Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR135618. The contractual start date was in May 2022. The final report began editorial review in March 2023 and was accepted for publication in June 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Sidhu et al. This work was produced by Sidhu et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Sidhu et al.
BRACE: The NIHR Birmingham, RAND and Cambridge Rapid Evaluation Centre
The NIHR BRACE Rapid Evaluation Centre (National Institute for Health and Care Research Birmingham, RAND and Cambridge Evaluation Centre) is a collaboration between the Health Services Management Centre at the University of Birmingham, the independent research organisation RAND Europe, the Department of Public Health and Primary Care at the University of Cambridge and National Voices. BRACE carries out rapid evaluations of innovations in the organisation and delivery of health and care services. Its work is guided by three overarching principles:
-
Responsiveness. Ready to scope, design, undertake and disseminate evaluation research in a manner that is timely and appropriately rapid, pushing at the boundaries of typical research timescales and approaches, and enabling innovation in evaluative practice.
-
Relevance. Working closely with patients, managers, clinicians and health-care professionals, and others from health and care, in the identification, prioritisation, design, delivery and dissemination of evaluation research in a co-produced and iterative manner.
-
Rigour. All evaluation undertaken by the team is theoretically and methodologically sound, producing highly credible and timely evidence to support planning, action and practice.
Chapter 1 Background, context and objectives
Summary of key points
-
The phase 2 rapid evaluation reported here follows up outstanding issues set out at the end of the report of phase 1 and addresses gaps in the literature on vertical integration in the context of the National Health Service (NHS) in England: understanding the extent of vertical integration between acute hospitals and general practices that has already taken place throughout the NHS in England; the impact on outcomes from the use of secondary care services, how service delivery has changed or is expected to change and the patient experience of vertical integration, with a particular focus on whether patients with multiple long-term conditions are affected differently from other patients.
-
Patient demand on general practices and patient dissatisfaction with general practitioner (GP; primary care physician) services are both growing.
-
Practices are merging and horizontally integrating in line with NHS primary care network (PCN) policy. The number of general practices is falling and the numbers of patients per practice is increasing nationally.
-
Policy focuses on horizontal rather than vertical integration. Vertical integration has not yet been part of government or NHS policy in England, although early in 2022 there was ministerial reference to it.
-
There is growing concern in policy discussions about meeting the particular requirements of patients with multiple long-term conditions, who are likely to be frequent users of health care and may particularly benefit from improved integration of health care.
Overview and scope
This report presents the second phase of a two-phase rapid evaluation of arrangements whereby NHS organisations operating acute hospitals have additionally taken over the running of general practices in locations in the NHS in the UK. This is a form of vertical integration: where one organisation provides care at different stages along the patient pathway. 1 We focus on cases where providers of secondary care in acute hospitals merge with providers of primary care (general practices). The setting of the rapid evaluation reported in the following pages is the NHS in England, but its findings are likely to be of interest internationally as forms of vertical integration have also occurred or could be introduced in other health-care systems.
The scope of the phase 2 rapid evaluation of vertical integration between acute hospitals and general practices starts from that of the phase 1 study, which is described and explained in full in chapter 2 of Sidhu et al. 20222,3 and is not repeated here. The phase 1 rapid evaluation was a qualitative study undertaken in 2019 and early 2020, which focused on the rationale, implementation and early impact of the vertical integration of acute hospitals with general practices in England and Wales. Prior to that study,2,3 there had been little systematic information on the rationale for, or desired impact of, vertical integration in a UK NHS setting, or on why it is being introduced in some places despite not being an explicit part of NHS policy. The phase 2 rapid evaluation reported here combines quantitative and qualitative evaluation methods to understand the extent of vertical integration in the NHS in England, its impact on patients’ use of hospital care, how service delivery has changed (or is expected to change) and the patient experience of vertical integration.
In the NHS in England, secondary health care is provided by organisations known as ‘trusts’. Some trusts provide acute hospital services, some provide community-based secondary care services, some provide mental health and/or learning disability services. Some trusts provide combinations of these types of services. For the purposes of the research reported here, we have grouped trusts into those that we refer to from here on as ‘acute trusts’ and those that we label ‘community trusts’. Any trust that provides acute hospital services we categorise as an ‘acute trust’, regardless of any further services that the trust may also provide. Other trusts that have taken on the running of general practices but do not provide acute hospital services we label for brevity as ‘community trusts’, although two trusts we label in this way are providers only of mental health and learning disability care. As in the phase 1 evaluation, we concentrate in this study on vertical integration of general practices with organisations that run acute hospitals, but we include reference to vertical integration of general practices with organisations providing other secondary care where that clarifies the analysis.
A novel aspect of the second phase evaluation reported in the following pages is that we have specifically analysed whether patients with multiple long-term conditions are affected by vertical integration differently from other patients. The rationale for this part of the present study is that changes in the organisational structure of primary care and its integration with secondary care may be expected to particularly affect those patients presenting with more than one single chronic condition. 4,5 These patients access care more frequently than others, are more complex in their needs and will often require access to and coordination of many different health-care providers not all operating from the same site. As far as we are aware, there has not yet been an evaluation of whether and how vertical integration affects people with multiple long-term conditions differently from other patients.
Throughout the phase 2 study we have attempted to allow for the disruptions resulting from the COVID-19 pandemic and the measures taken to combat it. The pandemic began in the UK in February 2020 and had a large initial impact on the volume of primary and secondary care activity. It has gone on to have a fundamental effect on how primary care is delivered. In particular there was an initial, large, step-change increase in the proportion of primary consultations conducted remotely (via digital or telephone consultations) rather than in person, although the remote proportion has dropped back to some extent more recently. 6 The quantitative analyses presented in the following chapters use data up to April 2021 to identify all locations in England where NHS hospitals are running general practices and the dates at which that first happened, and activity data up to February 2020 to estimate the impact of vertical integration on patients’ use of secondary care services and experience of primary care. Thus, for the analysis of secondary care usage we avoid the period when the pandemic affected hospital activity. The qualitative analysis is based on fieldwork conducted during the summer and autumn of 2022 and so is unavoidably affected by the changes to primary and secondary care brought about by the COVID-19 pandemic.
In the rest of this chapter, we summarise the institutional and policy context relevant to vertical integration in the NHS in England, which has three major aspects: (1) the challenges being faced by GP care in recent years; (2) the continuing attempts to better integrate health-care services; and (3) the particular needs of people with multiple (rather than single) long-term conditions. We then summarise what is known about vertical integration from the existing literature, including the main findings and conclusions of the phase 1 evaluation. 2,3 We finish the chapter by stating the aims of the phase 2 rapid evaluation reported here and the specific research questions, and by outlining the structure of the rest of the report.
Institutional background
Within the NHS, acute hospitals do not usually run general practices (nor other primary care services provided in community settings by dentists, pharmacists and opticians). GPs are contracted by the NHS to provide primary care medical services to the patients who register with them. Box 1 summarises the types of GP contract in use.
The general medical services (GMS) contract is agreed nationally. The contract is held (in perpetuity) by the practice, not by individual GPs. It provides the contracting general practice with an income stream to pay for the staff, premises and other costs of providing a menu of compulsory ‘essential’ services. Under the GMS contract, a practice may also voluntarily provide and be paid for ‘additional services’ and ‘enhanced services’. Around 70% of general practices operate under GMS contracts.
Personal medical servicesPersonal medical services (PMS) contracts are negotiated locally [formally with the local clinical commissioning group (CCG), now with the local integrated care board (ICB)]. These contracts are held by individual GPs rather than practices. They are held in perpetuity but can be terminated by the commissioner with six months’ notice. GPs contracted via PMS contracts are paid to provide a defined service as agreed locally. Around 25% of general practices operate under PMS contracts with their GPs.
Alternative provider medical servicesAlternative provider medical services (APMS) contracts are locally agreed and can be let to private sector – both commercial and voluntary – organisations as well as to traditional general practices. They are, unlike GMS and PMS contracts, time limited. This type of contract tends to be used in areas where it is difficult to recruit and retain GPs. Just 2% of general practices hold APMS contracts.
GPs also act as ‘gatekeepers’, referring patients to other, specialist (i.e. secondary care) NHS services, including those provided by acute hospitals. Despite these roles, the large majority of GPs are not employees of the NHS but instead are either contractors to the NHS or are salaried employees of organisations that are (e.g. partnerships of GPs who hold a contract with the NHS or private companies that do so). Practices employ not only GPs but also nurses and other health-care professionals, together with managers, administrative and reception staff. Many practices operate out of a single location, but some work from two or more sites. At the end of September 2022, there were 37,026 full-time equivalent (FTE) GPs (including trainees) in 6456 general practices in the NHS in England. 9 The number of general practices in England has been decreasing as individual practices merge with one another or close (the consequence of which is that their patients are then distributed across the remaining practices). In the 3 years to September 2022, the number of general practices in England fell 6.0% (from 6867 to 6456) and average practice list sizes rose 9.8% (from 8737 registered patients per practice in September 2019 to 9596 in September 2022).
Acute hospital trusts are providers of hospital-based, emergency and/or elective specialist health care. In England, acute hospitals are run by publicly owned organisations, which are either ‘NHS foundation trusts’ or ‘NHS trusts’ (hereafter referred to collectively as trusts). In September 2022, there were 142 acute hospital trusts in England. The services of acute hospitals are contracted for by both national and local NHS commissioners of care. In England, the commissioning organisations were, until 1 July 2022, NHS England (nationally) and 106 local clinical commissioning groups (England) (CCGs). Since July 2022, commissioning of health care for their resident populations has become the responsibility of 42 integrated care boards (ICBs), which have in effect absorbed the CCGs.
Some acute trusts in England now run general practices. Such vertical integration is a relatively new phenomenon in the NHS, occurring over the period since 2015, and rising over time. This kind of integration is distinct from horizontal integration, whereby organisations at similar stages along the patient pathway integrate or even formally merge with one another, such as when one acute hospital trust integrates or merges with another or when one general practice integrates or merges with another. There are many types of horizontal integration between general practices10 but this is not the main focus of the evaluation reported here. Nevertheless, each vertically integrated organisation that includes more than one general practice does necessarily also include a degree of horizontal integration between the practices that are owned by the same trust. Furthermore, we have found, as explained later in the report, that it sometimes happens that general practices are merged together (horizontally) at the time they are vertically integrated with a trust or subsequently. Consequently, any impacts of vertical integration may be seen as the combined result of both vertical integration between a trust and the practices it runs and horizontal integration between the practices that are run by the same trust.
As is explained in the report of our phase 1 evaluation,2 the concept and term ‘vertical integration’ is familiar to economists, although perhaps less so to health-care audiences. In the economics literature (e.g. Joskow et al. 200511 and, as applied to the health-care sector, Laugesen and France 201412) vertical integration is seen as having three main rationales: (1) as a way of increasing market power relative to other providers; (2) enabling better management of some risks (e.g. concerning the level of demand for an organisation’s services); and (3) to reduce transactions costs via better information sharing, monitoring and decision-making. In the health-care context, vertical integration has been defined as being along any or all of six types: organisational, functional, service, clinical, normative, systemic. 13 The examples of vertical integration studied in our phase 1 evaluation and now in the phase 2 evaluation mainly concern organisational and functional integration, together with some elements of service, clinical and normative integration. Interest in vertical integration is not limited to the UK NHS, other countries which have adopted this approach include Denmark, Spain and the United States. 14–17
Policy context
The phase 1 study2,3 highlighted (1) sustaining primary care in locations where practices were likely to close, and (2) better integration of care, as the two main drivers of vertical integration between acute hospitals and general practices in the NHS in England and Wales. The overall NHS context is one of persistently increasing demand and activity both in secondary care and primary care settings (about which we say more below). Indeed, our phase 1 study found that part of the motivation for hospital trusts to take on the running of general practices was the desire of trust management to maintain some control over the flows of patients to secondary care, especially accident and emergency department (A&E) attendances and emergency admissions. 2,3
Vertical integration in one of the two case study sites in England in the phase 1 evaluation had stemmed from an innovation in service provision aimed at people with multiple long-term conditions who were consequently frequent users of primary and secondary health-care services. Better meeting the needs of people with multiple conditions is an area of increasing policy concern. 18–20 The following paragraphs summarise the policy context in England with respect to the challenges for general practice-based care, integration of primary and secondary health care, and service provision for people with multiple long-term conditions.
Challenges for general practitioner primary care
The sustainability of primary care has for several years been the subject of increasing concern and debate for policy makers in England, as well as for health-care professionals, service managers and commissioners. In essence, demand for primary care is growing inexorably and the supply of GPs is not keeping pace with that demand. 19,21–25 GP FTEs in England grew by 6.6% in the 3 years to September 2022: from 34,729 in September 2019 to 37,026 in September 2022. This was a combination of a small decline in FTEs of fully qualified GPs (down 626 over that period from 28,182 to 27,556) and a large increase in GPs in training (up 44.6% over the same period from 6547 to 9470). 9 Over the same period, the total number of appointments at general practices increased by a similar amount: up 7.1% over the same 3-year period from 26,420,000 in September 2019 to 28,300,000 in September 2022. 26,27 The similarity between the two growth rates is perhaps unsurprising in a supply-constrained system (i.e. where potential demand exceeds available supply) given that the number of GP appointments is necessarily constrained by the number of FTE GPs available for patients to consult with. But it also suggests that employment in primary care practices of health-care professionals other than GPs did not greatly add to capacity for patient consultations over that period. 28
There has also been a rise in the number of patients with multiple long-term conditions, higher costs, developments in the consulting technology and tightening workforce constraints as result of GP recruitment and retention difficulties. 25,27,29,30 The gatekeeping role of GPs means that increasing difficulty with meeting patient demand in a primary care setting can lead to growing pressure on acute hospital emergency services. A desire on the part of managers at acute trusts to keep some control over the flow of patients to their hospitals was evident in our phase 1 evaluation. 2
The policy response has focused on increasing the numbers of GPs in training, as evidenced by the rapid growth in numbers of trainees mentioned earlier; on providing funding for new staff roles in general practice and on merging and integrating primary care practices horizontally with one another in the hope of increased efficiency (more and/or better patient services delivered per primary care staff member). 2,19,22,31 Nevertheless, patient experience and patient satisfaction with general practice services in England is falling, as summarised in the House of Commons Health and Social Care Select Committee report in October 2022 (quote taken from paragraph 25 of that report):25
Over several years the GP Patient Survey has shown declining access standards, albeit with satisfaction rates remaining high: from 2018 to 2020 the proportion of people who reported having a good overall experience of making an appointment fell slightly from 68.6% to 65.5%, but the proportion of people rating their care as good overall remained 81.8% in 2020. In the latest GP Patient Survey, however, the results are significantly worse and show the level of difficulty patients now face when trying to access general practice: the proportion of people who had a good experience of making an appointment has fallen sharply to 56.2% and the proportion of people rating their overall experience as good has also fallen significantly to 72.4%. 23,25 (Parliamentary Copyright House of Commons 2022. This material is reproduced under the terms of the Open Parliament Licence v3.0, which is published at: https://www.parliament.uk/site-information/copyright-parliament/open-parliament-licence)
Integrating health care
NHS policy has, over the past 10 years, repeatedly stressed an objective of more integrated patient care across primary health care, secondary health care and social care settings. 19,21–23 The policy focus on care integration led to the development of several recommendations in the 2014 NHS ‘five-year forward view’. 21 Among them was to seek stronger integration between primary and secondary care, in what were termed primary and acute care systems (PACS). Some piloting of PACS was funded as a result. The 2016 General Practice Forward View announced increased funding for GP services and plans for developing them further. 22 The 2019 NHS Long Term Plan19 set out the intention that all general practices in England should come together to deliver services as part of primary care networks (PCNs). This is a form of horizontal integration designed to cover populations of 30–50,000 patients per network. Since July 2019, all but a tiny number of practices have become horizontally integrated in that way with other practices, while remaining separate legal entities with separate contracts. Findings from a recent rapid evaluation of PCNs show that there have been a number of facilitators and challenges to horizontal integration to help achieve sustainable primary care, address growing workload issues and improve the availability and coordination of local primary care services. 10
Since 2015, a number of local initiatives have led to trusts running general practices but this was not in response to any particular policy stimulus. Apparently explicit policy-maker interest in NHS trusts running general practices emerged in early 2022. 32,33 The expectation was reported as being that functions, activities and organisations that provide different levels of patient care might be brought together under a single management and result in cost savings in secondary care, as had been reported at one vertical integration site by Yu and colleagues. 2,3,34 This policy-maker interest was despite the findings from our phase 1 evaluation that vertical integration in a health-care system worked when driven by local initiative (rather than central direction) and that many GPs evidently did not wish to become vertically integrated with trusts. 2,3
A subsequent ‘stocktake’ commissioned by NHS England of the state of integration in primary care and published in May 2022 made no mention of vertical integration as such. Instead, it focused on ‘building integrated teams’ at the level of PCNs but broadened the concept to:
teams from across primary care networks (PCNs), wider primary care providers, secondary care teams, social care teams, and domiciliary and care staff [working] together to share resources and information and form multidisciplinary teams (MDTs) dedicated to improving the health and wellbeing of a local community and tackling health inequalities. (Source: NHS England 2022, p. 6)31
Caring for people with multiple long-term conditions
The National Institute for Health and Care Excellence (NICE) defines multimorbidity as ‘the presence of two or more long-term health conditions, which can include:
-
defined physical and mental health conditions such as diabetes or schizophrenia
-
ongoing conditions such as learning disability
-
symptom complexes such as frailty or chronic pain
-
sensory impairment such as sight or hearing loss
-
alcohol and substance misuse.’35
The prevalence of people with two or more such long-term conditions has recently been estimated at 53% of the adult population in England. 36 People with multiple long-term conditions are higher users of NHS services than other members of the population and would particularly benefit from services focused around the individual patient rather than an individual condition. 24 The World Health Organization describes people with multimorbidity, compared with other members of the population, as facing:
more frequent and complex interactions with health-care services leading to greater susceptibility to failures of care delivery and coordination; the need for clear communication and patient-centred care due to complex patient needs; demanding self-management regimens and competing priorities; more vulnerability to safety issues … (p. 4)37
Multimorbidity is now a high-profile issue for consideration in NHS policy and practice. It is a major theme in the NHS Long Term Plan18 and the Academic Health Science Network, National Institute for Health and Care Research (NIHR) and NHS England report on priorities for innovation and research. 18 In July 2019, the Academy of Medical Sciences, NIHR, Department of Health and Social Care, Medical Research Council and Wellcome Trust jointly declared that: ‘Multimorbidity is recognised as an important priority across all our organisations and we all take a special interest in it’. 38
Evidence for vertical integration
It remains the case that relatively little evidence is available to inform policy makers about vertical integration between acute hospitals and general practices. Yu and colleagues34 found in a statistical study at one location, Wolverhampton in the West Midlands of England, using data from the period April 2015 to March 2019, that vertical integration between an acute hospital and 10 general practices was associated with a statistically significant, reduction in the rate of unplanned hospital admissions and readmissions, but not of A&E attendances. They estimated that this would imply an annual cost saving to the hospital of around £1.7 million. 34 We include in Chapter 4 a comparison of Yu and colleagues’ findings with our analysis for the same vertically integrated practices in Wolverhampton.
Our qualitative, phase 1 rapid evaluation of vertical integration at two locations in England and one in Wales revealed several noteworthy findings. It showed that key to achieving vertical integration is better clinical integration (coordination of treatment services for a patient) and functional integration (strengthening key support functions, such as financial management, human resources and strategic planning). Trust managers at case study sites anticipated that vertical integration would enable better management of patient demand for secondary care services, a view consistent with the findings of Yu and colleagues. 34 Vertical integration can lead to alterations in contractual arrangements and accountability, workforce recruitment, premises and care pathways, which in turn have the potential to create better care and outcomes for the patient. The phase 1 study also found potential downsides to vertical integration, including fears among GPs of loss of autonomy and having to interact with more bureaucratic and slower back-office processes in trusts (finance, procurement, human resources, estate management). It is certainly the case that even in locations where some general practices are integrated with an acute trust, many other general practices choose to remain outside any such arrangement. 2
Aims and research questions
In 2019–20, the phase 1 rapid evaluation of vertical integration investigated the implementation of acute hospitals managing general practices, as well as addressing questions relevant to scaling-up this model of integration in an NHS setting. That qualitative evaluation focused on understanding the rationale for, and the implementation and early impact of, vertical integration. It included the development of a theory of change, identifying what outcomes this model of vertical integration is expected to achieve in the short-, medium- and long-terms, and under what circumstances.
Phase 2 of the study of vertical integration, reported here, starts from the institutional and policy contexts described earlier and aims to address outstanding issues identified in phase 1. 2 These include: understanding the extent of vertical integration which has already taken place throughout the NHS in England; the impact on outcomes form the use of secondary care services; how service delivery has changed or is expected to change; and the patient experience of vertical integration, with a particular focus on whether patients with multiple long-term conditions are affected differently from other patients. To address these aims, the phase 2 rapid evaluation focuses on attempting to answer the following research questions:
-
How many general practices have already vertically integrated with NHS organisations running acute hospitals in England; when did the integration between general practices and acute hospitals take place, and what are the characteristics (in terms of geographical location, patient demographics and practice size/workforce) of those practices where vertical integration has taken place?
-
What impact is vertical integration having on the use of secondary care services [outpatient attendances, A&E attendances, all inpatient admissions, emergency inpatient admissions, inpatient admissions for ambulatory care sensitive conditions (ACSC), bed days, readmission within 30 days of discharge]? Does this impact differ for people with multiple long-term conditions compared with other patients without long-term conditions or living with a single condition?
-
What impact is vertical integration having on the patient journey with regard to access to and overall experience of care? How does the experience differ for people with multiple long-term conditions compared with those living with no or one long-term condition?
An overview of the methods used for the phase 2 evaluation is given in Chapter 2. The subsequent chapters then set out in turn the findings of work package (WP) 1, on the current extent of vertical integration in England; WPs 2 and 3, quantitative analyses of the impact of vertical integration on patient experience of primary care and utilisation of secondary care; and WP4, qualitative exploration of the patient journey and experience of care in three vertical integration case studies. These findings chapters are followed by a discussion and conclusions.
Chapter 2 An overview of the methods used in the evaluation
Summary of key points
-
Our phase 1 study in 2019 and early 2020 answered some of the pertinent questions about the introduction of vertical integration. However, it did not go so far as to investigate the impact on the use of secondary care services and patient experiences of vertical integration.
-
The research questions for the currently proposed project (phase 2) were designed to update and validate our theory of change for vertical integration.
-
We completed a mixed methods evaluation comprised of four WPs:
-
WP1: desk-based review of NHS trust annual reports, relevant literature and identified data sets, to understand the scale of vertical integration of general practices with acute NHS hospitals and other secondary care providers that has taken place across England.
-
WP2: development of the statistical analysis approach.
-
WP3: quantitative analysis of national data to explore the impact of vertical integration on hospital care and the financial implications of that, and on the patient experience of GP care as measured by a national survey of patients. The quantitative analysis investigated if there is any differential impact for people with multiple long-term conditions.
-
WP4: qualitative data collection and analysis with key stakeholders and patients across three case study sites in England to explore the impact of vertical integration on patient experience of care, particularly focusing on patients with multiple long-term conditions.
-
Protocol sign-off
An initial short pro forma outlining the study aims, methods and outcomes was submitted in December 2021 and was approved by NIHR Health and Social Care Delivery Research (HSDR). It was used as the basis for the full evaluation protocol, which drew on relevant literature and an online workshop with our user involvement group. The protocol was approved by NIHR HSDR in May 2022.
General approach
Our general approach to meeting the aims and answering the research questions was a cross-comparative case study mixed-methods evaluation comprising four WPs. The WPs were designed to overlap and thus inform each other to support analysis and triangulation between the quantitative and qualitative data. The study began with a desk-based review of NHS trust annual reports, relevant literature and identified data sets, to understand the scale of vertical integration of primary care practices with acute NHS hospitals that has taken place across England. Then, the study team completed a quantitative analysis of national hospital activity data to explore the impact of vertical integration on the use of secondary care services and the financial implications of that, and on the patient experience of GP care as measured by a national survey of patients. The quantitative analysis investigated if there is any differential impact on secondary care for people with multiple long-term conditions. We completed qualitative data collection and analysis with key stakeholders and patients across three case study sites to explore qualitatively the impact of vertical integration on patient experience of care, particularly focusing on patients with multiple long-term conditions. These four WPs are summarised in Table 1.
| WP | Description | Research questions |
|---|---|---|
| 1. Understanding the current scale of vertical integration | Establish the extent of vertical integration in England through a desk-based analysis of secondary care statutory financial reporting and primary care GP workforce data | 1 |
| 2. Development of the statistical analysis approach | Identifying the appropriate counterfactual or control sites and the appropriate approach to coding multiple long-term conditions | 1, 2 |
| 3. The impact of vertical integration on use of secondary care | Assess the impact of vertical integration overall and for patients with multiple long-term conditions for secondary care services for identified outcomes, for vertically integrated and control practices before and after vertical integration was introduced; and for patient experience of GP care as measured by a national survey of patients. Also report the financial implications based on the secondary care resource use data for vertical integrated and non-vertically integrated practices | 2, 3 |
| 4. Impact on the patient journey regarding access to and overall experience of care | Interviews and focus groups at each case study site, to which we invited key service managers and clinicians from the acute hospital, community care, and general practices. Primary qualitative research via interviews, capturing the views of patients from integrated general practices, to understand their experiences of the following where vertical integration models are present: what impact is vertical integration having on the patient journey with regard to access to and overall experience of care? How do models of vertical integration support patient transitions from primary care to acute care? How do patients experience services, more commonly found in secondary care, within a vertically integrated general practice setting? How does the experience differ for people with multiple long-term conditions compared with other patients? | 3 |
Learning from the BRACE phase 1 evaluation of acute hospitals managing general practices and the need for a follow-on phase 2 evaluation
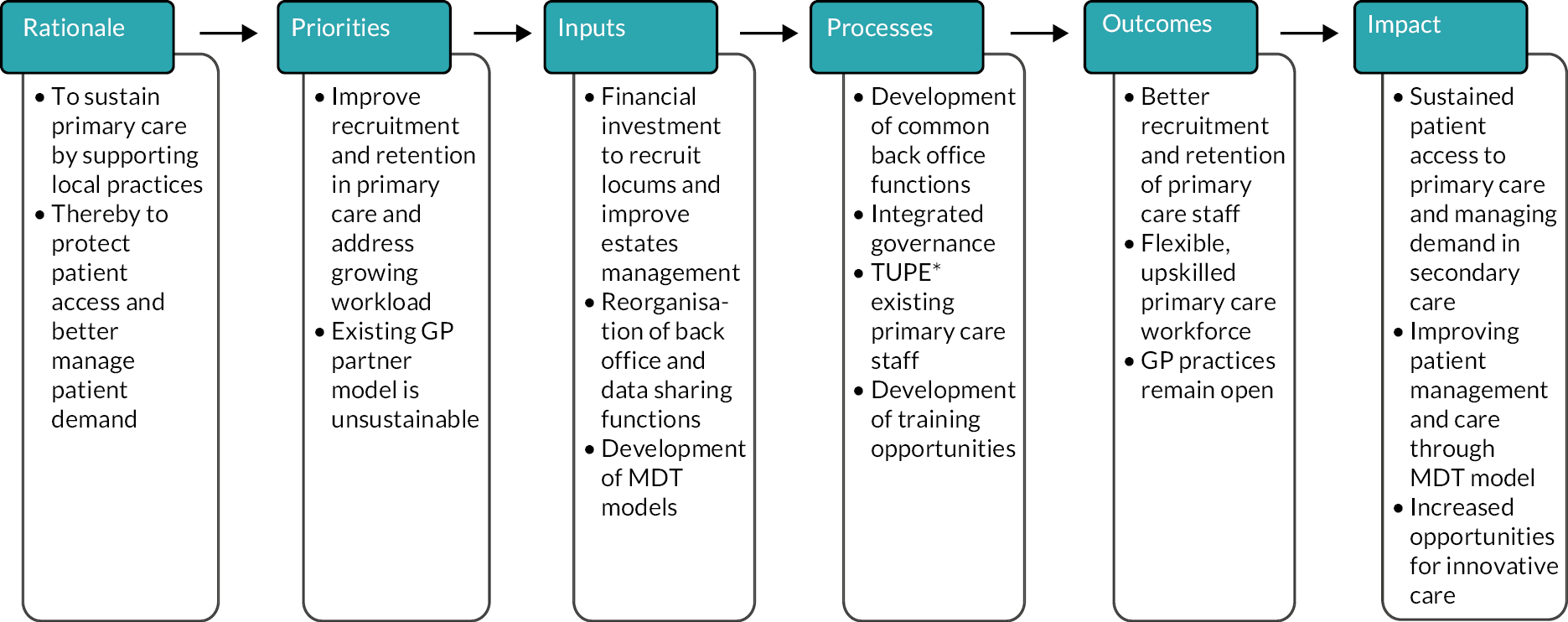
In 2019/20, Birmingham, RAND and Cambridge Evaluation Centre (BRACE) carried out a phase 1 rapid evaluation of arrangements in three case study areas where the NHS organisations operating acute hospitals had taken over the running of general practices at scale in England and Wales (i.e. a fully integrated model of vertical integration). 2 The aims of the phase 1 evaluation were to understand the early impact of vertical integration, namely: its objectives; how it is being implemented; whether and how vertical integration can underpin and drive the redesigning of care pathways; whether and how services offered in primary care settings change as a result; and the impact on the general practice and hospital workforces. The study team developed a theory of change for vertical integration, identifying the outcomes it is expected to achieve in the short, medium and long-term, and under what circumstances (see Figure 1). They found the single most important driver of vertical integration to be the maintenance of primary care local to where patients live. Vertical integration of general practices with organisations running acute hospitals has been adopted in some locations in England and Wales to address the staffing, workload and financial difficulties faced by some general practices. This phase 1 study answered some of the pertinent questions about the introduction of vertical integration. However, it did not go so far as to investigate the impact on secondary care and patient experiences of vertical integration. These interests are reflected in the research questions for the phase 2 project reported here.
FIGURE 1.
Overall vertical integration theory of change developed from the BRACE phase 1 rapid evaluation. 2 *TUPE, transfer of undertakings (protection of employment) – A ‘TUPE transfer’ happens when an organisation, or part of it, is transferred from one employer to another; a service is transferred to a new provider, for example when another company takes over the contract.
Co-designing the study approach and research questions with members from the BRACE patient and public involvement panel
Members of the study team met with the BRACE patient and public involvement (PPI) panel and discussed the ‘what’ questions (what is important to find out/know about) and the ‘how’ questions (how best to gather this information). Members of the PPI panel took part in two workshops across the duration of the study. A structured agenda was prepared in advance of each workshop and included time for presentation of findings, as well as time for discussion and feedback when sharing learning from data collected. As part of the first workshop (May 2022) members commented on our research questions, choice of methods and recruitment strategies, and participant facing study documentation. A second workshop (November 2022) was held to discuss preliminary findings whereby feedback fed into interpretation of data and supported synthesis of learning across data sets.
Overview of methods by work package
Work package 1: understanding the current scale of vertical integration in England
WP1 details the extent of vertical integration in England through a desk-based analysis of secondary care statutory financial reporting and primary care GP workforce data. There is triangulation of practices where vertical integration has been identified. Statistics that describe the characteristics of the vertically integrated practices are presented: number of acute hospital trusts managing general practices; the number of general practices managed by the acute hospital trust; practice sizes in terms of patient population, patient demographics and workforce descriptors.
Work package 2: development of a statistical analysis plan
As part of WP2, the study team identified appropriate control sites and an appropriate approach to coding multiple long-term conditions as part of a detailed plan of analysis. In addition, this WP addresses several methodological questions, for example how to deal analytically with general practices that have merged with other practices during the study time frame, and how to allow for the impact of the COVID-19 pandemic in the analyses of how patients use secondary care.
Work package 3: quantitative analysis of the impact of vertical integration on the use of secondary care services
As part of WP3, we assessed the impact of vertical integration on patients’ use of secondary care services both overall and more specifically for people with multiple long-term conditions. We examined the following outcomes: outpatient attendances, A&E attendances, all inpatient admissions, emergency inpatient admissions, inpatient admissions for ACSC, bed days, readmission within 30 days of discharge; for the identified practices and their controls before and after the identified practices were vertically integrated. We then discuss the financial implications in terms of an overall cost difference for secondary care use between vertically integrated and not vertically integrated practices. We additionally analysed the results of the GPPS questions relating to patient experience of primary care, comparing replies for vertically integrated practices with those for control practices.
Work package 4: staff and patient experiences of care delivery and provision across three purposively selected case study sites
We completed focus groups and interviews across three case study sites in England with key service managers and clinicians from the acute hospital, community care and general practices; and primary qualitative research via interviews, capturing the views of patients from integrated general practices, to understand their experiences of accessing services in areas where models of vertical integration are present.
We present more detailed methods and our findings in the next three chapters. Chapter 3 provides a description of the scale of vertical integration of primary care practices with acute and community trusts that has taken place across England. The subsequent chapter (Chapter 4) presents a quantitative analysis of national routine data to explore the impact of vertical integration on patient satisfaction and use of health-care services. Chapter 5 sets out an analysis of interviews and focus groups with key stakeholders and patients across three case study sites to explore qualitatively the impact of vertical integration on patient experience of care, particularly focusing on patients with multiple long-term conditions.
Chapter 3 Work package 1: understanding the current scale of vertical integration in the NHS in England
Summary of key points
-
We have compiled the first comprehensive list of trusts and general practices in England that are vertically integrated.
-
The process of identification of vertical integration is not straightforward and (at the time of writing this report February 2022) there is no organisation that holds information about the scale of vertical integration in England.
-
As part of WP1, we describe the characteristics of the vertically integrated practices including: number of acute hospital trusts managing general practices; the number of general practices managed by acute hospital trusts; practice sizes in terms of patient population, patient demographics and workforce descriptors.
-
As of March 2021, we identified 26 trusts in vertically integrated organisations, running a total of 85 general practices (i.e. with unique practice codes) across a total of 116 general practice sites (as some practices work from two or more locations). Vertically integrated practices do not appear to be ‘typical’ general practices but rather tend to be: poorer performing, located in more deprived areas and often with smaller patient numbers and fewer staff.
Methods
At the start of the phase 2 rapid evaluation, we undertook preliminary scoping work to assess the availability of data on trusts and general practices in vertically integrated arrangements. In addition to online searching, including the NHS Digital website, we contacted representatives of the British Medical Association, the Royal College of General Practitioners, NHS England and NHS Improvement. We found that none of these organisations holds such information systematically or comprehensively. The research team therefore compiled these data in the following way, which is represented schematically in Figure 2. In essence, we used trust annual reports as the main data source and then checked the robustness of that information by comparing with GP workforce data, general practice websites and other sources as listed in Figure 2 and described below.
FIGURE 2.
Flow chart of WP1 search process. *Using CQC data. 39 **Although vertical integration generally took place from 2015/16 onwards, we checked back to 2012/13 to allow for any earlier models of vertical integration which might have taken place.
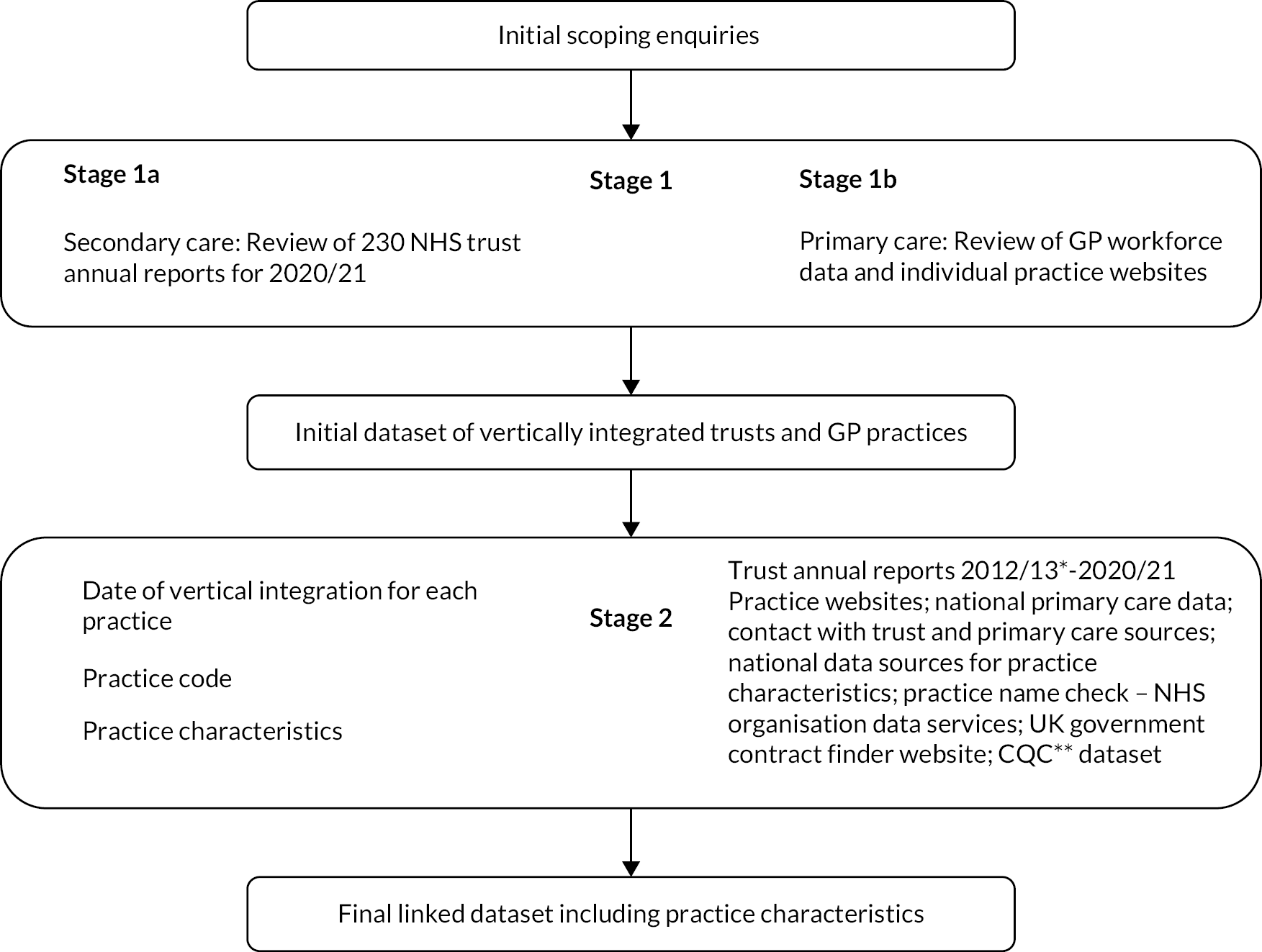
Stage 1a: secondary care statutory financial reporting
The principal source of information on vertical integration where trusts run general practices, was trusts’ annual reports. We hand searched the annual reports of all 230 NHS trusts listed on the nhs.uk website. 40 Each NHS foundation and non-foundation trust must publish annual reports and accounts to allow scrutiny of the year’s operations and outcomes. Trust annual reports are typically published in a PDF format on the trust’s website. 41 We first searched the reports from 2020/21 (the most recent available) and then backed this up by searching the reports from 2019/20, which revealed several additional vertical arrangements not evident from the later year’s reports.
One member of the research team (FO) used the ‘find and retrieve’ search option for the terms ‘general practitioner’, ‘GP’ ‘general practice’ and ‘primary care’ within each annual report and determined from the corresponding text whether the trust had reported a financial/ownership relationship with a provider of GP services, and thus would be considered vertically integrated with that practice or practices. For trusts with no vertically integrated practices, our expectation was that we would find less frequent use of the search terms in the report. We found that the search terms were frequently mentioned in the pension reporting sections but with no reference anywhere else in the report in question that indicated that the trust owned or managed any general practices. These were, consequently, not instances of vertical integration. The researcher (FO) was otherwise independent of the study and had no prior knowledge of vertically integrated practices, which helped to ensure an unbiased assessment of where vertical integration was present. All trust reports with identified vertically integrated general practices were then reviewed for a second time by another member of the research team. A further 20% of trusts identified by the first reviewer as not having vertically integrated practices were also second-reviewed as a control. The second review confirmed that these trusts were not integrated with general practices.
