Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the Health and Social Care Delivery Research Programme and managed by the Evidence Synthesis Programme as project number NIHR131593. The contractual start date was in June 2020. The final report began editorial review in November 2020 and was accepted for publication in May 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Al-Khudairy et al. This work was produced by Al-Khudairy et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Al-Khudairy et al.
Chapter 1 Background
The Department of Health and Social Care (DHSC) supported the introduction of social prescribing (SP) for people with long-term conditions, poor mental health and complex social needs. 1,2 SP in this context encourages health-care professionals to refer patients to a link worker, who will develop a personalised plan for each individual. Plans can include activities such as arts, gardening and physical activity, with the aim of improving an individual’s health and well-being. Referral to link workers can occur from:
. . . a wide range of local agencies, including general practice, pharmacies, multi-disciplinary teams, hospital discharge teams, allied health professionals, the fire service, police, job centres, social care services, housing associations and voluntary, community and social enterprise (VCSE) organisations. Self-referral is also encouraged.
There are several modes of SP, including signposting, direct referrals, the link worker model and the holistic model. 3 The Social Prescribing Network defines the link worker SP model as a facility that allows health-care professionals to refer a person to a link worker. A non-clinical social prescription is then co-designed by both the link worker and person referred. 4 NHS England (NHSE) defines SP as:
. . . a way for local agencies to refer people to a link worker. Link workers give people time, focusing on ‘what matters to me’ and taking a holistic approach to people’s health and wellbeing. They connect people to community groups and statutory services for practical and emotional support.
Link workers can support existing community groups, collaborate with local partners and support people to start new groups. 5 SP falls under the umbrella of NHS Universal Personalised Care,6 and the NHS Long Term Plan7 outlines proposals for a major expansion in the numbers of people referred to SP schemes. To support this, the 2019 general practitioner (GP) contract made provisions for all Primary Care Networks (PCNs) in England to employ one SP link worker from an allocated budget of £891M. This is a substantial investment in SP. 8
Description of the service under assessment
NHS England, in partnership with stakeholders, developed a standard model of SP, which is presented as Figure 1. NHSE worked with a range of stakeholders to develop its Social Prescribing Common Outcomes Framework to encourage consistent data gathering and measurement of the impact of SP because they were aware that locally driven approaches had emerged across England. The consensus reached was that the impact on the person, the impact on the health and care system and the impact on community groups should be measured. 5 In 2020/21, NHSE aimed to increase the number of link workers to build significant capacity to deal with higher uptake of the service (up to 900,000 referrals by 2023/24). 1 The DHSC wished to explore whether or not an evaluation of the link worker model of SP is possible. The Warwick Evidence Technology Assessment Review Team was commissioned to complete a feasibility analysis to understand what would be required and what is possible in a future impact evaluation study. The findings of our feasibility analysis are presented in this report.
FIGURE 1.
NHS England’s model elements of SP. Reproduced with permission from NHSE. 1 Contains public sector information licensed under the Open Government Licence v3.0.

Research questions
To complete the feasibility analysis the following research questions were proposed in the commissioning brief:
-
What are the most important evaluation questions that an impact study could investigate?
-
What data are already available at a local or national level and what else would be needed?
-
Are there sites delivering at a large enough scale and in a position to take part in an impact study?
-
How could the known challenges to evaluation (e.g. information governance and identifying a control group) be addressed?
Research objectives
To answer the four research questions, we developed the following objectives:
-
Undertake a rapid systematic review to better understand current models of SP, previous evaluations and evaluation questions that an impact study could investigate (research question 1).
-
Undertake qualitative interviews with those working in SP to identify:
-
data already collected at local and national levels and gaps in data availability (in particular outcomes data) to inform likely data availability for future evaluation (research question 2)
-
delivery sites, scale and processes of current service delivery and the number of sites available for future service evaluation (research question 3)
-
known challenges to evaluating the SP link worker model (e.g. information governance and identification of a control group) (research question 4)
-
-
Draw together findings and make recommendations for a future national evaluation of the SP link worker model (including feasibility, strengths and limitations) and how known challenges can be addressed.
Chapter 2 Methods
Evidence synthesis
We conducted a rapid systematic review9–12 to better understand the literature on previous evaluations and evaluation questions that an impact study could investigate and to inform the development and structure of our data collection. We searched MEDLINE® (National Library of Medicine, Bethesda, MD, USA) ALL [via Ovid® (Wolters Kluwer, Alphen aan den Rijn, the Netherlands)] from inception to 14 February 2019 (see Appendix 1) and the first 100 hits of a Google (Google Inc., Mountain View, CA, USA) search. We searched key studies for additional evidence. One reviewer screened potentially eligible studies and discussed with a second reviewer when in doubt. Studies were included if they included ‘social prescription’, ‘social prescribing’ or ‘social prescriber’. We included all study designs and study outcomes. Only studies published in the English language from 2015 were eligible. Two reviewers assessed studies for eligibility and data were extracted by two reviewers into summary tables. Key extracted data included study design, setting, definition of the link worker and outcomes reported. The evidence synthesis was analysed using a narrative approach and evidence summaries are provided in summary tables. A Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist was conducted.
Qualitative interviews
To capture the perspectives of people involved in the planning and delivery of SP, as well as those of patients, we conducted a series of semistructured interviews that were informed by the rapid systematic review, questions set out in the project commissioning brief, and the study protocol. The protocol was generated in collaboration with the National Institute for Health and Care Research (NIHR) and NHSE, and included the perspectives of other stakeholders including service experts, patient and public representatives and other relevant parties during the protocol planning phase of this study. We sought and received feedback, guidance and recommendations regarding the qualitative elements of our planned work during project stakeholder meetings and webinars. These were attended by a range of organisations and interested parties, including NHSE, voluntary sector organisations, link workers and other social prescribers, academics and members of the public. The supplementary information from the webinars was essential for facilitating discussions around the research gaps and potential areas for future work. A COnsolidated criteria for REporting Qualitative research (COREQ) checklist was carried out.
Ethics approval was obtained from the University of Warwick Biomedical and Scientific Research Ethics Committee (reference number BSREC 93/19-20). We did not deviate from the planned protocol.
Participants
Eligible interview participants were purposively sampled through the NHSE network and contacts of staff members at the University of Warwick (Coventry, UK). Subsequent participants were snowball sampled from these initial participants. We adopted an iterative approach, progressing to the next participants if information was not available from our primary target source. All participants were approached via e-mail by members of the research team (LAK, JH or IG). Targeted participants included (1) national SP leads identified through NHSE, (2) Social Prescribing Network regional leads (for East of England, London, North East, North West, South East, South West, West Midlands and Yorkshire and The Humber) and (3) sites delivering SP, both those with an established/mature link worker social prescribing model scheme and those that did not yet have a mature scheme.
In addition, we interviewed voluntary sector organisations involved in SP to understand what happens after people have been referred to voluntary sector service providers. We contacted people from five voluntary organisations and three people participated. In addition, we contacted project stakeholders, topic experts and academic colleagues to capture opinions and feedback regarding ongoing and completed SP evaluations. In total, we contacted 41 people (plus three academic researchers), of whom 28 participated in interviews (participants, n = 25; academics, n = 3; 68% participation rate).
Data collection
Qualitative data were collected using a semistructured interview topic guide that was informed by our rapid systematic review synthesis, questions set out in the project commissioning brief, and the study protocol (in collaboration with the NIHR and NHSE). The semistructured approach allowed for systematic data collection across participants and sites while ensuring flexibility in structuring the discussion.
The interview guide was peer reviewed by NHSE and colleagues at Warwick Medical School (University of Warwick) and piloted on one participant. Any questions that were not clear were amended as appropriate. Key areas of the interview topic guide included:
-
the nature of the service in terms of structure, models implemented, organisations involved and health domains covered
-
patient journey throughout the service
-
any measured outcomes
-
data collection methods and human resources
-
volume of service uptake
-
type of service utilisation (highest vs. lowest)
-
nature and length of follow-up
-
potential strengths and limitations of the current service
-
major enablers of and challenges to developing and implementing SP service
-
costs and savings when recruiting for and implementing SP service (for both PCNs and other organisations involved)
-
non-attendance data (e.g. resulting from people who do not take up their SP referral)
-
the make-up of people taking up SP (e.g. how they compare to the overall practice population and availability of social class data).
In addition, during the interviews we asked interviewees to comment on how the COVID-19 pandemic was affecting the implementation, provision and uptake of SP.
Interviews were conducted by four members of the research team (LAK, IG, JH or EM; three women and one man; 78% were conducted by IG). Two are senior research fellows, one is a research assistant and one a is medical student; all have previous experience or training in qualitative research methods. Most of the interviews were conducted on Microsoft Teams (Microsoft Corporation, Redmond, WA, USA) and only two were conducted over the telephone. Interviewers did not have a previously established relationship with interviewees at study commencement. A project brief was provided to each potential participant (either via e-mail or verbally) ahead of the interview, which described the research aims and objectives.
Interviews were audio-recorded with the interviewees’ consent, all audio-recorded data were manually transcribed and interview notes were generated by the interviewers. Interviews lasted for a mean of 51 minutes (range 31–147 minutes).
Virtual workshops
Two virtual workshops with researchers, people involved in delivering SP services, and patients and people with lived experience of SP services were undertaken to contribute to the specification and the focus of the recommendations for a future evaluation. The workshop attendees were grouped into two: nine experts focused on process evaluation and eight experts focused on impact evaluation. The workshops also considered the implications of COVID-19 for a future evaluation of SP.
Analysis
Of the 28 interviews that were conducted, 25 [which comprised interviews with link workers, social prescribers and voluntary community and social enterprise (VCSE) workers] were included in the main qualitative data analysis. The remaining three were academic colleagues, two of whom provided descriptions of their research projects to give us further insight into their work and experience in SP evaluations. Data from the academic participants do not follow the main topic guide and are discussed separately in Chapter 3, Ongoing studies of social prescribing: lessons learned from researchers. One academic colleague interview was excluded because their work was not appropriate to the research commissioning brief.
Interview data from the 25 non-academic participants were analysed using a pragmatic framework approach,13,14 using the interview guide as a framework to code and summarise the data into the key areas of interest. The framework was applied to and further developed as the subsequent transcripts were coded, and data were charted and summarised into the framework. Data manipulation and management were supported by NVivo 13 (QSR International, Warrington, UK) software and the framework was constructed in Microsoft Excel® (Microsoft Corporation). Analysis was performed by three members of the research team (AA, EM and IG). The immaturity of the data prevented any theoretical development and identification of reasons for the emergence of phenomena, beyond presentation of summary data in tables and example quotations.
Chapter 3 Results
Evidence synthesis
In this review we set out to identify evaluation questions, understand the nature of the existing evidence, identify outcome measures used in research and practice, and inform qualitative data collection. We screened 124 papers, of which 42 were assessed as relevant. Of these, 15 were excluded (seven protocols and eight editorials or clinical update reports). A total of 27 papers were included in the full-text review [see Appendix 1 for the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram]. 15 Primary studies included one randomised controlled trial (RCT),16 one trial within a cohort study,17 two cohort studies,18,19 two before-and-after studies,20–22 five mixed-methods studies,23–27 and six qualitative studies. 28–33
We identified various forms of secondary studies, including four systematic reviews,34–37 a realist review,38 a rapid review,39 two scoping reviews40,41 and two literature reviews. 42,43 The studies are described in detail below by study design and the key outcomes of studies are presented in Appendix 2. Included studies used a range of well-being measures, including the Warwick–Edinburgh Mental Well-being Scale (WEMWBS), the Hospital Anxiety and Depression Scale (HADS), General Anxiety Disorder-7 (GAD-7), the Patient Health Questionnaire-9 items (PHQ-9), Clinical Outcomes in Routine Evaluation-Outcome Measure (CORE-OM), the Work and Social Adjustment Scale (WSAS), the General Health Questionnaire-12 (GHQ-12), the EuroQol-5 Dimensions (EQ-5D), Recovering Quality of Life (ReQoL), the Dartmouth Primary Care Cooperative Information Project/World Organization of National Colleges, Academies and Academic Associations of General Practice/Family Physicians (COOP/WONCA) and the Rockwood Clinical Frailty Scale (RCFS).
In our summary we focus on the primary studies and briefly highlight the reviews (detailed study characteristics are available in Appendix 2). The classification of outcomes reported in studies is available in Appendix 3.
Randomised controlled trials
We identified one SP-intervention RCT. 16 The study was an evaluation of a smartphone application (app)-based well-being intervention involving 582 participants (54.2% of all selected participants) from Sheffield, UK. The app aimed to encourage appreciation of nature and was intended to be a potential social prescription. Primary outcome measures were the ReQoL and Inclusion of Nature with Self Scale. Secondary outcome measures were the Types of Positive Affect Scale (TPAS), Nature Relatedness Scale and Engaging with Nature Beauty Scale. The study participants were randomised to two different versions of the app, either intervention (green space) (n = 414, 70%) or control (built space) (n = 168, 30%). A total of 322 (55.1%) participants completed baseline measures and 164 (27.4%) completed the 1-month follow-up evaluation. The study reported an improvement in ReQoL score from baseline to follow-up for patients in the intervention group [mean score: baseline, 29.19 points, 95% confidence interval (CI) 28.53 to 29.85 points; follow-up, 32.05 points, 95% CI 30.93 to 33.18 points] but not in the control group (mean score: baseline, 28.67 points, 95% CI 27.69 to 29.65 points; follow-up, 30.69 points, 95% CI 28.90 to 32.47 points). Multivariate analysis showed no significant effect of condition (green vs. built space) [F(7, 118) = 0.964; p = 0.461; ηp2 = 0.054]. In summary, no overall clear benefit of the app was identified. The study was poorly designed because the discrepancy in group sizes (70% randomised to the intervention group and 30% to the control group) meant that the power of the study to detect differences was compromised. The minimum clinically important difference for the ReQoL is described as at least 5 points,44 which is larger than the differences that were observed in the paper reported. In addition, the study failed to recruit enough patients with common mental health problems (referred by a GP), had a high attrition rate for follow-up (the rate of retention from post intervention to follow-up was 27.36%) and reported that the app was only ‘moderately engaging’ to subjects.
Trials within cohorts studies
There was one study with a trials within cohorts (TWiCs) design. 17 The study evaluated telephone-based ‘health coaching’ among a cohort of 1306 older people with multimorbidity, of whom 504 were offered the health coaching intervention (intervention group) and the remaining 802 were not offered health coaching (the usual care group). This study measured patient-reported outcomes including patient activation, quality of life, depression, health-care utilisation and self-care. A cost-effectiveness analysis was also performed. There was no statistically significant improvement in patient activation, quality of life, depression and self-care in the intervention group compared with usual care. Use of planned services and overall costs increased and use of emergency care decreased in the intervention group. The incremental cost per quality-adjusted life-year (QALY) was £8049, and the probability that this intervention would be cost-effective at a cost-per-QALY threshold of £20,000–30,000 was 70–79%. The authors reported that the lack of significant improvement in primary outcomes may be due to the low level of uptake among those selected. The intention-to-treat study design included all patients who were offered health coaching in the intervention group regardless of whether or not they declined; therefore, the study estimates the effect of an ‘offer of treatment’ rather than the effect of receiving the treatment. Because only 41% of those selected consented to the intervention, 59% of participants in the intervention group did not receive health coaching, which substantially diluted the treatment effect.
Cohort studies
We identified two relevant cohort studies. 18,19 Munford et al. 18 assessed whether or not community assets participation is associated with better quality of life or lower costs of care among 4377 people aged ≥ 65 years with long-term conditions in Salford, UK. Outcomes assessed included QALYs, health-care costs and net benefits. Starting to participate in community assets was associated with a gain in QALYs of 0.056 (95% CI 0.017 to 0.094) at 18 months’ follow-up. The cumulative effect on care costs was –£453 (95% CI –£1366 to £461), for a net benefit of £1956 (95% CI £209 to £3703) per participant at 18 months. Stopping participation led to a change in QALYs of –0.102 (95% CI –0.173 to –0.031) and an increase in costs of £1335.33 (95% CI £112.85 to £2557.81) at 18 months. Overall, the study suggests that community assets participation was associated with improved quality of life and reduced costs of care. The study’s strengths include its longitudinal cohort design, use of statistical matching to address potential confounding and use of objective administrative data to collect health-care costs. However, it was conducted entirely in Salford, where significant investment in community groups has occurred, so results may not be generalisable to other regions. Furthermore, the study examined community assets participation (which may or may not be associated with SP schemes) rather than SP itself.
Sumner et al. 19 assessed factors associated with attendance, programme engagement and well-being change among 1297 patients with the ‘arts on prescription’ scheme in the south west of England. Higher baseline well-being was associated with successful attendance [odds ratio (OR) 1.030, 95% CI 1.006 to 1.054; p = 0.012] and increased likelihood of being engaged with the programme (OR 1.032, 95% CI 1.007 to 1.057; p = 0.012). However, higher baseline well-being also decreased the likelihood of improved well-being following the intervention (OR 0.961, 95% CI 0.933 to 0.989; p = 0.007). Considering deprivation level, participants in the medium deprivation quintile of the Index of Multiple Deprivation (IMD) reported more successful attendance (OR 2.080, 95% CI 1.092 to 3.963; p = 0.026) than participants of the lowest deprivation quintile of the IMD. Although the study had a large sample size, there was no control group, and the homogeneous socioeconomic status of participants reduced generalisability to other populations.
Before-and-after studies
There were two before-and-after studies. 20–22 Pescheny et al. 20,21 assessed change in mental well-being levels for 63 participants in the Luton SP programme, which involves link workers. Well-being, measured using the Short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS), improved statistically significantly from baseline to post intervention by 2.78 points (95% CI 1.68 to 3.88 points; p < 0.001). However, the study authors noted that the mean difference in scores was less than the minimal clinically significant difference of 3 points. The study assessed mental well-being outcomes by working status, sex and age. It used skew-normal regression, which is better aligned with the data than a paired t-test. However, problems included large loss to follow-up, a short follow-up period and lack of a control group. Elston et al. 22 evaluated the impact of ‘holistic’ link workers on 86 older adults with complex health needs. They assessed well-being, activation and frailty, and use of health and social care services and associated costs. Well-being, measured using the WEMWBS and Well-being Star,52 increased significantly, by 7.9 points (95% CI 6.1 to 9.7 points; p < 0.001) and 13.3 points (95% CI 10.6 to 15.9 points; p < 0.001), respectively. The total costs increased at the end of the study by £4212 (p < 0.001). Elston et al. 22 reported that 59% of this increase was attributable to 13 users with high costs due to morbidity and frailty. The study had high follow-up rates and comprehensive data collection, but with a lack of a control group it is difficult to confidently attribute the changes observed to the intervention.
Mixed-methods approaches
Five studies used a mixed-methods approach. 23–27 Four of these23–26 used patient outcomes and other service-related outcome measures such as service-related outcomes, barriers and facilitators, training needs, potential wider impact and programme effectiveness. Bird et al. 26 performed an evaluation of a community-based, 12-week physical activity programme for inactive adults with (or at risk of) long-term conditions. A total of 326 participants attended at least one 30-minute activity session, which accounted for 30.2% (1080) of the target population. The study reported a significant improvement in WEMWBS scores from baseline to 12-month follow-up (9.09 points, 95% CI 5.65 to 12.53 points; p < 0.001) and weekly physical activity increased from baseline to 12-month follow-up by an average of 158.60 minutes per week (95% CI 103.11 to 214.10 minutes per week; p < 0.001). Strengths of this study are its Reach, Efficacy, Adoption, Implementation, Maintenance (RE-AIM) study approach,45,46 which allows for transparent understanding and reporting of intervention planning, evaluation and outcomes, and multiple quantitative/qualitative measures to assess a broad range of outcomes that are relevant to SP. However, missing data for long-term follow-up (6.8% of participants completed 12 months’ follow-up), self-reported data and lack of a proper control group are the main drawbacks of the study.
Bowden et al. 25 evaluated the effects of asthma control therapy (the BreathStar Project) among children with breathing difficulties and the associated lifestyle and wider community consequences. The study recruited 7- to 12-year-old children from deprived and highly polluted communities. There were no statistically significant improvements in asthma control. However, interviews with four subjects reported improvements in self-esteem, enjoyment of participating in a choir and the importance of a family-centred approach. Lack of GP and NHS involvement, a small sample size (four children at baseline and the end of the study), local cultural factors and difficulties generalising the study findings to other SP settings are problems in this study. A pilot study evaluated the effectiveness of a structured 6-week nature-based intervention (NBI) in improving mental health (anxiety and/or depression) of 16 individuals. 24 The pilot study documented significant improvements in mental well-being (mean WEMWBS score: pre intervention, 37 points, post intervention, 41 points; p-value = 0.009). However, again the small homogeneous sociodemographic study sample limits the generalisability of the findings.
Woodal et al. 23 evaluated the service outcome and the process of delivery of SP provided by ‘well-being coordinators’ in the north of England. 23 The data summarised change in well-being, mental and physical health, loneliness and ability to manage long-term conditions among 342 participants. Well-being scores significantly improved by an average of 3.98 points (95% CI 3.41 to 4.55 points; p < 0.001). The role of well-being coordinators, who directed patients to community groups and services, was considered the key element of SP. Limitations included lack of a control group, the cross-sectional design and the presence of the service manager during interview data collection.
