Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR135660 as part of a series of evidence syntheses under award NIHR130538. The contractual start date was in October 2022. The draft manuscript began editorial review in August 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 de Bell et al. This work was produced by de Bell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 de Bell et al.
Chapter 1 Background
Globally, the population is ageing. By 2050, the proportion of people over the age of 60 years will have doubled. 1 Currently, this is occurring most rapidly in high-income countries; it is estimated that 22% of people in the UK will be aged over 65 years by 2023. 2 These shifting demographics have implications for the health and social care services, as both the type and number of health conditions that tend to develop as people age mean that older populations have different health and care needs. 3 Rates of non-communicable diseases are higher in older age groups,3 and older people are more likely to have multiple long-term health conditions. 1,4 In Wales, it is predicted that there will be a 38% increase in the number of older people with a long-term limiting illness by 2035, meaning another 120,000 people over the age of 65 years may need care and support. 5
Treatment for patients with multiple morbidities can be complex, often involving a number of health and social care services. 6 Providing the best possible care requires co-ordination and integration between health and social care organisations and professionals. 4 Integrated care can either be vertical, connecting generalists and specialists – for example, general practitioners (GPs) and hospital care – or horizontal, requiring broad-based collaboration such as between different community-based services, with both needed for whole system integration,7,8 enabling consistent and efficient delivery of care and services. The intended benefits of integrated care include improved clinical outcomes and patient and carer experience as well as cost-effectiveness. 8,9 Where barriers arise to integrated care, this may lead to inefficiencies in the provision of care, for example fragmentation of services10,11 or overlap;12 patients or their carers having to repeat their needs or stories to different professionals;9 intervention overload;13 and care ‘gaps’8 or missed opportunities, for example for co-ordinated care planning. 14
Additionally, it is important that care is tailored to the needs of older adults. 1 There has been an increasing focus on providing personalised care in the health and social services. 1,4 Yet older people often feel unheard when decisions are being made about their care and powerless in relation to health and social care professionals. 15 Older people’s autonomy needs to be respected and they should be involved in decision-making, with choice over treatment and place of care. 16
Integrating health and social care
The need for co-operation and co-ordination between health and social care has been recognised for a long time. In the UK, integrated working has been required by various pieces of legislation; these have included the Health and Social Care Act 2012 and the Care Act 2014. 17 More recently, there has been a move to Integrated Care Systems,17 which are supported by the NHS Long Term Plan. 4 Different ways of joint working have been tested through pilot programmes, including the Integrated Care Pilots, launched in 2008; the Integrated Care and Support Pioneers, which began in 2013; and the 2015 New Care Model Vanguards. 8 Within these programmes, information technology and data-sharing have consistently been identified as issues. 8,11 Informational continuity – the availability of relevant data or information on a patient to any professional involved in their care – is essential for care co-ordination. 9 Failure to ensure informational continuity and care co-ordination ‘… is likely to result in inefficient use of resources and relies on people or their family or carers, to coordinate care themselves’. 18
Data-sharing between health and social care
Although data-sharing is an aspect of communication, it has its own specificities. Initiatives and interventions aiming to improve communication between health and social care professionals may not necessarily lead to improvement in data-sharing. Data-sharing always has interorganisational and interprofessional aspects: even when information is shared between individual professionals, specific conditions (e.g. policy, legal and ethical frameworks, inter-institutional agreements and professional beliefs) need to be in place to make the exchange of information acceptable and desirable. Data-sharing is also a complex process that involves collecting, coding, storing and updating information which is then shared with or retrieved by other stakeholders, who interpret and make use of it. Stakeholders in the system are informationally dependent in the sense that they require data generated by other stakeholders to complete specific tasks and co-ordinate activities. They may differ in terms of information needs (e.g. content, format, access) as well as usage and contribution to the system’s maintenance (e.g. collecting, uploading and updating information).
Data-sharing can take different forms19 depending on whether it:
-
is between two or multiple stakeholders (e.g. telephone call vs. multidisciplinary team meetings or shared electronic record systems)
-
involves direct synchronous communication (e.g. face to face, telephone calls, multidisciplinary team meetings) or happens indirectly/asynchronously (e.g. making data available to other users on a shared electronic record system)
-
is formal (e.g. multidisciplinary team meetings) or informal (e.g. ‘corridor’ conversations)
-
involves patients and their families (e.g. patient-held paper-based records, patient access to an electronic record system)
-
involves technology (e.g. telephone, fax, e-mail, electronic record systems)
Different methods of data-sharing are often used in complementary ways (e.g. multidisciplinary team meetings and phone calls). The effectiveness of the process is further mediated by policy context, institutional boundaries and cultures, professional relationships and technological developments.
The provision of information systems that support data-sharing across organisational and professional boundaries has been identified as a key element in providing integrated care10,16 and is a long-standing policy objective in the UK. 20 Advances in technology increasingly enable electronic data-sharing; the NHS is tasked with using data and technology to improve health outcomes and is aiming to introduce a digital patient record accessible to health and social care professionals. 19
However, there are a range of challenges in sharing data between health and social care, occurring at both interorganisational and interprofessional levels. 6 Legislation such as the General Data Protection Regulation means that governance agreements need to be in place to allow data-sharing and also leads to concerns about what type of data can be shared and who it can be shared with. 6,8 Patient information is often inaccessible as different professions may not have access to the same records, or because of inconsistent documentation across organisations and professional boundaries. 6,21 Additionally, professional hierarchies lead to power asymmetries which can form a barrier to effective data-sharing. 16
Theories underpinning data-sharing
Data-sharing between health and social care organisations is a broad and complex phenomenon with multiple inter-related social and technical elements. There are numerous theories relating to different aspects of data-sharing, and the judgement of their relevance to the current project is to some extent subjective, reflecting the authors’ background, experience and preferences as well as input from different stakeholders. Since data-sharing is an aspect of communication, we considered communication theories most pertinent to our investigation. There are a wide range of communication theories and models; some focus on communication at different levels, such as between individuals or institutions, others on communication in different contexts. Here we provide a brief summary of the set of theories and concepts that we used as a starting point to explore further the conceptual landscape of data-sharing as a sociotechnical phenomenon.
Schramm22 presents one of the earliest interaction models of communication where communication is conceptualised as an interaction between active participants who encode, decode and interpret information, drawing on their respective ‘fields of experience’. Successful communication (and data-sharing) depends on the overlap of such ‘fields’ which concern not only language but, more broadly, the social context in which communicators operate. If there is not sufficient overlap of the ‘fields of experience’ of health and social care professionals, interpretation of shared data might be difficult and additional communication (e.g. further explanation and clarification) might be required. Such differences could be overcome by developing a common language and building a shared vision of reality. Similarly, Waring et al. 23 describe how knowledge boundaries between organisations and occupations can be understood in terms of differences and dependencies, with differences being the different forms of knowledge held and needed by specific groups, while ‘dependency’ refers to whether, and how much, the knowledge of a different group is needed to solve a particular problem. Where differences are small, standardised knowledge exchange is possible, for example, because language is shared. When differences are large and dependencies variable, however, semantic meanings and beliefs need to be translated across boundaries.
These theories are related to social constructionist models of communication, which suggest that communication is not a simple exchange of information but a meaning-making activity where shared understanding is the aim. Communication between health and social care professionals, which data-sharing is part of, helps to create a shared vision of the care process and develop knowledge of others’ roles and needs, thus changing the social reality in which data-sharing takes place. 24 A related concept is that of ‘systems awareness’: the aim of data-sharing is to improve the system’s performance as a whole, and therefore being aware of how the system works and the informational needs of all stakeholders makes the process of data-sharing more effective; one knows what information is needed, by whom and why. 25
While this provides a broad framing for understanding, and improving, communication between health and social care, data-sharing is a specific facet of communication, often involving the use of technology. The literature on technological change emphasises the additional layer this adds to the change process, with the need for both technical and adaptive, or behaviour-based, change. 26 Sociotechnical systems theory conceptualise the inter-related nature of technological and social elements in the workplace. 27 It considers organisations to be complex systems with intersecting social and technical elements, themselves operating within a wider system. 27,28 Whether introducing a new technology or implementing a programme of change within an organisation, it recognises that both technical and social factors are critical to the success of interventions. 29
There have been various developments of sociotechnical systems theory since it was initially conceptualised around 60 years ago. Davis et al. 27 represent the inter-related elements forming an organisation as goals, people, technology, buildings and infrastructure, culture, and processes and procedures, with the external factors that might have an influence including stakeholders, regulatory frameworks and economic circumstances. This framework is intended to support analysis of the relationships between these different social and technical elements. Sociotechnical systems theory has been used previously to understand conditions that support innovations in the healthcare system30 and responses of healthcare staff to the NHS National Programme for Information Technology. 31
Why it is important to do this review
The overall topic and area of uncertainty that the review focuses on was identified as a priority within a James Lind Alliance research prioritisation project. The overarching topic of the research prioritisation exercise was: How can we best provide sustainable care and support to help older people live happier and more fulfilling lives? The third of the ‘Top 10’ research priorities, prioritised by care workers, carers and older people, was:
How can social care and health services, including the voluntary sector, work together more effectively to meet the needs of older people?
This was viewed as a priority in order to ensure:
-
care workers and health professionals know about all the care and support available in their area and can signpost older people and their families to services
-
assessments in health services lead to the provision of appropriate social care and someone takes responsibility to check that all needs are met
-
funding and resources are distributed across all sectors to avoid voluntary services being forced to provide social care ‘on the cheap’
-
social care workers are members of multidisciplinary teams caring for older people in hospital
-
voluntary sector services are valued and respected for the essential care they provide
-
health professionals and care workers co-ordinate their care successfully to provide the best possible care for the older person
-
health and social care services communicate with each other, refer older people to each other’s services and provide seamless care. 32
The researchers involved in the priority-setting project stated:
there is a large existing evidence base (and several evidence syntheses) on integrated working but it is hard for practitioners to make sense of it. The key question is how to mobilise existing knowledge about integrated working… not just amongst health and Local Authorities, but also social care providers. 32
Overall, the project concluded that:
A new evidence synthesis is also needed on the mechanisms/interventions that local areas implement to improve communication between health services, social care services and social care providers. 32
This review addresses this need. Initial scoping searches found a wide-ranging body of evidence regarding communication between health and social care, including strategies aimed at organisations and individual professionals. Consultation with key stakeholders was used to focus the review on a specific aspect of communication: data-sharing.
Chapter 2 Research question
What are the factors perceived as influencing effective data-sharing between health care and social care, including private and voluntary sector organisations, regarding the care of older people?
Our specific research objectives were to:
-
identify factors that could potentially influence effective data-sharing between health care and social care, including private and voluntary sector organisations, relating to the care of older people
-
identify factors that could potentially influence effective data-sharing between care professionals who work in health care, social care or other organisations providing care for older people
-
identify factors that affect the successful adoption or implementation of initiatives to improve data-sharing between healthcare and social care organisations and/or care professionals.
Chapter 3 Methods
A protocol detailing inclusion criteria and methods for the review was developed and registered on PROSPERO (CRD42023416621).
Inclusion criteria
The criteria for the inclusion of studies in the review are described below and summarised in Table 1. Further detail can be found in Appendix 1, Table 8.
| Include | Exclude | |
|---|---|---|
| Study design | Qualitative studies or mixed-methods studies with a qualitative component. | Other study designs, including qualitative surveys. |
| Population | Older people, as defined by individual studies. Populations where it is reasonable to assume that the focus is on older people (e.g. people with dementia, people in residential care homes). Qualitative study participants could include both the service user population – older people – their family and carers, and health and social care professionals involved in their care. |
Studies focusing on other age groups or not reporting the results for older people separately. |
| Intervention | Data-sharing, defined as: information held by an organisation about an individual patient (e.g. an electronic patient record) which is transferred or made available between organisations or care professionals belonging to different organisations, where this is across the health and social care boundary. |
Studies investigating data-sharing within the same organisation, or which is not across the health and social care boundary. Informal data-sharing or sharing of aggregated and anonymised data. |
| Focus | Description or analysis of factors perceived as influencing effective data-sharing relating to the care of older people, including regarding the successful adoption or implementation of initiatives to improve data-sharing. | All other outcomes. |
Types of evidence
This review included qualitative studies designed to identify, explore and/or understand factors influencing effective data-sharing or the implementation of data-sharing improvement initiatives. Mixed-methods studies were included if the qualitative component was reported separately.
Type of service user population
We included studies where the service user population, the ultimate intended beneficiaries of the services and care organisations of interest, were older people. All studies that defined their service user population of focus as older people were included, regardless of the exact definition used. While we loosely defined an older person as someone over the age of 65 years, in line with NHS England’s ‘Improving care for older people’ guidance,33 this was used as a guiding principle when deciding on the inclusion or exclusion of studies where the service user population was not clearly defined as ‘older people’. Applying a strict definition was not always possible or desirable, as age does not necessarily relate to functional ability. 1,34
While there is no consensus on the key conditions associated with older age,35 studies were also included if it was reasonable to assume the majority of the population would be older people (e.g. people with dementia, multimorbidities, people in residential care homes). If the focus of a study was on a mixed population (i.e. of older and younger people), it was included if the results for older people were reported separately.
Type of study participant
As we were interested in data-sharing relating to the care of older people, we included studies where participants were health and social care professionals involved in the care of older people. Studies of older people and their families and carers were also included if they discussed data-sharing.
Types of intervention
Studies were included if they focused on data-sharing as related to the care of, or services for, older people. Data-sharing was defined as:
-
information held by an organisation about an individual patient or client (e.g. an electronic patient record or handwritten notes)
-
which is transferred or made available between organisations or care professionals belonging to different organisations, where this is across the health and social care boundary.
Studies were excluded if they investigated data-sharing within the same organisation, between different NHS or healthcare organisations (e.g. between primary and secondary care), or between different social care organisations (e.g. between social workers and care home staff). We also excluded studies focused on informal data-sharing, such as conversational sharing of knowledge about patients and their care, or the sharing of aggregated and anonymised data.
Focus of study
As the review includes qualitative studies, we included studies based on their focus rather than outcome measures. Studies were included if they contained:
-
description or analysis of factors perceived as influencing effective data-sharing relating to the care of older people
-
description or analysis of factors perceived as influencing the successful adoption or implementation of initiatives to improve data-sharing.
Types of location
Studies were limited geographically to those focusing on data-sharing between care organisations and care professionals in the UK. This was to ensure that the results from the review were relevant to improving data-sharing in the UK, and specifically for informing the policies and research of Health and Care Research Wales and Social Care Wales (who commissioned this work).
Types of setting
We included studies in any setting where data were shared between health and social care. This included secondary care, primary care and community settings such as the patient’s own home and care homes.
Search methods and sources
Electronic searches
The bibliographic database search strategies were developed using MEDLINE (via Ovid) by the information specialist (AB) in consultation with the rest of the review team. The search strategy combined search terms for data-sharing and qualitative research36 using both controlled vocabulary when available (e.g. Medical subject heading in MEDLINE) and free-text searching. A qualitative research filter informed our qualitative search terms. 37 To find studies conducted in the UK, a UK search filter,38,39 along with ‘United Kingdom’ and synonyms, was used as search terms in MEDLINE then adapted for the other databases (e.g. Web of Science, CINAHL), if required. The full search strategies can be found in Appendix 2.
We searched the following bibliographic databases in March 2023:
-
CINAHL Complete (EBSCOhost), 1937–present
-
EMBASE (Ovid), 1974–present
-
HMIC (Ovid), 1979–present
-
MEDLINE (Ovid), 1946–present
-
ProQuest Dissertations and Theses Global (ProQuest), 1637–present
-
Social Policy and Practice (SPP) (Ovid), 1890–present
-
Web of Science (Clarivate):
-
Science Citation Index (1990–present)
-
Social Science Citation Index (1990–present)
-
Arts and Humanities Citation Index (1975–present)
-
Conference Proceedings Citation Index – Science (1990–present)
-
Conference Proceedings Citation Index–Social Science and Humanities (1990–present)
-
Emerging Sources Citation Index (2015–present) (Clarivate).
-
-
Google Scholar using Publish or Perish (a software program that retrieves and analyses academic citations40).
Searching other resources
We searched relevant websites for publications in May 2023. The following websites were searched using these websites’ own search functions using the key words ‘data’, ‘information’ and ‘sharing’:
-
Age UK (www.ageuk.org.uk/)
-
Age Cymru (www.ageuk.org.uk/cymru/)
-
Older People’s Commissioner for Wales (https://olderpeople.wales/)
-
British Association of Social Workers (www.basw.co.uk/)
-
Royal College of General Practitioners (www.rcgp.org.uk/)
-
British Medical Association (www.bma.org.uk/)
-
Health Foundation (www.health.org.uk/)
-
Nuffield Trust (www.nuffieldtrust.org.uk/)
-
NHS Confederation (www.nhsconfed.org/)
-
Care Quality Commission (www.cqc.org.uk/)
-
Care Inspectorate Wales (www.careinspectorate.wales/)
-
Social Care Wales (https://socialcare.wales/)
-
NHS Wales (www.nhs.wales/)
-
NHS England (www.england.nhs.uk/)
-
Association of Directors of Adult Social Services (www.adass.org.uk/)
-
ADSS Cymru (www.adss.cymru)
-
Public Health Wales (https://phw.nhs.wales/)
-
IMPACT Centre (https://impact.bham.ac.uk/)
-
Skills for Care (www.skillsforcare.org.uk/Home.aspx)
Additionally, the term ‘older people’ was used in the search function on the websites of The Healthcare Improvement Studies Institute (www.thisinstitute.cam.ac.uk/) and the Centre for Care (https://centreforcare.ac.uk/). We browsed the publication lists for NHS Professionals (www.nhsprofessionals.nhs.uk/).
Manual checking of reference lists and forward citation searching using Scopus and Web of Science were conducted on studies that met our inclusion criteria in June 2023.
Screening and study selection
Stage 1: title and abstract
Once the search results were obtained, members of the review team (SDB, ZZ, JTC) independently applied the inclusion and exclusion criteria to a representative sample of citations (n = 100). Decisions were discussed in a group meeting, allowing clarification of the inclusion and exclusion criteria, and definitions updated where necessary. This enabled consistent reviewer interpretation and judgement of the criteria.
Following the initial calibration exercise, two reviewers (SDB, ZZ) independently applied the inclusion and exclusion criteria to the title and abstract of each identified citation. Results from MEDLINE were screened first, then citations from all databases apart from EMBASE. Our experience from previous health evidence syntheses and research41,42 suggested that searching EMBASE was unlikely to retrieve any unique results, particularly as we were searching for qualitative research,43,44 while considerably increasing the number of titles to screen (in this case up to 2725). Therefore, instead of screening all EMBASE results, we decided to carry out a precise search of the EMBASE records in End note using ‘older’ or ‘data sharing’ or ‘United Kingdom’ as keywords in the title field. There were 112 citations, which were single-screened by SDB. This also meant we had more time for citation searching, which has been found to be a lucrative method to find qualitative research. 44
Stage 2: full text
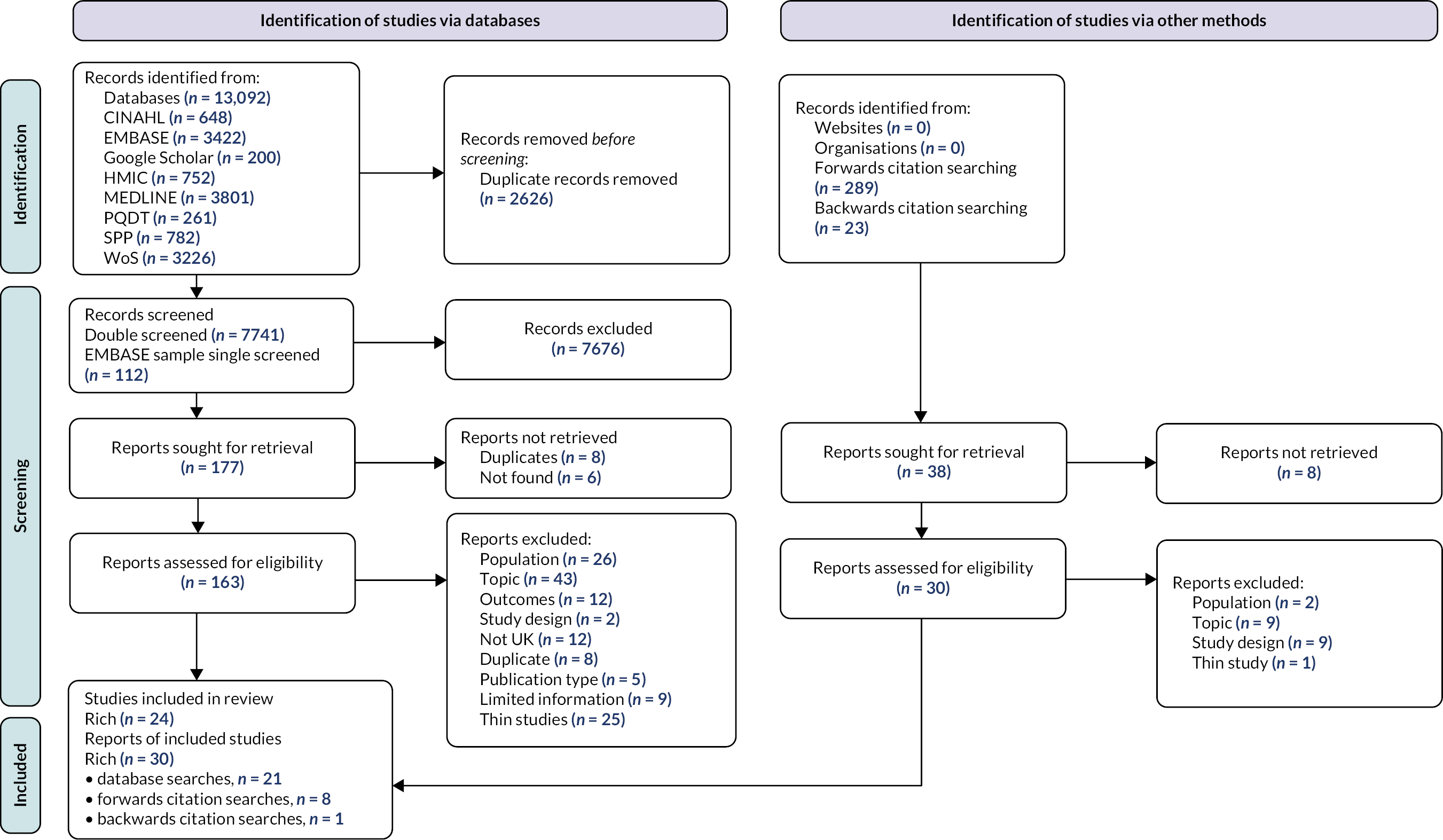
We obtained the full text of papers where either reviewer judged the title and abstract to meet the criteria. Two reviewers (SDB, ZZ) assessed the full-text publication of each record independently for inclusion, with disagreements settled through discussion and, where necessary, with the involvement of a third reviewer. The study selection process was detailed using a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-style flow chart (Figure 1), with a reason reported for exclusion of each record assessed at full text. 45
FIGURE 1.
PRISMA flow diagram of the screening process.
Data extraction and management
We considered multiple reports or publications which used the same data to be a single study. This meant that 49 studies met the inclusion criteria (reported in 54 papers, with 1 study reported in 6 papers and 1 study in 2 papers). In qualitative evidence syntheses, this poses a problem; unlike reviews of effectiveness, they do not aim for an exhaustive sample but to include variation in concepts. Also, a volume of qualitative data too large to allow familiarity with the content can reduce the quality of the synthesis. 46 We therefore used purposive sampling to identify the papers which would contain the most relevant data for the analysis. Consultation with stakeholders (as detailed in Stakeholder engagement) indicated their interest in data-sharing in a wide range of settings and populations, so we decided to use maximum variation sampling to ensure the broadest range of possible studies were included. 46 We began by mapping the included studies, identifying their aims and alignment with our review objectives, population of focus and the richness of the data in the study. 46,47 The richness of data was defined according to the scale developed by Ames et al. 47 where ‘thin’ studies had very little, and often only descriptive, qualitative data relating to our review objectives, while ‘rich’ studies had a large amount and depth of qualitative data relating to our objectives. Whether a study was ‘rich’ or ‘thin’ was decided independently by two reviewers (SDB, ZZ), with disagreements settled by discussion.
This exercise indicated that the majority of studies did not have aims which were closely aligned with our objectives and that over half the included studies had ‘thin’ data. We included all studies with ‘rich’ data (n = 24) in the analysis (and all studies with aims that corresponded more directly with the review objectives fell in this category). Studies with ‘thin’ data (n = 25) are reported in Appendix 3.
From the final sample, we extracted data on:
-
the characteristics of the study (e.g. study reference, aim, methods, service user population, study participants and findings)
To fully capture the characteristics of the included studies, we developed and piloted a data extraction form in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) based on templates developed by the National Institute for Health and Clinical Excellence. 48,49 This summarised contextual and methodological information as identified above and can be found in Report Supplementary Material 1.
-
themes identified by the study authors during the analysis (passages from the papers associated with the identified themes, including participants’ accounts and the authors’ interpretations, i.e. the Results, Discussion and Conclusions sections of the included studies)
Since the extraction of data related to the themes was part of the data analysis, we detail this in Data analysis. The full texts of all included studies were uploaded into NVivo v.12 (QSR International, Warrington, UK), and all data extraction tasks related to specific themes were managed using this software.
One reviewer (SDB or ZZ) performed data extraction for each study, with their data checked by a second reviewer (ZZ or SDB). Disagreements were settled through discussion.
