Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR129528. The contractual start date was in September 2020. The final report began editorial review in October 2022 and was accepted for publication in March 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Maben et al. This work was produced by Maben et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Maben et al.
Chapter 1 Introduction
The COVID-19 pandemic has rightly focused public attention on the extreme challenges of health-care work and the often-consequent psychological ill-health that can ensue. Yet, while the pandemic provided an intense and risky working environment, psychological ill-health in nurses, midwives and paramedics has been a considerable problem worldwide for many decades, but while considered important to address, it has not been given a high priority. One rare benefit of the pandemic is that it shone a light on the critical significance of the psychological well-being of healthcare staff, particularly those working on the front line, and the importance of supporting staff to care well.
The National Health Service (NHS) is the biggest employer in Europe and the world’s largest employer of highly skilled professionals with 1.6 million people, three-quarters of whom are women. 1 The NHS needs healthy, motivated staff to provide high-quality patient care; however, in recent years increasing workload due to workforce shortages and societal demand for healthcare services, combined with budget restraints and increasing external scrutiny of their work, has taken its toll on staff as well as patients. 1,2 Pre-pandemic, commentators described staff as ‘running on empty’ (Pearson Commission 2018, personal communication) and the ‘shock absorbers in a system lacking (the) resources to meet rising demands’2 and the COVID-19 pandemic has only added further to those pressures.
The most recent (2021) NHS staff survey reports 47% of staff have felt unwell because of work-related stress in the last 12 months (this figure has increased for four consecutive years, now more than 8% higher than in 2017). In addition, 55% of staff have gone into work in the last 3 months despite not feeling well enough to perform their duties (presenteeism). Overall, 34% of staff said they feel burnt out because of their work, with paramedics (51%) and registered nurses and midwives (41%) the highest across all professions. Organisational factors (service architecture) are likely causes, with only 43% of staff reporting being able to meet all the conflicting demands on their time at work (at a 5-year low), with 76.5% saying that they often have unrealistic time pressures and 73% that there are not enough staff at their organisation to enable them to do their job properly (a significant increase from 62% in 2020). Only 68% are happy with the standard of care provided by their organisation, a decrease of more than 6% from 2020 (74.2%). 3
Psychological ill-health is a major healthcare issue, leading to presenteeism, absenteeism and loss of staff from the workforce. 1,4,5 Multiple government and industry reports have highlighted the need to reduce stress and improve psychological health in NHS staff. 1,6–8 A recent report examining NHS staff and learner’s well-being highlights the high financial and personal costs of psychological ill-health and recognises that working and learning in the healthcare sector is like no other employment environment. Every day, staff are confronted with the extremes of joy, sadness and despair, with clinical staff retaining a collection of curated traumatic memories9, p. 13. A rapid evidence review and economic analysis of NHS staff well-being and mental health10 estimated that the cost of psychological ill-health to the NHS is at least £12.1 billion a year and that, by tackling this and reducing staff attrition, the NHS could save up to £1 billion.
High levels of stress and burnout among NHS staff can affect their ability to provide high-quality care. 11,12 Stress among healthcare staff is greater than in the general working population and explains more than 25% of staff absence;13 while depression, anxiety, and a loss of idealism and empathy are also reported by nurses. 14–16 It also has a significant impact on staff retention creating a vicious cycle of staff shortages potentially leading to more stress and burnout.
A word on ‘mental ill-health’ terminology
When we wrote the proposal for this study we used the term ‘mental ill-health’ to build on the work of care under pressure 1 (CUP-1)17 (the term they used) and also to distinguish from the broader term ‘well-being’, which has become ubiquitous and something of a catch-all term. We used a stakeholder meeting to discuss terminology with members noting the importance of language. Members suggested there was the possibility of ‘well-being’ becoming a less powerful term, with some ‘well-being washing’ seen in some organisations (a term that describes a superficial well-being strategy, which is ‘all talk and no action’,18 one size fits all and superficial). One paramedic stakeholder felt that ‘mental health’ (used colloquially to mean mental ill-health) was stigmatising and was felt to be more about patients with clinical diagnoses of mental illness, whereas many staff did not associate what they were experiencing with these diagnoses; another agreed that the term mental ill-health/mental health may be excluding those that do not relate to it. Burnout, for example, is recognised as an occupational hazard, rather than a form of mental illness, yet these forms of psychological distress are very serious for individuals and the broader healthcare system but may be missed if we framed our work as interventions to address mental ill-health. It was also felt that this risked attributing the distress to factors specific to the individual, rather than attributing a causal role to the broader context.
Others suggested well-being was very firmly embedded in the NHS architecture and was therefore useful and that ‘psychological well-being’ would make a useful distinction from physical well-being. Others preferred ‘psychological distress’ and ‘vicarious trauma’. What became clear from the literature and the stakeholder group discussions was that there are pros and cons to any choice of terminology in this area. 19,20 After this discussion and much consideration, we have chosen to use the terms ‘psychological ill-health’ and ‘psychological wellness’ throughout this report to distinguish between the broader well-being term that may also encapsulate physical health (important and inter-related though that is) and to distinguish from any pathologising of mental ill-health, and to remove any perceived stigma to appeal to as broad an audience of staff as possible.
Why nurses, midwives and paramedics?
Nurses, midwives and paramedics are the largest collective group of clinical staff in the NHS.
In 2020, nurses and midwives (n = 365,034) made up 27.9% of the NHS workforce and paramedics (n = 18,000) made up 1.4%. Therefore, in total nurses, midwives and paramedics comprise 29.3% of the total NHS workforce and over 56% of the clinical workforce. 4
Specific issues that may impact on psychological ill-health for these three professions include, for example, issues of power and autonomy for nurses; fear of significant litigation for midwives; and physical isolation for paramedics, community nurses and midwives. These professions may also have prolonged exposure to patients over long periods of time, and regular exposure to traumatic incidents; shift work; and heavy workloads. 21 Paramedic stakeholders told us they are exposed to unpredictable high stress caused by traumatic incidents, which create potential flashpoints, and prolonged exposure can compromise psychological health with staff going through a rollercoaster of emotions in every shift. Unique challenges (not faced in other countries) include the strict response targets in a climate with increasing demands and efficiency drives as well as unpredictable finish times, long hours of driving and unpredictable breaks (also affecting many nurses and midwives). 22
All three groups may be subject to verbal or physical assault, dealing with cognitively altered members of the public and patients with mental illness, which confers significant risk of post-traumatic stress disorder (PTSD). 21 Nurses are reported to be reluctant to report aggressive and violent incidents and emergency nurses considered violence to be part of their normal working day. 23 Amongst health professionals, the suicide rate is 24% higher than the national average, largely explained by the increased risk of suicide in female nurses (four times the national average) and in male paramedics. 24 Colleagues affected by suicide are at greater risk of psychological ill-health and suicide ideation. Significant stigma around disclosing psychological ill-health is known to exist in nurses, midwives and paramedics18,25 and in the paramedics’ culture in particular there is a narrative that once you’re damaged, you’re out, resulting in a culture of not disclosing mental health difficulties.
Nurses, midwives and paramedics faced with psychological ill-health are likely to either come to work when ill because they feel that they have to continue caring for patients in spite of their own difficulties (presenteeism); take sick leave (absenteeism), resulting in gaps in service and experience and leaving staff feeling guilty about the increased burden this places on colleagues; or leave the profession altogether (workforce attrition), either temporarily or permanently, creating more staff shortages. Nurses, midwives and paramedics have high rates of illness and sickness absence. 26–28
Discussions with individual nurses, midwives and paramedics suggested it is difficult to take breaks with little access to facilities, toilets, and places for food and drink; that work can be lonely and isolating and, as autonomous workers, midwives fear litigation.
In terms of support, nurses, midwives and paramedics have the same access to NHS Trusts’ HR and occupational health (OH) services as doctors, but they do not have access to the national ‘Practitioner Health Programme’ (a confidential self-referral service for doctors and dentists who are experiencing psychological ill-health or substance use difficulties). Participants at the Wounded Healer Conference (2018) noted ‘as bad as support is for doctors, it’s far worse for nurses, they are not allowed time off for treatment, not encouraged to seek help and don’t have the means to seek private help. ’29 Paramedics we spoke to echoed this with the provision of care for paramedics reported as poor with no consistency or support for paramedics with psychological ill-health. Some nurses felt they had no ‘voice’ and did not feel they could speak up if something was wrong. Finally, a nurse ward manager told us that the most important need was for proper psychological health training for managers and clear guidelines for what to do when a staff member reports mental health difficulty, a step-by-step guide that they can easily implement. Our study aims to develop and provide these resources.
Current interventions and evidence gaps
There is a large body of literature on interventions that offer prevention, support or treatment to nurses, midwives and paramedics experiencing psychological ill-health. 25,30,31 This literature tends to be discipline-specific and focuses on individual interventions placing responsibility for good psychological health with nurses, midwives and paramedics themselves. 25,32–34 Addressing the wider professional, organisational and structural contexts that ‘affect nurses’, ‘midwives’ and ‘paramedics’ psychological ill-health is less prevalent. 22,25,35,36 Therefore, there is a need for research approaches that are sensitive to the complexities and causes of psychological ill-health in nurses, midwives and paramedics, identifying what is unique within and between each profession and context.
This study builds directly on previous work: care under pressure (1): a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care17 sharing research team members (KM; DC; SB) across CUP-1 and care under pressure 2 (CUP-2) to address the following aims, objectives and research questions.
Methods
Project overall aim
To improve understanding of how, why and in what contexts nurses, midwives and paramedics experience work-related psychological ill-health; and determine which high-quality interventions can be implemented to minimise psychological ill-health in nurses, midwives and paramedics.
Our specific aims are to
-
A1. Understand when and why nurses, midwives, and paramedics develop psychological ill-health at work, and provide examples of where and how it is most experienced;
-
A2. Identify which strategies/interventions to reduce psychological ill-health work best for these staff groups, find out how they work and in what circumstances these are most helpful;
-
A3. Design and develop resources for NHS managers/leaders so that they can understand how work affects the psychological health of nurses, midwives and paramedics; and what they can do to improve their psychological health in the workplace.
Objectives
We will undertake a realist review to test and refine programme theories to meet A1 and A2 above to identify the following:
-
O1. How and why work has a positive or negative effect on the psychological health of nurses, midwives and paramedics and in what contexts these are most experienced and have impacted;
-
O2. The mechanisms at individual, group and professional levels by which strategies and interventions prevent or reduce the impact of work on the psychological ill-health of nurses, midwives and paramedics; and explain why, for whom and in which contexts these are most beneficial for these staff.
Using evidence from O1 to O2 above and informed by evidence-based implementation theory and stakeholder involvement we will
-
O3. Develop a range of resources to support NHS managers/leaders to understand better how work affects the psychological health of nurses, midwives and paramedics and identify what they can do to improve their psychological wellness in the workplace.
Chapter 2 Methodology
Introduction to realist synthesis
This study used realist synthesis methodology37–39 to scrutinise literature on workplace psychological ill-health for nurses, midwives and paramedics. Realist synthesis prioritises the development of explanatory theories postulating how, for whom and in which contexts interventions work to produce outcomes. The methodology is based in a realist philosophy of science, which acknowledges that ‘there is a (social) reality that cannot be measured directly (because it is processed through our brains, language, culture and so on), but can be known indirectly. ’40
Using realist synthesis methodology this investigation goes beyond simple lines of questioning, such as ‘do interventions to minimise psychological ill-health of nurses, midwives and paramedics work?’ Rather, we sought to understand how efforts to mitigate psychological ill-health work, for which staff, which organisations, and in what circumstances. We also sought to achieve this depth of analysis in relation to understanding causes of psychological ill-health. The analysis recognises the interwoven variables that operate at different levels in organisations. The realist approach to data collection in this study was driven by retroductive theorising, which is the ‘activity of uncovering underpinning mechanisms’. 41 Retroduction entails a logic of inference, which starts with that which is empirically observable and explains outcomes and events through identifying the underlying mechanisms which can produce them. 42
The literature retrieved in this synthesis (CUP-2) is based on theoretical prioritisation, in line with realist synthesis guidelines37,40 to further strengthen the context-mechanism-outcome configuration (CMOc) framework used in the analysis. A key component of the starting point for this theoretical prioritisation was the programme theory from CUP-1. 43 The search for papers for theoretical understanding has been inclusive of both primary and secondary empirical research papers as well as theory discussion and editorial publications, key reports on NHS staff well-being (particularly those that have focused on nurses, midwives and/or paramedics) that have been published in the last few years, and other non-traditional forms of data for realist synthesis. This is in line with realist synthesis methodology promoting the use of diverse forms of data to build ontologically deep insights into the analysis. 44 Middle-range theory documents were collected as an ongoing activity identified by team members and our own networks, through consultation with stakeholder group members, and citations in included papers.
The realist approach has assisted in synthesising evidence on organisational and structural contexts (e.g. community or hospital work) and profession-specific working practices (e.g. types of shift work, team or lone working) within each of these three professional groups, but also differences and similarities between the groups (e.g. by speciality, setting). By illuminating differences in context and working practices, we anticipated how they might influence the development of psychological ill-health and the uptake and success, or otherwise, of interventions aimed at supporting psychological wellness within and between these staff groups. This feature of the approach is particularly appealing because the causes and solutions to workplace psychological ill-health are complex and multifactorial. Realist methodology is also pragmatically focused on developing and testing programme theories that have more potential to be effective.
The CMOc39,45 is the central heuristic used in realist analysis and has been used in this review. The realist approach suggests that to infer a causal outcome (O) between two events (X and Y), one needs to understand the underlying mechanism (M) that connects them and the context (C) in which the relationship occurs. 45 These are usually represented as Context (C) + Mechanism (M) = Outcome (O). For example, to evaluate whether an intervention improves psychological ill-health in nurses, midwives and/or paramedics (O), we identified underlying mechanisms M (e.g. the resources offered by the intervention and how these might effect changes in participants through reasoning/response), and its contiguous contexts C (e.g. are there local skill shortages impacting on access to the intervention?). We draw on the work of Dalkin et al. 46 who discuss the importance of conceptualising mechanisms on an activation continuum, rather than a binary trigger (on/off switch). Theoretical explanations developed through realist review are referred to as ‘middle-range theories’, which ‘...involve abstraction... but (are) close enough to observed data to be incorporated in propositions that permit empirical testing’47 (cited in40). Table 1 provides a definition of terms of context, mechanism and outcome.
| Category | Definitiona |
|---|---|
| Context | Context includes elements of the background environment that impact whether mechanisms in interventions are enabled to produce outcomes. These operate at different ‘layers’ including individual, interpersonal, organisational and intrastructural (e.g. the prevailing NHS culture). |
| Mechanism | Mechanisms are usually hidden, sensitive to variations in context, and generate outcomes. They are a combination of (1) the resources offered interventions and (2) the reasoning and responses from people to these resources, which lead to outcomes. |
| Outcomes | Outcomes are any intended or unintended changes in individuals, teams or organisational culture generated by context-mechanism interactions. |
Study design
The design of CUP-2 builds upon similar prior work in CUP-1 with doctors only17,43 and adheres to our published protocol except minor deviations, which are described in Appendix 1, Table 13. An overview of the design is presented in Table 2, though note this was not a linear process as suggested by the table, with several different searches being folded into final analysis, as described further in the text.
| Review stage (as per project protocol) | Strategy | Description |
|---|---|---|
| Step 1a: Locate existing theories | Searching for middle-range theories and frameworks in key papers and reports. | Searching key papers and reports to extract relevant middle-range theories and frameworks. Examining outputs from CUP-1 to explore transferable lessons and possible reusable conceptual platform. |
| Step 1b: Understanding key contextual features that may impact on psychological ill-health | Systematic and comprehensive synthesis of NHS workforce data. | Comparative NHS workforce data for nurses, midwives, paramedics and doctors (in order to compare to CUP-1) in relation to demographics, service architecture, and well-being data. |
| Step 2: Searching for evidence | ||
| 2.1 Database searches and screening | Searches of bibliographic databases and Reverse Chronology Quota (RCQ) screening. | Establishing the number of papers to be retained in the round of screening; starting with the most recent publications, working in reverse chronology applying a screening tool until the established quota is met. |
| 2.2 Supplementary searching | Hand searching key journals when RCQ has not been met during database searching. | Consulting key journals (e.g. British Paramedic Journal) to retrieve relevant papers that may have been missed by the database searching due to journals not being indexed. |
| 2.3 Literature reviews and COVID-19 | Inclusion of literature reviews and electronic database searches for COVID-19 insights. | Literature reviews obtained in initial search were screened by two team members for inclusion and ten from each profession were retained (n = 30); COVID-19 database searches were conducted separately for the three professions: 50 most recent results were screened and ranked according to relevance, with the top ten retained in each profession (n = 30). |
| 2.4 Expert input | Inviting stakeholders and project team to suggest key papers/reports. | Project team, stakeholder and advisory group members (including patient and public representatives) supplemented database searching by suggesting key papers and reports that may be missed using key word searching in the databases. |
| Step 3: Assessing papers for inclusion | ||
| Developing and applying exclusion criteria, including two-person inter-rater scoring | Selection criteria development and application by two team members. | Selection criteria developed based on protocol and early theory sensitisation; two team members scored all papers using the selection criteria and agreement compared; disagreements arbitrated by a third member of the team. |
| Step 4: Extracting and organising data | ||
| 4.1 Descriptive extraction and analysis | Understanding article contents. | Capturing the type of papers (e.g. non-empirical/empirical, methodology used; description of causes and interventions architecture). |
| 4.2 Realist appraisal | Appraisal journaling. | Creation of journal entries for each paper that addresses (a) the important insights described or inspired from the document in relation to the overall analysis and (b) team member journal-on-journaling to build coproductive analysis. |
| 4.3 Realist data extraction | Data extraction. | Selection of key data that demonstrate causal insights mapped to the research questions. |
| Step 5: Synthesising the evidence and drawing conclusions | ||
| 5.1 Analysing the literature in stages | Realist analysis. | Building ontologically deep analysis from appraisal journal content; rereading papers and developing CMO configurations to produce the synthesis. |
| 5.2 Stakeholder group contributions to analysis | Emergent analysis shared and discussed with stakeholders. | Over the course of four meetings, findings were shared and discussed with stakeholders to check for relevance and importance. |
Step 1a: locating existing theories
The goal of this step was to identify theories that explain how and why work has a positive or negative effect on the psychological health of nurses, midwives and paramedics and in what contexts these are most experienced and have impacted most significantly. Also, to identify the theories explaining how and why interventions prevent or reduce psychological ill-health in nurses, midwives and paramedics; and explain why, for whom and in which contexts these are most beneficial.
For interventions to be successful in moderating the impact of psychological ill-health it is necessary to understand the relationship between the development of psychological ill-health at work for nurses, midwives and paramedics (the [causal] underpinning theory or theories), so that the interventions can be selected that may ‘intervene’ and minimise psychological ill-health. In realist terms, these are the programmes. Programmes are ‘theories incarnate’ (not always explicit or visible) – that is, underpinning the design of programmes or interventions, and include assumptions about why certain components are required and how they might work. These theories are often implicit; the designers of interventions have put them together in a certain way based on what needs to be done to get one or more desired outcomes. The realist researcher aims to make these more explicit and visible where possible.
The team began by building on the CUP-117,43 final programme theory as the initial programme theory for this study, and then took a specialised, inductive approach to go beyond what was already known (reviews of individual interventions) and determine a path through the potentially vast literature (see below). We also wanted to learn from and draw upon the knowledge and expertise of our stakeholder group.
Thus, an initial theory sensitisation stage consisted of the following activities. Members of the CUP-2 team
-
examined the CMO configurations and theories generated by our co-applicants (KM, DC, SB) in CUP-1. 17 Members of that project team (KM (principal investigator [PI] of CUP-1), DC and SB) are also co-investigators in CUP-2. When drawing on their findings in early discussions we identified some of the similarities and differences across professions. These led to the identification, extraction and comparison of nationally available data for demographics, service architecture (ways of working) and well-being outcomes for doctors, nurses, midwives and paramedics to underpin this work,4 see Step 1b below;
-
drew upon PI (JM) previous HS&DR funded study exploring patients’ experiences of care and the influence of staff motivation, affect and well-being (HS&DR-08/1819/213) and extended our understanding of psychological ill-health at work and the impact of staff psychological ill-health on patient care;
-
drew on PI’s (JM/CT) realist expertise from their previous HS&DR funded longitudinal evaluation of Schwartz Center Rounds as an intervention for enhancing compassion in relationships between staff and patients (HS&DR-13/07/49) – considering its findings in the context of other interventions for the improvement of psychological ill-health in nurses, midwives and paramedics;
-
consulted with experts representing multidisciplinary perspectives in our Stakeholder group (including our nurses, midwives, paramedics and patient and public involvement and engagement [PPIE] representatives);
-
considered findings from NIHR HTA project – facilitating return to work of NHS staff with common mental health disorders: a feasibility study (HTA-15/107/02) about the role of OH in supporting staff with psychological ill-health;
-
drew on key reports published by advisory and steering group members: Michael West’s King’s Fund report30 and Gail Kinman and Kevin Teoh Society of Occupational Medicine (SOM) report25; along with additional informal searching to identify causal explanations about how the programmes’ impact on staff mental health/well-being. Contextual factors (at different levels, for example, individual, organisational, economic, social) related to risk of psychological ill-health were extracted and synthesised, and preliminary CMOcs developed (see Appendix 2, Table 14 for an example).
This early activity allowed the team to explore the possible theoretical underpinnings, including structural features of work (which we called ‘service architecture’), on which programmes are based, in order to map out the conceptual and theoretical landscape of psychological ill-health causes and intervention outcomes and how they are supposed to work, for nurses, midwives and paramedics. This informal searching differs from the more formal searching process in Steps 1b and 2 in that it is more exploratory and aimed at quickly identifying the range of possible explanatory theories that may be relevant.
Step 1b: understanding key contextual features that may impact on psychological ill-health
The research team brainstormed key contextual features (important contributors to psychological ill-health for nurses, midwives and paramedics) and compared these to each other and to doctors, based on our own expertise and knowledge. We shared drafts of these demographic, service architecture and well-being features with our stakeholder group on two occasions requesting comments on their importance and to identify any omissions. Feedback suggested that the features we identified provided a useful summary of key statistics that could inform attempts to improve workforce well-being.
To understand the service architecture better, we next searched for whole NHS workforce data (focusing on hospital and community health services staff) where possible using NHS Digital NHS workforce statistics) and/or NHS England-related sources based on the whole NHS hospital or community services workforce in England. We prioritised the sources where data could be separated by the three professions of interest and compared with doctors. This was important because our review builds on CUP-1,17 which focused on doctors. We found limited data for the primary care workforce, so focused only on hospital and community health service settings in England. Sources were rated for their strength/accuracy of evidence, and comparability across professions and a summary of the key demographic, service architecture (structural features of work) and well-being indicators were produced. 4 See Chapter 4 and Report Supplementary Material 1 for full publication.
Step 2: searching for evidence
This step involved searching bibliographic databases, supplementary searching in profession-specific United Kingdom (UK) journals and input from stakeholder and team member experts.
Database screening
Reverse chronology quota sampling (RCQ) was applied to database screening by starting from the most recent date of publication and working backwards chronologically, applying a screening tool until a certain quota of papers had been met. Note: this strategy was used in conjunction with capturing literature by expert input through the stakeholder group and research team experts. RCQ was used in this study for several reasons:
-
to create roughly equal quotas (n ~ 30) in the initial database search for each of the professions and thereby a similar size body of evidence for each profession, thus not giving undue weight to one profession over another. This allowed us to capture the most up-to-date evidence, theories and frameworks with cross-comparisons across the professions and prevented nursing literature dominating over the smaller research fields in midwifery and paramedic science. We decided to limit the initial search to ~90 papers to allow adequate time for data immersion, knowing that more papers would be searched in subsequent rounds (see Initial database searching). The quota strategy aimed to retain ~30 papers in each of the professions as an approximation only. The final number of papers was determined by the combination of RCQ, eliminations of papers not relevant after full-text read, and the inclusion of additional papers through expert solicitation and purposive sampling at later stages of the analysis. The final number of papers and breakdown are presented in Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart (see Chapter 3).
-
to capture the most recent literature and thereby ensure that the most recent aspects of context were analysed (realist methodology prioritises a context-sensitive understanding of evidence). Thus, outdated aspects of NHS context in literature undertaken in the last 10 years were eliminated. This review also sought to collect and analyse a diverse array of intervention architectures related to workplace psychological ill-health (i.e. organisational, team-based and individual-level interventions). Taking the most recent papers meant locating the latest innovations given the proliferation of psychological ill-health interventions and the rapidly changing context (e.g. COVID-19 pandemic) in the current context of health service delivery. However, older seminal papers/reports were included through supplementary searching, and team and stakeholder expert input.
-
initial pilot searching revealed that the literature on psychological ill-health in healthcare staff, especially in the nursing literature is vast. Given the large scope of the research design and finite timeframe, screening a large volume of papers would have been extraordinarily time-consuming and inefficient. Reviewers of this grant proposal previously observed that ‘the research is very ambitious in its scope and the amount of work required seems to be considerable for a 20 month project’ and we responded that we would ‘take a pragmatic approach to the scope of data included in our review. As realist reviews can include a multitude of different data sources, deciding when we have “enough” data will be of critical importance’. Setting limits on the number of papers to be selected in iterative rounds of searching brought clarity on the boundaries of the review, and shortened the time needed during screening, which allowed for more time for data immersion and analysis.
Initial database searching
The CUP-2 database searches were managed and executed by our information specialist (SB). Three rounds of searching were conducted during the review. This included (1) a search across all three professions; (2) an expanded paramedic search due to a dearth in the initial search of all professions; and (3) a COVID-19-specific search. CUP-2 was funded pre-pandemic and so the additional contextual factors caused by the pandemic in relation to causes and interventions were not considered within our protocol. While we recognised the limitations of focusing ‘only’ on the COVID-19 literature (e.g. in terms of extraordinary contexts, and poor quality of evidence) we felt it important to include this literature as an additional component. The methods are therefore explained in this chapter, but findings presented in the Appendices (see Appendix 3, Box 3).
The search terms and method for searches (2) and (3) are described later (see Second round of database searching and selection: literature reviews and COVID-19).
For search (1), across all professions, initial search terms describing psychological ill-health and outcomes of psychological ill-health were taken from CUP-1. 17,43 Additional search terms were added to retrieve papers relevant to nursing, midwifery and paramedic practice. Three databases were searched: Medical Literature Analysis and Retrieval System Online Database (MEDLINE) ALL (via Ovid, which includes MEDLINE In-Process), Cumulative Index to Nursing and Allied Health Literature database (CINAHL) (via EBSCO) and Health Management Information Consortium Database (HMIC) (via Ovid). These three databases were selected because they covered the core health science literature (MEDLINE ALL), nursing and allied health professional literature (CINAHL) and grey literature (HMIC). The search strategies included terms for the populations of interest (nurses, midwives and paramedics), common psychological ill-health problems (e.g. stress, anxiety, depression) and outcomes of psychological ill-health (e.g. sick leave and burnout). Anticipating a large volume of returns (especially in nursing) and to maintain the study’s relevance to the UK’s NHS context, we limited our initial search to UK-based literature. To accomplish this, a published UK geographic search filter was added to the MEDLINE search. 49 CINAHL did not have a UK filter option; however, a function within the database was used to limit studies to the UK geographic region. This is accessed via the Refine Results menu on the left-hand panel within CINAHL, under the subheading ‘Geography’, and allows the searcher to limit results to studies pertaining to pre-specified geographic regions, including ‘UK and Ireland’. The HMIC database, which is published by the UK Department of Health, the Nuffield Institute for Health (Leeds) and the King’s Fund Library50 has a mainly UK focus. With filters applied where they could be, three searches were conducted for each profession, and these were exported to Endnote X9 reference management libraries for screening. No date limits were applied to searches. The exclusion criteria we applied to literature captured in this initial search are presented in Table 3.
| Exclusion criteria | Rationale |
|---|---|
| Healthcare staff physical health (i.e. not about psychological health) |
Papers reporting exclusively on the physical ill-health of healthcare staff is beyond the remit of this review |
| Undergraduate student context | Papers reporting predominantly on the undergraduate experience of healthcare trainees is outside review scope |
| Not UK context | Papers reporting research outside the UK context may lack relevance to the specific realities of working in the NHS; definition of midwife and paramedic varies worldwide |
| Papers reporting COVID-19 (excluded from the initial search) | Papers reporting on the psychological health of staff during the COVID-19 pandemic were initially excluded as it was assumed such papers would overwhelm the RCQ process, particularly in nursing, and the included set may contain only papers on COVID-19. A separate second search for COVID-19 papers was completed later (see Second round of database searching and selection: literature reviews and COVID-19) |
| Patient well-being (not health professional) | Papers reporting exclusively patient psychological ill-health were outside the scope of this review |
| Literature reviews | Literature reviews were set aside to be revisited at a later stage (see Second round of database searching and selection: literature reviews and COVID-19) |
| Publication date older than 2010 OR papers beyond the 30 most recent relevant papers (whichever comes first) | Older papers will begin to lack relevance to the most recent developments in the UK healthcare setting |
The initial searches were run in MEDLINE and CINAHL on 12 February 2021 and in HMIC on 26 February 2021. Appendix 4 describes the search process and results in detail (see also Appendix 4, Tables 17–20).
After screening, the initial database search for paramedic papers yielded a dearth of studies (n = 7). For this reason we ran an additional search with more sensitive search terms, informed by paramedic stakeholders and research experts and a published search filter for the paramedic field. 51 The revised search included a wider selection of medical subject heading (MeSH) terms and free-text terminology than the initial search, including terms such as ‘first responder’ and ‘emergency personnel’. Using these modifications, the second search for paramedic literature was undertaken in all three databases on 31 March 2021. Results from those searches are presented in Appendix 4, Tables 17–20.
Titles and abstracts for the total number of papers retrieved through the database searches were as follows: 1304 for nursing, 88 for midwifery and 79 for paramedics. These were exported to word files and filtered through a screening and selection process described in Step 3.
Supplementary searching
The initial database search was exhausted before we achieved the rough quota (n ~ 30) for midwifery and paramedics. Therefore, to meet the quota estimate, an additional 11 papers in midwifery and 23 papers in paramedics were identified through supplementary hand searching in relevant profession-specific UK journals. We selected this search method as it became apparent from contact with stakeholders that the database searches had not retrieved several papers that met our inclusion criteria, which were all published in a small number of midwifery and paramedic journals. There were a few possible explanations for this, including that (1) the CINAHL UK geographic filter erroneously excluded them, (2) the ‘outcomes of psychological ill-health’ terms did not pick them up; and (3) several of the papers did not have abstracts (e.g. commentaries, opinion pieces) which makes them harder to retrieve; (4) several may not have been indexed in the databases. After pilot testing the approach, we considered that the most efficient way of identifying relevant papers was to hand search the back issues of these journals. Starting from the most recent edition and using the same exclusion criteria, we searched the British Midwifery Journal, the Journal of Paramedic Practice, and the British Paramedic Journal. The PRISMA flowchart (see Chapter 3) presents the numbers of identified papers (see also Appendix 4). Two team members (JJ) and (CT) independently screened all papers for inclusion, with disagreements arbitrated by a third team member (JM).
Second round of database searching and selection: literature reviews and COVID-19
Literature reviews
Thirty of the most recent literature reviews identified (but set aside) in the initial database searches were included in this second round. Team members (CT) and (JM) independently reviewed titles and abstracts of each review and rated their inclusion based on a judgement of relevance to contribute to the emergent programme theory, and based on their knowledge of the literature and the potential for additional insights. Given the rich data found in the initial sample of papers, an additional 30 literature reviews were considered adequate to supplement the existing dataset (particularly as some key reports also contained recent systematic reviews or summaries of such reviews). The number of literature reviews in the quota was deliberately small, because secondary analysis in the included literature reviews contained fewer rich insights (thin data) for realist analysis in contrast to data found in the included primary literature, and most of the literature reviews were international (some not including any UK primary evidence), perhaps impacting relevance.
COVID-19
A second round of database searching was conducted on 7 December 2021, to supplement the ongoing work in building the synthesis with papers focused on COVID-19 and psychological ill-health in nurses, midwives and paramedics. The initial screening and selection of ~90 papers excluded papers on COVID-19 because we anticipated that the number of COVID-19 papers in the last 2 years might have ‘overwhelmed’ the RCQ screening, particularly in nursing. We also anticipated that COVID-19 papers might not contain the range or depth of service architecture insights related to the causes and solutions to workplace psychological ill-health, which have been in existence for many years prior to the pandemic.
Once a first draft of the analysis of the initial sample of included papers was complete (see below), the information specialist (SB) ran a second search for COVID-19 papers across three databases (MEDLINE ALL, CINAHL and HMIC), separately for the three professions. This search used the same professional and psychological ill-health terminology as the initial search, but replaced search terms for the outcomes of psychological ill-health with COVID-19 search terms developed by the UK Health Security Agency library services team (https://ukhsalibrary.koha-ptfs.co.uk/coronavirusinformation/). We applied a UK filter to the MEDLINE search but not to the CINAHL search, in view of shortcomings identified in the initial searches (see above, where some UK papers were missed by the CINAHL UK filter); however, we did prioritise inclusion of papers from the UK through the ranking system used for selection (explained below).
COVID-19 two-step identification stage inclusion/exclusion criteria
The exclusion criteria for the COVID-19 papers are presented in Table 4. The COVID papers were appraised differently given the aim to draw out COVID-19-specific causes rather than just exacerbation of known existing causes; and/or novel interventions and innovations. The search strategies used for each database are presented in Appendix 4.
| Step one exclusion criteria | Rationale |
|---|---|
| Healthcare staff physical health (i.e. not about psychological ill-health) |
Papers reporting exclusively on the physical ill-health of healthcare staff is beyond the remit of this review |
| Undergraduate student context | Papers reporting exclusively on the undergraduate experience of healthcare trainees is outside review scope |
| Patient, not professional psychological ill-health | Papers reporting on patient psychological ill-health during COVID-19 pandemic is outside review scope |
| Papers beyond the 50 most recent relevant papers | In the first stage, we retained 50 COVID papers for each of the professions |
| Step two exclusion criteria: ranking for inclusion | |
| 5 points | Paper cites a middle-range theory important for our analysis |
| 4 points | Paper is about COVID-19, UK-based, shows potential to make an important contribution to our current analysis regarding service architecture innovations (*only interested in papers ranked 4 and above unless there are less than ten 4 point papers, in which case the 3 point papers were rereviewed and the best selected) |
| 3 points | Paper is about COVID-19 but descriptive (about how bad circumstances are), lacks insight in service architecture, but UK-based or is about an underrepresented profession |
| 2 points | Paper is about COVID-19 but descriptive, lacks insight, not UK-based, not profession-specific |
The search for COVID-19 papers involved a two-step process. The initial step searched the 50 most recent COVID-19 papers in each of the professions to capture relevant information on the impact of the pandemic on psychological ill-health. The second step was a ranking process to select the top 10 papers in each of the professions for a total of 30 papers. As we anticipated, many COVID-19 papers reported only the acute negative state of psychological ill-health descriptively, rather than insight into the solutions developed in the context of the pandemic. The two-step selection process is described in Table 4.
Step 3: assessing papers for inclusion
As outlined above (and shown in Appendix 4), the database searches yielded a large literature for nursing and a smaller pool in midwifery and paramedic literatures. RCQ screening was applied to the sample, which meant that the most recent literature was prioritised over older literature.
Two members of the team (JJ) and (CT) used Excel spreadsheets to record their independent judgments about the inclusion/exclusion of all papers/articles and these decisions were compared. In almost all cases, discrepancies between JJ and CT were easily resolved; on three occasions, a third team member (JM) arbitrated on final inclusion. Appendix 5 provides a sample of the Excel sheet used with the inter-rater scoring process exemplified.
Step 4: extracting and organising data
Descriptive extraction and analysis
In a realist review, due to the ontological depth it seeks to reach – aiming to go beyond simply empirical observations and insights45 – the whole paper counts as ‘data’, including, for example, the introduction and discussion. As such, all included papers provided evidence of causes and potential interventions because in a paper focused on describing or evaluating intervention(s), the authors are likely to argue for the need for the intervention(s) by describing the problem (causes of psychological ill-health) that the intervention aims to mitigate; and in a paper identifying, describing and/or measuring causes, the authors are likely to discuss potential ‘solutions’ or interventions.
Included literature for description of causes
In relation to causes, the existing evidence base, based upon numerous general or profession-specific reports of psychological ill-health in NHS professionals, has predominantly focused on quantitative survey-based measures of sources of job stress (thereby limited to what can be ‘measured’ empirically). The theoretical insights that we aim to achieve with a realist synthesis places equal importance on qualitative and grey literature (such as commentaries and editorials) and, as such, may offer different and/or expanded insights to the current evidence base. We, therefore, used all included literature except COVID-19 literature, which is presented separately (see Appendix 3, Tables 15 and 16).
Included literature for description of interventions
While most of the included literature mentioned interventions/solutions to psychological ill-health (even if the predominant focus of the paper was to describe/explain causes), this descriptive exercise focused on including those sources most likely to inform our understanding of interventions that may have benefit, and thereby included the following:
-
papers from the initial search cycle where either the purpose was to evaluate an intervention (n = 10/75) or was an editorial or commentary that aimed to discuss what was needed to mitigate psychological ill-health in nurses, midwives and/or paramedics (n = 29/75). This thereby excluded 36 papers from the initial search that (1) solely or primarily focused on assessment or description of causes of psychological ill-health, or experiences of work (n = 27); or (2) ‘other’ types of papers, including discussion articles that did not include a specific focus on solutions/interventions (n = 352–54); conference abstracts (n = 255,56); study protocols (n = 157); continuous professional development/education resources (n = 258); and presentations (n = 159).
-
key reports (n = 7) and literature reviews (n = 24), excluding five that did not include interventions. 21,23,60–62
Data extraction
All included papers and reports (as described above) were read in full and any mention of causes and/or interventions was extracted to a study-specific spreadsheet that captured the type of paper, key focus of the paper (causes, interventions, or both), and for empirical papers, the methodological approach, method/design (including sampling), and overall results; and for interventions, the description of the interventions(s).
Descriptive analysis
Causes were described firstly using categories/language from the source paper and were also coded against the relevant domain(s) of the HSE Management Standards (https://www.hse.gov.uk/stress/standards/index.htm): demands, control, support, relationships, role and change. The HSE Management Standards were chosen as a framework for categorising the data due to their robust evidence base, being derived from syntheses of features of work relating to psychological ill-health across many occupations, including health care. 63 In addition to using this framework, data that contributed to an understanding of ‘who’ was most at risk of psychological ill-health (particularly focusing on work environment/role factors, rather than simply demographics), and ‘when’ psychological ill-health was most likely to develop was extracted, to plug the gap in the identified limitations of previous reviews. Following this first layer of categorical analysis, the causes were read and reread, and a coding framework was developed to thematically group the specific causes described in each paper. The data on causes were coded independently by two members of the team (NK and CT), going back to full manuscripts to supplement the data extraction where coding was uncertain or differed. The data on risk factors (‘who’ is at risk and ‘when’) were similarly collated thematically. This analysis was not intended to systematically extract every instance of a ‘cause’ in each paper but focused on gaining a nuanced understanding of causes and providing data to compare and contrast within and between the three professions. For example, we acknowledge that most papers included mention of the high demand, low control/support being causes, as already known in the pre-existing evidence base, but have only cited exemplar sources for this.
Interventions were categorised according to the following:
-
their aim/focus: following the methods for categorisation used by previous reports25,30 and in line with intervention theory such as the ‘Hierarchy of Controls’,64,65 interventions were categorised as primary, secondary, tertiary (or multifocal where they straddled two or more of these levels). The Hierarchy of Controls purports that the further upstream the interventions are, the more effective they will be at both preventing exposure and thereby disease. So, while secondary and tertiary level interventions are also needed, primary interventions will be the most effective at tackling psychological ill-health. Primary interventions aim to eliminate or reduce risk of psychological ill-health by intervening at the source of the risk and thereby target the healthcare work environment, often at a structural level. Such interventions usually target whole organisational, employer (e.g. NHS-wide) or wider societal levels. Secondary interventions aim to delay or reverse the harmful impact that exposure to ‘risky’ work environment factors may have by modifying how staff respond when exposed (e.g. mindfulness training), manage their work environment (e.g. time management training) or develop competence/confidence in specific aspects of their job. The target of these interventions is usually the individual worker. Tertiary interventions aim to intervene once harm has been identified to reduce or minimise the impact and allow the worker to return to normal functioning. As well as including psychological interventions such as counselling and therapy, this category also includes initiatives such as return to work programmes. Interventions that straddled more than one category (e.g. primary and secondary) were labelled as multifocal interventions.
-
Whether the interventions were single discrete interventions or were multiple combined interventions (e.g. a programme).
-
Whether the intervention(s) was formal or informal (or mixed). We defined formal interventions as those with a defined structure or plan, often designed for replication and evaluated, whereas informal interventions were those without formal structure or definition, nor necessarily aimed for replication/evaluation, often staff-led and ad hoc. We acknowledge that for some interventions there is a fine line between formal and informal, and that some informal interventions could easily be ‘formalised’, but felt it was important to capture the interventions that are being recommended/stated to be required/beneficial, even if they did not have a specific formalised structure or description.
Once causes and interventions had been categorised as described above, analysis according to type of paper (empirical vs. non-empirical) and across the three professions (nurses, midwives and paramedics) was conducted to understand the similarities and differences according to type of data source/paper, and profession; and also conducted a preliminary analysis of ‘fit’ between causes and interventions.
Realist appraisal and appraisal journaling
An initial analysis, including CMO configurations, was drafted from a subsample of retained papers (n = 49) and reviewed by all team members. Papers were folded into the analysis in stages. All papers were read, and details entered into an appraisal journal (see below) by the team. On occasion, a paper was eliminated (or moved to a different part of the project, e.g. literature reviews or COVID-19) after reading the full-text, due to not meeting inclusion criteria that were applied at screening. This occurred when we screened papers without abstracts and had to read the full-text paper to know whether the paper met our inclusion criteria.
Realist synthesis appraisal involves an assessment of relevance and rigour of included evidence in the synthesis. 37 Pawson suggests that relevance in realist appraisal means adjudicating content of articles to determine how and in what ways they are relevant to the research questions and theoretical framing of the inquiry. An included primary study in a realist synthesis need not be appraised in its entirety, but rather the specific parts of the paper should be subject to scrutiny. 37 Therefore, we searched articles for causal insights that could be retrieved anywhere in the publication. These insights were extracted to the appraisal journal and reviewed by the whole team. Appraisal journaling was introduced to the team by coauthor (JJ) for this study as a step to be conducted before the full analysis involving CMOcs. A general process for the appraisal journaling included the following steps:
-
the full paper was first read and annotated
-
a new MS Word document was created for the journaling exercise. Title and abstracts for papers were imported into that document
-
using a free-write approach, one member summarised any important insights from the paper along with additional thoughts in a reflexive manner after reading the full text
-
the wider team then added their own free-thinking insights, expertise and NHS experience, providing challenge and counterarguments. This second-layer ‘journaling-on-journaling’ became an ongoing written dialogue amongst team members and served to build the analytic process, including notes to link theory and ideas from papers. An example of a journal entry is found in Appendix 6
-
subsequently, parts of the journaling were progressed to an analysis document, including key direct quotes from papers, and from there, CMO configurations were drafted. Links across papers were made at this stage, with a specific focus on building ideas around tensions in the healthcare delivery architecture (see below)
-
after journaling, full-text papers were revisited as needed, to investigate whether insights were fully captured and to test developing analysis against new or different insights.
Data extraction
Extraction of important insights began in the journaling, which informed our analytical thinking alongside journaling content. The first draft of the synthesis was based on a small sample of the papers (n = 15, five for each profession) and included CMO configurations built from data extractions and insights from the journaling process. Subsequent papers were journaled in batches and then folded into the existing analysis. Team members (JJ and CT) read and reread papers in tandem with the emerging analysis to ensure that papers containing causal insights were not missed on the first read. Second and third reading of papers was beneficial over the course of building the synthesis to identify and sometimes fill gaps, in particular in looking across the three professions.
Step 5: synthesising the evidence and drawing conclusions
The literature synthesis began in the journaling stage (as described above). The journal entries were incorporated into the analysis document by the following: (1) editing the free writing to improve quality; (2) removing extraneous text; (3) incorporating important journaling insights from multidisciplinary team members; and (4) revisiting primary literature for further reflection, and possible data extraction. Through team discussions, coproduced appraisal journaling and expertise in psychological ill-health and realist methodology, the team agreed to look for ‘tensions’ in the healthcare service architecture to understand the causes and solutions to workplace psychological ill-health.
This idea was then advanced from initial insights drawn from the papers (key findings, possible interpretations of findings and rival explanations), triggering further team contributions leading to confirmation, challenge and new rival theories. We then studied all papers to reveal the (sometimes hidden, sometimes explicit) tensions in the health service architecture associated with healthcare staff psychological ill-health and extracted all instances in which a tension was identified. This helped reach an ontologically deep understanding of the causes and, thereby, solutions to workplace psychological ill-health and meet the expectations of a realist synthesis to go beyond a surface view of the evidence.
We continued to build, revise, and at times consolidate CMO configurations, using this theoretical framing to provide analytical clarity on the complex evidence in the dataset. At our third key stakeholder meeting in January 2022, we introduced a sample of these ‘tensions’ to receive expert feedback and to test the face validity of the emergent findings. Key stakeholders provided endorsement and expressed enthusiasm for the approach. Refined and revised tensions were then shared at the fourth stakeholder meeting in May 2022, where feedback from group members was that these were important and resonated with their experiences.
Analysing the literature in stages
After the initial set of papers had been synthesised from the database search, subsequent journaling and analysis of reports (n = 7), literature reviews (n = 29) and middle-range theories (n = 14) was undertaken. As more content from papers was added to the analysis, the headings were reorganised and CMO configurations expanded and modified to account for the full range of data entered into the analysis.
The COVID-19 papers were also journaled using the appraisal journal technique and drafted into a separate analysis (see Appendix 3). The aim of this work was to extract key insights in relation to the abrupt changes brought on by the 2020 global pandemic. In terms of the health service architecture, the COVID-19 analysis reflects considerable changes in service architecture, such as the sudden surge in intensity of healthcare delivery, sharp changes in resources and protocols, and new interventions to improve conditions for nurses, midwives and paramedics given the difficulties of pandemic-era health service delivery.
Stakeholder group contributions to analysis
Four stakeholder meetings were held during the review (December 2020, June 2021, January 2022 and May 2022). All meetings were held virtually (using Zoom) and included some core research team members (at minimum CT and JM) and Diana Bass, a psychotherapist whose role in the study was to provide psychological support to stakeholders should it be needed. Overall, these meetings provided confirmation that our developing analysis was resonating with stakeholders and provided suggestions regarding important areas to extend or improve our emerging analysis. Some alternative theories and challenges were also shared, which aided our thinking. All meetings (except the first where personal stories were shared) were recorded (with permission from all attendees), and meeting conversations and entries into the ‘chat’ function and on online whiteboards (Padlet, enabling anonymous contribution) were transcribed and reviewed in relation to the analysis to enrich and provide further support or challenge to the analysis. All stakeholders provided permission for their contributions to be used in this way, and contributions have been paraphrased and included anonymously in this report. Stakeholder meetings comprised a mix of presentation from the work-in-progress analysis as well as participants sharing stories and insights from their personal experience (see Table 5).
| Meeting #, (Date) | Number of attendees | Composition, N = nurse; M = midwife; P = paramedic | Activity relevant to data collection and/or analysis |
|---|---|---|---|
| 1 (Dec 2020) |
20 | Stakeholders: 20 - 10 staff by experience (5N, 3M, 2P) - 1 lay member - 9 other (e.g. Royal Colleges, Regulators) + Diana Bass |
Three of the stakeholders (a nurse, midwife and paramedic) shared their own particular poignant and traumatic experience story about ‘The day I questioned why I had chosen my profession.’ The rest of the group shared their reflections on the stories including common themes that they felt linked them in relation to causes of poor psychological ill-health and any specific issues related to the individual professional groups. This included the following: unpredictable/unexpected events; lone working; and wearing a professional ‘mask’ to protect self. |
| 2 (June 2021) |
24 | Stakeholders: 24 - 10 staff by experience (5N, 3M, 2P) - 1 lay member - 13 other + Diana Bass |
Subsequent to providing a progress update, including feedback and analysis of the stakeholder group contributions from meeting 1, the emerging ‘tensions’ were presented to the group for discussion. We also discussed the emerging findings about the existence of both ‘formal’ and ‘informal’ interventions and asked stakeholders to think about and tell us what has worked for you and why and how? In relation to well-being support. |
| 3 (Jan 2022) |
19 | Stakeholders: 19 - 7 staff by experience (3N, 1M, 3P) - 1 lay member - 11 other + Diana Bass |
Subsequent to providing a progress update, a short reminder regarding realist methodology was provided followed by an updated revised analysis of the ‘tensions’ presented as five key dilemmas – including draft C-M-O’s. Attendees also asked to help us with diversity in our group (age, gender, ethnicity, disability etc.). |
| 4 (May 2022) |
17 | Stakeholders: 17 - 9 staff by experience (3N, 2M, 4P) - 1 lay member - 7 other + Diana Bass |
Discussion on (a) the importance of terminology regarding psychological ill-health of healthcare staff; (b) key findings to date including a focus on three of the key tensions, including discussing the lack of intersectionality present in the literature, including menopause. Support for resonance and importance of uncovering the tensions; (c) comment on ideas for translating findings into recommendations and resources. Ideas were presented and discussed. |
Developing outputs
Our study outputs are in development, but we have developed recommendations for research, practice and policy (see Chapter 7). We worked with our stakeholder and advisory groups to turn our findings into recommendations and turn recommendations into practical guidance. This work is ongoing and due to be reported in Spring 2023. We held two advisory groups during the study (September 2021 and August 2022), and members provided academic input, lived experience and project oversight and governance. At our final advisory group in August 2022, we built on the responses from our stakeholder group in May 2022 to our suggested resources and presented refined ideas for comment and critique, which aided further refinement (see Chapter 7). We have also used the consolidated framework for implementation research (CFIR)66–68 to identify and attempt to mitigate implementation challenges in relation to the resources.
Ensuring rigour
Analytical rigour was supported by a number of strategies within the review process. This included the following:
-
the inclusion of empirical papers, grey literature, editorials and commentaries, reports and stakeholder as data sources to triangulate findings and create a robust analysis;
-
use of the realist and meta-narrative evidence syntheses: evolving standards (RAMESES) reporting guidelines (checklist uploaded to project webpage) to ensure rigour in the conduct and reporting of this realist synthesis;
-
whole-team appraisal engagement in reading papers, journaling-on-journaling that identified and confirmed the most important insights regarding tensions in the healthcare architecture to inform data analysis; and built on healthcare psychological ill-health knowledge and expertise in the group, resulting in the incorporation of wider relevant literature and middle-range theory;
-
a rigorous audit of the analysis conducted by team members (JM) and (CT) to ensure transparency from original source documents to the emergent tensions, including cross-checking consistency of key messages with the quotations/extracts used to inform analysis and CMO configurations, and searching across nurse, midwife and paramedic sources to ensure analysis was supported within the included literature;
-
consulting with the CUP-2 advisory and stakeholder groups on the relevance and richness of the analysis and receiving strong consistent messages from these groups that the analysis was relevant, important and provided new and needed insights.
