Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 15/136/67. The contractual start date was in November 2017. The final report began editorial review in June 2021 and was accepted for publication in November 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. This report has been published following a shortened production process and, therefore, did not undergo the usual number of proof stages and opportunities for correction. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Featherstone et al. This work was produced by Featherstone et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Authors et al.
Chapter 1 Context
There is increasing recognition that action is required to improve the experience and outcomes of people living with dementia (PLWD) admitted to hospital for an additional acute condition. 1–5 The Alzheimer’s Society (Plymouth, UK) has identified widespread poor care for PLWD in the acute setting, with the quality of care received varying widely. 6 This variation means that PLWD are ‘likely to experience poor care at some point along their care pathway’. 7
Prevalence of people with dementia in the acute setting
The acute hospital setting has become a key site of care for PLWD, with the Department of Health and Social Care recognising that between 25% and 50% of all acute hospital admissions are of people who are also living with dementia,6,8–12 representing high levels of unscheduled and emergency admissions (77%). 13 A diagnosis of dementia is associated with increased risk of hospitalisation,14 with potentially preventable conditions, such as pneumonia, sepsis, urinary system disorders and leg fractures,10,15 often the principal cause of admission.
Estimates are likely to be low because of under-reporting or late diagnosis of dementia in this population. 2 Previous screening studies suggest that, in the acute setting, approximately 50% of patients affected by dementia remain undetected and undiagnosed16 and do not yet have a formal diagnosis in their medical records;10,17,18 however, more recent figures suggest that this rises to two-thirds19,20 or even three-quarters12,21,22 of older people (i.e. patients aged > 65 years) during an acute hospital admission. A high prevalence of delirium (15.5%), undiagnosed delirium (72%)23 and comorbid mental health disorders among17 this patient population, as well as comorbid chronic conditions, such as diabetes,18 also potentially has an impact on cognitive function during an admission.
Impact on patient outcomes
People living with dementia are a highly vulnerable group, and their hospitalisation is associated with increased risk of deterioration,14,17 functional decline and a range of adverse outcomes,22,24 including delayed discharge25 and institutionalisation. 26 PLWD also have a markedly higher short-term mortality9,26–28 than similar patients without a dementia diagnosis.
Acute hospitals have been called ‘challenging’28 and ‘dangerous’29 places for older people and PLWD. Health-care-related harm and adverse events experienced by PLWD are typically associated with falls, delirium, incontinence and functional decline. 30 Associated iatrogenic impacts31 of an admission include incontinence,32 reduced mobility,33–35 increased agitation,36 delirium,37–40 longer admissions41 and distress. 42–46 These adverse events can result in further dependency, institutionalisation and, potentially, death during an acute admission. 31
Calls for transformation
In response to this evidence, there has also been recognition by policy-makers of the urgent need to improve care for PLWD in hospitals, particularly for admission to general hospitals for an unrelated condition. 28 A ‘transformation of dementia services’ (contains public sector information licensed under the Open Government Licence v3.0) has been called for in the Department of Health and Social Care national Living Well with Dementia: A National Dementia Strategy4 and by the Dementia Action Alliance. 47 In partnership with the NHS Institute for Innovation and Improvement (Coventry, UK), a key objective within the Dementia Action Alliance’s call to action47 is to design services around the person with dementia through the creation of dementia-friendly hospitals. These objectives are supported and reinforced by a wide range of policy recommendations. The Prime Minister’s Challenge on Dementia48 renewed the focus on dementia-friendly health and care, with the goal of every person with dementia obtaining the safest and best care in acute hospitals.
However, although acute hospitals have an increasing range of initiatives,8 even in institutions where high-quality acute care is identified, this is limited to specific wards, failing to reach across an organisation. 8 Overall, it is acknowledged that hospitals struggle to respond to the needs of an ageing population, with increasing hospital admissions among this group. 49
The social organisation and interactional context of care
Research draws attention to the social and organisational context of care in influencing front-line delivery in acute wards, with much research focused on the care of older people and PLWD. Meta-ethnography50 identifies that, despite nurses’ aspirations for a high standard of psychosocial care, a high standard of psychosocial care was largely dependent on ward-level social and organisational conditions.
National Institute for Health and Care Research (NIHR) studies report strong associations between ward cultures and care quality. Patterson et al. 51 found that positive patient and carer assessments of acute care for older patients were associated with higher staff ratings of a positive climate for care, which was mirrored in a second NIHR study that found that experiences of working in wards directly influenced patient experiences. 52 The impact of different shifts on work goals and priorities,53 a culture of reactivity,54 and austere ward environments and cultures that emphasise routines with few opportunities for communication restricted both patients and staff, and were associated with staff moral distress and burnout. 53,55,56 A systematic review of qualitative studies highlighted the importance of relational work in delivering high-quality care in acute wards57 and the importance of the nursing role in identifying and promoting dignity for older people with dementia. 56 However, given the increasing delegation of ‘hands-on’ care to health-care assistants (HCAs), an important focus needs to be this less-privileged58 and marginalised group, and how this group can influence how care is organised and delivered. 58,59
Despite PLWD representing a significant population in the acute setting, ward cultures can mean that delivering care appropriate to their needs is often viewed as ‘a disruption to core business’,60 as PLWD can be viewed as a group of patients who do not belong in the acute setting61 and should be transferred to other services. 62 Older people and family carers recognise that developing good relationships with staff powerfully informs and shapes their experience of a hospital admission. 63 Acute ward staff can fail to promote the identity and well-being of PLWD in their care, and may not recognise or respond to opportunities to deliver the recommended person-centred care,64 with patients who are viewed as ‘complex’ or ‘demanding’ receiving less personalised care. 56 As a result, the acute setting remains a potentially harmful location for this patient group.
Continence care: body work and ‘dirty work’ of the ward
Continence care is part of everyday intimate care to support PLWD, and has been described variously as ‘dirty work’, ‘elimination work’, ‘body work’ and ‘body labour’. These forms of paid work carried out on the bodies of others65 and their waste products are habitually regarded as low status, bordering on the polluted,66 and are often gendered. 66 This work poses a serious threat to formal caregivers’ sense of self and status, with higher-status workers distancing themselves from body work. 66–68 It is also invisible work,67 with body workers hiding ‘dirty work’ from others (e.g. by drawing screens around the bed,69 protecting the dignity of both the patient and the worker). Supporting patients to use the toilet supports the maintenance of dignity, as well as well-being and quality of life (QoL), which is a core nursing role. 70 Despite this, continence care is often described as ‘basic’, rather than ‘essential’, care. 71
Dementia, incontinence and stigma
A diagnosis of dementia is associated with significant levels of stigma and powerfully impacts on opportunities for social inclusion. 72 Incontinence is also powerfully stigmatising, particularly in care settings,73,74 discrediting an individual’s social identity and eliciting fear, stereotyping and social control. 75,76
The continued stigma, shame, social isolation and loss of integrity experienced by people living with incontinence is linked to a cultural disgust with urine and faeces. 77 Incontinence in older people can be viewed as a loss of control, a sign of incompetence that is incompatible with adulthood, putting them on the path to becoming a ‘non-person’. 78 Therefore, loss of continence has consequences that go far beyond the physical impairment, including casting strong doubt on a person’s social competence79 and disrupting privacy, as incontinence ‘threatens to expose the incompetence of the body to others’. 7
This stigma is further impacted by intersections of gender, race and ethnicity. 80,81 For example, older women with dementia are exposed to a ‘triple jeopardy’73 of age, sex and condition. Reviews examining the experiences of older women with incontinence identified microaggressions from others (e.g. subtle and insidious acts of aggression, such as impatience, intended to make the individual feel inferior), leading to social isolation. 80
Continence and dementia in the hospital setting
Urinary incontinence is one of the most commonly reported symptoms experienced in the last year of life, experienced by an estimated 72% of PLWD at this stage. 82 Key predictors of incontinence are the severity of cognitive impairment and degree of immobility. 83 Therefore, incontinence is typically a feature of the moderately severe and advanced stages of dementia. 84 Importantly, this does not reflect the continence status of the majority of PLWD admitted to acute wards, generally in the early and moderate stages of the disease, when incontinence should not be a typical feature of their dementia. However, in the acute setting, a UK national audit found that 71% of patients aged > 65 years (33% of whom had a diagnosis of dementia and 44% of whom had impaired mobility) were classified as incontinent of urine. 85 Similarly, a screening study of emergency admissions of patients aged > 70 years with cognitive decline found that 47% of patients were classified as incontinent,14 with 86% of patients identified as requiring supervision and assistance with toileting. 84
In the acute setting, PLWD are at high risk of ‘functional incontinence’, that is when their cognitive impairment, mobility problems or medication (associated with their admitting condition) means that they cannot reach the toilet in time84,86 as a result of their environment, rather than their dementia. 87 A small number88–90 of international audits in acute settings have identified that PLWD who are continent at admission are at significant risk of developing incontinence during admission, with this becoming permanent at discharge. An estimated 17%90 to 36%88 of previously continent PLWD will be clinically incontinent following an acute hospital admission. Carers report high dissatisfaction (60%) with continence care for PLWD during an acute admission, with hospital-acquired incontinence frequently reported as the key long-term post-discharge impact. 10
These high rates of hospital-acquired incontinence are associated with a number of hospital organisation and treatment factors. A primary provisional diagnosis of delirium, dementia or cognitive impairment is the most significant risk factor,89 more than doubling the risk of hospital-acquired incontinence. 91 Increased length of stay,88 advanced age (i.e. aged ≥ 85 years),89,91 gender (i.e. women identified as more at risk)91 and reduced mobility and physical functioning92 also increase risk. The use of continence pads, urinary catheters90 and chair restraints,91 and symptoms of drowsiness, daily pain and sleep problems,91 have all been associated with an increased risk of acquired incontinence following discharge. However, continence care, including new-onset incontinence among older adults and PLWD during their hospitalisation, is a significant and understudied phenomenon.
Continence care for PLWD in acute hospital wards is a continued concern for policy-makers,93 families and carers. 10,94–96 The systemic failure in the NHS to provide older and vulnerable patients with dignified continence care is widely highlighted in service reviews and inquiries. 94,95,97–99 Lack of dignity and privacy was a recurrent theme. 93,97,98
Dementia guidelines emphasise that incontinence is often treatable. 100 However, the small number of qualitative studies examining continence care for older patients in the acute setting identify containment (e.g. use of disposable pads and catheterisation) as key strategies,101,102 corroborated by national audits. 103
Incontinence is highly discrediting7,75 and can increase stigma and attack social status when combined with dementia. 74,104 A disparity exists between policy recommendations to improve care and actual implementation. Although incontinence care plans are common (83%) in care homes, only 37% of trusts have an integrated incontinence care pathway103 and only 18% of trusts have a continence nurse specialist,51 with low levels of continence training for ward staff. 49,102 Despite the growing population of PLWD and the significance of continence care in the acute setting,105 little is known about the appropriate management, organisation and interactional strategies for PLWD admitted to hospital. 8
The current paucity of evidence85 fails to support this population’s continence needs in this key site of care. 105 This presents a significant NHS challenge8 and new approaches are needed. Therefore, our research question is ‘how do ward staff respond to the continence care needs of PLWD being cared for in acute hospital wards, and what are the experiences of continence care from the perspectives of patients, their carers and families?’
Chapter 2 Research objectives
This in-depth ethnographic study aims to establish an empirically based conceptual and theoretical foundation to inform the development of innovative interventions in service organisation, delivery and training that will improve clinical care for PLWD, a large and growing, but often overlooked, population in acute hospital wards. This study focuses on an important, but poorly understood, feature of everyday care for PLWD, that is continence care.
Specific objectives are as follows:
-
To provide a detailed understanding and directly observed examples of the organisational and interactional processes that influence how acute hospital staff respond to continence management and the toileting needs of PLWD –
-
What are staff doing and why?
-
What caring practices are observable when interacting with this patient group?
-
How do staff respond to and manage continence needs?
-
What informs these approaches?
-
-
To provide a detailed understanding and concrete examples of the ward routines that have an impact on continence care for this group, specifically to examine the assessment, classification and management of patient toileting needs and their place in ward handovers, routines and schedules.
-
To examine and describe the experiences of incontinence, toileting and catheterisation care in the ward from the perspectives of PLWD and their carers.
-
To explore the relationship between continence needs and patient dignity to add to understandings of how continence care has an impact on person-centred care, patient dignity, the potential for dehumanisation, family experiences and staff morale.
-
To identify factors associated with the improved care of this patient population that are actionable, specifically what clinical care needs to look like to improve the quality and humanity of continence care for PLWD and their carers in acute hospital settings. This may include enhanced awareness of the risk of incontinence interventions and clinical management options.
-
To identify low-cost factors at the organisation level (e.g. staff training, ward practices and routines) that can lead to actionable change, and to explore barriers to and facilitators of implementing changes.
-
To provide a detailed foundation of knowledge to inform a longer-term programme to develop and evaluate interventions providing new or enhanced approaches to delivery of continence care to PLWD.
-
To transfer new knowledge to front-line providers of acute hospital care, including managers, service commissioners and the research community.
To the best of our knowledge, little empirical research has examined continence care for PLWD to inform practice in the acute setting. A systematic review85 has found a lack of evidence-based nursing interventions to manage continence care for PLWD. In addition, it cannot be assumed that interventions from long-term care can be transferred unproblematically to the acute setting. Therefore, we conducted a mixed-methods systematic review and thematic synthesis of the literature, alongside ethnographic fieldwork, to establish an empirical foundation from which interventions in acute care settings can be established.
Chapter 3 Methodology
Parts of this chapter have been reproduced with permission from Featherstone et al. 106 © Queen’s Printer and Controller of HMSO 2019. This work was produced by Featherstone et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health and Care Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
This study utilised an ethnographic approach, alongside a mixed-methods review. It focused on the routine work of continence care for PLWD admitted to acute hospital settings in the wider context of the everyday care carried out by nurses and HCAs. We provide a detailed understanding of social and institutional forces shaping and influencing continence care. Our ethnographic approach enabled us to understand how staff respond to the continence care needs of PLWD and to follow the consequences of their actions. We examined how staff account for and make sense of the needs of PLWD in these contexts. 107
Ethnography provides a sophisticated toolkit for exploring the complexities of the everyday, forging better understandings of daily meaning-making92 in organisational structures and settings. Ethnography delivers detailed understandings of organisational culture, organisational change and the inter-relationships between different elements of an organisation. In health-care settings, ethnography allows researchers to take into account perspectives across the clinical experience, exploring the perceptions of patients and carers; medical, nursing and care teams; and wider auxiliary, administrative and managerial staff. 108,109 It is particularly useful to examine research questions that aim to access the unspoken and tacitly understood, as well as complex and highly sensitive, topics that are not easy or appropriate to measure. 110
Our approach to ethnography is informed by the symbolic interactionist tradition, which aims to provide an interpretive understanding of the social world. This places an emphasis on interaction, understanding how action and meaning are constructed in a specific setting, and acknowledging the mutual creation of knowledge by both the researcher and those researched. 111 The study aimed to deliver understandings of everyday continence care for PLWD in the acute hospital setting, focusing on how the wide range of social actors in these settings (i.e. the large number of ward staff that patients will come into contact with during an admission) respond to continence care needs of PLWD and to follow the consequences of their actions. Ethnography allows us to examine these elements and, importantly, the interplay between them. Ethnography examines ‘up close and in person how work is organized and how the organizing organizes people’. 92
Ethnography, at its core, is the in-depth study of a small number of cases. By exploring people’s actions and accounts in their natural everyday settings, ethnographers can collect relatively unstructured data from a range of sources, including observation, informal interviews and documentary evidence. 112 Ethnographers ‘hold that an appreciation of the extraordinary-in-the-ordinary may help to understand the ambiguities and obscurities of social life’. 92 This approach provides a depth of understanding and theory generation. 113 There is long tradition of ethnography in health-care settings,111 and there are many examples of ethnographic studies that have had a significant impact on policy and practice. 114–117
Our aim in utilising ethnography was to explore the otherwise unnoticed details of everyday life, in other words what is tacitly acknowledged, but rarely discussed, around ordinary and, in the case of continence care, hidden activities. Starr118 notes the importance of examining organisational infrastructure and the ‘hidden mechanisms’ constructed and embedded in the technical and procedural work carried out within it. 118 The articulation work of people in organisational and institutional settings was examined (i.e. how people in organisational and institutional settings account for and make sense of their actions). An ethnographic approach allowed us to explore both the front-stage performance and also the backstage work practices,119 while always maintaining the dignity and privacy of both patients and staff.
In any organisation, there are groups of people whose everyday work is unrecognised formally, often unnoticed and invisible. 118 In the hospital setting, such groups include carers, nurses, HCAs and auxiliary staff, for example those working in domestic services. In the context of our research questions, ethnography can examine how social and institutional forces shape and influence the work of health-care providers (HCPs)120 and the everyday routine behaviours of individuals, both within and across multidisciplinary teams. 121
This study focuses on the routine work of continence care for PLWD admitted to acute hospital settings. This study considers the wider context of the everyday care carried out by nurses and HCAs, and provides a detailed understanding of the social and institutional forces that shape and influence continence care. Our ethnographic approach enables us to (1) understand how staff respond to the continence care needs of PLWD and (2) follow the consequences of their actions. We examine how staff make sense of the needs of PLWD in these contexts. 107 In presenting our findings, utilisation of ethnographic ‘thick description’ enables the reader to connect concepts, policies and practice to detailed empirical examples. 122 This approach allows the reader to develop not only a strong connection to the social world of these wards, but also an understanding of the complex social relations within them; the personal impacts of continence care on patient, carers and ward staff; and how this connects with wider issues in the organisation and delivery of care in these institutional settings. 122
Prior to data collection, in January 2018, Deborah Edwards and Jane Harden carried out a mixed-methods systematic review and thematic synthesis of the literature to identify successful strategies in care settings that could inform innovations in continence care for PLWD in the acute hospital setting. This approach bridged the gap between research, policy and practice123 and was useful in examining the complexities of health service settings. The generated synthesis was used to refine our approach to fieldwork and analysis, and to inform the development and feasibility of the interventions.
Chapter 4 Data sources
Parts of this chapter have been reproduced with permission from Featherstone et al. 106 © Queen’s Printer and Controller of HMSO 2019. This work was produced by Featherstone et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health and Care Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK. In addition, parts of this chapter have been reproduced with permission from Featherstone and Northcott124 under licence CC-BY-ND-4.0.
Ethnographic fieldwork
Multiple sites were used in this ethnography as an exercise in ‘mapping terrain’. The goal was not ‘representation’ or ‘comparison’, but ‘identification’ to reveal the social processes surrounding continence care for PLWD in the acute setting. Therefore, it was important to observe interaction and performance, how continence care work was organised and delivered, and how it was communicated between different actors. This moves beyond the traditional examination of verbal communication to exploring tacit and non-verbal interaction, that is the multiple, complex and nuanced, but everyday, interactions and strategies that occur around continence care, which often ‘communicat[e] many messages at once, even of subverting on one level what it appears to be “saying” on another’. 125 In these hospital settings, many such interactions are concealed and are part of backstage talk, veiled language, euphemism and informal conversations. Our approach remedies a common weakness in many qualitative studies, that is that what people say in interviews may differ from what they do or their private justifications to others, an issue that is exacerbated when the topic under discussion is taboo or concealed from everyday, public life. 126 Our approach allowed us to respond to this and to examine the impacts of the organisation and delivery of continence care on PLWD and those caring for them over time.
This ethnography was carried out in six wards in three hospitals across England and Wales. These wards were purposefully selected to represent a range of hospitals types, geographies and socioeconomic catchments. Across these sites, 180 days of observational ethnographic fieldwork were conducted in areas of acute hospital care known to admit large numbers of PLWD, including general medical wards (e.g. acute wards for older people) and medical admissions units (or variants thereof). Approximately 500,000 words of observational fieldnotes were collected, written up, transcribed, cleaned and anonymised by the ethnographers (KF and AN). To provide a detailed contextual analysis of the events observed, the expertise involved and the wider conditions of patient care, we also carried out ethnographic (during observation) interviews with ward staff (n = 562) on multiple occasions. Case study participants who were living with dementia (n = 10) and their family members and carers (n = 20) also took part in ethnographic interviews (n = 30) during their admission and, in some cases, following discharge. Given the scope of our data set, in this report, we focus on presenting our analysis of the observational data, examining key features of continence care in these wards, including the use of continence ‘pads’ in everyday bedside care, the impact of the use of the continence ‘pads’ on PLWD and ward staff, and the influence of continence ‘pads’ on shaping ward cultures. To fully present the analysis of other aspects of continence care (e.g. catheter care) and of other data sets (i.e. staff interviews and case studies following PLWD and their families), these will be published separately.
Multisited ethnography defines the object of study via a number of techniques or tracking strategies. In the fieldwork, we recognised the importance of focusing on the ‘busy intersections’127 and of seeking out sites of tension where a large number of interests and identities are expressed. It is at these points that identity and culture become articulated, enacted and constructed. We aimed to provide a detailed understanding of the clinical and interactional work and processes that influence ward teams, their response to the pressing continence needs of patients living with dementia and the organisation of continence care for multiple patients within and across shifts. We also explored the work of other clinical staff (e.g. specialist registrars, consultants, allied health professionals and staff with managerial responsibilities) and auxiliary staff (e.g. domestic services) involved in the care of PLWD and their continence. We observed their actions and accounts to explore how individuals, teams and institutions prepare for, respond to, communicate and organise continence care in these settings, and the cultures that are both produced and maintained by these approaches.
At each hospital (n = 3), we conducted 30 days of observation in each ward (n = 2) over a period of 8 weeks of detailed fieldwork. Care was observed during day and night shifts, on weekdays, weekends and, where possible, public holidays. Observation periods ranged in duration from 2 to 6 hours and were reactive to events in the wards during observation. These periods of observation were followed by a further 8 weeks of follow-up data collection (including case study interviews and additional observation) so that, where possible, we could examine the implications of continence care practices for discharge and long-term care trajectories. Fieldwork always preserved patient dignity (as this study did not need to go ‘behind the screen’ to observe intimate care) and the goal of our observational strategy was to provide an in-depth evidence-based analysis of the management and context of continence care in these wards:
-
The fieldwork used non-participant observation and concentrated on the visible work of nurses and HCAs who are responsible for continence care. Other health-care staff were also included, as they are involved in wider continence assessment and decision-making for this patient group.
-
The fieldwork focused on ward routines where continence care took place or was prompted, including observation rounds, personal care routines, medication rounds and mealtimes.
-
The fieldwork observed responses to personal alarms, calls for assistance and decisions to prioritise or defer to examine the classification, urgency and management of patient continence care needs when it disrupted ward routines and schedules.
-
Communication and language around continence care were examined, including everyday interactions and strategies used in the wards, communication between staff, and communication with PLWD and their families.
-
The fieldwork focused on ward practices of assessment and management of continence care for PLWD by ward staff (i.e. nurses and HCAs), the medical teams and other staff when they were involved in continence care, assessment and decision-making.
-
Shift handovers were observed to examine everyday ward classification practices of continence and incontinence, and explore how these classification practices informed the organisation and planning of patient care during shifts and how these classifications entered risk assessment and discharge planning.
-
The technical and procedural work around continence care management (e.g. types and use of pads), assessment and recording was examined.
-
The fieldwork focused on observing conversations with carers as opportunities for sharing information about continence and how these conversations might best be managed with regard to decisions about discharge and place of discharge.
-
The study collected routine ward data, providing a context and an understanding of the workload around both everyday care routines and continence care in these wards.
This in-depth evidence-based analysis enabled us to provide detailed understandings of organisational and interactional care processes that were having an impact on the responses to and the management and delivery of continence care for this patient group.
Working in acute wards required the researchers to adopt a range of observational practices and strategies. Observation time was spent standing, rarely sitting, reflecting the pace of work of the teams and the widespread hospital staff in them. Our practice was to stand in the corridor, usually close to an alcove, sink, trolley or equipment that was already blocking part of the walkway, where there was space to stand out of the way of the team, but we could still view areas of the ward and the events taking place there. We also shadowed and walked with individual members of staff and teams as they worked in the ward. The built environment of the observed wards was highly variable: some wards consisted of a central hub with satellite bays, whereas other wards took the form of a long corridor either with or without windows onto bays and rooms. In all wards the researchers positioned themselves appropriately in the corridors to maximise visibility while minimising obstruction.
Our strategy was comprehensive note-taking, with notes written up as more detailed accounts. The researchers wrote extensively during these periods of observation, using A4 spiral-bound notepads. Writing was typically carried out with the notebook in hand, writing as we were standing or walking. The fieldnotes recorded took the form of a running record of events and incidents and included details and near-verbatim text of conversations and interactions. The opposite side of the notebook remained clear of fieldnotes and was used to insert thoughts and any additional points or queries to follow-up on or expand later. Note-taking was clearly visible to all staff and patients in the wards, and both staff and patients had natural opportunities (and were offered opportunities by the team) to ask questions about our notes. Staff were granted access to look at the fieldnotes if they requested this.
Ethnographic interviews with ward staff
To provide a detailed understanding of the influences on HCPs’ response to continence care, ethnographic (during observation) interviews focused on and were predominantly carried out with nurses (across all grades), HCAs from a range of disciplines (e.g. clinical staff, foundation year doctors, junior doctors, registrars, consultants, physiotherapists, occupational therapists, pharmacists and specialist dementia teams), staff with co-ordinating responsibilities (e.g. ward clerk and discharge co-ordinators) and auxiliary staff (e.g. domestic services) where appropriate. These interviews (n = 562) with ward staff were carried out over multiple occasions and during and across shifts as staff cared for PLWD in each ward. These interviews had a broad focus on the organisation and delivery of everyday care and continence care, and allowed us to question routine practices, rationales and decision-making to understand what staff were doing and why:
-
What was the articulation work in acute ward settings and how did staff account for and make sense of their actions?
-
For staff working with PLWD and providing continence care, what were their experiences, what training was provide for this type of care and what informed their practices?
-
What aspects of caring were defined as difficult, demanding or rewarding, and were staff confident in caring for this patient group?
-
What were the barriers to and enablers of supporting PLWD?
-
What were the recognition and rewards from patients, relatives, colleagues and managers for providing care for this group?
Case studies
A number (n = 10) of patients were recruited for case studies. We aimed to follow individuals living with dementia and their family carers from initial admission to the acute ward through to being discharged home or to long-term care and to follow their short-term care pathways. However, we were not able to seamlessly identify and follow people through an admission. The organisation of hospital admissions, with patients admitted, transferred and discharged on these wards 24 hours per day, meant that identifying and tracing a patient was not always possible, requiring the availability of the nurse in charge of the ward to access systems on behalf of the researcher. These obstacles meant that we recruited 10 patients for case studies rather than 12, which was our objective, but these patients represented a range of diagnostic, prognostic and sociodemographic factors, including patients with a range of continence care needs, reflecting our aims of including people with diverse experiences.
The goal of our study was to support PLWD and their families, and to share their experiences of an acute hospital admission. However, the case studies provided limited data that specifically related to continence care. Nevertheless, these data contribute to our wider understandings of the experiences and perspectives of an acute admission and its consequences for PLWD and their families. To fully represent the experiences PLWD, and their families, a separate analysis will be published.
Sampling
Sampling in ethnography requires a flexible, pragmatic approach that involves using evidence from available literature and a range of variables that may influence the phenomena under observation. Probability sampling is inappropriate and, therefore, non-probability sampling was used to provide analytically, rather than statistically, generalisable findings. 128,129 Using this approach, the number of sites and participants in the sample was judged not on the basis of size, but by the nature and scope of the study aims, the findings of our syntheses, the quality and appropriateness of the sample, and the achievement of theoretical saturation of data. 129
Sampling of hospitals and ward sites
Hospital settings are well suited to an ethnographic approach. 130,131 We identified a range of variables that may influence the phenomena under observation using purposive and maximum variation sampling to include three sites that represented a range of hospital types, geographical location, expertise, interventions and quality. In these hospitals, we included sites of care (e.g. assessment units and general medical wards) that received a large number of patients living with dementia, with a wide range of continence care needs and who required acute medical attention. Detailed descriptions of these hospital sites and profiles of the participating wards can be found in Appendix 1.
Sampling in each acute hospital site
Although our sites (i.e. acute hospitals and wards) were standardised, with sequential and systematic data collection, there was some variation between sites. We applied theoretical sampling in sites to achieve robust analytic concepts in the analysis. Informed by grounded theory, sensitising concepts from the ongoing analysis fed into each stage of data collection, expanding the research process to capture emerging relevant aspects in the ongoing analysis. The focus was on ‘discovery’, ensuring the grounding of emerging concepts in data and the reality of the settings. 132
Sampling and recruitment of staff for observation and interviews
We followed the routine and everyday work of nurses and HCAs. We used purposive sampling to include a wide range of clinical grades and roles across the ward settings. In addition, we included other clinical staff, staff with co-ordinating responsibilities and auxiliary staff who were also involved in the care of PLWD and in continence care.
Sampling and recruitment of patients for observation
It was not possible to predict the type of patients who would be present in acute hospital wards during the fieldwork period. However, we were confident from our previous research106 that PLWD would constitute a significant population in these wards. Details of the populations in these wards are found in Appendix 1.
Ethics approvals
Research Ethics Committee (REC) approval for the study was granted by the NHS Research Ethics Service via the Wales REC 3 on 19 April 2018 (reference 18/WA/0033), with approval from the Health Research Authority (London, UK) and Health and Care Research Wales (Cardiff, UK) granted on 5 September 2018 [Integrated Research Application System (IRAS) 239618/protocol 4804]. The research project was approved for the purposes of the Mental Capacity Act 2005,133 confirming that it met the requirements of section 31 of the Act in relation to research carried out as part of this project on or in relation to a person who lacks capacity to consent to taking part in the project. Recruitment for the study was managed and recorded through the Central Portfolio Management System, beginning on 11 October 2018 and ending on 31 October 2019. A total of 108 participants were recruited to the study.
The safety of all participants was a key priority at each stage of the study. Before commencement, the ethics of observing care and of reporting, where necessary, what was observed was frequently discussed with the hospital sites and our carers group. In meetings with the REC that approved this study, it was clarified that, although neither of the researchers (KF and AN) had a clinical duty of care (i.e. being academics without clinical qualifications or professional affiliation), they would be bound to safeguard any patient participants observed during the project.
Prior to commencement, both researchers, experienced in both hospital ethnography and conducting research with PLWD, renewed their Good Clinical Practice certification and upgraded their existing Protection of Vulnerable Adults level 1 certification by completing Safeguarding Vulnerable Adults levels 1–3. The researchers were made aware of safeguarding and whistleblowing procedures at each site and had a named member of staff (i.e. the site principal investigator or a senior nurse on shift) to contact if malpractice or behaviour that put vulnerable patients at risk was observed. Both researchers underwent full occupational health checks, held honorary contracts with the NHS health boards and trusts, and had up-to-date Disclosure & Barring Service certification and NHS research passports.
Several months in advance of the period of observation at each ward, the research team visited the wards to introduce the study to the ward staff and to discuss the study aims with relevant staff. These meetings were repeated 24 hours before observations started, in handover meetings in week 1 of observations and to individuals throughout the study to ensure that ward staff were aware of the study, to answer questions and to recruit staff to the study.
Over the course of the observations, the researchers saw many aspects of everyday practice that would not be considered ‘best practice’ or in the interests of the individual patient. The examples of practice presented in this report were not isolated and formed part of systemic and established everyday routine practice in every ward at each hospital site. We never observed individual malicious behaviour or isolated incidents of deviance that placed a vulnerable adult at risk. Instead, we observed how the everyday routine organisation and delivery of continence care itself often placed the vulnerable person living with dementia at risk, as a part of the routine practices and established cultures of these hospitals and the wards within them. At no point did the researchers feel that any individual or ward team was acting in a way that necessitated escalating or whistleblowing.
The researchers did, however, frequently intervene to support PLWD and their families and carers, where necessary, to protect the comfort of the patient. PLWD would frequently tell the researchers that they wanted to go to the bathroom or that they were in pain, or share concerns about, for example, home, family or pets, or how to pay for their care. In response to disclosures, the researcher (with permission from the patient) would inform ward staff and ensure that this was attended to by the ward team.
The researchers were sometimes the only member of ‘staff’ spending uninterrupted time in a specific area of a ward and so would regularly ask patients if they needed anything. Sometimes, when ward staff were absent or could not be called quickly to a bay, the researchers provided immediate support. For example, were a patient at immediate risk of physical danger, the researchers would call staff and, if necessary, intervene. Similarly, the researchers would fetch cups of tea, pour glasses of water and carry out other simple tasks in these wards when requested and when permitted. Although the researchers accept that this may have, on occasion, contaminated the purity of their data, the welfare of those in the field of observation was always the priority.
Between sites, the emergent analysis was regularly presented to the research team, including nurses, clinicians, trust leads, PLWD and family carers, and, although it was agreed that the care observed could be detrimental or distressing to a person living with dementia, it was also recognised as routine and recognisable as the everyday practice of acute ward staff.
Although, in isolation, some of the descriptions of continence care presented in this report may appear to breach patients’ rights, we hope to have demonstrated in our analysis that these were not isolated incidents, but rather the everyday reality of the care delivery that each person living with dementia will experience during admission to acute hospital care. The results presented in this report also show that nurses and HCAs, likewise, experience distress, with little organisational support or recognition of the care required to respond to the continence needs of PLWD in ways other than those outlined here. The cultures of these wards prioritised risk reduction and timetabled routines over the comfort or preferences of PLWD. The actions of nurses and HCAs in response to continence needs presented in this report were carried out in good faith, attempting to protect the patient and the ward, and to respond to the policies and perceived expectations of the wider institution. We hope that the evidence presented here highlights the challenges faced by ward staff as they deliver care in the acute environment, and the need to better support both patients living with dementia and staff in this setting.
Chapter 5 Modes of analysis/interpretation
Parts of this chapter have been reproduced with permission from Featherstone et al. 106 © Queen’s Printer and Controller of HMSO 2019. This work was produced by Featherstone et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health and Care Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Data collection (in situ observations and interviews) and analysis was informed by the analytical tradition of grounded theory,132 which is a flexible approach for ethnographic research. 126 This approach utilises theoretical sampling and the constant comparative method, in which data collection and analysis are inter-related134,135 and conducted concurrently. 134,136 The flexibility and responsiveness of this approach were of particular significance, enabling us to increase the ‘analytic incisiveness’126 of the study. Preliminary analysis of data continued in parallel with data collection at later sites, informing the focus of further stages of data collection and subsequent concurrent analysis. The constant comparative method means that the coding of data into categories was a recurrent process. Data were examined in the context of previous fieldwork and analysis, which informed further strategies of data collection in subsequent sites, producing more focused stages of analysis. 126 The analytical concepts emerging were then further tested and refined to develop robust analytical concepts that transcend the local contexts of individual wards and sites, and identify broader structural conditions137 that influence continence care for PLWD in the acute setting.
Findings from our mixed-methods review informed the ethnography in various ways, with a focus on initiating the process of early thinking and theorising during data collection and analysis. The review aimed to increase our theoretical sensitivity to key areas of importance to explore during data collection, including communication, language and the importance of non-verbal cues. The review was conducted alongside data collection at the first site, with data at this site analysed as they were collected. The review and its findings were used to stimulate questions during the ongoing iterative analytical process. This affirmed our focus on issues of continence-related communication, language, privacy and dignity, combined with known routines and strategies of bedside care.
Corbin and Strauss135 caution that, in grounded theory, literature should not impede ‘discovery’, emphasising the importance of using it actively to identify potential areas to inform theoretical sampling. Therefore, we explicitly sought opportunities to identify examples of individualised care, planning and assessments, with the goal of improving the continence of PLWD during an acute admission and the use of promoted strategies, such as ‘prompting’ and other continence routines and schedules, identified in the review.
Grounded theory strengthens the ethnographic aims of achieving theoretical interpretation of data, whereas the ethnographic approach prevents a mechanistic and rigid application of grounded theory. 126 Ethnography can treat everything in a setting as data, leading to the ethnographer collecting large numbers of unconnected data and a heavily descriptive analysis. 129 Our approach provides a middle ground in which the ethnographer uses grounded theory to provide a systematic approach to data collection, with the analytic goal of developing theory to address the interpretive realities of the range of actors in these ward settings. 126 Data collection strategies explicitly supported ‘theoretical saturation’132 (i.e. where further data collection was no longer adding to the development of analytic concepts).
Analysis involved the development and testing of analytic concepts and categories. The strategies we used for the development of concepts and categories included careful reading of the data; looking for patterns and relationships; and noting surprises, inconsistencies and contradictions across the range of perspectives gathered. Line-by-line coding is inappropriate for field notes and, therefore, coding was selective, involving whole events or scenarios. 117 Initially, this produced a collection of ‘sensitizing concepts’138 and analytic memos that informed the later development of more refined and stable analytic concepts. At this stage, Katie Featherstone and Andy Northcott re-examined the raw data informed by the subsequent phases of analysis (re-coding where necessary), looking for examples and events to test the analysis. Emerging analytic concepts were tested and refined to develop (in collaboration with the wider research team) stable concepts that identified broader structural conditions135 influencing continence care.
Throughout this process, we drew on multiple perspectives (e.g. sociological, policy, clinical, patient and carer) to inform our analysis. This included the use of our mixed-methods systematic review, with the narrative syntheses generated (see Chapter 6) informing data collection strategies and the analysis. Credibility checks included presenting emergent analysis to ward staff (in participating sites) and to PLWD and carers (see Chapter 9) for discussion throughout this process.
Field notes of observation and near-verbatim text were hand-written and then transferred into Microsoft Word files (Microsoft Corporation, Redmond, WA, USA) following data collection. 139,140 All audio-recordings of observations and interviews (i.e. ethnographic and in-depth) were written up in Word files or transcribed verbatim by a professional transcription service. All sites and individuals, and the data collected, were anonymised and sorted in line with the UK General Data Protection Regulations as part of the Data Protection Act 2018. 141 Storage of the data was managed by the Information Security Framework of Cardiff University (Cardiff, UK).
Chapter 6 Findings from mixed-methods review and thematic synthesis
This chapter focuses on the mixed-methods systematic review and thematic synthesis. Parts of this chapter have been reproduced with permission from Edwards et al. 142 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Methods
This systematic review uses methods informed by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre). 143,144 A scoping exercise in January 2018 was followed by a targeted and in-depth review and synthesis. The protocol has been registered as PROSPERO CRD42018119495.
Scoping exercise
The scoping exercise asked ‘what is known about the management and practices of continence care (i.e. continence care, incontinence care, toileting and catheter care) for PLWD in acute, long-term and community health-care settings and home settings?’ Two databases (MEDLINE and PsycInfo®) were searched from inception to January 2018 for citations that focused on or contained an element relating to each of the following inclusion criteria:
-
PLWD, Alzheimer’s disease or cognitive impairment
-
acute, long-term and community health-care and home settings
-
urinary or faecal continence/incontinence, or toileting issues
-
conservative management or care practices (defined as any continence care practice that does not require medical or surgical intervention, including catheterisation145).
After title and abstract screening, 114 of the 1348 citations retrieved remained. After standard screening processes by two reviewers (DE and JH), 87 papers were included, including studies (n = 40, across 48 publications), discussion/opinion papers (n = 17), reviews (n = 13, across 17 publications), audits (n = 2), guidelines (n = 2) and a documentary analysis (n = 1). Studies or reviews published multiple times were treated as one and, therefore, the final number of included papers was 75.
In keeping with the EPPI-Centre approach, findings were presented to stakeholders to ascertain their views on the priority areas for the second phase of searching. All stakeholders (see Appendix 2), as part of this process, were asked to complete a priority-setting exercise, facilitated by answering the question ‘What do you think are five of the most important ways that continence could be managed for PLWD when they are in hospital?’. Responses were collated, coded and grouped together to generate a list of methods for managing continence in the hospital setting.
Descriptive maps of the findings from the scoping exercise and a summary of the consultation with the stakeholders were presented to the collaborative research/project team of co-applicants. Across both groups, the top two priority areas identified as most salient to informing and improving continence care in the acute setting were (1) ‘communication’ and (2) ‘individualised care planning’. This exercise informed the research question taken forward to the mixed-methods systematic review, that is ‘what is known about the management and practices of continence care in relation to communication and individualised care planning for PLWD in acute, long-term and community health-care settings and home settings?’
Mixed-methods systematic review
Objectives
The review aimed to:
-
explore carers’, family members’ and HCPs’ perceptions and experiences of communication and individualised care planning for PLWD with regard to toileting and continence
-
identify the communication strategies and the use of individualised care planning employed by carers, family members and HCPs to manage toileting and continence for PLWD.
Eligibility criteria
We used the PICOS (participants, interventions, comparisons, outcomes, study design)/PICO (population, intervention, control/comparison, outcome) framework to guide the inclusion criteria for participants, intervention/phenomenon of interest, comparators, outcome, study design and context (see Appendix 3).
Searching
Eight databases were searched from inception to June 2018 (updated August 2020), including MEDLINE, PsycInfo, EMBASE, Cumulative Index to Nursing and Allied Health Literature, Education Resources Information Center, Applied Social Sciences Index and Abstracts, British Nursing Index and Open Grey (see Appendix 4). Relevant organisational websites were searched for UK policy and guidance, and key journals were hand-searched (see Appendix 5). Reference lists of included studies were scanned, experts contacted and forward citation tracking performed using Web of Science.
Screening
All citations retrieved were imported into EndNote (Clarivate Analytics, Philadelphia, PA, USA) and duplicate references were removed. Two reviewers (DE and JH) conducted all screening processes, with disagreements resolved through discussion with a third reviewer. Multiple articles by the same authors reporting the same study were linked to help inform decisions on which studies to include.
Quality appraisal
Quality appraisal of the research material was conducted by two reviewers, with disagreements resolved through discussion with a third reviewer using the Mixed Methods Appraisal Tool (MMAT), version 2011. 146–148 Each study was assigned a score based on the number of criteria met (with 25% representing one criterion met and 100% representing all criteria met). Studies were excluded if they scored < 50% for quality (i.e. a maximum score of two out of four criteria). 146 Non-research evidence (e.g. policies and reports) were not subjected to quality appraisal.
Data extraction
Demographic data from the included primary research studies were extracted and entered into a series of electronic tables (see Appendix 6, Tables 4–6, and Appendix 7, Tables 7 and 8). Study findings for the primary research studies for the purposes of this review were all considered to be text labelled as results or findings. All such results were extracted and entered verbatim into Microsoft Word. Data for non-research material were extracted and entered directly into an electronic table (see Appendix 8). All non-research material was available as electronic documents, searched using keywords relevant to the priority areas (e.g. ‘communication’, ‘tailored’ and ‘individual’). These data were then considered to be findings and were extracted and entered verbatim into Microsoft Word. Data extraction was independently checked for accuracy and completeness by a second researcher (DE or JH), with any disagreements noted and resolved by consensus.
