Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/100/15. The contractual start date was in November 2018. The final report began editorial review in February 2020 and was accepted for publication in October 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Hannigan et al. This work was produced by Hannigan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Hannigan et al.
Chapter 1 Background and rationale
In this project, we undertook a rigorous synthesis of research and other evidence in the area of end-of-life (EoL) care for people with severe mental illness (SMI), conducted according to internationally agreed quality standards. The project has been within the remit of the National Institute for Health Research (NIHR) Health and Social Care Delivery Research (HSDR) programme in addressing quality, organisation and access in health services. In the context of calls for parity of esteem between mental health and physical health care,1 the health problem this project has addressed is a highly relevant but perhaps neglected one.
In preparing the original proposal supporting this project, an initial scoping review of literature was undertaken (with updated searches run in July 2018), and a targeted search was made for relevant policy documents across the four UK nations. A search of the database of NIHR projects was conducted to check for overlapping or related studies. Preliminary searches of four databases (combining ‘palliative care’, ‘mental health’ and ‘service provision’ terms) produced 4754 citations, within which were a number of relevant papers, including two previous literature reviews (from the UK and Canada, respectively), both now out of date, having been published over a decade ago. 2,3 Items discovered in this scoping search confirmed the timeliness and feasibility of a new, rigorous evidence synthesis, and particularly an EPPI (Evidence for Policy and Practice Information)-Centre-style review that is sensitive to the needs of stakeholders and that includes grey and non-research materials. 4 Items from this initial search, combined with general material addressing what is known about the burden of disease and the physical health of people living with mental health difficulties, have been used to inform this background and rationale (and subsequent) sections of this project report.
Burden of disease and costs
The overarching background for this project includes what is already known about the burden of SMI, cancer and end-stage lung, heart, renal or liver failure. Mental ill-health is a leading cause of years lived with disability around the world, with major depressive disorder the leading cause of years lived with disability in 56 countries and the second leading cause in a further 56. 5 Specific cancers, along with mental ill-health, neurological conditions, drug use disorders and specific organ diseases, all feature in the leading 20 causes of disability adjusted life-years in England for 2013. 6 The wider economic costs of mental illness in England were recently estimated at £105.2B each year. 7 This figure combines the direct costs of services, lost productivity at work and reduced quality of life, with the annual costs of the same in Wales estimated at £7.2B. 8
Meeting the physical health needs of people living with severe mental illness
The term ‘severe’ (or, often used interchangeably, ‘serious’, ‘serious and enduring’ or ‘serious and persistent’) mental illness, as used throughout this project, has longstanding currency in the fields of mental health policy, services and practice, dating back in the UK at least as far as the publication of Building Bridges: A Guide to Arrangements for Interagency Working for the Care and Protection of Severely Mentally Ill People. 9 It continues to be used in research10 and has currency with the NIHR Dissemination Centre, which published a themed review on SMI in 2018. 11 Building Bridges recognised the imprecision of the term ‘severe mental illness’ and endorsed a multidimensional framework definition encompassing five areas: safety, need for informal or formal care, disability, diagnosis and duration. Diagnosis is, therefore, an important, but not the only, dimension used in the identification of people with SMI and includes the International Classification of Diseases, Tenth Revision, diagnoses of schizophrenia, schizotypal and delusional disorders, bipolar affective disorder, and disorders of adult personality and behaviour,12 along with similar Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnoses, including schizophrenia spectrum and other psychotic disorders, bipolar and related disorders, and major depressive disorder. 13
The particular focus in this project on EoL care can also be set in the context of people with SMI having high comorbidities2 and experiencing higher mortality rates and reduced life expectancy than the general population. 14 Higher mortality and morbidity rates for this group have been found across all age groups,15 with a 10- to 20-year reduction in life expectancy reported. 16 Inequities, not limited to care at the EoL specifically, can be explained with reference to individual- and system-level factors. People with SMI are less likely to attend health screenings and may respond to symptoms differently. 17 They may delay or avoid seeking help, and are more likely to exhibit disruptive behaviours or miss contacts with health professionals,3,18 putting them at risk of delayed disease detection. 2 Inadequate support systems are also common among those with SMI, affecting their ability to access appropriate clinical care and navigate complex health systems. 19 Other factors influencing variations in mortality and morbidity for people living with SMI include poor previous experiences of seeking help from health-care professionals (HCPs), care staff’s incorrect attribution of physical symptoms to psychiatric disorder and the lack of experience by mental health professionals in determining how and when to refer people onwards to other appropriate services. 3,20
End-of-life care for people with severe mental illness
In this study, following the definition used by the General Medical Council,21 EoL care is used to refer to the care of people who have diagnoses of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and are likely to die within the next 12 months. It includes care provided in hospitals, hospices and other institutional settings (e.g. care homes, prisons and hostels) and care provided in the home and via outreach to people who may also be homeless.
Beyond the inequities identified above, commitments to parity of esteem demand that EoL care for people with SMI should be as timely and as high quality as it is for others. However, early evidence gathered in support of this initial project proposal suggests that this group is poorly served, with England’s Cancer Strategy 2015–2022 recognising that people with SMI need to be the focus of improvements diagnosis and care. Although the incidence of cancer among people living with SMI is similar to that of the general population, mortality rates among those with SMI are double. 23,24 This disparity may be related in part to late presentation and reduced use of interventions such as surgery, chemotherapy or radiotherapy. 25,26 The experience of SMI can delay detection and treatment of life-threatening physical disorders as people are less likely to seek treatment, to verbalise pain and to access timely health care. 27 Consequently, this patient cohort is more likely to present with more advanced cancers that are invariably more complex and costly to treat, with patients less likely to undergo invasive treatments and more likely to die. 28 Some cancers, other terminal conditions and/or related treatments may also compound mental illness and precipitate potential ‘problematic’ behaviours. 29 For many patients, therefore, palliative care is often the only meaningful treatment option available.
The original case for this evidence synthesis also built on the observation that, once people with SMI are in touch with EoL services, their symptoms may be poorly recognised and undertreated, with staff working in EoL services lacking knowledge, training and experience in this area. 30 Undetected and hence untreated mental illness can jeopardise treatment outcomes, reduce patient satisfaction and increase health-care costs. 31 Variable adherence can be a complicating factor,19 compounded by comorbid disorders, such as substance misuse, and social factors, such as homelessness, isolation or lack of transportation, all of which can exert an impact on planning for EoL care and treatment. 3,15 Assumptions about the capacity of people with SMI to make EoL decisions, and concerns that EoL discussions would be too distressing or would exacerbate mental health problems, may lead to inadequate consultation and advance care planning. 32 The case for this project included reference to the fact that people with SMI have a higher percentage of ‘do not resuscitate’ orders than other groups and are less likely to have had discussions about their explicit wishes for EoL care. 33
Palliative care
Although not all people at the EoL need palliative care, a review of the evidence34 confirmed inequities in palliative care provision for both cancer and non-cancer patient populations. In Wales, an estimated 24,000 of the 32,000 people who die per year would benefit from palliative care, but over one-quarter do not have access to it. 34,35 Access to palliative care services among people who die from cancer is 46%, compared with 5% among those dying from other conditions,36 including end-stage lung, heart, renal or liver failure.
The case for this project recognised that people with mental illness and advanced incurable cancer and/or lung, heart, renal or liver failure face inequities and discrimination35 and a lack of integrated care. 2 Some may be excluded from EoL care planning3, and even from hospitals or hospices entirely. 29 They may be referred back to mental health services, where staff are often inadequately prepared to provide appropriate EoL care. 3 Difficulties accessing appropriate services mean that for people with mental illness and a life-threatening disease palliative care may be the first line of treatment. 2 The specific provision of palliative care for people with SMI is known to be poorer than for the general population. People with SMI are approximately 50% less likely to access appropriate palliative care, including symptom control and pain relief. 3,20 Palliative care and hospice staff often feel unskilled,20 lacking confidence and training in conducting discussions about EoL care with people SMI. 32 Evidence gathered to inform the proposal for this synthesis also indicates that there is a lack of co-ordinated EoL care, and that access to appropriate psychosocial support is often limited. 2,3 Medical and nursing staff working in hospices have also been shown to be unprepared for working with people with SMI, basing their assessments on instinct rather than using evidence-based approaches. 37 In a survey of psychological services in hospices in the UK and the Republic of Ireland, only 30% of hospices had access to a psychiatrist, 41% had access to a clinical psychologist and 45% had neither. 38 Patient experience data underscore these observations, with England’s National Cancer Patient Experience Survey showing that people with a long-term mental health condition (2% of those surveyed; n = 1184) reported less positive experiences of cancer care. 39 In Wales, the most recent National Cancer Patient Experience Survey40 found that the lowest proportion of respondents reporting positive experiences of their cancer care were those identifying as also having mental health problems.
Evidence explaining why this research was needed
Research at the interface of physical and mental health care is recognised as a UK priority. 41 Against the background presented above, this project has created generalisable knowledge to improve EoL care and services for an underserved group. Policies from the four UK governments focus on improving EoL care, where diagnosis is immaterial. 42–50 These policies require the introduction of palliative and supportive care earlier in the illness trajectory, with patient surveys showing that this is rated very highly by those receiving it. 51 The charity Marie Curie (London, UK) identified triggers that should initiate palliative care for people with diagnoses other than cancer,52 but, apart from dementia, it does not mention those with pre-existing SMI. In national policy the needs of people with SMI who develop advanced incurable cancer and/or end-stage lung, heart, renal or liver failure are acknowledged poorly, or not at all. This group face the prospect of ‘disadvantaged dying’53,54 at a time when quality of care in the last months of life should be uniformly high for all groups.
Uniquely among the cancer, palliative and EoL strategies developed across the four countries of the UK, the Independent Cancer Taskforce’s Achieving World-class Cancer Outcomes: A Strategy for England 2015–202022 makes the specific recommendation that the NIHR commission research in the area of cancer care for people living with SMI. This project has responded to this call, and expanded it to also cover EoL care for people living with SMI and facing end-stage lung, heart, renal or liver failure. It has answered a question that is both timely and relevant: what evidence is there relating to the organisation, provision and receipt of care for people with SMI who have an additional diagnosis of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months?
This rigorously conducted evidence synthesis has brought together reports of approaches to service organisation, processes and interventions shown to both facilitate and hinder the provision of high-quality, accessible, equitable and acceptable EoL care to people with SMI. The project team has also gathered research and other evidence reporting the views and experiences of service users, families, and health and social care staff. Outputs from the project are intended to have an impact on services and practice, and plans are in place to present findings in accessible ways to NHS and other managers, practitioners and educators. It is anticipated that findings will inform future National Institute for Health and Care Excellence (NICE) guidelines, and thereby help shape the provision of services. Current relevant NICE guidance55–59 lacks standards or recommendations that particularly address EoL care for people with SMI.
A pre-project search of NIHR databases found studies that have investigated the physical health of people with SMI (e.g. Health Technology Assessment 12/28/0560), services for this group across organisations (e.g. HSDR 11/1023/1361) and care for people experiencing mental health difficulties after receiving cancer diagnosis (e.g. Health Technology Assessment 09/33/0262). As no research has been commissioned in the area addressed here, this project has effectively opened a new and important programme of work with value to the NHS and its partners. Having used a methodical, systematic and transparent approach, the MENLOC project team now plans to use this synthesis as the starting point for a programme of research that builds on what is already known, is designed with people who have experience of mental health difficulties and with people who have lived with cancer and have cared for family at the EoL, and generates new evidence of what works with value to the NHS and other relevant organisations.
Chapter 2 Working with stakeholders and defining parameters
In this chapter, the approach taken to working with stakeholders, including members of the public and people with personal experience of mental health and/or EoL care, is described. Reporting of this section is completed with reference to GRIPP2-SF standards. 63 The proposal for this evidence synthesis was shaped by people with experience of mental health problems, cancer and other long-term conditions, and by people with experience of caring. The original idea for the study arose following sustained and critical discussions between two co-investigators, Roger Pratt and Sally Anstey, who together identified that individuals with SMI are disadvantaged when diagnoses of advanced cancer or end-stage organ failure are made. Roger is a retired mental health social worker who lives with lymphoma (in long-term remission) and heart failure. He cared for his wife who died from advanced peritoneal cancer; she received specialist palliative care in the last year of her life and died in a hospice. This discussion observed that professional perceptions and misperceptions such as stigma and fear have an impact on management (e.g. pain control, supporting choice and place of care/death) in the case of people with SMI receiving EoL care. Alan Meudell later joined the project team as a mental health service user consultant and researcher. He has worked on two previous NIHR studies64,65 and one Health and Care Research Wales study66 and has led training for Health and Care Research Wales on involving service users in research. He is also interested in the physical health care of people living with mental health difficulties and in the provision of equitable services.
Throughout the project, building on these beginnings, the aim of public and patient involvement was to embed public and patient involvement perspectives into all aspects of the project, from the definition of search terms and parameters onwards to impact and dissemination. The role Alan Meudell played was equal partner in all stages of the research process except the literature search (which was led, uniquely, by Mala Mann as the team’s information services specialist). At his request, once the project had started, Roger contributed at stakeholder advisory group (SAG) meetings only, although both he and Alan Meudell participated in initial training that other investigators joined. They also contributed to the task of identifying carers and service users to join the project stakeholder group. Alan Meudell advised on the ongoing focus and direction of the study, and directly contributed to the screening of items for possible inclusion, the synthesis of materials and the accessible writing-up of this final report. In preparing an initial project proposal for submission to the HSDR programme, plans were also presented to the Patient Experience and Evaluation in Research (PEER) group at Swansea University (www.swansea.ac.uk/humanandhealthsciences/research-at-the-college-of-human-and-health/patientexperienceandevaluationinresearchpeergroup/; accessed 14 February 2020). The PEER group comprises people with experience of using health-care services and of caring and exists to provide a public and patient view of research proposals before they are submitted for funding. When the proposal was considered by the PEER group, members gave it a very positive response, stating that this was a much-needed project in an area that is largely ignored. People were particularly interested in plans for choosing members of the SAG and advised the project team to engage with charities such as Macmillan Cancer Support (London, UK), with hospices and with palliative care staff such as nurses. They also recognised the difficulty of actually recruiting SAG members from the target population but believed an attempt should be made to engage by offering opportunities for people with SMI and EoL diagnoses to participate in any way feasible for them. This advice was noted, and services in South Wales were approached to seek their agreement in principle to help put project team members in touch with service users and carers (as well as managers and practitioners) able to advise the study.
Populating the SAG was accomplished during the project set-up phase, with representatives drawn from the mental health and EoL fields. Members included professionals from a range of practitioner backgrounds based in NHS and charitable organisations, policy advisers and people with lived experience of mental health difficulties and of life-threatening disease. The full membership of the SAG is found in Appendix 1, and over the life of the study the combined project team and SAG met, in Cardiff, at three strategic time points. The first meeting was scheduled at the commencement of the project, with the focus on agreeing terms of reference (see Appendix 2) and then refining database search terms and wider search strategies, including the identification of online sources for the team to consult (see Appendix 3). The second meeting took place after the evidence searching and screening had been completed, which provided an opportunity to share work in progress (see Appendix 4). The final meeting was scheduled at the commencement of the whole-project synthesis and report-writing phase, with a focus on sharing preliminary findings and discussing plans for dissemination and maximising impact (see Appendix 5).
Defining the project’s parameters: ‘severe mental illness’ and ‘end of life’ (and related)
At the first, key, combined project team and SAG meeting, candidate database search strategies and search terms developed by the project team for both SMI (see Appendix 6) and EoL care (see Appendix 7) were distributed and discussed at length with the purpose of refinement.
Severe mental illness
Project team and SAG members recognised the imprecise nature of the phrase ‘severe mental illness’, but also the everyday currency of the term. It was recognised that the focus of this study was broadly on EoL care for adults over the age of 18 years who have used secondary, specialist, inpatient and/or community mental health services. At the meeting participants also discussed the inclusion of additional diagnoses [e.g. anorexia and post-traumatic stress disorder (PTSD)] not listed in the MENLOC protocol. It was noted that diagnostic manuals are extensive, and that listing new individual diagnoses at this point would open the door to including all diagnoses, making for unmanageable searches. It was decided, therefore, not to include such terms.
An intense dialogue was held around the diagnosis of depression as a result of the large numbers of outputs initially retrieved via the scoping search reporting on depression as a consequence of receiving an EoL diagnosis, as opposed to preceding such a diagnosis. The continuum of depression was also noted, and the project team agreed that outputs concentrating on people with mild, commonly experienced depression (and, by extension, anxiety) should be excluded. A consensus was to remove ‘depression’ as a search term or MeSH (medical subject headings) term but instead use ‘depression’ in conjunction with other terms such as ‘psychosis’ or ‘pre-existing’ or ‘severe’. This meant, therefore, using adjacency searching to retrieve accurate results. Project information specialist Mala Mann confirmed that older terms such as ‘melancholia’ would not need to be searched for, because database indexing combines outputs using these phrases with outputs using more contemporary terminology.
Project members reported that not all initial EoL care outputs retrieved made clear whether or not the mental health problems experienced preceded EoL diagnosis. Some discussion also took place on whether or not a fourth arm should be added to the search strategy, capturing the use of secondary services, in recognition of the fact that people with SMI are overwhelmingly people who use secondary mental health services. It was noted that a four-arm search would be too narrow, and that citations containing such terms would already be identified using the existing three-arm search (see Chapter 3).
A decision was made not to search specifically for the search terms ‘suicide’, ‘assisted death’, ‘assisted suicide’ and ‘euthanasia’ (noting that euthanasia may be seen by some people using services as the only possible option when all else fails), as papers in these areas would be found through existing search strategies.
End-of-life care
Suggestions from SAG members for search terms related to the EoL were noted, including ‘thanatology’ (the study of the theory, philosophy and doctrine of death); ‘best supportive care’/’enhanced supportive care’ (these being relatively new terms currently in use); ‘end-stage’, as a term to represent dying with chronic conditions; and ‘conservative management’ or ‘conservative treatment’. A consensus was to exclude ‘self-poisoning’ or ‘self-inflicted injuries’, as the goal of treatment likely to be reported in outputs was to sustain life. A consensus was also not to add into the search strategies terms attempting to establish the reasons for EoL care, but to include terms reflecting the closing down of active treatments: ‘withdrawing active treatment’, ‘withdrawing’ or ‘refusing’ treatments such as dialysis and ‘moribund’. It was noted that the ‘expected last six months of life’ is a term used in the USA and should be included.
At this first combined project team and SAG meeting, participants identified a group of conditions not previously considered by the project team, covering (for example) conditions broadly referred to in the meeting as ‘brain failure’. It was noted that ‘brain failure’ outputs would be captured under the term ‘organ failure’, and that a separate funding proposal was being prepared to synthesise the evidence in the area of EoL care for people with neurodegenerative conditions.
Finding grey literature, including non-research material
Websites to search that had already been identified by the project team were circulated (see Appendix 8), and in this first, key, meeting SAG members were invited to identify additional online sites. Suggestions made in the meeting or received thereafter included a Hospice UK (London, UK) report (KC), deaths in custody (SP), palliative care in prisons (NP) and searches on institutional repositories.
Chapter 3 Methods and description of included materials
This chapter describes the methods used in this evidence synthesis, and the materials finally included. At the commencement of the project a protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD42018108988). 67 The synthesis was conducted with the co-investigator involvement of an expert from the Cardiff Specialist Unit for Review Evidence (SURE). It followed guidance for undertaking reviews in health care published by the Centre for Reviews and Dissemination68 and in incorporating stakeholder views and non-research material used methods informed by the EPPI-Centre. 4 To ensure rigour, the review is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 69 Factors facilitating and hindering high-quality EoL care for people with SMI were identified, as was evidence relating to services, processes, interventions, views and experiences.
Aims and objectives
The aim of this project was to synthesise relevant research and other appropriate evidence relating to the organisation, provision and receipt of EoL care for people with SMI (including schizophrenia, bipolar disorder and other psychoses, major depression and personality disorder). Specifically, it answered the following question: what evidence is there relating to the organisation, provision and receipt of care for people with SMI who have an additional diagnosis of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months?
The specific objectives were to:
-
use internationally recognised, transparent literature review approaches to locate, appraise and synthesise the relevant research evidence relating to the organisation, provision and receipt of care in the expected last year of life (LYoL) for people with SMI who have additional diagnoses of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months
-
locate and synthesise policy, guidance, case reports and other grey and non-research literature relating to the organisation, provision and receipt of care in the expected LYoL for people with SMI who have additional diagnoses of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months
-
produce outputs with clear implications for service commissioning, organisation and provision
-
make recommendations for future research designed to inform service improvements, guidance and policy.
Inclusion criteria
Types of participants
This evidence synthesis considered all relevant evidence specifically relating to adult participants (> 18 years of age) with SMI who have an additional diagnosis of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months. SMI was defined as including but not limited to schizophrenia, schizophrenia spectrum and other psychotic disorders, schizotypal and delusional disorders, bipolar affective disorder, bipolar and related disorders, major depressive disorder and disorders of adult personality and behaviour.
Types of intervention and phenomena of interest
All citations were considered that addressed service organisation and the provision and receipt of EoL care for people with SMI who have an additional diagnosis of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months. Citations reporting the views and experiences of service users, families and health and social care staff were also included.
Context
All citations were considered with regard to organisation, provision and receipt of EoL care provided in hospitals, hospices and other institutional settings (e.g. care homes, prisons and hostels) and care provided in the home and via outreach to people who may also be homeless.
Types of evidence
Types of evidence sought included quantitative research, qualitative research and non-research material (e.g. policies, guidelines, reports of practice initiatives and clinical case studies). Searches were conducted for UK-only grey literature, including policies, guidance and related information, in recognition of the fact that the primary audience of decision-makers interested in the study’s key findings and implications is likely to be UK based. Materials published in the English language since the inception of databases were considered.
Exclusion criteria
-
As confirmed in a first combined project team and SAG meeting, where reporting allowed the distinction to be made, evidence relating to mental health problems (e.g. depression) as a consequence of terminal illness (e.g. cancer or chronic organ failure).
-
Evidence relating to EoL care for people with mental and behavioural disorders due to psychoactive substance use, except where these coexisted with SMI as specified above.
-
Evidence relating to EoL care for people with dementia or other neurodegenerative diseases, except where these coexisted with SMI as specified above.
-
Evidence from animal studies.
Developing the search strategy
The focus of the search strategy was to achieve high sensitivity and specificity for retrieving studies relevant to the review question. The search strategy was comprehensive and designed to ensure that all relevant literature was obtained, with the precise emphasis on concepts associated with the research question discussed in the first combined project team and SAG meeting, described in Chapter 2. Although some terminology remains equivocal in this area, the search strategy as it became finalised was designed to identify all relevant evidence relating to EoL care (i.e. in the LYoL) in those with SMI. Reflecting the importance of diagnosis in the framework definition of SMI,9 diagnostic terms included in the search strategy included schizophrenia, schizophrenia spectrum and other psychotic disorders, schizotypal and delusional disorders, bipolar affective disorder, bipolar and related disorders, major depressive disorder and disorders of adult personality and behaviour. Reflecting prevailing definitions of SMI (e.g. as used by the NIHR Dissemination Centre11), searches were not made for studies into mental and behavioural disorders due to psychoactive substance use or for studies into dementia or other neurodegenerative diseases, and items in these areas were not included in the review, except where participants’ diagnoses co-existed with the disorders included above.
Preliminary searching
Preliminary database searching using MEDLINE was carried out as part of initial scoping undertaken in preparation of the proposal for funding, with material from this drawn on in Chapter 1. The preliminary keywords that were used to inform these searches included the following:
Palliative care OR Hospice care OR Terminal care OR Terminally ill OR End of life care OR Last year of life
AND
Neoplasms OR Cancer OR heart failure, lung failure, liver failure or renal failure
AND
Mental health OR Depression OR Mental disorders OR Depressive disorder OR Personality disorders OR Bipolar disorder OR Schizophrenia OR Mental illness
An analysis of the text words contained in the titles and abstracts, and of the index terms used to describe each article, was undertaken. As a result of this, the search strategy was further developed, and in July 2018 the opportunity was undertaken to update and extend the preliminary scoping exercise across four databases. These were, on Ovid, MEDLINE® ALL, MEDLINE Epub Ahead of Print, In-Process and Other Non-Indexed Citations, PsycInfo and EMBASE. The MEDLINE search can be found in Appendix 9.
Comprehensive searching
A comprehensive search strategy was developed by Mala Mann following discussion at the first combined project team and SAG meeting (see Chapter 2). This search strategy was initially developed for MEDLINE (see Appendix 10) and PsycInfo (see Appendix 11). As a means of testing and refining this search strategy before applying it across multiple databases, Deborah Edwards first screened the citations retrieved across MEDLINE and PsycInfo to ensure relevance and to assess that the strategy was neither too broad nor too narrow. Once the project team was satisfied with the search strategy, this was tailored to the remaining eight databases, with searches run from each database’s inception. Databases searched included:
-
on the Ovid platform – MEDLINE ALL, EMBASE, HMIC (Health Management Information Consortium), PsycInfo and AMED (Allied and Complementary Medicine Database)
-
on the EBSCOhost platform – CINAHL (Cumulative Index to Nursing and Allied Health Literature) and CENTRAL (Cochrane Central Register of Controlled Trials)
-
on the ProQuest platform – ASSIA (Applied Social Sciences Index and Abstracts)
-
others – DARE (Database of Abstracts of Reviews of Effects) and the Web of Science.
Supplementary searches were undertaken to identify additional papers, information on studies in progress, unpublished research, research reported in the grey literature and personal blogs. Members of the SAG advised the project team as to which relevant websites to search (see Chapter 2), and a full list of websites searched along with the search terms utilised can be found in Appendix 12. Members of the SAG were also asked to inform the research team of any other publications of which they were aware that they thought might be relevant to the review. The principal investigator (BH) and the project manager (DE) followed a number of key EoL and mental health authors and organisations on Twitter (Twitter, Inc., San Francisco, CA, USA) to identify any material that could be potentially relevant to the evidence synthesis.
Searches were also conducted using Google (Google Inc., Mountain View, CA, USA), as described by Mahood et al. 70 The first 10 pages of each Google output were screened using the following terms:
-
“palliative care” and “mental illness”
-
“end of life” and “mental illness”
-
“end of life” and schizophrenia (searching the first five pages of output)
-
“end of life” and bipolar (searching the first five pages of output).
To identify published resources that had not yet been catalogued in electronic databases, recent editions of the Journal of Pain and Symptom Management, Cancer, Psycho-Oncology and BMJ Supportive & Palliative Care were hand searched. These journals were selected because a large number of outputs identified in database searches had been published in them. Reference lists of included studies were scanned and forward citation tracking was performed using the Web of Science.
Primary research citations retrieved from database searches
All citations retrieved from the 10 database searches were imported or entered manually into EndNote™ (Thomson Reuters, CA, USA) and duplicates were removed. The total numbers of hits retrieved for each database are displayed in Table 1.
| Database | Search interface | Hits |
|---|---|---|
| AMED | Ovid | 196 |
| ASSIA | ProQuest | 836 |
| CINAHL | EBSCOhost | 361 |
| CENTRAL | Wiley | 958 |
| DARE | CRD | 263 |
| EMBASE | Ovid | 7033 |
| HMIC | Ovid | 39 |
| MEDLINE alla | Ovid | 1302 |
| PsycINFO | Ovid | 663 |
| Web of Science | Clarivate Analytics | 125 |
| Total | 11,776 | |
Primary research citations identified from supplementary searching
All primary research citations identified as potentially relevant from across all supplementary sources (Table 2) were entered manually into EndNote. A total of 128 citations were identified.
| Source | Number of citations |
|---|---|
| Reference lists of included studies | 88 |
| Forward citation tracking of included studies | 15 |
| 4 | |
| 8 | |
| SAG | 2 |
| Trial registers | 0 |
| Hand-searching | 11 |
| Total | 128 |
Removing irrelevant citations
Once all of the primary research citations had been imported into EndNote, irrelevant citations were removed by searching for keywords in the title using the search feature of the EndNote software. The project team had previously agreed which keywords to use to identify papers that did not meet the review’s inclusion criteria. All hits for each keyword were screened by Deborah Edwards to ensure that they were, in fact, irrelevant before they were removed. The following keywords were used:
-
Abuse/substance
-
Adolescence/adolescent/youth
-
AIDS/HIV
-
Alcohol
-
Anxiety
-
Assessment
-
Bereav*
-
Bipolar diathermy/electrocautery
-
Book review
-
Child
-
Dementia/Alzheimer’s
-
Depression
-
Diabetes
-
Diagnos*
-
Fatigue
-
Grief
-
Incidence
-
Instrument/tool
-
Letter
-
Neonate/neonatal
-
Parent
-
Predict*
-
Prevalence
-
Prognosis/prognostic
-
Psychometric
-
Scale
-
Screen*
-
Sleep/insomnia
-
Smoking/tobacco
-
Spiritual/religious
-
Survival
-
Thesis
-
Validity/reliability/validation
-
Version.
At the end of this process, the remaining citations were exported as an XML file and then imported into the software package Covidence™ (Melbourne, VIC, Australia).
Title and abstract screening
All citations were independently assessed for relevance by two members of the review team using the information provided in the title and abstract using Covidence. Disagreements were resolved through discussion with a third reviewer, and, where needed for further clarity, the full text was retrieved to aid this discussion. Particular care was taken with citations referencing people experiencing depression. Depression is a commonly experienced mental health problem, but it is also one that can manifest as a severe mental health problem, requiring an urgent and potentially life-saving intervention. As our focus was on EoL care for people with pre-existing SMI, we excluded citations reporting on prior experiences of mild depression, and excluded items reporting on the identification of depression and its treatment among people who had experienced psychological distress subsequent to their EoL diagnosis. Only citations clearly reporting on EoL care for people who had pre-existing severe depression were included.
For citations that appeared to meet the inclusion criteria, or in cases in which a definite decision could not be made based on the title and/or abstract alone, the full texts of all citations that appeared to meet the review’s inclusion criteria by title and abstract screening were retrieved.
Full-text screening
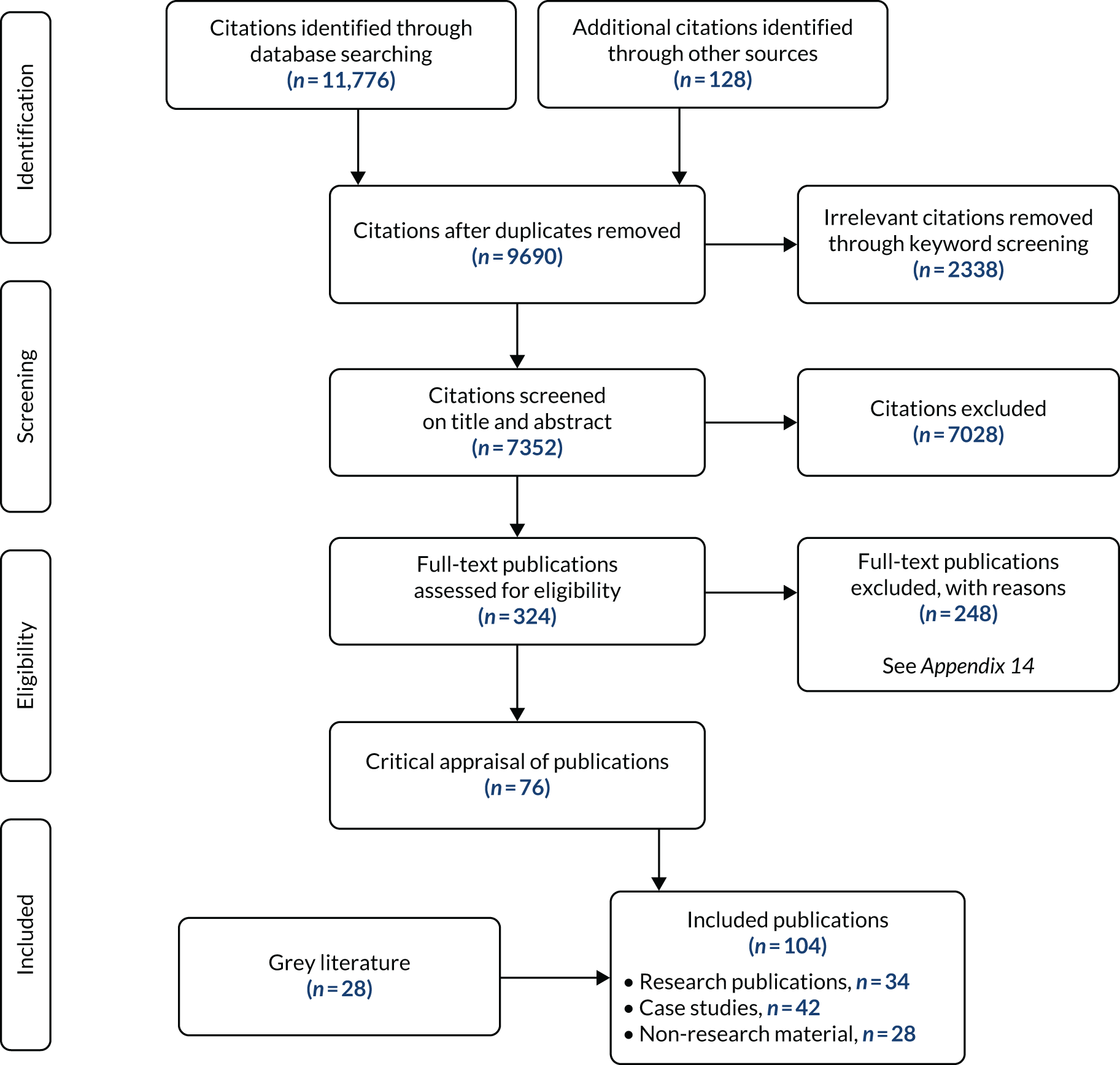
To achieve a high level of consistency, two reviewers screened each retrieved citation for inclusion using a purposely designed form (see Appendix 13). Disagreements were resolved through discussion with a third reviewer. All English-language items relating to the provision of EoL care to and the receipt of EoL care by people with SMI and an additional diagnosis of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure were included at this stage. The flow of citations through each stage of the review process is displayed in the PRISMA flow chart in Figure 1. 69
FIGURE 1.
The PRISMA flow chart. Reproduced with permission from Edwards et al. 71 © The Author(s) 2021 This article is distributed under the terms of the Creative Commons Attribution 4.0 License (https://creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Grey literature identified from supplementary searching
Sixty-eight grey literature citations were identified as potentially relevant from across all supplementary searches (Table 3), and these were all entered manually into EndNote. Policies and guidance, reports and other non-research materials found in the grey literature were also read by two members of the project team and considered against the topic inclusion criteria, with disagreements resolved as above. Forty were excluded (see Appendix 15), leaving a total of 28 that were assessed as relevant to the review (see Appendix 16). A test search for relevant information in renal-specific documents produced no material suitable to be included in the review. The decision was therefore made by the project team not to search within (the large number of) disease-specific policy and guidance documents for material concerned with the management of EoL care for people also with SMI.
| Source | Number of citations |
|---|---|
| Organisation websites | 47 |
| SAG | 16 |
| 3 | |
| E-mail alert for HQIP | 1 |
| Reference lists of included studies | 1 |
| Total | 68 |
Materials included in evidence synthesis
One hundred and four publications were included in the evidence synthesis, which consisted of research publications (n = 34), case studies (n = 42) and non-research policy and guidance material (n = 28).
Terminology and language use
Language is important (and sometimes contentious), and, as described in Chapter 2, Defining the project’s parameters: ‘severe mental illness’ and ‘end of life’ (and related), the variety of terms used in the mental health and EoL fields and in the materials included in this synthesis were recurring items at combined project team and SAG meetings. Across the items located and included in the synthesis, no agreed definitions could be discerned relating to the precise meanings of SMI or the content of EoL care or palliative care. Specialist palliative care could refer, particularly in the UK context, to care provided in any setting (hospice, home, care home or hospital) by a dedicated specialist team with additional education and skills in palliative care that enables them to support those at the EoL with any diagnosis who have complex, high-level needs, whatever the cause. Palliative care, however, could refer to care provided by all HCPs to those who are at the EoL (across all care settings) and do not have the additional complex needs that require additional specialist support. This clinical distinction may be similar across many countries with similarly developed health systems (e.g. the USA, Australia and Canada), but, in each case, the project team, having finalised the materials to include, noted the existence of different funding and organisational arrangements and varying standards for eligibility to access services. Discussion also took place between project team and SAG members on the language to be used in this report to describe people with SMI at the EoL. In recognition of people’s receipt of (or need for) integrated care crossing mental health and palliative care system boundaries, a decision was made at the third combined project team and SAG meeting to use the word ‘patient’.
Quality appraisal
Following searching and screening, information from research and case study publications was assessed independently for methodological quality by two reviewers using one of a number of agreed appraisal checklists. Alternative tools, which reflected the specific design and methods used in individual research outputs, were used as necessary when suitable Critical Appraisal Skills Programme (CASP) tools were not available. Any disagreement on quality was resolved through discussion with a third reviewer. No research items were judged to have been fatally flawed, and all were included. The policy and guidance documents and non-research reports were not subject to quality appraisal.
For qualitative studies, the appropriate checklist available from CASP was used. 72 For cross-sectional designs, the Specialist Unit for Review Evidence 12-item checklist73 (with responses ‘yes’, ‘no’, ‘can’t tell’) was used and an overall score reflecting the number of items answered ‘yes’ was generated.
Retrospective cohort studies were appraised using the Scottish Intercollegiate Guidelines Network’s Methodology Checklist 3: Cohort Studies. 74 This is a 14-item checklist (with responses ‘yes’, ‘no’, ‘can’t say’ and ‘does not apply’). Six items do not apply to this type of study design (statements 1.3, 1,4, 1,5, 1.6, 1.8 and 1.12). The overall assessment reflects how well a study has sought to minimise the risk of bias or confounders. The final rating is high quality (++), acceptable (+) or low quality (–). Reproduced from Scottish Intercollegiate Guidelines Network with permission. 74 These guidelines are licensed under the Creative Commons Attribution-Noncommercial-NoDerivatives 4.0 International Licence. This allows for the copy and redistribution of SIGN guidelines as long as SIGN is fully acknowledged and given credit. The material must not be remixed, transformed or built upon in any way. To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc-nd/4.0/
As retrospective designs are generally regarded as weaker, the authors of the checklist suggest that these should not receive a rating higher than ‘+’.
For case studies, the Joanna Briggs Institute critical appraisal checklist for case reports was used. 75 This is an eight-item checklist (with responses ‘yes’, ‘no’, ‘unclear’, ‘not applicable’) from which an overall score is generated reflecting the number of items answered ‘yes’.
Data extraction
All demographic data from the 76 research and case study publications were extracted directly into tables based on study design (see Appendices 17–20), following the format recommended by the Centre for Reviews and Dissemination. 68 The work was allocated to a member of the research team who extracted the relevant data, and a second reviewer (DE) independently checked the data extraction forms for accuracy and completeness. A record of corrections was kept. Where multiple publications from the same study were identified, data were extracted and reported as if from a single study.
Data analysis and synthesis
Following discussion at the second of the three combined project team and SAG group meetings, the decision was made to conduct a first analysis and synthesis for the combined research studies (n = 34) and policy and guidance documents (n = 28), and a second analysis and synthesis for the case studies (n = 42). The project protocol stated an intention to perform meta-analyses of data for included intervention studies. However, no intervention studies were found. All synthesised findings are therefore presented as narrative syntheses in Chapters 4 and 5.