Summary
Realist methodology was used to search, identify, appraise and synthesise the literature in relation to our aims to reach an ontologically deep understanding of causes and interventions to mitigate psychological ill-health in nurses, midwives and paramedics. Due to the broad mandate of this review, and the potential for locating insights across a diversity of literature in nursing, midwifery and paramedic professions, we used reverse chronology quota screening for the first round of database searching followed by more specific supplementary searching strategies, including hand searching journals and inviting expert solicitation of key papers. This was supplemented by literature reviews, and separate searches focused on COVID-19. The appraisal journaling technique permitted the multidisciplinary team to extract key insights, build on existing knowledge of literature and the NHS, and use these insights to formulate CMO configurations. Multiple rounds of analysis in consultation with stakeholders generated insights into a wide range of tensions facing nurses, midwives and paramedics and a range of interventions that might support their workplace psychological ill-health and wellness.
Chapter 3 Results: characteristics of included literature sources
The searches described in Chapter 2 resulted in inclusion of a total of 204 papers through cycles of searching and synthesis, as described in the Methods chapter and illustrated in the PRISMA flowchart (see Figure 1).
FIGURE 1.
PRISMA diagram for CUP-2 screening and selection of papers.
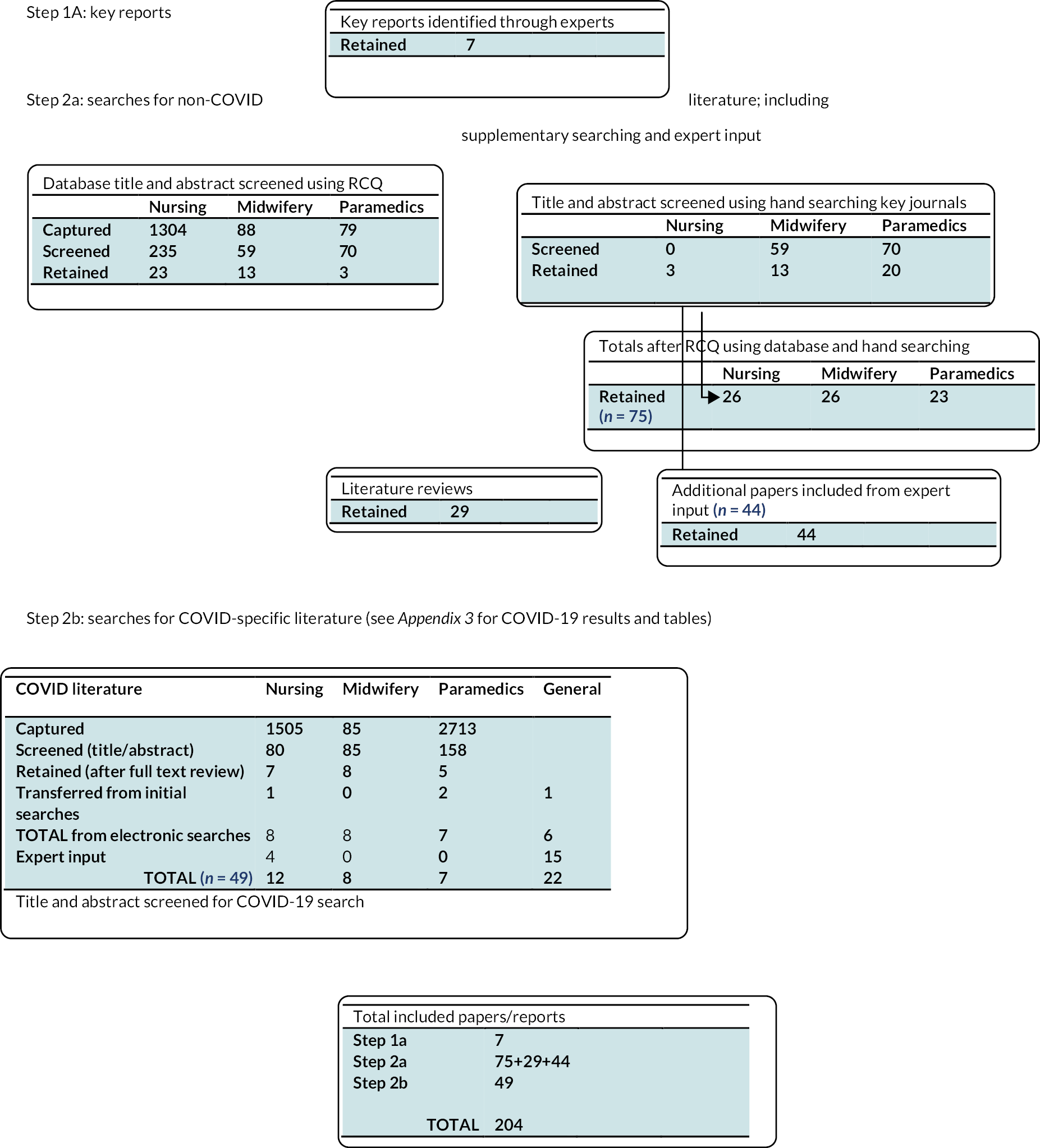
This included 75 papers in the first cycle of electronic database searches: 26 nursing; 26 midwifery and 23 paramedic; 7 key reports; and 29 literature reviews (see Appendix 7, Tables 21–25) and 49 COVID-19 focused papers, reports and literature reviews (see Appendix 3, Tables 15 and 16).
Of the 75 papers included in the first cycle of searches, 35 were empirical papers (18 nursing, 10 midwifery and 7 paramedic) and 40 non-empirical (e.g. editorials, commentaries and other types of papers and grey literature) (8 nursing, 16 midwifery, and 16 paramedic).
Across all 75 papers, 15 focused predominantly on causes (6 nursing, 4 midwifery, 5 paramedic); 38 on interventions (12 nursing, 16 midwifery, 10 paramedic); and the remaining 22 papers focused on both causes and interventions (8 nursing, 6 midwifery, 8 paramedic).
The included literature reviews were a range of different types of review, including systematic, narrative, integrative and scoping reviews (see Appendix 7).
Chapter 4 What are the causes of psychological ill-health in nurses, midwives and paramedics? A descriptive analysis
Introduction
This chapter reports on the ‘causes’ of poor mental health in nurses, midwives and paramedics, based upon descriptive analyses of the included literature. The overarching aim of our study was to understand ‘when’ and ‘why’ nurses, midwives and paramedics develop psychological ill-health at work and identify which nurses, midwives and paramedics are particularly affected (‘who’) in which specific contexts. This chapter is intended to provide descriptive analyses of the causes evidenced in our included literature to provide context for the realist synthesis of the included literature (see Chapter 6).
Our approach to understanding the causes of psychological ill-health is bio-psycho-social-cultural. We acknowledge that work-specific causes are only one part of the explanation for the development of psychological ill-health, but they are the focus of this project due to their potential power in explaining the excess levels of psychological ill-health in nurses, midwives and paramedics compared to the general population.
Decades of occupational stress research has confirmed the relevance of demand, control and support at work, as well as relationships, role clarity and how organisations manage change. 63,69,70 These features of work predict job stress in many different occupational settings, cross-culturally and internationally, and in turn job stress is a strong risk factor for psychological ill-health at work. The strong evidence supporting the relationship between these features of work and psychological ill-health led to them underpinning the UK HSE Management Standards on stress, which provides resources for risk-assessing and reducing work stress. 71 It is therefore not surprising that, in the literature about causes of psychological ill-health in nurses, midwives and paramedics, there is much discussion of these features. To advance our understanding still further and account for contextual differences, including within and between the different health professions, various authors have highlighted the need for research that takes different working environments into account. 25 In this chapter we have attempted to address the limitations of previous systematic reviews and reports to
-
describe the differences in demographic, structural features of work (service architecture), and well-being indicators between nurses, midwives and paramedics, and also compare to doctors to build on previous work (CUP-117);
-
provide a more detailed and nuanced understanding of why psychological ill-health develops in nurses, midwives and paramedics;
-
examine the literature to understand better ‘who’ is at risk and ‘when’, including identifying the differences within and between our three professions of nurses, midwives and paramedics, going beyond demographic and individual characteristics to also consider the impact of different work environments.
Please see Chapter 2, Descriptive analysis for the methods.
Results
Aim (a) to describe the differences in demographic, structural features of work (service architecture), and well-being indicators between nurses, midwives and paramedics, and also compare to doctors
We extracted and compared key demographic, service architecture (structural features of work) and well-being indicators for nurses, midwives and paramedics, as well as doctors. See Chapter 2, Step 1B for methods of the critical review we undertook, and Report Supplementary Material 1 for the full publication. 4 The comparison with doctors was important since this review built on CUP-1,17 which focused on doctors. Key differences that we found between the professions, that may be important to fully understand causes and interventions to mitigate psychological ill-health include the following:
-
Demographic
-
Gender: nursing and midwifery are female-dominated, whereas doctors and paramedics are more balanced. Various social and economic factors (e.g. being more likely to take on caring roles, live in poverty and experience domestic abuse) can put women at greater risk of psychological ill-health.
-
Age: nursing, midwifery and paramedic science have ageing populations – this ‘demographic timebomb’72 means many experienced professionals will be leaving the profession in the coming years.
-
Ethnicity: there is greater diversity among doctors and nurses than midwives and paramedics. Those with lower diversity have higher vacancy rates.
-
-
Service architecture
-
Turnover and retention remain problematic in all professions.
-
Nearly half of doctors were consultants, but much smaller proportions of staff held high-grade/band roles in nursing, midwifery and paramedic science.
-
Salaries were higher for doctors. There are significant gender and ethnicity pay-gaps across all professions.
-
-
Well-being
-
All reported high job stress, particularly midwives and paramedics.
-
Sickness absence rates for nurses, midwives and paramedics were three times those of doctors, and presenteeism nearly double.
-
We concluded that sociocultural factors known to increase risk of psychological ill-health may explain some of the differences between professions and that these factors should be considered when designing strategies to improve well-being. Other key recommendations are included at the end of this chapter and in Chapter 7.
Aim (b) to provide a more detailed and nuanced understanding of why psychological ill-health develops in nurses, midwives and paramedics
In this section, we consider each HSE domain in turn, describing the nuanced causes that sit beneath each domain.
Demands
The ‘demand’ causes identified in the literature were analysed and synthesised into nine distinct (albeit overlapping) ‘demands’ that were present across nursing, midwifery and paramedic literature (see Table 6). Unsurprisingly this included the well-reported staff shortages and high attrition in the professions [as reported above, within aim (a)], which could have knock on implications. For example,
| Risk factors for work-related stress (HSE Management Standardsa) | Specific ‘cause’ | Exemplar papers where cause has been cited | Profession-specific causes (N = nurses; M = midwives; P = paramedics) |
|---|---|---|---|
| Demands (workload, work patterns, work environment) |
Staff shortages and high attrition | 9,22,30,34,73–75 | Working on-call (M76,77) |
| Pressure of work in service in which demand continues to increase/unmanageable workload | 35,62,81–88 | Lack of continuity of care (N78 liaison psychiatric nurses, and P) | |
| Working long shifts with no/few breaks | 9,22,55,62,82,86,89–93 | Unnecessary call-outs (P55) | |
| Inadequate work-life balance | 60,74,83,94 | Heavy cognitive load/rapid decisions (P79 and M) Labour ward/home delivery (N emergency and critical care) | |
| Serve and sacrifice | 84,90,95–97 | ||
| Exposure to repeated episodes of trauma | 21,33,58,62,91,95,96,98–104 | High risk of sustaining injury (physical and psychological) (P80 likely to be similar in N: forensic/mental health settings and emergency nurses23) | |
| Experiencing death | 96,105–107 | ||
| Prolonged/cumulative stress | 35,94,98,108,109 | ||
| Emotional labour | 94,96,110–112 | Being a profession under scrutiny (N81) | |
| Control (how much say in the way you work) |
Lack of control/autonomy | 30,34,62,77,83,85,86,88,89,94,108,113 | |
| Support (encouragement, sponsorship and resources provided by org, line managers and colleagues) |
Not feeling supported/valued | 75,81,83,89,90,110,114–117 | Lone working (N,99,118,119 community/remote; P, critical care paramedics) |
| Stigma | 18,25,81,95,114,117,120–122 | ||
| Not having space/time to debrief after trauma or having inappropriate support | 9,30,82,91,95,96,103,105 | ||
| Not having basic ‘hygiene’ needs met | 9,30,34,74 | ||
| Relationships (promoting positive working to avoid conflict; dealing with unacceptable behaviour) |
Poor relationships with colleagues/incivility/bullying | 9,25,30,34,75,83,89,90,96,110,123 | Fear of assault/abuse from public/patients (P,124 but also N and M in some settings e.g. emergency nurses,23 secure forensic25,111) |
| Challenging relationships with patients, public, clients | 23,80,100,105,106,111,124,125 | ||
| Not feeling able to speak out | 9,83,90,94,114 | ||
| Role (clarity, not conflicting) |
Transition shock/reality shock (newly qualified) | 25,57,59,73,81,90,126,127 | None found |
| Values incongruence/theory-practice gap; moral distress | 30,62,75,90,128 | ||
| Unclear role boundaries/clarity | 25,52,56,62,91,99,129 | ||
| Role intensity | 22,99,101,130 | ||
| Change (organisational change management and communication) | Not being involved in change | 22,25,30,32,74,78,106,131 | None found |
one nursing paper focused on newly qualified nurses73 highlighted that this can mean regularly working with temporary staff (bank or agency staff) and/or being moved to other units (impacting teamwork and collegiality as well as knowledge of the systems and patients), and that such shortages can often mean being the only registered nurse on a shift, leading to feeling “vulnerable, and their units unsafe”73 (p. 3). Another commonly cited demand is having an unmanageable workload, relating to staff shortages and plugging gaps, but also from increased demands for care. This is ‘measured’ more easily in some settings than others, for instance, for paramedics there has been a well-documented increase in call volume over recent years. 82,132 In one review, the pressured decision-making and delivery of sometimes complex interventions in this context was cited as a key cause of psychological ill-health. 35 In a narrative review of impact of power and hierarchy on staff safety maternity services, one of the key themes was ‘dangerous workloads’ (p. 432) being linked to exhaustion, inflexibility, lack of breaks, low morale, poor communication and poor management. 83
Relevant to all three professions is the increasing move to working long shifts (12-hour shifts being increasingly the norm), and these long shifts were reported to often include very few opportunities for breaks (and/or unpredictable break patterns and times). Workplace culture means nursing and midwifery staff ‘tend to miss their breaks because of feelings of guilt, responsibility to colleagues or a sense that they are being most effective if they skip breaks’30 (p. 55). The nature of paramedic work frequently means unpredictable finish times, long hours driving and unpredictable breaks. 22 However, the literature reviewed by Ejebu et al. 62 suggests nurses often prefer working longer shifts attributing this to a greater work-life balance, higher numbers of days off and opportunities for greater continuity of care. Cull et al. 89 found likewise for midwives, though Ejebu et al. 62 concluded that despite this the shift patterns were ‘often organised in ways that are detrimental to nurses’ health and well-being, their job performance and the patient care they provide’ (p. 1), reporting that while days off might mitigate the adverse impacts of shift working, the impact varied according to personal characteristics and circumstances of the nurse. Inadequate work-life balance was reported across all three professions, being a key impact on recruitment and retention of community adult nurses in one review60 impacting on family-life in a paramedic review,94 and cited as a key stressor in the Work, Health and Emotional Lives of Midwives (WHELM) report. 74 Recent literature tended to focus more on arguing for the need for ‘time’ (for individual self-care and/or family activities), and thereby work-life balance is implied rather than explicit. The culture of ‘serve and sacrifice’ (see Chapter 6) was highlighted within all three professions, described in one midwifery review as a ‘culture of giving 100% … is a positive attribute but can be used negatively to persuade compliance to institutional needs’90 (p. 3), and in a nursing paper as ‘Nursing guidance, policies, reports, the media and nursing colleagues instilled the notion that patients take priority. While this was important for the role of a nurse, it was often interpreted in isolation without consideration of the nurse’s own needs, which were pushed aside in favour of others.’84 (p. 2).
It was perhaps not surprising that repeated exposure to trauma was mentioned in nearly all paramedic papers, but exposure to trauma and distressing incidents was also highlighted in many midwifery and nursing papers, and was the focus of a narrative review regarding secondary traumatic stress (STS) in emergency nurses98 (see Table 6). In one of the paramedic papers this exposure was described as an expected part of the job33 and in another, that there was “no way to avoid seeing sights that are difficult”95 (p. 225). One literature review reported predictors of PTSD, including the frequency and type of trauma exposure (e.g. proximity), and whether the threat to the worker was direct or indirect. 21 Arguably a subcomponent of exposure to trauma, although this could also be considered a separate stressor, is ‘experiencing death’ mentioned in papers for all three professions. Again, the impact of ‘death’ is often minimised due to being an expected part of the job and often only acknowledged as requiring support when it is unexpected (e.g. in the case of neonatal death) or particularly traumatic, or in the case of students or newly qualified staff when it may be their first experience of death and so not yet normalised. 96,105 The cumulative experience of stress (rather than just acute traumatic episodes), and the emotional labour of healthcare work caused by having to regulate emotions and remain ‘professional’ (called ‘wearing a professional mask’ in our stakeholder group) were cited as causes of psychological ill-health cited within papers across all three professions (see Table 6) and discussed in more detail and with a realist lens in Chapter 6. Some also cited feeling controlled as causal factors of psychological ill-health – both by the ‘politics’ of the organisation in which they worked or the wider healthcare system (i.e. administration, excessive paperwork, bureaucracy, inflexibility), and also by individuals (most often managers): “I felt very much under the control of management”34 (p. 27).
Profession-specific “demand” causes
There were some demand-related causes that were perhaps more profession-specific. One of these was working “on-call” (with unsociable hours), reported in a midwifery paper76 and a review article,77 the latter reporting findings from a Cochrane review of flexible working hours133 that found although negative experiences of ‘on call’ were reported, the midwives who worked on call had lower burnout scores. The authors attributed this to midwives ‘caseloading’, which provided opportunities for continuous care, building relationships with women and having autonomy over their work schedule. On-call working is common in medicine, but across our three professions is more likely in midwifery and – to our knowledge – not a model commonly used in nursing or by paramedics, though the role of the paramedic is rapidly expanding to many settings, including general practice, minor injuries units, and accident and emergency (A&E) departments (#not all paramedics wear green134), where on-call working may be more common. The impact of working ‘unsociable’ hours is relevant across all three professions due to the inherent need for healthcare delivery to be 24/7.
A feature of work highlighted as a cause of psychological ill-health (or at least work stress) was the lack of continuity of knowledge about patients’ health/well-being after being involved in their journey. This was specifically mentioned in a nursing paper about Liaison psychiatric nurses78 but is the nature of the job for paramedics who may care for and transport patients to hospital but not know the patient outcomes beyond this point. One paramedic paper also reported that the high number of unnecessary call-outs they have to respond to as a negative component of work, meaning that they cannot be elsewhere where they may be in greater need. 55 Another paramedic paper described “heavy cognitive load” due to the need to make rapid decisions, leading to a reliance on stereotypes and implicit bias,79 which while not mentioned in nursing or midwifery papers, is likely to be similar in other fast-paced ‘critical care’ environments such as labour wards for midwives, and A&E/critical care nursing. Indeed, in a recently published framework of nursing work, cognitive labour is one of four types of nursing work (alongside physical, emotional and organisational labour). 135 Paramedic-focused papers referred to feeling physically and emotionally drained because of their working conditions and environment,124,136 and also the high risk of sustaining a work-related injury (e.g. physical or psychological abuse, and concerns about the financial and psychological implications of sustaining an injury). 80 One of the nursing papers mentioned the Francis report and nursing being a ‘profession under scrutiny’81 as an aspect of the culture of nursing/health care that places additional pressure on individuals. While not present in any midwifery or paramedic literature in this review, the recent Ockenden review (midwives137) and the media focus on the consequences of growing ambulance waits138,139 makes it unlikely that this is a stressor unique to nurses.
Control
As expected, lack of control or autonomy was a key ‘causal’ factor in many of the included papers across all three professions, with nurses,85 and midwives83 described as experiencing ‘powerlessness’85 (p. 285) and ‘helplessness’83 (p. 432). Autonomy is one of the three core work needs in the ABC framework proposed by Michael West in a report about how to support high-quality care delivery by nurses and midwives. 30 When health professionals can control how they spend their time/how much time spent with patients, how they organise or control their workspace, and/or control over access to patients, this in turn can often relate to work satisfaction and staff being able to deliver the quality of care they want to deliver. In one midwifery paper,113 having autonomy regarding how to manage their midwifery unit was highlighted as a key protective factor, supporting earlier work,140 and midwifery papers also highlighted a preference for midwifery-led models of care (where midwives have a caseload of women and can provide continuity of care). 86 Across all three professions, the lack of control over working hours and shift patterns was regularly cited as problematic, with papers describing the subsequent impact on friendships, family life and hobbies/interests. 30,89,94 There were no profession-specific ‘control or autonomy’ features emergent in the literature.
Support
Not feeling supported and/or valued was a key cause highlighted in papers across all three professions. Lack of support related mostly to poor support from leadership/managers and organisational-level support, with one paramedic paper stating that it was a lack of confidence in support from employers that led paramedics to self-refer to their regulator. 114 However, one nursing paper highlighted the lack of support for leaders (senior nurses): ‘(it is) quite lonely at the top when you have no one to speak to’110 (p. 8), and a paramedic paper described the culture as sometimes being unsupportive if a colleague was struggling, referring to the military background of the profession and that there was consequently a very low tolerance for low standards amongst peers. 115 In one midwifery paper, midwives described feeling invisible and not being acknowledged,83 and another referred to the harsh mentorship they had received and lack of kindness from managers/mentors,116 with a third describing how midwives felt ‘scrutinised rather than supported by management’89 (p. e553). However, that same paper also describes how midwives in senior positions gain satisfaction from supporting others. Across all three professions, the lack of support when undergoing investigation or complaints processes was also highlighted (see Chapter 6, where this is discussed in more detail).
A relational-cultural cause mentioned in papers across all three professions was the stigma around talking about psychological health difficulties and accessing support. This was particularly prevalent in paramedic papers where it was stated that ‘disclosure of vulnerability in such a culture was perceived as a weakness’ (p. 9) and that the macho culture perpetuated not talking about mental health. 18 One paper talked about the bravado or stigma attached with the job ‘we all like to think we are infallible. We are there to support the public in (their) time of need, but we tend to not ask for help ourselves’95 (p. 226). All three professions described their concern that disclosing mental health difficulties may have a negative impact on their careers. One report highlighted that staff were particularly unlikely to access support services if situated in their own place of work and have concerns about confidentiality where staff are unable to self-refer. 25 A common theme in the midwifery and paramedic literature (as they were more likely to discuss exposure to trauma) was the lack of space and/or time to debrief after experiencing trauma (or generally having inappropriate support for this). One nursing paper96 described ‘disenfranchised grief’ for the way nurses may be made to feel after the death of a patient – that it was not their ‘place’ to feel loss or to grieve. Together with lack of spaces and/or time, across all three professions the lack of attention paid to basic ‘hygiene’ needs was highlighted (e.g. parking, food, water, bathroom breaks),9,30,34,89 with one report74 stating that this ‘appears to have become an accepted part of everyday practice’.
Profession-specific ‘support’ causes
Lone working was a specific (negative) feature of work mentioned in three nursing papers that focused on specific types of nurses [clinical nurse specialists for chronic conditions;118 emergency nurse practitioners (ENPs) based in minor injuries units;99 and children’s community nurses based in rural or remote areas],119 but this ‘cause’ is also relevant to any nurse, midwife or paramedic that works predominantly on their own (e.g. critical care paramedics who may spend most of their shift in a car on their own except for when attending incidents with other crews on scene; and nurses and midwives in rural/remote areas with a community caseload who may not often see their team members).
Relationships
Having poor relationships with colleagues and/or incivility and bullying was highlighted in papers across all three groups as being a causative factor for psychological ill-health. 9,34,83,123 In one midwifery review, they referred to the ‘cultural normalisation of dysfunctional relationships’83 (p. 433) to describe how such relationships have become expected and normalised rather than resolved. Such poor relationships can be within or between staff groups: in the midwifery literature, there was reference to challenges in multiprofessional relationships within teams or clinical areas in particular their relationships with obstetricians,89 as reflected in several high-profile maternity reviews,137,141 and in the nursing literature one paper described tensions between palliative and non-palliative staff. 110
Profession-specific ‘relationship’ causes
With regard to relationships with patients, while the nursing and midwifery literature was more likely to refer to the emotional impact of having empathic relationships with patients;100) in the paramedic literature the focus was on fear of assault and/or abuse from the public including physical abuse, intimidation, and sexual harassment. One paper described the physical and emotional stresses being common occupational hazards for paramedics. 124 This aspect of work was also reported in a paper focused on nursing in secure forensic units111 and emergency nurses in A&E departments. 23
Role
Newly qualified staff were a main ‘at risk’ group, identified particularly in the nursing and midwifery literature. The transition from being a student to being newly qualified is described as a ‘transition shock’ or ‘reality shock’. 142,143 One paper73 refers to nurses being uncertain about their competence, unrealistic expectations from managers, and not wanting to make mistakes; and another126 describes feeling unprepared. A related theme in the nursing and midwifery literature is values incongruence (also described as a ‘theory-practice gap’): whereby the work environment does not enable staff to practice how they thought they would and want to. 30,75,128 Issues in relation to role boundaries or clarity were mentioned across all three professions, some referring to a lack of understanding of role by others generally (e.g. lack of understanding of nursing work by others;87 unclear boundaries between midwives and colleagues;91 or in relation to particular subspecialisms such as EPNs feeling they had blurred role boundaries with doctors and advanced practitioners;99 prison nurses being a new/young specialty and describe feeling invisible: ‘literally hidden away from the world. This physical “hiddenness” appears to translate into a professional “hiddenness”’52 (p. 163). In the paramedic literature, a conference abstract referred to the conflict that managers feel between their varying roles as ‘manager, clinician, peer, referrer, adjudicator, parent figure, appropriate person and challenger’56 (p. 44), and the tension between performance management and staff support roles. ‘Role intensity’ was described in a nursing-focused literature review130 to capture the stress of work that goes beyond quantitative workload for example, satisfaction with workload, impact of disease acuity. In a blog, one midwife stated: ‘Many times I have cared for someone and thought “this is edging the limits of my training here”’101 (p. 398) describing the intensity caused by increasingly complex care needs due to the changing maternity population (e.g. women having babies later in life, high prevalence of obesity and associated health conditions, and women with more severe pre-existing health conditions having babies). There were no profession-specific ‘role’ causes evident in the literature.
Change
Organisational changes in healthcare provision, and in particular poor management or communication in relation to change – as well as the constant and rapid changes – was a cause of psychological ill-health reported across all three professions. This included the frequent changes in clinical practice reported in neonatal settings, due to medical advances;106 the need for greater involvement in change implementation – particularly in more junior front-line staff – to reduce their sense of ‘powerlessness’ and aid successful implementation of changes in acute mental health wards;78 and for paramedics, the ongoing changes to the scope of their role, and organisational and management changes having key impacts on psychological well-being. 22 In the King’s Fund report30 the hierarchical structures in health care were described as inhibiting ‘voice and influence’ (p. 37), and in the WHELM report,74 management were described as making changes as ‘knee jerk reactions to problems’ and ‘not listening to the staff … and valuing the resources that they have in their collective knowledge, skills and care that they give to women and each other’74 (p. 24).
Aim (c) to examine the literature to understand better ‘who’ is at risk and ‘when’ including identifying the differences within and between our three professions of nurses, midwives and paramedics, going beyond demographic and individual characteristics to also consider the impact of different work environments
Who is most at risk?
Individual characteristics
There have been many quantitative observational studies that have attempted to measure risk factors for burnout/psychological ill-health including individual predictors such as demographic factors. Methodological differences in measures and poor-quality studies make these challenging to synthesise, but in general, it is accepted that demographic variables are poor predictors of work-related psychological ill-health. 25
The exception to this is ethnicity, sexual orientation and/or gender identity, and disability: there is now increasing evidence, not least from the NHS Staff Survey and recent COVID-19 pandemic, that health-care staff from ethnic minority groups have greater exposure to aspects in their work that place them at greater risk of psychological ill-health. This includes that they are more likely to report experiencing physical and verbal abuse (from patients and relatives, have higher presenteeism rates, and are more likely to report working additional hours, as well as other inequities such as pay and promotion. 9,25,93 The Health Education England (HEE) NHS staff and learners’ mental well-being commission9 reported that additional risks for psychological ill-health existed for lesbian, gay, bisexual and transgender/transsexual people (LGBT+) and disabled staff. For staff identifying as LGBT+ the commission reported a wide disparity of experience, with staff in some Trusts facing hostility and discrimination that severely impacted their psychological health, and that many staff hid their sexual orientation for fear of bullying. A specific service architecture feature highlighted was the impact of rotational placements and/or lack of permanent team structure that exists in much healthcare provision, leading to staff having to constantly decide if/when/how to disclose their orientation. 9 Disabled staff are also more likely to report bullying/harassment from colleagues than other staff, and in the WHELM report74,128 midwives identifying as having a disability had higher levels of burnout.
Aside from mention in the reports cited above, we found no papers that focused specifically on ethnicity, sexual orientation, gender identity or disability; highlighting a major gap in our understanding of causes and interventions to mitigate psychological ill-health in these staff.
Professions and or subspecialties that may be at greater risk of psychological ill-health
In the included literature, there are several subgroups of the three professions that are presented as being at ‘high risk’. However, it should be noted that there are lots of articles written from the perspective of a particular profession/specialty, making the case for specific challenging features of their profession/specialty (possibly to justify publication), though as can be seen in Table 6, few of the ‘causes’ identified are unique and can be applied across all three professions. Below are some of the role/job related risk factors that have been identified in this review that may be worthy of further attention, particularly in relation to interventions.
Newly qualified nurses/midwives/paramedics
As mentioned earlier in this chapter, various papers discuss the ‘transition’ or ‘reality’ shock of being newly qualified, leaving student status behind and becoming a qualified health professional (see Table 6). 90,126 In part this is due to a ‘theory-practice gap’ (see early in chapter and Chapter 6),90,128 as well as a lack of confidence to speak out (when encountering bullying, lack of support, feeling out of control). 90 One review describes newly qualified nurses only becoming ‘insiders on the team’ (e.g. accepted/valued) when they are viewed as capable. 123 While many articles focused on the ‘newly’ qualified (first year or two of practice), evidence suggested that risks of psychological ill-health associated with being ‘less experienced’ continue for up to 10 years from qualification. 77
Location: hospital versus community
There was a suggestion in some of the literature that working within a hospital setting placed staff at greater risk of bullying, harassment and abuse,76 but this contrasted with other literature that highlighted the social and professional isolation that professionals in the community may experience together with the distinct environmental risks from providing care in the home or other non-clinical environments such as schools and thereby having fewer safeguards in place. 97,119
Being a ‘leader’
The issue of managers requiring support as well as undertaking the role of providing support was highlighted in a few papers. 110
Working in an ‘orphan’ specialty (distinct, young or neglected)
There were several papers focused on individual specialties that highlighted the distinct nature of their work and often their feelings of ‘invisibility’, where there has perhaps been less research or policy attention. This included district nurses97 and children’s community nurses in rural/remote areas. 119 There are also ‘new’ professions (including paramedic science, existing since the 1970s) or distinct subspecialties, such as prison nursing, where there has been much less research. Prison nursing has various unique features, not least the need to balance caring versus custody, lack of understanding of the role by others, and poor visibility of the profession both within nursing and to the wider public. 52 There are likely to be other such ‘orphan’ subspecialties omitted from the literature, and a gap-analysis should be undertaken to inform future research regarding causes and interventions.
Working with a ‘high-risk’ patient group
Several patient groups were positioned as being particularly ‘high risk’ in relation to causing stress and psychological ill-health. This included the following:
-
adult critical care nursing144 and end of life care:96 due to the emotional toll of exposure to death.
-
paediatric versus adult nursing: evidence here was conflicting, but several papers described the greater impact of paediatric care. For example, one paramedic paper describing a failed resuscitation attempt on a child saying ‘certain calls would affect me more than others’;95 and a nursing literature review93 describe paediatric nursing as positioning nurses at greater risk due to the high potential for empathic engagement and complexities in relationships with families93 and a review of neonatal nursing also describing this emotional labour as being a key part of what makes it a higher risk environment to work in106 due to advances in medicine leading to longer hospital stays (greater emotional support for parents) and more ethical dilemmas relating to end of life care resulting in MD.
-
Mental health nursing: papers focused on nursing in mental health inpatient settings describe the volatile, fluctuating environments with highly distressed patients as distinct stressors73,85 and thereby higher risk of psychological-ill health. One paper focused on burnout in high secure forensic psychiatric units, found rates to be comparable or lower than community or non-secure mental health nurses,145 suggesting perhaps that it is less about patient acuity and more about environmental factors linked to staff safety and support. However, a review of nursing in secure forensic mental health settings highlighted a unique feature of the environment relating to ‘gender and sexuality’: that although locked wards were single-sex, they had both male and female staff, which can sometimes leave female staff feeling vulnerable and marginalised. 111 Liaison psychiatric nurses78 may also have distinct features that place them at risk due to exposure to people with high levels of distress in the context of pressure for quick turnaround, multiple interfaces, liaison with gatekeepers, and little or no continuity after discharge.
-
Chronic illness: nursing provision for patients with chronic illness (e.g. inflammatory bowel disease118) was identified as a risk factor due to the increasing complexity of the treatment and management of patients, the emotional labour of the long-term relationship with patients, and lone working if they are the only specialist nurse in the hospital/setting.
-
emergency nurse practitioners: risk factors include99 exposure to trauma, not being taught to deal with death (unlike doctors), blurred role boundaries and identity and being expected to practice beyond their scope. ENPs may also feel geographically isolated if they work in a minor injuries unit that are distant from a hospital.
‘When’ are nurses, midwives and paramedics most at risk of psychological ill-health?
Several time points were identified when nurses, midwives or paramedics may be at increased risk of psychological ill-health. As well as when newly qualified (covered above), this included the following:
After trauma exposure
Several papers, particularly in the paramedic and midwifery literature, focused on the need for support and/or intervention after exposure to traumatic events or incidents (see Table 6). This is not surprising given the impact that such exposure is likely to have on staff and has been a major focus of some interventions (see Chapter 5). The priority placed on this, perhaps at the expense of a focus on cumulative ‘lower grade’ stress, is discussed in the realist synthesis chapter (see Chapter 6). There is also discussion in some papers about the timing of such intervention and following National Institute for Health and Care Excellence (NICE) guidance146 to ensure that intervention does not risk intervening with the natural process of recovery (risking development of PTSD).
When under investigation and/or during complaints
The significant impact on staff psychological well-being of being under investigation or during complaints processes is described in a number of papers147–149 and the role of the organisation and regulatory bodies in supporting staff versus ensuring safe patient care is described in depth in Chapter 6 where the tension between promoting staff well-being within a blame culture that focuses on the individual rather than collective responsibility.
Key findings
-
There are more similarities than differences in causes of psychological ill-health among nurses, midwives and paramedics.
-
Some causes may be more prevalent or exacerbated in certain professions, or roles within profession (rather than being profession-specific). In most cases it is the service architecture that can increase risk rather than the profession itself.
-
Some individual characteristics deserve greater focus in the literature to ensure greater understanding of causes and interventions. This includes ethnicity, sexual orientation and/or gender identity, and disability. Multi-level systems approaches are required that consider intersectionality and structural differences between professions.
-
There is a need for targeted interventions based on specific workplace settings/service architecture, to support particular staff groups, and at specific times when they may be at greater risk of psychological ill-health.
Chapter 5 Strategies and interventions proposed for mitigating psychological ill-health in nurses, midwives and paramedics: a descriptive analysis
Introduction
This chapter reports on a descriptive analysis of the interventions that have been evaluated and/or are recommended to mitigate psychological ill-health in nurses, midwives and paramedics in our sample of included literature. Our aim is to provide an overview of the interventions in the included literature, and to provide a contemporary update on the focus of intervention research in nurses, midwives and/or paramedics in recent years. There have been many systematic and comprehensive reviews of workforce well-being interventions,25,150 so the aim of this realist review was to build on that work and take a wider lens by including grey and non-empirical literature, which may identify different types of interventions and/or help explain why the existing evidence-based interventions are not yet making sufficient difference to the psychological ill-health of the workforce. Akin to Chapter 4, this chapter provides an overview and context for the realist synthesis of the included literature (see Chapter 6) and starts to answer a key aim stated in our protocol: to identify which strategies/interventions to reduce psychological ill-health work best for these staff groups, find out how they work and in what circumstances these are most helpful.
See Chapter 3 for the methods.
In this chapter we aim to
-
describe the interventions that are evaluated and/or recommended in the literature, according to
-
their intended level of action: primary, secondary or tertiary (or multifocal);
-
whether they are formal or informal interventions.
-
-
compare the types of interventions evaluated and/or recommended in the literature according to ‘type’ of paper, and professional group (nurse, midwife, paramedic);
-
assess the ‘fit’ of available interventions to the key causes identified in Chapter 3.
Results
The interventions were categorised according to their intended level of action (primary, secondary or tertiary) and whether they were formal or informal, though it was sometimes hard to attribute to these categories with confidence (see Tables 7–10).
In addition to the data presented in Tables 7–10, some of the papers described ‘negative’ or dysfunctional solutions to workplace stress, including leaving the profession105,148 or even suicide. 95,101,105,109 Many also included mention of the need for interventions for students/pre-qualification,9,34,114,151 including the need for universities and NHS to work collaboratively to reduce the theory-practice gap90 (see Chapters 4 and 6). Student well-being is outside the remit for this study, so these interventions are not included here, though are acknowledged as being an important focus for any strategy to mitigate mental ill-health in the healthcare workforce.
Very few papers described interventions that did not work or should not be used. This is not surprising given the likelihood of publication bias (negative findings being much harder to publish), but such studies would be extremely helpful. Commentaries and editorials were mostly focused on what needed to be actioned and happen. Ineffective interventions included critical incident stress debriefing (CISD), reported as ‘neutral at best and harmful at worst with respect to preventing PTSD’18 (p. 2) due to interfering with natural recovery; and psychological first aid, which has been shown to have an impact on raising awareness of psychological well-being, but is not effective at changing behaviour,25 and argued to be simply ‘not enough’ due to the multifocal approach required to tackle the systemic issues87 (p. 1). There was also debate regarding the utility of OH in being part of the solution, being described as ‘rarely utilised and is seen by most members of staff as being for extreme cases’91 (p. 21), and the SOM report acknowledged the low uptake (and need for more clarity about their role and processes) and called for OH staff to have ‘training, resources and tools to meet the needs of staff’25 (p. 8).
Aim 1: describe the interventions that are evaluated and/or recommended in the literature
A total of 115 different types of interventions were either evaluated and/or recommended in the included literature. These spanned primary (n = 52), secondary (n = 46), tertiary (n = 6) ‘levels’, and multifocal (n = 11) interventions. A total of 71 of these were classified as being ‘formal’ interventions (including all tertiary and multifocal interventions) and 44 ‘informal’ interventions (see Tables 7–10).
Note: virtually all empirical reviews of interventions (and key reports) concluded with strong caution about the limitations of the evidence-base, being based upon studies that had weak designs and/or measures (e.g. lack of control groups, measures that had low reliability and/or validity) and inability to synthesise due to heterogeneity between studies.
The interventions are presented in Tables 7–10 and discussed according to their intended level of action below.
Primary interventions
Formal
Formal primary interventions (see Table 7) included several interventions with a pre-existing evidence-base that were whole systems/healthcare models, including the Buurtzorg model30,87 (originating in the Netherlands, aimed at providing a devolved holistic care system where nurses have a flat hierarchy and autonomy to provide person-centred care across health and social care boundaries), and US Magnet Recognition Scheme, currently being evaluated in the UK. 30 Several papers also included reference to service/pathway models that enabled continuity of care and were associated with better staff well-being, such as the ‘caseload’ model in maternity;30,77,152 and three ‘good practice’ organisational interventions aimed at addressing inequality. 30 Several sources across the nursing, midwifery and paramedic literature referenced frameworks, toolkits or standards to be used/followed/implemented in order to mitigate psychological ill-health. Some were profession-specific, such as a work-life balanced code of practice proposed by the now defunct Larrey Society (Ambulance Service Think Tank, est-2017),153 and others were NHS-wide, including the NHS Health and Wellbeing Framework. 9,25,154
| Formal | Informal | |
|---|---|---|
| Primary: reduce risk at source | SYSTEMS/HEALTHCARE MODELS +/- CULTURE CHANGE Buurtzorg model30,87 Magnet Recognition Scheme30 Continuity/person centred care models, for example, caseload model (midwifery)34,77,152 Collaborative Care Model31 Rainbow Badge Project (LGBTQ+)9 Creating just cultures (Mersey Care NHS Trust)30 EDI (NE London NHS Trust) inc. reverse mentoring30 |
CULTURE CHANGE NHS (as employer) acknowledging/taking responsibility for role in supporting staff well-being156 Creating supportive/positive workplace culture81,87,96,130 Systemic approach to well-being74,101 Leadership training30,34,74,98,129,148,151 Mandate staff to challenge poor behaviour83 |
| FRAMEWORKS/TOOLKITS/STANDARDS NHS England’s Healthy Workforce Framework114 Safe Staffing Monitor and Planning155 RCN Healthy Workplace Toolkit25 RCN Caring For You campaign157 NHS Health and Wellbeing Framework9,25 NHS workforce well-being guardians and leaders48 Adoption of Larrey Society ‘work life balance code of practice’153 Adoption of ‘Thriving at Work’ (2017) mental health core standards9 Implement Boorman 5 whole system changes: identification/response to local need; engagement of all staff; involvement, visible leadership and upskilling of management and board staff31 |
FRAMEWORKS/TOOLKITS/STANDARDS Policy for managing stress/staff mental health with action plan and strategy for implementation25 Rapid access referral pathways (via primary care/occupational health)9 |
|
| WORKING CONDITIONS Tackle retirement barriers77,95,111 Flexible working/plan own workload77,94 Remove Pay Cap/restraints155 Ensure Student Bursary remains155 Assault on Emergency Workers Bill105 Zero tolerance policies123 Workplace social capital31 Mutual Aid approach to flexible staffing30 |
WORKING CONDITIONS Introduce minimum standards for facilities and working conditions; rotas based on realistic forecasting30,83 Deploy and develop alternative roles (e.g. admin support staff; maternity support workers)30 Planned time-out of setting111 |
|
| SUPPORT/CAREER PROGRESSION Mentorship32,82,90,116 CPD/Career Progression Programme for senior Children’s Palliative Care Nurses110 Community of Practice Clinical Network119 |
SUPPORT/CAREER PROGRESSION Chaplaincy service35,96 Social/professional networks and support158 Positive role models90,130,148 Additional support/mentoring for ‘critical moments’34 Support managers emotional well-being and needs74 |
|
| EDUCATION/TRAINING Implicit Bias Training79 Various diet and exercise related intervention programmes for example, Treatwell 5-a day campaign; wellness programme (walking)31 |
EDUCATION/TRAINING Learning and education throughout career30,83 Manager/employee training to recognise early signs/assist staff who disclose35,98,114,120,153 Mental health awareness for family, friends and loved ones94,114 |
|
| SOCIETAL World Suicide Prevention Day105 World Mental Health Day121 |
SOCIETAL Public showing kindness and compassion131 |
Primary interventions also included those focused on improving or changing working conditions, including tackling retirement barriers (e.g. reducing retirement age, allowing phased/partial retirement,77,95 and financial barriers to recruiting/retaining the workforce;155 and interventions that supported flexible working and/or gave workers more control over their work schedule. 77,94 Several sources also referenced the benefit of or need for policy-level intervention, including the Assault on Emergency Workers Bill105 and ‘zero tolerance’123 (to support safety of staff at work). In relation to support and/or career progression, several sources across all three professions described the provision of formal mentorship/community practice schemes;110,119 only one training course was categorised at ‘organisational’ level and that was ‘implicit bias training’ recommended in an editorial focused on tackling racism in healthcare provision and wider society. 79 At a societal level, two paramedic-focused editorials mentioned World Mental Health Day/World Suicide Prevention Day campaigns as ways of raising awareness of psychological ill-health in staff and/or encouraging action. 105,121
Informal
There were many different ‘informal’ primary interventions recommended in the included literature (see Table 7). By their informal nature, these usually lacked clarity regarding definition or content. These included recommendations for culture change: for the NHS to take responsibility as an employer for staff well-being; to create a supportive and/or positive workplace culture; for systemic change (including calls for changes in attitudes towards mental health, meaningful recognition of the importance of staff well-being, and systemic approaches to development and provision of initiatives that support better staff well-being and welfare) and role modelling, for example, about the importance of self-care. 81 ‘Good’ leadership was a key recommendation or intervention in many included sources, with ‘good’ being described variously as collective, shared, compassionate, person-centred, authentic, relational or sympathetic. While leadership training could be a formal intervention, and formal leadership courses exist for NHS staff, for example, HEE NHS Leadership Academy,159 and King’s Fund compassionate leadership training,160 no such ‘formal’ interventions were specially recommended or described in the included literature. In relation to frameworks, one high-profile report25 described the need for organisations to have a policy for managing stress/staff mental health with an action plan and strategy for implementation, highlighting the numerous previous ‘recommendations’ that have not been implemented as intended (or at all).
In the nursing and midwifery literature, there were various recommendations for changes to working conditions, including the introduction of minimum standards for facilities and working conditions;83 rotas based on realistic forecasting;30 and the development of alternative roles to support nurses and midwives (e.g. admin support staff, maternity support workers). 30 One paper (examining nursing staff experiences in high secure forensic mental health settings111 argued a need for planned ‘time-out of the setting’ (p. 2904) with high-frequency of violence/aggression, a suggestion that would be likely equally applicable to other professions, such as paramedics and adult dementia care. Having planned ‘time out’ as an intervention is not new, being common to medical training. 161 In relation to support/career progression, several sources described the often-overlooked role of the chaplaincy service in supporting staff well-being,35,96 and the importance of supporting the development of social and professional networks at work. 158 One paper specifically mentioned the need to ensure that additional support and/or mentorship was put in place for what they described as ‘critical moments’, for example, when newly qualified, exposed to trauma, or subject to investigation/complaint. 34 The importance that managers were provided with emotional support was highlighted in a further report. 74
A key report30 recommended that learning and education in relation to mental health and well-being should be a feature throughout careers, and several sources recommended that training staff to recognise and act upon early signs of psychological distress was important. 35,98,114,120,153 Two sources, both paramedic-focused, explicitly acknowledged the role of family, friends and loved ones in identifying, signposting and supporting staff impacted by experiences at work, and that they too should be offered such training. 94,114 There were also several interventions aimed at wider well-being: diet and exercise focused. 31 Finally, at the societal level, one paramedic-focused editorial131 acknowledged the positive impact of the general public showing kindness and compassion on emergency healthcare workers’ well-being (in relation to the Grenfell Fire major incident).
Secondary interventions
Formal
Formal interventions aimed at addressing essential needs at work were rare, but included one aimed at improving conditions and needs at work generally31 and specific initiatives regarding hydration and out of hours food for staff. 30
A range of formal psychosocial interventions, based on mindfulness, were evaluated and/or recommended within many of the included sources (see Table 8). This included specific applications or platforms aimed at supporting practice of reflection/mindful activity. In addition, several nursing-focused papers recommended various psychosocial education programmes, including stress-management91 and resilience training,32 and positive psychology training programmes. 106 These programmes included interventions such as ‘Three Good Things’106 and ‘Thankful Events’162 – both of which are underpinned by ‘positive psychology’ (Seligman163).
| Formal | Informal | |
|---|---|---|
| Secondary: modify response to exposure |
Essential needs at work: NHS workplace wellness intervention31 ‘Think to drink’ campaign (tackling dehydration)30 Access to food out-of-hours (Royal Free NHS Trust)30 Psychosocial Interventions Mindfulness training25,74,93,106,108,144,164,165 NHS In Mind (www.nhsinmind.co.uk)166 Calm App166 Headspace App166 |
Self-care: essential needs Space and time to care for self/self-compassion (and others)9,25,35,87,156,158 Exercise18,31,96,98,105,158 Hobbies/interest outside of work96,158 Good diet and nutrition31,96,98,158 Get enough sleep96,98 Take regular breaks/holidays from work9,158 Self-care: herbal remedies, message therapy158 Basic needs met at work: lockers, showers, food and drink etc.9 and personal safety23 |
| Psychosocial education Stress-management training22,91,106,112,122 Resilience training32,112 (Army) Care Provider Support Program32 Positive Psychology training106,122,162 PTSD prevention TRiM (Trauma Risk Management Training)9,18,33,35 Road to Mental Readiness Programme (Canada)114 Group reflection/debriefs Debriefs80,82,105 Reflective practice groups25,78 |
Stress-management Mindfulness practice81,87,96 Yoga/meditation32,96,162 Reflective practice (alone/group)87,124,167 Stress-management techniques/coping skills32,158,167 Cultivate/encourage positive beliefs and coping strategies87,156,158 Learn to say ‘no’ set boundaries98,156 Using Lego as art therapy/mindful activity168 Use of (dark) humour18,22,33,107,169 Coaching22 Time-out/downtime18,98 |
|
| Training in job-specific skills Communication skills112,162 Professional Identity Development Programme162 Job/role specific workshops93,162 Social support Tea and Empathy Group9 #WeCARE café30 Interdisciplinary teamwork (NHS Lanarkshire)30 Quality Improvement Collaborative Programmes (Royal College Paediatrics and Child Health)30 |
Social support Talking to family/friends18,80,158 Talking with colleagues/peer support/huddles9,18,32,35,82,95,98,130,156,167 Team culture/relationships with colleagues18,87,101,111,116,130 Access to psychologically safe, confidential spaces to socialise, share and discuss experiences, and rest/wobble room9,87 Managers checking in18 |
There were several interventions that were specifically focused on reducing the risk of PTSD after exposure to traumatic events. The most reported intervention, used as a standard intervention in many UK Ambulance Trusts, is trauma risk management training (TRiM). 9,18,33,35 Originating in the military, it is a trauma-focused peer support system based on ‘watchful waiting’ whereby trained ‘peers’ offer a first point of contact to share and discuss the traumatic event and signpost to professional help if needed.
