Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR129483. The contractual start date was in March 2021. The draft manuscript began editorial review in February 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Johnson et al. This work was produced by Johnson et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Johnson et al.
Chapter 1 Background
About this report
This report presents the results from research investigating the potential for adopting a command centre (CC) approach and related technology for hospitals in the UK NHS. We adopted a mixed-methods approach drawing on patient perspectives, relevant literature, qualitative research at a study and a control site and quantitative analysis of data drawn from the two sites. This chapter summarises the background and context to situate the research and its aims. Chapter 2 presents the overall methodology, including details of the methodology adopted for each sub-project. The results of our research are presented in Chapters 3–6. Chapter 3 summarises results from our patient and public engagement, Chapter 4 presents a detailed discussion of the literature on command and control approaches from our cross-industry review. Chapter 5 presents a case description of the CC implemented at the study site and comparisons with the control site. Chapter 6 presents the results of our data analysis from the two sites. We discuss the results from the different research methods and draw conclusions in Chapter 7.
The methods that we have adopted in this research may be useful to other researchers interested in evaluating CC approaches in hospitals in the UK NHS and more broadly and may be of general interest to researchers using mixed methods to evaluate complex sociotechnical implementations of digital health. Our results should be of interest to policy-makers and healthcare managers and practitioners keen to understand how technology can enable transformation in the management of complex healthcare service delivery.
Policy context
The introduction of electronic health record (EHR) has improved the patient care delivery process and quality of care, mainly through the easy access to comprehensive and rich patient data as well as minimising errors. 1 However, co-ordination of activities and sharing of real-time data from each department within hospitals are largely missing. 2 In fact, in most UK NHS hospitals, health service delivery is fragmented across multiple departments and services, with major implications for patient safety, efficiency and good patient care. Better use of digital technologies is a key feature of the NHS Long-Term Plan (2019), which sets out the basis in which ‘digitally enabled care will go mainstream across the NHS’ (chapter 9, page 91 onwards) and includes an emphasis on improving clinical efficiency and safety.
The 2019 plan set out a milestone that ‘By 2024, secondary care providers in England, including acute, community and mental healthcare settings, will be fully digitised, including clinical and operational processes across all settings, locations and departments’. While funds, leadership and national infrastructure have been provided to help achieve this, individual acute hospitals and their associated NHS trust organisations have been left to navigate their own path through the landscape of competing vendors, technologies, legacies and integration challenges. The result is that many acute hospitals continue to operate fragmented digital and semi-digital services even within different parts of the same hospital.
The fragmentation of the healthcare services is neither cost-effective nor safe for the delivery of patient care. 3,4 Such fragmentation can, however, be minimised by using health information management systems that consolidate data from disparate systems and disparate organisations. 5,6 One such technology that has attracted recent interest is the concept of a ‘command centre’ where data flow from various departments and services within a hospital are consolidated on centrally located digital displays in a room that is staffed with decision-makers able to co-ordinate the effective day-to-day operation of the hospital.
Hospitals in Canada, China, the UK, the USA and Saudi Arabia have reported implementing the command-centre approach using technology from a number of vendors in the last 6 years, but, to date, there has been limited empirical evidence to understand their impact and evaluate claims of success. The coronavirus-19 (COVID-19) pandemic has increased pressure on NHS hospitals to consider how best they can use digital technologies to provide faster, safer care with limited resources. It is becoming increasingly important to understand whether the CC approach should be adopted much more widely. Our research develops a detailed understanding of CC approaches to assist policy-makers in this vital area.
The concept of a ‘command centre’
Although the core transferable concepts of ‘command centres’, as they originate in non-healthcare domains, are the subject of a cross-industry review included in Chapter 4 of this report, it is useful to provide some background and context for the concept at this stage prior to describing the specific implementation of the CC at Bradford that forms the subject of our evaluation.
The modern concept of a CC was pioneered by the National Aeronautics and Space Administration for the purpose of managing space flights six decades ago. 7 The iconic image is of ranks of technical staff each managing vital components of the space flight mission organised in a sloping amphitheatre and facing a wall of visual images including live video of the space flight and real-time streaming data. Earlier forms of CC can be found throughout military history where generals in a central (safe) location typically gathered around a map of the campaign that was updated with information about the disposition of troops as it became available. The rationale for the approach is that locating the decision-makers in a central place enables them to all be updated with the same information at the same time and to work together as a team to co-ordinate the command and control (C2) of the various resources they are responsible for.
In the information-system literature, Holwell and Checkland8 provide a detailed analysis of the ingredients necessary for CCs in their chapter on ‘An Information System Won the War’ through a case study on the British Royal Air Force national network of CCs used to good effect during the Second World War. 8 With digital technology, information can be gathered, integrated, analysed and acted on at increasingly close to real-time speed and with fewer human actors needed. There is also the intriguing possibility that artificial intelligence (AI) can be used to make decisions faster and more efficiently than human actors, paralleled with concerns that such automation creates new moral, ethical and safety concerns.
Command centres can take many other names, including ‘command systems’, ‘control rooms’, ‘mission controls’, ‘security control’, ‘operation centres’, ‘command control’, ‘mission command’ and ‘dashboard monitoring’. However, in general, CCs can be defined as places (or departments) where information is centralised to improve communication and situational awareness within an organisation. 9,10 More generally the concept of ‘command and control’ is used to describe an approach to managing organisations and complexity drawn from military approaches to management. 11 The modern study of C2 is multidisciplinary, multidomain and has given rise to an extensive volume of scholarly literature encompassing conceptual commentary, case studies and empirical research. In our research, we define a Command Centre (capitalised) as a physical room or location that plays a central role in a C2 approach to organisational management but recognising that other interpretations and definitions exist. We describe a CC approach (not capitalised) as an organisational approach to management that includes a physical CC as its central feature. Our cross-industry review of C2 detailed in Chapter 4 provides a structured review of the relevant literature and subject-matter expertise in this area, including discussion of conceptual definitions, with a focus on translation for health care.
Different versions of the CC approach have been widely adopted in retail industries, finance and banking, automotive, manufacturing and transport industries. Health care has been a slow adopter of the CC approach with the notable exception of ambulance services. Even in the ambulance service where the real time co-ordination of ambulances is a matter of life and death there have been notable failures in the implementation of CC technology – a new CC system for the London Ambulance Service in 1992 resulted in days of chaos until the new system was decommissioned and the project has become a textbook case of information-system implementation failure. 12
There is a paradox here: digital technologies now enable information to be communicated instantaneously and everywhere yet the centralisation of decision-makers within a physical space may still be an essential ingredient in the shared experience of this information and mediate how it is interpreted, acted on and used to augment collective human and organisational intelligence. The concept of a CC would still appear to be relevant to many organisations despite digital technologies and, indeed, may be more relevant than ever with increasing amounts of big data and the data science and artificial intelligence tools to automate alerts and distil and represent patterns that emerge from complex data. In applications such as health care where operational decisions can have complex social, ethical and safety implications it may be increasingly important to have human-in-the-loop decision-makers.
Command centres in health care
Although the CC in the acute care setting that forms the focus of the present evaluation is of one specific model, it is useful to consider the range of models that have been implemented in health care:13 (1) Incidence responses – are activated when they are needed in the case of emergencies, for example, mass casualty events and pandemics; (2) security operations centres – perform surveillance as well as integrate services around threat detection and alarm management response; (3) facility operating centres – asset management systems, which can include real-time location systems and guided vehicles to deliver medication, linens, and meals to patients and (4) capacity management/care progression centres – which aim to improve allocation of resources and patient outcomes, boosting hospital financials and maximising organisational efficiency.
In the UK NHS the ‘Gold, Silver and Bronze’ model of major incident response command was well established before the COVID-19 pandemic and played a major role in the way that the health service organised its response and was supported by data dashboards such as QualDash. 14 The UK public became used to hearing references to ‘Gold Command’ in media reports of the government’s and NHS’s responses to the pandemic.
Many hospitals in the USA, UK and other countries appear to be using the ‘Capacity Management’ CC type. However, there appear to be variations in the designs and scale of the command-centres across these facilities (see Chapter 4 for more details and Appendix 1 for examples). To illustrate the variation, the UK Imperial College Healthcare Trust was reported as having one large video wall screen monitored by a single person,15 and the University Hospitals of Morecambe Bay NHS Trust16 and The Royal Wolverhampton NHS Trust17 report that they have multiple PC screens with video wall screens in front that are monitored by more than three people at a time. In the USA, AdventHealth18 and CHI Franciscan19 command-centres create one ‘common space’ by bringing data and staff from multiple hospitals; others such as the Bradford Command Centre represent only one hospital. 20
The use of command-centres in health care is a relatively new concept and its impact on patient care and safety has not been widely studied. However, preliminary reports suggest that command-centres have a positive impact on patient care and healthcare delivery process. 19,21–23 In this report we aim to generate a better understanding of the strengths and weaknesses and the opportunities and challenges inherent to the CC approach through in-depth evaluation of a recent implementation in a UK NHS hospital.
The Bradford Command Centre
In the UK, we identified at least four NHS hospital trusts who are piloting ‘command centres’, with others in early stages of planning. Bradford Teaching Hospitals NHS Foundation Trust (BTHFT) was an early adopter with the introduction, in 2019, of the ‘Command Centre’ at their Bradford Royal Infirmary (BRI) hospital. 20 The CC technology was provided by GE Healthcare based on adapting successful implementations in the USA. The software is based on a three-tier architecture comprising (1) an integration engine which draws data from hospital information systems, most notably the Trust’s Cerner Millennium EHR; (2) an application layer that implements rule-based algorithms to consolidate and interpret data in real time, including raising warnings and alerts; and (3) a presentation layer that presents information on display screens (also known as ‘tiles’) that provide real-time information on emergency and inpatient hospital services: overall hospital capacity, emergency department (ED) status, patient transfers, discharge tasks, care progression and patient deterioration. Information entered into the EHR and other hospital information systems flows through the integration engine to be interpreted and displayed on the screens in the Bradford Command Centre room. Tile usability is continually assessed, and iterations are made to content, alerts and displays in response to user feedback.
The business case for the Bradford Command Centre was to provide faster and safer care by providing decision-makers with up-to-date information that would allow them to address, anticipate and avoid bottlenecks in care delivery before they cause problems and so reduce unnecessary waiting. Patient flow through the hospital should be faster and patient safety should be improved. Through a proactive campaign of addressing ‘false alarms’ through root-cause analysis and correcting data on the source systems it was also believed that overall data quality would improve. The Trust embarked on the CC project with realistic expectations that service transformation would take time, hard work and strong leadership.
The introduction of the Bradford Command Centre occurred in four phases (Table 1). The first phase was the commencement of a broad change-management programme to emphasise the importance of patient flow in preparation for the technology implementation. The second phase was to incrementally develop and deliver CC ‘tiles’ populated with data from the hospital’s IT systems to gather feedback and refine the design of the system. The third phase commenced with the go-live of the CC complemented by a programme of hospital-wide engagement and training. The CC was in place and operational for several months before the global COVID-19 pandemic started to have an impact on UK NHS hospitals, at which point major rethinks in the operation and priorities of the hospital became a regular necessity as healthcare providers continued to adapt to meet the pressures of the pandemic. The final phase was the post-COVID-19 resumption of hospital-wide engagement, and training recommenced 14 months later.
| Date | Event |
|---|---|
| 1 July 2018 | Onset broad patient flow programme |
| 1 May 2019 | Command Centre tile roll-in |
| 1 December 2019 | Command Centre goes live and hospital-wide engagement and training commences |
| 1 May 2021 | Post-COVID-19 resumption of hospital-wide engagement and training |
The CC remains fully operational at BRI and is internally viewed as a successful intervention that played a significant role in the hospital’s response to the pandemic. There is less clarity on the extent to which it has met its original aims given the major impact of the pandemic shortly after its ‘Go Live’.
Why is this research needed now?
The Bradford Command Centre was styled as ‘the first of its kind in Europe’ by GE Healthcare, the supplier, and has received significant press and NHS attention. As an early adopter of the capacity management/care progression CC approach it merits detailed investigation to understand what it is, how it works and to evaluate its actual and potential contribution to improving the operation of NHS hospitals. We hypothesise that the implementation of an integrated and centralised hospital CC such as the example at Bradford can improve patient safety, patient flow and data quality. This report presents the results of our investigation.
Study aim and objectives
The aim of this study was to understand how the AI CC at Bradford impacts on the quality, safety and organisation of BRI to generate findings that can be applied to other hospitals in the UK. The objectives of the project were:
-
to evaluate the impact of the CC on patient safety, patient flow and data quality (quantitative evaluation and ethnographic study)
-
to understand the process of implementation and integration of the CC within the primary study site (qualitative process evaluation)
-
to elicit cross-industry perspectives on hospital C2 technologies to contextualise the findings (cross-industry review)
-
to synthesise findings into practical outputs to engage service stakeholders and inform future investment and practice.
About this study
This study was funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme through award NIHR129483; https://njl-admin.nihr.ac.uk/document/download/2036192. The project commenced on 1 March 2021 for 18 months with a 3-month extension to allow for contracts and staff recruitment; it ended on 31 November 2022. The research team are all co-authors on this report. The study protocol was published as McInerney et al. 24
The proposed protocol was planned prior to the COVID-19 pandemic, which caused substantial changes to the structures and processes used in healthcare systems, including those at the study and control sites. The pandemic also affected members of the research team and the ability to conduct effective research within UK health care. However, it also created opportunities to evaluate the ability of the health service teams to adapt and respond to the pandemic and specific opportunities to understand how the CC was used to support pandemic responses at the study site. Our research attempted to provide quantification of the influence of the CC implementation, but this report recognised that we were limited in our ability to distinguish the impact of the technology from impacts resulting from the COVID-19 pandemic and the health service responses.
Our mixed-method approach and involvement from our international study steering group helped to define the context of this turbulent period and to describe the processes of change in the hospitals studied. Under the epistemic constraints of our pre-COVID, funder-approved protocol, we have interpreted our research through these contextual descriptions.
Chapter 2 presents the methodology for the study as planned in the published protocol and as revised based on adapting to the opportunities and constraints experienced during the study period.
Chapter 2 Method
This chapter presents the methodology for the study including details of each of the substudies conducted as part of the research project. The original protocol was developed and agreed prior to the COVID-19 pandemic, and we necessarily adapted the approach to reflect the challenges and opportunities that this presented during the study period.
This study evaluates the implementation of the Bradford Command Centre as an exemplar of a real-time, centralised hospital CC. Our starting point was to recognise that the Bradford Command Centre represents a complex intervention within a complex adaptive system. We conducted a longitudinal mixed-method evaluation that was informed by public and patient involvement and engagement. We selected Huddersfield Royal Infirmary as a control site on the basis that it was broadly similar to the hospital in Bradford in terms of its geographic proximity, size, population demographics and in the maturity of its digital health systems. The pandemic affected all hospitals in the UK and the pressures felt by both the study site and control site can be broadly assumed to be similar.
Our mixed-method approach included interactions between the qualitative and quantitative workstreams through a number of iterations. Qualitative work combined ethnographic observations, qualitative process evaluation and quasi-experimental methods to study the evolving sociotechnical nature of the systems and processes within hospitals. Interviews and ethnographic observations informed iterations of quantitative data analysis that, in turn, helped to sensitise further qualitative work. Quantitative work identified relevant outcome measures from both the literature and pragmatically from data sets of routinely collected EHRs.
Our protocol was theoretically informed by contemporary safety-science theory concerning system resilience, human factors models of situational awareness and command and control in high-reliability organisations. The study protocol was approved by the NHS Health Research Authority (IRAS No.: 285933) on 1 April 2021. The study protocol was published as McInerney et al. 24 This is an open-access article distributed under the terms of the Creative Commons CC BY 4.0 license, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited. We have therefore reproduced much of the detail of this protocol here.
It was not possible to complete some parts of the protocol due to the impact of the pandemic on (1) the study sites, participants and study team and (2) consequential resource constraints at the end of the project. We describe the impact of the pandemic on the study and what parts of the protocol were not completed at the end of the chapter.
Our mixed-methods study design
System implementations such the Bradford Command Centre are complex interventions into complex adaptive systems that could provide improvements but might also result in emergent unforeseen consequences. 25,26 We conducted a longitudinal mixed-method evaluation informed by a multidisciplinary co-investigator team and public and patient involvement and engagement. A mixed-method approach is well suited to study complex interventions and the complex adaptive systems to which they are applied. Mixed-method approaches have been used to study information flow and organisational networks,27 integration of organisational interventions,28–30 effectiveness of service models30 and how health information technology affects communication,31 patient monitoring,32–34 care provision35 and clinical decision-making. 36
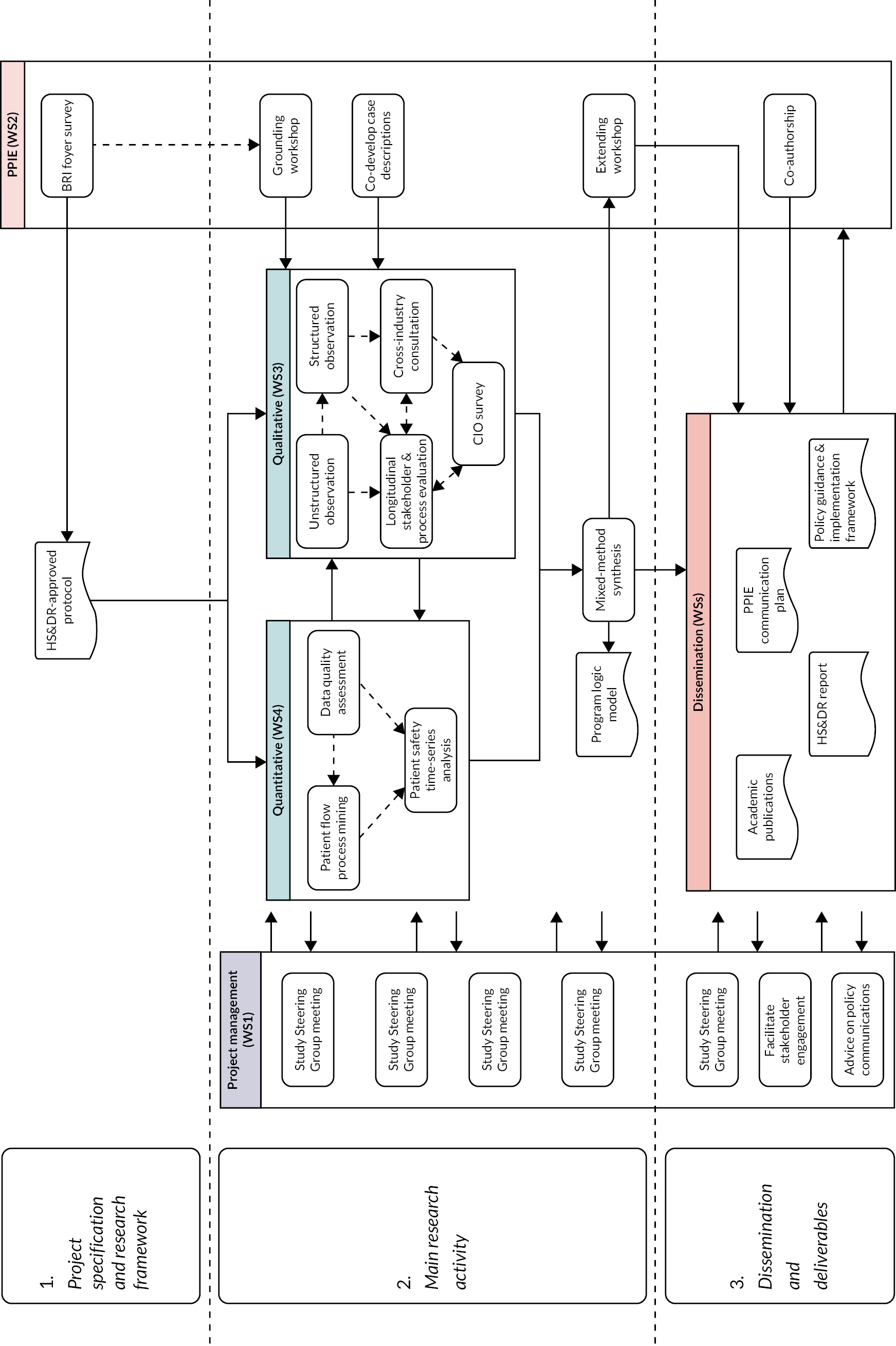
The study comprised five substudies across five workstreams (Figure 1). The five substudies were conducted by the qualitative and quantitative workstreams (WS3 and WS4). These workstreams mutually informed each other as part of an iterative synthesis of findings, rather than solely a summative synthesis. The main research activity was guided by the project’s Study Steering Group (see WS1) and by patient and public involvement and engagement (PPIE; see WS2). Our Study Steering Group was an independent body ensuring the project is conducted to the rigorous standards set out in the Department of Health’s Research Governance Framework for Health and Social Care and the Guidelines for Good Clinical Practice. 37 The Study Steering Group also facilitated stakeholder engagement in research and dissemination and advised on policy communications. Membership of our Study Steering Group includes clinical, technical, commercial and academic healthcare representatives from the UK, Canada, USA, China and Australia.
FIGURE 1.
Schematic overview of the research project’s components. CIO, chief information officer; HS&DR, National Institute for Health Research (NIHR) Health Service and Deliver Research funding programme; PPIE, patient and public involvement and engagement; WS, workstream.
Data sources
The mixed-method evaluation used multiple data sources, including EHRs, qualitative interviews, ethnographic field notes and documentary evidence. All data were managed according to a Data Management Plan approved by the University of Leeds and published as part of the study protocol.
Electronic health record data
The quantitative work was based on the analysis of routinely collected healthcare record data de-identified and processed by the hospitals’ data teams and accessed via Connected Bradford – a regional integration of health care and other data available for research purposes. 38
We conducted a retrospective cohort population-based study using EHR data from the systems at the study and control sites. Participants of the study were patients who visited accident and emergency (A&E) and inpatient departments of BRI hospital and in-patient departments of Calderdale & Huddersfield NHS Foundation Trust (CHFT) between 1 January 2018 and 31 August 2021. We used complete sampling of EHRs within relevant periods. The duration of relevant periods was informed by the initial case description and unstructured observations in the qualitative work, which sensitised us to the information handled by the CC. De-identified UK NHS Digital Secondary Use Services (SUS) data were used. The SUS data are patient-level NHS England data made available to support national tariff policy and secondary analysis. Construction of the SUS data was conducted by Connected Bradford, located at the Bradford Institute for Health Research (BIHR) in Bradford. 39 The team uploaded the SUS data into a secure Trusted Research Environment on the Google Cloud Platform where relevant data were processed before final outputs were extracted. The Connected Bradford data service had worked with data from BRI for several years and had only recently gained similar access to data from CHFT; there were therefore occasions where more detailed data were available for the study site than for the control site.
Ethnographic data collection
The qualitative workstream conducted an ethnographic study comprising non-participant observations (including opportunistic interviews) with staff at the study site working in and around the CC and related organisational processes, document analysis and formal interviews with key stakeholders. Data collection took place between July 2021 and August 2022. Methods included ethnographic observations, document analysis and qualitative research interviews. In total 78 hours of observations were conducted involving 36 staff members that included 22 opportunistic conversations with CC staff and compilation of 100 pages of field notes between July 2021 and March 2022. A total of 19 interviews involving 16 members of key staff relevant to the initiative (15 at study site and 4 at control site) took place between May 2021 and August 2022 and ranged in length from 14 to 71 minutes, with a median length of 38 minutes (9.5 hours).
Following delays in gaining access to the study control site, interviews with staff in comparable roles to those conducted in the study site took place between 8 June 2022 and 11 August 2022. Four participants were interviewed in total, in senior management positions responsible for patient flow (two matrons and two senior clinical managers). In addition, we reviewed 64 documents relevant to the CC programme at the primary study site.
We recruited relevant staff at the CC and control site in key roles. NHS staff working in and around the CC were asked to take part in ethnographic observations. Sampling was in accordance with qualitative research practices to maximise variation in stakeholder perspectives. Potential participants were identified through clinical leads and early observations. Participants were told that they did not have to take part in the research if they wished and that they could withdraw up to the point that their data were anonymised (< 2 weeks following research interviews; < 1 week following survey).
In the following sections, we describe how these data were managed and used and the study design for each of the five substudies.
Substudy 1: data quality
This substudy contributed to Objectives 1 (‘Impact Evaluation’) and 2 (‘Process Evaluation’) based on the hypothesis that the introduction of the CC will affect the awareness of, recording of and processing of electronic healthcare data, which are inextricably related to data infrastructure, operational efficiency, and organisational processes. We applied Weiskopf et al.’s 3 × 3 matrix to assess the quality of healthcare data. 40 This framework maps Patient, Variables and Time data items in terms of Completeness, Correctness and Currency (in other words, presence, accuracy and timeliness). Further detail on how to implement the 3 × 3 matrix is available in appendix B of Weiskopf et al. 40 Our initial identification of variables was informed by our qualitative substudies, and additional clinical input informed the expected attributes of the data, for example plausible ranges, regularity, expected completeness. We used a root cause analysis to trace potential data quality issues back to underlying systems to understand how data quality issues arose and how they were addressed or mitigated.
Although this substudy had planned to examine data quality of the hospital systems, we found that the majority of data quality issues resulted from the data quality issues in the ‘provenance chain’ of research data extraction and management rather than in the source data. Our research team traced multiple data quality issues through our own data management pipelines to the source at Connected Bradford and from there to the extraction services that they had used. This included discussions with the on-site data management team and clinical representatives within the two hospitals involved. Although the work to address data quality issues was substantial, we decided to subsume our investigation of data quality within the main qualitative and quantitative work areas and discontinue this substudy area. The methods for assessing data quality changes over time were developed within Substudy 3 (Patient Safety) and the discussions with staff on data quality are included within Substudy 4 (Ethnographic and Qualitative Interviews).
Substudy 2: patient flow
Approach
This substudy contributed to Objectives 1 (‘Impact Evaluation’) and 2 (‘Process Evaluation’) based on the hypothesis that operational efficiency, organisational processes and patient safety are affected by the flow of patients through the hospital. To study patient flow, we used process-mining methods41 to describe patients’ journeys through their hospital care. 42 Time-stamped data related to clinical events in individual patient journeys were extracted from the Connected Bradford data service and formatted to create event logs for patient cohorts of interest. An event log consists of a de-identified patient or hospital admission number, a date/time stamp showing the data and time an event occurred and an event or activity name. Typically, there are many events of potential interest within hospital systems and we worked iteratively with clinical domain experts to identify key events that ‘told the story’ of particular pathways of interest for patients at the two study sites.
Process mining
We constructed process models to represent patients’ log of clinical events (see Appendix 3) following a methodology our team had developed previously in dentistry,43 oncology,44 sepsis45 and primary care. 46 We evaluated these models by comparing their performance when constructed using various process-mining algorithms. The performance of the models was measured by:47
-
replay fitness, a measure of how many traces from the log can be reproduced in the process model, with penalties for skips and insertions; range 0–1
-
precision, a measure of how ‘lean’ the model is at representing traces from the log. Lower values indicate superfluous structure in the model; range 0–1
-
generalisation, a measure of generalisability as indicated by the redundancy of nodes in the model. The more redundant the nodes, the more variety of possible traces that can be represented; range 0–1.
We calculated conformance to a process model using the metrics defined in Fernandez-Llatas et al. 41 based on comparison between a normative model developed and agreed with domain experts and the actual events as found in the event log data. Conformance is measured as the proportion of moves-on-model and moves-on-log that ‘conform to’ the normative model against those that do not. One hundred per cent conformance suggests that all event logs fully comply with the normative model while 0% conformance suggests that the model is invalid in that none of the events follow the model. Our experience from previous work has been that few healthcare processes achieve 100% conformance due to the very individualised and personalised nature of patient care. We hypothesised that the CC should improve conformance to normative process models.
We identified process metrics of interest including process length and process conformance and calculated these for each month of the study to produce a time-series analysis to understand changes to process flow overtime. Patient flow as defined by the best-performing process model was described using the multilevel approach of Kurniati et al. ,48 which includes activity, trace and model measures. Where possible we conducted the same analysis between the study and control sites. Finally, we reviewed the results from our process flow investigation against the results from other parts of the study and reviewed these with clinical domain experts. The time-series results from our process mining are reported alongside the time-series data on Patient Safety (Substudy 3).
Substudy 3: patient safety
Approach
This substudy contributed to Objectives 1 (‘Impact Evaluation’) and 2 (‘Process Evaluation’) by directly evaluating the differences in patient safety outcomes before and after the implementation of the CC. The evaluation used longitudinal data analysis methods, for example including interrupted time-series analysis and latent growth modelling. We modelled trends in behaviour before, during and after the implementation of the CC, with consideration for the onset of the COVID-19 pandemic.
We approached the analysis in a responsive manner, revising the interruptions in response to discussions with the qualitative workstream as they identified key events from their discussions with the study site staff. We identified candidate variables of interest that included the Patient Safety Indicators from the Agency for Healthcare and Research Quality, for example pressure ulcer rate, in-hospital fall with hip fracture rate, postoperative sepsis rate. 49 We supplemented these with variables of interest identified by the qualitative research team and feedback from early PPIE workshops where patients identified measures that they considered important.
We assume that patient safety is influenced by the flow of patients and the quality of information (as encoded in EHRs) and therefore link data quality and patient flow metrics to those clinical outcomes logically related to patient safety.
In our protocol we had planned to handle unobserved confounders by comparison with the control site given that the control site was from the same geographical region, used the same EHR system, but did not have a CC. This was less successful than hoped as the pandemic response led to multiple changes in management style and approach at both study and control sites. Indeed, the control site reported that, part way through the pandemic, they had implemented a CC approach of their own using dashboard technology and insights from the study sight. Our longitudinal analysis considers those indicators that can be extracted from study and control sites that may provide insights into variations in data quality, patient flow and patient safety outcomes over time.
Metrics for patient safety, patient flow and data quality
We assume that patient safety is influenced by the flow of patients and the quality of information (as encoded in EHRs) and therefore link data quality and patient flow metrics to those clinical outcomes logically related to patient safety. Table 2 presents the initial list of proposed variables for analysis as published in our study protocol. 24
| Variable | Patient flow | Patient safety | Data quality | Study site | Control site |
|---|---|---|---|---|---|
| Ambulance diversion rates | X | ||||
| Ambulance handover rates | X | ||||
| Completeness | X | X | X | ||
| Correctness | X | X | |||
| COVID bed availability | X | ||||
| Currency | X | X | |||
| Diagnostic process time | X | X | X | ||
| Early discharges | X | X | X | ||
| Falls in hospital | X | ||||
| Hospital-acquired infections | X | ||||
| In-hospital transfers | X | X | |||
| Intensive care unit bed usage | X | X | |||
| Left without being seen rates | X | X | |||
| Length of stay | X | X | |||
| Marked ‘hospital discharge’ | X | X | X | ||
| Mortality in hospital | X | X | X | ||
| Mortuary crowding | X | ||||
| Number of patients awaiting surgery (inpatients and at home) | X | ||||
| Postoperative sepsis rate | X | X | |||
| Pressure sores in hospital | X | ||||
| Re-admission rates for same condition within 48 or 72 hours | X | X | X | ||
| Time to admission | X | X | X | ||
| Time to be seen | X | X | |||
| Time to discharge | X | X | X | ||
| Time to treat stroke patients | X | ||||
| Waiting time benchmarks (e.g. 4 hours A&E) | X | X |
Data constraints
Our longitudinal analysis considers those indicators that can be extracted from study and control site that may provide insights into variations in data quality, patient flow and patient safety outcomes over time. Patient safety, patient flow and data quality are not directly measurable. Hence, indicator variables were used as proxy measures for these outcomes. We identified a ‘long list’ of candidate indicators based on stakeholder discussion and relevant literature and shortened this to a ‘short list’ of what was feasible given data availability.
Indicators for patient safety
Three indicators from the BRI hospital, the study site (mortality, re-admissions within 72 hours and postoperative sepsis), and two indicators (mortality and re-admissions within 72 hours) from the CHFT hospital, the control site, have been used. The proportions of mortality and re-admissions in hospital were calculated as the total deaths and re-admissions, respectively, divided by the total number of emergency admissions. Postoperative sepsis was calculated by dividing the weekly count of patients with sepsis diagnostic codes in their records by the total count of surgical operations conducted in that week. The surgical operation codes were extracted from the UK Health Security Agency list of operation codes published document. 50 Postoperative sepsis occurrences were identified using T814 ICD10 code. 51
Indicators for patient flow
Four indicators of patient flow (length of stay, clinician seen time, waiting time and average transition time) were used and were only available from BRI hospital, the study site. Inpatient length of stay in emergency admissions (defined as the duration between date and time of admission and discharge), ‘clinician seen time’ (the duration between A&E date and time of arrival and seen by a clinician) and A&E waiting time (the duration between A&E date and time of arrival and treatment) were used as indicators for weekly patient flow patterns throughout the study period. In addition, average times taken between A&E transitions (arrival, assessment, treatment, visit conclusion and check-out) were used as indicators for patient flow patterns during the same period.
These indicators were subsequently supplemented by the inclusion of patient flow metrics derived from process mining of the data (Substudy 2) to produce a multidimensional perspective on patient flow.
Indicators for data quality
Four indicators of data quality were available from the BRI hospital data. The proportion of missing dates of treatment and clinician’s assessment, and proportion of records showing valid transition (arrival → assessment → treatment → visit conclusion → check-out) and ‘left-shift’ (arrival ← assessment ← treatment ← visit conclusion ← check-out) of patients in A&E care were used.
Other variables for quantitative analysis
Dummy variables were created for each of the intervention components (‘broad patient flow programme’, ‘command centre tile roll-in’, ‘command centre goes live’ and ‘hospital-wide engagement and training’), COVID-19 pandemic and spikes of COVID-19 pandemic. The components of the intervention were given a value of ‘1’ starting from the date of its introduction until the introduction of the next component or phase, then a value of ‘0’ for the rest of the period. ‘COVID-19 pandemic’ was given a value of ‘0’ through February 2020 and a value of ‘1’, thereafter. A spike dummy variable was also added by setting ‘1’ for the COVID-19 spike periods based on the UK data52 and ‘0’ throughout.
The intervention and baseline phases were also modelled using five continuous time variables. At the date that phases started, a covariate was encoded with ‘1’ and increased by one unit for every time step for the duration of the phase; the covariate was encoded as ‘0’, otherwise. For example, the ‘Command Centre tile roll-in’ phase is defined between 1 May 2019 and 1 December 2019. Each week from 1 May 2019 was encoded 1, 2, 3, …, 29, 30 until the week commencing 29 November 2019, and encoded as 0, 0, 0, … from then on. In addition, seasonality was modelled by including dummy variables for the number of weeks in a year.
Quantitative analysis methods
Two types of models were explored: ‘simple tech’ and ‘complex’ models. For the ‘simple tech’ models, a three-phase, interrupted time-series model was used that consisted of a pre-intervention (first phase), ‘Command centre tile roll-in’ component (second phase) and ‘Command centre goes live’ component (third phase). For the ‘complex’ model, a five-phase, interrupted time-series model was used that consisted of pre-intervention (first phase), ‘onset broad patient flow programme’ component (second phase), ‘command centre tile roll-in’ component (third phase), ‘command centre goes live’ component (fourth phase) and ‘hospital-wide engagement and training’ component (fifth phase).
Interrupted times-series linear regression analysis was used to assess the impact of the Command Centre on the patient safety, patient flow and data quality. First, linear time-series models were fitted to the data. Tests for serial autocorrelation of residuals were conducted and all tests were statistically non-significant. Hence, regression models with autoregressive integrated moving average (ARIMA) errors were not sought. The Akaike information criterion53 and the Bayesian information criterion54 were used in selecting the models best fitting to the data.
To estimate the average transition time between different stages of A&E care, and to map the destinations of A&E patients, a number of process-mining techniques were used. 55
A five-phase interrupted time-series was used for the main analyses. To explore if the technology alone would have had an impact on outcomes, three-phase interrupted time-series models were used as sensitivity analyses. The ‘broad patient flow programme’ and ‘hospital-wide engagement and training’ were assumed as independent events of the Command Centre and adjusted as independent dummy variables in the sensitivity analyses models. Five per cent significance level and 95% confidence intervals (CIs) were adopted throughout. Analyses were implemented in R (Version 4.0.2).
