Notes
Article history
The research reported here is the product of an HSDR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HSDR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HSDR journal.
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 16/138/31. The contractual start date was in March 2021. The final report began editorial review in October 2021 and was accepted for publication in March 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Sidhu et al. This work was produced by Sidhu et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Sidhu et al.
Chapter 1 Background, context and objectives
The key points of Chapter 1 are summarised in Box 1.
-
There are over 15,000 care homes in England, with an estimated combined capacity of approximately 450,000 beds and an average of slightly under 30 residents per home. Care homes in England employ an estimated 600,000 staff.
-
The majority of the care home resident population are older adults who have multiple long-term health conditions, and approximately 40% of the total care home population receive specialist dementia care. Care homes also provide accommodation and care for people with physical or learning disabilities of all ages.
-
During the COVID-19 pandemic, emergency procedures were introduced to free up bed capacity in NHS secondary care, including discharging some patients into care homes.
-
The NHS has included support for care homes in The NHS Long Term Plan,1 and this has been accompanied by development of the EHCH model. The EHCH model stipulates that all care homes should be aligned with a named PCN.
-
Although pulse oximeters may have been previously available in some nursing homes, there is evidence that increased and wider use of pulse oximetry in care home settings has been prompted by the COVID-19 pandemic.
-
We carried out a mixed-methods evaluation, combining qualitative and quantitative approaches, to understand the current level of use of pulse oximetry in the care home sector and the associated support provided to care homes.
EHCH, enhanced health in care homes; PCN, primary care network.
Some text in this chapter has been reproduced with permission from the following sources:
-
The King’s Fund. 2 [This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC-ND 4.0) license, which permits others to distribute for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc-nd/4.0/. The text below includes minor additions and formatting changes to the original text.]
-
Care Provider Alliance. 3 [This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text where cited.]
-
National Institute for Health and Care Research (NIHR). 4
-
Wessex Academic Health Science Network. 5
-
Keith et al. 6 [This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.]
-
The Health Foundation. 7
The study reported here is an extension to a concurrent evaluation of remote home monitoring models during the COVID-19 pandemic in England (see Report Supplementary Material 1, Box A). We begin the report by providing a short overview of adult social care and the care home sector in England.
Adult social care and the care home sector in England
According to The King’s Fund,2 adult social care covers a wide range of activities to support individuals who are older and frail, and living with a physical or mental impairment, to live independent lives. The King’s Fund2 states that adult social care includes ‘personal care’ (e.g. washing, dressing, social engagement) and ‘social care’ to allow people to live independently in their own homes, which may include sharing information and advice, as well as additional support for family carers. Social care can be both ‘short term’ (encouraging independence with limited need for ongoing support) and ‘long term’ (ongoing support in the form of nursing of community-embedded help), and is provided by local authorities using a range of health professionals.
Most publicly funded social care in England is available only to people with the highest needs and lowest assets (currently under review by the UK government). People with assets worth more than £23,250 are normally ineligible (in the case of residential care, this figure includes the value of a person’s property if they have one). 2 Local authorities are responsible for assessing people’s needs for publicly funded social care, which may also involve weekly top-up fees. Everyone else (i.e. people who do not qualify for publicly funded social care) must fund their own care, including places in care homes. In addition, housing-based services (e.g. extra care housing) in the form direct payments are a funding choice in personal budgets. Direct payments allow individuals to purchase their own care and support services, with the aim of maximising their involvement and control over how their needs are met. 8,9 Most social care services are delivered by independent domiciliary care and residential care providers, which are mainly for-profit companies, but also include some not-for-profit, voluntary sector organisations. In England, on 18 May 2021, there were 15,362 care homes registered with the Care Quality Commission (CQC) (London, UK). [The CQC registration data are live data, and they are available from the CQC website (URL: www.cqc.org.uk/about-us/transparency/using-cqc-data). The numbers reported here are from data downloaded on the 18 May 2021.] Just over one-quarter (27%) of these care homes are nursing homes, meaning that they have qualified nursing staff on site at all times. Seventy-two per cent of care homes are residential homes (i.e. without nursing staff) and 1% of care homes are dual residential and nursing. The total bed capacity of these care homes is approximately 450,000, implying an average capacity of just under 30 beds per home. Many care homes are parts of chains that have multiple individual sites. The six largest care home providers combined account for 11% of all UK care homes and 17% of UK care home beds. 10 Yet, despite the growth of care home chains, one-third of providers are businesses of one or two care homes, and almost 10% of the care home population in England are wholly funded by the NHS as continuing care recipients. 11 Long-term conditions, many of which linked to ageing, are all prevalent in the resident population of care homes, including arthritis, cancer, chronic heart disease, dementia, depression, diabetes, hypertension, respiratory disorders, stroke, cognitive impairment (not dementia) and hearing and vision loss. 12 At present, only 40% of long-term care providers offer specialist dementia care, despite 70% of older care home residents having cognitive loss/dementia. 12 Hence, the population living in care homes in England has a unique set of needs, and this directly affects who is responsible for assessment and how residents’ needs are recognised, communicated and documented.
English residential care homes facilities employ approximately 600,000 staff, of whom 85% are women. 13 The estimated annual turnover of directly employed staff working in the adult social care sector (which is broader than care home staff alone, but includes care home staff) is high. In 2019/20, the estimated annual turnover rate was 30.4%, meaning that at the end of the financial year nearly one-third of the staff had moved on from the employer they were with at the start of the financial year. Staff vacancy rates are also considerable, and it was estimated that in 2019/20 a total of 7.3% of roles in adult social care were vacant. 13
Providers of care homes are inevitably subject to financial pressures. Since 2015, the CQC has overseen the financial sustainability of around 65 difficult-to-replace care providers, representing around 30% of the overall care market by number of beds. 14 In addition, some providers with a sizeable regional or local presence may not be subject to the CQC’s oversight, but their failure would have a significant impact on the number of care home places available. In 2017, the Competition and Markets Authority (London, UK) concluded that care homes primarily accepting local authority-funded residents were unlikely to be sustainable at the rates local authorities paid. 11 Considering that 46% of care home residents in independent care homes were estimated to have received some form of state funding in 2018, this is a significant proportion of the sector. 10,11 Furthermore, the CQC’s State of Care 2019/20 report15 noted that many care homes were relying on higher prices for self-funders to remain viable (i.e. self-funders were subsidising publicly funded residents). 16
Challenges experienced by care homes in England during the COVID-19 pandemic
A survey of 9000 care homes in England found that 56% of the care homes had experienced at least one case of COVID-19 by July 2020. 17 Coronavirus was mentioned on the death certificate of 19,286 care home residents who died between mid-March and mid-June 2020. During the second wave of the pandemic (i.e. between 31 October 2020 and 5 February 2021), there were 16,355 COVID-19-related deaths registered among people in care homes. 18 Overall, during the first two waves of the pandemic in England, there was evidence to report that one-third of residents and one-quarter of care home staff had a COVID-19 infection. 19
The care homes sector also reported an increased demand for hospital discharge beds to support COVID-19 patients with high levels of dependence and acuity who, under other circumstances, would have been discharged to their own homes, following National Institute for Health and Care Excellence guidelines. 20 Notably, patient discharge from acute hospitals to care homes during the pandemic came under scrutiny. Many patients were discharged without having been tested for COVID-19 or having tested positive, or care homes were not notified of test results. 21 As a result, after negative reactions from the care home sector, residents’ families and some clinicians, official guidance from Public Health England (London, UK), NHS England (London, UK) and the Department of Health and Social Care (London, UK), in April 2020, abandoned the previous approach of rapid discharge of hospital patients to care homes without waiting for test results. 22
A survey of nearly 300 social care staff carried out in July 2020 found that staff felt that their job had left them feeling ‘tense, uneasy or worried’ more often since the onset of COVID-19. 12 In addition, a Queen’s Nursing Institute (2020) survey found that care home staff felt that their workload had risen since the onset of the pandemic, mainly as a result of covering for colleagues who had to self-isolate or having to train new volunteers. Staff turnover in 2020 was 29.6% in residential care and 36.8% in nursing facilities, indicating significant workforce pressures in both residential care contexts. 23
A report by Healthwatch with care homes in Barnet, north London, found that most care home managers reported that they had coped well during the first wave of the pandemic, although many care home managers noted that it had been an exceptionally stressful and challenging time for staff. 24 Many managers reflected that this was, to some extent, exacerbated by personal protective equipment coming 4 or 5 weeks too late, along with frustrations with accessing COVID-19 testing for staff and residents. The extra costs of personal protective equipment, a reduction in new admissions to care homes and the cost of COVID-19-related staff absences were all identified as key obstacles when dealing with the effects of the pandemic. In addition, care home staff had to accommodate the transition of routine health care for their residents to being predominantly provided digitally, with face-to-face consultations being carried out only if clinically necessary. Despite considerable nuanced learning coming from the Healthwatch report,24 such learning may be specific to the health system and care home network in Barnet, and may not be generalisable to other care home setting across England. Nevertheless, challenges remain, particularly the staffing shortfall in care homes across England (largely as a result of a post-Brexit economy) and the requirement for all care home workers to be fully vaccinated against coronavirus. The King’s Fund’s (2021)25 response to the Health and Social Care Committee report on workforce burnout and resilience in the NHS and social care stated that:
. . . the added pressure of the COVID-19 pandemic has left many staff physically and emotionally drained, but health and care services have been dogged by staff burnout and workforce shortages for many years.
As a result, the pandemic and years of funding shortfalls in social care have left the front-line workforce depleted, demoralised and feeling unvalued. These challenges can, at times, be exacerbated by how fragmented adult social care is, and how complex it is to try to deliver adult social care across many different providers working with NHS partners in different sectors of the economy. According to Skills for Care, an estimated 21,200 organisations (across 41,000 establishments) were involved in providing or organising adult social care in England, ranging from large national employers, large charities and local authority adult social services departments to small independent care services. 13 During the pandemic, policy-makers may have interpreted the term ‘care homes’ generically and not taken full account of local organisational NHS and non-NHS structures.
COVID-19 brought rapid change in hospital discharge, with ongoing concern about its immediate and longer-term consequences. Emergency procedures were introduced to free up beds in secondary care within days, and many patients were discharged to care homes without first being tested for COVID-19. The Public Accounts Committee reported that 25,000 people were discharged from hospital to care homes before the introduction of routine pre-discharge testing in mid-April 2020. 26
The NHS Five Year Forward View stated that the NHS in England was prioritising support for frail older people living in care homes,27 including a commitment to identify what changes were needed, as well as detailed prototyping of new care models of in-reach support (e.g. medical reviews, medication reviews and rehabilitation services). The NHS Long Term Plan1 built on this ambition by recommending that the NHS strengthen its support for the people who live in, and work in and around, care homes, using the enhanced health in care homes (EHCH) model. 3 The model was designed to be equally applicable to homes for people with learning disabilities and/or mental health needs as to care homes for frail older people. The EHCH model incorporates best practice with regard to moving away from reactive models of care delivery towards proactive individualised care. Key features of the EHCH model are described in Box 2.
-
Every care home is aligned to a named PCN.
-
Every care home has a named clinical lead.
-
A weekly ‘home round’ or ‘check-in’ with residents by an appropriate member of care home staff.
-
Within 7 days of re-admission/admission to a care home, a resident should have a person-centred holistic health assessment.
-
Within 7 days of re-admission/admission to a care home, a resident should have in place personalised care and support plan(s).
-
A requirement to prioritise care home residents who would benefit from a structured medication review.
To bring the EHCH service into being, Clinical Commissioning Groups (CCGs) have played a key role in aligning each eligible care home to an individual PCN. 3 PCNs built on the new ‘vanguard’ models of integrated health care that had been developed as a result of the Five Year Forward View. 27 Smith et al. 4 state that those vanguard models of care entailed pilots of significant integration of general practice and community health services; hospital, mental health, community and primary care; general practice and social care (particularly in providing support to residential care homes); and services focused on particular clinical conditions such as cancer.
In addition, the NHS in England is attempting to train and equip care home staff with necessary tools and skills to monitor the health of residents and to educate staff of when to escalate care. For instance, Recognise early soft signs, Take observations, Respond, Escalate (RESTORE2) is a physical deterioration and escalation tool for residential care/nursing homes based on nationally recognised methodologies. 5 The RESTORE2 tool is designed to support care home staff and health professionals to (1) identify those at risk of physical deterioration, (2) act in accordance with the resident’s care plan, (3) take the necessary physical observations to inform escalation, (4) communicate in a timely manner with health professionals and (5) provide a history of the resident’s escalation history so that they can make appropriate health-care decisions.
Stocker et al. ,28 in a qualitative study, explored the use of a National Early Warning Score (NEWS) intervention in care homes during the COVID-19 pandemic. They found that the NEWS tool improved the response of care home staff and health-care professionals to deterioration in residents’ health and that staff felt empowered by the NEWS tool, which provided a common clinical language that they could use to communicate concerns with external services, acting as an adjunct to staff intuition of resident deterioration. In addition, the British Geriatrics Society has emphasised the importance of care home staff having the skills, training and equipment to identify deterioration in residents. 29 However, embedding assessment technology in care homes and enabling care home staff to adequately engage to better identify residents who are deteriorating requires support from the wider health-care system to support scale-up. It remains important for care home staff to have access to trusted NHS professionals who can provide training on how to pick up on ‘soft signs’ (e.g. residents presenting reduced appetite), which, when combined with assessment technology, can lead to more robust decisions regarding escalating care. 30
The application of pulse oximetry during the COVID-19 pandemic in care homes
There is emerging evidence that using pulse oximetry, that is a non-invasive and painless test that measures a person’s blood oxygen saturation level, in community settings can accurately predict outcomes for individuals who have tested positive for COVID-19 with regard to mortality and intensive care unit admission. 28 Risk of severe disease and death from COVID-19 is known to be higher in people who are older and in those with certain underlying health conditions. 31
For nursing homes, pulse oximeters are part of a suite of standard clinical measurements that nursing staff have at their disposal. 32,33 Pulse oximeter usage is not mandated, and the decision to take the measurement is at the discretion of the clinician [e.g. general practitioner (GP) or nurse]. Information about the extent to which pulse oximeters are used in care homes is sparse. Therefore, the project team underwent a scoping process of mapping relevant literature and interviews with key experts to understand the extent of pulse oximetry use in care homes.
Identification of gaps in the literature
Although pulse oximeters may have previously been available in nursing homes, there is evidence that increased and wider use of pulse oximetry in care home settings has been prompted by the pandemic. Yet little is known about the introduction of pulse oximetry in other care home settings (specifically, residential care homes) that cater for a range of residents living with long-term health conditions, including dementia and learning disabilities. Furthermore, there is a paucity of evidence regarding support that the NHS has provided to care homes to administer pulse oximetry during the COVID-19 pandemic. Consequently, we carried out a mixed-methods evaluation, combining qualitative and quantitative approaches, to understand the current level of use of pulse oximetry in the care home sector and the associated support provided to care homes (Box 3).
-
Oxygen is carried around in your red blood cells by a molecule called haemoglobin. Pulse oximetry measures how much oxygen the haemoglobin in your blood is carrying, and this is called the oxygen saturation and is a percentage (scored out of 100). A pulse oximeter is a small medical device that is put on the tip of the finger to check someone’s oxygen levels.
-
Pulse oximeters are provided to patients as part of the NHS response to COVID-19. The NHS supports people at home and in care homes who have been diagnosed with coronavirus and are most at risk of becoming seriously unwell.
-
Advantages of pulse oximetry include that it is non-invasive and simple and can be used to evaluate trends.
-
Pulse oximetry can help with earlier detection of silent hypoxia, low oxygen levels in the absence of significant shortness of breath, and this can help ensure more timely hospital treatment if required.
-
Prior to the COVID-19 pandemic, pulse oximetry was used across a range of health-care settings to treat a number of health conditions.
-
During the first wave of the pandemic (between March and September 2020) there were over 30,500 excess deaths of care home residents. A total of 4500 additional deaths of domiciliary care users were also reported, a greater proportional increase in deaths than in care homes (225% vs. 208%).
-
The ability of social care services to deal with the crisis was affected by a severe staff shortage, a care system that is fragmented within complex national and local arrangements and a lack of good-quality data on what is happening in the sector.
Research questions
Following our mapping of the literature and scoping interviews with key experts, the research questions were identified as follows:
-
When and how is pulse oximetry being employed in care homes for managing the health care of residents with COVID-19 and other health conditions?
-
Which care home staff are involved in the set-up, delivery and monitoring of pulse oximetry in care homes?
-
What support are care homes receiving from primary, community and secondary care NHS teams with regard to the use of pulse oximetry, and is that support appropriate? Are there any weaknesses in providing that support that can be rectified?
-
-
What are the perceived benefits to residents (e.g. health-related outcomes, satisfaction with care received, hospital admission avoidance, impact on perceived anxiety) of using pulse oximetry in their care home?
-
What are the experiences of staff using oximetry in care homes, including barriers and enablers, and lessons learnt?
-
What training have care home staff received to deliver pulse oximetry in a range of care home settings?
-
What impact has the use of pulse of oximetry had on the well-being and confidence of care home staff?
-
What are the challenges faced by care home staff in delivering pulse oximetry and associated monitoring?
-
-
What are the views of senior care home staff and managers on the guidance and resource necessary to support and sustain the use of pulse oximetry in care homes?
-
What are the experiences of the primary, community and secondary care health-care staff involved in supporting the use of pulse oximetry in care homes, including, where relevant, as part of the national COVID Oximetry @home (CO@h) service?
The methods adopted for the rapid evaluation are described in Chapter 2.
Chapter 2 Design
The key points of Chapter 2 are summarised in Box 4.
-
We conducted a mixed-methods evaluation, combining qualitative and quantitative approaches. The evaluation comprised the following WPs:
-
scoping interviews and engaging with relevant literature, as well as co-designing the study approach and research questions with members from a User Involvement Group (WP1)
-
a national online survey that examines the application of pulse oximetry in care homes (WP2)
-
in-depth interviews at six case study sites (WP3)
-
synthesis, reporting and dissemination of study findings (WP4).
-
-
A survey was distributed to registered managers across 15,362 care homes (i.e. the total number of care homes in England registered with the CQC) to understand current practices regarding the use of pulse oximeters in patients with COVID-19 and other conditions.
-
We carried out semistructured interviews with a purposive sample of stakeholders in six selected (care home) sites. The sites were selected based on the principles of maximum variation and convenience sampling. Our analysis was guided by theoretical frameworks to understand staff engagement and adoption of pulse oximetry in care homes across England.
-
Our analysis was informed by CFIR and the Gale et al. 35 framework method for the analysis of qualitative data in multidisciplinary health research. The Gale et al. 35 framework method is a systematic method of categorising and organising data while continuing to make analytical and interpretive choices transparent and auditable.
-
We adopted the ‘following a thread’ approach put forward by O’Cathain et al. ,36,37 whereby synthesis of data takes place at the data analysis stage to identify key themes and data that warrant further analysis.
CFIR, Consolidated Framework for Implementation Research; WP, work package.
Aims of the evaluation
The study was conducted by the Birmingham, RAND and Cambridge Evaluation Centre (BRACE) and the Rapid Service Evaluation Team (RSET). Both BRACE and RSET have received funding from the NIHR Health and Social Care Delivery Research (HSDR) programme for a 5-year research programme that aims to rapidly evaluate health and care service innovations to produce timely findings of national relevance and immediate use to decision-makers. The topic of this report was identified through discussions between the NIHR HSDR programme and NHS England and NHS Improvement’s (NHSE&I’s) (London, UK) CO@h workstream. NHSE&I established a working group, which acted as a Project Steering Group to the evaluation (see Report Supplementary Material 2), to investigate the potential role of using pulse oximetry to support residents in care homes throughout the pandemic.
The rapid evaluation had two distinct aims:
-
To understand how pulse oximetry is used in care homes by care home staff and health-care professionals (including, but not limited to, through remote monitoring services run by NHS), and for which conditions and in which circumstances. The source of pulse oximeters, the nature of staff involved and their experience of using pulse oximeters, the level of training received by care home staff to deliver pulse oximetry and remote monitoring, the recording and storing of data, pathways for monitoring and escalation, and the level of support from primary, secondary and community NHS health-care teams were also considered.
-
To develop an understanding of how the use of pulse oximetry in care homes might be optimised, including an understanding of resources, approaches and activities necessary to sustain the use of pulse oximetry in care homes (e.g. support from national and regional bodies, such as CCGs, NHS trusts and local authorities).
We have carried out a mixed-methods evaluation, combining qualitative and quantitative approaches, to understand the current level of use of pulse oximetry in the care home sector and how that use might be optimised and supported in the future. The rapid evaluation comprised the following main steps: (1) scoping and designing the rapid evaluation by carrying out scoping interviews, engaging with the relevant literature and co-designing the study approach and research questions with members from a User Involvement Group (completed as part of a workshop delivered in February 2021); (2) a national, online survey sent to all registered care home managers in England, examining the application of pulse oximetry in care homes; (3) in-depth interviews with managers, staff and primary, community and secondary care providers at six purposively selected case study sites, plus interviews with national policy leads, alongside analysis of data and testing findings with members from a User Involvement Group (completed as part of a workshop delivered in May 2021); and (4) synthesising and reporting the findings and disseminating them to policy-makers, experts, academics and other key stakeholder groups to enable them to share and discuss the findings. These four work packages (WPs) are summarised in Table 1.
| WP | Description and activity | Research question |
|---|---|---|
| WP1: scoping interviews and engaging with the relevant literature, as well as co-designing the study approach and research questions with members of a User Involvement Group (as described in Chapter 1) |
To obtain an overview of the existing evidence on the use of pulse oximetry and remote monitoring in the care home sector and to inform the propositions to be tested through the national survey and interviews Interviews with key NHS leaders, care association directors and care home managers, mapping and engaging with relevant literature, and co-designing the study approach and research questions with a User Involvement Group (online workshop) |
1 (1.1 and 1.2) |
| WP2: a national online survey that examines the application of pulse oximetry in care homes |
A national online survey of care homes exploring the various aspects of pulse oximetry and remote monitoring use in care homes, including analysis of data and testing of findings with members from a User Involvement Group (online workshop) An online survey of all care homes in England on the use of pulse oximetry |
2, 3 (3.1, 3.2 and 3.3) |
| WP3: in-depth interviews at six case study sites | A series of interviews with managers and staff and at six purposively selected care homes, as well as with the NHS staff supporting them, exploring in depth the use of pulse oximetry and remote monitoring. WP3 includes further interviews with national policy experts, alongside analysis of data and testing of findings with members from a User Involvement Group (online workshop) | 2, 3 (3.1, 3.2 and 3.3), 4 and 5 |
| WP4: synthesising and reporting findings and disseminating them to policy-makers, practitioners, managers, academics and other key stakeholder groups to enable them to share and discuss findings |
To share and discuss findings generated from data collection from WP2 and WP3 and to develop recommendations for care homes, commissioners, health-care providers and policy-makers Workshops with NHSE&I’s CO@h and People Receiving Social Care groups |
5 |
We have used the Consolidated Framework for Implementation Research (CFIR) to guide and structure the rapid evaluation. 6 The CFIR is a conceptual framework that was developed to guide systematic assessment of multilevel implementation contexts to identify factors that might influence intervention implementation and effectiveness. The CFIR is well suited to guide rapid evaluation of the implementation of complex health-care delivery interventions because it provides a comprehensive framework to systematically identify factors that may emerge in various multilevel contexts to influence implementation. The five major domains of CFIR are presented in Box 5. The framework was used as a theoretical tool to provide a thread to synthesise, integrate and interpret data, and to present our key learning and findings. 6
-
Intervention characteristics, which are the features of an intervention that might influence implementation. Eight constructs are included in the domain of intervention characteristics (e.g. stakeholders’ perceptions about the relative advantage of implementing the intervention, complexity).
-
Inner setting, which includes features of the implementing organisation that might influence implementation. Twelve constructs are included in inner setting (e.g. implementation climate and leadership engagement).
-
Outer setting, which includes the features of the external context or environment that might influence implementation. Four constructs are included in the outer setting (e.g. external policy and incentives).
-
Characteristics of individuals involved in implementation that might influence implementation. Five constructs are related to characteristics of individuals (e.g. knowledge and beliefs about the intervention).
-
Implementation process, which includes strategies or tactics that might influence implementation. Eight constructs are related to implementation process (e.g. engaging appropriate individuals in the implementation and use of the intervention, reflecting and evaluating).
Reproduced with permission from Keith et al. 6 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original text.
Protocol sign-off
The study topic was identified and prioritised for rapid evaluation, with NIHR HSDR senior colleagues working with NHSE&I as part of a call to undertake a rapid evaluation. An initial short pro forma outlining the study aims, methods and outcomes was submitted (January 2021) and, once approved, was used as the basis for writing the full research protocol (February 2021), which drew on scoping interviews with key experts, relevant literature and an online workshop with our User Involvement Group (WP1).
Ethics approval
An application for ethics review to the University of Birmingham’s Research Ethics Committee was made by the project team and approval was gained in March 2021 (reference ERN_13-1085AP40). The project team received confirmation from the Head of Research Governance and Integrity, University of Birmingham, that this study was to be categorised as a service evaluation and, therefore, approval by the Health Research Authority or an NHS Research Ethics Committee was not required. At each of our six case study sites, we approached relevant research and development personnel/care home managers to confirm that all were content for the evaluation to proceed in their care home.
Method
The methods used in each of the evaluation WPs are described below. WPs 1–3 all included working with a User Involvement Group.
Co-designing the study approach and research questions with members from a User Involvement Group
Members of the study team met with a specially convened User Involvement Group. The User Involvement Group consisted of three members who were co-researchers who have either worked on previous care home sector-related studies and/or are currently supporting close family members in a care home (n = 2) and a member of the BRACE Patient and Public Involvement Group (n = 1). The User Involvement Group discussed the ‘what’ questions (e.g. what is important to find out/know about) and the ‘how’ questions (e.g. how best to gather this information). All members of the User Involvement Group took part in two workshops and two members attended a third workshop. 6 A structured agenda was prepared in advance of each workshop and included time for presentation of findings from the review of relevant literature and scoping interviews, as well as time for discussion and feedback when sharing learning from data collected. As part of the first workshop (February 2021), members of the User Involvement Group commented on our research questions, our choice of methods and recruitment strategies and the study’s participant-facing documentation. A second workshop (May 2021) was held to discuss preliminary findings whereby feedback fed into remaining data collection. A third workshop (June 2021) was held to refine interpretation of data and support synthesis of learning across data sets.