Quality assessment
Quality appraisal of included studies was performed by one reviewer (SDB or ZZ) and checked by a second (ZZ or SDB), with disagreements settled by discussion and, if required, a third reviewer (RA).
Studies were not excluded based on quality. However, the methodological quality of the included studies and the quality of reporting were considered in the interpretation of results. 50,51
Wallace criteria
The methodological strength and limitations of the included studies were assessed using the Wallace checklist,52 as adapted by Gwernan-Jones et al. 53 The latter included 14 questions which covered a range of domains, including research questions, context, data collection, data analysis, substantiation of findings, claims to generalisability, ethics and reflexivity. Each could be answered ‘yes’, ‘no’ or ‘can’t tell’. The checklist can be used to assess any qualitative research methodology, making it suitable for this review as studies came from a range of disciplines and used differing approaches. 54
In piloting the checklist, we found the following two questions difficult to interpret and apply consistently:
-
Is the theoretical or ideological perspective of the author explicit?
-
Has the theoretical or ideological perspective influenced the study design, methods or research findings?
To resolve the problem, we consulted the literature on methodological quality appraisal of qualitative studies and applied the questions to the included studies. After considerable deliberation in the team, we decided to exclude these questions from the final checklist. Our arguments are as follows:
-
It is not universally agreed that qualitative studies should be conducted from an explicit theoretical perspective; their logic could be purely inductive, aiming to develop a theory from the categories generated from the data. Whichever approach is taken, researchers’ particular understanding of the topic will always have a bearing on the way they investigate a specific research question. Such preconceptions need to be considered in relation to the design of the study and interpretation of results – which, within the Wallace checklist, is already covered by the question relating to reflexivity.
-
It is difficult to decide, in relation to our specific research question, what an ‘explicit ideological perspective’ means. All included papers start from the assumption, explicit or implicit, that health and social care interventions, data-sharing included, should result in better patient/client care; they also assume that such claims should be supported by research evidence rather than be taken for granted. These are core values in modern healthcare research in the UK and their explicit statement is usually unnecessary; not making them explicit does not constitute a failure of the authors to report their ideological perspective. As above, potential bias related to the authors’ endorsement of a specific policy or intervention (e.g. integrated care) should be dealt with in the reflexivity question and does not require a separate prompt.
As a result, the final checklist included 12 questions; we provide details of our interpretation of each question in Appendix 4, Table 9.
Data analysis
Framework analysis is a systematic method of analysing primary qualitative data. 55 This method has been developed for application in systematic reviews of qualitative evidence, where it is known as framework synthesis. 56 It is increasingly valued in the study of complex interventions and health systems,57 as it offers a highly structured but flexible approach to data analysis and can be used to map and compare the concepts under study, including identifying associations between themes. 56,58
Conducting framework synthesis involves five distinct stages:51
-
familiarisation with the topic
-
development of a ‘framework’ (i.e. initial set of themes)
-
indexing, where studies are screened and relevant data extracted using the initial framework
-
charting, where themes are revised according to data in the studies
-
mapping and interpretation
Developing the framework
In the first stages of the synthesis, we used a ‘best fit’ approach to develop an initial framework to analyse the data. 56,59 This involved identifying research detailing relevant theories and conceptual models in conjunction with searching for studies for inclusion in the review57 and consulting with stakeholders (as detailed in Stakeholder engagement).
The first iteration of the framework was based on sociotechnical systems theory. 27 This choice was informed by our initial scoping of the literature, which indicated that effective data-sharing between health and social care involves both social elements (e.g. trust in other professionals) and technical elements (e.g. interoperable IT systems). As described in the Introduction, sociotechnical systems theory considers organisations to be complex systems, with interacting social and technical elements. 27,28 The performance of the system as a whole depends on the ‘goodness of fit’ between the human and technical subsystems, which need to be treated as equally important and ‘jointly optimised’ in the iterative process of system design and redesign. Favouring one aspect of the system – for example, trying to get humans to adapt to a new technology without considering their specific requirements and needs – is likely to lead to undesired consequences and poor effectiveness. 28 Despite its origin in heavy industry, sociotechnical systems theory has gradually evolved and found a wide range of applications,28 including to support the design of large-scale IT projects for the NHS and social care. 60 Additionally, we consulted the Health Technology Assessment (HTA) core model; this is a key methodological framework used to evaluate the properties of health technologies and share information on their effects. 61 It contains nine domains which overlap with those of sociotechnical systems theory so indicated important factors to consider in the development of our framework, as well as extending our understanding by highlighting areas not specifically raised in sociotechnical systems theory, for example the legal context.
The six key domains of sociotechnical systems theory outlined by Davis et al. 27 formed the main themes in the framework. In Table 2, we describe our understanding of each theme, providing an indication of the subthemes we considered to fit within each. Specific subthemes (codes) were based on the HTA core model, as described above, and further scoping of the literature during the screening of the studies, which identified additional relevant theories and key points regarding data-sharing. For example, while screening, we considered the technology being used in studies, whether there were factors which were consistently mentioned related to technology, and discussed and agreed on factors (e.g. cybersecurity) that should be subthemes in the initial framework. Subthemes are not detailed further as the framework evolved rapidly during the process of indexing and charting, as described in the next section.
| Theme | Description |
|---|---|
| People | Various stakeholders are involved in the data-sharing process: health and social care professionals, care users and their informal carers. Their personal beliefs and attitudes, knowledge and skills, needs and relationships are likely to have a bearing on the data-sharing process. |
| Goals/metrics | Although the overarching goal of data-sharing is to improve care co-ordination leading to better patient outcomes, its focus will be slightly different in different settings; for example, to avoid undesirable medical procedures (e.g. cardiopulmonary resuscitation) and unnecessary hospital admissions in palliative care patients. |
| Processes/procedures | Successful data-sharing requires a complex set of inter-related processes and procedures, both internal to a care provider (e.g. data collection protocols and training) and external (e.g. policy context, legislation, funding, interagency agreements). |
| Technology | Technology is often involved in the process of data-sharing. In the past, paper records had to be copied and sent by mail or faxed. With the advent of new information and communication modalities, such as shared electronic record systems, the role of technology becomes crucial, impacting other aspects of the data-sharing process, for example interprofessional relationships. |
| Infrastructure | Infrastructure relates to the physical aspects of the data-sharing process. Examples of its impact include the physical implementation of information and communication technologies (e.g. interoperability of different systems) and the colocation of health and/or social care workers to facilitate collaboration and data-sharing. |
| Culture | Shared ideas, values and practices influence people’s behaviour and could act as a barrier or facilitator for effective data-sharing. An example is the often-observed asymmetry in data-sharing (e.g. care home staff should share information with GPs, while GPs may decide to share or not) underpinned by dominant ideas of professional hierarchy. |
Indexing and charting
After identifying and screening studies (as detailed in Search methods and sources and Screening and study selection), we moved to the indexing and charting stages of the synthesis. This involved coding the data from included studies (as defined in Data extraction and management) line by line using an iterative approach. 48 The initial framework served as a starting point for the coding process, with new codes generated to capture further details in the data not covered by the original framework. There was constant comparison of codes across studies,51 with the initial framework developed and changed to accommodate new data and evolving understanding of the phenomenon under study (data-sharing between care organisations and professionals).
The included studies were divided randomly between the reviewers, with half being coded first by SDB and the coding checked by ZZ, and the other half coded first by ZZ and checked by SDB. Data and themes were further explored and clarified through discussion with the wider review team. 62
Mapping and interpretation
Finally, we mapped and interpreted the data and codes, synthesising these to derive a final set of themes from the data using the iterative process described above, and to develop a conceptual model of the phenomenon under study. There were four main themes in this final framework: Goals; Processes and procedures; Technology and infrastructure; and Relationships (encompassing People and Culture from the initial framework). The final framework was compared to the original framework, recognising where themes had been merged and new subthemes which had been identified from the data added, and examining relationships between them (Table 3). 62 As detailed in Chapter 4, Findings, the theme of Goals identified five purposes of data-sharing in the included studies; studies were grouped into five clusters based on these purposes of data-sharing for further analysis. We mapped the themes in the form of a chart for each cluster of studies to aid interpretation. 56 Drawing on the final framework, we developed a conceptual model (detailed in Conceptual model of data-sharing between health and social care) that links together the macro-, meso- and micro-level factors identified in the studies and aims to explain the effectiveness and acceptability of data-sharing and data-sharing interventions.
| Theme | Subtheme (with examples) |
|---|---|
| Goals | Purpose of data-sharing; for example, for transitions from hospital to home |
| Implications of data-sharing; for example, benefits of data-sharing or consequences of not sharing data | |
| Processes and procedures | Translation of policy into procedure; for example, formal agreements for information governance (IG) |
| Implementation of procedures; for example, embedding data-sharing in ways of working | |
| Guidance and training; for example, protocols for data-sharing | |
| Type of record/data | |
| Technology and infrastructure | Method of data-sharing; for example, shared electronic system |
| Data protection and cybersecurity | |
| Access and availability; for example, whether different professional groups could log in to the same electronic system | |
| Update and accuracy; for example, perceptions of the quality of data in an electronic system | |
| Relationships | Interorganisational relationships; for example, culture of mistrust between organisations |
| Interprofessional relationships; for example, professional hierarchies, trust and respect | |
| Attitudes and perceptions; for example, knowledge and understanding of other professional roles, patient perceptions of data-sharing |
External engagement
The focus of this review – data-sharing between health and social care organisations and professionals in relation to the services they provide to older people – is naturally fraught with tensions and controversies. This is evidenced by the long history of local and national initiatives targeting collaboration between health and social care organisations. The results from the current review are intended to be of value to and impact on the lives or professional practices of various stakeholder groups, including older people and their carers, health and social care professionals, voluntary organisations, healthcare commissioners, social care commissioners, and policy-makers.
To ensure we adequately understood the complexity, and sometimes the technical nature of the topic, and considered different perspectives and interests, the review team engaged with professional stakeholders and public and patient involvement and engagement (PPIE) representatives at different stages of the work.
Stakeholder engagement
As commissioners of the research, Health and Care Research Wales and Social Care Wales were key stakeholders, but we also consulted a Professional Stakeholders Advisory Group (PSAG). The PSAG (n = 12) included representatives of health (n = 5) and social care organisations (n = 7) (e.g. social workers, doctors, managers, commissioners), focusing on those operating in Wales. Members of the group were recruited through relevant contacts in Wales and England and had different professional backgrounds and experiences:
-
Social Care Wales, including representation from IG and Mental Health
-
Age Cymru
-
All Wales Heads of Adults’ Services Group (AWASH – comprises heads of adult services from all local authorities in Wales)
-
Social Services Directorate, Welsh government
-
South West Academic Health Science Network
-
NHS Wales Delivery Unit
-
Livewell Southwest
-
Royal Devon University Healthcare NHS Foundation Trust
The PSAG met online twice to discuss progress and provide input to the following:
-
an understanding of data-sharing between health and social care organisations in Wales and how the review could provide impact
-
the framework for analysis and results of the review
-
dissemination of results
Decisions made as a result of consultation with the PSAG are detailed in the relevant sections of the report, with the group informing the focus of the review (see Why it is important to do this review), purposive sampling of studies (see Quality assessment) and feedback on the findings (see Implications/recommendations for future research).
Public and patient involvement
It was important to engage with patients, social care users and/or their carers as part of this project both because they often experience the consequences of poor data-sharing and, more fundamentally, because the data being shared are about them, that is, their personal data. The PPIE group included representatives of the relevant service user population – older people and their families and carers. Members of the group were recruited through relevant contacts in Wales and England following advice and support from the ARC South West Peninsula Patient and Public Engagement Group (https://arc-swp.nihr.ac.uk/patient-public-involvement-engagement/). We recruited four representatives of the service user population (three women and one man), each with different backgrounds and experiences. Three representatives were interested in the topic due to their own experiences, one as a result of their experiences as carer for a family member.
The PPIE group met once, to provide input into the topics detailed above in Stakeholder engagement, as well as providing feedback on the Plain language summary. Changes as a result of consultation with the PPIE group are detailed in Public and patient involvement and engagement.
Departures from the protocol
After screening results from all other databases that had been searched, we decided to refine the EMBASE search. This was due to the high volume of references which would have needed to be screened and because EMBASE has rarely been found to retrieve unique results in previous health evidence syntheses. 41,42 Further detail is given in Screening and study selection.
Due to the large number of relevant full-text articles initially identified for inclusion, we decided to use a purposive sampling method to focus the analysis on a smaller number of the most relevant studies. This is described more fully in Data extraction and management.
Chapter 4 Results
Results of the search and studies included in the review
A summary of the search and screening process is provided in Figure 1. The bibliographic database searches retrieved 13,092 records, with another 312 records then identified through citation-chasing and searches of websites. Following deduplication, we double-screened 7853 records from database searches and 312 records from other sources at title and abstract. This identified 192 reports which were eligible to be assessed at full text. Of these, 49 studies met our inclusion criteria, reported in 54 papers, with 1 study reported in 6 papers and 1 study in 2 papers. After purposive sampling, 24 studies were included in the analysis. Studies that met the inclusion criteria but were not included in the analysis (‘thin studies’) are reported in Appendix 3.
Studies excluded after screening at full text are listed in Report Supplementary Material 2, along with reasons for exclusion. The primary reasons for exclusion at this stage were that the population of focus was not older people (n = 28) or that the topic was not data-sharing (n = 50).
Summary of included studies
Of the 24 studies included in the review, reported in 29 papers and one report, the main settings or contexts in which data-sharing took place were primary care (n = 4 studies),9,12,20,63 the community (n = 8),18,64–70 transitional care (n = 5),14,23,71–73 palliative care (n = 5)19,21,74–76 or care home settings (n = 2). 77,78 Few studies (n = 5)14,20,66,71,77 reported demographic details regarding the service user population that data-sharing was intended to benefit. Most defined their population of focus as older people with care needs (Table 4), although some were conducted in specific populations, for example, adults with dementia (n = 2). 66,68 More details on service user populations, where provided, are given in the descriptions of the study clusters below.
| First author and date | Aim | Service users | Main points relating to data-sharing |
|---|---|---|---|
| Badger 201274 | To evaluate the impact of a training programme to improve end-of-life care in nursing homes on collaboration between nursing home staff and other health practitioners. | Nursing home residents (end-of-life care) | Implementation of the GSF for care homes training programme led to perceived improvement of collaboration between care home staff and other healthcare professionals (GPs, palliative care), and increased their confidence in seeking contact and sharing information. While shared vision supported improvement (GP practices who have implemented the GSF were supportive of the GSF for care homes, while out-of-hours GPs often failed to engage), interprofessional relationships and attitudes were more important. |
| Bailey 202263 | To compare social work in integrated teams with social-work-only teams to evidence the extent to which integration delivers cost-effective and quality outcomes (focusing on prevention of hospital admissions). | Adults aged 65 and over with complex care needs | One of the mechanisms through which integrated care achieved effectiveness was by facilitating communication and data-sharing between social workers and healthcare professionals, in the context of shared understanding of each other’s roles, trust and appreciation, and shared knowledge and information. ‘Embedding’ (which implied colocation and multidisciplinary team meetings) made data-sharing easier as health and social care professionals could build relationships. |
| Bower 201864 | To explore the process of implementation of the Salford Integrated Care Programme and the impact on patient outcomes and costs. | Adults aged 65 and over with long-term conditions | Facilitators of integrated care (and the Salford Integrated Care Programme) included establishing protocols for information-sharing, creating the necessary infrastructure (e.g. multidisciplinary team meetings), and a shared integrated record (acknowledging legal and technical limitations). |
| Chester 202120 | To evaluate the implementation of a shared electronic record system between nursing and adult social care practitioners in separate agencies and locations to inform assessment of need. | Adults referred to the continuing healthcare service team for assessment | The electronic system led to more timely and efficient service delivery and better partnership working (although the quantitative surrogate outcomes were inconsistent). Health and social care workers appreciated the new system; involvement in the design was suggested to be important in its success. Another reason was the lack of options for direct, face-to-face communication. |
| Care Quality Commission 201618 | The aim of this review was to independently assess integrated care within the fieldwork areas and build on existing information to better understand older people’s experiences of integrated care. | Older people (predominantly people with complex needs and comorbidity) | Data-sharing between health and social care providers varied across regions, reflecting levels of integration. It was discussed in relation to the identification and assessment of older people at increased risk of hospital admission, transition from hospital to community (including to care homes) and care management (e.g. duplication of care plans between providers). Data-sharing arrangements were a key element of good practice examples. |
| Dickinson 200665 | The evaluation aimed to produce information about the implementation, operation and effectiveness of the SAP pilot in order to inform and guide further action. | Older people | The implementation of SAP and data-sharing between health and social care professionals was affected by multiple factors including contradictions at programme level (e.g. between person-centred care and standardised assessment); ‘hurried up’ implementation without proper training and groundwork; interprofessional relationships and failure to address these in the implementation process; different managerial styles and attitudes; success/failure to engage with the development of the assessment tools which had implications for their adequacy and adoption; logistics of information-sharing (paper-based tools that had to be copied and faxed ‘across the border’). |
| Ellis-Smith 201877 | To understand the mechanisms of action of a measure to support comprehensive assessment of people with dementia in care homes; and its acceptability, feasibility and implementation requirements. | People aged over 65 with dementia | Care home staff identified barriers to communicating with external healthcare professionals; for example, shift work, staff turnover, differing expectations and lack of shared documentation. The measure was thought to have potential to support communication, particularly with mental health professionals, but GPs were unlikely to have time to read it. The form was paper-based but participants suggested that touch-screen technology could improve usability. |
| Holloway 200666 | To develop and implement a Care Pathway framework for people with Parkinson’s disease and their carers, involving a simplified referral system and more effective communication across health and social care, to facilitate more integrated care. | People with Parkinson’s disease | Elements of the Care Pathway (e.g. the clinic summary and service record) were felt to have potential to support consistent transfer of information between health and social care professionals. The service record needed to be brief enough to be completed by busy professionals but contain enough information to be useful. However, there was little evidence of either being used by other service providers and confusion on the purpose of these forms among patients, who did not ask professionals to fill them in. |
| Kharicha 200512 | To investigate perceptions of joint working in social services and general practice, identifying strengths, weaknesses and good practice. | Older people | Data-sharing was influenced by differences in professional identity and status. Face-to-face contact was seen as a solution to some problems of joint working, but social workers emphasised that this should be formal where possible; for example, multidisciplinary team meetings, which would encourage understanding of their roles. Health professionals saw the implementation of shared records and the restructuring of social care as more important. |
| Lewis 201367 | To describe the care practice in three virtual ward sites in England and to explore how well each site had achieved meaningful integration. | People at high risk of unplanned hospital admission | Patients at high risk of admission were typically cared for by multiple professionals, leading to fragmentation and failures of communication and care. Integrative processes were important; for example, multidisciplinary team meetings helped foster shared values (even where attending professionals were not organisationally aligned). Data-sharing and information management were key in all case studies; for example, in two, all virtual ward members could write in GP electronic records. |
| MacInnes 20209 | To support and monitor improvements to the Over 75 Service, an initiative delivering integrated health and social care. | Adults aged 75 or older, with multiple health and social care needs, living at home | The importance of interprofessional relationships and trust in sharing information were emphasised. Primary care and social services were not geographically aligned, which was a barrier to data-sharing, as were IT systems due to factors such as lack of interoperability and lack of understanding about what could be shared. Another important finding was that care plans were rarely used for data-sharing between professionals as the information they contained was not relevant for everybody. |
| Mahmood-Yousuf 200875 | To investigate the extent to which the GSF for palliative care influences interprofessional relationships and communication, and to compare GPs’ and nurses’ experiences and whether its implementation led to a change in the doctor–nurse relationship. | People with palliative care needs | The GSF enabled timely sharing of information about patients with palliative care needs; for example, from GP to nurse. It strengthened professional relationships and made information-sharing easier; for example, nurses were more likely to seek informal contact with GPs. Multidisciplinary team meetings were valued for information-sharing and felt to increase professional confidence but could be difficult to organise. The extra GSF paperwork was seen as a negative by some. |
| Patterson 201919 | To explore whether access to, and quality of, patient information affects the care paramedics provide to patients nearing end of life, and their views on a shared electronic record as a means of accessing up-to-date patient information. | People receiving end-of-life care | Social care was mentioned only in relation to the new electronic system; paramedics expressed the view that such a system could include social care data which would be helpful when dealing with patients at the end of life. |
| Petrova 201876 | To critically analyse EPaCCS, present a framework for comparing their features, contexts and outcomes, and suggest ways forward. | People receiving end-of-life care | Clinical IT systems need development, for example for interoperability. While these are being developed, temporary solutions are being used, many of which have problems. For example, IT systems external to all users require separate log-ins and double data entry. IG does not address many key issues for EPaCCS; there are communication difficulties in their development, for example between IT experts and professionals, and time is required for training and education. EPaCCS need national support and clinical leadership and projects need to be framed appropriately. |
| Piercy 201868 | To evaluate a new integrated service for postdiagnostic dementia care, assessing how well the service provided support, and understanding the opportunities, benefits and challenges associated with the model. | People with dementia and their families/carers | Information-sharing was a specific problem – securing permissions was a barrier and meant Admiral Nurses had no access to medical records (they were reliant on information from the referral process which was often inadequate). This meant potential risks and duplications of information. |
| Redwood 202371 | The study aim was to understand why delays in discharge from hospital occur and identify obstacles that may be amenable to local solutions that could also have wider application across other health and care systems. | Older people living with frailty | Hospital professionals had less time to collect patient information than social care staff. Information was recorded on paper and electronically, but this was often haphazard and non-systematic, with professionals unable to access information collected by others. Data were shared face-to-face, for example in multidisciplinary team meetings, which were important settings for care co-ordination. Social care information was rarely included in discharge summaries. Difficulties in accessing information led to delays in discharge. |
| Rwathore 200769 | To understand social workers’ and district nurses’ views about information flow, interagency working and SAP. | Older people living at home | Barriers to and facilitators of data-sharing in the context of SAP were discussed, including cultural aspects (e.g. mistrust between organisations/professionals), concerns related to feasibility (e.g. more paperwork) and preference for some forms of data-sharing (e.g. multidisciplinary team meetings were seen as more effective and having other benefits, such as building interprofessional relationships that enabled data-sharing, and overcoming technical and feasibility problems). |
| Shaw 201772 | To examine how and why macro-, meso- and micro-level influences inter-relate in the implementation of integrated transitional care out of hospital in the NHS. | Older people | The focus of the study was integrated transitional care, with this creating conditions for successful [implementation of] data-sharing or the effects of successful collaboration, implicitly including data-sharing. |
| Shenkin 202278 | To inform the development of a care home ‘data platform’ between social care and health for care home residents by (1) identifying what data are routinely collected as part of resident care and (2) collating care home managers’ views and experiences of collecting, using and sharing data. | Care home residents | Two main themes were identified: (1) the rationale for collecting data, and (2) the reality of collecting and sharing data. There were a range of barriers to data-sharing, including variation in practice, lack of standards and lack of agreement about what data should be collected and why. Linked to this were lack of interoperability and other technical issues. The reality of data collection and maintenance would depend on dedicated staff time, which has implications for data-sharing; for example, if data are not up to date or are incorrect, this may have an impact on the wider system when accessed from outside. |
| Standing 2020,21 202079 | To explore attitudes towards the potential of an EPaCCS solution for improving interdisciplinary information-sharing and co-ordination in end-of-life care and facilitating the delivery of care that meets patient preferences, focusing specifically on professional and organisational factors that promote or inhibit the acceptability, usefulness and integration of collaborative care planning across health and social care into service delivery and everyday practice. | People in need of end-of-life care | Poor information-sharing is a barrier to effective end-of-life care and frustrating for patients. Paper-based acute care planning documentation does not appear to be effective; for example, documents are often unavailable and variable in quality. Patients welcomed the idea of an EPaCCS that facilitated sharing of their information between health and social care services, and they did not report the same concerns about data protection and security issues that concerned clinicians. Perceived barriers to an EPaCCS were the increased demand on time and the lack of infrastructure in place to support the system. Care must be taken to ensure that information contained within the EPaCCS does not become overwhelming, particularly for emergency services, such as paramedics, who work under extreme time pressures. |
| Sutton 201673 | To characterise challenges in a project to improve transitions for older people between hospital and care homes. | Older people during periods of acute illness | One intervention implemented in the study was a summary discharge sheet. However, this solution was not co-produced with care home staff, and they did not feel it contained adequate information; this contributed to a negative relationship between hospital and care home staff. |
| Waring 2014,80 2015,81 2016,82 2019,23 2020;83 Bishop 201984 | To explore various aspects of the process of hospital discharge, including professionals’ and patients’ perceptions of threats to safety, the role and experiences of patients, and communication and co-ordination across multiple occupational and organisational boundaries, including investigation of three widely used interventions (information communication technologies, discharge co-ordinator roles and multidisciplinary care planning meetings) in enabling interprofessional knowledge-sharing and learning. | Orthopaedic hip fracture and stroke patients | Information and communication technology (particularly well-co-ordinated and easily accessible patient records), discharge co-ordinators (professionals with dedicated roles who work across institutional boundaries), and multiple-professional group formats (e.g. multidisciplinary team meetings) can facilitate data-sharing during discharge. They are complementary and each has its own advantages and disadvantages. Technology was not used consistently and seemed to support intra- rather than interorganisational activities, with fragmentation and duplication across different sites. |
| Wilberforce 201714 | To evaluate the implementation and potential value of an electronic referral system to improve integrated discharge planning. | Older people with complex care needs | The design and implementation of the electronic system affected data-sharing (e.g. the system had limited usability and did not duplicate the paper-based system forms that staff were familiar with and seemed to like; other issues included the time it took to load and the lack of interoperability/connection between services). However, staff were positive about potential benefits; for example, reducing the need to chase referrals. |
| Wright 199570 | To elicit potential clients’ views of new client-held joint health and social care records. | Older people | Older people found it difficult to conceptualise a shared health and social care record (some saw theoretical advantages, e.g. in emergencies) and were unwilling to contemplate their needs for social care. There were concerns about confidentiality and security. |
In 11 studies, study participants were health and social care professionals,12,14,19,20,67–69,73–75,78 11 studies included patients and carers as well as professionals,9,18,21,23,63–66,71,72,77,79–84 in 1 study participants were not clearly reported,76 while 1 study was conducted solely with older people. 70 Sample sizes ranged from 2 to 220 participants. A total of 13 studies9,14,18,20,53,64,66,68,70,74,76–78 used a mixed-methods approach and 11 were solely qualitative. 12,19,21,23,65,67,69,71,72,73,75,79,80–83 Interviews were used to collect data in all studies, with most obtaining additional data using other methods such as focus groups9,21,23,63,68,70,77,79–84 and participant observation. 23,63,65,69,71–73,75,77,80–85 Eight studies conducted document analysis or audits, for example of care plans. 9,14,20,64,68,69,72,76
Data were shared through face-to-face communication (between two or more care professionals, including formal communication, such as multidisciplinary team meetings, and informal communication e.g. ‘corridor’ conversations), technology-assisted interpersonal communication (e.g. telephone, e-mail, fax) and shared electronic record systems. The former two methods often involved paper-based records. In five studies, all of these methods were used. 12,14,23,64,69,80–84 Two studies focused only on shared electronic systems,21,68,79 one on multidisciplinary team meetings,72 and in two, the data were stored on paper-based forms. 65,74 In all other studies, multiple (but not all) methods of data-sharing were used (Table 5). Both health and social care data were shared in most included studies. 9,12,14,18,20,21,23,65,68–71,74,76,79–84
| First author | Method of data-sharing | Healthcare professionals | Social care professionals |
|---|---|---|---|
| Badger 201274 | Paper |
|
|
| Bailey 202263 | IT system, face-to-face, multidisciplinary team meetings |
|
|
| Bower 201864 | All (apart from fax) |
|
|
| Chester 202120 | IT system |
|
|
| Care Quality Commission 201618 | Unspecified |
|
|
| Dickinson 200665 | Paper |
|
|
| Ellis-Smith 201877 | Paper, face-to-face |
|
|
| Holloway 200666 | Paper, face-to-face |
|
|
| Kharicha 200512 | All (apart from fax) |
|
|
| Lewis 201367 | E-mail, IT system, multidisciplinary team meetings |
|
|
| MacInnes 20209 | E-mail, IT system, multidisciplinary team meetings, phone, face-to-face | Over-75 team:
|
Wider service delivery team:
|
Wider service delivery team:
|
|||
| Mahmood-Yousuf 200875 | Paper, phone, face-to-face, multidisciplinary team meetings |
|
|
| Patterson 201919 | Paper, IT system, face-to-face |
|
|
| Petrova 201876 | IT system |
|
|
| Piercy 201868 | Paper, IT system |
|
|
| Redwood 202371 |
|
|
|
| Rwathore 200769 | Paper, phone, face-to-face, e-mail, IT system, multidisciplinary team meetings |
|
|
| Shaw 201772 | Multidisciplinary team meetings |
|
|
| Shenkin 202278 | Paper, face-to-face, IT system |
|
|
| Standing 2020,21 202079 | Paper, IT system | All professionals involved in end-of-life care | |
| Sutton 201673 | Paper, phone |
|
|
| Waring 2014,80 2015,81 2016,82 2019,23 2020;83 Bishop 201984 | All | Acute hospital:
|
|
Community and primary care
|
|||
| Administrative | |||
| Wilberforce 201714 | All |
|
|
| Wright 199570 | Paper | Not specified | |
There were 13 studies investigating current practice,9,12,18,19,21,63,67,69,71,72,75,76,78,79 while 11 studies evaluated the implementation of initiatives focused either solely on improving data-sharing or on improving care delivery, of which data-sharing was a part (Table 4). 14,20,23,64–66,68,70,73,74,77,80–84 A range of health and social care staff shared data in the included studies (Table 5). Social workers were the social care professionals most often involved in data-sharing, with other professionals including social care assessors, representatives from the voluntary sector (e.g. dementia advisers) and care home staff. From the healthcare sector, nurses (district, community and/or specialist) shared data in the majority of studies, while other professionals included doctors (GPs, geriatricians and other specialists), occupational therapists, physiotherapists, mental health practitioners, paramedics and pharmacists.