Agaku et al. 27 explored barriers and facilitators related to the delivery and scale-up of the Ask, Advise, Assess, Assist, Arrange (5As) smoking cessation intervention programme. They used semistructured interviews with 21 programme directors and a quantitative survey of 120 clinic staff members. Barriers included time constraints, difficulty engaging patients and documentation challenges. Community referral resources were considered as a facilitator. Staff confidence in discussing treatment options (29%) and supporting relapsed patients was low (30%). Study limitations included the small number of participants, preventing intervention stratification by provider type; possible misclassification of clinics into 5As training status; and self-reported data from clinic staff, leading to misreporting.
Qualitative studies
We identified six qualitative studies. 28–33 Batt-Rawden and Anderson28 reported that singing in a choir can affect social inclusion and women’s perceptions of their own health and well-being. The researchers interviewed 19 female choir members in Norway and found that choir singing can support health and well-being in four ways: choir members can experience (1) joy when singing, (2) singing as essential for survival, (3) group singing as a route to social connection and (4) increased social inclusion. Participation in the study was via self-selection and, therefore, subject to selection bias. With the lack of follow-up, it is not possible to attribute improvement in well-being to taking part in the choir. In addition, men were not included and participants came from only two locations, which limits the generalisability of the findings. In a similar study, Redmond et al. 31 analysed open-ended survey responses from 1297 participants in a longitudinal study of an arts referral programme in general practices in the south-west of England. The study reported benefits across the thematic domains of ‘being with others’, ‘being on my own’, ‘doing something for me’, ‘losing oneself’ and ‘threshold’ (i.e. threshold opportunities to recognise personal growth). The study had a large sample size but generalisability to SP is limited because of the lack of attention to health outcomes.
Wildman et al. 33 conducted semistructured interviews to explore experiences of SP among people with long-term conditions 1–2 years after their initial engagement with a link worker. The study included 24 participants aged 40–74 years living in a socioeconomically deprived area of north-east England. Participants reported less social isolation and improved health-related behaviours and condition management. Barriers to SP were lack of onward referral options, unsuitable location or scheduling of activities, and language and cultural barriers. The authors suggested that an evaluation of SP requires longitudinal data collection because of the range of improvements and their episodic nature.
The remaining three qualitative studies explored organisational experiences of SP among small samples of participants conducted in single sites. 29,30,32 Payne et al. 30 focused on the mechanisms of SP. 30 They recruited 17 participants from a multiactivity SP organisation in Sheffield, UK, and identified five themes: (1) receiving professional support, (2) engaging with other participants, (3) developing new skills, (4) changing perceptions and becoming open to new futures and (5) developing a positive outlook on the present while moving forward. The study reported limitations related to participant recruitment and data coding for qualitative analysis. Bertotti et al. 29 conducted an interview-based realist evaluation of a SP pilot in London, UK, in the boroughs of Hackney and City of London. They aimed to explore the contextual factors and mechanisms that underpin the pathway linking primary care with the voluntary sector, especially via the SP coordinator. The authors subdivided the pathway into three stages: the GP referral process, consultation with the SP coordinator and interaction with the community/statutory organisations. Several challenges relating to the pathway were highlighted. This included ‘buy-in’ from some GPs, branding and funding for third-sector organisations. White et al. 32 interviewed 18 health-care professionals and 15 third-sector organisation workers involved in SP to explore the quality of the relationships with participants. The authors reported different representations of ‘health’ between the two groups, ‘mistrust of unknown third sector organisations’ by health-care professionals and the ‘lack of effective networks connecting the two groups’. The transferability of the study findings is limited by the single organisational recruitment, ‘socially desirable’ self-perceived response and the small number of GPs.
Reviews
We identified four relevant systematic reviews. 34–37 One of these reviews35 aimed to assess the outcomes of SP programmes based on primary care and involving navigators for service users. The review identified 16 studies of variable quality and reported that qualitative studies reported improved health and well-being outcomes but that quantitative studies reported mixed results. The authors suggested there is a need for more high-quality evaluations to accurately assess SP. Bickerdike et al. 37 reviewed 15 studies and reported that most of the studies were small in scale and assessed as being at high risk of bias. A review by Pescheny36 explored the barriers to and facilitators of the implementation and delivery of SP. This review included eight studies and identified barriers and facilitators related to legal agreements, leadership, stakeholder engagement and local infrastructure. The authors reported a lack of high-quality studies relevant to the review. The fourth systematic review sought to measure health and economic outcomes of SP for frail, elderly adults living in the community, but no papers met the selection criteria. 34 Other literature reviews (i.e. non-systematic)38–43 also highlighted the need for more high-quality studies.
Summary
In this rapid systematic review we have identified and summarised the growing literature surrounding SP. We screened 124 papers and included 27 in the final review. We identified various primary and secondary studies that used a range of research designs and methods. In summary, the key findings identified from the included systematic reviews are:
-
SP is a clinical priority and a key to the future provision of community care.
-
The available evidence reported mixed results; some evidence suggests improvement in well-being and health-related behaviour and some evidence does not.
-
The available evidence comes from small-scale studies that are mostly poor in design.
-
There is a lack of standardised and validated tools to measure the outcomes.
-
Studies have included short follow-up durations and high levels of missing data.
-
Service-related barriers include implementation approach, legal agreement, staff engagement, communication between partners and stakeholders, and local infrastructure.
Our review helped to identify appropriate evaluation questions for the evaluation of SP and to inform our qualitative data collection. It fed into the structure and content of the topic guide. Our review also helped the systematic assessment of anticipated and reported outcomes captured in the data collection section (see Qualitative interviews). In addition, the review highlighted a number of research challenges such as the low uptake of SP interventions, relatively small study sample sizes, frequent lack of a control group, heterogeneity of interventions and programmes and geographical variation of the evidence that limits generalisability.
Qualitative interviews
Findings from 25 interviews of people directly involved in SP (link workers, social prescribers and VCSE workers) are presented here. The findings are presented in line with the 12 categories that formed the framework developed in the data analysis. The framework was informed by the interview topic guide and project stakeholders during the protocol phase of the study. The 12 categories are provided, with a brief summary of each. For additional example quotations, see Appendix 4. The 12 categories were:
-
the nature of the service in terms of structure, models implemented, organisations involved and health domains covered
-
patient journey throughout the service
-
any measured outcomes
-
data collection methods and human resources
-
volume of service uptake
-
type of service utilisation (highest vs. lowest)
-
nature and length of follow-up
-
potential strengths and limitations of current service
-
major enablers of and challenges to developing and implementing SP service
-
costs and savings when recruiting for and implementing the SP service (for both PCNs and other organisations involved)
-
non-attendance data (for instance resulting from people who do not take up their SP referral)
-
the make-up of people taking up SP (e.g. how different are they to the overall practice population, availability of social class data).
In the light of the COVID-19 pandemic, during the interviews we asked participants to share their experiences of how the pandemic was affecting each of these areas.
Characteristics of study participants
A total of 25 participants (18 women and seven men) were included in the main analysis; descriptions of ongoing studies from the two academic researchers are provided in Ongoing studies of social prescribing: lessons learned from researchers. Participants’ roles covered several regions in England: the North East (n = 5), South West (n = 5), West Midlands (n = 4), South East (n = 3), North West (n = 2), East of England (n = 2), London (n = 2) and Yorkshire and The Humber (n = 1). One participant had a national role. Participants’ length of experience in SP-related roles at the time of the interview ranged from 4 months to 20 years.
The most common roles were social prescribers/link workers (n = 8), regional leads (n = 5) and learning coordinators (n = 3). The remaining participants covered a range of roles, and included one commissioner, one head of community well-being services, one community-linking project development manager, one chief executive, one operations director and one manager. Three VCSE workers were interviewed, one of whom was a programme manager for the VCSE who had a background as a health trainer and in a ‘health trainers in GP surgeries’ scheme from 2009. The programme manager worked in an organisation that had a link worker structure and served as an ‘umbrella organisation’ for several services, and sometimes supported patients directly or referred patients to an appropriate service. The remaining two VCSE interviewees were from organisations that deliver specific services (i.e. arts on prescription and mental well-being services). They are mainly dependent on volunteers and have their own policies in place in terms of referral acceptance from the link worker, self-referral or directly from general practices. One of them had worked as a freelance director of a voluntary organisation for 4 years and had previously worked as an artist. The other was managing a new service that provided telephone support, risk assessment and secondary referrals during the COVID-19 pandemic. The organisations were all located in the West Midlands. Participant characteristics are summarised in Table 1.
| Role in organisation | Length of practice in SP | Region |
|---|---|---|
| Lead | 14 years | South West |
| Stakeholder | 3 years | National |
| Lead | 20 years | South West |
| Lead | 5 years | London |
| Lead | ≥ 6 years | East of England |
| Link worker | > 1 year | South West |
| Link worker | < 1 year | South West |
| Stakeholder | 9 years | North East |
| Stakeholder | 5 years | North East |
| Stakeholder | 2 years | North East |
| Stakeholder | 9 years | Yorkshire and The Humber |
| Lead | 2 years | North West |
| Lead | 20 years | London |
| Stakeholder | 7 years | West Midlands |
| Link worker | 1.5 years | South East |
| Link worker | 4 months | North East |
| Link worker | 4 months | South East |
| Link worker | 5 months | South East |
| Stakeholder | 10 years | North East |
| Link worker | 2 years | East of England |
| Stakeholder | 10 months | North West |
| Link worker | 11 months | South West |
| Programme manager (voluntary sector) | 11 years | West Midlands |
| Freelance director (voluntary sector) | 4 years | West Midlands |
| Unknown role (voluntary sector) | 6 months | West Midlands |
Categories
In this section we provide a summary description of each of the 12 categories, with supporting example quotations from interview data.
1. The nature of the service in terms of structure, models implemented, organisations involved and health domains covered
Duration of services
Across the sample, the time since initiation of SP service operations ranged from 2 to 9 years. Some participants reported SP commencing in 2011; others (e.g. Gateshead) reported that it commenced 5 years previously; one clarified that a pilot started in 2015. Gloucestershire Clinical Commissioning Group (CCG) commissioned pilot community well-being services in 2017 but these services were not referred to as SP. SP commenced in 2018 in south Cambridgeshire, and seven participants (from Durham City, Kent, Berkley and Watton, Guildford and Waverly, Lewes and Ringmer, Barnstaple, and Yorkshire and The Humber) reported SP commencing in their area in 2019.
Types of services used (services patients are signposted to)
Participants reported a vast number of services that they could refer to according to patients’ needs. This included Citizens Advice (London, UK), well-being centres, gardening, walking groups, fishing groups and food banks. As reported by one participant:
We currently have a directory of over 3000 countywide . . . In terms of what is likely to be signposted to, it is varied as how many people we have on our books. And we try to offer a unique prescription to [suit the] needs [of the] person.
Stakeholder, 7 years, West Midlands
2. Patient journey throughout the service
Generally, GPs or nurses discussed SP with patients and obtained their consent for referral to link workers. The referral can be through clinical information technology (IT) platforms [such as EMIS (EMIS Health, Leeds, UK)], paper, e-mail or telephone. Our respondents reported that anyone can refer a patient and that self-referrals are made. Once a referral is received, the link worker contacts the patient, obtains a full assessment of their needs and completes any baseline questionnaires. Some participants reported that they prefer the initial contact with patients to be face to face, with initial meetings in the surgery for safety reasons (and subsequent sessions may be wherever the patient prefers). Other link workers hold the session in the patient’s home to facilitate a friendlier environment/insight into the patient’s living conditions.
During the initial assessment, the link worker works with the patient to highlight issues that are most important to them. Based on the patient’s goals, the link workers identify services to which to signpost the patient. Sometimes the link workers do not need to signpost patients to further services if the link worker is able to meet the patient’s goals themselves (e.g. help with completing forms). The length of time the link worker is engaged with patients and the number of sessions appeared to depend on the link workers’ assessments of the needs of the patient and their ongoing support requirements. A participant described the need to ‘move people’ on:
. . . people kind of click with you and people can’t move on. I am not good at managing expectations.
Link worker, > 1 year, South West
Communications received by voluntary community and social enterprises from link workers
The nature of communication between link workers and VCSEs varied. One organisation employed its own link workers embedded in general practices but also received external referrals. However, the participant noted that their organisation received more information about patients when referred by their own link workers than through external referrals. Link workers may communicate safety concerns to the organisation if, for example, a patient was at risk of suicide. Another organisation reported building positive communication with link workers at the time of referral and also after patients have made contact with the volunteer service activities (e.g. discussing concerns around individual patients). It appears that the nature and amount of information received from link workers may be influenced by the relationship between the link workers and the VCSE organisation.
Communications received by link workers/practices from voluntary community and social enterprises
The data feedback system varied among the services. One of the VCSE interviewees stated that they do not provide feedback to the link worker or GP, whereas others did. Generally, feedback included data such as patient attendance, referral made, referral accepted, referral declined and non-attended. Impact/outcomes data were not usually reported back to GPs.
3 and 4. Any measured outcomes, data collection methods and human resources
We found differences regarding data availability. Data collection was performed using a wide range of tools. There was inconsistency in the collection of outcome data, as can be seen in Table 2. Assessments were often made at the initial contact and sometimes repeated at the end of the process, but it was not always possible to capture the follow-up data and, therefore, it may not be possible to make an assessment about whether or not patients benefit from attending the service. Each locality appeared to have their own minimum data requirements and, whereas some localities reported collecting ‘standard outcome data’, some did not collect any outcome data.
| Variable | Additional comments |
|---|---|
| Name | – |
| Age | – |
| Sex | – |
| Marital status | – |
| Religion | – |
| Employment status | – |
| Long-term condition | – |
| Disability | – |
| Whether or not they have a carer | – |
| Whether or not they live alone | – |
| Contact details | – |
| General practice they are registered with | – |
| Contact with general practices | To see if consultation rates have been affected |
| Reason for referral | Includes various categories such as loneliness; social isolation; emotional well-being; being a carer; for exercise; to improve social skills and smoking and drug/alcohol problems; fire safety advice; and welfare benefits advice |
| Attendance/non-attendance | – |
| Number of contacts made | – |
| Time spent with patient/client | – |
| Number/type of goals | – |
| Number/type of sign postings | – |
| How long people are in the service | – |
Many participants (especially those based in general practices) recorded information about patients on clinical IT software, for example SystmOne (The Phoenix Partnership Ltd, Leeds, UK) or EMIS Health (Leeds, UK) software, which is accessible to the GP. The link worker was able to liaise directly with the GP in the event of issues or change of circumstances. Access to the clinical IT software meant that the link workers did not need to gather their own ad hoc data (e.g. patient demographics, contact details). Some participants reported using Systemized Nomenclature of Medicine (SNOMED) codes, although one participant pointed out that the SNOMED codes need to be reviewed, as the current codes do not fully capture what is being done in the service. Some participants reported using an Elemental Software (Liverpool, UK) system that has been developed for SP, while others developed their own systems.
Outcomes data collected included psychosocial health and well-being measures using questionnaires such as the Office for National Statistics four (ONS4) subjective well-being questions;47 WEMWBS;48 SWEMWBS;49 Patient Activation Measure (PAM);50 University of California, Los Angeles, Loneliness Scale;51 Well-being Star;52 and Measure Yourself Concerns and Wellbeing (MYCaW). 53 The ONS4 and PAM were the most frequently used among our interviewees. However, participants suggested that evaluation instruments were not necessarily relevant for patients. For example, the PAM is focused on patients with long-term conditions and not other, social, issues patients may have:
The trouble with PAM is [that it has] really very little relation to the sorts of issues that we would normally be discussing with the clients. It is a very health-based model. That isn’t the kind of issue that comes up for us with our clients, most of the time.
Link worker, 1.5 years, South East
Tools that examine aspects of an individual’s well-being, such as housing and income, were thought to be more relevant. Some services had developed their own data collection tools, perhaps because of the lack of content and face validity of existing tools. VCSE participants reported similar issues, finding that the assessment tools did not always capture outcomes that are relevant to patients:
The issue is there are so many patients who access social prescribing programmes who don’t have things like long-term conditions. And so you’re taking patients through an extra set of questions . . . not only interrupts the flow of what the service, what the person needs in their urgency on the delivery end, but also you end up with data which doesn’t really tell us a good picture.
Voluntary sector interviewee 1
To overcome these problems, bespoke data collection and patient assessment tools have been created, such as the How Are You? (HAY) tool. HAY covers aspects such as housing, relationships, finances and physical health and was designed with consideration of accessibility to potentially marginalised groups, for example those with literacy problems:
It’s a very simple chart to be used for those who may have literacy problems as well, and started as a good tool to start a conversation with a new referral. . . . It also helps the patient prioritise what’s important at that point in time.
Stakeholder, 2 years, North East
A problem with the outcomes measures and data collection methods was the wide range of services that patients are referred to. This makes it difficult to attribute individual outcomes to specific services. Some VCSEs seemed to have a structured approach using validated instruments whereas others did not. Follow-up data in VCSEs were mostly related to health, well-being and lifestyle outcomes in order to identify areas for possible improvement (using tools such as the ONS4, PAM and Well-being Star). One VCSE interviewee mentioned that they completed the WEMWBS at the beginning and end of the intervention and noted other relevant and predominant issues in their case notes:
And now when we get, when people register with us, we ask if they will have this, or having to consent to WEMWBS self-report measure. And then we review that [at] 2-week intervals. Up until when the client finishes working with us. On our case management system, we have a classification code, so that we can attach presenting issues.
Voluntary sector interviewee 3
Social prescribers often stated that these measures and methods do not capture patient health information, such as body mass index (BMI) and levels of glycated haemoglobin (HbA1c), as these are variables that are recorded by medical staff, but were available to view as required. Participants pointed out that the direct medical outcomes are not the focus of SP. One participant mentioned that collecting health information is not an ideal approach for SP because:
. . . it’s not a health relationship. Although it’s impacting on health, it’s about being person centred and we know about the barriers that can build it. The first couple of meetings, someone weighing you and taking your blood pressure, it’s, it’s largely not the approach social prescribing schemes want to take.
Stakeholder, 10 months, North West
However, some onward referral services may capture this health information, for example if a person is referred to a weight management programme. Interviewees pointed out that, since SP programmes are often patient led, there could be discrepancies in what GPs refer the patients for and what the patient decides to focus on when they have their consultation and perform goal-setting with the social prescriber.
Some link workers focus on progress through the action plan as an outcome measure, describing using case studies to assess the overall impact of the social prescription. One participant stated:
We’re usually just based around the action plans. Where the people are making progress or whether they change . . . direction . . . Progress on the action plan is the measure.
Stakeholder, 9 years, North East
There was variation in reports of the health-care service data collection by social prescribers, for example GP consultations, social care service used/currently being used and accident and emergency department attendance. Many social prescribers reported that they do not systematically collect data on service uptake (user compliance and adherence); however, others do collect data, such as how many sessions were attended and reasons for stopping. Many participants stated that ‘failed encounters’ (non-compliance) often remained uncollected (e.g. if they unsuccessfully tried to contact a patient over the phone). However, one participant stated that the terms ‘adherence’ and ‘compliance’ are not appropriate for SP. Another emphasised that adherence and compliance are not straightforward because the service aims to help patients achieve what they want to achieve, and this may change from time to time. One participant stated:
So if someone comes to you and says I’m really struggling with my violent partner, then you have to say, ‘Well, what do you want to do about it? How can I help you with that?’. They may want to leave them, they may not want to leave them, they may say they want to leave them and 1 week later they’re back with them. We want to stick with people . . . as opposed to, whether they comply or not. We’re not there to judge them, we’re not there to decide what’s best for them.
Stakeholder, 10 years, North East
When asked about frequency of outcome measurement, participants reported information collection for individual patient outcomes (e.g. contacts, referrals and case study data), whereas others reported service-level outcomes; for example, one participant stated that they report to the PCN monthly, whereas others conducted quarterly reports with an annual overview (and one reported weekly during the COVID-19 lockdown). One participant reported that Ways to Wellness (W2W) (Newcastle upon Tyne, UK) contacts clients for follow-up data collection every 6 months for a period of 2 years. Social prescribers would generally capture some data for individuals every time they met the client, but the data captured may not necessarily be individual outcome data. For example, one participant stated:
Data is captured at the beginning and ideally the end. Every time we have contact with a client we would record what happened within that contact and what was exchanged with the client on our case-recording system, but in terms of sort of measuring well-being, or measuring ongoing outcomes, then no, not really.
Link worker, 1.5 years, South East
There is also a considerable variability among VCSE organisations in how often outcomes are measured, depending on a patient’s needs and how often the patient is contacted. For example, one participant reported:
There are a lot of patients [that] need support prior to 4 months [i.e. the initial data collection point], so there’ll be ongoing appointments made with that patient depending on their need. We’ve allowed the patient and the link worker in their appointment to set their frequency for whatever the patient needs.
Voluntary sector interviewee 1
Difficulties in data collection have increased during the pandemic because there are increased challenges for patients (e.g. with literacy barriers) when link workers invite them to complete questionnaires remotely.
5. Volume of service and uptake
Mapping services
No standard system was used to map available onward referral services or their uptake. Some link workers created a database of available services that they shared with colleagues. Creating such databases is resource intensive, and such databases need to be constantly updated. Others used local directories from local authorities. However, local authority databases are not always comprehensive. Some link workers worked closely with VCSEs and had information on smaller local voluntary services (such as OurGateshead, Herts Direct and Connect Well). Others are based within voluntary organisations and, therefore, have the advantage of having access to information on available services. Link workers themselves have to map provisions in their area to identify what services are available and where they are located, and understand what they offer, for whom they are appropriate and which to refer to. This could involve Google (Google Inc., Mountain View, CA, USA) searches; WhatsApp (Meta Platforms, Inc., Menlo Park, CA, USA) groups; physically visiting community centres; e-mailing or visiting other organisations; having conversations with services regarding referral processes, policy and safeguarding; and collecting information leaflets. Some services (especially small groups such as knitting groups or tea groups) are extremely local, do not have an adequate online presence and are difficult to locate.