Substudy 4: ethnography and qualitative interviews
Rationale for the ethnographic approach
With a complex system like the Bradford Command Centre implementation, it is important that the researchers develop an understanding of behaviour in context including the meaning of those behaviours and interactions within the immediate operating culture that has developed within the system. Ethnographic enquiry was selected in order to facilitate deep understanding of the technology in its broader social and organisational context, including human experience, engagement and interaction. 56,57 Ethnographic methods are widely used for understanding situated practices with technology. 58–62
Context for the ethnography
Bradford Royal Infirmary implemented their CC based on a centralised location that brings together operators with varying functional roles, each with access to their own real-time data feeds. The main purpose of bringing the roles together is that they have access to shared data visualisation that represents the real-time hospital state for the broader system that they are trying to control. The CC is connected to the broader system so that staff operating within can affect inputs into the system and respond to intelligence that is developed within the CC.
Participation and consent during fieldwork
All hospital staff involved in the organisation and/or delivery of patient care relative to the CC were eligible to participate in the study. Site access was made possible through a local collaborator and the Medical Director of the CC. Prior to data collection, the study was introduced to key staff relative to the CC through a series of face-to-face briefings across multiple shifts delivered by two of the authors, JB and CM. In addition, the Clinical Lead for the CC circulated information about the study to all staff working in the Centre. Written informed consent was obtained from staff observed in the Centre and those involved in early qualitative interviews. Later interviews were conducted online where the consent process was recorded verbally.
Ethnographic observations
Phase 1: unstructured observations
As an initial step in developing the case study and in order to immerse and sensitise the research team to the context of hospital operational C2, the first phase of our work involved unstructured ethnographic observation within pre-specified observation periods, and system mapping. Observations comprised non-participant observation (documented as researcher field notes) and opportunistic conversations with staff in the CC, guided by a study-specific field note template informed by the literature on ethnographic methods in acute care settings and more broadly in healthcare and safety-critical industries. 58,59,61–65 The purpose of this approach was to capture contextual information and a chronological account of critical events, actions and researcher reflections as they took place in order to understand events and actions as they unfold from the actor’s perspective (and the meaning that CC users attach to them) drawing upon the Critical Incident Technique. 66 Researchers also recorded incidents of observer effects (e.g. staff asking ‘What are you writing?’) to allow analysis of whether participants’ awareness of the researchers’ presence changed over time. 67 Researcher field notes were generated both during and shortly after each observation period drawing upon substantive, reflective and analytic concepts. 68
Phase 2: structured observations
Following our initial observation period, ethnographic data collection moved to a more structured approach in order to explore the impact of the CC beyond the operations room and at all levels of the organisation, including micro-level (front-line clinical workflow in specific specialties), meso-level operational planning (e.g. bed management) and macro-level strategic planning (e.g. use of data in quality and safety governance). Our approach to structured observation drew upon engineering ‘use case’ methodology to understand usability of the system in context. 69 The approach taken was twofold: (1) followed key information through the system from modules in the CC visual displays (i.e. understanding the impact of the CC on certain ‘tracer issues’ at hospital level, such as detection and escalation for the deteriorating patient) and (2) formal shadowing of key professional roles, such as Clinical Site Matrons and operational leads as they utilised, acted upon and made decisions based upon CC data and intelligence. We produced six use cases (or vignettes) of specific tracer issues/professional roles that emerged from inductive analysis of data collected earlier in the study that represent interaction with CC processes and outputs.
Sampling
Sampling of observation periods was based on opportunistic access provided by key personnel and as agreed with CC Leads so as not to overburden staff. Observations took the form of approximately 4-hour windows with sampling of observations periods stratified in order to ensure representation of varied days of the week (including weekends), time of day and CC conditions (e.g. team handovers). As the study progressed, we used theoretical sampling for the ethnography to produce tracer issues and also for the interview participants to follow up emergent lines of enquiry. Initial observations were carried out by Carolyn McCrorie (CM) and Jonathan Benn (JB), and subsequently by CM, at different times of the day and on different days of the week. Researchers were situated within the CC room, usually towards the back of the room where there was available space (and to adhere to rules on social distancing required during the pandemic). As the study progressed, CM identified opportunistic moments within the staff workflow to carry out conversations with staff to check understanding and to explore what had been observed in more depth. CM and Josh Granger (JG) also observed the role of the CC in supporting operational planning meetings (silver tactical meetings) that took place at fixed times over the day.
Documentary analysis
We reviewed emerging hospital policies and guidance related to the CC (content reported in the original business case and CC set-up, reported impact on key performance indicators, activation programmes and training material for hospital-wide roll-out, iterations to the tiles and CC staff role descriptions) where practicable as an alternative to data collection involving staff to capture the ongoing implementation and monitoring process. A sampling framework to guide collection of documents (key documents and dates) was informed through earlier qualitative interviews with key members of staff and observations within and around the CC.
Qualitative research interviews
To complement our observational work, we conducted qualitative research interviews with key members of staff at multiple time points within the CC programme. Sampling was theoretically driven, based upon emerging insights from the observations and earlier interviews to include CC programme leads, key roles working in the CC, clinical leads in front-line areas interacting with the CC and organisational-level stakeholders representing operational strategy and clinical governance. We utilised the use cases (which emerged from observations within and around the CC) as a probe to compare operational planning, control and decision-making in specific priority areas, with and without the support of a centralised CC function, in order to enrich our understanding of how a CC operates within a health service context. An interview topic schedule with domains relevant to research aims was developed for use with programme leads and staff relative to hospital operational planning and patient flow and iterated throughout the study [including additional questions in light of feedback from patient and public (PPIE) representatives who attended our first patient-facing workshop and ongoing engagement with our PPIE co-applicant to ensure that the interviews covered topics relevant to patients]. Interviews were conducted by CM and JB either in person or online, audio-recorded, and professionally transcribed.
Data analysis
Data were anonymised and entered into the qualitative data analysis tool NVivo (Version 12.0) (QSR International, Warrington, UK) to facilitate data management. The analysis was an iterative and reflexive process and proceeded in parallel with data collection. Thematic analysis was undertaken on interview and ethnographic data, drawing upon concepts from Grounded Theory. 70,71
The coding frameworks were developed by the qualitative workstream research team (CM, JB, JG and RR) and included a framework for the interviews and a separate, complementary framework for the ethnographic data. Preliminary coding of sample ethnographic field notes was reviewed in research team meetings with feedback provided by RR and JB to the primary coder (CM). A process of open coding on the first four interview transcripts by CM and discussion of emerging concepts with the research team provided an initial inductive analysis framework. A second researcher (JG) independently coded the same four transcripts. Informal comparison of code patterns, using the constant comparative method for category and theme refinement, supported the development of conceptual code definitions and interpretations, which was discussed collectively in a series of researcher workshops (CM, JG and JB) and PPIE workshops (CM, JG and NS) and refined for consistency and focus by the workstream research team.
Six tracer issues were identified through frequency of referral to concepts during ethnographic observations, during interviews and in discussion within the research team. Theoretical sampling (analysis in parallel to sampling) informed subsequent data collection in order to build a comprehensive picture as to how intelligence is used to support operational planning, situational awareness and decision-making.
Data extracted from documents were analysed through an inductive process to capture key developments in design and functioning of the CC. The data were analysed in parallel to observation and interview data and informed lines of questioning for subsequent interviews (e.g. analyse the ‘official’ story vs. what happens in practice).
Through the coding and discussions regarding links and distinctions across transcripts, field notes and relevant documents and emerging themes mapped to the research aims, the later stages of our analysis followed the reflexive thematic analysis (RTA) process described by Braun and Clarke72,73 to produce a final inductive coding framework with a smaller number of selective codes.
Our PPIE co-applicant (NS) supported with qualitative data analysis for WS3, informed through reported best practice and discussion with colleagues within the CC on their recent experiences of related work. Involvement included a range of activities: (1) a training workshop on qualitative analysis (held in March 2022) based on an excerpt from one interview transcript collected eaconduct 40 interviews in totalrly in the evaluation Workshop 1; (2) a data analysis workshop (held in May 2022) based on the developing coding framework and exemplar quotes from interviews conducted at different phases of the process evaluation Workshop 2 and (3) an extended workshop (held in July 2022) to discuss data interpretation further from a lay perspective.
Data saturation
The value of data saturation as a guiding principle in RTA has been questioned;73 however, we did find the concept useful in guiding when we moved the focus of our enquiry between stages, for example from unstructured to structured observations and in terms of the main timepoints for the qualitative interviews.
The number of interviews and the scope for observation were significantly constrained by the restrictions imposed during the pandemic. We had planned to conduct 40 interviews in total, but the restrictions of the pandemic increased the time and complexity of organising and conducting interviews, leading to only 19 interviews in total. We would have like to conduct more than 15 interviews at the study site; specifically, we would have liked to do more follow-up interviews to discuss some of the findings, for example from the qualitative work. We would also have liked to have interviewed more than four people at the control site but even these four interviews had taken over 6 months to organise at the height of the pandemic. Limited access to the control site reduced our ability to investigate the comparisons between sites, which is disappointing as we surfaced interesting insights into how the control site had found different ways to meet the challenges of the pandemic but were unable to investigate these in detail.
We were allowed only one researcher to do ethnographic observation on site. They conducted 78 hours of observations at times and on days when we expected working patterns to vary as well as observing changing practice over time. This led to what we believe to be a comprehensive picture, but it would not be appropriate to claim data saturation given the complexity of the subject and its changing nature over time. Specifically, it would have been helpful to have more members of the study team involved in the observation to gain a range of perspectives, enable the team members to discuss the observations from their own direct observation and improve the depth of understanding across the research team.
Ethical issues
The study was approved by the NHS Health Research Authority (IRAS: 285933) on 1 April 2021. The Standards for Reporting Qualitative Research template was used to support complete, transparent reporting of qualitative research. 74
Substudy 5: cross-industry review
Rationale
With the increasing investment in, and implementation of, C2 centres in health care there is a need to develop a better understanding of the applicability of C2 principles to acute health care. Models of C2 were originally developed outside of health care, most notably in the military domain, and have long been the focus of research and development within these domains. C2 in health care, however, is a relatively new concept and as such there is a small but growing body of research in the area. Given this, there is a need to understand how acute health care can learn lessons from these mature safety-critical domains and how their C2 concepts and implementations can best be translated into the acute care environment. To understand this better, we planned and conducted a systematic scoping review supported by expert panel consultations to synthesise knowledge from across a range of non-acute healthcare domains to help inform the design and integration of C2 centres in hospital settings.
Review aims and objectives
The aim is to understand the principles of effective C2 as they have been developed in mature safety-critical industries and academic fields of enquiry, in order to synthesise and apply this knowledge in the development of hospital CCs in the acute healthcare setting. In doing so we scope and understand centralised C2 processes in safety-critical industries, including health care, and the key principles and contextual factors that may influence the applicability and transferability of C2 models and processes to a hospital setting. This review will help contextualise the findings from our qualitative and quantitative work.
Specific research objectives include the following:
-
To identify key principles/theories of effective C2 based upon expertise developed in mature, non-hospital safety-critical industries, including models of C2 implementations or theories of effective C2 processes
-
To describe and synthesise any available evidence for the efficacy of CC implementations in healthcare/high-risk industry
-
To develop transferable principles and recommendations for health care.
Study design
This systematic scoping review was developed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews. 75 A scoping review methodology was deemed suitable as the research aimed to map the key concepts underpinning centralised C2, technologies, implementations and evaluations across a heterogeneous collection of peer-reviewed and grey literature. The synthesis of knowledge gained from the scoping review was guided by a series of interviews with members of an expert panel on C2 in safety-critical operations.
Search strategy
We conducted formal database searches for any peer-reviewed articles that discussed or evaluated centralised C2 and one or more of the identified domains (Table 3). We conducted an initial scoping review on 9 April 2021 using five databases (EMBASE, Global Health, HMIC, MEDLINE and Transport) which found 7310 records of which 147 were considered potentially relevant. Key papers were shared among team members and helped the researchers to prepare for and contextualise the work, notably in Substudy 4.
| Domain | Categories covered |
|---|---|
| Defence | British Ministry of Defence Air defence Navy Ground Aerospace |
| Industry | Utility organisations Nuclear power Health and safety assurance in safety-critical installations (e.g. offshore; petrochemical) Logistics |
| Transport | Air traffic services Rail Road traffic |
| Emergency services | Ambulance Fire and rescue Police |
The search strategies were developed iteratively and comprised multiple search terms for centralised C2 and the domain respectively. The centralised C2 search terms were adapted from the Franklin et al. terms for CCs. 76 The domain search terms were developed with the research team, encompassing key terms within the domain identified through discussion, review of exemplar papers and review of preliminary search results for sensitivity and specificity. Four additional search strategies were used: to capture articles that more broadly review concepts of centralised C2, and to capture articles that cover any existing implementations of centralised C2 in a hospital or inpatient setting, to capture articles that cover centralised C2 and related concepts (e.g. high reliability or situational awareness) and to capture articles that cover centralised C2 and operations management.
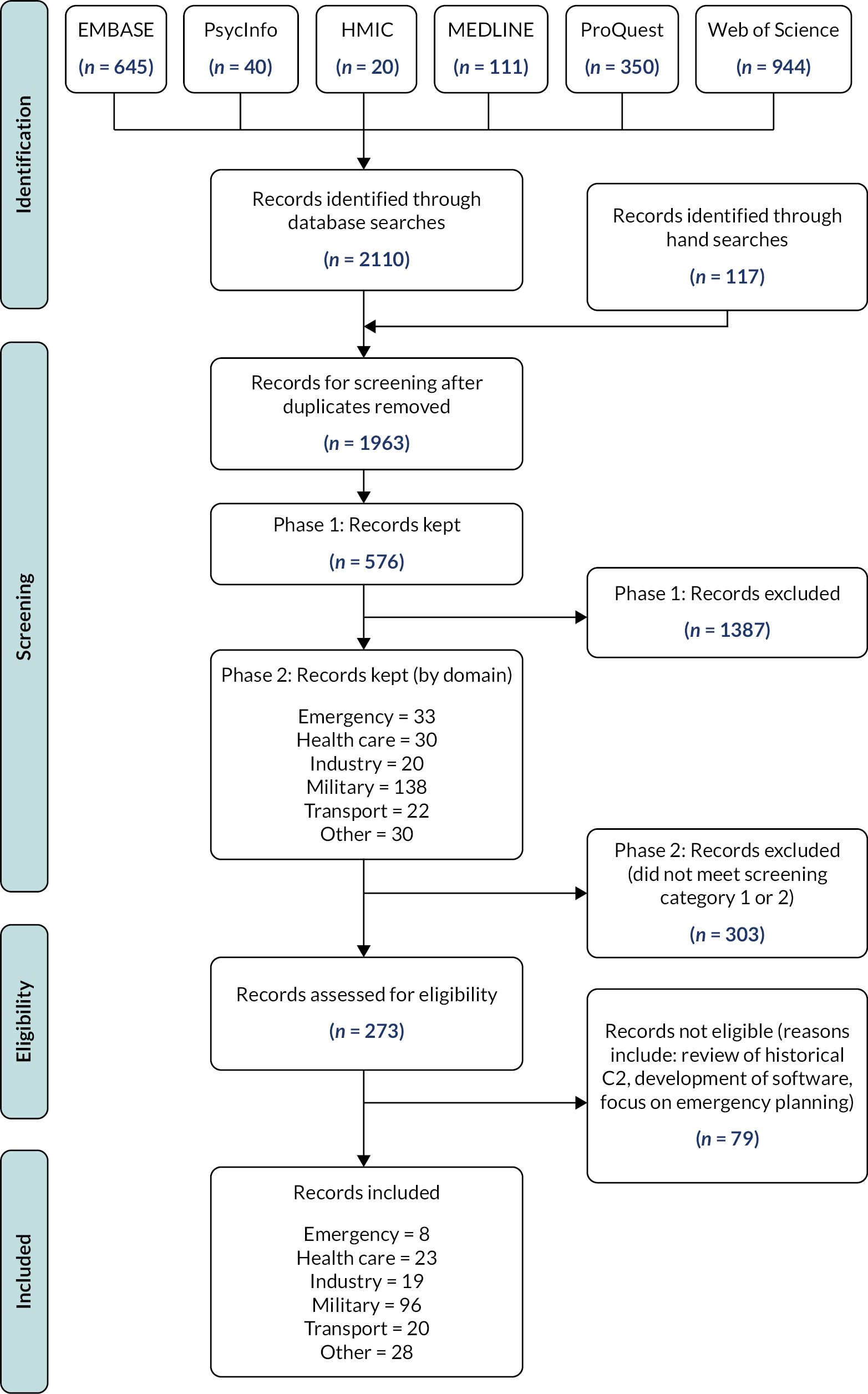
The search strategy from the cross-industry review is reproduced in Appendix 2 and is summarised in a PRISMA diagram in Figure 2. Six databases were searched: EMBASE, PsycInfo, HMIC, MEDLINE, ProQuest and Web of Science. Informal searches were also conducted to obtain grey literature (e.g. white papers and guidelines) and other relevant articles outside of the searched databases. All searches were limited to English and published between 1 January 2000 and the day of the search in order to cover contemporary research and processes. The last search was conducted on 14 June 2022. Search outputs were downloaded to EndNote for management and screening. Supplementary information and references were also gathered from expert panel interviews in which subject-matter experts were interviewed about their understanding and experiences of centralised C2. The additional article/resource recommendations from the interviews were added to EndNote for data extraction.
FIGURE 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for cross-industry review.
Inclusion and exclusion criteria
The target literature and subject-matter expertise for the scoping review was theoretical articles and commentary, empirical studies and evaluations of C2 implementations, domain-specific grey literature, and reported descriptive case studies across multiple safety-critical domains, including health care.
Two screening categories were defined in relation to the research aims and used to both categorise and screen the search results. These categories were defined as:
-
Reported cases and evaluations of operations CC implementations in safety-critical domains: any article that focuses on the design and/or implementation of a specific/named command/control centre (for operations in the target safety-critical domains) or operational control processes linked to a specific/named command/control centre in the target domain.
Excluded:
-
Instances of reported control centres the purpose of which is not for control of ‘operational activity’ within the domain (e.g. cancer control centres, control centres for remote monitoring of patient data, poison control centre).
-
Non-safety-critical operations (e.g. automated vehicle-fleet management, manufacturing supply networks or supply-chain control centres).
-
General literature, reviews, studies and theory about effective C2 in safety-critical domains: any article that focuses on C2 or related concepts as a topic within the target domains (either by referring to design, processes, related theory, research or reports of studies not linked to specific implementations).
Excluded:
-
Articles with a focus on more general concepts not specific to C2 systems or processes (e.g. leadership, general communication, role assignment, preparedness or focus on cost-effectiveness).
-
Reports on the development of methodology for studying or evaluating C2, without reporting evaluative criteria (i.e. don’t convey information about effective C2).
-
Research that focuses on a non-safety-critical domain such as urban management or animal health emergencies or has a specific focus on team performance that does not directly relate to C2 (e.g. focus on a single role).
-
The development, proposal or implementation of digital software/systems for information management or display/monitoring, or virtual CCs.
-
The published protocol related to this research.
Study screening and selection
An initial phase of screening was conducted using EndNote and assessed the titles of each record found across the searches (n = 1963). Records were excluded if they were clearly not relevant to the study; the eligibility criteria were used to inform this decision. A sample of the initial body of records was reviewed and discussed among three researchers for clarity and understanding through which a high level of agreement was achieved. The remaining volume was screened by one researcher. The records marked for retention (n = 576) were exported to an Excel spreadsheet for further screening.
A second phase of screening assessed both title and abstract against the eligibility criteria. Two researchers independently reviewed a sample of 50 records. These decisions were then compared and discussed, resulting in an agreed understanding and interpretation of the eligibility criteria with no significant disagreements. One researcher conducted screening on the remaining volume; any queries were marked and discussed with the other researchers. During this process, records marked for retention (n = 273) were also classified for article type and their domain (e.g. military) (see Figure 2). Any records without abstracts present were carried forward to be reviewed for eligibility.
The remaining volume (n = 273) were then assessed for eligibility against the research aims. This led to the exclusion of articles that met the screening categories but were not relevant to the research aims (e.g. reviews of historical C2 in naval warfare). The eligible volume (n = 194) was separated and retained for data extraction.
Data extraction
A subset of exemplar articles was identified from the included literature set and subjected to full text analysis to draw out the main themes in response to the research objectives. This was done using principles from a thematic analysis methodology. 72 The remaining articles were analysed for relevant information that could be applied to the established themes.
Expert interviews
In order to support the findings from the scoping review literature, subject-matter experts were invited to informal interviews. The experts were identified through preliminary reviews of the literature conducted prior to the formal database searches and through dialogue with members of our steering group representing expertise in human factors and safety science. Invites were sent out to seven individuals of whom three agreed to interview. One additional interview was conducted where the expert was identified through snowball sampling. All interviews were conducted remotely via Microsoft Teams and recorded with the verbal consent of the expert. The recordings were transcribed and input into NVivo for analysis.
Data analysis and synthesis
Using the themes elicited through the data extraction method described above, the data were analysed to answer the research aims. More specifically this was done to highlight prevailing definitions and models of C2 and then discuss how C2 features and is researched in each domain. The articles classified as ‘screening category 2’ were used to discuss specific implementations of CCs and create a table of researched implementations featured in our data set. These discussions resulted in the further highlighting of three broad themes that featured across C2 in all domains. These themes were then discussed by drawing on a wide range of information in a cross-domain synthesis. The healthcare literature was analysed and discussed separately. The cross-domain synthesis and healthcare literature analysis were ultimately brought together in the final discussion to support recommendations.
Revisions to the methodology during the study period
Our study protocol was planned prior to the COVID-19 pandemic but this study period coincided almost exactly with the pandemic. The impact of the pandemic necessitated changes to our methodology as a direct effect on the study team, for example in staff recruitment and working practices, and on the study itself as both the study site and control site reacted to the events and pressures of the pandemic as best they could. Specifically, we were unable to:
-
explore data-quality issues to the extent originally planned (Substudy 1)
-
conduct the survey of chief information officers (CIOs) attitudes to CCs
-
disseminate the outputs of the research as widely as planned within the timeline of the original planned study.
We describe the impact of the pandemic on the project and the reasons for not being able to complete these three aspects of the protocol in the following sections.
Impact of the coronavirus-19 pandemic on the project
The CC had only been live at Bradford a number of weeks prior to the pandemic impacting on UK NHS hospitals. We therefore followed the emerging use of the CC as it supported Bradford’s response, including the addition of new ‘tiles’ for COVID management and the swift reconfiguration of services and hospital rooms. Our substudies on data quality, patient flow and patient safety were intended to provide quantification of the influence of the CC implementation but will be limited in their ability to distinguish such contributions from those motivated by the response to COVID-19. Our mixed-method approach and involvement from our international Study Steering Group has helped to define the context of this turbulent period and to describe the processes of change in the hospitals studied. Under the epistemic constraints of our pre-COVID, funder-approved protocol, we interpret our research through these contextual descriptions.
The pandemic also affected the study team. We were fortunate in being allowed to continue observations throughout the study but with social distancing and associated restrictions. Despite this, we were able to conduct the planned interviews at the study site, using a combination of face-to-face and online interviews. Access to the control site was, however, significantly delayed and when the research team did gain access late in the project timeline, this limited the extent of interviewees that could be recruited and we therefore prioritised key operational roles. Patient group meetings largely took place online.
The study sites, patients, the clinical professionals and all involved in the study went through an extremely challenging time. We consider ourselves fortunate that the majority of the study has been completed successfully and largely within planned timescales. We were unable to complete:
-
Exploring data-quality issues to the extent originally planned (Substudy 1). Data quality proved significantly more complex to measure. Our approach was to construct a ‘long list’ of candidate data-quality metrics and reduce this to a ‘short list’ of those that our clinical advisers felt were most appropriate and our data scientist confirmed would be achievable. Our original plan had been to investigate a wider range of data-quality issues through root-cause analysis based on on-site interviews with the informatics team and front-line staff. We were unable to get clearance for on-site access for more of our team and it was agreed that the people we needed to meet with had higher priorities.
-
Conducting the survey of CIOs attitudes to CCs. This survey would have provided important insights. During the pandemic, we were advised that CIOs would find our survey an unhelpful distraction from important work dealing with the pandemic. With some staff ill or isolating and additional challenges of getting access to hospitals and healthcare workers, we deferred this task until later in the project. The resource scheduled to design and implement the survey was successful in gaining a new role and left the project. We did not have sufficient time to recruit a new resource with the underspent budget before the project completed. We are proposing a follow-on project to disseminate the results, including to CIOs and hope to include this survey in that dissemination.
-
Disseminating the outputs of the research as widely as planned within the timeline of the original planned study. Our approach through the pandemic was to prioritise the gathering of information on the use of the CC. This was a challenging time for the research team, the study and control sites and the wider NHS and society and the work took longer and took more resource than originally planned as a result. Dissemination activity scheduled at the end of the project had to be condensed in order to complete the project on time.
What was achieved despite the coronavirus-19 pandemic
Despite the pandemic, we have produced a set of results which provides a unique insight into the potential use of CCs in the UK NHS that will help inform future investments in the approach. The results are presented in the following chapters in terms of patient and PPIE (see Chapter 3), a cross-industry review of the literature on C2 concepts supplemented by interviews with a panel of subject-matter experts (see Chapter 4), the results from extensive ethnographic observation at the study site and a process evaluation based upon staff interviews at both the study and control sites (see Chapter 5), the results of a quasi-experimental analysis of hospital data against control for the study period (see Chapter 6) and synthesis of findings to construct intervention logic to support future CC implementations and research evaluation, along with reflection on the study limitations including the implications of the changes detailed above (see Chapter 7). The project has a significant underspend which we are hoping to still use for dissemination and, if approved, this would include the planned CIO survey and our plans for PPIE communication.
Chapter 3 Patient and public involvement and engagement
This chapter provides details of our PPIE.
Integrating patient and public involvement and engagement within our research
Integration of PPIE was an integral part of the study design, delivery and dissemination. Figure 1 shows how the PPIE workstream was engaged throughout all phases of the project.
Prior to commencement of the study our PPIE activity included working with a patient and public representative as co-applicant (NS), input on research design by the PPIE Research Fellow at the NIHR Yorkshire and Humber Patient Safety Translational Research Centre, and an informal survey of visitors to the hospital in which the CC was implemented. Our PPIE co-applicant was involved and engaged from the early stage of the development of the funding proposal and made key contributions to help develop and contribute to the design of the interview schedule and inform analysis of ethnographic data. NS also shared and advised the rest of the research team based on his experiences as a patient, including the analysis of the transition of changes to care practice and how effective change was cascaded in practice to the benefit of patients.
Early project PPIE activity included workshops to engage PPIE representatives to give lay perspectives on care co-ordination in hospitals, to inform the development of interview questions for hospital staff, and to suggest measures of patient safety. Our PPIE co-applicant supported qualitative data analysis through review and further development of emerging themes in the data set. Two workshops were hosted with PPIE representatives to help interpret findings and to draft a PPIE communication plan. Public and patient representatives were involved throughout all phases of the project. Details of the wider project’s PPIE are available in the published protocol. 24 Table 4 provides a summary of the engagement activities.
| Activity | Project phase | Description |
|---|---|---|
| PPIE co-applicant | 1 – Project specification | Patient and public representative as co-applicant throughout proposal and resubmission providing input on research questions, study design, project management and governance, and dissemination |
| Hospital foyer survey | 1 – Project specification | Informal survey of visitors to the hospital in which the CC was implemented asking their opinions on digital technologies being used to inform the management of patient journeys. Survey forms were positioned next to the mock-up CC display that was installed by the hospital to engage visitors |
| Grounding workshop | 2 – Main research activity | Online workshop asking PPIE representatives to give lay perspectives on care co-ordination in hospitals, to inform the development of interview questions for hospital staff, and to suggest measures of patient safety |
| PPIE interpretation of interview transcripts | 2 – Main research activity | PPIE co-applicant supporting qualitative data analysis through review and further development of emerging themes in the data set |
| Extending workshop | 2 – Main research activity | In-person workshop asking patients, public, and community-group representatives to help interpret findings and to inform a post-project communication plan |
| Co-authorship | 3 – Dissemination | PPIE co-applicant as co-author on all publications |
Patient and public involvement and engagement workshop outputs
We ran two workshops with patient representatives with the aim of gathering patient views on CC approaches and generating infographics which could be used to inform the research with hospital staff. We were interested in the extent to which staff shared patient concerns and whether they felt these were being adequately addressed in the operation of the CC.
Workshop 1: grounding workshop
Our first workshop in the PPIE workstream intended to:
-
gather lay perspectives on care co-ordination in hospitals
-
inform interview questions for hospital staff, as part of the qualitative workstream
-
contribute candidate measures of patient safety to the quantitative workstream.
The workshop output was summarised in an infographic (Figure 3) presenting the questions that should be asked of CC staff, and the measures of patient safety that should be analysed, in the qualitative and quantitative workstreams, respectively.
FIGURE 3.
Infographic produced by PPIE Workshop 1: grounding workshop.
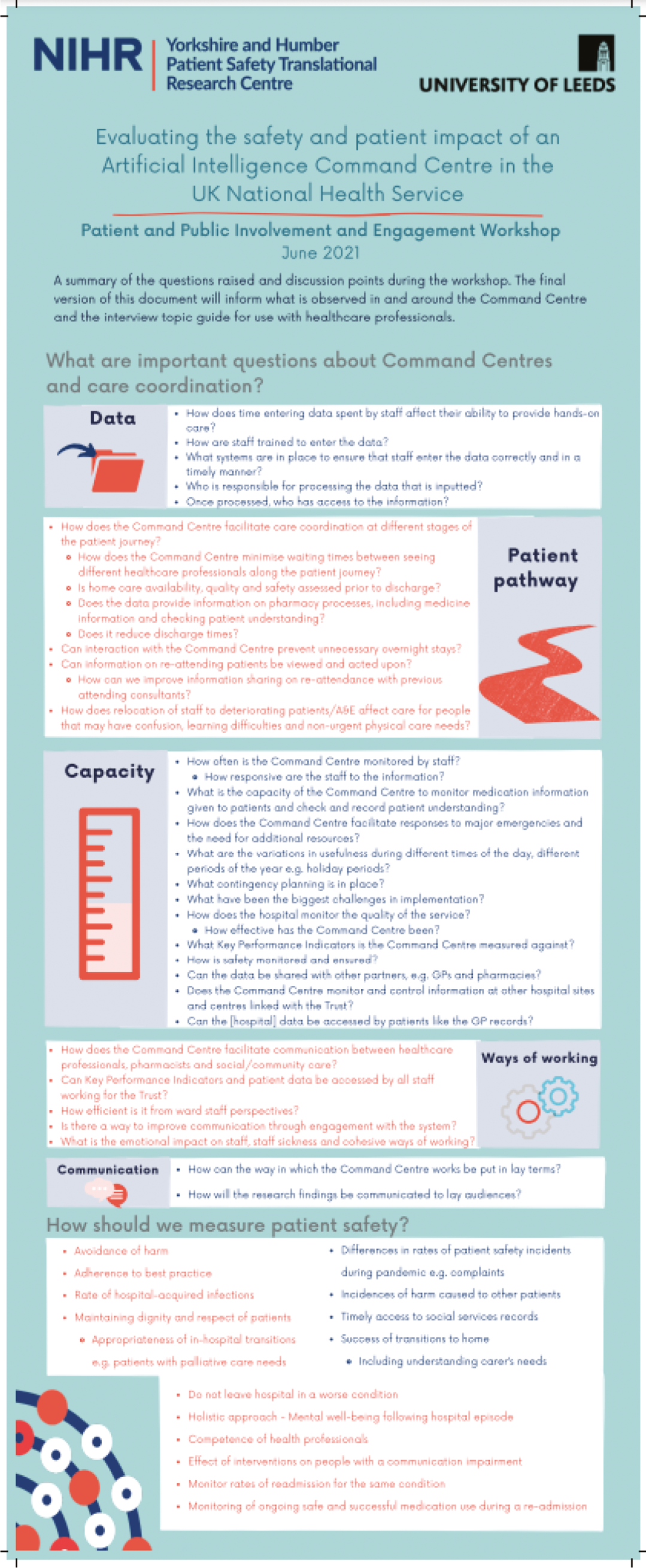
Another outcome of the workshop was the lessons learnt, which we integrated into the planning and delivery of our second workshop:
-
Minimise jargon and abbreviations.
-
Explain and check understanding of technical terms.
-
Provide pre-meeting reading for participants that details the agenda for the day and summarises the content that will be discussed.
-
Provide pre-meeting checks of IT equipment (perhaps days earlier or on the morning of the workshop, to allow time for remedies).
Workshop 2: extending workshop
Our second workshop in the PPIE workstream intended to:
-
communicate the outputs of the research to the patients and public who are the ultimate beneficiaries of the work
-
continue the collaboration with patient and public by integrating their perspectives into interpretation of research findings
-
co-produce a communication plan.
Components for our draft communication plan were:
-
A list of messages – What messages needs to be communicated?
-
A list of stakeholders – Who needs to know about these messages?
-
A list of justifications – Why do these audiences need to know?
-
A list of media for distribution – How will we reach these audiences?
The scope of the second workshop was constrained to informing the communication plan rather than enacting it. The communication plan was summarised in an infographic (Figure 4).
FIGURE 4.
Infographic produced by PPIE Workshop 2: extending workshop.
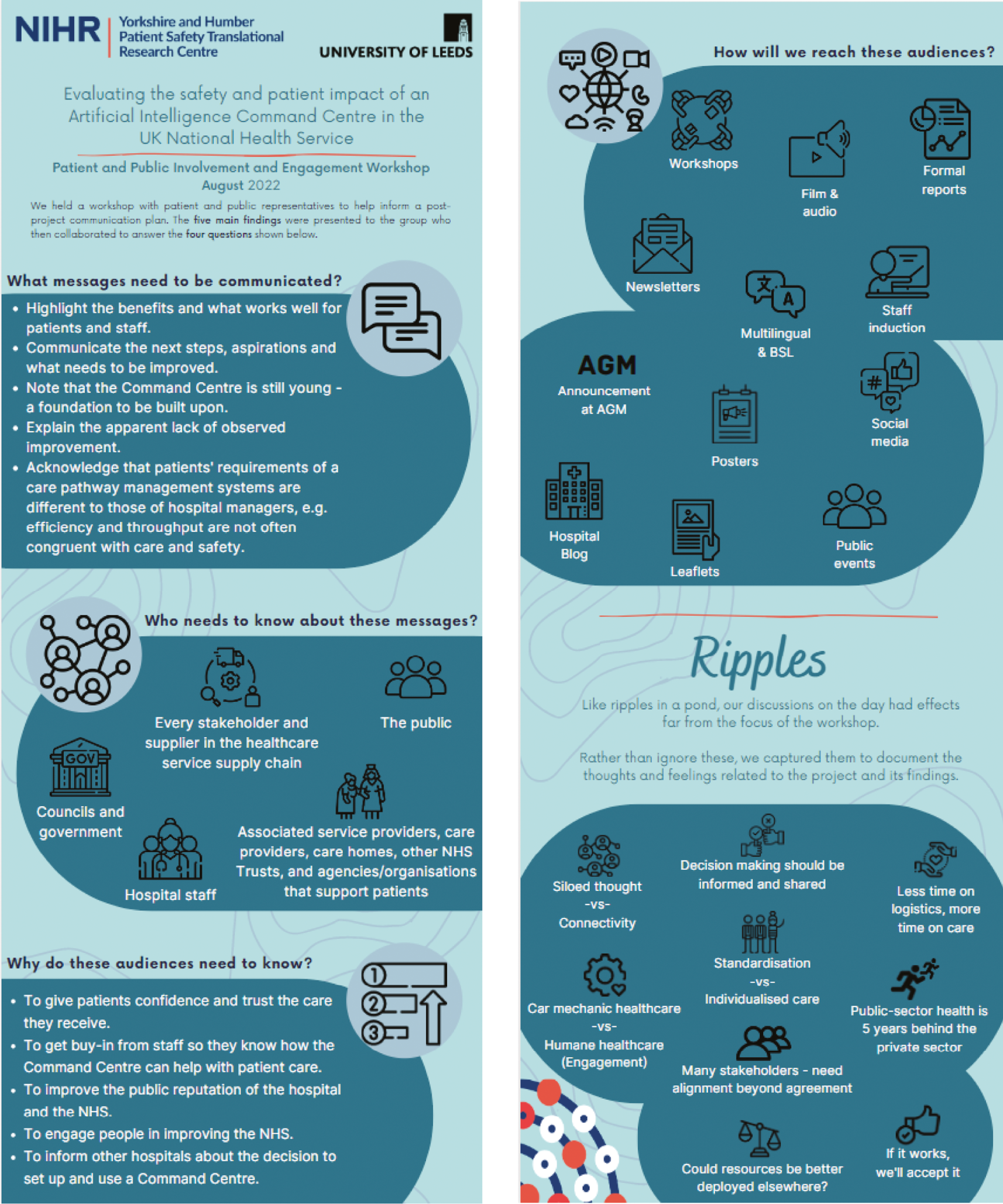
Chapter 4 Cross-industry perspectives
Rationale for a cross-industry perspective
In the introduction, we discussed some of the historical background to the CC approach and its use in military, government and industry, particularly in safety-critical industries where real-time, system-wide decision-making can be required to avert disaster. Our aims for the project included looking across these other industries to elicit perspectives that could help to contextualise the Bradford Command Centre and more generally the development of hospital C2 technologies. In this chapter, we summarise the results from our cross-industry review and describe dominant models for C2 and their adoption in other industries, and use these to surface emerging themes that may have implications for NHS hospitals interested in the CC approach.