It has been increasingly introduced to health care as an alternative to CISD, which has been shown to potentially cause harm (as mentioned earlier in this chapter). An alternative to TRiM mentioned in one paper is the Road to Mental Readiness Programme (originating in the Canadian military), consisting of mental health resilience education and training. 114
Formal group reflection and/or debriefs were also cited in a range of sources across the three professions (see Table 8). Debriefing mostly focused on ‘hot’ debriefs: short structured debrief immediately after events, intended to defuse and allow processing and learning from what had been experienced. 80,82,105 Reflective Practice Groups were also reported to support mental health and well-being: formal groups that facilitate reflection and critical thinking in a safe supportive environment. 25,78
In relation to training in healthcare job-specific skills, communication skills’ programmes were reported to be associated with well-being benefit in two reviews,112,162 with one also reporting positive benefit from a Professional Identity Development Programme. 162 Job-specific education/skills-training enhanced confidence and competence in the role according to two literature reviews (working with paediatric chronic pain for paediatric nurses,93 and assessment and treatment of schizophrenia for forensic nurses). 162
Several organisation-specific initiatives were identified in included reports, including a Tea and Empathy group (national peer-to-peer support on Facebook)9 and #weCARE café, providing a café and garden space for staff to decompress, socialise and have access to listeners who can refer for further support if needed. 30
Informal
Many of the sources referred to self-care in relation to the ‘essential’ elements of Maslow’s Hierarchy of Needs:170 the physiological needs (shelter, water, food, warmth, rest and health) at the bottom of the pyramid that need to be satisfied before individuals can attend to needs higher up the pyramid (including psychological). The importance of these needs being met was reinforced by many sources, with one report stating that a culture in which self-care is normalised is needed. 9 Essential self-care informal interventions included having space and time for food, hydration, exercise, sleep, and having breaks/holidays from work (see references in Table 8). One report highlighted that work-specific needs are often lacking in the workplace: having lockers to keep belongings safe; access to showers; access to food (ideally healthy, hot) 24/7 etc.;9 and personal safety referred to in another. 23
In relation to stress-management, many sources referred to the importance of using individual-focused relaxation, reflective and/or mindful practices, or using stress-management techniques and positive coping skills – and the benefit of such activities (without referencing specific formal interventions) (see references in Table 8). An informal intervention prevalent particularly in the paramedic literature (though also seen in nursing literature) was the use of humour – and dark humour – as a way of mitigating psychological ill-health. 18,22,33,107,169 Understood as an informal aspect of service architecture for staff mental well-being, dark humour is noted in the literature as requiring a sensitive adoption so as not to upset or offend patients, members of the public, or other colleagues, and may take some adaptation for newly qualified staff.
Across all three professions, many sources referenced the importance of social support in relation to informal conversations with family, friends and colleagues (peer-support); and the importance of a positive team culture and having good relationships with colleagues18,111,116 (akin to findings from CUP-1,17 and other previous research highlighting the importance of the ‘family at work’140). This included the importance of team stability to well-being,30 for example, paramedics having a regular ‘work partner’ (crew member in the ambulance). 18 Messaging such as ‘It’s OK to not be OK’ and ‘Be Kind’ were felt to be important messages to encourage a more open person-centred team culture. A ‘Going Home Checklist’ developed by Doncaster and Bassetlaw NHS Foundation Trust (https://www.dbth.nhs.uk/news/the-going-home-checklist/) suggests checking in with colleagues and texting a buddy as a way of perhaps attempting to formalise these important informal contacts. 156 Having access to spaces where staff can socialise, share, discuss experiences and rest (with reference to the essential self-care above) was a key recommendation in several sources, and discussed further in Chapter 6. In a qualitative synthesis of psychological ill-health and help seeking in trauma-exposed emergency service staff,18 the importance of managers simply ‘checking in’ with staff was reported, provided it was perceived as being genuine and authentic (and not ‘tick-box’, something that may be altered if such an intervention became formalised, see Chapter 6).
Tertiary interventions
No ‘informal’ tertiary interventions were found in the included literature (see Table 9). This is perhaps not surprising given that these interventions are targeting those in whom psychological ill-health has been identified, and there are robust evidence-based guidelines for treatments. 146,171 Interventions found in the NICE guidance were referenced as being helpful, such as cognitive–behavioural therapy (CBT), acceptance and commitment therapy (ACT), counselling and eye movement desensitisation and reprocessing (EMDR) (see references, Table 9). While several recommended counselling, one report stated the importance of this being independent from the employer,153 and an independent counselling service172 recommended in a commentary by a paramedic who had experienced psychological ill-health. 109
| Formal interventions | |
|---|---|
| Tertiary: reduce/minimise negative effect |
CBT/ACT22,32,112,120 Counselling95,109,124,153 Eye movement desensitisation and reprocessing (EMDR)22,114 Talking therapies91 Telephone support line/Samaritans9,18,87 SWAST: Staying Well Service109 Complementary/alternative therapies22,74,91 |
Several sources recommended the provision of 24/7 telephone support, with one report recommending the development of a national NHS ‘Samaritans’ emotional support service,9 which since COVID-19 has been introduced. 173 One paramedic-focused commentary recommended their Trust-specific ‘Staying Well Service’,174 which offers support and referral. 109 A few papers also recommended complementary/alternative therapies. 22,74,91
Multifocal interventions
Despite numerous reports over the past decade calling for systems approaches to well-being that target primary, secondary and tertiary levels25,150 we found relatively few interventions in the literature that had this aim, and no ‘informal’ interventions (see Table 10). Arguably the ‘intervention’ central to the NHS that should be primary, secondary and tertiary focused is OH, however as reported earlier in this chapter, OH is typically seen as being for extreme cases only and currently underutilised.
| Formal interventions | |
|---|---|
| Multifocal: mix of primary and/or secondary and/or tertiary |
Occupational Health9 Preceptorship Programme;175 peer support within preceptorship programme73,77,90 Clinical supervision: resilience-based;127 CBT-based;9,25,34,74,82,93,94,111,112,118,148,156; restorative supervision;32 FoNS person-centred resilience-based clinical supervision;87 professional midwife advocate156 Schwartz Rounds9,18,25,96 Blue Light Programme9,22,35,82,95,114 Beyond Blue (Australia)35 The Ambulance Services Charity (TASC) support for staff/families95 POPPY (PTSD Prevention Training)103 NHS workplace well-being intervention31 Workplace Social Capital Intervention31 Step-Ahead ecological intervention31 |
In relation to support for staff that straddled both primary (prevention) and secondary (mitigate impact of exposure) targets, several sources recommended and/or evaluated preceptorship programmes for newly qualified staff and clinical supervision models for all staff, particularly in nursing and midwifery. Preceptorship programmes have been found to vary widely,73 and a range of different supervision models were cited, including the following: resilience-based; CBT-based; restorative supervision; and person-centred resilience-based supervision models (see Table 10), as well as the professional midwife
advocate model (which has recently been adapted for nursing). 176 In some professions/roles, clinical supervision is mandated, but in others remains a voluntary component of the job, and there are calls for changing this to ensure supportive networks are in place for staff, for example. 156
Aside from these training and support interventions, there were some specific interventions and programmes recommended in the literature including Schwartz Rounds, a rare example of a whole organisation group reflection intervention that enables sharing and hearing of the emotional, ethical and social challenges of work in a safe, confidential, structured space. Schwartz Rounds have an evidence base demonstrating benefits at individual and organisational levels140,177 in relation to staff well-being and culture change (thereby straddling primary and secondary targets). In the paramedic-focussed literature, a key multifocal intervention cited by many sources is Mind’s Blue Light Programme178 providing information and advice as well as access to urgent help if needed (via a confidential helpline or text service to trained volunteers). Similar support is provided via The Ambulance Services Charity. 179 Finally in the midwifery literature an intervention called POPPY (Programme for the Prevention of PTSD in midwifery) has been evaluated positively,103 consisting of a stepped care process combining education and supportive resources, including access to trauma-focussed clinical psychology if required.
Aim 2: compare the types of interventions evaluated and/or recommended in the literature according to ‘type’ of paper, and professional group (nurse, midwife, paramedic)
Types of interventions in empirical literature versus non-empirical literature
Examination of the literature from the initial search that focussed on interventions to prevent/mitigate staff psychological ill-health (n = 39/75 sources) showed that empirical papers that evaluated interventions (n = 10/39 nursing = 7, midwifery = 3, paramedic = 0) focused on one single intervention (6/10) or intervention programme (4/10), compared to editorials/commentaries (n = 29/39) in which most (16/29) had a multifocal focus, recommending multiple interventions (range 1–10, mean 3.3 interventions per paper).
In addition, empirical papers all focused on ‘formal’ interventions (10/10) mostly aimed at individuals (6/10) (i.e. mindfulness training or clinical supervision/preceptorship), whereas only seven editorials and commentaries focused solely on formal interventions, most describing/recommending a mixture of formal and informal interventions (n = 15/29) (see Appendix 8, Tables 26–28).
In terms of interventions: three evaluated mindfulness training,108,144,164 four focused on clinical supervision or preceptorship,73,118,127,175 two evaluated interventions aimed at lessening the effects of exposure to work related trauma,78,103 and one was a career progression programme110 (see Appendix 8, Table 27).
The 29 literature reviews included in our review (which comprised qualitative evidence syntheses and those focused on explaining causes and solutions, as well as systematic reviews of interventions) revealed a different picture (see Appendix 8, Table 29). Five did not include reference to any interventions. Seven aimed to evaluate interventions, and of these all except one were focussed on secondary level interventions. The exception was Brand et al.,31 which aimed to identify and evaluate whole-systems approaches to well-being and identified a range of different multifocal programmes.
Types of interventions by professional group
The focus of included evaluation studies (either primary or secondary evidence) was predominantly secondary level (e.g. mindfulness, stress-management programmes) across all three professions. Of the ten empirical papers, three focused on newly qualified nurses/midwives; two on midwives, and five on a range of different types of nurses (see Appendix 8, Table 27). When including the wider literature from commentaries and editorials, there were few differences by professional group: though paramedic-focussed papers tended to focus on secondary level intervention (for trauma) more than nursing and midwifery papers (see Appendix 8, Table 28).
Aim 3: assess the ‘fit’ of available interventions to the key causes identified in Chapter 3
The identified interventions were mapped to the causes identified in Chapter 3, based on the intended key aim of interventions. We then graded the causes: red, amber or green according to the extent to which interventions that tackled these causes existed in the literature (see Appendix 9, Table 29).
Note: important caveats are that (1) the literature we included may not reflect what is actually happening on the ground; (2) we did not run searches specifically for interventions aimed at these causes; (3) the mapping and categorisation process require an element of judgement and may not be comprehensive but is intended as a starting point for identifying major gaps between causes and interventions.
The results of this process indicated that for the majority of the causes, there exist some formal and/or informal interventions but more evidence and work is needed; areas where intervention knowledge appears strongest are for exposure to trauma (including experiencing death); there are several identified causes of psychological ill-health where there may be no interventions currently, this includes many of the identified profession-specific causes (and thereby the ‘who’ and ‘when’ factors), including service architecture features such as working on call; lacking continuity of care; unnecessary call-outs; high risk of sustaining injury; being a profession under scrutiny; lone working; fear of assault/abuse from the public/patients. We also found no interventions aimed specifically at supporting staff through investigations or complaints despite this being a known key cause of psychological ill-health.
Key findings
The overarching findings from this descriptive analysis are as follows:
-
there are many ‘informal’ interventions that are cited to be beneficial or recommended, some of which have been formalised or could be formalised. These are perhaps informally developed to plug gaps in current provision and may help explain why current provision is not working to mitigate psychological ill-health;
-
interventions (both formal and informal) exist at primary, secondary and tertiary levels, most focus on individuals; very few interventions were profession specific;
-
few of the interventions that we found in this review were tertiary or multifocal ‘systems’ approaches, and we found no informal examples of these. Tertiary interventions are generally well evidenced (e.g. evidenced in NICE guidance), but our review suggests multifocal interventions are under-researched;
-
more attention needs to be paid to how the primary, secondary and tertiary levels can and should work together to provide a systems approach to prevent, mitigate, and treat psychological ill-health in staff;
-
most empirical papers evaluating interventions focussed on one single intervention, whereas most editorials and commentaries recognised the need for multi-level systems approaches;
-
interventions and strategies in the literature tended to focus on short-term goals, simplify and reduce issues and not take into account complexity, probably because this is practically and methodologically easier.
Chapter 6 Realist synthesis
Introduction
Previous chapters have mapped and described the literature on causes of psychological ill-health (see Chapter 4) and identified the range of interventions to prevent, reduce or treat psychological ill-health that have been evaluated and/or written about in the recent literature, including both formal and informal interventions (see Chapter 5). These chapters identify potential differences within and between professional groups, including who may be at greater risk of psychological ill-health, when and why. Despite the plethora of interventions in the literature, psychological ill-health remains prevalent in the NHS and, indeed is worsening. 3 This chapter explores and posits why this might be the case.
This chapter is thus drawing out the tensions we identified in the literature to explain
-
why psychological ill-health in healthcare professionals is still a huge and growing problem and has become entrenched in some settings;
-
why despite having interventions (some of which have an ‘evidence base’), the problem persists;
-
how we can optimise existing interventions, by analysing when and where they work suboptimally, as well as innovating and building upon what already exists.
Tackling staff psychological health is important for social, ethical and economic reasons. The IPPO report10 estimates the cost of staff psychological ill-health to the NHS as at least £12 billion a year, and as such, spending relating to staff well-being ‘should be thought of as an investment rather than expense’35 (p. 260). In this chapter, we present five key overarching findings and 14 tensions with 26 associated CMOcs.
In each ‘Key finding’ section we provide an overview of the finding, then CMOs are presented with supporting evidence following each CMO or group of CMOs. Mechanisms are reported as resources offered and responses to resources. Where responses are negative, this is indicated as (– response).
Key finding 1: interventions are fragmented, individual-focused and insufficiently recognise cumulative chronic stressors
Overview of key finding
Much previous literature has focused on descriptions or evaluations and syntheses of individual discrete interventions (potentially plug and play, ready for rollout), see Chapter 5. There is an implicit underpinning assumption that these alone may benefit well-being, without taking account of the wider context of the implementation of such interventions and the need for a dynamic ‘system’ of interventions contextualised to setting. We noted a prevalence of well-being solutions that are fragmented, individual-focused, with a non-aligned, incoherent approach, which conceptualises psychological ill-health as binary (ill or not) and focused on acute events rather than acknowledging any cumulative impact of work on psychological health. CUP-1 identified ‘It is also clear that complex problems require complex solutions, and so many interventions to tackle doctors’ mental ill-health are likely to be multi-dimensional and multi-level’17 (p. 57). CUP-2 found the same for nurses, midwives and paramedics and highlighted a dearth of multifocal system-level interventions (see Chapter 5), and despite many primary ‘organisation’ level interventions, many are policies or recommendations that should be implemented, rather than interventions that have already been implemented and evaluated. The ‘causes’ literature has often focused on acute traumatic incidents that lead to PTSD/secondary trauma, and by doing so has downplayed the cumulative impact and consequent ‘normalisation’ of low-level chronic stressors (see Chapter 4). We suggest a multilayered systems approach to psychological well-being is required; not a one-size-fits-all approach, but individualised and where everyday events, as well as acute events, are acknowledged as impacting staff psychological wellness.
One positive example was found in a review of support interventions for UK ambulance services staff22 who report that UK mental health charity Mind has undertaken more complex multipronged approaches to change culture in emergency services (including the emergency services psychological ill-health prevention and support the Blue Light Programme35,95 to try to get people to feel more able to talk about their psychological health and seek support. A second example was found within a report on nurse suicide36 Some of which suggested the need for evidence-based strategies to intervene at the personal, institutional and regulatory levels. The Blue Light Programme focuses on changing public perceptions of psychological health relating to front-line staff and seeking commitment for change from leaders, politicians and employers; setting up working groups and other activities designed to break down barriers and reduce stigma, as well as providing access to support via a confidential helpline. Another system-wide intervention strategy targeted at primary prevention (tackling the risk factors at their source) is the US Magnet programme now being implemented and evaluated in the UK. 180 This includes, for example, ‘shared governance’ and staff councils to enhance nurses’ and midwives’ roles in decision-making, fostering professional autonomy, exemplary professional practice and strong working relationships in multidisciplinary teams. Organisations that gain Magnet status have lower levels of staff burnout and provide safer patient care. Thus to support staff psychological ill-health often what is required is a long-term strategy to support culture change, not one-off discrete interventions. 30
Stakeholder contribution: investing in standalone discrete interventions or offering individual-level reactive interventions (e.g. counselling or mindfulness) is attractive to employers as it allows them to think something is being done, but in isolation, is unlikely to allow Trusts to meet their duty of care. Instead, it is important to tailor interventions to the individual (July 2022).
Everyone is on a continuum from good well-being to psychological ill-health and moves along this in a dynamic way. An effective well-being strategy must acknowledge that solutions need to be situated within a multilayered systems approach that considers psychological ill-health to be a fluctuating state (not binary ill-health/well-being) resulting from both singular/acute traumatic events and from ongoing cumulative chronic stressors.
Tension 1: the tension between a focus on individuals versus a focus on systemic issues
| CMOc#1: a focus on individuals blaming staff for systemic issues. |
| Context: workforce and resource shortages in a complex organisational context (where one event in the service architecture affects other parts of the system). |
| Mechanism: offering front-line staff access to individual-focused well-being interventions such as evidence-based mindfulness training (resource) to support them to individually manage stress in the absence of a systemic approach to well-being (resource) may send a message that the stress they are feeling is their fault and responsibility to resolve (–response). |
| Outcome: staff feel they have failed when unable to cope/do their job as expected (escalating psychological ill-health) or feel let down by their employer and disengage/leave the profession. |
Stakeholder contribution: it was noted that there is a predominant focus in the literature reviewed on ‘fixing’ the individual (Meeting 2), and one stakeholder highlighted that in other industries (e.g. nuclear industry) staff would not be expected to create their own suits to prevent contamination or carry their own boxes to tell them what is happening on the flight recorder (Meeting 3).
We identified a number of individually focused interventions, chief among them were mindfulness-type interventions (see Chapter 5), which do have an evidence-base regarding effectiveness54,108,144 and, in the absence of other wider organisational interventions, may be useful to some staff in the moment. However, while studies demonstrate that mindfulness training has positive impacts at an individual-level, and may result in cultural change through spread,165 these impacts potentially represent a myopic focus in terms of the causes and solutions to workplace psychological health. In one paper, mindfulness-based interventions are described as empowering staff to increase their psychological flexibility (capacity to make choices in accordance with authentic values despite symptoms), but not targeting symptom reduction. 108 This suggests mindfulness increases agency but does not clarify what happens when agency is increased, particularly when an organisation may be downshifting the burden of resource scarcity onto individual staff.
Mindfulness may therefore place the responsibility on the individual to manage their stress and psychological well-being when issues such as staff shortages and shift patterns are not in the power of the individual to change. By offering access to such training and support an organisation may inadvertently send a message to such staff that problems in the organisational system of service delivery falls on their shoulders and they should become psychologically and emotionally strong and flexible to handle the consequences of such problems. This can manifest as victim-blaming health-care staff for not being resilient enough in the face of insufficient support from leaders/managers/organisations/government. Maben and Bridges suggest: ‘Treating resilience as an individual trait is seen to “let organisations off the hook”’181 (p. 2742). Yet, resilience is commonly defined as an individual’s responsibility and the ability to ‘bounce back’ after difficulty. 32,167 Bouncing back implies that you might have fallen apart but also that you are able to get back up again.
A report about resilience in midwifery34 concurs with the need to avoid an individual focus, stating that resilience requires ‘deeper investment in creating sustainable ways of being and interacting’ and they ‘caution against the introduction of resilience programmes that focus on individual change and ignore the significance of context’ (p. 34) stating that in the current climate there is a danger such an approach could become a ‘convenient salve’ for managers; similarly the SOM report25 stated ‘focusing exclusively on secondary and tertiary initiatives not only means that the underlying causes of poor well-being are not addressed but also implies that protecting mental health and well-being is the responsibility of the individual, not the organisation’ (p. 32). Stacey and Cook32 report an ecological model of resilience, which ‘makes the assumption that there is a fundamental connection between the complexity of the world we live in and resilience as a way to navigate that complexity’ (p. 2). Thus, some tensions in the health service architecture we have identified may be a product of organisational systems that are not approaching resiliency from an ecological point of view.
Other literature reports broader aspects of work contributing to burnout and work-life balance so that individual interventions would be unlikely to have an impact. For example, Gribben and Semple130 review the literature on the impact of work colleagues and the culture of the working environment, stating the importance of good relations with colleagues as well as informal interventions such as positive feedback, peer support, debriefing, concise open communication and positive role modelling, which are considered as burnout protective factors (see also Key finding 5).
Few organisation-wide interventions that might create culture change were identified in our sample of the literature (but see also Appendix 3: COVID-19). There are exceptions, such as the various ‘good practice’ examples in recent reports, for example,30 and those reviewed in Brand et al. 31 One of the few is Schwartz Rounds,48 which are open to all staff and have been identified as creating a counter-cultural space (no blame, a supportive and psychologically safe and containing space to talk about the emotional social and ethical challenges of work where hierarchies are left at the door and where there is no pressure to have outcomes) that over time changes cultures and supports staff to process work challenges. 48 However, in a national evaluation177 it was noted as difficult for band 5/6 nurses and midwives to attend (since they have half-hour breaks and no control over schedule), and we conclude it is likely to be the same for paramedics and community-based staff, who would also have geographic barriers to attending.
Note that in Chapter 5 we have drawn on the language of primary, secondary and tertiary levels to indicate where the focus and action of the intervention operates. As there was also some discussion in the literature of where agency for the intervention lay, upstream and downstream language was also used, which we explore further here. Drawing on health equity language, this problem can be summed up as a focus on downstream interventions (individual behaviour change and treatments) as opposed to wider salutogenic and potentially preventative upstream interventions (contributing societal and organisational factors and prevention strategies for the whole community). 182 This river metaphor is often used in public health, ‘Upstream intervention is like building a bridge to healthier lives, whereas downstream intervention is throwing a life ring to someone who is already drowning’183 (p. 1).
In terms of psychological ill-health, Bosanquet87 comments on the need to rethink psychological interventions for nurses and those co-designed, with input from front-line staff may be the solution, further refining this tension. The author writes, ‘well-being initiatives continue to focus “downstream” (…) aimed at enabling individuals to continue gifting care and going the extra mile for their patients/work colleagues/families. Despite the short-term respite that such initiatives can bring, they are a “sticking-plaster” formulated (…), to maintain the status quo’ (p. 5).
Examining papers reporting on downstream interventions,77,84,96,127,165 some comment on the problem of implementing downstream interventions without upstream support and resources and interventions, and also that an individual lens or individual-focused project may not achieve wider change. For example, in an evaluation of resiliency-based clinical supervision,127 in which nurses felt empowered to speak up through the programme, but then the environment was not conducive to speaking out (see also below), militating against wider change.
| CMOc#2: messaging from leaders/managers to look after self at odds with the reality of work conditions |
| Context: work-related stressors, including poor staffing levels, lead to work regularly spilling over into home life. |
| Mechanism: when leaders/managers send messages regarding looking after self in and outside of work (resource), this can lead to staff feeling that managers are out of touch with reality and not acknowledging the impact of work on staff, and thereby lead to messages being ignored (–response). |
| Outcome: increased job dissatisfaction, reduced work engagement and morale. |
| CMOc#3: the importance of granting permission to practice self-care by managers and peers |
| Context: staff are exhorted to put patients first and hide needs and emotions. Thus, self-care is often not prioritised within the challenges and resource constraints of healthcare delivery due to staff feeling the burden of guilt and responsibility over the welfare of patients. |
| Mechanism: permission to be self-compassionately role modelled or at least granted by managers and peers (resource) allows staff to practice self-compassion (response). |
| Outcome: self-compassion leads to improved work satisfaction, better work practices and caretaking of self, reducing stress, and compassion for others and, ultimately, patients. |
CMOcs#2 and #3 present rival theories about the granting of permission by managers for self-care, with the same resource offered resulting in different outcomes.
Damage can result from messaging sent by managers/leaders to encourage staff to self-care as it can appear that they are out of touch with reality. There is a risk of significant cynicism from staff where messages from management (e.g. take time to reflect, take a break every hour etc.) are not met with the reality of work conditions. This mismatch makes people feel leaders are paying ‘lip service’ to the problem or implementing interventions in a ‘tick box’ fashion.
Some studies, for example, described managers encouraging staff to engage in healthy activities outside of work hours to improve their psychological well-being in the face of stressful work conditions. Cedar and Walker96 note that organisations should not put the onus on workers as often it is organisational stressors that need to be reduced. Comparing with doctors, CMOc#2 links to CUP-1 (focused on doctor’s psychological ill-health) findings, in particular, CMOc#9,17 where stakeholders suggested: ‘focusing also on quality of work (i.e. making work a functional and meaningful part of doctors’ lives and fostering a sense of meaning within, rather than outside work) appears to be a stronger strategy to tackle work pressures and mental ill-health’ (p. 36). Miller56 offers insights into the conflict for managers between the organisational metrics and targets for service delivery (which often put additional pressure on staff), and the staff psychological ill-health narrative. Thus, any disclosure of issues by staff may be impacted by the fact that managers (who have a responsibility for their well-being) also have responsibility for service delivery and may be performance managed on metrics of service delivery.
Staff often feel pressure to keep going even when they are resource-depleted because ‘The culture is that you suck it up and don’t have a break, or you’re made to feel like you can’t hack it.’30 This represents a tension in which the messaging for granting permission does not fit with resources available and, as we have identified above, a perceived requirement from ‘top’ to meet patients’ needs, meaning staff put their own needs second.
In support of the benefit of ‘granting permission’ as an informal intervention, Andrews and colleagues84 argue that for nurses to engage in self-care they often need permission from others, including colleagues and superiors. Giving permission can thereby be seen as a mechanism of the informal architecture of service delivery. In this sense, an embedded informal strategy of ‘granting permission’ as part of the informal architecture can come from the ‘grassroots’ where, for example, one staff member may reach out to colleagues who are struggling and say, ‘hey, it’s OK to cry if you need to. Take care of yourself.’
Compassion and kindness to self are also important. Many managers will have worked even longer hours than their teams, setting an example, or supporting the workload. As the airline safety briefing say: ‘you must put your own mask on before assisting others. 184
(p. 7)
It is possible that a culture of giving permission can grow from the grassroots, especially when resources are scarce, or during times of exceptional difficulty such as during the 2020 COVID-19 pandemic (see Appendix 3). These mechanisms can be understood in two ways. One, in terms of managers and healthcare leaders reaching out and granting permission to staff individually or collectively, and two, they may encourage the workforce to grant permission to each other (top-down mechanism triggering a lateral mechanism). This is akin to the ripple effects of Schwartz Rounds: that through the openness and honesty with which work challenges and emotional situations are discussed in Rounds slowly over time leads to changing of conversations/culture outside of Rounds. 177 Granting permission can be enhanced through role modelling, especially by those in senior positions (e.g. in Schwartz Rounds). 177
Granting permission is an important first step, but the action still needs to be feasible in the context of the realities of practice. People need to see how this can be prioritised and incorporated into busy work environments and timetables, which may require some other things not being done. For example, what will staff not do to practise self-compassion through, for example, attending a Schwartz Round (reflective space) or taking time out for recovery in everyday practice. Multiple concurrent strategies layered upon each other (such as granting permission for self-care and role modelling self-care, for example) can create a context, but only when self-care and self-compassion become the norm, which can only happen in truly psychologically safe working environments. Managers and colleagues may adopt a commitment to remind their workforce employees and their peers to take time out and be kind to self and others. Granting permission has been described above as an example of informal service architecture but can also be built into formal interventions, such as TRiM,185 where after exposure to trauma, staff are warned that it would be normal to struggle with sleep and other aspects of life in the days immediately following the event, and if that struggle does not resolve, further support should be sought. However, time away from work while experiencing the impact of exposure to trauma is not built into this intervention. Also, even with permission, nurses, midwives and paramedics may be ‘hard-wired’ to be caregivers,84 which may override efforts toward self-care. Organisations that create a culture of permission for self-care can balance the reality of being hard-wired as carers and the consequences of service-delivery that involves trauma exposure.
Tension 2: the tension between a focus on acute episodes of trauma versus recognising and supporting chronic cumulative stressors
| CMOc#4: there is a need to understand the cumulative nature of chronic trauma exposure. |
| Context: a considerable amount of trauma exposure is invisible because it is connected to chronic issues of patient suffering, resource scarcity and staff shortages. Staff who appear to ‘fall apart at the smallest little thing’ may be dealing with a lot more than is apparent. |
| Mechanism: managers may fail to recognise the cumulative nature of chronic low-grade trauma exposure (resource) and so may end up creating more harm by judging staff competency unfairly (–response), leading staff to experience secondary trauma due to lack of recognition (–response). |
| Outcome: worsening psychological health; job dissatisfaction; increased stress; attrition. |
Theory suggests that staff can experience STS and vicarious trauma in healthcare work,186 but that ‘Vicarious trauma can develop in people who are exposed to other people’s trauma over a prolonged period.’186 STS occurs when exposure to traumatic events result in staff exhibiting signs of trauma themselves. STS is defined as ‘the natural, consequent behaviours and emotions resulting from knowledge about a traumatizing event experienced by a significant other. It is the stress resulting from helping or wanting to help a traumatized or suffering person’ [Figley187 (p. 10)]. ‘The person with STS acquires symptoms by exposure to a traumatized individual and not from exposure to the traumatic event itself. ’188 STS appears similar to symptoms of primary trauma in terms of psychological and physical patterns, including potentially resulting in PTSD.
Furthermore, prolonged exposure to challenging service architecture such as low staffing, poor skill mix levels, unpaid overtime and steadily increasing work pressures is that staff: ‘make micro-adjustments to (…) work practices to cope with the increased work (…) (and) going the “extra mile” becomes expected, (…) by the time (they) realise that they have a problem, they may have already been seriously harmed by the system (the “boiling frog” effect)’. 189
(p. 1)
Chronic cumulative stressors and their effects on poor mental health need to be recognised just as much as acute traumatic episodes at work, and this non-acute trauma has been called everyday pressures:35,109
It is often the cumulative effect of less dramatic incidents rather than the major incident that impact our mental wellbeing... watching someone lose their independence, or escorting them from their home in the knowledge that they may never return can really hit home. 16
(p. 1)
It may take a while for the impact of these demands to manifest in terms of symptoms. 124
(p. 575)
In a paramedic literature review, Anderson94 reports Boyle (2007) identifying that ‘the most emotionally demanding are not those incidents involving the greatest physical trauma but the non-urgent ones, owing to the uninterrupted exposure to social emotions’. (p. 3)
Front-line staff and managers need to understand that both major and minor adverse events may trigger psychological health challenges and that the magnitude of the particular incident should not be the reason to judge the validity of the claim around lack of wellness. Staff also reported the need to move swiftly between very traumatic events (death of a child) to everyday stressors.
Stakeholder meeting (2): colleagues discussed the fact that staff move from this traumatic ‘stuff’ and then back to more ‘mundane’ (but still taxing) or more trivial bits. For example, in ED, staff move between CPR or an unexpected child death and then, minutes later, back to dealing with more trivial ‘normal’ work with no time to process.
Quaile95 reflects on the harm caused by seeing and experiencing difficult situations as a paramedic:
it may be one shocking call, or it may be a build up over time, but I believe we are all affected in some way by the things we see, by the emotion we experience but are forced to contain while dealing with our job. 95
(p. 225)
It may be the case that a minor incident triggers a big reaction, perhaps because the incident is just the final straw in a long string of experiences that involve secondary trauma. Or it may be that the staff member connects to it in some way, as acknowledged in the SOM report:25 ‘Events are more likely to have a traumatic impact when they are unexpected, involve children or patient suicide. Additional risk factors for post-traumatic stress are when nurses and midwives can personally relate to the situation in some way, either through their own or a family member or friends experience’ (p. 20). If a staff member breaks down at what seems to be ‘the slightest little thing’, managers and colleagues will need to have sufficient psychological health awareness and training in order to recognise the patterns at play, and not judge the incident against the severity of the reaction. This is never more important than following the COVID-19 pandemic, when there may be a long recovery time after such traumatic exposure, which may make staff appear to react to ‘little things’, which may be triggers or cumulative trauma.
| CMOc#5: there is a need to distinguish secondary trauma arising from acute dramatic versus chronic ‘low-level’ events. |
| Context: the work of nurses, midwives and paramedics involves being exposed to sudden dramatic, traumatic events as well as chronic low-grade trauma. |
| Mechanism: supervisory strategies for ensuring staff well-being may be more targeted to acute dramatic events (resource) and may or may not recognise the need for providing support to staff regarding chronic low-grade trauma exposure (resource). Staff may feel a sense of insecurity and inadequacy [and not know the signs to look for in themselves or others, or where to turn for support] when low-grade trauma exposure takes a toll on their (or their colleagues’) mental health (–response). |
| Outcome: staff psychological health is supported around the big events but may remain unchecked for the seemingly smaller events, which can have a cumulative impact, and where the expectation is either that staff can manage it on their own, or that it is not even recognised as being a problem needing support – instead ‘just part of the job’. |
Secondary traumatic stress (STS) occurs when exposure to traumatic events result in staff exhibiting signs of trauma themselves (see CMOc#5). Trauma exposure may be acute or chronic and supervision and well-being interventions may require adaption to need. STS can also trigger buried unresolved personal trauma from events outside of work events. For example, Quaile95 (p. 224) notes
It (poor mental health) started to manifest itself after a failed resuscitation attempt on a child(…) While there were low-level symptoms (…) and (…) certain calls that would affect me more than others, there was much more severe recurrence after witnessing the aftermath of a plane crash.
Supervisors and staff may grant themselves more permission for self-care when there is a dramatic incident such as a road accident. Although even here some psychological preparation is necessary as our first stakeholder group identified.
Stakeholder contribution (paramedic): when there is limited information available prior to arriving at an incident it is difficult for staff to mentally prepare for what they may see and experience. If staff know they are going to a traumatic event they can at least mentally prepare for this to some extent.
However, if trauma exposure accrues from more mundane events, it may be more difficult to provide recognition of the need for support and space to process trauma, and the chronic may also become ‘normalised’ so no longer seen as needing support. 108,109,158 The relationship between dramatic and low-level trauma events needs further unpacking. Clarke158 described a personal story of burnout written by a midwife. The author described that for decades working in the health service they had never experienced burnout but had often been a support to others who were. This then changed:
I can’t identify a particular trigger (…) It was probably just a combination of events, including a new and challenging job and a particularly upsetting and traumatic clinical incident (…) I became short tempered and difficult to live with. I felt weepy and weary.
(p. 16)
Importantly, there was not one trigger but rather a combination of different factors. It may be theorised that negative impacts of chronic exposure to patient suffering creates an invisible cumulation of trauma exposure. In a new job, less well-known support mechanisms, especially informal networks, may have made this midwife158 less able to process the acute traumatic event. In support of this theory, when discussing risk factors associated with PTSD, Naumann and colleagues117 note that
a perception of reduced social support can be a risk factor for PTSD following traumatic events. Although no causal link can be made (…), a lack of mentorship, support and appropriate team behaviours were reported. A holistic approach to addressing these would be required (…) to reduce risk to its employee.
(p. 519)
When a breakdown happens, there may be a trigger incident that is large or small – releasing emotional tension that has been suppressed over time. This understanding is important so that an outsider to the experience (e.g. a clinical supervisor) does not unfairly judge and misconstrue the secondary trauma as the staff member not being able to handle small stressors. Managers can then be empathetic and develop appropriate responses to the need for staff self-care, even if there is no ‘smoking gun’ incident that explains a lack of psychological wellness.
Key finding 2: it is difficult to promote staff psychological wellness where there is a blame culture
Overview of key finding
Healthcare organisational culture ‘is a metaphor for some of the softer, less visible, aspects of health service organisations and how these become manifest in patterns of care’190 (p. 364). Following the Francis report, Harry Cayton, chief executive of the Professional Standards Authority for Health and Social Care, said that although the government had taken steps ‘it had not done enough to make (the NHS) more accountable and to allow professional responsibility to flourish (…) a balance had to be struck between holding people and teams accountable for their actions and fostering a ‘toxic blame culture that would make it harder to raise (…) concerns’. 191 A blame culture is
… norms and attitudes within an organization characterized by an unwillingness to take risks or accept responsibility for mistakes because of a fear of criticism or management admonishment (…) (It) evolves out of a bureaucratic management style that is highly rule-oriented compliance-driven (…)assigning blame or accountability to individuals even for system-level failures. 192
(pp. 314–5)
It is the opposite of a psychologically safe culture and prevents people from both speaking up and taking accountability. Such an organisational culture can be predicated on poor leadership, a lack of visibility of leaders, a lack of resources, and lack of support. It is often left to front-line workers to accept responsibility and, even then, the weakest link in the chain, such as newly qualified staff, may receive most blame. Thus, the person with the least influence or power becomes the one required to speak up and, at times, convey the need for shared responsibility, often to no avail. The NHS states it is a ‘no-blame culture’ establishment, yet an understanding of the mechanisms by which such a culture is created and maintained is not immediately apparent. The recent introduction of ‘Freedom to Speak up Guardians’ in the NHS is one intervention to support raising concerns and a no-blame culture. Yet, many of these Guardians identified a lack of resources, especially time, which negatively and significantly impacted their ability to respond to concerns raised effectively and on their opportunities to learn from speaking-up data and develop a speak-up culture. 193 During times of extreme hardship, such as the COVID-19 pandemic, when resources are scarce, and the challenges in providing patient care are clearly beyond the capacities of any one person, the causal mechanisms involved in an instance of a medical error can be diffuse and hidden; yet, an organisation may choose to find blame in a single staff member or team.
Tension 3: the tension between a lack of collective accountability, which blames individual staff for errors, versus a team/system-based approach
| CMOc#6: attributing cause of blame to individual staff ignores the role of the wider system. |
| Context: front-line staff are most directly linkable to health service outcomes and medical errors. |
| Mechanism: the system is geared toward performance, measurement and individual accountability (resource) that precludes an acceptance of system-wide attribution of accountability for medical errors. Staff practice defensively to protect against blame falling squarely on their shoulders (–response). |
| Outcome: decreased workplace satisfaction, decreased autonomy in practice, reduced quality of patient care; increase secondary trauma and victimisation by downstream drift of accountability processes. |
The starting point should be an assumption that everyone is doing the best job they can in difficult circumstances, rather than ignoring the contextual factors and assuming an individual is to blame. A no-blame culture can help to encourage as much learning as possible, as in other safety-critical industries. Amy Edmondson’s work on psychological safety notes healthcare work can feel interpersonally risky – for example, ‘asking a question that might expose your ignorance to others, looking incompetent when admitting a mistake or a weakness, or appearing negative or critical when pointing out a flaw in a process worthy of improvement. ’194 Psychological safety is a factor in helping people to learn new behaviours and overcome defensive routines. A lack of psychological safety is often found at the root of significant organisational errors and failures in a variety of safety-critical industries. On the other hand: ‘A climate of psychological safety makes it easier for people to voice tentative thoughts (and) (…) can help people override a tendency to default to silence, instead encouraging or allowing them to offer ideas, report errors, and speak up in ways that are vital for health-care improvement’. 194
| CMOc#7: there are sometimes double standards in accountability. |
| Context: staff working in clinical areas that are known to organisational leaders and managers for poor standards of care. |
| Mechanism: a lack of accountability, attention, or inability to fix problems on the part of managers (resource) leads to a feeling of outrage at the injustice by staff who must remain professionally accountable for their actions in these clinical areas when others are not fulfilling their responsibilities (–response). |
| Outcome: workplace dissatisfaction due to a sense of double standards in accountability. Increased frustration, stress and burnout and staff leaving the profession. |
A related issue is the lack of a framework for collective accountability in the NHS. As a result, staff may practice defensively because they know they will get the blame if something goes wrong. This can lead to being overly cautious or overtreating rather than doing what they feel is right for a patient, although there may also be advantages to having a named person responsible for example, permission to intervene.
The WHELM study74 (p. 20) reports
Midwives vividly described their personal concerns about the level of responsibility they carried and their feeling of “being under the microscope”. Their accounts suggested that they did not feel well supported by managers (…) (and) were also concerned that a widespread culture of litigation fear impacted on the care that women received, with a default to medicalised care to ‘err on the safe side… When something goes wrong, which inevitably will always happen, as sadly not every pregnancy ends well, however good the care, midwives are treated appallingly, it is shocking and devastating to observe good hard-working midwives torn apart by the absolutely disgusting way that incidents are dealt with. Babies do and will die, and it is not always somebodies (sic) fault. Trusts persecute individual midwives in order to cover their own back as far as litigation. There is never any support, it is truly a horrific witch-hunt. I have met so many broken midwives, who then leave the profession.
(p. 21)
The literature suggests that health professions’ training is so geared up to measurement and individual accountability, that for many staff it is hard to change this way of thinking and move to more system- and team-based approach. In light of unavoidable negative clinical outcomes, a whole-culture, system-wide change is advocated to help staff in striving to provide the best possible care, without blaming individuals or finding scapegoats. Relatedly, accountability and blame issues, while different, also link to inaction and highlight the need to understand systemic power that is found at the managerial level as well as at the front line. Individual clinicians may be held accountable by their employing organisation, and/or professionally by their registering body [Nursing and Midwifery Council (NMC)/Health and Care Professions Council (HCPC)], yet in some instances managers and senior leaders were not felt to have the same accountability and some double standards may exist. The negative impacts when managerial support is lacking for front-line staff are evident in one report:75 ‘participants [nurses] were visibly outraged and frustrated (…) that certain clinical areas were known to have poor standards of care, (…) [but] not addressed by managers. Participants compared this to their own professional accountability, where they were held responsible for their own actions and omissions, whilst (…) others were not’ (p. 10).
| CMOc#8: investigation of medical errors can cause psychological ill-health in staff. |
| Context: investigation of medical errors rarely takes account of the wider context (e.g. understaffing, or toxic work environments) and thereby may focus on the individual rather than the wider system. |
| Mechanism: regulatory and organisational policies that focus on blaming the individual and dictate staff suspension from work and have protracted investigation processes (resource) lead to staff feeling guilty, unsupported, and isolated (–response). |
| Outcome: staff can feel broken, have worsening psychological health; possible suicidal ideation; and trauma can extend to friends and family. |
Highly empathic staff, especially those early in their careers may lack an awareness of larger systemic forces at play in service provision. However, they may still internalise and accept blame for events involving medical errors when, in fact, organisational leaders would also need to accept accountability. It can be hypothesised that the more self-reflective and empathic staff are, the more likely they will absorb blame for mistakes and internalise the effects of pressures, victim-blaming and bullying. Cull and colleagues89 describe the negative impact of blame culture on midwifery practice:
…many respondents commented on a perceived ‘blame culture’ in their workplaces, with a resulting impact on their mental health. One midwife described ‘coming home worrying about what I have missed, not documented, handed over [and] waking up with flashbacks’.
(p. e533)
Stakeholder contribution: while nurses, midwives and paramedics fear blame (and this may be particularly so for midwives as autonomous practitioners and where most litigation takes place), they also live with a lot of guilt and distress as the result of mistakes in practice, and risk protracted investigations (often suspended from work and unable to speak to colleagues).
Staff reflect on traumatic incidents and recognise that they were unprepared, thrown in at the deep-end, or unsupported. Healthcare is a complex workplace, and human error is inevitable. Nurses, midwives and paramedics in our stakeholder group told us that distress is often the result of feelings of guilt at mistakes and not being able to rectify them, as found in other reports and research papers. 28,83,137,195
It needs to be acknowledged that medical error and mistakes’ investigation is not about ‘protecting the interests of staff/staff well-being’ at all costs but about taking a contextualised view of the causes so that they are examined comprehensively. This needs to include an analysis of the context in which they happened, and the organisation needs to take responsibility and be accountable, as well as individual staff members. That way, there could be resolution for both patients and staff, and organisational learning.
Tension 4: the tension between needing to raise concerns to improve conditions and patient safety versus fitness-to-practice processes becoming an oppressive force
| CMOc#9: knowledge that the fitness-to-practice process is rarely supportive creates reluctance in staff to voice concerns about psychological health. |
| Context: public-facing healthcare staff are exposed to trauma and complex clinical decision-making daily, which can result in secondary trauma and burnout. Mistakes occur in safety-critical industries such as healthcare and psychological safety is important to allow disclosure of poor psychological health. Healthcare organisations are pressured to ensure staff are well enough to practice for the safety of all patients, but fitness-to-practice processes are known to rarely support staff. |
| Mechanism: the threat of potentially having to go through a fitness-to-practice process (resource) leads staff to feel reluctant to voice concerns about their mental health and its impact on their work for fear of losing their status, reputation or employment (–response). |
| Outcome: psychological health issues may remain undisclosed and unchecked. Some staff choose to self-refer rather than speak to supervisors about their performance and psychological health concerns. Missed opportunities to create a culture of shared learning, transparency and reflection and de-stigmatise mental health issues. |
The service architecture associated with patient safety and related fitness-to-practice concerns contains several inherent tensions. On the one hand, mechanisms to identify fitness-to-practice concerns are needed to ensure that people who are not fit to be handling the demands of the job are identified and offered the care they require and perhaps even taking time off. Yet, fitness-to-practice mechanisms, if not implemented with care and sensitivity can become an oppressive force, resulting in staff dealing with their psychological health issues on their own, or not dealing with them at all. This can increase stress, trauma and risk regarding psychological health concerns in staff149 and such health issues may only become apparent when a critical incident occurs.
In reviewing causes and solutions to psychological ill-health, paramedics114 note ‘Concerns over fitness to practise can result in a “culture of silence” whereby staff don’t talk to their employers…If employees don’t come forward, employers won’t necessarily be aware of the problem and things can get worse’. (p. 192)
One study has investigated why UK paramedics have a higher rate of self-referrals to the HCPC than other health professionals,115 resulting in convictions and cautions. Some of the reasons they give include a pressurised work environment, variable guidance, variable support from supervisors, and work cultures of fear and conflict. Interestingly, an additional insight given was the fact that many paramedics have origins in the military and that ‘paramedics may be more habituated to rules and protocols than some of their applied health professional colleagues’ (p. 205). They write: ‘the third (reason for higher self-referrals in paramedics) relates to work cultures predicated on blame and punishment rather than shared learning from errors’ (p. 209). A punitive culture may be more prevalent in paramedic workplaces, yet these issues would be similar for nurses and midwives. Golden54 notes
When a midwife is (…), referred to the regulatory authority(…) this can cause a breakdown in the relationship of trust and confidence with the employer, leading to stress, reactive depression and possibly nervous shock. Sadly, there have been cases of suicide.
(p. 63)
In nursing, Marran147 also suggests it is not what is done that has such a detrimental impact, but rather how an adverse event investigation is undertaken:
The purpose (…) is to understand what has happened, so that appropriate actions and learning can take place. However, some healthcare professionals perceive the focus (…) [is] on apportioning blame, a perception that contributed to Wu (2000)196 devising the term ‘second victim’.
(p. 5)
Stakeholder contribution: members spoke about how long-term sick leave due to stress could, in some instances, themselves become a trigger for performance management yet should not be and good workforce policies and attendance management can support long-term sickness.
| CMOc#10: the investigation of medical error can result in secondary victimisation and traumatic symptoms. |
| Context: medical errors happen in healthcare service delivery and require a psychologically safe climate for staff to facilitate open reporting and organisational learning. |
| Mechanism: the investigative process into medical errors provides an opportunity for the healthcare staff and wider organisation to understand and learn from mistakes by offering a respectful, psychologically safe no-blame process (resource), resulting in staff being willing to speak up, learn from any mistakes and continue to do better (response). However, an investigation may involve fear of public exposure and reputational damage and blame staff, thereby offering a psychologically unsafe process (–resource), creating feelings of guilt, shame, fear and silence (–response). |
| Outcome: increased secondary trauma if the investigative process is punitive; improved learning and performance if the process is fair and appropriate to the circumstances and staff may be identified and supported as ‘second victims’ of the error incident. |
In addition to the important relationship that staff have with line managers and organisational leaders, staff may also need to negotiate connection with external review processes in the context of medical errors, for example, to the NMC, and the HCPC. Such an external review may increase stress, as identified in CUP-1 for doctors43 and by registrants (including paramedics) referred to the HCPC. 28 A punitive approach and apportioning blame were identified in this paper149 for HCPC registrants undergoing fitness-to-practice investigations (FTP) where there was a significant psychological impact on many:
Their stories described influences on their wellbeing (...). A lack of information, long length of time for the process and poor support avenues (impacted) on the ability of registrants to cope with their experiences (…) (and) led to feelings of powerlessness, vulnerability and threat of ruin for many registrants. 149
(p. 1)
Recent changes in midwifery support and supervision were noted, as having increased stress for midwives. Previous in-house clinical supervision has stopped, and the supportive aspects of supervision have been replaced by the professional midwifery advocate model, which is non-mandatory and does not have any role in investigations. The regulatory role of supervisors is anticipated to lead to more involvement of the NMC as described by Barker:148
Currently, when incidents occur, midwives are investigated locally [and] (…) s concluded quickly [with] a plan introduced to (…) start the remediation process within weeks. When this is devolved to the NMC, it (…) may take up to 2 years to finalise, perhaps leading to more resignations.
(p. 826)
Secondary traumatic symptoms may also arise from medical error and the way organisations address issues around medical error. In a systematic review, Sirriyeh et al. 197 assess the effects of involvement in medical errors on healthcare professionals’ risk of psychological ill-health, noting an intense emotional response following an error with subsequent impact on the personal and professional lives of staff, particularly prevalent in blame cultures (see above). This includes acute stress disorder, suicidal thoughts or even suicide and these authors use the phrase ‘second victim’ to describe those who suffer emotionally when the care they provide leads to harm.
An incident that triggers traumatic memories from a personal life experience, or sudden and profound events, such as an unexpected patient death can have reverberating impacts that stay with healthcare workers long after the event resulting in them becoming ‘second victims’, with the incident leaving a ‘permanent imprint’ on them. 31 Marran147 reports shame, guilt, panic, shock and humiliation leading to self-doubt and loss of confidence as common feelings after making a mistake. She states that staff can feel personally responsible for any unintended harm to patients and doubt their clinical knowledge, and describes the term ‘second victim’ to denote
the negative psychological effects that making an adverse medical error can have (…) and the sense of alienation they can feel from their colleagues following the event (…). Second victims are doctors, nurses or other health-care professionals who have made errors relating to patient care and experienced psychological effects.
(p. e1)
Thus a second victim is a healthcare employee who experiences personal or professional impact as a result of involvement in a patient safety incident, or an error. 197 Marran147 also identifies the potential difficulty with healthcare professionals being identified as victims as
this may detract from the harm experienced by the patient (…) and suggests they lack accountability, yet (…)Lawton et al (2019) state they have rarely (…) encountered a healthcare professional who did not consider themselves accountable (…) and (such events) can result in significant harm to [them].
(p. 2)
A paramedic reflected on a child abuse case where the child died stating: ‘I’d often find myself just sat there not really doing anything but thinking about the job, and thinking about whether there was anything else I could have done. ’95 (p. 225)
Marran, in a literature review, describes a further example of a second victim, suggesting that the adverse event
left a ‘permanent imprint’ on them and the duration of the second victim’s recovery process may also be affected by any subsequent investigation, which can be protracted, uncomfortable and highly stressful. Second victims may fear making further errors, (…) (experience) loss of confidence, (…) all of which increase their risk of making further errors.
(p. e4)
She further suggests outcomes for staff can be poor: ‘Second victims often experience significant negative feelings and may question their skills and practice. This may result in unplanned absences from work, which places increased pressure on the rest of the workforce. In some cases, the healthcare professional involved may decide to leave their profession’147 (p. e4).
In midwifery there is significant fear of litigation and the WHELM report74 provides examples of midwives making second victim claims. Golden54 also notes that following a traumatic birth where the baby was significantly injured:
the midwife(…) makes a claim for nervous shock. The claim by the midwife is that the employer failed to protect her in her employment. The midwife claimed that the harm was reasonably foreseeable and that she was not party to the negligence that caused harm to the mother and baby.
(p. 62)
Litigation or fitness-to-practice processes implemented in a toxic work environment characterised by a lack of psychological safety and a blame culture may exacerbate symptoms of STS in staff who have made mistakes. However, Marran147 notes that when the process is well-designed, the majority of staff who have made an error report positive emotions such as ‘feeling motivated to improve their practice’ (p. e3).