All research papers were available in full-text form, and each was uploaded to a project created using the software package NVivo 12 (QSR International, Warrington, UK). All policy and guidance documents were available as electronic documents, and the content of each was searched using keywords relevant to the review (‘mental illness’ and ‘end of life’). Data retrieved in this way were extracted and entered verbatim into Microsoft Word (Microsoft 365 Apps for Enterprise; Microsoft Corporation, Redmond, WA, USA) documents, one for each policy and guidance item. Microsoft Word files containing the extracted data were then uploaded to the same NVivo project as the research items in preparation for analysis. All case studies were available in full-text form and were uploaded to a second NVivo project.
A thematic approach was employed to analyse and synthesise both sets of data,76 with work on the combined research and policy data set led jointly by Ben Hannigan and Deborah Edwards and work on the case study data set led by Michael Coffey. Using NVivo, in both cases inductive data-driven codes were generated and attached to segments of material through the line-by-line reading of documents. To aid discussion and refinement, and to support a visual appreciation of the overall character of the developing research and policy synthesis, codes and their relationships to each other were also reproduced on large sheets of display paper. In both thematic syntheses, codes were grouped into meaningful candidate themes (and, in the case of the research and policy synthesis, subthemes) reflecting the material being synthesised and the overarching objectives of the project. 4 These were shared with all members of the project team for review and further refinement, with no major disagreements noted. Themes and subthemes were then tabled at the third combined project team and SAG meeting, where the overarching thematic structure of both syntheses was discussed and approved. Both syntheses aimed to bring together reports of approaches to service organisation, processes and interventions shown to both facilitate and hinder the provision of high-quality, accessible, equitable and acceptable EoL care to people with SMI. The reporting of the separate analysis and synthesis of the combined research, policy and guidance items is contained in Chapter 4, and the reporting of the analysis and synthesis of the case study items is contained in Chapter 5. Figure 6 in Chapter 6 provides a visual overview of both thematic syntheses as a whole.
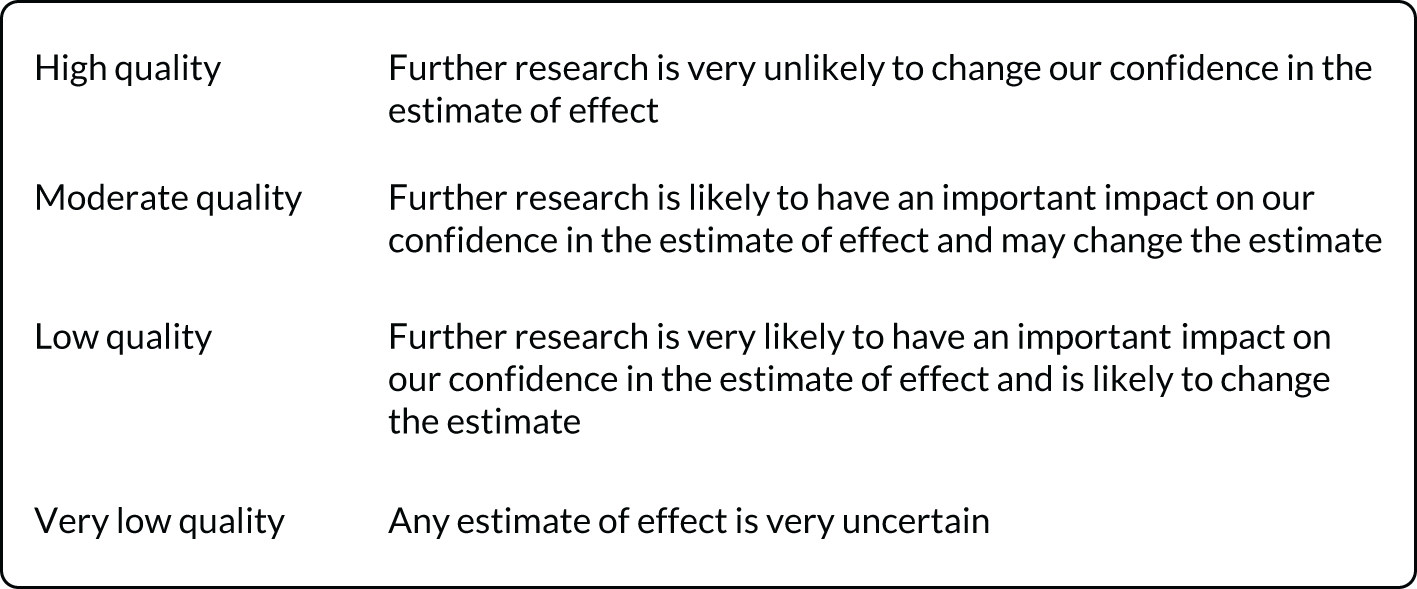
Assessing confidence
The assessment of the quality of evidence for retrospective cohort studies was conducted using the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach,77 and was conducted by Deborah Edwards and checked by Ben Hannigan. This approach rates the quality of a body of evidence as ‘high’, ‘moderate’, ‘low’ or ‘very low’ (Figure 2). 77 Explicit criteria, including study design, risk of bias, impression, inconsistency, indirectiveness and magnitude of effect, are used. As the studies retrieved for this evidence synthesis were observational as opposed to interventional, the initial quality of the body of evidence overall started off as low. 78 When the evidence base was rated specifically on study design (in particular retrospective cohort studies), this led to the ratings for all evidence generated using material from these types of study being downgraded from ‘low quality’ to ‘very low quality’.
FIGURE 2.
The GRADE quality of evidence and definitions. Reproduced from GRADE: an emerging consensus on rating quality of evidence and strength of recommendations, Guyatt G, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. , volume 336, pp. 924–6, 2008, with permission from BMJ Publishing Group Ltd. 77
The strength of the synthesised qualitative and non-intervention findings was assessed using the CERQual (Confidence in the Evidence from Reviews of Qualitative Research) approach,79 and this was again led by Deborah Edwards and Ben Hannigan. The original CERQual approach was designed for qualitative findings, but in this project a process previously used by members of the research team in HSDR 11/1024/0880 and in HSDR 08/1704/21181 was used. This approach involved using CERQual for the additional purpose of assessing confidence in findings synthesised from surveys and other non-intervention quantitative studies. The confidence in individual synthesised review findings is based on the assessment of four components: coherence, methodological limitations, relevance and adequacy. Overall assessments of confidence are then described using four levels – high, moderate, low or very low – as summarised in Figure 3, which draws on and adapts material previously published. 82
FIGURE 3.
The CERQual: applying high, moderate, and low confidence to evidence. Reproduced with permission from Lewin et al. 82 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. The figure includes minor additions and formatting changes to the original figure.

Description of research studies
Thirty-four publications covering 30 research studies were deemed suitable for inclusion in the review: 19 quantitative studies (reported across 21 publications), nine qualitative studies (reported across 11 publications) and two mixed-methods studies. Demographic information on the characteristics of included research studies is given in Appendices 17–20.
Country of research
Data were retrieved from 10 countries: the USA (n = 12, across 13 publications32,83–94), Canada (n = 4, across five publications95–99), New Zealand (n = 1100), Taiwan (Province of China) (n = 1101), Australia (n = 4, across six publications102–107), France (n = 1108), Belgium (n = 1109), the Netherlands (n = 2109–111), the UK (n = 337,112,113) and the Republic of Ireland (n = 1114).
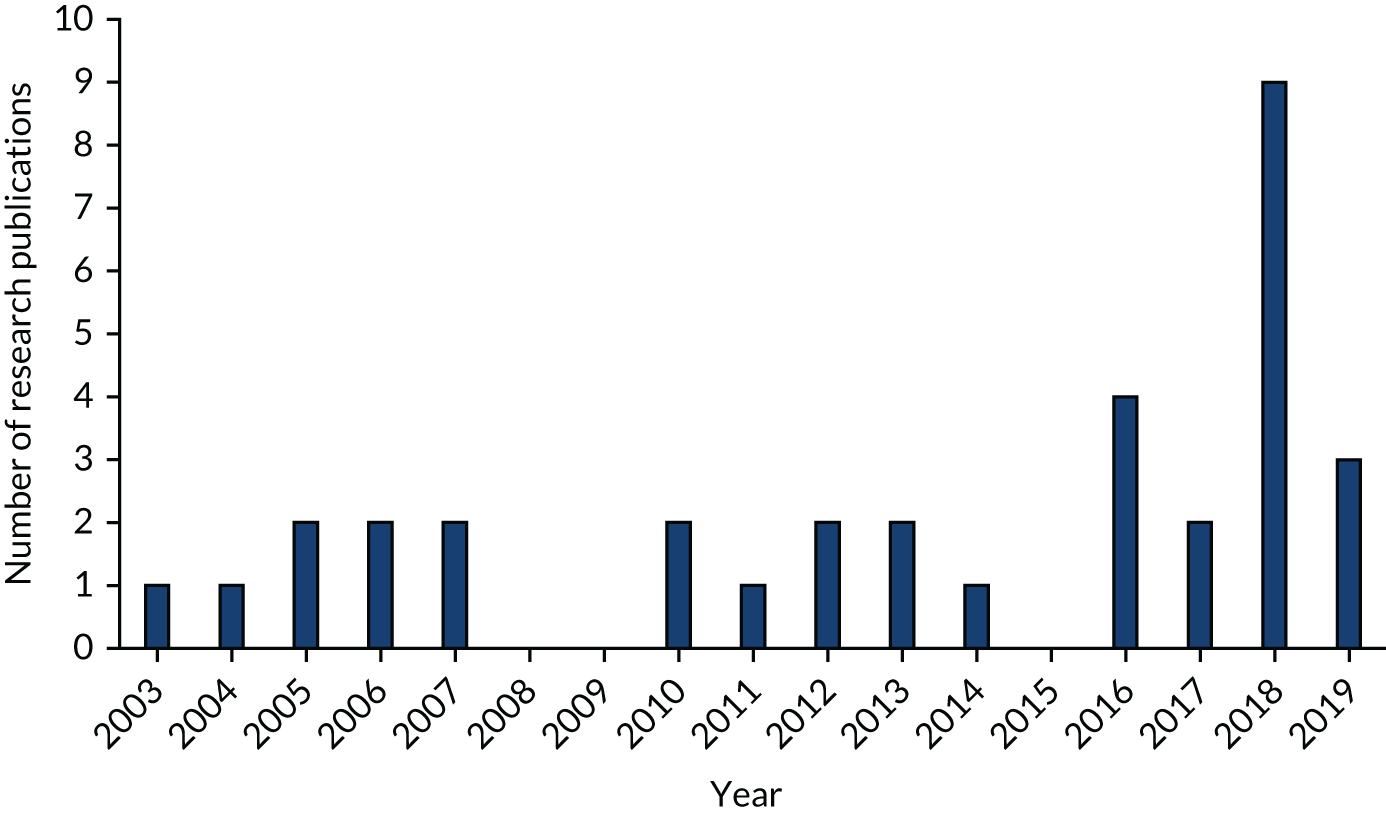
Year of publication
Figure 4 displays the year of publication of the 34 research study publications.
FIGURE 4.
Histogram of year of publication of research studies.
Study designs and methods
Among the quantitative studies, 12 studies (across 13 publications) were retrospective cohort studies,84,88–92,95,97,98,100,101,107,108 seven studies (across eight publications) were descriptive surveys83,85–87,93,94,96,111 and nine studies (across 11 publications) used a qualitative design. 32,37,99,102–106,109,112,113 Among the qualitative studies, five studies (across seven publications) were described as using a non-specific qualitative descriptive approach,102–106,112,113 two utilised grounded theory,37,109 one used ethnography99 and one used phenomenology. 32 Specific methods used to collect qualitative data included interviews (n = 6,32,37,102–106,109 across eight publications), focus groups (n = 1112), a combination of interviews and focus groups (n = 1113) and a combination of observation and interviews. 99 One mixed-methods study consisted of a retrospective review of patients’ medical records and a post-test evaluation of educational/training initiatives with HCPs, descriptive surveys and non-specific qualitative descriptive approaches using interviews. 110 The other mixed-methods study consisted of a descriptive survey and a qualitative descriptive approach using interviews. 114
Settings
The settings in which research studies were undertaken were described as follows: specialist palliative care services;100 palliative care consultation services;93 acute and psychiatric care;85,108 Veterans Administration medical centres/nursing homes;83,88,90 all medical care covered by one insurance company;101 acute care;91,92,96 all hospital and community based palliative care (n = 2 studies, across three publications);95,97,107 homeless/vulnerably housed;99,113 shelter-based hospice for the homeless;98 general practices and psychiatric practices;114 nursing/care homes;84,111 mental health and hospice/palliative care services32,94,112 including community, residential homes, supported accommodation and psychiatric hostels;106 mental health services (hospital and/or community based) (n = 5 studies, across eight publications);86,87,102–105,109,111 hospices;37 and not stated. 89
Participant characteristics
In 11 studies (across 12 publications) participants were decedents (people who had died) who were described as having had a diagnosis of severe and persistent mental illness,100 schizoaffective disorders,88,95,97,101,107,108 a pre-existing psychiatric illness,91 a mental health diagnosis,89 pre-cancer depression92 or PTSD. 90 One further study explored the views of family members of decedents who had PTSD. 83
Seven studies (across eight publications) directly involved patients and included:
-
residents in a nursing home with schizophrenia, bipolar disorder, or other psychosis84
-
homeless patients admitted to a shelter-based hospice with a range of mental health diagnoses98
-
homeless or vulnerably housed individuals (inferred that some would have had a mental health diagnosis) who were on a palliative trajectory and their support workers and formal service providers99
-
current or previous homeless individuals (inferred that some would have had a mental health diagnosis) and their health and social care providers, hostel and outreach staff113
-
adults with schizophrenia or other psychosis, mood disorders (major depression and bipolar disorder), personality disorders or PTSD who were receiving community-based services86,87
-
patients with severe and persistent mental illness96 or schizophrenia109 who were not at the EoL, but the study focused on future care preferences.
The remaining 12 studies (across 14 publications) were conducted with HCPs who worked with patients with SMI at EoL32,37,85,93,94,102–106,110–112,114 and these included mental health HCPs,85,102–104 EoL HCPs,37 mental health and EoL HCPs,32,94,106,112 psychiatrists105,114 and general practitioners (GPs). 114
Terminal or chronic condition/s or cause of death
A large number of research studies (n = 16, across 19 publications32,37,83–87,93,94,99,100,102–105,109,111,112,114) explored the perspectives of HCPs who cared for those with SMI at EoL and as a result did not refer to any specific terminal or chronic condition. The remaining studies reported cause of death (n = 6 studies across seven publications88,95,97,98,101,108,110), terminal condition(s) (n = 689,90,92,96,106,113) or chronic condition(s) (n = 291,107) and included the following:
Description of case studies
Forty-two publications consisted of 51 case studies of individuals who had an existing mental illness diagnosis and who went on to develop an EoL condition (see Appendix 20). In four case studies the purpose of the paper was to show the application of a particular model of care, such as dynamic system analysis115 or stepwise psychosocial palliative care. 116,117 Most of the case studies were published in peer-reviewed research journals (n = 38), along with two conference abstracts,118,119 one that appeared in a report120 and one that was in a first-person-account blog. 121 The case studies ranged in depth from discursive papers with little direct detail about the individuals involved, to those that focused mainly on the patient’s or patients’ physical illness and a substantive number that discussed issues of mental capacity and the ability of the person to express their choice to accept, refuse or abandon treatments.
Country of research
The majority of case study papers were published in the USA (n = 2826,116,117,121–145); followed by the UK (n = 4120,146–148), Canada (n = 3149–151), Australia (n = 115), France (n = 1152), Israel (n = 1153), Mexico (n = 1119), the Netherlands (n = 1115) and Singapore (n = 1154), with one conference abstract not stating the country in which the case study was located. 118
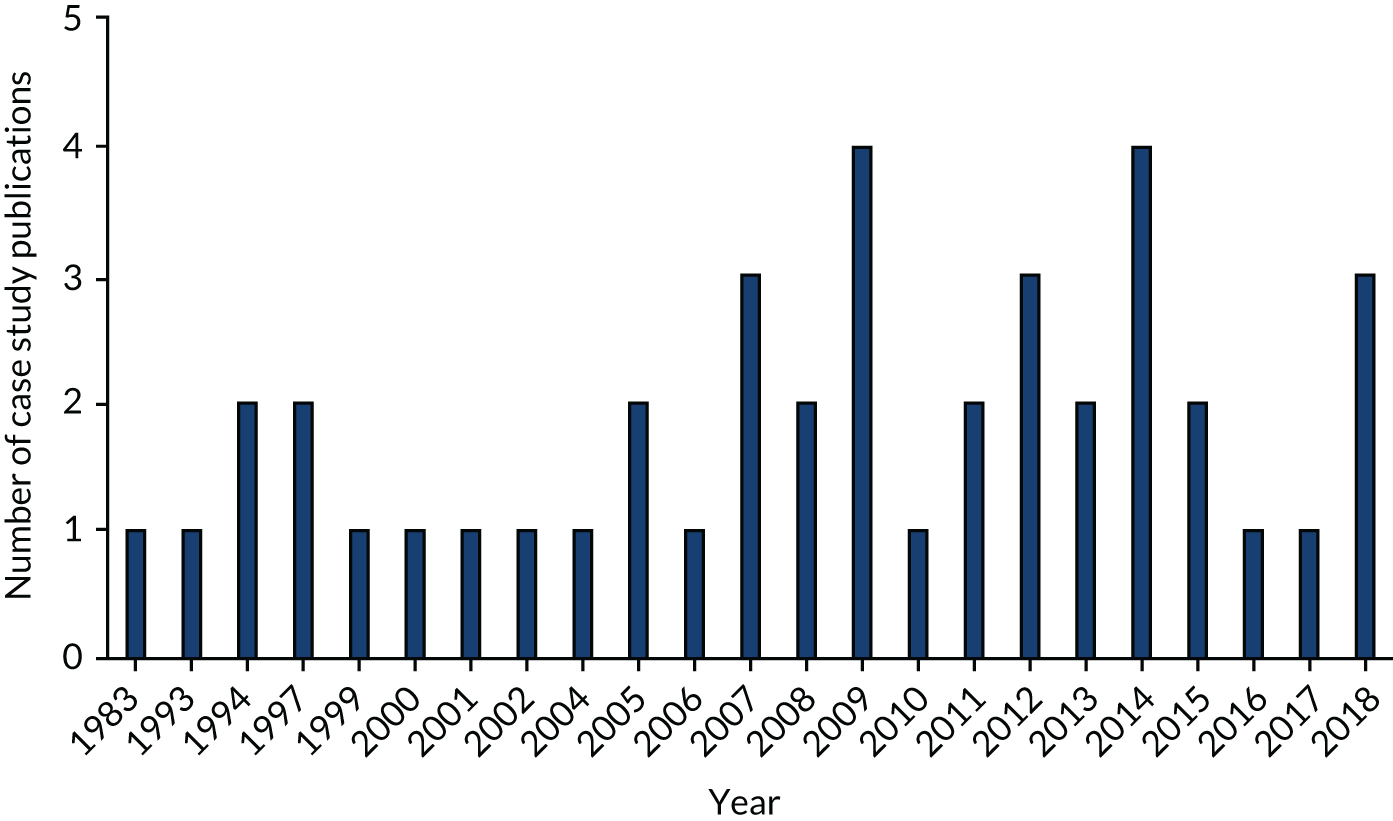
Year of publication
The earliest case study was published in 1983133 and outputs appeared regularly up until the end of the search period in 2019. 118,119,150 Figure 5 displays the year of publication of the 42 research study publications.
FIGURE 5.
Histogram of year of publication of case studies.
Attributes of service users
The case studies outlined, sometimes in very sparse detail, the individual attributes of the people with pre-existing mental health problems who were in the EoL trajectory. The age range across the case studies was 20–91 years (mean age 55 years) and was provided in all except two of the studies. 121,143 Women were the focus of 24 case studies. Diagnosis was reported for all case study individuals and included psychotic-type diagnoses (schizophrenia, psychosis, schizoaffective and bipolar conditions) (31 publications reporting 35 case studies15,26,115,118–121,124,127–130,132,133,135–147,149–154), personality disorder (five publications reporting five case studies122,123,125,131,132), PTSD (three publications reporting three case studies116,117,126) and anorexia nervosa (n = 2134,148). In the papers discussing the individuals with anorexia, the EoL condition was a direct result of that condition, leading to chronic fractures and organ failure. 134,148 These are then two outliers in that the EoL condition was a direct result of the mental health issue for those individuals. The vast majority of EoL conditions presented in the case study papers were cancer-related diagnoses, and organ failure [heart (n = 3 (across four publications115,126,129,130), liver (n = 1122) and kidney (n = 5131,139,146,150,154)] made up the remainder.
Results of quality appraisal
Critical appraisal scores for cohort studies
The methodological quality of each of the 12 cohort studies was judged against the relevant eight quality criteria derived from the Scottish Intercollegiate Guidelines Network’s Methodology Checklist 3: Cohort Studies checklist,74 and each study is summarised in Table 4. All the studies were judged to be of acceptable quality, indicating that some flaws in the study design were present, with an associated risk of bias. Seven studies did not provide confidence intervals (CIs) as part of the statistical analysis. 88–91,98,100,107
| Study (authors and year) | Q1 | Q2 | Q7 | Q9 | Q10 | Q11 | Q13 | Q14 | Overall assessment |
|---|---|---|---|---|---|---|---|---|---|
| Butler and O’Brien 2018100 | Y | Y | Y | Y | Y | Y | Y | N | Acceptable |
| Chochinov et al. 2012;95 Martens et al. 201397 | Y | Y | Y | Y | Y | Y | Y | Y | Acceptable |
| Ganzini et al. 201088 | Y | Y | Y | Y | Y | Y | N | N | Acceptable |
| Huang et al. 201789 | Y | Y | Y | Y | Y | Y | Y | N | Acceptable |
| Huang et al. 2018101 | Y | Y | Y | Y | Y | Y | Y | Y | Acceptable |
| Lavin et al. 201791 | Y | Y | Y | Y | Y | Y | Y | N | Acceptable |
| McDermott et al. 201892 | Y | Y | Y | Y | Y | Y | Y | Y | Acceptable |
| Podymow et al. 200698 | Y | Y | Y | Y | Y | Y | N | N | Acceptable |
| Spilsbury et al. 2018107 | Y | Y | Y | Y | Y | Y | N | N | Acceptable |
| Fond et al. 2019108 | Y | Y | Y | Y | Y | Y | Y | Y | Acceptable |
| Cai et al. 201184 | Y | Y | Y | Y | Y | Y | Y | Y | Acceptable |
| Kelley-Cook et al. 201690 | Y | Y | Y | Y | Y | Y | Y | N | Acceptable |
Critical appraisal scores for descriptive surveys
The methodological quality of seven descriptive studies and the survey component of two mixed methods studies110,114 were judged against the 12 quality criteria used in the SURE tool, and each study is summarised in Table 5. The authors of one study, reported in two companion papers,86,87 did not state the type of study that they had undertaken and were reporting on, but from the description of the methods this was classified as a quantitative descriptive project and, thus, was included in this section with other studies of this type. The quality of 9 of these 11 descriptive studies was high, with all nine meeting either 11 or all 12 criteria. The quality of the other two studies was significantly lower, with either the majority of quality criteria not being met or the account in the published paper being unclear. 85,94
| Study (authors and year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alici et al. 201083 | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Elie et al. 201896 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Evenblij et al. 2016110 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Evenblij et al. 2019111 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Foti 200385 | Y | Y | Y | U | N | Y | N | N | N | N | N | N |
| Foti et al. 2005;87 Foti et al. 200586 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Patterson et al. 201493 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Sheridan et al. 2018114 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Taylor et al. 201294 | Y | Y | N | N | U | N | N | N | N | N | Y | N |
Critical appraisal scores for qualitative studies
The methodological quality of each of the nine qualitative studies and the qualitative component of two mixed-methods studies110,114 were judged against the 10 quality criteria used in the CASP qualitative checklist,72 and each study is summarised in Table 6. In the case of two studies,106,113 the authors did not include a description of the type of study conducted, but from the description of the methods used these were classified as examples of qualitative descriptive studies. The quality of these 11 studies was high, with all bar one106 of the studies meeting at least 9 of the 10 quality criteria.
| Study (authors and year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Evenblij et al. 2016110 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Hackett and Gaitan 200737 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Jerwood 2018112 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| McGrath and Forrester 2006;104 McGrath and Holewa 2004;102 McGrath and Jarrett 2007103 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| McKellar et al. 2015105 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| McNamara et al. 2018106 | Y | Y | Y | U | Y | N | Y | Y | Y | Y |
| Morgan 201632 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Sheridan et al. 2018114 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Shulman et al. 2018113 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Stajduhar et al. 201999 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Sweers et al. 2013109 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
Critical appraisal scores for case studies
The methodological quality of each case study was judged against the eight quality criteria used in the Joanna Briggs Institute case report checklist,75 and each study is summarised in Table 7. As this shows, the quality of the studies varied overall. Twenty-five of the 42 case studies met either seven or all eight criteria; the single criterion missing from the majority of papers in this group related to the description of diagnostic tests or assessment methods and their results. Eight of the 42 studies met half or fewer of the eight quality criteria, but for the purposes of inclusivity all 42 studies were included in the subsequent narrative synthesis (see Chapter 5).
| Study (authors and year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Score |
|---|---|---|---|---|---|---|---|---|---|
| Ang et al. 2009154 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Badger and Ekham 2011122 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Bakker 2000115 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Boyd et al. 1997123 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Cabaret et al. 2002152 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Candilis and Foti 1999124 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Clements-Cortes 2004149 | Y | Y | Y | N | Y | Y | N | Y | 6/8 |
| Doron and Mendlovic 2008153 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Feely et al. 2013125 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Feldman and Petriyakoil 2006126 | Y | U | Y | N | N | Y | Y | N | 4/8 |
| Feldman et al. 2014116 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Feldman et al. 2017117 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Geppert et al. 2011127 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Gonzelez et al. 2009128 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Griffith 2007129 | Y | Y | N | Y | Y | Y | Y | Y | 7/8 |
| Griffith 2007130 | Y | Y | N | Y | Y | Y | Y | Y | 7/8 |
| Hill 2005131 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Irwin et al. 201426 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Kadri et al. 2018150 | Y | N | Y | N | Y | N | Y | Y | 5/8 |
| Kennedy et al. 2013120 | Y | U | Y | N | Y | Y | Y | Y | 6/8 |
| Kunkel et al. 1997132 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Levin and Feldman 1983133 | Y | Y | Y | N | Y | N | Y | Y | 6/8 |
| Lopez et al. 2010134 | Y | Y | Y | N | Y | Y | N | Y | 6/8 |
| Maloney et al. 2014121 | Y | Y | Y | N | Y | Y | Y | Y | 7/8 |
| Mason and Bowman 2018118 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| McCasland 2007135 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| McKenna et al. 1994136 | Y | N | U | N | Y | N | Y | Y | 4/8 |
| Mogg and Bartlett 2005146 | Y | N | N | N | Y | N | N | Y | 2/8 |
| Moini and Levenson 2009137 | Y | Y | Y | N | N | N | Y | Y | 5/8 |
| Monga et al. 2015138 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Muhtaseb et al. 2001147 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| O’Neill et al. 1994148 | Y | N | Y | N | Y | N | N | N | 2/8 |
| Picot et al. 201515 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Rice et al. 2012139 | Y | N | Y | N | Y | Y | Y | Y | 6/8 |
| Rodriguez-Mayoral 2018119 | Y | N | N | N | N | Y | Y | Y | 5/8 |
| Romm et al. 2009140 | Y | N | Y | N | N | N | Y | Y | 3/8 |
| Shah et al. 2008141 | Y | N | Y | Y | Y | Y | Y | Y | 7/8 |
| Stecker 1993142 | Y | N | Y | N | N | N | Y | Y | 4/8 |
| Steves and Willliams 2016143 | Y | N | N | N | Y | Y | Y | Y | 4/8 |
| Terpstra et al. 2014144 | Y | Y | Y | Y | Y | Y | Y | Y | 8/8 |
| Thomson and Henry 2012145 | Y | Y | N | N | N | N | N | Y | 2/8 |
| Webber 2012151 | Y | N | N | N | N | Y | Y | Y | 3/8 |
Chapter 4 Thematic synthesis of policy, guidance and research
This chapter presents a synthesis of policy, guidance and research included in the overall review. Material from the research studies and policy and guidance documents has been synthesised into four themes: structure of the system, professional issues, contexts of care and characteristics of people with SMI.
Structure of the system
Twenty-six policy and guidance documents22,30,55,120,155–176 and 18 research outputs32,85,88,91–94,97–99,103,105,106,108,110,112–114 contribute to this theme, which addresses the broad shape and structure of the EoL and mental health care systems. Material is organised under four subthemes: policy and guidance; separate commissioning, management and organisation; partnership; and no right place to die.
Policy and guidance
Nineteen policy and guidance documents22,30,156–161,163–170,172,174,175 and one research output contribute to this subtheme. 112
People with SMI are recognised as a group needing particular attention in the provision of EoL care in multiple independent UK reports and consultations,22,156–158,161,163–165 with the Care Quality Commission158 suggesting that many health-care providers have focused efforts on reducing premature death among people with a mental health condition rather than properly considering EoL care needs.
There is a lack of national and local policy guidance in the UK that addresses the EoL care of people with SMI;112 however, isolated examples of local policy do exist. 170 Evidence166 also exists that a majority (62%) of mental health providers have produced action plans to promote improvement in EoL care. Where this is in place, 92% of mental health providers have also reported forwarding this to clinical teams, and three-quarters (75%) have reported forwarding this to the trust/university health board. In the context of a lack of specific national and local policy, both mental health and palliative care nurses report concern about their legislative responsibility. 112
Standards of care for people with mental health problems should be the same as those for people with physical health problems, and this ideal is strongly emphasised across generic UK health policies,160,167–169 national mental health-specific policies159,172,175 and independent reports and guidance documents. 157,164 By extension, EoL care for people with SMI should be as good as the EoL care provided to others. 30 Aspirations that high-quality EoL care should specifically apply to people with SMI are found in Scottish mental health policy,172 and in Wales the current mental health strategy175 refers to supporting recovery and enablement through to the EoL with recent whole-system policy referring to equitable services for people with mental health difficulties and specifically improving EoL care. 174 Northern Ireland’s mental health service has a standard that people with incurable conditions should be supported at the EoL and to die in their preferred place of care. 159 English strategy identifies that there is a need to improve the provision of EoL care information in unscheduled care settings,168 and targets additional resources at homeless people. 167
Separate commissioning, management and organisation
Eleven policy and guidance documents30,120,157,158,162,164,166,169,170,173,176 and 11 research outputs32,85,93,94,99,103,106,110,112–114 contribute to this subtheme.
Accessing and navigating the system
All national health-care systems have obligations to provide access to palliative care for people with disabilities, including those associated with existing mental health difficulties. 176 In relation to access to hospice care specifically, a specific aim of the UK charity Hospices UK to make their services more available to people with serious mental illness. 162 Data reported in the National Audit of Care at the End of Life report,166 however, show that only 10% of mental health service providers have their own specialist palliative care service, in comparison with 95% of English and Welsh acute care providers. A majority of mental health providers report having access to specialist palliative care beyond their own hospital, however, with 16% having access to at least one EoL care facilitator, of which 40% are contained within a specialist palliative care team. Availability of specialist palliative care HCPs to mental health providers include 60% having face-to-face access to nursing staff during usual working hours across the whole week, and 49% having the same access to doctors. Other means of access to specialist palliative care reported include telephone contact, with doctors available at any hour to 57% of mental health providers and nurses available at any hour to 42% of mental health providers. 166
The separate organisation of mental health and EoL services means that many people with existing mental health issues do not receive treatment that is appropriate for them when they are eventually admitted to hospital. 164 Treatment also becomes more complicated if patients are receiving analgesia and other EoL medication. 164 Evidence brought together by the Social Care Institute for Excellence 2013173 is that people with mental health needs remain one of the groups missing out on equal access to EoL care. The needs of people with SMI are not always considered by commissioners and service planners, who have been described as lacking awareness of the EoL needs of people with SMI. 157
Accessing adequate and timely palliative care at the EoL for those with mental health problems, including in general hospital settings, is described as difficult for staff. 103,106,114 Psychiatrists report barriers when accessing physical health and palliative care services, even when services are co-located, with difficulties including communicating with physicians, being blocked by administrative staff, having to deal with multiple departments and working in systems where no single patient identifier is used to join up record-keeping. 114 Referral and consultation are reported as often being affected by patients’ past experiences of services and the impact of stigma. 106 Mental health staff have described people with mental illnesses at the EoL as not welcome in general hospitals, with the result that these patients are offered trial placements in appropriate settings but are then discharged or are simply refused care. 103
A considerable number of people with SMI have limited contact with their GPs, families and wider networks, and may be socially isolated. 30,106,110,170 This can be a challenge for them in terms of accessing, navigating and/or receiving appropriate EoL care, including making practical arrangements, such as travelling long distances to appointments and having enough funds to make this possible. 114
Access for homeless and vulnerable groups
Social isolation and disconnection from family, friends and services are particular concerns among people who are homeless, with around 50% of rough sleepers having mental health needs. 30,167 The social characteristics of homeless people include that they are unlikely to live in supported accommodation and may lead irregular lifestyles, with high levels of mental illness and drug and alcohol abuse, making them difficult for health and social care professionals to reach. 162
Homeless people, many of whom have SMI, have particular problems accessing EoL services and are often excluded from hospices and care homes, where they do not fit the profile of most people using such services. 113,158 Professionals describe difficulties placing homeless people with cancer in care homes or hospices even when they have no history of substance misuse. 113 Social services provide care for the ‘structurally vulnerable’ but typically view the provision of EoL care as beyond their remit of responsibility or expertise,99 and undertake assessments of need that take account only of homeless people’s immediate, current, needs such as during hospital admission or following detox from alcohol. 113 Guidance from St Mungo’s (London, UK), a charity for homeless people, is that hostel and project staff should carry out assessments supplementing those completed by HCPs and social care professionals in order that people can be supported as long as possible in their preferred place of care. 120
The siloing effect of services also means that homeless people (who generally have lower levels of health literacy, cognitive capacity and access to material resources such as telephones, the internet and transportation) are often unable to successfully navigate their way through multiple departments and agencies. They are, therefore, less likely to receive any meaningful palliative care and support whatsoever,99 and more likely to receive care in hostels where the support ethos is at odds with meeting needs at the EoL. 113
The Help the Hospices report162 suggests that people who are detained in prisons as a result of social exclusion and stigmatisation may have trouble accessing palliative care. Health care for prisoners has been described as focusing particularly on mental health and substance misuse programmes162 as opposed to including EoL care. To our knowledge, no research exists in these areas, but guidance is clear that detained people should be cared for with respect and dignity and should have choice. 161
Care co-ordination across systems
Separate commissioning, management and ways of organising both services and professionals create challenges for both mental health and EoL HCPs to co-ordinate high-quality care across mental health and EoL care systems. 112 National policy in England is clear on the importance of organising integrated services around the patient,169 and in Scotland clear emphases have been placed on services taking responsibility for care, negotiating working partnerships across palliative and mental health systems and involving families. 30 One example of local policy from NHS Lothian identifies the importance of strong linkages between different services in order that the wishes and needs of people with SMI at the EoL are considered and met. 170 This creates multiple co-ordination difficulties at a time when speed is critical so that people receive the care and support they need. 164
Lacking personal and material resources, homeless and vulnerable people at the EoL who require access to multiple health and social care services typically have to act as their own care co-ordinators to navigate the system. 99 The invisibility of vulnerable people means that they are liable to fall through the cracks between professional boundaries, with practitioners failing to take responsibility for meeting and co-ordinating palliative care needs and patients missing out on palliative care because they do not know where to go, who to see or when to find support99 or because professionals continue to work in ‘silos’. 112 Problems of fragmented services and a lack of continuity found in the care of homeless people are also associated with a lack of trust between practitioners and people using services. 113
Formal proposals to improve the organisation and coordination of care across palliative and mental health services include the following:
-
Identifying lead clinicians. 114
-
Having ‘liaison portfolios’ for designated members of existing care staff with specific responsibilities to advocate and act as a resource, to link mental health and palliative care services, to open channels of communication, to record-keep, to facilitate access to services for practitioners and to co-ordinate education sessions. 94
-
Designating link workers to develop care protocols and education and awareness-raising sessions crossing the mental health and EoL care systems. 30
-
Locating liaison mental health nurses, and resident mental health nurses in palliative care services, with liaison staff described as particularly well placed to develop close partnerships across services, broker collaborative care and offer support, education and supervision. 30
-
In circumstances such as these, supervision would be helpful. 32 One example of good practice reported in the Scottish system is a registered mental health nurse who provides clinical supervision for other members of the multidisciplinary team. 30
Resources
The lack of sufficient or suitably qualified staff in the usual residences of people with SMI drives people at the EoL to either acute hospital or nursing home care, and the strategy of employing non-professionals in community services is suggested as having depleted the capability of staff to care for people at the EoL. 114 A general absence of services and programmes to meet the EoL needs of people with SMI has been found in parts of the USA,85 alongside evidence of insufficient psychiatrist availability and inadequate resources to support people. 93
Partnership
Seven policy and guidance documents30,55,155,163,168,170,171 and seven research outputs85,103,105,106,110,112,114 contribute to this subtheme.
Funding and flexibility to work in partnership
Working in partnership across EoL and mental health services is important and when strong formal and informal partnerships between staff across the different settings exist then people with existing mental illnesses at EoL can be practically assisted with their palliative care needs. 85 However, some mental health and EoL HCPs report that they believe that the flexibility to work in partnership with other agencies has declined, with this attributed to reductions in funding and competitive commissioning arrangements. 112 This under-resourcing often means that EoL HCPs, including those working in hospitals, are not aware of the needs of people with SMI. 106 Funding systems requiring quick decisions also inhibit good care in the context of needs assessments taking time. 106
A lack of good relationships and partnership between mental health and EoL services specifically prevents adequate pain management85,112 and assessment of mental capacity. 112 Different approaches to improving this exist, which include building on the importance of identifying lead clinicians to improve care management, with one proposal being that the lead be whoever is best-placed: a GP, or a practitioner working in the area of the ‘dominant condition’. 114 Other flexible approaches include EoL services specifically training mental health staff to work full-time in their services, or vice versa. 30,103
Multidisciplinary teamwork
Interagency and interprofessional team working at the EoL is important30,55,163,168,170,171 and high levels of multidisciplinary care have been reported in the last days of life. 110 Mental health and EoL services have both been characterised as benefiting from a democratic multidisciplinary team ethos. 102 Outcomes have been found to improve when interprofessional care is in place, drawing on the contributions of staff in both mental health and palliative services with partnership and advocacy, ensuring that complex needs are met. 106
However, mental health staff report a lack of information on services provided by EoL HCPs, and vice versa,85 and consultant-level mental health staff are not always directly involved in the provision of EoL care, with junior staff leading instead. 105 Hospice staff have been advised to particularly focus their energies on the needs of people with the most complex problems155 and to improve communication and joint working across team boundaries. 163 However, in the absence of systems or structures designed to facilitate partnership, qualitative data show how ongoing mainstream service support for people with mental illnesses at the EoL is often accomplished only because of the ad hoc efforts of individuals. 103 Even in these cases, however, partnership working is described as limited to advice-giving or telephone support rather than the provision of hands-on care. 103
Ongoing interprofessional communication
Communication among practitioners working together to provide mental health and EoL care varies in intensity and effectiveness. Ongoing communication between partners in care is frequently given as a prerequisite for high-quality provision,30,55,164 with qualitative research pointing to the value of open and clear decision-making and interprofessional case conferences as a place for discussion of key issues such as advance care planning. 106 Practical examples of how ‘coalition building’ has benefited individual patients exist. 85 Missed opportunities have also been reported, with participants in one study describing limited or no space for health, social care, housing and other staff to meet, and a generally low quality of information being shared across boundaries, including in initial referrals. 112 GPs report rarely receiving updates from palliative care services. 114
No right place to die
Seven policy and guidance documents30,120,156–159,162 and 14 research outputs32,88,91,92,97–99,105,106,108,110,112–114 contribute to this subtheme.