Defining command and control and the ‘command centre’
Various definitions of C2 exist within organisational systems and research communities. A review of the literature describes C2 as ‘the recursive process of sharing the intent of decision-makers across organisations, turning intent into action, monitoring success, and adjusting goals to meet changing needs’. 11 C2 is understood as the process taken by teams and organisations to complete a shared goal, sometimes viewing this process as an information-processing chain as data flow across the organisation, the operating environment and the CC. 77,78 The systems involved are sociotechnical collections of human interactions, social norms and built technologies that enable this process. 78,79
Dominant models of command and control
The concept of C2 is often categorised as a sociotechnical model. There have been various proposed models of C2 across the literature. Stanton et al. provide a pertinent overview of a number of alternative models. 77 They state that C2 can be characterised with reference to, and understood from the following modelling perspectives, as:
-
an (open) system of interacting parts
-
a sociotechnical system of human and non-human agents and artefacts
-
a distributed system
-
a real-time system
-
an ‘intelligent’ system.
It is important to note that the authors suggest that the following models represent the evolving thought on C2 over the past two decades.
Process models
Adapted from Lawson’s model, the Process Model is rooted in the idea that the CC seeks a desired state. 80 Data are obtained from the environment, processed and then compared with the desired state. Any discrepancy between desired state and current state leads to the CC making decisions about how to rectify this, actions are taken and communicated to their own forces. The issues with this model are that the desired state is defined and/or described by quantitative, discrete data. It is unclear how the model would cope if the actual state was highly uncertain or if changes in the environment led to consequences outside of the limits of the discrete state. ‘The model does indicate the central issue that command can be thought of as working towards some specified effect or intent but suffers, however, from its apparent reliance on a deterministic sequence of activities in response to discrete events.’77
Contextual models
Arising from Hollnagel’s Contextual Control approach, this model describes C2 as ‘a constructive operation where the operator actively decides which action to take according to the context of the situation together with his/her own level of competence’. 81
Different modes of control are offered under this model:
-
Strategic Control – the ‘global view’, where the operator concentrates on long-term planning and higher-level goals.
-
Tactical Control – characteristic of a pre-planned action, where the operator will use known rules and procedures to plan and carry out short-term actions.
-
Opportunistic Control – characterised by a chance action taken due to time, constraints and again lack of knowledge or expertise and an abnormal environmental state.
-
Scrambled Control – in response to a completely unpredictable situation where the operator has no control and must act in an unplanned manner, as a matter of urgency.
Time is a main function of C2 in this model: with more time available the operator perceives, they can gain more control of the task/situation. Stanton et al. found that transitions between control modes were consistent with this model. 82
Decision models
Based on the works of Rasmussen and Vicente the Decision Model comprises two parts of the decision ladder, the observation of the current system state after the detection of the need for action and the planning and execution of tasks and procedures to achieve a target system state. 83,84 The ladder contains two types of nodes, information-processing activities and knowledge states.
Shortcuts can be applied to the ladder. For example, a diagnosis of a current system state signals a procedure to execute. Stanton et al. note ‘The path in which the operator moves through the ladder is dependent on a number of factors including: their workload, experience and familiarity with the current task’. 77
Functional models
Smalley’s85 functional model of C2 identified 7 operational and decision-support functions and 10 information-processing activities (primary situation awareness, planning, information exchange, tactical situation reports, current situation awareness, directing plan of execution, system operation, system monitoring, system status and internal co-ordination and communications).
This provides a distinction between command (command and planning, navigation and piloting and tactical decision-making) and control (communications, system monitoring, system operation and operational co-ordination), which are separate but connected. These occur in two different ways: internal operation of the system (command and planning, communications and system monitoring) and interfacing with the external environment (navigation and piloting, operational co-ordination and system operation).
Stanton et al. conclude ‘in contrast to the other three models, Smalley’s model offers much higher fidelity for command and control’. 77
Command and control in safety-critical domains: a narrative review of the literature
Command and control in defence
The concept of C2 is inherent in the operation of military organisations. Despite this there is no ‘authoritative formal UK or NATO definition for it’, which often results in a concept merged from the definitions of C2. 86 In a Joint Concept Note outlining, and titled, the Future of Command and Control, the British Ministry of Defence (MOD) offer a definition that describes C2 capability as ‘a dynamic and adaptive sociotechnical system configured to design and execute joint action’. 86
While the offered definition is comprehensive, the MOD also state that their approach to C2 has stemmed from industrial-era warfare and does not reflect the complex modern role of defence and military operations. In order to develop and progress, it is suggested that core thinking around C2 evolves with a view to increasing the agility of C2. Agile C2, or Edge C2, allows for an adaptive and responsive approach more relevant to the context of the operation or work at hand.
Edge C2 is suggested to be the most agile and advanced approach to C2 but is not the only approach. Other C2 approaches are named as conflicted C2, de-conflicted C2, co-ordinated C2 and collaborative C2. 86 It is important to note that these approaches are not mutually exclusive; they will interact across different organisations, and the different approaches will be appropriate for different situations. The ability to move between these as necessary in an informed and timely manner is dependent on the agility of the organisation and their ability to use de-centralised and adaptive C2 to improve synchronisation and maintain a drive towards unity of purpose.
In order to increase agility, the organisation requires the ability to collect and distribute data and transform them into intelligence for rapid decision-making across multiple domains and missions. 86 This highlights the need for sociotechnical integration in which people, structures, processes and technology are developed to be able to adapt to deliver a tailored system to meet the needs of a specific environment and context. Advances in technology will likely lead to the most significant changes in approach to C2. Development of a single information environment will enhance evidence-based decision-making at speed while allowing for humans and technology to be parts of a team. 86 Integration and use of interface technologies (i.e. command walls) will provide more natural interaction and improve situational awareness.
The introduction of technologies in this domain has already seen a shift in approach to operational control. Walker et al. suggest that there is a movement away from traditional C2 towards a network enabled capability (NEC) model. 87 In their study examining human performance under NEC and C2 systems, they present C2 as having a tight distribution of information in which ‘the commander is the only individual with an overall view of the situation’ and fire teams have a local view but otherwise work in isolation: ‘Everyone does not know everything’. 87 C2 also operates under a hierarchical structure in which individual roles can speak with the commander but not with each other and all decision-making rights rest with the commander, who could allocate autonomy, authority and discretion by defining and scripting the tasks of lower roles. Conversely, NEC has a broad distribution of information where fire teams receive regular situation updates from the system operator and can interact with their counterparts: ‘Everyone knows everything’. There is no communications hierarchy and collaborative working is encouraged and is facilitated by outcomes-based instructions and communications infrastructure.
Their findings suggest that utilising a traditional C2 structure resulted in accelerated task-completion times; however, this comes at a cost to other factors such as accuracy. While utilising a NEC structure was slower, there was a higher degree of accuracy and stability. The authors suggest that this trade-off is worth it when operating in a context with ‘inherent complexity, dynamism and asymmetry’ and allows the organisation to undertake more complex processes of optimisation; however, further research is warranted. 87
An alternative approach to integrating new technologies into a C2 model was reported by Hansberger and Barnette. 88 The United States Army Research Laboratory developed a model called ‘Command, Control and Communication: Techniques for the Reliable Assessment of Concept Execution’ (C3TRACE). This model represents ‘different organizational structures, individuals within those structures, the tasks and functions performed within a task, and the communication patterns between individuals in an organizational structure’. 88 While this model puts specific focus on communication in addition to C2, the key concepts remain the same as operator communication, workload, task times, situation awareness and decision-making were all reported variables. C3TRACE maintains a hierarchical structure but adopts a more flexible and adaptive workload-management process to facilitate information flow and reduce rates of dropped tasks. This model presents a more flexible and responsive form of C2 but does not go as far as the NEC model with regard to hierarchy of decision-making and instruction.
A common approach to understanding C2 systems is to utilise the Event Analysis for Systemic Teamwork (EAST) methodology. 89–94 EAST is described as ‘a macro-ergonomic method for extracting large scale systems level data on the emergent properties of C2 scenarios’. 79 The method does this by analysing the information flow and activity between three main network representations: Task Network, Knowledge Network and Social Network. 79 This provides insights into the participating agents and how they are arranged, how technology facilitates information flow, what tasks are enacted in response to which overarching goals, and the role of situational awareness. Situational awareness is one of the main focuses of EAST as it is defined as ‘one of the key emergent properties from command and control scenarios, and one of the major determinants of decision superiority’. 79 In Walker et al.’s research into applying EAST to emergent properties of C2 in a NEC scenario it was clear that situational awareness was dictated by the constraints placed on it by the facilitating communications technology and distributed among both social and technical agents within the system. 79 The social agents under this system had a degree of self-organisation provided by the distribution of situational awareness and cognition in tandem with the ability to adapt the technical agents to suit their needs and preferences. Eliciting these emergent properties of C2 provided insight into NEC C2 while also demonstrating the applicability and relevance of applying the EAST method to analysing C2 scenarios.
Command and control in transport
Systems of railway network control do not routinely use the language of C2 to describe the domain and work done. However, Farrington-Darby et al. ’s study elicited key features of the domain and there are obvious similarities with C2 systems. 95 For example, the study found that controllers manage a complex system with no direct interface and to do this they have to interpret the incoming data and form a mental model of the system. In C2 language, this would be referred to as situational awareness. At the time of the study, controllers were separated into distinct groups and located in control centres that varied in both physical set-up and make-up of the team present. There is some colocation of different roles, but this varies across different control centres, consequently a key part of the work is understanding the social distribution of both skill and knowledge across these teams. This requires not only expert knowledge of the processes and practices but also expert knowledge of the social relationships and responsibilities in the domain. Decision-making is distributed to each controller, who uses heuristics and guidance rules to aid their decision-making in order to achieve the high-level goals of the railway, for it to run safely and efficiently. It was also found that part of managing the railway involved responding and adapting to sudden increases to ‘full or overload situations’ resulting in a variable workload, some elements of which are safety-critical. 95 Operating successfully under these conditions requires resilience of the system and C2 agility.
The above findings were elicited using a naturalistic and ethnographically based field study. This approach allowed the researchers to observe the subtleties of the control room and understand the social elements of the work and the contextual nature of expertise in rail control centres. 95 The relevance of this social expertise was an unanticipated feature of the controller’s work that the researchers state is an example of the exploratory value of ethnographically derived methods.
Air traffic control (ATC) is another example of a transport domain where C2 systems are present. Walker et al. describe the C2 features of the work done by ATC as an example of distributed cognition in which the computational states (processes and knowledge used to achieve the goal) interact with the representational states (the environmental contributions to the total system), resulting in a highly complex and adaptive level of functioning. 96 As seen in other domains, situational awareness plays a key role within the system’s functioning. In this context, the controller forms a ‘picture’ of the airspace that arises from the interaction of several components. These components include designed parts of the system such as radar displays and communication channels and technology and incoming situational information such as a new aircraft entering the controlled airspace. The authors posit that applying distributed cognition to C2 scenarios requires a shift in approach to situational awareness from the traditional notions of individual situational awareness to the notion that situational awareness sits across the whole system; this includes the technical aspects of the sociotechnical system. 96 Additionally, it was found that the ATC domain has a diverging hierarchy that splits into groups further down the chain of command. This holds the benefits of a centralised hierarchical structure but allows for the flexibility and rapid response of localised decision-making which helps remove any delays that could occur from having to disseminate the relevant information throughout the hierarchy. 96
In the above research, the researchers adopted the EAST method seen used within the military domain. The paper describes using this method as going beyond ethnography. The strengths of an ethnographic approach are discussed (e.g. can be used to understand how information is used to support decision-making) alongside its drawbacks. Three overarching drawbacks are mentioned: the outputs from an ethnographic approach are often highly discursive and may not be easily reconciled with a non-social science audience, the requirement of being ‘imbued’ in the culture of the scenario can be incompatible with objectivity and validity in measurement, and their analyses are not always easily amenable to generalisation. 96 The researchers state that the EAST method can capture similar phenomena in a way that is appropriate and relevant to the designers of such systems by producing a systems-level description of the scenario. This method creates network diagrams that cover the social networks between agents, the dispersion of these agents, and a representation of the knowledge network in the domain that all include the non-human agents (i.e. technology) and the media that facilitate their communication. By doing this, the analysis has the following strengths: it avoids bias by focusing on objective and manifest phenomena, it is applicable to any domain and is comparable across and within domains, the outputs are graphical and easily interpreted, and it is underpinned by considerable detail that can be explored further. 96
In an article aimed at revealing potential areas for further improvement in reliability in the public transport domain, the dynamics and processes of operations control centres are discussed. 97 The authors focused their research on operations control centres in Germany and Singapore and their daily processes and procedures after the occurrence of an incident within the public transport network. Their findings were elicited through ethnographic methods: interviews, observations and documentary analysis.
One area highlighted for improvement by the research was communication. This includes both internal (between dispatchers and drivers) and external (with emergency services and passengers) communications. Internally it was recognised that incident situations can be challenging for drivers and dispatchers, and this negatively affects the level of communication between the two, which impacts the situational awareness within the system. It was suggested that additional training could be of benefit to the drivers and dispatchers and expanding the functionality of onboard computers to provide translations/subtitles of the conversations could help break down language barriers within the diverse workforce. 97 External communications are handled by dispatchers and in both instances (communication with emergency services and communication with passengers) could benefit from additional technology input to facilitate the sharing of information. Highlighting this area shows the importance of sharing information to aid situational awareness and how fundamental this is to the public transport operations system. It is also stated that the better the communication is, the better the dispositive measures are, which bolsters the resilience of the system. 97
The second area for improvement was the role/presence of automation in the domain. An increase in automated processes is suggested by the authors to both reduce the workload of the dispatchers and increase the quality and accessibility of relevant information. This would also be done by expanding the use of technology in the work done. The positives of better information-sharing and thus improved situational awareness are already apparent. The proposed automation would reduce the number of calls the dispatchers have to do in response to an incident, which gives them more time to concentrate on the dispositive measures needed and mitigate the negative effects on the service; this improves the resilience of the system. 97
The final area for improvement suggested by the authors was in the role of planning in the domain. It was recommended that the robustness of the timetables was evaluated. This has to do with the availability of services and the availability of replacement vehicles and staff in response to incidents that take staff or vehicles out of action. This availability is shown to have a large and significant impact on how negatively the incident can impact the service if no replacement is available. This recommendation is about the presence and quality of situational awareness in tandem with appropriate allocation of resources and how this can facilitate a timely response to a disruption in the service and maintain the resilience of the system in the highly dynamic task of incident management in the public transport domain. 97
Command and control in the power industry
Electricity power grid management is conducted from a central location, a CC, for real-time monitoring of grid conditions, assessing grid stability and maintaining system frequency. 98 Due to the physically dispersed nature of the power grid, situational awareness is essential for operations. This is achieved in this domain through technology that provides multiple streams of information such as spatial and geographical information, voltage levels, temporal information, functional information, substation information. Ready access to this information improves the operator’s capabilities and confidence to make timely and correct decisions.
Decision-making is informed by intelligent systems that perform model-based analytics which can quickly identify and recommend solutions to problems that may arise. The information from these analytics is readily available to a range of staff members (operators, engineers and managers) so that they can jointly assess a problem condition and together decide on the actions to take. This is a more collaborative decision-making process but still retains the traditional hierarchical structure we see under C2 models. Using model-based analytics further introduces the non-human agents seen in other forms of distributed situational awareness and distributed cognition above. These advances in technology adopted in a centralised CC provide grid operators with ‘wide-reaching visibility into the status of the grid, as well as the ability to predict and plan for potential problems’. 98
Salmon et al. studied this domain by utilising the already seen EAST method. 99 Their application of this methodology found support for distributed situational awareness between both human and non-human agents. It was found that by interacting with the non-human agents the operators could effectively and accurately update their individual situational awareness. There are notable differences in the form and level of individual situational awareness in this setting; however, these differences were observed to be complementary. For example, the CC operative held a very high-level overall picture of the scenario, whereas the field agent’s individual situational awareness was primarily focused upon the work they were engaged in at the time, working towards their own individual goals. This highlights the benefits of co-locating different roles and their respective pools of expert knowledge. Communication between centralised operators and field agents was found to be intrinsically structured by the knowledge that comprises the team’s distributed situational awareness, thus effectively coupling distributed systems. 99
The nuclear industry has been subjected to a vast amount of human factors and ergonomics research over the last 40 years and has benefited from this in areas such as the design and evaluation of processes, procedures and control rooms. It is arguably the source of safety culture that has highlighted the importance of management and organisational factors for the safety of nuclear power operations, and this has since been adopted by other safety-critical domains. While, like domains discussed above, the nuclear domain does not routinely use C2 language, it is clear that the key components of human factors as they pertain to safety in this domain have significant overlap with C2 terms and concepts.
A review on human factors engineering research into nuclear safety found that in research looking at groups and teams in nuclear operations, communication of the teams was a central focus and has seen increasing interest from 2010 onwards, looking at the communication structure in relation to operators’ activities with particular focus on overt behaviour and corresponding underlying cognitive processes. 100 This has been done by modelling team communication with a novel speech-act coding scheme to understand the difference between operator intention and enacted behaviour. This has included real-time feedback of individual actions to the wider team in order to enhance team situational awareness and increase team cohesion. Team situational awareness has also been adapted into computer-based systems with a view to improving team performance. Team resilience has seen a surge in focus in recent years, which has aimed to examine a team’s ability to adapt, co-ordinate and respond in abnormal operating conditions. This research has, however, been mostly conceptual in nature.
Research into the individuals involved in the operation of the nuclear plant has seen an increase in the areas of human error, human performance and situational awareness. Human-error research was prominent in the 80s and 90s, halted after 2000, but has seen a resurgence in the last decade. Cause classification methodologies have been used to try to identify contributing factors and provide explanations. Human performance research has highlighted the importance of experience and expert knowledge and their impact on executing tasks successfully. Situational awareness has seen greater focus since 2000 with the introduction of digital technologies spurring further interest in individual situational awareness. This has been recognised as an important factor when introducing increasingly advanced digital systems to aid operations. This importance and focus have prompted the creation of situational awareness reliability assessments to predict operators’ performance and reduce the chance of errors due to deficiencies in situational awareness. 100
Recently there has been research incorporating safety theory and methods from other domains into nuclear safety. For example, Teperi et al. have introduced a Safety II tool, a concept seen increasingly in health care. 101,102 This method highlights both successes and failures of operations in the nuclear industry to elicit a more accurate description of human-factor issues affecting operational events and provides learning related to resilience. The use of Safety II in the nuclear domain is novel and further research into its applicability and validity in this domain is needed.
Command and control in emergency services
While emergency services are closely linked to acute health care, they operate in different contexts and ways of working. Both situational awareness and distributed cognition have been researched in this domain using interviews, observations, documentary analysis and literature reviews. 103,104
Emergency medical dispatch, or ambulance control, is one such service. These services often operate regionally and independently, with size and structure varying depending on the location and area covered. Broadly, their work has two aspects: ‘call-taking, where calls for emergency medical assistance are received and prioritized, and controlling, where the most appropriate ambulance is dispatched to the emergency and ambulance resources are optimized in their areas of operations’. 104
Situational awareness in this context is twofold: operators maintain situational awareness of the control room (e.g. level of resources available, current allocation and location of ambulances), while also maintaining awareness of the wider world (e.g. other emergency services, local hospital capacity, major accidents). This awareness of the situation is critical to successful operation as ‘decisions are not made in isolation, but within the context of a dynamically changing situation’. 103 Senior operators utilise an ‘information hub’ strategy that allows them to be aware of changes in the areas under their control. Operators use situational awareness to form a mental model of the ambulance network and locations of allocated ambulances. It was reported that at times the operators did not use the mapping system they had to inform their decisions as they had an expert level of knowledge based on relevant static information (e.g. road network of their area) and could redirect ambulances based on this knowledge. Overall, their situational awareness has been described as a combination of this static information, dynamic information and a temporal component that they needed to keep track of. 103
The role of organisation structure has also been a focus within the emergency services domain. Ji and Ren discuss research into the application of C2 organisation theory to support emergency communication support organisation. 105 Broadly, the authors highlight support for the adoption of C2 systems. They state that the theory of C2 organisation can be applied to solve problems in the structure of organisations. Acknowledging the need for agility in response to dynamic mission environments, it is suggested that using C2 theory to establish the organisation structure and in parallel create organisational adaptation adjustment methods allows for a responsive and resilient communication support organisation. 105 However, it was found that using a three-stage method was too sensitive to a dynamic environment, resulting in wasted resources when utilising the adaptation methods. This highlighted the need to develop a more robust organisation structure that requires fewer adaptation methods in the face of dynamic situations. Further research is needed to develop the robust organisation structure but the authors state that the application of C2 organisation theory can help to ‘enhance the performance of emergency communications support command, to complete various tasks with high quality’. 105
As seen in other domains, C2 in emergency service operations has been studied using social network analysis. Houghton et al. used this method to elicit the differences in systems for fire services and the police. 106 Using Dekker’s command structure terminology, it was identified that the fire service adopted either distributed or centralised networks. 107,108 This was due to the need to have a central focus for conformation management but also allow for rapid response; this was more centralised in incidents where managing a mass of diverse information was required. 106 This demonstrates a need for agility in the C2 system of fire service response. In contrast, the police networks best matched the split network definition as the design arises from ‘procedures for eliciting well-defined information and clearly defined responses’. 106 The more procedural and legal nature of policing is likely responsible for this due to the need to maintain a log of the activities performed under police command. Distributed networks allow for more rapid response as agents work independently but the main advantages of using a centralised network are to manage information flow and co-ordinate response. The use of social network analysis has not only elicited this information but has also allowed the authors to represent this graphically for quick interpretation while also to reference both the emergent scenarios and the limited set of archetypes that are well defined. This method also allows for quantitative analysis provided by mathematical social network analysis techniques which provide subjective impressions from quantifiable statistics. Using this approach, even with relatively small networks and incidents for study, allowed the authors to identify issues relevant to C2 systems in general, such as ‘the balancing of speed of response against information quality and choosing between centralised and distributed command models’. 106
Command and control in health care
Although the literature on C2/CCs in health care is still at an early stage of development (especially in terms of robust research), there are already some emerging examples of C2 and CC use in the scholarly peer-reviewed literature. Most recently, C2 has been rapidly implemented in some settings in response to the COVID-19 pandemic. For example, Bruno and Petscavage-Thomas report on the introduction of a departmental CC for a radiology department in a US hospital in a response to change in ways of working during the peak of the pandemic. 109 Their CC included a well-defined hierarchy of roles and responsibilities that considered the need for some staff to work remotely due to the temporary social distancing requirements introduced at the time. It was ensured that the five staff members on-site covered all subspeciality areas needed and had a colocation of roles and expert knowledge. Additionally, the CC acted as a central communication hub and point of contact for the department. The centralisation of communication was aided by digital technologies, both in terms of ensuring the in-hospital communications came to this central point, but also so that staff working remotely had access to the relevant systems and information to continue working.
One example of this was the ability to hold daily meetings online both within the department and with clinical leads from other departments. This maintained situational awareness across the team and ensured that they could utilise all staff to distribute the workload and function effectively despite the novel remote-working requirements. Introducing a CC in response to the significantly abnormal operating environment (the pandemic) was deemed a success and responsible for the department being able to continue its clinical operations seamlessly. 109 In addition to aiding in the continuation of routine operations, using a CC also saw a sharp drop in safety incidents, ˂ 10% of prior levels, which the authors attribute to being able to communicate with other departments more readily (i.e. online), which led to more rapid identification and resolution of issues. The authors state that their ‘Command Center model enabled this success, which rested upon a robust IT infrastructure as well as clear, decisive leadership, with a high degree of autonomy afforded to each division, and open lines of communication at every level between all stakeholders’. 109
Successful use of C2 principles in response to the pandemic has been seen elsewhere, such as the reported use in Hutchings et al. , in which ‘the diverse and complex clinical situation that evolved at King’s College Hospital during the COVID-19 pandemic required an agile and dynamic C2 system with effective communication mechanisms’. 110
The use of C2 principles in acute health care has not been exclusively tied to the pandemic. Franklin et al. ’s scoping review into the use of hospital capacity CCs found that there were numerous anecdotal accounts of these centres being widely used in efforts to improve hospital patient flow and safety. 76 These centres are defined as involving the colocation of inter-disciplinary workgroups, the use of real-time data integrated from sources such as EHRs, and the management of two or more processes tied to patient flow. This demonstrates a centralisation of both situational awareness and decision-making, informed by the colocation of expert knowledge.
Table 5 summarises the specific CC implementations in health care we found with their target operations and implementation models. Additionally, the types of evidence offered in the related articles are noted. All the examples shown have been relatively recent adoptions showing a growth in use and interest of a centralised C2 approach in health care. Apart from one centre (the radiology command centre), all the centres have been introduced to manage operational functions (i.e. patient flow) rather than managing more localised medical functions and care. 109 It is also clear that technology has a significant role to play in command centres and may bolster their appeal as intelligent systems can provide enhanced situational awareness across the hospital. Another key feature of these implementations is the colocation of different teams and disciplines. As seen across other domains, this is a common feature of CCs and increases the ease of communication and decision-making, providing greater agility and resilience to the operations under the control of the centre.
| Publication source | Command centre/system name | Target operations | Implementation | Type of report |
|---|---|---|---|---|
| Alhaider et al. (2020) ‘Distributed situation awareness: a health-system approach to assessing and designing patient flow management’9 |
Carilion Transfer and Communications Center (USA) | Patient transfer and transportation communication | Mission control model with colocation of services and an electronic throughput and flow software system | Description of implementation |
| Collins (2021) ‘Use of high-reliability principles in the evolution of a hospital command centre’111 |
Humber River Hospital’s Command Centre | Patient access and flow | Command centre with real-time data integrated from multiple automated systems with predictive analytics | Descriptive overview of conceptual development |
| Davenport et al. (2018) ‘Integrating high-reliability principles to transform access and throughput by creating a centralized operations center’23 |
Un-named operations centre located southeast USA | Patient throughput and flow | Collaborative operations centre with colocated departments/services underpinned by a throughput and flow software platform | Description of 3-year implementation programme |
| Kane et al. (2019) ‘Use of systems engineering to design a hospital command center’112 |
Judy Reitz Capacity Command Centre | Capacity management | Command centre with colocation of teams, automated visual displays of real-time data, predictive analytics, standard work and rules-based protocols and a clear chain of command and guiding tenets | System description with performance statistics |
| Morris and Carter (2015) ‘A blended transfer and communications center: designing a state-of-the-art mission control’113 |
Carilion Transfer and Communications Center (USA) | Patient transfer and transportation communication | Mission control model with colocation of services and an electronic throughput and flow software system | Description of implementation |
| Bruno and Petscavage-Thomas (2021) ‘Brief communication: A departmental “command center” to facilitate staff safety and patient care during the peak of the COVID-19 pandemic’109 |
Radiology Command Centre | Radiology care and communications | Centralised Command Centre supported by communications technology and remote-working staff | Description of model introduction and shutdown and reported impact on services during COVID-19 pandemic |
| Krennerich et al. (2020) ‘Mission control: the development and centralization of an integrated communication center to facilitate intra-facility and inter-facility patient flow’114 |
Un-named integrated communication centre | Intra-facility and inter-facility patient flow | Centralised multidisciplinary hub with high-tech monitoring tools, a hospital census dashboard, transport electronic medical record, real-time ambulance and flight tracking systems and cameras on critical hospital areas (e.g. helipads, elevator bays and entryways) | System description with performance statistics |
Emerging themes and implications for health care
This scoping review has found a strong body of research to support the efficacy of adopting existing C2 principles and theory in CC applications in health care drawing upon evidence and experience across various safety-critical domains. These CCs are often stated to aid in the key components of C2 that are important for a successful and resilient organisation and as such they have the potential to enhance the reliability and effectiveness of operations management in acute care.
As seen across the domains covered, the overarching areas in which CCs, and thus C2, can offer support and enhancements are situational awareness, decision-making and team structure and workload. These areas are all supported by digital technologies tailored to the work done in the respective domain and contribute to system resilience with the main aim of successfully delivering safety-critical operations reliably over time and in the face of dynamic risks and variations in the operating environment and system conditions.
Most articles attribute performance improvements to the physical and functional features of the centres themselves; this often includes the use of technology to generate and display real-time and/or predictive data in the centres. An additional feature that emerges when adopting a CC approach is that the implementation process usually effects process and policy changes in the organisation. This can be because the implementation process provides an opportunity to review existing approaches and make changes to align with the CC approach. The influence of C2 principles can be seen in these changes. This can include introducing new ways of working and workload distribution or adding new roles into the organisational structure altering the existing hierarchy of decision-making and responsibility. The authors note, however, that peer-reviewed evidence regarding design and efficacy is in its earliest stages and it is unclear what proportion of reported improvements are attributable to the physical and functional aspects of the CCs versus the process and policy changes within the organisation that often arise out of the implementation process.
While there is emerging evidence that the core concepts of C2 may be transferable to acute health care, it is worth nothing that it may not be appropriate to transfer the language of C2 into a healthcare setting. Alberts suggests that the term ‘command and control’ has become a ‘significant impediment to progress’. 115 He states that this language is restrictive and prevents exploration of new approaches to C2 that are truly different. Using an example from the term’s traditional origins, the military domain, Alberts states that the term ‘command and control’ is unsuitable for coalition operations due to the differences between organisations. 115 Albeit not directly comparable, a similar issue may exist in transferring C2 terminology to health care due to the arrangement of departments and the staff under their direct responsibility in conjunction with the culture of autonomy on the clinical front line. The term ‘command and control’ is deeply ingrained in traditional military organisations; introducing this terminology to a new domain with a different ontological outlook or culture could be met with significant resistance. It has been seen across other domains that the language of C2 is not always used despite the principles of C2 being clearly present. This may be due to the lack of transferability of the terminology, and it is possible that this limitation will also apply to acute health care.
Reviewing this literature has highlighted the importance of having a clear model of the ‘stable’ C2 system state that includes protocolised levels of response to increasingly risky deviations, providing the system with both resilience and agility. This means the system has multiple modes of operation that can be spontaneously switched between in response to the level of risk and demands of the situation or current system state presented at any given moment. Effective C2 implementations are characterised by a strong sense of shared situational awareness within a team with a shared focus on specific focal points for intelligence and intensification of this focus as the threat level increases. System resilience is maintained in these implementations through simultaneous responsive and anticipatory strategies with variable resource allocation both for proactive planning for expected deviations and events with varying timescales, and for reactive adaptations that arise in response to detected unexpected deviations within the C2 system state.
Chapter 5 Ethnographic and interview study findings
Data integrated within the ethnography
We conducted 78 hours of observations involving 36 staff members that included 22 opportunistic conversations with CC staff and compiled 100 pages of field notes between July 2021 and March 2022. A total of 19 interviews involving 16 members of key staff relative to the initiative (15 at study site and 4 at control site) took place between May 2021 and August 2022 and ranged in length from 14 to 71 minutes, with a median length of 38 minutes (9.5 hours). In addition, we reviewed 64 documents relevant to the CC programme at the primary study site.
Observed participants and interviewees were staff in varying roles, including staff with dual clinical and operational planning responsibilities. Participants had a range of clinical, leadership and management backgrounds. Roles included senior clinical leadership (e.g. Command Centre Clinical leads, Operational leads), senior hospital leadership and management (e.g. chief information officer), clinical site staff (e.g. Matrons, Patient Flow Coordinators), staff in various clinical and non-clinical roles hospital-wide (e.g. Ward managers, Transport managers) and industry partners.
The results presented are derived from analysis of field notes, document analysis and interview data. We outline the case description including espoused rationale, design of the system and planned implementation model, then provide a descriptive account of organisational behaviour linked to C2 based upon ethnographic study of the CC.
Descriptive case summary
The descriptive case summary presented below represents an attempt to define the CC system and programme from a sociotechnical perspective based upon testimony from key informants during the interviews and ethnographic site visits, supplemented by review of documentary evidence. Such a description is important for the evaluation in that it describes, in detail, the intervention of concern, including the technological, social and programme elements (i.e. how the change was implemented), in order to establish an intervention model for comparison/replication. The case summary includes the espoused aims of the programme, technological design, planned development and implementation process, and the observed routine human and organisational work undertaken as part of CC operations.
Espoused aims of the programme
Based upon interviews with programme leads and programme documentation, the intention of the CC programme at the study site was to bring together real-time data from a multitude of source systems including the Cerner Millennium EHR system, process those data using advanced algorithms and display new intelligence on custom-built analytic applications (tiles). Visualisation of data that represent factors that impact care and patient throughput from a C2 and hospital oversight perspective would provide better understanding of current operational pressures than was currently available:
The main aims from a command and control and hospital oversight perspective were to give that understanding of what was happening from front to back door in a seamless way and the way that it was set-up originally was for the site team to have a visual aid for what was happening down in A&E, on the main hospital wards and also from a discharge point of view, so flow of patients move seamlessly from one area to the other.
Senior clinical leadership, 6/1
Remote access to the tiles was intended to support prioritisation of patient-related tasks at service or ward level, for example:
The ward link tile should be used for whatever that ward wants to call it, ward rounds, huddle, where you quickly flick through every patient and say, ‘right we’re going to see them first because they’re the sickest, but then actually they’re based on EDD, these ones are due over to go today so we’ll see them next, and then we’ll see all this lot in the middle’ and use that meaningfully.
Senior clinical leadership, 2/1
Design of the command centre technology: technical infrastructure and development
Key system components included a cross-system data feed that integrates data from all sources, a third-party data integration engine that converts data for display against the metrics and alerts displayed in the CC, visual display of data on tiles in the CC where each tile has a specific operational theme that can be filtered in different ways to support identification of issues and action and remote tile access across the hospital.
Development followed a human-centred design in the sense that each tile has a tile owner with expertise in the particular clinical areas that the tiles refer to and they worked closely with the developers to develop specifications. High-level ideas and priorities for development were informed at executive level:
The executives decided that they wanted a capacity snapshot, an ED status, the transfer tile, the three that were mandated from the executives at the time of purchase, the other ones were use cases brought forward by people in the organisation to say these are areas of concern where we think that the software would help us.
Senior clinical leadership, 1/1
… and through design sessions attended by the hospital management team:
All of the entire management team would’ve been invited. That kind of gave us the high-level ideas and the high-level priorities and then from there we got together all of the people involved in that topic to start co-design, what’s your real, what’s really your problem, not so much why doesn’t it work although I’m sure that came up, but what’s your problem and then what would help you and then how do we solve it.
Senior hospital leadership, 1/1
The CC system itself consisted of nine tiles consisting of real-time information and alerts (update approximately every 3 minutes) for patient care and intervention across the hospital site. The tiles are displayed on a Wall of Analytics in the CC room and can be accessed from desktops, mobiles and tablets linked to the hospital intranet. There are ongoing software development iterations to refine the tiles and their components. The main functions of the tiles are shown in Table 6.
| Tile name/date went live | Function |
|---|---|
| 01 Capacity snapshot | Visibility of inpatient bed capacity and demand across the hospital; provides users with a holistic view of the inpatient ward details such as census, occupancy, blocked beds, dirty beds, clean beds, available beds, targeted beds, transfers and discharges |
| 02 Patient transfers | Identifies patients who are waiting to move to a different care setting; view of the matching beds and the status of the beds that have been reserved |
| 03 ED Expediter upgraded in January 2022 |
Current operational state of the entire ED |
| 04 Discharge tasks | Identifies outstanding tasks necessary to complete patient discharges from the hospital |
| 05 Care progression | Identifies inpatients with outstanding tasks that may be causing delays to their care pathway |
| 06 Patient deterioration | Identifies patients with deteriorating NEWS2 scores and visible oversight of acuity at ward level |
| 07 Right patient right place | Displays inpatients who are outliers |
| 08 Ward link | Displays a ward-level summary of all alerts, tasks and risks related to the patients in a chosen ward |
| 09 COVID-19 June 2020 |
Visibility into demand and critical resources required to treat disease-specific patient population |
Staff reported some deviation in function from the original intention regarding certain tiles. CC staff reported that the care progression tile was not used as intended as ‘what that’s displaying we get through so many other tiles anyway’ (Senior clinical leadership 2/1) and that issues with data quality impacted ability to make use of the tile: ‘Data quality issues means that it is not as useful as it could be’ (Senior clinical leadership 6/2).
