.10 | t = 0.14, p = 0.9 | t = 3.62, p < 0.001 |
| Contact type: telephone/video (mean, SD) | t = 0.50, p = 0.62 | t = 0.24, p = 0.81 | t = 3.21, p < 0.01 | t = 4.97, p < 0.001 | t = 0.96, p = 0.3 | t = 6.00, p < 0.001 |
| Secondary outcomes: use of CMHT and other trust services by category | ||||||
| CMHT | t = 0.08, p = 0.94 | t = 1.11, p = 0.27 | t = 0.11, p = 0.91 | t = 1.76, p = 0.08 | t = 0.30, p = 0.76 | t = 1.78, p = 0.08 |
| Crisis resolution or home treatment team | t = 1.45, p = 0.15 | t = 4.15, p < 0.001 | t = 0.29, p = 0.77 | t = 1.06, p = 0.29 | t = 6.48, p < 0.001 | t = 50.03, p < 0.001 |
| Mental health support line | t = 1.02, p = 0.31 | t = 0.01, p = 0.99 | – | – | – | – |
Appendix 7 Qualitative coding framework
| Code name | Code description |
|---|---|
| A lack of support | Service users didn’t always feel appropriately supported and cared for on the PDU |
| Asking for help | What it was like to ask for help in a crisis and what it felt like to receive that help or not |
| Assessment process (in ED) | Lack of clarity around assessment process and location. The mechanics of the assessment process |
| Attitudes and assumptions of staff | Perceptions of staff towards people coming on to the unit |
| Balance between freedom and support | Both on the unit and in their everyday lives, service users experience the need for this balance. Independence on the unit can be appealing or felt as too much |
| Balance of people on the unit | Sense of camaraderie between service users helps people vs. distress of others can be challenging |
| Being supported and providing support | Importance of support networks (friends/family etc.). Feeling in a place where they can support others too |
| Boredom | Service users experiencing boredom in the PDU |
| Clarity around PDU service | How clearly defined the purpose, population and referral process for the PDU is |
| Cohort of the PDU | Who is coming to the PDU |
| Comparison with other services | How does the PDU compare to other services? |
| Connections with other services | How the PDU hooks into other services and the impact it has. How different services link in together |
| Environment | Physical structure of the PDU impacts facilities available and SU experience Atmosphere on the unit. Objects allowed/disallowed and the impact on safety |
| Experiences of and suggestions for other support post-discharge | Effectiveness of the unit dependent on services could signpost to Inadequate follow-up support Unaware of support available |
| Feeling safe on the unit | Kept safe in a crisis but questioning whether physical safety was enough |
| Holistic ways of working | Addressing all areas causing someone distress – housing, relationships, financial etc. |
| Impact of COVID-19 | Staffing shortages and stopping of services |
| Improvements to the PDU service | Suggestions for how to improve the service |
| In limbo | Service users on the PDU not high risk but not safe; uncertainty |
| Inappropriate use of the PDU service | Using the service inappropriately e.g. when there are not enough other services available or the service is used too frequently to be clinically beneficial |
| Lack of service capacity | Not enough space in services – this could be the PDU, A&E, inpatients wards, psychological therapies etc. |
| Mental health education | Educating staff and service users about mental health and mental health services |
| Positivity and optimism | PDU is the right service at the right time. A space apart from stressors |
| Relationship breakdown | The disintegration of close relationships, or the friction building within them, and how this contributes to a crisis |
| Someone to talk to | The importance of having someone to speak to – whether friends, family or formal support in the community. To feel listened to |
| Staff pressures | The pressures and demands staff deal with |
| Staff roles | Staff had different roles on the PDU; question around staff ability to administer medication. Staff roles that would benefit the PDU |
| Staff support | Whether staff on the PDU feel supported in their role and the support they provide to others in the team. Feeling able to challenge managerial decisions Ability to take responsibility/provide input |
| Suicidality and hopelessness | Feeling acutely suicidal. Pervasive sense of hopelessness, PDU could provide a respite |
| Talking with staff on a deeper level | Expectations of therapeutic input could exceed what was received on the PDU. Rationale behind differing levels of therapeutic input |