Quality of included studies
Wallace criteria
Table 6 shows the score of all studies for each item on the Wallace checklist. Overall, the methodological quality of the included studies was good. Only two studies scored ‘yes’ to all questions; however, 14 out of 24 studies scored ‘yes’ to 11 or more questions,12,19–21,23,63,66,68,69,71,73,74,77–79,81–84 and a further three scored ‘yes’ to 10 or more questions,9,64,75 indicating that most studies scored fairly highly. Of the remaining seven studies, three scored lower than the rest, with ‘yes’ for three or fewer questions. 18,67,76
| Author | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Total (Y, N, CT) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Badger 201274 | Y | Y | N | CT | Y | Y | Y | Y | Y | Y | Y | CT | 9, 1, 2 |
| Bailey 202263 | Y | Y | Y | Y | Y | Y | CT | Y | Y | Y | Y | N | 10, 1, 1 |
| Bower 201864 | Y | Y | Y | CT | CT | CT | Y | Y | Y | Y | Y | N | 8, 3, 1 |
| Chester 202120 | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | N | 9, 3, 0 |
| Care Quality Commission 201618 | Y | Y | N | CT | N | CT | N | Y | N | CT | CT | N | 3, 5, 4 |
| Dickinson 200665 | Y | Y | Y | N | N | CT | N | Y | Y | Y | Y | CT | 7, 3, 2 |
| Ellis-Smith 201877 | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N | 10, 1, 1 |
| Holloway 200666 | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | N | 9, 3, 0 |
| Kharicha 200512 | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11, 1, 0 |
| Lewis 201367 | Y | CT | N | CT | N | CT | N | CT | N | Y | Y | N | 3, 5, 4 |
| MacInnes 20209 | Y | Y | Y | CT | Y | Y | N | Y | CT | Y | Y | N | 8, 2, 2 |
| Mahmood-Yousuf 200875 | Y | Y | Y | CT | N | CT | Y | Y | Y | Y | Y | N | 8, 2, 2 |
| Patterson 201919 | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N | 10, 1, 1 |
| Petrova 201876 | CT | CT | Y | CT | N | CT | N | CT | N | Y | N | N | 2, 5, 5 |
| Piercy 201868 | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | 10, 2, 0 |
| Redwood 202371 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | CT | 11, 0, 1 |
| Rwathore 200769 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12, 0, 0 |
| Shaw 201772 | Y | Y | Y | CT | N | CT | CT | Y | N | Y | N | N | 5, 4, 3 |
| Shenkin 202278 | Y | Y | Y | CT | Y | Y | Y | Y | Y | Y | Y | N | 10, 1, 1 |
| Standing 2020,21 202079 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12, 0, 0 |
| Sutton 201673 | Y | Y | Y | CT | Y | Y | N | Y | Y | Y | Y | CT | 9, 1, 2 |
| Waring 2014,80 2015,81 2016,82 2019,23 2020;83 Bishop 201984 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12, 0, 0 |
| Wilberforce 201714 | Y | Y | Y | CT | N | CT | N | Y | Y | Y | Y | N | 7, 3, 2 |
| Wright 199570 | Y | Y | Y | CT | Y | Y | N | CT | N | Y | N | N | 6, 4, 2 |
| Total (Y, N, CT) | 23, 0, 1 | 22, 0, 2 | 21, 3, 0 | 6, 4, 14 | 16, 7, 1 | 16, 0, 8 | 12, 10, 2 | 21, 0, 3 | 17, 6, 1 | 23, 0, 1 | 20, 3, 1 | 3,17, 4 |
There were some questions for which the majority of studies scored ‘yes’. All included studies apart from one76 had a clear research question, and most used a suitable research design, with only two studies scoring ‘can’t tell’ for this question. 67,76 For ‘Do any claims to generalisability follow logically and theoretically from the data?’, only one study scored ‘can’t tell’,18 with all other studies scoring ‘yes’. Similarly, the majority of studies considered ethical issues; of the 24 studies, 1 study scored ‘can’t tell’18 and 3 ‘no’ to this question. 70,72,76
The criteria which were not met, or where the reported information was insufficient to make a decision, varied across studies and it was therefore difficult to judge their implications for the validity of the overall conclusions of the review. However, there were three criteria for which a large proportion of studies (≥ 50%) failed to score highly; these are discussed further below.
Only six studies21,23,63,68,69,71,79,80–83 provided sufficient evidence that their samples were adequate to explore the full range of perspectives relevant to their research question. Of the remaining 18 studies, 14 studies9,14,18,19,64,67,70,72–78 failed to report sufficient details to judge the adequacy of the samples. Studies may have faced practical limitations, such as the difficulties of accessing specific groups of busy healthcare professionals. However, data-sharing was not the focus of many of the included studies, and more than half of the studies were mixed-methods studies with multiple objectives, so the low scores of studies in this domain may be partly due to their definition of adequate sample being different from ours, for example in terms of types of health professionals. It could also reflect narrow understanding of the data-sharing flow, with only the ‘main protagonists’ (with higher professional status) being included in the research, thus reflecting the impact of professional hierarchies on data-sharing, as discussed further in Chapter 4, Findings. Although this means that individual studies might have failed to include all relevant stakeholder groups and reported on a limited range of perspectives, this is less of a problem for the review as a whole, as we included studies focusing on a wide range of perspectives and highlighted instances where evidence was limited or completely missing.
The second criterion relates to evidence for rigorously conducted data collection, with only 12/24 studies scoring ‘yes’,12,19,21,23,64,68,69,71,74,75,77,78,79,80–83 10 studies scoring ‘no’9,14,18,20,65,66,67,70,73,76 and 2 ‘can’t tell’. 63,72 Reasons for scoring ‘no’ included failure to identify and address factors that could have a potential impact on participants’ behaviour, such as recruitment of participants and setting of the interview, or failure to ensure rigorous recording and transcription of data. Again, these factors varied across studies and their impact should be judged on a case-to-case basis.
The third criterion for which there was a lack of evidence in included studies was reflexivity. There were only four studies where authors showed clear evidence of reflexivity;12,21,23,69,79,81–84 four others were scored ‘can’t tell’,65,71,73,74 with the majority of studies being ‘no’ (16/24). 9,14,18–20,63,64,66–68,70,72,75–78 Reflexivity involves critical examination of the impact of researchers’ own preconceptions and behaviour on the results of the study and their interpretation. Failure to do so may lead to biased results (e.g. through unintended influence on participants’ behaviour) or narrow interpretation favouring the researchers’ preferred explanations. Reflexivity has multiple aspects, and some guidelines caution against overcomplicated reporting resulting from being ‘too reflexive’. 86 Therefore, lack of evidence of reflexivity in some of the papers could be a reporting issue rather than failure of the researchers to be reflexive during the research process. However, the fact that 11/24 papers scored ‘no’ or ‘can’t tell’ on all three questions discussed here suggests that, at least for some of the studies, there was a failure to appreciate the potential impact of the researchers’ behaviour and choices on study results. Ignoring the importance of the specific choices that every researcher has to make (e.g. selection of sample; process of recruitment; choice of place and time for data collection) indirectly suggests limited reflexivity, rather than failure to report the relevant evidence. The implications of the quality of the included studies on the conclusions from the review are discussed further in Chapter 5, Limitations.
Findings
Initially, we coded different aspects of data-sharing and related mediating factors under broad headings derived from sociotechnical theory, as described in Chapter 3, Methods. As the analysis progressed and specific patterns in the data were identified, we observed that factors affecting data-sharing could be grouped into two broad categories: general factors common to all settings and uses of data-sharing, and factors specific to a particular care delivery process or setting. The latter was coded as ‘purpose of data-sharing’ within the overarching theme of Goals; five purposes were identified: joint assessment,14,20,64,65,67–69,72 integrated case management,9,12,18,63,64,66,68,70 transitions from hospital to home,14,18,23,69,71–73,81–84 data-sharing regarding residents of care homes18,21,73,74,77–79 and data-sharing for palliative care. 19,21,74–77,79 Studies were grouped into five clusters based on these purposes. There was some overlap between clusters; for example, joint assessment formed part of the process of integrated case management in some studies but, on the whole, each cluster focused on the process of data-sharing in relation to a specific care delivery process or context. 64,68 Table 7 shows the allocation of studies and the total number of papers and studies in each cluster.
| Study | Joint assessment | Integrated case management | Transition from hospital to home | Care homes | Palliative care |
|---|---|---|---|---|---|
| Badger 201274 | 0 | 0 | 0 | 1 | 1 |
| Bailey 202263 | 0 | 1 | 0 | 0 | 0 |
| Bishop 201984 | 0 | 0 | 1 | 0 | 0 |
| Bower 201864 | 1 | 1 | 0 | 0 | 0 |
| Chester 202120 | 1 | 0 | 0 | 0 | 0 |
| Care Quality Commission 201618 | 0 | 1 | 1 | 1 | 0 |
| Dickinson 200665 | 1 | 0 | 0 | 0 | 0 |
| Ellis-Smith 201877 | 0 | 0 | 0 | 1 | 1 |
| Holloway 200666 | 0 | 1 | 0 | 0 | 0 |
| Kharicha 200512 | 0 | 1 | 0 | 0 | 0 |
| Lewis 201367 | 1 | 0 | 0 | 0 | 0 |
| MacInnes 20209 | 0 | 1 | 0 | 0 | 0 |
| Mahmood-Yousuf 200875 | 0 | 0 | 0 | 0 | 1 |
| Patterson 201919 | 0 | 0 | 0 | 0 | 1 |
| Petrova 201876 | 0 | 0 | 0 | 0 | 1 |
| Piercy 201868 | 1 | 1 | 0 | 0 | 0 |
| Redwood 202371 | 0 | 0 | 1 | 0 | 0 |
| Rwathore 200769 | 1 | 0 | 1 | 0 | 0 |
| Shaw 201772 | 1 | 0 | 1 | 0 | 0 |
| Shenkin 202278 | 0 | 0 | 0 | 1 | 0 |
| Standing 2020,21 | 0 | 0 | 0 | 1 | 1 |
| Standing 202079 | 0 | 0 | 0 | 1 | 1 |
| Sutton 201673 | 0 | 0 | 1 | 1 | 0 |
| Waring 201480 | 0 | 0 | 1 | 0 | 0 |
| Waring 201581 | 0 | 0 | 1 | 0 | 0 |
| Waring 201682 | 0 | 0 | 1 | 0 | 0 |
| Waring 201923 | 0 | 0 | 1 | 0 | 0 |
| Waring 202083 | 0 | 0 | 0 | 0 | 0 |
| Wilberforce 201714 | 1 | 0 | 1 | 0 | 0 |
| Wright 199570 | 0 | 1 | 0 | 0 | 0 |
| Total number of papers | 8 | 8 | 11 | 7 | 7 |
| Total number of studies | 8 | 8 | 7 | 6 | 6 |
Our decision to think about the papers in clusters was based on the diversity of contexts in which data-sharing was described within the broad evidence base. Once the studies had been grouped into five clusters based on the purpose of data-sharing, the framework then provided a way of identifying common factors which were perceived to influence data-sharing across the clusters, as well as areas for which there were key differences between clusters. The final framework (Figure 2), which was developed iteratively from our initial framework (see Chapter 3, Wallace criteria), contained four themes – Goals, as defined above and Relationships, encompassing relationships between professionals as well as factors such as professional hierarchies; Processes and procedures, which included policy context, interorganisational relationships, and ways of working (e.g. guidance and training); and Technology and infrastructure, which details technical factors including the accessibility of different methods of data-sharing, as well as issues such as their accuracy and security.
FIGURE 2.
Themes in the final framework in relation to the clusters of studies.
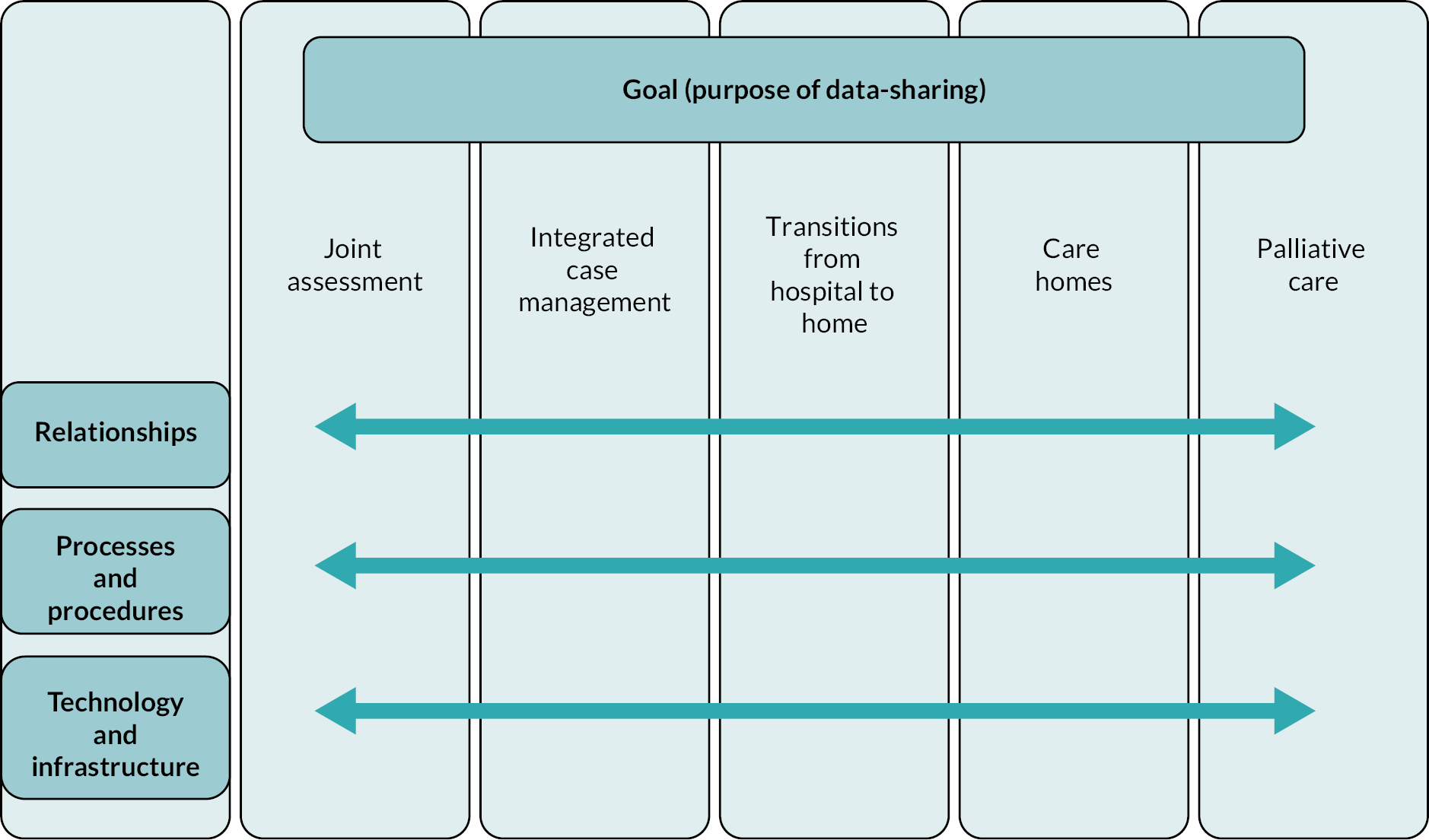
We used the Wallace criteria scores for each study (Table 6) to determine whether the quality of studies varied by cluster. We added up the number of ‘yes’ scores (criteria met) in each cluster and divided this by the number of studies included in that cluster. This gave us the mean number of criteria met per study for each cluster, which ranged from 7.63 to 8.83 (mean 8.3, standard deviation 0.45). This means that no clusters included only low-quality studies and the mean quality of studies (using the number of criteria met as a crude measure) was relatively high (8/12) across clusters.
We also considered Goals to encompass the perceived implications, or intended benefits, of data-sharing. We briefly summarise these benefits because an understanding of the aims of data-sharing in the included studies provides context to the factors perceived to influence data-sharing. Data-sharing provided a comprehensive ‘picture of the patient’ to all professionals involved in their care,67,76–78 while specific benefits were identified for some methods of data-sharing; for example, electronic systems improved transparency as professionals could access prior decisions in the system. 20 Data-sharing initiatives could change ways of working within formal working structures, improving collaboration,20,77 and lead to more timely and efficient delivery of services. 9,19,20,63 Additionally, data-sharing had the potential to reduce staff workload and support more co-ordinated and person-centred care;9,19,21,70,78,81 for example, patients did not have to repeat their stories or conversations about their care. 21,69,76
Below, we use the framework to explore themes which were common to each cluster of studies, before providing more detail on findings from each theme which are specific to each of the five clusters. Quotations are used to illustrate points; where these are from participants in the primary studies, this is indicated.
Overarching factors perceived to influence data-sharing
Within the theme of Relationships, interprofessional relationships were a key factor perceived to influence data-sharing across all clusters of studies. New ways of collaboration, including data-sharing, require changes to existing interprofessional relationships and belief systems. Mistrust,65,69 entrenched prejudices81 and professional hierarchies66–68,73,74,79,82,83 are likely to have a negative effect on data-sharing and interprofessional collaboration in general, and could be replicated in new practices and technological solutions,65,73 such as shared electronic record systems. For instance, Standing79 points out that ‘…lack of access to the new [EPaCCS] system could mark a loss to the professional jurisdiction of care home staff, further downgrading their occupational knowledge and competence’. However, shared records which were accessible to all could also support data-sharing. 11,55,58,65 Included studies emphasised the importance of trust and respect between professionals72,73 and the need to develop relationships between individuals. 23,63–65,69,74 Specific forms of data-sharing, particularly those involving face-to-face conversations such as multidisciplinary team meetings,9,72,75 can help challenge professional prejudice and hierarchies,12,64,66 provide a forum for professionals to build knowledge20 (e.g. develop systems awareness, as discussed under Technology and infrastructure) and build relationships to foster collaboration (including navigating conflict). 67,69,72
Two interlinked subthemes were evident as factors perceived to influence data-sharing within the wider theme of Processes and procedures. The first related to the wider context in which data-sharing was occurring, and the need for a policy context from which a shared vision of care, to which different organisations aspired, could be created. Processes and mechanisms encouraging data-sharing across institutional and professional boundaries were usually initiated as part of a wider integrated care initiative. Such initiatives created a shared vision of integrated care provision,20,65,67 sometimes with respect to a specific patient group (e.g. end-of-life patients74–76) and sometimes more generally. 18 These could then be translated into formal agreements,20,64,67,68 concerning issues such as mechanisms of data-sharing (including technical issues, e.g. interoperability), data governance and confidentiality, standardised assessment tools18 and so on. Aligning processes and practices, and providing the necessary resources, operationalised initiatives,20,67 supporting ways of working among professionals that enabled and encouraged data-sharing across organisational boundaries. Failure to do this led to a disconnect between policy ambitions and day-to-day reality. 14,23,64,65,67,73,78,79 As Rwathore69 put it in relation to the single assessment process (SAP) initiative: ‘Social workers believed that SAP was good in theory, but that it did not appear to be translating satisfactorily into practice’.
Two factors were perceived as important in influencing data-sharing across the clusters in the theme of Technology and infrastructure. The first was the use of technology as a tool for data-sharing, rather than a solution to all data-sharing problems. Successful implementation of a new technology depends on considering how that technology interacts with other elements of the data-sharing system, such as how professionals use the technology, whether it enhances data-sharing, and whether they have to overcome challenges to enable this, for example with usability14,64,67,69 and inaccessibility. 9,23,68,73,78 For instance, shared electronic record systems offer certain advantages by allowing multiple users to directly update the system and access data generated by other stakeholders. 14,21,67 This, however, requires standardised collection and representation of data (e.g. the type of data collected and in what form they are stored in the system). 20,23,64 By making it difficult to record contextual information on a patient’s ‘story’, this has implications for the provision of person-centred care. As different users will have different information requirements,9,19,21,79,87 it also raises questions about access and editing rights; these could reinforce existing professional hierarchies and prejudices, for example the higher value placed on clinical information. 71,78,81,82,84
The second factor was the need for systems awareness; to be able to share data effectively, health and social care professionals need to have an understanding of the care delivery system as a whole,65,76 to better understand each other’s role9,12,64 and accept their interdependence. 20 This also means understanding of each other’s information needs,14,23,73 what decisions the information is being used for, what language and format should be used to make data accessible and usable,23,69 and how logistical and informational processes align to create a seamless care delivery process23,69,72 (e.g. care home staff need to be aware of any changes in the patient’s condition, treatment and care needs before discharge from hospital, so they can make the necessary arrangements18,73).