Human work in the Command Centre
Staffing and roles
Staffing in the CC comprised the following senior strategic roles: Chief Operating Officer, Director of Operations Unplanned Care, Deputy Director of Operations Unplanned Care, CC Medical Director, Clinical Lead for Command Centre and Patient Flow (Senior clinical leadership 1/1). The original intended design comprised staff in varying roles, including staff with dual clinical and operational planning responsibilities consisting of a CC Medical Director, a Clinical Lead for patient flow and the hospital site team. At the start of the evaluation period, 22 members of staff worked in the CC. Their roles and responsibilities are shown in Table 7.
| Role | Responsibilities |
|---|---|
| Command Centre Medical Director | Executive-level leadership and management of all operational, developmental and strategic matters relevant to the CC |
| Command Centre Clinical Lead | General Manager and Lead Nurse for the CC and patient flow |
| Clinical Site Matrons | Day-to-day functioning of the CC including managing patient flow and teams of staff |
| Clinical Patient Flow Manager | Support CSM in hospital management and managing teams of staff |
| Patient Flow Coordinators | Support management of patient flow and escalate delays |
| Deputy Director of Operations | Executive-level leadership and management of strategic and daily decisions relevant to hospital operations |
| Emergency Planning Officer | Support leadership with resilience planning and emergency response |
| Transport Coordinator/Admin | Responsibility for co-ordinating transportation of patients and call-handling in the CC |
| Virtual Diagnostic Ward Coordinator | Co-ordinate patient flow through virtual ward |
The Medical Director is a medical doctor operating at executive level providing leadership and management of all operational, developmental and strategic matters relevant to the CC and its workforce since July 2019; they generally work in the CC 2 days per week, rotating in their role as Emergency Consultant Physician. Activities while in the CC include review of patient notes (and in some instances re-assessment of patients) whose wait time for a bed has breached (or is about to breach) key targets (identified through the ED expediter tile) for acuity and appropriate placement; review of patients notes ready for discharge that have been identified (through the ward link tile) as having outstanding tasks pre-discharge. This may include identification of a failure to update notes with completed tasks and a follow-up phone call or visit to the ward to prompt staff to discharge a patient or to carry out/prompt task completion related to the delayed discharge. Review of right patient right place tile to check for number of outliers and that they have been reviewed.
The Clinical Lead for CC and Patient Flow has been a General Manager and Lead Nurse for the CC since December 2019 and is present in the CC most weekdays. Also supports as Site Matron in response to low staffing levels. Has multiple roles within the hospital organisation, for example, manages the service side of the bed bureau, mortuary and multiagency integrated discharge team. Registered nurse who provides clinical input at ward/service level. Typical activities during the day include review of right patient right place tile to check for number of outliers and that they have been reviewed. The Deputy Director of Operations (or other nominated senior leadership role responsible for hospital management) is based in the CC weekdays.
Senior Clinical roles included Site Matrons (NHS Grade 8 +) acting as clinical site team lead for each shift responsible for managing the patient flow team, administration staff, virtual ward staff and bed bureau. A Grade 7 experienced nurse’s typical day starts with filtering the discharge tile for confirmed discharges for the day. This directs their attention to specific wards with confirmed discharges. The Site Matron visits the wards from around 09.00 hours to ensure that the patients are being prepared for discharge and to identify what can be done to assist them departing in a timely manner so that they can get early capacity. They return to the CC around 11.30 hours to compile the mid-day Situational Report (SitRep). Information from the capacity snapshot tile is used to manually populate the SitRep. This information is compared with information on the transfer tile and ED status to gather a complete picture of demand versus capacity.
Other operational roles included the Virtual Ward Coordinator. The Diagnostic ‘virtual ward’ was an earlier, successful intervention to improve patient flow and the patient experience by allowing low-risk patients to be physically sent home from hospital prior to being fully discharged as a patient. Patients transferred to the virtual ward remain under the care of the hospital until remaining diagnostic assessments are complete. The approach has proved popular with patients and reduces demand for in-hospital beds and resources.
Working routine
The CC operates 24 hours a day, every day. Staff work in 12-hour shift patterns. Typical staffing levels during the day are the Clinical Lead for patient flow, two Clinical Site Matrons (with the more senior staff member operating as shift leader), a Clinical Patient Flow Manager, a Patient Flow Coordinator, a Virtual diagnostic ward Coordinator and a member of Administrative Staff/Transport Coordinator (Senior clinical leadership 2/1; Field notes 1). The Medical Director operates in the CC between 08.00 and 16.00 hours 2 days per week and the Deputy Director of Operations is situated in the CC daily.
In terms of the observed daily routine, a typical morning in the CC starts with a handover at 07.30 led by shift leaders who assume oversight and responsibility for patient flow. Content is mainly focused on bed availability, projected discharges, ED SitRep and priority areas for staffing allocation. Figures are recorded onto a written pro-forma that is updated throughout the day as new information comes to light (Field notes 10). Working patterns of staff within the CC are composed of ward/department visits at regular intervals throughout the day/evening.
Handover for incoming shift leaders and site team consists of a team huddle for information exchange, recorded onto a paper-based pro forma that is used to document expected and actual patient movement during the shift:
After some personal talk amongst staff, they gathered around desk 1 for the site handover which focused on bed availability, projected discharges, ED SitRep, and priority area staffing levels (which CSM4 explained are AMU and ED). During this time, CSM4 added figures to a paper pro-forma on hospital-wide bed status which they explained is used whilst walking the wards to document expected and actual patient movement.
Field notes, 10
Programme timeline and implementation
Onset of the programme in July 2018 commenced with tile selection, design, configuration, testing and validation with incremental go-live of tiles from May to November 2019. A planned comprehensive integration programme for hospital-wide roll-out was developed in parallel. A central physical location for CC staff was purpose-built and opened in April 2019. The CC was part of a broader quality-improvement programme for process and capacity optimisation from onset. The COVID-19 pandemic interrupted roll-out throughout 2020 and into 2021. Resumption of hospital-wide roll-out took place in May 2021 through a Reactivation Programme.
Structured observation of ‘tracer issues’
Inductive analysis of data collected in the structured phase of the study used six use cases or specific tracer issues linked to five themes within the CC tiles and six themes based upon data integration for operational planning. Subsequent structured observations of the tracer issues and additional lines of questioning in later interviews supported understanding of how intelligence was used within and beyond the system, in connection with each identified tracer issue. Table 8 provides a description of the tracer issues, including source data.
| Tracer issue | Theme/tile function | Source data |
|---|---|---|
| Capacity snapshot tile | Visibility of inpatient bed capacity and demand across the hospital; provides users with a holistic view of the inpatient ward details such as census, occupancy, blocked beds, dirty beds, clean beds, available beds, targeted beds, transfers and discharges | Training material; senior clinical leadership 2/1 |
| Patient transfers tile | Identifies patients who are waiting to move to a different care setting; view of the matching beds and the status of the beds that have been reserved | Training material; senior clinical leadership 6/1 |
| ED expediter tile | Current operational state of the entire ED | Training material; senior clinical leadership 1/1; 6/1 |
| Patient deterioration tile | Identifies patients with deteriorating NEWS2 scores and visible oversight of acuity at ward level | Training material; senior clinical leadership 2/1 |
| Right patient right place tile | Displays inpatients who are outliers | Training material; senior clinical leadership 6/1 |
| Integration | Integration of tile data to support operational oversight and planning | Field notes; senior clinical leadership 6/1 |
Capacity snapshot tile: informing patient flow planning and control
The primary goals of the tile are to: (1) provide real-time visibility of occupancy, available, clean and dirty beds as well as planned admissions, discharges and transfers and (2) highlight areas where demand (incoming transfers and admissions) exceeds capacity (number of available beds) to facilitate unblocking and problem-solving. The tile also pulls estimated and predicted discharge dates (EDDs, PDDs) from the Cerner Millennium EHR and uses this information in addition to other criteria (e.g. medically/functionally fit) to identify patients who are meant to be going home on a given day. If a patient appears on the tile but is not likely to be going home, it is an expectation for ward staff to update the information to ensure that CC and ward staff have an accurate picture of capacity and demand.
Example tile actions include:
-
Review wards with net negative beds to identify bottlenecks and wards that are struggling with capacity:
-
Prioritise incoming patients for those beds and consider alternative locations for the lower priority patients.
-
Prioritise tasks to complete ‘pending’ discharges to discharge more patients to create capacity.
-
Identify available capacity for a specific attribute (e.g. side room).
-
Create capacity as required for incoming patients through review of patients currently occupying those rooms for requirements.
-
One example of the way in which information reported on the tile is used to inform decision-making around movement of patients waiting for admission from the ED to hospital wards is shown below. CC staff view bed availability on the tiles and, where identified, will seek additional information as to appropriateness of placement (through screening patient notes):
I open the tile to see how many bed waits we’ve got. And I look to see if I’ve got any downstream beds that I can move patients from assessment areas into them. So I do all that on the tiles. I might think there’s a few there [on the wards], I wonder why when we’ve got patients waiting in A&E? So then I’ll go into the patients’ notes just to make sure there’s no reason why we haven’t used that particular bed.
Senior clinical leadership, 2/1
This may also involve seeking additional information at ward level as to any plans for available beds and prompts to create capacity for incoming patients: ‘I might ring the ward and say, “This bed’s available, do you have you any idea why it hasn’t been used?”’ (Senior clinical leadership, 2/1).
Patient transfers tile: responsibility for transfers across the whole hospital system
This tile helps with understanding where and how long patients have been waiting. It also highlights opportunities for patients to move based on downstream ward availability.
Example tile actions included:
-
Flags when a patient has been assigned to a clean, available bed for 30 minutes or more as an indicator that the process of moving the patient has stalled. This prompts investigation into what barriers are preventing the move to be done.
-
When multiple patients have been targeted to the same ward, the tile shows this and supports prioritisation to decide patient placement in those situations.
An example of the way in which the patient transfer tile has changed oversight and responsibility for transfers is shown below:
Having someone having oversight of every single patient transfer for the whole hospital, not just for medicine or surgery or orthopaedics but of the whole hospital that’s really an important part …. One of the benefits of having a command centre is all those metrics are pulled together in one place and … making sure that there’s someone responsible not just for that one patient on a ward but for the whole patients in the whole hospital is for me the difference the command centre makes.
Senior clinical leadership, 6/1
Deteriorating patient tile: using acuity data to manage risk
The deteriorating patient tile helps to identify and prioritise patients with deteriorating NEWS2 scores. In the CC, staff may use information on the tile to inform decision-making with regard to patient placement. Through filtering the tile at ward level, CC staff can determine areas with high-acuity patients and make decisions about ward capacity and staff allocation:
When [ward staff] say to us, ‘I genuinely can’t take this patient, acuity’s too high’, we can filter the tile to that ward and say, ‘well actually you’ve only got one patient with a high NEWS, are you talking about dependency rather than acuity’? And that will help us to determine do we need to send them an extra RN to support or can we send them a healthcare because it’s actually heavy personal cares that are more the issue.
Senior clinical leadership, 02/1
At ward level, information on the tile can inform the order that ward rounds will take to ensure that sickest patients are seen quickest. Operational leads reported that the tile was frequently used by the anaesthetic outreach team to filter for sickest patients and deterioration so that they can review those patients earlier (Senior CC and operational planning clinical leadership, 01/2 and 02/1).
Emergency department expediter tile
This tile provides information on the overall situation of the department (and department zones) including occupancy, escalation level (state of the ED based on locally agreed factors) and time to triage. The tile flags specific patient delays in care including breaches of wait-time targets and patients waiting to move to a different care setting (Document: training material). At an operational level, the tile was used to inform current pressures in the ED at strategic meetings across the day (Senior clinical leadership, 6/1;2).
Right patient, right place tile: detection and management of medical outliers
This tile displays inpatients who are outlying from a specialist area and aims to facilitate the movement of patients to appropriate locations. At ward level, medical teams can identify where the patients that they are responsible for reside so that they can be reviewed by the appropriate team daily (Senior hospital leadership and management, 06/1).
Senior Clinical Leadership staff check daily the number of outliers across the hospital and whether they have been reviewed (Senior clinical leadership, 2/1). Instances of non-review are then flagged up to the appropriate medical team (either via e-mail/WhatsApp or telephone) and raised at the operational meetings taking place across the day.
During early implementation, attempts to make use of the tile information at ward level exposed issues with data quality relating to patients being put under the wrong treatment function code and then showing up on the wrong consultants list. This meant that the tile was not fit for purpose in some areas:
As it turns out the treatment function codes for consultants is a very complex issue and patients are often put under the wrong treatment function code and they show up on someone else’s list and they’re not on their list for example ….
Senior clinical leadership, 1/2
The main data quality issues were addressed, and the tile was included in the programme for hospital-wide roll-out in 2022.
Integration of tile data to support operational oversight and planning
In February 2022, tile data were embedded within silver command/operational huddles that took place online at regular intervals during the day. Information on the tiles was used to support discussion and raise awareness around issues relating to flow: ‘The tiles are contributing to the group awareness of what’s going on to a different degree than you would have without the display system, so I think that adds a different level of understanding’ (Senior clinical leadership, 1/2).
Command and control at the control site
Following delays in gaining access to the study control site, interviews with staff in comparable roles to those conducted in the study site took place between 8 June 2022 and 11 August 2022. Four participants were interviewed in total, in senior management positions responsible for patient flow (two Matrons and two Senior Clinical Managers). Table 9 provides examples of control site staff C2 behaviour.
| Theme | Reported behaviour | Illustrative quotes |
|---|---|---|
| Monitoring | Check electronic patient record to ensure actions are being taken. Visit wards to monitor/facilitate actions for flow. Use technology to inform workflow. |
‘So we go to the wards after the board rounds, especially on the acute floor, because we need to know where the query discharges are, etc, and what the actions are around those’ (Matron 1, 13) ‘We do a lot of troubleshooting, we do a lot of tactical kind of interactions and interventions around the hospital and, you know, we use our capacity management and FirstNet to use that. You know, we go through that, we look at patients’ notes. The whole team do that, we look at the patient’s notes through capacity management to see when they’re going home. Make sure then that when we follow-up with the wards, that they are actioning things that have been highlighted in the ward rounds, etc. TTOs, transport, etc, etc. So we do use, you know, the electronic part of our software, if you like, very much so as part of our job’ (Matron 1, 13) |
| Situational awareness | Information brought together to create awareness. View dashboard with key metrics. |
‘And then we would follow that up on the electronic patient record to make sure that those actions are being followed and that we can liaise with the nurses and the discharge co-ordinators through that. We’d give them a call’ (Matron 1, 13) ‘So the command centre really is just people kind of calling in and having that, you know, overview for the clinical site matron really’ (Senior Clinical Manager 2, 16) |
| Decision-making | Transformational leadership role. | ‘I guess making that command centre as the safe place, a safe place for staff to be able to come and say no, I don’t agree with that, but then you know, having that, empowering your staff on the wards to take back some of those decisions that actually no I don’t agree with that, these are the reasons why and being able to have that open, honest conversation with the command centre, not just, rather than it being a dictatorship it needs to be more of a transformational leadership, you’re transforming how those pathways are and you’re transforming the workload …’ (Matron 2, 19) |
Since the original conception of this study, by the point of gaining access, the control site trust had initiated their own CC programme through use of existing technology and software, in a model not dissimilar to the Bradford Command Centre, with which operational leads at the control site were familiar:
We’ve got Knowledge Portal and we’ve got Knowledge Portal + and we’ve also got, the OPEL score is live now as well. That’s part of the command centre software so that we, you know, it stays live and we can actually, if it’s not correct, we can interact on certain points on it that will be a write-back, so we can change that.
Matron 1, 13
So they’re a little bit like a mini-hub and we did a bit of a go-see at Bradford where they’ve got something very similar ….
Senior Clinical Manager 1, 14
In terms of C2 behaviour, the control site respondents reported use of electronic systems to monitor hospital capacity and make targeted interventions in follow up with wards. The sense of their CC being a central hub for focused decision-making and to resolve operational problems was additionally evident in the interview data. Ultimately, the control site aimed for a complete digital CC, integrating data on all key operational parameters including ED targets, similar to that at the study site:
I think theirs [Command Centre at BTHFT] is a little bit more polished than ours but ultimately, the ultimate vision for that will be a complete digital command centre which has got that oversight of all the different areas and sort of the key targets in ED that we work towards.
Senior Clinical Manager 1, 14
Respondents expressed an impetus to develop digital systems for monitoring key indicators centrally in addition to oversight by local clinical units and departments:
So this is a brand new role that I’m going into, but some of it will be about how we develop that digital side of it and look at those quality indicators, which is the ambulance handovers, the triage wait times, things like that, which we currently address in ED but there’s something about making sure we’ve got that wider target audience.
Senior Clinical Manager 1, 14
To support implementation of their CC, new roles were created with a similar team composition to that at BTHFT, but without medical support:
So the way that it’s currently set up at the moment is they have two lead nurses, which are Band 8 it is, and then under them there is a clinical commanding team, which is a set of Band 7s who manage all the patient flow aspects of it, and currently there is a band of 2s, so it’ll be one each site that go round and sort of do that bed counting, that physical go-round, walk round, what’s going on here.
Senior Clinical Manager 1, 14
We’ve just done a business case to change some of that so I’m putting that in and we’re calling those clinical site matrons, so they will take a lead on the sites and there’ll be one on each site and then there will be the Band 7 sat underneath that ….
Senior Clinical Manager 2, 16
Despite the emphasis placed upon digital evolution, one respondent put forward the view that C2 was predominantly a human-centred activity within a healthcare organisation.
I do feel though that the human aspect still needs to be in place throughout. You know, using electronic records as a supplement but we do still need to maintain that human approach to everybody because that’s the organisation, that’s the NHS, is a human organisation and we need to make sure that we maintain that but maximise the resources that we’ve got.
Matron 1, 13
Similarly, views were expressed that staff engagement and appropriate leadership behaviour towards front-line staff would be important in ensuring the successful implementation of C2 systems in the control site.
I think the staff engagement you know, and I think the staff work, and I guess that’s across all organisations, the staffing, I mean it’s no secret that nurse staffing and nursing there’s shortages everywhere so I think it’s just that engagement and that embedding and encouraging staff that actually what we’re doing is to improve patient safety, so being on the shopfloor, giving that physical clinical leadership of let’s do this together, let’s highlight any issues, how does it look, and giving them the confidence that you’ve got confidence and I definitely think it’s from that leading from above that really makes things happen.
Matron 2, 19
Thematic analysis of ethnographic field notes and interview data
The data gave rise to six main themes linked to enactment of C2 in the acute care setting and perceptions of the effectiveness of the CC programme in achieving intended and unintended outcomes: (1) generation and use of intelligence; (2) staff enactment of C2; (3) context and culture in the CC; (4) responding to unanticipated events and escalating pressures; (5) staff perceptions of impact of the CC and (6) challenges in implementation and operation. The first four themes are presented below as a synthesis of themes in the data representing C2 processes enabled by the programme. The last two themes are presented in the subsequent section on evaluative perspectives by way of an overview of key evaluative findings from the qualitative work.
Generation and use of intelligence
Information in the CC provided an up-to-date data feed that conveys current knowledge of hospital state for rapid decision-making and response. Intelligence was generated through tile activation and engagement with content, interaction with ward/department staff and discussion within teams.
Site position
Interaction with tile data at specific points during the day provided the site team with an up-to-date site position (creates awareness of where pressure points are): ‘Gives an update on the position at that moment in time … so are aware of where the pressure points are’ (Interview, senior clinical leadership, 4/1).
Multiple use cases for tile data
Staff working in the CC engaged with the tiles in different ways, depending on their role and function at any given time:
Each one of them [CC staff] uses each tile slightly differently. The basic principles are the same, but how I use them and the means for which I escalate from them is different to the way that maybe our Band 4 does.
Interview, senior clinical leadership, 2/1
Typical examples of the way in which staff interacted with tile information are shown in Table 10.
| Tile name | Information examples | Example interaction | Staff role(s) | Source |
|---|---|---|---|---|
| 01 Capacity snapshot | Bed state | Situational update × 4 daily Match bed waits to capacity downstream |
Clinical site matrons | Senior clinical leadership 2/1 |
| 02 Patient transfers | Patients who need to be in a different area | Inform decision-making about patient placement | Clinical site matrons | Senior clinical site staff 1/1 |
| 03 ED expediter | Patient numbers; transfers; admitted | Up to date site position | Clinical site matrons; senior clinical leadership | Senior clinical leadership 4/1 |
| 04 Discharge tasks | Confirmed discharges for the day | Visit/call wards to assist with timely discharge to facilitate early capacity | Clinical site matrons/patient flow co-ordinators | Senior clinical leadership 2/1; senior clinical site staff 1/1 |
| 05 Patient deterioration | Ward acuity level | Inform decision-making about patient placement | Clinical site matrons | Senior clinical leadership 2/1 |
| 06 Right patient right place | Number of outliers | Confirm that patients have been reviewed by appropriate medical team | Senior CC clinical leadership | Senior clinical leadership 2/1 |
| 07 Ward link | Expected date of discharge | Proactively plan for bed state | Clinical site matrons/improvement leads | Senior clinical staff 2/1 |
| 08 HID COVID-19 | Pop-ups | Trigger response to known positive case | Clinical Site matrons/senior CC clinical leadership/senior hospital leadership | Senior clinical leadership 1/1; senior clinical leadership 6/1 |
Response to tile information: walking the wards
Command Centre staff use tile information to identify potential bottlenecks in the system, for example delay discharges, and respond to issues arising by visiting wards/departments to offer in-person support:
They [CC staff] leave the Command Centre and go on a bit of an amble round, they’ll go and say, ‘you’ve got x number of patients on this ward, these are the names, what time are they leaving please? Is there anything we can do to assist them departing in a more timely manner so that we get that early capacity’?
Senior clinical leadership, 2/1
Staff enactment of command and control
Informed by emerging themes from the cross-industry review, our analysis of the C2 work that staff do can be understood through three main concepts: monitoring, situational awareness and decision-making. In terms of monitoring, staff constantly observed and checked site positions in terms of patient flow and took actions based upon intelligence. CC staff maintained situational awareness through continuous monitoring and sharing of information coming into the CC, through formal and informal means, watching out for what is going on in the hospital environment. The action or process of making important decisions was visible through frequent discussion between clinical and leadership roles in the CC and responsive problem-solving. Examples of the way in which CC staff enacted C2 behaviour are shown in Table 11.
| Subtheme | Example behaviours | Illustrative quotea |
|---|---|---|
| Monitoring | Directly support flow
|
Quote 1 Monitor capacity and demand ‘The matrons who populate the SITREPs four times a day use Capacity Snapshot tile because that’s telling us about our capacity at this moment in time, and then they can use that to marry up against what the transfer list’s looking like for patients coming in from ED, bed bureau, pre-admit, to be thinking, “crikey, demand is 30% higher than predicted capacity”’ (Senior clinical leadership, 2/1) Quote 2 Request to update data error ‘Clinical Site Matron (CSM) was on the phone asking for data to be amended as a patient has left the ED and is on the way to a ward but the electronic system states that they are returning to ED’ (Field notes, 15) Quote 3 In-person input for departments ‘Whilst walking through the hospital the CSM explained to me that they visited the assessment unit to check the current bed state and ensure that patients that could be moved from the unit into a ward were being moved. This would support with availability of beds during the night, should they be required’ (Field notes, 10) |
Monitor wait times and take action
|
Quote 1 Move patients themselves ‘CSM was on the phone asking someone to hurry up and move a patient as they were about to breach the 18-hour wait time for bed allocation. The CSM offered to move the patient themselves at one point. It appeared that the situation was resolved as they did not leave the room after the call’ (Field notes, 7) Quote 2 Prompt movement of more vulnerable patients ‘CSM was on the phone “an [older patient] had a 7-hour wait in the ED and the request was for a more comfortable place be found for the patient”. They also enquired if anyone could review the patient earlier (senior medical review). CSM then relayed the answer to the room “no consultant today and registrar on site is tied up in ENT”. CSM then asked the person on the phone, “do me a favour – ask around and see what can be done" (Field notes, 9) |
|
| Monitor outliers and take action | Quote 1 Right patient, right place tile identifies where outliers reside ‘The medical teams out in the organisation and senior clinical leads for the Command Centre, we use Right Patient Right Place because we want to check how many outliers have we really got, and have they been reviewed’ (Senior clinical leadership, 2/1) |
|
| Situational awareness | Hospital-wide
|
Quote 1 Seek and pass on information for situational awareness ‘CSM on the phone when she asked “How many green patients have you got? Ok, thanks. There’s one on route now, thank you”’ (Field notes, 1) |
Team awareness
|
Quote 2 Shared situational awareness ‘Often the staff member will speak out loud when reading data from screen either to make others aware or facilitate coordination (shared situational awareness) and another member at an adjacent workstation will pick up on a certain details and may then interact on critical points/coordination. Integration across roles within the same shared space is therefore a function of the command centre’ (Field notes, 6) |
|
| Decision-making |
|
Quote 1 Support decision-making ‘In the command centre we would use deteriorating patient where we’ve got a particularly challenging decision about, ‘can that ward take that patient into that last bed?’ And when they say to us, ‘I genuinely can’t take this patient, acuity’s too high’, we can filter the tile to that ward and say, ‘well actually you’ve only got one patient with a high NEWS, are you talking about dependency rather than acuity?’ And that will help us to determine do we need to send them an extra RN to support or can we send them a health care because it’s actually heavy personal cares that are more the issue’ (Senior clinical leadership, 02/1) Quote 2 Responsive problem-solving ‘Some discussion ensued about a need to deploy staff to the ED. The Patient Flow Coordinator suggested moving a staff member (who was speciallingb a patient on a ward who was at risk from falls). The CSM replied “We will see if that patient is settled before we think about moving that staff member again”. (I got the impression that they were looking out for the member of staff’s well-being whilst making this decision). Both staff then agreed to go to the ward to look for themselves at the situation and left the room’ (Field notes, 10) |
Context and culture in the Command Centre
The context and culture in the CC can be understood through artefacts staff engage with and intended purpose (environment), tempo of operations (speed and intensity of actions relative to the speed and intensity of unfolding events in the operational environment) and attitudes and values (culture of caring).
Variable data quality
Lag in some of the data presented in the CC and uncertainty regarding the current accuracy of information displayed in the tiles led to frequent activity to pursue up-to-date information and to manually check ‘real data’ sources. Staff working in the CC are almost constantly engaged with information-seeking and exchange through interaction with computers, telephones, staff coming into the CC, each other and conversations with staff in the ward environments. The majority of interactions observed concerned information regarding patient and bed figures; for example, ‘CSM1 on the phone when she asked “How many green patients have you got?” Ok, thanks’ (Field notes, 1) and ‘CSM4 was on phone with ED asking about figures’ (Field notes, 10). CC staff explained that the main purpose of telephone calls to the wards was to obtain up-to-date figures on bed state:
CSM4 stated to PCC1 ‘I’ll do Neonates and Covid shall I?’ To which they agreed. CSM4 then called around the wards to get their Covid figures. I asked why these were not available on the system in the centre to which they responded: ‘we need an up to date figure’.
Field notes, 1
Another example of the way in which data quality influenced intelligence and actions was observed in the silver command meetings:
Senior clinical leadership role stated that they reviewed the ward link tile and identified 24 patients with expired Expected Date of Discharge (EDD) and 62 patients with no EDD at all ‘so the information on Capacity Snapshot tile cannot be accurate’.
Meeting notes, 07/02
Tempo of operations and sense of pressure
Speed and intensity of actions relative to the speed and intensity of unfolding events in the operational environment.
In normal operations, pressure on CC staff was almost constant throughout the day and evening. Staff were always busy. As well as the routine work described earlier, unfolding events such as emerging pressures led to increases in intensity and speed of actions relative to the events. This often necessitated adapting ways of working:
On my arrival, a Senior clinical leader informed me: ‘It is already chaos. 105 people in ED following a big car crash. That’s why I am working at this (CSM) desk, to help get things moving quicker.
Field notes, 1
Emerging pressures for bed capacity gave rise to concern and tension for the team; for example, ‘During a silver command meeting discussion staff were discussing a situation where demand exceeded capacity, beyond that which was usual when CSM1-stated “I am nervous about the situation”’ (Meeting notes, 08/03). The researcher noted on these occasions that ‘the atmosphere was tense, air of panic’, for example (Meeting notes, 07/03).
Similar concerns were expressed in response to low staffing levels:
The member of staff stated to another ‘have you seen the RAG?’ sounded slightly panicked and concerned. I thought that this was in relation to the staffing levels RAG rating that had been circulated for the first time this morning. Levels indicated extreme pressures across the hospital.
Field notes, 15
During periods of reduced pressure, the atmosphere appeared relatively less tense, as seen in this example from field notes collected during an observation in the evening:
I noticed that there was relatively less tension/stress in the way in which the staff were working. Although there remained a constant workflow there was more interaction between staff unrelated to work in-between calls/data entry than I had noted previously (more relaxed, less formal on an evening? Related to relatively more beds available than I had observed on previous visits – see SitRep?).
Field notes, 10
Compassionate, personalised care for patients and staff
Staff working in the CC showed considerable compassion for patients and the staff working on the wards. Granular, personalised care for individual patients was apparent in many of their interactions; for example: ‘Patient needed to be moved but CC staff took into account the fact that the patient was diabetic and therefore needed to eat first’ and ‘Bless him, it’s his birthday [whilst referring to a patient due for admission]’ (Field notes, 6.2).
On occasions where CC staff interacted with ward staff in their departments, they provided support for staff experiencing difficult circumstances and shared their concern and response on negative outcomes:
The ED shift leader also discussed another patient of concern in the department. They mentioned that although vital signs were within acceptable limits that the patient did not look well at all (I got the impression that the situational update between staff was much more than numbers including tensions/concerns/atmosphere within the department that would not be captured within technical systems). When we returned to the Command Centre shortly after this, CSM4 checked up on the patient and informed me that the patient had been transferred to ICU and that there was likely to be a devastating outcome. The atmosphere at this time was flat as staff expressed sadness at the loss of a young patient.
Field notes, 10
Staff were observed to express gratitude, familiarity and warmth in their communication with ward staff: ‘CSM3 was on the phone and asked “can I have your bed please … thanks love, thank you … take care, bye”. Appeared to be asking for an update and expressing gratitude, familiarity, warmth in communication style’ (Field notes, 1).
Examples of the way in which CC staff were involved in personalised care interactions are shown in Table 12.
| Subtheme | Description | Illustrative quotesa |
|---|---|---|
| Environment | Which artefacts staff engage with and intended purpose | Quote 1 Manual collection of ‘real data’ ‘CSM4 stated to PCC1 “I’ll do Neonates and Covid shall I?” To which he agreed. CSM4 then called around the wards to get their Covid figures (I asked why these were not available on the system in the centre and did not really understand the response, e.g. “we need an up to date figure”. I had a similar experience with the CL yesterday when asked why the information on the tiles was not used and thought that perhaps I was asking the wrong question)’ (Field notes, 1) Quote 2 Paper-based bed board used ‘After some personal talk amongst staff, they gathered around desk 1 for the site handover. This was delivered by PCC1 (Is it usual practice for the Band 7 to lead the handover?) which was focused on bed availability, projected discharges, ED SitRep, and priority area staffing levels (which CSM4 explained are AMU and ED). During this time, CSM4 added figures to a paper pro-forma on hospital-wide bed status which she explained is used whilst walking the wards to document expected and actual patient movement’ (Field notes, 1) |
| Tempo of operations | Speed and intensity of actions relative to the speed and intensity of unfolding events in the operational environment | Quote 1 Adapt ways of working in response to emerging pressures ‘It is already chaos. 105 people in ED following a big car crash. That’s why I am working at this desk, to help get things moving quicker’ (Field notes, 1) Quote 2 Sense of panic at staffing levels ‘The member of staff stated “have you seen the RAG” sounded slightly panicked and concerned. I thought that this was in relation to the staffing levels RAG rating that had been circulated for the first time this morning. Levels indicate extreme pressures across the hospital’ (Field notes, 1) Quote 3 More relaxed on an evening (more relaxed when pressures not on) ‘I noticed that there was relatively less tension/stress in the way in which the staff were working. Although there remained a constant workflow there was more interaction between staff unrelated to work in-between calls/data entry than I had noted previously (more relaxed, less formal on an evening? Related to relatively more beds available than I had observed on previous visits – see SitRep?)’ (Field notes, 1) |
| Attitudes and values | Care culture (including granular personalised care for patients and looking out for staff) | Quote 1 Express friendliness and gratitude to ward staff ‘CSM3 was on the phone and asked “can I have your bed please … thanks love, thank you … take care, bye’” Appeared to be asking for an update and expressing gratitude, familiarity, warmth in communication style’ (Field notes, 1) Quote 2 Flat in response to devastating outcomes for patients ‘The shift leader also discussed another patient of concern in the department. They mentioned that although vital signs were within acceptable limits that the patient did not look well at all (I got the impression that the situational update between staff was much more than numbers including tensions/concerns/atmosphere within the department that would not be captured within technical systems). When we returned to the Command Centre shortly after this, CSM4 checked up on the patient and informed me that the patient had been transferred to ICU and that there was likely to be a devastating outcome. The atmosphere at this time was flat as staff expressed sadness at the loss of a young patient’ (Field notes, 1) Quote 3 Granular personalised care ‘Staff show considerable compassion for individual patients (e.g. ”… bless him. It’s his birthday …”). Individual needed to be moved but Command Centre staff took into account the fact that the patient was diabetic and therefore needed to eat first. Example of granular, personalised care delivered via the CC. Similarly, individual cases are discussed at a granular level. “Well where is she now?.... Standing by the front desk apparently…. Yeh, but she says she feels unwell.” Impressive level of operational knowledge for remote operation’ (Field notes, 1) |
Responding to unanticipated events and escalating pressure
Table 13 shows the themes derived from analysis of CC staff interactions when responding to unanticipated events and escalating pressures. During the evaluation period, staff were operating within an environment that was unprecedented due to the pandemic. Often, during silver command meetings, staff commented on the pressures for example: ‘Trying to fast forward flow as this winter is like nothing we have ever seen before’ (Meeting notes, 08/02:2) and ‘Staff commented that the last 24 hours was the most challenging of their career’ (Meeting notes, 08/03:1).
| Subtheme | Description | Illustrative quotesa |
|---|---|---|
| Unprecedented pressures | Pressure is more than it has ever been | ‘Trying to fast forward it as this winter is like nothing we have ever seen before’. Said last 24 hours was the most challenging of his career. ‘Know everyone is tired’. Currently at highest level of pressure in the hospital. |
| Collaboration triggered through identification of unexpected data | Sometimes CC staff will say out loud ‘well that’s strange …’ and this triggers collaboration on clarifying unexpected data or identifying an investigative action. | |
| Go out onto the wards to see for themselves (gather further information to support decision-making) | Some discussion ensued about a need to deploy staff to the ED. PCC1 suggested moving a staff member (who was speciallingb a patient on a ward who was at risk from falls). CSM4 replied ‘We will see if that patient is settled before we think about moving that staff member again’. (I got the impression that they were looking out for the member of staff’s well-being whilst making this decision – being a nurse). CSM1 and PCC1 then agreed to go to the ward to look for themselves at the situation and then left the room. |
Collaboration between staff members was often triggered by unexpected events; for example, ‘Sometimes CC staff will say out loud “well that’s strange …” and this triggers collaboration on clarifying unexpected data or identifying an investigative action’ (Field notes, 6.2).
On occasions where the information was not clear and/or the emerging issue could not be resolved immediately, CC staff would visit the ward/department to gather further information and support the situation:
Some discussion ensued about a need to deploy staff to the ED. PCC1 suggested moving a staff member (who was specialling a patient on a ward that was at risk from falls). CSM4 replied ‘We will see if that patient is settled before we think about moving that staff member again’. (I got the impression that they were looking out for the member of staff’s well-being whilst making this decision). CSM1 and PCC1 then agreed to go to the ward to look for themselves at the situation and then left the room.
Field notes, 10
Summative evaluative themes concerning the impact of the programme
In order to address the evaluative aims of the study, in addition to construction of narratives describing the CC programme as implemented and associated organisational behaviour at the study site, formal and informal interview transcripts were analysed to identify evaluative themes specific to the studied implementation. In the following sections, themes relating to the perceived impact of the CC (both intended and unintended) will be described followed by perceived challenges in implementation and operation.
Perceptions of the impact of the command centre on intended and unintended outcomes
In addition to observation of behaviour in and around the CC, during interviews with a range of staff connected to the CC programme, perceptions of the efficacy and impact of the CC in meeting its objectives were explored, along with potential impacts upon upstream operational management and organisational processes. Several themes emerged (Table 14) representing both intended and unintended consequences of CC implementation and operation.
| Sub-theme | Description | Illustrative quotesa |
|---|---|---|
| Staff perceptions of impact of the CC | In-hospital transfers; appropriate care | ‘The right patient’s in the right bed first time wherever possible, because that will lead to being looked after by the correct team’ (Clinical staff, 01). |
| Responsive problem-solving | ‘… and some of the things that are escalated to us, by staff who don’t know what to do or don’t know who to go to, end up coming through us’ (Clinical staff 21). | |
| Focal escalation point; co-ordinating across boundaries | ‘… previous to that the site coordinators were always in ED and so nobody ever thought to go, “I’m going to go talk to the site coordinator in ED” because you immediately think it’s an ED problem, but you might not have an ED problem, you might have a surgery problem …. I think, give people the confidence that there’s an escalation point and that you’re not going to spend five phone calls tracking down somebody to help you. You have somewhere to go to get help’ (Senior information officer 11) | |
| Situational awareness | ‘We’ve got oversight, from a safety point of view we can see notes much more easily. We can see when patients are deteriorating, we can see when patients are needing transfer’ (Clinical staff, 03). | |
| Real-time intelligence | ‘On the Covid Tile, we were pulling in feeds directly from their lab system. So patients who were being tested for Covid but might have been in a non-Covid ward, we were getting their Covid results immediately, and potentially before their own clinical teams were seeing them’ (Other roles, 07). | |
| Functional integration | ‘We co-located staff who were already working together in disparate sites and whose job it was to manage flow, and that actually had some benefit, just putting those people in the same room together …’ (Institutional Manager, 05). | |
| Data quality | ‘What we ended up finding was that implementation needs of the Command Centre actually drove correct use of the EPR … and better data quality’ (Institutional Manager, 04). |
Staff expressed views that the CC facilitated efficient bed and staff allocation, in-hospital transfers and planning for patient flow, not only easing flow but ensuring that patients were placed in the right destination initially to avoid the need for subsequent transfer. The perception of the CC was of a focal point for operational decision-making and problem-solving that extended beyond CC staff and operations managers. Front-line co-ordinators could contact or attend the CC in order to resolve complex operational issues that spanned functional areas and the view was expressed that the CC facilitated a system-wide perspective on these issues. This effect was enhanced through colocation of staff with different functional perspectives (namely clinical and operations management) in the same central location with access to system-wide data. The ethnography demonstrated substantial interactions between CC staff and multiple information systems as well as constant communication among the wider hospital services and wards. Characteristics that appear to support co-ordination and communication included the physical layout of the CC where site staff are located closer facilitating frequent informal communication and centralised access of diverse information (e.g. bed management software) for the site team to support co-ordination.
Respondent testimony suggested that the CC programme objectives to enhance the availability and use of real-time intelligence in hospital operations management had at least partially been met (see Table 14). The institutional response to the COVID pandemic was often cited as an example of effective use of real-time (or near real-time) data to monitor and respond to new cases of infection across both COVID and non-COVID wards. In broader areas of risk management, such as monitoring patient deterioration, views were expressed that the CC facilitated early detection and monitoring of at-risk patients, enhancing situational awareness. Finally, the implementation and subsequent operation of the CC had a secondary effect of enhancing data quality and awareness of data quality issues within the organisation.
Challenges in implementation and operation
In analysis of the interview data, we sought evidence of limitations of the CC system, both emergent and against espoused goals, along with narratives describing the inherent challenges of implementation and operation of this type of programme in an acute care setting.
An important unintended consequence of the CC implementation reported by both front-line and CC staff was a sense of being monitored among front-line units, sometimes leading to interventions (or fear of interventions) from the CC team that were perceived as unwelcome. This included sometimes challenging conversations about the importance of keeping electronic records up to date or acting on evidence of operational issues that were seen as being under local autonomy or ownership, rather than a centralised issue. It was suggested that front-line staff in some areas might delay updating records because they knew the CC team would be quick to respond with new allocations that would amount to increased local operational pressures. It was clear from subsequent interviews with both implementation and front-line staff that the reach of training on both electronic patient record (EPR) and on the intended function of the CC was limited. This may have influenced front-line staff engagement with the CC and the actions that they took, or not, to support functionality.
Data quality was a constant concern for staff working in and around the CC, and it was clear that there were limitations in how up to date and accurate (or complete) records were in the CC wall of analytics, often necessitating triangulation and verification from multiple sources and systems and discrepancy between what the CC wall of analytics displayed and what front-line staff reported. The added value of specific tiles was also questioned by front-line operations leads who believed that they already had access to real-time accurate data through alternative systems and that this had led to declined local uptake and use of the tile data. The design of the data integration pathways and systems additionally meant that certain conditions needed to be met by front-line units, in terms of updating electronic records and use of electronic systems, in order for displays and alerts to trigger properly in the CC. This necessitated some adjustments to human workflow at the data source. A summary of themes relating to perceived challenges in implementation is shown in Table 15 along with illustrative quotes.
| Subtheme | Description | Illustrative quotesa |
|---|---|---|
| Perceived challenges in implementation and operation | Front-line perceptions of being monitored | ‘In essence that can often result in quite a challenging discussion then by the Command Centre with the nurse in charge of that ward as to why the PDDs, EDDs haven’t been updated for that day …. I think they [front-line staff] probably feel like it’s a big stick that we’re trying to … so there probably is a big education piece to be done and maybe to go back to the original concept’ (Institutional manager, 06). |
| Data quality and availability | ‘So the main [issue] was … data quality of the primary bit of software, and we had to … revert to what’s the next best [metric] …. And in some cases that … didn’t really provide the exact use case that you went for originally …’ (Clinical staff, 01). | |
| Design limitations | ‘So in terms of the tiles, there’s one or two that I’ve still got issues with. So one of them was the ED tile. I don’t know who designed it, it’s not my business to know who designed it, but it doesn’t work for us here. Because basically it replicates everything we can get out of FirstNet that we’re looking at all day every day anyway’ (Senior clinical staff, 02). | |
| Challenging conversations | ‘In A&E … somebody would get to two and a half hours and no plans … we would go down, and we would say, ‘Right, what are you doing with this?’ …. And that just caused upset with everybody because it was as though we’re going and stepping on their toes’ (Clinical staff, 03). | |
| Data quality; impact on upstream work processes | ‘I’ll give you an example, transfers … there are different ways of doing it for valid reasons …. Nurses are great for workarounds and they found the shortest possible path to do it which wasn’t the path the software liked, so it didn’t trigger the transfer message properly … so that means the bed board wasn’t correct … so that has all sorts of downstream impacts … that was quite a big realisation … we had to unalign that process and say, no, and re-teach people this is the way you need to do it …’ (Senior information officer 11). | |
| Data quality; tile vs. live data | ‘I’ll take the live and the tile [data] and I’ll do the comparison on the form that we’ve created. And I’ll say, “The tile tells me this”, and then at the end I’ll say, “The [live data] tells me that”’ (Senior clinical staff, 02). |
Chapter 6 Quantitative analysis study findings
Introduction
This chapter summarises the results of substudies 1 (data quality analysis), 2 (patient flow) and 3 (patient safety). Collectively these three substudies formed the quantitative analysis work package which examined routine EHR data extracted from the study and control sites and analysed using data science methods including data visualisation, statistical and time-series analysis and process mining.
Results from the chapter have been published as Mebrahtu et al. 116
This is an open-access publication distributed under the terms of the Creative Commons CC BY 4.0 licence, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. The link to the licence is here: https://creativecommons.org/licenses/by/4.0/.
Descriptive summary of the data
We analysed EHR data extracted from the study site (BRI) and control site (CHFT) for the study period. There were a total of 203,807 inpatient emergency admissions and 34,625 operations performed in the BRI hospital and 291,018 inpatient emergency admissions in CHFT during the study period. The weekly mortality (as a percentage of weekly admissions) stayed below 3% and 5% (in BRI and CHFT, respectively) for most of the study period except a sudden increase in March–April 2020 when a spike in the hospital admissions associated with COVID-19 was reported in the UK. 52 The weekly deaths appear to be higher for the period after the COVID-19 pandemic when compared with the pre-pandemic period. Table 16 provides a summary of the patient safety indicators and Figure 5 shows the changing pattern over time.
| Period | Mortality (%),a mean (SD) | Re-admissions within 72 hours (%),a mean (SD) | Postoperative sepsis (%),b mean (SD) | ||
|---|---|---|---|---|---|
| BRI | CHFT | BRI | CHFT | BRI | |
| 1 January 2018–30 June 2018 (pre-intervention) | 1.5 (0.56) | 3.3 (1.1) | 8.2 (1.5) | 2.5 (0.7) | 3.8 (1.2) |
| 1 July 2018–30 April 2019 (Patient flow programme) | 1.1 (0.31) | 2.9 (0.78) | 6.8 (0.97) | 2.9 (1.22) | 4.2 (1.6) |
| 1 May 2019–30 November 2019 (CC tile roll-in) | 1.0 (0.29) | 2.5 (0.57) | 6.7 (0.62) | 5.6 (0.87) | 3.2 (1.2) |
| 1 December 2019–30 April 2021 (CC goes live) | 1.7 (0.94) | 4.3 (1.67) | 6.8 (1.1) | 5.2 (0.93) | 3.6 (2.1) |
| 1 May 2021–31 August 2021 (Engagement resumption) | 1.1 (0.38) | 2.9 (0.83) | 6.9 (0.81) | 4.5 (0.84) | 2.7 (1.2) |
FIGURE 5.
An overall pattern of patient safety indicators during the study period. CHH, Calderdale & Huddersfield Hospitals (CHFT). Postoperative sepsis data not available for CHH.
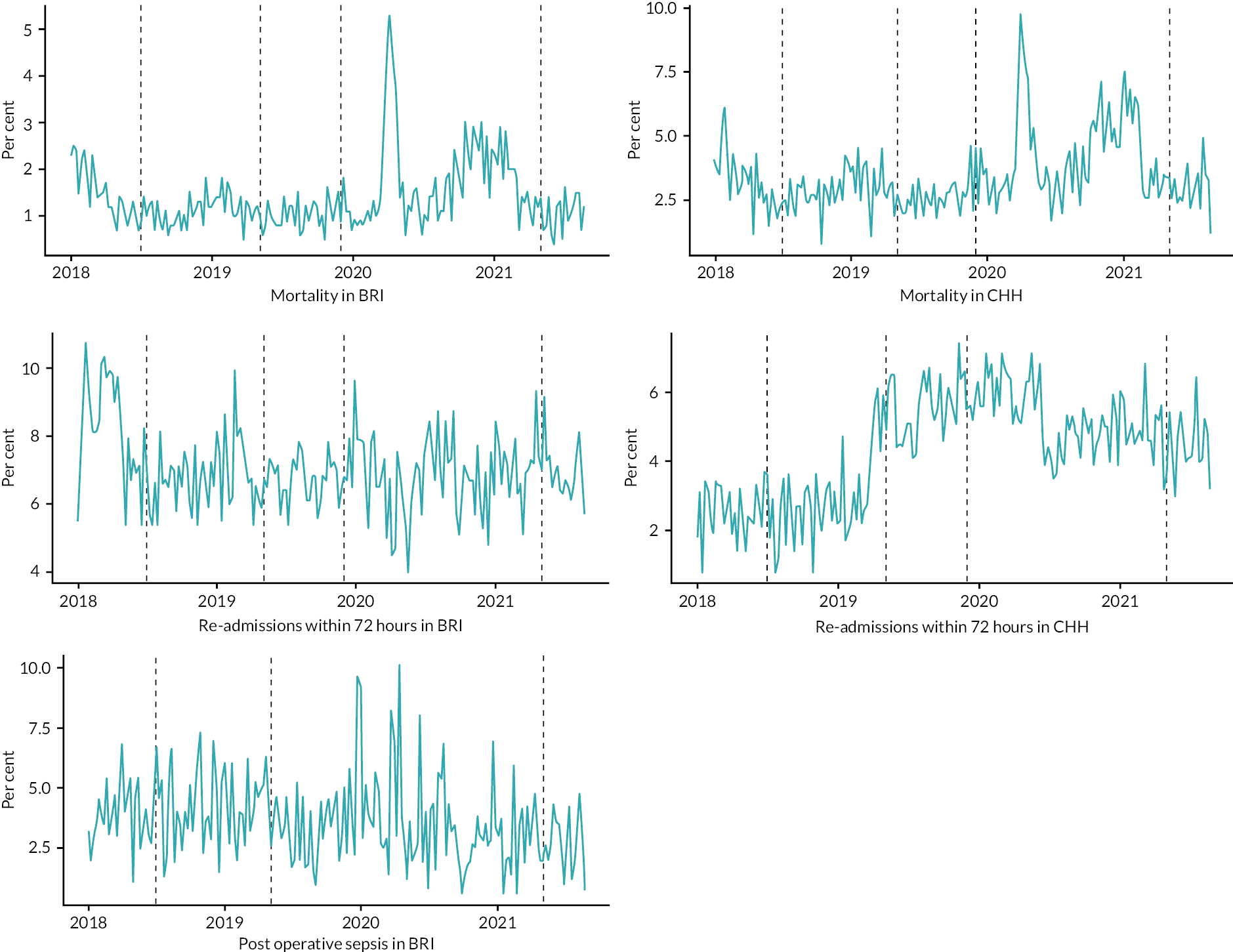
The weekly re-admissions within 72 hours (as a percentage of the total emergency admissions) remained above 6% and 4% (in BRI and CHFT, respectively) for the majority of the study period. The average re-admissions in BRI hospital were just over 8% during the first 6 months of the study period and stayed just under 7% throughout. On the other hand, the re-admissions in the CHFT were under 3% during the first 16 months then nearly doubled during the rest of the study period. The patterns of the weekly re-admissions do not appear to have been greatly affected by the pandemic.
The weekly post-operative sepsis (as a percentage of surgical operations performed) stayed between 1.5% and 6% for majority of the period, with occurrence of spikes during January and April 2020. The overall postoperative sepsis ranged between 0.6% and 10%, and it was below 5% during the study period on average. Postoperative sepsis data were not available for CHFT.
Table 17 provides a summary of the patient flow indicators and Figure 6 shows the changing pattern over time.
| Intervention phase | Mean (SD) | ||
|---|---|---|---|
| Length of stay (hours)a | Waiting time (hours)b | Clinician seen time (hours)b | |
| Pre-intervention | 77.2 (8.8) | 2.0 (0.17) | 0.57 (0.08) |
| PF programme | 76.0 (5.6) | 2.1 (0.21) | 0.55 (0.06) |
| CC tile roll-in | 79.6 (5.5) | 1.9 (0.20) | 0.55 (0.06) |
| CC goes live | 96.7 (13.6) | 1.2 (0.49) | 0.45 (0.15) |
| HW training | 87.5 (7.7) | 2.2 (0.32) | 0.51 (0.06) |
FIGURE 6.
Weekly pattern of patient flow indicators during the study period.
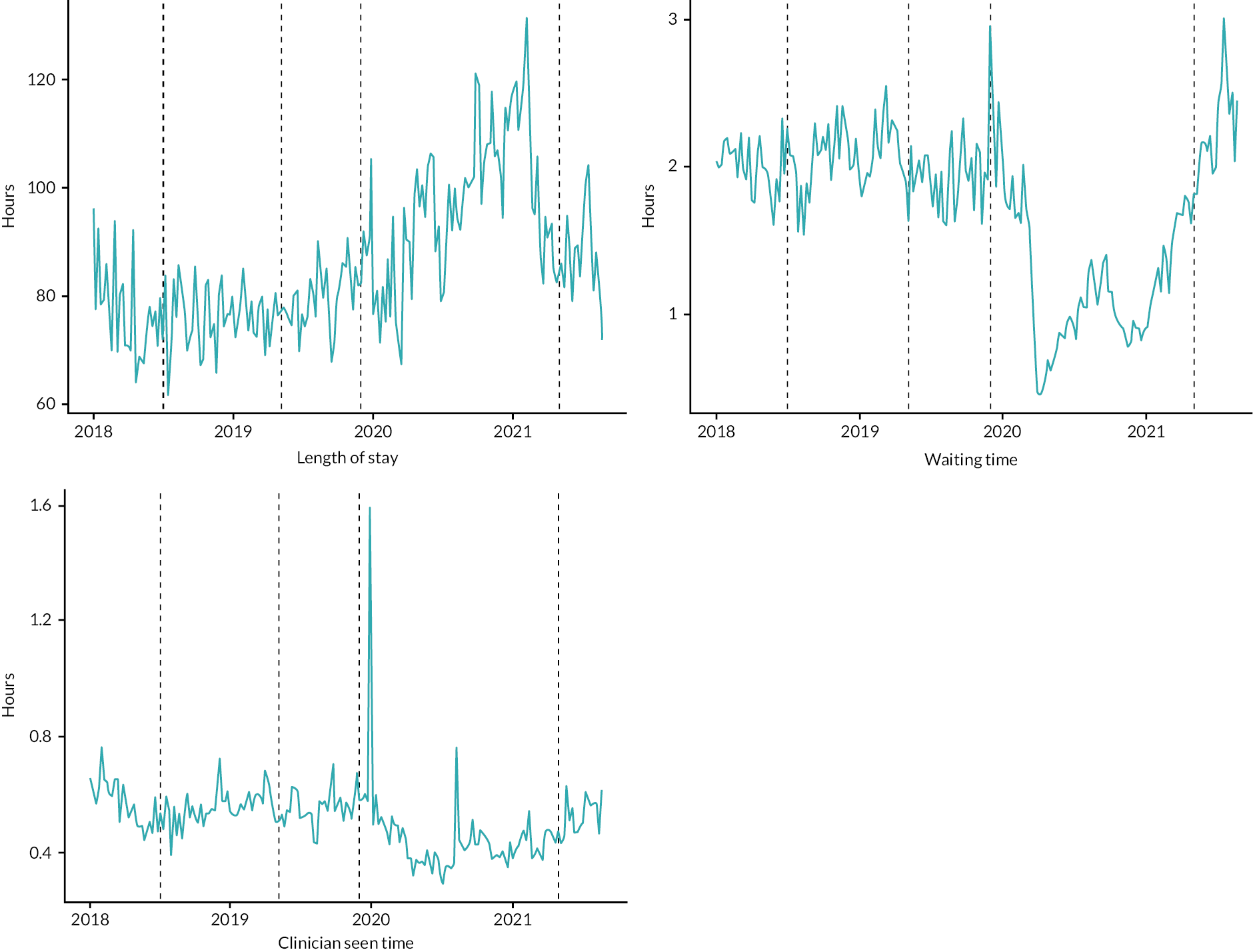
The weekly average waiting time (time until treatment) for A&E visiting patients was between 1.5 hours and 2.5 hours for the periods between January 2018 and November 2019, then increased to around 3 hours in the second week of December 2019. It then showed a steady drop until March 2020 to 0.5 hours, and then increased steadily until the end of the study. Although there was a significant variation of patterns between the pre and post-pandemic period, the average waiting time remained below the 4 hours mark117 in both periods. The weekly average clinician seen time (time until assessed by a clinician) stayed below 1 hour throughout the study period (Table 18).
| Intervention phase | Average time spent in minutes [mean (SD)] | |||
|---|---|---|---|---|
| Arrived → assessed | Assessed → treated | Treated → concluded | Concluded → checked out | |
| Pre-intervention | 33.5 (23.8) | 94.4 (64.6) | 89.6 (110.8) | 12.1 (60.3) |
| PF programme | 32.6 (22.1) | 100.3 (69.8) | 101.1 (39.5) | 26.1 (1234) |
| CC tile roll-in | 30.5 (21.2) | 99.1 (72.2) | 101.9 (100.3) | 16.2 (47.2) |
| CC goes live | 23.8 (73.2) | 73.4 (87.2) | 143.0 (402.4) | 13.0 (116.4) |
| HW training | 30.4 (21.7) | 104.6 (94.0) | 139.8 (164.1) | 11.7 (111.5) |
The average transition time between A&E care stages was largely similar between the pre-intervention and post-intervention periods except that there was a significant increase of transition time from treatment to conclusion of the visit during the ‘command centre going live’ and ‘hospital-wide engagement and training’ periods.
Data quality
A total of 197,084 A&E visits were included. Table 19 provides a summary of the data quality indicators and Figure 7 shows the changing pattern over time.
| Intervention phase | Mean (SD) | |
|---|---|---|
| Clinician seen date missing (%) | Treatment date missing (%) | |
| Pre-intervention | 25.5 (2.6) | 33.6 (2.5) |
| PF programme | 24.7 (3.3) | 37.1 (3.3) |
| CC tile roll-in | 23.6 (3.7) | 47.9 (5.7) |
| CC goes live | 20.8 (4.4) | 53.5 (19.3) |
| HW training | 28.5 (3.4) | 14.7 (1.9) |
FIGURE 7.
Weekly pattern of data-quality indicators during the study period.
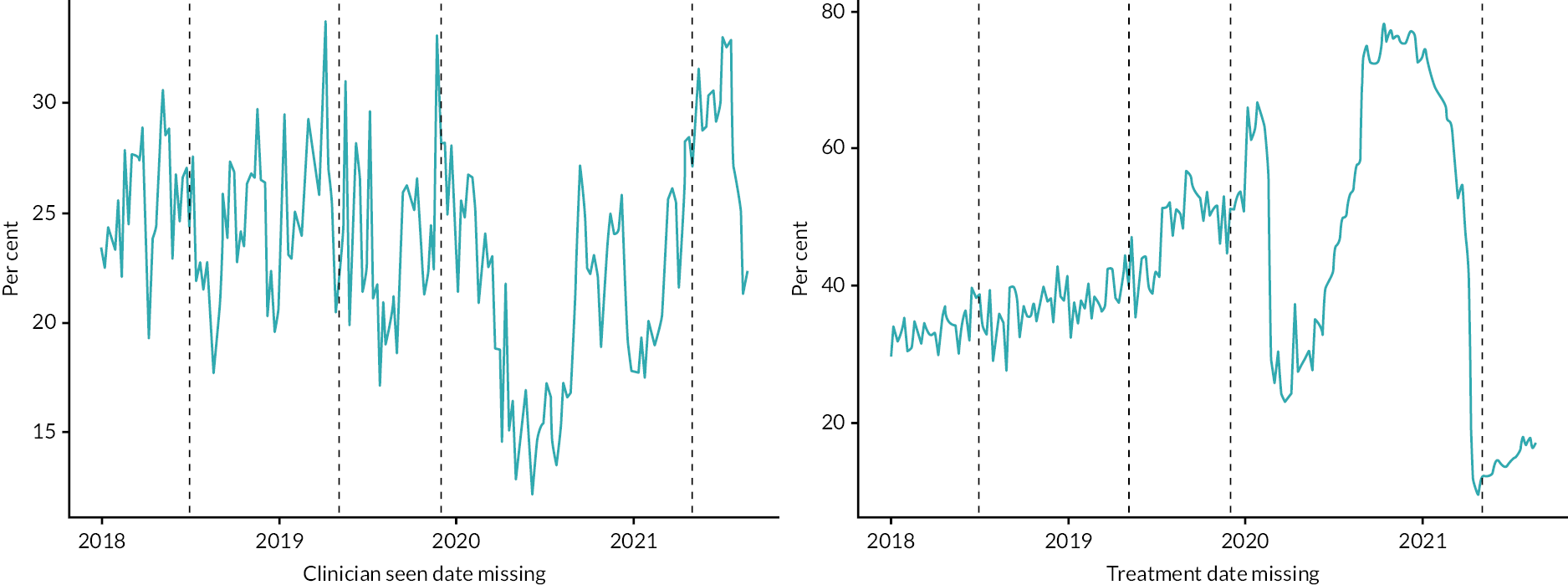
Overall, the proportion of missing clinician seen dates and treatment dates was 23.4% and 42.7%, respectively. The weekly per cent of clinician seen dates missing ranged between 12 and 34 during the follow-up period. Although the proportion of missing dates remained between 20% and 30% for the majority of the study period, there was a moderate decrease between March and May 2020. On the other hand, the weekly per cent of treatment dates missing showed a steady increase from January 2018 (30%) until February 2020 (67%) which then sharply decreased to around 25% in March 2020 before a sharp increase to over 75% in August–December 2020.
We examined the conformance of data on A&E visits to the standard process model. Specifically, we counted the number of cases that did not conform to the ‘rules’ and report these as percentages of the total cases in Table 20. We also identified cases where the patient journey through A&E experienced a ‘left-shift’. In process models the convention is for activities to flow from left to right so a ‘left-shift’ represents a return to an earlier activity, for example a re-admission to hospital or a return to ICU from a ward. In health care, these can be seen as indicators of adverse events if they are not part of the planned care model. We summarise the proportion of A&E care stages that have ‘shifted-left’ in Table 21.
| Intervention phase | Proportions (%) | |||
|---|---|---|---|---|
| Arrived → assessed | Assessed → treated | Treated → concluded | Concluded → checked out | |
| Pre-intervention | 86.5 | 60.7 | 91.2 | 92.7 |
| PF programme | 88.9 | 57.0 | 89.7 | 94.4 |
| CC tile roll-in | 89.5 | 42.6 | 83.2 | 96.0 |
| CC goes live | 86.5 | 28.1 | 65.5 | 92.2 |
| HW training | 90.1 | 70.1 | 79.8 | 96.4 |
| Intervention phase | Proportions (%) | |||
|---|---|---|---|---|
| Arrived ← assessed | Assessed ← treated | Treated ← concluded | Concluded ← checked out | |
| Pre-intervention | + 0.0 | 5.9 | 0.2 | 1.7 |
| PF programme | 0.0 | 7.2 | 0.2 | 1.7 |
| CC tile roll-in | + 0.0 | 12.6 | 0.2 | 3.6 |
| CC goes live | 0.0 | 24.8 | 0.2 | 6.9 |
| HW training | 0.0 | 7.0 | 0.3 | 3.0 |
The proportions of A&E visits progressing to the next ‘valid’ stage remained similar among the pre-intervention and post-intervention periods. Visits with records of consultation conclusion time were highly likely (> 92%) to have their check-out time recorded in all intervention periods. Visits with assessment time recorded were least likely (28–70%) to have their treatment time recorded for the same period. When the recorded times of A&E care stages were checked for a reversed sequence of events or ‘left-shift’, there was almost no assessment time that was recorded before arrival throughout the study period, as expected. However, treatment time and check-out time were recorded before their respective preceding care stages (assessment time and consultation conclusion time, respectively), contrary to what one would expect.
The effects of the command centre intervention
Impact on patient safety
Table 22 presents a summary of the key indicators for patient safety based on the five phases of the intervention.
| Outcome | Intervention phase | Change in BRI (95% CI)a | Change in CHH (95% CI)a | Difference between sites (BRI-CHH), 95% CI |
|---|---|---|---|---|
| Mortality (%)b | Pre-intervention | Reference | Reference | Reference |
| Patient flow programme | −1.4 (−1.9 to −0.8) | −2.0 (−3.1 to −0.9) | 0.6 (−0.6 to 1.9) | |
| Command centre tile roll-in | −1.5 (−2.1 to −0.9) | −2.3 (−3.5 to −1.1) | 0.8 (−0.6 to 2.2) | |
| Command centre goes live | −1.3 (−1.82 to −0.7) | −1.3 (−2.4 to −0.2) | 0.04 (−1.2 to 1.3) | |
| Engagement resumption | −2.5 (−3.4 to −1.7) | −3.1 (−4.8 to −1.4) | 0.6 (−1.4 to 2.5) | |
| Re-admissions within 72 hours (%)b | Pre-intervention | Reference | Reference | Reference |
| Patient flow programme | −2.7 (−3.8 to −1.7) | −0.6 (−1.5 to 0.2) | −2.1 (−3.4 to −0.7) | |
| Command centre tile roll-in | −2.5 (−3.6 to −1.4) | 2.6 (1.6 to 3.5) | −5.1 (−6.6 to −3.6) | |
| Command centre goes live | −2.02 (−3.0 to −1.0) | 3.6 (2.7 to 4.5) | −5.6 (−6.9 to −4.3) | |
| Engagement resumption | −0.70 (−2.3 to 0.9) | 2.2 (0.8 to 3.5) | −2.9 (−4.8 to −0.8) | |
| Postoperative sepsis (%) | Pre-intervention | Reference | – | – |
| Patient flow programme | 0.4 (−1.2 to 2.0) | – | – | |
| Command centre tile roll-in | −0.5 (−2.2 to 1.3) | – | – | |
| Command centre goes live | 1.31 (−0.3 to 2.9) | – | – | |
| Engagement resumption | −0.2 (−2.7 to 2.2) | – | – |
In BRI, when compared with the pre-intervention period, the weekly mortality decreased by 1.4% (95% CI 0.8% to 1.9%), 1.5% (95% CI 0.9% to 2.1%), 1.3% (95% CI 0.8% to 1.9%) and 2.5% (95% CI 1.7% to 3.4%) during the first (‘patient flow programme’), second (‘command centre tile roll-in’), third (‘command centre goes live’) and fourth (‘hospital-wide engagement resumption’) intervention periods, respectively. During the first, second and third intervention periods, the weekly per cent of re-admission within 72 hours also decreased by 2.7% (95% CI 1.7% to 3.8%), 2.5% (95% CI 1.4% to 3.6%), 2.0% (95% CI 1.0% to 3.0%) and 0.7% (95% CI 2.2% to 0.9%), respectively. The weekly postoperative sepsis data did not show a significant change during the study period.
In CHFT, compared to the baseline, the weekly mortality decreased by 2.0% (95% CI 3.1 to 0.9), 2.3% (95% CI 3.5 to 1.1), 1.3% (95% CI 2.4 to 0.2) and 3.1% (95% CI 4.8 to 1.4) for the respective intervention phases of BRI. However, except for the first intervention period, re-admissions within 72 hours showed a significant increase during the second (change = 2.6%, 95% CI 1.6 to 3.5), third (change = 3.6, 95% CI 2.7 to 4.5) and fourth (change = 2.2, 95% CI 0.8 to 3.5).
When BRI and CHFT are compared in regard to the indicator outcome changes during the study period, the weekly mortality significantly improved while the weekly re-admissions showed improvement in BRI hospital and otherwise in the CHFT.
Impact on patient flow
Table 23 presents a summary of results for patient flow. There was no significant difference in the weekly average of inpatient length of stay between the pre-intervention and the post-intervention periods. Table 24 shows the A&E waiting times and showed an increase of 62 minutes (95% CI 40 to 85 minutes) during the fourth (‘Hospital-wide engagement resumption’) intervention period when compared with the pre-intervention period. The first and second intervention periods also showed a decrease of 10 minutes (95% CI 4 to 16 minutes) and 9 minutes (95% CI 2 to 15 minutes) in the average A&E clinician seen time when compared with the pre-intervention period.
| Outcome | Intervention phase | Effect change (95% CI)a |
|---|---|---|
| Length of stay (hours)b | Pre-intervention | Reference |
| Patient flow programme | −8.8 (−17.6 to 0.08) | |
| Command centre tile roll-in | −8.9 (18.6 to 0.65) | |
| Command centre goes live | −1.67 (−10.3 to 6.9) | |
| Engagement resumption | −0.54 (−13.9 to 12.8) | |
| Waiting time (hours)c | Pre-intervention | Reference |
| Patient flow programme | −0.14 (−0.39 to 0.11) | |
| Command centre tile roll-in | −0.21 (−0.48 to 0.06) | |
| Command centre goes live | −0.19 (−0.43 to 0.06) | |
| Engagement resumption | 1.04 (0.67 to 1.42) | |
| Clinician seen time (hours)c | Pre-intervention | Reference |
| Patient flow programme | −0.16 (−0.26 to −0.06) | |
| Command centre tile roll-in | −0.14 (−0.25 to −0.04) | |
| Command centre goes live | −0.06 (−0.16 to 0.03) | |
| Engagement resumption | 0.01 (−0.14 to 0.15) |
| Intervention phase | Average transition time in minutes [mean (95% CI)] | |||
|---|---|---|---|---|
| Arrived → assessed | Assessed → treated | Treated → concluded | Concluded → checked out | |
| Pre-intervention | Reference | Reference | Reference | Reference |
| PF programme | −0.9 (−1.4 to −0.35) | 5.9 (3.9 to 7.9) | 11.5 (9.2 to 13.9) | 14.0 (−33.1 to 5.2) |
| CC tile roll-in | −3.0 (−0.3.5 to −2.4) | 4.7 (2.3 to 7.1) | 12.3 (8.7 to 15.9) | 4.1 (2.8 to 5.4) |
| CC goes live | −9.7 (−11.0 to −8.4) | −21.0 (−23.1 to −18.9) | 53.4 (48.1 to 58.7) | 0.9 (−1.2 to 3.0) |
| HW training | −3.1 (−3.5 to −2.7) | 10.2 (8.1 to 12.3) | 50.2 (47.5 to 52.9) | −0.4 (−2..4 to 1.6) |
The transition time from arrival to assessment consistently improved during the intervention period; there were decreases of 0.9 minutes (95% CI 0.35 to 1.4), 3 minutes (95% CI 2.4 to 3.5), 9.7 minutes (95% CI 8.4 to 11.0) and 3.1 minutes (95% CI 2.7 to 3.5) during ‘patient flow programme’, ‘command centre tile roll-in’, ‘command centre goes live’ and ‘hospital-wide training programme’, respectively. However, the transition time from assessment, treatment and visit conclusion to the next respective A&E stage of care had increased significantly.
Impact on data quality
The data quality did not change significantly during the study period, except the weekly proportion of missing clinician seen dates significantly worsened during the ‘hospital-wide engagement resumption’ period when compared with the pre-intervention period (change = 17%, 95% CI 10.4% to 32.5%). Likewise, there was a significant increase in the weekly proportion of treatment dates missing during the ‘command centre tile goes live’ period when compared with the pre-intervention period (Table 25).
| Outcome | Intervention phase | Change (95% CI)a |
|---|---|---|
| Clinician seen date missing (%)b | Pre-intervention | Reference |
| Patient flow programme | −1.5 (−4.75 to 1.76) | |
| Command centre tile roll-in | −0.85 (−4.38 to 2.69) | |
| Command centre goes live | 0.44 (−2.72 to 3.60) | |
| Engagement resumption | 17.2 (12.26 to 22.10) | |
| Treatment date missing (%)b | Pre-intervention | Reference |
| Patient flow programme | 3.0 (−8.37 to 14.38) | |
| Command centre tile roll-in | 10.2 (−2.16 to 22.54) | |
| Command centre goes live | 21.5 (10.4 to 32.5) | |
| Engagement resumption | 2.3 (−14.8 to 19.5) |
The proportion of arrivals and ‘concluded visits’ that progressed to the next ‘valid’ stage of A&E care (i.e. assessment and check-out, respectively) had largely improved during the intervention period. However, the proportions of those who were assessed or treated that progressed to the next ‘valid’ stage of A&E care (i.e. treatment and concluded visits, respectively) were consistently lower than the pre-intervention period (Table 26). However, the proportion of ‘reversal sequence of events’ or ‘left-shift’ (treatment to assessment and check-out to conclusion of consultation) worsened during the intervention period when compared with the pre-intervention period (Table 27).
| Intervention phase | Change in proportion of A&E activities following ‘rules’ (95% CI) | |||
|---|---|---|---|---|
| Arrived → assessed | Assessed → treated | Treated → concluded | Concluded → checked out | |
| Pre-intervention | Reference | Reference | Reference | Reference |
| Patient flow | 2.4 (1.7 to 3.2) | −3.7 (−4.8 to −2.6) | −1.5 (−2.4 to −0.7) | 1.5 (0.9 to 2.1) |
| CC tile roll-in | 3.0 (2.3 to 3.8) | −18.1 (−19.3 to −16.9) | −8.0 (−9.1 to −6.9) | 3.2 (2.7 to 3.8) |
| CC goes live | −0.0 (−0.0 to 0.0) | −32.6 (−33.5 to −31.7) | −25.7 (−26.5 to 25.0) | −0.5 (−0.9 to −0.0) |
| HW training | 3.7 (3.1 to 4.3) | 9.3 (8.4 to 10.2) | −11.4 (−12.0 to −10.7) | 3.7 (3.2 to 4.1) |
| Intervention phase | Change in proportion of A&E activities ‘left-shifted’ (95% CI) | |||
|---|---|---|---|---|
| Arrived ← assessed | Assessed ← treated | Treated ← concluded | Concluded ← checked out | |
| Pre-intervention | Reference | Reference | Reference | Reference |
| PF programme | −0.0 (−0.0 to +0.0) | 1.3 (0.6 to 2.0) | +0.0 (−0.0 to 0.0) | −0.0 (−0.3 to 0.3) |
| CC tile roll-in | +0.0 (−0.0 to +0.0) | 6.6 (5.4 to 6.4) | −0.0 (−0.0 to + 0.0) | 1.9 (1.5 to 2.3) |
| CC goes live | −0.0 (−0.0 to +0.0) | 18.9 (18.2 to 19.5) | −0.0 (−0.0 to + 0.0) | 5.2 (4.9 to 5.5) |
| HW training | −0.0 (−0.0 to +0.0) | 1.1 (0.5 to 1.6) | 0.1 (−0.0 to + 0.0) | 1.3 (1.1 to 1.6) |
Sensitivity analysis
Patient safety
When only the technology part of CC was assumed as the intervention, there was no significant difference between the pre- and post-intervention periods in the patient safety indicators. For example, mortality did not significantly change during the ‘command centre tile roll-in’ (change = −0.5%, 95% CI −1.3 to 0.3) and ‘command centre goes live’ (change = −0.3, 95% CI −1.0 to 0.4) periods when compared with the pre-intervention period (Table 28).
| Outcome | Intervention phase | Effect change (95% CI) |
|---|---|---|
| Mortality (%)a | Pre-intervention | Reference |
| Command centre tile roll-in | −0.50 (−1.3 to 0.27) | |
| Command centre goes live | −0.32 (−1.0 to 0.39) | |
| Re-admissions within 72 hours (%) | Pre-intervention | Reference |
| Command centre tile roll-in | −0.17 (−1.5 to 1.2) | |
| Command centre goes live | 0.36 (−0.9 to 1.6) | |
| Postoperative sepsis (%) | Pre-intervention | Reference |
| Command centre tile roll-in | −0.58 (−2.7 to 1.5) | |
| Command centre goes live | 1.17 (−0.8 to 3.1) |
Patient flow
When only the technology was assumed as part of the intervention, there was no meaningful difference between the pre- and post-intervention periods in the patient flow indicators (length of stay, waiting time and clinician seen time). However, the average transition time between A&E care stages significantly improved during the same period (Table 29). The data quality had, however, largely worsened during the intervention period (Table 30).
| Outcome | Intervention phase | Effect change (95% CI)a |
|---|---|---|
| Length of stay (hours)b | Pre-intervention | Reference |
| Command centre tile roll-in | −4.39 (−16.1 to 7.3) | |
| Command centre goes live | 3.2 (−7.6 to 14.0) | |
| Waiting time (hours)c | Pre-intervention | Reference |
| Command centre tile roll-in | −0.05 (−038 to 0.28) | |
| Command centre goes live | −0.02 (−0.32 to 0.28) | |
| Clinician seen time (hours)c | Pre-intervention | Reference |
| Command centre tile roll-in | −0.01 (−0.14 to 0.12) | |
| Command centre goes live | 0.07 (−0.05 to 0.19) | |
| Clinician seen date missing (%)c | Pre-intervention | Reference |
| Command centre tile roll-in | 3.4 (−0.86 to 7.8) | |
| Command centre goes live | 4.9 (0.9 to 8.9) | |
| Treatment date missing (%)c | Pre-intervention | Reference |
| Command centre tile roll-in | 10.7 (−4.0 to 25.5) | |
| Command centre goes live | 22.5 (8.8 to 36.2) |
| Intervention phase | Average time spent in minutes [mean (SD)] | |||
|---|---|---|---|---|
| Arrived → assessed | Assessed → treated | Treated → concluded | Concluded → checked out | |
| Pre-intervention | Reference | Reference | Reference | Reference |
| CC tile roll-in | −2.5 (−0.3.0 to −2.0) | −59.0 (−61.1 to −56.9) | −3.5 (−22.9 to 15.9) | −3.7 (−20.0 to 12.6) |
| CC goes live | −6.2 (−6.6 to −5.8) | −3.2 (−4.7 to −1.7) | 35.5 (16.2 to 54.8) | −7.5 (−12.0 to −3.0) |
Data quality
Table 31 summarises changes in data quality for just the three phases of the technology intervention. Table 32 summarises conformance to the ‘rules’ for A&E processes, as above, but just looking at the three phases of the technology intervention. The data quality had largely worsened during the intervention period, and we attribute this to the impact of the pandemic.
| Outcome | Intervention phase | Effect change (95% CI)a |
|---|---|---|
| Clinician seen date missing (%)b | Pre-intervention | Reference |
| Command centre tile roll-in | 3.4 (−0.86 to 7.8) | |
| Command centre goes live | 4.9 (0.9 to 8.9) | |
| Treatment date missing (%)b | Pre-intervention | Reference |
| Command centre tile roll-in | 10.7 (−4.0 to 25.5) | |
| Command centre goes live | 22.5 (8.8 to 36.2) |
| Intervention phase | Change in proportion of A&E activities following ‘rules’ (95% CI) | |||
|---|---|---|---|---|
| Arrived → assessed | Assessed → treated | Treated → concluded | Concluded → checked out | |
| Pre-intervention | Reference | Reference | Reference | Reference |
| CC tile roll-in | 1.6 (1.0 to 2.3) | −16.1 (−17.1 to −15.1) | −7.2 (−2.4 to −0.7) | 2.4 (2.0 to 2.9) |
| CC goes live | 0.4 (−0.1 to 0.7) | −11.6 (−12.2 to −11.0) | −15.9 (−16.4 to −15.4) | 0.5 (0.2 to 0.8) |
Chapter 7 Discussion and conclusions
In this chapter, we draw together the results presented in Chapters 3–6 with a synthesis of our research findings. We synthesise insights from the qualitative research and theoretical perspectives, including development of intervention logic to support future CC implementations and guide research evaluation. We then turn to the quantitative findings and their implications for evaluation of impact upon patient safety, patient flow and data quality. Finally, we consider the overall strengths and weaknesses of our mixed-method evaluation.
Synthesis of findings from the qualitative research and cross-industry review
The aims of the qualitative and theoretical research within this mixed-method study were to investigate the impact of the CC on patient safety, patient flow and data quality (aim 1), to understand the process of implementation and integration of the CC within the primary study site (aim 2) and to elicit cross-industry perspectives on hospital C2 technologies to contextualise the findings (aim 3) and provide practical recommendations for future development in this area (aim 4).
In response to these aims, a range of outputs were produced, including a detailed case description based upon extensive ethnography in and around the CC and triangulation of related data sources (aims 1 and 2, reported in Chapter 5), a qualitative process evaluation based upon interviews with staff concerning the implementation and impact of the initiative (aims 1 and 2, reported in Chapter 5), a cross-industry scoping review of C2 based upon a systematic search and screening of the published literature and guidance from a panel of industry experts (aim 3, reported in Chapter 4) and a theoretically informed synthesis of empirical findings and cross-industry perspectives, to construct intervention logic and inform future development and evaluation of healthcare operational C2 systems (aim 4, developed in the following synthesis within the present chapter).
In summary of the key qualitative findings, ethnographic observations and interviews with study site staff documented the complexity and challenges of developing, integrating and operating a system of this type in an acute care environment and how the CC, and crucially its experienced multi-professional team of combined clinical/operational staff, supported operational planning and control across the system. The CC additionally made a significant contribution to the organisation’s capacity to respond to the surges in service demand and operational challenges associated with the pandemic and represented a source of resilience at this time of deviation from ‘normal’ operating models. We found some evidence that organisational behaviour linked to the CC represented enhanced centralised operational monitoring and control, linked to established C2 functions identified through our cross-industry review, including acting as an effective hub to detect and resolve challenging and evolving operational issues. In addition, various unintended consequences emerged including occasional divergence in perspectives between the CC and front-line areas on operational issues and others affecting confidence in the quality of data available for decision-making. Despite tensions between centralised control and local autonomy, CC staff demonstrated the capacity to maintain granular, personalised care (facilitated by access to detailed patient information) in addition to system-wide oversight.
Theoretical description and application of transferable command centre functions
In order to develop transferable intervention logic for hospital CC programmes, we sought to integrate theoretical perspectives on effective C2 from our cross-industry review with insights from our empirical observations and from the testimony of key informants interviewed during the course of the study.
In considering the lessons from synthesis of cross-industry expertise and perspectives for a theory of effective C2 in health care, the following functions of effective CCs were identified (Table 33), along with sources of evidence and rationale for their efficacy.
| Command centre functions | Description | Source (interview/reference) | Rationale for effective C2 |
|---|---|---|---|
| Variable modes of operation/responsiveness to ‘operational tempo’ | Speed and intensity of actions relative to unfolding of events in the operational environment, sometimes seen as a shift in mode of operation | Busch (2001)118 Feigh and Pritchett (2010)119 Interview 01, 02, 03 |
Command and control should facilitate and not hinder the shift in operational tempo/mode to deliver effective service |
| Maintains a shared sense of situational awareness | Level of perception and understanding of environmental elements and events with respect to time or space | Buchler et al. (2016)10 McGuinness and Ebbage (2002)120 Interview 01, 02, 03, 04 |
Fundamental to support effective decision-making and action |
| Diversity in team composition and flexibility in decision hierarchy | Composition of operational team and flexible hierarchy of decision-making | Bell et al. (2013)121 Stanton et al. (2015)122 Interview 01, 02, 03 |
Operational team must consist of integrating multiple functions to facilitate effective control and have clear decision-making responsibilities with flexible hierarchy depending on the demands of the situation |
| System resilience | The ability to detect, quickly adapt and recover from any anticipated or unanticipated changes or events | Arbuthnot (2008)123 Hamer et al. (2021)100 Interview 01, 02, 03, 04 |
Essential to maintain service delivery in the face of dynamic adverse events or conditions |
| Expert knowledge | Domain-specific knowledge and understanding brought to bear upon operational issues | Hukill and Mortensen (2011)124 Walker et al. (2010)125 Interview 01, 03 |
Supports situational awareness for effective operation |
| Technology implementation | Introduction of new technologies and systems to the operating environment | Aniceto (2010)126 Kane et al. (2019)112 Interview 02, 03, 04 |
Potential to support situational awareness and decision-making |
The findings from the cross-industry review suggest the importance of developing a mature framework of protocols for the operation of a CC, in addition to the installation of requisite technological functions and the integration of diverse organisational roles in the approach to staffing the CC. As a controlling system, the CC’s operating protocols should be defined relative to a commonly understood model of the ‘stable’ system state (relating to the system under control). Operational behaviour within the CC may then switch between varying modes in response to detected variations in system state. In high-risk industries, the advantages of this approach to control are that the modes of operation may be rehearsed through operational experience, training and simulation in order to establish routines that are geared towards, for example, efficient information-seeking, effective intensification and direction of the focus of monitoring activity, division of resources to explore future contingencies over varying temporal horizons, and other behavioural routines that represent preparedness, resilient responses and agility in constructing an effective model of uncertain/novel/unstable situations.
Critical to maintaining situational awareness and the capacity for timely operational intervention is instantaneous presentation of information concerning system state (i.e. in real time without lag), the completeness of information (or having the right information), the accuracy of the information displayed as a true representation of the system state, and, where any of the aforementioned may be questionable, knowledge or awareness of the likely areas of discrepancy and hence its potential impact on the capacity to make effective responses (system transparency). While the example of a CC implementation that we studied in this project integrated a broad spectrum of data and information linked to a complex system, there were scenarios in which data completeness, accuracy and lag were not optimised, resulting in the team’s resources being consumed in secondary activities such as data validation and workarounds.
Intervention logic for a digitally enabled hospital command centre
In order to support future development, implementation and evaluation of CC programmes in health care, we synthesised key themes from the qualitative analysis, contextualised theory from the cross-industry review on C2 and constructs from Implementation Science theory describing known implementation factors to produce an intervention logic model (Figure 8). Here we refined themes into named variables and factors that we could subsequently classify according to a higher-level scheme representing causal sequence and processes or mechanisms driving outcomes. The framework was informed by constructs from the Consolidated Framework for Implementation Research, including consideration of the inner setting for the intervention (e.g. culture, implementation climate, structural characteristics of the organisation), outer setting (e.g. external policies and patient needs), implementation processes (e.g. engaging, executing) and nature of the innovation. 127,128
FIGURE 8.
An intervention logic model for digitally enabled hospital CC implementations. GPs, general practitioners; EDD, expected date of discharge.
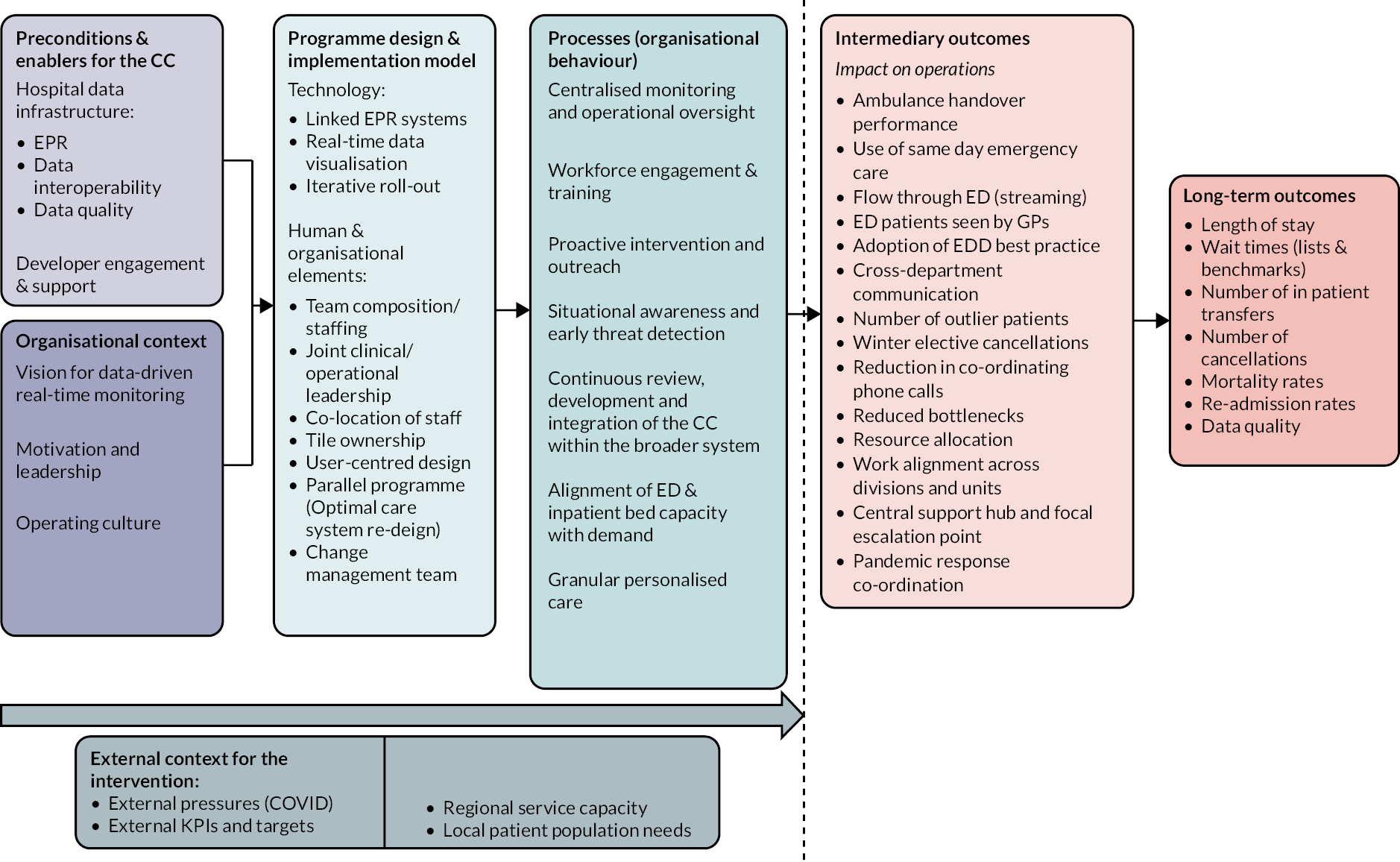
Implications of the logic model for evaluation of command centre implementations
In the structure of the model, ‘preconditions and enablers for the command centre’ and ‘organisational context’ refer to the factors identified within the study that enabled the CC programme to be initiated or that represented the impetus for the programme in the first place, including the requisite hospital data infrastructure, developer support, leadership vision and operating culture. We then represent factors concerning the programme design and implementation model within the framework, including both the key functional concepts (such as data integration, real-time visualisation and joint clinical–operational leadership) and development/implementation approach (e.g. iterative roll-out, user-centred design and change-management structures). Crucially, our ethnographic and qualitative investigations demonstrated the complex interplay between technical system design, the human and organisational dimensions of effective C2, and the implementation or change process undertaken to embed the system and promote uptake and engagement throughout the organisation.
The central category within the intervention logic model is concerned with organisational behaviour and more specifically the activities and processes that CC staff, programme leads and operations managers were engaged in during our ethnography. The daily business of CC operations included centralised, system-wide monitoring and operational oversight, including detection and mitigation of threats to the stable state of the system, in accordance with knowledge of C2 behaviours in organisational settings across a range of applications studied in our cross-industry review. The ethnography, however, additionally identified human activities and organisational behaviours in and around the CC that required a somewhat deeper immersion in the sociocultural context in order to understand their full significance and meaning. A considerable proportion of CC activity was undertaken to promote engagement across the front-line units of the organisation and develop or maintain relationships with key staff in front-line areas to promote effective two-way communication and co-ordination of activity. CC staff additionally made efforts to host visits to the CC from all areas of the organisation in an attempt to understand and resolve local operational issues and support staff in their remote operational roles. The CC therefore came to represent a focal point for escalation of what were often perceived to be hitherto intractable issues. It was additionally interesting to note that despite the high-level, centralised oversight afforded the CC team staff, and despite the high volume of individual patients represented in displays and metrics presented within the CC, the team showed particular diligence in providing a level of granular, personalised care for individual patients wherever the opportunity presented itself. This might include, for example, interrupting the flow of intrahospital transfer to delay an individual’s bed move until after a scheduled mealtime. Such behaviours demonstrate the value of including experienced front-line operational knowledge (in this case, nursing) in the CC team’s composition. It was suggested to the research team on more than one occasion by programme leads that the staffing composition and level of experience were critical if the team was to understand what the metrics displayed within the CC actually meant in operational terms on the ground.
Regarding evaluative outcomes from a CC programme of the type implemented in the study site, we have distinguished between intermediary (proximal) outcomes and long-term (distal or downstream) outcomes in our logic model. The rationale for this distinction is twofold. Firstly, the long-term outcomes tend to represent more pervasive, system-level parameters linked to quality, safety and efficiency of care within an acute trust and as such are subject to a broad range of influences (both within the control of the organisation and external to it, the pandemic being a prime example of the latter in this case). Secondly, specifying intermediary or proximal outcomes allows us to identify a range of factors that may be more directly influenced by the intervention itself drawing upon evidence from our investigations as to how organisational behaviour, decisions and intervention actions originating within the CC influence the broader system of care. Intermediary outcomes therefore represent, in many cases, the mechanisms by which the design and operation of the CC drive some proportion of variance in long-term outcomes. It should be noted, for example, that the CC operational focus was predominantly management of patient flow originating through emergency or non-elective admissions. We would not expect, therefore, to see effects of CC programme implementation or developments in certain service areas within the broader organisation, such as in maternity services. Similarly, high-level outcomes such as length of stay and wait times should be disaggregated to a level of granularity in which the impact upon specific service areas and waiting targets that are sensitive to this intervention can be evaluated.
An important finding from the study concerns the conception of a CC implementation which, based upon our experience in this study, should be regarded as a long-term programme of organisational development rather than a discrete technology deployment. In our logic model, a key process is ‘continuous review, development and integration of the CC within the broader system’. CCs require the capacity to evolve and procurement of off-the-shelf solutions with licensed support packages might actually hinder this process, by not being responsive enough to respond rapidly to emerging use cases, in comparison with ‘in-house’ developments. More specifically, each adopting organisation is likely to have specific user requirements and a specific data infrastructure profile that may make an off-the-shelf solution suboptimal for the needs of the organisation. Possessing ownership of the mechanisms for data integration (to facilitate rapid manipulation, troubleshooting and transparency in how metrics are compiled), our study suggests, is key to human confidence and trust in the system. Similarly, having uninhibited access to the organisations ‘raw’ data within an EHR would seem to be a prerequisite for organisations considering taking the step towards data-driven operational C2.
We observed certain instances where data lag and/or duplication of functions with parallel systems rendered data and flags within the CC obsolete and the team looking to alternative sources to maintain situational awareness. Effectively, the team’s mental model of system state tracked ahead of the presented data model of the system in the CC and drove interrogation of the presented data. The team essentially had developed ad hoc means of triangulating multiple data sources to arrive at a view in which they had confidence and in which the CC analytics was only one source of information. This was at odds with the system design rationale which was to create a real-time and accurate integrated source of information that would enhance decision-making by providing useful configurations of data with prioritisation flags to help guide attention and decision-making. Taking the CC system as a whole, there was a gap between what the underlying data model was delivering and what it might have contributed to support the human and organisational activity of operational C2; a gap that wasn’t quite closed, despite ongoing development efforts, by the end of our research involvement with the centre. This was in part due to local data-quality issues, but additionally inflexibility in systems that integrated and translated data streams and reliance on external providers to resolve suspected problems. In the design of the CC, where interplay between data presentation and human decision-making is concerned, consideration of system-level, in addition to tile-level, use cases and the human factors involved in interactions between the team and the CC system as a whole is implicated for future development.
Finally, a key finding from analysis of the many recorded narratives and field notes within our study was the emphasis placed upon the notion that effective digitally enabled hospital C2 was not just a technology-driven endeavour but a true sociotechnical system or intervention, in which the human and organisational work of C2 was of equal (perhaps even more) importance to the successful functioning of the system compared to the digital components. In practical terms, our intervention logic model therefore represents a sociotechnical framework for reasoning about the prerequisites, design elements, implementation factors, implicated organisational processes and proximal/distal outcomes for digital hospital CC implementations as long-term development programmes, based upon our experience in one such programme. Our observations and review of the programme at Bradford confirmed what the local developers and implementers knew at outset, that an undertaking of this nature was not simply a technology investment or informatics project, but a programme with considerable organisational change implications spanning all levels of the organisation and its front-line units.
As a complex organisational intervention, introducing centralised, digitally enabled hospital command systems may give rise to a range of intended and unintended consequences that affect human and clinical workflow across the system, in pursuit of data quality, as well as operational efficiency. The implementation of a system representing (even conceptually if not in actuality) a centralised system of close oversight, coupled with the capacity for reactive intervention in any area of the system, may challenge culturally engrained notions of clinical autonomy and self-regulation by front-line care teams. Again, this emphasises the importance of the right implementation model for such a system and crucially how its purpose and operation are presented to staff. The very language of military style ‘command and control’ may not be helpful here, as indicated by findings from our review, and there is considerable scope for additional work to understand how this type of initiative may be best adapted for the healthcare context through further robust evaluations of specific implementations and implementation models.
Discussion of quantitative findings and implications
In this pre- and post-intervention comparative study using EHR data, the findings indicate that introduction of the Bradford Command Centre may improve patient safety. However, given improvements in mortality have also been observed in the CHFT (control site) during the same period, the positive impacts seen in the BRI hospital may not be entirely due to the CC. In addition, there was no significant difference between pre- and post-intervention periods if only the software technology was considered part of the intervention. Furthermore, introduction of the CC was not observed to have a significant and consistent impact on patient flow and data quality.
Impact on patient safety
In the BRI hospital, when the process of change and technology were considered as a ‘whole package’, only two of the three patient safety indicators showed improvement during the post-intervention period when compared with the pre-intervention period. In particular, the mortality decreased by 1.4%, 1.5%, 1.3% and 2.5% after implementing a ‘patient flow programme’, ‘command centre tile roll-in’, ‘command centre goes live’ and ‘hospital-wide engagement and training’ programmes, respectively, compared to the pre-intervention period. Likewise, the re-admission within 72 hours also decreased by 2.7%, 2.5% and 2.0% for the ‘patient flow programme’, ‘command centre tile roll-in’ and ‘command centre goes live’ periods, respectively, when compared with the pre-intervention period. However, the same degree of improvement in mortality was also observed in the control site during the same period; 2.0%, 2.3%, 1.3%, 3.1% for the respective intervention phases of the BRI hospital.
Impact on patient flow
The introduction of the CC did not have a significant effect on the three out of three of patient flow indicators. The length of stay only showed a non-significant decrease of 8.8 hours [standard error (SE): 4.5], 8.9 hours (SE: 4.9), 1.7 hours (SE: 4.4) and 0.55 hours (SE: 6.8). The waiting (time taken until patient treatment), clinician seen time (time until patient is seen by a clinician) and A&E transition time (time taken to progress from one stage of A&E care to the next stage of A&E care) also did not significantly improve during the study period.
Impact on data quality
The state of the data quality, measured as the proportion of missing dates, A&E visits progress to the next stage of care and ‘reversal sequence of events’, was worse when the CC was introduced, albeit non-significant. On average, the proportion of missing in treatment date (42.7%) and clinician date (23.4%) was substantial. Moreover, the missing proportions were worse during the post-intervention periods than the pre-intervention period. For example, the missing in A&E visitor’s treatment date was higher by 3%, 10.2%, 21.5% and 2.3% when a ‘patient flow programme’, ‘command centre tile roll-in’, ‘command centre goes live’ and ‘hospital-wide engagement resumption’ programmes were implemented, respectively. These suggest that the use of a CC may not have had any measurable impact on data quality.
Comparison with other studies
There is a paucity of studies that investigate the impact of multidepartment hospital-based CCs on patient safety, patient flow and data quality. A recent report from the Saudi National Health Command Centre indicated that the use of a ‘smart centre’ had led to mortality rate below 2% and reduction of intensive care unit (ICU) lengths of stay by 10% in emergency admissions. 21 While the mortality is in line with the findings from BRI emergency admission data the ICU length of stay reported by Alharbi and colleagues21 disagrees with the findings of this study. In fact, the average ICU lengths of stay (as calculated separately) for pre-intervention and post-intervention periods are 91 and 108 hours, respectively, which is an increase of 18.7% after implementation of the CC. One notable difference between the study and Alharbi et al. ’s21 is that the Saudi Arabian Command Centre was a national hub and the data used were of the first wave of the COVID-19 pandemic whereas the Bradford Command Centre was used only in the BRI hospital and more than 3 years’ worth of data were used for analyses.
In a report by Johns Hopkins Hospital, transfers of patients from other hospitals were improved by 46%, ambulance dispatch times reduced by 43 minutes and bed allocations of emergency admission patient reduced by 3.5 hours. 22,129 In addition, the CHI Franciscan Mission Control Centre also reported that the lost cases were reduced by 20% in the first 6 months of the year. 19 However, we do not have comparable data in the study and these two CCs were used as hubs for their respective groups of hospitals, unlike the Bradford Command Centre, which only serves the BRI hospital.
Discussion on equality, diversity and inclusion
Both our project and our methodology were designed from the beginning with full consideration for equality, diversity and inclusion. This included involving local people in the research, being sensitive to the local population and its needs, reflecting on the research team’s composition and the consideration of participants in the research.
Our research group is based in BIHR and has developed a very strong place-based approach to equality, diversity and inclusion. The study site, BRI, is the primary hospital serving the population of Bradford. Bradford is one of the 20% most deprived areas of England, with 23% of its children being part of low-income families. Life expectancy, childhood obesity, tuberculosis, cancer, cardiovascular disease, violent crime and alcohol-related-harm hospital admissions are all worse than the England average. Social inequality is high; the most deprived areas have a life expectancy that is 9 years lower for men and 8 years lower for women compared to the least deprived areas, a distance of approximately 10 miles. Bradford has an increasing number of Black, mixed, Asian or British Asian people, with 25% being of Pakistani origin, the second largest proportion in England. Our control site, nearby Calderdale and Huddersfield, has similar patterns of ethnic diversity, inequality, social deprivation and related health issues. BIHR is a national leader in research directed at developing a better understanding of health and social inequalities with, for example, the Born in Bradford cohort study, which is directly engaging with local communities and has been successful in engaging under-represented groups.
Our research proposal was jointly developed with a patient co-investigator from an ethnic minority and with the support of the NIHR Yorkshire and the Humber Patient Safety Translational Research Centre, also based in BIHR and with a strong patient engagement team who follow the INVOLVE framework and are experts in engagement with local communities, particularly targeting under-represented groups. We have followed the INVOLVE framework for patient involvement in directing the research (see Chapter 3) and had a strong ‘Bradford-style’ emphasising inclusivity and celebrating diversity. Our patient advisers were drawn from the local community and were selected to represent diversity. The study built on early patient engagement by the hospital on the CC that had positively targeted the under-represented population with text and pictures that emphasise positive gender, ethnic and disability examples.
For the quantitative work, our data reflect the full diversity of patients attending the study and control sites, with 100% of patients with EHRs included in the study. For the qualitative work, the study participants were selected from the staff working at the study and control sites, so selected by role and involvement in CC work, and we were inclusive in that selection, for example, by interviewing more junior members of staff in a blame-free and confidential setting where they could talk freely about their experiences. This is a small study within a small, localised environment where the staff know each other so we did not consider it appropriate to collect details of gender, sexuality and ethnicity; however, it is worth noting that the gender and ethnic mix of the staff at both sites very closely reflects the gender and ethnic diversity of the local population and that our selection of study participants closely reflected this diversity.
Our research team did not reflect the diversity of the local population but did include male and female academics, ethnic minorities and non-British. The team included a range of experience and expertise including a clinician, a patient and senior professorial staff as advisers, mid-career academics leading the research and early-career researchers conducting much of the fieldwork. We are particularly proud of the development of the two early-career co-investigators who helped to conceive the work, took strong leadership roles in the project and have now progressed to more senior roles, largely as a result of the experience gained on this project.
Discussion on aims and objectives
The aim of this study was to understand how the AI CC at Bradford impacted on the quality, safety and organisation of BRI to generate findings that can be applied to other hospitals in the UK. The objectives of the project were:
-
to evaluate the impact of the CC on patient safety, patient flow and data quality (quantitative evaluation and ethnographic study)
-
to understand the process of implementation and integration of the CC within the primary study site (qualitative process evaluation)
-
to elicit cross-industry perspectives on hospital C2 technologies to contextualise the findings (cross-industry review)
-
to synthesise findings into practical outputs to engage service stakeholders and inform future investment and practice.
We were unable to evaluate the impact of the CC as fully as we had planned because the study was impacted by the COVID-19 pandemic. Hospital staff were extremely busy and access on site was challenging. The additional work negotiating access and the direct impact of the pandemic on our own team meant that we had fewer resources and were unable to complete all our objectives. We were able to observe how the CC helped support the hospital manage its operations through the pandemic and received strong positive evidence of its success. Complex demand challenges and rapid innovation to meet these challenges made it difficult to attribute outcomes to the specific intervention of the CC.
The disruptive effect of the pandemic made our data analysis significantly more challenging than we had anticipated. The study was not able to provide robust evidence that a digital hospital CC package which includes both technological (data display) elements and organisational components has a positive impact on patient safety. When the technology alone was considered as part of the intervention (CC), it does not appear to have a significant impact on patient safety indicators. When the control site was selected, they had no plans to implement a similar command centre approach and were planning to implement a decentralised digital dashboard instead. The decision by the control site to replicate aspects of a CC approach during the pandemic confounded some parts of the study plan but is also a strong indication that a CC approach is valuable, particularly at times of crisis such as during the pandemic.
Objective 1 – evaluation of the impact of the command centre
The CC was observed operating effectively throughout the study period. Our ethnographic observations and interviews with 15 study site staff provide documentary evidence of successful use in a complex environment. The CC made a significant impact on the management of the hospital through the pandemic, including through the introduction of a COVID-19 ‘tile’ which was used to manage COVID-19-specific processes. Our results from ethnographic interviews and observation describe how the CC, and its multi-professional team of combined clinical/operational staff, worked with the new technology to change the way that the hospital operates. We identified unintended consequences that included front-line staff developing a sense of being monitored and interventions (or fear of interventions) from the CC team that were perceived as unwelcome. Linked to this were challenging conversations about the importance of keeping electronic records up to date or acting on evidence of operational issues that were seen as being under local autonomy or ownership. Data quality was a constant concern for staff working in and around the CC and there were limitations in how up to date and accurate (or complete) records were, often necessitating triangulation and verification from multiple sources and systems and showing discrepancy between the data in the systems and what front-line staff reported. Compromise, goodwill and a shared sense of purpose were necessary to ensure the CC was effective.
We were able to extract time-series data on patient safety, patient flow and data quality from operational systems by selecting representative indicators and plotting these over time. We were able to measure changes in these indicators over time and evaluate statistically the long-term impact of the CC on these indicators. We were not able to isolate improvements in these indicators that could directly be attributed to the introduction of the CC. Similarly, we were unable to isolate noticeable improvements in these indicators between study and control site. When the study site and control site were compared, we found improvements in mortality and reduced rates of re-admission at the study site but caution against drawing conclusions from this at a time when the pandemic was raging. Some indicators, notably data quality, worsened rather than improved. We reason that the pandemic had such a profound impact on all aspects of operation that it is not possible to separate out and measure the impact of the CC. Similarly, the later adoption of a CC approach by the control site means we cannot use it to draw strong comparisons.
Objective 2 – understanding the process of implementation of the command centre
Our project started after the CC had been implemented so our results rely on staff recall of the implementation. We identified five phases in the implementation: (1) pre-intervention, (2) a patient flow change programme, (3) CC tile roll-in, (4) CC go-live and (5) post-intervention engagement. Phase 2 was an organisational change, Phase 3 represents a soft-implementation period of training and familiarisation and Phase 4 represents the hard implementation of the new technology and new ways of working. Staff interviews suggest that the overall implementation approach was effective but that they found the implementation challenging and identified some need for more training and software improvements. The intention had been for a period of post-intervention engagement to support staff in getting used to new ways of working and to adapt procedures and technologies to optimise the new approach. This was disrupted by the pandemic, which started to impact on hospital operations only a few months after Phase 4 was complete. Staff recollections are therefore mixed between the pandemic response and the new technology, but there is strong evidence that staff worked well together to find ways of working that were consistent with the CC approach while solving immediate challenges.
Analysis of time-series data on patient safety, patient flow and data quality at different stages of implementation revealed patterns of change in response to the implementation, but these were confounded by the impact of the pandemic on the same outcome measures. When only the technology part of CC was assumed as the intervention, there was no significant difference between the pre- and post-intervention periods in the patient safety and patient flow indicators. The data quality had largely worsened in the post-implementation phase, and we attribute this to the impact of the pandemic. Qualitative results show that the CC has had a long bedding-in process and that this is expected to be a long process as the hospital and its staff adapt to new ways of working. Our qualitative results suggest that major improvements in patient flow, patient safety and data quality have yet to be achieved.
Objective 3 – contextualising the findings using cross-sector and cross-industry perspectives
Results from the literature review found a strong body of research to support the adoption of a CC approach as part of a successful and resilient organisation. CCs are described as supporting situational awareness, decision-making, team structure and workload with the main aim of successfully delivering safety-critical operations reliably over time and in the face of dynamic risks and variations in the operating environment and system conditions. Digital technologies need to be tailored to the work done in the respective domain and should contribute to system resilience. Most articles attribute performance improvements to the physical and functional features of the centres themselves; this often includes the use of technology to generate and display real-time and/or predictive data in the centres. The implementation process usually affects process and policy changes in the organisation, including introducing new ways of working and workload distribution, adding new roles and altering the existing hierarchy of decision-making and responsibility. The literature advises caution in attributing improvements to the physical and functional aspects of the CCs versus the process and policy changes within the organisation that often arise out of the implementation process.
There is emerging evidence that a CC approach can be adopted in acute health care. Effective implementations are characterised by a strong sense of shared situational awareness within a team, with a shared focus on specific focal points for intelligence and intensification of this focus as the threat level increases. System resilience is maintained in these implementations through simultaneous responsive and anticipatory strategies with variable resource allocation for both proactive planning for expected deviations and events with varying timescales. One paper advised caution in using the term ‘command and control’, as it may overly restrict the exploring of new ideas and new approaches seen as important to meeting the specific needs of health care, hospitals and staff given the strong culture of autonomy on the clinical front line.