Data synthesis
Thematic synthesis was employed to bring together data from both qualitative and quantitative primary research studies and non-research material. 149
Assessing the certainty and confidence of the evidence
The confidence of the overarching synthesised findings derived from descriptive quantitative research (that had undergone qualitisation) and qualitative research were assessed using the Confidence in the Evidence from Reviews of Qualitative research (CERQual) approach,150 and the findings from quantitative experimental research were assessed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach. 151
Flow of studies through the review
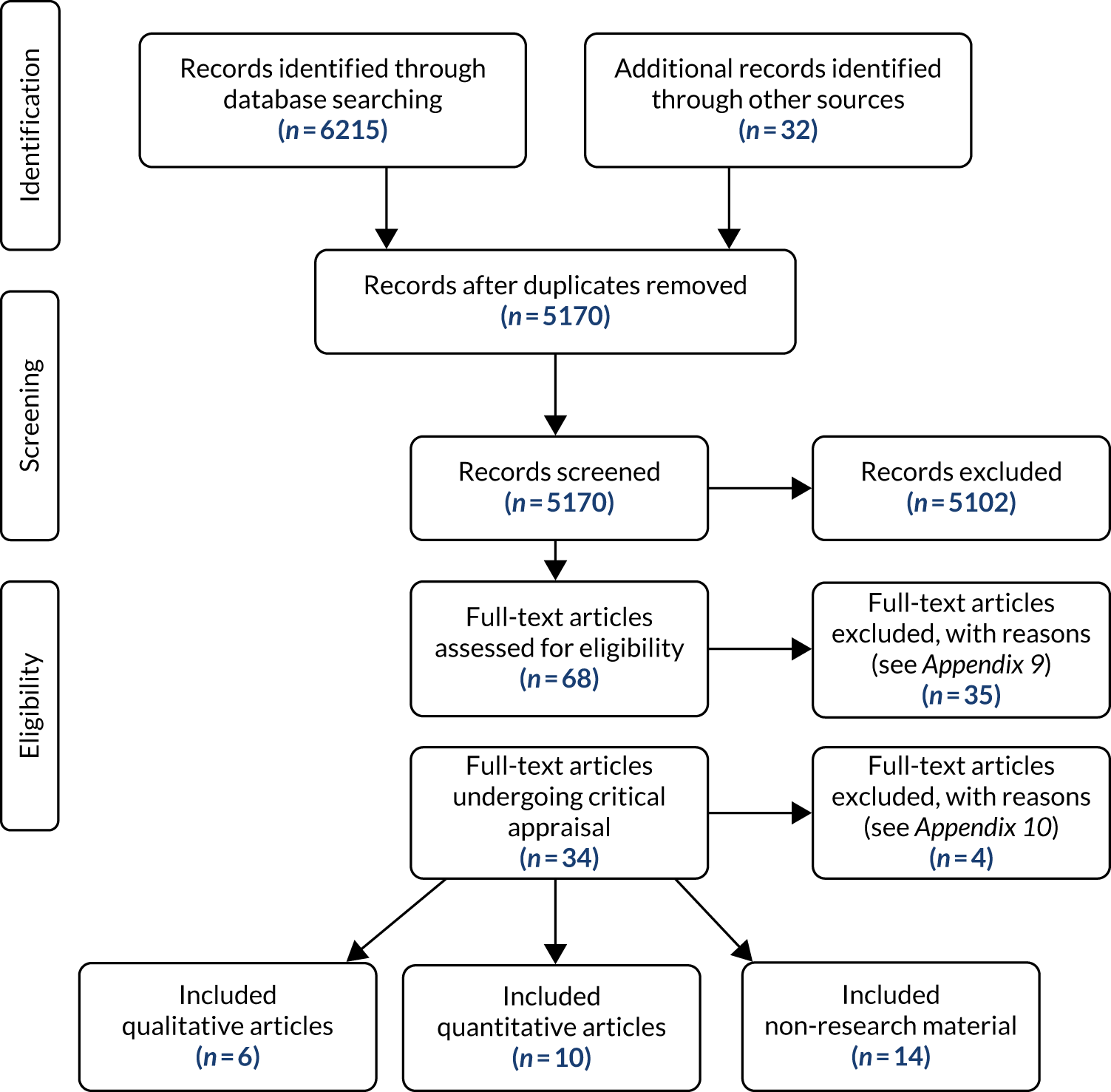
The database searches yielded a total of 5170 citations after removing duplicates (Figure 1). 149
FIGURE 1.
Flow of citations through the systematic review.
Characteristics of the included studies
The 30 included publications included quantitative research studies, qualitative research studies and non-research material studies and non-research material (Table 1).
| Study design | Number of studies and citation |
|---|---|
| Case series with non-concurrent multiple baselines | 2152,153 |
| Randomised controlled trial | 1154 |
| Pre test/post test | 1155 |
| Prospective cohort | 1156 |
| Post-intervention descriptive surveys | 2157,158 |
| Cross sectional survey | 2159,160 |
| Adapted three-stage Delphi consultation study | 1161 |
| Qualitative | 5 (across six publications)162–167 |
| Web pages/web booklets | 5168–172 |
| Guidelines | 21,87 |
| Reports | 2173,174 |
| Guidelines/guidance | 2175,176 |
| Framework | 1177 |
| Model | 1178 |
| Information sheets | 1179 |
The 15 research studies were conducted in seven countries (Table 2). Four publications of non-research material were published outside the UK: one European guideline,87 one international guideline,175 and a framework and model published by the same author from Australia. 177,178
| Country | Number of studies and citation |
|---|---|
| USA | 8 (across nine publications)152–154,157,158,162–164,166 |
| Australia | 2159,165 |
| UK | 1161 |
| Japan | 1155 |
| Taiwan (Province of China) | 1160 |
| Sweden | 1156 |
| Malta | 1167 |
The research studies were conducted across a variety of settings (Table 3).
| Setting | Number of studies and citations |
|---|---|
| Home care/community | 5154,157,158,161,162 |
| Nursing home | 2155,165 |
| Residential care facility | 1156 |
| Alzheimer’s disease rehabilitation centre | 2152,153 |
| Secondary care setting | 3160,166,167 |
| Alzheimer’s disease-specific day centre and home care setting | 1163 |
| Hostel care for ambulant people with dementia, aged care complex with hostel and nursing home facilities, and an acute hospital ward | 1159 |
| Day centre and long-term care facility | 1160 |
Methodological quality
The methodological quality is reported in Appendix 11.
Thematic synthesis
The findings from the quantitative and qualitative research, and from the included policy and guidance materials, were synthesised separately for each objective
Objective 1
The first objective was to explore carers’, family members’ and HCPs’ perceptions and experiences of communication, and the use of individualised care planning for PLWD with regard to toileting and continence. The objective comprised eight subthemes.
Communicating in a dignified way
The importance of protecting personal and social dignity163,165,166 during continence care was significant, and HCPs reported a belief that PLWD and their caregivers prefer not to talk about incontinence because it is a highly embarrassing165,166 and distressing issue. 178 HCPs believed that the provision of quality continence care for PLWD includes measures and approaches that conceal incontinence by creating situations that allow PLWD to go to the toilet in private and avoid communication that reveal their issues around incontinence or care dependence, which could cause them to feel embarrassed, ashamed or humiliated. 165
Respecting PLWDs’ right to privacy was also considered important. 163,165,178 To relieve PLWDs’ perceived embarrassment of accepting assistance,163,165 HCPs stressed the importance of building rapport and trust, using humour178 and ‘acting natural’163 when supporting continence needs. HCPs also felt that they should have the appropriate knowledge and skills to communicate with PLWD in ways that would minimise any emotional impact. 165 Other strategies to enhance privacy included whispering to the client about toileting issues165 and keeping these issues secret. 163 However, HCPs acknowledged that PLWD may have difficulties in recognising and communicating their continence needs, and PLWD not being verbally able to request toileting assistance was viewed as a barrier to protecting dignity. 165 Closely overlapping with this theme of communication is the issue of HCPs’ attitudes towards continence care.
The attitudes of health-care providers towards continence and continence care
The language used in a care environment is important with regard to continence care. 173,177 The language used was not always respectful;173 however, in situations in which staff had good knowledge of the people they cared for, staff were respectful and built good relationships with PLWD. 173 Ostaszkiewicz,177 discussing coercive continence care practices, described these practices as including ‘the use of verbal or physical force to wash a person, to accept wearing continence pads or other forms of incontinence containment and to accept continence checks’. 177 Ostaszkiewicz177 also suggested that chastising a person for being incontinent could be said to be a form of verbal abuse. Although some ward staff promote continence, this does not appear to happen consistently in acute settings. 167 Relatives expressed concern that, although PLWD would be happy to go to the toilet if assistance was provided, staff often encouraged them to ‘do it in the nappy’. 167 In addition, at times, for example when staff members were busy or appeared uncomfortable with or uninterested in providing support, routine toileting was avoided and cues ignored. 163,167 Ostaszkiewicz177 recognised that ‘[c]ommunicating therapeutically about incontinence with any person, including people with dementia, involves the demonstration of warmth, compassion and humanity’. 177 This requires both clinical knowledge and interpersonal and communication skills, which should all be included in education programmes. 178 Both formal caregivers and family carers would benefit from such programmes, which would also enable the development of ‘empathetic understanding’177 of the emotions that a person living with dementia has in response to incontinence and its care. 177
Presence of people living with dementia during outpatient consultations
There is no consensus as to whether or not PLWD should be present with their caregivers during outpatient consultations. 162,164,166 HCPs believed that care recipients should be present when discussing continence problems during consultations;166 however, caregivers expressed mixed opinions. 162,164 Caregivers who favour this approach view the HCP as an authority in this subject, with the result that they believe the PLWD would be more likely to co-operate with management strategies because they had been involved in the discussion. 162 By contrast, caregivers who opposed this reported that they did not want to upset or make their care recipient anxious by discussing a problem that the PLWD might not fully understand or be able to control. 162 Caregivers who were daughters felt the need to be sensitive to their parent’s privacy and feelings, preferring to discuss incontinence in greater depth with their HCPs, but this was not the case for caregiver spouses. However, time constraints or inability to meet alone with the HCPs prevented in-depth discussions from taking place. 164 Some caregivers suggested that HCPs could explain the problem and management options in simple terms when the care recipient was present in outpatient settings and then speak separately to the caregiver, providing more details. 162
Initiating conversations during outpatient consultations
There was a lack of consensus with regard to who caregivers thought should be responsible for initiating conversations about incontinence during dementia-related consultations in outpatient settings. 162,164,166 Caregivers believed that it is the responsibility of HCPs to initiate conversations about incontinence during both initial consultations and follow-up appointments. 162 However, there were differences depending on whether the care recipient was a parent or a spouse. Caregivers who were daughters or daughters-in-law would discuss incontinence with HCPs only when it became problematic to manage at home, whereas husbands tended to communicate their wives’ problems much sooner. 164 By contrast, HCPs thought that conversations about incontinence should be initiated by the caregiver. 162 However, when HCPs did initiate conversations about incontinence, they reported that this was appreciated by the caregiver, who was receptive and engaging in discussion around the topic. 166 However, in secondary care, not all HCPs saw addressing incontinence as a priority and many thought that the topic should be dealt with by the patient’s primary care providers, rather than during a specialist secondary care referral. 166
Extended family and friends who were caregivers reported that HCPs do not always ask about incontinence during consultations. 164 A lack of awareness of available resources and concerns about frightening patients/caregivers about potential problems before they occurred were suggested as possible explanations as to why HCPs do not routinely discuss incontinence and fail to initiate conversations about incontinence. 166 Time was the most common barrier to discussing incontinence reported by HCPs, as HCPs believed that a considerable amount of information needed to be covered during appointments and discussing incontinence issues needed more time than was typically allocated. 166 Possible solutions suggested by HCPs were for the patient/caregiver to have a follow-up appointment to discuss incontinence or to offer referrals to a nurse in continence care. 166
The language of incontinence during outpatient consultations
Caregivers prefer ‘straight talk’ from HCPs about incontinence and its management in relation to PLWD. 162 In a US study, Hispanic caregivers stressed that it is essential for providers to discuss incontinence using language that those with English as a second language can understand. These caregivers strongly supported having materials written in Spanish about incontinence in PLWD and the treatment plans available. 164 During outpatient consultations, caregivers rarely used the term incontinence and, instead, use terms such as having accidents, leaking, losing control, wetting or messing their pants, having a urine/bowel problem, urgency, diarrhoea, loose bowels, being unable to hold it and not getting there in time, difficulty in getting to the bathroom, and leaking and soiling themselves. 162,166 HCPs also tended to adopt these terms when discussing incontinence with family caregivers or patients. 166 Caregivers, when questioned, said that they did not know the right terms and did not want to be disrespectful to their care recipients. However, once caregivers were made aware of the term incontinence they were happy to use it. 162
Caregivers and HCPs suggested a number of different types of written information resources that could be provided to caregivers attending outpatient consultations,162,164,166 for example:
-
a guide to talking to a HCP about these problems, including definitions of common clinical terms162
-
a pre-visit checklist or written materials of some type to enable patients/caregivers to indicate whether or not incontinence is present, as this could then prompt the HCP to start a discussion during the consultation166
-
readily available handouts that would offer more detailed explanations of what had been covered during the appointment166
-
short and focused handouts that could stand alone and address a single concern. 166
The importance of non-verbal cues
People living with dementia are not always able to recognise and communicate that they need to go to the toilet or indicate that they need assistance. 87,152,153,157–159,162,163,165,166,171–173 Therefore, it is important to recognise the non-verbal signals, body language, facial expressions, behaviours and any signs that the PLWD use to communicate in such instances163,171–173 so that their wishes can be acknowledged. 173 Listening carefully to the words or phrases that PLWD use for describing the toilet,1,159,170,172,173 as well as being able to recognise familiar gestures,1,159,173 is seen as important. New staff should be trained to recognise the importance of toileting and on how to understand individual behaviours and non-verbal cues in relation to toileting. 163
A range of different non-verbal cues indicating need to go to the toilet have been observed or reported, include pulling/taking off clothing;87,160,171,179 making particular sounds, such as moaning or grunting;160,163,171 assuming a different posture;87 looking around;163 fidgeting;87,163,170,179 getting up and walking around or pacing;163,169,170,179 restlessness; 87,160 holding the crotch or stomach;87,163,170 various facial expressions, such as worry87 or sorrow;160 and going to the corner of the room. 170
Hutchinson et al. 163 also reported a number of affective cues, which included anger, profanity and acting in a frustrated and irritable manner. One study160 that investigated common behaviours when PLWD experience either bowel movement or urination needs found that anxiety, restlessness and taking off/putting on clothes inappropriately were exhibited by more than 30% of patients. 160
Finding the appropriate words and symbols to describe the toilet
Wilkinson et al. 159 sought to evaluate the comparative suitability of a range of words or symbols used to label toilets for PLWD. Among the 24 institutions surveyed, 16 used the label ‘toilet’ and x used the words ‘male/female’. Four institutions used no labelling. Only four institutions used symbols; one used the international symbols, one used a toilet symbols, one used yellow wrapping over the door and one used a ceramic plaque on which the word ‘toilet’ was written (n = 1). A further survey, among PLWD, found that the preferred word and symbol for toilet varied significantly (p < 0.05) according to mental status (assessed using the Folstein Mini-Mental State Exam and classified as normal, mild, moderate and advanced). The labels ‘Ladies’ and ‘Gents’ were preferred by those with no cognitive impairment and ‘toilet’ by those with moderate dementia. The international symbols was preferred by people with no cognitive impairment or mild dementia, whereas the toilet symbol was preferred by those with more advanced dementia. 159
The importance of individualised continence care
Targeted and individualised/person-centred continence care87,168,172,174,175,178 that is established after a thorough clinical assessment has taken place87,175,177,179 is seen as important, including the use of a bladder diary. 87 Individualised continence care means care that is best for the individual,87,172 avoiding harm87 and about promoting autonomy and independent living. 87
Objective 2
The second objective was to identify the communication strategies and the use of individualised care planning that carers, family members and HCPs have employed to manage toileting and continence for PLWD. This objective comprised five subthemes.
Strategies for improving communication
To reduce anxiety, fear and embarrassment, it is important to check HCPs’ awareness of good communication techniques when working with PLWD. 161 HCPs should consider:
-
getting to know the person with dementia, such as their previous routines, habits and lifestyle170–172 and how they communicate172
-
introducing themselves and seeking PLWD approval before performing tasks165
-
asking the person with dementia how they can help them manage their continence170
-
communicating with the family to determine usual behaviour patterns163
-
seeing the person as an individual and avoiding making assumptions. 172
Caregivers reported that they sought additional information about incontinence from the internet, but were concerned about the accuracy of the information retrieved and whether or not they could understand it. This also included concerns about their searching skills. 164 They wanted support and reassurance that they were providing the care that was required and they wanted information before any problems, such as incontinence, occurred so that they could feel prepared. 162
One further study described how nursing staff communicated with residents’ families about methods to manage incontinence when taking PLWD ‘on an outing’. 165 The advice included information about how to check and change continence pads, how to assist the resident to the toilet and how long continence pads could potentially last between changes. 165
Using technology to present instructions
Two pilot studies152,153 conducted by the same authors explored the effectiveness of verbal instructions presented automatically through simple technology in helping persons with mild to moderate Alzheimer’s disease recapture basic daily activities. Data from both studies152,153 showed that the use of basic technology to automatically present verbal instructions has the potential to be effective in helping people with mild to moderate Alzheimer’s disease recapture relevant daily activities, including toileting. 152,153
Components of individualised care plans
A number of different components that may be considered as part of individualised care plans have been identified, including being theory based,175 being concerned with the practical issues168 and involving multicomponents exploring both day-time and night-time care of incontinence. 175 There was a consensus that the needs of both PLWD and their caregivers need to be considered. 87,174–177 The advice given by the Alzheimer’s Society was that continence care plans should be tailored to the individual, with the intention of curing incontinence (or problems with toileting) whenever possible. 168 Other components to consider include changing medication,168 changes to lifestyle,168 exercise,168 skin care,175,177 manipulating the type, quantity and timing of food and drink,168 and advising of the support available from HCPs,168 as well as any accessible follow-up advice. 168
Ostaszkiewicz177 comments that nurses and care workers need support to develop individualised strategies to ‘optimize the care-dependent person’s rest/sleep in the context of the person’s concurrent need for continence and skin care’. 177 Three studies155,157,158 described individualised care plans as part of their interventions. One study155 was conducted in nursing homes, with one member of staff from each home selected to take part in a training programme. This person was then responsible for educating other staff members. The intervention used in this case was individualised comprehensive care that focused on providing adequate fluids and meals, encouraging patients to use toilets and reducing the size of their ‘diaper’ pads. This approach differed significantly from the usual urinary incontinence care in which ‘diapers’ would be changed at scheduled times only. Improvements across the different methods (e.g. ‘diapers’, chair, commode and urinary chamber pot) of urination were observed, with 11% of residents making improvements, but this finding did not reach levels of statistical significance. In addition, 19% of residents showed improvement during the night, changing from using ‘diapers’ to using the toilet, which was shown to be significant. Nevertheless, a large number of residents’ continence status remained static. 155
Two studies157,158 evaluated an environmental skill-building programme that involved a home-environment individualised intervention delivered by occupational therapists, which included toileting and incontinence. The intervention was designed to enhance the caregiver’s ability to problem-solve and to develop effective solutions to problematic situations. One of these studies was a pilot study158 in which 17 effective caregiver-initiated environmental solutions for incontinence were observed. Of these solutions, nine (53%) were accepted by the caregivers and integrated into their management routine by visit 5 of the intervention. In the later study,157 29% of caregivers identified continence as a problem area. Twenty-six attempted strategies that involved assistive devices were identified and, of these, 21 (81%) were used. Fifty-one attempted strategies that involved manipulating the type, quantity and timing of food and drink were identified and, of these, 46 (90%) were used.
One further study156 implemented a person-centred approach that focused on incontinence of residents with cognitive decline in residential treatment facilities. In this study,156 health workers were provided with training, but only 20 out of 100 health workers participated. The process outcomes were measured among all residents who agreed to participate in the study. There were no statistically significant mean differences in QoL scores before and after the intervention or between control and intervention participants. However, the quality of care improved for the intervention participants in that fewer aids were needed to manage incontinence and an increased number of urinary incontinence assessments were conducted.
Health-care providers and caregivers working in partnership
The importance of HCPs and caregivers working together to deliver individualised/person-centred continence care was a feature of three intervention studies154,157,158 and was encouraged in four pieces of non-research material. 168,172,174,176 In one intervention study,154 nurse practitioners worked with the carer to plan the schedule for PLWD, which was followed up with monthly telephone calls and bi-monthly visits. In a further two intervention studies,157,158 occupational therapists worked with the caregivers to deliver solutions to toileting and incontinence problems, and this involved five visits over 3 months158 or five 90-minute visits over 2 months. 157 Other HCPs that can work with PLWD and their caregivers include continence advisors168 or other HCPs specialising in continence care. 172 Working in partnership with caregivers and PLWD is important168,172,176 as it enables HCPs to gather personal stories of PLWD and their caregivers,174 helps HCPs to work out the best solutions for PLWD and their caregivers and ensures that specialist help can be accessed by caregivers when needed so that recommendations from HCPs are achievable. 168
Establishing a toileting routine in the home environment
The importance of developing a regular toileting schedule was discussed briefly in one study158 and one piece of non-research material87 and was the focus of one intervention study. 154 In a study by Jirovec and Templin,154 the intervention group was taught an individualised scheduled toileting procedure that compensated for cognitive impairment by providing ‘memory-impaired patients’ with toileting reminders. Initially, assignment was to one of two intervention groups. One group of participants was visited every 2 months and the other group after a 6-month interval. There was also a control group. At the 6-month follow-up, the two intervention groups did not differ with respect to urinary incontinence and so the original two intervention groups were combined, leaving a single intervention group and a control group. The authors154 conducted a completers-only analysis (with 28 of the 44 participants still in the study at 6 months) and reported that incontinence decreased in the intervention group, with almost no change in the control group. Further analysis of these data using the non-parametric sign test was conducted and a significant decrease was reported in the intervention group (z = −1.83; p < 0.05). The participants were coded according to any decrease in percentage of incontinent episodes, compared with staying the same or showing no improvement. However, two previous reviews180,181 that reported on this study conducted a reanalysis of the data and, although the results favoured the intervention groups, they were not statistically significant.
Synthesis summary statements
Twenty-six summary statements were produced, with associated levels of confidence using the CERQual and GRADE approaches (see Appendix 12). The experimental quantitative research that we retrieved were observational studies that were considered to be of poor design. As a result, the ratings for evidence from each outcome generated using material from these studies were downgraded from being rated as ‘low quality’ to ‘very low quality’. 182
Chapter 7 Findings from the ethnographic observations
This chapter explores the findings from the ethnographic observations in relation to continence care for PLWD during an acute hospital admission. Parts of this chapter have been reproduced with permission from Featherstone and Northcott124 under licence CC-BY-ND-4.0.
Our detailed analysis provides understandings of the complex social relations that occurred in these wards, including the ways in which the organisation and delivery of continence care at the bedside connected closely with and was informed by wider institutional expectations, policies and priorities, which, in turn, shaped the personal impacts of continence care for patients living with dementia and ward staff. Given the scope of our data set, in this report, we focus on presenting the five major themes that emerged from our analysis: (1) continence as a significant, visible and public phenomenon; (2) continence communication; (3) rationales of safety; (4) ‘pad cultures’; and (5) impacts of continence care.
Theme 1: continence as a significant visible and public phenomenon
Each of these wards and units possesses its own distinct and competing patterns and rhythms, that is the timetables of the wards. Despite organisational and environmental variants in tasks, across wards, the timetable dominates. This includes, but is by no means limited to, medication, diabetes checks (‘BMs’), personal care, changing sheets, toileting rounds, observation rounds, mealtimes, refreshing water jugs, the hot drinks round and the almost always hand-written recording practices that precede and follow each and every task.
Each team, care assistant, nurse and ward doctor, plus all the specialist and auxiliary teams external to the ward but temporarily present on them, has its own, often conflicting, timetable. This, in turn, powerfully shapes the timetables of the other groups in the ward, setting expectations and targets (e.g. personal care and bed-making must happen before the arrival of the breakfast trolley, meals must be cleared away before the medical rounds and care packages must be in place before the discharge team clock off).
These timetables dominated the ward and over-rode individual patterns of daily life, having a huge impact on continence care. For example, there was no room or opportunity for individual continence plans,142 which are known to be crucial to high-quality continence care in other care settings. These timetables reduced opportunities for individual ward staff to recognise the needs of the individual patient. Individual agency concerning waking up, getting dressed and, central to this study, going to the toilet were instead timetabled, reduced and limited to ‘toileting rounds’ and ‘pad rounds’.
Continence care was essential and very visible care in these acute wards. We found that continence care was a significant feature of the everyday routines of care, representing a considerable workload and being reflected in the pace of care work. In addition, continence care was evident in the soundscape and odour pervading these wards. The ‘privacy curtain’ (i.e. the partition to protect dignity and to allow a modicum of privacy between bedsides in these semipublic settings) did little to disguise the sounds and smells of ‘toileting’ as the everyday organisation and fast-paced delivery of other everyday ward routines (e.g. afternoon tea, bedside deliveries from the hot drinks trolley and lunchtime delivery of hot meals) continued and overlapped at close quarters:
The mealtime assistant has a tray to take into side room 1. She sees the door is closed and looks through the privacy window. It has a switch to change from opaque to clear and she decides to go in. She opens the door and reels back physically at the stench and exclaims. She then quickly composes herself and staying well away from the door looking in, cheerily shouts though the door to the person [recorded in notes as living with dementia] ‘Dinner! Beef curry!’
The medical team are cleaning their hands in the sink so she cannot get into the room yet. They leave and she goes in and puts it down in front of him on the bedside trolley [ . . . ] The medical team leave side room 1 and a nurse heads to the room with deodorising spray and sprays it liberally at the door and adds some more to the air around them as they walk away. The team of three medics and two nurses talking together at the nurses’ station, and all laugh as this nurse [with the room spray] says to [sister in charge] ‘Did [side room 1] open his bowels?’ They all snigger. ‘Oh my God, let’s say yes he certainly did! Don’t give him any more [laxative]. They all smile and laugh together as they head down the corridor together to the nurses’ station.
Site F, ward 12, day 2
Acute wards all had a distinct institutional smell, a cocktail of disinfectant mixed with cooked food slowly congealing on plates at the bedside. There was a general odour of bodies, mingled with something less pleasant, including smells of infection, the whiff of acetone mixed with an underlying cloying sweetness with hints of compost, the odour of concentrated urine, faeces and diarrhoea coming in waves from behind curtains, through closed doors and lingering at the entrances of vacated toilets. These toilets, often designed so that doors remain wide open when not in use, and the (typically) closed sluice room, produce strong smells of bodily waste mingled with disinfectant, which filled these overheated wards in regular and often overpowering waves throughout shifts. In addition, the wards wee subjected to the near-constant sounds of urgent care needs, the personal bedside alarms, unspecified cries and calls of ‘help’ for urgent care. Although one may assume that in a hospital setting these calls would relate to clinical or medical need, in these acute wards we found they overwhelmingly indicated the need for urgent continence support. Similarly, although we expected that the practice of drawing privacy screens and curtains would be primarily for medical consultations, examinations and procedures, for PLWD, the practice of screening beds was predominantly for intimate care and continence care. Although continence care may be concealed, the audio and visual cues of its practice are constant:
Bay A has a metal trolley parked outside of it. The bottom layer is stacked with folded clean hospital robes and pyjamas in pink and blue, the middle with towels and bed sheets, while the third holds a grey plastic box containing adult continence sheets and pads. A patient [bed 6] on bay A is taken a commode by a nurse, she is curtained for this, and the nurse talks to her behind the curtain. A health-care assistant walks purposefully down the busy corridor past both stations, with a full bedpan in each hand, literally full to the brim with urine, and walks around and sweeps past several staff on the way to the sluice room for disposal. An auxiliary returns to the ward carrying a very large cardboard box full of flat topped bedpans, which he takes past bays A–C to the store room.
Site F, ward 12, day 3
Continence care is an ever-present aspect of the routine activities undertaken by ward staff. It is a particular focus in the everyday care work of HCAs, but is also significant within the routines of nursing in these observed wards. In contrast, it was notably absent from the routines of the medical teams, even when it was associated with a patient’s admitting condition. Although small specialist continence teams worked at each of the sites observed, their caseloads included both inpatient and outpatient referrals in these hospital settings and, therefore, their presence on these wards was unusual.
Health-care assistants and nurses moved between bedsides, bays and sluice rooms, often crossing considerable distances in these wards, balancing full ‘pans’ containing urine and faecal matter to the sluice room for disposal. Each ward has a sluice room or ‘dirty utility’ dedicated to the disposal of human waste and the disposal or disinfection of associated equipment. This includes used disposables, such as incontinence pads, and reusable products, such as bedpans, which are cleaned and disinfected. Attempts to conceal bedside continence work behind privacy curtains and closed (and partly closed) doors were matched by the ritual practices of attempting to hide waste by covering bedpans and commodes for this journey to disposal. This was always a makeshift affair (typically covered with paper towels or with repurposed disposable plastic aprons) because concealment of waste on the journey to the sluice was not built into the design of the continence products used in these wards:
An HCA walks by me in the corridor on the way to the sluice room with a very full bedpan (it is clearly heavy, and she is focused on keeping it steady without spilling), the contents barely covered over by toilet roll. ‘Afternoon!’ she says, stopping to greet me. We chat briefly about the shift.
Site F, ward 12, day 17
The activity of these wards was punctuated with the coming and going of staff with distinct and recognisable continence equipment [e.g. bedpans (‘pans’), ‘bottles’, wipes, pads and larger equipment, such as commodes, ‘Stedys’ and hoists] to be used at the bedside or to support and/or transport patients to and from the toilets. The toilet doors are equally visible, labelled with brightly coloured signage and symbols, situated in the bays, the rooms and along the corridors of these wards. Nurses and HCAs (and sometimes the nurse in charge of these wards, particularly at the start of the day shifts) dragged bulky bags out of the bays and along the corridors for disposal and collection by other hospital services. These bags contained wet and soiled sheets and institutional clothing (e.g. gowns and pyjamas) stuffed into the semi-opaque coloured bags (an NHS colour-coding scheme indicates the location of contents and their disposal). These activities were a key feature of the routine and repetitive care work of these wards. Although this was typically viewed and described by ward staff as ‘heavy’ work carried out early in the morning or at specific points in the timetable of care work, in reality this continued throughout shifts:
On C bay the senior nurse is working as a ‘double’ with an HCA and they are with the woman in bed 2. ‘Can you turn over to me?’, the nurse asks. The HCA adds ‘You are too fast for us you are, at my age you need to take things easier, there we are, that’s better’. A groan can be heard from the patient as they do this, ‘It’s OK, it’s OK, we are going to sit you back up now’. They have changed her pad and this has included changing her gown and bed sheets. Throughout, they describe what they are doing and provide lots of reassurance. The HCA comes out from behind the curtain with a semi-opaque red plastic sack full of dirty linen, returning a minute later with arms full of clean linen, asking her, ‘Do you want a blanket as well?’
Site F, ward 12, day 16
The everyday and mundane aspects of this ongoing work in these wards could also be observed in the public nature of the, often loud, discussions surrounding it between individual staff and patients, and within and across bay teams. Staff often used a raised and slower ‘institutional’ tone of voice to talk to PLWD and shouted for help or with instructions to colleagues across bays:
In side room 23 the nurse in charge is talking to her patient, the conversation audible down the corridor: ‘did you go for a poo? Oh, you’ve got a pad on, did you do it on the bed? Lift your bum up for me’. RN2 [registered nurse] passes the room, so the nurse shouts for her to come in and help. As the nurse goes in she is instructed ‘Whole change, everything, pyjamas, pads, sheets’, suggesting the pad, or the failure of it, has created a lot of work (two nurses for approximately 10 minutes).
Site H, ward 16, day 22 (bold text represents shouting)
Importantly, here we can see that the nurse in charge of the ward shapes the continence care culture in this ward. In this instance, the nurse leads this ward by example and is actively supporting her team and contributing to bedside continence care; however, she is also demonstrating to staff in the ward the status of continence care (potentially as a form of interruption), how to talk to patients living with dementia (in a loud institutional tone of voice) and how continence care can be (re)prioritised when undertaken by a senior member of the ward team.
Visibility of continence care in the ward
The visibility and centrality of continence care can also be seen in the large number of toilets and signage, and the volume of everyday equipment, artefacts and continence products in these wards. The visible signs could be found everywhere across these wards, forming part of the detritus of medical records, bedside files, documents and forms across observation stations, and at patient bedsides on the mobile tray tables, often next to water jugs and trays of food. For example, urine ‘bottles’ could be seen everywhere (particularly in assessment units across these sites) and were typically left on tray tables or stacked on bedside cabinets waiting for personal use (with male patients frequently using bottles openly on the bay, under bed sheets or sitting or standing at the bedside):
I notice some male patients on bay B have cardboard ‘bottles’ next to the water bottles on their tray tables. They are clean and unused, but are striking next to food and drink. Most of the tray tables are stationed at the foot of the bed, so only accessible by the patient leaving the bed or by requesting it.
Site F, ward, 11, day 2
The sheer volume of continence products required in each ward made their visibility, to some extent, inevitable, but also meant that they became ubiquitous and taken for granted. Boxes of disposable continence products, labelled with both generic and recognised brand names, were evident in store and supply rooms, but also stacked in corridors, at each nursing station (the main station, but also the satellite small desks stationed at each bay) and on the mobile equipment trolleys attached to each of the bays:
There are two cupboards opposite bay C, one labelled as a store room, the other just with a number. Both are stacked full with continence products, including pads of all sizes, flat sheets, packs of wipes and catheter tubes, all sealed in white plastic packaging. Along this corridor there are also numerous toilets and bathrooms, some a single toilet or a disabled access toilet, with other doors propped open to multiple cubicles including showers, baths, sinks, and more toilets. Each toilet is clearly labelled, but there is no consistency to the signage used.
Site F, ward 11, day 2
Commodes and hoists stand in alcoves in the brief intervals between their frequent usage. There were usually a number of commodes (typically two or three that had to be shared across all of the bays and single rooms) and one hoist per ward, although there was some variation in the numbers of beds and the admissions, and the expected dependency of admitted patients. Therefore, equipment was typically in high demand, particularly at busy points in the shift, such as the morning, afternoon and evening routines of personal care and toileting, when continence care was part of bedside care timetabled across these wards, and when urgent continence needs were high for patients. Of note is the fact that during the periods of observation, there were shifts when all these wards were described as close to ‘running out’ of pads, reflecting the high usage of continence disposables and equipment in the care of PLWD in these wards:
17.10 Beep! [personal bedside alarm] coming from somewhere in bay 3. The person in bed 18 is back in bed again. 17 is still behind curtains, a mobile phone is ringing, possibly one of 15’s visitors. Senior member of the medical team, pharmacist, and the nurse in charge of the ward, are discussing the patient in bed 17. They are standing apart with the nurses’ station and a computer trolley between them. The doctor states that the person in bed 17 have got through three pads and filled two colostomy bags, the Sister is recording all this at the computer.
Site H, ward 16, day 28
There is, of course, some variation across the male and female bays. Continence technologies in the form of urine ‘bottles’ (i.e. a cardboard, sometimes plastic, curved tube) were highly visible and accessible in men’s bays. In female bays, the artefacts of continence care were less immediately visible at the bedside. Here, ‘pans’ to be used in bed, or commodes (i.e. a portable toilet on wheels that looks like a wheelchair and has a lid that can be removed to reveal a removable pan that needs to be emptied after each use) for use at the bedside, were the most common form of continence technology. Both ‘pans’ and commodes had to be requested (or prompted), brought onto the bay and taken to the bedside by staff to be used behind the curtain. The commode was also used as a mobility aid to transport the person to the nearest toilet. Therefore, to obtain, use and dispose of these methods required support from ward staff.
Continence must be observed and recorded
Continence is tacitly acknowledged as a bodily process that happens out of sight of others, an expectation in line with the emphasis placed on the dignity and privacy of patients found in the institutional policies governing these wards. However, this was rarely possible for PLWD (and older people) in these semipublic hospital spaces. Privacy was also over-ridden by the recording practices and required documentation of the wards (i.e. what, when, how often and what individuals have or have not ‘passed’), which must be viewed, assessed, described and recorded in patient notes. As a result, continence discussions and its assessment occurred openly in these wards and bays by ward teams across the semipublic ward spaces. We found that these assessments and the associated documentation appeared to be routinely applied during the care of PLWD (and older patients) compared with other patient groups (i.e. the very small number of working-age people in some of these wards). It was not uncommon for staff to publicly discuss a patient’s continence or the organisation of their continence care in hearing range of others, at the foot of beds, in the middle of bays or in the corridors that line each ward:
The handover sheet states the man in bed 19 has dementia, although there are no specifications of what type of dementia; the man in bed 22 has Alzheimer’s and ‘confusion’. It’s interesting that they have both been to the toilet today independently, while there was nobody on the bay to observe them doing it: it feels like together they are cheating the system, working in silent collaboration. The HCA is now helping the man in bed 22 to walk to the toilet. She seems very worried he will fall, so she gets him a walking frame to use and guides him in with an arm on his back and stays inside the toilet with him (even though he can walk there by himself when the nurse is not there). The man in bed 19 is now asleep on his bed. The HCA then comes off the bay and has a loud conversation with the nurse about his toilet trip: ‘Did he pass urine?’ ‘No, but he opened his bowels a little bit, at least I think that was his’. They discuss that they don’t know if anyone went to the toilet before him, so it could have been left in the toilet by someone else. I tell him that this man [bed 22] had walked to the toilet recently, assisted by the man in bed 19 who went after him. They were completely unaware of this and seem genuinely surprised that these patients, or indeed any patient in this bay, would go to the toilet without them.
Site H, ward 15, day 23
The visible, public and recorded nature of continence care was observable in other aspects of everyday hospital practices. As we can see from the example above, privacy was not, typically, considered by staff to be possible for PLWD, with their use of the toilets closely monitored. It was common practice for staff to stay in the bathroom or behind the curtain while a person living with dementia was using a toilet (or commode at the bedside). Toilet doors were commonly kept ajar or closed but unlocked and staff would stay present either inside with the person or just outside the door. This was also associated with managing risk and the fear of falls among staff, as this HCA explains to me, ‘[t]hey fall when you are not watching’:
The woman in bed 7 gets up and out of bed and tidies round her bedside picking up bits of paper from the floor. She is wearing a hospital gown and her large wrap-around pad is very visible. She suddenly holds onto her crotch, heads into the bathroom, and locks the door. The HCA comments to me, ‘She is very secretive she doesn’t like anyone looking at her bits and pieces’. She then tells me about another patient she has cared for, ‘A lovely lady, very independent, she wouldn’t let anyone look at her downstairs at all. I will leave her in there for a bit and then use the scissors to turn the lock (from the outside) and just check on her. I will just have a quick look’. The HCA uses scissors to open the lock and opens the door, the woman is standing at the door and she closes it and locks it, leaving the HCA outside. The HCA turns to me, ‘It’s not nice, but they fall when you are not watching!’
Site H, ward 16, day 14
This could lead to close monitoring and control of the person living with dementia. Here, the nurse supporting this man not only goes into the bathroom, but also repeatedly gives him instructions on how to use the bathroom (i.e. to sit rather than stand to urinate):
When the man in bed 19 wakes up, she brings him a frame so he can walk to the toilet. When she gets the frame to his bed, he immediately demands a cup of tea. ‘OK’, she says, ‘You were asleep till a minute ago!’ He responds, ‘Now what, I was getting up’. He seems quite irritated. He walks to the toilet using the frame, mentioning that his trousers are loose (hospital issue pyjamas that are far too big for him). He complains that the toilet light keeps getting left on but should be turned off when not in use. The nurse goes in with him and asks him to sit down to go to the toilet. This irritates him - ‘I’m standing up to do a jimmy riddle!’ he shouts, refusing to sit down. She explains that he keeps getting his trousers wet when he stands up, repeating this three or four times, standing in the doorway to the toilet, holding the door open. He refuses to sit down, so eventually she leaves and lets him do it as he wants.
Site H, ward 1,6 day 17 (bold text represents shouting)
Here, the close shadowing and instructions to wash her hands by this one-to-one carer clearly irritates this person living with dementia:
The one-to-one carer follows the woman in bed 4 into the bathroom, she is standing very close behind her, but they are very friendly and relaxed and both smiling as they walk through the bay. This woman has a diagnosis of dementia and the team tell me she also ‘has a touch of delirium’. She says firmly, ‘Don’t come in, I want to pee in peace!’ The one-to-one carer stops and they laugh together as she waits outside. As she comes out the one-to-one carer says, ‘Have you washed your hands?’ ‘Yes! I am not stupid!’
Site G, ward 14, day 29
Shouting instructions through doors and into bathrooms was an established practice, occurring frequently during shifts in these wards. The fact that these practices would draw public attention to a patient’s private continence and capabilities was neither recognised nor considered. Here, the team support this woman into the bathroom and check on her progress. Note that, although she is capable of reaching the bathroom using a walking frame (and this was a regular occurrence during this shift), the team use a wheelchair to return her to the bedside. This has consequences for the person (see Theme 5: impacts of continence care and ‘pad cultures’ on recognition of the person and understandings of dementia). Although using the frame was viewed as quicker and more efficient by the team (i.e. increasing the speed of continence care was often an explicit priority in staff discussions, informing the organisation of continence care and the rationales for their use of ‘Stedys’ and wheelchairs to transfer PLWD to or from the bathroom), this could deny patients opportunities for independence and lead to deconditioning:
17.00: The registered nurse from bay A is helping the patient from bed 5 walk to the toilet. She is wearing a pink dressing gown over her nightie, with blue slippers on her feet, and walking with support from a walking frame. She has two visitors (her sons) who move to the corridor to give her some privacy, where they stand talking to each other. She is walking very slowly with the frame, with the nurse now supporting her, leaning forward, and appears to be in danger of going over the frame without support. The HCA joins them, walking along with her, then helping her into the toilet once they reach it. ‘I got you’, prompts the HCA. Both the nurse and the HCA go into the toilet with her, before leaving with the frame. Opposite the toilet the nurse from Bay B is helping a patient from Bay C to the shower, pushing this patient’s i.v. [intravenous] drip along with her. After 5 minutes pass, the HCA knocks on the toilet door ‘Have we finished?’ then goes back into the toilet (the door was closed but not locked), taking a wheelchair in for her, wheeling her back rather than using the frame again. Getting 5 back to her bed is much quicker in the wheelchair. She smiles when she sees her visitors standing in the corridor.