Dying at home
Nurses have talked about there being ‘no right place to die’32 and that care for people with SMI at the EoL is lacking in all settings: psychiatric units, general medical units, and older people’s mental health and hospice/palliative care settings. 32 System features combine to prevent people with SMI at the EoL from dying in the place, and manner, of their choice, which for a lot of people with SMI and palliative care needs is at home158 or in a ‘home-like’ environment such as community-supported accommodation. 106,114 This is despite evidence that, with the right support from community-based services, people with SMI at EoL are able to stay at home. 157
Studies have explored whether decedents with SMI were more or less likely than those without SMI to have died at home,88,91,97 and have produced mixed findings. When all causes of death were considered, there were no differences in the likelihood of home deaths between decedents with and decedents without previous mental illness [odds ratio (OR) 1.02, 95% CI 0.92 to 1.14]. 91 For Lavin et al. 91 all causes of death included cancer, chronic obstructive pulmonary disease, coronary artery disease, congestive heart failure, peripheral vascular disease, liver failure, diabetes and renal failure. The evidence for cancer-specific deaths is contradictory, however, with the results of a smaller study demonstrating no differences in the likelihood of home deaths between decedents with and decedents without schizophrenia diagnoses (OR 0.88, 95% CI 0.48 to 1.62),88 whereas in a further study it was shown that decedents with schizophrenia diagnoses were 65% less likely to have died in a nursing home than decedents without (OR 0.35, 95% CI 0.28 to 0.44). 97
Dying in a mental health hospital
Opportunities for EoL care to be provided in mental health facilities are limited. 110 Older people’s mental health wards rarely include people with schizophrenia diagnoses, and few examples exist of people being cared for until death in mental health units. 32 One example shows a person with bipolar disorder, dementia and cardiac disease being repeatedly moved between services at the EoL. 32 Irrespective of any patient preferences on where they might be cared for, staff describe inpatient mental health services as poorly equipped to meet the EoL care needs of those with SMI. 112
Dying in a hostel
Many homeless people have combinations of long-term physical, mental health and substance misuse problems and have difficulties engaging with health-care practitioners. 120 Although the preference for many homeless people is to receive EoL care in a hostel setting, several challenges make this difficult to achieve. 98,99,113,156 Hostel staff express concern over the suitability of residents with advanced ill-health to receive support in hostel accommodation until death, with specific concerns including limited access to adequate support,113 lack of staff confidence,113 burden on staff,113 safeguarding concerns,113 no pain or symptom management98 and the fact that hostels are often noisy and chaotic. 113 Staff may also have concerns about providing hostel-based care because of the perceived risks associated with poor living conditions, overcrowding, drug or alcohol use and violence, even when such risks are probably negligible. 98,99,112 Storing and administering medication, particularly opiates, in hostels where many residents may have substance misuse problems and staff lack sufficient training or experience is also problematic. 99,113
Several models of good practice are reported in the literature. 98,99,162 The Mission Hospice Programme in Canada provided dedicated palliative care to homeless people in a shelter, where people could spend their remaining days surrounded by family, friends and volunteers. 162 This demonstrates what can be achieved with sufficient resources, training and support. One further study described a specific shelter-based hospice care programme, reporting that 57% of homeless individuals received a palliative care consultation; the programme achieved success in optimising pain and symptom management and was shown to save money compared with likely alternative care locations. 98
Dying in an acute hospital
National standards state that all people with advanced and incurable conditions should be able to die in their preferred place,159 but evidence from official reports includes the illustrative case study of a woman at the EoL being moved repeatedly between services before dying in an unfamiliar acute hospital environment. 158
Acute general hospitals often have a role in the EoL care provided to people with SMI, even though care in this context is described as in need of improvement. 30 Staff in acute hospitals report that they are often under-resourced and lack awareness of the particular needs of people with SMI at the EoL,106 or describe acute hospital admissions [particularly via emergency departments (EDs)] as undesirable and often explained by difficulties in accessing hospice care or physical care in mental health settings. 112
Many adults with SMI are ultimately transferred at the EoL to acute hospitals for EoL care,30,32,98,99,105,110,166 for care within palliative medical settings105 or for care in EDs,105,112 often because of the limited expertise of staff in mental health settings in EoL care114 or because patients’ physical health care needs cannot be met in a mental health establishment. 112 On other occasions patients may move from the community105 or from homeless shelters98,99 because of a lack of adequate support. 98,99,105 Many staff feel that transferring people at the EoL in this way leads to discontinuity and disruption. 105
Mixed results were observed across studies regarding the likelihood of dying in a hospital. 88,91,92,97,108 When all causes of death are considered, having a pre-existing mental illness was associated with a 33% lower chance of dying in a hospital than not having one (OR 0.67, 95% CI 0.60 to 0.75). 91 In the case of cancer-specific deaths, those with pre-cancer depression had 25% lower odds of dying in hospital than those without [adjusted odds ratio (aOR) 0.75, 95% CI 0.64 to 0.87],92 and those with a diagnosis of schizophrenia had 48% lower odds of dying in hospital than those without (OR 0.52, 95% CI 0.47 to 0.57). 97 One further study explored rates of death from cancer in the ED or intensive care unit (ICU), finding that having a schizophrenia diagnosis was associated with a 35% lower odds of dying in the ED or ICU than not having that diagnosis (aOR 0.65, 95% CI 0.56 to 0.76). 108 In comparison, findings from a smaller study found that rates of hospital deaths for those who died of lung cancer were comparable in those with and without schizophrenia diagnoses (OR 1.06, 95% CI 0.55 to 2.05). 88
Dying in a nursing home or residential facility
Consistent findings were reported across three studies88,91,97 regarding the increased likelihood of dying in a nursing home or residential facility among decedents with SMI. When all causes of death were considered, having any type of pre-existing mental illness was associated with 27% higher odds of dying in a nursing home than not having one (OR 1.27, 95% CI 1.09 to 1.49). 91 In the case of cancer-specific deaths, having a schizophrenia diagnosis was associated with significantly higher odds of dying in a nursing home than not having one (OR 49.33 95% CI 43.89 to 55.45). 97 In the case of lung cancer deaths, having a schizophrenia diagnosis was associated with higher odds than not having that diagnosis of dying in an assisted living facility (OR 3.16, 95% 1.33 to 7.49) or a skilled nursing unit (OR 1.31, 95% CI 0.59 to 2.89). 88
Dying in a hospice
One study91 found no significant differences in the likelihood of dying in a hospice between those with and those without a history of previous mental illness (OR 0.98, 95% CI 0.79 to 1.22).
Many hospices are not able to cope with the needs of homeless people as a result of complex behaviours related to chaotic lifestyles and substance abuse issues113,156 and the inexperience of staff. 113 Such issues often lead to homeless people leaving the ward setting, making delivering care difficult. 113 Care home and hospice staff find it challenging to find provision catering for this population group because of their typically young age, meaning that access to these services is uncommon. 99,113
Professional issues
Ten policy and guidance documents30,156,162–166,171,176,177 and 16 research outputs (reporting 14 studies)32,37,85,93,94,99,102–106,110–114 contribute to this theme, which addresses professional and practitioner issues. Material is organised under four subthemes: relationships between HCPs and people with SMI, mental health professionals doing EoL care, EoL care professionals doing mental health care, and training and education.
Relationships between health-care professionals and people with severe mental illnesses
Three policy and guidance documents30,164,176 and 11 research outputs (reporting nine studies)32,37,99,102–104,106,111–114 contribute to this subtheme.
Connecting relationships
Mental health nurses value connectedness. They emphasise the importance of building nurturing relationships that go beyond the usual nurse–patient relationship. 102,110 Nurses often describe themselves as a substitute family,32,104 especially when people with SMI have been receiving care for a long time, sometimes years. 102 Nurses describe this as part of their daily interactions, and that in their work they attend to patients’ daily needs. 102 Mental health nurses report that some people with SMI have limited social networks and, in some circumstances, no family contact. 104,110 In these circumstances mental health staff state that they often represent the interests of people living with mental health problems and do work that goes beyond health-care provision, such as assisting with money, shopping for clothing and looking after the home environment. 110 They have satisfaction and a belief that they make a difference. 102 However, some nurses also choose not to form close relationships of this type102 and staff who have built such relationships are reported as often being upset when people they have been caring for need to be relocated because of their increasing palliative care needs. 114
Talking about death and dying
Place of care and desired place of death are important topics of discussion between mental health staff and people with SMI,106 with global guidance recognising that people with life-limiting illnesses (including SMI) should be supported to make decisions at the EoL. 176 However, concerns over talking about EoL care, death and dying lead to the avoidance of such conversations. 112 This is particularly so with people who have histories of thinking about suicide and of attempting to take their own lives,112 as staff fear upsetting them and creating emotional instability or distress. 112 Some staff working in mental health facilities feel confident about their ability to engage in EoL communication with patients and their families. 111 Staff in care homes describe themselves as needing greater confidence in EoL communication. 111 Determinants of high self-efficacy in EoL care communication among staff are reported to include age (older), formal training in palliative care, number of years working in direct care (> 10 years) and knowledge of the definition of palliative care. 111
Good communication is vital when discussing care and support for people living with a terminal illness. 164 However, owing to the lack of appropriate skills and competence, staff are not always comfortable discussing EoL or mental health issues. Palliative care and mental health nurses report that when conversations arise about EoL care planning, patients appear to be willing and able to have conversations with them. 112 This supports the person to have choice and to die in a safe, home-like environment. 106 It is recognised that communicating about the EoL can be difficult and takes effort, time and experience, although in one study nurses stated that helpful EoL conversations are nonetheless possible. 110
Attitudes and beliefs of health-care professionals
Nurses and psychiatrists report that physical care providers are often unable or unwilling to deal with people living with SMI and that they are generally resistant to accepting those who are diagnosed with a mental illness and display an unwillingness to admit people with SMI to acute care hospitals. 110,114 In some cases people with mental disorders are reported to be unsuitable for hospices. 110 In other instances some mental health facilities have arrangements with nursing homes or hospices specialising in mental health care. 110
The negative views about people with SMI held by the general population may be held by staff working in palliative care and hospice services. 30,112 The underlying attitudes of HCPs serve as barriers to the provision of effective care, and are associated with prejudice and stigma about mental illness and death. 32,37,103,112 Caring for a person with SMI at the EoL is often associated with stigma and an inability among HCPs to see the person behind the illness. 103 Stigma manifests in how people with SMI are spoken with or written about, and underlying beliefs affect the exchange of information, care planning, involvement and management of risk. 112 Stigma and prejudice also influence care for those who are homeless or vulnerably housed,99,113 resulting in a lack of compassion. 113
Stigma is also reported to be attached not only to people with mental health problems but also to the HCPs who care for them. 103 Sometimes this stigma is generated by fear that the person with mental illness is going to be dangerous to themselves,32,103 leading to a fear of providing EoL care. 32 It is also associated with a lack of understanding about mental illness, especially schizophrenia. 32 Stigma also works in the opposite direction, with mental health staff holding stigmatising views about EoL care. 103
Professionals also hold particular views about people with mental health problems and their experiences of pain. Mental health nurses are reported as believing that people with anxiety disorders have a much lower pain tolerance, leading to a very high demand for care, and that people with SMI might express pain differently, hampering the interpretation of physical complaints by doctors. 110 They state that people living with schizophrenia often have a much higher pain tolerance and might not even recognise pain as such, meaning that they are at risk of waiting too long to visit a doctor. 110
Mental health professionals doing end-of-life care
One policy and guidance document30 and 10 research outputs (reporting eight studies)32,37,93,102–105,110–112 contribute to this subtheme.
Experience, knowledge and skills
One study reports that just over one-third of mental health nurses have experience of providing care to people living with mental illness at the EoL in the past 2 years. 110 A further study suggested that the willingness of mental health staff to be involved with people with SMI at EoL, and their ability to be compassionate, may also be related to personal as well as professional qualities. 102
Many mental health staff may know little about how EoL care is provided,30 how and when to refer, and how services are funded. 112 Although studies have shown that some mental health staff have a general understanding and awareness of what is involved in EoL care,102,111 others have found that they do not. 112 In terms of practical clinical skills to care for people with SMI at the EoL, mental health staff have questioned their ability to effectively deliver pain management or to provide psychosocial-spiritual support. 102,111
End-of-life care not being mental health work
Mental health staff have expressed a desire not to care for medically unwell patients at EoL,32,105 feeling that EoL care ‘falls outside the remit of a mental health service’112 and that it is not something that should be managed within specialised mental health services. 105 Some psychiatrists have been reported to display a lack of interest in working with palliative care services, or the observation has been made that the general approach that psychiatrists take to people with SMI may not always be appropriate for people receiving palliative care. 178 Specifically, in the Dutch health-care system, with the focus moving away from care in hospitals towards recovery-oriented care in the community, fewer people are now being admitted to mental health facilities, and when they are admitted they have a shorter length of stay. Consequently, palliative care is no longer seen as core business in mental health facilities. 110 A further factor eroding mental health staff members’ confidence in EoL care in Australia is that, to avoid investigations by coroners, people with SMI are transferred away from older adult mental health services to non-mental health clinical environments. 105 This is because laws require a coroner to investigate a death in psychiatric facilities, and the possibility of an inquiry causes anxiety about scrutiny, prompting staff to avoid patient deaths in their part of the health-care system. This avoidance compromises care for people at the EoL, and some psychiatrists feel frustrated and constrained in their roles. 105 Other mental health staff, however, see death as part of life and take the view that people with SMI should be supported from birth to death, which means embracing EoL care and not treating all psychological responses to impending death as evidence of mental illness. 105
Emotional distress
Staff who provide care over long periods to individuals with SMI need support in the face of terminal illness, and in bereavement. 30 Caring for individuals at the EoL can be stressful for mental health nurses,30,103 demonstrated in the way mental health nurses use words such as ‘hard’, ‘traumatising’, ‘angst’ and ‘stress’ to describe the experience. 103 Some nurses’ distress is exacerbated by issues of loss associated with the strong relationships that they develop with people with SMI, added to which are bureaucratic difficulties and a lack of resources. 103 In the hospice environment, mental health staff report becoming emotionally involved37 and find caring exhausting to the point that they have a sense of relief when people die. 32 Conversely, others who have long-term involvement with people with SMI report that they experience distress associated with grief. 104 For staff working in mental health institutions, stress is compounded when post-death inquiries (including those involving the police) are initiated, at exactly the time staff are already dealing with the grief of loss. 104 This knowledge that actions may be legally scrutinised increases the stress felt by staff, some of whom have reported traumatic coroners’ inquests. 104 Staff also report that they fear that providing the appropriate amount of pain relief could be seen as accelerating death rather than relieving pain and that they would then have to explain any decisions to a coroner’s inquest. 104
End-of-life health-care professionals doing mental health care
Two policy and guidance documents30,171 and five research outputs32,37,103,110,112 contribute to this subtheme.
It has been observed that people with SMI who develop cancer or other life-threatening conditions have insufficient attention paid to their palliative care needs. 30 Education, knowledge and skills are important, and in the case of EoL HCPs it is recognised that they must be prepared to fulfil roles caring for people with SMI even though they may not have the required skills,30 lack confidence37 and are not necessarily equipped for the task ahead106 in terms of training37,112 and experience. 103 This is particularly so in the case of new nurses who have yet to gain relevant experience. 32 EoL HCPs who report prior experience or training in mental health issues are more confident in dealing with this population group. 37
Staff in palliative care services feel poorly prepared to provide care and treatment to patients with long-term psychosis or active bipolar mood disorder, even though the underpinning principles applying to the care of these groups are similar to those applying to all other groups, with the consequence that the needs of these patients are not always well met. 171 One study reported that most nurses involved in palliative care (60%) had provided care to between one and three people living with mental illnesses in the past 2 years. 110 Staff are often unable, unwilling or not comfortable to deal with people with SMI178 and are reported to be sometimes ignorant of the needs of such people. 30,103
Many EoL HCPs report that they have limited understanding of the structure of their local mental health system, of different mental health diagnoses and how these may affect patients, and of how to contact relevant teams for additional information following referral. 112 They are also unfamiliar with the differences between a clinical psychologist and a counsellor. 37 It has been recommended that all hospices and palliative care staff become conversant with the major mental illnesses, including how they present, the signs of deterioration, the basics of care provision and how to assess people with SMI in emergencies. 30 It is also recommended that EoL staff be aware of the specific needs that present in this group of people at the EoL, and in doing so work closely with both mental health and social services. 30
Training and education
Eight policy and guidance documents30,156,162–166,177 and eight research outputs (reporting seven studies)32,37,85,93,94,102,104,106 contribute to this subtheme.
Educational needs
Similarities have been claimed in the ideals underpinning mental health and EoL care nursing, with both sharing commitments to holistic and non-judgemental care. 102,104 However, professionals also lack education, understanding and resources to make sure that people with SMI at the EoL are not lost to services. 106 These observations add to the case that education and training are important to better support the development of skills and collaborative working in palliative care among mental health staff, and to improve palliative care staff members’ understanding of mental health needs. 30,106,162 This is particularly the case for staff caring for homeless people at the EoL, who have significant training and personal support needs that enable them to provide personalised care in conjunction with relevant multidisciplinary teams. 156
General areas that education and training could focus on have been highlighted across the literature and include:
-
communication skills between HCPs and those with SMI at the EoL164
-
communication and shared understanding across EoL and mental health care teams32,163,165
-
palliative care skills for mental health staff,162–165 especially with regard to advance care planning skills among the mental health workforce85,162–165
-
addressing stereotypical beliefs about those with SMI30,32,106
-
mental health education to EoL HCPs that provides them with the basic skills needed for providing care. 30,37,162
More specific training needs have also been identified, for example formal differential diagnoses in the mental health field,37 cognitive–behavioural techniques and communication skills,37 and approaches to working with people with SMI and family members whose behaviour is seen as difficult to manage. 32,37 Differentiations have also been made between the training needs of nurses and the training needs of medical staff, with the latter requiring more detailed material to reflect their existing education. 37 Specific recommendations on education have been made for GPs, for whom continuing professional education might include the principles of palliative care to better enable them to provide high-quality primary care for people with SMI. 30
Core professional preparation
Education and training are important and offer ways of improving how different professionals work together. 30,164 This is particularly so in the context of core professional preparation, which lacks detail in some areas. An example is in psychiatry training, and programme directors of palliative care consult services have suggested that psychiatry training is inadequate in the categories of EoL care and issues related to death and dying. 178 The Leadership Alliance for the Care of Dying People sets out the underpinning competencies that it suggests should be part of the curriculum for doctors in training, including being able to address ethical and legal issues arising in the context of care for people with medical or mental health problems. 177 In one study, when talking about their core mental health training, some mental health staff pointed to their underpinning, person-centred training, and skills enabling them to be sensitive to individual needs, including at the EoL,102 and others spoke of how their preparation enables them to care for people with SMI, including during periods of physical illness. 103 In a further study, mental health nurses propose that their core education should consider how mental health practice might be adapted to medical and surgical areas. 32
In-service education
The Royal College of Physicians171 recommends improved training, including to better enable EoL care to be provided to vulnerable people who have pre-existing mental illnesses. This includes investing in liaison psychiatry, in education for specialist palliative care staff and in training to meet needs in the case of mental health emergencies. 171 Hospices have been described as focusing on education and training that remove barriers to access,162 and it has been suggested that hospices should develop training that equips staff and volunteers to better care for people with SMI, in the knowledge that education can improve services. 30
Marie Curie suggests that improvements are needed and that EoL care and bereavement training should be provided to all health and social care students and practitioners as routine both in core preparation and through ongoing post-qualification education. 164,165 Investments in education of this type are championed with the aim of developing all members of care staff to provide services to people with mental illness at the EoL. 164 However, education and training opportunities are patchy. One report166 found that, between 2017 and 2018, only 6% of mental health providers included EoL care training as part of their staff induction programme, with 13% saying that they included EoL care in their mandatory/priority training and 91% saying that they offered EoL care communication training. By contrast, among acute and community providers, 47% reported including EoL care in their mandatory training.
End-of-life and mental health staff learning from each other
End-of-life and mental health staff working together can improve knowledge and awareness, such as through the establishment of dedicated link positions with roles including the provision of education30 or through cross-training. 85,94 Hospice trainers can teach mental health providers about EoL care,85 and mental health providers use case examples to expose hospice and palliative care providers to typical mental health issues. 85,94 Evaluations from cross-training initiatives demonstrate that both mental health and EoL participants have greater confidence in their skills after the training,85,94 and palliative care staff report that they have a more positive regard for the lived experience of people with SMI. 94 In terms of approaches to learning, staff report valuing the use of real-life vignettes to illustrate practical approaches to complex problems. 85 Particularly appreciated by EoL HCPs is the chance to learn about commonly made mental health diagnoses, approaches to communicating bad news and how to manage mental health emergencies in people at the EoL. 85 Mental health staff feel that cross-training improved their confidence in caring for people at the EoL,94 giving them key insights, including into the importance of advance care planning. 85
Contexts of care
Eleven policy and guidance documents21,30,156,161–166,170,176 and 31 research outputs32,37,83–93,95–102,104–110,112–114 (reporting 28 studies) contribute to this theme, which addresses the organisation, provision and receipt of care. Material is organised under three subthemes: managing the interface between mental health and EoL care; health-care services and treatment utilisation in the LYoL, and meeting individual and family needs.
Managing the interface between mental health and end-of-life care
Two policy and guidance documents30,164 and eight research outputs37,93,95,105,106,110,112,114 contribute to this subtheme.
General practitioners managing care
Evidence suggests that GPs are the gatekeepers of enabling or hindering access to palliative care services, and in some instances manage the palliative care needs of people with SMI within their practice. 30,110,114 One study showed that just one-quarter of people with SMI were referred by a GP for palliative care assessment,114 and referrals to specialist palliative care services were mainly related to achieving admission to hospice, nursing home and intermediate care beds for further investigations or for community/specialist palliative care. 114
The role of medical specialists
The different types of specialists that people with SMI visit at the EoL include hospital specialists (medical, general surgery and surgical)95,110,114 as well as psychiatrists. 93,95,110,164 Palliative care HCPs are significantly more likely to refer people living with mental illnesses such as depression (r = 0.25; p < 0.01) and personality disorders (r = 0.23; p < 0.01) at the EoL to psychiatrists when their own comfort level with mental health is low. 93 The services psychiatrists provide include informal or ‘kerb-side’ consultations for the palliative care team without having patient contact, therapy, capacity evaluations and the management of delirium or behavioural disturbances. 93
Referral
When dealing with terminal illness, speed is of the essence. Whether someone has only a few years or, in many cases, a matter of months to live, they cannot afford to wait to get the support they need. Wherever possible, this means that support for people living with mental health issues and approaching the EoL must be fast-tracked or prioritised. 164 This is essential, given the importance of trusting relationships and mutual understanding for people with SMI. 106 However, staff acknowledge that referrals are not straightforward, particularly in the case of people with schizophrenia lacking someone to speak with and for them, or not having settled accommodation. 106 Inadequate quality of referrals of people with SMI can result in staff being unaware of vital information that would aid effective communication between them and the person using services. 112 Types of missing information include discussion of a patient’s mental ill-health, mental health history, symptoms, risk information relating to EoL care and advice on how best to work with the patient. 112
Mental health assessment at the end of life
Skilled assessment and care planning are important, as people with SMI require expert advice to manage their medication, to prevent crises and to receive appropriate help when crises do happen. 30 These are all areas in which staff can gain knowledge and skills. 30 Within mental health facilities, psychiatric assessment for those at the EoL is an important aspect of participants’ work, involving assessing patients for treatable psychiatric illness,112 decision-making capacity,105,112 pain112 and risks of harm. 105,112 Psychiatrists are described as working in a system that is focused on facilitating recovery and in supporting people at the EoL. 105 Evidence exists that people with SMI are not always offered assessments of their mental health needs in hospices. 37 It is important that hospices and specialist palliative care services have policies and procedures in place for assessing those with SMI at EoL so that there are no delays in accessing emergency psychiatric support if it is needed,30 and so that problems are not underdetected. 106,114 For those working in hospices, mental health issues are seen as a challenge, and staff express several fears and uncertainties acting as barriers influencing the assessment process for people with mental health difficulties at the EoL. 37 These barriers include separating physical and psychological symptoms, fear and limited ability to communicate. Time, trust and collegial support are facilitators of assessment and treatment processes. 37
Health-care services and treatment utilisation in the last year of life
Thirteen research outputs88–92,95,97,100,101,104,107,108,112 (reporting 12 studies) contribute to this subtheme.
Ambulatory visits to general practitioners or medical specialists
One retrospective cohort study95 explored the rates of ambulatory visits to the GP and medical specialists, and whether this was higher or lower for those with and those without schizophrenia diagnoses who had died from cancer. No differences were observed in rates of ambulatory visits to the GP within 6 months of death [adjusted relative risk (aRR) 1.03, 95% CI 0.96 to 1.11]. 95 However, in the 6 months to death decedents with schizophrenia diagnoses were 39% less likely than those without to visit medical specialists (aRR 0.61, 95% CI 0.54 to 0.69). 95
Palliative care services
Three studies compared rates of utilisation of palliative care among decedents with and decedents without schizophrenia diagnoses who died from cancer at different time points throughout the LYoL. One study conducted in New Zealand showed that decedents with SMI were 71% less likely to access specialist palliative care services (community and inpatient services) than those without SMI in the LYoL [relative risk (RR) 0.29, 95% CI 0.24 to 0.34]. 100 Huang et al. 101 found, in a nationwide population-based cohort from Taiwan (Province of China), no significant differences in the overall utilisation of palliative care services (hospice ward care, palliative care consultation and hospice home care) between those with schizophrenia diagnosis and those without at 3 months before death (OR 1.03, 95% CI 0.090 to 1.18) or at 1 month before death (OR 1.03, 95% CI 0.99 to 1.33). 101 However, they also demonstrated that people with SMI were 31% less likely to receive a palliative care consultation than those without during the last month of life (OR 0.59, 95% CI 0.43 to 0.82). 101 In a study from France, decedents with schizophrenia diagnoses and cancer were 61% more likely to have frequent admissions to palliative care units in the last 31 days before death (OR 1.61, 95% CI 1.45 to 1.80), 152% more likely in the last 3 days before death (OR 2.52, 95% CI 2.25 to 2.82) and to have had 36% more time from initiation of palliative care to death (ß 0.36; standard deviation 0.03) than matched controls. 108
Rates of hospice enrolment for people dying of cancer vary depending on the nature of the patient’s SMI. One study demonstrates no significant differences in the rates of hospice ward care between decedents with schizophrenia diagnoses and those without within 1 month of death (RR 1.15, 95% CI 0.99 to 1.33),101 and another found the same pattern regarding hospice enrolment for decedents with schizophrenia diagnoses and those without within 6 months of death (RR 11.3, 95% CI 0.63 to 2.01). 88 However, having depression ahead of a cancer diagnosis was found to be associated with a 19% higher hazard of hospice enrolment than not having depression ahead of a cancer diagnosis within the 30 days of death (subhazard ratio 1.19, 95% CI 1.11 to 1.28). 92 When looking at the length of stay once enrolled in hospice care, decedents with schizophrenia diagnoses had significantly longer hospice stays than those without (mean difference 44, 95% CI 5.16 to 82.84). 88 Having depression ahead of a cancer diagnosis has also been found to be associated with a 29% increased likelihood of longer hospice stays of ≥ 90 days than not having this (aOR 1.29, 95% CI 1.06 to 1.58). 92
General practitioners and psychiatrists believe that people with SMI are less likely than other groups to have their palliative needs identified, are less likely to be referred to specialist palliative care and are less likely to engage with or to use specialist palliative care services once they are referred. 114 Conflicting findings are found across studies exploring the rates of the use of specialist palliative care in the community for decedents with a schizophrenia diagnosis who died from cancer, depending on the time frame for which EoL care is measured. One study shows that decedents with schizophrenia diagnoses (where the cause of death meant that they were amenable to palliative care) were 66% less likely to receive hospital-based specialist palliative care (RR 0.34, 95% CI 0.26 to 0.44)107 and 62% less likely to have received specialist palliative care in the community than those without in the LYoL (OR 0.38, 95% CI 0.30 to 0.48). 107 Further analysis found that being enrolled in community-based specialist palliative care was associated with a 50% increased rate of hospital admission [hazard ratio (HR) 1.5, 95% CI 1.1 to 2.1] but no change in the rate of ED presentation (HR 1.2, 95% CI 0.8 to 1.7). Among decedents in the matched cohort, being enrolled in the service was associated with a 60% lower rate of emergency department admission (HR 1.6, 95% CI 1.2 to 2.4) but no difference in the rate of hospital admissions (HR 0.8, 95% CI 0.6 to 1.0). 107
Decedents with schizophrenia diagnoses who died of cancer were 29% less likely to have used specialist palliative care in the community than decedents without within 6 months of death (aRR 0.71, 95% CI 0.62 to 0.81)95 and also to have received significantly fewer days of specialist palliative care in the community on average (59.3 days compared with 76.2 days). 95 However, when looking within 1 month or 3 months of death, one study101 found no significant differences in rates between decedents with schizophrenia diagnoses for whom the cause of death was cancer and those without (OR 1.11, 95% CI 0.89 to 1.39, and OR 1.21, 95% CI 0.99 to 1.48, respectively). 101
Long-term institutional care
One study (reporting across two publications) explores the use of long-term institutional care (nursing homes, care homes) for those with and those without SMI at the EoL. 95,97 Decedents with schizophrenia diagnoses who died of cancer had a significantly increased rate of use of long-term institutional care than decedents without within 6 months of death, as demonstrated by a higher percentage residing in a nursing home (aRR 4.28, 95% CI 3.55 to 5.16). 95 They also had significantly longer lengths of stay than those without schizophrenia diagnoses in the 6 months before death, as demonstrated by the rate of days residing in a nursing home (per person) (aRR 5.19, 95% CI 3.60 to 7.78). 95 Decedents with schizophrenia diagnoses who died in a nursing home had significantly lower rates of inpatient hospital days than those without within with 6 months of death (aRR 0.80, 95% CI 0.67 to 0.95). 97 However, no significant differences were shown between cohorts for rates of GP visits (aRR 1.14, 95% CI 0.89 to 1.20),97 specialist visits (aRR 1.14, 95% CI 0.97 to 1.33) or hospital separation rates (RR 0.93, 95% CI 0.82 to 1.06) [separation from a health-care facility occurs any time a patient (or resident) leaves because of death, discharge, sign-out against medical advice or transfer. The number of separations is the most commonly used measure of the utilisation of hospital services]. 97
Acute care
With regard to inpatient separations, decedents with schizophrenia diagnoses who died of cancer had a significant reduction in the rate of inpatient hospital separations compared with decedents without such diagnoses within the 6 months before death (aRR 0.79, 95% CI 0.73 to 0.86). 95 Across all causes of death, one study91 found that decedents with pre-existing psychiatric illnesses were 41% less likely to have a hospital admission than those without within 1 month of death (OR 0.59, 95% CI 0.51 to 0.68). 91 A similar pattern was found when looking at cancer-specific deaths. Decedents with schizophrenia diagnoses were 27% less likely to have had more than one admission to acute care during the last 31 days of life (aOR 0.73, 95% CI 0.67 to 0.80). 108 In an exploration of rates of admission within 6 months of death, decedents with schizophrenia diagnoses had a 21% reduction in the rate compared with decedents without schizophrenia diagnoses (aRR 0.85, 95% CI 0.77 to 0.94). 95 Decedents with a schizophrenia diagnosis had a 40% reduction in the rate of admission compared with those without schizophrenia diagnoses (except for breast cancer) within the LYoL (aHR 0.6, 95% CI 0.5 to 0.8). 107 Lower rates of hospital admission were also observed for decedents with schizophrenia diagnoses who had heart failure (aHR 0.6, 95% CI 0.5 to 0.8),107 cirrhosis/liver disease (aHR 0.5, 95% CI 0.3 to 1.2)107 or renal disease/dialysis (aHR 0.6, 95% CI 0.3 to 1.2),107 but no differences were found for those who had died from chronic lower respiratory disease (HR 0.7, 95% CI 0.4 to 1.2). 107
With regard to length of stay, two studies showed no statistically significant differences between those with and those without SMI at EoL,91,95 and another showed that length of stay was longer for those with SMI than for those without SMI. 108 In the studies that showed no difference, the populations were those with schizophrenia diagnoses and those without schizophrenia diagnoses who died of cancer in the 6 months before death (aRR 1.00, 95% CI 0.85 to 1.19),95 and those with pre-existing mental illness and those without within 1 month of death across all causes of death (RR 0.93, 95% CI 0.86 to 1.00). 91 Conversely, Fond et al. 108 found that the median length of stay in acute care during the last 31 days of life was higher for decedents with schizophrenia diagnoses who died of cancer {median length of stay in acute care during the last 31 days of life [median (interquartile range) 16 (8–28), vs. 22 (11–31); p < 0.0001]}.
Intensive care unit admissions
When all causes of death were considered, decedents with pre-existing psychiatric illnesses were 59% less likely to be have been admitted for care in an ICU than those without pre-existing psychiatric illnesses within 1 month before death (OR 0.41, 95% CI 0.35 to 0.48). 91 This was also seen, albeit to a lesser extent (22%), for decedents with pre-cancer depression compared with those without pre-cancer depression within 1 month before death when the cause of death was lung cancer (aOR 0.78, 95% CI 0.67 to 0.90). 92 Conversely, it was found that having schizophrenia diagnoses and having died of cancer was associated with a 21% increased likelihood of having been admitted for care in an ICU compared with those without within 1 month of death (OR 1.21, 95% CI 1.07 to 1.36). 101 However, one further study found no association between having schizophrenia diagnoses and having died of cancer and at least one ICU admission during the last 31 days of life (aOR 0.92; 95% CI 0.91 to 1.09). 108 With regard to length of stay in the ICU, decedents with pre-existing mental illnesses spent significantly fewer days admitted than those without pre-existing mental illness in the 1 month prior to death (RR 0.88, 95% CI 0.79 to 0.97). 91
Emergency department visits
Studies investigated rates of visits to the ED and, again, the results were mixed. 91,92,107,108 Across all causes of death, having pre-existing psychiatric illnesses was associated with a 64% increased likelihood of visiting the ED at least once compared with not having one, within 1 month of death (OR 1.64, 95% CI 1.30 to 2.08). 91 One study demonstrated that having pre-cancer depression was associated with a 22% reduction in the likelihood of visiting the ED at least once compared with those without pre-cancer depression within 1 month of death (aOR 0.78, 95% CI 0.62 to 0.98),92 whereas another found no associations between having a schizophrenia diagnosis and attending the ED at least once during the last 31 days before death (OR 0.93, 0.91 to 1.09). 108
Where disease-specific analyses in relation to cause of death have been undertaken for decedents with schizophrenia diagnoses compared with those without, significantly higher rates of attending the ED within 1 month of death have been found for those dying from ischaemic heart disease (HR 1.1, 95% CI 1.0 to 1.4),107 heart failure (HR 1.0, 95% CI 0.8 to 1.3),107 chronic lower respiratory disease (HR 1.1, 95% CI 0.8 to 1.3),107 renal disease/dialysis (HR 1.1, 95% CI 0.8 to 1.5),107 cirrhosis/liver disease (HR 1.0, 95% CI 0.8 to 1.2)107 and cancer (HR 1.2, 95% CI 1.1 to 1.4). 107
Invasive interventions
End-of-life HCPs working in the UK feel that there is a lack of standard guidance on resuscitation,112 whereas staff in Australia report a legal requirement to always engage in cardiopulmonary resuscitation (CPR) in mental health settings. This is because of concerns about the validity of ‘do not resuscitate’ orders for people with SMI who may be judged as unable to consent to advance directives that might stipulate otherwise. 104 However, in one study it was found that no significant difference in orders about CPR existed between decedents with schizophrenia diagnoses and those without within 6 months of death at a Veterans Administration medical centre, in whom the cause of death was cancer (aRR 1.03, 95% CI 0.96 to 1.11). 88
Mixed findings were evident for a range of invasive interventions across studies. 101,108 In the month before death, decedents with schizophrenia diagnoses in whom the cause of death was cancer were significantly more likely than those without schizophrenia diagnoses to have had CPR (OR 1.34, 96% CI 1.15 to 1.57), endotracheal intubation (OR 1.22, 95% CI 1.08 to 1.38), mechanical ventilation (OR 1.15, 95% CI 1.03 to 1.29), urinary catheterisation (OR 1.19, 95% CI 1.07 to 1.32), or feeding tubes (OR 1.41, 95% CI 1.26 to 1.58). 101 However, in a second study108 no significant differences were found in artificial nutrition, tracheal intubation, mechanical ventilation, gastrostomy, dialysis, CPR and having at least one air extraction (sterile) chamber admission during the 31 days before death between those with schizophrenia diagnoses and those without. With regard to other procedures, the same study108 showed that decedents with schizophrenia diagnoses and cancer were less likely to have undergone surgery (aOR 0.71, 95% CI 0.63 to 0.80) or to have had blood transfusions (aOR 0.72, 95% CI 0.64 to 0.83) in the 31 days before death.