Some authors (reported by Marran147) have also suggested that healthcare organisations can become ‘third victims’: ‘because of the potential negative financial and reputational effects they experience(…). In addition, adverse events can affect people not directly involved in the event. This could include patient safety professionals or others who are responsible for investigating adverse incidents and service improvement and involve them (sic) potentially becoming third victims.’ (p. 4).
This can affect the ability to hear staff voices and be willing to be open to hearing mistakes and providing a supportive environment for staff to learn in the future having detrimental effects on staff psychological ill-health. It is rare for NHS organisations to come to the defence of individual staff members exposed for medical error in the media, most remain silent and allow staff to be individually targeted, without recognising the organisation’s role in allowing a psychologically unsafe culture to happen. The research into the consequences for third victims is scarce and the implementation of a crisis management plan and associated measures are suggested to limit potential damage to an organisation’s reputation. 198
Tension 5: the tension between encouraging staff to speak up versus the ‘deaf effect’ response from managers and hearers
| CMOc#11: encouraging staff to raise concerns can create problems if there is no action: a ‘deaf effect’ response. |
| Context: to identify and prevent harm to patients and staff, nurses, midwives and paramedics are encouraged to speak up or raise concerns to identify issues that need to be addressed. |
| Mechanism: in a non-learning organisation where it is not psychologically safe to speak up about mistakes and errors, and where senior leaders do not listen to staff concerns (‘deaf effect’) (resource), then staff will be scared of the consequences to them of speaking up or feel that no change will result (–response). |
| Outcome: decreased workplace satisfaction, poor staff retention, reduced quality of patient care; increased secondary trauma and victimisation and increased stress and helplessness at no changes observed. |
Healthcare staff who are encouraged to raise concerns and speak up play an important role in improving working conditions and in the detection and avoidance of harm to patients. 193 Yet, some staff feel unable to speak up and, if they do, their concerns may be ignored or responded to inappropriately. 199 Thus, fear of negative repercussions, organisational inaction, and the desire to ‘fit in’ can result in the silencing of employees’ voice. 193 In a recent review, Jones and colleagues (2021) also note the importance of ‘hearer courage’ to act on concerns. 193 There is some recognition in the literature that the culture in health care is not always that of a learning organisation where psychological safety is present in teams and where staff feel they can raise concerns without fear of retribution or consequences for their career. There is a long history of poor treatment of ‘whistle-blowers’ in the UK NHS. In the mid-Staffordshire scandal, for example, staff were accused of not speaking up but the inquiry found this not to be the case – staff were raising concerns and speaking up about poor care, but they were not being listened to, which authors in the field have labelled ‘the deaf effect’. 200 This term is used to describe the reluctance of those in authority to hear bad news from colleagues.
Stakeholder contribution: members spoke of trying to change things for the better – for staff and patients – yet feeling like they were ‘banging their head against a brick wall’. This inability to effect change was described as very wearing and dissatisfying aspect of work, causing staff to need to be extremely persistent to get their concerns heard at great personal costs or ‘give up’ and stop trying, both of which were reported by members as stressful.
This is reinforced by the following excerpt taken from Twitter:
In the NHS: the standards you keep challenging destroy your mental health from the moral injury of repeatedly not being able to deliver even the most basic intervention care being left undone as there is not enough of you to do it in a timely manner(…) nor any meaningful way to change any of it. I have taken to the streets with a placard, been an activist. Raised concerns formally. Blown the whistle, yet here we are watching the service implode as staff leave in an act of self-preservation.
(@spearce33801- nurse on Twitter 16.4.22)
Stakeholder meeting (3): a member suggested that immediate reactions to trauma in staff are often unrecognised and serve to create more trauma. Another highlighted the lack of visibility of well-being Guardians, and that in their organisation health and well-being is located within Human Resources with no clinical understanding or involvement to the perceived detriment to the service.
| CMO#12: supervision interventions (encouraging staff to voice concerns) may backfire and create burden if there is no organisational action. |
| Context: fragmented non-systemic approaches to supporting staff to deal with challenges at work caused by workforce and resource shortages. |
| Mechanism: interventions that give permission for staff to voice concerns (resource), lead to burden, frustration and guilt (–response of supervisors) and reduced staff satisfaction and trust in the supervisory model, feelings of isolation, abandonment, frustration (–response of staff) if they are not part of a wider systemic approach that welcomes and acts on speaking up. |
| Outcome: decreased workplace satisfaction and engagement (staff and supervisors), less likely to speak up (staff), lack of organisational learning and thereby reduced quality of patient care, psychological ill-health. |
Some interventions are aimed at enabling staff to process, have a voice and speak up about aspects of work that need to change through discussion, for example, various models of clinical supervision including resiliency-based supervision. 12 Such interventions may incur unintentional harm to staff and increase mistrust in the organisation if they are not part of a ‘systems’ approach to well-being that recognises the structural/organisational causes of psychological ill-health at work. If an intervention empowers staff to voice concerns when conditions of work are not adequate to need, this may lead to a backfiring effect if there are no organisational pathways to take and action such concerns.
For example, Stacey127 reports on an intervention called resilience-based clinical supervision, which is ‘underpinned by the principles of Compassion Focused Therapy. The aims of such clinical supervision are to alleviate work related stress and support individuals to reframe their experiences through structured and reflective discussion.’ (p. 1). A main finding from that study is that even though the intervention was designed to give nurses a voice through reflective discussion, the facilitating supervisors felt a sense of burden and guilt around the fact they could not really address the problems that the nurses were raising. The nurses gained a sense of empowerment but then face the difficult realisations about systemic problems that are beyond their control. This disparity in having a voice, but that voice not leading to any change, may backfire and be detrimental to staff satisfaction at work and impact negatively on their relationships with managers and leaders:
in organizations where the culture undermined a clear process or commitments to responding to the distress of preceptees, facilitators felt overwhelmed and saddled with holding the emotion of their group (…). without a clear sense of how issues could be escalated (…) leading to a feeling of isolation. 127
(p. 5)
Key finding 3: ‘serve and sacrifice’: the needs of the system often override staff well-being at work
Overview of key finding
Nurses, midwives and paramedics are often thought to have a ‘calling’ or a ’vocation’ to undertake the work that they do. They are exhorted to ‘put patients first’, which some have noted may suggest they often feel they need to put their own needs second, with a culture of giving 100%. 90 Choflet and colleagues36 suggest ‘The prevailing nursing culture is “patient over self” when prioritizing time’ (p. 21) and for paramedics, Quaile95 reports that when staff attend an incident that is particularly traumatic:
they are offered some ‘time out’ but many staff don’t take this up when they know there are patients out there waiting (…) We are there to support the public in [their] time of need, but we tend to not to ask for help ourselves.
(p. 226)
This can challenge the maintenance of good well-being in the face of intense and potentially traumatic work. As we have already outlined, these staff work in a context of high demand, where high workload and being present at work to support the team or for the patients may mean staff neglect their own health and needs.
In CUP-117 CMOc#2 noted a ‘Normalisation of a high workload’:
When high workload and its negative consequences (e.g. distress, burnout) are normalised (C), overworked or sick doctors may feel they are letting down their colleagues and patients (M). This can contribute to presenteeism (O) and associated negative consequences on mental health (O1) and workforce retention (O2).
The needs of the system override staff wellness, with high-quality patient care being the primary goal.
Tension 6: the tension between a professional culture that promotes a ‘serve and sacrifice’ ethos, which persuades staff to prioritise institutional needs, versus a culture that promotes self-care
| CMOc#13: a ‘serve and sacrifice’ professional ethos may be used to persuade compliance to institutional needs. |
| Context: high workload can become normalised, with breaks sacrificed. Nurses, midwives and paramedic roles are a calling or vocation with a desire to help, put patients first and go the extra mile. The maintenance of good psychological health in the face of challenging, intense and potentially traumatic work is therefore difficult. |
| Mechanism: management sending the message that healthcare professionals should give 100% to serve clients and patients (resource) yet provide little in the way of strategies and interventions to manage complex and distressing clinical situations (resource) reinforces compliance to institutional needs (response) to the detriment of staff psychological health, which feels like the required sacrifice (–response). |
| Outcome: increased stress, burnout and leaving the profession. |
The literature included in this review indicated that professional culture often sends a message that staff must adopt a ‘service and sacrifice’ ethos and give 100% at all times, working long shifts with few rest breaks. For example, Barker156 and Bacchus and Firth90 report a healthcare culture that asks newly qualified midwifery staff to participate in a culture of giving of themselves to the service, with the latter90 noting that
giving 100% or more to prove their worth is [considered] a positive attribute in the midwifery workforce but can be used negatively to persuade compliance to institutional needs. Midwives work long shifts with little or no breaks due to heavy workloads, which has been termed ‘service and sacrifice’90
(p. 3)
Barker156 notes that taking care of self often rests with the individual (as noted in Key finding 1) with the exhortation for midwives to take care of themselves in stressful and difficult situations, often without the necessary support in place:
midwives (are required to) be able to demonstrate at the point of registration that they (…) (can) work in stressful and difficult situations, that they are able to recognize signs of vulnerability in themselves and colleagues, and (…)can incorporate self-care (…) while employers are not required to [give]support.
(p. 210)
Stakeholder contribution: members suggested these issues highlighted by midwives would be the same for nurses and paramedics, with the responsibility for their own psychological health falling on their shoulders.
Other literature reports the ‘desire to help’ may work against nurses by putting them at risk of compassion fatigue and vicarious trauma and comments on the need to rethink the deployment of well-being interventions for nurses, which continue to focus on the individual nurse, with such initiatives being describe as ‘sticking-plasters’87 (p. 5), and goes on to note that
even if we can create more person-centred cultures, the traits that draw us to nursing may work against us. Once such characteristic, the desire to help may, may put nurses at risk of compassion fatigue and vicarious trauma. 87
(p. 54)
Tension 7: the tension between supporting existing staff in the context of staff shortages versus perceived coercion to fill vacant shifts beyond contracted hours
| CMOc#14: staff feeling unable to say no in a felt culture of coercion. |
| Context: managers face pressure to secure safe staffing levels in a context of staff shortages. |
| Mechanism: pressure communicated by managers to staff in the form of ‘begging’ for staff to agree to take on extra shifts (resource) and staff not feeling they can legitimately say ‘no’, leads to off-duty stress when they are not working, processing feelings of guilt and worry about colleagues (–response). |
| Outcome: pressure can lead to guilt and a feeling of letting the team down and to working even when meant to be off. Time off from work is not regenerative, leading to increased feelings of dissatisfaction and burnout. |
Linked to the serve and sacrifice ideas presented above there was also a sense of staff feeling coerced to cover shifts when there are gaps due to insufficient staff. Consequently, front-line staff shortages present a major concern for the mental well-being of nurses, midwives and paramedics and impact work-life balance. Particularly as most of these staff groups work routinely long 12-hour shifts, with a review by Ejebu et al. 62 finding that ‘Shift patterns are often organised in ways that are detrimental to nurses’ health and well-being’ (p. 21). For example, Cull89 highlights the negative impact of being asked to fill vacant shifts during severe staff shortages:
Midwives described managers ‘begging’ for them to work extra shifts. Even if they did not agree to these extra hours they felt guilty. The requests impacted on their enjoyment, on their days off and they began to dread phone calls or texts asking them to work overtime.
(p. e554)
In the context of understaffing and pressure for staff to work overtime, the messaging that they are desperately needed is something staff may take home with them. Even on their days off they may think of work and feel like they are working. Some may feel guilty for having days off and not answering the call to do extra shifts and empathise with the consequences of staff shortages on colleagues and patients. It is possible that being asked to fill vacant shifts creates presenteeism. In a literature review, Freeling et al. 61 suggests
Johns (2010)201 found that hospital cultures that exalt loyalty, teamwork and professional identity can unwittingly encourage presenteeism (…). Further possible causes are the caring nature of the profession, the suboptimal health of many nurses, and intense job demands.
(p. 2)
The importance of on-the-job, and off-the-job embeddedness – in protecting well-being – is discussed in one paper. 88 Embeddedness in this context means ‘the extent to which people are linked with others or to activities, the extent to which their jobs and communities fit with other aspects of their lives, and the ease with which their respective links can be broken – that is, what they would sacrifice if they left’ (p. 329). The authors argue that the more fulfilled staff feel in their personal lives, the greater the buffer to the emotional challenges of being off duty while there is a huge need for staffing.
Tension 8: the tension between the lived reality of staff shortages versus the wish to deliver high-quality patient care, which can result in moral distress
| CMO#15: staff shortages prevent staff from giving high-quality patient care. |
| Context: staff come into the profession to care well for people in need. Staff shortages mean there is less time to care for each patient. |
| Mechanism: institutional constraints (staff shortages) make it nearly impossible to pursue the right course of action (resource) staff feel dissatisfied with the care quality they can provide and care that is left undone (resource) and experience moral distress and injury (–response) causing them to experience anger, frustration, guilt and loss of the capacity to care (–response). |
| Outcome: staff become burned out and dissatisfied with work and leave the profession because they feel they can no longer give the quality of care that patients deserve. |
This is supported by findings from one study that many staff are leaving the profession because they feel they can no longer give the quality of care their clients deserve,155 supporting previous literature on this;16,202 and care ‘left undone’ by Ball and colleagues203 who report that 86% of nurses ‘reported that one or more care activity had been left undone due to lack of time on their last shift’ (p. 116).
| CMO#16: a vicious cycle of staff shortages leads to an unworkable situation for staff who remain. |
| Context: staff shortages create highly stressful under-resourced work environments. |
| Mechanism: with many people leaving the professions (resource), an unworkable situation for the staff who remain (–response) is created, who become more stressed and depleted (–response). |
| Outcome: these staff also eventually choose to leave, creating a further vicious cycle of staff depletion. |
Staff shortages create highly stressful under-resourced work environments, which can create a vicious cycle and increase burnout and intention to leave the workforce, with associated middle-range theories of MD, moral residue and moral injury.
Moral distress was defined in the nursing literature in the early 1980s as occurring when: ‘one knows the right thing to do, but institutional constraints make it nearly impossible to pursue the right course of action’204 (p. 6). More recently, Morley (2021) defined it as the combination of (1) the experience of a moral event, (2) the experience of ‘psychological distress’ and (3) a direct causal relation between (1) and (2)205 (p. 15). Morley and colleagues report that MD has been found to be associated with feelings of anger, frustration, guilt, loss of self-worth, sorrow, anxiety, misery, dread, anguish, depression and nightmares; it appears to cause a withdrawal from the bedside, the avoidance of patient contact and loss of the capacity to care, with MD reported as an additional factor for nurses leaving or intending to leave their place of employment and the profession altogether. 205 Brooks206 argues that ‘It is equally important for managers to acknowledge the suffering that goes along with MD and give nurses the resources to address it. In their study an ethicist was available to consult with nurses, which happened frequently’ and participants suggested it was ‘a very important resource, but managers need to be open with nurses about (...) MD (…). It is, to some degree, inescapable, but if nurses know what it is, and have resources to help deal with it, then it can be reduced.’ (p. 1).
Jones193 reports that while COVID-19 has brought MD to more people’s attention, it is not specific to the pandemic and could be brought about by staff’s reaction to inadequate staffing levels or an inappropriate skill mix. Lena-Riedel et al. 207 report the associated concept of moral residue, when individuals are repeatedly exposed to morally stressful situations, from which they may not fully recover from the distress they experience. 208 Prolonged MD, which develops into a moral residue, can lead to moral injury, which can increase staff’s risk of developing psychological health problems and manifest in the form of a loss of trust in self, authority, and systems.
We identified two interlinked challenges: the vicious cycle of staff shortages resulting in the need to work harder and more intensively, and the challenge of staff shortages causing staff to work outside of their scope of practice, both of which may increase intention to leave (see also Chapter 4). A ‘runaway’ effect can occur with so many people leaving the profession that it creates an unworkable void in the environment for the staff who remain (as seen during and post COVID-19 – see Appendix 3) and so more staff eventually choose to leave. The King’s Fund report30 discusses this in relation to district nurses:
The King’s Fund has identified a large and growing gap between capacity and demand in district nursing services: a significant increase in activity over recent years, both in terms of the number of patients and the complexity of care; a decline in staffing levels, particularly in senior ‘district nurse posts’ an increasingly task-focused approach to care; and a lack of continuity of care (...). Inevitably, this is having a negative impact on staff well-being, with unmanageable caseloads common and come district nurses leaving the service as a result. 30
(p. 17)
This was also highlighted as one of the key pressures facing the NHS in an Royal College of Nursing (RCN) report:209 ‘spikes in staff sickness rates put even more pressure on services and the ability of staff to deliver safe and effective care, as remaining staff are even more stretched as they try to cover for those off sick’.
| CMO#17: staff shortages may lead to an overextension of role scope. |
| Context: staff come into the profession to care well for people in need, to do a good job and expect to feel supported and well trained. |
| Mechanism: staff shortages can mean insufficient staff to perform all roles/tasks (resource) resulting in staff being asked to perform new tasks/undertake roles out of the scope of their practice and which they do not feel trained for or comfortable doing (–response) leading to anxiety and concern about the quality of care and potential mistakes (–response). |
| Outcomes: increased stress and risk of burnout, increased sickness absence and increased intention to leave or staff leaving the professions resulting in a vicious cycle of staff shortages. |
In our data, staff shortages led to further loss from the profession through another mechanism, in which staff are asked to perform tasks outside their role or job scope. For example,59 conducted qualitative research with midwives evaluating a preceptorship programme who suggested ‘understaffing means that you have to do more than you feel comfortable doing’ and that junior midwives ‘feel overwhelmed with responsibility and this can be a main factor that can impact on the sickness rate and staff retention’ (p. 10). Furthermore a paramedic systematic review21 highlighted: ‘it may be that staff shortages lead to an ambulance crew responding independently to a job that would otherwise require backup, making the job potentially more challenging and/or traumatic’ (p. 23). This was also reported in the SOM report25 and WHELM report74 where in the latter many midwives reported being moved around to plug gaps in service provision, making them feel undervalued, and causing stress and anxiety: ‘The perception that my role is not essential and the expectation that I can be used to plug gaps elsewhere means I am asked to work clinically in areas I’m very unfamiliar with, but where there is no support and it doesn’t feel safe’ (p. 19).
Undertaking tasks beyond their expertise and experience was particularly evident in staff who were redeployed during the COVID-19 pandemic (see Appendix 3) and by our stakeholders:
Stakeholder contribution: members noted that in 2020 healthcare professionals were increasingly being asked to take on extra or new responsibilities, opening themselves up to unfair pressure, affecting their confidence and making themselves vulnerable to psychological health issues.
Key finding 4: there are unintended personal costs of upholding and implementing values at work
Overview of key finding
Healthcare staff are known to have a desire to help others and hold strong professional values. Evidence tells us that empathy and compassion and professional values matter to patients and for high-quality care delivery. 11,210 In the UK, nurses, midwives and paramedics personal and professional values are underpinned by the NMC and HCPC professions’ codes of conduct and the NHS constitution and six values therein (working together for patients; respect and dignity; commitment to quality of care; compassion; improving lives and everyone counts). Like empathy (identification with and understanding of another’s situation, feelings and motives)211 compassion is something that is felt and is a deep awareness of the suffering of another coupled with the wish to relieve it. 210 Thus, health-care professionals are exhorted to care about patients to empathise and to show compassion. Yet compassion and high empathy can come at a high price for staff in terms of their own psychological ill-health resulting in vicarious or secondary trauma.
To deliver compassionate high-quality care, emotional labour is required; nurses, midwives and paramedics often have to suppress authentic feelings and regulate their emotions, which can impact staff psychological ill-health. Emotional labour can be defined as an outward appearance of calm that does not reflect inner turmoil while comforting patients. 212 A potential so-called theory-practice gap is reported to exist between the theory taught in healthcare education and the reality of healthcare delivery. 202,213 If staff cannot deliver care in line with their values (see CMOc#14 above) this can cause guilt and MD or moral injury.
Tension 9: the tension between the reality of healthcare delivery versus the taught theory and values, which can lead to guilt and moral and emotional distress
| CMOc#18: moral distress: the theory learned through formative training may not match real-world expectations at work. |
| Context: students in nursing and midwifery (and likely paramedics) may develop idealised visions of what work will be like when they qualify as professionals based on training that espouses high ideals. |
| Mechanism: pressures caused by staff shortages and other systemic factors may mean that day-to-day practices may not align with what students are taught (resource). Emotional and moral distress is felt when newly qualified staff are not able to practice in the profession in the way they anticipated during their training years (–response). |
| Outcome: reduced workplace satisfaction, stress and burnout and potential to leave the profession. |
CUP-1 programme theory17 identified that doctors did not feel able to do the job they were trained for or able to feel proud of the work they have done. Brooks21 suggests clinicians experience a high level of MD when they know they are not providing optimal care to patients. Our data also suggested the same was true, particularly for nurses and midwives with a theory-practice gap evident in a number of ways.
Published literature has alluded to the role of professional identity and role clarity as important determinations of psychological wellness for nurses and midwives. For example, a study on resiliency in midwifery214 in which they asked senior midwives what allows them to ‘bounce back’ after a difficult day. In that study, participants cited ‘having a strong sense of professional identity’ (p. 67), among other traits. Similarly, Goddard52 provides further insights into the role of professional identity formation on psychological health in the nurse workforce and issues of dissonance. In this study, they examined the prison nurse role and the challenges in maintaining a clear sense of professional identity in the face of incompatible ethos of prison administrative culture. They write ‘if there is a dissonance between what the nurse perceives to be essential values, ethos, and history and what which is encountered in the workplace, it could negatively impact on the growth of a positive professional identity’ (p. 165).
Some groups of staff seem to suffer more than others, with newly qualified staff often struggling the most, trying to implement theory and uphold ideals of care quality. 16 There is evidence to suggest that more experienced staff may have either had to compromise their ideals of care or left the professional because they had been crushed. 215 Hawkins et al. 123 in a review of the literature on new graduates describe the impact on them of working in unsupportive workplace cultures that have risk of
endemic bullying behaviour….aggressive acts are most often committed by nurses who are impacted by negative job characteristics, such as increased workload, emotional demands and role conflict (…) new graduate nurses (…) are often overwhelmed and stressed due to heavy workloads and inexperience.
(p. 42)
The reasons such staff are more at risk are because of their ‘inferior position within the nursing hierarchy (…) and the unrealistic expectation for new graduate nurses to hit the ground running’ (p. 42). They report that after 6 months of employment, nurses had their ‘ideal view of belonging to a noble profession replaced with being in a culture that eats their young’.
The literature on the causes of workplace-induced psychological ill-health (see Chapter 4) and solutions (see Chapter 5) point to the nature of job roles and the organisational conditions that form the basis of the work environment. A fundamental connection between job control and stress was summed up in79 in which the author states ‘Whether stress is perceived as positive or negative…is connected with a person’s ability to do something about the external stressor’ (p. 261). This implies that greater perceived autonomy over one’s work leads to a reduction of stress, burnout and attrition, as supported by the literature included in our causes chapter, and supported by organisational stress theory, for example, Karasek. 69
However, a tension also exists between the need for autonomous working conditions amongst team members and the resultant responsibility that comes with developing deeper relationships with patients and clients. For example, the midwifery literature has identified autonomous working conditions as an important factor in determining workplace psychological health. 34,74 Empirical survey findings from Yoshida76 revealed that ‘high levels of autonomy were a key protective factor of emotional exhaustion’ (p. 925). Autonomous working conditions can, in some instances, be compromised in the context of collaborating with other health professionals. In maternity care, this may involve a conflict in perspectives between obstetricians (medics) and midwives. Obstetric specialists may lead decision-making around maternal care from a medical perspective, which can be incongruent with midwifery practices, and poor teamwork between the multiprofessional members can lead to possible harms for the professionals and clients. Rocca-Ihenacho113 notes
organizational culture underpinned by teamwork, cooperation, and positive working relationships is a key characteristic of safe maternity units…maternity unit performance can suffer from a lack of focus on philosophy of care and that malfunctioning health care organizations with poor interprofessional relations are associated with catastrophic, avoidable harm to service users.
(p. 2)
Maben et al. 16 report nurses leaving due to an inability to implement their ideals and values:
On qualification nurses emerged with a coherent and strong set of espoused ideals around delivering high quality, patient-centred, holistic and evidence-based care (...) (yet) (…) within 2 years the majority experienced frustration and some level of ‘burnout’ as a consequence of their ideals and values being thwarted’
(p. 99)
This can cause MD and injury (see above). Newly qualified midwives can also experience cognitive dissonance between their original ideas around women-centred care provision and the reality in practice of the dominance of the medical model – the so-called theory practice gap202,213 – especially around issues of autonomous working:
…NQMs felt guilt and emotional distress at not being able to give woman-centred care…They were frustrated by their lack of autonomy and its effect on the women in their care, when taught at university to empower women to make their own decisions. 90
(p. 7)
Tension 10: the tension between the benefits of staff empathy to patients (ensuring quality care) versus the harms of staff empathy to staff (increasing risk of vicarious trauma or unhealthy/negative coping strategies)
| CMOc#19: empathic traits of staff members allows for better understanding of patient suffering and improved service provision but increases the risk of vicarious trauma. |
| Context: healthcare staff are recruited based on values (including compassion, which requires staff to be empathic), which may put them at more risk of burnout when faced with the expected exposure to traumatic events as well as chronic low-grade events, which can cause serious secondary trauma. Across the health service, some staff are more empathic than others, and a variety of factors influence risk of psychological ill-health, including frequency of traumatic events, lack of time to process and working in an unsupportive workplace environment. |
| Mechanism: staff who are genuinely empathic (resource) are better able to understand the pain and suffering of patients (response). Such staff may significantly identify with that suffering that may resonate to the point of negatively impacting emotionally and psychologically (–response). |
| Outcome: while empathy can improve patient experience and outcomes, it can also lead to vicarious trauma, burnout and staff leaving the profession. |
When ill, frightened and/or facing a difficult diagnosis, it is reasonable that patients want to be cared for and cared about by those looking after them. 215 There is evidence to suggest that a caring healthcare encounter is highly associated with patient satisfaction,216 better patient outcomes217,218 and facilitates healing. 219,220 Indeed Kenneth Schwartz (a patient who died aged 39 of lung cancer and founder of Schwartz Center Rounds) spoke not only of the need for care and validation but also spoke of the need for empathy: ‘I have learned that medicine is not merely about performing tests or surgeries, or administering drugs… For as skilled and knowledgeable as my caregivers are, what matters most is that they have empathized with me in a way that gives me hope and makes me feel like a human being, not just an illness’221 (p. 3).
We have noted the challenges of this work; that going the extra mile and caring for others is desirable but can readily be undermined by resource shortages and healthcare professionals need to bring their whole emotional selves to work each day. Yet, often there is no support or training on how they can protect their psychological well-being when faced with a daily exposure to trauma, to sadness and to loss. Healthcare staff are recruited for their caring values, and encouraged to empathise with patients, yet they can experience vicarious trauma, which ‘can develop in people who are exposed to other people’s trauma over a prolonged period’186 and which result in secondary trauma for nurses, midwives and paramedics as outlined above.
Although there are repeated calls for the professions to recruit more people who exhibit empathic traits and whose personal values align with professional demands, empathic staff are at risk due to their ability to resonate with patient suffering. High levels of empathy are reported in one study to put staff at risk of PTSD. 100 They write: ‘empathic engagement with women is fundamental in maternity care. However, it is recognised to increase vulnerability to traumatic stress responses’ (p. 5). And ‘the midwifery profession may risk losing the most empathic midwives following traumatic perinatal event exposure’ (p. 18).
Similarly, too much empathy for others may potentially exacerbate burnout, as found in another study. 104 They write ‘according to reviews examining predictors of secondary traumatic stress, findings were mixed, but suggested that empathy was not protective, such that empathy had either no relationship or a positive relationship with secondary traumatic stress’ (p. 2).
In trying to find resolution to this paradox, staff may engage in coping activities that suppress their natural empathic gifts. For many empathic staff members, being repeatedly exposed to hardships of caring for patients coupled with a lack of support from their organisations and superiors may mean ‘turning down the volume’ on empathy to be able to cope. There is evidence that staff are often recruited with the ‘right values’, yet compassion and empathy can become eroded over time by a toxic system and, in a vain attempt to help staff protect themselves, covert rules suggest they ‘do not get involved with patients’ (keep an emotional distance). 215 Without an outlet to express one’s empathic gifts in service delivery, the real rewards of providing care are missed, leading to decreased satisfaction with work and reduced personal accomplishment, which is one element of burnout.
| CMOc#20: staff adopt maladaptive strategies, controlling the environment or depersonalisation to cope with risks of secondary trauma and burnout. |
| Context: staff are exhorted to provide empathic and compassionate care in the context of limited healthcare resources despite the risk of secondary trauma and burnout, which can be exacerbated by a lack of organisational support or understanding for staff by employers. |
| Mechanism: everyday pressures may mean that empathy is depleted (–resource). Staff may engage in maladaptive strategies such as rigid task-oriented care, controlling the environment or depersonalisation to buffer against secondary trauma (response). |
| Outcome: worsening of STS symptoms, reduction of patient-oriented care, poor workplace satisfaction and further burnout. |
In the midwifery literature, there is an example of how midwives can at times establish processes that take control away from patients and their families to cope with the risks associated with providing care, and in particular to manage their ‘anxiety, loss of confidence, phobia and depression’ caused by the chronic stress they experience (p. 21). This need for control in the birthing process may be seen as a dysfunctional way of protecting against secondary trauma. Copp91 writes,
it is easier for a midwife to feel she has control in the birthing room, because this is her domain (…) and so she arranges for that to happen, unconsciously and through force of habit (…). So it seems that midwives can have a need to be orchestrating every person in the room
(p. 22)
Similarly, Barleycorn98 explains how staff may adopt a problem-solving approach void of empathy and connection to patients in order to cope. Although this may allow staff to function at work in the short-term, it may affect the patient’s (positive) experience, yet the underlying accumulation of secondary traumatic responses does not disappear and surfaces at some point. They write ‘emergency nurses will often have a problem-solving approach in emergency situations, this is termed as an ‘avoidant emotional coping strategy’ (a distraction) so they can carry on working. However, the long-term effects of this coping strategy can delay the recovery process and lead to the worsening of STS symptoms.’(p. 3). These examples and CMOc#20 link to middle-range theory developed by Isabel Menzies-Lyth (1960),222 whose classic paper on the structure of hospital nursing, (‘A case-study in the functioning of social systems as a defence against anxiety’). Menzies-Lyth suggested work in healthcare and social-care organisations entails significant anxieties for staff and that defences against this anxiety are part of organisational life. 222 Part of these defences (to defend against primitive anxieties aroused by contact with seriously ill patients), included depersonalisation, denial of the significance of the individual, detachment and denial of feelings and the attempt to eliminate decisions (and anxiety) by ritual task performance.
Tension 11: the tension between the excessive requirements for emotional labour inherent in healthcare practice versus the need to improve workplace psychological ill-health
| CMOc#21: excessive demands on using one’s emotional labour leads to burnout. |
| Context: exposure to horrific injury and other patient suffering has resonance and evokes natural emotions in healthcare staff such as repulsion, fear or distress. If such responses are not repressed, it can interfere with service provision and evoke extreme stress and upset in patients. Patients look to healthcare staff for clues about the seriousness of their circumstances and for calm reassurance. |
| Mechanism: nurses, midwives and paramedics need to find ways to regulate emotions to provide hope and positivity, and temporarily hide emotions such as revulsion, fear or distress (resource). This evokes feelings of trust, reassurance and hope in patients (response), but can impact negatively on the healthcare staff themselves if there are no informal or formal outlets for these emotions (–resource), leading to the felt emotion(s) building inside (–response). |
| Outcome: suppressed emotions may come out in other dysfunctional ways, for example, suppressing via alcohol, drugs, poor psychological well-being, job satisfaction, performance. |
The need to provide emotional labour and regulate emotions was identified in the literature as a requirement for the job, which has consequences for staff psychological well-being. 223 Hayes223 notes that emotional regulation occurs in two ways: the first is that staff have to provide positive emotional support to patients/relatives during times of acute crisis, regardless of what they may be feeling during those moments of crisis. At the same time, staff need to keep their genuine feelings at bay if they are experiencing secondary effects of trauma exposure. A midwifery paper reported that if midwives show distress and women see midwives crying this can impact on their feeling of safety, so midwives hide their emotions to support women in their care, which for staff further normalises these traumatic and distressing events. 224 Organisational expectations and pressures in the front-line emotional labour delivered by staff also play a role, as explained by Hayes et al. 223 in the context of paramedic practice:
An emotive response can appear insincere when it is acted, faked or actively modified to accommodate an organisational or societal norm (…) (however) certain human emotions (must) stay concealed; for example, revulsion at a horrific injury (…) this constitutes the effort that paramedics have to apply to their expressed behaviour.
(p. 320)
Stakeholder contribution (Meeting 2): building on the previous finding relating to chronic cumulative stressors impacting staff mental health (Key finding 1) a member stated that the emotional labour of moving between the continuum of emotion and experience (moving between traumatic and more mundane but still taxing everyday stressors) was intense and at times unmanageable, especially when there is not time to process it.
We are all affected in some way by things we see, by the emotion we experience but are forced to contain while dealing with our job. Showing any sign of emotion is still perceived as a weakness (…) and this is one of the things that needs to change. 95
(p. 225)
Anderson94 reports spaces in which different emotional rules apply for public and private performances of emotion for paramedics; with the on-stage performance with the public often using surface acting whereas the ‘debriefing in the vehicle or at the station – the off-stage arena – has been identified as an important coping mechanism employed by paramedics, providing a space to react “unprofessionally”’ (often with dark humour), with the backstage space at the home with family and friends. This draws on Goffman’s middle-range theory of dramaturgy, which uses the metaphor of theatre to explain human behaviour, describing front and back stages in presentation of self. Front stage is where individuals are expected to put on a costume and act differently when in front of an ‘audience’ and back stage is where individuals can relax and actions that would not be condoned in the front stage are free to be expressed. 225
Stakeholder contribution (Meeting 1): a member described that when they wear their professional mask they put their profession on a pedestal where there is no room for weakness – and that is where the naming and shaming comes in.
Oates and colleagues111 in a literature review on nursing in a secure forensic mental health setting describe nursing in this setting as ‘emotional hard labour’ due to the likelihood of assault and difficulty of working with a disturbed and distressed patient group. Citing the implications for practice they, like other literature points to the importance of workforce planning that allows for ‘time out’ of the setting or early retirement (see Chapter 5). However, these strategies could be seen to be not really addressing the problem, just ‘minimising the dose’ of exposure.
Key finding 5: it is challenging to design, identify and implement interventions to work optimally for diverse staff groups with diverse and interacting stressors
Overview of key finding
Our synthesis of the literature also revealed several tensions in terms of identifying the ‘right’ intervention for the ‘right’ circumstances at the ‘right’ time. We also noted that although there is a plethora of interventions (both formal and informal) as outlined in Chapter 5, aspects of the service architecture can impede (or facilitate) implementation and there is often an ‘implementation gap’. 25,226
CUP-117 (p. 42–46) note four CMOcs that related to implementation challenges for psychological health interventions. These included the need for
-
endorsement [CMOc#16]; if not endorsed by the employing organisation and senior leadership, doctors may lack trust in it and may also feel frustrated if they cannot access it because of work constraints
-
expertise [CMOc#17]; if those delivering interventions do not have specific training expertise recipients may be less likely to trust the intervention, which may be ineffective and/or harmful or not accessed at all
-
engagement [CMOc#18]; if doctors involved in the development and implementation of interventions (recipients are more likely to trust and feel ownership of the intervention resulting in more use and effectiveness
-
evaluation [CMOc#19]; if the outcomes of interventions and the well-being of the workforce are regularly reviewed and monitored and acted upon then doctors may feel more supported and engage with efforts to tailor these interventions.
These features fit with evidence-based Implementation Science frameworks such as the CFIR,66,67 which tells us the factors important for successful implementation of interventions, and also with conclusions from the King’s Fund report,30 which states interventions are most likely to work when they are tailored to specific contexts and needs of the staff group they affect, and when they involve and engage staff in shaping and implementing changes. 25,227 In our synthesis, we have also identified the importance of considering who when and how interventions are delivered, not just what they are. This includes the timing of delivery of interventions; the mandatory or voluntary nature of participation in wellness interventions, as well as top down versus peer-based interventions (building on the engagement feature identified in CUP-1).
Tension 12: the tension between making staff wellness interventions mandatory versus voluntary
| CMOc#22: mandatory participation in psychological wellness interventions may stigmatise staff and be inauthentic. |
| Context: delivering health care involves difficult emotional work every day and may involve exposure to trauma. Staff may respond and cope in different ways, and there are varying levels of psychological support in teams and organisations. |
| Mechanism: when there is an expectation by managers and peers that all staff should attend a wellness intervention (resource), this leads some people to benefit from the support of others (response) while others may be left feeling resentful, anxious and exposed at sharing emotions and possibly retraumatised by the requirement to disclose their emotional state to others. These staff may also feel stigmatised by their disclosures (–response). If mandated, these may become less authentic and a tick box response (resource), leading to staff feeling they are a management tool rather than caring for their wellbeing (–response) yet mandating such interventions could enable them to become normalised (resource), which may ultimately change culture regarding speaking about the emotional impact of work (response). |
| Outcome: mixed outcomes; where negative responses are triggered, staff are less engaged in work, feel less secure and safe, less likely to speak up, more likely to suppress/look for other means for support, which may be dysfunctional. Where positive responses are triggered, staff feel looked after and supported, believe their well-being matters are more likely to disclose, and culture change may follow. |
| CMOc#23: voluntary participation in wellness interventions provides choice but may reduce uptake. |
| Context: delivering health care involves difficult emotional work every day and may involve exposure to trauma. Staff may respond and cope in different ways, and there are varying levels of psychological support in teams and organisations. |
| Mechanism: offering debriefs or checking in as a voluntary/optional intervention (resource) means that those who wish to discuss/receive support can receive it (response) BUT may lead to some who needs support not accessing it due to fear of stigma, or not recognising they would benefit from it (–response). |
| Outcome: staff feel better supported and that their concerns are heard after challenging and stressful events (those who wish to receive it) but may leave others who do not want to access feeling unsupported and alone and unable to disclose or receive support. |
While we have identified the need for a dynamic ‘system’ of interventions and yet a prevalence of solutions that are individual-focused, which can make staff feel as if it is their responsibility alone for their psychological ill-health, we acknowledge that these interventions can be of benefit (within a suite of interventions) and some guidance about whether they should be mandatory versus optional, was identified in our synthesis. CMOCs#23 and #24 above present rival theories.
If an intervention is optional, some staff might not come forward even if they need help, perhaps due to perceived stigma associated with accessing help (e.g. one-to-one or group psychological therapy sessions). On the other hand, if an intervention is mandatory, some staff may feel forced to participate when they are not ready or feel the need to do so, or the offer of support may lack authenticity and feel ‘tick boxy’. This is explained in the following excerpt from a qualitative evidence synthesis of help-seeking in trauma-exposed emergency service staff:18
some participants resisted mandatory organizational mental health support following traumatic calls and Others, however, believed mandatory interventions would reduce stigma associated with their use and prevent delays to help seeking due to the stigma associated with disclosing vulnerability. 18
(p. 9)
Stakeholder contribution (Meeting 2): a group member said one of the issues that her organisation was struggling with is exactly this conflict; making wellness interventions mandatory or voluntary. While a paramedic in our third stakeholder group urged caution if mandating an intervention is conflated with ‘safety’ as just because it is mandated, does not mean it offers psychological safety.
It is known from the PTSD literature that psychological debriefing may interfere with natural recovery processes following a traumatic event18,35,103 and mandatory debriefing may not necessarily be the right intervention for a given staff member at a certain point in time. This potential harm is not always recognised by organisations, for example,
Midwives also reported an unhelpful organizational climate, and typically did not perceive responses from senior colleagues to be emotionally supportive. In addition, midwives who sought external input to help manage their responses to trauma were often referred to counselling services, despite counselling being contraindicated for the treatment of PTSD. 103
(p. 3)
Voluntary interventions may allow those who are most receptive to such interventions to take part and find benefit through connecting with peers and supervisors while allowing others to process emotional difficulty in different ways, such as through recreational activity, meditation and so on. Some voluntary interventions (e.g. Schwartz Rounds) may create a sense of psychological safety amongst the team/attenders whereby everyone knows no one is going to be forced into disclosing their difficulties (the audience can just listen and not share48,177). Normalising and attempting to de-stigmatise attention to and support for psychological health at work is also important, and if addressing/discussing well-being is a standing item on meeting agendas, appraisals, and other formal processes, and taken seriously and with good psychological safety then it may be helpful, but care needs to be taken that it is not just lip service, so how it is done is very important. In Duncan97 the authors argue ‘health and well-being concerns should be raised at staff meetings as a standing item, so it becomes normal practice for staff to think of their own health and well-being, as well as those of other team members’ (p. 480).
The theory here is that raising psychological health concerns as standard practice sends a message that people should monitor and reflect on their needs as part of normal everyday practice. Having group check-ins may also allow staff to think about their own and colleagues’ psychological health, which may increase recognition of the challenges everyone is facing across the workforce.
Tension 13: the tension between the need for spaces to debrief with managers/leaders so they hear and can thereby offer support versus the need for peer-led spaces for debriefing
| CMOc#24: psychologically safe spaces for processing work challenges can provide support and healing. |
| Context: trauma exposure and other stressors on the job may lead to supervisor-led check-ins as part of routine practice. |
| Mechanism: formal debriefing offered through occupational health (or the department, for example, hot and cold debriefs etc.) that have both organisational learning and staff support as their aim can provide the opportunity to process difficult experiences (resource); however, may not work if perceived as a management tool (–response). Peer-led spaces for debriefing can bring safety and willingness to disclose difficulties (response) if with trusted peers in a confidential and safe psychological space (resource) but may lead to managers/leaders being unaware of issues and thereby unable to act (–response). |
| Outcome: managers/formal: lack of uptake (if voluntary), or breakdown of trust if organisations use check-ins as a management tool, and therefore reduced disclosure from staff; but is an opportunity for managers to signpost/provide further support if needed. |
| Peer/informal: sharing of stories, psychological healing, not feeling so alone in feelings, improved teamwork if with trusted peers; but may not be signposted appropriately to support where needed. |
We need both interventions for organisational learning (e.g. hot and cold debriefs) and those for staff healing (peer-led informal spaces, and counter-cultural organisation-wide spaces such as Schwartz Rounds).
CUP-117 note two CMOcs that related to this tension. These included the need for
-
positive and meaningful workplace relations (CMOc#7): which can foster a sense of belonging between colleagues and towards the profession and lead to an increased capacity to work under pressure
-
‘organic’ spaces to connect (CMOc#11): with protected times and psychologically safe spaces to congregate staff can to bond over whatever is most important to them at that time, which may improve connectedness.
A recent review228 on shared social spaces on the wellness and learning of junior doctors identified four common attributes of positive social spaces: informal, safe, functional and legitimate, suggesting that informality was fundamental for a space to be positive for well-being and learning because
being away from the clinical ‘frontstage’ (…) allow(s) individuals to interact informally outside of the constraints of their usual roles (…) allowed social conversations to be ‘freewheeling’ and unguarded (...) (and) ‘backstage’ reflecting the degree of performance that must be enacted in the clinical environment.
(p. 6)
Our data support the benefit of spaces for staff to come together (see Chapter 5). It is known that over time such spaces and places for staff to eat and rest together have become eroded with break rooms often multipurpose rooms and not created with rests and recovery in mind, and ‘shared social spaces are in decline’ (Ulys under review). 228 Also, that certain contexts may make informal interventions more or less difficult to enact.
Stakeholder contribution (Meeting 2): a member highlighted that lone working makes ‘accidental’ or informal debriefing harder, but formal spaces are hard as you are told its ‘OK to share now’, which can be off-putting; another member described informal ad hoc support (e.g. while cleaning an ambulance) were important times for resetting mentally before the next job.
Thus, opportunities for staff to take lunch together or take breaks with other colleagues have been severely affected. This is particularly so for some specialist nurses,118 community nursing60 and midwifery staff and paramedics who are often lone workers and who may not see another colleague all shift, have less team support and perhaps more challenges around a manageable flow of patients. 60 While the importance of these informal spaces for peer-based support is acknowledged in the literature, so too is the importance of having support built into ‘the job’, as highlighted in our stakeholder group.
Stakeholder contribution (additional meeting, July 2022): one member described how all well-being initiatives should be built into the job and weaved into existing structures and routines – become routine practice rather than a separate initiative – because staff were continually exposed to occupational hazards that are part and parcel of the work.
Other papers suggested trauma is an expected part of the job33,100,229 and a paramedic paper suggested the intensity of this exposure is at complete odds with what member of the public may ever see, with the general public’s perception of ‘normal’ different to paramedics114 ‘paramedics and ambulance crews see incidents on a daily basis that the average person may only experience once in a lifetime’ (p. 192). A paramedic review paper18 reported that due to the potential stigma arising from disclosing in earshot of colleagues, most of this defusing occurs in the private space of the ambulance when returning to base or awaiting the next call, and referred to the shame and fear of repercussions of admitting to psychological health difficulties. This may be more prevalent in a male-dominated work environment with military roots such as the paramedic service perhaps94 (also see Appendix 3). Although Choflet and colleagues36 suggest it also applies to nurses due to
a culture of personal and institutional stigma against treatment of mental health conditions, fear of judgment by peers and supervisors, consequences of having mental health treatment or condition on their ‘record,’ and potential action by licensing boards. (…) Addressing stigma, confidentiality, and reliance on self are (…)critical barriers to help seeking.
(p. 21)
The other tension relevant to formal versus peer-led debriefs is clarity about the purpose of any given intervention – is it outcome-orientated and designed to create actions for organisational learning or is it primarily for staff healing, or both? If linked to organisational learning it may be perceived as a ‘management tool’. The conditions under which staff would perceive debriefing as a management tool versus a supportive intervention is not clear in the current literature retained, but it can be understood in relation to the objection to having their well-being ‘managed’, and also in relation to other ‘objectives’ that the interventions may be serving (e.g. patient safety/organisational learning etc.). In our stakeholder group, a paramedic member stated that ‘how’ managers checked in with them – and their tone – mattered in terms of working out whether managers were checking in to check whether paramedics are OK to go to work (being monitored, with service delivery at the root), or whether it was a supportive check-in, or simply a ‘tick box’ exercise. Alongside feeling their well-being is being ‘managed’, staff might feel that they are being monitored and judged by their superiors and their peers and suffer consequences to their job and possible reputation. Noting the key issue of stigma in the literature,18,35,36,230 issues may arise in terms of gaining a reputation of ‘being weak’ in the context of other staff who seem ‘resilient’.
This reaction against ‘management tools’ is proposed as one of the key rationales for the benefit of peer-to-peer spaces. Peer-to-peer community practice approaches to debriefing and wellness check-ins are recommended in a few papers,73,119,181,231 with a further paper suggesting them as an alternative to formal mentoring or supervisor-led check-ins:82
formal debriefing, particularly following critical incidents, is offered within ambulance services, usually from occupational health. Limitations can arise if ambulance staff perceive debriefing as a management tool, rather than a method of recognising and managing occupational stress, creating resistance to treatment.
(p. 1)
This also links to the need for spaces that are deemed to be independent (from managers, the organisation), raised in a few sources including a report about burnout in ambulance service staff by the Larrey society153 within which a key action was to ensure access to independent counselling services. Similarly, O’Neill and colleagues78 examined supervision with nurses that used reflective practice techniques, which illustrated the importance of confidentiality and psychological safety and an uninterrupted safe space free of management as important for group support. They found that participants preferred that managers were not present during the sessions because they felt
it changed the group as people were afraid of being judged or told how to think or act. There were also concerns that managers may follow-up conversations outside of the group, which they preferred to keep private.
(p. 8)
Thus, informal confiding and sharing of experiences is most likely with colleagues (or family) with whom staff share a bond of trust. Without trust staff risk reliving distressing events and their feelings being invalidated. 18 A national realist evaluation of Schwartz Rounds (one of the few organisation-wide, peer-led, team-based interventions) identified the importance of confidentiality and psychological safety as important mechanisms to ‘disclosure’ healing and self-compassion. Schwartz Rounds have specific ground rules carefully prescribed by the programme architecture and facilitators to make it a safe space with a flattened hierarchy that overcomes any risks regarding disclosures with managers present identified above by O’Neill and colleagues,78 despite being a ‘formal’ intervention. Schwartz Rounds are one intervention to use stories and Paranjape124 discusses value of casual storytelling for reflective practice and self-analysis, while Quaile95 reports ‘Talking to my peers has also been a massive help … it helps me realise that what I’m going through is normal, and that many people experience things like this from time to time’. Similarly, Jackson73 reports the importance of being listened to and of peer support (in feedback about a support group for newly qualified nurses), also supported within the HEE report9 emphasising the power of peer-to-peer support to help develop a strong team ethos and that both formal and informal methods can be useful.
The use of technology in providing peer-led spaces was also reflected in the literature, for example, Webster57 who reports on the implementation of an online peer support group for newly qualified nurses. The approach is to provide an online platform whereby nurses can feel supported emotionally and ‘collaborate with one another to reflect on their work, gain psychological support, share power and responsibility, and feel empowered’ (p. 1587). The peer-led and voluntary nature of the intervention are important facets of the programme architecture, leading to the idea that nurses need to have autonomy around the restorative interventions they are provided. Such peer-led interventions can be assumed to be advantageous as a downstream intervention in the sense of increased psychological safety and shaping their needs, voice concerns and gain a voice in what otherwise might be a silencing and oppressive work environment. Alternatively, peer-led interventions may not always ensure psychological safety if peers do not have trusting relationships with each other, or if the volunteer moderation of the forum does not create a safe and confidential space for people to disclose sensitive issues and receive support; and the informal nature of some peer-led approaches may lead to staff not being signposted for further support when it is needed.
| CMOc#25: the importance of kindness, listening and space to be heard by mentors. |
| Context: in the challenging experiences of delivering health care, staff may face chronic and acute trauma exposure that may not be understood by mentors and colleagues. |
| Mechanism: mentors offering kindness, listening and spaces to be heard (resource) allow staff to become stronger, recover and heal (response). |
| Outcome: staff feel supported and their trauma recognised, are able to carry on with their work and feel less alone and more supported. |
All staff, and especially mentors (who may be managers or people affiliated but not involved in line management) need to understand the impact of their actions on other staff who may be carrying secondary trauma. For example, the anonymous author of a blog116 writes about her struggles with psychological ill-health and how workplace mentorship has the power to cause and to heal deep wounds. She talks about how being yelled at by one of her mentors led to her spiralling down:
Sometimes it is the smallest thing that opens a crack, like a thorn in an open wound that is wiggled every time another ‘small comment’ is made, opening that space wider and allowing infestation and disease to spread deeper inward, until you are not quite sure who you are.
(p. 758)
The author described the impact of mentors being kind and patient, arguing that in some cases such acts of compassion can be more effective than resiliency training:
I think more effective than resilience is kindness, patience and gentleness. In my worst moments, I had kindness poured over me from hearts steadier than my own. I had ears that heard me and allowed me to speak, and many people who were willing to tread a path with me. This, more than anything, helped me to survive, heal and ultimately thrive. I am stronger, not by my own might, but by the strength of those that held me up when I couldn’t do it alone.