Site F, ward 12, day 9
This was a common feature of continence care in these wards, that is patient privacy was over-ridden by the expectation of close observation and instructions, recording and, often loud, public discussion. Discussing a patient’s continence was an everyday assessment made by ward staff. However, although we were not able to follow family discussions with the ward and medical teams elsewhere, we very rarely observed individual patients living with dementia involved in discussions about their continence care or preferences.
Theme 2: continence communication – silence, codes and the contracted language of continence care
Despite its apparent centrality in the everyday work of these wards, a fundamental way in which continence care for PLWD (and older patients) remained silenced, appearing almost unmentionable in these acute wards, was via the strategies of communication and language used. The naming of or failure to name body parts, in particular genitalia, bodily functions, urine and faecal matter; the naming and description of continence technology; and the language and etiquette of communicating continence needs during personal care for PLWD (and older patients more widely) were all notable. Some aspects of continence care were never discussed or discussed by using humour only, whereas other aspects were talked around or euphemisms were used. At the other extreme, particularly in discussions of clinical processes and technologies, coded institutional language was used, with the assumption made that everyone in these wards shared these understandings.
Although strategies of communication and language used were most notable during care at the bedside, this extended to include staff discussions of continence, for example in clinical meetings and team handovers, where body parts and genitalia were rarely named and euphemisms and infantile and informal language to describe continence predominated. The routine addition of humour and laughter that supplemented or emerged around discussions of continence also highlighted the discomfort of this topic, particularly during clinical discussions and team meetings. Descriptions of continence care often emphasised the impacts on staff and their intractable workloads, as can be seen in a handover meeting in a small cramped nursing office:
Night shift handover nurse: ‘I’ve dressed that (worried about the potential for a pressure ulcer and prevention), it’s intact [good] I put a convi [a urinary sheath] on as well’.
‘Last night he was soaking as well’ – the nurse demonstrates by putting her hands to her crotch, ‘So yes a convi is great’.
They discuss the woman living with dementia in the side room (SR7): she dressed herself and washed herself – ‘Can [discharge co-ordinator] confirm where she is going? We thought she was awaiting a package of care but she says she is going to live with her son, so she doesn’t need it’.
‘She does have a supportive son’.
They move on to discuss the man living with dementia in the next side room (SR8): ‘Doubly incontinent, he was in a mess’.
The day shift discuss that they are doing discharge planning with him [. . .]
They get to the man living with dementia in bay C (C2): ‘Loads better’.
A nurse on the day shift, ‘YESSS!’ She punches the air.
Night shift handover nurse: ‘He is piddling every hour in the night’.
They all chime in: ‘Lush man’ . . . ‘Beautiful’, ‘I know I love him’ [ . . . ]
They then move on to the man a few beds along (C4).
Night shift handover nurse: ‘He is 60 but looks 40’.
Nurse: ‘I know!’
Nurse in charge of the day shift: ‘He’s fine. He had a recent diagnosis of UTI, he’s a bit pussy around his catheter’.
Then to the nurse in charge of that bay: ‘Take a sample – he can do it, you don’t need to go down there!’
They all laugh.
Site F, ward 12, day 7 (bold text represents shouting)
Of note is how, at all sites, discussions of continence among staff typically focused on describing the levels of matter (e.g. ‘mess’) and wetness (e.g. ‘she’s wringing wet’ and ‘you are all wet’) of the person. In this discussion, there is celebration of a patient’s improved condition, and reluctance to carry out intimate care and contact with a man (without a diagnosis of dementia, but with a potential cognitive impairment diagnosis) who appears to the team to be much younger than his chronological age.
Silence at the bedside
It is important to note that continence care at the bedside was also often carried out in complete silence. This approach was routinely observed during the care of PLWD, particularly those who had difficulties in communicating verbally. Therefore, although staff would routinely announce what care was going to happen when they arrived at the bedside, the many procedures involved in carrying out intimate continence care on the body of the person often continued without explanations of what was happening to them, and seemed to assume tacit understanding and consent. Here, the team carry out intimate continence care in silence:
The patient in bed 18, who is living with dementia, is beginning to moan louder than previously. The team with her are giving no instructions, and are not talking through step by step what they are doing, in contrast to the other patients in this bay (they have been going round the bay in order from bed 13). They are just acting on her body, completing necessary tasks without talking to the patient. Her moans get louder and longer, but the work continues, with everything done in 5 minutes. The curtains are opened, and she is now lying flat on her bed, as if asleep. Her head is resting on the pillow. I think she is still awake, but her eyes are tightly closed, as if hiding. Her tray table is no longer over the bed and has been moved to the side, now out of her reach.
Site H, ward 16, day 23
This above exchange is additionally complicated for this patient because the absence of communication from the team also signalled a requirement (i.e. a taken-for-granted expectation) that this work must continue and involved the delivery of essential care. However, this approach was also problematic for PLWD and, as we can see in the tightly closed eyes of this person following the care, could lead to significant distress.
The language of continence care
The language used by ward staff to describe body parts, particularly during the delivery of intimate and personal care, was striking. The anatomical terms for genitalia appeared unmentionable and were rarely, if ever, used in these wards in discussion with patients, especially with PLWD (although this extended to other older people) and family visitors. Euphemisms would commonly be used for male genitalia in the discussions between staff and with patients during bedside continence care, and these were always juvenile in nature (e.g. ‘todgers’, ‘johnsons’ and ‘willies’), with expletive forms never used. Female genitalia were never named anatomically, always talked around and only euphemistically referred to (e.g. ‘your bits’, ‘bottom parts’, ‘lady parts’ and ‘bits and pieces’) or simply not referred to. The word ‘vagina’ was heard spoken by ward staff to a patient living with dementia only once during continence care over the 180 days of observation. More widely in these wards, ‘down below’ (or versions of this, e.g. ‘downstairs’) was the phrase most commonly used during the care of both women and men to describe and communicate intimate continence or personal care that was about to happen or was happening to the person. During timetabled personal care (which often included continence care) it was common for staff to describe (to each other and to patients) the routine of ‘give them a good wash down below’ or ‘we need to look downstairs to check if you are wet’, with the goal of such personal care explained as getting the person ‘nice and fresh’ and of ‘freshening up’ the person.
Continence care was often part of the wider personal and intimate care routines of washing the person, with a restricted range of language used to explain to PLWD what this entailed. Here, the team carrying out continence care as part of personal care describe to the person their goal of a ‘little freshen up’, with their notification to him that intimate care was about to take place described as ‘a little wash down below’. In addition, although the team talk about his continence, they do not involve him in these discussions and ignore his clear ‘no’ in response to being asked if he is ‘enjoying’ this:
The man in the side room (SR3) is a tiny extremely thin man with very thinning grey hair, he appears quite frail and has no front teeth, which makes him seem even more fragile (I wonder where his false teeth are as these can often go missing in the wards). The team (two HCAs) are working as a ‘double’ carrying out routine personal care at the bedsides and have now reached his side room. One HCA does all the talking although they are clearly doing all the work together:
‘Morning [they use his first name], did you sleep OK? You in a bit of a shape there!’ (He has been lying in what looks like a very uncomfortable angle in the bed with the sheets fairly tangled.) ‘Sore?’
He replies: ‘Yes’.
HCA: ‘You came in for a PEG [percutaneous endoscopic gastrostomy, an endoscopic medical procedure in which a tube is passed into a patient’s stomach through the abdominal wall, usually to provide nutrition when oral intake is not possible or adequate], can I see your tummy? You’re in a right little shape there! Can I have this arm my sweetheart? Work with us’.
They laugh together as they are taking his pyjama top off: ‘Ready one, two, three. Yes, there we go [they use his first name], getting somewhere . . . It’s warm in here! Watch your arm’.
‘It’s OK [they use his first name], relax my sweetheart I am going to give you a little freshen up’. She uses a wipe to wipe his face, ‘A bit cold and wet! Alright?’
As they work, the other HCA asks ‘Had he got a catheter?’
The first HCA responds: ‘No but he is doubly incontinent’ (she says this in a low tone) ‘Your wife coming in today?’
Patient: ‘I don’t know’.
‘I bet she is!’
[I can hear that they are pulling the side fasteners on his pad] and they say ‘You are determined to flash us! Are you helping?’
Patient: ‘Yes’.
‘Let’s have a little look at this butt. Lovely job’.
They are now drying him: ‘Are you ticklish on your feet! Are you enjoying that?’
Patient: ‘NO’ [he says this very firmly and clearly].
‘What did I do with that pad?’ She gets it from the chair. ‘Now a little wash down below’.
Site F, ward 12, day 7 (bold text represents shouting)
It is important to note that during the removal and replacement of clothes and pads, this man who is living with dementia is also described as ‘determined to flash’ them, suggesting that these ward staff are experiencing significant discomfort during this process, with this signalling that some intimate care was being viewed or experienced as potentially transgressive.
The language used by ward staff to describe continence care was often highly coded, with a taken-for-granted expectation that patients (and their families) already had a working understanding of and familiarity with ward practices and the everyday clinical jargon used within it. This was particularly problematic for PLWD (and older people), who often did not appear to recognise these terms, the technologies, such as the ‘bottles’ and ‘pans’, they were offered, or what the ‘pads’ (and catheters) attached to their bodies were or why they were wearing them.
Here, an everyday example of a HCA talking around continence technologies and care broadly referred to a continence pad as ‘it’, with the nurse using both highly contracted and coded language with this patient. The team become increasingly frustrated when this patient does not appear to recognise or respond to these requests as they try to find language to communicate, which included ‘change(s)’ and repetition of ‘leave it’. In addition, the team move from the word ‘dirty’ to eventually the more medicalised language of ‘opened your bowels’, rather than further explanation of what this care entailed:
The nurse walks down the corridor and comes back minutes later with an armful of packets of wipes. The HCA remains talking to the patient in bed 15. ‘Leave it alone now darling . . . leave it alone . . . leave it alone . . . leave it [pad] alone . . . We are going to change it . . . it’s dirty . . . leave it!’ She keeps repeating this until the nurse returns again, this time with a big yellow bowl full of soapy water. Throughout this, the only communication with this woman is to tell her to ‘leave it’ although not referring directly to her pad, and to warn her that ‘it’ is ‘dirty’. No introductions or explanations. It seems reasonable for this woman to want to remove the pad if it is wet or soiled. The nurse arrives and speaks to her more directly, saying her name five times until she has her attention, ‘We need to change you, you have opened your bowels, let me wash you’. Two minutes later I hear an exaggerated intake of breath and hushed giggles from the team behind the curtain.
Site H, ward 15, day 17
A key feature of the communication from ward staff to PLWD, in an attempt to rationalise the need for intimate continence care (e.g. cleaning the body and changing pads, clothes and sheets), was the emphasis on managing and containing ‘dirty’ (and ‘wet’, as we have seen earlier) bodies, beds and surfaces. The contracted phrase ‘it’s dirty’ was often used by staff and repeated to the person living with dementia during care, particularly when staff appeared anxious to speed up and complete continence care. The anxiety in this team (see above) appeared to increase when the woman tried to remove the continence pad herself, suggesting fear of not containing waste during continence care and the potential for contamination (and the additional personal care required) as an unsettling prospect. When patients appeared to resist this care, the team emphasised the institutional expectations and the fact that neither the patient nor the team had any choice in this, with the phrase ‘we need to change you’, as seen here, commonly used.
Although clinical terms were also used to discuss continence care and bodily processes, such as ‘bowel movements’ and ‘stools’, they were often highly coded, particularly during routine bedside personal and continence care. The terms used were often beyond the comprehension of many patients. These forms of coded language were commonly used when directed towards the technologies of continence care and, in particular, towards the use of continence ‘pads’. Staff would typically announce to the person living with dementia ‘we’re just going to change your pad’ [Site F, ward 12, day 1] before actively beginning to do so, often without context as to what the pad was, its purpose or location on the body. The routines of bedside continence care were typically abbreviated by ward staff to the point of jargon. Staff across these wards would routinely refer to ‘opening’, ‘passing’ or ‘voiding’, a shortening of ‘voiding his/her/your bowels’ or ‘passing [urine]’ in descriptions and instructions during, often fast-paced, bedside continence care. This could be especially problematic for PLWD. Here, two patients living with dementia do not respond when staff repeat these terms at the bedside; however, the team appear to assume that repetition will ensure the person’s recognition and comprehension (or that this is not possible for the person) and move on:
The HCA has taken two bottle bedpans to the man in bed 3. The female member of the medical team asks the HCA for ‘a sample to measure’, and then explains to the patient he is dehydrated so they want to ‘monitor intake’ and ‘how much he passes’, and explains that the consultant will be coming to see him later.
Site F, ward 11, day 17
HCA [A] and [B] are with the person in bed A1, who has a dementia diagnosis. They are doing the timetabled observations at each bedside in turn. ‘Any pain [name]?’ ‘When you went to the toilet [name] did you open your bowels by any chance?’ She repeats this question three times without rephrasing . . . ‘Did you open your bowels? Did you open your bowels? Did you open your bowels?’ A1 doesn’t answer.
Site F, ward 11, day 18
Importantly, as we can see in the example above, verbal responses to this coded language were also often required by ward staff to confirm a patient’s health status (and, in turn, could inform informal assessments of the person’s cognitive capacity). Ward staff typically used contracted speech and repetition of these key phrases to talk around continence, and these approaches indicated (to us, to PLWD and to the wider ward) staff understanding of the condition and that the compulsive repetition or slow annunciation of single words and phrases can aid comprehension. In contrast, our observations indicated that such loud repetition of contracted phrases often appeared to only increase distress in the person living with dementia.
Ward staff regularly used this coded language when communicating with PLWD who, subsequently, were expected to understand this language and to comply with instructions. Such institutional lingo, as characterised by Goffman,76 could be heard along with the host of wider acronyms, job titles, medical jargon and familiar words given new meaning, which all patients, including those living with dementia and their families, were expected to understand without explanation in these wards. More widely, names of areas of the hospital, the processes and procedures that take place within them, and the brand and common names of the equipment and technology used were spoken of without introduction or clear explanation. 124 For PLWD, this language could be particularly problematic, as assessment of their independence and mental acuity was based on their ability to appropriately recognise, respond and reply to unfamiliar jargon around unfamiliar processes.
Communication of continence needs: seeking permission – institutional and embodied forms of communication
A key aspect of the cultures informing continence care in these wards was the explicit requirement that PLWD must communicate and request continence care at the bedside or obtain permission to walk to a toilet, even if they were able to do so independently. However, for this patient group, the communication of an urgent continence care need was often not verbalised (through either difficulties in communication or embarrassment), but rather was embodied and could be identified only in their body language or via changes in their behaviour. It was unusual for staff to recognise or respond to these non-verbal forms of communicating an underlying continence care need.
During everyday care at the bedside, staff repeatedly emphasised to PLWD that they must communicate their care needs, including continence needs, using institutionally mandated forms of communication (e.g. through verbal requests and using the personal call button or ‘buzzer’ to seek help). Staff typically emphasised to all PLWD (and other older people in these wards) the risks of ‘falls’ and ‘falling’, the importance of waiting for assistance and of seeking permission to leave the bedside, even for those who were able to independently walk to and from the bathroom.
The requirement of ‘permissions’
The requirement of permissions was associated with the impacts of the built environment of these wards. Patients in each bay (usually with four to six beds) typically shared a bathroom cubicle that was attached to the bay or close by. There were always a number of additional toilets and bathrooms along the main corridor and throughout the wider ward, which is notable because, although, in principle, they were accessible to all, they were designated for use by the patients in the geographically closest bay (and, in some cases, the nearby side rooms). In addition, visitors and staff were prohibited from using these bathrooms (signs directed visitors towards public toilets outside the wards). This meant that some of these facilities were rarely, if ever, used.
People living with dementia were restricted by ward staff to the use of the specific toilet designated for their bay. These restrictions were typically tacit, although also sometimes clearly expressed by ward staff, who would not routinely support or permit the use of other toilets and bathrooms in these wards. Therefore, if the allocated bay toilet was in use, the person living with dementia would be expected to wait or was unsupported in leaving the bedside until their allocated toilet was vacated, regardless of the many alternatives typically available in the ward. This routine practice was associated with the typically fast pace of work carried out by the bay teams and the observable pressures ward staff experienced to stay in their designated bays (to monitor vulnerable patients). However, this could have a significant impact on PLWD:
With clouds low outside and lights dimmed down, it feels much later in the day than it is. The woman in bed 15 gets up to go to the toilet opposite the foot of her bed. She is younger than the other patients on the bay, but notes record her as having a non-specified cognitive impairment. All of the women on this bay have a record of cognitive impairment, dementia or queried dementia in the handover notes today. A large nappy-style continence pad is clearly visible under her backless hospital gown, despite her now demonstrated ability to get up and move to the toilet as required. The nurse tells her somebody is in the toilet and she responds by rattling the door, but the woman in bed 16 is in there. The nurse leads her off the bay, holding her hand. Rather than returning the patient to her bed the nurse and the patient go for a walk, giving the person in the bathroom time to finish. They go for a short loop of the unit, but do not go into any of the many vacant patient-only toilets they pass on this loop.
Site H, ward 15, day 17
This was also associated with an observable reluctance among PLWD to enter bathrooms independently, acting as if doing so was prohibited. PLWD in these wards appeared to quickly recognise that they were not permitted to act independently without seeking approval, particularly actions that involved leaving the bedside or the use of the bathrooms and toilets outside the immediate area of their bay:
One of the men from bay C is walking to the toilet. He is barefoot and has a small cut above his left eye. He looks in the toilet, but the housekeeper is in there cleaning, so he keeps going, walking towards the showers. The HCA and the housekeeper call him back and tell him it is OK to go in the toilet, which seems to confuse and startle him a bit, and so they again explain to him he is OK to go in. He doesn’t want to go in while the housekeeper is in there, but once she comes out, he is fine. After a few minutes HCA(B) knocks on the door to check that he is alright and reminds him to wash his hands when he is done. A different HCA working on the bay then comes and helps him to walk back to his bedside.
Site F, ward 12, day 13
This culture of permissions was pervasive. Ward teams clearly expected patients to ask to visit a bathroom and reacted in surprise when they found that PLWD had independently walked to the toilet without them, had not used their designated toilet or had used the ‘wrong’ toilet elsewhere in the ward. So engrained was this culture of permissions that unflushed toilets could lead to ward staff calling estates to report a ‘code brown’ (i.e. a blocked toilet), rather than consider if a patient had walked to the toilet without support or had used the ‘wrong’ toilet.
The permissions and privileges granted to PLWD around continence care and independence were closely associated with the cultures and understandings of risk and safety in these wards. A key concern in the care of PLWD was a risk of ‘falls’ during their care and managing and reducing this risk. If witnessed by ward staff, walking in the ward and looking for a bathroom or toilet would often be recognised as a risk and so it was common for ward staff to intercept patients attempting to leave their bedside, ask them to return to the bedside and offer alternatives:
8.30 a.m.: On bay 3 a female patient with a catheter tube visibly hanging between her legs is assisted by a nurse as she walks to the toilet. Minutes later another patient walks back from the toilet. She is walking using a frame, her hospital gown is open at the back, revealing a large nappy-style pad. When this patient is back at her bedside the nurse reminds her to tell her when she needs the toilet, and not to get up, emphasizing that if she does, she will fall. She then repeats this instruction to the neighbouring patient, showing her where the bedside buzzer (personal alarm) is so that she can call her if she is not there. This emphasis seems odd given that this nurse and I have observed both of these women independently get up and go to the toilet and show a clear awareness of their own continence needs.
Site H, ward 15, day 16
Theme 3: rationales of safety, reducing risk and deconditioning
The importance for ward staff of ensuring safety and reducing risk (particularly risk of ‘falls’) is significant. Minimising the risk of ‘falls’ often featured in discussions of continence care for PLWD. In contrast, we observed little discussion with PLWD of the importance of maintaining and increasing their mobility (a HCA in ward G was a notable exception to this) or recognition that keeping a person from leaving the bedside risked rapid deconditioning.
Here, the lead nurse from the night staff reports, during the handover to the day team, that, during the previous night shift, a patient was ‘incontinent in bed’, ‘confused’ and had ‘very loose’ stools. In addition, the lead nurse reported that the patient needed support washing and help to go to the bathroom, and the result was that ‘she went down’. A key emphasis in this description is that this fall was unavoidable:
Yesterday she [bed 3] was incontinent in bed, told [ward team] to monitor, very loose again and again had to shower her during the nights, she is confused. The nurse leading the handover whispers the continence episodes. ‘We helped her to the bathroom in the night, [the HCA] was behind her and I was next to her and she spotted another [walking frame] so left hold of her own [walking frame] and went to grab that one. And she went down, although she didn’t hit her head or anything. The doctor came up and asked why were we pushing fluids (via an IV) [intravenous line], and just to drink, so we pushed fluids that way’.
Site F, ward 12, day 13
During night shifts, when fewer members of staff were on duty, patients often became distressed or were assessed as ‘confused’. Although there were often long periods of ‘quiet’, it was not uncommon for staff to have to respond a number of simultaneous calls for urgent and competing patient continence care needs.
During the day, the ward could be a precarious place for PLWD (or, indeed, any patient with an acute condition) attempting to access the bathrooms, as they often walked more slowly and less confidently than the many staff members (sometimes up to 30) working in and striding through the wards and corridors at the same time. The pace adopted by staff reflected the impacts of the wider institutional cultures that valued speed and efficiency, which were felt powerfully by staff in these wards. Staff rarely paused as they moved around the wards, striding past those walking at a slower pace (i.e. the typically older and unsteady patients), avoiding eye contact and suggesting that these patients were viewed as potential obstacles to their work:
The woman in bed 4/5 is living with dementia and delirium and is walking along the corridor with a one-to-one carer who says ‘This way!’ and guides her back to her bedside. As she walks down the corridor a nurse and the senior registrar stride past her. They do not appear to register her or speak to her as they pass by almost touching, but both seem practiced in avoiding contact, both physical and eye contact, with patients in the corridors and they both walk at the same fast pace. She (4/5) walks past me down the corridor to the end of the ward and reaches the doctors’ office and peers in without entering. She had urinated on the floor in this office yesterday and I wonder if she is considering doing this again; she is looking thoughtful. The one-to-one carer is still shadowing her at a distance as she walks slowly back and says to me as she passes, ‘I am going back to bed’. The one-to-one carer has to take a sharps box 4/5 has picked up from a medication trolley on her on the way back to the bedside.
Site G, ward 14, day 4
However, there were some notable exceptions. For example, a HCA in ward G regularly encouraged mobility and had discussions with PLWD of the importance of maintaining and increasing their mobility. In one ward (site F), a locked general medical ward, staff were generally encouraging and supportive of PLWD (and older patients) walking independently within it. The everyday nature of walking independently within this ward can be seen in this afternoon observation of activity in a corridor, with older people, including those who are also living with dementia, moving freely in the ward to the bathroom and back. It was also notable for the encouragement and prioritisation of older patients walking at their own pace, with staff slowing their pace to support and encourage these older patients:
A woman (90 years old) wearing a long pink dressing gown is using a walking frame to go to the bathroom across the corridor and back. She does this slowly but steadily. As she walks, she is crossing a really busy part of the ward with lots of staff, opposite the nurses’ station. As a couple of staff pass her by, they do not rush past her, but slow down and give her plenty of space. Then one stops, smiles at her, and says ‘After you, my dear, are you OK?’
A man walks briskly from the bedside and across the corridor to the bathroom. He is a grey-haired older man in navy and red polka dots silk pyjamas using a walking frame in front of him with arms stiffly outstretched and locked. He marches swiftly across to the bathroom, his head down, a little later he marches back from the bathroom with the same stiff gait.
The woman from bed 23 walks slowly to the bathroom and back. She is wearing a large and extremely fluffy dressing gown with a patterns of large cartoon flowers all over it.
The woman from the next bay (22/3) is using her frame to walk to the bathroom. It is a very smart one that has been brought from home, with large wheels and brakes. She has short grey hair and is wearing a jumper and smart stay-pressed trousers and slippers. One of the nurses working in a different part of the ward goes over to her and reassures her, ‘You are doing really well’. I have not seen staff stop to recognise and encourage an older person walking in these wards before.
Site F, ward 12, day 26
The recognition of the person living with dementia (who was not ‘their’ patient) and the encouragement and support of this person’s steps in regaining independence was unusual and so notable that it is recorded in the fieldnotes as the first time this had been observed (despite many months of observations across other wards and sites for this study and other observational studies in wards this team member (KF) has been involved in. This incident also informed a follow-up discussion with the nurse in charge of this ward. The nurse believed that this was a recent change, possible only once the ward changed to a locked ward, which they had to ‘fight’ for, reporting that, previously, they had been constantly worried about ‘falls’ and patients ‘absconding’. The use of a locked door (with keypad access with the code 1-1-1-1) was credited with changing the atmosphere and to a more relaxed approach to PLWD walking in this ward. This was not the only locked ward in the study. Of note, however, was the different pace of work and bedside care in this ward, which was generally far slower and with a more relaxed tempo than the other wards.
Institutional forms of communication prioritised
We found that, for PLWD to successfully communicate an immediate and urgent continence care need that resulted in staff interrupting their timetabled care routines to attend to them, they needed to clearly articulate their request verbally or use the bedside personal call button. In the example below, this patient was able to verbally communicate their continence needs clearly and, in response, the HCA immediately interrupts timetabled care at another bedside to support her. Of note is that this woman is continent and independently mobile, but she is still helped to the bathroom and has a continence pad as routine. It is the removal and replacement of the continence pad that this woman needs support with, as she is able to walk to and from the bathroom independently:
For the first time in some time, I hear a clear request of ‘Help me’, coming from one of the side rooms. An HCA goes straight to this and assists the woman in question to walk to the disabled toilet opposite bay B. She goes in with her and closes the door, although their discussion is clearly audible from the corridor: ‘I’ll get you a clean pad, you just sit down there’. She returns to the corridor, gets a pad from the store room, and returns to the toilet with a pad, ‘Let’s get you up, let’s get this pulled up . . . ready now, let’s go back and have a wash’. The woman does not audibly respond but appears to follow the HCA’s instructions. They come out of the toilet and walk back down the corridor holding hands. The patient’s hospital gown is tied tightly all along the back hiding the continence pad from view.
Site F, ward 11, day 12
Many PLWD admitted to these wards, like the woman above, could clearly articulate their urgent continence needs. However, for others, verbal communication was not easy and was often restricted by their condition or by the quick responses of staff, which over-rode the person’s ability or opportunity to communicate themselves. In addition, although staff quickly responded to bedside alarms or ‘buzzers’, many PLWD found these difficult to access and use:
The woman in bed 15 is sitting up in her bedside chair aided by the physiotherapist who stops to explain the personal bedside alarm. The physiotherapist explains how it works then tests her comprehension. However, this woman appears to have no recollection when questioned about this button’s purpose or how to use it. The physiotherapist then puts it on the tray table in front of her and explains again, but when she repeats the test, this patient seems to become more confused. The physiotherapist then changes the subject, asking her if she wants to stay in the chair or get into bed. She responds that she would like to stay in the chair, then lifts up the button from her tray table to examine and asks the physiotherapist what it is for. After the physiotherapist leaves, this patient asks the HCA what the button in her hand is for.
Site H, ward 16, day 25
We found that, as researchers who were visible in these wards and, typically, in the corridor outside these bays, we (KF and AN) were regularly called over by PLWD (and older patients) to their bedside and asked for continence care and support. For example, PLWD would say to us ‘I want to wee’, would ask for support at the bedside (e.g. ‘Can you bring me a commode?’) or would request help to walk to the bathroom (e.g. ‘Can you help me get to the bathroom?’). These requests were typically made using more informal language (‘wee’ and ‘tinkle’) in hushed tones, but also contained a clear sense of urgency for the person. Here, two women on a ward for care of the elderly with cognitive impairment ask the ward team to call the researcher (KF) over to their bedsides. They have been admitted for a number of days and so we have spent quite a bit of time talking together during periods of observations. Of note is the fact that they bypass the ward team and ask the researcher (viewed quite reasonably as a ‘nurse’, despite being dressed in civilian clothing) for support:
5 p.m.: The HCA comes over, ‘The ladies are asking for you!’.
It is the ladies in beds 2 and 3 in this six-bedded bay and I head over and they both start talking to me at once. The woman in bed 2 is sitting up in bed. Her grey hair looks dishevelled and she has a cut on her lip (from her ‘fall’) and is wearing a pink hospital gown. She looks quite neatly tucked in the bed. The trolley next to her is very tidy and has a sip cup and water jug, a portion of cake and a packet of custard creams sealed in their wrappers laid out on it.
The woman in bed 3 is sitting in the chair, a tiny figure in a pink hospital gown and red hospital socks, a blue hospital blanket around her shoulders and an i.v. [intravenous] port in one arm leading to a mobile drip. The trolley is placed low in front of her and she has a glass of water and a water jug in front of her. They both talk quickly and at once.
The woman in bed 2 tells me ‘I’m not supposed to be here’. She giggles and shrugs nervously, ‘Something happened, I am not supposed to be there, I feel awful, embarrassed! I’m taking up space, taking up a bed meant for someone else, my husband is in [a small market town, south of the city], he won’t know where I am. I just came here as a visitor, I am not supposed to be here, something happened but I don’t know what’.
I listen to her and reassure her as best I can and tell her I will let the team know that she needs to contact her husband (I do that later).
At the same time the woman in bed 3 asks me, ‘Can you help me please, I want to wee, where is the commode can you help me nurse, I want the commode, where is it?’ I go to the team and they go to fetch the commode and wheel it to her bedside and close the curtain. I feel a certain discomfort that I seem to be the person these ladies feel they can speak to, bypassing the team.
Site G, ward 14, day 25
The woman in bay D (D1) opposite the nurses’ station, is a tiny woman with a silver–grey bob and had been described as ‘lush’ by the team in the morning handover. She is wearing blood-stained hospital issue pyjamas and is using a walking frame to leave the bedside and slowly making her way across the bay. In one of her hands she is clasping the walking frame, but also an extremely large wrap-around continence pad. She reaches the doorway and looks around. I smile at her and she beckons me over. She explains that she needs a pad and shows me what she has in her hand and explains that it is far too big. ‘Are you a doctor? Sorry?’
I explain who I am and that I will go and find someone who can help. I find the HCA in the corridor and explain, and we head to the store room together.
Site F, ward 12, day 5
Throughout the data collection period, we received many requests for continence support, in hushed and urgent tones, from PLWD and older patients. This patient group were not always able to recognise or use the call button, or to use it as instructed, but also faced the difficulties of publicly talking about or requesting continence care. In addition, given the fast pace of work on the wards, these difficulties and their attempts at communicating urgent care needs were often not recognised.
Bodily expressions of continence need
It was often not easy for PLWD to communicate their urgent care needs either verbally or via personal alarms. Instead, the communication or awareness of an urgent and pressing care need was often embodied. These embodied signs could be identified in the person’s body and changes in behaviour, which were typically subtle, at first, but, if unrecognised, often became overt, repetitive and increasingly urgent.
We identified several common patterns of embodied communication, which included touching, adjusting or trying to remove pads and catheters; displaying pads; looking increasingly uncomfortable in bed or in the bedside chair; repetitive drumming of hands or tapping of feet; and repeated attempts to get out of bed or the bedside chair and walk across the bay or into the wider ward. In addition, this could take the form of unarticulated moaning, calling or crying out, which was often prolonged and repetitive. These embodied expressions of underlying care needs were observable in almost every person living with dementia at some stage during their admission. As we could follow ward teams and their PLWD over time, we observed that the embodied expressions of continence needs could be missed or, if recognised, the ward staff did not understand the urgency of these needs when communicated, or they were interpreted as something to which the ward staff felt unable to respond given the expected pace of timetabled care.
Without early and prompt recognition and support, these underlying care needs, often related to pressing and urgent continence needs (i.e. needing the toilet, having a soiled or wet pad or bed), could quickly become more entrenched experiences and overt, audible and visible communication of distress. Yet even this distress could remain unrecognised and, instead, be understood by ward staff as a feature of the person’s dementia and, therefore, considered a behaviour that was without purpose and unremarkable in this setting. Consequently, continence needs remained overlooked.
In the example below, the patient’s embodied communication is neither subtle nor difficult for staff to interpret. The patient demonstrates her urgent continence needs by attempting to urinate on the floor in the ward day room. What is of note is that the nurse’s response to this is not to help the patient to go to the toilet, but, rather, to prevent the transgressive behaviour and exposure that appears to violate the expectations of decorum in these wards and the dignity of the person. As we have discussed, there was a powerful sense in all of these wards that continence care should remain hidden on the person and unseen by others in the wider ward. The immediate response of the ward team was to cover up the patient and return her to the bedside, neglecting the clearly expressed urgent continence need and distress communicated by the patient’s actions:
The patients in bay 7 to 10 all seem to be awake, handover is under way (this started at 7.30 a.m.) following the safety meeting in the seminar room. One person living with dementia (bed 20) is in the day room, accompanied by a nurse, who is now wearing a brown cardigan over her nursing scrubs, ready to go home after the night shift. The patient suddenly hitches up her pink hospital gown and squats to urinate. The nurse reacts by talking her out of what she is doing. The nurse is able to talk her out of going to the toilet on the day room floor, but then walks her directly back to her bed, passing the bay toilet.
Site H, ward 16, day 2
It is important to note that, although this was a less common example, it powerfully demonstrates the ways in which the organisation and delivery of care in these wards meant that staff could often not recognise or respond to the continence needs of their patients, even when they reflected an obvious physical and urgent need. It also reflects ‘pad cultures’ (see Theme 4: ‘pad cultures’ – conflicting urgencies and continence containment): the expectation that patients will use the pads they have been given to wear.
More commonly, PLWD attempting to leave the bed or bedside would be viewed as at risk of a ‘fall’, ‘wandering’ or ‘absconding’ and would be instructed to remain at the beside. PLWD would also typically be reminded of the risks of leaving the bedside. However, leaving the bed was often an unverbalised attempt to reach the bathroom. Here, this woman receiving one-to-one care, typically used for patients seen as ‘at risk’ or a ‘disturbance’ to the working of the ward, is restricted to the bed:
The one-to-one carer with the woman in bed 2/1 sitting opposite her. She is in the bed with the side rails up on the sides and she is slowly trying to place her legs over the rails.
In response the one-to-one carer says, ‘Where are you going? Stay inside please’. Putting her leg back in the bed the one-to-one carer hands her a little triangle of sandwich from the tray table. This woman takes it and throws it at the one-to-one carer, but she doesn’t have much strength and it reaches the end of the bed. She has also now pulled the sheets off. The HCA joins them and tells the one-to-one carer, ‘We have run out of sheets, we need to use the blankets’. They get a blanket and tuck her into the bed.
A little later the woman cries out, ‘I have wet the bed! I forgot!’ She sounds distressed.
The one-to-one carer responds, ‘Do you want to go for a number 2?’
She draws the curtains around the bed.
Site G, ward 14, day 29
Here, as this man walks unsteadily from the bedside, the team unsurprisingly focus on his immediate risk of falling; however, this means that the team do not recognise his need for independence and his underlying continence need. In addition, this is not easy for him to articulate this, and it takes him significant effort to walk independently and to express that he needs ‘a wee’:
A man (bed 15) comes into the corridor wearing hospital pyjamas and red socks, there is orange liquid smeared all over his face and top [orange juice or soup?] and he is walking very unsteadily in the corridor. The senior nurse is following him, ‘Do you want a wash?’ And the HCA with her pulls the visitor seat out into the hall in front of him [they are clearly worried he will fall] and he pushes it away.
He responds: ‘I don’t want any of your help!’
The team try to guide him back to the bay, but he looks at me though the glass and I say ‘Hello’. He walks towards me and the team. She tries to hold him and guide him back. He repeats, ‘I don’t want none of your help!’
I say ‘Hello’, and he is very unsteady and clinging onto the door frame to the day room and says to me, ‘I want to walk by myself’.
I say, ‘Of course, please join me’. He unsteadily and slowly sits down in one of the chairs opposite and I ask him how he is.
He tells me, ‘I would love it if they had asked me!’ He leans over and holds my hand and says, ‘I need a wee’.
I say, ‘I will get the team to help you’. I inform the nurse at the mobile workstation and ask her. She joins him and directs him to the bathroom in the corridor. She tries to hold him, but he pushes her away and gets quite frustrated when the team tries to hold his arm. She asks if he wants his frame. He says no to the frame. As he walks unsteadily, he gets halfway to the bathroom and stops, ‘I am doing it I am weeing’. He stands still. He doesn’t move but looks very alarmed.
He has a large pad on [wrap-around nappy style], which can be seen underneath his pyjamas. She waits, then leads him back to the bed and gets a plastic apron and closes the curtains.
Site H, ward 16, day 1
However, there were also examples of an embodied communication of need being recognised by ward staff. Here, a one-to-one agency HCA is walking with a person living with dementia. As they walk along the ward corridor, the patient holds her sides and fiddles with her waistband and, in response to this, the agency HCA asks whether or not she has a continence need and, instead, she reports pain:
The woman living with dementia (in bed 4/5) is walking along the corridor with a one-to-one carer by her side who says to her ‘This way!’ and guides her back to her bedside. As she moves, she holds onto the sides of her stomach and tells me she is in pain. She fiddles with the waistband and the one-to-one carer asks her if she wants to go to the bathroom, ‘Do you need the toilet?’
‘No!’ she is clearly irritated at being followed by the HCA.
A little later she stands at the medication trolley with the nurse as she does the medication round and says she is in a lot of pain holding her stomach, she does an extremely loud fart, which reverberates across the bay. She turns and points at me and exclaims to the room ‘she did it!’ We look at each other across the bay and laugh together.
Site G, ward 14, day 4 (bold text represents shouting)
In the example below, the HCA responds to a person becoming increasingly uncomfortable in her bed:
The woman in bed 2/6 is in bed, the side rails up.
She is a tiny figure with very white hair, wearing glasses. She is also wearing a cotton nightie covered in pretty blue sprigs of flowers. As she lies there, she starts to look increasingly uncomfortable. The HCA working in the bay sees this and heads over, ‘Are you OK?’
She replies: ‘I need a bedpan’.
The HCA immediately goes off the bay and gets one for her.
Site G, ward 14, day 19
A person living with dementia leaving the bed or bedside was almost always interpreted by ward staff as a risk to be managed. It was rare for staff to consider or investigate potential underlying reasons why a patient was repeatedly trying to climb over the side bars of the bed, trying to get out of the bed or the bedside chair, or pulling off their bed sheets. Instead, the ward team typically focused on the immediate behaviour, with the goal typically being to contain and reposition the patient in the bed or bedside chair. That these movements could (and often did) communicate urgent continence needs was often only recognised following a contracted pattern of staff repeatedly covering and repositioning in the bed, or returning a patient to the bedside or once the person had become incontinent.
Over time, we observed that these patterns repeated within and across these wards. A person living with dementia attempting to get up and stand was often found to be expressing an underlying and, eventually, urgent continence need. If unrecognised, this could transform into more entrenched patterns of conflict between a person and the ward team: the patient becomes distressed as they are constantly prevented from going to the toilet, whereas staff become frustrated by the management of what they perceive as behavioural features of the person’s dementia.
Theme 4: ‘pad cultures’ – conflicting urgencies and continence containment
On wards, ‘pads’ were by far the most common continence product and were widely used in the everyday bedside care of PLWD. In this report, we focus on ‘pads’ because of (1) their key role in continence care and (2) the significance of their use in informing wider ward cultures of care. These cultures were produced and reproduced in the organisation and delivery of everyday continence practices and in the expectations and language of continence care, which had wider impacts, particularly for the recognition and understandings of dementia, the needs of PLWD and opportunities of independence for PLWD in these wards.
What was most notable when first entering these wards was how visible ‘pads’ were, given their invisibility outside the wards and the ways in which these products are publicly marketed to consumers. Although the term ‘pad’ brings to mind the sanitary towel-style pads advertised as ‘discreet’ and ‘invisible’, the ‘pads’ used on these wards were far larger. These pads came in a range of sizes, from those that resembled extremely large sanitary pads (available in small, medium, large and extra-large sizes) to large padded absorbent flat square sheets, which were all used to produce a bulky ‘wrap-around nappy’ style on the person. None resembled the ‘pull-on’ style of continence pants that are available to purchase outside the hospital. In addition, the ‘pads’ did not provide self-sealable strips to aid fitting within underwear and, instead, were typically held in place with thin net or mesh pants.
These ‘pads’ were normal, mundane artefacts to be observed everywhere (e.g. in boxes and bags on the many trolleys in these wards). Mobile trolleys were typically parked in the corridor outside each bay (or just inside in newer builds, which typically had larger bays), standing ready for personal care. These trolleys were always kept stacked with piles of neatly folded laundered linen, sheets, towels and institutional gowns and pyjamas. Among these items, there were always multiple packets of disposable wipes (for use on the body), sachets of cleanser or soap, barrier cream (also sometimes built into the disposable wipes) and disposable water bowls. However, the key item that typically dominated these trolleys were the often precariously stacked piles of boxes and packs of continence pads. These boxes and packs of continence pads were made ready for the pace of use at the bedside, typically ripped open and spilling out of their packaging, or loose, balanced on top of the linen and in plain view to all. These ‘pads’ were also often unpackaged and sitting loose on tabletops at nurses’ stations and on top of files. Given their significance in continence care practices in these wards, the presence and visibility of these products may appear unremarkable and to be expected. However, they were so ubiquitous that they had, to some extent, lost their meaning as a medical device or technology, and were viewed as everyday mundane and familiar objects to be found unpacked and loose, not only on clinical and personal care stations, but left across workstations and bedsides:
The nurse sits at the small nurses’ station at the entrance to bay 3. There is a large pile of plastic folders with the bedside records for the six patients in the bay stacked up in a pile. On top of the pile in a large continence pad (unused) loose and out of its packaging. The nurse lifts it off, takes the first folder and replaced the pad on the files almost as a paper weight. She starts to update the first file.
Site G, ward 14, day 27
Pads could also be viewed when being carried around by ward staff as they moved between beds and bays. In some instances, this appeared to be a signal to others in the wards that continence care was being carried out, particularly when this was being carried out by senior nursing staff in these wards:
The sister in charge of the ward is wheeling a large shiny metal trolley outside of the row of three single-occupancy rooms. On the trolley there are large piles of sheets, blankets, hospital gowns, disposable bowls, large bags of continence pads, rolls of red and orange waste bags, and a large pack of continence pads open and spilling out ready for use. At each door in turn, she takes into the room a large pile of sheets and gowns, with a friendly, ‘Good morning, let me show you what we are doing this morning. Are you ready for a wash?’ She then goes back to the corridor, gets a disposable gown and gloves from the dispensers in the corridor and takes a large folded pad from the packet on the trolley and unfurls it at the doorway. It becomes a large square sheet as she shakes it out, like a large white flag unfurling in the corridor, and then heads back into the room.