Data-sharing for joint assessment
The eight studies in this cluster were published between 2007 and 2021. There was some overlap with other clusters, with two studies also appearing in the integrated case management cluster,64,68 and three in the transitions from hospital to home cluster. 14,69,72 Five focused on older adults living in the community,20,69 with some defining their population more specifically as those with complex needs14 or long-term conditions,64 or at risk of unplanned hospital admissions. 67 One study worked with adults with dementia. 68
Data-sharing occurred in the context of ‘joint’ assessments, that is, a process through which professionals aimed to identify a patient’s health and social care needs. 65 Various approaches are taken to assessments of health and/or social care need, including screening everyone within a particular population group or only those with particular risk factors. 14,20 The assessment can be reactive (undertaken in response to a situation such as hospital admission) or proactive. 69 Various policies have been developed to reduce the duplication of assessments between health and social care in the UK: the SAP from 2004,69 the Common Assessment Framework and the Better Care Fund. 14 All have aimed, either solely or as part of a broader remit, to enable ‘joint’ assessment, that is, assessments that can be conducted by health or social care professionals and shared between health and social care organisations. 14 In three studies, assessment was undertaken to enable co-ordinated care planning, including care on virtual wards,67 for transition from hospital to home,14 or for postdiagnosis dementia care. 68 In two studies, assessment was used to determine eligibility for health and social care, as part of the SAP,69 or through specific funding routes, such as NHS Continuing Healthcare or Registered Nursing Care Contribution. 20
Social workers and nurses were the professionals most often involved in data-sharing in the studies in this cluster. Multiple forms of data-sharing were used in most studies. Paper-based processes were used for referrals and to collate information; this also involved speaking to colleagues and using e-mail and fax. 14,64,65,68,69 Regular multidisciplinary team meetings were held,14,64,67,69 with paper records or paper copies of electronic records used to facilitate discussion. While electronic records for the two sectors were separate in some studies, shared electronic systems were also used, with two studies evaluating interventions involving the implementation of new systems. One was a local authority electronic record system prepopulated with information drawn from the national NHS spine system,14 the other a shared electronic record for nursing and adult social care practitioners in separate agencies and locations. 20
Within the theme of Relationships, factors perceived to influence data-sharing were identified at different structural levels. Interorganisational relationships, where organisations had worked to ‘harmonise aims and expectations’,20 facilitated data-sharing. 20,67 This was particularly the case for electronic information-sharing, which improved connection between agencies, and partnership working in the context of joint assessment. 20 Interagency mistrust resulted in poor communication,69 and cultural differences between health and social care prevented data-sharing65,67,68 for example, attitudes about the social services means-testing, ‘a practice that was seen by health service staff as conflicting with the National Health Service’s ethos’. 67 In some cases, there was the perception that information provided on service users from the social services was inadequate. ‘Basically you get the patient’s name and address and that’s what information the assessment starts with’ (study participant). 69
Positive relationships at the organisational level did not necessarily translate into interprofessional working: ‘I think managers do speak, do talk between health and social services. It’s not too bad maybe at higher levels, but the workers have no time and no opportunity’ (study participant). 65 At the interprofessional level, as identified in the overarching factors, knowledge and understanding and individual relationships were important. 14,64,65,67 Within these subthemes, electronic systems improved communication between individuals and aided understanding;20 their use ‘brought a greater appreciation of the process of assessment for continuing healthcare services funding by focusing attention on and clarifying the different responsibilities of the practitioner groups involved’. 20 However, other methods of data-sharing could also facilitate the process,67,69 with face-to-face contact or paper notes allowing professionals to place emphasis on particular aspects of patients’ data. 14
Barriers to data-sharing arose due to cultural differences, such as lack of a common language,69 and in relation to professional hierarchies. 65 Some social care practitioners raised concerns that nurses were not taking responsibility for moving assessments forward,20 while healthcare professionals appeared to view joint assessment as a social work activity. 69 Mistrust and fear could prevent data-sharing,65 with an unwillingness to share data arising from uncertainty over confidentiality rules. 69 There was also a lack of engagement by GPs with assessments:67 ‘The GPs, you can’t get them involved with anything’ (study participant). 65 However, colocation of social workers to GP practices enabled access to patient information and facilitated the SAP process, with some participants commenting that ‘… the GP-attached system might be a way forward for health and social services’. 69
While relationships between professionals are important for maintaining data-sharing, additional facilitators relating to the success of new initiatives were identified in the theme of Processes and procedures. The studies acknowledged that the implementation of electronic systems was setting- and time-specific14,20 and that looking at other data-sharing initiatives could provide contextual information to resolve problems. Co-production of new initiatives was emphasised as a facilitator:65 collaboration between health and social care agencies, and individual staff, to develop new ways of working together, led to ‘buy-in’: ‘I think we have been in control really… If the team weren’t happy… they would look at it again (health manager)’ (study participant). 20 Individuals were found to facilitate implementation of data-sharing initiatives, both internally20,65,67 – for example, managers acted as ‘change agents’, motivating and encouraging professionals – and externally, for example the use of consultants. 20 However, the complexity of data-sharing, in terms of the need to form IG agreements and secure information-sharing permissions, and develop mechanisms to operationalise these, was a barrier. 14,20 Guidance and training could facilitate data-sharing, clarifying the roles of health and social care and providing common standards to cover issues such as data confidentiality and care co-ordination. 67,69 Where these were inadequate, professionals could feel unprepared or unsure. 65
Ways of working were also identified as influencing data-sharing within the wider theme of Processes and procedures. 65 Moving from one form of data-sharing to another (e.g. from paper to electronic) necessarily changed working practices; embedding these new working practices as the normal way of doing things facilitated successful data-sharing. 20 However, this was time-consuming, with lack of time being a barrier for professionals to learn new ways of working and engage with guidance and training. 69 An additional barrier was identified relating to the difficulty of developing workarounds during the implementation of new data-sharing initiatives when parts of the process were not working properly. 14,64,67 These could have further consequences; for example, solutions to gain access to different IT systems led to inconsistent practice in different geographical areas. 67
Technology and infrastructure described how different technical aspects of data-sharing affected its success. Electronic systems were thought to facilitate data-sharing,64 by offering security,14 as well as accuracy due to ‘the capacity to update information over time’,14,67 and allow professionals to monitor referrals without contacting other staff. 14 Paper records could be a barrier for these reasons,65 as well as ‘the administrative and time costs of having to duplicate handwritten information’,14 and the need to use multiple methods of data-sharing, for example telephone to follow up. Data-sharing could also fail due to inadequacy of the available data,69 especially where forms were unsuitable for capturing information. 14,67,68 Some records were thought to be better than others; for example, GP records detail care over long periods of time and so provides rich information. In some cases, standardisation and transparency of the collection of information facilitated data-sharing. 20,64,65
There were specific problems identified with electronic systems. Their accessibility could be a barrier, with systems often inaccessible to different professions,14,64,67,69 for example, requiring an additional log-on, meaning that individuals were dependent on information provided by others. 68 This could lead to duplication, for example, taking paper copies to multidisciplinary team meetings as there was no internet access in meeting rooms. 14 For some systems, poor usability was a barrier:67,69 clunky interfaces were identified as a problem, contributing to systems being time-consuming to use, which made them impractical; for example, nurses did not have time to complete a whole form at once but when re-entering the system had to navigate through all sections to get back to their place. 14 While professionals identified advantages of electronic systems, as detailed above, the technology could also cause anxiety regarding the quality of data, whether the data had saved, or was correct. 14 The success of one electronic system was attributed to the separate locations of the staff using it,20 but with face-to-face data-sharing preferred to electronic if professionals were in the same location. 14
Data-sharing for integrated case management
There were eight studies in the integrated case management cluster: three were published between 1995 and 2006, five between 2015 and 2020. As noted above, two studies in this cluster were also discussed in relation to joint assessment, with one further study in this cluster occurring in the transitions from hospital to home and care home clusters. 18 Populations in these studies were similar to those in the joint assessment cluster: older adults12,70 with complex needs9,63 or long-term conditions. 64 One study focused on adults with Parkinson’s disease66 and one on adults with dementia. 68 While the focus of studies in the joint assessment cluster was the identification of patients’ health and social care needs, studies in the integrated case management cluster were concerned with the next stage in the process: the provision of care to those who had health and/or social care needs and ongoing monitoring of their health and well-being. Data-sharing was discussed in the context of ‘integrated’, ‘co-ordinated’ or ‘partnership working’ between health and social care professionals and organisations to provide this care – all long-standing goals on the policy agenda. 12,18,66 Integrated working is particularly important in the care of older people, who are more likely to need support with both health and social care needs,63 often as a result of multimorbidity. 64
Social workers and nurses were most often involved in data-sharing in these studies, along with doctors, particularly GPs. As well as shared electronic systems, regular multidisciplinary team meetings, telephone calls, and informal face-to-face meetings, colocation of health and social care professionals, and paper records held by patients were discussed in these studies.
As identified previously, relationships at different levels influenced data-sharing. At the interorganisational level, willingness to share information between organisations could be a facilitator:18 ‘It’s kind of working together and just sharing information, rather than thinking “Oh we’re the district nurses and that’s the GP surgery” and not sharing information’ (study participant),9 and seemed to be supported by some methods of data-sharing, such as colocation (e.g. having a social worker in the primary care team63) and regular multidisciplinary team meetings. 9 Relationships between individuals were also valued, with information-sharing often dependent on them. 9,63 In this cluster, professionals in dedicated linkage roles such as care co-ordinators were identified as important. 9,18,64 Data-sharing was both facilitated by and helped to build, trust and respect for other team members and professions. Some methods of data-sharing (e.g. multidisciplinary team meetings) acted as a place both for sharing and for professionals to increase their understanding of different roles. 9,12,64 Similarly, shared records could lead to successful partnerships between health and social care professionals. 12,18,64 Patient-held records were perceived to have the same potential,66,70 showing that everyone was important (reducing power dynamics) and working in the interest of patients:
by the patient carrying records to show to other health professionals and social services that they are as important in keeping the patient as well as we can in the community… I’m not trying to do their job but I’m aware that their job is as important as mine (study participant). 66
Although they were either not tested70 or not found to provide these benefits in practice. 66 While disconnected electronic systems were sometimes a barrier, they could facilitate data-sharing by strengthening relationships as they led to face-to-face and telephone communication between professionals. 9
However, in some studies, professional hierarchies were a barrier to data-sharing. They could lead to difficulty in engaging all professionals involved in a patient’s care in sharing data,18,66 and difficulties sometimes arose due to a lack of relationships between individuals, leading to conflict, for example due to differences of opinion on care decisions. The power dynamics between professions could lead to preferences for different methods of data-sharing. For example, Kharicha12 found that, as a higher-status professional group, GPs tended to prefer informal methods such as ‘corridor’ conversations, whereas social care professionals were more likely to prefer formal settings such as multidisciplinary team meetings, where they felt able to be heard. These differentials also led to the feeling among some GPs that social care needed restructuring to enable data-sharing, rather than changes to their working practices. 12 Additionally, a lack of understanding – whether of data-sharing tools18 or, as in the previous cluster, of what information could be shared – could prevent data-sharing.
An additional theme identified in this cluster related to patient experiences of data-sharing. Patients in an earlier study were not familiar with the concept of a shared health and social care record and tended to refer to medical rather than social care records, though they could see theoretical advantages. 70 More recent studies indicated that while some patients had concerns over confidentiality and security of data, especially financial, they typically expected data to be shared between health and social care. 9,12 They perceived electronic information systems as making data-sharing easier, but did not always feel data were being shared and did not like repeating information to different professionals, finding it ‘…very frustrating to be asked the same questions by different clinicians and providers’. 18 This sometimes meant they felt like they had to act as a co-ordinator with outside services. 9,12,18
Within Processes and procedures, as in the joint assessment cluster, context was identified as important, and the complexity of IG agreements and securing information-sharing permissions, particularly between organisations that have not previously shared processes or ways of working, was a barrier. 18,64,68 The studies suggested that agreeing common standards – for example, on data confidentiality and care co-ordination – between organisations to facilitate real-time data synchronisation between primary care, community care and social services was important and ensured quality. However, policies needed to be operationalised to facilitate data-sharing, for example through protocols, training or awareness-raising among professionals. 18 This could be through structural integration, such as colocation,12 but there was some indication that relationship-building was a more important factor. There was some overlap with factors identified in the previous cluster in this theme, including the need to develop workarounds when parts of the process were not working properly during the implementation of new data-sharing initiatives, and individuals facilitating improvements in data-sharing by acting as ‘change agents’. Partial or temporary funding,18 for example ‘no secure funding for the social care role and a perception that this role was not supported by management’, 63 was a barrier identified in this cluster but not others.
In terms of Technology and infrastructure, studies in this cluster discussed how different methods of data-sharing, such as opportunities for face-to-face communication – whether formal, for example multidisciplinary team meetings,64 or informal, for example through colocation64 – made other professionals more or less ‘accessible’ to each other, affecting their ability to share data. Geography was an aspect of this, with one study finding that the lack of alignment between the areas covered by primary care and social services caused difficulties. 9 The inaccessibility of electronic systems to different professions could also be a factor,9,18,68 particularly the lack of access to ‘local’ electronic patient records for external professionals,68 while ‘distant, telephone based communication between health and social services’12 created problems. When electronic systems were shared, this meant they contained irrelevant information – for example, ‘we’re all looking at slightly different things so, it’s of no interest to me how much money somebody’s got in the bank but that’s quite an inherent part of the social services assessment’ (study participant)9 – which was considered to be a problem due to concerns about IG and whether data could be shared; for example, social workers had concerns about the confidentiality of social data in a GP record. 9 For paper-based forms, the inadequate provision of information was considered an issue, due to ‘the difficulties of capturing relevant information from long and complex medical and social histories on a referral form’. 68
While data-sharing allowed consistent transfer of information around the health and social care system, some studies indicated a lack of trust in technology, leading to alternative methods of data-sharing being used, for example telephone calls. In contrast to findings from studies on joint assessment, perceptions of the quality of medical records were varied, with MacInnes9 finding ‘general practice records care episodes over long periods of time, which provides rich and comprehensive information about a user which has the potential to be shared’, whereas the Care Quality Commission suggested that medical records could be of poorer quality than social care records, particularly in relation to care planning, as ‘patient notes were not always added to their medical records. Where they were added they were often out of date’. 18
Transitions from hospital to home
There were seven studies in this cluster: one was published in 2007 and six between 2016 and 2023. Five studies were also discussed in other clusters: three in the joint assessment cluster,14,69,72 one in the care home cluster,73 and one was related to integrated case management and care homes. 18 Six focused on populations of older people,69,72 who in one study had complex needs. 14 One study, reported in six papers,23,80–84 focused on stroke and hip fracture patients. The purpose of data-sharing was slightly different in this cluster compared to the previous two clusters, as it was intended to facilitate continuity of care when patients were being discharged from hospital to home. Multiple health and social care professionals working both within and across organisational boundaries are involved in hospital discharge. 23,81 There are a number of complex processes involving co-ordination between individuals and the handover of information,73 such as conducting assessments for additional support and ensuring equipment and care packages are in place,71 that are essential to facilitate a safe transition. 23 There are multiple problems associated with hospital discharge, as noted in the Care Quality Commission report:
Although we were made aware of initiatives to improve older people’s transfer of care from hospital, in practice we saw delays in discharge from hospital, poor information for the receiving provider, and a lack of clarity of who was responsible for facilitating older people’s hospital discharge. 18
The co-operation of professionals in transitional care has been further complicated by legislation, such as the 2003 Delayed Discharges Act (now replaced by the Care Act 201488) which introduced fines when medically ready patients were not able to be discharged from hospital for reasons attributed to the social services,72 and other financial penalties, for example for hospital re-admissions. 73
As in the previous two clusters, social workers were the professionals who most often shared data from the social care sector. In the healthcare sector, a greater range of professionals were identified as being involved in data-sharing, with professionals from community, primary, and secondary care contributing to transitional care. In Shaw et al.,72 multidisciplinary team meetings were the sole method of data-sharing. While multidisciplinary team meetings were used to share data in all studies apart from Sutton73 and Care Quality Commission18 in this cluster, they were used in conjunction with other methods of data-sharing, including paper-based, telephone, e-mail and electronic systems. One study specifically evaluated the introduction of a new electronic system to replace a paper-based process. 14
In the theme of Relationships, the need for appropriate forums for data-sharing to be set up or supported at an organisational level was identified as facilitating data-sharing within the subtheme of interorganisational relationships. As in the integrated case management cluster, various methods were suggested as enabling professionals to share data. These included shared electronic records23,81,82 and more informal opportunities to relay information face-to-face, often using paper notes, allowing emphasis to be placed on important points. 14,23 Multidisciplinary team meetings were also important in certain contexts. 71,72,82 However, the presence of professional hierarchies, particularly power differentials between occupations, was a significant barrier in this cluster of studies. While multidisciplinary team meetings could be places where hierarchies were reduced through the renegotiation of differences, this was not always the case; sometimes ‘participants described difficulties of getting their voice heard and making a contribution to care planning, because of underlying professional hierarchies’. 82 This could be due to the distinctions being made between medical and social needs,83 or pressures to expedite discharge from hospital. 82 It was also the case for other methods of data-sharing, for example discharge summaries and other established records systems,81 as the information in these was not accessible to all professionals: ‘each [agency] has their own system, and you have to know what they each need, and when they need it’ (study participant). 23
Another factor which was identified in other clusters, but discussed by many studies in this cluster, was the connection between professional hierarchies and perceptions of different types of knowledge. 83 Generally, medical knowledge was considered more valuable than socio-psycho-experiential knowledge, despite the fact that ‘some participants… clearly described its importance and role in facilitating diagnosis, treatment decisions and discharge planning’. 71 This affected the dynamics of multidisciplinary team meetings and data-sharing (e.g. the contents of discharge summaries). 71,81 A related factor, specific to this cluster, was the different value occupational groups placed on planning transitional care,82 reflecting their different priorities, for example tolerance of risk71,73,84 or prevention of re-admissions:73,81,84
People working in primary and social care expressed strong views about the way in which staff in hospitals focused on what they needed to do and did not pay sufficient attention to others. Hospital staff said the same about primary and social care providers. 18
This meant information regarding discharge was often not relayed appropriately to social care and community teams, particularly care home staff. 18,73,83 The lack of a common language could be a problem,23 with the development of shared understanding,73 including knowledge of processes and ways of working23,69,72,73 and the specific needs of geriatric patients,71 suggested to facilitate data-sharing. Additionally, individuals could provide ‘translation’, particularly those in dedicated roles, for example discharge co-ordinators who could ‘retrieve and transmit’ data as necessary. 18,23,71
There were several factors common to previous clusters identified in the theme of Relationships. Mistrust and fear – whether between professionals,71,81 for example because ‘social workers were not aware of common information-sharing protocols’69 or at an interorganisational level,84 for example due to ‘inter-agency mistrust and a blame culture, relating to authority to access information and confidentiality rules’,69 or historically poor relationships between hospitals and care homes73 – prevented data-sharing. At the interprofessional level, a lack of relationships could stop professionals from sharing data;73 for example, ‘Ward staff and social workers do not know each other very well and therefore might be less willing to trust each other’s decisions [professional assessments]’. 71 Having appropriate forums for data-sharing gave professionals the opportunity to build relationships which facilitated data-sharing. 23,72 Studies discussed how this led to trust and respect, as emphasised by studies in the integrated case management cluster, but also discussed the need to ‘acknowledge their [relationships’] emotional nature, attending to the personal connections and conflicts that occur in the course of professional work such as integrated care’. 72 Conflict could arise as a result of differences in opinion regarding patient care, but relationship-building meant this could be resolved72 and reduced the presence of a fear culture, particularly in social care. 69
Various influencing factors identified in the theme of Processes and procedures related to differences in working practices between different groups of professionals. This was largely due to the greater involvement of healthcare professionals working in hospitals in this cluster. Time could be a barrier, whether this was due to low staffing and shiftwork in hospitals,71 misaligned working practices between hospital professionals and social care,82,84 or the time needed to implement new data-sharing initiatives,72 for example to read guidance, attend training, and set up new systems. 23,69 Additionally, improved data-sharing was seen by some professionals as increasing their workload by adding paperwork and admin. 69,71
Some factors that influenced the success of new data-sharing initiatives in the previous two clusters were also identified in the Processes and procedures theme in this cluster. These concerned the role of individuals acting as ‘change agents’ or ‘boundary spanners’, with particular individuals encouraging buy-in to new initiatives from other professionals. 23,72 The second related to the importance of relationship-building above policy or structural change in the successful implementation of data-sharing. 72,73 However, the wider landscape was still important, with a new electronic system trialled in one study considered to need revision to meet the requirements of the Care Act 2014 if it was reinstated,14 and a lack of protocols to support data-sharing suggested to be a barrier for professionals. 69 The need to develop workarounds during the implementation of new initiatives – for example due to professionals’ technical competence23 or clunky electronic systems14 – could lead to problems with data-sharing. Having separate electronic systems was also found to complicate communication in some cases,81 meaning multiple methods were needed to facilitate data-sharing.
As in previous evidence clusters, accessibility, in terms of the ability different methods of data-sharing gave professionals to connect with one another, was a subtheme within Technology and infrastructure. Being unable to contact other professionals directly could be a problem,84 whereas face-to-face methods, such as colocation69 and multidisciplinary team meetings,72 usually supported data-sharing. However, they could still be barriers to data-sharing, for example when meetings were held at times unsuitable for community professionals. 23 The inaccessibility of electronic systems was a barrier,14,69,71,82,84 as was the existence of multiple systems, most of them specialist, alongside paper records and informal communication, creating complexity as mentioned above. 23,84 Medical information, in connection to being seen as more valuable, was more likely to be recorded than information relevant for social care. 71
As there was overlap between the clusters, many influencing factors run across the integrated case management and transitions from hospital to home clusters in the theme of Technology. These include the ability of electronic systems to facilitate data-sharing, as they can be updated over time,14 due to their accuracy and security, and as electronic systems gave professionals the ability to access information easily71 and to track referrals reliably in near real time, unlike paper records. 14 The time-consuming nature of using unsuitable record systems, whether paper or electronic, was a barrier,14,23,69,71,84 and sometimes arose due to professionals’ lack of technical competence. 23 The way that information was collected, for example through ‘formulaic assessment processes’83 and the format in which it was presented, could be a barrier to the provision of adequate information. 14,23,69,73,84 This was the case both for health care, for example ‘community hospitals, community care teams and social care agencies requested the completion of different forms, care summaries or telephone questionnaires, causing confusion and frustration amongst ward staff’,82 and for social care,73 for example ‘community health and social care workers described how it was usual for care plans, devised by hospital staff, to neglect important information related to ongoing needs’. 83 However, both electronic and paper records could allow the flow of more standardised information. 23
Care homes
There were six studies in the care homes cluster, one published in two papers;21,79 other studies23,64,71,76,83 also mentioned care homes but provided too little detail to be included here. The studies were relatively recent, with one published in 2012, one in 2016, and the other three between 2018 and 2020. Studies in this cluster defined their populations as care home residents18,78 or focused on residents with specific needs: people during periods of acute illness,73 people with dementia and palliative care needs,77 and residents receiving end-of-life care. 21,74,79 The latter four studies are discussed again in relation to palliative care. Data were collected for various reasons: mainly to support person-centred care, but also to share information with internal staff and external professionals, to manage workforce and budget, and to record and evidence care for regulatory bodies. 78
Some studies focused on actual interventions, for example: training to improve end-of-life care;74 the implementation of IPOS-Dem, a brief comprehensive assessment tool for care home residents with dementia and palliative care needs ‘… for use in routine care by care home staff without a nursing qualification’;77 and improving transitions from hospital. 73 Standing21,79 explored attitudes towards the potential of Electronic Palliative Care Coordination System (EPaCCS) solutions to improve information-sharing in end-of-life care, while Shenkin78 investigated care home managers’ views and experiences of collecting, using and sharing data to inform the development of a care home data platform. As might be expected in this cluster, care home staff were the professionals most likely to be involved in data-sharing, rather than social workers as in other clusters. Fewer healthcare staff were discussed as being involved in data-sharing in this cluster; those who were tended to be GPs or district nurses.