(p. 758)
A key contextual factor here for mentors/managers (or those doing the checking in) would be their training needs and ensuring that they were properly trained to ask the right questions and offer or signpost to the required support.
For example, Duncan97 writes ‘If managers notice that a staff member is becoming withdrawn and quiet, they should create an appropriate confidential environment to let the staff member know they have noticed, and that they are concerned for their welfare (…) [This might] prevent a difficulty from escalating to a problem’ (p. 480).
Tension 14: the tension between the need to act and offer support versus providing interventions that are ineffective because they are too soon, reactive and/or single time point
| CMO#26: the importance of timing of psychological ill-health interventions. |
| Context: staff may experience stressors and trauma exposure that benefit from intervention but may require different support at different times in psychological ill-health journey or in working day (e.g. end of shift debriefing), yet staff are usually exhausted and drained at the end of their shifts. |
| Mechanism: in an immediate crisis, staff may need their immediate basic physiological and safety needs to be met (safety, shelter [resource]); once met, psychological support could be accessed (response). Debriefing interventions that occur at the end of shift (resource) provide a non-judgemental reflective space (resource). However, fatigue and exhaustion reduce motivation to attend such debriefings (–response). |
| Outcome: low uptake of psychological support if basic needs not met and low attendance at end-of-shift debriefing meetings and a less effective intervention/support for staff. |
Interventions and strategies to reduce stress, can also be affected by the timing of the intervention. There has been significant learning in the recent COVID-19 pandemic where in a longitudinal study of the Impact of COVID On Nurses (ICON), nurses reported not accessing interventions, such as mindfulness Apps, ‘wobble rooms’, online ‘zoom’ well-being sessions, counselling or psychology sessions. This was due to a variety of factors such as time constraints and not wishing to access resources outside of shift-hours (while recuperating), or because of physical barriers such as sessions not being set up on the site staff were working on. Another reason was that they were not the right intervention at the right time: they needed their essential safety and physiological needs to be met first. 232 Indeed, in terms of temporality, in the ICON study nurses reported requiring very different support at different times; in the immediate crisis, they needed their immediate basic physiological and safety needs to be met as per Maslow’s (1943)170 hierarchy of needs [food, safety (i.e. personal and protective equipment [PPE]), shelter]. Once these were met, and the threat receded, they could begin thinking of accessing psychological support (if required). Thus, timing matters. Bowen99 reports an evaluation of a debriefing intervention for ENPs and found debriefing was not helpful for everyone and made some feel worse. This is a known risk with psychological debrief interventions that may be designed to mitigate risk of PTSD (such as CISD) but now known to potentially increase risk of developing PTSD. Another discussion in the literature concerns when in the shift such interventions be implemented. Winter120 reported findings on a particular debriefing intervention in midwifery called ‘recognise and reflect’, which is a debriefing intervention led by a specialist registrar and senior midwife, that takes place at the end of shifts. They explain that while this intervention aimed to provide opportunities to discuss positive aspects and any issues arising, the intervention failed:
However, these were abandoned after five weeks due to a 50% attendance rate, with one midwife commenting ‘I personally found at the end of a 12-hour shift, most people are impatient to return home/exhausted/drained’.
(p. 802)
This points to the fact that timing matters in debriefing interventions and that debriefings after long shifts may not be suitable due to fatigue and the need leave the workplace, unless time is built into allowing them to happen prior to the end of a shift. After a long shift would seem like a time when staff are checking out, moving into a different mode outside of the workplace context. Other examples in the literature included interventions that were not successful due to not being needed or wanted78 and another where the introduction of the intervention (restorative supervision and helplines) were reported as ineffective and unwanted. 87 Both studies reinforce the need for involvement of front-line staff in planning designing and implementing interventions.
Chapter 7 Discussion
If the job is making doctors sick, why not fix the job rather than the doctors?233
Summary of key findings
Our aim in this review was to improve our understanding of how, why and in what contexts nurses, midwives and paramedics experience work-related psychological ill-health; and determine which high-quality interventions can be implemented to minimise psychological ill-health in nurses, midwives and paramedics. Through our analysis (see Chapters 4, 5 and 6) and discussions with our stakeholder group we realised there were some fundamental questions our work needed to answer. We therefore generated the following questions, which we have sought to address in Chapter 6, through our realist synthesis and our 14 tensions:
-
Why is psychological ill-health in healthcare professionals still a huge and growing problem which has become entrenched in some settings?
-
Why despite having interventions (some of which have an ‘evidence base’), does the problem persist?
-
How can we optimise existing interventions, by analysing when and where they work suboptimally, as well as innovating and building upon what already exists?
Our overall review findings are summarised in Box 1.
-
There are more similarities than differences in causes of psychological ill-health among nurses, midwives and paramedics; and very few interventions were profession-specific.
-
Some causes may be more prevalent or exacerbated in certain professions, or roles within profession (rather than being profession-specific). In most cases it is the service architecture that can increase risk rather than the profession itself.
-
Organisational prevention is under-represented and there is a focus on the traumatised (tip of the iceberg), rather than the essential needs of the majority.
-
Some individual characteristics (e.g. ethnicity, sexual orientation and/or gender identity, and disability) deserve greater focus to improve understanding of causes and interventions.
-
Empirical papers evaluating interventions mostly focus on one single intervention and do not account for complexity; editorial and commentaries tended to recognise the need for multi-level systems approaches.
-
Staff create informal interventions to plug gaps (in provision and suitability of interventions offered) but these are rarely recognised in formal syntheses/reviews.
-
Multi-level systems approaches – offering primary, secondary and tertiary solutions – are required that consider intersectionality and structural differences between and within professions and the ways they work, and to support particular staff groups at specific times when they may be at greater risk of psychological ill-health.
-
By surfacing tensions in the literature, we have identified aspects of work that are incompatible and affect psychological ill-health and we have learned that healthcare delivery and staff psychological health is a balancing act.
-
Interventions tend to be fragmented, focused on fixing the individual, reactive and insufficiently recognise cumulative chronic stressors.
-
It is difficult to promote staff psychological wellness where there is a blame culture.
-
‘Serve and sacrifice’: the needs of the system often override staff well-being at work.
-
There are unintended personal costs of upholding and implementing values at work.
-
It is challenging to identify the ‘right’ intervention for the ‘right’ circumstances at the ‘right’ time to work optimally for diverse staff groups with diverse stressors.
-
Implementation gaps may exist where interventions are not implemented well or sustained.
-
A long-term strategy and investment are required: some interventions take time to effect cultural change.
-
COVID-19 caused an exacerbation and acceleration of staff psychological ill-health from already difficult pre-pandemic conditions and continued investment is important to prevent further attrition.
-
Innovation increased during COVID-19 with new interventions adapted/established, though barriers to access (including stigma, stoicism and timing) were apparent, and required a focus on essential needs first.
We now summarise our main findings in relation to the three specific aims of our study.
Aim 1: understand when and why nurses, midwives and paramedics develop psychological ill-health at work, and provide examples of where and how it is most experienced
Our findings suggest that staff come into health care with high ideals, strong values and the desire to do a good job every day, yet many develop psychological ill-health as a result of their work. Our study suggests this is highly prevalent, and should be anticipated and prepared for, given the emotional, social and ethical aspects of the work. High degrees of empathy can also cause vicarious or secondary trauma. In short, delivering excellent care to patients can often come at a high price for staff in terms of their own psychological ill-health.
Our synthesis reveals that psychological ill-health in nurses, midwives and paramedics results from complex interactions between the individual, their professional role and values, the desire to deliver high-quality care and current working structures and conditions. These complex interactions – and resulting risk – are further exacerbated by intersectionality factors, such as gender, ethnicity, disability. It has always been challenging to provide prompt, high-quality, empathic care for patients, particularly when there are staff shortages, and this has been exacerbated by the COVID-19 pandemic. It is now even more challenging to provide excellent care and to ensure that the psychological health or nurses, midwives and paramedics is maintained and does not deteriorate further. Staff have gradually adapted their work behaviours and norms as conditions have got progressively worse. For example, gradually increasing overtime or work intensity can erode some protective mechanisms (such as job satisfaction and engagement and time with colleagues and family), resulting in harm to psychological health. This gradual worsening of working conditions has been compared to the ‘boiling a frog’ analogy (see Chapter 6; Tension 2) and can cause significant work dissatisfaction. Such work conditions Herzberg234 calls hygiene factors (see Figure 2). These are contextual extrinsic factors, including those deemed essential in Maslow’s hierarchy of needs, which we identified in the literature as causes of psychological ill-health.
FIGURE 2.
Herzberg’s two factor theory diagram (adaptation based on our data).
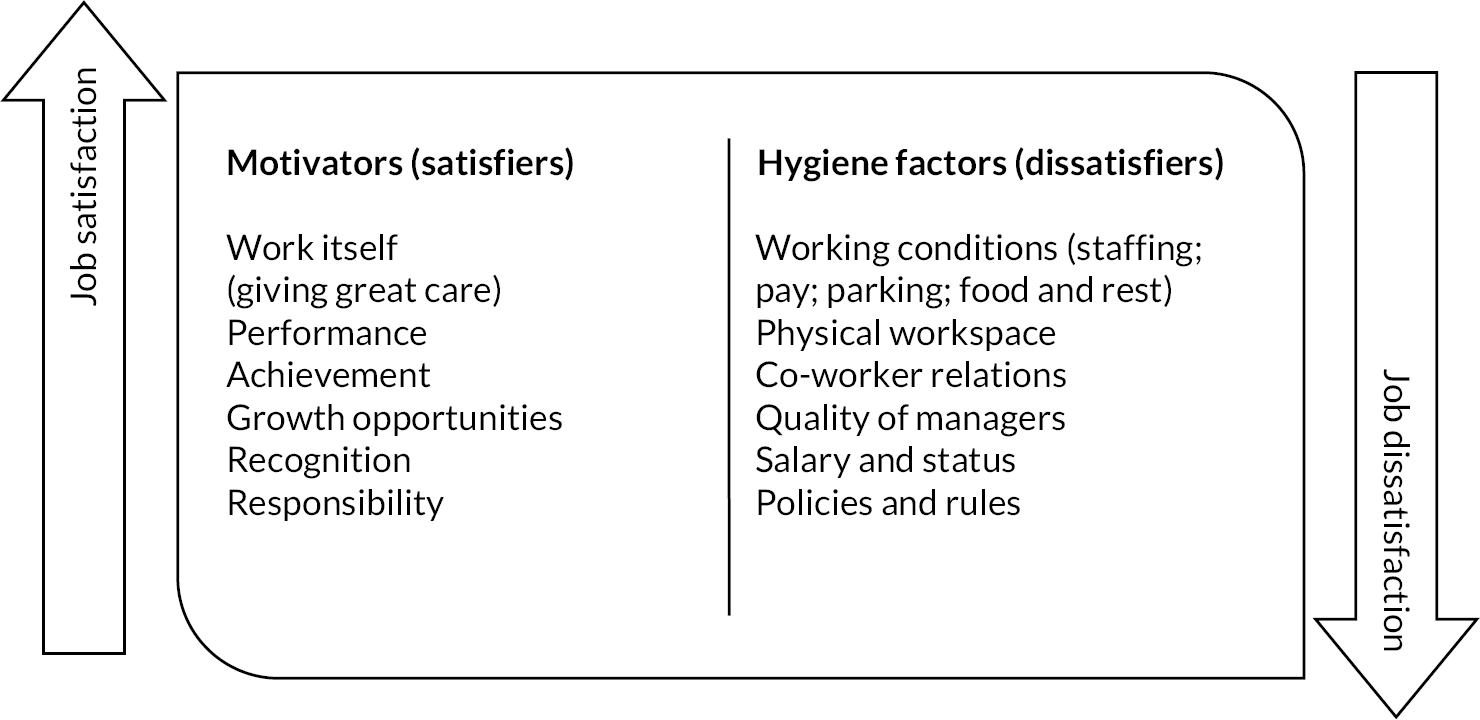
Our review has highlighted (see Box 1 for summary):
-
that trauma is not only acute, but can be chronic and cumulative, with seemingly benign events triggering psychological ill-health;
-
that collective blame is often attributed to individual staff and that there are double standards in accountability; and
-
that fitness-to-practice processes can be psychologically harmful and when staff do speak-up they can encounter a ‘deaf effect’ with no action.
Nurses, midwives and paramedics are often exhorted to ‘put patients first’ within a culture of giving 100%, which can send a message that their own psychological and physical needs come second, thus the needs of the system override staff wellness. There is also a professional culture that promotes a ‘serve and sacrifice’ ethos, which in the context of staff shortages can result in MD. Furthermore, excessive requirements for emotional labour can be at odds with messaging that well-being matters and exhortations to improve workplace psychological ill-health. This can cause some staff to feel they are failing at maintaining their own psychological health because they are not resilient enough, blaming themselves and individuals rather than work conditions and systemic forces identified above.
Secondary interventions that target individual nurses, midwives and paramedics to modify their response to stressors (and thereby prevent their psychological health deteriorating further) may address aspects of the causes identified in our review. However, our review has highlighted that these are fragmented (not part of a wider ‘well-being’ strategy that also focusses on primary prevention) and typically ignore the wider context. In doing so, offering such interventions can unintentionally backfire by sending a message that blames staff for their own psychological ill-health.
In terms of profession-specific issues, we identified more similarities than differences between nurses, midwives and paramedics. Most profession-specific causes we identified in the literature are likely to be applicable to other subspecialties (see Chapter 4, Table 6). The staff groups within our three professions that were most at risk included groups that were subject to discrimination at societal, structural or interpersonal levels, including ethnicities except White British, LGBTQ+, disabled staff and women. Structural features of work and working conditions may place certain staff at greater risk of psychological ill-health, including those with increased exposure to trauma, blurred role boundaries and geographic isolation. These features were mentioned for specific types of nurses (e.g. critical care; end of life; mental health inpatient setting; ENPs; district and community nurses; prison nurses) and are common to some midwives and paramedics. Leaders and managers were also identified as a group that may be particularly lacking support. In terms of stages of professional life where risk might be increased, this included staff in transition (e.g. newly qualified or new in post) or crises points (e.g. after trauma exposure or subject to investigation or complaints).
Aim 2: identify which strategies/interventions to reduce psychological ill-health work best for nurses, midwives and paramedics, find out how they work and in what circumstances these are most helpful
Our second aim focused on the strategies and interventions, which may operate differently in different contexts and for different staff groups. Our review found that the complex interactions that lead to psychological ill-health mean a reductionist ‘individual intervention’ approach would be inappropriate, and that identifying the ‘right’ intervention for the ‘right’ circumstances at the ‘right’ time is challenging.
Overall, our literature synthesis noted that individual-level interventions were unlikely to be enough to support staff due to systemic problems, and in the absence of a wider contextual lens could do more harm than good (potentially blaming staff for their own poor psychological health instead of intervening at the system level). However, individually focused interventions aimed at modifying response to stressors, such as mindfulness, are likely to be useful to some staff in the moment, and there is good evidence for some interventions aimed at wider organisational culture change such as Schwartz Rounds48 and the Blue Light Programme. 178 This key finding concurs with previous research arguing for systems approaches to psychological health at work. 65,235
Our review recommends avoiding implementing interventions into organisations without first understanding the service architecture, culture and work conditions that would impede or facilitate implementation (e.g. lone and/or community working or working night shifts affects access; trust, psychological safety, and compassionate leadership affects speaking up and disclosure of emotional support needs). We noted tensions in organisational priorities between
-
quick fixes and longer-term interventions, which may require patience and sustained support to produce their effects, and require non-quantifiable ways of showing benefit (e.g. Schwartz Rounds);
-
interventions focused on organisational learning versus staff healing; and
-
the need to act and offer support versus:
-
providing interventions that are ineffective because they are too soon, reactive and/or provided at a single time point;
-
protective strategies appearing as ‘lip service’ and managers perceived as ‘out of touch’ for recommending approaches when staff are not given time to access and participate in interventions.
-
Our synthesis suggests there are no easy ‘plug and play’ interventions that would result in significant change. The (interrelated) root causes of psychological ill-health that we have identified in this review are where interventions would likely have most benefit – with a system rather than individual cause lens. Building on organisational psychology approaches236 organisational interventions are most likely to be effective if there is first a focus on minimising demands and development resources – at individual, group, leader and organisational levels. Our research suggests this includes addressing staffing shortages, and hygiene factors to reduce job dissatisfaction, and changing culture to one that encourages and supports speaking up and listening, recognises the inevitable challenges of healthcare work and seeks to recognise staff psychological ill-health as the norm.
What is missing from the literature?
Key gaps in the literature include
-
there are few system-wide, multipronged interventions in the empirical literature: our review found that the literature is replete with individual often one-off interventions; with few multifocal system interventions although we did identify some (see Chapter 5 and Appendix 3). Few of these have been evaluated well, likely in part to be due to the complexity (in methods, expertise and time) required for evaluations of multicomponent/systems interventions
-
the empirical literature prioritised acute or one-off traumatic incidents, rather than acknowledging the cumulative impact of everyday stressors
-
we found very little focus on intersectionality in relation to causes or interventions, yet it is critical to underpin strategies aimed at mitigating psychological ill-health in the diverse healthcare workforce
-
although our search strategy was not explicitly designed to locate economic evaluations of interventions, very few papers included this. However, recent work has made a strong financial case for investment in staff psychological well-being that was noted in some sources. 10,35
CUP-2 programme theory
The 14 tensions highlight that healthcare delivery is a complex and dynamic balancing act. It is challenging to provide prompt, high-quality, empathic care for patients, especially in a context of staffing shortages, in a way that also concurrently maintains and even improves the health of the workforce. When we consider these tensions in relation to the five key findings, organisational ‘balancing acts’ came to the fore (see Figure 3); there are things that we need ‘more’ or ‘less’ of within our healthcare organisations and systems, based on the literature synthesised. It is worth noting that even too much of a ‘good’ intervention or strategy may be problematic (especially if not balanced with other elements). We deliberately focus the priorities for change at the organisational or systems level, rather than individual, given our learning from this review.
FIGURE 3.
Imbalances based on the tensions embedded within each of our five key findings.
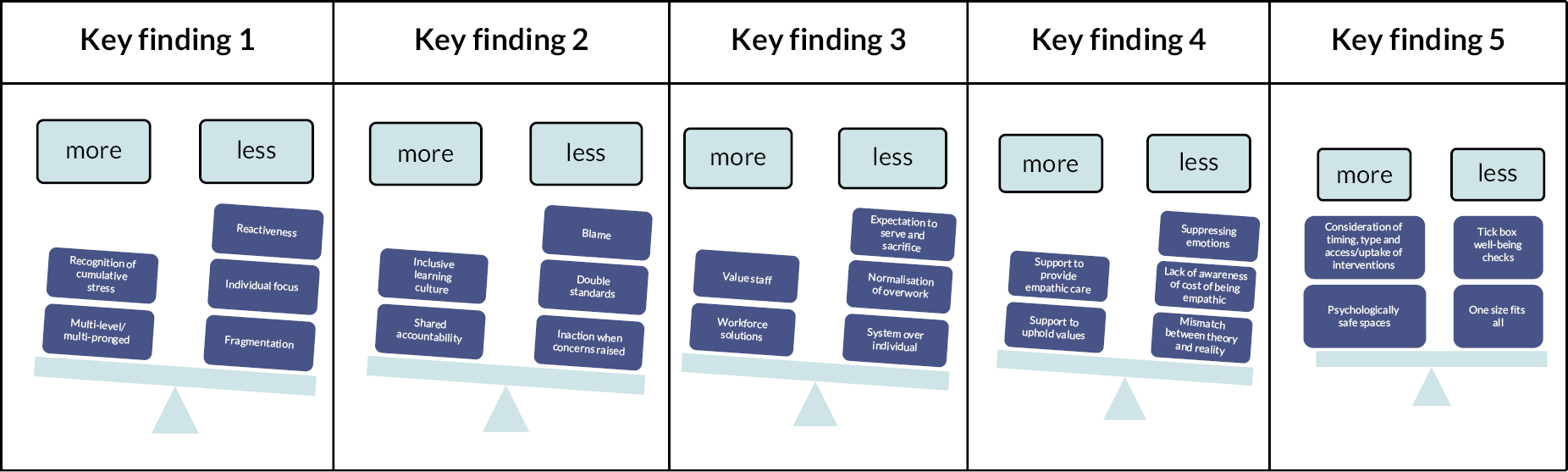
Figure 4 is based on our key findings (see above and Box 1), which has highlighted that a greater emphasis on self-care is a shared responsibility between individual staff, teams, managers, organisation, governing bodies, while being careful that this does not erode the high standards of patient care. The emphasis on patient care needs to be matched with an emphasis on staff psychological well-being; professional accountability needs to be matched by listening and responding to staff, with transparency of how staff input has translated into tangible changes and results. The emphasis on reacting and responding to events now needs to be balanced by more emphasis on prevention and the cumulative build-up of smaller stressors over a longer time period. And, perhaps most importantly, the predominant individual-focus of interventions, which can be perceived to place blame on the individual, must be balanced by interventions, which focus on organisational and system-wide change.
FIGURE 4.
Key focus areas to restore the balance. Each element on one side of the scale is in tension and needs to be balanced against the one on the opposite side.

Aim 3: design and develop resources for NHS managers/leaders so that they can understand how work affects the psychological health of nurses, midwives and paramedics; and what they can do to improve their psychological health in the workplace
The design and development of resources for NHS managers and leaders is in progress, due for completion and delivery to NIHR in Spring 2023. This section describes our progress to date towards meeting this aim.
The evidence and analyses presented in this review has been translated through an iterative process with stakeholder group, advisory group and policy-makers (as outlined in our protocol, see also Chapter 2), to produce eight overarching recommendations (see Box 2 below). These are targeted at Wellbeing Guardians and executive boards, those responsible for leading teams and/or those refining/designing interventional strategies to tackle nurses’ midwives’ and paramedics’ psychological ill-health. We have also begun to translate these recommendations for different audiences (noting that these are interdependent) (see Table 11).
| Audience | Recommendations |
|---|---|
| Nurses, midwives and paramedics |
|
| Team leaders/managers |
|
| Employers/executive boards |
|
| Other healthcare team members |
|
| Patients |
|
| Policy-makers |
|
| Regulators |
|
| Trade Unions and Royal colleges |
|
| Researchers |
|
| Those refining/designing interventions |
Consider our 8 Care Under Pressure 2 overarching recommendations, within an evidence-based implementation framework [such as the CFIR66 (see Box 2)]. |
-
Rebalance the service architecture and healthcare working conditions and the effects on staff psychological health (see Figures 3 and 4)
-
Invest in implementation and evaluation of multi-level systems approaches, including
-
Tailoring to local organisational and workforce needs (understand needs and intersectionality) and co-design with front-line staff and staff experts by experience.
-
‘Well-being bundles’ (primary to tertiary levels, individual to organisational focus).
-
Campaign for research funders and editors to prioritise evaluations of complex bundles/systems approaches (and for evaluations of individual-focused secondary interventions that ignore context to be de-prioritised).
-
-
Reduce stigma by implementing long-term plans and investment for well-being at organisational and individual levels:
-
Normalise experience of burnout/stress as an expectation of the job on a continuum/spectrum, not binary, and build in anticipatory planning to support staff’s psychological health from day one. Plan for it and support it.
-
Take a holistic lens to recognise trauma (not just work-related causes/triggers; not just acute incidents) to also consider cumulative exposure to healthcare work.
-
Consider risk to staff due to intersectionality; specific times in career (e.g. newly qualified; exposed to trauma; during investigations/complaints); subspecialties of staff with service architecture that places them at risk (e.g. lone workers).
-
-
Focus on essential needs (within Maslow’s hierarchy) and Herzberg’s hygiene factors in order of priority:
-
Hydration, food, parking, physical environment, break rooms (to rest, decompress and share work challenges with colleagues).
-
Consider needs and access for staff working shifts or with no work base.
-
-
The default position statement of the employer (NHS), leaders and managers should be that staff are doing the best job they can in difficult circumstances.
-
Identify and nurture future compassionate leaders and support them in the role:
-
Default position that everyone is a leader and training is required.
-
Support leaders to role model self-care and prioritise their own well-being and provide support for them too.
-
-
Challenge the ‘serve and sacrifice’ ethos to enable the needs of staff to be considered before the needs of organisation/system (not overridden by).
-
Use the NHSE/I Health and Wellbeing Framework154 or similar systems-based framework – to assess organisational need, plan and implement a staff well-being strategy.
To translate our project findings and recommendations (see Box 2 and Table 11) into solutions and resources we have also started working with our stakeholder and advisory groups to determine what could further support our various recommendations and develop our guide for managers (see Appendix 10). Our approach to designing and developing the resources is underpinned by the CFIR68 as shown in Table 12 (below).
| CFIR domain | Key considerations | Application to developing CUP-2 resources |
|---|---|---|
| Outer setting | What is there in the wider NHS to support the systemic change required? For example, patient needs/priorities; peer pressure; external policies/incentives |
|
| Inner setting | What are the barriers/facilitators from within Trusts/organisations and how can these be mitigated/capitalised upon? For example, networks/communications, culture, tension for change, compatibility, relative priority, organisational incentives/rewards, learning climate, readiness for implementation, leadership engagement, available resources |
|
| Characteristics of individuals | For example, knowledge/beliefs about the resources; self-efficacy |
|
| Intervention(s) – the resources | For example, evidence strength/quality; relative advantage compared to other things; adaptability; complexity; cost |
|
| Process of implementing | What is the strategy for implementing, sustaining and evaluating? For example, planning, engaging, opinion leaders, implementation leaders, champions, reflecting/evaluating |
|
CUP-2 strengths and limitations
There are several key strengths of this study. The use of realist methodology was beneficial for uncovering insights that went beyond the surface-level, well-established understanding of workplace psychological ill-health for three professional groups. It also helped us identify both causes and solutions comparing nurses, midwives and paramedics to identify important contextual factors, as well as subsets of individuals who were (more) affected within professional groups, and when. Our realist synthesis included different papers to other reviews such as commentaries and editorials, which offered rich insights that would usually be excluded in other review methodologies.
Realist methodology also allowed us to take an iterative flexible approach to searching and analysis, which meant that we were able to accommodate recent relevant data on COVID in a way that did not overwhelm the core study. We used the RAMESES quality standards for realist synthesis to ensure that the study design was rigorous and in line with principles of the realist approach. 40
The multidisciplinary skills and expertise of the core team (including experienced PIs and co-applicants, PIs immersed in the relevant literature, realist methods expertise, and an information specialist) and the linkage within the team with CUP-1 is a key strength of this project. This core team strength was supplemented by the expertise in our project advisory group, having both subject and methodological expertise, further strengthening the study, ensuring a robust approach and the inclusion of expert literature suggestions. We also had a diverse stakeholder group, which included staff experts by experience, providing diverse perspectives (multiprofessional and cross-professional and thereby ensuring discussions were not siloed). We ensured a supportive, safe and confidential environment by implementing many of the ground rules used in Schwartz Rounds (both JM and CT are experienced Schwartz Rounds facilitators), including clarity around confidentiality within the group, and enabling contribution in anonymous ways (using an online whiteboard [Padlet]). We also ensured the safety of members by providing the offer of psychological support (via Dr Diana Bass) to any members that may need it. Advisory and Stakeholder members critiqued and helped us make sense of the findings, which has strengthened the outputs and ensured relevance of the findings to the real-world problems faced in health care by nurses, midwives and paramedics and enabled translation of these findings into recommendations for practice.
Using retroduction (identification of hidden causal forces that lie behind identified patterns or changes in those pattern) we were able to develop complex findings around ‘tensions’ in healthcare architecture that help explain psychological ill-health in our staff groups. These tensions are underexamined in the literature and hold much potential for development in thinking about how to improve work conditions for the psychological health and well-being of healthcare staff. While this approach re-establishes and deepens our understanding of this topic it does not produce black and white answers. Furthermore, the cross-professional analysis (comparing nurses, midwives and paramedics, and also to doctors through comparison with CUP1) has significant benefits. Most previous research has tended to focus on whole healthcare workforces or one professional group (or a subset of that professional group), though a systems focus is essential to solutions to psychological ill-health as the healthcare system is inherently multiprofessional.
In term of limitations, due to the broad scope of the review, we analysed the data for nurses, midwives and paramedics separately and in some instances extrapolated these findings to apply across the professional groups, in discussion with our advisory and stakeholder groups. More research is needed regarding the role and service architecture features that may be distinct and place staff at greater risk. While there may have been generally patterned distinctions in the findings, there were always exceptions to the rule thus, further research will be necessary to build on this study.
The database searching for this review involved three separate searches for the three professions under study. The paramedic search terms were designed through iterative searches, in consultation with our stakeholder group, as the initial search retrieved a very limited set of papers. To ensure our review was as relevant to a UK context as possible, we applied database limiters, which in the CINAHL database were not as accurate as we would have liked, that is, some UK papers were not identified by the filter. However, we were still able to identify a focused sample of relevant UK papers and we were not aiming to search the literature comprehensively. We did not carry out citation searches, which are commonly used in realist reviews, as hand searching, and stakeholder/expert suggestions was an efficient way to identify papers that the database searches had failed to retrieve papers to approximate the quotas.
To ensure our review was up to date, and to manage the large literature (particularly in nursing) we used a reverse chronology screening. This enabled us to initially exclude the COVID-19 literature, and then subsequently return to this, and to stop searching at a pre-determined number of papers for each profession, for our initial analysis. The limitations of this approach means we might have missed significant literature, however, our subsequent inclusion of systematic and other reviews and use of key reports together with the subject expertise in the core team, advisory and stakeholder groups make this less likely but it remains a possibility. That said, a realist review is not intended to be exhaustive but takes a sample of literature for deeper insights going beyond the surface-level. The descriptive analyses of causes and interventions required an element of subjectivity for the categorisation into themes (HSE domains, informal/formal interventions and primary, secondary, tertiary target levels), and as such should be interpreted with caution. Furthermore, our review is limited in generalisability due to the key gaps in the literature (see p. 75) including lack of focus on intersectionality and how gender, ethnicity, disability and other factors (and their inter-relationships) may place individuals at greater risk of psychological ill-health.
Future research
Future research examining psychological ill-health in nurses, midwives and paramedics should build on our synthesis and
-
seek to evaluate and refine systemic interventional strategies already implemented that take account where possible of well-being bundles and/or systems approaches to intervention (primary to tertiary levels, and informal and formal approaches);
-
build future research programmes and design, implement and evaluate new interventional strategies, where possible tailoring to local organisational and workforce needs and co-designed with front-line staff and staff experts by experience;
-
seek funding that prioritises complex evaluations of whole systems approaches rather than only individual-focused secondary interventions;
-
identify and develop more sophisticated outcomes rather than those just easy to measure;
-
investigate further the tensions identified in this study, for example, cumulative impact of everyday stressors not only acute or one-off traumatic incidents;
-
explore the role of undergraduate education in preparing for psychological wellness throughout their career, including development and evaluation of anticipatory socialisation programmes or reflective spaces that are known to be beneficial;
-
investigate further the impact of equality diversity and inclusion issues, particularly the role of intersectionality on psychological ill-health;
-
continue to include health economic analysis in studies and investigate the cost-benefits on investing in staff psychological health.
Equality, diversity and inclusion
We have tried hard to address issues of equality, diversity and inclusion (EDI) in our study, but are limited by what has been published on these issues related to psychological ill-health in nurses, midwives and paramedics. We have used the lens of gender and ethnicity to explore both causes and to a lesser extent intervention. We were not able to retrieve relevant material directly relating to LGBTQ+ and disability issues in our sample for staff psychological well-being. We have included this as a focus for more research in this area and future studies may wish to use specific search terms in later cycles of realist synthesis to specifically search for EDI issues related to psychological ill-health. Our research team and stakeholder groups does include those from groups generally under-represented and there was a range of experience and expertise across the research team. Stakeholder participants and members of the public were recruited from across the country and involved representation of nurses, midwives and paramedics, some of whom had lived experience of psychological ill-health. We repeatedly discussed the diversity of the stakeholder groups with them and asked for their help to increase diversity, which resulted in more inclusion. Development opportunities and training were provided for research team members and psychological support was provided by Dr Diana Bass for experts by experienced members and as needed members of the team.
Patient and public involvement
Our engagement with the experts by experience (nurses, midwives and paramedics) and members of the public commenced before our study started with interviews with nurses, midwives and paramedics (n = 10) and this engagement continued throughout the study, as outlined in Chapter 2 (Stakeholder group contributions to analysis). We have held four project stakeholder group meetings and two project advisory group meetings. In each of these there has been public representation and representation of experts by experience (nurses, midwives and paramedics who have experienced psychological ill-health at work). This involvement had significant impact during the study; helping refine the project team’s ideas and thinking, providing a real-world perspective and challenging some of our suggestions (see Chapter 2, Table 5 in Stakeholder group contributions to analysis). In summary, our stakeholder PPIE members commented on and helped revise our theories, tensions and findings as the study progressed. Their views are embedded in the realist chapter and this report. They have also offered guidance on the dissemination of findings and how these can best have impact and we will be holding a dissemination event in December 2022/January 2023.
Conclusions
Our realist synthesis unequivocally suggests the need to improve the systemic working conditions and the working lives of nurses, midwives and paramedics to improve their psychological well-being. Individual, one-off psychological interventions are unlikely to succeed alone. Psychological ill-health is highly prevalent in these staff groups (and can be chronic and cumulative as well as acute) and should be anticipated and prepared for, indeed normalised and expected.
We expected to find variation between our three staff groups but found more similarities than differences. It is the way jobs are designed (service architecture) that can increase risk rather than the profession itself and these risks can be further exacerbated by intersectionality influences. Organisational and team cultures matter, and it is difficult to promote staff psychological wellness where there is a blame culture, and where the needs of the system override staff psychological health. We found that interventions are fragmented and individual-focused with an insufficient focus on systemic and hygiene issues (work dissatisfiers).
Synthesising the literature using a realist approach has allowed a nuanced and richer understanding of context and has enabled us to provide new insights into the body of evidence and make recommendations for practice and for policy. We had excellent engagement from our stakeholder groups, including nurse, midwife and paramedic experts by experience whose wise advice we have sought to heed. In the future, we anticipate the need for more research, particularly evaluation of system-wide, multipronged interventions. Due to their complexity these are difficult to evaluate well, yet vitally important for the systemic changes our study suggests are required if we are serious about supporting staff to care well as well as avoid psychological harms for themselves.
Acknowledgements
We would like to sincerely thank all those who supported this study. Specifically, members of our stakeholder and advisory groups, who so generously gave their time and expertise, even when personally psychologically difficult. These included (alphabetically by first name): Alison Marchbank; Alison Smith; Anna Conolly; Anna van der Gaag; Ash Brownett; Caitlin Wilson; Catherine Gamble; Dave Chuter (public member); Diana Bass (project psychologist); Dawn Querstret; Ellie Reynolds; Gemma Clay; Gill Adgie; Jennifer Lowe; Jennifer Woolf; Jo Mildenhall; Julia Williams; Kate Kirk; Katherine O’Neill; Katherine Timms; Kathryn Bamforth; Kathryn Grayling; Kellie Green; Kevin Teoh; Kim Tolley; Kirstie Brown; Laura Bridle; Lesley Wood; Lucas Hawkes-Frost; Mary Adams; Matthew Beadman; Mia Skelly; Naomi Nicholson; Niklas Auth; Nina Khazaezadeh; Rohan McCarty; Ruth Abrams; Ruth Riley; Sally Bassett; Sally Pezaro; Sarah Bolger; Simon Downs.
We would also like to thank the members of our Study Advisory Group (alphabetically by first name): Alex Aylward; Diana Bass; Elizabeth Barley (chairperson), Ellie Reynolds, Emma Wadey, Jane Leng (public member), Kathryn Grayling; Michael West, Nina Khazaezadeh Ruth Abrams; Ruth Riley; Sian Kitchen and Sue Shea for their excellent support, advice and guidance throughout.
Grateful thanks to Dr Evie Papavasiliou who supported our initial work and thinking, developing the initial report searching and literature reviewing. Finally, we would like to thank Elizabeth Campbell for her administrative support throughout the project and Dr Anna Conolly for her fantastic support with references and Endnote and document management.
Contributions of authors
Jill Maben (https://orcid.org/0000-0002-6168-0455) developed the research project, contributed to the formal search strategies, to screening, paper review and journaling, to the development and refinement of programme theory and CMOcs, provided methodological support and input, contributed theoretical ideas underpinning this analysis, facilitated patient and public involvement in the stakeholder group and drafted and revised the final report.
Cath Taylor (https://orcid.org/0000-0001-6239-4744) developed the research project, contributed to the formal search strategies, to screening, paper review and journaling, to the development and refinement of programme theory and CMOcs, provided methodological support and input, contributed theoretical ideas underpinning this analysis, facilitated patient and public involvement in the stakeholder group, led the causes and interventions analysis and drafted and revised the final report.
Justin Jagosh (https://orcid.org/0000-0001-6807-2957) (Research Fellow) provided realist methodology guidance on the study design; carried out the exploratory literature searches; contributed to the formal search strategies; screened the resulting references; developed and supported the team in appraisal journaling; applied a realist logic of analysis to the data; developed and refined the CMOcs; drafted and revised the methodology, realist chapters, and COVID-19 appendix in the final report.
Daniele Carrieri (https://orcid.org/0000-0002-3143-8430) (Lecturer in Public Health) developed the research project, contributed to the formal search strategies, to paper review and journaling, to the development and refinement of programme theory and CMOcs, provided relevant content and theoretical literature and revised the final report.
Simon Briscoe (https://orcid.org/0000-0002-6982-4521) (Information Specialist) developed and conducted the main and additional search strategies, and contributed to drafting and revising the methods chapter and strengths and limitations sections for the final report.
Naomi Klepacz (https://orcid.org/0000-0001-7552-8000) (Research Fellow) contributed to paper review and data extraction and causes and interventions analysis and revised the final report.
Karen Mattick (https://orcid.org/0000-0003-1800-773X) (Professor, Medical Education) developed the research project, contributed to the formal search strategies, to paper review and journaling, to the development and refinement of programme theory and CMOcs, provided relevant content and theoretical literature and revised the final report.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Ethics statement
This study did not require ethical approval as it was a secondary analysis of published papers. Contributions from our stakeholder groups were managed with care and adherence to ethical principle, but as these contributions do not constitute data, no ethical approval was required.
Information governance statement
This study did not handle any personal information.
Department of Health and Social Care disclaimer
This report presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, Medical Research Council, CCF, NIHR Evaluation, Trials and Studies Coordinating Centre, the Health Services and programme or the Department of Health.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Taylor C, Mattick K, Carrieri D, Cox A, Maben J. ‘The WOW factors’: comparing workforce organization and well-being for doctors, nurses, midwives and paramedics in England. Br Med Bull 2022;141(1):60-79. https://doi.org/10.1093/bmb/ldac003.
Taylor C, Maben J, Jagosh J, Carrieri D, Briscoe S, Klepacz N, Mattick K. Care Under Pressure 2: a realist synthesis of causes and interventions to mitigate psychological ill health in nurses, midwives and paramedics. BMJ Quality & Safety Published Online First: 04 April 2024. https://doi.org/10.1136/bmjqs-2023-016468
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS . The NHS Long Term Plan 2019.
- Ham C. UK Government’s autumn statement: no relief for NHS and social care in England. BMJ 2016;355. https://doi.org/10.1136/bmj.i6382.
- NHS . NHS Staff Survey 2021 National Results Briefing 2022.
- Taylor C, Mattick K, Carrieri D, Cox A, Maben J. ‘The WOW factors’: comparing workforce organization and well-being for doctors, nurses, midwives and paramedics in England. Br Med Bullet 2022;141:60-79.
- Johnson S. Burnout, depression and anxiety – why the NHS has a problem with staff health. The Guardian 2017. https://www.theguardian.com/wellbeing-at-work/2017/apr/25/burnout-depression-and-anxiety-why-the-nhs-has-a-problem-with-staff-health (accessed 8 February 2023).
- Limb M. Debriefing may help manage burnout among junior doctors, researchers say. BMJ 2015;350.
- Lords HO. The Long-term Sustainability of the NHS and Adult Social Care. London: NHS; 2017.
- Stevenson D, Farmer P. Thriving at work: the Stevenson/Farmer review of mental health and employers 2017. https://www.gov.uk/government/pubications/thriving-at-work-a-review-of-mental-health-and-employers (accessed 8 February 2023).
- England HE. NHS Staff and Learners’ Mental Health Commission. London: NHS; 2019.
- Daniels K. NHS Staff Wellbeing: Why Investing in Organisational and Management Practices Makes Business Sense. London: IPPO; 2022.
- Maben J. In praise of compassion. J Res Nurs 2010;15:9-13.
- Maben J, Adams M, Peccei R, Murrells T, Robert G. ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples’ experience of hospital care. Int J Older People Nurs 2012;7:83-94.
- Boorman S. NHS Health and Well-Being Review: Interim Report and Final Report 2009.
- Reiss H. Empathy in medicine: a neurobiological perspective. JAMA 2010;304:1604-5.
- Harvey SB. The Mental Health of Health Care Professionals: A Review for the Department of Health. London: Department of Health; 2009.
- Maben J, Latter S, Clark JM. The sustainability of ideals, values and the nursing mandate: evidence from a longitudinal qualitative study. Nurs Inq 2007;14:99-113.
- Carrieri D, Pearson M, Mattick K, Papoutsi C, Briscoe S, Wong G, et al. Interventions to minimise doctors’ mental ill-health and its impacts on the workforce and patient care: the care under pressure realist review. Health Serv Deliv Res 2020;8.
- Auth NM, Booker MJ, Wild J, Riley R. Mental health and help seeking among trauma-exposed emergency service staff: a qualitative evidence synthesis. BMJ Open 2022;12.
- Brady K, Trockel M, Khan C. What do we mean by physician wellness? A systematic review of its definition and measurement. Acad Psychiatry 2018;42:94-108.
- Bynum W, Varpio L, Teunissen P. Why impaired wellness may be inevitable in medicine, and why that may not be a bad thing. Med Educ 2021;55:6-22.
- Brooks D, Brooks R. A systematic review: what factors predict post-traumatic stress symptoms in ambulance personnel?. Br Paramed J 2021;5:18-24.
- Clark L, Fida R, Skinner J, Murdoch J, Rees N, Williams J, et al. Mental health, well-being and support interventions for UK ambulance services staff: an evidence map, 2000 to 2020. Br Paramed J 2021;5:25-39.
- McDermid F, Judy M, Peters K. Factors contributing to high turnover rates of emergency nurses: a review of the literature. Aust Crit Care 2020;33:390-6.
- Office for National Statistics (ONS) . Suicide by Occupation, England: 2011 to 2015 Analysis of Deaths from Suicide in Different Occupational Groups for People Aged 20 to 64 Years, Based on Deaths Registered in England Between 2011 and 2015 2017.
- Kinman G, Teoh K, Harriss A. The Mental Health and Wellbeing of Nurses and Midwives in the United Kingdom. London: Society of Occupational Medicine; 2020.
- Jones-Parry S. Exclusive: One in ten nurse sick days down to stress or depression in Nursing Standard 2017. https://rcni.com/nursing-standard/newsroom/analysis/exclusive-one-ten-nurse-sick-days-down-to-stress-or-depressio-118881 (accessed 8 February 2023).
- Campbell D. Paramedics taking tens of thousands of days a year off sick with stress. The Guardian 2017.
- RCM . State of Maternity Services Report 2018 – England 2018.
- 2018.
- West M, Bailey S, Williams E. The Courage of Compassion: Supporting Nurses and Midwives to Deliver High-Quality Care. London: The King’s Fund; 2020.
- Brand S, Coon JT, Fleming LE, Carroll L, Bethel A, Wyatt K. Whole-system approaches to improving the health and wellbeing of healthcare workers: a systematic review. PLOS ONE 2017;12.
- Stacey G, Cook G. A scoping review exploring how the conceptualisation of resilience in nursing influences interventions aimed at increasing resilience. Int Pract Develop J 2019;9:1-16.
- Daubney E. Emotional resilience in the ambulance service. J Paramed Pract 2018;10.
- Hunter B, Warren L. Investigating Resilience in Midwifery. Cardiff: Cardiff University; 2013.
- Dodd G. PTSD, available support and development of services in the UK Ambulance Service. J Paramed Pract 2017;9:258-63.
- Choflet A, Barnes A, Zisook S, Lee KC, Ayers C, Koivula D, et al. The nurse leader’s role in nurse substance use, mental health, and suicide in a peripandemic world. Nurs Admin Quart 2022;46:19-28.
- Pawson R, Bellamy J. Moving Beyond Effectiveness in Evidence Synthesis: Methodological Issues in the Synthesis of Diverse Sources of Evidence. London: National Institute for Health and Clinical Excellence; 2006.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7.
- Jagosh J. Realist synthesis for public health: building an ontologically deep understanding of how programs work, for whom, and in which contexts. Ann Rev Publ Health 2019;40:361-72.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Jagosh J. Retroductive theorizing in Pawson and Tilley’s applied scientific realism. J Crit Real 2020;19:121-30.
- Sayer A. Methods in Social Science: A Realist Approach. London: Routledge; 2000.
- Carrieri D, Mattick K, Pearson M, Papoutsi C, Briscoe S, Wong G, et al. Optimising strategies to address mental ill-health in doctors and medical students: ‘care under pressure’ realist review and implementation guidance. BMC Med 2020;18.
- Jagosh J, Stott H, Halls S, Thomas R, Liddiard C, Cupples M, et al. Benefits of realist evaluation for rapidly changing health service delivery. BMJ Open 2022;12.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34.
- Dalkin S, Greenhalgu J, Jones D, Cunningham B. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10.
- Merton R. On Theoretical Sociology. Five Essays, Old and New. New York: The Free Press; 1967.
- Maben J, Hoinville L, Querstret D, Taylor C, Zasada M, Abrams R. Realist evaluation of Schwartz rounds® for enhancing the delivery of compassionate healthcare: understanding how they work, for whom, and in what contexts. BMC Health Serv Res 2021;21.
- Ayiku L, Levay P, Hudson T, Craven J, Barrett E, Finnegan A, et al. The medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID medline. Health Info Libr J 2017;34:200-16.
- HMIC . HMIC Database n.d. https://www.wolterskluwer.com/en/solutions/ovid/hmic-database-99 (accessed 8 February 2023).
- Olaussen A, Semple W, Oteir A, Todd P, Williams B. Paramedic literature search filters: optimised for clinicians and academics. BMC Med Inform Decis Mak 2017;7.
- Goddard D, de Vries K, McIntosh T, Theodosius C. Prison nurses’ professional identity. Forensic Nurs 2019;15:163-71.
- Rowe A, Regehr C. Whatever gets you through today: an examination of cynical humor among emergency service professionals. J Loss Trauma 2010;15:448-64.
- Golden P. Who has a duty of care to keep midwives safe?. Br J Midwifery 2018;26:62-3.
- Miller E. The prevalence of stress and burnout in UK emergency ambulance service workers and its impact on their mental health and well-being. Br Paramed J 2021;5:62-3.
- Miller J. ‘We wear too many caps’: role conflict among ambulance service managers. Br Paramed J 2019;3.
- Webster N, Jenkins C, Oyebode J, Bentham P, Smythe A. Experiences of peer support for newly qualified nurses in a dedicated online group: study protocol. J Adv Nurs 2019;75:1585-91.
- Hollins Martin C, Beaumount E, Norris G, Cullen GL. Teaching compassionate mind training to help midwives cope with traumatic clinical incidents. Br J Midwifery 2021;29:26-35.
- Iaschi E. Preceptorship programme for newly qualified midwives. MIDIRS Midw Digest 2020;30:177-9.
- Chamanga E, Dyson J, Loke J, McKeown E. Factors influencing the recruitment and retention of registered nurses in adult community nursing services: an integrative literature review. Prim Health Care Res Develop 2020;21.
- Freeling M, Rainbow J, Chamberlain D. Painting a picture of nurse presenteeism: a multi-country integrative review. Int J Nurs Studies 2020;109.
- Ejebu OZ, Dall’Ora C, Griffiths P. Nurses’ experiences and preferences around shift patterns: a scoping review. PLOS ONE 2021;16.
- MacKay C, Copusins R, Kelly PJ, Lee S. ‘Management standards’ and work-related stress in the UK: policy background and science. Work Stress 2004;18:91-112.
- Centre for Disease Control and Prevention . Hierarchy of Controls 2023. www.cdc.gov/niosh/topics/hierarchy/default.html (accessed 8 February 2023).
- LaMontange A, Keegel T, Louie AM, Ostry A, Landsbergis PA. A systematic review of the job-stress intervention evaluation literature, 1990-2005. Int J Occup Environ Health 2007;13:268-80.
- Damschroder L, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4.
- Kirk M, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the Consolidated Framework for Implementation Research. Implement Sci 2016;11.
- CFIR . Consolidated Framework for Implementation Research 2022 2022. https://cfirguide.org/ (accessed 10 February 2023).
- Karasek RA. Healthy Work: Stress, Productivity and the Reconstruction of Working Life. New York: Basic Books; 1990.
- Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occupat Health Psychol 1996;1:27-41.
- HSE . What Are the Management Standards? 2022 2022. www.hse.gov.uk/stress/standards/ (accessed 10 February 2023).
- Nurses TICo . The Global Voice of Nursing in the Year of the Nurse and the COVID-19 Pandemic: 2020 Annual Report 2021.
- Jackson H. Retaining and valuing newly qualified nursing staff: evaluation of a peer support group. Ment Health Pract 2018;21:24-7.
- Hunter B, Henley J, Fenwick J. Work, Health and Emotional Lives of Midwives in the United Kingdom: The UK WHELM Study. Cardiff: School of healthcare Sciences, Cardiff University; 2018.
- Chesterton L, Tetley J, Cox N, Jack K. A hermeneutical study of professional accountability in nursing. J Clin Nurs 2021;30:188-99.
- Yoshida Y, Sandall J. Occupational burnout and work factors in community and hospital midwives: a survey analysis. Midwifery 2013;29:921-6.
- Welford C. What factors influence professional burnout in mid wives?. MIDIRS Midw Digest 2018;28:35-40.
- O’Neill L, Johnson J, Mandela R. Reflective practice groups: are they useful for liaison psychiatry nurses working within the Emergency Department?. Archiv Psychiat Nurs 2019;33:85-92.
- Mendes A. Are you ‘enhanced’ by your stress?. J Paramed Pract 2020;12.
- Mildenhall J. Protecting the mental health of UK paramedics. J Paramed Pract 2019;11:6-7.
- Best C. Building resilience in contemporary nursing practice. Pract Nurs 2019;30:400-4.
- Sibson L. Mental health in emergency care. J Paramed Pract 2017;9.
- Elliott-Mainwaring H. How do power and hierarchy influence staff safety in maternity services?. Br J Midwifery 2021;29:430-9.
- Andrews H, Tierney S, Seers K. Needing permission: the experience of self-care and self-compassion in nursing: a constructivist grounded theory study. Int J Nurs Stud 2020;101.
- Laker C, Cella M, Callard F, Wykes T. The impact of ward climate on staff perceptions of barriers to research-driven service changes on mental health wards: a cross-sectional study. J Psychiat Mental Health Nurs 2020;27:281-95.
- Albendin-Garcia L, Suleiman-Martos N, Cañadas-De la Fuente GA, Ramírez-Baena L, Gómez-Urquiza JL, De la Fuente-Solana EI. Prevalence, related factors, and levels of burnout among midwives: a systematic review. J Midw Women Health 2021;66:24-4.