Site H, ward 16, day 7
Other continence technologies were, of course, also visible and in constant use. For example, catheter bags were visibly hung from bedsides or from the back of chairs as patients were transported around the hospital and ‘Stedys’ and hoists took up considerable space along ward corridors. However, the sheer volume and visibly of pads was far more prominent. Their consistent use in the care of PLWD in these wards was a stable and unchanging feature of ward life. This suggests that, although pads are typically viewed as an ordinary, unremarkable and ubiquitous feature of both the landscape of these wards and the everyday bedside care work carried out by nurses and HCAs, their use is also of significance for PLWD, ward staff and the cultures of care in these wards.
Pads as standard practice for people living with dementia
Disposable continence products were universally referred to by ward staff as ‘pads’ and discussed with and described to patients in this way. For example, explanations at the beside were typically limited to ‘We just need to check your pad’, ‘We need to change your pad’ and ‘Don’t worry, you’ve got a pad on’. However, what a pad is, what a pad does, how a pad works and if the person had ever worn a pad previously was never explained or discussed with PLWD during our observations.
The standardised strategies of care at the bedside were typically accompanied by standardised and restricted language, which often took the form of incongruous or contracted phrases to describe continence products, care routines and practices. There was an assumption that these phrases would be immediately understood by all in these wards. Here, we can see that these explanations were typically made using contracted language that did not fully describe what was happening or about to happen to the person, and was delivered in a slow, enunciated and loud institutional tone of voice:
A member of staff is walking through the ward waving a continence pad and says out loud to the patient at the bedside, ‘we are just going to put you in a pad’.
Site F, ward 12, day 1 (bold text represents shouting)
The taken-for-granted language in these routine statements, as above, was assumed to be easily recognised and understood by PLWD in these wards. On occasion, there were a small number variants, such as ‘I’m just going to check your pad’ followed by an (often swift) intimate examination:
In side room 5, a patient is lying on their bed. They are quiet but have been awake the entire shift just looking out into the corridor. Two nurses (including the nurse in charge of the ward) put on latex gloves and go into the room. As they do this one says to the other ‘I’ll get a fresh pad [points to a pile on the nearby trolley], there’s some over there’. Having already walked into the room, the nurse in charge announces, ‘Can I come in? Hello, can we change your pad?’ They close the door behind them.
Site H, ward 16, day 23
(There were routine and regular checks to see if continence pads were ‘wet’ or ‘dirty’ and needed changing, using touch to evaluate this, see Theme 4: ‘pad cultures’ – conflicting urgencies and continence containment for details.)
This limited repertoire of phrases and descriptions was used across all these sites, with repetition, increased volume and slow enunciation of the same phrase used in response to a person’s apparent failure to recognise this routine care. In Theme 5: impacts of continence care and ‘pad cultures’ on recognition of the person and understandings of dementia, we explore how this could mean that PLWD may not expect the intimate care this involved, which could lead to significant distress for many patients.
‘Pads’: a routine precautionary strategy
The widespread and everyday use of pads in the care of PLWD was often explained and rationalised by ward staff (in discussion with patients, families, us and each other when organising care) as a precautionary strategy that is used ‘just in case’ (i.e. as a ‘safeguard’ for all, including those recognised as continent, ‘mobile’ and ‘self-caring’). Of course, many PLWD in these wards did have continence and mobility issues. However, we found that the widespread use of pads was not limited to those with identified continence issues associated with their dementia or their admitting condition. Rather, there was an expectation that the wider timetabled routines of care would mean that continence urgency could not be prioritised by ward staff and, therefore, these technologies were viewed as providing essential safeguards to ensure containment, prevent ‘accidents’ or incontinent episodes during a shift and to support the smooth running of the work of these wards. This precautionary ‘just-in-case’ approach to continence care for PLWD was deeply embedded and pervasive in all of the wards observed in this study.
Here, the bay team discuss one of its patients living with dementia, who is routinely ‘dressed’ in continence ‘pads’ by the team, even though she can walk to and from the bathroom independently (we observed her doing this), describing this practice as a ‘safeguard’:
I speak to a RN [registered nurse] and a HCA about continence amongst the patients living with dementia. A6 is continent but the HCA says she is still placed in pads. The RN interjects and says she isn’t, and the HCA says she just now changed her pad in the toilet, and has put it on as ‘a safeguard’. RN criticizes this, asking the HCA, ‘what’s the point’, and describes how it is not encouraging independence.
Site F, ward 11, day 20
This example also demonstrates that ward staff recognised that this precautionary approach had wider implications for this person, could have an impact on opportunities for rehabilitation and could lead to deconditioning and reduced independence. Ward staff (i.e. nurses and HCAs) often reflected (across the sites) this viewpoint in our discussions about continence care; however, they also described feeling powerless in having any influence to change these approaches, viewing it as a direct consequence of wider institutional pressures.
Justifying the use of ‘pads’ as a safeguard for PLWD who were otherwise continent was a common rationale used by ward staff to support their routine use. Here, this example demonstrates that this reflects wider expectations and understandings of poor QoL and dependency as inevitable in the context of a diagnosis of dementia in these wards:
The woman in bed 2 is eating chocolate from a large box on her tray table. I speak to the HCA about her, who tells me that she has put a pad on ‘just in case’, but confirms she is continent. Have conversation with RN [registered nurse] and HCA about this patient and the RN says she wouldn’t want to live that long, and the HCA talks about how lovely she is for her age, ‘she does seem with it’, despite her admission and dementia, and ‘she knows where she is’.
Site F, ward 11, day 25
The use of pads in the care of PLWD was so embedded in these wards that they were used even when other, often multiple, continence technologies were already in place to support the person. In many ways, ‘pad cultures’ were the most visible sign of the containment approach to continence care in these wards.
Cultures of containment: wearing a ‘pad’ informed expectations that they could and should be used
This use of ‘pads’ as a precautionary strategy had real and significant consequences for PLWD. Once adopted as a ‘just-in-case’ strategy, the routine use of pads in the care of PLWD resulted in the maintenance of continence being deprioritised, and the precautionary strategy became an expectation that PLWD not only wear pads, but that they could and should use the pad. We found that this expectation was a feature of all these ward cultures, regardless of an individual’s continence, independence or preference.
11.35: Inside side room 6 the visitor is explaining to the one-to-one carer that her father doesn’t like the continence pads. He finds them uncomfortable and they are too tight. No action is taken.
Site H, ward 15 day 7
Of course, many PLWD (and older people) did have episodes of incontinence or were incontinent, and, indeed, we observed many people call for assistance too late (i.e. after they had used their continence pad). However, we found that the use of pads as standard care for PLWD contributed to ward cultures and expectations of patients (and we also saw some slippage in the assessment of the person and their capabilities, which could lead to a recognition of the person as ‘bedbound’). This was not just because pads were associated with incontinence, but also because, once this patient group were placed in them, this, together with the associated visibility of the ‘pad’ on the person ‘wearing’ them, established a widespread culture that expected and instructed PLWD to actively use these pads.
The communication of a continence need and a request to go to the toilet by a person living with dementia was often answered by ward staff with the commonly used phrases ‘You’ve got a pad on’, a signal for the patient to remain in bed and to use the ‘pad’. Here, a nurse (who is covering the bay and tells me she does not know these patients) supports a woman living with dementia to the bathroom. It is clear that this woman is both mobile and continent, although she is lacking confidence in walking without support to the bathroom. We can also see that she appears not to have been to this bathroom before and, in her repeated thanks to the HCA, her relief in being able to reach and use it. However, as this example shows, supporting a patient to the bathroom was unusual and can be questioned:
After being told to stay in her chair, the woman in bed 17 asks the nurse from bay B, who is covering for the regular nurse’s break, if she can go to the toilet. 17 is really appreciative of the nurse for helping her with this, ‘Thank you. Oh, you have a little room’. They open the toilet door and it is as if she has not seen this toilet before, even though it is located within the bay. ‘Is there a light?’ The nurse turns the lights on for her, ‘Oh, thank you. Thank you so much’. The nurse explains to her that ‘When you are finished, pull the red one and I’ll come back’, pointing out the buzzer. 17 doesn’t seem to understand this. She responds, ‘Will you stay here and help me back, I’m almost finished’. ‘OK’, says the nurse and stays in the toilet with her. 17 finishes and they walk back to her bedside. As the nurse turns to leave, the other nurse returns from her break, so she lets her know 17 has just been to the toilet. The returning nurse responds questioning this, ‘Why? She’s got a pad on’.
Site H, ward 16, day 11
In all wards, in response to a person living with dementia asking for continence care, we identified staff reminding the person that they were wearing a pad and explicitly instructing them to use the pad. Later in the day, the same patient (as above) clearly states ‘I need the toilet’ and in response was reminded that she was wearing a pad and directed to use it, ‘You have a pad on, you can just go there’. This is extremely confusing for this woman who appears to interpret this as removing her pad and to use the bedside chair as a commode, which leads to high levels of distress for both the person and the team caring for her:
The woman in bed 17 gets up and moves to her bedside chair but remains standing up. She announces, ‘I need the toilet’, to which the response of the one-to-one HCA (who is closely monitoring this patient and the person in the bed next to it, bed 16) is to remind her that she has a pad on. This woman (bed 17) responds to this by reaching down and beginning to take the pad off. The one-to-one HCA tells her to pull it back up and again reminds her, ‘You have a pad on, you can just go there’. She (the woman in bed 17) appears to be confused by this and she again tries to take the pad off and sits on the bedside chair. The other team member in the bay suddenly shouts across the bay, ‘Wait a minute, that’s not the toilet! Wait a minute!’ She (the woman in bed 17) looks confused and says, ‘I can’t wait I need to go . . . I’m going to do it here’. The member of staff now keeps asking her to ‘sit down’.
Site H, ward 15, day 11
The routine use of ‘pads’ appeared to be informed by a number of institutional expectations and pressures powerfully felt by ward staff, particularly the expected pace of the organisation and delivery of bedside care for this patient group. As we can see here, ward staff emphasise to this person living with dementia that she must use the pad or ‘wait’ (i.e. her urgency must fit the timetables of wider care delivery that the team are working to) and they repeatedly instruct her to ‘sit down’, further emphasising the risks to the person of independently leaving the bed or bedside to reach the bathroom. It also appears to reflect a belief that it is possible to ‘use’ a pad, particularly for PLWD.
The families we spoke to often described their family member living with dementia experiencing these strategies of continence care during their admission. Here, two daughters join me in the day room and share their concerns about their parent’s continence care and the effects of the reliance on ‘pads’, the strategies of containment and the impacts for the person:
Dad [patient in bed 16 who is living with vascular dementia] gets agitated if he wants to go to the toilet or if his pad needs changing. I got here, there was a puddle in the bed so it hadn’t been changed in a while. I asked both nurses who said they were busy so I changed the sheets, stripped the bed, and put clean clothes on. When he gets sundowners he starts to swear. He was trying to get up and saying, ‘I am bursting for a piss, bursting for a piss’. I said to the nurse he wants to go to the toilet and she said, ‘He’s got a pad on!’ He doesn’t, it’s just for accidents, he has accidents, but he can walk to the bathroom! And we took him out to the bathroom the nurse said, ‘He can walk?’ Yes! They had been leaving him in bed and we got him up, it’s not good to be in bed and we walk him to the toilet. The nurse says, take him in a wheelchair, but no, he can walk. They think because they are in pads, they are toddlers and babies not adults. My brother does more, I am more squeamish, and he takes him to the toilet and changes his pad. But the nurse said, no, she will do it, but she was annoyed with him for doing it. She said to my dad ‘I am just going to change your nappy I am going to change your nappy’. That’s basic, that took all his dignity.
Daughter of 20 nods in agreement and tells us about her mum, ‘I could smell it, my mum can’t tell someone she needs changing. Oh my God, if I wasn’t here it could have been all day and until the night shift. I could smell it!’
Site H, ward 16, day 16
These ward cultures, which emphasise the organisation and delivery of timetabled bedside care and the strategies of ensuring patient safety and reducing risk, also appeared to constrain the power of staff to respond legitimately to urgent continence care needs, particularly if they involved supporting the person to leave the bedside, or promoting independence and continence.
These ward cultures emphasised pace, efficiency and busyness (as seen in the many examples above), with the need to maintain the daily organisational timetables of bedside care powerfully felt, creating a palpable source of tension among nursing and care staff. The fear and underlying anxiety of ‘falling behind’ during shifts was frequently discussed. Conversely, the sense of meeting or being ahead of the timetables or having time for a break was notable and a sign of a ‘quiet’ day (although to vocalise this was to ‘jinx’ it).
Continence care that supported the independence of PLWD was recognised by staff across these wards as requiring skilled interactional work, but also as a form of care that requires significant time and, in some cases, many members of staff. When unscheduled and driven by a person’s urgent needs, continence care was often perceived as taking ‘too long’ and a source of delay that could have an impact on other routinised timetabled aspects of bedside care. This shaped the dominant culture of continence care that we observed across all wards and sites (i.e. the ‘pad cultures’). Although pads would be rationalised as being used ‘just in case’, our observations revealed that the use of pads was an embedded practice in these wards, not only in response to incontinence in the person or as an (in)continence tool, but to support the wider organisation, management and delivery of the ward timetables of care that were institutionally mandated. These strategies were also reflected in the explanations and rationalisations staff provided to PLWD at the bedside and to their families. The standard use of pads removed the urgency of continence care, shifting the delivery of this care from one that interrupts these timetables to one that can fit within it. The use of pads transforms the continence care of PLWD into something that was perceived by staff as requiring a relatively quick and efficient set of care tasks contained at the bedside, preventing ward teams from ‘falling behind’ with the wider timetabled care that was perceived as more critical or closely monitored by the institution.
The pace of (expected and perceived) care at the bedside meant that the independence and autonomy of PLWD could become a reduced priority. Where staff perceived that they were ‘short’ (i.e. understaffed) or were ‘falling behind’ with the wider timetables of bedside care, the use of pads became prioritised over patient independence. At these junctures in shifts (we found that this typically occurred at some point during almost every shift), patterns of prompting and the procedures of assisting a person living with dementia to use a bathroom could become viewed as taking too long and perceived as clashing with and potentially delaying other institutionally mandated timetabled tasks of care (e.g. the timetables of other teams, including the arrival of medical teams or mealtime deliveries). Therefore, although staff in these wards discussed and recognised the importance of prompting patients to go to the toilet, particularly before or after a meal, in practice, these pad cultures dominated.
These pad cultures also created their own new routines and rituals in the wards, such as regular ‘pad rounds’ and ‘pad checks’ in which ward staff (typically HCAs) ‘checked’ on and prompted continence at points during the shift. These routines involved ward staff asking people at each bedside, in turn, about their continence needs. If a person was unable to respond verbally, then this could involve staff relying on detecting the smell of urine or faeces on the person, or by carrying out a physical examination at the bedside by swiftly lifting sheets, hospital gowns, robes and clothes and using touch to check if a person’s pad had been used. These pad checks would be carried out, in turn, for each person in a bay or carried out as part of other task-based bedside care throughout shifts, although this could also be less systematic, and varied depending on the individual staff and team approaches to bedside care and the pace, space and pressures on the timetables. In this way, continence care could be transformed and reduced to containment practices and the ‘checking’ and replacing of soiled or wet pads as part of other scheduled activities during a shift.
Conflicting urgencies and fear of falling behind
In wards, supporting independence and continence for PLWD was recognised as requiring expertise, as well as considerable time and resources (as with the person living with dementia in the example above). As we have described, the nurses and HCAs who supported a patient living with dementia to the toilet almost always stayed in or near the toilet, or in the bay, until that patient needed to be supported back to the bedside, where further personal care may be needed and clothing and/or bed sheets replaced. Supporting a person living with dementia from a bed or bedside chair onto a commode also involved a similar intensity of care work, which was generally carried out behind the curtain. Supporting independent or assisted continence typically took between 5 and 10 minutes, but could frequently take far longer, and included steps that often required additional support from the bay or wider ward team [sometimes requiring a ‘double’ of two members of staff in the team, requiring a ‘floating’ member of staff working across the ward (or ‘on the floor’) or, more commonly, taking staff away from their own bays and patients]. Such supportive care was observable throughout the shifts when this was a timetabled aspect of ward care, such as at the start of the morning handover or as part of the pre-breakfast personal care routines:
The HCA on bay 3 puts on a plastic disposable apron to go into the toilet to help the patient in there. It’s the woman from bed 16. ‘Why do you want to hit me?’ says the HCA loudly. She comes out and asks other staff for help, ‘She’s so aggressive’. As she does this, 16 dashes out of the toilet. She has a stumbling, lurching walk. Her hospital gown is pulled up high and she is holding up her large continence pad. The team try to talk her into going back into the toilet and tell her she is ‘showing herself’ to the unit and that men are going to walk past and ‘will see her’. It is only then that she turns around, before locking her legs and insisting that she wants to go back to her bed. They tell her that she needs to clean up, and manage to walk her back to into the toilet. The nurse comes out of the toilet and sighs, she is clearly tired at the end of the night shift, but goes immediately to support another patient who is calling out for help. Suddenly, the instructions change – previously the staff just wanted to get this woman (16) to go back into the toilet and now they are struggling to get her out of it. The HCA tries to reason with her and offer incentives, ‘Your breakfast is getting cold’, ‘Come and have your breakfast’. ‘Come out of there. Please come out of there’. At the same time the senior nurse helps the woman (bed 12) who is using a frame to walk from the bedside, he is directing her towards the toilet, she is very slow and he is being very patient. She is really struggling to use the frame, and looks terrified, and this senior nurse is supporting, holding the frame in front of her, but she starts to look distressed and the nurse calls out for a chair. The clerk at the nursing station tries to bring one but can’t get the chair brakes off and there is no one free to help and the clerk eventually forces the chair against brakes onto the bay, making a huge screeching sound. But she (12) then refuses to get on the chair, and continues to shuffle with the frame towards the toilet. She is very slow and shaky, but at the same time desperate to get there, and vocal about her worry and fear of ‘going’ before she gets there. The rear heel of her walking frame gets caught on the open toilet door, it takes a few minutes and I am convinced she is going to fall as they edge the frame around the door. She (12) turns to the nurse and says, ‘It’s difficult when you don’t know your way around!’ The nurse stays with her throughout and this takes around 10 minutes from bed to bowl.
Site H, ward 15, day 25
Continence care was also an important opportunity for staff to provide wider supportive care and comfort to the person, which could require more time than expected to see the person and to support their wider needs. Here, the HCA prompts support to reach the bathroom, despite this patient’s hesitancy, and, at the same time, she also responds to her wider needs, with a focus on her painful skin:
The woman in bed 8 asks the HCA, ‘Can I get out of bed a bit more today?’
The HCA replies, ‘Yes of course. Toilet first?’
‘We can try!’
The HCA takes the commode to her and drops the bed, puts fresh red hospital socks on her feet and helps her to sit and to move across to the commode. She is wearing a white gown [here they have the institutional logo printed across them] and has a large wrap-around pad on. They discuss how to swing her legs around from the bed because there are lots of skin breaks on her legs and she complains about her back being sore. The nurse gets some cream and rubs it across her back, working it into her skin.
This woman looks relieved: ‘Thank you nurse that’s much better’.
The HCA helps her onto the commode and takes her in to the bathroom, leaves her and returns to the bedside to make the bed and puts pillows on the bedside chair. She then heads back to the bathroom and wheels this woman out on the commode, locks it in place at the bedside and helps her out. ‘Have you got me?’
‘Yes.’
‘OK, lovely’.
Once she is in the bedside chair, the HCA puts pillows behind her back for support, arranges her gown straight and over her knees, and moves the bedside trolley next to her and in reach.
Site H, ward 16, day 7
However, outside these points in the organisation of the acute ward where continence was prioritised, the time required to support a person living with dementia from the bedside to the bathroom and back was often seen as significant, as taking too long and as interrupting the other timetabled demands. Continence care could then become deprioritised and overshadowed by pad cultures that enabled staff to focus on fulfilling the timetabled work of the ward, including the recordable and quantifiable aspects of their work. We had many discussions with ward staff about how they managed the timetabled routines of bedside care and the urgency of continence care needs for PLWD. One HCA described constant judgements on what to prioritise during a shift, highlighting the centrality of the observation routines:
There are six people in this bay, that’s a lot of attention, everyone needs the toilet so observation [timetabled rounds at each bedside that must be recorded at set points in each shift] or the toilet – or observation and wipe it up afterwards. I can only do what I can do. If I can do it, I do it, but you can’t do it all on your own. Some days I have 10 patients on my own.
Site G, ward 15, day 10
For ward staff, as we see in the example above, the organisational pressures that emphasise speed and pace resulted in concerns about ‘falling behind’ with the timetables of routine bedside care (e.g. observations, medications and mealtimes) and other routines of care that must be completed and recorded to meet internal and external institutional timetables, and the associated recording practices. Here, a HCA from a different site describes the recording of the timetabled observations (e.g. blood pressure, heart rate, temperature) as the institutional priorities and, as such, more pressing than other aspects of bedside care. Note how these institutional priorities trump urgent patient continence care needs:
We discuss continence care in the ward and the HCA tells me, ‘It’s important to stay in the zone, do the routine stuff and have tunnel vision, no interruptions to the routine observations, observations are more important, the priority, more important than someone sitting in poop. The happiest most productive nurses are the ones who stay in the zone. If anything happens to that patient then they will ask why weren’t the observations done, so the person sitting in poop has to wait, but at the same time if they sit in it for too long then they have skin issues and that comes up, but you only have two hands’.
Site H, ward 16, day 14
This could lead to staff carrying out these timetabled observations during continence care and over-riding concerns about the impact on (and potential immediate distress of) the individual person living with dementia:
2/5 is crying out. I thought the team were with her but no, she is by herself behind the curtain drawn around her bedside. The HCA goes over to her and asks her, ‘Do you want to wee?’
Another HCA joins them and repeats this: ‘Do you want to wee?’
The first HCA comes back with gloves on and a bedpan in her hands (it looks like a very large plastic shovel with a cardboard disposable insert fitted within it) and goes behind the curtain. This HCA tells her, ‘See if you can go, see if you can do a wee. I will just do your blood pressure while you are here’. She wheels the mobile BP [blood pressure] monitor in: ‘Which arm did you hurt?’
When they are finished this woman is lying flat in the bed, tucked into the bed, and looks calmer. The side rails are also up on the bed.
Site G, ward 14, day 7
These organisational pressures could inform cultures of continence care, which would mean that prompting and supporting independence and use of bathrooms become limited and withdrawn as non-essential, whereas continence pads (and bedside continence care) come to be relied on to ensure containment. Therefore, we regularly observed a team carry out fast-paced bedside care in a bay for 2–5 hours without seeing a single patient living with dementia leave the bedside and go to the toilet, including before and after mealtimes and drink rounds:
On bay A the man in bed 10 is up walking from the toilet to his bedside chair. Only the patients on this bay (younger, no dementia) have been up to go to the toilet during today’s observations.
Site H, ward 15, day 21
I stand between the nurses’ station and the toilet in the corridor and throughout the time I am here (9.30–11.30) no-one has used this toilet. It is the only one for the eight women in bays 3 and 4 opposite. This seems like a long time with no visits to the bathroom.
Site G, ward 13, day 1
This was associated with staff’s view that prompting PLWD to walk to the bathroom was possible during ‘quiet’ moments in the ward schedule only. However, quiet moments were rarely identified and acted on, and pad cultures allowed patients to be left while ward staff used these times to focus on the next timetabled task (or the required updating of patient records).
Containment, prompting and the prioritisation of urgent and visible continence care
Ward teams employed a range of strategies to manage their workloads and to try to keep pace with the expected timetables of care, including, prominently, continence care. If a ward team believed it was falling behind schedule, prompting independence was reduced. Calls for the toilet that were difficult for staff to respond to were replaced with reminders to patients of both the competing demands of the team’s workload and the continence technology available. Continence care that supported independence was replaced with containment.
Strategies of prompting
Toileting was regularly prompted at points across shifts, with prompting typically timed (informally) to support the wider organisation and delivery of routine bedside care and external institutional schedules entering the wards, such as meal delivery or medical rounds, to continue uninterrupted. Prompting and encouraging toileting independence was, in practice, often sporadic rather than routine, readily stalled if staff perceived they might ‘fall behind’. This would also reduce opportunities to respond to urgent continence care needs. Here, the team reassure a visitor that the person ‘has been seen’; however, this means that they find it difficult to recognise his continence care needs as legitimate outside these points in the timetable:
A visitor on the bay goes over to the clerk at the main nurses’ station and says one of the patients has been calling out for a nurse for a while. In response, the clerk says a nurse ‘has seen him’, but the visitor challenges this, saying the patient is uncomfortable and nobody has seen him. An argument of sorts starts, with the visitor adamant no nurse has been and that a nurse is needed, and the clerk saying the nurse has already been and will be back again soon. There hasn’t been a nurse on this bay for some time. ‘He’s not comfortable’ says the visitor, with an emphasis on urgency missing from staff interpretations of the situation. A nurse passing by says she will ‘come and see him next’.
Site H, ward 15, day 24
In discussions about continence care, ward staff typically talked about these strategies of prompting and continence promotion, but also the competing realities of the expected pace of care, the urgent needs of their patients and their fear of falling behind. Here, a nurse exemplifies this everyday challenge:
We go to all patients every 2–3 hours and if continent we will ask them if they want to go to the toilet, if incontinent we will check that pad, we promote continence [ . . . ] but we can’t always do it, we have acutely ill patients here, so we don’t always have the time to take them, the best time is when washing and dressing.
Site F, ward 11, day 21
Prompting was also typically timed to support the smooth delivery of the wider institutional systems and routines. This included organisational demands, such as staff clinical meetings and board rounds, and the schedules of specialisms, services and teams external to these wards, which were typically prioritised over the continence needs of PLWD. Here, the competing timetable of the external audiology service is explicitly prioritised over the personal and continence care needs of this person:
The man from C bay (C1) passes in the hall, he wears a hospital gown and is using a frame to walk to the bathroom and we smile to each other as he passes by. He later returns and looks a bit uncertain and I ask him if he is OK. He tells me, ‘I need a pad and a wash’. His pad is falling off him. It looks uncomfortably large and he is exposed because the hospital gown doesn’t cover his back. I go and find the nurse for this bay and tell her and she tells me he can’t [wash] yet because he needs to go to audiology. She goes over to him. He is now back in the bay sitting in the chair next to his bed. ‘I will get you a pad but you are going to audiology first’.
Site F, ward 12, day 5
The external timetabled order of food delivery could also conflict with the urgency of a patient’s continence care needs. Here, the prioritisation of the mealtime and the hot lunch (as with the schedule of the audiology department above) meant that ward staff appeared unable to recognise the urgency of the person’s need or the unpleasantness of this for the person:
A man in pale checked pyjamas walks gingerly and slowly down the corridor and he asks me where the bathroom is. I point him in the right direction. He is directly at the entrance to the bathroom so as I show him, he turns and goes in. When he comes out and heads down the corridor to the bay, I can see his pyjama bottoms are quite stained at the back. He does seem to be walking quite uncomfortably back to the ward. The nurse joins him and guides him back. She notices the stain but does not say anything [. . .]
Later he goes to the bathroom and the stain on the back of his pyjama bottoms is big. It’s definitely a large patch of faeces.
The same nurse sees the patch and leads him to the bedside: ‘Your food is here’.
[Later, after lunch, I can see the curtain is drawn and she is helping him change.]
Site F, ward 12, day 27
When ward staff attempted to fit the urgent continence needs of a person living with dementia into the timetabled order of bedside care, for whatever reason, this could lead to significant patient distress. Here, a distressed patient becomes viewed as requiring high levels of support that cannot be met by this ward, even when this shift is described by the nurse in charge as ‘well staffed’. Ward staff were constantly managing a number of conflicting organisational demands and patient care needs. In this case, compliance with the institutionally mandated recording practices is prioritised, with this person’s continence care needs managed through a strategy of ‘hourly checks’, with the nurse in charge also reassuring this patient. However, staff do not recognise the distress that this approach and the associated delays cause to patients:
As I enter the ward the woman (in bed 2/1) calls me over to her bedside. She seems very distressed as she holds her arms out to me: ‘Help me’. I go over to her and she tells me, ‘I want to wee, I am desperate, ooh, I am going to wee now, it is too late!’ She is wide eyed and looks extremely distressed as though she has been desperately holding on for a long time. I say I will find the nurse who is looking after her. She replies, ‘Please! I need the commode’.
I go over to the nurses’ station. The nurse who is writing updates in the medical notes, her head down, focused on completing the patient records, is her nurse, and I tell her about her patient, emphasising the urgency. She remains sitting at the desk and tells me, ‘She is very, very confused, we have dipped her urine, she came in with a fall so completely confused. We keep trying her on the commode but she won’t sit, she says it’s uncomfortable and she can’t go, so we are checking on her hourly. We are trying to satisfy her with something, but it’s constant, you can’t reply all the time to everything. You need to find a strategy for all the patients, we tried her on the bedpan but she won’t stay, you have to find a strategy that will help’.
As we talk, the nurse in charge of the ward passes and this woman also calls out to her, ‘Help me!’ She still sounds very distressed. The nurse in charge goes over to her and the nurse from that bay joins her. The nurse in charge tells this patient, ‘We are looking after you, I am going off shift now, you will soon feel better. She also tells her name and reassures her she is OK – she has an incredibly gentle manner.
However, when she leaves, this woman continues to call out her distress, ‘Please help me, please help me . . . ’
I follow the nurse in charge into the staff room as she leaves to ask her about this patient and the strategy. She tells me, ‘We are well staffed, so it’s easier to not get behind, but that’s going to change, I am going off I am on an early only (she gets her bag and coat) and they are moving (another very experienced nurse to cover another ward) now, so it’s going to get more chaotic from now on’.
I return to the ward and the woman is still distressed, it is affecting both me and also the other ladies in this bay, we are all starting to feel anxious for her.
Site G, ward 14, day 21
Importantly, as the continence needs of this person do not fit the routines of the wider ward, her behaviour and her high levels of distress become viewed as a feature of her dementia and of being ‘confused’. We will explore the impacts of continence care on understandings of ‘behaviour’ in Theme 5: impacts of continence care and ‘pad cultures’ on recognition of the person and understandings of dementia.
Prompted continence care as a ‘disturbance’ to the older person/patient
In these wards, the widespread culture of using pads as a precautionary strategy was associated with reduced prompting to support independent continence care for this patient group. Acute wards are typically fast-paced spaces, with an expectation of a sustained tempo (as a demonstration of efficiency) in the organisation and delivery of care within them. By contrast, for patients these wards are unstimulating places, particularly for PLWD, who did not typically have access to newspapers, books, television or radio. Although some wards had communal television screens (often fixed to a wall and tuned permanently to the same channel) or pay-per-view screens at the bedside, these were often inaccessible (as bedside screens were typically too complex to use). Few patients had devices or screens available for personal use in these wards. As a result, PLWD often sat in the bedside chair or in their bed for extended periods, with no stimulation. This produced a pervading sense of ennui, of patients left to wait and of sitting in ‘pads’:
It is so quiet, but even when there are empty beds and little to do, the patients admitted with dementia are dressed in continence pads and just left to sit unsupported in their beds. I have seen no prompting to go to the toilet. Fewer patients and fewer tasks do not seem translate to more engagement or more care, just to a quieter day. The team are either writing up notes at the nurses station or are not visible.
Site H, ward 16, day 24
This lack of stimulation meant that PLWD often appeared sleepy or drowsy and moved less, which, in turn, meant that individuals were less aware than usual of their immediate bodily needs (primarily continence, but also a wider range of care needs, e.g. hydration). At the same time, their immobility (which could be viewed as a feature of dementia) meant that these individuals were often conceptualised by the ward team as not needing prompted continence care, particularly in the context of the faster pace of care work on these wards. Combined with the precautionary strategy of pad use, this meant that prompting toileting and independence were often judged as non-essential or something that could be delayed for this patient group. This could inform other aspects of personal care where, in the fast pace of timetabled care work, PLWD who were ‘quiet’ could often be judged by ward staff (and other teams and services entering these wards) as not having obvious urgent support or care needs:
The patients in beds 19, 21 and 22 have all been on the unit for over a week. They seem to be bored, almost institutionalised, and are just sitting on their beds, propped up by pillows, staring forward blankly. 19 and 22 are just waiting for social workers to arrange discharge and safeguarding placements. This seems to take forever, both cleared to go home but seemingly no urgency for this.
Site H, ward 15, day 16
This could extend to recognition of intense faecal smells. Although this was a familiar and everyday odour in these wards, it was also masked by and mingled with the overpowering disinfectant smell of the institution, contributing to the everyday smell that ward staff were habituated to. It was customary for staff to comment on and note particularly intense and powerful odour, and, although this odour could alert staff to prioritise a patient and their continence needs, its source was not always identified until bed covers were disturbed for other routine care:
On bay 2 the patient in bed 14 is hidden behind the curtains. The nurse is at the bedside for what appears to be personal care, including washing and changing clothes and sheets. She admonishes this woman ‘Less of that’, who grumbles as the nurse continues, ‘We need to change you . . . your bed smells of urine . . . it doesn’t look good . . .’
Site H, ward 15, day 5
Therefore, the needs of PLWD could appear less visible to staff. In addition, ward and other external and auxiliary staff also appeared less comfortable approaching immobile older patients, with prompting potentially viewed as inappropriately ‘disturbing’ individuals appearing less alert. As a result, this could further distance the person living with dementia from social stimulation and care.
Strategies of containment
The ‘pad cultures’ we observed could create new, additional and unplanned work of their own. As continence ‘pads’ are designed to contain urine and faecal matter, it was common for staff to consider that ‘pads’ worked as a containment technology and that PLWD could remain in soiled or wet pads until staff judged that there was sufficient space in the timetables of care and the competing needs of other patients, as this was when staff felt able and permitted to attend the bedside and deliver continence care. However, when continence was not contained and became visible or noticeable on the body or at the bedside, this was recognised by all as requiring urgent and prompt care.
Our observations suggested that, despite their intended design, ‘pads’ rarely functioned as a containment technology for long, creating problems and work of their own. ‘Waste’ from continence ‘pads’ (and other technologies and equipment) that became visible in these wards was typically prioritised as urgent when recognised. Visible waste and ‘accidents’ were not tolerated in these wards, and were viewed as highly disturbing by staff in and entering these wards. Timetables would be interrupted and the cleaning of patients, surfaces and floors would be prioritised:
Bay 1 smells really strongly of faeces. I look in and there is a trail of faeces leading from the corridor along the floor back to bed 8. The NIC [Nurse in Charge] sees me looking at it and apologises about the mess. Two HCAs are crouched on the floor wiping it up with antibac [antibacterial] wipes. They tell me nobody had noticed until the ward sister slipped over in it.
Site H, ward 15, day 2
Such incidents often showed the failings of retroactive pad culture: changing a full set of bed clothes as well as cleaning a patient and changing their clothing, which was typically necessary, is generally more resource intensive for staff and distressing to patients (both immediately and in the longer term) than proactively supporting patient continence and independence. These impacts were, however, unrecognised (or unattributed) by ward teams. Rarely was there recognition of the distress experienced by a patient wearing a soiled pad, nor were immediate needs addressed with any sense of urgency or considering the practical implications of not doing so: that a person who had ‘used’ their pad would usually need urgent support with personal care.
The emphasis placed on the use of pads as a precautionary strategy of containment meant that, in these wards, optimum organisational efficiency was believed to be achieved when PLWD (and older people in these wards) were wearing pads and contained in bed and at the bedside. Here, the ward team were caring for a group of PLWD who were all wearing ‘pads’. The key focus of their work during this shift involved a strategy of containing these patients in their beds. In comparison with many shifts observed, this is an average team (i.e. one nurse to nine patients and one HCA to 13 patients); however, the demands of timetabled routine (perceived and expected) care and the support needs of this patient cohort meant that there appeared to be no potential for the team to prioritise care strategies that supported continence or independence more widely:
The nurse from bay 3 goes into bay 4, talking in whispers to the one-to-one agency HCA before shutting the door behind quietly. Two doctors in the corridor are preparing to go into the bay to see the patient in bed 21. They also repeat these actions, quietly closing the doors behind them. The nurse from bay 3 now seems primarily occupied with picking Elvis songs from YouTube [YouTube, LLC, San Bruno, CA, USA] to make sure the man in bed 15, (who is wearing a pad and had an additional large continence mat underneath him) stays in bed. The job of the one-to-one carer on bay 4 seems to be to simply keep the patients in bed and asleep, while the nurse is away from the bay. Another nurse is just trying to keep patient 14 at her bedside. Each staff member is on differing bays to the ones they were assigned at handover, covering for other staff, and concerned chiefly with containing individual patients at the bedside. There is little visible medical or personal care happening.
Site H, ward 15, day 17
The use of ‘pads’ in the care of PLWD, and the expectation of their use, would typically result in the patients needing support to ensure hygiene and cleanliness. These containment technologies regularly failed in their primary purpose (i.e. pads leak, smell and can damage skin), requiring significant personal care, including support with undressing, washing and changing, and a change of sheets. For staff, this also involved repeated trips to linen stores and sluice rooms, which were often located far from the patient’s room or bay. Therefore, the use of ‘pads’ often required care that was far more personally invasive and distressing than supporting the patient to the toilet:
The woman in bed 12 calls out, telling the team her pad needs changing, and the nurse and HCA go to her bedside and together decide that ‘the whole bed needs doing’. I wonder, are the pads ever effective? It is still tough to observe the bays today, everything is blocked by curtains. This woman’s (bed 12) visitor first reported she needed the toilet a long time ago. The visitor is still in the day room waiting.
Site H, ward 15, day 28
Prioritising the management of ‘dirty’ and ‘wet’ bodies
Judgements about the relative urgency of continence care typically emphasised to patients and the wider ward the importance of cleanliness and of managing ‘dirty’ and ‘wet’ bodies, beds and surfaces in the timetables of care. This organisational focus on responding to ‘dirty’ or ‘wet’ bodies (as with the urgency of responses to visible waste or ‘accidents’ described earlier) meant that other aspects of continence needs that are of importance to PLWD were hard for ward staff to recognise and respond to. Here, this patient clearly and repeatedly tells the team and the wider ward that she is ‘sore’ and needs barrier cream applied. However, because she has repeatedly been assessed as ‘dry’, it takes time for the ward team to recognise, understand and respond:
The woman in bed (4/6) calls me over with a movement of her hand and tells me, ‘Sore bottom, no cream, sore bottom, no cream . . . ’ repeating this.
I tell her the team are behind the curtain with another patient and I will let them know as soon as they come out. When they do I tell them, and the HCA draws the curtains around her and reports, ‘You are dry’. This is directed at this woman but also at me and the rest of the team. She comes out from the curtains and goes over to the nurse to discuss her: ‘I think she is clean but this is a constant issue, but I don’t have anyone to help me – she would need rolling, I’m new to this and it’s difficult’.
A bit later they meet again at this woman’s bedside and discuss the cream. They believe she has enough cream because it’s part of the cleansing wipes. They discuss whether this is the right type of cream for her or if it is enough.
Meanwhile this woman continues to plead with them: ‘Please nurse, nappy please . . . ’
The nurse tells her, ‘Don’t worry we will definitely do it’ [ . . . ]
Later during the medication round that day, she repeats her request, her body is now shaking: ‘Bottom sore’.
A nurse who can translate (this patient is of South Asian origin, although throughout she is clearly stating her needs in English) says, ‘She is happy for you to do it (give her the injection required during the medication round) but she wants cream on’. The nurse and HCA discuss and decide she needs extra cream: ‘I think she is used to having the cream on at home and we use the wipes so she is not used to it’. The nurse goes to get the cream and returns: ‘Here we go!’
The nurse turns to me: ‘The moisture cream is in the wipes, they are great, but she won’t be happy until we use this cream as well’. The nurse is very gently and sympathetic, and they both now have gloves and pinnies on and close the curtains, and as they do this they tell her again they have the cream.
Site G, ward 14, day 4
The distress of visible waste or ‘wet’ and ‘dirty’ bodies was also, unsurprisingly, a cause of great distress for families:
A couple come out of a side room (9) and see the nurse and they report, ‘She’s all wet’.
‘How did that happen?’
They add, ‘She’s just woken up and she’s wringing wet’.
‘OK we’ll be over to sort her out’. She asks other people in the team for help.
The family wait outside and the team head in and shut the door.
After a while the HCA is at the door, gloves on and brings out a red bag full of soiled linen, she talks to the family and they chat for a long time. She is lovely and friendly with the family.
Site F, ward 12, day 27
In bay 5–8, the one-to-one carer has been sitting and watching the room. The four women in the bay are all lying in bed and no one has moved all morning. The daughter of 8 arrives, she comes every day to care for her mum who is living with dementia. She comes out of the bay towards me looking incredibly distressed and she says to me in a low voice, ‘She is all wet’. The one-to-one carer and I join her at the bedside behind the curtain. The sheets that were covering her have been pulled back and the entire sheet and bed is completely soaking. The smell is overwhelming.
The one-to-one carer asks me to ‘watch the bay’ as she takes sheets in behind the curtain and offers to help the daughter who looks very unimpressed, but says yes. They are behind the screens together for a long time. When they are finished, the one-to-one carer drags a number of large heavy orange waste bags and linen bags out of the bay. The daughter washes the plastic wash bowl inside and out and then washes her hands, she looks very upset.
Site H, ward 16, day 20
The failure of containment strategies could also cause distress to ward staff. Here, a student nurse seeks support from a more experienced HCA:
An HCA heads over to the other more senior HCA in the team: ‘We need your help with [side room 3]’.
‘Why? Who is with them?’
She tells her, ‘It’s [the student nurse]. Diarrhoea it’s gone everywhere all over the floor and we need more pads’.
The student nurse joins them, she is looking very stressed, ‘We need more pads! Diarrhoea everywhere!’
The senior HCA: ‘Do we need to wash her?’
‘Yes’.
‘Get a bowl and towels and let’s start from scratch’.
The student nurse gets a bowl and towels and they head into the room, the HCA ahead. The student nurse looks scared, but able to face it with the HCA.
Site G, ward 14, day 11
The isolation and impacts of being responsible for continence care
A key feature of discussions with ward staff about continence care was their experience of it as a ‘heavy’ burden, continence care being described by all ward teams as ‘heavy work’, ‘heavy nursing’ and a ‘heavy load’, expressing the perceived dependency of the patients and the physically demanding nature of this care. Continence care for PLWD was also typically described by ward staff as ‘demanding’ and requiring ‘doubles’ (i.e. two members of staff at the bedside):
It’s lack of nursing care, lack of bedside care. Filling in forms rather than nursing, that’s the biggest change in the profession. They [patients] are very disabled, very demented, incontinent, it takes time and it’s heavy nursing, if you add all these together, it’s all about time.