Work package 1: scoping interviews and engaging with relevant literature, as well as co-designing the study approach and research questions with members of our User Involvement Group
Members of the study team carried out seven telephone interviews, using a semistructured topic guide informed by the literature and revised iteratively following preliminary interviews with key stakeholders, including key NHS leaders, representatives of national care associations and senior care home managers. The interviews had two purposes: (1) to gather stakeholders’ initial insights and views on the use of pulse oximetry and remote monitoring in care homes and (2) to help define the scope of the work regarding the maturity of the use of pulse oximetry in care homes before and during the COVID-19 pandemic.
Following the review of the literature (see Description of review strategy for grey literature search and summary of findings from scoping work) and the initial scoping interviews, the research team held a workshop with the Project Steering Group, which comprised members from NHSE&I and from the Care Provider Alliance (which represents most care homes in England). In addition, the research team held a separate event with the User Involvement Group. Both groups suggested that further investigation was required on the feasibility of including residents in the rapid evaluation. During initial evidence searching for this further investigation, a systematic review from 2016 was identified and further engagement with more recent relevant literature was guided by key experts. 38 Concurrently, members of the study team completed telephone/online interviews, again, using a structured topic guide, with a range of key experts (n = 5) with vast experience of working in and/or carrying out research with residents in care facility settings. A summary of key themes and messages from our scoping work can be found in Boxes 6 and 7.
To scope the evaluation, we captured learning from BRACE and RSET’s rapid systematic review in 2021 of remote home monitoring models set up during the COVID-19 pandemic38 and performed an additional evidence review of grey literature identified in the 12 months between January 2020 and January 2021, following principles outlined by Munn et al. 39 Grey literature is non-academic literature that is published in sources such as reports and/or working papers from policy groups or committees. 38,40,41 The full details of the evidence mapping are given in the following sections and Boxes 6 and 7.
As part of the scoping phase of the project, the study team engaged with relevant literature to:
-
collate published literature, including grey literature (i.e. research that is either unpublished or has been published in non-academic form), using a selective systematic approach to searching on the use of pulse oximetry and remote monitoring in care homes in the England
-
provide a descriptive summary of our findings
-
inform our study design, research questions and methods.
Description of review strategy for grey literature search and summary of findings from scoping work
The evidence review strategy included grey literature identified in the 12 months between January 2020 and January 2021, using the search terms ‘remote monitoring’ OR ‘oximetry’ AND ‘Covid-19’ (including synonyms) AND ‘Care home’ (including synonyms).
The search was performed by the HSMC Knowledge and Evidence Service at the University of Birmingham on 21 January 2021. The search used the Health Management and Policy database, from the Healthcare Management Information Consortium, and Google (Google Inc., Mountain View, CA, USA). The search was re-run on 27 January 2022 to identify any new literature (identifying one additional publication).
Material was considered eligible if it detailed the use of oximetry and/or remote monitoring in a care home setting during the COVID-19 pandemic or in the 12 months prior. Seventy-nine sources were identified (excluding three duplicate sources), of which 63 items were reviewed. These sources were all reviewed by one member of the research team (JRT), with learning shared during weekly team meetings, allowing input from all authors. Sources included a variety of media, including newspapers, guidance, evaluation plans and product videos focusing on care homes for older adults, with none sources mentioning other types of care homes, such as homes for people with sensory or learning disabilities. In addition, the search identified a variety of supportive guidance from NHSE&I, NHS Digital (Leeds, UK), NHSX (London, UK), Public Health England, the Local Government Association (London, UK) and the British Geriatric Society (London, UK). Data from sources were extracted using a thematic framework, which was shaped by early evaluation research questions and was iteratively updated alongside learning captured from scoping interviews completed as part of WP1. A subteam of authors (JRT, JB, IL and MS) came together as part of an online meeting to identify cross-cutting themes from both scoping interviews (n = 7) and mapping of the relevant literature and agreed final themes.
Box 6 summarises what we found from the scoping work.
-
Variation in the care home sector, with nursing and residential homes having different skill sets in the use and interpretation of pulse oximetry.
-
Localised variation in IT infrastructure and networks of relationships with the NHS (across primary, secondary and community care).
-
Workload changes as a result of the pandemic and also due to pulse oximetry accompanying other elements of service change, such as new IT systems, which were likely to have an impact on staff perception of pulse oximetry as a tool generally.
-
Some expert interviewees felt that the CO@h programme was well advertised to the care home sector; however, some interviewees from the care sector remained unaware.
-
The comfort and understanding of residents with pulse oximetry was variable and dependent on pre-existing conditions, such as dementia and familiarity with health technology.
-
IT, information technology.
Inner and outer settings: considerations for care homes when introducing pulse oximetry
Interviews with key experts indicated that there was a great deal of variation in the care home sector, with nursing and residential homes having different skill sets in the use and interpretation of pulse oximetry, with care home staff varying in their familiarity with administering pulse oximetry to a range of residents living with long-term conditions, including dementia. Within care homes, staff undertaking routine measurements were likely to be senior, but pulse oximetry was perceived as a form of monitoring accessible by any member of staff. The issue of localised variation in information technology (IT) infrastructure and networks of relationships between care homes and the NHS (across primary, secondary and community care) was raised, and many of the staff interviewed felt that there should be a better and more nuanced understanding of how care homes operate across different regions in England. Notably, information on care home relationships with local general practices, PCNs, CCGs and acute hospital trusts was limited; however, there was mention of tools to support appropriate escalation by interviewees for care home residents [e.g. National Early Warning Score 2 (NEWS2) and RESTORE241]. In addition, one study mentioned that decisions by central government can result in resource constraints and additional work and, consequently, sometimes impair the ability of care home staff and managers to make decisions regarding the care of their residents. 42
Characteristics of individuals involved in the administration of pulse oximetry
Admissions to hospital of care home residents decreased substantially during the pandemic, with 11,800 fewer admissions during March and April in 2020 than in previous years. In addition, there were numerous reports of a reluctance among GP, ambulance and hospital staff to accept care home residents as patients during the pandemic. 7 Expert interviewees highlighted workload changes as a result of the pandemic and the introduction of pulse oximetry accompanying other elements of service change, such as new IT systems. These factors were likely to have an impact on staff perception of pulse oximetry as a tool generally. Concern for staff working across care home settings throughout the pandemic was voiced by a number of staff interviewed, and it was clear that the ability of care home staff to engage with programmes like CO@h was likely to be compromised as a result of increased workload and pressure, especially during the first wave of the pandemic.
The implementation process, relative advantages and sustainability of remote monitoring and pulse oximetry in care homes
Remote monitoring was mediated in a variety of ways, including via online platforms, paper-based systems with telephone calls or (less frequently) through wearable sensors. Remote monitoring models based on telephone calls were considered more inclusive than paper-based systems alone. 38
Which care home staff members took readings and how they were submitted to NHS contacts varied between systems and care home type, as did the type of training available for staff using pulse oximetry with residents. Some care home staff were described as having low skill and confidence levels and were, therefore, nervous of using new devices. Developing these skills was identified as key to utilising new technologies to reduce infection transmission risk. 20 Some expert interviewees felt that the CO@h programme was well advertised to the care home sector and was being locally adapted to account for differing clinical pathways for residents; however, some interviewees from the care sector remained unaware. Some care homes may be benefiting from the programme, but associate the programme with wider support services from their GP, PCN, CCG or initiatives derived from the EHCH programme, rather than knowing it as the CO@h programme.
Some interviewees mentioned the benefits of using pulse oximetry to manage conditions such as chronic obstructive pulmonary disease (COPD) or to manage frail patients near the end of life. Expert interviewees also highlighted that the level of care home residents’ comfort with, and understanding of, pulse oximetry was variable and dependent on pre-existing conditions, such as dementia, and on familiarity with health technology.
Exploration of including data collection with care home residents
Following a review of relevant literature and interviews with experts, the project team found that research with care home residents would require significant support from care home staff, social workers and/or family members to help the resident understand the purpose of the research and to help make clear to the researcher what might be meant by the resident (i.e. communicating resident experiences as the resident intends as best as possible), as well as requiring informed consent. It would have been time-consuming and problematic to obtain such support during the pandemic. Box 7 summarises the key challenges and issues in collecting data from care home residents.
-
The use of pulse oximeters is often accompanied by the use of other physiological monitoring methods. Therefore, separating the use of pulse oximeters specifically from the wider experience of care home resident monitoring may miss the wider context of care in these unique environments.
-
Residents’ capacity to share their views and recall their experiences may be a challenge across some groups of residents who encounter greater difficulty around memory and recall, as well as capacity to consent.
-
Residents’ capacity to be involved and provide consent could vary from day to day. In addition, many residents have sensory impairments (visual/hearing) and and/or speech impairments that would make it difficult to collect data remotely.
-
Among residents with cognitive issues, periods of lucidity can be irregular and, therefore, flexibility and more elapsed time needs to be built into the research process. 43
-
In the COVID-19 era, care homes require all visitors, including researchers, to be fully vaccinated and tested. In addition, each participating home needs to invest significant time in encouraging resident participation.
-
Interviews would be possible, but could be subject to significant bias if family members and care home staff were facilitating conversations or answering questions on behalf of their relative/resident without first relaying questions.
It was agreed by the project team and the Project Steering Group (see Work package 1: scoping interviews and engaging with relevant literature, as well as co-designing the study approach and research questions with members of our User Involvement Group) that a rapid evaluation could not address the main knowledge gaps with regard to capturing the experience of care home residents.
In addition, members of the study team established a Project Steering Group. This was made up of senior policy leads at NHSE&I, policy directors from two national care associations (part of the Care Provider Alliance) who have supported the identification of research evidence, and key experts related to the use of pulse oximetry and remote monitoring in care homes. A descriptive summary of the findings was provided to the Project Steering Group for comment and discussion. In addition, the project team set up a workshop with the project-specific User Involvement Group (see Co-designing the study approach and research questions with members from a User Involvement Group). The workshop was held in March 2021, and at this workshop it was agreed that further scoping on the involvement of residents in the evaluation of pulse oximetry in care homes was required.
Work package 2: national survey of care homes
The main objective of the survey was to understand current practices relating to the use of pulse oximeters in care homes to monitor COVID-19 and other conditions, and the extent to which care homes were receiving support and guidance from the NHS about the use of pulse oximeters. Therefore, the survey was designed to understand the potential impacts of the use of pulse oximeters, and the associated support, on (1) outcomes for care home residents, such as the extent to which residents appear to be reassured; (2) the delivery of health and social care services in care homes; (3) the organisational workflow and workforce capacity of care home staff; and (4) residents’ use of health-care services, including emergency department attendance and hospital admission.
Specifically, the survey explored the following:
-
the conditions for which pulse oximetry are used (e.g. management of COVID-19 and other conditions)
-
the procedures and processes involved in the use of pulse oximetry (e.g. implementation, monitoring and escalation) and if and how procedures and processes differ by type of care home setting and characteristics of residents
-
the experiences of staff delivering pulse oximetry and their perspectives on residents receiving pulse oximetry (e.g. deciding which patients should receive pulse oximetry, taking readings, monitoring residents, deciding when to escalate residents to acute care, and working with NHS staff if appropriate).
-
the competencies (skills) and training needs of care home staff in the use of pulse oximetry in care homes, and staff capacity to deliver pulse oximetry
-
staff knowledge and engagement with the NHS CO@h service in care home settings
-
the expected impact on residents’ attendance at hospital emergency departments, admission to hospital or other use of health-care resources
-
the expected impact on residents’ health outcomes.
The survey questionnaire was designed collaboratively with the Project Steering Group, informed by scoping interviews with key experts and feedback received from members of the User Involvement Group during a workshop in March 2021. To reduce burden and to improve response rates, the online survey was designed so that it would take no longer than 20 minutes to complete.
Based on discussion with representatives from the Care Provider Alliance, managers of care homes were considered the most relevant survey respondents. Each care home has an assigned registered manager who has overall knowledge of all of the processes and procedures implemented in the care home that they manage. The CQC agreed to advertise, and provide a link to, the survey in its fortnightly online bulletin that is sent to all registered care home managers in England.
The survey was disseminated using the online platform SmartSurvey (SmartSurvey Ltd, Tewkesbury, UK) and was piloted between 23 and 26 February 2021 with a small number (n = 6) of key stakeholders identified by the research team. The survey questionnaire was revised slightly based on feedback from the pilots.
Key organisations were contacted by the research team to support survey distribution and to encourage care home managers to respond. Several organisations supported the online survey throughout March and April 2021:
-
The CQC distributed the survey via its fortnightly electronic bulletin to all 15,362 registered care homes in England. A message inviting care home managers to take part in the survey was included in two CQC bulletins (11 March 2021 and 25 March 2021).
-
The Care Provider Alliance supported survey dissemination by means of separate e-mail communications to its members, which includes associations representing the majority of care homes in England.
-
NHSX included a message about the survey in its March 2021 newsletter.
-
The Association of Directors of Adult Social Services included information about the survey in its March newsletter.
The study team monitored the survey response rate frequently. As the survey response rate was low, the study team implemented additional methods of reaching out to registered home managers. A variety of additional stakeholders were approached and asked to support the survey link distribution:
-
The study team contacted all members of the Skills for Care Registered Manager Network whose e-mail addresses were listed on that organisation’s website, asking them in turn to share the survey link with their contacts in care homes.
-
In April, the NIHR Applied Research Collaborations circulated a survey link by e-mail among members of the care home researcher network.
-
The NIHR ENRICH (Enabling Research in Care Homes) Research Ready Care Home Network shared the survey link with its members.
-
My Home Life England sent the survey link to its members.
-
NHS England and Improvement sent the survey to stakeholder associations.
Participants were able to access the survey between 8 March 2021 and 30 April 2021 (inclusive). The original plan had been to close access to the survey on the 6 April; however, given the low participation rate, the survey data collection phase was extended to the end of April 2021. Despite the extended survey period, and the considerable assistance of several organisations (as described above), the response rate finally achieved was only 1.5% (i.e. 232 out of 15,362 care homes). The demands on care home managers were very high throughout the survey period as a result of the roll-out of the COVID vaccination programme, exacerbation of staff shortages due to the pandemic and continued restrictions on visits from residents’ families. Responding to our survey is likely to have been a low priority for many care home managers in the circumstances. The survey provided useful insights into how care homes (with a wide variety of different residents) were using pulse oximeters. The survey also provided useful information regarding care home managers’ experiences of using pulse oximeters. However, the low response rate means that the survey results cannot be assumed to be representative of all care homes.
In early May 2021, the survey data were downloaded from the survey website and were cleaned before being analysed. The research team developed an analysis plan describing how to best analyse and present the information emerging from the survey to answer the research questions. The analysis was carried out in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), which was adequate in relation to the number of respondents.
Analysis included descriptive statistics and identification of patterns and trends in the data. The analysis was conducted in two stages. First, the team performed descriptive analysis (i.e. frequency distributions) of each question individually. Second, cross-tabulations for group analysis were carried out to compare similarities and differences in experiences in the use of pulse oximetry by different groups (i.e. frequency distributions of the grouped variables). 44 These analyses were conducted for the following groups:
-
type of care home (residential, nursing or dual residential and nursing).
-
size of care home (by number of beds)
-
length of use of pulse oximeters (< 12 or ≥ 12 months).
Work package 3: in-depth case studies of staff experience based on interviews
The aim of this workstream was to explore the use of pulse oximetry in care homes, using the experiences of a range of stakeholders involved in delivering this technology in care homes; the factors influencing this delivery, including the communication to care homes about use of pulse oximetry and the level of support offered by NHSE&I and by local primary and secondary care providers; the range of conditions for which pulse oximetry is considered a beneficial component of a resident’s care (including residents who have tested positive for COVID-19); any variation the use of pulse oximetry across different care home settings (e.g. nursing or residential, size, location); perceptions of residents’ experience; and, finally, the potential to optimise the use of pulse oximetry and other remote monitoring approaches in the longer term.
Data collection followed a rapid qualitative research design, involving teams of field researchers and iterative data collection and analysis. 45 Three researchers (JRT, IL and MS) with a background in the social sciences and public health, and with a record of undertaking qualitative data collection with a range of stakeholders, carried out semistructured interviews with a purposive sample of stakeholders in six selected (care home) sites, with the aim of ensuring an appropriate variety of sites and giving opportunity to complete a significant number of interviews to achieve a depth of understanding to answer our evaluation questions. 46
Care home sites were selected purposively based on the principles of maximum variation (i.e. sampling for heterogeneity by selecting a small number of case study sites to understand a phenomenon from the perspective of a range of stakeholders in different settings relevant to our research questions) and convenience sampling, taking a pragmatic approach with the aim of selecting care homes that are, taken together, able to address many of the following criteria in combination: nursing, residential and learning disability care homes, funding model, size, geographic location (with regard to socioeconomic deprivation) and mechanism [e.g. application (app), paper based or both] for remote monitoring7 (Table 2). We did not have prior data on how long pulse oximeters had been used across care homes and, therefore, this was not taken into account when sampling for case study sites, but we did account for CQC ratings. Recruitment of case study sites was aided by NIHR-funded ENRICH facilitators, who approached care homes across their clinical research network on the study team’s behalf. In addition, the NHSE&I Project Steering Group supported the identification of care homes administering pulse oximetry with the support of the NHS CO@h programme’s primary and secondary teams. In all, seven care homes were identified (five care homes by ENRICH and two care homes with the support of the NHSE&I Project Steering Group). One care home was excluded, as another care home from the same care home group was already included in our study sample. An overview of our case study sites is presented in Chapter 3.
| Variable | Description |
|---|---|
| User group |
Without dementia or learning disability With dementia With learning disability |
| Type of care home |
Nursing Residential |
| Organisation size | Number of places |
| Mechanism for patient monitoring |
Paper based App |
| Geographic location |
Urban Rural |
Interviewees comprised a purposive sample of study participants, who were selected in relation to the sampling framework outlined in Box 8 using snowball/convenience sampling. 47 We aimed to carry out interviews with five staff members with various levels of responsibility and experience (managers, care assistants, employees involved in the set-up, implementation and/or delivery of care using pulse oximeters, etc.) at each site.
Senior managers from care home associations (e.g. Care England, National Care Association, Nursing Homes Association, National Care Forum).
Care home manager.
Staff using the service with nursing or clinical training.
Staff using the service with no nursing or clinical training (including staff working day and/or night shifts).
Where relevant, NHS staff (primary, community or secondary care) supporting the care home’s use of oximetry.
To achieve this, the evaluation team planned to carry out 37 interviews across the six care homes (with a minimum of four per care home) or until data saturation (meaning that, once data were triangulated, no new emerging information was being discovered during data analysis, only data that confirmed existing themes and conclusions). 9 We interviewed a range of care home staff and senior managers in the care home sector and related care associations, plus NHS health-care professionals across primary, community and secondary care who are currently working with care homes, as well as senior national policy leads. Data collection was carried out between March and May 2021. The point of saturation was agreed by all members of the qualitative subteam (MS, IL and JRT), along with the co-principal investigators (JS and RM). Fieldwork, with regard to interviews, was carried out in some care homes sooner than others owing to difficulties in arranging interviews in some homes. Ian Litchfield was responsible for communicating with three care homes, Jamie-Rae Tanner was responsible for communicating with two care homes and Manbinder Sidhu was responsible for communicating with the final care home.
Individuals participated in a semistructured interview with one member of the study team (JRT, IL or MS). Interviews were carried out at a time convenient to the individual (e.g. during or outside working hours) via telephone, Zoom (Zoom Video Communications, San Jose, CA, USA) or Microsoft Teams (Microsoft Corporation, Redmond, WA, USA). Each participant was provided with a participant information sheet at least 48 hours in advance of the interview to enable them to make an informed decision regarding whether or not to participate. Interviewees had the opportunity to ask questions about the study and/or wider BRACE-related work. Participants signed a consent form prior to participating in the interview. This also required them to say whether or not they consented to the recording of the interview. Participants were informed that they were entitled to withdraw from the study at any time and were given information about how to find out more about the study and how to raise any concerns about its conduct. In total, the study team approached 42 potential interviewees across the six sites, and 34 agreed to participate. Those who chose not to participate cited other, more important, commitments as the reason for doing so. Salient characteristics of stakeholders interviewed across our six case study sites are provided Table 3.
| Type of care home/participant | Generic description of role | Number of participants |
|---|---|---|
| Senior managers from national care associations and national policy leads | Senior managers from care home associations (e.g. Care England, the National Care Association, the Nursing Homes Association, the National Care Forum) | 3 |
| Nursing | Care home manager | 3 |
| Staff using the service – with nursing or medical training | 4 | |
| Staff using the service – with no nursing or clinical training (including those working day and/or night shifts) | 4 | |
| NHS staff (primary, community or secondary care) supporting the care home’s use of oximetry | 1 | |
| Residential | Care home manager | 5 |
| Staff using the service – with nursing or medical training | 0 | |
| Staff using the service – with no nursing or clinical training (including those working day and/or night shifts) | 13 | |
| NHS staff (primary, community or secondary care) supporting the care home’s use of oximetry | 1 | |
| Total | 34 |
An interview guide was piloted at a workshop with our User Involvement Group and with two scoping interviewees to determine whether or not the guide was designed appropriately to answer the evaluation questions. The guide was used by researchers as an aide memoire during the interviews.
The interviews lasted approximately 30–60 minutes. The interviews were audio-recorded (subject to consent being given), transcribed verbatim by a professional transcription service, anonymised and kept in compliance with the General Data Protection Regulation 2018 and Data Protection Act 2018. 48
Given the short time frame of this rapid evaluation, the study team adopted a pragmatic approach to the comprehensive analysis of the data, with a shorter timescale than traditional qualitative analysis, undertaken in two stages. First, data collection and analysis of interview data were carried out in parallel and facilitated through the use of rapid assessment procedure (RAP) sheets, as explained in Vindrola-Padros et al. 49 RAP sheets were developed for each case study site to facilitate cross-case comparisons and per population (i.e. to make comparisons between subgroups). The categories used in the RAP sheets were structured in accordance with the interview topic guide, maintaining flexibility to add categories as the data collection proceeded. The interviewers (JRT, IL and MS) completed site-specific RAP sheets following each interview, noting key points from the data under the agreed categories. The researchers (JRT, IL and MS) held weekly 1-hour meetings to discuss emerging learning and relayed this learning to other members of the study team during weekly team meetings throughout the duration of the study. A virtual workshop meeting was held in May 2021 and was attended by all researchers. The meeting aimed to develop and establish themes drawn from the data (both survey and interviews) and to ensure that all research questions had been addressed.
Following the virtual workshop, the second stage of analysis began with further interrogation of interview data by Jamie-Rae Tanner, Ian Litchfield and Manbinder Sidhu. The analysis was informed by the CFIR and the Gale et al. 35 framework method for the analysis of qualitative data in multidisciplinary health research. The Gale et al. 35 framework is a systematic method of categorising and organising data while continuing to make analytical and interpretive choices transparent and auditable. Specifically, the Gale et al. 35 framework facilitated constant comparison across the six case studies. There are seven stages to the analysis:
-
transcription of interviews
-
familiarisation with the interview/observation/documentary material
-
coding
-
developing a working analytical framework
-
applying the analytical framework
-
charting data in a framework matrix
-
interpreting the data.
Stage 1: transcription
All interviews across the six case study sites were transcribed verbatim through a professional, outsourced transcribing company. A single organisation, specialising in transcribing health-related qualitative interviews, was used for all interviews. The quality of transcriptions was checked by having one of member of the research team (MS) check one transcript against the audio-recording.
Stage 2: familiarisation with the material
Three members of the project team (JRT, IL and MS) established familiarity with the data by each reading four transcripts from across the six case study sites (based on type of stakeholder interviewed) and by holding weekly data analysis meetings while data collection was still ongoing/near completion (May to June 2021). During each meeting, team members were able to reflectively discuss and share thoughts and impressions of early findings.
Stages 3 and 4: coding and developing a working analytical framework
Stages 3 and 4 of the analysis took place in tandem. The study team applied an inductive approach, having developed predefined codes that focus on specific areas of interest identified from our interview topic guide, RAP sheet and CFIR. The codes were reviewed, refined and added to. One interview transcript was independently coded, with a further 11 interview transcripts coded by all three project team members (JRT, IL and MS). The remaining 22 transcripts were read to ensure that no emerging learning was missed, to identify deviant cases, to draw out relevant quotes to support conclusions and to ensure that no important aspects of the data were missed. NVivo 12 (QSR International, Warrington, UK) was used for coding. After the first data analysis workshop meeting (May 2021) and the independent coding of one transcript, an analytical coding framework was agreed (see Report Supplementary Material 3). The codes were categorised under the following broad themes of the CFIR framework (i.e. the five overarching domains). Note that not all 39 constructs of the framework emerged from our data. Each domain, with its existing construct (with definition) and emerging issues, is summarised in turn and illustrated by exemplar quotes under thematic headings. The analytical coding framework was reviewed at subsequent data analysis meetings between Jamie-Rae Tanner, Ian Litchfield and Manbinder Sidhu, as well as with the wider study team.
Stage 5: applying the analytical framework
The working analytical framework was then applied by indexing by Jamie-Rae Tanner, Ian Litchfield and Manbinder Sidhu across a sample of 12 interview transcripts [i.e. the systematic generation of codes (n = 37)].
Stage 6: charting codes
The project team took a novel, rapid approach to charting codes, by developing a matrix based on summaries of each code and using the CFIR (once the analytical framework had been applied to the 12 transcripts). This process was led by a single researcher within the project team (IL), with input from the other team members (JRT and MS). The matrix was structured according to research questions and how best to develop integrative themes. As a result, summarised codes were merged together to support the development of themes with respect to overarching CFIR domains under newly devised thematic headings.