- Bosanquet J. Providing not prescribing: fostering a culture of wellbeing in nursing. J Res Nurs 2021;26:367-75.
- Fasbender U, Van der Heijden B, Grimshaw S. Job satisfaction, job stress and nurses’ turnover intentions: the moderating roles of on-the-job and off-the-job embeddedness. J Adv Nurs 2019;75:327-37.
- Cull J, Hunter B, Henley J, Fenwick J, Sidebotham M. “Overwhelmed and out of my depth”: responses from early career midwives in the United Kingdom to the Work, Health and Emotional Lives of Midwives study. Women Birth 2020;33:e549-57.
- Bacchus A, Firth A. What factors affect the emotional well-being of newly qualified midwives in their first year of practice?. MIDIRS Midw Digest 2017;27:444-50.
- Copp E, Morton N. Attention: calm and relaxed midwives at work!. Pract Midw 2011;14:21-3.
- Rodriguez Santana I, Anaya Montes M, Chalkley M, Jacobs R, Kowalski T, Suter J. The impact of extending nurse working hours on staff sickness absence: evidence from a large mental health hospital in England. Int J Nurs Stud 2020;112.
- Buckley L, Berta W, Cleverley K, Medeiros C, Widger K. What is known about paediatric nurse burnout: a scoping review. Hum Resour Health 2020;18:1-23.
- Anderson L. The impact of paramedic shift work on the family system: a literature review. Coll Paramed 2019;3.
- Quaile A. Ambulance staff contemplate suicide due to stress and poor mental health. J Paramed Pract 2016;8:224-6.
- Cedar SH, Walker G. Protecting the wellbeing of nurses providing end-of-life care. Nurs Times 2020;116:30-4.
- Duncan M. Managing sickness absence and declared disabilities in a district nursing team. Br J Commun Nurs 2019;24:478-81.
- Barleycorn D. Awareness of secondary traumatic stress in emergency nursing. Emerg Nurs 2019;27:19-22.
- Brett Bowen A. How do emergency nurse practitioners experience managing acutely unwell patients in minor injury units? An interpretative phenomenological analysis. Internat Nurs 2019;43:99-105.
- Sheen K, Spiby H, Slade P. Exposure to traumatic perinatal experiences and posttraumatic stress symptoms in midwives: prevalence and association with burnout. Int J Nurs Stud 2015;52:578-87.
- Axcell C. Mental health and the midwife. Br J Midwifery 2019;27.
- Higgins J, Okoli C, Otachi J, Lawrence J, Bryant ED, Lykins A, et al. Factors associated with burnout in trauma nurses. J Trauma Nurs 2020;27:319-26.
- Slade P, Sheen K, Collinge S, Butters J, Spiby H. A programme for the prevention of post-traumatic stress disorder in midwifery (POPPY): indications of effectiveness from a feasibility study. Eur J Psychotraumatol 2018;9.
- McDonald MA, Meckes SJ, Lancaster CL. Compassion for oneself and others protects the mental health of first responders. Mindfulness 2021;12:659-71.
- Mendes A. How does your job impact your health?. J Paramed Pract 2018;10.
- Bresesti I, Folgori L, De Bartolo P. Interventions to reduce occupational stress and burn out within neonatal intensive care units: a systematic review. Occupat Environ Med 2020;77:515-19.
- Lancaster C, Phillips P. How does the use of humour in the UK ambulance service affect a clinician’s well-being?. Br Paramed J 2021;6:26-33.
- Warriner S, Hunter L, Dymond M. Mindfulness in maternity: evaluation of a course for midwives. Br J Midw 2016;24:188-95.
- Johnston S. My time as a paramedic and why mental health matters. J Paramed Pract 2018;10.
- Whiting L, O’Grady M, Whiting M, Petty J. Factors influencing nurse retention within children’s palliative care. J Child Health Care 2020;25:587-602.
- Oates J, Topping A, Ezhova I, Wadey E, Marie RA. An integrative review of nursing staff experiences in high secure forensic mental health settings: implications for recruitment and retention strategies. J Adv Nurs 2020;76:2897-908.
- Foster A, Wood E, Clowes M. Identifying the evidence base of interventions supporting mental health nurses to cope with stressful working environments: a scoping review. J Nurs Manag 2021;29:1639-52.
- Rocca-Ihenacho L, Yuill C, McCourt C. Relationships and trust: Two key pillars of a well-functioning freestanding midwifery unit. Birth 2020;48:104-13.
- Gilroy R. Mental health: caring for the paramedic workforce. J Paramed Pract 2018;10:192-3.
- van der Gaag A, Jogo R, Austin Z, Zasada M. Why do paramedics have a high rate of self-referral?. J Paramed Pract 2018;10:205-10.
- Team BE. A comment on kindness. Br Midwifery 2018;26.
- Naumann D. Acute stress and frontline healthcare providers. J Paramed Pract 2017;9:516-21.
- Younge L, Sufi H, Dibley L. Regular clinical supervision to enhance wellbeing in inflammatory bowel disease specialist nurses: a small pilot study. Gastrointest Nurs 2020;18:36-42.
- Dunlop S, Maunder E. Developing and nurturing a community practice clinical network for community children’s nurses in Wales. Br J Nurs 2019;28:782-6.
- Winter G. Dealing with burnout. Br J Midw 2019;27.
- Peate I. The workplace and mental wellbeing. J Paramed Pract 2017;9.
- Webster N, Oyebode JR, Jenkins C, Bicknell S, Smythe A. Using technology to support the emotional and social well-being of nurses: a scoping review. J Adv Nurs 2019;76:109-20.
- Hawkins N, Jeong S, Smith T. New graduate registered nurses’ exposure to negative workplace behaviour in the acute care setting: an integrative review. Int J Nurs Stud 2019;93:41-54.
- Paranjape A. Taking care of the practising paramedic. J Paramed Pract 2016;8.
- Michael T, Streb M, Häller P. PTSD in paramedics: direct versus indirect threats, posttraumatic cognitions, and dealing with intrusions. Int J Cogn Therap 2016;9:57-72.
- Beryl R, Davies J, Völlm B. Lived experience of working with female patients in a high-secure mental health setting. Int J Mental Health Nurs 2018;27:82-91.
- Stacey G, Cook G, Aubeeluck A, Stranks B, Long L, Krepa M, et al. The implementation of resilience based clinical supervision to support transition to practice in newly qualified healthcare professionals. Nurs Educ Today 2020;94.
- Hunter B, Fenwick J, Sidebotham M, Henley J. Midwives in the United Kingdom: levels of burnout, depression, anxiety and stress and associated predictors. Midwifery 2019;79.
- Cummings G, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud 2018;85:19-60.
- Gribben L, Semple C. Factors contributing to burnout and work-life balance in adult oncology nursing: an integrative review. Eur J Oncol Nurs 2020;50.
- Paranjape A. Helping the helpers: how paramedics were cared for. J Paramed Pract 2017;9.
- Plewes J. NHS Confederation Analysis: November Release of NHS Performance Statistics 2021. www.nhsconfed.org/articles/system-under-pressure-november-release-nhs-performance-statistics (accessed 10 February 2023).
- Joyce K, Pabayo R, Critchley J. Flexible working conditions and their effects on employee health and wellbeing. Cochr Datab Syst Rev 2010;2010.
- Paramedics Co . Become a Paramedic 2022. https://collegeofparamedics.co.uk/COP/Become_a_Paramedic/COP/BecomeAParamedic/Become_a_Paramedic.aspx?hkey=f10838de-b67f-44a0-83b7-8140d8cdba83 (accessed 10 February 2023).
- Jackson J, Anderson A, Maben J. What is nursing work? A meta-narrative review and integrated framework. Int J Nurs Stud 2021;122.
- Treglown L, Palaiou K, Zarola A, Furnham A. The dark side of resilience and burnout: a moderation-mediation model. PLOS ONE 2016;11.
- Care DoHaS . Final Report of the Ockenden Review: Findings, Conclusions and Essential Actions from the Independent Review of Maternity Services at the Shrewsbury and Telford Hospital NHS Trust 2022.
- Aspinall A, Bagot M. Man, 87, forced to wait 15 HOURS for ambulance as family says ‘system is broken’. Mirror 2022.
- Editorial . The Guardian view on ambulance waiting times signs of a collapsing NHS. The Guardian 2022.
- Maben J. Exploring the Relationship between Patients’ Experiences of Care and the Influence of Staff Motivation, Affect and Wellbeing. Southampton: NIHR Service Delivery and Organisation Programme; 2012.
- RCM . Improving Maternity: Learning from Reviews of Maternity Services, in The Solution Series 2021.
- Kramer M. Reality Shock. St. Louis, MO: Mosby; 1974.
- Conolly A, Rowland E, Abrams R, Harris R, Kelly D, Kent B, et al. ‘There was a pivotal moment’. The dynamics, transitions, adaptions and trajectories of nursing at the front-line in the UK during the COVID-19 pandemic: a longitudinal qualitative study. PLOS ONE 2023.
- Anderson N. An evaluation of a mindfulness-based stress reduction intervention for critical care nursing staff: a quality improvement project. Nurs Crit Care 2020;26:441-8.
- Berry S, Robertson N. Burnout within forensic psychiatric nursing: its relationship with ward environment and effective clinical supervision?. J Psychiat Ment Health Nurs 2019;26:212-22.
- National Institute for Health and Care Excellence (NICE) . Post-Traumatic Distress Disorder 2018.
- Marran E. Supporting staff who are second victims after adverse healthcare events. Nurs Manag 2019;26:36-43.
- Barker K. Reasons why midwives leave. Br J Midw 2016;24.
- Maben J, Hoinville L, Querstret D, Taylor C, Zasada M, Abrams R. Living life in limbo: experiences of healthcare professionals during the HCPC fitness to practice investigation process in the UK. BMC Health Serv Res 2021;21.
- Bajorek Z, Holmes J. Health and Wellbeing Interventions in Healthcare: A Rapid Evidence Review. London: Institution for Employment Studies; 2020.
- Byrne I. Is the perfect midwife attainable in modern maternity care?. MIDIRS Midw Digest 2018;28:28-34.
- Rajamohan S, Porock D, Chang Y. Understanding the relationship between staff and job satisfaction, stress, turnover, and staff outcomes in the person-centered care nursing home Arena. J Nurs Scholar: Off Publ Sigma Theta Tau Int Honor Soc Nurs 2019;51:560-68.
- David D. The ‘Ambulance Burnout’ Issue. London: The Larrey Society; 2015.
- NHS . NHS Health and Wellbeing Framework 2021.
- Warwick C. Midwives can no longer keep services afloat. Nurs Stand 2016;31.
- Barker K. Giving midwives some ‘me’ time. Br J Midw 2019;27.
- Leversidge A. Caring for midwifery staff will ensure better care for women. Br J Midw 2016;24.
- Clarke E. Toasted, fried or frazzled? Burnout and stress in midwifery practice. Midw Matters 2013;139:15-6.
- Academy NL. Develop Your Career, Connect With Peers, Grow As a Leader 2022. www.leadershipacademy.nhs.uk/ (accessed 10 February 2023).
- West MA. Compassionate Leadership: Sustaining Wisdom, Humanity and Presence in Health and Social Care. London: Swirling Leaf Press; 2021.
- Barber Z, Jones C, Dobbs T. Taking time out of training. BMJ 2015;351.
- Aryankhesal A, Mohammadibakhsh R, Hamidi Y, Alidoost S, Behzadifar M, Sohrabi R, et al. Interventions on reducing burnout in physicians and nurses: a systematic review. Med J Islamic Republ Iran 2019;33.
- Seligman M, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol 2000;55:5-14.
- Delaney MC. Caring for the caregivers: evaluation of the effect of an eight-week pilot mindful self-compassion (MSC) training program on nurses’ compassion fatigue and resilience. PLOS ONE 2018;13.
- Hunter L. Making time and space: the impact of mindfulness training on nursing and midwifery practice: a critical interpretative synthesis. J Clin Nurs 2016;25:918-29.
- Mendes A. Protecting your mind amid crisis. J Paramed Pract 2020;12.
- Yu F, Raphael D, Mackay L, Smith M, King A. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud 2019;93:129-40.
- Barker K. Building bricks and resilience. Br J Midw 2018;26.
- Daubney E. Use of dark humour as a coping mechanism. J Paramed Pract 2019;11.
- Maslow AH. A theory of human motivation. Psychol Rev 1943;50:370-96.
- National Institute for Clinical Excellence (NICE) . Depression in Adults: Treatment and Management 2022.
- theredpoppycompany 2022. https://www.theredpoopycompany.couk/ (accessed 7 September 2022).
- Samaritians . Wellbeing Support Line for Health and Social Care Workers 2022 n.d. www.samaritans.org/how-we-can-help/health-and-care/here-listen-support-line-nhs-people/ (accessed 10 February 2023).
- SWAST . Staying Well Service for Staff Staying Well Service 2022 n.d. www.swast.nhs.uk/welcome/staying-well-service-for-staff/staying-well-service (accessed 10 February 2023).
- Wain A. Examining the lived experiences of newly qualified midwives during their preceptorship. Br J Midw 2017;25:451-7.
- NHS . National Professional Nurse Advocate Implementation Guide 2021.
- Maben J. A Realist Informed Mixed-Methods Evaluation of Schwartz Center Rounds® in England. Southampton: NIHR; 2018.
- Mind . Blue Light Programme 2022. www.mind.org.uk/news-campaigns/campaigns/blue-light-programme/ (accessed 10 February 2023).
- ASC . The Ambulance Services Charity 2022. www.theasc.org.uk/ (accessed 10 February 2023).
- Editorial . The attraction of working in a Magnet hospital: why UK hospitals are trialling the US model and what its staff well-being goals mean for nurses and patients. Nursing Standard 2021;2021:19-21.
- Maben J, Bridges J. COVID-19: Supporting nurses’ psychological and mental health. J Clin Nurs 2020;29:2742-50.
- Williams O, Fullagar S. Lifestyle drift and the phenomenon of ‘citizen shift’ in contemporary UK health policy. Soc Health Illness 2019;41:20-35.
- NIHR . Why Do Health Policies Designed to Reduce Health Inequalities Increase Them Instead? 2022. https://arc-w.nihr.ac.uk/news/why-do-health-policies-designed-to-reduce-inequalities-increase-them-instead/#:~:text=‘Downstream’%20interventions%20focus%20on%20things,as%20housing%2C%20employment%2C%20education (accessed 10 February 2023).
- Vogel S, Flint B. Compassionate leadership: how to support your team when fixing the problem seems impossible. Nurs Manag 2021;28:32-41.
- TRIM . Trauma Risk Management: March on Stress 2022. www.marchonstress.com/page/p/trim (accessed 10 February 2023).
- Davies N. Vicarious trauma in nursing. Independent Nurse 2021.
- Figley CR. Secondary Traumatic Stress: Self-Care Issues for Clinicians, Researchers, and Educators. Lutherville, MD: Sidran; 1999.
- Beck C. Secondary traumatic stress in nurses: a systematic review. Archiv Psychiat Nurs 2011;25:1-10.
- Hewett M. Ethics and toxic high-workload work environments. Br J Gen Pract 2022;76:227-8.
- Mannion R, Davies H. Understanding organisational culture for healthcare quality improvement. BMJ 2018;363.
- Limb M. Need for accountability should not result in “toxic” blame culture in NHS, conference hears. BMJ 2014;348.
- Khatri N, Brown GD, Hicks LL. From a blame culture to a just culture in health care. Health Care Manage Rev 2009;34:312-22.
- Jones A, Blake J, Adams M, Kelly D, Mannion R, Maben J. Interventions promoting employee “speaking-up” within healthcare workplaces: a systematic narrative review of the international literature. Health Pol 2021;125:375-84.
- Maben J, Ball J, Edmondson A. Workplace Conditions (Elements of Improving Quality and Safety in Healthcare). Cambridge: Cambridge University Press; 2022.
- Ockenden D. Ockenden Report: Emerging Findings and Recommendations from the Independent Review of Maternity Services at the Shrewsbury and Telford Hospital NHS Trust. London: House of Commons; 2020.
- Wu AW. Medical error: the second victim – the doctor who makes the mistake needs help too. BMJ 2000;320:726-7.
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Coping with medical error: a systematic review of papers to assess the effects of involvement in medical errors on healthcare professionals' psychological well-being. Qual Saf Health Care 2010;19.
- Mira J, Lorenzo S, Carrillo I, Ferrús L, Pérez-Pérez P, Iglesias F, et al. Interventions in health organisations to reduce the impact of adverse events in second and third victims. BMC Health Serv Res 2015;15.
- Abrams R, Conolly A, Rowland E, Harris R, Kent B, Kelly D, et al. Speaking up during the COVID-19 pandemic: Nurses' experiences of organizational disregard and silence. J Adv Nurs 2023;79:2189-99. https://doi.org/10.1111/jan.15.
- Jones A, Kelly D. Deafening silence? Time to reconsider whether organisations are silent or deaf when things go wrong. BMJ Qual Saf 2014;23:709-13.
- Johns G. Presenteeism in the workplace: a review and research agenda. J Organ Behav 2010;31:519-42.
- Maben J, Latter S, Clark JM. The theory–practice gap: impact of professional–bureaucratic work conflict on newly-qualified nurses. J Adv Nurs 2006;55:465-77.
- Ball J, Murrells T, Rafferty AM, Morrow E, Griffiths P. ‘Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf 2014;23.
- Jameton A. Nursing Practice: The Ethical Issues. Englewood Cliffs, NJ: Prentice Hall; 1984.
- Morley G, Bradbury-Jones C, Ives J. What is ‘moral distress’ in nursing? A feminist empirical bioethics study. Nurs Ethics 2019;27:1297-314.
- Brooks D. Acknowledge pandemic driven moral distress, mitigate harmful effects. ED Manag 2021;33:1-2.
- Riedel PL, Kreh A, Kulcar V, Lieber A, Juen B. A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. Int J Environ Res Public Health 2022;19.
- Epstein EG, Whitehead PB, Prompahakul C, Thacker LR, Hamric AB. Enhancing understanding of moral distress: the measure of moral distress for health care professionals. AJOB Empir Bioeth 2019;10:113-24.
- Royal College of Nursing (RCN) . 10 Unsustainable Pressures on the Health and Care System in England 2021.
- Chochinov H. Dignity and the essence of medicine: the A, B, C, and D of dignity conserving care. BMJ 2007;335:184-7.
- Spiro H. What is empathy and can it be taught?. Ann Intern Med 1992;116:843-6.
- Hochschild A. The Managed Heart: Commercialization of Human Feeling. Berkeley, CA: The University of California Press; 2012.
- Safazadeh S, Irajpour A, Alimohammadi N, Haghani F. Exploring the reasons for theory-practice gap in emergency nursing education: a qualitative research. J Educ Health Promot 2018;7.
- Power A. Midwifery in the 21st century: are students prepared for the challenge?. Br J Midw 2016;24:66-8.
- Maben J. The art of caring: invisible and subordinated? A response to Juliet Corbin: ‘is caring a lost art in nursing?’. Int J Nurs Stud 2008;45:335-8.
- Park C, Kim N, Chung J, Feldman SR. Patients’ Perceptions of Physicians’ Caring Attitude Is the Critical Factor in Determining Patient Satisfaction 2014.
- Gupta A, Harris S, Naina HV. The impact of physician posture during oncology patient encounters. J Cancer Educ 2015;30:395-7.
- Hillen MA, de Haes HCJM, Stalpers LJA, Klinkenbijl JHG, Eddes EH, Butow PN, et al. How can communication by oncologists enhance patients’ trust? An experimental study. Ann Oncol 2014;25:896-901.
- Scott J, Cohen D, Dicicco-Bloom B, Miller WL, Stange KC, Crabtree BF. Understanding healing relationships in primary care. Ann Fam Med 2008;6.
- Churchill LR, Schenck D. Healing skills for medical practice. Ann Intern Med 2008;149:720-4.
- Schwartz K. A patient’s story. Boston Globe Magazine 1995.
- Menzies IEP. A case-study in the functioning of social systems as a defence against anxiety: a report on a study of the nursing service of a general hospital. Hum Relat 1960;13:95-121.
- Hayes C, Corrie I, Graham Y. Paramedic emotional labour during COVID-19. J Paramed Pract 2020;12:319-23.
- Pezaro S, Pearce G, Bailey E. Childbearing women’s experiences of midwives’ workplace distress: patient and public involvement. Br J Midw 2018;26:659-69.
- Goffman E. The Presentation of Self in Everyday Life. New York: Anchor Books: A Division of Random House; 1980.
- Miller J. The well-being and productivity link: a significant opportunity for research-into-practice. J Organ Effect: People Perf 2016;3:289-311.
- Gray P, Senabe S, Naicker N, Kgalamono S, Yassi A, Spiegel JM. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: a realist review. Int J Environ Res Publ Health 2019;16.
- Uys C, Carrieri D, Mattick K. The impact of shared social spaces on the wellness and learning of junior doctors: A scoping review. Med Educ 2023;57:315-30. https://doi.org/10.1111/medu.14946.
- Smith M. What is your ‘normal’?. J Paramed Pract 2021;11.
- Gardiner M, DeMuy A, Tran NK. Here4HealthCare: a response to the emerging mental health crisis of the frontline healthcare workforce. Can J Commun Ment Health 2020;39:85-8.
- Maben J, Conolly A, Abrams R, Rowland E, Harris R, Kelly D, et al. Impact of COVID On Nurses (ICON) Survey Research Group . ‘You can’t walk through water without getting wet’ UK nurses’ distress and psychological health needs during the COVID-19 pandemic: a longitudinal interview study. Int J Nurs Stud 2022;131.
- Maben J, Conolly A. Lessons for Structure, Workplace Planning and Responding to Emergencies from Nurses in the COVID-19 Pandemic in Pandemics, Major Incidents and Mental Health: The Psychosocial and Mental Health Aspects of Health Emergencies. Cambridge: Cambridge University Press; 2023.
- Chambers R, Maxwell R. Helping sick doctors. BMJ 1996;312:722-3.
- Herzberg FI. Work and the Nature of Man. New York: Wiley; 1966.
- Sanz-Vergel A, Nielsen K. Virtual issue: psychological interventions in the field of work and organizational psychology. Appl Psychol 2021;2021:1-6.
- Nielsen K, Christensen M. Positive participatory organizational interventions: a multilevel approach for creating healthy workplaces. Front Psychol 2021;12.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage; 2013.
- Ustun G. COVID-19 Pandemic and Mental Health of Nurses: Impact on International Health Security. Contemporary Developments and Perspectives in International Health Security, Vol. 2. London: IntechOpen; 2021.
- Falatah R. The impact of the Coronavirus disease (COVID-19) pandemic on nurses’ turnover intention: an integrative review. Nurs Rep 2021;11:787-810.
- Sampaio F, Sequeira C, Teixeira L. Nurses’ mental health during the COVID-19 outbreak: a cross-sectional study. J Occup Environ Med 2020;62:783-7.
- Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during COVID-19. Occup Med 2021;71:62-7.
- Vera San Juan N, Aceituno D, Djellouli N, Sumray K, Regenold N, Syversen A, et al. Mental health and well-being of healthcare workers during the COVID-19 pandemic in the UK: contrasting guidelines with experiences in practice. BJPsych Open 2021;7.
- Williams R, Ntontis E, Alfadhli K, Drury J, Amlôt R. A social model of secondary stressors in relation to disasters, major incidents and conflict: implications for practice. Int J Disas Risk Reduct 2021;63.
- Ntontis E, Luzynska K, Williams R. The Impact of COVID-19 on the Psychosocial and Mental Health Needs of NHS and Social Care Staff: The Final Report on Literature Published to Mid-2021 2021.
- Wong A, Pacella-LaBarbara ML, Ray JM, Ranney ML, Chang BP. Healing the healer: protecting emergency health care workers’ mental health during COVID-19. Ann Emerg Med 2020;76:379-84.
- Vera San Juan N, Clark SE, Camilleri M, Jeans JP, Monkhouse A, Chisnall G, et al. Training and redeployment of healthcare workers to intensive care units (ICUs) during the COVID-19 pandemic: a systematic review. BMJ Open 2022;12.
- Maloney L, Wilson J. MINDING THE MIND OF EMS, PART 2: here’s how to help employees’ mental well-being. EMS World 2021;50:36-41.
- Rees N, Smythe L, Hogan C, Williams J. Paramedic experiences of providing care in wales (UK) during the 2020 COVID-19 pandemic (PECC-19): a qualitative study using evolved grounded theory. BMJ Open 2021;11.
- Singleton G, Dowrick A, Manby L, Fillmore H, Syverson A, Lewis-Jackson S, et al. UK healthcare workers’ experiences of major system change in elective surgery during the COVID-19 pandemic: reflections on rapid service adaptation. Int J Health Policy Manag 2021;11:2072-82.
- Rengers A, Day E, Whitfield S. Describing a 12-hour ambulance shift during a second wave of COVID-19 in London. Australas J Paramed 2021;18:1-4.
- Uytenbogaardt A. COVID-19’s effect on midwives’ mental health. Br J Midw 2020;28.
- Maloney L, Hoffman J, Pepe P. Minding the mind of EMS - Part I. EMS World 2020. https://www.hmpgloballearningnetwork.com/site/emsworld/article/1225094/minding-mind-ems-part-i (accessed 8 February 2023).
- Hoernke K, Djellouli N, Andrews L, Lewis-Jackson S, Manby L, Martin S, et al. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open 2021;11.
- Llop-Gironés A, Vračar A, Llop-Gironés G, Benach J, Angeli-Silva L, Jaimez L, et al. Employment and working conditions of nurses: where and how health inequalities have increased during the COVID-19 pandemic?. Hum Res Health 2021;19:1-11.
- Williamson V, Murphy D, Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occup Med 2020;70:317-9.
- Williams R, Murray E, Neal A, Kemp V. The top ten messages for supporting healthcare staff during the COVID-19 pandemic n.d. https://doi.org/10.13140/RG.2.2.13439.76968.
- Mitchinson L, Dowrick A, Buck C, Hoernke K, Martin S, Vanderslott S, et al. Missing the human connection: a rapid appraisal of healthcare workers’ perceptions and experiences of providing palliative care during the COVID-19 pandemic. Palliat Med 2021;35:852-61.
- Oshikanlu R. How we rose to the leadership challenges of COVID-19: five black nursing professionals describe how the pandemic affected their work, teams and patients as they strived to ensure equal access to healthcare and minimise disruption to services for vulnerable groups. Nurs Stand 2021;36:40-3.
- Regenold N, Vindrola-Padros C. Gender matters: a gender analysis of healthcare workers’ experiences during the first COVID-19 pandemic peak in England. Soc Sci 2021;10.
- Blake H, Gupta A, Javed M, Wood B, Knowles S, Coyne E, et al. COVID-well study: qualitative evaluation of supported wellbeing centres and psychological first aid for healthcare workers during the COVID-19 pandemic. Int J Environ Res Public Health 2021;18.
- Muscat H, Morgan L, Hammond K. Staff burnout: how a nurse advocate course can help: programme uses a model of restorative clinical supervision proven to boost well-being and patient outcomes. Learn Disab Pract 2021;24:13-4.
- Dowrick A, Mitchinson L, Hoernke K, Mulcahy SS, Cooper S, Martin S, et al. Re-ordering connections: UK healthcare workers’ experiences of emotion management during the COVID-19 pandemic. Sociol Health Illn 2021;43:2156-77.
- McFadden P, Ross J, Moriarty J, Mallett J, Schroder H, Ravalier J, et al. The role of coping in the wellbeing and work-related quality of life of UK health and social care workers during COVID-19. Int J Environ Res Publ Health 2021;18.
- Trepanier S, Henderson R, Waghray A. A health care system’s approach to support nursing leaders in mitigating burnout amid a COVID-19 world pandemic. Nurs Admin Quart 2022;46:52-9.
- Vindrola-Padros C, Andrews L, Dowrick A, Djellouli N, Fillmore H, Bautista Gonzalez E, et al. Perceptions and experiences of healthcare workers during the COVID-19 pandemic in the UK. BMJ Open 2020;10.
- Barden A, Giammarinaro N. Team Lavender: supporting employee well-being during the COVID-19 pandemic. Nursing 2021;51:16-9.
- Jakimowicz S, Maben J. “I can’t stop thinking about it”: Schwartz Rounds® an intervention to support students and higher education staff with emotional, social and ethical experiences at work. J Clin Nurs 2020;29:23-4.
- Greenberg N. “Going for Growth”: An outline NHS staff recovery plan post-COVID19 (Outbreak 1). London: Royal College of Psychiatrists; 2020.
- Conolly A, Abrams R, Rowland E, Harris R, Couper K, Kelly D, et al. “What is the matter with me?” or a “badge of honor”: nurses’ constructions of resilience during COVID-19. Glob Qual Nurs Res 2022;9.
- Eagen-Torkko M, Altman MR, Kantrowitz-Gordon I, Gavin A, Mohammed S. Moral Distress, trauma, and uncertainty for midwives practicing during a pandemic. J Midw Women Health 2021;66:304-7.
- Adams M, Kelly D, Maben J, Mannion R, Banks C, Jones A. How do “heroes” speak up? NHS staff raising concerns during COVID-19 n.d. https://blogs.bmj.com/bmj/2020/08/11/how-do-heroes-speak-up-nhs-staff-raising-concerns-during-covid-19/ (accessed 8 February 2023).
- Baldwin S, George J. Qualitative study of UK health professionals’ experiences of working at the point of care during the COVID-19 pandemic. BMJ Open 2021;11.
- Labrague L. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag 2021;29:893-1905.
- World Health Organization . Action Required to Address the Impacts of the COVID-19 Pandemic on Mental Health and Service Delivery Systems in the WHO European Region: Recommendations from the European Technical Advisory Group on the Mental Health Impacts of COVID-19 2021.
- Kosyluk K, Baeder T, Tran JT, Egan M. Using a chatbot to address psychological distress among first responders, American congress of rehabilitation medicine (ACRM) annual conference (virtual), September 24−29, 2021. Archiv Phys Med Rehab 2021;102.
- Cunningham T, Pfeiffer K. Posttraumatic growth as a model to measure and guide implementation of COVID-19 recovery and resiliency. Nurs Admin Quart 2022;46:81-7.
- Team LE. Aged care staff cop the blame for vaccine bungling. Lamp 2021:20-1.
- Clancy G, Gaisser D, Wlasowic G. COVID-19 and mental health: self-care for nursing staff. Nursing 2020;50:60-3.
- Hall S, White A, Ballas J, Saxton SN, Dempsey A, Saxer K. Education in trauma-informed care in maternity settings can promote mental health during the COVID-19 pandemic. J Obst Gynecol Neonat Nurs 2021;50:340-51.
- Selçuk Tosun A, Akgül Gündoğdu N, Taş F. Anxiety levels and solution-focused thinking skills of nurses and midwives working in primary care during the COVID-19 pandemic: a descriptive correlational study. J Nurs Manag 2021;29:1946-55.
- Murphy P. Midwifery in the time of COVID-19. J Midw Women Health 2020;65:299-300.
- Teoh K, Kinman G, Harriss A. Supporting nurses and their mental health in a world after COVID-19. Occup Health Wellb 2020;72:26-9.
- Laker C, Cella M, Callard F, Wykes T. Why is change a challenge in acute mental health wards? A cross-sectional investigation of the relationships between burnout, occupational status and nurses’ perceptions of barriers to change. Int J Ment Health Nurs 2019;28:190-8.
- Sanford N, Lavelle M, Markiewicz O, Reedy G, Rafferty AM, Darzi A, et al. Capturing challenges and trade-offs in healthcare work using the pressures diagram: an ethnographic study. Appl Ergon 2022;101.
- Newman L. Bullying: the issue in (and beyond) midwifery. Br J Midw 2019;27.
- Brintworth K. Listening in: a survey of supervisors of midwives in London. Br J Midw 2014;22:432-7.
- Wild J, Smith KV, Thompson E, Béar F, Lommen MJJ, Ehlers A. A prospective study of pre-trauma risk factors for post-traumatic stress disorder and depression. Psychol Med 2016;46:2571-82.
- Peate I. The workplace and mental wellbeing. J Paramed Pract 2021;9.
- Sibson L. Mental health in emergency care. J Paramed Pract 2021;9.
Appendix 1 Protocol comparison and divergence table
| Protocol divergence summary: | ||
Divergence between the CUP-2 protocol and actual review process was minimal but included the following changes:
|
||
| Protocol item description | Completed? (yes/no) | Additional comments |
| Step 1: Locate existing theories | ||
| (1.1) Draw on our preliminary discussions with nurses, midwives, paramedics and patients and the public. | yes | |
| (1.2) Draw on the CMO configurations and theories generated by our co-applicants (KM, DC, SB) study (Care Under Pressure (1): a realist review to tackle doctors’ mental ill-health) and their final evidence informed programme theory and test and explore these with nurses, midwives and paramedics. | yes | |
| (1.3) Consult with key content experts representing multidisciplinary perspectives in our Stakeholder Group (including our nurses, midwives, paramedics, and PPIE representatives). | yes | |
| (1.4) Draw on the literature we are already familiar with (PI and co-applicant previous NIHR research reviews; endnote databases etc.), along with additional informal searching to identify causal explanations about how the programmes impact on staff mental health/well-being. | yes | |
| (1.5) Consult our information specialist (SB) regarding a tightly bound search of the grey literature, for example, Nursing Times, Academy of the Fabulous (https://fabnhsstuff.net/), King’s Fund and Health Foundation Reports, The Health Management Information Consortium (HMIC) database, and others in consultation with our stakeholders. | yes | Key reports known to the PI and co-investigator team and our stakeholders were retrieved during this step and examined for potential theoretical framings. A formal search of grey literature through the HMIC database was undertaken in step 2 during the time in which the information specialist was searching other databases including MEDLINE and CINAHL. This was done to streamline the process of database searching. |
| (1.6) We will use English language papers from 2000−2019. | no | We changed the date parameters to 2010−current, with the rationale that papers older than 2010 would be less relevant given changes in context and interventions for workplace mental well-being and given the huge volume of data (which we were asked to actively manage by the HS&DR board in the commissioning process following review). |
| Step 2: Search and screen for evidence | ||
| (2.1) Working with our information specialist (SB) we anticipate that we may need to search the following databases: MEDLINE-in-Process, CINAHL, PsycINFO, Maternity and Infant Care, the Cochrane Library and ASSIA, and any other relevant databases identified by the Information. | yes | We consulted MEDLINE In-Process, CINAHL, and HMIC databases in the initial round of searching. Due to the fact that hand searching provided rich content for the analysis, additional database searching using other databases including PsychINFO, The Cochrane Library and ASSIA was not undertaken. |
| (2.2) We will also undertake forward citation searches and search the citations contained in the reference lists of relevant documents. | no | We were open to the possibility of undertaking forward citation searches but used hand searching as an alternative supplementary search method due to our recognition (from stakeholder recommendations) that there were a few select journals that would be particularly valuable to search. |
| (2.3) We anticipate that we will search the databases using free text terms for terms relating to the following: (a) the staff groups of interest: “nurs*”, midwi*” “paramedic*”; (b) outcomes of interest: ‘mental health’, ‘wellbeing’ ‘absent*’, ‘presenteeism’ ‘attrition’ and ‘workforce’ and ‘retention’; and (c) the specific organisational/structural issues and working practices identified in step 1. | yes | |
| (2.4) Study design: all study designs | yes | |
| (2.5) Types of settings: all healthcare settings (acute, primary care, community). | yes | |
| (2.6) Types of participants: all studies that included registered nurses, midwives and/or paramedics. Focus: identify how and why work has a positive or negative effect on the mental health of nurses, midwives and paramedics and in what contexts these are most experienced and have impacted (includes at least one example of impact of work on staff mental health). |
yes | |
| (2.7) Types of strategies/intervention: all studies that included any strategies/interventions designed to improve mental health of nurses, midwives and paramedics and minimise its impacts Focus: identify which groups of staff these have been used with and whether they are operating at individual, team or organisational levels and allows identification of the mechanisms by which strategies and interventions prevent or reduce the impact of work on mental ill-health. |
yes | |
| (2.8) Outcome measures: mental ill-health (e.g. stress; anxiety, burn out; moral distress; depression; psychological distress; psychiatric morbidity; PTSD etc.) and its impacts (e.g. presenteeism, absenteeism, workforce retention quality of relationships and work with colleagues and patients, errors, and mistakes; alcoholism, substance misuse and other self-harm, suicide [parasuicide]) – all studies that focused on one or more of these aspects. | yes | |
| (2.9) Screening will be undertaken by the Research Fellow who will be recruited/appointed if this proposal is successful. A 10% random subsample of the citations retrieved from searching will be reviewed independently for quality control (by CT). Any disagreements will be resolved by discussion between the RF and the second reviewer (CT) and the PI (JM). If disagreements remain then a third member of the team will review (e.g. KM/DC) and any disagreements will be resolved through further review/discussion. | yes | We did much more than 10% random sample of double reviewing. Two members of the team (JJ and CT) reviewed 100% of papers, with any disagreements resolved by PI (JM). |
| (2.10) An important process in realist reviews is finding additional data needed to confirm, refine, or refute aspects of developing programme theory. In other words, more searches will be undertaken if we find that we require more data to develop and confirm, refute, or refine certain subsections of the programme theory. | yes | |
| (2.11) If we do not have sufficient material for any of our staff groups, we may also look at literature about nurses, midwives and paramedics working in other countries, other groups of healthcare professionals working in the UK such as other Allied health professionals with similar pressures, and professions outside health care who experience the same broader societal organisational and structural changes but in a different industry. | yes | The initial set of 80 papers were limited to the UK Context. Once preliminary analysis of these papers was drafted, we conducted additional searches for literature reviews and COVID-19, in which we searched outside of the UK context and included papers describing other professions or the healthcare workforce generally. |
| Step 3: Article selection | ||
| (3.1) Documents will be prioritised and selected based on relevance (whether data can contribute to theory building and/or testing) and rigour (whether the methods used to generate the relevant data are credible and trustworthy). However, papers will not necessarily be excluded based on rigour as they may generate important insights regarding, for example, context and mechanisms, which will not be dependent on the same criteria for rigour as for study outcomes. Included papers would be divided into those which can make ‘major’ or ‘minor’ contributions to our research questions. | yes | |
| (3.2) Major: Studies that contribute to the study aims and are conducted in an NHS context; or, Studies that contribute to the study aims and are conducted in contexts (e.g. universal, publicly funded health-care systems) with similarities to the NHS; or Studies that contribute to the study aims and can clearly help to identify mechanisms, which could plausibly operate in the context of the NHS. Minor: Studies conducted in health-care systems that are markedly different to the NHS (e.g. fee-for-service, private insurance scheme systems) but where the mechanisms causing or moderating mental ill-health could plausibly operate in the context of nurses, midwives and paramedics working in the NHS. |
yes | We included papers that were specific to the professions as well as papers that were not specific by profession (e.g. about doctors or health-care staff generally) but had insights that could be extrapolated for our nurse, midwife and paramedic analysis. |
| (3.3) Classification decisions will be checked between two reviewers (RF & CT) and discussed with the rest of the team. The RF will read all included papers and finalise article selection by including documents or studies that contain data relevant to the realist analysis – that is, those that could inform some aspect of the programme theory. Decisions will be made regarding whether a paper is to be included in the study or not based on a combination of relevance (based on inclusion criteria above) and rigour (e.g. how trustworthy the study is). This will allow us to determine whether papers make a major or minor contribution. | yes | |
| (3.4) We will use the RAMESES guidelines for reporting realist synthesis to guide us in what to report.40 | yes | |
| (3.5) Following an initial random sample of documents being reviewed together (10%); selected, assessed and discussed between the RF and CT to ensure that decisions for final inclusion have been made consistently, the remaining 90% of decisions re rigour will be made by the RF (though a number of these may require further discussion/joint reading between the RF, second reviewer and other co-applicant (JM/CT/KM/DC) and/or the wider project team as there may be uncertainty over issues of relevance and/or rigour). We will employ the same decision-making process as outlined above in step 2. Article selection for any additional searches will follow the process described above. | yes | As above, two members of the team (JJ and CT) reviewed 100% of papers, with any disagreements resolved by PI (JM). |
| Step 4: Extracting and organising data | ||
| (4.1) The full texts of the included papers will be uploaded in a reference manager software tool (Mendeley). Relevant sections of texts that have been interpreted as related to contexts, mechanisms and/or their relationships to outcomes will be coded and organised in Excel or NVivo. This coding will be both inductive (codes created to categorise data reported in included studies) and deductive (codes created in advance of data extraction and analysis as informed by the initial programme theory). These will be analysed separately and then brought together in further iterative analysis cycles. Each new element of relevant data will be used to refine aspects of the programme theory, and as it is refined, included studies and documents will be rescrutinised to search for data relevant to the revised programme theory that may have been missed initially. The characteristics of the studies will be extracted separately into an Excel spreadsheet to provide a descriptive overview. | no | We used Endnote and Dropbox for data management and MSWord for appraisal journaling and extracting the data. In appraisal journaling members of the team read papers and journaled their thoughts on the most important aspects of the papers that were salient to the emerging analysis. Other team members read all the journal entries and provided further comment and insight. From this process papers were read again on a case-by-case basis to determine best selection of quotes from the data to be added to the analysis. Quotes from papers were entered directly into a MSWord document that was used to build the analysis CMO configurations were then constructed from the extracted quotes. The characteristics of the studies, and descriptive details on causes and interventions were extracted separately into an Excel spreadsheet to provide a descriptive overview. |
| (4.2) We will start the coding and analysis process by using the literature that has been deemed to make a ‘major’ contribution to the research questions to start building and refining our programme theory, while progressively focusing the review. Articles categorised as providing ‘minor’ contributions will be analysed to address particular aspects of the programme theory where necessary. The aim of the review will be to reach theoretical saturation in achieving the objectives, rather than to aggregate every single study that exists in the area. Decisions about whether a study can have a ‘major’ or ‘minor’ contribution may change over the course of the project, as the analysis progresses. All changes will be documented and recorded as part of an audit trail to increase transparency and ensure consistency. | yes | |
| Step 5: Synthesising the evidence and drawing conclusions | ||
| (5.1) Our data analysis will use realist logic to make sense of the initial programme theory. A realist logic of analysis builds context + mechanism = outcome configurations (CMOCs) for the programme theory. To achieve this, the data will be interpreted to ascertain if it pertains to context (C), mechanism (M), outcome (O), the relationships between C, M, and O and/or the relationships between CMOCs. | yes | |
| (5.2) In addition, evidence will also be subject to analysis by observed outcomes (by comparing interventions where reducing mental ill-health has been ‘successful’ against those which have not, to understand how the mechanism of the intervention and context have impacted positively vs. negatively on mental health). We will also compare any differences between our professional groups or settings (so where the impact of a change has been more or less beneficial in paramedics and not with nurses for examples or in acute care and not community care). This type of analysis will enable us to understand how the most relevant and important mechanisms work in different contexts, thus allowing us to build more transferable CMOCs. | no | We did not systematically examine observed outcomes in studies and compare them across cases to unearth mechanisms. This is because we found that context between studies varied significantly, and that evidence showed a tension between offering interventions that ‘work’ downstream vs. fixing structural problems in the healthcare setting that cause poor working conditions in the first place. The realist analysis unpacked this complexity, and it was only after immersion in the data that we felt this would be a better approach. |
| (5.3) Finally, during our data analysis we will use the following analytic processes to make sense of our data [as in Mattick et al.’s protocol who draws on the work of Pawson (2013)237]: Compare and contrast sources of evidence – for example, where evidence about interventions in one paper or report allows insights into evidence about outcomes in another paper. Reconciling of sources of evidence – where results differ in apparently similar circumstances, further investigation is appropriate in order to find explanations for why these different results occurred. Adjudication of sources of evidence – on the basis of methodological strengths or weaknesses. Consolidation of sources of evidence – where outcomes differ in particular contexts, an explanation can be constructed of how and why these outcomes occur differently. |
yes | Although this step was not a formalised process in the analysis, when we extracted data and assembled these across different ‘tensions’, we juxtaposed data segments that enabled us to compare and contrast sources of evidence to improve the articulation of CMO configurations. The CMO configurations in early stages of the analysis were advanced as more data was incorporated into the work-in-progress, thus allowing for further comparing and contrasting as the analysis matured. |
Appendix 2 Initial theory of context-mechanism-outcome factors in paramedics
| Mechanisms | Interventions | Outcomes | ||
|---|---|---|---|---|
| Feelings/emotions Attitudes Preferences Values Beliefs Norms Awareness/knowledge Motivation Reasoning |
Training initiatives:
Awareness initiatives:
Schemes/programmes:
Other sources of support:
|
Health outcomes | Non-health outcomes | |
Symptoms:
|
Action:
|
Presenteeism Absenteeism High attrition rates Resilience Sick leave |
||
| Illustrative CMO configurations | ||||
| Exposure to traumatic or distressing incidents (C) can make paramedics feel overwhelmed (M1) or deeply disturbed (M2) falling into high range for post-traumatic stress symptoms (O) | Increasing demands (C1) and strict response times (C2) make it more challenging for paramedics to take time to gather their thoughts or talk to peers (M). This may result in experiencing emotional fatigue (O1) and burnout (O2) | |||
| The longer paramedics serve (C1), the more likely they are to feel the negative impact (M) of workload pressures (C2), making them an important audience for poor mental health (O) | Providing mental health training to new recruits (C) can help build their awareness (M1) and their understanding (M2) of different ways to build resilience (O) | |||
| Listening to colleagues’ negative experiences of accessing mental health support within the organisation (C) can make paramedics feel reluctant (M1) or put them off (M2) using these services in the future. As a result, mental ill-health problems may remain unresolved or exacerbate (O) | These is still some stigma attached to disclosing a mental health problem to a line manager within the ambulance services (C1), potentially because of fears it may impact detrimentally upon career progression (C2). Consequently, paramedics may feel it is hard to talk to their managers about their mental health issues (M), making them more vulnerable to ill-mental health (O) | |||
| Organisational upheaval (C) can add to the pressures that paramedics feel in their line of work (M), making them more susceptible to poor mental health (O) | There is still taboo around talking about mental health issues in the workplace (C) because of fear of being treated differently (in a negative way) if mental health issues are disclosed (M). This may lead paramedics to continue going into work even when unwell (O) | |||
Appendix 3 The effects of COVID-19 on nurses’, midwives’ and paramedics’ psychological wellness
Introduction
As outlined in the methods chapter (see Chapter 2), due to our reverse chronological screening process and the risk of including only COVID-19 literature if we did not exclude in the first cycle of searching, we excluded such literature at first, but decided to come back to the COVID-19 related literature towards the end of this study. This was to ensure we were able to incorporate any extraordinary causes of psychological ill-health that may still be relevant to consider (given the pandemic is not yet over and has long-term impacts); and capture any innovative interventions to mitigate psychological ill-health that may differ from those pre-pandemic, and provide important learning. This short appendix presents a synthesis of this literature.
As shown in the PRISMA statement (see Chapter 3, Figure 1) we included a total of 49 COVID-19 papers in this cycle of searching and synthesis. These are summarised in Table 15 below, with a longer version provided at the end of this appendix (see Table 16). Twenty-two papers related to a range of healthcare professionals, some of whom may have been nurses or midwives or paramedics, but also include doctors and support workers and other staff (labelled general); 7 paramedic papers, 12 nurses and 8 midwife papers (some of which are both nurses and midwives). Table 16 (at the end of the appendix) details descriptors of author, date, year, country and type of paper. Table 15 below details a summary of the types of papers included.
| Empirical | Commentary | Lit review paper | Editorial | Discussion paper | Theory paper | Report | TOTAL | |
|---|---|---|---|---|---|---|---|---|
| General | 11 | 1 | 3 | 3 | 2 | 1 | 1 | 22 |
| Paramedic | 2 | 3 | 2 | 7 | ||||
| Nursing | 3 | 1 | 1 | 7 | 12 | |||
| Midwifery | 1 | 1 | 2 | 2 | 2 | 8 | ||
| TOTAL | 17 | 5 | 6 | 6 | 13 | 1 | 1 | 49 |
| Ref # | Author | Year | Title | Aim/focus | Type of paper | Paper focus (cause vs. intervention) | Which profession (N, M, P or general) | Country setting | |
|---|---|---|---|---|---|---|---|---|---|
| General/mixed papers | |||||||||
| 1 | 266 | Barden and Giammarinaro | 2021 | Team Lavender: Supporting employee well-being during the COVID-19 pandemic | Team based peer support model | Empirical (survey) | Intervention | General | USA |
| 2 | 230 | Gardiner et al. | 2020 | Here4HealthCare: A response to the Emerging Mental Health Crisis of the Frontline Healthcare Workforce | Programme for front-line healthcare workers: (1) website of mental health resources (2) service pathways for workers | Commentary | Intervention | General | Canada |
| 3 | 245 | Wong et al. | 2020 | Healing the Healer: Protecting Emergency Health Care Workers’ Mental Health During COVID-19 | Details challenges in pandemic and compares to other pandemics and strategies that may be useful for staff at different stages | Editorial | Causes and interventions | General | USA |
| 4 | 273 | Labrague and Leodoro | 2020 | Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. | A literature review of quantitative COVID-19 studies | Empirical systematic review | Causes and interventions | General | China, Oman |
| 5 | 180 | Nursing Standard journalist (no author identified) | 2022 | The attraction of working in a Magnet hospital: Why UK hospitals are trialling the US model and what its staff well-being goals mean for nurses and patients. | Reports new research study evaluating Magnet hospitals in UK/Europe – creating places where nurses want to work. | Editorial/short report | Intervention | General- nurses and others | USA |
| 6 | 263 | McFadden et al. |
2021 | The Role of Coping in the Wellbeing and Work-Related Quality of Life of UK Health and Social Care Workers during COVID-19 | Impacts of COVID-19 and coping strategies on health and social care workers’ well-being. | Empirical [survey] | Interventions | General | UK |
| 7 | 256 | Williams et al. | 2020 | The top ten messages for supporting healthcare staff during the COVID-19 pandemic |
Summarises ten core messages to aid managers and staff re how to reduce staff requiring additional assistance. | Discussion paper | Causes and interventions | General | UK |
| 8 | 246 | San Juan et al. | 2022 | Training and redeployment of healthcare workers to intensive care units (ICUs) during the COVID-19 pandemic: a systematic review | Captures redeployment and training strategies and the needs of redeployed healthcare workers | Empirical; systematic review | Causes and interventions | General | UK team; International literature |
| 9 | 265 | Vindrola-Padros et al. | 2020 | Perceptions and experiences of healthcare workers during the COVID-19 pandemic in the UK | A review of UK healthcare policies; mass and social media and in-depth interviews with frontline staff | Empirical; rapid appraisal | Causes | General | UK |
| 10 | 244 | Ntontis et al. | 2021 | The impact of COVID-19 on the psychosocial and mental health needs of NHS and social care staff: The final report on literature published to mid-2021 | To direct the attention of the People Directorate in NHSE/I to reliable new information about effective care for staff during the pandemic | Empirical literature review | Causes | General | UK |
| 11 | 242 | San Juan et al. | 2021 | Mental health and well-being of healthcare workers during the COVID-19 pandemic in the UK: contrasting guidelines with experiences in practice | Qualitative study – rapid appraisal of applicability of well-being guidelines in practice, and interviews with frontline staff during current and future pandemics | Empirical | Causes and interventions | General – mostly Drs but 3 nurses | UK |
| 12 | 241 | Greenberg et al. | 2021 | Mental health of staff working in intensive care during Covid-19 | Identify rates of probable mental health disorder in staff working in ICUs in nine English hospitals; June/July 2020 | Empirical survey | Causes | General- includes nurses | UK |
| 13 | 255 | Williamson et al. | 2020 | COVID-19 and experiences of moral injury in front-line key workers | Discussion of moral injury on healthcare staff | Editorial | Causes | General | UK |
| 14 | 268 | Greenberg | 2020 | ‘Going for Growth’ An outline NHS staff recovery plan post-COVID19 | Recovery plan guidance Royal College of Psychiatrists | Editorial/guidance | Interventions | General | UK |
| 15 | 249 | Singleton et al. | 2021 | UK Healthcare Workers’ Experiences of Major System Change in Elective Surgery During the COVID-19 Pandemic: Reflections on Rapid Service Adaptation | Qualitative study of surgical staff (interviews) | Empirical | Causes | General- sample includes 4 nurses | UK |
| 16 | 253 | Hoernke et al. | 2021 | Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal | Rapid assessment of media and front-line staff interviews | Empirical | Causes | General – 8 nurses in sample | UK |
| 17 | 257 | Mitchinson et al. | 2021 | Missing the human connection: A rapid appraisal of healthcare workers’ perceptions and experiences of providing palliative care during the COVID-19 pandemic | Identify barriers to delivering end-of-life care | Empirical- rapid appraisal and interviews | Causes | General | UK |
| 18 | 259 | Regenold and Vindrola-Padros |
2021 | Gender Matters: A Gender Analysis of Healthcare Workers’ Experiences during the First COVID-19 Pandemic Peak in England | How gender shapes HCWs’ personal experience | Empirical; interviews | Causes | General – 10 nurses in sample | UK |
| 19 | 260 | Blake et al. | 2021 | COVID-Well Study: Qualitative Evaluation of Supported Wellbeing Centres and Psychological First Aid for Healthcare Workers during the COVID-19 Pandemic | Qualitative interviews assessing well-being centres in NHS trust | Empirical; interviews | Interventions | General – 3 nurses in sample | UK |
| 20 | 272 | Baldwin and George |
2021 | Qualitative study of UK health professionals’ experiences of working at the point of care during the COVID-19 pandemic | Front-line health professionals’ experiences of working during the COVID-19 pandemic | Empirical; interviews | Causes | General – 8 nurses in sample | UK |
| 21 | 243 | Williams et al. | 2021 | A social model of secondary stressors in relation to disasters, major incidents and conflict: Implications for practice | Theoretical examination of primary and secondary stressors with new theoretical approach | Theoretical paper | Causes and interventions | General | UK |
| 22 | 274 | World Health Organization (WHO) | 2021 | Action required to address the impacts of the COVID-19 pandemic on mental health and service delivery systems in the WHO European Region | Recommendations from the European Technical Advisory Group on the mental health impacts of COVID-19 | Report | Causes | General | Europe |
| Paramedic papers | |||||||||
| 23 | 275 | Kosyluk et al. | 2021 | Using a chatbot to address psychological distress amongst first responders | Chatbots (TABATHA) used to screen and refer front-line workers to care for example, mindfulness apps (conference poster) | Empirical | Intervention | Paramedic (first responders) | USA |
| 24 | 247 | Maloney et al. | 2021 | Minding the mind of Emergency medical responders (EMS), Part 2 | Examples of resources – for example, CODE Lavender programme (team alerted and follows up with responders after tragic/stressful incident) | Discussion | Causes | Paramedic (EMS) | USA |
| 25 | 248 | Rees et al. | 2021 | Paramedic experiences of providing care in Wales (UK) during the 2020 COVID-19 pandemic (PECC-19): a qualitative study using evolved grounded theory | Paramedic experiences (interviews) of providing care during COVID-19 pandemic | Empirical | Causes | Paramedic | UK |
| 26 | 250 | Rengers et al. | 2021 | Describing a 12-hour ambulance shift during a second wave of COVID-19 in London | Case report, of 12-hour emergency ambulance dayshift in central London during the second COVID-19 wave | Commentary | Causes | Paramedic | UK |
| 27 | 252 | Maloney et al. | 2020 | Minding the Mind of EMS—Part I | Challenges of pandemic for emergency responders – including letting people down and stoicism | Discussion paper | Causes | Paramedics (EMS) | UK |
| 28 | 166 | Mendes | 2021 | Protecting your mind amid a crisis | Discusses quick/easy interventions for front-line workers freely accessible on NHS in Mind platform | Commentary | Interventions | Paramedics | UK |
| 29 | 223 | Hayes et al. | 2021 | Paramedic emotional labour during COVID-19 | Review of literature (not systematic) to raise awareness of the concept of emotional labour in the role of paramedics | Commentary | Causes | Paramedics | UK |
| Nurse papers | |||||||||
| 30 | 36 | Choflet et al. | 2022 | The Nurse Leader’s Role in Nurse Substance Use, Mental Health, and Suicide in a Peri-pandemic World | Reviews nurse suicide; promising interventions and practices, for example, Healer Education Assessment and Referral (HEAR) and peer support | Discussion paper | Causes and interventions | Nurses | USA |
| 31 | 276 | Cunningham and Pfeiffer | 2022 | Post-traumatic Growth as a Model to Measure and Guide Implementation of COVID-19 Recovery and Resiliency | Suggests use of and Posttraumatic Growth (PTG) Inventory to guide leaders; identifies three science-based interventions to increase PTG | Discussion paper | Interventions | Nurses | USA |
| 32 | 264 | Trepanier et al. | 2022 | A Health Care System’s Approach to Support Nursing Leaders in Mitigating Burnout Amid a COVID-19 World Pandemic | Organisational approach to support – focused coaching/support to leaders and teams experiencing the highest stress levels. Also offers concrete interventions to consider for example, NOCA | Discussion paper | Interventions | Nurses | USA |
| 33 | 206 | Brooks | 2021 | Acknowledge Pandemic-Driven Moral Distress, Mitigate Harmful Effects | Reports nurses’ moral distress and how managers can work to reduce it | Discussion paper | Causes | Nurses | USA |
| 34 | 277 | The Lamp [NSW Nurses and Midwives’ Association magazine – Editorial team] | 2022 | Aged care staff cop the blame for vaccine bungling | Reports issues arising from mandating vaccinations for aged care facilities in NSW Australia | Editorial | Causes | Nurses | Australia |
| 35 | 278 | Clancy et al. | 2020 | COVID-19 and mental health: Self-care for nursing staff | Discusses the pandemic and effects on nurses and some strategies to support | Discussion paper | Causes and interventions | Nurses | USA |
| 36 | 258 | Oshikanlu | 2021 | How we rose to the leadership challenges of COVID-19 | Five black nurses report the affects on the pandemic on them and their work | Discussion paper/report | Causes and interventions | Nurses | UK |
| 37 | 238 | Ustun | 2021 | COVID-19 Pandemic and Mental Health of Nurses: Impact on International Health Security | To identify literature to prevent and address psychological ill-health in nurses and identify strategies. | Empirical narrative review | Causes and interventions | Nurses | International |
| 38 | 232 | Maben and Connolly |
In press | Chapter 39: lessons for structure, workplace planning and responding to emergencies from nurses in the Covid- 19 Pandemic |
COVID-19 experiences of nurses (book chapter) | Empirical; interviews | Causes and interventions | Nurses | UK |
| 39 | 231 | Maben et al. | 2022 | ‘You can’t walk through water without getting wet’ UK nurses’ distress and psychological health needs during the Covid-19 pandemic: A longitudinal interview study | COVID-19 experiences of nurses | Empirical; interviews | Causes and interventions | Nurses | UK |
| 40 | 269 | Conolly et al. | 2022 | ‘What Is the Matter With Me?’ or a ‘Badge of Honor’: Nurses’ Constructions of Resilience During Covid-19 | COVID-19 experiences of nurses | Empirical; interviews | Causes | Nurses | UK |
| 41 | 184 | Vogel and Flint | 2021 | Compassionate leadership: how to support your team when fixing the problem seems impossible. | Discussion paper examining the need for compassionate leadership because of COVID-19 | Discussion paper | Causes and intervention | Nurses | UK |
| Midwife papers | |||||||||
| 42 | 270 | Eagen-Torkko et al. | Moral Distress, Trauma, and Uncertainty for Midwives Practicing During a Pandemic | Reports on moral distress in midwifery practice | Commentary | Causes | Midwives | USA | |
| 43 | 279 | Hall et al. | 2021 | Education in Trauma-Informed Care in Maternity Settings Can Promote Mental Health During the COVID-19 Pandemic | Reports need for education on trauma-informed care to support mental health of pregnant women, and staff | Discussion paper | Causes and interventions | Midwives | USA |
| 44 | 254 | Llop-Girones et al. | 2021 | Employment and working conditions of nurses: where and how health inequalities have increased during the COVID-19 pandemic? | Aims to explain why nurses are exposed to multiple risks and/or poorer health as a result of inequalities | Empirical [Literature Review] | Causes | Nurses and midwives | Spain and international |
| 45 | 261 | Muscat et al. | 2021 | Staff burnout: how a nurse advocate course can help | Examines new professional nurse advocate role (PNA) and A-Equip model | Discussion paper | Intervention | Midwives | UK |
| 46 | 280 | Selçuk et al. | 2021 | Anxiety levels and solution-focused thinking skills of nurses and midwives working in primary care during the COVID-19 pandemic: A descriptive correlational study | To determine the state–trait anxiety levels and solution-focused thinking skills of primary care nurses/midwives during COVID-19 pandemic | Empirical (survey) | Causes and interventions | Nurses and midwives | Turkey |
| 47 | 281 | Murphy | 2020 | Midwifery in a time of COVID-19 | Personal reflection in time of pandemic | Editorial | Causes | Midwives | USA |
| 48 | 282 | Teoh et al. | 2020 | Supporting nurses and their mental health in a world after COVID-19 | Reports Teoh, K. Kinman, G. and Harriss, A. SOM literature review in summary and reflects on this in light of pandemic | Empirical literature review | Causes and interventions | Midwives and nurses | UK |
| 49 | 251 | Uytenbogaardt | 2020 | COVID-19’s effect on midwives’ mental health | Reports Couper et al. ICON COVID survey and response from RCM | Editorial | Causes | Midwives | UK |
The literature indicates that the COVID-19 pandemic has significantly impacted the psychological health of staff, in an almost entirely negative way. 238–240 For example, a recent study reported NHS intensive care staff suffered double the rates of PTSD during the pandemic compared to British military veterans deployed in Afghanistan in a combat role. 241 Nurses made up over half of the sample (57%) of 6080 respondents in this study, with younger, less experienced nursing staff most likely to report probable change to psychological health. One of the few benefits that the pandemic offered was the focus on staff health and psychological well-being. There has been a proliferation of research in this area and considerable resources on offer for support and interventions. However, as described in this chapter, many of the interventions had unintended negative consequences and much of the research was undertaken at pace and unfunded, and is therefore typically cross-sectional, descriptive and of poor quality. As in non-pandemic times, some authors note the importance of a whole-systems approaches to understanding the impact of COVID-19 on staff well-being, (e.g. Vera San Juan and colleagues). 242
This chapter provides a synthesis of the included COVID-19 literature. We have organised this into three sections as follows and highlighted our key findings (see Box 3) before presenting each of these sections in turn:
-
exacerbation and acceleration of staff mental distress from already difficult pre-pandemic conditions;
-
innovation and immediate interventions introduced during the pandemic;
-
sustained, longer-term changes and interventions arising from the pandemic.
-
Exacerbation and acceleration of staff psychological distress from already difficult pre-pandemic conditions specifically caused by the following:
-
Redeployment and new duties without sufficient training
-
‘Deathscapes’; high numbers of deaths and distressing end of life care
-
Unfiltered, constantly changing global stream of information, government rules and clinical protocols
-
Fear of contagion and virus spread
-
Impact of inadequate PPE access/PPE wearing especially for interpersonal communications
-
‘Tragic choices’, which caused moral distress and injury
-
An inability to always provide excellent care
-
Reports of losing the human side of care during the pandemic
-
The pandemic exposed health, global and societal inequalities
-
Staff feeling undervalued and embittered leading to workforce attrition
-
-
Innovation and immediate interventions introduced during the pandemic
-
National interventions were initially accessed minimally, healthcare staff preferring peer support and to connect with each other talk and be heard
-
Access to psychological well-being services was limited with no paid allocated time and a reluctance to access in time off
-
Provision of formal psychological support did not always reduce stigma and some staff felt the need to be stoic and conceal feelings
-
Some taboos broken around staff psychological ill-health enabling staff to prioritise their health and talk about their experiences
-
COVID-19 well-being guideline development placed greater emphasis on well-being at an individual level rather than organisational level
-
Some innovative interventions were adopted or adapted during the COVID pandemic in the US, three that were multifocal in approach [primary, secondary and/or tertiary levels: Code Lavender; HEAR and No One Cares alone (NOCA)]
-
-
Sustained, longer-term changes and interventions arising from the pandemic
-
The pandemic has shone an important spotlight on staff psychological wellness and the importance of primary prevention
-
On-going psychological health requires support and investment for sustainability
-
The pandemic provided an opportunity to change professional norms and for staff to reclaim autonomy and power and speak up and raise concerns, although these were not always heard
-
Intervention timing is important (in COVID-19): meeting essential needs in the immediate crisis with access to psychological support required later
-
An increased sense of camaraderie and pulling together during the pandemic with calls for this to be harnessed to increase cooperation and collaboration going forward
-
Innovation increased and new interventions were established and, while others that were not useful need to stop and be de-invested in.
-
1. Exacerbation and acceleration of staff mental distress from already difficult pre-pandemic conditions
As indicated in previous chapters there was already substantial evidence pre-pandemic to indicate that nurses, midwives and paramedics were under considerable strain, with their psychological health suffering. Reasons included existing secondary stressors and Williams243 highlight ‘The huge importance of camaraderie, taking adequate breaks, having conversations with peers, reducing hassles over parking and eating, for example, demonstrated a decade ago, was re-emphasised’ (p. 7). The included literature provides strong indication that the conditions of healthcare delivery presented during the COVID-19 pandemic created an exacerbation and acceleration of staff psychological distress in relation to pre-pandemic workplace conditions,231,232,238,244 describe in one paper as the ‘perfect storm of psychosocial stress’245 (p. 380). We explore the reasons for this below.
Redeployment and new duties without sufficient training: staff experienced increased stress from being redeployed (being assigned a new role and/or moved to a new setting or area; usually to a COVID-19 ward or intensive care unit) in which they were required to work in unfamiliar environments and teams, often at short notice and without adequate training. 231,246
‘Deathscapes’; high numbers of deaths and distressing end of life care: nurses reported ‘Deathscapes’ (COVID-19 environments with high mortality rates) where care could not be well-planned, relatives and friends could not be present during/at end of life and so farewells were by telephone or video, with nurses present in intimate moments they would not have been before, and unable to hold patients’ hands or offer comfort as usual231 (48JM-CV). Other papers also highlighted the stress on paramedics, ‘where death has so frequently characterised the most severe cases of the virus’223 (p. 319).
Unfiltered, constantly changing global stream of information, government rules and clinical protocols: several included papers described the impact of constantly changing and differing messaging and protocols. 245,247,248 With Wong et al. 245 highlighting that COVID-19 was the first pandemic in an age of deep digital integration. Staff reported being exposed to constant streams of unfiltered clinical information and government rules and messaging that was constantly changing, reinforcing emotions of angst, confusion and despair, and frustration at the shifting and differing guidance at local and national levels: ‘Our clinical environment faces relentless increases in patient volume and acuity while we experience unprecedented physical and psychological hardship. In addition, conflicting and rapidly changing information regarding personal protective equipment fuels our ongoing fears of exposure and uncertainty about our own safety in the workplace’245 (p. 379).
Constantly changing directives led to great uncertainty in staff:
We were getting different information every day from different sources, from Europe, within maternity, within the Trust, from PHE (Public Health England), and I think everything felt very, very different…I found that a bit stressful, this conflicting advice and nobody being quite sure what’s the right thing to do. Do we break the Trust rules and do what we think is right ourselves?249
(p. 6)
The unique paradox of simultaneous global digital interconnectedness and social and physical isolation also shifted normal systems of coping. Front-line workers (e.g. paramedics) were being challenged to ‘both grapple individually with our emotions and to work collectively to support resilience among our colleagues.’245 (p. 379). Paramedics expressed frustration with the media scaring people into not calling for emergency support when they had valid reasons to seek help unrelated to COVID-19. 250 At the same time, they were being called to homes of people who were in a state of fear and confusion from watching the news and needed professional reassurances that they were not sick or dying.
Fear of contagion and virus spread: in the Impact of COVID on Nurses (ICON) study, nurses and midwives experienced considerable stress in terms of the fear around spreading the virus to their families and members of their households. 251 Similarly, paramedics reported developing traits close to obsessive compulsive disorder around cleaning and sanitising stations. 248 Furthermore, the ‘protect me to protect you’ messaging to staff, while emphasising the collective efforts needed to prevent transmission and interdependence of teams to practice COVID-19 safety, also highlighted the heavy burden of responsibility that all staff were facing. 248 The literature highlighted the sense of ‘guilt’ that nurses, midwives and paramedics felt if they were infected, firstly in terms of letting patients down, even when they were not at fault; and secondly letting each other down, for example, those sent home to quarantine may feel like they’re letting co-workers down. 252
Impact of inadequate PPE access/PPE wearing especially for interpersonal communications: COVID-19 was reported as causing greater and different psychological issues (to those pre-pandemic) due to concerns over safety (lack of sufficient PPE), staffing unpredictability and moral injury. 162 Maloney and colleagues247 discussed the psychological impact of high rates of patient mortality and the need for more specialised training for emergency medical staff around death and dying.: ‘even before COVID-19, performing death notifications was associated with increased burnout among EMS professionals. Appropriate targeted training in death notification procedures can mitigate this effect and may have become particularly important over the past year, with many areas seeing profound increases in unresuscitable cardiac arrest cases during the pandemic’ (p. 3).
Numerous papers discussed the impact of inadequate PPE. 231,245,247,253 Paramedics described feeling scared to transmit the virus from their patients to their loved ones, particularly due to fear caused by ill-fitting PPE, or being told to use PPE that was old and out of date. 248 Llop-Girones et al. 254 similarly discusses the lack of adequate PPE and how shifting policy around PPE put staff at risk. They write
Lack of PPE was commonly reported by many health workers globally, also in rural areas and the private health sector … Evidence shows that nurses who do not consider the availability and quality of PPE to be adequate had significantly higher levels of depression, anxiety, and stress.
(p. 11)
Various papers described the taxing use of PPE by nurses and midwives and paramedics during the pandemic. 250 This included the difficulty taking breaks and eating, going to the bathroom, and the additional time and labour caused by the need to don and doff PPE. 250 Paramedics often had to stay in full PPE for several hours while transporting a patient to hospital and waited for admission, and then had to spend further time and labour to decontaminate the ambulance after a COVID-19 patient transport, while concurrently receiving calls for more emergencies. Donning and doffing PPE often had to happen inside the ambulance en-route to patients and different patient cases required different levels of PPE based on a tiered system. 250
‘Tragic choices’ caused moral distress and injury: staff experienced MD in relation to making difficult choices with limited resources206,255 and those working on the front lines in ICU departments experienced high rates of mental health disorders and thoughts of self-harm. 241 The literature indicated that staff experienced heightened distress during the pandemic due to making ‘tragic choices’;248 personal; organisational and societal. Rees et al. 248 draw on the theory of Calabresi and Bobbitt who explored how societies allocate tragically scarce resources and make such ‘tragic choices’. Examples of tragic choices meant that inevitably some patients would not receive treatment.
An inability to always provide excellent care: paramedics and nurses reported feeling they were unable to deliver the standard of care they would usually provide and described how this could result in MD and injury,248,256 resulting in the following key message intended to aid managers to support staff:
It is important to acknowledge facing the moral strain and distress that staff suffer now and later when they are unable to do everything possible for all patients. This includes advising staff not to fill gaps by heroic actions that place them at greater moral and physical risk and not to raise their expectations of what should be done for patients. 256
(p. 8)
Rees et al. 248 discussed the rise of MD for paramedics when conducting home visits. Paramedics experienced decision fatigue and ethical dilemmas around advising (non-COVID-19) patients to go to hospital. One paramedic noted ‘I would say at least about 50% (of patients) are refusing to go in…so you are really having to convince and weigh up the balance of fighting against that, because if you do take them in and they do catch it and they do die, it’s weighing up the responsibility of that as well’ (p. 6). Mitchinson et al. 257 described the challenging circumstances in treating dying patients in intensive care:
Nurses struggled with the changes to care delivery: ‘as a gut feeling, as a nurse, you didn’t feel it was right what you were doing’ (Nurse, Palliative Care). Palliative specialists who would do anything to enable a good death and perceived themselves as ‘rule breakers’ (Nurse, Palliative Care) were now required to enforce policies which contradicted their care beliefs (p. 6).
Reports of losing the human side of care during the pandemic was prevalent across all our professional groups,231,238 illustrated for paramedics here
their interaction pre-pandemic with people with mental health issues was often tactile, involving holding hands and using nonverbal communication. Participants explained how the pandemic had significantly changed this: ‘the human side of our job has been taken away, and its really put into sharp contrast how much humanity we usually have in our job…personally I have found it really difficult leaving relatives behind and especially when you have got time-critical, possibly not going to survive patients. We had a lady with a very dense CVA (an early sign of ischemic stroke) the other day…and had to leave her daughter standing crying on the side of the road. 248
(p. 6)
The pandemic exposed health, global and societal inequalities. Several papers highlighted how the pandemic disproportionately impacted on those staff with minority backgrounds and revealed significant gender differences,258,259 yet we know that there is a link between inclusive environments and staff psychological well-being. 160 A Nursing Standard practice feature258 described reflections from black nurses and the extra risks that COVID-19 provided for this population, many of which were hidden and not talked about. ‘As a profession we are good at what we do, but not always good at sharing our problems with others’ (p. 41).
Gender, social class, ethnicity/race, age and migrant status were described as inequality axes254 that act as key relational mechanisms explaining why nurses (and often their families) are exposed to multiple risks and poorer health. They also highlighted other inequities such as pay rises being offered to many other public sector workers, including doctors and dentists but not to nurses. Similarly, inequalities were noted with regard to PPE:253 ‘Many health care workers (HCWs) reported failing their respirator fit-test and a lack of alternatives meant that they proceeded caring for patients with COVID-19 with these masks or used a lower level of protection. This was especially the case for female HCWs who experienced a lack of small sized masks and scrubs. Media analysis found reports of greater PPE supply problems for black, Asian and minority ethnic (BAME) HCWs. Powered air purifying respirator hoods (an alternative for HCWs with beards unable to shave for religious reasons) were especially lacking’ (p. 8). One paper noted that in some cases, stigma became associated with ethnic minority communities due to the higher rate of infection in those people. 260 This created an additional layer of stress of staff from ethnic minority backgrounds: ‘For a minority (of non-BAME staff), the apparent disproportionate impact of COVID-19 on BAME staff and patients generated a certain level of fear and stigma. A few non-BAME participants admitted that at some point during the pandemic, they had perceived themselves to be at greater risk of contracting COVID-19 from BAME colleagues and patients’ (p. 9).
Staff feeling undervalued and embittered leading to workforce attrition: the pandemic accentuated nurses extremely difficult working conditions and left many nurses, midwives and paramedics feeling undervalued and embittered. This caused some professionals to prioritise their own well-being or job-hop to try and find improved work conditions and intrinsic value in their work, which some had lost. 143
Innovation and immediate interventions introduced during the pandemic
The COVID literature highlighted both the on-going deficits in psychological support for staff, as well as some innovative calls-to-action that were established quickly as the pandemic emerged. Over the course of the acute phase of the pandemic (2020–2022), numerous interventions were made available nationally. 261 These included free access to mindfulness Apps and online interventions such as an online mental health forum SilverCloud;251 a network of NHS staff mental health and well-being hubs to support staff, which includes self-referral to NHS psychological talking therapies; and the implementation of the Professional Nurse Advocate (PNA) role (adapted from midwifery, providing ‘a safe and confidential space to allow time to reflect on and make sense of workplace issues’261 (p. 14) and restorative supervision. 261
During the difficulties of COVID-19, the literature indicates at least in some instances organisations improving their workplace culture and co-operation through rapid innovation, for example: ‘... the pandemic context appears to have simulated a significant amount of innovation and cooperation. For instance, the organisation initiated more provision of clinical support, better information, communication and digitalisation, factors which may have created an environment for improved professional growth. It should be recognised that such accelerated innovation and growth was forced rather than discretionary, which can occur to ensure the organisation’s survival and because it had to’248 (p. 9).
2a. National interventions were initially accessed minimally, healthcare staff preferring peer support and to connect with each other talk and be heard: online Apps and interventions were difficult for staff to access in their working hours and at home they often wanted to switch off and not think about work. Consequently, uptake was low,251 in one study only 12% of nurses and midwives reported using well-being apps to cope with the crisis; 17% reported making use of timeout rooms; and only 1% used the online mental health forum, SilverCloud. Instead, staff reported wanting peer support and opportunities to meet and speak with each other and such support was gained virtually through WhatsApp or Facebook groups:232 ‘What has been shown to help healthcare staff is peer support; opportunities for staff to connect with each other and share experiences, talk to each other and be heard by those who understand as well as more formal one-to-one talking therapy support as needed in due course.’ (p. 5). 232 The PNA role is relatively new to nursing and has not yet been nationally evaluated, but local evaluation from the first cohorts of PNA’s has been overwhelmingly positive with many reporting how the training had helped them become more self-compassionate. 261 A key barrier is that the time for providing support to others is not protected or built into workforce budgets, and staff need to undertake these roles on top of their day job. 261
2b. Access to psychological well-being services was limited with no paid allocated time and a reluctance to access in time off: the lack of paid allocated time to access psychological well-being services was highlighted in one paper:259
many HCWs had to take time out of their busy work schedules to access this [psychological] support, which was nearly impossible for overburdened HCWs. A consultant anaesthetist expressed her concern about the impact of this on certain groups, ‘I was quite surprised that there wasn’t (psychological support) particularly for the high-risk groups, so the ITU nurses and all the ward staff who are being pushed into ITU, stretching their skills in a very upsetting environment, weren’t being given allocated time, even on a fortnightly basis, paid to be there to get this psychological input and support.
(p. 7)
2c. Provision of formal psychological support did not always reduce stigma and some staff felt the need to be stoic and conceal feelings: the pandemic highlighted the importance of well-functioning mental health service provision, yet existing stigma and under-resourced provision prior to the pandemic had undermined this. For example, in a qualitative study on staff emotional well-being,262 it was noted that while hospitals increased the provision of formal psychological support available to staff, some (study) participants perceived a paradox, with implicit institutional rules that they should be stoic and conceal feelings that would enable them access to this support:
They used to do this (traffic) light system, like ‘amber’ and ‘red’, for how you were feeling, and you were encouraged to put your hand up in front of a hundred people to say how you were feeling. I think the pressure was for everyone to be ‘green’ at the beginning of a shift. It’s the wider feeling right now, to feel either amber or red every day when you come to work. But no one was amber or red. In a hundred people. I found it very weird.
(p. 14)
2d. Some taboos broken around staff psychological ill-health enabling staff to prioritise their health and talk about their experiences: one important positive finding included the breaking of taboos around staff mental health challenges so that people could start talking about what they were experiencing. Informally, the pandemic has created new norms for discussing psychological health amongst teams and networks of professionals. For example, McFadden et al. 263 noted that the pandemic helped to start new conversations around mental health in the healthcare workforce precisely because the changes in circumstances caused by the pandemic were so substantial that previously stigmatising disclosures of ‘not being able to cope’ became so common-place that the fear of being stigmatised was lost. Maloney and colleagues247 writing in the USA, talk about the stoic narrative, seeing the pandemic as an opportunity to ‘replace the traditional and stoic EMS culture of “be in control, suck it up, and move on”’ (p. 1) and a chance to advocate for emergency professionals’ own health and reflect together on the work they do: ‘Needing help and reassurance from others is human. Advocating for our own health must be seen as an intrinsic part of our duties to ourselves—and to others. This is not a call for non-productive criticizing and complaining, but rather more reflecting and confiding’252 (p. 2).
Trepanier et al. 264 report being inspired by the idea of the need for ‘psychological PPE’ advocated by the Institute for Healthcare Improvement in the US. The model includes encouraging individuals to take a day off and create space between work and home life; avoid unnecessarily publicity and media coverage about COVID-19; receive mental health support during and after the crisis; facilitate opportunities to demonstrate gratitude and reframe negative experiences. It also offers actionable interventions for leaders such as limiting staff time on site; clear roles and leadership with visible leadership key; educating managers to be aware of key risk factors and monitor signs of distress; instituting a buddy system and offering peer support services. 264
2e. COVID-19 well-being guideline development placed greater emphasis on individual level than organisational level interventions: akin to Key finding 1 in our realist synthesis (see Chapter 6), the COVID-19 literature placed emphasis on individual secondary and tertiary interventions. For example: ‘Box breathing is just one of eight quick and easy interventions designed specifically out of concern for the mental health of front-line workers during the current pandemic’166 (p. 177). The literature we reviewed was replete with discussion papers and reviews summarising what was known and developing guidelines. These guidelines placed greater emphasis on well-being at an individual level, as did other papers,167 rather than actions that should/could be taken at an organisational level, with few providing recommendations for both levels. 242 Vindrola-Padros et al. 265 recognise the benefit of organisations remaining agile in providing psychological support in times of acute distress for staff, but also the importance of adapting to the needs of local contexts:
…we would argue that these (well-being) guidelines need to be developed without losing sight of the realities of HCWs working on the ground, where fatigue and work pressures might not allow them to visit group support meetings or make use of quiet rooms for relaxation.
(p. 6)
Some innovative interventions were adopted or adapted during the COVID pandemic: in terms of innovative practices, there were several noted in the literature, including three that provide multifocal level (primary, secondary and tertiary) support at the team and organisational wide levels (Code Lavender,266 Healer Education Assessment and Referral (HEAR)36 and NOCA:264
‘Code/Team Lavender’ is an example of a programme that existed pre-pandemic but was adopted by more organisations in the USA to support staff during the pandemic. 153,247 ‘Team Lavender’153 is a hospital team-based peer support psychological health intervention that includes an interdisciplinary group of healthcare professionals dedicated to supporting co-workers during time of stress and/or hardship…and ‘although it does not replace the services of an employee assistance programme or mental health and psychiatric counselling, the approach provides dedicated time and space for initial emotional peer support, offering team members a moment of pause, reflection, and teamwork’ (p. 16).
The programme reported by Maloney and colleagues247 has two key components: (1) a proactive team is alerted and performs follow-up with involved responders after tragic or exceptionally stressful incidents or responses; and (2) a continuous pan-agency emphasis on both individual and group wellness, both physical and mental well-being, creating that safe harbour. When alerted, Code Lavender team members determine if they need to meet staff in person immediately after an incident, or if following up by phone or text is reasonable. ‘Importantly, this follow-up process extends for several days, if not weeks, beyond the initial call’247 and access to other (tertiary) resources, including therapy and support from chaplains, for example, was facilitated.
Healer Education Assessment and Referral was originally developed as a suicide prevention programme for doctors, but expanded to nurses in 2016 and other health workers soon after, and recommended in one paper as a promising intervention to mitigate psychological ill-health in a ‘peripandemic world. ’36 HEAR is a multifocal (primary prevention as well as secondary and tertiary referral) including a comprehensive educational programme, proactive screening for high distress and suicide risk coupled with ‘warm’ referrals, crisis intervention and critical incident debriefing for clinical units and their individual providers under duress, a peer support programme as a first-line intervention, and Schwartz Center Rounds, to share and discuss social, emotional and ethical challenges of their work in a safe space. 36
‘No One Cares Alone’ is a system-wide caregiver support programme123 within which coaching and support is provided by licensed behavioural health providers (BHPs), targeting leaders and the teams experiencing the highest stress levels. ‘Leaders are paired up with BHPs who can help navigate various available resources and develop a plan in partnership with their caregivers’123 (p. 57). The programme aims to be proactive, removing barriers to engaging help and interventions are bespoke and tailored, ‘It starts with creating space for conversation and taking the time to listen’ (p. 58).
In the UK face-to-face Schwartz Rounds were adapted at speed in 2020, to online sessions I called ‘Team Time’. These online sessions were shorter, more focused on specific teams (not organisation wide as Schwartz Rounds) and included sharing of more recent experiences and stories. 267 Gardiner et al. 230 highlighted a new programme (called Here4HealthCare) developed by a mental health association in Canada for healthcare staff. Such new efforts may improve the delivery of specialist psychological resources into healthcare settings and build bridges between mental health and healthcare sectors. The authors state: ‘Our case study should serve as a call to action for the governments at all levels to play a larger role in uniting capacity of our mental healthcare system and crafting a coordinated response to the emerging mental health crisis.’ (p. 88).
Sustained, longer-term changes and interventions arising from the pandemic
The COVID literature we reviewed described how the exposure of inequities and staff psychological health challenges led to calls for longer-term positive change to workplace conditions for staff psychological well-being. 238,268
3a. The pandemic has shone an important spotlight on staff psychological wellness and the importance of primary prevention: the pandemic has also exposed the importance of understanding staff psychological well-being through a wider holistic lens rather than solely individualised perspective. 269 Indeed, the pandemic has provided more visibility for the upstream causes and the need for organisation-wide prevention interventions. Maben and Bridges181 note that the health and well-being of the nursing and midwifery workforce had previously been considered important but not always an absolute essential priority. The COVID-19 pandemic changed this, by shining a light on the critical significance of the psychological well-being of healthcare staff, particularly nurses working on the front line. The immense challenges and trauma that nurses, midwives and paramedics experience during their working lives was finally being recognised and acknowledged with the hope that ‘When health care is back to ‘normal,’ ongoing support for nurses’ well-being will remain critically important’181 (p. 7).
3b. On-going psychological health requires support and investment for sustainability:
several papers noted the need for long-term/continued provision of support. 230,247,260,268 There was concern expressed about supportive provisions being scaled back, whereas the need for psychological support would increase postpandemic:260
Staff had felt valued by their employer during the pandemic and wanted to retain this feeling (...). However, almost all staff interviewed had concerns about supportive provisions being reduced in the future when the pandemic subsides, and they used terms such as ‘slipping back’ and services ‘dropped off’ when ‘the NHS goes back to more normal operating standards’. Most staff alluded to the impacts of the pandemic on staff mental health as long-term and they were worried about the emergence of more serious psychological problems later down the line once the immediate threat of COVID had subsided: ‘there’s gonna be a lot of, delayed stress, guilt, mental health impact, because people have been in survival mode for crisis.’
(p. 10)
Maloney and colleagues247 concur, highlighting the reality that the effect of witnessing tragedy does not go away overnight. Long after the public stop applauding healthcare staff as heroes, there will still be those who suffer the negative impacts of what they witnessed. Maloney and colleagues speak also of the guilt that can accompany healthcare work, when patient outcomes are less than optimal (through no-ones ‘fault’): ‘Not only do all of us need to find better ways to acknowledge and “forgive” ourselves for the human feelings of guilt, fear, betrayal, defeat, and the moral- and morale-injuring moments we experience, we also need to do the same for others and encourage a culture of safe zones among colleagues as we journey together through our challenges, past, present and future.’247(p. 1)
Neil Greenberg268 similarly advocates for the importance of adequate post-pandemic mental health resources for staff and a realistic longer-term plan, writing
A poorly implemented post-COVID-19 plan, leading to seemingly false promises of support or of time to readjust to the new normal or managers making high work demands on staff who have been working ‘flat out’ has the potential to derail staff support efforts to date and to cause serious psychological harm. Put another way, the unwritten psychological contract between NHS staff, their managers, and the public, has been that staff members will give their all to save lives and in return the nation will give them the support, and time they need, to be able to recover.
(p. 1)
3c. The pandemic provided an opportunity to change professional norms and for staff to reclaim autonomy and power and speak up and raise concerns: several papers noted the positive changes caused by COVID-19. For example, stimulating innovation and cooperation: ‘the pandemic context seems to have stimulated a significant amount of innovation, and cooperation. For instance, the organization initiated more provision of clinical support, better information, communication and digitalisation, factors which may have created an environment for improved professional growth.’248 (p. 9). Eagen-Torkko et al. 270 reflected on the impact of the rapid implementation of pandemic-related policies without much evidence, stating that it provided an important moment for staff (midwives in this case) to voice concerns and be heard. They write
It is not enough to note the effects of the pandemic on midwives and patients with a restrained clinical eye. Instead, midwives are ethically obligated to speak up, and speak loudly, when these policies create additional or unintended harms. Identifying and giving voice to harmful policies or practices creates the opportunity to resolve moral distress, by directly addressing the tension between what one can do, and what one should do, and to reclaim the sense of autonomy and power that is often lost in trauma (…) raising one’s voice can promote positive change for health systems, patients, and themselves. The sweeping wave of new policy brought by COVID-19 has the potential for harm but also the opportunity to enact change, and midwives can be at the forefront of that change.
(p. 306)
Yet it was not always easy for staff to speak up and raise concerns and challenge policies. Adams et al. 271 writes ‘The COVID-19 crisis has laid bare the question for healthcare professionals over how—and to what effect—they can raise concerns for themselves and their patients’ (p. 1) yet ‘some have reported cases of workplace bullying, retaliation, or threats of disciplinary action when raising legitimate concerns’ (p. 1). Abrams et al. 199 also report nurses’ and midwives’ fear of repercussions when speaking up and of organisations ‘deaf’ to those who did raise concerns (see also Chapter 6).
3d. Intervention timing is important (in COVID-19) – meeting essential needs in the immediate crisis with access to psychological support required later: the COVID-19 literature draws attention to the importance of timing of interventions and temporality. Citing Maslow’s hierarchy of needs and relating this to immediate and then longer-term needs in relation to the pandemic several authors note the importance of the right intervention at the right time. Wong et al. 245 note
(Maslow) provides a hierarchic context for how individuals prioritize their needs, starting from the most fundamental (physiologic and safety) and progressing to more abstract and complex needs once more basic ones are met (love and belonging, esteem, and self-actualization). 245
(p. 382)
This thinking has been applied to the pandemic by Maben and colleagues, following research with nurses during COVID-19,232 writing ‘Staff in our study required very different support at different times. Thus, in the immediate crisis, staff needed their immediate basic physiological and safety needs to be met as per Maslow’s (1943) hierarchy of needs (…). Only when these were met, and the threat receded, could they begin to access psychological support to meet these needs’170 (p. 12). Supporting this, Williams et al. 256 provide guidance for supporting staff during COVID-29, using a phased approach to understanding the needs of staff and what might be required to support them.
3e. An increased sense of camaraderie and pulling together during the pandemic with calls for this to be harnessed to increase cooperation and collaboration going forward: Baldwin and George272 noted the increased sense of camaraderie seen across the front-line health professionals because of the pandemic, and how this could benefit staff longer-term:
The pandemic has created a special professional bond among the staff where they felt that they were fighting this war together. In the military, bonds between team members have been reported to build resilience among troops, which echoes the messages from the participants in this study. Health professionals working together across professional boundaries is a welcomed move which will hopefully continue beyond the COVID-19 pandemic, resulting in more collaborative working among nurses, doctors and allied health professionals.
(p. 9)
Appendix 4 Bibliographic database search strategies and results
Initial Database Search
Database: MEDLINE
Host: Ovid
Issue: 1946 to February 10, 2021
Date searched: 12/2/2021
Searcher: SB
Hits: 405 (nurses); 40 (midwives); 6 (paramedics)
Strategy:
-
(nurse or nurses or nursing).tw.
-
nursing/
-
exp specialties, nursing/
-
or/1-3
-
(midwif* or midwives).tw.
-
Midwifery/
-
5 or 6
-
paramedic*.tw.
-
Emergency Medical Technicians/
-
8 or 9
-
(‘mental health’ or ‘mental ill health’ or stress* or distress* or anxiety or anxious or depression or depressed or ‘wellbeing’ or wellbeing or resilienc*).tw.
-
(pressure* adj3 (work* or ‘patient* demand*’)).tw.
-
*Mental Health/
-
Stress, Psychological/
-
*Depression/
-
*Anxiety/
-
or/11-16
-
(retention or presenteeism or absenteeism or ‘sick leave’ or burnout or ‘burn* out’).tw.
-
Presenteeism/
-
*Absenteeism/
-
*Sick Leave/
-
or/18–21
-
exp United Kingdom/
-
(national health service* or nhs*).ti,ab,in.
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab.
-
(gb or ‘g.b.’ or britain* or (british* not ‘british columbia’) or uk or ‘u.k.’ or united kingdom* or (england* not ‘new england’) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or ‘south wales’) not ‘new south wales’) or welsh*).ti,ab,jw,in.
-
(bath or ‘bath’s’ or ((birmingham not alabama*) or (‘birmingham’s’ not alabama*) or bradford or ‘bradford’s’ or brighton or ‘brighton’s’ or bristol or ‘bristol’s’ or carlisle* or ‘carlisle’s’ or (cambridge not (massachusetts* or boston* or harvard*)) or (‘cambridge’s’ not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (‘canterbury’s’ not zealand*) or chelmsford or ‘chelmsford’s’ or chester or ‘chester’s’ or chichester or ‘chichester’s’ or coventry or ‘coventry’s’ or derby or ‘derby’s’ or (durham not (carolina* or nc)) or (‘durham’s’ not (carolina* or nc)) or ely or ‘ely’s’ or exeter or ‘exeter’s’ or gloucester or ‘gloucester’s’ or hereford or ‘hereford’s’ or hull or ‘hull’s’ or lancaster or ‘lancaster’s’ or leeds* or leicester or ‘leicester’s’ or (lincoln not nebraska*) or (‘lincoln’s’ not nebraska*) or (liverpool not (new south wales* or nsw)) or (‘liverpool’s’ not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (‘london’s’ not (ontario* or ont or toronto*)) or manchester or ‘manchester’s’ or (newcastle not (new south wales* or nsw)) or (‘newcastle’s’ not (new south wales* or nsw)) or norwich or ‘norwich’s’ or nottingham or ‘nottingham’s’ or oxford or ‘oxford’s’ or peterborough or ‘peterborough’s’ or plymouth or ‘plymouth’s’ or portsmouth or ‘portsmouth’s’ or preston or ‘preston’s’ or ripon or ‘ripon’s’ or salford or ‘salford’s’ or salisbury or ‘salisbury’s’ or sheffield or ‘sheffield’s’ or southampton or ‘southampton’s’ or st albans or stoke or ‘stoke’s’ or sunderland or ‘sunderland’s’ or truro or ‘truro’s’ or wakefield or ‘wakefield’s’ or wells or westminster or ‘westminster’s’ or winchester or ‘winchester’s’ or wolverhampton or ‘wolverhampton’s’ or (worcester not (massachusetts* or boston* or harvard*)) or (‘worcester’s’ not (massachusetts* or boston* or harvard*)) or (york not (‘new york*’ or ny or ontario* or ont or toronto*)) or (‘york’s’ not (‘new york*’ or ny or ontario* or ont or toronto*))))).ti,ab,in.
-
(bangor or ‘bangor’s’ or cardiff or ‘cardiff’s’ or newport or ‘newport’s’ or st asaph or ‘st asaph’s’ or st davids or swansea or ‘swansea’s’).ti,ab,in.
-
(aberdeen or ‘aberdeen’s’ or dundee or ‘dundee’s’ or edinburgh or ‘edinburgh’s’ or glasgow or ‘glasgow’s’ or inverness or (perth not australia*) or (‘perth’s’ not australia*) or stirling or ‘stirling’s’).ti,ab,in.
-
(armagh or ‘armagh’s’ or belfast or ‘belfast’s’ or lisburn or ‘lisburn’s’ or londonderry or ‘londonderry’s’ or derry or ‘derry’s’ or newry or ‘newry’s’).ti,ab,in.
-
or/23-30
-
(exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp asia/or exp australia/or exp oceania/) not (exp United Kingdom/or europe/)
-
31 not 32
-
4 and 17 and 22 and 33[Nursing literature]
-
7 and 17 and 22 and 33[Midwifery literature]
-
10 and 17 and 22 and 33[Paramedics literature]
Database: CINAHL
Host: EBSCO
Issue: n/a
Date searched: 12/2/2021
Searcher: SB
Hits: 844 (nurses); 60 (midwives); 16 (paramedics)
Strategy: Available on request from the authors.
Notes: EBSCO UK/Ireland geographic limit applied.
Database: HMIC
Host: Ovid
Issue: 1974 to January 2021
Date searched: 26/2/2021
Searcher: SB
Hits: 243 (nurses); 9 (midwives); 3 (paramedics)
Strategy: Available on request from the authors.
| Nurses | Midwives | Paramedics | |
|---|---|---|---|
| MEDLINE | 405 | 40 | 6 |
| CINAHL | 844 | 60 | 16 |
| HMIC | 243 | 9 | 3 |
| Total records | 1492 | 109 | 25 |
| Duplicate records | 188 | 21 | 2 |
| Unique records | 1304 | 88 | 23 |
| Profession | Papers selected through database search | Papers selected through key journals hand search | Papers included through expert input including empirical papers and reports |
|---|---|---|---|
| Nursing | 30 of 235 | 0 | 8 |
| Midwifery | 19 of 59 | 11 | 5 |
| Paramedics | 7 of 70 | 23 | 5 |
Revised paramedic search
Database: MEDLINE
Host: Ovid
Issue: 1946 to March 30, 2021
Date searched: 31 March 2021
Searcher: SB
Hits: 24
Strategy:
-
paramedic*.tw.
-
(emergency adj2 (attendant* or personnel or responder* or technician*)).tw.
-
(ems or emt).tw.
-
(prehospital or ‘pre hospital’).tw.
-
‘first responder*’.tw.
-
‘emergency services’.tw.
-
ambulance*.tw.
-
HEMS.tw.
-
‘field triage*’.tw.
-
‘out of hospital’.tw.
-
(‘trauma risk management’ or TRIM).tw.
-
Emergency Medical Technicians/
-
Emergency Medical Services/
-
Emergency Responders/
-
Ambulances/
-
Air Ambulances/
-
or/1-16
-
(‘mental health’ or ‘mental ill health’ or stress* or distress* or anxiety or anxious or depression or depressed or ‘wellbeing’ or wellbeing or resilienc*).tw.
-
(pressure* adj3 (work* or ‘patient* demand*’)).tw.
-
*Mental Health/
-
Stress, Psychological/
-
*Depression/
-
*Anxiety/
-
or/18-23
-
(retention or presenteeism or absenteeism or a ‘sick leave’ or burnout or ‘burn* out’).tw.
-
Presenteeism/
-
*Absenteeism/
-
*Sick Leave/
-
or/25-28
-
exp United Kingdom/
-
(national health service* or nhs*).ti,ab,in.
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab.
-
(gb or ‘g.b.’ or britain* or (british* not ‘british columbia’) or uk or ‘u.k.’ or united kingdom* or (england* not ‘new england’) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or ‘south wales’) not ‘new south wales’) or welsh*).ti,ab,jw,in.
-
(bath or ‘bath’s’ or ((birmingham not alabama*) or (‘birmingham’s’ not alabama*) or bradford or ‘bradford’s’ or brighton or ‘brighton’s’ or bristol or ‘bristol’s’ or carlisle* or ‘carlisle’s’ or (cambridge not (massachusetts* or boston* or harvard*)) or (‘cambridge’s’ not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (‘canterbury’s’ not zealand*) or chelmsford or ‘chelmsford’s’ or chester or ‘chester’s’ or chichester or ‘chichester’s’ or coventry or ‘coventry’s’ or derby or ‘derby’s’ or (durham not (carolina* or nc)) or (‘durham’s’ not (carolina* or nc)) or ely or ‘ely’s’ or exeter or ‘exeter’s’ or gloucester or ‘gloucester’s’ or hereford or ‘hereford’s’ or hull or ‘hull’s’ or lancaster or ‘lancaster’s’ or leeds* or leicester or ‘leicester’s’ or (lincoln not nebraska*) or (‘lincoln’s’ not nebraska*) or (liverpool not (new south wales* or nsw)) or (‘liverpool’s’ not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (‘london’s’ not (ontario* or ont or toronto*)) or manchester or ‘manchester’s’ or (newcastle not (new south wales* or nsw)) or (‘newcastle’s’ not (new south wales* or nsw)) or norwich or ‘norwich’s’ or nottingham or ‘nottingham’s’ or oxford or ‘oxford’s’ or peterborough or ‘peterborough’s’ or plymouth or ‘plymouth’s’ or portsmouth or ‘portsmouth’s’ or preston or ‘preston’s’ or ripon or ‘ripon’s’ or salford or ‘salford’s’ or salisbury or ‘salisbury’s’ or sheffield or ‘sheffield’s’ or southampton or ‘southampton’s’ or st albans or stoke or ‘stoke’s’ or sunderland or ‘sunderland’s’ or truro or ‘truro’s’ or wakefield or ‘wakefield’s’ or wells or westminster or ‘westminster’s’ or winchester or ‘winchester’s’ or wolverhampton or ‘wolverhampton’s’ or (worcester not (massachusetts* or boston* or harvard*)) or (‘worcester’s’ not (massachusetts* or boston* or harvard*)) or (york not (‘new york*’ or ny or ontario* or ont or toronto*)) or (‘york’s’ not (‘new york*’ or ny or ontario* or ont or toronto*))))).ti,ab,in.
-
(bangor or ‘bangor’s’ or cardiff or ‘cardiff’s’ or newport or ‘newport’s’ or st asaph or ‘st asaph’s’ or st davids or swansea or ‘swansea’s’).ti,ab,in.
-
(aberdeen or ‘aberdeen’s’ or dundee or ‘dundee’s’ or edinburgh or ‘edinburgh’s’ or glasgow or ‘glasgow’s’ or inverness or (perth not australia*) or (‘perth’s’ not australia*) or stirling or ‘stirling’s’).ti,ab,in.
-
(armagh or ‘armagh’s’ or belfast or ‘belfast’s’ or lisburn or ‘lisburn’s’ or londonderry or ‘londonderry’s’ or derry or ‘derry’s’ or newry or ‘newry’s’).ti,ab,in.
-
or/30-37
-
(exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp Asia/or exp australia/or exp oceania/) not (exp United Kingdom/or Europe/)
-
38 not 39
-
17 and 24 and 29 and 40
Database: CINAHL
Host: EBSCO
Issue: n/a
Date searched: 31 March 2021
Searcher: SB
Hits: 56
Strategy: Available on request from the authors.
Notes: EBSCO UK/Ireland geographic limit applied.