Across all databases there were concerns about information going out of date. One of the participants pointed out that link workers cannot rely on directories:
[Link workers] can’t just rely on directories. They have to have confidence in services [to refer] their clients to, and therefore they have to actually get to know the organisations. Referring clients to an organisation that you have no knowledge of [is risky]. [Link workers] need to have a much closer understanding of the organisations.
Lead, 20 years, London
Voluntary community and social enterprise organisations reported engaging in active efforts to disseminate information about their services to link workers and general practices. For example, one participant said that they organise meetings with all the general practices to tell them about their services. Another reported that information about service activities is available in a database that could be shared with link workers. However, they did acknowledge that it is challenging for the link workers to signpost clients appropriately to the services available. For example, one interviewee stated that:
. . . [it’s] time-consuming to try and assess [services] on behalf of the client. Which of these range of services that seems to be offering the same service would be most appropriate we don’t know – how good they are – how professional they are. We, you know, we don’t necessarily have that information.
Interviewee 3
Capturing uptake
Link workers often have records of how many people have been referred to them and how many contacts they have had with each patient. One participant stated that they ask onward referral services to fill in attendance sheets, which they collect from the individual services. Link workers record this information on spreadsheets or upload it to clinical systems such as an EMIS Health system. The challenge faced by link workers was capturing uptake data beyond the point of referral, because uptake varies according to the person’s action plan and the type of service they are referred to. As a result, referral data may not be useful in an assessment of impact. A participant highlighted that referral and uptake outcomes are not comparable across different services:
And we certainly don’t do anything across the region to compare different types of interventions, because every intervention is slightly different, and every individual is different. But they would keep records of how outcomes are improving or otherwise at a global level, at a locality level.
Lead, 2 years, North West
Many link workers do not capture data beyond the point of referral. One participant stated that one of the reasons that data are not captured in the voluntary sector is the lack of incentive to capture uptake data: it may not be a priority for the organisation because it may not be linked to funding. The participant stated:
[Data are] rarely captured at the community level . . . because in most cases the community sector does not get paid for it. So they don’t have much incentive to capture the data. And if it’s captured, it is captured by those people who deliver the sessions, who manage the sessions.
Lead, 5 years, London
6. Type of service utilisation (highest versus lowest)
The most common referral services reported by link workers were services to help with social isolation, finance, housing, increasing physical activity, healthier living and weight management. Organisations included Citizens Advice (especially for benefits and housing), Campaign Against Living Miserably (CALM) (London, UK) and People Potential Possibilities (P3) (Ilkestone, UK). Informal groups included gardening groups, craft groups, lunch groups, working groups and coffee morning groups. Other types of organisations included bereavement counselling group therapy, art prescription and exercise on prescription. Some activities were also delivered on an individual basis such as telephone befriending. Some groups provide support for carers of people with specific conditions such as dementia, Alzheimer’s and cancer care. Participants reported changes in service use due to the COVID-19 pandemic, during which there were few face-to-face services available, reduced resources and increased social isolation.
7. Nature and length of follow-up
The nature and length of follow-up depended on a wide range of factors such as patient need, level of intervention implemented, goals to achieve, types of approaches to address needs, and local commissioning variation. One VCSE interviewee stated that clients were followed up by the link worker who had made the initial referral. Another stated that patients are generally not followed up by their GPs. The open-ended nature of many services means that establishing a discrete period of intervention with follow-up can be challenging. Participants highlighted this in their responses:
. . . we can move on with that person long term, we don’t have a time limit, in terms of how long we support somebody, so we don’t necessarily see a cut-off point.
Stakeholder, 2 years, North East
One participant described the development of a bespoke system to generate outcome data and report them to the GP. In these more formal arrangements, the link workers did an initial assessment and engaged for an active intervention period of one to six sessions for a maximum of 6–12 weeks. Follow-up sessions were described as follows:
We are funded to follow up for [the] long term. . . . Follow-ups are face to face in [the] first 6 months and come to 12 months depending on patient’s need.
Stakeholder, 5 years, North East
The two most reported challenges to follow-up and data collection were lack of communication and time:
Often, [it’s] not possible to always find out what’s happened. And, you know, communications may be difficult, they may be difficult to get hold of that person again.
Lead, 20 years, London
Across the VCSE organisations, follow-up generally included measurements of patient well-being. One interviewee reported that they also requested feedback on the service from the patients during follow-up, with this often being done remotely and taking a less formal approach (e.g. no specific structure or data collection tools used).
8. Potential strengths and limitations of current service
One strength mentioned by participants is that link workers give more time to patients (appointments of up to 1 hour) than is possible from GPs. Participants said that SP targets what is important to the patient and focuses on empowering individuals to achieve their health and well-being goals holistically:
We’ve got time to speak to the patients, [we] identify things that wouldn’t necessarily have come up in a 10-minute GP appointment. . . . We’re in a really unique position to actually talk to patients and see what matters to them and make a difference to those things that aren’t necessarily the medical and clinical.
Link worker, 2 years, East of England
One participant reported that SP has the potential to reduce GP workload and potentially save costs for the NHS:
The best value is that it will essentially save the NHS funding in the future. Also reduce the demands and dependence, and also reliance on GPs, it’s very person centred. So they have a voice, they’re empowered to make choices, and it works.
Link worker, 11 months, South West
Participants stated that SP has the ability to unite communities, identify community needs and grow and develop the voluntary sector in the community:
[SP] has the ability to bring communities together, and grow and develop the voluntary sector if done well, so that communities are thriving and there’s much more activity happening on the ground, much more opportunity for people to come together and take part in activities which we know improve health and well-being, because we know the opposite of that is isolation and loneliness, which is detrimental to health and well-being.
Stakeholder, 10 months, North West
Social prescribing also provides a bridge between the health-care and social care systems:
There is a divide between those and they’re almost two separate worlds [health care and social care] and I think social prescribing is a method to enable the coming together of those two things. We know that 90% of the factors that affect people’s health are rooted within communities. But, we give all the energy to the system, which only deals with a small portion of that.
Stakeholder, 10 months, North West
Participants suggested that being embedded in the primary-care team is of great benefit, particularly if they have access to referral systems that are easy to use. One participant was located in a Healthy Living Centre where there are four general practices and also a large community charity with 80 skilled and experienced staff. The link workers were able to be a part of both the GP team and the voluntary organisations delivering the service. Acceptance by voluntary organisations and community areas and link worker support peer networks were viewed as important strengths:
We have [a SP] steering group which has membership from all 10 localities, and enables us to share best practice. Find out what’s going on in different areas. People talk to each other and share information across the 10 localities, which I think is very good.
Lead, 2 years, North West
9. Major enablers and challenges to developing and implementing social prescribing service
Social prescribing is a relatively new concept, and sometimes patients do not want to engage with the service. Consequently, one of the main challenges highlighted was the acceptability of the non-clinical model that forms the basis of SP. Interviewees suggested that more communication around SP to increase awareness of the service would be beneficial. They also suggested that clear definition of the role of link workers in relation to other types of roles in the health-care system is important. One participant recommended that co-facilitation and co-delivery be maximised through linking with experts, patients and patient participation groups. Connecting directly to clinical IT platforms (such as EMIS systems) is also an important enabler. This allows the GPs to see what social prescribers are doing and, in the process, they can learn more about the role of a social prescriber.
During the interviews there was incongruence between models designed to improve well-being and those that were health related. Some participants mentioned that a lot of health-care professionals and patients still do not understand SP. For example, one participant reported as follows:
The challenge is convincing the health service and other referrers of the value and the worth in the community sector and the weight of that, actually going into a singing group is as powerful to health outcomes as medicine. I think it’s our chance to really change things and root people’s health in communities, and that medicine and structured health is something that fewer people need and rely on. But we need everyone to buy into that and that needs to be the first point of call if we’re going to crack this.
Stakeholder, 10 months, North West
Often a lack of GP engagement was reported, especially in cases where workers were not based in general practices. It was reported that practice managers do not always understand issues relating to caseload management and so difficulty was reported around the social prescriber being understood and having the support in place to be able to do their job effectively. As a result of the lack of acceptance, practice staff and charity staff are also sometimes hostile towards link workers, as described by two participants:
GPs just aren’t particularly interested in SP and unless the link workers are based in the surgery running clinics and actually interacting with GP colleagues and attending MDT [multidisciplinary team] meetings and practice meetings, then it’s very easy for the service to be pretty much sidelined.
Link worker, 1.5 years, South East
The charity become anxious the link worker may take some of their jobs. Those charities that provide one-to-one support become hostile and concerned that you are here to do their job, and patients don’t know how engagement with the link worker could be worth their time.
Link worker, 4 months, North East
Participants reported role boundary problems and difficulty getting other professional groups to understand exactly what a link worker does. For example, participants reported the need to define the difference between a link worker and a social worker and described the misleading nature of the term:
It’s a very unfortunate term because people think they’re going to be prescribed something, they need to tell them something they could do or something they can have. When in fact it’s not that at all, it’s much more coaching model.
Link worker, 1.5 years, South East
There were reported challenges relating to funding SP, such as high workloads, the need for increased numbers of link workers and the problem of short-term-funded and underfunded VCSEs for onward referral. This led to challenges in locating appropriate services to signpost patients to. There was a reported lack of adequate training for social prescribers and those addressing the needs of the community in VCSEs. A link worker and a national stakeholder describe the issues below:
When you look at NHSE guidelines for what a link worker is expected to do without any training except a 3-hour online course from Health Education England, its frankly ludicrous. The model tends to talk about coaching and motivational interviewing. . . . Well, that’s all very well and good, but people are trained for years to be able to do that. And I certainly haven’t had any training on it. I don’t think most of my colleagues have either.
Link worker, 1.5 years, South East
My view is that Health Education England regionally being commissioned to provide the training packages, leaning on the support of the organisations and the voluntary sector organisations and NALW [National Association of Link Workers] to understand what that training looks like. So there needs to be more collaborative approach between the experts in the sector . . . to develop what that package should look like.
Stakeholder, 3 years, National
One participant described the problem of conflicting salaries for workers recruited by the voluntary sector and those recruited by the NHSE:
We found that the introduction of NHS SP destabilised the local market because they were offering salaries far in excess of the current rate locally for that level of job. Most experienced staff have moved to those roles as they are paying higher rates. At that time the commissioners, local authorities, do not have money to pay that value loss of experienced staff and have to build that back again.
Stakeholder, 9 years, North East
The organisation of the link worker model potentially increases link workers’ isolation and lack of peer support. This may make their work challenging and may be detrimental to their own well-being:
The model that the NHS adopted was to assign one link worker per Primary Care Network. It means that link workers can be very isolated. They have no contact with other link workers, they’re not able to share practice and learn from others. And they have no peers to talk to. . . . Feeling not supported, or not having access to the support that they need.
Lead, 20 years, London
To minimise isolation, offering peer support was seen as helpful. Some participants described online forums where link workers can talk to others and receive peer support. One participant suggested that link workers should be employed as teams:
They have team meetings together, they have team training and learning opportunities together, they are able to contact each other. And therefore they feel supported, they’re able to grow and develop together. And they’re able to help each other, you know, when they come across a patient who’s got a problem that they’ve never come across before.
Lead, 20 years, London
One of the participants summarised the enablers of the link worker model using relationships, resources and research:
You need to get the relationships right, right within the GP practices, and the Primary Care Networks. . . . You need that relationship with patient. The public or the person that the service user needed the relationship certainly with the local health professionals, whether they are GP and GPs, are crucial to it. But you also need the relationship with the volunteer community sector to manage that. You also needed the resources, in terms of money and people. And you need the resources out there in the sector. And then, finally, you needed the research, in order to demonstrate the work to get social prescribing implemented, but you also needed some research as to what effect it has got because you were asking systems to make very difficult decisions with limited money.
Stakeholder, 9 years, Yorkshire and The Humber
10. Costs and savings when recruiting for and implementing the social prescribing service (both to Primary Care Networks and to other organisations involved)
Participants reported that SP funding was limited to funding direct employment costs and that there were different elements of the service that were not costed or were undercosted. One larger organisation reported having a link worker’s salary reimbursed by the NHS (i.e. PCN). However, many participants raised concerns about lack of support for overheads, management, training, coordination of link workers and costs on the voluntary sector. A participant from a VCSE infrastructure organisation reported as follows:
That was a big problem when it first started because all the money covered the direct employment costs. It didn’t cover all the costs of employing people, so there was a massive issue around management costs and overhead costs. It didn’t include training. So we had to beg, steal and borrow for training. They need some sort of management structure in place. That wasn’t covered.
Stakeholder, 9 years, Yorkshire and The Humber
Some link workers reported having no office or administrative support because of a lack of funding for overheads and service management. Some link workers reported having no access to a computer or telephone. One of the participants said that the salary provided by the PCN for social prescribers was not acceptable, so they paid their SP more than the PCN recommended:
The problem is, that’s not quite enough to fund a good standard of social prescribing link worker. So we’ve paid our social prescriber a bit more than the PCN allow, so we’re paying a little bit over what they give money for.
Lead, 20 years, South West
The limited funding for SP was similar in the VCSEs, where funding is often short term and limited (by value or time). One of the interviewees reported receiving funding from the local council for up to 2 years, but others reported struggling to get further funding as they do not have robust case data. This causes problems for SP if ongoing referral services are limited:
If the NHS are giving funding for social prescription workers, that’s pointless if there’s no funding for community groups.
Interviewee 2
Some VCSE organisations reported receiving COVID-19 response funding until the end of December 2020.
11. Non-attendance data (for people who do not take up their social prescribing referral)
Link workers usually collate data on patients’ non-attendance because this is required as part of their service contract. However, as described, they do not collect non-attendance data for the services patients are referred on to. For example, one participant reported as follows:
Well, OK, so non-attendance data in social prescribing when seeing the link worker is recorded through ‘did not attend’ recording. Trying to capture the data, beyond the link worker, when they get referred to services is probably the weakest link in the data chain. So understanding what percentage of patients who get referred to services actually go to those services is quite a challenge.
Lead, 20 years, London
Some participants reported that they do not have good records of non-attendance, which may be a consequence of poor recording processes. At times, patient cases are closed after a number of unsuccessful contact attempts:
The only thing we do is contact a client three times. And if we cannot contact them at all after the third attempt, then we close the case. And we would refer that back to the, to the referrer, and that would be, well, it should be recorded on the GP computer systems that referral has been declined.
Link worker, 1.5 years, South East
One link worker reported pushing back the responsibility to engage to the patient after a first failed contact attempt. However, non-attendance may signify other problems that need to be reported, for example if social prescribers are concerned about safeguarding issues. In general, non-attendance data collection is heterogeneous across schemes. Some data may have been recorded in clinical IT systems and other schemes may have unsystematic data collection, as described by one participant:
. . . in some cases, it is reasonably sophisticated, a referral is made into the system. So, if a service is using Elemental they are able to bring that up [at] almost a touch of a button, so how many people [who were] referred in the past took off, and how long they stayed on that system. For others, those schemes that are a little bit less mature, it’s much more difficult because for example [they] don’t have [a] current case management system. So a lot of it is done by spreadsheets. It would be quite difficult to draw that information off at a population level or at a cohort level.
Lead, 2 years, North West
The interviewees from the voluntary sector recorded attendance data regularly, but non-attendance data collection was more ad hoc. For example, participants from one medium-sized organisation reported that they used a ‘reporting card’ to capture attendance. In this case, staff monitored attendance, number of referrals received, appointments conducted, those who did not turn up and those they tried to contact but could not reach on a monthly basis. VCSEs reported using non-attendance data for their own tracking and case-reporting purposes or to evaluate their model of service delivery. For example, one interviewee stated as follows:
I will record [that they] didn’t attend, didn’t answer in our workflow, but I will usually accompany my case record with whatever follow-up that time, so normally that would be maybe a text message, and what seems to be their preferred method of communication.
Interviewee 3
12. The make-up of people taking up social prescribing (e.g. how different they are to the overall practice population, availability of social class data)
Participants reported varied demographics of the local population and people taking up SP. Although health inequalities were not formally assessed across SP services, the descriptions of people taking up SP revealed overlapping dimensions with people often falling into various combinations of socioeconomic status and deprivation, age, sex, race, disability, vulnerable groups and location (urban vs. rural areas). One participant commented that their service use was representative of their area:
Our practice is [in] a very deprived area, one of the most deprived areas of the county, and older, more affluent people. It tends to be pretty fairly split. We don’t have a large number of black and minor[ity] ethnic group patients but to be honest we don’t have a large black and ethnic minority group. . . . it is not a very diverse population.
Link worker, 4 months, North East
Participants reported that patients often have long-term conditions and mental health conditions and are unemployed. They also reported that more women than men use the service. Others suggested that patients were often from more deprived areas and were vulnerable users, mostly older adults/elderly people. For example, a participant reported that about half of the people they see are between the ages about 45 and 64 years, whereas another reported that they mostly see people aged ≥ 85 years who live alone. Other participants suggested that the people accessing SP may be frequent consulters and the demographics do not necessarily reflect the demographics of the general practice where the link worker is based. One participant noted that living alone is an important predictor of seeing the link worker, rather than social class, although it is not clear which specific group was examined:
Now, interestingly, social class, we looked into this heavily really, so social class doesn’t really seem to particularly apply. Living alone was a risk factor for seeing the link worker, and older people were more likely to be referred, so elderly living alone was the most referred group.
Lead, 20 years, South West
It was noted that the COVID-19 pandemic had led to changes in the demographics of people accessing services. For example, one of the VCSEs had seen a significant increase in the age of participants because general practices had provided a list of vulnerable patients to work with. The same interviewee reported that before COVID-19 a higher proportion of service users were from ethnic minority communities, but post COVID-19 a lot more work was taking place in areas that are predominantly white British and wealthy.
Barriers to and enablers of a social prescribing impact evaluation
During the interviews we asked participants about what they considered to be the main barriers to and enablers of an impact evaluation/future research in SP. To facilitate SP impact evaluation, several enablers were reported. Some participants suggested using case studies and routine data collection, and others emphasised the importance of familiarisation with the relevant people beforehand to mitigate the resistance that can result from being continually evaluated/monitored. Building relationships with health-care professionals and personnel from relevant organisations was often referred to. It was reported that organisations like the Social Prescribing Institute would also be good steering groups for future research.
Key enablers of a SP impact evaluation:
-
an interested and active workforce of link workers
-
a system that is gradually becoming more mature and, therefore, potentially more evaluable
-
some robust data systems
-
a desire and need by link workers and those providing SP funding to understand the impact of the service.
Key barriers of a SP impact evaluation:
-
heterogeneous link worker service provision (participants reported wide variation in services even within the same county)
-
large differences in terms of available onward referral services and engagement with the PCN
-
the precarious financial and organisational nature of some onward referral services
-
heterogeneous data collection, reporting and data monitoring by different social prescribers
-
commissioners do not usually ask social prescribers to use standardised assessment tools
-
lack of agreement across schemes regarding the key outcomes that need to be measured
-
services are individualised because SP filters into so many aspects of health and social care and patients’ well-being.
Participants’ views on evaluating SP can be found in Appendix 5.
Ongoing studies of social prescribing: lessons learned from researchers
To gain insight into ongoing SP research, we interviewed three researchers who had undertaken or were conducting research studies in the field of SP. Unfortunately, one data set was unusable because the research did not align with our commissioning brief (e.g. it provided a generic description of SP, not experiences of SP service provision), so we present data from the remaining two. One researcher was a social scientist who had been working in SP since 2014. Another had worked for Public Health England (PHE) for a decade before moving into research. The researchers gave detailed examples of the types of research they had conducted in SP and lessons they had learned.
Researcher 1: exploring approaches to evaluate the use and impact of social prescribing using electronic health records
The project led by this research team aimed to assess the feasibility of a quantitative evaluation of SP and focused on the link worker model. The researchers were using the Royal College of General Practitioners (RCGP) Research and Surveillance Centre data to explore approaches to evaluating the use and impact of SP. 54 The Research and Surveillance Centre included more than 500 (nationally representative) general practices across the country. Approximately 350–400 out of 500 GPs upload their entire electronic health record (EHR) report to PHE on a weekly basis using three codes for SP: SP offered, SP referral made and SP/social prescription declined.
The researchers extracted those codes, as a starting point, to understand use of those codes. Thereafter, they created a taxonomy and ontology for those codes because the existing codes were broadly generic and did not indicate whether or not individuals completed a prescribed programme or indicate any outcomes that could be used to evaluate whether or not that intervention had any impact. The aim was that, with this taxonomy and ontology coding, specific outcome sets could be associated with different presenting complaints. For example, if a patient was referred to a support service for domestic abuse and there was a code for that, then automatically the outcome measure would be whether or not the domestic abuse was resolved (without necessarily knowing the details of intervention). With these codes the researchers would explore the use of SP and its impact. The problem was that individual needs vary and in order to define outcomes they suggested that we first need to understand the presenting complaint and the social need. Afterwards, an intervention to tackle the specific social need could be identified/developed. They suggested that this is the reason that it is difficult to get a standard outcome set for all social need.
Researcher 2: evaluating Ways to Wellness
The second researcher described their work evaluating a specific SP intervention called W2W. 55 W2W is a SP service for people aged 40 to 74 years with specific long-term conditions (i.e. chronic obstructive pulmonary disease, asthma, diabetes, heart diseases, epilepsy or osteoporosis, with or without anxiety or depression) attending any participating general practice in Newcastle upon Tyne. W2W started in April 2015, with a developmental phase of 8 years that included scoping work with potential service users and voluntary sectors and collaboration between the voluntary sector and the health sector. The researcher mentioned that initial discussion with the people delivering the service highlighted that a RCT did not appear to be possible in the W2W setting. Exploratory qualitative work was conducted, including focus groups with link workers delivering the intervention. This was followed by a feasibility before-and-after study of outcome measurement using outcome data collected by the link workers.