Site H, ward 16, day 6
In our discussions with these teams, nurses typically focused on prioritising the timetabled care they were responsible for, particularly the completion of the medication rounds, viewing continence care as primarily the role of the HCAs. Here, I ask a nurse about the previous day shift, during which I observed her interrupting the medication round to respond to urgent care requests and to support her team in attending to those she describes as ‘heavy’ highly dependent patients and the unremitting ‘heavy load’ of providing continence care at the bedside (note that, in many sites, nurses wear red tabards, indicating ‘do not disturb’, during the medication round, although in practice disturbances do still occur):
Yes, the drug round there are the six rules you have to go through and, yes yesterday I wanted to change my name, there were too many calls! It’s so busy and the patients here are heavy so you need help. If there are not enough HCAs, we have to step up and wash and toilet on the ward but sometimes it doesn’t allow the nursing role to the gold standard. Toileting – it’s a heavy load.’
Site G, ward 14, day 25
The HCAs often described feeling abandoned and left on their own with the ‘heavy load’ responsibility of caring for bays of PLWD who needed highly supportive continence care:
Staffing for the past few days with [HCA colleague] has not been bad. But nurses are bad. We find we are on our own. We struggle with the heavy load. Everyone in bay 1 is very needy. They are calling for the toilets every 5 minutes. With commodes and pans I have just done five washes on my own with no help.
Site G, ward 13, day 13
I discuss the shift with a small group of HCAs during their short break. A HCA who looks exhausted (and not yet half-way through a 12-hour shift) describes her cohort of 10 patients (the majority living with dementia) as including four ‘doubles’ and three who need support at mealtimes:
We discuss the shift in the little break room.
I’ve done one double and three more doubles to do, I have done the rest on my own but then it will be lunchtime and I have three to feed.
She sounds exhausted. It is the lunch break and while everyone else eats she doesn’t eat or drink anything. She continues ‘I have 10 patients, six and three and a side room. Seven patients – six in the bay and one side too, it’s enough and it means the other three (in the next door six-bedded bay) get forgotten. One into 10 patients does not go! You need two’.
Yes that’s why they lose people, they don’t want to do it – but we old fogies we just crack on! Sometimes you get held up because there is no one to help you – I have two doubles to do but no one to help. I had one shift where I did the last wash at 7 p.m., I told the lady she was really patient.
Site G, ward 14, day 26
This also reflects the perceived status of continence care in these wards and in these teams. In the teams, higher status is defined by those whose role does not involve intimate continence care. Here, a ward clerk becomes agitated when she is required to leave her computer desk at the nurses’ station and visit a bedside. Likewise, the dementia specialist team also delegate this care to the HCA in the bay:
The ward clerk is now vigorously washing her hands at the sink next to me.
She tells me, ‘I’m keeping my head down. I have to engage. But I’m not wiping no one’s bum. You know what I mean? I have to engage with families. But I’m not here to wipe bums’ [ . . . ]
The [dementia specialist team] has been with a patient in this bay and as she leaves, she tells the HCA, ‘She now needs to go to the bathroom’.
The HCA takes a walking frame and heads to the bedside.
Site G, ward 14, day 13
Those outside the team entering the ward could identify and report when continence care or cleaning was required, but would not consider carrying this out themselves. Here, a member of a medical team enters the ward to examine a patient:
It has been silent during this night shift, the lighting is dimmed, and no one is around as I stand by the nurses’ station. Screaming has started to come from one of the bays. The locked door bangs open and some light enters from the hallway and a medic in scrubs strides in. We acknowledge each other and she says, ‘Interesting night here!’
As she heads into the bay to see the patient [bed 9] we both suddenly see there is faeces smeared all over the floor in the middle of the bay. It is unclear whose it is. After stepping around it to examine the patient she steps gingerly around it and says firmly to me, ‘There is faeces on the floor someone needs to clean it up’. She marches off. There are no other members of staff around or in view and she leaves the ward.
A little later the nurse in charge and an HCA are in and out, and both carefully step around it to reach the bedsides. It feels like we are all pretending it is not there. Eventually they identify some more near the sink and the HCA clears it all up.
Site H, ward 16, day 21 (night shift)
The isolation of decision-making around continence care, assessing who and what to prioritise against the demands of everyday timetabled care, meant that, for staff, exhaustion and burnout developed over shifts and rotations:
I chat to the nurse. She is sitting at the small nurses’ station by bay 3. There are two huge piles of folders on the desk. On the top of one is a further pile of fresh (but unpacked) continence pads. She is going through the folders and filling the bedside records within the files for both bays 3 and 4 and tells me, ‘I am trying to do everything but most of these patients need two [members of staff] so I have to go and find an HCA and then someone needs me and needs something and I just can’t do it all! It’s also so hot!’ (The heat in this ward is oppressive and a nurse fainted on the previous day shift). She goes to side room 4 and returns with a disposable bowl covered with a paper towel and heads to the sluice.
The HCA tells me, ‘I have the pad round to do, I have a loose routine in my head and when it goes like this you re-enter yourself (in the routine) at the next person you see . . . it’s like the patients don’t lose out too much because we run around like idiots, so in the long run we pay the price’.
As we talk, we look over to the nurse at the nurses’ station who is about to start the medication round and is adjusting some i.v. equipment. She doesn’t look well and the HCA calls over, ‘Are you OK?’.
She says she needs to sit down: ‘But I don’t have time!’.
‘I will get you some water’, and heads to the kitchen and gets her some water.
When she returns, she then decides between answering the phone and continence pads, looking from one to the other she chooses continence pads. She tells the student nurse to have a drink of water as well.
She opens the bedside curtains and wheels out a commode, the lid is balanced on the seat and there is tissue poking out. As she wheels it to the sluice room, she turns to me, ‘People don’t understand, but there is not enough of me, I haven’t stopped, I think it’s an alright day when everyone is OK, but not if someone is poorly’.
The nurse adds: ‘When you are doing the drug round and have three people who want to go to the toilet then what do you prioritise!’.
Site G, ward 14, day 16
Theme 5: impacts of continence care and ‘pad cultures’ on recognition of the person and understandings of dementia
In the previous sections, our observations revealed that continence care for PLWD was viewed as a source of unscheduled, conflicting and ‘heavy’ care work in these acute wards. Staff must find ways to incorporate continence care into the wider institutional timetables of care delivery, without creating risk (i.e. the fear of falls) and without affecting the pace and schedule of care during each shift (i.e. ‘falling behind’). In response, ‘pad cultures’ dominated these acute wards, with a focus on containing continence care to fit the wider schedules governing the organisation and delivery of bedside care. In many ways, ‘pad cultures’ reduced the act of continence to the biological (i.e. the patient producing waste that required containment, removal and disposal). By conceptualising continence in this way, the personal impacts of continence care on PLWD can remain unrecognised. The expected pace of work could mean that ward staff did not always have opportunities to recognise patients’ unarticulated and embodied care needs or consider the impacts of routine continence care practices on the person. The impacts on the ward staff responsible for delivering this care also appeared unrecognised in these wards and by the wider institutions.
This characterisation of the dependency of PLWD in these acute wards had wider and significant impacts on the person, and these impacts were intrinsically linked to ‘pad cultures’. Placing a person into ‘pads’ and institutional gowns, and containing them at the bedside, could lead to the reclassification of these individuals and people (both PLWD and older people) grouped together in a given bay or ward area. This could also extend to recognition and understandings of behaviour. Walking to the bathroom could become understood by staff as ‘wandering’, no longer a sign of continence, capacity and capability, but a risk of ‘falls’ or ‘absconding’, and recognised by staff as a sign of confusion or resistance to ward care. Distress at experiencing intimate continence care from strangers, often carried out in silence or without adequate warning, could quickly become perceived as ‘aggression’. Forms of embodied communication of continence care needs could be viewed as transgressive or as a form of behaviour constituting a feature of a patient’s dementia, rather than an expression of underlying need.
Clothing, contagion and the recognition of ‘high dependency’
Although there was some variation, it was common practice for PLWD who were wearing pads (and this often extended to older patients) to also be dressed in hospital-issued institutional gowns (with ties at the back) and pyjamas in these acute wards. These items of clothing were typically ill-fitting and loose; they were also easily removed and replaced, which aided the use, checking and changing of ‘pads’ at the bedside.
Staff preferred patients to wear institutional gowns rather than their won day clothes, as this improved access to continence technologies. However, institutional gowns are another way in which (in)continence is highly visible in these wards, othering older patients, and particularly those living with dementia, from the general patient population. The everyday use of gowns was also a response to the routine failure of pads as a containment technology (i.e. soiled clothing and people running out of clean clothes brought in by family). Therefore, the requirements and failures of the pad technology itself are, as expected, normalised and prioritised. These practices could become applied to a wider group of older patients in a bay or a ward as they become viewed as equally high dependency:
Posters in the hall state – ‘[Hospital] is working to end PJ paralysis – get dressed, get up, get better, get moving’. All the patients in the ward are wearing hospital issue gowns and pyjamas and I have yet to see anyone wearing their own clothes other than a cardigan or jumper over the top of a gown. Only one person has left the bedside today and I have seen him get up and walk to the bathroom, the HCA tells me: ‘The only patient who is continent is 22, he is continent’.
Site H, ward 16, day 25
This institutional clothing also exposed the body, which meant that these ‘pads’ were highly visible. The wearing of these typically bulky continence products was readily apparent to everyone in these wards. The combination of ‘pads’ and institutional clothing was a marker that staff recognised PLWD as representing high-dependency patients. This could overshadow individuals and their capabilities:
I note that on the semi-public admissions board 11 of the 23 patients have a flower symbol (representing dementia) attached to them. The nurse in charge of the ward tells me: ‘95% of people on here all wear pads, it’s just an age thing, this is really a dementia ward, it’s general medicine, but it’s mainly people who have falls and dementia. Thursday we had four one-to-one carers because they were confused, frightened, want to leave, need to be watched. We wanted four but only got three’.
The HCA adds, ‘We have a new lady really poorly and scoring 8, she’s ever so confused, she had an accident all over the floor because she’s confused, but all of them are incontinent, every single one of them and we only have two nurses on so you can’t do a lot, because as soon as I have done the washes it’s time to turn them and do their pads’.
The woman in bay 3 (4) has been sitting in the bedside chair all morning. She is wearing a pink hospital gown with a white cardigan over the top and red hospital socks on her feet. She gets the walking frame by her bed and walks steadily across the bay to the bathroom opposite.
Site G, ward 14, day 5
Institutional clothing in hospital wards affects both the male and female body, is a significant feature of the presentation of the ageing body in these wards and has a powerful role in reinforcing understandings of PLWD.
This further reinforced to all in the ward that the use of pads was usual practice in the care of PLWD, that is the ‘ways things are done’ in these wards.
These ‘pad’ practices had significant consequences in these wards and at the bedside. We identified processes of contagion and spread in their use in the care of PLWD, the recognition and application of continence care, and the category of who was believed to be ‘incontinent’, of ‘reduced mobility’ or of ‘high dependency’ in these wards. The established routine care practices believed to be appropriate for one group (i.e. patients who had a formal classification or diagnosis of incontinence) could quickly become attached to a wider group of PLWD and older people in these wards.
This could be exacerbated by common practices of ‘zoning’ or ‘corralling’ patients who shared specific attributes (e.g. by assessments of dependency, condition or age) being placed together in these wards and bays. This often resulted in older people living with and without dementia being grouped side by side in bays and areas of these wards. Therefore, the routine organisational practices and delivery of bedside care believed to be appropriate for one group could quickly become recognised and applied as standard care for a larger and heterogeneous group of PLWD and older patients aged ≥ 65 years, but who were understood to be a homogeneous population with similar care needs in these wards.
We found that in these ‘high-dependency’ bays, all patients could become placed in continence pads, regardless of their continence status prior to and during their admission. Here, a nurse discusses continence assessments of patients in what is categorised as a ‘high-dependency’ bay only in the context of the wider capabilities and dependencies of her patients. The mobility of her patients, not being ‘mobile’ or ‘reduced mobility’, is central to her assessments and is associated with the expectation that wearing ‘pads’ was an essential feature of their bedside care:
Speak to the RN [registered nurse] on bay A. Reading from her hand-written handover notes she tells me about the patients (only asked about 3 and 4) on this bay. She tells me: ‘3 is usually mobile with assistance from a frame, but vastly reduced at the minute. 4 is really not well, has dementia but also blind, not mobile. 5 has reduced mobility and cognitive function, but the other patients are fine’. She is reluctant to discuss continence, talking around this with mobility. She did not confirm but suggests that 3, 4 and 5 are all wearing pads (I know that 3 is for certain as it has been visible).
Site F, ward 11, day 16
Importantly, continence cultures on the wards explicitly extended to the routine and standard practice of using ‘pads’ in the care of PLWD, even if they were continent. Here, a woman living with dementia was able (with some support) to use a frame to walk the short distance (approximately 3 metres) from her bedside to the toilet opposite the bay and back. Despite this, she is expected by the ward team to wear a continence ‘pad’ at all times. This was observable and highly visible to the wider ward through the open-backed hospital gowns that she and the other patients in this bay were wearing:
On bay 3 the woman in bed 17 is up and out of bed. As she goes to the toilet, 18 is still on the phone, and 16 is awake, looking across the bay towards bed 18. The nurses’ buzzer red light is on above the door of bay 3. The nurses have not seen this as they are talking in the corridor besides the nurses’ base and the huddle of computer trolleys. 17 opens the toilet door and calls for help. The HCA goes over to her and 17 tells her, ‘I got giddy when I stood up’. With the door open, the HCA helps her up from the toilet to her frame. 17 is then able to support herself walking back to her bedside chair. Through the back of her open hospital gown a large clean pad is visible, despite what seems obvious continence and mobility.
Site H, ward 15, day 16
It was also a widespread practice for a wider group of older patients to be placed in continence pads, reflecting their routine use in these wards. However, staff also recognised that this did not reflect best practice. Here, this senior ward nurse reflects a widely held view among staff in these wards that ‘we shouldn’t use them’ and describes this standard use of pads as something that she recognises as undesirable, but feels unable to change:
The nurse in charge arrives. She is very friendly and welcoming. We discuss and tell her about the study. She picks up on continence products: ‘I do the order but I tend to underorder the full continence pads because I hate them being used. We use them with the confused patients, the wrap-around nappies, but they shouldn’t use them. One woman came in confused and she woke up and found herself in a wrap-around nappy and she was very upset to find she had been put in this. It’s one of my bugbears’.
Site F, ward 11, day 1
Continence technologies also restrict the person in more subtle ways. Given their size and bulkiness, pads appeared difficult to walk in, hampering the patient’s ability to move. This could mean that patients who were previously independently mobile now need to request assistance to leave the bedside to walk short distances. In addition, patients often required support in their application and removal of pads, creating a new level of dependence. These impacts were recognised by staff:
In the break room discussing continence pads with the HCAs on a break. We talk about the large wrap-around ones and one of the HCAs says, ‘They are the last resort, they take away their liberty, it’s a choice you are taking away’.
Site F, ward 12, day 17
Understandings of behaviour: ‘wandering’
Attempts by PLWD to leave the bedside and walk could also be quickly understood by ward staff not as a trip to or a search for the toilet, but as ‘wandering’, a behaviour without purpose and potentially a feature of their dementia diagnosis. As we have described earlier (see Clothing, contagion and the recognition of ‘high dependency’), leaving the bedside was typically discouraged for PLWD and patients aged ≥ 65 years. In contrast, the small number of working-age people in these wards were typically able to walk around unrestricted, use the bathrooms and leave the wards unchallenged by staff.
We observed that ward staff would regularly return PLWD to the bedside and rarely considered that they could be leaving the bedside because they had urgent continence needs. This could sometimes result in patterns of the person being returned to their bedside (or reminded to remain in their bed or at the bedside) multiple times during a shift, which could cause anxiety and frustration for ward teams and increasing distress in the person, who was not able to communicate their needs in the way staff recognised or understood:
Handover is finishing. As staff come out into corridors, I notice the woman from bed 20 quite far down the corridor, walking with the frame. She is 97 and has delirium with suspected (but undiagnosed) dementia and is wearing a large nappy-style pad, which is visible through the material of her hospital gown. A one-to-one carer stands in front of her, saying loudly ‘no, this way’, pointing with her arm back to the bay, her arm thrust out and pointing straight ahead. She calls the patient ‘mama’, ‘no mama, this way’. She does not explain to this patient, just repeats this command. The patient mutters under her breath throughout, turns slightly and walks in the other direction, the one-to-one carer stops her, so she turns and walks to the nurses’ station, leaving her frame. She sits down on one of the chairs, then stands and repeatedly tries to climb up on to the desk to sit, while the HCA admonishes her, warning that she will fall. The phlebotomist approaches, and takes this woman’s bloods at the nurses’ station, the one-to-one carer continuing to call her ‘mama’ as she talks through the process and reassures her. The patient whimpers as bloods are taken, but she does not resist the process. Afterwards she says, ‘Oh my God’ before muttering incoherently again. The one-to-one carer says, ‘Come on, back to your bed’ and this time she gets up and goes with her. [ . . . ] The one-to-one is still with her, still addressing her as mama, and insisting she stays in her bed. The one-to-one sits with her back to her, updating the bedside records on a computer on a mobile stand at the foot of her bed.
Site H, ward 15, day 2 (bold text represents shouting)
In the instance above, the act of leaving the bedside and ‘wandering’ eventually leads to the patient’s needs being recognised and her being permitted to walk to the toilet. We observed how these cultures of recognition and responses to ‘wandering’ were deeply engrained. The act of physically leading a patient back to the bedside was usually also accompanied by the repeated use of contracted set phrases and commands including ‘sit down’, ‘leave things alone’, ‘stay’ in bed or ‘turn around’. This also demonstrates the restricted understandings of the needs of PLWD, rather than a recognition that these patterns could reflect underlying discomfort, urgency or distress for the person or simply a desire to walk.
Reactions to intimate care perceived as ‘challenging behaviour’
Distress at experiencing intimate continence care from strangers, often carried out in silence, could become quickly perceived as ‘aggression’. These responses could be understood by staff as the impacts of dementia, but also as a wilful disregard for the routines of continence care and essential care more widely in these wards.
Here, the team carry out routine pad checks at each bedside of a bay, in turn. When they reach the second bed, they inform the patient that they are going to ‘check’ her ‘bottom’. As they do this, they switch from providing reassurance and instructions to the patient to talking to each other about the patient, her continence and what care is required, as though she is not there. Intimate care is necessary, and, although discussed between these two staff members, is not explained to the patient, who is clearly unhappy with this procedure:
The team discuss (3/2) as they head to her bedside.
[They use her first name] ‘Shall we stand you? We came to check and make sure you are clean’. They draw the curtains. ‘Stand up for us [first name], we are going to check your bottom’. They discuss her as they get gloves and a fresh pad: ‘Will she be wet?’ And they head back behind the screen, saying to her, ‘Sorry darling you don’t like it’.
‘She was soiled yesterday, I think they are giving her laxatives, we will probably have to change her’.
‘Sit down for us now, well don’t, there you go’.
‘It’s definitely from the laxatives’.
‘Can you sit back in the chair for me?’
‘Aaah don’t put your hand in it’.
‘Get more wipes . . . ’
The HCA heads out taking a large folded pad out to the sluice.
Site F, ward 12, day 21
Although staff were often very reassuring during continence care, they were also limited by the restricted language used in the care of PLWD in these wards. Here, the nurse in charge, while delivering continence care to a patient with dementia, repeatedly reminds the patient that she is ‘in hospital,’ as a way to prepare her for this intimate care:
The nurse has been incredibly busy. She is the nurse in change and also leads care within this bay. She has been reassuring the woman in 2/1 intermittently all day as she passes her bed, talking to other families, bagging and lugging large bags of dirty laundry through the ward. She gets a plastic pinny and a pad and closes the curtains around 2/1. She is very reassuring and gentle in her tone as she approached the bedside: ‘You are in hospital, you are in hospital, we are not going anywhere’.
In the background the radio is playing, ‘Now I’ve had the time of my life, No, I never felt like this before, Yes I swear it’s the truth, And I owe it all to you . . . ’
I realise this is Dirty Dancing. As this plays, care continues behind the curtains, everyone is silent in the wider bay apart from a regular sound of snoring from the bedsides.
Site G, ward 14, day 12
Patterns of distress were notable during the routine bedside rounds of personal care, particularly when PLWD required staff to support personal and intimate continence care. Staff would typically focus on and describe this care as checking and changing the ‘pad’, which was often carried out using restricted language or in silence. However, this did not prepare the patients (most often female) for this intimate contact. This could result in responses to care from PLWD that ward staff could interpret as ‘aggression’ or ‘refusal’, which could, however, be defensive reactions to unexpected or unprompted intimate contact.
In the example below, a patient in her 90s, admitted with a diagnosis of dementia, was observed on a cohorted bay of older women, many of whom also had a diagnosis of dementia and/or delirium. The patient had been admitted to this bay for several days, receiving one-to-one supervision, which was imposed because of her ‘wandering’ (the patient was able to walk independently but was considered a fall risk) and her ‘aggression’, which included punching and scratching at staff. We repeatedly observed staff describing her as ‘aggressive’ during the timetabled rounds of continence and personal care. The example below describes an incident where this does not happen, and, in contrast to other observed personal care she had received, the communication used by the nurse throughout clearly lets this woman know step by step what is going to happen and what is happening to her:
With the woman in bed 16 the nurse continues to talk the patient through every step. She is being really clear and focusing on each individual part of the process. There is a real focus on keeping the patient calm and informed. ‘I’m going to wash your face’. ‘I’m going to wash your legs’. ‘No, no, you don’t want that. It’s rubbish’. ‘I’m going to have to change your sheets, we will have to wash your pyjamas’. ‘Lie down. I have to wash your vagina’. She repeats this three times. ‘Is it OK? Can you lift yourself up? I’ll have to wash your bottom as well. Yes, it’s very wet. I’ll get it dried off’. The talking trails off as the wash continues. I’m surprised to hear talking so directly about washing her genitals. Normally this is not described by staff. But in explaining what she is going to do, there’s no shock and this patient, who is usually quite distressed during personal care, doesn’t cry. With the wash finished the nurse goes through the same process to get the patient dressed and back into bed. ‘Just going to put your new pad on. Let’s get your pyjamas on’. When this is finished the curtain is drawn back and the patient looks comfortable and appears to be falling asleep.
Site H, ward 15 day 12
The language of staff in these wards to describe body parts was so significant (see above) that when anatomical terms were used it was striking. In this example, it is notable that, when the body part was explicitly named, the patient, who was previously said by ward staff to be highly ‘aggressive’ during personal care, appeared able to recognise what the nurse was doing and why, and, consequently, fully co-operated with intimate care that had resulted in distress and resistance on prior occasions. However, more commonly, the challenges of communicating continence needs and the resulting distress could be observed among both PLWD and ward staff.
Chapter 8 Discussion
Parts of this chapter have been reproduced with permission from Featherstone and Northcott124 under licence CC-BY-ND-4.0.
This study aimed to deliver detailed understandings of the everyday practices and impacts of continence care for PLWD following an unscheduled admission in the acute hospital ward setting. Utilising ethnography permitted examination of those details of everyday life in acute wards that were, to the best of our knowledge, previously unexamined in the literature. In addition, ethnography allowed the investigation of the seemingly hidden and undiscussed activities and phenomena of the hospital ward, while placing them in the wider context of everyday care. We were able to examine the ‘hidden mechanisms’,119 the organisational infrastructures and the rationales embedded in the technical and procedural work of continence care as it was delivered in these wards. In addition, we observed how ward staff account for and make sense of the continence needs of PLWD, and how staff respond to and rationalise these needs and the consequences of their actions over time. We have presented findings that provide an original and detailed understanding of the social and institutional forces that shape and influence everyday organisation and delivery of continence care in these acute wards for this significant patient population.
The use of ethnographic ‘thick description’ in presenting our detailed empirical findings permits the reader to develop a strong connection to the social worlds of these wards. We shine a light on the multiple nuanced, complex and skilled everyday interactions involved in the practices of continence care carried out by ward staff (predominantly nurses and HCAs). Our detailed analysis provides understandings of the complex social relations occurring in these wards, and the ways in which the organisation and delivery of continence care at the bedside connects closely with and is informed by wider institutional expectations, policies and priorities,122 which, in turn, shape the personal impacts of continence care for both PLWD and ward staff.
Our analytic goal was one not of ‘representation’ or ‘comparison’, but rather of ‘identification’ (i.e. to reveal the social processes underpinning and informing the everyday practices of continence care for PLWD in these acute ward settings). This allowed us to identify the significance of continence ‘pads’ in shaping the cultures of care for PLWD.
In this report, we have focused on presenting our analysis on continence ‘pads’, which, we believe, is the most common and ubiquitous continence product on these wards. These ‘pads’ are widely used in the everyday bedside care of PLWD and have significance in informing wider cultures of care for PLWD in this setting. These products both produce and reproduce cultures of care, including the organisation and delivery of everyday continence practices. These products also have wider impacts, particularly for shaping staff understandings of dementia as a condition, the recognition of the needs of PLWD in these wards, and PLWD’s status in the organisational and wider institutional priorities.
The ‘pad cultures’ identified in these wards emphasised the routine use of continence ‘pads’ as a precautionary ‘just-in-case’ strategy (i.e. a ‘safeguard’ in preventing, but also containing, ‘accidents’ or incontinent episodes at the bedside) for PLWD admitted to these wards. ‘Pads’ were used regardless of independence, mobility, capacity and functionality. Importantly, we identified processes of contagion and spread in the recognition and application of this category of patient, which meant that this practice typically informed care for a wider group, including not only PLWD recognised as continent, ‘mobile’ and ‘self-caring’, but also the large numbers of older people in these wards.
This strategy was recognised as routine across these wards, legitimising care practices with real and significant consequences for the dignity, rights and outcomes for PLWD, and their status in the wider cultures of care in these wards. ‘Pads’ were transformed beyond a precautionary strategy into a routine feature of continence care. In turn, this allowed the practices to support maintaining continence (e.g. mobility, walking to and support to the toilets in these wards) to become deprioritised and no longer expected or required of the PLWD. Instead, there was an expectation (often explicitly stated by ward staff, but also embedded in other routine timetabled care practices at the bedside) that the person would not only wear the pad, but use it. This strategy was a feature of continence care across all of the wards observed and would often become a feature of care regardless of an individual’s continence, independence or preference.
The timetables of the ward and bedside care are critical. Expectations of maintaining the daily organisational timetables of bedside care were powerfully felt and were a palpable source of tension among nursing and health-care staff. An underlying anxiety of ‘falling behind’ during shifts was frequently discussed and universally feared. The development of these ‘pad cultures’ represents not a malicious act or poor care on the part of ward staff but, rather, a solution or ‘workaround’ to achieve the (both perceived and expected) pace of work, the institutionally mandated timetabled ‘rounds’ of routine and essential care, and the associated recording and monitoring practices at the bedside. The use of pads as a precautionary and containment strategy was not only a response to a person’s incontinence or their inability to independently walk to a toilet in these wards, but was believed to be necessitated by organisational constraints. The timetabled organisation and delivery of care during shifts appeared not to allow for urgent continence care needs to be prioritised by staff over other routine care or the associated recording practices. In turn, this organisational strategy acted to create urgency by discouraging PLWD from leaving the bedside and walking to the bathroom. Similarly, the use of pads as containment mean that incontinence or ‘accidents’ could remain undiscovered or concealed on the person and at the bedside until the timetable allowed.
According to ward staff, it was only by adopting such approaches that they could complete their timetabled routines of care and their recording practices, meaning there were reduced opportunities to respond to (or prioritise) the unpredictable and significant care involved in supporting the continence needs of the large numbers of PLWD in these wards. This informed understandings, expressed by staff across these wards, that this approach to continence care for PLWD was both legitimate and institutionally mandated. Many ward staff did recognise the significance of these approaches and the potential for the rapid deconditioning of PLWD, but did not see other ways of working that supported continence and independence as possible. This rationale was expressed by staff to the research team, and also to each other, and was also evident in staff explanations and rationalisations to PLWD and to their families at the bedside.
The goal of reducing the risk of ‘falls’, particularly for this patient population, was deeply embedded in the rationales supporting ‘pad cultures’. This risk is legitimate for many PLWD; however, staff were motivated to reduce this risk not simply for its own sake, but also because they were universally fearful of the sanctions (for the ward and themselves) that would be imposed if a person living with dementia fell while in their care. Therefore, containment at the bedside through the use of continence ‘pads’ saw continence care transformed into a form of restrictive practice in these wards, lessening perceived risk by reducing or eliminating the requirement to leave the bedside at the expense of or despite the preferences and needs of the person. In these wards, a person living with dementia independently trying to get out of bed or walking to the bathroom (including using a walking frame) could provoke high levels of anxiety in ward staff and was a form of independence that was generally discouraged and often forbidden (although we identified notable exceptions to this).
This ethnographic study has revealed that continence care represented a significant and central aspect of care work for staff in these wards. A key feature of discussions with ward staff about continence care was their experience of it as ‘heavy nursing’. When explaining the ‘heavy’ burden and the ‘heavy load’, staff described the physically demanding nature of this care and also the experience of feeling abandoned and of being isolated with the responsibility of caring for large numbers of PLWD who required highly supportive care. Staff were further isolated by the perceived status of this care work. Much has been written about continence care and its status in nursing. 67 In these wards, continence care was typically invisible to teams and services entering these wards and was viewed as low-status work to be delegated to others, with little effect on the experiences and outcomes of their patients. As we have discussed throughout our findings, ward staff were aware that the continence care strategies adopted on these wards did not reflect the care they wanted to provide to their patients. However, more widely, there were no indications in these wards and their cultures that continence care was recognised by these institutions as critical for care quality and having significant implications for the individual person living with dementia in their care.
Time is of significance here. Continence care that supported the independence of PLWD was often viewed as taking ‘too long’ and a source of delay that could have an impact on other routinised timetabled aspects of bedside care. Our synthesis142 identified the difficulties of communicating continence needs and the importance of health-care staff having the time to recognise and respond to the non-verbal and affective cues PLWD may use to convey their need; however, these ‘pad cultures’ included the requirement of ‘permissions’. Strategies of containment and the requirement for continence care to be carried out at the bedside, in turn, also generated significant care needs and care work.
As we have described in Chapter 7, Containment, prompting and the prioritisation of urgent and visible continence care, the large wraparound continence pads typically used in these wards regularly failed in their primary purpose (e.g. pads leak, smell and can damage skin) with the result that it was necessary not only to remove and replace ‘pads’, but also to carry out significant personal and intimate care (e.g. undressing, washing, changing clothes and changing sheets). For staff, this involved repeated trips to linen stores and sluice rooms, which were often located far from the patient’s room or bay. This also required care that was far more personally invasive than if the patient had been supported to the toilet, invasiveness that routinely caused significant distress to patients. In addition, even the use of pads in the care of PLWD who were assessed as ‘mobile’ and ‘self-caring’ created care work. The bulky nature of the wraparound pads and the dexterity needed to change them meant that PLWD (and also many older people without a diagnosis of dementia) required additional support in walking to toilets and in changing pads, which, in at least some cases, was unnecessary.
The pace of (expected and perceived) care at the bedside meant that the independence and autonomy of PLWD could become a reduced priority. When staff perceived that they were ‘short’ (i.e. understaffed) or were ‘falling behind’ with the wider timetables of bedside care, the opportunities for patient independence became reduced and a reliance on the use of ‘pads’ became further prioritised. At these junctures in shifts (although we found that this typically occurred at some point during almost every shift), patterns of prompting and the procedures of assisting a person living with dementia to use a bathroom could quickly become perceived as too time-consuming, clashing with and potentially delaying other institutionally mandated timetabled tasks of care (e.g. observation, medication rounds and the timetables of other teams, including the arrival of medical teams or mealtime deliveries). Although staff in these wards discussed and recognised the importance of providing care that supported independence, at these points in the shift, these routines could become ‘tightened’53,124 and reduced to the use of a more limited range of (verbal and physical) techniques and approaches with a focus on increasing their efficiency, with pads used to contain both continence and the PLWD at the bedside. Instead of ‘prompting’, ‘pad checks’ or a reliance on containment came to the fore until the timetables permitted staff to attend to continence care.
This ‘tightening’ also created its own forms of continence routines and rituals (e.g. ‘prompting’, ‘pad rounds’ and ‘pad checks’) in these wards where ward staff (typically HCAs) prompted continence and ‘checked’ if ‘pads’ required changing at points during shifts. In practice, in these wards, these routines appeared to have transformed from ‘prompted voiding’ (i.e. an established approach that combines a schedule to support toileting with ‘prompting’ from health-care staff or carers for people with cognitive impairment)183 into more limited routines and practices at the bedside. These routines reduced opportunities for flexibility and for staff to see and respond to an individual’s urgency. These routines also appeared to have transformed into the far more restrictive practice of ‘pad checks’, which emphasised the centrality of checking and replacing continence pads at the bedside. ‘Pad checks’ could also become a more sporadic and ad hoc practice, which could be interrupted or stalled during shifts once staff perceived they were at risk of ‘falling behind’ or could be deprioritised and become viewed as possible only during ‘quiet’ points in the shifts. Therefore, continence care often became transformed and reduced to containment practices and the ‘checking’ and replacing of soiled or wet pads as part of other scheduled activities during a shift.
When ward staff attempted to fit the urgent continence needs of a person living with dementia in the timetabled order of bedside care, this could lead to significant patient distress, either through difficulties in recognising care needs and responding to urgency or through the level of intimate continence care required. There also appeared to be little recognition of the urgency or distress for the person of being unable to reach a bathroom, being unable to avoid using a continence pad or of wearing the soiled pad, and of the immediate needs or the practical considerations once a person had ‘used’ or soiled their pad. Importantly, such distress could also become viewed as a feature of a person’s dementia and could cause distress for family members and visitors. Our synthesis identified the significance of health-care staff attitudes to continence care and incontinence. 142
By reducing continence care to these forms of prompting and checks, the important opportunity that continence care provides for staff to provide wider supportive care and comfort to the person was overlooked (i.e. care and comfort that requires time to see the person and to support their wider needs). Our synthesis142 also identified the importance of language, and the need to incorporate interpersonal and communication skills into the context of continence care in training for those staff working with this patient group. Despite its apparent centrality in the everyday work of these wards, continence care for PLWD (and older patients) was often carried out in silence or with staff using a restricted repertoire of language to communicate continence care and to explain and describe the intimate care that was happening or about to happen. The naming or failure to name body parts, particularly genitalia, bodily functions, urine and faecal matter, the naming and description of continence technology, and the language and etiquette of communicating continence needs during personal care for PLWD (and older patients more widely) was notable. Some aspects of continence care were not discussed at all or by using humour only, whereas other aspects were talked around or euphemisms were used. Importantly, there was little evidence that staff were able to check the person’s comprehension or vary language to suit the individual.
Robustness of the results and limitations
This study set out to explore and establish how ward staff account for and make sense of the continence needs of PLWD, how staff respond to and rationalise these needs, and the consequences of staff actions over time. As a result, we have presented findings that provide an original and detailed understanding of the social and institutional forces that shape and influence everyday organisation and delivery of continence care in these acute wards for this significant patient population.
By collecting 180 days of observational data across six acute wards in three hospital sites, which included a range of institutions, geographies and patient demographics, we were able to respond to the potential limitations of transferability. This long-term ethnographic engagement with these ward settings meant that we were able to move our analysis beyond individual incidents and a descriptive account to build up an analysis that was grounded in observations. This analysis allowed us to achieve a theoretical interpretation of the data to deliver understandings of the cultures that shaped and reshaped the practices of continence care and the wider care of PLWD across these institutional settings. Although the staffing, teams, technologies, expertise and interventions to support PLWD varied across sites and wards, in these ward settings the organisation and delivery of continence care, the prominence of ‘pad’ technologies and the ‘pad cultures’ identified in this report remained relatively stable as embedded practices of everyday bedside care for PLWD.
Our aim in using ethnography to examine everyday continence care, a complex and highly sensitive topic, was to access unspoken and tacitly understood aspects of such care. 110 The ethnographic approach enabled us to take into account the perspectives of ward staff, patients and families, and wider clinical and hospital staff108,109 in these acute wards. However, as experienced ethnographic researchers, the team working in these ward settings was also acutely aware of the potential for the presence of observers to influence practice and contaminate data. Prior to the research, we did consider the potential for the Hawthorne effect or ‘participant reactivity’ and acknowledged that staff behaviour may be changed by the researcher’s presence in the wards.
In response, and based on our prior research in acute wards,106 our design included extended periods of observation in each ward, with each individual ward setting observed for 30 days over 8 weeks, with periods of observations lasting from 2 to 6 hours. This time frame meant that staff became used to the presence of and developed relationships of trust with the researchers (KF and AN), which we hoped would mitigate the potential for observations to influence practice. 184 However, we recognise that the behaviour of the teams and individual members of staff working in these wards may have been changed by the researchers’ presence in these wards.
It is not possible to eliminate the impacts of the presence of observers; however, a key strength of an ethnographic approach is that any performance observed, regardless of how it is staged or influenced by the researcher presence, can reveal critical insights by displaying how people see themselves and how they want to be seen. 184,185 By adopting a grounded theory approach, we were able to carry out theoretical sampling in these ward sites, and this also enabled us to focus on the representativeness and consistency of events and concepts, rather than individuals and people. To identify and understand everyday practice, we observed multiple rotations of staff, patient admissions and events in these wards that had the potential to influence care delivery. In situ ethnographic interviews with staff, PLWD and their families also provided the opportunity to test and refine our analysis during observations, in line with our grounded theory approach. This reflects a key strength of ethnography, and remedies a common weakness in many qualitative studies, which is that what people say in interviews may differ from both what they do and their private justifications to others. 126 These approaches were central to collecting high-quality data to achieve methodological rigour and aid theoretical interpretation of the data.
As can be seen in the results presented, during our extended engagement in these wards, PLWD (and older people in these wards) would frequently tell us that they wanted to go to the bathroom. In addition, these people would ask for support and, more widely, would often share their concerns (which were not always related to their admitting condition or present comfort, but, instead, about loved ones, possessions, family and pets, or how they would afford to pay for their food or their care). The research team (with patient consent) would inform ward staff of these concerns. The researchers were often the only people present on or around these wards for uninterrupted periods of time. As a result of this, sometimes, when ward staff were not present or able to be called quickly to a bay, we provided immediate support and help. For example, if we observed a patient placing themselves at immediate risk of falling, injuring themselves or leaving the ward, we would call staff or, if necessary, intervene to protect the patient. Although we accept that this may have, on occasion, contaminated the purity of this research, the welfare of the people in these wards was always our priority.
Practical limitations presented themselves throughout the research. As a result of the ethics and governance permissions granted to the study, the team was unable to follow or track patients once they were transferred to other sites in these hospitals. This was mitigated by the inclusion of medical assessment units (where people are admitted for assessment and are either discharged or transferred elsewhere) and general medical ‘care of the elderly’ wards (which typically have additional support and services in them for PLWD), which enhanced the potential for data collection to include PLWD at admission, following transfer and at discharge. The inclusion of these units and wards also allowed the study to explore whether or not there were variations in the organisation and delivery of continence care PLWD received across these acute settings.
The researchers could observe and take fieldnotes for only a limited number of hours and shifts at each site. It was rarely possible for the researchers to continue observations in the wards for the extended period required to see a patient’s response to and the impacts of continence care over the entire period of a shift or their admission. It was also not uncommon to arrive at a ward and be told that we had missed an incident. However, these incidents and events often represented the extraordinary and not the everyday practices and cultures we wanted to explore. These incidents also reflected that, although staff knew of the purpose of our research and our goal to improve care, staff often misinterpreted the context of our observations and data collection.
A significant limitation of this study, which could not be predicted at the time of data collection and analysis, was the outbreak of COVID-19 during the production of this report. All data were collected between October 2018 and October 2019. Therefore, these data reflect everyday acute ward organisation, culture and practice prior to the outbreak of the COVID-19 pandemic and the resulting changes to the delivery of care. Owing to infection control measures, the researchers have not conducted any observations during the pandemic and cannot say if the measures taken to control the spread of COVID-19 in these wards have changed the ways in which continence care is delivered and the continence needs of PLWD are met.
Recommendations for future research
In this study, we had hoped to explore if continence care was further impacted by the intersections of gender, race and ethnicity,84 and we have identified some complexities in continence care and its impacts and interactions with gender. We have included within the data collection the experiences of people in ethnic minority communities who were living with dementia and did explore these individual experiences of care to inform our broader analysis. However, to bring the experiences of the small number of individuals from diverse communities together within our analysis lacked methodological rigour. We do not want to further contribute to the longstanding ‘black box’ research approach of grouping the experiences of individuals from diverse communities together, which has been widely critiqued. 186–188 Although research in the field has provided generalised understandings, it has yet to adequately address the specific needs of diverse populations186,189 that are also living with dementia. We believe research is required that focuses on the experiences of specific communities. This research should explore the complexity of intersectional experiences of living with dementia. We are currently working to support researchers to take the lead in this research.
Our findings indicate a pressing need for a programme of research that examines the timetabled organisation and delivery of task-based routine bedside care carried out by nursing staff and HCAs. The modern hospital is typically represented as a site of great technological advancements. However, there was little evidence of new knowledge or interventions in these acute wards, or of their use in the organisation and delivery of care at the bedside. The routine and timetabled practices of bedside care work do not appear to be recognised or valued, have remained relatively stable and constant in their mode of delivery, and remain relatively unexamined. A programme of research is required to deliver the evidence base needed to inform the timetabled organisation and delivery of care (and care cultures) for these seemingly invisible routines of care work delivered to significant populations of vulnerable acute older patients, as this care work has powerful iatrogenic and longer-term impacts on both experiences and outcomes of PLWD (and older people) in the acute setting, including the potential for deconditioning and mortality.
Review of evidence and implication for decision-makers
-
Ward staff expressed the experience of feeling abandoned and of being isolated with the responsibility for continence care and for caring for large numbers of PLWD who required highly supportive care. In response, we urge greater institutional recognition of the importance of continence care as dignified and essential care work that has significance not only for clinical outcomes, but also the humanity of care and the personhood of PLWD, as well as other vulnerable populations in the acute setting.
-
Training and resources are required to support ward staff, and hospital staff more widely, working across the acute setting. This training should include how to talk about the body, its management and the intimate care and care needs to PLWD and older people during an admission. Training in communication and in the interactional expertise required at the bedside must reflect ‘work as done’ rather than ‘work as imagined’. Training should recognise and respond to the discomfort for staff across the acute setting in discussing body parts, processes and the practices surrounding intimate care, particularly with older people.
-
The education of continence care is not a significant part of the undergraduate nursing curriculum, which typically does not provide ‘skill-based teaching’ for what is widely perceived to be a practical routine task to be learnt predominantly at the bedside during clinical placements and in practice. This produces and reproduces current cultures of ward care as standard practice, instead of delivering evidence-based training in a significant aspect of care in the acute ward setting and this, as we have presented in the findings of this research, can have significant impact on both PLWD the ward staff caring for them. The results of this study indicate that there is an urgent need to invest in the development and delivery of evidence-based nursing education in continence care and in the care of PLWD in the acute setting in nursing education.
-
In this study, staff often expressed the view that, although they wanted to support their patients’ continence, they believed it was not possible to work in other ways. NHS organisations need to support wards and ward teams to develop ways of working, particularly in the organisation and delivery of bedside care for PLWD, that supports continence and that respond more flexibly to patients’ care needs, and to their mobility and independence more widely.
-
The reduction of risk for this patient population, particularly of ‘falls’, was deeply embedded in the rationales supporting ‘pad cultures’. Falls are a legitimate risk for many PLWD; however, staff were not simply motivated to reduce this risk for its own sake, but were universally fearful of the sanctions (for the ward and for themselves) of a person living with dementia falling while in their care. The NHS and hospital institutions must recognise that the introduction of such policies and the associated sanctions can have unintended consequences on care cultures. Institutions need to monitor whether or not these policy interventions are informing the cultures of care in acute wards, in what ways and with what consequences.
Outputs and dissemination
We are using this research to develop and deliver outputs focused on service organisation and training staff in the acute setting. In response to COVID-19 restrictions, we focused our attention on delivering outputs that informed policy and connected with and developed networks of practice, taking full advantage of remote methods to offset access difficulties.
To inform policy, we have worked with the Welsh Assembly Government. Katie Featherstone attends the Welsh Assembly Government Cross-Party Group on Dementia, having been invited to join in March 2021. Study findings have contributed to the Cross-Party Group report into hospital care for PLWD (yet to be published). Katie Featherstone is also a member of the Dementia Partners National Steering Group (Welsh Assembly Government), chaired by Innovate Cymru, Public Health Wales, which contributes directly to the dementia care programme to improve care in Wales. Paula Boddington has been appointed as a member of the European Commission Committee’s Atomium European Institute AI4People 2020 Committees, including the Committee on Healthcare, which makes recommendations on the implementation and deployment of ethical artificial intelligence in the health-care sector. Our NIHR research directly informed and is cited in the national Wales Safeguarding Procedures for Children and Adults at Risk of Abuse and Neglect, which was published in April 2020. 190
The team have presented the study to a wide range of audiences, with invitations to speak to acute clinical staff, allied health professionals, PLWD and academics nationally, including:
-
the East Midlands Dementia Education Day (December 2021)
-
Continence Team, Aneurin Bevan University Health Board (October 2021)
-
the All Wales Inpatient Falls Network (November 2021)
-
the Clinical Board of Dementia Champions, Cardiff and Vale University Health Board (July 2021)
-
NIHR Applied Research Collaboration North Thames and the Centre for Health Care Innovation Research (June 2021)
-
Alzheimer’s Society, Dementia Action Alliance and Public Health Wales event to support the Dementia-Friendly Hospital Charter (Wales) (March 2021)
-
Framing Ageing: A Clinical, Cultural and Social Dialogue, Trinity College, Dublin (March 2021)
-
East Midlands Medical Sociology Group, British Sociological Association (February 2021)
-
the Salford Institute for Dementia (March 2021)
-
Wales international conference Advancing Dementia Care Cymru, a collaboration between Public Health Wales Improvement Cymru, The Royal College of Psychiatrists (Wales) Old Age Faculty and key partners from across Wales (February 2021)
-
Medicine, Science and Culture Group, Cardiff University (December 2020)
-
Centre for Research in Communication and Culture Seminar Series, Loughborough University (November 2020)
-
3 Nations Dementia Working Group: Our Experiences of Hospital Care During a Pandemic (November 2020)
-
World Hospice and Palliative Care Day event, De Montfort University (October 2020).
A primary research goal was to update existing ward-based recommendations for models of care and the organisation of nursing and HCA care work to ensure support for the quality and humanity of continence care. This includes integrating continence care in existing risk assessment (e.g. falls), rehabilitation strategies and discharge planning. In response, we have worked with key dementia care, clinical and policy networks to deliver new knowledge that has informed and contributed to the following:
-
The development of the Dementia-Friendly Hospital Charter (supported by Welsh Assembly Government). The Charter sets out the standards for all hospitals in Wales to create dementia-friendly environments for PLWD and their families and carers. The Charter’s purpose is to focus on improvement and to support the embedding of the dementia-friendly principles in hospitals. Katie Featherstone was a committee member and was invited to present the research to inform the discussion of what is required to improve care for PLWD in the acute setting, with the Charter drawing directly on this NIHR research.
-
Presentations and discussions with the All Wales Inpatient Falls Network (November 2021). The goal, here, was to develop awareness of the role of risk management and policies in ward cultures of continence care for PLWD.
-
Presentations and discussions with clinical boards and dementia champions to discuss ways to improve continence care in acute wards.
-
Presentations and discussions with the Executive Director of Nursing, Associate Director of Nursing and Continence Team, in a participating Health Board. We are working together to develop and deliver training to support ward staff using an improvement collaboratives approach.
-
Presentations and discussions with the Welsh Ambulance Service and the Mental Health and Dementia Steering Group to discuss risk assessment, how to prevent inappropriate hospital admissions and how to improve ambulance environments for PLWD (March and May 2021).
Another goal was the identification of factors in organisation and ward culture (e.g. practices, routines and interactional styles) that can improve or worsen the experiences and outcomes of PLWD who have continence needs. This may include approaches to facilitate the integration of key elements in handovers and observation rounds. In response, we have carried out the following:
-
We have worked closely with one of our participating NHS sites to collaborate with and support the continence team. The research and development director has recognised that the team and this NIHR research has ‘supported nursing leadership around dementia care within our acute hospital care settings [which serve a population of 600,000] and promoted the research culture and capacity within our organisation’.
-
We have collaborated with Dementia UK (London, UK) and admiral nurses. Dementia UK’s head of research has communicated that the team and this NIHR research ‘have been particularly influential in helping us to refine the admiral nurse “offer” in supporting the acute sector to deliver person-centred care . . . the numbers of acute care partnerships we have are increasing exponentially as a result’.
-
We have supported individual dementia specialist nurses working in the acute setting, providing remote support via e-mail and Zoom (Zoom Video Communications, San Jose, CA, USA) to support the development of organisational interventions to improve care for PLWD in the wards.
The research team are in discussions with Dementia UK to establish a community of practice focused on the care for PLWD in the acute setting. Networks and individuals in the acute setting will be invited to join when this is launched in 2022.
A further goal was to create training targeted at acute staff (i.e. nurses, HCAs and allied health professionals), carers and families to support continence care for PLWD, including organisational and interactional techniques that facilitate the quality and humanity of continence care. In response, we achieved the following:
-
As a direct result of the research, Public Health Wales Improvement Cymru and NHS Cymru, invited Katie Featherstone, Andy Northcott and Jane Harden to design and deliver a training programme for all seven NHS health boards in Wales. This was accompanied by training for nursing and ward staff from three NHS trusts in collaboration with Dementia UK. Pilot training took place in one health board in November 2019. Nine further sessions were scheduled to take place from March 2020 onwards, but were postponed because of COVID-19.
-
In collaboration with NHS health boards in Wales and NHS specialist teams in continence care, the research has directly contributed to and is cited in the development of the NHS e-learning module ‘Continence’. This will be available to all NHS staff via the electronic staff record portal for Wales. Prior to our involvement, this portal did not contain any specific advice on continence care for PLWD, including the interactional or communication skills required.
-
Masterclasses (via video and factsheets) were held for hospital staff on continence care, decision-making and management for PLWD and integrated into undergraduate nursing and allied health professional curricula, including –
-
a 3-hour masterclass on dementia care, patient safety and risk via a postgraduate nursing module at Cardiff University (November 2020)
-
a 3-hour masterclass on ‘caring for the person with dementia in acute settings’ for undergraduate (first-year) nursing students at Cardiff University (December 2020)
-
a 2-hour masterclass on ageing and health for 360 third-year undergraduate students via the De Montfort University (Leicester, UK) Health and Wellbeing in Society programme.
-
Capacity building
The researchers believe that this study could have a significant impact on improving continence practice, raising continence awareness and improving the experience PLWD have during a hospital admission:
-
Discussions are under way with Innovation Cymru, Public Health Wales, Dementia UK and members of acute hospital trusts in England and Wales to use the study findings to pilot interventions to improve continence care.
-
Katie Featherstone developed and co-ordinated a training network to support early career researchers and mid-career academics working in the field of dementia research via the NIHR Dementias Portfolio Development Group (NIHR funding). This involved a series of monthly (2019–21) online workshops that delivered research training and mentoring to a cohort of 12 early career researchers. The series was rated highly by participants and, in response, Alzheimer’s Research UK contacted Katie Featherstone to discuss how to build on this initiative and expand its reach to develop a larger programme to support the development of early career researchers working in the field of dementia research. In addition, Katie Featherstone was invited to present the programme to The Dementia Research Funders Forum in January 2021.
-
We have developed a research network with leaders in the field of continence care and dementia, which includes international collaborations with colleagues in Australia, New Zealand and Finland, to build on this study, with further research and publications in development.
A publication strategy is in place following this report, which will target high-impact journals in nursing, sociology and dementia.
Theoretical developments from this research are expanded in Wandering the Wards: An Ethnography of Hospital Care and its Consequences for People Living with Dementia. 124 To date, this open-access publication has been in the top 10 anthropology books on the Amazon Kindle store (URL: www.amazon.co.uk/kindle-store-ebooks-newspapers-blogs/b?ie=UTF8&node=341677031) since publication. In addition, the publication was shortlisted for the 2021 Foundation for the Sociology of Health and Illness Book Prize. 191
Chapter 9 Patient and public involvement
Patient and public involvement (PPI) was central to and integrated within all stages of this study, and our overarching goal was to ensure that we included a wide range of experiences of living with dementia, which includes supporting those who are often under-represented in research or who may find verbal communication difficult. We were also aware that the experiences of PLWD and carers may be very personal and have often been silenced, with traditional research methods or public consultation approaches, in turn, eliciting emotions that can be hard to express. In response, we employed four interlocking and integrated approaches to support involvement:
-
We worked closely with our Carer Steering Group and Study Steering Group, which included PLWD and carers, to facilitate regular involvement in the direction and governance of the research.
-
We organised large-scale consultation events, attended by 60 PLWD and carers (Cardiff, UK, 2018 and 2019), which involved regular discussions between PLWD, family carers, researchers and the wider team about the direction of the research, the analysis and development of the findings.
-
Participants engaged in an arts-for-health enquiry in which they collaborated with an artist to produce creative pieces (n = 25) reflecting their personal experiences of being in hospital or caring for someone with dementia who has been hospitalised. This involved an opportunity to record their stories (n = 7) on camera in collaboration with filmmakers to raise awareness through sharing their personal stories.
-
We delivered five engagement events in Cardiff, which involved 80 older people and PLWD from within ethnic minority; lesbian, gay, bisexual and transgender; and disability communities to discuss dementia care and involvement preferences in the research. In addition, we developed collaborative relationships with organisations with a specific remit to support communities living with dementia that are often excluded from research, including Diverse Cymru (Cardiff, UK), Alzheimer’s Society, Women Connect First (Cardiff, UK), British Deaf Association (London, UK), Down’s Syndrome Association (London, UK), Royal National Institute for Deaf People (London, UK), Stonewall Cymru (Cardiff, UK), the Mentor Ring (Cardiff, UK), Nubian Life (London, UK) and the Sub-Saharan Advisory Panel (Cardiff, UK). The principal investigator lead (SV) also conducted 20 in-depth interviews (face to face, by telephone or on Zoom) to explore the experiences of PLWD, as well as those of their families and carers.
Across these activities, key experiences and concerns for PLWD and family carers were identified, and these are discussed below.
Continence care
Participants reported that ward staff expected all PLWD to be incontinent. A significant belief across these groups was that PLWD who were previously continent became incontinent as a result of a hospital admission, and that this was caused by these assumptions and the clinical care they received during an admission. During the workshops, a carer tells her story through the collage to depict the obstacles her mother faced in regaining mobility and self-care during her last stay in hospital. The groups strongly believed that these approaches to continence care were a result of poor staffing and high staff turnover in acute wards caused by NHS funding cuts. Carers also reported a lack of dignity in the continence care provided to PLWD, with continence care for this patient group witnessed as public and visible to others in the wards.
Discharge delays
The groups described that becoming incontinent during an admission had long-term implications for the person, the organisation of their social care support and their opportunities to return home. Carers were key advocates in the discharge of PLWD from hospital; however, they expressed frustration at how long this took and how much pressure was required to get a relative living with dementia discharged. During the workshops, one carer described how her mother believed she was in an asylum while in hospital and her delayed discharge was likened to the transition from darkness to light, to going from the ‘mess and tangle’ of ‘hell’ back to a luxurious ‘feather bed’ of home surrounded by the warmth of those who knew and loved her.
The experience of stigma associated with a diagnosis of dementia
Participants spoke about the invisibility of living with dementia as both a physiological and a social experience. Hospital staff were described as not seeing the person, but instead labelling patients by their condition (i.e. ‘dementia’). Carers reported that staff responses to a diagnosis of dementia included giving memory tests (e.g. the Montreal Cognitive Assessment or a mini mental test) to the person when they were acutely ill, whereas other acute admitting conditions remained undiagnosed or diagnosed late. One carer noted that ward and medical staff assumed all symptoms were related to a person’s dementia, which meant that other common conditions, such as sepsis and delirium, remained undiagnosed. In the workshops, experiences of depersonalisation and invisibility of the person living with dementia during an admission were depicted in black and white drawing to represent the loss of identity in institutions. One family carer shaped her creative piece to resemble a form of loudspeaker, covered with the phrases she heard repeated by her mother’s during her hospital admission, including ‘What are you doing to me’, ‘Help!’, ‘What do you want?’ and ‘Where am I?’.
Communication
Once a diagnosis of dementia was discussed, the groups believed that this overshadowed all interactions. In the workshops, a person living with dementia created an art piece named ‘Empty Boxes? Look Inside’ to reflect his experiences of ward staff seeing only his dementia diagnosis and to emphasise his individuality: ‘These boxes might look the same, but people are very different from each other. Don’t put me in a box because I have a label of dementia’. PLWD felt that their diagnosis meant that they were treated with less respect than other patients, with staff spending less time explaining procedures to them and, instead, continuing with care delivery without taking time to introduce or explain procedures to the person. The communication of ward staff with PLWD was described by carers as emphasising prohibitions and reinforcing what they were not allowed to do. Carers also reported a lack of awareness among ward staff that PLWD often communicate non-verbally, which meant that ward staff did not recognise or respond to non-verbal cues indicating underlying care needs. The therapeutic value of touch was identified as important, but lacking, in the acute setting. In the workshops, a man living with dementia chose an image depicting a hug to represent supportive care, whereas a family carer traced her own hands with blue chalk, writing around it ‘hands in dementia provide assurance, comfort, safety, security, friendship and stability’, and she became visibly moved and emotional as she described its significance to the wider group.
Restrictive practice
During his admission, one man living with early-onset dementia described the experience of observing ward staff regularly shouting at another patient living with advanced dementia, which made him fear for the future. Carers also believed that there was an overuse of antipsychotic medication in the care of PLWD during an admission because it suited the hospital environment, rather than reflecting a person’s medical need.
Feelings of fear and vulnerability during a hospital admission
Overall, across the groups, there was a lot of fear about hospital admissions. One person living with dementia described feeling very scared and vulnerable during her admission. This woman described that, when her husband could not visit and there was nobody to talk to, staff would not spend time with her or comfort her, even when she was crying. Across these groups, carers raised significant concerns and fears about what happened when they were not there. A carer described their fear of witnessing screaming behind closed doors and finding bruising on their partner living with dementia during an admission. Creative pieces during the workshops reflecting these feelings included a woolly string placed in a pile in the middle of the paper with the description ‘Life all tangled up, trying to cope, a mess’. In addition, a ballpen drawing of a rose reflected the vulnerability and helplessness experienced by PLWD and their family carers.
Carers
Carers described wanting to be more involved in their partners care during a hospital admission, but believed that they were not listened to, did not have rights in the acute ward setting and could be kept away from the ward. In the workshops, letters in the screw-top glass jar represented the ‘communication nightmare’ of trying to convey the care needs of a person living dementia to ward staff and the difficulty of the person in finding words to make their care needs known during an admission. One carer noted that there was antipathy towards carers on the ward, even though their presence could minimise anxiety in a person living with dementia and, instead, wards prefer to use expensive agency one-to-one staff. Being ignored on a ward was a familiar experience for these carers and, during the workshops, the destabilising impact of this experience was represented by the stitched felt portrait pressed onto to a cold and hard surface.
Diversity and dementia
We delivered five engagement events in Cardiff, which involved 80 older people and PLWD from within ethnic minority; lesbian, gay, bisexual and transgender; and disability communities to discuss their experiences and involve them in the research. In addition, we developed collaborative relationships with organisations with a specific remit to support communities living with dementia that are often excluded from research, including Diverse Cymru, Alzheimer’s Society, Women Connect First, the British Deaf Association, the Down’s Syndrome Association, the Royal National Institute for Deaf People, Stonewall Cymru, the Mentor Ring, Nubian Life and the Sub-Saharan Advisory Panel.
The consultation process led to the development of three collaborative performances that explored dementia and ethnicity, hearing loss and sexuality, informed by the research findings and co-produced with people with lived experiences who actively contributed to script development. Although we heard many positive stories of care, many PLWD and carers reported negative and discriminatory experiences, including microaggressions and discriminatory language used by ward staff across care settings. These PLWD and family carers described feeling additionally vulnerable during a hospital admission and we have explored these in the following co-produced films:
-
Next of Kin explores the issues raised by the Deaf/deaf community. 192
-
More Time explores the issues raised by the ethnic minority community and ethnic minority health-care workers. 193
-
Back in the Closet explores the issues for lesbian, gay, bisexual and transgender older adults raised by the lesbian, gay, bisexual and transgender community. 194
For her work developing this programme, Sofia Vougioukalou was awarded the Alzheimer’s Society Cymru Dementia Friendly Diversity Award winner 2021 and the Public Involvement Award by Health and Care Research Wales. 195
Chapter 10 Conclusions
Our detailed analysis provides understandings of the complex social relations occurring in these wards, and the ways in which the organisation and delivery of continence care at the bedside connects closely with and is informed by wider institutional expectations, policies and priorities, which, in turn, shape the personal impacts of continence care for both PLWD and ward staff. Given the scope of our data set, in this report, we focus on presenting the five major themes that emerged from our analysis: (1) continence as a significant, visible and public phenomenon, (2) continence communication, (3) rationales of safety, (4) ‘pad cultures’ and (5) impacts of continence care.
Theme 1: continence as a significant, visible and public phenomenon
Continence was a significant, visible and public phenomenon, representing a considerable aspect of care for PLWD in the everyday bedside care routines predominantly carried out by HCAs, but also significant in the routines of nursing. Considerations of privacy were often over-ridden by the recording practices and required documentation of these wards. This could also lead to close monitoring and control of the person living with dementia at the bedside.
Theme 2: continence communication
Despite its apparent centrality in the everyday work of these wards, communication was significant in the silencing of continence and the work of continence care. The discomfort surrounding continence care for ward staff could be seen in the strategies of communication and the language used in these wards during bedside care for PLWD, but also extended to staff discussions of continence in team meetings. Euphemisms, particularly for genitalia, bodily functions, urine and faecal matter, were notable during intimate personal care, as was a restricted repertoire of language used to communicate intimate continence and personal care to PLWD. Importantly, there was little evidence that staff were able to check the person’s comprehension or vary language to suit the individual.
In these wards, there was the explicit requirement that PLWD must communicate urgency and request continence care at the bedside using institutionally recognised forms of communication (e.g. through verbal requests and using the personal call button to seek help). Permission was also required to leave the bedside and walk to a toilet, even if the person was able to do so independently. For PLWD, the communication of an urgent continence care need was often not verbalised (either through difficulties in communication or embarrassment), but rather was embodied and could be identified in the body and via changes in behaviour only. It was unusual for staff to recognise or respond to these non-verbal forms of communicating an underlying continence care need.
Theme 3: rationales of safety
Ensuring safety and minimising risks often featured in discussions of continence care for PLWD. A person living with dementia leaving or repeatedly attempting to leave the bed or bedside was always interpreted by ward staff as a risk to be managed, and ward staff typically focused on the immediate behaviour, with the goal of containing and repositioning the patient in the bed or bedside chair. This focus on immediate risks of falling may reduce one risk, but meant that staff typically did not recognise immediate continence needs, other potential impacts on the person or the reduced opportunities for independence and rehabilitation, such as regaining the ability to walk.
Theme 4: ‘pad cultures’
We identified ‘pad cultures’ as the routine use of continence pads in the care of a wider group of PLWD as a precautionary strategy (regardless of a person’s continence and independence). This was viewed as being essential to provide safeguards, ensure containment and prevent ‘accidents’ or incontinence episodes, but had an expectation that PLWD not only wear pads, but that they could and should use the pads. These cultures enabled wards to reduce unscheduled interruptions and ensure containment at the bedside. This approach meant that continence care could become reduced to containment practices and the ‘checking’ and replacing of soiled or wet pads as part of other scheduled task-based bedside care during a shift. Ward staff described continence care as a ‘heavy’ burden, and a ‘heavy load’, which expressed not only the physically demanding nature of this care, but also the experience of isolation and of feeling abandoned with the responsibility of caring for large numbers of PLWD who required highly supportive care.
Theme 5: impacts of continence care
This characterisation of the dependency of PLWD in these wards had wider and significant impacts on the person and their identities. These impacts were intrinsically linked to ‘pad cultures’.
Placing a person into ‘pads’ and institutional gowns, and containing them at the bedside, could lead to the reclassification of these individuals and people (both PLWD and older people) grouped together in a given bay or ward area. The everyday use of institutional gowns was also a response to the routine failure of ‘pads’ as a containment technology, which meant that clothing also needed to be routinely changed along with pads. Therefore, the requirements and failures of the pad technology itself were expected, normalised and prioritised.
The characterisation of the dependency of PLWD could also extend to recognition and understandings of individual behaviour. Walking to the bathroom could be understood by staff as ‘wandering’ and no longer a sign of continence, capacity and capability, but a potential risk of ‘falls’ and recognised by staff as a potential sign of confusion or resistance to ward care. Distress at experiencing intimate continence care from strangers, often carried out in silence or without adequate warning, could also become quickly perceived as ‘aggression’. Forms of embodied communication of continence care needs could be viewed as transgressive or as a form of behaviour constituting a feature of their dementia, rather than an expression of urgent and underlying need.
This study identified ‘pad cultures’ as an embedded practice in these acute wards. We recognise that the use of continence ‘pads’ was often required to support PLWD in response to incontinence. However, ‘pad cultures’ refers to the routine use of continence pads in the care of a wider group of PLWD (regardless of continence and independence) as a precautionary strategy that is essential to provide safeguards, ensure containment and prevent ‘accidents’ or incontinent episodes. In addition, ‘pad cultures’ have an expectation that PLWD not only wear pads, but that they could and should use the pad. These cultures enabled wards to reduce unscheduled interruptions to the timetabled work of these wards and encouraged containment at the bedside. This approach meant that continence care could become reduced to containment practices and the ‘checking’ and replacing of soiled or wet pads as part of other scheduled task-based organisation and delivery of bedside care during a shift.
These ‘pad cultures’ had significant impacts on PLWD and ward staff. These practices informed wider understandings and characterisations of PLWD (both cohorted individuals and groups) in these wards as being highly dependent, which had wider and significant impacts on the person and their identity. In turn, ward staff described continence care as a ‘heavy’ burden, and a ‘heavy load’, which expressed not only the physically demanding nature of these ‘pad cultures’, but also the experience of isolation and of feeling abandoned with the responsibility of caring for large numbers of PLWD. Staff also often expressed the view that, although they wanted to support their patients’ continence, they believed that it was not possible to work in other ways.
Acknowledgements
We thank our External Oversight Group for the incredibly stimulating and encouraging meetings: Jackie Askey (chairperson), Chris Roberts (activist and living with dementia), Jayne Goodrick (activist and carer), Lorraine Edmunds (Dementia Strategy, Welsh Government, UK), Alexandra Feast (University College London, UK), Paula Saukko (Loughborough University, UK), John Vorhaus (University College London), Laura Cole (King’s College London, UK) and Chris Chatterton (academic and activist).
We thank our Carers Steering Group; its involvement has been vital in both highlighting the acute setting as a key area of urgent need and in shaping our research agenda. The Carers Steering Group has continued to support us throughout our project, commenting on the appropriateness of our methods and discussing and debating our analysis and findings. We particularly thank Rosie Tope, Jackie Askey, Anne Davies, Peggy Martin, Viv Morgan, Julie Stacey, Betty Roderick, David Jones, Lynne Jeffrey, Chris Jones, Joan Gabe-Jenkin and all the members of the Carers Steering Group for all their support and for keeping us focused on our goal of this research. We also remember George Askey whose experiences continue to inform our work.
We are, of course, extremely grateful to all the PLWD, their families and carers, and the nurses, HCAs and medical teams who have shared their stories, supported our work and given us the encouragement to use our ethnography to improve care for PLWD, and to improve the working lives of nurses and HCAs working in the acute setting. We would like to acknowledge them all individually, but are required to preserve their anonymity.
Contributions of authors
Katie Featherstone (https://orcid.org/0000-0003-4999-8425) was principal investigator for this project, conducted data collection and analysis, was responsible for significant editing of this report and was a primary author of this report.
Andy Northcott (https://orcid.org/0000-0003-3030-9861) was research lead for this project, conducted data collection and analysis, was responsible for significant editing of this report and was a primary author of this report.
Paula Boddington (https://orcid.org/0000-0002-0859-3678) contributed significantly to data analysis and to the writing, editing and reviewing of the report.
Deborah Edwards (https://orcid.org/0000-0003-1885-9297) was responsible for the scoping and review, was responsible for significant editing of this report and was the primary author of the mixed-methods review and thematic synthesis (see Chapter 6).
Sofia Vougioukalou (https://orcid.org/0000-0003-0788-0373) provided patient and carer insight, contributed to the PPI events and was primary author of the PPI section of this report (see Chapter 9).
Sue Bale (https://orcid.org/0000-0001-5648-0072) provided nursing and clinical expertise throughout the analytic process and in the production of the report.
Karen Harrison Dening (https://orcid.org/0000-0001-7635-644X) provided patient and carer insight, and contributed to the PPI events and to the production of the PPI section of this report (see Chapter 9).
Karen Logan provided expertise in clinical continence care throughout the analytic process and production of the report.
Rosie Tope (https://orcid.org/0000-0003-4300-1532) provided nursing and clinical expertise throughout the analytic process and in the production of the report, gave patient and carer insight, and contributed to the PPI events and to the production of the PPI section of this report (see Chapter 9).
Daniel Kelly (https://orcid.org/0000-0002-1847-0655) provided nursing and clinical expertise throughout the analytic process and in the production of the report.
Aled Jones (https://orcid.org/0000-0002-2921-8236) provided nursing and clinical expertise throughout the analytic process and in the production of the report.
Jackie Askey provided patient and carer insight, and contributed to the PPI events and to the production of the PPI section of this report (see Chapter 9).
Jane Harden (https://orcid.org/0000-0001-8158-6450) was responsible for the scoping and review, and provided nursing and clinical expertise throughout the analytic process and in the production of the report.
Data-sharing statement
This is a qualitative study and, therefore, the data generated is not suitable for sharing beyond that contained in the report. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Collaborating Centre for Mental Health . A NICE–SCIE Guideline on Supporting People With Dementia and Their Carers in Health and Social Care. Clinical Guideline [CG42] 2007.
- National Audit Office . Improving Services and Support for People Living With Dementia 2007.
- House of Commons Public Accounts Committee . Sixth Report of Session 2007–8: Improving Services and Support for People With Dementia 2008.
- Department of Health and Social Care (DHSC) . Living Well With Dementia: A National Dementia Strategy 2009.
- The Health Foundation . Spotlight on Dementia Care: A Health Foundation Improvement Report 2011.
- Alzheimer’s Society . Fix Dementia Care: Hospitals 2016.
- Kelly D. Changed men: the embodied impact of prostate cancer. Qual Health Res 2009;19:151-63. https://doi.org/10.1177/1049732308328067.
- Royal College of Psychiatrists . National Audit of Dementia Care in General Hospitals 2012–2013: Second Round Audit Report and Update 2013.
- Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61-6. https://doi.org/10.1192/bjp.bp.108.055335.
- Lakey L. Counting the Costs. Caring for People with Dementia on Hospital Wards. London: Alzheimer’s Society; 2009.
- Department of Health and Social Care (DHSC) . Dementia: A State of the Nation Report on Dementia Care and Support in England 2013.
- Crowther GJ, Bennett MI, Holmes JD. How well are the diagnosis and symptoms of dementia recorded in older patients admitted to hospital?. Age Ageing 2017;46:112-18. https://doi.org/10.1093/ageing/afw169.
- Alzheimer’s Research UK . Cost of Dementia for Hospitals in England Doubles in a Decade 2020. www.alzheimersresearchuk.org/cost-of-dementia-hospitals-england-doubles/ (accessed 18 June 2021).
- Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA 2012;307:165-72. https://doi.org/10.1001/jama.2011.1964.
- Pinkert C, Holle B. People with dementia in acute hospitals. Literature review of prevalence and reasons for hospital admission. Z Gerontol Geriatr 2012;45:728-34. https://doi.org/10.1007/s00391-012-0319-1.
- Shenkin SD, Russ TC, Ryan TM, MacLullich AM. Screening for dementia and other causes of cognitive impairment in general hospital in-patients. Age Ageing 2014;43:166-8. https://doi.org/10.1093/ageing/aft184.
- Goldberg SE, Whittamore KH, Harwood RH, Bradshaw LE, Gladman JR, Jones RG. Medical Crises in Older People Study Group . The prevalence of mental health problems among older adults admitted as an emergency to a general hospital. Age Ageing 2012;41:80-6. https://doi.org/10.1093/ageing/afr106.
- Russ TC, Shenkin SD, Reynish E, Ryan T, Anderson D, Maclullich AM. Dementia in acute hospital inpatients: the role of the geriatrician. Age Ageing 2012;41:282-4. https://doi.org/10.1093/ageing/afs048.
- Gordon A, Hu H, Byrne A, Stott DJ. Dementia screening in acute medical and geriatric hospital admissions. Psychiatr Bull 2009;33:52-4. https://doi.org/10.1192/pb.bp.107.016550.
- Jackson TA, MacLullich AM, Gladman JR, Lord JM, Sheehan B. Diagnostic test accuracy of informant-based tools to diagnose dementia in older hospital patients with delirium: a prospective cohort study. Age Ageing 2016;45:505-11. https://doi.org/10.1093/ageing/afw065.
- Briggs R, Dyer A, Nabeel S, Collins R, Doherty J, Coughlan T, et al. Dementia in the acute hospital: the prevalence and clinical outcomes of acutely unwell patients with dementia. QJM 2017;110:33-7. https://doi.org/10.1093/qjmed/hcw114.
- Timmons S, Manning E, Barrett A, Brady NM, Browne V, O’Shea E, et al. Dementia in older people admitted to hospital: a regional multi-hospital observational study of prevalence, associations and case recognition. Age Ageing 2015;44:993-9. https://doi.org/10.1093/ageing/afv131.
- Collins N, Blanchard MR, Tookman A, Sampson EL. Detection of delirium in the acute hospital. Age Ageing 2010;39:131-5. https://doi.org/10.1093/ageing/afp201.
- Dewing J, Dijk S. What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia 2016;15:106-24. https://doi.org/10.1177/1471301213520172.
- Barker A, Bullock R. Delayed discharge in older people’s mental health beds. Old Age Psychiatr Newsl 2005;9.
- Lehmann J, Michalowsky B, Kaczynski A, Thyrian JR, Schenk NS, Esser A, et al. The impact of hospitalization on readmission, institutionalization, and mortality of people with dementia: a systematic review and meta-analysis. J Alzheimers Dis 2018;64:735-49. https://doi.org/10.3233/JAD-171128.
- Care Quality Commission . The State of Health Care and Adult Social Care in England in 2013 14 (Vol. 763) 2016.
- Sampson EL, Leurent B, Blanchard MR, Jones L, King M. Survival of people with dementia after unplanned acute hospital admission: a prospective cohort study. Int J Geriatr Psychiatry 2013;28:1015-22. https://doi.org/10.1002/gps.3919.
- Mathews SR, Epperson N, Arnold SE. Hospitalization and cognitive decline: can the nature of the relationship bet deciphered?. Am J Psychiatry 2013;22:465-80. https://doi.org/10.1016/j.jagp.2012.08.012.
- George J, Long S, Vincent C. How can we keep patients with dementia safe in our acute hospitals? A review of challenges and solutions. J R Soc Med 2013;106:355-61. https://doi.org/10.1177/0141076813476497.
- Thornlow DK, Anderson R, Oddone E. Cascade iatrogenesis: factors leading to the development of adverse events in hospitalized older adults. Int J Nurs Stud 2009;46:1528-35. https://doi.org/10.1016/j.ijnurstu.2009.06.015.
- Hofmann H, Hahn S. Characteristics of nursing home residents and physical restraint: a systematic literature review. J Clin Nurs 2014;23:3012-24. https://doi.org/10.1111/jocn.12384.
- Evans D, Wood J, Lambert L. A review of physical restraint minimization in the acute and residential care settings. J Adv Nurs 2002;40:616-25. https://doi.org/10.1046/j.1365-2648.2002.02422.x.
- Borbasi S, Jones J, Lockwood C, Emden C. Health professionals’ perspectives of providing care to people with dementia in the acute setting: toward better practice. Geriatr Nurs 2006;27:300-8. https://doi.org/10.1016/j.gerinurse.2006.08.013.
- Moyle W, Kellett U, Ballantyne A, Gracia N. Dementia and loneliness: an Australian perspective. J Clin Nurs 2011;20:1445-53. https://doi.org/10.1111/j.1365-2702.2010.03549.x.
- White N, Leurent B, Lord K, Scott S, Jones L, Sampson EL. The management of behavioural and psychological symptoms of dementia in the acute general medical hospital: a longitudinal cohort study. Int J Geriatr Psychiatry 2011;20:1445-53.
- Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet 2014;383:911-22. https://doi.org/10.1016/S0140-6736(13)60688-1.
- Pan Y, Jiang Z, Yuan C, Wang L, Zhang J, Zhou J, et al. Influence of physical restraint on delirium of adult patients in ICU: a nested case-control study. J Clin Nurs 2018;27:1950-7. https://doi.org/10.1111/jocn.14334.
- McCusker J, Cole M, Dendukuri N, Belzile E, Primeau F. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ 2001;165:575-83.
- Voyer P, Richard S, Doucet L, Cyr N, Carmichael PH. Precipitating factors associated with delirium among long-term care residents with dementia. Appl Nurs Res 2011;24:171-8. https://doi.org/10.1016/j.apnr.2009.07.001.
- Bai X, Kwok TC, Ip IN, Woo J, Chui MY, Ho FK. Physical restraint use and older patients’ length of hospital stay. Health Psychol Behav Med 2014;2:160-70. https://doi.org/10.1080/21642850.2014.881258.
- Powers BA. Ethnographic analysis of everyday ethics in the care of nursing home residents with dementia: a taxonomy. Nurs Res 2001;50:332-9. https://doi.org/10.1097/00006199-200111000-00002.
- Gallinagh R, Slevin E, McCormack B. Side rails as physical restraints in the care of older people: a management issue. J Nurs Manag 2002;10:299-306. https://doi.org/10.1046/j.1365-2834.2002.00319.x.
- Flannery RB. Restraint procedures and dementia sufferers with psychological trauma. Am J Alzheimers Dis Other Demen 2003;18:227-30. https://doi.org/10.1177/153331750301800408.
- Saarnio R, Isola A. Use of physical restraint in institutional elderly care in Finland: perspectives of patients and their family members. Res Gerontol Nurs 2009;2:276-86. https://doi.org/10.3928/19404921-20090706-02.
- De Bellis A, Mosel K, Curren D, Prendergast J, Harrington A, Muir-Cochrane E. Education on physical restraint reduction in dementia care: a review of the literature. Dementia 2013;12:93-110. https://doi.org/10.1177/1471301211421858.
- Dementia Action Alliance . Dementia Friendly Hospital Charter 2012.
- Department of Health and Social Care (DHSC) . Prime Minister’s Challenge on Dementia 2015.
- Harari D, Husk J, Lowe D, Lourtie J. Pilot Audit Evaluation Report 2012.
- Bridges J, Nicholson C, Maben J, Pope C, Flatley M, Wilkinson C, et al. Capacity for care: meta-ethnography of acute care nurses’ experiences of the nurse-patient relationship. J Adv Nurs 2013;69:760-72. https://doi.org/10.1111/jan.12050.
- Patterson M, Nolan M, Rick J, Brown J, Adams R, Musson G. From Metrics to Meaning: Culture Change and Quality of Acute Hospital Care for Older People 2011. www.semanticscholar.org/paper/From-Metrics-to-Meaning%3A-Culture-Change-and-Quality-Patterson-Nolan/e5d916503a2b57e9b1777865d5b514021fd6fd19 (accessed 17 November 2021).
- Maben J, Adams M, Peccei R, Murrells T, Robert G. ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples’ experience of hospital care. Int J Older People Nurs 2012;7:83-94. https://doi.org/10.1111/j.1748-3743.2012.00326.x.
- Featherstone K, Northcott A, Bridges J. Routines of resistance: an ethnography of the care of people living with dementia in acute hospital wards and its consequences. Int J Nurs Stud 2019;96:53-60. https://doi.org/10.1016/j.ijnurstu.2018.12.009.
- Tutton E, Seers K. Comfort on a ward for older people. J Adv Nurs 2004;46:380-9. https://doi.org/10.1111/j.1365-2648.2004.03005.x.
- Wolf A, Ekman I, Dellenborg L. Everyday practices at the medical ward: a 16-month ethnographic field study. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-184.
- Bridges J, Flatley M, Meyer J. Older people’s and relatives’ experiences in acute care settings: systematic review and synthesis of qualitative studies. Int J Nurs Stud 2010;47:89-107. https://doi.org/10.1016/j.ijnurstu.2009.09.009.
- Bridges J, Wilkinson C. Achieving dignity for older people with dementia in hospital. Nurs Stand 2011;25:42-7. https://doi.org/10.7748/ns2011.03.25.29.42.c8402.
- Daykin N, Clarke B. ‘They’ll still get the bodily care’. Discourses of care and relationships between nurses and health care assistants in the NHS. Sociol Health Illn 2000;22:349-63. https://doi.org/10.1111/1467-9566.00208.
- V Lloyd J, Schneider J, Scales K, Bailey S, Jones R. Ingroup identity as an obstacle to effective multiprofessional and interprofessional teamwork: findings from an ethnographic study of healthcare assistants in dementia care. J Interprof Care 2011;25:345-51. https://doi.org/10.3109/13561820.2011.567381.
- Gladman J, Porock D, Griffiths A, Clisset P, Harwood RH, Knight A, et al. Better Mental Health: Care for Older People With Cognitive Impairment in General Hospitals. Final Report 2012.
- Tadd W, Hillman A, Calnan M, Calnan S, Read S, Bayer A. From right place – wrong person, to right place – right person: dignified care for older people. J Health Serv Res Policy 2012;17:30-6. https://doi.org/10.1258/jhsrp.2011.011118.
- Moyle W, Olrenshaw R, Wallis M, Borbasi S. Best practice for the management of older people living with dementia in the acute care setting: a review of the literature. Int J Older People Nurs 2008;3:121-30. https://doi.org/10.1111/j.1748-3743.2008.00114.x.
- Arthur A, Aldus C, Sarre S, Maben J, Wharrard H, Schnieder J, et al. Can Health-care Assistant Training improve the relational care of older people? (CHAT) A development and feasibility study of a complex intervention. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05100.
- Clissett P, Porock D, Harwood RH, Gladman JR. The challenges of achieving person-centred care in acute hospitals: a qualitative study of people with dementia and their families. Int J Nurs Stud 2013;50:1495-503. https://doi.org/10.1016/j.ijnurstu.2013.03.001.
- Wolkowitz C. The social relations of body work. Work Employ Soc 2002;16:497-510. https://doi.org/10.1177/095001702762217452.
- Twigg J. Carework as a form of bodywork. Ageing Soc 2000;20:289-411. https://doi.org/10.1017/S0144686X99007801.
- Jervis LL. The pollution of incontinence and the dirty work of caregiving in a US nursing home. Med Anthropol Q 2001;15:84-99. https://doi.org/10.1525/maq.2001.15.1.84.
- Bolton SC. Women’s work, dirty work: the gynaecology nurse as ‘other’. Gend Work Organ 2012;12:169-86. https://doi.org/10.1111/j.1468-0432.2005.00268.x.
- Lawler J. Behind the Screens: Nursing, Somology and the Problem of the Body. Edinburgh: Churchill Livingstone; 1991.
- Health H. The nurse’s role in helping older people to use the toilet. Nurs Stand 2009;24:43-7. https://doi.org/10.7748/ns2009.09.24.2.43.c7266.
- Cornwell J. The Care of Frail Older People with Complex Needs: Time for a Revolution. London: The King’s Fund; 2012.
- Mukadam N, Liningston G. Reducing the stigma associated with dementia: approaches and goals. Aging Health 2012;8:377-86. https://doi.org/10.2217/ahe.12.42.
- Graham N, Lindesay J, Katona C, Bertolote JM, Camus V, Copeland JR, et al. Reducing stigma and discrimination against older people with mental disorders: a technical consensus statement. Int J Geriatr Psychiatry 2003;18:670-8. https://doi.org/10.1002/gps.876.
- Bamford SM, Walker T. Women and dementia – not forgotten. Maturitas 2012;73:121-6. https://doi.org/10.1016/j.maturitas.2012.06.013.
- Brittain KR, Shaw C. The social consequences of living with and dealing with incontinence – a carers perspective. Soc Sci Med 2007;65:1274-83. https://doi.org/10.1016/j.socscimed.2007.04.002.
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. East Rutherford, NJ: Penguin; 1963.
- Dombrowsky TA. Continence and incontinence: a concept analysis. J Theory Constr Test 2012;16:31-7.
- Lothian K, Philp I. Maintaining the dignity and autonomy of older people in the healthcare setting. BMJ 2001;322:668-70. https://doi.org/10.1136/bmj.322.7287.668.
- Horrocks S, Somerset M, Stoddart H, Peters TJ. What prevents older people from seeking treatment for urinary incontinence? A qualitative exploration of barriers to the use of community continence services. Fam Pract 2004;21:689-96. https://doi.org/10.1093/fampra/cmh622.
- Heintz PA, DeMucha CM, Deguzman MM, Softa R. Stigma and microaggressions experienced by older women with urinary incontinence: a literature review. Urol Nurs 2013;33:299-305. https://doi.org/10.7257/1053-816X.2013.33.6.299.
- Sange C, Thomas L, Lyons C, Hill S. Urinary incontinence in Muslim women. Nurs Times 2008;104:49-52. https://doi.org/10.1016/S0084-4071(08)79182-6.