While interprofessional relationships and attitudes73 were identified as a common factor in the theme of Relationships in all clusters, professional hierarchies were particularly significant in relation to care homes,74 as care staff were viewed as lower status by other professionals. 79 This had an impact on collaboration even between top-level staff, such as GPs and home managers,74 and had a negative impact on data-sharing even when care homes and health organisations had a shared vision of care [e.g. gold standards framework (GSF)] for palliative care. 74 Despite the fact that care assistants usually have better knowledge of residents’ day-to-day lives and preferences,77,79 these hierarchies mean their knowledge has often been ignored and not included in the data collection process. 74,78 An additional problem related to the influence of knowledge on data-sharing, as there was a lack of understanding regarding care home priorities and ways of working among healthcare professionals. For example, in the case of discharge from hospital:18,73 ‘they [care home staff] needed notice and particular information to receive an older person into their care safely. Hospital staff were not always aware of this’. 18 This contributed to the lack of success of an initiative to improve data-sharing in one study. 73
Training was identified as a factor that influenced data-sharing in the theme of Processes and procedures. While training was discussed in some other clusters, for example joint assessment, it was significant in the care home cluster. 73,74 This finding may relate to the levels of qualification held by most care home staff and poor understanding of terminology, with subjective assessments and variable definitions also contributing to the need for training. 78 Training made nursing home staff more confident in contacting other healthcare professionals, sharing information, and contributing to decision-making [e.g. the advance care planning (ACP) process]. 74
Several factors related to ways of working were identified as specific to the care home cluster, including ‘… shift work, high healthcare staff turnover, time limitations, differing expectations, and lack of shared documentation’77 preventing the sharing of data with healthcare professionals. 21,73,77,79 Standardisation, such as through the use of measurement tools like IPOS-Dem,77 and programmes, such as the GSF for Care Homes,74 were perceived as having the potential to address these issues and lead to general improvement of communication with healthcare staff. 77 Time was an issue for care home staff, in that they found data collection time-consuming so it was often done retrospectively. 78 It was also a problem for healthcare professionals, with care home staff feeling ‘there was uncertainty as to whether GPs would have time to read documents’. 77
Within the theme of Technology and infrastructure, a significant factor perceived to influence data-sharing was the inaccessibility, or inability, of systems or processes to share data:73,78 ‘Although care homes possessed valuable information that is wanted, and needed, by other services, systems did not facilitate a two-way exchange of information, in and out of the care home’. 79 Interoperable electronic systems were rarely present,78,79 but a larger issue was poor use of other methods and channels of communication by care home staff and healthcare professionals. Transitions from hospital to home, or vice versa, were identified as a particular problem, with care home residents arriving at hospital with little medical information,73 and care home staff rarely provided with information which was important in providing care, for example changes in medication, when residents were discharged. 18,73
A factor unique to this cluster related to the types of data being collected and the implications for providing person-centred care. Shenkin78 identified 15 core data items routinely collected by care homes through a range of different tools and assessment protocols, with very little harmonisation. Additionally, a ‘reactive approach to identifying and responding to risk and complex needs’18 meant that people at risk were normally identified by an external health professional. Managers stressed that a care home data platform should have a ‘… context built in to ensure appropriate analysis and interpretation’,78 and expressed concerns about a task-oriented tick-box culture and focus on clinical data leading to important information about a resident not being recorded. The need ‘… to construct a holistic understanding of a resident’s changing needs’78 and encourage a cultural shift from task-oriented to person-centred care was also recognised in other studies,77,79 with the need to build a ‘picture of the person’. 77 Related to the type of data collected was the reality of data collection: data accuracy was a problem, with inconsistencies and human error due to illegible writing and spelling on paper records, and the fact that for some care workers English was not their first language. 77,78
Palliative care
Six studies, published between 2008 and 2020, were included in the palliative care cluster. In terms of population, three included patients in care homes,21,74,77,79 one of which specifically addressed the needs of patients with dementia;77 the rest had a more general scope. 19,75,76 Palliative care requires a close collaboration between multiple health and social care providers, patients and their families ‘… to ensure care is coherent and aligned with patient preferences’. 79 Data-sharing plays a crucial role in this process as the quality of care often depends on various professionals being able to access reliable and up-to-date information generated by other stakeholders in a timely manner, for example when paramedics make decisions about attempting a cardiopulmonary resuscitation. Over the past 20 years, there have been a series of policy initiatives to improve collaboration and co-ordination between different care providers, with the patients and their families placed at the heart of this process. Notable examples in the UK include the implementation of the GSF, a programme aimed at facilitating primary palliative care and later extended to care homes;74,75 and EPaCCS –
an umbrella term covering a number of different electronic solutions that aim to capture patient wishes and preferred place of death and improve coordination of care in real time, through enabling the sharing of information across health and social care services. 21
Two studies investigated the implementation of the GSF in primary care75 and in care homes;74 one study investigated IPOS-Dem, a brief comprehensive assessment tool for use in care homes;77 one study focused on the implementation of EPaCCS;19 and the other two studies (one of which was reported in two papers) explored the views and experiences of different stakeholders in relation to current palliative care provision and future implementation of EPaCCS. 21,76,79 Participants in the studies were care home staff, social workers, hospital doctors, GPs, out-of-hours services, paramedics, district and specialist nurses, patients and their families, and other supporting professionals (e.g. managers, coroner).
For palliative care, the number of different health and social care services that needed to collaborate was greater than in other clusters; this was identified as a factor influencing data-sharing within the theme of Relationships. The implementation of EPaCCS, for example, would involve nine key service types and hundreds of individual settings and teams ‘… GP practices, emergency telephone lines, ambulance services, GP out-of-hours services, hospitals, community nursing teams, specialist palliative care services, hospices and care homes’,76 while out-of-hours services were more likely to be involved than in other clusters. 21,74,76,79 As in previous clusters, data-sharing through direct interprofessional communication was positively influenced by ‘… a variety of processes aimed at formalising communication…’. 75 In this cluster, policy initiatives74,75 such as the GSF were key to the initiation of this process, although preference for, and effectiveness of, specific forms of verbal data-sharing depended on local arrangements, practical considerations and interprofessional relationships. Multidisciplinary team meetings in primary care ‘… were generally valued, and were felt to provide a formal channel of communication for sharing knowledge, discussing treatment, and keeping colleagues informed ’,75 offering time for professionals to gain a better understanding of each other’s role and informational interdependency. They were particularly appreciated by district nurses as they allowed them access to busy GPs, made them feel appreciated and part of a multidisciplinary team. 75 In addition, formal meetings enabled a review of all palliative care patients, irrespective of their most recent contact, meaning that ‘all practice staff became aware of patients receiving palliative care, encouraging a multidisciplinary approach to management’. 75 Informal communication also played an important role in co-ordinating care74 and was particularly valued by GPs as it allowed district nurses who ‘… were recognised as often being better informed about patients’ day-to-day condition…’75 to ‘… alert the GP when a patient is deteriorating and might require greater attention’. 75
An additional factor unique to this cluster concerned the potential for implementation of data-sharing initiatives to be a ‘… barrier for change’79 by reinforcing interprofessional hierarchies. For EPaCCS, Standing concluded that ‘… if different health and social care professional groups were to be afforded varying access and editing rights… this new system could be seen as a reflection on the value of a profession, reinforcing professional boundaries and hierarchies’. For instance, ‘… lack of access to the new system could mark a loss to the professional jurisdiction of care home staff, further downgrading their occupational knowledge and competence’. 21
As in the integrated case management cluster, patient perceptions were identified as a factor influencing data-sharing. However, in this case they were a challenge to data-sharing, as perceptions of EPaCCS as ‘death registers’ presented a significant obstacle to their uptake. 76 Patient-held ACP documents, intended to help paramedics and out-of-hours services to make decisions such as resuscitation and hospital admission, were supposed to be kept ‘visible’ in the patient’s home (e.g. on the mantlepiece). Similarly to EPaCCS, this was problematic from the patients’ and families’ point of view as they perceived them as a constant reminder of the patient’s imminent death. 21
Within the theme of Processes and procedures, policy was particularly important in the palliative care cluster. Palliative care needed national support and strong leadership, with policy initiatives such as the ones described above playing an important role in creating a context for interprofessional collaboration and supporting the systemic nature of palliative care provision. 74–76 While the legal context influenced data-sharing in other clusters, there were particular challenges related to IG in the palliative care cluster: ‘The IG documents… [listed in the paper]… add up to 629 pages, yet they do not address many of the IG issues associated with an EPaCCS’76 which meant that ‘… rules need to be ‘bent’ or controversially interpreted so that EPaCCS projects are not obstructed or abandoned, while the lawfulness of decisions is ensured within broader legal and governance frameworks’. 76
Further factors related to implementation were identified in this theme. Teams starting EPaCCS could find themselves transforming systems and cultures, with projects becoming ‘… complex, long-term, resource hungry initiatives that need to uncover and optimise existing care pathways, change workflows, patterns of collaboration and culture, educate health professionals and break new ground in data-sharing’. 76 Tapping into congruent initiatives (e.g. Direct Enhanced Service for avoiding hospital admissions) and expanding the concept of EPaCCS (e.g. towards ‘Urgent Care Plans’ for all patients with complex needs) could help. 76 Gaining clinician commitment to data-sharing for end-of-life care was also key,19,21,79 through appealing to the core values of users (improvement of patient care rather than cost savings) and extensive information provision and awareness-raising activities. 76
In the theme of Technology and infrastructure, different methods of data-sharing interacted in specific ways with other elements of the system and had important implications for the success or failure of the process. One method for improving palliative care delivery recommended in the GSF was the use of patient-held paper-based records. Such records are routinely produced,76 for example as part of the ACP, which is the process of discussing and documenting the treatment preferences of patients with a palliative diagnosis, and might include a written summary of care preferences and a Do Not Attempt Cardiopulmonary Resuscitation order. 21,79 As in other clusters, there was a move away from paper records, and patient-held ACP documentation was found to be ineffective, at least in terms of enabling paramedics and out-of-hours services to make adequate decisions. 19 Electronic data-sharing, in the form of EPaCCS, was seen as a potential or actual improvement on the current arrangements, but not a solution to all challenges related to the provision of well-co-ordinated multidisciplinary end-of-life care. 19,21,76 For all types of record, paramedics attending end-of-life calls shared that the usefulness was limited by the ‘… time taken to access, level of detail, and accuracy’,19 which meant they often ‘… felt that in such situations [lack of up-to-date information] they had no choice but to admit the patient’,21 and ‘… fear of litigation meant [they] often “err on the side of caution”’. 19,79 They expected that EPaCCS would improve ‘… their decision-making (in terms of speed and quality), supporting them to arrange community-based care more frequently, and improving their confidence in managing the care of patients nearing end of life’. 19
However, actual and potential technical and practical issues of EPaCCS were discussed,76 such as the reliability of mobile devices and electronic systems. 19 EPaCCS will only be useful if the information on the system is accurate and up to date. Yet the responsibility for updating the system is not equally distributed across all users. Paramedics and out-of-hours services were ‘information-poor’ users with virtually no responsibilities for updating patient records; GPs and nurses, on the other hand, were ‘information-rich’ users. 19,21 The responsibility for keeping the records up to date would fall mostly on them, explaining some of the resistance that GPs showed in engaging with yet another electronic record system which is not fully interoperable with the existing ones and will require duplication of tasks. 21,79
Another factor was the divergent information needs of different users. 21,79 EPaCCS should be designed considering the specific information that different health and social care professionals require as well as the format in which data are stored and the speed of retrieval: ‘[. . . An electronic record] would be beneficial [for paramedics], but you’ve got to have the time to access it, and technical competency and ability to actually drag the data out…’ (study participant). 19 Additionally, the use of prespecified measures could empower staff. For example, collecting individual patient data using prespecified GSF forms and validated assessment tools, such as IPOS-Dem, empowered care home staff to be more confident when seeking advice and communicating information about residents to health and social care professionals. 74,77
Chapter 5 Discussion
Summary of findings
Twenty-four studies were included in the review. Most studies focused on populations of older people with complex needs, for example people with multimorbidity; some included specific populations, such as people with dementia, end-of-life patients or people living in care homes. Social workers were the professionals most often involved in data-sharing from the social care sector, while healthcare professionals included nurses, doctors and occupational therapists, among others. Data-sharing tended to occur using multiple methods; in most cases, data were drawn from paper-based or local electronic systems, while shared electronic systems were less common and generally limited to pilot projects and initiatives.
The framework used to synthesise the studies comprised four overarching themes: Goals, Relationships, Processes and procedures, and Technology and infrastructure. Within Goals, we identified five purposes of data-sharing: joint (health and social care) assessment; integrated case management; transitions from hospital to home; care homes; and palliative care. Studies were grouped into five clusters based on these purposes of data-sharing. Within the other three themes, some of the factors perceived to influence effective data-sharing were more general and applied across these clusters of studies (e.g. the impact of professional hierarchies), while others were context-specific (e.g. patients’ and families’ perceptions of EPaCCS as a ‘death register’).
In relation to our original objectives, which were to identify factors that could potentially influence effective data-sharing between health and social care (1) organisations and (2) individuals and (3) in relation to new data-sharing initiatives, we found that evidence in included studies was interlinked. Effective and seamless data-sharing between individual health and social care professionals depended on intraorganisational factors – for example policies and protocols, resources (e.g. means and allocated time), organisational culture – and interorganisational arrangements (agreements, channels of communication and technology) which, in their turn, were mediated by macro-level factors (e.g. policy initiatives, legislation, funding). On the other hand, the success of interorganisational arrangements for data-sharing, such as shared electronic records, was highly dependent on the behaviour of individual health and social care professionals as determined by their needs, perceptions, knowledge and skills. For instance, failure to allocate time for uploading data on a shared database led to higher-priority tasks taking precedence and poor and inconsistent quality of records. When the needs, knowledge and perceptions of (different groups of) database users were not considered during the development process, they were reluctant to engage with the system. The reasons included finding it unhelpful to their day-to-day tasks; not having the necessary knowledge and skills to use it effectively; not being encouraged and enabled to do so or because they couldn’t ‘see the bigger picture’ (i.e. the importance of the information they shared to other decision-makers and the overall impact on patients). Data-sharing initiatives that failed to appreciate the complexity and systemic nature of the process or were too vulnerable to contextual factors, such as short-lived policy programmes and funding, struggled to achieve their goals and lead to sustainable changes in practice.
Overarching factors perceived to influence data-sharing
Within the theme of Relationships, good interprofessional relationships were identified as essential to effective data-sharing, with evidence from studies in all clusters. The existence of professional hierarchies contributed to less effective data-sharing, whereas forms of data-sharing which allowed hierarchies to be challenged and professionals to develop trust and respect for one another (e.g. multidisciplinary team meetings) had the potential to foster effective data-sharing. Without addressing the quality of interprofessional relationships, interventions and technological solutions are likely to replicate existing problems leading to ineffective data-sharing.
In Processes and procedures, the creation of a policy context was identified as an important subtheme. This referred both to the need for formal agreements (e.g. regarding data governance and confidentiality) to enable data-sharing across institutional and professional boundaries and to the need for a shared interorganisational vision regarding the provision of care. Interorganisational relationships were also a factor perceived to influence effective data-sharing, by contributing to the translation, or operationalisation, of formal agreements into aligned processes and practices that allowed data-sharing across institutional boundaries. This included providing the required resources, helping professionals to understand new practice (e.g. through protocols or training), and embedding new process in day-to-day practice.
Finally, two main factors relating to Technology and infrastructure were perceived as influencing effective data-sharing across all clusters. Firstly, technology should be seen as a tool which has the potential to improve data-sharing alongside other processes and conditions, rather than as a stand-alone solution to all data-sharing problems. Successful development and implementation of such tools requires stakeholder involvement and consideration of how professionals interact with the technology and with each other. Secondly, systems awareness: in order to share data effectively, health and social care professionals need to understand the care delivery system as a whole. This leads to recognition of each other’s information needs, the decisions different stakeholders make using the provided information and the interdependence of different processes within the system, helping professionals share data in a suitable language and format and contributing to the provision of co-ordinated care.
Context-specific factors perceived to influence data-sharing
Studies also reported various context-specific factors related to more effective data-sharing. For instance, concerns related to data governance and confidentiality were reported across all settings, but the lack of legal frameworks to enable data-sharing between multiple care providers was particularly important in the context of end-of-life care, where EPaCCS connected multiple stakeholders including patients and families. Other issues specific to end-of-life care relate to the large number of stakeholders that need to be connected, the central role of the patient and family in all data-sharing arrangements, and the potential that patients/families perceive EPaCCS as a ‘death register’ and are then reluctant to engage with it.
Data-sharing between care homes and external care professionals also had its specific challenges. Care homes ‘… were identified as a site of informational isolation, where information does not easily flow in or out’. 79 Although care home staff were expected to collect information to be shared with other care professionals, in most cases there was no reciprocal expectation. Collecting data was also a challenge as care homes often used different assessment tools or no tools at all, staff often lacked the necessary training and/or language skills, and data were sometimes recorded retrospectively and inconsistently. External professionals often dismissed information provided by care home staff, most likely due to the lower value placed on their professional status and expertise.
Data-sharing in the context of patients transitioning from hospital to community was affected by the priority and value placed on this process by hospital and community-based professionals. These reflect not only beliefs about one’s professional responsibilities but also the fact that both settings are commonly stretched to capacity and under-resourced, and so thinking beyond one’s immediate responsibilities is often a challenge.
In the context of joint assessment and integrated case management, cultural differences between organisations and professions, and professional hierarchies, were often an issue. For instance, successful implementation of the SAP was often challenged because needs assessment was perceived as a ‘social work thing’ beyond the remit of healthcare professionals. Multidisciplinary team meetings could help to overcome entrenched professional prejudices, develop trust and understanding, and lead to overall improvements in data-sharing. However, their effectiveness depended on contextual factors, such as leadership and team dynamics, as well as lack of staff availability and geographical proximity, which could be barriers as they prevented attendance at meetings.
Conceptual model of data-sharing between health and social care
From our analysis, we developed a conceptual model of data-sharing between health and social care providers which also considers the involvement of patients/users and their informal carers. By ‘data-sharing’ we mean the collection, coding, storing and updating of information about individual patients/service users which is then conveyed, transmitted or made available to other care providers (or individual care professionals belonging to other institutions) across the health/social care boundary. Such data-sharing systems may or may not involve patients/users and their informal carers (either in terms of holding, passing on or having access to their own data). Below we provide a brief description of the model, which is also illustrated in Figure 3.
FIGURE 3.
Diagram summarising the main factors that affect data-sharing at macro, meso and micro levels. Light blue arrows represent the level of alignment of vision, policy and practice between stakeholders while navy arrows represent interpersonal and interprofessional relationships as a mediating factor; the orange arrows of different thickness represent the fact that stakeholders differ in terms of information needs, usage and contribution to the data-sharing system. Patients/clients and informal carers are represented as separate stakeholders as their relationship is likely to affect their participation in data-sharing.
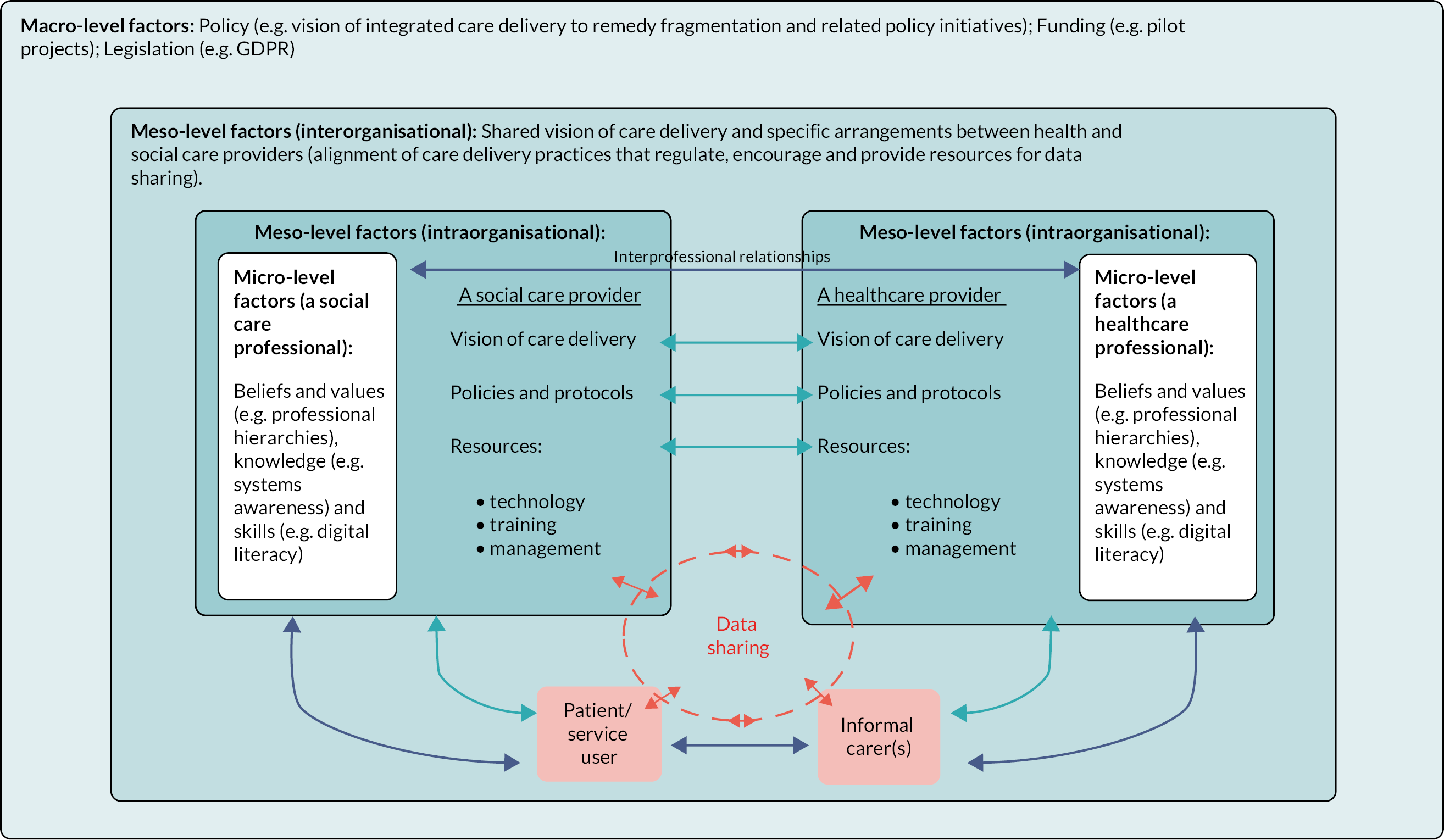
The overarching aim of data-sharing between health and social care providers is to enable care co-ordination by ensuring informational continuity. The specific Goals of data-sharing and related metrics of effectiveness will depend on the specific context in which it takes place. For instance, the aim of EPaCCS is ‘… to capture patient wishes and preferred place of death and improve coordination of care in real time, through enabling the sharing of information across health and social care services’,21 with the most prominent measure of effect being the proportion of users who die in their preferred place of death. 76
Various macro-, meso- and micro-level factors could have a bearing on the effectiveness and acceptability of initiatives aiming to improve data-sharing (either alone or within a broader remit). At a macro level, dominant policy discourses and related initiatives (e.g. integrated care) play an important role in creating a policy and service delivery context in which health and social care providers feel enabled and incentivised to create conditions for data-sharing at a ground level. Related to this is the provision of resources, with the need for long-term sustainable funding mechanisms and the availability of a legal framework that enables data-sharing. Frequent policy changes, ‘pilot fatigue’ (i.e. negativity towards ‘yet another’ new initiative), a lack of sustainable funding and the need to create workarounds to deal with the inadequacies of the current legislation were often identified as barriers to successful implementation of data-sharing initiatives.
At a meso level, factors relating to the different institutional cultures and practices that health and social care organisations have developed over the years need to be changed and aligned across organisational boundaries. Organisations need to develop a shared vision of care provision, often in relation to a specific setting (e.g. transition from hospital to community) or patient group (e.g. patients with palliative care needs) and update their data-related policies and protocols to reflect this new vision. In particular, they need policies and protocols relating to the collection, recording and sharing of information about individual patients/users. Such changes require a systems view of the data-sharing process and co-production involving all system users. This helps to depart from the traditional model where different care providers are concerned only with their own informational needs while data-sharing is seen as a subsidiary activity of little importance. Co-production could help users better understand each other’s decision-making processes and informational needs as well as dealing with issues such as differences in culture and language.
Another crucial factor at this level is the availability of resources to support the transition to new ways of working and their long-term sustainability. These resources include technology and infrastructure (e.g. interoperable or shared electronic record systems; office space and technology for team meetings and colocation), redesigning protocols to allow sufficient time for data-sharing and providing training and managerial support. The latter two relate not only to new data-sharing processes but to support for a broader cultural change, in line with the shared vision of care agreed between participating organisations at the macro level.
Co-production concerns not only the initial design of the system but also its further calibration and development. Evidence suggests that data-sharing systems, such as shared electronic patient records, rarely behave or are used as expected. They may have a wide range of undesired ‘side effects’ (e.g. encourage a ‘task-focused’ care)78 and without robust audit mechanisms in place may have disastrous consequences. 89 Co-production could also help with another resource-related issue: the different levels of contribution to and usage of the system by different stakeholders. ‘Information-rich’ users might be reluctant to engage with a data-sharing system if they have to collect additional information, enter data in multiple systems and frequently update records, without the provision of additional resources.
New technology, such as shared electronic patient records, is often seen as a silver bullet for data-sharing. Yet, there is very little evidence that a single technology could solve all data-sharing problems, many of which relate to human behaviour. In line with the sociotechnical theory underpinning our analysis, the development of a data-sharing system should be guided by the joint optimisation principle, where technology and human elements are considered together, and their interaction and ‘goodness of fit’ determines the performance of the system as a whole. 28 Different combinations of data-sharing methods (e.g. shared records, multidisciplinary team meetings, colocation) and technological solutions (shared electronic systems, video-conferencing etc.) could provide ‘best fit’ in different settings.
At the micro level, factors relate to the behaviour of health and social care professionals, and patients and informal carers, reflecting their beliefs and values as well as knowledge and skills. For instance, to be able to share data effectively, health and social care professionals need to develop a systems awareness of the data-sharing system and the system of care provision more generally. Understanding the decisions other professionals make and the information they need could guide them in collecting and sharing data. Although changes in organisational culture and ways of working (meso level) are expected to change individuals’ behaviour, this will depend on their consistency over time, the provision of resources and leadership, and the time required for such changes to take place.
Fostering interpersonal relationships, through forums such as multidisciplinary team meetings and colocation, is an important mediating factor that seems to have a considerable impact on the success of data-sharing interventions. These relationships help address interprofessional barriers, such as professional hierarchies and prejudices, and seem to play an important role in developing solutions when the ‘official system’ is transitioning or not working as expected. They are also important for the involvement of patients and informal carers who may have concerns about engaging with the system and participating in the data-sharing process.
There is limited evidence of the involvement of patients/users and their informal carers in the data-sharing process, and where evidence does exist, it is limited to specific contexts, such as palliative care. There is no question that the involvement of service users in the development of such systems is highly desirable. However, while having access to their health and social care records and directly contributing information may lead to empowerment, engagement and better co-ordinated and more person-centred care, it will also require considerable changes in current health and social care practices, to avoid misuse, misunderstanding and undesired effects. Future research is required to identify effective system designs and understand the implications of such involvement.
Findings in context
Data-sharing, and evidence about data-sharing, should be considered within the broader context of health and social care integration and collaborative working. From an analysis of four international case studies of integration in health care, Rosen et al. 90 suggest that there are six processes – clinical, organisational, informational, financial, administrative and normative – that support integration within teams and between organisations. Among these, informational integration was identified as a particularly challenging process. 90 Furthermore, all of these processes interact, with wider literature suggesting that a lack of integration at one level, such as the absence of an information system shared between organisations, can restrict integration at other levels, such as the delivery of co-ordinated care at a clinical level. 10 Within studies included in the review, and across the clusters, different forms of data-sharing had their own advantages and disadvantages. As can be seen in the discussion of different methods of data-sharing below, these processes were present, and their interaction contributed to the success of different methods in different contexts.
Multidisciplinary team meetings provided a systematic method of data-sharing, with all participants receiving the same information. They were also a forum for relationship-building (e.g. developing trust) and made participants aware of their informational interdependence and specific information needs, thus facilitating data-sharing. Individual relationships are particularly important in the context of data-sharing, as power (im)balances between professions can result in individuals deciding what they think others need to know. 91 Reducing and resolving these divisions facilitate data-sharing, with an essential component being the development of a shared language and common understanding of terms and processes. 15,16 Multidisciplinary team meetings enabled health and social care professionals to present information in a form accessible to, and usable by, other team members (e.g. by ‘translating’ professional jargon); to provide context to the information they shared; to focus on important details and explain the implications of specific information; and allowed team members to ask ‘data keepers’ for clarification and further information. On the other hand, the effectiveness of multidisciplinary team meetings was limited by a number of practical and relational factors, such as lack of time and geographical distance (an obstacle that could now be overcome with the new information and communication technologies), interprofessional relationships (with the presence of occupational hierarchies at the professional level being a problem identified in other studies6,16), team dynamics and poor leadership. Also, multidisciplinary team meetings are, by definition, costly in terms of the numbers of staff committing time to them.
Direct communication between individual health and social care professionals (verbally or by telephone, fax or e-mail) provided a more flexible and effective way of data-sharing, and often complemented multidisciplinary team meetings. Similarly to the latter, it allowed care professionals to ‘negotiate’ the information they shared and received. The effectiveness of direct data-sharing depended on relational factors, such as trust, understanding and acceptance of each other’s role, skills and expertise. Of the processes identified above, leadership and effective governance arrangements were found to be particularly important,90 and we found that individuals acted as ‘change agents’ in facilitating data-sharing in studies included in the review. While institutional arrangements that sanctioned and facilitated data-sharing (e.g. arrangements around confidentiality and data governance) were significant, relationship-building was a greater facilitator. There were practical limitations to direct communication (e.g. paramedics were often unable to get hold of the patient’s GP to check end-of-life arrangements).
Colocation facilitated direct interprofessional communication and offered similar advantages, for example: creating an opportunity to build relationships and better understand other stakeholders’ roles and institutional environment; offering more opportunities and time to discuss patients with each other. At the same time, there was a risk of the colocated professionals losing their professional autonomy and having their role misinterpreted and transformed to fit in the culture of the ‘host institution’ (e.g. social workers colocated to GP practices felt sometimes as if they were there to serve GPs’ requests rather than as autonomous care professionals).
There is a typical assumption that information technology will improve data-sharing, and while shared electronic record systems were welcomed by most participants, they were not seen as a solution to all data-sharing problems. They were perceived as helpful in co-ordinating the care of specific patient groups (e.g. end-of-life patients) and offered various advantages, such as direct access to data generated by multiple stakeholders; remote and mobile access (highly important for some providers, such as ambulance and out-of-hours services); and continuous update of patient records by multiple stakeholders including, in some cases, patients and families (e.g. end-of-life care).
However, research included in our synthesis also provided evidence that they were challenging to implement and even more challenging to maintain over time. Sociotechnical systems theory emphasises the importance of the interaction between technical and social,29 and the scepticism in the older literature on electronic systems is often linked to poor design and technical problems. 16 While the importance of technical aspects such as interoperability, cybersecurity and access to mobile internet was acknowledged in the included studies, they also reported on the impact of the social factors discussed earlier, such as:
-
cultural issues; for example, different levels of access and editing rights could reflect professional hierarchies and prejudice rather than stemming from pragmatic or professional reasons
-
complex data management involving multiple stakeholders updating the system and thus increasing the risk of human error, incompleteness and failure to keep the records updated
-
users’ perceptions and attitudes, such as trust in the validity and accuracy of the data
-
possible misinterpretation due to limited or no contextual information and lack of an ‘interpreter’ (an advantage of multidisciplinary team meetings and direct interprofessional communication)
-
an inadequate legal framework
Our findings correspond with those of the wider literature, which suggest that when new technology is underused or poorly embedded or implemented in a workplace, it does not result in the transformation which is intended or assumed by policy. 11,23 Influencing factors revealed by the included studies could be mapped onto different stages and elements of the data-sharing process, again indicating the importance of interaction between different processes, for example informational and administrative. 90 Collecting, coding and storing data to be shared with other stakeholders required understanding of their information needs and requirements (e.g. what decisions the data will be used for, by whom, level of detail, language, format). Data shared directly by health and social care professionals (via interpersonal communication and multidisciplinary team meetings) are usually retrieved from each profession’s own local paper-based or electronic record systems and have been collected, coded and stored to meet their own information needs. External users (i.e. users from outside of the data-recording organisation) have no direct access to such patient records and rely on those who retrieve the relevant data to present it in a way that makes it usable, for example the presentation of information related to a service user’s health condition by a district nurse to a social worker in a multidisciplinary team meeting. This may involve a process of translation, clarification and contextualisation with the need, as noted above, for a shared language. Along with accessing the information, participants also learn about each other and build relationships, supporting the development of a shared language and understanding.
In comparison, data collected and uploaded to a shared electronic record system sometimes include limited contextual information, and electronic systems (with standard and limited data fields) may offer fewer opportunities for clarification, so data are therefore at higher risk of misinterpretation. For instance, data collection may not be standardised and may involve the use of heterogenous methods and practices, resulting in inconsistent data. For example, one study reported that assessment tools and definitions used by care homes to collect data on their residents were highly heterogenous. 78 Another study reported different assessment protocols followed by social workers and district nurses within the joint assessment process. 69 Users of the system might be ignorant of such inconsistencies, which will lead to further variation in practice. Information may also be recorded in such a way that it makes it ‘unusable’ by other stakeholders (e.g. paramedics often found ACP documentation too vague and ambiguous to help them make decisions about resuscitation or hospital admission of end-of-life patients). Therefore, shared electronic record systems should be designed to meet the specific information needs of all potential users, involving them in the conceptualisation, definition and development of the system from the very start. As the system is continuously updated, with different users contributing information, having a shared vision, systems awareness of the care provision, understanding of each other’s information needs and learning from each other’s experience become crucial for maintaining its function.
Not only do different care providers have different information needs, but they also differ in terms of usage and expected contribution to a joint records system. For instance, ambulance and out-of-hours services considered access to EPaCCS highly beneficial when attending a patient receiving palliative care as this could help them make an informed decision about resuscitation and hospital admission. Yet they access such information infrequently while contributing limited or no information at all that could benefit other users. On the other hand, ‘information-rich’ professionals, such as GPs or care home staff, might make regular updates of a patient record, including information that will benefit mostly other users. Again, this is different from usual practice where professionals only collect and store information they need in a format that serves their information needs and share with others only what is available. This ‘contribution/usage imbalance’ was one of the reasons that GPs were less enthusiastic about the implementation of EPaCCS, especially when the system was not interoperable with the other electronic record systems they were using (so they had to enter the same information multiple times).
Furthermore, some participants (notably GPs and care home staff) expressed concerns that ‘information hungry’ systems requiring extensive data collection are likely to encourage a bureaucratic care culture, and therefore distract them from focusing on patients/clients. Care home staff were concerned that focusing on data related to specific tasks could lead to ‘task-oriented’ care, while limiting the type of information that is collected (e.g. restricting electronic data collection to prepopulated fields rather than contextual information on a patient’s story). Focusing on medical information could also encourage further medicalisation and formalisation of care with less attention being paid to the patient’s quality of life, experience and overall well-being. As the provision of person-centred care is a key aim within the NHS,4 data-sharing initiatives need to ensure they are enabling this.
Access-related issues also differed between direct interprofessional data-sharing and shared electronic record systems. When sharing data directly (between individuals and in multidisciplinary team meetings), health and social care professionals felt in control of what was shared and could use their professional judgement to decide on the relevance and appropriateness of disclosing specific information. This provided some reassurance that even when they were uncertain about the legality of such decisions, they could justify them from an ethical point of view. Effective sharing, especially of sensitive data, through such forums required time to gain trust and understanding of each other’s role and appreciate the informational interdependence of care providers. Building personal relations facilitated the process as care professionals shared data because they had a shared vision of care and were convinced that it would help patients/clients, despite legal uncertainties or gaps in institutional policies.
In contrast, shared electronic record systems (if used without other channels of communication) typically lack such a ‘human interface’ that could facilitate more nuanced or tailored data-sharing across professional and institutional boundaries. This needs to be considered in their design but also in the broader context of interprofessional and interorganisational communication by providing ways to counteract such deficiencies. They also face challenges related to access and editing rights. Decisions over whether to make all patient data accessible to all users or limit access and editing rights not only create serious legal challenges76 but present ethical dilemmas to health and social care professionals who might be uncertain about what data should and should not be uploaded to the system – especially when the system is also accessible to patients and families. On the other hand, limiting the access and editing rights of certain professional groups could perpetuate existing professional prejudices and hierarchies, stymie engagement with the system and limit its effectiveness. Accessing data that have not been ‘translated’ or summarised for specific users (e.g. social workers accessing medical data) could also increase the risk of misinterpretation and error.
While the design of electronic systems centres on their use by professionals, the people whom these systems are intended to benefit – the patients and their informal carers – are often forgotten. Very few studies included patients’ and informal carers’ perceptions of data-sharing by professionals, or of access to their own records. However, where this was investigated, patients and carers usually had a positive attitude towards data being shared between health and social care providers, assumed this was already taking place and, compared to care professionals, were less concerned about confidentiality and data protection.
Paper-based patient-held records were considered potentially helpful by patients and families but less so by care providers. There were issues with updating the record and using it to make clinical decisions. An example of this was paper-based ACP records which contain information about patient preferences in relation to end-of-life care. Being placed on such a record was often seen by patients and families as being placed on the ‘death register’; keeping the record ‘visible’ in the patient’s home was also undesirable and perceived as a reminder of imminent death. Even when ACP documentation existed, paramedics struggled to find it in the limited time they had, and often found the information too vague and ambiguous to help them make a decision; confirming its validity and meaning (e.g. by calling the patient’s GP) was rarely an option.
While paper-based patient-held records are designed mainly for the benefit of the patient/family and have a relatively limited role in care professionals’ decision-making (e.g. whether or not to carry out cardiopulmonary resuscitation), patient and/or carer access to a shared electronic record system raises a whole new set of questions, for instance: which part of the record the patient should be allowed to access and edit; in what circumstances informal carers should have access to the patient’s record; and whether such information needs to be presented in a language that is accessible to patients and families. Additionally, patient/carer access to relevant information in these records may have an impact on the confidence and quality of care professionals’ decision-making. 19,74,77 Some EPaCCS are already providing access for patients who are able to enter their preferences about end-of-life care, but no research investigating this issue met the criteria for inclusion in this review.
Implications/recommendations for future research
Technology is advancing rapidly, facilitating innovations which may support more widespread and more effective data-sharing. With the NHS Long Term Plan setting out goals for the use of technology in the NHS in England, including the use of electronic patient records systems in all care settings,4 further research is needed to ensure the successful use of different types of technology. Our findings suggest that while shared electronic patient record systems have been in use for some time now (e.g. in palliative care), the evidence on their implementation and use is limited and of poor quality. 76 Generating better-quality evidence that captures both objective outcomes and stakeholders’ experience could inform the effective implementation of electronic systems more widely.
There are other uses of technology, such as holding meetings virtually, which have been driven by the COVID-19 pandemic. 92 Technology could be key to resolving some of the barriers identified in this review, for example by allowing community professionals to attend multidisciplinary team meetings held on hospital sites. However, more research is needed to assess whether technologies implemented as pragmatic solutions to problems raised by the pandemic, with a focus on factors such as speed, are also the most effective solutions to the barriers to data-sharing. For example, studies on the use of technology in primary care have tended to focus on GPs; the experiences of other care professionals need to be investigated as they may be different. 93 Similarly, research from primary care indicates that certain types of technology are preferred by professionals (e.g. telephone consultations), despite the range of technologies available. 93 Understanding how health and social care professionals are sharing data post COVID-19, and why these methods are being used, including the impact of policies such as the Digital and Data Strategy for Health and Social Care in Wales,94 could ensure that current methods are achieving their intended outcomes and inform the development of initiatives to improve the effectiveness of data-sharing.
Another more recent technological advancement, artificial intelligence (AI), is also likely to change the landscape of care co-ordination and data-sharing. For instance, the option to interact with AI-powered databases using natural language will change the way health and social care professionals collect, retrieve and share data, and overcome long-standing problems, such as the need for technical skills to interact with electronic databases. Rather than being yet another digital tool, AI will soon become a central player in the process of collecting, storing, retrieving and sharing data as well as using data to make decisions about the person’s life. An example of this is the use of smart homes for people with various chronic conditions, where AI can constantly collect data (monitoring) and make decisions related to safety, well-being, medical and social care needs. Therefore, future studies looking at the role of AI in health and social care need to consider its impact on care co-ordination and data-sharing, not only in terms of the technical aspects of the process but also with respect to its impact on human relations.
With few studies reporting on patient experiences of different types and levels of data-sharing, this area clearly needs further investigation. In particular, there is very little evidence on shared patient record systems where patients and informal carers have access to and are able to update their records. Limited data from EPaCCS projects show the complexity and challenges involved in creating and maintaining such systems. However, further research is needed to understand the impact they might have on health and social care practices (e.g. the way in which care professionals record and share data).
Similarly, there was a gap in the evidence regarding data-sharing between healthcare and private and voluntary sector organisations, and a related lack of evidence from care homes. The ageing population means that more people will need social care, or become care home residents, in the future, and are likely to receive care from professionals employed by private or voluntary sector organisations. Consultation with our stakeholder group also identified this as an area for which they wanted more information. As discussed in this review, public sector health and social care organisations face difficulties sharing data; given the additional barriers private and voluntary sector organisations face, research is needed on successful data-sharing initiatives including these types of organisations. For example, NHS England’s Enhanced Health in Care Homes model has been shown to result in 23% fewer emergency admissions among care home residents in test sites. 4 The model mandates better communication (including data-sharing) within the care system, so evaluation could indicate factors involved in successful data-sharing between public and private and voluntary sector organisations. There is also a need to explore what works and for whom – whether organisational, whole teams, or for individual professionals or patients – to inform the design and implementation of systems that consider equity and digital inclusion. 92
The reviewed literature suggests that data-sharing is often perceived as something that ‘comes naturally’ to care professionals and the only thing needed is motivation. However, the complexity of data-sharing, and the various challenges and uncertainties associated with the process, indicates that preparing care workers and supporting them in the process is of paramount importance. The scope of training should be extended to include elements such as shared vision of care, systems awareness and legal aspects of data-sharing. We found very little evidence on successful training and management programmes to support the process of care co-ordination and data-sharing, but plenty of evidence that failure to provide this is likely to lead to poor outcomes.
Last but not least is the importance of further research into the legal aspects of data-sharing. Lack of clarity in this area was identified as a major problem across settings and levels of communication, from the experience of care professionals to difficulties encountered by multiagency initiatives such as EPaCCS, where ‘… IG rules need to be “bent” or controversially interpreted so that EPaCCS projects are not obstructed or abandoned, while the lawfulness of decisions is ensured within broader legal and governance frameworks’. 76
Implications for policy and practice
Our findings indicate that no single factor or change is enough to facilitate effective data-sharing; a combination of approaches and a systems view of the whole care management and delivery process are needed to enable the effective sharing of information across service and professional boundaries. 23 Initiatives to improve data-sharing should consider this in their design, ensuring that professionals are able to share information in multiple ways. Additionally, while some agreement regarding governance was necessary between health and social care organisations, the evidence in our review showed that organisational support for relationship-building was a greater facilitator of data-sharing than formal organisational or information systems integration. The use of methods of data-sharing that allow relationship-building is therefore important, as is the development of knowledge and understanding, whether of different professional roles or of processes and ways of working.
When designing new initiatives or systems, studies where staff were consulted were more likely to lead to effective data-sharing, a finding echoed in the healthcare system more widely; for example, a report by the Health Foundation found that although the experiences of NHS staff with the increased use of technology during the COVID-19 pandemic were generally positive, they were particularly positive for those who had been personally involved in implementation. 92 Following from this finding, co-production approaches may be a component in the success of new initiatives. 95 Co-production means the design, implementation and long-term management of initiatives or systems collaboratively by all those who will use or be affected by them. 95 We found that processes at interorganisational and interprofessional levels influenced data-sharing, suggesting that co-production would need to occur at both levels. At the organisational level, co-production might involve agreeing on the processes of collecting, storing and sharing data. At the professional level, co-production approaches can determine what works in the specific contexts in which teams or individuals are working,96 which for data-sharing initiatives might regard the provision of adequate resources such as time (e.g. to learn new systems), functional technological solutions and training. Additionally, involvement in intervention development can result in a sense of ownership, with studies of co-production of other workplace interventions, such as to reduce sedentary behaviour, indicating this improved acceptability and uptake. 97,98 We found allowing time for solutions to be developed to problems that may arise during the implementation of data-sharing initiatives was important; a sense of ownership of the intervention might aid professionals in this iterative process. The wider co-production literature suggests that the success of co-production can be challenged by institutional rigidity and differing values between organisations. 96 These were also barriers to data-sharing, particularly at the organisational level, so would need to be considered if co-production approaches were used to develop data-sharing initiatives.
Limitations
We found a relatively large number of qualitative studies that met our inclusion criteria, which meant that we used a purposive sampling approach. While studies were included on the basis of their data richness, it is possible this approach means that we missed insights contained in some ‘thin’ studies; for example, where they focused on settings for which we found fewer data-rich studies, such as care homes. The ‘thin’ studies identified from our search are accessible in a list in Appendix 3. We found several reports from the grey literature which met our inclusion criteria (both rich and thin studies); these came from citation-chasing and, while they were also identified during our searches of the websites of relevant organisations, we did not find any additional grey literature meeting our inclusion criteria. Although the fact we found grey literature already included in the review while searching websites suggests we were using suitable search terms, it is possible that some grey literature was missed due to the limited search functions offered by organisations’ websites.
Studies tended to focus on data-sharing within the context of wider working practices or interventions, for example integrated care programmes. While this context is part of the complex story surrounding data-sharing, it meant that only a small number of studies specifically investigated data-sharing. As the included studies contained few findings explicitly about data-sharing, we had relatively little information to include in the analysis for some factors perceived to influence effective data-sharing, which sometimes made it difficult to draw out detailed findings. A related limitation is that we found few studies focusing on patient and carer experiences of data-sharing that met our inclusion criteria. While studies of the views of professionals, who are the ones sharing data, are likely to contain the most relevant information on this topic, this evidence gap is significant, as the opinions of patients may influence the effectiveness or implementation of data-sharing between health and social care, for example the perception of EPaCCS as a ‘death register’.
No publication year limit was placed on studies included in the review and, surprisingly, we found no relevant studies on data-sharing during or post the COVID-19 pandemic. As noted above, technology and the routine use of technology has advanced rapidly and the COVID-19 pandemic has had a significant impact on working practices, so this lack of evidence is a limitation of the review. Yet despite the increasing priority being placed on the use of electronic systems in health and social care,19 a key finding of the review is that technology is neither a panacea nor a simple substitute for interpersonal data-sharing, and that multiple methods of data-sharing are needed. While the results of earlier studies in the review may be less relevant today, they still contain information that could inform data-sharing practices.
The methodological quality of the included studies was relatively good and similar across clusters. This provides some reassurance that both the findings related to more general factors and those related to cluster-specific factors are based on good-quality evidence. However, the reviewed evidence has important limitations that need to be considered when interpreting the results. Most of the studies failed to provide evidence of reflexivity and many had limitations or uncertainty related to adequacy of samples and methods of data collection. For some of these studies, this might be a reporting issue rather than a failure to adhere to the accepted standards for conducting qualitative research. Others, however, seem to have genuine limitations which cast doubt on the validity of their findings. While we believe that the overall conclusions of the review are valid and reflect observations that are consistent across studies and settings, specific findings might be biased, incomplete and based on interpretations that failed to consider the complexity of data-sharing and the full range of perspectives relevant to this topic. Therefore, the validity of specific findings (e.g. patients’ and carers’ perceptions of palliative care co-ordination systems as ‘death registers’) should be judged in the context of the primary studies that report them and not taken for granted because they are included in the review and ‘make sense’.
We used framework synthesis as our method of analysis. Framework synthesis was suitable given that our topic – data-sharing – is complex, as it allows flexibility, using both a deductive and inductive approach to identifying themes across included studies. 56 However, the construction of the initial framework relies on existing literature and theories which can lead to limitations, as pre-existing frameworks may contain gaps, with categories not filled by included studies, or information in included studies not fitting into categories in the framework. 57 While iterative development ensured all information in included studies fitted into the framework, there may be gaps where we did not find studies, for example data-sharing regarding mental health. Our consultations with stakeholders were intended to understand whether important areas may have been missed, and if so, to document and identify these as areas for further research.
Equality, diversity and inclusion
We used the NIHR-INCLUDE guidelines99 to reflect on equality, diversity and inclusion while designing the protocol for the review and writing the final report. Our population focus was older people, with age being a PROGRESS-Plus characteristic100,101 that has been identified as being associated with discrimination. 91 Few studies explored older people’s experiences of data-sharing in relation to their health and/or social care records (although this might be a side effect of our inclusion criteria, as acknowledged in Limitations), or the impacts of poor or improved data-sharing, so we have identified this as an area for further study. While not all data-sharing uses technology, both members of the public and NHS staff aged over 55 years have been found to be more likely to report negative experiences of using technology in the NHS. 92 Technological competence of staff was discussed in one included study,23 and the need for training was also identified within the theme of Processes and procedures. Further research into digital inclusion of different care professionals may be needed, as it is important that staff and patients are supported to prevent digital exclusion in the workplace.
Another equity issue highlighted by our research is the common imbalance between those care professionals who produce and enter data into electronic record systems, and those who use the systems and their data. There seemed to be few mechanisms for incentivising or compensating those care professionals who might be expected to invest time in providing data for systems, yet who may not be the primary beneficiaries of having a shared or integrated patient/user record system.
Public and patient involvement and engagement
We consulted PPIE representatives while searching for studies and developing the framework for analysis. They shared their views of data-sharing between health and social care and their experiences, for example, of arrangements being made for social care provision after a stay in hospital. While these discussions made some contribution to our understanding of the topic and key issues regarding data-sharing which informed the framework, they highlighted the challenges of discussing a topic which focuses primarily on professional working practices with service users. PPIE representatives generally thought that data should be shared between health and social care and provided examples of how it had impacted them when this had been done well or had not happened. However, they were unaware of the methods that professionals had used to share data. This raised questions in the research team around the value of eliciting service user views on the topic, as PPIE representatives were more concerned with whether the relevant data had been shared than the method used to do this. We acknowledge that we were unable to involve PPIE representatives in all stages of the review, due to a lack of time and resource; additional meetings might have enabled richer discussions.
Later consultation focused on the plain language summary of the review and ensuring that this conveyed the findings of the review in an accessible way.
Chapter 6 Conclusions
This review identified five clusters of studies focused on different purposes of data-sharing across the health and social care boundary, and in relation to the care of older people: joint assessments; integrated case management; transitions from hospital to home; care homes and palliative care. Factors perceived to influence effective data-sharing were identified running across the clusters, within three main themes, relating to different methods of data-sharing, and across different parts of the data-sharing process. There were also specific factors identified within each theme.
Within Relationships, interprofessional relationships were found to be the most significant factor influencing data-sharing, with methods of data-sharing such as multidisciplinary team meetings and other opportunities for direct communication being particularly important in supporting them. These forums allowed professionals to build trust and respect but also afforded knowledge and understanding of other professionals’ roles and information needs. Professional status was often a barrier to data-sharing, having a negative influence on data-sharing, for example, decisions being made on who is given access to data based on their profession.
Processes and procedures supported data-sharing and were essential in the implementation of new data-sharing initiatives. While policies and formal agreements were required, these needed to be operationalised to facilitate data-sharing. Providing the necessary resources and embedding new ways of working by taking into account existing working practices was an important aspect of operationalisation.
While data-sharing often relied on Technology and infrastructure, technology facilitated data-sharing most effectively when it was considered in the context of broader interprofessional communication, that is, as a tool, to be used to support, or in conjunction with, other methods of data-sharing. Studies indicated a need to consider interactions, whether of professionals with technologies or of technology with the care processes and decisions for which professionals needed it, for example, the language used to record data in electronic record systems. Professionals’ awareness of the care delivery system as a whole was also an important influencing factor.