Subsequently, the research team was commissioned to evaluate a community-based diabetes intervention using a mixed-methods study. The study included a quantitative before-and-after study (1 year follow-up) assessed against the EQ-5D. The qualitative component was an ethnography study that involved the observation of the daily routine practices of the service users (recruited into the intervention) and the practices of the link workers for 18 months. The researcher stated that the main concerns regarding data were (1) obtaining the data and (2) defining the comparison group and how these would be identified in each of the organisations taking part. The researcher also highlighted that the organisations providing the intervention were different, which meant that the intervention delivered may vary between organisations. Furthermore, link workers found it challenging to administer the outcome measure, the EQ-5D, as they have other priorities. The researcher highlighted that the link workers usually use the Well-being Star to monitor progress; however, the Well-being Star is not a validated tool to measure improvement in well-being in outcomes. Researchers also reported that obtaining GP data for other outcomes was a lengthy process (i.e. taking around 24 months).
Additional data from network meetings held during this project, where key challenges to research in SP were discussed in more detail, are available in Appendix 6.
Summary
We collected interview data from 25 participants (and three academic researchers; data reported separately) over 6 months (April 2020 to September 2020). In addition, views of topic experts, patient and public representatives, stakeholders and academic colleagues were captured during network meetings (see Appendix 6).
The findings are presented in a pragmatic framework. A brief narrative summary is provided here, with key area in parentheses and related headings in italics.
We identified several delivery sites. Participants were based in different regions (key area 1) in England, including the South West, South East, North West, North East, West Midlands, East Midlands and London, which demonstrates distribution of SP sites. The service (key area 1) has a holistic nature that covers several domains, such as social isolation, housing, healthier living and weight management. SP is a complex intervention and there is heterogeneity in service delivery (e.g. routes to referral, services offered, outcomes assessed, number of link workers and training provided to link workers); services vary widely even in the same county. SP is an open-ended service and link workers have varied backgrounds; variations were also reported in types of services available and engagement with the PCN. The link worker model had been running for approximately 2 years; however, other forms of SP had been operational for longer. Training programmes provided to link workers differed and high turnover of link workers was reported. The voluntary sector plays a major role in service delivery. The patients’ journey (key area 2) starts with referral. Referral routes to link workers include GPs, nurses or self-referral. Following a needs assessment, the link worker can either deliver the intervention or refer the client to the appropriate service.
Outcome measures (key areas 3 and 4) were collected using a wide range of tools in SP services and across sites. We found significant heterogeneity in data availability and outcome assessment. Each locality had its own core data collection method using a wide range of tools and recording databases. We found not consistent criteria for outcome data collection; as a result, there is considerable inconsistency in the data collected. Social prescribers usually collect data on non-attendance as they are contractually obliged, but these are collected in different formats across different sites. Non-attendance data for the services patients are referred to are not routinely collected. Findings from our rapid systematic review and interviews suggest that well-being is an appropriate outcome to capture the impact of SP.
Volumes of service and uptake (key area 5) are not recorded in standardised systems. Sites have their own databases. Link workers have their local referrals and contact records, but do not capture data beyond the point of referral. Mapping of the services relies heavily on the link workers’ efforts and the voluntary sector presence. Services utilised (key area 6) are those that help with social isolation, finance, housing, increasing physical activities, healthier living and weight management. These services are often underfunded or funded for a short period of time. Length of follow-up (key area 7) varied across sites and there were differences in the follow-up measures and frequency of outcome measurement. Follow-ups and outcome measures were seen as client dependent and, therefore, not comparable. Interviewees highlighted that significant challenges to follow-up and data collection were lack of communication and time.
Strength and limitations (key area 8) included the increase in time that link workers can dedicate to address patient needs (compared with GPs) and that SP in general has the potential to reduce GP workload. The service enables health-care service providers to look holistically at the needs of people (e.g. beyond medical health) and to unite communities, identify community needs and develop the voluntary sector. Service implementation was limited by the mismatch between patient needs and what providers considered appropriate. A further limitation was the reported lack of a comprehensive directory of services, making it difficult to know where to signpost patients, although some clearly had substantial local knowledge. Barriers and enablers (key area 9) included the relatively new concept of the link worker, which affected service awareness and acceptance from both patients and those referring. Adequate training of link workers was seen as an important enabler of SP, and peer support as a helpful mechanism to limit link workers’ isolation.
A variety of costs and savings (key area 10) issues were described by participants, including concerns about lack of support for ‘additional costs’ such as overheads, training and voluntary sector costs. The SP service relies heavily on the voluntary sector, where funding models may be unstable. Non-attendance (key area 11) data were not systematically collected for onward referral services. Instead, link workers kept their own limited records. The voluntary sector generally records attendance data, but not systematically, to facilitate comparison and transfer to a third party. People who take up social prescribing (key area 12) were understood as being from more deprived areas and were vulnerable, mostly older adults and individuals living alone.
COVID-19 changed the service in terms of delivery mode, service uptake, client recruitment and client demographics. There was a clear push from service providers, stakeholders, topic experts and academics for mixed-methods research to improve our understanding of whether or not the current model is effective and how.
Mapping the current social prescribing model
The current SP link worker model is complex and difficult to map and quantify. However, drawing on our rapid systematic review and interviews, we have mapped the current service model and its different pathways (Figure 2).
FIGURE 2.
Current link worker model: social prescribing pathway. a, SNOMED code 103; b, SNOMED code 106.
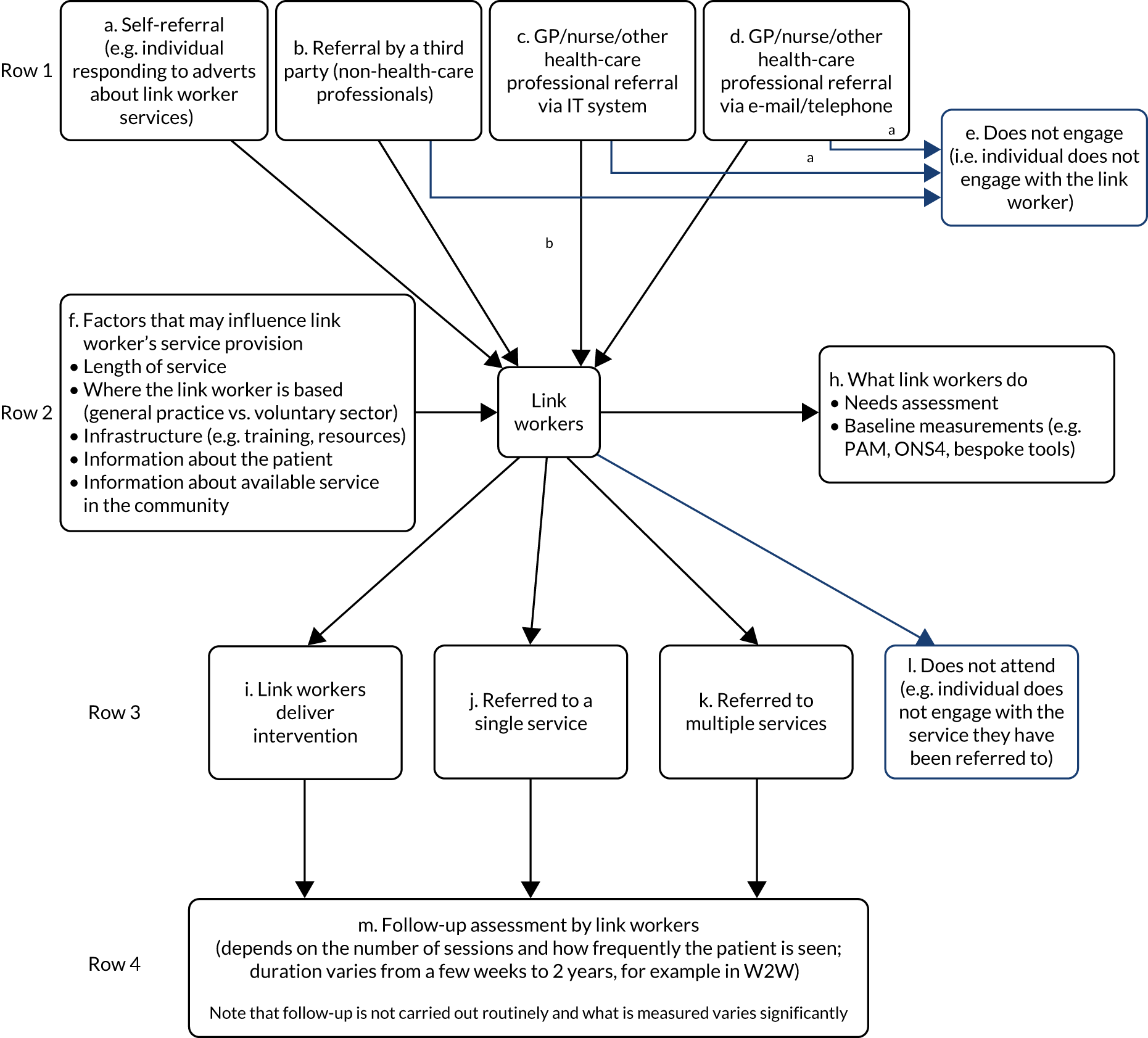
Stage 1
Row 1 of Figure 2 illustrates potential referral pathways by which the client can access a link worker. For instance, through referral from a health-care provider (such as a GP, nurse or health-care professional). This referral can take place using an established IT system or other modes (such as by telephone or e-mail). The health-care provider can document this process using the relevant SNOMED code (106 for referral made and 103 for declined or not required). In some instances, ‘Nil’ (no code used) may be recorded, which indicates that there was no clear reason available or given for declining the referral. It is worth noting that the ‘reason’ for referral may vary; for instance, a GP might refer a client to control their diabetes but the underlying condition may be a financial issue that is picked up in stage 2 (by a link worker’s assessment of needs).
Stage 2
Row 2 of Figure 2 illustrates the factors (see box f) that may influence link worker service delivery: the covariates that should be considered in an evaluation. Figure 2, box h, describes the client measures that are captured by the link worker at the initial visit, also known as baseline measures or time zero (T0). These measures often include a needs assessment (involving a dialogue with the client to understand their needs and what issues are most important to them) and well-being measures, such as ONS4, WEMWBS and the PAM, which includes 13 questions to quantify four levels of ‘activation’: disengaged and overwhelmed; becoming aware but still struggling; taking action; and maintaining behaviours and pushing further. 56 Additional measures include hopes and goals, and what barriers a client might envisage. These assessments vary across sites and some sites have developed their own assessment tools (e.g. the HAY tool covers aspects such as housing, relationships, finances and physical health). These measures are usually made at the initial contact.
Stage 3
Row 3 of Figure 2 illustrates the service available to the client. The link worker can provide this service themselves or refer the client on to the voluntary sector. The type and number of services a client is referred to may vary depending on the client’s needs. For instance, a client may require a service to support them with weight loss, whereas another may require services for weight loss, housing issues and diabetes. In addition, referral to services is highly dependent on the locally available services, knowledge of services and relationships with the voluntary sector. The link worker usually captures the number of referrals and number of contacts with each client (including the number of contacts across the service). They are also able to capture who has been signposted to what service and may be able to assess if the patient achieved their goals if follow-up data are collected (stage 4).
Stage 4
This is the stage where the client is engaged in the onward referral services, including the voluntary sector. Many link workers do not capture data beyond the point of referral (i.e. after stage 3). However, if they do, they would potentially recapture the same measures collected at stages 2 and 3, such as well-being, number of contacts across services and reasons for referral. There may be some communication between the link worker and the voluntary sector, and this is determined by a number of factors. For instance, if the link worker is based in the voluntary sector, data capture would be different from that in the case of a general practice-based link worker. The relationship between the voluntary sector and the link worker would also influence data capture. The IT infrastructure that connects the link worker to the voluntary sector is also important at this stage. The maturity of the service is important: more mature services will have a stronger infrastructure. The voluntary sector records attendance data regularly. However, how they record non-attendance varies, because there is no standardisation of this process. Post-referral data that may be collected by the voluntary sector before the start of the intervention are related to patient health and well-being, interest and lifestyle. Follow-up data are mostly related to health, well-being and lifestyle to identify possible improvements (using tools such as the ONS4, PAM and Well-being Star). There is also a considerable level of variability in how often outcomes are measured, depending on the service undertaking the measurement, its assessment of patient needs and how often the patient is contacted.
Chapter 4 Options for completing a social prescribing impact evaluation
Social prescribing can be described as a complex intervention:36 it is composed of a number of components that may interact independently and interdependently. 57 These components may include behaviours, features of an intervention or context, and the methods and processes of organising these components at different levels. 58 For example, SP may have an effect at individual patient level, organisational or service level or population level (or in some circumstances, all levels).
Drawing on our rapid systematic review and interviews, we propose a number of different possible options for undertaking an assessment of the effectiveness and cost-effectiveness of the link worker SP model (Table 3). These are either informed by current service data (where available) and large routine data sets or require additional data collection or more controlled research settings.
| Recommendation | Methodology | Strengths and limitations | Example assessment that could be undertaken |
|---|---|---|---|
| Retrospective matched cohort analysis |
|
Strengths:
|
|
| A mixed-methods pre and post design |
|
Strengths: Limitations: |
|
| A realist evaluation |
|
Strengths:
|
|
| A CUA |
|
Strengths: Limitations: |
|
| A pragmatic cluster randomised trial (potentially plus CUA and realist or process evaluation) |
|
Strengths:
|
|
Using current service data (where available) and large routine data sets
Retrospective matched cohort analysis
Our feasibility study demonstrated the scale and shape of the current link worker SP service. Our data highlighted that outcomes relevant to well-being and SP are currently recorded using different tools and different systems and vary by site and region. Therefore, running a national evaluation informed by current record-keeping is potentially extremely problematic. An alternative approach is to use anonymised individual-level primary health-care data between 2018 and 2019 (i.e. time cut-offs informed by when the link worker model was implemented) using EHRs, such as from the IQVIA Medical Research database (IQVIA Inc., Danbury, CT, USA) (these data sets include participating general practices to capture routine EHRs of patients managed in primary health care). This analysis would need to be condition controlled (e.g. diabetes only or obesity only or depression only). Patients with a social prescription code (e.g. SNOMED 106: social prescribing made) could be compared with matched controls. The two retrospective cohorts (i.e. intervention and matched control) could be matched based on several characteristics, such as age, sex, postcode, ethnicity and socioeconomic status, to generate a less heterogeneous sample. The intervention would be whether or not a referral to a social prescription was made. Outcomes would include clinical outcomes relevant to the health condition of the cohort (e.g. glucose measures, adiposity measures or prescriptions). Exploratory outcomes could include GP appointments and PAM scores. 50 However, the levels of uncertainty around the effect of the link worker per se would be wide. It would be almost impossible to reliably attribute outcomes to the link worker model. This approach will investigate only the effect of a SP referral rather than the uptake of the social prescription. The clinical outcomes (e.g. glucose measures, adiposity measures or prescriptions) that are routinely collected may not reflect the ‘effect’ of the intervention. Our data highlight the holistic nature of SP; therefore, well-being outcomes may be more appropriate to detect change.
It may be unwise to proceed with this approach for two reasons: first, the link worker model is a relatively new model and this will reduce the retrospective time points of the evaluation; second, a premature evaluation may not produce clinically meaningful or statistically significant changes in clinical outcomes (e.g. HbA1c level or weight). In addition, clinical outcomes may have multifaceted determinants, making it difficult to infer causation.
Colleagues in Oxford, UK, are working on harmonising the SP codes for routine data. 54 This work aims to extrapolate codes related to social needs and social interventions that are more relevant to SP. This work is ongoing, though it may eventually help inform an evaluation using ‘homogeneous’ retrospective routine data.
Controlled research settings
A mixed-methods pre and post design
Our systematic review and interview data suggest that well-being is a key outcome for the current model (see Figure 2). However, it is not possible to systematically pool available data on a national level. We have demonstrated through this feasibility assessment the complexity of the service, the potential factors that may influence the link worker model and the heterogeneity of service provision (see Figure 2). Therefore, we consider that a mixed-methods case study might be a valuable option, with a pre- and post-test design, with baseline and possibly with 6-week and 6-month data points for quantitative measures of well-being, and with qualitative data collected midway through the follow-up period to understand participants’ lived experience of the services. The time points are suggestive, although they are informed by this feasibility assessment (described in Chapter 3 and Figure 2), reflecting academic colleagues’ experience in primary research in this area and taking into account the balance between an ‘ideal’ scenario and a ‘feasible’ scenario.
The holistic nature of SP would suggest a need for quantitative measures around quality of life, well-being, depression, anxiety, hope, loss of control, social support and social networks. A primary outcome would be identified to inform the sample size calculation and the remaining outcomes would serve as secondary outcomes. Additional data could include baseline characteristics, sociodemographics, type of services used and number of sessions attended. Self-reported outcomes would be collected using validated and unified tools that would be introduced to capture quantitative measures at three separate time points. Outcomes would be completed by the link worker to account for any illiteracy (as demonstrated by our findings) or other barriers and to reduce the research burden on clients. However, link worker incentives may be necessary. Qualitative data would include a semistructured approach to capture both client and link worker experiences of the process. Baseline characteristics of clients can be used for stratification to evaluate the differences across groups. Additional subgroup analysis can be carried out using the number of link worker visits (i.e. dose) or number and type of services referred on to. For instance, subgroup analysis would be considered for the three levels of the intervention (i.e. link worker, single service and multiple services). Factors (i.e. covariates) influencing the link worker service would be captured and accounted for. Non-attendance data would be captured to better understand the reasons behind attrition. Mean differences across outcomes would be reported at different time points. It should be noted that, in the light of COVID-19, the ‘service’ is rapidly changing across England. For instance, the service is now reaching out to people rather than relying on the traditional referral route. The mode of delivery and outcome assessment has switched over the course of 2020 from being face to face to virtual or by telephone. This may negatively affect people with literacy issues or lack of access to devices. In addition, the demographics and priorities of people taking up SP have changed.
A realist evaluation
What we have demonstrated through this feasibility assessment is that we do not yet know what types of SP services are more successful for whom and in what circumstances, nor do we know how successful programmes are over time. Our data highlight the vast heterogeneity in the delivery of SP, which has a range of consequences, with different participants valuing different outcomes.
To acknowledge and attempt to cut through the complexity, and to explore the active ingredients of SP, it would be important to focus on theories that underlie this social intervention. 60 Therefore, we consider that some form of realist evaluation may be beneficial. The aim of the realist evaluation is to provide an explanatory analysis of how and why SP works (or does not work) in particular contexts or settings. 61
The realist evaluation process will be staged, although the process is iterative and would involve significant back and forth between the data, emerging programme theory and literature. 61 The stages involve the identification of a programme theory or theories. Programme theories represent the proposed mechanism of action and give an indication as to the active ingredients of SP programmes and how they are expected to work. This would be informed by other research components, existing realist reviews and a project stakeholder group. Similar to the context–mechanism–outcome (CMO) configurations described by Tierney et al. ,62 the programme theory will be used to guide the evaluation. The later stages will involve the exploration and testing of the programme theory across a range of contexts (e.g. different patient groups and implementation chains) to examine whether or not and how they work, and if it is in the manner anticipated. This will be achieved through the primary data collection stage, where multiple data collection methods (e.g. interviews, focus groups, observations and document analysis) will be performed across multiple sites in England. The aim of the primary data collection is to conduct up-close, in-depth and detailed investigation of each comparative ‘case’ and its related contextual position. The cases (i.e. the units of investigation) could range from one link worker and one general practice to one region delivering SP, depending on the level of analysis required. Building on the findings of our feasibility assessment (see Figure 2), we propose following the route of referral as the justification for the selection of cases. Each of the four types of referral (i.e. self-referral, third party, IT system, e-mail/telephone) could be used as a tracer and examined in detail during the realist evaluations. This approach would provide excellent opportunities to compare and contrast the different modes of service delivery, testing the programme theory across each. The number of comparative cases would be limited by the resources available, but we suggest that at least four would be required to assess each referral route.
Once the data are analysed using appropriate methods for each type of data collected, the evaluation would be completed by refining the original programme theory, which will be informed by the primary data (e.g. how we thought it would work compared with what we found in practice). This would be refined further using mid-range social science theory to support explanations of how and why SP does or does not achieve the intended outcomes. It will be important to build on the findings of Tierney et al. ,62 who suggest areas for further empirical investigation, including the need to focus on link worker integration, sustainability of impact on patient well-being, and cost-effectiveness.
The realist method is not intended to be formulaic, with the goal of determining the effectiveness of an SP intervention. Instead, it is a logic of enquiry that is characteristically pluralist and flexible. 61 The planned realist evaluation could contain both qualitative and quantitative methods, formative and summative analysis and prospective and retrospective understanding. This would be informed by members of a project stakeholder team (including professionals and patients) who act as the ‘insiders’ with knowledge of SP; the project team can then test programme theories and findings. Therefore, the approaches used in the realist evaluation would differ significantly from those used in the other research scenarios (see A mixed-methods pre and post design and A cost–utility analysis). However, this element of the evaluation will maximise learning across policy, disciplinary and organisational boundaries to enable a more in-depth understanding of SP from those directly involved in its delivery.