- McCarthy M, Addington-Hall J, Altmann D. The experience of dying with dementia: a retrospective study. Int J Geriatr Psychiatry 1997;12:404-9. https://doi.org/10.1002/(SICI)1099-1166(199703)12:3<404::AID-GPS529>3.0.CO;2-2.
- Rose A, Thimme A, Halfar C, Nehen HG, Rübben H. Severity of urinary incontinence of nursing home residents correlates with malnutrition, dementia and loss of mobility. Urol Int 2013;91:165-9. https://doi.org/10.1159/000348344.
- O’Connell B, Orr J, Ostaszkiewicz J, Gaskin CJ. Nursing care needs of patients with and without dementia admitted to hospital with fractured neck of femur. Int J Orthop Trauma Nurs 2011;15:136-44. https://doi.org/10.1016/j.ijotn.2010.12.004.
- Hägglund D. A systematic literature review of incontinence care for persons with dementia: the research evidence. J Clin Nurs 2010;19:303-12. https://doi.org/10.1111/j.1365-2702.2009.02958.x.
- van Houten P. The Relationship Between Incontinence, Toileting Skills and Morbidity in Nursing Homes 2008.
- Alzheimer’s Europe . Guidelines on Continence Care for People With Dementia Living at Home 2014.
- Furlanetto K, Emond K. ‘Will I come home incontinent?’ A retrospective file review: incidence of development of incontinence and correlation with length of stay in acute settings for people with dementia or cognitive impairment aged 65 years and over. Collegian 2016;23:79-86. https://doi.org/10.1016/j.colegn.2014.09.013.
- Mecocci P, von Strauss E, Cherubini A, Ercolani S, Mariani E, Senin U, et al. Cognitive impairment is the major risk factor for development of geriatric syndromes during hospitalization: results from the GIFA study. Dement Geriatr Cogn Disord 2005;20:262-9. https://doi.org/10.1159/000087440.
- Zisberg A, Sinoff G, Gary S, Gur-Yaish N, Admi H, Shadmi E. In-hospital use of continence aids and new-onset urinary incontinence in adults aged 70 and older. J Am Geriatr Soc 2011;59:1099-104. https://doi.org/10.1111/j.1532-5415.2011.03413.x.
- Rabinowitz T, Martin L, Montague P, Hirdes JP. Prevalence and correlates of urinary incontinence in a large cohort of psychiatric inpatients. Psychiatr Serv 2011;62:97-100. https://doi.org/10.1176/ps.62.1.pss6201_0097.
- Ybema S, Yanow D, Wels S, Kamsteg FH. Organizational Ethnography: Studying the Complexity of Everyday Life. London: SAGE Publications Ltd; 2009.
- National Institute for Health and Care Excellence and Social Care Institute for Excellence . Operating Framework for the NHS 2006.
- Patients Association . Patients . . . Not Numbers, People . . . Not Statistics 2009.
- Department of Health and Social Care (DHSC) . A New Ambition for Old Age Next Steps in Implementing the National Health Service Framework for Older People – A Report from Professor Ian Philp 2006.
- Alzheimer’s Society . Counting the Cost of Care: Caring for People With Dementia on Hospital Wards 2009.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary 2013.
- House of Lords, House of Commons Joint Committee on Human Rights . The Human Rights of Older People in Healthcare Eighteenth Report of Session 2006–07 2007.
- Nottingham City and Nottinghamshire County Joint Health Scrutiny Committee . Report of the Overview and Scrutiny Manager (Nottingham City Council). Review of Dementia Care in Hospital – Summary of Findings to Date 2010. www.nottinghamshire.gov.uk/DMS/Document.ashx?czJKcaeAi5tUFL1DTL2UE4zNRBcoShgo=42s%2B5roEcK2FBrZ20nispHOiVJG7CeEVTaOtu8%2FOkCoKZpivJfuHOQ%3D%3D&mCTIbCubSFfXsDGW9IXnlg%3D%3D=hFflUdN3100%3D&kCx1AnS9%2FpWZQ40DXFvdEw%3D%3D=hFflUdN3100%3D&uJovDxwdjMPoYv%2BAJvYtyA%3D%3D=ctNJFf55vVA%3D&FgPlIEJYlotS%2BYGoBi5olA%3D%3D=NHdURQburHA%3D&d9Qjj0ag1Pd993jsyOJqFvmyB7X0CSQK=ctNJFf55vVA%3D&WGewmoAfeNR9xqBux0r1Q8Za60lavYmz=ctNJFf55vVA%3D&WGewmoAfeNQ16B2MHuCpMRKZMwaG1PaO=ctNJFf55vVA%3D (accessed 25 November 2021).
- National Institute for Health and Care Excellence (NICE) . Urinary Incontinence: The Management of Urinary Incontinence in Women. Clinical Guideline [CG40] 2006.
- Dingwall L, McLafferty E. Do nurses promote urinary continence in hospitalized older people?: An exploratory study. J Clin Nurs 2006;15:1276-86. https://doi.org/10.1111/j.1365-2702.2006.01381.x.
- Booth J, Kumlien S, Zang Y, Gustafsson B, Tolson D. Rehabilitation nurses practices in relation to urinary incontinence following stroke: a cross-cultural comparison. J Clin Nurs 2009;18:1049-58. https://doi.org/10.1111/j.1365-2702.2008.02688.x.
- Wagg A, Harari D, Husk J, Lowe D, Lourtie J. National Audit of Continence Care. London: Royal College of Physicians; 2010.
- Bamford S-M, Holley-Moore G, Watson J. A Compendium of Essays: New Perspectives and Approaches to Understanding Dementia and Stigma. London: ILCUK; 2014.
- DuBeau CE, Kuchel GA, Johnson T, Palmer MH, Wagg A. Incontinence in the Frail Elderly. 4th International Consultation on Incontinence. Recommendations of the International Scientific Committee: Evaluation and Treatment of Urinary Incontinence, Pelvic Organ Prolapse and Faecal Incontinence. Paris: Health Publication Ltd; 2009.
- Featherstone K, Northcott A, Harden J, Harrison Dening K, Tope R, Bale S, et al. Refusal and resistance to care by people living with dementia being cared for within acute hospital wards: an ethnographic study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07110.
- Atkinson P, Delamont S, Housley W. Contours of Culture: Complex Ethnography and the Ethnography of Complexity. Lanham, MD: Rowman Altamira; 2008.
- Hammersley M. Ethnography: problems and prospects. Ethnogr Educ 2006;1:3-14. https://doi.org/10.1080/17457820500512697.
- Caracelli VJ. Enhancing the policy process through the use of ethnography and other study frameworks: a mixed-method strategy. Res Sch 2006;13:3-14.
- Dixon-Woods M. What can ethnography do for quality and safety in health care?. Qual Saf Health Care 2003;12:326-7. https://doi.org/10.1136/qhc.12.5.326.
- Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handb Qual Res 1994;2.
- Hammersley M, Atkinson P. Ethnography: Principles in Practice. London: Routledge; 1989.
- Hammersley M. What’s Wrong with Ethnography. Methodological Explorations. London: Routledge; 1987.
- Popay J, Williams G. Qualitative research and evidence-based healthcare. J R Soc Med 1998;91:32-7. https://doi.org/10.1177/014107689809135S08.
- Lauder H, Brown P, Halsey AH. Sociology and political arithmetic: some principles of a new policy science. Br J Sociol 2004;55:3-22. https://doi.org/10.1111/j.1468-4446.2004.00002.x.
- Hammersley M. Action research: a contradiction in terms?. Oxf Rev Educ 2004;30:165-81. https://doi.org/10.1080/0305498042000215502.
- Black N. Why we need qualitative research. J Epidemiol Community Health 1994;48:425-6. https://doi.org/10.1136/jech.48.5.425-a.
- Starr SL. The ethnography of infrastructure. Am Behav Sci 1999;43:377-91. https://doi.org/10.1177/00027649921955326.
- Goffman E. The Presentation of Self in Every Day Life. Scotland: Doubleday; 1959.
- Greenhalgh T, Swinglehurst D. Studying technology use as social practice: the untapped potential of ethnography. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-45.
- Quinlan E. The ‘actualities’ of knowledge work: an institutional ethnography of multi-disciplinary primary health care teams. Sociol Health Illn 2009;31:625-41. https://doi.org/10.1111/j.1467-9566.2009.01167.x.
- Vaughan D. On the relevance of ethnography for the production of public sociology and policy. Br J Sociol 2005;56:411-16. https://doi.org/10.1111/j.1468-4446.2005.00074.x.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. York: ESRC Methods Programme; 2006.
- Featherstone K, Northcott A. Wandering the Wards: An Ethnography of Hospital Care and its Consequences for People Living with Dementia. New York, NY: Taylor and Francis; 2021.
- Turner V, Bruner E. The Anthropology of Experience. New York, NY: PAJ Publications; 1986.
- Charmaz K, Mitchell RG, Atkinson P, Coffey A, Delamont S, Lofland J, et al. Handbook of Ethnography. London: SAGE Publications Ltd; 2001.
- Rosaldo R. Culture and Truth: The Remaking of Social Analysis. Boston, MA: Beacon; 1989.
- Curtis S, Gesler W, Smith G, Washburn S. Approaches to sampling and case selection in qualitative research: examples in the geography of health. Soc Sci Med 2000;50:1001-14. https://doi.org/10.1016/s0277-9536(99)00350-0.
- Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ 2000;320:50-2. https://doi.org/10.1136/bmj.320.7226.50.
- van der Geest S, Finkler K. Hospital ethnography: introduction. Soc Sci Med 2004;59:1995-2001. https://doi.org/10.1016/j.socscimed.2004.03.004.
- Goodson L, Vassar M. An overview of ethnography in healthcare and medical education research. J Educ Eval Health Prof 2011;8. https://doi.org/10.3352/jeehp.2011.8.4.
- Glaser B, Strauss A. The Discovery of Grounded Theory. Strategies for Qualitative Research. London: Weidenfeld and Nicholson; 1967.
- Great Britain . Mental Capacity Act 2005 2005.
- Suddaby R. From the editors: what grounded theory is not. Acad Manage J 2006;49:633-42. https://doi.org/10.5465/amj.2006.22083020.
- Corbin J, Strauss A. Grounded theory research: procedures, canons and evaluative criteria. Qual Sociol 1990;13:3-21. https://doi.org/10.1007/BF00988593.
- Green J. Commentary: grounded theory and the constant comparative method. BMJ 1998;316:1064-5. https://doi.org/10.1136/bmj.316.7137.1060.
- Coffey A, Atkinson P. Making Sense of Qualitative Data: Complementary Research Strategies. London: SAGE Publications Ltd; 1996.
- Blumer H. What is wrong with social theory?. Am Sociol Rev 1954;19:3-10. https://doi.org/10.2307/2088165.
- van Maanen J. Tales of the Field: On Writing Ethnography. Chicago, IL: University of Chicago Press; 2011.
- Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. Chicago, IL: University of Chicago Press; 2011.
- Great Britain . Data Protection Act 2018 2018.
- Edwards D, Harden J, Jones A, Featherstone K. Understanding how to facilitate continence for people with dementia in acute hospital settings: a mixed methods systematic review and thematic synthesis. Syst Rev 2021;10. https://doi.org/10.1186/s13643-021-01743-0.
- EPPI-Centre . EPPI-Centre Methods for Conducting Systematic Reviews 2007.
- Gough D, Oliver S, Thomas J. An Introduction to Systematic Reviews. London: Sage Publications Ltd; 2017.
- Hay-Smith J, Berghmans B, Burgio K, Dumoulin C, Hagen S, Moore K, et al. Incontinence: 4th International Consultation on Incontinence, Paris, July 5–8, 2008. Paris: Health Publications Ltd; 2009.
- Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49:47-53. https://doi.org/10.1016/j.ijnurstu.2011.07.002.
- Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. Int J Nurs Stud 2009;46:529-46. https://doi.org/10.1016/j.ijnurstu.2009.01.009.
- Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, et al. Proposal: A Mixed Methods Appraisal Tool for Systematic Mixed Studies Reviews. Montréal, QC: McGill University; 2011.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med 2009;151. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
- Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001895.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. https://doi.org/10.1136/bmj.39489.470347.AD.
- Lancioni GE, Pinto K, La Martire ML, Tota A, Rigante V, Tatulli E, et al. Helping persons with mild or moderate Alzheimer’s disease recapture basic daily activities through the use of an instruction strategy. Disabil Rehabil 2009;31:211-19. https://doi.org/10.1080/09638280801906438.
- Lancioni GE, La Martire ML, Singh NN, O’Reilly MF, Sigafoos J, Pinto K, et al. Persons with mild or moderate Alzheimer’s disease managing daily activities via verbal instruction technology. Am J Alzheimers Dis Other Demen 2008;23:552-62. https://doi.org/10.1177/1533317508328181.
- Jirovec MM, Templin T. Predicting success using individualized scheduled toileting for memory-impaired elders at home. Res Nurs Health 2001;24:1-8. https://doi.org/10.1002/1098-240X(200102)24:1<1::AID-NUR1001>3.0.CO;2-R.
- Tanaka Y, Hanata K, Tanaka T, Kuwano K, Endo H, Otano T, et al. Can an individualized and comprehensive care strategy improve urinary incontinence (UI) among nursing home residents?. Arch Gerontol Geriatr 2009;49:278-83. https://doi.org/10.1016/j.archger.2008.10.006.
- Wijk H, Corazzini K, Lindstrom K, Kinnander A, Alexiou E, Swedberg K. Person-centrered incontinence care in residential care facilities for older adults with cognitive decline. J Gerontol Nurs 2018;44:11-9. https://doi.org/10.3928/00989134-20181010-04.
- Corcoran MA, Gitlin LN. Family caregiver acceptance and use of environmental strategies provided in an occupational therapy intervention. Phys Occup Ther Geriatr 2001;19:1-20. https://doi.org/10.1080/J148v19n01_01.
- Gitlin LN, Corcoran MA. Expanding caregiver ability to use environmental solutions for problems of bathing and incontinence in the elderly with dementia. Technol Disabil 1993;2:12-2. https://doi.org/10.3233/TAD-1993-2104.
- Wilkinson TJ, Henschke PJ, Handscombe K. How should toilets be labelled for people with dementia?. Australas J Ageing 1995;14:163-5. https://doi.org/10.1111/j.1741-6612.1995.tb00727.x.
- Shih YH, Wang CJ, Sue EP, Wang JJ. Behavioral characteristics of bowel movement and urination needs in patients with dementia in Taiwan. J Gerontol Nurs 2015;41:22-9. https://doi.org/10.3928/00989134-20150414-01.
- Iliffe S, Wilcock J, Drennan V, Goodman C, Griffin M, Knapp M. Changing practice in dementia care in the community: developing and testing evidence-based interventions, from timely diagnosis to end of life (EVIDEM). Programme Grants Appl Res 2015;3. https://doi.org/10.3310/pgfar03030.
- Bliss D, Rolnick C, Jackson J, Arntson C, Mullins J, Hepburn K. Health literacy needs related to incontinence and skin damage among family and friend caregivers of individuals with dementia. J Wound Ostomy Continence Nurs 2013;40:515-23. https://doi.org/10.1097/WON.0b013e3182a3ff24.
- Hutchinson S, Leger-Krall S, Skodol Wilson H. Toileting: a biobehavioral challenge in Alzheimer’s dementia care. J Gerontol Nurs 1996;22:18-27. https://doi.org/10.3928/0098-9134-19961001-12.
- Mullins J, Bliss DZ, Rolnick S, Henre CA, Jackson J. Barriers to communication with a healthcare provider and health literacy about incontinence among informal caregivers of individuals with dementia. J Wound Ostomy Continence Nurs 2016;43:539-44. https://doi.org/10.1097/WON.0000000000000263.
- Ostaszkiewicz J, Tomlinson E, Hutchinson AM. ‘Dignity’: a central construct in nursing home staff understandings of quality continence care. J Clin Nurs 2018;27:2425-37. https://doi.org/10.1111/jocn.14293.
- Rolnick S, Bliss DZ, Jackson JM, Arntson C, Mullins J, Hepburn K. Healthcare providers’ perspectives on communicating incontinence and skin damage information with patients with dementia and their family caregivers: a descriptive study. Ostomy Wound Manage 2013;59:62-7.
- Scerri A, Scerri C, Innes A. The perceived and observed needs of patients with dementia admitted to acute medical wards. Dementia 2020;19:1997-201. https://doi.org/10.1177/1471301218814383.
- Alzheimer’s Society . Continence and Using the Toilet, Factsheet 502LP 2016. www.alzheimers.org.uk/sites/default/files/migrate/downloads/factsheet_continence_and_using_the_toilet.pdf (accessed 7 July 2018).
- Gray C. Support and Care for People with Dementia at Home: A Guide for Homecare Workers. London: Alzheimer’s Society; 2014.
- Dementia UK . Continence 2017. www.dementiauk.org/wp-content/uploads/2018/06/Continence_FINAL_WEB_JUNE-2018.pdf (accessed 7 July 2018).
- Social Care Institute for Excellence . When People With Dementia Experience Problems Related to Using the Toilet 2015.
- Care Inspectorate . Promoting Continence for People Living With Dementia and Long Term Conditions 2015. www.careinspectorate.com/index.php/guidance/9-professional/2613-promoting-continence-for-people-living-with-dementia-and-long-term-conditions (accessed 7 July 2018).
- Care Quality Commission . Cracks in the Pathway. People’s Experiences of Dementia Care As They Move Between Care Homes and Hospitals 2014.
- Thompson R, Health H, Mills N. Dementia: Commitment to the Care of People with Dementia in Hospital Settings. London: Royal College of Nursing; 2013.
- Abrams P, Cardozo L, Wagg A, Wein A. 6th International Consultation on Incontinence. Bristol: ICI-ICS. International Continence Society; 2017.
- Potter P. Excellence in Continence Care; Practical Guidance for Commissioners, Providers, Health and Social Care Staff and Information for the Public. Reading: NHS England; 2015.
- Ostaszkiewicz J. Reframing continence care in care-dependence. Geriatr Nurs 2017;38:520-6. https://doi.org/10.1016/j.gerinurse.2017.03.014.
- Ostaszkiewicz J. A conceptual model of the risk of elder abuse posed by incontinence and care dependence. Int J Older People Nurs 2018;13. https://doi.org/10.1111/opn.12182.
- Alzheimer’s Scotland . Continence Management – Advice for Carers of People With Dementia 2009.
- Ostaszkiewicz J, Johnston L, Roe B. Timed voiding for the management of urinary incontinence in adults. Cochrane Database Syst Rev 2004;1. https://doi.org/10.1002/14651858.CD002802.pub2.
- Drennan VM, Greenwood N, Cole L, Fader M, Grant R, Rait G, et al. Conservative interventions for incontinence in people with dementia or cognitive impairment, living at home: a systematic review. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-77.
- Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401-6. https://doi.org/10.1016/j.jclinepi.2010.07.015.
- Newman DK. Prompted voiding for individuals with urinary incontinence. J Gerontol Nurs 2019;45:14-26. https://doi.org/10.3928/00989134-20190111-03.
- Monahan T, Fisher JA. Benefits of ‘observer effects’: lessons from the field. Qual Res 2010;10:357-76. https://doi.org/10.1177/1468794110362874.
- Paradis E, Sutkin G. Beyond a good story: from Hawthorne Effect to reactivity in health professions education research. Med Educ 2017;51:31-9. https://doi.org/10.1111/medu.13122.
- Bhopal R. Is research into ethnicity and health racist, unsound, or important science?. BMJ 1997;314:1751-6. https://doi.org/10.1136/bmj.314.7096.1751.
- Moriarty J, Sharif N, Robinson J. Black and Minority Ethnic People with Dementia and Their Access to Support and Services. London: Social Care Institute for Excellence; 2011.
- Botsford J, Clarke CL, Gibb CE. Research and dementia, caring and ethnicity: a review of the literature. J Res Nurs 2011;16:437-49. https://doi.org/10.1177/1744987111414531.
- Manthorpe J, Hettiaratchy P. Ethnic minority elders in the UK. Int Rev Psychiatry 1993;5:173-80. https://doi.org/10.3109/09540269309028308.
- Welsh Government . Wales Safeguarding Procedures for Children and Adults at Risk of Abuse and Neglect n.d. www.safeguarding.wales/int/i1/i1.p1.html (accessed 22 November 2021).
- British Sociological Association . Foundation for the Sociology of Health and Illness Book Prize n.d. https://bit.ly/3DbqS7d (accessed 22 November 2021).
- YouTube . Next of Kin: D Deaf Communication, Dementia Care and Family in Hospital Settings 2021. www.youtube.com/watch?v=RImvuBAcr0w&list=PLEPkwdTAlW1Hs7vaTZ7Fg4Y7MZKMQ3hiE&index=4&t=8s (accessed 29 November 2021).
- YouTube . More Time: Cultural Competence and Person-Centred Dementia Care in Community Settings 2021. www.youtube.com/watch?v=7w_3INWqRWE&list=PLEPkwdTAlW1Hs7vaTZ7Fg4Y7MZKMQ3hiE&index=2 (accessed 29 November 2021).
- YouTube . Back In The Closet: Homophobia, Human Rights and Organisational Cultures of Dementia Care 2021. www.youtube.com/watch?v=sY6cy8K-tEo&list=PLEPkwdTAlW1Hs7vaTZ7Fg4Y7MZKMQ3hiE&index=5 (accessed 29 November 2021).
- Health and Care Research Wales . Three Awards Celebrate Life-Changing Research at Health and Care Research Wales Conference 2021 n.d. https://bit.ly/2ZoveZS (accessed 23 November 2021).
Appendix 1 Profiles of observations sites
Assessment units
Assessment units are units where unscheduled patient admissions arrive for assessment after being referred from accident and emergency (A&E), the outpatient department clinic or a general practice. Following assessment, patients are discharged, transferred to a specialist centre or admitted to an inpatient bed. Assessment units are high-turnover settings, designed to manage the bottlenecks associated with A&E, with the goal of discharging or transferring patients within 24 hours. There is a different routine in this setting, with staff geared to manage acute admissions with a fast turnaround, with a lack of apparent continuity or personalised care, and often a chaotic atmosphere. Carers in the Carer Steering Group reported poor experiences of this setting and found their stay there a frightening time in which they felt they were not listened to and were often separated from their partners.
General medical wards
General medical wards are where patients are transferred to following an emergency admission or assessment in an assessment unit. These wards usually provide greater continuity and more structured routines. However, despite an increasing number of admissions of PLWD in general medical wards, these wards are typically not designed for this patient population. A routine admission for PLWD is 10–20 days; however, for many, this is much longer. 8 Carers in the Carer Steering Group reported poor experiences of this setting and found that general wards did not understand the needs of their partners with dementia.
Observation sites
Site F
Site F is a district general hospital (containing 200 beds) located in a town of approximately 10,000 people and serves a largely rural population. However, the hospital also serves a wider population of small towns and villages, representing both rural and post-industrial communities. The hospital was built entirely in the second half of the twentieth century. Although the town in which the hospital is based is relatively affluent, the surrounding areas have significant wealth inequalities and areas of deprivation. Patient admissions are largely white British, with English as a first language. This hospital has a specialist frailty unit for the treatment of older people. Staff at this hospital are largely drawn from the area and staff often know patients (or their families) from previous admissions or through local social networks. There is ample free parking for visitors at this hospital. This site is not under the jurisdiction of the Care Quality Commission (London, UK).
Emergency assessment unit
The emergency assessment unit contained 30 beds (i.e. four bays of six beds and six side rooms) plus a triage bay. Three neighbouring bays along one corridor were used for older patients. Rates of dementia diagnosis and cognitive impairment in this emergency assessment unit were high. A final bay was reserved for ambulatory and younger patients. Four toilets lined the corridor. It is an open, unlocked unit with three entry/exit points. A RAID (rapid assessment, intervention and discharge) team was in place for older patients admitted to the unit. Each bay has a designated registered nurse and a HCA. Deprivation of Liberty Safeguards and one-to-one care interventions were rarely used.
Acute medical ward
The acute medical ward is a 32-bed Nightingale-style ward (containing four bays of six beds and eight side rooms). The acute medical ward has two main intakes from cardiology and gastroenterology and, therefore, includes patients with heart and liver failure (both alcohol and non-alcohol related); however, the majority of admissions are for general acute conditions, including falls, urinary tract infections and ‘confusion’. The ward was typically staffed by one nurse in charge of the ward, four registered nurses and three HCAs during a day shift, with high continuity across the ward team. All toilets and bathrooms were in the corridor running through the ward. There is a small, plainly decorated day room with a communal television that also doubles as a meeting room for multidisciplinary teams. Patients are typically in their 70s or 80s, with a minority of patients (up to 10) in their 60s and a smaller number of patients (two or three) in their 90s. On average, approximately 10–12 patients have a formal diagnosis of dementia in the board handover notes each day. Only a small number of patients (i.e. two or three) are identified as having continence issues in the handover notes. This is a locked ward with one entrance, accessed via a code or buzzer. Deprivation of Liberty Safeguards and one-to-one care were rarely used.
Site G
Site G is a teaching hospital (containing 900 beds) that is situated in a regional city with an urban/suburban population of approximately 500,000 people. The hospital is typical of many large NHS hospitals, comprising a mix of very new and very old buildings and units, linked by corridors and walkways. The city itself has significant economic inequalities and areas of deprivation, whereas the surrounding areas are affluent. Patient admissions were representative of the demographics of the city and its outlying areas, meaning a multicultural mix of patients, with a range of first languages spoken by patients and staff. This hospital had recently built a number of specialist assessment units for older people, serving one of the largest A&E units in the UK. Staff were from heterogeneous backgrounds and served by nursing and medical schools at two large local universities. There was ample parking for visitors, but this was quite expensive.
At the time of observations, hospitals in this trust were classified by the Care Quality Commission as requiring improvement, in part because of a lack of understanding around mental capacity assessments at the site. This trust has since been reclassified as good.
Acute frailty unit
The acute frailty unit contains 16 beds (i.e. three bays of four beds plus four side rooms) and is set around a small central hub, from which beds cannot be seen. Each bay and bedroom has its own toilet. This is a locked ward with two entrance/exits, with one leading from A&E and towards an exit and the other leading to ‘memory lane’, an area painted to look like a promenade with a fake coffee shop at one end. Both entrances/exits are accessed via security card or intercom. This unit is next to, but is separated from, the main medical assessment unit. The unit is for older patients and has an aim of discharge or transfer within 24 hours of admission. Each bay [plus neighbouring side room(s)] is designated to a registered nurse and a HCA.
Acute older people ward
The acute older people ward has acute intakes of older people with a range of admitting conditions (e.g. pneumonia, sepsis, urinary system disorders, fractures from ‘falls’ and ‘confusion’). The ward has an old-build Nightingale-style design with 32 beds (i.e. four bays of six beds plus eight side rooms). The bays and single rooms are dissected by a long corridor, with a large and busy nurses’ station in the centre of the corridor. The ward is typically staffed by one nurse in charge, three nurses, one discharge co-ordinator and four HCAs; however, nursing staff were often ‘transferred’ to other wards during shifts, which meant that the number of staff was sometimes reduced to as low as three nurses and two HCAs ‘on the floor’ [the institutional staffing levels for this ward are six nurses (i.e. one nurse in charge, four nurses and one discharge coordinator) and four HCAs]. This is a large team with some continuity of longstanding staff members, but also includes a large number of agency staff and a high use of one-to-one agency staff (often two or three per day shift). All toilets and bathrooms were also in the main corridor. There is a large day room decorated with and containing a large amount of ‘dementia-friendly’ resources. Most patients are in their 70s and 80s, but sometimes there can be as many as five patients in their 90s. On average, approximately 10, but up to 15, patients have a formal diagnosis of dementia in the board handover notes, but staff anecdotally report ‘all’ patients as having the condition. On average, 7–10 patients are identified as having continence issues in each day’s handover notes, but staff describe the ‘majority’ as incontinent or ‘doubles’. This is a locked ward with one entrance accessed via a code or buzzer.
Site H
Site H is a teaching hospital (containing 800 beds) in a major metropolitan city with an urban population of over 1,000,000 people. This hospital was entirely rebuilt very recently and is set in an area of significant social deprivation. Patient admissions were multicultural/national, with a range of first languages spoken. A significant number of admissions spoke only Bengali, a language not commonly spoken by ward staff. This hospital had specialist teams in general units and wards. Staff were from heterogeneous backgrounds and served by nursing and medical schools from several local universities. Staff typically did not live near the hospital or have a connection with the local area, commuting considerable distances to work. There was no parking for visitors and visitors were encouraged to use public transport.
At the time of observations, this trust and site were classified by the Care Quality Commission as good, which included direct inspection of the acute assessment unit and of older people’s care.
Acute assessment unit
The acute assessment unit has 26 beds (i.e. four bays of four beds plus 10 side rooms) set around a long horseshoe-shaped corridor. The unit is next to a similar unit, also with 26 beds, which typically admits younger patients, with staff rotated and shared across the two units. The unit is on a double-digit floor of a large tower that is accessed by a single hub of lifts or a staircase. The unit is staffed by five registered nurses, each assigned five or six beds that cut across physical bays. Two HCAs are allocated 13 beds each between two bays and the neighbouring side rooms. The unit is a locked ward and is accessed via intercom or security card.
Care of the elderly ward
The care of the elderly ward contains 26 beds and has acute intakes of older people with a range of admitting conditions (e.g. pneumonia, sepsis and urinary system disorders). It is a new build, approximately double the size of traditional wards, with four large bays with four patients, each bay also with its own large bathroom. There are 10 single-occupancy rooms, each with a large en-suite bathroom. There are additional toilets in the hall. The ward is typically staffed by one nurse in charge (plus a full-time discharge co-ordinator), four nurses and four HCAs during the day shifts, although they were often ‘short’ (the institutional staff levels for this ward is nine, i.e. five nurses and four HCAs for a day shift). There was some continuity of staff in this ward. There are two nursing stations situated within a large and wide circular corridor. The patients are typically in their 70s and 80s, with anywhere from four to 10 patients having a formal diagnosis of dementia in the handover notes each day. Similar numbers are recorded for continence issues in the handover. However, overall, ward staff describe ‘all’ patients as incontinent, highlighting singular continent patients as exceptions. There is a small ‘dementia-friendly cafe’ for patients and visitors. This is a locked ward with one entrance accessed via identification cards or buzzer.
Appendix 2 Stakeholders who took part in the consultation exercise
| Stakeholder | Source of contact |
|---|---|
DCAs:
|
A service in the local university health board, which exists to provide support to carers and those diagnosed with dementia, depression or severe later-life mental illness. The aims of the service include help to prevent admission to hospital and prevent deterioration in relation to being in hospital |
| DCAs (n = 2) | Liaison psychiatry: a service that covers wards in the general hospital setting. Its role is to help PLWD when they are in hospital if they are struggling, anxious or agitated and are exhibiting behaviours that are challenging, such as walking around a lot, and the staff are not able to cope |
Continence service team:
|
NHS continence service: an outpatient-based service. The role of the team is to accept and take referrals from primary care general practitioners, district nurses and others to see patients with incontinence and to assess and put in place a suitable management plan for them |
| Occupational therapist (n = 1) | Facebook: currently works on an elderly ward with both functional patients and PLWD. Previous employment was on a specific dementia ward in a community hospital |
|
PLWD (n = 2) Family carers (n = 11) DCAs (n = 10) Activities co-ordinator of local care home (n = 1) Volunteer from the Alzheimer’s Society (n = 1) |
Public consultation event:a a whole-day event in which issues around toileting and continence were explored through narrative and creative presentations (including pictures, poems and artistic expression, arts and discussion) |
Appendix 3 Inclusion criteria
| Category | Criterion |
|---|---|
| Participants |
People living with dementia or cognitive impairment and/or carers or family members, and HCPs of people living with dementia or cognitive impairment All dementia subtypes were included (e.g. Alzheimer’s disease, vascular dementia, frontotemporal dementia) |
| Interventions/phenomena of interest |
Any communication strategy or individualised care plan(s) that carers, family members and HCPs have employed to manage toileting and continence for PLWD Perceptions and experiences of communication and/or individualised care planning for PLWD with regard to toileting and continence |
| Comparators | All comparisons were considered |
| Outcomes | All outcomes as presented across the primary studies that related to communication and individualised care planning |
| Study designs | All quantitative and qualitative research studies and non-research material [e.g. policies (UK only), guidelines, reports of practice initiatives and clinical case studies] |
| Context | A person living with dementia and all those involved in their care in acute, long-term and community health-care settings and home settings |
Appendix 4 Search strategies for systematic review
Ovid MEDLINE(R) all
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
dement*.mp.
-
alzheimer*.mp.
-
exp Dementia/)
-
((cognit* or memory* or mental*) adj3 (declin* or impair* or los* or deteriorat*)).mp.
-
exp DEMENTIA, MULTI-INFARCT/
-
exp FRONTOTEMPORAL DEMENTIA/
-
exp DEMENTIA, VASCULAR/
-
exp senile dementia/
-
exp Alzheimer Disease/
-
exp Cognition Disorders/
-
exp mild cognitive impairment/
-
(“limited cognitive disturbance*” or “mild cognitive disorder*”).mp.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
exp urinary incontinence/
-
(incontinen$ or continen$).tw.
-
exp fecal incontinence/
-
((fecal or faecal) adj2 (incontinen$ or continen$)).tw.
-
(stool$ adj2 (incontinen$ or continen$)).tw.
-
(Conservative adj2 (intervention$ or measure$)).ti,ab.
-
(Continence adj2 restoration).ti,ab.
-
(Continence adj2 care).ti,ab.
-
((UI or Incontinence) adj2 (care or manag$ or reduc$ or assess$ or contain$)).tw.
-
toilet training/
-
toilet$.tw.
-
14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24
-
exp NONVERBAL COMMUNICATION/or exp COMMUNICATION/
-
(cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language or visual or language or expression* or voice).ti,ab.
-
(discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*).ti,ab.
-
26 or 27 or 28
-
13 and 25 and 29
-
limit 30 to English language.
Individualised care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
dement*.mp.
-
alzheimer*.mp.
-
exp Dementia/
-
((cognit* or memory* or mental*) adj3 (declin* or impair* or los* or deteriorat*)).mp.
-
exp DEMENTIA, MULTI-INFARCT/
-
exp FRONTOTEMPORAL DEMENTIA/
-
exp DEMENTIA, VASCULAR/
-
exp senile dementia/
-
exp Alzheimer Disease/(
-
exp Cognition Disorders/
-
exp mild cognitive impairment/
-
(“limited cognitive disturbance*” or “mild cognitive disorder*”).mp.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
exp urinary incontinence/
-
(incontinen$ or continen$).tw.
-
exp fecal incontinence/
-
((fecal or faecal) adj2 (incontinen$ or continen$)).tw.
-
(stool$ adj2 (incontinen$ or continen$)).tw.
-
(Conservative adj2 (intervention$ or measure$)).ti,ab.
-
(Continence adj2 restoration).ti,ab.
-
(Continence adj2 care).ti,ab.
-
((UI or Incontinence) adj2 (care or manag$ or reduc$ or assess$ or contain$)).tw.
-
toilet training/
-
toilet$.tw.
-
14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24
-
exp Patient Care Planning/
-
(Individual* adj3 plan*).tw.
-
(Personal* adj3 plan*).tw.
-
26 or 27 or 28
-
13 and 25 and 29
-
limit 30 to English language.
Cumulative Index to Nursing and Allied Health Literature
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
S1 TI dement* OR AB dement*
-
S2 TI alzheimer* OR alzheimer*
-
S3 TI (cognit* W2 declin*) OR AB (cognit* W2 declin*)
-
S4 TI (cognit* W2 deteriorat*) OR AB (cognit* W2 deteriorat*)
-
S5 AB (cognit* W2 fail*) OR TI (cognit* W2 fail*)
-
S6 TI (cognit* W2 los*) OR AB (cognit* W2 los*)
-
S7 TI (cognitive impairment*) OR AB (cognitive impairment*)
-
S8 TI MCI OR AB MCI
-
S9 TI (cognitive disorder*) OR AB (cognitive disorder*)
-
S10 (MH “Dementia, Vascular+”)
-
S11 (MH “Delirium, Dementia, Amnestic, Cognitive Disorders+”)
-
S12 (MH “Dementia, Multi-Infarct”)
-
S13 (MH “Dementia, Presenile”)
-
S14 (MH “Dementia, Senile”)
-
S15 (MH “Alzheimer’s Disease”)
-
S16 (MH “Cognition Disorders+”)
-
S17 (MM “Cognition”)
-
S18 TX (incontinen* or continen*)
-
S19 TX (fecal OR faecal) N2 (incontinen* OR continen*)
-
S20 TX stool* N2 (incontinen* or continen*)
-
S21 MH urinary incontinence+
-
S22 MH fecal incontinence+
-
S23 TI (Conservative W2 (intervention* or measure*)) OR AB (Conservative W2 (intervention* or measure*))
-
S24 TI Continence N2 restoration OR AB Continence N2 restoration
-
S25 TI Continence W2 care OR AB Continence W2 care
-
S26 TX (UI or Incontinence) N2 (care or manag* or reduc* or assess* or contain*)
-
S27 (MM “Toilet Training”)
-
S28 TX toilet*
-
S29 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17
-
S30 S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28
-
S31 (MM “Communication+”) OR (MM “Nonverbal Communication+”) OR (MH “Communication Skills”)
-
S32 ((TI discour* or TI dialog* or TI disclos* or TI intera* or TI communica* or TI talk* or TI speak* or TI verbal or TI non-verbal or TI interpersonal or TI convers*or TI relation*) OR (AB discour* or AB dialog* or AB disclos* or AB intera* or AB communica* or AB talk* or AB speak* or AB verbal or AB non-verbal or AB interpersonal or AB convers*or AB relation*))
-
S33 S31 OR S32
-
S34 S29 AND S30 AND S33
-
S35 S29 AND S30 AND S33 (Limit English).
Individualised care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
S1 TI dement* OR AB dement*
-
S2 TI alzheimer* OR alzheimer*
-
S3 TI (cognit* W2 declin*) OR AB (cognit* W2 declin*)
-
S4 TI (cognit* W2 deteriorat*) OR AB (cognit* W2 deteriorat*)
-
S5 AB (cognit* W2 fail*) OR TI (cognit* W2 fail*)
-
S6 TI (cognit* W2 los*) OR AB (cognit* W2 los*)
-
S7 TI (cognitive impairment*) OR AB (cognitive impairment*)
-
S8 TI MCI OR AB MCI
-
S9 TI (cognitive disorder*) OR AB (cognitive disorder*)
-
S10 (MH “Dementia, Vascular+”)
-
S11 (MH “Delirium, Dementia, Amnestic, Cognitive Disorders+”)
-
S12 (MH “Dementia, Multi-Infarct”)
-
S13 (MH “Dementia, Presenile”)
-
S14 (MH “Dementia, Senile”)
-
S15 (MH “Alzheimer’s Disease”)
-
S16 (MH “Cognition Disorders+”)
-
S17 (MM “Cognition”)
-
S18 TX (incontinen* or continen*)
-
S19 TX (fecal OR faecal) N2 (incontinen* OR continen*)
-
S20 TX stool* N2 (incontinen* or continen*)
-
S21 MH urinary incontinence+
-
S22 MH fecal incontinence+
-
S23 TI (Conservative W2 (intervention* or measure*)) OR AB (Conservative W2 (intervention* or measure*))
-
S24 TI Continence N2 restoration OR AB Continence N2 restoration
-
S25 TI Continence W2 care OR AB Continence W2 care
-
S26 TX (UI or Incontinence) N2 (care or manag* or reduc* or assess* or contain*)
-
S27 (MM “Toilet Training”)
-
S28 TX toilet*
-
S29 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17
-
S30 S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28
-
S31 TX ((patient-cent* W3 care) or (patient-cent* W3 toilet*))
-
S32 TX ((person-cent* W3 care) or (person-cent* W3 toilet*))
-
S33 TX ((person-cent* W3 care) or (person-cent* W3 toilet*))
-
S34 TX ((individual* W3 care) or (individual W3 approach*) or (individual* W3 intervention*) or (Individual* W2 program*) or (Individual* W3 plan*))
-
S35 TX ((personal* W3 care) or (personal* W3 plan*) or (personal* W3 approach*) or (personal* W3 intervention*) or (personal* W3 plan*))
-
S36 TX ((tailor* N3 care) or tailor* N3 plan* or (tailor* N3 approach*) or (tailor* N3 intervention*))
-
S37 (MM “Patient Centered Care”)
-
S38 (MM “Patient Care Plans+”) OR (MM “Nursing Care Plans+”)
-
S39 S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38
-
S40 S29 AND S30 AND S39
-
S41 S29 AND S30 AND S39 (Limit English).
EMBASE
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
dement*.mp.
-
alzheimer*.mp.
-
exp Dementia/
-
((cognit* or memory* or mental*) adj3 (declin* or impair* or los* or deteriorat*)).mp.
-
exp DEMENTIA, MULTI-INFARCT/
-
exp FRONTOTEMPORAL DEMENTIA/
-
exp DEMENTIA, VASCULAR/
-
exp senile dementia/
-
exp Alzheimer Disease/
-
exp Cognition Disorders/
-
exp mild cognitive impairment/
-
(“limited cognitive disturbance*” or “mild cognitive disorder*”).mp.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
exp urinary incontinence/
-
(incontinen$ or continen$).tw.
-
exp fecal incontinence/
-
((fecal or faecal) adj2 (incontinen$ or continen$)).tw.
-
(stool$ adj2 (incontinen$ or continen$)).tw.
-
(Conservative adj2 (intervention$ or measure$)).ti,ab.
-
(Continence adj2 restoration).ti,ab.
-
(Continence adj2 care).ti,ab.
-
((UI or Incontinence) adj2 (care or manag$ or reduc$ or assess$ or contain$)).tw.
-
toilet training/
-
toilet$.tw.
-
14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24
-
exp *interpersonal communication/
-
(cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language or visual or language or expression* or voice).ti,ab.
-
(discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*).ti,ab.
-
26 or 27 or 28
-
13 and 25 and 29
-
limit 30 to English language.
Individualised care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
dement*.tw.
-
alzheimer*.tw.
-
exp Dementia/
-
((cognit* or memory* or mental*) adj3 (declin* or impair* or los* or deteriorat*)).tw.
-
exp DEMENTIA, MULTI-INFARCT/
-
exp FRONTOTEMPORAL DEMENTIA/
-
exp DEMENTIA, VASCULAR/
-
exp senile dementia/
-
exp Alzheimer Disease/
-
exp Cognition Disorders/
-
exp mild cognitive impairment/
-
(“limited cognitive disturbance*” or “mild cognitive disorder*”).tw.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
exp urinary incontinence/
-
(incontinen$ or continen$).tw.
-
exp fecal incontinence/
-
((fecal or faecal) adj2 (incontinen$ or continen$)).tw.