We further arranged and linked these factors together in a conceptual model that could be used for analysing and designing interventions that aim to improve data-sharing between health and social care providers.
These findings have implications for designing and implementing initiatives to improve data-sharing between health and social care. They suggest a need for further research given the rapid implementation of technologies that allow data-sharing both during the COVID-19 pandemic and in response to the NHS Long Term Plan and policy initiatives in the other UK nations to utilise digital solutions more effectively. In terms of data-sharing initiatives, they highlight the need for initiatives which support multiple, complementary methods of data-sharing and allow different professionals to build relationships. Additionally, they indicate the importance of co-production to understand how data-sharing and shared data systems can be made more effective, whether within, or by changing, current ways of working.
Additional information
Acknowledgements
The Exeter HS&DR Evidence Synthesis Centre team would like to acknowledge and thank Health and Care Research Wales and Social Care Wales for their support in developing this review and the members of the PSAG and PPIE group for their valuable feedback. We would also like to thank Sue Whiffin and Jenny Lowe for administrative support throughout this review.
This report presents independent research funded by the National Institute for Health Research (NIHR). This review (award NIHR135660) was commissioned by the Health Services and Delivery Research (HSDR) programme as part of a series of evidence syntheses under the award NIHR130538 and supported by the NIHR Applied Research Collaboration South West Peninsula. For more information, visit https://fundingawards.nihr.ac.uk/award/NIHR135660 and https://fundingawards.nihr.ac.uk/award/NIHR130538.
CRediT contribution statement
Siân de Bell (https://orcid.org/0000-0001-7356-3849): Conceptualisation (equal), Formal analysis (equal), Writing – original draft (lead), Writing – editing and reviewing (equal). Zhivko Zhelev (https://orcid.org/0000-0002-0106-2401): Conceptualisation (equal), Formal analysis (equal), Visualisation (lead), Writing – original draft (supporting), Writing – editing and reviewing (equal). Alison Bethel (https://orcid.org/0000-0002-0963-9201): Conceptualisation (equal), Writing – editing and reviewing (equal). Jo Thompson Coon (https://orcid.org/0000-0002-5161-0234): Conceptualisation (equal), Funding acquisition (equal), Project administration (equal), Writing – editing and reviewing (equal). Rob Anderson (https://orcid.org/0000-0002-3523-8559): Conceptualisation (equal), Funding acquisition (equal), Project administration (equal), Writing – editing and reviewing (equal).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/TTWG4738.
Primary conflicts of interest: Siân de Bell declares none. Zhivko Zhelev declares none. Jo Thompson Coon is a member of the NIHR HTA General Board (2019–23) and was a member of NIHR PRU Commissioning Panel 2022. Jo Thompson Coon and Alison Bethel are also supported by the National Institute for Health Applied Research Collaboration South West Peninsula. Rob Anderson declares none.
Data-sharing statement
This is an evidence synthesis study based on published primary research; it did not generate new data. All data extracted from the primary studies, along with links to each publication, can be found in the Appendices to the report. Further information can be obtained from the corresponding author.
Ethics statement
This was an evidence review, based on published primary studies, so ethical approval was not required.
Information governance statement
This study did not involve primary research or, therefore, the handling of any personal information.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- World Health Organization . Ageing and Health 2021. www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed July 2023).
- Centre for Ageing Better . Summary Report: The State of Ageing 2022 2022.
- GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. https://doi.org/10.1016/S0140-6736(20)30925-9.
- NHS England . The NHS Long Term Plan 2019.
- Milsom S, Breeze C. Delivering Transformation Grant Programme 2019–20. Rebalancing Social Care: A Report on Adult Services. Abercynon: Association of Directors of Social Services Cymru; 2020.
- Mitchell C, Tazzyman A, Howard SJ, Hodgson D. More that unites us than divides us? A qualitative study of integration of community health and social care services. BMC Fam Pract 2020;21. https://doi.org/10.1186/s12875-020-01168-z.
- Thomas P, Meads G, Moustafa A, Nazareth I, Stange KC, Donnelly Hess G. Combined horizontal and vertical integration of care: a goal of practice-based commissioning. Qual Prim Care 2008;16:425-32.
- Lewis RQ, Checkland K, Durand MA, Ling T, Mays N, Roland M, et al. Integrated Care in England – what can we learn from a decade of national pilot programmes?. Int J Integr Care 2021;21. https://doi.org/10.5334/ijic.5631.
- MacInnes J, Baldwin J, Billings J. The Over 75 Service: continuity of integrated care for older people in a United Kingdom primary care setting. Int J Integr Care 2020;20. https://doi.org/10.5334/ijic.5457.
- MacAdam M. Frameworks of Integrated Care for the Elderly: A Systematic Review. Ontario: Canadian Policy Research Networks; 2008.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English Integrated Care Pilots. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.982.
- Kharicha K, Iliffe S, Levin E, Davey B, Fleming C. Tearing down the Berlin wall: social workers’ perspectives on joint working with general practice. Fam Pract 2005;22:399-405. https://doi.org/10.1093/fampra/cmi010.
- Chase M, Lloyd CEM, Peters BJ, Chase E, Lee K. Joining the dots: day to day challenges for practitioners in delivering integrated dementia care. Health Soc Care Community 2021;29:1061-71. https://doi.org/10.1111/hsc.13140.
- Wilberforce M, Hughes J, Clarkson P, Whyte D, Chester H, Davies S, et al. An electronic referral system supporting integrated hospital discharge. J Integr Care 2017;25:99-109. https://doi.org/10.1108/JICA-09-2016-0034.
- Jobe I. Reflections of the collaborative care planning as a person-centred practice. Nurs Philos 2022;23. https://doi.org/10.1111/nup.12389.
- Payne S, Kerr C, Hawker S, Hardey M, Powell J. The communication of information about older people between health and social care practitioners. Age Ageing 2002;31:107-17. https://doi.org/10.1093/ageing/31.2.107.
- Miller R, Glasby J, Dickinson H. Integrated health and social care in England: ten years on. Int J Integr Care 2021;21. https://doi.org/10.5334/ijic.5666.
- Care Quality Commission . Building Bridges, Breaking Barriers: How Care Is Integrated Across Health and Social Care and the Impact on Older People Who Use the Service and Their Families and Carers 2016.
- Patterson R, Standing H, Lee M, Dalkin S, Lhussier M, Exley C, et al. Paramedic information needs in end-of-life care: a qualitative interview study exploring access to a shared electronic record as a potential solution. BMC Palliat Care 2019;18. https://doi.org/10.1186/s12904-019-0498-2.
- Chester H, Hughes J, Bowns I, Abendstern M, Davies S, Challis D. Electronic information sharing between nursing and adult social care practitioners in separate locations: a mixed-methods case study. J Long Term Care 2021:1-11. https://doi.org/10.31389/jltc.16.
- Standing H, Patterson R, Lee M, Dalkin SM, Lhussier M, Bate A, et al. Information sharing challenges in end-of-life care: a qualitative study of patient, family and professional perspectives on the potential of an electronic palliative care co-ordination system. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-037483.
- Schramm W. The Process and Effects of Mass Communication. Champaign, IL: University of Illinois Press; 1954.
- Waring J, Bishop S, Marshall F, Tyler N, Vickers R. An ethnographic study comparing approaches to inter-professional knowledge sharing and learning in discharge planning and care transitions. J Health Organ Manag 2019;33:677-94. https://doi.org/10.1108/JHOM-10-2018-0302.
- Trenholm S. Thinking Through Communication: An Introduction to the Study of Human Communication. New York: Routledge; 2020.
- Cabrera D, Cabrera L. Learning, Design, and Technology: An International Compendium of Theory, Research, Practice, and Policy. Cham: Springer International Publishing; 2019.
- Maguire D, Evans H, Honeyman M, Omojomolo D. Digital Change in Health and Social Care. London: The King’s Fund; 2018.
- Davis MC, Challenger R, Jayewardene DN, Clegg CW. Advancing socio-technical systems thinking: a call for bravery. Appl Ergon 2014;45:171-80. https://doi.org/10.1016/j.apergo.2013.02.009.
- Abbas R, Michael K. TheoryHub Book. 2023.
- Greenlagh T. How to Implement Evidence-based Healthcare. Hoboken, NJ: Wiley Blackwell; 2017.
- Marjanovic S, Altenhofer M, Hocking L, Chataway J, Ling T. Innovating for improved healthcare: sociotechnical and innovation systems perspectives and lessons from the NHS. Sci Public Policy 2020;47:283-97. https://doi.org/10.1093/scipol/scaa005.
- Eason K. Local sociotechnical system development in the NHS National Programme for Information Technology. J Inf Technol 2007;22:257-64. https://doi.org/10.1057/palgrave.jit.2000101.
- Health and Care Research Wales, Social Care Wales, James Lind Alliance . How Can We Best Provide Sustainable Care and Support to Help Older People Live Happier and More Fulfilling Lives? 2021. www.jla.nihr.ac.uk/priority-setting-partnerships/setting-priorities-for-social-care-research-in-wales/downloads/Setting-priorities-for%20social-care-research-in-Wales-project-background-English%20.pdf (accessed 27 March 2024).
- NHS England . Improving Care for Older People n.d. www.england.nhs.uk/ourwork/clinical-policy/older-people/improving-care-for-older-people/ (accessed July 2023).
- Public Health England . Guidance 7. Living Well in Older Years 2019. www.gov.uk/government/publications/better-mental-health-jsna-toolkit/7-living-well-in-older-years#references (accessed July 2023).
- Melzer D, Delgado JC, Winder R, Masoli J, Richards S, Ble A. The Age UK Almanac of Disease Profiles in Later Life: A Reference on the Frequency of Major Diseases, Conditions and Syndromes Affecting Older People in England 2015. https://editorial.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/health-wellbeing/age_uk_almanac_final_9oct15.pdf (accessed 27 March 2024).
- McMaster University . Health Information Research Unit 2022. Hedges Project 2022. https://hiruweb.mcmaster.ca/hkr/hedges/embase/ (accessed July 2023).
- Canadian Health Libraries Association . Qualitative Research 2018. https://extranet.santecom.qc.ca/wiki/!biblio3s/doku.php?id=concepts:recherche-qualitative (accessed 21 November 2023).
- Fulbright H, Stansfield C. Applying Geographic Limits Within the Web of Science Platform, Using the UK as an Example n.d.
- Ayiku L, Levay P, Hudson T, Finnegan A. The NICE UK geographic search filters for MEDLINE and EMBASE (Ovid): post-development study to further evaluate precision and number-needed-to-read when retrieving UK evidence. Res Synth Methods 2020;11:669-77. https://doi.org/10.1002/jrsm.1431.
- Harzing AW. Publish or Perish 2007. https://harzing.com/resources/publish-or-perish (accessed July 2023).
- Bethel AC, Rogers M, Abbott R. Use of a search summary table to improve systematic review search methods, results, and efficiency. J Med Libr Assoc 2021;109:97-106. https://doi.org/10.5195/jmla.2021.809.
- Halladay CW, Trikalinos TA, Schmid IT, Schmid CH, Dahabreh IJ. Using data sources beyond PubMed has a modest impact on the results of systematic reviews of therapeutic interventions. J Clin Epidemiol 2015;68:1076-84. https://doi.org/10.1016/j.jclinepi.2014.12.017.
- Subirana M, Solá I, Garcia JM, Gich I, Urrútia G. A nursing qualitative systematic review required MEDLINE and CINAHL for study identification. J Clin Epidemiol 2005;58:20-5. https://doi.org/10.1016/j.jclinepi.2004.06.001.
- Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0249-x.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- Cochrane Effective Practice and Organisation of Care . EPOC Qualitative Evidence Syntheses Guidance on When to Sample and How to Develop a Purposive Sampling Frame 2019. https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/qes_guidance_on_sampling.pdf (accessed July 2023).
- Ames HM, Glenton C, Lewin S, Tamrat T, Akama E, Leon N. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis. Cochrane Database Syst Rev 2019;10. https://doi.org/10.1002/14651858.CD013447.
- Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, et al. Cochrane Qualitative and Implementation Methods Group guidance series – paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol 2018;97:49-58. https://doi.org/10.1016/j.jclinepi.2017.06.020.
- National Institute of Health and Care Excellence . NICE Process and Methods Guides. Methods for the Development of NICE Public Health Guidance 2012.
- Carroll C, Booth A, Lloyd-Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012;22:1425-34. https://doi.org/10.1177/1049732312452937.
- Carroll C, Booth A, Leaviss J, Rick J. ‘Best fit’ framework synthesis: refining the method. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-37.
- Wallace A, Baldwin S, Croucher K, Quilgars D. Meeting the challenge: developing systematic reviewing in social policy. Policy Polit 2004;32:455-70. https://doi.org/10.1332/0305573042009444.
- Gwernan-Jones R, Lourida I, Abbott RA, Rogers M, Green C, Ball S, et al. Understanding and improving experiences of care in hospital for people living with dementia, their carers and staff: three systematic reviews. Health Serv Deliv Res 2020;8. https://doi.org/10.3310/hsdr08430.
- Noyes J, Booth A, Cargo M, Flemming K, Harden A, Harris J, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane; 2022.
- Ritchie J, Spencer L. The Qualitative Researcher’s Companion. Thousand Oaks, CA: Sage Publications; 2002.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009;9. https://doi.org/10.1186/1471-2288-9-59.
- Brunton G, Oliver S, Thomas J. Innovations in framework synthesis as a systematic review method. Res Synth Methods 2020;11:316-30. https://doi.org/10.1002/jrsm.1399.
- Pope C, Ziebland S, Mays N. Qualitative Research in Health Care. Malden, MA: Blackwell Publishing; 2006.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-39.
- Clegg C, Shepherd C. The biggest computer programme in the world… ever!’: Time for a change in mindset?. J Inf Technol 2007;22:212-21. https://doi.org/10.1057/palgrave.jit.2000103.
- EUnetHTA Joint Action 2: Work Package 8 . HTA Core Model ® Version 3.0 2016. www.htacoremodel.info/BrowseModel.aspx (accessed August 2023).
- Carroll C, Booth A, Cooper K. A worked example of ‘best fit’ framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-29.
- Bailey D, Mutale GJ. Social work’s contribution to integrated primary health care teams in the UK for older adults with complex needs. J Integr Care 2022;30:263-75. https://doi.org/10.1108/JICA-10-2021-0053.
- Bower P, Reeves D, Sutton M, Lovell K, Hann M, Howells K, et al. Improving care for older people with long-term conditions and social care needs in Salford: the CLASSIC mixed-methods study, including RCT. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06310.
- Dickinson A. Implementing the single assessment process: opportunities and challenges. J Interprof Care 2006;20:365-79. https://doi.org/10.1080/13561820600807270.
- Holloway M. Traversing the network: a user-led care pathway approach to the management of Parkinson’s disease in the community. Health Soc Care Community 2006;14:63-7. https://doi.org/10.1111/j.1365-2524.2005.00600.x.
- Lewis G, Vaithianathan R, Wright L, Brice MR, Lovell P, Rankin S, et al. Integrating care for high-risk patients in England using the virtual ward model: lessons in the process of care integration from three case sites. Int J Integr Care 2013;13. https://doi.org/10.5334/ijic.1150.
- Piercy H, Fowler-Davis S, Dunham M, Cooper C. Evaluation of an integrated service delivering post diagnostic care and support for people living with dementia and their families. Health Soc Care Community 2018;26:819-28. https://doi.org/10.1111/hsc.12592.
- Rwathore SA. An Intervention to Detect and Manage Health Problems in Community-Dwelling Older People: Assessing the Evidence Base Prior to Implementation 2007.
- Wright F, Young E. Focusing on client-held joint health and social care records. J Interprof Care 1995;8:321-8.
- Redwood S, Brant H, Maluf A, Combes G, Neubauer K, Thomas C, et al. How latent patterns of interprofessional working may lead to delays in discharge from hospital of older people living with frailty – ‘Patient more confused than usual?’. Ageing Soc 2023;43:576-97. https://doi.org/10.1017/S0144686X21000805.
- Shaw JA, Kontos P, Martin W, Victor C. The institutional logic of integrated care: an ethnography of patient transitions. J Health Organ Manag 2017;31:82-95. https://doi.org/10.1108/JHOM-06-2016-0123.
- Sutton E, Dixon-Woods M, Tarrant C. Ethnographic process evaluation of a quality improvement project to improve transitions of care for older people. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010988.
- Badger F, Plumridge G, Hewison A, Shaw KL, Thomas K, Clifford C. An evaluation of the impact of the gold standards framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation. Int J Nurs Stud 2012;49:586-95. https://doi.org/10.1016/j.ijnurstu.2011.10.021.
- Mahmood-Yousuf K, Munday D, King N, Dale J. Interprofessional relationships and communication in primary palliative care: impact of the gold standards framework. Br J Gen Pract 2008;58:256-63. https://doi.org/10.3399/bjgp08X279760.
- Petrova M, Riley J, Abel J, Barclay S. Crash course in EPaCCS (electronic palliative care coordination systems): 8 years of successes and failures in patient data sharing to learn from. BMJ Support Palliat Care 2018;8:447-55. https://doi.org/10.1136/bmjspcare-2015-001059.
- Ellis-Smith C, Higginson IJ, Daveson BA, Henson LA, Evans CJ. BuildCARE . How can a measure improve assessment and management of symptoms and concerns for people with dementia in care homes? A mixed-methods feasibility and process evaluation of IPOS-Dem. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0200240.
- Shenkin SD, Johnston L, Hockley J, Henderson DAG. Developing a care home data platform in Scotland: a mixed methods study of data routinely collected in care homes. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afac265.
- Standing H, Patterson R, Dalkin S, Exley C, Brittain K. A critical exploration of professional jurisdictions and role boundaries in inter-professional end-of-life care in the community. Soc Sci Med 2020;266. https://doi.org/10.1016/j.socscimed.2020.113300.
- Waring J, Marshall F, Bishop S, Sahota O, Walker M, Currie G, et al. An ethnographic study of knowledge sharing across the boundaries between care processes, services and organisations: the contributions to ‘safe’ hospital discharge. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02290.
- Waring J, Marshall F, Bishop S. Understanding the occupational and organizational boundaries to safe hospital discharge. J Health Serv Res Policy 2015;20:35-44. https://doi.org/10.1177/1355819614552512.
- Waring J, Bishop S, Marshall F. A qualitative study of professional and carer perceptions of the threats to safe hospital discharge for stroke and hip fracture patients in the English National Health Service. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1568-2.
- Waring J, Bishop S. Health States of Exception: unsafe non-care and the (inadvertent) production of ‘bare life’ in complex care transitions. Sociol Health Illn 2020;42:171-90. https://doi.org/10.1111/1467-9566.12993.
- Bishop S, Waring J. From boundary object to boundary subject; the role of the patient in coordination across complex systems of care during hospital discharge. Soc Sci Med 2019;235. https://doi.org/10.1016/j.socscimed.2019.112370.
- Bower F. Caring for Patients with Dementia in Acute Physical Health Settings. Leicester: University of Leicester; 2017.
- Ho L, Limpaecher A. Delve . The Importance of Reflexivity in Qualitative Research 2022. https://delvetool.com/blog/reflexivity (accessed 20 November 2023).
- Professional Record Standards Body for Health and Social Care . Care Home Information Flow Consultation Report 2017.
- Department of Health . Care Act 2014 2014.
- White S, Wastell D, Broadhurst K, Hall C. When policy o’erleaps itself: The ‘tragic tale’ of the Integrated Children’s System. Crit Soc Policy 2010;30:405-29. https://doi.org/10.1177/0261018310367675.
- Rosen R, Mountford J, Lewis G, Lewis R, Shand J, Shaw S. Integration in Action: Four International Case Studies. London: The Nuffield Trust; 2011.
- Alaszewski A, Billings JR, Coxon K. Integrated Health and Social Care for Older Persons: Theoretical and Conceptual Issues. University of Kent: Centre for Health Services Studies; 2003.
- Horton T, Hardie T, Mahadeva S, Warburton W. Securing a Positive Health Care Technology Legacy from COVID-19. London: The Health Foundation; 2021.
- Anderson H, Scantlebury A, Galdas P, Adamson J. Remote and technology-mediated working during the COVID-19 pandemic: a qualitative exploration of the experiences of nurses working in general practice (the GenCo Study). J Adv Nurs 2023. https://doi.org/10.1111/jan.15921.
- Welsh Government . Digital and Data Strategy for Health and Social Care in Wales 2023. www.gov.wales/digital-and-data-strategy-health-and-social-care-wales-html (accessed 8 October 2023).
- NHS England . Improving Experience of Care: A Shared Commitment for Those Working in Health and Care Systems 2022. www.england.nhs.uk/long-read/improving-experience-of-care-a-shared-commitment-for-those-working-in-health-and-care-systems/ (accessed July 2023).
- Beckett K, Farr M, Kothari A, Wye L, le May A. Embracing complexity and uncertainty to create impact: exploring the processes and transformative potential of co-produced research through development of a social impact model. Health Res Policy Syst 2018;16. https://doi.org/10.1186/s12961-018-0375-0.
- Cameron J, Pidd K, Roche A, Lee N, Jenner L. A co-produced cultural approach to workplace alcohol interventions: barriers and facilitators. Drugs: Educ Prev Policy 2019;26:401-11. https://doi.org/10.1080/09687637.2018.1468871.
- Mackenzie K, Such E, Norman P, Goyder E. Using co-production to develop ‘Sit Less at Work’ interventions in a range of organisations. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18157751.
- National Institute for Health and Care Research . Improving Inclusion of Under-Served Groups in Clinical Research: Guidance from the NIHR-INCLUDE Project 2020.
- O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014;67:56-64. https://doi.org/10.1016/j.jclinepi.2013.08.005.
- Cochrane Methods Equity . PROGRESS-Plus n.d. https://methods.cochrane.org/equity/projects/evidence-equity/progress-plus (accessed July 2023).