Objective 4 – synthesis of research findings to inform future investment and practice
The results of our qualitative investigation correspond to themes identified in the cross-industry review. Tensions between the CC and local decision-making within hospital departments were evident throughout the interviews and observations and closely reflect existing literature from other industries. Digital technology should make operational activities transparent for all, but the literature emphasises the importance of systems that are closely tailored to needs and information that are reliable. We identified two major challenges: (1) a strong culture of local autonomy in operational, as well as clinical, decision-making and (2) concerns that data within systems may not be sufficiently accurate or up to date to reflect the reality on the ground. Both challenges are widely recognised in the healthcare literature but are less dominant in other industries with stronger traditions of C2 and well-established, centralised systems. Our quantitative work reflected the data challenge – it was time-consuming and difficult to extract operational data and compare performance metrics and our approach is relatively novel in the literature and for the study site.
The implementation of the CC at Bradford has been a success in changing the operational approach. We found evidence that the approach to implementation was broadly successful but that benefits take time, and significant additional innovation to realise. We consolidate our learning as an intervention logic model that can be used by other hospitals planning an implementation of a digitally enabled hospital CC. This study was limited by the pandemic and further work would be needed to make stronger recommendations for investment and policy.
Reflections on the strengths and limitations of this study
Our ethnographic and qualitative investigations were possessed of the usual limitations of this mode of enquiry, namely access constraints, subjectivity in interactions, data collection and interpretation and the potential for bias in the presentation of the initiative and its impact at the study site. The presentation and impacts of these potential limitations will be discussed below. In conducting this study, we were additionally faced with a number of operational challenges for the project as a result of variations in project staff resources, the timing of the project relative to the pandemic and external challenges in accessing the control site.
The substantial timescale over which a programme like a CC implementation evolves was a challenge for the research for a number of reasons. The pandemic had interrupted, altered and prolonged the implementation timeline and this affected recall of key informants as to key events, sequences and the historic rationale for design decisions. This was somewhat exacerbated by the fact that the programme substantially pre-dated the research team’s presence on site, resulting in some key staff being unavailable or having moved outside the organisation at the point of data collection. Fortunately, the research team had access to a broad range of programme documentation which allowed the timeline to be reconstructed, supplemented by the accounts of programme leads and staff involved. Being able to follow the programme from onset via an action-research-style partnership would perhaps have been preferable to relying on retrospective description and recall, however.
As with all ethnographic work, there is a risk that the presence of researchers within the context being studied might affect behaviour. This may have manifested itself in two ways: firstly, at the level of team behaviour within the CC during observation periods and, secondly, during interviews with informants. In consideration of the first point, it became clear quite quickly with the high volume of observations that the researchers were accepted within the context and operating culture of the CC, as was evident by developing rapport with staff and admission to the full range of team briefings and meetings at all levels of command. This did require a considerable resource to sustain in terms of researcher time on site, however. During interviews, it was possible that perceived pressure from the organisation to achieve a demonstrable return on its substantial investment in the CC programme might have led to inflated presentation of benefits. However, analysis of the transcripts by the research team revealed a willingness to disclose and reflect upon both positive and negative aspects of the CC programme, including what might have been regarded as design oversights and implementation challenges, tending towards a balanced view in the opinion of the researchers, who were also able to explore common themes with multiple informants. In order to account for subjectivity in the analysis of the qualitative data, the research team observed best practices in qualitative research, including multiple iterative stages of coding, theoretically informed analysis, researcher reflexivity, frequent reviews of emerging themes by multiple coders with diverse backgrounds, search for counterfactual evidence, triangulation with multiple data sources, and, in follow-up interviews with key informants, presentation of emerging themes to check relevance and interpretation.
A strength of the cross-industry review work was that it became clear early on in the project that due to the dispersion of relevant literature across multiple domains, a systematic search and screening process would be preferable as the basis for the subsequent scoping review and narrative synthesis. Contributions by subject-matter experts and members of our steering group and co-investigator team with specific expertise in human factors and safety science considerably enhanced the identification of relevant concepts and themes to inform our review. Due to resource constraints in the form of movement of research project staff at a late stage in the project, coupled with late-running data collection at the control site, completion of the intended survey of chief information officers, a component of the cross-industry review, could not be completed before finalisation of the data analysis. While the omission of informatics professionals’ perspectives on CC implementation in health care was a limitation of our review work, we were still able to complete a comprehensive review of industry perspectives, including health care, using a large volume of literature resources and interviews with healthcare experts on CC operations. We additionally identified and described all cases of CC healthcare implementations that met our inclusion criteria, as part of our review. While the majority of peer-reviewed literature on C2, especially in non-military applications, tends towards descriptive case studies and conceptual articles, rather than robust evaluations, it was possible with the application of a systematic process involving multiple screeners to classify this complex body of evidence and draw out translatable themes for synthesis. Development of frameworks for evaluation of CC initiatives in health care, such as the intervention logic model presented in this report, will serve to support future robust evaluations and strengthen the evidence base.
An important consideration in understanding the strengths and limitations of the project concerns insights into the status of the control site gained during the qualitative research. Since the original conception of this study, due to prolonged delays in gaining access to the control site as a result of changes in leadership and COVID-19 pressures at the site, the control site trust had initiated their own CC programme through use of existing technology and software by the time we gained access. Qualitative data collected at the control site indicated that key operational leads there were aware of the Bradford Command Centre, had visited it and were using it as a model for development of their own C2 systems. From an experimental paradigm this represents clear contamination of the control site, which no longer represented in this case any pre-centralised/digitally integrated CC-style control structures, processes or behaviour and hence limited the value of the control site as a comparator for the study site CC effects and processes.
Our experience as qualitative researchers interacting with the control site, however, did lead to some important observations, namely that:
-
The CC model was seen as an effective means of addressing various operational and environmental challenges concerning patient flow through the hospital system and that this rationale was common to both study and control sites.
-
There was an impetus at the control site, just as had been reported at the study site, to capitalise on the digitisation of operational data and the opportunities afforded by investment in contemporary, system-wide data integration and reporting systems.
-
The experience of managing the operational pressures and requirements for rapid iterative service reconfigurations associated with the pandemic had a profound effect on both organisations, including rapid change in operational control structures and processes. In such an environment and at such a time, the notion of being able to access and capture any ‘clean’, ‘normal’ or ‘stable’ operational command system for comparison with our CC model, which itself had to rapidly adapt to the post-COVID operational environment, was probably unrealistic.
From the perspective of the quantitative, quasi-experimental evaluation, the study had certain limitations. First, health service delivery was significantly affected by the COVID-19 pandemic resulting in rapid and system-wide effects which may have impacted on the pool of patients and capacity management in both hospitals. Cancellation and postponement of surgical operations were common due to reallocation of resources during the peaks of the pandemic. Although we attempted to control for the effects of the pandemic in our time-series models, the proximity of the activation of the CC with the onset of the pandemic surge makes it difficult to isolate the effect of the intervention or control for the pandemic without masking potentially interesting variation.
Second, apart from the CC, it has been assumed that the intervention site (BRI hospital) and control site (CHFT) are equivalent in other factors, which may not necessarily be the case. The control site showed considerably higher initial mortality, which might have led to subsequent reduction in mortality rates or local interventions to reduce mortality, acting as a confounding factor in attempts to isolate the effect of the CC intervention. Re-admission rates additionally showed widely different trends between the study and control sites.
Another potential limitation of the study concerns the focus of this quantitative evaluation on a small number of outcome indicators for what was a system-wide initiative designed to impact many areas. Although informing our intervention models using qualitative research at the study site is a strength in our design, qualitative investigation additionally revealed the complexity of this type of intervention and the challenges of implementation within a pressured acute care environment. This may have influenced the study outcome in a number of ways. Staff recall of the historical implementation timeline was variable (especially for piloting and roll-in of intervention components, including organisational in addition to technological elements). There were suggestions that colocation of staff in the CC room preceded the roll-in and activation phase for CC displays, so the team may have already been established and co-ordinating functions sooner than the intervention timeline suggests, leading to under-specification of our model. When considering the challenges observed in implementing the technological aspects of the intervention, including data quality, there may have been significant time lag between activation of components and any impact upon patient safety outcomes. Given the complexity in our intervention model we did not seek to control for lagged effects of intervention implementation (the time it takes for an intervention to start to influence detectable outcomes). Rather, we presumed that the effects of the intervention components were instantaneous.
Finally, due to data-access limitations we were not able to explore all outcomes identified for analysis in the study protocol. Furthermore, although minimal, errors during data entry and processing prior to our receipt of the SUS data cannot be ruled out.
Nonetheless, the strengths of the study are threefold. First, we have used a large sample size for the analyses: a total of 203,807 inpatient visits and 34,625 surgical operations. Second, the use of EHRs data minimises the inherent biases and errors in other types of observational data. Third, we employed a quasi-experimental design using repeated time-series measurement.
Conclusions
Our case study demonstrates that a hospital-wide CC approach can be successfully adopted by a large UK NHS hospital. However, this study was affected by the pandemic and does not provide sufficient evidence to demonstrate major benefits for widespread adoption of command-centre approaches across the NHS. The introduction of the Bradford Command Centre did not have a statistically significant effect on patient flow indicators or mortality when compared with the control site, and data quality was statistically non-significantly worse. Both sites innovated as best they could to manage complex changing pressures from the pandemic, making it challenging to link observable changes in outcomes at the two sites to the specific technology interventions.
Ethnographic observations and testimony from staff were suggestive of more positive benefits of the CC approach, along with the challenges inherent in implementation and adoption of this type of technology. Staff emphasised that benefits came from the way they adapted to and used the new technology rather than the technology per se, a conclusion that is reflected frequently in the health technology literature. Synthesis of qualitative and theoretical perspectives on this technology enabled construction of intervention logic to support future development and evaluation in this area.
The study has presented a case study of a successful implementation of a CC in the UK NHS. There has been growing interest in hospitals adopting a CC approach as part of attempts to improve hospital operations. One major constraint has been the availability of suitable digital systems that can support this form of centralised approach.
The Bradford Command Centre demonstrates that systems are available, but it also reveals challenges in the reliability, timeliness and quality of these data that reduce transparency and limit confidence. Management and staff have managed to overcome many of these challenges through determination, negotiation and gradual improvements while also dealing with the pandemic. There was a strong sense that the CC had been invaluable during the pandemic but we were not able to empirically validate this.
Recommendations
Our recommendations fall into several categories. In further work, we plan to continue longitudinal study of the Bradford Command Centre as it continues to evolve. The study highlights success factors and challenges for other organisations considering implementation of a CC approach. We also highlight the need for further research to more fully understand the optimum approach to realise the benefits of the potential transformation in operational management of UK NHS hospitals that the CC approach offers.
Continued study of the Bradford Command Centre
As the first of type in the UK NHS, the Bradford Command Centre should be a national reference point for other NHS hospitals considering similar approaches. Our report contains many details that should be of interest to the stakeholders involved in similar projects and the management team at Bradford have been open to showcasing their approach to colleagues. Continued study of the evolving adoption of the CC technology and working practices at Bradford should provide a longitudinal perspective that goes beyond the decision to adopt a CC by generating learning about how to sustain success in the long term.
We recommend:
-
Further dissemination of the study findings through a wider range of academic and non-academic channels. Specifically, the lessons learnt from the study should reach policy-makers, clinical and management decision-makers, NHS staff, patients and the general public via informative videos, infographics, presentations and workshops at NHS conferences, CIO and associated networks, invited talks and social media. We will work with NIHR and others to actively disseminate this impact.
-
A follow-up study at repeated intervals of approximately 2 years should be able to track the evolution of the Bradford Command Centre and ‘tell its story’ with lessons learnt to inform other adopters. This should be achievable with a ‘light touch’ by repeating our mixed-method study design combining ethnographic observation within the CC and follow-up interviews with previous study participants and others in relevant roles. Having built the infrastructure for our quantitative analysis using routine data from the Connected Bradford Data Service repeating the data analysis involves relatively little additional cost. There is potential for Bradford, as the first of its type in the UK, to continue to help inform the NHS for many years to come.
Implementation of command centres in National Health Service hospitals
In common with many organisations, the NHS has a tendency to look for efficiency savings to fund capital investment and widespread organisational change while retrospective evaluation tends to focus on the effectiveness that was achieved. This case study shows that effectiveness can be achieved.
We recommend:
-
Command centres are a viable approach to improving hospital management that should be considered for future investment and practice.
-
The technology prerequisite for a successful CC is that it must be built on a foundation of reliable, modern hospital-wide information systems. Poor systems integration, poor usage and above all poor data quality will undermine implementation if not addressed. A new CC system is unlikely to be right first time so software changes should be anticipated and budgeted for.
-
The organisational prerequisite for a successful CC is that the strategic leadership team are prepared to sustain support for an investment in organisational change as well as the additional technology and estates cost. Our case study shows that higher visibility of patient flow and centralisation of decision-making can be uncomfortable for staff, local management and potentially patients too. At Bradford, incremental, responsible and responsive change backed by enthusiastic leadership has proved successful and is an approach that is likely to be effective elsewhere.
Further research on the potential for command centres to transform National Health Service operational management
This study was not able to provide definitive evidence to demonstrate major benefits for widespread adoption of CCs. It does, however, provide a base for others to do so. Our cross-industry review demonstrates solid benefits to operational management that CCs have provided to other industries where either safety is a major concern or where flow needs to be efficiently managed. NHS hospitals require both safety and efficient flow. They are, however, highly complex relative to other industries that have implemented CCs so it is reasonable to conclude that it will take time and considerable study to find the best way that CC approaches can be adopted before their full potential can be realised.
We recommend:
-
Further studies will be needed to prove a more extensive assessment of the critical success factors and benefits case for NHS CCs. Such studies would do well to follow a mixed-methods approach rather than relying on just quantitative data (we have found it hard to attribute longitudinal change to specific interventions) or qualitative data (we have found this rich in anecdotal evidence and learning but insufficient to be conclusive). Specifically, a benefits-management approach could be embedded within new CC implementations and linked directly to the research methods employed in the study following an action-research philosophy.
-
Our work developing a long list and then a short list of indicators for patient safety, patient flow and data-quality merits further development. In our limitations we noted that a wider list of indicators would have been more effective and access to richer data would be a benefit. Data analytics using routine EHR data is becoming more firmly established with new machine learning and AI techniques able to identify, learn from and potentially act autonomously on changes in trends in time-series data. Process-mining proved useful in understanding, mapping and measuring flow and has the potential to be used for the evaluation of CC interventions and, in time, can be built into more advanced CC systems as process-aware intelligence. Standardisation on indicators between hospitals and across CCs would allow comparison across more hospitals and support the evaluation of other implementations.
-
An NHS CC implementors network would allow researchers and practitioners who are interested in understanding the challenges and potential of CCs to share learning, research methods and critical success factors. An approach that embeds research about CCs with NHS activity implementing them is likely to support rapid adoption and transformation of the NHS more dynamically than long studies that develop an evidence base before action.
Additional information
Acknowledgements
Study participants
First and foremost, we thank the NHS staff working in and around the Command Centre at Bradford Teaching Hospitals NHS Foundation Trust and in key operational roles across both the study site and the control site, for giving up their valuable time to be interviewed by the research team and for supporting our ethnographic work on site during what was an unprecedented period of demand and challenge for the service. We hope that the insights generated within the research will help to replicate their commitment and innovation in future service developments elsewhere.
Study Steering Group
We thank members of the Study Steering Group who have provided invaluable insight, guidance and motivation throughout the project: Iain Buchan (Chair), Hilary Thompson (PPI representative), Paul Charnley, Sarah Cindy Fedell, Hamish Fraser, Charles Koo, Farah Magrabi, Sue Mason, Mark Sujan, Sean White, Patrick Waterson. The Workstream 3 team in particular would like to thank Hilary Thompson for her help in securing access to the control site and Patrick Waterson and Mark Sujan for generously making their expertise in human factors and safety science available to the cross-industry review work.
Patient and public involvement and engagement
We thank members of the Yorkshire Quality and Safety Research group patient panel and participants of our patient and public workshops for providing patient and public perspectives on the design, interpretation and communication of the study.
Contributions of authors
Owen Ashby Johnson (https://orcid.org/0000-0003-3998-541X) (Senior Fellow in Computing, Digital Health) was principal investigator and led the project and Workstream 1 (Project Management), Workstream 3 (Quantitative Analysis) and Workstream 5 (Dissemination); he is corresponding author for the report and collated contributions from other authors.
Carolyn McCrorie (https://orcid.org/0000-0002-2673-6839) (Senior Lecturer in Nursing, Health Science Research) was the only member of the team allowed on site during the pandemic; she performed the majority of the ethnographic investigation (WS3) including interviews and observation and the writing of Chapter 5.
Ciarán McInerney (https://orcid.org/0000-0001-7620-7110) (Research Fellow in Primary Care Medicine, Data Science) supported the project management (WS1) including finance, ethics, data access, the steering groups and PPIE engagement (WS2).
Teumzghi F Mebrahtu (https://orcid.org/0000-0003-4821-2304) (Senior Research Fellow at Born in Bradford, Statistical Epidemiology) was the lead data scientist and performed the majority of the quantitative analysis (WS3), the writing of Chapter 6 and the associated publications.
Josh Granger (https://orcid.org/0000-0002-0925-8345) (Research Assistant in Psychology, Research Methods) performed the majority of the cross-industry review and the writing of Chapter 4.
Naeem Sheikh (Patient) was our patient co-investigator and led Workstream 2 (PPIE); he contributed to drafts of the report including the Plain language summary and Chapter 3 (PPIE) and reviewed drafts from a patient’s perspective.
Tom Lawton (https://orcid.org/0000-0003-1351-8127) (Consultant in Critical Care and Anaesthesia, Digital Health) supported the project with clinical, safety systems and digital health expertise respectively and contributed to reviewing drafts of the report.
Ibrahim Habli (https://orcid.org/0000-0003-2736-8238) (Associate Professor in Computing, Safety Science) supported the project with clinical, safety systems and digital health expertise respectively and contributed to reviewing drafts of the report.
Rebecca Randell (https://orcid.org/0000-0002-5856-4912) (Professor of Digital Innovations in Healthcare, Digital Health) supported the project with clinical, safety systems and digital health expertise respectively and contributed to reviewing drafts of the report.
Jonathan Benn (https://orcid.org/0000-0001-5919-9905) (Associate Professor in Psychology, Patient Safety) was joint co-investigator and deputy lead for the project; he led Workstream 3 (Qualitative Analysis) and contributed to drafting of the report including leading the cross-industry review (Chapter 4), qualitative method and results (Chapters 2 and 5), and the construction of the logic model (Chapter 7).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/TATM3277.
Primary conflicts of interest: All co-authors are linked to the NIHR Yorkshire and Humber Patient Safety Translational Research Centre. Owen Ashby Johnson was previously a Director of X-Lab Limited (2005–20), a software company providing digital health products for care-pathway modelling and pathology messaging. Tom Lawton is a Consultant in Critical Care & Anaesthesia at Bradford Teaching Hospitals NHS Trust. Tom Lawton reports funding from Medical Protection Society Foundation Funding for AI research, Assuring Autonomy International Programme, European Health Data Evidence Network and Health Data Research UK. Rebecca Randell was a member of the HSDR Researcher-Led Panel (2017–20), HSDR Unmet Need Sub-Committee (November 2019) and HSDR Funding Committee (Seacole) (2020–1).
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. We thank Kuldeep Sohal, John Birkinshaw and the Connected Bradford team for working closely with us to provide our project with patients’ electronic healthcare data securely and respectfully. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
The University of Leeds data repository, https://archive.researchdata.leeds.ac.uk, holds deposited data for a minimum of 10 years and data sets are associated with digital object identifiers (DOIs). All available data can be obtained from the corresponding author.
Ethics statement
Ethical approval for this study was obtained from the UK NHS Health Research Authority (IRAS No.: 285933, REC Reference: 21/HRA/0960, approved on 1 April 2021) and the University of Leeds Faculty of Engineering and Physical Sciences Research Ethics Committee (Reference: MEEC 20-016, approved on 30 June 2021).
Information governance statement
The University of Leeds is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, The University of Leeds is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: https://dataprotection.leeds.ac.uk/.
Department of Health and Social Care Disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy 2011;4:47-55.
- Pilosof NP, Barrett M, Oborn E, Barkai G, Pessach IM, Zimlichman E. Telemedicine implementation in COVID-19 ICU: balancing physical and virtual forms of visibility. HERD 2021;14:34-48. https://doi.org/10.1177/19375867211009225.
- Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med 2009;7:100-3.
- Castro-Sánchez E, Charani E, Drumright LN, Sevdalis N, Shah N, Holmes AH. Fragmentation of care threatens patient safety in peripheral vascular catheter management in acute care – a qualitative study. PLOS ONE 2014;9.
- Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform 2014;83:779-96.
- Lau F, Bartle-Clar J, Bliss G. Improving Usability, Safety and Patient Outcomes with Health Information Technology: From Research to Practice. Amsterdam: IOS Press; 2019.
- National Aeronautics and Space Administration . Johnson Space Center’s Mission Control Center 2013. www.nasa.gov/johnson/jsc-mission-control-center/ (accessed 8 February 2022).
- Holwell S, Checkland P. An information system won the war. IEE Proc Softw 1998;145:95-9.
- Alhaider AA, Lau N, Davenport PB, Morris MK. Distributed situation awareness: a health-system approach to assessing and designing patient flow management. Ergonomics 2020;63:682-709. https://doi.org/10.1080/00140139.2020.1755061.
- Buchler N, Fitzhugh SM, Marusich LR, Ungvarsky DM, Lebiere C, Gonzalez C. Mission command in the age of network-enabled operations: social network analysis of information sharing and situation awareness. Front Psychol 2016;7. https://doi.org/10.3389/fpsyg.2016.00937.
- Eisenberg DA, Alderson DL, Kitsak M, Ganin A, Linkov I. Network foundation for command and control (C2) systems: literature review. IEEE Access 2018;6:68782-94. https://doi.org/10.1109/access.2018.2873328.
- Beynon-Davies P. Information systems ‘failure’: the case of the London Ambulance Service’s Computer Aided Despatch project. Eur J Inf Syst 1995;4:171-84.
- HealthSpaces . The Evolution of the Healthcare Command Center 2020. https://info.healthspacesevent.com/blog/the-evolution-of-the-healthcare-command-center (accessed 13 June 2022).
- Randell R, Alvarado N, Elshehaly M, McVey L, West RM, Doherty P, et al. Design and evaluation of an interactive quality dashboard for national clinical audit data: a realist evaluation. Health Soc Care Del Res 2022;10:1-156.
- Imperial College Healthcare Trust . How We Implemented a Command Centre to Tackle Winter Pressures 2020. www.imperial.nhs.uk/about-us/blog/command-centre-winter-pressures (accessed 14 June 2022).
- University Hospitals of Morecambe Bay NHS Trust . Trust’s Award-Winning Analytical Command Centre Adopted by Seven NHS Organisations in London 2020. https://www.uhmb.nhs.uk/news-and-events/latest-news/trusts-award-winning-analytical-command-centre-adopted-seven-nhs-organisations-london (accessed 14 June 2022).
- TeleTracking . The Royal Wolverhampton NHS Trust: Enabling Technologies 2014. www.teletracking.com/resources/the-royal-wolverhampton-nhs-trust-enabling-technologies/ (accessed 14 June 2022).
- AdventHealth . A Look Inside AdventHealth’s Massive New Command Center 2020. https://healthtechmagazine.net/article/2020/02/look-inside-adventhealths-massive-new-command-center (accessed 14 June 2022).
- Schlicher J, Metsker MT, Shah H, Demirkan H. From NASA to healthcare: real-time data analytics (mission control) is reshaping healthcare services. Perspect Health Inf Manag 2021;18.
- Bradford Teaching Hospitals . Command Centre 2019. www.bradfordhospitals.nhs.uk/command-centre/ (accessed 8 February 2022).
- Alharbi M, Senitan M, Ohanlon T, Smith S, Mominkhan D, Alqahtani S, et al. 27 Healthcare in the time of a pandemic and beyond: the innovative large-scale and integrated Saudi national health command centre. BMJ Specialist Journals 2021;5:A10-1.
- Kane EM, Scheulen JJ, Püttgen A, Martinez D, Levin S, Bush BA, et al. Use of systems engineering to design a hospital command center. Jt Comm J Qual Patient Saf 2019;45:370-9.
- Davenport PB, Carter KF, Echternach JM, Tuck CR. Integrating high-reliability principles to transform access and throughput by creating a centralized operations center. J Nurs Adm 2018;48:93-9. https://doi.org/10.1097/NNA.0000000000000579.
- McInerney C, McCrorie C, Benn J, Habli I, Lawton T, Mebrahtu TF, et al. Evaluating the safety and patient impacts of an artificial intelligence command centre in acute hospital care: a mixed-methods protocol. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-054090.
- Sturmberg JP, O’Halloran DM, Martin CM. Understanding health system reform – a complex adaptive systems perspective. J Eval Clin Pract 2012;18:202-8.
- Sturmberg JP. Want improved quality? Improve your systems. J Eval Clin Pract 2020;26:1530-3.
- Grove A, Clarke A, Currie G, Metcalfe A, Pope C, Seers K. Advancing clinical leadership to improve the implementation of evidence-based practice in surgery: a longitudinal mixed-method study protocol. Implement Sci 2020;15:1-10.
- Ha NHL, Chan I, Yap P, Nurjono M, Vrijhoef HJM, Nicholas SO, et al. Mixed-method evaluation of CARITAS: a hospital-to-community model of integrated care for dementia. BMJ Open 2020;10.
- Schmidt B, Watt K, McDermott R, Mills J. Assessing the link between implementation fidelity and health outcomes for a trial of intensive case management by community health workers: a mixed methods study protocol. BMC Health Serv Res 2017;17:1-6.
- Mann R, Beresford B, Parker G, Rabiee P, Weatherly H, Faria R, et al. Models of reablement evaluation (MoRE): a study protocol of a quasi-experimental mixed methods evaluation of reablement services in England. BMC Health Serv Res 2016;16:1-9.
- Manojlovich M, Adler-Milstein J, Harrod M, Sales A, Hofer TP, Saint S, et al. The effect of health information technology on health care provider communication: a mixed-method protocol. JMIR Res Protoc 2015;4.
- Allan S, Mcleod H, Bradstreet S, Beedie S, Moir B, Gleeson J, et al. Understanding implementation of a digital self-monitoring intervention for relapse prevention in psychosis: protocol for a mixed method process evaluation. JMIR Res Protoc 2019;8.
- Sun Y, Luo R, Li Y, He FJ, Tan M, MacGregor GA, et al. App-based salt reduction intervention in school children and their families (AppSalt) in China: protocol for a mixed methods process evaluation. JMIR Res Protoc 2021;10.
- Ward M, McAuliffe E, Wakai A, Geary U, Browne J, Deasy C, et al. Study protocol for evaluating the implementation and effectiveness of an emergency department longitudinal patient monitoring system using a mixed-methods approach. BMC Health Serv Res 2017;17:1-10.
- Farre A, Cummins C. Understanding and evaluating the effects of implementing an electronic paediatric prescribing system on care provision and hospital work in paediatric hospital ward settings: a qualitatively driven mixed-method study protocol. BMJ Open 2016;6.
- van Huizen LS, Dijkstra P, Halmos GB, van den Hoek JG, van der Laan KT, Wijers OB, et al. Does multidisciplinary videoconferencing between a head-and-neck cancer centre and its partner hospital add value to their patient care and decision-making? A mixed-method evaluation. BMJ Open 2019;9.
- Department of Health . Research Governance Framework for Health and Social Care 2005. www.gov.uk/government/publications/research-governance-framework-for-health-and-social-care-second-edition (accessed 19 February 2024).
- Bradford Institute for Health Research . Connected Yorkshire 2022. www.bradfordresearch.nhs.uk/our-research-teams/connected-bradford (accessed 11 November 2022).
- Sohal K, Mason D, Birkinshaw J, West J, McEachan RR, Elshehaly M, et al. Connected Bradford: a whole system data linkage accelerator. Wellcome Open Res 2022;7.
- Weiskopf NG, Bakken S, Hripcsak G, Weng C. A data quality assessment guideline for electronic health record data reuse. EGEMS 2017;5.
- Fernandez-Llatas C, Munoz-Gama J, Martin N, Johnson O, Sepulveda M, Helm E. Interactive Process Mining in Healthcare. Cham: Springer; 2021.
- Mans RS, van der Aalst WM, Vanwersch RJ. Process Mining in Healthcare: Evaluating and Exploiting Operational Healthcare Processes. Cham: Springer; 2015.
- Mans RS, Reijers HA, van Genuchten M, Wismeijer D. Mining Processes in Dentistry n.d.:379-88.
- Baker K, Dunwoodie E, Jones RG, Newsham A, Johnson O, Price CP, et al. Process mining routinely collected electronic health records to define real-life clinical pathways during chemotherapy. Int J Med Inform 2017;103:32-41.
- Mannhardt F, Blinde D. Analyzing the trajectories of patients with sepsis using process mining. RADAR+ EMISA@ CAiSE 2017;1859:72-80.
- Williams R, Ashcroft DM, Brown B, Rojas E, Peek N, Johnson OA. Process Mining in Primary Care: Avoiding Adverse Events Due to Hazardous Prescribing n.d.
- van der Aalst W, Adriansyah A, van Dongen B. Replaying history on process models for conformance checking and performance analysis. WIREs Data Min Knowl Discov 2012;2:182-9.
- Kurniati AP, McInerney C, Zucker K, Hall G, Hogg D, Johnson O. A Multi-Level Approach for Identifying Process Change in Cancer Pathways 2019;362:595-607. https://doi.org/10.1007/978-3-030-37453-2_48.
- McDonald KM, Romano PS, Geppert J, Davies SM, Duncan BW, Shojania KG, et al. Measures of Patient Safety Based on Hospital Administrative Data: The Patient Safety Indicators. Rockville, MD: Agency for Healthcare Research and Quality; 2010.
- UK Health Security Agency . Updated Operating Procedure Codes Supplement (OPCS) and Protocol for the Surveillance of Surgical Site Infection (Derived From: NHS Digital Health and Social Care Information Centre OPCS-4.8 to OPCS-4.9) 2022.
- World Health Organization . ICD-10 Version:2010 2010. https://icd.who.int/browse10/2010/en#/T81.4 (accessed 9 May 2022).
- UK Health Security Agency . Coronavirus (COVID-19) in the UK 2022. https://coronavirus.data.gov.uk/details/cases?areaType=overview&areaName=United%20Kingdom (accessed 25 February 2022).
- Sakamoto Y, Ishiguro M, Kitagawa G. Akaike Information Criterion Statistics. Dordrecht: Springer; 1986.
- Schwarz G. Estimating the dimension of a model. Ann Statist 1978;6:461-4. https://doi.org/10.1214/aos/1176344136.
- van der Aalst W. Process mining: overview and opportunities. ACM Trans Manag Inform Syst 2012;3:1-17.
- Greenhalgh T, Swinglehurst D. Studying technology use as social practice: the untapped potential of ethnography. BMC Med 2011;9:1-7.
- Holloway I. Qualitative Research in Health Care. Maidenhead: Open University Press; 2005.
- Bailey S, Hunt C, Brisley A, Howard S, Sykes L, Blakeman T. Implementation of clinical decision support to manage acute kidney injury in secondary care: an ethnographic study. BMJ Qual Saf 2020;29:382-9.
- Blandford A, Berndt E, Catchpole K, Furniss D, Mayer A, Mentis H, et al. Strategies for conducting situated studies of technology use in hospitals. Cogn Technol Work 2015;17:489-502.
- Bonaconsa C, Mbamalu O, Mendelson M, Boutall A, Warden C, Rayamajhi S, et al. Groote Schuur Hospital Antimicrobial Stewardship and Surgical Study Group . Visual mapping of team dynamics and communication patterns on surgical ward rounds: an ethnographic study. BMJ Qual Saf 2021;30:812-24.
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15.
- Pope C, Halford S, Turnbull J, Prichard J, Calestani M, May C. Using computer decision support systems in NHS emergency and urgent care: ethnographic study using normalisation process theory. BMC Health Serv Res 2013;13:1-13.
- DeVault ML. Introduction: what is institutional ethnography. Soc Probl 2006;53.
- Morgan-Trimmer S, Wood F. Ethnographic methods for process evaluations of complex health behaviour interventions. Trials 2016;17:1-11.
- Pink S, Morgan J. Short‐term ethnography: intense routes to knowing. Symb Interact 2013;36:351-61.
- Flanagan JC. The critical incident technique. Psychol Bull 1954;51:327-58.
- McDonald S. Studying actions in context: a qualitative shadowing method for organizational research. Qual Res 2005;5:455-73.
- Phillippi J, Lauderdale J. A guide to field notes for qualitative research: context and conversation. Qual Health Res 2018;28:381-8.
- Kulak D, Guiney E. Use Cases: Requirements in Context. Boston, MA: Addison-Wesley; 2012.
- Corbin JM, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol 1990;13:3-21.
- Strauss A, Corbin JM. Grounded Theory in Practice. Thousand Oaks, CA: SAGE; 1997.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11:589-97.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73. https://doi.org/10.7326/m18-0850.
- Franklin BJ, Mueller SK, Bates DW, Gandhi TK, Morris CA, Goralnick E. Use of hospital capacity command centers to improve patient flow and safety: a scoping review. J Patient Saf 2022;18:e912-21. https://doi.org/10.1097/PTS.0000000000000976.
- Stanton N, Walker G, Jenkins D, Salmon P, Young M, Aujla A. Engineering Psychology and Cognitive Ergonomics. EPCE 2007. Lecture Notes in Computer Science. Berlin: Springer; 2007.
- Walker GH, Stanton NA, Salmon PM, Jenkins DP. A review of sociotechnical systems theory: a classic concept for new command and control paradigms. Theor Issues Ergon Sci 2008;9:479-99. https://doi.org/10.1080/14639220701635470.
- Walker GH, Stanton NA, Stewart R, Jenkins D, Wells L, Salmon P, et al. Using an integrated methods approach to analyse the emergent properties of military command and control. Appl Ergon 2009;40:636-47. https://doi.org/10.1016/j.apergo.2008.05.003.
- Lawson JS. Command control as a process. IEEE Control Syst Mag 1981;1:5-11.
- Hollnagel E. Human Reliability Analysis: Context and Control. Cambridge, MA: Academic Press; 1993.
- Stanton MA, Prichard J, van Vuget M, Connely V. Assessing the effects of location media and task type on team performance. J Defen Stud 2002;7:29-41.
- Rasmussen J. The Human Data Processor as a System Component: Bits and Pieces of a Model No. 1722. Roskilde: Risø National Laboratory; 1974.
- Vicente KJ. Cognitive Work Analysis: Toward Safe, Productive, and Healthy Computer-Based Work. Mahwah, NJ: Lawrence Erlbaum; 1999.
- Smalley J. Handbook of Cognitive Task Design. Boca Raton, FL: CRC Press; 2003.
- Joint Concept Note 2/17: Future of Command and Control. Swindon: The Development, Concepts and Doctrine Centre; 2017.
- Walker GH, Stanton NA, Salmon PM, Jenkins DP. Human performance under two different command and control paradigms. Appl Ergon 2014;45:706-13. https://doi.org/10.1016/j.apergo.2013.09.011.
- Hansberger JT, Barnette D. Human performance modeling for operational command, control and communication. Proc Hum Fact Ergon Soc Annu Meet 2005;49:1182-5. https://doi.org/10.1177/154193120504901218.
- Roberts A, Stanton NA, Fay D. The command team experimental test-bed phase two: assessing cognitive load and situation awareness in a submarine control room. Adv Hum Asp Transp 2017;484:427-37. https://doi.org/10.1007/978-3-319-41682-3_36.
- Roberts APJ, Stanton NA, Fay DT. Go deeper, go deeper: understanding submarine command and control during the completion of dived tracking operations. Appl Ergon 2018;69:162-75. https://doi.org/10.1016/j.apergo.2018.02.003.
- Stanton NA, Robert APJ. Better together? Investigating new control room configurations and reduced crew size in submarine command and control. Ergonomics 2020;63:307-23. https://doi.org/10.1080/00140139.2019.1654137.
- Stanton NA, Roberts APJ. Examining social, information, and task networks in submarine command and control. IEEE T Hum-Mach Syst 2018;48:252-65. https://doi.org/10.1109/THMS.2017.2720659.
- Stanton NA, Roberts APJ, Fay DT. Up periscope: understanding submarine command and control teamwork during a simulated return to periscope depth. Cogn Technol Work 2017;19:399-417. https://doi.org/10.1007/s10111-017-0413-7.