-
(stool$ adj2 (incontinen$ or continen$)).tw.
-
(Conservative adj2 (intervention$ or measure$)).tw.
-
(Continence adj2 restoration).tw.
-
(Continence adj2 care).tw.
-
((UI or Incontinence) adj2 (care or manag$ or reduc$ or assess$ or contain$)).tw.
-
toilet training/
-
toilet$.tw.
-
14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24
-
exp Patient Care Planning/
-
exp *Patient-Centered Care/
-
((patient-cent* adj3 care) or (patient-cent* adj3 toilet*)).tw.
-
((person-cent* adj3 care) or (person-cent* adj3 toilet*)).tw.
-
((individual* adj3 care) or (individual adj3 approach*) or (individual* adj3 intervention*) or (Individual* adj2 program*) or (Individual* adj3 plan*)).tw.
-
((personal* adj3 care) or (personal* adj3 plan*) or (personal* adj3 approach*) or (personal* adj3 intervention*) or (personal* adj3 plan*)).tw.
-
((tailor* adj5 individual) or (tailor* adj3 patient*) or (tailor* adj3 person*)).tw.
-
26 or 27 or 28 or 29 or 30 or 31 or 32
-
13 and 25 and 33
-
limit 34 to English language.
PsycInfo
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
exp urinary incontinence/
-
(incontinen$ or continen$).tw.
-
exp fecal incontinence/
-
((fecal or faecal) adj2 (incontinen$ or continen$)).tw.
-
(stool$ adj2 (incontinen$ or continen$)).tw. (10)
-
(Conservative adj2 (intervention$ or measure$)).ti,ab.
-
(Continence adj2 restoration).ti,ab.
-
(Continence adj2 care).ti,ab.
-
((UI or Incontinence) adj2 (care or manag$ or reduc$ or assess$ or contain$)).tw.
-
toilet training/
-
toilet$.tw.
-
dement*.mp.
-
alzheimer*.mp.
-
exp Dementia/
-
((cognit* or memory* or mental*) adj3 (declin* or impair* or los* or deteriorat*)).mp.
-
exp DEMENTIA, MULTI-INFARCT/
-
exp FRONTOTEMPORAL DEMENTIA/
-
exp senile dementia/
-
exp Alzheimer Disease/
-
(“limited cognitive disturbance*” or “mild cognitive disorder*”).mp.
-
exp presenile dementia/
-
exp semantic dementia/
-
2 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11
-
exp *VERBAL COMMUNICATION/or exp *INTERPERSONAL COMMUNICATION/or exp *NONVERBAL COMMUNICATION/or exp *COMMUNICATION/or exp *COMMUNICATION SKILLS/
-
(cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language or visual or language or expression* or voice).ti,ab.
-
(discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*).ti,ab.
-
25 or 26 or 27
-
23 and 24 and 28
-
limit 29 to English language.
Individualised care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
exp urinary incontinence/
-
(incontinen$ or continen$).tw.
-
exp fecal incontinence/
-
((fecal or faecal) adj2 (incontinen$ or continen$)).tw.
-
(stool$ adj2 (incontinen$ or continen$)).tw.
-
exp *Urinary Function Disorders/
-
(Conservative adj2 (intervention$ or measure$)).tw.
-
(Continence adj2 restoration).tw.
-
(Continence adj2 care).tw.
-
((UI or Incontinence) adj2 (care or manag$ or reduc$ or assess$ or contain$)).tw.
-
toilet training/(
-
toilet$.tw.
-
dement*.tw.
-
alzheimer*.tw.
-
exp Dementia/
-
((cognit* or memory* or mental*) adj3 (declin* or impair* or los* or deteriorat*)).tw.
-
exp DEMENTIA, MULTI-INFARCT/
-
exp FRONTOTEMPORAL DEMENTIA/
-
exp senile dementia/
-
exp Alzheimer Disease/
-
(“limited cognitive disturbance*” or “mild cognitive disorder*”).tw.
-
exp presenile dementia/
-
exp semantic dementia/
-
13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
-
((patient-cent* adj3 care) or (patient-cent* adj3 toilet*)).tw.
-
((person-cent* adj3 care) or (person-cent* adj3 toilet*)).tw.
-
((individual* adj3 care) or (individual adj3 approach*) or (individual* adj3 intervention*) or (Individual* adj2 program*) or (Individual* adj3 plan*)).tw.
-
((personal* adj3 care) or (personal* adj3 plan*) or (personal* adj3 approach*) or (personal* adj3 intervention*) or (personal* adj3 plan*)).tw.
-
((tailor* adj3 care) or tailor*adj3 plan* or (tailor* adj3 approach*) or (tailor* adj3 intervention*)).tw.
-
25 or 26 or 27 or 28 or 29
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
24 and 30 and 31
-
limit 32 to English language.
British Nursing Index/Applied Social Sciences Index and Abstracts
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
ti(dementia OR Alzheimer*) OR ab(dementia OR Alzheimer*) AND ti(cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language OR visual OR language OR expression* or voice or discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*) or aB (cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language OR visual OR language OR expression* or voice or discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*) AND ti(toilet* OR incontinen* OR continen*) OR aby (toilet* OR incontinen* OR continen*)
Individualised care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
(ti(dementia OR Alzheimer*) OR ab(dementia OR Alzheimer*)) AND (ti(toilet* OR incontinen* OR continen*) OR aby (toilet* OR incontinen* OR continen*)) AND (ti(patient-cent* NEAR/3 care) OR (patient-cent* NEAR/3 toilet*) OR (person-cent* NEAR/3 care) OR (person-cent* NEAR/3 toilet*) OR (individual* NEAR/3 care) OR (individual NEAR/3 approach*) OR (individual* NEAR/3 intervention*) OR (personal* NEAR/3 care) or (personal* NEAR/3 plan*) or (personal* NEAR/3 approach*) or (personal* NEAR/3 intervention*) or (personal* NEAR/3 plan*) OR (tailor* NEAR/3 care) or tailor*NEAR/3 plan* or (tailor* NEAR/3 approach*) or (tailor* NEAR/3 intervention*) (Individual* NEAR/2 program*) OR (Individual* NEAR/3 plan*) OR ab(patient-cent* NEAR/3 care) OR (patient-cent* NEAR/3 toilet*) OR (person-cent* NEAR/3 care) OR (person-cent* NEAR/3 toilet*) OR (individual* NEAR/3 care) OR (individual NEAR/3 approach*) OR (individual* NEAR/3 intervention*) OR (Individual* NEAR/2 program*) OR (Individual* NEAR/3 plan*) or (personal* NEAR/3 care) or (personal* NEAR/3 plan*) or (personal* NEAR/3 approach*) or (personal* NEAR/3 intervention*) or (personal* NEAR/3 plan*) OR (tailor* NEAR/3 care) or tailor*NEAR/3 plan* or (tailor* NEAR/3 approach*) or (tailor* NEAR/3 intervention*))
Web of Science
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
Indexes = SCI-EXPANDED, Social Sciences Citation Index (SSCI), Emerging Sources Citation Index (ESCI).
TOPIC: (dementia OR Alzheimer*)
AND
TOPIC: (toilet* OR incontinen* OR continen*)
AND
TOPIC: (cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language OR visual OR language OR expression* or voice or discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*).
Individualised care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
Indexes = SCI-EXPANDED, SSCI, ESCI.
TOPIC: (dementia OR Alzheimer*)
AND
TOPIC: (toilet* OR incontinen* OR continen*)
AND
TOPIC: (cues or behavio?r* or word* or signs* or signage or promp* or reassur* or speak* or reinforc* or language OR visual OR language OR expression* or voice or discour* or dialog* or disclos* or intera* or communica* or talk* or speak* or verbal or non-verbal or interpersonal or convers*or relation*).
Education Resources Information Center
Communication
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
S1 TI dement* OR AB dement*
-
S2 TI alzheimer* OR alzheimer*
-
S3 TI (cognit* W2 declin*) OR AB (cognit* W2 declin*)
-
S4 TI (cognit* W2 deteriorat*) OR AB (cognit* W2 deteriorat*)
-
S5 AB (cognit* W2 fail*) OR TI (cognit* W2 fail*)
-
S6 TI (cognit* W2 los*) OR AB (cognit* W2 los*)
-
S7 TI (cognitive impairment*) OR AB (cognitive impairment*)
-
S8 TI MCI OR AB MCI
-
S9 TI (cognitive disorder*) OR AB (cognitive disorder*)
-
S10 TX (incontinen* or continen*)
-
S11 TX (fecal OR faecal) N2 (incontinen* OR continen*)
-
S12 TI (Conservative W2 (intervention* or measure*)) OR AB (Conservative W2 (intervention* or measure*))
-
S13 TI Continence W2 care OR AB Continence W2 care
-
S14 TX toilet*
-
S15 ((TI discour* or TI dialog* or TI disclos* or TI intera* or TI communica* or TI talk* or TI speak* or TI verbal or TI non-verbal or TI interpersonal or TI convers*or TI relation*) OR (AB discour* or AB dialog* or AB disclos* or AB intera* or AB communica* or AB talk* or AB speak* or AB verbal or AB non-verbal or AB interpersonal or AB convers*or AB relation*))
-
S16 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9
-
S17 S10 OR S11 OR S12 OR S13 OR S14
-
S18 S15 AND S16 AND S17
-
S21 S21 AND S22.
Care plans
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
-
S24 S15 AND S16 AND S23
-
S23 S17 OR S18 OR S19 OR S20 OR S21 OR S22
-
S22 TX ((tailor* N3 care) or tailor* N3 plan* or (tailor* N3 approach*) or (tailor* N3 intervention*))
-
S21 TX ((personal* W3 care) or (personal* W3 plan*) or (personal* W3 approach*) or (personal* W3 intervention*) or (personal* W3 plan*))
-
S20 TX ((individual* W3 care) or (individual W3 approach*) or (individual* W3 intervention*) or (Individual* W2 program*) or (Individual* W3 plan*))
-
S19 TX ((person-cent* W3 care) or (person-cent* W3 toilet*))
-
S18 TX ((person-cent* W3 care) or (person-cent* W3 toilet*))
-
S17 TX ((patient-cent* W3 care) or (patient-cent* W3 toilet*))
-
S16 S10 OR S11 OR S12 OR S13 OR S14
-
S15 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9
-
S14 TX toilet*
-
S13 TI Continence W2 care OR AB Continence W2 care
-
S12 TI (Conservative W2 (intervention* or measure*)) OR AB (Conservative W2 (intervention* or measure*))
-
S11 TX (fecal OR faecal) N2 (incontinen* OR continen*)
-
S10 TX (incontinen* or continen*)
-
S9 TI (cognitive disorder*) OR AB (cognitive disorder*)
-
S8 TI MCI OR AB MCI
-
S7 TI (cognitive impairment*) OR AB (cognitive impairment*)
-
S6 TI (cognit* W2 los*) OR AB (cognit* W2 los*)
-
S5 AB (cognit* W2 fail*) OR TI (cognit* W2 fail*)
-
S4 TI (cognit* W2 deteriorat*) OR AB (cognit* W2 deteriorat*)
-
S3 TI (cognit* W2 declin*) OR AB (cognit* W2 declin*)
-
S2 TI alzheimer* OR alzheimer*
-
S1 TI dement* OR AB dement*.
OpenGrey
Date range searched: inception to August 2020.
Date searched: August 2020.
Search strategy
dementia AND communication and toilet or continence.
dementia AND care plans and toilet or continence.
Appendix 5 List of organisational websites searched and key journals hand-searched
Organisational websites
-
Alzheimer Europe (Luxembourg).
-
Alzheimer’s Society.
-
British Geriatrics Society (London, UK).
-
Care Quality Commission.
-
Care Inspectorate (Dundee, UK).
-
Dementia UK.
-
NHS England.
-
Department of Health and Social Care (London, UK).
-
The King’s Fund (London, UK).
-
National Collaborating Centre for Mental Health (London, UK).
-
National Institute for Health and Care Excellence (London, UK).
-
Northern Ireland Executive (Belfast, UK).
-
Royal College of Nursing (London, UK).
-
Royal College of Physicians (London, UK).
-
Scottish Executive (Edinburgh, UK).
-
Scottish Intercollegiate Guidelines Network (Edinburgh, UK).
-
Social Care Institute for Excellence (London, UK).
-
The Queen’s Nursing Institute (London, UK).
-
Welsh Government (Cardiff, UK).
-
United Kingdom Continence Society (Romsey, UK).
-
International Continence Society (Bristol, UK).
Journals hand-searched within past year
-
Journal of Gerontological Nursing.
-
American Journal of Alzheimer’s Disease & Other Dementias.
-
Journal of the American Geriatrics Society.
-
Journal of Wound, Ostomy, and Continence Nursing.
Appendix 6 Characteristics of included studies: communication
| Author, country and aim | Setting and participants | Demographic details for PLWD | Methods and MMAT score |
|---|---|---|---|
|
Study 1 Bliss et al. 162 Country USA Aim To describe health literacy needs related to incontinence and skin care among family or friend caregivers of individuals with AD and develop supportive and educational materials that address these |
Setting Home Participants Family/friend adult caregivers (n = 48), including spouses (44%), daughters (31%), or extended family members/friends (25%) Recruited from community-based agencies |
Gender Female (75%) Age (mean ± SD) 64 ± 14 years Mental status AD or dementia |
Methods Focus groups and interviews MMAT score 100% |
|
Study 1 Mullins et al. 164 Country USA Aim To examine barriers to communicating with health-care professionals and health literacy about incontinence among different types of informal caregivers of individuals with AD |
See Bliss et al.162 | See Bliss et al.162 | See Bliss et al.162 |
|
Study 2 Hutchinson et al. 163 Country USA Aim To address the range and variation of toileting problems, including management strategies used by family and employed caregivers |
Setting AD-specific day centre Home Participants Family members who participated in the centre support groups (n = 16) and staff members employed at the day centre (n = 13) |
Demographic characteristics of patients with AD who attended the day centre were not reported Mental status AD |
Methods Participant observation at the day centre, clients’ home and support groups Interviews with families and staff members Based on qualitative ethology MMAT score 75% |
|
Study 3 Rolnick et al. 166 Country USA Aim To examine HCPs’ perspectives regarding improving communication with patients and their caregivers about incontinence and dementia |
Setting Secondary care providers Participants Physicians (n = 8), nurse practitioners (n = 2) and a pharmacist (n = 1) Potential participants suggested by advisory committee |
Not applicable Mental status Dementia |
Methods Interviews MMAT score 100% |
|
Study 4 Ostaszkiewicz et al. 165 Country Australia Aim To explore nursing home staff members’ beliefs and expectations about what constitutes ‘quality continence care’ for people living in nursing homes |
Setting Nursing home Participants Nursing home staff (n = 19), registered nurses (n = 8), enrolled nurses (n = 4) and personal care workers (n = 7) Recruited using snowballing technique, selective placement of information in print and electronic media, and information sessions at several nursing homes |
Not applicable Mental status Most nursing home residents were cognitively impaired |
Methods Interviews Naturalistic inquiry using a qualitative exploratory descriptive research approach MMAT score 100% |
|
Study 14 Scerri et al. 167 Country Malta Aim To categorise the perceived and observed needs of persons with dementia admitted in acute medical wards and to explore whether or not these needs are being or have been met |
Setting Acute medical wards (n = 3) Participants PLWD and their family members (n = 12) |
Age Mean 84.7 years; range 71–93 years Mental status Dementia |
Methods Interviews Observations using dementia care mapping MMAT score 75% |
| Author, country and aim | Setting, participants and demographic details for PLWD | Intervention | Data collection, outcome measure and MMAT score |
|---|---|---|---|
|
Study 5 Lancioni et al. 152 Country USA Aim The present three pilot studies that assessed the effectiveness of verbal instructions (presented automatically through simple technology) in helping persons with mild-to-moderate AD recapture basic daily activities |
Setting Alzheimer rehabilitation centre Participants Residents with AD (n = 3) Gender Female: 100% Age 79, 81 and 86 years Mental status AD MMSE scores 10, 19 and 22 |
Intervention Baseline: pilot study 1 – the participants were to perform the bathroom routine without the help of the technology and related verbal instructions Intervention: pilot study 1 – the participants performed all bathroom routine steps with the help of the technology, which presented the instructions. There were 17 steps in total and step 1 was ‘to sit on the toilet’ |
Data collection The participants’ performance of a step was recorded as ‘correct’ if it matched the description of the step (and the instruction available for it during the intervention) and occurred independent of prompting by research assistants Outcome measures Percentage of correct steps performed MMAT score 100% |
|
Study 6 Lancioni et al. 153 Country USA Aim To assess the effectiveness of verbal instructions (presented automatically through simple technology) in helping persons with mild or moderate AD perform daily living activities |
Setting Alzheimer rehabilitation centre Participants Residents with AD (n = 4) Gender Female: 100% Age 59, 76, 79 and 85 years Mental status AD MMSE scores 11, 12, 16 and 20 |
Intervention Same as Lancioni et al. 152 Four studies, with the first study aimed at replicating pilot study 1 from Lancioni et al. 152 Efforts directed at re-establishing the performance of morning bathroom routine |
Data collection Same as Lancioni et al. 152 Outcome measures Same as Lancioni et al. 152 MMAT score 100% |
| Author, country and aim | Setting and participants | Demographic details for PLWD | Data collection, outcome measures and MMAT score |
|---|---|---|---|
|
Study 7 Wilkinson et al. 159 Country Australia Aim To evaluate the comparative suitability of a range of words or symbols to label a toilet for people with dementia |
Setting Phase 1: hostel care for ambulant people with dementia (n/N = 24/28, RR 86%) Phase 2: aged care complex with hostel and nursing home facilities (n = 28) and an acute hospital ward (n = 20) Participants Phase 1: 24 institutions Phase 2: 24 patients |
Gender No details provided Age 80.4 (95% CI 77.1 to 83.1) years Mental status Folstein MSE Normal cognition: n = 21 Mild dementia: n = 11 Moderate dementia: n = 16 Severe dementia: excluded The study comprised two phases and questionnaires were used in both |
Data collection Phase 1: questions posed to hostel management on what word and/or symbols were already in use in that institution to label toilet and/or bathroom facilities Phase 2: questions asking preference for toilet door labelling Outcome measures Preferred symbol according to cognitive state Preferred word according to cognitive state MMAT score 100% |
Appendix 7 Characteristics of included studies: care planning
| Author, country and aim | Setting, participants and demographic details for PLWD | Intervention | Data collection, outcome measures and MMAT score |
|---|---|---|---|
| Randomised control trials | |||
|
Study 8 Jirovec and Templin154 Country USA Aim To evaluate the effectiveness of an individualised scheduled toileting programme on incontinent, memory-impaired elders being cared for at home |
Setting Home Participants Caregivers (n = 118) and memory-impaired elders (n = 118) Randomised to intervention: n = 77 Randomised to control: n = 41 Recruited through announcements in newsletters, flyers on bulletin boards and newspaper advertisements asking for volunteers who were caring for a memory-impaired elder Gender Female: 69% Age (mean ± SD) 79.89 ± 7.93 years Mental status SPMSQ: mean 6.69 ± 2.28 |
Intervention Individualised scheduled toileting programme The intervention group was taught an IST procedure that compensated for cognitive impairment by providing memory-impaired patients toileting reminders Initially, assignment was to one of two intervention groups: one group of participants was visited every 2 months and the other group after a 6-month interval. There was also a control group At 6-month follow-up, the two intervention groups did not differ with respect to urinary incontinence. The original two intervention groups were combined, leaving a single intervention group and a control group |
Data collection Incontinence was calculated as the percentage of time the patient was incontinent by dividing the incontinent episodes by the total number of voiding episodes, both continent and incontinent Voiding record Outcome measures Decrease in percentage of incontinent episodes vs. staying the same or not showing improvement in incontinence Incontinence frequency Mobility Consistency in implementing the IST protocol MMAT score 75% |
| Pre/post test | |||
|
Study 9 Tanaka et al. 155 Country Japan Aim To investigate whether or not a system of individualised and comprehensive care was able to increase the intake of fluids and food, and to reduce the proportion of nappy users and the size of their nappy pads, therefore, leading to an enhanced QoL |
Setting Nursing homes (n = 17) Participants Nursing home residents (n = 122) Gender Female: 85.2% Age (mean) 85.2 years Mental status Dementia |
Intervention Individualised and comprehensive care that focused on providing adequate fluids and meals, encouraging patients to use toilets and reducing the size of their nappy pads. This approach would differ significantly from the usual urinary incontinence care in which nappies would be changed at scheduled times only |
Data collection methods Water intake volume, condition of nappies (i.e. dry or wet) and when residents wet their nappies were recorded in residents check sheets by staff Hours spent in wet nappies were calculated by subtracting the total time spent in dry nappies from 24 hours Types of pants or nappies (e.g. cloth pants, training pants, nappy, cloth nappies) and the size of pads (e.g. small, medium, large, extra large, 2 × extra large) Method of daytime urination (e.g. toilet, commode chair, urinary chamber pot, nappy) Outcome measures Mean water intake volume Time spent in wet nappies (hours/day) Changing types of pants or nappies and the size of pads during daytime Change in method of daytime night-time urination MMAT score 100% |
| Post-intervention descriptive surveys | |||
|
Study 10 Gitlin and Corcoran158 Country USA Aim To describe the use of the home environment by 17 spouse caregivers to manage problems associated with bathing and incontinence |
Setting Home Participants Spouse caregivers of elderly with dementia (n = 17) Recruited from a network of local social services agencies Demographic characteristics of elderly PLWD not provided Mental status Physician’s diagnosis of dementia |
Intervention Individual treatment strategies delivered by an OT and designed to enhance the caregiver’s ability to problem-solve about their environment and to develop effective solutions to situations they considered problematic Data collection Data recording form completed by OT |
Outcome measures The number of solutions that were implemented by a caregiver The number of solutions deemed ineffective and eliminated by the caregiver MMAT score 75% |
|
Study 11 Corcoran and Gitlin157 Country USA Aim To describe the specific aspects of treatment that were accepted and utilised by 100 family caregivers |
Setting Home Participants Family caregivers in the treatment arm of a randomised controlled trial (n = 100) Recruited using media announcements and social service referrals Demographic characteristics of elderly PLWD not provided Mental status Physician’s diagnosis of dementia |
Intervention Environmental skill-building programme Home environment intervention delivered by OTs and included toileting and incontinence (same as Gitlin and Corcoran158) Data collection Interviews to ascertain the specific problems areas that were addressed in the intervention, the specific strategies that the caregiver indicated a willingness to try (attempted) and the strategies the caregiver actually used |
Outcome measures The number and type of problem area Strategies for specific problems Strategies by environmental layers Acceptance and use of environmental strategies MMAT score 75% |
|
Study 15 Wijk et al. 156 Country Sweden Aim To operationalise, assess and evaluate the feasibility and preliminary effects of implementing a person-centred approach to incontinence care for older adults with cognitive decline in residential care facilities in Sweden |
Setting Residential care facilities (n = 3) Participants Health-care workers (n = 20) and residents with cognitive decline (n = 54) Gender Female: 59.9% Age (mean + SD) 83.9 + 8.72 years Range 68 to 99 Mental status Cognitive decline MMSE score of 9.28 ± 7.94 |
Intervention Person-centred approach focused on assessment and care planning to incontinence care over a 10-month period Training was provided over five sessions to teach participants how to tailor a person-centred incontinence plan At the end of the 10-month period, the participants created guidelines to make change towards person-centred incontinence care sustainable |
Data collection Health-care records assessed by research team at baseline, immediately after and at 6 months Process outcome measures of the person-centred approach Impact outcome measures of participants’ QoL Impact outcome measures of participants’ quality of care Outcome measures QoL in late-stage dementia Continence status [totally independent (i.e. using the toilet with no need of any containment product); partly continent (i.e. continent if assisted when needing to go to the toilet with or without use of a containment product); and totally incontinent (i.e. being dependent on containment products 24/7 and not managing by oneself)] Has basal assessment of incontinence been conducted? Have person-centred actions been taken regrading incontinence? Has the resident been given adapted continence aids? MMAT score 75% |
| Author, country and aim | Setting and participants | Demographic details for PLWD | Methods and MMAT score |
|---|---|---|---|
| Cross-sectional surveys | |||
|
Study 12 Shih et al. 160 Country Taiwan (Province of China) Aim To understand and compare the behavioural characteristics of bowel movement and urination needs in patients with dementia |
Setting Long-term care facilities (n = 8) and a day centre (n = 1) Participants Residents (n = 187) |
Gender Female: 59% Age Mean ± SD 80.1 ± 9.6 years; range 70–90 years Mental status AD: 38.5% Unspecified dementia: 32.6% Vascular dementia: 18.7% Other dementia: 10.2% |
Data collection Behaviour checklist for bowel and urination developed for the study Outcomes measures Symptoms and signs of bowel movement and urination expressed by the patient MMAT score 100% |
| An adapted three-stage Delphi consultation study | |||
|
Study 13 Iliffe et al. 161 Country UK Aim The aim of this study was to develop and test a continence assessment tool and supporting resources for people with dementia to be used by primary care professionals and primarily community nurses |
Setting Community Participants Stage 1: carers and professionals (n = 10) Stage 2: carers and professionals (n = 10) and specialist continence professionals (n = 10) Stage 3: carers (n = 8), general practitioners (n = 2), a geriatrician/psychogeriatrician (n = 1), continence nurse specialists (n = 3), district nurses/community nurses (n = 7), occupational therapists (n = 2) and other (n = 3) RR = 26/50 |
Not applicable Mental status Dementia |
Data collection Stage 1: face-to-face consultations were facilitated to describe a broad range of principles and issues that would underpin an assessment tool designed to address the needs of people with dementia Stage 2: a prototype dementia-focused continence assessment tool was developed using the data generated in stage 1, asking for agreement or disagreement to items, plus suggestions for further items. This was used to consult, in writing, both the expert group in stage 1 and also a further group of carers and specialist continence professionals. The prototype was further adapted Stage 3: a different, wider group of experts (including carers and professionals) was consulted in writing. The group was sent the draft dementia-focused assessment tool together with a questionnaire to test its face and content validity Outcome measures Recipients were asked (1) whether or not the tool would improve recognition of the problems (face validity) and (2) to rate each item for importance and identify missing or unnecessary items (content validity) MMAT score 75% |
Appendix 8 Details of included grey literature
| Document details | Focus of material relevant to the review |
|---|---|
| Web page: Alzheimer’s Society168 | Individualised care planning |
| Book: Alzheimer’s Society and Gray169 | Communication |
| Web page: Dementia UK170 | Communication |
| Web page: Social care Institute for Excellence171 | Communication |
| Guideline: Alzheimer’s Europe87 | Individualised care planning and communication |
| Guideline: Collaborating Centre for Mental Health1 | Communication |
| Report: Thompson et al.174 | Individualised care planning |
| Guidance: Potter176 | Individualised care planning |
| Report: Care Quality Commission173 | Communication |
| Web-based booklet: Care Inspectorate172 | Individualised care planning and communication |
| Framework: Ostaszkiewicz177 | Individualised care planning and communication |
| Model: Ostaszkiewicz178 | Communication |
| Guideline: Abrams et al.175 | Individualised care planning |
| Information sheet: Alzheimer’s Scotland179 | Communication |
Appendix 9 Studies excluded after full-text screening
| Study | Reason for exclusion |
|---|---|
| Burkhard FC, Bosch JLHR, Cruz F, Lemack GE, Nambiar AK, Thiruchelvam N, et al. Clinical Guideline for the European Association of Urology: Urinary incontinence. 2018. URL: https://uroweb.org/guideline/urinary-incontinence/ (accessed 24 November 2021) | No data on PLWD, Alzheimer’s disease or cognitive impairment within the guideline |
| Billing J, Alaszewski H, Wagg A. Privacy and Dignity in Continence Care Project. London: Royal College of Physicians; 2009 | Sample was people aged > 65 years who had the cognitive and linguistic ability to participate |
| National Institute for Health and Care Excellence (NICE). Faecal Incontinence in Adults. Clinical Guideline 49. London: NICE; 2014 | No data on communication of individualised care plans in the section relevant for PLWD |
| Royal College of Psychiatrists. National Audit of Dementia Care in General Hospitals 2016–2017. Third Round of Audit Report. London: Royal College of Psychiatrists; 2017 | Continence mentioned in relation to assessment only |
| Royal College of Physicians. National Audit of Continence Care. London: Royal College of Physicians; 2010 | No data on for PLWD, Alzheimer’s disease or cognitive impairment within the guideline |
| Albert SM. The caregiver as part of the dementia management team. Dis Manag Health Out 1999;5:329–37 | Not about toileting or incontinence |
| Allwood R, Pilnick A, O’Brien R, Goldberg S, Harwood RH, Beeke S. Should I stay or should I go? How healthcare professionals close encounters with people with dementia in the acute hospital setting. Soc Sci Med 2017:191:212–25 | Not about toileting or incontinence |
| Burgener SC, Jirovec M, Murrell L, Barton D. Caregiver and environmental variables related to difficult behaviors in institutionalized, demented elderly persons. J Gerontol 1992;47:242–9 | Not about communication in relation to toileting |
| DiZazzo-Miller R, Samuel PS, Barnas JM, Welker KM. Addressing everyday challenges: feasibility of a family caregiver training program for people with dementia. Am J Occup Ther 2014;68:212–20 | Research covers communication in relation to nutrition and transfer and toileting, but not about communication in relation to toileting |
| Ghatak R. A unique support model for dementia patients and their families in a tertiary hospital setting: description and preliminary data. Clin Gerontol 2011;34:160–72 | Support programme for dementia carers and not about communication in relating to toileting |
| Lanciono GE, Singh NN, O’Reilly MF, Sigafoos J, Renna C, Ventrella M, et al. Supporting daily activities and indoor travel of persons with moderate Alzheimer’s disease through standard technology resources. Res Dev Disabil 2013;34:2351–9 | Not about communication in relation to toileting |
| Moyle W, Bramble M, Bauer M, Smyth W, Beattie E. ‘They rush you and push you too much . . . and you can’t really get any good response off them’: A qualitative examination of family involvement in care of people with dementia in acute care. Australas J Ageing 2016;35:E30–4 | Not about communication in relation to toileting |
| Norbergh KG, Asplund K, Rassmussen BH, Nordahl G, Sandman PO. How patients with dementia spend their time in a psycho-geriatric unit. Scand J Caring Sci 2001;15:215–21 | Not about communication in relation to toileting |
| Panella J. Toileting strategies in day care programs for dementia. Clin Gerontol 1986;4:61 | Discussion article |
| Perilli V, Lancioni GE, Hoogeween F, Caffo A, Singh N, O’Reilly M, et al. Video prompting versus other instruction strategies for persons with Alzheimer’s disease. Am J Alzheimers Dis Other Demen 2013;28:393–402 | Not about communication in relation to toileting |
| Tales A, Burholt V, Nash P, Bichard J, Clayton-Turner A. Dementia-friendly public toilets. Lancet 2017;390:552–3 | Correspondence piece |
| Uchimoto K, Yokoi T, Yamashita T, Okamura H. Investigation of toilet activities in elderly patients with dementia from the viewpoint of motivation and self-awareness. Am J Alzheimers Dis Other Demen 2013;28:459–68 | Not about communication in relation to toileting |
| Warkentin R. Implementation of a urinary continence program. J Gerontol Nurs 1992;18:31–6 | Not about communication in relation to toileting |
| Williams GO, Gjerde CL, Haugland S, Darnold D, Simonton LJ, Woodward PJ. Patients with dementia and their caregivers 3 years after diagnosis. A longitudinal study. Arch Fam Med 1995;4:512–17 | Not about communication in relation to toileting |
| Svedas K, Wise K. Improving bowel care in residential aged care facilities. Aust N Z J Continence 2012;18:46–51 | Not about individualised care plans and continence care |
| Bucci AT. Be a continence champion: use the CHAMP tool to individualise the plan of care. Geriatr Nurs 2007;28:120–4 | Discussion article |
| Rogers JC, Holm MB, Burgio LD, Granieri E, Hsu C, Hardin M, McDowell BJ. Improving morning care routines of nursing home residents with dementia. J Am Geriatr Soc 1999;47:1049–57 | Not about individualised care plans and continence care |
| Corcoran M, Gitlin LN, Levy L, Eckhardt S. An occupational therapy home-based intervention to address dementia-related problems identified by family caregivers. Alzheimers Care Today 2002;3:82–90 | No data regarding individualised care plans and continence care |
| Prizer LP, Zimmerman S. Progressive support for activities of daily living for persons living with dementia. Gerontologist 2018;58:S74–87 | Not about individualised care plans and continence care |
| Drennan VM, Manthorpe J, Iliffe S. Meeting the needs of older people living at home with dementia who have problems with continence. Qual Ageing Older Adults 2017;18:246–53 | Not about individualised care plans and continence care |
| Olthof-Nefke MWLJ, Kruse H, Derksen E, de Swart BJM, Nijhuis-van der Sander MWG, Kalf JG. Improving communication between persons with mild dementia and their caregivers: qualitative analysis of a practice-based logopaedic intervention. Folia Phoniatr Logop 2018;70:124–33 | Not about communication in relation to toileting |
| Soderman M, Rosendahl S, Sallstrom C. Caring and uncaring encounters between assistant nurses and immigrants with dementia symptoms in two group homes in Sweden – an observational study. J Cross Cult Gerontol 2018:33:299–317 | Not about communication in relation to toileting |
| Dahlke S, Hunter KF, Negrin K, Reshef Kalogirou M, Fox M, Wagg A. The educational needs of nursing staff when working with hospitalised older people. J Clin Nurs 2019;28:221–34 | Not about the care of PLWD |
| Foster S, Balmer D, Gott M, Frey R, Robinson J, Boyd M. Patient-centred care training needs of health care assistants who provide care for people with dementia. Health Soc Care Community 2019;27:917–25 | Not about toileting or incontinence |
| Samuelsson C, Ekstrom A. Digital communication support in interaction involving people with dementia. Logoped Phoniatr Vocol 2019;44:41–50 | Not about communication in relation to toileting |
| Stanyon M, Thomas S, Gordon A, Griffiths A. Effects of care assistant communication style on communicative behaviours of residents with dementia: a systematic multiple case study. Scand J Caring Sci 2019;33:207–14 | Not about communication in relation to toileting |
| Mariana E, Chattat R, Ottoboni G, Koopmans R, Vernooig-Dassen M, Engels Y. The impact of a shared decision-making training program on dementia care planning in long-term care. J Alzheimers Dis 2018;64:1123–35 | Not about toileting or incontinence |
| Villar F, Celdran M, Vila-Miravent J, Serrat R. Involving institutionalised people with dementia in their care-planning meetings: lessons learnt by the staff. Scand J Caring Sci 2018;32:567–74 | Not about toileting or incontinence |
| Yenisehir S, Citak Karakaya I, Gurhan Karakaya M. Knowledge and practice of nursing home caregivers about urinary incontinence. Eur Geriatr Med 2019;10:99–105 | Not about toileting or incontinence |
Appendix 10 Studies excluded on critical appraisal
| Study | Reason for exclusion |
|---|---|
| Tarrier N, Larner S. The effects of manipulation of social reinforcement on toilet requests on a geriatric ward. Age Ageing 1983;12:234–9 | MMAT146 score of 50% with the following questions being answered no:
|
| Colling J, Ouslander J, Hadley BJ, Eisch J, Campbell E. The effects of patterned urge-response toileting (PURT) on urinary incontinence among nursing home residents. J Am Geriatr Soc 1992;40:135–41 | MMAT146 score of 25% with the following questions being answered no:
|
| Williams R. Hospital programme for dementia-specific care. Nurs Older People 2011;23:14–17 | MMAT146 score of 0% and all questions were given an answer of no |
| Duncan K. Development of a continence management chart for carers of people with dementia who have functional incontinence. World Council Enterostom Ther 2002;22:21–3 | MMAT146 score of 0% and all questions were given an answer of no |
Appendix 11 Methodological quality
Qualitative studies
Four162,164–166 of the six qualitative studies162–167 fulfilled all four quality criteria on the MMAT, with the remaining two studies163,167 fulfilling three of the quality criteria; however, these studies did not report whether or not the researchers’ role might influence the outcome of the study.
Quantitative studies
One study154 was a quantitative randomised controlled trial that fulfilled three out of the four quality criteria, with complete outcome data (i.e. ≥ 80%) not reported. There were six quantitative non-randomised studies152,153,155–158 and of these studies three152,153,155 fulfilled all four quality criteria. In the remaining three studies, the response rate for the sample was unclear in two studies157,158 and the authors did not compare the baseline characteristics between those in the control and those in the intervention groups in one study. 156 Three studies were quantitative descriptive. 159–161 Two159,160 of these studies fulfilled all four criteria and we were unable to ascertain what the response rate was for the sample in one study that that did not fulfil all four criteria. 161
Appendix 12 CERQual and GRADE summary statements
1. PLWD and their carers find talking about incontinence distressing and embarrassing.
CERQual: moderate – studies 2,163 3166 and 4. 165
2. HCPs to build trust and rapport through using humour, having appropriate knowledge and skills by speaking quietly and keeping incontinence issues secret.
CERQual: moderate – studies 2,163 3166 and 4. 165
The attitudes of HCPs towards continence and continence care3. HCPs often ignore toileting requests or avoid routine toileting, citing being busy or being uncomfortable with or disinterested in toileting.
CERQual: moderate – studies 2163 and 14. 167
4. Staff in acute settings do not consistently promote continence.
CERQual: very low – study 14. 167
5. HCPs having respect-building relationships and using appropriate language.
CERQual: very low – study 2. 163
6. Interpersonal and communication skills are important and should be a focus of education programmes. 177,178
Non-research: ungraded.
The importance of non-verbal cues7. PLWD are not always able to recognise and communicate that they need to go to the toilet or indicate that they need assistance87,171–173 and they can use a variety of non-verbal cues. 1,87,170,172,173,176,178
CERQual: high – studies 1–7152,153,159,162–166 and 10–12,157,158,160 and non-research (ungraded).
8. HCPs checking PLWD’s awareness of communication techniques, including non-verbal cues through communicating with the family.
CERQual: moderate – studies 2163 and 13. 161
9. HCPs being able to recognise the non-verbal signals, body language, facial expressions, behaviours and signs that PLWD use to communicate that they need to go toilet is crucial,170–172 and this should be a focus education programmes for new staff.
CERQual: moderate – studies 2163 and 12,160 and non-research (ungraded).
Finding the appropriate words and symbols to describe the toilet10. Finding out what words or phrases PLWD use for describing the toilet is seen as important. 1,170,172,173
CERQual: very low – study 7159 and non-research (ungraded).
11. People living with moderate dementia preferred the word toilet compared with those with no cognitive impairments and those with advanced dementia preferred the international symbols for toilet compared with those with mild dementia or no cognitive impairment.
CERQual: very low – study 7. 159
Strategies for improving communication12. HCPs introducing themselves and seeking approval of PLWD before performing tasks.
CERQual: very low – study 4. 165
13. A range of strategies have been identified that include getting to know PLWD and how they communicate and manage their continence, communicating with the family, prompting, seeing the person has an individual and checking HCPs communication skills. 1,87,171–173
CERQual: moderate – studies 4165 and 13,161 and non-research (ungraded).
Using technology to present instructions14. Verbal instructions presented automatically through simple technology have the potential to be effective in helping persons with mild or moderate Alzheimer’s disease go to the toilet independently by presenting simple stepwise sequential instructions.
Grade: very low – studies 5152 and 6. 153
Theme 2: communication during outpatient appointments Presence of PLWD during outpatient consultations15. Caregivers felt that having the PLWD with them during outpatient consultations could cause unnecessary anxiety.
CERQual: very low – study 1. 162,164
16. Caregivers felt that having PLWD with them during outpatient consultations would allow greater co-operation with management strategies.
CERQual: very low – study 1. 162,164
17. HCPs felt that it was important that PLWD were present at appointments.
CERQual: very low – study 3. 166
Initiating conversations during outpatient consultations18. Uncertainty over who should initiate conversations during consultations.
CERQual: very low – study 3. 166
19. HCPs suggested developing a pre-visit checklist to prompt conversation during consultations.
CERQual: very low – study 3. 166
The language of incontinence during outpatient consultations20. Incontinence and management options are often explained in terms that caregivers find difficult to understand.
CERQual: low – studies 1162,164 and 3. 166
21. Caregivers and HCPs suggested a variety of written information resources that could be provided.
CERQual: low – studies 1162,164 and 3. 166
Theme 3: delivering individualised continence care Importance of individualised continence care22. Targeted and individualised/person-centred continence care that is established after a thorough assessment has taken place is seen as important. 87,168,172,174,175,177–179
Non-research (ungraded).
23. Individualised continence care is about what is best for the person living with dementia and avoiding harm, and is about promoting autonomy and independent living. 87
Non-research (ungraded).
Components of individualised care planning24. Individualised care planning should consider the needs of both PLWD and their caregivers and involve multicomponents. Exploring both daytime care and night-time care of incontinence are helpful in addressing incontinence in the home care setting. 87,168,174–177
Non-research (ungraded).
25. An intervention that involved individualised and comprehensive care for residents in a care home that focused on providing adequate fluids and meals by encouraging patients to use toilets was effective for 19% of residents in reducing the proportion of continence pads used.
Grade: very low – study 9. 155
26. An intervention that involved individual treatment strategies delivered by an occupational therapist and designed to enhance the caregiver’s ability to problem-solve about their environment. A post-intervention survey reported that this approach enabled caregivers to develop effective solutions to situations they considered problematic, which included toileting.
CERQual: low – studies 10158 and 11. 157
27. An intervention that involved training health workers in person-centred care was effective in improving the quality of care and reducing the number of aids needed to manage incontinence.
GRADE: very low – study 15. 156
Health-care professionals and caregivers working in partnership28. It is important that HCPs and caregivers work together to deliver individualised/person-centred continence care. 168,172,174,176
Non-research (ungraded).
Establishing a toileting routine in the home environment29. The importance of developing a regular toileting schedule was highlighted by caregivers. 87
CERQual: very low – study 10158 and non-research (ungraded).
30. An individualised scheduled toileting programme that compensated for cognitive impairment by providing memory-impaired patients with toileting reminders was not shown to have any significant benefits in terms of improving the number of incontinent episodes for PLWD in a home care setting.
Grade: very low – study 8. 154
List of abbreviations
- A&E
- accident and emergency
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- EPPI-Centre
- Evidence for Policy and Practice Information and Co-ordinating Centre
- ESCI
- Emerging Sources Citation Index
- GRADE
- Grading of Recommendations, Assessment, Development and Evaluation
- HCA
- health-care assistant
- HCP
- health-care provider
- i.v.
- intravenous
- MMAT
- Mixed Methods Appraisal Tool
- NIHR
- National Institute for Health and Care Research
- PLWD
- people living with dementia
- PPI
- patient and public involvement
- QoL
- quality of life
- REC
- Research Ethics Committee
- SSCI
- Social Sciences Citation Index