Appendix 1 Inclusion and exclusion criteria
| Include | Exclude | |
|---|---|---|
| Population | Older people, as defined by individual studies. Studies will be included if data-sharing relates to care or services for the above population. If the study focuses on a mixed population, will include it if the results for older people are reported separately. We will also include studies of populations where it is reasonable to assume that the focus is on older people (e.g. people with dementia, multimorbidities, people in residential care homes). |
Studies focusing on other age groups or not reporting the results for older people separately. |
| Study participants | Health and social care professionals, volunteers, older people, and their families and carers. | Focusing on professionals within a single type of organisation, for example within primary and secondary healthcare.
|
| Interventions | Data-sharing, defined as:
|
Studies not focusing on data-sharing, or investigating data-sharing within:
|
Evaluation of types of healthcare/strategies that are likely to be relevant:
|
Informal data-sharing for example conversational sharing of knowledge about patients or their care. Sharing of aggregated and anonymised data. Interprofessional education. |
|
| Study focus | Description or analysis of factors perceived as influencing effective data-sharing relating to the care of older people OR Description or analysis of factors perceived as influencing the successful adoption or implementation of initiatives to improve data-sharing. |
All other outcomes. |
| Study design | Qualitative studies or mixed-methods studies with a qualitative component designed to identify, explore and/or understand factors influencing effective data-sharing or the implementation of data-sharing improvement initiatives. | Other study designs. Qualitative surveys were excluded. Relevant systematic reviews will be excluded from the review but will be used to identify additional titles and will be listed in an appendix. |
| Context | Studies focusing on data-sharing between UK care organisations and care professionals will be considered first. If necessary (e.g. only a small number of relevant studies identified), this criterion will be expanded to include studies conducted in other countries with similar health and social care systems. This is to ensure that the results from the review are relevant to Health and Care Research Wales who commissioned this work. Studies of multiple countries were included if results from the UK were reported separately. |
Non-UK studies unless only a small number of UK studies have been identified. The decision on whether non-UK studies need to be included to complement the UK-based evidence will be made through discussion with stakeholders. If there are specific gaps in the UK evidence, we will conduct focused searches for relevant non-UK studies. |
| Publication type | Only studies reported in English or Welsh will be included. If the number of hits exceeds our capacity, we will restrict the inclusion to studies published in the most relevant time period, defined after discussion with our stakeholder groups. Both journal articles and grey literature (e.g. evaluation reports) will be included, but we will exclude conference abstracts or similarly short publications which do not provide sufficient information on the methods and results of the study. |
Studies not reported in English or Welsh. |
Appendix 2 Search strategy and databases
CINAHL Ultimate
(((TI semi-structured OR AB semi-structured OR SU semi-structured) OR (TI semistructured OR AB semistructured OR SU semistructured) OR (TI unstructured OR AB unstructured OR SU unstructured) OR (TI informal OR AB informal OR SU informal) OR (TI in-depth OR AB in-depth OR SU in-depth) OR (TI indepth OR AB indepth OR SU indepth) OR (TI face-to-face OR AB face-to-face OR SU face-to-face) OR (TI structured OR AB structured OR SU structured) OR (TI guide OR AB guide OR SU guide)) N3 ((TI discussion* OR AB discussion* OR SU discussion*) OR (TI questionnaire* OR AB questionnaire* OR SU questionnaire*)))
OR
((TI “focus group*” OR AB “focus group*” OR SU “focus group*”) OR (TI qualitative OR AB qualitative OR SU qualitative) OR (TI ethnograph* OR AB ethnograph* OR SU ethnograph*) OR (TI fieldwork OR AB fieldwork OR SU fieldwork) OR (TI “field work” OR AB “field work” OR SU “field work”) OR (TI “key informant*” OR AB “key informant*” OR SU “key informant*”) OR (TI interview* OR AB interview* OR SU interview*))
OR
(MH “Qualitative Studies+”)
AND
(((TI share* OR AB share*) OR (TI sharing OR AB sharing) OR (TI integrat* OR AB integrat*)) N2 ((TI data OR AB data) OR (TI organisat* OR AB organisat*) OR (TI organizat* OR AB organizat*)))
OR
((TI integrat* OR AB integrat*) N1 ((TI care* OR AB care*) OR (TI health* OR AB health*)))
OR
(((TI interprofession* OR AB interprofession*) OR (TI ‘inter profession*’ OR AB ‘inter profession*’) OR (TI organisat* OR AB organisat*) OR (TI organizat* OR AB organizat*) OR (TI interagency* OR AB interagency*) OR (TI agenc* OR AB agenc*)) N1 ((TI communicat* OR AB communicat*) OR (TI share* OR AB share*) OR (TI sharing OR AB sharing) OR (TI integrat* OR AB integrat*)))
OR
(((TI data OR AB data) OR (TI digital* OR AB digital*)) N1 ((TI link* OR AB link*) OR (TI system* OR AB system*) OR (TI access OR AB access) OR (TI information* OR AB information*) OR (TI exchange* OR AB exchange*)))
AND
AF “united kingdom” OR SU “united kingdom” OR TI “united kingdom” OR AB “united kingdom” OR TI britain OR AB britain OR SU britain OR AF britain OR TI england OR AB england OR SU england OR AF England
OR
AF wales OR SU wales OR TI wales OR AB wales OR TI scotland OR AB scotland OR SU scotland OR AF scotland OR TI “northern ireland” OR AB “northern ireland” OR SU “northern ireland” OR AF “northern ireland”
OR
(MH “United Kingdom+”) OR (MH “Great Britain+”)
EMBASE search strategy
Database: EMBASE <1974 to 2023 March 21>
Search strategy:
------------ ------------- ------------- ------------ ---------- ---------------
-
exp qualitative research/ (113,853)
-
((“semi-structured” or semistructured or unstructured or informal or “in-depth” or indepth or “face-to-face” or structured or guide) adj3 (discussion* or questionnaire*)).tw. (49,954)
-
(focus group* or qualitative or ethnograph* or fieldwork or field work or key informant* or interview* or experience*).tw. (2,512,755)
-
1 or 2 or 3 (2,546,302)
-
((share* or sharing or integrat*) adj2 (data or organisat* or organizat*)).tw. (34,626)
-
(integrat* adj2 (care* or health*)).tw. (38,525)
-
((interprofession* or inter profession* or organisat* or organizat* or interagency* or agenc*) adj2 (communicat* or share* or sharing or integrat*)).tw. (5901)
-
((data or digital*) adj2 (link* or system* or access or information* or exchange*)).tw. (123,953)
-
(electronic* adj2 record*).tw. (112,902)
-
(patient* adj2 record*).tw. (118,943)
-
(share* or sharing or integrat* or access*).tw. (2,118,154)
-
9 or 10 (217,083)
-
((share* or sharing or integrat* or access*) adj2 ((electronic* adj2 record*) or (patient* adj2 record*))).tw. (3086)
-
5 or 6 or 7 or 8 or 13 (197,865)
-
interdisciplinary communication/ (13,450)
-
14 or 15 (210,857)
-
4 and 16 (35,185)
-
exp United Kingdom/ (459,762)
-
(national health service* or nhs*).ti,ab,in,ad. (465,861)
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. (58,823)
-
(gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jx,in,ad. (3,712,789)
-
(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*”or ny or ontario* or ont or toronto*))))).ti,ab,in,ad. (2,893,846)
-
(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in,ad. (119,041)
-
(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in,ad. (398,020)
-
(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in,ad. (55,330)
-
or/18-25 (4,533,426)
-
(exp “arctic and antarctic”/or exp oceanic regions/ or exp western hemisphere/or exp africa/ or exp asia/) not (exp united kingdom/ or europe/) (3,484,679)
-
26 not 27 (4,278,686)
-
17 and 28 (5868)
-
(share* or sharing or integrat* or data or organisat* or organizat* or care* or health* or interprofession* or inter profession* or interagency* or agenc* or communicat* or data or digital* or link* or system* or access or information* or exchange*).ti. (3,815,833)
-
29 and 30 (2725)
MEDLINE search strategy
Database: Ovid MEDLINE(R) ALL <1946 to March 22, 2023>
Search strategy:
UK terms
-
exp United Kingdom/ (388,603)
-
(“national health service” or nhs).ti,ab,in. (260,214)
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. (48,240)
-
(gb or “g.b.” or britain or (british not “british columbia”) or uk or “u.k.” or united kingdom* or (england not “new england”) or northern ireland* or nothern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jw,in. (2,405,575)
-
(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in. (1,708,882)
-
(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in. (68,641)
-
(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in. (251,789)
-
(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in. (32,940)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 (3,018,117)
-
(exp africa/ or exp americas/ or exp antarctic regions/ or exp arctic regions/ or exp asia/ or exp oceania/) not (exp great britain/ or europe/) (3,295,923)
-
9 not 10 (2,858,092)
-
((“semi-structured” or semistructured or unstructured or informal or “in-depth” or indepth or “face-to-face” or structured or guide) adj3 (discussion* or questionnaire*)).tw,kf. (36,908)
-
(focus group* or qualitative or ethnograph* or fieldwork or field work or key informant* or interview*).tw,kw. (667,263)
-
Interviews as Topic/(66,807)
-
Focus Groups/(35,344)
-
Narration/(9993)
-
exp Qualitative Research/ (80,131)
-
12 or 13 or 14 or 15 or 16 or 17 (718,664)
-
((share* or sharing or integrat*) adj2 (data or organisat* or organizat*)).tw. (26,495)
-
(integrat* adj2 (care* or health*)).tw. (27,399)
-
((interprofession* or inter profession* or organisat* or organizat* or interagency* or agenc*) adj2 (communicat* or share* or sharing or integrat*)).tw. (4668)
-
((data or digital*) adj2 (link* or system* or access or information* or exchange*)).tw. (86,093)
-
interdisciplinary communication/ (18,127)
-
*“Delivery of Health Care, Integrated”/(10,678)
-
*interprofessional relations/ (22,423)
-
*interdisciplinary communication/ (6687)
-
(electronic* adj2 record*).tw. (57,094)
-
(patient* adj2 record*).tw. (64,397)
-
(share* or sharing or integrat* or access*).tw. (1,659,487)
-
(((electronic* adj2 record*) or (patient* adj2 record*)) adj2 (share* or sharing or integrat* or access*)).tw. (1995)
-
(information adj2 (share or sharing)).tw. (8576)
-
19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 30 or 31 (192,839)
-
11 and 18 and 32 (3768)
HMIC search strategy
Database: HMIC Health Management Information Consortium <1979 to January 2023>
Search strategy:
--------- ---------- ----------- ----------- ------------ ----------- -----------
-
(focus group* or qualitative or ethnograph* or fieldwork or field work or key informant* or interview*).tw. (25,366)
-
((“semi-structured” or semistructured or unstructured or informal or “in-depth” or indepth or “face-to-face” or structured or guide) adj3 (discussion* or questionnaire*)).tw. (875)
-
exp qualitative research/or mixed-methods research/ or qualitative analysis/ or qualitative techniques/(1710)
-
1 or 2 or 3 (25,870)
-
((share* or sharing or integrat*) adj3 (data or organisat* or organizat*)).tw. (745)
-
(integrat* adj2 (care* or health*)).tw. (3081)
-
((interprofession* or inter profession* or organisat* or organizat* or interagency* or agenc*) adj2 (communicat* or share* or sharing or integrat*)).tw. (532)
-
((data or digital*) adj2 (link* or system* or access or information* or exchange*)).tw. (1709)
-
exp Access to information/(2159)
-
exp Information transfer/(2053)
-
(electronic* adj2 record*).tw. (1372)
-
(patient* adj2 record*).tw. (1564)
-
(share* or sharing or integrat* or access*).tw. (35,836)
-
11 or 12 (2411)
-
((share* or sharing or integrat* or access*) adj2 ((electronic* adj2 record*) or (patient* adj2 record*))).tw. (159)
-
5 or 6 or 7 or 8 or 9 or 10 or 15 (9552)
-
4 and 16 (1001)
-
(share* or sharing or integrat* or data or organisat* or organizat* or care* or health* or interprofession* or inter profession* or interagency* or agenc* or communicat* or data or digital* or link* or system* or access or information* or exchange*).ti. (146,652)
-
17 and 18 (556)
SPP search strategy
Database: SPP <202210>
Search strategy:
--------- ----------- ----------- ---------- ---------- ----------- --------
-
(focus group* or qualitative or ethnograph* or fieldwork or field work or key informant* or interview*).tw. (43,060)
-
((“semi-structured” or semistructured or unstructured or informal or “in-depth” or indepth or “face-to-face” or structured or guide) adj3 (discussion* or questionnaire*)).tw. (607)
-
((share* or sharing or integrat*) adj3 (data or organisat* or organizat*)).tw. (936)
-
(integrat* adj2 (care* or health*)).tw. (3534)
-
((interprofession* or inter profession* or organisat* or organizat* or interagency* or agenc*) adj2 (communicat* or share* or sharing or integrat*)).tw. (811)
-
((data or digital*) adj2 (link* or system* or access or information* or exchange*)).tw. (1410)
-
(electronic* adj2 record*).tw. (206)
-
(patient* adj2 record*).tw. (178)
-
(share* or sharing or integrat* or access*).tw. (60,232)
-
7 or 8 (340)
-
((share* or sharing or integrat* or access*) adj2 ((electronic* adj2 record*) or (patient* adj2 record*))).tw. (27)
-
1 or 2 (43,306)
-
4 or 5 or 6 or 11 (5629)
-
12 and 13 (564)
PQDT search strategy
(((((TI,AB(semi-structured) OR TI,AB(semistructured) OR TI,AB(unstructured) OR TI,AB(informal) OR TI,AB(in-depth) OR TI,AB(indepth) OR TI,AB(face-to-face) OR TI,AB(structured) OR TI,AB(guide)) NEAR/3 (TI,AB(discussion*) OR TI,AB(questionnaire*))) OR (TI,AB((“focus group” OR “focus groups”)) OR TI,AB(qualitative) OR TI,AB(ethnograph*) OR TI,AB(fieldwork) OR TI,AB(“field work”) OR TI,AB((“key informant” OR “key informants”)) OR TI,AB(interview*))) AND (((TI,AB(share*) OR TI,AB(sharing) OR TI,AB(integrat*)) NEAR/2 (TI,AB(data) OR TI,AB(organisat*) OR TI,AB(organizat*))) OR ((TI,AB(interprofession*) OR TI,AB((“inter professional”)) OR TI,AB(organisat*) OR TI,AB(organizat*) OR TI,AB(interagency*) OR TI,AB(agenc*)) NEAR/2 (TI,AB(communicat*) OR TI,AB(share*) OR TI,AB(sharing) OR TI,AB(integrat*))) OR ((TI,AB(data) OR TI,AB(digital*)) NEAR/2 (TI,AB(link*) OR TI,AB(system*) OR TI,AB(access) OR TI,AB(information*) OR TI,AB(exchange*))) OR (((TI,AB(electronic*) NEAR/2 TI,AB(record*)) OR (TI,AB(patient*) NEAR/2 TI,AB(record*))) NEAR/2 (TI,AB(share*) OR TI,AB(sharing) OR TI,AB(integrat*) OR TI,AB(access*))) OR (TI,AB(information) NEAR/2 (TI,AB(share) OR TI,AB(sharing))))) AND ulo((gb OR g.b. OR britain OR uk OR u.k. OR “united kingdom*” OR england OR “northern ireland*” OR scotland* OR wales))) AND (title(health) OR title(social))
Web of Science (all databases listed) search strategy
# Web of Science search strategy (v0.1)
# Database: Web of Science Core Collection
# Entitlements:
-
- WOS.SCI: 1900 to 2023
-
- WOS.AHCI: 1975 to 2023
-
- WOS.ESCI: 2015 to 2023
-
- WOS.ISTP: 1990 to 2023
-
- WOS.SSCI: 1900 to 2023
-
- WOS.ISSHP: 1990 to 2023
# Searches:
-
TS=((semi-structured OR semistructured OR unstructured OR informal OR in-depth OR indepth OR face-to-face OR structured OR guide) NEAR/3 (discussion* OR questionnaire*))
-
TS=(“focus group*” or qualitative* or enthograph* or fieldwork or “field work” or “key informant*” or interview*)
-
#2 OR #1
-
(TI=((share* OR sharing OR integrat*) NEAR/2 (data OR organisat* OR organizat*)) OR AB=((share* OR sharing OR integrat*) NEAR/2 (data OR organisat* OR organizat*))) Date Run: Wed Mar 22 2023 11:45:16 GMT+0000 (Greenwich Mean Time) Results: 101793
-
(TI=(integrat* NEAR/2 (care* OR health*)) OR AB=(integrat* NEAR/2 (care* OR health*)))
-
(TI=((interprofession* OR “inter profession*” OR organisat* OR organizat* OR interagency*OR agenc*) NEAR/2 (communicat* OR share* OR sharing OR integrat*)) OR AB=((interprofession* OR “inter profession*” OR organisat* OR organizat* OR interagency* OR agenc*) NEAR/2 (communicat* OR share* OR sharing OR integrat*)))
-
(TI=((data OR digital*) NEAR/2 (link* OR system* OR access OR information* OR exchange*)) OR AB=((data OR digital*) NEAR/2 (link* OR system* OR access OR information* OR exchange*)))
-
(TI=(electronic* NEAR/2 record*) OR AB=(electronic* NEAR/2 record*))
-
(TI=(patient* NEAR/2 record*) OR AB=(patient* NEAR/2 record*))
-
(TI=(share* OR sharing OR integrat* OR access*) OR AB=(share* OR sharing OR integrat*OR access*))
-
#8 OR #9
-
#10 AND #11
-
#12 OR #7 OR #6 OR #5 OR #4
-
#13 AND #3
-
TS=(“national health service” or nhs)
-
OO=(“national health service” or nhs)
-
AB=((english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) NEAR/5 (english))))
-
TS=(gb or “g.b.” or britain or (british not “british columbia”) or uk or “u.k.” or united kingdom*or (england not “new england”) or northern ireland* or nothern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*)
-
CU=(gb or “g.b.” or britain or (british not “british columbia”) or uk or “u.k.” or united kingdom*or (england not “new england”) or northern ireland* or nothern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*)
-
SO=(gb or “g.b.” or britain or (british not “british columbia”) or uk or “u.k.” or united kingdom*or (england not “new england”) or northern ireland* or nothern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*)
-
CI=(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts*or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*)))))
-
OO=(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*)))))
-
CI=(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”)
-
OO=(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”)
-
CI=(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”)
-
OO=(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”)
-
CI=(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”)
-
OO=(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”)
-
#15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28
-
#29 AND #14
-
TS=(health* NEAR/5 (care* or social))
-
#31 AND #30
-
TS=(older NEAR/2 (people* or person* or adult* or patient*))
-
TS=(elderly or senior* or aging or ageing or geriatric*)
-
#33 OR #34 Editions:WOS.SCI,WOS.SSCI,WOS.AHCI,WOS.ESCI Date Run:Wed Mar 22 2023 12:13:39 GMT+0000 (Greenwich Mean Time) Results:4280476
-
#35 AND #30
-
#32 OR #36
-
TI=(share* or sharing or integrat* or data or communicat* or information*)
-
#38 AND #30
-
#39 OR #37
Appendix 3 List of ‘thin’ studies
Beech R, Henderson C, Ashby S, Dickinson, A, Sheaff, R, Windle, K, et al. Does integrated governance lead to integrated patient care? Findings from the innovation forum. Health Soc Care Community 2013;21:598–605. https://doi.org/10.1111/hsc.12042
Bielinska AM, Archer S, Soosaipillai G, Riley J, Darzi LA, Urch C. Views of advance care planning in caregivers of older hospitalised patients following an emergency admission: a qualitative study. J Health Psychol 2022;27:432–44. https://doi.org/10.1177/1359105320926547
Carnes Chichlowska S, Burholt V, Beech C, Dobbs C. A Realistic Evaluation of Integrated Health and Social Care for Older People in Wales, to Promote Independence and Wellbeing: Interim Report. Cardiff: Welsh Government Social Research; 2013. URL: www.gov.wales/sites/default/files/statistics-and-research/2019-07/131015-evaluation-integrated-health-social-care-older-people-interim-report-en.pdf (accessed July 2023).
Chase M, Lloyd CEM, Peters BJ, Chase E, Lee K. Joining the dots: day to day challenges for practitioners in delivering integrated dementia care. Health Soc Care Community 2021;29:1061–71. https://doi.org/10.1111/hsc.13140
Christiansen A, Roberts K. Integrating health and social care assessment and care management: findings from a pilot project evaluation. Prim Health Care Res Dev 2005;6:269–77. https://doi.org/10.1191/1463423605pc247oa
Community Health Partnerships, Integrated Care Network, Institute of Public Care. From the Ground Up: A Guide to Integrate Service Delivery and Infrastructure: Part 3: Case Studies. 2010. URL: https://ipc.brookes.ac.uk/files/publications/From_The_Ground_Up_-_A_guide_to_integrated_care_and_delivery_Final_Nov.pdf (accessed July 2023).
Cook G, McNall A, Thompson J, Hodgson P, Shaw L, Cowie D. Integrated working for enhanced health care in English nursing homes. J Nurs Scholarsh 2017;49:15–23. https://doi.org/10.1111/jnu.12261
Dambha-Miller H, Simpson G, Hobson L, Olaniyan D, Hodgson S, Roderick P, et al. Integrating primary care and social services for older adults with multimorbidity: a qualitative study. Br J Gen Pract 2021;71:e753–e61. https://doi.org/10.3399/BJGP.2020.1100
Douglas N, Mays N, Al-Haboubi M, Manacorda T, Thana L, Wistow G, Durand MA. Observations of community-based multidisciplinary team meetings in health and social care for older people with long term conditions in England. BMC Health Serv Res 2022;22:758. https://doi.org/10.1186/s12913-022-07971-x
Henderson L, Bain H, Allan E, Kennedy C. An exploratory multi-case study of the health and wellbeing needs, relationships and experiences of health and social care service users and the people who support them at home. Int J Integr Care 2023;23:11. https://doi.org/10.5334/ijic.7003
Kupeli N, Leavey G, Harrington J, Lord K, King M, Nazareth I, et al. What are the barriers to care integration for those at the advanced stages of dementia living in care homes in the UK? Health care professional perspective. Dementia 2018;(London) 17:164–79. https://doi.org/10.1177/1471301216636302
Levin KA, Miller MA, Henderson M, Crighton E. Implementing a step down intermediate care service. J Integr Care 2019;27:276–84. https://doi.org/10.1108/JICA-08-2018-0056
Lhussier M, Dalkin S, Hetherington R. Community care for severely frail older people: developing explanations of how, why and for whom it works. Int J Older People Nurs 2019;14:e12217. https://doi.org/10.1111/opn.12217
Llewellyn M, Garthwaite T, Blackmore H, McDonald M. Working for a Shared Common Purpose: Experiences of Health and Social Care Integration in Wales. Welsh Institute for Health and Social Care, University of South Wales for UNISON Cymru/Wales; 2018. URL: https://cymru-wales.unison.org.uk/content/uploads/sites/9/2018/05/Working-for-a-Shared-Common-Purpose-11.5.18-1.pdf (accessed July 2023).
McCormack B, Mitchell EA, Cook G, Reed J, Childs S. Older persons’ experiences of whole systems: the impact of health and social care organizational structures. J Nurs Manag 2008;16:105–14. https://doi.org/10.1111/j.1365-2834.2007.00823.x
Moore KJ, Candy B, Davis S, Gola A, Harrington J, Kupeli N, et al. Implementing the compassion intervention, a model for integrated care for people with advanced dementia towards the end of life in nursing homes: a naturalistic feasibility study. BMJ Open 2017;7:e015515. https://doi.org/10.1136/bmjopen-2016-015515
Professional Record Standards Body. Care Home Information Flow Consultation Report. Professional Record Standards Body; 2017. URL: https://theprsb.org/wp-content/uploads/2018/02/Care-home-information-flow-consultation-report-v1.4-3.pdf (accessed July 2023).
Riste LK, Coventry PA, Reilly ST, Bower P, Sanders C. Enacting person-centredness in integrated care: a qualitative study of practice and perspectives within multidisciplinary groups in the care of older people. Health Expect 2018;21:1066–74. https://doi.org/10.1111/hex.12803
Ruaux S, Chadborn N. A qualitative exploratory study of training requirements for general practitioners attending older people resident in care homes. J Integr Care 2023;31:64–74. https://doi.org/10.1108/jica-11-2021-0060
Scantlebury K, Bixley M, Williamson I. Exploring accounts of collaborative working between speech and language therapists and stroke association communication support coordinators following stroke. J Interprof Care 2018;32:490–500. https://doi.org/10.1080/13561820.2018.1446921
Smith H, Grindey C, Hague I, Newbould L, Brown L, Clegg A, et al. Reducing delayed transfer of care in older people: a qualitative study of barriers and facilitators to shorter hospital stays. Health Expect 2022;25:2628–44. https://doi.org/10.1111/hex.13588
Stocker R, Bamford C, Brittain K, Duncan R, Moffatt S, Robinson L, Hanratty B. Care home services at the vanguard: a qualitative study exploring stakeholder views on the development and evaluation of novel, integrated approaches to enhancing healthcare in care homes. BMJ Open 2018;8:e017419. https://doi.org/10.1136/bmjopen-2017-017419
Sudbury-Riley L, Hunter-Jones P. Facilitating inter-professional integration in palliative care: a service ecosystem perspective. Soc Sci Med 2021;277:113912. https://doi.org/10.1016/j.socscimed.2021.113912
Sutcliffe CL, Jasper R, Roe B, Jolley D, Crook A, Challis DJ. Inter-professional perspectives of dementia services and care in England: outcomes of a focus group study. Dementia (London) 2016;15:1002–20. https://doi.org/10.1177/1471301214548692
Tyson SF, Burton L, McGovern A. Multi-disciplinary team meetings in stroke rehabilitation: an observation study and conceptual framework. Clin Rehabil 2014;28:1237–47. https://doi.org/10.1177/0269215514535942
Woodward A, Ruston A. Empowerment of care home staff through effective collaboration with healthcare. J Interprof Care 2023;37:109–17. https://doi.org/10.1080/13561820.2022.2047015
Appendix 4 Adapted Wallace criteria
| Question | Interpretation |
|---|---|
| 1. Is the research question clear? | ‘Yes’ or ‘no’ based on the reviewer’s judgement. |
| 2. Is the study design appropriate to answer the question? | ‘Yes’, if the question(s) could be answered by qualitative methods; for mixed-methods studies, the suitability of methods was assessed separately for the qualitative and quantitative components of the study. |
| 3. Is the context or setting adequately described? | ‘Yes’ or ‘no’ based on the reviewer’s judgement. |
| 4. Is the sample adequate to explore the range of subjects and settings, and has it been drawn from an appropriate population? |
|
| 5. Was the data collection adequately described? | Description of data collection should include the whole process and setting, for example where and when the interviews/observations took place, interview schedule and its sources and development, recording and transcription, field notes. This description should be methods-specific for example interviews, focus groups, observations. |
| 6. Was data collection rigorously conducted to ensure confidence in the findings? | Factors that might have bearing on participants behaviour have been identified and addressed (e.g. those related to recruitment such as whether this happened through official organisational channels, managers, etc.), confidentiality (addressed prior to interview), setting (interviews conducted in a ‘safe space’), researcher’s relationship to the organisation to which the participant belongs (clarified before the interview); recording and transcription; field notes to complement and contextualise transcript. |
| 7. Was there evidence that the data analysis was rigorously conducted to ensure confidence in the findings? | Type of analysis is stated and the process described in sufficient detail (audit trail, including interplay between data collection and analysis); credibility/validity of findings is ascertained using a range of methods, such as parallel coding, peer review, reflexivity, triangulation, or member checking. |
| 8. Are the findings substantiated by the data? | ‘Yes’, or ‘no’ based on the reviewer’s judgement; factors such as the use of quotations to support findings were taken into consideration. |
| 9. Has consideration been given to any limitations of the methods or data that may have affected the results? | ‘Yes’, if (any) limitations reported. |
| 10. Do any claims to generalisability follow logically and theoretically from the data? | ‘Yes’, if claims followed logically from the data or if no claims to generalisability were made. |
| 11. Have ethical issues been addressed and confidentiality respected? | ‘Yes’, if an ethical approval has been granted by a legitimate institutional body or all relevant ethical issues have been addressed. |
| 12. Is/are the author(s) reflexive? | ‘Yes’, if authors explicitly consider the impact that their subjectivity (e.g. beliefs), behaviour (e.g. language) and context (e.g. gender) might have had on the design, data collection and analysis, and formulation and reporting of findings. As reflexivity is difficult to ‘quantify’ any evidence of reflexivity will lead to ‘yes’. |
List of abbreviations
- ACP
- advance care planning
- AI
- artificial intelligence
- EPaCCS
- Electronic Palliative Care Coordination System
- GP
- general practitioner
- GSF
- gold standards framework
- HTA
- Health Technology Assessment
- IG
- information governance
- PPIE
- public and patient involvement and engagement
- PSAG
- Professional Stakeholders Advisory Group
- SAP
- single assessment process
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/TTWG4738).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