We checked the websites of practices identified by this process to confirm their connections with NHS trusts. We additionally searched via Google for press mentions of trusts taking over the running of general practices. Finally, we cross-checked the findings of the blinded reviews against study team knowledge of areas where vertical integration is occurring and found that all instances of vertical integration previously known to members of the research team had been identified, plus some further instances.
Stage 1b: validation via primary care general practitioner workforce data and practice websites
A key finding from our phase 1 evaluation2 was that vertical integration was a way of sustaining local primary care, and one form of vertical integration was for a trust to employ GP staff directly. We therefore inspected the GP workforce data published by NHS Digital at 31 March 2021,42 which reports all types of GP employment contracts. Our focus for searching was on GPs categorised as ‘other’ (i.e. not salaried GPs, GP partners, trainees or locum practitioners). A preliminary review of these data identified 243 practices where one or more ‘other’ GPs were employed. We then searched on the practice names to find and review the corresponding individual practice websites for further indications of possible vertical integration with a trust. Practice names were cross-checked against information provided by NHS Digital. 43
Further robustness checks were provided by reviewing all general practices with alternative provider medical services (APMS) contracts on the UK government contract finder website to identify those where acute or community trusts hold the contract. 44 This revealed no further examples of vertical integration for our analysis. We also cross-checked our findings of vertically integrated practices with the Care Quality Commission register of general practices39 filtered by ‘location primary inspection category’ and ‘provider type/sector’.
Stage 2: finalisation of linked dataset
The second main stage in the identification process was to return to the annual reports of those trusts that had been found to be running general practices, to enable identification of practice level details including the individual practice code (the ‘organisation code’ which identifies any NHS organisation uniquely). The practice code is required to be able to link the study outcomes (described in Chapter 4) with the vertically integrated practices. We also needed to identify the practice name and the date that it became vertically integrated into a trust. Practices entering a vertical integration arrangement with a trust are undergoing an organisational change and may consequently have a change in their practice code. We found that there were sometimes practice mergers occurring around the time that practices became part of vertically integrated organisations. To help us track which preintegration practices had merged into which post-integration practices and when that happened, we took note of information about the sites (geographical locations) from which vertically integrated practices were working. A site becoming a location for a practice with a different practice code than previously, is an indication that the practice working from that site has merged with another. All this information gathering entailed hand-searching the annual reports of each of the vertically integrated trusts, starting with the 2020/21 annual report in each case and then working backwards preceding year by preceding year, noting all mentions of general practices and/or practice sites being vertically integrated (and whether they were merged at any point or left the vertically integrated organisation at any date) until the date of the first vertical integration event (the first general practice whose management was taken over by the trust).
Details on models of integration at the practice or trust level are not always stated clearly in trust annual reports, specifically the date when the change happens and what happens to the practice codes at that date. Where practice code, name and date of integration were not mentioned or were otherwise unclear in trust annual reports, the following detailed search process was followed in hierarchical order:
-
Visited individual practice websites and carried out online searching for date of entry into vertical integration; we then visited local and national media sources.
-
Used NHS Digital ‘GP and general practice related data’ sources for two separate years (2022 and 2016; 2022 was chosen as the first year to identify practice codes as it was the most up-to-date version available. We also used an archived version from 2016 as being around the start of vertical integration and would enable us to identify any practice codes which might since have changed due to mergers, closures and so on) to identify the practice code using the data files for both GP practices (epraccur) and branch surgeries (ebranchs). 43,45–47 The datasets include all general practices active in that year. We searched on practice name to match to practice code. Where there was uncertainty, practice address was used for confirmation of a match.
-
Contacted trust or practice contacts, where research team members had those, to ask for practice code and date of entry into vertical integration.
During our preliminary work we identified that horizontal integration (where general practices join with one or more practices) would be a methodological challenge for the quantitative analysis in our study. We therefore undertook a two-step approach to identifying where horizontal general practice mergers had taken place.
In step 1, we used person-level outpatient data from the Hospital Episode Statistics (HES), held under the BRACE data sharing agreement. We used data from the financial year April 2013/14 to the financial year April 2019/20 (i.e. April 2013–March 2020). In each year, we selected practices with at least 1000 patients and then identified practices in the following financial year where over 50% of patients from the previous financial year were now registered. For example, if 100 individual patients with the same practice code in the HES data for 1 year are again treated in hospital the following year but more than 50 of those patients all now have the same practice code, that is different from the practice code they had the previous year, then we may reasonably assume that the first practice has been merged into the second. We also looked in the data set from April 2018/19 for practices where the majority of patients were registered previously and cross-checked the practice codes from the two approaches.
In the second step, we used practice-level data on branch surgeries listed by the NHS Organisation Data Service via NHS Digital40 and matched current practice codes for branch surgeries with historic practice codes for practices at the same postcode (where a postcode was unique by practice) but which no longer had registered patients. This would indicate that a surgery that was previously the base for one practice has become a branch surgery for a practice based elsewhere and thus is likely to have merged with that practice.
Once we had identified the general practice codes before and after vertical integration of all practices integrated vertically with trusts, whether acute or community trusts (by our definition, as described in Chapter 1) we retrieved data on practice characteristics from general practice level data sources provided by NHS Digital at the national level. Further details are provided in the following ‘data and sources’ section. The datasets were extracted as raw CSV files from the primary source and imported into STATA® Se version 17 (StataCorp LP, College Station, TX, USA). The required variables from each of the data sources were then merged, matching on the practice code. The dataset we had created detailing vertically integrated trusts and their general practices was then merged into the practice characteristics dataset, again using the practice code as the identifier.
Data and sources
We constructed a cross-sectional dataset for March 2021 for all general practices in England and with all the relevant characteristics of the sites from which the vertically integrated practices operate, as follows.
-
Practice code – an organisation code that uniquely identifies each general practice in England.
-
VI – a binary variable which has a value of 1 if it is a vertically integrated NHS trust or general practice. Identified from the search process described earlier.
-
NHS trust type – NHS trusts are publicly owned organisations providing health care to NHS patients and are either NHS foundation trusts or NHS trusts. For the purposes of our work, we refer to them collectively as ‘trusts’. Trusts can take different forms: acute, community, mental health – and any combinations of those – or ambulance trusts. For the purposes of our study, we define an acute hospital trust is one providing acute hospital-based secondary health care, whether solely that or in combination with community and/or mental health services. An acute trust can have more than one acute hospital site within it. In March 2021, there were 230 trusts in England, with 144 of them being acute hospital trusts. 41 For our analysis, we split the trust type into a binary variable with a value of 1 if an acute hospital trust or a combined trust including acute hospital services, and a value of 0 if any other type of trust. For brevity we label this second category as ‘community trusts’, as explained in Chapter 1.
-
Date of vertical integration – This is the date that the first general practice was integrated with that trust. This is retrieved from the primary data source: the trust annual report or the general practice website.
-
Practice list size – This is defined as the number of patients who are registered at a general practice on the first day of each month. These data are nationally available at the practice level via the NHS Digital website. 48 For the purpose of this analysis, the list size data are retrieved for March 2021.
-
Contract type – general practice services are contracted by NHS commissioners (until July 2022, these bodies were known as CCGs; since July 2022, NHS commissioners are ICBs) following national guidelines for the practice to provide general medical services for the population registering with them, who are typically resident locally to the general practice’s premises. Most practices are run by at least two, and usually more, GPs alongside other health-care professionals such as practice nurses and physiotherapists who work within the same building. One or more of the GPs may own a stake in the practice business, although practices can also be owned by companies and via other ownership models. 8 Each practice holds an NHS contract to run the practice, of which there are three different types as described in Box 1 in Chapter 1: general medical services (GMS), personal medical services (PMS) and APMS. We obtained the contract type for each practice from NHS Digital ‘NHS Payments to General Practice’ for 2021/22. 49
-
GP workforce – We obtained the number of FTE GPs at the general practice level using NHS Digital data on GP workforce. 42 We also retrieved data on the number of GPs funded by ‘other’ as defined by NHS Digital (i.e. those GPs who are neither salaried, nor partners, trainees or locum practitioners). We did this in case GPs employed by trusts would be recorded in this category.
-
Quality and Outcomes Framework (QOF) score – Quality and outcomes indicators are agreed as part of the NHS GP contract negotiations every year. These indicators have points attached that are awarded according to how well general practices do against them, and so the QOF score is a proxy measure for the quality of the practice. We retrieved data on practice level QOF scores from NHS Digital,50 and specifically whether each practice achieved a QOF score within 25% of the total quality points achievable.
-
Index of Multiple Deprivation (IMD) code – The IMD is the official measure of relative deprivation for small areas in England based on seven different domains to produce an overall relative measure of deprivation. 51 It provides a rank from 1, which is the most deprived area to 32,844, the least deprived area. Using the ranks, decile 1 represents the most deprived 10% of areas nationally and at the other end of the scale, decile 10 represents the least deprived 10% of areas nationally. We report the percentage of practices in the most deprived decile as of March 2021. We obtain IMD codes for the postcode of each general practice in our dataset using the ‘English indices of deprivation’ 2019 online tool. 51
-
Rural or urban classification – We distinguish rural and urban areas, where the classification defines areas as rural if they fall outside of settlements with more than 10,000 resident population. 52 We retrieved data on the rural or urban classifier through the NHS Digital, ‘NHS Payments to General Practice for England dataset 2019/2020’,49 which we then linked to our practice level dataset using the practice code.
Findings
Number of vertically integrated general (medical) practitioner practices
As of March 2021, we identified 26 trusts in vertically integrated organisations, running a total of 85 general practices (i.e. with unique practice codes) across a total of 116 general practice sites (as some practices work from two or more locations). The locations of these vertically integrated practices are scattered across England (see Figure 3). There are concentrations of vertically integrated practices in several locations, but with no particular geographical pattern, although we note that there are few instances in London.
FIGURE 3.
Locations of vertically integrated general practices in England, March 2021.

We initially identified 26 vertically integrated trusts from financial year 2020/21 trust annual reports and a further 7 from the 2019/20 reports. Further in-depth checking of these 33 annual reports by a second researcher, confirmed that 7 of the total number of apparently vertically identified trusts from this search process were not in fact cases of vertical integration. The reasons why these trusts were incorrectly identified was most commonly because the trust was either in a joint working arrangement with a general practice or was using primary care premises for some trust activity. The final total number of vertically integrated trusts identified from the annual reports identified in Stage 1a of our analysis was thus 26.
Stage 1b confirmed many of the instances of vertical integration that we found by inspecting trust annual reports and did not reveal any additional instances. The resulting list of vertically integrated trusts and general practices included all of those that had been known to the members of the research team (which includes two researchers who had taken major roles in the phase 1 evaluation of vertical integration) prior to the analysis. This triangulation encourages confidence that the list of 26 vertically integrated trusts with 85 practices operating from 116 sites obtained from the search of trust annual reports is robust and reliable.
During the search process, it became evident that there is not a single criterion for identifying vertically integrated general practices, and that identification can prove complex, for example:
-
One general practice we identified is co-owned by both an acute and a community trust and is included in our dataset as owned by the acute trust only.
-
Five practices owned by acute hospitals and identified in this process were serving populations of homeless people or provided services for patients who are otherwise unable to access primary care and had been running in a similar structure for over 20 years. These practices are excluded from the analysis in this chapter.
There is also heterogeneity in the ownership arrangements for practices who become vertically integrated; for example, practices may undergo vertical integration at the same time as the acute or community trusts takes on the APMS contract. For some practices within a vertically integrated model, their GMS contracts are retained, although for some they are not. Ownership of practices can be taken on directly by the trusts or in some cases the trust sets up a wholly owned subsidiary company, which then owns the vertically integrated practices within the trust. However, the biggest challenge was in identifying the practice codes and the date of which the vertical integration of a practice took place (as detailed in the methods section).
Our preliminary scoping work revealed that general practices may undergo several stages of reorganisation as part of the vertical integration process, for example initially becoming a vertically integrated practice, and then undergoing horizontal mergers with other vertically integrated practices within the same trust. Although horizontal mergers have been a feature of primary care nationally, it has become evident that they are also a particular feature of vertically integrated general practices. The fact that practice codes within vertically integrated practices are particularly susceptible to change has meant that being able to reliably identify horizontal integration as well as vertical integration of primary care is an important methodological step for this evaluation (Appendix 1 provides further details of the process of identifying horizontal integration and the application to vertical integration of general practices into NHS trusts).
Linking to general practitioner practice characteristics
The next stage in constructing the dataset was to link it to data on general practice characteristics using NHS Digital GP primary care data sources as described in Chapter 2. Appendix 2, Table 23 provides a tabular overview of the linkage process in more detail.
The data set of vertically integrated practices initially contained 119 unique practice codes, 66 of these practices were run by acute hospital trusts and 53 were by community hospital trusts. Just 5 of the 119 practices were identified as homelessness practices or provided services for patients who are otherwise unable to access primary care. These practices were excluded from the analysis for WP1 because some had been established more than 20 years ago and all had been created specifically to serve those special populations. For the analysis in this chapter, we have used a cut off time point of March 2021. Thus, three further practices were excluded from the analysis in this WP, as their date of vertical integration took place after March 2021. Finally, a further 28 practices were excluded as they had either closed or merged with another practice before the cut-off point of end-March 2021 (2 of these 28 practices were homeless practices and thus had already been excluded). This gave us dataset of 85 general practices still operating as of March 2021 (see Table 2).
| Trusts/general practices | Trusts | General practices |
|---|---|---|
| Total (n) | 230 | 6576 |
| Of which vertically integrated, n (% of total) | 26 (11) | 85 (1) |
| Of which: | ||
| Acute hospital, n (% of all vertically integrated) | 15 (58) | 52 (61) |
| Community, n (% of all vertically integrated) | 11 (42) | 33 (39) |
The mean number of practices run by each trust was 3.3 (median 2.5; range 1–12) with community trusts (mean 3.0; median 2.0; range 1–8) running slightly fewer practices on average than acute trusts (mean 3.5; median 2; range 1–12). The largest group of practices was run by an acute trust, Yeovil District Hospital NHS Foundation Trust, which has a wholly owned subsidiary company called Symphony Healthcare that is responsible for running 12 general practices across the south-west of England. The second largest group of practices was also run by an acute trust: the Royal Wolverhampton NHS Trust, which manages 10 practices as part of the trust. By contrast, 11 of the vertically integrated trusts were each only running one practice (see Table 3).
| Trust | Practice sitesa | Unique practice codes (April 2021)a | Date first practice joinedb |
|---|---|---|---|
| Acute hospital trusts | |||
| Chesterfield Royal NHS Foundation Trust | 7 | 3 | May 2015 |
| Epsom and St Helier University Hospitals NHS Trust | 1 | 1 | October 2019 |
| Gateshead Health NHS Foundation Trust | 4 | 4 | January 2021 |
| Great Western Hospitals NHS Foundation Trust | 2 | 2 | November 2019 |
| Imperial College Health NHS Trust | 1 | 1 | July 2016 |
| Northumbria Healthcare NHS Foundation Trust | 9 | 8 | April 2015 |
| Royal Devon University Healthcare NHS Foundation Trust | 1 | 1 | January 2018 |
| Sandwell and West Birmingham Hospitals NHS Trust | 7 | 3 | May 2019 |
| Somerset Foundation NHS Trust | 3 | 3 | September 2016 |
| St Helens and Knowsley Teaching Hospitals NHS Trust | 1 | 1 | April 2020 |
| The Royal Wolverhampton NHS Trust | 11 | 10 | June 2016 |
| University Hospitals Birmingham NHS Foundation Trust | 1 | 1 | July 2020 |
| University Hospitals of Morecombe Bay NHS Foundation Trust | 1 | 1 | October 2016 |
| West Suffolk NHS Foundation Trust | 1 | 1 | June 2020 |
| Yeovil district hospital NHS Foundation Trust | 16 | 12 | April 2016 |
| Community trusts | |||
| Cheshire and Wirral Partnership NHS Foundation Trust | 4 | 3 | July 2015 |
| Derbyshire Community Health Services NHS Foundation Trust | 5 | 3 | May 2016 |
| Dudley Integrated Health and Care NHS Trust | 1 | 1 | April 2020 |
| East London NHS Foundation Trust | 5 | 2 | May 2013 |
| Humber Teaching NHS Foundation Trust | 9 | 8 | June 2015 |
| Lincolnshire Community Health Services NHS Trust | 3 | 2 | April 2019 |
| North Staffordshire Combined Healthcare NHS Foundation Trust | 2 | 1 | June 2018 |
| Sheffield Health and Social Care NHS Foundation Trust | 6 | 4 | June 2015 |
| Solent NHS Trust | 4 | 1 | October 2017 |
| Southern Health NHS Foundation Trust | 4 | 1 | April 2017 |
| Sussex Community NHS Trust | 7 | 7 | March 2019 |
| Totals (26 trusts) | 116 | 85 | |
Figure 4 plots the number of general practices by the date when they became vertically integrated. It shows that the first case of vertical integration between a trust and a general practice recorded in our dataset occurred in 2015.
FIGURE 4.
Date of vertical integration by number of general practices.
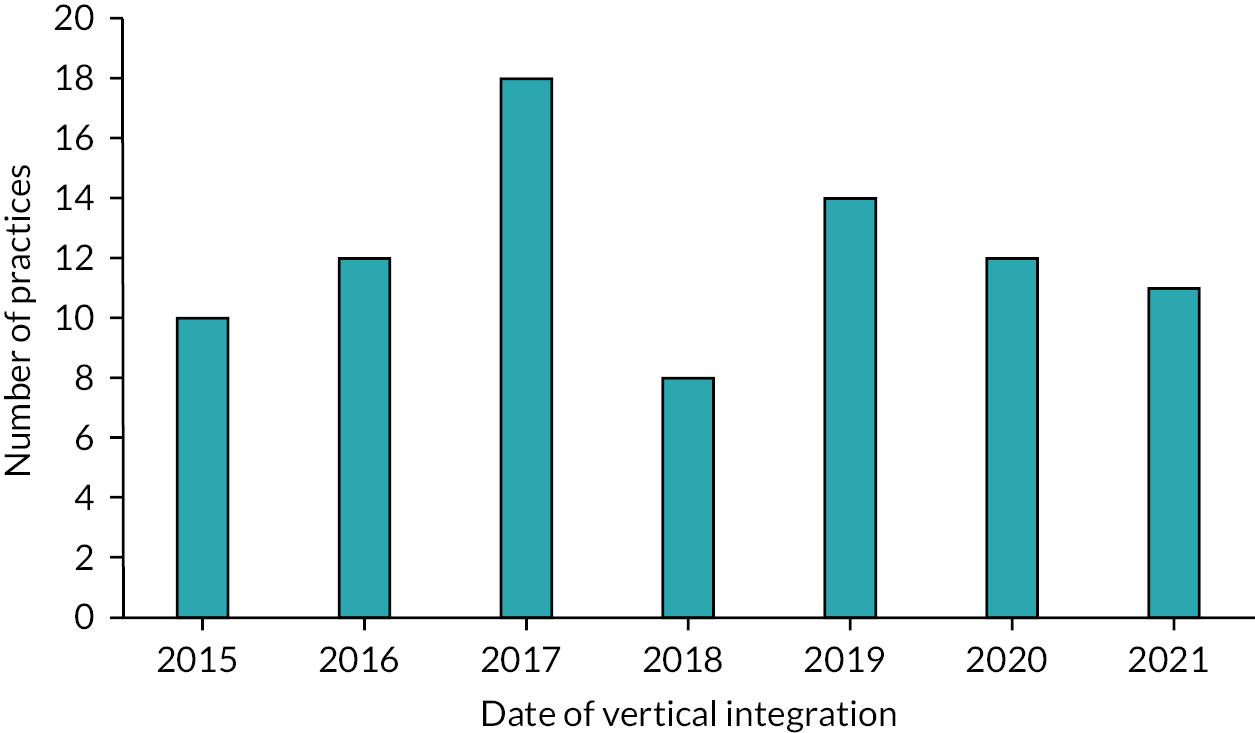
Table 4 reports descriptive statistics (as of March 2021) comparing vertically integrated with other general practices and disaggregating vertically integrated practices according to whether they are integrated with an acute or community trust. Overall, vertically integrated general practices are smaller than other practices on average, with a median list size of 6794 patients (mean 8902) at vertically integrated practices against a median list size of 8028 patients (mean 9245) at other practices. There is not much difference in size between practices integrated with acute trusts and those integrated with community trusts, although the latter are on average slightly larger in terms of median patient list sizes as of March 2021. The phase 1 study2 found that one reason (though by no means universal) for a general practice to become vertically integrated with an acute trust was due to a practice with one or two remaining GP partners (i.e. probably a smaller than average practice) finding it difficult to recruit new GPs when the existing GP(s) were contemplating retirement. This rationale is consistent with finding that vertically integrated practices are smaller than other practices on average.
| General practice characteristics | Category | Vertically integrated | Not vertically integrated | ||
|---|---|---|---|---|---|
| Total | Acute | Community | |||
| List size, median (IQR) | 6794 (5177–10,273) | 6647 (5390–10,430) | 6927 (4406–9,507) | 8028 (5195–11,734) | |
| IMD, n (% in most deprived decile)a | 16.4 | 11.5 | 24.2 | 15.2 | |
| Contract type, n (%)b | APMS | 12 (14.1) | 6 (11.5) | 6 (18.2) | 150 (2.3) |
| GMS | 50 (58.8) | 33 (63.5) | 17 (51.5) | 4567 (70.5) | |
| PMS | 23 (27.1) | 13 (25) | 10 (30.3) | 1763 (27.2) | |
| Rural/urban, n (%)c | Rural | 22 (27.5) | 18 (34.6) | 4 (14.3) | 1052 (16.6) |
| Urban | 58 (72.5) | 34 (65.4) | 24 (85.6) | 5302 (83.4) | |
| QOF (% achieving top 25% score)d | 58.90 | 63.50 | 51.59 | 75.80 | |
| GP FTEs, median (IQR)e | 3.6 (2–6) | 3.4 (2–5.5) | 3.8 (2–6.1) | 4.3 (2.3–7.2) | |
| GP FTEs employed in the practice on an ‘other’ contractf (%) | 21 | 25.40 | 15 | 2.50 | |
| Practices that have undergone a merger between 2013 and 2021 (%) | 24.4 | 20.7 | 30.3 | 23.1 | |
Table 4 shows that, in terms of social deprivation levels where they are located, vertically integrated practices are very slightly more likely to be in the most deprived decile when compared with non-vertically integrated practices (16–15% respectively). Disaggregating the vertically integrated practices further by acute and community trusts reveals that those located in community trusts are far more likely to be in deprived areas (24% compared with 11% for acute trusts).
Vertically integrated practices are more likely to have GMS than PMS or APMS contracts (see Box 1 in Chapter 1), but this pattern is weaker than among other practices. Vertically integrated practices are considerably more likely to be on APMS contracts than are other practices: only 2% of other practices have APMS contracts but 14% vertically integrated practices do. Practices integrated with community trusts are rather less likely to hold GMS contracts than do practices integrated with acute trusts.
A higher proportion of vertically integrated practices are in rural areas (26%) than is the case for other practices (16%) and this difference is entirely due to those practices that are integrated with acute trusts. This result is skewed by the vertically integrated trust with by far the most general practices being located in a rural area (Yeovil District Hospital NHS Foundation Trust, which ran 12 general practices by April 2021).
Three-quarters (75%) of practices that are not vertically integrated achieved a QOF score within 25% of the total quality points achievable. The performance of vertically integrated practices, as measured by QOF scores, was weaker: only 59% of the vertically integrated practices achieved QOF scores of at least 75% of the possible maximum. This result is further emphasised for practices that are integrated with community trusts, of which only 52% are achieving a QOF score within 25% of the maximum possible score. These findings are suggestive of practices with greater performance issues being more likely to be vertically integrated. The direction of causation is not known, but the phase 1 study2 noted that a rationale for practices to vertically integrate with an acute hospital was because the practice was struggling to keep going on its own.
In line with the finding that vertically integrated practices have, on average, smaller patient list sizes than other practices, Table 4 shows that vertically integrated practices also employ fewer GPs on average: a median of 3.6 compared with 4.3 in other practices. Average list size per FTE GP is similar in vertically integrated as compared with other practices. The numbers for acute and community trusts’ practices are very similar. We note that practices that are not vertically integrated employ just 2.5% of their GPs on ‘other’ arrangements (i.e. other than being salaried, partners, trainees or locum practitioners) but this proportion is considerably higher, at 21%, among vertically integrated practices. We made use of this difference when checking the robustness of our initial search for vertically integrated trusts and practices (see Stage 1b: validation via primary care GP workforce data and practice websites).
In summary, this is, to our knowledge, the first time that the extent of vertical integration of NHS trusts running general practices in England has been determined. We have developed and tested a robust and comprehensive method using a two-stage process. In doing so, we have identified that as of March 2021 there were 26 NHS trusts, running 85 general practices with 116 sites. We have been able to provide summary statistics about these practices, revealing that practices in vertically integrated organisations with NHS trusts are, compared with other practices in England: on average smaller with fewer GPs and fewer patients; less likely to be on GMS contracts; more likely than other practices to be on APMS contracts; and to have a higher proportion of their GPs on ‘other’ terms of employment than being partners, salaried, trainees or locum GPs.
Chapter 4 Work packages 2 and 3: quantitative analysis of the impact vertical integration has on primary care patient experience and use of secondary care services
Summary of key points
-
In this chapter, we present the methods and results for the quantitative part of the impact evaluation of vertical integration providing evidence to answer research questions 2 (What impact is vertical integration having on secondary care utilisation) and 3 (What impact is vertical integration having on the patient journey), also considering specifically the experiences of people living with multiple long-term conditions.
-
We contrast this impact with the impact of horizontal mergers between general practices and with the impact of switching to APMS contracts not associated with vertical integration.
-
We find that the impact of vertical integration on patient experience is small, with the exception of the effect on continuity. Horizontal mergers have minimal impact on patient experience while switching to an APMS contract is associated with slightly worsening patient experience for continuity, access and satisfaction.
-
Regarding the use of secondary care services, we find that vertical integration is associated with modest reductions in rates of A&E attendances (–2%), outpatient attendances (–1%), emergency admissions (–3%) and emergency readmissions (–5%) after it is introduced, with no impact on length of stay, overall inpatient admissions or inpatient admissions for ACSC. The falls in A&E and outpatient attendance rates are temporary, as the rates resume growing at faster rates than for practices that held GMS contracts throughout the study period.
-
We found little difference between the impact of vertical integration with acute hospital trusts and vertical integration with community trusts, although we note that in the 2 years following vertical integration outpatient attendances increase faster in practices that have merged with an acute hospital trust.
-
We find no evidence that the impact of vertical integration is differential for people living with multiple long-term health conditions compared with people with a single or no long-term health conditions.
Introduction
Evaluations of integrated care in the NHS over the past two decades that have considered the impact on hospital admissions and costs have rarely found the a priori expected result of fewer admissions and consequent cost savings. 53 Possible explanations for this are: that the particular model of integration evaluated was not designed to have that effect, or it may not have been well implemented (or scaled), or the evaluation itself may not have been methodologically rigorous. 54,55 In contrast, a quantitative impact evaluation of the introduction in Wolverhampton of vertical integration of general practices with an acute hospital found reductions in emergency hospital admissions and readmissions, and hence reduced hospital costs. 34 Building on these earlier analyses, and on earlier qualitative evaluation in three sites,2 this chapter describes our methodological approach to and findings from a national evaluation of vertical integration in England.
We test the logic2 for and impact of the introduction of vertical integration across the patient journey, including access to and satisfaction with primary care, outpatient attendances in secondary care, A&E attendances, and inpatient admissions, to understand where along the patient pathway impact might or might not occur. We include vertical integration sites from across England and consider the context of vertical integration, by comparing the impact of vertical integration with the impact of other types of contract changes or integration in primary care. We additionally compare the impact of vertical integration where general practices integrate with an acute hospital trust compared with where practices integrated with a community trust. This allows us to explore the impact of practices being integrated specifically with an acute hospital as distinct from integration with any type of trust, noting that all trusts have considerably larger financial resources than an individual general practice.
In our evaluation protocol,56 we identified several methodological questions that this rapid evaluation would need to answer to deliver a rigorous quantitative evaluation of vertical integration. These include how to code multimorbidity, how to define the most appropriate counterfactual, and how to incorporate the impact of COVID-19 in the analysis framework. Following this preliminary methodological work, and building on the work presented in the preceding chapter identifying the scale and scope of vertical integration across England, we use routine health-care data to answer the following research questions:
-
2: What impact is vertical integration having on secondary care utilisation (outpatient attendances, A&E attendances, all inpatient admissions, emergency inpatient admissions, inpatient admissions for ACSC, length of stay, readmission within 30 days of discharge)? Does this impact differ for people with multiple long-term conditions compared with other patients without long-term conditions or living with a single condition?
-
3: What impact is vertical integration having on the patient journey with regard to access to, and overall experience of, care? How does the experience differ for people with multiple long-term conditions compared with those living with no or one long-term condition?
Preliminary methodological work
In the protocol for this evaluation, we identified two main issues which would need resolving:
-
The coding of patients with multiple long-term conditions (i.e. multimorbidity) in secondary care data to allow us to answer the research questions about whether the impact of vertical integration differs for people with multiple long-term conditions compared with other patients without long-term conditions or living with a single such condition.
-
The most appropriate counterfactual approach to use in the impact evaluation.
We additionally identified that (horizontal) general practice mergers, and the impact of COVID-19 on the outcomes for this study (use of secondary care and patient experience), were further areas where additional methodological thinking would be required.
To develop approaches to address these questions we sense-checked our analysis plans with GPs, analysts, statisticians and other research teams, and carried out focused literature reviews to understand best analysis practice in the current policy context. The statistical analysis plan was developed in the light of the WP1 findings and was critically reviewed by an experienced health statistician. There was no change to the outcomes or to the overarching approach from that described in the protocol.
As a result, we have coded multimorbidity using Charlson score codelists shared by the NIHR Rapid Evaluation Service Team. 57 The Charlson score is a multimorbidity score which predicts the use of primary and secondary care and mortality. 58–61 In our analyses of HES, we considered people with one single condition included in the Charlson score or with two or more conditions.
Early evaluations described a large impact of COVID-19 on primary62 and secondary63 care activity. It would be very difficult currently to disentangle the impact of vertical integration from these changes. We therefore end our statistical analyses on 1 February 2020. The time period for this evaluation starts on 1 April 2013 (the earliest secondary care data held by the BRACE team).
We describe our preliminary work exploring general practice mergers in Report Supplementary Material 1 and describe how this had an impact on the choice of counterfactual in the following methods section.
Data and methods
This section provides details of the data and analysis for the evaluation of the quantitative impact of the introduction of vertical integration on primary care patient experience and use of secondary care services, and whether this impact is different for people living with multiple long-term health conditions. In the following paragraphs, we describe the two national data sources used: the GPPS and HES; including the particular measures of outcomes we have included and how they are coded for our analyses. Subsequent paragraphs describe our approach to selection of controls: that is the general practices we compare with those that have been vertically integrated with trusts. We describe how the existence of multiple long-term conditions for individual patients was coded for both data sources (GPPS and HES). Finally, we set out the descriptive and multivariable analysis framework for our quantitative evaluation, separately for patient experience and hospital utilisation, and explain how the analyses answer different parts of our research questions 2 and 3.
Data
General Practice Patient Survey
The GPPS is an annual survey on behalf of NHS England that is sent to patients in every general practice in the country. 64 The survey collects information on patient experience of access to care, continuity of care, communication with the practice, and overall patient satisfaction, together with data on patients’ sociodemographic characteristics and their long-term health conditions.
Hospital Episode Statistics
The HES is a database containing details of all inpatient admissions, A&E attendances and outpatient appointments at NHS hospitals in England. 65 These data are collected during an episode of clinical care in hospital and are then processed by NHS Digital, which releases data for secondary uses, including evaluation. In this evaluation, we use data from HES to explore the impact of vertical integration on the use of secondary care services by patients at vertically integrated and control practices.
Follow-up and inclusion criteria
For GPPS, we include data from the 10 most recent survey waves, from July 2011 to January 2021. For HES, we have data available from April 2013 and for our analysis have used them to February 2020 (i.e. stopping at the commencement of the COVID pandemic in the UK). In our vertical integration group (also the groups of practices which have undergone horizontal mergers and those which have swapped to an APMS contract), we include only practices that have data available to permit a full 2 years’ follow up before and after the date of the intervention. In other words, we analyse patient data only from practices with a date of vertical integration or other intervention (merging horizontally with another practice or commencing an APMS contract) occurring on or after 1 April 2015 and on or before 1 February 2018.
Data sharing
General Practice Patient Survey data were shared with the evaluation team (data held at the University of Cambridge) by NHS England under a data sharing agreement. HES data were shared with the evaluation team by NHS Digital (data held at RAND Europe) under a separate data sharing agreement.
Outcomes
General Practice Patient Survey
We included six measures of patient experience covering access, continuity and satisfaction with primary care across the patient journey. We selected all items that had consistent question wording across all 10 survey years. Likert response options from very good to very poor experiences were recoded as a continuous variable on a 0 (least positive) to 100 (most positive) scale, with non-evaluative responses coded as missing. Full question wording is presented in Table 5.
| Outcome | Full question wording |
|---|---|
| Helpfulness of receptionists | How helpful do you find the receptionists at your general practice? Very helpful, Fairly helpful, Not very helpful, Not at all helpful, Don’t know |
| Ability to get through on the phone | Generally, how easy is it to get through to someone at your general practice on the phone? Very easy, Fairly easy, Not very easy, Not at all easy, Haven’t tried |
| Time taken to see or speak to a GP | How long after initially trying to book the appointment did the appointment take place? On the same day, On the next day, A few days later, A week or more later, Can’t remember |
| Overall experience of access | Overall, how would you describe your experience of making an appointment? Very good, Fairly good, Neither good nor poor, Fairly poor, Very poor |
| Continuity | How often do you see or speak to your preferred GP when you would like to? Always or almost always, A lot of the time, Some of the time, Never or almost never, I have not tried |
| Overall satisfaction | Overall, how would you describe your experience of your general practice? Very good, Fairly good, Neither good nor poor, Fairly poor, Very poor |
Hospital Episode Statistics
We included seven measures of use of secondary care covering A&E attendances, inpatient admissions and outpatient attendances. Details of outcome coding are presented in Table 6.
| Outcome | Details |
|---|---|
| A&E attendances | All A&E attendances at all types of emergency care departments and providers were included. For financial year 2019/20 we used data from HES A&E data rather than the new ECDS data set, to maintain consistency across the whole analysis time frame. Multiple attendances on the same day were only included once |
| Outpatient attendances | Only outpatient appointments that were marked as having been attended were included |
| Inpatient admissions | Inpatient admissions are recorded in HES as a series of ‘finished consultant episodes’ (i.e. time spent under a particular consultant’s care). Sometimes a patient’s stay in hospital includes successive periods under the care of different consultants. We linked these episodes together to form single admissions using the University of York Centre for Health Economics Continuous Inpatient Spell definition. Because the person identifier for HES changed during the 2019/20 financial year, we used the mapping files provided by NHS Digital to allow for continuous inpatient spells that started in financial year 2018/19 but finished in 2019/20 (the date across files where the person identifier changed) to be correctly included |
| Inpatient admissions (with an ambulatory care sensitive condition) | Admissions were flagged if they were related to an ACSC based on the classification used by Bardsley et al.66 |
| Emergency inpatient admissions | Admissions were defined as emergency admissions based on the HES data classification |
| Emergency readmissions | We used the University of York Centre for Health Economics definition for readmissions within 30 days of discharge, and included only emergency coded admissions for this outcome |
| Length of stay | Length of stay, measured in days, was calculated for the continuous inpatient spells, and included based on the date of admission |
Intervention and control practices
In primary care, vertical integration is one of several new models that have developed and spread in the 2010s. Horizontal merger of primary care (general practice mergers) is a second model, where previously separate practices merge to work together in larger organisational units. Other new models include private ownership of primary care practices, either directly or through umbrella companies, and the use of APMS contracts. To evaluate the impact of vertical integration, and particularly in terms of identifying the most appropriate counterfactual, it is important to be able to distinguish the effects associated with vertical integration from these other changes in primary care in England that have occurred over the last decade. Our findings from WP1, identifying and describing where vertical integration is occurring, highlighted that vertical integration general practices across England are also more likely than other practices to have merged horizontally and are more likely to have APMS contracts.
An impact evaluation tries to understand whether what has happened in the intervention group after the intervention has occurred is different from what would have happened had the intervention not taken place. In randomised studies this is controlled by assigning intervention and control groups at random. However, in real world implementation of health-care service change (including vertical integration) this is not possible. Rather there is sequential roll-out and with selection into the intervention rather than random allocation. Consequently, thought is required to identify an appropriate control. For example, we know from the phase 1 evaluation of vertical integration that practices often struggled with staffing before switching to a vertical integration model,2 and this is the kind of context it is important to try to match on, but that is not possible in practice because information on the extent of difficulties with staffing is not routinely available.
Data driven matching (such as propensity score matching) and synthetic control approaches are two approaches to addressing this issue. They try to find the most similar set of controls for an intervention group that cannot be randomised, and for which no obvious control can be identified, and do this by matching the trends in the outcomes of interest in the time period before an intervention (in this study, the switch over of a general practice to a vertically integrated approach). Using synthetic controls67 can give different results compared with analyses of the same intervention using alternative (difference in difference) approaches. 68,69 Synthetic control approaches are designed to better match pre-intervention trends and have been found to be less biased in simulation analyses when some of the assumptions about changes in both the intervention group and the control group over time before the intervention takes place are not met. 70 A synthetic control approach was used in the analysis of vertical integration between an acute hospital trust and general practices in Wolverhampton, England. 34
We concluded that the use of matched control practices (such as propensity score matching or use of generalised synthetic controls) would not be feasible for this evaluation of the impact of vertical integration nationally, as these approaches depend on matching stable practices over time. By contrast, vertical integration practices are more likely than other practices to merge horizontally, or to switch to APMS contacts, and we wanted to be able to distinguish between all these changes explicitly in our analyses. We used publicly available annually reported data from NHS Digital to characterise changes in general practices’ contract types over time, taking the date of the first change during the study period as the date of the intervention. We identified general practice horizontal mergers for both vertically and non-vertically integrated practices through a two-stage approach, tracing the general practices of registered patients attending hospital outpatient services, where the practice codes of those patients subsequently disappeared. We additionally looked at the postcodes of practices that had closed, exploring whether their postcodes were linked to practices which are still open as branch surgeries, and identified these also as mergers (see Report Supplementary Material 1).
Hence, in all analyses we consider four different groups of general practices:
-
all vertical integration practices and additionally, separately:
-
practices vertically integrated with acute trusts
-
practices vertically integrated with community trusts
-
-
non-vertical integration practices that have undergone a horizontal merger
-
non-vertical integration practices that have changed to an APMS contract
-
GMS practices that have not changed contract, undergone a horizontal merger, or vertically integrated.
We therefore carried out three separate analyses for each outcome, describing the impact of vertical integration, of horizontal merger (without becoming vertically integrated and not switching to APMS contracts), and of switching to APMS contracts (but not undergoing horizontal merger or vertical integration) compared with a random sample of general practices with GMS contracts that did not change or merge at all during the study period using a difference in difference framework, adjusting for differences in pre-intervention trends as part of the modelling framework. Terminology varies slightly across disciplines: in our analysis the pre- and post-intervention slopes are modelled (rather than the assumption of parallel trends being tested) and this is sometimes alternatively known as a controlled interrupted time series approach.