Veterans with existing, but unspecified, mental health conditions, among whom over half had a terminal condition of cancer (30.1%) or heart disease (20.1%) at the time of death, were 20% less likely to have an intravenous infusion (OR 0.80; p = 0.001) than those without and 23% more likely to have both a do-not-resuscitate order (OR 1.23; p = 0.002) and physical restraints (OR 1.23; p = 0.004) than those without. 89
Physician orders for life-sustaining treatment are orders that stay with the patient regardless of care setting and are most often used to limit life-sustaining treatments, artificially delivered nutrition and even transport to hospital. 88 Decedents with schizophrenia diagnoses who died of cancer were 267% more likely to have physician orders for life-sustaining treatment in place (OR 3.67, 95% CI 1.38 to 9.72). 88
Chemotherapy
Findings are mixed relating to chemotherapy presented across studies. 89,92,108 Decedents with schizophrenia diagnoses in whom the cause of death was cancer were 45% less likely to have chemotherapy than those without within 1 month of death (OR 0.55, 95% CI 0.48 to 0.63)89 or 47% less likely in the last 14 days of life (aOR 0.53, 95% CI 0.46 to 0.62). 108 In a study of people dying of lung cancer, no association was found between having depression ahead of a cancer diagnosis and not having depression ahead of diagnosis in the use of chemotherapy in the last 14 days of life (aOR 0.89, 95% CI 0.74 to 1.07). 92
Advanced diagnostic examinations
Studies investigated whether those with SMI at the EoL were more or less likely to have received a number of different advanced diagnostic examinations. 101,108 Decedents with schizophrenia diagnoses in whom the cause of death was cancer were less likely to have had computed tomography, magnetic resonance imaging/sonography (OR 0.80, 95% CI 0.71 to 0.89), bone scans (OR 0.62, 95% CI 0.50 to 0.76) or positron emission tomography scans (OR 0.37, 95% CI 0.15 to 0.96) than those without within 1 month of death. 101 There were no differences in the use of pan-endoscopy (OR 0.98, 95% CI 0.84 to 1.15) or colonoscopy (OR 1.02, 95% CI 0.74 to 1.41) between the groups. 101 Decedents with schizophrenia diagnoses and cancer were less likely to have had imaging (OR 0.66, 95% CI 0.59 to 0.73) or endoscopy (OR 0.85, 95% CI 0.74 to 0.97) in the 31 days before death. 108
Use of medications at the end of life
Decedents with schizophrenia diagnoses who died of cancer were 44% less likely to have used analgesia than those without in the 6 months prior to death, as demonstrated by the total days and rate per person-year of receiving analgesics (aRR 0.66, 95% CI 0.54 to 0.81). 95 However, there was no significant difference in the number of different drugs used between those with schizophrenia diagnoses who died from cancer and those without within 6 months of death as demonstrated by the number of different drugs (per person-year, for those on at least one prescription in the 6 months) (aOR1.02, 95% CI 0.96 to 1.08). 95
Contrary to one study’s hypothesis, veterans with schizophrenia diagnoses where the cause of death was cancer were no less likely than those without to receive opioid medications before hospice enrolment in the last 6 months of life (73% vs. 81%; OR 0.64, 95% CI 0.33 to 1.26). 88 A further study showed a significant association between a lifetime diagnosis of PTSD and the medications needed at the EoL, where there was found to be a higher use of medications (in particular hypnotics and antidepressants) at the EoL among terminally ill veterans with PTSD than among those without PTSD. 90
Meeting individual and family needs
Eleven policy and guidance documents21,30,156,161–166,170,176 and 20 research outputs (reporting 18 studies)32,37,83–88,90,93,96,98,99,102,104,106,109,110,112,113 contribute to this subtheme.
Spiritual and psychosocial support
It is recognised that people with SMI have particular vulnerabilities arising from their mental health experiences, and will often lack support from personal networks. 176 This means that programmes and services for people with SMI at the EoL require a comprehensive team approach incorporating symptom relief (pain control),30,37,98,110 psychological support (clinical psychology, counsellors and support groups),37,164 psychosocial support (social worker)30,90,102,104,106,110 and spiritual care (chaplain or spiritual counsellors),30,90,98,102,104,106,110 whether in the mental health or the EoL setting. Nurses working in mental health settings highlight the importance of spiritual care for a peaceful death. They report that at the EoL many people with SMI tend to reflect on the meaning of their lives and frequently aim to resolve old issues. 110 One study shows that there are no significant differences in the likelihood of receiving a social work, chaplain or psychologist visits between veterans with and veterans without PTSD. 90
Families and their involvement
In the mental health setting, HCPs report on the impact and challenges of chaotic family systems,32,110,112 prior family estrangement98,102,104,106,110 and family members also having a mental health diagnosis. 32 Attempting to negotiate contact with estranged family members is an important aspect of palliative care98,102,104,110 as people with SMI often have less family support. This has implications for reduced advocacy and for reduced liaison with staff in the context of making shared treatment decisions, both of which serve as barriers to good EoL care. 112
Among veterans with and veterans without PTSD, the majority (72%) received consultations before being referred for hospice care, including a family meeting. These consultations included most aspects of advance care planning, such as pain concerns, goals of care, feeding, hydration and symptom management. No significant differences were reported in the likelihood of family meetings occurring between veterans with and veterans without PTSD. 90 However, some family members of veterans with PTSD reported unmet needs for emotional support, especially in the last month of life, linked to poor communication with care providers. Family members also felt that their relatives were not treated with dignity and they were generally not satisfied with the level of care that their relative had received. 83
Advocacy
Having an advocate that can support a person with SMI throughout their cancer journey, including at the EoL, is important. 30,162 Staff report that people with SMI being referred to palliative care and receiving services, such as pain control, is not straightforward and appears to be based on the presence or absence of a strong advocate. 32,106,112 HCPs have suggested that an advocate can be a family member, friend, health professional (e.g. a GP or a member of mental health staff), a public advocate,106 an identifiable carer32 or a case manager who has a history with the person using services. 112 People fulfilling this role can ensure that the needs of people with SMI at the EoL are recognised and met,30 can support the development of palliative care skills among mental health staff and can improve the palliative care team’s understanding of people’s mental health needs. 162 Without such advocates, people with SMI may become ‘lost in the system’. 106,156 Palliative care experts have a responsibility to act as advocates for people with SMI at the EoL, ensuring that they are not passed across agencies and do not fall through the gaps. 30
Not having strong external social supports, and possibly having experienced family estrangement, means that people with SMI can lack access to advocacy to help navigate the complex EoL trajectory. 30,32,106,110,112,156,161,162 Those most at risk may have additional vulnerabilities, including being homeless or living on their own in boarding house accommodation,106,156 or having mental health and/or learning disabilities. 161 In these circumstances, when admitted to hospital in crisis they may have nobody to speak on their behalf or to give their history and background,156 and, as a result, ‘ill-informed decisions are made about their care and discharge’(p. 8; contains public sector information licensed under the Open Government Licence v3.0). 156
End-of-life care preferences
All countries are expected to have mechanisms in place to support people with disabilities to make decisions, and to use these mechanisms in preference to substitute decision-making processes. 176 It is in this context particularly that anticipatory, or advance, planning for people with mental health issues at the EoL is important,164,165 along with the need for improved working across palliative care and mental health services and better education and training to support anticipatory care-planning skills. 163 Ninety per cent of mental health providers in England and Wales report having advance care planning processes in place, with 75% saying that they have a care plan that supports priorities for care compared with 97% of acute and community providers. 166 However, discussing EoL care wishes is often problematic for people who have SMI,32,106,110,113,156,170 especially for those who are homeless. 113,156 Nursing staff report that it is sometimes difficult to have realistic conversations32 and to distinguish reality from delusions when trying to explore the EoL care wishes of those with SMI. 110 Nursing staff have also expressed concerns that some patients with SMI may react differently to ‘bad news’ and, consequently, establishing EoL care preferences may be difficult. 110 It is therefore essential for HCPs to take sufficient time to assess the person properly, particularly if that person is unable to express their needs clearly. 106
It is important not to assume that mental capacity is lacking;21 however, the fluctuating or limited capacity of people with SMI at the EoL can challenge care,106,112 and EoL HCPs are not always comfortable determining patients’ capability to make medical decisions. 93 As a consequence, both palliative care and mental health nurses have a tendency to assume that mental capacity is lacking, with the consequence that discussions around advance care planning are avoided. 112
Three studies examined scenario-based preferences regarding medical advance care planning among persons with SMI who were not at the EoL. 86,87,96 People with SMI were able to designate treatment preferences in response to EoL health state scenarios and felt comfortable talking about EoL matters. 86,96 Some people with SMI had thought about their medical treatment preferences in the event that they became seriously medically ill, but very few had discussed these preferences. 87 Others believed that someone should be designated to make medical health-care decisions for a person who is too sick to make or communicate these decisions themselves. 87 A further study into the EoL care perspectives of people with schizophrenia diagnoses (including those experiencing cognitive and emotional deficits) found that they were open to the idea of talking about EoL care and found this reassuring and sometimes beneficial. 109
A retrospective medical records review85 in the USA shows that, despite federal legislation being in place to support the use of a health proxy for patients with SMI, only 1 out of 344 patients whose care records were examined had a proxy in place. As a result, people were not assisted with advance care planning or with their preferences for medical treatment if they became seriously ill, despite this being identified as a right for persons with mental illness. Mental health and EoL nurses who work with people with SMI at the EoL report that people are capable of completing advance care planning documents without undue distress85,110 and are able to make advanced decisions about medical treatments and decide who should make decisions if they become unable. 110 This is more likely to occur when open communication exists between people with SMI and practitioners. 106 However, professionals working with the homeless population at EoL (many of whom also have SMI) report that they often lack confidence in having such conversations and express concerns regarding the fragility and vulnerability of many homeless people. 113 Stajduhar et al. 99 report that homeless people are likely to experience oppression, poverty and inadequate housing, which usually makes the ‘survival imperative’ more important than accessing palliative care, and, as a result, advance care planning, the provision of palliative care or discussions about death and dying are not issues of importance in their everyday lives. 99 When EoL care was discussed with those residing in a homeless shelter-based hospice, most requested or agreed do-not-resuscitate orders and specifically declined emergency ambulance and hospital transfer. 98
The authors of one study88 hypothesised that veterans with schizophrenia diagnoses and advanced cancer would be less likely than those without schizophrenia diagnoses to complete advance directives. However, no differences were found (OR 1.29, 95% CI 0.72 to 2.32). Findings from another study84 found that having a diagnosis of SMI was significantly associated with 24% lower odds of having any advance directives in a nursing home after controlling for a variety of resident and family characteristics (aOR 76, 95% CI 0.66 to 0.87).
Living with severe mental illness
Eight policy and guidance documents22,30,156–158,161,162,170 and 11 research outputs32,37,85,99,102,103,106,110,112–114 (reporting 10 studies) contribute to this theme, which addresses the individual and social characteristics of patients with SMI. Material is organised under three subthemes: complexities of EoL care, familiarity and trust, and recognising physical decline.
Complexities of end-of-life care
Two policy and guidance documents156,170 and seven research papers32,37,103,106,110,112,113 contribute to this subtheme.
Providing EoL care to people with SMI is challenged by patients’ behaviour associated with their mental health difficulties. 32,37,103,106,110,112,113,156,170 Many HCPs often find it difficult to address mental health issues at the EoL, particularly if the person affected demonstrates complex or interpersonally challenging behaviour, anger or aggression, hostility or paranoia32,37,112,113,156 and/or are uncommunicative or have limited communication. 37,106,110,112,156,170 EoL care HCPs typically report that they are challenged by both care-seeking and care-rejecting behaviours, unusual presentations, and angry and aggressive outbursts. 112 Unpredictable and potentially dangerous side effects arising from combined medications associated with SMI and EoL management are also challenges in EoL care for people with SMI. 106
Familiarity and trust
Four policy and guidance documents156,161,162,170 and nine research outputs32,85,99,102,103,106,112–114 (reporting eight studies) contribute to this subtheme.
Trust and rapport
Early referral to palliative care services is important so that health-care staff can build trust and rapport with people with SMI. 106 There is also a need for greater integrated care, shared care-planning and better communication between specialist health and social care services to ensure that appropriate EoL care is provided in a familiar environment (where practicably possible) for those with SMI. 85,170 People with SMI who are living in supported accommodation, living in community-based residences, receiving institutional mental health care and/or are homeless may see ‘home’99,102,103,112,114 as linked with staff and residents they know and trust. 103,114
Supporting people in familiar environments
People with SMI benefit from care in environments with which they are familiar, surrounded by people they know and trust. However, they often need to leave their familiar, supported accommodation at the EoL. 114 It is likely that staff offering usual mental health support will not be suitably qualified to provide EoL care. 99,102,103,113,114 Studies give examples of how staff in mental health establishments are able to care for people with SMI at EoL in mental health establishments. One showed how mental health staff sought advice from colleagues at local hospice/palliative care organisations so that patients could die in a familiar environment. 85 Another reported how opportunities for palliative care staff to visit people in mental health facilities were preferable to transferring people for palliative care because it prevented the problem of people becoming distressed in an unfamiliar environment. 102,103 Staff also talked about becoming a substitute family to the person with SMI and appreciated being able to care for them at the EoL. 102
Providing palliative care in hostels is challenging, but as residents see these as ‘home’ this may make them a better choice than hospital at the EoL on the grounds of compassion and choice. 113 However, some residential staff have been reported as ignoring the subsequent pressure to transfer residents to acute care settings, often putting themselves at significant risk, simply to ensure that residents can, where possible, remain in an environment familiar to them at the EoL. 99 In the case of homeless people, even though hospitals are better suited to meet the physical needs of dying people, the benefits of enabling a person with SMI at the EoL to remain in a familiar hostel often outweigh the challenges. 113 However, significant deteriorations in EoL-related physical health commonly result in the homeless person being admitted to hospital in a crisis, when they may be unable to advocate for themselves and have nobody to speak on their behalf, and may also be experiencing language barriers, substance misuse problems, emotional volatility, social anxiety and other mental health issues. 156 Consequently, ill-informed decisions may be made about their care and subsequent discharge. 156 Furthermore, as and when the homeless person enters the EoL phase, hospitals and hospices may be unable to adequately support their complex physical and mental health needs and any associated issues such as chaotic lifestyles and addictions. 113,156
Recognising physical decline
Six policy and guidance documents22,30,156–158,161 and six research99,106,110,112–114 outputs contribute to this subtheme.
Identifying signs of declining health
A key to good palliative care is the early recognition of declining physical health and a gradual awareness of the impending potential of death. However, the physical health needs of those with pre-existing SMI may not be identified and, as a result, care is often inadequate. 30,161 Death is often perceived as sudden, but in reality there are usually missed signs of deterioration,156 including on the part of patients themselves.
People with schizophrenia often find it difficult to articulate their physical health needs to those who care for them, and they may not identify the significance of escalating physical symptoms that indicate a decline in their own health,106,114 causing them to present late to services. 106,110 Access to quality health care is often diminished114 and the commonality of previously unsatisfactory health-care encounters adds to delays in medical help-seeking. 106 This typically affects disease progression, delays the diagnosis process and has an impact on treatment and outcomes. 22,112 Many people with SMI die within 2 years of presentation with a serious physical health issue and initial deterioration. 114 Not only do those with SMI often not recognise the decline of their own health, but when they do they often experience difficulty in having their physical symptoms taken seriously30,110 and, because of a history of such experiences, they end up making limited contact with primary care. 106
The impact of late diagnosis
All of the factors cited above can, in turn, lead to a delayed/late diagnosis for people with SMI, and this presents a challenge in organising and providing quality EoL care as people are often not identified as approaching the EoL until a late stage of life-limiting physical disease such as cancer. 106,158 As a result, the timely provision of palliative care is hampered,30,110 which ultimately results in people with SMI having little time to plan their EoL care. 157 This is particularly an issue for those who are homeless, as symptoms are not recognised by staff and it is difficult to predict disease trajectories as their health is often poor and their needs complex. 113
Identifying an end-of-life care trajectory for those who are homeless
People who are homeless do not always see accessing EoL care and/or attending medical appointments as a priority, and HCPs often do not appreciate this, as the priority for patients is more about simply surviving. 99 Given the large number of fatalities from substance misuse among this group, death is often normalised, and as a result palliative care needs are relatively invisible. 99 Given this, and the chaotic lifestyle of many homeless people, predicting and even identifying an EoL care trajectory is problematic, especially when care is provided outside the formal health-care system, where workers have very little health or palliative care knowledge, experience and training. 99
However, identifying deteriorating health in a timely manner is essential to allow time to plan appropriate care and support and may help to avoid crisis-driven hospital deaths. 156 Hostel staff and HCPs are reported as answering ‘no’ to what has been described as the ‘surprise question’ (‘Would you be surprised if this person were to die in the next 6–12 months?’) asked about many homeless people. 113 This is in the context of homeless people being hard to assess for palliative care because of their complex needs and generally poor health, with prognostically uncertain conditions commonly experienced by many, including liver disease resulting from substance misuse or hepatitis C. 113 There is also evidence to suggest that when a homeless person is identified as dying (primarily from cancer) by health-care providers who better understand the social determinants of health, access to and provision of palliative care is improved. 99
Chapter 5 Thematic synthesis of case studies
This chapter thematically synthesises material from included case studies. Many of these report on key episodes, or critical junctures,179 in the lives of people with SMI at the EoL. They include instances of people presenting to health services and then disappearing again, or pivotal decisions being made with profound impact for patients and others. Material from the case studies has been synthesised into five themes as follows: diagnostic delay and overshadowing, decisional capacity and dilemmas, medical futility, individuals and their networks, and care provision.
Diagnostic delay and overshadowing
Although the case studies ranged across many countries, they nevertheless show a consistent picture of delayed or late diagnosis and what might be termed diagnostic overshadowing. Complex and enduring mental health problems are often described as contributing to this. This is signalled in case studies as arising from the mental illness of the individual who fails to recognise the seriousness of their plight, and presents to services only when their condition is advanced and treatment options are limited. 124,132,133,137,144 Kunkel et al. 132 present four case examples of individuals with existing mental health problems, including that of Ms A, a 38-year-old African American woman with an unspecified psychosis presenting with a 20 cm mass in her right breast that was adhering to the chest wall. Investigations revealed a significant cancer with lymph node involvement but, despite the late presentation, there were no metastases. Ms A was treated with chemotherapy and surgery but then failed to attend for radiation treatment and considered the new lesions as nothing more than ‘haematoma’. She later presented to the ED in respiratory distress and with large, presumably malignant, effusions, asked not to be resuscitated and died soon after. The case study paper labels Ms A’s difficulty with accepting her situation and similar behaviours as ‘maladaptive denial’.
This tendency to impute the mental conditions of individuals as a source of late presentation, or indeed of deciding not to continue with treatment, is a recurring feature of this literature. Other case study examples suggest how diagnosis and treatment of serious life-threatening or life-limiting physical conditions are complicated by untreated mental illness and the beliefs and behaviours arising from this. 132,133,137 A number of papers also appear to elide behavioural aspects of presentations with mental ill-health and position these as problematic in the delivery of care and treatment, with terms used such as ‘malingering’, ‘manipulative’, ‘dominance and aggression’ and ‘demanding’,115,122,123,125 or problems for staff who ‘struggled with how best to provide care’. 126
Denial by people with SMI, or seeming to have a lack of insight, is a possible complicating factor. It is not unknown for any persons diagnosed with serious conditions to deny the gravity of their situation, and for people with pre-existing mental health conditions it appears that this is no different. 132 Feldman and Periyakoil126 note that specific issues arise in cases of people with PTSD, where ‘the threat to life inherent in terminal illness may mimic the original trauma’, leading to an exacerbation of the psychological symptoms associated with the condition, including anxiety, anger, denial, avoidance and distrust of authority, impeding medical adherence and resulting in the refusal of treatment.
There are also examples of individuals with long histories of pre-existing mental health problems, often in long-stay facilities, who, despite their access to HCPs, experience delayed or late diagnosis of conditions that placed them on the EoL trajectory. 26,119,127,138,151–153 Terpstra et al. 144 present the case of a 61-year-old man with a longstanding diagnosis of schizophrenia, living in an adult foster home and under legal guardianship. The man was seen every 2 weeks at a mental health clinic and attended a primary care provider to report a new-onset cough. His examination was documented as benign, but 1 week later he complained of hypotension and left-sided weakness. A detailed examination revealed advanced bladder cancer and multiple brain metastases that had not been spotted until this last presentation. The authors locate the problem in the mental condition of the person and suggest that people with conditions such as schizophrenia do not willingly verbalise pain or related symptoms. It is, however, difficult to escape the issue that extended contact with health-care services could have included some monitoring of the physical health of the person.
Decisional capacity and dilemmas
Many of the case studies feature a concern about the decisional capacity of individuals to consent to treatment and/or to refuse treatments offered, and implicate professional dilemmas of determining the value of attempting curative treatments compared with palliation. 118,120,122,127,132,133,146,147,154 Romm et al. 140 argue that mental health staff have a particular duty to ensure that the interests of people with SMI are defended via treatments targeting potentially distorted states of mind, adding that although SMI can impair decisional capacity this should not be assumed and should be thoroughly assessed. 140 In some case study examples, the conclusion arrived at was that the person retained the capacity to determine their treatment choices, and that these choices were then respected. 120
Treatment refusal is highlighted numerous times. 120,124,127,128,133,136,139,140,143,145–147 Past refusals seem to prompt treatment teams to impute future problems. 139 For example, Gonzalez et al. 128 present the case of an 86-year-old with a 20-year history of mastectomy for cancer and refusal of medical care who re-presented with a bleeding and ulcerating mass on the chest wall. The case study reported that the patient was not a case for curative treatment even though there was no evidence of metastases. The reasons for lack of curative efforts were indicated as:
curative treatment was not feasible based on a geriatric evaluation, which considered the patient’s severe cognitive decline, advanced age of the patient’s caregiver, and the expectations of the patient and his family.
Gonzalez et al. 128
In some cases, treatment refusal is reported as arising from psychiatric symptomatology, such as fixed beliefs about damnation or that thoughts could be read by physicians, rather than being related to capacity to understand and make decisions based on available information. 26
Approaching the courts for guidance is reportedly made in a variety of contexts, including where major concerns exist relating to a patient’s capacity or best interests and for declarations on treatment in the case of patients lacking decision-making capacity. 146. Shah et al. 141 report an example of treatment refusal by a man with decisional incapacity where the review of the medical ethics committee concluded that even with full decision-making capacity a person might refuse the radical procedures being proposed because of the risks involved and the deforming nature of the surgery.
Fluctuating mental capacity requiring multiple assessments118,146 is also reported. In some reports, the option to review and return to previous decisions is implied in case examples. 141
The absence of previously declared wishes on life-saving treatments appears to be a recurring issue and suggests one area for future intervention testing. 150 The absence of any declaration on treatment may mean that teams seek agreement of a substitute decision-maker, such as a family member,139,140 sometimes with power of attorney, but the patient may indicate their refusal in their actions, for example repeatedly removing life-saving treatments such as catheters in renal dialysis150 or not agreeing to take medication. 132 Enforcing medical treatment of a person who is actively refusing is not supported in this literature and it is argued that doing so may complicate future alliance building. 139
Medical futility
Some case studies reveal, in the example of people with anorexia nervosa, how experience of this condition can exhaust the optimism of those doing the caring, and the language used, such as ‘refractory’ and ‘incurable’, reflects this. 148 Lopez et al. 134 describe the case of Ms A, a 30-year-old woman with a diagnosis of anorexia nervosa, where ‘neither forcing her into involuntary treatment nor waiting for her to voluntarily engage in treatment appeared likely to resolve her illness, return her to a state of life-sustaining clinical stability or provide her a decent quality of life’. 134 The paper invokes the concept of medical futility, and the case demonstrates an example of the use of palliation and referral to hospice care for this psychiatric condition. In this case, it is also reported that the option of an out-of-state eating disorder treatment programme, which was acceptable, was eventually rejected on cost grounds, implying that perhaps the situation was less futile than indicated. Nevertheless, the treatment team and the ethics committee concluded ‘that her physical and psychiatric impairments were likely to lead to her death, despite any plausible attempts at aggressive intervention’. 134 The palliative care team therefore commenced involvement with the consent of both the patient and the family.
Individuals and their networks
For many people with SMI the availability of support networks in their communities is crucial, and the absence of these supports is implicated in delayed treatment seeking. Some case studies refer to family involvement,115,129,130,135,145,154 whereas others indicate the lack or absence of such support. 122,124,180 The EoL condition in some circumstances appears to have led to the re-emergence of family support,152 or that teams actively support the person to reconnect with distant family. 120 In some instances, tensions in family involvement are reported,123,131 and in one example family dynamics are situated as the source of subsequent mental health-related troubles. 148 Other case studies identify the reciprocal nature of support, and report the concerns of the individual with the EoL condition for their family. 129,130 EoL care places an additional set of demands on families, such as learning to manage symptoms,116 and some conditions appear to result in exhausted or burned-out family members. 134 An additional demand on support networks can arise from the absence of advance decisions or where decisional capacity is in question so that, for instance, families may be involved in discussions on treatment and with do-not-resuscitate decisions for which they may be ill-prepared. 127,132,139,140,150 Families also show some concern that their family member’s mental health problems are overlooked by the palliative care team. 145
Care provision
Where case studies report on the ongoing delivery of care to individuals with pre-existing SMI and subsequent EoL condition, they advocate the benefits of a transdisciplinary approach involving palliative care specialists, psychiatric specialists (preferably the team whose members already know the person) and wider community members (e.g. religious ministers). 15,26,119,120,134,140,148 Stecker142 provides an example of drawing on a specialist in both oncology and psychiatry to advise an inpatient mental health nursing team.
Liaison consultation and collaboration is reported as beneficial for hospice staff. Examples include learning from psychiatric consultation,125 learning from psychologists on how to alter the environment to reduce distress116 and a hospice nurse being supported by a psychiatric nurse. 131 Case reports note the mutual benefits of hospice and mental health nurses working together in EoL care, and the similarities in their work, but they also note a need for hospice staff to be better informed about mental health conditions. 145 Case studies also demonstrate the interest that mental health teams have in learning from their colleagues working in palliative care. 152
Some case study papers present models of care, although these are small scale and may not indicate either transferability or generalisability. Examples include treatment models such as dynamic system analysis,115 stepwise psychosocial palliative care116,117 and the patient, provider, systems model. 26
Case studies reveal issues in the provision of care for treatment teams, such as how to handle psychiatric presentations. 115,123,139,145 Case studies also report examples of what has worked in supporting people with mental health problems at the EoL, including building rapport and trust, especially with people with PTSD;116 using music therapy at the EoL;149 having conversations about death;26,129,130,152 initiating hospice at home;26,129,130 and providing multidisciplinary mental health care and palliative care at home. 120
An array of places for the provision of EoL care is proposed and supported in case studies. In almost every example the place of care and treatment is positioned as one arising from the preferences of the individual. These include palliative care provision in mental health institutions,127,152,153 hospice care for mental health patients,125,135,144,148 acute hospital15 and home care. 120 Repeated transfer between settings related to psychiatric and/or physical symptomatology is also evident,139 suggesting potential challenges to continuity of care.
Challenges reported in this literature include mental health staff being emotionally unprepared for caring for people who are terminally ill,142 an observation that it is suggested supports the need for staff to become aware of feelings that may interfere with their therapeutic functioning. Where people with SMI receive EoL care in hospices, palliative care staff are reported as experiencing strong emotions, such as anger and frustration. 116 Case study papers also occasionally offer psychodynamic interpretations of staff–patient interactions and care. 115,131,142
Treatment challenges are reported in managing some mental health-related medication alongside the provision of chemotherapy. Two case study papers report issues with the prescription of clozapine, as this is implicated in depressing white blood cell counts, which, in consequence, could precipitate a life-threatening infection. 136,138 Treatment challenges also arise from people with SMI at the EoL absconding or being lost to follow-up. 137,147 One paper reports a concern regarding suicide risk assessment in EoL care, although this is not a feature directly relevant in the case presented. 145 A further challenge is in providing palliative care to patients who, despite being provided with careful explanation, continue to believe that they are not going to die. 134
Chapter 6 Overarching summary and conclusion
This chapter summarises the main findings from both of the thematic syntheses and presents assessments of the confidence in the summaries of the synthesised findings reported in Chapter 4. Implications for service commissioning, organisation and provision are outlined and recommendations are made, drawing on both syntheses, for future research.
Summary of what has been learned
Figure 6 summarises the main findings from the two thematic syntheses, the first drawing on research, policy and guidance and the second drawing on case studies.
FIGURE 6.
Summary of thematic syntheses.
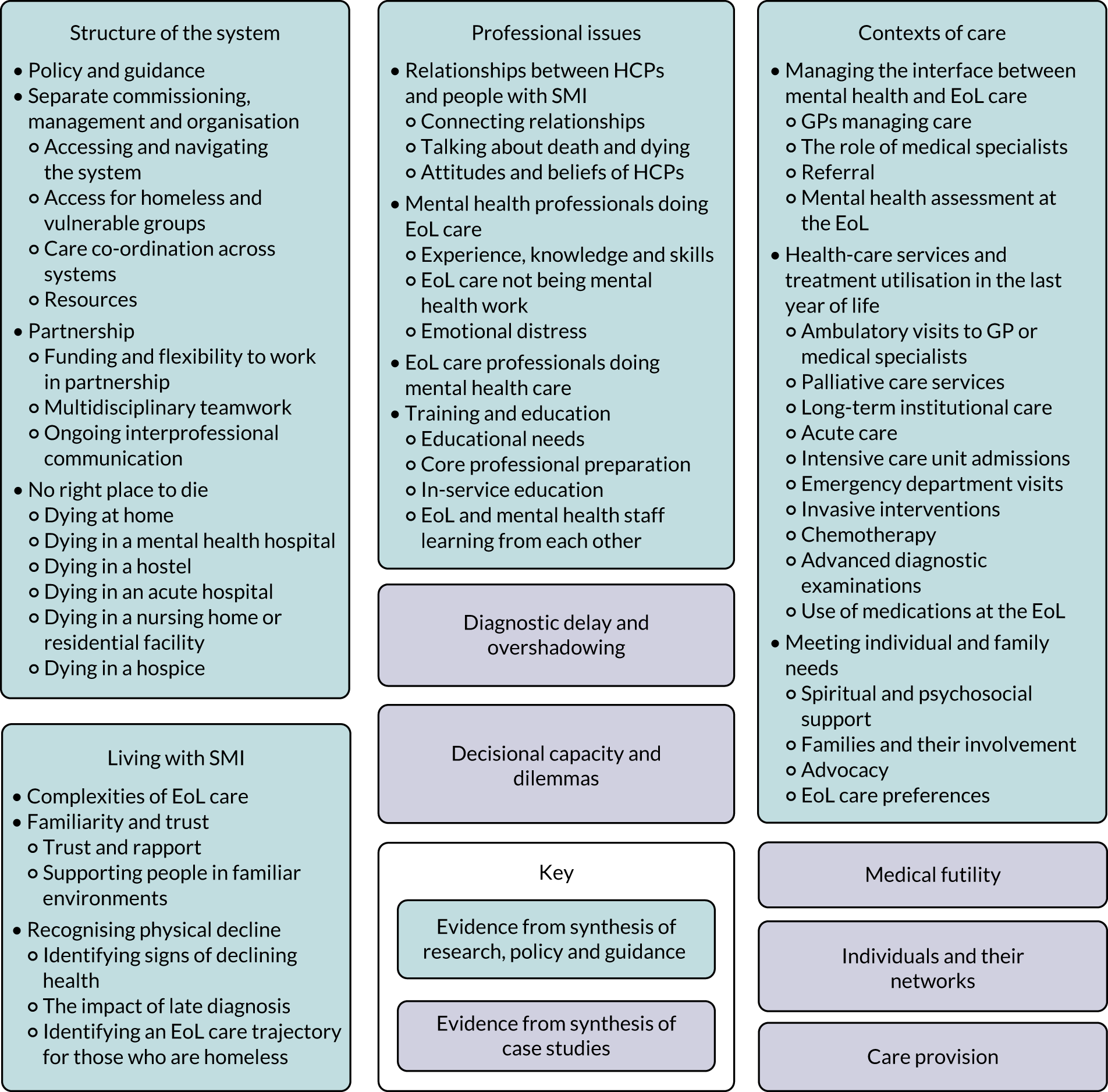
Overarching summary of first synthesis
This section presents an overarching summary of the first synthesis (see Chapter 4) complete with an assessment of confidence. The qualitative and non-intervention findings were assessed for confidence using the CERQual (Table 8) approach. The quality of evidence derived from retrospective cohort studies also included in this first synthesis was assessed using the GRADE approach. Appendices 21–24 include the detail of how the CERQual statements were generated, along with the detail of the ungraded summary statements derived from policy and guidance material.
| Summary of review finding | Studies contributing to review finding | CERQual confidence |
|---|---|---|
| Synthesis 1: structure of the system | ||
| Policy and guidance | ||
| 1. Owing to a lack of national and local guidance regarding EoL care and mental health care, palliative care nurses report concerns about their legislative responsibility | 112 | VL |
| Separate commissioning, management and organising | ||
| 2. HCPs recognise that accessing and navigating EoL care for those with SMI is a challenge and many obstacles exist | 102–104,106,114 | M |
| 3. Homeless people are often excluded from hospices and care homes, and HCPs report difficulties in placing homeless people with cancer | 99,113 | M |
| 4. Separate commissioning, management and ways of organising both services and professionals creates challenges for both mental health and EoL HCPs to co-ordinate high-quality care across mental health and EoL care systems | 112 | VL |
| 5. The invisibility of homeless and vulnerable people, and the fragmented character of care systems, means that they often have to act as their own care co-ordinators | 99,112,113 | M |
| 6. Multiple proposals have been made to improve the co-ordination of care for people with SMI at the EoL, mostly involving the identification of staff with clear responsibilities | 32,94,114 | M |
| 7. HCPs feel that there is a lack of resources in terms of services and trained professionals who are able to meet the needs of those with SMI at EoL | 85,93,114 | M |
| Partnership | ||
| 8. Working in partnership across EoL and mental health services is important, and when flexibility and solutions to work in partnership across agencies exist then EoL care for those with SMI can be facilitated | 85 | M |
| 9. A lack of good relationships and partnership working, influenced by reductions in funding and competitive commissioning, inhibit good care, especially with regard to pain management, needs assessments and assessment of mental capacity | 106,112,114 | M |
| 10. HCPs report that formal (and sometimes ad hoc) multidisciplinary teamwork can improve patient outcomes | 85,102–106 | M |
| 11. Coalition-building and formal opportunities to meet and discuss care are essential and must ensure that information is made available to primary care and social services partners | 85,93,112,114 | H |
| No right place to die | ||
| 12. Mental health and EoL staff recognise that allowing people to die in the location of their choice (which is often a home or home-like environment) is important, but staff also talk about how appropriate care is often lacking in all settings | 32,106,114 | H |
| 13. Mental health services rarely care for people with SMI at the EoL as they are poorly equipped to meet their needs, and as a result patients are frequently moved between services | 32,110,112 | H |
| 14. Multiple challenges exist for EoL care to take place in a hostel, including a lack of staff preparedness, the chaotic environment, and concerns over risks and the safe storage of medication | 98,113 | M |
| 15. Providing EoL care in the community, in mental health settings or in homeless shelters can be difficult and as a result those with SMI are often transferred into acute settings at the EoL, but providing mental health care in acute settings also poses challenges | 32,105,106,110,112,114 | M |
| 16. Staff working in hospices report that hospices are ill-prepared to care for the needs of homeless people at the EoL and require more help in dealing with substance misuse and the alternative lifestyles of what is mostly a younger age group | 99,113 | M |
| Synthesis 2: professional issues | ||
| Relationships between HCPs and people with SMI | ||
| 1. Some mental health staff feel that building nurturing relationships is important, especially for those with limited social networks and no family contact. However, others choose not to form such relationships, finding it too upsetting when patients are transferred for EoL care | 32,102–104,106,110,114 | H |
| 2. Some mental health staff find conversations about death and dying challenging, but those who feel able to have these have found that patients are receptive | 106,110,112,114 | H |
| 3. The underlying stigmatising and prejudicial attitudes of EoL HCPs towards those with SMI, including those who are homeless, can affect decisions around EoL care | 32,37,99,102–104,112–114 | H |
| Mental health professionals doing EoL care | ||
| 4. Mental health staff feel that they have limited experience of caring for patients with SMI at the EoL, and although some feel able to deliver care others feel that they lack the knowledge and skills, particularly with regard to pain management and psychosocial or spiritual support | 102–104,110,112 | M |
| 5. Some mental health staff report that they do not feel able, are not interested or avoid caring for people with SMI at the EoL, whereas others embrace caring for them | 32,93,105,110,112 | M |
| 6. Mental health staff report that caring for those with SMI at EoL can be distressing and emotionally draining, and some fear being scrutinised following the death of patients | 32,37,102–104 | M |
| EoL HCPs doing mental health care | ||
| 7. EoL HCPs feel that they lack knowledge and understanding of mental health diagnoses and services. As a result, they report that they are not always confident, willing or comfortable to care for patients with SMI at the EoL | 32,37,93,102–104,106,110,112 | M |
| Training and education | ||
| 8. Mental health and EoL HCPs have highlighted a wide range of educational needs | 37,85,102–104 | M |
| 9. Palliative care programme directors have suggested that psychiatry training is inadequate in the categories of EoL care and issues related to death and dying | 93 | VL |
| 10. Although some mental health nurses feel that that their core professional preparation enables them to care for people with SMI during periods of physical illness and at the EoL others feel that this is something that can be improved | 32,102–104 | M |
| 11. EoL and mental health staff learning from each other, such as through cross-training, has been positively evaluated | 85,95 | VL |
| Synthesis 3: contexts of care | ||
| Managing the interface between mental health and EoL care | ||
| 1. GPs are the gatekeepers in enabling or hindering access to palliative care services and in some instances they manage the palliative care needs of people with SMI within their practice | 110,114 | M |
| 2. People with SMI are reported to visit a number of different types of physician specialists as well as psychiatrists at EoL | 93,110,114 | M |
| 3. Both EoL and mental health staff acknowledge that referrals are often complicated and lack vital information that would facilitate communication between themselves and those with SMI at the EoL | 106,112 | L |
| 4. Both EoL and mental health HCPs across a variety of settings report that mental health assessments at the EoL can be a challenge and that they need help to deal with their fears and uncertainties | 37,105,112,114 | M |
| Health-care services and treatment utilisation in the LYoL | ||
| 5. GPs and psychiatrists believe that people with SMI are less likely than other groups to make use of specialist palliative care | 110 | VL |
| 6. EoL HCPs working in the UK feel that standard guidance on resuscitation is lacking for people with SMI at EoL | 112 | VL |
| 7. EoL professionals in Australia have concerns about capacity to consent in relation to resuscitation orders for people with SMI at EoL | 102–104 | VL |
| Meeting individual and family needs | ||
| 8. Programmes and services for people with SMI at EoL require a comprehensive team approach incorporating symptom relief, psychological and psychosocial support, and spiritual care | 37,90,98,102–104,106,110 | H |
| 9. HCPs report challenges in handling contact with families, especially when years of estrangement have occurred or where family members also have mental health conditions | 32,98,102–104,110,112 | M |
| 10. Veterans with a diagnosis of PTSD were just as likely to receive a family consultation regarding advance care planning as those without a diagnosis of PTSD | 90 | VL |
| 11. When families were involved in the care of veterans with a diagnosis of PTSD, they reported unmet needs for emotional support and felt generally that their relatives were not treated with dignity and were unsatisfied with the level of care received | 83 | VL |
| 12. HCPs report that being referred to palliative care and receiving services appears to be based on the presence or absence of a strong advocate | 32,106,112 | H |
| 13. People with SMI can lack access to advocacy to help navigate the complex EoL trajectory because of limited social and family support and, as a result, they can become ‘lost in the system’ | 32,106,110,112 | H |
| 14. HCPs have concerns about negotiating EoL care preferences with people with SMI for fear that mental health symptoms may influence understanding and expectations or that such discussions may lead to further distress | 32,106,110,113 | M |
| 15. HCPs report that they are not always comfortable with determining patients’ capability to make medical decisions and that they tend to assume that mental capacity is lacking and as a result discussions around advance care planning are avoided | 93,106,112 | M |
| 16. Findings from scenario-based preferences regarding medical advance care planning suggest that people with SMI are able to designate treatment preferences in response to the EoL and are open to discussing EoL care | 86,96,109 | M |
| 17. People with SMI conditions are capable of completing advance care plans for the EoL but even where legislation is in place to support this it rarely appears to be standard practice | 85,98,110 | M |
| 18. A lack of confidence to have open communication and experience among HCPs, especially when working with homeless people, may explain the absence of advance care planning for those with SMI at the EoL | 98,99,106,113 | M |
| Living with SMI | ||
| Complexities of EoL care | ||
| 1. Challenging behaviours, communication issues and side effects of combining SMI and EoL medications make it difficult to address mental health issues at the EoL | 32,37,102–104,106,110,112 | M |
| Familiarity and trust | ||
| 2. Early referral to palliative care helps build trust and rapport between staff and people with SMI at the EoL | 37,85,99,102–104,112,114 | M |
| 3. Although people with SMI often leave environments with which they are familiar at the EoL, mental health and palliative care staff can work together to support people without the need for moving | 99,102–104,113,114 | M |
| 4. Hostel staff report that they try to ensure that palliative care can be provided in a familiar environment for as long as possible as they feel that the benefits outweigh the challenges | 99,113 | M |
| Recognising physical decline | ||
| 5. Staff report that people with SMI are not always able to recognise their own declining health, and it is felt that, because of previous unsatisfactory health-care encounters, they often present late to services | 106,110,112,114 | M |
| 6. The timely provision of palliative care can be hampered when people with SMI (especially those who are homeless) are not identified as approaching the EoL until the late diagnosis of life-limiting physical disease | 106,110,113 | H |
| 7. People who are homeless are often more concerned with day-to-day survival than with keeping appointments with HCPs, and this makes it difficult to identify EoL trajectories and to provide palliative care | 99,113 | M |
A high degree of confidence was judged to apply to 10 of the 52 synthesis summary statements, distributed across all four major themes (Structure of the system, Professional issues, Contexts of care and Living with severe mental illness). All 10 were summary statements synthesised from generally well-conducted, relevant studies in which there was a high degree of coherence. A moderate degree of confidence was judged to apply to 32 of the statements, denoting concerns relating to one or more of the dimensions assessed in the underpinning evidence (methodology, coherence, relevance and adequacy), with the confidence in the remaining 10 summary statements judged as being either low or very low.