A cost–utility analysis
This feasibility assessment has demonstrated that assessing the cost-effectiveness of link worker SP in the current systems is likely to be problematic. The health economic objective is to estimate the comparative cost-effectiveness of the link worker model against a ‘traditional/standard care’ model. To achieve this, a cost–utility analysis (CUA) could be conducted to capture resource use costs and quality-of-life outcomes at a patient level. It would then be analysed by intention-to-treat principles for each treatment pathway (depicted in Figure 2). The difference between overall costs and QALYs for each pathway is then used to calculate the incremental cost-effectiveness ratio (ICER) and established cost-effectiveness of the link worker model.
For the purpose of economic evaluation, to facilitate more robust comparison between pathways, the ‘traditional/standard care’ pathway is limited to GP-initiated referrals to external services (see Figure 2, boxes c and d) and compared with the ‘current’ SP pathway of a GP referring directly to a link worker who then refers on to external services. Simplification of this ‘traditional’ route by removal of self-referral by individuals and non-health-care professionals is important, as establishing baseline costs/quality-of-life measures in this cohort would be highly problematic.
Similarly, establishing a condition-controlled cohort, where participation is limited to those with a specific ‘health/issue’ rather than from a holistic approach would improve baseline heterogeneity. For instance, a cost-effectiveness evaluation would be performed of clients presenting with a primary issue of ‘obesity’ who then transition through either of the two pathways and on to appropriate external services.
This would be a resource-intensive research project conducted on a national level and assumes that there are a sufficient number of sites across England still implementing the ‘traditional/standard’ pathway of GP referral direct to the voluntary sector (this can be assessed by a preliminary scoping assessment).
Economic evaluation would ideally be conducted from both an NHS and Personal Social Services perspective, with resource use, and costs of services accessed by clients, collected at each stage. This will include number and length of patient consultations with GP and/or link worker, number of external services referred on to (both NHS funded and in the voluntary sector) and administration time/communication between referrer and service(s). Different approaches will be used for data collection, including routine data sources (e.g. for frequency and length of patient consultations) and appropriate resource use measurement questionnaires, such as those detailed on the Database of Instruments for Resource Use Measurement (DIRUM) website (URL: www.dirum.org; accessed 1 November 2021). Outcome measures in the form of quality-of-life, well-being and clinical measures would also be collected to estimate the difference in QALYs between those who receive SP and those who do not. Both resource use and outcome data would ideally be collected regularly, for example at baseline and 3, 6 and 12 months. This would be completed by trained researchers at each stage to account for literacy barriers and reduce the research burden on both the client and GP/link worker.
It is noted that 1 year’s follow-up may be challenging, but given successful SP ‘research-controlled’ evaluations, such as the W2W evaulation and the Rotherham evaluation, indicate that these timelines may be possible.
A pragmatic cluster randomised controlled trial
A pragmatic cluster randomised controlled trial (cRCT) (potentially plus CUA and realist evaluation) would control for unmeasured confounders between clients who are and are not offered SP, therefore making it more likely that some element of causation can be inferred if differences in outcomes are observed.
General practices would be cluster randomised to either enhanced link worker input or to standard care (which includes the current model with a link worker for each PCN), and the unit of assessment would be the practice. Standardised GP and link worker protocols for all activity would be required and stratification would be needed for practice size, geographical area and practice deprivation.
Adults with GP-assessed social prescription needs would be recruited and the primary outcome would be a measure of well-being (e.g WEMWBS score). Additional outcomes could include, for example, EuroQol-5 dimensions, five-level version (EQ-5D-5L), score with, for example, 18 months’ follow-up. Allocation of general practice would not be revealed to individual patients until their consent and baseline measures had been collected. An intention-to-treat population analysis should be undertaken.
The strengths of this approach are its unbiased nature, and outcomes relevant to SP could be collected. In addition, the cRCT could be undertaken with a simultaneous mixed-methods/realist process evaluation and alongside a CUA, furnishing more accurate data for the understanding of processes and further implementation as well as data on costs and QALYs and, therefore, for an ICER.
One limitation of this approach is that it is highly resource intensive. To work even as a pragmatic trial it would have to set up a slightly artificial model of link worker practice. This is because standardised protocols for GP and link worker activity would be needed and the inevitable substantial heterogeneity of onward referral would be a problem.
Perhaps more importantly for generalisability, the cRCT would need to trial an enhanced service in general practice as each PCN currently has a link worker; a design with controls who had no link worker input would lack equipoise. Patient selection would also be a problem and would need standardisation, but pragmatic evaluation would require an open approach to inclusion criteria that match current practice as far as possible. Inclusion criteria could be based on the 3D trial63 approach to selecting patients with chronic/long-term conditions, although it would be important to restrict the patient groups selected as little as possible from the point of view of clinical as opposed to social prescription need. There may be problems in the statistical design and sample size assessments because the intraclass correlation coefficient (ICC) would not be known [although there may be previous useful trials to build on, e.g. the WISE (whole system informing self management engagement) trial59].
Summary
-
A retrospective, matched cohort analysis using existing data would save time and cost compared with the other study designs discussed. This would not introduce additional burden to the current service. This evaluation would be restricted to specific health conditions and look at routinely collected process and clinical outcomes. Clinical outcomes may not reflect the effect of SP. This approach would investigate only the effect of a SP referral rather than the uptake of the prescription. Clinical outcomes may not precisely capture the effect of the intervention. The link worker model is relatively new; therefore, the retrospective time points of evaluation will be reduced and the study may be underpowered.
-
A mixed-methods pre and post design using a combination of quantitative and qualitative methods would allow outcomes to be consistently collected and uploaded at different time points.
-
Quantitative outcomes would include measures that are relevant to the intervention, such as well-being. Qualitative outcomes would capture both client and link worker perspectives. However, this would be subject to observational design critique. In the light of COVID-19, the mode of delivery for SP changed from face-to-face to remote, and this may negatively affect assessments in people with literacy issues or lack of access to devices or the internet.
-
An interactive realist evaluation that aims to provide an explanatory analysis of how and why SP works (or does not work) in particular contexts or settings may maximise learning across policy, disciplinary and organisational boundaries to enable more in-depth understanding of SP from those directly involved in its delivery.
-
A cost–utility evaluation would aim to capture resource use costs and quality-of-life outcomes at a patient level and then be analysed by intention-to-treat principles for each treatment pathway. The difference between overall costs and QALYs for each pathway is used to calculate the ICER. The cost-effectiveness of the link worker can be established, allowing for comparison with other health and social care interventions. However, this is a resource-intensive approach.
-
Research-controlled environments with a robust study design, such as in a cRCT, and, importantly, alongside CUA, can help us understand any potential causal relationship between SP and patient outcomes. However, this will require the introduction of more uniform tools, methods and timelines across sites to properly answer the research question.
COVID-19 impact
COVID-19 is changing SP in terms of delivery mode, service uptake, client recruitment and client demographics. SP services have transitioned activities and support online and/or are operating at reduced capacity, affecting their ability to respond to referrals. Link workers are more engaged in outreach to identify those most at risk of isolation and providing one-to-one virtual support. Online questionnaires and methods of data collection have caused accessibility issues for some patients, meaning some outcomes go unrecorded. There is a clear push from service providers, stakeholders, topic experts and academics for mixed-methods research to increase understanding about whether or not the current model is effective and how.
Chapter 5 Discussion
Statement of principal findings and comparison with previous literature
This was a feasibility study that aimed to investigate whether or not an evaluation of the national link worker model of SP is possible. We undertook a rapid systematic review and conducted qualitative interviews across different sites in England. The sites included in this evaluation followed the NHSE link worker model for SP. We interviewed 25 participants involved in different aspects of SP (i.e. social prescribers/link workers, regional leads, learning co-ordinators, commissioners, managers and those working in the voluntary sector across several regions in England) and three academics. We identified a number of factors that influence link worker service delivery that will require consideration in any future evaluation and a number of possible methods for undertaking an evaluation.
We found that the current service model is a complex intervention with several interacting components. 64 SP programmes were not singular or finite interventions and set-up of a link worker-mediated SP service involved entire services across health and social care and the voluntary sector. In addition, we found that the current link worker model of SP is running in a substantially heterogeneous manner across the country.
The link worker model has been running for approximately 2 years, although other forms of SP have been running for longer. The current service is patient focused and includes a needs assessment with a degree of flexibility or tailoring to meet patient needs. Onward referral services include services to help with social isolation, finance, housing, increasing physical activity, healthier living and weight management. These services may be small and financially precarious, for example underfunded or funded only in the short term. These services have an array of goals, with many activities and many actors. This is one of the major challenges of the current model, in that it relies heavily on small charities and voluntary organisations, which in turn depend on intermittent external funding. In line with the 2020 National Voices report,65 we found that link workers suffer from a lack of financial support to address additional costs such as overheads, management, training and coordination with link workers locally. This creates an additional financial burden on voluntary services that also host link workers.
Link workers and stakeholders are concerned about the systematisation of link workers’ roles, training and career structures. Information available to link workers to support the most appropriate onward referral was seen to be heavily dependent on local knowledge and circumstances. Turnover among link workers was reported to be high.
For the purpose of considering evaluation, a number of measures are captured at a local level, such as service uptake, well-being, sociodemographics and social and behavioural aspects. However, there is clear heterogeneity in IT infrastructure, data access, tools and paper assessment and outcome forms across sites, and no centralised mechanism for their collation. Local assessment tools have been developed to capture different social aspects, such as housing, relationships, finances and physical health. These tools seem to capture the main components of the holistic nature of SP. For example, each locality has its own core elements of data to be recorded (and non-attendance data are almost always recorded). There appears to be very little data collection by link workers about outcomes from onward referral agencies or services. We are aware of work to establish a minimum data set for SP and of the work of the Oxford National Social Prescribing Observatory. 5 Although there are ‘accepted’ measures using routine data (e.g. SNOMED), they do not cover the health and well-being outcomes important to SP.
The quantitative literature on the effectiveness of SP tends to focus on specific conditions, to evaluate specific services and to be carried out at a local or regional level. Some routine measures and databases exist, but these do not necessarily relate to the most appropriate outcomes for a SP intervention. A number of condition-controlled evaluations (e.g. aimed at weight reduction only) have been undertaken and may be useful to inform future, more generic evaluation. However, such evaluations will require a research setting and currently available routine data will need to be supplemented with specifically collected additional research data.
Previous researchers have undertaken realist examinations of SP in the form of realist reviews. 38,62 Tierney et al. 62 conducted the most recent review of SP in primary care to identify how connector schemes (e.g. link workers) work, for whom, why and in what circumstances. They generated CMO configurations programme theories, which drew on 118 documents, that highlighted the essential role of ‘buy-in’ and connections. The programme theories were further refined by drawing on social capital and patient activation theories. The secondary research has warranted further investigation of SP;62 in particular:
-
how a link worker is best integrated so that ‘buy-in’ can be developed,
-
how to recruit the ‘right’ people, able to develop connections, and what training/support they require
-
sustainability of impact on patient well-being (long-term follow-up)
-
cost-effectiveness of different components of the link worker model.
Husk et al. 38 highlighted the importance of developing research alongside SP practice but noted the difficulty of doing this robustly in such a complex system. 38 However, they did note some key ways in which this could be achieved, for example using evidence to inform elements of the patient pathway, reporting contextual factors and being realistic about what outcomes are relevant and useful. One of our proposed research recommendations is a realist evaluation to provide a depth of understanding regarding what mechanisms support link workers working in various delivery contexts to achieve outcomes in the delivery of SP programmes and how these outcomes are achieved.
COVID-19 has exacerbated pressures on voluntary sector resources, particularly in poorer communities, which tend to have lower levels of voluntary sector activity. We heard that COVID-19 had strengthened working relationships and processes between primary care, link workers and the voluntary sector in some areas because SP services are being utilised in local responses to the pandemic. However, COVID-19 has created additional capacity issues for link workers and voluntary organisations in terms of caseload and ability to follow up with patients, as well as shifting the nature of the support offered. As recommended by our workshop participants, a future evaluation should take into account how SP is evolving in the context of COVID-19 and the legacy of the pandemic on voluntary and community sector capacity.
Strengths and limitations of the study
This was a rapid systematic review of the published evidence and qualitative interviews with purposively sampled stakeholders to investigate the feasibility of evaluation of the link worker model of SP. The work was designed to give a rapid overview of the issues involved in evaluation. In this rapid review we did not undertake systematic quality assurance of the included studies, although we have made comments on the quality of studies in our narrative synthesis where appropriate. The rapid review was systematic although restricted to publications in English from 2015.
Our interviewees included several sites across different regions in England and included data from link workers and those involved in managing the service at a local, regional and national level as well as from academics in the field. For the qualitative interviews, we describe a snowballing method of purposive sampling. This approach took advantage of existing networks, availability and convenience of participation in a short recruitment time period. This was deemed the most appropriate method given the difficult conditions under which this study took place. All interviews were undertaken remotely via sound and video link and our methods of establishing connections with relevant stakeholder organisations were restricted. The scope of the work in general also precluded a more systematic and routine method of sampling and recruitment.
Despite the COVID-19 outbreak, which had a significant impact on the shape of the service, the mode of service delivery, health priorities and the capacity of staff, we were able to conduct our interviews between April 2020 and September 2020. This limited our interview sample size while SP organisations focused on responding to the pandemic. Nevertheless, we managed to recruit a range of perspectives and roles in our purposive sample of link workers, SP practitioners and VCSE organisations. Interviews were scheduled at a time most convenient to participants to minimise disruption to front-line services. We asked participants during interviews to reflect on how COVID-19 was affecting current service delivery and activities and recorded their responses.
We were unable to identify a number of important elements that might be valuable for any future evaluations. These include a more in-depth mapping of the heterogeneous current service pathways, which would need further investigation to better understand how and why link worker SP might and might not work. Examples of the problems include understanding the difference between clients who are self-referred and those who are referred by health-care professionals, and understanding differences in referral rates from individual practitioners, practices and PCNs. It would also be important to identify barriers to referral and what would need to be done in terms of education and training to overcome those barriers.
In addition, SP link workers are a new workforce and there are clearly issues with their career structures, training and support management arrangements, which we were not able to examine in any depth. We were not able to examine quality assurance in the system.
We were also not able to examine the potential causal mechanisms in any detail. For example, it is not clear whether it is the relationship that the link worker builds with the patient or client or the activities that clients then pursue following onward referral that is the key variable in a successful outcome. From our interviews, we consider that this may vary considerably and may depend very much on local and regional structures and availability (or not) of comprehensive VSCSE input.
We drew on previous research studies, our interviews and discussion with academics and stakeholders in the field to recommend different possible methods of researching the effectiveness and cost-effectiveness of the link worker model of SP (see Table 3). In our report we detail the strengths and limitations of a number of research methods. Evaluation of this complex intervention is itself complex. We considered recommending further in-depth impact evaluation of discrete interventions with defined target groups that might be expected to benefit from SP and we consider that this would make a more satisfactory evaluation project; however, the nature of our brief was to view the link worker model of SP generically (i.e. not in relation to any one condition or set of conditions), since there are already a number of evaluations of SP in specific conditions. If a national overarching evaluation is to be undertaken, then restrictions to groups with specific conditions will not answer the overarching questions of the value of the link worker model overall.
It might be considered that multiple studies are needed to evaluate the link worker model of SP because a single study will inevitably be extremely complex. We believe that it is possible to reflect the link worker approach in one evaluation but acknowledge that this may be a very difficult and resource-intensive evaluation to undertake.
The stated aim of the link worker model is to improve health and well-being and, fortunately, there are a number of generic measures of health and well-being that could be used in any future evaluations (e.g EQ-5D-5L and WEMWBS). Other outcomes that may be considered relevant include changes in demand on GP and hospital services. Studies in this area are fraught with problems of attribution error. However, despite the lure of potentially more easily accessible routine data, improvements in health and well-being might plausibly lead to either an increase or a decrease in GP attendances, as expectations for better health are raised. It was beyond our scope to investigate a relationship between improved quality of life and demand for services, although this may have implications for service design and the length of time the link worker remains in contact with the client.
It can be challenging to evaluate complex health and public health interventions. Often, the difficulty is in determining whether or not the components refer to the same things and whether or not the measures researchers use to evaluate the components are comparable. It can also be challenging to determine which features of an intervention and its context are important in influencing key outcomes and determining the suitability and sustainability of an intervention. 58 Unpicking the interactions between intervention and context (e.g. recipient and provider of SP) has frequently been reported as difficult in reviews of evaluation studies. 58 It was also beyond our scope to assess the relevant data that might be needed across all components and levels, alongside detailed descriptions of the context ‘systems’ and how this may affect the intervention required. With Datta and Petticrew58 we consider that an evaluation of the link worker model of SP might usefully include a ‘multicriteria’ form of assessment acknowledging the multiple objectives of this complex intervention.
It was also beyond the scope of this investigation to consider investigating policy research in this area and the possibility that investigation into policy instruments and tools to enhance SP (e.g. in relation to the organisation of social care and the integration of the health and social care sectors) might be valuable.
COVID-19 impact
As discussed in Chapter 4, COVID-19 is changing SP service in a number of ways: delivery mode, service uptake, client recruitment and client demographics have all changed. Services have moved to online provision. Link workers are more likely to be undertaking outreach. Gathering outcomes data has become more difficult. This transition may be permanent or temporary, depending on how the COVID-19 pandemic continues. However, these changes mean that there has been significant discontinuity in this relatively new service, which may affect methods and optimal timing of evaluation.
Implications for policy and practice
In this section we highlight some of the implications for policy and practice that have emerged from our work. Our conclusions regarding potential future research approaches are presented in Chapter 6.
We have identified key enablers of and barriers to evaluation of the link worker model of SP, which will need to be addressed at both policy and practice levels.
Key enablers:
-
an interested and active workforce of link workers
-
a system that is gradually becoming more mature and, therefore, potentially more evaluable
-
some robust data systems
-
a desire and need by link workers and those providing SP funding to understand the services and their impact.
Key barriers:
-
substantially heterogeneous service provision models
-
large differences in available onward referral services and engagement with the PCN
-
the precarious financial and organisational nature of some onward referral services
-
heterogeneous data collection, reporting and data monitoring by different social prescribers
-
commissioners do not usually ask social prescribers to use standardised assessment tools
-
there is no agreement across schemes regarding the key outcomes that need to be measured
-
there is a clear need for harmonisation of data collection; for instance, some clear direction is required to encourage programmes to use common validated well-being measures
-
mature data are currently not available; there needs to be agreement across schemes on how and when to follow up referrals
-
previous evaluations have often concentrated on individual (or a small, selected subgroup of) health conditions, but if a national overarching evaluation is to be undertaken then restriction to groups with specific conditions will not answer the overarching questions of the value of the link worker model overall.
Chapter 6 Conclusions
Synthesis of conclusion in relation to research questions
In this chapter we summarise our conclusions in relation to the questions posed in the commissioning brief.
1. What are the most important evaluation questions that an impact study could investigate?
We identified the following most important evaluation questions:
-
What is the effectiveness of the national link worker SP scheme in terms of its stated outcomes of improving health and well-being?
-
What is the cost-effectiveness of the national link worker SP scheme?
-
How do geographical and organisational differences in the link worker model of SP (e.g. differences in setting and availability of onward referral sites) impact the effectiveness of SP?
-
Do SP referrals and outcomes vary between different deprivation areas or different population groups?
-
What outcomes are associated with the link worker role in SP? What mechanisms are at work to produce these outcomes and under what contexts are they triggered?
-
Does SP impact routinely collected process measures (such as GP attendance, hospital admission and readmission) and how do these relate to underlying well-being?
-
What policy instruments and tools enhance and advance the effectiveness of the SP link worker scheme?
2. What data are already available at a local or national level and what else would be needed?
We identified that the research infrastructure available to allow for an evaluation of the link worker model was not robust. Any evaluation would span health care (particularly primary care), social care and the voluntary sector. The multiplicity of organisations, sites, data and data collection methods (which can vary by individual social prescriber) would make sufficient harmonisation across multiple heterogeneous organisational and geographical sites extremely challenging. Although there is an NHS national outcomes set5 related to the link worker model of SP, this reflects only process measures (e.g. attendance/non-attendance) and these measures are not sufficient to evaluate the link worker model of SP in terms of its stated outcomes of improving health and well-being. A multiplicity of outcome measures is currently used, with few pointers as to the best method for current assessment. Data needed are those that can be collected to measure harmonised well-being outcomes across all link workers and NHS SP organisations. Data are also required on costs and resources use. We recommend that CUA is undertaken to allow for evaluation of cost-effectiveness. The only way to undertake this (even inside a research-controlled environment) will be via a painstaking collation of costs and resource use data across the disparate sites and link worker SP organisational set-ups. Even in mature sites data are not mature because follow-up ranges from between 3 to 6 months and is rarely longer.
It is also the case that additional harmonised data collection would enhance evaluations, for example of patient experience of services.
3. Are there sites delivering at a large enough scale and in a position to take part in an impact study?
There are a number of mature sites delivering the link worker model of SP that would be in a position to take part in an impact study. However, it is clear that the heterogeneous nature of the link worker model of SP (i.e. the variety of organisational set-ups and of relationships with and quality and size of onward referral agencies) means that standardisation to allow for a national evaluation will be extremely difficult and the problem of lack of harmonisation of data collection remains problematic. The precarious financial situation of many onward referral agencies is a concern for the sustainability of services in the future.
4. How could the known challenges to evaluation (e.g. information governance, identifying a control group) be addressed?
We have highlighted throughout this report the problems of harmonising the data currently collected in a way that would allow for meaningful evaluation of the link worker model of SP. At present this process of harmonisation would be hugely costly and time-consuming, although it may eventually be required as interventions such as SP become more mainstream. In the meantime, we consider that the only way to address the known challenges is to use a research-controlled environment to undertake an evaluation. Therefore, we recommend a pragmatic cRCT with an additional realist evaluation to understand the underlying programme theory. This will be extremely valuable and could be undertaken before or simultaneously with an outcome/impact evaluation.