We included an additional sensitivity analysis considering only vertical integration practices and compared the impact of the introduction of vertical integration with acute hospital trusts on the one hand with the introduction of vertical integration with community trusts on the other. This, by design, matches preintervention period in practices undergoing vertical integration, as only vertical integration practices are included, but allows the specific impact of integration with acute hospitals to be tested, compared with practices that have undergone vertical integration but with community trusts rather than acute hospital trusts.
The geographical distribution of included intervention and control practices are presented in Figure 5.
FIGURE 5.
All included vertical integration practices (X) and APMS controls (orange), stable GMS practices (light blue) and horizontally merged practices (green).
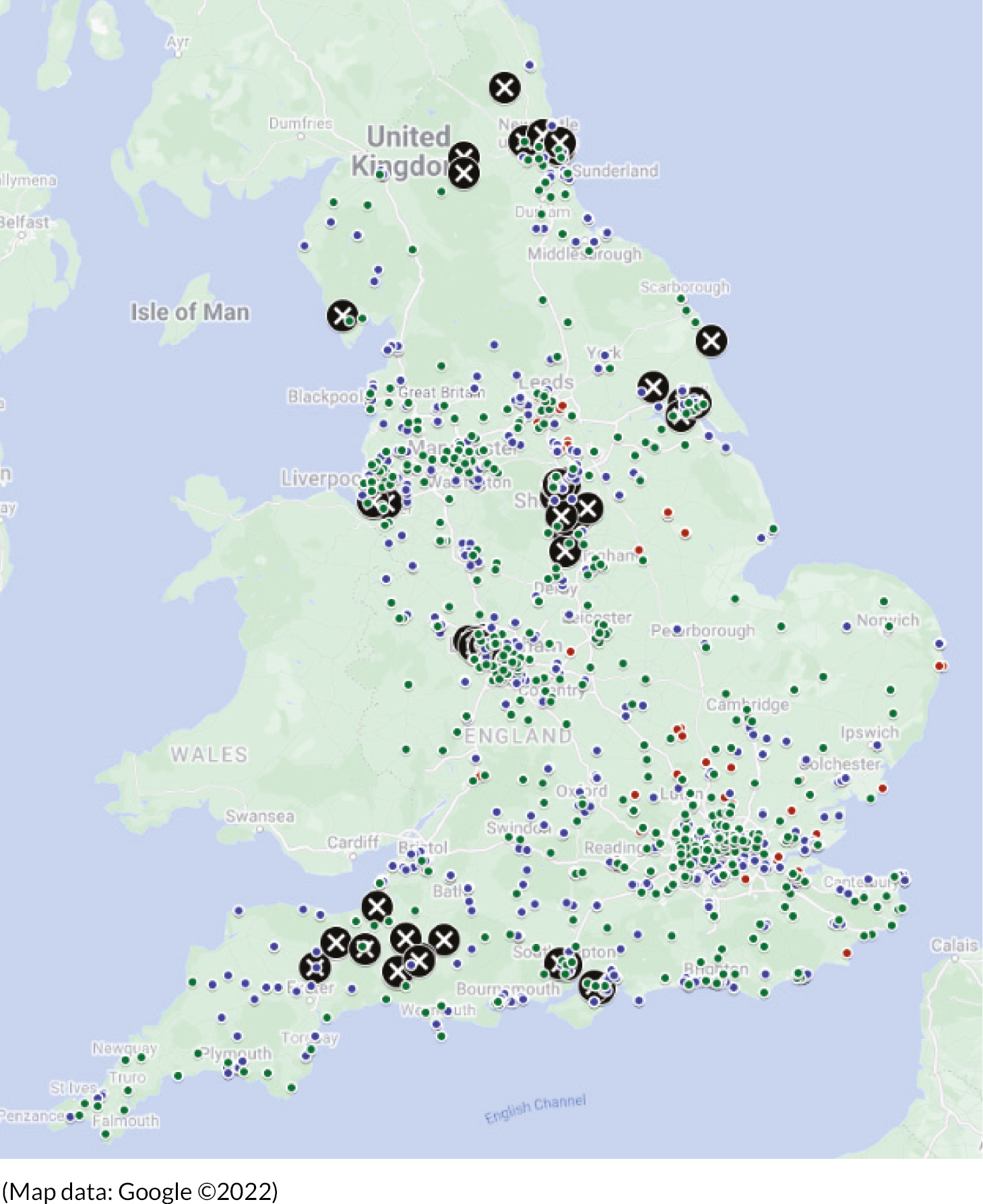
Multimorbidity
General Practice Patient Survey
We used responses to the question in the GPPS asking about long-term health conditions to define multimorbidity (2021 wording): ‘Which, if any, of the following long-term conditions do you have? Alzheimer’s disease or other cause of dementia, arthritis or ongoing problem with back or joints, autism or autism spectrum condition, blindness or partial sight, a breathing condition such as asthma or chronic obstructive pulmonary disease (COPD), cancer (diagnosis or treatment in the last 5 years), deafness or hearing loss, diabetes, a heart condition such as angina or atrial fibrillation, high blood pressure, kidney or liver disease, a learning disability, a mental health condition, a neurological condition such as epilepsy, a stroke (which affects your day-to-day life), another long-term condition or disability.’ Responses were added together coding people as having reported 0, 1, 2, 3 or 4 or more long-term conditions in response to the survey question, (this is consistent with the approach used in another rapid evaluation). 71 Question wording changed slightly across the time period of the survey. We applied the same coding of 0–4 or more conditions used across all years, (although the included conditions changed slightly over the years, this is negligible for the purposes of our analysis).
Hospital Episode Statistics
We coded 17 long-term health conditions included in the Charlson multimorbidity score using inpatient admission data from HES using the coding approach below (see Table 7). 72 We defined that a person was living with multimorbidity if they had two or more of these 17 long-term conditions recorded during an inpatient hospital admission while registered at any of the intervention or control practices at any time from 1 April 2013 to 31 March 2020. On this basis, 65% of all individuals with any hospital inpatient admission recorded in these practices had no long-term conditions recorded at any time, 18% had one, and 17% more than one (although this translated into more admissions among people living with long-term conditions).
| Condition | ICD-10 codes |
|---|---|
| Myocardial infarction | I21, I22, I252 |
| Congestive heart failure | I43, I50, I099, I110, I130, I132, I255, I420, I425, I426, I427, I428, I429, P290 |
| Peripheral vascular disease | I70, I71, I731, I738, I739, I771, I790, I792, K551, K558, K559, Z958, Z959 |
| Cerebrovascular disease | G45, G46, I60, I61, I62, I63, I64, I65, I66, I67, I68, I69, H340 |
| Dementia | F00, F01, F02, F03, G30, F051, G311 |
| Chronic pulmonary disease | J40, J41, J42, J43, J44, J45, J46, J47, J60, J61, J62, J63, J64, J65, J66, J67, I278, I279, J684, J701, J703 |
| Connective tissue disease-Rheumatic disease | M05, M32, M33, M34, M06, M315, M351, M353, M360 |
| Peptic ulcer disease | K25, K26, K27, K288 |
| Mild liver disease | B18, K73, K74, K700, K701, K702, K703, K709, K717, K713, K714, K715, K760, K762, K763, K764, K768, K769, Z944 |
| Diabetes without complications | E100, E101, E106, E108, E109, E110, E111, E116, E118, E119, E120, E121, E126, E128, E129, E130, E131, E136, E138, E139, E140, E141, E146, E148, E149 |
| Diabetes with complications | E102, E103, E104, E105, E107, E112, E113, E114, E115, E117, E122, E123, E124, E125, E127, E132, E133, E134, E135, E137, E142, E143, E144, E145, E147 |
| Paraplegia and hemiplegia | G81, G82, G041, G114, G801, G802, G830, G831, G832, G833, G834, G839 |
| Renal disease | N18, N19, N052, N053, N054, N055, N056, N057, N250, I120, I131, N032, N033, N034, N035, N036, N037, Z490, Z491, Z492, Z940, Z992 |
| Cancer | C00, C01, C02, C03, C04, C05, C06, C07, C08, C09, C10, C11, C12, C13, C14, C15, C16, C17, C18, C19, C20, C21, C22, C23, C24, C25, C26, C30, C31, C32, C33, C34, C37, C38, C39, C40, C41, C43, C45, C46, C47, C48, C49, C50, C51, C52, C53, C54, C55, C56, C57, C58, C60, C61, C62, C63, C64, C65, C66, C67, C68, C69, C70, C71, C72, C73, C74, C75, C76, C81, C82, C83, C84, C85, C88, C90, C91, C92, C93, C94, C95, C96, C97 |
| Moderate or severe liver disease | K704, K711, K721, K729, K765, K766, K767, I850, I859, I864, I982 |
| Metastatic carcinoma | C77, C78, C79, C80 |
| AIDS/HIV | B20, B21, B22, B24 |
Analysis framework
In this section, we describe our preliminary analysis work, the main analysis framework for all outcomes, and the analysis details separately for GPPS and HES.
Preliminary analysis
We carried out a series of preliminary analyses. In our first such analysis, we explored the trade-off between length of follow-up before and after the introduction of vertical integration, general practice mergers and contract changes, on the one hand, and the sample size of practices that would then be available for analysis, on the other. We found that during the study period 68 vertically integrated practice sites had at least 1 year of pre-intervention and 1 year of post-intervention follow-up, 59 sites had at least 1 year of pre-intervention and 2 years of post-intervention follow-up, 59 had at least 2 years of pre-intervention and 2 years of post-intervention follow-up and 29 sites had at least 2 years of pre-intervention and 3 years of post-intervention follow-up. The impact of vertical integration on patient experience and use of secondary care outcomes is not expected to be immediate, and an adequate follow-up period is required. In the final analysis, we included only practices with 2 complete years of follow-up before and after the switch to vertical integration, to horizontal merger or to an APMS contract in our intervention groups.
The date of vertical integration for each intervention practice was identified in WP1. The date of horizontal merger was defined as the first month in which either of two practices which had been identified as having merged had fewer than 1000 patients in their recorded list size. 73,74 Where more than one practice horizontally merged, we included the date of the first merger only as the date of the intervention. The date of a switch to an APMS contract was defined as 1 April of the year that the practice was first reported as having this contract type. 73,74 This length of follow-up using the HES data held by BRACE (from 1 April 2013) up to 1 February 2020 (the study period’s end being a month before any expected impact of COVID-19 on secondary care) meant that we included practices where the intervention had occurred between 1 April 2015 and 1 February 2018. Although patient experience data from 2021 were included in the final analysis framework (and so a potentially slightly longer period could have been included for patient experience outcomes), for consistency, the same set of practices were included in analyses for all outcomes.
In a second set of preliminary analyses, we explored the most appropriate modelling approach to include horizontally merged general practices. We originally explored using combined denominators (adding together list sizes from merged practices before and after the date of merger) but preliminary analyses identified that in the months around the date of a merger many merged practices either had temporarily high or low recorded list sizes as patient lists transferred across and may have been duplicated or disappeared for short periods. We additionally explored the use of historic codes in secondary care data and found that merged codes that disappeared from NHS Digital lists continued to appear in HES for some time, while gradually tailing off. This may reflect delays in hospital trusts’ patient details being updated. We therefore used denominators from a single fixed point in time for descriptive analyses of rates across all practices and did not use denominators in multivariable analysis. We assumed that the multilevel model with the random effect for merged practices and adjusting for overall secular trends, having identified where practices do merge, would account for the within-practice changes.
We initially considered and explored analytically three sets of multilevel models for the analysis framework: a random effect for the original practice code in all time points, for the merged practice code in all time points and including original codes nested within merged codes over time. In final analyses, we took the second approach: considering all practices that have undergone horizontal mergers, both practices in the vertical integration intervention group and practices in the horizontal merger intervention group, as if they were a single practice across the whole study time period. This choice was made because including only original codes gave potentially biased estimates; longitudinal follow-up for practices where the codes disappeared was incorrectly truncated in the analysis at the date of merger rather than included as part of the same organisation post merge. Including original codes nested within merged codes was computationally challenging and in preliminary analyses we were unable to get these models to converge. In addition, we could not follow up these previously merged codes post practice merger, and so the model would only add additional insight about within practice variation for the pre-intervention period.
In a final set of preliminary analyses, we explored the quality of secondary care data across the intervention time period, and visually inspected trends over time for any obvious data quality issues. For 19 practices (including three vertical integration practices) there were obvious errors, suggesting that trusts had in those cases been unable to code any use of a service to particular practice codes during periods of change (temporary codes are likely to have been used, but these are non-identifiable). We identified these 19 practices through initial descriptive and visualisation work, exploring trends in use over time. We excluded these practices from analyses for all HES outcomes, although they are included in the GPPS analysis. It is unlikely that these exclusions are completely at random, as data quality issues are likely to be more prevalent when a practice is undergoing organisational change. However, we believe that making these exclusions is the correct approach as otherwise use would be inappropriately measured as much lower in practices during periods when data quality issues were occurring. The limitation in our approach is that we are restricting the analysis to practices that have undergone organisational change and that do not have any issues with data quality.
Main analysis framework
In our first analysis, we describe the characteristics of people registered at intervention (vertical integration, horizontal merger and APMS) and control (stable GMS contracts) practices during the period before the intervention dates (March 2014–April 2015) using data from the GPPS. We describe survey reported age, gender, ethnicity, deprivation and multimorbidity for the groups of general practices included in the analysis:
-
all vertical integration practices, and separately
-
vertical integration community
-
vertical integration acute
-
-
merged (non-vertical integration) practices
-
APMS (non-vertical integration) practices
-
stable GMS practices (controls).
In our second set of analyses, we describe the median and the interquartile range (IQR) for each outcome (both patient experience and HES) across practices for the same six groups of practices during the same pre-intervention period (April 2014–April 2015).
In our third set of analyses, we describe unadjusted changes in the outcomes over time, for intervention practices during the two years before and after the date of the intervention for all vertical integration practices, horizontally merged non-vertically integrated practices and non-vertically integrated practices that switched to APMS contracts.
Analyses four and five are the main set of analyses that answer the parts of the research questions 2 and 3 about the quantitative impact of vertical integration on patient experience in primary care and use of secondary care. In our fourth set of analyses, we use a difference in difference framework in multivariable analysis, adjusting for age, gender, deprivation, calendar month and year, and using a separate categorical flag for each month to account for both secular trends and seasonal variation, a flag for whether practices were intervention or control practices and a flag (in intervention practices) for whether the time period included was before or after the date of the intervention. We adjusted separately for time (as a linear variable) before and after the date of the intervention in intervention practices to adjust for and characterise differences in pre-intervention trends in intervention practices compared with control practices. We additionally included a random effect for practice (merged practices included in a single group), and for outcomes from the use of secondary care, a random slope for the intervention, to allow the impact of the intervention to vary between practices, and a random slope for year to allow trends over time to vary between practices. We included the random slopes a priori in the modelling framework based on our expectation that there would be heterogeneity in the impact of vertical integration across practices and wanting to explicitly include this. The primary aim was not to optimise model fit; this is a modelling framework where we are interested in most appropriately estimating the impact of the intervention within integrated general practices, rather than developing a series of predictive models for the evaluation outcomes. In equation form, this model would be represented as follows:
where y is the outcome being predicted from the model, the β terms are the coefficients from the fixed portions of the model, and the u terms are the matrices for the random parts. In the same way that β0 is the intercept for the fixed part of the model, u0j is the random intercept (the random effect for practice); u1j x1ij + u2j x2ij are the two random slope terms, associated with coefficients β1 and β2. The other coefficients in the fixed part of the model do not have random slopes associated.
In the fifth analysis, a similar multivariable difference in difference analysis framework is used, but only vertical integration practices are included and practices that switch to a vertical integration model with an acute hospital trust are compared directly with practices that switch to a vertical integration model with a community trust. This analysis matches on all the processes and decisions that a practice might undergo before choosing a vertical integration model, and tests the specific impact of being part of an acute trust, while controlling for other factors such as the financial and workforce stability that comes with moving to a vertical integration model described in the phase 1 evaluation. 2 This analysis controls for measured and unmeasured confounding of factors that influence the decision to switch to a vertical integration model (as vertical integration practices are compared with each other) but only tests for the specific impact of integrating with an acute trust, rather than for the overall impact of vertical integration compared with not becoming vertically integrated with a trust.
Analysis six answers the parts of research questions 2 and 3 about the impact of vertical integration for people living with multiple long-term health conditions. In analysis six, we use the same difference in difference frameworks, but additionally explore whether the impact of vertical integration is differential for people living with multiple long-term health conditions, compared with people living with a single condition, or people without long-term health conditions. We do not consider horizontal mergers or practices that change to APMS contracts in this analysis. In the GPPS/patient experience analysis, we additionally include multimorbidity in the multivariable model using an interaction term with the intervention. This is a similar modelling framework to the framework described in detail for a BRACE rapid evaluation of the impact of telephone triage for people living with multiple long-term health conditions. 71 In the secondary care use analysis, because multimorbidity is defined from inpatient admission data across the whole study period, we only consider the outcomes that are coded from inpatient data. We have excluded the ACSC analysis because of co-linearity. Instead of an analysis that tests the differential impact of vertical integration among people living with multiple long-term conditions, we carried out a stratified analysis including only people with a single condition at any point during the study period (in both intervention and control practices) and then only people with multiple long-term conditions in two separate models. We compared these with the overall findings from the main impact analysis.
Specific analysis details
For the GPPS analyses of patient experience outcomes, we have used linear mixed models with each outcome coded on a 0–100 scale, so coefficients can be interpreted as a percentage point change in the outcome. We included all periods for both intervention and control practices in the analysis. We adjusted for survey reported age (in 10-year age groups), gender, deprivation (in five groups based on the postcode of survey responders) and ethnicity (in five groups).
For the analyses of secondary care outcomes using HES we initially grouped counts of all outcomes by age (in 10-year age groups), gender and deprivation (in five groups, based on the IMD coded in the data), and calendar month in a similar approach to earlier work. 75 Where a group (age, gender, deprivation and calendar month) had zero counts we included this zero count explicitly in the data set. We used Poisson models for all count outcomes and a linear model for length of inpatient stay. For intervention practices we only included the 2 years of follow-up before and after the intervention (i.e. a 4-year window) but for control practices we included all periods to allow adjustment for secular trends.
Sensitivity analyses
In a series of sensitivity analyses, we explored the impact of vertical integration in practices that integrated in Wolverhampton only. This enabled us to compare our results directly with those of the only other quantitative analysis so far published of an acute hospital trust running some general practices. 34
Statistical software
All data cleaning and analysis of GPPS data was carried out using Stata 15.1. Initial data processing for HES data was carried out using SQL (Microsoft Corporation, Redmond, WA, USA) in line with our data sharing agreement with NHS Digital, and processing of the secondary care outcomes was carried out using Stata 17.0. Multivariable models for all secondary care outcomes used SAS® 9.4 (SAS Institute Inc., Cary, NC, USA. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries. ® indicates USA registration).
Results
Included practices
Building on the work from WP1, we present the numbers in England of vertical integration practices, horizontally merged practices and practices that switch to an APMS contract in Table 8; the final numbers of practices included in our analyses are then shown in Table 9. After excluding practices with shorter follow up than the required 2 years before and after the date of vertical integration, we are left in the final analysis with 59 practices (becoming 42 merged practices by February 2020) that had switched to a vertical integration approach; 33 vertically integrated with acute hospital trusts and 26 with community trusts. Correspondingly, we included 42 practices that switched to an APMS contract and 964 practices that merged horizontally (becoming 331 merged practices by the end of the study).
| All | Stable GMS contracts | Vertical integration | Vertical integration acute | Vertical integration community | APMS | Merge horizontally | |
|---|---|---|---|---|---|---|---|
| Practices (n) | 8046 | 3272 | 119 | 66 | 53 | 352 | 1861 |
| Practice merged groups (n) | 6969 | 3272 | 92 | 54 | 38 | 324 | 784 |
| Practice codes in February 2020a (n) | 6727 | 3272 | 91 | 54 | 37 | 216 | 787 |
| Trusts (n) | 26 | 15 | 11 | ||||
| Practice months (n) | 608,808 | 268,222 | 8520 | 4919 | 3601 | 24,350 | 109,719 |
| Switch to vertical integration | Switch to vertical integration acute | Switch to vertical integration community | Switch to APMS | Merge horizontally | |
|---|---|---|---|---|---|
| Practices (n) | 59 | 33 | 26 | 42 | 964 |
| Included practice codes in February 2020, n (multivariable analysis sample) | 42 (39)a | 26 (25)a | 16 (14)a | 35 | 331 |
| Trusts | 15 | 8 | 7 | ||
| Practice months (n) | 4020 | 2449 | 1571 | 3195 | 56,541 |
Analysis 1 – characteristics of patients at vertically integrated, horizontally merged, alternative provider medical services and control practices
In analysis 1, we describe the characteristics of patients at vertically integrated and non-vertically integrated practices using survey data from GPPS. In the same way as for our findings in WP1, patients at vertical integration practices (particularly practices vertically integrated with community trusts) are more likely to be living in the most deprived parts of the country. Levels of multimorbidity are similar across all intervention and control practices (see Table 10).
| Characteristic | Vertical integration practices (all) (N = 5368) |
Vertical integration (Community trusts) (N = 2085) |
Vertical integration (Acute trusts) (N = 3283) |
Horizontally merged general practices (N = 78,748) |
APMS practices (N = 6301) |
‘Stable’ practices with GMS contracts (N = 48,818) |
|---|---|---|---|---|---|---|
| Age (years), n (%) | ||||||
| 18–24 | 208 (9.8) | 94 (12.9) | 114 (8.2) | 2713 (9.1) | 252 (10.8) | 1767 (9.9) |
| 25–34 | 430 (15.1) | 179 (15.9) | 251 (14.8) | 6256 (16.8) | 617 (18.2) | 3734 (15.5) |
| 35–44 | 566 (16.2) | 239 (15.9) | 327 (16.3) | 8712 (16.9) | 821 (17.6) | 5223 (15.8) |
| 45–54 | 836 (17.8) | 339 (17.6) | 497 (17.8) | 13,016 (18.6) | 1015 (17.6) | 8185 (18.9) |
| 55–64 | 1104 (16.0) | 390 (14.0) | 714 (17.0) | 16,250 (15.4) | 1210 (13.5) | 10,083 (15.7) |
| 65–74 | 1207 (13.7) | 450 (12.9) | 757 (14.1) | 17,645 (12.7) | 1349 (12.4) | 10,985 (13.2) |
| 75–84 | 769 (8.3) | 298 (7.8) | 471 (8.5) | 10,768 (7.6) | 766 (6.8) | 6739 (7.9) |
| 85+ | 248 (3.2) | 96 (3.1) | 152 (3.3) | 3388 (3.1) | 271 (3.1) | 2102 (3.1) |
| Gender, n (%) | ||||||
| Female | 3036 (51.3) | 1158 (50.3) | 1878 (51.8) | 44,340 (50.6) | 3525 (51.0) | 27,625 (51.2) |
| Male | 2332 (48.7) | 927 (49.7) | 1405 (48.2) | 34,408 (49.4) | 2776 (49.0) | 21,193 (48.8) |
| Ethnicity,a n (%) | ||||||
| White | 4997 (90.7) | 1903 (87.4) | 3094 (92.4) | 70,393 (88.1) | 5372 (86.0) | 43,934 (89.4) |
| Mixed | 29 (0.7) | 8 (0.4) | 21 (0.9) | 517 (0.9) | 54 (0.9) | 350 (0.9) |
| Asian | 170 (4.3) | 87 (6.3) | 83 (3.2) | 3892 (5.3) | 377 (5.7) | 2266 (4.9) |
| Black | 66 (1.8) | 33 (2.6) | 33 (1.4) | 1728 (2.5) | 258 (3.8) | 991 (1.9) |
| Other | 106 (2.6) | 54 (3.3) | 52 (2.2) | 2218 (3.3) | 240 (3.7) | 1277 (2.9) |
| Deprivation, n (%) | ||||||
| Least deprived | 790 (12.7) | 294 (12.0) | 496 (13.1) | 13,321 (18.0) | 1074 (17.9) | 10,270 (21.9) |
| 4 | 1267 (22.4) | 371 (19.1) | 896 (24.2) | 15,430 (18.9) | 738 (14.6) | 10,200 (19.4) |
| 3 | 1059 (18.9) | 345 (13.9) | 714 (21.5) | 17,193 (20.6) | 1335 (20.7) | 10,326 (20.6) |
| 2 | 1042 (21.4) | 434 (23.1) | 608 (20.5) | 16,459 (20.7) | 1345 (25.3) | 9364 (19.6) |
| Most deprived | 1210 (24.6) | 641 (31.9) | 569 (20.7) | 16,345 (21.9) | 1809 (21.6) | 8658 (18.5) |
| Long-term health conditions, n (%) | ||||||
| 0 | 1911 (45.5) | 730 (45.5) | 1181 (45.5) | 29,561 (48.6) | 2378 (49.2) | 18,760 (48.8) |
| 1 | 1775 (30.9) | 690 (32.1) | 1085 (30.3) | 26,024 (30.5) | 2046 (30.1) | 16,172 (30.4) |
| 2 | 989 (14.0) | 374 (12.8) | 615 (14.6) | 13,657 (12.7) | 1048 (11.9) | 8288 (12.8) |
| 3 | 446 (6.2) | 184 (6.2) | 262 (6.2) | 5979 (5.2) | 518 (5.7) | 3585 (5.1) |
| 247 (3.3) | 107 (3.3) | 140 (3.4) | 3527 (3.0) | 311 (3.1) | 2013 (2.8) | |
Analysis 2 – evaluation outcomes during the year April 2014–March 2015 (pre-intervention in all practices)
In our second set of analyses, we described the patient experience and outcomes from the use of secondary care services during the pre-intervention period in all groups of practices (see Table 11). Patient experience outcomes (particularly continuity) were lowest in practices that went on to become vertically integrated with community trusts or switched to APMS contracts, and highest in control and horizontally merged practices. A&E attendance rates were highest in practices that went on to be vertically integrated with community trusts but similar across all other groups of practices. Outpatient attendance rates and inpatient admission rates were lowest in practices that switched to APMS contracts but were similar across all other types of practices.
| Outcome | Vertical integration practices (all) (N = 39) |
Vertical integration (community trusts) (N = 14) |
Vertical integration (acute trusts) (N = 25) |
Horizontally merged general practices (N = 331) |
APMS practices (N = 35) |
‘Stable’ practices with GMS contracts (N = 492) |
|---|---|---|---|---|---|---|
| Patient experience; responses, n (mean on a 0–100 scale) | ||||||
| Helpfulness of receptionists | 5342 (79.7) | 2075 (78.0) | 3267 (80.6) | 78,379 (81.4) | 6274 (79.0) | 48,578 (81.1) |
| Ability to get through on the telephone | 5344 (67.0) | 2077 (64.6) | 3267 (68.2) | 78,436 (70.6) | 6283 (67.7) | 48,615 (69.2) |
| Time taken to see or speak to a GP | 4306 (56.7) | 1634 (54.2) | 2672 (58.0) | 63,713 (56.0) | 4855 (54.0) | 39,774 (56.8) |
| Overall experience of access | 5130 (69.8) | 1999 (66.9) | 3131 (71.4) | 75,710 (73.2) | 6029 (68.7) | 46,910 (72.7) |
| Continuity | 2700 (60.9) | 966 (54.9) | 1734 (63.8) | 40,123 (63.5) | 2702 (60.4) | 27,115 (64.6) |
| Overall satisfaction | 5311 (78.3) | 2062 (76.6) | 3249 (79.3) | 78,032 (80.5) | 6251 (76.4) | 48,404 (80.7) |
| Use of secondary care; rate per person per year median (IQR across practices in each group) | ||||||
| A&E attendances | 0.31 (0.26–0.39) | 0.33 (0.29–0.40) | 0.30 (0.25–0.39) | 0.31 (0.26–0.36) | 0.31 (0.24–0.38) | 0.29 (0.24–0.36) |
| Outpatient attendances | 1.27 (1.15–1.59) | 1.24 (1.15–1.58) | 1.32 (1.15–1.59) | 1.28 (1.14–1.47) | 1.18 (1.06–1.40) | 1.27 (1.12–1.47) |
| Inpatient admissions | 0.29 (0.26–0.31) | 0.29 (0.25–0.31) | 0.29 (0.28–0.32) | 0.27 (0.23–0.30) | 0.24 (0.22–0.30) | 0.26 (0.22–0.29) |
| Inpatient admissions (ACSC) | 0.03 (0.02–0.04) | 0.03 (0.02–0.04) | 0.03 (0.02–0.04) | 0.03 (0.02–0.03) | 0.02 (0.02–0.03) | 0.02 (0.02–0.03) |
| Emergency admissions | 0.09 (0.08–0.11) | 0.10 (0.08–0.11) | 0.09 (0.09–0.12) | 0.08 (0.07–0.10) | 0.08 (0.06–0.10) | 0.08 (0.07–0.10) |
| Emergency readmissions (per 100 people per year) | 1.82 (1.50–2.63) | 1.96 (1.39–2.76) | 1.78 (1.69–2.41) | 1.74 (1.43–2.14) | 1.52 (1.22–2.24) | 1.70 (1.33–2.07) |
| Length of stay; mean days per admission median (IQR across practices in each group) | ||||||
| Length of stay | 2.84 (2.62–3.21) | 2.78 (2.46–3.39) | 2.84 (2.69–3.21) | 2.87 (2.51–3.19) | 2.69 (2.16–3.04) | 2.94 (2.57–3.35) |
Analysis 3 – unadjusted changes over time before and after the intervention in practices that vertically integrate, practices that merge horizontally, and practices that switch to alternative provider medical services contracts
For the unadjusted (descriptive) analyses of patient experience in the 2 years before and after the date of the general practice changes in, outcomes declined for all groups in a manner that was consistent with national trends. 76 In general, consistent with the pre-intervention period, patient experience was lowest both before and after the change, in those practices that switched to APMS contracts (see Figures 6–11). No outcome showed a large step change after the vertical integration, horizontal merger or switch to an APMS contract by the practice.
FIGURE 6.
Helpfulness of receptionists.
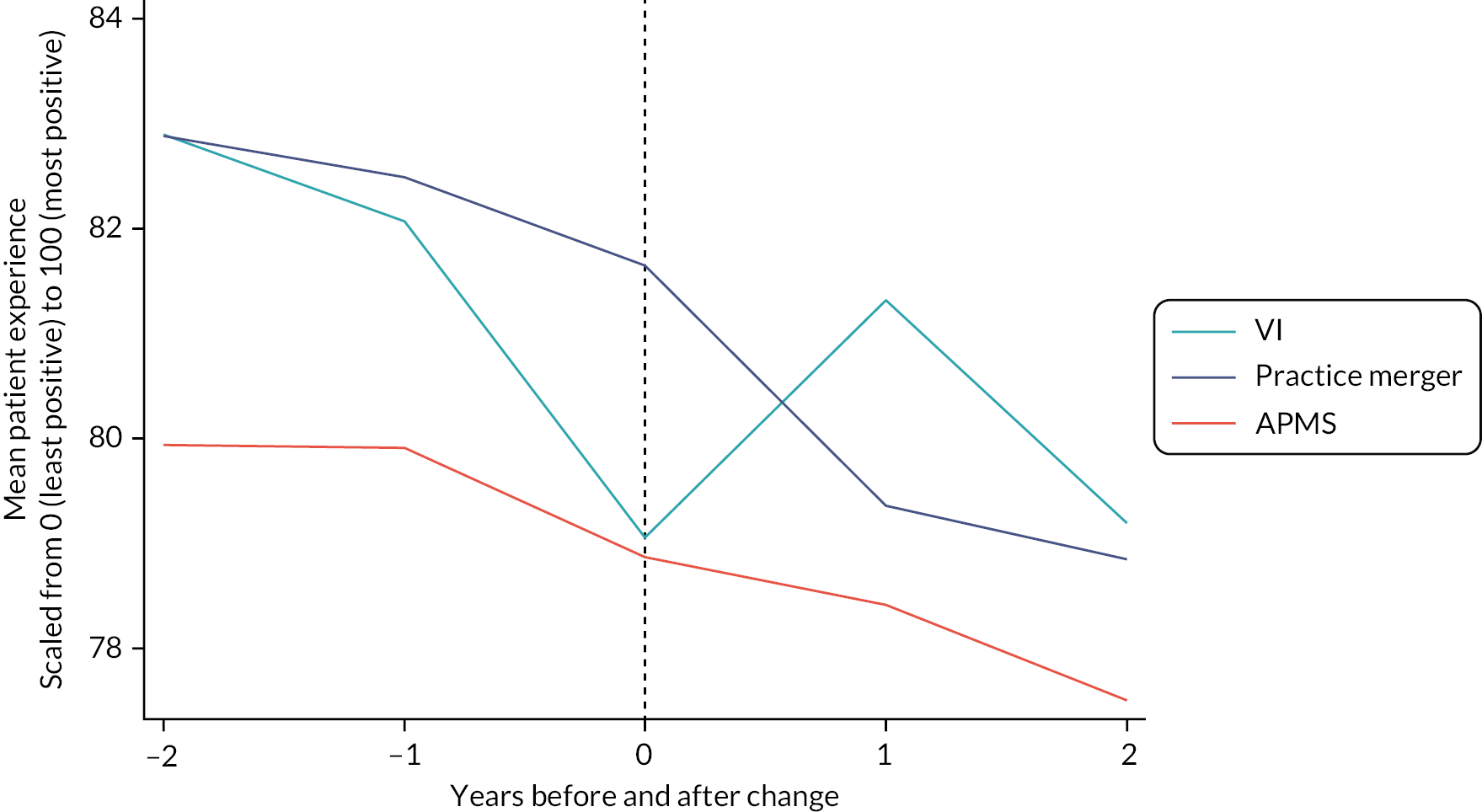
FIGURE 7.
Ability to get through on the phone.
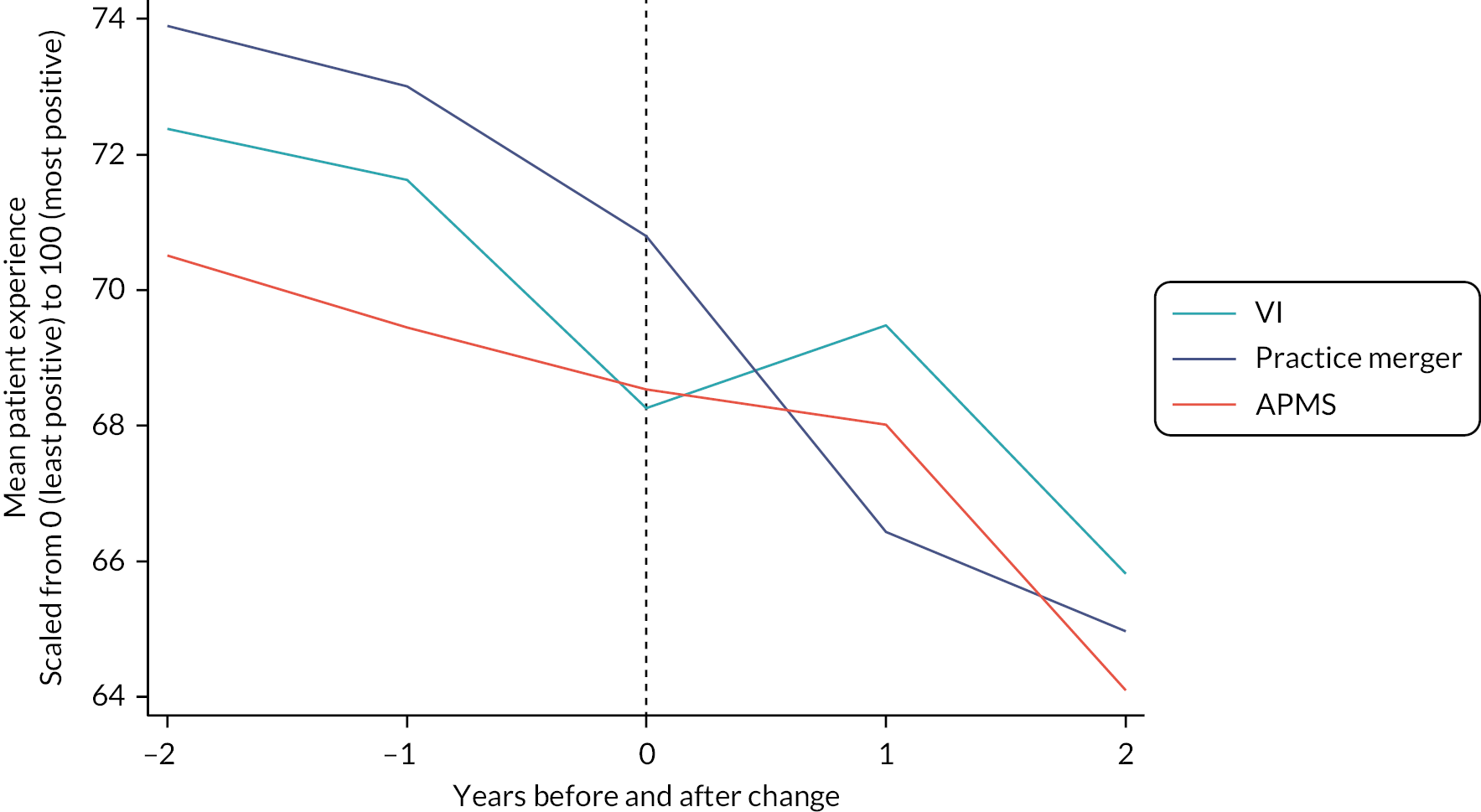
FIGURE 8.
Time taken to see or speak to a GP.
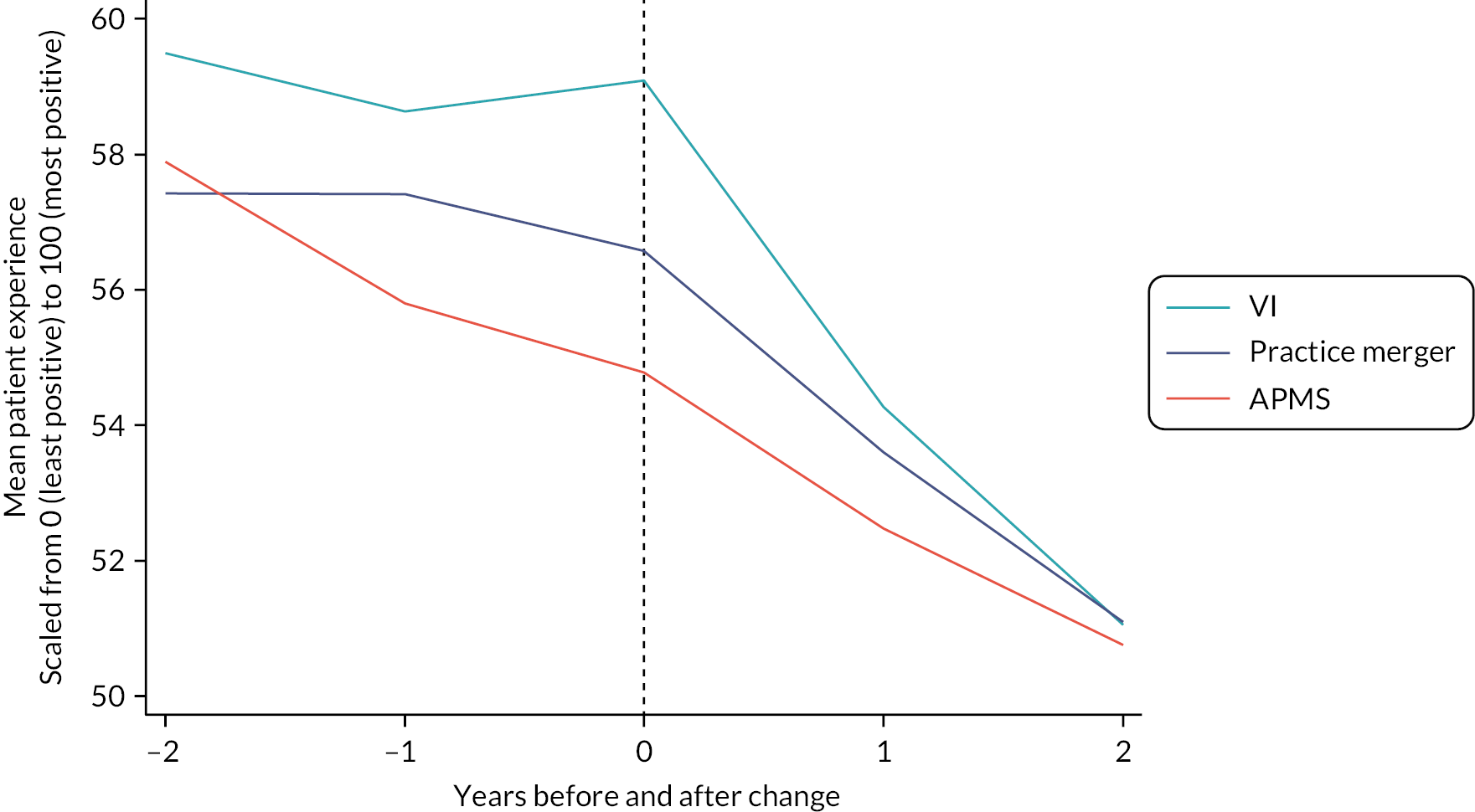
FIGURE 9.