- Walker GH, Stanton NA, Jenkins D, Salmon P, Young MS, Beond A, et al. How network enabled capability changes the emergent properties of military command and control. Proc Hum Fact Ergon Soc Annu Meet 2006;50:2492-6. https://doi.org/10.1177/154193120605002306.
- Farrington-Darby T, Wilson JR, Norris BJ, Clarke T. A naturalistic study of railway controllers. Ergonomics 2006;49:1370-94. https://doi.org/10.1080/00140130600613000.
- Walker GH, Stanton NA, Baber C, Wells L, Gibson H, Salmon P, et al. From ethnography to the EAST method: a tractable approach for representing distributed cognition in Air Traffic Control. Ergonomics 2010;53:184-97. https://doi.org/10.1080/00140130903171672.
- Air force awards command and control modernization program contract. Microw J 2000;43:41-2.
- Giri J, Parashar M, Trehern J, Madani V. The situation room control center analytics for enhanced situational awareness. IEEE Power Energy Mag 2012;10:24-39. https://doi.org/10.1109/MPE.2012.2205316.
- Salmon P, Stanton N, Walker G, Green D. Situation awareness measurement: a review of applicability for C4i environments. Appl Ergon 2006;37:225-38. https://doi.org/10.1016/j.apergo.2005.02.001.
- Hamer R, Waterson P, Jun GT. Human factors and nuclear safety since 1970 – a critical review of the past, present and future. Saf Sci 2021;133. https://doi.org/10.1016/j.ssci.2020.105021.
- Teperi A-M, Puro V, Kannisto H. Applying a new human factor tool in the nuclear energy industry. Saf Sci 2017;95:125-39. https://doi.org/10.1016/j.ssci.2017.02.013.
- Hollnagel E, Wears R, Braithwaite J. From Safety-I to Safety-II: A White Paper. London: NHS England; 2015.
- Blandford A, Wong BLW. Situation awareness in emergency medical dispatch. Int J Hum Comput. Stud 2004;61:421-52. https://doi.org/10.1016/j.ijhcs.2003.12.012.
- Furniss D, Blandford A. Understanding emergency medical dispatch in terms of distributed cognition: a case study. Ergonomics 2006;49:1174-203. https://doi.org/10.1080/00140130600612663.
- Ji YW, Ren XJ. A summary of the application and research of the command and control organization theory in emergency communication support. Proc Int Conf Commun Inform Manag Netw Sec 2016;47:8-11.
- Houghton RJ, Baber C, McMaster R, Stanton NA, Salmon P, Stewart R, et al. Command and control in emergency services operations: a social network analysis. Ergonomics 2006;49:1204-25. https://doi.org/10.1080/00140130600619528.
- Dekker A. Applying social network analysis concepts to military C4ISR architectures. Parameters 2002;24.
- Dekker AH. C4ISR Architectures, Social Network Analysis and the FINC Methodology: An Experiment in Military Organisational Structure. Edinburgh, SA, Australia: Commonwealth of Australia; 2002.
- Bruno MA, Petscavage-Thomas J. Brief communication: a departmental ‘command center’ to facilitate staff safety and patient care during the peak of the COVID-19 pandemic. Clin Imaging 2021;74:19-21. https://doi.org/10.1016/j.clinimag.2020.12.015.
- Hutchings SD, Perry J, Mills A, Bartley F, Bartley M, Park CL. Command, control and communication (C3) during the COVID-19 pandemic; adapting a military framework to crisis response in a tertiary UK critical care centre. J Intensive Care Soc 2021;23:162-9. https://doi.org/10.1177/1751143720982191.
- Collins BE. Use of high-reliability principles in the evolution of a hospital command centre. Healthc Quart 2021;23:46-52. https://doi.org/10.12927/hcq.2020.26393.
- Kane EM, Scheulen JJ, Puttgen A, Martinez D, Levin S, Bush BA, et al. Use of systems engineering to design a hospital command center. Jt Comm J Qual Patient Saf 2019;45:370-9. https://doi.org/10.1016/j.jcjq.2018.11.006.
- Morris MK, Carter KF. A blended transfer and communications center: designing a state-of-the-art mission control. Nurs Adm Q 2015;39:357-61. https://doi.org/10.1097/NAQ.0000000000000129.
- Krennerich EC, Graf JM, D’Ambrosio D, McPherson ML. Mission control: the development and centralization of an integrated communication center to facilitate intra-facility and inter-facility patient flow. Pediatrics 2020;146:506-7. https://doi.org/10.1542/peds.146.1MA6.506.
- Alberts DS. Agility, focus, and convergence: the future of command and control. Int C2 J 2007;1:1-30.
- Mebrahtu TF, McInerney CD, Benn J, McCrorie C, Granger J, Lawton T, et al. Effect of a hospital command centre on patient safety: an interrupted time series study. BMJ Health Care Inform 2023;30.
- Nuffield Trust . Indicators: A&Amp;E Waiting Times 2022. https://www.nuffieldtrust.org.uk/resource/a-e-waiting-times (accessed 31 March 2022).
- Busch TE. Use of modern control theory in military command and control. Enabl Tech Simul Sci 2001;4367:326-9. https://doi.org/10.1117/12.440036.
- Feigh KM, Pritchett AR. Modeling work for cognitive work support system design in operational control centers. J Cogn Eng Decis Mak 2010;4:1-26. https://doi.org/10.1518/155534310X495564.
- McGuinness B, Ebbage L. Proceedings of the 2002 Command and Control Research and Technology Symposium, May 2002. Monterey, CA: Department of Defense Command and Control Research Program (DoD CCRP); n.d.
- Bell ER, Badillo V, Coan D, Johnson K, Ney Z, Rosenbaum M, et al. Mission control team structure and operational lessons learned from the 2009 and 2010 NASA desert RATS simulated lunar exploration field tests. Acta Astronaut 2013;90:215-23. https://doi.org/10.1016/j.actaastro.2012.11.020.
- Stanton NA, Rothrock L, Harvey C, Sorensen L. Investigating information-processing performance of different command team structures in the NATO problem space. Ergonomics 2015;58:2078-100. https://doi.org/10.1080/00140139.2015.1046499.
- Arbuthnot K. A command gap? A practitioner’s analysis of the value of comparisons between the UK’s military and emergency services’ command and control models in the context of UK resilience operations. J Contingencies Crisis Manag 2008;16:186-94. https://doi.org/10.1111/j.1468-5973.2008.00549.x.
- Hukill JLC, Mortensen DRD. Developing flexible command and control of airpower. ASPJ 2011;25:53-6.
- Walker GH, Stanton NA, Salmon PM, Jenkins DP, Rafferty L, Ladva D. Same or different? Generalising from novices to experts in military command and control studies. Int J Ind Ergon 2010;40:473-83. https://doi.org/10.1016/j.ergon.2010.04.003.
- Aniceto HAR. Integrated real-time information to use in commercial, logistics and operational activities provided by the National Control Center Operation of TRANSPETRO. Proc ASME Int Pipel Conf 2010;3:523-9.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci 2022;17. https://doi.org/10.1186/s13012-022-01245-0.
- Johns Hopkins . Capacity Command Center Celebrates 5 Years of Improving Patient Safety 2021. www.hopkinsmedicine.org/news/articles/capacity-command-center-celebrates-5-years-of-improving-patient-safety-access (accessed 7 February 2022).
Appendix 1 List of suppliers and consumers of command centres in health care
| Supplier’s name | Customer’s name | Customer’s location/country | Features of the technology | Purpose of use | |
|---|---|---|---|---|---|
| Wall of analytics | Room orientation | ||||
| Qlik Sense: www.qlik.com/us/products/qlik-sense | Imperial college healthcare trust: www.imperial.nhs.uk/about-us/blog/command-centre-winter-pressures | UK | Yes | One video wall in front | Patient flow management |
| University hospitals of Morecambe bay NHS Trust: www.uhmb.nhs.uk/news-and-events/latest-news/trusts-award-winning-analytical-command-centre-adopted-seven-nhs-organisations-london | UK | Yes | Multiple PC screens and video walls in front | Patient flow management | |
| Teletracking: www.teletracking.com/health-system-operational-command-center | Spread across 36 states: www.teletracking.com/health-system-operational-command-center | USA | Yes | Multiple PC screens and video walls in front | Patient flow management |
| The Royal Wolverhampton NHS Trust: www.royalwolverhampton.nhs.uk/ | UK | Yes | Multiple PC screens and video walls in front | Patient flow management | |
| The Countess of Chester Hospital NHS Foundation Trust: www.coch.nhs.uk/ | UK | Yes | Multiple PC screens and video walls in front | Patient flow management | |
| GE Healthcare: www.gehealthcare.com/ | Bradford Teaching Hospitals: www.bradfordhospitals.nhs.uk/command-centre/ | UK | Yes | Multiple PC screens and video walls in front | Patient flow management |
| Johns Hopkins hospital: www.hopkinsmedicine.org/the_johns_hopkins_hospital/ | USA | Yes | Multiple PC screens and video walls in front | Patient flow management | |
| AdventHealth-representing hospitals across eight states in the US: https://healthtechmagazine.net/article/2020/02/look-inside-adventhealths-massive-new-command-center | Yes | Multiple PC screens and video walls in front | Patient flow management | ||
| CHI Franciscan (representing hospitals in Washington state): https://www.biospace.com/article/releases/chi-franciscan-activates-first-ai-powered-hospital-mission-control-center-in-washington-state/ | Yes | Multiple PC screens and video walls in front | Patient flow management | ||
| Rush University Hospital: www.rush.edu/ | Yes | Multiple PC screens and video walls in front | Patient flow management | ||
| Oregon Health & Science University (OHSU): https://news.ohsu.edu/2019/10/31/ohsu-mission-control-offers-modern-high-tech-solution-to-historic-challenge | Yes | Multiple PC screens and video walls in front | Patient flow management | ||
| Humber River hospital: www.hrh.ca/2022/07/28/humber-river-hospitals-command-centre-and-generation-3/ | Canada | Yes | Multiple PC screens and video walls in front | Patient flow management | |
| Epic: www.epic.com/ | Yale New Haven Hospital: www.ynhh.org/ | USA | Yes | Patient flow management | |
| Oracle: www.oracle.com/applications/ | Texas Children’s Hospital: https://texaschildrensannualreport.org/2017/news/page-1.html | USA | Yes | Multiple PC screens and video walls in front | Patient flow management |
| Barco: www.barco.com/en/products/video-walls | Erasmus University Medical Center, Rotterdam: https://www.barco.com/en/inspiration/customer-stories/erasmus-university-medical-center | Netherlands | Yes | Multiple PC screens and video walls in front | Security operations |
| Philips: www.philips.co.uk/healthcare/clinical-solutions/clinical-operations-center | Centres for Veterans Affairs (VA), spread across all the states: www.limburger.nl/cnt/dmf20200708_00167415 | USA | No | Multiple PC screens | Telecare |
| Nationwide virtual cardiology network (cardiology departments of eight hospitals): www.zawya.com/mena/en/press-releases/story/Philips_highlights_growing_role_of_command_center_approach_for_managing_healthcare_at_Arab_Health-ZAWYA20200127101706/ | Saudi Arabia | No | Multiple PC screens | Telecare | |
| Centralized tele-ICU: www.zawya.com/mena/en/press-releases/story/Philips_highlights_growing_role_of_command_center_approach_for_managing_healthcare_at_Arab_Health-ZAWYA20200127101706/ | Saudi Arabia | No | Multiple PC screens | Telecare | |
| University of Kentucky | USA | No | Multiple PC screens | Telecare | |
| Cerner: www.cerner.com/solutions/command-center#section2 | Northern Light Health: https://northernlighthealth.org/Contact-Us | USA | No | Multiple PC screens | Patient flow management |
| GMV: www.gmv.com/en/Sectors/Healthcare/ | Hospital General Universitario Gregorio Marañón: www.comunidad.madrid/hospital/gregoriomaranon/ | Spain | No | One screen | Telecare |
| Splunk: www.splunk.com/en_us/solutions/industries/healthcare.html | New York-Presbyterian Hospital: www.nyp.org/ | USA | No | Individual screens | Patient flow management |
Appendix 2 Search strategies from the cross-industry review
| Domain | Search strategy |
|---|---|
| Command centres | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) |
| Healthcare | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (flow OR capacity OR safety) AND (healthcare OR health care OR patient care OR hospital OR acute care OR secondary care OR inpatient OR in-patient OR COVID-19 OR pandemic) |
| Military | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (army OR military OR air force OR navy OR naval OR marine* OR space OR aerospace OR defence OR defense OR warfare) |
| Industry | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (nuclear power OR nuclear plant OR chemical industr* or chemical process* or petrochemical or offshore or petroleum) (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND logistics |
| Emergency services | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (fire or rescue or police or ambulance or emergency services or emergency response) |
| Transport | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (air traffic control OR airport OR airline OR rail network OR rail OR railway OR road traffic control OR vehicular traffic OR traffic management OR aviation OR transport) |
| Centralised C2 and core concepts | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (high reliability or situational awareness or (command adj2 control) or resilience or distributed cognition or safety 2 or safety-critical OR safety critical) (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND (operations management OR operations monitoring OR operational sensitivity) |
| Command-centre reviews | (‘command adj2 control’ OR ‘command cent*’ OR ‘operation* cent*’ OR ‘control cent*’ OR ‘management cent*’ OR ‘mission control’ OR ‘transfer cent*’ OR ‘access cent*’) AND review.ti. |
Appendix 3 Process-mining descriptive graphs
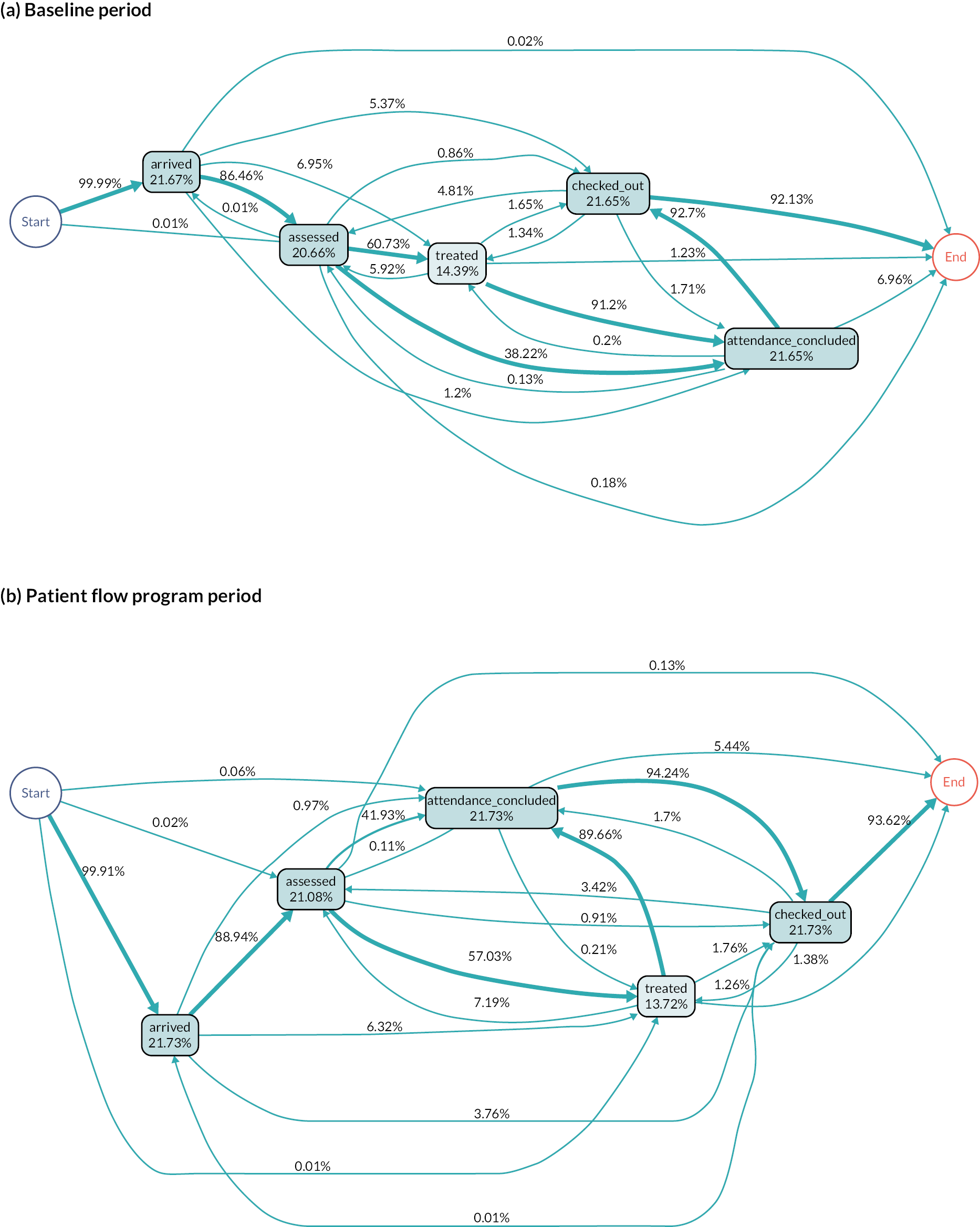
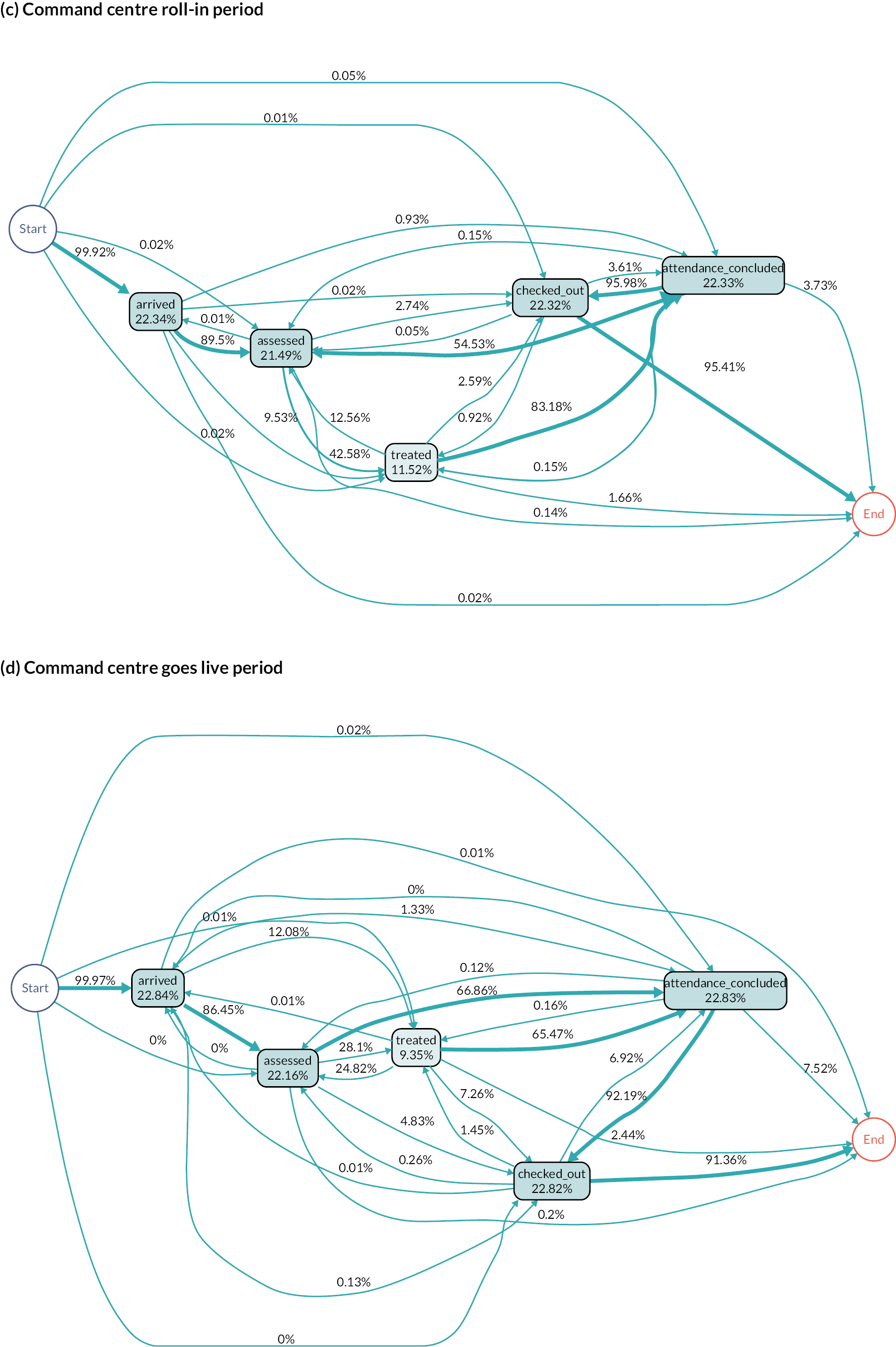
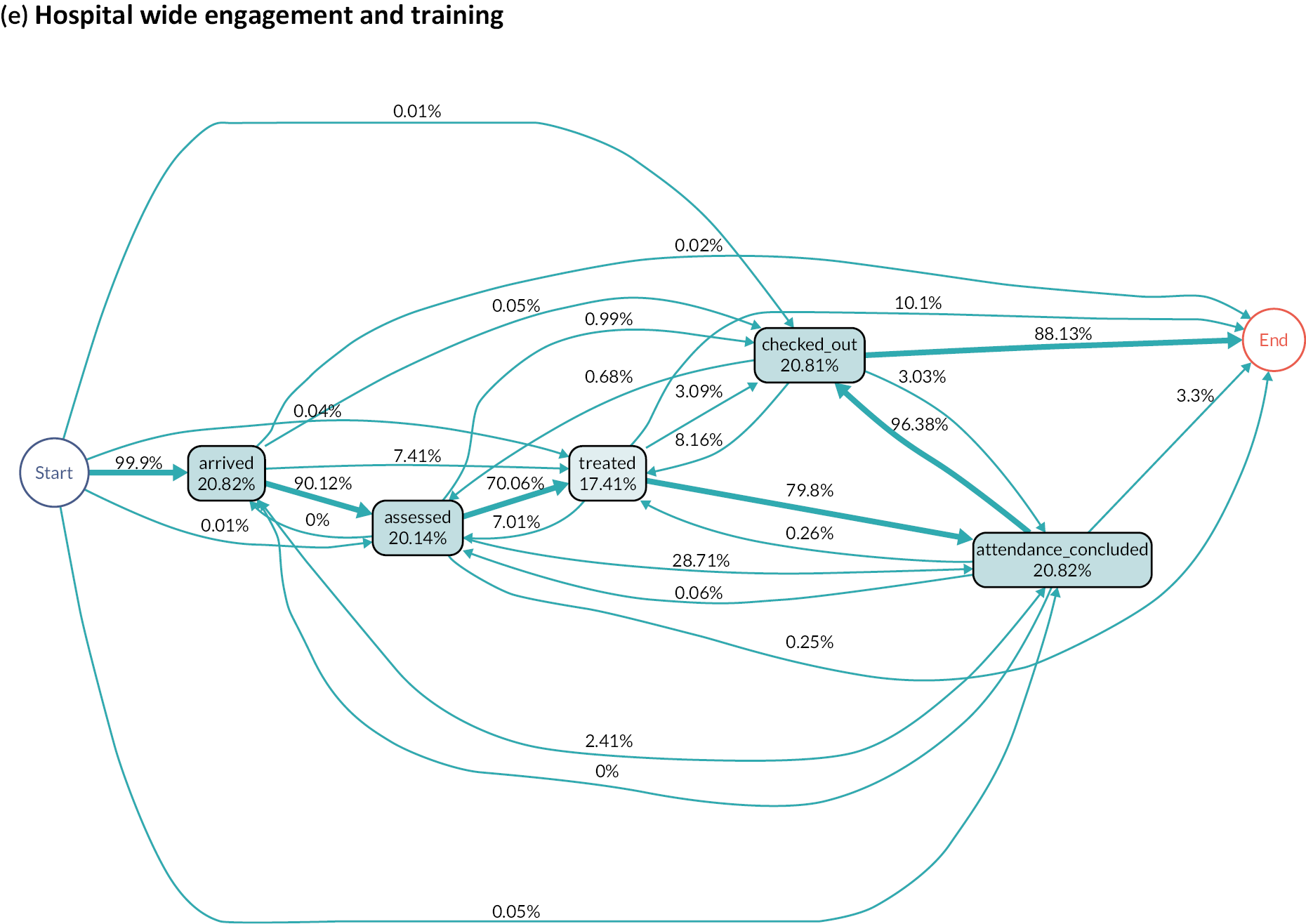
Appendix 4 Model output graphs
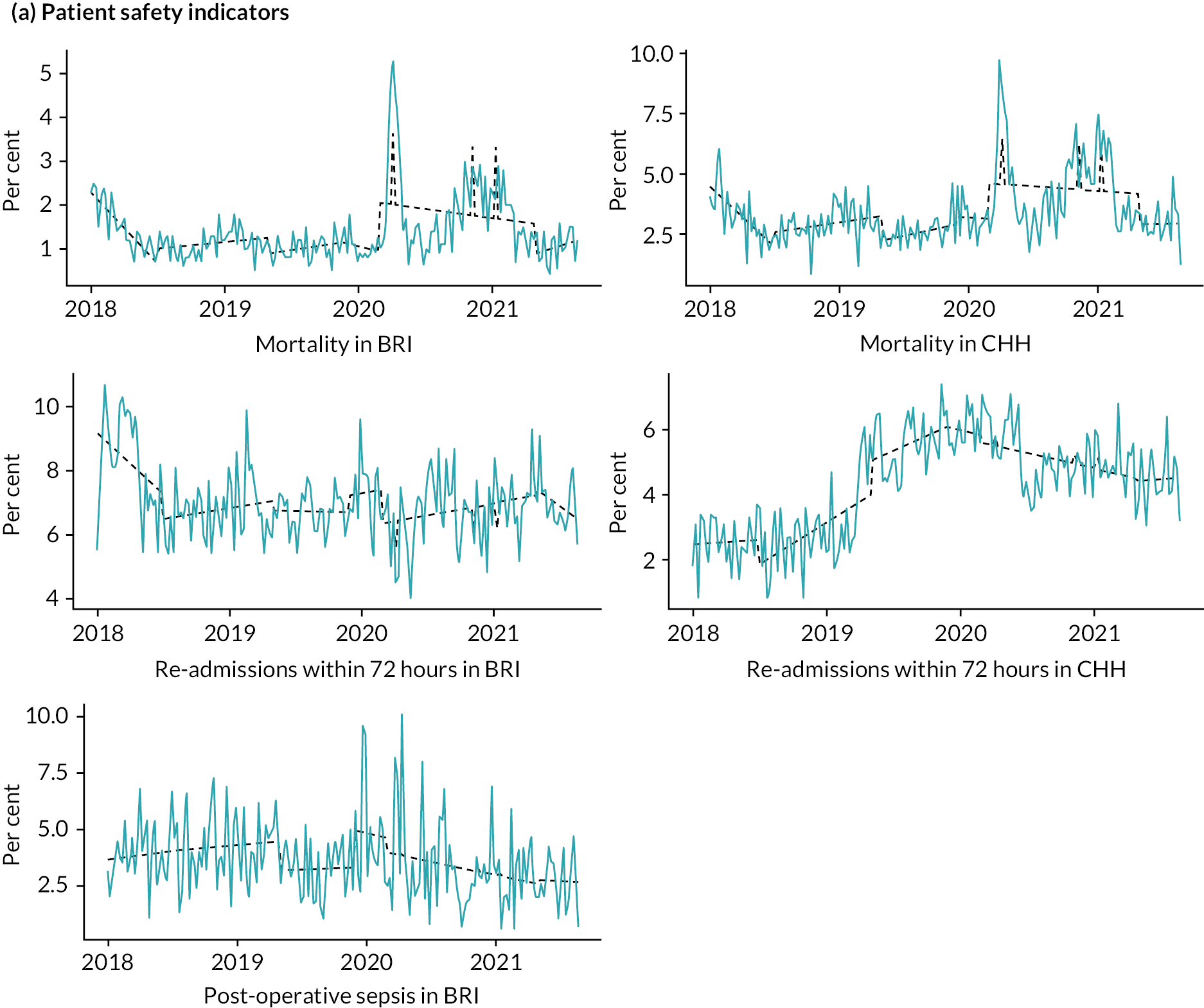
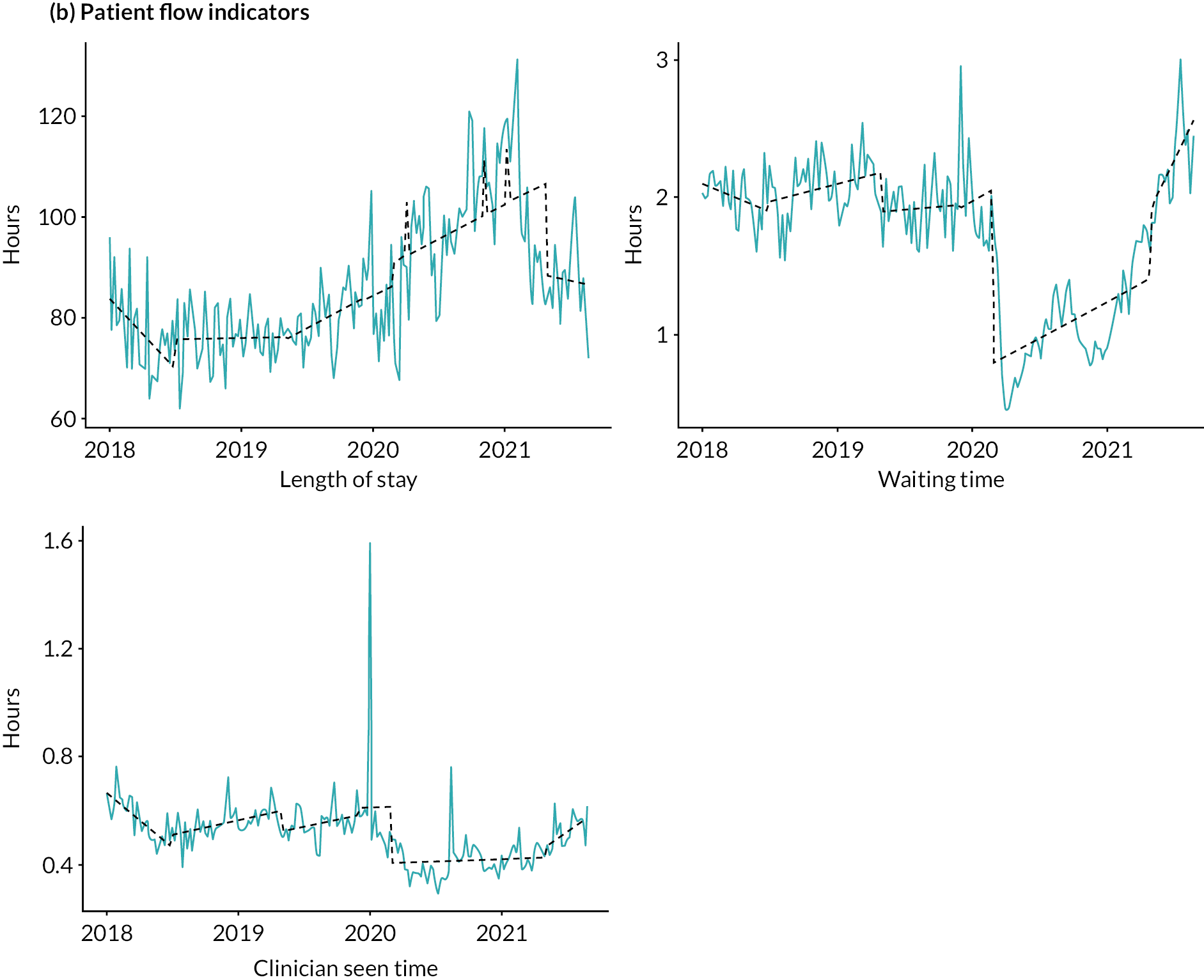
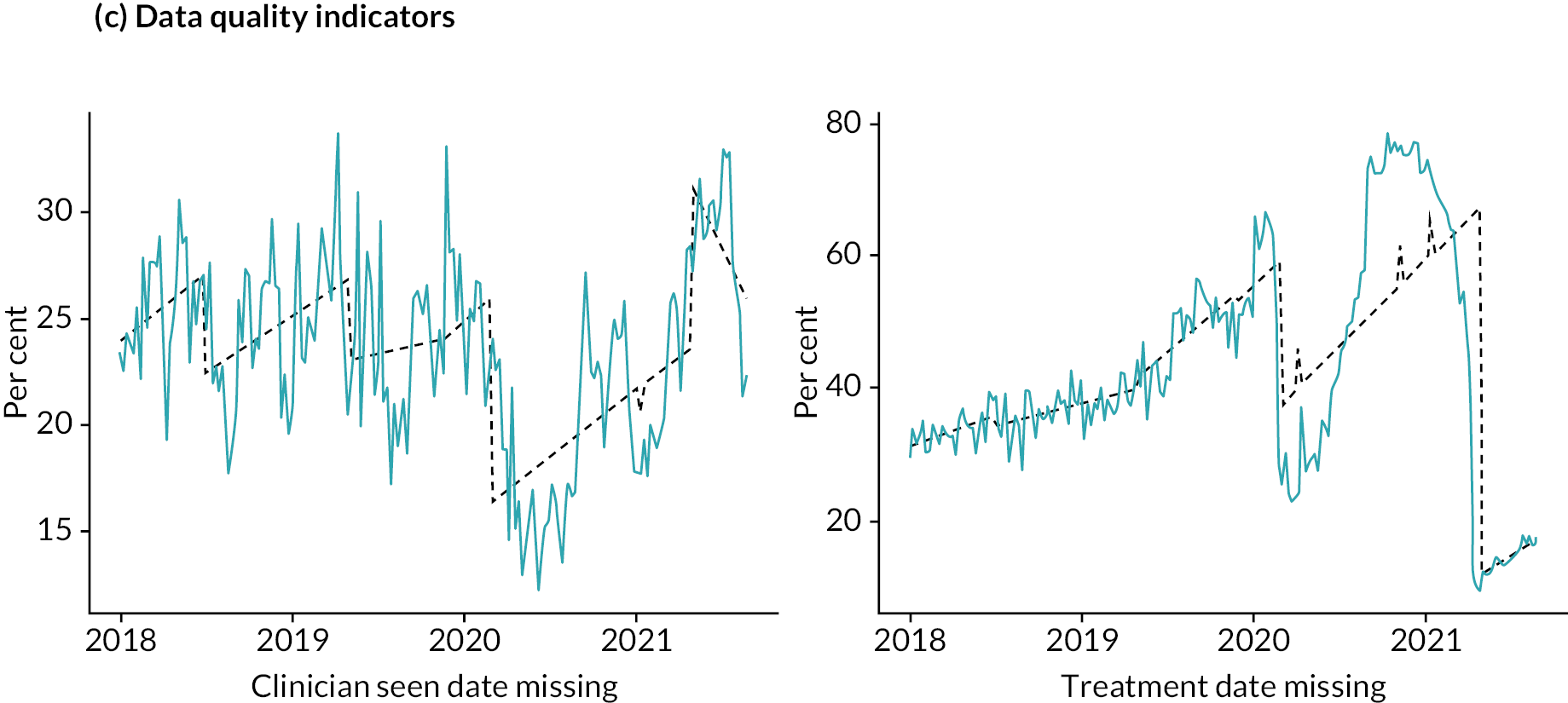
List of abbreviations
- A&E
- accident and emergency
- AI
- artificial intelligence
- ATC
- air traffic control
- BIHR
- Bradford Institute for Health Research
- BRI
- Bradford Royal Infirmary, the main hospital managed by BTHFT
- BTHFT
- Bradford Teaching Hospitals NHS Foundation Trust
- C2
- command and control, an approach to managing organisations and complexity
- C3TRACE
- Command, Control and Communication: Techniques for the Reliable Assessment of Concept Execution
- CC
- command centre, specifically the Command Centre implemented at BRI
- CHFT
- Calderdale & Huddersfield NHS Foundation Trust
- CIO
- chief information officer
- EAST
- Event Analysis for Systemic Teamwork
- ED
- emergency department
- EHR
- electronic health record
- EPR
- electronic patient record, sometimes used as a synonym for EHR
- MOD
- British Ministry of Defence
- NEC
- network enabled capability
- PPIE
- patient and public involvement and engagement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RTA
- reflexive thematic analysis
- SUS
- UK NHS Digital Secondary Use Services
- WS
- workstream