In summary, we have identified that, although an evaluation of the link worker model of SP is possible and that there are a number of different methods, each has its own drawbacks. Only a RCT would allow for adequate attribution of SP outcomes, although the problem of generalisability to the current model of SP is a concern.
We consider that a cost-effectiveness analysis is key because this is the metric with which public programmes such as this are compared in allocating scarce health and social care resources. We also consider that the investigation of relevant processes (e.g using a simultaneous realist evaluation) would be beneficial. Although the use of routine data is an attractive approach, it will not shed light on the cost-effectiveness of the SP link worker model.
Research recommendations
As a result of our work, we describe three possible models of evaluation of effectiveness to inform future research. We also describe three possible modes of evaluation of cost-effectiveness that are complementary to the evaluations of effectiveness. All have drawbacks that will require ingenuity to overcome.
Models of evaluation of effectiveness
-
Evaluation based on currently available, routinely collected health-care data. This will require:
-
assembly of generic (not condition-specific) relevant process and outcome measures, including those available from national routinely collected primary and secondary health-care data
-
development of a deep understanding of the multiplicity of ‘clinical’ pathways followed by clients receiving link worker interventions in order to understand what is being evaluated
-
development of evaluative models allowing for restricted follow-up, heterogeneity of delivery modes and effects of confounding.
-
-
Evaluative mixed-methods research to better capture the complexity of SP through understanding the CMO configurations across comparative settings.
-
Interventional evaluative research, for example a cRCT focused on the link worker approach per se rather than (as is presently being undertaken) focused on individual conditions.
Models of evaluation of cost-effectiveness
-
Using routinely available costing and outcomes data as in effectiveness evaluation 1.
-
Using routinely available costing and outcomes data where possible and supplementing these with ad hoc data collection.
-
Attachment to a cRCT, entailing ad hoc data collection as part of the design, as in effectiveness evaluation model 3.
Acknowledgements
This study was undertaken in collaboration with, and with the advice of, the NHSE Social Prescribing Unit.
We would like to thank Mary Jordan and Peter Auguste, Division of Health Sciences, Warwick Medical School, University of Warwick, for their advice on health economics; Jill Colquitt, Effective Evidence LLP (Waterlooville, UK), for editorial support; Anne Devrell, Research Champion, CRN West Midlands, for her work as a PPI contributor to this report; and Sarah Abrahamson, Division of Health Sciences, Warwick Medical School, University of Warwick, for her project management support.
Patient and public involvement
A patient and public involvement (PPI) contributor was recruited to the project team to help shape the research and ensure that no decisions were made about the project without the inclusion of patient voices. The PPI contributor met with members of the research team at key stages of the project to consider the most important questions that an evaluation of SP could answer, develop the fieldwork design, help interpret findings and comment on draft versions of the report. The PPI contributor was supported in her role by Dr Jenny Harlock. Communication was maintained between key project meetings via e-mail and telephone to provide progress updates, particularly regarding changes to the proposed fieldwork and time frame for the project caused by the COVID-19 pandemic. During the project, people with lived experience of SP services were invited to two online workshops, held in June 2020 and September 2020, and hosted by NHSE, to consider the most important questions that an evaluation of SP could answer, and methods and types of data collection most appropriate for such an evaluation. Discussions from the workshops have been recorded and are included in Appendix 6. Following discussions with our PPI contributor and from the workshops, we decided to expand the original scope of our fieldwork design to include voluntary and community organisations that are key providers for SP services. We also reflected in our findings that the evidence collected by SP schemes may not always reflect the outcomes that are most important to patients. Our PPI contributor read and commented on draft versions of our final report and helped to draft the Plain English summary.
Contributions of authors
Lena Al-Khudairy (https://orcid.org/0000-0003-0638-583X) (Senior Research Fellow) was the principal investigator, contributed to the inception of the work, design, methodology, data collection and project oversight and lead the write-up of the final report.
Abimbola Ayorinde (https://orcid.org/0000-0002-4915-5092) (Research Fellow) supported the analysis of the data, evidence synthesis and write-up of the report.
Iman Ghosh (https://orcid.org/0000-0002-7073-7468) (Research Assistant) supported the data collection, evidence synthesis, transcription and revision of the final report.
Amy Grove (https://orcid.org/0000-0002-8027-7274) (Associate Professor) contributed to the inception of the work, design, methodology and write-up of the final report.
Jenny Harlock (https://orcid.org/0000-0002-2300-750X) (Senior Research Fellow) contributed to the inception of the work, design, data collection, PPI and write-up of the final report.
Edward Meehan (https://orcid.org/0000-0002-9340-819X) (Public Health Trainee) supported the evidence synthesis and analysis of the data.
Adam Briggs (https://orcid.org/0000-0002-2314-1039) (Honorary Associate Professor) contributed to the inception of the work and design.
Rachel Court (https://orcid.org/0000-0002-4567-2586) (Information Specialist) supported the electronic searches.
Aileen Clarke (https://orcid.org/0000-0001-8299-3146) (Professor) provided senior clinical oversight and contributed to the inception of the work, design, methodology and the write-up of the final report.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS England . Social Prescribing n.d. www.england.nhs.uk/personalisedcare/social-prescribing (accessed 4 October 2020).
- Drinkwater C, Wildman J, Moffatt S. Social prescribing. BMJ 2019;364. https://doi.org/10.1136/bmj.l1285.
- Brandling J, House W. Investigation into the Feasibility of a Social Prescribing Service in Primary Care. Bath: University of Bath and Bath and North East Somerset NHS Primary Care Trust; 2007.
- The Social Prescribing Network . The Social Prescribing Network n.d. www.socialprescribingnetwork.com (accessed 4 October 2020).
- NHS England and NHS Improvement . Social Prescribing and Community-Based Support: Summary Guide 2020. www.england.nhs.uk/publication/social-prescribing-and-community-based-support-summary-guide/ (accessed 3 March 2021).
- NHS England . Delivering Universal Personalised Care n.d. www.england.nhs.uk/personalisedcare/upc (accessed 4 October 2020).
- NHS England . NHS Long Term Plan n.d. www.longtermplan.nhs.uk (accessed 4 October 2020).
- Alderwick H, Dixon J. The NHS long term plan. BMJ 2019;364. https://doi.org/10.1136/bmj.l84.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141-6. https://doi.org/10.1097/XEB.0000000000000050.
- Peters MDJ, Godfrey C, McInerney P, Baldini Soares C, Khalil H, Parker D, et al. Joanna Briggs Institute Reviewers’ Manual. Adelaide, SA: The Joanna Briggs Institute; 2017.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2003.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73. https://doi.org/10.7326/M18-0850.
- McEwan K, Richardson M, Sheffield D, Ferguson FJ, Brindley P. A smartphone app for improving mental health through connecting with urban nature. Int J Environ Res Public Health 2019;16. https://doi.org/10.3390/ijerph16183373.
- Panagioti M, Reeves D, Meacock R, Parkinson B, Lovell K, Hann M, et al. Is telephone health coaching a useful population health strategy for supporting older people with multimorbidity? An evaluation of reach, effectiveness and cost-effectiveness using a ‘trial within a cohort’. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1051-5.
- Munford LA, Wilding A, Bower P, Sutton M. Effects of participating in community assets on quality of life and costs of care: longitudinal cohort study of older people in England. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-033186.
- Sumner RC, Crone DM, Baker C, Hughes S, Loughren EA, James DVB. Factors associated with attendance, engagement and wellbeing change in an arts on prescription intervention. J Public Health 2020;42:e88-e95. https://doi.org/10.1093/pubmed/fdz032.
- Pescheny JV, Gunn LH, Pappas Y, Randhawa G. The impact of the Luton social prescribing programme on mental well-being: a quantitative before-and-after study. J Public Health 2019;43:e69-e76. https://doi.org/10.1093/pubmed/fdz155.
- Pescheny JV, Gunn LH, Randhawa G, Pappas Y. The impact of the Luton social prescribing programme on energy expenditure: a quantitative before-and-after study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-026862.
- Elston J, Gradinger F, Asthana S, Lilley-Woolnough C, Wroe S, Harman H, et al. Does a social prescribing ‘holistic’ link-worker for older people with complex, multimorbidity improve well-being and frailty and reduce health and social care use and costs? A 12-month before-and-after evaluation. Prim Health Care Res Dev 2019;20. https://doi.org/10.1017/S1463423619000598.
- Woodall J, Trigwell J, Bunyan AM, Raine G, Eaton V, Davis J, et al. Understanding the effectiveness and mechanisms of a social prescribing service: a mixed method analysis. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3437-7.
- Maund PR, Irvine KN, Reeves J, Strong E, Cromie R, Dallimer M, et al. Wetlands for wellbeing: piloting a nature-based health intervention for the management of anxiety and depression. Int J Environ Res Public Health 2019;16. https://doi.org/10.3390/ijerph16224413.
- Bowden L, Long T, Henry H. Evaluation of a choir as a non-medical intervention for children with asthma: BreathStars. Compr Child Adolesc Nurs 2020;43:128-41. https://doi.org/10.1080/24694193.2019.1607629.
- Bird EL, Biddle MSY, Powell JE. General practice referral of ‘at risk’ populations to community leisure services: applying the RE-AIM framework to evaluate the impact of a community-based physical activity programme for inactive adults with long-term conditions. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-7701-5.
- Agaku IT, Olaiya O, Quinn C, Tong VT, Kuiper NM, Conrey EJ, et al. A mixed-methods assessment of a brief smoking cessation intervention implemented in Ohio public health clinics, 2013. Matern Child Health J 2015;19:2654-62. https://doi.org/10.1007/s10995-015-1786-y.
- Batt-Rawden K, Andersen S. ‘Singing has empowered, enchanted and enthralled me’ – choirs for wellbeing?. Health Promot Int 2020;35:140-50. https://doi.org/10.1093/heapro/day122.
- Bertotti M, Frostick C, Hutt P, Sohanpal R, Carnes D. A realist evaluation of social prescribing: an exploration into the context and mechanisms underpinning a pathway linking primary care with the voluntary sector. Prim Health Care Res Dev 2018;19:232-45. https://doi.org/10.1017/S1463423617000706.
- Payne K, Walton E, Burton C. Steps to benefit from social prescription: a qualitative interview study. Br J Gen Pract 2020;70. https://doi.org/10.3399/bjgp19X706865.
- Redmond M, Sumner RC, Crone DM, Hughes S. ‘Light in dark places’: exploring qualitative data from a longitudinal study using creative arts as a form of social prescribing. Arts Health 2019;11:232-45. https://doi.org/10.1080/17533015.2018.1490786.
- White JM, Cornish F, Kerr S. Front-line perspectives on ‘joined-up’ working relationships: a qualitative study of social prescribing in the west of Scotland. Health Soc Care Community 2017;25:194-203. https://doi.org/10.1111/hsc.12290.
- Wildman JM, Moffatt S, Steer M, Laing K, Penn L, O’Brien N. Service-users’ perspectives of link worker social prescribing: a qualitative follow-up study. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-018-6349-x.
- Smith TO, Jimoh OF, Cross J, Allan L, Corbett A, Sadler E, et al. Social prescribing programmes to prevent or delay frailty in community-dwelling older adults. Geriatrics 2019;4. https://doi.org/10.3390/geriatrics4040065.
- Pescheny JV, Randhawa G, Pappas Y. The impact of social prescribing services on service users: a systematic review of the evidence. Eur J Public Health 2020;30:664-73. https://doi.org/10.1093/eurpub/ckz078.
- Pescheny JV, Pappas Y, Randhawa G. Facilitators and barriers of implementing and delivering social prescribing services: a systematic review. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-2893-4.
- Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-013384.
- Husk K, Blockley K, Lovell R, Bethel A, Lang I, Byng R, et al. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc Care Community 2020;28:309-24. https://doi.org/10.1111/hsc.12839.
- Jensen A, Stickley T, Torrissen W, Stigmar K. Arts on prescription in Scandinavia: a review of current practice and future possibilities. Perspect Public Health 2017;137:268-74. https://doi.org/10.1177/1757913916676853.
- Pilkington K, Loef M, Polley M. Searching for real-world effectiveness of health care innovations: scoping study of social prescribing for diabetes. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.6431.
- Mossabir R, Morris R, Kennedy A, Blickem C, Rogers A. A scoping review to understand the effectiveness of linking schemes from healthcare providers to community resources to improve the health and well-being of people with long-term conditions. Health Soc Care Community 2015;23:467-84. https://doi.org/10.1111/hsc.12176.
- Leavell MA, Leiferman JA, Gascon M, Braddick F, Gonzalez JC, Litt JS. Nature-based social prescribing in urban settings to improve social connectedness and mental well-being: a review. Curr Environ Health Rep 2019;6:297-308. https://doi.org/10.1007/s40572-019-00251-7.
- Rempel ES, Wilson EN, Durrant H, Barnett J. Preparing the prescription: a review of the aim and measurement of social referral programmes. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017734.
- ReQoL . ReQoL: Interpretation of Scores n.d. www.reqol.org.uk/p/scoring.html (accessed 16 March 2021).
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Jauregui E, Pacheco AM, Soltero EG, O’Connor TM, Castro CM, Estabrooks PA, et al. Using the RE-AIM framework to evaluate physical activity public health programs in México. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-1474-2.
- Office for National Statistics (ONS) . Personal Well-Being User Guidance 2018. www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/methodologies/personalwellbeingsurveyuserguide (accessed 17 March 2021).
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Vaingankar JA, Abdin E, Chong SA, Sambasivam R, Seow E, Jeyagurunathan A, et al. Psychometric properties of the short Warwick Edinburgh mental well-being scale (SWEMWBS) in service users with schizophrenia, depression and anxiety spectrum disorders. Health Qual Life Outcomes 2017;15. https://doi.org/10.1186/s12955-017-0728-3.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. https://doi.org/10.1111/j.1475-6773.2004.00269.x.
- Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess 1996;66:20-4. https://doi.org/10.1207/s15327752jpa6601_2.
- Good A, Lamont E. Outcomes Star™ Psychometric Factsheet: Well-being Star™. Hove: Triangle Consulting Social Enterprise Ltd; 2019.
- Paterson C, Thomas K, Manasse A, Cooke H, Peace G. Measure Yourself Concerns and Wellbeing (MYCaW): an individualised questionnaire for evaluating outcome in cancer support care that includes complementary therapies. Complement Ther Med 2007;15:38-45. https://doi.org/10.1016/j.ctim.2006.03.006.
- Royal College of General Practitioners . RCGP Research and Surveillance Centre n.d. www.rcgp.org.uk/clinical-and-research/our-programmes/research-and-surveillance-centre.aspx (accessed 27 October 2020).
- Moffatt S, Steer M, Lawson S, Penn L, O’Brien N. Link Worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015203.
- NHS England/Personalised Care Group/Patient Activation . PAM Implementation Quick Guide 2018. www.england.nhs.uk/wp-content/uploads/2018/04/patient-activation-measure-quick-guide.pdf (accessed 27 October 2020).
- Medical Research Council (MRC) Health Services Public Health Research Board . A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health 2000.
- Datta J, Petticrew M. Challenges to evaluating complex interventions: a content analysis of published papers. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-568.
- Kennedy A, Bower P, Reeves D, Blakeman T, Bowen R, Chew-Graham C, et al. Implementation of self management support for long term conditions in routine primary care settings: cluster randomised controlled trial. BMJ 2013;346. https://doi.org/10.1136/bmj.f2882.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. Manchester: University of Manchester, ERSC Research Methods Programme; 2004.
- Pawson R, Tilley N, Chelimsky E, Shadish WR. Evaluation for the 21st Century: A Handbook. Thousand Oaks, CA: SAGE Publications Ltd; 1997.
- Tierney S, Wong G, Roberts N, Boylan AM, Park S, Abrams R, et al. Supporting social prescribing in primary care by linking people to local assets: a realist review. BMC Med 2020;18. https://doi.org/10.1186/s12916-020-1510-7.
- Man MS, Chaplin K, Mann C, Bower P, Brookes S, Fitzpatrick B, et al. Improving the management of multimorbidity in general practice: protocol of a cluster randomised controlled trial (The 3D Study). BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011261.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Cole A, Jones D, Jopling K. Rolling Out Social Prescribing: Understanding the Experience of the Voluntary, Community and Social Enterprise Sector. London: National Voices; 2020.
Appendix 1 MEDLINE search strategy
Database: Ovid MEDLINE ALL.
Date range of search: 1946 to 14 February 2020.
Date of search: 14 February 2020.