Stage 7: interpreting the data
The project team held a final weekly meeting in July 2021 to finalise the development of themes. Key to this meeting was to understand the characteristics of the implementation of pulse oximetry in care homes across the six case study sites and the differences across qualitative and survey data, interrogating theoretical concepts relational to our research questions, and mapping connections across our themes. In September 2021, the research team circulated a summary of findings (via a digital slide deck) to each case study site, and gave them the opportunity to provide comments (i.e. member validation). In addition, emerging data were shared in an online workshop with key stakeholders and the Project Steering Group (including members of NHSE&I, care provider associations and of the User Involvement Group).
Work package 4: synthesising findings from qualitative and quantitative components of the evaluation
A virtual workshop meeting of the research team was held in July 2021. Jon Sussex, Barbara Janta, Giulia Maistrello, Ian Litchfield and Manbinder Sidhu attended the meeting to discuss how to thematically synthesise findings across survey and qualitative interviews, guided by the CFIR framework. The ‘following a thread’ approach put forward by O’Cathain et al. 36,37 was adopted, whereby synthesis of data takes place at the data analysis stage to identify key themes and data that warrant further analysis. 36,37 Hence, following the identification of key themes within each data set, the researchers used the CFIR’s five overarching domains to create a ‘thread’ to organise the findings. As part of the workshop, colleagues took an iterative approach, going back and forth across both sets of themes (for survey and interview data) to draw out key messages that were consistent with answering research questions and also most pertinent within the data. For example, during the workshops, members of the team would begin with findings from the survey, identify corresponding learning that supported and/or deviated from the data, and then iteratively return to the relevant literature, both policy and theoretical, to identify key learning from both sets of data. In addition, the team presented findings and recommendations to the User Involvement Group (May and October 2021), at the NHSE&I CO@h – Evaluation Workshop (September 2021) and to the NHSE&I People Receiving Social Care Group (May, July and October 2021). The accumulated outputs of these workshops will lead to a slide deck of findings, which will be disseminated across the NHS and into the public domain.
In summary, we followed an adapted rapid qualitative analysis approach, including the use of RAP sheets, interrogation of transcripts, application of a theoretical lens, using a framework approach, including repeated discussion across the whole research team and calling on additional national experts, in the development of our findings. We used a COREQ (consolidated criteria for reporting qualitative research) checklist to add rigour to our reporting. Throughout this chapter, we have detailed processes for protocol sign-off and ethics approval, and described the nature of our scoping work (both with literature and key experts) and the methods used with regard to how we collected data using an online survey and interviews.
We present our synthesised findings for both the survey and interview study in the next two chapters (Chapters 3 and 4). The first of these chapters (Chapter 3) covers domains I, II and III of the CFIR, that is, the characteristics of the intervention we are evaluating and the outer and inner settings into which the intervention is introduced. Therefore, Chapter 3 provides a description of the use of pulse oximetry in care homes, including a description of the care homes included in our sample, the application of pulse oximetry in care homes and how the use of pulse oximetry relates to routine practice and care pathways. The subsequent chapter (Chapter 4) covers domains IV and V of the CFIR, looking at staff experiences of pulse oximetry and staff views on the impact on residents of implementing pulse oximetry in care homes.
Chapter 3 The use of pulse oximetry and the care pathways associated with its delivery in care homes
The key points of Chapter 3 are summarised in Box 9.
-
There are more than 15,000 care homes operating in England. Following repeated reminders that were distributed to all care homes, and with the assistance of the CQC, the Care Provider Alliance and other organisations in contact with care homes, we received survey responses from 232 (1.5%) care homes.
-
We undertook interview-based case studies in six care homes, two nursing homes and four residential homes, the key characteristics of which are described in this chapter.
-
Owing to the low survey response rate, our findings cannot be assumed to be representative of the picture nationally in England. However, the proportions of residential homes and of smaller care homes (i.e. care homes with fewer than 40 beds) in our sample were close to the national figures and, therefore, we provide here a small snapshot of views from the adult social care sector. The findings provide insights into the use of pulse oximeters in care homes during the COVID-19 pandemic, including the interaction between care homes and the NHS.
-
The survey of care home managers indicates that pulse oximeters are used routinely in care homes and, in the majority of cases, had been in use before the COVID-19 pandemic. Pulse oximetry is useful for a range of, mainly respiratory, conditions and not limited to COVID-19. Just over one-quarter of care homes responding to the survey had been using pulse oximeters for 12 months or less.
-
Pulse oximeters were not uncommonly purchased, either prior to or during the pandemic, by the care homes themselves, although a smaller number of care homes had been provided with oximeters by the NHS (with some homes having pulse oximeters from both sources).
-
Care home managers reported that a variety of care home staff received training on all aspects of pulse oximetry usage. Two-thirds of respondents indicated that staff did not require any further training or support in the use of pulse oximetry, and just under one-third of responding care home managers expressed a view that further training or support for staff may be required.
-
Pulse oximeters were reported as easy to use and could be readily accommodated alongside the recording of other routine clinical measurements, such as temperature and blood pressure.
-
A number of training materials are available, yet routine or systematic training in the use of pulse oximeters in residential homes was not universal, with staff describing how they had learned to use them through experience.
COVID-19 Oximetry @home services for care home residents: programme theory
The CO@h and the Covid Virtual Ward (CVW) programmes (see Report Supplementary Material 1) both describe an enhanced package of care for individuals with confirmed or suspected COVID-19 who are at risk of future deterioration, including residents of care homes.
A key motivation underlying the introduction of CO@h into care homes was addressing the disproportionate impact of COVID-19 on care home populations by equipping care home staff with, and through the supported use of pulse oximetry. Clinicians, including GPs, nurses and clinicians working in hot hubs (i.e. GP-led sites providing a place to see patients with coronavirus symptoms face to face) or working with community teams, are expected to identify care home residents who would benefit from oximetry at home.
Referrals can be referred to CO@h by the NHS 111 COVID Clinical Assessment Service, by NHS Test and Trace or by hospital emergency departments. In the case of the CVW programme, residents are referred by a hospital clinician and are discharged to the care home with a pulse oximeter and a discharge pack. Alternatively, care home staff can contact their designated GP if they want a resident to be considered for the service. Care home managers should be informed of the CO@h service by their local CCG. Figure 1 illustrates a resident’s journey on the CO@h service.
FIGURE 1.
Resident journey (adapted with permission from Care Provider Alliance CO@h guidance for care homes3).

In the first quarter of 2021, when the study reported here commenced, there were more than 15,000 care homes operating in England. Following repeated reminders that were distributed to all care homes, and with the assistance of the CQC, the Care Provider Alliance and other organisations in contact with care homes, we received survey responses from 232 (1.5%) care homes. A low response rate was not unexpected, given the exceptional pressures on care homes, their managers and staff at this time when the COVID vaccination programme was being rolled out, staff shortages were exacerbated by the pandemic and care homes were still operating with restrictions on contact between residents and their families.
We undertook interview-based case studies in six care homes. The key characteristics of the six care homes are described in Table 4.
| Care home ID | Region of England | Type of care home/CQC rating | Types of residents cared for (in addition to frail and elderly) | Number of beds (maximum capacity) | Staff numbers (nurses/care staff) | Part of CO@h programme? | Nature of care home ownership | Funding model | Number of interviews carried out |
|---|---|---|---|---|---|---|---|---|---|
| Care home 1 | North West | Nursing/good | Dementia, including Alzheimer’s disease, learning disabilities, physical disabilities, hearing impairment and visual impairment | 30 | Seven nurses and 18 other care staff | No | For-profit | Self-funded, social services/local authority with top up, NHS | 6 |
| Care home 2 | Midlands | Residential/good | Dementia | 35 | One nurse and 32 care staff | No | For-profit | Self-funded, social services/local authority with top up, NHS | 6 |
| Care home 3 | Midlands | Nursing/good | Has a specialist dementia care unit, including Alzheimer’s disease, Parkinson’s disease, stroke, palliative care, respite care and physiotherapy | 52 | Seven nurses and 45 care staff | No | Not-for-profit | Self-funded, charitable donations | 6 |
| Care home 4 | South | Residential/good | Dementia, including Alzheimer’s disease, Parkinson’s disease and respite care | 39 | Eight senior carers and 20 other care home staff | Yes | For-profit | Self-funded, social services/local authority with top up, NHS | 4 |
| Care home 5 | North East | Residential/outstanding | Dementia, including Alzheimer’s disease, multiple sclerosis, stroke, mental illnesses, physical and sensory impairment, respite care, and a separate specialist dementia care unit | 90 | One nurse providing clinical oversight across this care home and five other care homes, eight senior care leads and 24 care staff | No | For-profit | Self-funded, social services/local authority with top up, NHS | 4 |
| Care home 6 | South West | Residential/good | Dementia, including Alzheimer’s disease | 36 | Four senior care team leaders and a further 20 care staff | Yes | Not-for-profit | Self-funded, charitable donations | 5 |
Owing to the small numbers of respondents in both parts of the rapid evaluation data gathering, our findings cannot be assumed to be representative of the picture nationally in England. However, our findings do provide a snapshot of views from the adult social care sector on important policy and practice, as well as the topic of interest, during unprecedented times and when under considerable pressure. The findings provide valuable insights into the use of pulse oximeters in care homes during the COVID-19 pandemic, including interaction between care homes and the NHS.
Descriptions of the six care homes where we undertook interviews are presented in Table 4, including type of care home, the characteristics of residents cared for, bed capacity, staff model, ownership and funding models. Concise descriptions of the circumstances for using pulse oximetry at each case study site during the pandemic are described in Table 5.
| Care home ID | Relationship with primary, community and secondary care (prior to and during the pandemic) | Experience of using pulse oximeters (prior to and during the pandemic) | Provision/purchasing of pulse oximeters |
|---|---|---|---|
| Care home 1 | Limited to having remote access to a GP via the telephone, although staff had some limited face-to-face contact with the district nursing team in the area | The care home had prior experience of using pulse oximeters with residents before the onset of the pandemic. During the pandemic, pulse oximetry was used to monitor all patients, whereas previously the focus had been on residents diagnosed with respiratory illnesses | Pulse oximeters were purchased by the care home from an online supplier for use by their staff |
| Care home 2 | A well-established relationship with a local GP who was readily accessible via telephone, video calls and e-mail. The care home also works closely with members of the district nursing team, who were responsible for treating residents with recurring chest infections | The care home had pre-pandemic experience of using pulse oximeters in residents with chronic respiratory conditions such as COPD. When the pandemic started, the use of pulse oximetry was extended to all residents | Pulse oximeters were provided to the care home by their GP and administered to residents by the care home manager and senior care staff |
| Care home 3 | A well-established relationship with a local GP, who pre pandemic would conduct a weekly check-in with care home staff and residents. In between check-ins the GP could be contacted via e-mail to raise any pressing concerns | During the pandemic, pulse oximetry was used to monitor residents who were diagnosed with COVID-19, alongside the continuing routine monitoring of COPD patients | Pulse oximeters (n = 8) were purchased by the care home directly via a supplier identified using the internet |
| Care home 4 | In response to an outbreak of COVID-19 at the home, the local CCG’s clinical lead for care homes invited the care home to participate in the NHS CO@h programme | Limited pre-pandemic experience of using pulse oximeters, which were predominantly used by senior staff under the direction of the home’s GP | As part of the CO@h programme, pulse oximeters were provided to the home, alongside guidance on their use and on the process for escalating patients whose blood oxygen saturation fell. The oxygen saturation of all residents was measured, recorded and reported to the CO@h team three times a day |
| Care home 5 | Working with their local general practice, care home staff used pulse oximeters twice daily to monitor blood oxygen saturation, alongside blood pressure and temperature observations | Prior experience of using pulse oximeters with residents before the onset of the pandemic, but increased the use of pulse oximeters for COVID-19-positive residents across two separate outbreaks | Pulse oximeters (n = 5) were purchased by the care home from an online supplier very early during the pandemic to accommodate increased levels of monitoring |
| Care home 6 | Throughout the pandemic, the care home received continued support from its local GP, who was no longer able to undertake ward rounds in person. The GP was sent twice-daily pulse oximetry readings. The care home was also receiving support from a CVW run by its local NHS trust to monitor residents discharged from hospital to the residential home after being diagnosed with COVID-19 | No prior experience of using pulse oximeters, or blood pressure or temperature monitoring, prior to the pandemic. The local NHS trust was also responsible for delivering in-person RESTORE2 training (February 2020) and online RESTORE2 refresher training (March 2021) | A designated general practice provided the care home with two pulse oximeters, and infrared temperature sensors were purchased directly by the home |
Types of care homes responding to the survey
In total, 256 care home managers – one per care home – responded to the survey by opening the survey link and providing responses to (at least) some questions. During the data cleaning, the study team examined the partial responses (i.e. data provided by 72 respondents who replied to some of the survey questions but not all of them) to determine the best inclusion/exclusion approach. 50 Only a small number of questions were mandatory for respondents. Therefore, it was possible for respondents to skip some questions and to move on to a next question. Consequently, the actual number of survey respondents varied, to some degree, per question. The analysis did not show any systematic bias in the survey dropout rates, suggesting that dropouts were probably simply due to survey fatigue. The thematically related, detailed questions in the survey started with question 5, which asked about the use of pulse oximetry (i.e. ‘Do you use pulse oximeters routinely in your care home?’), which was answered by 222 respondents, and followed by question 6, which asked about the length of time the home had been using pulse oximetry (i.e. ‘How long have you been using pulse oximeters for?’) which was answered by 232 respondents. As the number of respondents was larger for question 6 than for question 5, we have included in the analysis all respondents who provided an answer to question 6. Consequently, information received from 232 respondents (i.e. 1.5% of the total number of care homes in England) is included in the analysis.
Table 6 and Figure 2 present descriptive statistics for the survey respondents. Table 6 shows that among the 228 survey participants who stated the type of care home:
-
68% (n = 155) of participants were from residential homes
-
19% (n = 44) of participants were from nursing homes
-
13% (n = 29) of participants had a dual residential and nursing registration.
| Data source | Type of home, n (%) | Number of beds, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total available answers | Residential | Nursing | Dual | Total available answers | < 20 | 20–39 | 40–59 | 60–99 | > 100 | |
| Survey respondents | 228 | 155 (68) | 44 (19) | 29 (13) | 229 | 69 (30) | 88 (38) | 45 (20) | 22 (10) | 5 (2) |
| CQC database | 15,362 | 10,987 (72) | 4160 (27) | 215 (1) | 15,350 | 6511 (42) | 4162 (27) | 2553 (17) | 1906 (12) | 218 (2) |
FIGURE 2.
Types of care home taking part in the online survey compared with types of care homes in England, according to the CQC database. (a) Online survey of care home managers (n = 228); and (b) CQC database (n = 15,362).
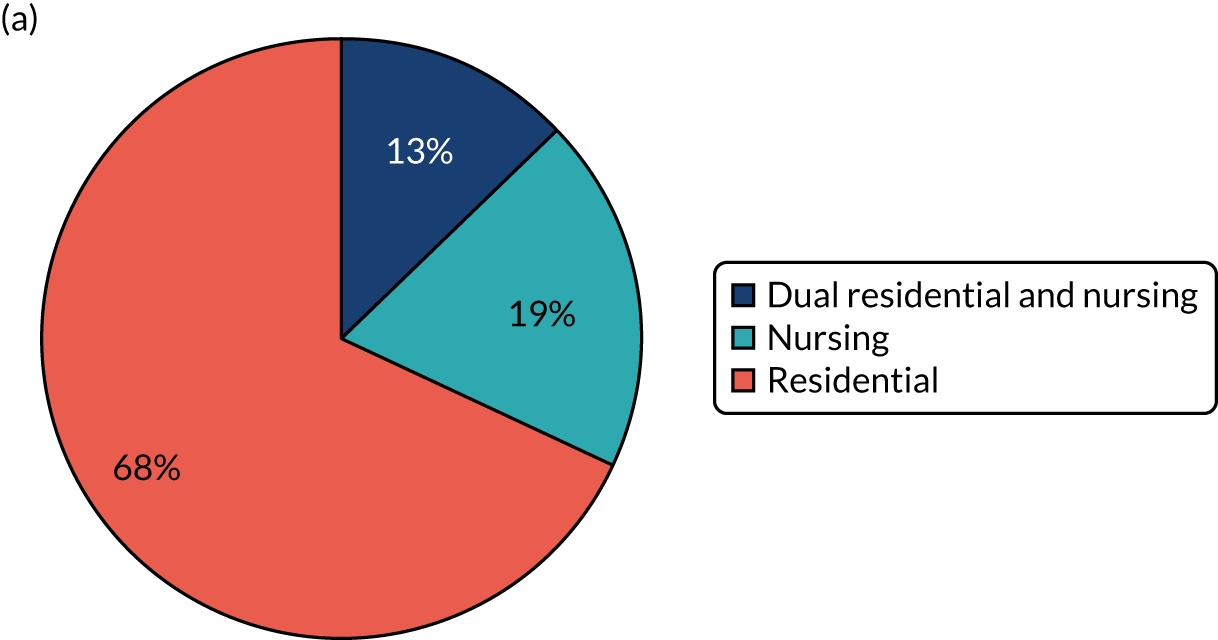
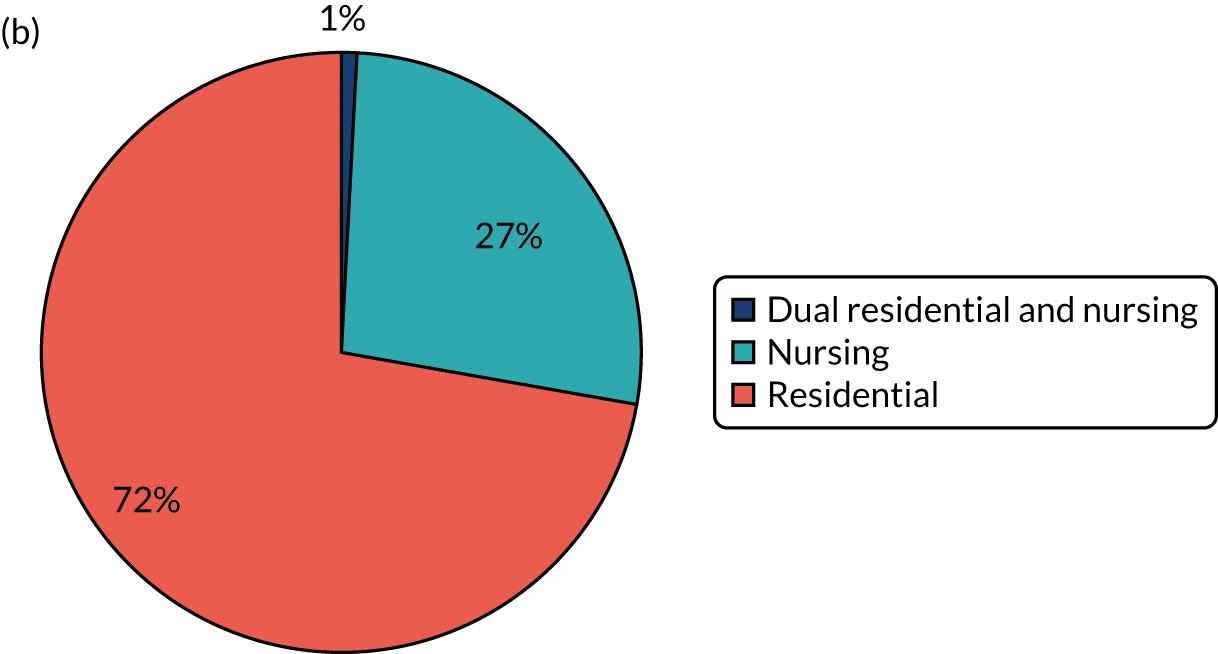
To understand how representative survey respondents were of the overall population of care homes in England, we conducted an analysis of CQC registration data. [The CQC registration data, which are available for every care home in England, are live data and are available from the CQC website: www.cqc.org.uk/about-us/transparency/using-cqc-data (accessed 17 August 2022). The comparative analyses were conducted on CQC data downloaded on 18 May 2021.] As shown in Table 6 and Figure 2, the proportion of residential homes that participated in the survey reflected the overall share of residential care homes as recorded in the CQC registration data. The proportion of surveyed nursing homes was somewhat lower than the figure represented in the CQC registration data, and the share of dual residential and nursing homes was higher. We also separately analysed the 13 responses that were from care homes that cater exclusively for residents with learning disabilities. This analysis was inevitably circumscribed by the small number of responses in this group. No significant differences in answers were found relative to the rest of the responses.
Most care homes in our sample had fewer than 40 beds, with around one-third of care homes having fewer than 20 beds and one-third having 20–39 beds (see Table 5 and Figure 3). Compared with the CQC registration data, the proportion of the smallest homes (i.e. care homes with fewer than 20 beds) was lower in our survey population. When considering the cumulative share of homes with fewer than 40 beds, the survey and CQC registration data display similar proportions, with 68% of care homes in our survey and 69% of CQC registrations, respectively, having fewer than 40 beds.
FIGURE 3.
Number of beds in care homes participating in the online survey compared with all care homes in England registered with the CQC. (a) Online survey of care home managers (n = 229); and (b) CQC database (n = 15,362).
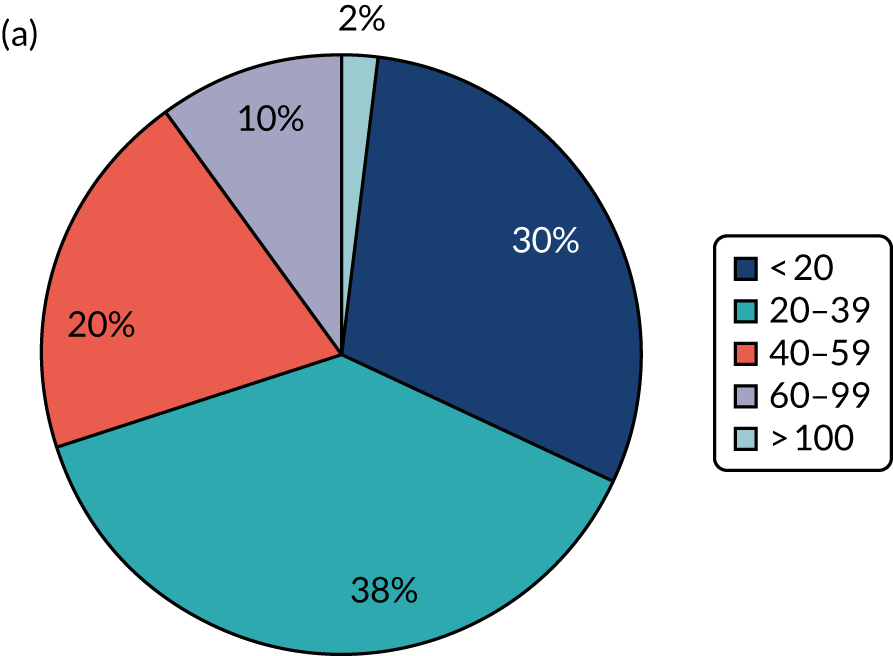
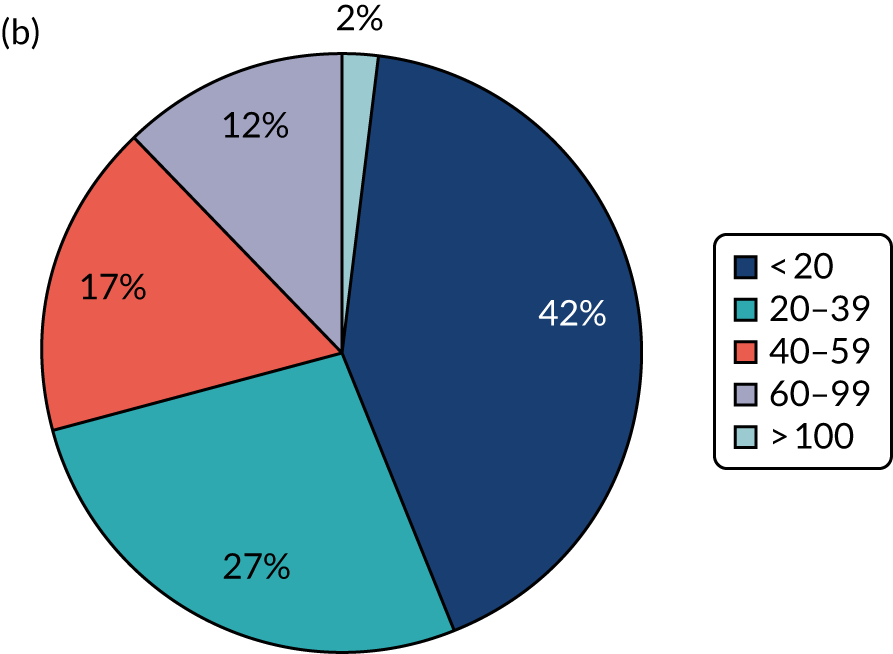
The smaller care homes among our survey were mostly residential, with more than 80% of respondents from residential homes representing homes with fewer than 40 beds, whereas nursing homes or homes that were dual residential and nursing homes were more likely to have 40 or more beds (Figure 4).
FIGURE 4.
Number of beds in care homes per care home type: online survey of care home managers (n = 227).