Structure of the system: confidence in the evidence
This evidence synthesis found that there is a lack of national and local guidance in the UK regarding EoL care and mental health care, and that palliative care nurses report concerns about their legislative responsibility (CERQual – very low).
Health-care professionals recognise that the separate commissioning, management and organisation of mental health and EoL services often result in those with SMI having trouble accessing and navigating the system (ungraded – non-research) and that many obstacles exist (CERQual – moderate). Access to health care is particularly difficult for homeless and vulnerable groups, who are often isolated and disconnected from family and friends (ungraded – non-research). Homeless people are also often excluded from hospices and care homes, and HCPs report difficulties in finding suitable placements for homeless people who have cancer (CERQual – moderate).
It is important that care is co-ordinated and integrated across services so that the needs of those with SMI at the EoL are met, although it is acknowledged that this is difficult to achieve (ungraded – non-research). The separate commissioning, management and ways of organising both services and professionals create challenges for both mental health and EoL HCPs in co-ordinating high-quality care across mental health and EoL care systems (CERQual – very low). The invisibility of homeless and vulnerable people, and the fragmented character of care systems, means that they often have to act as their own care co-ordinators (CERQual – moderate). Multiple proposals have been made to improve the co-ordination of care for people with SMI at the EoL, mostly involving the identification of staff with clear responsibilities (CERQual – moderate). HCPs feel that a barrier to being able to meet the needs of those with SMI at the EoL is a lack of resources in terms of appropriate services and trained professionals (CERQual – moderate).
Working in partnership across EoL and mental health services is important, and when flexibility and solutions to work in partnership across agencies exist then EoL care for those with SMI can be facilitated (CERQual – very low). However, a lack of good relationships and partnership working, influenced by reductions in funding and competitive commissioning, inhibit good care, especially with regard to pain management, needs assessments and the assessment of mental capacity (CERQual – moderate). Interagency and interprofessional team working at the EoL is important (ungraded – non-research) and HCPs report that formal (and sometimes ad hoc) multidisciplinary teamwork can improve patient outcomes (CERQual – moderate). Ongoing communication between partners is a key element of high-quality care (ungraded – non-research) and coalition-building and formal opportunities to meet and discuss care are essential and must ensure that information is made available to primary care and social services partners (CERQual – high).
With the right support from community-based services, people with SMI at the EoL are able to stay at home, and both mental health and EoL staff recognise that allowing people to die in the location of their choice (which is often home or a home-like environment) is important, but staff also talk about how appropriate care is often lacking in all settings (CERQual – high). However, results across the retrospective cohort studies are mixed regarding the likelihood of decedents with SMI having died at home compared with that of those without SMI at the EoL (GRADE – very low), but studies consistently report that decedents with SMI were significantly more likely than those without SMI to have died in a nursing home or residential facility (GRADE – very low). Results across the retrospective cohort studies were mixed regarding the likelihood of decedents with SMI having died at home compared with those without SMI (GRADE – very low). Retrospective cohort studies consistently reported that decedents with SMI were significantly more likely to have died in a nursing home or residential facility than those without SMI (GRADE – very low). In reality, people with SMI at the EoL are often moved between services and mental health services rarely care for them as they are poorly equipped to meet their needs (CERQual – high).
With regard to those who are homeless with SMI at the EoL, although one shelter-based hospice care programme was cost-effective and successful in delivering EoL care,98 it is acknowledged that multiple challenges exist for EoL care to take place in a hostel, including lack of staff preparedness, the chaotic environment, and concerns over risks and the safe storage of medication (CERQual – moderate). Providing EoL care in the community, within mental health settings or homeless shelters, can be difficult and, as a result, those with SMI are often transferred into acute settings at the EoL, but providing mental health care in acute settings also poses challenges (CERQual – moderate). However, results across retrospective cohort studies are mixed regarding the likelihood of decedents with SMI having died in a hospital compared without SMI at the EoL (GRADE – very low). Staff working in hospices report that hospices are ill prepared for caring for the needs of homeless people at the EoL, and require more help in dealing with substance misuse and the alternative lifestyles of what is mostly a younger age group (CERQual – moderate). For people with SMI more generally, one retrospective cohort study found no significant differences in the likelihood of dying in a hospice between those with and those without a history of mental illness (GRADE – very low).
Professional issues: confidence in the evidence
A number of different aspects of the relationships between HCPs and people with SMI have been explored. Mental health staff feel that building nurturing relationships between HCPs and people with SMI is important, especially for those who have limited social networks and no family contact. However, others choose not to form such relationships, finding it too upsetting when patients are transferred for EoL care (CERQual – high). Being able to talk about death and dying is crucial if people with life-limiting illnesses (including people also living with SMI) are to be supported to make decisions at the EoL, and good communication is an important aspect of this (ungraded – non-research). Even though some mental health staff find conversations about death and dying challenging, those who feel able to do so have found that patients are receptive (CERQual – high). Relationships, however, can be hindered by the attitudes and beliefs of HCPs. This includes the underlying stigmatising and prejudicial attitudes of EoL HCPs towards those with SMI, including those who are homeless, which can affect decisions around EoL care (CERQual – high).
Mental health staff feel that they have limited experience of caring for patients with SMI at the EOL and although some feel able to deliver care others feel that they lack the knowledge and skills, particularly with regard to pain management and psychosocial or spiritual support (CERQual – moderate). Some feel that EoL care is not mental health work and they report that they do not feel able to, are not interested in or avoid caring for people with SMI at the EoL, whereas others embrace caring for people with SMI at the EoL. They also report that caring for those with SMI at the EoL can be distressing and emotionally draining, and some fear being scrutinised following the death of patients (CERQual – moderate). It is recognised that staff who provide care to this group of patients will need support (ungraded – non-research). When it comes to EoL HCPs delivering care to those with SMI, they feel that they lack knowledge and understanding of mental health diagnoses and services. As a result, they report that they are not always confident, willing or comfortable to care for patients with SMI at the EoL (CERQual – moderate). As a consequence of this, the needs of people with SMI at the EoL are not always well met (ungraded – non-research). It is widely recognised that education and training opportunities across professional groups who care for people with SMI at the EoL are important, that core professional preparation could be improved (ungraded – non-research) and that greater opportunities could be provided for in-service education (ungraded – non-research). Mental health and EoL HCPs have highlighted a wide range of educational needs (CERQual – moderate). With regard to core professional preparation, palliative care programme directors have suggested that psychiatry training is inadequate in the categories of EoL care and issues related to death and dying (CERQual – very low). Although some mental health nurses feel that that their core professional preparation enables them to care for people with SMI during periods of physical illness and at the EoL, others feel that this is something that could be improved (CERQual – moderate). However, it is recognised that in-service education opportunities for HCPs to develop skills and knowledge in EoL care are patchy, particularly in organisations providing mental health care, and could be developed (ungraded – non-research). One solution is for EoL and mental health staff to work together so that knowledge and awareness can be improved, such as through the establishment of dedicated link positions with roles including the provision of education (ungraded – non-research). Another solution that has been positively evaluated is EoL and mental health staff learning from each other through initiatives, such as cross-training (CERQual – very low).
Contexts of care: confidence in the evidence
General practitioners are the gatekeepers at the interface between mental health and EoL care and can enable or hinder access to palliative care services and, in some instances, manage the palliative care needs of people with SMI in their practice (CERQual – moderate). However, one study showed no significant differences in the rates of ambulatory visits to the GP within 6 months of death between those with schizophrenia and those without schizophrenia who died from cancer (GRADE – very low). People with SMI are also reported to visit a number of different types of physician specialists as well as psychiatrists at the EoL (CERQual – moderate), and one study showed that decedents with schizophrenia were significantly less likely to visit a medical specialist than those without schizophrenia (GRADE – very low). Regardless of the initial point of contact, support for people living with mental health issues and approaching the EoL must be fast-tracked or prioritised (ungraded – non-research). Both EoL and mental health staff acknowledge that referrals are often complicated and lack vital information that would facilitate communication between professionals and people with SMI at the EoL (CERQual – low). Once a person with SMI has been referred successfully, skilled mental health assessment at the EoL is required so that care can be planned and they can be helped to manage their symptoms and other needs (ungraded – non-research). Both EoL and mental health HCPs across a variety of settings report that mental health assessments at the EoL can be a challenge and that they need help to deal with their fears and uncertainties (CERQual – moderate).
With regard to health-care service utilisation at the EoL, GPs and psychiatrists believe that people with SMI are less likely than other groups to make use of specialist palliative care (CERQual – very low). However, findings across retrospective cohort studies are inconsistent regarding the rates of utilisation of palliative care or specialist palliative care in the community among decedents with and decedents without schizophrenia diagnoses who died from cancer at different time points throughout the LYoL (GRADE – very low). When looking at hospices, significant differences were seen in rates of enrolment for decedents with a schizophrenia diagnosis who died of cancer (GRADE – very low), although one study showed that having depression ahead of a cancer diagnosis was associated with a significantly increased rate in hospice enrolment and in length of stay (GRADE – very low).
At the EoL, people with SMI use long-stay, hospital, ED and ICU care in different ways from people without SMI, but findings from research in this area are inconsistent (GRADE – very low). One study shows that decedents with a schizophrenia diagnosis who died of cancer had a significantly increased rate of use long-term institutional care and longer lengths of stay than those without within 6 months of death (GRADE – very low). However, studies consistently report that people with SMI who died from cancer, heart failure cirrhosis/liver disease or renal disease/dialysis were significantly less likely to have been admitted to hospital at the EoL than those without SMI, but no differences were noted for those who died from chronic lower respiratory disease (GRADE – very low).
At the EoL, people with SMI receive invasive interventions such as analgesia or opioid medication, chemotherapy and advanced diagnostic examinations in different ways from people without SMI, but findings from research in this area are inconsistent (GRADE – very low). One study shows that decedents with schizophrenia diagnoses who died of cancer were significantly more likely to have physician orders for life-sustaining treatment (GRADE – very low). A further study shows that veterans with pre-existing, but unspecified, mental health conditions where over half had a terminal condition of cancer or heart disease were more likely to receive care that was directed at controlling symptoms or supporting do-not-resuscitate orders (GRADE – very low). EoL HCPs working in the UK feel that standard guidance on resuscitation is lacking for people with SMI at EoL (CERQual – very low), and EoL professionals in Australia have concerns about capacity to consent in relation to resuscitation orders for people with SMI at the EoL (CERQual – very low). Only one study explored rates of CPR and found no significant differences between those with and those without SMI at the EoL (GRADE – very low).
Meeting individual and family needs is an area that has been explored. People with SMI have particular vulnerabilities arising from their mental health experiences, and programmes and services for people with SMI at the EoL require a comprehensive team approach (ungraded – non-research). Programmes and services for people with SMI at the EoL require a comprehensive team approach incorporating symptom relief, psychological and psychosocial support, and spiritual care (CERQual – high). On exploring families and their involvement, HCPs report challenges in handling contact with families, especially where years of estrangement have occurred or where family members also have mental health conditions (CERQual – moderate). Some work has been conducted with veterans with a diagnosis of PTSD at the EoL that shows that their families were just as likely to receive a consultation regarding advance care planning as those without a diagnosis of PTSD (CERQual – very low). However, when families were involved in the care of veterans with a diagnosis of PTSD they reported unmet needs for emotional support, felt generally that their relatives were not treated with dignity and were unsatisfied with the level of care received (CERQual – very low).
Having an advocate who can support a person with SMI throughout their cancer journey, including at the EoL, is important, and such advocates can prevent people with SMI from falling through gaps in the system (ungraded – non-research). HCPs report that whether or not people with SMI are referred to palliative care and receive services appears to be based on the presence or absence of a strong advocate (CERQual – high). However, people with SMI can lack access to advocacy to help them navigate the complex EoL trajectory owing to limited social and family support and, as a result, they can become ‘lost in the system’ (CERQual – high).
End-of-life care preferences, such as advance care planning, for people with SMI at the EoL are important, and mechanisms should be in place to support these people to make their own decisions, although it is recognised that this can be problematic (ungraded – non-research). HCPs have concerns about negotiating EoL care preferences with people with SMI because of the fear that the person’s mental health symptoms may influence their understanding and expectations or that such discussions may lead to further distress (CERQual – moderate). Another issue with this population group is mental capacity and in the context of making decisions it is important not to assume that this is lacking (ungraded – non-research). HCPs report that they are not always comfortable with determining patients’ capability to make medical decisions and that they tend to assume that mental capacity is lacking and, as a result, discussions aound advance care planning are avoided (CERQual – moderate). Findings from scenario-based preferences regarding medical advance care planning suggest that people with SMI are able to designate treatment preferences in response to the EoL and are open to discussing EoL care (CERQual – moderate). People with SMI are capable of completing advance care plans for the EoL, but even where legislation is in place to support this it rarely appears to be standard practice (CERQual – moderate). Results from retrospective cohort studies are inconsistent regarding the likelihood of people with a diagnosis of SMI having completed an advance directive (GRADE – very low). A lack of confidence in having open communication and experience among HCPs, especially when working with homeless people, may explain the absence of advance care planning for those with SMI at the EoL (CERQual – moderate).
Living with severe mental illness: confidence in the evidence
Providing EoL care to people with SMI can be challenged by patients’ behaviour associated with their mental health difficulties (ungraded – non-research). The complexities of care for people living with SMI, such as challenging behaviours, communication issues and the side effects of combining SMI and EoL medications, make it difficult to address mental health issues at the EoL (CERQual – moderate). A number of factors can facilitate addressing mental health issues at the EoL and include the person with SMI being referred early to palliative care so that trust and rapport can be built between staff and people with SMI at the EoL (CERQual – moderate). Another facilitator is the ability to support people with familiar environments and, although people with SMI often leave environments with which they are familiar at the EoL, mental health and palliative care staff can work together to support people without the need for movement (CERQual – moderate). For those who are homeless and vulnerable this is not as easy as deteriorations in EoL-related physical health commonly results in the homeless person being transferred to hospital in crisis, where their needs are poorly met (ungraded – non-research). However, hostel staff report that where possible they try to ensure that palliative care can be provided in a familiar environment for as long as possible, as they feel that the benefits outweigh the challenges (CERQual – moderate).
It is acknowledged that not being able to recognise the physical health needs of, and the signs of physical deterioration in, those with pre-existing SMI can be a barrier to the receipt of adequate EoL care (ungraded – non-research). Staff report that people with SMI are not always able to recognise their own declining health and because of previous unsatisfactory health-care encounters it is felt that they often present late to services (CERQual – moderate). As a result, the timely provision of palliative care can be hampered when people with SMI (especially those who are homeless) are not identified as approaching the EoL until the late diagnosis of life-limiting physical disease (CERQual – high). People who are homeless are often more concerned with day-to-day survival than with keeping appointments with HCPs, and this makes it difficult to identify EoL trajectories and to provide palliative care (CERQual – moderate).
Implications for policy, services and practice
The purpose of assessing confidence in summaries of synthesised findings is to better support decisions by policy-makers, managers and senior practitioners, including in the areas of policy and guideline development. 82 The GRADE and CERQual assessments presented above are explicitly drawn on in this section. Particular weight is given to the 10 GRADE and CERQual summary statements, derived uniquely from research studies included in the review, and therefore not from case studies, policy or guidance, in which there is a high degree of confidence.
The key implications are as follows:
-
This evidence synthesis points with a high degree of confidence to the importance of formal and informal partnership opportunities being taken and encouraged. Partnerships can involve the building of coalitions across the whole system, including mental health, EoL, primary care, social care and other services. This is necessary to support the exchange of information in the integrated care of people with SMI at the EoL. In a context in which there is often ‘no right place to die’ and in which mental health staff are often poorly equipped to care for people at the EoL, and where people with SMI at the EoL face frequent moves between services, finding ways of supporting people to die in the location of their choice is a priority.
-
This synthesis also has implications for professional practice. Many people with SMI have limited social networks and little or no family contact, but even though mental health staff value the quality of their relationships with patients, some find it difficult to invest in relationships with people with SMI at the EoL because of the upset caused when patients are transferred to other facilities for EoL care. Mental health staff, many of whom find talking about death and dying with patients difficult, find that when opportunities are found patients are receptive. In the case of HCPs working in EoL care, stigmatising and prejudicial attitudes towards people with SMI and people who are homeless can affect EoL decision-making. All of these summary statements have clear implications for the future education, support and supervision of all care staff working across both the mental health and the EoL care systems.
-
A high-confidence synthesis summary from the contexts of care domain is that programmes and services for people with SMI at the EoL require a comprehensive team approach that incorporates symptom relief, psychological and psychosocial support, and spiritual care. Comprehensive services of this type are exactly as should be expected by all members of the population, but their importance for people with SMI at the EoL is worth restating for the purposes of promoting parity of esteem. Capable advocates are able to increase the numbers of people with SMI at the EoL who are referred to palliative care services, and to help make sure that palliative care is provided and received. Not having an advocate risks people with SMI who are lacking social and family support becoming ‘lost in the system’. Taken together, these synthesis summaries have important implications for the identification of roles for members of the care team in co-ordinating services across boundaries, advocating for and on behalf of patients, and providing direct care.
-
A final high-confidence summary statement is derived from the evidence synthesised in the area of living with SMI. This review has found that the timely provision of palliative care can be hindered when people with SMI, and particularly those who are homeless, receive delayed diagnoses of their EoL-related conditions. This has implications for the proactive provision of physical health care to groups of people who might not recognise the seriousness of their condition and who might miss out on routine health assessments.
Recommendations for future research
The case studies synthesised in Chapter 5 demonstrate the complexities and the ethical dilemmas associated with the provision of care to people with SMI at the EoL. Many are stark in revealing the challenges presented by delayed diagnosis, patients’ fluctuating capacity to make decisions and the futility of treatment. Case studies also demonstrate, as does the included research, the unpreparedness of professionals to meet patients’ multiple needs. Synthesised case study findings also show the dangers of ascribing delays in mobilising (or continuing with) palliative care services in response to what are often described, in written reports, as patients’ challenging presentations, or even their wilfully difficult behaviour.
Among the research publications from which data were synthesised in Chapter 4, only three originate from the UK, and across all included research studies very few include either patients or family members as participants. The consequence of this is that information on the experiences of people with SMI at the EoL features most prominently in the synthesis of case studies, making this a wide-open area for future well-designed research. Significantly, none of the included research publications reported on intervention studies, and no research was found in the area of EoL care provided to people with SMI in the prison setting.
In this context of a paucity of research evidence, key recommendations for future studies arising from this evidence synthesis are as follows:
-
Patient- and family-facing studies should be commissioned to examine the experiences of people with SMI at the EoL, and the experiences of their surrounding paid and unpaid carers and those important to them, to establish the factors that help and hinder care in the UK-specific context.
-
A programme of research should be commissioned comprising studies that explicitly co-produce, introduce and evaluate new ways of providing and organising EoL care for people with SMI with both cancer and other life-threatening conditions. This programme should include studies involving support for structurally disadvantaged groups, including people with SMI at the EoL who are also homeless or who are in prison. Candidate interventions include advance care plans, advocacy and improved education for professionals, along with the development of new or enhanced roles for practitioners and the introduction of models of integrated provision spanning the mental health, EoL and related care systems.
Limitations
All 30 research studies reported in 34 publications included in this review were undertaken in high-income countries with developed health systems, but only three were completed in the UK. 37,112,113 All three UK studies used qualitative methods, but only one113 included people who had experience of using services and none evaluated interventions to improve care. Although implications for policy, services and practice arising from this project have been drawn from all 30 studies, it is recognised that contextual differences in global health and social care systems (e.g. relating to the funding of services) need to be borne in mind when the transferability of findings and summary evidence statements are considered. In addition, it is recognised that the search for policy and guidance was limited to the UK only, rather than being extended to other countries around the world, including those with broadly comparable health systems. With only English-language items included in this project, the possibility also exists that important research and other evidence of relevance has been neither identified nor included. Finally, as no intervention studies were located, no meta-analysis could be performed.
Conclusion
This rigorously conducted evidence synthesis has brought together policy, guidance, research and case studies in an important but neglected area: EoL care for people with SMI. Although findings from this review are of immediate and direct relevance in this very specific area, they also have relevance for the EoL care of other disadvantaged groups in which health inequalities persist. Reflecting approaches developed through the EPPI-Centre, a strength of this synthesis is the inclusion of both research and non-research material, coupled with the exclusive use of research evidence to inform the project’s overall implications for policy, services and practice. The project was launched in response to a need identified by people with lived experience of mental health and EoL services, one of whom proceeded to work as a full member of the project team doing work that included reviewing and approving this full report and its Scientific and Plain English summaries. The establishment of a SAG populated by senior professionals, government advisors, and people with direct experience of service use and of caring was key, and this was a further vehicle for a public and patient voice to be heard at strategic points during the lifetime of the project.
Outputs written for internationally leading journals will follow, reporting main and other findings from this full NIHR Journals Library report along with the production of an accessible summary for wide dissemination. Presentations are planned at key conferences, and with help from the project’s SAG key policy-makers, managers, professionals and organisations these will be targeted to make sure that the findings reach people who are able to make full use of them. With this evidence synthesis designed as the starting point for a programme of research, further projects are planned, including studies involving people with SMI at the EoL and their carers and studies evaluating new ways of providing and organising care.
Acknowledgements
The team is grateful to Roger Pratt for his contribution to generating the ideas underpinning this project, as reported in Chapter 2. The team is also grateful to all members of the SAG (named in Appendix 1), and particularly to the group’s independent chairperson, Dr Nikki Pease, for their time, energy and expertise.
Contributions of authors
Ben Hannigan (https://orcid.org/0000-0002-2512-6721) (Professor of Mental Health Nursing) contributed to the development of the protocol; screened, selected, appraised and synthesised materials; and wrote for and edited the final report.
Deborah Edwards (https://orcid.org/0000-0003-1885-9297) (Research Associate) contributed to the development of the protocol; screened, selected, appraised and synthesised materials; and wrote for and edited the final report.
Sally Anstey (https://orcid.org/0000-0003-2295-3761) (Senior Lecturer in Adult Nursing) contributed to the development of the protocol; screened, selected, appraised and synthesised materials; and wrote for and commented on the final report.
Michael Coffey (https://orcid.org/0000-0002-0380-4704) (Professor of Mental Health Care) contributed to the development of the protocol; screened, selected, appraised and synthesised materials; and wrote for and commented on the final report.
Paul Gill (https://orcid.org/0000-0003-4056-3230) (Senior Lecturer in Adult Nursing) contributed to the development of the protocol; screened, selected, appraised and synthesised materials; and wrote for and commented on the final report.
Mala Mann (https://orcid.org/0000-0002-2554-9265) (Information Specialist) contributed to the development of the protocol, and searched for materials and wrote for and commented on the final report.
Alan Meudell (https://orcid.org/0000-0001-8138-4744) (Independent Service User Researcher) contributed to the development of the protocol, screened materials, and wrote for and edited the final report.
Publications
Edwards D, Anstey S, Coffey M, Gill P, Mann M, Meudell A, Hannigan B. End of life care for people with severe mental illness: mixed methods systematic review and thematic synthesis (the MENLOC study). Palliat Med 2021;35:1747–60.
Coffey M, Edwards D, Anstey S, Gill P, Mann M, Meudell A, Hannigan B. End of life care for people with severe mental illness: mixed methods systematic review and thematic synthesis of published case studies (the MENLOC study). BMJ Open 2022;12:e053223.
Data-sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HSDR programme or the Department of Health and Social Care.
References
- Mental Health Taskforce . The Five Year Forward View for Mental Health 2016.
- Ellison N. Mental Health and Palliative Care. Literature Review. London: Mental Health Foundation; 2008.
- Woods A, Willison K, Kington C, Gavin A. Palliative care for people with severe persistent mental illness: a review of the literature. Can J Psychiatry 2008;53:725-36. https://doi.org/10.1177/070674370805301104.
- Gough D, Oliver S, Thomas J. An Introduction to Systematic Reviews. London: SAGE Publications Ltd; 2017.
- Global Burden of Disease Study 2013 Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743-800.
- Newton JN, Briggs AD, Murray CJ, Dicker D, Foreman KJ, Wang H, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2257-74. https://doi.org/10.1016/S0140-6736(15)00195-6.
- Centre for Mental Health . The Economic and Social Costs of Mental Health Problems in 2009–10 2010.
- Friedli L, Parsonage M. Promoting Mental Health and Preventing Mental Illness: The Economic Case for Investment in Wales. Cardiff: All Wales Mental Health Promotion Network; 2009.
- Department of Health and Social Care . Building Bridges: A Guide to Arrangements for Interagency Working for the Care and Protection of Severely Mentally Ill People 1995.
- Kronenberg C, Doran T, Goddard M, Kendrick T, Gilbody S, Dare CR, et al. Identifying primary care quality indicators for people with serious mental illness: a systematic review. Br J Gen Pract 2017;67:e519-30. https://doi.org/10.3399/bjgp17X691721.
- National Institute for Health Research (NIHR) . Forward Thinking: NIHR Research on Support for People With Severe Mental Illness 2018.
- World Health Organization . ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines 1992.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-V) 2014. https://doi.org/10.1176/appi.books.9780890425596.
- Thornicroft G. Premature death among people with mental illness. BMJ 2013;346. https://doi.org/10.1136/bmj.f2969.
- Picot SA, Glaetzer KM, Myhill KJ. Coordinating end of life care for individuals with a mental illness – a nurse practitioner collaboration. Collegian 2015;22:143-9. https://doi.org/10.1016/j.colegn.2013.12.007.
- Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 2014;13:153-60. https://doi.org/10.1002/wps.20128.
- Carney CP, Jones L, Woolson RF. Medical comorbidity in women and men with schizophrenia: a population-based controlled study. J Gen Intern Med 2006;21:1133-7. https://doi.org/10.1111/j.1525-1497.2006.00563.x.
- Millman J, Galway K, Santin O, Reid J. Cancer and serious mental illness – patient, caregiver and professional perspectives: study protocol. J Adv Nurs 2016;72:217-26. https://doi.org/10.1111/jan.12812.
- Knapik GP, Graor CH. Engaging persons with severe persistent mental illness into primary care. J Nurse Pract 2013;9:283-7. https://doi.org/10.1016/j.nurpra.2013.02.019.
- Shalev D, Brewster K, Arbuckle MR, Levenson JA. A staggered edge: end-of-life care in patients with severe mental illness. Gen Hosp Psychiatry 2017;44:1-3. https://doi.org/10.1016/j.genhosppsych.2016.10.004.
- General Medical Council . Treatment and Care Towards the End of Life: Good Practice in Decision Making 2010. www.gmc-uk.org/-/media/documents/treatment-and-care-towards-the-end-of-life---english-1015_pdf-48902105.pdf (accessed 5 March 2019).
- Independent Cancer Taskforce . Achieving World-Class Cancer Outcomes: A Strategy for England 2015–2020 2015.
- Howard LM, Barley EA, Davies E, Rigg A, Lempp H, Rose D, et al. Cancer diagnosis in people with severe mental illness: practical and ethical issues. Lancet Oncol 2010;11:797-804. https://doi.org/10.1016/S1470-2045(10)70085-1.
- Batty GD, Whitley E, Gale CR, Osborn D, Tynelius P, Rasmussen F. Impact of mental health problems on case fatality in male cancer patients. Br J Cancer 2012;106:1842-5. https://doi.org/10.1038/bjc.2012.150.
- Desai MM, Bruce ML, Kasl SV. The effects of major depression and phobia on stage at diagnosis of breast cancer. Int J Psychiatry Med 1999;29:29-45. https://doi.org/10.2190/0C63-U15V-5NUR-TVXE.
- Irwin KE, Henderson DC, Knight HP, Pirl WF. Cancer care for individuals with schizophrenia. Cancer 2014;120:323-34. https://doi.org/10.1002/cncr.28431.
- Foti ME, Chochinov HM, Breitbart W. Handbook of Psychiatry in Palliative Medicine. Oxford: Oxford University Press; 2012.
- Ishikawa H, Yasunaga H, Matsui H, Fushimi K, Kawakami N. Differences in cancer stage, treatment and in-hospital mortality between patients with and without schizophrenia: retrospective matched-pair cohort study. Br J Psychiatry 2016;208:239-44. https://doi.org/10.1192/bjp.bp.114.156265.
- McCormack P, Sharp DMM. Palliative care for people with mental health problems. Eur J Palliat Care 2006;13:198-201.
- Addington-Hall J. Positive Partnerships: Palliative Care for Adults with Severe Mental Health Problems. Occasional Paper 17. Northampton: National Council for Hospice and Specialist Palliative Care Services and Scottish Partnership Agency for Palliative and Cancer Care; 2000.
- Zabora JR, Loscalzo M, Smith E, Abeloff MD, Armitage JO, Lichter AS, et al. Clinical Oncology. New York, NY: Churchill Livingstone; 2000.
- Morgan BD. ‘No right place to die’: nursing attitudes and needs in caring for people with serious mental illness at end-of-life. J Am Nurses Assoc 2016;22:31-42. https://doi.org/10.1177/1078390316629960.
- Warren MB, Lapid MI, McKean AJ, Cha SS, Stevens MA, Brekke FM, et al. Code status discussions in psychiatric and medical inpatients. J Clin Psychiatry 2015;76:49-53. https://doi.org/10.4088/JCP.13m08912.
- Dixon J, King D, Matosevic T, Clark M, Knapp M. Equity in Provision of Palliative Care in the UK. London: London School of Economics and Marie Curie; 2015.
- Hughes-Hallet T, Craft A, Davies C. Palliative Care Funding Review: Funding the Right Care and Support for Everyone. London: Department of Health and Social Care; 2011.
- Marie Curie and the Bevan Foundation . Death and Dying in Wales 2014.
- Hackett A, Gaitan A. A qualitative study assessing mental health issues in two hospices in the UK. Int J Palliat Nurs 2007;13:273-81. https://doi.org/10.12968/ijpn.2007.13.6.23739.
- Price A, Hotopf M, Higginson IJ, Monroe B, Henderson M. Psychological services in hospices in the UK and Republic of Ireland. J R Soc Med 2006;99:637-9. https://doi.org/10.1177/014107680609901213.
- Department of Health and Social Care . National Cancer Patient Experience Survey Programme: 2010 National Survey Report 2010.
- Picker Institute Europe . Wales Cancer Patient Experience Survey 2016: National Report 2017.
- Department of Health and Social Care . A Framework for Mental Health Research 2017.
- Department of Health and Social Care . Our Commitment to You for End Of Life Care: The Government Response to the Review of Choice in End of Life Care 2016.
- Department of Health, Social Services and Public Safety . Living Matters Dying Matters. A Palliative and End of Life Care Strategy for Adults in Northern Ireland 2010.
- Scottish Government . Better Cancer Care: An Action Plan 2008.
- NHS Scotland . Living and Dying Well. A National Action Plan for Palliative and End of Life Care in Scotland 2008.
- Scottish Government . Improving the Health and Wellbeing of People With Long Term Conditions in Scotland: A National Action Plan 2009.
- Welsh Assembly Government . Designed for Life: Creating World Class Health and Social Care for Wales in the 21st Century 2005.
- All Wales Palliative Care Planning Group . Report to Minister for Health and Social Services on Palliative Care Services – Sugar Report 2008.
- All Wales Palliative Care Planning Group . Implementation of Palliative Care Report: Palliative Care Services Funding 2008 to 2009 - the Finlay Report 2009.
- Welsh Government . Together for Health: Delivering End of Life Care 2013.
- Drakeford M. Palliative Care Services in Wales Are Making an Enormous Difference to People’s Quality of Life 2014. www.wired-gov.net/wg/news.nsf/articles/Palliative+care+services+in+Wales+are+making+an+enormous+difference+to+peoples+quality+of+life+Mark+Drakeford+28102014162040?open (accessed 24 June 2021).
- Marie Curie . Triggers for Palliative Care. Improving Access to Care for People With Diseases Other Than Cancer: Implications for Wales 2015.
- Exley C. Review article: the sociology of dying, death and bereavement. Sociol Health Illn 2004;26:110-22. https://doi.org/10.1111/j.1467-9566.2004.00382.x.
- Payne S. From here to there: reaching out for palliative care. Eur J Palliat Care 2011;18:264-5.
- National Institute for Health and Care Excellence (NICE) . Guidance on Cancer Services Improving Supportive and Palliative Care for Adults With Cancer 2004.
- National Institute for Health and Care Excellence (NICE) . End of Life Care for Adults in the Last Year of Life: Service Delivery 2019.
- National Institute for Health and Care Excellence (NICE) . Psychosis and Schizophrenia in Adults: Prevention and Management 2014.
- National Institute for Health and Care Excellence (NICE) . Care of Dying Adults in the Last Days of Life 2015.
- National Institute for Health and Care Excellence (NICE) . Service User Experience in Adult Mental Health: Improving the Experience of Care for People Using Adult NHS Mental Health Services 2011.
- Holt RIG, Hind D, Gossage-Worrall R, Bradburn M, Saxon D, McCrone P, et al. Structured lifestyle education to support weight loss for people with schizophrenia, schizoaffective disorder and first episode psychosis: the STEPWISE RCT. Health Technol Assess 2018;22. https://doi.org/10.3310/hta22650.
- McCrone P, Wright S, Zala D, Radhakrishnan Kartha M, Koeser L, Ashworth M, et al. Location of care for people with serious mental illness (LOCAPE): implications for service use and costs using a mixed-methods approach. Health Soc Care Deliv Res Res 2016;4. https://doi.org/10.3310/hsdr04340.
- Serfaty M, King M, Nazareth I, Moorey S, Aspden T, Tookman A, et al. Manualised cognitive behavioural therapy in treating depression in advanced cancer: the CanTalk RCT. Health Technol Assess 2019;23. https://doi.org/10.3310/hta23190.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
- Simpson A, Hannigan B, Coffey M, Jones A, Barlow S, Cohen R, et al. Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP). Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04050.
- Simpson A, Coffey M, Hannigan B, Barlow S, Cohen R, Jones A, et al. Cross-national mixed-methods comparative case study of recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings (COCAPP-A). Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05260.
- Coffey M, Hannigan B, Meudell A, Jones M, Hunt J, Fitzsimmons D. Quality of life, recovery and decision-making: a mixed methods study of mental health recovery in social care. Soc Psychiatry Psychiatr Epidemiol 2019;54:715-23. https://doi.org/10.1007/s00127-018-1635-6.
- National Institute for Health Research . PROSPERO: International Prospective Register of Systematic Reviews n.d. www.crd.york.ac.uk/prospero/ (accessed 1 November 2018).
- Centre for Reviews and Dissemination . CRD’s Guidance on Undertaking Reviews in Health Care 2009.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
- Mahood Q, Van Eerd D, Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods 2014;5:221-34. https://doi.org/10.1002/jrsm.1106.
- Edwards D, Anstey S, Coffey M, Gill P, Mann M, Meudell A, et al. End of life care for people with severe mental illness: mixed methods systematic review and thematic synthesis (the MENLOC study). Palliat Med 2021;35:1747-60. https://doi.org/10.1177/02692163211037480.
- Critical Appraisal Skills Programme . CASP Checklists 2017. https://casp-uk.net/casp-tools-checklists/ (accessed 24 June 2021).
- Specialist Unit for Review Evidence . Questions to Assist With the Critical Appraisal of Cross-Sectional Studies 2018. www.cardiff.ac.uk/insrv/libraries/sure/checklists.html (accessed 20 January 2019).
- Scottish Intercollegiate Guidelines Network . Methodology Checklist 3: Cohort Studies 2019. https://www.sign.ac.uk/media/1712/checklist_for_cohort_studies.rtf (accessed 28 June 2021).
- Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. JBI Manual for Evidence Synthesis. JBI; 2020.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. https://doi.org/10.1136/bmj.39489.470347.AD.
- Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401-6. https://doi.org/10.1016/j.jclinepi.2010.07.015.
- Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001895.
- Hannigan B, Edwards D, Evans N, Gillen E, Longo M, Pryjmachuk S, et al. An evidence synthesis of risk identification, assessment and management for young people using tier 4 inpatient child and adolescent mental health services. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03220.
- Edwards D, Noyes J, Lowes L, Haf Spencer L, Gregory JW. An ongoing struggle: a mixed-method systematic review of interventions, barriers and facilitators to achieving optimal self-care by children and young people with type 1 diabetes in educational settings. BMC Pediatr 2014;14. https://doi.org/10.1186/1471-2431-14-228.
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0688-3.
- Alici Y, Smith D, Lu HL, Bailey A, Shreve S, Rosenfeld K, et al. Families’ perceptions of veterans’ distress due to post-traumatic stress disorder-related symptoms at the end of life. J Pain Symptom Manage 2010;39:507-14. https://doi.org/10.1016/j.jpainsymman.2009.07.011.
- Cai X, Cram P, Li Y. Origination of medical advance directives among nursing home residents with and without serious mental illness. Psychiatr Serv 2011;62:61-6. https://doi.org/10.1176/ps.62.1.pss6201_0061.
- Foti ME. ‘Do It Your Way’: a demonstration project on end-of-life care for persons with serious mental illness. J Palliat Med 2003;6:661-9. https://doi.org/10.1089/109662103768253830.
- Foti ME, Bartels SJ, Van Citters AD, Merriman MP, Fletcher KE. End-of-life treatment preferences of persons with serious mental illness. Psychiatr Serv 2005;56:585-91. https://doi.org/10.1176/appi.ps.56.5.585.
- Foti ME, Bartels SJ, Merriman MP, Fletcher KE, Van Citters AD. Medical advance care planning for persons with serious mental illness. Psychiatr Serv 2005;56:576-84. https://doi.org/10.1176/appi.ps.56.5.576.