Search strategy
-
social prescrib*.mp. (115)
-
social prescrip*.mp. (32)
-
social referral*.mp. (9)
-
1 or 2 or 3 (143)
-
community prescrib*.mp. (66)
-
community prescrip*.mp. (25)
-
community referral*.mp. (156)
-
5 or 6 or 7 (243)
-
4 or 8 (378)
-
link worker.mp. (33)
-
link* scheme*.mp. (44)
-
community navigator*.mp. (12)
-
well-being coordinat*.mp. (1)
-
(patient navigator* and (social or community or wellbeing or well-being)).mp. (241)
-
10 or 11 or 12 or 13 or 14 (328)
-
9 or 15 (695)
-
(systemat* or realist or literature or evidence).mp. (2,726,055)
-
16 and 17 (176)
-
limit 16 to ‘review articles’ (54)
-
18 or 19 (193)
-
limit 20 to yr = ‘2015 -Current’ (129)
-
limit 21 to english language (129)
The PRISMA flow diagram

Appendix 2 Description of included studies
| Author(s), year of publication | Location | Description of SP | Outcome measured | Tool used | Strengths and limitations (reported by authors) |
|---|---|---|---|---|---|
| Randomised control trial | |||||
| McEwan et al., 201916 | Sheffield, UK |
Smartphone app to notice the good things about urban nature or built spaces and thereby increase nature connectedness and positive affect Signposting approach |
Primary outcome: recovering quality of life Secondary outcomes: types of positive affect, nature relatedness, engagement with natural beauty |
Self-reported measures of well-being and nature connectedness at baseline, post intervention and at 1-month follow-up |
The app could be enhanced, more engaging Sample selected with the baseline assessment of recovering quality-of-life score – true testing of social prescription is required Small sample for ‘common mental health problem’ group Barriers for app: research response Attrition rate high for long-term follow-up |
| Trial within a cohort | |||||
| Panagioti et al., 201817 | North-west England, UK |
The PROTECTS intervention delivered by a ‘health advisor’; includes ‘telephone health coaching’ involving support and encouragement for the patient to adopt healthy behaviours SP involved links to resources: W2W |
Primary outcome: self management; quality of life (leads to cost-effective analysis) Secondary outcomes: depression; self-care |
Self-reported data |
Strengths: large sample size; focused multimorbidity; TWiCs design Limitations associated with the TWiCs design: non-adherence; time constraint for effect estimation; missing data The trial cannot answer the question of whether or not health coaching is effective and cost-effective for multimorbidity in the longer term The study area consists of white patients – ethnic variation not measured |
| Cohort studies | |||||
| Munford et al., 202018 | Salford, north-west England, UK | Community asset participation, health and health-care utilisation | QALYs, health-care costs and social value estimated using net benefits | Questionnaires | Limitations: use of longitudinal cohort data, statistical matching, health-care cost estimated from linked administrative cost, data from a single geographic area, data estimated the natural changes |
| Sumner et al., 202019 | Gloucestershire, south-west England, UK | Arts on prescription is a type of social prescription that refers patients to participate in courses of art | Attendance at and engagement in the programme; well-being changes for the involved patients | WEMWBS completed by the participants on the first and last session |
Strengths: large data set; longer follow-up Limitations: no control group; lack of diversity in sample in terms of socioeconomic status |
| Before-and-after studies | |||||
| Pescheny et al., 201921 | Luton, UK |
A referral from a GP to a link worker. The link workers do an individual assessment to identify the non-medical needs of service users, motivational interviewing and continuous personalised support, and link service users with non-medical sources of support, to help to improve their health and well-being Link worker approach |
The quantitative study to assess the mental well-being of patients was based on a repeated-measures design | WEMWBS |
Strengths: association between mental health and SP and association by age and sex; data analysis – used skewed normal regression; provides important information and guidance for policy-makers, commissioners and providers planning to implement in the UK and beyond; identifies the research needs Limitations: missing data; high loss to follow-up; a short follow-up period; lack of control group |
| Elston et al., 201922 | South Devon, UK |
The coordinators hold an initial 30- to 40-minute conversation to determine need and decide whether signposting or a more in-depth ‘holistic’ conversation is required Well-being coordinator is holistic Link worker approach |
Health outcome at the point of entry and exit Data on the use of health and social care services Cost |
Well-being Star, PAM, WEMWBS, RCFS |
Strengths: conceptually clearer than previous studies, with a specific focus on referrals; included all the relevant outcomes that are not mentioned elsewhere; had good participation and excellent follow-up rates in relation to outcomes and long-term follow-up of health and social care activity data and costs; allowed some provisional exploration of which patient characteristics on programme entry might be associated with positive outcomes Limitations: lack of a control group – findings could be biased positively; no outcome or attendance data; data-quality issues precluded an analysis of GP contacts data; local costing data were used – did not include the average cost per person of the holistic element of the well-being coordination service because contact time was not recorded, nor were the wider societal benefits of the programme |
| Mixed-method studies | |||||
| Agaku et al., 201527 | OH, USA | Smoking cessation intervention (the 5As) for low-income pregnant and postpartum women | Implementation-related barriers to and facilitators of training needs and staff confidence in delivering the 5As | Semistructured interviews with programme directors and staff members |
Strengths: several opportunities to deliver smoking cessation counselling to pregnant and postpartum smokers; service delivery can be improved using different media (e.g. video, social media) Limitations: implementing the 5As service in all three stages; service delivery; time constraints; varying knowledge of the clinic directors; smoking cessation interventions were not stratified by provider type because of small sample size; attrition of staff; self-reported response to the online survey; no data were collected regarding staff perception of the quality of the training received Future requirements: adherence and enhanced implementation; additional training; resources for diversity of people; regular update of resources; quality improvement; toolkit development; treatment specialist |
| Bird et al., 201926 | South-west England, UK |
Individuals referred to community-based physical activity by a primary health-care professional A signposting approach |
From participants:
|
Follow-up questionnaires, qualitative interviews and programme-related documentation, including programme cost data |
Strength: RE-AIM study approach Limitations: lack of control or comparison group; sample lacks individuals who have not participated in the ‘CLICK into Physical activity’ session; low 6- to 12-month follow-up response rates limits understanding of long-term effects; self-reported data – increased bias; difficult to measure the exact effects on long-term diseases/conditions |
| Bowden et al., 202025 | North-west England, UK |
Participant are recruited through local schools, health-care services and art and community organisations The children met weekly for an hour’s singing, initially at a local high school Signposting approach |
Effect of the programme on the community, children and family: asthma control; impact on family Measurable difference in asthma: compliance; other reported measurable impacts Unintended consequences: positive experience of the programme; perception of game and activity; acceptance of the intervention; importance of family-centred approach; wider impact; community benefit |
Childhood Asthma Control Test Qualitative interviews with participants and their family using both audio- and video-recordings Telephone interviews with other stakeholders Postcards containing qualitative questions from participants and family about their experience of attending BreathStars |
Strengths: pleasant and fulfilling experience for the participants; the positive experience caused wider changes in the context of greater confidence, improved behaviour and raised mood and self-esteem; the establishment of the group in the locality, the informal atmosphere and the family focus; improvement in asthmatic control reported by children, siblings and parents, notably reduction in the need for inhalers, less coughing and less disturbance during the night; pressure on participants; wider community impact Limitations: the area in which the project was located was known to have particular cultural and demographic features which made recruitment and engagement difficult; attrition from intervention group; lack of GP and NHS involvement |
| Maund et al., 201924 | Gloucestershire, UK | Nature-based health interventions: a pilot study of a 6-week intervention, aiming to engage individuals with wetland nature for the treatment of anxiety and/or depression |
|
Questionnaires, focus groups and semistructured interviews |
Limitations: small sample size; participants were relatively homogeneous in sociodemographic characteristics and did not reflect the diversity of the wider population experiencing anxiety and/or depression Pilot study specifically design for NBI project |
| Woodall et al., 201823 | North of England, UK |
The service operates through ‘well-being coordinators’ who offer support to individuals and provide advice on local groups and services in their local community – the activities individuals can be referred to include mental health and counselling advice, physical fitness classes, support for physical or emotional difficulties, finance and debt advice, and creative groups A holistic approach |
Change in well-being, mental and physical health, social isolation and loneliness as well as ability to manage long-term conditions |
|
Mixed-methods study design and no control group Interview bias is mentioned as strength and limitation |
| Qualitative studies | |||||
| Batt-Rawden and Andersen, 202028 | Norway | Singing in a choir | Grounded theory approach: well-being (joy and vitality), life supporting (survival), social connection (belonging and identity) and social inclusion and cohesion | Open-ended focus group interview; the sample was selected purposively |
Strengths: underlying assumptions about health, well-being and singing were the subject of much internal critique and discussion, which contributes to the depth of the study; personal ‘style’, enthusiasm and interest in doing the fieldwork may have influenced the participants in a positive manner; included the researcher’s self-reflection, which contributes to trustworthiness and credibility Limitations: sample was not representative – a self-selected group, not selected by the researcher; there were no negatives to group singing identified here, so more research is warranted to examine this area; the results only represent a snapshot of the participants’ views as they were not followed up over time; only two locations were compared, and they were within the same country – not a generalisable result; only two focus groups were carried out, one by each researcher; the study excluded men |
| Bertotti et al., 201829 | London UK | This is a realist evaluation of SP (for reducing social isolation and improving well-being) in the boroughs of Hackney and City of London, identifying the specific experience of SP by testing the CMO approach |
Overall outcome: beneficial outcome for patients results from the combination of multiple stages working together effectively Measured in three stages: GP referral process; consultation with SPC; interaction with the community |
GP online survey; qualitative interviews of stakeholders, SP co-ordinators and patients; thematic analysis | |
| Payne et al., 202030 | Sheffield, UK |
Clients are referred by local health-care professionals and triaged by telephone or at an initial consultation. Following triage, clients are signposted to relevant community groups or within the organisation to advocacy, health trainers, and social cafés A signposting approach |
The thematic analysis produced five key themes: receiving professional support for social problems; engaging with others through participation in socially prescribed activity; learning different ways to relate to others and developing new skills; changing perceptions by realising personal assets and becoming open to the possibility of new futures; and developing a positive outlook on the present while moving forwards in pursuit of future goals and better health | Semistructured face-to-face interviews |
The study tried to recruit a diverse sample but no participant was aged < 45 years, and the majority of participants were white British despite the wealth of cultural diversity in the local area Strengths: coding process reviewed regularly; the interviews and analysis were conducted alongside integration of themes from published literature Limitations: only two participants were engaged in advocacy work alone, which limited the ability to explore how advocacy relates to some of the broader mechanisms; several participants demonstrated a keen awareness of lack of funding |
| Redmond et al., 201931 | South-west England, UK |
Using a variety of art as a vehicle to support patients referred from a range of primary-care-based health-care professionals Referral criteria included low mood, recent bereavement and being socially isolated An arts on prescription approach |
‘Patient satisfaction form’ – feedback from individual who attended the service-thematic analysis | ||
| Wildman et al., 201933 | Newcastle upon Tyne, north-east England, UK |
W2W: patients with long-term conditions (e.g. COPD, DM 1/2, CHD, asthma), aged 40–74 years and from socioeconomically deprived area are referred to link workers. Link workers are trained in behaviour change methods and help service users identify which areas of their lives they wish to change and how A link worker model following a holistic approach |
Experiences of SP among people with long-term conditions 1–2 years after their initial engagement with a SP service, reduced social isolation and improvements in their condition management and health-related behaviours | Semistructured interview |
Limitations: attrition rate; data from participants who are engaged for a shorter time A ‘methodologically flexible’ approach was used to investigate the impact of SP |
| White et al., 201732 | South-west Scotland, UK |
Link worker made contact with patient to assess and match their health and well-being needs with the available community resources and to subsequently facilitate and ultimately monitor this interaction A single point of contact model |
|
One-to-one structured interview | Limitations: limitation in transferability of the findings; relied on self-report and study participants |
| Reviews | |||||
| Husk et al., 202038 | NA | Studies focusing on the transfer between primary care and community-based activities | Enrolment, engagement and adherence | Included both empirical and non-empirical, quantitative and qualitative studies |
Strengths: realist approach to the surface mechanism (the process of SP); breadth of the evidence included Limitations: time and resource constraints meant that it was not possible to consider all the statements in detail; findings also limited by the majority of the studies relating to exercise prescriptions, particularly those identified through database searches, with pockets of evidence relating to specific activity type |
| Mossabir et al., 201541 | NA | A social intervention was defined as an intervention that aims to improve health and/or well-being by facilitating contact with other people, groups and community organisations; the review focused on the linking mechanisms of social interventions | Reasons for referral; types of referral methods; health outcome – reduction in mental health problems; social outcome –reduction in social isolation; barriers to implementation; cost-effectiveness |
Strengths: use of the scoping review methodology, enabling a review of a wide range of both peer-reviewed and grey literature Limitations: heterogeneity of interventions and populations in the literature; very few peer-reviewed papers; included articles did not differentiate between the impacts of different types of community-based resources that participants were referred to |
|
| Pilkington et al., 201740 | UK and Ireland | The interventions and services identified included structured group educational programmes, exercise referral schemes and individualised advice and support, with signposting of health-related activities in the community | Range of intervention; evidence | Limitations: referral criteria; exclusion of studies that do not use SP as key work; limited to UK and Ireland; online information only; no contact with service providers | |
| Jensen et al., 201739 | Sweden, Norway, Denmark and the UK | Art on prescription; art and culture for rehabilitation | Based on data availability: follow-up anxiety, stress, depression level, mental health, etc. | Rapid review including peer reviewed and grey literature in English and Scandinavian languages | |
| Leavell et al., 201942 | NA | Nature-based social prescriptions that included a clinical referral to outdoor activity; includes green prescription | The study identified three broad categories – intrapersonal process, interpersonal process and perceived environment – to motivate lasting changes |
Strengths: valuable opportunity to help adults and children find ways to feel more socially connected and be part of their larger community and natural environment; a low-cost, creative intervention to strengthen social networks, reduce stress and facilitate social connectedness among participants and providers without requiring expensive gym memberships or special clothing to access a local park or natural area with friends, family or groups Limitations: more research is needed to understand non-dominant communities’ access to and connection with natural areas, including but not limited to minority and low-income populations and recent immigrants; providers do not have a reliable mechanism for recording patient behaviour (SP software in future may resolve this); need to evaluate the range of interventions across different demographic and social groups to understand the uptake of the intervention by high-risk populations |
|
| Rempel et al., 201743 | NA | Reported the assessment of a referral programme of patients from a health context to a social context. A health context was considered to be any form of health or mental care, for example emergency departments, primary care and mental health-care professionals. A social context was considered to be any form of community programme, including cultural programmes, arts classes and community groups. This excluded programmes evaluating a single programme, for example a diabetes health management course | Aims of social referral; measures of social referral; strengths and weaknesses |
Limitations: UK specific; cannot guarantee that all specific studies have been included Strength: inclusion of both grey and published literature and non-academic reports |
|
| Bickerdike et al., 201737 | Studies conducted in the UK | Included only studies where referral was made from a primary care setting to a coordinator, link worker or facilitator of SP | Health and well-being outcomes; health-care usage outcome; patient experience; cost; experience and lessons learnt |
Strengths: first study to assess effectiveness in UK; relevant setting; literature included from 2000; published and grey literature Limitation: local evaluations not included |
|
| Pescheny et al., 201836 | Studies based in the UK | SP services based in general practice and involving a navigator | Facilitators of and barriers to SP service |
Limitations: potential publication bias Strengths: generalisation of findings; all eligible records were included in the review independently of their appraised methodological quality |
|
| Pescheny et al., 201920 | UK based |
Navigator model In this model, general practice staff refer patients for non-medical needs to a navigator, who assesses the needs and refers or signposts to sources of support in the third sector |
Health and well-being; health-related behaviour; self-concepts and feelings; social interactions; day-to-day functioning | Various quantitative tools and statistical methods were used to assess the various service user outcomes; 14-item WEMWBS |
Strength: comprehensive search strategy Limitations: meta-analysis not done because of diverse study design included; publication bias; generalisation of findings; quality of the included studies; did not consider the differences in the delivery models including the workforce model (i.e. voluntary/paid off) |
| Smith et al., 201934 | No paper is eligible for review | Limitation: paucity of evidence | |||
Appendix 3 Classification of outcomes reported in studies
| Outcome(s) | Code(s) |
|---|---|
| Health related |
|
| Cost and effectiveness | Programme effectiveness (generally from the stakeholder or service provider perspective) |
| Service use/patients declining | Patient engagement; activity group attendance; service uptake; acceptance of the intervention; relationship with service-provider; patient’s experience; health-care usage; compliances |
| Challenges | Strength and weaknesses of services; barriers and facilitators; lessons learnt |
| Health inequality and wider impact | Effect of the programme on the community (e.g. children and family) |
| Qualitative health- and social-related outcomes | ‘Joy and vitality’; ‘survival’; ‘social connection’; ‘belonging and identity’; ‘social inclusion and cohesion’ |
Appendix 4 Extract framework with additional example quotations
| Category | Quotation(s) |
|---|---|
| Patient journey through the service | And we actively encouraged first appointments, and either in the home or in a community setting, unless there are any potential safeguarding issues. And, we, one of the challenges we have within surgeries is lack of space [to] see patients in the surgery. Well, I guess [from the] SP point of view the idea is to take people away from health settings to engage them with a community. But I think the feedback we get loud and clear from our team is that you do get a much better understanding of somebody’s position through a visit. And they are much more willing to reach, and share whatever issues or experiences they happen, because once they get what a link worker’s role is and that it is a non-medical, you know that the strength of the purpose of the link worker is the relationship and the trust you build up with that patient to understand what the issues [are] that they’re going throughStakeholder, 2 years, North EastSo the referral is just a simple task which is just an e-mail, really on the system to the link worker, and that can come from any member of the practice team, it doesn’t have to be [a] GP. It can be the nurse receptionist admin. And interestingly, in the [?] where we’ve been longest established we have the highest number of self-referrals, because patients are more aware of that service or are more inclined to contact the link worker direct, which is exactly what we want, the bypassing [of] the GP . . . The GP can’t help them with their housing or debt or whatever it may be. And so yeah, it’s a very simple straightforward process in terms of the differenceStakeholder, 2 years, North EastA lot of it [the self-referral process] [has] been word of mouth where you know a neighbour or relative has access to the service and recommended it. And we haven’t necessarily had to proactively advertise the service, we’ve never had a shortage of referrals. And because I think if you get a good GP and a good practice, get social prescribing, it’s a win–win. It happens automatically. And it’s just because of the simplicity of the referral process. And we get to steady flowStakeholder, 2 years, North EastAnd also there are drop-in centres or drop-in cafes. So for example in [location]. There are several . . . drop-in cafes. Essentially there are places like a cafe where young people can turn up and meet other young people, but at the same time, they’ve access to a link worker who can support them, and then help them out and perhaps refer them to other support if needed. So that their referral sources can be quite a fewLead, 5 years, LondonDoctors, nurses or anybody can self-refer and [it] comes to her via SystmOne. They fill [in] the referral form and she sends a task. . . . There are self-referrals but [the] person must be a patient of the GP service and the process is, self-refer to the reception and [be] picked up by the link workerLink worker, 4 months, South EastSome schemes also take self-referral[s]. And that can be via telephone, via drop-in, and some schemes have a self-referral button on the website as wellStakeholder, 10 months, North West |
| Costs of recruiting social prescribers and of implementing service | . . . there’s a lot of additional on-costs, not quite as straightforward. And we know that the Primary Care Network funding is quite restricted in terms of what that cost can be used for. But there are additional on-costs, which means that we’ve had to find commissioned and funding from other [sources]Stakeholder, 7 years, West MidlandsOne issue that came up for our service was the fact that [it] only covered salary costs. There was no overhead, there’s no admin costs. And that has been an issue for us because we don’t have office space, we don’t have administrative support. So, yeah, I think that was an issue for the GP, they were a bit surprised that NHS England was only providing them with a salary and no overheadsLink worker, 1.5 years, South EastAnd we know this through our regional work that there are link workers [at] the moment who don’t have access to a laptop, who don’t have a phone. We’re obviously expected to be in the surgery using equipment there. And because the surgeries aren’t doing that stuff at the moment, they’ve not been able to function as well during COVID . . . So I think the only way we were able to make this work was that the NHSE told us back in May last year that we could use money that wasn’t reimbursed to the PCN and it became discretionary money for the CCG. We could then thereby use it as these fees, which we’ve done. And as a result, we’ve now got 13 link workers out of 16 within the voluntary sector. And three directly employed by [the] PCN who aren’t part of a strategic approachLead, ≥ 6 years, East of EnglandAnd we felt really strongly that actually if you were going to refer on to a voluntary community sector organisation, then you had to help support that voluntary community sector organisation with its costs. I think there was some movement before COVID-19 on agreement that management costs to some of that was starting to get covered. There still was no resolution on how they would support the voluntary community sector . . . [The] Rotherham scheme that we ran for the long-term conditions . . . the cost was 560, about 550k a year. Roughly 60% of that went out to the voluntary community sector in contracts, roughly two-thirds went out to support each subcontracted . . . The other third covered things like employment evaluation trading, that sort of stuffStakeholder, 9 years, Yorkshire and The Humber. . . but as a small charitable organisation we’ve had very little resource made available to see for example my cost and the operational lead, which for me now are crucial now that the team’s expanded to have that infrastructure that support link worker. . . . I think that would be, the time and effort to recruit and induct and get somebody embedded in the surgery is quite intense for a small charityStakeholder, 2 years, North EastThere are different financial models in the history up until now with very different evidence of its impact in terms of the value to the third sectorLead, 14 years, South West. . . part of what we were looking to do, pre COVID again, was to have a sort of a volunteer call within the service, more to do the sort of referral and the admin, but obviously that would have come under its own confidentiality agreements and DBS [Disclosure and Barring Service] checks and all that sort of thing for anybody coming into the practice, but we were looking at a volunteer role within the practice as well as the paid roleLink worker, 2 years, East of EnglandWe have a complicated financial modelStakeholder, 5 years, North East |
| Data collection methods for an individual’s outcomes during the journey | In terms of outcomes, we use a range of . . . off-the-shelf standard outcomes across [location]. There isn’t at the moment one consistent one. But that’s something we’re hoping to develop. And so each locality, scheme, uses their own that they’ve developed themselves as a bespoke measure, or one of the kind of nationally recognised off-the-shelf onesLead, 2 years, North WestSo we will ask five questions based on those sorts of assessments at the beginning. And then we would ask them again at the end of the process, when possible, but as I said it’s not always possible to follow people up. I would also add, and this may be outside the remit of what you’re trying to capture, but, well-being evaluations, my experience of doing [them], they’re clunky and never seem to be relevant to the conversation you’re having with somebody. So I find them unsatisfactoryLink worker, 1.5 years, South EastWe use our own tool that we developed. And that works very well for us. Actually, and we’ve showed it to a number of other link workers as well across the region who also really like it. And my manager has been on PAM training, because I know that there is a lot of talk at the moment about link workers using PAM. We found it very clinically related, which didn’t really fit very well with a lot of the work that we were doing. It’s very much focused around long-term conditions. Now, not all of their patients have got long-term conditions, and neither are we qualified to advise on those or, you know, network, even though we appreciate the work that we do around the wider determinants of health will have an impact on those long-term conditions. So, we have not adopted PAM, although it may be [adopted] next year. It does look as though we’re going down a mandated route, which I am reluctant about. . . . It’s a tool called SIGNAL or CLEAR SIGNAL [Transit Enterprise, Gateshead, UK], which is a web-based tool that looks at sort of various measures around housing, poverty, income and so on, which I thought was really helpful. And probably much more in line with the kind of conversations that link workers are having with people than PAMStakeholder, 10 years, North EastWe haven’t pulled any of that information off as yet, as I say, because that wasn’t a focus of the model, it was the social isolation and the inactivity . . . but we do have access to all that data on SystmOne, so it’s something we can do at any point if we wanted toLink worker, 2 years, East of EnglandWe don’t routinely collect things like social care use, that isn’t one of our standard parameters that we would collect in the beginning, but if obviously an individual shares that during the course of the conversation that they have a social worker, or that they are in sort of a certain service, we’d obviously make that noted. I mean, obviously if the referral comes through from a social worker then it’s fairly obvious that they . . . don’t have a social worker, but we don’t routinely collect clinical informationLead, 2 years, North WestOne GP has started to capture [data with a] satisfaction survey and patient’s satisfaction survey. But we haven’t done it regularly as we have the [university] researchers doing a lot of patient interviews . . . This is in high demand. Therefore, we want to respect that and do much by ourselves . . . We have done a patient satisfaction survey; we’ve mailed out hundreds of surveys and got back [can’t remember the exact number] 2 years ago, but we do have some informationStakeholder, 5 years, North EastYeah, I think pre referral. It’s just the appointment usage, and the contact with the surgery we’ve been concentrating on because a lot of the work initially was to see if we could take some of the work off the GP or affect that at all. And so we tend to capture the contact with the surgery sort of 12 weeks prior to our intervention, and then 12 weeks post intervention, to see if there is a difference. And some of the data we’ve managed to capture has shown that we can see up to a 20% decrease in GP attendanceLink worker, 2 years, East of England |
