Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR127709. The contractual start date was in September 2019. The final report began editorial review in October 2021 and was accepted for publication in June 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Clibbens et al. This work was produced by Clibbens et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Clibbens et al.
Chapter 1 Introduction
Background and rationale
Mental health crises cause significant disruption to the lives of individuals and their families and can be life-threatening. 1,2 The need for community crisis care is driven by international deinstitutionalisation of mental health care,3 whereby hospitalisation is a last resort and community services are available to respond to mental health need, including in times of crisis. 4 Crisis resolution services originated in the USA5,6 and Australia7 and were later implemented in the United Kingdom (UK)4 and some other countries in the rest of Europe. 8,9
Since the implementation of statutory crisis services in 2000,4 UK crisis services have seen the development of a proliferation of community-based services for people experiencing acute crises embodied in a complex range of service providers, service designs, referral routes and interventions. The voluntary sector has grown significantly in response to gaps in statutory crisis services,10 but this growth has contributed to the confusing array of care pathways, which can be difficult to access and navigate. 11,12 Evaluation study data suggest that too many people are unable to access timely crisis support and are dissatisfied with the help they receive. 12–14
Previous research in this field has, for the most part, focused on evaluating and developing the fidelity of NHS Crisis Resolution Teams (CRTs),15–17 scoping the range of crisis services available nationally (including alternatives to hospital admission)18,19 and understanding the role of the voluntary sector in crisis care. 10,20 This collage of evidence leaves substantial gaps in our understanding about how or why these different crisis services work for people in different circumstances.
A mental health crisis can be defined in different ways,10 including as a relapse in a psychiatric condition, characterised by increased symptom severity (such as voice-hearing, suicidal thoughts and risky behaviours) and decreases in social functioning (including reduced self-care). 21,22 Irrespective of psychiatric diagnoses, a mental health crisis can also be defined as a reaction to adverse life events, leading to increasing disruption for the person and their family whereby their usual coping strategies have failed. 23 Being in a state of crisis can also be conceived as an opportunity for change and may enable people to develop new ways of coping. 24
Mental health crises are serious, are sometimes life-threatening and are often associated with increased risks to the safety and well-being of the person or others. 11,25 The nature of a crisis varies between individuals and has a complex aetiology linked to factors including general health; life stresses; treatment adherence; coping skills; and social situation, including family, work, income, social support and housing. 9,22 This can result in a complex array of health problems related to mental, physical and social well-being that can, if people are unsupported, lead to catastrophic outcomes, such as suicide. 25 Social stigma and a lack of public awareness about mental health contribute to delays in contacting services because of fear of being coerced into treatment or negatively labelled,26 and may influence how and from whom people seek help in a crisis. The complexity of service structures and referral routes may also present a barrier, resulting in people failing to access the most appropriate or timely crisis care for their needs. 12
The Crisis Care Concordat27 was a national response in England to a need for urgent improvement in mental health crisis care. A key part of this strategy has been the development of local plans that bring together multiple agencies through local implementation that is co-ordinated nationally. The Crisis Care Concordat has influenced improvement in crisis services, including more people being seen quickly, more people reporting being taken seriously and fewer people describing their care as poor or having their first contact with the police. 28 Our review of the Crisis Care Concordat27 web pages (www.crisiscareconcordat.org.uk/) identified that the information-sharing component had not been active since 2016 and that many of the data contained there were of poor quality or incomplete. The Five Year Forward View for Mental Health,29 which followed the Crisis Care Concordat, sets out the broad mental health policy direction and highlights the importance of effective crisis services.
Crisis services across health, social care, local government and the voluntary sector are shaped by health priorities, including increasing community-based care that is close to home, available urgently 24/711,30 and situated in an appropriate safe place. 31 The involvement of people and their family members in decisions about crisis care2 and improved access for marginalised communities are also important. 11,30 Associated policy priorities include suicide prevention32 and reducing pressure in both hospital bed use and accident and emergency (A&E) attendances. 33
Mental health crisis care is delivered through two main commissioned care pathways: the acute mental health care pathway34 and the urgent care pathway. 35 In theory, CRTs play a central role in co-ordinating crisis care, often through a single point of access (SPA) service. 36 The function of CRTs has been summarised as follows:9
-
assess all patients being considered for acute psychiatric hospital admission and act as gatekeeper
-
initiate home treatment as an alternative to hospital admission until the crisis has been resolved
-
refer to other services for ongoing support
-
facilitate early discharge for those requiring a hospital admission.
In practice, implementation of CRTs appears to be highly variable. According to reports published between 2015 and 2018, less than half of CRTs in England provide 24/7 services,12 the number of referrals varies between 42 and 430 per 100,000 of the population across England,37 and some core CRT functions are inconsistently implemented. 11,38 CRTs have, however, been shown to reduce the cost of crisis care (although estimates vary between 17% and 30%39,40), and they work well for many people. 13,16 Despite this, areas where CRTs fall short of expectations include the lack of a consistent care worker; the timing, duration and frequency of visits; and the tendency for interventions to focus excessively on risks and medicine management. 41,42 A fundamental reason for this variability appears to be the lack of evidence for each of the specific interventions delivered by CRTs, or indeed consensus about what these, or any other crisis intervention, should comprise.
The voluntary sector has a long history of delivering crisis care services alongside statutory care and has gained recognition over the past decade as providing an alternative or an adjunct service, as well as occupying the gaps left by statutory services. 10 Voluntary sector crisis care was, initially, largely focused on providing alternatives to acute inpatient care;43 it has increasingly focused on community interventions such as crisis cafés, night-time drop-in services and services to improve access for marginalised communities. 44 Increasingly, community crisis care is jointly funded between local government, the NHS and voluntary sector organisations, as evidenced in the range of investment in crisis care via NHS non-recurrent funding. 45
Currently, in England, access to mental health crisis services is postcode dependent and a diverse array of different services are available, for example:
-
A&E departments
-
ambulance and paramedic services
-
crisis cafés
-
crisis drop-in services
-
crisis houses
-
CRTS
-
day treatment services
-
mental health liaison teams
-
NHS 111
-
NHS 999
-
out-of-hours teams
-
place of safety suites
-
police
-
specialist home treatment teams
-
street triage teams
-
telehealth
-
general practitioners (GPs).
It is unclear what each of these services offers (and how provision may vary in different contexts), or which mechanisms (such as safety, trust, community involvement) are most effective for whom and in which circumstances.
Study justification
Identified need
There is a drive in the UK to improve experiences of crisis care and to design services and interventions that are effective, timely and accessible to all those in need,30 including services that are able to respond with urgency that equals that of responses to physical health emergencies. 29 It is therefore vital to develop complex interventions from a theoretical understanding of the mechanisms that produce the desired outcomes and in which contexts these work best. The Crisis Care Concordat27 identified a need for crisis care to be developed across multiple agencies, including statutory and voluntary sectors; for crisis care to be largely community based; and for improved implementation across the UK, to avoid crisis care being postcode dependent. Attention has been focused on service providers and settings, but there is currently a lack of evidence about the mechanisms that underpin effective mental health crisis care and how these are activated to resolve crises across a range of contexts. A focus on underpinning theoretical development would enable commissioners to invest in a range of services designed to include the mechanisms that produce the best outcomes across service designs and providers.
Health services are under ongoing financial pressures, and inpatient care is not only undesirable in many cases, but is expensive37 and scarce. 33 Community-based crisis care presents an opportunity for cost-effectiveness, provided that interventions can successfully be developed, tested and implemented to enable improved prediction of outcomes. 46 The development of effective community crisis care may also help to alleviate pressure in the urgent care pathway, particularly in A&E departments.
Previous work
Prior to the commencement of the current study, the review group’s consultations with people who have accessed community crisis care [patient and public involvement (PPI)] showed that these services resemble a tangled web of overlapping services with complex referral routes and blurred functions. PPI participants endorsed a focus on community crisis services on the grounds that they are generally preferred; they provide the respite, information and support that people ask for; and they avoid the need to be away from home and family. These experiences echoed the published evidence in respect of mixed experiences of CRTs, and lent weight to the need to improve understanding of how services work to resolve crises. This could improve people’s ability to access the right care at the right time. 12
Aim
The aim of this study was to identify mechanisms to explain how, for whom and in what circumstances community crisis services for adults work to resolve crises, with a view to informing current and future intervention design and development.
Objectives
-
Use stakeholder expertise, current practice and research evidence to develop programme theories to explain how different crisis services work to produce the outcome of resolution of mental health crises.
-
Use a context, intervention, mechanism and outcome (CIMO) framework to construct a sampling frame to identify subsets of literature within which to test programme theories.
-
Iteratively consult with stakeholders via a series of consultations with an expert stakeholder group (ESG) and individual interviews with diverse stakeholders to test and refine programme theories.
-
Identify and create pen portraits of UK crisis services that provide exemplars of the programme theories to explain how mental health crisis interventions work to explore and explain contextual variation.
-
Synthesise, test and refine the programme theories, and, when possible, identify mid-range theory, to explain how crisis services work to produce the outcome of resolution of the crisis, and hence provide a framework for future empirical testing of theories in the pen portraits and for further intervention design and development.
-
Produce dissemination materials that communicate the most important mechanisms needed to trigger desired context-specific crisis care outcomes to inform current and future crisis care interventions and service designs.
Chapter 2 Review methodology and methods
Introduction to methodology and methods
This chapter outlines how the research team used stakeholder expertise, research evidence and current practice to develop programme theories to explain how, for whom and in what circumstances different community mental health crisis services for adults work to resolve crises. The chapter was developed as per the publication standards for Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES). 47 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline48 for reporting systematic reviews has been used to structure flow charts representing the process of identification and selection of included records.
Patient and public involvement and engagement
Prior to commencement of the study, members of the public, people with lived experience of crisis care, their carers and other stakeholders in statutory and voluntary sector services were consulted to help formulate the general aims and direction of the research. This was achieved through telephone consultations with key voluntary sector service managers, attendance at team meetings of CRTs and a focus group with people who had recently accessed crisis services for themselves or a family member. Visitors from two voluntary sector services involved in pre-protocol PPI consultation continued their involvement through membership of the ESG.
Ethics approval
Following favourable review by an NHS Research Ethics Committee, approval was granted on 8 January 2020 [Integrated Research Application System (IRAS) reference number: 261486; Research Ethics Committee reference number: 19/YH/0347]. Approvals were obtained for recruitment and consent of members to the ESG and individual interviews (see project web page: www.journalslibrary.nihr.ac.uk/hsdr/TWKK5110).
Study design and rationale
A four-phase realist evidence synthesis design was developed, comprising (1) identification of initial programme theories (IPTs); (2) iterative group and individual interviews to prioritise, test and refine programme theories; (3) focused reviews of prioritised IPT ; and (4) synthesis to mid-range theory. The focus of the realist synthesis was to develop programme theories to explain how different elements of crisis mental health care work provide appropriate and effective responses to mental health crises. Figure 1 summarises the study design.
FIGURE 1.
Summary of study design.

Realist synthesis
The synthesis design drew on realist expertise within the research team. Realist synthesis is a theory-driven approach for understanding existing diverse multiple sources of evidence relating to complex interventions. 47,49 A realist approach aims to understand the interaction between an intervention and its context, mechanisms and outcomes. 47 It draws on realist philosophical ideas to answer a generative causal question that, rather than asking ‘Does “A” lead to “B”?’, instead asks ‘What is it about “A” that results in “B” happening, for whom and in what circumstances?’,50 in other words, how the context (the situation around a person) affects any mechanism (the resources and human responses) to generate an outcome (intended or not). 47,51
How people respond to the resources offered by an intervention is conceptualised in realist syntheses as a ‘mechanism’. Realist programme theories are theories about what an intervention is expected to do and how it is expected to work. Realist synthesis uses both iterative and purposive sampling from a wide range of evidence to develop, refine and test theories about how an intervention works, for whom and in what circumstances. 52
Application of realist methods to explore complex interventions
The current study conceptualised crisis resolution services as heterogeneous, complex interventions, as defined by the Medical Research Council. 46 Complex interventions activate multiple human responses that interact in non-linear ways to produce highly context-dependent outcomes. 47 Realist review offers an optimal approach for exploring how and why complex programmes involving human actions and decisions, such as crisis mental health services, may or may not work, and to inform the theoretical development of intervention(s). 46,47
Theory testing
Outcomes of interventions are causally activated by multiple context-sensitive mechanisms. They happen not only because of what is done in an intervention, but also because of how people respond. 47,51,53 The realist approach offers a participatory method of synthesis that allows for, and indeed capitalises on, continual testing and refinement of emergent programme theories against empirical evidence, data from policy documents and primary data (e.g. from engagement with stakeholders). 49 The involvement of consumers of health care is central to this type of research. 54,55
A theory-driven approach strengthens the potential to inform commissioning, service design and delivery that are sensitive to context across diverse service designs and providers. 56 From the perspective of patients and the public, the theory testing provides a platform for future empirical testing of service designs, thereby improving access and experience of crisis care. This research aims to inform the ongoing development and evaluation of existing mental health community crisis services and interventions.
Programme and mid-range theories
Realist synthesis offers a lens through which a research team can make sense of what is occurring within a complex intervention, particularly in understanding the circumstances in which it is more or less likely to be effective through the identification and testing of programme theories. 47,49,57
‘Programme theory’ is conceived as a fairly concrete set of ideas and observations that explain how different elements of a specific intervention (or programme) interact to produce the intervention outcomes. In contrast, mid-range (or middle-range) theories represent intermediaries between programme theories and ‘all-inclusive speculations comprising a master conceptual scheme’. 56,58 Mid-range theory considers the theoretical and practical issues simultaneously, thus applying theory to practice. Mid-range theories are therefore useful frameworks to guide development of interventions and make generalisations about their application.
In the context of realist synthesis, these ‘minor working hypotheses’ are labelled ‘programme theories’ or explanations for how the programme or intervention works. Mid-range theories are often useful ‘as frameworks for understanding a problem or as guides to develop specific interventions’. 56 According to Pawson et al.,49 mid-range theories can be a product of the realist synthesis process. However, the world of health, social and behavioural research is so densely populated with mid-range theories that it is common to find confirmation of programme theory findings in existing mid-range theory. Although it has not yet proved possible to harvest these theories in a systematic way, realist synthesis harnesses theories identified via the expertise and knowledge of the review team and its experts, through theories referenced in included studies and through a body of theorisation published alongside included studies.
Study methods
Overview of methods
As realist research is essentially iterative,49 decisions about how to proceed are informed by emerging insights into how best to explore the research question. These methods do not readily fit with a linear narrative and so the following description of methods aims to provide a transparent and clear account of the study components, rather than a strict chronology.
A preliminary search of the literature sought to identify IPTs about how UK crisis interventions and crisis services work. Expert stakeholders were consulted to refine the IPTs and to agree research priorities and the scope for the review. These processes resulted in three prioritised IPTs and were the focus for three focused reviews. Consultation with the ESG and individual interviews facilitated further sense-making, theory testing and refinement. A final search was undertaken to synthesise the programme theory components with mid-range theory. Pen portraits were used to formulate exemplars of service user journeys through the system, to convey generative causal logic, to connect the theory components with real-world experiences of stakeholders and to explain how mental health community crisis interventions work. Figure 2 illustrates the study process, highlighting how the focus contracted and expanded throughout the review.
FIGURE 2.
The scope and focus across the life of the synthesis.

Changes to the study plan, including in the context of the COVID-19 pandemic
This research commenced in September 2019 and was largely conducted during the COVID-19 pandemic. The pandemic precipitated ongoing adjustments to the project milestones and timeline: delaying ethics approval, prolonging uncertainties about the feasibility of face-to-face meetings and interviews, limiting options for recruitment of participants, restricting access to practitioners and service users, challenging continued engagement of stakeholders and resulting in unexpected absences among the research team. Hence, these challenges were addressed in the context of national restrictions on accessing practice areas and delays in communication due to the reduced capacity of many organisations. For example, the ESG was established before the start of the government restrictions. They met face to face in February 2020. Subsequent delays, postponements or cancellations and a switch to video link may all have affected the ESG contribution.
The original plan to interview up to 50 experts in crisis care from across the UK was modified. After postponement of interview recruitment, it was planned to include 25 participants; finally, 19 participants were recruited to 20 interviews. In addition, issues related to gaining ethics approval during the COVID-19 pandemic restricted recruitment to three NHS health trusts and one NHS ambulance trust in England. The planned six pen portraits was reduced to three, linked to each of the three prioritised programme theories. The original plans to support the ESG members to produce a short animation to share the findings with a wide audience has not been achieved owing to delays earlier in the project delivery and funding limitations.
Focus of the review
The research team focused the review59 using the definitions of crisis stated in the Crisis Care Concordat,27 which highlights the architecture of crisis services, summarised as follows:
Access to support before crisis point . . .
Urgent and emergency access to crisis care . . .
Quality of treatment and care when in crisis . . .
Recovery and staying well . . ..
Crisis Care Concordat27
The review focused on ‘Urgent and emergency access to crisis care’ and ‘Quality of treatment and care when in crisis’, specifically on initial contact and access via the crisis aspect of services, thereby excluding home treatment and onward referral.
Expert stakeholder group engagement, recruitment and membership
Following ethics approval via IRAS/the Health Research Authority, expert stakeholders (n = 15) were recruited through NHS trusts, the voluntary sector and service user/carer networks. The ESG members included professional and user/carer expertise. Two research team members (JT and NC) maintained contact with two voluntary sector organisations following the pre-protocol PPI, which aided engagement and recruitment of those with lived experience to the ESG. Michael C Ashman led and co-ordinated the recruitment of all stakeholders and co-chaired the group with Jill Thompson.
The ESG membership comprised six people with lived experience of using crisis services, a carer, a peer support worker, a consultant psychiatrist, a mental health nurse, an NHS crisis service manager, a mental health social worker with approved mental health professional (AMHP) experience, a voluntary sector manager, a mental health services commissioner and a mental health policy specialist.
Membership of the ESG reflected diverse community crisis care services, recognising that no single individual or group holds all knowledge about crisis care. 60 All were based in England at the time of the consultation. Many participants described dual roles: the peer support worker had (of necessity) crisis service lived experience, but many others had acquired lived experience, either personally or through carer responsibilities. Membership of the ESG remained largely stable throughout the study, with the following exceptions: one service user dropped out, commissioner expertise was covered by two people, and a voluntary sector manager was replaced by their new manager. Table 1 charts the composition of the ESG.
| ESG rolea | Number of individuals |
|---|---|
| Carer | 1 |
| Commissioner | 2 |
| Consultant psychiatrist | 1 |
| Mental health nurse | 1 |
| Mental health policy specialist | 1 |
| Mental health social worker/AMHP | 1 |
| NHS crisis service manager | 1 |
| Peer support worker | 1 |
| Person with lived experience | Initially 6, reduced to 5 during course of project |
| Voluntary sector manager | 1 |
| Total number of individuals in ESG | 15 |
Expert stakeholder group consultations were held in February, September and December 2020 and April 2021. The first ESG meeting was face to face and was recorded through photographs and audio-recordings; subsequent meetings were via recorded video link.
The realist searches
The search followed the six principal procedures for a realist search61 (Box 1). Search strategy development was supported by expert guidance from an information specialist.
-
Formulate specific questions as lines of inquiry.
-
Ascertain previously published research, refining the research question as necessary.
-
Identify theories as hypothetical explanatory accounts of how an intervention works in order to identify programme theories.
-
Identify empirical evidence for context–mechanism–outcome configurations to test and refine the programme theories.
-
Respond to new information needs as they emerge during testing and refining of the IPT.
-
Explicit and transparent documentation of the search process.
Adapted from Booth et al. 61
Search for initial programme theories
The search for IPTs sought to find data to develop IPTs related to the architecture of crisis interventions and crisis services in the UK context. 61 During August and September 2019, an information specialist conducted the search using Google Scholar (Google Inc., Mountain View, CA, USA) (see Appendix 3 and Report Supplementary Material 1). 47 As programme theories may be located in the title, abstract and sections other than the results,62 the search strategy was designed to identify programme theories by screening full texts.
Eligibility criteria
Inclusions
Literature was included if it related to people aged ≥ 16 years accessing adult mental health services for a crisis related to mental health, relevant to the UK context. Reports from the European Union, the USA, Canada and Australasia, with similar structures and a shared history of development, were also considered relevant. Settings included health services, voluntary sector, social care and police crisis services based in community settings. Published articles, reports, theses and book chapters were considered eligible if they were published in the English language. No date limits were used for the theory scoping searches, but focused reviews included documents published between 2000 and 2021.
Exclusions
General hospital inpatient care and acute inpatient mental health care, including acute mental health wards, psychiatric intensive care and short-stay acute wards, were excluded. Literature related to crises without a mental health focus and crisis services specifically commissioned for children and young people aged <16 years was outside the study scope and not eligible. Records that did not contain relevant theory were not eligible.
Search terms: initial programme theory identification
The research team identified 25 relevant terms relating to setting (Box 2). Each setting was combined with a filter for identifying logic models together with terms related to mental health and crisis care. Logic models are representations of programme theory that include a focus on steps in the explanatory causal chain including inputs, processes, outputs and outcomes. 52
-
NHS 111.
-
NHS Direct (Wales).
-
24 hours.
-
Helpline.
-
Crisis line.
-
Accident & emergency (A&E).
-
Hospital.
-
999 (telephone number for emergency services in the UK).
-
GP.
-
Liaison psychiatry service.
-
Local on-call mental health services.
-
Social services.
-
Local Community Mental Health Team.
-
Crisis houses.
-
Crisis teams (CRHT).
-
Café.
-
Drop in.
-
Day services.
-
Day treatment.
-
Police.
-
Street triage.
-
Crisis resolution teams (CRTs).
-
Community.
-
Decision.
-
CRHT, Crisis Resolution and Home Treatment Team.
The first 50 results for each of the 30 systematic searches carried out in Google Scholar were reviewed. When at least one potentially relevant result was found, a further 50 records were scanned; summary search terms are shown in Appendix 3 and full search terms are in Report Supplementary Material 1.
Initial programme theory identification
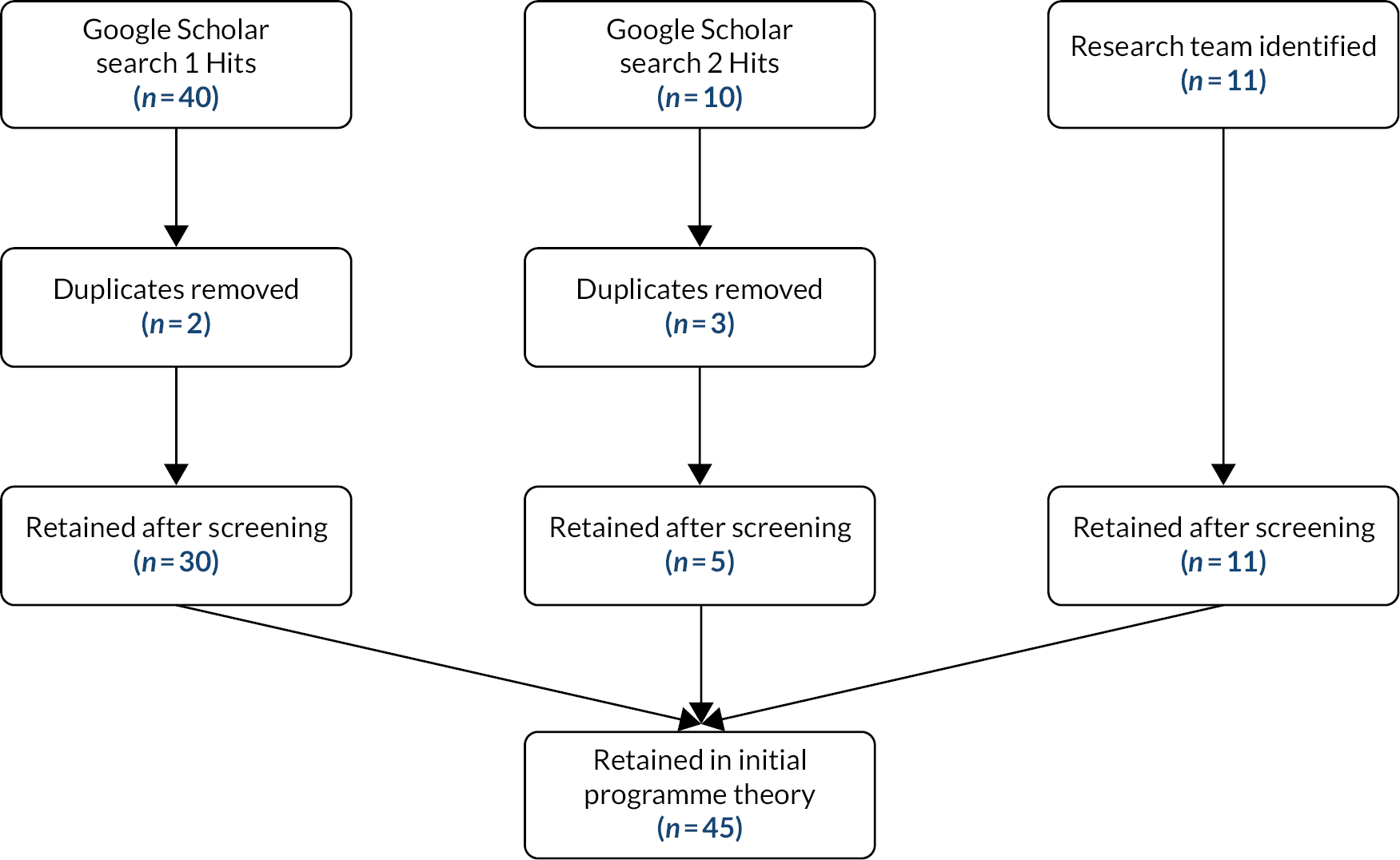
Selected records were used to construct a long list of IPTs. 61 All articles, reports, doctoral theses and book chapters identified by the information specialist (n = 55) were read in full by three researchers independently (KB, LS and NC). Disagreements were resolved through discussion and resulted in 10 records being excluded because they were out of the scope of the study (n = 5) or contained no relevant theory (n = 5). Data on CIMOs were extracted to a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet from 45 records (see Appendix 1). The results of the search for IPTs is shown in a flow chart in Figure 3. 48
FIGURE 3.
Results of search for IPTs.
Data extraction from 45 included documents to an Microsoft Excel spreadsheet (see Appendix 1) according to the CIMO framework resulted in a total of 247 incomplete lines of IPT. At this stage, not all aspects of the CIMO framework were complete in each line of theory. Members of the research team (NC, LS and KB) used a sense-making exercise to compare, contrast and synthesise the initial theories from the extracted data. The extraction and synthesis processes were supported by regular discussions with all members of the research team. Once the research team reached consensus on 11 embryonic IPT areas (see Box 3), these were discussed with the ESG.
-
A mature multi-agency approach and joint commissioning.
-
Urgency of response.
-
Compassionate care.
-
Involvement.
-
Access to crisis care and treatment.
-
Culturally relevant care and treatment.
-
Ability to meet the needs of vulnerable groups.
-
Service configuration.
-
Therapeutic intervention.
-
Sustaining professionals/staff.
-
Professional/staff skills and knowledge.
Involvement of the expert stakeholder group
The ESG worked in partnership with the research team to discuss, refine and test theories, and to prioritise topics for focused review. Subsequently, the ESG scrutinised the focused review outcomes and contributed to the overall synthesis. Four ESG consultation meetings took place. Engagement with stakeholders took place at key stages of the research to ensure that important, yet potentially hidden, subtle contextual conditions were not missed. 63
Expert stakeholder group involvement in agreeing on the focus and priorities
In the first meeting, held face to face in December 2019, ESG members were introduced to the project and methods, and were provided with information about taking part and the opportunity to ask questions before providing written consent. One lived experience participant declined involvement in the ESG, but requested to be invited to take part in an individual interview.
Expert stakeholder group members worked in small groups of mixed expertise to use their expertise to make sense of, debate and rank the importance of the 11 embryonic IPT areas (see Box 3). This was achieved using the Diamond-9 consensus and prioritisation approach, which encourages participants to work together, developing and exposing thinking. 64 A template used for the exercise is shown in Figure 4 and a photographic image of the ESG group deliberations shown in Figure 5. Each of the programme theory areas were printed onto individual cards along with blank cards to facilitate new ideas from the ESG deliberations. The stakeholders organised themselves into four groups so that they could prioritise, reject, or amalgamate any of the 11 embryonic programme theory areas using a card sort process. Each of the four groups included experts by lived and professional experience. Expert views and rankings were aggregated across the groups to generate overall agreement on refined and prioritised IPTs.
FIGURE 4.
Diamond-9 prioritisation template.
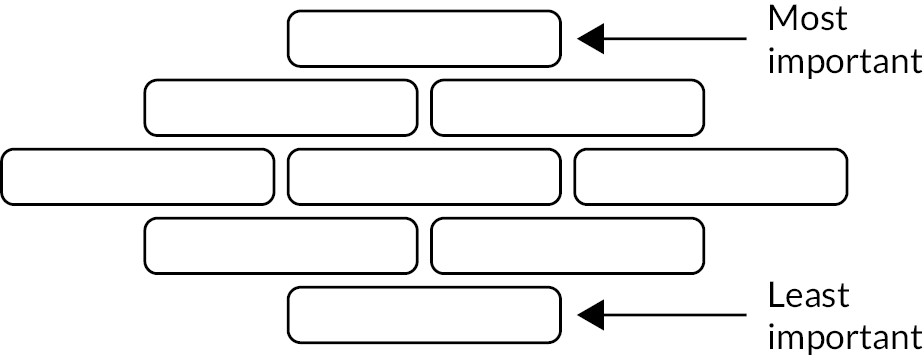
FIGURE 5.
Photograph of ESG members deliberating IPT using Diamond 9.
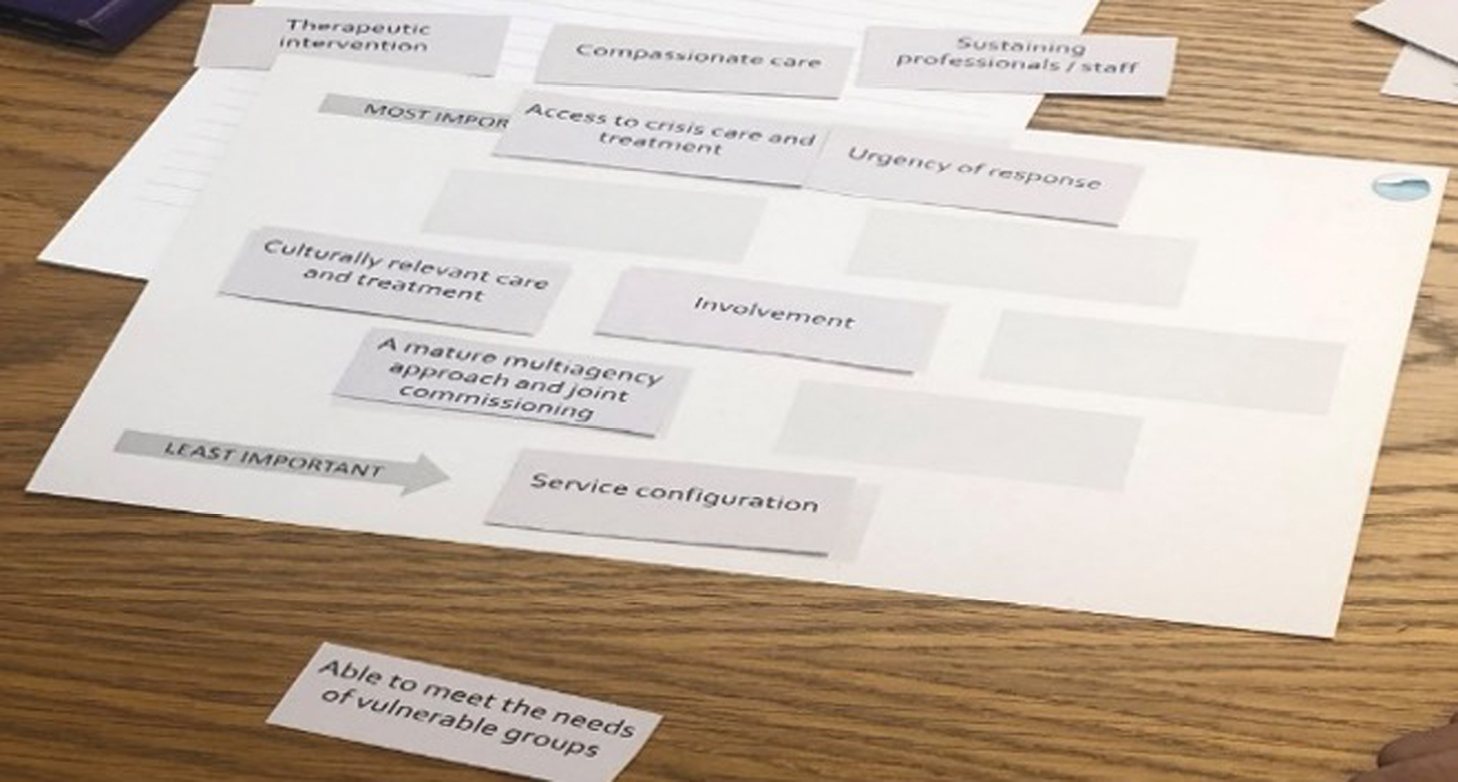
The results of the ESG discussions and Diamond-9 process showed that the most important priority for the ESG members was ‘urgency of response’. The pivotal role of urgency and easy access was highlighted by one ESG member:
. . . if that’s wrong, everything goes out of line because things aren’t happening at the right time with the right people.
The theories, ranked in descending order of importance following urgency of response, were compassionate care, access to crisis care and treatment, culturally relevant care and treatment, and involvement. Sustaining professionals/staff was identified as the least important.
The initial theories ‘service configuration’ and ‘mature multi-agency approach and joint commissioning’ were not prioritised by the ESG. However, after discussion between the research team and the ESG, the research team retained the ‘mature multi-agency approach and joint commissioning’, considering it integral to the architecture of crisis services and fundamental to the research focus. Through an iterative process of discussion and deliberation between the research team and ESG members, a reduced and refined set of five IPTs were agreed. These IPTs were developed from the data extracted and recorded in the Microsoft Excel spreadsheet (see Appendix 1). These are outlined as a narrative summary in Table 2.
| Context | Mechanism | Outcome |
|---|---|---|
| IPT 1: crisis services can be accessed urgently | ||
| When community crisis services are adequately resourced, work together across agencies, are known to people and are easy to access . . . | People are more satisfied with the service and are more motivated to engage . . . People believe that the service is ‘for them’ . . . |
Which results in people seeking help earlier in the crisis. People understand what is on offer and make informed choices about where to seek help. Expectations for timely support are met |
| Staff trust that they have the resources to respond | Staff use resources to provide timely responses according to need | |
| IPT 2: care in a crisis is compassionate and therapeutic | ||
| When community crisis services provide compassionate and therapeutic care that is non-judgemental, dignified and safe, and such care is provided by staff who have relevant therapeutic skills, knowledge and support . . . | People feel listened to and taken seriously, and trust staff . . . | Which results in reduced distress (and duration of distress) and in therapeutic engagement |
| Staff trust the organisation and their peers and believe that they have the skills and resources needed for compassionate care | Staff retain compassion, have confidence | |
| IPT 3: community crisis agencies work together | ||
| When community crisis services work effectively and seamlessly together across agencies and providers . . . | People have a sense of connection that prompts trust. People in crisis and the staff experience a sense of ownership and affiliation . . . Staff are prompted to have a wider systemic understanding and learn together . . . |
Which results in shared decision-making, improved communication between agencies, improved knowledge of services across the system Which results in reduced likelihood of traumatic repeat assessments Which results in transitions between services that are seamless and timely |
| IPT 4: community crisis services are culturally relevant | ||
| When community crisis services are culturally relevant, by employing people who share characteristics of the local population, and when they train staff in knowledge and appreciation of culture and ethnicity in relation to health and mental health . . . | People are less stigmatised and stereotyped, prompting trust and willingness to engage . . . | Which results in people seeking crisis support sooner and being less likely to require hospitalisation or involvement from the criminal justice services |
| Staff are confident, aware and sensitive to issues of culture and ethnicity | Staff have skills and knowledge that enable cultural sensitivity; they adapt interventions and refer appropriately across the crisis care system | |
| IPT 5: community crisis services are developed and delivered with involvement of service users | ||
| When there is meaningful involvement of people with lived experience of crises and their family and friends, that is recognised by those designing, leading and delivering services and is appropriately resourced . . . | People recognise the service as being for them; they trust services and believe that the service reflects their expectations . . . | Which results in increased engagement and community recognition and acceptance of the service |
| There is ownership and affiliation. Equalising of power is facilitated | People have an increased sense of personal control (agency) | |
Defining the scope for the focused review
Following the RAMESES guidance on defining and refining the study scope,47,53 the ESG and research team jointly discussed the scope of the review and the selection of IPTs for focused review. First, an overarching focus on the initial stages of a person in crisis seeking help and securing support and the quality of the support provided (key intervention points in the architecture of crisis services as identified in the Crisis Care Concordat27,28) was agreed. Although the term ‘multi-agency’ was initially adopted, it was replaced by ‘inter-agency’ in the course of the team discussions because of the perceived synergy between agencies that work together effectively in crisis care. The two terms can be interpreted as broadly synonymous. 65
Figure 6 illustrates the process used to refine the scope of the study and identify the IPTs for focused review: from 11 embryonic IPT areas (see Box 3) to five IPTs (see Table 2) and, finally, resulting in three IPTs retained for focused review. The deliberations between the ESG and the research team resulted in amalgamation of ‘urgency of response’ and ‘access to crisis care’ into IPT 1 (crisis services can be accessed urgently) as they were felt to be inherently linked. The ESG and research team also combined compassionate and therapeutic care into IPT 2: care in a crisis is compassionate and therapeutic. The third and final programme theory combined multi-agency working and joint commissioning, amalgamated to IPT 3: inter-agency working.
FIGURE 6.
Figurative illustration of the decision-making process to prioritise and refine the scope of the review.
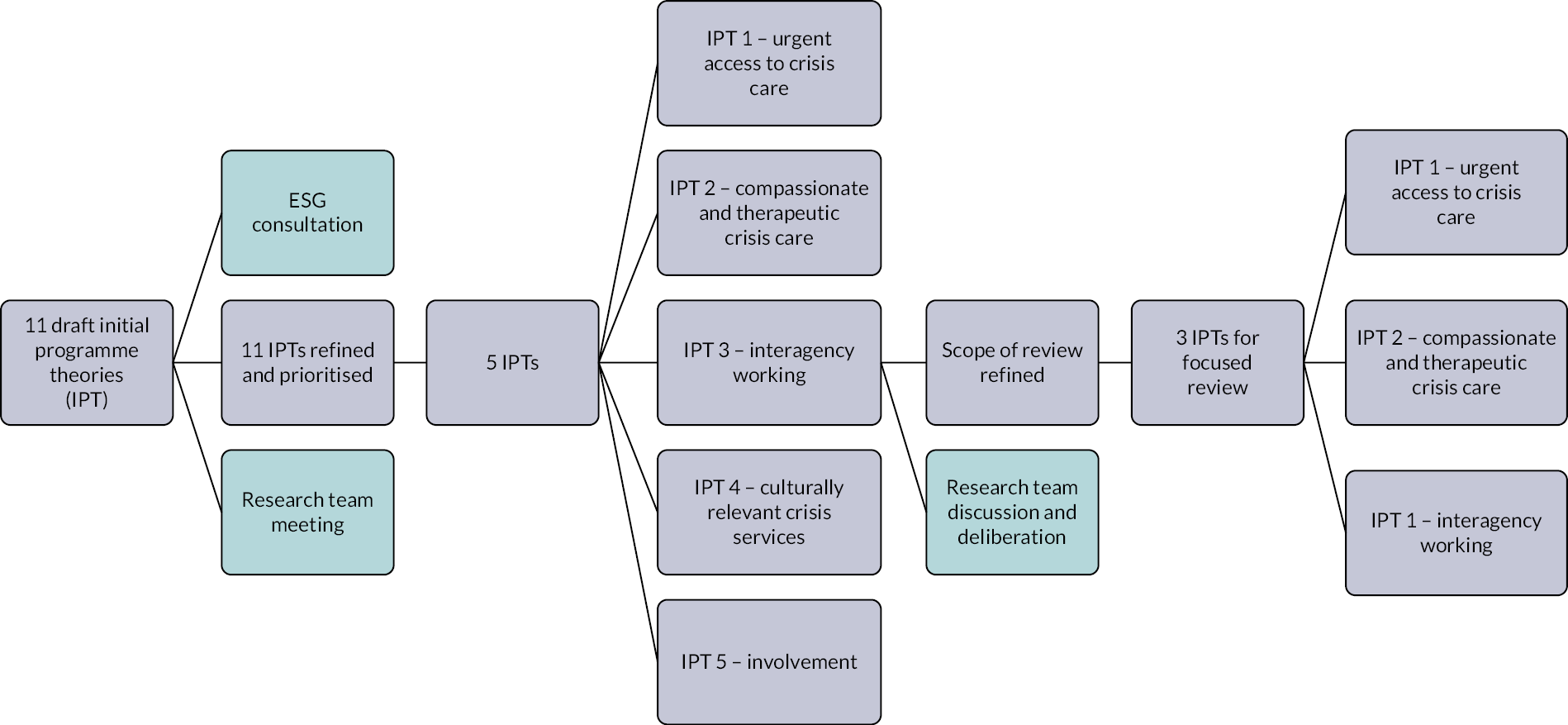
IPT 4, culturally relevant care (although highly relevant), was acknowledged to require consideration beyond the scope of the current study. Our initial searches revealed little published evidence focused on culturally relevant crisis care at a level that was sufficiently granular to provide adequate explanation. It was decided that IPT 4 would benefit from a future primary realist evaluation to generate new explanatory evidence. Data pertaining to cultural relevance, when identified as relevant to causal explanations, have been included in IPTs 1–3. IPT 5, involvement, was felt to be cross-cutting and has been reported when causally linked to concepts in focused reviews for IPTs 1–3.
Pen portraits
At the fourth and final ESG meeting, a pen portrait method was used to support theory development. Pen portraits offer an analytic method to focus large volumes of qualitative data while maintaining richness. 66 In ESG meetings, brief vignettes (see example in Report Supplementary Material 2) were used to structure discussions. These vignettes enabled the ESG members to use their expertise to relate the evidence from the included documents to real-world experiences. Discussions took a realist perspective that sought to explain and identify causal links.
Pen portraits were developed once the focused reviews were more fully developed, and provided an illustration from a real-world perspective of the causal link between mechanism and outcomes. They were constructed using synthesised data to map components of crisis interventions structured around the Template for Intervention Description and Replication (TIDieR)67 (see Box 10 and Appendix 2), together with context, mechanisms and outcomes, and to inform future empirical testing of the programme theory. The use of vignettes and pen portraits facilitated discussions with ESG members throughout the research, enabling theory to be presented to stakeholders in an accessible way, and to test and refine the understanding of CIMO in crisis services.
Rather than a description of any individual experience, the pen portraits provide examples of people experiencing crises, their circumstances and the crisis responses. Three pen portraits were developed (i.e. one drawn primarily from each focused review) to illustrate real-world examples of the theories in action; they were subsequently refined following ESG consultation and through the process of synthesis across focused reviews and mid-range theory. The draft pen portraits were discussed between research team members to ensure that the stories effectively linked to IPTs 1–3 (see Table 2) and interventions described in TIDieR Lite (see Box 10 and Appendix 2) before presenting them to ESG members. At the fourth and final online meeting between the ESG and the research team, ESG members were asked to sense-check three draft pen portraits, by moving between three subgroups. Discussions were recorded and reviewed by members of the research team (NC, KB and LS) and used to refine the pen portraits.
The discussions told us that the pen portraits were recognisable to ESG members, who endorsed them as exemplars of good crisis care. Some found them somewhat idealistic and were not convinced that the system could respond as the pen portraits described. Discussion of the final pen portrait versions is included in the three focused review chapters: Chapter 3, IPT 1 pen portrait: urgent and accessible crisis services; Chapter 4, IPT 2 pen portrait: compassionate and therapeutic crisis services; and Chapter 5, IPT 3 pen portrait: community crisis agencies work together.
At this final meeting, ESG members were invited to complete an ESG evaluation; the template for feedback and a summary of the evaluation results are in Report Supplementary Material 2, with a blog providing a personal account of participating in the ESG.
Testing and refining the initial programme theory via focused review
Focused searches were conducted to identify literature to test the IPTs61 between January and July 2020 by an information specialist (Ruth Wong). Iterative cluster searching was carried out by the researcher in each focused review up to March 2021 (NC, KB, LS). Included documents were published between 2000, when community crisis services were first mandated by the UK government,9 and March 2021.
Sources for empirical testing
Ten academic databases were searched: MEDLINE, EMBASE, Web of Science Core Collection (Science Citation Index, Social Sciences Citation Index, Conference Proceedings Citation Index – Science and Conference Proceedings Citation Index – Social Science & Humanities), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cumulative Index to Nursing and Allied Health Literature, PsycINFO, Applied Social Sciences Index and Abstracts (ASSIA), ProQuest Dissertations & Theses Abstracts and Indexes (A&I), and Health Management Information Consortium (HMIC).
Search strategies combined mental health keywords with keywords for crisis and keywords for each programme theory, together with a highly sensitive and published geographical UK filter,68 using the AND Boolean operator. The filter was applied to all database searches except ASSIA, ProQuest Dissertations & Thesis A&I and HMIC. All searches were restricted to English-language studies. The search results were managed using EndNote (X9 version 3.3) [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] (see Appendix 3 for a summary of search strategies and see Report Supplementary Material 1 for the full search strategies).
Theory-orientated searches
Theory-orientated, focused review searches were conducted from February to March 2020, with supplementary searches conducted in July 2020. The intention was to sample, rather than to identify an exhaustive body of literature. 69 A Google Custom Search (Google Inc.) was created to facilitate supplementary searching of grey literature sources across 32 UK websites (January–April 2020), with particular attention paid to NHS England publications, the Royal College of Psychiatrists and the Centre for Mental Health (see Appendix 3 for a summary of grey literature searches).
Cluster searching
The search strategy was developed iteratively and revisited at predetermined milestones, using different permutations and additional concepts. 69 As each focused review progressed, the lead author considered how each document contributed to the aims and objectives of the realist synthesis and to theory development. When relevant, lead authors deployed ‘cluster searching’, an innovative purposive sampling approach, to identify ‘clusters’ of related publications. This approach added to the conceptual richness and contextual thickness of the studies identified through topic-based searching. 69 Sibling (i.e. outputs directly linked to a single study) and kinship (i.e. papers sharing a common contextual/conceptual legacy) reports were sought to add richness while preserving rigour and relevance. 69 The research team pursued citation networks, using Google Scholar and Web of Science. The iterative approach enabled the research team to search for data beyond the literature particular to community crisis services, but also to test veracity in the context of UK community crisis interventions. The theory was continually tested and refined through expert consultation and individual interviews. The ESG also recommended records, based on its expertise. Searching continued until sufficient data were found (‘theoretical saturation’) to conclude that the programme theory components were coherent and plausible. 53,70
Screening
Retained records included primary research, reports, policy documents and expert opinion. Using EndNote (X9), retrieved records were screened for relevance by three members of the research team (LS, KB and NC). Full texts of the selected records were obtained and screened (see Figures 7–9). A list of the retained records from the searches for initial theory is provided in the Appendix 4.
Appraisal of relevance and rigour
A modified realist appraisal tool (Dr Justin Jagosh, director of the Centre for the Advancement of Realist Evaluation and Synthesis, visiting professor at the University of the West of England, Bristol, and a research fellow at the University of Surrey, personal communication, 2021) was used to appraise relevance and rigour across all the retained records (see Report Supplementary Material 3). Relevance was determined to be less substantial, medium or high. A document was considered highly relevant when the framing of the research and the research questions closely matched the review questions. Rigour was assessed by quality appraisal of the study methods, using the Mixed Methods Appraisal Tool (MMAT)71 (see Report Supplementary Material 3), in all documents where a methodology was available for assessment (J Jagosh, personal communication). 53
Data extraction
An analytical framework was created by the research team; the data extracted included the publication type, origin, type of service or intervention, and influencing factors (i.e. theoretical perspective). When it was possible to make inferences, the data extracted were attributed to context, mechanism or outcome. Data suggesting explanatory links between context and mechanism, between mechanism and outcome or between context and outcome were also extracted. Relevant data from the retained records were coded against the analytical framework (i.e. deductive coding) or by identifying new codes (i.e. inductive coding). 47,49,53 Data were extracted into a Microsoft Excel spreadsheet (see Appendix 1) and coded in NVivo version 12 (QSR International, Warrington, UK).
Individual realist interviews
The realist interviews were theory driven, and used conversation to explore participant views, with the specific aim of investigating ‘how, where when and why programmes are and are not effective’. 59 Ethics approval was obtained for individual interviews, as outlined in Study design and rationale (see project web page: www.journalslibrary.nihr.ac.uk/hsdr/TWKK5110).
Recruitment
Purposive strategies were used to identify mental health service users, carers and professionals from diverse organisations including the NHS, local authorities, universities and the voluntary sector. Expertise not represented in the research team or the ESG was prioritised. Representation was sought from urban and rural areas, as well as mental health trusts, ambulance trusts and the police force. Study information was distributed to potentially eligible participants, who could contact the research team if they wanted to participate.
Sample
Following revision of the size and scope of the sample frame, in view of the 2020 COVID-19 pandemic, study recruitment targeted an updated intended sample size of 25. The final sample comprised 20 interviews, with 19 expert interviewees (one participant took part in two interviews). Table 3 details the sample profile, along with the corresponding interviewee codes.
| Interviewee background | Interviewee context | Code | Participants (N = 19) (n) | |
|---|---|---|---|---|
| 1 | 2 (where relevant) | |||
| Academic | Voluntary sector | KB4 | 1 | |
| Ambulance emergency care assistant | Ambulance trust | LS3, LS4, LS5 | 3 | |
| Carer | Paramedic | Carer accessing crisis care and ambulance trust | NC3 | 1 |
| Manager | CRT manager | KB6, LS1 | 2 | |
| Mental health nurse | SPA, CRT, A&E liaison | LS2, LS6, NC1, NC2 | 3 | |
| Paramedic | Ambulance trust | KB2, NC4 | 2 | |
| Police | Street triage | KB1 | 1 | |
| Policy expert | Social worker | CMHT, AMHP | KB3 | 1 |
| Psychiatrist | CRT | KB5, LS7 | 2 | |
| Service user | Crisis services | JT1, JT2, JT3 | 3 | |
Strategy for realist interviews
A bank of semistructured interview questions, formulated in accordance with a realist interviewing approach,72 was agreed within the research team (see Report Supplementary Material 4). Interview participants were asked to comment on the evidence and on how thinking in the research team was developing. Participants were selected for interview based on their expertise in one or more programme theories. All interviewers had access to all interview questions and could opt for relevant questions as the interview progressed (see Report Supplementary Material 4).
Participants were invited to take part via Microsoft Teams (Microsoft Corporation), Zoom (Zoom Video Communications, San Jose, CA, USA)73 or telephone, and were provided with a participant information sheet and consent form in advance. Verbal consent was audio-recorded before the interview; interviews lasted up to 1 hour.
Four research team members conducted the interviews (NC, LS, KB and JT). Interviews were recorded and saved to a secure, password-locked server accessible by the research team. The interview recordings were reviewed, and detailed notes transcribed by each interviewer and shared with the research team. Following discussion between the research team members, a deductive coding process was used to connect interview data with the IPTs in the focused reviews. Interview data were used to test the veracity of the IPTs, particularly where there were gaps in the published evidence, but also to strengthen real-world understanding of the architecture of crisis services and causal links between context, mechanism and outcome. Excerpts from the interviews are reported throughout the focused review chapters in the form of discussion and direct quotations. After the completion of 20 interviews, it was agreed that there were sufficient data to inform the programme theories.
Data synthesis and theory refinement
Data from the focused review chapters, which included contributions from ESG and individual interviews, were synthesised to refine the programme theories. The synthesis enabled the team to identify important mechanisms that need to be ‘activated’ in a programme or intervention, together with links between the contexts and the key mechanisms. Synthesised context–mechanism–outcome (CMO) configurations are presented in table in Appendix 5. Confidence in the synthesised findings was assessed using the Grading of Recommendations Assessment, Development and Evaluation – Confidence in the Evidence from Reviews of Qualitative research (GRADE-CERQual). 74 GRADE-CERQual assesses confidence at the level of findings in four domains: (1) methodological, informed by the MMAT;71 (2) relevance, supported by realist appraisal (J Jagosh, personal communication); (3) coherence, the extent to which the finding is grounded in the data; and (4) adequacy, the degree of richness and quantity of data. 74 Discussion about the relationship between intervention strategies and their underpinning mechanisms is provided in Chapter 6.
Developing a mid-range theory
A final search was undertaken to link the three programme theories with mid-range theory. 61 Mid-range theories were identified relating to inter-agency collaboration,75,76 feeling in control,77 breaking point,78 a strengths perspective,79 compassionate care80,81 and protection motivation theory. 82
Evidence sources
Sources of evidence for the study are summarised in Table 4.
| Source | Use |
|---|---|
| Literature (academic; grey, including websites and reports) | Background search for logic models and candidate programme theories |
| ESG consultation | Selection of broad theory areas for focused review; theory testing |
| Literature (academic; grey, including websites and reports) | Focused reviews to test programme theories for urgency and accessible care, compassionate and therapeutic care, and inter-agency working |
| Individual interviews with experts | Theory testing |
Summary
This chapter provides the rationale for undertaking the realist synthesis, documenting the search for IPTs, the procedures for scoping the literature and identifying the IPTs, the search for empirical evidence, and the strategy for finalisation and synthesis of the programme theories. 61 It supplies additional detail on how the expert stakeholders contributed through the collection and analysis of primary data and the use of pen portraits to connect the theories to real-world stakeholder experience, facilitating the assessment of quality and rigour,61 following RAMESES publication standards47 (see Report Supplementary Material 5).
Structure of review chapters
Chapters 3–5 report the three focused reviews to test and refine IPTs 1–3 (see Table 2): IPT 1, crisis services can be accessed urgently; IPT 2, care in a crisis is compassionate and therapeutic; and IPT 3, community crisis agencies work together.
Chapters 3–5 are structured to follow the realist CMO convention. The context is reported first, followed by outcomes and unintended consequences, and, finally, mechanisms and conclusions. The IPTs are explained from three circumstances: the person in crisis and their family, front-line staff and the crisis care system. Each chapter concludes with an ‘if – then – leading to’ statement and a pen portrait to illustrate the IPT from a real-world perspective. Synthesis across the findings from IPTs 1–3 and mid-range theory is discussed in Chapter 6.
Chapter 3 Focused review for initial programme theory 1: crisis services can be accessed urgently
Introduction
This chapter examines the first of the three IPTs (i.e. crisis services can be accessed urgently), identified from the initial searches outlined in Chapter 2.
If crisis services are adequately resourced, work together across providers, are known to people and use shared decision-making, then there is satisfaction with crisis care that meets expectations for urgency, people believe in the service and there is trust, leading to people accessing urgent help that is timely and appropriate to their individual needs.
This chapter first describes the characteristics of urgent and accessible services, including interventions and intervention components identified in the literature to enhance their development and delivery. The evidence base for urgent and accessible services, the outcomes of urgent and accessible services and the unintended consequences when key components are not in place or are not effective are described. Next, the chapter describes the mechanisms for urgent and accessible services, demonstrating how they may be facilitated at different points within mental health community crisis care. A narrative drawn from the literature is supported by contributions from the ESG discussions and interviews. The chapter concludes with an overview of how urgent and accessible services can enhance mental health crisis care, using the ‘if – then – leading to’ convention.
Context: urgent and accessible crisis care
The theory component ‘urgent and accessible care’ was prioritised through discussion between the research team and the ESG. Feedback from one breakout group of ESG members emphasised the primary importance of urgent access:
Without urgent access to services in a mental health crisis, nothing else will work.
The National Institute for Health and Care Excellence (NICE), the National Collaborating Centre for Mental Health and NHS England35 define ‘emergency’ and ‘urgent’ situations as follows:
An emergency is an unexpected, time-critical situation that may threaten the life, long-term health or safety of an individual or others and requires an immediate response. An urgent situation is serious, and an individual may require timely advice, attention or treatment, but it is not immediately life threatening.
NICE, the National Collaborating Centre for Mental Health and NHS England. 35Contains public sector information licensed under the Open Government Licence v3.0.
Policy and published evidence state that crisis interventions should be ‘timely’ or ‘urgent’,35,83,84 yet this has been poorly defined in a mental health context. 83,84 The focus on waiting times excludes some agencies providing crisis care, contrary to the aspiration for multi-agency collaboration of the Crisis Care Concordat. 28,86 The risks to safety posed by a failure to respond in a timely way have driven the development of clinical decision tools. 86–88 Clinical approaches including decision tools are not, however, universally accepted by people using services or by all types of community crisis service. 10
Uncertainty as to what constitutes a mental health crisis, uncertainty as to the intervention required10,85,89,90 and the heterogeneity of the population seeking crisis support85,89 means that people access crisis services via a complex range of routes. 10,15,78,89,91–93 The route into crisis care is different for those known to mental health services than for people seeking crisis support for the first time. 89
Services have been developed to improve urgent access in a range of settings, including in A&E,94 with the police,92 with ambulance services95 and in voluntary organisations. 10 The UK government invested in the development of mental health crisis resolution services (i.e. CRTs) and a body of research has resulted in a service fidelity model. 16,17 There is a long history of telephone support in crisis services, and planned development of telehealth has been fast-tracked as a result of the COVID-19 pandemic. 84 Shared decision-making, information-sharing and skilled front-line staff have been identified in studies of stakeholder perspectives as indicators of good crisis services. 83,96 Inter-agency working is important to providing urgent access and has been identified as an IPT explored in detail in Chapter 5. Box 4 lists contextually important intervention strategies that facilitate urgent access to community crisis mental health care.
The evidence
Approach to identification of studies for review
Three iterative database searches were conducted: the first used search terms related to urgency and access, the second search used terms related to waiting and delay and the third focused on mental health triage. The results of these searches were combined. After exclusions on the grounds of relevance to IPT 1, urgent and accessible crisis care, 33 records were retained [13 from academic databases, five from grey literature (websites and reports) and 15 from hand-searching]. Backward citation searching of 18 records identified in database and grey literature searches produced a further 14 records, of which five were retained. In total, 38 records were included. The flow chart in Figure 7 shows the process of identification of studies for this review. 48
FIGURE 7.
Search results of the focused review: IPT 1, urgent and accessible crisis services.
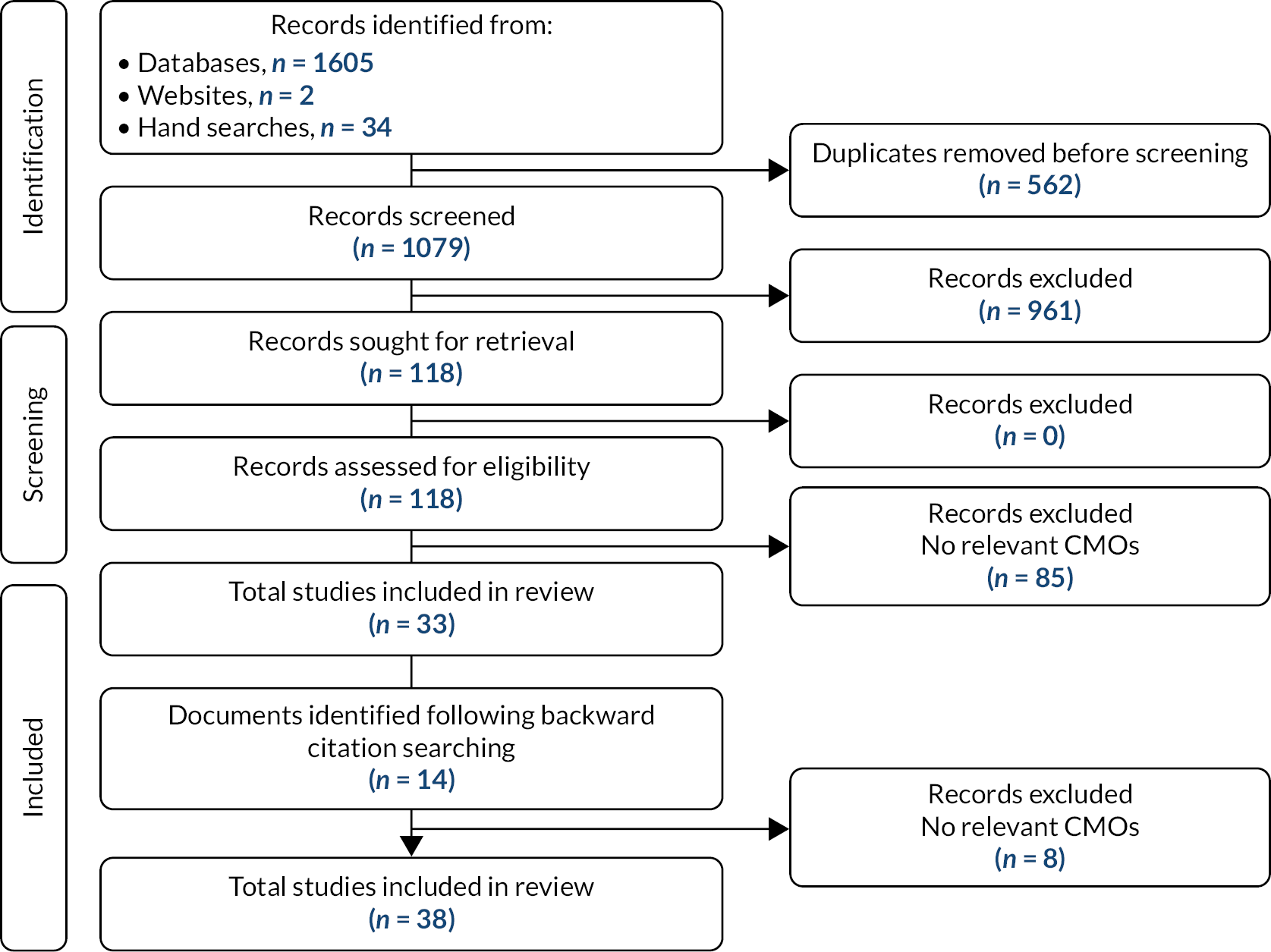
Retained records
Details of the 38 retained records for the urgency- and accessibility-focused review are provided in Appendix 4.
Settings
The research settings reported included all community mental health services,90,99,102,106,108–117 community crisis services,2,10,15,83,85,96–98,100 integrated services with the police,78,89,92 integrated services with paramedics,95 emergency departments93,94,103–105 and telehealth. 84,87,88,101,107
Focus
Included documents were focused on joint crisis planning,110–117 crisis response models,78,83,85,94,102 gatekeeping and referral processes,97,99,107 triage and decision-making,87,88,98,101,103 waiting times,103,105,106 service user perspectives of crisis services,2,10,15,78,96,100,104,109 carers’ experiences of mental health services,90 co-location models,78,89,95 interventions in rural areas,108,109 telehealth,84,87,88,107–109 experiences of black and minority ethnic groups accessing crisis services100 and the voluntary sector contribution to crisis services. 10 Companion documents containing findings from the same study focused on joint crisis planning112–114,117 and on telephone triage. 87,8
Appraisal of relevance and rigour
All included documents were appraised for relevance and richness using a modified realist appraisal tool (J Jagosh, personal communication) (see Report Supplementary Material 3). Documents containing primary research data were also appraised for rigour using the MMAT71 (see Report Supplementary Material 3). The combined appraisal of relevance and rigour identified that the evidence supporting IPT 1, urgent and accessible crisis services, is based on studies of mixed quality.
One mixed-methods multisite study of the voluntary sector contribution to crisis care was highly matched to the theory component, providing a rich description of context, mechanism and outcome. 10 This study was methodologically rigorous and highly relevant, and was included as a key document.
Included documents reporting randomised controlled trials (RCTs) were all focused on joint crisis plans (JCPs). 110,111,116,117 These studies provided context and outcome but provided less substantial theoretical relevance. One study of JCPs reported the economic data drawn from the RCT, but the small sample size and lack of quality-of-life measures limited the rigour of these findings. 110 All included RCTs reported methodological problems, including small sample sizes110 due to under-recruitment;111 a lack of reliability in the measures;116 and inadequate staff training, causing intervention implementation problems. 117
The included mixed-methods evaluations reported small samples, mostly limited to a single site; lacked comparators; and did not consistently synthesise across methods, but provided less substantial95,115 to moderate89,92,93,98,102 framing of context, mechanism and outcome.
The included qualitative studies were theoretically rich, despite problems of rigour related to small samples that lack variance. 78,88,104,112,113 Included qualitative studies with less substantial theoretical relevance were rigorous. 15,87,90,96,97,99,114 One qualitative study provided context, but lacked rigour. 108
A scoping review85 and a realist review91 provided less substantial relevance, and one systematic review provided moderate relevance, to the theory. 94 A case study design provided less substantial relevance and rigour, but was retained because of its specific focus on triage decisions. 101
Expert reports were not assessed for rigour. Appraisal of these documents for relevance found that documents moderately framed to the theory provided context and mechanism. 2,103 Documents with less substantial theoretical relevance provided context. 83,100,105 Three documents were retained because they provided specific contextual relevance from policy or services, but were less substantially relevant. 84,106,107
Outcomes
This section discusses outcomes relating to service users, staff and systems. Included studies often focused on service and organisational outcomes over outcomes at an individual level. The documents contained few outcome data, often based on studies with methodological limitations.
Service user outcomes
Urgency and timeliness of response
Service users want to be seen the same day. 15 From a service user perspective, rapid referral to a mental health intervention, a feature of CRTs,15 A&E liaison94 and NHS 111 services,107 is viewed as the most helpful feature of crisis services. 15 Rapid referral15,94 and co-response models such as street triage92 result in people reaching a mental health assessment more quickly, but may not improve urgent access to a mental health intervention. 10,94
Accessibility of crisis services
The timeliness of response of crisis services is linked to accessible service designs. An independent review of acute and crisis services concluded that people who experience a crisis are more willing to access crisis services in the future if they have a positive experience of initial access to crisis support. 2 Successfully navigating to appropriate crisis support led to people feeling believed and hopeful, which, in turn, enabled them to manage their distress. 104
When people lack information about mental health services83 or have physical health concerns, they are more likely to contact their GP78 or attend A&E. 91,93,102 Open access (including self-referral) is highly valued by service users and families15,98 and is a feature of voluntary sector services. 10 Open access to NHS crisis services is a policy aspiration;83,86,98 currently, open-access options are often available only to people already engaged in a mental health service. 89 Walk-in services, mostly available via A&E and some voluntary sector services, provide black men with an access route they prefer and are more likely to use,10 thus avoiding delays in seeking help because of stigma related to both racial stereotypes and mental ill health. 100
Service users valued co-response models providing joint assessments by mental health staff and other agencies such as police, ambulance staff or A&E staff, especially in situations where risk of violence or suicide were high. 78,92,95 Joint responses also helped avoid the stigma related to being taken into custody. 89 Although policy emphasises the need to provide services close to home, time away from the context of the crisis, in a community setting, allows some people to ‘take stock of the situation’10 and regain control of the crisis. 10,112
Accessibility of crisis care was linked to service users and family carers being involved in decisions through gatekeeping,97 the use of video-conferencing in rural areas109 and JCPs. 116 JCPs developed with the involvement of a patient advocate, when compared with those developed by clinical staff alone, were more comprehensively completed and specific about individual needs. 116 Shared decision-making facilitated by JCPs with people with personality disorder provided a greater sense of control and improved relationships with their care provider. 111 Despite RCTs findings that JCPs had no significant impact on treatment effects or cost, when compared with a control,110,117 a difference according to ethnicity was observed. This difference suggested a higher probability of cost-effectiveness with black (90%) service users than with white (30%) or Asian (10%) service users. 117 These findings suggest that JCPs may provide a sense of trust for black people, who often report experiencing higher levels of fear, stigma and marginalisation. 100,117
When people have personal resources, such as family support, they often seek support from them first (JT2, service user), but some people are concerned about being a burden to their family. 10 A less clinical approach, involving peer support, seems to act as a proxy for family and friends by providing support in comfortable environments and through an approach that:
. . . is not kind of saying ‘I’m making you better, it is my job to make you better’. There is something about ‘we’re in it together, you and I’.
Newbigging et al. 10
Access to peer support as part of joint crisis planning generated a sense of being understood. 113 In addition, people from black and minority ethnic communities reported that peer support enabled them to ‘learn about themselves and have a new perspective on their situation’. 10 This was linked to a distal outcome through their recognition of opportunities to volunteer, which gave meaning and hope. 10
Services were perceived as more approachable when front-line staff provide immediate interventions, including supportive counselling88 and active listening; this conveyed hope and encouragement, thus engendering a sense of relational safety. 10 Relational safety improved therapeutic relationships,110,117 thereby calming the crisis situation and enabling the person to deal with their crisis. 10,104 People with lived experience report that this leads to a distal outcome of being more likely to access the service again in the future. 2
Front-line staff outcomes
Urgency and timeliness of response
Outcomes related to the timing of crisis responses were highly theoretical. Front-line staff viewed urgency of response as important and linked this to response times stated in policies of between 1 and 24 hours, depending on assessed urgency of need. 15,86 Staff in CRTs value the role of gatekeepers, originally intended to reduce hospital admissions, but also viewed by staff as controlling workload by reducing inappropriate referrals,97 although their success in achieving these outcomes is unclear. Fears about being overwhelmed by referrals and about resource pressures made NHS front-line staff reticent about open-access service designs. 97
Accessibility of crisis services
Being able to access a crisis service required front-line staff to have skills to create a sense of trust and safety that facilitates the person being able to communicate their needs. 10 This was achieved when front-line staff had skills in supportive counselling that enabled them to be flexible and responsive to the individual needs of the person seeking help. 87 Compassionate staff were more collaborative, providing a sense of involvement that people in crisis value, thereby supporting the immediate stabilisation of the crisis,96,109 even by telephone. 88 A service user interviewee explained the important link between the interpersonal approach of staff and the development of trust:
Their approach is very person centred [and I have] more trust in that service. They might not be able to solve your problem, but sometimes it is just being able to speak to someone.
JT3, service user
Front-line staff deal with trauma, distress and decision-making in often pressured situations, putting them at risk of the ill effects of stress, including compassion fatigue and burnout. Access to clinical leaders and systems of support and supervision is linked to staff being less fearful of blame or competency issues, and being more likely to seek out support98 and to sustain compassionate engagement. 10 When staff are supported, decision-making improves98,101,109 and staff stress is decreased, including when support is provided via telephone or video conference. 87,92,109
System outcomes
Urgency and timeliness of response
Data related to clinically relevant waiting times in mental health crisis care are lacking. 85 The rationale for current waiting time standards is not understood by front-line staff:
. . . some of the standards recommend a time frame, ‘see people within 24 hours’, [the] new standard is 4 hours. I would like an explanation of where that target comes from, what is the clinical reason and evidence for that.
LS6, mental health nurse
The time people wait for a mental health assessment is linked to availability of resources,15,94 even when services are available 24 hours a day, 7 days a week. 89,92 Co-locating mental health practitioners in emergency control rooms improves the timeliness of responses because the most appropriate service can be despatched or issues can be dealt with using telehealth. 92,95 Co-location in emergency control rooms has been found to be cost-effective, and therefore sustainable in the longer term,92 but has not been fully evaluated.
Joint or parallel assessments improves collaboration between staff,94 and leads to more rapid responses92,94,95,104 and fewer people failing to reach a mental health intervention. 94 According to one interviewee, parallel assessments, as well as saving time, are more accurate and avoid the discomfort of multiple assessments for service users105 (NC1, mental health nurse).
A mental health triage tool, adapted for use in the UK, has been ‘subject to preliminary validity and reliability testing’. 87 Following front-line staff training, triage approaches have been linked to more timely and appropriate service responses88,98 and improved accuracy in identification of suicidality. 98 The outcomes of service thresholds on timely access to crisis care have not been fully evaluated. ESG members and an interviewee explained that how services manage access thresholds may have more impact on urgent access than assessment and triage processes:
I think once you get through to the triage element and the assessment, you’re kind of in. It’s . . . thresholds that I think is quite a barrier to people.
NC1, mental health nurse
Accessible crisis services
We found no published evaluation of SPA sercvices. 83,106 One interview participant suggested that a SPA helps to manage staff resources by separating roles between triage calls and crisis intervention follow-up (LS1, manager). Telephone access has a long history in crisis services and has been used as an alternative to face-to-face contact during the pandemic. The UK Government fast-tracked implementation of dedicated 24/7 NHS mental health crisis helplines in 2020 to mitigate barriers to access to A&E during the COVID-19 pandemic. Ease of access was prioritised and the new telephone lines received 3 million calls during the pandemic,84 suggesting uptake, although individual and service outcomes from these calls have not yet been reported.
The availability of sufficient resources to CRTs15 and in A&E influences the time available to carry out initial assessments. 105 If organisations value involvement of service users and families in their care, providing resources that ensure that staff have time for assessment enables greater attention to the person’s own interpretation of their crisis and the likelihood of negotiation and participation in treatment decisions. 99 Time spent in this way may reduce the number of times individuals attend for urgent support, and therefore have the potential for cost-effectiveness and improved individual experience,93 as one interviewee explained:
It feels like you’ve had your call now if you call the NHS. So, if I reach that point again in the night, then it is more likely to go down the harm route and I am more likely to then end up in A&E.
JT3, service user
Organisations where staff burnout and compassion fatigue are addressed through training and support are more likely to have improved service user experience and may reduce service use for those who access services frequently. 88,93
Information-sharing and shared decisions related to joint crisis planning were limited to those already known to mental health services. 112,114,117 Acknowledged problems of engagement of clinical staff with JCPs suggest that organisational support for sustained change and implementation at organisational level is needed. 117 Information-sharing and shared decision-making have shown improved service co-ordination in a crisis for those known to services,115 especially where there is a risk of relapse or frequent need for support, such as for people with personality disorder. 111 An interviewee explained it as follows:
It does make a difference when they know a little bit about who you are. If they know my diagnosis and what treatment I have had, they can then relate stuff that is meaningful.
JT2, service user
Unintended consequences
Service users
Urgency and timeliness of response
Gaps between services mean that the link between access to a rapid assessment and people reaching a rapid mental health intervention is not consistent. 92 Service users and families describe waiting for their crisis to escalate to be accepted into services. 99 Crisis service provision has been historically situated in secondary mental health services, but these services are difficult to access because of high service thresholds. Primary care services designed to meet the needs of those requiring lower-intensity interventions88 have not traditionally accepted crisis care referrals and have long waiting times for interventions. 10 People in crisis report that waiting for services to respond feels pointless when there is no accurate information about what they are waiting for. 104
Accessibility of crisis services
Complex referral processes, such as gatekeeping, are viewed by service users as a barrier. 99 Gaps between different agencies and services result in people having multiple assessments, which causes unnecessary distress,99 results in no intervention10,15 or results in circling in the system, with repeat attendances. 93,104 Not being taken seriously leads to withdrawal from services, isolation and an increase in negative beliefs about services. 2,99
Service users described being perplexed when directed to attend A&E by their GP or community-based crisis providers,93,103 who they believed ought to be able to provide more appropriate crisis support. Referral processes between agencies in crisis care are biased towards statutory services. 10 Often, rather than a referral to a voluntary service, people are signposted, leaving the process of accessing the service to the person or their family member to co-ordinate. 10 As a result, service users and families are often unaware of voluntary sector services and discover them only by word of mouth. 10 An ESG member explained that a CRT had not felt right for their needs. They met a friend locally who provided information about a bespoke black, Asian and minority ethnic crisis service in the voluntary sector. They wished they had been referred to the service sooner.
Failure to secure appropriate crisis support leaves family members feeling abandoned; they lose trust in mental health services and resort to calling emergency services or attending A&E. 90 Although A&E is an uncomfortable environment for many people in crisis, those who attend are guaranteed to be seen. 91 An interviewee explained that this guarantee makes the wait for treatment more tolerable than the frustration of circling the system (NC1, mental health nurse).
Failures in the crisis care system, including an inability to provide timely responses, and gaps between services that prevent continuity when coupled with individual factors such as perceptions of urgency and the nature of the crisis,10,93 lead to people circling the system and making repeat attendances. When people attend services frequently,93,103,104 service users believed that front-line staff ‘regarded them as “a nuisance” or, worse, seeing them as a diagnosis or behavioural category rather than a person’. 89 An interviewee explained that they had experienced that staff with negative attitudes provided inadequate risk assessment, made assumptions about a person’s circumstances (NC3, carer) and people were discharged too hastily, which led to further self-harm, escalating behaviour105 and, ultimately, further repeat attendances. 104
Although access to telephone support was valued as part of crisis services,15 it may not provide the sense of relational safety identified as important. 10,93 A service user interviewee explained the need for telephone responders to have skills in supporting mental health:87
Generic answers from NHS lines are not helpful and . . . can make things worse.
JT3, service user
Front-line staff
Urgency of access to services
Differences in perceptions about urgency87 and definitions of crisis10,90,103 can lead to disputes about responsibility between front-line staff from different agencies providing crisis services. 10 When staff are not clear about how different agencies work together to respond urgently, the result can be multiple assessments that are distressing for service users, ‘exacerbate the crisis’ (JT1, service user) and cause delays in reaching an intervention. 104 Resource pressures can lead to responsibility for crisis care being pushed to the urgent care pathway, the police and to secondary mental health community teams, as one interviewee explained:
I personally I found it more challenging to get someone referred . . .. So, on duty [in a community mental health team], we pick up a lot more of the work that might have been done by the home treatment team and underlying that is . . . how resources have changed and reduced.
LS2, mental health nurse
Staff interviews suggest that a SPA service, that is, triage and referral of callers by front-line staff, is challenging, as it can be difficult to secure appropriate and timely support for callers, who often expect more than is on offer (NC2, mental health nurse). A service user interviewee (JT1) was sceptical that a SPA improved access and believed that people in crisis are still sent ‘from pillar to post’. A lack of confidence that services will be available is stressful for front-line staff and service users and leads to difficulties in developing trust and therapeutic relationships. When staff are stressed about resources, they fear being overwhelmed and act to protect resources, as explained by an interviewee:
And this is to do with resources, where people just want to protect their own. So, they’re like ‘We’re not taking that referral because XYZ’. There’s always a reason why you can say no to accepting referral.
LS2, mental health nurse
Although telephone interventions have been prioritised, partly in response to the pandemic, to ensure timely access to a mental health assessment, an over-reliance on telephone consultations in a crisis may lead to front-line staff being complacent or less responsive to risks because their assessment is less detailed,92 or to needs being missed. 112 A lack of face-to-face presence of mental health staff may mean that the police are more likely to rely on the use of emergency sections of the Mental Health Act 1983118 and the Mental Health Act 2007119 to expedite a mental health assessment. 92
Accessibility of crisis services
A mental health nurse interviewee described an experience in a SPA service when they were unable to secure any follow-up service after several referrals to follow-up services. Despite each service providing services appropriate to the needs of the caller, the referrals were rejected because of ‘resource pressures’ or ‘not meeting the service threshold’. This resulted in the SPA nurse providing follow-up interventions, outside their role, to keep the person safe (NC2, mental health nurse). When staff are unable to work within their role, they lack belief that the service has the resources to respond in a timely way. 15,102
The pressure to dispatch callers to an appropriate follow-up service is compounded by imposed maximum waiting times: clinical priorities can become distorted, staff may aim for hasty assessment and discharge,105 and communication may lack empathy and collaboration. 99 Staff become dissatisfied with their role, believing that they are being forced to work outside personal or professional ideals (NC2, mental health nurse). Staff who are exposed repeatedly to situations where there are system gaps lose motivation and experience compassion fatigue and ‘avoid contact with mental health calls’ (NC4, paramedic).
An unintended consequence of the time spent on mental health calls by ambulance personnel, particularly in rural areas, is a lack of available ambulances, causing delays for other emergencies (NC3, paramedic; LS4, emergency care assistant) and increased resentment between agencies providing mental health crisis care:
I’ve been stuck on these kind of jobs for 3 or 4 hours. The crews get incredibly frustrated with these jobs because . . .they don’t feel it’s their role, they don’t feel they are adequately trained, and they don’t feel they get any support or help.
NC4, paramedic
Interviewees (NC2, mental health nurse; NC4, paramedic) described frequent attenders in mental health crisis teams as ‘the hardest to deal with for staff’ (NC2) and explained that low levels of support for staff when dealing with frequent attenders lead to resentment and, ultimately, unhelpful attitudes towards service users. Staff perceive frequent visits as unnecessary, although the person may be objectively as unwell as other non-frequent attenders. 103 Beliefs about crisis being a single episode10 perpetuate front-line staff attitudes about those who seek support from service more than once, as a service user interviewee explained:
I felt taken seriously the first time, but not the second. Feels that professionals expect that you can deal with it the second time, but the first time is seen as more legit.
JT1, service user
Negative staff attitudes experienced by service users in A&E lead to people being afraid or unwilling to attend again. This can cause delays in transfer by ambulance staff to follow-up crisis care:
Quite a lot of the patients get quite upset with going to A&E, especially if they have been there before.
LS5, emergency care assistant
When people stayed away from A&E during the pandemic, negative attitudes of A&E staff towards people attending in a mental health crisis increased:
. . . during the lockdown . . . pressure was placed on people [experiencing a mental health crisis] not to go to A&E. [I] have experienced attitudinal changes in the A&E staff who were quite clear that it meant that the people that didn’t come had been time wasters before, rather than necessarily appreciating that what we have seen is a huge deterioration [in] people.
NC1, mental health nurse
Ambulance paramedic staff in interviews talked about a lack of clarity about their role in transporting people to crisis services. When a service other than A&E was the most suitable for the person, ambulance personnel were conflicted about whether or not this constituted an emergency, and therefore felt it may not be their role to provide transport to these services. In these situations, ambulance staff were also not always aware of the range of community crisis services available or if they were permitted to refer to these services (NC3, carer/paramedic; NC4, paramedic).
Front-line staff are ambivalent about the use of JCPs as a means to shared decision-making, believing them to be another layer of bureaucracy115,117 and that service users may not choose the most appropriate intervention, fearing that this may adversely affect staff accountability or contradict best practice. Staff also believed that JCPs may give false hope about the interventions available in a crisis. 113,115 When staff do not engage with JCPs, service users feel disempowered and the crisis plan is not activated. 112,113,117 Organisational cultures centred on professional power over therapeutic relationships115 and a lack of staff resources create barriers to shared decision-making. 113 A crisis service manager explained that when staff fail to engage with crisis planning, crisis care becomes paternalistic and people are more likely to be referred to the urgent care pathway, resulting in a ‘cautious or paternal response, ringing ambulances . . .’ (LS1, manager).
System
Urgency of access
The combined pressure of limited resources and waiting time standards may push staff to focus on meeting the waiting time standard, to comply with policy, over focusing on the individual needs of service users. Practice experts believe that waiting time standards could be linked with increased avoidable admissions, inadequate risk assessment, avoidable restrictive practices due to rushed assessments105 and reduced involvement in treatment decisions that service users believe lead to increased likelihood of misinterpretation of their crisis. 99
Complex commissioning boundaries for the different agencies involved, for example between ambulance services, A&E, police and mental health crisis services, can result in delays, as explained by paramedic interviewees (NC3, paramedic; LS4, emergency care assistant). A lack of multi-agency agreement about responsibility for transport and systems to support transition between agencies95 caused disputes between staff,10 resulting in delays for service users.
Co-location of mental health staff in emergency control rooms reported potential for positive outcomes for timely access to mental health assessment and dispatch of appropriate resources;92 however, interviewees discussed limitations in the adoption of the control room model. Sometimes police personnel had already detained the person before seeking support via the control room:
The reality . . . it’s [control room triage] being used after the event, so the service phone the control room triage to just say, well, ‘we’ve put this person under 136’ [section 136 (emergency police power of detention) of the Mental Health Act 1983].
KB6, manager
Ambulance staff noted that the control room triage system may not be sensitive to mental health, meaning that, without an accompanying serious physical health problem, the triage assessment would result in a long wait for an ambulance:
Decisions about who attends are made via triage in the control room. Calls will be graded 1–5, Cat[egory] 1s are the most serious. A lot of mental health problems, unless it involves harm or loss of consciousness, would be downgraded to 2, 3 or even 4, but quite low-grade calls.
NC4, paramedic
Furthermore, mental health expertise in control rooms may not be available 24/7:
My understanding is that sometimes you can get put onto a mental health nurse, but not very often and invariably, like Sod’s law, not there when you want one. Usually, 3 a.m., and . . . when you really need somebody, you can’t get them.
NC4, paramedic
Accessibility of crisis services
The interface between the array of different agencies providing crisis responses is characterised by variation in definitions of crisis. 10 Crisis was described by a service user when interviewed as ‘an ill-defined thing’ (JT2). Differences in how a crisis is defined could be tolerated within a multi-agency system. 101 Where there is a lack of multi-agency collaboration, agreements about different approaches and boundaries are not reached, leading to fragmentation. 2,10,89 Fragmented services result in people failing to secure the support they seek; interventions lacking continuity; and people having to make frequent contact with services, often via the urgent care pathway. One interviewee explained that poor communication from services led to a perception that services were unresponsive:
I think we should be more responsive . . . some of that’s about resources, but some of it is about communication. I feel like these different parts of the service are completely not integrated.
LS2, mental health nurse
Fragmentation is compounded by a lack of stability in service availability. In the voluntary sector, this is often due to time-limited funding, particularly for smaller organisations. 10 Instability in statutory services is caused by resource pressures89 and is managed by having high thresholds for access. Services are then focused on protecting resources, rather than being responsive to need. 10 An ESG member talked about their frustration and feeling of abandonment when told by a crisis service that had supported them previously that the similar mental health issues they were experiencing did not now meet the threshold for access.
An A&E department is commonly believed to be unsuitable for people seeking crisis support, yet a lack of responsiveness in statutory services pushes people to the urgent care pathway. 89,102,104 A paramedic believed that some people, ‘. . . phone 999 because they know they’ll get a response’ (KB2, paramedic). Attendance at A&E is also guaranteed to produce a response:91
. . . that is why often people will go to an emergency department . . . you are guaranteed to be seen . . ..
NC1, mental health nurse
Presentation to A&E is believed to be appropriate for people in crisis who have physical health concerns, but this assumes that the person is aware that they have a physical health issue, or that the systems in place to assess this identify it. 112 One interviewee was concerned that identifying physical needs in a mental health crisis over the telephone, such as via NHS 111, may result in potentially unnecessary referral to the urgent care pathway:
The [telephone responder’s] first response is to send an ambulance anyway because they are not confident diagnosing over the phone.
NC4, paramedic
Equally, a failure to identify physical health issues may put people at increased risk of missed care:
. . . diversion away from A&E doesn’t necessarily work because lots of people have actually got a medical reason. We’ve seen lots of people that would have got missed if they’ve been diverted.
NC1, mental health nurse
Gatekeeping in the crisis care pathway provides an example of unintended barriers to access perceived by service users2,97,102 and staff:
And I know [gatekeeping] also creates complexity and duplication, so I might decide [in A&E] that someone needs an admission. The crisis team still insists on doing another assessment. And we’ve had situations where, as a consultant nurse, and the consultant psychiatrist say yes [to admission]. A band five [crisis team] could say no.
NC1, mental health nurse
Conceptualisation of mental health crises as single events, rather than as a series of points in a recovery process,10 makes the continuity that service users seek difficult to provide. 2,99,101 Conceptualising crises as single events, as well as failing to meet expectations for continuity, may perpetuate negative staff attitudes about those who seek crisis support on more than one occasion. 10,93 A carer (NC3) explained in an interview, ‘A crisis is always there, it’s just when it bubbles over’, and a nurse theorised in an interview:
. . . suicide is a chronic, relapsing condition, rather than acute crisis every time. I think there’s very few people that have that kind of spontaneous combustion moment where it’s the last straw. I guess you do get that, but I think it’s rare.
NC1, mental health nurse
Fast-track implementation of crisis telephone lines in England aimed to provide an alternative to A&E. 84 This was prioritised despite evidence that telephone contact does not meet all crisis needs10,15 and telephone access was already offered via NHS and voluntary sector services, creating further complexity. There are also reports of individual experiences of people failing to reach services via telephone calls,96 as an interviewee explained:
In an ideal world, an urgent response would be when you call someone up, they would answer the phone. But that is not the reality. SPA never called me back. It is invalidating and it means I will need the help for longer and longer.
JT2, service user
One service manager noted that the regional telephone lines may be a barrier to the continuity of supports that service users want:
. . . there is now a regional 24-hour helpline number . . .. What we find is that service users who have rung our service for a long time are not always that keen on ringing somewhere different and prefer our response . . . it takes time to build up people’s confidence in different services.
LS1, manager
Digital poverty and poor mobile phone coverage (especially in rural areas) requires freephone systems or local systems to overcome barriers to telephone access. 108 An interviewee described people telephoning 999 when seeking crisis support because they had no phone credit, the call was free and the number was known to them:91
How will people know that those crisis lines are in place? . . . people will always default to what they know, which ultimately is going to be 999 or 111.
NC1, mental health nurse
Mechanisms
Service users
Services that people perceive as providing a guaranteed response91,104 (resource) (e.g. urgent care services) engender trust,10,15,90,91,102 a sense of safety2,10,90 and a belief that the service can help102 (response). Complex referral routes, delays in responses and failure to secure crisis responses reinforce a sense that crisis care is not guaranteed, driving people to contact urgent care services, despite the likelihood of having to wait. People in crisis and their families have a reduced sense of urgency and can tolerate the discomfort of waiting for an intervention or follow-up91,104 (response) when information is shared with them about the nature of the follow-up and the timing of interventions104 (resource). People kept waiting without accurate information may become increasingly desperate for support and contact other services or leave without treatment. People are reassured and have a reduced sense of urgency (response) when crisis services require little effort to navigate and are available 24/7 (resource). 2,10,15,91,92 Access to crisis services with low financial and social burden, by having no cost91,95 (e.g. freephone,108 not requiring travel or fee-paid transport10,92) and with minimum disruption to family life through agreed timing and venue of visits10,92,109 (resource), encourages people to make contact sooner and choose mental health crisis services rather than urgent care services (response).
The person’s (or their family’s) perception of the urgency of the crisis is acknowledged,2,90,96,112,113 and front-line staff acknowledge that the person may have already used their personal resources or that their own resources (such as family) are not available (such as during the night),89,112 or are perceived as unavailable because they do not wish to be a burden to family members10,112 (resource). When these acknowledgements are made by front-line staff, there is mutual understanding, open communication,87,88,91,98 a sense of collaboration104 and respect112 (response). Support from family and friends in a crisis may also generate continuity not available in some crisis services. Safe and welcoming community spaces with peer support2,10 provide a proxy for family and friends, generating a sense of safety and belonging. 10 Consistency, continuity and relational safety are critical factors for people in crisis10,102 (resource), giving an increased sense of safety, control and a reduced sense of urgency,110,112–114 and motivating people to make contact with the service again in future crises2,10,104 (response).
When a mutual agreement about the support required is agreed alongside negotiation about the timing of any intervention (shared decision-making)112 (resource), there is motivation to engage, relational safety10 and a reduced sense of urgency,2,10,88,115 and people are less likely to feel patronised (response). Shared decision-making requires front-line staff to have positive attitudes,2,10,100 mental health knowledge, and interpersonal and therapeutic skills87,96 (resource) so that the person in crisis and their family can have a sense of safety and an ability to communicate their need,10 and so that trust can be developed2 (response). When there is trust in front-line staff, a therapeutic alliance is developed whereby immediate supportive interventions to reduce distress can be provided,89 such as active listening and supportive counselling10,87 (resource), the crisis experience is validated. The person feels believed, that their concerns have been taken seriously,2,10,83,109 that they have been prioritised,104 respected and able to engage in their care117 (response).
Front-line staff
When front-line staff have mental health knowledge appropriate to their role and have knowledge about the role of other agencies83 through access to training appropriate to the context in which they encounter people in crisis,87,98,117 they provide immediate interventions to reduce distress104 (resource). Staff invest in shared decision-making10,92,112,113 and are confident in their role89 (response). Confident staff are open, flexible and able to take account of the views and experiences of a person in crisis113,117 and their family,10,90 thereby empowering service users during the decision process. 117 They understand the importance of providing explanations to the person and their family, including proactively supporting people as they wait for follow-up87,98 (response). Referral, liaison and transitions to follow-up care (resource) are achieved through mutual understanding and negotiation between front-line staff,85,92 the person experiencing the crisis112,113,117 and their family/carer,90 enabling a shared commitment to the decisions made109,110 (response).
Front-line staff have access to support, supervision10,98 and consultation about decisions and debriefing10,87 (i.e. immediately available to them, by telephone, face to face98 or video call109) from peers10 and leaders10,98 (resource). Staff are less stressed; have improved emotional well-being;10,98 and believe that seeking advice and support is an accepted norm10 that creates a working environment with a sense of safety, tolerance and acceptance between staff98 (response). When responsibility is shared in high-risk situations (resource), staff are confident with decision-making, less inhibited by fear of blame98,117 and less paternalistic in their attitudes to service users (response).
Systems
Service thresholds, staff resources needed to manage workload15,108 and systems to deliver care across complex commissioning boundaries have been planned for (resource), allowing front-line staff to confidently liaise and refer people in crisis in a supportive and timely way108 (response). Morale98 and motivation enable staff to believe in the service and trust that services are available to respond urgently to referrals10,89 (response).
There is investment in a shared approach to maintaining up-to-date information across agencies, which is easily accessible to members of the public83,91 and includes all types of crisis service10,83,89 (resource). People in crisis, their families and front-line staff can make informed decisions about sources of support appropriate to individual circumstances102 (response).
IPT 1 pen portrait: urgent and accessible crisis services
The pen portrait shown in Box 5 provides an illustration of the CIMO framework identified in the focused review through a narrative characterisation of a person in crisis. The pen portrait was drafted from the chapter findings and through discussion with the research team. A draft version was discussed with ESG members and edited in the light of their feedback. The pen portrait of ‘Nimra’ did not sufficiently convey a sense of proactive follow-up that the ESG members felt was important in providing a sense of safety. One ESG member also commented that men from minority ethnic groups would not receive the same positive response as the woman described in the pen portrait.
It was midnight,2,10,83,88,91 and Nimra was feeling frightened and that her mental health was getting so bad she couldn’t manage any more. Nimra’s mum was really worried. 10,89,90,96,103,108 Nimra had received treatment from a mental health service before and had information82 about getting help urgently. Nimra phoned NHS 111 for advice and was automatically given an option to speak with someone from a mental health service. 1,10,15,82,83,85,88,97,105,106 Although Nimra felt anxious as she waited for someone to answer the phone, she felt it was an easy way to reach help. 10,15,90 Nimra’s mum was relieved that they didn’t have to go out of the house at night to get help. 10,83,90,91,94,101,107,120
Nimra’s call was answered by Jobe, a staff member trained in helping people who are distressed over the telephone. 116,121–125 Jobe introduced himself and explained what would happen during the call. Jobe listened as Nimra talked about what had happened that day. Jobe asked questions about what was happening to Nimra91,95,121,125 and about family and friends86,87,90,97,103,111 and how quickly Nimra thought she needed someone to help her. 2,89,95,98,111,112,124 He also asked what Nimra thought would be helpful. 99,116 Nimra felt able to talk to Jobe, who seemed to understand what she was saying, and she believed he wanted to help. 10,103,110,115
Nimra was still feeling distressed and very tired, but unable to sleep. Jobe stayed on the telephone with her until they had talked about ways to feel calmer and get some sleep. 98,121,123–125 Nimra was worried about still feeling like this the next day. During the call, Jobe arranged an appointment for the morning, guaranteeing that Nimra would see someone. 90,103,126 He also provided Nimra with a telephone number to call back overnight if needed87,92 and the address of a walk-in service1,10,15,82,83,85,88,97,105 open during the day for additional support. He offered to call Nimra back later, but Nimra preferred to try to get some sleep. Jobe also spoke with Nimra’s mum, who wrote down the appointment and contact details. 111,109,115,116 Nimra felt safer and that she was welcome to call back if needed. 2,10,15,89,90,101
Nimra didn’t get much sleep, but remembered what she had talked about with Jobe, whom she trusted,10,15,90,101 and this helped her to feel able to wait for her appointment in the morning. Nimra looked up the walk-in service on her phone and thought it looked like a place she might like because it has a meeting group for women and a café. 10,127,128,129 Nimra wondered if this service might feel welcoming and homely and be able to help in a way similar to how her family and friends help. 10,112,129
Conclusions
People experiencing a crisis choose to access services they perceive as providing a guaranteed response, that are easy to navigate to and that fit with their definition of the crisis. Although the timing of responses remains unclear in relation to outcomes, what is clear is that people feel safer and have a reduced sense of urgency when they trust services. Trust is established through compassionate interactions and proactive management of transitions and waiting. Involvement of the person and their family or support network in decisions supports a sense of trust and relational safety, which may help meet a need for continuity for some.
To sustain compassion, front-line staff need access to support for themselves, as well as resources to deliver crisis care that meets their personal and professional ideals. Training in the knowledge, skills and values required for compassion can build confidence in front-line staff in all agencies. System leaders must provide resources and communicate an expectation for compassionate engagement so that it becomes the norm for staff to seek support.
Mental health crisis care is provided by a complex array of agencies, each with different definitions of crises, different values about the nature of interventions and different approaches to prioritisation. This is further complicated by multiple overlapping service boundaries. What is apparent is that these differences can be accommodated within an inter-agency system only if information and decisions are shared from commissioning through to front-line delivery. Conceptualisations of crises as single events or as the sole responsibility of statutory secondary mental health systems are unhelpful and generate fragmentation, leading to gaps and delays for those seeking crisis care and frustration for leaders and front-line staff. Access to services for those known and new to services need to be planned for to avoid overemphasis on one over the other.
If–then programme theory: urgent and accessible crisis services
If
Commissioning focuses on maximising access and delivering seamless transition between agencies. Waiting time standards are linked to interventions and desired outcomes. There is information-sharing and shared decision-making. There are agreements about prioritisation and service thresholds that minimise gaps and delays. Systems to assess urgency (e.g. triage) are agreed between agencies and are evidence based. The person’s (or their family’s) perception of urgency is considered. Gatekeeping and referral systems operate to facilitate ease of access. Evidence-based technology and telehealth are used to enhance access and provide support during any waiting. Transition and transportation between agencies are managed proactively and waiting is actively managed. Access to an intervention appropriate to need is guaranteed. Resources enable time for therapeutic engagement, collaboration, support and learning.
Then
Front-line staff are confident and trust leaders and agencies in the crisis care system. Staff are confident that there are resources available and are confident in their ability to provide a response linked to need. Staff are confident and skilled in using decision aids and technology. Training is appropriate to staff role. There is immediate access to support for decision-making from peers and leaders. There is a culture of support rather than blame. Staff are proactive in providing information, supporting people as they wait and facilitating transitions. Staff engage with systems of planning and shared decision-making. Compassion is prioritised and fatigue prevented.
Service users and their family or support network believe that a crisis response is guaranteed. People in crisis believe that they have been believed and prioritised. They invest in relationships with agencies and their staff. They feel safe and supported to wait. People reach an intervention. There is low financial, social and emotional burden when accessing crisis care.
Leading to
People attending urgent care services when it is the right service for their needs, such as when they have physical health concerns during a crisis. Ease of access and guaranteed responses in crisis care reduce the need for people to attend A&E. There is a reduction in repeat attendances. People contact crisis services sooner, reducing the likelihood of restrictive care. People experience faster access to support that reduces their distress. Staff are supported and have skills appropriate to delivering compassionate crisis care. There is improved experience of crisis services and relationships between communities and services.
Chapter 4 Focused review for initial programme theory 2: care in a crisis is compassionate and therapeutic
Introduction
This chapter examines the second of the three IPTs, compassionate and therapeutic care, identified from the initial scoping searches outlined in Chapter 2:
If services provide compassionate and therapeutic care that is non-judgemental, dignified and safe and delivered by well-supported staff with requisite skills and knowledge, then there is trust, and people feel listened to and taken seriously, leading to reduced distress and duration of distress, and engagement in services that are delivered by compassionate staff.
The chapter first describes the characteristics of compassionate and therapeutic care, including interventions and intervention components identified in the literature to enhance the development and delivery of such care. The evidence base for compassionate and therapeutic care, the outcomes of compassionate and therapeutic care, and the unintended consequences when key components are not in place or are not effective are described. Subsequently, the chapter describes the mechanisms for compassionate and therapeutic care, demonstrating how it may be facilitated at different points within mental health community crisis care. A narrative drawn from the literature is supported by contributions from the ESG discussions and interviews. The chapter concludes with an overview of how compassionate and therapeutic care can enhance mental health crisis care, using the ‘if–then–leading to’ convention.
Context: compassionate and therapeutic care
At the individual level, compassion can be understood as being open to others’ suffering, being affected emotionally and sometimes cognitively, and acting or feeling motivated to help. 130 Compassionate organisations operate person-centred cultures, which prioritise structures and systems, in which high levels of distress can be contained, managed and alleviated, thereby facilitating compassionate care. 131 Compassionate organisations value employees and allocate ample resources to supporting and developing the workforce, thereby building a compassionate organisational culture. 132
The consensus of the ESG was ‘compassionate care comes from the top’: organisational leaders being the ‘brain’ of services, and front-line staff mirroring the organisational values –
Trusts need to look after their staff, they’re the best asset they’ve got.
ESG member
Nevertheless, the ESG agreed that, although most organisations identified as compassionate and would say they were committed to compassionate leadership and compassionate care, the salient question was whether or not the care was truly compassionate. ‘Organisational commitment and leadership’ and ‘psychologically safe models of care’ were seen as core issues for activating compassionate and therapeutic care and were used as a lens through which to explain compassionate and therapeutic care; the review scope was refined to include only documents focused on these aspects of compassionate care. A list of contextually important intervention strategies of IPT 2 were identified from the included documents and confirmed through discussion between the research team and the ESG, listed in Box 6.
The evidence base
Sixty-six records were identified as part of the preliminary theory component ‘compassionate and therapeutic care’ [54 from academic literature, seven from grey literature (websites and reports) and five from hand-searching]; after exclusions on the grounds of irrelevance to theory, 11 were retained. Backward citation searching of these 11 identified a further 13, of which five were not relevant and seven were included. In total, 18 study records were retained. Figure 8 illustrates the identification of new studies for this review.
FIGURE 8.
Search results focused review IPT 2, compassionate leadership.

Retained records
Details of the 18 retained records for the compassionate and therapeutic care focused review are in Appendix 4.
Settings
The research settings reported in included documents were as follows: all health care,127,134–136 adult social care,137 the NHS in England,138 hospitals,131,132 primary care,139 community mental health services,118,125,126,129,133,140 the ambulance service128 and the voluntary sector. 10,130
Focus
The included documents investigated lived experiences of crisis,130,137 fostering compassionate care through Schwartz Rounds,125 culture of care,127 crisis planning,118 care quality,128,138,139 care planning and co-ordination,118,129 compassion,126,134–136 the impact of waiting,132 risk management,133 therapeutic relationships131 and team functioning. 140
Appraisal of relevance and rigour
All included documents were appraised for relevance and richness using a modified realist appraisal tool72 (J Jagosh, personal communication) (see Report Supplementary Material 3). Documents containing primary research data were also appraised for rigour using the MMAT73 (see Report Supplementary Material 3). The combined appraisal of relevance and rigour identified that the evidence supporting IPT 2, compassionate and therapeutic care, is based on studies of mixed quality.
Three records had high relevance, in that they were highly matched to the theory and provided a rich description of mechanisms and context. 10,126,133 A high-quality mixed-methods study of the voluntary sector contribution to crisis services was methodologically rigorous. 10 A qualitative study provided rich accounts of lived experience from a small sample that was limited by a lack of ethnic diversity. 133 The expert report was strongly linked to theory related to practice, but reported no method. 126
Most documents were moderately framed to the theory, reporting different, but related, phenomena, and containing multiple relevant areas of interest. 125,127–129,134,136,138–140 Of these, four were mixed-methods or multimethod studies127,129,136,138 reporting rigorous methods, but limited by low response rates to a survey,129 the narrow focus of the research setting,127,138 a stated limitation of the interpretative nature of the study risking biases from the research team,138 and a lack of detail in the stated method and approach to sampling. 136 A realist evaluation125 provided rich data related to mechanism, but had limitations in linking these and any reported outcomes specifically to Schwartz Rounds within a complex clinical setting. Two qualitative studies provided in-depth rich data limited by small samples that lacked variation139,140 and data that were more than 5 years old. 140
There were four relevant articles in which the pertinent context, mechanisms and outcomes were less substantial;118,130–132 a further two less substantially framed documents were retained on the basis of their contribution to understanding risk137 and leadership. 135 Of these, a meta-synthesis lacked a focus on community settings,131 and two qualitative studies provided in-depth rich data from small samples. 118,130 The remaining documents were expert reports with no stated methods. 132,135,137
Outcomes
Many of the included documents were highly theoretical in their treatment of effectiveness and the relationships between the contexts, mechanisms and reported outcomes. There appeared to be little in the literature to support the identification of outcomes of compassionate organisations and leadership, linked with psychologically safe crisis care.
Service user, staff and system outcomes
Where organisations prioritise reducing coercive practices, described as ‘measures such as compulsory admission, restraint and forced medication’, people in crisis are supported to keep themselves safe, and risk reduces. 133 Front-line workers feel valued, engaged, respected, less isolated and less exposed when they are fully supported by their organisation. 125,139 When front-line workers feel supported, staff groups are more stable and staff turnover is reduced. 126 Hence, compassionate treatment, of both people in crisis and front-line staff, produces better service user and organisational outcomes. Furthermore, in interviews, front-line staff provided insights into how favourable outcomes may depend on how individual staff respond:
Compassionate response is completely dependent on the individual officer. Looking back on my own behaviour, I used to be quite by the book. I wouldn’t consider and reflect and alter my behaviour at the time, but I don’t recognise myself even looking back 5 years. I’ve changed so much and that’s moving from a response officer to a community behaviour, it really brought about a sea change.
KB1, police officer
Furthermore, the well-being of the staff has an impact on how able they are to provide compassionate responses:
My personal mental health experience shapes how I deal with people. I notice how much patience I have depends on how tired I am, how hungry I am, whether I’ve had a break . . .
KB2, paramedic
At times, the behaviour of the person and the escalating nature of some crises make staying compassionate difficult for staff. The ability of staff to retain compassion relies on staff members’ ability to draw on their personal resources and resilience:
Some people will be deliberately antagonistic and aggressive – people shouting, screaming and swearing, trying to push me out of the room. They are going to be threatened with police involvement; they are going to get a very different response than those sitting quietly. Even if aggression is a result of distress, I don’t want to be hit!
KB2, paramedic
Unintended consequences
The reality of mental health crisis care was perceived by many stakeholders to be not compassionate and psychologically safe. This reflects literature suggesting that service deficiencies may currently affect help-seeking behaviour,10 for example leaving emergency departments before treatment. 132 Other concerns around services include increased use of the Mental Health Act 1983118 and 2007,119 particularly among black, Asian and minority ethnic groups;10 the use of restrictive interventions;132 more incidents of self-harm;131 and the potential for negative experiences of crisis care to increase trauma and suicide risk. 130,133
Service users
The crisis care experienced by some people in crisis appears, in many ways, to lack compassion, being experienced as humiliating, invasive,; traumatising and, in some instances, reminiscent of previous abuse. 133 Service users have reported being domineered by front-line workers. 118 They describe feeling dehumanised and losing trust. 130 Loss of trust in services and workers may affect self-confidence, abilities, activities and thoughts, and lead to isolation and anxiety. 130 Inadequate responses and rejection from services has been reported to lead to increasingly desperate people:10
If they ever offered me any support at all, I might have trust in them [crisis services].
JT2, service user
NHS services, such as CRTs, working to the national model may not be able to offer continuity. A service user interviewee (JT1) reported that the lack of continuity was distressing and prevented them from establishing rapport with workers; this point was further explained by a mental health nurse:
A criticism we get is consistency of staff: when people come to the CRHT [Crisis Resolution and Home Treatment Team], they see different nurses each time. It is really hard for them to connect with people. We try to allocate the same worker to the same service user if we can. But with holidays and breaks in shifts, it’s really hard to do. They are having to tell the same story. However much we document things, they feel we ask the same questions, and, in many ways, we are, we ask about risk and medication.
LS6, mental health nurse
A lack of investment in suitable safe spaces for people in a mental health crisis130 is a challenge for the delivery of compassionate and therapeutic care. Service users may have no choice other than to attend the emergency department, where care and assessment may not routinely be trauma-informed:132
I have to be in a very bad place to present at A&E. I find it triggers me there. It is not a helpful place to be.
JT2, service user
If someone is stressed, anxious and suffering, to put them in a stressed and anxious environment is not going to help.
LS6, mental health nurse
Front-line staff
Poor leadership at the level of middle management has been identified as detrimental to delivering compassionate care. 129 Compassionate and therapeutic care delivery can be challenged by continuous tension between meeting the day-to-day demands of working in health care, developing and supporting teams, and embedding structures and policies. 140 Organisational policies may not support the workforce to make decisions. 138 Lines of accountability can be unclear within multidisciplinary mental health teams, with the result that it may be less apparent who is in charge, or unhelpful power dynamics may undermine operational and clinical decisions,140 leading to poor communications and disengagement:
It is hard to know whose opinion is the top one . . . so that can cause tensions.
LS1, operational manager
Workload pressures on clinical team leaders may limit their availability to team members. 136 This may be particularly noticeable when things go wrong, as identified by one interviewee:
Everyone’s a bit unsure where to go when there have been incidents.
LS7, psychiatrist
Inherent conflicts within the leadership role may paralyse the decision-making of clinical team leaders. This can lead to a tendency to resist innovation and constructive criticism; to label staff who raise concerns as disruptive or complainers; and to resort to blaming any service problems on either external circumstances or front-line staff, thus absolving themselves of responsibility. 135 In response to these tensions, clinical leaders may also display power and superiority,140 and engage in bullying to drive change. 134 Ultimately, these processes may diminish the capacity of a clinical team to deliver compassionate care. 134,140
Staff morale
Clinical leadership approaches may impose solutions that create resentment and resistance at the front line. 140 In working environments where there is a lack of autonomy, exposure to severe health problems, limited social support and limited opportunities for constructive feedback, workplace stress is common. 135 Front-line workers can also feel frustrated and powerless to enact change, resulting in low motivation and morale, and consequent disengagement from their teams and from the goals of their organisation:138,139
I don’t necessarily feel well supported or trusting of more senior [colleagues]. I’d like to feel like I can trust managers a bit more.
LS2, mental health nurse
Disengagement of staff from their employing organisation’s goals can be linked to high levels of staff turnover,126 resulting in staff shortages, heavy workloads and unclear priorities. 135,138 These pressures are compounded by increasing level of need and complexity in UK mental health care,129 and the fact that, in health care, when there are workforce gaps, the work still needs to be done. Interviewees expressed feelings of frustration around the gap between what they felt was needed and what they were able to deliver:
NHS services stretch and stretch to meet impossible demands until the whole system fails.
NC2, mental health nurse
It’s leading more towards, you know, not helping people and not supporting people as much as I’d like to.
LS2, mental health nurse
Front-line staff who attempt to speak up risk being vilified by clinical leaders and might learn not to complain, leading to failure to escalate concerns. 136 Some front-line workers learn helplessness or focus exclusively on keeping immediate line managers happy for survival and advancement. 136 Some emulate bad role models, leading to undesirable behaviours. 135
Quite early in their career, front-line workers may become traumatised by the emotional demands of the job, which can limit their personal resources for compassion. 134 They may deal with unresolved emotional burden by distancing themselves from work and colleagues:134
How we maintain standards is to disconnect [emotionally] so that you can maintain that standard of care.
LS4, ambulance care assistant)
Management of risk
In some areas, systemic failings are driving skills deficits at the front line,138 especially if there are limited opportunities for professional development. 129 A lack of therapeutic skills and the inability to provide interventions may result in an excessive focus on the mitigation of risk129 and the prioritisation of medicines and short-term physical safety. 133 If front-line workers fear making the wrong decision and being blamed for the consequences of that decision,137 anxiety may drive behaviours in individuals and teams that are not conducive to providing high-quality compassionate care. 126 In the crisis context, a lack of confidence may paralyse decision-making. 128 The effect may be that decisions around risk assessments do not involve the people directly affected by the risk:137
We have adopted a more litigious approach to society . . . so for anything neglectful or for omissions, there is a high degree of fear in organisations. It makes the formal relationship between the organisation and the service user cautious and risk averse.
LS3, emergency medical technician
Front-line workers may justify taking coercive actions in challenging situations, on grounds of risk. 128,131 Concern about paramedics taking people to hospital by force following self-harm, irrespective of motives or severity, has been highlighted in the light of the known likelihood that such action can escalate risk, particularly following self-harm. 128 An interviewee reflected on the value of interpersonal skills for risk management:
Understanding, rapport and de-escalation are soft skills that are important, but aren’t taught or given the time to be appreciated or reflected on in busy working environments.
LS7, psychiatrist
Coercive practices undermine the development of trusting relationships. 133 The lack of a trusting relationship may generate fear in staff around risk and decision-making,137 thereby increasing levels of coercion. Front-line workers may also respond to risk with complacency, for example ‘He’s not going to do it because he’s never done it yet’ (NC3, carer). Alternatively, they may engage in ‘positive risk-taking’:
Positive risk-taking can be kind of a little bit of a buzzword that we use when we’re talking about, you know, justifying why we’re not responding to something.
LS2, mental health nurse
Systems
There is potential for tensions between financial and performance management agendas and the delivery of compassionate and psychologically safe crisis care,138 because the systems for regulation, inspection and commissioning across the health-care system may directly undermine compassion in organisations. 136 The issue appears to relate to health quality improvement strategies that involve comparative indicators and external audits. It has been observed that evaluation strategies are underpinned by an assumption that public sector organisations cannot be trusted to manage performance, leading to an imposition of standardised quality assurance approaches across organisations. 125 Furthermore, strategies to drive out bad practice based on what can be measured and regulated may actually restrict the ability of staff to meet service user need:125,134
Sometimes you feel like you are governed by performance reporting and the things the commissioners want. You would hope that is about service user outcomes, but sometimes it feels like it does restrict you as opposed to free you . . ..
LS1, operational manager
The current institutional and regulatory environment requires public sector health-care organisations to achieve targets, measures and standards; to seek financial incentives; and to report compliance to multiple overlapping authorities. The obligation to supply metrics in different formats to multiple external organisations is costly and distracting and may lead to fragmented knowledge, competing and ambiguous priorities, diffusion of responsibility and a lack of innovation. 138 Some service user priorities, such as compassion and psychological safety, are difficult to measure,125,136 and may not be reflected in outcome data that focus on quantifiable aspects of care. This suggests that there may be better ways to approach service evaluation:
What we are not doing is using the data intelligently to improve outcomes.
KB4, researcher
Voluntary sector systems have been described as relatively compassionate and humane, compared with the public sector,10 although similar organisational dynamics appear to be affecting their potential for delivery of compassionate care. Numerous and diverse funding arrangements and relationships between the public and voluntary sectors are contingent on complex factors such as organisational ethos, mission and strategic objectives. 10,130
A key informant study in this review10 investigated the contribution of voluntary sector organisations to mental health crisis care and highlighted the complexity of commissioning decisions concerning voluntary sector mental health crisis care, particularly in the context of austerity and cuts to services. The authors concluded that the quality of services in the voluntary sector can be inhibited, similarly to the public sector, when commissioners operate a business model;10 however, in other ways, business models can be beneficial to voluntary organisations:
There are large ones [voluntary sector organisations] that are now run like businesses and well-off, others that are local and grassroots and struggle.
KB4, researcher
Prioritising finance and performance management over people appears to lead to a lack of investment in the following: peer support services; physically and psychologically safe and calm alternatives to admission (e.g. crisis houses, safe spaces and walk-in services);10 and safe, short-term options for people who are intoxicated or distressed. 132,133
An NHS England report136 identified a risk that organisational leaders feed reports and metrics to system leaders without any genuine oversight and interpretation of the data, thereby reducing the potential for outcome data to inform better service delivery. For example, the interpersonal and relational aspects of care may be less visible (and hence of lower priority) to organisational leaders because they are not readily captured, measured and reported:139
I don’t think there’s much connection between, sort of, ground-level staff and the directorate any more.
LS2, mental health nurse
Therefore, arguably, if primacy is given to achieving financial objectives and to rationalisation, the main unintended consequence of prioritising measurable organisational ‘business’ outcomes is that health-care delivery may become unduly performance and task orientated. 125,127 Employees may be required to operate as units of production,126 with little regard for the relational or compassionate aspects of care. 125 The Royal College of Psychiatrists has argued that hierarchical organisational structures may be unhelpful, especially if the organisation is not clinically led. 126 In an interview, a psychiatrist conveyed the frustrations of having to work with the system:
Your MDT [multidisciplinary team] time, your team meetings, governance meetings, those are important. If you don’t get the support, it can’t happen. They just look at numbers and go ‘you reached that target’.
LS7, psychiatrist
Managers are equally likely to be frustrated by performance target cultures, as explained by one interviewee:
There are things you might want to do more work on, but . . . it doesn’t fit your current performance target.
LS1, operational manager
An extensive comparative mixed-methods study of mental health teams across six NHS sites in England and Wales129 found a discernible gap between national policy aspirations for recovery-focused mental health care, and practice. The authors raised concerns about a lack of vision among leadership teams and the impact on front-line services as a consequence of budget cuts, under-resourcing and bureaucracy. 129 They highlighted a need to ensure that organisational aims and operations were consistent with supporting staff and service users. 129 The ESG discussions identified that organisational priorities determined ‘how well staff are looked after’ and ‘how well staff know what is expected of them’, that is were focused on staff rather than service users. 64
Although the systems, processes, practices and disciplines within organisations are reported to determine the boundaries of action, when the organisational structure is fragmented, or a product of isolated decisions and workarounds, there is potential for toxic cultures and unhelpful norms to emerge. 136 Increasing demands create conditions for defensive and reactive responses from organisational leaders, leading to quality improvement efforts that may not use robust methods, or findings that are not subject to scrutiny. There may be ‘magical thinking’138 and indiscriminate use of particular approaches. One interviewee described investing time in a quality improvement project only for ideas to be ‘rubbished’ (LS2, mental health nurse) by organisational leaders, providing an example of how a perceived lack of support risks discouraging front-line workers from engagement in quality improvement initiatives.
Mechanisms
Service users
Service users have the opportunity to form supportive trusting relationships130 and retain control118 and their safety is balanced with independence in a collaborative way. 133,137 A consistent and stable staff group enables early signs of deterioration to be noticed, and service users trust the opinion of front-line workers who raise concerns133 (resource). Trust in front-line workers provides a sense of belonging to service users in crisis;130 front-line workers provide consistency and service users feel that front-line staff are interested in the psychosocial context of their distress and prioritise emotional safety, healing and relationships;133 service users are not turned away if they identify that they need help;137 treatments are individually tailored;118 there is freedom, control and privacy; and service users can engage in meaningful social and occupational activities and maintain social roles and relationships that are important to their well-being during a mental health crisis (response).
Staff
Front-line workers
Front-line workers emulate and practise prosocial behaviours and skills that are modelled by clinical leaders. 134 Teams interact and take lunch breaks, and there is an opportunity to be social135 (resource). Employees are connected to their humanity, the goals of the organisation and their core purpose. 136 Relationships are based on shared values, openness126 and mutual trust. 140 Professional and personal values are aligned, and the staff feel more satisfied at work. 139 There are good relationships at all levels and there is active engagement with organisational and clinical leaders138 (response):
It’s really important part of my professional practice to work alongside people in their own care.
LS2, mental health nurse
There is communication and teamwork. 131 Speaking to colleagues about difficult encounters prompts feedback and discussion. 135 Good relationships with peers are important to be able to be able to reflect in real time and after events. There are valued support structures, such as supervision, debriefing, reflective practice131 and communities of practice139 (resource).
The provision of formal clinical supervision with ‘someone senior who has more experience than you’ safeguards against the ‘echo chamber you get with peers’ (LS7, psychiatrist). In these circumstances, front-line staff feel empowered to act,140 they engage in ongoing problem-solving,126 they challenge bullying and blaming,126 and they speak up if the behaviour of leaders falls below expectations136 (response). Front-line workers are compassionate, are able to tolerate distress, and are empathetic and non-judgemental:125,126
We are a very reflective station; some of the stations there is no reflective practice, they are quite burnt out. They just take people to hospital. There is no reflection or thought.
LS5, ambulance care assistant
Front-line workers are motivated to care rather than coerce or be rule bound126 (response). There is recognition of the key role played by relationships and the potential for coercive measures to be retraumatising. 133 There is trust and recognition of the central role of power, choice and control in the development of, and recovery from, mental distress. 133,137 Decisions about risk are made with the people directly affected by the risk and the tension between ensuring safety and enabling rights is managed by understanding and negotiating. 137 Front-line workers understand accountability; implement clear and predictable boundaries, which maintain safety;131 and deploy ‘the least restrictive intervention’ (LS7, psychiatrist). Anxieties about risk are managed through clear organisational structures and procedures and working collaboratively131 (resource). There is greater tolerance of risk, and respect for individual freedoms,137 particularly following self-harm. 131 Front-line workers are recognised, rewarded and thanked for remaining compassionate in difficult and pressurised times135 (response):
We take risks in collaboration with service users and carers. We try to work out risks they are comfortable with and support them with that.
LS6, mental health nurse
Clinical leaders/middle managers
A culture of care in which staff and service users are regarded compassionately is achieved when there are shared values and objectives between leaders at all levels and the front line. 138 Clinical leaders promote ‘healing environments’135 in which there is affiliation within teams and between teams,126,127 and front-line workers are supported, treated humanely125 and respected. 140 The Royal College of Psychiatrists, in its report on the importance of compassionate care,126 stresses the benefits of flat workforce structures in which clinical leaders are visible, accessible and compassionate. There is a culture of being ‘at service’. 135 The role of the operational manager is to buffer external demands and to make the work of front-line workers easier,126 to enable them to care:
Leadership is massively important and visible . . . that’s, for me, integral. The quality of a good leader is someone people go to when things get hard. You would like to go to a leader to debrief and have that trusting relationship.
LS7, psychiatrist
Education may include listening, legal frameworks, mentalising, reflection, humanities, ethics, awareness of unconscious processes and how to address the barriers to compassion. 126 Education ‘should involve everyone from support workers to consultants’ (LS7, psychiatrist) (resource):
First and foremost, education, increases confidence
LS3, emergency medical technician
Compassionate leaders implement balanced governance, which carefully facilitates support and accountability. 138 Leaders ensure that roles and expectations are clear131 and they hold front-line workers to account for values and performance. 136 Practising senior clinicians provide the clinical direction. 126 Clinical leaders may role-model prosocial behaviours and skills to front-line workers. 134 Clinical leaders foster growth and make time for staff development129,131,139(response).
Systems
Organisational leaders
Organisational leaders create the conditions for compassionate care and set the tone. 138 There is a strong focus in compassionate organisations on supporting a culture that benefits service users and on addressing system problems. 138 Compassionate organisations have a clearly articulated vision, which maps on to a realistic number of goals for quality and safety, and an achievable strategy. 138 They are transparent about their philosophy (e.g. of recovery and personalisation129) and they communicate ‘what’s going on’ (LS2, mental health nurse) (resource). A culture of reflective practice is embedded in the organisation and reflective practice is considered fundamental, not only for clinicians but also for those in leadership roles139 (response).
For example, compassion is central to recruitment and selection processes. 126 Values, standards and behaviours are incorporated into job advertisements, job descriptions, job plans, appraisals, complaints and compliment forms (resource). Governance is carefully balanced for delivering accountability and support. 138 There are clear structures, procedures and standards to support employees to respond to risk133,137 (response).
Performance management aims to motivate and align values with the values of the organisation and strategies include creating opportunities for professional networking, sharing knowledge, reflection, team development and developing peer-negotiated standards. 139 Clear evidence-based guidelines offer decision-making support and ensure that employees can be held accountable. 126 However, governance arrangements are sufficiently flexible to avoid institutional responses to risk (resource), ensuring that decisions can be made on an individual basis by front-line workers in collaboration with service users137 (response).
There is status and recognition for those who provide compassionate care, especially in pressured circumstances. 126,135 Compassionate organisations openly acknowledge human resource limitations126 (resource). Compassionate organisational leaders do their utmost to ensure that there are resources to meet unpredictable demands, for example that the staffing levels and skills mix are adequate. 138 Compassionate organisational leaders reduce the burden of administrative tasks as much as possible to enable front-line workers to care. 126 They promote affiliation across institutional boundaries and a culture of care in which staff and service users are regarded compassionately126,127 (response).
Intelligence is generated using a range of methods and organisations are not reliant on mandated measures. 138 Quality improvement uses robust methods, and the findings are monitored and critically evaluated, avoiding the potential for indiscriminate use of particular approaches and magical thinking. 138 An executive and a non-executive director may be elected to take a special interest in compassion, with ‘critical friends’ (e.g. non-executive directors, governors or Patient Advice and Liaison Service staff) invited to undertake formal observations of the care and staff support, reporting directly back to the board. 135 Other recommendations in the literature include using mystery shoppers, shadowing peers and swapping roles for a short period138 (resource). These approaches may enable problems to be identified early and for staff who are compassionate to be identified and recognised. 135 Service user and staff feedback is heard, even when the content is uncomfortable or challenging126,136,138 (response).
System leaders
Compassionate leadership is required across arm’s-length, assurance and oversight bodies. 136 Compassionate commissioning, regulation and inspection can reinforce compassion in organisations. System leaders have a duty of care and must not collude with distorted objectives. 136 There is a need to recognise the tension between efficiency and mass production and the importance of the interpersonal and relational aspects of care139 (resource). Compassionate system leaders offer governance that balances control and support, which is demonstrable in policy and across regulatory systems, and ultimately improves the experiences of service users138 (response). A member of the ESG said, ‘Quality needs to be more than a tick box’. 64
Compassionate system leaders drive investment in services, which are valued by service users, such as those that provide physically and psychologically safe and calm alternatives to admission to hospital (response). Examples in the literature include crisis houses, peer support, safe spaces, walk-in services10,133 and women-only environments133 (resource). NHS clinicians who interact with non-clinical services generally view them favourably. However, there may be stringent access criteria, compared with the NHS. One interviewee (JT3, service user) described experiencing a crisis house as being very person-centred, inspiring trust. However, were other interviewees who believed that staff from voluntary organisations may be ‘overinvolved’ and sometimes have unrealistic expectations about what can be done (NC2, mental health nurse):
My impression is that you go there [voluntary sector services] and they haven’t got a checklist of things they need to do for somebody. They don’t ask much of people.
LS6, mental health nurse
Co-production (resource) ensures that the aspirations of service users are encapsulated in the delivery, monitoring and evaluation of services across the system137 (response). Co-creating services with the benefit of systemic, relational and experiential knowledge is reported to drive quality. 139 However, an interviewee cautioned that there could be a tension if the service users involved in co-producing services do not have contemporary experiences of using services (LS1, manager). There may be a need for active recruitment of service users to this role and enhanced remuneration. There also seems to be a need for more service user consultation at this level. An interviewee perceived that people might be ‘unwilling to talk to services’ but would be ‘more likely to feed back to outside organisations’ (JT3, service user):
If the community services are commissioned and work like they should, the numbers [attending the emergency department] should be reduced.
LS7, psychiatrist
IPT 2 pen portrait: compassionate and therapeutic crisis services
Although ESG members endorsed the central importance of compassion, some stakeholders found it challenging to engage with the pen portrait for IPT 2(see Box 7), compassionate and therapeutic care, especially in relation to how compassionate organisations and leaders might forge compassionate and psychologically safe crisis care at an individual level.
Maxine’s GP and alcohol worker wanted her to go into hospital. A community mental health nurse arrived at Maxine’s house to do an initial assessment. The nurse talked to Maxine about why people were concerned and asked what she thought. 122,127,129,131,135,136 Maxine did not want to go into hospital. The nurse recognised that going to the hospital might be traumatic for Maxine because of her history, but was worried about Maxine’s safety. 10,122,129,131 Maxine and the nurse considered the options together. 115,121,122 Maxine’s partner did not think the hospital was right for Maxine either. Maxine, her partner, who lives at the address, and the nurse negotiated an individual plan115,117,118 so that Maxine could remain at home safely. 10,89,96,97,100,107,113,144 Maxine and the nurse knew each other well and there was mutual trust. 10,97,100,118 Maxine knew that the nurse would be open and honest with her and that, if her mental health deteriorated, she could pick up the telephone and would not be turned away. 93,98,109,116,120,142
The nurse went back to the office and communicated the assessment to the team. The nurse felt anxious about the decision to support Maxine at home because the GP had been so concerned that they had initially wanted to call the police. The GP was insistent that Maxine was unable to keep herself safe. 15,92,93,97,103 The nurse trusted his colleagues and felt able to voice his concerns in the office. 10,97,100,103,122 Although the nurse’s colleagues said they would have reached the same conclusion based on the assessment, they all agreed that it would be valuable to take the discussion to the team reflective practice session, as they thought it would be helpful for the wider team to reflect on some specific issues. 134,136,138
The next day, the alcohol worker called the office to complain about the decision to support Maxine at home. The team manager listened to the concerns flagged by the alcohol worker and wondered how they might work more collaboratively. 127,134,136,138 The team manager spoke to the nurse to see if they could offer any support. The nurse knew the team manager respected him and felt comfortable in voicing his distress. In the past, the nurse had been well supported at work by the team manager. 123,133,138
The nurse asked the team manager if they could do a joint visit; as a practising senior clinician, the team manager was pleased to accompany the nurse to see Maxine later that day. The nurse called Maxine to let her know that he would be visiting with the team manager in the afternoon. The nurse asked Maxine if she would like him to do a joint visit with her alcohol worker later in the week. 127,132,133,136,138
Conclusions
Some of the evidence included in this chapter presents a dichotomous view of a system that either prioritises finance and performance management or prioritises compassionate and psychologically safe crisis care. The reality appears to be more of a mixed picture.
It is apparent from this part of the evidence synthesis that the conditions for compassionate and psychologically safe crisis care must be created by compassionate leaders. Compassion shown to front-line staff by leaders leads to compassionate care. A tension between exerting control and providing support was evident at all levels. As integrated care systems are introduced, there is an aspiration that strategic partnerships will reduce competing priorities, which appear to be debilitating to organisations. Alongside these strategic partnerships, there is a need for coherent local strategies for compassionate and psychologically safe crisis care, cognisant of the fact that high-quality care can co-exist alongside the worst examples of care in the same organisation. 127 Strategies should include how compassionate and psychologically safe crisis care is provided to people who may be currently excluded from a range of crisis services, such as people who use alcohol or drugs and people who self-harm.
If–then programme theory
If
System leaders streamline expectations and operate governance that balances oversight and assurance with support. They engage in co-production, which is actively resourced. System leaders recognise the value in services in which performance data are less readily captured, for example crisis houses and peer support. They use diverse data to monitor services and inform decision-making, and trust organisational leaders to deliver high-quality services. There is investment in compassionate and psychologically safe services that service users value.
Then
Organisational leaders have a clear vision, philosophy and values that map onto a realistic organisational strategy. There is transparency. There is affiliation across institutional boundaries and a culture of care in which staff and service users are regarded compassionately. Status is given to compassionate people. There is a culture of addressing system problems. Intelligence is generated using a range of methods, and organisations are not reliant on mandated measures. Quality improvement uses robust methods. Compassion is central to recruitment. There is a compassionate workforce strategy and contingency to meet unpredictable needs. There is governance that balances accountability and support, and facilitates decision-making at the front line. There is evidence-based decision support. Reflection is embedded throughout the organisation. There is staff and service user engagement, and willingness to hear uncomfortable feedback. Performance management is focused on motivating and aligning values.
Clinical leaders/middle managers share values and objectives with organisational leaders and seek to align the values of front-line workers. There are flat workforce structures and practising clinical leaders who role-model prosocial behaviours and skills. There is a culture of being at service and of making the work of front-line clinicians easier. Clinical leaders foster growth and make time for reflective practice and staff development. There is affiliation across institutional boundaries and a culture of care in which staff and service users are regarded compassionately. Clinical leaders/middle managers implement balanced governance, which carefully facilitates support and accountability. Clinical leaders aim to motivate rather than control, but they ensure that roles and expectations are clear. They hold front-line workers to account for values and performance. There is open and honest communication and clinical leaders support decision-making at the front line.
Front-line workers are connected to the goals of their organisation and their core purpose. There are shared values and there is valued reflective practice and opportunities for development. Staff groups are more stable, turnover may be reduced and there is more time. There is open communication, relationships and trust, and front-line workers confidently engage with the leadership team, each other and service users. Front-line workers practise prosocial behaviours and are motivated to care, rather than being rule bound. Front-line workers are empowered to speak up and to act. There is the capacity to tolerate personal discomfort. Front-line workers prioritise relationships, seek to understand, negotiate and offer choice. Front-line workers trust service users and are compassionate.
Leading to
Trust that facilitates belonging. Emotional safety and healing are prioritised, and decisions are made collaboratively. Social roles and relationships are prioritised, and safety is balanced against independence. Freedom, control and privacy are maintained. Treatment and support are personalised. People in crisis are not turned away.
Chapter 5 Focused review of initial programme theory3: community crisis agencies work together
Introduction
This chapter examines the third of the three IPTs, community crisis agencies working together, identified from the initial scoping searches outlined in Chapter 2:
If there is effective seamless inter-agency working, then there is trust, a sense of connectedness, ownership and affiliation, prompting systemic understanding of the crisis care system, leading to improved shared decision-making and communication without repeated assessment or delay.
Inter-agency working occurs when multiple agencies contrive to work jointly to deliver crisis care. The term ‘multi-agency’ occurs frequently in the literature, and is often used synonymously,65 but, for this study, it was decided that the term ‘inter-agency’ was preferable as it conveys a stronger sense of agencies working closely together, rather than in parallel, and will be used from this point forward.
The inter-agency programme theory differs from the others as it was considered of low priority by the ESG members. Following discussion between the ESG and the research team on the basis of their prior knowledge of the inter-agency nature of crisis responses, the IPT focused on inter-agency working was retained. Indeed, the review findings highlight the extent to which the sharing of knowledge and practices between agencies supports all aspects of adult community crisis care.
This chapter first describes the characteristics of inter-agency working, including interventions and intervention components identified in the literature to enhance inter-agency crisis care. The evidence base for inter-agency working in crisis care, the outcomes of inter-agency care and the unintended consequences when key components are not in place, or are not effective, are described. Subsequently, the chapter describes the mechanisms for inter-agency crisis care, demonstrating how it may be facilitated at different points within mental health community crisis care. A narrative drawn from the literature is supported by contributions from the ESG discussions and interviews. The chapter concludes with an overview of how inter-agency working can enhance mental health crisis care, using the ‘if–then–leading to’ convention.
Context: inter-agency working
The context of inter-agency working in mental health crisis care is a complex one. 65,81 The nature of mental health crisis means that agencies from statutory sectors within and outside the health sector are involved, including, commonly, the police,141 but also emergency departments,142 the NHS 111 telephone or online advice service143 or paramedics. 142 Non-statutory services, such as voluntary organisations, are also frequently involved:10
. . . you want this independence from the stat[utory] sector because you want to be able to pick up the people who aren’t going to turn up or whose behaviour might be a risk, so in an ecosystem you want all of this range – and some of these were people in an urgent state.
KB4, academic
Agencies responding to people experiencing mental health crises require links across the whole system. These links are subject to temporal changes as services are commissioned and decommissioned and relationships between staff develop or diminish. 10 Inter-agency working operates at a range of levels, from joint decision-making with limited shared resources to more complex and fully integrated systems. 81 There is no single model of integrated care; what matters is that the integration is primarily designed and co-ordinated around the needs of individuals, rather than to serve the needs of organisations. 144
Inter-agency working is seen as a way to co-ordinate complex systems of care and was initiated across England in the context of mental health crises by the Crisis Care Concordat. 27,28 It is currently implemented at area commissioning level, enabling community crisis services to be designed to meet local population need. 30,92 More recently, inter-agency crisis care has been described as comprising four categories: (1) community-based crisis services, (2) blue-light services, (3) liaison mental health services and (4) age-specific services. 89 Organisations employ many strategies to deal with the inherent complexities of crisis care systems; ultimately, the commissioning of inter-agency crisis care must support the principles of intervention being ‘everyone’s job’ and there being ‘no wrong door’. 145 Contextually important intervention strategies of inter-agency working that supports community crisis service delivery were identified and are shown in Box 8.
The evidence base
For the theory component ‘inter-agency working’, 721 new records were identified from electronic database searches and nine from iterative hand-searching. Of these, 22 were retained. A further four were retained from a backward citation search of the 22 new included documents.
In view of the emerging insight into the core relevance of inter-agency working, the results of focused review searches 1 (urgent access) and 2 (compassionate and therapeutic care) were iteratively hand-searched, generating an additional 11 included records for this review (inter-agency working). Six of these 11 records are appraised in Chapter 3, The evidence. 2,15,94,101,106,118 The remaining five are appraised in Chapter 4, The evidence base. 55,131,132,134,140 In total, 26 new records and 11 previously identified records were retained. Figure 9 illustrates the identification of studies for this review.
FIGURE 9.
Search results of the focused review for IPT 3: inter-agency crisis services.

Retained new records: inter-agency working
Details of the 26 new retained records for the focused review on inter-agency working are in Appendix 4.
Settings
The research settings reported in the retained new records (n = 26) were as follows: inter-agency crisis services,27,28,30,89,155 and specific inter-agency collaborations, including between mental health services and the police81,98,141,146,148,150–152 and between mental health services and paramedics. 142 Other settings included voluntary sector services,10,156 integrated mental health services,147,157 integrated health services,144,149,153,154 commissioning health services145,158 and crisis mental health services. 143
Focus
The retained records reported on models of integrated service design,81,98,144,151–153,156,157 policy guidance,27,28,30,145 good-practice guidelines,89,147,154,155 service user experiences,146 voluntary sector contribution,10 staff experiences,149,150 decision-making,148 commissioning,158 inter-agency self-harm interventions142 and NHS access to urgent crisis help. 143
Appraisal of relevance and rigour
All included documents were appraised for relevance and richness using a modified realist appraisal tool72 (J Jagosh, personal communication) (see Report Supplementary Material 3). For this review, records were scrutinised for relevance to inter-agency working in mental health crisis services. Documents containing primary research data were also appraised for rigour using the MMAT73 (see Report Supplementary Material 3). The combined appraisal of relevance and rigour identified that the evidence supporting IPT 3, inter-agency working, is based on studies of mixed quality.
Two documents were highly matched to the theory component: they provide rich descriptions of context, mechanism and outcome and were key documents focusing on voluntary sector crisis services10 and inter-agency crisis care between police and health services. 98 Both studies reported rigorous mixed-methods studies limited only by being at the level of description10 and reporting inconsistencies in analysis related to limitations in clinical data recording. 98
One mixed-methods study evaluated the impact of implementation of the Crisis Care Concordat and was rich in context and outcome, providing moderate relevance to the theory component, although limited by evaluating data from 12 months of implementation. 28 Two further mixed-methods studies were less substantially relevant to the theory component, providing mostly context. 148,153 An included survey provided less substantial relevance and was limited by a small sample size. 149
Included qualitative studies provided rich descriptions of context related to integrated police and health services, with some reference to outcomes, but very little mechanism, and were moderately framed to the theory. 150,152 Both studies were limited by a lack of lived-experience perspective,150,152 and one study describes a model of inter-agency crisis care not available in the UK. 152 A further qualitative study was less substantially relevant to the theory, providing mostly context, with limited mechanism or outcome. This study reported a very small sample, with resulting lack of variation. 146 Two literature reviews, a scoping review81 and a meta-synthesis,142 were less substantially relevant, providing only context.
Expert reports containing rich descriptions of context and mechanism were moderately framed to the theory. 89,144,147 Expert reports less substantially relevant were limited to providing inter-agency context. 141,151,154,156–158 Included policy documents were moderately framed when they contained specific context related to inter-agency crisis services27,30 and were less substantially relevant when they were limited to local context155 or had a context wider than mental health. 145 Expert reports and policy documents were not appraised for rigour as they reported limited or no information on method.
Outcomes
Inter-agency working
Service user outcomes
As there are numerous agencies that can become involved in trying to provide support for a person experiencing mental health crisis, it is inevitable that they will not all have staff with expert mental health knowledge and experience. One of the benefits of inter-agency working is providing a range of expert input to meet different health needs. 147 What is important to those accessing services is co-ordination: people are often less aware of how services integrate unless a failure to integrate results in discontinuity. 154 People seek a ‘single trusted point of liaison’. 154 An interviewee explained that continuity depends on the availability of a ‘key contact’ responsible for planning and relaying information (JT1, service user).
A focus on joining up statutory health services with non-health services (such as housing) and non-statutory organisations, such as the voluntary sector, is a stated priority, although a lack of outcome data makes assessing the extent to which current inter-agency working achieves this difficult. 10,145 From a practice services delivery perspective, improvements in street triage models have prioritised development of systems to foster inter-agency links, as explained by an interviewee:
. . . so, they’ve got a vulnerable person’s hub . . . with links to safeguarding and to local authority and our emergency duty team . . ..
KB6, manager
Inter-agency systems that include providing more user-focused interventions show promise in improving outcomes related to the experience of people in crisis by providing interventions including shared decision-making, peer support, befriending and advocacy. 10,89,155 Good-practice documents suggest that co-produced crisis care is an aspiration that requires inter-agency working. 89
In-depth qualitative analysis of service user narratives identified that inter-agency working between police and mental health staff in a street triage model provided more immediate access to specialist support in a setting suited to the person’s circumstances, but also minimised unnecessary, and potentially traumatic, retelling;146 care was experienced as more dignified, less restrictive and less disruptive to the lives of the person and their family when staff were working within defined roles and across integrated agencies. 152
Service users want front-line staff to have two key areas of knowledge. 154 First, they want staff to know about them as individuals and, second, they want staff to know how to help and from where help can be reached. 154 To achieve this, staff require knowledge about different parts of the inter-agency system, there needs to be information-sharing and meaningful communication between staff in different agencies.
An interviewee explained how having meaningful communication is helpful:
Sometimes it does help as you can mainline the supervisor and we are [usually] very strict on chain of command . . . but having that relationship, you can bypass that and go straight to the person you know.
KB1, police officer
Activities that facilitate interpersonal contact between staff in different agencies, such as through job shadowing, joint training and cross-agency meetings,145 have been linked to improvements in knowledge about different agencies, information-sharing and inter-agency communication. 10,145,148 This can improve immediate referral of people in crisis to the most appropriate service through a more streamlined process with fewer ‘closed doors’ and, ultimately, greater satisfaction with crisis support for the service user. 147 Improved communication and information-sharing between police and mental health services facilitated improved care planning that helped to reduce repeat presentations in services, and reduced the use of police time. 148,150
People in crisis view co-location and co-response models favourably, although this was not necessarily related to the agencies being based at the same location. 98 An interviewee stated that being co-located in ‘neutral spaces’ produced better outcomes (KB6, manager). Service users focused more on joined-up and seamless receipt of care that met their individual needs. 145 Inter-agency working can provide a stability in the delivery of crisis care that can lead to better outcomes; this has been emphasised in policy as especially important for people presenting with multimorbidity or complex needs, such as substance use and mental ill health. 145 The findings from a national evaluation of integrated care found that, after service integration, service users had received their care plans more frequently and that their care was better co-ordinated. 153
Staff outcomes
In a national evaluation of integrated care, staff reported taking on greater responsibility within their roles, which made their jobs more interesting. They did, however, identify a need for additional training to support integrated working. 153 Importantly, 53% of front-line staff respondents considered service integration to have improved patient care, and only 1.1% believed that care had got worse. 153
Joint training can, most obviously, lead to a better knowledge of the services that make up the complex network of crisis services in a locality and how that network operates. 10,150 Front-line staff who have knowledge of available services are better able to help service users navigate more smoothly to the most appropriate services. 147 Joint training can improve relationships between staff in different agencies, leading to improved information-sharing98 through a mutual understanding of different roles and by providing an avenue for exploring different values within an inter-agency system. 10 Successfully integrated care relies on the attitudes of the staff within the system and the relationships between them. 150 These relationships, alongside inter-agency leadership, are more important to successful inter-agency working than the structural aspects of the system. 147
Joint training programmes enhanced knowledge of the options available to police officers, resulting in deceases in detentions using section 136 of the UK Mental Health Act 1983. 98,118 The design and content of joint training is less clear, but established inter-agency forums at managerial and front-line service delivery levels provide a platform for co-design of training. 27,30
Job shadowing, whereby staff from one agency shadow staff from another agency that they will be frequently in contact with, is promoted by some multi-agency systems. 98 Interpersonal contact between staff in different agencies can lead to more streamlined processes and, ultimately, greater user satisfaction with crisis support. When services are more streamlined, there is the potential for reduced service costs, as inappropriate referrals cost resources and cause distress. 153
Police having immediate access to expert mental health advice by telephone was shown in a local service evaluation to be highly valued by police in helping them respond to challenging situations, such as when a person has self-harmed or is suicidal. 148 Evaluation findings concluded that access to telephone advice in this way improved decisions and co-ordination of multi-agency responses, especially during the night, and reduced police time spent attending the call. 148
System outcomes
The Crisis Care Concordat27,30 identified continuity of care as an important factor in producing desired outcomes in crisis care, yet this has been identified as difficult to provide in a system that conceptualises crises as single events. 10 The Crisis Care Concordat27 also set targets to reduce costly and distressing out-of-area placements. This has been achieved through inter-agency collaboration and, when successful, has enabled diversion of cost savings to improvements in community crisis interventions. 157 A reduction of up to 32% in the use of section 136 of the Mental Health Act 198327,118,150 has been observed through implementation of street triage (an inter-agency response between police and mental health). 146 Other beneficial outcomes included reduced transportation to places of safety by ambulance and police services101 and reduced attendances at emergency departments. 98,146
Health and social care services form a complex system. The commissioning and contracting out of health services has been the dominant model, leading to a range of providers delivering services,158 each with different organisational boundaries. A police force area might cover several NHS trust areas, whereas a small voluntary organisation service might serve only one town in this area. Thus, in any given region of the UK, there will be a network of specialist and non-specialist agencies that respond to people experiencing mental health crisis across different sectors. 10 Sometimes only one agency can respond to the crisis (a first response), but it is more likely that an immediate referral will be made to another agency (a second response). 152
Specified first- and second-responder roles were highlighted in an Australian inter-agency model as important to improve the outcomes related to transition between services within an inter-agency system. 152 The terms ‘first’ and ‘second’ responder are not usually associated with crisis mental health service design in UK settings, as explained by an interviewee:
This is where it gets quite complicated if you use the term first responders, it’s actually a programme [of volunteers] in the ambulance sector. The ambulance and police would normally say ‘first on scene’. I think this is where language is really important, because yeah, they do mean different things. I guess they just need to be clear, because if they’re calling themselves first responders, they could be mistaken for volunteers.
NC1, mental health nurse
Despite the potential for confusion, the term ‘first response’ is beginning to appear in more recent UK descriptions of good practice in inter-agency crisis care models,151,157 for example ‘Receives a first response in the community’. 89
The voluntary sector can have a unique role as the main provider in supporting communities, especially for those who report long-standing poor relationships with, or low expectations of, statutory services;10,64,106 for example, the Health and Wellbeing Alliance is a voluntary organisation that supports communities that experience health inequalities:156
This is key – there’s a normative assumption that integration with public services is helpful, but some people have had contact with public services, e.g. Afro Caribbean men, and they don’t have a lot of truck with them, so organisations supporting them might want to keep their independence, people who’ve been multiply sectioned.
KB4, academic
A typology of voluntary sector services providing mental health crisis care shows that co-location or jointly commissioned service models between voluntary sector and statutory services have provided a platform for inter-agency working. 10 Co-location models have been linked with more efficient use of resources in police and ambulance/paramedic contexts by enabling faster transfer of care to an appropriate service, following an immediately accessible, expert, mental health assessment. ‘Downtime’ for police or ‘time taken for call’ for ambulance paramedics is reduced and cost efficiency improved. 98,101 Joint response services between police and mental health have been found to be most effective when covering a smaller area with a dense population, compared with the greater reach of mental health support via the emergency control room. 98,150
Mental health staff located with police resulted in reduced need to transport people to A&E or places of safety and to use section 136 of the Mental Health Act 1983. 98,118 A UK local service evaluation of a pilot mental health ambulance car reported that the proportion of people transported to A&E had reduced by one-third, with associated cost savings suggested. 101
Multi-agency forums were highlighted by the Crisis Care Concordat as beneficial to mental health crisis services,30 and the importance of multi-agency leadership and co-ordination has been endorsed as key to positive outcomes in crisis care. 10,15,64,108,154 As recommended by the Crisis Care Concordat27,30 a SPA service can enhance effective inter-agency working. SPA is an arrangement whereby all services, provided by multiple agencies, are channelled through one referral process, and may be accessed simply, for example by phoning a single telephone number. The effectiveness of a SPA relies on people with knowledge of the whole system, who can connect or reconnect people to the best service to meet their needs. Although there is a paucity of published evidence on the efficacy of SPA interventions, there is some tentative evidence that staff acting as navigators for a person experiencing a crisis improved the knowledge of providers and helped staff feel more confident when co-ordinating crisis responses. 157
Staff systemic understanding of the remit of different services was improved through well-maintained ‘warm networks’ facilitated by job shadowing, focused induction programmes for staff that include different agencies and inter-team meetings. 98 An ESG member described the link between these warm networks and what they termed ‘warm handovers’, whereby good interpersonal relationships encourage front-line staff to invest in information-sharing between agencies. 64
For inter-agency working to succeed, there is a need to focus on improving team working both ‘within and between organisations’. 153 The degree of engagement between staff across agencies is a predictor of organisational performance. 147 Co-ordination of inter-agency working is considered most important where there is complexity and/or urgent need; it can improve outcomes in health care generally144 and has been shown to have positive impacts on crisis services. 28 Co-ordination is also identified as important to how service users experience services. 154
In terms of distal outcomes and future policy aspirations, inter-agency collaboration is a prerequisite for co-produced crisis services as it provides a platform for all voices to be heard. 89,154 Inter-agency approaches that facilitate quality improvement approaches that are instigated from commissioning through to delivery and evaluation have the best chance of enabling co-production. 89
Although there is no single model of integrated care, leaders should focus on removing barriers and adopting change models that are not overly prescriptive about how integration is achieve. 144 The greatest impact on individual outcomes is likely to be achieved when integration is focused on meeting the needs of people where co-ordination is at its weakest,144 such as in crisis services. Although integration can improve the process of care, it is not guaranteed to reduce costs. 153 The success of inter-agency systems relies on having goals that form part of a shared vision, led through engagement that empowers all partners. 157
Unintended consequences
Inter-agency working
Service user
In response to the many ways in which mental health crises manifest, there are a range of different agencies that can be called on to respond. 89 The responder depends partly on the location and circumstance of the person in crisis, and whether they or their family actively seek help, and from whom. Staff working within this network of different agencies might not have a ‘systemic understanding’ of the network they are part of, particularly where there is high staff turnover and frequent service reconfiguration. 10
For many people and their families, this system complexity might mean not knowing how and where to seek help and might affect the chances of them being directed to the most appropriate place for their situation. It might also result in people having continually to repeat traumatic details to different people, adding to their already acute distress. 146 System navigators are needed to pull together integrated care;147 in the context of crisis care, this function may not be best provided by existing systems of care co-ordination, particularly for those new to services.
An interviewee explained that a crisis care system that is provided by multiple agencies should improve outcomes, but the benefits are not realised unless the system operates in an integrated way:
. . . you would think that the model that is in place at this moment in time is much better and it’s actually not. It’s too detached and I think that’s always been the problem . . . when I interviewed all of the service users [inter-agency working] . . . was the one thing that they all said was useful.
KB6, manager
Added to this complexity are differences in the route into crisis care linked to ethnicity and cultural beliefs. 106 A failure to accommodate this variation in routes to crisis care can result in people being delayed in reaching services and more distressed at first contact. This delay contributes to increased likelihood of hospitalisation, detention and restrictive interventions. 106 Inter-agency collaboration is needed to ensure that the aspiration for ‘no wrong door’ is a reality for minority groups who are more likely to be marginalised by mainstream services. 10 Interviewees explained that some cultural groups access services via different routes and have different beliefs about seeking help that can act as a barrier:
In the south Asian community, people are less likely to contact the police or mental health. Some cultures naturally don’t involve the authorities and the same with mental health.
KB1, police officer
A good example is the Imams and community leaders take the place of social workers and decision-makers, they resolve domestic and criminal matters . . . the number of things that are brushed under the carpet . . . not just in Asian but in non-indigenous white communities.
KB1, police officer
BAME [black, Asian and minority ethnic] groups are less likely to come to A&E or any service really and that’s to do with different systemic factors, structural inequalities, racism, suspicion of services seen as for the white majority, not seen as culturally sensitive, different beliefs about health and health care and a more close-knit family environment which tends to manage crises at home rather than access outside help.
KB5, psychiatrist
A lack of integration results in fragmented services, which may lead to ‘responsibility cordons’ with gaps in support, resulting in service users being ill-informed, distressed and potentially at risk. 10,138 Services users place great importance on continuity; if this is lacking during a mental health crisis, the stress people experience is increased. 118 An interviewee (JT1, service user) reported that when they ask for things, they are commonly told it is somebody else’s job. This is a phenomenon described by a participant in a mixed-methods study of the voluntary sector contribution to crisis care as services playing ‘responsibility tennis’. 10
Integration does not always produce positive outcomes: service users reported that, after integration, they found it harder to see a nurse of their choice, were listened to less frequently and felt less involved in their care. 153 Furthermore, these disadvantages were most evident for people who were considered at highest risk,153 such as people experiencing a mental health crisis.
Staff
Staff identity and role clarity
Barriers to inter-agency working relate to the beliefs of staff in different agencies about their role in mental health crisis care; for example, a review of street triage reported that some police officers are critical of mental health systems, believing that dealing with mental health crises is not within the remit of the police service and they are called on to fill gaps in services. 151 In a study of paramedic responses to people who self-harm, one respondent reported that, when they took time to talk to an individual in crisis, they were criticised by other paramedics who believed that this is the job of a social worker. 142 Police officers reported a lack of clarity about their own role and the role of staff from other crisis response agencies, leading to a reduced ability to make decisions about risk and delay in getting help for the affected individual. 149 These examples appear to suggest that mental health care is on the periphery of, rather than central to, the role of blue-light services,142 even though these services routinely come into contact with people in crisis. 89 This can result in these staff being conflicted in their role when attending mental health calls. This conflict is driven by culture of their organisation and their profession and can act as a barrier to optimal mental health crisis care:
The service users I talked to said that the police . . . are really lovely, really caring, really kind when they were with them in A&E, or when they were talking to them on a bridge, [and] in the car having a chat. But they weren’t nice when they were in the police cells.
KB6, manager
Although co-location models have provided a platform for collaborative working between blue-light services,98 the voluntary sector10 and statutory mental health services, this approach may not be universally supported by the staff in these agencies. The ESG members,64 and some staff in a study of the voluntary sector,10 reported that they believe that the unique value and independence of the different agencies risk being lost if organisations become too closely aligned with statutory services. Joint training may provide a forum for articulating differences between values and perceptions by:
. . . offering a radical critique of public sector services, which may not be well received by the public sector and may challenge the development of collaborative relationships, inadvertently fuelling unhelpful stereotypes.
Newbigging et al. 10
However, training framed as ‘joint’, but which lacks a sense of collaboration, can cause frustration; an interviewee explained that they had volunteered for a workshop with the police, but found it:
. . . so disappointing; it was joint ambulance–police and was dealing with absconded patients, which is now an ambulance service job. [But] instead of being a workshop, a police officer that said, ‘we’re not doing this [dealing with absconded patients] anymore’ and that was that. No practical useful work. We get no info[rmation] and have to go [back to the ambulance team] with no other information. Incredibly difficult.
KB2, paramedic
Furthermore, if the training has no mechanism for sharing the learning with others across agencies, then the knowledge is embodied in one individual, who is not always available:
. . . they don’t always cascade the knowledge down, so you end up with silos of knowledge and experience and then they are off sick or leave . . ..
KB1, police officer
Co-ordination across agencies
A lack of inter-agency working leads to mistrust and suspicion, resulting in reduced collaboration or co-operation between staff groups151 and an overly dismissive approach to referrals from some agencies. 64 Differences in the approach to onward referral between NHS and voluntary organisations have been described as the subtle but important differences between signposting, whereby the person and their family have to co-ordinate and navigate to the service, and referral, whereby access is facilitated by services. 10 A limitation of co-response models from the perspective of police was an inability to co-ordinate attendance between agencies, often because of poor systems of communication. 149
When resources are not co-ordinated or properly resourced, partner agencies have difficulty knowing how to respond. 149 Slow responses, or high thresholds for access from crisis teams, often as a result of resource pressures, are perceived by police as system failings and can breed resentment, which is a barrier to inter-agency collaboration. 149 Difficulties sharing information were attributed to information technology (IT) systems not being integrated, as one interviewee explained:
The inoperability of the IT systems was a complete nightmare, data-sharing and all that . . .
KB6, manager
The effect of staff burnout
Front-line workers may not trust service users,134 each other140 or clinical and organisational leaders, and may also resist inter-agency working. A lack of inter-agency working can leave individual front-line staff feeling that they are powerless and unable to help, and they commonly become frustrated,132 demonstrating negative attitudes, anxiety and avoidance. 131 High staff caseloads in crisis care can have a profound impact on staff morale and their ability to work collaboratively within an inter-agency system. 147 If there is an absence of support, there is a strong risk staff will become cynical136,159 and they may engage in conflict. 138 A lack of support generates defensiveness, weak communication and poor teamwork140 within agencies, making inter-agency working less likely.
System
Commissioning and evaluating inter-agency systems
A search of the Crisis Care Concordat web pages, originally used as a repository of good practice in crisis care across England, revealed that data were last updated in 2016 and the quality of the data held there was inconsistent. 30 As this website has also been a communication hub for national co-ordination of crisis care in England, there is currently little evidence of ongoing national co-ordination, and it remains unclear how inter-agency crisis care has been co-ordinated in the other nations of the UK. Although policy has stipulated that inter-agency systems are required in crisis care, and some have been established, there is a sense that implementation has been inconsistent. 144
Regionally devolved responsibility for inter-agency crisis care has contributed to large variations in the system of agencies involved in delivering crisis services and how these agencies operate together. 157 These differences may be accounted for, at least in part, by commissioning responses to local population need or geographic differences, but, as a result, meaningful evaluation of what is working is very complex. A failure to design and commission services to meet the needs of local populations taking account of the geography can create barriers to collaboration between staff,150 as one interviewee explained:
. . . it’s so big, the geographical area is . . . nobody’s bought into it ’cause nobody benefits from it, you know? I absolutely understand why they think . . . strategically, ‘put the investment into one big centre’ . . . so it works for them [police] because they only have one control room triage, that’s fine. Don’t work for us [working across] three mental health providers that go over [the whole geography].
KB6, manager
NHS regulation focuses on individual organisational performance, rather than across the system,144 making evaluation of inter-agency working lower priority and potentially producing fragmented data. An absence of joint commissioning that reaches beyond crisis care services risks gaps and delays for people needing more than one agency to respond. 147 Poor co-ordination of inter-agency services results in people becoming lost in the system, where their care is delayed or duplicated, the quality of care declines and the service is less cost-effective. 144
Devolved commissioning and contracting out of health services can lead to the dual and often competing aims of cutting costs and responding to local need. 158 These commissioning processes often mean that the configuration of service availability frequently changes and, as a result of contract changes, the (often related) appearance and disappearance of providers. 10
Impact of inter-agency systems on service delivery
A failure to include all relevant agencies in the inter-agency system can contribute to delays and disputes about responsibility. 10 This can be especially difficult when the excluded agency has a statutory responsibility, such as for transporting people in crisis. If ambulance teams are excluded from inter-agency agreements about transportation,101,160 and this is coupled with a failure to acknowledge the important contribution that ambulance staff make beyond transportation, ambulance staff believe they are treated like a taxi service,142 breeding resentment and resulting in responsibility disputes. 10,149
The specialisation of teams can lead to staff becoming protective of their service, creating barriers to inter-agency collaboration. This can result in polarisation of agencies in the system, generating systemic inflexibility that prevents access and transition through the system. 161 Polarised services within the system can create service silos that are unable to meet all the needs of people in crisis because they are not able to operate beyond the boundary of their own service, something that has been noted as a particular challenge for people with more complex needs. 161
In IPT 1, believing that a crisis service provided a guaranteed response was linked to how people make decisions about where and from whom to access help in a crisis. 97 Inconsistencies in these guarantees, such as for an agreed care plan, a named care co-ordinator and telehealth, have been identified as an artefact of policy variations, rather than an issue about spending,144 and may therefore have the greatest negative impact on those with complex needs requiring responses from multiple agencies. A further organisational issue is that, among these multiple agencies, there are not always coterminous operational boundaries and this can lead to one agency having to network with several others performing the same role, depending on the precise location and needs of the person requiring support. 150
Co-location models highlight tensions between providing services that are adequately resourced 24/7 and having periods of wasteful inactivity that can lead to staff being redeployed to other parts of the service, rendering them unavailable for crises that occur after redeployment. 98 Findings show that co-response models result in efficiencies for the non-mental health service (police, A&E, ambulance). although there are significant methodological limitations in these health economic calculations. 98,101 There is, however, a lack of data related to the impact on cost and resources in mental health services as part of co-response models, and doubts have been expressed as to whether or not simply placing professionals together in the same location is enough to ensure collaborative service delivery. 147 An interviewee described these problems:
I’m not a fan of nurses in police cars. The only reason being is you’re always in the wrong place. So . . . you can only have one nurse ever on at a time. The problem [is] if you say you’ve got a nurse in a car that will respond to every mental health incident, you haven’t! Because you’ve only got one nurse here . . . you just can’t deliver that as a consistent service. And that’s the problem. You will always have police officers and that go, ‘well I rang and [the nurse] weren’t there’. And then [they] just stopped believing in it and stop engaging in it ’cause it didn’t work for them.
KB6, manager
Mechanisms
Service users
When people recognise crisis services as being relevant for them (response) by having been developed with involvement from their community106 (resource), people have a sense of connectedness to the service2,10 (response). Inter-agency working that is planned and delivered with involvement with those who access services (resource) generates mutual trust and shared ownership89,147 (response). Inter-agency services that demonstrate culturally sensitive values106 by being staffed by people who represent the diversity within the community they serve, have had training to improve cultural awareness and use language and communication that avoids stigma and racial stereotyping89,106 (resource) promote a sense of belonging and shared values, which, in turn, lead to reduced fear or shame about accessing the service118 (response). When people are less afraid (or stigmatised), they take an active role in their own recovery,2,10 engendering a sense of ownership and pride that enables them to take an active role in their community, for example through volunteering or providing peer support, and challenging negative attitudes10,64 (response).
When an inter-agency system of crisis services provides user-focused interventions including peer support, befriending, advocacy and less clinical services, such as those delivered in the voluntary sector (resource), then people in crisis recognise services as being ‘for them’, providing a sense of safety that fosters engagement10,89,145,155 (response). Within a complex inter-agency system when individuals are provided with a ‘single trusted point of liaison’154 (resource), they feel confident to navigate the system and are able to build trust that provides the sense of continuity and relational safety that people seek10,147 (response).
Staff
When staff have attended training suited to their specific role in providing support in a mental health crisis, staff have increased knowledge, improved skills and increased confidence in providing crisis care, and there is more interpersonal contact between the person and staff member (resource). This can lead to practice that is less risk averse and restrictive. 98,147 The person in crisis is more likely to feel supported and trust the service to keep them safe by providing care that people value, staff are happier and have more confidence in their crisis response (response).
Clarity about how the pieces of the system fit together help to reduce concerns about, for example, a perceived shift from a more psychosocial focus to a biomedical and risk-focused approach15 (resource). Role clarity, coupled with system knowledge, within inter-agency services (resource) supports staff to hold a more balanced perspective between legitimate concerns about the nature and timing of responses and an informed acceptance that the spectrum of care is available across the system. This enables front-line staff to understand where their role fits, allowing each part of the system to ‘play to its strengths’ (response). 10 Clarity about how their role fits within the wider service enhances front-line staff confidence that they are working within an accepted role and enhances their belief that their contribution is valued, reducing suspicion and cynicism about other front-line staff roles10 and enabling improved communication161 (response).
Inter-agency working needs stable internal team-working, facilitated by leaders who drive integration147 (resource) to enable different agencies to operate collaboratively (response). When team-working is stable within and across agencies (resource), front-line staff are able to create a positive team culture that is open to ‘being challenged’10 (response). Openness and challenge within and across teams provide opportunities for professional and user debate that facilitates scrutiny and advocacy, (response), especially where this involves voluntary sector teams10 (resource).
Increasing interpersonal contact and rapport between staff in different agencies by facilitating gatherings at which people share experiences and perspectives,28,150 including through joint training10,94,98,149 and job shadowing27 (resource), fosters mutual understanding and respect for differences in values and approaches to crisis care10,15,153 (response). Mutual understanding achieved through interpersonal contact (resource) can help to facilitate the development of shared goals and understanding of each agency’s role, and the overall ‘landscape of demand’28 on all parties149,150 (response).
Learning together (resource) creates new lines of communication and a sense of collaboration and a shared language that can overcome communication difficulties caused by jargon98,104,149 (response). This means that, in future contact, they might know the person they are liaising with; this goodwill on both sides can make the process go more smoothly, with agreements being able to be made and negotiation over who will provide what (response). Leaders and staff within each agency have new perspectives (resource) through which they develop improved understanding of how demands on their services differ (response); through sharing (resource), new ways of responding could be fostered28 (response), and warm handovers provide opportunities for improved information-sharing between agencies64,161 (resource).
The presence of colleagues with different expertise in the same office or car, or by rapid remote access over video calls or telephone (co-location and co-response), provides instant access to specialist advice (resource) and can help the spread of good practice30,98 (response). Co-location and co-response models (resource) promote collaborative decision-making between staff in different agencies (response) by drawing on a range of expertise, including being able to draw on each other’s established knowledge of, and links to, services. Being able to share expertise in these ways helps to support decision-making regarding the appropriateness of onward referral (resource). The social contact of sharing a car, or office, responding to calls together and getting to know each other promotes professional trust and respect for the other’s expertise (response).
Systems
Agreements about shared procedures between agencies, including assessment, prioritisation processes and information-sharing that is supported by integrated IT systems147,150 (resource), enable staff to ‘buy into’ the system10,94,147 (response). Shared agreements such as these provide clear boundaries for staff (resource), thereby allowing them to overcome anxieties regarding rules about data protection and confidentiality, improving confidence when communicating between agencies and improving motivation to do so from all involved96 (response). Shared assessment processes (resource), streamlined communication and improved decision-making98 between agencies ensure that the assessment gathers all the information needed by each agency, so that each agency can quickly access the information it requires and reduce the number of times people in crisis have to repeat themselves64 (response).
When commissioners and leaders across agencies work to co-produce and co-design crisis care informed by local population and geographic data,64,158 in collaboration with representation from all stakeholders89 (resource), different values and definitions of crises are accommodated, and problem-solving is conducted across the system (response). When evaluation is carried out using methods that incorporate inter-agency data (resource), commissioning is informed by a whole-system approach153,161 (response). By taking a whole-system approach to commissioning, organisations, particularly smaller voluntary sector organisations, can have a stable presence10 and there is system-wide understanding of the resources required. A system-wide understanding helps to avoid the detrimental impact of agencies operating in silos and being focused on protecting resources, thereby improving the ability of the whole system to maintain the flow of people through the complex pathway. 147 There are links between national policy expectations and co-ordination of inter-agency crisis service commissioning and local delivery27,30,89,152 (resource). There is legitimacy for inter-agency quality improvement, evaluation and research direction for system leaders10,28 (response).
IPT 3 pen portrait: community crisis agencies work together
Discussions with ESG members identified that the pen portrait for IPT 3, Karl’s story (Box 9), was limited to providing one example of inter-agency crisis care amid a vast array of possible inter-agency responses. Although ESG members recognised Karl’s experience as representing one experience of inter-agency crisis care, a limitation of using pen portraits in this programme theory was the limitless possibilities for inter-agency configurations that cannot realistically be represented in this way.
At 9 p.m., Karl is in a very distressed state in the town centre near where he lives; he is shouting and gesticulating at passers-by. A staff member at a corner shop calls 999, worried that Karl is a risk to others; she thinks he might be drunk or on drugs. 2,10,15,89,94,97
A police officer arrives at the corner shop and is shown in which direction Karl has headed. The police officer finds Karl leaning over the edge of a bridge over the railway. He tries to approach Karl, but Karl threatens to climb over the side of the bridge if the officer comes any nearer. From what he says, the police officer suspects that Karl might be experiencing a mental health crisis. The police have a street triage service, so the officer is able to immediately telephone for support from a mental health nurse. 97 The nurse is located in the emergency control room, but is also able to attend in person. 97,141,147
The nurse goes to the bridge, where she recognises Karl from when she worked in a previous role in mental health services. She also knows the police officer from being based in the same building and attending training together. 124,125,129,137 They are quickly able to work collaboratively to decide on a plan for Karl. 97,115,121,122,151 They decide it is best if the police officer keeps his distance, while the nurse approaches Karl, addressing him by name. 122,129 She can see how upset he is and reassures him that he won’t be in trouble with the police. After taking time to talk with Karl, he eventually sits on the ground, making it safer for the nurse to approach him. 127,128,131,135,136,138
Karl tells her that someone has broken into his flat and stolen his money; he feels overwhelmingly upset and angry. The nurse asks Karl who supports him these days, and if he has any support at home. 95,96 Karl says that he sees his community nurse once a month, he goes to a service user-run café every few days and he has regular contact with his brother. The nurse knows the café; it’s run by a voluntary organisation that also has a crisis drop-in until midnight, which she has taken people to before. 10,128,130,153 She asks Karl what would best help him now. They decide he needs help getting his door secured and tidying up his flat; he’s also worried about who has broken in. 10,95,108 They agree that the priority is for Karl to feel calmer, so the nurse suggests that they go to the crisis drop-in service. 122
Karl agrees for the nurse to explain the situation to the police officer. Karl passes on the name of the housing association so the police can contact them to arrange a locksmith. 118,120 The police officer leaves the scene to follow up on the break-in. The nurse accompanies Karl to the crisis drop-in and, with permission from Karl, explains what has happened. 10 The nurse agrees with Karl that she will also update his community nurse, who is also his care co-ordinator, about what’s happened and ask him to contact Karl to check he’s OK. 136,142,145,151,152
Once he feels calmer, a peer worker10,153 at the crisis drop-in helps Karl contact his brother, who goes to meet the police at the flat and then comes to collect Karl and take him to his house for the night. 10,95,96,102,109,114 The voluntary organisation makes an appointment with Karl for the next afternoon with a support worker, and also gives him a number to ring if he needs help before then. 10,89,96,97,100,107,113,144 Karl is glad he hasn’t had to keep repeating himself110,117,131 and he’s really glad he wasn’t arrested, as he has had bad experiences with the police in the past. 10,97,100,129,130,131
Conclusions
Inter-agency working provides mechanisms that trigger seamless service delivery through improved communication and collaboration. For this system to work, representation from all agencies and stakeholders is needed. National co-ordination at policy level ensures that investment is appropriately targeted and that important strategic aspirations are met. National co-ordination should steer, but not dictate, local configurations of the agencies needed. Local crisis services should be configured to meet the crisis care needs of local populations within their geography, taking account of any marginalised individuals or communities they serve.
Commissioning for inter-agency working needs a focus on managing complex boundaries and transitions across agencies to avoid gaps and disputes. Attention is also needed as to how the inter-agency crisis system engages with wider systems important to resolution of crises, including, for example, housing, police, local authority, safeguarding and the justice system. Ultimately, the inter-agency system needs to aim for there being no wrong door for accessing mental health crisis care and, once in a service, navigation should be facilitated via a single trusted point of liaison.
Leaders need to drive team-working within and across agencies. Different values and definitions of crisis are accommodated, allowing challenge and debate to become accepted as an opportunity to drive quality improvement. Evaluation is not restricted by organisational boundaries and aims to provide data that take account of how the whole inter-agency system is operating. This is achieved when there is interpersonal contact between all levels of worker, from commissioning to front-line delivery, that facilitates learning, communication and appreciation of different roles. Furthermore, co-production and co-design of crisis care can be facilitated within the inter-agency system, enabling crisis care to be recognised and valued by the community it serves.
If/then/leading to
If
Crisis services operate within an inter-agency system that supports information-sharing, communication and interpersonal contact between agencies and staff. Technology operates across agencies. There is shared decision-making across agencies and with people in crisis and their support network. Leaders drive inter-agency collaboration and support team-working within and across agencies. Staff relationships and leadership have equal emphasis to the structure of the inter-agency system. Specialisation of services and staff is balanced with flexibility that allows inter-agency co-operation. Staff understand how their role fits within an inter-agency system. Training is co-designed and shared between agencies and with involvement from communities and individuals. Services are designed with the communities they serve and reflect their diversity. There is cultural awareness. There are system navigators and co-ordinators with knowledge of the whole system and resources to support people to make seamless transitions into and through crisis care. Crisis care operates to national guidance with local configuration. There is stability in services and funding.
Then
The inter-agency system is co-ordinated and operates to meet national, local and individual expectations and aspirations for good crisis care. Differences in definition of crises and values about interventions are accommodated. There is co-operation between agencies. There is a platform for co-production and co-design of services. System problems are tackled collectively. Commissioning takes account of gaps and transitions, and operates to resource the whole system. Boundaries between different agencies are proactively managed at commissioning and supported by system leaders. Services are stable and wasteful duplication is reduced. There is investment in joint training and interpersonal contact between staff across agencies. There are open channels of communication between agencies. Staff retention is improved.
Front-line staff have clarity about how their role fits within the whole crisis care system. Staff trust leaders. They have access to information about roles of agencies other than their own and the staff working within them. Trust between staff and different agencies facilitates a culture of learning. It is safe to challenge and debate. Staff understand their role within the wider system. Staff are open to new roles and ways of working. Joint training is meaningful. Staff are culturally aware. Staff rely less on restrictive approaches and seek support from across the inter-agency system. Staff invest in information-sharing, providing warm handovers. They are less stressed, better informed and can sustain compassion. Decision-making is safer.
Service users, family and support networks find it easy to access crisis care that is trusted and guarantees a response appropriate to perceived needs. Crisis care is provided with minimum disruption and burden to the person and their family or support network. There is an identified trusted person to support navigation and communication. Involvement in decisions is the norm. Service users can and have contributed to the design and delivery of the crisis inter-agency system. The crisis care system reflects the characteristics and needs of the community it serves. There are services that are recognisable and trusted as ‘for me’ within the inter-agency system.
Leading to
Nationally led and locally designed crisis care that has been commissioned across agencies. There is stability for agencies, staff and people in crisis. Relationships and leadership are prioritised. Information is shared, decisions are collaborative and people from communities are involved and invested in their crisis services. Wasteful duplication is minimised, and cost-effectiveness improved. Staff believe in the service and trust system leaders, and staff retention is improved. Service users and their support networks are not turned away. There is a single trusted point of liaison. Multiple and complex needs can be accommodated. People reach an intervention suited to their needs, values and expectations.
Chapter 6 Discussion
In this synthesis chapter, findings from the urgent and accessible compassionate care and the inter-agency-focused reviews are synthesised. These cumulative explanations are used to refine the realist programme theory and to identify mechanisms that might operate across multiple interventions to ‘activate’ an appropriate treatment response.
Summary of key findings
Our aim in this review was to improve understanding of how, why and in what contexts mental health crisis services for adults can be designed to optimise mental health outcomes and service user satisfaction. A synthesis across the three focused reviews identified 39 causally linked CMO configurations (see Appendix 5). The confidence in each of these 39 review findings has been assessed using the GRADE-CERQual,80 summarised in Table 5 (for the full assessment of confidence, see Appendix 6). These findings were synthesised with mid-range theory and linked to interventions using the TIDieR Lite,67 summarised in Box 10 and reported in full in Appendix 5.
| Summary review finding | Studies contributing to the review finding | CERQual80 assessment of confidence | Explanation of CERQual assessment |
|---|---|---|---|
| Routes into crisis services 1. (C1) People in crisis who have physical health concerns or (C2) who lack information about crisis services (M) seek help from services they know, trust and are easy to access, (O) making it more likely that they will attend A&E, call 999 or 111, or see a GP |
10,84,89,90,97,99,108,118,143 | Moderate confidence | Moderate methodological limitations and minor concerns about coherence, adequacy and relevance |
| Guaranteed service response 2. (C) People in crisis believe that a service provides a guaranteed response. (M) They have a reduced sense of urgency, feel safer and trust that the service can help. The guarantee of a response makes them more likely to choose the service and tolerate waiting. (O) If crisis services guarantee a response, then people are less likely to attend A&E |
2,10,15,84,89,96,97,99,108,118,143,144 | Moderate confidence | Moderate methodological limitations, no concerns about adequacy and minor concerns about coherence and relevance |
| Safe spaces 3. (C) When people in crisis access safe spaces away from home, (M) they are less fearful and can take stock of their situation, thereby regaining control over their situation, managing their distress and (O) have improved experiences of services |
10,118,130,133,138,155 | Low confidence | Moderate methodological limitations, moderate concerns about coherence and adequacy and minor concerns about relevance |
| Non-clinical safe spaces, open access and peer support 4. (C1) Non-clinical safe spaces in communities (C2) have open access and (C3) include peer support; (M) the service seems to act as a proxy for family support by providing a sense of safety, belonging and being understood. People in crisis seek this support sooner (O1), improving engagement, reducing distress and (O2) attendance at A&E |
10,106,110,118,130,132 | Moderate confidence | Moderate methodological limitations, minor concerns about adequacy and no concerns about coherence or relevance |
| Early navigation to help 5. (C) People in crisis successfully navigate to help in the early stages of a crisis; (M) they feel believed and hopeful; they regain control over their situation and manage their distress. (O) People in crisis have increased willingness to seek help in the future |
2,10,15,96,97,109,112,146 | Moderate confidence | Moderate methodological limitations; minor concerns about coherence, adequacy and relevance |
| Services fit around personal circumstances 6. (C) People in crisis receive a response that fits around their personal circumstances with minimal disruption to usual life, with no social or financial burden. (M) They perceive the service to be easy to access and designed for them, prompting help-seeking sooner in the crisis. (O1) People have personal control and are (O2) less likely to access crisis support via the urgent care pathway |
1,2,10,15,90,95,97,98,101,108,110,112,114,115,146,147 | Moderate confidence | Moderate methodological limitations; minor concerns about coherence, adequacy, and relevance |
| Ease of access and referral 7. (C1) Crisis services can be accessed without complex referral routes; (C2) this was particularly important for black men, who prefer open-access services. (M) People in crisis, especially black men, perceive open-access services to be easy to access and designed for them. More generally, people in crisis who find access easy experience reduced fear and services are accessed sooner. (O1) People are less distressed at first contact and (O2), particularly black men, are less likely to experience coercive responses |
1,10,15,89,90,95,97,104,106,112,130–133 | Low confidence | Serious concerns regarding methodological limitations, moderate concerns about adequacy of data and minor concerns about coherence and relevance |
| Gatekeeping 8. (C) Front-line crisis staff (particularly in statutory services) value gatekeeping. (M) Gatekeeping seems to provide reassurance to staff, who are less fearful of being overwhelmed; they feel able to control their workload (O1), minimising the impact of inappropriate referrals and (O2) reducing the number of hospital admissions. (O3) Resource pressures are managed |
2,15,95,103,105,108,112 | High confidence | Minor methodological limitations, and minor or no concerns about coherence, adequacy and relevance |
| Shared decision-making 9. (C) Decisions are reached through negotiation between staff across agencies and involve the person in crisis, which is especially important for black people. (M) People in crisis trust the service and have personal control; the perception of the person and their family of the crisis is acknowledged, and there is a shared commitment to decisions, (O) improving relationships between services and people in crisis |
1,2,96,102,103,116–119,122,123 | High confidence | Minor methodological limitations, and minor or no concerns about coherence, adequacy and relevance |
| Organisational culture and therapeutic relationships 10. (C) The organisational culture is centred on therapeutic relationships. (M1) Front-line staff trust shared decision-making, take a collaborative approach and prioritise shared decisions. (M2) People in crisis feel respected, and engage, (O) improving people’s experience of crisis services |
115–123,131,133 | Low confidence | Moderate methodological limitations and concerns about coherence. Minor concerns about adequacy and relevance |
| Therapeutic skills, risk and relational safety 11. (C) Front-line staff have therapeutic skills and provide compassionate crisis interventions. (M) Front-line staff deliver care that is balanced between mitigating risk and providing care that promotes relational safety. (O1) People in crisis are more likely to be involved in decisions and (O2) have improved experience of, and satisfaction with, crisis care |
10,129,133,137,138,147 | Moderate confidence | Minor methodological limitations, and minor or no concerns about coherence, adequacy and relevance |
| Peer support 12. (C1) When peer support is available to all people in crisis, (C2) particularly for black and minority ethnic people, to reduce stigma and a sense of marginalisation, (M1) people believe that they have been able to learn about themselves through having a new perspective and feeling understood. (M2) This new perspective helps them recognise opportunities to contribute to their community and this results in a greater sense of (O) hope and meaning |
10 | Very low confidence | Minor methodological limitations, serious concerns about coherence and adequacy and no concerns about relevance |
| A proxy for family 13. (C) When the support of family and friends is not available, or is perceived to be unavailable, people can access a proxy for family via peer support provided in non-clinical safe spaces. (M) People in crisis have a sense of connectedness and trust. (O) The person in crisis feels safe and has reduced guilt about being a burden to family and friends |
10,96,118,119,133,155 | Moderate confidence | Minor methodological limitations, and minor concerns about coherence, adequacy and relevance |
| Family and friends first 14. (C) When people have access to support from family and friends, (M) they have a sense of connectedness, trust and safety that enables collaboration in decisions and mutual respect. The person seeks help from family and friends first and (O) secures help quickly |
10,93,94,96,97,103,104,110,115,118 | Moderate confidence | Moderate methodological limitations, and minor or no concerns about coherence, adequacy and relevance |
| Immediate supportive responses 15. (C) Front-line staff have skills that enable them to provide immediate supportive responses, including active listening and counselling. (M1) Staff are more flexible and responsive. (M2) People in crisis experience relational safety, hope and encouragement, and can communicate their needs, regain control and manage their distress, and believe that the service can help. (O) The person is more likely to contact the service again in the future |
2,10,93,102,110,117,118,122,129,133,138 | Moderate confidence | Moderate methodological limitations. Minor or no concerns about coherence, adequacy and relevance |
| Compassionate crisis responses 16. (C) Front-line staff are compassionate in their responses (in person or via telehealth) to people in crisis and their family and friends. (M) People in crisis are valued, believed, respected and involved in their care. (O1) People in crisis experience relational safety, (O2) stabilisation of the immediate crisis and (O3) improved service user experience, and (O4) there is improved job satisfaction for staff |
10,102,113,115,118,122,125,126,129,130,132–134,139,140,147 | Moderate confidence | Minor methodological limitations. Minor concerns about coherence, adequacy and relevance |
| 24/7 access and same-day responses 17. (C) Crisis services are available 24/7 and provide same-day responses. (M) The expectation of people in crisis (and their family) for an urgent response is met; they trust the service and have a reduced sense of urgency. (O) People in crisis access a mental health assessment quickly |
2,10,15,90,95,97,98,100,110,116,118–120 | Moderate confidence | Minor methodological limitations. Minor concerns about coherence, adequacy and relevance |
| Trauma-informed parallel assessment 18. (C) Crisis services provide co-response models that include parallel assessment. (M) People in crisis experience less fear (of traumatic retelling) and a greater sense of personal control. (O1) People in crisis experience a reduced number of assessments and related traumatic retelling and (O2) have faster access to a mental health assessment that is holistic and more accurate |
98,100,101,111,118,133,143,149 | Low confidence | Moderate methodological limitations. Moderate concerns about coherence and adequacy; minor concerns about relevance |
| Inter-agency co-location 19. (C) Co-location of mental health staff in emergency control rooms where non-mental health specialist staff (e.g. police, ambulance) and specialist mental health staff share workspaces. (M) Non-mental health specialist staff are more confident in responding and feel supported in decisions. (O1) Services are more cost-effective and sustainable. (O2) People in crisis experience faster responses to mental health calls because of improved decision-making and appropriate onward referral. (O3) There is a reduced likelihood of people in crisis being taken to (or choosing to attend) A&E or coercive responses being implemented (e.g. Mental Health Act 1983118 and 2007119) by clinical staff or police |
98,100,101,110 | Low confidence | Minor methodological limitations. Serious concerns about adequacy; minor concerns about coherence and relevance |
| Supportive clinical leaders 20. (C) Front-line staff have access to clinical leaders and systems of support (e.g. clinical supervision). (M) Front-line staff are less fearful of blame, and seeking support is an accepted norm that facilitates acceptance and tolerance between staff. (O1) Front-line staff sustain compassion and are more confident in decision-making, and staff stress is reduced. (O2) Staff job satisfaction is increased, and staff turnover is reduced |
10,93,104,107,115,125,126,139,147 | Moderate confidence | Moderate methodological limitations, and minor concerns about coherence, adequacy and relevance |
| Decision-making 21. (C) Decision-making is supported by evidence-based decision aides that are understood across the inter-agency crisis care system (e.g. triage tools) and decisions are linked to available services. (M1) Front-line staff have confidence in decisions and there is mutual trust across agencies. (M2) Staff have less fear of referring to other agencies and a sense of role clarity. (O1) Accuracy in identification of urgency and need (e.g. suicidality) is improved. (O2) Improved decisions enable improved inter-agency service co-ordination and more accurate resource allocation. (O3) There are reduced disputes about responsibility between staff and agencies |
10,15,93,94,98,101,104,123 | Low confidence | Moderate methodological limitations and moderate concerns about coherence. Minor or no concerns about adequacy and relevance |
| Leaders buffer external demands 22. (C1) Front-line staff in ‘first-response’ roles have immediate access to clinical leaders to support and manage resource pressures and disputes about responsibility across the inter-agency system. (C2) Leaders focus on buffering external demands and pressures. (M) Front-line staff are confident in decisions, have role clarity and can focus on the person in crisis. (O1) Disputes about responsibility are reduced. (O2) Front-line staff are focused on the person in crisis, rather than resource pressures and disputes, enabling them to retain their compassion and make decisions that are collaborative and safe |
10,92,102,104,107,115,126,129,135,136,139,152 | Moderate confidence | Moderate methodological limitations and moderate concerns about coherence. Minor or no concerns about adequacy and relevance |
| Definitions, values and inter-agency affiliation 23. (C) Multiple definitions of crises are understood across agencies. (M1) Front-line staff accept, have a sense of ownership of, and work with different values across the crisis care system. (M2) Commissioners and leaders design services that accommodate different approaches to crises, allowing healthy challenge and debate (that challenges, e.g., unhelpful stereotyping and operational or professional silos). (M3) Inter-agency affiliation facilitates improved communication, information-sharing and engagement. (O) Staff work flexibly across agencies, reducing gaps and delays |
10,96,106,109,126,127,138–140,147,156 | Low confidence | Serious methodological limitations. Moderate concerns about coherence and adequacy, and minor concerns about relevance |
| Crises as part of recovery 24. (C) Mental health crises are conceptualised as part of a recovery journey, rather than as single events. (M1) Front-line staff are accepting of people who may require multiple crisis interventions and are confident to refer and liaise across the crisis system. (M2) People in crisis feel confident when contacting crisis services more than once without fear of rejection. (O1) Front-line staff retain compassion. (O2) People in crisis requiring multiple crisis responses are more likely to engage and less likely to escalate risky behaviour. (O3) There is a reduction in repeat attendances and people leaving the service without treatment |
2,10,89,94,99,106,109–111,115,123,132 | Low confidence | Serious methodological limitations. Moderate concerns about coherence and adequacy, and minor concerns about relevance |
| Time for assessment 25. (C) Front-line staff have time to assess people in crisis. (M) Staff are less pressured for time and are enabled to focus on the person’s interpretation of the crisis and to involve them in decisions. (O1) Comprehensive assessment is more likely to be accurate, with appropriate onward referral, reducing the need for repeat attendances. (O2) People in crisis are more likely to reach an appropriate intervention and experience a reduced likelihood of escalation of distress and harm. (O3) There is improved cost-effectiveness and service user experience |
2,10,94–96,99,102,105,109–111,118,119 | Moderate confidence | Minor methodological limitations, and no or minor concerns about coherence, adequacy and relevance |
| Implementation and change 26. (C1) Organisational strategy and operational leadership drive sustained engagement with information-sharing and shared decision-making. (C2) Crisis planning and information-sharing are particularly important for people known to services or who attend services frequently. (M1) Front-line staff are engaged and adopt changes in practice. (M2) People in crisis perceive that the service knows something about them, and they are more engaged in their care. (O) There is improved service co-ordination, faster responses and sustained change |
117,119,121,123 | Very low confidence | Moderate methodological limitations. Serious concerns about coherence, moderate concerns about adequacy and minor concerns about relevance |
| Managed waiting 27. (C) A focus on compassionate and psychologically safe crisis care drives proactive management of waiting at strategic, operational and clinical levels. (M1) Front-line staff provide information about waiting times to people in crisis, what the wait is for and what the person can do to stay safe during the wait. (M2) There is a shared understanding of waiting time policy and staff act to meet the standard. (M3) People in crisis and their family can tolerate waiting and the sense of urgency is reduced. (O1) People in crisis are less likely to disengage from services without treatment or to circle the system. (O2) People in crisis experience reduced distress and harmful behaviour is less likely to escalate |
2,10,15,91,93,94,97,105,110,130,132,133 | Moderate confidence | Moderate methodological limitations, and minor concerns about coherence, adequacy and relevance |
| Boundary management 28. (C) Commissioning takes account of how complex boundaries between agencies (including thresholds for access) affect service delivery and service user and family experience. (M1) Commissioners and leaders drive inter-agency agreement about geographic and service remit boundaries. (M2) Staff believe in the service and act to collaborate across organisational and geographic boundaries. (O1) Gaps, delays and disputes about responsibility are reduced. (O2) Staff morale is improved. (O3) There is improved service delivery and cost-effectiveness. (O4) People in crisis are less likely to experience coercive crisis responses |
10,15,27,95,104,114,141,142,146,147,149,150,151,157 | Low confidence | Serious methodological limitations, moderate concerns about coherence, and minor concerns about adequacy and relevance |
| Continuity and stability 29. (C) Crisis services are commissioned to provide continuity and have a stable presence in communities. (M) People in crisis and crisis staff know their local crisis services and can navigate to them. (O1) Front-line staff are responsive to the needs of people in crisis (rather than focused on protecting scarce resources). (O2) Resources are available to provide continuity at service and individual levels |
2,10,95,104,105,116,118–120,128,139,147,149,157,158 | Moderate confidence | Minor methodological limitations. Moderate concern about adequacy; minor or no concern about coherence or relevance |
| Co-production and stigma reduction 30. (C) Co-production (including co-design of training) is actively resourced. (M1) The aspirations of service users (communities) are incorporated into design, delivery and evaluation of services across the inter-agency system. (M2) People in crisis recognise the service as designed for them, have a sense of ownership and affiliation, and talk positively about crisis care. (O1) People in communities become aware of local crisis services. (O2) There is reduced fear and shame about accessing crisis services (stigma). (O3) The quality of crisis care is improved |
2,10,89,106,118,137,139,147,156 | Very low confidence | Serious methodological concerns. Serious concerns about coherence, moderate concerns about relevance and minor concerns about adequacy |
| Diversity and inclusion 31. (C) Crisis services are designed and delivered with involvement from the communities they serve, and the staff reflect local diversity. (M1) Staff use language and communication that avoids racial and other stereotypes. (M2) People from black and minority ethnic populations recognise the crisis service as being for them. (O1) There is reduced fear and shame about accessing services (stigma). (O2) The quality of crisis care is improved |
2,10,89,106,118,139,147 | Low confidence | Moderate methodological limitations, minor concerns about coherence, moderate concerns about relevance and serious concerns about adequacy |
| Evaluating inter-agency crisis services 32. (C) Diverse data are used to monitor services and inform decision-making, including data from across agencies and aspects of service delivery that are harder to measure (e.g. relational safety and compassion). (M) End users of services are involved in evaluating services from multiple perspectives, and commissioners and leaders are focused on shared priorities (rather than competing priorities). (O) Quality of care is understood from multiple perspectives, including the priorities of service users and the communities served |
10,137–139,145,147 | Low confidence | Moderate methodological limitations; concerns about coherence and relevance. Serious concerns about adequacy |
| Technology and information-sharing 33. (C) Technology operates across crisis agencies to support information-sharing. (M) Front-line staff are confident to communicate across different agencies; they ‘buy into’ the system and trust is established. (O1) Improved information-sharing reduces the number of assessments and related risk of trauma. (O2) Improved communication systems help to reduce barriers to information-sharing caused by rules about confidentiality and boundary disputes. (O3) People in crisis experience faster access and transition through different agencies |
10,94,96,98,143,147,150 | Low confidence | Moderate methodological limitations, and concerns about coherence, adequacy and relevance |
| Inter-agency staff support 34. (C1) There is equal emphasis on inter-agency leadership and staff relationships as there is to the operational structure of the inter-agency system. (C2) Clinical leaders and middle managers are focused on support that balances the day-to-day demands of service delivery with attention to the needs of staff. (C3) Workloads allow leaders to be available to staff. (M) Staff are clear about lines of accountability and seek support with clinical decisions. (O1) Improved morale among leaders and staff; staff retention is improved. (O2) Front-line staff retain compassion. (O3) Resources are managed effectively, sustaining clinical priorities. (O4) Staff are empowered (rather than helpless) |
126,129,134,135,136,138,139,140,147 | Low confidence | Serious methodological limitations. Minor or no concerns about coherence, adequacy and relevance |
| Compassionate leadership 35. (C) There are shared values and objectives between leaders, who model compassion. (M1) There is affiliation within and between teams; there is a flat structure and leaders make themselves accessible and visible; expectations are clear. (M2) Staff are regarded compassionately and humanely, and are respected; there is staff development and (joint) training that fosters growth. (O1) Compassionate leaders set the tone for compassionate care, and people in crisis experience reduced distress and increased satisfaction with crisis services. (O2) There is greater likelihood that services are cost-effective |
98,125,126,127,129,131,135,138–140,147,153 | Moderate confidence | Moderate methodological limitations and minor concerns about coherence, adequacy and relevance |
| System navigators 36. (C) There are system navigators and co-ordinators with knowledge of the whole crisis system. (M) People in crisis experience continuity through trusted points of liaison. (O1) Police time spent dealing with crises is reduced. (O2) People in crisis are more likely to transition through agencies seamlessly |
138,143,144,147,148,153,154 | Very low confidence | Serious methodological limitations, moderate concerns about adequacy and minor concerns about coherence and relevance |
| Inter-agency commissioning 37. (C) There is a system-wide approach to commissioning crisis services. (M) There is a system-wide understanding of the resources required, and agencies operate to manage complexity across the system (rather than operating in silos to protect resources). (O1) There is greater likelihood of cost-effectiveness through more streamlined processes across the system and a reduced focus on resolving disputes. (O2) Inter-agency systems that provide seamless crisis services are more likely to reduce distress and increase satisfaction with crisis services |
10,81,98,147,153,161 | Moderate confidence | Minor methodological limitations; minor concerns about coherence, adequacy and relevance |
| National standards and local implementation 38. (C) Crisis care operates to national standards with local implementation. (M1) Leaders engage with quality improvement; they set standards (nationally and locally) and lead the delivery of crisis services that meet these standards and expected outcomes. (M2) Commissioners and leaders pay attention to local populations, making service design responsive to local need. (O) Crisis services have potential for cost improvements through reduced use of the urgent care pathway |
27,28,30,89,98,106,146,152,157 | Low confidence | Serious methodological limitations. Moderate concerns about adequacy and minor concerns about coherence and relevance |
| Inter-agency role clarity 39. (C) Staff understand how their role fits within an inter-agency system. (M) Staff across agencies have confidence (rather than concern) that the spectrum of care is available across the inter-agency system. (O) Suspicion and mistrust between different agencies are reduced and there is improved communication between staff and between agencies |
10,15,142,149,151,161 | High confidence | Minor methodological limitations and minor concerns about coherence, adequacy and relevance |
| C, context; M, mechanism; O, outcome. | |||
The findings from this realist review reveal that community mental health crisis services share a requirement to provide an urgent response that is perceived as accessible by people in crisis and their family or friends. The immediate response needs to be delivered within a culture of compassionate concern, which can be largely, but not exclusively, shaped by the service leadership. Accessible and responsive services delivered compassionately according to this leadership imprint are necessary, but are not sufficient on their own.
Extending beyond the remit and capacity of each individual organisation is a requirement for inter-agency interaction and joint working, facilitated by interventions such as improved communication, information-sharing, joint training, sharing of values, and shared understanding of systems and service thresholds. Evidence suggests that joint working may witness an eroding of traditional stereotypes whereby it is only health professionals who have a capacity for compassion. 162 While compassion for service users is critical, this cultural attribute relates strongly to having an empathetic attitude towards staff from other agencies. 163 Inter-agency working does not relate simply to allowing staff from different agencies to access a common knowledge base; it also includes learning about how to communicate effectively across organisations, understanding the respective roles of different agencies and developing new relationships while learning side by side. 163 Figure 10 illustrates the overarching programme theory for this synthesis.
FIGURE 10.
Conceptual diagram illustrating overarching programme theory. The red line indicates the focus of the realist review.

However, this apparently linear relationship for crisis management is potentially misleading, given that compassionate leadership may shape the quality of inter-agency interactions. Similarly, the perceived accessibility of the response depends on the configuration of the collective inter-agency response. When collaboration works well, it can lead to an improved understanding of roles and responsibilities in the ‘other’ agency and lead to the development of local agreements for information-sharing. 150 Furthermore, referral to existing services is a key function150 that may require a response that bypasses repeated contact, and reinforcement of relationships within the same single agency, requiring instead targeted, co-developed responses from multiple agencies. This complexity extends to interventions such that joint training may include mutual understanding that facilitates appropriate referral and may also help in extending a compassionate and caring environment beyond an organisation’s peripheries to its points of contact and interactions with other agencies. Nevertheless, tensions may arise as agencies working towards a common goal find themselves competing for available resources. 150
Summary of interventions
Box 10 provides a summary of the interventions identified through our research using the TIDieR Lite framework. 67 A table showing the full detail of the TIDieR Lite interventions is in Appendix 2. Contextually important intervention strategies operating within the interventions identified in the TIDieR Lite were synthesised to three levels of intervention, namely system, organisational and service levels, and linked to each of the three programme theories in Table 6.
-
Ambulance/paramedic response car. 101
-
Crisis house. 133
-
Culture-of-care barometer. 127
-
The Mental Health Act 1983, section 136 (England and Wales). 95,141
-
Models of crisis care. 91
-
Recovery-focused care planning. 129
-
Risk management. 137
-
Schwartz Rounds. 125
-
Short hospital stay. 105
-
Suicide triage. 104
-
Team-working. 129
-
Voluntary sector crisis services. 10
| System level | Organisational level | Service level |
|---|---|---|
| Information-sharing (1)102,118,121,123 Inter-agency meetings (3)10,27,28,98,153 Referral processes (1)10,15,89,91,100,103–105 Shared decision-making (1)10,95,105,115–123 Staff training, supervision and support (1, 2, 3)10,93,94,104,107,123,129 Telehealth (1)15,93,94,98,113–115 Immediate supportive interventions (1)93–95,104,105,110 Triage and prioritisation (1)91,93,94,100,104,109,110 Waiting time standards (1)111,112 Joint training, job shadowing and networking (3)10,15,27,147,149,150,153,154 Care co-ordinators and system navigators (3)144,147,153 |
Co-response, co-location and parallel assessment (1, 3)10,84,95,98,100,101,108–110,141,146,148–152 Team-working (2)126 Leadership (2, 3)118,125,126,134–136 Peer support (2, 3)132 Psychologically safe models of care (2)10,129,132,133 Safe environments (2)132 Support for family and friends (2)10,129 Role clarity and role allocation (3)98,118,147,153 |
Continuity of care (1)10,105,107,108 Therapeutic relationships (2)129 Individualised care (2)118,129 Safety planning (2)129 |
Comparison with existing literature
The literature on community mental health crisis services is predominantly descriptive. This facilitates an exploration of contextual variation, but offers less evidence to resolve debate about the most effective interventions with which to address the needs of service users or on the outcomes produced. This synthesis can add to the important developing body of literature identified for the review by contributing a realist perspective, thus considering contextual and generative mechanisms across diverse processes and stages potentially relevant to community crisis services across provider agencies.
We acknowledge that this report conceives a mental health crisis as an urgent event with a limited time window within which the first point of contact must demonstrate accessibility and a circumscribed view within which a responding organisation must reveal its response as compassionate and caring. Others have chosen to represent a mental health crisis as a biographical disruption. 10 While some of this difference may be attributed to contrasting individual and service provider perspectives, and further explained by differing emphases on a collective inter-agency versus voluntary organisation response, we contend that, once beyond the initial issue of access, a compassionate and supportive environment can similarly accommodate a biographical disruption model.
When considering the pathway of a service user through a crisis service (the ‘therapeutic itinerary’), as delivered by multiple agencies, one can assume one of three perspectives:164 the first is focused on the patient’s perception about illness and how it affects help-seeking (patient viewpoint). The second is focused on identifying barriers to and gaps in health system accessibility and referral arrangements (system viewpoint). Finally, a third integrative approach situates patient actions within a socioeconomic context that iteratively produces the preferred choices for service users, carers and service providers (contextual approach).
What this study adds to existing knowledge
This analysis and synthesis of the literature revealed several important theoretical constructs associated with our programme theories. These constructs helped us to develop our thinking and to establish the relevance of our inquiry within a wider body of theoretical literature beyond the documents reviewed. We identified relevant theories by iterative reading of the data, alongside theoretical literature from across multiple disciplines, and through discussions within the research team and with the ESG. By mapping how our programme theories correspond with substantive theories, we were able to strengthen our propositions regarding causal explanations. This section presents the mid-range theories relevant to each of the three reviews (see Table 7).
| Programme theory/ies | Mid-range theory | Explanation |
|---|---|---|
| PT1: crisis services can be accessed urgently | Goffman’s165 (1981) sociological theory, forms of talk Outram et al.166 (2004), accessing professional help for psychological distress |
The talking encounter entered into by a mental health practitioner and a patient is an example of ‘interactional talk’, an arrangement whereby people come together, sustaining conversation and mutual attentiveness that holds them in an ‘intersubjective world’.165 The social setting for the encounter sets the scene, providing not only context, but also partially determining the structure of the interaction. For a potentially sensitive discussion to take place successfully, certain conditions, individual to those within the encounter, must be fulfilled. Previous unsuccessful interactions can set the tone for future talking encounters,165 leading to service users becoming disinclined to express themselves and reluctant to seek help166 |
| Ball et al.83 (2005), theory of mental health crisis. Feeling in control | ‘Underlying vulnerability sets the stage for crisis occurrence which involves feeling overwhelmed and lacking control and manifests as agitation/anger/aggression, being low, feeling anxious, or euphoria. Immediate responses to crises involve getting help or managing alone and numerous factors contribute to crisis resolution and prevention’83 | |
| Caplan’s168 (1964) crisis theory. Breaking point Subsequent theory development by: Hobbs174 (1984), Caplan24 (1989), Ball175 (2003), Ball et al.83 (2005), Brennaman176 (2012) and Boscarato et al.84 (2014) |
‘Crises can occur when a person encounters an overwhelmingly stressful situation that might exceed their capacity to cope, resulting in feelings of helplessness and tension’.84 ‘Disorganization and confusion might be subsequently experienced, leading to a “breaking point”, characterized by psychological decompensation and disturbed or destructive behaviour’.174 When this occurs, crisis intervention might be required. Ball175 extended Caplan’s168 crisis theory to differentiate the experience of crisis for individuals with SPMIs from the experience of crisis for the rest of the population.83 Ball83,175 identifies an ‘underlying vulnerability’ that mental illness creates as the primary precipitating factor. His explanation of crisis is comparable to Caplan’s168 crisis theory, although mental illness usually requires professional care.176 Opportunities for growth and the development of new coping skills are present in the resolution of the crisis24,175 | |
| Mirabito85 (2017). Strengths perspective. Breaking point | Crisis intervention uses the strengths perspective to help individuals mobilise their ‘own strengths, assets, and capacities as well as to identify the resources and supports that exist in their environments, including within families, social networks, neighbourhoods, and communities. In combination with the strengths perspective, an empowerment approach is used to help people access and use inner and environmental resources’85 | |
| PT1: crisis services can be accessed urgently PT2: compassion and leadership |
Recovery alliance theory: Shanley and Jubb-Shanley167 (2007), and Wright et al.177 (2007) | Stresses the importance of therapeutic rapport and compassion. The issue of common humanity has been shown to be essential in the recovery process.177 Individuals are social beings who share a common humanity, which, via interaction with others, helps us to develop as individuals.167 If professionals exhibit dehumanising behaviour, the resultant social rejection and professional distance merely serves to increase the likelihood of harmful behaviour |
| PT2: compassion and leadership | Protection motivation theory: Allen and Campbell88 (2018) | ‘The protection motivation theory proposes that people protect themselves based on four factors: the perceived severity of a threatening event, the perceived probability of the occurrence, or vulnerability, the efficacy of the recommended preventive behaviour, and perceived self-efficacy’88 |
| The compassionate mind training model: McEwan et al.86 (2020) and Gilbert178 (2014) | Humans are profoundly social beings, with compassion linked to caring and attachment.178 Because compassion operates through, and depends on, social bonds and relationships, it is also context dependent. Different organisational systems can either facilitate or inhibit it. Compassion in mental health means the creation of contexts within which compassion competencies can flourish. ‘Compassionate care involves providing a welcoming environment, promoting bidirectional compassion, providing training in compassion and creating supportive organizations’86 | |
| Compassion in psychotherapy: Vivino et al.87 (2009) | Compassion in psychotherapy is a broad construct that encompasses elements of therapy process, therapist variables and other important components of psychotherapy, and functions to facilitate client change87 | |
| PT 2: compassion and leadership PT3: community crisis agencies work together |
Social innovation model (specifically the ecosystem for innovation model): Bason179 (2010) and Hartley170 (2005) | Social innovation involves taking new knowledge, combining existing knowledge in new ways or applying it to new contexts. It seeks to create positive social change, and improve social relations and collaborations to address a social demand, defined by an emphasis on public value and social need.170 ‘The Ecosystem for Innovation model179 sets out four interdependent dimensions: Consciousness: Degree to which organizational leaders are aware of “innovation” and consciously strive towards achieving innovation when developing new interventions. Capacity: Degree to which structures within organizations allow social innovation to take place. Co-creation: Collaborative processes that allow the cross fertilization of ideas across different agency perspectives and which are necessary for innovative ideas to develop. Courage: The leadership environment required to facilitate the above dimensions’179 Professionals may be considered social innovators, implementing and expanding on new ideas within their own organisations and across systems170 |
| PT3: community crisis agencies work together | Activity system framework evolved from sociocultural learning theory: Vygotsky180 (1978), Engeström181 (2001) and Hean et al.182 (2009) | The learning that takes place during an activity is not only a function of an individual’s own cognition.180 It is also mediated by factors external to the individual within the social world. Activity theory (systems) and boundary crossing that operationalises this theory181 have been used to underpin joint training workshops182 |
| The inter-group contact hypothesis: Carpenter and Hewstone171 (1996), Hewstone et al.173 (1996) and Dickinson and Carpenter183 (2009) | Establishing contact between agencies is a recognised mechanism in building relationships and minimising inter-group stereotypes and prejudice. However, contact alone is not enough.173,183 ‘Inter-agency placements, visits, and shadowing opportunities provide contact. Positive effects of contact require four key conditions: equal status, common goals, inter-group cooperation and support by social and institutional authorities’.171 If contact opportunities are left unmanaged, then contact may have unintended consequences, with stereotypes being reinforced and inter-agency relationships harmed173 | |
| Inter-agency collaboration models: Parker et al.81 (2018) | ‘Inter-agency collaboration involves three core principles of information sharing, joint decision making and coordinated intervention. Inter-agency collaborations involving the police aim to improve health and social care outcomes for individuals with mental ill health and the cost and effectiveness of services’81 | |
| Polivka’s82 (1995) theoretical model of community inter-agency collaboration | ‘Collaboration is a function of environmental conditions, organizational situations, and task characteristics. Discusses transactional patterns including intensity, formalization, inter-relational patterns, and structured relationships as well as outcomes pertaining to organizations, interorganizational relations, clients, and communities’82 |
In the mid-range theory of Goffman165 (forms of talk), interpersonal communication and therapeutic relationships are confirmed as central to understanding the relationship between the mental health practitioner and the service user. Outram et al. 166 have observed that attitudinal barriers are more likely to prevent individuals from seeking treatment than structural barriers. Framed in terms of our programme theory, the perception of whether or not a service and service providers are accessible carries more of an inhibitive effect than the way that the service is actually organised. Further work might therefore usefully examine how intervention components and service configurations (different contexts) are perceived by service users, rather than trying to isolate which permutation of intervention components is most likely to achieve optimal effectiveness. Past encounters with services carry a strong imprint in relation to perceived future accessibility and urgency. The relational aspect of service provision is further affirmed by a mid-range recovery alliance theory. 167 With an emphasis on rapport and compassion, professionals are encouraged to exhibit positive behaviours that mitigate against the dehumanising and stigmatising attitudes that service users may perceive when they encounter a service, and that may precipitate or exacerbate a crisis.
A further mid-range theory, feeling in control,83 also serves to highlight the key role of first contact within crisis management services. People perceive a crisis when they feel overwhelmed and anxious and when they perceive that they lack a sense of control. Familiar contacts and a welcoming environment, coupled with reassurance, can help to shape their perception of the service but, more importantly, can help to reduce agitation and aggression, thereby making them more likely to respond to suggested strategies or inter-agency referrals. This theory is very much reinforced by the work of Caplan,168 from the mid-1960s, who similarly asserted that crisis occurs when the stress being encountered by an individual exceeds their capacity to cope. Viewed in this way, crises represent a particular ‘breaking point’ at which an individual feels unable to manage without extra support. From this perspective, complex systems theory would not only recognise the need for a service to recognise the urgency of this breaking point, and to be accessible at this critical time, but would see an important role in delaying or preventing this breaking point, or diverting the need to mitigating resources for coping, whether from the individual themselves or from informal care networks. These mitigating resources constitute an important contributor to a strengths perspective, such that past service users are empowered to access and use inner and environmental resources.
Fundamental to our programme theories is the role of compassion. Although this characteristic may be incorporated within specific interventions, such as the compassionate mind training model,86 the focus of our programme theory is not on the individual therapeutic encounter itself, although undoubtedly important,87 but on the contribution that leadership can make towards becoming a compassionate organisation. Focusing on compassion at this level helps to shape a context within which many different interventions might operate. A leader’s contribution to compassionate care entails providing a welcoming environment, promoting bidirectional compassion, providing training in compassion and creating supportive organisations. 86 Strong enabling leadership is similarly important in inter-agency working, such that escalation can take place when organisational barriers are encountered. 169
The fact that a leader can shape the culture or environment within which care is delivered recognises the potential insights that can be gained from social innovation. In meeting the social demand from service users, service leaders can increase the capacity of their organisation to allow the ‘innovation’ (in this case, compassionate care) to take place. 170 This may extend to building collaborations, making contacts and broadening networks for inter-agency working. One reason why the impact of the Crisis Care Concordat27 has proved less than that anticipated may be a focus on the characteristics required, such as compassion, at the possible expense of mechanisms, such as compassionate leadership and social innovation, that might disrupt the current context and therefore increase the likelihood of change and innovation.
As an intervention to facilitate inter-agency working, joint learning can engage with sociocultural learning theory; it represents a practical instance of boundary-crossing,169 further enhanced by shadowing and job swaps, that improves understanding of other agencies and helps to envisage the physical and situational context within which partner agencies are having to respond and reciprocate. Outside the learning context, the inter-group contact hypothesis (see Table 7) attests to the value of contact between partner agencies. However, contact by itself is not sufficient; it must be strengthened by certain prerequisites such as equal status, common goals, inter-group co-operation and external support. 171–173
In the absence of these enabling factors, any inter-agency initiative may simply provoke the unintended consequences of reinforcements of stereotypes and existing cliques, causing lasting damage to future working. At a more instrumental level, inter-agency co-operation requires such practicalities as information-sharing, joint decision-making and co-ordinated intervention. 81 Noticeably, Polivka’s82 model of community inter-agency collaboration operates across the same three levels [environmental, organisational and task (i.e. intervention)], as highlighted in our programme theories (see Table 6).
How does urgency and accessibility of services determine what happens during a mental health crisis?
Although urgency (linked to perceived need) and accessibility (linked to a response that meets that need) are conceptually different, they are very closely related in the minds of service users. Service users adopt strategies to negotiate access to mental health care when emotions become overwhelming and harmful behaviours become likely. 184 These strategies may include contact with police services when health services fall short of the response times that users themselves expect. Urgency may increase when there are delays in accessing services. Services that are seen as accessible are less likely to be accessed prematurely or on a ‘just-in-case’ basis. Dissatisfaction with access to crisis care in England has driven a national service improvement programme and the introduction of the Crisis Care Concordat27 in 2014. New models aimed at offering improved access are discussed elsewhere within this report and include ‘crisis cafes’ (‘safe havens’ or ‘recovery cafes’), walk-in services, stand-alone community crisis assessment teams and 24-hour crisis lines. Inconsistency of coverage remains an important issue, with some people having improved access to numerous alternative forms of community crisis care, whereas others have access to the same CRTs that have been standard in the UK for the past 20 years.
However, when services are designed to be accessible, they may be accessed for convenience at the expense of those who most need them at that specific point in time. Conversely, access to regular health services, for example to GPs, by mental health service users may be limited, out of respect for appointment requests by other patients. 162 Queuing theory suggests that services that are accessible will be increasingly accessed until they stop being accessible, after which usage will drop until the service is used little enough to once more offer a timely response. In reality, service users want a just-in-time, not a just-in-case, response. However, a further complication in planning the accessibility of services is the fact that needs that are not addressed early may become exacerbated and require a more extensive, prolonged or resource-intensive response. Managing these processes is challenging because it not only requires a knowledge of the needs of an individual service user, but it also requires an overview situation report of the current usage and availability of the service as a whole.
With new crisis care models continuing to emerge, with the potential to improve access and service user satisfaction, it remains important to establish the evidence base for these models and, in line with the complexity approach assumed by this review, to explore the implications of these new models within the broader local crisis care system. 185
What is compassionate care during a mental health crisis and why is it important?
This review has confirmed that compassionate care is an important feature of a crisis management response. Kindness and compassion are highly valued by people in crisis:
A kind, compassionate, caring, and effective response followed by the right support can transform lives for the better.
(Lynch and Persaud, Lived Experience Commentary) Dalton-Locke et al. 185
Yet these attributes are often lacking in mental health crisis care. 12 It is worth noting that the Francis Inquiry181 put much store on remedial documentation and communication when users reported a basic ‘lack of compassion’;186 crisis mental health services would do well to avoid a similar pitfall. In particular, police services may resort to coercive powers in transporting service users to a location where they can access mental health services. This initial contact may serve to ‘frame’ the service user’s subsequent perceptions of crisis mental health services.
According to the theoretical model associated with compassion, compassion includes offering a welcoming environment. This link between programme theories 1 (urgent and accessible services) and 2 (compassionate leadership) suggests that the identity of an organisation as compassionate can be perceived from early contact and contributes positively to impressions of accessibility. Similarly, recovery alliance theory, which requires professional and service user rapport, can be seen as a facilitator of access to staff, and requires a compassionate environment. Person-centred care approaches strongly resonate with our analysis (e.g. recovery alliance theory;167 Goffman’s165 sociological theory, forms of talk;165 and compassion in psychotherapy87).
Perhaps what is unique from these findings is the realisation that compassion is not simply an attribute of individual staff with whom service users come into contact. Organisation leaders hold the potential to influence the culture of their organisation: to make it more compassionate. Routes to achieving culture change lie within social innovation theory, whereby organisation leaders consciously strive to innovate: they do this within structures that facilitate change; they are open to cross-fertilisation of ideas, including from other agencies; and they drive forward the movement towards change.
How does inter-agency working influence the service response to people experiencing a mental health crisis?
Our findings suggest that a fragmented and disjointed cross-agency response may serve to exacerbate the challenges of the first response. 187 This can operate at a practical level in terms of delays in referral2 or in having to repeat one’s history multiple times to different agencies. When police officers contribute to a mental health response, service users experience agencies working in isolation and being hastily referred from one agency to the next. 2 Equally, a disjointed response may be perceived to symbolise that the concerns of the service user or their significant others are not important or are not being taken seriously. 2 The transfer of mental health care into emergency health services or police custody has seen increasing interest in how services work together to offer help-seeking pathways to support people in crisis with mental health disorders. 149
Two approaches to help-seeking pathways have been distinguished: the ‘contingency’ approach, which describes and correlates service use with clinical and sociodemographic profiles of patients, and the ‘process-oriented’ view, which focuses on social and interpersonal processes that affect help-seeking behaviour in the community and in the health system. 188 The same research has shown that client pathways to mental health services are divergent and can be a product of choice, coercion or simply ‘muddling through’; the ‘muddling through’ approaches conflict with the demand for urgent and accessible service responses. 189
Evidence from novel models of police collaboration, such as crisis intervention teams and street triage,84,190 suggests that collaborative models between police and health-care professionals may achieve some success in improving service user experience.
Strengths and limitations
We recognise that this synthesis holds several limitations. First, the quality of any review is only as robust as the primary studies on which the synthesis is based. A major constraint is that the majority of the studies included in our review give only a cursory description of the context and content of the crisis management services described. Outcomes extracted, particularly at an individual level, were highly theoretical and often based on methodologically limited studies. Unlike systematic reviews, analysis requires purposive approaches to retrieval and analysis of included studies. Nevertheless, our use of iterative searching and citation tracking and our close adherence to documented realist search methodologies has increased our confidence that we have optimised data inclusion. Familiar caveats relate to the limited extent to which all aspects of the explanatory theories identified in this report can be applied to all contexts in which crisis management is delivered. Examination of internal records and service specifications, not in the public domain, might have yielded richer, detailed descriptions of the interventions and permitted a more nuanced analysis of contextual barriers and facilitators. Subsequently, our testing of our mid-range theories and propositions may have been more selective than greater detail would have permitted. Nevertheless, we have been able to focus our inquiry on those areas considered as most important to stakeholders, including service users and commissioners, and we have been able to identify mid-range theories to explain how these interventions might work.
Realist synthesis, being a largely interpretative process, may have been influenced by the composition and individual expertise and disciplinary background of the team. In answering the same research questions, a different group of researchers may have prioritised different primary sources and made different judgements about their rigour, richness and relevance. Reflexivity is not yet considered a key component of realist reporting and yet lessons remain to be learned for interpretative variants of qualitative evidence synthesis. Although each lead author steered the direction of one of the three individual programme theories, the wider team put in place procedures to mediate the individual effects of each author’s idiosyncratic approach. These included using common procedures and presentation structures, themed meetings at which each lead author presented on a shared aspect of activity, and close liaison and communication among the lead authors during analysis and write-up. However, we continue to acknowledge, as highlighted previously, that each programme theory addresses a different interventional, organisational, social or environmental context. This may have required different approaches to the evidence base and diverse analytical procedures. Most importantly, each reviewer’s interpretative judgements are integral to the synthesis process and can never fully be ‘controlled’ or rationalised. The presence of several procedures for ‘sense-checking’, as effected throughout the synthesis process, does, however, allow for resonance with stakeholder and larger research team experience and expertise.
Deviations from the protocol
The original plan to interview up to 50 experts in crisis care from across the UK was modified: after postponement of interview recruitment, we planned to include 25 participants, and recruited a total of 19 participants for 20 interviews. In addition, issues related to gaining ethics approval during the COVID-19 pandemic restricted recruitment to three NHS health trusts and one NHS ambulance trust in England. The planned six pen portraits were reduced to three linked to each of the three prioritised programme theories. The original plans to support the ESG members to produce a short animation to share the findings with a wide audience has not been achieved owing to delays earlier in the project delivery and funding limitations.
Our plans to engage with UK-wide stakeholders was limited by the impact of the COVID-19 pandemic. Difficulties obtaining ethics approvals delayed recruitment to interviews and a pragmatic decision was taken to recruit participants via three NHS trusts and one ambulance trust in England. Attempts to recruit lived experience participants from across the UK were also hampered by the pandemic. We made a pragmatic decision to continue to work with the stakeholders already recruited to the ESG to provide a stable and familiar online environment for discussion.
Conclusion
This chapter has briefly synthesised findings from the three programme theories and sought mid-range theory that seeks to explain at least one theory, if not multiple theories. It is noticeable that no one mid-range theory explains all three programme theories. This is not a rare occurrence within the context of realist synthesis, although it is partly explained in this instance by the fact that the three chosen programme theories lie across the system, organisation and intervention levels of our analysis.
Chapter 7 General conclusions and recommendations
General conclusions
The pathway to help in a crisis is complex, and this is unlikely to change because of varied definitions of crisis and the heterogeneous nature of the population and the mental health concerns people face in a crisis. The findings showed that this complexity can be managed through greater clarity at the boundaries of services and how they operate together, making referral and transition seamless and timely. This would also enable crisis responses to be guaranteed, easy to navigate, and trusted by the people and communities they serve.
Inter-agency working is known to improve accessibility of crisis care, but requires commitment and leadership to succeed. Inter-agency crisis care works best when there is a strong steer at policy level, and delivery is driven by local commissioning, enabling service delivery that supports collaboration within and between different agencies. When inter-agency crisis care is designed to meet the needs of the local population it serves within the local geography, more attention can be paid to the specific local needs of individuals and communities, with particular attention to those who are marginalised from crisis services owing to stigma, racial stereotypes and diagnostic labels.
This synthesis shows that a shared acknowledgement that there is no single definition of a mental health crisis and that crises are rarely single events may help facilitate inter-agency working, thus accommodating different values and facilitating support for people who require interventions from more than one source. However, a lack of role clarity (for agencies and individual staff within them), coupled with resource pressures, fuels disputes about responsibility. As a result, people in crisis may find themselves circling the system while staff lose their ability to provide compassionate responses.
Compassionate care is central to positive outcomes in crisis care and relies on staff having appropriate support to enable them to respond with compassion and hope. Those who respond first in a crisis require interpersonal skills and values that help to calm and reassure the person. This includes acknowledging the person’s sense of urgency, explaining any waiting and being clear about what the person is waiting for. When staff respond in this way, people in crisis trust the service and their sense of urgency is reduced.
It is unrealistic to expect stressed staff to retain their compassion, but resourcing pressures can create barriers for staff who might otherwise have access to support to prevent stress, burnout and compassion fatigue. Compassion starts with leaders, who have influence over the culture of organisations. Therefore, compassion is as relevant from commissioning processes through to leaders and front-line staff as it is to the service user experience.
Interpersonal contact between front-line staff within an inter-agency system through joint training, cross-agency meetings and job shadowing can improve communication, generate positive values and generate an understanding of different responsibilities and roles across the whole crisis delivery landscape. Co-location, co-response models and parallel assessments provide a platform for staff to share information, build relationships, and share knowledge and skills, making access to services smoother and more timely. When services respond together in these ways, crisis care can avoid the added trauma of multiple assessments.
Research recommendations
Inter-agency working
This study identified several important causal links between inter-agency models of crisis care and optimal outcomes. These outcomes are at times theoretical and have been subjected to limited testing in primary research. There are a number of different models of inter-agency working operating in UK crisis services, providing an opportunity for mixed-methods case study approaches to evaluate these models to facilitate implementation of models that produce optimal outcomes in different contexts. An important, but neglected, area of focus for this research should be on efficacy of models for rural populations.
Inter-agency models involving police and other ‘blue-light’ responders are rapidly evolving. Crisis interventions involving police and mental health services have a growing body of evidence; however, there is a lack of evidence for co-response models involving ambulance paramedic staff or emergency control rooms.
Technology
Information-sharing and communication are important to facilitate inter-agency working, involvement and shared decision-making. A lack of effective and shared technology was identified as a barrier to implementation of these important intervention strategies.
Stakeholders talked about the use of mobile apps and web pages to support self-care and self-management during a crisis, but no evidence was located on their use or efficacy. Research evaluating implementation of technology such as this would be a useful addition, particularly to support people as they wait for call-backs, visits or referrals.
The use of telephone and video-call technology has increased during the COVID-19 pandemic for initial contact and triage. Although some evidence was included in the review to show that important mechanisms such as relational safety and trust can be established using telehealth approaches in crisis care, there is a lack of UK evaluations of crisis lines, SPA, telephone triage and video-call assessment.
Meaningful stakeholder involvement
Meaningful co-production with service users and other expert stakeholders enhances the relevance of research and should be incorporated routinely into research design and delivery.
Marginalised populations accessing crisis services
Initial searches did not identify data at a granular enough level to allow exploration of the experiences of black and minority ethnic people and their experiences of accessing crisis services within the scope of this study. Despite this, it has been possible to identify some important contexts and mechanisms that improve the outcomes of crisis care for these populations, including shared decision-making, open access and non-clinical safe spaces. A realist evaluation is needed to explore in more depth the factors influencing access to and transition through crisis care for black and minority ethnic populations.
Although psychiatric or any other diagnoses have not been used to contextualise data in this study, some of the included evidence pointed to some diagnoses, or health conditions, generating additional barriers to access, for example substance use or alcohol use problems, personality disorders, physical health conditions and autistic spectrum disorders. There is a need to design research to identify effective crisis interventions for people marginalised by these diagnostic complexities.
Evaluating individual-level outcomes
It was notable in the conduct of this review that outcomes from crisis care are largely expressed in service outcomes such as reduction in hospital admissions, use of sections of the Mental Health Act 1983118 and 2007,119 and attendances at A&E. There is a lack of focus on individual or recovery outcomes. This review highlights the importance of mechanisms such as psychological and relational safety, compassion and trust in producing optimal crisis outcomes. Research is needed to develop evaluation approaches to measure the presence and impact of these mechanisms in crisis care.
Mental health triage
Mental health triage appears to be a promising approach, but has a limited evidence base. Future research could explore and test the implementation and effect of mental health triage systems. There is a paucity of research exploring the link between decisions in triage and access to appropriate crisis responses across an inter-agency system and how this is experienced by people in crisis and their family or friends. Taking an inter-agency approach to such research may uncover important insights into differences in values driving decisions and support closing of gaps and reduction of delays between services.
Implications for practice
Inter-agency working
Inter-agency working is very important to the delivery of optimal community mental health crisis care. Policy-makers might consider strengthening national leadership of inter-agency crisis care, such as previously provided by the Crisis Care Concordat,27 to provide a framework for the development of agreed standards; to drive improvement; and, importantly, to provide a platform where expectations for inter-agency working can be shared. Within a national policy framework, support for local decisions about commissioning of community crisis services ensures that the needs of local populations are served, cognisant of local demographic characteristics, population size and dispersion. Further research could help improve understanding of how the geographic location of crisis services affects service delivery. There is, for example, limited evidence focused on inter-agency models of crisis care in rural UK communities.
Within an inter-agency crisis care system, cross-agency agreements about how services operate across traditional service boundaries, including information-sharing agreements, trigger mechanisms such as affiliation and shared goals, which, the evidence suggests, improve experiences of receiving crisis care. Advances in digital and telehealth technology used in crisis care, fast-tracked as a result of the COVID-19 pandemic,90 provide additional flexibility needed to improve cross-boundary information-sharing. Evidence focused on the use of technology to support delivery of crisis care was, however, sparse, and often not based on UK service designs. Future research could focus on understanding if telehealth is an acceptable intervention strategy and how these technologies contribute to producing optimal crisis outcomes. Although current technology provides a means for intervention and information-sharing, our review found that information was not shared evenly across the crisis system and that limitations with the technology itself led to frustrations among front-line staff. We also located very little in the evidence about how information-sharing supports families (or friends) during a crisis, with or without technology, despite availability of guidance for carer support in England,188 and the knowledge that families take a great deal of responsibility for providing support during crises.
Policy-makers and researchers might consider how inter-agency working can trigger distal outcomes such as stigma reduction, increased likelihood of co-production and reduction in restrictive responses. Co-production triggers mechanisms such as community engagement. When communities are engaged in local crisis services, people recognise the crisis service as ‘designed for them’ and this may reduce stigma and fear. When there is less fear, especially in marginalised and minority communities, the evidence suggests that people access crisis care sooner. When people access crisis care sooner, they may be less distressed at first contact, and this could be a way for services to reduce the likelihood of using restrictive approaches to care.
Co-production provides opportunities to design services that can accommodate the diverse ways in which people define mental health crises, including the different values and expectations people have about crisis responses. The evidence suggests that, to accommodate this diversity within any inter-agency crisis system, service commissioners might consider designing inter-agency crisis services that include services perceived as ‘clinical’ (including, e.g., CRT and A&E liaison), services perceived as ‘non-clinical’ (e.g. safe havens, crisis cafés) and ‘non-health’ services (such as interventions delivered by the police).
These findings suggest that inter-agency services are more likely to produce optimal outcomes when they are designed in ways that facilitate co-operation across service boundaries, such as between statutory and voluntary sectors, primary and secondary care, urgent care and crisis care, health and social care, justice systems and local authorities. The evidence suggests that, when crisis services prioritise opportunities for joint endeavour across agencies (including shared meeting structures, shared service evaluation, joint training), mutual understanding between leaders and staff in different agencies may improve. At the front line of service delivery, parallel assessment provides an opportunity for joint working, but also improves the accuracy of assessment and reduces the likelihood of traumatic retelling, known to risk further harm to those in crisis. Our findings conclude that joint working in these ways provides a platform for delivery of inter-agency crisis care that may reduce the stress, distress, delays and service gaps caused by boundary and responsibility disputes.
Although this synthesis identified important mechanisms triggered by interpersonal contact between staff in different agencies, mid-range theory identified that contact alone may not be sufficient to generate co-operative inter-agency working. What is also needed is equal status across different providers, common goals and external support such as through national policy co-ordination. Without these, there is a risk of reinforcing difference and of siloed thinking, leading to lasting damage to inter-agency working. 82,169,170 This is not to suggest that inter-agency working requires services to operate with the same values, but rather the approach to inter-agency collaboration may be required to accommodate different values to optimise outcomes. This synthesis also identified the importance of retaining the unique identity of services (particularly the voluntary sector), thereby facilitating challenge and debate that may protect the crisis care system from unhelpful attitudinal barriers to service delivery.
Stability and continuity
We concluded from evidence that commissioners of inter-agency crisis care are faced with the challenge of, on one hand, enabling voluntary sector providers (for example) to retain their unique identity, and therefore their ability to challenge attitudes, and, on the other hand, enabling these services to have a stable presence in the crisis care landscape. Policy-makes and commissioners might therefore consider novel ways to sustainably fund voluntary sector services while also enabling them to retain their values and independence. The stable presence of different crisis services across an inter-agency system may also enable the system-level mechanism of continuity through stable thresholds for access to services, which enable people in crisis to navigate to timely help.
Continuity was identified in the evidence as an important mechanism for optimal crisis care and was often conceptualised in the synthesis in terms of individual front-line workers who are known, trusted and co-ordinate service responses. Although care co-ordination is an existing feature of UK mental health services, and provides a degree of continuity, further consideration of how care co-ordination operates to support people to navigate crisis services, especially for those new to mental health services, may help to provide the sense of continuity people in crisis seek.
Although we located limited evidence focused on the role of family and friends during a mental health crisis, it was clear from the synthesis that, when family and friends are present and available for support, people in crisis often seek their help first; as a result, continuity may be best provided by them. When family support is not available, our review identified that peer support in non-clinical services may be conceptualised as providing a proxy for family support, further emphasising the importance of non-clinical crisis services having a stable presence in the crisis care system.
Compassion
The focused review of compassionate and therapeutic crisis care identified the importance of compassion throughout the crisis care system. The mechanism activated by compassionate leadership was that leaders set the tone for service delivery, influencing the culture of services and, as a result, how staff operate at the front line. If compassionate leadership supports front-line staff to retain their compassion, it may logically lead to improved experience for those accessing crisis care. The causal link between compassionate leaders and improved service outcomes is somewhat theoretical, in part because compassion is not easily measured. Future evaluation of compassionate leadership might focus on the support needs of leaders, as well as those of front-line staff. Furthermore, evaluation of crisis services more generally may be most impactful when conducted across the inter-agency crisis system, as people in crisis often encounter multiple agencies, thus providing a more complete picture of crisis services.
Decision-making, referral and transition
The evidence focused on accessing crisis care showed that first impressions of crisis services have a lasting impact on how people perceive crisis services (stigma and fear), and seem to then affect how individuals and families choose their route to help in future crises. These attitudinal barriers may be maintained by services having complex referral systems; coupled with service boundaries and thresholds that lack transparency, these seem to lead to more people circling the system (multiple assessments and no intervention) or accessing help via the urgent care pathway. Designing services that guarantee that a person will access a service (such as A&E or some voluntary sector crisis services) increases the likelihood of people in crisis prioritising that service for first contact.
Continued emphasis on commissioning of community crisis services with streamlined access routes, transparent thresholds for access and cross-boundary agreements may facilitate earlier access to crisis support for anyone in crisis, but are very important to people from minority ethnic groups, for whom stigma and fear present the greatest barriers to access. Although this review located limited evidence focused on crisis care for people who are black or from minority ethnic backgrounds in the UK, the use of joint crisis planning to facilitate shared decision-making showed more promising results in trials for black and minority ethnic populations than for other ethnic groups, and may be an important consideration for future intervention development and evaluation.
Difficulties accessing crisis care appropriate to perceived need was linked to inconsistent application of decision processes between services, often resulting in disputes about responsibility. Decision tools used in crisis care lack robust evidence regarding their measurement efficacy; this is an area recommended for future research. Support from leaders who operate close to the front line of crisis service delivery was an important mechanism to improve decision-making and confidence of front-line staff, enabling them to feel more in control of workload and retain their compassion. Commissioning of crisis services might consider development of clinical leadership roles and design these roles in ways that assure their availability to provide support to front-line crisis staff.
Final remarks: delivery of study objectives
The study achieved its objectives (see Table 8), despite unexpected difficulties resulting from the effects of the COVID-19 pandemic, owing to an agile and committed research team and support from the funders. Project milestones were adjusted to accommodate the changing context of the study.
| Number | Objective | Outcome | Reported |
|---|---|---|---|
| 1 | Use stakeholder expertise, current practice and research evidence to develop programme theories to explain how different crisis services work to produce the outcome of resolution of mental health crises | Diverse sources of expertise and information about community mental health crisis services were synthesised to prioritise three programme theory components: (1) urgent and accessible, (2) compassionate leadership and (3) inter-agency working | Chapters 2–6 |
| 2 | Use a CIMO framework to construct a sampling frame to identify subsets of literature within which to test programme theories | A sampling frame, developed using the CIMO framework, was used during the realist searches to steer identification and selection of literature for theory testing | Chapter 2 |
| 3 | Iteratively consult with stakeholders via a series of ESG consultations and individual interviews with diverse stakeholders to test and refine programme theories | Expert stakeholders were actively and meaningfully involved in selecting, testing and refining the programme theories. A range of interviews generated further insights for theory testing and refining | Chapter 2 |
| 4 | Identify and create pen portraits of UK crisis services that provide exemplars of the programme theories to explain how mental health crisis interventions work in order to explore and explain contextual variation | Each programme theory component generated a pen portrait that may be used as an exemplar to illustrate how mechanisms trigger outcomes in different contexts linked to aspects of crisis care intervention and the service user perspective and experience | Chapter 2 |
| 5 | Synthesise, test and refine the programme theories, and, when possible, identify mid-range theory, to explain how crisis services work to produce the outcome of resolution of the crisis, and hence to provide a framework for future empirical testing of theories in the pen portraits and for further intervention design and development | Insights into context, mechanisms and outcomes for prioritised theory components presented in relation to three focused reviews, generating an overall synthesis. Pen portraits illustrate the mechanisms required for optimal crisis service delivery from a real-world perspective. Synthesised CMO configurations provide a framework for empirical testing in Chapter 6 | Chapters 3–6 |
| 6 | Produce dissemination materials that communicate the most important mechanisms needed to trigger desired context-specific crisis care outcomes, to inform current and future crisis care interventions and service designs | A number of in-project dissemination activities have been undertaken. These include methodological papers and posters, webinars to lay and professional audiences, and presentations to clinical and commissioning teams. A Twitter (Twitter, Inc., San Francisco, CA, USA) presence has been maintained throughout the project delivery and two blogs have been posted online during the project | |
| Post-project dissemination materials are in development, including international conference presentations and academic journal papers |
Acknowledgements
Study sponsor
Sheffield Health and Social Care NHS Foundation Trust.
Other acknowledged contributions
The members of the ESG, who were generous with their knowledge and expertise on this project.
Dr Ruth Wong (Information Specialist) School of Health and Related Research, University of Sheffield, who designed and conducted the electronic searches.
Georgia Greaves (undergraduate student), University of Sheffield, undertook a review of the data held in the Crisis Care Concordat web pages.
Contributions of authors
Dr Nicola Clibbens (https://orcid.org/0000-0002-9047-6496) (Associate Professor of Mental Health Nursing) was the chief investigator, led the project, contributed to the development of IPTs, led and conducted one focused review, contributed to stakeholder consultation, conducted individual interviews, contributed to the report and led dissemination activities.
Dr John Baker (https://orcid.org/0000-0001-9985-9875) (Professor of Mental Health) was a co-applicant; provided leadership support to the new chief investigator; and contributed topic expertise to the development of candidate programme theories, to the focused reviews and to the development of dissemination materials.
Dr Andrew Booth (https://orcid.org/0000-0003-4808-3880) (Professor in Evidence Synthesis) was a co-applicant, provided expert methodological advice on realist evidence synthesis, contributed to the development of candidate programme theories, supported the delivery of three focused reviews, led the delivery of synthesis to mid-range theory, and contributed to report writing and dissemination materials.
Dr Kathryn Berzins (https://orcid.org/0000-0001-5002-5212) (Senior Research Fellow) was a co-applicant, led on administration and the ethics approval process, provided mentorship to a co-applicant who is an independent consultant and visiting research assistant, contributed to stakeholder consultations, conducted individual interviews, developed candidate programme theories, delivered one focused review, led on in-project communications with stakeholders, and contributed to report writing and dissemination materials.
Mr Michael C Ashman (https://orcid.org/0000-0003-4195-0208) (Independent Consultant and Visiting Research Assistant) was a co-applicant; co-chaired the ESG; and contributed to the development of programme theories, focused literature reviews, report writing and dissemination materials.
Dr Leila Sharda (https://orcid.org/0000-0002-8427-4310) (Research Assistant) contributed to stakeholder consultations; recruited to and conducted individual interviews; developed candidate programme theories; delivered one focused review; and contributed to mid-range theory synthesis, report writing and dissemination materials.
Dr Jill Thompson (https://orcid.org/0000-0001-9256-1208) (Lecturer) was a co-applicant; co-chaired the ESG; conducted individual interviews; and contributed to the development of candidate programme theories, focused reviews, report writing and dissemination materials.
Dr Sarah Kendal (https://orcid.org/0000-0001-8557-5716) (Research Fellow) led and contributed to report writing.
Dr Scott Weich (https://orcid.org/0000-0002-7552-7697) (Professor of Mental Health) was a co-applicant; provided leadership support to the new chief investigator; and provided topic expertise to the development of candidate programme theories, focused reviews and dissemination materials.
Data-sharing statement
All available data relevant to this report are either included as an appendix to the report or can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
Appendix 1 Data extraction templates
Identification of initial programme theory template (example)
| Study | Relevance | Theory ID | Rigour | Screening and extraction | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Year | Country | Search ID | Focus | Intervention(s) | If (C) | Then (M) | Leading to (O) | KB | LS | AB | NC | |
| Frisina and Evans189 | 2016 | Canada | RW theory v3 | Logic model for street-dwelling youth mental health services for those aged 16–21 years (p. 228) | Refers to specific pathways that include DBT, global functioning focus, skills for life, psychoeducation | Referral and triage approach feeds into a stepped care system with defined pathway of care | Resource: resources can be used effectively to meet individual needs despite complexity Response: provide a service that is responsive to need and specific population |
Increased ability to reach hard-to-reach group, increased capacity to endure challenging situations, manage emotional instability, improved QoL | Book chapter reporting ethnographic study (p. 221) | ✓ | 7 November 2019 | ||
| Frisina and Evans189 | 2016 | Canada | RW theory v3 | Logic model for street-dwelling youth mental health services for those aged 16–21 years (p. 228) | Refers to specific pathways that include DBT, global functioning focus, skills for life, psychoeducation | If the referral and triage process uses a range of communication approaches | Resources: in-person communication, e-mail, text messaging and social media Response: people more likely to be able to maintain contact with the service |
Increased ability to reach hard-to-reach group | Book chapter reporting ethnographic study (p. 221) | ✓ | 7 November 2019 | ||
Focused review data extraction template (example)
| Date | Extracted by | Report title | Document type | Author | Year | Origin | Intervention | Context | Mechanism | Outcome | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resources | Responses | Proximal | Distal | |||||||||
| 1: urgent and accessible care | ||||||||||||
| 15 July 2020 | NC | Embedding an evidence-based model for suicide prevention in the National Health Service: A Service Improvement Initiative | Research paper | Brown104 | 2020 | UK and USA | Suicide triage | People presenting in A&E or to crisis mental health services as suicidal | Staff training in suicide risk assessment, history-taking, urgent medical treatment, help-seeking behaviour and pathways through services | Staff more objective about suicide and rating of risk | Improved decisions and accurate signposting to follow-up | Faster access to mental health service |
Appendix 2 Table of interventions: Template for Intervention Description and Replication Lite
| Intervention name | Document ID | Detail of intervention (What?) | Where is it used (Where?) | When is it used? Dose? (When? How much?) | Who uses it? (Who?) | IPT |
|---|---|---|---|---|---|---|
| Ambulance/paramedic response car | NHS England101 2020 | Mental health joint response car with additional staffing. Responded to call from control centre to people experiencing a mental health crisis. Aimed to use the skills of the mental health nurses and paramedics to provide a complete biopsychosocial assessment at the earliest point pre hospital. Convey or refer to most appropriate services, avoiding hospital when possible | South London | Six cars ran 11.00–23.00 7 days a week from 2018 | 13 mental health staff seconded to the ambulance service working alongside 22 paramedics. Paired mental health nurses with paramedics in a vehicle | 1 |
| Compassionate care and leadership | NHS England136 2014 | 10 most important characteristics of compassionate leadership: emotional intelligence, integrity, listening, trust, authenticity, openness, caring, reflective, committed and genuine | Health services UK | Not reported | All health services leaders | 2 |
| Cole-King and Gilburt134 2011 | Multimodal compassionate mind training | Not reported | Not reported | For all health-care staff | 2 | |
| Firth-Cozens and Cornwell135 2009 | Components of compassion | UK acute hospitals | Not reported | For all acute hospital health-care staff | 2 | |
| Royal College of Psychiatrists126 2015 | 10 components of compassionate care. Description of evidence-based actions to deliver on compassion. As an individual: mindfulness; improve self-awareness; self-compassion. Organisationally: compassionate organisations; culture change | UK mental health services | Advocated for everyday practice | For organisations, leaders and health-care staff | 2 | |
| Crisis House | Prytherch et al.133 2020 | Trauma-informed approach in an NHS-commissioned crisis house. Alternative to hospital admission. Staff trained in trauma-informed approaches and recruited based on attitudes and values, rather than qualifications. Work closely with local crisis team. Risk is managed through psychological interventions, safety planning, check-ins and one-to-one time with staff. The service is co-designed. Self-referral. Staff receive support and supervision | London | 24/7, 4-week maximum stay, average stay 2 weeks | For women with a previous history of hospital admissions who are vulnerable owing to trauma. Female staff in crisis house and requested for all external liaison staff | 2 |
| CRT | Begum and Riordan103 2016 | Mental health crisis response service with responsibility for decision-making on the most appropriate treatment and pathway of care. The gatekeeping role aims to reduce hospital admissions and facilitate early discharge. Provides assessment, involvement of family and the person in crisis, referral, liaison and negotiation of care with multi-agency mental health services, avoiding hospital admission when possible | Crisis resolution and home treatment services | All crises where there is a risk of hospital admission | Health professionals working in crisis resolution mental health services | 1 |
| Chilman et al.102 2021 | To provide intensive community support to people experiencing a mental health crisis and to reduce the need for hospital admission | UK model; intervention not fully reported | Not reported | Not reported | 1 | |
| Morant et al.15 2017 | CRT provided rapid assessment and intensive home treatment for people experiencing a mental health crisis. Direct access, multidisciplinary gatekeeping, referrals for inpatient care, providing a range of interventions including medication, practical help with daily tasks, family/carer support and interventions to increase resilience and prevent relapse | Provided in community settings across England | 24 hours, 7 days per week | Delivered by a multiprofessional team in a mental health organisation to people experiencing a mental health crisis | 1 | |
| Culture-of-care barometer | Rafferty et al.127 2017 | Culture-of-care barometer. A measurement tool to assess the culture of care in health settings. A 4-factor scale focusing on macro-organisational culture, meso team culture and micro relationships with colleagues and micro constraints of job | Scale developed and validated in the UK | Not reported | For use in health-care organisations | 2 |
| Integrated services | Association of Mental Health Providers156 2021 | An alliance between voluntary sector providers to support the two-way flow of information between communities, the voluntary sector and policy leads | England | Not reported | NHS England, voluntary organisations delivering health and well-being interventions | 3 |
| National Voices154 2013 | Good integrated care included the following: care co-ordination, information-sharing, shared decisions and care planning, support for medicines and self-management, transitions managed, supported at home, residential care options | Across all health care and health-care settings | Not reported | All agencies/staff involved in delivery of health and social care | 3 | |
| NHS England157 2018 | Integrated mental health first-response service. A collaborative, multi-agency partnership approach to out-of-hours crisis response services. Local Crisis Care Concordat group developed a shared vision. First responses closer to home through crisis response lines, single point of referral | Bradford District Care NHS Foundation Trust | 24/7 availability of first response | Co-ordinated responses from all services providing crisis care in the Bradford district Involved all mental health services, police, voluntary sector, EDs, occupational health, commissioners and local authority |
3 | |
| RAND Europe et al.153 2012 | Integrated care pilots. Each site provided a different population focus and approach to integration for evaluation. Approaches to integration included macro-organisational level, meso level and micro level. Most integration was horizontal between community services rather than vertical, for example between primary and secondary services | Bournemouth and Poole, Cambridge, Sunderland, North Cornwall, Cumbria, Durham, Northamptonshire, Newquay, Norfolk, North Tyneside, Northumbria, Nottinghamshire, Tameside and Glossop, Torbay, Tower Hamlets, Wakefield | Not reported | Not reported | 3 | |
| Jespersen et al.108 2016 | A service redesign to integrate crisis mental health services within general community mental health teams | Victoria, Australia | Not reported | All patients are seen by the same team, regardless of their stage of treatment | 1 | |
| Goodwin et al.144 2012 | Integrated health-care approaches. Modelling a focus on resolving policy and organisational barriers | UK | Needs large populations (cover large geography) | Advocating wide systemic involvement of multiple stakeholders | 3 | |
| Mental Health Foundation147 2013 | Nine factors that facilitate good integrated care: information-sharing, shared protocols, joint funding and commissioning, co-located services, multidisciplinary teams, liaison services, navigators, research and reduction in stigma | UK | Not reported | Advocating wide systemic involvement of multiple stakeholders | 3 | |
| Bowles and Jones161 2005 | Refocusing acute mental health services. Whole-system working that enables systemic understanding for staff. People are able to use their specialist skills; warm networking | UK mental health inpatient wards | Not reported | All professional staff working across the whole system of acute mental health care across inpatient and community settings | 3 | |
| Inter-agency crisis services | Boscarato et al.84 2014 | Integrated mental health responses, including ride-along model, crisis intervention team model, embedded model, separate response model | Community settings Police setting Police and community settings |
Response to crisis calls When police encounter a person experiencing a mental health issue, specialist mental health services based in police setting provide immediate crisis responses. Bidirectional referral between police and crisis services as needed |
People experiencing a mental health crisis. People who encounter police when experiencing a mental health crisis. All people experiencing a mental health crisis in a police setting. As-needed referral in a mental health crisis | 1 |
| Crisis Care Concordat27 2014 Crisis Care Concordat30 2021 |
A joint statement from all stakeholders in mental health crisis delivery in England. Signatories agreed to deliver the principles agreed in a national document and to drive local implementation plans shared via an open-access website | England, all mental health crisis services across agencies | Concordat signed 2014 | Association of Ambulance Chief Executives, Association of Chief Police Officers, Association of Directors of Adult Social Services, Association of Directors of Children’s Services, Association of Police and Crime Commissioners, British Transport Police, Care Quality Commission, Royal College of Emergency Medicine, College of Policing, The College of Social Work, Department of Health and Social Care, Health Education England, Home Office, Local Government Association, Mind, NHS Confederation, NHS England, Public Health England, Royal College of General Practitioners, Royal College of Nursing, Royal College of Paediatrics and Child Health, Royal College of Psychiatrists | 3 | |
| Gibson et al.28 2015 | An England-wide agreement between different agencies and services involved in responding to people experiencing, or at risk of experiencing, a mental health crisis. Agreed formally through a multi-agency signatory | England. Across health, social care, voluntary sector, social enterprise, local authority, and criminal justice services | Signed in 2014. The agreement had been in place for 12 months at the point of evaluation | Evaluated by an independent organisation | 3 | |
| Healthy London Partnership155 2016 | Combined urgent care and crisis care to provide clarity on the crisis pathway and a more consistent approach across London. Collection of baseline data on places of safety, bed use and section 136 detentions. Implementation of health needs assessment | London, crisis care pathway | Not reported | NHS England and NHS mental health trusts and justice system strategic clinical network | 3 | |
| Hollander et al.149 2012 | Mobile CATTs. CATTs operate independently of police, but are responsive to requests from police for shared management. Protocols exist for delivery of the service not stated in this document. Police had received additional training in mental health | Melbourne, VIC, Australia | Not reported | Multidisciplinary community-based mental health crisis service (CATT) and local police | 3 | |
| McKenna et al.152 2015 | NPACER. Operates a ‘second response’ model whereby a mental health clinician and a police officer respond to an initial ‘first response’ that identifies a need for a joint assessment. The NPACER team provides assessment and intervention to reduce behavioural escalation and provide a better outcome for people with mental health needs. Focused on diversion away from EDs | Australia | 7 days a week between 15.00 and 23.30 | Team consists of one police officer and one nurse on duty, drawn from a wider pool of appropriately skilled mental health staff and police personnel | 3 | |
| Parker et al.160 2018 | Pre-arrest diversion – first-response police; co-response model Post booking jail diversion and court diversion, information-sharing agreement models, co-location model, comprehensive systems model, consultation model, service integration model, special protective measures, re-entry programmes |
Delivered mostly in developed countries including the UK, the USA, Canada, Australia and mainland Europe | Availability of models varied by country and type | Delivered in collaboration with police and mental health services. Many models engage with wider health, social care, local authority and criminal justice services | 3 | |
| Joint crisis planning | Barrett et al.116 2013 Farrelly et al.118,120 2014 Farrelly et al.119 2015 Thornicroft et al.123 2013 (CRIMSON study) |
Development of a JCP to provide advance decisions about what the person wishes to happen should they experience a crisis/relapse in the future. JCP is disseminated to MDT and anyone else nominated by the participant. JCP facilitators received 1 week of training in JCP facilitation and received weekly supervision Control: treatment as usual received via a community mental health team delivered to both the treatment participants in the JCP arm and the control arm |
Generic and specialist community mental health teams in three geographical areas in England | Two meetings convened by the JCP facilitator between nurse and participant to develop the JCP. Meetings were at least 1 week apart. A review meeting was offered after 9 months Meeting 1: introduction to principles of JCP and the JCP menu, which included a list of items the participant may wish to include in their JCP. Meeting 2:the JCP is finalised |
Adults aged > 16 years with a history of relapsing psychotic illness with at least one admission to hospital in previous 2 years and registered under the care programme approach as requiring enhanced care. Delivered by senior mental health nurses. A relative of the participant could also attend the meetings Treatment as usual delivered by any staff in community mental health team |
1, 2 |
| Borschmann et al.117 2013 | Participants provided with a blank JCP template and a list of topics to be considered for inclusion. The participant chose if family or other key workers attended the meeting in which the content of the JCP was discussed. The JCP was finalised by the participant, written in their words, distributed to individuals stipulated by the participant and attached to their medical record with consent. Participants in the JCP intervention also received standard care. Control: treatment as usual from community mental health team | Community mental health team in London, UK | 1 week after the participant received a JCP template and a list of suggested topics for inclusion, a 1-hour meeting to agree the content of the JCP was held. Within 24 hours of the meeting, the JCP is distributed to all agreed individuals and, if the person agrees, attached to the medical record | People who experienced crises, self-harming behaviour in the previous 12 months with a diagnosis of borderline personality disorder (DSM-IV-TR). Accessing community mental health teams in UK, aged ≥ 18 years | 1 | |
| Lequin et al.121 2021 | JCP intervention not described in detail | Inpatients in Switzerland | Not reported | Inpatients | 1 | |
| Ruchlewska et al.122 2014 | Focused on crisis prevention and the provision of practical information for future psychiatric emergency care. The information is summarised on a small ‘crisis card’. The crisis plan is not legally binding. Compared two types of crisis plan: (1) created between a patient advocate and the patient and (2) created between a clinician and a patient. Both had the same format. Covered four domains: (1) relapse indicators and daily functioning; (2) what to do in times of crisis; (3) medical information, including medication, and (4) information about all relevant people involved in the crisis plan, including family, friends and services. All participating clinicians and advocates received training in the crisis plan. The completed plan was signed by the patient, and all involved in their crisis plan. The plan was then summarised on a crisis card | Mental health teams and mental health hospitals in Rotterdam, the Netherlands | Meetings with clinician or advocate at least twice to develop plan. Annual review of plan | Clinicians who were mostly registered nurses and advocates who were social workers Delivered with patients who had psychosis or bipolar disorder and had contact with mental health services over the previous 2 years (crisis contact or hospital admission) |
||
| Liaison mental health | Eales110 2013 | Mental health liaison service in general acute hospital setting | Based in acute general hospitals covering A&E and acute general wards | 24-hour access by referral | Delivered to any person in an acute hospital setting requiring a mental health assessment or intervention. Delivered by specialist mental health practitioners in a mental health liaison service based in the acute hospital | 1 |
| Evans et al.100 2019 | Models of mental health liaison: Co-located in A&E departments Arrangements for response from existing in-hospital mental health service Emergency mental health services delivered at a specialist mental health site |
A&E department Hospital-wide mental health service Specialist emergency mental health unit |
24 hours | All models were delivered by specialist mental health staff, including psychiatrists, nurses and social workers | 1 | |
| Mental Health Act 1983118 (England and Wales) section 136 | Bendelow et al.95 2019 | Police power of detention for a person suspected to be experiencing a mental health condition requiring treatment in a public place Police can convey a person to a place of safety for assessment of their mental health |
In a public place in England and Wales | When a person comes into contact with the police in a public place and requires assessment of their mental health | Police in a public place | 1 |
| Griffith141 2018 | Collaborative care from district nurses related to the use of emergency sections of the Mental Health Act,118 including sections 135 and 136 | In a public place or private residence in England and Wales | When a person is being cared for by district nurses and is subject to sections 135 or 136 | District nursing | 3 | |
| Mental health triage | Edmondson and Cummins148 2014 | RAID team based in mental health liaison available to community police officers who needed mental health advice during attendance at an incident | Telephone triage service delivered in Oldham from Royal Oldham Hospital near A&E department for local community police officers attending an incident where they suspect a person is experiencing a mental health problem | 24-hour telephone triage | Telephone triage service staffed by mental health liaison RAID team. Telephone advice provided to community police | 3 |
| Grigg et al.107 2007 | Mental health triage used to rapidly assess the acuity and deployment of resources to meet needs in a mental health crisis. Applied in a range of settings where an urgent response is needed | Australian mental health services. Three case studies in which triage decisions are made | 24 hours, face to face and telephone | Any person seeking urgent help in a mental health crisis. Delivered by specialist mental health staff from a range of professional groups | 1 | |
| Sands et al.93,94 2013 | Mental health triage services provide a SPA to specialist mental health services. Provide access to assessment, support, advice and referral for people of all ages experiencing a mental health problem Referrals to triage are made after an initial screening assessment by telephone to determine the nature and urgency of the problem and the best course of action. Mental health triage scale to assess urgency in three domains: (1) urgency, (2) response time and (3) descriptor Cases are divided into seven categories from emergency immediate response through to advice only with no stated response time |
Co-located in either mental health teams, EDs, psychiatric units or in call centres in Australia | 24 hours a day | People of all ages experiencing a mental health problem Delivered by a MDT of mental health expert clinicians |
1 | |
| Models of crisis care | Sunderji et al.91 2015 | 10 programmes of care. Hospital based: rapid response outpatient team, rapid response model, urgent consultation clinic, urgent follow-up clinic, paediatric crisis clinic, ED mental health nurse practitioner outpatient service and interim crisis clinic. Community based: mental health urgent care service, quick response team and urgent assessment service | Based in mental health services or EDs. Hospital based: Quebec, Ontario, Sydney and New York. Community based: Alberta and the UK | Response times for hospital-based programmes ranged between 2 and 10 days, average 7 days. Community services were similar; one provided a walk-in service | Psychiatry, nursing, social work and psychology Heterogeneous population and inability to safely await routine ambulatory care because of suicide risk, self-harm or clinical deterioration |
1 |
| Recovery-focused care planning | Simpson et al.129 2016 | A case management approach to delivery of care planning. Requires providers to comprehensively assess health and social care needs, develop a written care plan in collaboration with the service user and carer, allocate a care co-ordinator and regularly review care. Care panning should be personalised and recovery focused | Community mental health teams in England and Wales | All eligible people receiving secondary mental health care | Staff in mental health services and all eligible people with a mental health condition requiring a care plan | 2 |
| Risk management | Faulkner137 2012 | Approaches to risk management focused on key components, including a rights-based approach, responsibility, regulation of services, adult safeguarding, balancing power and co-production | UK mental health services | Not reported | Multiple stakeholders engaged in understanding their role in management of risk | 2 |
| Schwartz Rounds | Farr and Barker125 2017 | Interdisciplinary reflective groups to enable staff to share experiences and vulnerabilities, to support each other and to enhance connections between caregivers and patients The Rounds standard procedure starts with a mixed staff panel discussing a patient or a work-related theme, to which all participants can then respond. Rounds use an evidence-based model with trained facilitators moderating the group discussion. A steering group oversees the development and process of running Rounds |
Community and mental health services Case A: a large foundation trust, delivering mental health, community and specialist services to adults and children. Case B: a large and complex community foundation trust covering a wide, rural geographical area. Case C: a foundation trust that provided mental health services. It had a mixed rural and urban geography |
Monthly Schwartz Rounds. Observed for 1 hour, although duration of rounds unclear | Multidisciplinary clinical staff. Schwartz Rounds are open to all staff, including non-clinicians, and may focus on themes made up of a number of stories or different perspectives on one particular case | 2 |
| Short hospital stay | Gudde et al.105 2013 | People known to mental health services can choose to have a short hospital admission of 1–5 days if they experience a mental health crisis | Norwegian acute mental health services for people with psychosis or bipolar disorder experiencing a crisis | Short hospital admission of 1–5 days | Service users choose an admission if they identify a mental health crisis | 1 |
| Street triage | Carson146 2018 | Street triage added to existing RAID model in crisis services in EDs. Telephone response to request for immediate support and advice on mental health from police on scene | By telephone via ED | 24 hours a day, 7 days per week | All mental health presentations encountered by police in Oldham and Greater Manchester Intervention delivered by mental health nurses and social workers |
3 |
| Horspool et al.150 2016 | Street triage interventions that have departed from the UK Department of Health and Social Care initial pilot models implemented and evaluated as part of the Crisis Care Concordat | England, two locations, urban and urban/rural: Study location 1: joint response car, integrated recovery programme for high users of police time, joint training Study location 2: joint response car, mental health workers in the emergency control room, joint training |
Availability of the interventions was reliant on opening times, which varied for the different components of the service in each area. The availability of the intervention was also linked to the density of the population, the geography, and the complexity of boundaries between different health and social care organisations in each location | Delivered by specialist mental health staff from a range of professions and the police | 3 | |
| Lancaster et al.151 2016 | Overview of different models of joint police and health responses to mental health crisis. Joint responses or rapid referral between mental health and police for people experiencing a mental health crisis. NPACER, DeKalb CSB, COAST, street triage | Australia USA Canada UK |
15.00–23.00 15.00–23.00 24 hours 14.00–00.00 |
NPACER: one police officer and one mental health clinician DeKalb CSB: four police officers and two nurses COAST: one police officer and one psychiatric nurse Street triage: psychiatric nurse paired with unknown number of police officers |
3 | |
| Reveruzzi and Pilling98 2016 | Nine pilot sites delivering five models of street triage in England: Control room telephone response Control room and face to face Mental health practitioner responding when requested by an officer Police officer and mental health practitioner responding together Mental health practitioner, police and paramedic responding together |
British Transport Police, Devon and Cornwall Police; London mental health trust, West Yorkshire Police, North Yorkshire Police, Sussex Police, Thames Valley Police, Derbyshire Constabulary, West Midlands Police | Not reported | Control room staff, mental health staff, police, paramedic | 1, 3 | |
| Suicide triage | Brown et al.104 2020 | CAMS. Completion of a SSF comprises self-completion section and therapist assessment section. A treatment plan is generated and the SSF is used as a progress measure. When three SSF measures show self-management of suicidal thoughts, feelings and behaviours, intervention stops. CAMS training for staff with clinical supervision | Crisis and home treatment services and mental health liaison in one region of England | Presentations at crisis services and mental health liaison provided CAMS triage for all suicidal and self-harm presentations. High-risk service users received the CAMS intervention. Suicide management intervention targets individual defined suicide risks over 4–12 sessions | All high-risk suicide and self-harm presentations at crisis and mental health liaison services. Staff who have received the CAMS training and supervision | 1 |
| Telephone crisis line | Cambridgeshire and Peterborough NHS Foundation Trust113 2016 | Mental health advice, support and treatment to anyone experiencing a mental health crisis. Phone NHS 111 and select option 2. Direct contact; no referral needed. Refer, make an appointment or dispatch a first responder urgently. Provide support, prescribe medication and refer to a sanctuary run by Mind. Link to children’s services, learning disability services and older people’s services. The service is confidential. Interpreters are available | By telephone in Cambridgeshire, England | 24 hours, 7 day per week. Refer to a sanctuary run by Mind 18.00–01.00 | Anyone in Cambridgeshire who feels that they need urgent mental health support, including service users, family and friends Calls answered by a ‘telecoach’ who was a psychological well-being practitioner. First responders are mental health nurses and social workers, sometimes accompanied by an emergency services worker |
1 |
| NHS England90 2021 | Crisis helplines for anyone experiencing a mental health crisis or friends and family making a call on behalf of someone in crisis. The lines are also open to professionals such as police and paramedics when they encounter someone in crisis. Connected to NHS 111. Provides immediate response and referral to other services, which may include phone, video and in-person consultations | England | Implemented in 2020, available 24/7 | For a person in crisis, or their family or friends. Professional staff encountering someone in crisis such as police and ambulance. Staffed by mental health professionals | 1 | |
| Trondsen et al.115 2014 | On-call video conferencing in rural Norway for psychiatric emergencies. Rural areas without access to a local psychiatrist can have real-time video consultations Available to consult following referral by regional ambulatory mental health teams or hospital wards | Video call facilities installed in three psychiatric centres (offices or homes of six psychiatrists) in Norway | Available 24/7 | Access to psychiatrist in consultation with rural mental health centres that included nurses. Psychiatrist 24-hour rotational on-call system. Direct consultations carried out supported by nurses at the centre with the patient | 1 | |
| Saurman et al.114 2014 | Telehealth intervention where there are no local mental health specialist staff or services. Existing telehealth access to specialist mental health services for rural communities extended to support access in an emergency mental health situation. The service operates a ‘no wrong door’ philosophy whereby no caller is turned away. Four private video rooms are available from the control room to take emergency calls. Calls are initiated by a triage assessment and followed up by video interventions to provide a more comprehensive assessment, information, advice, help with medication, well-being and safety. Onward referral can be to emergency services including flying doctors, police and ambulance, or to mental health services for follow-up or further assessment | Rural and remote mental health services in western New South Wales, Australia Calls handled from a mental health triage control room. Callers must be in a local hospital facility to receive the video assessment |
24 hours every day of year | Delivered by mental health nurses and psychiatrists based in a mental health service in the same state. Staff work 12-hour shifts with 8 hours overlapping. Two nurses on duty at any one time. Support provided by a manager, a nurse consultant and administrator | 1 | |
| Team-working | Simpson129 2007 | Components of good team-working: structure and procedures, interpersonal communication and contact between members of MDT, humour and social encounters used to relieve tension in the team, safe environment to explore difficulties, support from team members | Community mental health teams, London, England | Not reported | Multiprofessional teams working in community mental health | |
| Voluntary sector mental health crisis services | Newbigging et al.10 2020 | Voluntary sector services providing crisis care. Five types of voluntary sector crisis service: Provides crisis support. Provides peer support, listening services, safe spaces, signposting and liaison General mental health support and crisis support. Wide range of services including courses, counselling, skills development, welfare and benefits advice, advocacy and awareness-raising General support to a specific population including crisis support. Promoting rights, welfare support, counselling, accessing health and social care, campaigning and education, interpreters Support for specific life event or social issue, which can be associated with a crisis. Counselling, welfare support, housing and health advice. Signpost to local health and social care Community and social organisations. Wide range of social support including welfare, housing, social connection. Signposting to health and social care |
England Helplines, crisis houses, safe spaces, and sanctuaries Covering a specific geography or population (defined by characteristics such as age, ethnicity or mental health condition). Open access at an identified location Covering specific population (defined by age, gender, ethnicity, faith, health condition). Open access Addressing specific issues including rape, domestic violence, bereavement, gambling, homelessness, pregnancy Societies, clubs, faith groups |
Varied availability across the sector, type and location of the service | Delivered by a range of specialist staff, volunteers, peer support workers | 1, 2, 3 |
| Waiting times | Haslam111 2019 | The 4-hour ED wating time standard and its applicability to people experiencing a personality disorder attending EDs | EDs in the UK | Waiting times in EDs for people attending who have a personality disorder | People attending EDs who have a personality disorder | 1 |
| Judkins et al.132 2019 | 4-hour wait in EDs | Australia | Not reported | Focus on people presenting to EDs with mental health needs | 2 | |
| NHS England112 2021 | Policy outline: for an ‘urgent’ referral to a community-based mental health crisis service, seen within 24 hours of referral, across all ages. For a ‘very urgent’ referral to a community-based mental health crisis service, seen within 4 hours of referral, for all age groups. Patients referred from A&E should be seen face to face within 1 hour, by mental health liaison or children and young people’s equivalent service | Crisis services and EDs | Urgent within 24 hours Very urgent within 4 hours ED 1 hour |
Crisis services and mental health liaison staff | 1 | |
| National Collaborating Centre for Mental Health and Positive Practice in Mental Health89 2020 | Crisis care services provide an immediate, short-term response to alleviate a crisis and prevent hospital admission. Crisis services are described in four ways: Community based – CRTs, telephone lines, primary care, voluntary sector, drug and alcohol services, homelessness services, social care, NHS 111, crisis cafés Blue-light services – police, ambulance, fire and rescue Liaison mental health – provided in physical care settings, including hospitals and EDs Age-specific services – children and young people and older adults |
Online access to support, and the ability to receive online support. Local crisis telephone numbers, helplines or text lines run by either statutory or non-statutory services. Local crisis team directly using their telephone number. Walk-in crisis services. SPA
NHS 999 or NHS 111. Presenting in person to A&E |
24 hours a day, 7 days a week | Delivered by a range of statutory and voluntary sector services and the ‘blue-light’ services, including police, ambulance, and fire and rescue | 1, 3 | |
| Duggan et al.109 2020 | Standard setting for A&E departments to address the excessively long waiting times for people presenting with mental health issues. Appropriate resources to respond with urgency. Equal priority to physical health. Integrated services | Australia | Not reported | All-age mental health responses in ED | 1 |
Appendix 3 Summary search strategy
Search strategy: initial theory scoping searches
Google Scholar
| Concept | Terms |
|---|---|
| A logic model filter* | V1: “logic model” OR “theory of change” OR “theory of action” OR “outcomes chain” OR “program* theory” OR “program* logic” OR “logical framework*” V2: “model” |
| AND | |
| Mental health | Mental health OR mental health |
| AND | |
| Setting | 1. NHS 111 2. NHS Direct (Wales) 3. 24 hour 4. Helpline 5. Crisis line 6. Accident & emergency (A&E) 7. Hospital 8. 999 9. GP 10. Liaison psychiatry service 11. Local on-call mental health services 12. Social services 13. Community 14. Local community mental health team 15. Crisis houses 16. Crisis teams (CRHT) 17. Café 18. Drop in 19. Day services 20. Day treatment 21. Police 22. Street triage 23. Crisis resolution teams (CRT) 24. Community 25. Decision |
Summary Google Scholar search strings (full version in Report Supplementary Material 1)
-
((“logic model” OR “theory of change” OR “theory of action” OR “outcomes chain” OR “program* theory” OR “program* logic” OR “logical framework*”) AND (“mental health crisis”) AND (communit*)
-
to 30. ((AND (“24 hour*”); AND (“crisis house*”); AND (“helpline*”); AND (“crisis teams”); AND (“day service” or “day treatment”); AND (“police”); AND (“street triage”); AND (“home”); AND (“cafe*”); AND (“drop in”); AND (crisis or crises or acute or emergenc*); AND (“crisis line”); AND (GP); AND (“Accident and Emergency”); AND (“NHS 111”); AND (“NHS direct”); AND “hospital”; AND “liaison psychiatry”; AND “on-call”; AND “social service*”; AND “community mental health*”; AND “crisis team*”; AND “day service*”; AND “street triage”; AND “crisis resolution team*”; AND “crisis team*”; AND triage; AND crisis AND triage; AND crisis AND decision*
Summary search strategy: focused reviews for initial programme theories 1–3 (full search strategy in Report Supplementary Material 1)
Three focused programme theories were searched between February and March 2020:
-
urgent and accessible care
-
compassionate and therapeutic care
-
inter-agency working.
Academic databases
-
MEDLINE (Ovid, 1946 to 2020)
-
EMBASE (Ovid, 1974 to 2020)
-
Web of Science Core Collection (Clarivate Analytics)
-
Science Citation Index Expanded (1900–2020)
-
Social Science Citation Index (1956–2020)
-
Conference Proceedings Citation Index – Science (1990–2020)
-
Conference Proceedings Citation Index – Social Science & Humanities (1990–2020)
-
Cochrane Library
-
Cochrane Database of Systematic Reviews (1996–2020)
-
Cochrane Central Register of Controlled Trials (1898–2020)
-
-
Cumulative Index to Nursing and Allied Health Literature (EBSCO, 1974–2018)
-
PsycINFO (Ovid, 1806–2018)
-
ASSIA (ProQuest, 1987–2018)
-
ProQuest Dissertations & Theses A&I (ProQuest, 1743 to 2020)
-
HMIC (NICE Healthcare Databases Advanced Search, 1979–2020).
Database search limits
-
A highly sensitive filter (Ayiku et al. 68) was applied to all database searches except ASSIA, ProQuest Dissertations & Thesis A&I and HMIC.
-
All searches were restricted to English-language studies.
-
2000 to present.
Grey literature searches
-
Anxiety UK (www.anxietyuk.org.uk/get-help/crisis-support/).
-
Breathing Space (Scotland), 0800 83 85 87 (https://breathingspace.scot/)).
-
C.A.L.L. Helpline (Wales), 0800 132 737 (www.callhelpline.org.uk/).
-
Centre for Mental Health (www.centreformentalhealth.org.uk).
-
College of Paramedics (www.collegeofparamedics.co.uk/).
-
Cornerstone Counselling Service (www.ccscounselling.org.uk/).
-
Exclusive Secure Care Services (www.securecareservices.co.uk/).
-
Inspire Wellbeing (www.inspirewellbeing.org/).
-
Lifeline Helpline (Northern Ireland), 0808 808 8000 (www.lifelinehelpline.info/).
-
Live Well Leeds (https://livewellleeds.org.uk/crisis-support/).
-
Mental Health At Work (www.mentalhealthatwork.org.uk).
-
Mental Health Crisis Care Concordat (www.crisiscareconcordat.org.uk).
-
Mental health crisis helplines in the UK (2018) (www.youthemployment.org.uk/list-of-mental-health-crisis-helplines-in-the-uk/).
-
Mental Health Foundation(www.mentalhealth.org.uk/).
-
Mental Health Resource (www.mentalhealthresource.org.uk/).
-
Mental Health Today (www.mentalhealthtoday.co.uk/).
-
Mind (www.mind.org.uk).
-
New Hope (www.newhope.org.uk/mental-health).
-
NHS England publications (www.england.nhs.uk/publication/).
-
Navigo (www.navigocare.co.uk/).
-
Papyrus Prevention of Young Suicide HOPEline UK, 0800 068 41 41 (https://papyrus-uk.org/hopelineuk/).
-
Porthedon (https://portheden.org/).
-
Protect Life 2 – Suicide Prevention Strategy (www.health-ni.gov.uk/protectlife2).
-
Royal College of Psychiatrists (www.rcpsych.ac.uk/).
-
Samaritans, 116 123 (www.samaritans.org/).
-
SANE (www.sane.org.uk/).
-
Shout (www.giveusashout.org/).
-
Stress Project (www.stressproject.org.uk/).
-
Sunflowers Suicide Support (www.sunflowerssuicidesupport.org.uk/).
-
Touchstone (www.touchstonesupport.org.uk/).
-
Turning Point Crisis Support (www.turning-point.co.uk/services/mental-health/crisis-support.html).
-
Young Minds (https://youngminds.org.uk/).
Search terms: MEDLINE (full database searches and supplementary searches in Report Supplementary Material 1)
IPT 1: urgency and accessibility
| Number | Searches | Results (n) |
|---|---|---|
| 1 | (mental* or psychiatric or psychotic or schizophren* or bipolar or personality disorder* or anxiety or anxio* or panic or suicid*).mp. | 1,115,928 |
| 2 | ((deliberat* or self*) adj2 (destruct* or harm* or injur* or mutilat* or poison*)).mp. | 20,760 |
| 3 | (crisis or crises or acute or emergenc* or urgen*).tw. | 1,587,418 |
| 4 | (1 or 2) and 3 | 77,045 |
| 5 | Health Services Accessibility/ | 72,509 |
| 6 | (access or accessible or accessing or accessibility).tw. | 417,262 |
| 7 | (availab* adj2 (service* or staff)).tw. | 6287 |
| 8 | or/5-7 | 461,036 |
| 9 | (emergency adj2 service*).tw. | 16,230 |
| 10 | (emergency care or urgent care or rapid).tw. | 644,928 |
| 11 | (after-hour* or 24 hour* or 24hour* or twenty-four-hour* or out-of-hour*).tw. | 155,691 |
| 12 | (open* hour* or open* time* or operating hour*).tw. | 2985 |
| 13 | (walk-in or walk in or drop-in or drop in).tw. | 26,792 |
| 14 | ((place based or place-based) adj5 (care or service*)).tw. | 23 |
| 15 | (local care or local service* or community service* or community care or immediate care or responsive service*).tw. | 10,291 |
| 16 | (telephone* or phone or hotline* or helpline* or call centre*).tw. | 77,735 |
| 17 | (nhs 111 or nhs111 or “999” or “accident and emergency” or ambulance* or paramedic* or “blue light” or “crisis resolution team*” or police* or triag* or liaison).tw. | 82,165 |
| 18 | or/9-17 | 989,130 |
| 19 | 4 and 8 and 18 | 902 |
| 20 | Case report.tw. | 304,411 |
| 21 | Letter/ | 1,065,756 |
| 22 | Historical article/ | 356,956 |
| 23 | 20 or 21 or 22 | 1,711,557 |
| 24 | 19 not 23 | 888 |
| 25 | limit 24 to english language | 843 |
| 26 | exp Great Britain/ | 361,115 |
| 27 | (national health service* or nhs*).ti,ab,in. | 188,463 |
| 28 | (english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. | 94,070 |
| 29 | (gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jw,in. | 2,021,964 |
| 30 | (bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in. | 1,370,356 |
| 31 | (bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in. | 53,786 |
| 32 | (aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in. | 204,042 |
| 33 | (armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in. | 25,305 |
| 34 | or/26-33 | 2,601,287 |
| 35 | (exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp asia/or exp oceania/) not (exp great britain/or europe/) | 2,818,198 |
| 36 | 34 not 35 | 2,457,091 |
| 37 | 25 and 36 | 165 |
IPT 2: compassionate and therapeutic care
| Number | Searches | Results (n) |
|---|---|---|
| 1 | (mental* or psychiatric or psychotic or schizophren* or bipolar or personality disorder* or anxiety or anxio* or panic or suicid*).mp. | 1,117,876 |
| 2 | ((deliberat* or self*) adj2 (destruct* or harm* or injur* or mutilat* or poison*)).mp. | 20,798 |
| 3 | (crisis or crises or acute or emergenc* or urgen*).tw. | 1,590,953 |
| 4 | (1 or 2) and 3 | 77,228 |
| 5 | (compassion* adj3 (care or caring or therapeutic or therapy or treatment*)).tw. | 2106 |
| 6 | ((understanding or empathy or listened or listening or genuineness or helping or helpful or kind or kindness or respect or dignity or keeping privacy or tolerance or acceptance or affirmation) adj3 (compassion* or care or caring or therapeutic or therapy or treatment*)).tw. | 37,020 |
| 7 | ((support* or non-judgemental or non-stigmatising or anti-stigma or unprejudiced) adj3 (compassion* or care or caring or therapeutic or therapy or treatment*)).tw. | 64,955 |
| 8 | ((good or friendly or trust-based or appropriate or efficient) adj3 communication).tw. | 4075 |
| 9 | (staff adj1 (attitude* or skill*)).tw. | 1564 |
| 10 | (cultural* adj2 sensitiv*).tw. | 4820 |
| 11 | (values based care or recovery orientated practice or recovery-orientated practice).tw. | 20 |
| 12–32 | As IPT 1 | 228 |
IPT 3: inter-agency working
| Number | Searches | Results (n) |
|---|---|---|
| 1 | (mental* or psychiatric or psychotic or schizophren* or bipolar or personality disorder* or anxiety or anxio* or panic or suicid*).mp. | 1,110,148 |
| 2 | ((deliberat* or self*) adj2 (destruct* or harm* or injur* or mutilat* or poison*)).mp. | 20,589 |
| 3 | (crisis or crises or acute or emergenc* or urgen*).tw. | 1,578,178 |
| 4 | (1 or 2) and 3 | 76,533 |
| 5 | Interinstitutional Relations/ | 10,621 |
| 6 | (interagenc* or inter-agenc* or interinstitution* or inter-institution*).mp. | 13,935 |
| 7 | ((integrated or joint) adj commission*).tw. | 3556 |
| 8 | ((coordinated or co ordinated or joint* or joined up) adj3 (care or healthcare or service* or partnership* or working)).tw. | 5275 |
| 9 | (colocat* or co-locat*).tw. | 2660 |
| 10 | ((policy or policies or procedure* or agreement*) adj2 (joint or share* or sharing)).tw. | 1931 |
| 11 | (strategic adj (collaboration or service*)).tw. | 62 |
| 12 | whole system*.tw. | 2398 |
| 13 | concordat.tw. | 25 |
| 14 | integrat* governance.tw. | 28 |
| 15 | ((share* or sharing) adj2 (working or training or technolog* or “point of access”)).tw. | 545 |
| 16 | ((interprofession* or inter profession*) adj2 (work* or relation*)).tw. | 1025 |
| 17–36 | As IPT 1 | 68 |
Appendix 4 Retained records
Retained records of theory scoping searches
| Number | Reference |
|---|---|
| 1 | Amrhein C, Barber-Rioja V. Jail Diversion Models for People with Mental Illness. In Estrine SA, Hettenback RT, Arthur H, Messina M, editors. Service Delivery for Vulnerable Populations: New Directions in Behavioral Health. New York, NY: Springer Publishing Company; 2011. pp. 329–52 |
| 2 | Aubry T, Pantin S, Riesin E, Runnels V, Swenson R, MacPhee C, et al. An Evaluation of the Ottawa Shared Mental Health Care (SHARE) Project: Final Report. 2006. URL: www.researchgate.net/profile/Vivien-Runnels/publication/253363120_An_Evaluation_of_the_Ottawa_Shared_Mental_Health_Care_SHARE_Project_Final_Report/links/02e7e529651c00fc3f000000/An-Evaluation-of-the-Ottawa-Shared-Mental-Health-Care-SHARE-Project-Final-Report.pdf (accessed 24 October 2022). |
| 3 | Aubry T, Lebel M, Hodgson S, Bouchard D. Development of an Outcome Monitoring System for Crisis Telephone Services of the Distress Centre of Ottawa and Region & Tel-Aide Outaouais: Final Report. Ottowa: Distress Centre of Ottawa and Region & Tel-Aide Outaouais; 2005 |
| 4 | Ball JS, Links PS, Strike C, Boydell KM. ‘It’s overwhelming . . . everything seems to be too much’: a theory of crisis for individuals with severe persistent mental illness. Psychiatr Rehabil J 2005;29:10–17 |
| 5 | Bird KS, Vigurs C, Quy K. What Works: Crime Reduction Systematic Review Series No. 7: Police Pre-Arrest Diversion of People with Mental Health Issues: A Systematic Review of the Impacts on Crime and Mental Health. London: EPPI Centre, UCL Department of Social Science, University College London; 2017 |
| 6 | Brennaman L. Crisis emergencies for individuals with severe, persistent mental illnesses: a situation-specific theory. Arch Psychiatr Nurs 2012;26:251–60 |
| 7 | British Columbia Schizophrenia Society. Police Intervention In Emergency Psychiatric Care: A Blueprint For Change. Vancouver, BC: British Columbia Schizophrenia Society; 2006 |
| 8 | Chan P. Consumers’ Mental Health Recovery in a Psychiatric Outreach Program: A Process and Outcome Evaluation. Masters thesis. Waterloo, ON: Wilfrid Laurier University; 2008 |
| 9 | Clark F, Khattak S, Nahal J, Linde K. Crisis Resolution and Home Treatment: The Service User and Carer Experience. London: National Audit Office; 2008 |
| 10 | Collin B. Outcomes for Mental Health Services What Really Matters? London: The King’s Fund; 2019 |
| 11 | Connery L, Brekke J. A home-based family intervention for ethnic minorities with a mentally ill member. Alcohol Treat Q 1999;17:149–67 |
| 12 | Rockar E, Yurkow S. A Turning Leaf on Mental Illness: A Formative Evaluation of a Community-Based Response. Winnipeg, MB: University of Manitoba; 2014 |
| 13 | de Boer C. Right Here, Right Now Drop-In Counselling Clinic: Program Evaluation. St John’s, NL: St. John’s Status of Women Council/Women’s Centre and the School of Social Work, Memorial University; 2017 |
| 14 | Engel RS, Worden RE, Corsaro N, McManus HD, Reynolds D, Cochran H, et al. Alternatives to Arrest. The Power to Arrest: Lessons from Research. Cham: Springer International Publishing; 2019. pp. 75–122 |
| 15 | Frisina C, Evans C. Vignette: A Transdisciplinary Community Mental Health Program Providing Clinical Care to Street-involved Youth in Hamilton. In Nichols N, Doberstein C, editors. Exploring Effective Systems Responses to Homelessness. Toronto, ON: The Homeless Hub; 2016. pp. 221–232 |
| 16 | Gibson S, Hamilton S, James K. Evaluation of the Crisis Care Concordat Implementation: Final Report. London: McPin Foundation for Mind; 2016 |
| 17 | Godrey M. Leeds Partnership for Older People Pilot: Whole System Change in Later Life Mental Health: Final Report. Leeds: Leeds Institute of Health Sciences, University of Leeds; 2009 |
| 18 | Graham BA. Documenting and Analyzing the Contribution of the Gatekeeper Strategy for Enhancing Health Care Access in a Midwestern City. PhD thesis. Lawrence, KA: University of Kansas; 2005 |
| 19 | Healthy London Partnership. London’s Mental Health Crisis Care Programme Update. London: Healthy London Partnership; 2018 |
| 20 | Heyeres M, Kinchin I, Whatley E, Brophy L, Jago J, Wintzloff T, et al. Evaluation of a residential mental health recovery service in North Queensland. Front Public Health 2018;6(123) |
| 21 | Department of Health and Social Care, Concordat signatories. Mental Health Crisis Care Concordat – Improving Outcomes for People Experiencing Mental Health Crisis. London: HM Government; 2014 |
| 22 | His Majesty’s Inspectorate of Constabulary and Fire & Rescue Services (HMICFRS). Policing and Mental Health: Picking Up the Pieces. Birmingham: HMICFRS; 2018 |
| 23 | House A, Guthrie E, Walker A, Hewsion J, Trigwell P, Brennan C, et al. A programme theory for liaison mental health services in England. BMC Health Serv Res 2018;18:742 |
| 24 | Johnson S. Crisis resolution and home treatment teams: an evolving model. Adv Psychiatr Treat 2013;19:115–23 |
| 25 | Lamb D, Lloyd-Evans B, Fullarton K, Kelly K, Goater N, Mason O, et al. Crisis resolution and home treatment in the UK: A survey of model fidelity using a novel review methodology. Int J Ment Health Nurs 2020;29:187–201 |
| 26 | Maguire R, Baraki B. Blue Light Programme Impact on the Public: Exploratory Research. London: Mind; 2018 |
| 27 | King County MIDD Advisory Committees. Mental Illness and Drug Dependency 2 Evaluation Plan: Attachment A. Seattle, WA: King County; 2017 |
| 28 | Miewald CG. Process Evaluation on Crisis Services in Northern Idaho. Boise, ID: Boise State University; 2016 |
| 29 | Mind. Mental Health Crisis Care: Commissioning Excellence: A Briefing for Clinical Commissioning Groups. London: Mind; 2012 |
| 30 | Molfenter T, Connor T, Ford JH, II, Hyatt J, Zimmerman D. Reducing psychiatric inpatient readmissions using an organizational change model. WMJ 2016;115:122–8 |
| 31 | Murphy G, Draper J, McKeon R. Following Up With Individuals At High Risk For Suicide: Developing A Model For Crisis Hotline And Emergency Department Collaboration. New York, NY: National Suicide Prevention Lifeline; 2010 |
| 32 | Murphy SM, Irving CB, Adams CE, Waqar M. Crisis intervention for people with severe mental illnesses. Cochrane Database Syst Rev 2015;12:CD001087 |
| 33 | Naylor C, Taggart H, Charles A. Mental Health and New Models of Care: Lessons from the Vanguards. London: The King’s Fund and Royal College of Psychiatrists; 2017 |
| 34 | Murdoch C, Farmer P, Cumisky S. NHS Mental Health Implementation Plan 2019/20–2023/24. Leeds: NHS England; 2019 |
| 35 | East Midlands, West Midlands and East of England Mental Health Clinical Networks. Urgent and Emergency Mental Health Pathway Compendium of Case Studies 2018/19. East Midlands Clinical Network; 2019 |
| 36 | National Institute for Health and Care Excellence, National Collaborating Centre for Mental Health, NHS England. Achieving Better Access to 24/7 Urgent and Emergency Mental Health Care – Part 2: Implementing the Evidence-based Treatment Pathway for Urgent and Emergency Liaison Mental Health Services for Adults and Older Adults – Guidance. Leeds: NHS England; 2016 |
| 37 | Quinnett P. QPR Gatekeeper Training for Suicide Prevention: The Model, Rationale and Theory. Spokane, WA: QPR Institute; 2007 |
| 38 | Reifels L, Too LST, Ross A, Reavley N, Pirkis J. Evaluation of the Lifeline ‘Pause.Call.Be Heard’ Campaign in the Rail Environment. Melbourne, VIC: TRACKsafe Foundation and Lifeline Research Foundation, Centre for Mental Health, Melbourne School of Population and Global Health, University of Melbourne; 2018 |
| 39 | Rodgers M, Thomas S, Dalton J, Harden M and Eastwood A. Police-related triage interventions for mental health-related incidents: a rapid evidence synthesis. Health Serv Deliv Res 2019;7(20) |
| 40 | Sjølie H, Karlsson B, Kim HS. Crisis resolution and home treatment: structure, process, and outcome – a literature review. J Psychiatr Ment Health Nurs 2010;17:881–92 |
| 41 | Stolk Y. Development and Evaluation of a Training Program in Cross-cultural Psychiatric Assessment for Crisis Assessment and Treatment Teams (CATTs). PhD thesis. Melbourne, VIC: University of Melbourne; 2005 |
| 42 | Sylvestre J, Sundar P, Jamshidi P, Manion M. Evaluating the early implementation of a community crisis bed program for people experiencing a psychiatric emergency using key component scaling. Can J Program Eval 2009;24:157–78 |
| 43 | Trewin M. We Need to Talk about Social Care: Social Care and the Mental Health Forward View: Ending Out of Area Placements. London: Centre for Mental Health; 2017 |
| 44 | Vingilis E, Hartford K, Diaz K, Mitchell B, Velamoor R, Wedlake M, et al. Process and outcome evaluation of an emergency department intervention for persons with mental health concerns using a population health approach. Adm Policy Ment Health 2007;34:160–71 |
| 45 | White C, Goldberg V. Hot spots of mental health crises. Policing 2018;41:401–14 |
Included studies for IPT 1, urgent and accessible crisis services
| Authors | Year of publication | Study setting | Country | Participant number and characteristics | Method of data collection | Date of data collection | Method of analysis |
|---|---|---|---|---|---|---|---|
| Barrett et al.116 | 2013 | Community mental health services | UK | Participants aged > 16 years with relapsing psychosis, at least one hospital admission over previous 24 months. Excluded if under Mental Health Act118 or 2007.119 Sample analysed in treatment, n = 285; control, n = 284 | Economic evaluation within RCT. Adult Service Use Schedule completed 3 months prior to randomisation and 18 months after | August 2008 to September 2011 | Economic analyses adjusted for site and baseline costs. Cost-effectiveness calculated through incremental ratios |
| Begum and Riordan103 | 2016 | CRT | UK | Six nurses working in two CRTs | Semistructured individual interviews | Unclear | Thematic analysis |
| Bendelow et al.95 | 2019 | Police, street triage | UK | 62 people with lived experience of being detained using section 136 of the UK Mental Health Act118 in 2012, three of whom were family members of a detained person Police, mental health services and voluntary sector staff took part in interviews and focus groups; sample size unclear |
Mixed methods: individual interviews with service users, carers and staff, focus groups, 250 hours of observed practice, data from medical records of all patients detained under section 136 in 2012 in one region of England | Qualitative data: 2013–2016; quantitative data: 2012. Stakeholder focus groups and workshops: unclear | Retrospective analysis anonymised patient data Qualitative thematic analysis Stakeholder involvement |
| Boscarato et al.84 | 2014 | Police and crisis assessment teams | Australia | 11 mental health consumers who had experienced at least one crisis that involved a response from police and mental health services | Individual semistructured interviews using open questions and a vignette and visual images to stimulate responses | Unclear | Thematic analysis |
| Borschmann et al.117 | 2013 | Community Mental Health Teams | UK | Community-dwelling people aged > 18 years with personality disorder (DSM-IV-TR). Target population had experienced crises and engaged in self-harm in the previous 12 months. Randomised to treatment + TAU (n = 46) or control TAU (n = 42) | Parallel-group TAU-controlled randomised trial. Self-report questionnaire and secondary clinical outcomes measured in interview using nine standardised questionnaires | Unclear | Primary outcome assessed using a logistic regression model with treatment and stratification factors including alcohol use and depression. Results were summarised as odds ratios and effect sizes at 6 months’ follow-up with 95% confidence intervals Cost variables were compared descriptively with no statistical analysis |
| Brown et al.104 | 2020 | Crisis resolution and home treatment service | UK | 14 interviews (seven with service users and seven with clinical staff) with people who had delivered or received the suicide triage intervention | Mixed methods, recording and reporting suicide rates in one region of the UK. Standard health-care service use data. Interviews with service users and clinical staff | Quantitative data unclear, qualitative data collected from October 2019 | Statistical analysis of service data and suicides before and after implementation of a suicide triage model Qualitative analysis not reported |
| Cambridgeshire and Peterborough NHS Foundation Trust113 | 2016 | Crisis telehealth | UK | Information bulletin | Not applicable | Not applicable | Not applicable |
| Chilman et al.102 | 2021 | Crisis resolution services | UK | 500 randomly selected tweets relevant to CRTs Qualitative data from previously published study of CRTs with services users (n = 41), carers (n = 20) and CRT clinical staff (n = 137) |
Twitter advanced search using hashtags related to CRTs | Tweets collected after June 2018 for the date range January 2010 to June 2018. Qualitative data collection date unclear | Tweets were selected at random and 100 tweets at a time were organised into descriptive categories following principles of content analysis. Thematic analysis of tweets. Refutational synthesis was used to compare themes emerging from tweets and from the qualitative study of CRTs |
| Duggan et al.109 | 2020 | Emergency departments | Australia | A summit of > 170 delegates representing health professionals and those with lived experiences | Unclear | October 2018 | Unclear |
| Eales110 | 2013 | Mental health liaison in emergency departments | UK | 17 people who has accessed liaison mental health services in one emergency department. Time between attendance and interview was between 3 and 25 weeks | Semistructured interviews | September 2000 to June 2001 | Grounded theory secondary analysis |
| Evans et al.100 | 2019 | Mental health liaison in emergency departments | UK | Systematic review of impact of liaison mental health services on emergency departments 17 papers included |
Systematic review | September 2016 and repeated in April 2018 | Data extraction by two independent blinded researchers. Risk-of-bias assessment. Mixed-methods synthesis |
| Farrelly et al.118 | 2014 | Community mental health services | UK | 221 participants from a control group with a history of psychosis | Audit of JCPs using a bespoke assessment tool | Unclear | Summary statistics were calculated for levels of individualisation in the JCP and compared with clinical data from the trial |
| Farrelly et al.120 | 2014 | Community mental health services | UK | 50 JCPs | Records from meetings between the service user, a psychiatrist and a JCP facilitator | Unclear | Inductive thematic analysis of service user treatment preferences |
| Farrelly et al.119 | 2015 | Community mental health services | UK | 51 service users, 29 care co-ordinators, 16 psychiatrists. All participants had taken part in the trial of JCPs | Focus groups Individual semistructured interviews |
Unclear | Constructivist grounded theory analysis |
| Grigg et al.107 | 2007 | Mental health triage | Australia | Three case studies. Individual interview sample size unclear | Routine data related to mental health triage in three case study sites. Semistructured interviews with staff, consumers, GPs | Unclear | Mixed-methods analysis not fully described |
| Gudde et al.105 | 2013 | Crisis services | Norway | 19 people with major mental disorder who have experienced a crisis | Semistructured interviews | August 2010 to May 2011 | Giorgi’s190 phenomenological analysis |
| Haslam111 | 2019 | Emergency departments | UK | Clinical commentary | Not applicable | Not applicable | Not applicable |
| Jespersen et al.108 | 2016 | Integrated CMHT with crisis services | Australia | Service data baseline 2006/7 and comparator 2007/8 to 2012/13. Survey of service users (n = 26), carers (n = 31) (service user and carer, n = 9) and staff (n = 55) Focus groups of staff (n = 38) |
Mixed methods: routine service data, and postal surveys to staff, service users and carers. Staff focus groups | Unclear | Descriptive statistical analysis of service data and survey responses Analysis approach to focus group data qualitative, but not fully described |
| Lequin et al.121 | 2021 | JCP | Switzerland | 184 JCPs 12 patients and 12 providers were interviewed. No family members were included |
Data extracted from records of JCPs. Semistructured interviews | 2016, and January–April 2017 | Qualitative and quantitative content analysis of JCPs. Inductive and deductive analysis of content of interviews. Descriptive statistical analysis of sample characteristics |
| Mind2 | 2011 | Acute and crisis mental health services | UK | 350 responses from people with experience of receiving acute and crisis care and their family members or carers, nurses, social workers, managers, advocates and organisations | Web-based survey of experiences. Panel meetings with experts | Survey: September–November 2010 and April–May 2011 Panel meetings: August 2011 Individual consultations: March–June 2011 |
Analysis unclear |
| Mind106 | 2013 | Acute and crisis mental health services | UK | All mental health trusts in England | Freedom of information requests Mental Health Minimum Data Set 2011–2012 |
August 2012 | Analysis unclear |
| Morant et al.15 | 2017 | CRT | UK | 20 carers and 42 service users who had experience of crisis resolution services within previous 3 months 147 practitioners with experience of delivering crisis resolution services from 10 mental health trusts in England Stakeholder group: 13 service users, seven carers and eight clinicians |
Individual semistructured interviews with carers, service users and nine staff. A total of 26 focus groups with staff Consultations with stakeholder steering group |
Unclear | Thematic analysis using inductive and deductive reasoning with support of stakeholder group |
| National Collaborating Centre for Mental Health and Positive Practice in Mental Health89 | 2020 | Crisis mental health services | UK | Multi-agency, user-led collaborative of 75 UK organisations. All-age crisis care | Methods not reported | Unclear | Methods not reported |
| Newbigging et al.10 | 2020 | Voluntary sector crisis mental health services | UK | 171 voluntary sector mental health crisis organisations; between 13 and 27 individual stakeholder interviews in each of four case study sites. Two focus groups (30 service users and 22 carers). Narrative interviews (47 service users and 11 carers). Brief questionnaire (43 service users) | Mixed methods: National survey Mapping services, case studies |
Survey: May 2017 to August 2018. Other data collection: not stated | Database analysis, thematic analysis, framework analysis. Descriptive statistical analysis of database and survey data |
| NHS England112 | 2021 | Mental health access standards | UK | Not applicable: web-based policy | Not applicable | Not applicable | Not applicable |
| NHS England90 | 2021 | Telephone access in a crisis | UK | Not applicable: web page content | Not applicable | Not applicable | Not applicable |
| NHS England and NHS Improvement101 | 2020 | Joint response ambulance car | UK | 240 cases | Routine data from one NHS ambulance service Clinical notes from staff attending mental health cases |
January to July 2020 | Mixed-methods analysis of routine health data, descriptive statistics presented with summaries of qualitative data. Health economic descriptive summaries. Methods not fully outlined |
| O’Cathain et al.97 | 2020 | Emergency department | UK | 32 + 29 documents included | Realist evidence synthesis | February to March 2017 | Realist evidence synthesis according to RAMESES standards |
| Olasoji et al.96 | 2017 | Community mental health | Australia | 19 caregivers of people living with mental illness | Five focus groups | Unclear | Inductive thematic analysis |
| Reveruzzi et al.98 | 2016 | Street triage | UK | Nine pilot street triage scheme reports and related service data. Six individual interviews with senior staff | Routine service data; documentary evidence of the service designs; interviews with health and police staff, service users and family members | Unclear (data from pilot services: 2013–2018) | Retrospective statistical analysis of service data from nine teams Synthesis of qualitative service data from reports from nine pilot schemes. Thematic analysis of additional interviews with senior organisation staff |
| Ruchlewska et al.122 | 2014 | Community mental health services | The Netherlands | 212 JCPs | Randomised study of comparison of scores between clinician-facilitated JCP and patient- and/or advocate-facilitated JCP using a JCP checklist score | November 2007 and March 2011 | Statistical analysis using a statistical software package to measure internal consistency, distribution and group and individual differences. Descriptive statistical mean scores were used to compare quality of completion of JCP. Effect size calculated using pooled variance of the two means |
| Sands et al.93 | 2013 | Mental health triage | Australia | 18 clinicians, 16 nurses, two social workers 197 observations of telephone calls |
Inter-rater reliability testing on 42 validated hypothetical mental health triage scenarios Observations of calls to a mental health telephone triage service using a 58-item data collection tool |
Observations: January to March 2011 | Inferential statistical analysis of reliability between raters, descriptive analysis of observational data, qualitative data subject to qualitative content analysis |
| Sands et al.94 | 2013 | Mental health triage | Australia | 197 observations of telephone calls | Observations of calls to a mental health telephone triage service using a 58-item data collection tool | January–March 2011 | Descriptive analysis of observational data; qualitative data subject to qualitative content analysis |
| Saurman et al.114 | 2014 | Mental health emergency care rural access programme | Australia | 11 days of observations of 14 staff | Routine service data, notes from live observation, documentary evidence from policy and services | April 2013 | Qualitative ethnographic observational analysis |
| Sunderji et al.91 | 2015 | Urgent ambulatory psychiatric assessment | Canada | 16 studies included | Scoping review of studies describing a specific programme providing rapid access to psychiatric assessment | Unclear (studies included from January 1993 to June 2014) | Donabedian’s framework for quality of care |
| Thornicroft et al.123 | 2013 | Community mental health team | UK | 569 participants randomised: 285 in the intervention group and 284 in the control group. Participants had at least one psychiatric admission within 2 years and were on Enhanced Care Programme Approach register | Data collected at baseline and 18 months. Rating of JCP meetings using Likert scale; clinical records to measure primary outcome; psychometric measures via four questionnaires; DSM-IV global assessment of functioning Semistructured interviews and focus groups |
Unclear | Statistical analysis modelled on intention-to-treat principles. Comparison between groups used t-test, and logistic regression carried out. Linear regression for continuous outcomes. Controlled for site and missing data. Analysis repeated for black subgroup Inductive thematic analysis using constant comparative methods |
| Trondsen et al.115 | 2014 | Rural telehealth assessment | Norway | 29 patients, psychiatrists and nurses who had taken part in video call psychiatric assessment | Semistructured interviews | July 2012 and June 2013 | Exploratory, stepwise deductive–inductive analysis to identify themes |
| Wise-Harris et al.99 | 2017 | Emergency departments | Canada | 166 adults with five or more visits to emergency department in previous 6 years, with at least one visit for mental health or substance use 20 participants who had received the intervention were interviewed |
Service use and baseline self-report data. In-depth interview | August–December 2013 | Descriptive statistics to summarise baseline self-report data and emergency department use Thematic analysis |
| CMHT, Community Mental Health Team; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; TAU, treatment as usual. | |||||||
Included studies for IPT 2, compassionate leadership
| Authors | Year of publication | Study setting | Country | Participant number and characteristics | Method of data collection | Date of data collection | Method of analysis |
|---|---|---|---|---|---|---|---|
| Bögle and Boden130 | 2019 | Mental health charities providing peer support | UK | Seven people with recent first crisis in psychosis and attended peer support group | Semistructured interviews | Unclear | Hermeneutic phenomenological, multimodal qualitative analysis |
| Cole-King and Gilburt134 | 2011 | Health services | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Dixon-Woods et al.138 | 2014 | English NHS services | UK | 304 staff interviews, 650 hours of observation, 715 survey responses, two focus groups and 10 interviews with patients and service users; performance data from 621 clinical teams; 793 documents from 71 NHS trusts over 18 months | Interviews, observation, survey, focus groups, performance data, NHS documents | Post Mid Staffordshire report181 publication; dates unclear | Narrative synthesis of findings from mixed-methods study |
| Farr and Cressey139 | 2015 | Primary care NHS trust covering urban and rural communities | UK | 21 health-care staff | In-depth interviews | Unclear | Grounded theory thematic analysis |
| Farr and Barker125 | 2017 | Community mental health services | UK | 22 staff interviews, 206 evaluation forms, observations of five Schwartz Rounds at three case study sites | Interviews, observations and evaluation forms | 2014–2015 | Realist evaluation |
| Farrelly et al.118 | 2014 | Community mental health teams | UK | 50 JCPs | Records from meetings between the service user, a psychiatrist and a JCP facilitator | Unclear | Inductive thematic analysis of service user treatment preferences |
| Faulkner137 | 2012 | Adult social care | UK | 17 stakeholder discussions | Discussions with stakeholders from diverse backgrounds and review of published evidence | Unclear | Synthesis of personal reflections, stakeholder discussions and published literature |
| Firth-Cozens and Cornwell135 | 2009 | Hospital care | UK | Unknown | Literature review, data from written anonymised contributions of participants at a workshop | 2008 | Unclear |
| Judkins et al.132 | 2019 | Emergency departments | Australia | Not applicable | Not applicable | Not applicable | Not applicable |
| Newbigging et al.10 | 2020 | Voluntary sector crisis mental health services | UK | 171 voluntary sector mental health crisis organisations; between 13 and 27 stakeholder individual interviews in each of four case study sites. Two focus groups with 30 service users and 22 carers. Narrative interviews with 47 service users and 11 carers. Brief questionnaire (43 service users) | Mixed methods: National survey Mapping services, case studies |
Survey: May 2017 to August 2018. Other data collection not stated | Database analysis, thematic analysis, framework analysis. Descriptive statistical analysis of database and survey data |
| NHS England136 | 2014 | National Health Services England | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| O’Connor and Glover131 | 2017 | Hospital staff | UK | Nine included papers | Literature review | February 2015 | Qualitative meta-synthesis |
| Prytherch et al.133 | 2020 | NHS crisis house | UK | Eight women with experience of the crisis house | Semistructured interviews | Unclear | Thematic analysis |
| Rafferty et al.127 | 2017 | Hospital and community health care | UK | Item generation n = 34 health-care staff; pilot test n = 467; full validation n = 1698 | Mixed methods: focus groups and questionnaires | Full validation: June–August 2014 | Factor analysis; Cronbach’s alpha reliability test |
| Royal College of Psychiatrists126 | 2015 | Mental health services | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Rees et al.128 | 2017 | Ambulance paramedic services | UK | 11 paramedics | Semistructured interviews | Unclear | Grounded theory, constant comparative analysis |
| Simpson140 | 2007 | Community mental health teams | UK | 200 interviews with CMHT staff and service users. Observations of 71 meetings and analysis of service documents | Non-participant observation, semistructured interviews, questionnaire | January 1999 and February 2001 | Constant comparative analysis to generate themes |
| Simpson et al.129 | 2016 | Acute inpatient mental health settings | UK | 19 mental health wards on six NHS sites in England. Interviews with 301 service users and 290 members of staff. Case study interviews with mixed stakeholders (n = 76); 51 care plans; 12 meetings | Mixed methods: narrative synthesis of policy and evidence, service user survey, staff survey, embedded case study interviews, documentary review of care plans and meetings | Quantitative analysis of measures from surveys at site level, cross-site comparisons, covariance and correlational analyses provided outcomes related to recovery Qualitative analysis using framework approach within and across sites |
Summary table of included documents for IPT 3, inter-agency working
| Author(s) | Year of publication | Study setting | Country | Participant number and characteristics | Method of data collection | Date of data collection | Method of analysis |
|---|---|---|---|---|---|---|---|
| Association of Mental Health Providers156 | 2021 | Voluntary sector | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Bowles and Jones161 | 2005 | Mental health acute inpatient settings | UK | Fourteen health-care staff from different professional backgrounds with experience of acute mental health care | One focus group and field notes | Unclear | Thematic analysis |
| Carson146 | 2018 | Street triage | UK | Three individuals with experience of accessing street triage | Individual narrative interviews | Unclear | Narrative analysis |
| Crisis Care Concordat30 | 2021 | All crisis mental health service providers in England | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Department of Health and Social Care and Concordat signatories27 | 2014 | All crisis mental health service providers in England | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Edmondson and Cummins148 | 2014 | Street triage | UK | Six months of service data, including 673 incidents referred to the pilot intervention; 17 individual interviews with police and health staff; group interviews (unclear sample) | Mixed methods: qualitative service data, individual and group interviews and consultations | December 2013 to May 2014 | Descriptive statistical analysis of service data; thematic constant comparative analysis |
| Gibson et al.28 | 2016 | All crisis mental health service providers in England | UK | 32 crisis service action plans; observations of eight key meetings in four local areas; 16 interviews with local and national steering group stakeholders; two surveys of crisis experiences: survey 1, n = 391; survey 2, n = 140 | Service-level crisis action plans; observations of meetings; two surveys of experiences using crisis services | Observations: July–October 2014 Survey: October 2014 to December 2015 |
Thematic analysis of action plans. Descriptive analysis of change over time in survey data |
| Goodwin et al.144 | 2012 | Integrated health care | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Griffith141 | 2016 | Primary care | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Healthy London Partnership155 | 2016 | NHS London | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Hollander et al.149 | 2012 | Police and crisis services | Australia | 44 police and 13 crisis services staff | Questionnaire | Unclear | Descriptive statistical analysis of Likert responses. Non-parametric tests to control for differences is sample size between groups |
| Horspool et al.150 | 2016 | Street triage | UK | 14 police and mental health staff involved in delivering street triage interventions | Semistructured interviews | September 2014 to January 2015 | Framework analysis |
| Iacobucci158 | 2015 | NHS | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Lancaster151 | 2016 | Joint police and mental health crisis responses | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| McKenna et al.152 | 2015 | Northern Police and Clinical Emergency Response Team | Australia | 17 participants with experience of NPACER model (six service users/carers and 11 staff from police and health) | Individual interviews | January–July 2014 | Inductive thematic analysis |
| Mental Health Foundation147 | 2013 | Integrated mental health care | UK | 31 seminar participants; 1200 responses to a call for evidence | Literature review, seminar, call for evidence | April 2012 to June 2013 | Unclear |
| National Collaborating Centre for Mental Health89 | 2020 | Crisis mental health services | UK | Multi-agency, user-led collaborative of 75 UK organisations. All-age crisis care | Methods not reported | Unclear | Methods not reported |
| National Voices154 | 2013 | Integrated care | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Newbigging et al.10 | 2020 | Voluntary sector crisis mental health services | UK | 171 voluntary sector mental health crisis organisations; between 13 and 27 stakeholder individual interviews in each of four case study sites. Two focus groups with 30 service users and 22 carers. Narrative interviews with 47 service users and 11 carers. Brief questionnaire (n = 43 service users) | Mixed methods: National survey Mapping services, case studies |
Survey: May 2017 to August 2018. Other data collection: not stated | Database analysis, thematic analysis, framework analysis. Descriptive statistical analysis of database and survey data |
| NHS England157 | 2018 | Integrated 24/7 multi-agency mental health first-response service | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| NHS143 | 2020 | Web page advice on seeking help in a crisis | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| Parker et al.81 | 2018 | Inter-agency mental health with police | UK | 125 studies included | Systematic scoping review | Unclear | Arksey’s literature mapping framework |
| Public Health England145 | 2017 | Mental health and alcohol/drug use | UK | Not applicable | Not applicable | Not applicable | Not applicable |
| RAND Europe et al.153 | 2012 | Integrated care | UK | 16 sites included: 223 interviews with staff and 82 with patients; cost estimate pro forma to 16 sites | Mixed methods: staff interviews; patient questionnaires; staff questionnaires; routine health data, service documents and local evaluations conducted on included sites; cost analysis | Autumn 2009 to autumn 2011 | Quantitative regression analysis and McNemar’s test for clustering. Costs calculated using 12 months of categories of cost and resources |
| Rees et al.142 | 2015 | Ambulance paramedic services | UK | 11 paramedics | Semistructured interviews | 2014–2016 | Evolved grounded theory approach |
| Reveruzzi and Pilling98 | 2016 | Street triage | UK | Nine pilot street triage scheme reports and related service data. Six individual interviews with senior staff | Routine service data; documentary evidence of the service designs; interviews with health and police staff, service users and family members | Unclear (data from pilot 2013–2018) | Retrospective statistical analysis of service data from nine teams Synthesis of qualitative service data from nine pilot scheme reports. Thematic analysis of additional interviews with senior organisation staff |
Appendix 5 Synthesised context–mechanism–outcome configurations
| (Context) If . . . | (Mechanism) Then . . . | (Outcome) Leading to . . . | Programme theory |
|---|---|---|---|
| People in crisis have physical health concerns83,118 | People in crisis seek help from known and easy-to-access services that they trust10,97 | There is increased likelihood of people in crisis attending A&E or their GP or phoning NHS 111/NHS 99984,89,97,99,108,143 | 1, 3 |
| People in crisis or their family members lack information about sources of help in a mental health crisis90 | 1 | ||
| People in crisis or their family members believe that the crisis service guarantee a response97,120,143,144 | People in crisis have a reduced sense of urgency, feel safer,2,10,96 trust that the service can help,10,15,96,97,108 engage with the service and tolerate waiting | There is reduced A&E use84,89,97,99,108 | 1 |
| People in crisis can access help in a safe space130,155 away from home10 | People in crisis are less fearful and can take stock of their situation10 | People in crisis can regain control118 over their situation, manage their distress,133 and have improved experiences of crisis services138 | 1,3 |
| Non-clinical, safe spaces in communities have open access (e.g. crisis café, haven) that include peer support10,130,132,155 | People in crisis access a service, as a proxy for family and friends, that provides a sense of safety and belonging10,155 and being understood.119 People seek support sooner in the crisis10,106 | Engagement with the service is improved and distress is reduced.110 Reduced use of A&E 132 | 1, 2, 3 |
| People successfully navigate to crisis help in the early stages of a crisis2,10,15,97,98,112,147 | People in crisis and their family members feel believed and hopeful110 | People in crisis can regain control over their situation and manage their distress110 | 1 |
| There is increased willingness from people in crisis to seek help in a future crisis2 | |||
| People in crisis receive a response that fits around their personal circumstances with minimal disruption to usual life and accessing causes no financial or social burden10,90,97,98,101,108,114,146 | People in crisis or the person seeking help (often family) perceive the service to be easy to access97 and designed for them,1 prompting them to make contact sooner in the crisis10,106 | People in crisis and those seeking help on their behalf have a sense of personal control.115 Reduced urgent care use95,108,110 | 1, 2 |
| Crisis services can be accessed without complex referral routes (particularly important to black men, who often experience stigma, fear and racial stereotyping)1,10,15,89,90,95,104,106,112 | The service is perceived as easy to access,97 available and designed to meet the needs1 of people in crisis. People in crisis experience less fear and crisis responses are accessed sooner | People in crisis, particularly black and minority ethnic people and men, are less distressed at first contact and the response is less likely to be coercive10,130,131,132,133 | 1, 2 |
| Front-line staff in crisis services (particularly in statutory services) value referral that includes gatekeeping2,103,105,108,112 | Front-line staff are less fearful of being overwhelmed15,103 | Reduction in hospital admissions.103 Reduction in inappropriate referrals and controlled workload.15 Resource pressures are managed95,103 | 1 |
| Black and minority ethnic people in crisis have been involved in shared decision-making106,123 | Black and minority ethnic people experience trust and personal control117,122 | Improved relationships between services and people in crisis117,122 | 1, 2 |
| Decisions are reached through negotiation between staff in different agencies and involve the person in crisis (shared decision-making)116,122,123 | The person’s (and family’s) interpretation of the crisis is acknowledged;2,96,102,103,118,119 there is a shared commitment to decisions115,116 | ||
| The organisational culture is centred on therapeutic relationships (over professional power)123,131 | Front-line staff trust joint decision-making to produce appropriate crisis plans and take a collaborative (rather than paternalistic) approach to shared decisions,118,119,121,123 which they prioritise.116,122,123 People in crisis are hopeful and feel respected, encouraging them to engage with services115,116,117,122 | There is improved service user experience of services133 | 1, 2 |
| Front-line staff have therapeutic skills and ability to provide compassionate crisis interventions129,133,137,138 | Front-line staff deliver care that is balanced between focusing on mitigating risk and relational safety.10,129,133 People in crisis are involved in decisions about their care137 | There is improved satisfaction with crisis care10,147 | 1, 2 |
| Black and minority ethnic people receive peer support10 | People who are black or identify as being from an ethnic minority, learn about themselves and gain a new perspective10 | People who are black or identify as being from an ethnic minority have an immediate sense of being understood and a distal recognition of opportunities to contribute that gave meaning and hope10 | 1 |
| The support of family and friends is not available (or perceived to not be available).96 People can access a proxy via peer support, often provided via voluntary sector non-clinical services10,155 | People in crisis have a sense of connectedness, trust and safety10,119 | The person feels safe, with reduced guilt about being a burden to family and friends10,118,119,133 | 1, 3 |
| People have access to support from family or friends, and their family and friends are available for support; the person believes that accessing their support is reasonable, rather than burdensome10,96,97,103,110,115 | People in crisis experience connectedness, trust and a sense of safety. People in crisis can collaborate in decision-making; there is respect93,94,97,104,110,118 | The person in crisis seeks help from family and friends first and secures support quickly10 | 1 |
| People in crisis experience continuity of support | |||
| Front-line staff have skills that enable them to provide immediate supportive responses, such as active listening and counselling93,102,129,138 | People in crisis experience relational safety, hope and encouragement. Staff are more flexible and responsive10 | The person in crisis can communicate their needs, can regain control, can manage their distress and believes that the service can help10,117,118,122,133 | 1, 2 |
| In the longer term, the person in crisis is more likely to contact the service again2,10,110 | |||
| Front-line staff are compassionate in their responses (in person or via telehealth) to people in crisis and their family and friends10,112,118,126,129,130,132,133,134,140 | People in crisis feel valued, believed, respected10,130 and involved in their care115,122 | People in crisis experience relational safety and stabilisation of the immediate crisis.10,103,130 People in crisis report improved experience of crisis services.133 Improved job satisfaction for crisis services staff125,139 | 1, 2 |
| Crisis services are available 24/72,10,90,95,98 and provide same-day responses15 | The expectations of people in crisis (and their families) for an urgent response are met; they trust the service and have a reduced sense of urgency96,110,116,118,119,120 | People in crisis access a mental health assessment more quickly and are less likely to circle the system10,100 | 1 |
| Crisis services provide co-response models that include parallel assessment98,143,149 | People in crisis experience less fear (of traumatic retelling) and a greater sense of personal control118,133 | People in crisis experience a reduced number of assessments and related traumatic retelling.111 People in crisis experience faster access to a mental health assessment that is holistic and more accurate100,101 | 1, 2, 3 |
| Mental health staff are co-located in emergency control rooms98 | Non-mental health specialist staff (e.g. police, ambulance) are more confident in responding to crises and feel supported in making decisions98 | Cost-effective and sustainable crisis services.98 Faster response to mental health calls with improved decision-making and onward referral.98,100,101,110 Reduced likelihood of people in crisis being taken to or choosing to go to A&E or of coercive responses being implemented (e.g. Mental Health Act 1983118 and 2007119) by clinical staff or police98,101 | 1, 3 |
| Front-line staff have access to clinical leaders and systems of support10,93,104,115 | Front-line staff are less fearful of blame and seeking support is an accepted norm.104 There is acceptance and tolerance between staff104 | Front-line staff sustain compassion and are more confident in decision-making; staff stress is reduced. Staff turnover is reduced and job satisfaction increased107,125,126,139,147 | 1, 2, 3 |
| Decision-making is supported by evidence-based decision aides that are understood across an inter-agency system of crisis care (e.g. triage tools) and are linked to available services (e.g. service access thresholds)15,93,94,98,104 | Front-line staff have confidence in their decisions and there is mutual trust across agencies.10,98,101 Front-line staff have less fear in referring to other agencies and have a sense of role clarity within the crisis system104,123 | Inter-agency service co-ordination98,101 is improved and leads to accurate resource allocation. Accurate identification of urgency and need (e.g. suicidality).93,94,98,104 Reduced disputes about responsibility between staff and between agencies10 | 1, 3 |
| Front-line staff in ‘first-response’ roles (the first staff member to speak with the person in crisis) have immediate access to clinical leaders to support and manage resource pressures and disputes about responsibility across the inter-agency system10,104,129,135,139,152 | Leaders focus on buffering external demands and pressures.126 Front-line staff are confident in decisions and can focus on the person in crisis136 | Disputes about responsibility are reduced and front-line staff retain compassion.10 Decisions are collaborative and safe10,93,102,107,115 | 1, 3 |
| Multiple definitions of crises are understood and accepted across agencies10,96,109 | Front-line staff accept, have a sense of ownership of, and work with different values across the crisis care system.10,106,126,139,140,147 Commissioners and leaders design services that accommodate different approaches to crises. There is challenge and debate10,156 | Inter-agency affiliation facilitates improved communication, information-sharing and engagement.10,126,127 Staff work flexibly across agencies, reducing gaps and delays10,138,147 | 1, 3 |
| Mental health crises are conceptualised as part of a recovery journey rather than as single events10,95,109 | People in crisis feel confident when contacting crisis services more than once without fear of rejection.95,110,111 Front-line staff are more accepting of people who may require multiple crisis interventions and are confident to refer and liaise across the crisis system109,110 | Front-line staff retain compassion irrespective of how frequently a person has attended the service.94,99 People in crisis requiring multiple crisis responses are more likely to engage and less likely to become desperate and escalate risky behaviour.89,110,111,115,123 Reduction in repeat attendances110,111 and people leaving the service without treatment132 | 1, 2, 3 |
| Front-line staff have positive attitudes that are not labelling or stereotyping people in crisis, irrespective of the number of times they have attended2,10,106 | |||
| Front-line staff have time to assess people in crisis105 | Staff focus on the person’s interpretation of the crisis and involvement in decisions2,96,102,118,119 | Reduced number of attendances for crisis support.94,99,110,111 Reduced escalation of distress and harm.95 Improved cost-effectiveness and service user experience10,99,109,110 | 1 |
| Organisational strategy and operational leadership drive sustained engagement with information-sharing and shared decision-making123 | Front-line staff engage in information-sharing and shared decision-making and adopt changes into practice. People in crisis feel able to engage in their care and that the service knows something about them119,121 | Improved service co-ordination, faster responses for people who attend services frequently or are known to services117,121 | 1, 3 |
| Sustained change123 | |||
| A focus on compassionate and psychologically safe crisis care drives proactive management of waiting at strategic, operational and clinical levels.10,91,94,105,110 Front-line staff provide information about waiting times, what the wait is for and what the person can do to stay safe during the wait110 | There is a shared understanding of waiting-time policy and staff act to meet the standard. People in crisis and their families can tolerate waiting; the sense of urgency is reduced.97,110,111 Front-line staff use systems of prioritisation to support decision-making about appropriate waiting time based on urgency of need93,94 | People in crisis are less likely to disengage from services without treatment or circle the system.2,10,15,105,132 Distress and harmful behaviour are less likely to escalate110,130,133 | 1, 2 |
| Commissioning takes account of how complex boundaries between agencies are (e.g. between urgent care, police, crisis services, voluntary sector services), including how thresholds for access affect service delivery and service user and carer experience (e.g. transport, transitions, service thresholds)10,15,95,114,141,157 | Commissioners and policy-makers lead a systemic drive for inter-agency agreement about geographic and service remit boundaries.147 Staff believe in the service and act to collaborate across organisational and geographic boundaries142,151 | Gaps, delays and disputes about responsibility are reduced.10,149 Staff morale is improved.104 There is improved service delivery and cost-effectiveness.157 There is a reduction in use of coercion27,146,149 | 1, 3 |
| Crisis services are commissioned to provide continuity and have a stable presence in communities2,10,95,105,158 | Front-line staff are responsive to the needs of people in crisis (rather than focused on protecting scarce resources).128 People in crisis know their local crisis services and navigate to them.10,116,118,119,120 Front-line staff are familiar with available services10,147 | Gaps, delays and disputes about responsibility are reduced.10,149 Staff morale is improved.104 There is improved service delivery and cost-effectiveness.157 Quality of crisis care is improved139,147 | 1, 3 |
| Co-production (including co-design of training) is actively resourced2,10,106,158 | The aspirations of service users is incorporated into design, delivery and evaluation of services across the inter-agency system.137 Service users recognise the service as designed for them; there is ownership and affiliation89,147 | Quality of crisis care is improved.139 There is reduced fear and shame about accessing services (stigma)2,118 | 2, 3 |
| Services are designed with the communities they serve and reflect their diversity89,106 | People from minority groups recognise the service as being for them; staff use language and communication that avoids racial and other stereotypes10,89,106 | Quality of crisis care is improved.139 There is reduced fear and shame about accessing services (stigma)2,118 | 3 |
| Diverse data are used to monitor services and inform decision-making, including data drawn from across agencies and including aspects of service delivery that are harder to measure (e.g. relational safety, compassion)10,145 | End users of services are involved in evaluating services from multiple perspectives137 and commissioners and leaders are focused on shared priorities138 (rather than competing priorities) | Quality of care is understood from multiple perspectives, including priorities of service users and communities served138,139 | 2, 3 |
| Technology operates across crisis agencies143,147,150 | Information-sharing facilitates communication and confidence between staff in different agencies, staff buy into the system and trust is established10,94,98,147 | Improved information-sharing.147,150 Reduced number of assessments and reduced trauma.98 Reduced barriers caused by rules about confidentiality and boundary disputes.10,96 Faster access to and transition through agencies98 | 1, 3 |
| There is equal emphasis on the leadership of, and relationships between, staff across agencies, and the structure of the inter-agency system129,138,140 | Leaders of crisis services balance the day-to-day demands of service delivery with attention to the needs of staff. Workloads allow leaders to be available to staff.136 Staff are clear about lines of accountability and seek support with clinical decisions138,140 | Front-line staff retain compassion.134,140 Improved morale among leaders and staff; staff retention is improved.126,138,139 Change is initiated and sustained.134,138,139,147 Resources are managed effectively, sustaining clinical priorities.135,138 Staff are empowered (rather than helpless)138 | 2, 3 |
| There are shared values and objectives between leaders, who model compassion136,139 | There is affiliation within and between teams.126,127 There is a flat structure and leaders make themselves accessible and visible;126 expectations are clear.131 There is staff development and (joint) training that fosters growth129,131,139,147 | Staff are regarded compassionately135 and humanely125 and are respected140 | 2, 3 |
| Cost-effectiveness through streamlined processes and referral.98,153 People in crisis experience reduced distress and increased satisfaction with crisis services153 | |||
| There are system navigators and co-ordinators with knowledge of the whole crisis system138,144,147,153 | People in crisis experience continuity through trusted points of liaison154 | Reduced time for police dealing with crises.148 People in crisis experience transition through agencies seamlessly154 | 3 |
| There is a system-wide approach to commissioning crisis services153,161 | There is stability in funding and resources;10 smaller organisations have a stable presence. There is a system-wide understanding of the resources required and agencies operate to manage complexity across the system (rather than operating in silos to protect resources)81,147 | Services are cost-effective through streamlined processes and referral.98,153 People in crisis experience reduced distress and increased satisfaction with crisis services153 | 3 |
| Crisis care operates to national standards with local implementation27,30,89,152 | Crisis services operate to meet standards and expected outcomes from crisis care nationally and locally.27,28,30 Attention to local populations drives commissioning that is responsive to local need30,106 | Crisis services have the potential for cost improvements.157 People in crisis are less likely to attend A&E 98,146 | 3 |
| Staff understand how their role fits into an inter-agency system140,149,151 | Staff across agencies have confidence (rather than concern) that the spectrum of care is available across the inter-agency system10,15 | Suspicion and mistrust between different agencies and staff groups is reduced and there is improved communication between staff and between agencies10,161 | 1, 3 |
Appendix 6 GRADE-CERQual assessment of confidence in findings: full assessment
| Summary finding | Studies | Methods | Coherence | Adequacy | Relevance | CERQual assessment | Explanation of CERQual |
|---|---|---|---|---|---|---|---|
| Routes into crisis services: 1. (C1) People in crisis who have physical health concerns or (C2) lack information about crisis services (M) seek help from services they know, trust and are easy to access, (O) making it more likely that they will attend A&E, call 999 or 111 or see their GP |
10,84,89,90,97,99,108,118,143 | Moderate methodological limitations (two studies with moderate methodological limitations in analysis; one study minor methodological limitations in analysis; one study reported no method) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (six studies that together offered rich or very rich data; one report offered moderately rich data) | Minor concerns about relevance (one study setting not mental health) | Moderate confidence | Moderate methodological limitations and minor concerns about coherence, adequacy, and relevance |
| Guaranteed service response: 2. (C) If people in crisis believe that a service provides a guaranteed response, (M) they have a reduced sense of urgency, feel safer and trust that the service can help. The guarantee of a response makes them more likely to choose the service and tolerate waiting. (O) If crisis services guarantee a response, then people are less likely to attend A&E |
2,10,15,84,89,96,97,99,108,118,143,144 | Moderate methodological limitations (two studies with moderate methodological limitations in analysis; two studies with minor methodological limitations in analysis; three studies reported no or limited method) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | No concerns about adequacy | Minor concerns about relevance (two studies’ setting not mental health) | Moderate confidence | Moderate methodological limitations, no concerns about adequacy and minor concerns about coherence and relevance |
| Safe spaces: 3. (C) When people in crisis access safe spaces away from home, (M) they are less fearful and can take stock of their situation, thereby regaining control over their situation, managing their distress and (O) have improved experiences of services |
10,118,130,133,138,155 | Moderate methodological limitations (one study with moderate methodological limitations in analysis; two studies minor methodological limitations in sample and analysis; one study reported no method) | Moderate concerns about coherence (concerns about the fit of two studies to the review finding) | Moderate concerns about the adequacy of the outcomes in this review finding | Minor concerns about relevance | Low confidence | Moderate methodological limitations, moderate concerns about coherence and adequacy, and minor concerns about relevance |
| Non-clinical safe spaces, open access and peer support: 4. (C1) Non-clinical safe spaces in communities (C2) have open access and (C3) include peer support; (M) the service seems to act as a proxy for family support by providing a sense of safety, belonging and being understood. People in crisis seek this support sooner, (O1) improving engagement, reducing distress and (O2) reducing attendance at A&E |
10,106,110,118,130,132 | Moderate methodological limitations (one study with moderate methodological limitations in analysis; three studies reported limited or no method) | No concerns about coherence | Minor concerns about adequacy (one study had thin data) | No concerns about relevance | Moderate confidence | Moderate methodological limitations, minor concerns about adequacy and no concerns about coherence or relevance |
| Early navigation to help: 5. (C) People in crisis successfully navigate to help in the early stages of a crisis. (M) They feel believed and hopeful; they regain control over their situation and manage their distress. (O) People in crisis have increased willingness to seek help in the future |
2,10,15,96,97,109,112,146 | Moderate methodological limitations (two studies with moderate methodological limitations in analysis; two studies reported limited or no method) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (two studies offered thin data) | Minor concerns about relevance (one study setting not mental health) | Moderate confidence | Moderate methodological limitations; minor concerns about coherence, adequacy, and relevance |
| Services fit around personal circumstances: 6. (C) People in crisis receive a response that fits around their personal circumstances, with minimal disruption to usual life and no social or financial burden. (M) They perceive the service to be easy to access and designed for them, prompting help-seeking sooner in the crisis. (O1) People have personal control and are (O2) less likely to access crisis support via the urgent care pathway |
1,2,10,15,90,95,97,98,101,108,110,112,114,115,146,147 | Moderate methodological limitations (eight studies with minor methodological limitations in analysis, sampling and mixed-methods synthesis; three studies reported limited or no method) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (three studies offered thin data) | Minor concerns about relevance (one study setting not mental health) | Moderate confidence | Moderate methodological limitations; minor concerns about coherence, adequacy, and relevance |
| Ease of access and referral: 7. (C1) Crisis services can be accessed without complex referral routes; (C2) this is particularly important for black men, who prefer open-access services. (M) People in crisis, especially black men, perceive open-access services to be easy to access and designed for them. More generally, people in crisis who find access easy experience reduced fear and services are accessed sooner. (O1) People are less distressed at first contact and (O2), particularly black men, are less likely to experience coercive responses |
1,10,15,89,90,95,97,104,106,112,130,131,132,133 | Serious concerns regarding methodological limitations (six studies reported limited or no method; one study had serious methodological limitations in reporting of design, sampling and analysis; and one study had minor limitations in analysis and synthesis) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Moderate concerns about adequacy (although nine studies together provided rich or very rich data, five studies provided thin data) | Minor concerns about relevance (one study setting not mental health) | Low confidence | Serious concerns regarding methodological limitations, moderate concerns about adequacy of data and minor concerns about coherence and relevance |
| Gatekeeping: 8. (C) Front-line crisis staff (particularly in statutory services) value gatekeeping. (M) Gatekeeping seems to provide reassurance to staff, who are less fearful of being overwhelmed; they feel able to control their workload, (O1) minimising the impact of inappropriate referrals and (O2) reducing the number of hospital admissions. (O3) Resource pressures are managed |
2,15,95,103,105,108,112 | Minor methodological limitations (two studies report limited or no method, two studies have minor limitations in analysis) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (one study provided thin data) | No concerns about relevance | High confidence | Minor methodological limitations and minor or no concerns about coherence, adequacy and relevance |
| Shared decision-making: 9. (C) Decisions are reached through negotiation between staff across agencies and involve the person in crisis, which is especially important for black people. (M) People in crisis trust the service and have personal control; the perception of the person and their family of the crisis is acknowledged and there is a shared commitment to decisions, (O) improving relationships between services and people in crisis |
1,2,96,102,103,116,117,118,119,122,123 | Minor methodological limitations (three studies reported limited or no methods; three studies had minor methodological limitations related to intervention fidelity and analysis) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (trial studies reported limited data to inform mechanism) | No concerns about relevance | High confidence | Minor methodological limitations and minor or no concerns about coherence, adequacy and relevance |
| Organisational culture and therapeutic relationships: 10. (C) The organisational culture is centred on therapeutic relationships. (M1) Front-line staff trust shared decision-making, take a collaborative approach and prioritise shared decisions. (M2) People in crisis feel respected, and engage, (O) improving people’s experience of crisis services |
115,116,117,118,119,120,121,122,123,131,133 | Moderate methodological limitations (five studies report minor methodological limitations related to sample variation and analysis; three studies report moderate methodological limitations related to intervention fidelity, selection bias and blinding) | Moderate concerns about coherence in relation to the specific fit of the studies to the finding | Minor concerns about adequacy | Minor concerns about relevance (studies not centrally focused on organisational culture) | Low confidence | Moderate methodological limitations and concerns about coherence. Minor concerns about adequacy and relevance |
| Therapeutic skills, risk and relational safety: 11. (C) Front-line staff have therapeutic skills and provide compassionate crisis interventions. (M) Front-line staff deliver care that is balanced between mitigating risk and providing care that promotes relational safety. (O1) People in crisis are more likely to be involved in decisions and (O2) have improved experience of and satisfaction with crisis care |
10,129,133,137,138,147 | Minor methodological limitations (two studies reported limited or no method, two studies reported minor methodological limitations related to appraisal and analysis) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy. Studies provide rich data, but are limited in number | No concerns about relevance | Moderate confidence | Minor methodological limitations and minor or no concerns about coherence, adequacy and relevance |
| Peer support: 12. (C1) Peer support is available; (C2) this is particularly important to black and minority ethnic people, who (M1) believe that they have learned about themselves and gained a new perspective, giving a sense of being understood and (M2) recognised opportunities to contribute that (O) gave hope and meaning |
10 | Minor methodological limitations | Serious concerns about coherence | Serious concerns about adequacy (single study with very rich data) | No concerns about relevance | Very low confidence | Minor methodological limitations, serious concerns about coherence and adequacy, and no concerns about relevance |
| A proxy for family: 13. (C) When the support of family and friends is not available, or perceived to be unavailable, people can access a proxy for family via peer support provided in non-clinical safe spaces. (M) People in crisis have a sense of connectedness and trust. (O) The person in crisis feels safe and has reduced guilt about being a burden to family and friends |
10,96,118,119,133,155 | Minor methodological limitations (one study reported limited or no method; three studies reported minor methodological limitations related to sampling and analysis.) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (one study provides thin data) | Minor concerns about relevance | Moderate confidence | Minor methodological limitations and minor concerns about coherence, adequacy and relevance |
| Family and friends first: 14. (C) When people have access to support from family and friends, (M) they have a sense of connectedness, trust and safety that enables collaboration in decisions and mutual respect. The person seeks help from family and friends first and (O) secures help quickly |
10,93,94,96,97,103,104,110,115,118 | Moderate methodological limitations (moderate concerns in one study related to analysis and reporting of method; six studies had minor limitations in analysis) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | No concerns or minor concerns about adequacy (studies report rich data) | No concerns about relevance | Moderate confidence | Moderate methodological limitations and minor or no concerns about coherence, adequacy or relevance |
| Immediate supportive responses: 15. (C) Front-line staff have skills that enable them to provide immediate supportive responses, including active listening and counselling. (M1) Staff are more flexible and responsive. (M2) People in crisis experience relational safety, hope and encouragement, and can communicate their needs, regain control, manage their distress, and believe that the service can help. (O) The person is more likely to contact the service again in the future |
2,10,93,102,110,117,118,122,129,133,138 | Moderate methodological limitations (one study reported limited or no method, moderate limitation in one study related to blinding and validity of measures, minor limitations in four studies related to sampling and analysis) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | No concerns or minor concerns about adequacy (studies report rich data) | No concerns about relevance | Moderate confidence | Moderate methodological limitations. Minor or no concerns about coherence, adequacy or relevance |
| Compassionate crisis responses: 16. (C) Front-line staff are compassionate in their responses (in person or via telehealth) to people in crisis and their family and friends. (M) People in crisis are valued, believed, respected and involved in their care. (O1) People in crisis experience relational safety, (O2) stabilisation of the immediate crisis (O3) and improved service user experience, and (O4) there is improved job satisfaction for staff |
10,102,113,115,118,122,125,126,129,130,132,133,134,139,140,147 | Minor methodological limitations. Four studies reported limited, or no, method and five reported minor methodological limitations related to sampling and analysis | Minor concerns about coherence (some concerns about the fit from some studies and the review finding) | Minor concerns about adequacy. Most documents provide rich data, limited to thin data in two studies) | Minor concerns about relevance (one study not focused on mental health setting) | Moderate confidence | Minor methodological limitations. Minor concerns about coherence, adequacy or relevance |
| 24/7 access and same-day responses: 17. (C) Crisis services are available 24/7 and provide same-day responses. (M) The expectation of people in crisis (and of their families) for an urgent response are met; they trust the service and have a reduced sense of urgency. (O) People in crisis access a mental health assessment quickly |
2,10,15,90,95,97,98,100,110,116,118,119,120 | Minor methodological limitations (two studies report limited or no method, minor limitations related to analysis in five studies and moderate limitation related to blinding in one study) | Minor concerns about coherence (some concerns about the fit from studies and the review finding) | Minor concerns about adequacy (one study provides thin data) | Minor concerns about relevance (one study not focused on mental health setting) | Moderate confidence | Minor methodological limitations. Minor concerns about coherence, adequacy or relevance |
| Trauma-informed parallel assessment: 18. (C) Crisis services provide co-response models that include parallel assessment. (M) People in crisis experience less fear (of traumatic retelling) and a greater sense of personal control. (O1) People in crisis experience a reduced number of assessments and related traumatic retelling and (O2) have faster access to a mental health assessment that is holistic and more accurate |
98,100,101,111,118,133,143,149 | Moderate methodological limitations. (Lack of methodologically robust studies. Studies with no or limited reported method or minor methodological limitations related to sampling and analysis) | Moderate concerns about coherence (concerns about the fit from the studies and the review finding) | Moderate concerns about adequacy. Studies report single site evaluations and others report thin data) | Minor concerns about relevance | Low confidence | Moderate methodological limitations. Moderate concerns about coherence and adequacy, minor concerns about relevance |
| Inter-agency co-location: 19. (C) Co-location of mental health staff in emergency control rooms where non-mental health specialist staff (e.g. police, ambulance) and specialist mental health staff share workspaces. (M) Non-mental health specialist staff are more confident in responding and feel supported in decisions. (O1) Services are more cost-effective and sustainable. (O2) People in crisis experience faster responses to mental health calls because of improved decision-making and appropriate onward referral. (O3) There is a reduced likelihood of people in crisis being taken to (or choosing to attend) A&E or coercive responses being implemented (e.g. Mental Health Act 1983118 and 2007119) by clinical staff or police |
98,100,101,110 | Minor methodological limitations in all studies related to sample and analysis | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Serious concerns about adequacy. Limited number of studies, some with thin data | Minor concerns about relevance | Low confidence | Minor methodological limitations. Serious concerns about adequacy; minor concerns about coherence and relevance |
| Supportive clinical leaders: 20. (C) Front-line staff have access to clinical leaders and systems of support (e.g. clinical supervision). (M) Front-line staff are less fearful of blame and seeking support is an accepted norm that facilitates acceptance and tolerance between staff. (O1) Front-line staff sustain compassion and are more confident in decision-making; staff stress is reduced. (O2) Staff job satisfaction is increased, and staff turnover is reduced |
10,93,104,107,115,125,126,139,147 | Moderate methodological limitations (one study reported no method, one study had serious limitations in analysis and reporting of method, one study had moderate limitations in analysis and three studies had minor limitations related to analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Minor concerns about adequacy | Minor concerns about relevance | Moderate confidence | Moderate methodological limitations and minor concerns about coherence, adequacy and relevance |
| Decision-making: 21. (C) Decision-making is supported by evidence-based decision aides that are understood across the inter-agency crisis care system (e.g. triage tools) and decisions are linked to available services. (M1) Front-line staff have confidence in decisions and there is mutual trust across agencies. (M2) Staff have less fear in referring to other agencies and a sense of role clarity. (O1) Accuracy in identification of urgency and need (e.g. suicidality) is improved. (O2) Improved decisions enable improved inter-agency service co-ordination and more accurate resource allocation. (O3) There are reduced disputes about responsibility between staff and agencies |
10,15,93,94,98,101,104,123 | Moderate methodological limitations (one study serious concerns relating to analysis and reporting; five studies have minor limitations in relation to analysis and intervention fidelity) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | Minor concerns about adequacy, studies provide rich data, although few in number | No concerns about relevance | Low confidence | Moderate methodological limitations and moderate concerns about coherence. Minor or no concerns about adequacy and relevance |
| Leaders buffer external demands: 22. (C1) Front-line staff in ‘first response’ roles have immediate access to clinical leaders to support and manage resource pressures and disputes about responsibility across the inter-agency system. (C2) Leaders focus on buffering external demands and pressures. (M) Front-line staff are confident in decisions, have role clarity and can focus on the person in crisis. (O1) Disputes about responsibility are reduced. (O2) Front-line staff are focused on the person in crisis, rather than resource pressures and disputes, enabling them to retain their compassion and make decisions that are collaborative and safe |
10,92,102,104,107,115,126,129,135,136,139,152 | Moderate methodological limitations (no or limited method reported in three studies, serious and moderate limitations in two studies related to analysis, and minor limitations in analysis in two studies) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | No concerns about adequacy; all studies provided rich data | Minor concerns about relevance (one study not focused on mental health settings) | Moderate confidence | Moderate methodological limitations and moderate concerns about coherence. Minor or no concern about adequacy and relevance |
| Definitions, values, and inter-agency affiliation: 23. (C) Multiple definitions of crises are understood across agencies. (M1) Front-line staff accept, have a sense of ownership of, and work with different values across the crisis care system. (M2) Commissioners and leaders design services that accommodate different approaches to crises, allowing healthy challenge and debate (e.g. challenging unhelpful stereotyping and operational or professional silos). (M3) Inter-agency affiliation facilitates improved communication, information-sharing and engagement. (O) Staff work flexibly across agencies, reducing gaps and delays |
10,96,106,109,126,127,138,139,140,147,156 | Serious methodological limitations (five studies report no or limited methods; three have minor methodological limitations related to analysis and appraisal) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | Moderate concerns about adequacy. Rich data related to this finding in three studies. Remaining studies report thin data | Minor concerns about relevance (two studies are not reporting a mental health setting) | Low confidence | Serious methodological limitations. Moderate concerns about coherence and adequacy, and minor concerns about relevance |
| Crises as part of recovery: 24. (C) Mental health crises are conceptualised as part of a recovery journey rather than as single events. (M1) Front-line staff are accepting of people who may require multiple crisis interventions and confident to refer and liaise across the crisis system. (M2) People in crisis feel confident when contacting crisis services more than once that they will not be rejected. (O1) Front-line staff retain compassion. (O2) People in crisis requiring multiple crisis responses are more likely to engage and less likely to escalate risky behaviour. (O3) There is a reduction in repeat attendances and people leaving the service without treatment |
2,10,89,94,99,106,109,110,111,115,123,132 | Serious methodological limitations (six studies report no or limited methods, two studies report moderate limitations related to analysis and synthesis, four studies report minor limitations related to analysis) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | Moderate concerns about adequacy. Rich data related to this finding in eight studies. Remaining studies report thin data | Minor concerns about relevance (two studies have limited focus on the finding) | Low confidence | Serious methodological limitations. Moderate concerns about coherence and adequacy, and minor concerns about relevance |
| Time for assessment: 25. (C) Front-line staff have time to assess people in crisis. (M) Staff are less pressured for time and are enabled to focus on the person’s interpretation of the crisis and involve them in decisions. (O1) Comprehensive assessment is more likely to be accurate with appropriate onward referral, reducing the need for repeat attendances. (O2) People in crisis are more likely to reach an appropriate intervention and experience a reduced likelihood of escalation of distress and harm. (O3) There is improved cost-effectiveness and service user experience |
2,10,94,95,96,99,102,105,109,110,111,118,119 | Minor methodological concerns (three studies reported limited or no methods; seven studies had minor concerns related to analysis and recruitment bias) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Minor concerns about adequacy | No concerns about relevance | Moderate confidence | Minor methodological limitations and no or minor concerns about coherence, adequacy and relevance |
| Implementation and change: 26. (C1) Organisational strategy and operational leadership drive sustained engagement with information-sharing and shared decision-making. (C2) Crisis planning and information-sharing are particularly important for people known to services or who attend services frequently. (M1) Front-line staff are engaged and adopt changes into practice. (M2) People in crisis perceive that the service knows something about them, and they are more engaged in their care. (O) There is improved service co-ordination, faster responses and sustained change |
117,119,121,123 | Moderate methodological limitations (two studies have moderate limitations related to blinding, sampling and selection bias; one study has minor limitations related to intervention fidelity) | Serious concerns about coherence (concerns about the fit from the studies and the review finding) | Moderate concerns about adequacy (small number of studies) | Minor concerns about relevance | Very low confidence | Moderate methodological limitations. Serious concerns about coherence, moderate concerns about adequacy and minor concerns about relevance |
| Managed waiting: 27. (C) A focus on compassionate and psychologically safe crisis care drives proactive management of waiting at strategic, operational, and clinical levels. (M1) Front-line staff provide information about waiting times to people in crisis, what the wait is for and what the person can do to stay safe during the wait. (M2) There is a shared understanding of waiting-time policy and staff act to meet the standard. (M3) People in crisis and their families can tolerate waiting and the sense of urgency is reduced. (O1) People in crisis are less likely to disengage from services without treatment or circle the system. (O2) People in crisis experience reduced distress and harmful behaviour is less likely to escalate |
2,10,15,91,93,94,97,105,110,130,132,133 | Moderate methodological limitations (four studies report no or limited methods; five studies have minor limitations related to sampling, analysis and recruitment bias) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Minor concerns about adequacy | Minor concerns about relevance | Moderate confidence | Moderate methodological limitations and minor concerns about coherence, adequacy and relevance |
| Boundary management: 28. (C) Commissioning takes account of how complex boundaries between agencies (including thresholds for access) affect service delivery and service user and family experience. (M1) Commissioners and leaders drive inter-agency agreement about geographic and service remit boundaries. (M2) Staff believe in the service and act to collaborate across organisational and geographic boundaries. (O1) Gaps, delays and disputes about responsibility are reduced. (O2) Staff morale is improved. (O3) There is improved service delivery and cost-effectiveness. (O4) People in crisis are less likely to experience coercive crisis responses |
10,15,27,95,104,114,141,142,146,147,149,150,151,157 | Serious methodological limitations (five studies report no method, one study has serious limitations related to analysis and reported method, and three studies have minor limitations in analysis and synthesis) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | Minor concerns about adequacy | Minor concerns about relevance | Low confidence | Serious methodological limitations, moderate concerns about coherence and minor concerns about adequacy and relevance |
| Continuity and stability: 29. (C) Crisis services are commissioned to provide continuity and have a stable presence in communities. (M) People in crisis and crisis staff know their local crisis services and can navigate to them. (O1) Front-line staff are responsive to the needs of people in crisis (rather than focused on protecting scarce resources). (O2) Resources are available to provide continuity at service and individual levels |
2,10,95,104,105,116,118,119,120,128,139,147,149,157,158 | Minor methodological limitations (three studies report no or limited methods, three studies have minor limitations related to analysis and one study has moderate limitations related to blinding) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Moderate concerns about adequacy. Rich data related to this finding in six studies. Remaining studies report thin data | No concerns about relevance | Moderate confidence | Minor methodological limitations. Moderate concern about adequacy, minor or no concern about coherence or relevance |
| Co-production and stigma reduction: 30. (C) Co-production (including co-design of training) is actively resourced. (M1) The aspirations of service users (communities) are incorporated into design, delivery and evaluation of services across the inter-agency system. (M2) People in crisis recognise the service as designed for them, have a sense of ownership of and affiliation with the service, and talk positively about crisis care. (O1) People in communities become aware of local crisis services. (O2) There is reduced fear and shame about accessing crisis services (stigma). (O3) The quality of crisis care is improved |
2,10,89,106,118,137,139,147,156 | Serious methodological limitations (six studies report no or limited methods, one study reports minor limitations related to analysis) | Serious concerns about coherence (unclear that the data provide a convincing explanation) | Minor concerns about adequacy (most studies provide rich data) | Moderate concerns about relevance. Studies are inconsistently related to the finding | Very low confidence | Serious methodological concerns. Serious concerns about coherence, moderate concerns about relevance and minor concern about adequacy |
| Diversity and inclusion: 31. (C) Crisis services are designed and delivered with involvement from the communities they serve, and the staff reflect local diversity. (M1) Staff use language and communication that avoids racial and other stereotypes. (M2) People from black and minority ethnic populations recognise the crisis service as being for them. (O1) There is reduced fear and shame about accessing services (stigma). (O2) The quality of crisis care is improved |
2,10,89,106,118,139,147 | Moderate methodological limitations (two studies report limited or no methods; one study has minor limitations related to retrospective data) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Serious concerns about adequacy. (Two studies report rich data related to this finding. Remaining studies report thin data) | Moderate concerns about relevance | Low confidence | Moderate methodological limitations, minor concerns about coherence, moderate concerns about relevance and serious concerns about adequacy |
| Evaluating inter-agency crisis services: 32. (C) When diverse data are used to monitor services and inform decision-making, including data from across agencies and aspects of service delivery that are harder to measure (e.g. relational safety and compassion), (M) end users of services are involved in evaluating services from multiple perspectives and commissioners and leaders are focused on shared priorities (rather than competing priorities). (O) Quality of care is understood from multiple perspectives, including priorities of service users and communities served |
10,137,138,139,145,147 | Moderate methodological limitations (two studies report limited or no methods; a review provided inadequate appraisal) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | Serious concerns about adequacy (two studies report rich data related to this finding. Remaining studies report thin data. There are a small number of studies related to this finding) | Moderate concerns about relevance | Low confidence | Moderate methodological limitations, concerns about coherence and relevance. Serious concerns about adequacy |
| Technology and information-sharing: 33. (C) Technology operates across crisis agencies to support information-sharing. (M) Front-line staff are confident to communicate across different agencies; they ‘buy into’ the system and trust is established. (O1) Improved information-sharing reduces the number of assessments and related risk of trauma. (O2) Improved communication systems help to reduce barriers to information-sharing caused by rules about confidentiality and boundary disputes. (O3) People in crisis experience faster access to and transition through different agencies |
10,94,96,98,143,147,150 | Moderate methodological limitations (two studies report limited or no methods; three studies report minor limitations related to sampling, analysis and retrospective data) | Moderate concerns about coherence (concerns about the extent to which the data provide a convincing explanation) | Moderate concerns about adequacy. Rich data related to this finding in three studies. Remaining studies report thin data | Moderate concerns about relevance | Low confidence | Moderate methodological limitations and concerns about coherence, adequacy and relevance |
| Inter-agency staff support: 34. (C1) There is the same emphasis on inter-agency leadership and staff relationships as there is on the operational structure of the inter-agency system. (C2) Clinical leaders and middle managers are focused on support that balances the day-to-day demands of service delivery with attention to the needs of staff. (C3) Workloads allow leaders to be available to staff. (M) Staff are clear about lines of accountability and seek support with clinical decisions. (O1) Improved morale among leaders and staff; staff retention is improved. (O2) Front-line staff retain compassion. (O3) Resources are managed effectively, sustaining clinical priorities. (O4) Staff are empowered (rather than helpless) |
126,129,134,135,136,138,139,140,147 | Serious methodological concerns (four studies report limited or no method; two studies have minor limitations related to a lack of appraisal in a review and analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | No concerns about adequacy | No concerns about relevance | Low confidence | Serious methodological limitations. Minor or no concerns about coherence, adequacy or relevance |
| Compassionate leadership: 35. (C) There are shared values and objectives between leaders, who model compassion. (M1) There is affiliation within and between teams. There is a flat structure and leaders make themselves accessible and visible; expectations are clear. (M3) Staff are regarded compassionately and humanely, and are respected; there is staff development and (joint) training that fosters growth. (O1) Compassionate leaders set the tone for compassionate care and people in crisis experience reduced distress and increased satisfaction with crisis services. (O2) There is greater likelihood that services are cost-effective |
98,125,126,127,129,131,135,138,139,140,147,153 | Moderate methodological limitations (four studies report no or limited method, three studies report minor limitations related to sampling, retrospective data and analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Minor concerns about adequacy: although most documents provide rich data, three are thin on data for this finding | Minor concerns about relevance | Moderate confidence | Moderate methodological limitations and minor concerns about coherence, adequacy and relevance |
| System navigators: 36. (C) There are system navigators and co-ordinators with knowledge of the whole crisis system. (M) People in crisis experience continuity through trusted points of liaison. (O1) Reduced time for police dealing with crises. (O2) People in crisis are more likely to transition through agencies seamlessly |
138,143,144,147,148,153,154 | Serious methodological limitations (four studies report no or limited methods, one study has minor limitations related to reporting of methods and one study has moderate concerns related to analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Moderate concerns about adequacy. Few studies and thin data | Minor concerns about relevance | Very low confidence | Serious methodological limitations, moderate concerns about adequacy, and minor concerns about coherence and relevance |
| Inter-agency commissioning: 37. (C) There is a system-wide approach to commissioning crisis services. (M) There is a system-wide understanding of the resources required, and agencies operate to manage complexity across the system (rather than operating in silos to protect resources). (O1) There is greater likelihood of cost-effectiveness through more streamlined processes across the system and a reduced focus on resolving disputes. (O2) Inter-agency systems that provide seamless crisis services are more likely to reduce distress and increase satisfaction with crisis services |
10,81,98,147,153,161 | Minor methodological limitations (three studies have minor limitations related to age of data and analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Minor concerns about adequacy: although most documents provide rich data, one is thin on data for this finding. Small number of studies | Minor concerns about relevance | Moderate confidence | Minor methodological limitations; minor concerns about coherence, adequacy and relevance |
| National standards and local implementation: 38. (C) Crisis care operates to national standards with local implementation. (M1) Leaders engage with quality improvement; they set standards (nationally and locally) and lead the delivery of crisis services that meet these standards and expected outcomes. (M2) Commissioners and leaders pay attention to local populations, making service design responsive to local need. (O) Crisis services have potential for cost improvements through reduced use of the urgent care pathway |
27,28,30,89,98,106,146,152,157 | Serious methodological concerns (six studies report no or limited method; two studies report minor limitations related to age of data and analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Moderate concerns about adequacy. Three studies are thin on data | Minor concerns about relevance | Low confidence | Serious methodological limitations. Moderate concern about adequacy, and minor concerns about coherence and relevance |
| Inter-agency role clarity: 39. (C) Staff understand how their role fits within an inter-agency system. (M) Staff across agencies have confidence (rather than concern) that the spectrum of care is available across the inter-agency system. (O) Suspicion and mistrust between different agencies are reduced and there is improved communication between staff and between agencies |
10,15,142,149,151,161 | Minor methodological limitations (one study reported no or limited method, two report minor limitations related to age of data and analysis) | Minor concerns about coherence (concerns about the fit from the studies and the review finding) | Minor concerns about adequacy: although three documents provide rich data, there is a small number of studies | Minor concerns about relevance | High confidence | Minor methodological limitations and minor concern about coherence, adequacy and relevance |
| C, context; M, mechanism; O, outcome. | |||||||
Glossary
- Approved mental health professional
- UK-qualified mental health professionals approved to carry out certain duties under the Mental Health Act 1983 (Great Britain. Mental Health Act 1983. London: The Stationery Office; 1983) and the Mental Health Act 2007 (Great Britain. Mental Health Act 2007. London: The Stationery Office; 2007). They are responsible for co-ordinating assessment and admission to hospital in the case that an individual is to be detained under the Mental Health Acts 1983 and 2007.
- Community Mental Health Team
- UK teams providing a range of community based care and treatment for mental health conditions experienced by adults.
- Crisis Resolution Team/Crisis Resolution Home Treatment Team
- UK NHS providing interventions to people seeking urgent support for a mental health problem.
- Mental Health Act 1983
- UK law applying in England and Wales, designed to give health professionals conditional powers to detain, assess and treat people with mental disorders, in the interests of their health or the safety of the public.
- Mental Health Act 2007
- Amended the Mental Health Act 1983.
- Mid-range theory
- A level of theory that bridges overarching theory and empirical findings.
- Programme theory
- Explains components and mechanisms of an intervention or programme; programme theory is often used in evaluation studies. Clarifies rationale and assumptions underpinning the programme.
- Section 136 (emergency police power of detention) of the Mental Health Act 1983
- UK police power to remove someone from a public place and take them to a place of safety, if they believe that the individual has a mental illness and requires immediate ‘care or control’.
List of abbreviations
- A&E
- accident and emergency
- A&I
- Abstracts and Indexes
- AMHP
- approved mental health professional
- ASSIA
- Applied Social Sciences Index and Abstracts
- CIMO
- context, intervention, mechanism and outcome
- CMHT
- Community Mental Health Team
- CMO
- context–mechanism–outcome
- CRT
- Crisis Resolution Team
- ESG
- expert stakeholder group
- GP
- general practitioner
- GRADE-CERQual
- Grading of Recommendations Assessment, Development and Evaluation – Confidence in the Evidence from Reviews of Qualitative research
- HMIC
- Health Management Information Consortium
- IPT
- initial programme theory
- IRAS
- Integrated Research Application System
- IT
- information technology
- JCP
- joint crisis plan
- MH-CREST
- Mental Health-Crisis Realist Evidence SynThesis
- MMAT
- Mixed Methods Appraisal Tool
- PPI
- patient and public involvement
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- RCT
- randomised controlled trial
- SPA
- single point of access
- TIDieR
- Template for Intervention Description and Replication
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.10.3310/TWKK5110).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