- Ganzini L, Socherman R, Duckart J, Shores M. End-of-life care for veterans with schizophrenia and cancer. Psychiatr Serv 2010;61:725-8. https://doi.org/10.1176/ps.2010.61.7.725.
- Huang C-HS, Kvale E, Bailey FA, Goode P, Burgio K. Association between mental health diagnoses and process of care at the end of life: findings from the BEACON trial (S771). J Pain Symptom Manage 2017;53. https://doi.org/10.1016/j.jpainsymman.2016.12.282.
- Kelley-Cook E, Nguyen G, Lee S, Edwards TM, Sanchez-Reilly S. Medication needs vary for terminally ill Vietnam era veterans with and without a diagnosis of PTSD. Am J Hosp Palliat Care 2016;33:625-32. https://doi.org/10.1177/1049909115586556.
- Lavin K, Davydow DS, Downey L, Engelberg RA, Dunlap B, Sibley J, et al. Effect of psychiatric illness on acute care utilization at end of life from serious medical illness. J Pain Symptom Manage 2017;54:176-85.e1. https://doi.org/10.1016/j.jpainsymman.2017.04.003.
- McDermott CL, Bansal A, Ramsey SD, Lyman GH, Sullivan SD. Depression and health care utilization at end of life among older adults with advanced non-small-cell lung cancer. J Pain Symptom Manage 2018;56:699-708.e1. https://doi.org/10.1016/j.jpainsymman.2018.08.004.
- Patterson KR, Croom AR, Teverovsky EG, Arnold R. Current state of psychiatric involvement on palliative care consult services: results of a national survey. J Pain Symptom Manage 2014;47:1019-27. https://doi.org/10.1016/j.jpainsymman.2013.06.015.
- Taylor J, Swetenham K, Myhill K, Picot S, Glaetzer K, Loon Av. IMhPaCT: an education strategy for cross-training palliative care and mental health clinicians. Int J Palliat Nurs 2012;18:290-4. https://doi.org/10.12968/ijpn.2012.18.6.290.
- Chochinov HM, Martens PJ, Prior HJ, Kredentser MS. Comparative health care use patterns of people with schizophrenia near the end of life: a population-based study in Manitoba, Canada. Schizophr Res 2012;141:241-6. https://doi.org/10.1016/j.schres.2012.07.028.
- Elie D, Marino A, Torres-Platas SG, Noohi S, Semeniuk T, Segal M, et al. End-of-life care preferences in patients with severe and persistent mental illness and chronic medical conditions: a comparative cross-sectional study. Am J Geriatr Psychiatry 2018;26:89-97. https://doi.org/10.1016/j.jagp.2017.09.018.
- Martens PJ, Chochinov HM, Prior HJ. Where and how people with schizophrenia die: a population-based, matched cohort study in Manitoba, Canada. J Clin Psychiatry 2013;74:e551-7. https://doi.org/10.4088/JCP.12m08234.
- Podymow T, Turnbull J, Coyle D. Shelter-based palliative care for the homeless terminally ill. Palliat Med 2006;20:81-6. https://doi.org/10.1191/0269216306pm1103oa.
- Stajduhar KI, Mollison A, Giesbrecht M, McNeil R, Pauly B, Reimer-Kirkham S, et al. ‘Just too busy living in the moment and surviving’: barriers to accessing health care for structurally vulnerable populations at end-of-life. BMC Palliat Care 2019;18. https://doi.org/10.1186/s12904-019-0396-7.
- Butler H, O’Brien AJ. Access to specialist palliative care services by people with severe and persistent mental illness: a retrospective cohort study. Int J Ment Health Nurs 2018;27:737-46. https://doi.org/10.1111/inm.12360.
- Huang HK, Wang YW, Hsieh JG, Hsieh CJ. Disparity of end-of-life care in cancer patients with and without schizophrenia: a nationwide population-based cohort study. Schizophr Res 2018;195:434-40. https://doi.org/10.1016/j.schres.2017.10.029.
- McGrath P, Holewa H. Mental health and palliative care: exploring the ideological interface. Int J Psychosoc Rehabil 2004;9:107-19.
- McGrath P, Jarrett V. The problem of stigma during end-of-life care at a psychiatric institution. Int J Psychosoc Rehabil 2007;11:19-30.
- McGrath PD, Forrester K. Ethico-legal issues in relation to end-of-life care and institutional mental health. Aust Health Rev 2006;30:286-97. https://doi.org/10.1071/AH060286.
- McKellar D, Ng F, Chur-Hansen A. Is death our business? Philosophical conflicts over the end-of-life in old age psychiatry. Aging Ment Health 2016;20:583-93. https://doi.org/10.1080/13607863.2015.1031636.
- McNamara B, Same A, Rosenwax L, Kelly B. Palliative care for people with schizophrenia: a qualitative study of an under-serviced group in need. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0309-1.
- Spilsbury K, Rosenwax L, Brameld K, Kelly B, Arendts G. Morbidity burden and community-based palliative care are associated with rates of hospital use by people with schizophrenia in the last year of life: a population-based matched cohort study. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0208220.
- Fond G, Salas S, Pauly V, Baumstarck K, Bernard C, Orleans V, et al. End-of-life care among patients with schizophrenia and cancer: a population-based cohort study from the French national hospital database. Lancet Public Health 2019;4:e583-91. https://doi.org/10.1016/S2468-2667(19)30187-2.
- Sweers K, Dierckx de Casterlé B, Detraux J, De Hert M. End-of-life (care) perspectives and expectations of patients with schizophrenia. Arch Psychiatr Nurs 2013;27:246-52. https://doi.org/10.1016/j.apnu.2013.05.003.
- Evenblij K, Widdershoven GA, Onwuteaka-Philipsen BD, de Kam H, Pasman HR. Palliative care in mental health facilities from the perspective of nurses: a mixed-methods study. J Psychiatr Ment Health Nurs 2016;23:409-18. https://doi.org/10.1111/jpm.12320.
- Evenblij K, Ten Koppel M, Smets T, Widdershoven GAM, Onwuteaka-Philipsen BD, Pasman HRW. Are care staff equipped for end-of-life communication? A cross-sectional study in long-term care facilities to identify determinants of self-efficacy. BMC Palliat Care 2019;18. https://doi.org/10.1186/s12904-018-0388-z.
- Jerwood J, Phimster D, Ward G, Holliday H, Coad J. Barriers to palliative care for people with severe mental illness: exploring the views of clinical staff. Eur J Palliat Care 2018;25:20-5.
- Shulman C, Hudson BF, Low J, Hewett N, Daley J, Kennedy P, et al. End-of-life care for homeless people: a qualitative analysis exploring the challenges to access and provision of palliative care. Palliat Med 2018;32:36-45. https://doi.org/10.1177/0269216317717101.
- Sheridan A, Coughlan B, Frazer K, Walsh S, Bergin JA, Crawley L, et al. The Palliative Care Needs of People with Serious Mental Illness in Ireland. Dublin: School of Nursing, Midwifery and Health Systems, University College Dublin; 2018.
- Bakker TJ. Palliative care in chronic psycho-geriatrics: a case-study. Patient Educ Couns 2000;41:107-13. https://doi.org/10.1016/S0738-3991(00)00120-8.
- Feldman DB, Sorocco KH, Bratkovich KL. Treatment of posttraumatic stress disorder at the end-of-life: application of the Stepwise Psychosocial Palliative Care model. Palliat Support Care 2014;12:233-43. https://doi.org/10.1017/S1478951513000370.
- Feldman DB. Stepwise psychosocial palliative care: a new approach to the treatment of posttraumatic stress disorder at the end of life. J Soc Work End Life Palliat Care 2017;13:113-33. https://doi.org/10.1080/15524256.2017.1346543.
- Mason EN, Bowman EH. Determination of capacity in a critically ill patient with long standing mental illness. J Am Geriatr Soc 2018;66.
- Rodriguez-Mayoral O. Bipolar disorder and cancer. Management at end of life. Case report. Bipolar Disord 2018.
- Kennedy P, Sarafi C, Greenish W. Homelessness and End of Life Care. Practical Information and Tools to Support the Needs of Homeless People who are Approaching the End of Life, and those who are Bereaved. London: Marie Curie Cancer Care and St Mungo’s; 2013.
- Maloney K. Opinion: my husband refused to believe he had bipolar disorder, and denial destroyed him. The Journal 2014.
- Badger JM, Ekman Ladd R. Conflicting voices: Withhold treatment or not for a patient with chronic self-destructive behavior?. JONAS Healthc Law Ethics Regul 2011;13:79-83. https://doi.org/10.1097/NHL.0b013e31822ab019.
- Boyd CO, Cantone J, Gambino P, Harris T, Malone EN. When the hospice patient is manipulative. Hosp J 1997;12:1-16. https://doi.org/10.1080/0742-969x.1997.11882839.
- Candilis PJ, Foti ME. Case presentation: end-of-life care and mental illness: the case of Ms. W. J Pain Symptom Manage 1999;18:447-8. https://doi.org/10.1016/S0885-3924(99)00116-5.
- Feely MA, Havyer RD, Lapid MI, Swetz KM. Management of end-of-life care and of difficult behaviors associated with borderline personality disorder. J Pain Symptom Manage 2013;45:934-8. https://doi.org/10.1016/j.jpainsymman.2012.04.004.
- Feldman DB, Periyakoil VS. Case discussions in palliative medicine posttraumatic stress disorder at the end of life. J Palliat Med 2006;9. https://doi.org/10.1089/jpm.2006.9.213.
- Geppert CM, Rabjohn P, Vlaskovits J. To treat or not to treat: psychosis, palliative care, and ethics at the end-of-life: a case analysis. Psychosomatics 2011;52:178-84. https://doi.org/10.1016/j.psym.2010.12.003.
- Gonzalez MR, Marcelo CD, Stringer M. Hospice care for 86 year old male with recurrent breast cancer: a case report. Cases J 2009;2. https://doi.org/10.4076/1757-1626-2-8357.
- Griffith LJ. Good palliative care for a patient with schizophrenia dying of emphysema and heart failure. Psychiatry 2007;4:61-5.
- Griffith LJ. Brief supportive psychotherapy for a patient with chronic schizophrenia who is dying. Psychiatry 2007;4:49-54.
- Hill R. End-of-life care for the patient with borderline personality disorder. J Hosp Palliat Nurs 2005;7:150-63. https://doi.org/10.1097/00129191-200505000-00007.
- Kunkel EJ, Woods CM, Rodgers C, Myers RE. Consultations for ‘maladaptive denial of illness’ in patients with cancer: psychiatric disorders that result in noncompliance. Psycho-Oncology 1997;6:139-49. https://doi.org/10.1002/(SICI)1099-1611(199706)6:2<139::AID-PON256>3.0.CO;2-O.
- Levin SM, Feldman MB. Terminal illness in a psychiatric patient – issues and ethics. S Afr Med J 1983;63:492-4.
- Lopez A, Yager J, Feinstein RE. Medical futility and psychiatry: palliative care and hospice care as a last resort in the treatment of refractory anorexia nervosa. Int J Eat Disord 2010;43:372-7. https://doi.org/10.1002/eat.20701.
- McCasland LA. Providing hospice and palliative care to the seriously and persistently mentally ill. J Hosp Palliat Nurs 2007;9:305-13. https://doi.org/10.1097/01.NJH.0000299313.99514.0c.
- McKenna RC, Bailey L, Haake J, Desai PN, Prasad BR. Clozapine and chemotherapy. Hosp Commun Psychiatry 1994;45. https://doi.org/10.1176/ps.45.8.831.
- Moini B, Levenson JL. A forgotten diagnosis: simple schizophrenia in a patient with breast cancer. Psychosomatics 2009;50:87-9. https://doi.org/10.1176/appi.psy.50.1.87.
- Monga V, Broucek M, Amani M, Ramaswamy S. Clozapine and concomitant chemotherapy in a patient with schizophrenia and new onset esophageal cancer. Psycho-Oncology 2015;24:971-2. https://doi.org/10.1002/pon.3744.
- Rice TR, Dobry Y, Novakovic V, Appel JM. The importance of patient-provider communication in end-of-life care. J Bioeth Inq 2012;9:439-41. https://doi.org/10.1007/s11673-012-9397-4.
- Romm S, Combs H, Poeschla B. Psychiatry and palliative care: thoughts on collaboration. J Hosp Palliat Nurs 2009;11:79-81. https://doi.org/10.1097/NJH.0b013e31819b003d.
- Shah HA, Lee HB, Nunery WR. Neglected basal cell carcinoma in a schizophrenic patient. Ophthalmic Plast Reconstr Surg 2008;24:495-7. https://doi.org/10.1097/IOP.0b013e31818be843.
- Stecker E. The terminally ill patient on an acute psychiatric unit. A case study. J Psychosoc Nurs Ment Health Serv 1993;31:13-5. https://doi.org/10.3928/0279-3695-19930501-05.
- Steves F, Williams T. Enhancing end-of-life care for terminally ill psychiatric patients. Nursing 2016;46:54-8. https://doi.org/10.1097/01.NURSE.0000484964.08605.37.
- Terpstra TL, Williamson S, Terpstra T. Palliative care for terminally ill individuals with schizophrenia. J Psychosoc Nurs Ment Health Serv 2014;52:32-8.
- Thomson K, Henry B. Oncology clinical challenges: caring for patients with preexisting psychiatric illness. Clin J Oncol Nurs 2012;16:471-80. https://doi.org/10.1188/12.CJON.471-480.
- Mogg A, Bartlett A. Refusal of treatment in a patient with fluctuating capacity – theory and practice. J Forensic Psychiatry Psychol 2005;16:60-9. https://doi.org/10.1080/14789940412331290049.
- Muhtaseb M, Olver JM, Constantine S. Massive basal cell carcinoma in a schizophrenic patient: treatment options and constraints. Br J Ophthalmol 2001;85:117-18. https://doi.org/10.1136/bjo.85.1.110h.
- O’Neill J, Crowther T, Sampson G. A case study: anorexia nervosa. Palliative care of terminal psychiatric disease. Am J Hosp Palliat Care 1994;11:36-8. https://doi.org/10.1177/104990919401100609.
- Clements-Cortes A. The use of music in facilitating emotional expression in the terminally ill. Am J Hosp Palliat Care 2004;21:255-60. https://doi.org/10.1177/104990910402100406.
- Kadri A, Blackmer J, Ibrahim M. Obtaining consent to a life-sustaining treatment for a patient with a major psychiatric illness. CMAJ 2014;186:1087-9. https://doi.org/10.1503/cmaj.130714.
- Webber T. End of life care for people with mental illness. J Ethics Ment Health 2012;7:1-4.
- Cabaret W, Krerbi Y, Saravane D. Palliative care in psychiatric institutions. Eur J Palliat Care 2002;9:150-2.
- Doron A, Mendlovic S. Dying in the psychiatric ward. Isr J Psychiatry Relat Sci 2008;45:141-4.
- Ang A, Loke PC, Campbell AV, Chong SA. Live or let die: ethical issues in a psychiatric patient with end-stage renal failure. Ann Acad Med Singap 2009;38:370-4.
- Addicott R, Ashton R. Delivering Better Care at the End of Life: The Next Steps. London: The King’s Fund; 2010.
- Care Quality Commission . A Second Class Ending: Exploring the Barriers and Championing Outstanding End of Life Care for People Who Are Homeless 2017. www.cqc.org.uk/sites/default/files/20171031_a_second_class_ending.pdf (accessed 24 January 2019).
- Care Quality Commission . A Different Ending: Addressing Inequalities in End of Life Care 2016. www.cqc.org.uk/sites/default/files/20160505%20CQC_EOL CARE_OVERVIEW_FINAL_3.pdf (accessed 18 February 2019).
- Care Quality Commission . People With a Mental Health Condition: A Different Ending: Addressing Inequalities in End of Life Care 2016. www.cqc.org.uk/sites/default/files/20160505%20CQC_EOLC_MentalHealth_FINAL_2.pdf (accessed 24 January 2019).
- Department of Health . Service Framework for Mental Health and Wellbeing 2018–2021 2018.
- Department of Health and Social Care . Health and Wellbeing 2026. Delivering Together 2016.
- Department of Health and Social Care . End of Life Care Strategy. Promoting High Quality Care for All Adults at the End of Life 2008.
- Help the Hospices . Hospice and Palliative Care – Access for All 2006.
- Marie Curie . Marie Curie Briefing: Inequities in Palliative Care – Mental Health 2017. www.mariecurie.org.uk/globalassets/media/documents/policy/briefings-consultations/scotland-briefings/marie-curie-briefing-inequities-mental-health.pdf (accessed 20 February 2019).
- Marie Curie . Marie Curie Response: Mental Health Strategy for Scotland 2016. www.mariecurie.org.uk/globalassets/media/documents/policy/briefings-consultations/scotland-briefings/marie-curie-response-mental-health-strategy.pdf (accessed 20 February 2019).
- Marie Curie . Marie Curie Briefing: Mental Health and Terminal Illness 2016. www.mariecurie.org.uk/globalassets/media/documents/policy/policy-publications/october-2016/marie-curie-briefing-mental-health.pdf (accessed 20 February 2019).
- NHS Benchmarking Network . National Audit of Care at the End of Life. First Round of the Audit (2018 19) Report England and Wales 2019.
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/publication/nhs-long-term-plan/ (accessed 4 April 2019).
- NHS England . Next Steps on the NHS Five Year Forward View 2017. www.england.nhs.uk/publication/next-steps-on-the-nhs-five-year-forward-view/ (accessed 2 February 2019).
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 2 February 2019).
- NHS Lothian . Living and Dying Well in Lothian 2010. www.nhslothian.scot.nhs.uk/OurOrganisation/Strategies/ladwinlothian/Documents/Palliative%20Care%20Strategy%202010%20-15%20VER%2023%20FINAL.pdf (accessed 2 February 2019).
- Royal College of Physicians . Palliative Care Services: Meeting the Needs of Patients. Report of a Working Party 2007 2007.
- Scottish Government . Mental Health Strategy: 2017–2027 2017.
- Social Care Institute for Excellence . Dying Well at Home: Research Evidence 2013.
- Welsh Government . A Healthier Wales: Our Plan for Health and Social Care 2018.
- Welsh Government . Together for Mental Health: A Strategy for Mental Health and Wellbeing in Wales 2012.
- Worldwide Palliative Care Alliance . Building Integrated Palliative Care Programs and Services 2017. www.thewhpca.org/resources/category/building-integrated-palliative-care-programs-and-services (accessed 30 January 2019).
- Leadership Alliance for the Care of Dying People . One Chance to Get It Right: Improving People’s Experience of Care in the Last Few Days and Hours of Life 2014. http://wales.pallcare.info/files/One_chance_to_get_it_right.pdf (accessed 24 January 2019).
- Patterson C, Procter N, Toffoli L. Situation awareness: when nurses decide to admit or not admit a person with mental illness as an involuntary patient. J Adv Nurs 2016;72:2042-53. https://doi.org/10.1111/jan.13024.
- Hannigan B, Evans N. Critical junctures in health and social care: service user experiences, work and system connections. Soc Theory Health 2013;11:428-44. https://doi.org/10.1057/sth.2013.16.
- Nikoletti S, Young J, King M. Evaluation of an electronic monitoring device for urinary incontinence in elderly patients in an acute care setting. J Wound Ostomy Continence Nurs 2004;31:138-49. https://doi.org/10.1097/00152192-200405000-00008.
- Abdullah KN, Janardhan R, Hwang M, Williams CD, Farasatpour M, Margenthaler JA, et al. Adjuvant radiation therapy for breast cancer in patients with schizophrenia. Am J Surg 2015;209:378-84. https://doi.org/10.1016/j.amjsurg.2014.07.004.
- Ahearn E. The loneliness of mental illness at the end of life. WMJ 2018;117.
- Akechi T, Nakano T, Akizuki N, Nakanishi T, Yoshikawa E, Okamura H, et al. Clinical factors associated with suicidality in cancer patients. Jpn J Clin Oncol 2002;32:506-11. https://doi.org/10.1093/jjco/hyf106.
- Akechi T, Okuyama T, Sugawara Y, Nakano T, Shima Y, Uchitomi Y. Major depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients: associated and predictive factors. J Clin Oncol 2004;22:1957-65. https://doi.org/10.1200/JCO.2004.08.149.
- Alexander P. An investigation of inpatient referrals to a clinical psychologist in a hospice. Eur J Cancer Care 2004;13:36-44. https://doi.org/10.1111/j.1365-2354.2003.00441.x.
- Alexopoulos GS. Problem-Solving Therapy for People With Major Depression and Chronic Obstructive Pulmonary Disease 2008.
- Ann-Yi S, Bruera E, Wu J, Liu DD, Agosta M, Williams JL, et al. Characteristics and outcomes of psychology referrals in a palliative care department. J Pain Symptom Manage 2018;56:344-51. https://doi.org/10.1016/j.jpainsymman.2018.05.022.
- Anquinet L, Rietjens J, van der Heide A, Bruinsma S, Janssens R, Deliens L, et al. Physicians’ experiences and perspectives regarding the use of continuous sedation until death for cancer patients in the context of psychological and existential suffering at the end of life. Psycho-Oncology 2014;23:539-46. https://doi.org/10.1002/pon.3450.
- Aragona M. Tolerability and efficacy of aripiprazole in a case of psychotic anorexia nervosa comorbid with epilepsy and chronic renal failure. Eat Weight Disord 2007;12:e54-7. https://doi.org/10.1007/BF03327643.
- Atkin N, Vickerstaff V, Candy B. ‘Worried to death’: the assessment and management of anxiety in patients with advanced life-limiting disease, a national survey of palliative medicine physicians. BMC Palliat Care 2017;16. https://doi.org/10.1186/s12904-017-0245-5.
- Azhar A, Wong AN, Cerana AA, Balankari VR, Adabala M, Liu DD, et al. Characteristics of unscheduled and scheduled outpatient palliative care clinic patients at a comprehensive cancer center. J Pain Symptom Manage 2018;55:1327-34. https://doi.org/10.1016/j.jpainsymman.2018.01.015.
- Azuero C, Allen RS, Kvale E, Azuero A, Parmelee P. Determinants of psychology service utilization in a palliative care outpatient population. Psycho-Oncology 2014;23:650-7. https://doi.org/10.1002/pon.3454.
- Baile WF, DiMaggio JR, Schapira DV, Janofsky JS. The request for assistance in dying. The need for psychiatric consultation. Cancer 1993;72:2786-91. https://doi.org/10.1002/1097-0142(19931101)72:9<2786::aid-cncr2820720942>3.0.co;2-2.
- Baker A. Palliative and end-of-life care in the serious and persistently mentally ill population. J Am Psychiatr Nurses Assoc 2016;11:298-303. https://doi.org/10.1177/1078390305282209.
- Balaban ÖD, Aydin E, Keyvan A, Yazar MS, Tuna Ö, Devrimci Özgüven H. Psychiatric comorbidity, sexual dysfunction, and quality of life in patients undergoing hemodialysis: a case-control study. Noro Psikiyatr Ars 2017;54:137-42. https://doi.org/10.5152/npa.2016.12677.
- Balogun RA, Abdel-Rahman EM. Successful maintenance hemodialysis in nonagenarians with end-stage renal disease and preexisting comorbidities. J Am Geriatr Soc 2009;57:174-5. https://doi.org/10.1111/j.1532-5415.2009.02045.x.
- Bang SM, Park SH, Kang HG, Jue JI, Cho IH, Yun YH, et al. Changes in quality of life during palliative chemotherapy for solid cancer. Support Care Cancer 2005;13:515-21. https://doi.org/10.1007/s00520-004-0708-0.
- Bannink M, Van Gool AR, van der Heide A, van der Maas PJ. Psychiatric consultation and quality of decision making in euthanasia. Lancet 2000;356:2067-8. https://doi.org/10.1016/S0140-6736(00)03407-3.
- Barth J, Delfino S, Künzler A. Naturalistic study on the effectiveness of psycho-oncological interventions in cancer patients and their partners. Support Care Cancer 2013;21:1587-95. https://doi.org/10.1007/s00520-012-1700-8.
- Bartlett VL, Kiliu C, Finder S, Hackner D. Clinical ethics in the ICU: a case of attempted suicide. ICU Dir 2010;1:312-7. https://doi.org/10.1177/1944451610392520.
- Bassirpour G, Mahr G, Lee B, Torres M. The use of hospice care in end-stage psychiatric patients. J Palliat Med 2011;14:107-8. https://doi.org/10.1089/jpm.2009.0431.
- Battersby M, Kidd MR, Licinio J, Aylward P, Baker A, Ratcliffe J, et al. Improving cardiovascular health and quality of life in people with severe mental illness: study protocol for a randomised controlled trial. Trials 2018;19. https://doi.org/10.1186/s13063-018-2748-7.
- Bauer RL. Ethical considerations regarding end-of-life planning and palliative care needs in patients with chronic psychiatric disorders. Am J Psychiatry 2016;11:4-6. https://doi.org/10.1176/appi.ajp-rj.2016.110503.
- Baumrucker SJ, Sheldon JE, Stolick M, Oertli RK, Harrington D, Vandekieft G, et al. Ethics roundtable. Providing care in an unacceptable environment. Am J Hosp Palliat Care 2009;26:493-9. https://doi.org/10.1177/1049909109352230.
- Beechem MH. Maria: developing a culturally-sensitive treatment plan in pre-hospice south Texas. Hosp J 1995;10:19-34. https://doi.org/10.1080/0742-969x.1995.11882789.
- Beernaert K, Deliens L, Pardon K, van den Block L, Devroey D, Chambaere K, et al. What are physicians’ reasons for not referring people with life-limiting illnesses to specialist palliative care services? A nationwide survey. PLOS 2015;10. https://doi.org/10.1371/journal.pone.0137251.
- Bekelman DB, Allen LA, McBryde CF, Hattler B, Fairclough DL, Havranek EP, et al. Effect of a collaborative care intervention vs usual care on health status of patients with chronic heart failure: the CASA Randomized Clinical Trial. JAMA Intern Med 2018;178:511-19. https://doi.org/10.1001/jamainternmed.2017.8667.
- Bekelman DB, Johnson-Koenke R, Bowles DW, Fischer SM. Improving early palliative care with a scalable, stepped peer navigator and social work intervention: a single-arm clinical trial. J Palliat Med 2018;21:1011-16. https://doi.org/10.1089/jpm.2017.0424.
- Bergquist H, Ruth M, Hammerlid E. Psychiatric morbidity among patients with cancer of the esophagus or the gastro-esophageal junction: a prospective, longitudinal evaluation. Dis Esophagus 2007;20:523-9. https://doi.org/10.1111/j.1442-2050.2007.00741.x.
- Berlim MT, Mattevi BS, Duarte AP, Thomé FS, Barros EJ, Fleck MP. Quality of life and depressive symptoms in patients with major depression and end-stage renal disease: a matched-pair study. J Psychosom Res 2006;61:731-4. https://doi.org/10.1016/j.jpsychores.2006.04.011.
- Bernard M, Strasser F, Gamondi C, Braunschweig G, Forster M, Kaspers-Elekes K, et al. Impact of Existential and Psychological Determinants on the Perceived Quality of Life in Palliative Care Patients n.d.
- Black C, Hanson E, Cutcliffe J, Goward P. Palliative care nurses and mental health nurses: Sharing common ground?. Int J Palliat Nurs 2001;7:17-23. https://doi.org/10.12968/ijpn.2001.7.1.9039.
- Block SD, Billings JA. Patient requests to hasten death. Evaluation and management in terminal care. Arch Intern Med 1994;154:2039-47. https://doi.org/10.1001/archinte.1994.00420180041005.
- Block SD. Perspectives on care at the close of life. Psychological considerations, growth, and transcendence at the end of life: the art of the possible. JAMA 2001;285:2898-905. https://doi.org/10.1001/jama.285.22.2898.
- Block SD. Psychological issues in end-of-life care. J Palliat Med 2006;9:751-72. https://doi.org/10.1089/jpm.2006.9.751.
- Bloomer MJ, O’Brien AP. Palliative care for the person with a serious mental illness: the need for a partnership approach to care in Australia. Prog Palliat Care 2013;21:27-31. https://doi.org/10.1179/1743291X12Y.0000000033.
- Borowiak E, Al Harbi A, Bayoumi M, Al-Suwaida K, Al Ghonaim M, Mishkiry A. Quality of life of chronic hemodialysis and peritoneal dialysis patients. Clin Exp Med Lett 2009;50:37-42.
- Bove DG, Lavesen M, Jellington MO, Marsaa KB, Herling SF. First year experiences with a palliative out-patients structure for patients with COPD: a qualitative study of health professionals’ expectations and experiences. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0369-2.
- Bradley N, Davis L, Chow E. Symptom distress in patients attending an outpatient palliative radiotherapy clinic. J Pain Symptom Manage 2005;30:123-31. https://doi.org/10.1016/j.jpainsymman.2005.02.015.
- Braiteh F, El Osta B, Palmer JL, Reddy SK, Bruera E. Characteristics, findings, and outcomes of palliative care inpatient consultations at a comprehensive cancer center. J Palliat Med 2007;10:948-55. https://doi.org/10.1089/jpm.2006.0257.
- Bramstedt KA, Arroliga AC. On the dilemma of enigmatic refusal of life-saving therapy. Chest 2004;126:630-3. https://doi.org/10.1378/chest.126.2.630.
- Brandt HE, Deliens L, Ooms ME, van der Steen JT, van der Wal G, Ribbe MW. Symptoms, signs, problems, and diseases of terminally ill nursing home patients: a nationwide observational study in the Netherlands. Arch Intern Med 2005;165:314-20. https://doi.org/10.1001/archinte.165.3.314.
- Braverman DW, Marcus BS, Wakim PG, Mercurio MR, Kopf GS. Health care professionals’ attitudes about physician-assisted death: an analysis of their justifications and the roles of terminology and patient competency. J Pain Symptom Manage 2017;54:538-45.e3. https://doi.org/10.1016/j.jpainsymman.2017.07.024.
- Breitbart W, Jacobsen PB. Psychiatric symptom management in terminal care. Clin Geriatr Med 1996;12:329-47. https://doi.org/10.1016/S0749-0690(18)30230-1.
- Breitbart W, Bruera E, Chochinov H, Lynch M. Neuropsychiatric syndromes and psychological symptoms in patients with advanced cancer. J Pain Symptom Manage 1995;10:131-41. https://doi.org/10.1016/0885-3924(94)00075-V.
- Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Nelson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho-Oncology 2010;19:21-8. https://doi.org/10.1002/pon.1556.
- Breitbart W, Poppito S, Rosenfeld B, Vickers AJ, Li Y, Abbey J, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol 2012;30:1304-9. https://doi.org/10.1200/JCO.2011.36.2517.
- Breitbart W, Pessin H, Rosenfeld B, Applebaum AJ, Lichtenthal WG, Li Y, et al. Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: a randomized controlled trial in patients with advanced cancer. Cancer 2018;124:3231-9. https://doi.org/10.1002/cncr.31539.
- Brennan F, Collett G, Josland EA, Brown MA. The symptoms of patients with CKD stage 5 managed without dialysis. Prog Palliat Care 2015;23:267-73. https://doi.org/10.1179/1743291X14Y.0000000118.
- Brown R, Chambers S, Rosenberg J. Exploring palliative care nursing of patients with pre-existing serious persistent mental illness. Prog Palliat Care 2019;27:117-21. https://doi.org/10.1080/09699260.2019.1619964.
- Browne E. A Case of Breast Cancer in a Patient With Antipsychotic-Induced Hyperprolactinaemia n.d.
- Bruhn H, Bond CM, Elliott AM, Hannaford PC, Lee AJ, McNamee P, et al. Pharmacist-led management of chronic pain in primary care: results from a randomised controlled exploratory trial. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-002361.
- Buda F, Basello E, Lugano A, Pagani L. Psycho-emotional experience and the critical factors in 80 elderly patients undergoing terminal cancer stage. Asia Pac J Clin Oncol 2012;8.
- Buss MK, Lessen DS, Sullivan AM, Von Roenn J, Arnold RM, Block SD. Hematology/oncology fellows’ training in palliative care: results of a national survey. Cancer 2011;117:4304-11. https://doi.org/10.1002/cncr.25952.
- Byock I, Twohig JS, Merriman M, Collins K. Promoting excellence in end-of-life care: a report on innovative models of palliative care. J Palliat Med 2006;9:137-51. https://doi.org/10.1089/jpm.2006.9.137.
- Calderón C, Jimenez-Fonseca P, Jara C, Hernández R, Martínez de Castro E, Varma S, et al. Comparison of coping, psychological distress, and level of functioning in patients with gastric and colorectal cancer before adjuvant chemotherapy. J Pain Symptom Manage 2018;56:399-405. https://doi.org/10.1016/j.jpainsymman.2018.05.010.
- Campo-Engelstein L, Jankowski J, Mullen M. Should health care providers uphold the DNR of a terminally ill patient who attempts suicide?. HEC Forum 2016;28:169-74. https://doi.org/10.1007/s10730-015-9289-1.
- Candilis PJ, Foti ME, Holzer JC. End-of-life care and mental illness: a model for community psychiatry and beyond. Community Ment Health J 2004;40:3-16. https://doi.org/10.1023/b:comh.0000015214.24404.cc.
- Capozzo MA, Schillani G, Aguglia E, De Vanna M, Grassi L, Conte MA, et al. Serotonin transporter 5-HTTLPR polymorphism and response to citalopram in terminally ill cancer patients: report of twenty-one cases. Tumori 2009;95:479-83. https://doi.org/10.1177/030089160909500412.
- Carter GL, Clover KA, Parkinson L, Rainbird K, Kerridge I, Ravenscroft P, et al. Mental health and other clinical correlates of euthanasia attitudes in an Australian outpatient cancer population. Psycho-Oncology 2007;16:295-303. https://doi.org/10.1002/pon.1058.
- Check DK, Kwan ML, Chawla N, Dusetzina SB, Valice E, Ergas IJ, et al. Opportunities to improve detection and treatment of depression among patients with breast cancer treated in an integrated delivery system. J Pain Symptom Manage 2019;57:587-95. https://doi.org/10.1016/j.jpainsymman.2018.11.024.
- Chochinov HM. Palliative care: an opportunity for mental health professionals. Can J Psychiatry 2004;49:347-9. https://doi.org/10.1177/070674370404900601.
- Chou FH, Tsai KY, Wu HC, Shen SP. Cancer in patients with schizophrenia: what is the next step?. Psychiatry Clin Neurosci 2016;70:473-88. https://doi.org/10.1111/pcn.12420.
- Choudhry A, Srinivasan S, Bouknight JG. Comorbid mental health disorders in hospice consultation in geriatric psychiatry training: a retrospective review. Am J Geriatr Psychiatry 2015;23:S104-6. https://doi.org/10.1016/j.jagp.2014.12.105.
- Close H, Reilly J, Mason JM, Kripalani M, Wilson D, Main J, et al. Renal failure in lithium-treated bipolar disorder: a retrospective cohort study. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0090169.
- Cohen M, Dembling B, Schorling J. The association between schizophrenia and cancer: a population-based mortality study. Schizophr Res 2002;57:139-46. https://doi.org/10.1016/S0920-9964(01)00308-5.
- Craun MJ, Watkins M, Hefty A. Hospice care of the psychotic patient. Am J Hosp Palliat Care 1997;14:205-8. https://doi.org/10.1177/104990919701400409.
- Crump C, Sundquist K, Winkleby MA, Sundquist J. Comorbidities and mortality in bipolar disorder: a Swedish national cohort study. JAMA Psychiatry 2013;70:931-9. https://doi.org/10.1001/jamapsychiatry.2013.1394.
- Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry 2013;170:324-33. https://doi.org/10.1176/appi.ajp.2012.12050599.
- Davie E. A social work perspective on palliative care for people with mental health problems. Eur J Palliat Care 2006;13:26-8.
- den Boer K, de Veer AJE, Schoonmade LJ, Verhaegh KJ, van Meijel B, Francke AL. A systematic review of palliative care tools and interventions for people with severe mental illness. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2078-7.
- Dinnen T, Armstrong H, Perkins P. Managing an intentional overdose in a hospice. BMJ Support Palliat Care 2018;8:189-90. https://doi.org/10.1136/bmjspcare-2016-001219.
- Doering P. End-of-life care and serious persistent mental illness. Reg Palliat Care Serv 2018.
- Donald EE, Stajduhar KI. A scoping review of palliative care for persons with severe persistent mental illness. Palliat Support Care 2019;17:479-87. https://doi.org/10.1017/S1478951519000087.
- Dube G. Excellent outcomes of kidney transplant in patients with bipolar disorder. Am J Transplant 2013;13.
- Durkin I, Keorney M, O’Slorain L. Psychiatric disorder in a palliative care unit. Palliat Med 2003;17:212-18. https://doi.org/10.1191/0269216303pm670oa.
- Evenblij K. Palliative Care for Patients With and Without Psychiatric Illness: A Nationwide Survey Study in The Netherlands 2018.
- Fairman N, Irwin SA. Palliative care psychiatry: update on an emerging dimension of psychiatric practice. Curr Psychiatry Rep 2013;15. https://doi.org/10.1007/s11920-013-0374-3.
- Farasatpour M, Janardhan R, Williams CD, Margenthaler JA, Virgo KS, Johnson FE. Breast cancer in patients with schizophrenia. Am J Surg 2013;206:798-804. https://doi.org/10.1016/j.amjsurg.2012.06.013.
- Feldman DB. Posttraumatic stress disorder at the end of life: extant research and proposed psychosocial treatment approach. Palliat Support Care 2011;9:407-18. https://doi.org/10.1017/S1478951511000435.
- Filiberti A, Ripamonti C, Totis A, Ventafridda V, De Conno F, Contiero P, et al. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. J Pain Symptom Manage 2001;22:544-53. https://doi.org/10.1016/S0885-3924(01)00295-0.
- Flick RJ. Palliative care, if not in name: a compassionate violation of opioid prescribing guidelines. J Gen Intern Med 2018;33.
- Forster BC, Proskurin H, Kelly B, Lovell MR, Ilchef R, Clayton JM. Psychiatry trainees’ views and educational needs regarding the care of patients with a life-limiting illness. Palliat Support Care 2017;15:231-41. https://doi.org/10.1017/S1478951516000365.
- Frei A, Schenker TA, Finzen A, Kräuchi K, Dittmann V, Hoffmann-Richter U. Assisted suicide as conducted by a ‘Right-to-Die’-society in Switzerland: a descriptive analysis of 43 consecutive cases. Swiss Med Wkly 2001;131:375-80.
- Fried TR, Gillick MR. Medical decision-making in the last six months of life: choices about limitation of care. J Am Geriatr Soc 1994;42:303-7. https://doi.org/10.1111/j.1532-5415.1994.tb01756.x.
- Fujioka JK, Mirza RM, McDonald PL, Klinger CA. Implementation of medical assistance in dying: a scoping review of health care providers’ perspectives. J Pain Symptom Manage 2018;55:1564-76.e9. https://doi.org/10.1016/j.jpainsymman.2018.02.011.
- Fukunishi I, Kitaoka T, Shirai T, Kino K, Kanematsu E, Sato Y. Psychiatric disorders among patients undergoing hemodialysis therapy. Nephron 2002;91:344-7. https://doi.org/10.1159/000058418.