Database: HMIC
Host: Ovid
Issue: 1979 to January 2021
Date searched: 31 March 2021
Searcher: SB
Hits: 7
Strategy: Available on request from the authors.
| Database | Hits |
|---|---|
| MEDLINE | 24 |
| CINAHL | 56 |
| HMIC | 7 |
| Total records | 87 |
| Duplicate records | 8 |
| Unique records | 79 |
COVID search
Database: CINAHL
Host: EBSCO
Issue: n/a
Date searched: 7/12/2021
Searcher: SB
Hits: Nurses: 1355; midwives: 75; paramedics: 227
Strategy:
-
TI (nurse or nurses or nursing) OR AB (nurse or nurses or nursing)
-
(MH ‘Nurses+’)
-
S1 OR S2
-
TI (midwif* or midwives) OR AB (midwif* or midwives)
-
(MH ‘Midwifery+’)
-
S4 OR S5
-
TI paramedic* OR AB paramedic*
-
TI ((emergency N1 (attendant* or personnel or responder* or technician*))) OR AB ((emergency N1 (attendant* or personnel or responder* or technician*)))
-
TI (ems or emt) OR AB (ems or emt)
-
TI (prehospital or ‘pre hospital’) OR AB (prehospital or ‘pre hospital’)
-
TI ‘first responder*’ OR AB ‘first responder*’
-
TI ‘emergency services’ OR AB ‘emergency services’
-
TI ambulance* OR AB ambulance*
-
TI HEMS OR AB HEMS
-
TI ‘field triage*’ OR AB ‘field triage*’
-
TI ‘out of hospital’ OR AB ‘out of hospital’
-
TI ((‘trauma risk management’ or TRIM)) OR AB ((‘trauma risk management’ or TRIM))
-
(MH ‘Emergency Medical Technicians’)
-
(MH ‘Emergency Medical Services+’)
-
(MH ‘Ambulances’)
-
S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20
-
TI (‘mental health’ or ‘mental ill health’ or stress* or distress* or anxiety or anxious or depression or depressed or ‘wellbeing’ or wellbeing or resilienc*) OR AB (‘mental health’ or ‘mental ill health’ or stress* or distress* or anxiety or anxious or depression or depressed or ‘wellbeing’ or wellbeing or resilienc*)
-
TI (pressure* N2 (work* or ‘patient* demand*’)) OR AB (pressure* N2 (work* or ‘patient* demand*’))
-
(MM ‘Mental Health’)
-
(MH ‘Stress, Psychological’)
-
(MM ‘Depression’)
-
(MM ‘Anxiety’)
-
S22 OR S23 OR S24 OR S25 OR S26 OR S27
-
TI ((coronavirus* or coronovirus* or coronoravirus* or coronaravirus* or ‘corono virus*’ or ‘corona virus*’)) OR AB ((coronavirus* or coronovirus* or coronoravirus* or coronaravirus* or ‘corono virus*’ or ‘corona virus*’))
-
(MH ‘Coronavirus’)
-
(MH ‘Coronavirus Infections’)
-
TI ((‘COVID-19’ or ‘CORVID-19’ or ‘2019nCoV’ or ‘2019-nCoV’ or ‘WN-CoV’ or nCoV or ‘SARS-CoV-2’ or ‘HCoV-19’ or ‘novel coronavirus’)) OR AB ((‘COVID-19’ or ‘CORVID-19’ or ‘2019nCoV’ or ‘2019-nCoV’ or ‘WN-CoV’ or nCoV or ‘SARS-CoV-2’ or ‘HCoV-19’ or ‘novel coronavirus’))
-
(MH ‘COVID-19’)
-
(MH ‘SARS-CoV-2’)
-
(MH ‘COVID-19 Testing’)
-
(MH ‘COVID-19 Vaccines’)
-
S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36
-
S3 AND S28 AND S37 (Nurses)
-
S6 AND S28 AND S37 (Midwives)
-
S21 AND S28 AND S37 (Paramedics)
Database: MEDLINE ALL
Host: Ovid
Issue: 1946 to December 06, 2021
Date searched: 7/12/2021
Searcher: SB
Hits: nurses: 210; midwives: 15; paramedics: 55
Strategy:
-
(nurse or nurses or nursing).tw.
-
nursing/
-
exp specialties, nursing/
-
or/1-3
-
(midwif* or midwives).tw.
-
Midwifery/
-
5 or 6
-
paramedic*.tw.
-
(emergency adj2 (attendant* or personnel or responder* or technician*)).tw.
-
(ems or emt).tw.
-
(prehospital or ‘pre hospital’).tw.
-
‘first responder*’.tw.
-
‘emergency services’.tw.
-
ambulance*.tw.
-
HEMS.tw.
-
‘field triage*’.tw.
-
‘out of hospital’.tw.
-
(‘trauma risk management’ or TRIM).tw.
-
Emergency Medical Technicians/
-
Emergency Medical Services/
-
Emergency Responders/
-
Ambulances/
-
Air Ambulances/
-
or/8-23
-
(‘mental health’ or ‘mental ill health’ or stress* or distress* or anxiety or anxious or depression or depressed or ‘wellbeing’ or wellbeing or resilienc*).tw.
-
(pressure* adj3 (work* or ‘patient* demand*’)).tw.
-
‘emergency services’.tw.
-
*Mental Health/
-
Stress, Psychological/
-
*Depression/
-
*Anxiety/
-
or/25-30
-
(coronavirus* or coronovirus* or coronoravirus* or coronaravirus* or ‘corono virus*’ or ‘corona virus*’).tw.
-
Coronavirus/
-
Coronavirus Infections/
-
(‘COVID-19’ or ‘CORVID-19’ or ‘2019nCoV’ or ‘2019-nCoV’ or ‘WN-CoV’ or nCoV or ‘SARS-CoV-2’ or ‘HCoV-19’ or ‘novel coronavirus’).tw.
-
COVID-19/
-
SARS-CoV-2/
-
COVID-19 Serological Testing/
-
COVID-19 Nucleic Acid Testing/
-
COVID-19 Testing/
-
COVID-19 Vaccines/
-
or/33-42
-
exp United Kingdom/
-
(national health service* or nhs*).ti,ab,in.
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab.
-
(gb or ‘g.b.’ or britain* or (british* not ‘british columbia’) or uk or ‘u.k.’ or united kingdom* or (england* not ‘new england’) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or ‘south wales’) not ‘new south wales’) or welsh*).ti,ab,jw,in.
-
(bath or ‘bath’s’ or ((birmingham not alabama*) or (‘birmingham’s’ not alabama*) or bradford or ‘bradford’s’ or brighton or ‘brighton’s’ or bristol or ‘bristol’s’ or carlisle* or ‘carlisle’s’ or (cambridge not (massachusetts* or boston* or harvard*)) or (‘cambridge’s’ not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (‘canterbury’s’ not zealand*) or chelmsford or ‘chelmsford’s’ or chester or ‘chester’s’ or chichester or ‘chichester’s’ or coventry or ‘coventry’s’ or derby or ‘derby’s’ or (durham not (carolina* or nc)) or (‘durham’s’ not (carolina* or nc)) or ely or ‘ely’s’ or exeter or ‘exeter’s’ or gloucester or ‘gloucester’s’ or hereford or ‘hereford’s’ or hull or ‘hull’s’ or lancaster or ‘lancaster’s’ or leeds* or leicester or ‘leicester’s’ or (lincoln not nebraska*) or (‘lincoln’s’ not nebraska*) or (liverpool not (new south wales* or nsw)) or (‘liverpool’s’ not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (‘london’s’ not (ontario* or ont or toronto*)) or manchester or ‘manchester’s’ or (newcastle not (new south wales* or nsw)) or (‘newcastle’s’ not (new south wales* or nsw)) or norwich or ‘norwich’s’ or nottingham or ‘nottingham’s’ or oxford or ‘oxford’s’ or peterborough or ‘peterborough’s’ or plymouth or ‘plymouth’s’ or portsmouth or ‘portsmouth’s’ or preston or ‘preston’s’ or ripon or ‘ripon’s’ or salford or ‘salford’s’ or salisbury or ‘salisbury’s’ or sheffield or ‘sheffield’s’ or southampton or ‘southampton’s’ or st albans or stoke or ‘stoke’s’ or sunderland or ‘sunderland’s’ or truro or ‘truro’s’ or wakefield or ‘wakefield’s’ or wells or westminster or ‘westminster’s’ or winchester or ‘winchester’s’ or wolverhampton or ‘wolverhampton’s’ or (worcester not (massachusetts* or boston* or harvard*)) or (‘worcester’s’ not (massachusetts* or boston* or harvard*)) or (york not (‘new york*’ or ny or ontario* or ont or toronto*)) or (‘york’s’ not (‘new york*’ or ny or ontario* or ont or toronto*))))).ti,ab,in.
-
(bangor or ‘bangor’s’ or cardiff or ‘cardiff’s’ or newport or ‘newport’s’ or st asaph or ‘st asaph’s’ or st davids or swansea or ‘swansea’s’).ti,ab,in.
-
(aberdeen or ‘aberdeen’s’ or dundee or ‘dundee’s’ or edinburgh or ‘edinburgh’s’ or glasgow or ‘glasgow’s’ or inverness or (perth not australia*) or (‘perth’s’ not australia*) or stirling or ‘stirling’s’).ti,ab,in.
-
(armagh or ‘armagh’s’ or belfast or ‘belfast’s’ or lisburn or ‘lisburn’s’ or londonderry or ‘londonderry’s’ or derry or ‘derry’s’ or newry or ‘newry’s’).ti,ab,in.
-
or/44-51
-
(exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp asia/or exp australia/or exp oceania/) not (exp United Kingdom/or europe/)
-
52 not 53
-
4 and 32 and 43 and 54 (Nurses)
-
7 and 32 and 43 and 54 (Midwives)
-
24 and 32 and 43 and 54 (Paramedics)
Database: HMIC
Host: Ovid
Issue: 1979 to September 2021
Date searched: 7/12/2021
Searcher: SB
Hits: nurses: 3; midwives: 0; paramedics: 0
Strategy: as per MEDLINE without MeSH (available on request from author)
| Nurses | Midwives | Paramedics | |
|---|---|---|---|
| MEDLINE | 210 | 15 | 55 |
| CINAHLa | 1355 | 75 | 227 |
| HMIC | 3 | 0 | 0 |
| Total records | 1568 | 90 | 282 |
| Duplicate records | 63 | 5 | 9 |
| Unique records | 1505 | 85 | 273 |
Appendix 5 Sample of Excel spreadsheet
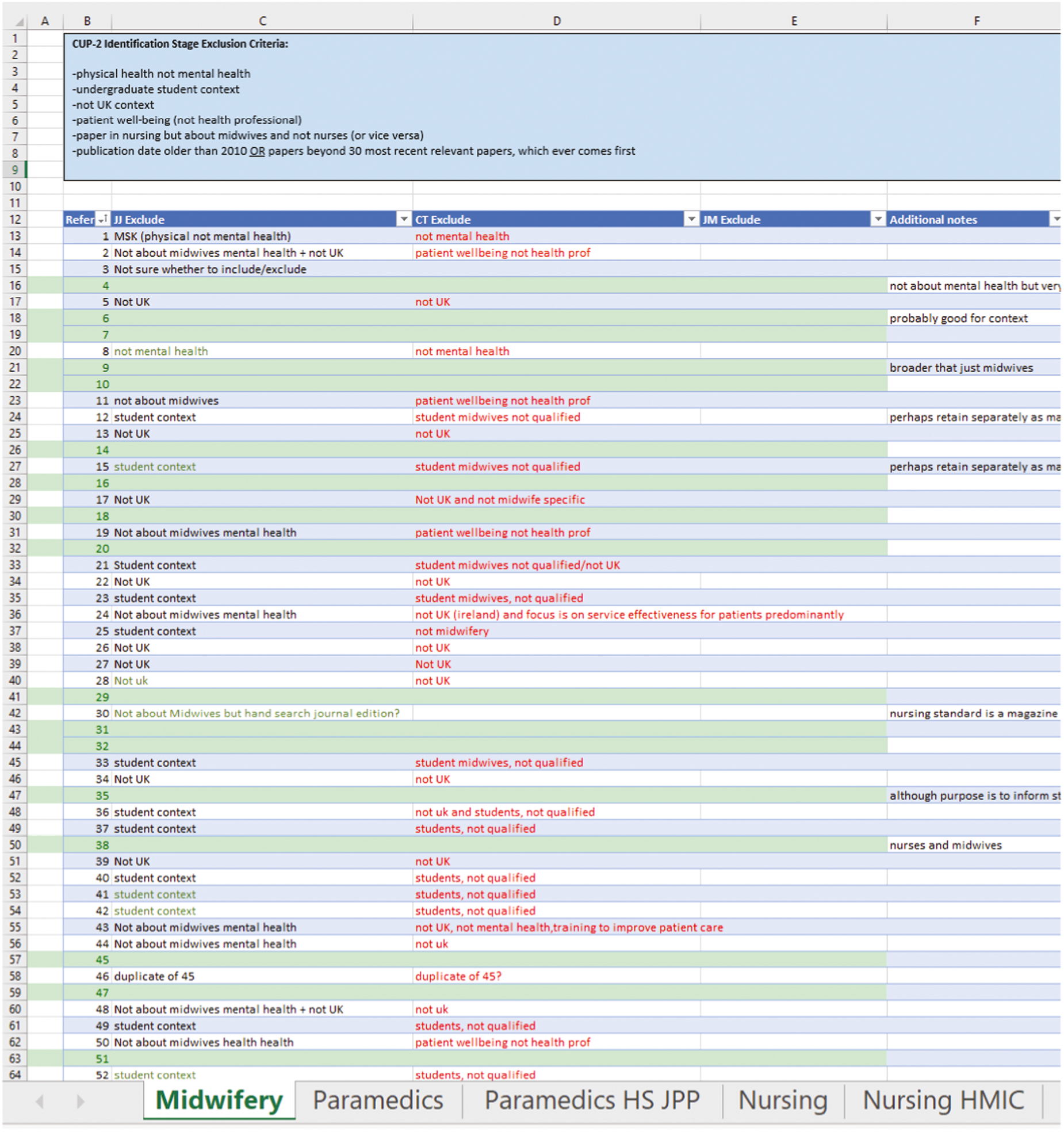
Appendix 6 Sample from appraisal journal
[20M-HS] How do power and hierarchy influence staff safety in maternity services?
Background: there are considerable tensions for healthcare staff between their employee allegiance and contracts, patient safety, and their responsibilities to codes of conduct within professional registration, and the NHS Constitution. Aims: the research aim was to identify how power and hierarchy influence staff safety in maternity services and this was achieved by reviewing research papers concerned with personal narratives of staff experiences and perspectives of employment in their profession. Methods: this systematic narrative review was based on the approach of a narrative synthesis, with papers coded using Nvivo software. Findings Power and hierarchy influence staff safety in maternity services by creating challenges to staff safety, which appear to essentially derive from poor communication. The workplace adversity described by participants seems to be linked with (1) psychological vulnerability, (1.1) anxiety about the job, and (1.2) dysfunctional relationships, alongside (2) working conditions (2.1) poor organisational and structural conditions (2.2) institutional normalisation of dysfunctional relationships and (2.3) interpersonal elements feeding into an obstructive culture. Conclusion: the negative influences of the cultural concepts of power and hierarchy on staff safety are significant within maternity services. Disconfirmation findings, those which stood out as different from the rest, evidenced the possibilities that healthy, psychologically safe working conditions could offer for healthcare staff in improving their prevailing culture.
This research paper took a systematic narrative approach to investigating how power and hierarchy influence staff safety in maternity wards. The findings are disturbing and in line with other findings from the maternity literature. (Karen: this also resonates with some of the medical literature, particularly with junior doctors that is when viewed from the bottom of the hierarchy Jill: and definitely nurses – we have signposted phrase of nurses eating their young!!). The review cites a very hostile environment for midwives, which is characterised by psychological vulnerability DC signposting that we discussed psychological safety. (Jill: yes Amy Edmondson work). This is fuelled by a lack of support by supervisors, cultural normalisation of dysfunctional relationships, poor working conditions, bullying, threats and lying. The research suggested that 80% of midwives who have left the profession said they would return if the working conditions improved (Jill: suspect v sim for N and P). It was interesting to note that bullying was experienced by frontline staff, both by superiors as well as clients: ‘so much is done to support the clients, that clients then believe they have the right to abuse staff (Cath: interesting that these are linked – that we provide good care and this leads to abuse?) so that generally staff felt unsupported from both managers and patients’ p. 434. This presents an important tension about the need for patient-centeredness, but the potential negative impacts of patient-centeredness on staff when there are staff shortages. (Karen: very interesting point, that patient-centeredness can be at the cost of staff well-being- Jill: yes indeed have written about this!) DC – I think the move from ‘triple’ to ‘quadruple aim’ (which I mentioned elsewhere in this journal – and if not see here Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. The Annals of Family Medicine. 2014 Nov 1;12(6):573-6) may be quite relevant to contextualise and discuss this tension. Jill: agree DC (Cath: agree and also the shift to consumerist language in health care in the last decades – setting expectations that cannot be met). The report cites cover-ups around bad births that are due to staff shortages and individual midwives are targeted as the cause. (Karen: individuals ‘paying’ for deficiencies in the system) ‘the abuses of both power and hierarchy are feeding into a system so much so that it has become commonplace institutional behaviour with staff left unsupported and yet still held accountable, threatening their safety on a professional register. This was powered by the terror of potential emergencies and poor outcomes during deliveries’ p. 435. The paper should be revisited (Jill: yes sounds v important and an important new tension) as there is a lot of information about the toxic work environment faced by midwives. DC this may link to ‘moral injury’ as well. (Jill: agree and we have a lot of data re this in current ICON study – impact of COVID on nurses (and midwives!) (Cath: there has been lots of publicity around things like this in doctors and other professions: that individuals are blamed when mistakes are made but actually those mistakes are due to organisational systemic issues – another tension to bring out? That you are accountable for the quality of care provided but have little/no power/authority to ensure appropriate resources, staffing, training, systems etc)
Appendix 7 Tables of included papers in the synthesis
| Citation | Type of paper | Paper focus: causes, interventions or both | Approach (if empirical) | Brief method (if empirical) |
|---|---|---|---|---|
| Chesterton et al.75 | Empirical | Both | Qualitative | Phenomenological design |
| Anderson144 | Empirical | Intervention | Quantitative | Pre/post-intervention evaluation |
| Andrews et al.84 | Empirical | Both | Qualitative | Constructivist grounded theory |
| Cedar and Walker96 | Commentary | Intervention | N/A | N/A |
| Higgins et al.102 | Empirical | Causes | Quantitative | Secondary analysis of a cross-sectional survey |
| Laker et al.85 | Empirical | Both | Quantitative | Random-effects models |
| Rodriguez Santana et al.92 | Empirical | Both | Quantitative | Causal analysis |
| Stacey et al.127 | Empirical | Intervention | Qualitative | Service evaluation |
| Whiting et al.110 | Empirical | Intervention | Mixed-methods | Appreciative inquiry (AI) approach |
| Younge et al.118 | Empirical | Intervention | Qualitative | Exploratory qualitative approach |
| Berry and Robertson145 | Empirical | Intervention | Quantitative | Cross-sectional design |
| Best81 | Commentary | Causes | N/A | N/A |
| Brett Bowen99 | Empirical | Causes | Qualitative | Interpretative phenomenological analysis (IPA) |
| Duncan97 | Commentary | Both | N/A | N/A |
| Dunlop and Maunder119 | Commentary | Intervention | N/A | N/A |
| Marran147 | CPD exercise | Both | N/A | N/A |
| Fasbender et al.88 | Empirical | Causes | Quantitative | Survey |
| Goddard et al.52 | Discussion article | Both | N/A | N/A |
| Laker et al.283 | Empirical | Causes | Quantitative | Randomised controlled trial (RCT) |
| O’Neill78 | Empirical | Intervention | Qualitative | Thematic analysis |
| Webster57 | Study protocol | Intervention | Qualitative | Qualitative design |
| Delaney164 | Empirical | Intervention | Mixed-methods | Observational pilot study (single group design) |
| Jackson73 | Empirical | Intervention | Qualitative | Service evaluation |
| Bosanquet87 | Editorial | Both | N/A | N/A |
| Sanford et al.284 | Empirical | Causes | Qualitative | Ethnography |
| Beryl et al.126 | Empirical | Intervention | Qualitative | Thematic analysis |
| Citation | Type of paper | Paper focus | Approach (if empirical) | Brief method (if empirical) |
|---|---|---|---|---|
| Rocca-Ihenacho et al.113 | Empirical | Intervention | Qualitative | Critical realist ethnography |
| Iaschi59 | Grey literature | Intervention | Mixed-methods | N/A |
| Cull et al.89 | Empirical | Causes | Qualitative | Thematic analysis |
| Hunter et al.128 | Empirical | Causes | Quantitative | Cross-sectional |
| Slade et al.103 | Empirical | Intervention | Quantitative | Feasibility study |
| Byrne151 | Commentary | Both | N/A | N/A |
| Warwick155 | Commentary | Both | N/A | N/A |
| Warriner et al.108 | Empirical | Intervention | Quantitative | Survey |
| Power214 | Commentary | Both | N/A | N/A |
| Sheen et al.100 | Empirical | Causes | Quantitative | Survey |
| Yoshida and Sandall76 | Empirical | Intervention | Quantitative | Survey |
| Clarke158 | Commentary | Intervention | N/A | N/A |
| Copp and Morton91 | Commentary | Intervention | N/A | N/A |
| Hollins Martin et al.58 | CPD exercise | Intervention | N/A | N/A |
| Winter120 | Commentary | Intervention | N/A | N/A |
| Axcell101 | Commentary | Both | N/A | N/A |
| Newman285 | Editorial | Causes | N/A | N/A |
| Barker156 | Commentary | Both | N/A | N/A |
| Barker168 | Commentary | Intervention | N/A | N/A |
| Anonymous blog116 | Commentary | Intervention | N/A | N/A |
| Pezaro et al.224 | Empirical | Intervention | Qualitative | PPI |
| Golden54 | Commentary | Intervention | N/A | N/A |
| Wain175 | Empirical | Intervention | Qualitative | Interpretive phenomenological analysis (IPA) |
| Barker148 | Commentary | Both | N/A | N/A |
| Leversidge157 | Commentary | Intervention | N/A | N/A |
| Brintworth286 | Empirical | Intervention | Mixed-methods | Online survey |
| Citation | Type of paper | Paper focus | Approach (if empirical) | Brief method (if empirical) |
|---|---|---|---|---|
| McDonald, Meckes104 | Empirical | Both | Quantitative | Online Survey |
| Treglown, Palaiou136 | Empirical | Causes | Quantitative | Online Survey |
| Wild, Smith287 | Empirical | Causes | Quantitative | Structured Clinical Interview |
| Mendes79 | Editorial | Intervention | N/A | N/A |
| Daubney169 | Commentary | Intervention | N/A | N/A |
| Smith229 | Commentary | Intervention | N/A | N/A |
| Mildenhall80 | Commentary | Both | N/A | N/A |
| Daubney33 | Commentary | Intervention | N/A | N/A |
| Mendes105 | Editorial | Intervention | N/A | N/A |
| Johnston109 | Commentary | Intervention | N/A | N/A |
| van der Gaag, Jago115 | Empirical | Intervention | Mixed-Methods | Mixed methods Design |
| Gilroy114 | Commentary | Intervention | N/A | N/A |
| Naumann, McLaughlin117 | Empirical | Causes | Mixed-Methods | Cross-sectional observation study |
| Peate121 | Commentary | Both | N/A | N/A |
| Sibson82 | Editorial | Both | N/A | N/A |
| Paranjape131 | Editorial | Both | N/A | N/A |
| Paranjape124 | Editorial | Both | N/A | N/A |
| Quaile95 | Commentary | Both | N/A | N/A |
| Miller55 | Conference Abstract | Causes | Mixed-methods | Online Survey |
| Miller56 | Conference Abstract | Intervention | Qualitative | Semi-structured Interviews |
| Rowe and Regehr53 | Discussion Paper | Intervention | N/A | N/A |
| Michael, Streb125 | Empirical | Causes | Quantitative | Postal Questionnaire |
| Maben, Hoinville149 | Empirical | Both | Qualitative | Semi-structured Interviews |
| Citation | Profession | Report type | Overview of contents | Causes/interventions/both |
|---|---|---|---|---|
| NHS Health Education England: NHS Staff and Learners’ Mental Wellbeing Commission9 | N,M,P | Commissioned report | Aim: Identify and review organisational good practice examples of NHS staff and learners’ mental well-being. Recommendations: 33 recommendations addressing NHS culture, staff well-being, NHS support to learners. |
Both |
| Royal College of Nursing: 10 unsustainable pressures on the health and care system in England209 | N,M,P | Report by Royal College of Nursing (RCN) | Context: The RCN has identified 10 areas reliant on nursing that demonstrate unsustainable, untenable conditions within the health and care system across England. Recommendation: Government must invest in core areas to sustain nursing workforce supply to meet the needs of the population now and in the future. |
Both |
| Hunter and Warren: Investigating Resilience in Midwifery34 | M | Funder report | Aim: Explore midwives understanding and experiences of resilience; model the concept in collaboration. Method: A two stage exploratory qualitative study. Key findings: Midwives described adverse workplace situations leading to resilience; practical coping strategies. |
Both |
| Hunter et al.: Work, Health and Emotional Lives of Midwives in the UK (UK WHELM Study)74 | M | Funder report | Aim: Explore relationship between work environment and emotional well-being of UK midwives. Method: The WHELM survey Key findings: UK’s midwifery workforce is experiencing significant levels of emotional distress. Recommendations: System level changes in resourcing and provision of maternity care are required. |
Both |
| West et al.: The courage of compassion: supporting nurses and midwives to deliver high-quality care30 | N,M | Commissioned report | Aim: Examine workplace stressors, organisational cultures, working contexts and leadership styles that impact on nurses and midwife’s mental well-being. Method: Literature review, secondary analysis of data, semi-structured interviews, focus groups. Recommendations: 8 key recommendations on working environment and contexts for nurses and midwives. |
Both |
| Kinman et al.: The mental health and well-being of nurses and midwives in the UK25 | N,M | Commissioned report | Aim: Review research related to the mental well-being of nurses and midwives working in the UK. Method: Systematic review of 100 studies from last 10 years; Delphi Study Findings: UK’s nurses and midwives are struggling with their mental well-being Recommendations: 45 recommendations with 8 highlighted as key priorities |
Both |
| Larrey Society: The ‘Ambulance Burnout’ Issue153 | P | Membership survey | Purpose: Canvass member views and the future direction of The Larrey Society Priority issues: Education and training, commissioning, burnout. Proposed actions: Organisations to implement Society’s 7-point code on Work-Life Balanced. |
Both |
| Citation | Profession: M,N,P subgroup) | Type of review | Aim of review | Causes/interventions/both | Number of papers included (UK) |
|---|---|---|---|---|---|
| Brand31 | Whole NHS | Systematic | Whole system approaches/interventions | Interventions | 11 (1) |
| Albendin-Garcia86 | M (all) | Systematic | Burnout: prevalence related factors | Causes | 27 (4) |
| Welford77 | M (all) | Narrative | Burnout: factors influencing | Both | 4 (0) |
| Bacchus90 | M (newly qualified) | Systematic | Factors affecting emotional well-being in newly qualified midwives | Both | 4 (2) |
| Hunter165 | M (all) | Critical interpretive synthesis | Evaluation of Mindfulness | Intervention | 5 (0) |
| Elliott-Mainwaring83 | M (all) | Systematic narrative | Impact of power and hierarchy on staff safety | Both | 10 (np) |
| Breseti106 | N (neonatal intensive care) | Systematic | Interventions to reduce occupational stress | Both | 6 (1) |
| Buckley93 | N (paediatric nurses) | Scoping | Burnout in paediatric nurses | Both | 78 (0) |
| Chamanga60 | N (community) | Integrative | Recruitment and retention of adult community nurses | Causes | 10 (1) |
| Freeling61 | N (all) | Integrative | Presenteeism | Causes | 17 (0) |
| Gribben130 | N (adult oncology) | Integrative | Burnout and work-life balance: factors contributing | Both | 20 (0) |
| McDermid23 | N (emergency nurses) | Thematic analysis | Factors contributing to turnover | Causes | 20 (0) |
| Oates111 | N (high secure forensic) | Integrative | Experiences and implications for recruitment/retention | Causes | 15 (6 UK) |
| Webster122 | N (all) | Scoping (Protocol) | Using technology for social and emotional well-being | Interventions | 0 (0) |
| Aryankhesal162 | N (all) – and physicians | Systematic | Interventions to reduce burnout | Interventions | 18 (2) |
| Hawkins123 | N (newly qualified) | Integrative | Exposure to negative workplace behaviour | Both | 16 (0) |
| Rajamohan152 | N (nursing home) | Integrative | Relationship between staff and job satisfaction, stress, turnover | Both | 11 (0) |
| Stacey32 | N (all) | Scoping | Influences of nurse resilience conceptualisation on educational interventions | Interventions | 16 (2) |
| Yu167 | N (all) | Systematic | Personal and work-related factors associated with resilience | Causes | 38 (np) |
| Cummings129 | N (all) | Systematic | Leadership styles and outcomes | Both | 129 (0) |
| Foster112 | N (mental health) | Scoping | Interventions to support coping with stressful work environments | Both | 18 (3) |
| Ejebu62 | N (all) | Scoping | Experiences and preferences about shift patterns | Causes | 30 (7) |
| Barleycorn98 | N (emergency nursing) | Narrative | Awareness of secondary traumatic stress | Both | 12 (np) |
| Dodd35 | P (ambulance service – all) | Methodical literature search | Post-traumatic stress disorder (PTSD) | Both | np |
| Anderson94 | P (all) | Systematic literature | Impact of shift work on family system | Both | 22 (np) |
| Lancaster107 | P (ambulance service – all) | Thematic analysis | Use of humour | Both | 4 (np) |
| Brooks21 | P (ambulance – all) | Systematic | Predictors of PTSD | Causes | 18 (np) |
| Clark22 | P (ambulance – all) | Evidence mapping methodology | Mapping well-being and Interventions for UK ambulance service staff | Both | 45 (45) |
| Auth18 | P (emergency service staff) | Qualitative evidence synthesis | Mental health and help seeking in trauma- exposed emergency service staff | Both | 24 (5) |
Appendix 8 Interventions in included documents
| Citation | Professional group N/M/P | Intervention(s) (description) | Target: primary/secondary/tertiary or multifocal | Formal/informal | Single/programme (or multiple interventions) |
|---|---|---|---|---|---|
| Anderson 144 |
N (critical care) |
Mindfulness-based stress reduction (MBSR) | Secondary | Formal | Single |
| Stacey 127 |
N (newly qualified) |
Resilience-based clinical supervision with compassion focused therapy (in addition to standard preceptorship) | Multifocal (primary and secondary) | Formal | Single |
| Whiting 110 |
N (children’s palliative care) |
CPD/Career Progression Programme for Children’s Palliative Care Nurses London (CHaL) comprising Mary Seacole Leadership and Action Learning Sets (ALSs) 6-month programme for senior nurses | Primary | Formal | Programme |
| Younge 118 |
N (inflammatory bowel CNSs) |
CBT-based clinical supervision for inflammatory bowel disease clinical nurse specialists | Multifocal (primary and secondary) | Formal | Single |
| O’Neill 78 |
N (liaison psychiatry) |
Psychologist-facilitated reflective practice groups (liaison psychiatry nurses) | Secondary | Formal | Single |
| Delaney 164 |
N (all/mixed) |
Mindful self-compassion training | Secondary | Formal | Single |
| Jackson 73 |
N (newly qualified) |
Facilitated peer support within preceptorship programme | Multifocal (primary and secondary) | Formal | Programme |
| Slade 103 |
M – all | POPPY (PTSD prevention training) for midwives | Multifocal (secondary and tertiary) | Formal | Programme |
| Warriner 108 |
M – all | Mindfulness training | Secondary | Formal | Single |
| Wain 175 |
M (newly qualified) |
Preceptorship programme | Multifocal (primary and secondary) | Formal | Programme |
| Citation | Professional group N/M/P | Intervention(s) (description), primary/secondary/tertiary/multifocal | Target: primary/secondary/tertiary/multifocal | Formal/informal/both | Number of interventions |
|---|---|---|---|---|---|
| Cedar 96 |
N (end of life) |
Primary: chaplaincy service; creating positive workplace culture; positive role models Secondary: exercise; hobbies/interest outside work; diet and nutrition; sleep; mindfulness; yoga/meditation Multifocal: Schwartz Rounds |
Multifocal | Both | 10 |
| Best 81 |
N (all) |
Primary: creating positive workplace culture, mentorship Secondary: mindfulness practice; talking with colleagues/peer support |
Multifocal | Both | 4 |
| Dunlop 119 |
N (children’s N in rural/remote community locations) |
Primary: community of practice clinical network | Primary | Formal | 1 |
| Bosanquet 87 |
N (all) |
Primary: Buurtzorg; creating positive workplace culture; Secondary: space and time to care for self/self-compassion; mindfulness practice; reflective practice; cultivate/encourage positive beliefs/coping; team culture/relationships with colleagues; access to safe confidential spaces. Tertiary: telephone support line Multifocal: clinical supervision |
Multifocal | Both | 10 |
| Byrne 151 |
M (all) |
Primary: leadership training | Primary | Informal | 1 |
| Warwick 155 |
M (all) |
Primary: safe staffing monitor and planning; remove pay cap/restraints; ensure student bursary remains | Primary | Formal | 3 |
| Clarke 158 |
M (all) |
Primary: social/professional networks and support Secondary: space/time to care for self; exercise; hobbies/interest outside work; diet/nutrition; breaks/holidays; self-care herbal remedies/massage; stress-management/coping; positive beliefs/coping; talking to family/friends; |
Multifocal | Informal | 10 |
| Copp 91 |
M (all) |
Secondary: stress-management training Tertiary: talking therapies; complementary therapies |
Multifocal | Formal | 3 |
| Winter 120 |
M (all) |
Primary: manager/employee training to recognise early signs Tertiary: CBT/ACT |
Multifocal | Both | 2 |
| Axcell 101 |
M (all) |
Primary: systemic approach to well-being Secondary: team culture/relationship with colleagues |
Multifocal | Informal | 2 |
| Barker 156 |
M (all) |
Primary: NHS acknowledge/take responsibility; Secondary: space/time to care for self/others; cultivate positive beliefs/coping; learn to say ‘no’/boundaries; talk with colleagues/peer support; Multifocal: clinical supervision |
Multifocal | Both | 6 |
| Barker 168 |
M (all) |
Secondary: Lego as art therapy | Secondary | Informal | 1 |
| Anonymous 116 |
M (all) |
Primary: mentorship Secondary: team culture/relationships with colleagues |
Multifocal | Both | 2 |
| Barker 148 |
M (all) |
Primary: leadership training; positive role models Multifocal: clinical supervision |
Multifocal | Both | 2 |
| Leversidge 157 |
M (all) |
Primary: RCN Caring for You campaign | Primary | Formal | 1 |
| Mendes 79 |
P (all) |
Primary: implicit bias training | Primary | Formal | 1 |
| Mendes 166 |
P (all) |
Secondary: NHS in Mind; Calm App; Headspace App; talking to family/friends Tertiary: telephone support line |
Multifocal | Both | 5 |
| Daubney 169 |
P (all) |
Secondary: humour | Secondary | Informal | 1 |
| Smith 229 |
P (all) |
Secondary: reflective practice | Secondary | Informal | 1 |
| Mildenhall 80 |
P (all) |
Secondary: debriefs; talking to family/friends | Secondary | Both | 2 |
| Daubney 33 |
P (all) |
Secondary: TRiM; humour | Secondary | Both | 2 |
| Mendes 105 |
P (all) |
Primary: Assault on Emergency Workers Bill; World Suicide Prevention Day Secondary: debriefs; exercise |
Multifocal | Both | 4 |
| Johnston 109 |
P (all) |
Tertiary: counselling; SWAST Staying Well Service | Tertiary | Formal | 2 |
| Gilroy 114 |
P (all) |
Primary: NHS England Healthy Workforce Framework; manager/employee training to recognise early signs; mental health awareness for family, friends, loved ones Secondary: Road to Mental Readiness Programme Tertiary: EMDR Multifocal: Blue Light Programme |
Multifocal | Both | 6 |
| Paranjape 131 |
P (all) |
Primary: public showing kindness and compassion | Primary | Informal | 1 |
| Paranjape 124 |
P (all) |
Secondary: reflective practice Tertiary: counselling |
Multifocal | Both | 2 |
| Peate 288 |
General workforce | Primary: World Mental Health Day | Primary | Formal | 1 |
| Sibson 289 |
Emergency care workforce | Primary: mentorship Secondary: debriefs; talking with colleagues/peer support Multifocal: clinical supervision; Blue Light Programme |
Multifocal | Both | 5 |
| Quaile 95 |
Ambulance staff | Primary: tackle retirement barriers. Secondary: talking with colleagues/peer support Tertiary: counselling Multifocal: Blue Light Programme; TASC |
Multifocal | Both | 5 |
| TOTALS |
Multifocal: 16
Primary: 7 Secondary: 5 Tertiary: 1 |
Formal: 7
Informal: 7 Both: 15 |
Range 1–10 (Mean 3.3) | ||
| Citation | Profession | Type of review | Focus of review | Intervention(s) (number of included papers), primary/secondary/multifocal | Target: primary/secondary/tertiary or multifocal |
Formal/informal/both | Evaluated or emergent finding? |
|---|---|---|---|---|---|---|---|
| Brand 31 |
Whole NHS | Systematic review | Whole systems approaches/interventions | Primary: implement Boorman whole system changes; collaborative care model; Secondary: mindfulness; exercise; diet/nutrition; Multifocal: NHS workplace well-being intervention; Workplace Social Capital Intervention |
Multifocal | Formal | Evaluation |
| Albendin-Garcia 86 |
M (all) |
Burnout: Prevalence related factors | Primary: caseload model; leadership (protective) | Primary | Formal | Emergent | |
| Welford 77 |
M (all) |
Burnout: factors influencing | Primary: caseload model; tackle retirement barriers; flexible working Multifocal: preceptorship |
Multifocal | Formal | Emergent | |
| Bacchus90 | M (newly qualified) |
Factors affecting emotional well-being in newly qualified midwives | Primary: mentorship; positive role models Multifocal: preceptorship |
Multifocal | Both | Emergent | |
| Hunter 165 |
M (all) |
Evaluation of Mindfulness | Secondary: mindfulness | Secondary | Formal | Evaluation | |
| Elliott-Mainwaring 83 |
M (all) |
Systematic narrative review | Impact of power and hierarchy on staff safety | Primary: mandate staff to challenge poor behaviour; introduce minimum standards for working conditions; rotas based on realistic forecasting; learning and education throughout career | Primary | Informal | Emergent |
| Bresesti 106 |
N (neonatal intensive care) |
Interventions to reduce occupational stress | Secondary: mindfulness, stress-management training, positive psychology training | Secondary | Formal | Evaluation | |
| Buckley 93 |
N (paediatric nurses) |
Scoping | Scoping review about burnout in paediatric nurses | Secondary: mindfulness; job/role specific workshops Multifocal: clinical supervision |
Multifocal | Formal | Emergent |
| Chanmanga 60 |
N (community) |
Recruitment and retention of adult community nurses | NONE | ||||
| Freeling 61 |
N (all) |
Presenteeism | NONE | ||||
| Gribben130 | N (adult oncology) |
Integrative review | Burnout and work-life balance: factors contributing | Primary: positive workplace culture; positive role models; Secondary: talking with colleagues/peer support; team culture/relationships with colleagues |
Multifocal | Informal | Emergent |
| McDermid 23 |
N (emergency nurses) |
Factors contributing to turnover | NONE | ||||
| Oates 111 |
N (high secure forensic) |
Integrative review | Experiences and implications for recruitment/retention | Primary: tackle retirement barriers; planned time out of setting Secondary: team culture/relationships with colleagues Multifocal: clinical supervision |
Multifocal | Both | Emergent |
| Webster 122 |
N (all) |
Scoping review | Using technology for social and emotional well-being | Secondary: mindfulness; stress-management training; positive psychology training | Secondary | Formal | Evaluation |
| Aryankhesal 162 |
N (all) – and physicians |
Systematic review | Interventions to reduce burnout | Secondary: mindfulness; positive psychology training; communication skill; professional identity development programme; job/role specific workshops; yoga/meditation | Secondary | Both | Evaluation |
| Hawkins 123 |
N (newly qualified) |
Integrative review | Exposure to negative workplace behaviour | Primary: zero tolerance policies; leadership training | Primary | Both | Emergent |
| Rajamohan 152 |
N (nursing home) |
Relationship between staff and job satisfaction, stress, turnover | Primary: caseload model (person centred care model) | Primary | Formal | Emergent | |
| Stacey 32 |
N (all) |
Scoping review | Nurse resilience conceptualisation | Primary: mentorship Secondary: resilience training; care provider support programme; yoga/meditation; stress-management techniques;talking to colleagues/peer support Tertiary: CBT/ACT; restorative supervision |
Multifocal | Both | Emergent |
| Yu 167 |
N (all) |
Systematic Review | Personal and work-related factors associated with resilience | Secondary: coping skills; social support | Secondary | Informal | Emergent |
| Cummings 129 |
N (all) |
Systematic review | Leadership styles and outcomes | Primary: leadership training | Primary | Informal | Emergent |
| Foster 112 |
N (mental health) |
Scoping review | Interventions to support coping with stressful work environments | Secondary: mindfulness; stress-management; resilience training; communication skills; Tertiary: CBT/ACT Multifocal: clinical supervision |
Multifocal | Formal | Evaluation |
| Ejebu 62 |
N (all) |
Scoping review | Experiences and preferences about shift patterns | NONE | |||
| Barleycorn 98 |
N (emergency nursing) |
Awareness of secondary traumatic stress | Primary: leadership training; manager/employee training to recognise early signs Secondary: exercise; diet/nutrition; sleep; learn to say no/boundaries; time-out/downtime; talking with colleagues/peer support |
Multifocal | Informal | Emergent | |
| Dodd 35 |
P (ambulance service – all) |
PTSD | Primary: chaplaincy service; manager/employee training to recognise early signs Secondary: TRiM; talking with colleagues/peer support; space/time for self-care Multifocal: Blue Light Programme; Beyond Blue |
Multifocal | Both | Emergent | |
| Anderson 94 |
P (all) |
Impact of shift work on family system | Primary: flexible working/plan own workload; mental health awareness for family/friends Multifocal: clinical supervision |
Multifocal | Both | Emergent | |
| Lancaster 107 |
P (ambulance service – all) |
Use of humour | Secondary: humour | Secondary | Informal | Emergent | |
| Brooks 21 |
P (ambulance – all) |
Predictors of PTSD | NONE | ||||
| Clark 22 |
P (ambulance – all) |
Interventions for UK ambulance service staff | Primary: mindfulness; humour; coaching; Tertiary: CBT/ACT; EMDR; complementary therapies Multifocal: Blue Light Programme; |
Multifocal | Formal | Evaluation | |
| Auth 18 |
P (emergency service staff) |
Qualitative evidence synthesis | Mental health and help seeking in trauma-exposed emergency service staff | Primary: regular work partner; Secondary: exercise; TRiM; humour; time out/downtime; talking to friends/family; talking with colleagues/peer support; managers checking in Tertiary: telephone support line Multifocal: Schwartz Rounds |
Multifocal | Both | Emergent |
Appendix 9 Mapping interventions to causes
| Risk factors for work-related stress (HSE Management Standards*) | Specific ‘cause’ | Interventions: formal | Interventions: informal |
|---|---|---|---|
| N/M/P causes | |||
| Demands (workload, work patterns, work environment) |
Staff shortages and high attrition | Primary
|
Primary
|
| Pressure of work in service in which demand continues to increase/unmanageable workload | Primary
|
Primary
|
|
| Working long shifts with no/few breaks | Secondary
|
Primary
|
|
Secondary
|
|||
| Inadequate work-life balance | Primary
|
|
|
| Serve and sacrifice | Multifocal
|
|
|
| Exposure to repeated episodes of trauma | Secondary
|
|
|
|
|
||
Secondary
|
|||
| Experiencing death |
|
|
|
| Prolonged/cumulative stress |
|
|
|
| Emotional labour | |||
| Profession-specific causes (potentially) | |||
| Working on-call | |||
| Lack of continuity of care | |||
| Unnecessary call-outs | |||
| Heavy cognitive load/rapid decisions | Secondary: stress-management | Secondary: stress-management | |
| High risk of sustaining injury | |||
| Being a profession under scrutiny | |||
| Control (how much say in the way you work) |
Lack of control/autonomy | Primary:
|
|
| Support (encouragement, sponsorship and resources provided by org, line managers and colleagues) |
Not feeling supported/valued |
|
|
| Stigma |
|
|
|
| Not having space/time to debrief after trauma or having inappropriate support |
|
|
|
| Not having basic ‘hygiene’ needs met |
|
|
|
| Profession-specific causes (potentially) | |||
| Lone working |
|
||
| Relationships (promoting positive working to avoid conflict; dealing with unacceptable behaviour) |
Poor relationships with colleagues/incivility/bullying | Primary
|
Primary
|
| Challenging relationships with patients, public, clients | Secondary
|
||
| Not feeling able to speak out |
|
||
| Profession-specific causes (potentially) | |||
| Fear of assault/abuse from public/patients | |||
| Role (clarity, not conflicting) |
Transition shock/Reality shock (newly qualified) |
|
|
| Values incongruence/theory-practice gap; moral distress | |||
| Unclear role boundaries/clarity |
|
||
| Role intensity |
|
||
| Change (organisational change management and communication) | Not being involved in change | ||
| Other risk factors | |||
| WHO? | Ageing population | Tackling retirement barriers | |
| Gender | |||
| Ethnicity | Zero tolerance; implicit bias training; EDI projects | ||
| Sexual orientation/gender identity | Zero tolerance; implicit bias training; Rainbow Badge and EDI projects. | ||
| Disability | Zero tolerance; implicit bias training | ||
| WORK CONDITIONS | Pay | Remove pay caps/restraints; ensure student bursary remains | |
| Promotion opportunities | |||
| ROLE/TYPE OF JOB | Newly qualified | Preceptorship programmes | |
| Leaders |
|
||
| Working in orphan specialties | |||
| Working with high-risk patient groups | |||
| WHEN | After trauma exposure | As per above exposure to trauma/death/cumulative stress POPPY |
As per above exposure to trauma/death/cumulative stress |
| When under investigation/during complaints |
Appendix 10 Practical proposed solutions co-developed with stakeholders and advisory group for further development into project guide
(To be aligned with the People Plan and the NHS Health and Wellbeing Framework)
-
Normalise and anticipate psychological ill-health (burnout/stress) as normal outcome of the job – on a continuum or spectrum not binary and requiring anticipatory planning, offer support, prioritise skills development:
-
At induction for all staff: support at individual, team, organisational levels for well-being (culture and expectations – ‘its difficult work and we’re here to help you with it’ messaging)
-
At key points: career decision-making and recognise need for ‘job-hopping’ and breaks from some clinical specialities
-
Start early: within undergraduate curriculum (consider introducing Schwartz Rounds/other safe spaces to process work challenges – also for newly qualified staff)
-
Normalising psychological health-checking-in with colleagues – how are you today?
-
-
Develop practical ‘how to do/implement interventions’ case study examples with others of well-being bundles; individual to organisational and prevention to treatment
-
Consider organisation psychological health credential quality mark re psychological health: signalling a good place to work re psychological wellbeing – for example, Magnet or NHS organisations pledge [like Blue Light Pledge (Mind, 2016)] to show commitment to tackle stigma and implement organisation wide interventions to support staff etc.
-
Industrial injury/risk – HSE approach to well-being: collect and report on health and well-being ‘near misses’ – develop thinking around this and consider how feasible to collect these and report on staff psychological well-being
-
Prioritise Maslow’s hierarchy of needs and Herzberg’s hygiene factors – hydrated, food, break rooms, parking, physical environment (no base, shifts and sleep?); salary/reward
-
Upside down Maslow – address the base of pyramid as strong foundations
-
Consider concierge for staff
-
Parking – reduced rates/disabled parking for staff not just patients
-
Access to good/hot food – nohungrystaff.com especially out of hours
-
-
Long-term organisational and individual plans to acknowledge and manage risk:
-
Individual level: design and implement all staff psychological health personal development plans to anticipate and prevent stress/burnout, but particularly
-
new starters (at all levels of seniority) and newly qualified staff
-
jobs with high risk of exposure to trauma
-
minority groups at risk of discrimination/exclusion
-
-
meaningful, ongoing and regularly revised (not tick box!)
-
Well-being conversations (People Plan)
-
Organisational level: multi-level systems approach needed – well-being bundles, modelling complexity (case studies and examples, guidelines)
-
Risk assessment for impact on well-being in same way as impact on equality, etc., impact of changes in one discipline/profession on another
-
Bringing staff from different professions together – for example, Schwartz Rounds; and networks for health and well-being leads within and across orgs to cover different professions/rotation of professions
-
Wellbeing Guardians to hold responsibility for plans with whole board (not just Guardians alone)
-
-
-
Leadership: identify and nurture future compassionate leaders and support in role: everyone is a leader – role modelling/senior leaders defining the culture
-
Organisational approach to talent spotting
-
Support
-
Role modelling job
-
Prioritising development of skills from student onwards/invest in trainees – long-term approach
-
-
Provide further information on the ‘informal’ and ‘promising’ interventions in the literature.
Glossary
- COVID-19
- A highly contagious respiratory disease caused by the SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus 2). The disease SARS-CoV-2 causes is called coronavirus disease 2019 (COVID-19).
- Context-mechanism-outcome configurations
- Relationships between the building blocks of realist analysis (i.e. how mechanisms are triggered under specific contexts to cause particular outcomes).
- Contexts
- Settings, structures, environments, conditions or circumstances that trigger behavioural and emotional responses (i.e. mechanisms) in those affected.
- Mechanisms
- The way in which individuals and groups respond to and reason about the resources, opportunities or challenges offered by a particular programme, intervention or process. Mechanisms are triggered in specific contexts and lead to changes in behaviour.
- Outcomes
- Impacts or behaviours resulting from the interaction between mechanisms and contexts.
- Programme theory
- A set of theoretical explanations or assumptions about how a particular programme, process or interventions is expected to work.
- Retroduction
- Identification of hidden causal forces that lie behind identified patterns or changes in those patterns.
- Retroductive
- The activity of uncovering underpinning mechanisms.
List of abbreviations
- A&E
- accident and emergency
- ACT
- acceptance and commitment therapy
- BME
- black, Asian and minority ethnic
- CBT
- cognitive–behavioural therapy
- CFIR
- consolidated framework for implementation research
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CISD
- critical incident stress debriefing
- CMOc
- context-mechanism-outcome configuration
- CPD
- continuous professional development
- CUP-1
- care under pressure 1
- CUP-2
- care under pressure 2
- EMDR
- counselling and eye movement desensitisation and reprocessing
- ENP
- emergency nurse practitioner
- HCPC
- health and care professions’ council
- HCW
- healthcare workers
- HEE
- Health Education England
- HMIC
- Health Management Information Consortium Database
- HR
- human resources
- HSE
- Health and Safety Executive
- LGBT+
- lesbian, gay, bisexual and transgender/transsexual people
- MEDLINE
- Medical Literature Analysis and Retrieval System Online Database
- MeSH
- medical subject heading
- NHS
- National Health Service
- NHSE/I
- NHS England and NHS Improvement
- NICE
- National Institute for Health and Care Excellence
- NMC
- Nursing and Midwifery Council
- OH
- occupational health
- PI
- principal investigator
- PPE
- personal and protective equipment
- PPIE
- patient and public involvement and engagement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analysess
- PTSD
- post-traumatic stress disorder
- RAMESES
- realist and meta-narrative evidence syntheses: evolving standards
- RCQ
- reverse chronology quota sampling
- SOM report
- Society of Occupational Medicine
- TRiM
- trauma risk management training
- UK
- United Kingdom
- WHELM report
- Work, Health and Emotional Lives of Midwives in the United Kingdom
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/TWDU4109).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