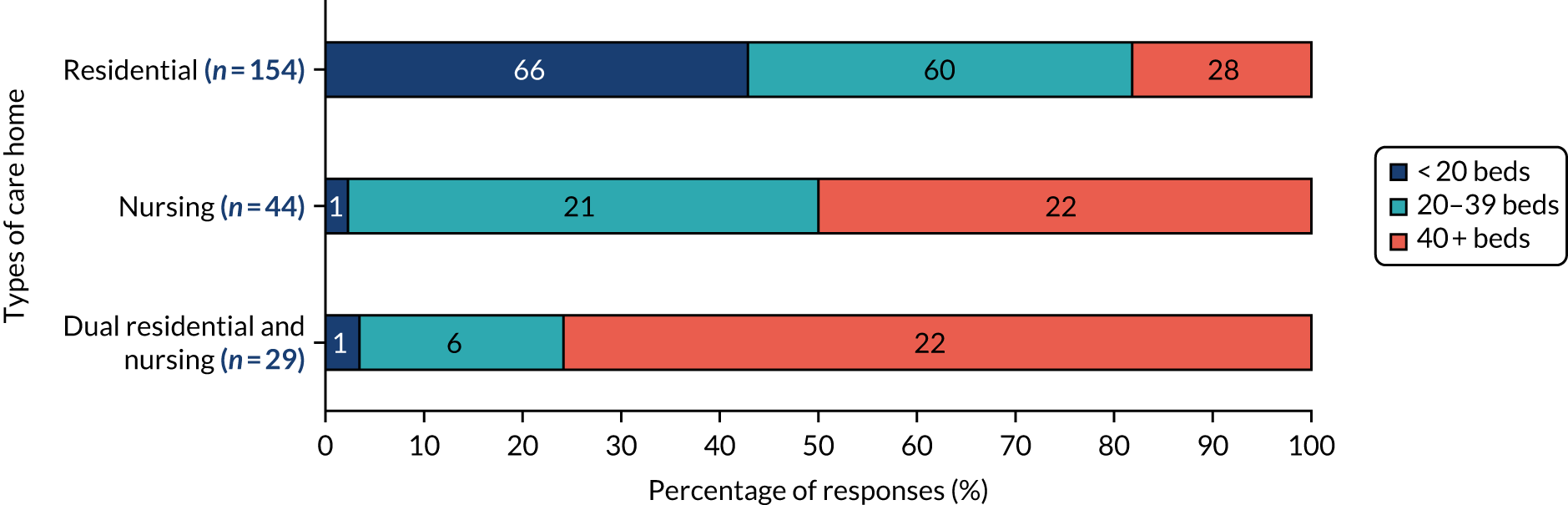
The most common characteristics of residents living at responding care homes included older residents and residents with dementia, physical disabilities, complex needs and/or learning and sensory impairments (Figure 5). However, comparing the resident populations of our surveyed homes with the populations of CQC registered homes data was not possible because of different terminologies and classifications used.
FIGURE 5.
The most common characteristics of care home residents: online survey of care home managers (n = 231).
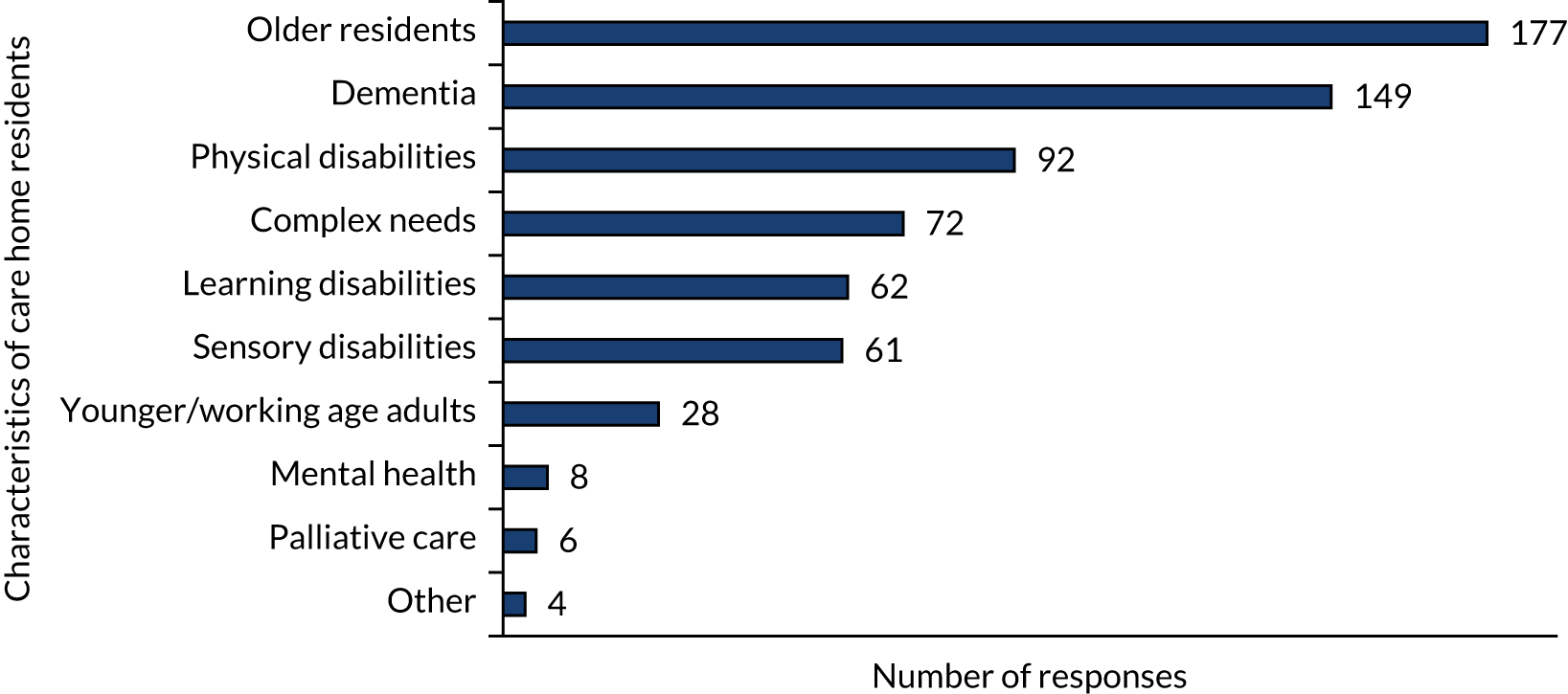
Group analysis revealed no differences for category of resident per type of care home, with the exception of residents with learning disabilities, who are more prevalent in residential homes (n = 53) than in dual (n = 4) and nursing homes (n = 3).
In the following sections of this chapter, we present the findings from the survey and the interviews. The findings are organised according to the themes that emerged from the synthesis and analysis of the combined information that was undertaken by the research team at an internal workshop in July 2021.
Implementation and use of pulse oximetry
The following three themes present data and analysis with regard to procurement and maintenance of pulse oximeters, their use as part of providing routine care to residents and staff perception of use, as well as descriptions of training received.
Theme 1: procurement and maintenance of pulse oximeters by care homes
Theme 1 relates to research question 1 about when and how pulse oximetry is used in care homes, and to research question 4 about guidance and resource needed to sustain that use. According to the survey results, pulse oximeters were often purchased by the care homes themselves (78%, 170 respondents). A smaller number of care homes had been provided with oximeters by the NHS (33%, 73 respondents). (Please note that research question 1 was a multiselect question and respondents were able to select all applicable pulse oximetry sources and, therefore, the answers do not add up.) In total, 219 respondents answered research question 1, of whom 73 reported that they were provided with pulse oximeters by the NHS and 42 also selected ‘another source(s)’ of pulse oximeters (13 respondents already had it in the home, 36 respondents noted that pulse oximeters were purchased by the care homes themselves and one respondent received it as part of a trial/pilot).
Some care homes had both purchased pulse oximeters themselves and received oximeters from the NHS. In 42 (19%) care homes, the pulse oximeters being used were reported as having already been available to use in the home before the COVID-19 pandemic (Figure 6). Group analyses indicate that care homes that had used pulse oximetry for less than 12 months were more likely than other care homes to have been provided with the pulse oximeters by the NHS. In addition, small care homes (i.e. care homes with fewer than 20 beds) were more likely than larger care homes to be provided with pulse oximeters by the NHS. Notably, residential homes were more likely than nursing homes to have been provided with pulse oximeters by the NHS. All of these findings need to be caveated as being in the context of a low survey response rate and, therefore, cannot be assumed to apply to the total population of care homes in England.
FIGURE 6.
Source of pulse oximeters: online survey of care home managers (n = 219). Note that the answers do not add up to 219, as the question was a multiselect question and respondents were asked to select all options that apply.
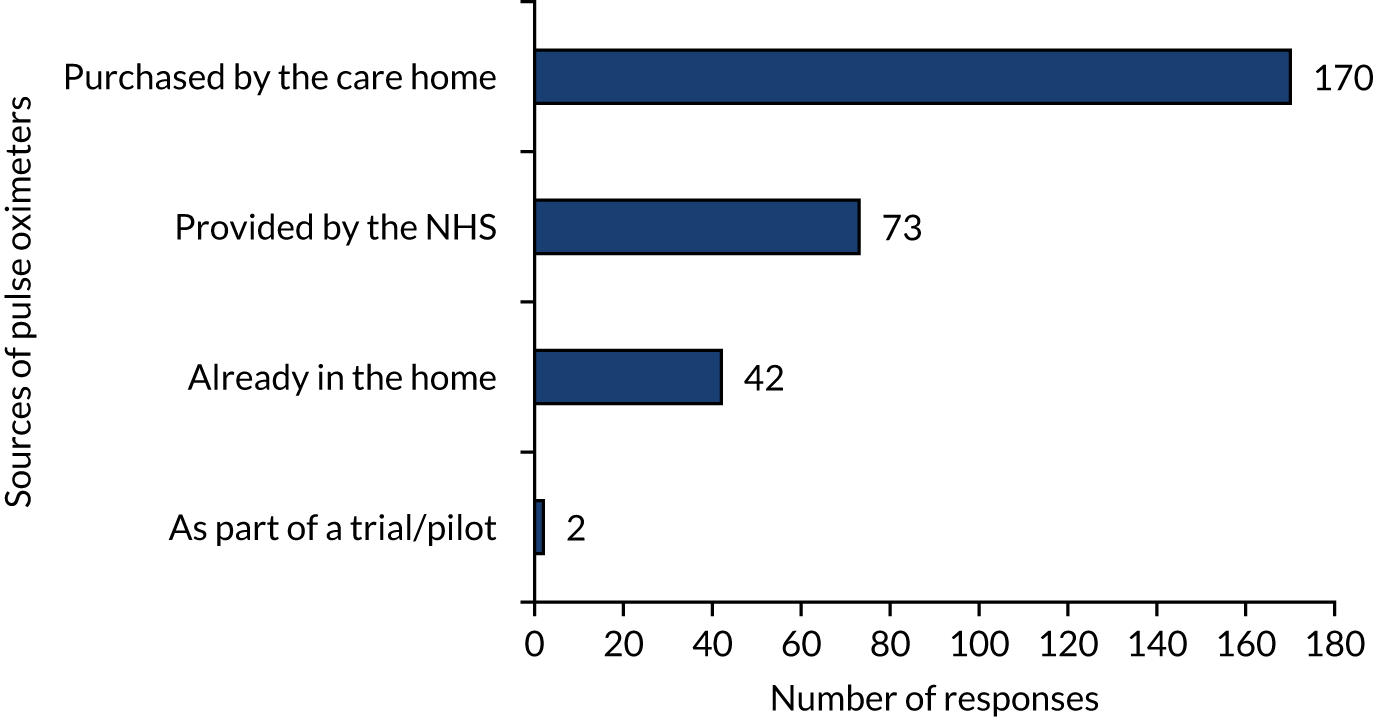
One theme that was evident in the open-text comments that were provided by survey respondents was that pulse oximeters are helpful and simple tools, and use of pulse oximeters can readily become part of the daily routine.
Several of the case study sites had purchased their own pulse oximeters, which were considered relatively inexpensive, whereas other care homes were provided with pulse oximeters by their local CCG; however, there was a mixture of care homes that had bought their own pulse oximeters either prior to or during the pandemic and care homes that were given devices by their local CCG through their GP. Where care homes purchased their own pulse oximeters, they did so without consultation with their NHS partners and, instead, relied on the discretion of the care home manager to identify a reliable and reasonably priced device. Care home staff reported that they could monitor a care home with over 50 beds with between five and eight pulse oximeters. It was also reported that the culture of thoroughly cleaning any shared equipment , already embedded before the pandemic, was further emphasised and acknowledged when the COVID-19 pandemic began:
. . . on each floor there’s like a basket and it’ll have a blood pressure cuff, temperature probe and an oximeter . . . I’ve always got spare ones. I’m looking . . . I’ve got three new ones . . . I’ve bought them off Amazon [Amazon.com, Inc., Seattle, WA, USA] in the past, I’ve bought them for £10 off Amazon.
Registered manager, nursing home (site 3)
Pulse oximeters were considered reliable and straightforward to maintain. Some, but not all, sites mentioned the importance of calibration checks, which should be performed on all pulse oximeters purchased independently by care homes, with pulse oximeters supplied by the NHS not requiring initial calibration but needing recalibration checks after 12 months from first use. Open-text comments by a few survey respondents referred to inaccuracies and technical difficulties when using pulse oximeters, including using pulse oximeters on residents with darker skin pigmentation. No case study sites reported a formal maintenance schedule for the upkeep of pulse oximeters. Instead, if staff felt that a measurement was erroneous, then they would take another reading using another oximeter or replace the batteries. If a particular oximeter caused problems regularly, then they would replace it:
If you’re taking someone’s oxygen levels and they’re like 87, 90 and they’re not COPD, you’ll want to retake again to make sure. Normally I’ll try another one. Say I’m using an oximeter and it’s giving me like a low level, I’ll try another one just to see if they’re both saying the same thing and then you act on that.
Qualified nurse 1, nursing home (site 3)
A small number of care home staff stated that when they first started using pulse oximetry they had a limited understanding of some of the key issues (e.g. cold hands, dark nail varnish) that might affect the accuracy of the reading, akin with learning from a recent rapid review. 51,52
Theme 2: routine use of pulse oximeters in care homes
Theme 2 provides further insights into research question 1, about when and how pulse oximetry is used in care homes, and research question 4 about guidance and resource needed to sustain that use. Among the care homes that responded to our survey, 91% (202/222 respondents) reported using pulse oximeters routinely at the time of the survey (in spring 2021). The highest prevalence of pulse oximetry use was reported by nursing homes (98%, 43 respondents), followed by dual residential and nursing homes (93%, 27 respondents) and then residential homes (89%, 132 respondents). (We are reporting percentage values using answers from care home managers who reported using pulse oximeters, taking the total number of care home type as a denominator.) Care homes with fewer than 20 beds, as well as care homes that started using pulse oximetry less than 12 months ago, were slightly less likely than other care homes to use pulse oximeters routinely. [Note that, in general, we report group analysis results only if the differences between groups of care homes (e.g. by care home type, care home size and the length of time for which the care home had been using pulse oximetry) were ≥ 10%. However, when the absolute values in some of the group analyses were small (i.e. fewer than 20 care homes in a given category), we report differences only of around ≥ 20%.]
Pulse oximetry had been in use for less than 12 months in just over one-quarter of the care homes that replied to the survey (67 respondents), for 1–5 years in around 40% of care homes (93 respondents) and for 5 or more years in nearly 3 in ten care homes (63 respondents) (Figure 7). The remaining 4% of care homes ( respondents) were not using pulse oximetry.
FIGURE 7.
Length of time using pulse oximetry in care homes: online survey of care home managers (n = 232).
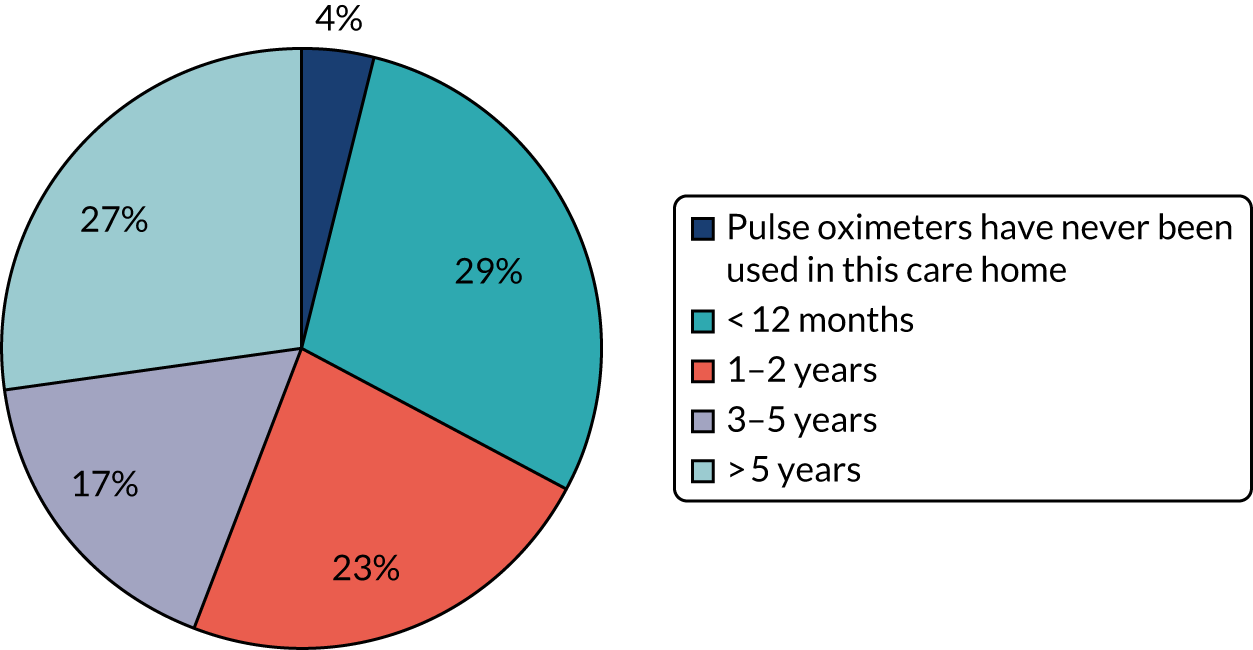
The majority of nursing homes and of dual residential and nursing homes that responded to the survey had been using pulse oximetry for 5 or more years. By contrast, a large majority of the residential homes had used pulse oximetry for less than 2 years. Indeed, 41% (63 respondents) of residential homes had used pulse oximetry for less than 12 months (Figure 8). The majority of small care homes (care homes with fewer than 20 beds) had used pulse oximeters for less than 12 months. (The usual caveat relating to the low survey response rate applies to these results.)
FIGURE 8.
Length of time of use of pulse oximetry in care homes by care home type: online survey of care home managers (n = 228).
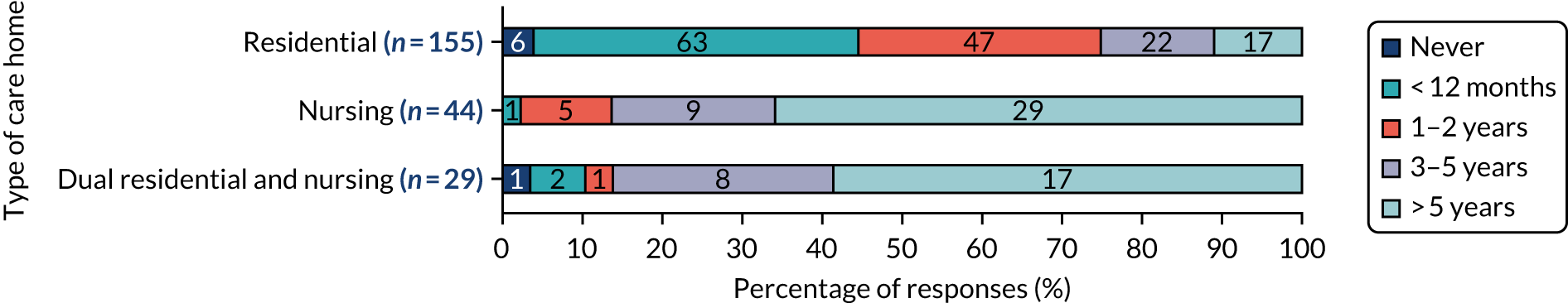
In 91% of care homes where pulse oximetry had been used for less than 12 months (60 of 66 respondents), pulse oximetry was introduced specifically in response to the COVID-19 pandemic. In care homes where pulse oximetry had been used for more than 12 months, it was used for a variety of conditions, including chest infections or pneumonia (128 respondents), COPD (108 respondents), asthma (82 respondents) and heart attack or heart failure (73 respondents) (Figure 9).
FIGURE 9.
Conditions for which pulse oximeters were being used in care homes where pulse oximetry had been used for more than 12 months: online surveys of care home managers in March and April 2021 (n = 153). Note that the answers do not sum to 153 as the question was a multiselect question and respondents were asked to select all options that apply.
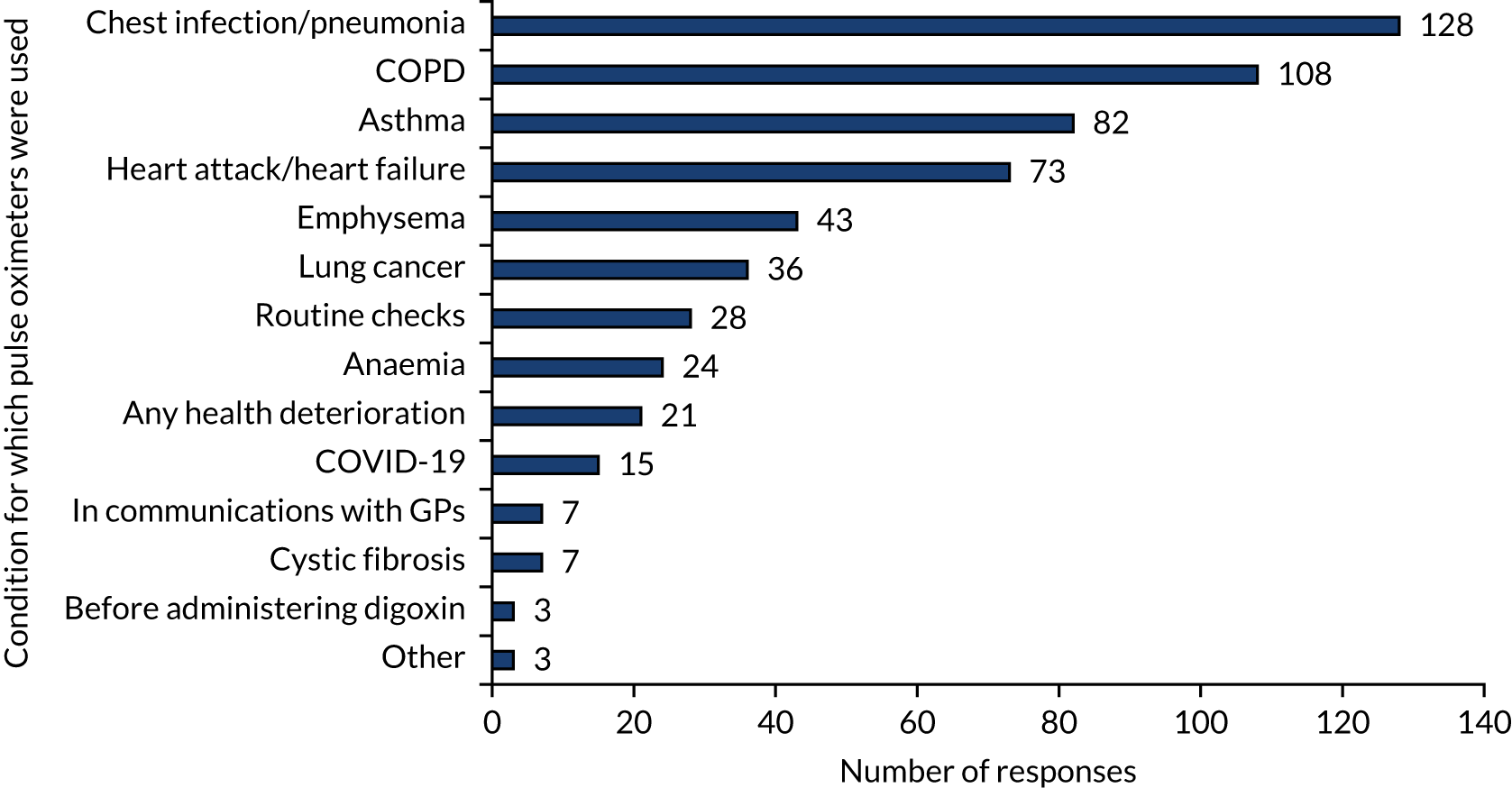
Staff at residential homes reported that, before the COVID-19 pandemic, they would use pulse oximetry only as prescribed by their local NHS partners (e.g. GP, PCN, district nursing team, Virtual Ward Team), and this would include direction on how frequently a measurement might be taken (e.g. twice-daily in the case of residents with a COPD exacerbation) and the length of time for which a resident would be monitored (e.g. days or weeks):
. . . it’s like could we monitor them like over a week, or over a few days, sometimes it can be medication which can affect that . . . Or different illnesses and things like that, so like monitor them over the weekend or over a week and then they’ll use them results.
Senior carer, residential home (site 5)
In one nursing home where pulse oximetry was regularly used in the routine care of residents before the COVID-19 pandemic, a qualified nurse explained how the home had used pulse oximetry for a number of years, incorporating pulse oximetry into the monthly monitoring of residents:
It’s something that we’ve always done. I mean I’ve been here for 9 years and since I’ve started our care manager got us all our own oximeters . . . so that’s something that they’ve always done here actually. Obviously with COVID they’re more hot on it but yeah, definitely, we’ve always used oximeters.
Qualified nurse, nursing home (site 3)
In interviews, we found that care home staff appreciated the benefits of capturing an additional physiological measurement that could more precisely inform the clinical management of a resident by the care home, with regard to COVID-19 and respiratory conditions, and that could also be used to further inform any discussions about a particular resident with their clinical partners and colleagues from across the NHS:
Main positive is that we get the care for the resident that they need a lot quicker than they was before. It gives us a better view of what’s going on as well so that when we’re speaking to health professionals we’ve got a better understanding and better communication with them, whereas before it was like we were stumbling over ourselves trying to explain to the doctor what was going on, or to the paramedics on the phone what was going on, whereas now we’ve got that reading we can speak to them and the communication’s more effective and it gets the care that the resident needs a lot quicker.
Senior carer 1 residential home (site 6)
We’ll use them regular and I can probably count on my hand the amount of times that we’ve probably saved someone’s life going from the SATS [saturation] and getting that emergency call in straightaway, rather than thinking oh well we’ll just see it goes, no, let’s get the readings first and let’s just, you know, get the treatment that way where the symptoms could worsen and it could end up quite fatal really.
Senior carer 3, residential home (site 5)
Staff would use a number of cues to assess a resident’s health and well-being during the pandemic. By establishing residents’ usual behaviour, staff could more readily identify a resident who potentially had health issues:
. . . it’s the same girls that work the floor so they kind of know the residents and they’ve been there quite a while, so they’ll just say ‘look, can you just call – she’s not right – there’s just something not – can you just come and have a look’, you know, ‘yeah, yeah, fine I’ll come down’.
Senior carer 2, residential home (site 5)
For nursing homes, the clinical training of the nursing staff meant that they possessed a broad understanding of the clinical value of monitoring oxygen saturation in a variety of circumstances and for a number of conditions, including the impact of a fall, exacerbations as a result of chronic respiratory conditions or for the prescription of antibiotics. In addition, staff at one nursing home had independently learnt of the value of monitoring oxygen saturation specific to COVID-19 in identifying silent hypoxia:
So that’s how we could kind of distinguish . . . those that had COVID and those that are just normal regular chest infections . . . say half a dozen residents in, looking back on the information, you can see that there was an indicator within the NEWS2 score that the blood saturation levels were really low, in the 80s so . . . once someone was COVID positive, even if they had no underlying other health issues.
Nursing care manager, nursing home (site 3)
Following the onset of the COVID-19 pandemic, staff in residential care homes also had an awareness of how measuring oximetry could help detect silent hypoxia:
If somebody’s displaying symptoms of COVID we’ll then start doing, checking the oxygen levels because purely one of the issues is like with the breathing, so we’ll check the oxygen levels every 4 hours and we have, obviously using the oximeter, noticed some of the saturation levels that have dropped and we have then recommended residents being put forward for oxygen, so that’s helped us in that way because obviously it’s not something we would have been able to easily pick up on without it.
Senior carer 1, residential home (site 5)
Staff described how pulse oximetry was only one factor in determining the health of a resident, alongside soft signs. For example, the demeanour of the resident would provide an additional indication as to their condition:
I think on one occasion it was obviously the oxygen was very low but also they were very cold, their temperature was quite low and they just seemed more confused . . . Obviously we know our residents so we kind of know what their best day is, if that makes sense?
Assistant manager, residential home (site 4)
Theme 3: ease of using pulse oximeters and availability of training
In relation to research question 3.1 about training received by care home staff, we found from the survey responses that many, but not all, care workers and care home managers had received training in aspects of using pulse oximetry (Table 7). Out of a total of 186 care home managers who provided answers to research question 3.1, between 126 and 146 respondents, depending on the specific oximetry-related activity, reported that staff and managers at their care home had received training relating to pulse oximetry.
| Category of staff | Training received for the following activities (n) | ||||||
|---|---|---|---|---|---|---|---|
| Deciding when to use pulse oximeters | How to take pulse oximetry readings | Recording a pulse oximetry reading | Monitoring a resident’s progress | Escalating patients when necessary | Cleaning pulse oximeters | Storing pulse oximeters | |
| Care workera | 126 | 146 | 142 | 128 | 130 | 144 | 137 |
| Care home nurse | 62 | 64 | 64 | 64 | 64 | 58 | 56 |
| Registered manager | 138 | 141 | 141 | 134 | 141 | 128 | 127 |
| Other | 20 | 17 | 17 | 16 | 16 | 17 | 14 |
Most care home managers (69%, 123 respondents) reported that care home staff who used pulse oximetry with residents did not require further training or support in respect of its use. However, 31% (55 respondents) said that further training or support for staff may be required, with 37% of residential homes reporting such a need, compared with 14% of nursing homes that responded and 23% of dual residential and nursing homes. Managers in care homes that had been using pulse oximetry for less than 12 months, as well as residential homes managers, were more likely to report a need for further training and support. However, there were no major differences between different-sized care homes in the reported need for further training or support.
Staff at the case study sites typically viewed pulse oximeters as non-invasive, quick and relatively simple to use, enabling pulse oximeters to be readily integrated into existing care regimens. For example, one senior carer at a residential home described how they used oximeters while measuring the resident’s temperature and blood pressure:
It’s only a matter of minutes, well not a minute even, until you get a reading, even if you need to do a couple just to be sure, it doesn’t actually take that long.
Senior carer 2, residential home (site 5)
The pulse oximetry measurements would be either written down and entered into the resident’s care record later or immediately transcribed into the personalised care plan held on a software-based clinical management system that was hosted by the home. The software-based data management systems included the functionality to prompt and record pulse oximetry measurements:
Yeah, so each resident has their own care plan on a New Age system what we use, so they have like different drop-down tabs. So for each resident it would be recorded within their care plan. If they had to have, if it was somebody who had to have their oxygen levels measured every 4 hours, that would be wrote within the care plan as well so that everybody knew that that needed to happen and then all the readings would be wrote under the observations tab. If it was to do with coronavirus you’d document it under the coronavirus tab . . . The seniors more often do it on the computers but all the care staff have access via phone system, so the mobile phone system is all linked to the New Age. So each carer’s given a mobile phone each morning and they’ll use that for the data document, anything to do with any resident . . .
Senior carer 3, residential home (site 5)
Nurses working in nursing homes had received training in delivering pulse oximetry as part of their nursing qualification and so were comfortable and confident in taking and interpreting measurements:
Obviously with our training, with the hospital, you use them quite regularly. Their machines are a lot different to here but I mean our care manager just shows you how to do it and then I haven’t had any recent training or needing updates because it’s quite a simple thing to do, isn’t it?
Nurse 1, nursing home (site 3)
At some sites, there was a lack of awareness of the training resources available for staff available from NHS CO@h, CCGs and local NHS trusts, and there was also a lack of time to access this training. At one residential care home that had systematically trained its staff, the care home manager described difficulties in co-ordinating training and the challenges they had to overcome to ensure that a trained member of staff was available on both day and night shifts. As a result, the training took a number of weeks to prepare and complete, early in the pandemic:
It did take about a month really, I would say, of getting everything sorted, getting everybody trained to know exactly what they were looking for when they did the pulse oximetry, the levels that they did, explaining sometimes that you know if they come back a bit low, we would have to go back, let’s have another look at this, let’s not just take this, you know have they put it on the finger correctly, have they waited long enough. So I would say it’s probably taken us about a good month to get everybody up to scratch and my idea was that including weekends, there would always be somebody on shift that would be able to do this effectively.
Registered manager, residential home (site 5)
Care home staff and managers from two case study sites had received training in using RESTORE2 (a physical deterioration and escalation tool designed in the NHS for use in care homes, and which includes oximetry):
After COVID, I think it’s just a normal thing now, you literally just grab all of that stuff, so you grab the oximeter, you grab the thermometer, you grab the blood pressure machine, you get the RESTORE2 form, because it’s easier with a RESTORE2 form now that they’ve come in, because that’s what they ask you as well, so it’s easier to have it all together.
Senior carer, residential home (site 4)
I’ve got the staff trained and the competency signed off, then we were looking to do the RESTORE2 Programme. We’ve done the RESTORE-mini but we would like to go on and do the full course, to be able to do the blood pressures and that, to monitor properly, for any deterioration.
Registered manager, residential home (site 6)
In the absence of concerted training in several instances, carers had learned to use pulse oximeters by watching either their colleagues or visiting clinicians:
. . . to be honest with you, I’ve just watched other people and what I’ve picked up myself, yeah, we haven’t had any specific training on – it’s like if we’ve had like the GPs in and things, there was one time I rang the GPs because somebody’s beats per minute was quite high and then when they came in and they actually said to us, ‘you do know you need to leave it for a couple of minutes so that it does get to have a true reading’, so it’s just things like that, guidance from other professionals really.
Senior carer 3, residential home (site 5)
I was shown how to use, yeah, I never worked in a care setting before this one, so when I started here everything is new to me and, yes, so I was shown by one of the nurses.
Senior care assistant, nursing home (site 3)
Since the pandemic began, a number of training and educational materials specifically relating to pulse oximetry in care homes have been made available by NHS and other organisations via multiple online platforms (see Report Supplementary Material 4), although much of the material appeared only towards the end of the second wave of the pandemic:
The NHS did put quite a lot of effort into kind of trying to explain it. I don’t think – I mean things vary so much at a local level because the landscape of how things operate and where the support comes from seems to be quite different – so some of the things that the NHS team put into place were around kind of very simple guides, user friendly explanations of how to use the pulse oximeters, how to record that information, how to make sure that the escalation routes, the reporting routes were right . . .
National lead interview
The need for straightforward messaging and clear guidance about the introduction and application of pulse oximetry in care homes (both nursing and residential) was commented on. Interviewees suggested that guidance should be co-ordinated across care home policy-makers and disseminated in a manner that is accessible to care homes:
. . . one of the things was this kind of lack of clarity coming from all different sectors so, you know, Public Health England would publish something, NHS would publish something, DoH [the Department of Health and Social Care] would publish something and it was really confusing to this sector. So publishing a very simple, one-side guide which incorporated some of the Department of Health and some of the NHS and some of the Public Health England measures specifically for care homes: top line ‘how you do things, do it well’ – would add that clarity.
National leader (NHS)
The need for a greater awareness of what the pulse oximeter readings meant was reported. This awareness would enable staff to speak to their NHS partners with more confidence if they suspected that there was an issue with a resident:
. . . to me it would be a handy tool for care staff, well all staff in care homes, to have that knowledge [of pulse oximetry], so that they can, you know, do it themselves, understand that there’s a problem and not have to wait around, you know, you can ring a GP, you know, ‘I’ve been trained in this, I’ve taken blood pressure, pulse, temperature and these are my findings, I really recommend that, you know, I need some advice or could you come and see?’
Senior carer, residential home (site 5)
In summary, this study has used the survey and case study interview data to describe how pulse oximeters have been obtained and used to help look after care home residents before and during the COVID-19 pandemic. The study has found that pulse oximetry was frequently used in managing residents with a variety of conditions, either independently in the case of nursing homes or as directed by their NHS partners. Pulse oximetry was described as being easy to use within the daily routine of the care home and as useful in supporting care home staff to communicate more effectively with clinicians working in the NHS. Staff needed to be trained to use pulse oximeters, and this was not without challenges when the use of pulse oximeters was introduced or when use increased, as it did in some care homes when the COVID-19 pandemic began.
Chapter 4 describes staff experiences and views on the impact on residents of implementing pulse oximetry in care homes.
Chapter 4 Analysis of the experiences of how pulse oximetry was introduced in care homes and the impact on residents and staff
The key points of Chapter 4 are summarised in Box 10.
-
Pulse oximetry was quickly expanded or introduced in care homes during the pandemic, as it was viewed as a useful tool to help residents.
-
Care homes had varying degrees of involvement with primary and secondary care practitioners at a local level when treating residents with COVID-19, which has, in part, influenced the extent of awareness and subsequent uptake on implementing pulse oximetry as part of the CO@h programme.
-
The NHS CO@h programme was implemented across England, but with variations in relation to its reach and adoption in care homes.
-
The activities associated with pulse oximetry were usually not challenging for care home staff.
-
Nevertheless, some aspects of using pulse oximeters were seen as having at least a slight degree of challenge. For example, 45% of survey respondents felt that deciding when to escalate patients was a challenge to some degree.
-
Most of the survey respondents (care home managers) did not feel that pulse oximetry affected their workload or the workload of their staff, although some respondents reported slight increases in workload.
-
When assessing impact on staff stress levels, the responses were nearly equally divided between respondents reporting no impact and respondents reporting improved (reduced) stress levels.
-
Most care home managers indicated that pulse oximetry was improving their own job satisfaction and the job satisfaction of their staff (60% of respondents), with just under one-third of respondents selecting the ‘no impact’ option.
-
Most survey respondents and interviewees considered that pulse oximetry was reassuring to residents, or at least did not increase their anxiety, but some reported that some patients were made more anxious by the use of pulse oximetry.
-
Pulse oximetry was also perceived, on average, to be leading to fewer hospital admissions and accident and emergency attendances.
-
Many care home managers, although fewer than half of those responding to the survey, felt adequately supported by the NHS when asked about support with how to use pulse oximeters, how to communicate readings to the NHS and when/how to escalate cases appropriately. A similar number of care home managers responded that they had not received such support from the NHS. However, as many care homes were already using pulse oximeters pre pandemic, and many staff did not find pulse oximeters challenging to use, it is unclear if support was not received because it was not sought. A minority of care home managers reported receiving some support from the NHS, ‘but not enough’.
-
Forty per cent of survey respondents were aware of the CO@h service, and two of the six case study sites were part of the CO@h programme.
-
CO@h support was considered beneficial at the two sites that were actively engaged with the programme, especially with regard to making appropriate and timely care decisions about COVID-19-positive residents.
Theme 4: staff attitudes and level of challenge when undertaking pulse oximetry with residents
Within this theme, we present evidence that addresses research questions 3.2 and 3.3, which concern challenges experienced by staff associated with using pulse oximeters and the impact on staff well-being and confidence. It seems from both the interviews and the survey responses that the activities associated with pulse oximetry were usually not challenging for care home staff. When asked about the level of challenge for staff to carry out the activities associated with taking, recording and reporting pulse oximetry measurements, as well as acting on the results, respondents (i.e. care home managers) indicated that, overall, these activities were not deemed unduly challenging for staff (Figure 10).
FIGURE 10.
Level of challenge for staff to carry out activities relating to pulse oximetry: online survey of care home managers. Note that the number of answers differed per option, as indicated in the figure.
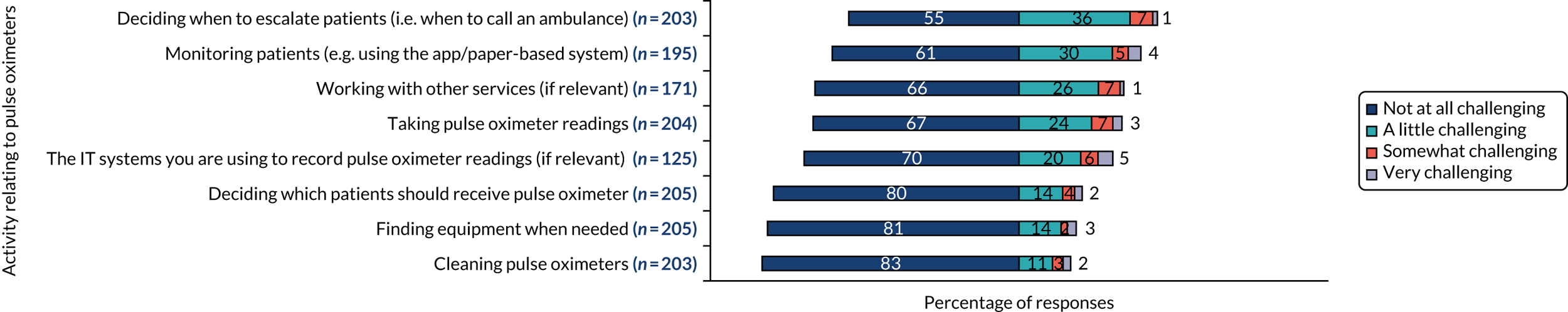
Nevertheless, some aspects of pulse oximetry were seen as having at least a slight degree of challenge. For example, nearly half of survey respondents (45%, 91 respondents; cumulative answer for respondents selecting ‘a little’, ‘somewhat’ and ‘very’ challenging) felt that deciding when to escalate patients was a challenge and 39% (77 respondents) found it challenging to monitor patients. Around one-third of respondents found working with other services (34%, 58 respondents), taking pulse oximetry readings (33%, 68 respondents) and using the IT systems to record pulse oximetry readings (30%, 38 respondents) to be challenging (see Figure 10).
Most care home managers (93%, 180 respondents) reported having the staff capacity required to use pulse oximeters in their care home, and this did not vary by care home type, care home size or the length of time for which the care home had been using pulse oximetry. Only a small number of respondents reported that they did not have enough capacity (4%, eight respondents) or were unsure if they had enough capacity (3%, five respondents).
Overall, most of the survey respondents (i.e. care home managers) did not that feel pulse oximetry affected their workload (61%, 112 respondents) or the workload of their staff (53%, 97 respondents) (Figure 11). However, some respondents did report a slight increase in their own workload (35, 19% of respondents) and/or their staff’s workload (47, 26% of respondents). The low response rate to the survey means, however, that we cannot assume that these views are representative of all care homes in England.
FIGURE 11.
Impact of pulse oximeters on staff workload, stress and satisfaction: online survey of care home managers. Note that the number of answers differed per option, as indicated in the figure.
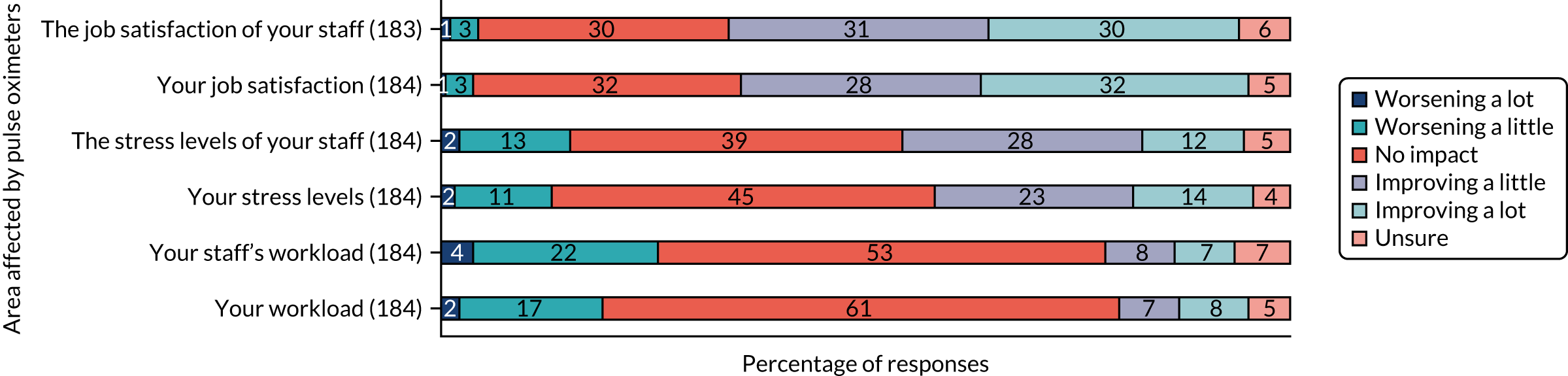
When assessing impact on staff stress levels, the responses were nearly equally divided between respondents reporting no impact and respondents reporting improved (reduced) stress levels. Forty-five per cent of care home managers (83 respondents) reported that pulse oximetry had no impact on their own stress levels and 39% (72 respondents) reported that it had no effect on the stress levels of their staff. In fact, 38% of care home managers (69 respondents) reported that pulse oximetry was improving (i.e. reducing) their own stress levels and 40% (74 respondents) said that it improved their staff’s stress levels (cumulative number for ‘improving a little’ and ‘improving a lot’ answers).
Finally, most care home managers indicated that pulse oximetry was improving their own job satisfaction and the job satisfaction of their staff (60%, 110 respondents) (cumulative number for ‘improving a little’ and ‘improving a lot’ answers), with just under one-third of care home managers selecting the ‘no impact’ option with regard to improving their own job satisfaction (32%, 58 respondents) and the job satisfaction of their staff (30%, 54 respondents). It is worth noting that between 4% and 7% of responding care home managers (i.e. between 8 and 12 respondents) selected the ‘unsure’ option.
Group analyses indicate that care homes that had used pulse oximetry for more than 12 months reported slightly higher levels of improvement in workload, stress levels and job satisfaction. However, no major differences were reported between care homes with different numbers of beds.
Carers and managers across care homes understood the vulnerability of residents to COVID-19 and silent hypoxia and, consequently, placed a priority on protecting and monitoring residents throughout the pandemic. As a result, a range of care home staff, including those without clinical training, were prepared to assume responsibility for measuring pulse oximetry. In nursing homes, responsibility for pulse oximetry was typically (if not exclusively) performed by qualified nurses. In residential homes, responsibility for pulse oximetry tended to fall to senior carers, although during the pandemic a broader range of staff became involved as the use of pulse oximetry increased and staffing levels varied:
I don’t see it as a pressure. I think it’s perfectly reasonable for us to do it because at the end of the day, like I said, we don’t want to sit back and know that we could have got help sooner had we known what was actually wrong.
Senior carer, residential home (site 5)
Pulse oximetry quickly became assimilated into the new working practices brought about by the pandemic. In contrast, pre pandemic, the need for competency-based training and sign-off would result in implementation taking longer. The time and effort to undertake pulse oximetry was minimal and pulse oximetry could be performed along with other observational/clinical measurements, such as temperature and/or blood pressure. At site 4, staff numbers during an outbreak were reduced by nearly 60% and, consequently, all remaining senior carers and care assistants were involved in administering pulse oximetry. As staff understood the importance of pulse oximetry in the context of COVID-19, as well as the threat of silent hypoxia, they were happy to accept this additional responsibility:
I think to start off with it felt like it was just like an extra bit, but then you just get used to it and you have to do it because at the end of the day that’s what you’re here for, you’re here to look after them [residents].
Senior carer, residential home (site 4)
However, it should also be noted that, based on a few open-text responses to our survey, it was evident that some care home staff considered pulse oximetry potentially unhelpful (e.g. because their care home did not have oxygen available) and that it may, on occasion, have resulted in unnecessary hospitalisation (e.g. residents being taken into emergency secondary care when they could have been cared for in a care setting).
In general, care staff (both those working in nursing homes and those working in residential homes) appeared confident when administering pulse oximetry:
I think as a team we’re quite confident in it. – I think it’s about four weeks in total where was doing it daily, so everybody had a good knowledge of what to do when they suspected anything.
Senior carer, residential home (site 6)
I am, [confident] yes, it’s quite simple and if you know what you’re looking for, how to read it, yeah, it’s I think very simple to use.
Senior care assistant, nursing home (site 3)
There were mixed attitudes towards accepting the additional responsibility of taking and recording pulse oximetry measurements (or any other similar observations) on a range of clinical management systems, as some interviewees believed that any mistakes in the data uploaded could put a resident’s well-being at risk:
It’s just they’re like ‘I don’t understand why you can’t do blood pressures or whatever because you could go to Boots [Boots UK Limited, Nottingham, UK] and have it done’. But they don’t understand that what if we were to do it wrong then we’re putting a vulnerable resident at risk.
Senior carer, residential home (site 6)
The same staff member conveyed their nervousness and perceived greater accountability when using pulse oximetry:
Thinking oh my God, actually it’s quite nerve wracking. I know it’s just like easy thing of like putting it on your finger, but what if we haven’t read it properly.
Senior carer, residential home (site 6)
However, other care staff were content to increase the frequency of the pulse oximetry measurements and to accept the additional responsibility, within the wider context of CQC guidance:
It doesn’t take long at all, it’s not an issue and if it’s something that needs to be done then it’s something that needs to be done.
Care assistant, residential home (site 4)
Since the onset of the COVID-19 pandemic, the use of pulse oximetry had increased and become embedded as part of routine care in both nursing and residential care home environments:
. . . after COVID, I think it’s just a normal thing now, you literally just grab all of that stuff, so you grab the oximeter, you grab the thermometer, you grab the blood pressure machine, you get the RESTORE2 form, because it’s easier with a RESTORE2 form now that they’ve come in, because that’s what they ask you as well, so it’s easier to have it all together.
Senior carer, residential home (site 4)
Theme 5: how pulse oximetry affects care home residents
Within the constraints imposed by the pandemic, and because of the nature of a rapid evaluation, we were unable to include interviews with residents and their families. However, to address question 2 about perceived impacts on residents, we asked care home managers for their views on how the use of pulse oximetry affected the residents in the homes they managed. A substantial minority (40–46%) of care home managers who responded to the survey considered that pulse oximetry had neither increased nor decreased the anxiety or reassurance felt by residents. The remaining respondents felt that pulse oximetry was more likely to reassure residents, rather than make residents feel anxious (Figure 12). Nearly half of care home managers agreed (cumulative number for ‘agree’ and ‘strongly agree’ answers) that residents felt reassured by the use of pulse oximetry (49%, 89 respondents). Similarly, nearly half of care home managers disagreed (cumulative number for ‘strongly disagree’ and ‘disagree’ answers) with the suggestion that residents may have felt anxious because of the use of pulse oximetry (43%, 78 respondents). However, 17% of care home managers (32 respondents) thought that residents would have felt anxious by the use of pulse oximeters. It is perhaps noteworthy that there were 17 respondents who reported that residents have felt both reassured and anxious by the use of pulse oximetry, which may indicate that they felt that, although some residents were reassured, other residents were left more anxious.
FIGURE 12.
Care home managers’ perceptions of residents’ feelings towards pulse oximetry: online survey of care home managers (n = 177).

Nearly all care homes (91%, 166 respondents) indicated that the use of a pulse oximeter facilitates timely identification of deterioration of a resident’s health. In addition, care home managers reported that pulse oximeters had a reassuring function for staff (85%, 156 respondents) and the ability to provide reassurance for residents (66%, 121 respondents) (Figure 13).
FIGURE 13.
Impact and benefits of using pulse oximeters, for residents and staff: online survey of care home managers. Note that the number of answers differed per option, as indicated in the figure. There were five ‘unsure’ answers per option and these answers are not shown in the figure. Owing to small numbers, the answers ‘strong negative impact’ and ‘negative impact’ have been merged and the figure shows a cumulative value for these two answers.

Group analyses did not show any major differences between answers provided by care homes of particular care types or of different sizes, or with regard to length of time of pulse oximeter use.
In addition, we looked at whether or not answers differed according to the needs of the residents, in particular for residents living with dementia or with a learning disability (see Figure 4). Overall, out of a total of 231 respondents who answered the question about the most common needs of care home residents, 13 reported that they manage care homes that accept only residents with learning disabilities. The overall number of respondent care homes where at least some residents have learning disabilities was 62. Nearly two-thirds (149/231) of the care home managers who replied to the survey question about the needs of care home residents stated that at least some of their residents were living with dementia.
As part of our survey, care home managers were asked about the impact of pulse oximetry on residents’ health. Respondents were divided in their views and indicated that pulse oximetry either reduces health crises or deterioration, or is not having an impact (Figure 14). Half of the care home managers reported that pulse oximetry is reducing residents’ frequency of attending a hospital accident and emergency department (50%, 91 respondents) and of residents being admitted to hospital (46%, 84 respondents). This is important because our qualitative findings showed that staff felt that the majority of residents prefer to remain in their care home and not to be unnecessarily escalated to emergency secondary care if their physical health deteriorates. In addition, this finding means that unnecessary demand on NHS hospitals is reduced.
FIGURE 14.
Perceptions of impact of pulse oximeters on key health parameters of residents: online survey of care home managers. Note that he number of answers differed per option, as indicated in the figure.
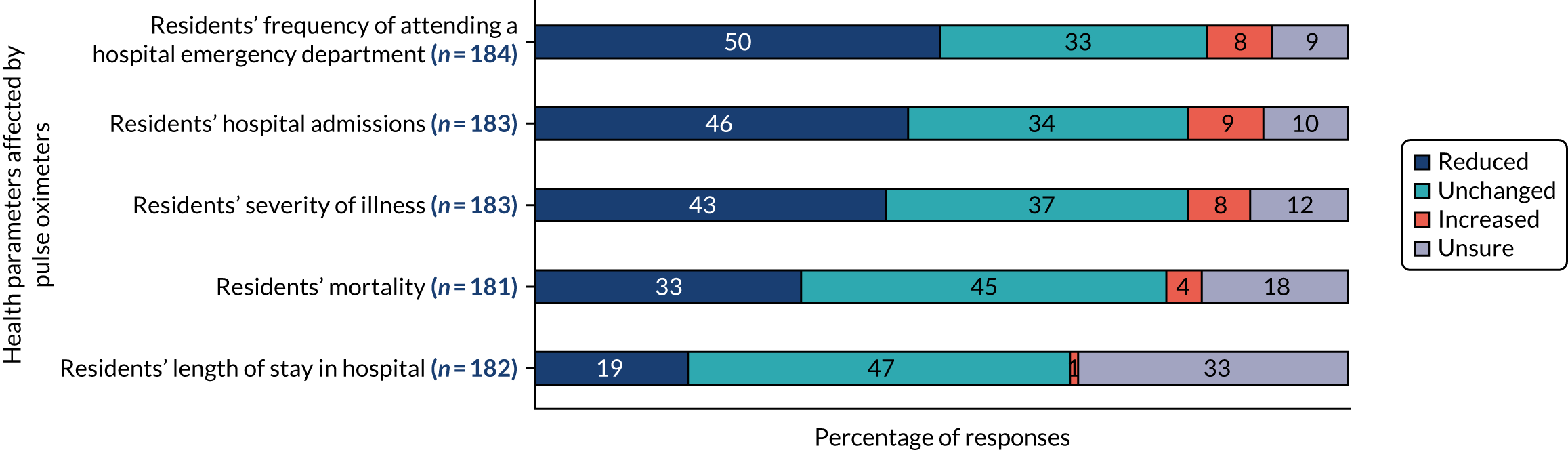
In the survey, we asked care home managers if they thought that the use of pulse oximeters in care homes would affect the length of time their residents would stay in a hospital once admitted there. Nearly half of the care home managers who responded thought that pulse oximetry would not change residents’ length of stay in hospital, and one-third of respondents were unsure about this either way. Nearly all of the remaining respondents thought that pulse oximetry would reduce hospital length of stay, with only 1% of all respondents considering that hospital length of stay would increase as a result of care homes using pulse oximetry.
One-third of the care home managers responding to the survey thought that using pulse oximeters in their care homes was improving residents’ survival. Just under half of respondents thought that it was making no difference to residents’ mortality and another 18% were unsure. Only 4% of respondents thought that the use of pulse oximeters was increasing mortality.
Group analyses indicate that residential care home managers and managers of care homes that had been using pulse oximetry for less than 12 months were slightly more unsure about the impact of pulse oximetry on residents than were the managers of nursing and dual nursing and residential care homes and the managers of care homes that had been using pulse oximetry for more than 12 months.
The open-text comments provided by some survey respondents summarised pulse oximeters as effective and simple tools that provide reassurance to residents, their families and to staff, and benefit residents’ health.
Pulse oximetry was considered by respondents as having a positive impact on reassuring residents. In addition, pulse oximetry was felt to provide timely identification of deterioration of a resident’s health. In interviews, staff in both nursing and residential homes reported that care home residents would readily accept staff taking these routine pulse oximetry measurements, but always with the resident’s consent:
You say hello and ‘morning’ or whatever, ‘can I do your oxygen level please?’ and then some are like ‘what’s that?’, ‘just to measure your breathing’. So that’s it. And they’ll just give you their finger. You say ‘can I have a finger?’ and they’ll just give it. But you do get consent, you don’t just go and pop it on.
Qualified nurse 1, nursing home (site 3)
Some residents would go on to enquire as to the precise reading and its implications, with care home staff requiring some additional time to provide explanations:
They’d go ‘oh, is it OK?’ and you’d say ‘yeah, it’s . . . ’, you know, you’d say the number and they’d go ‘oh, if it’s not OK, what would it be?’ and I’ll just say ‘92 or below’ and they always accepted that and they were fine with that.
Care assistant, residential home (site 4)
During the pandemic, care home staff appreciated the heightened concern of residents’ families and loved ones unable to visit and how reporting pulse oximetry measurements would help to reassure them:
You do have to communicate to let them know what’s happening and to let them know what’s done. Say you do the oxygen levels because the GP wanted it, you have to let them know that the GP requested it and this is what it is and stuff like that, yeah. You do relate to family.
Qualified nurse 1, nursing home (site 3)
There were occasional issues with compliance among residents with dementia or learning difficulties who, failing to understand what was happening, would remove the pulse oximeter before a reliable reading could be taken, occasionally becoming confused and/or agitated in the process. In this instance, care staff would return later or a ‘favourite’ member of staff (i.e. a member of staff who had established a particular rapport with a resident) would try again:
. . . the people that have got the capacity, we can speak to them more about it but . . . there’s quite a lot in our home got dementia and some of it’s quite bad, so trying to explain anything to them is just in one ear and out the other I’m afraid to say . . .
Care supervisor, residential home (site 2)
So obviously we have a lot of residents with dementia. A lot of them are fine with it on their finger but some of them will try and get it off.
Qualified nurse 2, nursing home (site 3)
Theme 6: NHS and other external support for pulse oximetry received by care homes
Within this theme are insights that are relevant to research question 1.2 about NHS support provided to care homes and their staff. As we were able to obtain only very few interviews with NHS practitioners working with care homes, we were not able to address research question 5.
NHS support
When asked whether or not their care home had received adequate support from the NHS in administering pulse oximetry, a majority of the care managers who responded to our survey reported either ‘no support’ or ‘some support but not enough’, with a substantial minority of care managers describing their support as adequate (Figure 15). It is not clear from the survey responses if the answer ‘no support’ indicates that such support was required and not received by care homes or if support was felt to be unnecessary, given that respondents also reported that most care home staff did not find using oximeters challenging. An expressed desire for more training and support from the NHS was also a theme of the open-text comments provided by some care home managers.
FIGURE 15.
Perceived level of support from the NHS: online survey of care home managers. Note that the number of answers differed per option, as indicated in the figure.

Among the 185 respondents who answered in respect of all four types of NHS support listed in Figure 15, 48 (26%) reported having received adequate support of all four types. Eighty-six (46%) respondents reported having received either no support or some support but not enough in any of the four categories. The other 28% of respondents received adequate support in at least one area, but also said that they received no support in at least one of the other four areas.
There were no major differences between the answers provided by different care home types; however, managers of care homes that had used pulse oximetry for more than 12 months or had more than 20 beds were slightly more likely to report ‘no support’, whereas managers of care homes that had been using pulse oximetry for less than 12 months were slightly more likely to report some support, but not enough.
When support provided by the NHS was described as ‘adequate’, the support mostly related to escalation of patients (45%, 85 respondents) and communicating readings to the NHS (44%, 82 respondents), and these were the same pulse oximetry-related activities that respondents had described as the most challenging.
The precise nature of the support reported being received from NHS partners pre pandemic varied across the care home case study sites. Some staff reported that their care home was associated with a single general practice, as part of a PCN, and had regular contact with a GP who would conduct regular weekly rounds. As the senior care manager at a nursing home that received such visits explained:
Myself and the GP, we’re in constant e-mail communication, so if someone’s poorly outside of a Tuesday we can still be requesting things and we get sorted within that day, so if I’ve got anybody that feels, kind of, having an infection or whatever we get the clinical obs [observations] sent over by e-mail and he’ll do a prescription for antibiotics. But the GP was looking at doing something where we had antibiotics on standby for each resident, a prescription that we could kind of cash in if so he trusts our knowledge and our clinical skills to identify infection and cash this prescription in if we need it.
Care manager, nursing home (site 2)
At other care homes, the residents moving into the home retained the services of their existing GP. Therefore, one of our care homes was associated with seven GPs across three practices; however, we were unable to determine whether or not these three practices were part of the same PCN. Each GP visited only in response to the needs of the individual patient(s) who were registered with them. Consequently, despite NHSE&I introducing the NHS Framework for EHCH in March 2020, alignment between care homes and PCNs appeared to be still evolving:
. . . you’ve got several general practices, so you’ve got – I think there’s – off the top of my head you’ve got about three or four different GP practices – all quite established GP practices as well, do you know, they’re not little, there’s not just like one or two GPs, there’s quite a lot. So, yeah, there was different GP practices. And we do give residents the choice of which one they want to register with.
Registered manager, residential home (site 5)
During the pandemic, owing to the restrictions imposed on face-to-face consultations in care homes, regular contact with GPs was reduced and other models of care evolved. One residential home was supported via a local paramedic service organised through its local PCN. The paramedics would visit regularly and consult with the GP if an issue arose:
So they introduced in late 2019 paramedic practitioners as part of the primary care networks, so what we used to do, or what they still currently do, is if there’s anybody that they’re concerned about on that day they’ll ring the paramedic practitioners who come that day to review them and then they’d communicate with the GP and decide the best course of action from there, whether it be antibiotics, whether it be just monitoring, it might be that they need to be admitted to hospital and the paramedics also did like ward rounds, so they’d come round on a routine basis just to check everybody over really.
Senior carer 1, residential home (site 5).
At another site, where, due to the pandemic, they no longer received the weekly visit by the local GP, a community nurse supported the home:
Our team has done a lot to deliver the ward rounds and work closely with the homes between, like a sort of middleman between the homes and GPs. So by working alongside the GPs within you know delivering ward rounds and patient care within the home, I think we’ve been able to better signpost where some residents need to be.
Community nurse, residential home (site 2)
At this site, when the community nurse was unavailable, care home staff consulted NHS 111, and then, if it seemed necessary, contacted the local GP, so as to avoid unnecessary hospitalisation and the associated anxiety related to hospital admission for the resident concerned (particularly during the pandemic):
The registered manager likes us to get in touch with her first before we do anything like ring 111 now, because of COVID, because a lot of the families are a bit worried about them going into hospital so, I mean, we will get the doctor out if it is, you know, quite worrying.
Care supervisor, residential home (site 2)
In the context of the pandemic, several participants said that they would have welcomed increased support from their NHS partners to manage COVID-19 outbreaks:
Personally, I think care homes have been overlooked through the whole thing with regards to training, the support we have, this isn’t just through [place 1], this is for all care homes, some of the support they’ve received obviously not having the training to look out for the indications of COVID because I know testing wasn’t in place to start with, which caused quite a bit of [COVID] outbreak in care homes, I think if the testing was brought in a lot quicker with the use of pulse oximetry it could have prevented a lot of deaths.
Senior carer, residential home (site 6)
Since COVID, one of the things that’s been highlighted is that care homes have been sort of left out on their own.
Community nurse, residential home (site 2)
Before the onset of the COVID-19 pandemic in the UK in February 2020, there was no specific national guidance or advice, from NHSE&I or other national bodies, on the use of pulse oximetry in care homes. However, CQC guidance, published in 2015, suggested that non-medical care home staff should not be using pulse oximetry for ‘spot’ recording. 53 The CQC did, however, clarify the application of its guidance to state that non-clinically trained care home staff could administer pulse oximetry during the pandemic, but should stop to undertake training if pulse oximetry was to be used as part of routine monitoring for the longer term. Not all care home managers were fully aware of the most recent CQC guidance for pulse oximetry, with one care home manager reporting having been dissuaded from using pulse oximetry because it is considered a clinical task and beyond the scope of carers’ responsibilities:
. . . there’s quite a lot of conflict going on at the moment between medical professionals and care homes because some GPs, some paramedics, some nurses are quite happy for you to take the set of observations, whereas others say ‘well you shouldn’t be taking that because you don’t understand the readings that you’re getting’.
Registered manager, residential home (site 5)
This mixed messaging was acknowledged by one of the national leads we spoke to:
. . . so the workforce might perceive that using these bits of equipment goes beyond their regulatory limits and that’s a myth, but it’s not well understood, so that prevents the adoption and the use of the oximeters because we’re doing this through proxy, through the staff who are delivering. So I think that was definitely a barrier that we felt.
National lead (NHS)
From a national perspective, a number of strategies were employed to encourage and support implementation of pulse oximetry in nursing and residential care homes. The strategies included creating and maintaining a series of national and local leadership cohorts, a reliance on collaborative management and open communication within these groups, and utilising the shared motivation to accelerate change due to a common goal (which is a difficult task, given that the care home sector is not embedded within the NHS):
. . . the real difference it makes is that collaborative leadership so when you’ve got three or four people saying ‘yeah, we’re going to do this . . . and you think about other people in your kind of leadership cohort who you can work collectively with to make a big difference, so that was a really key feature of the oximetry . . . there were lots of other people who had lots of other agendas. We just got together and collaborated to get the work done.
National lead interview
In the absence of clear messaging or support, the registered manager at one care home, who was a trained nurse by background, described how they had independently driven the implementation of routine pulse oximetry with the support of local district nursing teams, that is, independent of external support:
. . . it’s me as a manager wanting to do this anyway, pushing ahead with it, . . . I have a good relationship with the district nurses so yeah, we’ve kind of a collaboration although I would say I’ve led it really myself here, pushed it.
Registered manager, residential home (site 3)
The NHS COVID oximetry @home programme in care homes
At a national level, a key motivation underlying the introduction of the NHS CO@h programme into care homes was addressing the disproportionate impact of COVID-19 on care home populations by equipping care home staff, through the supported use of pulse oximetry, to make appropriate and timely care decisions:
I was very keen right at the beginning of the thoughts around COVID oximetry to make sure that older people living in care homes and also those who are vulnerable from learning disabilities were front and centre of an offer of support, so that we don’t increase the health inequalities agenda, so we actually reduce the health inequalities agenda by specifically targeting and specifically supporting that approach.
National leader
There appeared to be marked variation in the recruitment of care homes to the CO@h programme. Of the care home managers who replied, only 40% said that they were aware of the CO@h programme. In our interviews, a GP who had been supporting patients in the community as part of his involvement in CO@h was not aware that the service could be extended in care homes to support staff and residents as part of their PCN:
Through our primary care network we were asked to have a look at this COVID Oximetry @home . . . where we’ve identified patients who’ve been reviewed face to face that are kind of at risk of re-admission, we send them home with a pulse oximeter to stay on what’s called the ‘COVID Management Service . . . it’s not been a care home discussion’.
GP, nursing home (site 3)
Two of the sites reported receiving support to implement and deliver pulse oximetry from the CO@h programme, one by its CCG and the other by its local NHS foundation trust. In both instances, sites were contacted directly and key principles of the programme were described to a senior member of staff:
I think obviously [CCG clinical lead care homes] informed us about . . . the COVID hub and then the next thing, it was either her or someone else delivered a big box of oximeters and all the paperwork and everything like that.
Senior carer 2, residential home (site 4)
Care homes that were aware of and became part of the CO@h programme received pulse oximeters as part of it:
The Oximetry at Home team delivered, I think they delivered 20 or 25 oximeters so that we had one for every resident who needed one, so we weren’t sharing . . . It was one each.
Registered manager, residential home (site 4)
Care homes received a set of instructions in a specific format, with wording locally adapted from the standard operating procedure for CO@h, created by NHSE&I, and this set of instructions included instructions on how to use the pulse oximeter and also as to how pulse oximeters were to be used as part of the CO@h programme (e.g. the various stages of escalation if oxygen levels started to drop). Care home managers, from both case study sites, found these resources valuable:
They sent us information, so we had a kind of a checklist of what to do and when. So when somebody was unwell or if we suspected they had COVID, we had a checklist of what we had to go through. So for example they told us if a person’s oxygen SATS [saturation] were below 94% then it was an ambulance call, if it was between 94 and 97 we should speak to the GP. So they gave us all that information.
Registered manager, residential home (site 4) [note that this extract does not align with NHS guidance, as detailed in Novel Coronavirus (COVID-19) Guidance Note: COVID Oximetry @home54]
They sent over links to, I think it was just YouTube videos [YouTube, LLC, San Bruno, CA, USA], demonstrations on how to use the oximetry correctly. And I think it was just information leaflets and bits and pieces they sent over. But they also sent over a poster of who our contact was. There was a lady and a gentleman, a clinical nurse, so I’ve got posters in the staff room now for the team to call if they need to with their contact numbers.
Registered manager, residential home (site 3)
We basically were told obviously to take their oxygen three times a day and that obviously you guys would then call in the morning and then just check during the day and obviously let us know if you feel like there was any concerns and vice versa, we could call you guys as well.
Senior carer 2, residential home (site 4)
For residential care homes that had experienced a COVID-19-related outbreak and were part of CO@h programme, the advantages of repeated pulse oximetry in conjunction with readily accessible clinical support were marked:
. . . we were in chaos really, we had so many residents who were very unwell, we had so many staff who were off sick . . . everyone worked really well together and we needed the support from Oximetry at Home, from the CCG and from social services.
Registered manager, residential home (site 4)
It was just the knowing that someone else was going to make – not make a decision for you – but someone else was going to give you advice if you needed it . . . it’s just that little bit of backup.
Senior carer, residential home (site 4)
They were really supportive. I couldn’t fault them at all. Any questions we had we would call them up and they’d kind of give us the correct information on how to read the oximeter machines properly and what result we should be looking at. We didn’t even know you had to kind of remove nail varnish and things like that for it to work properly. So they supported us through all of that.
Registered manager, residential home (site 6)
The CO@h programme also facilitated close links with a range of supporting groups, as a registered manager at one such care home explained:
I was in contact with – obviously I’ve had to report on our outbreak to CQC and to Public Health England . . . As part of our outbreak we had a lot of support from the CCG and from social services, so I was having regular Zoom and Microsoft Teams meetings with various people, so we had a lot of support from afar as it were.
Registered manager, residential home (site 4)
Staff believed that, because pulse oximetry was implemented with help from the CO@h programme and, therefore, the oversight of NHS practitioners, this offered additional reassurance to the families of residents:
We explained to them that this is what we’re doing, we’re taking their oxygen levels three times a day, if anything was to drop below 93 then obviously help would be there, we’d call it through. We also told them that you guys with the COVID hub and stuff will call us as well to check and obviously if you then had any concerns you would them send someone out, so yeah I think it was reassuring for them as well knowing that it was us and another third party as well and obviously the paramedics and stuff helping them, so yeah, I think it was reassuring for the family members as well to know that we had that extra help because it was tough!
Senior care assistant 2, residential home (site 4)
One residential care home that was receiving support as part of the CO@h programme reported difficulties in replacing staff who had left or were sick. The severe staff shortage that resulted meant that the care home struggled to fulfil the requirement to monitor all residents several times a day, or could do so only by adding to the workload of the remaining staff:
The one thing I said at our CCG afterwards was that COVID had been happening for almost a year when we got our outbreak and there was no real plan for what to do when you’ve got a really serious outbreak and it all comes on so suddenly and where do you go for staff? There was no sort of contingency plan . . .
Registered manager, residential home (site 4)
One manager reported that it was sometimes difficult to carry out oximetry across the entire resident population before they received the next call from members of the CO@h support teams:
Because I had so many people off sick, there were a few times definitely where we felt that actually they were on the phone, they were demanding these obs [observations] and it was very difficult because we were just running round like blue-tailed flies trying to keep up with everything and they’re on the phone to us asking for obs. So sometimes it felt like we just didn’t have time to do it but actually when we could sit back and reflect on it, it was an important part of what we were doing and it did help us to focus on who was deteriorating or who was stable.
Registered manager, residential home (site 4)
Non-NHS support
The NHS is not the only source of support for care homes implementing pulse oximetry. Care homes are linked through regional and local forums, local authorities, partnerships and care associations. In many cases, these links are in addition to the links with other care homes owned by the same parent company, as many care homes are parts of chains of homes within the same ownership. The strength of these links varied across case study sites. For example, several care homes actively engaged in sharing learning with others, particularly as the pandemic took hold in the early part of 2020:
We started talking a lot more about the use of oximetry in the early days of COVID. So kind of March, April, May time last year, 2020, because a number of our providers when they – we had a kind of – we started lots of networking, weekly networking calls with members in March, early March last year as everything was starting to ramp up and so pulse oximetry was something that they were starting to talk about amongst themselves as helpful to detect soft signs of COVID, particularly in the absence of access to testing, regular testing.
Care supervisor, residential home (site 2)
One nursing home manager described the value of a regular e-mail from the homes local authority, which was introduced at the beginning of the pandemic. This e-mail was deemed useful because it collated key messages from multiple national and local groups to provide a concise update of the policy and practice changes relevant to care homes:
Well, to date, this morning, I’ve probably had 40 e-mails! but anything that comes from the government or the CCG or [place 1] city council always automatically go into a ‘read’ folder, so I make sure that I read all those that come in . . . every week since we’ve had COVID [pandemic], we have from [place 1] city council ‘market intelligence’, so in yesterday’s one that came, there’s [updates on] care home visiting, schools and care staff, [place 1] city council referral pathway. So it covers a lot of things, it’ll cover government and CCG guidance.
Registered manager, nursing home (site 3)
In summary, we have found that implementation of pulse oximetry was not usually perceived by care managers and staff as challenging. Pulse oximetry was also seen as more likely to be reassuring to residents (and staff) than as a source of increased anxiety. In addition, pulse oximetry was commonly considered to be beneficial to residents. Views on the adequacy of NHS support for care homes varied, and not all care homes were aware of the CO@h support programme for care homes.
In Chapter 5 we discuss some of the issues that have raised by the findings reported in Chapter 3 and in this chapter.
Chapter 5 Discussion
The key points of Chapter 5 are summarised in Box 11.
-
Despite the historic and recent challenges facing care homes, participants in this study reported being able to introduce, sustain and/or expand the deployment of pulse oximetry.
-
Inner-setting factors that contributed to the adoption of pulse oximetry were the belief that pulse oximetry was of benefit to residents, particularly in the light of the pandemic, and the active leadership of care home managers. Wider functions within the care homes, such as workforce development, information technology and finance, also had roles in the implementation.
-
Registered nurses felt most comfortable in using pulse oximetry, but other staff were also willing to do so if the homes had a supportive culture and they had access and time to engage with required training and development.
-
Although pulse oximeter devices were seen as relatively easy to operate, there were uncertainties and challenges regarding the outer-setting context in relation to wider clinical pathways and how and when to seek support from health professionals.
-
Prior to the COVID-19 pandemic, most homes purchased their own devices and few homes had robust processes in place to maintain and calibrate them for long-term use. The guidance and provision of devices through the CO@h programme was seen as helpful for care homes that participated in the programme.
-
Support from health professionals was vital, and in many areas (particularly for homes involved in the CO@h programme) was positive and sufficient; however, a proportion of care home staff did not feel that they received adequate support.
-
Pulse oximetry should continue to be deployed within care home settings, including within residential care homes.
-
Guidance from the CQC on the competences required of staff to use oximetry would provide clarity for care managers on assessing suitability and what training would be appropriate.
-
Accessible training packages that are tailored to the care home context and updated in line with changing guidance should be made available.
-
Policy and practice initiatives to ensure that there is better collaboration between care homes and primary care should incorporate escalation of pulse oximetry results.
-
Integrated care systems should consider how they can support care homes in relation to the purchase and use of such devices, and in achieving quality improvement in general.
-
Across all six case study sites, the number of interviews carried out was smaller than intended, in part because of participant unavailability (especially clinical colleagues from the NHS supporting care homes) but also because some interviews were cancelled at short notice as a result of other commitments related to the COVID-19 pandemic. Access to such data would have strengthened the robustness of our findings, as would direct observation of the administration of pulse oximetry.
-
Another limitation was the need to go through a number of organisations independent from the NHS to reach care homes to complete the online survey. Although these organisations were very cooperative in disseminating the survey, the team had to work in accordance with organisation policy on routes for dissemination, formatting of study adverts and frequency of promoting the survey. The team received a lot of help from these organisations in advertising the survey, but the response rate was low (1.5%). Throughout the pandemic, care homes may have been asked to complete a number of surveys from other research and/or regulatory bodies, which may have contributed to this.
-
Owing to anonymity, the research team were unable to determine the range of care homes responding to the survey across variables such as location, financial budget and CQC rating.
Summary of principal findings
This study sought to understand how pulse oximetry has been employed in care homes before and during the COVID-19 pandemic, the factors that support the use of pulse oximetry by staff in this setting and the external supports that are required. This rapid evaluation presents survey responses from 232 care homes and detailed case studies at six sites. As there are more than 15,000 care homes operating in England, it is recognised that this is a small sample size and that our findings cannot, therefore, be assumed to be generalisable to all care homes across England. Furthermore, researching during a pandemic, with the connected restrictions on access, additional hygiene measures and scale of concerns about the well-being of care home residents, meant that the wider context was far from normal. With those caveats, a number of findings were able to be drawn. A majority of care homes were already procuring pulse oximeters before March 2020. The use of pulse oximeters to help to monitor the health of residents was common, but not universal, practice in care homes in England before the COVID-19 pandemic, and this was particularly the case in nursing homes but was also common in many residential homes. A range of care home staff were evidently already using pulse oximeters with the residents they were looking after and, consequently, there was less need for NHS support for sourcing and using pulse oximeters in response to the pandemic in those cases compared with the minority of care homes where oximetry was introduced in response to the COVID-19 pandemic.
Pulse oximetry is used routinely in care homes to monitor patients for COVID-19 and a variety of other conditions, mainly respiratory conditions (e.g. chest infections, COPD, asthma, emphysema), but also heart failure. Although we did not explicitly ask about other diagnostics being used in care homes, it seems from the interviews that pulse oximetry is not used in isolation, but rather is one of a number of ways (including taking temperature or measuring blood pressure) in which the staff of care homes monitor the health of residents. In most care homes responding to our survey, and where we undertook interviews, the use of pulse oximeters was not seen as challenging for staff, nor as adding significantly to their, or their managers’, workloads or stress levels. This was in a context, however, of the COVID-19 pandemic having already added greatly to the workload and stresses falling on care home staff and, therefore, we can suppose that, when set against such a background, the use of pulse oximetry may have seemed a minor issue for many people working in care homes. Training care home staff in the use of pulse oximetry and in when to escalate cases was widely reported as having been received, although a minority of care home managers in our sample evidently wanted further training for their staff.
We found that many care home managers, although fewer than half of those responding to the survey, felt adequately supported by the NHS when asked about support with how to use pulse oximeters, how to communicate readings to the NHS and when/how to escalate cases appropriately.
A similar number of care home managers responded that they had not received much support from the NHS. However, given that many care homes were already using pulse oximeters pre pandemic, and many staff did not find it challenging to do so, it is not clear to what extent this was because help was not wanted and not sought. A minority of care home managers reported receiving some support from the NHS, ‘but not enough’. The NHS CO@h programme that was implemented across England seems to have been well received and beneficial at the sites in contact with it. However, 60% of care home managers responding to the survey were unaware of the CO@h programme and the support that it could provide. We do not know how many of those care home managers (i.e. the 60%) would have liked to receive support from the programme had they known about it; however, this finding does at least imply that there is scope for increasing knowledge of the programme in the care homes sector. Beyond that programme, where NHS support was deemed to be ‘not enough’, we do not know if this was because of the desired support being unavailable or if it was potentially available but that was unknown to some care homes.
Finally, in the large majority of cases in our sample, residents seem (in the views of care home managers and staff) to have been untroubled by pulse oximeters being used and were much more likely, than not, to have been reassured as a consequence of their use. Furthermore, among the care home managers responding to the survey, half thought that use of pulse oximeters had probably resulted in fewer accident and emergency attendances by their residents, and just under half thought that there had been fewer hospital admissions of residents. Most of the remaining respondents thought there had been no change to those impacts on NHS hospital activity. Therefore, the indications are that the use of pulse oximeters in care homes is considered by managers and staff to have been, in most cases, beneficial to care home residents.
All of these findings from the rapid evaluation are subject to the important caveats that the survey response rate was low (i.e. just 1.5%) and that our interview-based case studies were limited to 31 interviews across six sites (i.e. six out of a possible 15,362 care homes in England).
Implications for practice and policy
Many challenges to embedding innovations within the care home sector have been recognised, including the diversity of organisation forms, the fragmented market with both private and public purchasers, and considerable financial and demand pressures on providers. 55,56 Furthermore, the considerable turnover of workforce across the sector and the correspondingly high level of staffing vacancies can be disruptive in maintaining the quality of care and embedding of new practices. Adoption of pulse oximetry appeared to be aided by the fact that care home staff believed that the associated procedures could be of benefit to their residents and did not put them at harm or cause them distress. Pulse oximetry could, therefore, be seen as compatible with the common underlying values of care staff to provide a better quality of life for their residents, and this has been previously recognised as a core motivation for social care staff to actively participate in such initiatives. 52,54–57 Although not all home managers were convinced about the tangible impacts of pulse oximetry, the device was also not seen as troublesome to introduce or as causing undue stress to staff and, therefore, not a major distraction from other activities.
Care home managers appeared central to the process of implementation through ensuring that there was good communication within the homes regarding the purpose of the device and that staff felt supported and trained in its use. Good communication covers clarity towards the introduction of pulse oximetry, the benefits for both care home staff and patients, and detailing how taking readings can be embedded in daily routine ward rounds. Care home staff with prior experience of taking routine clinical readings felt more comfortable with taking pulse oximeter measurements as part of routine ward rounds. In addition, it was imperative for care home staff to have knowledge of how best to seek oversight or how best to share information about residents in cases of deterioration, and this reflects previous knowledge on the importance of leadership by care home managers to the general running of care facilities and the successful implementation of quality improvement in this context. 58–60 Opportunities for care home managers to strengthen their leadership abilities and to learn about improvement techniques would, therefore, seem vital. It is important to note that successful implementation did not involve only managers: there were also contributions from, for example, staff in workforce development (in relation to training), IT (in relation to adapting electronic records) and finance (in relation to procurement). This observation, alongside the fact that external bodies also have a role to play, emphasises that the introduction of even a simple technology can involve considerable complexity. The COVID-19 pandemic strengthened the internal case for prioritising the introduction of oximetry, including within those homes whose residents did not have long-term conditions previously requiring such monitoring. The changing guidance from the CQC regarding which staff could undertake pulse oximetry53 did provide some uncertainty, and it would be helpful for this to be clarified post pandemic. It would also be useful for this guidance to provide a rationale for which staff would be seen as having the necessary competence to use pulse oximetry so that care home managers can plan accordingly.
Cultural issues, such as a shared understanding of the value of an innovation, trust between different staff groups and a common purpose, enable better implementation of new technologies in care homes. 61 In non-nursing homes, prior to the pandemic, it was largely senior care staff who would use pulse oximetry; however, as a result of the disruption caused by COVID-19 and the resulting pressures on the care home workforce, this responsibility was widened to other care staff. This change in responsibility suggests a culture in which staff are willing to be flexible in their duties to respond to new demands and wider contextual risks to the residents. It is recognised that care home staff who are not qualified nurses will need to gain new knowledge and skills to use oximeters. Again, the culture in the homes is encouraging, as it seems that staff have both the time and opportunity to access relevant learning opportunities, including virtual training packages and observing more qualified or experienced colleagues using the device. Those respondents who were familiar with undertaking and interpreting readings associated with pulse oximetry largely felt unfazed by its introduction in residential homes. Going forward, it will be important for all care homes that will be using pulse oximetry to have easy access to up-to-date training for relevant staff. It would be helpful if both stand-alone training (i.e. just on oximetry) and integrated training (i.e. within a wider training package such as RESTORE2) reflected the learning needs of staff. In addition, it might be beneficial, if use of pulse oximetry is to become standard practice in residential homes as well as in nursing homes, to include the skills needed to use pulse oximetry in formal care qualifications. Care home staff varied in their level of anxiety about taking on additional responsibilities for monitoring residents’ physical well-being and, therefore, it will be important to ensure that staff have the opportunity to express concerns through supervision so that associated support and guidance can be provided as appropriate.
The characteristics of pulse oximetry supported its adoption. Pulse oximetry was described as being simple to use and not intrusive, and its results were clearly displayed. However, there were complexities regarding the related care pathways. In particular, 45% of survey respondents thought it challenging to assess when it is appropriate to escalate patient care to a health professional, and 34% of survey respondents reported difficulty in working with other services. The case study sites that were part of the CO@h programme described good collaboration with the associated health-care teams, suggesting that such pathway issues can be addressed with clearer processes and by establishing closer working relationships. 62 Reporting of results and escalating concerns appeared to be largely via telephone, which was simple to undertake. Digital reporting options could be more efficient, with potential for NHS systems to connect directly with electronic recording systems when these are available within care homes. Such connectivity of personal health records is a broader issue for the interface between social care providers and health services, and this requires a more fundamental reform of the underpinning electronic recordings systems and associated information-sharing agreements, with new approaches being developed with some localities. A historical challenge, which is still found in many areas, is the lack of linked population-level data sets between health and social care regarding care home residents, and this limits strategic analysis and planning for this population and contributed to its seeming invisibility at the start of the pandemic. Integrated personal health and care records, as well as population-level data sets for care home residents, should, therefore, be a focus for integrated care systems.
Pulse oximeters are low-cost items that appear to be readily available from multiple suppliers and, therefore, the expectation that care homes would be purchase them directly does not seem to be unreasonable. However, there could be opportunities to improve the purchasing arrangements across the sector and/or within regions. Not all homes will be well placed to assess the benefits and limitations of different models or suppliers and may, therefore, benefit from more standardisation and guidance. A coordinated procurement approach over a number of homes may result in lower costs and consistency in the specifications being used. It was not also clear if homes understood what was required to adequately maintain the devices for long-term use, and this is of potential concern, particularly when linked to the reports from the case studies that the staff perceived that devices could provide apparently erroneous measurements. However, there may be no issues regarding calibration as such, and the low cost of devices does suggest that they can be easily replaced. Nevertheless, the uncertainty that this may generate regarding the accuracy of results and the corresponding anxiety for staff suggests that more guidance and standardisation of processes would be beneficial. More of the homes that had introduced oximetry in the last 12 months had received guidance from the NHS than was the case for homes that had been using pulse oximeters for longer. Staff within the CO@h sites received written guidance about how pulse oximeters should be used and the connected pathways for escalation, both of which were seen as positive supports to successful embedding in practice.
As highlighted above, the recent social and policy environment has been turbulent because of the pandemic, and such turbulence would normally be seen as disruptive to the introduction of new technologies. In respect of pulse oximetry, COVID-19 has made the adoption of pulse oximeters a greater priority within national policy. There has also been encouragement from the leadership of national care organisations and government bodies regarding their adoption. The CO@h programme has provided helpful practical support through the distribution of oximeters, the provision of detailed guidance on their use and escalation procedures, and collaboration with homes in relation to the well-being of individual residents. It is not clear what role, if any, commissioners played in the implementation of pulse oximetry, either before or during the pandemic. As this is a health-related procedure, the decision to advocate and support use of pulse oximetry in care homes is one that would primarily be for NHS commissioners to take. However, as local authorities have the lead responsibility for overseeing local care home markets and for public health, there is a rationale for collaboration between local authority and NHS commissioners to better support care homes with securing and deploying such devices and, indeed, responding to such major changes to their operating environment. 63 The benefits of care homes being able to provide peer support through provider networks were mentioned in many case study sites. Such arrangements have potential to be developed into more formal quality improvement collaboratives for care homes, bringing together implementation leads from different care homes and external professionals to share insights and learning. 64
NHS policy over the past decade has recognised that strengthening support provided to care homes from general practice and wider community health services has considerable potential to improve the overall well-being of this population, reduce emergency admissions and enable swifter discharges from hospital, and this reflects studies highlighting long-standing variabilities in the support provided to care homes by NHS services and the potential for corresponding inequalities of access and poor health outcomes. 65,66 For example, Iliffe et al. 67 reported a lack of consensus about how primary care services could be best structured in relation to care homes, with only 55% of staff reporting that residents received sufficient support from general practice.
Difficulties in securing access to specialist health professionals, including geriatricians, old age psychiatrists and palliative care teams, was also highlighted by care home managers. Pulse oximetry underlines the importance of collaboration between care homes and primary care, and that more work still has to be carried out to ensure that this is seen as sufficient by care homes. Interpretation of the ‘no support’ responses by care home managers cannot be taken to suggest that care home managers wanted more assistance, but had not been able to access it. However, given that less than 50% (and in one case only 33%) of responses by home managers regarding forms of support stated that care homes had ‘adequate support’, this does suggest that further collaboration with primary care is necessary. The continued variation in the arrangement of support from general practice to care homes reported by the case studies cannot be helpful in this regard. The CO@h programme was seen to address many of the difficulties in relation to the use of pulse oximeters. It is to be hoped that, when fully implemented, the EHCH model will provide a stronger foundation, in general, for the relationship between primary care and care homes. To do so, the EHCH model will need to respond to barriers previously identified, such as a failure of health professionals to recognise the knowledge and skills of care staff, and being seen as acting in a ‘policing’ rather than a ‘collaborating’ capacity. 66
Feedback workshops with policy-makers at NHS England and Improvement
The study team gave four presentations (between May to September 2021) to senior policy leads at NHSE&I, both as part of the CO@h and People Receiving Social Care workstreams, to feed back results from the rapid evaluation and for the study team to learn more about how pulse oximetry was being used as part of the NHS’s response to the COVID-19 pandemic. Attendees, in general, agreed with the findings presented (following our thematic approach detailed in Chapters 3 and 4), but provided a few additional comments relating to the following:
-
The need to assess further the relationship between general practices and care homes. This relationship/support may be different from provisions for the general public, as evaluation findings highlight the importance of communication and of assessing practices to better understand this relationship between general practices and care homes.
-
The fact that, although the NHS provided a large number of pulse oximeters to care homes during the pandemic, respondents from our survey and from our case study sites reported purchasing their own devices.
-
The nature of additional support (if any) that would be welcomed by care homes to manage residents as part of their response to the pandemic.
-
The need to be clear that NHS-provided pulse oximeters do not need to be calibrated in the first 12 months of use and, therefore, the need for calibrated devices refers to devices that were independently purchased by care homes.
-
Clarity with regard to whether or not any of the interviewees thought that the use of pulse oximeters had saved lives. Although pulse oximetry helped care home staff to make more informed decisions about residents’ care and well-being, there was no evidence of the use of a pulse oximeter saving a life.
Reflections on the robustness of the results
Strengths
The study team completed a mixed-methods rapid evaluation, following established methodology and guided by previous evidence of implementation, while engaging iteratively with published literature. The robustness of our findings has been shown in a number of ways throughout the evaluation. 68,69 The use of mixed methods (i.e. collecting data through interviews and online survey analysis) enabled the team to develop a comprehensive understanding of the introduction and experience of implementing pulse oximetry to monitor residents in care homes. 70 At a time when care home staff were under great pressure, we nevertheless completed a good number of interviews (n = 34), with a range of stakeholders across a variety of care home settings and with national policy figures. (However, note that we had fewer interviews with clinical staff working primary and secondary care.) The quality across these interviews varied. Despite recruitment of interviewees being guided by local gatekeepers within care homes, fewer completed interviews of primary and secondary care professionals, and the low response rate, we are confident data saturation was achieved. 71
Member validation occurred throughout data analysis and among study team members, the Project Steering Group, the User Involvement Group, senior members of the BRACE executive team and external colleagues with expertise of the adult social care who acted as critical friends. 72 In addition, our considerations for policy-maker theories of change were developed with significant input from care home policy leads (external from NHSE&I) and consolidated with numerous data analysis workshops (however, these have not been confirmed/checked by case study sites).
The team encountered a number of challenges that resulted in a longer than anticipated period to complete the evaluation (i.e. 9 months between the submission of a short proposal and the completion of the report). Notably, the team encountered difficulties identifying case study sites that had been receiving support for the administration of pulse oximetry as part of the national CO@h programme, despite working with ENRICH and members of the Project Steering Group. In addition, our attempts to increase our survey response rate, using varied avenues of dissemination, pushed project timescales. With respect to project management, a large team (i.e. three principal investigators, one project manager, one administrator and fiver researchers) with clear hierarchy, roles and responsibilities, which was largely consistent throughout the project (with two members leaving during the project, one in May and one in June), was a significant positive, as was weekly communication with the larger BRACE and RSET CO@h team to facilitate rapid working (with four members working across both projects).
Limitations
Our rapid evaluation has a number of limitations.
Perhaps the most obvious limitation is the low response rate to the survey, with just 1.5% of care homes responding, despite repeated reminders and helpful publicity by a number of organisations. The survey for the rapid evaluation was conducted at a time when care home managers and staff remained under great and exceptional pressure as a result of the COVID-19 pandemic, which is likely to have made responding to our survey a low priority for many. Furthermore, throughout the pandemic, care homes may have been asked to complete a number of surveys from other research and/or regulatory bodies, which would have affected our response rate.
A methodological limitation was the need to go through a number of organisations that were independent of the NHS to reach all care homes to complete an online survey. Despite these organisations being very cooperative when disseminating the survey, the team had to work in accordance with each organisation’s policy (i.e. routes for dissemination, formatting of study adverts, frequency of promoting the survey).
Owing to anonymity requirements, the research team was unable to determine the range and type of care homes responding to the survey across a range of variables (e.g. size by staff employed, financial budget, CQC rating). Finally, owing to the ongoing COVID-19 pandemic, all data collection occurred using online/virtual mediums, as well as data analysis workshops and meetings with policy experts.
The team found it challenging to determine the scope of this rapid evaluation and the nature of exploration that could be completed in a relatively short timescale which was responsive to NHS health care policy. Following the project design workshop, research questions were identified and, alongside discussions with senior members of the BRACE and RSET centres, Project Steering Group, User Involvement Group and policy leads at NHSE&I, it was decided not to include residents in our evaluation. In comparison with the wider BRACE and RSET programmes, this rapid evaluation has informed our continued learning on best practice with regard to engagement with stakeholders in relation to design, patient and public involvement, and data collection, as well as the resources required when undertaking rapid evaluations. Across all six case study sites, a smaller than intended number of interviews were completed partly because of participant unavailability (especially clinical colleagues from the NHS supporting care homes) and partly because some interviews were cancelled at short notice as a result of other commitments related to the COVID-19 pandemic. Access to such data would have further strengthened the robustness of our findings. Similarly, being able to directly observe care home staff using pulse oximeters with residents would have provided helpful insights into the use of pulse oximetry in practice; however, the restrictions relating to COVID-19 made such data gathering unfeasible.
The success of our interviewing approach was largely dependent on the relationships that members of the study team established with gatekeepers (i.e. care home managers) over a relatively short period of time. In addition, the success of our recruitment approach also depended on the strength of the relationship between the gatekeeper and the interviewee. Hence, this may explain why the study team had limited success in recruiting NHS colleagues working outside care homes. The lack of interviews with NHS colleagues may also reflect the variation of support received by care homes from primary, secondary and community care colleagues. On reflection, the team does not believe that this imbalance across care home and primary and secondary participants influenced the overall data set but, rather, focused our interpretation on the most pertinent purpose for pulse oximetry in care home settings (i.e. an additional tool that can be used by care home staff to make more informed choices with regard to providing best possible care for residents). Notably, some potential interviewees may have prioritised care tasks over taking part in an interview.
We note that there are a both advantages and drawbacks of using the CFIR to structure this evaluation. The CFIR approach provides a rigorous systematic method of organising findings for implementation evaluations and takes into account the nature of intervention, stakeholders both outside and within the intervention setting, and contextual factors. However, we recognise that the study team has taken an adapted approach when using the framework, using it as a lens to guide the evaluation, rather than a more encompassing application of the framework with reference to each of the numerous subdomains within it.
Reflections on the experience of conducting a rapid evaluation
We have summarised our experiences of conducting a NIHR-funded rapid evaluation as defined by our three overarching principles (i.e. responsiveness, relevance and rigour), including the context of the data being gathered during the pandemic.
Responsiveness
The team carried out a mapping exercise to identify relevant literature relating to our aims and research questions, as opposed to a traditional systematic review, which saved both time and resource. However, there was limited published and grey literature on the topic of using pulse oximetry to support residents in care home settings in general and more specifically relating to COVID-19. The speed at which the evaluation was undertaken affected the study team’s ability to provide real-time feedback to the case study sites, especially case study sites seeking to learn from our findings to inform practice within their own care homes. The evaluation has taken longer to complete than was stated in the original protocol because of (1) a delay in gathering data using an online survey and interviews and (2) additional demands on potential participants due to the COVID-19 pandemic. However, many participants (and study team researchers) felt that using media such as Zoom, Skype™ (Microsoft Corporation, Redmond, WA, USA) and Microsoft Teams made it easier to complete interviews more readily amid the context of a global pandemic,49 and this may also be the case outside such circumstances, as virtual media can offer greater flexibility, with a potential blending of in-person and virtual approaches.
Relevance
There has been continued and close collaboration with the Project Steering Group and the User Involvement Group to discuss the priority of our evaluation, and to receive comment on our participant-facing material (e.g. information sheets) and input into our emerging findings. The involvement of key experts to support our study scoping activity ensured that the team answered the most appropriate research questions with regard to current adult social care policy changes. Hence, collaboration from stakeholders has been in the form of both consultation and co-production (i.e. scoping interviews with key experts), and this was particularly important as the context and measures relating to the pandemic changed, as the research team could respond in a timely manner because of the good level of communication with experts.
Rigour
The team iteratively engaged with theoretical- and policy-relevant literature throughout the design, data collection and analysis/interpretation stages of the evaluation. A key learning from undertaking this rapid evaluation was the value of member validation with appropriate policy stakeholders. For example, presenting findings at workshops with policy experts increased the rigour of findings and helped us to present the findings appropriately within this report. Nevertheless, we have proceeded cautiously when synthesising our findings.
Chapter 6 Conclusions
The key points of Chapter 6 are summarised in Box 12.
-
Pulse oximeters (along with other diagnostic tools) were in use in many, but not all, responding care homes before the pandemic, and use of pulse oximeters widened during the pandemic.
-
Pulse oximeters were reported in the survey and interviews as not being a major challenge for care home staff to use, and usually not adding to staff workload or stress levels.
-
In some cases, support from the NHS, including training, was sought, but was not always available to the full extent desired.
-
In the view of most care home managers, residents benefited from the use of pulse oximeters and residents were more often reassured than made anxious.
-
Use of pulse oximetry is thought by care home managers to have, on average, reduced accident and emergency attendances and hospital admissions of care home residents.
-
The NHS CO@h programme was well received and beneficial at the care home sites in contact with it. However, 60% of care home managers responding to the survey were unaware of the programme.
-
Future research should include learning about the experiences of care home residents and their families. In addition, research should find out more about interactions with care home staff, from an NHS perspective.
-
The low cost of the equipment and the positive impacts that pulse oximetry is thought to have are grounds for optimism that pulse oximetry in care homes is clinically effective and cost-effective. Research to investigate cost-effectiveness of pulse oximetry in care homes would, nevertheless, be worthwhile.
-
Further research to establish the net costs and health impacts and, hence, the cost-effectiveness or otherwise of the CO@h in Care Homes programme would be desirable.
-
Continued policy focus on strengthening collaboration between care homes, primary care and wider health services is supported, including digital means of sharing patient information.
Conclusion
During fieldwork for this study, the COVID-19 pandemic was in its second wave, generating pressures on health and care services. Care homes were supporting their residents and their families to cope with the extended period of separation due to the lockdown restrictions, as well as having to share tragic news with numerous families who lost loved ones through the much higher than normal mortality rates in many homes,55,73 and these circumstances were likely to have affected the psychological well-being of care home staff. Home managers faced the practical challenges of increased staff absences due to COVID-19 infections and self-isolation procedures, as well as the debilitating impacts of long COVID. Women and those from minority ethnic groups who make up higher proportions of the care workforce than in the general population were particularly affected by the extended forms of COVID 19. Finally, the care home sector was insufficiently supported at the start of the pandemic, with the priority from national government being to prevent acute care from being overwhelmed. 42
Considering this context, the overall findings of the evaluation are positive. Pulse oximeters appear to be used routinely in care homes and in the majority of cases had been in use before the COVID-19 pandemic. The care homes responding to our survey and where we conducted interviews seemed able to introduce care oximetry with relative ease before and during the pandemic, including homes with and without nursing registration, smaller and larger homes, and homes in all types of ownership. Deploying the technology and associated pathways were not seen to have major implications on the capacity or stress of the workforce, even during recent times of such disruption and societal anxiety. Although views were divided among care home managers regarding the relationship between pulse oximetry and hospital admissions for residents, over 90% of care home managers thought that the use of pulse oximetry facilitated the timely identification of health deterioration of residents. In addition, the use of pulse oximetry was seen as helping to ease the worry of families, as staff were able to evidence that they were monitoring the well-being of residents. From the perspectives of study participants, pulse oximetry yielded benefits for care home residents and it was not challenging to embed the devices and associated pathways successfully within the daily routines of care.
The need for the rapid evaluation to be conducted during the COVID-19 pandemic is likely to have been a major factor in limiting engagement with the survey and interviews, and the evaluation findings have to be seen in this context. Nevertheless, the evaluation has provided valuable insights.
Policy in England continues its focus on greater integration of health and social care with the introduction of integrated care systems across the county. The experience of care homes regarding pulse oximetry supports this direction of focus, but also emphasises that the focus must be more strategic in its intent and must also respond to the practical issues that make it more difficult for care staff and health professionals to collaborate successfully. System issues, such as sharing of personal health and care records and development of common population data sets, may not be headline-grabbing, but are essential enablers of efficient communication and care coordination. Similarly, the case for the EHCH model is also strengthened, as it is the relationship between primary care and care homes that is central to promoting the well-being of residents. The positive experience of care homes of the CO@h programme shows that care homes and health professionals can collaborate well, even in the most difficult of contexts. Alongside further integration, there is continued need for the fundamental reform of adult social care. Care homes in this study seemed able to support their residents, despite the financial and workforce challenges, which emphasises their commitment and ability. Improving the quality of care and introducing innovations will be greatly helped by a more stable financial position and a connected continuity of staffing.
Recommendations for future research
A major gap in this evaluation was in not being able to listen to the views of residents within care homes regarding the use of pulse oximetry. We had hoped to acquire the views of residents so that their experiences could be revealed and to determine if use of oximeters might beneficially be adapted in any way. However, this was not possible because of the rapid design of the evaluation and the context of the pandemic, but should be made a priority for future studies. Future studies could include qualitative and ethnographic methods, and should involve people who use alternative methods of communication. Direct observation of the interaction between residents and care staff in the use of pulse oximeters and of decision-making in relation to engaging health-care services would be beneficial. The views of family carers should be researched, as family carers can provide invaluable insights into both the experiences of their loved ones and their own experience of communication with the care homes regarding pulse oximetry. Other important stakeholder perspectives are that of health professionals, including community nurses, paramedics and GPs. Obtaining views from family carers and health professionals would avoid the risk of overlooking important ways to improve appropriate use of oximeters in care homes.