| Tensions | Tension between human, caring experience of PDUs vs. ticking boxes and moving people on from the service |
| Time | Issues around lack of time/too much time. Also the positives of expanded sense of time on the PDU. Support not being received at the right time, when the SU needs it |
| Treated with care and compassion on the PDU | Positive relationships with staff. Use of humour |
| Unsafe | Something about the unit itself or the way it is run that makes service users unsafe |
Appendix 8 Additional economic analyses
| Description | Unit cost (£) | Source | Notes |
|---|---|---|---|
| Cost per inpatient psychiatric day | 493.91 | 1 | SPMHS, other specialist mental health services, admitted patient |
| Liaison psychiatry (per contact) | 238.72 | 1 | MHSTAEA ED mental health liaison services, adult and elderly |
| ED attendance (per attendance) | 188.25 | 1 | Reference costs A&E weighted, and is a weighted average cost for A&E attendance (using values from HRG codes VB01Z–VB11Z), covering all attendances including scenarios both where investigation and treatment are received, and where they are not received |
| Ambulance conveyance (per visit) | 292.09 | 1 | Ambulance, see treat and convey (ASSO2) |
| Acute hospital inpatient admission (per episode) | 742.09 | 1 | Reference costs weighted for all poisoning related short-stay admissions WHO4A to WHO4E |
| CMHT (per contact) | 246.81 | 1 | MHSTOTHA other mental health specialist teams, adult and elderly |
| Home treatment teams (per contact) | 246.81 | 1 | MHSTOTHA other mental health specialist teams, adult and elderly |
| CRHT teams (per contact) | 246.81 | 1 | MHSTOTHA other mental health specialist teams, adult and elderly |
| Perinatal teams (per contact) | 207.84 | 1 | SPHMSMBUCC specialist perinatal mental health services, community contacts |
| Criminal diversion teams (per contact) | 277.27 | 1 | MHSTCJA criminal justice liaison services, adult and elderly |
| Mental health nurses (per hour) band 5 | 40 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 37.5 hours |
| Mental health nurses (per hour) band 6 | 50 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 37.5 hours |
| Mental health nurses (per hour) band 7 | 60 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 37.5 hours |
| HCA (per hour) band 2 | 24 | 3 | Assumed to have same proportion of oncosts etc. as band 4 |
| HCA (per hour) band 3 | 27 | 3 | Assumed to have same proportion of oncosts etc. as band 4 |
| HCA (per hour) band 4 | 30 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 37.5 hours |
| Consultant psychiatrist (per hour) | 116 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 43.3 hours |
| Support workers (per hour) band 2 | 24 | 2 | Assumed to have same proportion of oncosts etc. as band 4 |
| Service manager (per hour) band 8a | 69 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 43.3 hours |
| Unit administrator (per hour) (band 4) | 30 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 37.5 hours |
| Social worker (per hour) | 51 | 2 | Includes salary oncosts, overheads, ongoing training, capital overheads, assuming working week 37 hours |
| Psychologist per hour (band 8a) | 71 | 2 | Includes salary oncosts, overheads, capital overheads, assuming working week 37.5 hours |
| BSMHFT | LPFT | SWLSTG | STHFTa | |
|---|---|---|---|---|
| PDU cost | 928,560 | 1,296,480 | 1,909,680 | 2,102,400 |
| ITS cost impacts | ||||
| Inpatient costs | 0 | −38,887 | −63,052 | 0 |
| Liaison psychiatry | −4208 | −5687 | 0 | 0 |
| Acute hospital ED visits | −1431 | 1056 | 0 | 2194 |
| Ambulance/police conveyance | 0 | 0 | 0 | 1702 |
| Acute hospital inpatient admissions | 0 | 1918 | 2582 | 3952 |
| Total impacts | −5640 | −41,599 | −60,470 | 7848 |
| Synthetic control impacts | ||||
| Inpatient costs | 0 | 0 | −164,589 | 0 |
| Acute hospital ED visits | 0 | 0 | 0 | −245,775 |
| Ambulance/police conveyance | 0 | −96,740 | 0 | 0 |
| Acute hospital inpatient admissions | 0 | 0 | 0 | 0 |
| Total impacts | 0 | −96,740 | −164,589 | −245,775 |
| Overall costs averted | −5640 | −138,339 | −225,059 | −237,927 |
| Return on investment | −0.61% | −10.67% | −11.79% | −11.32% |
| Cost | BSMHFT | SE | BCa 95% CI | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Mean difference | Lower | Upper | p-value | ||
| Inpatient stays | 1021 | 5718 | −4697 | 843 | −6421 | −3163 | 0.000 |
| Liaison psychiatry | 328 | 347 | −19 | 19 | −62 | 19 | 0.333 |
| CMHTs | 779 | 1423 | −643 | 112 | −909 | −414 | 0.000 |
| Crisis teams | 1888 | 3383 | −1494 | 262 | −2039 | −960 | 0.000 |
| Nurses | 5 | 9 | −4 | 3 | −12 | 2 | 0.303 |
| Psychologist | 4 | 18 | −14 | 4 | −23 | −6 | 0.010 |
| Social workers | 0 | 0 | 0 | 0 | 0 | 0 | 0.135 |
| Perinatal team | 43 | 96 | −54 | 42 | −142 | 23 | 0.208 |
| Criminal diversion | 41 | 61 | −20 | 16 | −53 | 11 | 0.215 |
| All non-inpatient | 3089 | 5337 | −2249 | 288 | −2841 | −1667 | 0.000 |
| Total cost | 4110 | 11055 | −6945 | 892 | −8760 | −5264 | 0.000 |
| Cost | LPFT | SE | BCa 95% CI | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Mean difference | Lower | Upper | p-value | ||
| Inpatient stays | 922 | 5981 | −5059 | 953 | −7224 | −3173 | 0.001 |
| Liaison psychiatry | 135 | 90 | 45.46 | 14 | 19 | 73 | 0.001 |
| CMHT | 1115 | 2406 | −1291 | 238 | −1807 | −852 | 0.001 |
| Crisis teams | 1265 | 2417 | −2152 | 267 | −2706 | −1651 | 0.000 |
| Nurses | 21 | 26 | −6 | 6 | −18 | 6 | 0.328 |
| Psychologists | 4 | 4 | 0 | 4 | −10 | 8 | 0.969 |
| Social workers | 3 | 1 | 2 | 1 | 0 | 4 | 0.101 |
| Perinatal team | 41 | 73 | −32 | 36 | −127 | 28 | 0.481 |
| Criminal diversion | 48 | 3 | 45 | 34 | −2 | 123 | 0.315 |
| All non-inpatient | 2632 | 6019 | −3387 | 375 | −4176 | −2666 | 0.000 |
| Total cost | 3554 | 12,000 | −8446 | 1028 | −10,670 | −6365 | 0.000 |
| Cost | SWLSTG | SE | BCa 95% CI | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Mean difference | Lower | Upper | p-value | ||
| Inpatient stays | 160 | 3832 | –3671 | 735 | –5261 | –2264 | 0.001 |
| Liaison psychiatry | 266 | 134 | 132 | 22 | 83 | 177 | 0.000 |
| CMHT | 791 | 1851 | –1059 | 165 | –1412 | –726 | 0.000 |
| Crisis teams | 1071 | 2267 | –1196 | 208 | –1642 | –788 | 0.000 |
| Nurses | 63 | 50 | 13 | 10 | –9 | 34 | 0.255 |
| Psychologist | – | – | – | – | – | – | – |
| Social workers | 7 | 10 | –3 | 5 | –13 | 7 | 0.609 |
| Perinatal team | 7 | 26 | –20 | 12 | –50 | 2 | 0.178 |
| Criminal diversion | – | – | – | – | – | – | – |
| All non-inpatient | 2206 | 4338 | –2132 | 296 | –2761 | –1512 | 0.000 |
| Total cost | 2367 | 8170 | –5803 | 890 | –7735 | –4073 | 0.000 |
| Cost | SHSCFT | BCa 95% CI | |||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Mean difference | SE | Lower | Upper | p-value | |
| Inpatient stays | 1455 | 6634 | –5179 | 1408 | –8200 | –2495 | 0.004 |
| Liaison psychiatry | 364 | 340 | 24 | 74 | –154 | 160 | 0.753 |
| CMHT | 3863 | 5181 | –1319 | 508 | –2328 | –369 | 0.008 |
| Crisis teams | 2128 | 3389 | –1261 | 489 | –2236 | –349 | 0.011 |
| Nurses | – | – | – | ||||
| Psychologist | – | – | – | ||||
| Social workers | – | – | – | ||||
| Perinatal team | – | – | – | ||||
| Criminal diversion | – | – | – | ||||
| All non-inpatient | 6645 | 9374 | −2729 | 763 | −4247 | −1346 | 0.000 |
| Total cost | 8100 | 16,008 | −7908 | 1635 | −11,405 | −4862 | 0.000 |
List of abbreviations
- A&E
- accident & emergency
- AfC
- Agenda for Change
- BSMHFT
- Birmingham and Solihull Mental Health NHS Foundation Trust
- CI
- confidence interval
- CMHT
- community mental health team
- CRHT
- crisis resolution and home treatment
- ED
- emergency department
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FCE
- finished consultant episode
- FOI
- freedom of information
- GLM
- generalised linear modelling
- GRADE
- grading of recommendations, assessment, development and evaluations
- GSC
- generalised synthetic control
- HCA
- healthcare assistant
- HCP
- hospital catchment population
- HES-APC
- Hospital Episode Statistics admitted patient care
- HES-EC
- Hospital Episode Statistics emergency care
- ICD
- International Classification of Diseases
- IQR
- interquartile range
- IRR
- inter-rater reliability
- LEAP
- Lived Experience Advisory Panel
- LOS
- length of stay
- LPFT
- Lincolnshire Partnership NHS Foundation Trust
- MHT
- mental health trust
- NIHR
- National Institute for Health and Care Research
- OR
- odds ratio
- PDU
- psychiatric decision unit
- PEER
- Peer Expertise in Education and Research
- PES
- psychiatric emergency service
- PLE
- psychiatric liaison episodes
- RCT
- randomised controlled trial
- ROBINS-I
- Risk of Bias in Non-Randomised Studies
- RoI
- return on investment
- SD
- standard deviation
- SGUHFT
- St George’s University Hospital NHS Foundation Trust
- SHSCFT
- Sheffield Health and Social Care NHS Foundation Trust
- SPSS
- Statistical Product and Service Solutions
- STHFT
- Sheffield Teaching Hospital NHS Foundation Trust
- SWBHFT
- Sandwell and West Birmingham Hospitals NHS Foundation Trust
- SWLSTG
- South West London and St George’s Mental Health NHS Trust
- UHBT
- University Hospitals Birmingham NHS Foundation Trust
- ULHFT
- United Lincolnshire Hospitals NHS Foundation Trust
- WP
- work package