Overall experience of access.
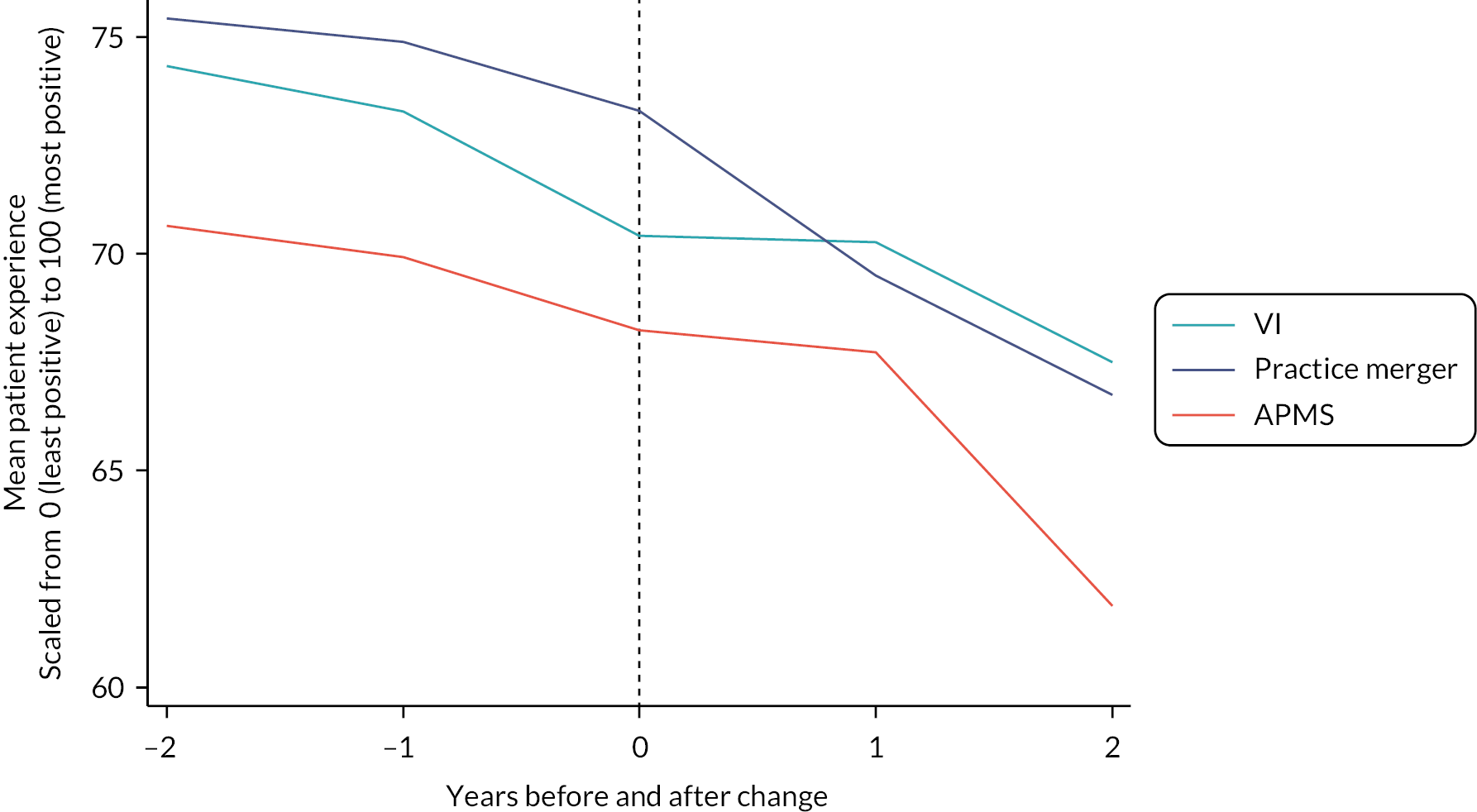
FIGURE 10.
Continuity.
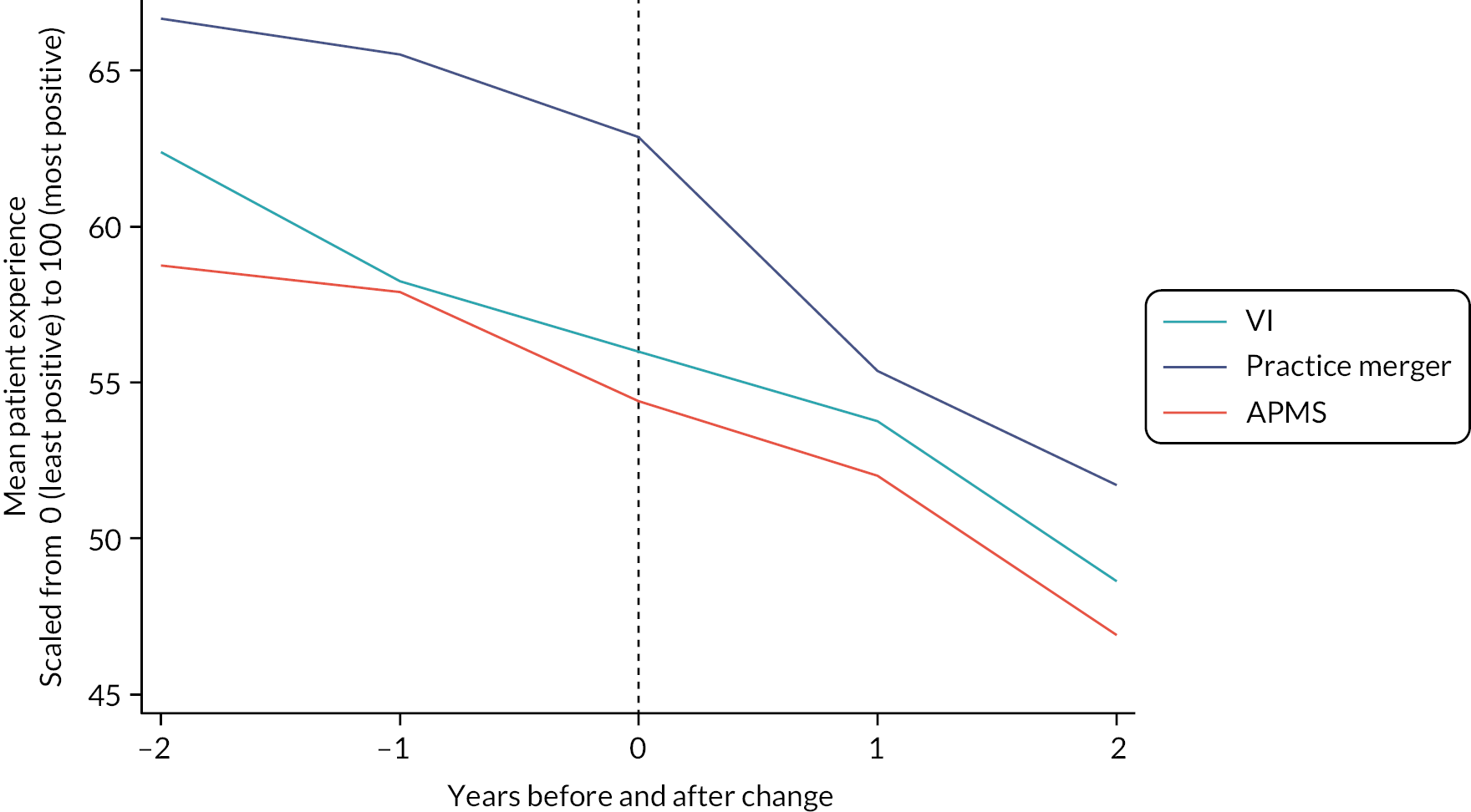
FIGURE 11.
Overall satisfaction.

For the seven secondary care utilisation outcomes (see Figures 12–18) differences between the three intervention groups were least for length of stay in hospital (see Figure 18) and greatest for rates of emergency inpatient admissions (see Figure 16) and A&E attendances (see Figure 12). For no outcome was there a ‘step change’ after the date of the intervention. Secondary care utilisation before and after the intervention was highest among vertical integration practices and lowest among practices that underwent horizontal mergers.
FIGURE 12.
Accident and emergency (department) attendances.
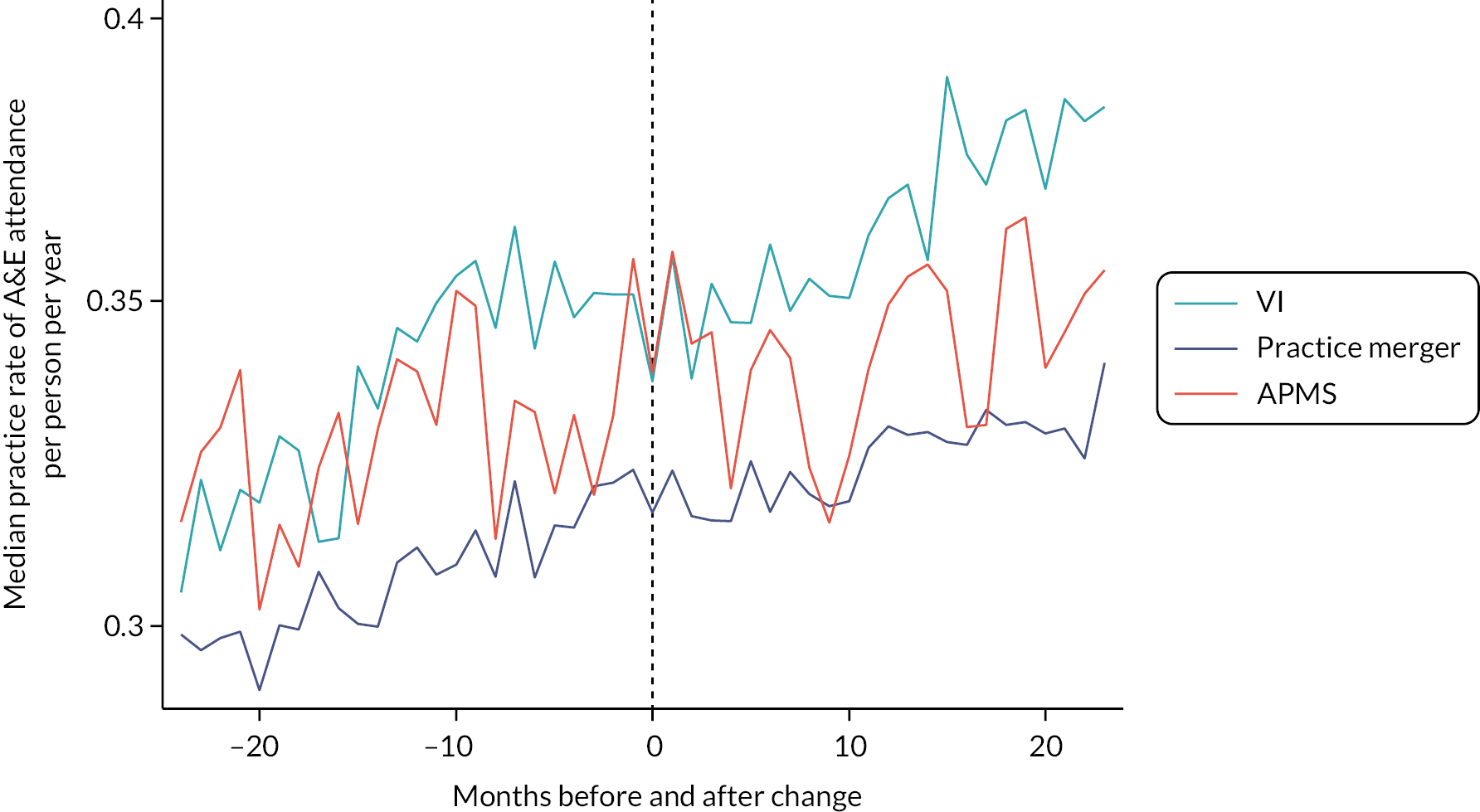
FIGURE 13.
Outpatient attendances.
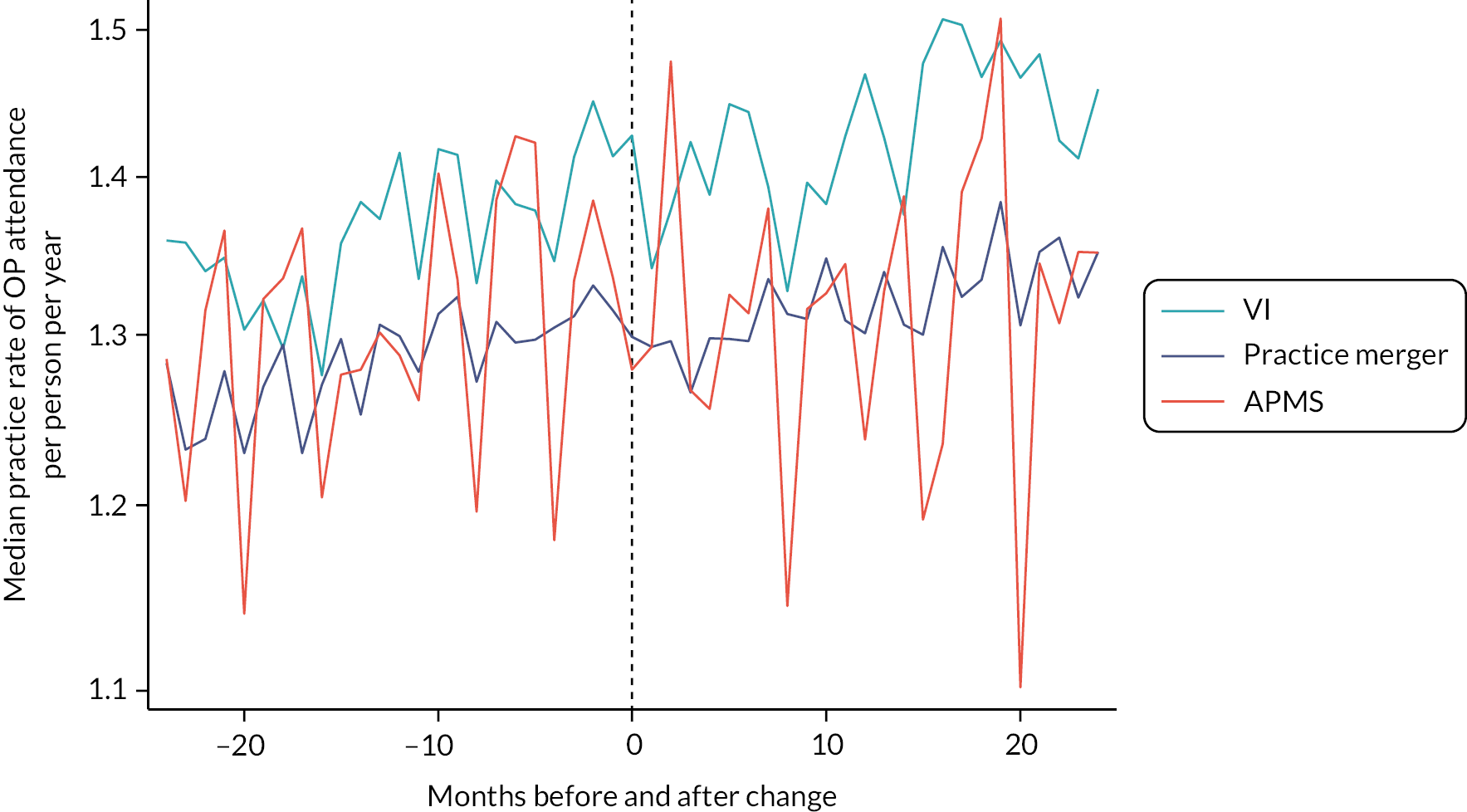
FIGURE 14.
Inpatient admissions.
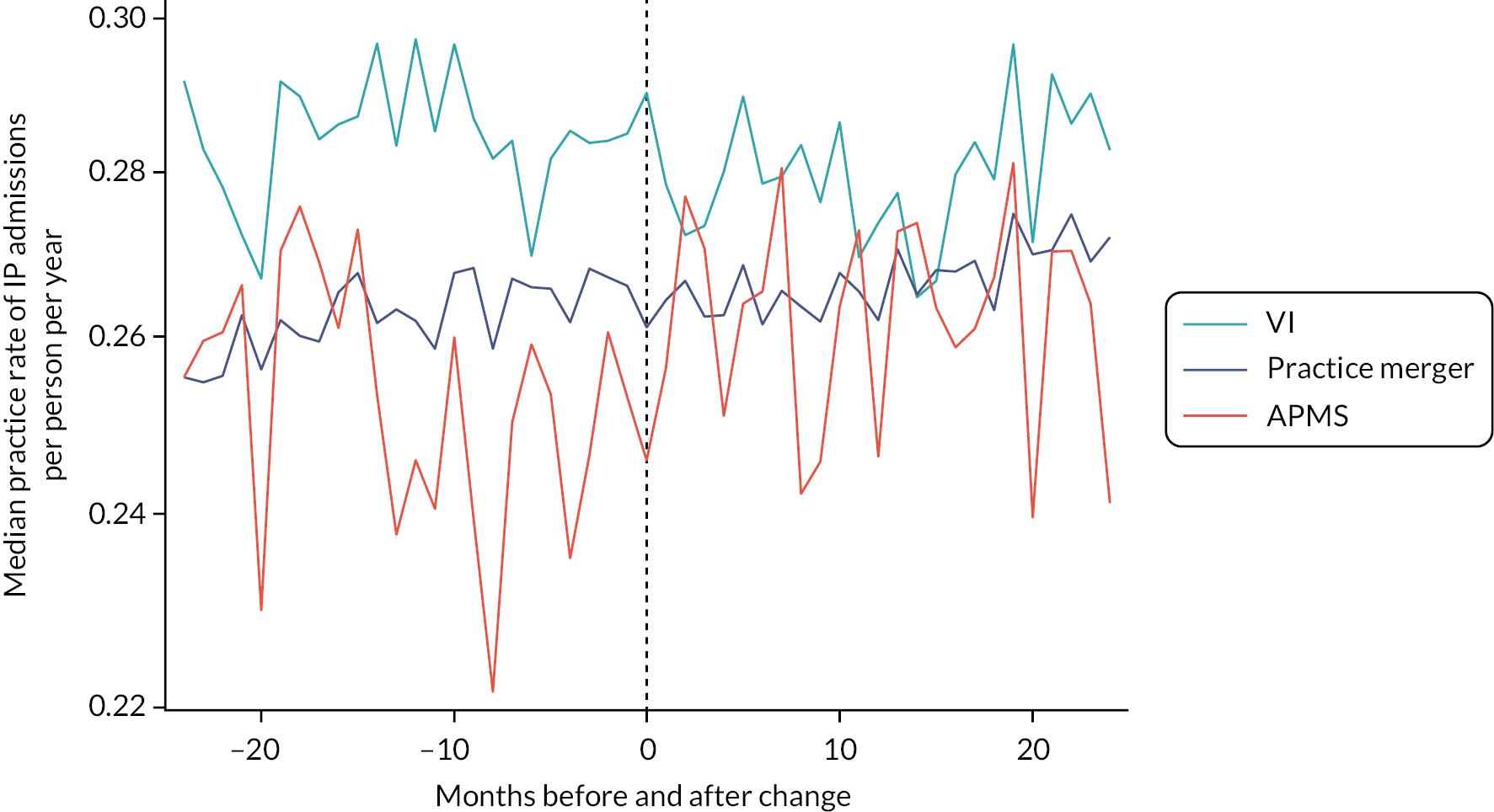
FIGURE 15.
Inpatient admissions for ACSC.
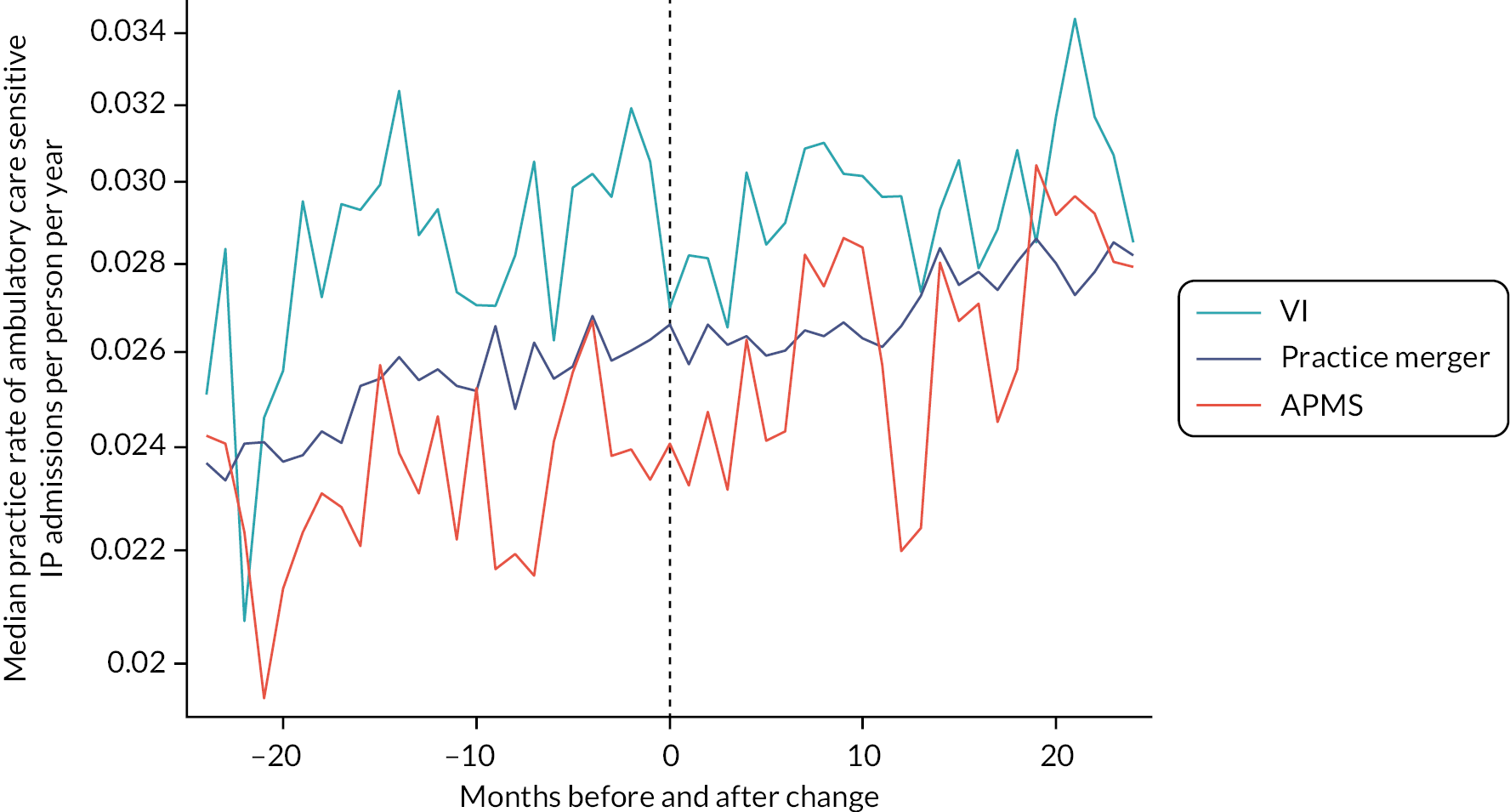
FIGURE 16.
Emergency inpatient admissions.
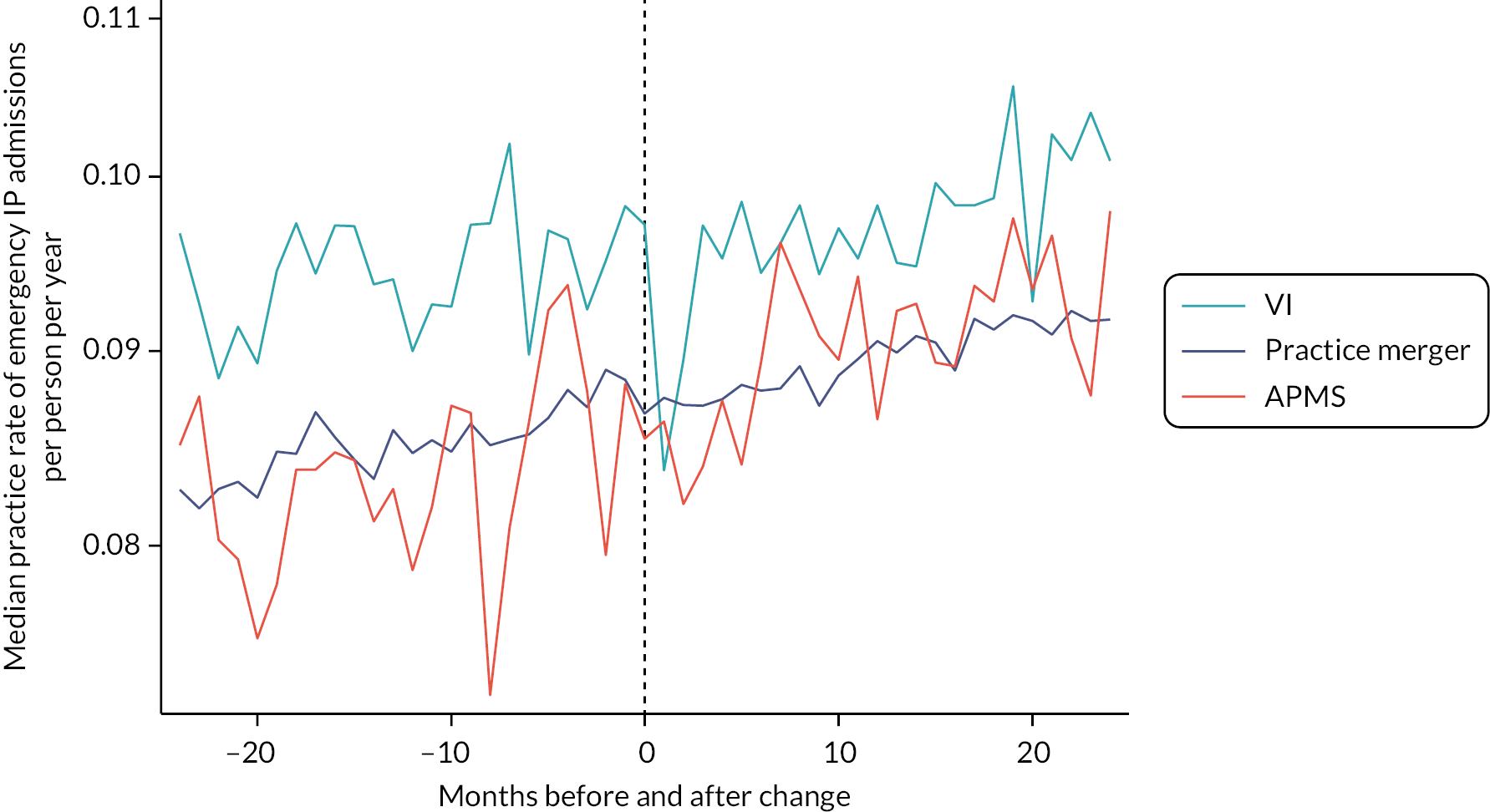
FIGURE 17.
Emergency inpatient readmissions.
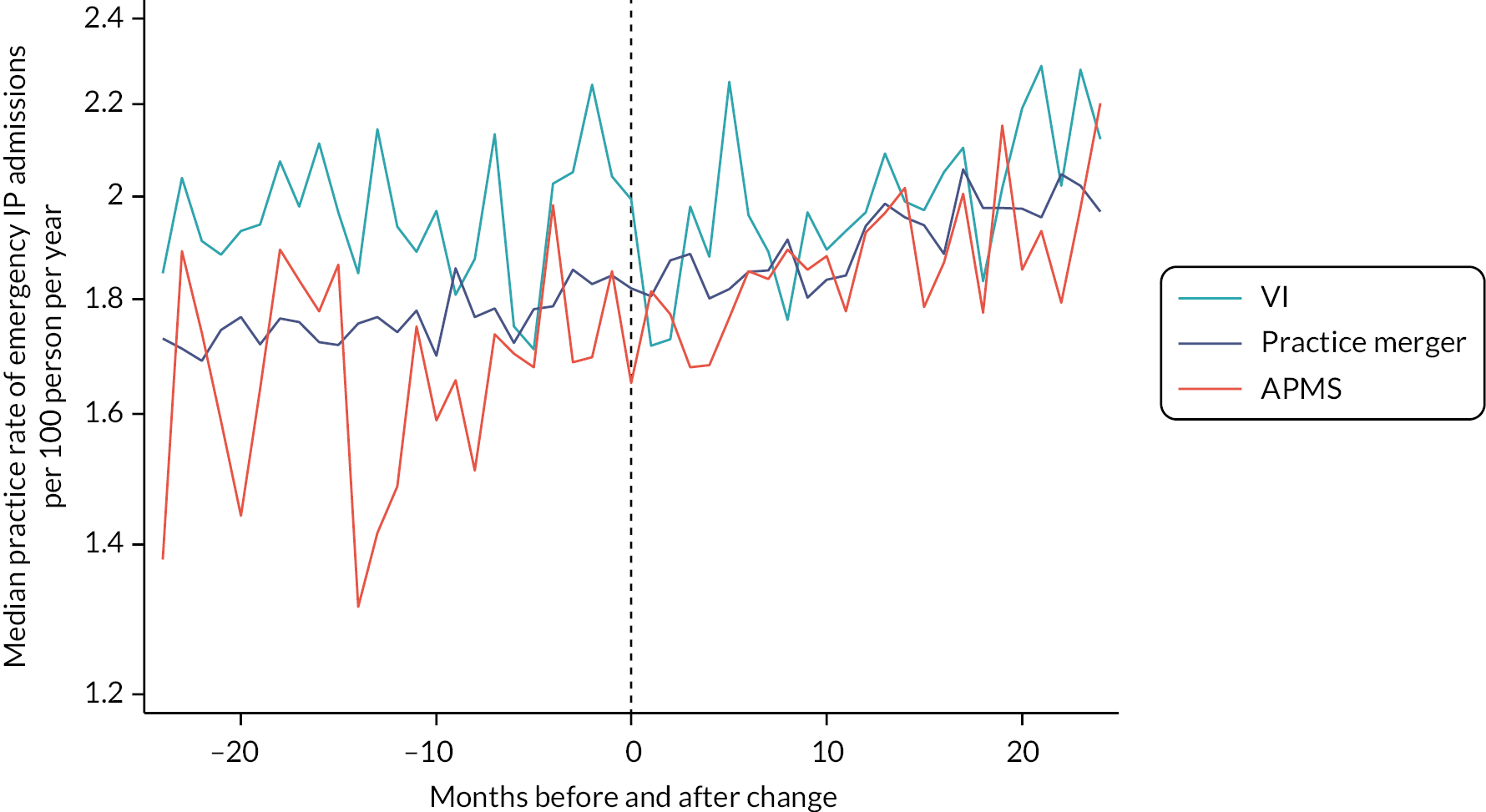
FIGURE 18.
Length of stay.
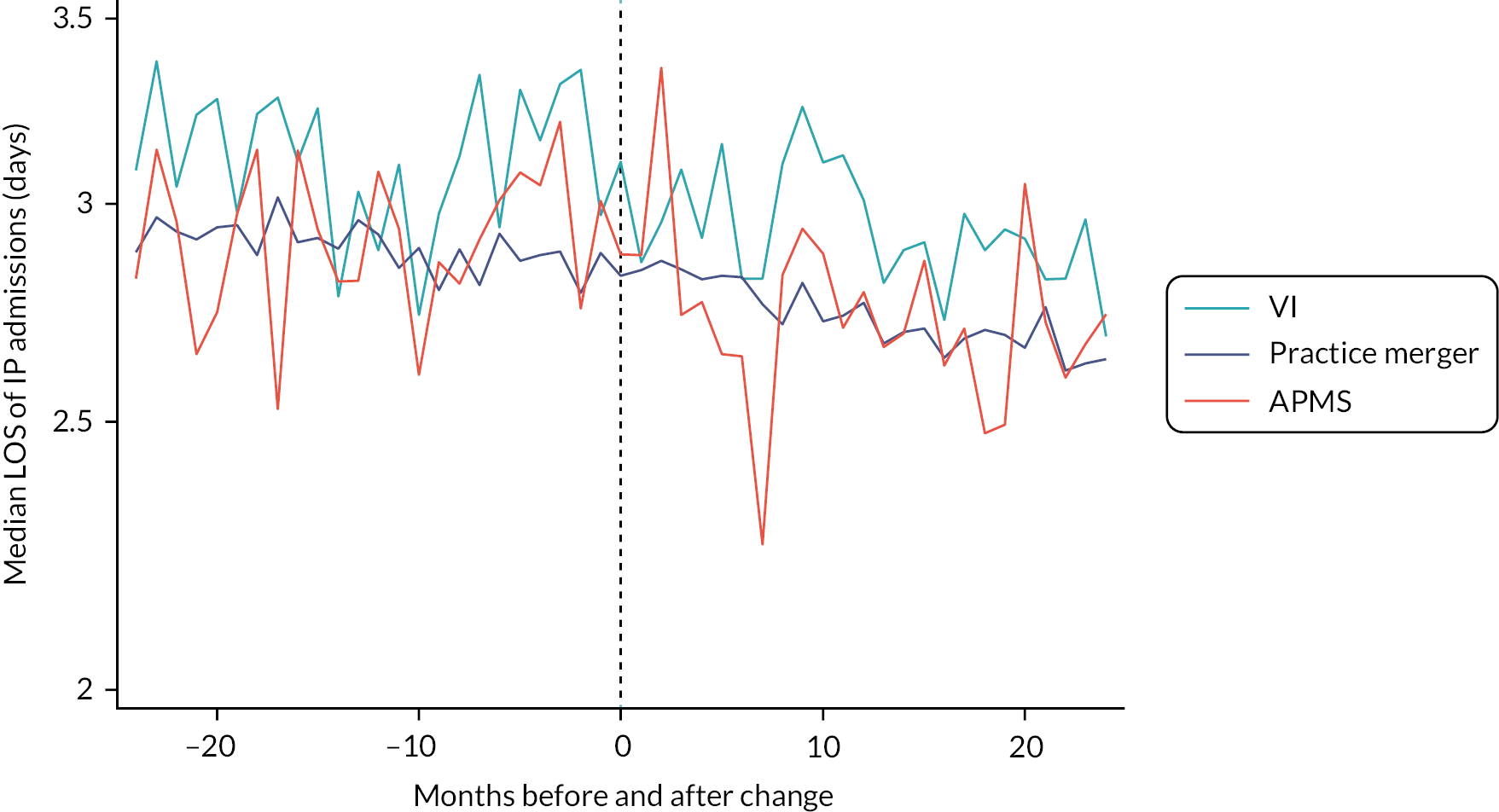
Analysis 4 – impact of vertical integration, horizontal practice mergers and switching to an alternative provider medical services contract on patient experience in primary care and on the use of secondary care
The results of these analyses are presented in Table 12 (patient experience) and Table 13 (use of secondary care services).
| Patient experience | Additional percentage point change per year before vertical integration compared with ‘stable’ GMS practices | Percentage point step change at time of vertical integration compared with ‘stable’ GMS practices | Additional percentage point change per year after vertical integration compared with ‘stable’ GMS practices | |||
|---|---|---|---|---|---|---|
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | Difference (95% CI) | p-value | |
| Helpfulness of receptionists; 0–100 scale | ||||||
| Vertical integration | −0.8 (−1.4 to −0.1) | 0.02 | −1.3 (−2.9 to 0.4) | 0.13 | −0.9 (−1.7 to −0.2) | 0.01 |
| APMS contract change | −0.7 (−1.3 to −0.0) | 0.04 | −1.9 (−3.4 to −0.4) | 0.01 | −0.2 (−0.9 to 0.5) | 0.59 |
| Horizontal integration | −0.4 (−0.6 to −0.2) | < 0.0001 | −0.0 (−0.6 to 0.6) | 0.94 | −1.1 (−1.3 to −0.9) | < 0.0001 |
| Ability to get through on the ‘phone; 0–100 scale | ||||||
| Vertical integration | −1.3 (−2.1 to −0.6) | 0.0007 | −1.6 (−4.7 to 1.5) | 0.31 | −2.5 (−3.4 to −1.7) | < 0.0001 |
| APMS contract change | −0.2 (−1.0 to 0.5) | 0.53 | −1.9 (−4.7 to 0.8) | 0.16 | −1.7 (−2.6 to −0.9) | < 0.0001 |
| Horizontal integration | −1.0 (−1.2 to −0.8) | < 0.0001 | 0.5 (−0.7 to 1.7) | 0.39 | −1.7 (−2.0 to −1.4) | < 0.0001 |
| Time taken to see or speak to a GP; 0–100 scale | ||||||
| Vertical integration | −0.0 (−1.4 to 1.4) | 0.96 | 1.0 (−2.6 to 4.5) | 0.59 | −2.8 (−4.3 to −1.2) | 0.0004 |
| APMS contract change | −0.9 (−2.3 to 0.5) | 0.19 | −2.1 (−5.3 to 1.1) | 0.19 | −0.7 (−2.3 to 0.8) | 0.36 |
| Horizontal integration | −0.1 (−0.4 to 0.3) | 0.80 | 0.4 (−0.9 to 1.8) | 0.56 | −1.0 (−1.5 to −0.6) | < 0.0001 |
| Overall experience of access; 0–100 scale | ||||||
| Vertical integration | −0.5 (−1.4 to 0.3) | 0.22 | −2.5 (−5.3 to 0.3) | 0.08 | −2.5 (−3.4 to −1.6) | < 0.0001 |
| APMS contract change | −0.7 (−1.5 to 0.1) | 0.10 | −4.4 (−6.9 to −1.8) | 0.0007 | −2.1 (−3.0 to −1.1) | < 0.0001 |
| Horizontal integration | −0.9 (−1.1 to −0.7) | < 0.0001 | −0.5 (−1.6 to 0.6) | 0.35 | −2.0 (−2.3 to −1.7) | < 0.0001 |
| Continuity; 0–100 scale | ||||||
| Vertical integration | −1.1 (−2.5 to 0.3) | 0.14 | −6.6 (−10.6 to −2.6) | 0.001 | −2.4 (−4.1 to −0.7) | 0.005 |
| APMS contract change | −1.8 (−3.3 to −0.2) | 0.03 | −7.4 (−11.1 to −3.8) | 0.0001 | −0.8 (−2.8 to 1.1) | 0.39 |
| Horizontal integration | −0.9 (−1.3 to −0.5) | < 0.0001 | −1.2 (−2.7 to 0.3) | 0.11 | −2.8 (−3.3 to −2.3) | < 0.0001 |
| Overall satisfaction; 0–100 scale | ||||||
| Vertical integration | −0.4 (−1.1 to 0.2) | 0.20 | −1.4 (−3.4 to 0.5) | 0.16 | −0.9 (−1.6 to −0.2) | 0.02 |
| APMS contract change | −1.3 (−1.9 to −0.6) | 0.0001 | −5.5 (−7.3 to −3.7) | < 0.0001 | −2.1 (−2.9 to −1.4) | < 0.0001 |
| Horizontal integration | −0.5 (−0.7 to −0.3) | < 0.0001 | −1.0 (−1.8 to −0.3) | 0.008 | −1.2 (−1.4 to −0.9) | < 0.0001 |
| Secondary care use | Additional yearly change in the pre-intervention period | Step change at time of intervention compared with ‘stable’ GMS practices | Additional yearly change after the intervention | |||
|---|---|---|---|---|---|---|
| IRR (95% CI) | p-value | IRR (95% CI) | p-value | IRR (95% CI) | p-value | |
| A&E attendances (rate) | ||||||
| Vertical integration | 1.03 (1.01 to 1.05) | 0.0008 | 0.98 (0.96 to 0.99) | < 0.0001 | 1.02 (1.00 to 1.04) | 0.012 |
| APMS contract change | 0.95 (0.93 to 0.96) | < 0.0001 | 1.01 (0.99 to 1.02) | 0.36 | 1.02 (1.01 to 1.04) | 0.0091 |
| Horizontal integration | 1.00 (0.99 to 1.00) | 0.37 | 0.99 (0.99 to 0.99) | < 0.0001 | 0.99 (0.98 to 1.00) | 0.024 |
| Outpatient attendances (rate) | ||||||
| Vertical integration | 1.03 (1.02 to 1.05) | < 0.0001 | 0.99 (0.99 to 1.00) | 0.0061 | 1.02 (1.00 to 1.03) | 0.0064 |
| APMS contract change | 1.01 (1.00 to 1.03) | 0.040 | 0.98 (0.97 to 0.99) | < 0.0001 | 0.94 (0.93 to 0.95) | < 0.0001 |
| Horizontal integration | 1.00 (0.99 to 1.00) | 0.28 | 0.99 (0.98 to 0.99) | < 0.0001 | 0.99 (0.98 to 1.00) | < 0.0001 |
| Inpatient admissions (rate) | ||||||
| Vertical integration | 0.97 (0.96 to 0.98) | < 0.0001 | 1.00 (0.99 to 1.01) | 0.94 | 0.97 (0.96 to 0.99) | 0.0002 |
| APMS contract change | 0.95 (0.94 to 0.97) | < 0.0001 | 1.06 (1.04 to 1.07) | < 0.0001 | 1.00 (0.99 to 1.02) | 0.76 |
| Horizontal integration | 0.99 (0.98 to 0.99) | < 0.0001 | 0.99 (0.99 to 1.00) | 0.0026 | 0.99 (0.99 to 1.00) | 0.0012 |
| Inpatient admissions – ACSC (rate) | ||||||
| Vertical integration | 1.01 (0.98 to 1.04) | 0.36 | 0.98 (0.94 to 1.01) | 0.23 | 0.98 (0.96 to 1.01) | 0.24 |
| APMS contract change | 0.98 (0.95 to 1.01) | 0.18 | 1.00 (0.96 to 1.05) | 0.84 | 1.02 (0.99 to 1.06) | 0.18 |
| Horizontal integration | 1.00 (0.99 to 1.01) | 0.43 | 0.98 (0.97 to 1.00) | 0.0051 | 1.00 (0.99 to 1.01) | 0.54 |
| Emergency admissions (rate) | ||||||
| Vertical integration | 0.98 (0.96 to 1.00) | 0.03 | 0.97 (0.95 to 0.99) | 0.0062 | 1.00 (0.98 to 1.01) | 0.61 |
| APMS contract change | 0.99 (0.97 to 1.01) | 0.46 | 1.01 (0.99 to 1.04) | 0.43 | 1.01 (0.99 to 1.03) | 0.43 |
| Horizontal integration | 0.99 (0.99 to 1.00) | 0.076 | 0.99 (0.99 to 1.00) | 0.014 | 0.99 (0.99 to 1.00) | 0.12 |
| Emergency readmissions (rate) | ||||||
| Vertical integration | 0.97 (0.94 to 1.00) | 0.093 | 0.95 (0.91 to 1.00) | 0.039 | 1.01 (0.97 to 1.04) | 0.74 |
| APMS contract change | 0.99 (0.95 to 1.03) | 0.67 | 1.03 (0.97 to 1.09) | 0.29 | 1.00 (0.96 to 1.03) | 0.84 |
| Horizontal integration | 1.00 (0.98 to 1.01) | 0.52 | 0.99 (0.98 to 1.01) | 0.25 | 1.00 (0.99 to 1.01) | 0.77 |
| Length of stay (days); difference (95% CI) | ||||||
| Vertical integration | 0.01 (−0.07 to 0.09) | 0.81 | 0.09 (−0.11 to 0.28) | 0.51 | −0.03 (−0.11 to 0.05) | 0.51 |
| APMS contract change | 0.12 (0.03 to 0.21) | 0.12 | −0.09 (−0.23 to 0.06) | 0.25 | −0.02 (−0.11 to 0.08) | 0.72 |
| Horizontal integration | 0.02 (0.00 to 0.05) | 0.076 | −0.05 (−0.12 to 0.03) | 0.24 | 0.01 (−0.01 to 0.04) | 0.34 |
Patient experience
There is no statistically significant step change in patient experience before and after practices switch to a vertically integrated model compared with control practices for five of six of the patient experience outcomes (those concerning access and overall satisfaction). However, after practices switch to vertical integration, continuity (ability to make an appointment with a preferred GP) becomes differentially poorer by 6.6% points (p = 0.001; see Table 12. Patients of practices switching to an APMS contract experience a similar worsening of continuity, by 7.4% points (p = 0.0001).
We find no meaningful impact of horizontal mergers on patient experience. But for non-vertically integrated practices that switch to APMS contracts, patient experience worsens by 2–7% points for helpfulness of receptionists, overall experience of access, continuity, and overall satisfaction after the change.
For all three types of general practice change, experience worsens slightly faster in the intervention practices compared with more stable GMS control practices for all outcomes both before and after the date of the intervention. This change is small (0–2% points per year) but slightly faster after the change than before.
Secondary care
We find that vertical integration is associated with a 2% reduction in the rate of A&E attendances [incidence rate ratio (IRR) 0.98, 95% confidence interval (CI) 0.96 to 0.99; p < 0.0001], a 1% reduction in the rate of outpatient attendances (IRR 0.99, 95% CI 0.99 to 1.00; p = 0.0061), a 3% reduction in the rate of emergency inpatient admissions (IRR 0.97, 95% CI 0.95 to 0.99; p = 0.0062) and a 5% reduction in the rate of emergency readmissions (IRR 0.95, 9%% CI 0.91 to 1.00; p = 0.039) when it is introduced (see Table 13). There was no impact on length of inpatient stay. The falls in A&E and outpatient attendance rates appear to be temporary, as the rates resume growing at faster rates than for practices that held GMS contracts throughout the study period.
In comparison, we additionally find 1% reductions in use of secondary care services after non-vertically integrated practices undergo horizontal mergers (IRR 0.99) for A&E attendances, outpatient attendances, all inpatient admissions and emergency inpatient admissions; and we find a 2% reduction (IRR 0.98) for ACSC admissions; with no impact on emergency readmissions, nor on length of inpatient stay (see Table 13).
When practices switch to APMS, we found a 2% reduction (IRR 0.98) in the rate of outpatient attendances and a 6% increase in the rate of inpatient admissions (IRR 1.06). Again, there was no impact on length of stay (see Table 13).
Differential pre- and post-intervention trends vary between outcomes, with some evidence that inpatient admission rates are differentially reducing before the dates of practice change compared with control practices (p < 0.0001 for all interventions) but in general differential yearly changes in use are small and not in consistent directions.
Analysis 5 – comparison of the impact of vertical integration with acute hospital trusts compared with vertical integration with community trusts, for both patient experience and secondary care use
We present our findings from analysis 5 in Table 14 for both patient experience and secondary care use. We find no evidence of a differential impact of vertical integration with an acute hospital trust compared with vertical integration with a community trust for any of the six patient experience outcomes.
| Patient experience | Step change post vertical integration acute compared with community VI | Additional yearly change after the intervention for acute compared with community vertical integration | ||
|---|---|---|---|---|
| Percentage point step change for acute compared with community vertical integration practices | Percentage point step change for acute compared with community vertical integration practices | |||
| Difference (95% CI) | p-value | Difference (95% CI) | p-value | |
| Helpfulness of receptionists; 0–100 scale | 0.3 (−2.3 to 2.9) | 0.81 | −1.1 (−2.6 to 0.5) | 0.17 |
| Ability to get through on the telephone; 0–100 scale | −1.9 (−5.0 to 1.1) | 0.22 | 0.3 (−1.5 to 2.2) | 0.71 |
| Time taken to see or speak to a GP; 0–100 scale | 0.7 (−4.8 to 6.2) | 0.80 | 1.1 (−2.2 to 4.5) | 0.50 |
| Overall experience of access; 0–100 scale | −0.9 (−4.4 to 2.6) | 0.60 | −0.6 (−2.7 to 1.5) | 0.58 |
| Continuity; 0–100 scale | 0.1 (−5.9 to 6.1) | 0.97 | −1.7 (−5.3 to 2.0) | 0.38 |
| Overall satisfaction; 0–100 scale | −0.3 (−3.0 to 2.5) | 0.85 | −1.2 (−2.8 to 0.5) | 0.16 |
| Secondary care use | IRR (95% CI) | p -value | IRR (95% CI) | p -value |
| A&E attendances | 0.97 (0.95 to 0.99) | 0.010 | 1.02 (0.98 to 1.06) | 0.32 |
| Outpatient attendances | 1.00 (0.99 to 1.01) | 0.72 | 1.13 (1.03 to 1.24) | 0.013 |
| Inpatient admissions (rate) | 1.04 (1.01 to 1.06) | 0.0095 | 1.15 (0.92 to 1.45) | 0.22 |
| Inpatient admissions (ACSC) | 1.02 (0.95 to 1.10) | 0.64 | 0.95 (0.70 to 1.29) | 0.75 |
| Emergency admissions | 1.02 (0.98 to 1.06) | 0.32 | 0.82 (0.65 to 1.04) | 0.10 |
| Emergency readmissions | 1.02 (0.95 to 1.11) | 0.56 | 1.09 (0.86 to 1.37) | 0.49 |
| Length of stay | Difference (95% CI) | p -value | Difference (95% CI) | p -value |
| Length of stay (days) | −0.08 (−0.23 to 0.06) | 0.26 | −0.08 (−0.23 to 0.07) | 0.31 |
We find that the rate of A&E attendances differentially falls by 3% more in vertical integration with acute hospital trusts (IRR 0.97, 95% CI 0.95 to 0.99; p = 0.01) compared with vertical integration with community trusts, after the practices switch to vertical integration. Conversely, the rate of inpatient admissions increases by 4% more in vertical integration with acute hospital trusts (IRR 1.04, 95% CI 1.01 to 1.06, p = 0.0095) compared with vertical integration with community trusts (see Table 14).
Although we find no differential impact between the two types of trusts at the date of vertical integration with respect to outpatient attendances, we note that in practices that vertically integrate with acute hospitals the post-integration rate of outpatient attendances does increase over the next two years at a considerably faster rate than in practices that integrate with community trusts (IRR 1.13, 95% CI 1.03 to 1.24, per year; p = 0.013; see Table 14).
Analysis 6 – impact of vertical integration for people living with multiple long-term health conditions
Overall, before a practice vertically integrates, we found that people living with multiple long-term health conditions, relative to other patients, reported better experience of the helpfulness of general practice receptionists, ability to get through on the telephone and continuity, but with poorer experiences overall of access to primary care, and with mixed (although small) differences for time taken to see or speak to a GP and for overall satisfaction (see Table 15).
| Conditions | Before | After | Change | Differential change | p-value |
|---|---|---|---|---|---|
| Patient experience | |||||
| Helpfulness of receptionists (0–100 scale) | |||||
| 0 | Reference | Reference | −1.2 (−2.9 to 0.5) | Reference | 0.10 |
| 1 | 2.6 (2.5 to 2.8) | 2.7 (2.0 to 3.4) | −1.1 (−2.8 to 0.6) | 0.1 (−0.6 to 0.7) | |
| 2 | 2.8 (2.6 to 3.0) | 2.7 (1.9 to 3.5) | −1.3 (−3.0 to 0.5) | −0.1 (−0.9 to 0.7) | |
| 3 | 2.6 (2.4 to 2.9) | 2.5 (1.4 to 3.6) | −1.3 (−3.2 to 0.6) | −0.1 (−1.2 to 0.9) | |
| 4+ | 2.1 (1.8 to 2.3) | 0.3 (−0.9 to 1.6) | −2.9 (−4.9 to −0.9) | −1.7 (−3.0 to −0.5) | |
| Ability to get through on the telephone (0–100 scale) | |||||
| 0 | Reference | Reference | −1.6 (−4.7 to 1.5) | Reference | 0.20 |
| 1 | 2.2 (2.1 to 2.4) | 2.4 (1.6 to 3.2) | −1.5 (−4.6 to 1.6) | 0.2 (−0.6 to 1.0) | |
| 2 | 2.3 (2.1 to 2.5) | 2.4 (1.5 to 3.4) | −1.5 (−4.7 to 1.7) | 0.1 (−0.8 to 1.1) | |
| 3 | 2.2 (1.9 to 2.5) | 2.6 (1.3 to 3.8) | −1.3 (−4.5 to 2.0) | 0.4 (−0.9 to 1.6) | |
| 4+ | 2.0 (1.7 to 2.3) | 0.4 (−1.1 to 1.9) | −3.3 (−6.6 to 0.1) | −1.6 (−3.2 to −0.1) | |
| Time taken to see or speak to a GP (0–100 scale) | |||||
| 0 | Reference | Reference | 1.8 (−1.9 to 5.4) | Reference | 0.04 |
| 1 | −2.3 (−2.6 to −2.0) | −4.0 (−5.4 to −2.5) | 0.1 (−3.6 to 3.8) | −1.7 (−3.2 to −0.2) | |
| 2 | −1.9 (−2.3 to −1.6) | −3.4 (−5.1 to −1.7) | 0.4 (−3.4 to 4.1) | −1.4 (−3.2 to 0.3) | |
| 3 | −0.6 (−1.1 to −0.1) | −2.1 (−4.4 to 0.1) | 0.2 (−3.9 to 4.3) | −1.6 (−3.9 to 0.8) | |
| 4+ | 1.9 (1.3 to 2.4) | 3.5 (0.8 to 6.3) | 3.4 (−0.9 to 7.8) | 1.7 (−1.1 to 4.4) | |
| Overall experience of access (0–100 scale) | |||||
| 0 | Reference | Reference | −1.9 (−4.8 to 0.9) | Reference | 0.05 |
| 1 | −0.1 (−0.3 to 0.1) | −0.5 (−1.4 to 0.4) | −2.3 (−5.2 to 0.5) | −0.4 (−1.3 to 0.5) | |
| 2 | −0.9 (−1.1 to −0.7) | −2.0 (−3.0 to −0.9) | −3.0 (−6.0 to −0.1) | −1.1 (−2.1 to −0.0) | |
| 3 | −1.8 (−2.1 to −1.5) | −3.2 (−4.6 to −1.8) | −3.4 (−6.4 to −0.3) | −1.4 (−2.8 to 0.0) | |
| 4+ | −3.0 (−3.4 to −2.6) | −4.9 (−6.6 to −3.3) | −3.9 (−7.1 to −0.7) | −1.9 (−3.6 to −0.3) | |
| Continuity (0–100 scale) | |||||
| 0 | Reference | Reference | −6.5 (−10.6 to −2.3) | Reference | 0.06 |
| 1 | 3.4 (3.1 to 3.6) | 3.5 (1.9 to 5.1) | −6.3 (−10.4 to −2.2) | 0.2 (−1.5 to 1.8) | |
| 2 | 4.0 (3.7 to 4.4) | 4.4 (2.6 to 6.2) | −6.1 (−10.3 to −1.9) | 0.4 (−1.4 to 2.2) | |
| 3 | 4.1 (3.6 to 4.5) | 3.5 (1.2 to 5.7) | −7.1 (−11.5 to −2.7) | −0.6 (−2.9 to 1.7) | |
| 4+ | 3.5 (3.0 to 4.1) | 0.2 (−2.4 to 2.7) | −9.9 (−14.4 to −5.3) | −3.4 (−6.0 to −0.8) | |
| Overall satisfaction (0–100 scale) | |||||
| 0 | Reference | Reference | −1.0 (−3.0 to 1.0) | Reference | 0.07 |
| 1 | 0.4 (0.2 to 0.5) | −0.1 (−0.8 to 0.6) | −1.4 (−3.4 to 0.6) | −0.5 (−1.2 to 0.2) | |
| 2 | 0.0 (−0.1 to 0.2) | −0.7 (−1.5 to 0.1) | −1.7 (−3.7 to 0.4) | −0.7 (−1.6 to 0.1) | |
| 3 | −0.3 (−0.5 to −0.1) | −1.7 (−2.8 to −0.6) | −2.4 (−4.5 to −0.2) | −1.4 (−2.5 to −0.3) | |
| 4+ | −1.3 (−1.6 to −1.1) | −2.4 (−3.7 to −1.2) | −2.1 (−4.4 to 0.2) | −1.1 (−2.4 to 0.2) | |
We find that when practices vertically integrate with trusts any differential impact for people living with multiple long-term health conditions compared with people living with a single condition or no conditions, is either not significant or of very small magnitude for the measures of patient experience.
Use of secondary care services
For all the secondary care outcomes we investigated we found that the size and direction of impact of vertical integration for people with a single long-term condition, and with two or more long-term conditions (see Table 16), were closely similar to the size and direction of impact for all patients taken together (see Table 13).
| Secondary care utilisation | Change in the pre-intervention period | Step change compared with ‘stable’ GMS practices | Additional yearly change after the intervention | |||
|---|---|---|---|---|---|---|
| IRR (95% CI) | p-value | IRR (95% CI) | p-value | IRR (95% CI) | p-value | |
| IP admissions; rate | ||||||
| People with 1 condition | 0.97 (0.96 to 0.99) | 0.0007 | 1.00 (0.99 to 1.02) | 0.75 | 0.97 (0.96 to 0.99) | 0.0017 |
| People with ≥ 2 conditions | 0.97 (0.95 to 0.99) | 0.0012 | 1.01 (0.99 to 1.03) | 0.37 | 0.95 (0.94 to 0.97) | < 0.0001 |
| Emergency IP admissions; rate | ||||||
| People with 1 condition | 1.00 (0.98 to 1.02) | 0.89 | 0.97 (0.95 to 1.00) | 0.046 | 0.99 (0.97 to 1.01) | 0.39 |
| People with ≥ 2 conditions | 0.99 (0.97 to 1.02) | 0.57 | 0.98 (0.95 to 1.01) | 0.22 | 0.98 (0.96 to 1.00) | 0.12 |
| Emergency readmissions; rate | ||||||
| People with 1 condition | 1.00 (0.96 to 1.03) | 0.81 | 0.96 (0.91 to 1.02) | 0.18 | 1.00 (0.97 to 1.04) | 0.91 |
| People with ≥ 2 conditions | 0.99 (0.95 to 1.04) | 0.75 | 0.97 (0.91 to 1.03) | 0.35 | 0.98 (0.94 to 1.03) | 0.47 |
| Length of stay (days); difference (95% CI) | ||||||
| People with 1 condition | −0.01 (−0.13 to 0.10) | 0.80 | 0.05 (−0.14 to 0.23) | 0.62 | 0.00 (−0.12 to 0.12) | 0.98 |
| People with ≥ 2 conditions | −0.01 (−0.16 to 0.15) | 0.92 | 0.08 (−0.16 to 0.32) | 0.52 | 0.01 (−0.14 to 0.17) | 0.86 |
Sensitivity analysis
In our sensitivity analysis considering only practices from Wolverhampton, our results were broadly consistent with the main analysis including all vertical integration practices, albeit with smaller effect sizes overall and often lacking statistical significance, reflecting the smaller sample size. We note that when considering vertical integration practices in Wolverhampton alone we do not see a statistically significant overall impact of vertical integration on the rate of A&E attendances, outpatient attendances, inpatient admissions or length of stay (see Table 17). However, in contrast with the analysis including all vertical integration practices (see Table 13), the impact of vertical integration on the rate of emergency readmissions is a larger reduction than for the main analysis: a 12% reduction in Wolverhampton (IRR 0.88) compared with a 5% reduction (IRR 0.95) nationally.
| Secondary care use (Wolverhampton) | Change in the pre-intervention period | Step change compared with ‘stable’ GMS practices | Additional yearly change after the intervention | |||
|---|---|---|---|---|---|---|
| IRR (95% CI) | p-value | IRR (95% CI) | p-value | IRR (95% CI) | p-value | |
| A&E attendances (rate) | ||||||
| Vertical integration | 1.07 (1.04 to 1.11) | 0.0001 | 1.00 (0.98 to 1.02) | 0.96 | 0.97 (0.93 to 1.00) | 0.051 |
| Outpatient attendances (rate) | ||||||
| Vertical integration | 0.98 (0.96 to 1.01) | 0.18 | 1.00 (0.99 to 1.02) | 0.68 | 0.99 (0.97 to 1.02) | 0.63 |
| Inpatient admissions (rate) | ||||||
| Vertical integration | 0.94 (0.91 to 0.97) | <0.0001 | 0.97 (0.94 to 1.00) | 0.055 | 0.96 (0.93 to 0.99) | 0.0041 |
| Inpatient admissions – ACSC (rate) | ||||||
| Vertical integration | 0.92 (0.86 to 0.98) | 0.0086 | 0.96 (0.87 to 1.05) | 0.38 | 0.92 (0.86 to 0.98) | 0.014 |
| Emergency admissions (rate) | ||||||
| Vertical integration | 0.92 (0.88 to 0.96) | <0.0001 | 0.96 (0.91 to 1.01) | 0.15 | 0.98 (0.94 to 1.02) | 0.33 |
| Emergency readmissions (rate) | ||||||
| Vertical integration | 0.88 (0.81 to 0.95) | 0.001 | 0.88 (0.78 to 0.98) | 0.025 | 1.05 (0.97 to 1.14) | 0.21 |
| Length of stay (days); difference (95% CI) | ||||||
| Vertical integration (Wolverhampton) | −0.05 (−0.25 to 0.15) | 0.62 | 0.22 (−0.10 to 0.54) | 0.17 | 0.07 (−0.14 to 0.27) | 0.52 |
Discussion of quantitative findings
Summary of findings
In this quantitative analysis, we explore the impact on patient experience and secondary care use of a practice becoming vertically integrated compared with a control group of practices that have not undergone organisational change.
We contrast this impact with the impact of horizontal mergers between general practices and with the impact of switching to APMS contracts not associated with vertical integration. We additionally compare practices that vertically integrate with acute trusts to practices that vertically integrate with community trusts.
We found that the impact of vertical integration on patient experience was small, except for the effect on continuity where there was a 6.6% points worsening of patient experience. Horizontal mergers have minimal impact on patient experience, while switching to an APMS contract was associated with slightly worsening patient experience for continuity, access and satisfaction (i.e. for three of the six included outcomes). Patients of practices switching to APMS contracts reported the worst (albeit still small) declines in their experience in all categories, compared with vertically integrated or horizontally integrated practices.
Regarding use of secondary care services, we found that vertical integration was associated with a small reduction in rates of A&E attendances (−2%), outpatient attendances (−1%), emergency admissions (−3%) and emergency readmissions (−5%) after it was introduced, with no impact on length of stay, overall inpatient admissions or inpatient admissions for ACSC. The falls in A&E and outpatient attendance rates appeared to be temporary, as the rates resumed growing at faster rates than for practices that held GMS contracts throughout the study period. We additionally found small reductions in secondary care use after non-vertically integrated practices underwent horizontal mergers for A&E attendances, outpatient attendances, emergency inpatient admissions and ACSC admissions; with no impact on readmissions. When practices switch to APMS we found no impact on secondary care use except for an increase in inpatient admissions. For none of the interventions was there any impact on length of stay.
We found little difference between the impact of vertical integration with acute hospital trusts and vertical integration with community trusts, although we note that in the 2 years following vertical integration, outpatient attendances increased faster in practices that had merged with an acute hospital trust. Differential pre- and post-intervention trends varied between outcomes but, in general, differential yearly changes in use were small and not in consistent directions. We found no evidence that the impact of vertical integration was differential for people living with multiple long-term health conditions compared with people with a single or no long-term health conditions.
How findings relate to previous research
Our findings are broadly consistent with an earlier statistical evaluation of vertical integration in Wolverhampton;34 and we extend their work by considering a larger number of vertical integration sites, longer follow up, and additional outcomes, both patient experience and secondary care use. When considering only outcomes used in this earlier evaluation, we found overall (small) reductions in inpatient admissions, emergency readmissions and A&E attendances when practices changed to a vertical integration approach. This impact on A&E attendances was not found by the earlier Wolverhampton analysis. Our sensitivity analysis considering Wolverhampton practices alone suggests that this is a feature of vertical integration in Wolverhampton rather than of methodological differences between the two evaluations, as we similarly did not find an impact on A&E attendances in these Wolverhampton practices when considered in the sensitivity analysis.
This highlights that the impact of vertical integration is likely to be heterogeneous across the country. Two early evaluations of APMS contracts found that practices performed more poorly on measures of clinical quality and patient experience compared with GMS and PMS practices. 77,78 Previous research suggests that continuity may reduce when general practices undergo horizontal mergers,79 and although we did find a small reduction, we note that this was not as large as the reduction in continuity associated with vertical integration or when practices switch to an APMS contract.
Chapter 5 Work package 4: staff and patient experiences of care delivery and provision as part of a vertically integrated model
Summary of key points
-
This WP aimed to answer the following question: what impact is vertical integration having on the patient journey with regard to access to and overall experience of care?
-
Our general approach to answering the research question was a cross-comparative case study qualitative evaluation comprising: (1) focus groups or one-to-one interviews in each case study site, to which we invited key service managers and clinicians from the acute hospital and general practices; (2) one-to-one interviews, capturing the views of patients from integrated and non-integrated general practices, to understand their experiences of vertical integration models.
-
We have used the Sustainable intEgrated care modeLs for multimorbidity: delivery, FInancing, and performancE (SELFIE) framework80 as a lens to guide our qualitative study. Our analysis was conceptually informed by the notion of the sociology of ‘work’, informed by Corbin and Strauss. 81,82
-
Vertical integration between acute trusts and general practices is supported by the introduction of novel ways of clinically integrating care across primary, community and secondary care to meet the needs of all patients locally, but specifically those at risk, have complex, and/or multiple long-term conditions.
-
Health service improvements are driven by local acute trusts, in collaboration with clinicians in general practice, and focus on health service changes that can improve population health for all patients locally using vertically integrated practices to test services before encouraging wider local roll out to non-vertically integrated practices.
-
Following the COVID-19 pandemic and the introduction of new health services, patients with multiple long-term conditions encounter significant ‘navigation work’ concerned with choosing and accessing health provision with diminishing continuity of care with the onset and scaling up of multidisciplinary team (MDT) working; however, this holds true for both vertically integrated and non-vertically integrated general practices nationally.
Introduction
Despite previous research on vertical models of integration, there is a paucity of evidence on staff perspectives on how best to serve complex patients and understanding patient experiences of accessing and navigating health services, especially for patients with multiple long-term conditions living in England. We have augmented evidence in this area via qualitative research, as explained in this chapter. We have used the SELFIE framework80 as a lens to guide our qualitative study. The framework structures concepts and features of how best to design and deliver integrated care for patients living with multiple long-term conditions. The framework is structured into six components (service delivery, leadership and governance, workforce, financing, technologies and medical products, and information and research), across three levels (micro, meso and macro). We have used this framework as a starting point to aid our understanding of the nature of implementation of vertical integration and service redesign across three case sites that are heterogenous with respect to their local contexts. An illustration of the SELFIE framework is provided in Figure 19.
FIGURE 19.
Description of the SELFIE framework. Source: Leijten et al. 201880 (reproduced in accordance with terms of the CC BY-NC-ND licence: https://creativecommons.org/licenses/by-nd-nc/4.0).
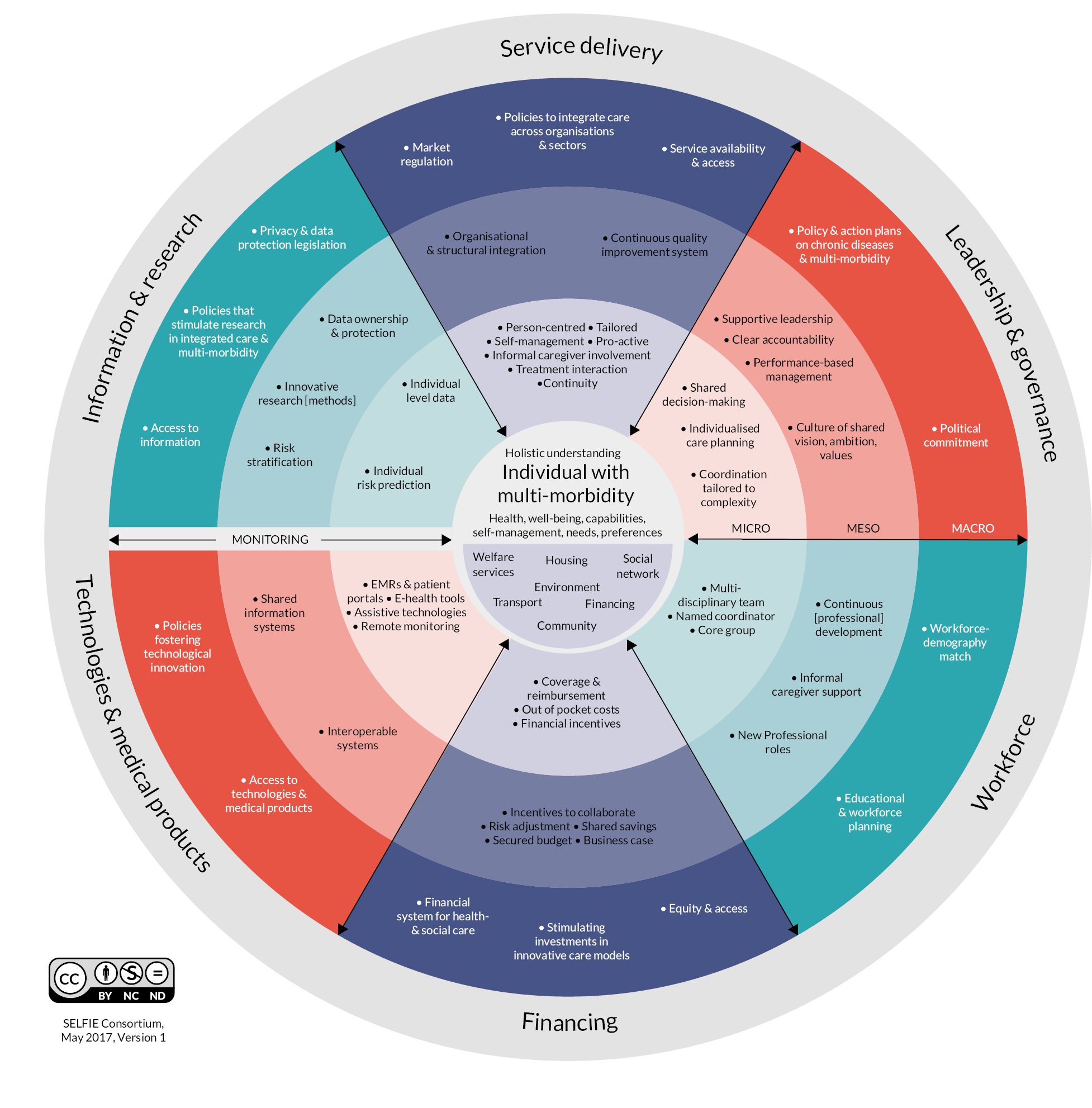
Our analysis was conceptually informed by the notion of the sociology of ‘work’ as in Corbin and Strauss’s seminal paper on three lines of work (illness work, everyday life work and biographical work) when managing chronic illness. 81,82 The most pertinent and relevant of the three lines of work for the purposes of this study was part of illness work: namely the navigation work undertaken by patients and related sense-making and decision-making in the face of an integrated model of care local to where they live. Hence, we considered the range of services available to patients and their sense making of how best to engage with primary, secondary and community care, in addition to patient decision-making concerning routine and urgent care. We also assessed the impact vertical integration has upon continuity of care.
Research questions
Our research attempts to address gaps in the literature regarding how service delivery and coordination changes following the implementation of vertical integration and the patient experience of vertical integration, with a particular focus on whether patients with multiple long-term conditions are affected differently from other patients. This WP aimed to answer the following research questions:
-
3: What impact is vertical integration having on the patient journey with regard to access to and overall experience of care?
-
3.1: How do models of vertical integration support patient transitions from primary care to acute care?
-
3.2: How do patients experience services, more commonly found in secondary care, within a vertically integrated general practice setting?
-
3.3: How does the experience differ for people with multiple long-term conditions compared with other patients?
-
Methods
A detailed description of the methods for the qualitative analysis is set out below.
Design
Our general approach to answering the research questions was a cross-comparative case study qualitative evaluation comprising: (1) focus groups or one-to-one interviews in each case study site, to which we invited key service managers and clinicians from the acute hospital and general practices; (2) one-to-one interviews capturing the views of patients from integrated and non-integrated general practices to understand their experiences of vertical integration models; and (3) refining and validating an overall theory of change for this model of vertical integration, starting from that emerging from our phase 1 study,2 following feedback from case study sites.
Selection of case study sites
We recruited case studies at three vertical integration sites. We focused on sites in England to correspond with the scope of the quantitative analysis (WPs 2 and 3). The research team already had (through BRACE) access to the requisite NHS activity data for England but was unable to acquire corresponding data for Northern Ireland, Scotland or Wales within the timeframe of this rapid evaluation. We returned to the two phase 1 case study sites in England (Urbanville and Greenvale) and recruited one additional vertical integration site in England to undertake further qualitative data collection and analysis. During WP1 (see Chapter 3), the research team identified NHS trusts in England where vertical integration between an acute hospital and general practices was already being delivered. Members of the study team undertook a purposive approach to identify the third case study site, with the aim of ensuring variation in our sample in terms of: (1) geographical location; (2) population served; (3) legal and governance arrangements; and (4) time elapsed since vertical integration was introduced. Members of the study team (JS and MS) emailed to vertical integration organisational strategic or clinical leads (or their equivalent) at two potential case study sites, and following initial informal conversations with both regarding participation, one site agreed to take part. One site declined to participate because they were in the process of addressing pertinent local challenges about the contractual and ownership model of vertical integration.
All three case study sites sent formal confirmation of participation letters/emails. Table 18 summarises key characteristics of the three sites as of September 2022.
| Case study site | Location | Date of commencement of vertical integration | No. of general practices |
|---|---|---|---|
| Urbanville | Central England | July 2018 | 8 |
| Greenvale | South of England | April 2016 | 16 (across 20 sites) |
| Townshire | Central England | July 2015 | 4 |
Interviewing staff across case study sites
We planned to complete focus groups and/or interviews at each case study site, inviting key strategic and service level managers and clinicians from both primary and secondary care. The aim was to understand the model of vertical integration in operation and whether/how it has evolved since it was first established, and what (if any) elements of the current model are expected to improve the care and support of people with multiple long-term conditions. The evaluation team planned to complete one to two focus groups and six to eight interviews at each case study site or until data saturation (meaning that, once data were triangulated, no new emerging information was being discovered during data analysis, but only data that confirmed existing themes and conclusions). The point of saturation was agreed by discussion with all members of the full research team. Fieldwork was completed in parallel across all three case study sites (May–September 2022) by four members of the research team with experience of undertaking interviews and qualitative data analysis (IL, GM, led by MS). MS was responsible for all communication at two sites and, with IL, undertook data collection there, while GM was responsible for communication and data collection at the third site. As part of bimonthly team meetings, early findings were shared by IL, GM, MS and FW to provide the principal investigator (JS) and quantitative team members (CD, CS) the opportunity to embed themselves appropriately within the data collection process to better inform data analysis and subsequent synthesis.
Participants for interview were purposively sampled and were approached through each case study site’s gatekeeper via email invitation, including a participant information sheet (see Project website document). 83 A gatekeeper was defined as a person based at our case study sites who could act as an intermediary between a researcher and potential participants with the authority to deny or grant permission for access to potential research participants. 84 Informants included directors (clinical and non-clinical) and other NHS managerial staff (related to strategy, delivery of health-care services, financial and governance-related management); GPs, PCN leads and other primary care staff who had implemented the vertical integration model in each area.
Individuals participated in a focus group or one-to-one semistructured interview, completed at their place of employment, via telephone or Microsoft Teams® (Microsoft Corporation, Redmond, WA, USA) or Zoom (Zoom Video Communications, Inc., San Jose, CaA, USA). Each participant was provided with the participant information sheet at least 48 hours in advance to enable them to make an informed decision regarding whether to participate or not. Interviewees had the opportunity to ask questions about the study and/or wider BRACE-related work. Participants signed a consent form (see Project website document) prior to participating in the interview, including whether they consented to the audio recording of the interview. Participants were informed that they were entitled to withdraw from the study at any time and were given information about how to find out more about the study and how to raise any concerns about its conduct.
In total, the study team approached 26 potential participants to complete an interview across all 3 sites with 22 agreeing to take part (9 participants took part in 3 focus groups, 13 completed one-to-one interviews). Salient characteristics of staff interviewed across the three case study sites are provided in Table 19.
| Area of specialism | Generic description of role | Number of participants (participant identifiers) |
|---|---|---|
| Primary care | Clinical | A5, A7, A8 |
| Organisational management | B2, C3 | |
| Clinical and managerial | A1, B6, C1 | |
| Primary and secondary care | Clinical | C6 |
| Clinical and managerial | B1, B3 | |
| Organisational management | B7 | |
| Secondary care | Clinical | B4 |
| Clinical and managerial | A2, C2, C4 | |
| Organisational management | A9 | |
| Senior Management | C5 | |
| Community care | Clinical | A3, A4, A6, B5 |
| Total | 22 |
A topic guide was developed and used by researchers as an aide memoire during the interviews (see Project website document). The main themes the topic guide covered were: understanding the rationale behind the implementation of vertical integration (or whether the drivers have changed since we last collected data in the two areas involved in the phase 1 study); understanding the experiences of staff involved with the delivery of this model; what outcomes this model is expected to deliver in the short, medium and long term and what data are collected to monitor them.
Interviews were audio recorded (subject to consent being given), transcribed verbatim by a professional transcription service, anonymised and stored securely in compliance with the General Data Protection Regulation 2018 and the Data Protection Act 2018.
Interviewing patients with multiple long-term conditions across case study sites
The evaluation team planned to complete up to six to eight interviews with patients living with multiple long-term conditions across each case study site or until data saturation (N = 24). We used the definition of ‘multimorbidity’ from the NICE (2016), which defines multimorbidity as ‘the presence of two or more long-term health conditions’, which NICE states can include:
-
defined physical and mental health conditions such as diabetes or schizophrenia
-
ongoing conditions such as learning disability
-
symptom complexes such as frailty or chronic pain
-
sensory impairment such as sight or hearing loss
-
alcohol and substance misuse. 35
To identify patients with multiple long-term conditions who could be invited to be interviewed, we asked gatekeepers to facilitate communication between members of the study team (IL, GM and MS) and leads at the PCNs that the vertically integrated practices at each site are part of (Urbanville = 1 PCN, Greenvale = 10, Townshire = 2). We sought to engage with members from patient participation groups (PPGs) of vertically integrated practices and of practices not part of a vertically integrated arrangement. The rationale for working with PCNs was to work with a group of practices that may include those that are integrated and not integrated as part of local vertical integrated arrangements, and hence may expedite access for researchers into case study sites. Where PCNs were entirely created from integrated practices, then the study team asked the case study site gatekeeper to facilitate communication with local neighbouring PCNs to identify suitable patients for interview.