| Data link workers have about available services | . . . within our service we maintain a database, which is supported by a wide range of volunteers who contact groups and organisations to check the information that we’ve got is up to date and relevant. And the information that we collect is . . . so that we can search based on when somebody is available, the price of activity, location of activity, day of the week [of] activity, that kind of thing. So we collect information around making sure what the name of the group is, the provider, and a description of the activity, contact details, location, how much it costs and communication information. And they put relevant policies and procedures in place. If there’s a waiting list, capacity, [a] particular age limit, and when the activity [has] any access issues to note, or availability of access requirements . . . we make a note . . .Stakeholder, 7 years, West MidlandsThere are people talking about creating other, very clever IT platforms that will draw their data from any number of directories into a single search function. If all the different directories use common data standards, as one way of trying to overcome this problem. But it’s a problem that I have been hearing about for well over a decade. And it’s, it’s also very difficult. Organisations that provide services often don’t update their entries about services so that the information goes out of dateLead, 20 years, London |
| How data from different types of SP or community groups are captured | Yeah, I mean obviously we go out to collect the data about onward referrals, so we’ve got all of that. And, but it’s not necessarily all that useful, because everybody’s different, they want different things clearly, things like [Citizens Advice] for money advice is actually up there, there is art carer support. Age UK [London, UK] for older people. But there are not a lot of people who don’t want to go through each day, but they want something different, etc. But we do have that data and obviously that’s useful in terms of commissioning and will become more useful as . . . we get more of that data, and we’re hoping to get a decent system, at some point, which is specifically for social prescribing, but we haven’t got oneLead, ≥ 6 years, East of EnglandI think generally the community group element is not well recorded. I think after they get referred on to a community group, that’s when the data goes a bit skew-whiff and we’re hoping . . . Elemental [will] help [with] that because that allows community groups to record data on it, but currently that’s not captured. So, the data, the well-being outcomes, and where they go on to, which I do, by the way, and then recorded with the scheme on whatever their, their system is basically. But we need to get better at recording what happens after people get linked into community groupsStakeholder, 10 months, North West |
| Length and nature of the follow-up | . . . it is something for them to think about from service to service, depending on what is commissioned, and there is [an] in-built 6-weeks review regardless of the trigger episodes, something that changes the pathway or journey, [a] life event or whatever that might be, and that for me automatically trigger some sort of review . . . depend[ing] on the tracking system . . .Stakeholder, 3 years, NationalTime points vary generally again, but more often than not you would have the baseline and 3-months then 6-months stage, and then depending on the intervention or the service it may go on longer, depending on how people, what their needs are, and so onLead, 2 years, North WestVaries [by] strength of local social prescribing and also sort of difficulties with it . . . just a variety. I can see that it would be really nice for the simple system, but it’s not, and it’s all developed locally and it’s all slightly different locally, so it’s a bit like herding cats, trying to get all the different schemes togetherStakeholder, 9 years, Yorkshire and The HumberIn our system, Elemental – we’re just about to launch, in fact. Our first locality is going live in about a month or so. . . . We’ll be able to have that push back that will allow a limited amount of data to come back in to the GP system, so that the next time they’re sitting down with that individual in front of them, they’ll be able to see, oh! . . . [they] went to this gardening club. I see that you attended. And the GP will be able to talk that through with the individual. That’s still in its early stages, because what we do need to do is to work out what exactly we’re going to refer. That’s the anticipation, we’ll be able to have that push backLead, 2 years, North West |
| Non-attendance data | I don’t think we’ve got particularly good information about that, and that’s for a couple of reasons. So, first of all, we don’t have a lot of non-attendance because we visit people at home, so that would be refusing to open the door, and on the whole our link workers will come back another day and check. Because obviously, [it] can be quite concerning if people won’t respond having said they would. There is a certain amount of having to reorganise because people have changed their mind, or can’t do it on that particular day, something happens, but we tend to persevere because we know that some of the people who need the help most are the ones most likely to kind of get cold feet and cancel. In terms of once they start attending groups and stuff really, that comes back to what I was saying about policy from the bat. So if it’s a carer, and they joined a carers’ group, and we’re assuming that the carers’ group will keep an eye on them and check what happens to them, if they stopped turning up and stuff, so we wouldn’t normally be collecting the data on that, I don’t thinkLead, ≥ 6 years, East of EnglandAnd then after the case is live with a link worker, and all schemes will have a case management system or a way of recording cases and planned appointments, ‘failed to attend’ will be recorded. Usually after a number of ‘failed to attend’ the case is closed. And then that’ll be reported back to the referrer. But [if] it was closed because [they were] no longer in contact or were out of contact, and if it’s suspicious, I worry and then usually that’s flagged as some kind of safeguard onto the referrer as wellStakeholder, 10 months, North WestEverything goes to EMIS, if they do not attend it goes to EMIS as ‘did not attend’. If someone attended but [they] do not engage, then it will be coded as ‘SP declined’Link worker, 4 months, North East |
| Potential strength (or benefit) of the current service | I think [this] is threefold. So, the opportunities to develop people and help them to grow and meet their own goals and improve their health and well-being, which in turn can start to improve the health outcomes and reduce health inequalities. So, people, that’s the strength, social prescribing. And it truly speaks to what that person sees is important, not what anyone else sees is important, like BMI, smoking. It is important, but social prescribing is very much about what that person sees. Going back to some of the theory around Maslow’s hierarchy of needs and recognising that if people have got problems with money and housing and family, they’re not going to be in a position to start to address[ing] unhealthy behaviours such as weight, diet, exercise . . . Really recognising that everybody’s at a different place and working with people where they are, to move forward on what their goals are, and giving people the power and choice over thatStakeholder, 10 months, North West |
| Potential limitations of current service/major challenges in developing and implementing link workers | I think a lot of people don’t know what SP is. People in the system understand what it is but for common people, nine out of 10 don’t know and thinks it is a type of medication. When they are into the service they feel relaxed and liked itLink worker, < 1 year, South WestI think in terms of challenges, there’s a lot to be honest. The way we’ve got such variety of models is good . . . we still don’t know what are the key elements that are really strong in SP models. What are the things that we need to replicate and not only what but how? So what are the key elements of that? So we’ve got various models from voluntary-sector-led models, primary-care-led models, different models that focus heavily on health outcomes, we’ve got ones that don’t. We’ve got factors like self-referral that some schemes are really passionate about, some schemes don’t recognise that as kind of an important element of social prescribingStakeholder, 10 months, North West. . . there’s a mismatch between what clients want and what NHS England thinks they should have. So, it’s all about what matters to me. When I look at NHS England literature it strikes me that what matters to you, it’s fine as long as what matters to you is eating less, exercising more, being less diabetic and being less fat. If those are not your priorities, you know, then I’m not quite sure how the NHS England model is going to workLink worker, 1.5 years, South EastI think in some areas, a challenge is actually knowing what’s out there. Sometimes we spoke about directories a little bit. But I think that, it’s not just knowing where somebody can be referred to, but what the availability of that is, and making sure that there’s a good availability across an area, so maybe some, more asset mapping might be useful to, to help that side of things. And we’ve spoken about the digital, I think that has been a challenge. Some areas haven’t collected the information in a way that’s easy to access activity and look at outcomes. I think we’re on a journey with that one, I think that one’s getting better. But it’s still, not quite there with it. But I think that that is definitely improvingLead, 2 years, North WestSo the biggest problems are VCS [Voluntary and Community Sector] are underfunded . . . And, therefore, the language I use is we’re getting more and more travel agents, but we’re not getting any more holidays, and that is starting to become an issueLead, ≥ 6 years, East of England |
| Major enablers of developing and implementing link workers | One other challenge I would say is probably clinicians’ own education. We need to really change, you know, clinicians who go through medical school for, Lord knows, a decade, are taught a very . . . medical understanding of health. And if we want clinicians to really fully understand social prescribing, we need to change what they’re taught in medical schools. We need to get them to be taught what some of us call a social model of health. And this is very difficult if you spend a decade training somebody to understand, health, or something very biomedical, then expect them to unlearn a large portion of what they’ve spent 10 years learning . . . We would do better to start off with the teaching of a social model of health in medical school, but that is a challenge for social prescribingLead, 20 years, LondonBut I think eventually BBB [Bromley By Bow Centre (London, UK)] helps to deliver one of the only accredited training programmes for link workers, which is a level 3 qualification. I think we need to massively scale up the delivery of training for link workers. I think it’s also important because they need to be safe. They need to know how to do their job well. They will be dealing with particularly vulnerable people. They will undoubtedly come across significant safeguarding issues, but the people they work with, they need to know exactly what to do in those situations. And I think that, you know, training is really important for them [link workers]. I think also it’s important in terms of their own professional esteem. They are part of a system, full of very highly qualified people, doctors and nurses and health-care systems. And I think it’s helpful if social prescribing eventually has a widespread workforce with . . . qualifications, because then that will gain more recognition from the other colleagues within the health system as well. Having said that, I wouldn’t want it to be a requirement that all link workers had to have a qualification. I think there are some people who work in our communities who would make [an] absolutely brilliant link worker who may struggle to do a qualification for whatever reason. So I don’t think it has to be a requirement, but I do think we do need to move towards having a more qualified workforce amongst the workersLead, 20 years, London |
| Potential challenges of evaluating SP | . . . it’s measuring the softer things, like just feeling a greater sense of belonging, so . . . how do you effectively measure that? I think that’s going to be one of the key challenges because it’s so subjective. If you do an outcome measurement with somebody, they might have [had] bad news, you might be feeling well that day, that measurement is that point in time, it doesn’t measure how that person feels, in general, and they may have improved things, but they still feel bad, or feel bad at that point in time. I think it’s really hard to measure that holistic pictureStakeholder, 10 months, North WestWhat we found in [location] the evaluation that [university] did . . . it did impact on service reduction, it did reduce any attendances, it did reduce hospital admissions, and it did reduce GP appointments, Whether it could be completely categorically down to social prescribing intervention, it’s hard to tellStakeholder, 9 years, Yorkshire and The Humber |
| Suggestions on how to address some of the challenges in evaluating SP | Make sure kick-off data is sufficiently good and well collected. What link workers are telling us is that they are collecting data and what they see in a report at a CCG [is] completely different [from] what they thought they told them in the first place. There is a big underestimation of people getting interventionLead, 14 years, South WestI suppose also what you want to capture is not just the numbers. This is one of my big soapbox . . . so I was trying not to go on a rant about it, but qualitative information in these surveys is really key. Not just constitute information, because I can see if you want me to see 350 patients a week and give them all the leaflet and say that I’ve done social prescribing, then of course that looks great, doesn’t it? From a quantitative point of view I’ve got 350-people throughput a week. When it’s actually achieving very little. Those people will still be coming back to the gym, again and again and again, and the problems are not getting sorted out. So this is about quality of service as well, the quality of time and investment. And I feel strongly that [we] need to capture, you know, the quality of the work, not just the quantity of the work, because there’s a tendency to love numbers [more] than [the] alphabetStakeholder, 10 years, North East |
Appendix 5 Interview participants’ views on evaluating social prescribing
The quotations below detail some of the participants’ views on evaluating SP. The first addresses the issue of outcome measurement:
[The] first challenge is everybody measuring different things, it is a struggle. [The] NHS model is looking at PAM or ONS around well-being. . . . [The] underlying root of [the] problem is how do you measure something that is different for each person? We are delivering [an] individualised and personalised service and so [it’s] tricky to measure the individualised outcome which is more qualitative. How do you measure something that is quite nebulous and qualitative? And it is really important.
Stakeholder, 5 years, North East
Another participant described a need to capture the impact of SP on a community as a whole rather than on individuals, suggesting as follows:
We need to be measuring things like number of community groups, attendance at community groups, resilience of community groups, size of voluntary actions. We kind of have only a record in social prescribing within the realm of the impact on an individual rather than a community as a whole. You put it out. I don’t know how you measure that.
Stakeholder, 10 months, North West
Another participant suggested measuring socioeconomic outcomes such as how many people got back to work or how many are no longer in debt:
What we know isn’t happening is [to] measure how many people got back into work, how many people have got their benefits sorted out, that’s all happening. And, again, that data will be collected by the people who have had the baton passed on to them.
Lead, ≥ 6 years, East of England
Regarding outcome measures, one participant suggested that SP might cause an increase in GP usage and that this should be captured positively in an assessment:
Individuals may for a time see their GP more once social issues are under control, because they’ll be able to start talking about how to manage their physical health, mental health, because they actually decided they do want to try and manage their diabetes rather than just ignoring it. And so that’s a positive, but it might look like a negative, which is why you’ve got a look at all this data in the round as well.
Lead, ≥ 6 years, East of England
One participant thought that an individual’s experience of SP depends a lot on relationships with link workers and, therefore, questioned the system-level assessment of the scheme:
. . . people tend to look at the world in terms of systems. And that’s not actually how the world works. We have some link workers [who] are absolutely amazing. And everybody thinks they may have some others who aren’t quite so amazing . . . It’s nothing to do with the link worker role itself, it’s to do with how it’s done by that particular person. A lot of this is about making sure that the right skills are in the right place at the right time.
Lead, ≥ 6 years, East of England
Participants also highlighted the difficulty of determining cause and effect in SP when considering individuals. For example, one participant commented as follows:
People talk about reduction in hospital visits, reduction in GP appointments. But I think it’s really hard to determine cause and effect – if somebody sees their GP a lot and then suddenly doesn’t start to see [them] . . . how do you attribute that to social prescribing, how [do] you actually demonstrate that in quantifiable terms?
Lead, 2 years, North West
Other areas suggested by participants that might be assessed included how many people are engaging with SP and how much GP time is saved by SP. Suggestions were varied and mixed, and provided a starting point in helping to understand how SP could be evaluated.
Summary of key challenges in social prescribing research
We identified the following challenges that need to be considered in future research studies.
-
The complexity of SP as an intervention:
-
It may not be possible to consider SP as a single intervention.
-
SP is an open-ended service; there may be difficulty in determining cut-off points.
-
There is variation in link workers’ backgrounds and training, which may affect services delivered.
-
Approaches to the link worker role vary; link workers may act as a signposter or as a health coach. Most link workers refer patients on to onward referral services.
-
The onward referral services vary enormously, from very small community knitting groups that may be financially precarious to large, sophisticated regional or national VCSE organisations.
-
-
Heterogeneous service delivery:
-
There is substantial variation in SP within regions and across the country.
-
There appears to be a high turnover of link workers.
-
Some organisations have been delivering SP before adaptation by the NHS, which is perceived as destabilising the previous delivery systems.
-
Link workers have to be able to find onward referral services to which to refer the patients and to be conscious of the quality of those services.
-
Communication between agencies can be poor (e.g. between the VCSE and PCN).
-
Problems in data capture.
-
Link workers may not be able to administer (or administer consistently) outcome measures deemed suitable by researchers.
-
Outcome measures are not measured routinely in practice and, where they are, they are not necessarily measured systematically.
-
Some outcome measurement may not be possible given a lack of communication or harmonisation of data collection systems.
-
Reporting mechanisms, and additional contracts and funding, would be needed to support the additional workload of obtaining reliable process and outcome data from the voluntary sector.
-
-
In addition to problems of harmonisation of data collection and communication between organisations, the underlying rationale for such collection needs to be accepted by each of the organisations (particularly by the VCSE) involved.
-
Resources and access:
-
The training programmes provided to link workers varied.
-
Some institutions (such as the University of East London) have been commissioned to design and deliver training courses. This includes a ‘detailed version’ for link workers who will be working as a health coach, and a lighter version for those who act mainly as signposters. This may facilitate the standardisation/formalisation of link worker training programmes.
-
Information available to the link workers varies. For example, some link workers have access to GP EHRs whereas others do not.
-
PCNs may target specific patient groups. This could create issues for national evaluation.
-
There is no consistent funding set aside for the VCSE organisations that deliver the service, and their financial status can be precarious.
Appendix 6 Social prescribing evaluation workshop
Social prescribing evaluation workshop (30 June 2020)
The first network meeting, which took place on 30 June 2020, involved 17 people, including people with lived experience of SP services, people working in SP, researchers, regional leads and the national team. The objectives of the workshop were to contribute to the specification and the focus of the evaluation. The workshop attendees were grouped into two: nine experts focused on process evaluation and eight experts focused on impact evaluation. The key suggestions from the discussions are summarised in this appendix.
Focus for the evaluation
Generally, the attendees suggested that the process evaluation should focus on how SP link workers have been embedded in PCNs and their multidisciplinary teams (MDTs). Another important focus they identified is whether or not the embedding of link workers in primary care is sustainable and has had a transformational effect on the local systems, particularly in areas that are just starting up. They noted that a process evaluation would be invaluable in showing how well NHSE’s investment had been taken up and could be used to continually develop the policy in real time.
Below are the questions raised during the discussion:
-
Are the practitioners (and/or patients) doing what they are supposed to be doing?
-
What happens to the users when they access activities?
-
How frequently do users access what activities and does it work?
-
How can we optimise the presentation of referral to a SP link worker to a patient to ensure that the referral is accepted by the patient?
-
Do patients know what being referred to a link worker means?
-
How do we retain link workers, what support are they being offered and do they feel part of a MDT?
-
What helps people take up a referral?
-
What are the factors that may encourage people to stay as a link worker?
-
What is the effect of SP on primary care?
-
What is not working, where is it not working and why?
-
Which sites are not engaging in research?
-
How will this process be rolled out to communities that do not have many assets such as outdoor areas?
-
Has SP had an impact on reducing inequalities?
-
How will link workers make SP effective in areas that have a high level of inequalities?
-
Has community infrastructure changed since COVID-19?
-
What are the gaps within communities?
-
Has cultural change been brought to the NHS in delivery of services, in terms of coproduction in partnership with local communities and people?
Potential impact of COVID-19 on the focus of evaluation
With the prevailing COVID-19 pandemic, the group agreed that there is a need to evaluate how link workers have responded to the pandemic, particularly whether or not their role has supported VCSEs to link with primary care better during this time. It was also highlighted that link workers are uniquely placed to reassure those referred that services across the health and care system are still accessible and that this should be considered in an evaluation. It is important to capture the hard work that SP link workers have put in during the COVID-19 period and showcase the impact of their role. A real-time assessment of how SP contributes to the response to COVID-19 (over the next 18 months to 2 years) would be useful.
Accounting for health inequalities
There was also a discussion on how an evaluation should take account of the experiences of ethnic minority groups and other people affected by health inequalities. The group noted that link workers were well placed to work with those with the greatest health inequalities, especially ethnic minority groups. The work of the link worker enables them to work across the breadth of health inequalities and local context should be taken into account (for example urban vs. rural context). There was agreement in the group that there was a need to evaluate whether or not SP is reaching the populations that are known to have health inequalities, if link workers were supporting the right people at the right time and if different approaches are needed for different people. There is a need to consider how SP will be effectively implemented in areas with poorer infrastructure (e.g. no green spaces and community assets). There was also concern that inequalities will become considerably worse as a result of the current national situation (e.g. high levels of unemployment and debt and poor housing and security).
Potential approach to impact evaluation
The group suggested that evaluation should be based on a logic model that clarifies the outcomes that SP is expected to achieve and what to measure. This can also help to understand unintended consequences, for example where initiatives lead to increased secondary care use because they uncover unmet need. It is important to have clearly defined target groups based on referral criteria.
Potential challenges to evaluation and possible solutions
The diverse nature of SP schemes makes evaluation of impact very challenging. The group also highlighted that it will not be possible to evaluate SP in a randomised trial. The outcome measures suitable for research may be of limited value for practitioners. There is a lack of follow-up data on what happens to people after a referral; for example, do they actually take up community-based activities?
Considering the challenges to evaluation, the group suggested that a well-designed process evaluation (rather than an impact evaluation) might be a better way to understand how SP is functioning. This can make use of routinely collected data (such as GP visits, use of medication and what activities and support options people take up through SP) and help us to understand how SP is working. Primary care indicators will be more measurable and realistic to collect compared with the impact on patients’ health and well-being. This includes GP appointments, number of prescriptions, number of visits and number of visits with link workers.
Outcome measures should be extended to cover issues specific to the intended outcomes of SP, such as improvement in confidence, ability to manage one’s health, feeling connected and not feeling isolated. This could be done by creating a bespoke tool. Provision of an interface that links to SP and voluntary sectors will be useful to facilitate data sharing, particularly for feeding data back from the voluntary sector. Having an information management system is also useful in improving the quality and consistency of routine data.
Finally, though it may not be possible to carry out an impact study nationally, there is a possibility of assessing impact on defined client groups in places where service can be structured to have fewer variables.
Social prescribing evaluation workshop (16 September 2020)
This workshop was to obtain feedback on the findings of the interviews. The main issues from our findings were discussed, that is, variation in services and challenges related to outcome measures. Overall, the feedback was consistent with that from the interviews. There were suggestions for standardised outcomes but also acknowledgement that standardised outcomes will also require standardised referrals. Inherent variations in outcomes by location should also be considered when trying to standardise outcome measures between PCNs. For example, one participant commented that, for ONS4 and WEMWBS, pre and post outcomes vary according to where people reside (e.g. it was mentioned that the baseline for SWEMWBS for people in a city is as much as 5 points lower than for people in a rural community). Clearly adjusted outcomes would need to be considered. Because SP is a personalised care programme, a personalised measurement such as MYCaW was suggested. Attendees also mentioned the lack of relevant SNOMED codes for outcomes and suggested ensuring that there are relevant SNOMED codes for recording outcomes once those outcomes are agreed. Attendees also mentioned the importance of capturing routine qualitative data.
List of abbreviations
- app
- application
- BMI
- body mass index
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- cRCT
- cluster randomised controlled trial
- CUA
- cost–utility analysis
- DHSC
- Department of Health and Social Care
- EHR
- electronic health record
- EQ-5D
- EuroQol-5 dimensions
- EQ-5D-5L
- EuroQol-5 dimensions, five-level version
- GP
- general practitioner
- HAY
- How Are You?
- HbA1c
- glycated haemoglobin
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- MDT
- multidisciplinary team
- MYCaW
- Measure Yourself Concerns and Wellbeing
- NBI
- nature-based intervention
- NHSE
- NHS England
- NIHR
- National Institute for Health and Care Research
- ONS4
- Office for National Statistics four
- OR
- odds ratio
- PAM
- Patient Activation Measure
- PCN
- Primary Care Network
- PHE
- Public Health England
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta-Analyses
- QALY
- quality-adjusted life-year
- RCFS
- Rockwood Clinical Frailty Scale
- RCT
- randomised controlled trial
- ReQoL
- Recovering Quality of Life
- SNOMED
- Systemized Nomenclature of Medicine
- SP
- social prescribing
- SWEMWBS
- Short Warwick–Edinburgh Mental Well-being Scale
- TWiCs
- trials within cohorts
- VCSE
- voluntary community and social enterprise
- W2W
- Ways to Wellness
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale
