Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR128070. The contractual start date was in January 2020. The draft manuscript began editorial review in February 2023 and was accepted for publication in August 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Baker et al. This work was produced by Baker et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Baker et al.
Chapter 1 Context
Safety within mental health services
Mental health services report high levels of safety incidents1,2 that involve both patients and staff. This is a key concern of the Care Quality Commission3 and an NHS priority. 4,5 According to UK government records for 2020–1, 300,703 incidents were reported to have occurred in a mental health service in England. 6 More detailed data from acute mental health wards show that the most frequently occurring incidents in this setting involve violence and self-harm. 7 On acute mental health wards, safety incidents are often associated with increased costs, including the costs of restraint, seclusion, rapid tranquilisation and increased one-to-one nursing and physical and psychological harm to the patient, which may increase length of stay and have a negative impact on their health-related quality of life. 8 In some cases, injuries to staff may occur, with associated costs of replacement staff and staff support. 9
A further safety issue on acute mental health wards is that one incident may increase the probability of further incidents occurring, via a disturbed ward milieu and social contagion. 10 Social contagion is a mechanism by which an influence or idea spreads from person to person. For example, self-harming behaviours can spread among people on a mental health ward through behavioural contagion (a type of social contagion11–13),14,15 so successfully avoiding one incident may bring further positive benefits by reducing the probability of future incidents. 14–17
Previous work examining contributory factors to safety incidents in secondary care hospital settings produced the Yorkshire Contributory Factors Framework (YCFF). 18 The YCFF describes 20 separate domains, such as team factors, supervision and leadership. In response to the recognition of patient safety as an under-researched but important aspect of mental health care, researchers19 adapted the YCFF to focus on contributory factors within a mental health setting. Further qualitative work exploring patient perspectives on safety highlighted wider issues than those currently captured via incident reporting systems; for example, factors such as ‘not being listened to’ or not feeling psychologically safe. 20
Discourses on safety
Patient discourses around safety in the mental health literature suggest that inpatient mental health settings perceived by patients to be safe are places where it is not dangerous to be vulnerable,21 patients have a sense of being recognised as a whole person22 and they have some feeling of control within an uncertain world. 23 However, the organisational perspective tends to dominate, and this prioritises identification and risk management of violence, aggression, self-harm or suicide by patients. 24–27 Furthermore, patient safety as an academic discipline has traditionally focused on acute physical health care settings, both empirically and theoretically. It is widely acknowledged that patient safety in mental health care contexts has been a neglected area of research. 28–30
Service-oriented perspectives tend to omit patients’ definitions of safety. 20,31,32 Consequently, incident reporting systems fail to capture the spectrum of patients’ safety concerns, for example, around bullying, intimidation, racism, aggression, drug and alcohol use, or theft of personal property. 33 This in turn obscures the extent and impact of physical and psychological harm caused by restrictive practices. 31,34,35 Psychological consequences for those involved directly or indirectly (e.g. as witnesses)36 can include anger, fear, anxiety and symptoms suggestive of post-traumatic stress disorder.
In addition, where organisations focus on the avoidance of risk, ward cultures can be characterised by defensive practices that are ineffective and potentially harmful. 32,37 Safety incidents can include iatrogenic harm even when procedures are correctly followed and best practice38,39 is observed. 31,34,35,40,41 Given their far-reaching impact, it could be argued that restrictive practices, which are intended to prevent harm,42 are simply sanctioned violence. 43
Various frameworks and sets of guidance for the appropriate use of restraint have been produced. 38,39,44–47 Nonetheless, ongoing abuses in mental health wards and other institutional settings have attracted media attention. 48–51 For instance, in 2022, an undercover journalist recorded evidence of harmful use of restrictive practices in a UK mental health unit,50 in a narrative that resonates with other witness accounts of abuse, for example, Reese (2021). 52
Behavioural contagion
Behavioural contagion is a type of social contagion. 11–13 The term refers to the tendency for people to repeat a behaviour after others have performed it,53 in a process similar to the transfer of emotions between staff and patients in a healthcare setting. 54 Behavioural contagion has been identified in studies of self-harm, aggression and assaults,14–16,55 and suicide and deliberate self-harming behaviour. 14,55,56 Parents and health professionals have expressed concerns that adolescents in mental health settings may acquire destructive behaviours in hospital, for example, self-harm and suicide. 57 Their perspectives are supported by the results of a study exploring the dynamics of violence on adult mental health wards, which found that patient aggression and self-harm incidents clustered temporally, both within a specific day and also in adjacent days, indicating that behavioural contagion was a factor. 15
Milieu
The milieu of a mental health ward is something in the environment or setting, beyond formal treatment, that is potentially beneficial to mental health inpatients. 58,59 It has been described as the interaction between the physical environment, social structures and social interactions. 60 Some research on mental health wards has linked the use of physical space61,62 or noise levels63–65 with agitation and aggression. According to Gunderson,66 a therapeutic milieu is one that reassures patients that they are physically safe and cared for; it makes ‘conscious efforts … to make people feel better and improve their self esteem’ (p. 329); has predictable and helpful structures (e.g. of routines, roles and activities), invites patients to be involved in the social environment and validates each individual. Conversely, a ward milieu that is less therapeutic may feature unstructured periods, denial of privileges, high noise and activity levels, threatening language and authoritarian, inflexible or confrontational staff. 67
Improving therapeutic milieu has been associated with reduction in violent incidents and restrictive practices (e.g. seclusion and mechanical restraint) and staff and patient injury. 67 The trend towards short inpatient stays, however, may prioritise achieving measurable safety targets over building community and therapeutic relationships;58 making it harder for patients to heal. 67 When short inpatient stays are the norm, potentially helpful and feasible factors include therapeutically minded nurses,58 thoughtful tolerance of risk68 and a move away from a coercive culture. 69 Therefore, ward milieu seems to be highly relevant to patient safety interventions development for acute mental health wards.
Patient perspectives on safety
Patient involvement is a priority for mental health research. 29 Indeed, the need to involve patients and their families in improving the quality and safety of health care is recognised as a cornerstone of policy and practice. 70 Previously, the Berwick report on how to improve services in the wake of care failures at Mid Staffordshire NHS Foundation Trust had concluded that, ‘the patient voice should be heard and heeded at all times’ (p. 18);71 yet it has been argued that this report may not have had a clear impact72 and, in 2022, the British Broadcasting Corporation50 showed a poor mental health ward environment in which patients did not appear to have opportunities to offer feedback to service providers.
Patients and staff have been shown to have different perspectives on safety, and despite the policy focus, very few patient-reported safety data are collected in the health services. 73 Patients have pointed out that healthcare staff prioritise physical safety, often at the cost of psychological safety. 31 The commonly accepted World Health Organization definition of ‘the prevention of errors and adverse effects to patients associated with health care’74 could arguably be enhanced through the inclusion of patients’ perspectives on safety. 19,20,31,75 Furthermore, adverse incident reporting mechanisms in NHS hospitals may not effectively identify all such incidents. 76,77 The submission of organisational incident data to the National Reporting and Learning System is largely voluntary to encourage openness and continual increases, and should be seen as indicative rather than precisely accurate (p. 18). 78
Barriers to participation of experience experts (patients, service users, carers) in mental health research
Lay perspectives from experience experts (e.g. patients, carers, lived experience advisory groups, patient and public involvement and engagement (PPIE) groups and non-executive director roles) is a valuable and relevant component of mental health research. 20,79 It can be perceived to meet the requirements of the equality, diversity and inclusion agenda80 and in some contexts is a mandatory element of a research funding application. 81 However, these groups may have limited influence other than to help secure funding. 81 There are many structural and personal factors that discourage experience experts from participating in mental health research, whether or not they are currently patients (i.e. actively receiving care). They may feel too unwell to participate in research; alternatively, their opinion may be given less weight than that of other experts, because it is assumed that they have unreliable judgement. 20,82–85 Even when specifically invited to offer a perspective, a patient may have difficulty articulating their view, and/or may not be given a genuine opportunity to speak up. 86 Individuals may be deterred from participatory research roles because of feelings of shame (e.g. Femi-Ajao et al. 87; Roodt et al. 88) and hence, an ongoing fear of judgement. 89 Better training and preparation for health professionals can mitigate these barriers90 and can encourage lay experts to share their perspectives to improve health care and health research.
Patients and carers also struggle to raise safety concerns because of fear of repercussions from raising concerns and because the processes are onerous, particularly for someone experiencing poor mental health. 20 Therefore, staff may be unaware of the psychological harms occurring on wards, whether caused by staff behaviour, treatment or other patients. Patients may consequently experience harm while resident on acute mental health wards and also have difficulties raising concerns with staff. If patients were given the opportunity to report safety issues in real time, staff could potentially respond and intervene before situations escalate.
The need for more patient involvement in mental health safety research
Research studies in general hospital settings have found that patients can be a valuable source of safety information and that participating in such activities is both acceptable and feasible for patients. 20,91,92 Generally, there appears to be little empirical evidence concerning interventions that enable staff to use patient feedback about safety to improve service-level safety performance, although The Patient Reporting and Action for a Safe Environment (PRASE) intervention18,93 offers a theory and evidence-based approach to the systematic collection of hospital inpatient feedback about safety and a framework to help staff interpret and act on that feedback. Furthermore, research on the potential for ward staff to respond to patient feedback about safety is limited and appears to be restricted to secondary care hospital settings. Two studies found that ward staff required additional support to respond to patient feedback;75,94 other research found that real-time data support staff to respond proactively to safety issues. 95 A stronger research base in this field can inform how these findings might be applied to an acute mental health ward.
Proactive safety monitoring
Two emerging ideas within the literature on safety in health settings are the notion of safety ‘monitoring’ as opposed to solely ‘measurement’, alongside awareness that prospective clinical surveillance may have potential as a means of promoting safety within organisations. 96,97 Prospective clinical surveillance is particularly important within the acute mental health context, since there can be rapid fluctuations within the dynamic of the inpatient group and between patients, staff and the environment, such that individual patient needs create immediate knock-on effects for other patients, their quality of care and their safety.
In previous98 national level initiatives, such as the NHS Safety Thermometer,99 monthly data relating to mental health ward safety were collected from patients by staff; however, a recognised limitation of this measure was its ‘snapshot’ nature, which in this case was an opportunity sample of patients on one predetermined day per month. There are established strategies for measuring harms that have already occurred but approaches to understanding safety of care in real time are more limited. 100 Incident data are often reviewed retrospectively but this precludes the opportunity for anticipation and prevention; that is, data are ‘lagging’, rather than ‘leading’. 100
Alignment with the measurement and monitoring of safety framework
In 2014, Vincent et al. published the Measurement and Monitoring of Safety Framework (MMSF),100 a theoretical framework for the measurement and monitoring of safety in health care. This framework proposed a shift of focus from the measurement of past harm towards the prevention of future harm, through assessment of current safety. It involved co-design with service users and was evaluated in a range of healthcare services, including mental health services. The MMSF has five domains:
-
Past harm: has patient care been safe in the past?
-
Reliability: are our clinical systems and processes reliable?
-
Sensitivity to operations: is care safe today?
-
Anticipation and preparedness: will care be safe in the future?
-
Integration and learning: are we responding and improving?
The current study is aligned with the MMSF100 domain ‘sensitivity to operations’. This domain highlights the crucial but often overlooked activity of monitoring the safety of care as it is delivered in real time, recognises patients and families as important sources of information, and highlights the need for staff to develop a collective awareness of the workings of the service and to be sensitive and responsive to subtle changes and disturbances. Proactive day-to-day monitoring of patient perspectives could potentially bring greater benefits than the traditional reactive approaches relying on retrospective review and could be part of a broader vision of how to improve ward safety.
Mechanisms for patient feedback
At present, there is no mechanism by which leading (i.e. moment to moment) safety data from patients on acute mental health wards can be captured and made available to staff in real time. There are different potential mechanisms for patient feedback about safety to be received and discussed by ward staff in an acute mental health ward. For example, in the PRASE intervention,92 feedback was collected over a 3- to 4-week period, and staff came together to consider the feedback report and produce action plans. 20,91,92
Routine shift handover meetings between outgoing and incoming staff can successfully be modified to incorporate standard items such as evidence. 101 Another option is ‘safety huddles’,102 which originated in secondary care as short daily meetings to brief staff on immediate safety issues. They were found to facilitate real-time identification of, and response to, safety concerns,103 and have been implemented successfully in a mental health setting. 102
Implementation of innovations in health settings
Innovations can meet resistance in acute mental health settings104,105 and implementation was carefully considered in the current study. Staff burnout is one contributing factor; its effect may be mitigated when staff can influence the change,103 leading to improvements in feasibility and acceptability. Leadership appears to be another moderating factor, since managers in acute mental health care have been found to be more positive than their ward staff about change. 101
Feasibility and acceptability are consistently identified as key concepts within implementation theory, although with varying relative importance. For instance, Allen et al. 106 groups feasibility, fidelity, acceptability, sustainability and adoption together as the principal determinants of implementation, whereas Hernan et al. 107 identifies feasibility as the overarching concept, with acceptability, fidelity, enablers, barriers, scalability and process of data collection as measurable components.
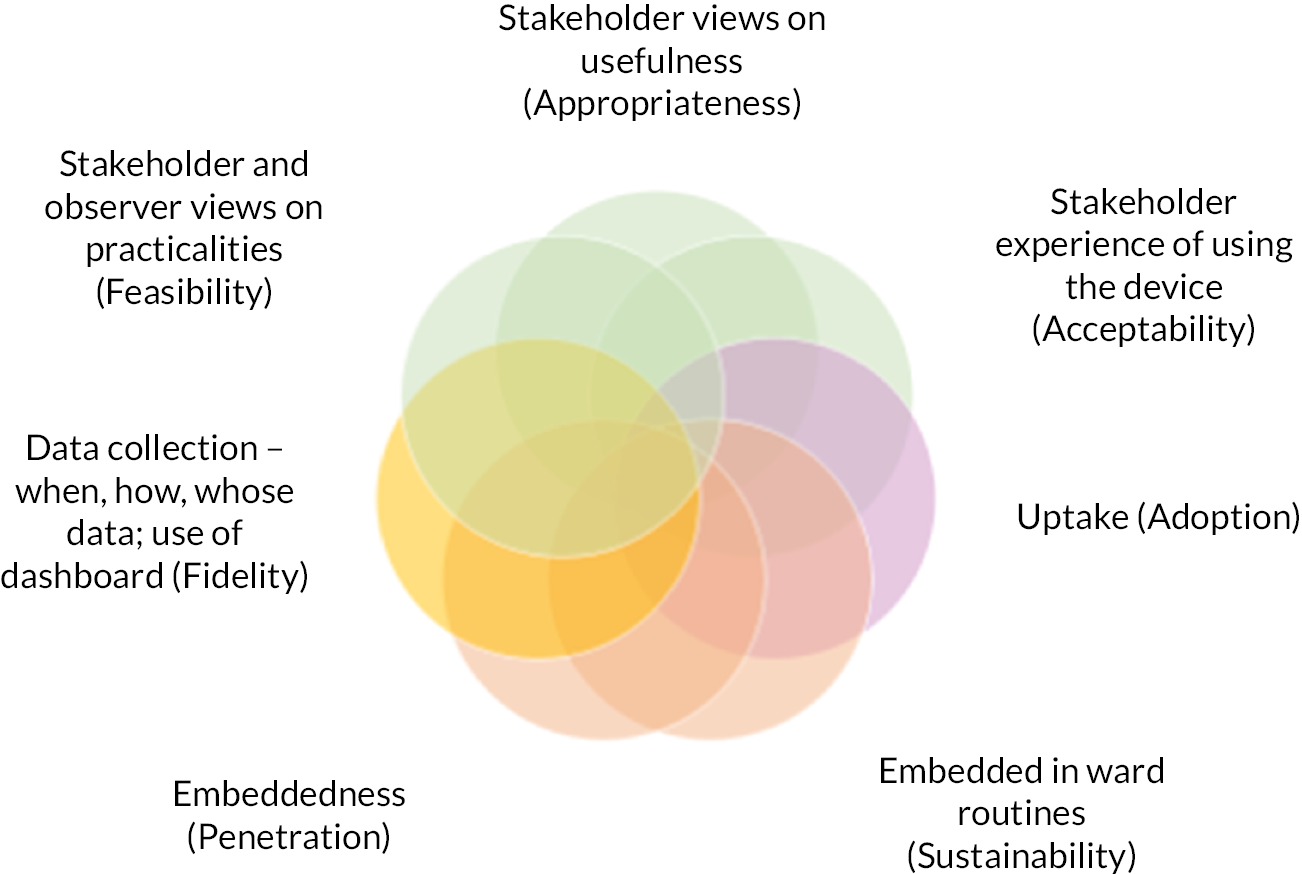
An implementation outcomes taxonomy produced by Proctor et al. 108 was a useful framework for thinking about implementation within the current study. It comprises eight primary influences on innovation implementation within a health setting (Table 1). In this model, implementation outcomes are seen as preconditions for successful service, system and clinical outcomes, and should be understood before progressing to a larger study.
| Implementation components | |
|---|---|
| Acceptability | Stakeholder perception of satisfactoriness |
| Adoption | Stakeholder willingness to adopt intervention |
| Appropriateness | Stakeholder perception of suitability and usefulness of intervention in the specific setting |
| Cost | The cost/effort of the intervention |
| Feasibility | The degree to which the innovation can be used or implemented successfully |
| Fidelity | The degree to which the intervention was implemented as intended |
| Penetration | The degree to which the intervention is embedded within the systems |
| Sustainability | The degree to which the intervention is normalised |
Focus of the current study
Using the MMSF100 as the theoretical foundation, the focus of the current study was to develop a monitoring tool for collecting and monitoring real-time data directly from patients on acute mental health wards using digital technology and to explore whether staff could use this information on a daily basis to anticipate and avoid developing incidents, thereby proactively managing safety in acute mental health settings. Our focus mapped closely to the vision for data on mental health inpatient settings recently published by the UK Department of Health and Social Care,109 ‘where the potential of data and evidence is fully exploited so that the healthcare system is able to ensure the highest standards of care in all mental health inpatient wards and pathways’ (p. 8).
Chapter 2 Design overview
This was a two-phase mixed-methods study. The design was theoretically informed by a triangulation approach, which employs multiple methods to understand a phenomenon. 110,111 Phase 1 focused on development and Phase 2 on evaluation. The study was characterised by iterative co-design, information gathering, review and reflection.
Although the structure of the current report may suggest a linear timeline, the research was essentially iterative. For example, PPIE activities were concurrent with, informed, and were informed, by other parts of the research.
Aims and objectives
The study had two principal aims:
-
To co-design a monitoring tool to improve patient safety on acute mental health wards, through the collection of daily data about the patients’ perceptions of safety, to support staff in monitoring and improving the safety of the clinical environment (Phase 1).
-
To implement the tool and explore its feasibility and acceptability (Phase 2).
The following objectives were identified:
-
To co-design with service users and staff a digital innovation that will allow real-time monitoring of safety on acute mental health wards.
-
To explore the feasibility and acceptability of capturing real-time feedback from service users about safety.
-
To explore how staff use this information when reported during daily handovers (or other mechanism).
-
To explore how the resulting data are related to quality and safety metrics.
-
To explore how these data can be used longitudinally to promote safety.
The study objectives and corresponding issues to explore are indicated in Table 2 and revisited in Chapter 10.
| Phase | Objective | Corresponding issues | Chapter | |
|---|---|---|---|---|
| Phase 1 | 1 | With service users and staff, co-design a digital intervention, to allow real-time monitoring of safety on acute mental health wards. It was envisaged that the intervention would involve use of a tablet computer device (hereafter referred to as a ‘tablet’ or ‘device’). | Does the intervention allow real-time monitoring of safety (i.e. how/when do staff circulate the tablet; do/how do patients engage with the tablet; do staff access data; what do staff do with the data; do they/how do they action it?) | 4–7 |
| Phase 2 | 2 | Explore the feasibility and acceptability of capturing real-time feedback from patients about safety | What are patient and staff attitudes/expectations? What practical issues come up in using the device? | 8–9 |
| 3 | Explore how staff use this information when reported during daily handovers (or other mechanism) | How do staff use the data in practice? | 8 | |
| 4 | Explore how the resulting data are related to quality and safety metrics | How do the resulting data relate to quality and safety metrics? | 9 | |
| 5 | Explore how these data can be used longitudinally to promote safety | How can these data be used longitudinally to promote safety (i.e. what conditions context and culture are needed to improve safety using the data?) | 8 | |
Design
This was a mixed-methods design in two phases, developed and refined to suit the context. The approach taken to reporting the study adhered to key principles of reporting guidance described in the literature. 112
Phase 1 design
Phase 1 consisted of overlapping stages progressing towards conceptual clarification, as illustrated in Figure 1, followed by technical specification and delivery of a testable intervention. Key theoretical concepts underpinning the development of the tool were the MMSF domain ‘sensitivity to operations’, contagion and milieu. These were explored in the literature at an early stage in the study113 to aid conceptual clarity and inform the research design.
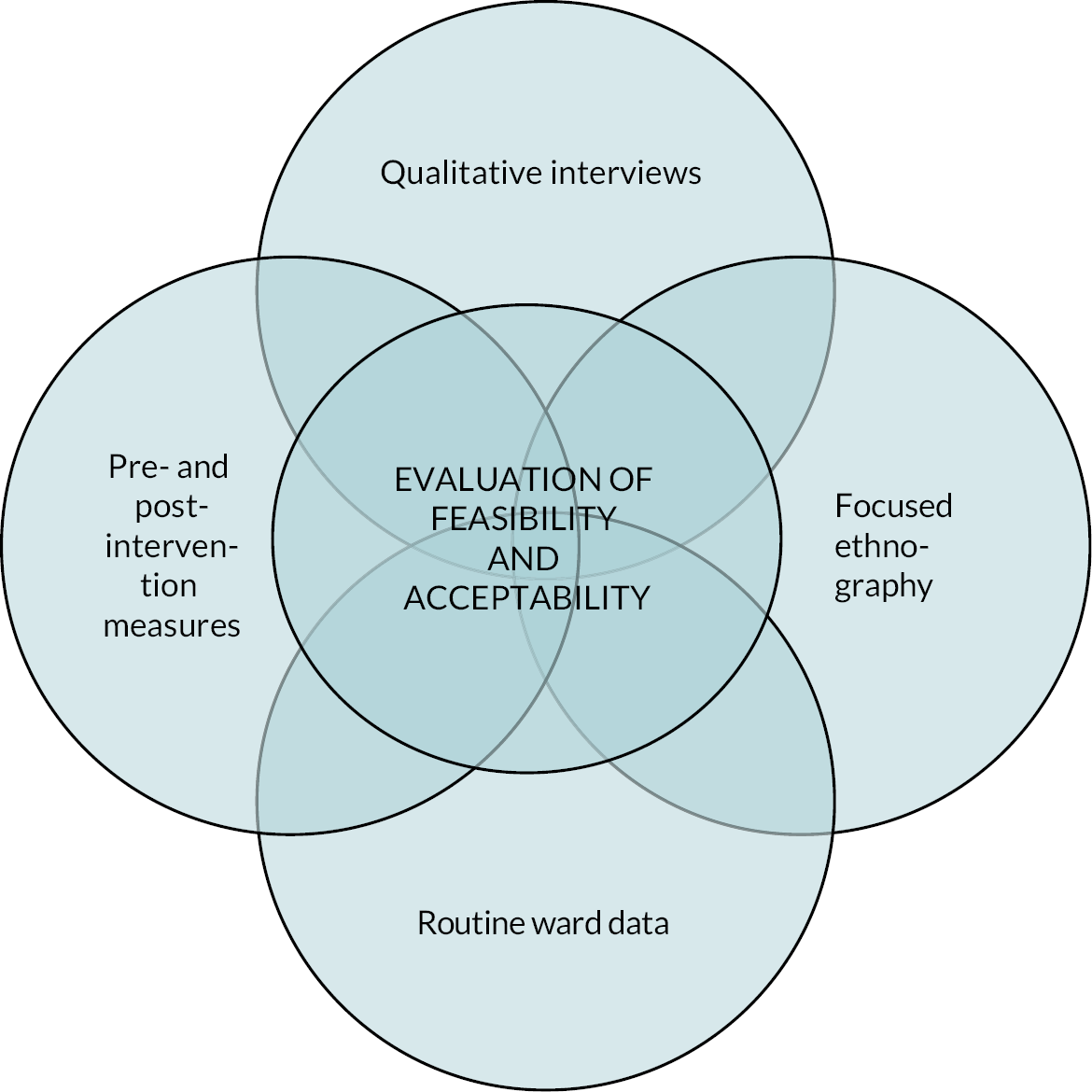
FIGURE 1.
Phase 2 data categories synthesised for evaluation of feasibility and acceptability.
Specific Phase 1 components were:
-
A co-design approach.
-
A series of consultations with patient advisory groups, current inpatients and health professional staff to explore possible conceptualisations of the intervention and refine prototypes.
-
A review of the literature on patient involvement in safety interventions in acute mental health care.
-
An evidence scan of the use of digital technology in mental health contexts.
-
Semistructured qualitative interviews with mental health patients and health professional staff, to elicit their views on ward safety.
-
Ongoing engagement with stakeholders to guide and inform concept development and refine technical iterations.
-
Development of a logic model and programme theory to act as a framework for organising and refining ideas about a safety monitoring tool.
-
Technical development of a testable tool that uses patient feedback for proactive safety monitoring.
Phase 1 resulted in a testable monitoring tool that used a tablet computer device for real-time safety monitoring of patients’ perceptions of safety on the ward.
Phase 2 design
Phase 2 was a mixed-methods process evaluation of the feasibility and acceptability of the monitoring tool via four categories of data (qualitative interviews, focused ethnography, pre- and post-intervention measures, real-time measures and routinely collected ward data; Figure 1).
Specifically, these categories were:
-
A focused ethnography to explore how staff communicate and use safety data; this included on-site observations by researchers.
-
Qualitative interviews with patients and staff (health professional staff).
-
Simultaneous collection of routine data (i.e. incidents, workforce and ward occupancy).
-
Pre- and post-intervention measures relating to staff perceptions of safety culture and ward atmosphere, together with real-time measures of these concepts.
-
Analysis of data from all the above.
Collaborating partners
The core research team worked with collaborating partners to deliver specific pieces of work. Two NHS mental health trusts in the UK supported the project throughout. One of these trusts was directly involved in the Phase 1 intervention development activities. Other collaborators were the co-design specialists ‘Thrive by Design’114 and the digital product developers ‘Ayup Digital’. 115
Promoting equality, diversity and inclusion through patient and public involvement and engagement activity
In the current study, the PPIE work reflected the research team’s intention to promote equality, diversity and inclusion. Patient and public involvement and engagement116 is key to effective and relevant health research82 and was integral to WardSonar. The whole project development was informed by stakeholder and lay input, specifically through discussions with patients and co-applicants with lived-experience expertise. The original PPIE strategy involved convening and engaging a lived experience advisory group. It was developed on principles of co-design and incorporated multiple face-to-face discussions with different groups, but necessary revisions were made to the original design to try to accommodate the original objectives (see Coronavirus disease 2019 amendments to project design below). The PPIE plan was revisited and replaced with an alternative stakeholder engagement plan that was feasible during the coronavirus disease 2019 (COVID-19) pandemic. A member of the core research team with experience expertise established links and facilitated a series of sessions with two pre-existing stakeholder groups hosted by a mental health trust in the north of England.
Technological co-design
The intervention technical development in this study was co-produced by Thrive by Design and Ayup Digital in consultation with service user networks, healthcare staff and wider stakeholders, using a collaborative, human-centred and sprint-based/agile approach. 117–119 Ayup Digital was involved in co-design, put the technical brief into operation and provided technical support during the implementation of the intervention. Cycles of co-design activities were led by Thrive by Design and included workshops and activities with patients and staff on two wards, in addition to more opportunistic in-person discussions with health professionals at one NHS trust.
Coronavirus disease 2019 amendments to project design
The project commenced in 2020 in the very early stages of the COVID-19 pandemic. This context had a considerable impact on plans for stakeholder engagement. The original intention behind convening a lived-experience advisory group was for the group to consider the emerging evidence from the early phases of the project and to contribute to deciding how the evidence should inform the development of the tool. Once there was broad agreement on what the monitoring tool would be, we intended to run a series of co-design discussions, with separate discussions for staff and patients (approximately 12 participants per discussion) on different sites and with different groups, facilitated by up to three co-design experts.
However, a significant amount of non-COVID-19 related research was paused, and it was not thought appropriate to advertise (e.g. via social media) to convene a new group. Various alternatives were considered. For example, at the co-design stage, a hybrid approach was suggested in which patients in stakeholder roles were gathered in a room on the ward, facilitated by staff, and the co-design team joined them remotely via video link. Difficulties relating to poor connectivity, limitations on physical space, and COVID-19 restrictions around patients mingling and going off the ward meant that this was not feasible. In brief, pragmatic adjustments were made to the co-design plan to produce a feasible alternative in which a single NHS trust permitted limited visits from a clinical collaborator familiar with the local protocols, who was able to gather ad hoc views and opinions from patients and staff passing through a communal space. The PPIE work is described in more detail in Chapter 5. In addition, following discussion with the funders, timescales were adjusted and a decision was made to remove a phase of small-scale testing.
Subsequent waves of COVID-19 infection had significant impact on the testing of the monitoring tool, particularly in the early months of 2022. These caused delays in accessing sites, unusual staff to patient ratios and considerable challenges to the researchers involved in observing the implementation of the monitoring tool.
The development of the WardSonar monitoring tool is describe in more detail in Chapter 5.
Ethical approval
Ethical approval for Phase 1 was obtained in November 2020 from the University of Leeds, School of Healthcare Ethics Committee, reference HREC 19-028 (health professional arm of the study) and South Central – Berkshire B Research Ethics Committee, reference 20/SC/0360 (patient arm of the study).
Ethical approval for Phase 2 was obtained in November 2021 from East Midlands – Nottingham 2 Research Ethics Committee (IRAS project ID: 300833; REC reference: 21/EM/0247).
Chapter 3 Literature reviews
Objective
Patient safety in acute mental health care is a pressing concern48,120 and patient involvement in safety research is crucial to addressing the issue. 121 The development of a patient safety monitoring tool was informed by exploration of the literature around: (1) patient involvement in safety research in acute mental health care and (2) the application of digital technology in mental health contexts. The literature reviews aimed to provide background information to inform processes outlined in objective 1; that is:
-
With service users and staff, co-design a digital intervention, to allow real-time monitoring of safety on acute mental health wards.
Methods
The literature reviews comprised a scoping review of the literature on patient involvement in safety interventions and an evidence scan of the application of digital technology in mental health contexts.
Scoping review of the literature on patient involvement in safety interventions
The team conducted a scoping review of the literature on patient involvement in safety interventions in an acute mental health setting. The Smits ‘Involvement Matrix’122 was applied to classify and assess patient involvement in development, implementation and/or evaluation of relevant research and interventions. The following section contains a summary of the review. Further information is available in the published report in Appendix 1. 123
Methods
Search strategy and study selection
Systematic searches of academic databases (CINAHL, PsycINFO, MEDLINE, EMBASE, Web of Science and Scopus) and grey literature were designed using medical subject headings and the research question: ‘To what extent are patients involved in interventions to improve patient safety in acute mental health care?’ Searches (2000–20) were conducted during March–June 2020 (last academic database search 1 April 2020; last grey literature search 19 June 2020).
Grey literature was included because of the likelihood of finding unpublished research around safety in acute mental health conducted by clinical teams. Additionally, 14 mental health-specific sources (e.g. Centre for Global Mental Health) and 25 non-mental health-specific sources (e.g. Royal College of Nursing) were explored, together with the National Institute for Health and Care Excellence (NICE) evidence database, ProQuest Thesis and Dissertations database, and three social media platforms (Twitter, Facebook, YouTube). Additional grey literature sources of interest identified by authors’ expertise and hand searching were screened. Review papers produced by the search were scanned for potentially relevant papers. Duplicates were identified and removed using EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) bibliographic software.
The same eligibility criteria applied to both academic and grey literature. Eligible studies involved patients in active research and/or patient or staff safety improvement role, as classified by the Involvement Matrix. 122 Eligible outcomes related to patient involvement in patient safety research or interventions. Eligible settings were inpatient mental health care contexts. All study designs were eligible for inclusion.
Search results were exported to Covidence (Melbourne, Australia) for screening at title, abstract and full text level by two researchers. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart124 is shown in Figure 2.
FIGURE 2.
Preferred reporting items for systematic reviews and meta-analyses flow chart.

Data extraction used the Covidence online tool and was informed by the Joanna Briggs Institute reviewers’ manual. 125 Study quality was appraised using the Mixed-Methods Appraisal Methodology Tool (MMAT),126 which is suitable for assessing diverse study designs. Patient involvement was evaluated using Smits et al.’s Involvement Matrix. 122
Results summary
A total of 52 studies from the grey and published literature were included. They were conducted in the UK, United States, Canada, Finland, New Zealand and Europe. The majority (n = 33) focused on reducing staff use of restrictive practices. About half of the studies reported only limited patient participation in the research, and the involvement of patients as decision-makers was reported in only four studies.
Safety interventions ranged from system change at the organisational level, through operational decision-making at ward level to interventions for individuals, such as a smartphone application (app). Patients were involved mainly as co-thinkers, advisers and partners rather than decision-makers. The more extensive their involvement, the more likely they were to have active roles in the research. Research with high patient involvement tended to focus on forensic mental health and to be associated with reduction in restrictive practices. Low patient involvement tended to be associated with less reduction in restrictive practices.
Narrative synthesis of the included literature identified a possible association between studies with high levels of patient involvement and more effective safety interventions, but methodological quality of the surveyed papers was inconsistent. The review findings were incorporated into the ongoing synthesis of all data and learning from Phase 1.
Evidence scan of the application of digital technology in mental health contexts
Methods
To further inform the development of a safety monitoring tool, an evidence scan127–129 of the literature around digital technology in a mental health context, was conducted in November 2020, using the databases CINAHL, PsycINFO and Web of Science. The search terms and included studies detail can be found in Appendix 1.
Results
Research in the field of application of digital technology in mental health contexts appears to be concentrated primarily on therapeutic interventions, such as assessment of suicidal ideation or suicidal risk, and psychological support therapies, such as counselling. A limited body of research on telecare and the design of mental health apps for use in various other contexts was identified but digital technologies specifically related to mental health care are relatively new. Many digital technologies for health (mainly apps) have been designed within the tech industry, not always using mental health expertise. 130
Regarding technology design, there was an emphasis on usability and accessibility and some concerns around confidentiality. Poor digital literacy is seen as a barrier to utility and some degree of personalising technology to the user was seen as potentially helpful. Preferred design features included images and the use of colour. Other themes included the possibility of under- or over-reporting by patients and the impact of the technology on staff. Establishing a threshold for staff action and building it into the technology to trigger an appropriate response were considered important. The reviewed literature also indicated that patients’ cognitive abilities, health status and confidence in the technology affect their engagement and that, provided that the digital technology does not cause patients any harm, it is seen as potentially helpful and useful to them.
Factors that support successful technology implementation and staff engagement included connectivity (e.g. access to a reliable internet connection), training for people who may be using the technology, the provision of technical support, and ensuring effective communication about the technology so that its rationale is understood.
Conclusions to literature reviews
Interrogation of the literature clarified that there was an evidence gap regarding meaningful patient involvement in mental health safety research. It further indicated potential priorities for the development and design of digital mechanisms to improve ward safety from patient perspectives. These conclusions were incorporated into Phase 1 data synthesis.
Chapter 4 Phase 1: qualitative interviews
Objective
Phase 1: qualitative interviews relate to objective 1, that is:
-
With service users and staff, co-design a digital monitoring tool, to allow real-time monitoring of safety on acute mental health wards.
Semistructured interviews were conducted in Phase 1 to explore patient and staff perspectives on safety issues and how patients and health professionals can contribute towards the measurement and monitoring of ward safety in an acute mental health setting. Access to patients for interview was greatly affected by COVID-19 restrictions. Ultimately, 8 patients and 17 mental health professionals participated in interviews. The intention was to use learning from the interviews to inform overall data synthesis and hence intervention development.
Methods
Recruitment
Two NHS mental health trusts in the north of England (NHS trust 1 and NHS trust 2) supported the overall project and facilitated recruitment of patients. Patients were recruited via posters placed in NHS trust premises. Patients who were interested in taking part notified designated health professionals, who passed on contact details to the researchers. Health professionals were recruited via advertisements on social media (Twitter, now X, X Corp., San Fransisco, CA, USA) inviting them to contact the research team about the study. Potential interviewees were provided with further information and consent forms. Before commencing each interview, researchers explained the purpose and process of the interview to the participant, read the consent form out loud and recorded consent verbally. Interviews took place via the telephone/Microsoft (MS) Teams (Microsoft Corp., Redmond, WA, USA). Patients who were interviewed received a £10 shopping voucher as a thank you for their time.
Data collection
A topic guide was used to explore participants’ views about safety issues in acute adult mental health inpatient services and was adapted as interviews progressed so that pertinent topics were raised with subsequent participants. Appendix 2a contains the interview topic guide. Staff participants were asked to describe their job role and experience in acute adult inpatient mental health services. All interviewees (patients and staff) were prompted to discuss what they considered to be the features of safe and unsafe wards, their experience (or otherwise) of sensing that an incident had occurred or was about to occur, and their understanding of why safety incidents appeared to be temporally clustered. Interviews were audio recorded, anonymised and transcribed professionally.
Analysis
Members of the core research team coded the transcripts and jointly developed a coding framework based on inductive open coding of transcripts and deductive application of codes relating to the research questions and the topics covered in the interview. The constant comparison technique131 was used throughout, and analyses were conducted by hand and in Nvivo 12 (QSR International, Warrington, UK) software. Thematic analysis informed by Braun et al. 132 identified themes that cut across the descriptive categories.
Results
Sample
A sample of 25 patients and mental health professionals participated in semistructured interviews via telephone or video link. Patient interviews were conducted between November 2020 and April 2021. Health professional interviews were conducted September–November 2020. Interview duration was driven by the interviewee and ranged between 15 and 71 minutes. The interview sample is summarised in Table 3.
| Patient | Health professional | All | |
|---|---|---|---|
| Female | 2 | 11 | 13 |
| Male | 6 | 6 | 12 |
| Total | 8 | 17 | 25 |
A total of eight patients (female n = 2; male n = 6) over the age of 18 years with current or recent experience (during the past 2 years) of being an inpatient on an acute mental health ward were recruited for interview after responding to publicity material displayed in clinical areas. They made contact with the researcher and received further details about the study with a consent form. This sample was smaller than originally intended, with many fewer patients than staff. It is likely that the COVID-19 restrictions and the general social context influenced patients’ motivation to participate in interviews.
From health professionals, 17 (13 nurses, a psychologist, a psychiatrist, a speech and language therapist and a social worker) were recruited for interview. All had experience of working in UK inpatient psychiatric settings; 12 were based in one UK region and 11 were female; 8 were currently working in an acute mental health inpatient setting. Experience of working in mental health inpatient settings ranged from under 5 years to over 15 years.
Thematic data analysis133 explored aspects of contagion and milieu, highlighting the relationship between the milieu and contagion, and identifying themes of contagion via risk amplification, contagion via therapeutic depletion and contagion via increased exposure to safety incidents. Individual factors, the social and physical environments, and wider service factors (such as staffing levels) were considered as influences on safety.
The relationship between behavioural contagion and the milieu
Participant accounts of the physical, cultural and therapeutic space that constitutes a mental health ward described a complex, multilayered milieu in which attributes such as the social interactions of patients and staff and the wider service context were important influences. Their narratives suggested three mechanisms by which the milieu contributed to behavioural contagion: amplification of risk; a diminished therapeutic milieu; and increased exposure to safety incidents.
The extract below illustrates how different layers of the milieu and the interactions between them may be seen as facilitating, if not directly causing, perceived clusters of safety incidents.
When I enter a ward, I’m often told, you know, so-and-so has become distressed and then it’s set off someone else … I wonder whether, as professionals, we put that [interpretation] on the situation, because we’re trying to make sense of it ourselves, … You know, if someone becomes distressed, it then, kind of, ruminates with another person [and] they then feel upset. I think there might be a little bit of trauma stuff behind that, in terms of seeing someone be distressed is really upsetting … I also wonder whether there’s a relationship between that availability of staff. So, you know, if someone’s distressed because they haven’t been able to see the doctor, then it’s very likely that another person is going to get distressed, because they also can’t see the doctor. So I wonder whether there’s a more tangible reason why more than one person might be upset at that time.
Senior leadership team member
In this extract, the participant described being briefed about an incident (‘so-and-so has become distressed’) resulting in contagion (‘set off someone else’). She offered two explanations for contagion: (1) individuals’ characteristics (rumination, retraumatisation or increased sensitivity due to trauma, difficulty interpreting, regulating and expressing emotions); (2) the service context; specifically, that a diminished therapeutic milieu might frustrate patient attempts to access care (‘they haven’t been able to see the doctor’), leading to unmet needs and distress for that individual and potentially others.
Perspectives on safety
Participants referred to safety incidents that they said stemmed from patients and/or staff, and/or deficiencies within the service context. Aggression, violence, absconding, self-harm, suicidal behaviour, bullying, intimidation, substance use, property damage and use of restrictive practices were seen as safety issues.
Staff also referred to other events as having implications for safety, such as unexpected admissions or meetings, a chaotic patient, boredom, a fire alarm in the night, missed patient leave or staff being perceived (by patients) as acting unfairly. Many staff acknowledged that individual-level interpretations of service-level policy might vary between patients and staff or even different professions and that some incidents ‘never get recorded because it’s not recognised as an incident by a clinician’ (social worker, patient safety lead). This reflects differences in perspectives of patients, staff and organisational processes.
The quotation below illustrates how bullying by patients, staff behaviour and the wider service context combine to influence safety.
There was a lot of bullying. I felt really uneasy with some patients’ company, I spent a lot of my time in the activity room or in my own room, [or] on the occasions when I could get out, [in] the communal garden … Sometimes it was behind your back, if I was in the activity room but as soon as staff leave you could feel that uneasiness, you know what I mean, and there was one occasion when a member of staff went in and the panic alarm started but this female patient was always bullying people and the staff literally didn’t know how to handle her. It was so understaffed but the lack of staff, staff cannot be everywhere patrolling the wards, and they’re escorting patients and doing medication.
Patient 6, F
Patients drew on personal experience and gave examples indicating a broader range of the factors affecting physical and psychological safety. Other patients were a potential safety issue, as some were wary of the possibility of being attacked, without being protected by staff:
You get attacked in the hospital, by other patients and the staff don’t do nothing about it … I did get attacked in the hospital and they did nothing about it … I rung the police but the staff were saying he’s a liar.
Patient 3, M
Various norms and values around safety and risk were expressed, forming an impression of the cultural aspects of the milieu from reflections on policy, training, individual interpretations and staff–patient relations. Staff described shifts in attitudes to risk, safety and the use of restrictive practices (e.g. physical restraint, as-needed medication) had shifted over the past decade. They recalled feeling safe when ‘we could all restrain people and we had access to medications and that there were loads of staff’ (ward manager 1) and how the focus of post-incident reviews had shifted from explaining ‘why the incident occurred from our perspective’ (nurse 4) to considering patients’ psychological safety.
Staff also revealed how qualities they associated with a safe milieu could produce harm and clusters of behaviours they interpreted as ‘contagion’. For example, being ‘risk averse’ or performing well-intentioned efforts to prevent anticipated safety incidents could actually increase risk and safety incidents by imposing a culture perceived as oppressive: ‘the more restrictions we put on people, the more chance we’ve got of violence’ (ward manager 2). To add to the complexity of the context, it was possible that, if staff were out on the ward, visibly monitoring safety, patients could interpret this as a sign of disinterest in the patients:
I just think that they’re too busy, they’re moving around constantly, they’re not really putting the patients first.
Patient 5, M
Temporal clustering
One feature of social contagion is ‘temporal clustering’,134 where incidents of a behaviour are clustered together over a short period of time, like a ‘chain reaction’ (patient 2, M). Staff reported temporal clustering of incidents using terms such as ‘knock-on’ (ward manager 2) and ‘ripple’ (nurse 2). Arguably, this type of language represents a view that fails to consider contextual factors (such as staff shortages or subsequent COVID-19 restrictions).
Staff shared their perspectives on how patient aggression may be amplified and incidents of one type (violence, shouting) might have consequences (patient traumatisation, staff redeployment, patients need support, patients’ needs go unmet) that lead to incidents of another type (self-harm, leaving the ward without permission):
If a patient is very violent and aggressive on a ward, you may see a contagion for other violence and aggression … you may also see an incidence of increasing self-harm because people are distressed.
Social worker, patient safety lead
If you ever get a violent incident, you always end up with knock-on events … people requiring more one-to-one input [but] they can’t get it because the staff are redeployed somewhere else so that … it has a massive effect on the ward. And it’s traumatic, isn’t it, if you see something like that and people really struggle …
Ward manager 2
Information sharing between staff was seen as integral to constructing and maintaining a predictable, safe milieu, and indicative of a good team. Handovers between shifts provided an opportunity for outgoing staff to update incoming staff but could also ‘set off a chain of reaction with [staff]’ (nurse 6).
You get people going, oh you might as well go home, you’re going to have a terrible shift, it’s been a bloody horrible day, so-and-so’s been awful. You just think, for God’s sake, I don’t need this, this is not going to help me.
Ward manager 2
Although sharing patient information might help the team to feel prepared and safe, it could also lead staff to make negative assumptions, create anxiety and impact on how they interpret and respond to that patient.
Oh, Helen’s [name changed] been on this ward before and she’s really violent and then suddenly the next four people get this narrative of this person. And then […] maybe you’re scared or you’re unsure of what to do or your experiences inform how you interact with Helen.
Ward manager 1
Through their hypervigilance and information sharing, staff were primed to interpret cues based on their experience of previous instances that felt similar, information about patients, patients’ diagnoses and unconscious biases. Participants reflected that preparedness could be almost self-fulfilling: ‘when you’re expecting that situation, it can almost create that situation’ (social worker). They described how thinking about ‘scenarios that might arise, and how you’re going to manage them’ (nurse 4) generated feelings of tension and anxiety which affected relations with patients and also within the clinical team and could produce a ‘never-ending kind of spiral round of frustration, agitation and aggression’ (social worker, patient safety lead). Participants also described how they might arrive for a shift ‘already on the defensive’ (nurse 2) and full of ‘dread’ and this influenced how they processed information.
Staff interpretation of patient sensitivity
Health professionals observed that patients were ‘very perceptive as to what’s going on’ (nurse 8 manager) and inevitably affected by disruptions such as patient departures and arrivals and staff changeovers. Patients suggested that if other patients were ‘calm and settled’ (patient 4, M), this would help them to feel safe themselves. However, while staff saw their own hypervigilance as a marker of skill and expertise, they associated patients’ hypervigilance with hypersensitivity and impaired perceptions, judgements and abilities attributable to, for example, paranoia, poor emotional regulation, sensory issues and substance use.
Patients said that staff could misinterpret their behaviour, as these two examples show:
If you stay in your room they say you’re isolating or you could walk the corridors and take your chances but it’s a very violent environment … you couldn’t sit down and watch the telly or anything like that because if they got a telly the patients would smash it up. I couldn’t stay in my room because they said I was isolating myself.
Patient 8, M
I got a day release and I come home but then I got stuck in traffic so I phoned them up to say I was setting off back but it took me an hour and half because of the traffic and I got locked up for a week … I phoned up three times, I phoned from [city] in rush hour, stuck in traffic but the staff didn’t really tell that, and the doctor said lock him up. I was extremely pissed off.
Patient 1, M
Furthermore, whereas staff did not reflect on patients’ perceptions of how staff were feeling, this seemed to be important to patients.
If the staff are not warm and empathetic, that can really affect how you feel.
Patient 4, M
The importance of predictability
The belief that safety incidents are predictable and contagious was pervasive; for example, participants repeatedly demonstrated their conviction that a safe milieu was a predictable milieu: ‘you need to know what’s going on in order to have that safety and be able to practice safely’ (nurse 3). Participants proposed that structure, stability and predictability, ‘knowing what’s coming next’ (ward manager 1), were essential for staff and patients to feel safe.
Staff knowledge and experience of all aspects of the milieu at all three levels (service context, social and physical environment and individual) informed planning and preparedness for ‘what possible situations can arise’ (nurse 4), increasing incident predictability and therefore preventability. Staff were expected to know and understand many formal procedures and processes, policies and guidelines, to perform regular activities completing care plans, handovers, meetings, training in de-escalation and restraint, safety huddles,102 including structured risk assessments of patients to calculate ‘how risky they are to us, to our other patients’ (ward manager 2). They were expected to be familiar with patients’ triggers and ‘calm down methods’ (nurse 6), the whereabouts of ligature points and blind spots on the ward, be ‘trained in conflict and violence management’ (ward manager 2), de-escalation and ‘able to use physical restraint’ when necessary (nurse 7).
‘Ground level work’ (ward manager 2) was also required; that is, being with patients, meeting their needs and providing meaningful activities were thought to help build therapeutic relationships and, ultimately, safety: ‘you feel safe, they feel safe’ (social worker). There was a tension for staff between planning for anticipated risks and spending time with patients, however:
[Staff] feel like they’re going to get in trouble if they’ve not done a care plan, … But don’t realise that maybe if they’d sat out with the [patients] for a few hours that morning, you’ve probably managed about a million incidents … that are not going to happen because you’ve spent that time and had a cuppa with someone.
Ward manager 1
Staff claimed that ‘there’s always something like a precursor’ (nurse 4) and there were few safety incidents ‘we could never have predicted’ (psychologist). They interpreted safety incidents and other behaviours that occurred over the course of one or more days as causally related, ‘suddenly there’s three [incidents] in a day, that’s just not going to be chance’ (psychiatrist).
Staff described how their interpretation of what was expected in terms of safety led them to be in a constant state of ‘sensory awareness’ (SW, patient safety lead) or ‘hypervigilance’ (nurse 2) for anything that jarred with their notion of a safe, predictable milieu. There was a common belief that staff could sense ‘tension in the air’ (nurse 7) or ‘that feeling when you come on the ward’ (nurse 1), either from intuition or ‘micro-cues’.
I don’t really believe that it’s something that’s in the air. But it’s something about the situation that’s not the same and I suppose people who work in mental health, and people who have mental health issues, they’re more acutely attuned to those micro-changes in behaviour, in environment.
Nurse 1
These digressions were conceptualised as ‘disruptions’ in the milieu: something unexpected or out of the ordinary, ranging from shouting, alarms sounding or police presence to silence, an absent administrator or empty lounge. Disruptions were significant because participants interpreted them as cues: ‘it was like you knew something was going on’ (nurse 7). Claims about the ‘atmosphere’ or ‘vibe’ of the ward could be traced to disruptions in the physical or embodied milieu: visual and auditory ‘micro-cues’ (nurse 1), ‘subconscious stimuli’ or ‘environmental signals’ (nurse 2), such as changes in behaviour or body language, or the presence or absence of people. For example, one staff believed that patients ‘set the tone for the ward’ through their body language (relaxed or tense) and ‘what they’re saying, how they’re saying things, what they’re doing’ (nurse 9, practice development).
Patients said they did not think staff noticed everything. ‘Patients are more vigilant … got to look after themselves’ (patient 1, M). They emphasised how easily a small irritation can escalate:
Usually it builds up, you know? Starts with a disagreement over something or other, petty little thing and then escalates. For an example when I was in XXX, this lad … came in [to the TV room] to make himself a cup of tea … anyway he came in and went back out and then came in again and he says to me you pinched my phone. I said don’t talk daft I haven’t pinched your phone, look round for it … he found his phone and he didn’t apologise for that, so I just went in my room, I thought, the bastard just accused me, excuse my language, I were seething.
Patient 2, M
Impact of physical layout
Safety at the service-context level could be facilitated by the physical layout and visibility. Poor lines of sight and blind spots were considered ‘unnerving’ (nurse 9 practice development) by staff; patients tended to agree:
[Ward T] has four corridors that all join in the middle in the nurses’ office, I thought that were one of the best layouts. They can stand outside the office and turn 180 degree and see down all corridors, from that junction. They can keep an eye on people. First time I’ve come across that, other wards are corridors with little rooms coming off it where things could happen and people couldn’t see.
Patient 3, M
The milieu as a physical place brings patients who might ‘rub each other up the wrong way’ (psychologist) into proximity, whereby even one person ‘can completely change the dynamics of the ward’ (psychiatrist). Health professionals thought that, in some services, particular conditions (e.g. learning disability, personality disorder, autism) and patient mix affected safety by increasing the likelihood of ‘unpredictable’ behaviours.
When we have a lot of people with bipolar and everybody’s a little bit manic then what’s happening is everybody’s looking at somebody and saying are you having a go at me, are you looking at me. You’re looking at me strange. And being very high in their activity, more reactive to just normal cues or more reactive to other people being unwell. And getting involved in each other’s care.
Nurse 1
Although ‘patients really want to help each other out’, whether by ‘trying to soothe someone’ or ‘someone else is upset about something and they go, “oh yes and me”' (ward manager 2), this could lead them to become distressed or create additional challenges for staff. Although patient communities and friendships were beneficial, they could also facilitate the development of shared behaviours and goals.
If one [patient] would become difficult or challenging or if one would become upset for whatever reason, it would spread to the other two [patients], or the other two would be quite obstructive, or they would become quite difficult to engage.
Nurse 9, practice development
A physical layout that facilitated visibility made both intentional and inadvertent witnessing of incidents and staff and patient behaviours possible. Participants suggested that patients could be ‘distressed by witnessing’ (SW, patient safety lead) and/or hearing incidents. ‘I think when someone sees [an incident] it infuriates someone else’ (patient 4, M). This could reportedly facilitate the spread of fear, anxiety and distress, ‘like an infection’ (nurse 1).
[A patient] said he’d smash the ward up worse than the guy next door to me if you don’t let me out. It was then that ripple effect of he’d seen or heard what happened next door and thought well I want to leave, and maybe the only way I can leave is by doing what he’s done.
Nurse 7, staff nurse
Attempts to minimise the impact of witnessing an incident by dispersing patients could have their own negative implications. Staff suggested that patients encouraged to stay in their rooms may ‘feel more and more frustrated and concerned’ (nurse 8, manager), while one-to-one observation might be experienced by patients as ‘unhelpful’ (ward manager 2) or ‘unsafe’ (senior leadership team member). Similarly, the use of alarms to signal for assistance caused stress in both staff and patients across ‘the entire service’ (nurse 8, manager).
Patients described the impact on their mental health of the layout, cleanliness and general appeal of the physical environment.
Interviewer: Why did you not feel safe?
It was dirty … The cleaners were good and the morning clean was good, but it’s not enough. In my room there was snot on the walls, I had to clean it off myself … They cleaned in the morning but after that it were left, you know what I mean, it was constant, people making a mess, flooding toilets, staff saying ‘it’s not my job’.
Patient 1, M
One explained the significance of having their own room:
If you’re not feeling safe then go to your room and read a book or something. People have their own tellies and whatnot … their own private space so if you’re feeling a bit dodgy or irritated then go to your room.
Patient 2, M
Another patient was very clear about the importance of fresh air and space, in a dialogue that suggests these preferences were independent of the impact on wards of COVID-19.
Interviewer: What kind of things make you feel unsafe?
Patient: An unpleasant physical … environment, yeah. If there’re not enough windows and sort of fresh sunlight. Yeah, I’d say that.
Interviewer: Anything else about the kind of physical environment?
Patient: If it’s not spacious enough.
Interviewer: Right, so space and natural light, windows, that kind of thing?
Patient: Yeah.
Patient 4, M
As a physical space, the milieu could be said to bring similar individuals and similar behaviours together, creating the impression that patients’ behaviour is clustered because it occurs in broadly the same spatio-temporal context of the milieu. This phenomenon has been interpreted as the ‘convergence model of group influence’135 (p. 746), in which individuals within a group (e.g. patients on a ward) become more similar to each other as a result of the influence of group norms over time. Participants thought that this could increase the likelihood of patients upsetting each other and their vulnerability to contagion. Also, ward design with its emphasis on visibility intended to facilitate staff surveillance of patients in the pursuit of safety, and enabled patients to witness and be affected by the behaviour of staff and other patients, further facilitating contagion.
Contagion via therapeutic depletion
Therapeutic environments can become depleted when target-driven care models are prioritised over holistic philosophies of care. 136,137 Participants viewed the therapeutic potential of the milieu as another fundamental component of safety, suggesting that without it, ‘everything starts to fall to pieces’ (nurse 8, manager) and the ward becomes merely a ‘holding pen’ (senior leadership team member). Some pointed out that a depleted therapeutic milieu was harmful because ‘you’re leaving people just in their own distress or disturbance’ (ward manager 1) and creating an opportunity for aggression and unrest to develop.
They might sit for a couple of hours longer in the bedroom and then something that might have been quite easily resolved earlier on becomes another incident, whether it be self-harm or whether they go AWOL [absent without leave] or it could be anything.
Nurse 5
If you’re not allowing people to have access to leave, access to activities, access to things that make them feel well, you’re going to find that it’s going to be more unsafe because people are going to be more aggressive, people … there’s going to be a lot of unrest, people are going to be unsettled.
Ward manager 2
Furthermore, staff who looked disinterested or unhappy could influence the whole milieu:
[There should be something for staff] to remind themselves why they’re actually there, they’re there to help people, you know, to help those in need. Some having that negative, very down, low attitude, it’s going to translate into the team and translate into the patients.
Patient 5, M
It should be included in their training about showing empathy and compassion with patients no matter what their situation is because some of them can be really dismissive and just not interested … I think again it comes down to like, you know, more staff, attentive staff, staff that are not overworked to really sort of help dissipate these sorts of problems.
Patient 4, M
Patients were also sensitive to a ward milieu that made life difficult for staff.
A patient punched [a nurse] in a private area and all she did was go into the toilet and cry about it and then come back out and get on with her job … She should have reported. I mean if you’re a female in a hospital and you get touched inappropriately by a patient then you should report it. There were another female nurse that happened to, it were the same patient.
Patient 3, M
The topic of smoking was particularly highlighted, as restrictions on smoking could build up tension within the milieu without staff noticing.
This lad who kicked off, they wouldn’t let him have a smoke and that wound him up.
Patient 1, M
One of the examples of what staff don’t know about is smoking. In xxx you have to get an e-cig off one of the nurses and smoke it. I smoke myself and when I were in xxx I got fed up of asking for cigs so for a week I ended up on [nicotine] chewing gum, but that were the same, and every time I asked it were like ‘ten minutes’, ‘not now’, and it ended up they were like that with the chewing gum as well … I think that annoys people, not having a cigarette it affects people in different ways, some of those misunderstandings come from not having a cigarette.
Patient 2, M
Safety could be considered therapeutic in itself: ‘a vital thing for somebody to feel well’ (nurse 1). The therapeutic potential of the milieu could be diminished via exposure to an incident, or due to staff availability/unavailability, because of redeployment to an incident or retreat to their offices. Staff saw enormous potential for patients to feel ‘pissed off’ (nurse 8, manager), ‘rejected’ (nurse 7) and unsafe which may lead them to ‘self-harm or to try and abscond’ (nurse 7) or to try to elicit care, by using ‘verbal aggression’ (nurse 5) and ‘competing for volume’ (ward manager 2). These processes would damage trust: ‘it ruptures the patient–staff relationship hugely’ (psychologist).
Contagion via increased exposure to safety incidents
Potentially, exposure to safety incidents can create a norm whereby even in quiet periods, everyone within the milieu is anticipating the next incident, with resulting tensions contributing to the likelihood of it developing. When they do occur, the impact is widespread.
All the staff, kind of, run away into an office and say, are you alright, is everyone alright, and we’re all checking with each other. But we forget that we’ve got 20 guys either on the ward or in the bedrooms that are probably just as terrified or unsure of what’s happened, but we’ve left them to dwell in it. And then they don’t know what to do with it so then … we get that ripple effect of incidents.
Nurse 2
Finally, staff and patients shared concerns about the impact on patients of asking them to monitor their feelings of safety:
It is important to give feedback of any experiences, but … it is extra stress to be on the lookout for anything, you know, bad going on, having to report it and take the responsibility of reporting it, and everything.
Patient 4, M
One phenomenon in the data that can be interpreted as behavioural contagion was anxiety. Anxiety could be transmitted between staff and between patients and staff, leading to an overall increase in anxiety across the ward. The data presented here also included examples that did not qualify as contagion. For example, convergence, in which group norms lead to increased similarity, may be seen in the hypervigilance that stemmed from shared norms around the predictability of safety incidents.
Implications for development of the monitoring tool
The socioecological model (e.g. 138, 139) explains how levels of a setting interact to affect the development of an individual or organisation. In view of the staff interview data, it can be argued that the pervasive risk culture of the psychiatric milieu (context) primes staff attitudes, behaviours and interpretations of patients’ behaviours and safety incidents as contagious through a process of risk amplification which staff transmit between each other (priming).
Safety discourse in psychiatry often focuses on individual-level patient risk (e.g. reducing incidents of violence or self-harm) rather than on ward culture and staff characteristics and behaviours. 24,25,27 Risk culture drives staff to engage in practices that examine patient characteristics and past and recent incidents and individualise safety incidents such as risk assessment, care planning, debriefing and post-incident review. By shifting the focus to patients, this dominant conceptualisation of risk obscures the potential harm caused by associated risk management or safety promotion strategies. Risk culture also facilitates the anticipation and prevention of future incidents, encourages the retrospective attribution of linear cause and effect, and reinforces staff perceptions of incidents as predictable, preventable and contagious.
The harm caused by risk management strategies such as restraint and seclusion was acknowledged by staff, but the data presented here suggest that staff are also implicated in contagion (despite this usually being attributed to patient behaviour). Practices such as handovers between shifts or sharing information with other staff about patients could negatively prime staff’s expectations and interpretations of patients’ behaviour. Like staff, patients are tuned in to the atmosphere of the ward33,140 and value predictability and structure. 22,141 Seemingly innocuous staff practices such as the constant process of looking for and responding to disruptions in the milieu could therefore contribute to further disruption and provoke patients142,143 with potential implications for patients’ psychological safety and their perception of the milieu as a therapeutic space.
Thus, the milieu may act as a ‘depleting barrel’, not only eroding resources144 (p. 3), but also resulting in therapeutic depletion, and according to participants, therapeutic depletion could also contribute to contagion. By prioritising specific types of risk and safety staff are diverted away from therapeutic work, leading to unmet needs among patients. Yet patients’ conceptualisations of safety risks as including ‘not being listened to’, ‘not feeling psychologically safe’, understaffing and diminished therapeutic relationships19,20 suggest that therapeutic depletion is potentially harmful and may contribute to contagion. This was observed by Kang et al.,145 who reported that lack of support and emotional distress preceded ‘behaviours of concern’. A snapshot of the interim data (i.e. discussions around applying interview data to the development of the monitoring tool) is available in Appendix 2c.
Conclusion
The analysis of these interviews revealed dominant safety ideologies that shaped the perceptions and interpretations of individual staff, the consequences of which were played out in staff–patient relations, particularly in how staff interpreted and responded to patients’ characteristics and behaviours and how they sought to prevent and manage safety incidents. The data suggest that it is not only patients’ exposure to safety incidents that triggers further incidents. Instead, participants’ accounts indicate that any kind of disruption detected in the microsocial dynamics of the milieu could act as a cue for staff or patient behaviours that may subsequently be interpreted as a safety incident and/or contagion.
These findings illuminate the hitherto unexplored influence of staff and the psychiatric milieu on contagion via the proposed mechanisms of disruption, priming (risk amplification), involuntary convergence and therapeutic depletion. Kindermann and Skinner’s135 proposed criteria for identified contagion were limited by the lack of direction regarding how to define the attribute being transmitted, with clear implications for the over- or under-identification of contagion. In this study, identification of contagion must also be treated with caution. Although multiple examples of ‘contagion’ were identified by participants, their interpretation of disruptions in the milieu were informed by dominant cultural beliefs around the identifiability of risk, predictability of safety incidents and inevitability of contagion. Moreover, it is possible that contagion is also more likely to be identified in spatiotemporal contexts where individuals with shared characteristics and identities are gathered, subject to contextual confounds. 135 Previous studies of contagion among professionals have tended to focus on employee misconduct and ‘bad apples’,144,146 and even references to context such as the ‘corrupting barrel’ imply fault. 144,147,148 Analysis of staff views on ward safety, however, suggests that in their enactment of risk culture and the pursuit of safety and predictability, staff are capable of causing harm in their execution of care.
Chapter 5 Patient and public involvement and engagement in the development of the digital monitoring tool
Patient and public involvement and engagement in the current study addressed the principles of equality, diversity and inclusion. It was not a discrete piece of work but integrated into all the development and design processes. However, the narrative has been structured for readability. This chapter focuses on stakeholder consultations and co-design activities.
Supporting people to ensure that they have a meaningful experience of participation is vital to health services research and in this study was led by lived-experience experts on the core research team with collaborators ‘Thrive by Design’ (co-design specialists) and ‘Ayup Digital’ (digital product developers).
Objective
The digital monitoring tool development work addressed objective 1:
-
With service users and staff, co-design a digital intervention, to allow real-time monitoring of safety on acute mental health wards.
Overview
The purpose of this development work was to establish user requirements for the patient safety data recording interface. Co-design activities were led by Thrive by Design. They employed techniques such as ‘personas’ (typical users with specific characteristics including experience of disability and low digital skills); storyboards (to elicit user goals), service user journey mapping (the path of an individual patient and healthcare staff member on an ward), user stories (to elicit specific user requirements), prototyping (rapid creation of paper prototypes of a digital tool) and prioritisation (exercise to create constraints so top features are prioritised). These co-design activities identified goals, requirements, barriers and design preferences.
The content of each activity was synthesised to prioritise outputs that were acceptable to end users, technically feasible and efficacious. These priorities informed the technical prototype development. Divergent requirements (e.g. a specific feature important to service users but disliked by healthcare staff) were noted and discussed with the core research team, including experience experts.
The first cycle of co-design activities generated requirements for the digital tool; subsequent activities tested and refined the tool as it developed and considered its use within the clinical workflow of the ward environment.
Process
Table 4 outlines the timescales for stakeholder engagement.
| Date | Activity | Output |
|---|---|---|
| August 2020 | Virtual discussions with two stakeholder groups | Stakeholder perspectives on acute mental health ward safety, communication about ward safety, and factors to consider in the development of a digital tool to improve ward safety |
| September 2020–April 2021 | Interviews with patients and mental health professionals | Perspectives on safety issues and how patients and health professionals can contribute towards the measurement and monitoring of ward safety in an acute mental health setting |
| December 2020 | Steering group | Discussion and synthesis of outputs so far |
| December 2020 | Ward visit for face-to-face engagement with patients and staff of two acute mental health wards | Feedback on draft ideas for digital monitoring tool |
| January 2021 | Ward visit for face-to-face engagement with patients and staff of two acute mental health wards | Feedback on several potential digital products |
| July 2021 | Virtual discussions with two stakeholder groups | Feedback on prototype version 3 |
Potential ideas for the digital products were drafted to facilitate discussion with stakeholders. User stories were created to guide development of the products (see the technical development detail in Appendix 2d). The sessions used a collaborative, human-centred and sprint-based/agile approach117–119 aimed at facilitating a good experience for the group members, as well as generating high-quality research outputs to feed into the overall data synthesis.
The original intention with this PPIE work was to convene and engage a lived experience advisory group and also to deliver a series of co-design workshops, with separate discussions for staff and patients (approximately 12 participants per discussion).This plan was revisited and replaced with an alternative stakeholder engagement plan that was feasible during the pandemic. The lived experience advisory group was replaced with virtual stakeholder engagement sessions. Regarding the co-design workshops, fortunately, NHS trust 1 was able to approve controlled, on-site visits from a member of one of the project collaboration teams (Thrive by Design) for a limited amount of stakeholder engagement. The reworked stakeholder co-design activities included a face-to-face discussion, opportunistic in-person feedback from patients and staff and e-mail feedback (from health professionals).
Pre-prototype discussions: virtual stakeholder engagement sessions
In the summer of 2020, virtual stakeholder engagement sessions were facilitated by a member of the core research team with each of two stakeholder groups already established and hosted by an NHS trust (‘trust A’). One 30-minute session was held with a group that has a monthly meeting for people who currently access or have accessed trust services and their relatives, friends and carers. The second session (60 minutes) was held with a forum that provides researchers with an opportunity to involve public, service user and patient and carer involvement in research. These sessions focused on three key areas of discussion:
-
How to phrase or ask patients about whether wards feel safe or unsafe.
-
How best to talk about patient safety (e.g. the use of language, words or phrases that should or should not be used).
-
Suggestions for what to consider when developing a digital intervention to be used on acute mental health wards.
One example of the impact of stakeholders is in preferences around language. For example, in the academic literature there are clear distinctions between the two concepts of milieu, with its therapeutic potential, and atmosphere, which is widely perceived as a measurable construct. 60,149,150 Atmosphere has been defined as the ward’s psychosocial climate,60 although it is argued that physical factors are important and should not be overlooked. 151 Milieu and atmosphere are closely connected concepts60,152 and are sometimes used interchangeably. 152
In the current study, stakeholder consultations concluded that the word ‘milieu’ was linguistically and conceptually challenging outside academic spheres; service-user networks preferred to refer to ‘atmosphere’ and ‘ward atmosphere’ as more familiar and self-explanatory terms. The use of inaccessible language can have an alienating effect. 153,154 In view of the stakeholder feedback, the term ‘atmosphere’ was applied in a broad sense within the user-facing components of the WardSonar project. It was agreed that it was more important to use language that was inclusive to diverse groups, than to complicate the syntax to avoid conflation of technical terms.
Ward visits to discuss prototypes 1 and 2
In late 2020, NHS trust A permitted a clinical team member of Thrive by Design to visit two wards (‘ward X’, male, and ‘ward Y’, female), to meet with staff and patients, on two occasions. This approach meant that contributions were made at a time and place that suited patients and ward staff. The permission was granted because this team member was also an occupational therapist who was familiar with the infection control policies and personal protective equipment in the trust. The first ward visits were in December 2020 and focused on prototype 1 of a digital product. The second ward visits were in January 2021 and focused on prototype 2 of the digital product.
Wards X and Y shared a reception area. Ward X was a working-age adult acute ward caring for males aged 18–65 years. In the reception area, six people from ward X contributed opportunistic feedback (three patients and the clinical team manager, ward staff of all grades, including administrative staff). Ward Y was a working-age adult acute ward caring for females aged 18–65 years. Opportunistic feedback from ward Y was elicited in the reception area from five patients, the clinical team manager and 12 other ward staff (clinical and administrative). The difference in participation between wards X and Y was due to overall engagement from each separate ward, particularly with respect to ward Y’s clinical team manager, who was very keen to be part of the work and ensured that staff were well informed about the visit and its purpose. In addition, three members of ward staff and five patients participated in co-design workshop activities (approximately 40 minutes’ duration) at the end of an existing meeting forum.
Feedback from these two ward visits was collated and prioritised jointly by co-design partners ‘Thrive by Design’ and developers ‘Ayup Digital’ using the MoSCoW method (Must have; Should have; Could have; Won’t have this time). 155
A bank of user stories was collected during the co-design activities to guide the conceptual and technical development of the tool. A sample is shown in Table 5. The full set is available in Appendix 2d.
| As a (role) | I want (to do …) | So that (goal) | MoSCoW |
|---|---|---|---|
| Staff | it to all look and sound the same | I can use it on any ward | M |
| Staff | to record positive responses also | it isn’t all negative | M |
| Staff | to look at a daily screen | we can use it in our process now | |
| Service user | a graded approach to inputs/outputs | I can express myself better | M |
| Service user | to use touch screen | it’s the same as my phone | S |
| Service user | option to be anonymous | I don’t have to describe why I feeling like that | S |
| Service user | it to express my mood now | staff know how I’m feeling | S |
| Service user | to flag to staff when there are issues | it doesn’t reduce time spent with staff | |
| Staff | like it to be used everywhere on the ward | so that people in isolation can access | M |
| Service user | to understand current perceptions of safety | concerns about COVID-19 safety are captured | |
| Service user | maybe an artificial intelligence element | I use a concept familiar to me | C |
| Service user | messages that are secure | I know where the information is going | M |
| Service user | private messages | my feelings aren’t shared on a board | S |
| Service user | to report on other things like there are no cups | I don’t become agitated about it | C |
Ward visit 1: prototype 1
The first prototype patient recording interface formed the basis of discussions in ward visit 1 in December 2020 (Figure 3). Draft ideas for the digital ‘products’ (i.e. patient recording interface, health professional dashboard) and the potential for a public-facing ward interface were presented and discussed, for example, with regard to wording, format, colour and how they would work in relation to existing systems. People wrote comments and fed back on all aspects of the design. Health professionals were consulted on whether the visuals looked like materials already in use, to avoid unintended consequences arising from confusion.
FIGURE 3.
Prototype 1.
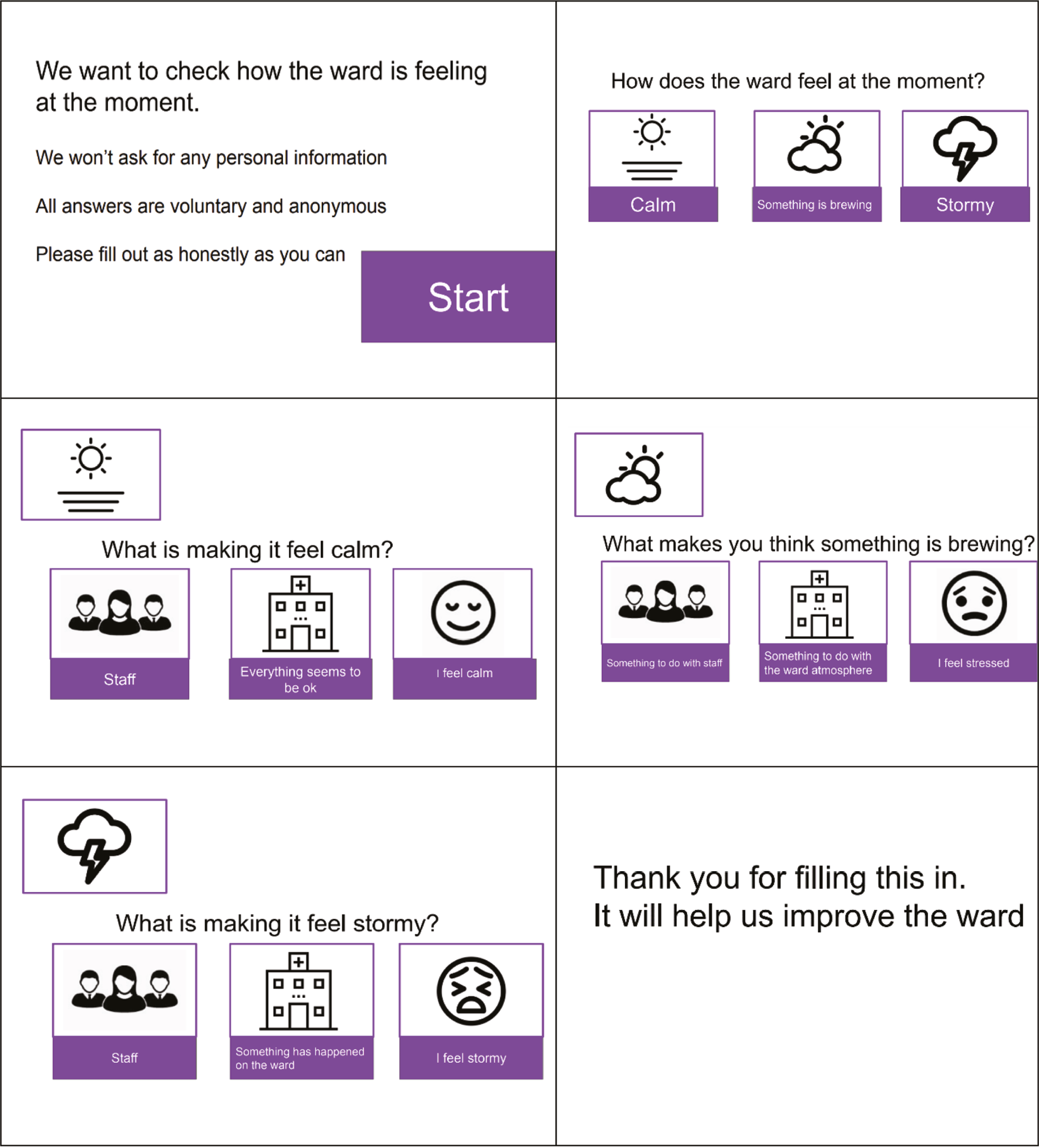
Staff were keen on the use of colour and traffic light systems, as these elements would align with other systems. Following the first set of ward visits, the feedback and discussion content was represented in a spreadsheet as user stories, as described in Methods, to facilitate prioritisation to guide development.
Key areas where decisions were made following this first visit included that people suggested having different ways to be able to express how the ward was feeling, including pictures, text and being able to write in specifics. It was thus agreed to include free-text options. It was also suggested that more options for how the ward was feeling could be helpful to reflect that this is often more than ‘good, bad and okay’ and that the feeling is more of a spectrum. Consequently, it was agreed to have five options in the tool to describe how the ward was feeling, and that an additional question would be included to show the direction things are moving in (i.e. getting better, worse or staying the same; see Figure 3).
Ward visit 2: prototype 2
Ward visit 2 took place in January 2021 and focused on prototype 2 (Figure 4). Multiple versions of the latest iteration of digital ‘products’ were presented and feedback elicited from the patients, clinical staff and administrative staff, in addition to revisiting discussions from visit 1. People commented on components including the wording, icons, colours and representations (e.g. was it what they imagined?). The ward staff perspective on the requirements of the health professional dashboard were revisited, and the patient and ward staff perspective on the acceptability of a public-facing ward interface was considered (see Figure 4).
FIGURE 4.
Example content of prototype 2.
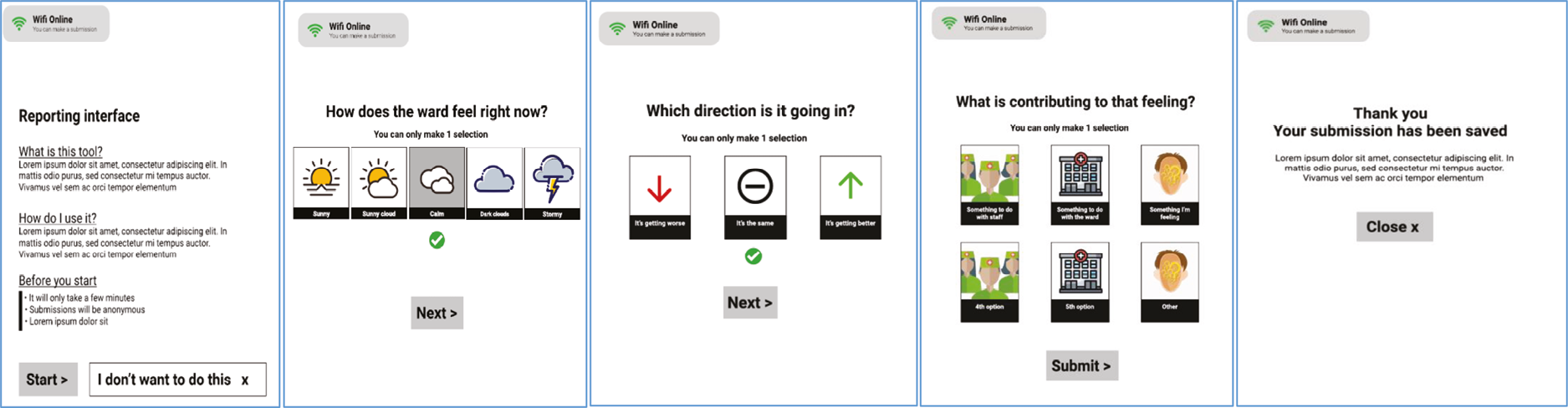
In this second ward visit, prototype 2 (see Figure 4) was viewed as a set of slides on a digital tablet. (When implemented on the wards, the tablet computers used in the study were often referred to as ‘devices’ to avoid confusion with pharmaceutical tablets.) As there was a high turnover of patients, many new patients were involved, although many of the same staff contributed, which enabled discussions from the first visits to be revisited.
People shared general perspectives on the prototypes and commented on wording and visual components, for example, the hospital image in prototype 2 was deemed to be confusing, as it looked like a church, and the weather descriptor ‘sunny’ was considered to be the wrong word and was subsequently changed to ‘calm’.
Practicalities of using a tablet on the ward was also discussed. The idea of using patients’ personal mobile phones had been rejected as unfeasible, but many staff raised concerns around the security of the tablets and who would have responsibility for them. This discussion led to key development decisions. Whereas it was not reasonable to rely on all patients having a smartphone and data, the NHS trusts did not permit use of iPads® (Apple Inc., Cupertino, CA, USA) or the hospital Wi-Fi, so options for the monitoring device were limited to Android computer tablets and the patient Wi-Fi.
Around the time of this visit, the team also met to agree how and when the tool would be distributed to patients (three times a day facilitated by a member of staff), and this information was included within the introductory information in the tool itself.
Prototype 3 discussions
Following the ward visits, a third prototype of the patient recording interface was produced that incorporated the feedback and key decisions. Further virtual stakeholder engagement sessions with the two stakeholder groups focused on this prototype. These sessions centred on the following areas of discussion:
-
The design of the patient interface: would you feel comfortable completing it?
-
Could you say why you would feel more or less comfortable?
-
Do you think completing a report on the ward atmosphere on a digital tablet like the example in the pictures would make you feel less or more distressed?
-
Ward facing interface: how would you feel about this being displayed on a ward?
The group also discussed the idea of conducting ethnography on acute mental health wards.
Prototype 3 was approved by the two stakeholder groups, who particularly liked the simplicity of the patient interface and the anonymity it provides, as well as the use of weather icons to indicate the milieu (referred to in the user interface as ‘ward atmosphere’ following advice from the stakeholders). The groups also discussed issues around whether it was reasonable to ask patients for real-time data without building in an immediate response from staff, when there was an urgent need such as self-reported suicidal feelings. Overall, people felt that the patient interface would be a safe space to report concerns.
The final versions of the patient user interface and staff dashboard are presented in Figure 7 in Chapter 7. Further illustrations and the full technical report are available in Appendix 2d.
Chapter 6 Design of the safety monitoring tool
Objective
The design of the safety monitoring tool addressed objective 1:
-
With service users and staff, co-design a digital intervention to allow real-time monitoring of safety on acute mental health wards.
Methods
Data from Phase 1 included the review of patient involvement in safety interventions,123 the evidence scan of the use of technology in mental health settings, patient and mental health professional interviews, virtual stakeholder engagement sessions and ward-based co-design visits. These were discussed on an ongoing basis between the core research team (including two co-applicants with lived experience), service user research advisory groups, the wider research group (including technical and co-design partners) and the project steering group. Findings and insights were discussed routinely among the core research team, the collaborating partners and the wider stakeholders. Commencing with the first ward visit in December 2020, Thrive by Design and Ayup Digital met fortnightly with the core research team to interrogate and interpret the feedback on the evolving interpretation of a digital product that addressed requirements identified from information gathering in Phase 1.
Discussions were collaborative and enabled an iterative approach to data synthesis. This led ultimately to the development of a series of prototypes for a digital product, as described in Chapter 5. These discussions centred on framing the findings to inform intervention development and formulate an idea of a real-time patient safety monitoring tool that could be put into operation. They considered what the ‘must haves’ were; for example, health professionals said that it was important to capture whether patients felt the atmosphere was changing, and if so, whether deteriorating or improving. They also considered how many of the ‘must haves’ could realistically be implemented and noted where there was consensus on what to exclude or change, such as ambiguous language or imagery. Potential unintended consequences and challenges were highlighted; for example, stakeholders said that patients might feel unsettled if they saw that the public-facing ward interface displayed a ‘stormy’ or deteriorating ward atmosphere.
Discussion of findings
The synthesis of the findings from the literature reviews, patient and mental health professional interviews and early stakeholder engagement sessions were ultimately organised around seven themes that underpinned the further development of the monitoring tool in subsequent stakeholder engagement sessions: conceptualisation of safety; anonymity; milieu (ward atmosphere), contagion and incidents; digital technology on the ward; involving patients in measuring safety; feeding data back; and unintended consequences. Each theme had its own implications for the intervention development phase. The theme descriptions below are principally informed by facilitator notes from the stakeholder consultations.
Conceptualisation of safety theme
Facilitator notes from the stakeholder consultations demonstrated that although some service users said that the tablet would be a safe way to report safety issues, many remarked that reporting safety information on a digital tablet could create its own safety concerns, for example, it might be ‘bad’ for their mental health or could make other service users suspicious.
Physical, mental and emotional safety were all relevant: ‘It was noted that safety might at first be assumed to be physical [an example of tripping over the cleaner’s bucket was mentioned]’ (facilitator notes). Alternative terms representing safety were suggested: ‘reassurance, recovery caring, security, calm, responsive, comfortable, protect, concern, and safeguard’ (facilitator notes).
There was general agreement that it was important to report matters to staff in person, regardless of digital monitoring, and the suggestion that using the technology could reduce the amount of time staff spend actually checking in with patients: Please make sure it’s clear from the start that it is an optional extra NOT a replacement.
Facilitator notes
A group participant mentioned the difficulty in distinguishing ‘what is in my head and what is the atmosphere’ – this would make answering the question ‘other patients/staff/how I’m feeling/ward environment’ very difficult.
Facilitator notes
Implications for intervention development
-
Allow for a multifaceted conceptualisation of safety.
-
Consider how the word ‘safety’ may be misinterpreted – provide a clear and accessible description to enhance readability for diverse groups including individuals with cognitive difficulties.
Anonymity theme
Stakeholders reinforced the need for anonymity, as a prerequisite for safety.
It’s not safe – if someone has an issue with another patient and it’s known about.
Stakeholder feedback
The tablet was seen to enable anonymous feedback: for instance:
If particular staff create an atmosphere – this method will pick this up.
Stakeholder feedback
This is great, feel more comfortable anonymously saying how I feel, I probably wouldn’t say otherwise.
Stakeholder feedback
Implications for intervention development
-
Anonymity is essential.
-
Reinforce that feedback is anonymous and that everyone’s experience is important and all feedback is valued.
-
Give clear information about the use and purpose of collecting information via digital technology.
Milieu (ward atmosphere), contagion and incidents theme
The term ‘milieu’ was discussed and rejected by the stakeholders:
All agreed to the removal of the word ‘milieu’ from the interface. The group agreed that ‘atmosphere’ is more understandable and that using plain English is important.
Facilitator notes
Stakeholders also noted that if there was a bad atmosphere or the ward was understaffed, there would less likely be support with the device and so in that situation, some people would not be heard (facilitator notes); however, the device could encourage reporting:
I would feel more comfortable being able to say how safe I feel on a ward without queuing at a desk or not reporting at all out of fear.
Stakeholder feedback
Stakeholders expressed that an atmosphere in which alarms are going off and staff are running to an incident feels unsafe, so prevention was preferable. The need to capture whether the direction was changing that is ‘getting worse’ or ‘getting better’ was felt to be really important from a health professional perspective.
On the subject of placing researchers on the ward as observers, one stakeholder group advised that: patients would not be uncomfortable but that staff may feel they are being monitored and that they may not want patients to say they are uncomfortable on the ward, the staff might behave differently and it wouldn’t be representative of the norm.
Facilitator feedback
Implications for intervention development
-
The technology needs to be sensitive to subtle changes in a negative direction to anticipate the potential for an incident occurring.
-
Explore whether the technology can be sensitive to context; for example, highlighting when a safety incident has recently occurred.
-
Location: potential for the technology to be sensitive to location within the ward; for example, increased anxiety or input activity by patients into the technology (prior to and after an incident).
-
Night and day: the technology needs to recognise night and day as different contexts.
-
The technology may need to account/recognise ward profiles (e.g. all male, all female, mixed wards).
-
The technology may need to account/recognise differences between individual patients.
Digital technology on the ward theme
Stakeholders discussed the advantages and disadvantages of introducing a digital monitoring tool to the ward. There was a feeling among stakeholders that the device could be an unhelpful introduction on the ward as a digital system could potentially feel intrusive. It was also noted that some people might need help using the device.
Comments included:
Some people with mental health conditions dislike using technology, have suspicions or are affected by the digital divide, e.g. ‘If someone was tapping on a device – I would think it was about me’.
(Stakeholder feedback). Medication can also affect the ability to take in information and remember it – relating to using a digital system.
People need to know that input is anonymous otherwise (ironically) reporting ward atmosphere might not be a safe thing to do.
It needs to be explained when people first arrive on the ward including that is for everyone’s benefit – patients shouldn’t just need to figure it out or be told by other service users.
Most people like a screen but staff would need to support people not used to digital devices. It was pointed out that if there was a bad atmosphere or the ward was understaffed – there would less likely be support with the device and so in that situation, some people would not be heard.
Facilitator notes
Implications for intervention development
-
Ensure the purpose of the monitoring tool is clearly described to patients and staff.
-
The technology needs to be inclusive across a wide range of patients and digital abilities.
-
Staff may need support with using the technology and with data interpretation.
-
Consider multiple mechanisms for data collection other than a single device/reporting ‘point’.
-
Consider other relevant systems in place by staff.
Involving patients in measuring safety theme
With some exceptions, stakeholders agreed they would be happy to complete the survey and that the weather buttons were useful for determining an atmosphere.
Facilitator feedback
Apart from the possibility of triggering individuals’ symptoms (see Unintended consequences theme), concerns that were raised related to potential adverse impact on relationships between patients.
Stakeholders pointed to some of the implications of collecting patient perspectives on safety, such as: ‘If someone was on the device and someone else had their lighter taken off them by staff – the person with the lighter might think it’s related’ (stakeholder feedback).
The stakeholders also generated some ideas for sensitively crafted phrases explaining what the device was for, which it was felt would reassure people, for example: ‘We want you to have a good stay, we want to create a calm and responsive environment and to help you to feel safe’.
Implications for intervention development
-
Technology needs to incorporate the input of quantitative and qualitative data to give patients choice about the level of detail they provide.
-
Explore using language/imagery that is universal and include a free-text option to expand.
-
Consider levels of providing feedback, for example, level 1 reporting – a colour or smiley face; level 2 – more detailed information.
-
Explore whether thresholds need to be built into the system to trigger alerts/action.
-
Consider how the phrases used to describe safety converge with those used by other relevant organisations.
-
Consider the location of data collection and timings.
-
Consider implications of type of ward.
Feeding data back theme
Feedback included that the digital feedback method would be good for people who didn’t want to make a fuss. That if particular staff create an atmosphere – this method will pick this up.
Facilitator notes
The group asked what would be done with the findings – I said that the research is to see what difference it made having real-time feedback of how safe the ward feels. The group asked if the research team would be expecting the ward staff to act on the dial if the mood was turning on a ward to improve the situation before it gets ‘stormy’.
Facilitator feedback
They also agreed that if safety information is gathered it must be responded to in a timely way.
Implications for intervention development
-
The technology and mechanism of feeding data back need to work within existing trust and ward infrastructures.
-
Explore frequency/timing of monitoring the data to ensure staff can be responsive.
-
Consider approaches to displaying the data.
-
Consider who can see the data and when.
-
Staff may need support with data interpretation and action.
Unintended consequences theme
There was some critique of the possible impact of the device on how patients felt, such as:
[I]f the dial pointed to ‘stormy’ it would affect how [patients] felt; they also reflected on the impact on patients if the dial reflected something different from how they felt.
Facilitator notes
One stakeholder said, ‘I don’t like it – it’s triggering’. Another explained, ‘I would feel less safe because of it – I remember using a mobile phone on a ward and it triggered someone’s symptoms and I got water thrown over me’ (stakeholder feedback).
Implications
-
It is important to provide choice and freedom on when to provide feedback.
-
We may need to offer different levels of providing feedback.
-
Consider how the technology sits alongside verbal information and feedback.
Logic model and programme theory
A logic model was generated to articulate how the various components of WardSonar related to each other (Figure 5). This model was informed by patient safety theory and the previous phases of research. In conjunction with the logic model, a programme theory was developed to explain how WardSonar could work in ward settings. Table 6 illustrates an iteration of the programme theory explaining how WardSonar might facilitate change in proximal and distal outcomes, leading to change in practice.
FIGURE 5.
Capturing real-time data about safety from service users on acute mental health inpatient wards to support staff in monitoring and improving the safety of the clinical environment: a logic model to demonstrate programme theory. a, e.g. gender, ethnicity, disorder, digital literacy. b, e.g. qualification, gender. c, e.g. skill mix, staffing levels.
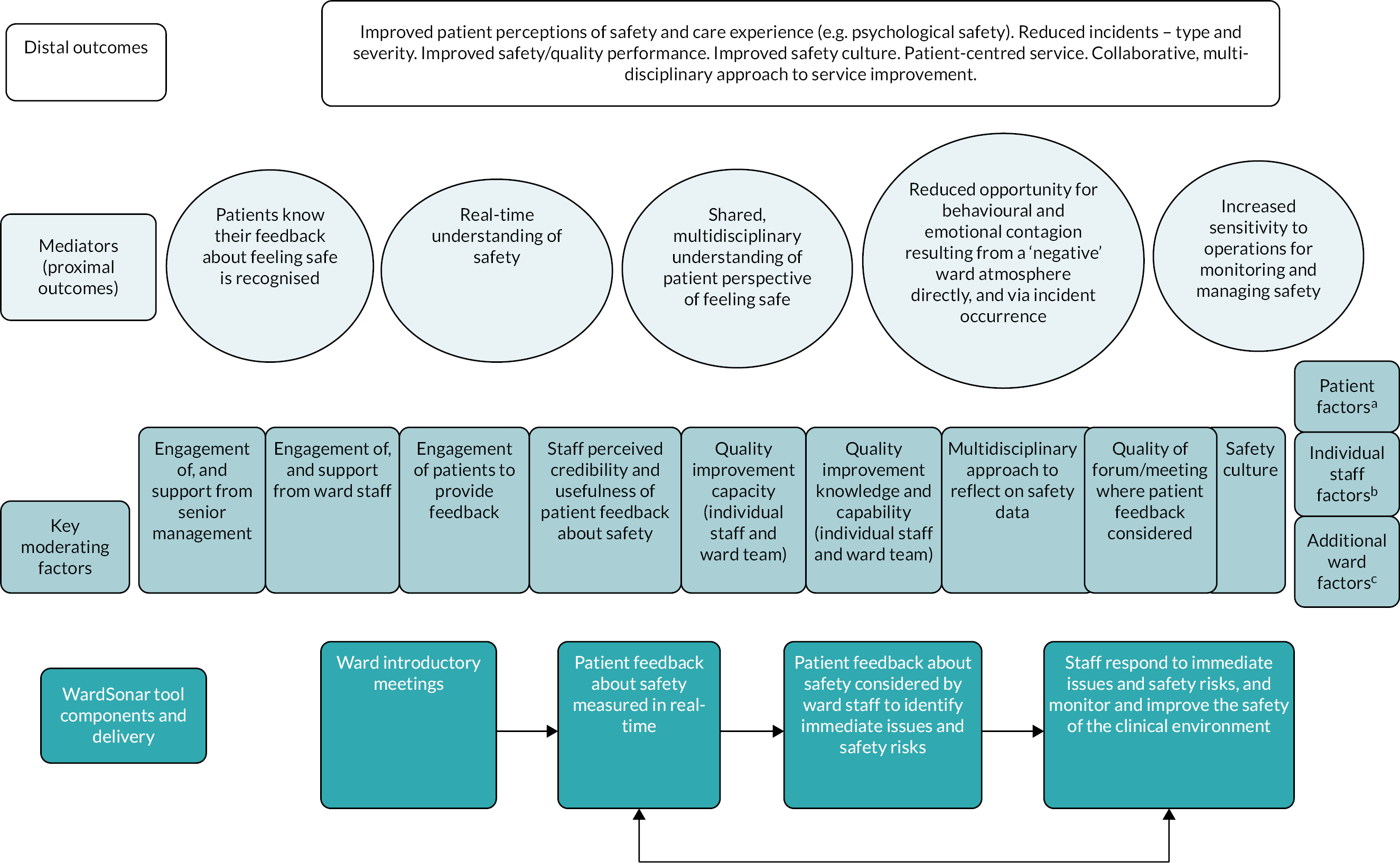
| Study component | How WardSonar could work in a ward setting |
|---|---|
| Ward introductory meetings | The implementation of the WardSonar monitoring tool includes start-up meetings/visits to wards. These meetings address the rationale for development of a monitoring tool and discuss how the tool might help maintain and/or improve the safety of the ward by recognising patients as a key source of safety information in real time. Staff will be trained in how to use the handheld devices (referred to in this report as ‘devices’) to facilitate collecting feedback from patients and on how to interpret the information available on the staff dashboard. |
Relevant moderating factors:
|
|
| Patient feedback about safety measured in real time | Staff invite patients to complete anonymous questions at multiple time points per day via the patient recording interface on the handheld device. This generates real-time information about the patient perspective of safety/ward atmosphere. The introductory information provided to patients on the handheld device emphasises the purpose of the monitoring tool and that patients are recognised as a key source of safety information. This aims to generate a more complete understanding of safety as we know patients and staff may conceptualise safety differently (physical, emotional and mental aspects of safety). Gender is also relevant here and the tool recognises differences between forensic/non-forensic contexts and all male/all female wards, as we know contagion may occur differently on male, female and mixed wards. |
Relevant moderating factors and mediators (proximal outcomes):
|
|
|
|
| Patient feedback about safety considered by ward staff to identify immediate issues and safety risks. Staff respond to immediate issues and safety risks, and monitor and improve the safety of the clinical environment | The staff dashboard displays the information collected from patients in real time. How the information is displayed emphasises the current ratings from patients, as well as how this has changed since the last round of feedback was collected (i.e. the direction and information about what is making patients feel this way) to help direct staff in deciding on when and what action/intervention to take. At any given time, this would support staff to be able to better anticipate and respond to shifts in the safety dynamic as close to real time as possible, which in turn may allow more effective management of the safety and quality of care via existing mechanisms. This facilitates ‘a collective awareness by staff of the workings of the service and their ability to be sensitive and responsive to subtle changes and disturbances’ as described in the MMSF definition of the domain sensitivity to operations which the monitoring tool was developed to sit within. We know that a negative ward atmosphere or an incident occurring can have a ‘ripple effect’, having a more real-time understanding of the feel of the ward aims to reduce the opportunity for behavioural and emotional contagion which can have a lasting effect on the ward over hours and days, as well as potential to transfer from shift to shift. Relevant moderating factors: |
|
|
|
|
| Relationship between mediators (proximal outcomes) and postulated distal outcomes | Improved patient perceptions of safety and care experience (e.g. psychological safety). Reduced incidents-type and severity. May reduce overall number of incidents; particular types of incidents; severity of incidents. Improved safety/quality performance. Improved safety culture. Patient-centred service. Collaborative multidisciplinary approach to service improvement. |
The development processes in Phase 1 resulted in the WardSonar monitoring tool, which aims to collect daily information from patients on acute mental health wards about how safe they feel on the ward in the moment, with the aim of providing real-time information for health professionals to use for monitoring and improving the safety of the clinical environment.
Digital tool design
The development process resulted in agreement that WardSonar would take the form of a digital tool with three primary interfaces. First, a patient interface to record their perspectives. Service user groups and patients on the wards preferred a combination of pictures, multiple choice questions and free text, to express their subjective view on how the ward was feeling and the direction in which things were moving (e.g. ‘getting better’ or ‘getting worse’). The second interface was a health professional dashboard with functionality to interrogate the data at different levels.
The third component was a public-facing ward interface, which was developed but ultimately not tested on the wards (unlike the patient recording interface and staff dashboard). This was partly due to doubts about the availability of screens in ward areas; additionally, there were concerns that accessing and displaying it on a tablet could compromise data security. Additionally, stakeholder discussions had presented mixed views on the possible adverse effects for patients, such as triggering,156 if they could see the ward atmosphere measure displayed in real time.
Figure 6 is a diagrammatic overview of how it was hypothesised that by tapping into the ward atmosphere from the patient perspective, real-time monitoring of perceptions of safety could prevent incidents and subsequent contagion. Contagion and milieu were considered alongside the MMSF domain ‘sensitivity to operations’,100 with the aim of understanding how perceptions of ward safety in real time might be captured. The premise was that developing a monitoring tool to understand how the ward atmosphere (i.e. the milieu) feels at any given time would support health professionals, better to anticipate and respond to changes in the safety dynamic as close to real time as possible, which in turn might allow more effective management of the safety and quality of care via existing mechanisms. Examples of existing mechanisms are staff handovers, staff meetings, or – a relatively new mechanism – ‘safety huddles’, which are brief, ward-based meetings focused on safety. 102
FIGURE 6.
Diagrammatic overview of how a real-time intervention could prevent incidents and subsequent contagion.
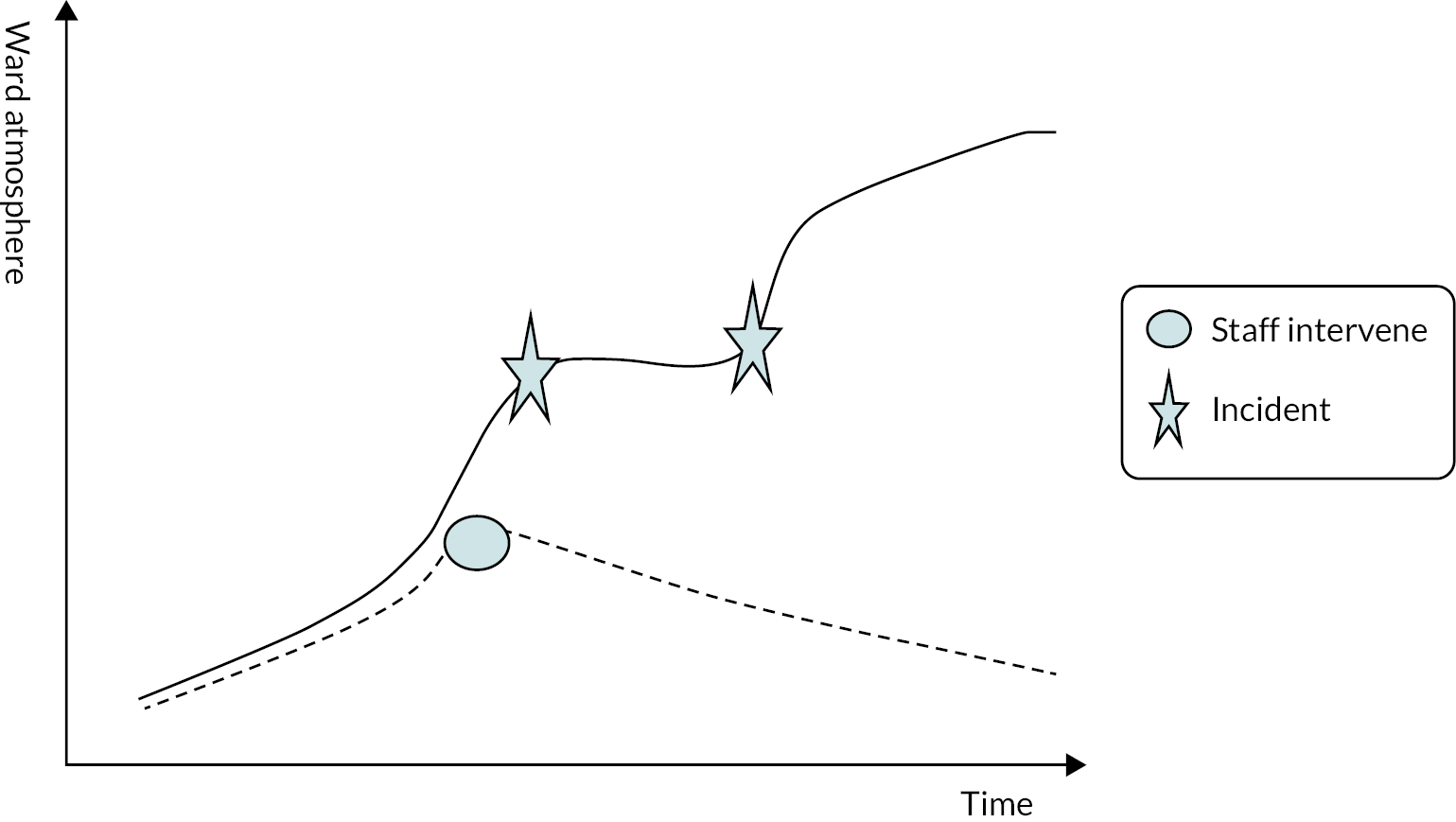
Development of a digital tool prototype
The development process resulted in a digital tool with three primary interfaces: First, a patient interface to record their perspectives. As previously discussed (see Chapter 5), stakeholders who discussed the prototypes explained that they preferred a combination of pictures, multiple choice questions and free text, to express their subjective view on how the ward was feeling and the direction in which things were moving, for example, ‘getting better’ or ‘getting worse’. The second interface was a health professional dashboard with functionality to interrogate the data. The third component was a public-facing ward interface, as discussed in Digital tool design.
Conclusion
Synthesis of data produced during Phase 1 generated an idea for a monitoring tool that could be built by technical developers, put into operation and refined in response to further feedback. Embedding the principles of WardSonar within the MMSF,100 and within the domain sensitivity to operations specifically, produced a safety monitoring tool which recognises patients as a key source of safety information and facilitates health professionals being aware of subtle changes and disturbances.
As described Discussion of findings, the synthesis brought together the findings from a scoping review, evidence scan, interviews with patients and health professionals, and stakeholder engagement, to inform a cycle of design activities. This process highlighted broad themes that were revised further within the subsequent design phase, that is the meaning of ward safety; the importance of patient anonymity; patients’ experience of the ward ‘atmosphere’ (i.e. the ward milieu); involving patients in improving ward safety; how best to feedback data once collected; and potential unintended consequences.
Chapter 7 Technical development
This chapter summarises the technical report that the technical developers, Ayup Digital, produced with regard to operationalising the ideas that came out of the design process. The full technical report is available in Appendix 2d.
Technical development of the safety monitoring tool addressed objective 1:
-
With service users and staff, co-design a digital intervention to allow real-time monitoring of safety on acute mental health wards.
Note that Aim, User stories, Key considerations, Appearance and use of the WardSonar tool, The recording interface, The staff dashboard and Ward interface contain Ayup Digital’s description of the operational processes post development, but prior to deployment, and are therefore written in the present tense.
Aim
Ayup Digital’s overall aim as technical developers is to develop a suite of digital products that facilitate the anonymous collection of real-time patient safety data and measures within acute mental health wards. All data collected should then be computed and presented to ward staff for real-time analysis and to inform their decision-making with any interventions they might make; and should be made available to research staff for detailed analysis after the end of the implementation period.
User stories
Three key user stories underpin the digital products:
As a service user, I want to easily and anonymously report how I am feeling on the ward, so that staff are aware and can take action.
As a member of staff, I want a secure and easy to use dashboard to review data submitted, so that I can get a gauge of the ward atmosphere.
As a researcher, I want to be able to see all collected data points, so that I can perform detailed analysis on how the digital products were adopted and what impact they might have had.
Key considerations
Key considerations are that the suite of digital products should:
-
Be co-designed with stakeholders to test assumptions and validate designs.
-
Have strong user experience design and be simple, easy to use and accessible.
-
Be secure and anonymous.
-
Use existing open-source technology wherever possible.
-
Be developed technology in line with NHS standards where possible (see National Health Service standards).
-
Have an ‘opt-in’ approach to usage.
-
Consider potential issues such as Wi-Fi dead-spots and technology constraints within clinical settings.
-
Collaborate with Information Governance leads to conform to Information Governance and data protection standards.
Appearance and use of the WardSonar tool
The developed ‘app’ will be loaded and accessed on a device that will be stored on the ward throughout the intervention. The tablet device will be taken around the ward by a member of staff to patients one at a time. Patients will be able to opt in or opt out of providing data. Data inputted by patients will be recorded via the app and automatically sent back in real time to the central database. If Wi-Fi is temporarily unavailable on the ward, the inputted data will be stored locally on the device in ‘offline’ mode. When the device comes back into Wi-Fi range the data will be submitted to the central database automatically.
Patient data will be monitored through a ‘staff dashboard’ which only authorised members of staff are able to access, via the tablets, a desktop or laptop computer displaying real-time patient-inputted data, charts and metrics.
Figures 7 and 8 indicate what the WardSonar tool looked like to the end user. Patients accessed screens represented in Figure 7 and staff accessed the dashboard represented in Figure 8.
FIGURE 7.
Final prototype of patient interface.
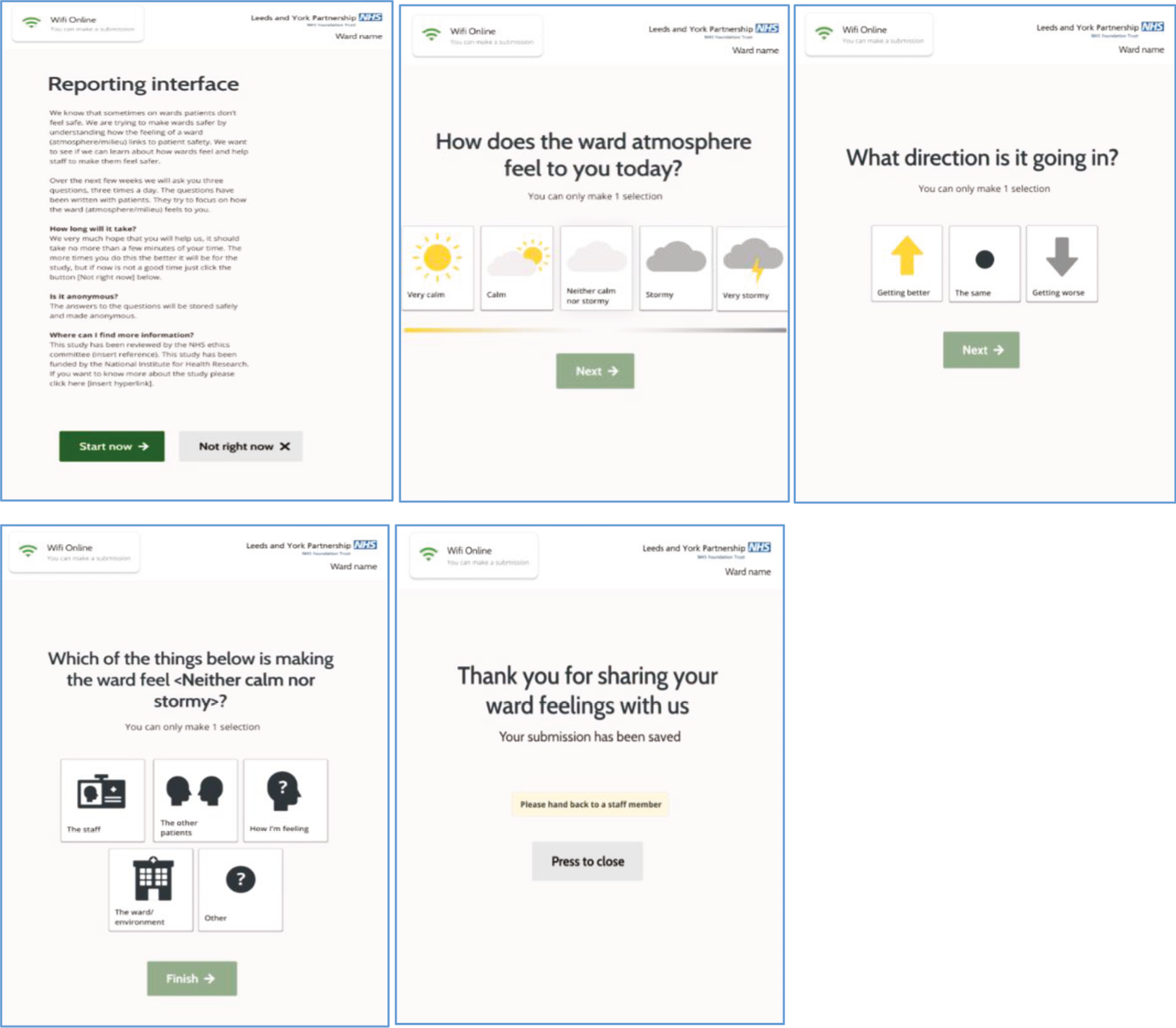
FIGURE 8.
Screenshot of a ward staff dashboard. The barometer value is the mean of values entered per time period.
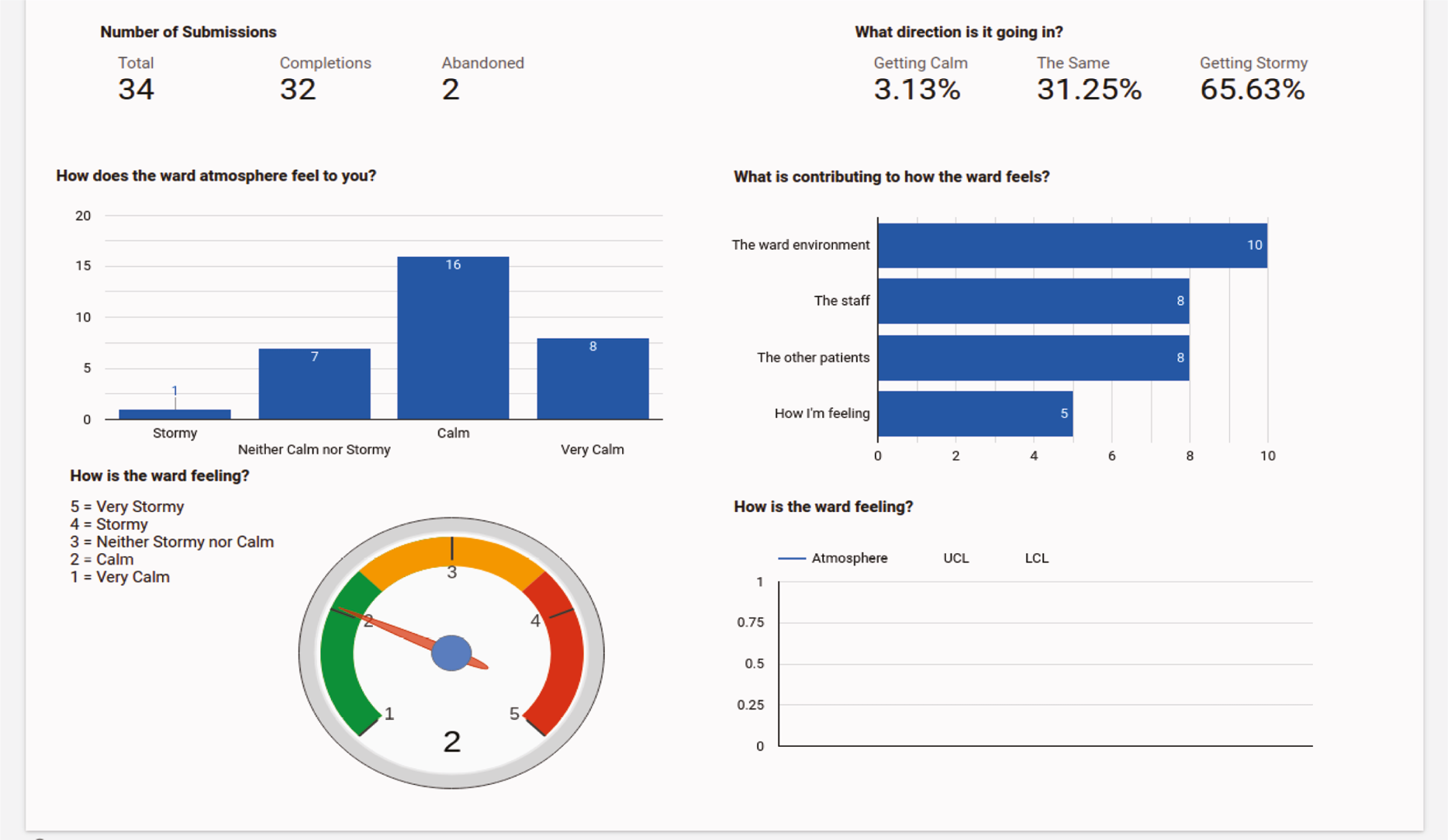
The recording interface
This facilitates the collection of patient safety data and measures within acute mental health wards. The interface is presented as an app on a device on which patients are asked to answer a few simple questions about how safe they feel on the ward. No patient data are collected, and all data collected on the interface are anonymous.
Data are recorded in real time and sent to an application programming interface for data processing. The questions that patients are asked on the interface were determined from the environmental scan findings and co-design workshops. Particular attention has been paid to the user experience, especially in understanding contextual constraints and pressures that patients may be experiencing (e.g. location when entering data, what device they will be using, what their mental state might be at the time of data entry). Similar attention to detail with respect to accessibility is also important to ensure the interface can be used by a wide range of users with varying abilities.
The interface has been built to Web Content Accessibility Guidelines (WCAG) 2.1 AA standards (to improve accessibility of web content for people with disabilities). 157 It is usable across most modern devices, platforms, operating systems and internet browsers. Patients are able to respond via a device supplied by ward staff.
Each ward has its own unique deployment of the core recording interface product. The recording interface is completely separate from other wards and accessible via a unique uniform resource locator (URL) to ensure an easy-to-use experience for patents submitting data. This approach also helps to eliminate the potential of malicious data submissions across wards.
The staff dashboard
The main interface used by staff to view data submitted by patients is the staff ‘dashboard’. It is primarily accessed in specific, authorised locations, such as the ward office, and provides real-time snapshot data and other information through the use of interactive data visualisations.
Co-design work with healthcare staff, statisticians and researchers determined the exact requirements of how data should be represented on the dashboard, including barometer-style visualisation of ‘How is the ward feeling’, through charts and graphs and the potential for a statistical process control chart to enabled tracking of ‘ward feeling’ over time. Monthly/weekly/daily/shift aggregated data are extractable and can be compared with historical time periods.
Each ward has their own staff dashboard independent of other wards, so no data can be exposed between wards. The dashboards are behind a layer of authentication and can only be accessed by authorised staff members with login credentials.
Ward interface
The ward interface presents a snapshot on the question: ‘How does the ward atmosphere feel today?’ The information is displayed in the form of a barometer and shows the average milieu rating for the current shift; specifically, the barometer value is the mean of values entered per time period.
The ward interface has been designed to be displayed on a television, desktop computer monitor or tablet device. Simple prototypes were tested with stakeholders before the final prototypes were approved. Each participating ward has two devices with the recording interface preloaded. This is taken in person to them by a project team member, who also provides documentation and guidance to help ward staff to set up the device. The staff dashboard is accessible through existing computers on each ward.
Aim, User stories, Key considerations, Appearance and use of the WardSonar tool, The recording interface, The staff dashboard and Ward interface summarise key points about the developed product from the perspective of the user. Ayup Digital’s full technical report is available in Appendix 2d. The technical report also identifies post deployment challenges which, for the purpose of narrative clarity, are included in the Discussion (see Chapter 10).
The next section addresses NHS governance and related considerations for development of digital health tools.
Technical considerations in health and care context
At this early stage of design, development and testing, in which the aim was to create a prototype digital monitoring tool, the team took an approach that prioritised and balanced the needs of users (identified through development work described in Chapters 3–6), the safety of those engaging with the tool during the implementation testing (risks and mitigations identified through steering group meetings and documented in ethical approvals), and key technical considerations relating to the use of digital tools in a health and care context.
National Health Service standards
Technical considerations were discussed early and embedded in decision-making to lay the foundations for steps that would be required, should the WardSonar suite of digital products be deployed for use within NHS settings in the future. This includes the standards that NHS commissioners and funders will require to assess the adoption of the tools, namely the digital technology assessment criteria (DTAC),158 which bring together the baseline standards that digital tools need to meet for use within the NHS.
The standards include the following key areas: clinical safety, technical assurance, data protection, interoperability, usability and accessibility. The DTAC overlaps with guidance and standards around medical devices,159 data protection regulation [UK General Data Protection Regulation (GDPR)],160 Data Protection Act 2018;161 evidence and benefits [National Institute for Health and Care Excellence Evidence Standards Framework (NICE-ESF)]162 and data security and governance (NHS Data Security and Protection Toolkit). 163
Product developers creating technology for use in health and care are encouraged to gather evidence to meet these standards from the earliest stages. The evidence required is extensive. The steps taken and information generated from this study, including co-design, technical development and evaluation data all contribute to the evidence and documentation required for future use and deployment of the WardSonar products.
Approvals
Approvals for use of the digital products in Phase 2 implementation in the current study were managed through ethical and site approval steps. They were preceded by discussions with key stakeholders from the participating NHS trusts during the co-design process, including research and development, service/ward managers, information technology (IT) and information governance. These discussions supported hardware purchasing decisions that would meet trust policies and avoid any network restrictions. They also informed key functional and non-functional requirements for the tools alongside the co-design findings, such as:
-
The requirement for the tool to be anonymous and not collect any personal information. There was a discussion around mitigating risk by not including any ‘free-text’ entry boxes within the user interface. Service users expressed a preference for a free-text option, however, so this was included.
-
The requirement for the tool to allow for data collection in all areas of the ward environment. Risk here was mitigated by ensuring the tool had an offline option to mitigate against any potential data loss within areas of the wards that had patchy or no Wi-Fi access. Wi-Fi maps were provided to inform this.
-
The requirement for data to be secure. Risk was managed by ensuring data could only be accessed by key personnel with login credentials.
Medical device classification
A medical device classification assessment was completed in June 2021, based on the features of the products that were intended to be used in Phase 2. The assessment referred to Medicines and Healthcare products Regulatory Agency guidance for software159 and concluded that the products do not classify as medical devices. Preliminary assessments against the NICE-ESF suggest that WardSonar would be classified as a tier B product. Full assessment against this framework was not completed during the study as this is not a requirement for tools used within research but would be required in the future to support deployment.
The steps taken during this study go some way to supporting the WardSonar suite of products to be ‘DTAC ready’; however, this is an ongoing process of evidence generation and documentation that will need to continue past the current study, should the product be developed further for use within NHS settings.
The changing context of National Health Service technology standards
It is relevant to note that there is an ever-changing landscape for use of technology within the NHS and the frameworks and standards that are applicable. Over the time that the current study was running, significant changes occurred that affected this landscape, including the merger of NHS Digital with NHS England. This particular change affected who is responsible and accountable for these standards and for iterations to the standards, frameworks and assessments. For example, the DTAC was previously the Digital Assessment Questionnaire, which was a self-assessment tool for product developers, but the responsibility for assessment is now held by the commissioning organisation.
Chapter 8 Qualitative evaluation
Objectives
The evaluation processes addressed the following study objectives:
-
Objective 2: explore the feasibility and acceptability of capturing real-time feedback from patients about safety.
-
Objective 3: explore how staff use this information when reported during daily handovers (or other mechanism).
-
Objective 5: explore how these data can be used longitudinally to promote safety.
Methods
Qualitative evaluation methods combined ethnographic observations on six adult acute mental health wards to understand the context for implementation and adoption of the WardSonar tool, with qualitative interviews with patients and staff to explore perspectives on WardSonar. The data were synthesised using a pen portrait analytical process and statistical analysis methods.
Access and implementation
The WardSonar monitoring tool was implemented during the first half of 2022 on six acute adult mental health inpatient wards: three in each of two NHS trusts in the north of England. The study was subject to various ward-specific delays and interruptions stemming from COVID-19 outbreaks and/or restrictions and some wards experienced more interruptions than others, but on each site a 4-week baseline period (weeks 1–4) was followed by 10 weeks of WardSonar implementation (weeks 1–10).
The study team made preparatory visits to the participating wards to explain to ward managers how WardSonar worked and the rationale behind it. Ward managers agreed that staff would attempt to take the devices around to the patients on their ward, optimally three times per day, so that they could enter real-time data regarding how they were feeling about ward safety at that moment. When they used the device, a patient would find brief, illustrated, multiple choice questions based on a weather analogy, for example, ‘How does the ward atmosphere feel to you today? Very calm; calm; neither calm nor stormy; stormy; very stormy’ (see Figure 7).
On commencement of the study, each ward manager took charge of two tablet computers (Galaxy Tab A7, Samsung, Suwon-si, South Korea). The WardSonar screens (see Figures 7 and 8) were accessed on the tablet via a web app.
Data collection
Pseudonyms are used here to protect the identity of individuals, wards and organisations.
Two health researchers (R1 and R2) with psychology backgrounds were each allocated to one of the NHS trusts to conduct ethnography-informed observations164 and qualitative interviews with staff and patients. R1 was allocated to wards Apple, Cherry and Elderflower in NHS trust 1. R2 was allocated to wards Bramble, Damson and Fir in NHS trust 2.
The implementation period was 10 weeks (weeks 1–10). It was preceded by a 4-week baseline period (weeks 1–4) that allowed for the wards to get used to the monitoring tool (Figure 9). R1 and R2 visited their respective wards during weeks 1–4 to conduct baseline interviews and observations to start to build an impression of the ward and the views of staff and patients. They subsequently visited their wards at weeks 4, 6 and 9 for further interviews and observations. At each visit, they tried to encourage ward managers and other ward staff to use the device as agreed. Additionally, they conducted post-implementation interviews with the ward managers.
FIGURE 9.
Schedule for ward-based implementation and evaluation of the WardSonar monitoring tool.
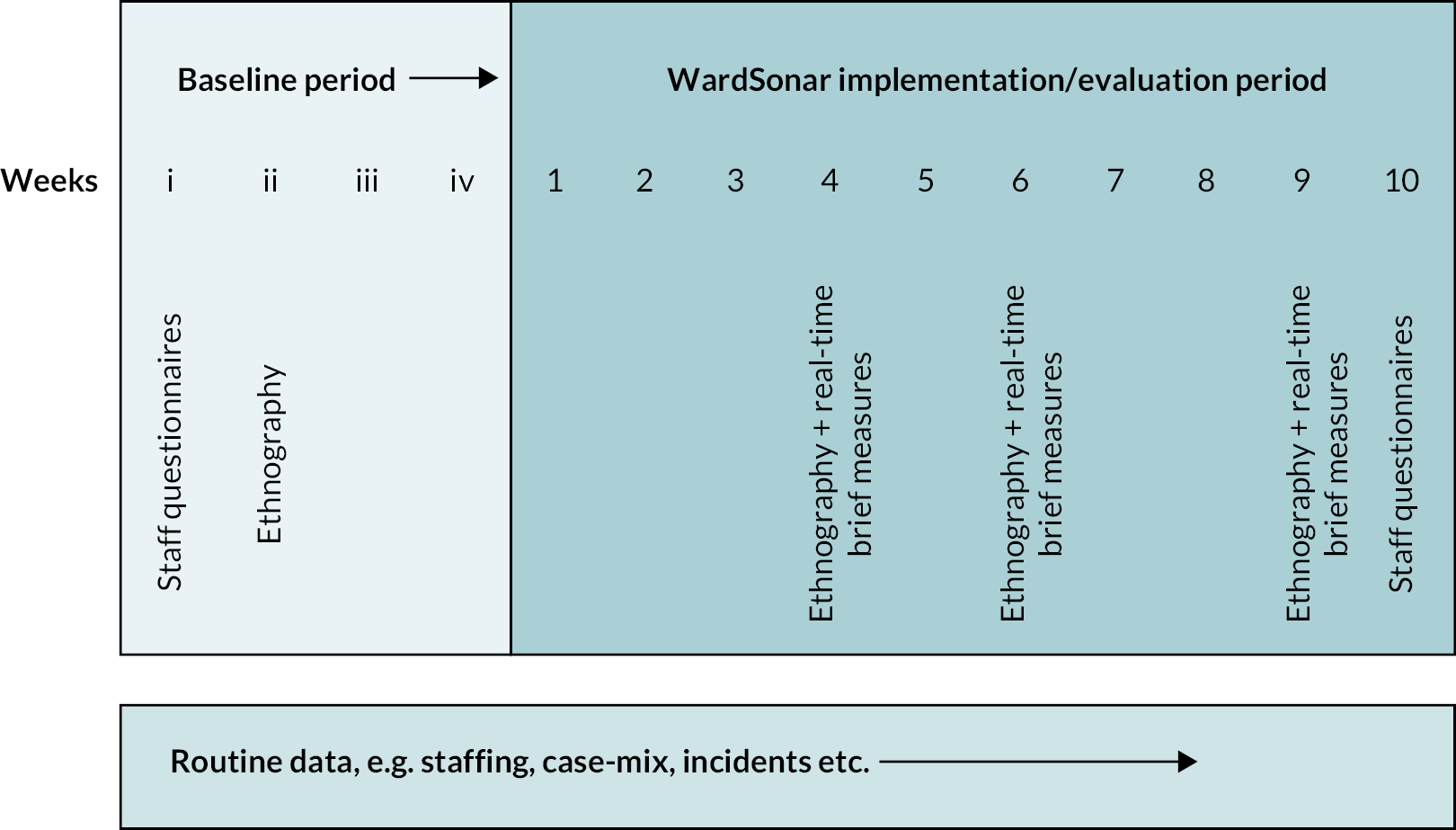
Each ethnographic observation involved being present on the ward for 4–6 hours on two occasions in that week and taking detailed fieldnotes. The aim was to develop insights into each ward’s milieu to understand the context for implementation.
The purpose of the qualitative interviews with staff and patients was to understand technology adoption and elicit perspectives on feasibility and acceptability. R1 and R2 were advised by staff on which patients they could approach to invite to participate in an interview. Staff could be approached directly to invite to participate. Interviews focused on patient or staff experience and views on using the device. The Phase 2 interview topic guide is available in Appendix 2a.
Additionally, the technology automatically recorded ‘dashboard completions’ (see Figure 8), that is occasions when a patient entered real-time data about their perspective on the ward milieu. Other categories of data were gathered and subjected to statistical analysis (see Chapter 9).
Interviews were professionally transcribed. Observations were either written or audio recorded by the observer. Audio recordings of observations were professionally transcribed to MS Word®165 documents. Each transcript and observation were allocated a unique number. Original and anonymised audio files and transcripts were stored in the (organisation detail removed for peer review) secure drive. Only anonymised files were permitted to be downloaded from the secure drive.
All transcripts were imported into a Nvivo 12+project to support data management, retain links to source data during analysis, and to facilitate within- and between-case exploration of the data.
Analysis
Each of the six wards was a study site (i.e. a case) for analysis. Qualitative data collection and analysis were concurrent. Researchers R1 and R2 met frequently with other research team members to start preliminary data interpretation while the study was ongoing. This meant that their data collection could be responsive to questions suggested by the data. The statistical data analysis and qualitative data analysis informed each other to generate a rounded interpretation of WardSonar’s feasibility and acceptability. Data were examined across and within cases.
Pen portrait analytical process
A pen portrait analytical process was used to help clarify and communicate key messages found across the observations, interviews and dashboard completions. Pen portraits are familiar tools for humanities scholars wishing to convey a sense of how different strands of data interact within the complete data set. 166,167 The use of pen portraits is consistent with key analytical strategies for qualitative data, including framework,168 constant comparisons131 and Template Analysis. 169 In health services research, however, they are still an emerging method170 for working with multidimensional data sets. 75,170–172
Sheard et al. (2019)170 argued that the study of change has often focused on individual patients over time, and they recommend considering a broader data set. They identified a need for broad guidelines that researchers can draw on for the synthesis and reporting of multidimensional data, suggesting that this could replace study-specific bespoke methods, while enhancing methodological rigour via a consistent and theoretically sound approach. 173 The pen portraits in Sheard et al. (2019)170 broadly consist of tabulated summaries of fieldnotes, taped discussions, follow-up interviews and comments on how the ward engaged with the study, but the structure is adapted to differences between ward data sets. Louch et al. 75 used a more narrative style with commentary and quotations.
The guidance offered in Sheard et al. (2019)170 is a four-stage application of pen portraits to analysis of longitudinal data from qualitative health research:
-
Understand and define what to focus on.
-
Design a basic structure relevant to the data set in question.
-
Populate the content.
-
Interpret the data. 170 (p. 5)
Each of the two pen portrait exemplars in Sheard et al. (2019)170 is a one- or two-page, tabulated, chronological account of what happened and what it means. There is no rigid formula, and the exemplars illustrate how the proposed guidelines can be used to suit the particular data set. This flexible approach was applied to the analysis of qualitative data in the current study.
Findings
Data set
Of the six acute adult mental health inpatient wards, two were psychiatric intensive care units (PICUs); two were all female, one was all male, two were mixed (partly as a response to COVID-19) and one changed from mixed to all male during the study. The number of beds per ward ranged from 12 to 21. The impact of COVID-19 meant that some of these wards were underoccupied at times, so the number of beds did not always reflect the number of patients. To protect the identity of the trusts, wards and individual participants, some detail has been aggregated and names have been removed or changed.
Table 7 summarises the data set used for qualitative evaluation. R1 and R2 conducted 39 observations and 67 interviews. Each observation was for a minimum of 3 hours; total observation was 145.45 hours. Interview duration depended on each interviewee’s (patient or staff) preference and availability. Staff interviews ranged from 4 to 12 minutes (mean 8.3 minutes). Patient interviews ranged from 5 to 15 minutes (mean 7.8 minutes). Mean interview duration was 8.3 minutes (staff) and 7.8 minutes (patients). In total, 602 dashboard completions were recorded.
| Hospital ward | Apple | Bramble | Cherry | Damson | Elderflower | Fir | All |
|---|---|---|---|---|---|---|---|
| NHS Trust | 1 | 2 | 1 | 2 | 1 | 2 | |
| Ward profile | Acute F | Acute M | PICU M + F | PICU M + F | Acutea | Acute F | |
| Data source | Total | ||||||
| Observations | 8 | 5 | 8 | 5 | 8 | 5 | 39 |
| Staff interviews | 5 | 5 | 7 | 6 | 5 | 5 | 33 |
| Patient interviews | 5 | 3 | 7 | 3 | 9 | 7 | 34 |
| All interviews | 10 | 8 | 14 | 9 | 14 | 12 | 67 |
| Dashboard completions (n) | |||||||
| Week 1 | 11 | 12 | 65 | 18 | 8 | 9 | 123 |
| 2 | 13 | 2 | 47 | 3 | 0 | 20 | 85 |
| 3 | 13 | 11 | 25 | 26 | 13 | 23 | 111 |
| 4 | 5 | 3 | 24 | 27 | 6 | 27 | 92 |
| 5 | 10 | 0 | 8 | 10 | 12 | 0 | 40 |
| 6 | 0 | 5 | 8 | 5 | 0 | 0 | 18 |
| 7 | 15 | 0 | 15 | 5 | 0 | 0 | 35 |
| 8 | 0 | 7 | 14 | 6 | 17 | 0 | 44 |
| 9 | 0 | 0 | 7 | 0 | 2 | 1 | 10 |
| 10 | 0 | 5 | 3 | 5 | 0 | 31 | 44 |
| N/A | 0 | 0 | 1 | 0 | 0 | 10 | 11 |
| Total (excl. N/A) | 67 | 45 | 216 | 105 | 58 | 111 | 602 |
Pen portraits
Six pen portraits, one per ward, were constructed from these data. Several possible pen portrait structures were considered. The research team experimented with focus, length and level of detail,75,170 before finally agreeing on the format presented below. A high proportion of quotations was included to highlight the richness of the data. 174 The approach was underpinned by well-established principles for analysis of qualitative data, in which, for example, the researcher differentiates between semantic content and latent meaning. 175
The pen portrait for Elderflower ward is presented in Timeline below, as an exemplar. All six pen portraits are available in Appendix 4.
Elderflower ward pen portrait (exemplar)
Emotional contagion was most obvious on this ward, usually due to service users regularly congregating in groups outside the staff room to ask for an e-cigarette refill. Half the service users sat in communal areas and the other half stayed in their rooms. Service users on this ward sometimes argued and, on several occasions, physical fights needed to be deescalated. I would describe the atmosphere on this ward as tense. Staff were very busy but were visible most of the time.
R1 reflection
Timeline
At baseline, R1 noted that the ward felt clean and cheerful with friendly and helpful staff and patients who approached her, assuming she was staff herself.
-
In week 4, the ward had changed from mixed to all male and was notably busy. R1 noted that the use of the device was not 5 into ward routines:
I can see the devices are on the table and I say, oh, [staff name], I’ll just show you how to use them, but they’re both out of battery … Staff were a bit reluctant today to have an interview. It felt like they have their hands full.
R1 fieldnotes, week 4
However, in interview, a member of staff was clearly supportive of using the device, saying that it was facilitating useful conversations.
I think with the ward going through quite a hostile period before this time … [patients] were keen to give that feedback.
Staff interview, week 4
-
In week 6, the ward atmosphere was volatile at times. Staffing levels were low:
The nurse in charge said that there are only five members of staff on the ward today, and there are meant to be double this.
R1 fieldnotes, week 6
Some staff were trying hard to collect data, although most were unfamiliar with the dashboard. There were mixed views about using the device. Some staff told R1 that patients saw it as pointless and rolled their eyes when asked to complete it repeatedly, but others said it was useful to have patient views and the device prompted conversation:
Actually, it did prompt conversation because one or two people were really unhappy on the ward. So, I was like, why have you put that score kind of thing and then they would answer, if they were annoyed at someone or annoyed at the staff.
Staff interview, week 6
A comment from one staff member raised the question of whether a light-hearted reaction from staff could influence patients’ reports of the ward atmosphere (e.g. by seeming to not take it seriously, or alternatively, by making it easier to report staff tensions by introducing levity):
It was good to see how they were feeling, well to see how they felt the ward was … a lot of them said staff [were causing tensions], so I would just have a bit of a laugh and a bit of a joke, so it prompted conversation.
Staff interview, week 6
Technical issue that arose included, on one visit, R1 saw that the battery was flat in one device, and a software update needed in the other.
-
In week 9, R1 noted several new patients. The ward was busy and R1 had difficulty engaging with the ward manager. R1 noted that the dashboard was not working properly. However, a student nurse told R1 that she had been taking the device round to the patients:
She said some patients don’t want to use it, some do, and that it is very straightforward to use.
R1 fieldnotes, week 9
A patient explained their view on using digital technology, suggesting that they would not easily use the device without help.
I’m not very tech savvy. I’m more still in analogue rather than digital. So I struggle quite a lot with my dyslexia … I can use a mobile phone just about, and my device I can use just about, if I’m signed in. Sometimes I have to get people to sign me in … I find it a bit confusing, ’cause like … I’m like 50. I’m not like you young ones who can text like 90 miles an hour.
Patient interview, week 9
-
At the end of the implementation period, the ward manager emphasised that a main issue with implementation was reminding and motivating staff to use the device. They explained how general busyness had affected adoption of the technology.
When we started the study, it was very busy, we were very short staffed … the ward being shut and COVID-19 isolation, and the routine of the ward was very different. Whereas as we’re finishing it, we’re actually starting to come into a time where the ward is a bit more of a normal routine and structure.
Ward manager, post-implementation interview
Acceptability and feasibility
The ward manager also reflected that they had intended to use the device data in safety huddles,102 but:
We still haven’t started the safety huddles again, so through other circumstances on the ward, we didn’t end up being able to bring it but I think, going back to wards where I’ve previously worked where they did use the safety huddles regularly, I think it would have been really helpful to bring into that.
Ward manager, post-implementation interview
When asked about using the dashboard data, the ward manager recalled:
I know I showed quite a few [staff] the staff dashboard, I don’t know how many people checked it regularly but they did find it interesting when I pointed it out to them … [and] a lot of the patients really valued being asked about their thoughts on things.
Ward manager, post-implementation interview
The ward manager had a generally positive view of the study. Even just taking the device round the ward to patients helped staff to think about patient perspectives:
We had some quite interesting discussions about improving services and I suppose it led to a lot more conversations about patients being involved and that sort of thing, which was really good.
Ward manager, post-implementation interview
The user interface was seen to be inclusive.
[The questions] were good because they were simple … if the questions had been a bit more complicated, we probably wouldn’t have approached certain people because they wouldn’t have been in the mindset to engage with it.
Ward manager, post-implementation interview
R1 observed that patients were happy to answer questions using the device but much less inclined to leave additional feedback (as open text comments). It seemed to be valued by patients and staff:
I think with the ward going through quite a hostile period before this time … [patients] were keen to give that feedback.
Staff interview, week 4
Suggestions for further development
Staff suggested that real-time data could be helpful to plan where staff should be, such as more of them in communal area if patients report feeling unsettled.
The comment below represents a commonly expressed view from staff and patients that collection of patients’ views could be both unfeasible and unacceptable if too frequent.
Like if they are nagging [for] the information, or just [sometimes] I guess don’t feel comfortable because it’s too often.
Patient interview, week 9
Focused ethnography
Overview
The focused ethnography made a valuable contribution to understanding the context for adoption of the technology. For example, R1 and R2 learnt that staff were involved in helping patients to enter their data and were using the moment to engage with patients. Patients who said they might need help from staff to use the device did not seem to be deterred by the absence of privacy when staff entered data on their behalf or asked them about what they had written. Additionally, staff on two of the wards (Damson and Cherry) were using the device to enter their own data. R2 reported being told by staff that,
Patients on PICU wards don’t always fill out the device, they decline to do most things anyway, so to do this was a big ask. She also said how staff had been completing the questions instead. I did say that it’s just for patients.
R2 fieldnotes, Damson ward, week 6
In an interview with R1, a member of staff remarked that they had:
Basically showed patients [what to do with the device] and used it myself to try to see what it was like.
Staff interview, Cherry ward, week 9
Therefore, the observations revealed and explained some issues around the representativeness of the patient data.
The observations also provided insights into the impact of COVID-19 on the implementation process. For example, the number of staff interviews was fairly even across wards. Not all wards were at full capacity the whole time, and sometimes wards received admissions in quick succession, which would suggest a high proportion of individuals who were unwell and potentially not available to enter data on the device or be interviewed. Access to the wards was affected by ward closures and restrictions consequent to COVID-19 outbreaks, in addition to the everyday complexities of ward life, so it is unclear whether the wards’ perceived engagement and fidelity to the study protocol (or otherwise) was reflected in reality.
It was noted that patients appreciated being given a shopping voucher as a thank you for participating in an interview and understood that patients told each other about this and it acted as an incentive to agree to be interviewed. Generally, patients did not raise any concerns about confidentiality, although two patients did tell the interviewers that this was their reason for not engaging with study.
R1 and R2, who conducted the observations, were different from other people in the settings in the sense that they were not there to provide or receive care. They noted phenomena that might have been unremarkable to seasoned mental health clinicians, such as restless and bored patients, patients asleep during the day or patients not wearing shoes; expressed unease when realising that there was only one qualified nurse present during a shift; recorded a sense of ‘enough’ or ‘not enough’ staff; felt agitated if nurses were not visibly responding to alarms or else were ‘rushing around’; and reflected on seeing that qualified staff stayed in the nursing office while support workers were out on the wards. Arguably, all these factors in the milieu were everyday occurrences and unremarkable to ward staff. They did seem to become less noteworthy to the researchers over the course of the study.
The researchers reported that a tense ward atmosphere or hostile staff created a barrier to promoting use of the WardSonar tool. Another frustration was that one of the two researchers (R2) was required to wear hospital scrubs, which she found caused some staff or patients to assume they were a member of staff. However, regardless of scrubs, the neutral position of researchers as observers in the field meant that they were not able to take action if anyone asked for help. This could leave them feeling frustrated, especially if patients were trying to attract attention of staff.
From these researchers’ perspectives, engagement with the study differed across the wards; positive engagement when staff and patients were actively supporting the study contrasted with occasions where staff were perceived as uninterested or even hostile.
I feel [nursing staff] on this particular ward to be very rude and dismissive and will only speak to me if the ward manager asks them to [but] healthcare support workers [are] more friendly.
R2 fieldnotes, Fir ward
Access to the device
Access to the devices was subject to technical and practical problems including uncharged devices, missing devices, software updates required, poor Wi-Fi connections to the patient Wi-Fi and absence of visible dashboard data. The latter issue was a problem for researchers attempting to demonstrate to staff how they might benefit from using the tool.
I can see the devices are on the table and I say, oh, [staff name], I’ll just show you how to use them, but they’re both out of battery.
R1 fieldnotes, Elderflower ward
Concerns about protecting the study hardware meant that the devices were liable to be locked away, meaning less opportunity for data collection.
Additionally, COVID-19 outbreaks, periods of busyness and malfunctioning equipment seemed to be deterrents to taking the device round the patients. Patients frequently acknowledged how busy and overworked the staff were and understood this to be one of the reasons why they might not get to use the device. Ward managers seemed to agree that unless the device use was embedded into routines, staff would be unlikely to remember to take it round the patients. Figure 10 summarises challenges affecting opportunities for patients on the wards to enter real-time data on the WardSonar device.
FIGURE 10.
Challenges to collecting real-time safety data from patients.
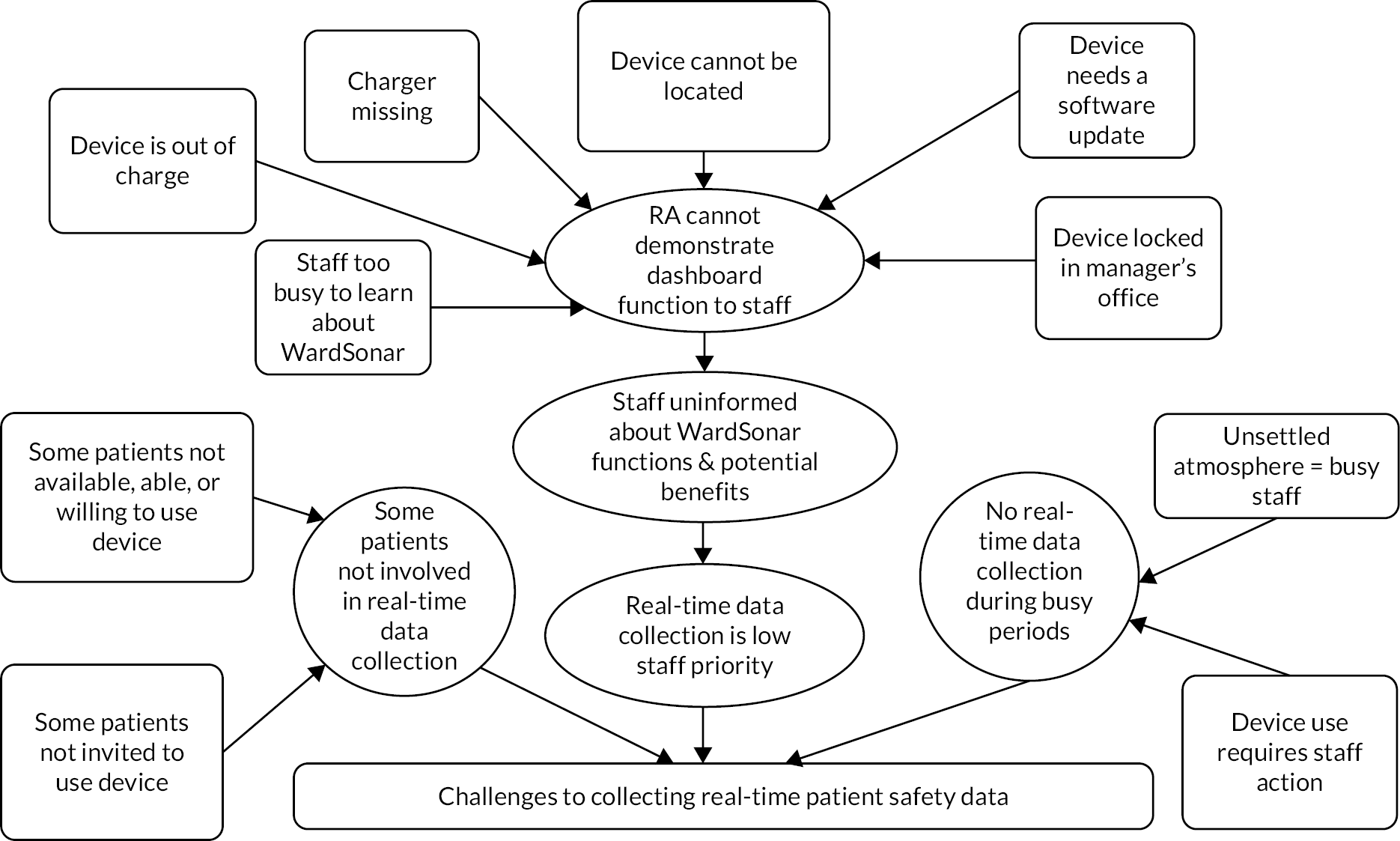
Neither patients nor staff saw with data collection three times daily as feasible, and some did not see it as necessary. One member of staff said that low patient numbers meant each patient was approached too often with the device and lost interest in it; generally, however, staff cited the busyness of the ward as a barrier.
Information dissemination
Staff response to the WardSonar study was mixed. Some staff did not know about the tool or the project; most did not know about the dashboard data and/or did not look at it, and the dashboard data was not used to inform safety strategies. Despite not being used as intended, the dashboard data was perceived as useful by staff who knew about it.
R2: Have you been able to use [the dashboard data] in any meetings or any handovers?
Ward manager: I haven’t so far … I don’t know a lot about it to be honest.
Staff, Damson ward
Ward managers reflected on the study in post-intervention interviews. Dissemination to all staff was reported as difficult, so not all staff were properly informed about the study. Without understanding the study, they were unmotivated, so they never saw it as a priority task. One ward manager was sceptical about value of WardSonar tool except to help with engaging patients (i.e. by prompting conversation between staff and patients). Alternative viewpoints were that lack of routine and habit was a difficulty, or the specifics of a ward may have affected engagement; for example, patients were not interested and it was not a priority for most staff.
Differences between patient and staff perspectives
The data from the focused ethnography and interviews highlighted some differences between patient and staff perspectives. Patients and staff approved of the design features and, despite some staff’s reservations, patients were able to understand the phrasing and work with the weather analogy.
I felt it was like a way to let people know how I was feeling. And it was, like, an easy way.
Patient, Apple ward
Compared with patients, staff seemed less likely to believe that WardSonar would add to their understanding about how the patients were feeling on the ward.
Patients and staff explained that patients’ interest in using the device was likely to fluctuate and that people who were unwell were unlikely to engage with WardSonar; however, patients appeared to like the device despite staff reports that they did not want to use it.
In interviews, patients suggested that some staff created tensions when they come on shift, but there was some evidence that staff did not accept this perspective. R1 made the following note:
A patient keeps asking, who is on tomorrow? And when the nurse names the member of staff who will be working on the following day, the patient says, oh, I don’t like [Name], and refers to them as Rottweiler. The nurse just says that all staff members are nice, and then the service user says, no, they are not.
R1 fieldnotes
Similarly, when a member of staff described their experience of bringing the device round the patients and encouraging them to record their feelings on it, they said that talking about using the device prompted further conversation, a point made by other staff.
They wrote a lot of daft stuff, but some of them did write how they were feeling.
Staff, Damson ward
This suggests a possibility that staff did not believe that patients described their views accurately, which may potentially question the validity of any rapport between them. It appears that staff were often privy to what patients wrote, often because they were helping or encouraging them to write something, so it seems possible that staff response could influence a patient’s motivation to share their views via the device. For example, if a patient perceives staff to be dismissive of patient data, they may feel they do not want to share their views.
Alternatively, the staff may take the data very seriously, which could be an incentive to share, or equally, a deterrent, if the patient was relying on anonymity:
I was shocked when one of the patients put in that it is stormy, when I asked what is happening, he couldn’t tell me. If he could tell me I could have given him one to one [i.e. a private conversation]. But today we are short staffed.
Staff, Cherry ward
The above quotation also highlights how staffing issues can directly affect staff–patient communications.
Do staff know how patients feel?
The issue of taking the device round three times per day was frequently discussed. All interviewees, both staff and patients, said that this was too much; either it irritated patients or staff could not facilitate it. However, patients did say that they valued being asked for their views and some said they would tolerate the inconvenience of frequent data collection.
Patients liked the purpose of the tool and they suggested that staff may not be aware of their views. They saw the point of the dashboard data to help staff to make timely safety interventions.
If it was ‘very stormy’, the staff might come out and talk to the patients and see what was happening, and why they are feeling that way.
Patient, Fir ward
There were inconsistencies between staff and patient perspectives on whether staff understood how patients were feeling. Some staff said that they did not need any help with this. This was especially true on the psychiatric ICUs.
[Staff] don’t obviously see the utility in [WardSonar], given they feel that they are used to or already privy to whether people feel safe or not on the ward.
Ward manager, Cherry ward
Some patients told interviewers they felt differently about this.
RA: Did you like being asked about how you felt the ward was feeling at the time?
Patient: Yeah. ‘Cause they don’t really ask much.
Apple ward
Engagement
Ward engagement fluctuated during the study. Fewer observations were possible in NHS trust 2 than trust 1.
Patients were fairly consistent in grasping the purpose of the tool, including the dashboard. They said they liked to be approached by staff to be asked how they were feeling and to have their views recorded and taken seriously. They liked the user interface and, in contrast with comments from some staff, did not find it confusing. Some staff were openly unenthusiastic about taking the device round and it was seen as just a task to be got through like any other. As on other wards, no staff member would take the device round unless specifically instructed. Staff were wary that repeatedly asking patients to use the device might harm therapeutic alliances. One ward manager explained that the ward was dealing with a group of new admissions, affecting staff availability for WardSonar. All ward managers highlighted efforts they had made to support the study, despite the difficult contexts they were working in.
What’s really hard is getting staff motivated to do it, especially with the acuity and [COVID-19] and everything else … it’s like you’ve got to force them … Sometimes it didn’t get used at all, we tried to put names in the diary to do it but it is difficult.
Ward manager, Bramble ward
Although staff were not accessing the dashboard data, it would appear they were aware of what patients inputted, perhaps through helping patients.
Staff could volunteer to be interviewed, whereas the study protocol required staff to indicate potential patients to interview. Therefore, interviewing either staff or patients depended on the availability and motivation of staff.
An example of the advantage of concurrent data collection and analysis is that by week 6 of the implementation period, it was evident that dashboard completions had dropped off. This was potentially an acceptability issue, if the cause was lack of engagement by either staff or patients; or alternatively a potential low feasibility issue, if the cause was a technical or structural problem. As can be seen from the pen portraits, it was possible to explore both possibilities in interviews and observations. The ward manager interviews tended to be reflective, offering explanations for much of what was recorded in fieldnotes.
Fidelity
The occasions (reported in Overview) when R1 and R2 reported that staff were apparently entering their own perceptions of safety into the device, introduced some uncertainty about whether the data reflected patient perspectives.
The way that the device was used on the wards meant that data collection tended to be clustered into certain times of day. Data did not seem to be collected when staff were busy, especially if they were dealing with tense or difficult situations, but more typically during typically the quiet periods when patients were present in communal areas. Staff and patients both pointed out that a patient’s mood could change quickly; therefore, the fact that the real-time data may reflect only snapshots of calm periods and a limited range of time during the day, limits the story the data can tell.
The context was generally one of staff promoting the project, helping patients to enter data, and acknowledging patients’ feelings; however, it compromised confidentiality (although data were anonymised once entered).The observational and interview data suggested that staff reacted to what patients wrote as they wrote it, so may have influenced what patients chose to write; for example, a patient may not wish to record data implicating staff in ward tensions or, alternatively, may feel better because staff approached them to talk about their feelings.
Conclusion
The qualitative work addressed objectives 2, 3 and 5. Implementation and technology adoption were successful in terms of gaining support from many patients and staff. Both alone and when considered together with the statistical results described in the following chapter, these qualitative findings provide valuable insights that can inform future iterations, implementation and testing of the monitoring tool. The implementation period of 10 weeks limited opportunities for longitudinal data collection and therefore objective 5 was only partly met.
Chapter 9 Phase 2: quantitative evaluation of WardSonar
Objective
The quantitative evaluation (pre- and post-implementation analyses and real-time analyses) addressed:
-
Objective 2: explore the feasibility and acceptability of capturing real-time feedback from patients about safety.
-
Objective 4: explore how the resulting data are related to quality and safety metrics.
The related research questions were:
-
Does collecting data from patients and feeding it back to staff in real-time improve the safety of the ward?
-
Is it feasible and acceptable to capture real-time feedback from patients about safety?
-
Do data collected from patients accurately reflect the safety of the ward?
Introduction
The focus of the quantitative evaluation was to examine whether incidents can affect atmosphere beyond the duration of the incident and whether responses are more likely when the atmosphere is different from usual, that is whether the volume of WardSonar responses are as indicative of ward atmosphere as the readings themselves.
The WardSonar monitoring tool was implemented on each of the six wards after a 4-week baseline/pre-implementation period (hereafter referred to weeks 1–4). The tool was then made available and used on the wards for 10-week implementation period (hereafter referred to weeks 1–10) (see Figure 9). The focus of much of the analysis is on these 10-week periods. Overall, this study ran from January to May 2022, with staggered start dates for each ward.
Pre- and post-implementation analyses: staff questionnaires
Research question:
-
Does collecting data from patients and feeding it back to staff in real-time improve the safety of the ward?
Data sources
This part of the quantitative evaluation used a pre- and post-implementation design, focusing on staff perceptions of safety culture and ward atmosphere. Measurements were taken at baseline (week 1) and at the end of the implementation period. Staff across the six wards were invited to complete a paper questionnaire on these two occasions. The staff questionnaire is available in Appendix 2b.
Staff perceptions of ward atmosphere were measured using the EssenCES scale. 176 This measure has three subscales: patients’ cohesion, experienced safety and therapeutic hold. Respondents indicate the extent to which they agree with 15 statements on a 5-point Likert scale from 1 = not at all to 5 = very much.
Staff perceptions of safety culture were measured using the Agency for Healthcare Research and Quality (AHRQ) Hospital Survey on Patient Safety Culture (HSOPSC). 177 Despite recognised issues surrounding the assessment of safety culture,178 the AHRQ HSOPSC is a suggested tool for evaluating the cultural impact of patient safety initiatives and interventions. 177 This survey includes 10 composite measures and two additional measures – number of events reported and patient safety rating. the composite measures include teamwork, staffing and work pace, organisational learning – continuous improvement, response to error, supervisor, manager or clinical leader support for patient safety, communication about error, communication openness, reporting patient safety events, hospital management support for patient safety, handoffs and information exchange. Respondents indicate the extent to which they agree with statements on a 5-point Likert scale from 1 = strongly disagree to 5 = strongly agree. The single item ‘number of events reported’ asks respondents to indicate the number of patient safety events they have reported in the last 12 months, and the single item ‘patient safety rating’ asks respondents to provide an overall patient safety rating from ‘excellent’ to ‘poor’.
Data preparation and statistical analyses
EssenCES
Prior to calculating the subscale scores, the appropriate questionnaire items were reverse scored. To compute each subscale score, the corresponding items for each respondent were summed. Where a response was missing to a questionnaire item, the corresponding subscale score was not calculated for that respondent and was recorded as missing. The patient cohesion and experienced safety subscale scores were approximately normally distributed, so mean average scores were calculated pre- and post-implementation. Change over time (pre vs. post-implementation) in the mean subscale scores was assessed using a Welch two sample t-test and p-values were considered at the 0.05 significance level. This test was appropriate as different respondents completed the questionnaires pre- and post-implementation with different sample sizes at each time point. For one ward (Apple), no post-implementation questionnaires were completed. The therapeutic hold subscale scores were negatively skewed, so the median average score was calculated pre- and post-implementation and change over time was assessed using a Wilcoxon rank-sum test, with p-values considered at the 0.05 significance level.
Agency for Healthcare Research and Quality Hospital Survey on Patient Safety Culture
Average per cent positive scores were calculated for each item of the AHRQ HSOPSC. For positively worded items, the per cent positive was the percentage of respondents who answered strongly agree (5) or agree (4), or always (5) or most of the time (4). For negatively worded items, it was the percentage of respondents who answered strongly disagree (1) or disagree (2), or never (1) or rarely (2). For each of the 10 composite measures, the average per cent positive was computed as the total number of positive responses to all questions in the corresponding measure, divided by the total number of valid responses to all questions in that measure. Average percentage positive scores were calculated by composite measure pre and post WardSonar implementation. Change over time (pre vs. post-implementation) was assessed by a test of proportions and a Bonferroni-corrected p-value of 0.005 was used as the significance threshold, to account for multiple testing.
The two additional AHRQ HSOPSC items – number of events reported and patient safety rating – were analysed as categorical data. Counts and percentages are reported, and a Fisher’s exact test was used to assess change over time (pre vs. post-implementation). This was considered the most appropriate test, given the data type and sample size anticipated.
Results
A total of 124 questionnaires were completed by staff from across the six wards. Invalidated questionnaires were removed, leaving 119 questionnaire responses for analysis. Table 8 shows the number of valid questionnaire responses, split by ward and pre/post WardSonar implementation. There were 84 questionnaires completed pre implementation and 35 questionnaires completed post-implementation across the six wards. The number of responses varied by ward with the most responses on Cherry ward (n = 29) and the fewest responses on Apple ward (n = 12). Given the small sample size, analyses were not conducted at the individual ward level.
| Ward | Pre | Post | Total |
|---|---|---|---|
| Apple | 12 | 0 | 12 |
| Bramble | 14 | 6 | 20 |
| Cherry | 22 | 7 | 29 |
| Damson | 9 | 5 | 14 |
| Elderflower | 15 | 8 | 23 |
| Fir | 12 | 9 | 21 |
| Total | 84 | 35 | 119 |
Table 9 shows the mean average scores for each of the three EssenCES subscales, pre and post WardSonar implementation. The EssenCES patient cohesion and experienced safety scores were approximately normally distributed; however, the therapeutic hold score had a skewed distribution. There was a slight increase in the average scores of each subscale post-implementation, compared with pre implementation, but this difference was not statistically significant for any of the subscales.
| Pre | Post | ||
|---|---|---|---|
| n = 84 | n = 35 | p-value | |
| EssenCES subscale | |||
| Patients’ cohesion | 9.27 (3.34)a | 9.97 (4.10)a | 0.39b |
| Missing | 3 | 2 | |
| Experienced safety | 10.00 (3.89)a | 10.12 (3.51)a | 0.88b |
| Missing | 6 | 1 | |
| Therapeutic hold | 17 (3.75)c | 17.5 (3.5)c | 0.13d |
| Missing | 6 | 1 |
Table 10 shows the average percentage of positive responses pre and post WardSonar implementation for each of the 10 AHRQ HSOPC composite measures. The measures with the highest per cent positive responses pre-implementation were: reporting patient safety events (74%), communication openness (74%), teamwork (73%), communication about error (73%) and supervisor, manager or clinical leader support for patient safety (73%). The measure with the fewest per cent positive responses was staffing and work pace, for which only 32% of responses were positive. There was an increase in the average percentage positive responses for 5 of the 10 composite measures, but none of these differences were statistically significant at the 0.005 significance level.
| Composite measure | Pre % | Post % | Differencea % | p-value |
|---|---|---|---|---|
| Teamwork | 73.09 | 70.87 | −2.22 | 0.6717 |
| Staffing and work pace | 32.22 | 32.86 | 0.64 | 0.8925 |
| Organisational learning – continuous improvement | 67.35 | 59.80 | −7.54 | 0.1792 |
| Response to error | 59.13 | 55.40 | −3.74 | 0.4554 |
| Supervisor, manager or clinical leader support for patient safety | 72.65 | 71.15 | −1.50 | 0.7749 |
| Communication about error | 72.84 | 79.81 | 6.97 | 0.1701 |
| Communication openness | 73.75 | 83.58 | 9.83 | 0.0239 |
| Reporting patient safety events | 74.21 | 75.00 | 0.79 | 0.901 |
| Hospital management support for patient safety | 64.29 | 56.19 | −8.10 | 0.1512 |
| Handoffs and information exchange | 66.53 | 68.57 | 2.04 | 0.7092 |
Table 11 shows the responses for the items number of events reported and patient safety rating pre and post WardSonar implementation. For number of events reported, pre implementation, the most common response was either no events reported (29%) or 1 or 2 events reported (25%). post-implementation, the most common response was 11 or more events (28%), which was an increase from 18% pre implementation; however, these differences were not statistically significant. The most common response to the overall patient safety rating question both pre- and post-implementation was ‘very good’ (49% and 40% of respondents, respectively). The proportion of respondents rating patient safety ‘excellent’ increased from 15% pre implementation to 26% post-implementation; however, these differences were not statistically significant.
| Prea | Posta | ||
|---|---|---|---|
| n = 84 | n = 35 | p-valueb | |
| Number of events reported | 0.7 | ||
| None (%) | 22 (29) | 6 (19) | |
| 1–2 (%) | 19 (25) | 7 (22) | |
| 3–5 (%) | 11 (14) | 6 (19) | |
| 6–10 (%) | 10 (13) | 4 (13) | |
| 11 or more (%) | 14 (18) | 9 (28) | |
| Missing | 8 | 3 | |
| Patient safety rating | 0.6 | ||
| Poor (%) | 3 (4) | 2 (6) | |
| Fair (%) | 11 (13) | 3 (9) | |
| Good (%) | 16 (19) | 7 (20) | |
| Very good (%) | 41 (49) | 14 (40) | |
| Excellent (%) | 13 (15) | 9 (26) |
Discussion of results
With respect to the research question ‘Does collecting data from patients and feeding it back to staff in real time improve the safety of the ward?’ there were no statistically significant differences in staff perceptions of ward atmosphere or safety culture pre and post WardSonar implementation. Therefore, WardSonar implementation did not improve staff perceptions of ward safety. A limitation of the work is that due to the sample size, analyses were not conducted at the individual ward level.
Real-time analyses
Real-time analyses addressed the following research questions:
-
Does collecting data from patients and feeding it back to staff in real time improve the safety of the ward?
-
Do the data collected from patients accurately reflect the safety of the ward?
-
Is it feasible and acceptable to capture real-time feedback from patients about safety?
Data sources
Patient perceptions of ward atmosphere (data from WardSonar monitoring tool)
Patients were invited by staff to feed back about their perception of ward atmosphere via the WardSonar device up to three times a day during the implementation period. The patient interface of the WardSonar monitoring tool collected data on perceived ward atmosphere (very calm, calm, neither calm nor stormy, stormy, very stormy), ward atmosphere direction (getting calm, the same, getting stormy) and the reasons for the ward atmosphere (the staff, the other patients, how I’m feeling, the ward/environment, other). Multiple reasons could be given. There was also a free-text box to record additional comments. The date and time of the WardSonar submissions were captured by the devices.
Real-time staff questionnaire data
Staff on the six wards were asked to complete paper questionnaires (see Appendix 2b) and return them via a secure drop box in staff-only ward areas, on weeks 4, 6 and 9 of the implementation period. The aim was to capture ‘real-time’ staff perceptions of ward atmosphere, safety culture and ability to act as a safe practitioner. The date and time when the questionnaires were completed were recorded.
The single patient safety rating item from the AHRQ HSOPSC177 was used to assess staff perceptions of safety culture.
To assess staff perceptions of ward atmosphere, items from the EssenCES scale176 were selected. Two items were selected for each of the three subscales (patients’ cohesion, experienced safety and therapeutic hold), informed by a previous factor analysis. 179
A further one-item measure on a 5-point Likert scale (from 1 = not at all to 5 = very much) was included to assess the extent to which staff felt they were able to act as a safe practitioner, given the conditions on that particular shift. 180
All real-time staff questionnaire items were phrased to capture perceptions ‘right now’.
Routine incident data
The two NHS trusts provided routine incident data for the six wards for 1 January to 31 May 2022. The data contained information on the date the incident occurred, the date the incident was reported, the location where the incident occurred, the type of incident and level of harm caused by the incident.
Staffing data
The two NHS trusts provided staffing data for the six wards. The data contained the aggregate number of staff on each shift pattern on each day between 1 January and 31 May 2022. The counts of staff were split by registered nurse, unregistered nursing assistants or other, and whether they were permanent ward staff or employed via the trust staff bank register or external agency. Staffing data were ultimately not used in the regression analysis because they were not reliable for half of the wards.
Case mix data
Daily patient occupancy data for the period 1 January to 31 May 2022 were requested from the NHS trusts, but only received for the three wards in trust 1: Apple, Cherry and Elderflower. This included information on the number of patients on each ward, split by gender and ethnic group, for each day. Aggregated monthly occupancy data were provided for the remaining three wards.
Data preparation and statistical analyses
WardSonar monitoring tool data
WardSonar monitoring tool data included test data that were identified from the date and time of the submissions and removed prior to data analysis.
The dates of WardSonar patient submissions were converted to study time based on the 10-week WardSonar implementation period. The start date was taken as the date on which the devices were deployed to the wards (week 1) and study time calculated in days from the start date to the date of each submission. On some wards, there was a lag between the date of deployment and the date of the first recorded submission.
For the statistical analysis, the data were analysed by hour. The number of WardSonar submissions per ward was compiled for each hour of each day across the 10-week implementation period. The count was split by completed and abandoned submissions – abandoned submission refers to submissions with a time stamp but without recorded information on patient-perceived ward atmosphere. Ward atmosphere and direction scores were recorded for each hour at which there was a completed WardSonar submission. Where there were multiple completed submissions during a 1-hour period, the median average score was computed.
Real-time staff questionnaire data
In total, 163 real-time staff questionnaires were completed. Five questionnaire responses were missing time (but not date) information, and two responses were missing date (but not time) information. One further response was after the 10-week implementation period. Excluding these responses left a total of 155 responses for analysis. The number of responses varied by ward. Cherry had the most responses (n = 33) and Bramble had the fewest responses (n = 22).
The six items from the EssenCES scale were reverse scored if appropriate, combined by EssenCES subscale (two items per subscale) and an average score taken. Along with the single patient safety rating item from the AHRQ HSOPSC and the one-item safe practitioner measure, they were linked by hour of each day across the 10-week implementation period. Where more than one staff member responded to the real-time staff measures within a 1-hour period, a median average score for each measure was calculated.
Incident data
This consisted of a total of 1522 incidents reported across the six wards between 1 January and 31 May 2022. For the psychiatric ICU wards, incidents that occurred in the seclusion ward were combined with those on the main ward for the analysis.
Date, location, category and level of harm were recorded for all incidents, but time of incident was missing in 301 cases (20% of sample). The proportion of records missing time varied by ward: 34.8% (Bramble), 30.4% (Damson), 16.5% (Apple), 9.4% (Elderflower), 7.5% (Fir) and 4.3% (Cherry).
Multiple imputation techniques were used to assign incidents with missing time to specific 1-hour time slots, for inclusion in the statistical analysis. Time was represented in hours as a categorical variable (0–23 hours), as this was the level at which the analysis was carried out (so time in minutes and seconds was not required). The chosen imputation method was the proportional odds model which is suitable for variables with ordered categories. Variables that were to be included in the statistical modelling were included in the imputation model (date of incident, ward, incident type and level of harm). The imputation was stratified by trust as the incident data were categorised differently at each trust; 30 imputations were used.
Harm was measured as a dichotomous variable where 0 = no harm and 1 = harm, derived from the incident harm measures used by the two trusts. The no harm category was a combination of ‘no harm caused’ and ‘near miss – incident prevented’ and ‘near miss (action prevented harm)’ and ‘none (no harm)’, the harm category was a combination of ‘harm caused’ and ‘psychological harm’ and ‘minor (minimal harm requiring minor treatment)’ and ‘moderate (significant but not permanent harm)'. The incident data were filtered to the corresponding 10-week implementation period for each ward. Study time was calculated in days between the start of the implementation period and the date of the incident. The incident date rather than the reported date was used as in some cases the incident was not reported for a number of days after the incident occurred.
The selection of only certain time periods in the analysis (i.e. the 10-week implementation period) means that the number of imputed incidents used in the analysis fell to 126 (20% of the 624 incidents during the 10-week implementation period).
Staffing data
Staffing data consisted of the number of staff on each ward by hour, which was calculated based on the shift times for each shift type, as provided by the NHS trusts, and the number of staff on each shift by date. Where a shift pattern started or ended at half past the hour (e.g. a night shift from 19.30 to 07.30), a staff count of one was allocated to the 1-hour period.
Case mix data
This consisted of counts of patients by date and ward for each day during the 10-week implementation period and were compiled by ward.
Data matrix
A matrix of counts by ward of patient, staff, incidents, real-time staff questionnaire data and WardSonar submissions per hour for each day in the 10-week implementation period was compiled. Additional variables were derived. For the three wards with available case mix data, the staff to patient ratio was calculated at each hour and compared with the mean average staff to patient ratio for the period. In terms of WardSonar response variables, a nominal WardSonar atmosphere response variable (positive atmosphere, negative atmosphere, medium atmosphere, no response), a WardSonar atmosphere direction response variable (getting better, getting worse, the same, no response), a volume of responses count and a recording of the ‘worst’ atmosphere response were created and used in a regression analysis. The hours were allocated to four time periods: morning 08:00–10:59; midday 12:00–14:59; afternoon 15:00–19:59 and evening 20:00–22:00.
WardSonar submissions, incidents (by harm) and staffing levels were summarised by ward across the 10-week implementation period. Summaries were split by day (08:00–22:00) and night (22:00–08:00).
The data were organised by hour. The night-time period (22:00–08:00) was excluded from the statistical analysis as there were very few WardSonar submissions during this period and the relationship between explanatory variables and dependent variable is expected to differ across night and day periods.
One of the planned analyses was to examine real-time staff perceptions of safety culture, ward atmosphere and ability to act as a safe practitioner alongside WardSonar submission data to understand whether data collected from patients accurately reflected the safety of the wards. However, across the wards, the matrix of counts indicated minimal overlap between real-time staff questionnaire data time periods and WardSonar submission periods. Therefore, the real-time staff questionnaire data were not included in the statistical modelling.
Statistical modelling
A number of statistical models were used to explore the relationships between wards, WardSonar use and occurrence of incidents over time. Owing to differing types of outcome measures, different types of models were used, ranging from zero-inflated negative binomial models for count data with a high proportion of zero counts to ordinal logistic regression for ordered response data. However, the underlying structure of the explanatory variables, the design matrix, was consistent across all models and consisted of fixed effects to capture time-invariant ward-specific effects, time of day variables and lagged values of incidents of WardSonar responses, depending on whether the model was explaining current incidents or current response. A simple linear trend was also included to determine any systematic deviation in use or response over time. Patient to staff ratios were not included in the analysis as the data were not considered universally valid.
Results
WardSonar submissions, incidents and staffing data
There were 627 WardSonar submissions (602 completed submissions and 25 abandoned submissions) across the 6 wards over the 10-week implementation period. Table 12 shows average hourly volumes and case mix for staffing and patients, the total observed incidents, the number of WardSonar submissions and average hourly WardSonar scores by ward, split by day and night periods.
| Ward | Time of day | Average staff | Average registered staff | Average unregistered staff | Average patients | Average patient–staff ratio | Incidents | Incidents Harm | Completed WardSonar submissions | Abandoned WardSonar submissions | Average ward atmosphere | Average ward direction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Apple | Day | 7.3 | 2.6 | 4.7 | 22.5 | 3.5 | 119 | 42 | 66 | 2 | Calm | The same |
| Apple | Night | 6.2 | 2.0 | 4.3 | 22.5 | 3.9 | 37 | 14 | 1 | 1 | NA | NA |
| Bramble | Day | 8.0 | 2.3 | 5.7 | NA | NA | 58 | 18 | 41 | 1 | Calm | The same |
| Bramble | Night | 8.2 | 2.0 | 6.3 | NA | NA | 12 | 2 | 4 | 0 | NA | NA |
| Cherry | Day | 9.4 | 2.7 | 6.6 | 11.7 | 1.4 | 31 | 9 | 211 | 8 | Calm | The same |
| Cherry | Night | 7.1 | 1.5 | 5.6 | 11.7 | 1.8 | 2 | 0 | 5 | 0 | NA | NA |
| Damson | Day | 10.8 | 2.9 | 7.9 | NA | NA | 79 | 19 | 105 | 6 | Calm | The same |
| Damson | Night | 11.9 | 2.2 | 9.7 | NA | NA | 13 | 2 | 0 | 1 | NA | NA |
| Elderflower | Day | 7.2 | 2.4 | 4.8 | 21.3 | 3.4 | 48 | 6 | 58 | 2 | Calm | The same |
| Elderflower | Night | 6.5 | 2.0 | 4.5 | 21.3 | 3.7 | 18 | 3 | 0 | 0 | NA | NA |
| Fir | Day | 8.7 | 2.5 | 6.3 | NA | NA | 71 | 29 | 108 | 4 | Calm | The same |
| Fir | Night | 8.6 | 1.7 | 6.9 | NA | NA | 10 | 5 | 3 | 0 | NA | NA |
There were some instances of multiple submissions at exactly the same date and time. Insights from the qualitative data suggest data entry patterns may reflect ward routines (e.g. group meetings, shift changes), so there may be a group of service users entering data all during the same short period of time (potentially multiple entries inputted within one minute). There also appears to be some repeat submissions (with the same comments), but as they are indistinguishable from duplicates or different service users entering the same information, these records were retained within the analysis data set.
The number of completed WardSonar submissions varied by ward. The most submissions were on Cherry ward (n = 216) and the fewest were on Bramble ward (n = 45). On average, across the implementation period, the perceived ward atmosphere was calm on all six wards during daytime hours (8:00–22:00). Average WardSonar scores for the night-time hours were not calculated as there were either no, or very few, completed submissions during this period. On average, there was no perceived change in ward atmosphere on any of the six wards.
In total, 624 incidents were reported during the 10-week implementation period. Of these, 126 cases (20%) were missing information about the time the incident occurred, leaving 498 cases containing the time of the incident. Apple ward had the highest number of (complete case) incidents (n = 156) and Cherry ward had the fewest (n = 33). Of the incidents with complete case information, 149 (30%) were classed as causing harm. The proportion varied by ward, with 42% (n = 34) of incidents on Fir ward classed as causing harm, compared with 14% (n = 9) of incidents on Elderflower ward.
Average patient to staff ratios were slightly higher during night-time hours than during daytime hours on Apple, Cherry and Elderflower wards. On all six wards, the average number of registered staff was higher during daytime hours compared with night-time hours; but on Bramble, Damson and Fir wards, the average number of unregistered staff was higher during night-time hours than during daytime hours. On the smaller Cherry ward, with an average of 12 patients, the patient to staff ratio was lower (on average 1.5 patients to each nurse during the day) compared with the larger wards (Apple and Elderflower wards, with an average of 23 and 21 patients, respectively) which had an average day time ratio of 3.5 and 3.4 patients to each nurse, respectively.
Figure 11 shows WardSonar submissions (across the 10-week implementation period) by time of day. There were very few, if any, submissions during night-time hours on any of the six wards. There is some variation by ward in the pattern of submissions by time of day. Apple, Cherry and Fir wards appear to have peaks in submissions at particular time points during the day (i.e. in the morning, in the middle of the day and in the early evening). This trimodal pattern could reflect the stated intention to take the WardSonar devices around the wards three times a day. In contrast, Bramble ward has a single peak in the morning. Submissions on Elderflower ward are concentrated in the afternoon and on Damson ward around the middle of the day. Apple, Bramble, Cherry and Fir wards all have a peak in submissions in the morning around 8–10 a.m. (which from some of the earlier qualitative insights may correspond with a morning meeting).
FIGURE 11.
WardSonar submissions on each ward by hour of the day.

The pattern of submissions by day of week (Figure 12) also varied by ward. There were no submissions on Elderflower ward (and very few on Fir ward) Friday to Sunday. Apple ward recorded very few submissions during the beginning of the week (Monday–Wednesday) and Bramble ward had no submissions on Mondays and very few on Saturdays. Submissions on Cherry and Damson ward were more spread out across the week, with peaks on Cherry ward on Tuesdays and Thursdays and on Damson ward on Mondays and Fridays.
FIGURE 12.
WardSonar submissions on each ward by day of week.
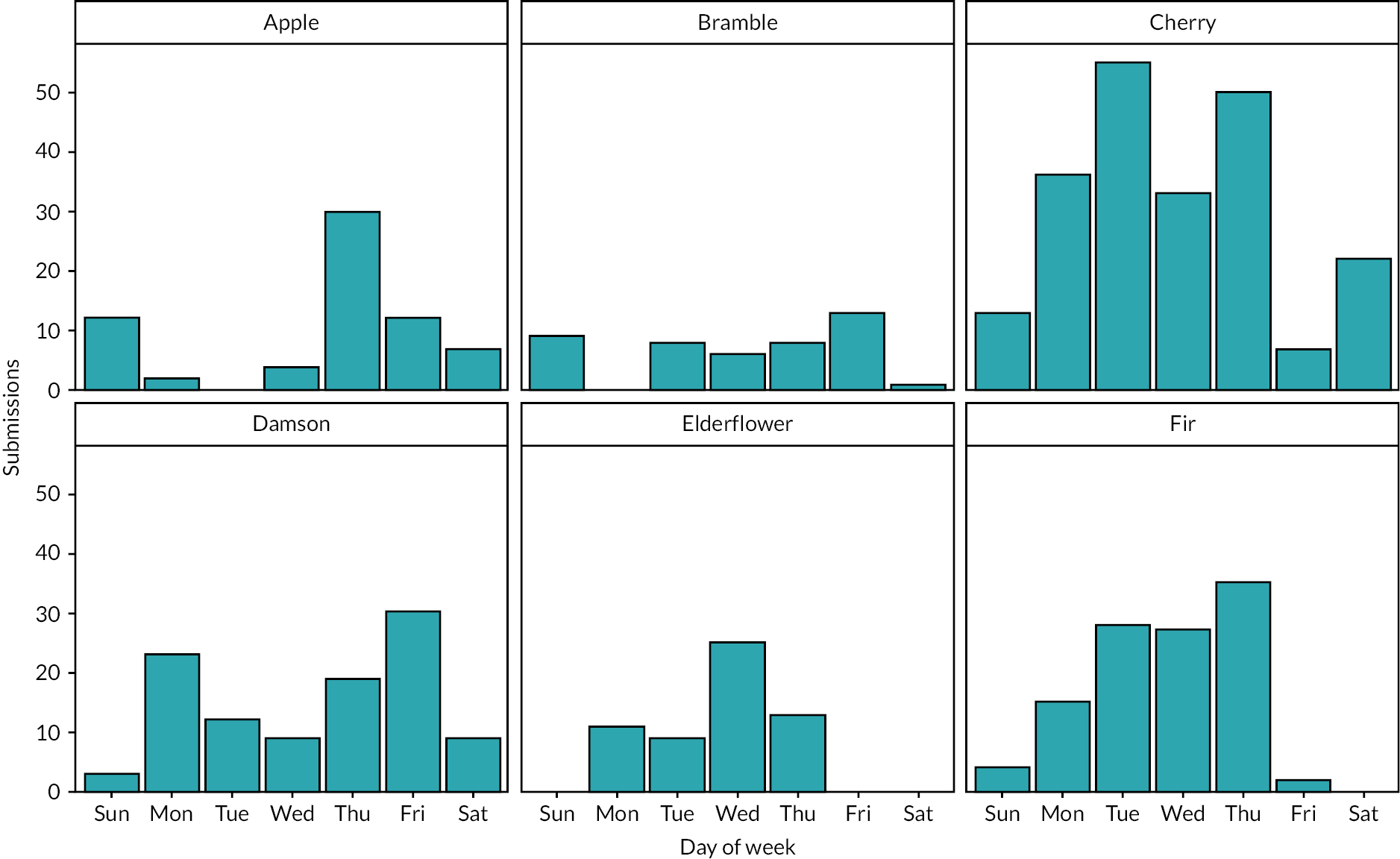
As with submissions, there were also fewer incidents during night-time hours compared to during daytime hours on all six wards (Figure 13). There was, however, some variation by ward in the pattern of incidents by time of day. While there were fewer incidents during the night-time hours on Damson and Elderflower wards, the number of incidents throughout the rest of the day was fairly flat. In contrast, there was a peak in incidents on Apple ward in the evening and on Bramble ward in the late afternoon. Cherry and Fir wards had smaller peaks in incidents in the late morning.
FIGURE 13.
Incidents on each ward by hour of the day.
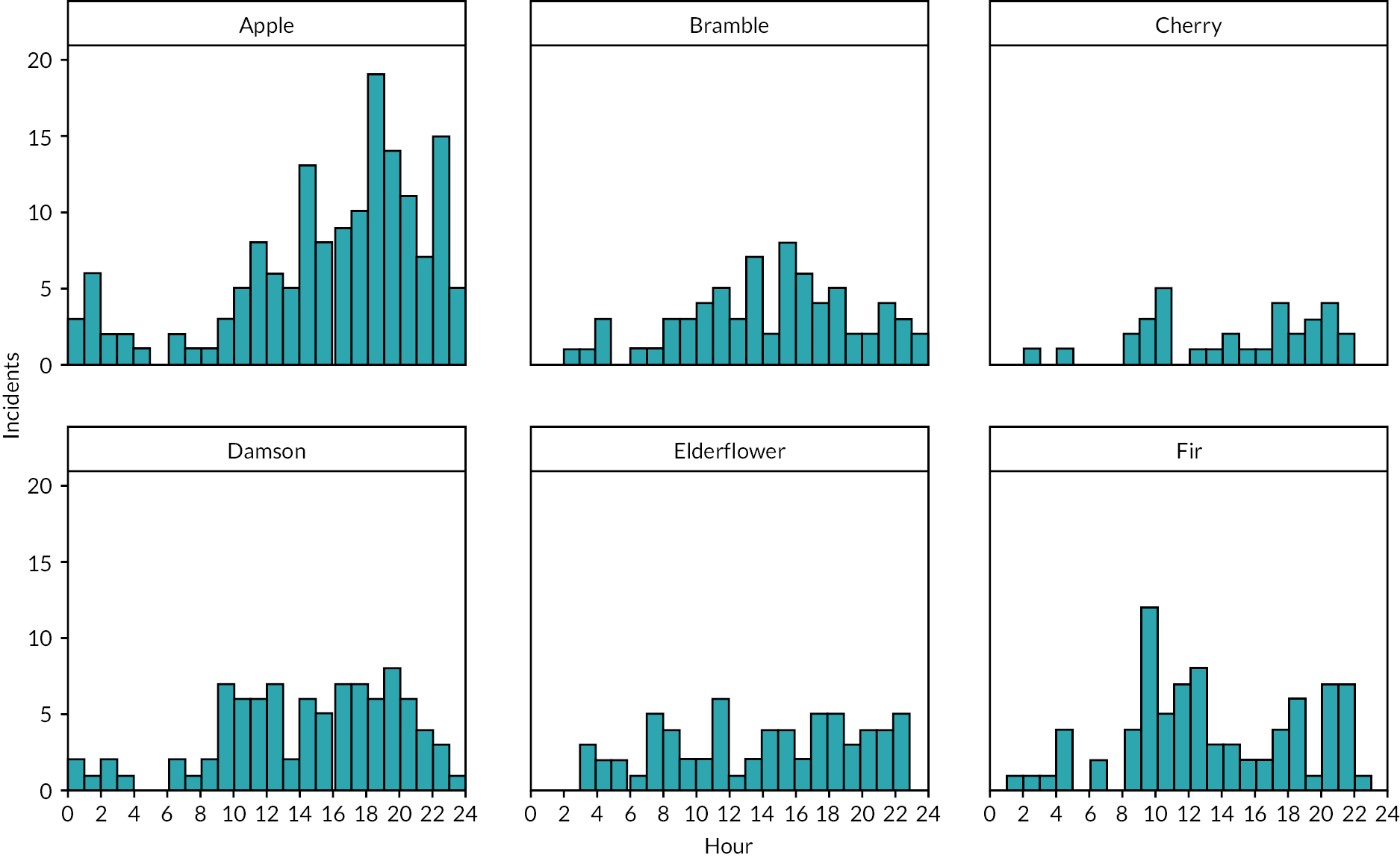
Figure 14 shows ward atmosphere responses by ward and week over the WardSonar implementation period. There was a general decline in responses over time on all wards. The most common response on all wards over the entire 10-week time period was that the atmosphere was ‘calm’ and the least common response was ‘very stormy’. However, Figure 14 shows that there was variation in the ward atmosphere rating within each week, with responses recorded across the five categories. This could reflect change in the perception of the ward atmosphere throughout the week or the differing perception of the ward atmosphere by different patients.
FIGURE 14.
Ward atmosphere over time by ward.
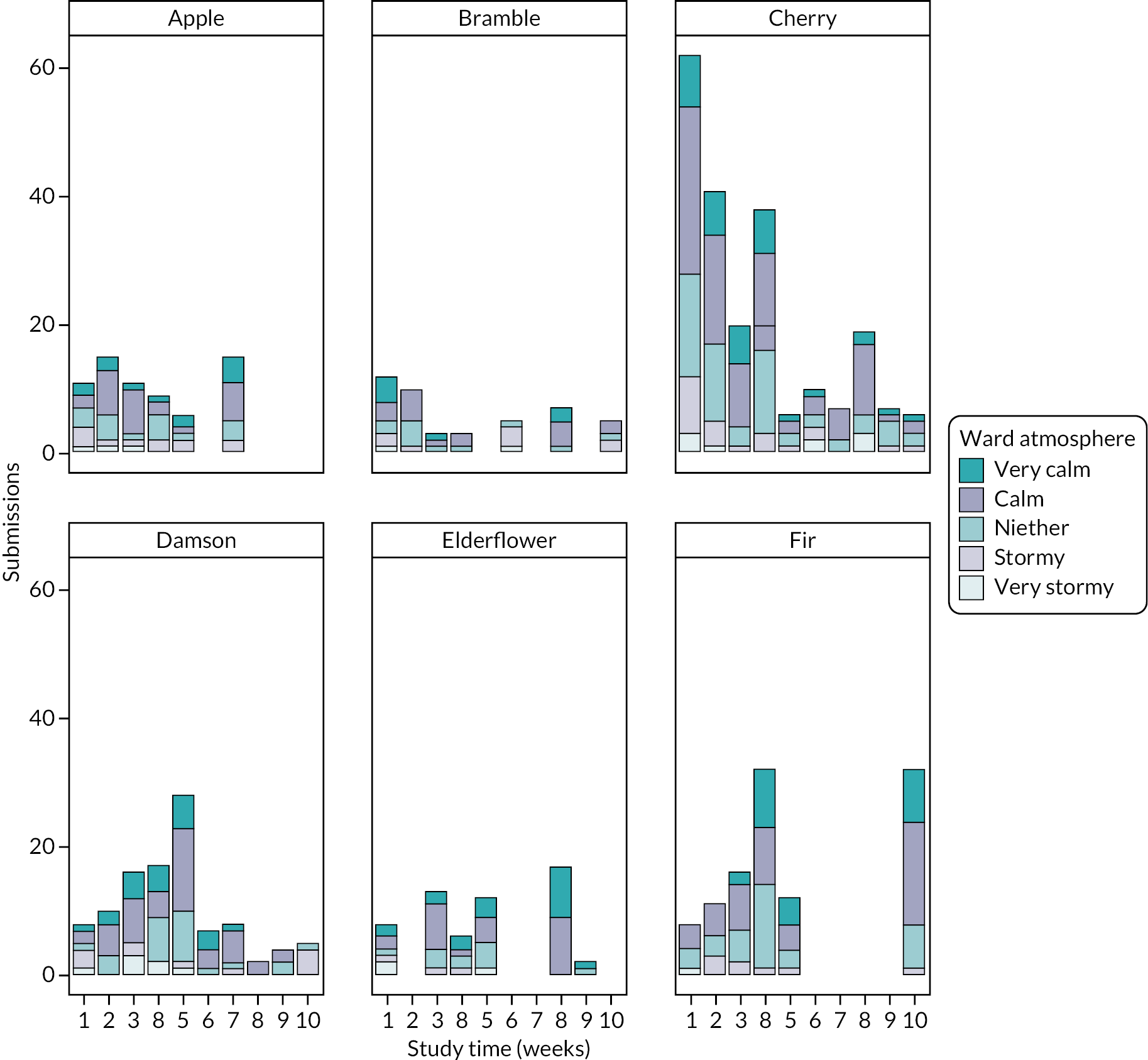
Figures 15 and 16 show the reasons given for the WardSonar submissions on each ward, split by ward atmosphere (see Figure 15) and direction of ward atmosphere (see Figure 16). When the ward atmosphere was rated as calm (‘calm’ or ‘very calm’ categories combined), the most common reason given for this on all but one ward was ‘the staff’. On Apple ward, the most common reason given was ‘the ward’. Similarly, the most common reason given for the ward direction ‘getting calm’ on all wards, apart from Apple ward, was ‘the staff’, although this was more pronounced on some wards (Cherry, Elderflower and Fir) than others. On Apple ward, the most common reason given was ‘the ward’.
FIGURE 15.
Reason for ward atmosphere by ward.

FIGURE 16.
Reason for direction in ward atmosphere by ward.

In contrast, when the ward atmosphere was rated as stormy (‘stormy’ or ‘very stormy’ categories combined), the most common reason on all but one ward was ‘the other patients’. On Fir ward, the most common reason given for a stormy atmosphere was ‘how I’m feeling’. The most common reason given for the ward direction ‘getting stormy’ on all wards was ‘the other patients’, although on Cherry ward this was closely followed by ‘how I’m feeling’.
Figure 17 shows WardSonar submissions and incidents by ward over the 10-week WardSonar implementation period. Cherry ward had the most WardSonar submissions but the number of submissions tailed off over the implementation period. Submissions on Apple ward increased over the first couple of weeks of the implementation period, dropped off and then increased again in week 7, after which no more submissions were recorded. Submissions did not appear to follow any clear pattern on the other wards and there were gaps in data collected during which no WardSonar submissions were recorded. In particular, there were large periods with no submissions on Fir and on Elderflower ward. Where there are peaks in incidents, there appear to be few (if any) WardSonar submissions.
FIGURE 17.
WardSonar device submissions and incidents by ward over 10-week WardSonar implementation period.

Exploratory regression analysis
Exploratory regression analysis was used to identify any systematic patterns between wards, time, incidents, submissions and types of submission. Of primary interest is whether information obtained from tool submissions may be used to predict the likelihood of incidents above and beyond alternative information, such as knowledge of recent previous incidents and whether or not there is any evidence of a contagion effect that persists after an incident has occurred.
All models were estimated using SAS® 9.4 (SAS Institute Inc., Cary, NC, USA) analytical software.
Graphical inspection of the volume of submissions revealed differing patterns across wards, time of day and duration of study; alongside a mix of other notable factors such as a lack of submissions during weekend for Fir ward and long periods of non-response within the implementation period (e.g. Apple ward after 44 days, Bramble between 25 and 38 days, Elderflower between 34 and 54 days and Fir between 33 and 63 days). Submissions also tended to be made in clusters when any submission was made. Given the large number of periods where no submissions were made, combined with a clustering of submissions, conventional ‘count’ models (Poisson and negative binomial) were considered. Owing to the overdispersion of zero counts, zero-inflated Poisson and negative binomial models were also estimated, in which there were two models: a logistic regression looking at the probability of any submission and a count model conditional on there being a submission.
All estimations were conducted across all 30 imputed data sets with within and between variation synthesised using Rubin’s rule. The analysis data consisted of all ward by hour observations for which the WardSonar tool was in systematic use (i.e. excluding the hours after 22:00 and before 08:00) and also excluding those systematic periods for which the tool seemed to be unused or unavailable (e.g. Apple ward after 44 days). Thus, the results should be interpreted as conditional on the WardSonar tool being in general use. A sensitivity analysis was run in which only night-time data were excluded. The reduced data set contained 4695 ward by hour observations and the fuller data set contained 6300 observations.
Explanatory variables included: fixed effect/dummy variable for each ward to capture time-invariant underlying tendencies; a dummy variable for time of day (morning 08:00–10:59 hours; midday 12:00–14:59 hours; afternoon 15:00–19:59 hours and evening 20:00–23:00 hours); a weekend dummy variable to capture any systematic impact of weekends; a Fir ward by weekend interaction dummy variable to accommodate the noticeable, but not total, drop in submissions on Fir ward during weekends; and a series of lagged variables indicating whether an incident had occurred in each of the previous 5 hours. The rationale for the lagged incidents variables was to determine whether there was any evidence of social or behavioural contagion. Patient to staff ratios were not measured systematically across wards and so were excluded from the analysis. Finally, a days since trial started (days elapsed) category was included as a measure of time on the study. A positive (or negative) coefficient on this variable indicated whether the tool was being used more (or less often) over time.
For the fuller data set containing periods of systematic zero counts additional ad hoc dummy variables were included, indicating whether the data refer to an Elderflower ward weekend (Friday–Sunday) and/or a period in which no data submissions were made. These are only included in the zero-prediction stage of the zero-inflated models.
Table 13 shows the best fit zero-inflated negative binomial model (Zinf). Because of the large proportion of zero counts, the negative binomial distributional assumption is preferred to the Poisson and the two-stage zero-inflated strategy preferred to the standard traditional count models. The table shows the coefficient values and standard errors for both stages of the model with logistic model for predicting zero counts having coefficient prefixed by Zinf for the zero-inflation part of the model. Positive coefficients in the negative binomial part of the model represent increased volume of responses given a response, but as the zero-inflation part of the model models probability of a zero count then positive Zinf coefficients imply a lower count. Thus, the sign of the estimates should be interpreted differently, depending on which part of the model is being considered.
| Parameter | Daytime w/o systematic non-use (n = 4695) | Full daytime sample (n = 6300) | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | Pr > |t| | Estimate | Std error | Pr > |t| | |
| Apple ward | 1.120 | 0.329 | 0.00 | 1.120 | 0.329 | 0.00 |
| Bramble ward | 0.341 | 0.368 | 0.35 | 0.341 | 0.368 | 0.35 |
| Cherry ward | 0.566 | 0.242 | 0.02 | 0.566 | 0.242 | 0.02 |
| Damson ward | 0.567 | 0.273 | 0.04 | 0.567 | 0.273 | 0.04 |
| Elderflower ward | 1.172 | 0.349 | 0.00 | 1.172 | 0.349 | 0.00 |
| Fir ward | 0.911 | 0.321 | 0.00 | 0.911 | 0.321 | 0.00 |
| Weekend | −0.223 | 0.262 | 0.40 | −0.223 | 0.262 | 0.40 |
| Weekenda Fir ward | −5.854 | 1.453 | < 0.0001 | −5.854 | 1.453 | < 0.0001 |
| Morning | 0.484 | 0.213 | 0.02 | 0.484 | 0.213 | 0.02 |
| Afternoon | 0.333 | 0.217 | 0.12 | 0.333 | 0.217 | 0.12 |
| Evening | 0.015 | 0.580 | 0.98 | 0.015 | 0.580 | 0.98 |
| Any incident lag 1 hour | 0.450 | 0.285 | 0.11 | 0.450 | 0.285 | 0.11 |
| Any incident lag 2 hours | −0.407 | 0.463 | 0.38 | −0.407 | 0.463 | 0.38 |
| Any incident lag 3 hours | 0.234 | 0.461 | 0.61 | 0.234 | 0.461 | 0.61 |
| Any incident lag 4 hours | −0.082 | 0.495 | 0.87 | −0.082 | 0.495 | 0.87 |
| Any incident lag 5 hours | −0.373 | 0.527 | 0.48 | −0.373 | 0.527 | 0.48 |
| Days elapsed | −0.002 | 0.005 | 0.73 | −0.002 | 0.005 | 0.73 |
| Zinf intercept | 1.444 | 0.281 | < 0.0001 | 1.444 | 0.281 | < 0.0001 |
| Zinf Apple ward | 1.175 | 0.348 | 0.00 | 1.175 | 0.348 | 0.00 |
| Zinf Bramble ward | 0.841 | 0.354 | 0.02 | 0.841 | 0.354 | 0.02 |
| Zinf Cherry ward | −0.412 | 0.265 | 0.12 | −0.412 | 0.265 | 0.12 |
| Zinf Damson ward | 0.328 | 0.287 | 0.25 | 0.328 | 0.287 | 0.25 |
| Zinf Elderflower ward | 1.058 | 0.361 | 0.00 | 1.058 | 0.361 | 0.00 |
| Zinf Fir ward | 0.000 | 0.000 | – | 0.000 | 0.000 | – |
| ZInf weekend | 0.397 | 0.244 | 0.10 | 0.397 | 0.244 | 0.10 |
| Zinf weekenda Fir ward | −4.523 | 5.463 | 0.41 | −4.523 | 5.463 | 0.41 |
| Zinf weekenda Elderflower | 17.585 | 0.235 | – | |||
| Zinf morning | 0.382 | 0.210 | 0.07 | 0.382 | 0.210 | 0.07 |
| Zinf afternoon | 0.997 | 0.211 | < 0.0001 | 0.997 | 0.211 | < 0.0001 |
| Zinf evening | 2.472 | 0.484 | < 0.0001 | 2.472 | 0.484 | < 0.0001 |
| Zinf any incident lag 1 hour | −0.491 | 0.317 | 0.12 | −0.491 | 0.317 | 0.12 |
| Zinf any incident lag 2 hours | −0.339 | 0.409 | 0.41 | −0.339 | 0.409 | 0.41 |
| Zinf any incident lag 3 hours | 0.086 | 0.436 | 0.84 | 0.086 | 0.436 | 0.84 |
| Zinf any incident lag 4 hours | −0.026 | 0.479 | 0.96 | −0.026 | 0.479 | 0.96 |
| Zinf any incident lag 5 hours | −0.057 | 0.497 | 0.91 | −0.057 | 0.497 | 0.91 |
| Zinf days elapsed | 0.016 | 0.004 | 0.00 | 0.016 | 0.004 | 0.00 |
| Zinf system not in use | 19.671 | 0.222 | ||||
| _Alpha | 0.632 | 0.201 | 0.00 | 0.632 | 0.201 | 0.00 |
For the zero-inflation part of the model there was substantial heterogeneity between wards with, all other things being equal, Apple, Bramble and Elderflower were all more likely to post zero submissions at any time of the study and Cherry ward least likely to post zero submissions. There were also systematic differences across the time of day, with all periods more likely to have zero submissions compared with midday, and a response much less likely to occur during evenings. As indicated by the graphs, the positive and significant coefficient on Zinf days elapsed indicates a higher likelihood of zero submissions over time.
The coefficients for the lagged incident variables in the zero-inflation part of the model were mostly negative but not statistically significant. The 1-hour lagged variable was of the largest magnitude and had the predicted sign and was the closest to being statistically significant.
In terms of the conditional count second part of the model, significant differences across wards were again observed. However, in this case, wards Apple and Elderflower were more likely to have higher numbers of submissions, if any submissions should occur. Bramble ward, on the other hand, was not only most likely to submit zero responses, but also submitted the lowest volume, even when a submission was made. There were no time effects bar a slightly increased rate of submissions for morning, when at least one submission was made.
The expected coefficient sign for lagged incidents is positive, but only two of the five lagged variables had a positive coefficient and none was statistically significant. The coefficient for the lag of 1 hour, as in the zero-inflated regression, was of the hypothesised direction, largest magnitude and the closest to being statistically significant.
The days elapsed variable was not significant for the second part of the model.
The addition of the periods in which there were no submissions with accommodating dummy variables did not change the results. The estimated coefficients on the systematic non-use and Elderflower weekend demonstrated predictable signs of quasi-complete separation.
Conclusion to explanatory variables analysis
The observed variation in response rates across wards observed in the descriptive plots were found to persist in a multivariate statistical analysis. Similarly, there was a trend for submission rates to become lower over time, and for greater numbers to be submitted at midday. The two-part statistical model looking at WardSonar responses identified that much of the variation in overall number of reports was due to differences in an underlying probability to submit rather than in the volume or clustering of reports when any submission is made.
The estimated coefficients for lagged incidents was a notable finding. Although nothing was statistically significant in the model, the 1-hour lag was of the expected direction, had the largest magnitude and was closest to being statistically significant. This finding is broadly true across all estimation models estimated (including those not reported). Indeed, in the non-zero-inflated models, the coefficient attached to incidents lagged by one was always significant and positive, indicating that a response was more likely in the hour following an incident, all other things being equal. It is only when the mechanism of count generation is split into two in the zero-inflated models that significance is lost. Thus, in the exploratory analysis it is concluded that there is weak evidence to suggest that incidents may increase the probability of a response in the following hour, but no evidence to suggest that the effect has a longer duration.
Ward atmosphere
This section addresses the type of response for ward atmosphere and atmosphere direction, given that a response has been made. It represents a secondary part of the analysis considering the impact of ward characteristics on response. This regression used all 602 complete submissions and adopted a set of explanatory variables similar to that used to estimate volume of responses. Table 14 shows the estimated coefficients.
| Ward atmosphere | Atmosphere direction | |||||
|---|---|---|---|---|---|---|
| Estimate | SE | Pr > |t| | Estimate | SE | Pr > |t| | |
| Intercept1 | −1.44 | 0.28 | < 0.0001 | −0.45 | 0.30 | 0.13 |
| Intercept2 | 0.47 | 0.28 | 0.09 | 2.44 | 0.32 | < 0.0001 |
| Intercept3 | 1.86 | 0.29 | < 0.0001 | |||
| Intercept4 | 3.22 | 0.33 | < 0.0001 | |||
| Apple ward | −0.20 | 0.31 | 0.52 | −0.39 | 0.33 | 0.24 |
| Bramble ward | −0.19 | 0.35 | 0.58 | −1.32 | 0.38 | 0.00 |
| Cherry ward | −0.19 | 0.24 | 0.42 | −0.68 | 0.25 | 0.01 |
| Damson ward | −0.13 | 0.28 | 0.65 | −0.82 | 0.30 | 0.01 |
| Elderflower ward | 0.33 | 0.32 | 0.29 | −0.46 | 0.35 | 0.18 |
| Fir ward | 0.00 | 0.00 | ||||
| Weekend | −0.26 | 0.23 | 0.26 | −0.38 | 0.26 | 0.14 |
| Morning | −0.05 | 0.20 | 0.81 | −0.26 | 0.21 | 0.22 |
| Afternoon | −0.16 | 0.20 | 0.42 | −0.03 | 0.22 | 0.89 |
| Evening | −1.87 | 0.60 | 0.00 | −0.75 | 0.61 | 0.22 |
| AnyiIncident lag 1 hour | −0.17 | 0.25 | 0.50 | 0.13 | 0.28 | 0.65 |
| Any incident lag 2 hours | −0.71 | 0.44 | 0.10 | −0.07 | 0.50 | 0.88 |
| Any incident lag 3 hours | −0.09 | 0.46 | 0.85 | −0.38 | 0.54 | 0.48 |
| Any incident lag 4 hours | −0.25 | 0.46 | 0.59 | −0.45 | 0.59 | 0.44 |
| Any incident lag 5 hours | −0.28 | 0.47 | 0.55 | 0.44 | 0.60 | 0.47 |
| Days elapsed | 0.01 | 0.00 | 0.04 | 0.01 | 0.00 | 0.10 |
In both cases, the response category was treated as ordered with five categories for ward atmosphere (very calm, calm, neither calm nor stormy, stormy, very stormy) and three for atmosphere direction (getting calmer, no change/same, getting stormy). The ordered regression model also estimated thresholds between these categories within each regression (four thresholds for the five categories in ward atmosphere and two thresholds for the three categories).
Positive coefficients represent higher probabilities of calmer outcomes.
In the atmosphere model, very little was statistically significant. There appeared to be no variation across wards. Lagged incidents appear to have no impact. The negative and significant coefficient attached to evening indicates that stormier atmospheres were more likely to be reported later in the day. The statistically significant coefficient for days elapsed suggest that although the number of submissions declined over time (see previous analysis) they were more likely to report a calmer atmosphere.
For the atmosphere direction, significant differences were found across wards with Fir ward responses being more proportionately likely to report the atmosphere is getting calmer than other wards and Bramble ward being more likely to report the atmosphere deteriorating. No other variable was significant.
Overall, in terms of volume and types of display, there is evidence to suggest greater variation in volume of response rather than type of response across wards and time of day with weaker evidence that an incident occurring in the previous hour and only previous hour increases the likelihood and volume of response.
The final set of regression models looks at whether lagged WardSonar responses can help predict the likelihood of future incidents. Such a link would support the argument that measurements of ward atmosphere can be a proactive instrument in reducing ward incidents.
This relationship was explored by looking at the probability of an incident occurring as a function of fixed ward effects, time of day, the lag of previous incidents (up to 5 hours) and had four models of lagged WardSonar responses: mean ward atmosphere, mean ward atmosphere direction, volume of WardSonar submissions and the lowest atmosphere reading. Owing to the categorical nature of lagged responses and the low volume of some observed values, quasi-complete separation meant that lags of more than 1 hour could not be estimated in the data.
All non-night observations were used. This included periods when the WardSonar tool appeared not to be in use at all. To accommodate this an additional category was created for the WardSonar response ‘WardSonar not in systematic use’. The coefficient attached to this variable was intended to capture whether the periods for which the tool was not used happened to be periods of high incident occurrence. A significant result could suggest underlying tensions which cause incidents and may also affect the use of the tool. Tables 15 and 16 together summarise the lagged WardSonar responses.
| Parameter | Lagged mean WardSonar atmosphere | Lagged mean WardSonar atmosphere direction | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | Pr > |t| | Estimate | SE | Pr > |t| | |
| Apple ward | −2.26 | 0.15 | < 0.0001 | −2.26 | 0.15 | < 0.0001 |
| Bramble ward | −2.57 | 0.15 | < 0.0001 | −2.57 | 0.15 | < 0.0001 |
| Cherry ward | −3.89 | 0.23 | < 0.0001 | −3.89 | 0.23 | < 0.0001 |
| Damson ward | −2.42 | 0.15 | < 0.0001 | −2.42 | 0.15 | < 0.0001 |
| Elderflower ward | −3.25 | 0.19 | < 0.0001 | −3.25 | 0.19 | < 0.0001 |
| Fir ward | −2.84 | 0.16 | < 0.0001 | −2.84 | 0.16 | < 0.0001 |
| Weekend | 0.03 | 0.11 | 0.7848 | 0.03 | 0.11 | 0.7898 |
| Morning | 0.01 | 0.16 | 0.9504 | 0.01 | 0.16 | 0.9466 |
| Afternoon | 0.18 | 0.13 | 0.1683 | 0.18 | 0.13 | 0.1676 |
| Evening | −0.03 | 0.16 | 0.8508 | −0.03 | 0.16 | 0.8509 |
| Any incident lag 1 hour | 0.44 | 0.16 | 0.0073 | 0.44 | 0.16 | 0.0073 |
| Any incident lag 2 hours | 0.23 | 0.18 | 0.2164 | 0.23 | 0.18 | 0.2152 |
| Any incident lag 3 hours | 0.48 | 0.17 | 0.0061 | 0.48 | 0.17 | 0.0061 |
| Any incident lag 4 hours | 0.40 | 0.18 | 0.026 | 0.40 | 0.18 | 0.0266 |
| Any incident lag 5 hours | 0.15 | 0.22 | 0.4787 | 0.15 | 0.22 | 0.4843 |
| Sonar not in systematic use | 0.17 | 0.12 | 0.1737 | 0.17 | 0.12 | 0.1743 |
| Mean atmosphere calm lag 1 hour | 0.31 | 0.37 | 0.4121 | |||
| Mean atmosphere medium lag 1 hour | −0.05 | 0.75 | 0.9478 | |||
| Mean atmosphere stormy lag 1 hour | 0.06 | 1.07 | 0.9522 | |||
| Getting calmer lag 1 hour | 0.28 | 0.63 | 0.6595 | |||
| No change lag 1 hour | 0.19 | 0.44 | 0.6673 | |||
| Getting stormier lag 1 hour | 0.17 | 0.76 | 0.8198 | |||
| Parameter | Lagged WardSonar submissions | Lagged worst WardSonar atmosphere | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | Pr > |t| | Estimate | SE | Pr > |t| | |
| Apple ward | −2.27 | 0.15 | < 0.0001 | −2.26 | 0.15 | < 0.0001 |
| Bramble ward | −2.58 | 0.15 | < 0.0001 | −2.57 | 0.15 | < 0.0001 |
| Cherry ward | −3.90 | 0.23 | < 0.0001 | −3.89 | 0.23 | < 0.0001 |
| Damson ward | −2.42 | 0.15 | < 0.0001 | −2.41 | 0.15 | < 0.0001 |
| Elderflower ward | −3.22 | 0.18 | < 0.0001 | −3.24 | 0.19 | < 0.0001 |
| Fir ward | −2.84 | 0.16 | < 0.0002 | −2.84 | 0.16 | < 0.0001 |
| Weekend | 0.04 | 0.11 | 0.6762 | 0.03 | 0.11 | 0.7869 |
| Morning | 0.01 | 0.16 | 0.9495 | 0.01 | 0.16 | 0.9755 |
| Afternoon | 0.18 | 0.13 | 0.1666 | 0.17 | 0.13 | 0.1823 |
| Evening | −0.03 | 0.16 | 0.8613 | −0.03 | 0.16 | 0.8495 |
| Any incident lag 1 hour | 0.44 | 0.16 | 0.0073 | 0.44 | 0.16 | 0.0072 |
| Any incident lag 2 hours | 0.22 | 0.18 | 0.2399 | 0.23 | 0.18 | 0.2135 |
| Any incident lag 3 hours | 0.48 | 0.17 | 0.0054 | 0.48 | 0.17 | 0.0059 |
| Any incident lag 4 hours | 0.39 | 0.18 | 0.0296 | 0.40 | 0.18 | 0.0269 |
| Any incident lag 5 hours | 0.16 | 0.22 | 0.4665 | 0.15 | 0.22 | 0.5053 |
| Sonar not in systematic use | 0.17 | 0.12 | 0.1702 | 0.17 | 0.12 | 0.1694 |
| Any submissions lag 1 hour | 0.08 | 0.06 | 0.1495 | |||
| Any submissions lag 2 hours | −0.01 | 0.08 | 0.9002 | |||
| Any submissions lag 3 hours | 0.04 | 0.07 | 0.5013 | |||
| Any submissions lag 4 hours | −0.03 | 0.09 | 0.6977 | |||
| Any submissions lag 5 hours | −0.01 | 0.09 | 0.9195 | |||
| Min atmosphere very calm lag 1 hour | 0.71 | 1.05 | 0.4971 | |||
| Min atmosphere calm lag 1 hour | 0.11 | 0.60 | 0.8482 | |||
| Min atmosphere neutral lag 1 hour | −0.17 | 0.71 | 0.81 | |||
| Min atmosphere stormy lag 1 hour | 0.88 | 0.51 | 0.0832 | |||
| Min atmosphere very stormy lag 1 hour | −14.60 | 20436 | 0.9994 | |||
As discussed, a positive (or negative) coefficient on the series of lagged variables indicated whether the tool was being used more (or less often) over time. In all four regressions, the results of the common variables were very consistent. There was significant variation in the rate of incidents between wards. There was no impact of time of day. Importantly there was compelling evidence that lagged incidents increase the probability of an incident in the current period – with statistically significant positive coefficients for 1, 3 and 4 hours. The lack of significance for 2 hours is puzzling but, overall, the data showed clear evidence of a lingering effect of previous incidents.
In all models, the ‘WardSonar not in use’ category was not statistically significant. This indicates that the periods for which the tool appeared never to have been used were not different from the other periods in terms of numbers of incidents.
In all, there was little evidence that lagged WardSonar responses were predictive of future incidents. No category for median atmosphere nor median atmosphere direction showed any statistical power in predicting incidents from the omitted no response category; and nor were the coefficients in the hypothesised directions. For example, the ‘calm’ category for ward atmosphere had a positive coefficient when a negative coefficient would have been expected. Furthermore, the size of the positive coefficient is greater than that for the ‘stormy’ category. A value that predicted fewer incidents when calm compared with stormy would have been expected.
There was a positive relationship between the 1-hour lag of volume of submissions and an increased rate of incidents, but it was not statistically significant. However, there was weak evidence (significant at 10%) that any reporting of a stormy atmosphere in a period leads to a higher likelihood of an incident in the following hour than if no response. The estimated coefficient for ‘very stormy’ as the lowest response showed clear signs of quasi-complete separation.
Discussion of results
There is substantial and significant variation in the use of the device across wards, both in terms of the likelihood of any submission at a given time and the number of submissions. There does appear to be a time element, with more responses in the morning. There is weak evidence to suggest that submissions are more likely in the hour following an incident. There is evidence to suggest that the use of the device declines over time; that is, that any submission is less likely over the duration of the study.
In terms of the type of responses for both direction and current atmosphere, although a response appears to be more likely given a recent incident, the type of response is not sensitive to whether or not there has been an incident. In terms of atmosphere, the only seemingly related factor was that evenings lead to greater likelihood of a worse atmosphere being reported, given a submission was made. Although the volume of submissions decreased over time, the probability of a submission reporting a better atmosphere increased slightly. There was surprisingly no variation across wards. In terms of direction of atmosphere, there was significant differences across wards, but this was the only significant variable.
The most important regressions look at the ability of the tool responses in terms of predicting future incidents. However, this did not generate useful insights, especially in comparison with the information that a recent lagged incident gives. This can be viewed in four ways while also allowing non-response as a predictor: (1) as a function of median reported atmosphere; (2) median reported direction; (3) volume of submissions; and (4) as a function of the worst reported atmosphere reading. Given the nature of the data, it was only possible to look back at a 1-hour lag each time. Lagged incidences (up to 5 hours) were included and the analysis allowed for time-invariant ward characteristics.
In summary, there were substantial significant differences in the probability of an incident happening across wards, which is consistently measured across all models. Similarly, there was strong evidence to suggest that incidences happening up to 3–4 hours prior adversely affected (i.e. increased) the probability of an incident occurring in the current hour. This was consistent across all models and offers a measure of the duration of contagion. There is nothing to suggest that the medians of responses are useful for predicting the likelihood of an incident in the current period. However, there is weak evidence to suggest that if the volume of submissions is high in the past hour, then an incident is more likely, and slightly stronger evidence (significance at 90% confidence interval) to suggest that if there is a single ‘stormy’ atmosphere reported then an incident is more likely.
Chapter 10 Discussion
Introduction
Background to study
The WardSonar patient safety monitoring tool uses proactive real-time safety monitoring rather than traditional retrospective data review and is part of a broader vision for ward safety. Previous studies have found differences between patient and staff perceptions of the milieu in psychiatric settings. 31,150,179–181 The WardSonar study was partly a response to evidence gaps around the large numbers of reported and unreported safety issues on acute mental health wards; common practice is that data are collected retrospectively and almost none of the data relate to the patient perspective. Our data illustrate the relevance of this point, in suggesting patients may perceive that a ward is not safe on the basis of the interpersonal dynamics they are experiencing, but staff may take the absence of visible disruptions to the milieu as a mark of ward safety.
The current study preceded the recent publication by the UK Department of Health and Social Care of a review of data on mental health inpatient settings. 109 The review sets out ‘a vision for the future where the potential of data and evidence is fully exploited so that the healthcare system is able to ensure the highest standards of care in all mental health inpatient wards and pathways’. 109
Five themes were identified in the review:
-
measuring what matters;
-
patient, carer and staff voice;
-
freeing up time to care;
-
getting the most out of what we have;
-
data on their own are not enough.
These are closely consistent with the aims and findings of the WardSonar study, thus demonstrating the currency and relevance of our work.
The study plan was disrupted by the COVID-19 pandemic. One possible consequence of this was low uptake of the tool, affecting data validity.
Study outputs
The study’s outputs were the development and evaluation of a co-designed monitoring tool to improve patient safety on adult acute mental health wards, through the collection of daily data about the patients’ perceptions of safety, to support staff in monitoring and improving the safety of the clinical environment and to test the intervention and explore its feasibility and acceptability.
The study delivered on its aims, which were to co-design a monitoring tool to improve patient safety on acute mental health wards, through the collection of daily data about the patients’ perceptions of safety, to support staff in monitoring and improving the safety of the clinical environment (completed in Phase 1); and to implement the tool and explore its feasibility and acceptability (completed in Phase 2).
The five study objectives are mapped to their corresponding report chapters below:
-
Objective 1, to co-design with service users and staff a digital innovation that will allow real-time monitoring of safety on acute mental health wards. Chapters 4–7 address objective 1.
-
Objective 2, to explore the feasibility and acceptability of capturing real-time feedback from service users about safety. Chapters 8 and 9 address objective 2.
-
Objective 3, to explore how staff use this information when reported during daily handovers (or other mechanism). Chapter 8 addresses objective 3.
-
Objective 4, to explore how the resulting data are related to quality and safety metrics. Chapter 9 addresses objective 4.
-
Objective 5, to explore how these data can be used longitudinally to promote safety. A barrier to achieving objective 5 was the compressed time-scale for the study following pragmatic revisions to the protocol in the context of COVID-19. Chapter 8 partly addresses objective 5.
Insights from statistical analysis
General patterns
Statistical analysis highlighted some patterns in the data, and construction of an hour-by-hour data set over each ward permitted detailed analysis of the use of the WardSonar tool over the duration of the trial and the relationship with recorded incidents. This approach revealed substantial variation in the use of the tool over time across wards, particularly in the volume of reports generated from the tool rather than the levels of ward atmosphere recorded. Peaks in incidents appeared to correspond with time periods where there were few or no WardSonar submissions. The reasons patients gave for the ward atmosphere varied by whether the atmosphere was perceived as calm (often attributed to staff) or stormy (often attributed to other patients).
Tool use was most common in the middle of the day and there was a small but systematic general trend to using the tool less over the duration of the trial. There were very few (if any) submissions during night-time hours; devices were used less during the weekend (and not at all or very rarely on some wards). Additionally, device use reduced over time and there were occasions during which there were no submissions for days or weeks at a time.
Predictive potential of WardSonar
There was strong evidence that an incident leads to increased probability of further incidents in the next 4 hours. This supports the idea of social/behavioural contagion and puts a measure on the extent to which the contagion persists. There is weak evidence to suggest that an incident leads to a greater use of the WardSonar tool in the following hour but does not appear to influence the type of response. There is no evidence to suggest that mean atmosphere nor changes in atmosphere predict the likelihood of future incidents; however, the presence of any individual ‘stormy’ response or an increased volume of submissions in a hour is associated with an increased likelihood of an incident in the next hour, but is not as strong a signal as is given by recent incidents.
Further work
Further work could explore relationships between high levels of staff sickness and ward atmosphere and between ward atmosphere and the reason for sickness, such as anxiety or stress. A separate analysis of seclusion incidents could explore possible contagion affecting how incidents in the seclusion room impact staff and patients on the main ward. The finding that use of the tool trailed off over time on most wards may suggest a need to review implementation processes in future work.
Qualitative analysis
Use of pen portraits
As suggested in the literature,75 pen portraits were an effective tool for highlighting barriers to, and facilitators of, the implementation processes, and generated an holistic interpretation of how the monitoring tool was perceived and adopted on the wards. 75,166,167
These pen portraits supported the presentation of large quantities of data from a range of sources in a concise format. They facilitated rapid appraisal of rich data findings across and between cases, helping with data management, data familiarisation, synthesis, comparison, clarity around semantic ideas and latent themes, and summarising. The use of NVivo qualitative analysis software allowed an efficient approach to maintaining navigable trails between source and context, similar to the framework method. 168
Focused ethnography and researcher positionality
Focused ethnography is characterised by clear research positioning182 and reflexivity,183 a concept that is highly relevant, since researcher subjectivity shapes data interpretation,184 especially in qualitative research. 185,186 Theoretical frameworks for analysis of multimodal data can overlook researcher positionality, but it is critical to the process,187 as reflexivity helps to understand complexities of the context. 193 As insiders in terms of being familiar with WardSonar, and outsiders in terms of limited previous exposure to mental health wards, the researchers conducting the focused ethnography brought the valuable perspective of what Barnes describes as ‘the liquid inbetweener’182 (i.e. occupying a different space somewhere between the two extremes).
In this study, the focused ethnography facilitated a narrative in which the observers’ perspectives changed as they became used to the wards and the ward communities became used to them. ‘Othering’ theory suggests ‘three types of shocks — those based on a violation of a social taboo, those deriving from professional role reversal, and those that are based on stereotypes’ (p. 950). 189 The observers started out as ‘other’189 – strangers who did not know what is normal in this environment but, over time, they settled into the ward culture. A possible unfortunate effect of evolving observer perspectives over time may be that the observers became accustomed to and tolerant of ‘rudeness’ from some staff. This may have wider significance, as acceptance of unpleasant behaviour from colleagues can be one of the factors contributing to toxic nursing cultures. 190–194
The observations therefore offer a lay view, but an evolving one, on the ward milieu. The fieldnotes showed changes in the observers’ interpretation of the ward milieu. Wolgemuth and Donohue195 refer to ‘a beneficial shift from dualistic, categorical, and entrenched subjective positionality to a more ambiguous engagement with social reality’ (p. 1022), another phenomenon that can be seen in the observer fieldnotes. During their observations, the researchers occupied, both physically and conceptually, a space of work and treatment. They attempted to remain neutral and uninvolved in ward daily life. But from a patient perspective, the ward was home, however temporary, so some of the things that appeared noteworthy to the observers (one example might be idiosyncratic dress), may have been of no particular significance to patients or staff. Analysis of these data by other members of the core research team reinforced the importance of understanding researcher positionality.
Reflections on implementation and evaluation
The mixed-methods design contributed to a rounded understanding of the implementation and evaluation of WardSonar, demonstrating the value of a mixed-methods design. The development processes (Phase 1) were extensive and involved multiple partners, such that the WardSonar tool was created from a wide range of perspectives and expertise.
Possible contextual influences on implementation and evaluation
Qualitative analysis provided potential explanations for the data patterns identified through statistical analysis. For example, patients’ positive overall response to WardSonar seemed to be linked with patients’ views that staff do not really know how they feel or what is going on among the patients; staff tended to have limited understanding of the WardSonar tool’s facility to aggregate and display patient reports; there was a positive response from staff as well as patients to the design features of WardSonar; it seemed important to have an engaged ward manager who would enthuse the rest of the staff to use the tool.
The qualitative analysis offered potential explanations for the fluctuations in submissions, such as that the tool was not much used during busy times when staff were dealing with incidents, and if the device was lost or out of action, the tool was unavailable for use. This appears to explain a common tendency for staff to collect patient submissions at quiet times, and when patients were gathered in communal areas such as during the mornings. Additionally, it raises questions about data quality (i.e. the extent to which the submissions genuinely reflect patients’ perceptions of ward atmosphere).
The insights described above add to the literature concerning how research studies can best be implemented in hospital settings196–199 and can inform a future iteration of WardSonar implementation and evaluation.
Implementation taxonomy
We adapted and applied Proctor et al. ’s taxonomy108 to help understand the implementation of WardSonar (Table 17 and Figure 18). Table 17 sets out the eight components of the taxonomy108 with comments on what was highlighted by the evaluation of the WardSonar monitoring tool and what this means for future implementation. According to Hernan et al.,107 one fidelity indicator could be the data collection processes (i.e. the entries on the devices for each ward); however, our evidence highlighted non-adherence to the protocol, for example a member of staff entering their own data, or staff potentially influencing the data entered by patients.
| Implementation component | WardSonar evaluation (n.b. COVID-19 context) | Implication | |
|---|---|---|---|
| Acceptability: stakeholder perception of satisfactoriness | Favourable response to user interface and design features | Collaborative design process resulted in well-designed product | Impact of COVID-19 |
| Adoption: stakeholder willingness to adopt intervention | Mixed response; patients consistently supportive, staff ambivalent | Staff willingness to adopt may be enhanced by knowing more about WardSonar | |
| Appropriateness: stakeholder perception of suitability and usefulness of intervention in the specific setting | Mixed response; considered suitable for the setting in relation to general design and as a way of encouraging conversation between staff and patients. Some patients and staff expect WardSonar to alert staff about safety issues. Considered unsuitable in relation to staff effort involved in gathering patient perspectives. Staff who knew about the dashboard functions generally saw more potential for WardSonar to improve ward safety, though this was less true on PICUs. Some patients expected prompt staff response to the concerns they raised. No indications that WardSonar caused friction between patients | WardSonar aimed to improve patient safety with minimal effort for staff, i.e. by asking patients to tell staff what the atmosphere is like and the direction it is going in. By facilitating early intervention, it could potentially reduce the emotional and physical work of staff, thus freeing them to engage in a higher proportion of activities that contribute to a milieu perceived by patients as therapeutic | |
| Cost: the cost/effort of the intervention | Not evaluated | Cost and effort could be evaluated in future studies | |
| Feasibility: the degree to which the innovation can be used or implemented successfully | WardSonar was implemented successfully in all 6 wards | Future implementation strategies can be informed by current study outputs | |
| Fidelity: the degree to which the intervention was implemented as intended | Analysis highlighted possibility of staff in adding or influencing patient safety information. Dashboard information not used in staff meetings. Data rarely collected 3× daily | Better staff awareness of WardSonar rationale and study protocol may improve fidelity | |
| Penetration: the degree to which the intervention is embedded within the systems | Penetration depended to a great extent on the ward managers; additionally, they highlighted difficulties communicating WardSonar to staff | Review of strategy for preparing wards for WardSonar may aid penetration once implemented. Patients as well as staff could be better informed about WardSonar’s rationale and functionality | |
| Sustainability: the degree of normalisation | WardSonar did not become normalised over the study period. Some staff and patients said this would be possible in a longer study or when the wards were settled for a prolonged period. They suggested revised implementation strategies (e.g. reviewing role of staff in bringing device round to patients) | Review how WardSonar is introduced to wards, and ensure all individuals understand it |
Figure 18 maps the results from Phases 1 and 2 WardSonar study to the taxonomy; that is, whether stakeholders perceived WardSonar to be useful for improving ward safety, and suitable for the ward settings; personal responses to using the device to enter or access data; the extent to which WardSonar was accepted and integrated into ward routines and norms; the challenges and successes of data collection; and other practicalities such as whether the device was physically available (i.e. not locked away and with a charged battery and internet connection).
These implementation issues resonate with the conclusions of the evidence scan that formed part of Phase 1 of the current study, for example, the importance of connectivity, and effective communication about the technology so that its rationale is understood.
Engagement issues in digital health care
Data from the current study showed reductions in research engagement over time. The implementation context appeared to be profoundly shaped by the effects of COVID-19; however, staff burnout, which is a documented effect of the pandemic,200–205 has been highlighted previously as a barrier to change in health contexts. 192,197 Analysis of log data is an emerging field in health technology research that may improve understanding of these processes. 206
Digital health care seems more likely to succeed where it suits individual patient needs and preferences. 207 There are some indications that provision of personalised support may be a useful strategy to promote patients’ engagement with health technology;199,208–210 yet overall, the wider digital health literature suggests that engagement with digital health technology is not well evaluated and its mechanisms are poorly understood. 211–214 Further research into this field could support effective engagement strategies.
Tentative conditions for successful implementation of WardSonar
The evaluation of WardSonar highlighted conditions that appeared to enhance how the WardSonar study was perceived and implemented and perceived across the six sites. Broadly, these conditions may be summarised as:
-
The design features are acceptable to staff and patients.
-
Staff and patients alike understand the study’s purpose and the study protocol.
-
Staff perceive that using the device will benefit patients and/or enhance ward safety.
-
Patients perceive that using the device will benefit staff, patients, or the ward in general.
-
The process of entering and accessing data via the WardSonar device is user friendly.
-
The device works with minimal hitches.
-
Ward leaders including managers and nurses in charge of shifts, are positive about and engaged with the study.
It seems that where the conditions are not met, adoption of the technology is adversely affected. Figure 19 illustrates similarities and differences between factors affecting patients’ and staff’s individual motivation to use the device.
FIGURE 19.
Factors affecting motivation to engage with the WardSonar device.

Technical assessment of challenges and further development
The prototype tool was designed as a standalone web app that did not receive or send information to any other systems during its implementation during the study. This was for several reasons:
-
During discussions with the first NHS site involved in the co-design, it became apparent that the timescales for developing a tool that connected with existing systems would have created unmanageable delays to the study timelines.
-
Different systems were used across different sites.
-
At the early stage of design, it was not clear which systems the tool would need to talk to; that is, which systems would support use of the tool and where data collected by the tool may need to be transferred to.
The developers created an application programming interface that links the digital products together with the underlying data storage engine. This was developed using an open data format standard so that the data could be interoperable with other systems/products in the future, recognising that this is of importance to NHS staff and also a requirement of the DTAC. 161 More information is available in the technical report (see Appendix 2d).
Post-deployment challenges
This section highlights selected challenges reported to the core research team by the technical developers. A detailed account of post-deployment challenges is available in the technical report (see Appendix 2d).
-
Connectivity issues: at times, certain wards were unable to connect their devices to the Wi-Fi:
-
What we did: issues resolved by trust IT department.
-
Future recommendations: more investigation/testing on wards before deployments and deployment of higher capacity servers. Map the coverage of the patient Wi-Fi across the wards. Ensure that staff know the patient Wi-Fi login details.
-
-
Some dashboards were showing a ‘no data’ error:
-
What we did: this was because the date range ‘remembered’ what date was selected previously. We updated the dashboard logic so the date defaulted to ‘today’ to avoid confusion.
-
Future recommendations: investing in training users of the dashboard prior to use.
-
-
Two of the devices were lost on ward A:
-
What we did: change the password on the Google account to limit data access.
-
Future recommendations: consider other security measures.
-
Considerations for further development of WardSonar technology
Technology considerations
The tools developed within the study used existing technology that was within budget and suitable for the exploratory nature of the work. Many of the challenges faced with the staff dashboard were related to the use and limitations of the data visualisation platform (Google Data Studio, Google Inc., Mountain View, CA, USA). Google Data Studio was used to create the staff dashboard, and this was a standalone product that did not receive or send information to any other systems during the trial. Some challenges of the technology may be attributable to the limitations of this tool for data visualisation. Despite its limitations, it was deemed to be the most appropriate piece of technology to use. Potentially, a bespoke dashboard would overcome the challenges and create a simpler, more refined experience. However, this is budget dependent. A future step may be to develop a bespoke dashboard, which might further support interoperability with relevant IT systems.
Findings from this study would support reviewing user needs for this dashboard and how the dashboard might share and receive information with other clinical systems. This is a potentially complex area, given that different NHS trusts have different systems; however, interoperability is a key consideration for digital tools within health and care, both in terms of the documentation required for commissioning (DTAC)158 and regarding acceptability to staff.
Further development of the WardSonar technology would be informed by the technical challenges described above in addition to insights from the implementation analysis. In the original study design, small-scale testing followed by a phase of design iteration was scheduled prior to the implementation study but this was removed as part of the adjustments to make the study feasible during the COVID 19 pandemic. The Phase 2 study outputs are therefore a new opportunity to further refine the outputs from co-design work.
The study results suggest that further technical design iterations could maintain a focus on refining the staff dashboard and also the model for deploying the tools in the ward environment.
Intellectual property
Currently, intellectual property for the technology rests with the institution that sponsored the research. In addition to funding, further development would require some key decisions relating to ownership of the technology, and who would support its development now and maintain it longer term. Key to this would be to further complete the evidence generation and documentation needed for digital products intended to be commissioned within the NHS, including the DTAC. 158 Completing the DTAC will, in fact, prompt many of the questions that need to be considered to assess future direction.
Sustainability
Funding and support of the technology longer term may be enabled through different models and the pros and cons of each would need to be assessed. Working at a local level initially, for example, with one NHS trust or a number of NHS trusts that are already connected (e.g. a provider collaborative or trusts that are part of an integrated care system) to support further testing and development may be supportive in the first instance. Gathering support and input from key stakeholders such as Academic Health Science Network colleagues, NHS England (in particular colleagues responsible for digital mental health and the transformation directorate) may help to understand alignment with current NHS strategic priorities and identify possible opportunities to further develop and support the tool in the short and longer term.
The user interface
It was important that the user interface was easy for everyone to understand,157 therefore it was intentionally simple. The design budget was small, so freely available images were used. The screenshots included in the current report demonstrate the development of a prototype of the digital monitoring tool’s user interface. This was iterated on during the study and based on user feedback. The design drew from NHS Service Standard components (notably the green button used to move between pages) and was built to WCAG 2.1 AA standards157 for accessibility.
Use of the tool during the study suggested that the user interface design was accepted by those that used it, that the questions were simple to answer and there were no challenges highlighted that related to the user interface design (from service users; a small number of comments relating to staff perceptions of the questions in the tool could be considered). Refinements could, of course, be made and further tested with service users and staff, as is best practice during the lifecycle of a product. However, a focus on refining the staff dashboard and also the model for deploying the tools in the ward environment may be more valuable in response to the findings.
Readiness for implementation
Ward-based implementation workshops facilitated by the research team prior to deployment would have reduced some of the friction and challenges faced, as a number of the issues were down to understanding/education about the system and its usage, not necessarily bugs or issues with the technology itself.
Conclusion: considerations for data interpretation
The idea that all data are socially constructed215 challenges the notion of objective reality in analysis. Gelman and Hennig184 propose eight markers (‘virtues’) of high-quality analysis that avoid using categories of subjectivity and objectivity: transparency, consensus (i.e. drawing on knowledge and providing rationales), impartiality (considering bias and alternative points of view), correspondence to observable reality, by connecting theory with empirical observation and creating conditions for reproducibility and testing, awareness of multiple perspectives; awareness of context dependence and investigation of stability (i.e. considering how conclusions might have been different if different decisions had been made). Therefore, in the current study, as with all categories of data,184 contexts for data collection and interpretation were subject to decisions about methods and meaning.
Figure 20 summarises possible influences on the data collected in Phase 2; for instance, what patients decided to report or not report, and why. This is a further consideration for data interpretation. It is possible that the context for entering data into the WardSonar monitoring tool was a mediating factor (e.g. whether or not staff and other patients were helping, watching, interested or reactive). Our work in Phase 1 of the current study highlighted that patients may be concerned that other patients think they are reporting on them or be reluctant to report that staff are creating tensions. This is consistent with the well-established argument that privacy preferences are an important driver of social interaction and behaviour. 216 Additionally, there seemed to be a possibility that staff could challenge patients’ perceptions (e.g. by assuming they were joking or expressing shock at what they had written). This possibility is supported by an observation in Salmon and Young,217 that ‘patients can regard being asked about care as an occasion to show gratitude rather than appear critical’ (p. 1516).
FIGURE 20.
Influences on the data; considerations for data interpretation.

Therapeutic milieu on wards
A therapeutic milieu may reduce violent incidents on a psychiatric ward. 67 The concept is not new59 and has evolved since first being proposed. Components of a therapeutic milieu may include reassurance, predictability and validating the individual;66 community and therapeutic relationships;58,59 careful risk tolerance68 and minimal coercion. 69
The current study found many highly motivated staff, but also a dominant sense of busyness, staffing issues including low staff numbers, high proportions of agency staff, and some staff who were tired and perhaps demoralised. Short stays and a target-oriented management culture58 may be part of the problem; the ongoing impact of the COVID-19 pandemic is undoubtedly another; and the political frameworks also have an impact.
As the NIHR puts it:
Nurses’ workload and staff shortages can make it difficult to create a calm environment. Many wards rely on agency staff who do not know the service users personally. As a result, many acute wards do not meet the needs of either service users or staff. Service users can feel disregarded and dehumanised, while nurses can feel unsupported and unsafe. 218
The current study showed that patients were sensitive to whether staff are personable or not. Although staff may be unlikely to engage with patients in this type of conversation, it is well reported in the media (e.g. 50) and discussed in the literature. 144,146
Searle et al.’s (2017) analysis focuses on systemic issues rather than individuals, that is poor conduct is attributable to the corrupting influence of professional or institutional norms – the cellar or barrel is bad, rather than individual apples. 144 However, findings from the current study reinforce conclusions of McAllister et al. 219 that, from the patient perspective, there are simple things that staff can do to enhance the therapeutic potential of the ward environment, for example, by not being dismissive towards patients, explaining the reasons behind decisions, giving patients their time and attention, and validating each patient as a person. Unhelpful staff behaviours included being unavailable, not offering privacy for one-to-one conversations and not providing personalised care. These findings are similar to perspectives highlighted in the Phase 1 interviews reported in Chapter 4 Phase 1; for example, when staff are constantly moving around it can make patients feel as though they are a low priority. Staff priorities were around improving team working and communications with service users. 219
Contagion
As discussed earlier in this report, various manifestations of behavioural contagion can emerge on a mental health ward. The hour-by-hour analysis of incident data showed that that the occurrence of one incident leads to increased probability of further incidences in the next four hours. This not only reflects what is reported by the literature10,15,135 and by stakeholders in the current study, reported, but also develops the literature on contagion and also narrows the suggested time periods for measuring contagion suggested by Beck et al. 15 from 1 day to 4 hours.
The harm caused by risk management strategies, such as restraint and seclusion, was acknowledged by staff, but the data presented here suggest that staff are also implicated in contagion (despite usually being attributed to patient behaviour). Staff interviews in the current study also suggest that staff returning from violent incidents bring contagion back to the wards, for example, in the form of low expectations of a calm atmosphere and heightened sensitivity to disruptions in the atmosphere, and general feelings of tension and stress. This reflects patient accounts of the psychological harms that can result from being in the vicinity during incidents even if not directly involved. 36
Impact of COVID-19 on the study
The COVID-19 pandemic had a considerable impact on the research plan, forcing a revision of the stakeholder engagement strategy and targets for data collection for staff and patients. Nationally, a significant amount of research was paused. 220 Pragmatic adjustments to the research design made it possible to deliver the WardSonar study. The monitoring tool was implemented during a significant wave of infections which undoubtedly influenced our ability to access wards, collect data and undertake implementation activities.
All wards reported some kind of disruption to normal routines, stemming directly or indirectly from the COVID-19 pandemic. Differences in ward size, population and acuity do not seem to suggest patterns or trends that could help predict feasibility or acceptability in a future study; except that PICU staff explained that PICU wards are very safety focused, such that the WardSonar tool was unlikely to add anything useful in that regard. The absence of obvious links between how welcome the researchers on the wards felt, and how much data was collected on each ward, suggests that a cool reception from individual staff may not be indicative of an unsupportive study site.
No wards were using the dashboard data as planned. The WardSonar tool was designed to elicit real-time safety data that staff could feed into ‘safety huddles’ and similar meetings, but safety huddles were not taking place and the observers perceived that dashboard data were not used in any other staff meetings. We have reported how some interviewees had a general idea about how the tool worked for data entry, but most expressed surprise and interest when they were shown the dashboard. According to Hernan et al.,107 one fidelity indicator could be the data collection processes (i.e. the entries on the devices for each ward); however, the evidence highlighted non-adherence to the protocol, for example, a member of staff entering their own data, or staff potentially influencing the data entered by patients.
The complex stresses affecting health staff during and after the 2020 COVID-19 pandemic221,222 should be emphasised. The fact that this study remained feasible is testament to their dedication and commitment to improving patient care.
Strengths and limitations of the study
The WardSonar monitoring tool has a strong patient perspective, which arguably gives it particular relevance for addressing patient safety. It was co-designed to be used without training. This was part of brief for the developers and our evaluation suggests that the tool was easy to use. The core research team included experience experts, and mental health service users and professionals were involved in co-design activities. The WardSonar study responded to evidence gaps around the large numbers of reported and unreported safety issues on acute mental health wards, in which data are collected retrospectively, and almost none of the data relate to the patient perspective. The stakeholder perspectives fundamentally impacted on the conceptualisation and operationalisation of WardSonar, adding to its validity. Equally, the separate components of the mixed-methods design were mutually beneficial, resulting in greater insights into the study data.
The use of a mixed-methods design supported good insights into the tool’s potential to improve ward safety, including strong evidence to support the idea of behavioural contagion between incidents on the ward. The technology was pragmatically adapted for use within an NHS context, but issues arose with connection of the devices via freely accessible patient Wi-Fi, and with Google Data Studio. While the inputting of data did not seem to be affected, this did cast doubt on the reliability of the monitoring tool.
Throughout this report we have emphasised ways in which the WardSonar study was disrupted by COVID-19. The pandemic not only affected access to the wards, data collection and implementation, but also meant the wards were experiencing considerable flux in staffing and patient numbers. A limitation of the study is that objective 5 was not fully met. This may be chiefly due to the amended research design with compressed implementation phase.
A further potential consequence of the pandemic for the quantitative analysis involves both the volume and content of the WardSonar responses. As a minimum the lower volume of responses may have severely limited the power of the statistical analyses to identify statistically significant relationships between responses and outcomes. In addition, the observation that tool use declined over time may simply be an artefact of the pandemic. We note that the volume of routinely collected data was not affected and it is those data in which we find significant findings.
The pandemic may also have influenced the types of responses that were recorded and we may have observed a period in which the usual relationship between ward atmosphere and events was temporarily superseded by a COVID-specific relationship. Specifically, it may be possible that ward atmosphere was heavily influenced by a large exogenous factor that was independent of tensions within the ward and therefore less likely to lead to events like violent incidents. If the same type of atmosphere readings had been observed at a different time without external contamination, then there may have been different outcomes and a different relationship estimated. We recognise that the research environment was severely atypical and can only speculate on the impact on results.
Data were gathered from interviews with patients, staff and observations on each ward at selected time points, but because interviews were opportunistic, it is unclear how much the interviewees represented the perspectives of the staff and patient populations. The views of people not interviewed are unknown. Likewise, little information was collected concerning personal demographic characteristics of participants, because that type of information was not considered relevant to understanding the study data.
With regard to the range of data collected, it may have been valuable to include patients in the pre/post evaluation EssenCES and AHRQ assessments, and this is something the team considered when designing the study. However, within the WardSonar implementation plan, patients may have been invited to provide feedback up to three times per day, and they may have been invited to participate in interviews throughout the evaluation period. Therefore, inviting patients to also complete pre/post evaluation EssenCES and AHRQ assessments was felt to be burdensome.
Furthermore, one of the aims of assessing patient safety culture via the staff-facing AHRQ measure was to explore composite measures (i.e. organisational learning – continuous improvement, response to error; supervisor, manager, or clinical leader support for patient safety; communication about error; communication openness; reporting patient safety events; hospital management support for patient safety; patient safety rating) over time that linked to factors within the logic model and programme theory around how the staff dashboard may support staff in monitoring and improving the safety of the clinical environment.
In addition, the analysis highlighted several unknowns, including relationships between ward atmosphere and staff stress or absence due to sickness, contagion between incidents in the seclusion room and impact on staff and patients on the main ward, and implementation processes affecting reduction in use of tool over time. These could be explored in future studies.
In this iteration of WardSonar, only the English language was used. No health economic analysis was conducted.
Implications for research
This project provides several implications for future research. Moving forward with these issues would be highly pertinent to addressing recent government recommendations on making the most of data on mental health inpatient settings. 109
Future development of WardSonar:
-
Developing an approach whereby patients can input data more freely rather than when prompted may improve the accuracy of the tool and reduce variation in use.
-
In view of the need to intervene if patients report a deteriorating ward milieu, future WardSonar research could address approaches to accessing and responding to patient concerns about safety in a timely manner.
-
WardSonar would benefit from more use of longitudinal design with repeated measures and a clear implementation plan, ideally without the disruption of COVID-19.
This project also highlights some more general directions for future research and implementation:
-
It may be useful to test whether outcomes are influenced by directly feeding back perceptions of data to patients.
-
Intervention studies should consider those factors which contribute towards feelings of being safe or unsafe on wards, such as factors that are important to patients on wards.
-
There are substantial uncertainties around how the safety experience is related to ethnicity, diversity and inclusion and the influence of milieu and contagion on safety.
-
Further research on the implementation of digital interventions in inpatient mental health wards is needed, such as how to adapt patient safety theory and interventions to the context of mental health services prior to testing.
Implications for decision-makers
The study results have highlighted a range of factors influencing safety improvement initiatives on adult acute mental health wards. Consideration of these may improve the safety of wards:
-
Prompting patients to discuss their perception of safety may be beneficial to patients.
-
Staff could be encouraged to consider how patient perceptions about safety may be different from their own perceptions.
-
Using real-time data may enable a shift from reactive to proactive care delivery.
-
Social contagion may occur and is likely to be influenced by staff and patients alike.
-
Staff returning to wards after responding to incident may influence the ward milieu.
-
Incidents on wards influence the feeling of safety, therefore, post-incident milieu management for all patients, not just those directly affected, may prove beneficial for preventing future incidents.
-
Staff may need additional support with technology to enable maximum benefit to be obtained from it.
Equality, diversity and inclusion
WardSonar is an example of how to design mental health research in which there is meaningful involvement of patients. The design is based on principles of equality, diversity and inclusion consistent with the INCLUDE guidance,80 as can be seen from the descriptions of the PPIE work in Chapters 2 and 5. The conceptual starting point for design was that it would be inclusive and easy to understand. The research was developed in genuine collaboration with stakeholders, including co-applicant experience experts and a service user network that includes people with learning disabilities. Language (English only) and pictures were carefully selected and tested for accessibility. A limitation of this phase of development is that no materials were translated into other languages; however, experience experts scrutinised the text and images used in the project documentation and an experience expert/co-applicant in the core research team approved the lay summary of this report.
Current patients contributed their perspectives to the development and implementation evaluation phases through recording their sense of ward safety via the WardSonar monitoring tool or sharing their views in interviews with researchers. The WardSonar monitoring tool was developed to be inclusive and easy for everyone to understand, and was deployed on whole wards, that is not targeted groups of patients.
The development phase worked up an idea into a testable tool for mental health wards, using co-design processes that relied on the involvement of service users or healthcare providers. The study found that patient perspectives differ from staff perspectives around ward safety, so is consistent with the literature. It seems noteworthy that patients were more likely than staff to express a view that staff were not always aware of safety issues affecting the patients, which further emphasises the importance of patient perspectives in identifying research priorities.
Apart from the location of the participating trusts, demographic data (on race, gender, geography, sexuality, sex, age, social and socioeconomic status and health status) were not requested from any of the participants. This was a conscious omission based on consideration of pertinent ethical issues around demographic data collection223–226 and it was intended to promote inclusiveness and encourage research participation; however, it meant that these demographic factors could not inform the analysis. There remain many gaps in knowledge regarding how the safety experience relates to ethnicity, diversity and inclusion.
Conclusions
As far as can be ascertained by the research team, this is the first project to apply a theoretical framework for improving patient safety to a mental health inpatient context. The project has provided additional insights into the nature of milieu and contagion in inpatient settings. It has developed, tested and implemented a digital patient-focused monitoring tool across acute mental health wards and PICUs. As such, it provides a deeper understanding of issues related to technological adoption in an NHS context, and qualitative observations about the dynamic nature of patient safety, milieu and contagion. The ability to monitor patient perspectives in real time provides an additional proactive approach to safety which is novel and unique. The analysis indicates the WardSonar potentially is measuring contagion and might identify the likelihood of future incidents occurring.
The abnormal patient mix and staffing arrangements may have reduced potential uptake of WardSonar and does impact on the validity of the study findings.
Developing an approach whereby patients can input data more freely rather than when prompted may improve the accuracy of the tool and reduce variation in use. More research is required into the implementation of the monitoring tool, particularly in wards not disrupted by COVID-19. Future trials of WardSonar would need to be conducted on a larger scale, across different mental health contexts and with longer timescales for implementation. This would allow a proper period of familiarisation for both patients and staff and a deeper exploration of both initial response and experience of WardSonar over time. Staff, for instance, might come to value WardSonar as they see how easy it is for patients to raise concerns when they feel anxious on the ward and so prevent escalation of problems and potential serious incidents.
Additional information
Acknowledgements
Thanks are due to Leeds and York Partnership NHS Foundation Trust Service User Network and Help from Experts by Experience for Researchers, for sharing their wisdom and advice. The project was supported by the NIHR Yorkshire and Humber Patient Safety Translational Research Centre (PSTRC).
We also thank the Patient and Public Involvement and Engagement networks at NIHR Yorkshire and Humber PSTRC Lay Leaders and Citizen Participation Group, Leeds University, participating NHS trusts and service users and staff.
Ayup Digital (https://ayup.agency) were commissioned to work on this project and collaborated with us in the development phase. They subsequently built the tool and provided technical support during implementation. There is no associated intellectual property or declaration of interests.
Contributions of authors
John Baker (https://orcid.org/0000-0001-9985-9875) Professor of Mental Health Nursing led the study, contributed all aspects of the monitoring tool development, and collection and analysis of the data, and contributed to the writing of the report.
Sarah Kendal (https://orcid.org/0000-0001-8557-5716) Research Fellow, mental health, contributed to qualitative analysis and prepared the report.
Chris Bojke (https://orcid.org/0000-0003-2601-0314) Professor of Health Economics Specialising in Health Technology Assessment oversaw and helped conduct quantitative analysis of data and contributed to writing of report.
Gemma Louch (https://orcid.org/0000-0001-6946-3693) Senior Research Fellow, patient safety, led the intervention development write up, contributed to the quantitative analysis and contributed to the writing of the report.
Daisy Halligan (https://orcid.org/0000-0003-0354-759X) Research Assistant, healthcare services research, contributed to data collection.
Saba Shafiq (https://orcid.org/0000-0001-5506-8692) Research Assistant, psychology and health, contributed to data collection on hospital wards.
Charlotte Sturley (https://orcid.org/0000-0001-8415-352X) Research Fellow in Health Data Analytics carried out the quantitative analysis and contributed to the corresponding report sections.
Lauren Walker (https://orcid.org/0000-0003-2459-7860) Lived Experience Co-applicant conducted the PPIE work and gave lived-experience advice to the study team.
Mark Brown (https://orcid.org/0000-0002-0633-8745) Development Director, Social Spider CIC co-applicant contributed lived experience and discussion.
Kathryn Berzins (https://orcid.org/0000-0001-5002-5212) Senior Research Fellow contributed to design of research, conducted qualitative data collection and analysis, reviewed and commented on final report.
Lyn Brierley-Jones (https://orcid.org/0000-0003-0395-9447) Research Fellow contributed to Phase 1 literature reviews and led the write up of the published review, led Phase 2 qualitative work, and reviewed and commented on the final report.
Jane K O’Hara (https://orcid.org/0000-0001-5551-9975) Professor of Healthcare Quality and Safety provided expertise on patient safety theory, patient and public involvement, and health services research delivery.
Kirstin Blackwell (https://orcid.org/0000-0002-8215-4040) Deputy Director, Thrive by Design, co-design, contributed to co-design, tool development and stakeholder engagement during Phase 1, and report writing.
Gemma Wormald (https://orcid.org/0000-0003-0560-6557) Co-design Facilitator/Occupational Therapist led onsite stakeholder co-design activities and contributed to description of tool development during Phase 1.
Krysia Canvin (https://orcid.org/0000-0001-6571-6411) Senior Research Fellow, mental health, contributed to qualitative analysis and report writing.
Charles Vincent (https://orcid.org/0000-0003-0270-0222) Professor of Psychology, University of Oxford, contributed to design of research and reviewed and commented on final report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/UDBQ8402.
Primary conflicts of interest: John Baker: Selection Committee Chair for the HEE/NIHR ICA programme from March 2022, committee member of NIHR Advanced Fellowship panel until July 2022. Chris Bojke: Committee member of NIHR HS&DR funding panel up to 30 September 2021.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Phase 1: IRAS project 242683
The health professional arm of the Phase 1 interview study received ethical approval from the University of Leeds, School of Healthcare Ethics Committee (reference: HREC 19-028) and the patient arm of the Phase 1 interview study received ethical approval from South Central – Berkshire B Research Ethics Committee (reference: 20/SC/0360).
Phase 2: IRAS project 300833
Phase 2 received ethical approval from East Midlands – Nottingham 2 Research Ethics Committee (reference: 21/EM/0247).
Information governance statement
The University of (detail withheld for peer review process) is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679.
Under the Data Protection legislation, the University of (detail withheld) is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (detail withheld).
Department of Health and Social Care disclaimer
This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Brierley-Jones L, Ramsey L, Canvin K, Kendal S, Baker J. To what extent are patients involved in researching safety in acute mental healthcare? Res Involv Engagement 2022;8(1):8.
Canvin K, Brierley-Jones L, Ramsey L, Baker J, Berzins K. Safety and contagion in acute psychiatric wards: How the milieu is implicated in the occurrence of clustered safety incidents. Theory Psychol 2023; in press. ISSN:0959-3543.
Kendal S, Louch G, Walker L, Shafiq S, Halligan D, Brierley-Jones L, Baker J. Implementing and evaluating patient-focused safety technology on adult acute mental health wards. J Psychiatr Ment Health Nurs 2024; in press. Online ISSN:1365-2850.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS England . Report a Patient Safety Incident 2023. www.england.nhs.uk/patient-safety/report-patient-safety-incident/#:~:text=Patient%20safety%20incidents%20are%20any,action%20to%20keep%20patients%20safe (accessed 29 January 2023).
- Rotherham Doncaster and South Humber National Health Service Foundation Trust (RDASH) . Incident Reporting Policy 2016.
- Care Quality Commission . Care Quality Commission (CQC) The Independent Regulator of Health and Social Care in England 2021. www.cqc.org.uk (accessed 4 May 2021).
- NHS England . NHS Mental Health Implementation Plan 2019 20–2023 24 2019.
- NHS England . NHS Patient Safety Strategy: 2021 Update 2021. www.england.nhs.uk/publication/nhs-patient-safety-strategy-2021-update (accessed 24 October 2022).
- NHS England . NRLS National Patient Safety Incident Reports: Commentary (September 2021) 2022. www.england.nhs.uk/publication/nrls-national-patient-safety-incident-reports-commentary-september-2021 (accessed 6 June 2023).
- Berzins KM, Louch G, Albutt A, Baker J. Conference: Improving Patient Safety: New Horizons, New Perspectives. Leeds: Cloth Hall Court; 2019.
- Thapa PB, Palmer SL, Owen RR, Huntley AL, Clardy JA, Miller LHPRN. (As-needed) orders and exposure of psychiatric inpatients to unnecessary psychotropic medications. Psychiatr Serv 2003;54:1282-6. https://doi.org/10.1176/appi.ps.54.9.1282.
- Evidence Generation and Dissemination Unit . Mental Health Patient Safety: A Rapid Literature Review 2019.
- Edwards D, Evans N, Gillen E, Longo M, Pryjmachuk S, Trainor G, et al. What do we know about the risks for young people moving into, through and out of inpatient mental health care? Findings from an evidence synthesis. Child Adolesc Psychiatry Mental Health 2015;9. https://doi.org/10.1186/s13034-015-0087-y.
- Broly P, Deneubourg J-L. Behavioural contagion explains group cohesion in a social crustacean. PLOS Comput Biol 2015;11. https://doi.org/10.1371/journal.pcbi.1004290.
- House T. Modelling behavioural contagion. J R Soc Interface 2011;8:909-12. https://doi.org/10.1098/rsif.2011.0014.
- Sprague DA, House T. Evidence for complex contagion models of social contagion from observational data. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0180802.
- Cawthorpe D, Somers D, Wilkes T, Phil M. Behavioral contagion reconsidered: self-harm among adolescent psychiatric inpatients: a five-year study. Can Child Adolesc Psychiatr Rev 2003;12:103-6.
- Beck NC, Tubbesing T, Lewey JH, Ji P, Menditto AA, Robbins SB. Contagion of violence and self-harm behaviors on a psychiatric ward. J Forens Psychiatry Psychol 2018;29:989-1006. https://doi.org/10.1080/14789949.2018.1516230.
- Rosen PM, Walsh BW. Patterns of contagion in self-mutilation epidemics. Am J Psychiatry 1989;146:656-8. https://doi.org/10.1176/ajp.146.5.656.
- Delaney KR. Calming an escalated psychiatric milieu. J Child Adolesc Psychiatr Nurs 1994;7:5-13. https://doi.org/10.1111/j.1744-6171.1994.tb00199.x.
- Lawton R, McEachan RR, Giles SJ, Sirriyeh R, Watt IS, Wright J. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Qual Saf 2012;21:369-80. https://doi.org/10.1136/bmjqs-2011-000443.
- Berzins K, Baker J, Brown M, Lawton R. A cross-sectional survey of mental health service users’, carers’ and professionals’ priorities for patient safety in the United Kingdom. Health Expect 2018;21:1085-94. https://doi.org/10.1111/hex.12805.
- Berzins K, Louch G, Brown M, O’Hara JK, Baker J. Service user and carer involvement in mental health care safety: raising concerns and improving the safety of services. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3455-5.
- Eldal K, Veseth M, Natvik E, Davidson L, Skjølberg A, Gytri D, et al. Contradictory experiences of safety and shame in inpatient mental health practice – a qualitative study. Scand J Caring Sci 2019;33:791-800. https://doi.org/10.1111/scs.12674.
- Eldal K, Natvik E, Veseth M, Davidson L, Skjølberg A, Gytri D, et al. Being recognised as a whole person: a qualitative study of inpatient experience in mental health. Issues Ment Health Nurs 2019;40:88-96. https://doi.org/10.1080/01612840.2018.1524532.
- Holmes S, Baumhover M, Lockwood J. Safety unseen: leveraging design to improve inpatient mental health-care practices. Creat Nurs 2020;26:e48-55. https://doi.org/10.1891/crnr-d-20-00030.
- Crowe M, Carlyle D. Deconstructing risk assessment and management in mental health nursing. J Adv Nurs 2003;43:19-27. https://doi.org/10.1046/j.1365-2648.2003.02669.x.
- De Santis ML, Myrick H, Lamis DA, Pelic CP, Rhue C, York J. Suicide-specific safety in the inpatient psychiatric unit. Issues Ment Health Nurs 2015;36:190-9. https://doi.org/10.3109/01612840.2014.961625.
- Royal College of Psychiatrists . Assessment and Management of Risk to Others 2016. www.rcpsych.ac.uk/members/supporting-your-professional-development/assessing-and-managing-risk-of-patients-causing-harm (accessed 6 June 2023).
- Slemon A, Jenkins E, Bungay V. Safety in psychiatric inpatient care: the impact of risk management culture on mental health nursing practice. Nurs Inq 2017;24. https://doi.org/10.1111/nin.12199.
- Brickell TA, McLean C. Emerging issues and challenges for improving patient safety in mental health. J Patient Saf 2011;7:39-44. https://doi.org/10.1097/PTS.0b013e31820cd78e.
- Dewa L, Murray K, Thibaut B, Ramtale S, Adam S, Darzi A, et al. Identifying research priorities for patient safety in mental health: an international expert Delphi study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021361.
- D’Lima D, Crawford MJ, Darzi A, Archer S. Patient safety and quality of care in mental health: a world of its own?. BJPsych Bull 2017;41:241-3. https://doi.org/10.1192/pb.bp.116.055327.
- Berzins K, Baker J, Louch G, Albutt A. A qualitative exploration of mental health service user and carer perspectives on safety issues in UK mental health services. Health Expect 2020;23:549-61. https://doi.org/10.1111/hex.13025.
- Cutler NA, Moxham L, Stephens M. The meaning of safety in acute mental health inpatient services. Aust Nurs Midwifery J 2015;22.
- Jones J, Nolan P, Bowers L, Simpson A, Whittington R, Hackney D, et al. Psychiatric wards: places of safety?. J Psychiatr Ment Health Nurs 2010;17:124-30. https://doi.org/10.1111/j.1365-2850.2009.01482.x.
- Cusack P, Cusack FP, McAndrew S, McKeown M, Duxbury J. An integrative review exploring the physical and psychological harm inherent in using restraint in mental health inpatient settings. Int J Ment Health Nurs 2018;27:1162-76. https://doi.org/10.1111/inm.12432.
- Valenti E, Giacco D, Katasakou C, Priebe S. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics 2014;40:832-6. https://doi.org/10.1136/medethics-2011-100370.
- Advonet; CHANGE . Lived Experience of Restraint, Seclusion and Segregation (RSS): Stories and Recommendations for Safer Care 2020.
- Royal College of Psychiatrists . Rethinking Risk to Others in Mental Health Services 2017.
- Welsh Government . Reducing Restrictive Practices Framework: A Framework to Promote Measures and Practice That Will Lead to the Reduction of Restrictive Practices in Childcare, Education, Health and Social Care Settings 2019.
- Ashcraft L, Bloss M, Anthony WA. Best practices: the development and implementation of ‘no force first’ as a best practice. Psychiatr Serv 2012;63:415-7. https://doi.org/10.1176/appi.ps.20120p415.
- Butterworth H, Wood L, Rowe S. Patients’ and staff members’ experiences of restrictive practices in acute mental health in-patient settings: systematic review and thematic synthesis. BJPsych Open 2022;8. https://doi.org/10.1192/bjo.2022.574.
- Social Care Local Government and Care Partnership Directorate . Positive and Proactive Care: Reducing the Need for Restrictive Interventions 2014. www.gov.uk/government/publications/positive-and-proactive-care-reducing-restrictive-interventions (accessed 6 June 2023).
- Equality and Human Rights Commission . Human Rights Framework for Restraint: Principles for the Lawful Use of Physical, Chemical, Mechanical and Coercive Restrictive Interventions 2019. www.equalityhumanrights.com/human-rights/human-rights-framework-restraint?return-url=https%3A%2F%2Fwww.equalityhumanrights.com%2Fsearch%3Fkeys%3DHuman%2BRights%2BFramework%2Bfor%2BRestraint%26f%255B0%255D%3Dcontent_type%253Apublication (accessed 6 June 2023).
- McKeown M, Thomson G, Scholes A, Jones F, Downe S, Price O, et al. Restraint minimisation in mental health care: legitimate or illegitimate force? An ethnographic study. Sociol Health Illn 2020;42:449-64. https://doi.org/10.1111/1467-9566.13015.
- HM Inspectorate of Prisons . Behaviour Management and Restraint of Children in Custody: A Review of the Early Implementation of MMPR by HM Inspectorate of Prisons 2015.
- Ministry of Justice; National Offender Management Service; Youth Justice Board for England and Wales . Minimising and Managing Physical Restraint: Safeguarding Processes, Governance Arrangements, and Roles and Responsibilities 2012. www.gov.uk/government/publications/minimising-and-managing-physical-restraint (accessed 6 June 2023).
- Positive and Active Behaviour Support Scotland (PABSS), Challenging Behaviour Foundation (CBF) . Reducing Restrictive Intervention of Children and Young People: Update of Case Study Results 2020.
- Restraint Reduction Network . Post-Incident Debriefing Guidance: For Staff Working in Inpatient Settings With Children and Young People 2022. https://restraintreductionnetwork.org/resource/rrn-launches-post-incident-debriefing-and-support-toolkit (accessed 6 June 2023).
- Care Quality Commission . Modernising the Mental Health Act: Increasing Choice, Reducing Compulsion. Final Report of the Independent Review of the Mental Health Act 1983 2018.
- Gregory A. Mirror. 2017.
- British Broadcasting Corporation . Panorama: Undercover Hospital: Patients at Risk 2022. www.bbc.co.uk/programmes/m001ckxr.
- Weiss EM. Deadly restraint: a Hartford courant investigative report. Hartford Courant 11–15 October 1998 n.d. www.charlydmiller.com/LIB05/1998hartforddata.html (accessed 30 November 2023).
- Reese J. Psychiatric Hospital Left Me Suicidal and Homeless – We Need a Human Rights-based Approach to Mental Health Care [blog post]. National Survivor User Network 2021. www.nsun.org.uk/psychiatric-hospital-left-me-suicidal-and-homeless-we-need-a-human-rights-based-approach-to-mental-health-care (accessed 4 November 2022).
- Baumeister R, Vohs K. Encyclopedia of Social Psychology. Thousand Oaks, CA: SAGE Publications Ltd; 2007.
- Petitta L, Jiang L, Härtel CEJ. Emotional contagion and burnout among nurses and doctors: do joy and anger from different sources of stakeholders matter?. Stress Health 2017;33:358-69. https://doi.org/10.1002/smi.2724.
- Taiminen TJ, Kallio-Soukainen K, Nokso-Koivisto H, Kaljonen A, Helenius H. Contagion of deliberate self-harm among adolescent inpatients. J Am Acad Child Adolesc Psychiatry 1998;37:211-7. https://doi.org/10.1097/00004583-199802000-00014.
- Cheng Q, Li H, Silenzio V, Caine ED. Suicide contagion: a systematic review of definitions and research utility. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0108724.
- Hannigan B, Edwards D, Evans N, Gillen E, Longo M, Pryjmachuk S, et al. An evidence synthesis of risk identification, assessment and management for young people using tier 4 inpatient child and adolescent mental health services. Health Serv Deliv Res 2015;3:1-228. https://doi.org/10.3310/hsdr03220.
- Mahoney JS, Palyo N, Napier G, Giordano J. The therapeutic milieu reconceptualized for the 21st century. Arch Psychiatr Nurs 2009;23:423-9. https://doi.org/10.1016/j.apnu.2009.03.002.
- Jones M. The concept of a therapeutic community. Am J Psychiatry 1956;112:647-50. https://doi.org/10.1176/ajp.112.8.647.
- Røssberg JI, Friis S. A suggested revision of the Ward Atmosphere Scale. Acta Psychiatr Scand 2003;108:374-80. https://doi.org/10.1034/j.1600-0447.2003.00191.x.
- MacAllister L, Bellanti D, Sakallaris BR. Exploring inpatients’ experiences of healing and healing spaces: a mixed methods study. J Patient Exp 2016;3:119-30. https://doi.org/10.1177/2374373516676182.
- Sakallaris BR, Macallister L, Voss M, Smith K, Jonas WB. Optimal healing environments. Glob Adv Health Med 2015;4:40-5. https://doi.org/10.7453/gahmj.2015.043.
- Brown B, Rutherford P, Crawford P. The role of noise in clinical environments with particular reference to mental health care: a narrative review. Int J Nurs Stud 2015;52:1514-24. https://doi.org/10.1016/j.ijnurstu.2015.04.020.
- Brown J, Fawzi W, Shah A, Joyce M, Holt G, McCarthy C, et al. Low stimulus environments: reducing noise levels in continuing care. BMJ Qual Improv Rep 2016;5. https://doi.org/10.1136/bmjquality.u207447.w4214.
- Camuccio CA, Sanavia M, Cutrone F, Marella I, Gregio M, Cabbia C, et al. Noise levels in an acute psychiatric unit: an exploratory observational study. Issues Ment Health Nurs 2019;40:493-502. https://doi.org/10.1080/01612840.2018.1557301.
- Gunderson JG. Defining the therapeutic processes in psychiatric milieus. Psychiatry 1978;41:327-35. https://doi.org/10.1080/00332747.1978.11023992.
- Espinosa L, Harris B, Frank J, Armstrong-Muth J, Brous E, Moran J, et al. Milieu improvement in psychiatry using evidence-based practices: the long and winding road of culture change. Arch Psychiatr Nurs 2015;29:202-7. https://doi.org/10.1016/j.apnu.2014.08.004.
- Glyn J. Don’t tell me I’m normal: inpatient psychotherapy of a severely abused patient at the Cassel Hospital. Psychoanal Psychother 2016;30:240-55. https://doi.org/10.1080/02668734.2016.1178035.
- Paterson B, McIntosh I, Wilkinson D, McComish S, Smith I. Corrupted cultures in mental health inpatient settings. Is restraint reduction the answer?. J Psychiatr Ment Health Nurs 2013;20:228-35. https://doi.org/10.1111/j.1365-2850.2012.01918.x.
- O’Hara JK, Lawton RJ. At a crossroads? Key challenges and future opportunities for patient involvement in patient safety. BMJ Qual Saf 2016;25:565-8. https://doi.org/10.1136/bmjqs-2016-005476.
- Berwick D. A Promise to Learn: A Commitment to Act: Improving the Safety of Patients in England. London: National Advisory Group on the Safety of Patients in England; 2013.
- Hammond P. NHS England’s depressing response to Berwick Review. Dr Phil Hammond 2013. www.drphilhammond.com/blog/2013/08/21/private-eye/nhs-englands-depressing-response-to-berwick-review/ (accessed 20 December 2022).
- Armitage G, Moore S, Reynolds C, Laloë PA, Coulson C, McEachan R, et al. Patient-reported safety incidents as a new source of patient safety data: an exploratory comparative study in an acute hospital in England. J Health Serv Res Policy 2018;23:36-43. https://doi.org/10.1177/1355819617727563.
- World Health Organization Europe . Patient Safety n.d. www.who.int/europe/health-topics/patient-safety#tab=tab_1 (accessed 12 September 2022).
- Louch G, Mohammed MA, Hughes L, O’Hara J. ‘Change is what can actually make the tough times better’: a patient-centred patient safety intervention delivered in collaboration with hospital volunteers. Health Expect 2018;22:102-13. https://doi.org/10.1111/hex.12835.
- Bovis JL, Edwin JP, Bano CP, Tyraskis A, Baskaran D, Karuppaiah K. Barriers to staff reporting adverse incidents in NHS hospitals. Future Healthc J 2018;5:117-20. https://doi.org/10.7861/futurehosp.5-2-117.
- Trbovich P, Vincent C. From incident reporting to the analysis of the patient journey. BMJ Qual Saf 2019;28:169-71. https://doi.org/10.1136/bmjqs-2018-008485.
- National Reporting and Learning System . NRLS Organisation Patient Safety Incident Reports: Commentary 2022. www.england.nhs.uk/patient-safety/national-patient-safety-incident-reports/national-patient-safety-incident-reports-13-october-2022/ (accessed 30 November 2023).
- Greenhalgh T, Hinton L, Finlay T, Macfarlane A, Fahy N, Clyde B, et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect 2019;22:785-801. https://doi.org/10.1111/hex.12888.
- National Institute for Health Research . Improving Inclusion in Under-Served Groups in Health and Care Research: Guidance from the NIHR-INCLUDE Project 2020. www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 (accessed 30 November 2023).
- Jackson T, Pinnock H, Liew SM, Horne E, Ehrlich E, Fulton O, et al. Patient and public involvement in research: from tokenistic box ticking to valued team members. BMC Med 2020;18. https://doi.org/10.1186/s12916-020-01544-7.
- Ocloo J, Garfield S, Franklin BD, Dawson S. Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health Res Policy 2021;19:1-21. https://doi.org/10.1186/s12961-020-00644-3.
- Fox J. Experiences of user involvement in mental health research: exploring reflections from a service user researcher using auto-ethnography. Mental Health Rev J 2020;25:281-94. https://doi.org/10.1108/MHRJ-11-2019-0040.
- Mjøsund NH, Eriksson M, Espnes GA, Haaland-Øverby M, Jensen SL, Norheim I, et al. Service user involvement enhanced the research quality in a study using interpretative phenomenological analysis – the power of multiple perspectives. J Adv Nurs 2017;73:265-78. https://doi.org/10.1111/jan.13093.
- Tambuyzer E, Van Audenhove C. Service user and family carer involvement in mental health care: divergent views. Community Ment Health J 2013;49:675-85. https://doi.org/10.1007/s10597-012-9574-2.
- Alikhanizadeh M, Hartley C, Kendal S, Neill L, Trainor G. Voices in the History of Madness: Personal and Professional Perspectives on Mental Health and Illness. Cham: Springer Publishing; 2021.
- Femi-Ajao O, Kendal S, Lovell K. A qualitative systematic review of published work on disclosure and help-seeking for domestic violence and abuse among women from ethnic minority populations in the UK. Ethn Health 2020;25:732-46. https://doi.org/10.1080/13557858.2018.1447652.
- Roodt CA, Turner M, Edmondson A, Keeley P, Kendal S. A qualitative study exploring international experiences of seeking treatment for adults with trichotillomania: a story of frustration and unmet need. J Patient Exp 2021;8. https://doi.org/10.1177/23743735211060792.
- Jones AC. Stigma and shame: conceptualisations and views concerning service use and health care provision: a literature review and commentary. J Clin Med Res 2019;1.
- Bower P, Roberts C, O’Leary N, Callaghan P, Bee P, Fraser C, et al. A cluster randomised controlled trial and process evaluation of a training programme for mental health professionals to enhance user involvement in care planning in service users with severe mental health issues (EQUIP): study protocol for a randomised controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0896-6.
- Lawton R, O’Hara J, Sheard L, Reynolds C, Cocks K, Armitage G, et al. Can staff and patient perspectives on hospital safety predict harm-free care? An analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf 2015;24:369-76. https://doi.org/10.1136/bmjqs-2014-003691.
- O’Hara JK, Lawton RJ, Armitage G, Sheard L, Marsh C, Cocks K, et al. The patient reporting and action for a safe environment (PRASE) intervention: a feasibility study. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1919-z.
- Improvement Academy . Patient Reporting and Action for a Safe Environment: PRASE 2022. www.improvementacademy.org/resource/patient-reporting-and-action-for-a-safe-environment-prase (accessed 12 September 2022).
- Sheard L, Marsh C, O’Hara J, Armitage G, Wright J, Lawton R. The patient feedback response framework – understanding why UK hospital staff find it difficult to make improvements based on patient feedback: a qualitative study. Soc Sci Med (1982) 2017;178:19-27. https://doi.org/10.1016/j.socscimed.2017.02.005.
- Chatburn E, Macrae C, Carthey J, Vincent C. Measurement and monitoring of safety: impact and challenges of putting a conceptual framework into practice. BMJ Qual Saf 2018;27:818-26. https://doi.org/10.1136/bmjqs-2017-007175.
- Wong BM, Dyal S, Etchells EE, Knowles S, Gerard L, Diamantouros A, et al. Application of a trigger tool in near real time to inform quality improvement activities: a prospective study in a general medicine ward. BMJ Qual Saf 2015;24:272-81. https://doi.org/10.1136/bmjqs-2014-003432.
- Thomas EJ. The future of measuring patient safety: prospective clinical surveillance. BMJ Qual Saf 2015;24:244-5. https://doi.org/10.1136/bmjqs-2015-004078.
- NHS Digital . NHS Safety Thermometer 2022. digital.nhs.uk/services/closed-services/nhs-safety-thermometer (accessed 22 December 2022).
- Bojke C, Castelli A, Grasic K, Mason A, Street A. Accounting for the Quality of NHS Output. York: Centre for Health Economics, University of York; 2018.
- Vincent C, Burnett S, Carthey J. Safety measurement and monitoring in healthcare: a framework to guide clinical teams and healthcare organisations in maintaining safety. BMJ Qual Saf 2014;23:670-7. https://doi.org/10.1136/bmjqs-2013-002757.
- Poh CL, Parasuram R, Kannusamy P. Nursing inter-shift handover process in mental health settings: a best practice implementation project. Int J Evid Based Healthc 2013;11:26-32. https://doi.org/10.1111/j.1744-1609.2012.00293.x.
- Improvement Academy . Using Safety Huddles in Mental Health (Violent and Aggressive Incidents) – The Experience of Bradford and District Care Trust 2016. www.improvementacademy.org/patient-safety/mental-health.html (accessed 30 November 2023).
- Rodriguez HP, Meredith LS, Hamilton AB, Yano EM, Rubenstein LV. Huddle up!: the adoption and use of structured team communication for VA medical home implementation. Health Care Manage Rev 2015;40:286-99. https://doi.org/10.1097/HMR.0000000000000036.
- Evlat G, Wood L, Glover N. A systematic review of the implementation of psychological therapies in acute mental health inpatient settings. Clin Psychol Psychother 2021;28:1574-86. https://doi.org/10.1002/cpp.2600.
- Laker C, Callard F, Flach C, Williams P, Sayer J, Wykes T. The challenge of change in acute mental health services: measuring staff perceptions of barriers to change and their relationship to job status and satisfaction using a new measure (VOCALISE). Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-23.
- Allen P, Pilar M, Walsh-Bailey C, Hooley C, Mazzucca S, Lewis CC, et al. Quantitative measures of health policy implementation determinants and outcomes: a systematic review. Implement Sci 2020;15. https://doi.org/10.1186/s13012-020-01007-w.
- Hernan AL, Giles SJ, Beks H, McNamara K, Kloot K, Binder MJ, et al. Patient feedback for safety improvement in primary care: results from a feasibility study. BMJ Open 2020;10:e037887-87e. https://doi.org/10.1136/bmjopen-2020-037887.
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Mental Health Serv Res 2010;38:65-76. https://doi.org/10.1007/s10488-010-0319-7.
- Strathdee G. Rapid Review into Data on Mental Health Inpatient Settings: Final Report and Recommendations. London: Department of Health and Social Care; 2023.
- Creswell JW, Plano Clark VL. Designing and Conducting Mixed-methods Research. Thousand Oaks, CA: SAGE; 2007.
- Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed-methods Approaches. Newbury Park, CA: SAGE; 2017.
- O’Cathain A, Murphy E, Nicholl J. The quality of mixed-methods studies in health services research. J Health Serv Res Policy 2008;13:92-8. https://doi.org/10.1258/jhsrp.2007.007074.
- Paré G, Kitsiou S. Handbook of eHealth Evaluation: An Evidence-based Approach. Victoria, BC: University of Victoria; 2017.
- Thrive by Design . Thrive by Design 2022. www.thrivebydesign.org.uk (accessed 24 October 2022).
- Ayup . Ayup 2022. https://ayup.agency (accessed 24 October 2022).
- National Institute for Health Research . Patients, Carers and the Public 2023. www.nihr.ac.uk/patients-carers-and-the-public (accessed 20 January 2023).
- Cooke JL. PRINCE2 Agile An Implementation Pocket Guide: Step-by-step Advice for Every Project Type. Ely: IT Governance Publishing; 2016.
- Sangiorgi D, Prendiville A, Ricketts A. Mapping and Developing Service Design Research in the UK. Cologne, Germany: Service Design Research UK Network; 2014.
- Zomerdijk LG, Voss CA. Service design for experience-centric services. J Serv Res 2010;13:67-82. https://doi.org/10.1177/1094670509351960.
- Care Quality Commission . The State of Care in Mental Health Services 2014 to 2017 2017.
- Davis RE, Jacklin R, Sevdalis N, Vincent CA. Patient involvement in patient safety: what factors influence patient participation and engagement?. Health Expect 2007;10:259-67. https://doi.org/10.1111/j.1369-7625.2007.00450.x.
- Smits D-W, Meeteren K, Klem M, Alsem M, Ketelaar M. Designing a tool to support patient and public involvement in research projects: the Involvement Matrix. Res Involv Engagement 2020;6:1-7. https://doi.org/doi:10.1186/s40900-020-00188-4.
- Brierley-Jones L, Ramsey L, Canvin K, Kendal S, Baker J. To what extent are patients involved in researching safety in acute mental healthcare?. Res Involv Engagement 2022;8. https://doi.org/10.1186/s40900-022-00337-x.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- JBI Manual for Evidence Synthesis. JBI Collaboration; 2020.
- Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed-Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers 2018;34:285-91. https://doi.org/10.3233/EFI-180221.
- Bamber J, de Silva D. No 23: Improving Quality in General Practice. London: Health Foundation; 2014.
- Brannon PM, Weaver CM, Anderson CA, Donovan SM, Murphy SP, Yaktine AL. Scanning for new evidence to prioritize updates to the Dietary Reference Intakes: case studies for thiamin and phosphorus. Am J Clin Nutr 2016;104:1366-77. https://doi.org/10.3945/ajcn.115.128256.
- Scanning for New Evidence on the Nutrient Content of Human Milk: A Process Model for Determining Age-specific Nutrient Requirements. Washington, DC: National Academies Press; 2020.
- Marshall JM, Dunstan DA, Bartik W. Smartphone psychology: new approaches towards safe and efficacious mobile mental health apps. Prof Psychol Res Pract 2020;51:214-22. https://doi.org/10.1037/pro0000278.
- Hallberg LRM. The ‘core category’ of grounded theory: making constant comparisons. Int J Qual Stud Health Well-Being 2006;1:141-8. https://doi.org/10.1080/17482620600858399.
- Braun V, Clarke V, Gray D. The Palgrave Handbook of Critical Social Psychology. Palgrave Macmillan/Springer Nature; 2017.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Carcach C, Goldney R, Grabosky P, Strang H. Temporal clustering of child homicide: contagion or illusion?. Aust N Z J Criminol 2001;34:182-92. https://doi.org/10.1177/000486580103400206.
- Kindermann TA, Skinner EA. Is psychology suffering from an epidemic of ‘contagion?’ Moving from metaphors to theoretically derived concepts and methods in the study of social influences. Theory Psychol 2019;29:739-56. https://doi.org/10.1177/09593543198571.
- The Therapeutic Milieu Under Fire: Security and Insecurity in Forensic Mental Health. London: Jessica Kingsley; 2012.
- Millar D. The therapeutic milieu under fire: security and insecurity in forensic mental health by John Adlam. Psychodyn Pract 2013;19:336-40. https://doi.org/10.1080/14753634.2013.807988.
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979.
- Dishion TJ, Dodge KA. Peer contagion in interventions for children and adolescents: moving towards an understanding of the ecology and dynamics of change. J Abnorm Child Psychol 2005;33:395-400. https://doi.org/10.1007/s10802-005-3579-z.
- Kanyeredzi A, Brown SD, McGrath L, Reavey P, Tucker I. The atmosphere of the ward: attunements and attachments of everyday life for patients on a medium-secure forensic psychiatric unit. Sociol Rev 2019;67:444-66. https://doi.org/10.1177/0038026119829.
- Katz P, Kirkland FR. Violence and social structure on mental hospital wards. Psychiatry 1990;53:262-77. https://doi.org/10.1080/00332747.1990.11024508.
- Hamilton BE, Manias E. Rethinking nurses’ observations: psychiatric nursing skills and invisibility in an acute inpatient setting. Soc Sci Med 2007;65:331-43. https://doi.org/10.1016/j.socscimed.2007.03.025.
- Thomson AE, Racher F, Clements K. Caring for the entire unit: psychiatric nurses’ use of awareness. J Psychosoc Nurs Ment Health Serv 2019;57:17-23. https://doi.org/10.3928/02793695-20190528-03.
- Searle RH, Rice C, McConnell AA, Dawson JF. Bad Apples? Bad Barrels? Or Bad Cellars? Antecedents and Processes of Professional Misconduct in UK Health and Social Care: Insights into Sexual Misconduct and Dishonesty. Coventry: University of Coventry; Professional Standards Agency; 2017.
- Kang M, Bushell H, Lee S, Berry C, Hollander Y, Rauchberger I, et al. Exploring behaviours of concern including aggression, self-harm, sexual harm and absconding within an Australian inpatient mental health service. Australas Psychiatry 2020;28:394-400. https://doi.org/10.1177/1039856220926940.
- Muzio D, Faulconbridge J, Gabbioneta C, Greenwood R. Organizational Wrongdoing: Key Perspectives and New Directions (Cambridge Companions to Management). Cambridge: Cambridge University Press; 2016.
- Ingram JR, Paoline Iii EA, Terrill W. A multilevel framework for understanding police culture: the role of the workgroup. Criminol Interdiscip J 2013;51:365-97. https://doi.org/10.1111/1745-9125.12009.
- Quispe-Torreblanca EG, Stewart N. Causal peer effects in police misconduct. Nat Hum Behav 2019;3:797-80. https://doi.org/10.1038/s41562-019-0612-8.
- Friis S. Measurements of the perceived ward milieu: a reevaluation of the Ward Atmosphere Scale. Acta Psychiatr Scand 1986;73:589-99. https://doi.org/10.1111/j.1600-0447.1986.tb02729.x.
- Tomlin J, Tonkin M. The EssenCES measure of ward atmosphere: Mokken scaling, confirmatory factor analysis, and investigating patient-level characteristics. Int J Forensic Ment Health 2022;22:199-20. https://doi.org/10.1080/14999013.2022.2134946.
- van der Schaaf PS, Dusseldorp E, Keuning FM, Janssen WA, Noorthoorn EO. Impact of the physical environment of psychiatric wards on the use of seclusion. Br J Psychiatry 2013;202:142-9. https://doi.org/10.1192/bjp.bp.112.118422.
- Nicholls D, Kidd K, Threader J, Hungerford C. The value of purpose built mental health facilities: use of the Ward Atmosphere Scale to gauge the link between milieu and physical environment. Int J Ment Health Nurs 2015;24:286-94. https://doi.org/10.1111/inm.12138.
- Woolston C. Words matter: jargon alienates readers. Nature 2020;579. https://doi.org/10.1038/d41586-020-00580-w.
- Kirkpatrick E, Gaisford W, Williams E, Brindley E, Tembo D, Wright D. Understanding Plain English summaries. A comparison of two approaches to improve the quality of Plain English summaries in research reports. Res Involv Engagement 2017;3. https://doi.org/10.1186/s40900-017-0064-0.
- Hatton S. Early Prioritisation of Goals. Advances in Conceptual Modeling – Foundations and Applications. Berlin: Springer; 2007.
- Ponte K. Understanding mental illness triggers 2022. www.nami.org/Blogs/NAMI-Blog/January-2022/Understanding-Mental-Illness-Triggers (accessed 17 November 2022).
- The World Wide Web Consortium . Web Content Accessibility Guidelines (WCAG) 2.1 2023. www.w3.org/TR/WCAG21 (accessed 27 June 2023).
- NHS England Transformation Directorate . Digital Technology Assessment Criteria (DTAC) 2021. https://transform.england.nhs.uk/key-tools-and-info/digital-technology-assessment-criteria-dtac (accessed 23 June 2023).
- Medicines and Healthcare Products Regulatory Agency . Guidance: Medical Device Stand-Alone Software Including Apps (including IVDMDs) v1.10e 2023. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1157146/Medical_device_stand-alone_software_including_apps.pdf (accessed 23 June 2023).
- Information Commissioner’s Office . UK GDPR Guidance and Resources 2023. https://ico.org.uk/for-organisations/uk-gdpr-guidance-and-resources (accessed 23 June 2023).
- Data Protection Act 2018 2018. www.legislation.gov.uk/ukpga/2018/12/contents (accessed 30 November 2023).
- National Institute for Health and Care Excellence . Evidence Standards Framework (ESF) for Digital Health Technologies 2023. www.nice.org.uk/about/what-we-do/our-programmes/evidence-standards-framework-for-digital-health-technologies (accessed 23 June 2023).
- NHS England . Data Security and Protection Toolkit 2023. www.dsptoolkit.nhs.uk (accessed 23 June 2023).
- Cruz EV, Higginbottom G. The use of focused ethnography in nursing research. Nurse Res 2013;20:36-43. https://doi.org/10.7748/nr2013.03.20.4.36.e305.
- Microsoft . Microsoft Trading and Brand Guidelines 2022. www.microsoft.com/en-us/legal/intellectualproperty/trademarks (accessed 22 March 2022).
- Hollway W, Jefferson T. Doing Qualitative Research Differently: Free Association, Narrative and the Interview Method. London: SAGE; 2000.
- Sutton P, Gates B. Giving voice to adults with intellectual disabilities and experience of mental ill-health: validity of a psychosocial approach. Nurse Res 2019;26:19-26. https://doi.org/10.7748/nr.2018.e1520.
- Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. JOAAG 2009;4.
- King N. Welcome to the Template Analysis Website. Huddersfield: University of Huddersfield; 2022.
- Sheard L, Marsh C, Mills T, Peacock R, Langley J, Partridge R, et al. Using patient experience data to develop a patient experience toolkit to improve hospital care: a mixed-methods study. Health Serv Deliv Res 2019;7:1-104. https://doi.org/10.3310/hsdr07360.
- Sheard L. Can patient improvement improve patient safety? A cluster randomised control trial of the Patient Reporting and Action for a Safe Environment (PRASE) intervention. BMJ Qual Saf 2017;26:622-31. https://doi.org/10.1136/bmjqs-2016-005570.
- Sheard L, Marsh C, O’Hara J, Armitage G, Wright J, Lawton R. Exploring how ward staff engage with the implementation of a patient safety intervention: a UK-based qualitative process evaluation. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014558.
- Denzin NK, Lincoln YS. Collecting and Interpreting Qualitative Materials. Thousand Oaks, CA: SAGE; 2003.
- Ritchie J, Lewis J. Qualitative Research Practice. A Guide for Social Science Students and Researchers. London: SAGE; 2005.
- Braun V, Clarke V. Thematic Analysis. n.d.
- Schalast N, Redies M, Collins M, Stacey J, Howells K. EssenCES, a short questionnaire for assessing the social climate of forensic psychiatric wards. Crim Behav Ment Health 2008;18:49-58. https://doi.org/10.1002/cbm.677.
- Westat R, Sorra J, Yount N, Famolaro T, Gray L. Rockville, MD: Agency for Healthcare Research and Quality; 2021.
- Pronovost P, Sexton B. Assessing safety culture: guidelines and recommendations. Qual Saf Health Care 2005;14:231-3. https://doi.org/10.1136/qshc.2005.015180.
- Howells K, Tonkin M, Milburn C, Lewis J, Draycot S, Cordwell J, et al. The EssenCES measure of social climate: a preliminary validation and normative data in UK high secure hospital settings. Crim Behav Ment Health 2009;19:308-20. https://doi.org/10.1002/cbm.745.
- Louch G, O’Hara J, Gardner P, O’Connor DB. The daily relationships between staffing, safety perceptions and personality in hospital nursing: a longitudinal on-line diary study. Int J Nurs Stud 2016;59:27-3. https://doi.org/10.1016/j.ijnurstu.2016.02.010.
- Corbetta M, Corso B, Camuccio CA. Rules and ward climate in acute psychiatric setting: comparison of staff and patient perceptions. Int J Ment Health Nurs n.d.;31:611-24. https://doi.org/10.1111/inm.12980.
- Barnes G-J. Researcher positionality: the Liquid Inbetweener. Practice 2021. https://doi.org/10.1080/25783858.2021.1968280.
- Byrne D. A worked example of Braun and Clarke’s approach to reflexive thematic analysis. Qual Quant 2022;56:1391-412. https://doi.org/10.1007/s11135-021-01182-y.
- Gelman A, Hennig C. Beyond subjective and objective in statistics. J R Stat Soc Ser A Stat Soc 2017;180:967-1033. https://doi.org/10.1111/rssa.12276.
- Dean J, Furness P, Verrier D, Lennon H, Bennett C, Spencer S. Desert island data: an investigation into researcher positionality. Qual Res 2018;18:273-89. https://doi.org/10.1177/1468794117714612.
- Mao L, Mian Akram A, Chovanec D, Underwood ML. Embracing the spiral: researcher reflexivity in diverse critical methodologies. Int J Qual Methods 2016;15. https://doi.org/10.1177/1609406916681005.
- Bosco A, Paulauskaite L, Hall I, Crabtree J, Soni S, Biswas A, et al. Process evaluation of a randomised controlled trial of PBS-based staff training for challenging behaviour in adults with intellectual disability. PLOS O 2019;14. https://doi.org/10.1371/journal.pone.0221507.
- Mosselson J. Subjectivity and reflexivity: locating the self in research on dislocation. Int J Qual Stud Educ 2010;23:479-94. https://doi.org/10.1080/09518398.2010.492771.
- Sands RG, Krumer-Nevo M. Interview shocks and shockwaves. Qual Inq 2006;12:950-71. https://doi.org/10.1177/1077800406288623.
- Weberg DR, Fuller RM. Toxic leadership: three lessons from complexity science to identify and stop toxic teams. Nurse Leader 2019;17:22-6. https://doi.org/10.1016/j.mnl.2018.09.006.
- Özkan A, Çamlica T, Kartal H. An analysis of the effect of nurse managers’ toxic leadership behaviours on nurses’ perceptions of professional values: a cross-sectional survey. J Nurs Manag 2022;30:973-80. https://doi.org/10.1111/jonm.13597.
- Laker C, Cella M, Callard F, Wykes T. The impact of ward climate on staff perceptions of barriers to research-driven service changes on mental health wards: a cross-sectional study. J Psychiatr Ment Health Nurs 2020;27:281-95. https://doi.org/10.1111/jpm.12577.
- Kim Y, Lee E, Lee H. Association between workplace bullying and burnout, professional quality of life, and turnover intention among clinical nurses. PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0226506.
- Farghaly Abdelaliem SM, Abou Zeid MAG. The relationship between toxic leadership and organizational performance: the mediating effect of nurses’ silence. BMC Nurs 2023;22. https://doi.org/10.1186/s12912-022-01167-8.
- Wolgemuth JR, Donohue R. Toward an inquiry of discomfort: guiding transformation in ‘emancipatory’ narrative research. Qual Inq 2006;12:1012-21. https://doi.org/10.1177/1077800406288629.
- Cowie J, Nicoll A, Dimova ED, Campbell P, Duncan EA. The barriers and facilitators influencing the sustainability of hospital-based interventions: a systematic review. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05434-9.
- Laker C, Cella M, Callard F, Wykes T. Why is change a challenge in acute mental health wards? A cross-sectional investigation of the relationships between burnout, occupational status and nurses’ perceptions of barriers to change. Int J Ment Health Nurs 2019;28:190-8. https://doi.org/10.1111/inm.12517.
- Strudwick G, Booth RG, Bjarnadottir RI, Rossetti S, Friesen M, Sequeira L, et al. The role of nurse managers in the adoption of health information technology: findings from a qualitative study. J Nurs Adm 2019;49:549-55. https://doi.org/10.1097/NNA.0000000000000810.
- Umstead CN, Unertl KM, Lorenzi NM, Novak LL. Enabling adoption and use of new health information technology during implementation: roles and strategies for internal and external support personnel. J Am Med Inform Assoc 2021;28:1543-7. https://doi.org/10.1093/jamia/ocab044.
- Alkhamees AA, Assiri H, Alharbi HY, Nasser A, Alkhamees MA. Burnout and depression among psychiatry residents during COVID-19 pandemic. Hum Resour Health 2021;19:46-9. https://doi.org/10.1186/s12960-021-00584-1.
- Foye U, Dalton-Locke C, Harju-Seppänen J, Lane R, Beames L, Vera San Juan N, et al. How has COVID-19 affected mental health nurses and the delivery of mental health nursing care in the UK? Results of a mixed-methods study. J Psychiatr Ment Health Nurs 2021;28:126-37. https://doi.org/10.1111/jpm.12745.
- Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs 2021;77:3286-302. https://doi.org/10.1111/jan.14839.
- Karcz E, Zdun-Ryżewska A, Zimmermann A. Loneliness, complaining and professional burnout of medical personnel of psychiatric wards during COVID-19 pandemic – cross-sectional study. Healthcare 2022;10.
- Labrague LJ, Santos JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag 2021;29:395-403. https://doi.org/10.1111/jonm.13168.
- Liberati E, Richards N, Willars J, Scott D, Boydell N, Parker J, et al. A qualitative study of experiences of NHS mental healthcare workers during the Covid-19 pandemic. BMC Psychiatry 2021;21. https://doi.org/10.1186/s12888-021-03261-8.
- Sieverink F, Kelders S, Poel M, van Gemert-Pijnen L. Opening the black box of electronic health: collecting, analyzing, and interpreting log data. JMIR Res Protoc 2017;6.
- Yeager CM, Benight CC. If we build it, will they come? Issues of engagement with digital health interventions for trauma recovery. Mhealth 2018;4. https://doi.org/10.21037/mhealth.2018.08.04.
- Borghouts J, Eikey E, Mark G, De Leon C, Schueller SM, Schneider M, et al. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J Med Internet Res 2021;23. https://doi.org/10.2196/24387.
- Patel S, Akhtar A, Malins S, Wright N, Rowley E, Young E, et al. The acceptability and usability of digital health interventions for adults with depression, anxiety, and somatoform disorders: qualitative systematic review and meta-synthesis. J Med Internet Res 2020;22. https://doi.org/10.2196/16228.
- Saleem M, Kühne L, de Santis KK, Christianson L, Brand T, Busse H. Understanding engagement strategies in digital interventions for mental health promotion: scoping review. JMIR Ment Health 2021;8. https://doi.org/10.2196/30000.
- Lipschitz JM, Van Boxtel R, Torous J, Firth J, Lebovitz JG, Burdick KE, et al. Digital mental health interventions for depression: scoping review of user engagement. J Med Internet Res 2022;24. https://doi.org/10.2196/39204.
- Gan DZQ, McGillivray L, Larsen ME, Christensen H, Torok M. Technology-supported strategies for promoting user engagement with digital mental health interventions: a systematic review. Digit Health 2022;8. https://doi.org/10.1177/20552076221098268.
- Escriva Boulley G, Leroy T, Bernetière C, Paquienseguy F, Desfriches-Doria O, Préau M. Digital health interventions to help living with cancer: a systematic review of participants’ engagement and psychosocial effects. Psychooncology 2018;27:2677-86. https://doi.org/10.1002/pon.4867.
- Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual Research Review: digital health interventions for children and young people with mental health problems – a systematic and meta-review. J Child Psychol Psychiatry 2017;58:474-503. https://doi.org/10.1111/jcpp.12663.
- Gergen KJ, Gergen M. The SAGE Handbook of Social Science Methodology. Thousand Oaks, CA: SAGE; 2007.
- Altman I. The Environment and Social Behavior: Privacy, Personal Space, Territory, and Crowding. Pacific Grove, CA: Brooks/Cole; 1975.
- Salmon P, Young B. Qualitative methods can test and challenge what we think we know about clinical communication – if they are not too constrained by methodological ‘brands’. Patient Educ Couns 2018;101:1515-7. https://doi.org/10.1016/j.pec.2018.07.005.
- National Institute for Health Research . How can acute mental health wards be improved? [plain English summary of https://doi.org/10.1111/inm.12835] 2021. https://evidence.nihr.ac.uk/alert/how-can-acute-mental-health-wards-be-improved/ (accessed 24 November 2022).
- McAllister S, Simpson A, Tsianakas V, Robert G. ‘What matters to me’: a multi-method qualitative study exploring service users’, carers’ and clinicians’ needs and experiences of therapeutic engagement on acute mental health wards. Int J Ment Health Nurs 2021;30:703-14. https://doi.org/10.1111/inm.12835.
- Mitchell R. How to overcome the challenges of doing research during Covid-19 [blog post]. Institute of Development Studies 2021. www.ids.ac.uk/opinions/how-to-overcome-the-challenges-of-doing-research-during-covid19/ (accessed 27 October 2022).
- Chen R, Sun C, Chen JJ, Jen HJ, Kang XL, Kao CC, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs 2021;30:102-16. https://doi.org/10.1111/inm.12796.
- Li TM, Pien LC, Kao CC, Kubo T, Cheng WJ. Effects of work conditions and organisational strategies on nurses’ mental health during the COVID-19 pandemic. J Nurs Manag 2022;30:71-8. https://doi.org/10.1111/jonm.13485.
- Slade T, Gross DP, Niwa L, McKillop AB, Guptill C. Sex and gender demographic questions: improving methodological quality, inclusivity, and ethical administration. Int J Soc Res Methodol 2021;24:727-38. https://doi.org/10.1080/13645579.2020.1819518.
- Hasnain-Wynia R, Taylor-Clark K, Anise A. Collecting race, ethnicity, and language data to identify and reduce health disparities: perceptions of health plan enrollees. Med Care Res Rev 2010;68:367-81. https://doi.org/10.1177/1077558710382549.
- Damianakis T, Woodford MR. Qualitative research with small connected communities: generating new knowledge while upholding research ethics. Qual Health Res 2012;22:708-18. https://doi.org/10.1177/1049732311431444.
- Call CC, Eckstrand KL, Kasparek SW, Boness CL, Blatt L, Jamal-Orozco N, et al. An ethics and social-justice approach to collecting and using demographic data for psychological researchers. Perspect Psychol Sci 2022;18:979-95. https://doi.org/10.1177/17456916221137350.
Appendix 1 Detail of literature reviews
Scoping review of patient involvement in safety research
Full report in: Brierley-Jones L, Ramsey L, Canvin K, Kendal S, Baker J. To what extent are patients involved in researching safety in acute mental healthcare? Res Involv Engagement 2022;8(1):8. https://doi.org/10.1186/s40900-022-00337-x
Evidence scan of the application of digital technology in mental health contexts
Date: 5 November 2020
Search string <mental health AND digital technology AND safety>
Databases accessed: CINAHL, PsycINFO, Web of Science.
Search results
The included papers are listed in Table 18.
General
-
Most research in this area appears to be concentrated on therapeutic interventions, such as detecting suicidal ideation/risk or offering psychological support therapies, such as counselling. There is also a focus on telecare, but the design of apps for a variety of uses in mental health is also a feature.
-
It is acknowledged in the literature that digital technologies are in their infancy in specific relation to mental health. Nevertheless, concerns exist around the plethora of digital technologies (mainly apps) that have been primarily designed by the tech industry, often with little or no mental health professional input.
Technology design
-
Usability and accessibility is emphasised for both staff and patients.
-
Patient anonymity is frequently suggested (but this is mainly in the context of delivering therapeutic interventions via technology and the input of personal data).
-
Devices most frequently used in a mental health setting are apps for smartphones, tablets and websites (in that order of preference).
-
Text and images are suggested as means of communication via technology.
-
Assessment of efficiency of any technology should use multiple baseline single-case designs (this is because many interventions are therapeutic, but this may apply to individual patients’ notions of safety). General message is that some kind of base-lining is important.
-
Design features are important such as colour scheme, SOS facility.
-
Context important: do patients over or under report safety incidents in real time?
-
There is contradictory evidence regarding age as a barrier to take up.
-
Patients expressed concern over confidentiality.
-
Any technology needs to facilitate existing workflows (not hinder them).
-
Staff consider apps better than computer interventions.
-
Detecting risk situations depends on: a. Input type from user (e.g. free text or closed questions?). b. Establishing a threshold for action.
-
‘Contagion’ means certain questions and phrases should only be used once a risk situation has been identified.
-
Technology should be personalised wherever possible (perhaps in relation to subjects’ previous responses).
-
Early service user involvement in design means that any digital technology is less likely to be seen as a nuisance, or worse still, as paternalistic.
Technology implementation
-
Staff, and even patient, training is a recurrent theme. Staff technology champions are also seen as effective for implementation.
-
Consistent availability is considered crucial for ongoing staff and patient participation. This includes Wi-Fi connectivity but also swift repair if and when things go wrong. The NHS is noted as not being great for technology implementation or maintenance. Consistent availability of the technology is considered vital for ongoing patient engagement.
-
Members of research team being on ward to trouble is shoot seen as crucial, especially in pilot phase/early days.
-
Positive collaborations are important between research team, data scientists and technicians for continuous data flow.
Technology engagement
Staff
-
Initial set-up meetings and constant negotiation with staff improves engagement.
-
Staff confidence and comfort in technology usage also requires addressing.
-
Staff worried about devices when dealing with aggressive patients, for example, could be snatched and used as a weapon.
-
Staff need to be aware that patients may misinterpret device usage.
-
Staff worry about deskilling.
-
Any technology has to be easily accessible by staff.
-
Staff expressed concerns over patients from disadvantaged socioeconomic backgrounds underusing the technology.
-
Staff fear a constant stream of data to which they cannot respond and they remain cautious about real-time monitoring.
Patients
-
Cognitive, language and literacy skills of patients are highly varied; raised by staff as a concern with technological engagement (our staff interviews bring this out too).
-
Psychological morbidity is also considered a factor for patient engagement (e.g. some patients will experience increased anxiety from technology use). Staff believe smartphone may exacerbate patient symptoms.
-
There is potential harm to patients reported.
-
Any technology must be suitable for those with intellectual disabilities (our staff interviews brought this out too). Many use only basic functions. Can often have physical disabilities too affecting both fine and gross motor skills. Sensory impairment may mean small mobile screens are not suitable for these patients.
-
Most studies reported little or no damage or loss of equipment during use.
-
Patients reported fears of being recorded or pictures taken without their knowledge/consent (reported as paranoia). They also expressed fears about reporting impacting their care or leave.
-
Good communication with patients and carers vital for uptake.ie what the technology is and what it is used for.
-
Digital technology can increase patient empowerment.
-
Digital technology is good for patients who may dislike face-to-face interaction/confrontation.
| No. | Authors | Title | Source | Year | Summary |
|---|---|---|---|---|---|
| 1 | Barrera et al. | Introducing artificial intelligence in acute psychiatric inpatient care: qualitative study of its use to conduct nursing observations | Original Research: Digital Mental Health 23:34–8. hrrps://doi.org/10.1136/ebmental-2019-300136 | 2020 | The aim of this project was to establish whether it is safe to conduct nursing observations remotely from the nursing office using a novel digital technology. The use of Oxehealth® (Oxford, UK) sensors, which employ a software that uses computer vision, signal processing and AI techniques removed the need for nurses to directly observe patients at night and thus disturb them. All staff were trained on the new protocol, emphasising that they should always check patients in person if they felt that anything might not be right. Thus, if the nursing staff using the sensors had any concerns (e.g. patient on the floor, pacing or another person in the room), the member of the staff is prompted to go and check the patient in person. |
| Two thousand seven hundred and forty-nine nursing observations using the sensors were done. There were no significant gaps or drops in usage, suggesting that staff were using them even when the project team’s presence was less intense. On a few nights, usage was slightly lower than expected, so some staff members became ‘sensors champions’ ensuring all staff were trained each night shift. Ten members of the staff were surveyed, and all reported that the sensors were easy and fast to use and had had a positive impact on patient and staff experience. Forty-three patients were surveyed about their experience at night. While most comments from patients were not related to the sensors, the comments that did mention them were all positive, and some described their impact on sleep. | |||||
| 2 | Melvin et al. | Evaluating the feasibility and effectiveness of an Australian safety planning smartphone application: a pilot study within a tertiary mental health service | Suicide and Life Threatening Behaviour 49: 846–58 | 2019 | The majority of participants reported accessing the BeyondNow app during the study, either to edit their safety plan or to view it to manage their suicidal crisis. Google Analytics data revealed that the app was accessed over 200 times by participants across the trial. The highest number of entries was observed within the warning signs and internal coping sections, and fewer entries were entered into the external coping strategy sections. Also shown to be feasible given the high level of usability, with a vast majority of participants reporting that they were able to set up and navigate the BeyondNow app without difficulty. All participants at follow-up reported that they would recommend the app to a friend. |
| Qualitative analysis also revealed a high regard for the app’s utility. App feasibility was also supported by the finding that participants developed a sense of hope and connection from using the app. The intervention was associated with increased knowledge of, and confidence in using, strategies to help cope with suicidal thoughts. The frequency of engagement with adaptive strategies to help cope with suicidal thoughts increased over the trial. Contrary to expectations, no change in suicide resilience was observed across the trial period, which contrasts the related construct of suicide-related coping. It is possible that suicide resilience might change slowly over time, perhaps with insufficient change detectable over the period of the current trial. It was also hypothesised that the App + TAU intervention would be associated with reduced suicidal thinking. The results support this prediction, showing a significant reduction in the severity and intensity of suicide ideation across the trial period. | |||||
| 3 | Dewa et al. | What do young people think about using technology to detect worsening mental health? | PLOS ONE 14:e0222655. www.nationalelfservice.net/treatment/digital-health/young-people-using-technology-to-detect-worsening-mental-health/ | 2019 | Most participants agreed that monitoring their mental health using technologies such as apps, wearables and social media could be possible for spotting signs of mental health deterioration earlier. Additionally, participants believed that while monitoring and flagging warning signs was needed, acting on these was vital. Suggested actions included displaying helplines, calling an ambulance or other emergency services, having immediate online access to a designated psychiatrist or psychologist or going to hospital. |
| 4 | Christie S | Big White Wall: transforming mental health services through digital technologies | Mental Health and Social Inclusion Journal 17: 202–5 | 2013 | ‘Big White Wall’ (BWW) uses digital technologies and social networking to provide safe, anonymous online support in mental health. BWW has been designated a high impact innovation by the NHS, and offers digital assessment: an online tool to assess common mental health problems and co-morbid physical conditions. ‘SupportNetwork: a community of peers which enables safe, anonymous support through talking therapies and creative self-expression.’ (posting comments on the ‘wall’). GuidedSupport: a range of self-managed and facilitated programmes for individuals and groups. Programmes include anxiety, depression, sleep, smoking and alcohol use. |
| LiveTherapy: a range of real-time therapies by instant text, audio or video from a panel of approved BWW therapists offering CBT, interpersonal therapy, person-centred counselling and integrative counselling. Alternatively local services can provide tele-health services using their own clinicians through this platform. BWW services a number of markets including health care, military, employers and education. It has contracts that cover 22% of the UK population aged 16 years and over. Everyone on BWW gets access to the SupportNetwork service, where members can receive peer and professional support. It’s staffed 24/7 by trained counsellors, who facilitate and moderate to keep the community safe. Members can express themselves in words and images, by creating vibrant bricks that are added to the wall. Up to 95% of members report increased well-being after using the SupportNetwork. | |||||
| 5 | Sheehan and Hassiotis | Digital mental health and intellectual disabilities: state of the evidence and future directions | BMJ Evidence Based Mental Health 20:107–11. https://doi.org/10.1136/eb-2017-102759 | 2017 | This review paper discusses the intelligent integration of digital technologies into mental health care which can support a cultural shift to the recovery model and increase service user empowerment in mental health care. Approximately 1 million adults in England have an intellectual disability.4 People with intellectual disability have lifelong deficits in cognitive and adaptive functioning that impinge on a variety of everyday activities.5 As clinicians working with people with intellectual disability, we are interested in the potential of digital mental health to deliver improved methods of engaging with service users and managing mental health. The Review also considers how technology might be designed and implemented to achieve maximum benefit for all, ensuring that no one is left behind. |
| Relevant literature published in English was identified by Medline and Google Scholar searches up to 31 May 2017. Best estimates indicate that between one-quarter and one-half of people with intellectual disability access the internet.10,11 The use of mobile phone is lower among people with intellectual disability than in the general population and people with intellectual disability tend to use the basic functions of devices rather than more sophisticated operations.12 Uptake of newer devices (such tablet computers and smartwatches) by people with intellectual disability has not been studied in any depth but is likely to similarly lag behind use in the wider population. | |||||
| The gap between those who have access to information and communication technologies and those who do not has been termed the ‘digital divide’. In addition to the cognitive obstacles faced in accessing digital technologies, many people with intellectual disability have physical limitations that can affect fine and gross motor skills and the ability to use keyboards or a traditional computer mouse. Sensory impairments are common and can hinder the viewing of information on the small screens of mobile devices. | |||||
| Universal design (alternatively known as ‘design for all’) is the design of products and environments usable by all people, to the greatest extent possible, without the need for adaptation.28 People with intellectual disability are able, and willing, to use digital technologies. | |||||
| 6 | Marshall et al. | Smartphone psychology: new approaches towards safe and efficacious mobile mental health apps | Professional Psychology: Research and Practice 51:214–22. https://doi.org/10.1037/pro0000278 | 2020 | Like most articles in this area, this paper investigates the safety of mental health apps as therapeutic devices. However, the article does raise some interesting issues vis a vis technology use in mental health, regardless of its purpose. The article states that there is disparity about an acceptable methodology for examining the effectiveness of a mental health app and proposes a new approach to incorporate multiple baseline single-case designs to increase the amount of evidence and to guide larger-scale randomised controlled trials, something that could and should include practicing psychologists. This novel approach also proposes that mental health apps undergo a new ‘certification’ process with the participation of app store marketplaces. |
| 7 | Hoffman et al. | Augmenting mental health in primary care: a 1-year study of deploying smartphone apps in a multi-site primary care/behavioural health integration programme | Frontiers in Psychiatry 10: 94 | 2019 | Although this study relates to primary care, if an app is being considered for WardSonar its findings may be relevant. Their findings indicate mental health apps are applicable and relevant to patients within integrated primary care settings in safety-net health systems. Behavioural health providers perceive the clinical value of using these tools as part of patient care, but require training to increase their comfort level and confidence applying these tools with patients. To increase provider and patient engagement, mobile apps must be accessible, simple, intuitive and directly relevant to patients’ treatment needs. |
| 8 | Bruen et al. | Exploring suicidal ideation using an innovative mobile app-strength within me: the usability and acceptability of setting up a trial involving mobile technology and mental health service users | JMIR Mental Health 7:e18407. https://doi.org/10.2196/18407 | 2020 | This study reports the practicalities and acceptability of setting up and trialling digital technologies within an inpatient mental health setting in the UK and highlights their implications for future studies. Service users were recruited from six inpatient wards in the north west of England. Service users who were eligible to participate and provided consent were given an iPhone and Fitbit for 7 days and were asked to interact with a novel phone app, SWiM. Interaction with the app involved journaling (recording daily activities, how this made them feel, and rating their mood) and the option to create safety plans for emotions causing difficulties (identifying strategies that helped with these emotions). Participants also had the option to |
| allow the study to access their personal Facebook account to monitor their social media use and activity. In addition, clinical data (i.e. assessments conducted by trained researchers targeting suicidality, depression, and sleep) were also collected. Overall, 43.0% (80/186 response rate) of eligible participants were recruited for the study. Of the total sample, 67 participants engaged in journaling, with the average number of entries per user being 8.2 (SD 8.7). Overall, only 24 participants created safety plans and the most common difficult emotion to be selected was feeling sad (n = 21). This study goes into some detail on design and use of the app (but bear in mind this app was for therapeutic purposes and not all points apply). | |||||
| Several participants identified the ease of using an app on a phone; you ‘don’t always have pen and paper, but you always have your phone’. Participants commented on improvements they would like to see in the app, such as changing the colour scheme, including uplifting quotes, having self-help links, and an SOS (an abbreviation for distress) button for helpful contact numbers. The staff at the participating sites expressed concerns about giving service users iPhones and Fitbits for the duration of the study, suggesting that the equipment would either be stolen or damaged. They were also concerned about who would be responsible for monitoring the devices. However, out of 18 iPhones and Fitbits, only one phone and one Fitbit were lost and one phone was accidently damaged. All other devices were returned intact. | |||||
| Pros and cons of apps: one of the advantages of using digital technology is that it has the potential to be an efficient and cost effective However, there are cost issues that might hinder the adoption of health apps within services such as access to smartphones, connectivity, development and regular updates of apps, and the maintenance of the technology. | |||||
| This study found that 4G connectivity was essential for reliable and continuous access to the SWiM app. An important element in this study was capturing people’s thoughts in real time and fluctuations in mood. This required participants to be able to journal at any time without the worry of loss of connectivity and journal entries not being saved. Future studies using mobile apps should strive for as much connectivity as possible to allow for consistent functionality. Although this may have financial implications for research budgets, it is a vital consideration for future research not only to ensure continued participation in studies in part for security reasons. | |||||
| Of the total sample, 12 participants were affected by technological issues, with one service user being unable to take part. This study illustrates the importance of having the research team available in participating wards to trouble shoot issues in a timely manner. It also demonstrates the significance of having positive working collaborations within the research team, including data scientists and technicians, to ensure a continuous flow of data. This is supported by previous research that emphasises the importance of collaborative partnerships between researchers, clinicians, app developers, and service users. The initial cost of the devices and the | |||||
| possibility of having to replace them were concerns in this study that proved to be unfounded. A concern raised by staff in the context of this study was that smartphones would be broken, lost or stolen. Clear policies about responsibilities and implementation could help avoid these issues. In this study, a contract with the service user placed the responsibility for the iPhone and Fitbit on the participant. The extent to which the contract influenced how a participant took care of the devices is unclear. It is possible, in general, that people are more responsible about other people’s equipment than we give them credit for. | |||||
| Establishing good working relationships between research and clinical staff before commencing recruitment and then maintaining them is vital to building enthusiasm for study trials. In line with this, the value of developing positive working relationships with frontline workers is equally important. Although having an initial set-up meeting was critical for the study to begin, having constant negotiations with the staff maintained the profile of the study with staff. It has been suggested that key engagement strategies should be employed with frontline staff in the design and rollout of a study to improve engagement. Positive relationships are crucial for effective recruitment. Future research should consider the most effective ways of engaging with the wider clinical team to enhance recruitment to studies. | |||||
| In this study, several participants reported that they experienced suicidal thoughts on which they had no intention of acting. This raises the question of whether in clinical practice there is a tendency to over-rely on personal expression of suicidal thoughts, which may lead to premature and unnecessary intervention in the lives of service users. Careful consideration needs to be given to the ways in which people think and feel in the context of suicide if digital apps are to be designed to accurately predict the risk of suicide. In contrast to previous research that suggests older people may have difficulties with mental health apps, this study included people aged 18–61 years, and there were no reports from participants about difficulty in using iPhones or Fitbits. | |||||
| Age does not appear to be a factor that affects a participant’s interest or ability to use mental health apps, research in digital apps should therefore not assume that older people will not be interested in participating. Given the ageing population, research, using mobile phone apps should allow for the participation of adults across a wide range of age groups and should not just focus on younger people. | |||||
| 9 | Marshall et al. | Smartphone psychology: new approaches towards safe and efficacious mobile mental health apps | Professional Psychology-Research and Practice 51:214–22. https://doi.org/10.1037/pro0000278 | 2020 | The use of mobile mental health applications (apps) is a contentious issue in the therapeutic context because a large proportion of such apps has been developed by individuals who are not mental health experts. The shortcomings of mental health apps include suboptimal use of the available technological features of smartphones but also a lack of technology literacy on the part of some users, particularly the elderly, who may struggle to operate apps and smartphones generally. Single-case designs have advantages over RCTs. More information about individual participants can be captured in a single-case design, as compared with RCTs where only group means are reported. Therefore, it is possible to make more informed hypotheses about how peripheral issues may have influenced results. Also, data can be collected at more time intervals |
| in single-case designs, more precisely identifying when outcomes change in respect to changes in treatment. These designs also offer the opportunity for real-time monitoring and therefore tailoring to the responses from individuals. Finally, data can be collated and analysed faster in single-case designs compared to larger RCTs, a crucial point in the world of mobile apps, where development and listing on app stores happen at rapid speeds. As a practical exercise for clinicians (and researchers), the following is a simplified demonstration of how such a protocol might look and how research on a mental health app may progress using the methodology of a multiple baseline across-subjects in a practice setting. Five individuals are asked to use a specific app. A baseline period is established to confirm a series of stable readings across time (and this allows each individual to act as their own control). | |||||
| 10 | Brimblecombe et al. | A mixed-methods survey to explore views of staff and patients from mental health wards prior to introduction of a digital early warning system for physical deterioration | Journal of Psychiatric and Mental Health Nursing 26:65–76 | 2019 | This study adds to the existing evidence by reporting specific staff and patient concerns about a technological development in an inpatient mental health setting. ‘Early warning systems’ are increasingly used in inpatient mental health services to detect physical deterioration in patients and prompt staff to take appropriate action. Using a questionnaire survey, this project gathered views from staff and patients on a planned change from a paper-based ‘early warning system’ to one using handheld electronic devices (tablets). Some patients were concerned about confidentiality of data entered onto tablets. While were either positive or neutral in attitude to the planned change some staff raised concerns that electronic devices could be used as weapons, and also that patients or visitors might misinterpret their use. Views of staff and patients must be considered when introducing new technology into clinical practice, in order to make the change successful and sustainable. Inadequate or unclear information about the use and purpose of electronic devices may lead to misunderstandings as to their purpose and the security of their data, particularly in mental health settings. Eighty-two staff and 26 inpatients completed questionnaires. Some inpatients expressed concerns about data confidentiality. Most staff were neutral or positive about the planned change, but raised possible safety risks and the risk of electronic recording being misinterpreted by patients. The implementation plan was modified in response to this information, principally by improving communication processes with patients. The authors cite several studies but two most relevant appear to be: |
|
|||||
| Technology designed to allow staff to record patient observations into a mobile device (such as an electronic tablet), quickly and at the point of care. Such mobile observations are typically termed ‘eObs’. The information is automatically uploaded into an electronic patient record system. ‘eObs’ may feature predefined algorithms (procedures for solving a problem, based on conducting a sequence of specified actions) to alert staff that an identified action is required in response to observations. The first such development planned by the trust was designed to improve compliance with escalation processes indicated by the early warning system when physical health deterioration is identified, for example, calling medical staff or increasing observation. | |||||
| Aimed to collate views of staff and inpatients related to prospective use of eNEWS to inform the plan for implementation. Risks associated with using handheld devices on mental health ward-several described the potential for an aggressive patient to snatch a device from staff and assault staff or other patients with it. Some felt that patients might experience paranoid ideas about the devices, ‘they may think that they are being recorded or pictures taken’ or that visitors to the ward might believe that staff were using the tablets for personal use; for example, looking at Facebook. General concerns were associated with previous negative experience with IT systems, such as slow processing time and frequent network problems. Changes to the project arising from patient and staff comments. A number of modifications were made to the detailed project plan for the implementation of eNEWS in response to views elicited in the surveys and discussion groups (see Table 5). These focused largely on improving communication to patients and carers about the purpose and processes of eNEWS. | |||||
| The main concern of patients was that data entered into the tablet could easily be lost or illicitly accessed. This reflected a lack of information provided to patients at that point in time as to the mechanism of eObs. This detail was included in future communications about the introduction of eNEWS. Patients viewed increased frequency of physical observations as related to their personal experience of delays to leave commencing due to poorly timed physical observations on the ward. As a result, an increase in physical health observations was seen as potentially further delaying their leave. This highlighted the need to understand context users’ concerns in the local context to successfully engage them with development projects. The findings are | |||||
| congruent with the concepts of the Technology Acceptance Model (Davis 1989), whereby acceptance and use of technology depends on perceptions of ease of use and usefulness. The most frequent expectation for improvement related to features inherent in the eNEWS’ system design, such as improving the calculation of risk scores, while other more speculative improvements, such as improving staff/service use interaction, were seen as less likely. The caution expressed by patients as to the use of electronic recording devices suggests that mental health staff may need to be aware of possible misinterpretations of technological developments and to ensure that information provided is clear and consistent. | |||||
| Reference: Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13:319–40. https://doi.org/10.2307/249008 | |||||
| 11 | Bucci et al. | ‘They are not hard-to-reach clients. we have just got hard-to-reach services’. staff views of digital health tools in specialist mental health services | Frontiers in Psychiatry 10:344. https://doi.org/10.3389/fpsyt.2019.00344 | 2019 | Staff working in specialist early intervention for psychosis services found digital tools on the whole acceptable in mental health service provision, but raised a number of concerns that will likely affect implementation of such systems into routine service delivery and practice. Thirteen recommendations are made in this paper as a result of the themes generated in these data. Implementing of digital systems needs to be simple and uncomplicated and improve clinical workflows for staff rather than hinder and increase clinical workflows. Furthermore, organisational support with a clear plan for implementing technological innovations is required for successful adoption of digital systems. Consideration of staff views around digital systems is important if successful adoption and implementation of such systems are to occur. Staff barriers: |
|
|||||
|
|||||
|
|||||
|
|||||
| 12 | Myrthe et al. | Considering patient safety in autonomous e-mental health systems – detecting risk situations and referring patients back to human care | BMC Medical Informatics and Decision Making 19:47 | 2019 | Risk detection model: Exactly how to detect a risk situation depends on two factors that might differ per AEMH system. The first factor is what type of input the AEMH system gets from the user. Some systems allow free-text input from the user and work as a type of chatbot, while others work with closed questions and questionnaires. A system with free-text input is capable of screening the input on keywords and phrases related to risk situations. Additionally, it might include specific questions for risk screening. A system without free-text input would need to rely on the second screening method. To determine how to detect a risk, the second factor is whether there is a measure for the risk situation that can be used to establish a threshold for referral. The exact threshold score needs to be established in concord with clinical specialists. It might also be necessary to adapt the threshold during use if it becomes clear that too many or too few situations are detected. It is important to note that posing questions to establish risk thresholds might only be appropriate after a possible risk situation has already been detected, which is why this action is not located in the detection part of this model. Especially for suicide, posing unwarranted questions about suicidal ideation might not be the preferred approach. Suicide contagion is a well-studied phenomenon where hearing about suicide prompts suicidal people to commit suicide. This means that care should be taken to only pose suicide question when the situation already indicates this might be a problem. |
| 13 | Depp et al. | Mobile interventions for severe mental illness design and preliminary data from three approaches | Journal of Nervous and Mental Disease 198:715–21. https://doi.org/10.1097/NMD.0b013e3181f49ea3 |
2010 | This study provides the rationale, design, and preliminary data from three clinical trials of mobile interventions developed for bipolar disorder or schizophrenia. There was no evidence for overriding operational and logistic barriers (e.g. loss of devices), rates of adherence to mobile interactions were similar to that seen in other populations, and qualitative feedback from consumers indicated perceived usefulness. There are several commonalities among the three pilot studies that likely enhanced the capacity of individuals to learn to use and to accept mobile devices. Multimodal training procedures and extensive pilot testing may help to increase feasibility and reduce the likelihood of implementation problems in the field. We found that many participants did not have familiarity with mobile devices, particularly in the two studies enrolling patients with schizophrenia, and training participants in the use of devices combined of modelling, practice, and printed manuals. Manuals made use of ‘worked examples’ (Paas et al. 2004), |
| which are diagrams or screenshots that describe user actions. Careful attention to operational problems is essential, as particularly in experience sampling, participants view the same questionnaire many times over the course of the study – therefore small problems or annoyances are amplified (Shiffman et al. 2008). In terms of increasing acceptance of mobile devices, we observed that early involvement of consumers and other stakeholders assists in fitting intervention with consumer preferences, helping to promote attitudes toward mobile device as a helpful tool rather than a nuisance, or worse, paternalistic. Increasing the perceived value of mobile devices can also be achieved by enabling participants to use other device features (e.g. cell phone calls, games, calendar functions). Permitting participants to schedule when prompts or phone calls occurred provides some user control over the experience. Rapid prototyping (Kinzie et al. 2002) that combines needs assessments, qualitative interviews, focus groups, and iterative truncated developmental trials in the population is an applicable approach to intervention development. | |||||
| References: Kinzie M, Cohn W, Julian M, et al. A user-centred model for web site design: needs assessment, user interface design, and rapid prototyping. J Am Med Informatics Assoc 2002;9:320. https://doi.org/10.1197/jamia.M0822 Paas F, Renkl A, Sweller J. Cognitive load theory: instructional implications of the interaction between information structures and cognitive architecture. Instruct Sci 2004;32:1–8. https://doi.org/10.1023/B:TRUC.0000021806.17516.d0 Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Ann Rev Clin Psychol 2008;4:1–32. https://doi.org/10.1146/annurev.clinpsy.3.022806.091415 |
Appendix 2 Project documents
Appendix 2a: Phase 2 interview topic guide
FIGURE 21.
Phase 2 interview topic guide.
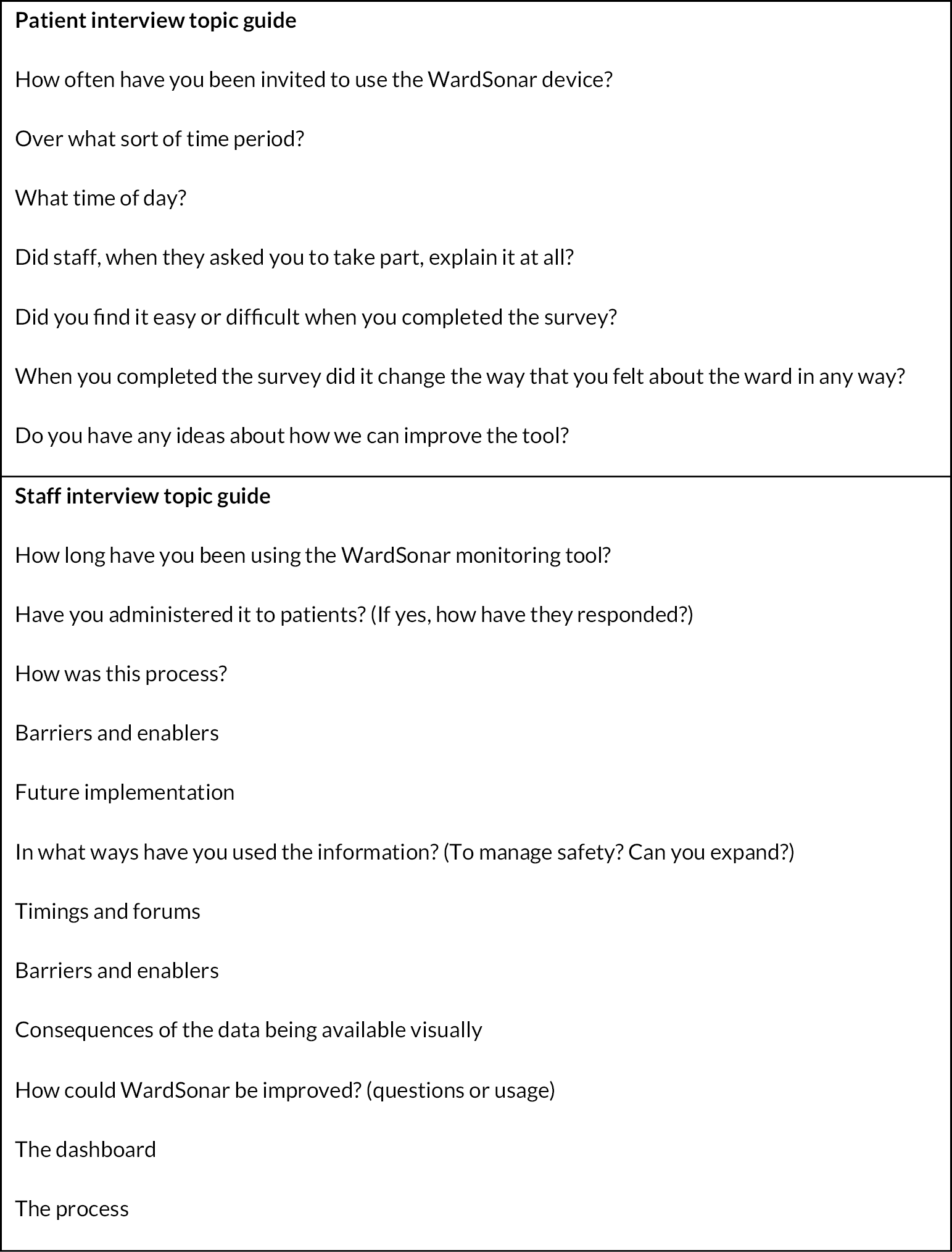
Appendix 2b: Staff questionnaire for pre- and post-implementation analyses
Questionnaire Booklet
(Staff)
PLEASE RETURN COMPLETED BOOKLETS TO THE BOX LOCATED IN THE STAFF AREA OR HAND BACK TO A WARDSONAR RESEARCHER ON THE WARD
The #WardSonar research team are asking all staff on the ward to complete this questionnaire booklet on two occasions during the study (beginning and end). You will also be invited to complete a much shorter questionnaire on three occasions during the study (beginning, middle and end).
The questionnaires are completely anonymous. There are some questions about you followed by questions about how safe the ward feels.
The booklet will take about 10 minutes to complete.
Please tick the box by the answers you want to give.
Please only give one answer for each question.
You can add any other comments at the end.
About you
| Age | |
| Gender | |
| Ethnicity | |
| Role (e.g. nurse; HCA) | |
| How many years have you been doing this job? | |
| Approximately how long have you worked on this particular ward? | |
Please tick one response to each statement about the ward.
| I agree | |||||
|---|---|---|---|---|---|
| Not at all | A little | Somewhat | Quite a lot | Very much | |
| This ward has a homely atmosphere | |||||
| The patients care for each other | |||||
| Really threatening situations can occur here | |||||
| On this ward patients can openly talk to staff about all their problems | |||||
| Even the weakest patient finds support from his/her fellow patients | |||||
| There are some really aggressive patients on this ward | |||||
| Staff take a personal interest in the progress of patients | |||||
| Patients care about their fellow patients’ problems | |||||
| Some patients are afraid of other patients | |||||
| Staff members take a lot of time to deal with patients | |||||
| When patients have a genuine concern, they find support from their fellow patients | |||||
| At times, members of staff are afraid of some of the patients | |||||
| Often, staff seem not to care if patients succeed or fail in treatment | |||||
| There is good peer support among patients | |||||
| Some patients are so excitable that one deals very cautiously with them | |||||
| Staff know patients and their personal histories very well | |||||
| Both patients and staff are comfortable on this ward | |||||
This next section asks for your opinions about patient safety issues, medical error and event reporting.
-
‘Patient safety’ is defined as the avoidance and prevention of patient injuries or adverse events resulting from the processes of healthcare delivery.
-
A ‘patient safety event’ is defined as any type of healthcare-related error, mistake or incident, regardless of whether or not it results in patient harm.
Please tick one response to each statement.
How much do you agree or disagree with the following statements about your unit/work area?
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| In this unit, we work together as an effective team | |||||
| In this unit, we have enough staff to handle the workload | |||||
| Staff in this unit work longer hours than is best for patient care | |||||
| This unit regularly reviews work processes to determine if changes are needed to improve patient safety | |||||
| This unit relies too much on temporary, float or staff as needed | |||||
| In this unit, staff feel like their mistakes are held against them | |||||
| Strongly
disagree |
Disagree | Neither agree nor disagree | Agree | Strongly agree | |
| When an event is reported in this unit, it feels like the person is being written up, not the problem | |||||
| During busy times, staff in this unit help each other | |||||
| There is a problem with disrespectful behaviour by those working in this unit | |||||
| When staff make errors, this unit focuses on learning rather than blaming individuals | |||||
| The work pace in this unit is so rushed that it negatively affects patient safety | |||||
| In this unit, changes to improve patient safety are evaluated to see how well they worked | |||||
| In this unit, there is a lack of support for staff involved in patient safety errors | |||||
| This unit lets the same patient safety problems keep happening |
How much do you agree or disagree with the following statements about your immediate supervisor, manager or clinical leader?
| Strongly disagree |
Disagree | Neither agree nor disagree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| My supervisor, manager, or clinical leader seriously considers staff suggestions for improving patient safety | |||||
| My supervisor, manager, or clinical leader wants us to work faster during busy times, even if it means taking shortcuts | |||||
| My supervisor, manager, or clinical leader takes action to address patient safety concerns that are brought to their attention |
How often do the following things happen in your unit/work area?
Think about your unit/work area:
| Never | Rarely | Sometimes | Most of the time | Always | |
|---|---|---|---|---|---|
| We are informed about errors that happen in this unit | |||||
| When errors happen in this unit, we discuss ways to prevent them from happening again | |||||
| In this unit, we are informed about changes that are made based on event reports | |||||
| Never | Rarely | Sometimes | Most of the time | Always | |
| In this unit, staff speak up if they see something that may negatively affect patient care | |||||
| When staff in this unit see someone with more authority doing something unsafe for patients, they speak up | |||||
| When staff in this unit speak up, those with more authority are open to their patient safety concerns | |||||
| In this unit, staff are afraid to ask questions when something does not seem right |
How often do the following things happen in your unit/work area?
Think about your unit/work area:
| Never | Rarely | Sometimes | Most of the time | Always | |
|---|---|---|---|---|---|
| When a mistake is caught and corrected before reaching the patient, how often is this reported? | |||||
| When a mistake reaches the patient and could have harmed the patient, but did not, how often is this reported? |
In the past 12 months, how many patient safety events have you reported? (Please circle one option).
-
None
-
1–2
-
3–5
-
6–10
-
11 or more
Patient Safety Rating
| Poor | Fair | Good | Very good | Excellent | |
|---|---|---|---|---|---|
| How would you rate your unit/work area on patient safety? (Please tick one option) |
How much do you agree or disagree with the following statements about your hospital?
Think about your hospital:
| Strongly disagree |
Disagree | Neither agree nor disagree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| The actions of hospital management show that patient safety is a top priority | |||||
| Hospital management provides adequate resources to improve patient safety | |||||
| Hospital management seems interested in patient safety only after an adverse event happens | |||||
| When transferring patients from one unit to another, important information is often left out | |||||
| During shift changes, important patient care information is often left out | |||||
| During shift changes, there is adequate time to exchange all key patient care information |
| Your comments |
| Please feel free to provide any comments about how things are done or could be done in your hospital that might affect patient safety. |
Thank you for completing this questionnaire.
Please put it in the box located in the staff area or return to a WardSonar researcher on the ward.
Staff questionnaire for real-time analyses.
Real-Time Questionnaire
(Staff)

THIS QUESTIONNAIRE WILL TAKE 2 MINUTES TO COMPLETE. PLEASE RETURN THE COMPLETED QUESTIONNAIRE TO THE BOX LOCATED IN THE STAFF AREA OR HAND BACK TO A WARDSONAR RESEARCHER ON THE WARD
About you
| Age | |
| Gender | |
| Ethnicity | |
| Role (e.g. nurse; HCA) | |
| How many years have you been doing this job? | |
| Approximately how long have you worked on this particular ward? |
What shift pattern are you on right now? (Please tick)
| Early | Late | Long day | Night | Other (please specify) |
|---|---|---|---|---|
Please add the current date and time
| Date (dd/mm/yyyy) | |
| Time (e.g. 10.25 a.m.) |
Please tick one response to each statement.
| Poor | Fair | Good | Very good | Excellent | |
|---|---|---|---|---|---|
| Right now, how would you rate your unit/work area on patient safety? |
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree | |
|---|---|---|---|---|---|
| Right now, my practice is not as safe as it could be because of work related factors/conditions (e.g. staffing, patient factors, teamwork) |
Please tick one response to each statement about how the ward feels right now.
| I agree | |||||
|---|---|---|---|---|---|
| Right now … | Not at all | A little | Somewhat | Quite a lot | Very much |
| Really threatening situations can occur here | |||||
| On this ward patients can openly talk to staff about all their problems | |||||
| There are some really aggressive patients on this ward | |||||
| Staff take a personal interest in the progress of patients | |||||
| Patients care about their fellow patients’ problems | |||||
| When patients have a genuine concern, they find support from their fellow patients | |||||
Appendix 2c: Example of an interim report for technical developers
Introduction
The mental health literature indicates that staff, patients and carers all perceive safety slightly differently. Staff and carers are far more likely to focus upon physical safety, for example, avoidance of self-harm, whereas patients view emotional and psychological safety as equally, if not more, important.
What is reported below has emerged from interviews with mental health staff only. Each section follows the same format: headline findings, followed by an illustrative quotation(s), followed by what this means (potentially) for any technological development.
-
Staff see patients as more sensitive to safety concerns than they are (this is both positive and negative).
-
Threshold for safety is higher for staff than patients because staff know what is going to happen next to deal with an incident, patients don’t.
-
Patients don’t have preloaded knowledge of other patients, they haven’t read the case notes, so an incident can be more scary for patients than staff.
-
Staff see patients' feelings about safety as relating to their pathology, for example paranoia. Feeling unsafe can be seen as a proxy for suicidal intent.
-
Staff see patients as having trauma responses and which leads them to having highly sensitive sensory reactions. This can be seen as positive or negative by staff, that is patients can be seen as informative or over reactive.
-
Staff normalise distress, whereas patients, especially new patients, do not.
-
‘The Safety Thermometer [was flawed as there were] … thousands of reasons that patients didn’t feel safe … they’d … be absolutely distracted by everything else in the world that didn’t make them feel safe, whether those be symptoms or otherwise. So I don’t think something like that worked because it was far too vague’.
And
-
‘[Patients pick up on safety issues] … much earlier than we do. I’m always astounded by how … patients know exactly what’s going on … [they] pick up on the controlling nature of the micro interactions’.
-
What this means.
-
Any safety data fed through to staff might need to be anonymised (so it can’t be linked to a particular patient pathology).
-
Safety data need to be specific, not simply asking about feelings of safety/lack of safety.
-
Data need to be salient so that staff take them seriously: it needs to trigger the staff threshold for safety.
-
Safety is a multifaceted concept that can mean different things to staff depending upon their professional role and career stage.
-
Safety can be seen as primarily a nursing concern, whereas it is the responsibility of all staff, from consultants to domestics.
-
Staff understandings of safety relate to experience of handling previous safety incidents and a building of confidence in doing so.
-
Safety relates to having the skill set required to deal with incidents, for example, de-escalation and communication techniques.
-
Safety relates to working with knowledgeable and engaged staff that can be relied upon, that is not too many bank/agency staff who may have no alignment to the ward.
-
My experience of safety has definitely changed, my understanding, research, models of the interventions that we use more than when first trained which isn’t long ago compared to other people that I work with.
What this means
Any technology should allow for a multifaceted conception of safety according to role and career stage so that individual staff reading the data will recognise something as a safety concern.
Safety incidents are often preceded by micro-cues but in the context of complexity:
-
Word slip
-
‘A look’
-
Demeanour
-
Way someone walks-with their ‘head down’
-
Voice – -both tone and content
-
A lot of activity or movement/noise on the ward
Space: how it is being used on the ward by both staff and patients. Are all patients in one place on the ward (or nowhere to be seen?)-sometimes referred to as ‘retreat and swarm’. Are staff visible on the ward? Where? (or nowhere to be seen).
Deviation from the normal, for example someone in their room who is normally in communal areas, or vice versa; someone eating in their room who normally eats in the dining room, or eating faster than normal in the dining room, or a norm breached by patients or staff.
Language changes, from proactive to reactive, staff become more directive:
-
‘[if the] patient is acting different to usual … [gives example of patient who unusually sat in TV lounge] escalated through the day and she became more and more withdrawn and … isolative and then that wasn’t picked up by the staff and she was found ligatured in the lounge’.
And
-
‘The wards are so complex … lots of things contribute to it … lots of small things … that then become a big thing … it’s pattern recognition as well’.
And
-
‘when there’s some social norm that’s been breached, by the patient maybe but also by the staff’.
What this means
-
These micro-cues could be held in a database and if/when input into a digital technology by patients they can alert staff to a potential incident unfolding, particularly if multiple cues or ‘patterns’ are identified.
-
Staff may not respond to one cue but may need evidence of several before they intervene. (Thus, this can be conceptualised in synchronic terms, as events at one point in time, or as diachronic, as events that develop one after another that significantly alter the milieu, that is the ripple/domino effect.)
-
Cues could be differentially weighted.
-
Safety incidents and micro-cues are gendered.
-
Men more often elicit intimidating, violent and aggressive behaviours whereas women tend to withdraw or want increased staff attention.
-
Mixed wards can have a differ dynamic to single sex wards: either, sexual safety can be an issue on mixed wards, with both male and female patients reporting feeling safer on single sex wards, or, they can have more balance with men and women using informal controls to check each other's behaviour.
-
Men are more likely to get in the middle of an ongoing incident.
-
Women are more likely to self-harm.
-
A female staffed male ward can present particular safety challenges.
-
‘men generally, I think, act more intimidating. And a lot of the ladies kind of retreat and go quiet, or will want to spend more and more time with you’.
And
-
[on an] acute male ward … when you have people … on the sex offenders register … they tend to be put on our ward … and we’re a largely female staffed ward … sometimes that actually affects our personal safety … we end up having to brief everyone from the domestic about not going in to rooms on their own.
What this means
-
All female, all male and mixed wards may all need different metrics to trigger a safety concern to reflect the gender composition of each.
-
Gender mix between patients and staff is another context variable to consider.
Milieu and contagion.
-
All staff seemed to agree that milieu and contagion exist even if they found these hard to articulate.
-
Many metaphors were used for contagion: ripples, pressure, domino effect etc. For milieu-environment, atmosphere, a feeling.
-
There was overall agreement that one safety incident could lead to others and that this effect could last from an hour up to 2 days on the ward. It was recognised that it can be transferred from shift to shift.
-
There are often differences between night and day shifts (the latter is more difficult).
-
One person can upset a whole ward, in part by diverting resources from other patients. Restraints particularly upset the ward.
-
Contagion spreads differently on male and female wards (men get aggressive/interfere, women withdraw or seek staff support).
-
Contagion can be more acute on wards with patients with learning disabilities:
-
[it lasts] probably an hour or two … sometimes it’ll go into the nightshift … it carries on again because then there’s more people available … that are refreshed … it’s not intentional, people don’t intentionally think right, we’ll just drain these new staff, that’s not the way it works, it’s just that’s human behaviour, isn’t it, that’s what happens.
And
-
In my head 2 days is the maximum to it. I think sometimes.…resentments rumble on and then there’s retaliatory things but usually after 2 days things are starting to calm down, that arousal curve, again.
And
-
‘I definitely saw the difference between day and nights … [so I] speak to people straight away, start turning the lights down a little bit, ask people if they want a brew and a toast, you know, it’s late at night, you start putting those routines in place plus it’s quieter, there’s not as many people around, it’s a bit easier’.
And
-
The whole ripple goes through the whole ward … so, it doesn’t take long for everybody to know that XXXX was restrained and … that then causes upset for everybody
And
-
I think [contagion] … depends on the dynamic of the service users … some … love to get involved in an incident … [others will just]. … listen, and if you ask them to move away from the situation …
And
-
As soon as we have one lady going up there, everybody else is jumping in and either competing for volume or trying to soothe someone …
What this means
-
Any technology may have to incorporate an alert status (for up to 2 days) when a safety incident has occurred. The technology may have to become more sensitive during this period.
-
The technology would need to be able to pick up and collate input from patients perhaps in different areas of the ward to indicate that an incident was spreading, for example, increased anxiety or input activity by patients into the technology.
-
The technology needs to see night and day as different contexts and incorporate that into any alerts.
-
Milieu and contagion operate according to ward profile thus the technology would ideally incorporate this factor (e.g. all male, all female, mixed wards).
A digital technology on the ward: divided opinion.
There is some variation between trusts in the capacity for a digital technology to be incorporated into ward life some have superb Wi-Fi, others don’t have enough computers and are still using pens and paper.
Views were divided over the usability of iPads and phones by patients to input safety data. Some felt that patients could easily do this, whereas others highlighted that some patients cannot read and write.
Direct patients to bespoke website.
Not all patients speak English or have English as their first language.
Any technology would have to be very structured and focused to work.
A simple technology of smiley/sad faces or traffic light system was thought a good idea by some and usable by patients, though others thought patients would report in the negative all of the time with such a system.
A mixture of words, pictures and sound clips was suggested.
It is no good knowing that patients feel unsafe staff need to know why.
Most staff thought that patients could report on ward safety.
Some staff would struggle with interpreting the data.
Any technology may need to operate independently from nursing staff.
There’s a … role there for education because it’s that assumption … patients know how to work these things. Some … can’t even read or write, so how can we expect [them to] engage with technologies [they need] … skills to engage with it meaningfully.
And
-
… we have to embrace digital ways of working as we move forward because that’s the way the world is moving … that’s the way younger people understand the world and they’re going to be the newly qualified nurses of tomorrow … the Band 6s … [and] Band 7s of the future.
And
-
We take a photo of the QR code for their friends and family and then they fill out our surveys on the iPads and they’re quite receptive to that, I think that’s probably better than paper and pens, I don’t know if you could maybe develop a QR code that directs you to a website and just do it that way? … we’ve got amazing Wi-Fi.
What this means
-
Any technology is going to have to engage with a wide range of patients and abilities, making it accessible to those without reading/digital skills but not being too simplistic and potentially patronising for more able patients.
-
Some staff would struggle to interpret the data and may need training or more training than others. Potentially problematic for staff qualified a long time.
Measures of safety
-
Both quantitative and qualitative measures would be needed.
-
Some cues might be given more weight, numerically, than others.
-
Data should be collected daily and sent to an app (for patients/staff) or a dashboard/computer (for staff).
-
Numerical scores could be assigned to feelings of safety by patients.
-
Safety can be measured in language both body and verbal when safety is diminishing language becomes more reactive and here and now. Staff may become ‘shouty’.
-
Patient reporting activity is a valid construct in itself and indicates safety concerns, even if the reporting is incorrect in the detail.
-
‘having a threshold where … a nought to ten scale where once you hit four, that triggers a safety huddle, once you get to six or eight … that triggers an MDT discussion. I think the issue … with that though is … to have that huddle or … MDT discussion because if you’ve got to … the higher end of the scale … the likelihood is that you need staff on the ward, observing to maintain people safety’
What this means
-
Any technology needs to incorporate the input of quantitative and qualitative data, perhaps giving patients the choice of drilling further and further into how they are feeling. Some may want to give basic information.
-
Stress for patients should be considered.
-
Thresholds/scales need to be built into the system, triggering alerts to action.
What to do with the data
There appear to be four options to streaming the data to staff that staff interviewees thought would work:
-
Live, continually and directly to staff phones via apps while on the ward.
-
At daily meetings huddles and handovers this could be via phones or existing computer systems.
-
Digital display boards.
-
Direct patients to bespoke website.
-
At weekly meetings-reporting, community meetings, mutual help meetings, again adapted to existing computer systems
-
At monthly meetings – ‘community’ – often involve patients.
-
Data could be displayed in the patient lounge.
-
Every ward is different.
-
There was recognition that any technology would be experimental at first.
Live, continually and directly to staff by phone app
-
A lot of us on our ward, use our phones all the time … ’cause we use it with patients, whether we’re listening to music, discussing things, you know? So we’re quite open with our mobile phones. If I didn’t answer e-mails on my mobile phone, I probably wouldn’t answer a lot. Our ward it’s not seen as a negative that staff do actually have their phones, ’cause they’re interacting with service users for their use. I don’t know, sometimes 10 minutes can be enough for you to and intervene …’.
To existing computer systems/digital display boards
-
[I don’t see] see why we couldn’t pull up your daily … screen for your safety huddle …
And
-
I wonder whether there’s a digital display board when you walk on the ward and staff can check out on it and check in on it as well.
Daily meetings: huddles and handovers (from one shift to another)
-
Handovers would be really good. You could say, such and such has said this, or the data that’s come through on the app has shown this, this and this, and then plan … we need to be more vigilant, you need to spend one-to-one time with such and such, we need to keep da, da, da, separate. … if it was drugs coming on the ward, we need to be better with searches, so definitely handover. Safety Huddles, great when you’ve got the staff in numbers to be able to pull people off the floor ….
And
-
You would want something that comes through … and you can discuss it in your safety huddle … this is what the patients are telling you … having something that you could then pick up on a daily basis and use as a team.
And
-
We have another huddle at tea time again and that would probably be the best one that I would … use to talk about things that we’ve done through the day, how’s it going … we call it a havoc huddle.
At weekly review meetings
-
Even if it’s a summary … we do weekly [meetings] … being able to talk about that would be quite useful and say, we … understand that last week was a really difficult week, particularly over the weekend …
Information needs to go to patients
-
[We] ... should be able to feed that back to the patients and say … you told us this and this is what we’re going to do … if patients don’t see any change … then they’re just going to stop filling out that information. So it needs to be something that goes maybe both to the staff but also to the patients.
And
-
[Feeding back to service users] … would be helpful … it might help people take a little bit of responsibility for their contribution to the environment …
Every ward is different
-
[E]ven though they talk about policies and procedures, systems and processes, every ward does everything differently … nothing is in the same place. They don’t even do the handovers the same way … there’s inconsistency there.
Any tech experimental at first
-
I think you’d have to try … a few different things.
What this means
-
Whichever route is chosen, or chosen for any ward, means it would have to work within existing ward and trust systems. There may have to be several versions of the same technology, or a suitably plastic technology, to adapt to different wards structures, systems and conditions.
Potential harm to patients.
-
Only 1 of 10 of the respondents mentioned potential harms to patients but it worth considering.
-
We spend our time trying to … help patients relax and … slow down their thoughts and process … it can only harm them, to … say, your job today is watchman of the ward … that constant stress state that they’re going to be in, it’s going to harm them psychologically, it’s going to harm them physically.
What this means
-
We may need to offer patients different levels of engagement so that the most vulnerable to stress can contribute (or not) as they feel able to.
Appendix 2d: Technical report
Technical development report for WardSonar
Prepared by
Michael Stephens (mike@ayup.agency) and Steven Taylor (ste@ayup.agency)
Contents
Technical brief
High-level summary
Key user stories
Key considerations
Proposed scenario usage
Technical approach
High-level technical architecture overview
Developed digital products
Recording interface
Technologies used
Infrastructure
Staff dashboard
Technologies used
Infrastructure
Ward interface
Technologies used
Application Programming Interface (API)
Technologies used
Infrastructure
Database schema
Development approach and resources
Key personnel resource
Deployment process
Post Deployment challenges
Challenges faced
Challenge 1
Challenge 2
Challenge 3
Challenge 4
Challenge 5
Challenge 6
Challenge 7
What we’d do differently
Annex (a) to technical report: user stories
Annex (b) to technical report: device set-up guide
Technical brief
High-level summary
The overall aim is to develop a suite of digital products that facilitate the anonymous collection of real-time patient safety data and measures within acute mental health wards.
All data collected:
-
should then be computed and presented to ward staff for real-time analysis and to inform their decision-making with any interventions they might make.
-
should be made available to research staff for detailed analysis after the implementation period comes to an end.
Key user stories
The three key user stories that underpin the digital products are as follows:
-
As a service user, I want to easily and anonymously report how I am feeling on the ward, so that staff are aware and can take action.
-
As a member of staff, I want a secure and easy to use dashboard to review data submitted, so that I can get a gauge of the ward atmosphere.
-
As a researcher, I want to be able to see all collected data points, so that I can perform detailed analysis on how the digital products were adopted and what impact they might have had.
Key considerations
The suite of digital products should:
-
be co-designed with stakeholders in order to test assumptions and validate designs;
-
have strong UX design – they need to be simple, easy to use and accessible;
-
be secure and anonymous;
-
use existing open-source technology wherever possible;
-
be developed technology in line with NHS standards where possible;
-
have an ‘opt-in’ approach to usage;
-
consider potential issues such as Wi-Fi dead-spots and technology constraints within clinical settings;
-
collaborate with information governance leads to conform to information governance and data protection standards.
Proposed scenario usage
The developed ‘app’ will be loaded and accessed on a tablet device which will be stored on the ward throughout the intervention.
The tablet device will be taken around the ward by a member of staff to patients one at a time. Patients will be able to opt-in or opt out of providing data. Any inputted data by patients will be recorded via the app and will be automatically sent back in real time to the central database. If Wi-Fi is temporarily unavailable on the ward, then the inputted data will be stored locally on the device in ‘offline’ mode. When the device comes back into Wi-Fi range the data will be automatically submitted to the central database.
Patient data will be monitored through a ‘staff dashboard’ which authorised members of staff only are able to access, via a desktop or laptop computer, that displays real-time patient-inputted data, charts and metrics.
Technical approach
High-level technical architecture overview
The digital products developed will be built using open web standard technologies (e.g. HTML5, CSS3, JavaScript, PHP) in a componentised and scalable way, to allow modifications and future developments to easily happen.
All digital products will be hosted in a custom cloud environment built on top of the Amazon Web Services (AWS) Infrastructure. Technical details of the infrastructure are described below attached to each of the digital product's descriptions.
Figure 22 shows all of the digital products to be developed, how they interact with each other and sit within the wider context.
FIGURE 22.
Digital products in context.
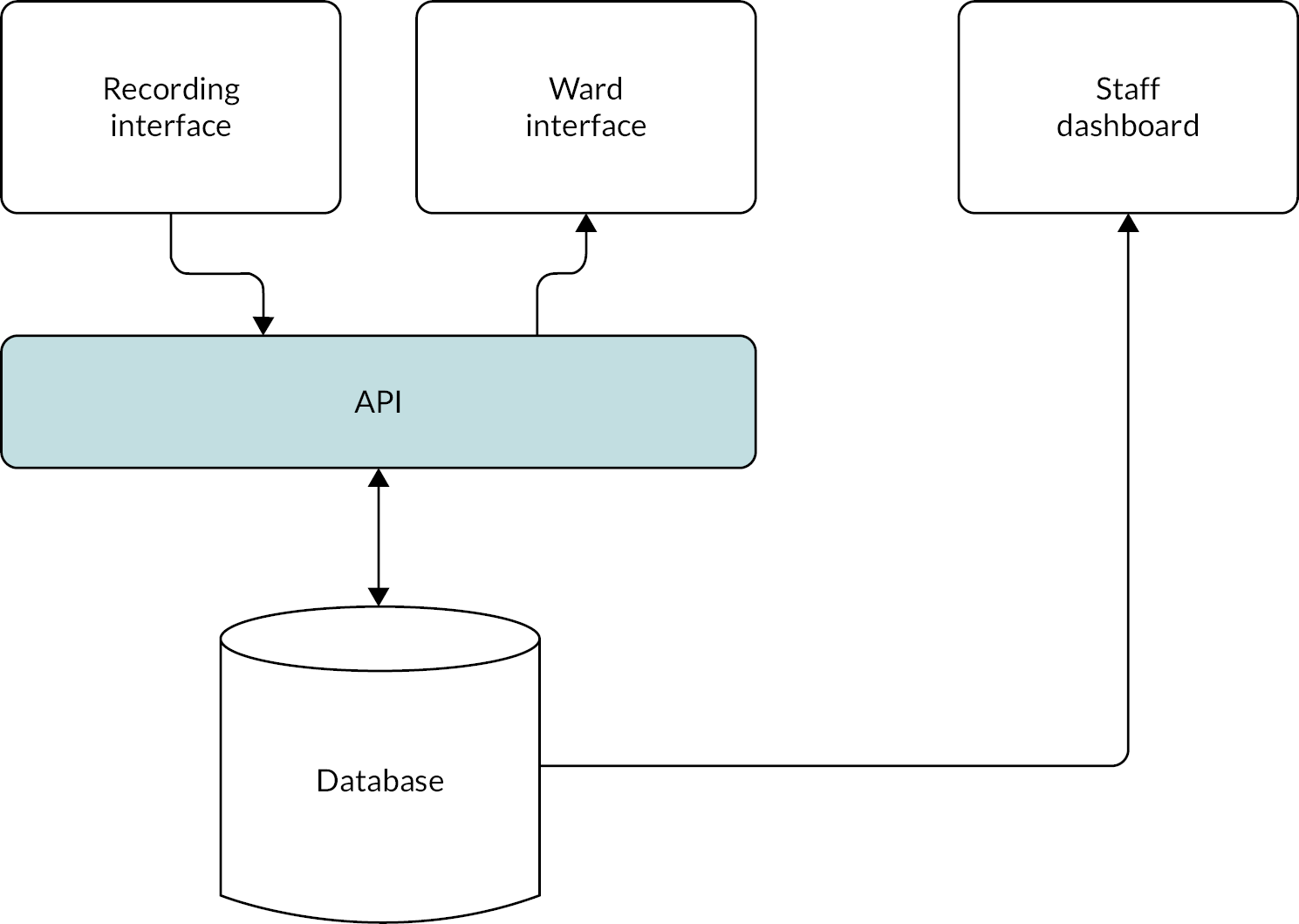
Developed digital products
Recording interface
The recording interface facilitates the collection of patient safety data and measures within acute mental health wards. The interface is presented as an app on a tablet device on which patients are asked to answer a few simple questions about how safe they feel on the ward. No patient data is collected and all data collected on the interface is anonymous
Data are recorded in real time and sent to an API (see below) for data processing. The questions that patients are asked on the interface were determined from the environmental scan findings and co-design workshops. Particular attention has been paid to the UX of the interface, especially in understanding contextual constraints and pressures that patients may be experiencing (e.g. location when entering data, what device they will be using, what might their mental state be at the time of data entry). Similar attention to detail with respect to accessibility is also important to ensure the interface can be used by a wide range of users with varying abilities.
The interface has been built to WCAG 2.1 AA standards and is device agnostic (i.e. it is usable across most modern devices, platforms, operating systems and internet browsers). Patients are able to respond via a device supplied by ward staff.
Technologies used
The core technologies used to develop the recording interface are:
-
HTML/CSS (HyperText Markup Language/cascading style sheets) – the underlying technologies of the web. HTML and CSS were used to develop the core structure and provide visual styling.
-
ReactJS 17+ – an open-source JavaScript framework for building component-driven web applications and user interfaces.
-
MaterialUI 4.11 – an open-source comprehensive suite of user interface tools that can be reused to develop interfaces faster and with consistency.
Infrastructure
Each ward has its own unique deployment of the core recording interface product with each ward having its own unique ‘instance’. The recording interface is completely separate from other wards and accessible via a unique URL to ensure an easy-to-use experience for patents submitting data and to avoid increasing the number of questions asked, for example, ‘which ward are you on?’. This approach also helped to eliminate the potential of malicious data submissions across wards.
Each ward has its own subdomain which is automatically generated using a random string of characters as the subdomain. For example, ‘{4–6 char}.wardsonar.co.uk’.
The instances of the product are stored in an S3 Bucket fronted with a Cloudfront distribution to handle caching and SSL termination. Route 53 DNS records have been updated automatically through a Cloudformation script which generates the unique subdomain values. Secrets manager has also been used to store API keys, credentials and configuration values for the recording interface.
FIGURE 23.
Patient interface.
Staff dashboard
The staff dashboard is the main interface used by staff to view data submitted by patients. It is primarily accessed in specific, authorised locations, such as the ward office and provides real-time snapshot data and greater informational insights through the use of interactive data visualisations.
Co-design work with healthcare staff, statisticians and researchers determined the exact requirements of how data should be represented on the dashboard, including barometer-style visualisation of ‘How is the ward feeling’, SPC charts, graph and statistical metrics. Monthly/weekly/daily/shift aggregate data is available and comparable to historic time periods.
Each ward has their own staff dashboards independent of other wards, so no data can be exposed between wards. The dashboards are behind a layer of authentication and can only be accessed by authorised staff members with login credentials.
FIGURE 24.
Screenshot of the ward F staff dashboard (identifiers removed).
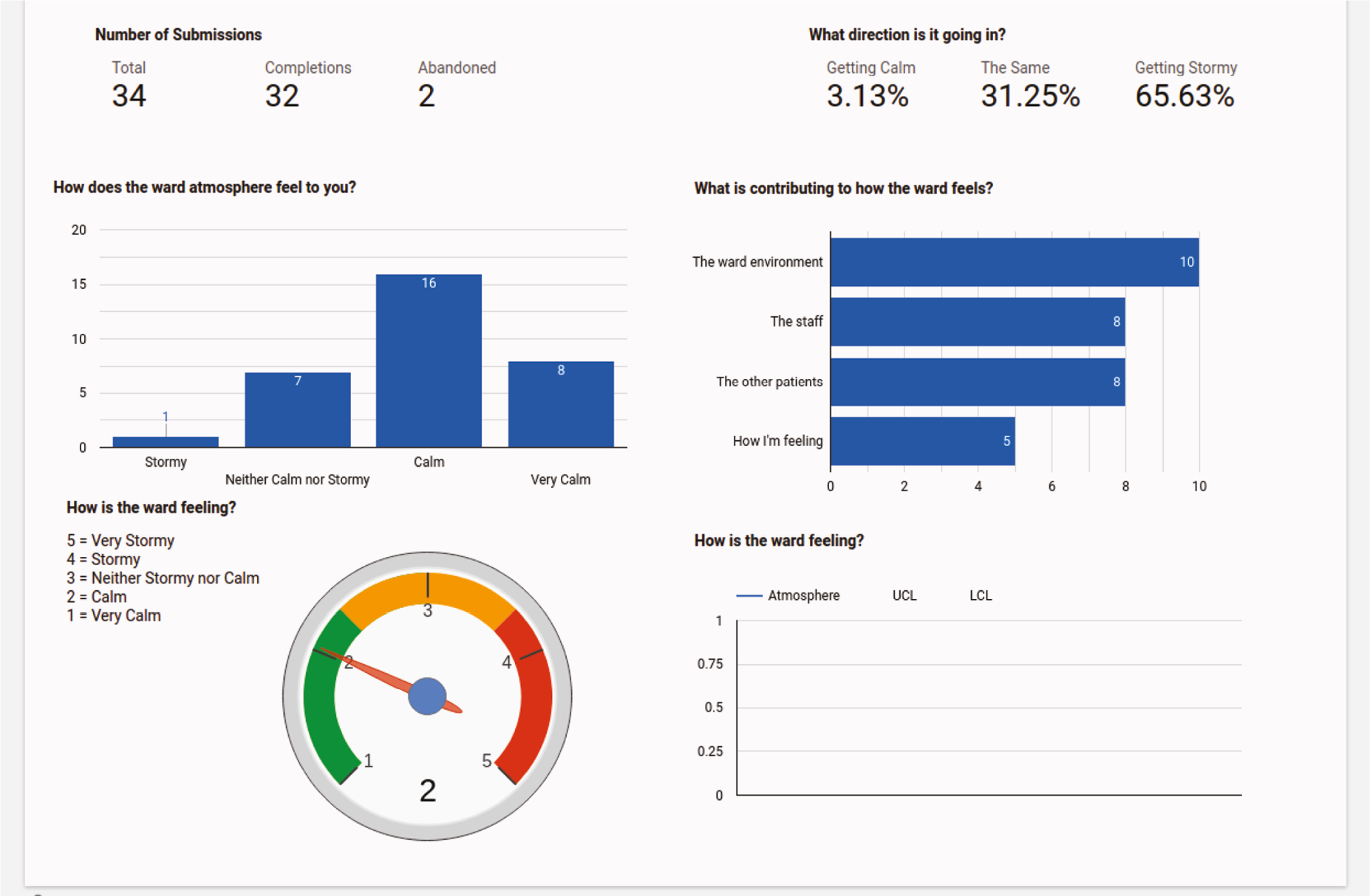
Technologies used
The staff dashboards have been developed within the openly available Data Studio tool, which is produced and provided by Google. Budget and time constraints meant that an ‘off the shelf’ product for data visualisation – a scan of the market highlighted Google Data Studio as the most appropriate and cost effective.
Data Studio was connected securely to the underlying database where the raw data recorded by patients was held. This enabled much greater control over reporting and presenting of the data than would be possible through the relatively simple API that was created.
Having access directly to the raw data set meant data was able to be computed, reformatted and presented with the in-built scripting language, in the ways which the co-design work highlighted.
Infrastructure
The staff dashboards are hosted directly within the Google Infrastructure, however a couple of alterations to our infrastructure were required in order to achieve a stable and secure connection from Google to our database:
-
A read-replica MySQL database was deployed – this is a read-only and real-time version of the live database but is exclusively used for data computation and reporting. Using a read-replica means these high resource intensive tasks do not affect the performance or stability of the master database.
-
By default, the database within our infrastructure is not accessible publicly and is behind several layers of network security and firewalls. For the dashboards to connect, a secure link had to be created to allow Google servers to connect. This was achieved through whitelisting a set of intellectual properties that belong to Google, which allowed access into Virtual Private Cloud to connect to read-replica database instance.
Ward interface
The ward interface communicates the output from a specific measure for public consumption. Through co-design work, the specific outcome measure was determined to be ‘How does the ward atmosphere feel today?’. The outcome measure is displayed in the form of a barometer and shows the average milieu rating for the current shift.
The ward interface has been designed to displayed on a television, desktop computer monitor or tablet devices.
FIGURE 25.
Screenshot of the ward F interface (identifiers removed).
Technologies used
The ward interface is a subsection of the recording interface product, accessed by appending/dashboard to the URL and thus uses the exact same technologies.
Using the same code base for the ward interface allowed us to entirely reuse code and develop the interface much quicker, especially as the existence of the ward interface product was unknown from the start and something that co-design informed.
Application programming interface
An API, that is central to the digital products, has been developed in line with as many best practice government and health standards as feasible. The API is used to link all of the digital products together with the underlying data storage engine. It facilitates data recording, processing, representation and exporting. Where possible, we used an open data format standard so that the data can be interoperable with other systems/products (e.g. JSON, REST, OpenAPI).
The API has a one public endpoint (/stats) which returns a single computed payload that is used to power the ward interfaces. The rest of the API endpoints require a simple authentication bearer token which is unique to each ward. This token identifies where submissions are coming from, as well providing an authentication layer.
Technologies used
The core technologies used to develop the API are:
-
PHP 7.2 – The underlying programming language used to create the API.
-
Laravel 8.12 – An open-source application framework written in PHP that provides some reusable code for common tasks (e.g. validation).
-
MySQL 5.7 – The central database engine used where all data is stored and accessed.
-
PHPUnit: 9.3 – A library to help with automated testing of the API.
Infrastructure
The API is hosted on a dynamically sized group of application servers, fronted with a load balancer. All requests to the API first are forwarded to load balancer which then decides which application server to send the request to. This model allows for automatic scaling to handle traffic spikes.
The API code is packaged up into a Docker container (a unit of software which contains the application code and all of its dependencies) which is deployed to the application servers via the CI/CD pipeline Travis.
We make use of CloudFormation which allows most of the infrastructure to be templated and scripted, which automates all of the tasks of deployment.
Application programming interface exist at the endpoint (api.wardsonar.co.uk).
FIGURE 26.
Database schema extract.
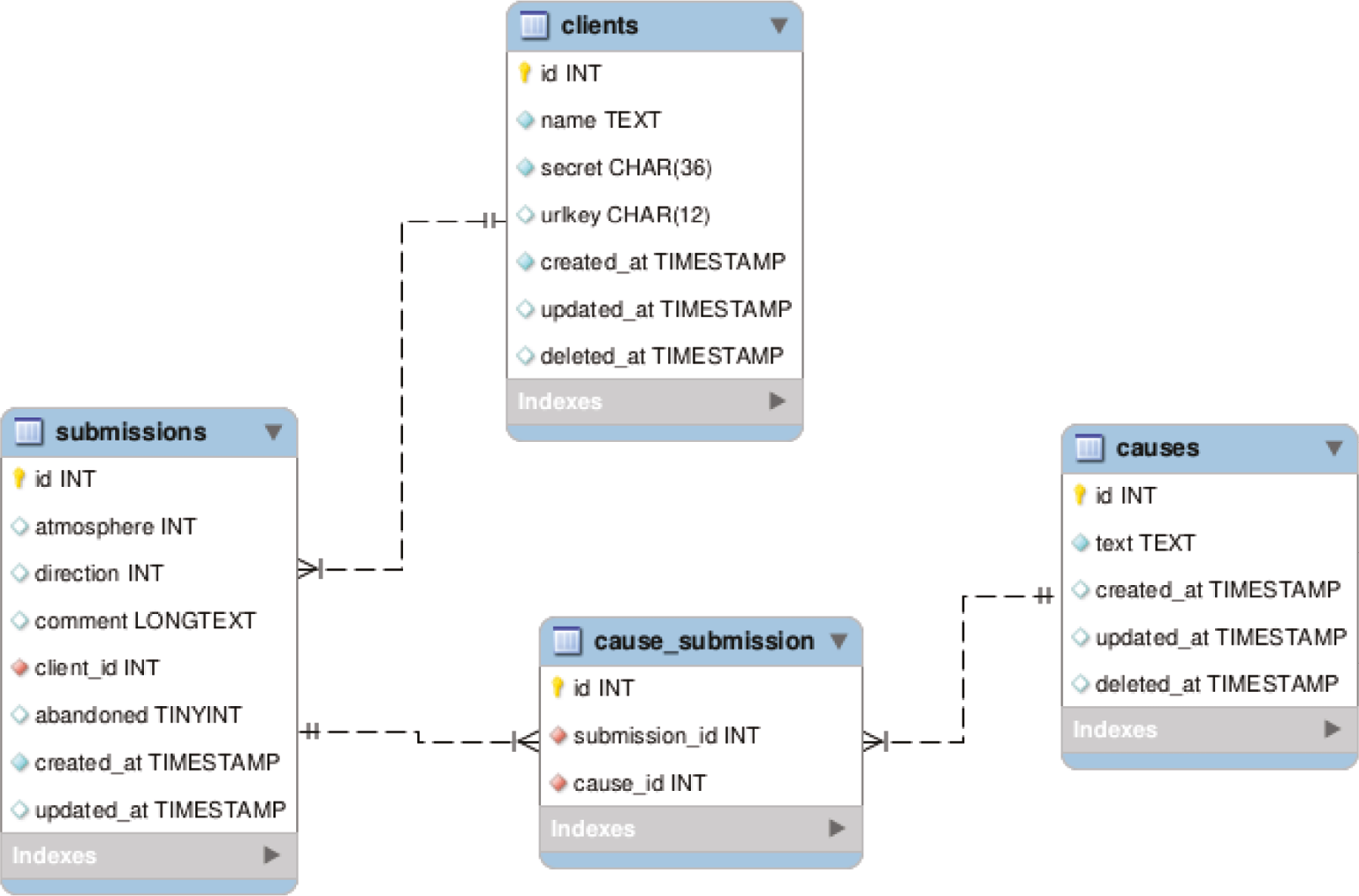
| Table name | Description |
|---|---|
| clients | Clients = wards. Each ward has an entry in this table with a unique id, secret (for authentication) and urlkey (random 4–6 char which forms the URL for the recording interface) |
| submissions | The main table where all user submissions are stored. Each submission is tied to a client_id (the ward they are on). If abandoned indicates a user didn’t want to submit data. Atmosphere and direction fields store the value of the user selection – see below data structure for the options. |
| causes | A populated table with predetermined options of ‘valid’ reasons/causes |
| cause_submission | A table that stores the reason/cause responses by users. Maps submissions to causes via their unique ids |
Database schema
The database engine used to store all data across all products is MySQL. Below (see Figure 5) is an extract from the database schema which shows the main tables and data styles used to store the submission data.
How does the atmosphere feel to you today? (Database field: atmosphere)
-
−2 Very calm;
-
−1 Calm;
-
0 Neither calm nor stormy;
-
1 Stormy;
-
2 Very stormy.
Is the feeling of the ward atmosphere changing? (Database field: direction)
-
−1 Getting calm;
-
0 The same;
-
1 Getting stormy.
Which of the things below is making the ward feel xxx
-
1 The staff;
-
2 The other patients;
-
3 How I’m feeling;
-
4 The ward;
-
5 Other (Database field: comment).
Development approach and resources
In developing the digital tools, we followed an agile, co-creation, human-centred, data-driven and iterative approach based on the Government Digital Service Agile Delivery methodology framework and NHS Standards.
Working with mHabitat (aka Thrive by Design) we designed simple prototypes to test with stakeholders. Design iteration took place after every round of testing until final digital designs were created. Following the design stage, a series of technical development sprints moved the simple prototypes into technical prototypes for stakeholders to test via their browsers.
Further testing and feedback were carried out before the final prototypes were approved by the working group.
Key personnel resource
-
Technical architect – to produce and oversee the technical approach and blueprint.
-
Designer – to produce high-fidelity wireframes that can go straight into frontend development based on an existing framework (e.g. material user interface). Only concerned with the design of the recording interface and ward interface.
-
Frontend developer – to create the two/three products (recording interface and ward interface). To use frontend framework as per designs/wireframes and use a JavaScript frontend framework to communicate with the API.
-
Backend developer – to create the API. Needs to be a very simple way of authenticating and accessing/exporting the data.
-
Data intelligence developer – to create the ‘admin dashboard’ using Google Data Studio.
-
Project manager – to oversee the project and ensure delivery.
Deployment process
The process of deployment the digital tools on the wards was as follows:
-
The patient recording interface was installed on the ‘Samsung Galaxy Tab A’ device by the project team.
-
The patient recording interface was fully tested on the device and a dummy setup was performed.
-
Each participating ward had one device with the recording interface preloaded. This was taken in person to them by a member of the project team.
-
Documentation and guidance was created for device setup and disseminated to the ward.
-
ward staff setup the device by following the documentation guide [see Annex (b) to technical report: device set-up guide] with assistance from team.
-
The staff dashboard – accessible through existing computers on their ward.
Each ward had their own instances of the recording interface, ward interface and staff dashboards. This meant all wards were in essence completely separate from each other thus restricting the potential of data access or submission from other wards. However, underlying all wards share the same central API and database but use authentication tokens/IDs to distinguish between them.
Post deployment challenges
Throughout the deployment of the technology onto the wards and throughout the intervention, a small number of challenges came up. We highlight the main challenges faced here, along with what action was taken and future recommendations.
As the technology partner we provided a service level agreement throughout and were on-hand throughout the deployment and implementation process.
To aid with troubleshooting and debugging, application and infrastructure level monitoring was implemented through BugSnag and AWS respectively, to proactively monitor the application and platform for any issues.
Challenges faced
Challenge 1
Problem
Sharing ward-specific Google accounts with multiple people caused Google to flag as suspicious activity.
What we did
Disabled as much verification checking as possible as a temporary measure.
Future recommendations
Every person to have their own account/login and for them not to be shared.
Challenge 2
Problem
Ward was unable to connect their devices to the Wi-Fi @ ward F.
What we did
Issue was resolved by trust IT department.
Future recommendations
More investigation/testing on wards before deployments.
Challenge 3
Problem
‘Data set configuration error’ appeared throughout the dashboards. Connection issues at the start of deployment.
What we did
The read-replicate server needed to be upgraded to cope with all the database queries that Google Data Studio was sending. Anticipated just a few connections per dashboard but learnt that Data Studio doesn’t ‘reuse’ existing connections and establishes new ones.
Some of the issues occurred due to the data needing to be ‘refreshed’ on Google Dashboard.
Future recommendations
Deploy higher capacity servers.
Challenge 4
Problem
Some dashboards were showing a ‘no data’ error.
What we did
This was because the date range ‘remembered’ what date was selected previously. We updated the dashboard logic so the date defaulted to ‘today’ to avoid confusion.
Future recommendations
Investing in training users of the dashboard prior to use.
Challenge 5
Problem
Two of the tablet devices were lost.
What we did
Change the password on the Google account to limit data access.
Future recommendations
The ‘reporting interface’ app is not password protected/locked down (to reduce barrier on users entering data). Could look at introducing restrictions/authentication.
Challenge 6
Problem
While the ‘ward dashboard’ was viewable outside of the ‘staff dashboard’ – the one included within the ‘staff dashboard’ required users to click a ‘proceed’ button to view it.
What we did
No updates – this is a security precaution enforced by Google.
Future recommendations
Further training on how to use/access the dashboards.
Challenge 7
Problem
Dashboards taken offline – users reported ‘can’t access report’.
What we did
Temporary Google Data Studio outage which meant the connections had to be re-established.
Future recommendations
Have some monitoring tools in place to detect when this happens?
What we’d do differently
Many of the challenges faced with the staff dashboard were related to the use and limitations of Google Data Studio, which was developed for much different use cases to this study. However, in terms of minimum required functionality and cost, it was deemed to be the most appropriate piece of technology to utilise.
Developing a bespoke dashboard that is designed around this specific use case should overcome the challenges and create a simpler, more refined experience. However, this clearly is budget dependent and would require investment.
Investing in training workshops on the wards facilitated by the technology partner prior to deployment would have reduced some of the friction and challenges faced – as a number of the issues were down to understanding/education about the system and its usage, not necessarily bugs or issues with the technology itself.
Annex (a) to technical report: user stories
| As a (role) | I want (to do …) | So that (goal) | MoSCoW |
|---|---|---|---|
| Staff | it to all look and sound the same | I can use it on any ward | M |
| Staff | it to either be consistent or able to match the individual wards | it works | |
| Staff | to record positive responses also | it isn’t all negative | M |
| Staff | to look at a daily screen | we can use it in our process now | |
| SU | A graded approach to inputs/outputs | I can express myself better | M |
| SU | to use touch screen | it’s the same as my phone | S |
| SU | option to be anonymous | I don’t have to describe why I feeling like that | S |
| SU | it to express my mood now | staff know how I’m feeling | S |
| Staff | I want to be able to see/review patterns of behaviours | ||
| SU | to flag to staff when there are issues | it doesn’t reduce time spent with staff | |
| Staff | like it to be used everywhere on the ward | so that people in isolation can access | M |
| SU | to understand current perceptions of safety | concerns about COVID safety are captured | |
| SU | maybe an AI element | I use a concept familiar to me | C |
| SU | messages that are secure | I know where the information is going | M |
| SU | private messages | my feelings aren’t shared on a board | S |
| SU | to report on other things like there are no cups | I don’t become agitated about it | C |
| SU | press a ‘suicidal’ button | Staff are aware | C |
| SU | staff to use pagers | they are aware of the situation/triggers | C |
| SU | alert a member of staff too my safety that’s more specific than the nurse call button | I can express my safety | C |
| SU | say how I feel about other SU – it’s not shown on there | I can say why the ward is like this | M |
| Staff | to be sure I’m using the information | Su don’t feel unheard – negative reinforcement | M |
| SU | it support used systems e.g. triangle of care | it enhances them | |
| Staff | to understand all the small complexities | I can recognise a pattern | |
| Staff | it to be aware of shift patterns – day vs. night | I can look at differences | |
| Staff | to use it to review the days/weeks data | so we can reflect | |
| Staff | to use it to review with SU | reflects feedback/collaboration | |
| CTM | the outputs to be meaningful to staff | handover/sharing of information is supported | S |
| CTM | outcomes to be meaningful to support clinical interventions | patients have better care/improved safety | M |
| CTM | outcomes to be meaningful to support embedding into ward culture | S | |
| CTM | to be able to see/read outputs | endure all staff are able to understand the outcomes/implications | |
| CTM | experienced staff to be able to demonstrate their clinical reasoning | experience is shared and taught | |
| Staff | to not rely on a scale to instigate a response | I don’t lose my clinical reasoning skills | C |
| Staff | look at the information | I can use it to review with Su or in groups | M |
| Staff | to be able to show Managers/CQC the information | conditions are improved | C |
| Staff | a tool that triggers reactions | actions are proactive/we can plan | |
| CTM | capture staff feelings of safety | staff feel safe | S |
| CTM | capture staff feelings of safety | Staff side interventions are proactive | S |
| Staff | it to understand SU individuals’ ‘norms’ | interventions are proactive/appropriate | |
| Staff | it to be aware of shift pattern/implications on staff | ||
| Staff | to record individuals’ ‘usual’ reactions to incidents | plans/interventions can be improved | |
| SU | 1 to 1 conversations with staff | I am heard | M |
| Staff | the role of it to be fully explained to the SU | there are no detrimental effects on SU | |
| Service user | have some control over my time/responses | I don’t feel pressured | S |
| CTM | to encourage least restrictive practice | SU benefit | S |
| CTM | to capture the feelings across the whole ward | interventions are proactive | M |
| Service user | put my feeling in when I want to | I can express myself when I want to | S |
| Service User | it to be chained/secured to the wall | it’s not thrown at me | C |
| Staff | SU to be able to input then they want | they have a sense of mastery | S |
| Staff | SU to be able to input when they like | we get a true sense of feelings | S |
| Staff | reassurances that I am not responsible for breakages/it being stolen etc. | I don’t have to worry about devices on the ward | S |
| Staff | devices to be safe/protected e.g. boxed in | everyone is safe, compliant with policies | M |
| Staff | SU to be able to record when they want to | they don’t have to ‘save’ their views for groups or other processes | M |
| Staff | there to be enough Wi-Fi for it to work | it can do all it promises | M |
| Staff | SU to have lots of opportunities to be heard | M | |
| Staff | it to be in a booth | it isn’t stolen/damaged | S |
| Staff | SU to be able to say what they are feeling when they choose | they have choice | S |
| Staff | like to use the system in established processes e.g. Pipa, Safety huddles, staff meetings | it has some meaning and we can explore reasons why and/or be proactive | M |
| Staff | like to use it to support safety plans | interventions are collaborative | S |
| Staff | to know how to respond | my actions are appropriate | C |
| Staff | it to be safe e.g. the wards computers and lounge TV are housed | M | |
| Staff | it to understand the potential difference between male/female SU | awareness is better | |
| Staff | to use it in everyday established processes e.g. safety huddle | we improve practice/embed it in culture | |
| Staff | to understand what I’m supposed to do with the information | my actions/care plans are right | M |
| SU | to be able to add things anytime of the day/night | it shows how I’m feeling | S |
| SU | like to use my own words | I can say things how I want | C |
| SU | use a drop-down box of phrases | I don’t always have to put my feelings into words | C |
| SU | it to capture individual concerns but also general ones | ||
| CTM | for it to support containment | it increases safety | C |
| CTM | to lessen the impact of a large screen with only negative outputs | SU/Staff feel safe | S |
| CTM | to encourage staff presence on the ward | SU feel Staff are available | M |
| CTM | to support the ward culture of ‘containment’ | staff work cohesively | S |
| Staff | to see the same as SU | we are talking about the same things | S |
| Staff | it to be viewable to all | we take a shared responsibility in the actions | M |
| Staff | everyone to be able to look at a large screen | everyone is aware of what’s happening | |
| Staff | understand how the SU see’s/feel’s the ward as they ‘know exactly what’s going on’ | I can learn the nature of the micro interactions | |
| Staff | the devices to be safe – ward phones get stolen | its achievable | M |
| Service user | to use the internet | I can do things/look things up | C |
| Staff | no other functions | it can’t be messed with | S |
| SU | to use my own phone, I have unlimited data | I have control | M |
| SU | to use my own phone, I have unlimited data | I don’t have to use the slow computers here | S |
| Staff | ensure data about all SUs are captured | The ‘quiet’ SU doesn’t get ignored/parity of care | S |
| SU | to ensure my friends are ok on this ward | I don’t have to worry about them | C |
| SU | to ensure my friends are ok on other wards | I don’t have to worry about them | C |
| SU | use my name | staff know it’s me | S |
| Staff | specifics about what is causing the unsafe feelings | I understand what is causing the feelings | |
| Staff | to know if the displays are recorded | we can use them later for formulations | S |
| Staff | a longer-term record of events | debriefings/actions are effective | |
| Staff | SU who can’t read or write to be able to use it | everyone can use it | |
| Staff | only see my wards information | I can concentrate on my ward | C |
| CTM | staff engagement | safety is better for staff and SU | S |
| Staff | education on how to use it/technology | I can use it properly | |
| Staff | everyone to chip in | the tool is adopted | S |
| Staff | any pictures to be more than RAG (red/amber/green), e.g. weather symbols or a rainbow colour system | people aren’t just ok, middle or not safe | S |
| SU | it to show the time as there are no clocks here | I know what time of day it is | M |
| SU | it to be explained properly – it is an optional extra NOT a replacement for human contact | it does not replace human contact | |
| Staff | know what’s the data collected for? | I understand why we’re doing it | S |
| Staff | to be able to see the whole ward and individuals in real time | I have a good overview of the environment | S |
| Staff | to maybe use emojis | people are familiar and can express themselves | C |
| Staff | the tablet to be robust | I don’t have to worry about them | M |
| Staff | tech that people already know how to use | it’s easy to use | |
| Staff | to use a mobile device/phone | its natural | |
| Staff | ensure there’s Wi-Fi | it works | M |
| Staff | no camera | Su aren’t worried about being recorded | S |
| SU | like it to be easy/familiar to use | I don’t have to learn new things | S |
| SU | to use my own words | I don’t have to use ‘hospital’ words | S |
| SU | Use patient-based words | they describe feeling better e.g. ‘worried’ ‘scared’ ‘fearful’ | S |
| SU | words that I use/no jargon | it has meaning for me | M |
| SU | language that isn’t condescending | I feel like a person | M |
| SU | to use bright colours | they match the ward | C |
| SU | input using picture and words | I can express myself even when I’m distressed/have jumbled thoughts | M |
| SU | it to use pictures as well as words | people who don’t speak English can use it | M |
| Staff | outputs may be in colours | its graded to support care plans/discharge | C |
| Staff | to be able to highlight poor environmental conditions e.g. plaster coming off the wall | the environment is improved | C |
| Staff | to look at factors influencing the atmosphere – how much details? | I can understand what is happening | C |
| Staff | to know who else is aware | we work together | S |
| Staff | ALL staff to benefit/understand the system | everyone is safe | |
| Staff | observe the ripple effect | I can understand it better | |
| SU | my world to be safe | I can get better | C |
| SU | to comment on noise and chaos of the ward | staff can do something about it | S |
Annex (b) to technical report: device set-up guide
| WardSonar – device setup |
|---|
| This guide assumes that each deployment in a ward will consist of two tablet devices. One for the patients to use within the ward to record their feelings and another for the staff within the ward to monitor/view responses. There are some connect set-up steps to do on both versions of the tablets and then specific instructions to setup each tablet with the correct applications. |
| Setup required on both tablets |
| These steps are aimed at reducing the amount of distractions, clutter and other third-party software on the devices, so that the respective users will have very limited opportunity to deviate from the primary objective of using the webapp. |
|
|
Settings
Open up the Settings app and navigate and apply the following settings: |
|
|
|
Uninstall applications
We want to remove all unnecessary applications from the device. Since the devices will exclusively be used to access a web application via the internet, almost all applications can be uninstalled. |
|
|
Delete home screen shortcuts
We want the home screen of the tablets to be completely free of all distractions and options – we just want a single application to be presented to the user who can simply press on it to load |
|
| Turn off app suggestions |
|
| Update the devices |
|
| Expected experience |
|
| Setup required for the user tablet |
|
| Staff tablet |
|
Prepared by Michael Stephens (mike@ayup.agency) and Steven Taylor (ste@ayup.agency)
Appendix 3 Example of the application of interview data to the data pool
During the various stages of Phase 1, a number of briefings were drafted to keep the steering group, stakeholders and technical developers, Ayup, apprised of growing insights from the data. For example, a technical briefing was drawn up following completion of the health professional interview data analysis. Key messages drawn from these data at this stage are summarised below:
-
Staff see patients as more sensitive to safety concerns than they are (this is both positive and negative): The threshold for safety is higher for staff than patients, because staff know what’s going to happen next in order to deal with an incident, and patients do not have that information. They also do not have information about other patients, so they can be more scared by an incident than staff are. In addition, staff see patients as having trauma responses and which leads them to having highly sensitive sensory reactions; and staff normalise distress whereas patients, especially new patients, do not.
-
Safety is a multifaceted concept that can mean different things to staff depending upon their professional role and career stage, and it is a shared responsibility for all staff regardless of role.
-
Safety incidents are often preceded by micro-cues (such as ‘a look’), but the context is complex and therefore subject to interpretation by staff.
-
Safety incidents and micro-cues are gendered. Men more often elicit intimidating, violent and aggressive behaviours, whereas women tend to withdraw or want increased staff attention. The social dynamics of a mixed ward can differ from that of a single sex ward. Mixed wards can have a different dynamic to single sex wards, for example, a mix of genders can facilitate social checks and balances on behaviour; but there can be more concerns about sexual safety on mixed wards.
-
Milieu and contagion: all staff seemed to agree that milieu and contagion exist even if they found these hard to articulate.
-
Opinions are divided about the introduction of a digital safety technology on the ward. For example, the quality of ward-based Wi-Fi is inconsistent and some wards do not have enough computers and rely heavily on handwritten records. Views were divided over the usability of digital tables and phones by patients to input safety data. Some felt that patients could easily do this, whereas others highlighted that some patients cannot read and write.
-
Both quantitative and qualitative strategies would be needed to evaluate safety.
-
In deciding how best to stream real-time safety data to staff, it was emphasised that every ward is different, and recognised that any technology would be experimental.
-
Few respondents mentioned potential harms to patients, although it was pointed out that asking patients to monitor safety could induce state of constant stress.
Appendix 4 Pen portraits
Apple ward pen portrait
Sometimes this ward was very quiet and other times it was chaotic, often because one patient felt restless and wanted to go outside for a walk but there weren’t enough staff to do this. The staff were consistently extremely busy and understaffed with the majority of visible staff on the wards being bank support workers who were very tired. I think the atmosphere on the ward was very changeable, often with a feeling of unsettledness. I would say this ward had a risk tolerant culture.
R1 reflection, 6 months post-implementation
Timeline
At baseline, R1 noted a ‘stifling’ atmosphere caused by COVID restrictions combined with a spell of hot weather. Patients could not go off the ward and there were no ward-based activities for them.
In week 4, it was clear that the device was only used when the ward manager was on duty, and the study was low priority.
[The ward manager] came out and met me in the corridor and looked a bit guilty, in a jokey way, and said, ‘we’re really bad at doing the WardSonar Device’.
R1 fieldnotes, week 4
Staff were starting to describe some of the challenges of using the device, for example, one mentioned that patients could become suspicious if repeatedly asked to answer the same questions. Patients were broadly supportive of the study:
R1: Did you like being asked about how you felt the ward was feeling at the time?
Patient: Yeah. ‘Cause they don’t really ask much.Patient interview, week 4
In week 6, the ward was very busy with several acutely ill patients. However, some ward activities for patients had resumed.
R1 noted that five support workers had still not heard of WardSonar, but also this week, the ward manager ensured that use of the device was at the top of the handover agenda and gave R1 a slot in the staff meeting to talk about the study. Some staff members expressed positive opinions about the study, for example:
I think [patients] quite like having a mechanism to feed back to us because I think sometimes obviously, they can get quite frustrated in here and don’t feel listened to.
Staff interview, week 6
One patient explained,
I felt it was like a way to let people know how I was feeling. And it was, like, an easy way.
Patient interview, week 6
Therefore, the ward manager was promoting WardSonar and staff seemed to be a little more familiar and comfortable with it.
R1 had struggled to find people to interview this week, and noted
I think this might have something to do with … the ward manager, not being present.
R1 fieldnotes, week 6
In week 9, R1 observed,
Generally, staff do not have a good understanding of the study.
R1 fieldnotes, week 9
One of the devices had gone missing. The ward manager decided to keep the other somewhere safe, but this meant that it was less available for use.
[The ward manager] said that she was worried … that one of the members of staff might have taken it but there is no way of knowing this. I say, have you been able to use the other device okay? And then she says, well we’re keeping it in my room, just to try and be a bit safer with it.
R1 fieldnotes, week 9
A patient said,
We did get asked [to use the device] quite a lot [a few weeks ago] but it’s just completely stopped now … When the staffing got really bad.
Patient interview, week 9
Some staff expressed reservations about the study, such as:
It’s a bit hard to just intervene in situations that are not going well on the ward, holding a device and asking them questions.
Staff interview, week 9
At the end of the implementation period,
The ward manager told R1 ‘I didn’t have a clue that there was that bit [i.e. the dashboard]’.
They also highlighted the importance of embedding the study in ward routines:
… Regular staff, if they know that there’s a project going on, are more likely to use their own initiative to go and do it; whereas, if it’s bank and agency staff, they needed to be told to go and do it … maybe it’s something that not all of the staff were on board with and so it didn’t get embedded …
Ward manager, post-implementation interview
Once a change is embedded into the culture, then it’s more likely to happen. And if the staff understand the rationale for it and they’re part of that and, kind of, on board with it, then they’d be more likely to do it … We probably didn’t get the time to do some of the preparation work that we, perhaps, would have liked.
ward manager, post-implementation interview
I suppose the whole purpose of it was to get to different points of the day to see if there was variation across and what those variations were. If you’re just doing once a day, it wouldn’t feel like you were gathering the right amount of information.
Ward manager, post-implementation interview
Acceptability and feasibility
One staff member explained,
Some patients experience paranoia … So, it’s not really received well by certain patients.
R1 fieldnotes, week 4
Staff and patients also expressed positive opinions, for example
The questions were right straightforward. And I like the pictures on it as well.
Patient interview, week 4
The ward manager emphasised the importance of embedding WardSonar into routines.
[if] it was busy, then [taking the device round] probably wasn’t getting done. Which is, perhaps, the times that you wanted it to be done … think at the time that you actually started, it was a really chaotic time on the ward … a lot going on in terms of COVID … it wasn’t on the highest agenda.
Ward manager interview, post-implementation
Suggestions for further development
Patients and staff made constructive suggestions. One much discussed topic was how frequently to take the device round to patients to collect their views on the ward atmosphere. A commonly expressed view was that three times a day was too much. As one patient put it, ‘Sometimes you’re in a mood'. (patient interview, week 4).
Supporting this point, a member of staff suggested:
Probably, best one is weekly, especially when we’re not having the time to do it a lot of the time, if it’s daily then, there might be days where we don’t actually do it at all, so it’s a bit pointless doing daily.
Staff interview, week 4
To make the device more accessible, staff suggested,
We were thinking, if there was a way that it could be on, like, a stand, sort of thing, say in the kitchen or something like that, so when patients are coming to get their food, they can … while they’re in the queue, they can, maybe, do it at the same time.
Staff interview, week 4
Bramble ward pen portrait
This ward was usually very busy, with a high number of patients admitted. Staff were not very accommodating and often rude and dismissive of others, including patients. This often led to emotional contagion. For example, when one patient requiring something from a member of staff member was dismissed, it led to others also questioning the members of staff and huddling up outside the staff base. This then caused unrest between the staff and patients, until patients’ needs were met. The staff on the ward were usually bank staff, as like other wards it too was short staffed. The atmosphere on this ward majority of the time was quite tense and staff weren’t always visible. Generally, staff remained in the staff base and patients in communal areas or their rooms.
R2 reflection, 6 months post-implementation
Timeline
At baseline, there were two patients in COVID-19 isolation and the ward was closed to new admissions. Patient facilities were reduced because space was required temporarily to accommodate female patients (this is a male only ward).
R2 was told she could not move around the ward because of safety issues, so when the devices were in the ward manager’s office she was unable to access them for checking or charging.
In week 4, the ward was busy and the alarm kept going off, with staff ‘running around’ (R2 fieldnotes, week 4) in response.
R2 learnt from staff that that low staffing and the use of bank/agency staff (i.e. new people to get used to) makes patients uneasy, and they get a sense that the environment is unsafe.
Device use was driven by the ward manager and it was not used when the ward manager was off duty. During this week there was no sign of the device on the ward and R2 thought it might be locked in the ward manager’s office. Despite this, the staff seemed generally engaged, and positive about the user interface and design.
Staff were largely unfamiliar with dashboard, although R2 was told that the dashboard data are considered in weekly meetings.
A member of staff said,
Asking [patients] multiple times, they tend to get annoyed.
Staff interview, week 4
A patient pointed out that,
It’s been very easy … simple questions …, and the way it’s laid out [but] say for more unwell patients …yeah, [the device] might get a bit too complicated … I helped another patient because he’d found it difficult to write a comment in the last bit.
Patient interview, week 4
In week 6, R2 heard from staff that they thought the user interface was well designed, because it was simple, brief and the pictures seemed to be important. The ward manager said they did not think the device is helpful; however, although the ward manager planned to incorporate the dashboard date into morning meetings, this had not yet happened.
Another staff member explained a specific difficulty with taking the device round:
I’m finding that, sometimes, because of the acuity of the ward, it’s getting missed, and it’s mainly because we don’t want to be carrying a tablet round even though it’s in a heavy duty case, I just don’t want it getting lamped against the wall or being used as a weapon. So, that’s why some shifts, it can be a bit of a hindrance.
Staff interview, week 4
R2 noted that there was some training on the device this week, though this seemed to her to be quite late in the implementation period.
In week 9, there had been a COVID-19 outbreak. Staff were busy working out strategies for COVID-19 isolation. Additionally, the roof in the visiting area was broken and there was a leak in the staff office. The device was only being used when the ward manager was on duty.
At the end of the implementation period, the ward manager clarified why the devices had been locked away at times during the implementation period:
If it goes on a ward, it will get broken.
Ward manager, post-implementation interview
They described strategies they had tried to encourage use of the device:
We have tried using it a couple of times when it’s busy [but] sometimes it didn’t get used at all, we tried to put names in the diary to do it but it is difficult … We have tried putting the device in the clinic, so … [patients] can just touch it when they’ve had their physical obs[ervations] done, which we trialled a couple of times. Sometimes it didn’t get used at all, we tried to put names in the diary to do it but it is difficult.
Ward manager, post-implementation interview
The ward manager emphasised the importance of finding ways to motivate staff to engage with the study and use the device:
What’s really hard is getting staff motivated to do it, especially with the acuity and COVID-19 and everything else … it’s like you’ve got to force them. So, when you’re [i.e. R2] not here, it gets missed … If it doesn’t have a purpose, they’re not interested … I think they’ll need to see the outcome to understand it fully.
Ward manager, post-implementation interview
Acceptability and feasibility
Notwithstanding the reservations they expressed, staff appeared to see potential value in data that highlights patterns in behaviour. They recognised that patients can often feel things building up that staff do not sense, and also may not want other patients to know how they feel.
Staff: A lot of the time the patients can feel what we might not necessarily feel building up and if you ask them, well why do you feel like that and they do explain, they might have had an altercation or something has been mentioned and it does help us because we’re more aware of what’s actually going on there.
R2: Do you think the device has helped to record that?
Staff: I would say so, yes when they’re doing games, you can sit down with them and do it and it’s a way of almost having an engagement with them when they don’t always feel like they’re having to talk because a lot of the time, they don’t want to do, what they call, grassing each other up and they will talk to you about why they feel like that.
Staff interview, week 4
With regard to the device, the ward manager’s comments reflected views expressed by staff and patients:
The device in itself, in terms of what it’s like, is good because you can reflect back and say, we’ve had three good summer days and we’ve had two stormy days.
Ward manager, post-implementation interview
Suggestions for further development
To engage staff, the ward manager suggested creating a video presentation about the study to give them a clearer understanding of the study background.
A patient suggested improving access to the device and simplifying the user interface to reduce the need for staff input:
The device could use pictures instead of words- then if staff are really busy, in which they are, like, pretty much 24/7 … that’s probably why I haven’t filled it out or other patients, you know. Yeah, it could be fixed onto the wall. Certainly, in a room … it couldn’t be, like, the corridors or something in case someone punched it.
Patient interview, week 4
Regarding how often data could be collected, staff agreed that three times daily was excessive:
Twice a day would possibly work, but I think it would be better just doing it once a day with just multiple patients instead.
Staff interview, week 6
Cherry ward (psychiatric intensive care unit) pen portrait
This ward was the most calm and settled with a strong staff presence felt at all times. There were occasions where one service user might be acting aggressively but staff were so quick to deescalate situations that I don’t think emotional contagion was as noticeable compared to other wards. I would describe the culture on this ward as risk averse. Regular staff were on this ward and, in general, patients and staff had good rapport.
R1 reflection, 6 months post-implementation
Timeline
At baseline, R1 observed that staff were tired. A cleaner told R1 that they had been working back-to-back shifts and also helping out with lunches because the cook was ill with COVID-19. R1 was asked to wear a mask and goggles. The staff and patients were friendly.
In week 4, R1 noted that there was a high proportion of very unwell patients, and also staff shortages. For instance, a translator was needed but there was none available. Staff were visibly taking the device round the patients.
R1: Have there been any times when you’ve not been able to bring it round to service users?
Staff: Just if there’s no one around, or if they’re in bed obviously I wouldn’t disturb them, but if they’re out on communal areas, then we’ll go and ask them.
Staff interview, week 4
Staff however were not necessarily seeing potential value in using the device
I can see how it could have some utility and maybe bring up some things in the future, but as it stands I think, yeah, it’s telling us what we already know.
Staff interview, week 4
In contrast, one patient explained that they liked to use the device, because,
I felt good in telling people that, like a lot of staff are really good people.
Patient interview, week 4
In week 6, the ward felt generally calm and quiet, though R1 struggled to find people to interview and the ward manager seemed to be ‘rushing around’ (R1 fieldnotes, week 6).
R1 found that the dashboard was not working and could not fix it or access technical support on this occasion, so was unable to demonstrate it to staff to explain its potential.
In week 9, R1 felt that the atmosphere was calm. A member of staff told R1 that with one exception, the patients were ‘a very settled group’, who would be ‘quite happy’ to speak with her (R1 fieldnotes, week 9). R1 learnt that one of the devices had been kept in a cupboard throughout the study, and found that staff tended to be sceptical about the potential of the collected data to be useful to them.
One member of staff described an interaction they had with a patient while taking device round, explaining that patients have views they wish to express even if they are not able to articulate them to staff:
I was shocked when one of the patients put in that it is stormy, when I asked what is happening, he couldn’t tell me. If he could tell me I could have given him one to one. But today we are short staffed.
Staff interview, week 9
Another staff member revealed they had added their own perceptions of the atmosphere to the data set,
Basically showed patients and used it myself to try to see what it was like.
Staff interview, week 9
At the end of the implementation period, the ward manager concluded that using the device had had a relatively small impact.
I genuinely thought that it might spark more conversations about whether patients felt safe and that would be an in to have a conversation about why that was and whether we could do anything about it, in terms of altering care plans …
Ward manager interview, post-implementation
Acceptability and feasibility
The ward manager particularly highlighted the assessments that take place on a PICU ward.
I think they’ve found it very easy to use and very easy to understand but don’t obviously see the utility in it, given they feel that they are used to or already privy to whether people feel safe or not on the ward. … on a PICU … everybody is seen in review, every single day by at least a doctor and a nurse and often by more people, and discussing their safety is a feature of that review every single day[so] some patients got a little bit irritated about it and were like, why are you asking me again.
Ward manager interview, post-implementation
Cherry ward’s routines seemed to make it difficult to circulate the device.
Suggestions for further development
I guess it would be good to do it in, like, in busy times of day like lunchtime, teatime, stuff like that.
Staff interview, week 4
Maybe just, like, if it was not handed out by staff but, like, hooked to a wall or something, you know, in a rugged case, so it can’t be broken.
Patient interview, week 4
In contrast to other interviewees across the study, the ward manager suggested a review of the user interface:
I think sometimes the cognitive deficiency that psychotic people have is an inability to think abstractly and by the very nature of using the analogy of weather with feelings could be confusing … I wonder, what is the disadvantage just to use plain, concise English?
Ward manager interview, post-implementation
Damson ward (psychiatric intensive care unit) pen portrait
This ward was a PICU ward. Although there were staff shortages the ward did have regular bank staff, allowing for rapport building with some patients. However, the atmosphere on this ward was unpredictable. Many patients were ‘high risk’ and the atmosphere could change rapidly. This was a mixed gender ward, but male patients would generally stay in their room and the female patients in the communal tv room. The only time groups of male and female patients would interact was when an incident took place. This is when emotional contagion was evident, especially when an incident occurred between staff and a patient. Staff and patients had many confrontations, generally because of patients feeling unheard or dismissed when knocking on the door of the staff base.
R2 reflection, 6 months post-implementation
Timeline
At baseline, it was notably busy, with alarms going off frequently. There were some very unwell patients and a member of staff described the ward as ‘quite chaotic’ (R2 fieldnotes). Tensions between staff were diffused by the ward manager. R2 was largely ignored by staff.
In week 4, R2 noted,
[Staff are] saying … people want to know how patients feel about ward safety, but what about staff safety and neglect?
R2 fieldnotes, baseline
A member of staff reported that the device helped to elicit patient perspectives and complements existing processes; for example, it could capture data that patients did not feel they could say directly to staff. Staff generally appeared to understand and value what the device was for, though it was unclear whether they were using the dashboard.
In week 6, R2 observed:
[A member of staff says that] patients on PICU wards don’t always fill out the device, they decline to do most things anyway, so to do this was a big ask. She also said how staff had been completing the questions instead. I did say that it’s just for patients…
R2 fieldnotes, week 6
One staff member questioned the trustworthiness of the information contributed by some patients:
They wrote a lot of daft stuff, but some of them did write how they were feeling.
Staff interview, week 6
Additionally, the ward was using a lot of agency staff who were not familiar with the device.
In week 9, staff seemed, in principle, to be open to using device, but did not know much about it, in contrast to observations made in week 4. R2 wanted to demonstrate how to use the dashboard, but it was not working.
Some staff suggested that using the device can feed into paranoid thinking, so may discourage some patients. R2 also learnt that staff were not using the data in team meetings; however, individuals did seem to be using the device to help them get an accurate sense of the atmosphere:
[Staff] mentioned … at the moment [the device] is only used for staff themselves to get an idea of the ward atmosphere.
R2 fieldnotes, week 9
At the end of the implementation period, the ward manager stated that they did not know much about the dashboard functions.
R2: Have you been able to use [the dashboard data] in any meetings or any handovers?
ward manager: I haven’t so far … I don’t know a lot about it to be honest.Ward manager, post-implementation interview
Staff engagement had also been a challenge:
I think on a few occasions, there’s been difficulties with staffing, trying to get the device out but I know a select few of the staff have been quite passionate about going round with it.
Ward manager, post-implementation interview
Staff report that patient’s perceptions of ward atmosphere is affected by their mood and their mood can change rapidly, and suggest that snapshot data could give an inaccurate impression. According to the ward manager, some of the barriers to adopting the technology stem from the level of acuity on the ward and the fact that it was unsettled for months up to the start of the study.
Acceptability and feasibility
Patients appeared to like both the concept and application of the device:
It’s straightforward. It’s not elaborated text, it’s just simple for my understanding, you see … It’s asking about my experience of being on the ward what is happening really and I think that’s good, we’re giving that information in as patients.
Patient interview, week 6
Not all patients wanted to engage however. The ward manager explained that,
The males, they just want to be left alone, so when you go in, they do get frustrated with you.
Ward manager, post-implementation interview
Some staff say patients approach them to report concerns, but also that the device may help those not willing to do so.
It’s definitely provided insight into how service users are feeling which is obviously always good, because it might not be something they’d want to tell us outright.
Staff interview, week 4
Suggestions for further development
The ward manager had wondered whether allocating use of the device to a single member of staff could increase uptake, but a member of staff suggested that this could be counterproductive:
If somebody is suffering from paranoia and you’re coming back with the same questions, seeing the same face, then it could bring issues.
Staff interview, week 9
It was generally agreed that the use of the device should be less frequent, as patients might be unavailable, and were often asleep. Staff and patients suggested that once per day would be suitable.
Elderflower ward pen portrait
Emotional contagion was most obvious on this ward, usually due to service users regularly congregating in groups outside the staff room to ask for an e-cigarette refill. Half the service users sat in communal areas and the other half stayed in their rooms. Service users on this ward sometimes argued and, on several occasions, physical fights needed to be deescalated. I would describe the atmosphere on this ward as tense. Staff were very busy but were visible most of the time.
R1 reflection, 6 months post-implementation
Timeline
At baseline, R1 noted that the ward felt clean and cheerful with friendly and helpful staff and patients who approached her, assuming she was staff herself.
In week 4, the ward had changed from mixed to all male and was notably busy. R1 noted that the use of the device was not incorporated into ward routines:
I can see the devices are on the table and I say, oh, [staff name], I’ll just show you how to use them, but they’re both out of battery … Staff were a bit reluctant today to have an interview. It felt like they have their hands full.
R1 fieldnotes, week 4
However, in interview, a member of staff was clearly supportive of using the device, saying that it was facilitating useful conversations.
I think with the ward going through quite a hostile period before this time … [patients] were keen to give that feedback.
Staff interview, week 4
In week 6, the ward atmosphere was volatile at times. Staffing levels were low:
The nurse in charge said that there are only five members of staff on the ward today, and there are meant to be double this.
R1 fieldnotes, week 6
Some staff were trying hard to collect data, though most were unfamiliar with the dashboard. There were mixed views about using the device. Some staff told R1 that patients saw it as pointless and rolled their eyes when asked to complete it repeatedly, but others said it was useful to have patient views and the device prompted conversation:
Actually it did prompt conversation because one or two people were really unhappy on the ward. So, I was like, why have you put that score kind of thing and then they would answer, if they were annoyed at someone or annoyed at the staff.
Staff interview, week 6
A comment from one staff member raised the question of whether a light-hearted reaction from staff could influence patients’ reports of the ward atmosphere (e.g. by seeming to not take it seriously or, alternatively, by making it easier to report staff tensions by introducing levity):
It was good to see how they were feeling, well to see how they felt the ward was … a lot of them said staff [were causing tensions], so I would just have a bit of a laugh and a bit of a joke, so it prompted conversation.
Staff interview, week 6
Technical issues
On one visit, R1 saw that the battery was dead in one device and a software update needed in the other.
In week 9, R1 noted several new patients. The ward was busy and R1 had difficulty engaging with the ward manager. R1 noted that the dashboard was not working properly, and that staff told her it had not been working ‘for weeks’. R1 could not fix the problem or access technical support, which meant it remained out of use for the time being. However, a student nurse told R1 that she had been taking the device round to the patients:
She said some patients don’t want to use it, some do, and that it is very straightforward to use.
R1 fieldnotes, week 9
A patient explained their view on using digital technology, suggesting that they would not easily use the device without help.
I’m not very tech savvy. I’m more still in analogue rather than digital. So I struggle quite a lot with my dyslexia. … I can use a mobile phone just about, and my device I can use just about, if I’m signed in. Sometimes I have to get people to sign me in … I find it a bit confusing, ’cause like … I’m like 50. I’m not like you young ones who can text like 90 miles an hour.
Patient interview, week 9
At the end of the implementation period, the ward manager emphasised that a main issue with implementation was reminding and motivating staff to use the device. They explained how general busyness had affected adoption of the technology.
When we started the study, it was very busy, we were very short staffed … the ward being shut and COVID-19 isolation, and the routine of the ward was very different. Whereas as we’re finishing it, we’re actually starting to come into a time where the ward is a bit more of a normal routine and structure.
Ward manager, post-implementation interview
Acceptability and feasibility
The ward manager also reflected that they had intended to use the device data in safety huddles,102 but,
We still haven’t started the safety huddles again, so through other circumstances on the ward, we didn’t end up being able to bring it but I think, going back to wards where I’ve previously worked where they did use the safety huddles regularly, I think it would have been really helpful to bring into that.
Ward manager, post-implementation interview
When asked about using the dashboard data, the ward manager recalled,
I know I showed quite a few [staff] the staff dashboard, I don’t know how many people checked it regularly but they did find it interesting when I pointed it out to them … [and] a lot of the patients really valued being asked about their thoughts on things.
Ward manager, post-implementation interview
The ward manager had a generally positive view of the study. Even just taking the device round the ward to patients helped staff to think about patient perspectives:
We had some quite interesting discussions about improving services and I suppose it led to a lot more conversations about patients being involved and that sort of thing, which was really good.
Ward manager, post-implementation interview
The user interface was seen to be inclusive.
[The questions] were good because they were simple … if the questions had been a bit more complicated, we probably wouldn’t have approached certain people because they wouldn’t have been in the mindset to engage with it.
Ward manager, post-implementation interview
R1 observed that patients were happy to answer questions using the device but much less inclined to leave additional feedback (as open text comments). It seemed to be valued by patients and staff:
I think with the ward going through quite a hostile period before this time … [patients] were keen to give that feedback.
Staff interview, week 4
Suggestions for further development
Staff suggested that real-time data could be helpful to plan where staff should be, such as more of them in communal area if patients report feeling unsettled.
The comment below represents a commonly expressed view from staff and patients that collection of patients’ views could be both unfeasible and unacceptable if too frequent.
Like if they are nagging [for] the information, or just [sometimes] I guess don’t feel comfortable because it’s too often.
Patient interview, week 9
Fir ward pen portrait
This generally was a quiet and calm ward. Staff were regular, with regular bank staff too. The visible presence of both nursing and healthcare support workers made the atmosphere supportive and relaxed. Staff and patients appeared to have a strong rapport; however, the atmosphere did often change. Other than at mealtimes or to smoke patients didn’t really leave their rooms. This may have been due to COVID on the ward numerous times, and a reduced level of communal activities/games. Incidents often did take place where a patient acted aggressively, but they were quickly resolved and other than one incident involving two patients and a fight, I do not recall any obvious emotional contagion. This risk levels on this ward appeared to be low.
R2 reflection, 6 months post-implementation
Timeline
At baseline, it was busy, with alarms going off, and staff delivering food to patients located in isolation area. Patients and staff were enduring COVID-related disruptions, loss of amenities and communal space. R2 noted tensions between staff, and that some staff were quite abrupt and rude with her.
In week 4, R2 was asked to don additional personal protective equipment, including goggles. She sensed that that the ward manager and assistant ward manager were avoiding her. She did not see any sign of the device being used; it was in a corner in the staff base out of sight, no one really encourages staff to use it (R2 fieldnotes, week 4).
One patient mentioned how they don’t get given the device because, they suggested, they ‘might damage it’.
In week 6, many staff did not appear to know why R2 was present on the ward, although the ward manager had explained to R2 that all staff had been informed about the study. There was no sign of the device.
When I was trying to speak to the ward manager, he said he’d bring [the device], but he didn’t … I feel [nursing staff] on this particular ward to be very rude and dismissive and will only speak to me if the ward manager asks them to … healthcare support workers [are] more friendly.
R2 fieldnotes, week 6
Many patients were asleep in their rooms during the day and therefore were not available to be approached for an interview.
In week 9, there were several new patients. R2 continued to try to engage with the ward manager, without success.
I can see that there is one of the devices that’s been left on the staff desk … it looks like it’s just been used. It’s next to a student nurse [who said], some patients don’t want to use it, some do, it really depends. She says it’s very straightforward to use.
R2 fieldnotes, week 9
At the end of the implementation period, the ward manager said that use of the device was not prioritised during a busy period.
I’ll be honest with you, I haven’t done any of [the dashboard] … it is useful, but apologies that I forgot that it was on the device … I feel like, about 2 weeks ago, for a week we had COVID-19 on the ward, so it was really busy … we’ve had an influx of admissions and within those admissions, we’ve had quite a few poorly people. During that 2-week period, we had two serious assaults on the ward … So, there was possibly a week and a half, 2 weeks period where we’ve not completed any.
Ward manager, post-implementation interview
However, they indicated that it had been useful to prompt conversations, and emphasised the importance of embedding use of the device in daily routines:
We had some quite interesting discussions about improving services and I suppose it led to a lot more conversations about patients being involved and that sort of thing, which was really good.
Ward manager, post-implementation interview
It’s more the routine of remembering to hand it out, which I think we struggled with.
Ward manager, post-implementation interview
Acceptability and feasibility
R2 repeatedly found herself explaining to staff why she was present on the ward. Compared with other wards, some patient interviews were very brief, as interviewees had difficulty concentrating.
Device availability depended on the ward manager and the device was not necessarily available to be used. R2 also observed that staff were not prompted to use device and that there was often no sign that it was in use or had recently been used. Nevertheless, despite an apparent lack of enthusiasm for the study, team leaders facilitated observations and interviews, which helped R2.
The ward manager explained that when they were busy, they were less likely to use the device; but equally, low ward occupancy meant patients may be approached with device too often:
… people did find it a little bit repetitive, they were finding that three times a day, the service users felt was too much.
Ward manager, post-implementation interview
Staff may be reluctant to risk damage to device, and may not offer it to all patients.
Once the interview stopped, the patient mentioned how they don’t get given the device because they might do something with it, they might damage it.
R2 fieldnotes, week 4
There was a mixed response from patients; some engaged, some refused, some wanted staff to put their answers in for them, and some anticipated a prompt staff response when they looked at the data.
Well, for example, if it was very ‘stormy’, the staff might come out and talk to the patients and see what was happening, and why they are feeling that way.
Patient interview, week 9
Patient: I just left it to the staff to fill it in for me. Yes.
Patient interview, week 6
The design of the user interface was generally liked:
It’s quite simple and straightforward, the questions … It just makes you think, what is making you feel that way … I just found it easy to navigate.
Patient interview, week 4
I think [the questions] were good because they were simple enough for people who were in the earlier stages of their admission to understand.
Ward manager, post-implementation interview
Suggestions for further development
R2: So, initially the device was asked to be used three times a day …
Patient: Three times a day for the same person? … How is that going to change, why do you want it three times a day?
Patient interview, week 6
A patient suggested that ‘if staff had like a rota for who’s going to go round and use it at different times, that would be really useful’ (patient interview, week 4).
Glossary
Acute adult mental health ward Inpatient facility for working-age adults currently experiencing a severe crisis in their mental health.
Clustering In this context, clustering is a result of behavioural contagion – multiple similar incidents occur during the same time period; for example, agitation in one individual may be sensed by another, who then feels agitated themselves.
Milieu In this context, milieu involves the interaction between the physical environment, social structures and social interactions.
Patient In this study, the term ‘patient’ means someone who is currently receiving health care, for example, as an inpatient a mental health ward.
Safety huddle Daily focused brief meetings between ward staff.
Service user In this study, ‘service user’ means a person who has experience of using hospital mental health services but may not currently be doing so. Social contagion Ideas and behaviour that spread through social contact.
Steering group The project steering group included co-investigators and key collaborators leading the intervention development phase: a digital design group (Ayup Digital) and co-production specialists (Thrive by Design). Steering group meetings informed the development and evaluation phases.
Tablet/device Terms used in this study for the digital tablet computer used by patients to enter data about their perceptions of ward safety in real time.
WardSonar The study reported here sits within the WardSonar programme of research to develop a service user-centred, co-designed patient safety intervention for acute mental health wards.
Web app Application programme accessed via a web browser.
List of abbreviations
- AHRQ
- Agency for Healthcare Research and Quality
- DTAC
- digital technology assessment criteria
- IT
- information technology
- MMSF
- Measurement and Monitoring of Safety Framework
- PICU
- psychiatric intensive care unit
- PPIE
- patient and public involvement and engagement
- PRASE
- Patient Reporting and Action for a Safe Environment
- YCFF
- Yorkshire Contributory Factors Framework
- Zinf
- zero-inflated negative binomial model