We have found that most care home managers believe that there is a benefit to residents of using pulse oximetry to detect hypoxia in those with COVID-19 or other, especially respiratory, diseases. The implication is that pulse oximetry is likely to continue in most care homes. The rapid evaluation reported here was not designed to determine the cost-effectiveness of using pulse oximetry in care homes or the cost-effectiveness of NHS support to care homes to increase use of pulse oximetry. The low cost of the equipment, the fact that pulse oximetry was frequently reported to have little or no impact on staff workload and stress and the assessment that use of hospital services may have declined, on average, and that residents are usually more reassured than anxious as a result of pulse oximetry, are all supportive of optimism that pulse oximetry in care homes would be found to be clinically effective and cost-effective on further investigation. Such quantitative investigation would, nevertheless, be worthwhile.
The cost-effectiveness of maintaining, expanding or reducing the NHS programme of support for pulse oximetry in care homes that was implemented in response to the COVID-19 pandemic is currently unclear. Evidently, many care homes are successfully using pulse oximetry, and care homes are necessarily doing so with some degree of interaction with the NHS. However, we have found evidence of some care home managers and staff being unaware of the NHS support available. This is alongside the finding that some care home managers, albeit a minority of care home managers who responded to our survey, felt in need of more support from the NHS than they were currently receiving, in respect of pulse oximetry. Therefore, research to establish the net costs and health impacts and, hence, the cost-effectiveness or otherwise of the current CO@h programme for supporting pulse oximetry in care homes, as well as options for expanding the programme so that it reaches a greater proportion of care homes, is desirable. This research could be extended to consider implementation and benefits of similar models being applied in other health and care systems.
Equality, diversity and inclusion
Participant and case study site representation
Throughout our evaluation, the study team ensured that case study sites were as representative as possible of the care home sector. Likewise, participants who were purposively selected for interview were from a range of professional backgrounds and differing levels of seniority, including senior managers, care staff with and without clinical training, staff who were and were not supported by the CO@h programme and, where relevant, NHS staff (primary, community or secondary care) supporting the care home’s use of oximetry.
Site characteristics
We sent our online survey to all registered care homes in England. For the case studies, we interviewed staff at six care homes that were selected purposively (see Chapter 2, Design) from across England, from both rural and urban settings. The six care homes represented a range of ownership and funding models, and treated diverse populations with varying needs (see Table 4).
Strategies to improve representation
The study team used a range of strategies to promote inclusivity. Given that data collection occurred during the middle of the COVID-19 pandemic (March to June 2021), the team offered care homes across England an electronic survey, as opposed to a paper survey, for ease of completion (i.e. removing the need for printing and postage). The survey was intentionally designed to be quick to complete (approximately 10 minutes) so as not to take care home staff away from their caring responsibilities. Given workforce constraints, we offered interviewees different modes of interview (e.g. telephone, Microsoft Teams or Zoom) and various times for interviews to ensure accessibility for as many people as possible. We offered incentives to both the care homes (£250.00) and participants (£20.00 Amazon voucher) as a thank you for taking part in the interviews.
Participant characteristics
The survey data (see Chapter 3) show that the sample of care homes that responded to our survey, with respect to type of care home (i.e. residential, nursing or mixed), size (based on bed capacity) and range of residents cared for (i.e. older residents and residents with dementia, physical disabilities, complex needs and/or learning and sensory impairments), were representative when compared with CQC care home registration data. Nevertheless, our survey response rate was low (1.5%).
Care home staff taking part in interviews varied in their professional role, clinical and non-clinical skill set and location, as well as in the nature of training they had received to deliver pulse oximetry within a care home setting. The study team did not collect data relating to staff personal demographics (e.g. gender, age, ethnicity) as the study focused on professional characteristics.
Research topics relating to equality, diversity and inclusion
Our evaluation had a clear focus on inclusivity in relation to capturing the experience of those working across the care home sector, a group that, in the past, has been overlooked by health service researchers when evaluating services delivered across the NHS in a range of settings. In addition, we recommend that further research with residents and family members would be beneficial to understand experiences of receiving care, including pulse oximetry.
Reflections on research team and wider involvement
Research team
The study team consisted of researchers across two NIHR-funded rapid evaluation teams (i.e. RSET and BRACE). The study team was a small, mixed-methods, multidisciplinary team from many different disciplines (e.g. statistics, sociology, applied health research, health psychology, health economics and project management) and team members differed in seniority (e.g. professors, experience research fellows, early career researchers). The research team was balanced with regard to gender and ethnicity. Two team members took paternity/maternity leave during the evaluation, and another two members left the team to take employment elsewhere; however, all contributions were recognised and team members were given opportunities to review drafts of the report.
Throughout, the team held weekly meetings to discuss project management, data collection, analysis and write-up, with additional workshops to shape interpretation of findings. All members of the team have been involved in varying capacities with data collection and analysis, as well as with dissemination of findings [i.e. both written (chapters) and oral (meetings with policy stakeholders from NHSE&I)]. All researchers were supported by the joint principal investigators (JS, RM and NF).
Wider involvement
Throughout the evaluation, the team sought the advice of experts experienced in undertaking research with care homes (Dr Alys Griffiths, University of Liverpool; and Dr Denise Tanner, University of Birmingham), a Project Steering Group composed of three care association leads, and a project-specific patient and public involvement group with whom we piloted data collection and shared findings in real time, thereby helping to shape our data analysis.
Acknowledgements
We are very grateful to all of the participants in this study and to our contacts at each case study site who helped to coordinate our interactions with interviewees. We thank our BRACE and RSET colleagues and members of the BRACE Steering Group and User Involvement Group for their input and constructive comments throughout the duration of the study. In addition, we thank our colleagues from Care England, the National Care Forum and NHSE&I for their contributions at the project design, data collection, analysis and presentation of findings stages. Specifically, we thank Professor Jon Glasby (University of Birmingham) and Dr Alys Griffiths (University of Liverpool) for advising on our study protocol and final report; Ann Evans (BRACE Administrator, University of Birmingham) for reviewing our Plain English summary; and Dr Adrian Hayter (NHSE&I), David Bramley (NHSE&I), Professor Jonathan Benger (NHS Digital) and Professor Judith Smith (University of Birmingham) for undertaking critical review of drafts of the report. Any errors in the report are the responsibility solely of the authors.
An application for ethics review to the University of Birmingham’s Research Ethics Committee was made by the project team and approval was gained in March 2021 (ERN_13-1085AP40).
Patient and public involvement
The evaluation protocol was reviewed by one member from the User Involvement Group. Three meetings were held with members of the User Involvement Group to discuss study design and the inclusion of the care home residents, sharing preliminary and final findings. The Plain English summary of the report was reviewed by another User Involvement Group member. In addition, we will seek the advice of those members concerning how best to communicate the evaluation’s findings to patient and public audiences.
The NIHR Birmingham, RAND and Cambridge Rapid Evaluation Centre
The NIHR BRACE Rapid Evaluation Centre is a collaboration between the Health Services Management Centre at the University of Birmingham, the independent research organisation RAND Europe, the Department of Public Health and Primary Care at the University of Cambridge, and National Voices. BRACE carries out rapid evaluations of innovations in the organisation and delivery of health and care services. BRACE’s work is guided by the following three overarching principles.
Responsiveness
Researchers are ready to scope, design, undertake and disseminate evaluation research in a manner that is timely and appropriately rapid, pushing at the boundaries of typical research timescales and approaches, and enabling innovation in evaluative practice).
Relevance
Researchers work closely with patients, managers, clinicians and health-care professionals, and others from health and care, in the identification, prioritisation, design, delivery and dissemination of evaluation research in a co-produced and iterative manner.
Rigour
All evaluation undertaken by the team is theoretically and methodologically sound, producing highly credible and timely evidence to support planning, action and practice.
The Rapid Service Evaluation Team
Members of the RSET, comprising health service researchers, health economists and other colleagues from University College London and the Nuffield Trust, have come together to rapidly evaluate new ways of providing and organising care. RSET have been funded by the NIHR HSDR)programme for 5 years, starting on 1 April 2018.
The RSET is carrying out rapid evaluations with respect to:
-
the impact of services on how well patients do (e.g. their quality of life, how likely patients are to recover)
-
whether or not services give people the right care at the right time
-
whether or not these services are good value for money
-
how changes are put into practice, and what patients, carers and staff think about how the changes happened and if they think the changes made a difference
-
what lessons there are for the rest of the NHS and care.
Contributions of authors
Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Research Fellow, University of Birmingham) was the project manager and a researcher for the study; contributed to the conception and design of the study, to the theoretical framework, to data collection and to the overall data analysis and interpretation; made critical revisions to the report for important intellectual content and approved the final manuscript; and is the lead author of the final report, contributing to all chapters.
Ian Litchfield (https://orcid.org/0000-0002-1169-5392) (Research Fellow, University of Birmingham) was a researcher for the study; contributed to the conception and design of the study, to the theoretical framework, to data collection and to the overall data analysis and interpretation; and is a co-author of the final report, contributing to Chapters 1–4.
Robin Miller (https://orcid.org/0000-0003-2646-5589) (Professor, University of Birmingham) was a co-principal investigator for the study; contributed to the conception and design of the study, to the theoretical framework and to overall data analysis and interpretation; made critical revisions to the report for important intellectual content and approved the final manuscript; and is a co-author of the final report, contributing to Chapters 3–5.
Naomi J Fulop (https://orcid.org/0000-0001-5306-6140) (Professor, University College London) was a co-principal investigator for the study; contributed to the conception and design of the study, to the theoretical framework and to overall data analysis and interpretation; made critical revisions to the report for important intellectual content and approved the final manuscript; and is a co-author of the final report, providing critical review of the final report.
Barbara Janta (https://orcid.org/0000-0003-2908-8758) (Senior Analyst, RAND Europe) was a research analyst for the study; contributed to the conception and design of the study, to data collection and analysis of survey data and to interpretation of synthesised findings; and is a co-author of the final report, contributing to Chapters 2–4.
Jamie-Rae Tanner (https://orcid.org/0000-0003-0177-3518) (Public Health Trainee, University of Birmingham) was a researcher for the study; contributed to the conception and design of the study, to the theoretical framework, to data collection and to overall data analysis and interpretation; and is a co-author of the final report, contributing to Chapters 1–4.
Giulia Maistrello (https://orcid.org/0000-0002-2099-006X) (Analyst, RAND Europe) was a research analyst for the study; contributed to the data collection and analysis of survey data, and to interpretation of synthesised findings; and is a co-author of the final report, contributing to Chapters 2–4.
Jenny Bousfield (https://orcid.org/0000-0002-5671-2336) (Analyst, RAND Europe) was a research analyst for the study; contributed to the conception and design of the study, and to data collection; and is a co-author of the final report, contributing to Chapter 1.
Cecilia Vindrola-Padros (https://orcid.org/0000-0001-7859-1646) (Senior Research Fellow, University College London) was a researcher for the study; contributed to the conception and design of the study, to the theoretical framework, to data collection and to overall data analysis and interpretation; and is a co-author of the final report, providing critical review of the final report.
Jon Sussex (https://orcid.org/0000-0001-8970-4546) (Chief Economist at RAND Europe and Co-Director of the Cambridge Centre for Health Services Research, a collaboration between RAND Europe and University of Cambridge) was a co-principal investigator for the study and led the study; contributed to the conception and design of the study, to the theoretical framework, and to overall data analysis and interpretation; made critical revisions to the report for important intellectual content and approved the final manuscript; and is the corresponding author of the final report, contributing to all chapters.
Data-sharing statement
Data from interviews and observations will be accessible to participants who took part in this rapid evaluation following GDPR, RAND Europe and University of Birmingham data protection guidelines upon request. All data requests should be sent to Dr Manbinder Sidhu (m.s.sidhu@bham.ac.uk) in the first instance. Due to the consent process for data collection at case study sites and as part of the survey within this evaluation, there are no data that can be shared.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS . The NHS Long Term Plan 2021 n.d. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 15 August 2022).
- The King’s Fund . Key Facts and Figures About Adult Social Care 2021. www.kingsfund.org.uk/audio-video/key-facts-figures-adult-social-care (accessed 11 October 2021).
- The Care Provider Alliance . Enhanced Health in Care Homes: A Guide for Care Homes 2021. www.careprovideralliance.org.uk/enhanced-health-in-care-homes-cpa-guide (accessed 15 October 2021).
- Smith J, Parkinson S, Harshfield A, Sidhu M. Early evidence of the development of primary care networks in England: a rapid evaluation study. Health Soc Care Deliv Res 2022;10.
- Wessex Academic Health Science Network . RESTORE2 Programme: Patient Safety Collaborative n.d. www.wessexahsn.org.uk/projects/329/restore2 (accessed 2 July 2021).
- Keith RE, Crosson JC, O’Malley AS, Cromp D, Taylor EF. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0550-7.
- Shembavnekar N, Allen L, Idriss O. How Is COVID-19 Impacting People Working in Adult Social Care? 2021. health.org.uk/news-and-comment/blogs/how-is-covid-19-impacting-people-working-in-adult-social-care (accessed 15 October 2021).
- Age UK . Factsheet 24: Personal Budgets and Direct Payments in Social Care 2020.
- Henwood M, McKay S, Needham C, Glasby J. From Bystanders to Core Participants? A Literature and Data Review of Self Funders in Social Care Markets. Birmingham: University of Birmingham; 2018.
- Competition and Markets Authority . Care Homes Market Study: Summary of Final Report 2017.
- Blakeley G, Quilter-Pinner H. Who Cares? The Financialisation of Adult Social Care 2019. www.ippr.org/files/2019-09/who-cares-financialisation-in-social-care-2-.pdf (accessed 11 October 2021).
- Macdonald A, Cooper B. Long-term care and dementia services: an impending crisis. Age Ageing 2007;36:16-22. https://doi.org/10.1093/ageing/afl126.
- Skills for Care . Care Homes Without Nursing in the Adult Social Care Sector 2020.
- Hussein S. The Impact of COVID-19 on Social Care Workers’ Workload, Wellbeing and Ability to Provide Care Safely: Findings from the UK. 2020. www.pssru.ac.uk/blog/the-impact-of-covid-19-on-social-care-workers-workload (accessed 29 July 2021).
- Care Quality Commission . State of Care 2019 20 n.d. www.cqc.org.uk/publications/major-report/state-care-201920 (accessed 15 August 2022).
- Davies G. The Adult Social Care Market in England. London: National Audit Office; 2021.
- Office for National Statistics . Coronavirus (COVID-19) Related Deaths by Disability Status, England and Wales: 2 March to 14 July 2020 2020. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbydisabilitystatusenglandandwales/2marchto14july2020 (accessed 2 July 2021).
- Office for National Statistics . Impact of Coronavirus in Care Homes in England: 26 May to 19 June 2020 2020. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/impactofcoronavirusincarehomesinenglandvivaldi/26mayto19june2020 (accessed 2 July 2021).
- Krutikov M, Palmer T, Tut G, Fuller C, Borscha A, Giddings R, et al. Prevalence and duration of detectable SARS-CoV-2 nucleocapsid antibodies in staff and residents of long-term care facilities over the first year of the pandemic (VIVALDI study): prospective cohort study in England. Lancet Healthy Longev 2022;3:e13-21. https://doi.org/10.1016/S2666-7568(21)00282-8.
- National Institute for Health and Care Excellence (NICE) . Social Care Guideline Scope 2016.
- Local Government Association . COVID-19: Local Examples of Care Technology Approaches 2020. www.local.gov.uk/covid-19/covid-19-local-examples-care-technology-approaches (accessed 2 July 2021).
- O’Dowd A. COVID-19: Official figures ‘underestimate’ deaths caused by discharging patients into care homes. BMJ 2021;373. https://doi.org/10.1136/bmj.n1415.
- The Queen’s Nursing Institute . The Experience of Care Home Staff During Covid-19: A Survey Report by the QNI’s International Community Nursing Observatory 2020. www.qni.org.uk/wp-content/uploads/2020/08/The-Experience-of-Care-Home-Staff-During-Covid-19-2.pdf (accessed 5 October 2021).
- Healthwatch Barnet . A Report Into the Experiences of Barnet Care Homes During the First Wave of the COVID-19 Pandemic 2020.
- The King’s Fund . ‘Bitter Irony’ That Health and Care Staff Are Made Ill by Their Work: The King’s Fund Response to the Commons Committee Report on Workforce Burnout and Resilience n.d. www.kingsfund.org.uk/press/press-releases/bitter-irony-health-care-staff-made-ill-committee-report-workforce-burnout-resilience (accessed 18 August 2022).
- House of Commons Public Accounts Committee . Readying the NHS and Social Care for the COVID-19 Peak 2020.
- NHS . Five Year Forward View 2014.
- Stocker R, Russell S, Liddle J, Barker RO, Remmer A, Gray J, et al. Experiences of a National Early Warning Score (NEWS) intervention in care homes during the COVID-19 pandemic: a qualitative interview study. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-045469.
- British Geriatrics Society . COVID-19: Managing the COVID-19 Pandemic in Care Homes for Older People 2020. www.bgs.org.uk/resources/covid-19-managing-the-covid-19-pandemic-in-care-homes (accessed 11 October 2021).
- Spilsbury K, Devi R, Griffiths A, Akrill C, Astle A, Goodman C, et al. SEeking AnsweRs for Care Homes during the COVID-19 pandemic (COVID SEARCH). Age Ageing 2021;50:335-40. https://doi.org/10.1093/ageing/afaa201.
- Inada-Kim M, Chmiel FP, Boniface MJ, Pocock H, Black JJM, Deakin CD. Validation of home oxygen saturations as a marker of clinical deterioration in patients with suspected COVID-19. MedRxiv 2020. https://doi.org/10.1101/2020.11.06.20225938.
- Singh A, Kataria S, Das P, Sharma A. A proposal to make the pulse oximetry as omnipresent as thermometry in public health care systems. J Glob Health 2020;10. https://doi.org/10.7189/jogh.10.0203102.
- Oliver D. David Oliver: Let’s be open and honest about COVID-19 deaths in care homes. BMJ 2020;369. https://doi.org/10.1136/bmj.m2334.
- Deeny S, Dunn P. The Devastating Impact of COVID-19 on Social Care in England 2020. blogs.bmj.com/bmj/2020/08/12/the-devastating-impact-of-covid-19-on-social-care-in-england (accessed 19 September 2021).
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- O’Cathain A, Murphy E, Nicholl J. Multidisciplinary, interdisciplinary, or dysfunctional? Team working in mixed-methods research. Qual Health Res 2008;18:1574-85. https://doi.org/10.1177/1049732308325535.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- Vindrola-Padros C, Singh KE, Sidhu MS, Georghiou T, Sherlaw-Johnson C, Tomini SM, et al. Remote home monitoring (virtual wards) for confirmed or suspected COVID-19 patients: a rapid systematic review. EClinicalMedicine 2021;37.
- Munn Z, Stern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-017-0468-4.
- Vindrola-Padros C, Sidhu MS, Georghiou T, Sherlaw-Johnson C, Singh KE, Tomini SM, et al. The implementation of remote home monitoring models during the COVID-19 pandemic in England. EClinicalMedicine 2021;34. https://doi.org/10.1016/j.eclinm.2021.100799.
- Marshall F, Gordon A, Gladman JRF, Bishop S. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr 2021;21. https://doi.org/10.1186/s12877-021-02053-9.
- Daly M. COVID-19 and care homes in England: what happened and why?. Soc Policy Adm 2020;54:985-98. https://doi.org/10.1111/spol.12645.
- InHealthcare . Reducing Non Elective Admissions With Digital Care Home Monitoring Telehealth in Care Homes 2020. www.inhealthcare.co.uk/digital-health-services/long-term-conditions/digital-care-home (accessed 2 July 2021).
- Bernard HR . Social Research Methods: Qualitative and Quantitative Approaches 2000.
- McNall M, Foster-Fishman PG. Methods of rapid evaluation, assessment, and appraisal. Am J Eval 2007;28:151-68. https://doi.org/10.1177/1098214007300895.
- Silverman D. Doing Qualitative Research: A Practical Handbook. Thousand Oaks, CA; 2013.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Great Britain . Data Protection Act 2018 2018.
- Vindrola-Padros C, Chisnall G, Cooper S, Dowrick A, Djellouli N, Symmons SM, et al. Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID-19. Qual Health Res 2020;30:2192-204. https://doi.org/10.1177/1049732320951526.
- Bryman A. Social Research Methods. Oxford: Oxford University Press; 2004.
- NHS Race and Health Observatory . Pulse Oximetry and Racial Bias: Recommendations for National Healthcare, Regulatory and Research Bodies 2021.
- Greenhalgh T, Knight M, Inda-Kim M, Fulop NJ, Leach J, Vindrola-Padros C. Remote management of COVID-19 using home pulse oximetry and virtual ward support. BMJ 2021;372. https://doi.org/10.1136/bmj.n677.
- Care Quality Commission . GP Mythbuster 102: Pulse Oximetry and Monitoring Vital Signs Outside the GP Practice Setting n.d. www.cqc.org.uk/guidance-providers/gps/gp-mythbuster-102-pulse-oximetry-monitoring-vital-signs-outside-gp-practice (accessed 5 October 2022).
- NHS England . Novel Coronavirus (COVID-19) Guidance Note: COVID Oximetry @home n.d. www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/11/C1671_COVID-Oximetry-@home-Novel-coronavirus-COVID-19-guidance-note.pdf (accessed 18 August 2022).
- Szczepura A, Nelson S, Wild D. Improving Care in Residential Care Homes: A Literature Review. York: Joseph Rowntree Foundation; 2008.
- McArthur C, Bai Y, Hewston P, Giangregorio L, Straus S, Papaioannou A. Barriers and facilitators to implementing evidence-based guidelines in long-term care: a qualitative evidence synthesis. Implement Sci 2021;16. https://doi.org/10.1186/s13012-021-01140-0.
- Miller R, Freeman T, Davidson D, Glasby J. Managing Change in Social Care. Birmingham: University of Birmingham; 2015.
- Kelley R, Griffiths AW, Shoesmith E, McDermid J, Couch E, Robinson O, et al. The influence of care home managers on the implementation of a complex intervention: findings from the process evaluation of a randomised controlled trial of dementia care mapping. BMC Geriatr 2020;20. https://doi.org/10.1186/s12877-020-01706-5.
- Damery S, Flanagan S, Jones J, Jolly K. The effect of providing staff training and enhanced support to care homes on care processes, safety climate and avoidable harms: evaluation of a care home quality improvement programme in England. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18147581.
- Newbould L, Ariss S, Mountain G, Hawley MS. Exploring factors that affect the uptake and sustainability of videoconferencing for healthcare provision for older adults in care homes: a realist evaluation. BMC Med Inform Decis Mak 2021;21. https://doi.org/10.1186/s12911-020-01372-y.
- Devi R, Chadborn NH, Meyer J, Banerjee J, Goodman C, Dening T, et al. How quality improvement collaboratives work to improve healthcare in care homes: a realist evaluation. Age Ageing 2021;50:1371-81. https://doi.org/10.1093/ageing/afab007.
- Davies SL, Goodman C, Bunn F, Victor C, Dickinson A, Iliffe S, et al. A systematic review of integrated working between care homes and health care services. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-320.
- Needham EBaC . Implementing the Care Act 2014: A Synthesis of Project Reports on the Care Act Commissioned by the NIHR Policy Research Programme 2021.
- Devi R, Hinsliff-Smith K, Goodman C, Gordon AL. The COVID-19 pandemic in UK care homes: revealing the cracks in the system. J Nurs Home Res Sci 2020;6:58-60. https://doi.org/10.14283/jnhrs.2020.17.
- Gordon AL, Goodman C, Achterberg W, Barker RO, Burns E, Hanratty B, et al. Commentary: COVID in care homes – challenges and dilemmas in healthcare delivery. Age Ageing 2020;49:701-5. https://doi.org/10.1093/ageing/afaa113.
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-based Care: How do we Know What Works?. London: Nuffield Trust; 2013.
- Iliffe S, Davies SL, Gordon AL, Schneider J, Dening T, Bowman C, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Prim Health Care Res Dev 2016;17:122-37. https://doi.org/10.1017/S1463423615000250.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Lamont T, Barber N, de Pury J, Fulop N, Garfield-Birkbeck S, Lilford R, et al. New approaches to evaluating complex health and care systems. BMJ 2016;352. https://doi.org/10.1136/bmj.i154.
- Flick U, Flick U, von Kardorff E, Steinke I. A Companion to Qualitative Research. London: SAGE Publications; 2004.
- Fusch P, Ness L. Are we there yet? Data saturation in qualitative research. The Qualitative Report 2015;20:1408-16. https://doi.org/10.46743/2160-3715/2015.2281.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-6. https://doi.org/10.1136/bmj.320.7227.114.
- Chadborn NH, Devi R, Hinsliff-Smith K, Banerjee J, Gordon AL. Quality improvement in long-term care settings: a scoping review of effective strategies used in care homes. Eur Geriatr Med 2021;12:17-26. https://doi.org/10.1007/s41999-020-00389-w.
List of abbreviations
- app
- application
- BRACE
- Birmingham, RAND and Cambridge Evaluation Centre
- CCG
- Clinical Commissioning Group
- CFIR
- Consolidated Framework for Implementation Research
- CO@h
- Covid Oximetry @home
- COPD
- chronic obstructive pulmonary disease
- CQC
- Care Quality Commission
- CVW
- COVID Virtual Ward
- EHCH
- Enhanced Health in Care Homes
- ENRICH
- Enabling Research in Care Homes
- GP
- general practitioner
- HSDR
- Health and Social Care Delivery Research
- IT
- information technology
- NEWS
- National Early Warning Score
- NEWS2
- National Early Warning Score 2
- NHSE&I
- NHS England and NHS Improvement
- NIHR
- National Institute for Health and Care Research
- PCN
- Primary Care Network
- RAP
- rapid assessment procedure
- RESTORE 2
- Recognise early soft signs, Take observations, Respond, Escalate
- RSET
- Rapid Service Evaluation Team
- WP
- work package
Notes
-
The study reported here is an extension to a concurrent evaluation of remote home monitoring models during the COVID-19 pandemic in England
-
Membership of the NHS England & Improvement COVID oximetry in care homes steering group
-
Key educational materials supporting COVID oximetry in the care home sector
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/PQWC3425).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