Study team members asked gatekeepers to identify suitable patients from PPGs for interview, using the following inclusion criteria:
-
18 years or older
-
living with at least two long-term health conditions (in accordance with NICE guidance)
-
accessed primary and/or secondary health-care services within the past 12 months
-
not on a palliative care pathway
-
capable of giving informed consent
-
not prevented from being able to take part in an interview due to their ill-health.
To support uptake at Urbanville, MS gave a presentation of the study at an online monthly PPG meeting (September 2022) while the site gatekeeper sent an invitation to all patients registered to receive their PPG newsletter. At Greenvale, IL and MS gave a presentation of the study to all PPG leads for practices that were part of the integrated arrangement local to the area (online, August 2022) with follow-up emails sent by the site gatekeeper. At Townshire, GM worked closely with the site gatekeeper to identify suitable members for interview. Study team members purposively recruited patients based on a convenience sampling strategy due to a low response rate.
Each patient was emailed a participant information sheet (see Project website document) prior to commencing the interview and given at least 48 hours to decide whether they would participate. Prior to commencing the interview, interviewees were given the opportunity to ask questions about the study and about what taking part would involve (either at the end of online recruitment meetings or direct with a named site-specific study team member at any time during the duration of the study). Participants signed a consent form (electronic via email) or provided verbal consent before participating in the interview, including whether they consented to the recording of the interview. Participants were permitted to withdraw from the study at any time without having to offer a reason for doing so, though none did so, and they were given information about how to find out more about the study or to raise concerns about its conduct.
The main themes covered by the topic guide for the patient interviews were: recent experiences of accessing care within their local health-care system including both primary and second care; coordination of care; communication and care planning between clinicians and the patient; speed of access to care; range of clinicians and allied health professionals to whom patients had access; barriers to and facilitators of accessing care (accounting for the COVID-19 pandemic); and perceived quality of care and care-related decision making by patients.
In total, the study team approached 24 potential patients to complete an interview across all three sites with 14 agreeing to take part (Urbanville = 8, Greenvale = 2, Townshire = 4). Despite a low response, the patients interviewed represented a varied sample of high and low users of primary and secondary care, gender, ethnicity, age and range of long-term conditions (see Table 20). The team also interviewed two participants who were both patients living with multiple chronic conditions and carers. No patients from non-integrated practices were interviewed from across the three sites. There were challenges in gatekeepers encouraging non-integrated practices to take part due to pressures faced by primary care staff during the period of data collection. Study team members (IL, GM and MS) completed semistructured interviews either by online (Zoom, Microsoft Teams) or by telephone. Interviews lasted between 20 and 75 minutes.
| Demographic characteristic | Number of participants (participant identifiers) | |
|---|---|---|
| Case study site | Urbanville | 8 (A10–17) |
| Greenvale | 2 (B8, B9) | |
| Townshire | 4 (C7–10) | |
| Gender | Male | 3 (B8, C7, C9) |
| Female | 3 (B9, C8, C10) | |
| Age | < 50 years | 3 (A13, A17, C10) |
| 50–64 years | 2 (A10, A11) | |
| 65–79 years | 7 (A14, A15, A16, B8, B9, C7, C9) | |
| ≥ 80 years | 2 (A12, C8) | |
| Ethnicity | White British/English/Welsh/Scottish/Irish or any other white background | 12 (A10, A12, A14–17, B8, B9, C7–10) |
| Black/African/Caribbean/black British or any other black background | 1 (A11) | |
| Asian/Asian British or any other Asian background | 1 (A13) | |
| Range of long-term conditionsa | Breast cancer, CVD, Chronic pain, Asthma, Lupus, Epilepsy, Bipolar disease, ADHD, Long COVID, Type 2 diabetes mellitus, Arthritis, Underactive thyroid, Irritable bowel syndrome, Myopia | |
| Total | 14 | |
Analysis
Validation and refinement of a theory of change
As part of our phase 1 evaluation, JS and MS developed a working theory of change, following principles from Weiss and Vogel. 85,86 They produced a diagrammatic representation and accompanying narrative of vertical integration in the UK, presenting the causal chains, assumptions and contextual conditions that influence how vertical integration works. As part of our phase 2 evaluation, we revisit the working theory of change and refine our understanding of vertical integration and how this leads to a desired impact. We understand that the contribution towards refining the theory of change from our qualitative work needs to be caveated according to several limitations. First, we have replaced one case study site from our phase 1 evaluation and all three case study sites remain heterogenous regarding the breadth of multiple services delivered across health sectors comprising multiple processes, causal chains and outcomes. Second, because our samples of staff and patients are small, study team members are careful not to overestimate participant narratives about both positive and negative experiences of delivering, accessing and receiving care following the implementation of vertical integration. In addition, most staff interviewed in phase 2 differ from those interviewed in phase 1, so may vary in their accounts when distinguishing between the expected and aspirational outcomes which vertical integration is expected to achieve and how they have evolved since the COVID-19 pandemic.
We held three data analysis workshops between September to November 2022 to develop interpretation of findings and refine the overall theory of change, with input from all members of the research team and from colleagues with expertise in evaluating integrated models of care within the BRACE partner organisations. As part of the workshops, study team members reconsidered the rationale, priorities, inputs, processes, outcomes and impacts of vertical integration in the light of the accumulating qualitative evidence. Rather than wholesale revisions to the theory of change, the refined version (see Chapter 6, Discussion) is now more nuanced and considers how models of vertical integration are responsive to both nationally set health-care policy and local population needs. Akin to phase 1, the theory of change was validated as part of site-specific feedback sessions once data collection and analysis were complete.
Data analysis
Between September and December 2022, the insights gained through interviews with staff and patients were analysed for each case study site.
A qualitative analysis subteam (IL, GM, MS and FW) held bimonthly 1-hour telephone meetings for the duration of data collection, analysis and write-up (June–December 2022) to discuss project progress and emerging findings and to shape theoretically informed interpretation. Collectively, all members of the study team partook in three analysis workshops from September to November 2022 (including, as described above, discussion regarding refining the theory of change) to discuss data in the context of findings from across all WPs. We took steps to consider how data gathered from focus groups may differ from interview data with respect the nature of participants involved based on their professional role. As a result, one focus group, with senior clinicians and managers, focused more on rationale and the drivers of vertical integration, while the two remaining focus groups, with primary and community care service leads, centred on implementation and delivery. As part of the analysis, we considered how participant accounts in focus groups built on each other based on reciprocity of understanding of vertical integration locally compared with interview data that was more reflective and based on individual experiences.
Our interview analysis was informed by the Gale et al. framework method for the analysis of qualitative data in multidisciplinary health research. 87 This is a systematic method of categorising and organising data while continuing to make analytical and interpretive choices transparent and auditable. Specifically, it facilitated constant comparison across the three case studies. There are seven stages to the analysis:
-
transcription of interviews
-
familiarisation with the interview/observation/documentary material
-
coding
-
developing a working analytical framework
-
applying the analytical framework
-
charting data in a framework matrix
-
interpreting the data.
Stage 1: transcription – all interviews were transcribed verbatim through a professional, outsourced transcribing company. A single organisation, specialising in transcribing health-related qualitative interviews, was used for transcribing all interviews. The quality of transcriptions was checked against recordings by one of member of the project team (MS) on two transcripts, which also supported early immersion and familiarity with the data.
Stage 2: familiarisation with the material – members of the qualitative subteam (GM, MS and FW) established familiarity with the data by each reading and writing short memos on one transcript from each case study site on the nature of vertical integration while data collection was still continuing (August 2022). During a meeting, GM, MS and FW were able to reflectively discuss and share preliminary thoughts and impressions of early findings. This was fed back into the conduct of how members of the qualitative subteam completed further interviews.
Stage 3: coding and stage 4: developing a working analytical framework – these stages of the analysis took place in tandem. The study team applied a deductive approach, having developed predefined codes focusing on specific areas of interest identified from: (1) our phase 1 evaluation findings; (2) our research questions; and (3) engagement with policy-informed and theoretical frameworks, specifically the SELFIE framework. 80 These codes were reviewed, refined and added to throughout data analysis by members of the qualitative subteam. One interview transcript from each of the three case study sites was independently coded by three project team members (GM, MS and FW) to ensure no important aspects of the data were missed by applying predefined codes. NVivo 12 (Lumivero, Denver, CO, USA) was used for coding. After independent coding of transcripts, an analytical coding framework was agreed with all project team members (see Appendix 3, Table 24). The codes were categorised under the following broad themes: delivery, coordination and health service improvement; patient experience of accessing and navigating local integrated health-care systems; description of current models of integration including rationale and drivers; impact of the implementation of vertical integration on strategic leadership and culture; alignment of vertical integration with other horizontal models of primary care; and continuity of care.
The analytical coding framework was reviewed at bimonthly study team and data analysis meetings throughout October to November 2022.
Stage 5: applying the analytical framework – the working analytical framework was then applied by indexing by three project team members (GM, MS and FW) across all interview transcripts, that is the systematic application of codes (n = 30) from the agreed analytical framework to the whole qualitative dataset using the existing categories and codes.
Stage 6: charting codes – the project team took a novel rapid approach to charting codes by developing a framework based on summaries of each code (once the analytical framework had been applied to all transcripts). The framework was structured according to the SELFIE framework,80 research questions and how best to develop integrative themes. As a result, summarised codes were merged together to support the development of themes.
Stage 7: interpreting the data – the qualitative subteam (GM, MS and FW) engaged with policy-relevant literature and theoretical concepts relational to our research questions and identified connections across our themes and with learning from our quantitative analysis (see Chapter 4). Once all members of the qualitative subteam agreed on the final themes, writing up of the findings commenced. The project team circulated a summary of findings (digital slide deck) to each case study site providing them with an opportunity to give comments; that is, member validation (February 2023).
We have completed a Consolidated Criteria for Reporting Qualitative Research checklist.
Results
Findings
Description of current models of integration including rationale and drivers
Description of organisational arrangements
Townshire initially took over three struggling practices on a caretaker arrangement at the request of NHS England and NHS Improvement on APMS contracts in 2015. The acute trust currently holds contracts for four general practices. All four practices were experiencing financial challenges at the time of integration with the local trust. The individual contracts are directly held by the trust via a newly created primary care division, driven by improving key service provision performance indicators (across primary, community and secondary care). Thus, Townshire has a centralised organisational model of governance:
It is run as a standalone business within the overall trust organisation. So it has a clinical director, I think the official title is divisional director, so that’s a doctor. And it has a managing director, so that’s [de-identified name 2] and [de-identified name 3], respectively, who are on a day-to-day basis responsible for running the organisation. (C2, secondary care, clinical and managerial)
The acute trust has, until recently, managed general practices at a significant financial deficit; but in the financial year 2021/22 broke even. Notably, a senior executive at Townshire acute trust (C1, primary care, clinical and managerial) stated that they are willing to integrate further general practices as part of their arrangement. Although Townshire acute trust directly holds general practice contracts, it has considered adopting a similar model to Greenvale (see below) and establishing an arm’s-length limited company wholly owned by the trust. They may reconsider this alternative model in future if they increase the number of practices they manage.
The organisational and governance model at Urbanville is a primary care division within the acute trust overseen by a governance team, comprising both primary care clinicians and secondary care managerial staff. The governance team is responsible for: (1) organisational governance, (2) structural governance, and (3) fiscal governance [i.e. meeting the ‘true cost of primary care’ (A2, secondary care, clinical and managerial)]. The Urbanville trust currently manages eight general practices (two further practices have left since March 2020 as former partners in now-integrated practices decided to leave the vertical integration arrangement) treating approximately one-third of the local primary care population.
The Greenvale model takes the form of the acute hospital trust 100% owning a limited company, which by late 2022 held 16 general practice contracts covering 20 sites (following mergers between some practices). The trust-owned primary care company reports directly to the trust board. Greenvale was supported by an NHS ‘vanguard’ programme, which meant that there was funding in place that was helpful to support the integration of practices in 2016.
Drivers for continued integration between primary, community and secondary care
The fundamental rationale for vertical integration in Townshire and Greenvale was to sustain primary care local to where patients live, as it is likely that without support from the local acute trust, those practices that have integrated would have closed. The principal rationale for vertical integration in Urbanville was for the acute trust to work more closely with primary care to improve local population health outcomes through collaborative working.
Each case study site has taken a nuanced approach on the best strategy to support practices and manage patient demand across local health economies. Townshire acute trust continues to recruit GPs with special interests such as respiratory medicine to deliver COPD clinics and to get more consultant input to work with primary care clinicians to redesign patient pathways.
The Urbanville acute trust has shifted its rationale to focus on improving patient-centred care delivered in general practice by a multidisciplinary workforce (i.e. GPs, advanced nurse practitioners, pharmacists, physiotherapists, healthy ageing coordinators, social prescribers and mental health practitioners):
The different way of doing it is not to have one monolithic organisation, but to be sure that you create collaboration between service provision with patient centric care. Patient-centric care isn’t about one person, it’s about a whole population, so inside that embedded population health principles. (A2, secondary care, clinical and managerial)
Senior managers and executives from acute trusts from all three of our case study sites felt that vertical integration could continue to improve the sustainability of general practice and improve services local to where patients live because the rationale was driven by delivering high-quality care rather than financial incentives.
Challenges with respect to implementation and/or sustaining integration
All three case study sites continue to experience challenges regarding recruitment and retention of GPs, akin to general practices nationally. Specifically, recruiting full- and part-time GPs remains difficult and there is significant long-term dependency on locum clinicians, which is expensive. As a result, acute trusts across the three case study sites offer a range of incentives to GPs in addition to what they hope are competitive salaries, including portfolio careers (i.e. offering GPs the opportunity to hold multiple jobs/roles within their working week) and opportunities for further training in clinical specialisms.
Senior clinicians from the acute trusts and general practices in Urbanville and Greenvale spoke at length about the attempts made to bridge the understanding of how best to deliver health services in general practice. As a result, conversations were held by senior managers and clinicians to understand the pressures and challenges faced in general practice and how a collaborative effort could alleviate or address such pressures.
In Townshire, interviewees leading the vertically integrated model from the acute trust reported that they had continued to face challenges from their local commissioner, previously the CCG and now the integrated care system (ICS) and ICB, who are not keen on vertical integration being adopted to support general practice in their area:
It is a strange CCG environment, which doesn’t help. And the politics at the minute around the ICS, the ICB, primary care, there’s just a lot of angst in the system and I think some of the politicians, medical politicians, just don’t want the noise. (C1, primary care, clinical and managerial)
Senior primary care clinicians from Greenvale remained unsure what impact the local ICS and ICB would have upon their vertical integration model. However, Urbanville acute trust interviewees felt that the ICS would not aid the success of their model because of a lack of understanding of how the acute trust is attempting to break boundaries on ways of working between primary and secondary care to provide joined-up care that is preventative, high quality and efficient:
The death of this venture will be the ICS, because the ICS is one size fits all, yeah, it totally doesn’t understand it. (A2, secondary care, clinical and managerial)
A senior executive and a GP in Urbanville considered that the acute trust’s strategy had evolved. Thus, they were in agreement with Townshire interviewees that any approach to vertical integration should be driven by meeting population needs, with the acute trust acting as an ‘anchor’ (A2, secondary care, clinical and managerial) organisation, which underwrites the financial risk for integrated working between acute, community and primary care.
Across all three case study sites, important aims of vertical integration were to bring stability to general practice, continue to support health-care redesign following acquisition and facilitate integrated working across their local health economy, largely by bringing secondary and primary care working closer together.
see ourselves as being in a period of consolidation, so we’ve got that outstanding that we’ve worked so hard for so long and desperately been trying to get. So, for us now, it’s consolidating and making sure that we maintain those levels. (B2, primary care, organisational management)
Alignment of vertical integration with horizontal models of primary care
There was recognition by acute and primary care interviewees from Townshire, Greenvale and Urbanville that vertical integration is one model of many that imply horizontal integration via practice mergers, a PCN model of provision, or both. Thus, vertical integration can establish a model where the acute trust acts as an anchor organisation, who can then work with PCNs as an organisational medium to work at scale across general practice. That can make it easier to invest in the primary care workforce and take the financial risks entailed in introducing innovative approaches to improving health services across both vertically integrated and not vertically integrated general practices in the area.
Where PCNs are composed of a mix of vertically integrated and not vertically integrated practices, there can be tension about how care should be delivered in the local health economy. Thus, how best to balance between improving population health (or at least targeting those living with multiple long-term conditions who are higher users of primary and secondary services) or supporting the financial stability of general practices by maximising incentives attached to the NHS direct enhanced services (DES) contract (i.e. NHS-funded support for practices that enables wider working with neighbouring practices and build a multidisciplinary workforce to deliver services to meet population needs). In Townshire, the acute trust working with both vertically integrated and not vertically integrated practices as part of a PCN thought that they had missed opportunities for greater care coordination for complex patients:
So what the primary care network wanted to do was to bring in a specialist nurse who would see all of these patients but these nurses would be I think band 4, so they’re the nursing associates. I didn’t agree with it because these nursing associates are just ticking a box, whereas when I’m using my trained practice nurses they’re seeing the links between ‘Has this learning disabilities lady had a smear lately?’ ‘No she hasn’t, she’s actually overdue let’s talk to them and encourage them to do it.’ (C3, primary care, organisational management)
In Greenvale, where the acute trust manages general practices that are distributed across several PCNs across a wide geographical distance, a key challenge was the lack of control over how much financial investment generated via the NHS DES contract leads to improvement in patient care for integrated practices and alleviates workforce pressures:
We have absolutely no real power per se with some of the other PCNs, particularly we have one single practice, very small practice for example, you’ve got three or four others, so sometimes it can be really hard to understand some of the decision making or even influence that, (B6, primary care, clinical and managerial)
This contrasts significantly with Urbanville, where colleagues felt the PCN was an effective meso level organisational model to establish relationships with practices and learn about working practices in general practice and understand the challenges clinicians faced. The PCN in Urbanville that consisted solely of vertically integrated practices was used as a test bed where service innovations could be trialled and, if successful, scaled up by working with neighbouring PCNs, albeit with integrated practices still receiving preferential treatment:
It is an [acute trust] service so it does work across all the city’s PCNs. To an extent, when we did the GP home visiting then the VI services I think got a preferential service. (A3, community care, clinical)
Primary care recruitment and retention
Despite the implementation of vertical integration, challenges remained regarding recruitment and retention of GPs as well as increased use of locums. At Greenvale, some vacancies for salaried GPs were left unfilled for extensive periods:
And similarly with the GP, we’ve had this vacancy since May (four months prior to interview), and we haven’t been able to fill it. (B2, primary care, organisational management)
All three case study sites have attempted to introduce incentives to recruit salaried GPs including offering portfolio careers, joint roles across primary and secondary care, ‘golden hello’ payments (i.e. incentive payments made at the point of recruitment or following a period of service), and opportunities to explore special interests. All three acute trusts felt well-placed to provide support to salaried GPs in relation to skills training with peer support, mentoring, leadership opportunities and continuous clinical professional development. However, additional remuneration and career development opportunities meant that salaried GPs were asked to accept increased responsibilities akin to GP partners; hence, working beyond designated hours and taking greater responsibility in the management of a given practice.
It remains difficult to recruit allied health professionals without the commitment of salaried GPs willing to supervise trainees. For example, one primary care clinician cited that advanced nurse practitioners needed to complete 140 prescribing hours with the support of GPs (B6, primary care, clinical and managerial). However, primary care clinicians in Urbanville and Greenvale felt that general practices that were not integrated with a trust had an advantage when attracting potential non-clinical and clinical staff because they were not tied to Agenda for Change (except for GPs who are not covered) and hospital doctor bandings and pay rates, and so can offer more generous remuneration packages:
particularly the admin and clerical front of house teams who we are now competing with supermarkets [for] because the pay differentials on that and the hassle factor are sort of tipping people away. (B7, primary and secondary care, organisational management)
Impact of the implementation of vertical integration on strategic leadership and culture
Across case study sites, interviewees described a focus on realising more of the expected potential operational and clinical benefits of vertical integration. To do so, acute trust leadership had to effectively manage both macro and meso level influences on the implementation of vertical integration. In earlier sections, we discussed both positive and negative influences at the macro level, including PCNs and ICSs/ICBs in the local health economy. In this section, we present findings related to the organisational level.
Acute trust and GP leadership across the sites described the importance of establishing and developing working relationships with general practices in the local area. Interviewees described two areas of priority: (1) building trust between general practices and acute trust leadership; and (2) senior trust managers and clinicians understanding the complexities of operating in primary care, both in terms of understanding the funding mechanisms and how best to re-organise service provision. Undoubtedly the two approaches are linked and mutually reinforcing; for example, efforts by senior trust managers and clinicians to understand the intricacies of primary care operations led to increased trust by general practice managers and clinicians. This led to a greater willingness of general practice staff to support changes that resulted from vertical integration. Across case study sites, a major challenge during early stages of vertical integration was to overcome perceptions that the acute trust was taking over primary care. It was reported as important to show that the acute trust had the interests of primary care in mind and was not an ‘avaricious takeover beast’ (A2, secondary care, clinical and managerial):
Well at least we now have the credibility, we have many GPs, well respected, who know their mates, they know that we didn’t shaft them, we didn’t destroy them, we poured resource into them, we continue to talk the language of primary care. (A2, secondary care, clinical and managerial)
Acute trust staff described the importance of achieving credibility in terms of trusting the acute trust to act in primary care interests; that is, to prove that an acute trust was capable of managing and delivering primary care services. There were examples where credibility was enhanced by giving primary care clinicians roles as part of vertical integration arrangements, thereby giving greater legitimacy to changes being introduced in general practice after vertical integration. Acute trust interviewees acknowledged their initial lack of understanding of challenges facing general practice and how best to resolve them. One senior manager in Greenvale acute trust shared their experience more broadly:
I think our learning was trying to bring primary care into a much bigger organisation and put its people, clinical and financial governance on top of that – [it] just didn’t work. The practices themselves struggled with working in that bigger environment and the processes that were there, because they thought they were bureaucratic and out of sync of what they normally did. And likewise, I think we had a lack of understanding of some of the intricacies of primary care. (B7, primary and secondary care, organisational management)
Nevertheless, tensions remain between primary and acute care due to differences in attitudes and perceptions of the other and to different ways of working. Examples relating to clinical pathway development between the two care settings highlighted this tension. A few interviewees described the dynamic of the acute trust wanting to protect pathways into secondary care to avoid burdening staff in acute settings and better serve patients in the community. Yet, one senior clinician leading the vertical integration model in Townshire also acknowledged a perceived culture of protectionism established in general practice, to protect their own capacity to meet patient needs irrespective of integrated working with an acute trust. This is one example – in general, there remains across sites a cultural tension between secondary and primary care, which hinders the extent of collaborative working that is possible:
I think there was also an undercurrent of: ‘GPs are a bit crap and I’m sure we can make them work a bit better’, which is not an uncommon attitude for secondary care. (C1, primary care, clinical and managerial)
Such tensions added to the degree of apprehension with respect to what the key priorities should be for local vertical integration models. However, staff were also positive about the overall progress of vertical integration locally, including ways in which general practices, community-based care providers and the acute trust were working towards a shared vision, ambition and values:
Our new role is a journey of an acute trust to understand what primary and community care is. I think we’ve made that journey – to help community and primary care to understand us, define the ‘we’ word, get the culture in the organisation right… (A1, primary care, clinical and managerial)
There were ways in which case study sites described their process of developing their respective vertical integration model as highly relational. For example, staff accounts appeared to support relational coordination,88 a theory used to understand coordination within and across organisations. Relational coordination is based on three dimensions of work relationships: (1) shared goals, (2) shared knowledge or understanding, and (3) mutual respect and four dimensions of communication (timely, frequent, accurate and problem-solving communication). These dimensions of work relationships and communication are mutually reinforcing; high levels of such dimensions can lead to closer working and more effective performance across organisations.
The following excerpt from an interview in Townshire illustrates how shared understanding of each other’s operational intricacies translated into more realistic expectations of the other and more thoughtful, considerate working relationships:
And being sure that primary care also don’t get overloaded because hospitals are really quite good at saying ‘Oh the GPs can do this’ without really thinking about what the GPs can do and without actually thinking ‘Well general practice and their work force, they’ve got a certain amount of resource and is their time best spent doing what they think it is or what we think it is’. So we have to talk to them and be much more robust in working together basically (C4, secondary care, clinical and managerial)
Co-location (i.e. practitioners from primary, community and acute care working in a single setting) helped to increase both the frequency and timeliness of communication to implement innovation projects and health service changes in general. One Urbanville respondent described benefits of being physically present, but also why that is not always realistic:
I think there’s a distinct difference between where we’re present in a surgery and where we’re not. I think that’s one thing that we notice. You’re a small team … So when you’re not present in a building I think that makes a difference as well and I’m not sure what the solution is because some of it is building dependent, there just isn’t space for all of the team to be in there. (A3, community care, clinical)
In Greenvale co-location was also viewed positively as enhancing efforts toward coordinated care and improving working relationships. In the primary care setting, there was a concerted effort to address patient needs for complex patients living with long-term conditions by co-locating secondary care clinicians such as specialist diabetes nurses, physiotherapists and pharmacists.
A small number of clinicians in our sample of interviewees felt that the cultural and organisational working gap between primary and secondary remained too large to close. Thus, beyond administrative and operational efficiencies there were only limited service provision improvements that could be realised by establishing working relationships between primary and acute care:
I think what you risk doing is putting the demands of secondary care onto primary care and actually you lose the real value of primary care, which is about the continuity, it’s about holistic care, it’s a much less transactional process than secondary care is and the rules and regulations of secondary care may fit when you’re counting your numbers of your outpatient appointments or the surgeries that you’ve done, but they don’t fit [primary care]. (B4, secondary care, clinical)
Delivery, coordination and health service improvement: a bottom-up, collaborative model of service redesign
Coordination and delivery of care
Despite patient interviewees being part of PPGs, which might assume an extra level of understanding about primary care and, indeed, vertical integration, interviewees across all case study sites found it difficult to attribute service improvements specifically to vertical integration or to primary care in general. In the following themes, we refer to specific examples of vertical integration improvements in the following context, with this caveat in mind.
We found that vertical integration facilitated health service improvements for patients largely because of a bottom-up, collaborative approach to redesigning patient care between colleagues across primary, community and hospital care. For example, across case study sites, GPs referred patients directly to community and secondary services, with GPs and secondary care consultants working in MDTs, which improved coordination:
So, we’ve got some of the consultants that are due to come out into primary care. So, they’re coming to do clinics out in primary care, to try and prevent patients that actually could be dealt with in primary care with the input of a consultant, actually ending up in secondary care. (B5, community care, clinical)
In Urbanville, a MDT coordinator role at practice level was employed to support health-care professionals. As a result, health-care professionals felt better equipped to treat patients with higher support needs in a holistic manner; for example, working with colleagues across social care and housing. A further benefit of the MDT was oversight of patients who had high A&E use. There was a danger that without well planned coordination, duplication of care could arise in vertically integrated sites:
Because you could say ‘well I think this is a home visit’ and that’s fine, but as frequently happened, what the GPs thought would be a single visit, single problem, in and out in 40 minutes and GPs can do it. If you send a nurse in, they tend to do everything holistically and do the whole lot. So where does this acute episode end, versus how do I hand it onto the relevant services and get out without doing it too quickly? (A5, community care, clinical)
Yet there were challenges introducing new services brought forward by acute trusts with respect to PCN working local to case study sites. Indeed, we heard from a senior GP in Townshire (C1, primary care, clinical and senior manager) that because of the different approaches to meeting patients’ needs (i.e. PCNs working together to provide improved care across their area) compared with the vertically integrated approach where patients registered to integrated practices predominantly benefited from new services, full clinical integration and coordination of care between primary and secondary settings remained challenging.
Delivery of care for patients in Townshire was described by one senior GP as reflecting a continuous quality improvement system where the vertically integrated approach was intended to be pre-emptive of local population health needs, rather than responsive. Hence, the acute trust working with integrated practices has adopted a targeted approach to improve health outcomes for patients living with multiple long-term conditions, living with complex needs, or at high risk of developing illness, with the goal of reducing the propensity for patients to access both primary and secondary care services more regularly:
It’s opening that flexibility to our patients, which we can do. We have a GP who does an ENT [ear, nose and throat] clinic every other week. Now any patient on our list can go there, you know. He can touch base with the ENT consultants at the drop of a hat if he needs to (C3, primary care, organisational management)
Greenvale has established a shared medication workflow hub for managing medication requests centrally, bringing in specialists to the primary care setting so that GPs can refer patients directly to the right clinician has improved services for patients.
Provision for patients living with multiple long-term conditions
At Urbanville and Greenvale, vertical integration provided new opportunities to assess the needs and outcomes of individuals with multiple long-term conditions and support those needs through a coordinated and holistic approach using a MDT model and enhanced access to specialists and disease-specific clinics. The coordinated approach to treating patients with complex needs at both sites signalled a drive to improve patient care while simultaneously aiming to reduce A&E attendance:
In the room at the time, we’ve got housing in there, so the local authority in terms of housing; we’ve got our community nursing teams, whether that’s rapid intervention or somebody that’s involved in that patient care; social prescriber is in there; the mental health team will be in there because we’ve just appointed a mental health worker. So, it’s a whole range of individuals that are either involved in that patient or equally not involved in that patient but have got something to contribute to the wider discussion (A9, secondary care, organisational management)
The introduction and application of digital health tools to enhance support for people with multiple long-term conditions was a feature across case study sites, although to varying degrees. Also, this was directly applicable to primary care in general and not vertical integration. However, vertical integration was crucial in acting as a test site for the introduction of the digital health tools, which then enabled non-vertically integrated practices to roll out the digital improvements. For example, at Urbanville, a digital dashboard was trialled to enable practices to share data across their sites and was made available to all practices in the area during the pandemic.
At Urbanville specific service improvements included provision of primary care clinics at weekends. A well-established dashboard was used to help clinicians identify patients with multimorbidity and higher supports needs and monitor patients who are high users of care services. The focus at Urbanville was earlier detection of patients with multiple long-term conditions and prevention of secondary care usage. The data collated from the dashboard was also used in planning clinician time and formalising processes to support patients with multiple long-term conditions. At Greenvale, the acute trust has introduced Brave AI (Brave Artificial Intelligence Laboratory, Navi Mumbai, India), an artificial intelligence application that assigns to each patient a score for how complex their health needs are and monitors their wellbeing and risk level for potential hospitalisation. In Townshire, virtual wards providing patients with remote care at home are being used to monitor individuals with cardiology and respiratory support needs. Patients also had increased access to specialist knowledge due to consultants working directly with vertically integrated practices:
So being able to very quickly and easily talk to a respiratory physician, respiratory nurses, and one of the things I’m looking at is having a respiratory nurse into one of my areas where we know we’ve got a massive amount of COPD, so again talking to the trust to share resources (C3, primary care, organisational management)
Adopting an innovative approach to health-care delivery
All three case study sites displayed elements of innovation in health-care delivery. Innovation in health-care delivery is generally accepted as including new/improved service delivery, reimagined ways of working and new technologies. 89,90 Senior GPs at Urbanville described changes to health-care delivery as ‘innovation projects’, which were conceptually categorised in two groups: process (improving internal working practices to better support health-care delivery) and structure (changes to internal or external infrastructure and creation of new models of working). 91 Process change included stratifying the patient population and conducting analyses to assess patient needs across the health economy, as well as implementing home visiting support for very vulnerable and housebound patients. Structural innovations included enhancing the workforce through a clinical fellowship programme, which included the recruitment of GPs who were then made available to both vertically integrated and not vertically integrated practices in the area, and a pharmacy hub that managed repeat prescriptions to alleviate GP time, as well as an integrated telephone system introduced across vertically integrated practices to manage appointments:
We’ve created a digital model, today [a colleague] and I are going to meet all the other PCN leads to try and take an innovation project … to them to see if they will join in it, now this project is about [risk] stratifying the whole population from a primary care perspective and then supporting, aiding primary care clinicians to undertake needs analysis (C3, primary care, organisational management)
Like Urbanville, Townshire described structurally led innovation projects, including the development of a community midwifery team located in the same building with GPs. Yet, there were several challenges to introducing innovation projects to improve service delivery, notably from the local ICB. It was reported by one participant that a recent initiative in Townshire to introduce a renal clinic with consultant input did not materialise because of concerns from the ICB about equity of access for patients from non-vertically integrated practices:
I’m getting really frustrated at the fact I’ve got all these fantastic innovative things that we want to be doing to make sure the patient population, particularly the most deprived patients in [de-identified place], are better cared for and yet I’m fighting the system. I’m fighting national policy because it is not geared up for models like ours. It’s geared up to help traditional primary care practices (C3, primary care, organisational management)
In Greenvale, process led innovation projects centred around (but are not limited to) patients living with multiple long-term conditions and built on learning from the recent NHS Vanguard programme there to support patients in community settings with complex needs:
We did start to look at doing some shared work with the community nursing team in two of the practices to say ‘well look, how about we try to for a time to set up almost like a one team where we have our community nurses coming into the practice to learn much more about long-term conditions so when they’re seeing patients in their homes they’ve got much more knowledge about that and any practice nurses who want to go out into the community’ (B4, secondary care clinical)
Overall, it appears that structural and process innovation projects to improve health service delivery across vertically integrated practices are effective at the local level through collaborative working with primary and community care staff, with expertise and oversight from clinicians in secondary care.
Navigation work: accessing urgent and routine care as part of an integrated health-care system
Patient access
Difficulty in accessing primary care is a long-standing issue. Increased GP workloads, patients presenting with complex needs and shortfalls in capital investment have attributed to such difficulties. 92–94 These issues have exacerbated post COVID-19 with a push towards digital platforms to improve access. 94 Across all three case study sites we found issues with access not exclusive to vertical integration but common across primary care in general. Patients were offered various points of access to primary care including, but not limited to, in-person, on the telephone and digital via smartphone applicationss and online. The level of navigation work undertaken by patients across case study sites was high due to the convoluted nature of the different access routes, whereby many resorted to using in-person techniques to obtain urgent appointments while using digital media for routine care. Overall, patients felt that access to appointments to consult with a GP was challenging:
So, I literally called on the dot of 8 o’clock this morning and there were five people in front of me and I managed to get an appointment for this morning … Again, you have to go at certain times to make an appointment for the following day or something. I don’t know, it’s a little bit confusing but basically getting an appointment can be really very difficult but it’s not something I have to do often, but if I can set up on that patient portal access, not the [online platform] one, I would opt to do it through that because you can choose your times then and it’s just less time consuming (A10, Urbanville, patient)
Patients across case study sites also experienced an extra layer of navigation work, common across primary care, to access appointments in general practice with the added element of new triage systems introduced following the COVID-19 pandemic. 94 This additional layer of navigation led to confusion among some patients but, for others, it was a welcome introduction:
I had a haematology appointment on the phone this afternoon, so I have accessed … It’s frustrating having a phone appointment first, because he’s like, oh, I need to see you face to face because it’s a problem with your neck, and I’m like, you could have probably worked that out from the referral letter, and we could have been a lot more efficient having a face-to-face appointment first. (A17, Urbanville, patient)
I’m quite comfortable with [digital provider] telephone triage. What I would like, and I’ve been trying to ask my surgery to do this, I think actually that video triage is better … I’ve had a video consultation with the [de-identified person] at [de-identified place] and actually it is quite … It’s face to face, you can see the interaction. I think you have a better conversation as well. (B9, Greenvale, patient)
There is the potential to improve access to urgent appointments in vertically integrated practices due to innovations in central booking systems, which have enabled prioritisation of urgent appointments more easily, as implemented in Urbanville. While these innovations could be introduced in non-vertically integrated practices as well, what was unique to vertically integrated practices was the rapidity and flexibility that acute trusts had when introducing service-level changes, together with their greater financial resource compared with non-vertically integrated practices.
Patient satisfaction in accessing primary and secondary care services
Patient satisfaction in primary care was mixed across the three case study sites. We have established that access to primary care across the vertically integrated sites was challenging. This is indicative across primary care and therefore not a limitation of vertical integration. However, patient experiences of the quality of care received across primary and secondary care was positive:
Just before COVID landed I had a really, really, really bad chest infection. It was very bad and she saw me very quickly. She listened to all the lobes on my chest, on my lungs, took my temperature and she looked a bit worried and went off to see a doctor but the thing is because I did dentistry, I know a bit about thoroughness and she was thorough, and she was really really good you know (B8, Greenvale, patient)
Patients contextualised their accounts of accessing primary care around the well-established narrative regarding the lack of GPs. 95,96 As a result, patients questioned whether to access care given the lack of GPs:
Impact on me? I think there have been times when I’ve thought over a couple of things, perhaps I ought to contact the doctor about it and I think maybe not (B8, Greenvale, patient)
Patient satisfaction with secondary care across the sites was also varied. At Townshire and Greenvale it was noted that, post vertical integration, the patient transition from primary to secondary care via referral was efficient. Also, the introduction of specialist clinics in the pre-hospital space (e.g. for physiotherapy) may have positively influenced patient satisfaction. Treatment was also considered to be good once patients were seen in secondary care:
No, I’ve got to say it must be better now. In my own feelings and experience at talking to other people, it’s far easier to get to see a consultant at [de-identified place] than it was prior to the takeover. You’d got that system where the GP had got to write to the hospital, wait for a reply to come back and then went down that path to get an appointment. That doesn’t seem to happen now as much, it seems that they’re able to press a button on their computer, that has then gone instantly to the consultant’s secretary, and it gets dealt with fairly quickly (C8, Townshire, patient)
Despite positive experiences of care, there were accounts that were less positive around access to hospital care, although this is not described as being worse due to vertical integration. Patients experienced long waits to be seen and operated on (C7 and C10, Townshire, patients) and poor communication around appointment cancellations. Patients interviewed cited examples concerning mental health care in Townshire and rheumatology in Greenvale:
Several years ago, when my GP first thought I’d got lupus, there was a hideously long waiting list at the local hospital and I was in really quite a bad way. He said I think you’d better pay and just go to the [place] (B8, Greenvale, patient)
We found that patients at Townshire and Urbanville displayed a change in navigation behaviour once access had been gained to secondary care. Due to the improved communication and referral processes attributed to increased integration between vertically integrated practices and secondary care, it is possible to suggest that patients’ behaviour change is a result of vertical integration. For example, patients reported bypassing general practice and going directly to a named referral clinic or consultant assigned to them rather than waiting for intermediary support from their GP; a feature of care that was thought to be positive by patients in our sample:
Yeah. As I say, the hospital and the Macmillan support centre at the hospital was all very supportive, so I wasn’t lacking in psychological support, but I wasn’t getting it from primary care. I got it from secondary care (C9, Townshire, patient interview)
Overall, the landscape of navigation and illness work shifted for patients across the three case study sites, as it did across the whole country during the pandemic, with many reporting that the care they received was predominantly via remote methods, thus speaking with clinicians in primary and secondary care by telephone, online platforms and e-mail. While most patients in our sample felt comfortable with this shift in care, there was an emerging narrative around the nuances in the type of care provided. The dichotomy between in-person and remote care was interpreted by patients through the lens of thoroughness. With the former providing a ‘full assessment’ (A10, Urbanville, patient) and the latter acting as a triage or a shorter consultation appointment. Patients varied in their opinions about the introduction of remote care during the pandemic, but inevitably increased the intensity of the navigation work completed by patients prior to receiving care:
Well, I think they’re trying to put you off going there. They don’t seem to want to see you as readily as they did before, especially if you want an appointment during, when we did have the restrictions; you couldn’t get in the practice. You had to stand at the door and wearing masks and this, that and the other, which to some extent I can understand – not too against that. But I think it has made the whole process less personal and harder to access (C10, Townshire, patient)
In Urbanville and Greenvale during the pandemic, community teams were used to establish COVID-19 related services, including vaccination hubs. Vertical integration in this context was seen as having a beneficial impact, with practices stating that their general practice workforce was vaccinated sooner compared with staff in non-integrated practices (who were supported by the ICB) in the area. In addition, staff in vertically integrated practices thought they were better prepared to manage demand with respect to infections in the population as they were able to move staff across sites more readily.
Overall, the pandemic had a significant impact on the reorganisation of care and integrated services across the health sector. Importantly, patients thought the introduction of remote care and digital platforms increased the extent of illness and navigation work required to access care to address their needs. These changes cannot be directly attributed to vertical integration as there were wide ranging changes to care being made across local health economies to address COVID-19 challenges generally.
The influence of vertical integration on continuity of care
Patients with multiple long-term conditions whom we interviewed strongly welcomed continuity of care when accessing any health service in their local area, but particularly in primary care. In several of our patient interviews, references were made to repeatedly sharing illness narratives with multiple professionals, with the assumption that they had not read the patient notes prior to consultations. Preventing instances of repeating illness narratives was the primary reason stated by patients living with multiple long-term conditions for wishing to see the same clinician each time:
GPs at your surgery have an awareness of your conditions and your history. And that in itself makes for efficiency because if you’re seeing a random GP at odd intervals they will have to spend, I don’t know, fifteen, twenty minutes, looking at your case file before they could even talk to you sensibly about what your problem is. (A14, Urbanville, patient)
While some patients spoke of care continuity as a desire, others felt that it was a central component of receiving quality care:
They know you and they know your history. I think it’s very very important to have continuation in your care rather than going from one person to another person to another person to another person. I think things could get missed or you have to explain all over again what your problems are. (A16, Urbanville, patient)
At Townshire, one patient stated that continuity of care varies depending on the type of clinician and/or health professional, being less likely with GPs and nurses but more likely with allied health professionals:
The only continuity I had was the, whatever she was, probably a nursing assistant of some sort taking the blood, she was the same woman who took the blood every three weeks. So she was saying to me, ‘How are you getting on?’ but, you know, nothing from the nurses and doctors in the way of continuity. (C9, Townshire, patient)
In addition, patients were aware that continuity of care was impacted by workforce challenges in general practice, which had led to widespread use of locums. One patient was disparaging in their views of locums:
There’s your problem, a lack of GPs, and … it’s made far worse by locums. Locums breeze in, they see the patients, they breeze out and have an afternoon on the golf club or something. (C8, Townshire, patient)
Overall, patients across case study sites presented a strong preference for continuity of care with GPs as opposed to any other professional working across primary, community and secondary care, whereby patients saw the GP as a central figure in the long-term self-management of their chronic conditions. Notably, staff at Urbanville felt that the level of continuity of care delivered in the past was no longer realistic or achievable in primary care across the whole country:
The chances of many patients getting that continuity of care that they used to have has probably gone, which is a great shame. But, you know, I think that’s just the way general practice has changed really. (A8, primary care, clinical)
Discussion
Summary of findings
Analysis of interviews with staff and patients showed that vertical integration remains one model of integrated care that can help general practices remain open. Vertical integration between acute trusts and general practices is supported by the introduction of novel ways of clinically integrating care across primary, community and secondary care to meet the needs of all patients locally, but specifically those at risk, have complex, and/or multiple long-term conditions. However, there are some caveats. First, health service improvements driven by local acute trusts in collaboration with clinicians in general practice focus on health service changes that can improve population health for all patients locally and may use vertically integrated practices to test services before encouraging wider local roll out to non-vertically integrated practices. Notably, health service improvements are introduced following a significant period of cultural interchange (i.e. colleagues from acute and primary care understanding ways of working, challenges to delivering provision and aligning back office functions). Second, health service improvements were not only between primary and acute care, but also primary and community care, with clinicians from community and acute care becoming more embedded in providing services in general practice. Finally, following the pandemic and the introduction of new health services, patients with multiple long-term conditions encounter significant ‘navigation work’ concerned with choosing and accessing health provision with diminishing continuity of care with the onset and scaling up of MDT working; however, this holds true for both vertically integrated and non-vertically integrated general practices nationally.
How findings relate to previous research
There is growing interest in understanding how vertically integrated models of care can meet population and workforce needs in primary care from across the UK. Findings from this chapter extend the literature on understanding the drivers for vertical integration and the impact on the patient journey regarding their overall experience of treatment between primary, community and secondary care. Shortell et al. 97 identified several factors that need to be considered before commencing vertical integration. These included (but are not limited to): the need to establish trust among clinicians and institutions and consensus on practice and care delivery guidelines. Further, Shortell’s more recent work on accountable care organisations98 has detailed the importance of vertical integration to be physician led given their perceived legitimacy among clinicians and knowledge of local patient needs. Across our three sites, we found considerable engagement between GPs and secondary care clinicians and managers in attempt to understand how vertical integration could support and alleviate pressures faced in primary care, especially in relation to addressing workforce challenges and delivering services within community settings. The acute trusts in our study attempted to establish an almost bottom-up approach to engaging with primary care clinicians and attempt to understand organisational practices, historical challenges to providing care, and culture; nevertheless, tensions remained. Interviews with members of staff revealed how long the process of relationship building and cultural understanding has taken and how it entailed differing components of integration;99 we relate such findings to Gittell et al. ’s relational coordination theory and its associated dimensions. 88 Thus, akin to our phase 1 findings, organisational and functional integration takes a considerable length of time, whereby clinical integration (e.g. introduction of a range of services across primary, community and secondary care) has only recently been attainable.
Robinson and Casalino100 go further, highlighting that vertical integration focuses on integration between acute care and larger primary care entities (rather than solo physician or small physician practices) because of advantages such as increased efficiency in services for hospitalised patients, reduction in duplication of services, improved transitions across care settings, as well as facilitating cooperation where financial incentives across settings are not aligned. Similarly in our work, we found examples where vertically integrated primary care services were enhanced through greater horizontal integration of primary care. All examples of vertical integration between acute trusts and general practices include a degree of horizontal integration (either through practices merging or working as part of a network). Such a model can provide opportunities to redesign patient pathways to deliver care more efficiently.
Data from our qualitative study shows that vertical integration provides opportunity to embed clinicians from secondary and community care into primary care settings and also target patients at greatest need as well as those living with multiple long-term conditions, predominantly with the introduction of MDT working. Yet, it remains difficult to decipher whether changes to patient services resulted directly from vertical integration arrangements or due to increased horizontal collaboration amongst general practices, which also comes with additional resource (e.g. NHS DES contact as part of PCNs). Although, ‘innovation projects’ as described in this chapter demonstrate the greater level of flexibility and autonomy vertically integrated trusts have to deliver new services that are more responsive to local population needs and are not nationally prescribed.
Lastly, we build on Turnbull et al.’s82 application of navigation work encountered by patients and their sense making strategies and help-seeking behaviours and applied their understanding on interpreting patient journeys as part of vertically integrated models of care. We found that patients continued to face challenges accessing care and showed a preference to seek clinicians who understood their illness narratives. Although, much of the navigation work completed by patients was not specific to vertically integrated models of care but how the primary care landscape has changed since the COVID-19 pandemic.
Chapter 6 Discussion
Summary of key points
-
Identifying all instances of vertical integration, where a trust runs one or more general practices, is not a simple task. There was no dataset that could be interrogated to determine this, so we created one.
-
General practices that have vertically integrated with a trust do not appear to be ‘typical’ general practices but are smaller and performing less well against QOF criteria than other practices.
-
Some general practices would probably have closed if they had not been vertically integrated with trusts. We cannot determine what would have happened to patient care and use of hospital services in that eventuality. We have compared the outcomes where practices were vertically integrated with general trends. The findings need to be interpreted accordingly.
-
Among vertically integrated practices we have found modest reductions in patient use of hospitals at the time of vertical integration, which imply some cost savings. For the 39 vertically integrating practices included in this part of the quantitative analysis, the total estimated annualised hospital cost saving amounts to £1.9–6.7 million.
-
Overall, vertical integration is associated with a slight worsening in continuity of GP care for patients but with no impact on access to primary care or on satisfaction with primary care generally. This is alongside association with some positive service innovations and some improvement in mutual understanding between primary and secondary care staff.
-
We have found no evidence of any difference in the impact of vertical integration on use of hospital services between patients with multiple long-term conditions and other patients.
-
We have found examples of service innovations in vertically integrated practices that were focused particularly on supporting people with multiple long-term conditions but it is unclear whether they would have happened also in the absence of vertical integration.
-
Our phase 2 evaluation findings confirm many of our phase 1 findings, reported in Sidhu et al. 2022,2 and do not contradict any of them. The theory of change for vertical integration has been confirmed and elaborated but not fundamentally revised.
-
Our analysis approach has limitations; for example, restricted fewer than intended interviews were completed and the coding of ‘multiple long-term conditions’ in the analysis of hospital use data, but overall the mixed methods approach has yielded robust findings.
Synthesis of findings
The research team brought together the findings from all the WPs iteratively and cumulatively by means of a series of online team workshop meetings. These took place in October, November and December 2022 and in January 2023. Although WP1 necessarily preceded the quantitative analyses in WPs 2 and 3, the qualitative research at three case study sites (WP4) ran in parallel with the quantitative data preparation and the analyses of GPPS data, (i.e. alongside the earlier parts of the quantitative research).
The following discussion of the findings of all WPs taken together is organised under the headings of the three research questions we set out to answer. We specify to what extent the findings are similar or different for patients with multiple long-term conditions compared with other patients. The overall findings are then compared with the theory of change for vertical integration that was established in the BRACE phase 1 evaluation,2 and some refinements are proposed. The chapter concludes with a discussion of the strengths and limitations of our research, and with some reflections on the experience of conducting a rapid evaluation in the way that we have done.
Research question 1
-
1: How many general practices have already vertically integrated with NHS organisations running acute hospitals in England; when did the integration between general practices and acute hospitals take place; and what are the characteristics (in terms of geographical location, patient demographics and practice size/workforce) of those practices where vertical integration has taken place?
Identifying all instances of vertical integration, where a trust runs one or more general practices, proved challenging. There was no single dataset that could be interrogated to determine this, so we created one, drawn mainly from the annual reports and accounts published by each trust individually. We have established that, at the end of March 2021, 26 trusts (15 acute hospital trusts and 11 community trusts), which is roughly 1 in 10 trusts in England, were each running one or more general practices, 85 in total, which is equal to somewhat over 1% of all general practices with significant variation in how many general practices each trust has vertically integrated. The number of vertically integrated general practices in England has been increasing annually since 2015 in a steady trickle: vertical integration is an established approach to organising care in some places, but it is far from being common. The number of practices run by each trust ranges from just a single practice in several cases, to as many as 12 practices in the largest vertically integrated group.
The geographical spread of vertical integration is broad. It occurs across the whole of England, in both urban and rural geographies. Measures of population deprivation are similar in vertically integrated areas to the average in the rest of the country (a higher percentage of practices vertically integrated with community trusts are in deprived areas compared with acute trusts). However, practices that vertically integrate are below average size in terms of numbers of registered patients and FTE GPs. Practices that vertically integrate are also, on average, doing less well than other practices in terms of QOF scores. Our qualitative findings corroborate this position. Townshire’s and Urbanville’s approaches to vertical integration were predominantly to sustain primary care close to where patients live but also improve key service provision performance indicators (across primary, community and secondary care). These findings are consistent with our findings in the phase 1 study, and internationally, that practices that enter vertical integration include some that are struggling. 101 In short, practices that have vertically integrated with a trust do not appear to be ‘typical’ general practices.
Research question 2
-
2: What impact is vertical integration having on secondary care (outpatient attendances, A&E attendances, all inpatient admissions, emergency inpatient admissions, inpatient admissions for ACSC, bed days, readmission within 30 days of discharge)? Does this impact differ for people with multiple long-term conditions compared with other patients without long-term conditions or living with a single condition?
Our findings relating to this question are largely, but not solely, from the quantitative analyses we undertook of HES data. We restricted those analyses to the instances of vertical integration that were supported by reliable, monthly, hospital activity data for 2 years before the date of vertical integration and 2 years afterwards. We compared patient use of hospital services for these practices with use by patients of ‘stable’ practices that had held GMS contracts throughout the period. We thereby identified some statistically significant, but modest in magnitude, impacts of vertical integration on use of hospital services.
Our interviews did not reveal any perceptions of notable changes in rates at which patients of vertically integrated practices accessed hospital services. Our quantitative analyses however revealed modest, statistically significant falls in rates of A&E attendances, outpatient attendances, emergency inpatient admissions and emergency readmissions, at the time of vertical integration, and no increases in any broad category of hospital activity. But, in respect of A&E attendances and outpatient attendances, vertically integrating practices had faster growth in hospital activity than for ‘stable’ practices, both before and after the date of vertical integration. A consequence is that the modest reductions in A&E and outpatient activity at the time of vertical integration are temporary; soon erased by increased activity subsequently. For emergency inpatient admissions and readmissions, vertically integrating practices’ trends in hospital activity were not significantly different from those of other practices, so the reductions in emergency admission and readmission rates may persist (at least for the 2 years post-vertical integration that our analyses covered).
We have paid particular attention to analysing whether the impact of vertical integration on the use of hospital services differs for people with multiple long-term conditions compared with patients with one or no long-term conditions. We have found no evidence of any difference in impact on that part of the patient population. Nevertheless, evidence from interviews with staff and patients from across our three case study sites shows acute trusts are prioritising improved coordination of care for those living with multiple long-term conditions. Improved coordination of care includes an increased presence of consultants in general practice, MDT working and improved access to screening services available in community settings. Such service level improvements may also have some bearing on hospital utilisation in the medium to long term. We have compared our results with the only previously published quantitative analysis of the impact of vertical integration on patients’ use of hospital services. Our data include those analysed by Yu et al. 202034 for the effect of vertical integration in one location: Wolverhampton. However, we have taken a different statistical approach and have more data, from the whole country. We are reporting a total effect across all vertical integration sites where there are reliable data for 2 years before and 2 years after the date of vertical integration. In that context, our findings can be seen as broadly consistent with those of Yu et al. 34 They report hospital cost savings resulting from reductions in emergency inpatient admissions and readmission. We have additionally found, when looking beyond Wolverhampton, small reductions in A&E attendances and outpatient attendances.
Our analysis suggests that at the time of vertical integration there are small but significant downward shifts in some hospital activity for the patients of the integrating practices. These reductions appear to persist for vertically integrated practices relative to other general practices in the following 2 years in respect of emergency admissions and readmissions. However, at the vertically integrating practices the rates at which patients were attending A&E and outpatients departments of hospitals were growing faster than at stable practices before the date of vertical integration, and they resumed this relatively faster rate of growth after vertical integration. Thus, the saving in amount of hospital A&E and outpatient activity is temporary. Figure 20 provides a schematic illustration of this effect.
FIGURE 20.
Conceptual depiction of the pattern of A&E attendance rates and outpatient attendance rates for patients of practices that vertically integrate with trusts.

Financial implications following the implementation of vertical integration
The combined effect of the reductions in hospital activity that we have found at the point of vertical integration are summarised in Table 21. The table shows the approximate activity impact and consequent financial impact on the vertically integrated trusts in our analysis. The financial estimates cannot be extrapolated to all general practices; our evaluation has made clear that practices that vertically integrate are not typical or average, so it cannot be assumed that the effects seen there would be replicated widely were vertical integration to be implemented across the country.
| Activity | Step change compared with stable GMS practices, IRR (95% CI) | Total VI secondary care use per year (N = 39 practices) pre VI | Change in secondary care use post VI | Annualised cost saving across all VI practices (N = 39) post VI (£) | Mean cost saving per practice after VI (95% CI), £ |
|---|---|---|---|---|---|
| A&E attendances | 0.98 (0.96 to 0.99) | 126,312 | 2526 | 460,000 | 12,000 (£8900 to 14,600) |
| Outpatient attendances | 0.99 (0.99 to 1.00) | 487,253 | 4873 | 660,000 | 17,000 (£13,000 to 21,000) |
| Emergency inpatient admissions | 0.97 (0.95 to 0.99) | 33,553 | 1007 | ||
| If short stay | 610,000 | 16,000 (£12,000 to 19,000) | |||
| If long stay | 3,400,000 | 87,000 (£68,000 to £106,000) | |||
| Emergency readmissions | 0.95 (0.91 to 1.00) | 7092 | 355 | ||
| If short stay | 210,000 | 5,500 (£4200 to 6700) | |||
| If long stay | 1,200,000 | 31,000 (£24,000 to 37,000) | |||
| Total | 1,940,000–6,720,000 | 50,500 to £147,000 |
We estimate any potential cost reductions in secondary care utilisation resulting from the introduction of vertical integration, using the unit cost per activity provided by the NHS National Schedule of References Costs for the year 2019/20102 and the Unit Costs of Health and Social Care 2020. 103 We use the IRR for the step change in secondary care use for vertically integrated practices compared with ‘stable’ GMS practices, to calculate the change in our chosen secondary care outcomes. This then enabled us to multiply the unit cost for each outcome measure by any statistically significant change at the point where vertical integration is introduced. The results of these calculations are reported in Table 21, which is for all secondary care outcome measures where the step change compared with ‘stable’ vertical integration practices was statistically significant, namely for A&E attendances, outpatient attendances, emergency inpatient admissions and inpatient readmissions.
We find that at the point of vertical integration, there is a reduction of 2526 A&E attendances per year among the patients of vertically integrating practices. This results in a cost saving of £460,000, based on a unit cost of £182 per A&E attendance. 102 There is also a reduction of 4873 outpatient appointments equating to a cost saving of £660,000, based on a unit cost of £135 per outpatient attendance (the weighted average cost of all outpatient attendances as reported in Curtis and Burns 2020). 103 Emergency inpatient admissions drop by 1007, equating to a cost saving of £610,000 if these were short-stay emergency admissions (unit cost of £602 per admission) or £3,400,000 (unit cost of £3366 per admission) if these were long-stay emergency admissions. 103 Likewise, inpatient readmissions drop by 355, equating to a cost saving of £210,000 if they were short-stay readmissions and £1,200,000 if they were long stay readmissions. 103 In total, for the 39 vertically integrating practices we were able to include in this part of the quantitative analysis, the estimated annualised hospital cost saving from the initial reductions in hospital activity seen for the patients of those practices amounts to £1.9–6.7 million.
Research question 3
-
3: What impact is vertical integration having on the patient journey with regard to access to, and overall experience of, care? How does the experience differ for people with multiple long-term conditions compared with those living with no or one long-term condition?
It is important to note first that the vertically integrated practices stayed open and continued to provide primary care to their local populations. Our evaluation is unable to determine how many of those practices would have closed had they not integrated with a trust, but our phase 1 study2 showed that it is highly likely that at least some practices would have ceased to operate. The consequence of that would have been the patients of the affected practices being redistributed to the lists of other practices, presumably less convenient (on average) for patients and adding to the demand pressures and need for recruitment at the receiving practices.
We have used data from the national GPPS to evaluate quantitatively the impact of vertical integration on the patient experience of primary care and we have conducted interviews with 14 patients and 22 staff to obtain qualitative data. The analysis of GPPS data looked at six measures related to patient experience, all of which are measured on a 0–100 scale with a higher score equating to a better patient experience: helpfulness of receptionists; ability to get through on the telephone; time taken to see or speak to a GP; overall experience of access; continuity; and overall satisfaction. The interviews were able to explore the views of patients and staff in a broader way, allowing respondents to raise issues they considered noteworthy.
The analysis of GPPS data found that patient experience of care was worsening gradually over the study period for vertically integrated practices but that this was in line with national trends. We found no statistically significant step change in patient experience before and after practices switch to a vertically integrated model compared with control practices for five of six of the patient experience outcomes (those concerning access and overall satisfaction). We did find a statistically significant though modest worsening relative to ‘stable’ practices in continuity of GP care for patients (ability to make an appointment with a preferred GP) after practices became vertically integrated. Our qualitative findings show that continuity of care in vertically integrated practices remains a challenge. For instance, patients living with multiple long-term conditions are likely to receive care from a range of allied health professionals working as part of a MDT and this may be despite patient preferences to see a preferred GP.
The interviews we conducted revealed that vertical integration is associated with some service innovations and improved clinical integration, including examples where vertically integrated practices had pioneered initiatives and thereby encouraged other practices in the area to do likewise. We found that, where this was happening, vertical integration facilitated service improvements for patients largely because of a bottom-up, collaborative approach to redesigning patient care between colleagues across primary, community and hospital care. It is unclear whether the innovations could be directly attributed to vertical integration, but circumstantial evidence shows vertical integration as at least driving and supporting innovation in these cases. However, we also found at one of the three case study locations examples of where changes in service provision sought by vertically integrated practices were opposed by others locally.
Despite evidence that integrating health and social care improves access and patient experience for people with complex needs, they continue to experience a lack of coordination across teams and wider community resources. 104 We identified two related but distinct elements of vertical integration which appears to be necessary for innovations in health-care service delivery to thrive: relational coordination and service coordination towards delivery of care. We found that vertical integration is highly relational and the coordination within and across organisations is facilitated by: (1) shared goals, (2) shared knowledge or understanding, (3) mutual respect and (4) increasing opportunities for communication. Despite concerted efforts to establish closer working relationships across primary, community and secondary as part of vertically integrated models, cultural differences remained and hinder the extent of collaborative working that was possible. Yet we heard reports of increased shared understanding between secondary care and primary care staff of each other’s operational intricacies, which helped to determine expectations of what colleagues could achieve as part of vertically integrated model of care. On both a macro and micro level, aspects of relational coordination can contribute to an environment where health-care service provision can deliver timely and appropriate care.
Further still, improvements in relational coordination can lead to better co-ordinated care (e.g. bringing consultants into general practice, the use of MDTs and application of digital tools). Such examples that suggest coordination of care in vertically integrated models of care can be proactive,82 to treat patients in primary care and away from emergency secondary care.
Informed by Corbin and Strauss’ concept of the ‘work’, our approach to understanding patient navigation builds on existing literature which suggests that help-seeking behaviour is a social process with exogenous factors (external to the patient) and influenced by health-care professionals and models of health-care provision. 105 Although we found examples where patients’ ‘work’ was increased (e.g. patients using digital tools for remote consultations), we also identified examples where patients’ navigation work was reduced at the intermediary level due to improved access for appointments in general practice and improved transitions between primary and secondary care. The overall picture of the impact that vertical integration is having on patient access to, and overall experience of care, relative to the national picture across all practices, is that it is associated with a slight worsening in continuity but with no impact (for better or worse) on access to primary care or satisfaction with primary care generally. As a result, those considering introducing vertically integrated models of care need to ensure any changes in health-care provision is underpinned by the importance of continuity and the need to prioritise or incentivise this alongside other developments in health care.
We specifically analysed in the quantitative work whether patients with multiple long-term conditions were affected differently by vertical integration compared with other patients. All 14 of the patients we interviewed had multiple long-term conditions. It would not have been practical within the constraints of a rapid evaluation (a point reinforced by the difficulties we encountered in recruiting patients, as discussed earlier) to interview the much larger number of patients that would have been needed to undertake a comparative qualitative study. The interviews revealed examples of some service innovations in vertically integrated practices that were focused particularly on supporting people with multiple long-term conditions. It is unclear the extent to which these would have happened in the absence of vertical integration. For example, in Greenvale innovative support for patients with multiple long-term conditions had been a focus of a ‘new model of care’ vanguard initiative that was implemented 1 year before the vertical integration started and continued alongside it. However, as our phase 1 study highlighted, sustaining practices via vertical integration at least provides the opportunity for service innovation to happen, including innovations particularly aimed at patients with multiple long-term-term conditions. Yet, akin to existing literature, evidence on the impact of models of integrated care on cost and health-care use remains unclear. 106
Our quantitative analysis of GPPS data showed that when practices vertically integrate with trusts any differential impact for people living with multiple long-term health conditions compared with people living with a single condition or no conditions, is either not significant or of very small magnitude for the measures of patient experience.
Revisiting the theory of change
The phase 1 evaluation enabled us to define an initial theory of change for vertical integration. In the light of the phase 2 evaluation, we can confirm the continued applicability of that theory of change and add some refinements. Figure 21 reproduces from the phase 1 evaluation2 the diagram illustrating the theory of change and with the further additions and refinements identified by the phase 2 evaluation shown in bold font.
FIGURE 21.
Updated overall theory of change for vertical integration.
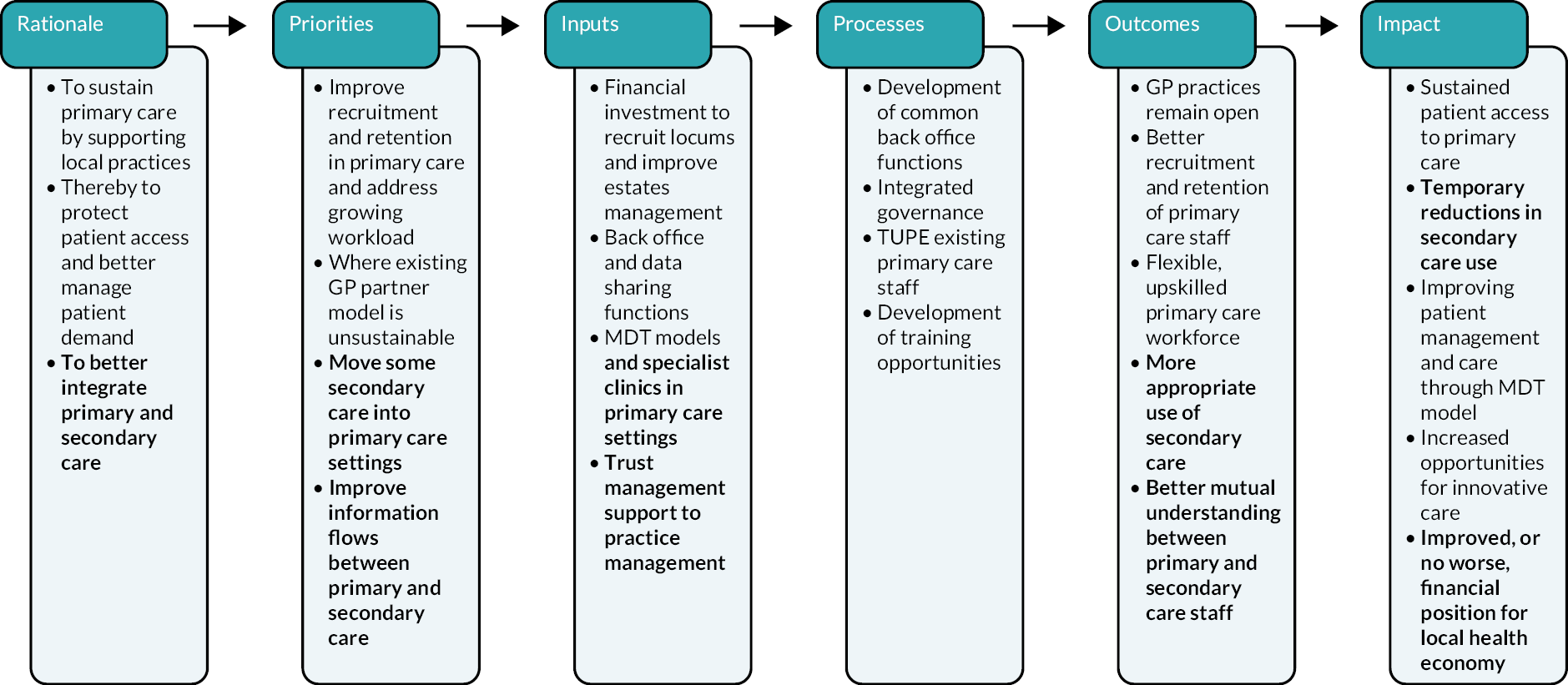
The context remains that NHS policy stresses horizontal integration in primary care, though not necessarily merger, and is silent on trusts running general practices. However, there has been a publicised period of ministerial interest in this type of vertical integration in early 2022 and it has become a topic of policy discussion again in early 2023. 107
Our phase 2 evaluation findings confirm many of our phase 1 evaluation findings and do not contradict any of them. The rationale for vertical integration is focused on sustaining primary care, managing demand for secondary care services and better integrating secondary and primary care. With respect to the last of these, the main priorities are to provide some specialist services in primary care settings and, more generally, to improve information flows between primary care and secondary care providers. The managerial integration of vertically integrated practices, either directly with trust management arrangements or via a trust-owned company managing primary care, has not been without challenges, as noted in both phases of the evaluation. Bringing two very different cultures – primary care and secondary care – together is not easy but we have heard encouraging reports of better mutual understanding coming out of vertical integration. We have discussed at some length above the limited extent to which vertical integration has had an impact on patients’ use of secondary care and the consequent temporary financial savings that it might yield. Owing to the impossibility of knowing the counterfactual had vertical integration not occurred where it did, we cannot tell whether more lasting financial savings may result, but we know from the phase 1 study that trust managers expect that they will.
Strengths of the evaluation
This report presents the second phase of a two-phase evaluation of vertical integration between general practices and secondary care trusts in the NHS in England. The first phase took place in 2019 and early 2020 and is reported in full elsewhere. 2 The second phase, reported here, commenced more than 2 years after the end of phase 1 and was completed during 2022. Returning to the same evaluation topic, and indeed to two of the same case study sites, has the advantage that even though each phase of evaluation is conducted rapidly we can allow time to elapse and impacts to emerge in a way that would not be possible in a single, rapid study.
The study team completed a mixed methods rapid evaluation following established methodology (and guided by previous evidence of implementation), while engaging iteratively with published literature. Using mixed methods – secondary analysis of large, national, routinely collected data sets and collecting data through interviews – enabled the team to develop a comprehensive understanding of the scale and impact of vertical integration in England. At a time when primary and secondary care staff were under great pressure, we nevertheless completed a good number of interviews (13 interviews and 3 focus groups with 22 members of staff and 14 patient interviews) with a range of stakeholders across three case study sites. Given the extent of our data collection and analysis we are confident that within the scope of the evaluation data saturation was achieved: additional interviews were, by the end of the study, adding no further fresh insights.
As has been described earlier in this report, the quantitative analysis was thorough in identifying all instances of vertical integration and in disentangling horizontal mergers between general practices from vertical integrations with trusts. The analysis made use of a range of comparators for practices that vertically integrated (with acute hospital trusts or with community trusts, separately identified); including practices merging horizontally, practices taking on APMS contracts, and ‘stable’ practices that retained GMS contracts and did not merge throughout the study period.
Member validation occurred throughout data analysis amongst study team members, the BRACE Steering Group, BRACE PPI panel, senior members of the BRACE executive team, and external colleagues with expertise on integrated care acting as critical friends. In addition, our analysis across all parts of the study were conducted iteratively and cumulatively in research team data analysis workshops.
Limitations
An unavoidable issue in the analysis is that we do not know what would have happened in the counterfactual (i.e. if the practices had not integrated with a trust). It is likely that some of the practices that are providing primary care to patients today would have closed if they had not been vertically integrated with trusts. None of our analyses can determine what would have happened to patient care, including use of hospital services, in that eventuality. But we have compared the outcomes where practices were vertically integrated with general trends. The findings must be interpreted accordingly.
Our analysis shows that general practices that vertically integrate with trusts are probably not average practices but rather are atypical. Hence, an inevitable limitation of the evaluation, despite the range of comparators we deployed (listed earlier), is that we could not replicate the counterfactual of what would have happened had practices not merged with trusts (in those places where they did, in fact, merge with trusts). Our results are interesting for what they say about the impact of vertical integration where it has been implemented, but we cannot extrapolate from them to the hypothetical case of vertical integration being rolled out to general practices generally.
The phase 2 evaluation reported here, commenced 2 years into the COVID-19 pandemic, which has changed so much, so rapidly, about how health care, and especially primary care, is provided. These large COVID-19 related effects make it hard to distinguish in what we heard in patient interviews what might be the, probably more subtle, impacts of vertical integration on their experience of care following the COVID-19 pandemic. As a result, we have taken a cautious approach when synthesising quantitative and qualitative findings, given that data were captured prior, during and post the COVID-19 pandemic, and we have developed our implications for policy makers accordingly.
There are limitations to the use of the GPPS to explore the impact of vertical integration on patient experience, and we acknowledge these limitations. We were only able to explore access, continuity and overall satisfaction in our analyses, as measures of doctor and nurse communication quality changed across the study time period and so could not be included. We also acknowledge that the survey response rate is low (between 34% and 38% across the study period). In mitigation, we used survey weights that account for sampling and non-response in our estimates of descriptive statistics; we adjusted for age, gender, ethnicity and deprivation in our analysis; and included general practice as a random effect in our multivariable models; which will mitigate in part the impact of where these characteristics are associated with both patient experience and survey non-response. We were able to explore in part patient experience in our qualitative work and these findings are consistent with the quantitative analyses.
The team encountered difficulties identifying and recruiting interviewees across case study sites despite identifying gatekeepers and working with PPGs. Consequently, we have a modest number of interviews completed with patients (14 of an intended 24), and with more patients recruited from one site compared with the other two sites (Urbanville N = 8, Greenvale N = 2, Townshire, N = 4). The evaluation accessed patients from PPGs which may have limited the reach of which patients were made aware of the study, while those patients who tend to be more engaged with PPGs are using older, less ethnically diverse (predominantly white British), more educated and have greater awareness of navigating local health economies in relation to care co-ordination and self-management.
A methodological limitation was, arguably, the need to go through a gatekeeper to identify appropriate members of staff to take part in focus groups or interviews. The success of our interviewing approach was largely dependent upon the relationships that members of the study team established with gatekeepers (senior managers) over a relatively short period of time. But our recruitment approach also depended upon the strength of the relationship between the gatekeeper and the interviewee. Such a method of identifying staff can introduce bias when putting forward individuals for interview. This may explain why the study team had limited success in recruiting clinical NHS colleagues. The team does not believe this imbalance across primary, community and secondary participants influenced the overall data set but rather focused our interpretation on the most pertinent issues for integrated models of care local to each area.
Focus groups were completed at one site only, with staff across other sites opting for one-to-one interviews, which may signify levels of comfort staff felt sharing their experiences of vertical integration amidst colleagues. In addition, there was imbalance with respect to the number of focus groups and interviews, with only three focus groups completed in person with the remaining interviews all completed using Microsoft Teams, Zoom or telephone.
We note that there are a both advantages and drawbacks of using the SELFIE framework to structure learning from this evaluation. The approach provides a rigorous systematic method of organising findings for impact evaluations and considers the nature of coordination of care for people living with multiple long-term conditions. Yet we recognise that the study team has taken an adapted approach when using the framework; using it as a lens to guide the evaluation rather than a more encompassing application of the framework with reference to each of the numerous sub-domains within it.
Finally, we have sought to determine whether vertical integration affects patients with multiple long-term conditions differently from other patients. We note, in respect of the quantitative analysis of HES data on hospital use, that we adopted the commonly used Charlson Comorbidity Index conditions to code ‘multiple long-term conditions’. This has the weakness that it excludes mental health-related diagnoses. Hence, all the patients we coded as having multiple (two or more) long-term conditions certainly had multiple conditions, but we will have omitted some patients with one or more mental health long-term conditions plus one or no physical health long-term conditions. We acknowledge that throughout this report we have used three interpretations of multiple long-term conditions (GPPS, HES and NICE). Although the presence of two or more long-term conditions is the widely acknowledged definition, the way in which multiple long-term conditions is measured varies. 108 We use more than one definition of multimorbidity in this report. All are count based metrics rather than more nuanced weighted scores. We acknowledge the limitations of this approach but note that there is no standard approach. 109 One strength of this study is that we have used data from more than one source, but the limitation of course is that the definitions of included conditions, and therefore multimorbidity, vary between sources. In mitigation, we have considered dose–response relationships (in secondary care use considering people with 0, 1, or 2 or more conditions, and in the analysis of patient experience 0, 1, 2, 3, 4 or more conditions); although the specific impact of multimorbidity may vary between definitions, we would expect relationships with increasing numbers of long-term conditions to be less sensitive to bias and for interpretation of these across data sets to be more comparable.
Reflections on the experience of conducting a rapid evaluation
We noted earlier that a two-phase approach, with each phase conducted as a rapid evaluation, is useful to allow time for longer-term impacts to become evident, without the expense of maintaining an evaluation actively throughout. The research team would advocate consideration of this approach for other evaluations where major elements of the expected impact are likely to emerge over a few years rather than be evident in the shorter term.
A particular feature of the analysis reported here was the ability to use routine national datasets of hospital activity and patient experience of GP services. Having ‘on the shelf’ HES and GPPS data enabled extensive quantitative analysis to be commenced rapidly, without adding months of delay to the evaluation timescale while data permissions were obtained from scratch.
But some aspects of this evaluation were more time consuming than the research team had initially expected. In particular the process involved in tracking down all instances of vertical integration was prolonged. So too was the process of identifying where horizontal mergers between (which) general practices had taken place.
We summarise our experiences of conducting a rapid evaluation, including the context of the data being gathered during the pandemic, as follows:
-
Responsiveness: the team continued to build and revisit a mapping exercise to identify relevant literature related to our aims and research questions which two authors (JS and MS) had undertaken for our phase 1 evaluation, which saved time and resource. The speed at which the evaluation was undertaken has impacted on the study team’s ability to provide real-time feedback to our case study sites, especially those sites seeking to learn from our findings to inform practice local to their site. There was a preference amongst interviewees (as well as study team researchers) to use media such as Zoom and Microsoft Teams to complete interviews via video link, which supported flexibility in arranging interviews compared with in-person interviews while permitting a fuller interaction during the interview itself than would be possible by telephone.
-
Relevance: there has been continued and close collaboration with the BRACE Steering Group and BRACE PPI group to discuss the priority of our evaluation, comment on our participant-facing material (e.g. information sheets) and input into our emerging findings. The involvement of key experts to support ensured that the team answered the most appropriate research questions about current integrated models of care. Hence, collaboration from stakeholders has been in the form of both consultation and co-production.
-
Rigour: the team iteratively engaged with theoretical and policy relevant literature throughout the design, data collection, and analysis/interpretation stages of the evaluation. Combining quantitative and qualitative analyses has helped to challenge and test the robustness of findings in both directions. Nevertheless, we have proceeded cautiously when synthesising our findings.
With respect to project management, a team with a clear hierarchy, roles and responsibilities (one principal investigator, one project manager and six researchers) operating over a time period of a year from starting work on the protocol to submitting this project report, was a significant positive; alongside monthly communication with BRACE governance teams to facilitate rapid working.
Chapter 7 Conclusions
Summary of key points
-
Vertical integration can be beneficial for particular general practices and trusts, but our analysis does not reveal a case for widespread roll-out of the approach.
-
Implications for policy and practice include:
-
That routinely recorded general practice details should in future include whether each practice is owned by another organisation, and if so whether that organisation is an NHS trust, another public body, or a private organisation.
-
For vertical integration to be successful, there is a need for an initial period of trust and relationship building as part of the cultural transformation for both primary and secondary care.
-
Practitioners and managers in vertically integrated arrangements could usefully consider how changes in the provision of care can help to reduce the extent of ‘navigation’ and ‘illness work’ that patients have to undertake and which are greatest for those living with multiple long-term conditions.
-
The effects of vertical integration take time to build up and initial impacts may not last. Hence patience is needed to allow vertical integration to develop where it is attempted.
-
-
Further research in future would be worthwhile to investigate:
-
If vertical integration improves recruitment and retention of primary care staff, including GPs?
-
The extent (if any) of economies of scale in provision of back-office functions?
-
The longer-term impact of vertical integration on hospital usage and more certain and precise estimation of the magnitudes of any effects.
-
Quantitatively, the impact of vertical integration on patient use of primary care.
-
More extensively, patient and carer experiences of secondary care and of navigating care overall as part of vertically integrated models of care.
-
From the perspective of primary and secondary care clinicians, service managers and other staff, to understand the rationale and drivers for service level improvements; the indicators that would represent effective integration between primary, community and secondary care; and how agendas to meet local needs can best be agreed and addressed.
-
The rapid evaluation reported here and undertaken in 2022 returned to a topic we first evaluated in 2019 and early 2020. In this phase 2 evaluation, we have found that vertical integration is widespread but affects (at end March 2021) only 10% of trusts and a little over 1% of general practices. Where vertical integration has occurred, it was not as a result of top-down national policy but rather of bottom up local initiatives. In these places, vertical integration serves the purposes identified in our phase 1 study of sustaining primary care and providing a platform for some service innovation and integration. We have detected statistically significant reductions in hospital activity, of the order of 1–5%, at the time of vertical integration which imply annualised savings of £1.9–6.7 million in the costs of those hospitals affected. These reductions appear short-lived for A&E attendances and outpatient attendances, but more persistent for emergency inpatient admissions and readmissions. There appears to be little impact of vertical integration, either for better or for worse, on patient experience of care as measured by the answers to questions in the GPPS, apart from a small reduction in the continuity of care (patient being able to see their preferred GP). Patients with multiple long-term conditions are affected in very similar ways to patients with single or no long-term conditions.
Thus, vertical integration is one model of integrated care that can help general practices remain open by introducing novel ways of clinically integrated care across primary, community and secondary care to meet the needs of all patients locally. The success of this model of care is reliant on stakeholders across primary and secondary care trusting and understanding their counterparts and working collaboratively while acknowledging drivers and challenges to providing health services in each sector. While patients welcomed easier transitions of care between primary and secondary care, there was acknowledgement of some diminishing in continuity of GP care.
Implications for policy makers and decision makers
This study prompts the following recommendations for policy and practice. It proved far from straightforward to determine which trusts and general practices are parts of vertically integrated organisations. We discovered that there was no database that permits ready determination of this. We therefore recommend that routinely recorded general practice details should in future include whether each practice is owned by another organisation, and if so whether that organisation is an NHS trust, another public body, or a private organisation (and, in the last case, whether for profit or not for profit).
Following a sustained period of embedding, which includes addressing system level changes to improve organisational and functional integration,13 vertically integrated models have shown success in establishing collaborative working across health sectors local to their area. Hence, clinical and non-clinical staff from secondary care were more likely to achieve changes to clinically integrated patient pathways if a bottom up, facilitative approach built on trust was present with colleagues from primary care. Thus, for vertical integration to be successful in bringing about service level change, there is a need for an initial period of trust and relationship building as part of the cultural transformation happening for both primary and secondary care.
Achieving improvement in outcomes occurs in stages, which may overlap in sequence: (1) contractual and legal changes to enable acute trusts to hold GMS, APMS or PMS contracts either directly or via a subsidiary company; (2) organisational and functional integration (human resources, finance, estates) and alignment of back office functions; (3) cultural understanding and trust building among colleagues from secondary and primary care with the development of shared goals; and (4) developing and introducing innovative practices to improve clinical care and pathways, with explicit consideration given to the needs of patients with multiple long-term conditions in some clinical areas to meet local population needs. Practitioners and managers working in vertically integrated arrangements could usefully consider how changes in the provision of care can help to reduce the extent of ‘navigation’ and ‘illness work’ that patients have to undertake and which are greatest for those living with multiple long-term conditions.
Our analysis has not revealed a case for vertical integrated to be rolled out nationally. Yet, it continues to be a potentially valuable option to keep available to trusts and general practices wherever they consider that local circumstances make it attractive. We have learned that some effects take time to build up and that initial impacts may not last. Hence patience is needed to allow vertical integration to develop where it is attempted.
Implications for future research
At the end of the phase 1 rapid evaluation of vertical integration the research team proposed the future research should address several questions. 2 We have addressed some of those questions in the phase 2 rapid evaluation reported here, but the following two were not and consequently remain on the future research agenda:
-
Is vertical integration improving recruitment and retention of primary care staff, including, but not limited to, GPs?
-
Are there economies of scale in provision of back-office functions?
Our quantitative analysis of hospital utilisation data showed that initial reductions in A&E and outpatient attendances at hospital following vertical integration of a general practice with a trust did not appear to last. While reductions in emergency admission and readmission rates appear to persist. However, we followed up only for 2 years after vertical integration, and even for that modest a follow-up period our sample of practices that could be analysed was merely 39. Further quantitative follow-up in future would not only permit investigation of the longer-term impact of vertical integration on hospital usage but would also enable more certain and precise estimation of the magnitudes of any effects. Additional analyses of secondary care activity data in a future study could investigate whether there are differential impacts of vertical integration for patients with various combinations of long-term conditions, and for extending the list of relevant conditions to include mental health issues.
In the present study, we have not sought or analysed quantitative data on patients’ use of primary care. Quantitative investigation of the impact of vertical integration on primary care usage, alongside analysis of the impact of horizontal mergers of general practices, changes in contract (e.g. to APMS contracts), an of general practice closures on the affected patients’ use of primary care, would be an interesting avenue for future research.
More extensive interviewing of patients and their carers could provide qualitative evidence of the impact of vertical integration on patient experience of secondary care. It could also yield better evidence about patient experiences of navigating care as part of vertically integrated models of care compared with care outside vertical integration models, including patients with multiple long-term conditions and patients managing mental health conditions to give greater nuance to our analysis. For example, speaking to patients with combinations of multiple long-term conditions or those recently diagnosed compared with patients who have lived with their conditions for much longer could give greater insight into navigating care across health-care systems where vertically integrated models are present. In addition, speaking to patients receiving care outside of vertically integrated models would allow for some comparability; providing opportunities to observe which changes in care can be attributed directly to vertical integration between primary and secondary care. Finally, from the perspective of primary and secondary care clinicians, service managers and other staff, further exploration is warranted to understand the rationale and drivers for service level improvements; the nature of and range of indicators that would represent effective integration between primary, community and secondary care (e.g. patient experience of access to general practice, continuity, satisfaction of care, patient experience of access to secondary care, A&E attendance rates, emergency and non-emergency inpatient admission rates, length of stay in secondary care; quality and speed of communication between primary care and secondary care professionals); and to understand how agendas to meet local needs can best be agreed and addressed in collaboration across primary and secondary, including community, care.
Equality, diversity and inclusion
Participant and case study site representation
Throughout our evaluation the study team ensured case study sites were, despite all being examples of vertically integrated models of care, heterogenous while participants purposively selected for interview were from a range of professional backgrounds and differing levels of seniority including clinicians, senior managers, and patients living with a range of multiple long-term conditions.
Site characteristics
For quantitative analysis, we decided to compare vertical integration practices with: (1) practices that have horizontally merged with other practices but have not merged with hospitals; (2) practices that have changed the type of contract they hold (GMS, PMS, APMS) and those who have not; (3) and practices integrated with acute hospitals compared with those integrated with community trusts.
For the case studies, we interviewed staff and patients across three sites selected purposively (see Chapter 5) from across England from both rural and urban settings, representing a range of vertically integrated models, as well as treating diverse populations with varying needs (see Table 20, Chapter 5).
Strategies to improve representation
Within our evaluation the study team used a range of strategies to promote inclusivity. The team offered interviewees different modes of interview (telephone, Microsoft Teams or Zoom) and different times depending on participants’ preferences and to ensure accessibility for as many people as possible given workforce constraints.
Participant characteristics
Primary, community and secondary care staff taking part in interviews varied in their professional role, clinical and non-clinical skill set, location, duration in position, and the nature of their responsibilities with respect to their vertically integrated arrangement. The study team did not collect data relating to staff personal demographics (e.g. gender, age, ethnicity) as we focused on professional characteristics. Patients recruited from general practice PPGs varied with respect to age, gender, ethnicity and type of multiple long-term conditions they were currently living with at the time of the interview (see Table 20, Chapter 5).
Research topics relating to equality, diversity and inclusion
Our evaluation had a clear focus on inclusivity in relation to capturing the experience of those serving and living with multiple long-term conditions, a group which in the past has been identified as a priority when designing and coordinating care across the NHS in a range of settings. In addition, we recommend that further research with patients to understand experiences of receiving care as part of a vertically integrated model.
Reflections on research team and wider involvement
Research team
The study team was a small, mixed-methods, multidisciplinary group from many different disciplines (statistics, sociology, applied health research, health economics and project management); team members differed in seniority with respect to senior fellows and research associates to early career researchers. The research team was balanced regarding gender and ethnicity. Two team members left the team to continue with other research projects elsewhere and outside of BRACE; however, all contributions were recognised, and team members were given opportunities to attend analysis workshops and review drafts of the report.
Throughout, the team held bimonthly meetings to discuss project management, data collection, analysis and write up, with additional workshops to shape interpretation of findings. All members of the team have been involved in varying capacities with data collection and analysis, as well as dissemination of findings – both written (chapters) and oral (meetings and academic conferences). All researchers were supported by the principal investigator and project manager (JS and MS).
Wider involvement
Throughout the evaluation, the team sought the advice of: experts experienced in undertaking research across the care interface in the UK (Professor Judith Smith; Dr Joanna Ellins, University of Birmingham), the BRACE Steering Group, and members of the BRACE PPI panel, with whom we shared data collection instruments with and preliminary findings, thereby helping to shape our data analysis. In addition, CS and CD sought quantitative advice from Marc Elliot (senior statistician, RAND Europe), researchers at the Strategy Unit West Midlands and NHS Confederation with regard to analysis completed as part of WP 1–3.
Acknowledgements
We are very grateful to all of the participants in this study and to our contacts at each case study site who helped to coordinate our interactions with interviewees. We thank our BRACE colleagues and members of the BRACE steering group and PPI panel for their input and constructive comments throughout the duration of the study and for their contributions regarding project design, data collection, analysis and presentation of findings stages. Specifically, we thank Professor Russell Mannion and Professor Judith Smith (both University of Birmingham) for advising on our study protocol and final report; Dr Marc Elliott (RAND) for discussing our statistical analysis plan and Dr Katherine Morley (RAND Europe) for critically reviewing it; Ann Evans (BRACE Administrator, University of Birmingham), for reviewing our plain language summary in this report; and Dr Joanna Ellins (University of Birmingham) for undertaking critical review of drafts of the report. Any errors in the report are the responsibility solely of the authors.
Ethical approval
An application for ethical review to the University of Birmingham’s Research Ethics Committee was made by the project team and approval was gained in March 2021 (ERN_13-1085AP48). The project team received confirmation from the Head of Research Governance and Integrity, University of Birmingham, that this study was to be categorised as a service evaluation and therefore approval by the HRA or an NHS Research Ethics Committee was not required.
Information governance
University of Birmingham is committed to handling all personal information with regard to all qualitative data and RAND Europe for all quantitative data in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679.
Publications
Davies C, Saunders CL and Sussex J, ‘The extent of acute hospitals managing general practice (vertical integration) and its impact on secondary care utilisation in the NHS’. Presented at the Health Economics Study Group (HESG) Winter Conference, 11–13 January 2023.
Patient and public involvement
The evaluation protocol was reviewed by one member from the BRACE PPI panel. Two meetings were held with members of the panel to discuss study design, sharing preliminary and final findings. The panel advised on the strengths and limitations of using large primary care data sets with respect to understanding patient experience; shaping our research questions appropriately when speaking with patients living with multiple long-term conditions; how the recruitment of participants using a gatekeeper and PPGs may bring bias into our data, including discussion of how to address this as part of our analysis and how best to validate findings with case study sites as part of workshops. The plain language summary of the report has been reviewed by the same member of the panel. We will seek the advice of those members concerning how best to communicate the evaluation’s findings to patient and public audiences.
Contributions of authors
Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Associate Professor, University of Birmingham) was the project manager and a researcher for the study. He contributed to the conception and design of the study, the theoretical framework, data collection, and overall data analysis and interpretation, and he is the lead author of the final report. He led on work package 4 and contributed to all chapters.
Catherine L Saunders (https://orcid.org/0000-0002-3127-3218) (Senior Research Associate, University of Cambridge) was a statistician for the study. She contributed to the conception and design of the study, data analysis, interpretation of individual and synthesised findings, and she is a co-author of the final report. She led on work packages 2 and 3 and contributed to all chapters.
Charlotte Davies (https://orcid.org/0000-0003-4388-6676) (Senior Analyst, RAND Europe) was a research analyst for the study. She contributed to the conception and design of the study, data analysis of survey data, interpretation of individual and synthesised findings, and she is a co-author of the final report. She led on work package 1 and contributed to all chapters.
Gemma McKenna (https://orcid.org/0000-0001-8261-0598) (Fellow, University of Birmingham) was a researcher for the study. She contributed to the theoretical framework, data collection, and overall data analysis and interpretation of qualitative findings, and she is a co-author of the final report. She contributed to work package 4.
Frances Wu (https://orcid.org/0000-0002-9951-6626) (Senior Analyst, RAND Europe) was a research analyst for the study. She contributed to overall data analysis and interpretation of qualitative findings, and she is a co-author of the final report. She contributed to work package 4.
Ian Litchfield (https://orcid.org/0000-0002-1169-5392) (Senior Research Fellow, University of Birmingham) was a researcher for the study. He contributed to the conception and design of the study, the theoretical framework, data collection and overall data analysis and interpretation of qualitative findings, and he is a co-author of the final report. He contributed to work package 4.
Fifi Olumogba (https://orcid.org/0000-0002-6032-562X) (Research Assistant, RAND Europe) was a research assistant for the study. She contributed to the data collection and data analysis, and she is a co-author of the final report. She contributed to work package 1.
Jon Sussex (https://orcid.org/0000-0001-8970-4546) (Chief Economist at RAND Europe and Co-Director of the Cambridge Centre for Health Services Research, a collaboration between RAND Europe and University of Cambridge) was a principal investigator for the study and led the study. He contributed to the conception and design of the study including all work packages, the theoretical framework and overall data analysis and interpretation, and he is corresponding author of the final report. He contributed to all chapters.
All authors contributed to integrating the findings of the study. JS and MS made critical revisions to the report for important intellectual content and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Funding
This project was funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme (BRACE Project no. 16/138/31) and will be published in full in Health and Social Care Delivery Research; Vol. 11, No. 17. See the NIHR Journals Library website for further project information.
Department of Health and Social Care disclaimer
This report presents independent research commissioned by the NIHR. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, or of the NIHR or the Department of Health and Social Care.
Ethics statement
Ethical approval was received from the University of Birmingham Research Ethics Committee (ERN_13-1085AP48).
Data-sharing statement
Data supplied under specific data sharing agreements cannot be made available by the study team. Sources for data that are already publicly available are supplied either in the text or the references.
Data from interviews will be accessible to participants who took part in this rapid evaluation following GDPR, RAND Europe and University of Birmingham data protection guidelines upon request. All requests will be sent to MS in the first instance. To protect anonymity of interviewees, the data are not publicly available. Further information can be obtained from the corresponding authors.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Rumbold B, Shaw S. Horizontal and vertical integration in the UK: lessons from history. J Integr Care 2010;18:45-52.
- Sidhu M, Pollard J, Sussex J. Vertical integration of general practices with acute hospitals in England and Wales: rapid evaluation. Health Soc Care Deliv Res 2022;10:1-106.
- Sidhu M, Pollard J, Sussex J. Vertical integration of primary care practices with acute hospitals in England and Wales: why, how and so what? Findings from a qualitative, rapid evaluation. BMJ Open 2022;12.
- King’s Fund . Long-Term Conditions and Multi-Morbidity n.d. https://www.kingsfund.org.uk/projects/time-think-differently/trends-disease-and-disability-long-term-conditions-multi-morbidity (accessed 5 January 2023).
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43.
- NHS Digital . Appointments in General Practice 2022. https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/september-2022 (accessed 28 November 2022).
- Healthcare Financial Management Association . NHS Finance 2022.
- King’s Fund . GP Funding and Contracts Explained 2020. https://www.kingsfund.org.uk/publications/gp-funding-and-contracts-explained (accessed 28 December 2022).
- NHS Digital . General Practice Workforce 2022. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/30-september-2022 (accessed 28 December 2022).
- Smith J, Parkinson S, Harshfield A, Sidhu M. Early evidence of the development of primary care networks in England: a rapid evaluation study. Health Soc Care Deliv Res 2022. https://doi.org/10.3310/hsdr-tr-129678.
- Joskow PL. Handbook of New Institutional Economics. New York, NY: Springer; 2005.
- Laugesen MJ, France G. Integration: the firm and the health care sector. Health Econ Policy Law 2014;9:295-312.
- Ramsay A, Fulop N, Edwards N. The evidence base for vertical integration in health care. J Integ Care 2009;17:3-12.
- Blom A, von Bülow LL. Vertical integration across hospital acute care and on-call general practitioners. an evaluation of a cross sectional cooperation model at Odense University Hospital, southern region of Denmark. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.1481.
- Schwartz PM, Kelly C, Cheadle A, Pulver A, Solomon L. The Kaiser Permanente Community Health Initiative: a decade of implementing and evaluating community change. Am J Prev Med 2018;54:S105-9. https://doi.org/10.1016/j.amepre.2018.02.004.
- Comendeiro-Maaløe M, Ridao-López M, Gorgemans S, Bernal-Delgado E. A comparative performance analysis of a renowned Public Private Partnership for health care provision in Spain between 2003 and 2015. Health Policy 2019;123:412-8.
- Comendeiro-Maaløe M, Ridao-López M, Gorgemans S, Bernal-Delgado E. Public–private partnerships in the Spanish National Health System: the reversion of the Alzira model. Health Policy 2019;123:408-11.
- Academic Health Science Network . National Survey of Local Innovation and Research Needs of the NHS: Full Report 2019. https://arc-em.nihr.ac.uk/resources/national-survey-local-innovation-and-research-needs-nhs (accessed 6 July 2023).
- NHS England . The NHS Long Term Plan 2019. https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan (accessed 6 July 2023).
- Whitty CJM, MacEwen C, Goddard A, Alderson D, Marshall M, Calderwood C, et al. Rising to the challenge of multimorbidity. BMJ 2020;368.
- NHS England . Five Year Forward View 2014. https://www.england.nhs.uk/publication/nhs-five-year-forward-view (accessed 6 July 2023).
- NHS England . General Practice Forward View 2016. https://www.england.nhs.uk/gp/gpfv (accessed 6 July 2023).
- NHS England . GP Patient Survey, 2022 National Report 2022. https://www.england.nhs.uk/statistics/2022/07/14/gp-patient-survey-2022 (accessed 6 July 2023).
- Aiden H. Multimorbidity: Understanding the Challenge. London: Richmond Group of Charities; 2018.
- Health and Social Care Committee . The Future of General Practice. Fourth Report of Session 2022–23 2022. https://publications.parliament.uk/pa/cm5803/cmselect/cmhealth/113/report.html (accessed 6 July 2023).
- NHS Digital . General Practice Workforce 2021. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/30-november-2021 (accessed 13 September 2022).
- King’s Fund . General Practice: Our Position 2020. https://www.kingsfund.org.uk/projects/positions/general-practice (accessed 5 January 2023).
- McDermott I, Spooner S, Goff M, Gibson J, Dalgarno E, Francetic I, et al. Scale, scope and impact of skill mix change in primary care in England: a mixed-methods study. Health Soc Care Deliv Res 2022;10:1-148.
- Nuffield Trust . General Practice on the Brink 2022. https://www.nuffieldtrust.org.uk/comment-series/general-practice-in-trouble (accessed 6 July 2023).
- Shembavnekar N, Buchan J, Bazeer N, Kelly E, Beech J, Charlesworth A, et al. Projections: General Practice Workforce in England. London: Health Foundation; 2022.
- NHS England . Next Steps for Integrating Primary Care: Fuller Stocktake Report 2022. https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake-report (accessed 6 July 2023).
- Iacobucci G. Government wants more GPs to be employed by hospital trusts, says news report. BMJ 2022;376.
- Limb M. What’s behind the government’s plan for hospitals to employ more GPs?. BMJ 2022;376.
- Yu V, Wyatt S, Woodall M, Mahmud S, Klaire V, Bailey K, et al. Hospital admissions after vertical integration of general practices with an acute hospital: a retrospective synthetic matched controlled database study. Br J Gen Pract 2020;70:e705-13.
- National Institute for Health and Care Excellence . Multimorbidity: Clinical Assessment and Management 2016. https://www.nice.org.uk/guidance/ng56 (accessed 6 July 2023).
- Head A, Fleming K, Kypridemos C, Schofield P, Pearson-Stuttard J, O’Flaherty M. Inequalities in incident and prevalent multimorbidity in England, 2004–19: a population-based, descriptive study. Lancet Healthy Longev 2021;2:e489-97. https://doi.org/10.1016/S2666-7568(21)00146-X.
- World Health Organization . Multimorbidity 2016. https://www.who.int/publications/i/item/9789241511650 (accessed 6 July 2023).
- Academy of Medical Sciences, Medical Research Council, National Institute for Health Research, Department of Health and Social Care, Wellcome Trust . Taking Multimorbidity Out of the ‘Too Difficult’ Box 2019. https://acmedsci.ac.uk/more/news/taking-multimorbidity-out-of-the-too-difficult-box (accessed 29 December 2022).
- Care Quality Commission . Active Locations for Providers Registered Under the Health and Social Care Act (HSCA) 2022.
- NHS Digital . Organisation Data Service 2023. https://digital.nhs.uk/services/organisation-data-service (accessed 6 July 2023).
- NHS Improvement . NHS Foundation Trust Annual Reporting Manual 2020 21 2021. https://www.england.nhs.uk/publication/nhs-foundation-trust-annual-reporting-manual/#heading-2 (accessed 6 July 2023).
- NHS Digital . General Practice Workforce 2021. https://digital.nhs.uk/data-and-information/publications/statistical/general-practice-workforce-archive/31-march-2021 (accessed 6 July 2023).
- NHS Digital . GP and GP Practice Related Data – Epraccur 2022.
- GOV.UK . Contracts Finder 2022. https://www.gov.uk/contracts-finder (accessed 12 July 2023).
- NHS Digital . GP and GP Practice Related Data – Ebranchs 2016.
- NHS Digital . GP and GP Practice Related Data – Epraccur 2016.
- NHS Digital . GP and GP Practice Related Data – Ebranchs 2022.
- NHS Digital . Patients Registered at a GP Practice 2021. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice (accessed 7 July 2023).
- NHS Digital . NHS Payments to General Practice, England 2021. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-payments-to-general-practice (accessed 7 July 2023).
- NHS Digital . Quality and Outcomes Framework 2021. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/general-practice-data-hub/quality-outcomes-framework-qof (accessed 7 July 2023).
- Noble S, McLennan D, Noble M, Plunkett E, Gutacker N, Silk M, et al. The English Indices of Deprivation 2019 – Research Report 2019. https://www.gov.uk/government/publications/english-indices-of-deprivation-2019-research-report (accessed 7 July 2023).
- Department for Environment Food and Rural Affairs . Rural Urban Classification 2021. https://www.gov.uk/government/collections/rural-urban-classification (accessed 13 September 2022).
- Lewis RQ, Checkland K, Durand MA, Ling T, Mays N, Roland M, et al. Integrated care in England – what can we learn from a decade of National Pilot Programmes?. Int J Integr Care 2021;21. https://doi.org/10.5334/ijic.5631.
- Kumpunen S, Edwards N, Georghiou T, Hughes G. Why do evaluations of integrated care not produce the results we expect?. Int J Care Coord 2020;23:9-13.
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-Based Care: How Do We Know What Works? Research Report 2013.
- Davies C, Sidhu M, Saunders C, Sussex J. Acute Hospitals Managing General Practice Services (Vertical Integration) – Study Protocol for Impact Evaluation 2022. https://fundingawards.nihr.ac.uk/award/NIHR135618 (accessed 27 February 2023).
- NIHR . Research Award: Rapid Service Evaluation Research Team: RSET 2018. https://fundingawards.nihr.ac.uk/award/16/138/17 (accessed 27 February 2023).
- Payne RA, Mendonca SC, Elliott MN, Saunders CL, Edwards DA, Marshall M, et al. Development and validation of the Cambridge Multimorbidity Score. CMAJ 2020;192:E107-14.
- Crooks CJ, West J, Card TR. A comparison of the recording of comorbidity in primary and secondary care by using the Charlson Index to predict short-term and long-term survival in a routine linked data cohort. BMJ Open 2015;5.
- Brilleman SL, Salisbury C. Comparing measures of multimorbidity to predict outcomes in primary care: a cross sectional study. Fam Pract 2013;30:172-8.
- Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med 2012;10:134-41.
- Curtis HJ, MacKenna B, Croker R, Inglesby P, Walker AJ, Morley J, et al. The OpenSAFELY Collaborative . OpenSAFELY NHS Service Restoration Observatory 1: primary care clinical activity in England during the first wave of COVID-19. Br J Gen Pract 2022;72:e63-74.
- Rocks S. Why is the NHS Really Under ‘Record Pressure’?. London: Health Foundation; 2022.
- GP Patient Survey . About the Survey 2023. https://www.gp-patient.co.uk/about (accessed 27 February 2023).
- NHS Digital . Hospital Episode Statistics (HES) 2023. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed 27 February 2023).
- Bardsley M, Blunt I, Davies S, Dixon J. Is secondary preventive care improving? Observational study of 10-year trends in emergency admissions for conditions amenable to ambulatory care. BMJ 2013;3.
- O’Neill S, Kreif N, Grieve R, Sutton M, Sekhon JS. Estimating causal effects: considering three alternatives to difference-in-differences estimation. Health Serv Outcomes Res Methodol 2016;16:1-21.
- Sutton M, Nikolova S, Boaden R, Lester H, McDonald R, Roland M. Reduced mortality with hospital pay for performance in England. N Engl J Med 2012;367:1821-8.
- Kristensen SR, Meacock R, Turner AJ, Boaden R, McDonald R, Roland M, et al. Long-term effect of hospital pay for performance on mortality in England. N Engl J Med 2014;371:540-8.
- O’Neill S, Kreif N, Sutton M, Grieve R. A comparison of methods for health policy evaluation with controlled pre-post designs. Health Serv Res 2020;55:328-38.
- Saunders CL, Gkousis E. Impact of telephone triage on access to primary care for people living with multiple long-term health conditions: rapid evaluation. Health Soc Care Deliv Res 2022. http://www.doi.org/10.3310/UCCE5549.
- Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson comorbidity index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits 2019;12:188-97.
- NHS Digital . Series/Collection:/NHS/Payments/to/General/Practice 2022. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-payments-to-general-practice (accessed 27 February 2023).
- NHS Digital . Series/Collection:/Patients/Registered/at/a/GP/Practice 2022. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice (accessed 27 February 2023).
- Newbould J, Ball S, Abel G, Barclay M, Brown T, Corbett J, et al. A ‘telephone first’ approach to demand management in English general practice: a multimethod evaluation. Health Serv Deliv Res 2019;7:1-158.
- Saunders CL, Flynn S, Massou E, Lyratzopoulos G, Abel G, Burt J. Sociodemographic inequalities in patients’ experiences of primary care: an analysis of the General Practice Patient Survey in England between 2011 and 2017. J Health Serv Res Policy 2021;26:198-207.
- Cowling TE, Laverty AA, Harris MJ, Watt HC, Greaves F, Majeed A. Contract and ownership type of general practices and patient experience in England: multilevel analysis of a national cross-sectional survey. J R Soc Med 2017;110:440-51.
- Greaves F, Laverty AA, Pape U, Ratneswaren A, Majeed A, Millett C. Performance of new alternative providers of primary care services in England: an observational study. J R Soc Med 2015;108:171-83.
- Forbes LJ, Forbes H, Sutton M, Checkland K, Peckham S. Changes in patient experience associated with growth and collaboration in general practice: observational study using data from the UK GP Patient Survey. Br J Gen Pract 2020;70:e906-15.
- Leijten FRM, Struckmann V, van Ginneken E, Czypionka T, Kraus M, Reiss M, et al. SELFIE consortium . The SELFIE framework for integrated care for multi-morbidity: development and description. Health Policy 2018;122:12-2. https://doi.org/10.1016/j.healthpol.2017.06.002.
- Corbin J, Strauss A. Managing chronic illness at home: three lines of work. Qual Sociol 1985;8:224-47. https://doi.org/10.1007/BF00989485.
- Turnbull J, McKenna G, Prichard J, Rogers A, Crouch R, Lennon A, et al. Sense-making strategies and help-seeking behaviours associated with urgent care services: a mixed-methods study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07260.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE; 2013.
- Andoh-Arthur J. SAGE Research Methods Foundation. London: SAGE; 2020.
- Weiss CH. New Approaches to Evaluating Community Initiatives: Concepts, Methods and Contexts. New York, NY: Aspen Institute; 1995.
- Vogel I. Review of the Use of “Theory of Change” in International Development: Review Report 2012.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Gittell JH. Relational Perspectives in Organizational Studies: A Research Companion. Northampton, MA: Edward Elgar Publishing; 2006.
- Lansisalmi H, Kivimaki M, Aalto P, Ruoranen R. Innovation in healthcare: a systematic review of recent research. Nurs Sci Q 2006;19:66-72.
- Omachonu VK, Einspruch NG. Innovation in healthcare delivery systems: a conceptual framework. Innov J n.d.;15.
- Varkey P, Horne A, Bennet KE. Innovation in health care: a primer. Am J Med Qual 2008;23:382-8.
- Baird B. Is General Practice in Crisis? Big Election Questions. London: King’s Fund; 2018.
- Levene L, Seidu S, Greenhalgh T, Khunti K. Pandemic threatens primary care for long-term conditions: change is required to ensure effective care during and after COVID-19. BMJ 2020;371. https://doi.org/10.1136/bmj.m3793.
- Paddison CAM, McGill I. Digital Primary Care: Improving Access for All? Rapid Evidence Review. London: Nuffield Trust; 2022.
- Baird B, Holmes J. Why Can’t I Get a Doctor’s Appointment? Solving the Complex Issue of GP Access. London: King’s Fund; 2019.
- British Medical Association . Pressures in General Practice Data Analysis 2022. https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed 27 February 2023).
- Shortell SM, Gillies RR, Anderson DA, Erickson KM, Mitchell JB. Integrating health care delivery. Health Forum J 2000;43:35-9.
- Shortell SM. Themed issue: accountable care organizations and vertical integration. Health Care Manage Rev 2019;44:91-2. https://doi.org/10.1097/HMR.0000000000000244.
- Singer SJ, Kerrissey M, Friedberg M, Phillips R. A comprehensive theory of integration. Med Care Res Rev 2020;77:196-207. https://doi.org/10.1177/1077558718767000.
- Robinson JC, Casalino LP. Vertical integration and organizational networks in health care. Health Aff (Millwood) 1996;15:7-22.
- Machta RM, Maurer KA, Jones DJ, Furukawa MF, Rich EC. A systematic review of vertical integration and quality of care, efficiency, and patient-centered outcomes. Health Care Manage Rev 2019;44:159-73. https://doi.org/10.1097/HMR.0000000000000197.
- NHS England . NHS Schedule of NHS Costs 2019 20. 2019 20 National Cost Collection Data Publication 2022. https://www.england.nhs.uk/publication/2019-20-national-cost-collection-data-publication/ (accessed 23 January 2023).
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2020. Canterbury: Personal Social Sciences Research Unit, University of Kent; 2020.
- Davidson L, Scott J, Forster N. Patient experiences of integrated care within the United Kingdom: a systematic review. Int J Care Coord 2021;24:39-56. https://doi.org/10.1177/20534345211004503.
- McKenna G, Rogers A, Walker S. The influence of personal communities in understanding avoidable emergency department attendance: qualitative study. BMC Health Serv Res 2020;20.
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3161-3.
- Fisher B, Alderwick H. Reforming the GP partnership model?. BMJ 2023;380. https://doi.org/10.1136/bmj.p134.
- Skou ST, Mair FS, Fortin M, Guthrie B, Nunes BP, Miranda JJ, et al. Multimorbidity. Nat Rev Dis Primers 2022;8. https://doi.org/10.1038/s41572-022-00376-4.
- Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012;10:142-51.
Appendix 1 Taking account of horizontal integration
For many practices, once a horizontal merger occurred, it took several months before the original practice code disappeared or for patients to move general practice lists. Where more than one practice merged, this often meant that practices joined at different times.
We have presented practice codes as at the end of the quantitative analysis period in 2020 (see Chapter 4); that is, the most recent practice code reported but have also recorded all previous codes that we identified as having merged into this final code. We also recorded the first and last dates for which the practice code at the study end and the previous codes were present in the data. We included 8065 practices with at least 1000 patients registered on 1 April on any year between 2013 and 2021. There were 6987 unique practice codes at the study end; 6199 of 8065 (77%) of practices did not undergo any mergers. The remaining 1874 practices underwent at least one horizontal merger (see Table 22).
| Size of general practice merger: original practices per merged practice | Number of general practices in such mergers |
|---|---|
| 2 | 1184 |
| 3 | 417 |
| 4 | 136 |
| 5 | 50 |
| 6 | 48 |
| 7 | 21 |
| 8 | 8 |
| 10 | 10 |
Application to vertical integration of general practices into NHS trusts
To combine the horizontal general practice mergers dataset (described above) with the dataset containing information on where trusts have taken over the running of general practices, we merged the list of vertically integrated practice codes into the horizontal merger data set. This included the list of current and previous practice codes. Three of the vertically integrated practice codes could not be matched for the following reasons:
-
One of the overarching practice group codes did not have patient ‘list size’ associated.
-
There was a historic code from a practice which closed before 1 April 2013.
-
One ‘homelessness practice’ had fewer than 1000 patients.
We also made the following decisions:
-
To exclude one of the NHS trusts where the practice is vertically integrated with two separate trusts.
-
Four general practices reported different dates of vertical integration for two different trusts. In this case, we recorded the earliest date reported.
-
For single practice codes that have more than one date of vertical integration, we included the earliest date of vertical integration of the approximately 119 practices identified in our search process.
Appendix 2 Practice characteristics variables
| Practice characteristic variables | Source | Link | Observations not successfully mergeda |
|---|---|---|---|
| GP list size | Patients registered at a general practice – NHS digital | Patients Registered at a GP Practice – NHS Digital | 104 |
| IMD | English indicates of deprivation 2019, Ministry of Housing Communities and Local Government | English indices of deprivation 2019: postcode lookup (opendatacommunities.org) | 0 |
| Contract type | NHS Payments to General Practice, England 2021 – NHS digital | https://digital.nhs.uk/data-and-information/publications/statistical/nhs-payments-to-general-practice/england-2021-22 | 34 |
| Rural/urban indicator | NHS Payments to General Practice, England 2021 – NHS digital | https://digital.nhs.uk/data-and-information/publications/statistical/nhs-payments-to-general-practice/england-2021-23 | 0 |
| Quality and outcomes indicator | QOF, 2019–20 – NHS digital | QOF, 2019–20 – NHS Digital | 19 |
| GP FTE (%) | General Practice Workforce – NHS digital | General Practice Workforce – NHS Digital | 19 |
| GP employed in the practice on an ‘other’ contract (%) | General Practice Workforce – NHS digital | General Practice Workforce – NHS Digital | 0 |
Appendix 3 Qualitative coding framework
| Code | Description | SELFIE component | Micro, Meso, Macro |
|---|---|---|---|
| 1. Rationale for integration | What was the rationale from the perspective of the acute trust/health board and/or general practices? Has the rationale changed since the model was first implemented? Who initiated this model of vertical integration? |
Service delivery: policies to integrate care across organisations and sectors | Macro |
| 2. Patient access | What has been the impact on patients accessing services across the care interface? | Service delivery: service availability and access | Macro |
| 3. Drivers of integration | Factors that are encouraging closer working between primary and secondary care (including advantages) | Service delivery: organisational and structural integration | Meso |
| 4. Challenges to integration | Factors that are hindering closer working between primary and secondary care (including disadvantages) | Service delivery: organisational and structural integration | Meso |
| 5. Current strategy of vertical integration | The current vision set out by strategists of what the vertical integration model is intended to achieve (short-, medium-, and long-term) | Leadership and governance: culture of shared vision, ambition and vales | Meso |
| 6. The role and impact of the PCN | The future of the current vertical integration model in the context of developing PCN working/collaboration arrangements in England | Service delivery: organisational and structural integration | Meso |
| 7. Current model and maturity | Please describe the current model of the acute trust/health board taking over and directly managing general practice services. When did it first take place? | Service delivery: organisational and structural integration | Meso |
| 8. Number of practices | How many practices are involved? Has this increased/decreased since implementation? | Service delivery: organisational and structural integration | Meso |
| 9. Selection process | How are practices selected to join the model? Against what criteria are they measured? | Service delivery: organisational and structural integration | Meso |
| 10. Coordination and delivery of care | How has the delivery of services changed in given settings (primary and secondary care, and wider community services)? | Service delivery: person-centred; tailored; treatment interaction; continuity | Micro |
| 11. Provision to care for patients living with long-term conditions | Introduction of new services/clinical pathways to support patients, especially those with long-term conditions | Service delivery: person-centred; tailored; treatment interaction; continuity | Micro |
| 12. Patient satisfaction with primary care | Levels of approval of current primary care | Service delivery: person-centred; tailored; treatment interaction; continuity Technologies and medical products: e-health tools; shared information systems |
Micro, Meso |
| 13. Patient satisfaction with secondary care | Levels of approval of current secondary care | Service delivery: person-centred; tailored; treatment interaction; continuity Technologies and medical products: e-health tools; shared information systems |
Micro, Meso |
| 14. Patient experience of primary or care | Patient accounts of recent primary care experiences | Service delivery: person-centred; tailored; treatment interaction; continuity | Micro |
| 15. Patient experience of secondary care | Patient accounts of recent secondary care experiences | Service delivery: person-centred; tailored; treatment interaction; continuity | Micro |
| 16. Continuity of care | Relationships with health professionals, care providers across the interface | Service delivery: continuity | Micro |
| 17. Impact of the pandemic | Impact of COVID-19 on care provisions across the interface | Service delivery: tailored | Micro |
| 18. General practice culture and context | Information/reflections on the current context and culture of general practice | Leadership and governance: political commitment | Macro |
| 19. Impact between acute trust and/or GPs | How has the vertical integration model impacted governance, contractual and legal arrangements between acute trust/health board and the general practices? | Leadership and governance: supportive leadership | Meso |
| 20. Culture | The lack of understanding of the working of primary care compared with secondary care | Leadership and governance: culture of shared vision, ambition and vales | Meso |
| 21. Tension | Have there been issues of tension amongst stakeholders? | Leadership and governance: clear accountability | Meso |
| 22. Success | How is ‘success’ being determined and/or measured? What process measures are being considered? | Leadership and governance: performance based management | Meso |
| 23. Intended outcomes | What are the intended outcomes (clinical and non-clinical)? | Leadership and governance: performance based management | Meso |
| 24. Unintended outcomes | Have any unintended outcomes occurred? What are they? | Leadership and governance: performance based management | Meso |
| 25. Impact on recruitment and retention | What has been the impact of the recruitment and retention across both primary and secondary care? | Workforce: MDTs; new professional roles | Micro, meso |
| 26. Financial implications | Financial implications of this model? | Financing: stimulating investments in innovative care models | Macro |
| 27. Anything else? | Is there anything else you wanted to tell us about that has not already been covered in the interview? | N/A | N/A |
| 28. Gold dust | Great quote to use in the final report | N/A | N/A |
| 29. People with multiple long-term conditions | Is this group of the population mentioned, especially with respect to differential impact compared with other patients? | Service delivery: person-centred; tailored; treatment interaction; continuity | Micro |
| 30. Innovations | Innovate methods of working to support care for people living with multiple long-term conditions | Service delivery: person-centred; tailored; treatment interaction; continuity | Micro |
List of abbreviations
- A&E
- accident and emergency
- ACSC
- ambulatory care sensitive conditions
- APMS
- alternative provider medical services
- BRACE
- Birmingham, RAND and Cambridge Evaluation Centre
- CCG
- clinical commissioning group (England)
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- DES
- direct enhanced services
- FTE
- full-time equivalent
- GMS
- general medical services
- GP
- general practitioner
- GPPS
- General Practice Patient Survey
- HES
- Hospital Episode Statistics
- HSDR
- Health and Social Care Delivery Research
- ICB
- integrated care board
- ICS
- integrated care system
- IMD
- index of multiple deprivation
- IQR
- interquartile range
- IRR
- incidence rate ratio
- MDT
- multidisciplinary teams
- NHS
- National Health Service
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PACS
- primary and acute care systems
- PCN
- primary care network
- PMS
- personal medical services
- PPG
- patient participation group
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- SELFIE
- Sustainable intEgrated care modeLs for multimorbidity: delivery, FInancing, and performancE
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/PRWQ4012).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