- Gao Y, Wei Y, Yang W, Jiang L, Li X, Ding J, et al. The effectiveness of music therapy for terminally ill patients: a meta-analysis and systematic review. J Pain Symptom Manage 2019;57:319-29. https://doi.org/10.1016/j.jpainsymman.2018.10.504.
- Gardner-Sood P, Lally J, Smith S, Atakan Z, Ismail K, Greenwood KE, et al. Cardiovascular risk factors and metabolic syndrome in people with established psychotic illnesses: baseline data from the IMPaCT randomized controlled trial. Psychol Med 2015;45:2619-29. https://doi.org/10.1017/S0033291715000562.
- Garrido MM, Prigerson HG, Neupane S, Penrod JD, Johnson CE, Boockvar KS. Mental illness and mental healthcare receipt among hospitalized veterans with serious physical illnesses. J Palliat Med 2017;20:247-52. https://doi.org/10.1089/jpm.2016.0261.
- Gil F, Costa G, Pérez FJ. Does chemotherapy reduce stress?. Palliat Support Care 2010;8:455-60. https://doi.org/10.1017/S1478951510000337.
- Gillick MR, Mendes ML. Medical care in old age: what do nurses in long-term care consider appropriate?. J Am Geriatr Soc 1996;44:1322-5. https://doi.org/10.1111/j.1532-5415.1996.tb01402.x.
- Ginieri-Coccossis M, Theofilou P, Synodinou C, Tomaras V, Soldatos C. Quality of life, mental health and health beliefs in haemodialysis and peritoneal dialysis patients: investigating differences in early and later years of current treatment. BMC Nephrol 2008;9. https://doi.org/10.1186/1471-2369-9-14.
- Glick DM, Cook JM, Moye J, Kaiser AP. Assessment and treatment considerations for post traumatic stress disorder at end of life. Am J Hosp Palliat Care 2018;35:1133-9. https://doi.org/10.1177/1049909118756656.
- Granek L, Nakash O, Ariad S, Shapira S, Ben-David M. Strategies and barriers in addressing mental health and suicidality in patients with cancer. Oncol Nurs Forum 2019;46:561-71. https://doi.org/10.1188/19.ONF.561-571.
- Grigoletti L, Perini G, Rossi A, Biggeri A, Barbui C, Tansella M, et al. Mortality and cause of death among psychiatric patients: a 20-year case-register study in an area with a community-based system of care. Psychol Med 2009;39:1875-84. https://doi.org/10.1017/S0033291709005790.
- Groenewoud JH, van der Maas PJ, van der Wal G, Hengeveld MW, Tholen AJ, Schudel WJ, et al. Physician-assisted death in psychiatric practice in the Netherlands. N Engl J Med 1997;336:1795-801. https://doi.org/10.1056/NEJM199706193362506.
- Güth U, Myrick ME, Reisch T, Bosshard G, Schmid SM. Suicide in breast cancer patients: an individual-centered approach provides insight beyond epidemiology. Acta Oncol 2011;50:1037-44. https://doi.org/10.3109/0284186X.2011.602112.
- Habraken JM, ter Riet G, Gore JM, Greenstone MA, Weersink EJ, Bindels PJ, et al. Health-related quality of life in end-stage COPD and lung cancer patients. J Pain Symptom Manage 2009;37:973-81. https://doi.org/10.1016/j.jpainsymman.2008.07.010.
- Harris J, Xiang M, Chang D, Pollom E. The burden of mental health disorders among elderly patients with gastrointestinal malignancies. Int J Radiat Oncol Biol Phys 2019;103:E30-1. https://doi.org/10.1016/S0360-3016(19)30470-5.
- Hawkins M. Breaking the silence – the terminally ill mental health client. Aust Nurs Midwifery J 2016;24.
- Hay JL, Passik SD. The cancer patient with borderline personality disorder: suggestions for symptom-focused management in the medical setting. Psycho-Oncology 2000;9:91-100. https://doi.org/10.1002/(SICI)1099-1611(200003/04)9:2<91::AID-PON437>3.0.CO;2-8.
- Henderson JM, Ord RA. Suicide in head and neck cancer patients. J Oral Maxillofac Surg 1997;55:1217-21. https://doi.org/10.1016/S0278-2391(97)90170-1.
- Henoch I, Bergman B, Gustafsson M, Gaston-Johansson F, Danielson E. The impact of symptoms, coping capacity, and social support on quality of life experience over time in patients with lung cancer. J Pain Symptom Manage 2007;34:370-9. https://doi.org/10.1016/j.jpainsymman.2006.12.005.
- Henriksson MM, Isometsä ET, Hietanen PS, Aro HM, Lönnqvist JK. Mental disorders in cancer suicides. J Affect Disord 1995;36:11-20. https://doi.org/10.1016/0165-0327(95)00047-X.
- Hietanen P, Lönnqvist J, Henriksson M, Jallinoja P. Do cancer suicides differ from others?. Psycho-Oncology 1994;3:189-95. https://doi.org/10.1002/pon.2960030305.
- Hindley G, Stephenson LA, Ruck Keene A, Rifkin L, Gergel T, Owen G. Why have I not been told about this?’: a survey of experiences of and attitudes to advance decision-making amongst people with bipolar. Wellcome Open Res 2019;4. https://doi.org/10.12688/wellcomeopenres.14989.2.
- Hinton J. Psychiatric consultation in fatal illness. Proc R Soc Med 1972;65:1035-8. https://doi.org/10.1177/003591577206501164.
- Holmes ACN, Adams SJ, Hall S, Rosenthal MA, Drummond KJ. Liaison psychiatry in a central nervous system tumor service. Neurooncol Pract 2015;2:88-92. https://doi.org/10.1093/nop/npv001.
- Hwang M, Farasatpour M, Williams CD, Margenthaler JA, Virgo KS, Johnson FE. Adjuvant chemotherapy for breast cancer in patients with schizophrenia. Oncol Lett 2012;3:845-50. https://doi.org/10.3892/ol.2012.560.
- Iachina M, Ljungdalh PM, Sørensen RG, Kaerlev L, Blaakær J, Trosko O, et al. Influence of prior psychiatric disorders on the treatment course of gynaecological cancer – a nationwide cohort study. Clin Oncol 2019;31:115-23. https://doi.org/10.1016/j.clon.2018.11.006.
- Inagaki T, Yasukawa R, Okazaki S, Yasuda H, Kawamukai T, Utani E, et al. Factors disturbing treatment for cancer in patients with schizophrenia. Psychiatry Clin Neurosci n.d.;60:327-31. https://doi.org/10.1111/j.1440-1819.2006.01509.x.
- Iordanidis P, Alivanis P, Iakovidis A, Dombros N, Tsagalidis I, Balaskas E, et al. Psychiatric and psychosocial status of elderly patients undergoing dialysis. Perit Dial Int 1993;13:192-5. https://doi.org/10.1177/089686089301302S46.
- Irwin SA, Rao S, Bower K, Palica J, Rao SS, Maglione JE, et al. Psychiatric issues in palliative care: recognition of depression in patients enrolled in hospice care. J Palliat Med 2008;11:158-63. https://doi.org/10.1089/jpm.2007.0140.
- Irwin SA, Montross LP, Bhat RG, Nelesen RA, von Gunten CF. Psychiatry resident education in palliative care: opportunities, desired training, and outcomes of a targeted educational intervention. Psychosomatics 2011;52:530-6. https://doi.org/10.1016/j.psym.2011.08.002.
- Irwin KE, Park ER, Shin JA, Fields LE, Jacobs JM, Greer JA, et al. Predictors of disruptions in breast cancer care for individuals with schizophrenia. Oncologist 2017;22:1374-82. https://doi.org/10.1634/theoncologist.2016-0489.
- Jackson AJ, Colombo R, Baer S, Young L, Waller J, Kheda M, et al. Risk Factors for Mortality in Patients With Schizophrenia and End-Stage Renal Disease 2018.
- Jamison NK, Holmes EG. A case of mast cell leukemia: a review of the pathophysiology of systemic mastocytosis and associated psychiatric symptoms. Psychosomatics 2018;59:517-21. https://doi.org/10.1016/j.psym.2018.02.002.
- Jarero IN, Lucina A, Susana U, Garcia LE. The EMDR integrative group treatment protocol for patients with cancer. J EMDR Pract Res 2016;10:199-207. https://doi.org/10.1891/1933-3196.10.3.199.
- Jeffery DD, Art Ambrosio L, Hopkins L, Burke HB. Mental health comorbidities and cost/utilization outcomes in head and neck cancer patients. J Psychosoc Oncol 2019;37:301-18. https://doi.org/10.1080/07347332.2018.1519626.
- Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand 2008;118:169-71. https://doi.org/10.1111/j.1600-0447.2008.01211.x.
- Kadan-Lottick NS, Vanderwerker LC, Block SD, Zhang B, Prigerson HG. Psychiatric disorders and mental health service use in patients with advanced cancer: a report from the coping with cancer study. Cancer 2005;104:2872-81. https://doi.org/10.1002/cncr.21532.
- Kaerlev L, Iachina M, Trosko O, Qvist N, Ljungdalh PM, Nørgård BM. Colon cancer patients with a serious psychiatric disorder present with a more advanced cancer stage and receive less adjuvant chemotherapy – a Nationwide Danish Cohort Study. BMC Cancer 2018;18. https://doi.org/10.1186/s12885-018-4879-3.
- Kardinal CG, Porter GH. The psychologic care of the cancer patient. Compr Psychol Care Cancer Patient 1981;7:65-70.
- Kaufman KR. Lamotrigine and hemodialysis in bipolar disorder: case analysis of dosing strategy with literature review. Bipolar Disord 2010;12:446-9. https://doi.org/10.1111/j.1399-5618.2010.00818.x.
- Kelly BD, Shanley D. Terminal illness and schizophrenia. J Palliat Care 2000;16:55-7. https://doi.org/10.1177/082585970001600210.
- Kim SY, De Vries RG, Peteet JR. Euthanasia and assisted suicide of patients with psychiatric disorders in the Netherlands 2011 to 2014. JAMA Psychiatry 2016;73:362-8. https://doi.org/10.1001/jamapsychiatry.2015.2887.
- Kimmel PL, Thamer M, Richard CM, Ray NF. Psychiatric illness in patients with end-stage renal disease. Am J Med 1998;105:214-21. https://doi.org/10.1016/S0002-9343(98)00245-9.
- King DA, Heusel MJ, Lyness JM. Assessment and psychological treatment of depression in older adults with terminal or life-threatening illness. Clin Psychol Sci Pract 2005;12:339-53.
- Kisely S, Sadek J, MacKenzie A, Lawrence D, Campbell LA. Excess cancer mortality in psychiatric patients. Can J Psychiatry 2008;53:753-61. https://doi.org/10.1177/070674370805301107.
- Kisely S, Crowe E, Lawrence D. Cancer-related mortality in people with mental illness. JAMA Psychiatry 2013;70:209-17. https://doi.org/10.1001/jamapsychiatry.2013.278.
- Kisely S, Forsyth S, Lawrence D. Why do psychiatric patients have higher cancer mortality rates when cancer incidence is the same or lower?. Aust N Z J Psychiatry 2016;50:254-63. https://doi.org/10.1177/0004867415577979.
- Kissane DW, Smith GC. Consultation-liaison psychiatry in an Australian oncology unit. Aust N Z J Psychiatry 1996;30:397-404. https://doi.org/10.3109/00048679609065005.
- Kissane DW, Grabsch B, Love A, Clarke DM, Bloch S, Smith GC. Psychiatric disorder in women with early stage and advanced breast cancer: a comparative analysis. Aust N Z J Psychiatry 2004;38:320-6. https://doi.org/10.1080/j.1440-1614.2004.01358.x.
- Kleiboer A, Bennett F, Hodges L, Walker J, Thekkumpurath P, Sharpe M. The problems reported by cancer patients with major depression. Psycho-Oncology 2011;20:62-8. https://doi.org/10.1002/pon.1708.
- Lacy TJ, Higgins MJ. Integrated medical-psychiatric care of a dying borderline patient: a case of dynamically informed ‘practical psychotherapy’. J Am Acad Psychoanal Dyn Psychiatry 2005;33:619-36. https://doi.org/10.1521/jaap.2005.33.4.619.
- Lamers WM. Symptom control in end-of-life care: pain, eating, acute illnesses, panic attacks, and aggressive care. J Pain Palliat Care Pharmacother 2005;19:71-5. https://doi.org/10.1080/J354v19n04_12.
- Lawrence D, Kisely S. Inequalities in healthcare provision for people with severe mental illness. J Psychopharmacol 2010;24:61-8. https://doi.org/10.1177/1359786810382058.
- Legler A, Bradley EH, Carlson MD. The effect of comorbidity burden on health care utilization for patients with cancer using hospice. J Palliat Med 2011;14:751-6. https://doi.org/10.1089/jpm.2010.0504.
- Lehto R, Miller S, Flanigan M, Wyatt G. Psychological well-being in patients with advanced cancer at the end of life. Psycho-Oncology 2019;28:77-8.
- Lent B, Brown-Bradley K. Case report: treating a mentally ill patient with serious medical problems. Can Fam Physician 1999;45:1743-4.
- Levine PM, Silberfarb PM, Lipowski ZJ. Mental disorders in cancer patients: a study of 100 psychiatric referrals. Cancer 1978;42:1385-91. https://doi.org/10.1002/1097-0142(197809)42:3<1385::aid-cncr2820420349>3.0.co;2-0.
- Levinson P. Obstacles in the treatment of dying patients. Am J Psychiatry 1975;132:28-32. https://doi.org/10.1176/ajp.132.1.28.
- Lichtenthal WG, Nilsson M, Zhang B, Trice ED, Kissane DW, Breitbart W, et al. Do rates of mental disorders and existential distress among advanced stage cancer patients increase as death approaches?. Psycho-Oncology 2009;18:50-61. https://doi.org/10.1002/pon.1371.
- Liu CH, Yeh MK, Weng SC, Bai MY, Chang JC. Suicide and chronic kidney disease: a case-control study. Nephrol Dial Transplant 2017;32:1524-9. https://doi.org/10.1093/ndt/gfw244.
- Lloyd-Williams M, Friedman T, Rudd N. A survey of psychosocial service provision within hospices. Palliat Med 1999;13:431-2. https://doi.org/10.1191/026921699672181597.
- Lloyd-Williams M, Abba K, Crowther J. Supportive and palliative care for patients with chronic mental illness including dementia. Curr Opin Support Palliat Care 2014;8:303-7. https://doi.org/10.1097/SPC.0000000000000064.
- Macleod AD. Palliative medicine and psychiatry. J Palliat Med 2013;16:340-1. https://doi.org/10.1089/jpm.2013.9517.
- Madeira N, Albuquerque E, Santos T, Mendes A, Roque M. Death ideation in cancer patients: contributing factors. J Psychosoc Oncol 2011;29:636-42. https://doi.org/10.1080/07347332.2011.615381.
- Madrigal M. Understanding end-of-life care in schizophrenia mortality, stigma, and innovations. Int Soc Psychol Treat Schizophr Psychoses-US Chap Newsl 2010;11:202010-11.
- Maguire P, Walsh S, Jeacock J, Kingston R. Physical and psychological needs of patients dying from colorectal cancer. Palliat Med 1999;13:45-50. https://doi.org/10.1177/026921639901300106.
- Martiny C, e Silva AC, Neto JP, Nardi AE. Psychiatric disorders in patients with end-stage renal disease. J Ren Care 2012;38:131-7. https://doi.org/10.1111/j.1755-6686.2012.00261.x.
- Masel EK, Berghoff AS, Mladen A, Schur S, Maehr B, Kirchhoff M, et al. Psyche at the end of life: psychiatric symptoms are prevalent in patients admitted to a palliative care unit. Palliat Support Care 2016;14:250-8. https://doi.org/10.1017/S1478951515000899.
- Maull F. Dying in prison: sociocultural and psychosocial dynamics. Hosp J 1991;7:127-42. https://doi.org/10.1080/0742-969x.1991.11882695.
- McDaniel JS, Stoudemire A, Riether AM, Firestone S, Cohen-Cole SA, Cobbs BW. Terminal cardiomyopathy, splitting, and borderline personality organization. Gen Hosp Psychiatry 1992;14:277-84. https://doi.org/10.1016/0163-8343(92)90099-V.
- Medenica S, Racic M, Vukovic M, Ristic S, Karic J. The role of the psychiatrist in obtaining informed consent from patients with somatic and mental comorbidity: report of one case. Rev Med Chil 2014;142:512-15. https://doi.org/10.4067/S0034-98872014000400014.
- Meyer F, Block S. Personality disorders in the oncology setting. J Support Oncol 2011;9:44-51. https://doi.org/10.1016/j.suponc.2011.02.002.
- Meyer AA, Hwang M, Farasatpour M, Janardhan R, Margenthaler JA, Virgo KS, et al. Metastatic breast cancer in patients with schizophrenia. Mol Clin Oncol 2013;1:359-64. https://doi.org/10.3892/mco.2012.44.
- Miller L. A Multi-Disciplinary Systemic Approach to Caring for the Complex Patient With Serious Mental Illness During Chemotherapy (Including Tips for Safely Managing Psychotropics and Steroid Therapy) n.d.
- Miovic M, Block S. Psychiatric disorders in advanced cancer. Cancer 2007;110:1665-76. https://doi.org/10.1002/cncr.22980.
- Morasso G, Capelli M, Viterbori P, Di Leo S, Alberisio A, Costantini M, et al. Psychological and symptom distress in terminal cancer patients with met and unmet needs. J Pain Symptom Manage 1999;17:402-9. https://doi.org/10.1016/S0885-3924(99)00034-2.
- Moskowitz EH. Mental illness, physical illness, and the legalization of physician-assisted suicide. Fordham Urban Law J 1997;24:781-94.
- Moss D. Transient paranoia and the ‘gift’ in terminal illness. Br J Med Psychol 1980;53:155-9. https://doi.org/10.1111/j.2044-8341.1980.tb01431.x.
- Mucsi I, Bansal A, Jeannette M, Famure O, Li Y, Novak M, et al. Mental health and behavioral barriers in access to kidney transplantation: a Canadian cohort study. Transplantation 2017;101:1182-90. https://doi.org/10.1097/TP.0000000000001362.
- Muir-Cochrane E. Medical co-morbidity risk factors and barriers to care for people with schizophrenia. J Psychiatr Ment Health Nurs 2006;13:447-52. https://doi.org/10.1111/j.1365-2850.2006.01002.x.
- Mulder ME, Verwey B, van Waarde JA. Electroconvulsive therapy in a terminally ill patient: when every day of improvement counts. J ECT 2012;28:52-3. https://doi.org/10.1097/YCT.0b013e3182321181.
- Myhill KJ. In their hour of need - addressing issues of psyche and soma at end of life. J Pharm Pract Res 2014;44:75-7. https://doi.org/10.1002/jppr.1023.
- Nash M. Mental healthcare training needs of oncology nurses in Ireland. Cancer Nurs Pract 2017;16:32-8. https://doi.org/10.7748/cnp.2017.e1348.
- Neely KJ, Roxe DM. Palliative care/hospice and the withdrawal of dialysis. J Palliat Med 2000;3:57-6. https://doi.org/10.1089/jpm.2000.3.57.
- Ng PN. Consultation Liaison and Integrated Care for COPD Patients With Psychiatric Co-Morbidity 2012.
- Ng CG, Dijkstra E, Smeets H, Boks MP, de Wit NJ. Psychiatric comorbidity among terminally ill patients in general practice in the Netherlands: a comparison between patients with cancer and heart failure. Br J Gen Pract 2013;63:e63-8. https://doi.org/10.3399/bjgp13X660797.
- Ng CG, Boks MP, Roes KC, Zainal NZ, Sulaiman AH, Tan SB, et al. Rapid response to methylphenidate as an add-on therapy to mirtazapine in the treatment of major depressive disorder in terminally ill cancer patients: a four-week, randomized, double-blinded, placebo-controlled study. Eur Neuropsychopharmacol 2014;24:491-8. https://doi.org/10.1016/j.euroneuro.2014.01.016.
- Nipp RD, El-Jawahri A, Moran SM, D’Arpino SM, Johnson PC, Lage DE, et al. The relationship between physical and psychological symptoms and health care utilization in hospitalized patients with advanced cancer. Cancer 2017;123:4720-7. https://doi.org/10.1002/cncr.30912.
- O’Connor M, Fisher C, Guilfoyle A. Interdisciplinary teams in palliative care: a critical reflection. Int J Palliat Nurs 2006;12:132-7. https://doi.org/10.12968/ijpn.2006.12.3.20698.
- Ogawa A, Shimizu K, Akizuki N, Uchitomi Y. Involvement of a psychiatric consultation service in a palliative care team at the Japanese cancer center hospital. Jpn J Clin Oncol 2010;40:1139-46. https://doi.org/10.1093/jjco/hyq147.
- O’Mahony S, Bines S, Gerhart J, Bagwell E, Marlene M, Card A. Managing pain in patients with chronic medical illnesses and serious mental illnesses. Am J Hosp Palliat Care 2018;35:825-8. https://doi.org/10.1177/1049909117739300.
- Onishi H, Okuno S, Yae S, Sairenji M, Onose M, Mizuno Y, et al. Brief psychotic disorder mimicking the symptoms of cerebrovascular attack evoked by symptoms that symbolized death in a patient with terminal stage stomach cancer: case report and review of the literature. Palliat Support Care 2006;4:87-9. https://doi.org/10.1017/s147895150606010x.
- Owen C, Tennant C, Jones M. Cancer patients’ attitudes to final events in life: wish for death, attitudes to cessation of treatment, suicide and euthanasia. Psycho-Oncology 1994;3:1-9. https://doi.org/10.1002/pon.2960030103.
- Ozenli Y, Giray S, Sagliker Y, Adam SM. A controlled study of psychiatric manifestations and electroencephalography findings in chronic kidney disease patients with Sagliker syndrome. J Ren Nutr 2010;20:51-5. https://doi.org/10.1053/j.jrn.2010.06.001.
- Paice JA. Managing psychological conditions in palliative care. Am J Nurs 2002;102:36-42. https://doi.org/10.1097/00000446-200211000-00023.
- Parkerson GR, Gutman RA. Perceived mental health and disablement of primary care and end-stage renal disease patients. Int J Psychiatry Med 1997;27:33-45. https://doi.org/10.2190/PWUP-AB1N-2YPL-KDG8.
- Payne S, Haines R. The contribution of psychologists to specialist palliative care. Int J Palliat Nurs 2002;8:401-6. https://doi.org/10.12968/ijpn.2002.8.8.10684.
- Payne A, Kelleher MJ, O’Brien T. Liaison psychiatry in palliative care. Ir J Psychol Med 2004;21:25-7. https://doi.org/10.1017/S0790966700008132.
- Pengelly M, Purnell D. An audit of levels of psychological support referrals for cancer patients. Cancer Nurs Pract 2009;8:34-8. https://doi.org/10.7748/cnp2009.02.8.1.34.c6840.
- Perr IN. Right to refuse treatment and delayed medical care for psychiatric patients. Am J Psychiatry 1985;142. https://doi.org/10.1176/ajp.142.9.1127b.
- Peteet JR, Meyer F, deLima Thomas J, Vitagliano HL. Psychiatric indications for admission to an inpatient palliative care unit. J Palliat Med 2009;12:521-4. https://doi.org/10.1089/jpm.2009.0015.
- Phongtankuel V, Meador L, Adelman RD, Roberts J, Henderson CR, Mehta SS, et al. Multicomponent palliative care interventions in advanced chronic diseases: a systematic review. Am J Hosp Palliat Care 2018;35:173-83. https://doi.org/10.1177/1049909116674669.
- Popa-Velea O, Cernat B, Tambu A. Influence of personalized therapeutic approach on quality of life and psychiatric comorbidity in patients with advanced colonic cancer requiring palliative care. J Med Life 2010;3:343-7.
- Quentzel SJ, Levine S. Aggressive lithium treatment for mania in a hemodialysis patient with end-stage renal disease. Psychosomatics 1997;38:398-9. https://doi.org/10.1016/S0033-3182(97)71453-1.
- Quipourt V, Jooste V, Cottet V, Faivre J, Bouvier AM. Comorbidities alone do not explain the undertreatment of colorectal cancer in older adults: a French population-based study. J Am Geriatr Soc 2011;59:694-8. https://doi.org/10.1111/j.1532-5415.2011.03334.x.
- Rajmohan V, Kumar SK. Psychiatric morbidity, pain perception, and functional status of chronic pain patients in palliative care. Indian J Palliat Care 2013;19:146-51. https://doi.org/10.4103/0973-1075.121527.
- Ramos K, Fulton JJ. Integrating dignity therapy and family therapy in palliative care: a case study of multiple sclerosis, depression, and comorbid cancer. J Palliat Med 2017;20. https://doi.org/10.1089/jpm.2016.0495.
- Rasmussen KG, Richardson JW. Electroconvulsive therapy in palliative care. Am J Hosp Palliat Care 2011;28:375-7. https://doi.org/10.1177/1049909110390203.
- Rayner HC, Pisoni RL, Bommer J, Canaud B, Hecking E, Locatelli F, et al. Mortality and hospitalization in haemodialysis patients in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 2004;19:108-20. https://doi.org/10.1093/ndt/gfg483.
- Rayner L, Price A, Evans A, Valsraj K, Hotopf M, Higginson IJ. Antidepressants for the treatment of depression in palliative care: systematic review and meta-analysis. Palliat Med 2011;25:36-51. https://doi.org/10.1177/0269216310380764.
- Reeve J, Lloyd-Williams M, Dowrick C. Depression in terminal illness: the need for primary care-specific research. Fam Pract 2007;24:263-8. https://doi.org/10.1093/fampra/cmm017.
- Reinke LF, Slatore CG, Udris EM, Moss BR, Johnson EA, Au DH. The association of depression and preferences for life-sustaining treatments in veterans with chronic obstructive pulmonary disease. J Pain Symptom Manage 2011;41:402-11. https://doi.org/10.1016/j.jpainsymman.2010.05.012.
- Relyea E, MacDonald B, Cattaruzza C, Marshall D. On the margins of death: a scoping review on palliative care and schizophrenia. J Palliat Care 2019;34:62-9. https://doi.org/10.1177/0825859718804108.
- Rhondali W, Ledoux M, Sahraoui F, Marotta J, Sanchez V, Filbet M. Management of psychiatric inpatients with advanced cancer: a pilot study. Bull Cancer 2013;100:819-27. https://doi.org/10.1684/bdc.2013.1796.
- Riquin E, Hubault P, Baize N, Lhuillier JP, Duverger P. Specificities of support palliative care of a patient suffering from schizophrenia in psychiatric hospital. Ann Med Psychol 2017;175:140-5. https://doi.org/10.1016/j.amp.2016.06.003.
- Sanders J, Berrier A, Nshuti L, Lindvall C, Tulsky J. Differences by race, religion, and mental health in preferences for life-prolonging treatment in adverse health states: results from a national sample of Medicare beneficiaries. J Pain Symptom Manage 2019;57:378-9. https://doi.org/10.1016/j.jpainsymman.2018.12.059.
- Saracino RM, Jutagir DR, Cunningham A, Foran-Tuller KA, Driscoll MA, Sledge WH, et al. Psychiatric comorbidity, health-related quality of life, and mental health service utilization among patients awaiting liver transplant. J Pain Symptom Manage 2018;56:44-52. https://doi.org/10.1016/j.jpainsymman.2018.03.001.
- Sato K, Higuchi H, Yoshida K, Takahashi H, Shimizu T, Watanabe J. Milnacipran treatment of a terminally ill cancer patient with major depressive disorder. Hum Psychopharmacol 2004;19:431-2. https://doi.org/10.1002/hup.605.
- Scott JK, Taylor DM, Dudley CRK. Intravenous drug users who require dialysis: causes of renal failure and outcomes. Clin Kidney J 2018;11:270-4. https://doi.org/10.1093/ckj/sfx090.
- Shalev D, Brewster KK, Levenson JA. End-of-life care for patients with schizophrenia #332. J Palliat Med 2017;20:787-8. https://doi.org/10.1089/jpm.2017.0164.
- Sharma A, Ngann S, Nandoskar A, Lowdell C, Lewis JS, Hogben K, et al. Schizophrenia does not adversely affect the treatment of women with breast cancer: a cohort study. The Breast 2010;19:410-2. https://doi.org/10.1016/j.breast.2010.04.001.
- Sharma TR, Baker GM, Kline DB. ‘Holes in my head’: a case of primary delusional parasitosis in a patient with end-stage renal disease. Prim Care Companion J Clin Psychiatry 2012;14. https://doi.org/10.4088/PCC.11l01229.
- Shipman C, Gysels M, White P, Worth A, Murray SA, Barclay S, et al. Improving generalist end of life care: national consultation with practitioners, commissioners, academics, and service user groups. BMJ 2008;337. https://doi.org/10.1136/bmj.a1720.
- Snyder DK, Whisman MA. Treating distressed couples with coexisting mental and physical disorders: directions for clinical training and practice. J Marital Fam Ther 2004;30:1-12. https://doi.org/10.1111/j.1752-0606.2004.tb01218.x.
- Spencer RJ, Ray A, Pirl WF, Prigerson HG. Clinical correlates of suicidal thoughts in patients with advanced cancer. Am J Geriatr Psychiatry 2012;20:327-36. https://doi.org/10.1097/JGP.0b013e318233171a.
- Stedeford A, Bloch S. The psychiatrist in the terminal care unit. Br J Psychiatry 1979;135:1-6. https://doi.org/10.1192/bjp.135.1.1.
- Stein GL, Leff V, Pincus HA, Remke SS, Hilliard R. Providing palliative care to patients and families with pre-existing mental health and substance use issues. J Pain Symptom Manage 2018;55:550-1. https://doi.org/10.1016/j.jpainsymman.2017.11.067.
- Talbott JA, Linn L. Reactions of schizophrenics to life-threatening disease. Psychiatr Q 1978;50:218-27. https://doi.org/10.1007/BF01064712.
- Tate FB, Longo DA. Death and dying: implications for inpatient, psychiatric care. Palliat Support Care 2005;3:239-43. https://doi.org/10.1017/s1478951505050364.
- Taylor EJ, Golas L, Martel JR, Martel JB. Advanced basal cell carcinoma in a patient with schizoaffective disorder: constraints and management. Ophthalmic Plast Reconstr Surg 2013;29:e49-51. https://doi.org/10.1097/IOP.0b013e31826a24cb.
- Taylor C, Fertal JC, Liao S. Refractory schizophrenia, attempted suicide, and withdrawal of life support: a clinical ethics case report. J Pain Symptom Manage 2018;56:153-7. https://doi.org/10.1016/j.jpainsymman.2018.02.014.
- Terpstra TL, Terpstra TL. Hospice and palliative care for terminally ill individuals with serious and persistent mental illness: widening the horizons. J Psychosoc Nurs Ment Health Serv 2012;50:28-34. https://doi.org/10.3928/02793695-20120807-02.
- Trachsel M. The ethical importance of assessing end-of-life care preferences in patients with severe and persistent mental illness. Am J Geriatr Psychiatry 2018;26:98-9. https://doi.org/10.1016/j.jagp.2017.09.026.
- Trachsel M, Irwin SA, Biller-Andorno N, Hoff P, Riese F. Palliative psychiatry for severe persistent mental illness as a new approach to psychiatry? Definition, scope, benefits, and risks. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0970-y.
- Trachsel M, Hodel MA, Irwin SA, Hoff P, Biller-Andorno N, Riese F. Acceptability of palliative care approaches for patients with severe and persistent mental illness: a survey of psychiatrists in Switzerland. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2091-x.
- Udo I, Gash A. Challenges in management of complex panic disorder in a palliative care setting. BMJ Case Rep 2012;2012. https://doi.org/10.1136/bcr-2012-006800.
- Unseld M, Vyssoki B, Bauda I, Felsner M, Adamidis F, Watzke H, et al. Correlation of affective temperament and psychiatric symptoms in palliative care cancer patients. Wien Klin Wochenschr 2018;130:653-8. https://doi.org/10.1007/s00508-018-1400-6.
- van der Lee ML, van der Bom JG, Swarte NB, Heintz AP, de Graeff A, van den Bout J. Euthanasia and depression: a prospective cohort study among terminally ill cancer patients. J Clin Oncol 2005;23:6607-12. https://doi.org/10.1200/jco.2005.14.308.
- Vehling S, Kissane DW, Lo C, Glaesmer H, Hartung TJ, Rodin G, et al. The association of demoralization with mental disorders and suicidal ideation in patients with cancer. Cancer 2017;123:3394-401. https://doi.org/10.1002/cncr.30749.
- Verschuur EML, Nogarede RFC, Krol RJA, van der Sande R. Consulting Palliative Care Nurses in Long-Term Care Settings for People With Intellectual Disabilities, Mentally Ill and Elderly n.d.
- Walker S, Walker J, Richardson G, Palmer S, Wu Q, Gilbody S, et al. Cost-effectiveness of combining systematic identification and treatment of co-morbid major depression for people with chronic diseases: the example of cancer. Psychol Med 2014;44:1451-60. https://doi.org/10.1017/S0033291713002079.
- Walling A, Coscarelli A, Simon W, Wenger N, Pietras C, Ahmed K, et al. Engaging oncologists toward integrating a Shared Mental Model (SMM) for palliative oncology within a large academic oncology practice. J Pain Symptom Manage 2018;55:581-2. https://doi.org/10.1016/j.jpainsymman.2017.12.046.
- Ward J, Smith J. Management of mood disorders in patients with advanced illnesses. Br J Hosp Med 2009;70:204-7. https://doi.org/10.12968/hmed.2009.70.4.41622.
- Warmenhoven F, Bor H, Lucassen P, Vissers K, van Weel C, Prins J, et al. Depressive disorder in the last phase of life in patients with cardiovascular disease, cancer, and COPD: data from a 20-year follow-up period in general practice. Br J Gen Pract 2013;63:e303-8. https://doi.org/10.3399/bjgp13X667150.
- Waterman LZ, Denton D, Minton O. End-of-life care in a psychiatric hospital. BJPsych Bull 2016;40:149-52. https://doi.org/10.1192/pb.bp.114.049833.
- Wei R, Chang A, Rockoff A. Polyglandular autoimmune syndrome disguised as mental illness. BMJ Case Rep 2013;2013. https://doi.org/10.1136/bcr-2012-008541.
- Weinstein LC, Stefancic A, Cunningham AT, Hurley KE, Cabassa LJ, Wender RC. Cancer screening, prevention, and treatment in people with mental illness. CA Cancer J Clin 2016;66:134-51. https://doi.org/10.3322/caac.21334.
- Wen FH, Chen JS, Chou WC, Hsieh CH, Chang WC, Shen WC, et al. Quality of life and psychological distress are differentially associated with distinct symptom-functional states in terminally ill cancer patients’ last year of life. Psycho-Oncology 2018;27:2111-18. https://doi.org/10.1002/pon.4775.
- White C. Jack: a study in anguish. Nurs Times 1985;80:24-6.
- Wilson KG, Chochinov HM, McPherson CJ, Skirko MG, Allard P, Chary S, et al. Desire for euthanasia or physician-assisted suicide in palliative cancer care. Health Psychol 2007;26:314-23. https://doi.org/10.1037/0278-6133.26.3.314.
- Wilson KG, Chochinov HM, Skirko MG, Allard P, Chary S, Gagnon PR, et al. Depression and anxiety disorders in palliative cancer care. J Pain Symptom Manage 2007;33:118-29. https://doi.org/10.1016/j.jpainsymman.2006.07.016.
- Wilson KG, Dalgleish TL, Chochinov HM, Chary S, Gagnon PR, Macmillan K, et al. Mental disorders and the desire for death in patients receiving palliative care for cancer. BMJ Support Palliat Care 2016;6:170-7. https://doi.org/10.1136/bmjspcare-2013-000604.
- Wilson R, Hepgul N, Higginson IJ, Gao W. End-of-life care and place of death in adults with serious mental illness: a systematic review and narrative synthesis. Palliat Med 2020;34:49-68. https://doi.org/10.1177/0269216319867847.
- Woersching J, Van Cleave JH, Haber J, Chyun D. Mental health and substance use disorders in patients diagnosed with cancer: an integrative review of healthcare utilization. Oncol Nurs Forum 2019;46:365-83. https://doi.org/10.1188/19.ONF.365-383.
- Woodhead C, Ashworth M, Broadbent M, Callard F, Hotopf M, Schofield P, et al. Cardiovascular disease treatment among patients with severe mental illness: a data linkage study between primary and secondary care. Br J Gen Pract 2016;66:e374-81. https://doi.org/10.3399/bjgp16X685189.
- Harari D, Husk J, Lowe D, Wagg A. National audit of continence care: adherence to National Institute for Health and Clinical Excellence (NICE) guidance in older versus younger adults with faecal incontinence. Age Ageing 2014;43:785-93. https://doi.org/10.1093/ageing/afu056.
- Social Care Institute for Excellence . Dying Well at Home: The Case for Integrated Working 2015. https://www.scie.org.uk/publications/guides/guide48/ (accessed 28 June 2021).
- Royal College of Psychiatrists . Liaison Psychiatry for Every Acute Hospital: Integrated Mental and Physical Healthcare 2013.
Appendix 1 List of stakeholder advisory group members
-
Dr Nikki Pease (chairperson), Consultant in Palliative Medicine, Velindre University NHS Trust, Cardiff.
-
Dr Idris Baker, Lead Palliative Care Clinician for Wales and Consultant in Palliative Care, Abertawe Bro Morgannwg University Health Board, Swansea.
-
Dr Liz Davies, Head of Mental Health and Vulnerable Groups Division, Welsh Government.
-
Hazel Powell, Nursing Officer for Mental Health and Learning Disability, Welsh Government.
-
Pam Penman, Practice Development Facilitator, Marie Curie Hospice, Cardiff and the Vale.
-
Dr Helen Noble, Reader, Queen’s University Belfast.
-
Professor Ian Jones, Director of the National Centre for Mental Health, Cardiff.
-
Kathleen Caper, Head of Policy and Advocacy, Hospice UK, London.
-
Niamh Brophy, previously Palliative Care Coordinator at St Mungo’s, London.
-
Dr Stephanie Perrett, Lead Nurse for Health and Justice, Public Health.
-
Roger Pratt, public and patient representative.
-
Sian Jones, public and patient representative.
-
Huw Davies, public and patient representative.
Appendix 2 Terms of reference for stakeholder advisory group
Background
MENLOC aims to synthesise relevant research and other appropriate evidence relating to the organisation, provision and receipt of end-of-life care for people with SMI who have an additional diagnosis of advanced incurable cancer and/or end-stage lung, heart, renal or liver failure and who are likely to die within the next 12 months.
Project team and stakeholder advisory group: membership
The MENLOC project team comprises people with backgrounds in mental health services and end-of-life care research and practice, health services research, evidence review and information sciences, and lived experience of mental health difficulties and of surviving cancer.
The MENLOC SAG comprises people drawn from communities with interests in the project and its findings, including HCPs, mental health and end-of-life care researchers, service managers from the NHS and charitable sector, and people with experience of using services and of caring for people using services.
Stakeholder advisory group: terms of reference
The SAG will be independently chaired and will provide guidance to the project team over the lifetime of the study. The SAG will specifically:
-
receive information on the aims and objectives of MENLOC, and provide guidance on key definitions (e.g. ‘severe mental illness’), the corresponding refinement of search terms and strategies for evidence searching and review
-
review MENLOC’s progress and receive preliminary findings and provide a final round of guidance on evidence searching and review
-
advise the project team on the dissemination of findings, the promotion of impact and the identification of future research questions.
Working together
It is anticipated that members of the MENLOC project team and the SAG will meet on three occasions in Cardiff. In addition to participating in these meetings, members of the SAG can expect to spend approximately 1–2 hours in preparation. Members of the SAG will also be welcomed to the MENLOC end-of-project launch event.
Funding acknowledgement
MENLOC is funded by the NIHR Health and Social Care Delivery Research programme (project number 17/100/15).
Department of Health and Social Care disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Appendix 3 Notes from first combined project team and stakeholder group meeting
Appendix 4 Notes from second combined project team and stakeholder group meeting
Appendix 5 Notes from third combined project team and stakeholder group meeting
Appendix 6 Definitions and search terms: ‘severe mental illness’
Appendix 7 Definitions and search terms: ‘end of life’
Appendix 8 Searching for grey literature and non-research material
Appendix 9 Ovid MEDLINE® all: initial search strategy
Date range searched: 1946 to 5 July 2018. Last date searched: 6 December 2019
-
exp Palliative care/ (48,615)
-
exp Hospice care/ (5807)
-
exp Terminal Care/ (47,347)
-
exp Terminally ill/ (6150)
-
(“palliative care” or “hospice care” or “end of life care” or end-of-life).tw. (38,005)
-
((hospice or terminal*) adj3 (care or caring or ill*)).tw. (12,527)
-
(“last year of life” or LYOL or “end of life” or “end of their lives”).tw. (19,101)
-
(end-stage disease* or end stage disease* or end-stage ill* or end stage ill*).tw. (1112)
-
or/1-8 (104,642)
-
exp Neoplasms/ (3,055,654)
-
(cancer* or tumo?r* or neoplas* or malignan* or carcinoma* or adenocarcinoma* or adeno?carcinoma* or choriocrcinoma* or leukemia* or leukaemia* or metastat* or sarcoma* or teratoma* or lymphoma).tw. (3,168,623)
-
exp Multiple Organ Failure/ (10,043)
-
Organ failure.tw. (16,597)
-
Pulmonary Disease, Chronic Obstructive/ (32,992)
-
(Chronic obstructive pulmonary disease or COPD).tw. (53,007)
-
Heart Failure/ (105,052)
-
Renal Insufficiency/ (14,550)
-
Liver Failure/ (6735)
-
(“cardiac failure” or “liver failure” or “kidney failure” or “renal failure”).tw. (114,515)
-
Chronic Disease/ (248,675)
-
Health service utilization.mp. (1502)
-
lifestyle-related factor*.mp. (337)
-
or/10-22 (4,430,236)
-
exp Bipolar Disorder/ (37,229)
-
exp Schizophrenia/ (97,818)
-
(bipolar or mania or Schizophrenia).tw. (148,564)
-
exp Depression/ (102,372)
-
exp Mental Disorders/ (1,125,241)
-
(“mental illness” or “mental disorder*” or depression).tw. (333,320)
-
mental health condition*.tw. (1794)
-
exp Depressive Disorder/ (99,383)
-
exp Mental Health/ (31,108)
-
exp Personality Disorders/ (39,084)
-
(severe and persistent mental illness).mp. (304)
-
severe mental illness.mp. (3558)
-
or/24-35 (1,3902,77)
-
9 and 23 and 36 (2648)
-
(dementia or Alzheimer).tw. (106,344)
-
(Algeria$ or Egypt$ or Liby$ or Morocc$ or Tunisia$ or Western Sahara$ or Angola$ or Benin or Botswana$ or Burkina Faso or Burundi or Cameroon or Cape Verde or Central African Republic or Chad or Comoros or Congo or Djibouti or Eritrea or Ethiopia$ or Gabon or Gambia$ or Ghana or Guinea or Keny$ or Lesotho or Liberia or Madagasca$ or Malawi or Mali or Mauritania or Mauritius or Mayotte or Mozambiq$ or Namibia$ or Niger or Nigeria$ or Reunion or Rwand$ or Saint Helena or Senegal or Seychelles or Sierra Leone or Somalia or South Africa$ or Sudan or Swaziland or Tanzania or Togo or Ugand$ or Zambia$ or Zimbabw$ or China or Chinese or Hong Kong or Macao or Mongolia$ or Taiwan$ or Belarus or Moldov$ or Russia$ or Ukraine or Afghanistan or Armenia$ or Azerbaijan or Bahrain or Cyprus or Cypriot or Georgia$ or Iran$ or Iraq$ or Jordan$ or Kazakhstan or Kuwait or Kyrgyzstan or Leban$ or Oman or Pakistan$ or Palestin$ or Qatar or Saudi Arabia or Syria$ or Tajikistan or Turkmenistan or United Arab Emirates or Uzbekistan or Yemen or Bangladesh$ or Bhutan or British Indian Ocean Territory or Brunei Darussalam or Cambodia$ or India$ or Indonesia$ or Lao or People’s Democratic Republic or Malaysia$ or Maldives or Myanmar or Nepal or Philippin$ or Singapore or Sri Lanka or Thai$ or Timor Leste or Vietnam or Albania$ or Andorra or Bosnia$ or Herzegovina$ or Bulgaria$ or Croatia$ or Faroe Islands or Greenland or Liechtenstein or Lithuani$ or Macedonia or Malta or maltese or Romania or Serbia$ or Montenegro or Svalbard or Argentina$ or Belize or Bolivia$ or Brazil$ or Chilean or Colombia$ or Costa Rica$ or Cuba or Ecuador or El Salvador or French Guiana or Guatemala$ or Guyana or Haiti or Honduras or Jamaica$ or Nicaragua$ or Panama or Paraguay or Peru or Puerto Rico or Suriname or Uruguay or Venezuela or developing countr$ or south America$).ti,sh. (1,190,707)
-
Academic Dissertations/ (0)
-
thesis.tw. (7038)
-
book.pt. (0)
-
Books/ (3122)
-
or/38-43 (1,303,105)
-
37 not 44 (2373)
-
limit 45 to (English language and humans and “all adult (19 plus years)”) (1387)
Appendix 10 Ovid MEDLINE: final search strategy
Date range searched: 1946 to 6 December 2018. Last date searched: 6 December 2019
-
exp Palliative care/ (49,655)
-
exp Hospice care/ (5949)
-
exp Terminal Care/ (48,040)
-
exp Terminally ill/ (6227)
-
(“palliative care” or hospice or “end of life care” or end-of-life).tw. (43,896)
-
((hospice or terminal*) adj3 (care or caring or ill*)).tw. (12,766)
-
(“Irreversible condition” or “terminal condition” or fatal illness).tw. (791)
-
(“last year of life” or LYOL or “end of life” or “end of their lives” or “last six months of life” or “last 6 months of life”).tw. (19,924)
-
(end-stage disease* or end stage disease* or end-stage ill* or end stage ill* or end-stage or end stage).tw. (60,633)
-
(expected adj3 die).tw. (215)
-
(imminent adj3 death).tw. (561)
-
(“Dying soon” or “expected death” or “imminently dying” or Moribund).tw. (2493)
-
conservative treatment/ (1401)
-
(conservative adj2 (treatment or management)).tw. (42,831)
-
Withholding Treatment/ (10,909)
-
Treatment Refusal/ (11,477)
-
(Refus* adj3 (treat* or care or intervention or dialysis)).tw. (4855)
-
((withdrew or withdraw* or withhold*) adj3 (treat* or car* or intervene* or therap* or dialysis or transplant*)).tw. (15,455)
-
or/1-18 (244,771)
-
exp Neoplasms/ (3,107,101)
-
(cancer* or tumo?r* or neoplas* or malignan* or carcinoma* or adenocarcinoma* or adeno?carcinoma* or choriocrcinoma* or leukemia* or leukaemia* or metastat* or sarcoma* or teratoma* or lymphoma).tw. (3,243,976)
-
(“Enzymatic disease*” or “enzyme disease*”).tw. (25)
-
Genetic Disease, Inborn/ (13,207)
-
(“duchenne muscular dystrophy” or “amyotrophic lateral sclerosis” or ALS).tw. (40,207)
-
amyotrophic lateral sclerosis/ (16,921)
-
Muscular dystrophy, Duchenne/ (4706)
-
(“Genetic disease” or “genetic condition”).tw. (7305)
-
Cystic Fibrosis/ (33,150)
-
(“cystis fibrosis” or CF).tw. (36,968)
-
exp Multiple Organ Failure/ (10,209)
-
(“Organ failure” or “chronic organ failure”).tw. (17,137)
-
Pulmonary Disease, Chronic Obstructive/ (34,379)
-
(“renal insufficiency” or “serious physical illness”).tw. (21,134)
-
(Chronic obstructive pulmonary disease or COPD).tw. (54,881)
-
(chronic adj3 (illness or condition or disease*)).tw. (250,692)
-
“chronic medical condition”.tw. (382)
-
Heart Failure/ (107,446)
-
Renal Insufficiency/ (14,803)
-
Liver Failure/ (6828)
-
(chronic adj2 (“cardiac failure” or “liver failure” or “kidney failure” or “end-stage renal disease” or ESRD or “renal failure” or “heart failure”)).tw. (44,143)
-
Chronic Disease/ (251,517)
-
Health service utilization.mp. (1569)
-
lifestyle-related factor*.mp. (354)
-
or/20-43 (4,717,135)
-
exp Bipolar Disorder/ (37,764)
-
exp Schizophrenia/ (99,011)
-
(schizo* or “mood disorder*” or “personality disorder*” or psychotic* or psychosis or psychoses).tw. (197,049)
-
(bipolar or mania or Schizophrenia).tw. (151,754)
-
(Depression adj2 (psychosis or psychotic or severe or major)).tw. (28,840)
-
exp Mental Disorders/ (1,143,274)
-
mental health condition*.tw. (1954)
-
exp Personality Disorders/ (39,433)
-
exp psychotic disorders/ (48,805)
-
exp schizoaffective disorder/ (48,805)
-
exp psychosis/ (48,805)
-
Paranoid Disorders/ (3987)
-
(“severe mental illness” or “persistent mental illness”).tw. (3969)
-
((chronic* or sever* or serious or persistent* or enduring or debilitating) adj2 (mental* or psychological*) adj2 (ill* or disorder* or health)).tw. (12,556)
-
exp Mentally Ill Persons/ (5926)
-
(SPMI or SMI).tw. (3830)
-
or/45-60 (1,239,759)
-
(dementia or Alzheimer).ti. (52,380)
-
(bipolar electrocoagulation or bipolar radiofrequency or bipolar tumour probe or bipolar diathermy).tw. (1123)
-
(“respiratory depression” or “marrow depression” or “hematologic* depression”).tw. (6399)
-
(child* or adoles* or pediatric or paediatric).tw. (1,520,041)
-
(Algeria$ or Egypt$ or Liby$ or Morocc$ or Tunisia$ or Western Sahara$ or Angola$ or Benin or Botswana$ or Burkina Faso or Burundi or Cameroon or Cape Verde or Central African Republic or Chad or Comoros or Congo or Djibouti or Eritrea or Ethiopia$ or Gabon or Gambia$ or Ghana or Guinea or Keny$ or Lesotho or Liberia or Madagasca$ or Malawi or Mali or Mauritania or Mauritius or Mayotte or Mozambiq$ or Namibia$ or Niger or Nigeria$ or Reunion or Rwand$ or Saint Helena or Senegal or Seychelles or Sierra Leone or Somalia or South Africa$ or Sudan or Swaziland or Tanzania or Togo or Ugand$ or Zambia$ or Zimbabw$ or China or Chinese or Hong Kong or Macao or Mongolia$ or Taiwan$ or Belarus or Moldov$ or Russia$ or Ukraine or Afghanistan or Armenia$ or Azerbaijan or Bahrain or Cyprus or Cypriot or Georgia$ or Iran$ or Iraq$ or Jordan$ or Kazakhstan or Kuwait or Kyrgyzstan or Leban$ or Oman or Pakistan$ or Palestin$ or Qatar or Saudi Arabia or Syria$ or Tajikistan or Turkmenistan or United Arab Emirates or Uzbekistan or Yemen or Bangladesh$ or Bhutan or British Indian Ocean Territory or Brunei Darussalam or Cambodia$ or India$ or Indonesia$ or Lao or People’s Democratic Republic or Malaysia$ or Maldives or Myanmar or Nepal or Philippin$ or Singapore or Sri Lanka or Thai$ or Timor Leste or Vietnam or Albania$ or Andorra or Bosnia$ or Herzegovina$ or Bulgaria$ or Croatia$ or Faroe Islands or Greenland or Liechtenstein or Lithuani$ or Macedonia or Malta or maltese or Romania or Serbia$ or Montenegro or Svalbard or Argentina$ or Belize or Bolivia$ or Brazil$ or Chilean or Colombia$ or Costa Rica$ or Cuba or Ecuador or El Salvador or French Guiana or Guatemala$ or Guyana or Haiti or Honduras or Jamaica$ or Nicaragua$ or Panama or Paraguay or Peru or Puerto Rico or Suriname or Uruguay or Venezuela or developing countr$ or south America$).ti,sh. (1,225,437)
-
Academic Dissertations/ (0)
-
thesis.tw. (7167)
-
book.pt. (0)
-
Books/ (3174)
-
or/62-70 (2,653,676)
-
19 and 44 and 61 (2434)
-
72 not 71 (2126)
-
limit 73 to (english language and humans and “all adult (19 plus years)”) (1217)
Appendix 11 Ovid PsycInfo: final search strategy
Date range searched: 1806 to December week 1 2018. Last date searched: 6 December 2019
-
exp Palliative Care/ (11,016)
-
Hospice/ (3062)
-
exp Terminally Ill Patients/ (4562)
-
exp HOSPICE/ (3062)
-
(“palliative care” or “hospice care” or “end of life care” or end-of-life).tw. (15,589)
-
((hospice or terminal*) adj3 (care or caring or ill*)).tw. (6333)
-
(“Irreversible condition” or “terminal condition” or fatal illness).tw. (216)
-
(“last year of life” or LYOL or “end of life” or “end of their lives” or “last six months of life” or “last 6 months of life”).tw. (9038)
-
(end-stage disease* or end stage disease* or end-stage ill* or end stage ill* or end-stage or end stage).tw. (2002)
-
(expected adj3 die).tw. (44)
-
(imminent adj3 death).tw. (272)
-
(“Dying soon” or “expected death” or “imminently dying” or Moribund).tw. (235)
-
(conservative adj2 (treatment or management)).tw. (460)
-
Treatment Withholding/ (462)
-
Treatment Refusal/ (730)
-
(Refus* adj3 (treat* or care or intervention or dialysis)).tw. (1811)
-
((withdrew or withdraw* or withhold*) adj3 (treat* or car* or intervene* or therap* or dialysis or transplant*)).tw. (3579)
-
or/1-17 (28,620)
-
exp NEOPLASMS/ (47,829)
-
(cancer* or tumo?r* or neoplas* or malignan* or carcinoma* or adenocarcinoma* or adeno?carcinoma* or choriocrcinoma* or leukemia* or leukaemia* or metastat* or sarcoma* or teratoma* or lymphoma).tw. (76,722)
-
(“Enzymatic disease*” or “enzyme disease*”).tw. (0)
-
Genetic Disorders/ (4048)
-
(“duchenne muscular dystrophy” or “amyotrophic lateral sclerosis” or ALS).tw. (13,477)
-
Amyotrophic Lateral Sclerosis/ (3551)
-
Muscular Dystrophy/ (1293)
-
(“Genetic disease” or “genetic condition”).tw. (611)
-
Cystic Fibrosis/ (854)
-
(“cystis fibrosis” or CF).tw. (3217)
-
“Multi* Organ Failure*”.tw. (71)
-
(“Organ failure” or “chronic organ failure”).tw. (203)
-
exp Chronic Obstructive Pulmonary Disease/ (1272)
-
(“renal insufficiency” or “serious physical illness”).tw. (319)
-
(Chronic obstructive pulmonary disease or COPD).tw. (2277)
-
(chronic adj3 (illness or condition or disease*)).tw. (28,394)
-
“chronic medical condition”.tw. (196)
-
Heart Disorders/ (8989)
-
Kidney Diseases/ (2001)
-
Liver Disorders/ (1145)
-
(chronic adj2 (“cardiac failure” or “liver failure” or “kidney failure” or “end-stage renal disease” or ESRD or “renal failure” or “heart failure”)).tw. (866)
-
Chronic Illness/ (10,804)
-
lifestyle-related factor*.mp. (51)
-
or/19-41 (139,563)
-
exp Bipolar Disorder/ (25,413)
-
exp SCHIZOPHRENIA/ (85,758)
-
(schizo* or “mood disorder*” or “personality disorder*” or psychotic* or psychosis or psychoses).tw. (208,100)
-
(bipolar or mania or Schizophrenia).tw. (137,089)
-
(Depression adj2 (psychosis or psychotic or severe or major)).tw. (34,922)
-
exp Mental Disorders/ (566,262)
-
mental health condition*.tw. (1698)
-
exp Personality Disorders/ (33,638)
-
exp Schizoaffective Disorder/ (2961)
-
exp Psychosis/ (109,879)
-
“Paranoia (Psychosis)”/ (1215)
-
“Severity (Disorders)”/ (15,885)
-
“severe mental illness”.tw. (4681)
-
“persistent mental illness”.tw. (799)
-
((chronic* or sever* or serious or persistent* or enduring or debilitating) adj2 (mental* or psychological*) adj2 (ill* or disorder* or health)).tw. (16,725)
-
Mentally Ill Persons.mp. (805)
-
(SPMI or SMI).tw. (1991)
-
or/43-59 (637,058)
-
(dementia or Alzheimer).ti. (30,336)
-
(bipolar electrocoagulation or bipolar radiofrequency or bipolar tumour probe or bipolar diathermy).tw. (5)
-
(“respiratory depression” or “marrow depression” or “hematologic* depression”).tw. (407)
-
(child* or adoles* or pediatric or paediatric).tw. (811,926)
-
(Algeria$ or Egypt$ or Liby$ or Morocc$ or Tunisia$ or Western Sahara$ or Angola$ or Benin or Botswana$ or Burkina Faso or Burundi or Cameroon or Cape Verde or Central African Republic or Chad or Comoros or Congo or Djibouti or Eritrea or Ethiopia$ or Gabon or Gambia$ or Ghana or Guinea or Keny$ or Lesotho or Liberia or Madagasca$ or Malawi or Mali or Mauritania or Mauritius or Mayotte or Mozambiq$ or Namibia$ or Niger or Nigeria$ or Reunion or Rwand$ or Saint Helena or Senegal or Seychelles or Sierra Leone or Somalia or South Africa$ or Sudan or Swaziland or Tanzania or Togo or Ugand$ or Zambia$ or Zimbabw$ or China or Chinese or Hong Kong or Macao or Mongolia$ or Taiwan$ or Belarus or Moldov$ or Russia$ or Ukraine or Afghanistan or Armenia$ or Azerbaijan or Bahrain or Cyprus or Cypriot or Georgia$ or Iran$ or Iraq$ or Jordan$ or Kazakhstan or Kuwait or Kyrgyzstan or Leban$ or Oman or Pakistan$ or Palestin$ or Qatar or Saudi Arabia or Syria$ or Tajikistan or Turkmenistan or United Arab Emirates or Uzbekistan or Yemen or Bangladesh$ or Bhutan or British Indian Ocean Territory or Brunei Darussalam or Cambodia$ or India$ or Indonesia$ or Lao or People’s Democratic Republic or Malaysia$ or Maldives or Myanmar or Nepal or Philippin$ or Singapore or Sri Lanka or Thai$ or Timor Leste or Vietnam or Albania$ or Andorra or Bosnia$ or Herzegovina$ or Bulgaria$ or Croatia$ or Faroe Islands or Greenland or Liechtenstein or Lithuani$ or Macedonia or Malta or maltese or Romania or Serbia$ or Montenegro or Svalbard or Argentina$ or Belize or Bolivia$ or Brazil$ or Chilean or Colombia$ or Costa Rica$ or Cuba or Ecuador or El Salvador or French Guiana or Guatemala$ or Guyana or Haiti or Honduras or Jamaica$ or Nicaragua$ or Panama or Paraguay or Peru or Puerto Rico or Suriname or Uruguay or Venezuela or developing countr$ or south America$).ti,sh. (128,851)
-
thesis.tw. (24,537)
-
book.pt. (476,469)
-
exp BOOKS/ (6110)
-
or/61-68 (1,332,511)
-
18 and 42 and 60 (838)
-
70 not 69 (609)
Appendix 12 Supplementary searches
All websites last accessed 8 March 2019.
Trial registers
| Trial register | Search terms |
|---|---|
| ClinicalTrials.gov | “end of life” or palliative and mental |
| metaRegister of Controlled Trials | Not applicable |
| UK Clinical Trials Gateway | “last year of life” or LYOL or “end of life” or “end of their lives” in mental |
| WHO ICTRP Search Portal International (www.who.int/ictrp/en/) | “end of life” or “end of their lives” and mental |
Charity websites
| Website | Search type | Search terms |
|---|---|---|
| Cancer Research UK (www.cancerresearchuk.org/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and mental illness/health” | ||
| Cancer Research Wales (www.cancerresearchwales.co.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and mental illness/health” | ||
| Tenovus Cancer Care (www.tenovuscancercare.org.uk/) | Electronic search: main website | “end of life” and “mental illness” |
| Mental Health Foundation (www.mentalhealth.org.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| Manual search: policy publications | “palliative care” and mental illness/health” | |
| As per reviews inclusion criteria | ||
| Centre for Mental Health (www.centreformentalhealth.org.uk/) | Electronic search: policy publications | “end of life” and “mental illness/health” |
| “palliative care” and mental illness/health” | ||
| National Kidney Foundation (www.kidney.org/) | Electronic search: main website | “end of life” and “mental illness/health” |
| Manual search: policy publications | “palliative care” and mental illness/health” | |
| As per reviews inclusion criteria | ||
| British Liver Trust (www.britishlivertrust.org.uk/) | Electronic search: publications | “end of life” and “mental illness” |
| “palliative care” and mental illness” | ||
| (mental health too broad a term) | ||
| British Renal Society (http://britishrenal.org/) | Electronic search: conference abstracts | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| The Renal Association (http://britishrenal.org/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| British Heart Foundation (http://britishrenal.org/) | Electronic search: main website | “last year of life” or LYOL or “end of life” or “end of their lives” and “severe mental” and “Healthcare professionals” |
| “palliative care” and “mental illness” | ||
| (mental health too broad) | ||
| British Lung Foundation (www.blf.org.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| Hospice UK (www.hospiceuk.org/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| Marie Curie (www.mariecurie.org.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| Manual search: briefings | “palliative care” and “mental illness/health” | |
| As per reviews inclusion criteria | ||
| Macmillan Cancer Support (www.macmillan.org.uk/) | Electronic search: main website | “last year of life” or LYOL or “end of life” or “end of their lives” and “severe mental” |
| “palliative care” and mental illness/health” | ||
| Bipolar UK (www.bipolaruk.org/) | Electronic search: main website | “end of life” and “mental illness/health” |
| Palliative | ||
| MIND (www.mind.org.uk/) | Electronic search: main website | “end of life care” and “mental illness/health” |
| Palliative | ||
| Rethink Mental Illness (www.rethink.org/) | Electronic search: main website | “end of life care” and “mental illness/health” |
| Palliative | ||
| Sova (www.sova.org.uk/) | Electronic search: main website | “end of life care” and “mental” |
| Palliative | ||
| Hafal: for recovery for serious mental illness (www.hafal.org) | Electronic search: main website | “end of life care” and “mental” |
| Palliative and mental | ||
| Age Concern (www.ageuk.org.uk) | Electronic search: main website | “end of life care “ and “mental” |
| Palliative and mental | ||
| Salvation Army (https://salvationarmy.org.uk) | Electronic search: main website | “end of life care” and “mental” |
| Palliative and mental | ||
| Dying Matters (www.dyingmatters.org/) | Electronic search: main website | “end of life “ and “mental” |
| “palliative care” and “mental illness/health” | ||
| Care Not Killing (www.carenotkilling.org.uk/) | Electronic search: main website | “end of life care” and then searched within results for the term “mental” |
| “palliative care” and then searched within results for the term “mental” | ||
| Northern Ireland Hospice (www.nihospice.org/) | Electronic search: main website | “end of life care” and “mental” |
| Palliative | ||
| Mental Health UK (www.mentalhealth-uk.org/) | No search facility or publications page | |
| Heads Together (www.headstogether.org.uk/) | No search facility or publications page | |
| Kidney Research UK (www.kidneyresearchuk.org/) | Electronic search: main website | “end of life care” and “mental” |
| Palliative | ||
| National Kidney Federation (www.kidney.org.uk/) | Electronic search: main website | “end of life care” and “mental” |
| Palliative | ||
| St Mungo’s (www.mungos.org/) | Electronic search: main website | “end of life“ |
| Palliative | ||
| “mental illness” | ||
| Samaritans (www.samaritans.org/) | Electronic search: main website | “end of life” and “severe mental” |
| Palliative and “severe mental” | ||
| Llanmau (www.llamau.org.uk/) | Electronic search: main website | |
| SSAFA (www.ssafa.org.uk/) | Electronic search: main website | |
| Community Housing Cymru (https://chcymru.org.uk/) | Electronic search: main website | |
| National Housing Federation (www.housing.org.uk/) | Electronic search: main website | |
| Shelter Cymru (https://sheltercymru.org.uk/) | Electronic search: main website | |
| Shelter (www.shelter.org.uk/) | Electronic search: main website | |
| Gofal (www.gofal.org.uk/) | No search function checked projects and services page but no relevant reports | As per reviews inclusion criteria |
| Compassionate Communities (www.compassionate-communitiesuk.co.uk/) | No search function checked projects but no relevant reports | As per reviews inclusion criteria |
| Byw Nawr (www.dyingmatters.org/wales) | Electronic search: main website | |
| Combat Stress (www.combatstress.org.uk/) | Electronic search: main website | |
| Royal British Legion (www.britishlegion.org.uk/) | Electronic search: main website |
Organisation websites
| Website | Search type | Search terms |
|---|---|---|
| NHS England (www.england.nhs.uk/cancer/strategy/; www.england.nhs.uk/EoLC/resources/-; http://endoflifecareambitions.org.uk/) | Electronic search: main website | “mental illness” |
| NHS Wales (www.wales.nhs.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| Advanced search: title field only | “palliative care” and “mental illness/health” | |
| Welsh Government (https://gov.wales/) | Electronic search: main website | “end of life” and “mental illness/health” |
| Advanced search: limited to health and social services | “palliative care” and “mental illness/health” | |
| Department of Health and Social Care (www.gov.uk/) |
Electronic search: publications Limited by: Department of Health and Social Care Topic: Health and Social Care Subtopic: end of life |
“end of life” and “mental illness/health” “palliative care” and “mental illness/health” |
| Department of Health: Northern Ireland (www.health-ni.gov.uk/) | Electronic search: publications | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| Department of Health, Social Services and Public Safety: Northern Ireland (www.health-ni.gov.uk/) | Electronic search: publications | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| Ministry of Justice (www.gov.uk/) |
Electronic search: publications Limited by: Ministry of Justice Topic: health and social care Subtopic: end of life |
“end of life” and “mental illness/health” “palliative care” and “mental illness/health” |
| Care Inspectorate Wales (www.qcs.co.uk/wale)s/ |
Searching available only with practitioner registration E-mailed – no relevant publications |
|
| Care Quality Commission (www.cqc.org.uk/) | Electronic search: publications | “end of life” and “severe mental” |
| “palliative care” and “mental illness” | ||
| Prisons and Probation Ombudsman (www.ppo.gov.uk) |
Electronic search: main website Manual search: fatal incident reports over a 1-year period between June 2017 and 2018 Limited by: deaths of natural causes |
“end of life” |
| As per reviews inclusion criteria | ||
| Royal College of Psychiatrists (www.rcpsych.ac.uk/) | Manual search: college reports | As per reviews inclusion criteria |
| Royal College of Physicians (www.rcplondon.ac.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health” | ||
| The Worldwide Hospice and Palliative Care Alliance (www.thewhpca.org/) | Manual search: resources | As per reviews inclusion criteria |
| European Association of Palliative Care (www.eapcnet.eu/) | Manual search: national guidelines (UK countries only) | As per reviews inclusion criteria |
| Scottish Partnership Agency for Palliative Care (www.palliativecarescotland.org.uk/) | Electronic search: main website | “end of life care” and “mental illness” and evaluation |
| “palliative care” and “mental illness/health” | ||
| National Council for Palliative Care (www.ncpc.org.uk/) | Electronic search: main website | “end of life” and “mental illness/health” |
| “palliative care” and “mental illness/health”“ | ||
| Social Care Institute for Excellence (www.scie.org.uk/) | Electronic search: main website | “end of life” and “mental illness” |
| “palliative care” and “mental illness” | ||
|
Health Improvement Scotland (www.healthcareimprovementscotland.org/) Covers publications by NHS Scotland, Scottish Government and Healthcare Improvement Scotland |
Electronic search: main website | “end of life” and “mental illness” |
| “palliative care” and “mental illness” | ||
| NICE (www.nice.org.uk/guidance) | Electronic search: main website | “end of life” or “palliative care” |
| “mental illness” | ||
| Royal College of Nursing (www.rcn.org.uk/clinical-topics/end-of-life-care) | Manual search through section on clinical topics end of life | As per reviews inclusion criteria |
| Gold Standards Framework (www.goldstandardsframework.org.uk/) | Manual search through library resources | As per reviews inclusion criteria |
Appendix 13 Screening tool
Appendix 14 Table of studies excluded from the review
| Study | Reason for exclusion |
|---|---|
| Abdullah et al. 2015181 | Not about EoL care – radiotherapy |
| Ahearn 2015182 | No evidence of any participants with pre-existing SMI |
| Akechi et al. 2002183 | No evidence of any participants with pre-existing SMI |
| Akechi et al. 2004184 | Prevalence of mental health concerns post-cancer diagnosis |
| Alexander 2004185 | Patterns of referral to a hospice and not about EoL care |
| Alexopoulos 2008186 | Not about EoL care – problem-solving therapy |
| Ann-Yi et al. 2018187 | No evidence of any participants with pre-existing SMI |
| Anquinet et al. 2014188 | Pre-existing psychological problems, namely depression and anxiety, and not SMI |
| Aragona 2007189 | Not about EoL care – tolerability and efficacy of aripiprazole |
| Atkin et al. 2017190 | Anxiety assessment and management as a consequence of advanced life-limiting illness |
| Azhar et al. 2018191 | No evidence of any participants with pre-existing SMI |
| Azuero et al. 2014192 | No evidence of any participants with pre-existing SMI |
| Baile et al. 1993193 | No evidence of any participants with pre-existing SMI |
| Baker 2016194 | Review article – all relevant citations screened |
| Balaban et al. 2017195 | Not about EoL care – haemodialysis |
| Balogun and Abdel-Rahman 2009196 | No evidence of any participants with pre-existing SMI |
| Bang et al. 2005197 | No evidence of any participants with pre-existing SMI |
| Bannink et al. 2000198 | No evidence of any participants with pre-existing SMI |
| Barth et al. 2013199 | No evidence of any participants with pre-existing SMI |
| Bartlett et al. 2010200 | Not about expected LYoL – normal health until emergency |
| Bassirpour et al. 2011201 | Review article – all relevant citations screened |
| Battersby et al. 2018202 | Not about expected LYoL – cardiovascular health |
| Bauer 2016203 | Review article – all relevant citations screened |
| Baumrucker et al. 2009204 | No evidence of any participants with pre-existing SMI |
| Beechem 1995205 | No evidence of any participants with pre-existing SMI |
| Beernaert et al. 2015206 | Dementia; no other SMI |
| Bekelman et al. 2018207 | No evidence of any participants with pre-existing SMI |
| Bekelman et al. 2018208 | No evidence of any participants with pre-existing SMI |
| Bergquist and Hammerlid 2007209 | No evidence of any participants with pre-existing SMI |
| Berlim et al. 2006210 | No evidence of any participants with pre-existing SMI |
| Bernard et al. 2016211 | No evidence of any participants with pre-existing SMI |
| Black et al. 2001212 | Employing registered mental health nurses in palliative care settings |
| Block and Billings 1994213 | Review article all relevant citations screened |
| Block 2001214 | Focuses on one person who does not have any pre-existing SMI |
| Block 2006215 | No evidence of any participants with pre-existing SMI |
| Bloomer and O’Brien 2013216 | Review article – all relevant citations screened |
| Borowiak et al. 2009217 | Excluded patients with psychiatric disorders |
| Bove et al. 2018218 | Palliative care for people with COPD and not SMI |
| Bradley et al. 2005219 | No evidence of any participants with pre-existing SMI |
| Braiteh et al. 2007220 | No evidence of any participants with pre-existing SMI |
| Bramstedt and Arroliga 2004221 | No evidence of any participants with pre-existing SMI |
| Brandt et al. 2005222 | No evidence of any participants with pre-existing SMI |
| Braverman et al. 2017223 | HCPs’ attitudes towards physician-assisted suicide |
| Breitbart and Jacobsen 1996224 | No evidence of any participants with pre-existing SMI |
| Breitbart et al. 1995225 | No evidence of any participants with pre-existing SMI |
| Breitbart et al. 2010226 | No evidence of any participants with pre-existing SMI, and participants with psychosis excluded |
| Breitbart et al. 2012227 | No evidence of any participants with pre-existing SMI, and participants with psychosis excluded |
| Breitbart et al. 2018228 | No evidence of any participants with pre-existing SMI, and participants with psychosis excluded |
| Brennan et al. 2015229 | No evidence of any participants with pre-existing SMI |
| Brown et al. 2019230 | Review article – all relevant citations screened |
| Browne 2017231 | Not about expected LYoL – treatment |
| Bruhn et al. 2013232 | Not about expected LYoL – pain management |
| Buda et al. 2012233 | No evidence of any participants with pre-existing SMI |
| Buss et al. 2011234 | Not about meeting the needs of people with pre-existing SMI at the EoL |
| Byock et al. 2006235 | Review article – all relevant citations screened |
| Calderón et al. 2018236 | No evidence of any participants with pre-existing SMI at the EoL |
| Campo-Engelstein et al. 2016237 | Not about meeting the needs of people with pre-existing SMI at the EoL |
| Candilis et al. 2004238 | Not about meeting the needs of people with pre-existing SMI at the EoL |
| Capozzo et al. 2009239 | No evidence of any participants with pre-existing SMI |
| Carter et al. 2007240 | No evidence of any participants with pre-existing SMI |
| Check et al. 2019241 | The paper addresses post-cancer diagnosis depression |
| Chochinov 2004242 | Review article – all relevant citations screened |
| Chou et al. 2016243 | Not about EoL care – general discussion about cancer in patients with schizophrenia |
| Choudry et al. 2015244 | No evidence of any participants with pre-existing SMI |
| Close et al. 2014245 | Not about expected LYoL – lithium exposure and renal failure in people with bipolar disorder |
| Cohen et al. 2002246 | Not about EoL care – association schizophrenia and cancer |
| Craun et al. 1997247 | Review article – all relevant citations screened |
| Crump et al. 2013248 | Not about EoL care – comorbidities and mortality in bipolar disorder |
| Crump et al. 2013249 | Not about EoL care – comorbidities and mortality in schizophrenia |
| Davie 2006250 | No evidence of any participants with pre-existing SMI |
| den Boer et al. 2019251 | Review article – all relevant citations screened |
| Dinnen et al. 2018252 | No evidence of any participants with pre-existing SMI |
| Doering 2018253 | Review article – all relevant citations screened |
| Donald and Stajduhar 2019254 | Review article – all relevant citations screened |
| Dube 2013255 | Not about EoL care – kidney transplants |
| Ita et al. 2003256 | Prevalence study |
| Evenblij 2018257 | Prevalence study |
| Fairman and Irwin 2013258 | Review article – all relevant citations screened |
| Farasatpour et al. 2013259 | Not about EoL care – treatment delay |
| Feldman 2011260 | Review article – all relevant citations screened |
| Filiberti et al. 2001261 | Psychological autopsy but none of the cases had obvious pre-existing SMI |
| Flick 2018262 | No evidence of any participants with pre-existing SMI |
| Forster et al. 2017263 | No evidence of any participants with pre-existing SMI |
| Frei et al. 2001264 | Prevalence study |
| Fried and Gillick 1994265 | No evidence of any participants with pre-existing SMI |
| Fujioka et al. 2018266 | A scoping review of the perspectives of professionals on assisted dying. Nothing about SMI |
| Fukunishi et al. 2002267 | Not about EoL care – haemodialysis |
| Ganzini 201888 | No evidence of any participants with pre-existing SMI |
| Gao et al. 2019268 | No evidence of any participants with pre-existing SMI |
| Gardner-Sood et al. 2015269 | Not about EoL care – cardiovascular risk factors and metabolic syndrome in people with established psychotic illnesses |
| Garrido et al. 2017270 | Not about EoL care – serious physical illness |
| Gill et al. 2010271 | Prevalence study |
| Gillick and Mendes 1996272 | No evidence of any participants with pre-existing SMI other than dementia |
| Ginieri-Coccossis et al. 2008273 | No evidence of any participants with pre-existing SMI |
| Glick et al. 2018274 | Review article – all relevant citations screened |
| Granek et al. 2019275 | Not EoL care – emotional distress and suicidal ideations |
| Grigoletti et al. 2009276 | Prevalence study |
| Groenewoud et al. 1997277 | Not about EoL care –incidence study of assisted suicide |
| Güth et al. 2011278 | Not about EoL care – suicide |
| Habraken et al. 2009279 | No evidence of any participants with pre-existing SMI |
| Harris et al. 2019280 | Not EoL care – incidence of gastrointestinal cancers |
| Hawkins 2016281 | Opinion/review article – all relevant citations screened |
| Hay and Passik 2000282 | Not about EoL care – symptom management |
| Henderson and Ord 1997283 | No evidence of any participants with pre-existing SMI |
| Henoch et al. 2007284 | Excluded patients with psychiatric disorders |
| Henriksson et al. 1995285 | Not about EoL care – suicide |
| Hietanen et al. 1994286 | Not about EoL care – suicide |
| Hindley et al. 2019287 | Not about EoL care – advance decision-making for mental health crisis |
| Hinton 1972288 | Psychological problems arose during their terminal illness |
| Holmes et al. 2015289 | No evidence of any participants with pre-existing SMI |
| Howard et al. 201023 | Review article – all relevant citations screened |
| Hwang et al. 2012290 | Not about EoL care – chemotherapy |
| Iachina et al. 2019291 | Not about EoL care – treatment |
| Inagaki et al. 2006292 | Not about EoL care – treatment |
| Iordanidis et al. 1993293 | Older people with end-stage renal disease |
| Irwin et al. 2008294 | No evidence of any participants with pre-existing SMI |
| Irwin et al. 2011295 | Psychiatry resident education in palliative care |
| Irwin et al. 2017296 | Not about EoL care – treatment |
| Ishikawa et al. 201628 | Not about EoL care – screening, treatment and 30-day mortality |
| Jackson et al. 2018297 | Not about EoL care – dialysis |
| Jamison and Holmes 2018298 | No evidence of any participants with pre-existing SMI |
| Jarero et al. 2016299 | No evidence that PTSD was pre existing |
| Jeffery et al. 2019300 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Jones et al. 2008301 | Not about EoL care – diagnostic overshadowing |
| Kadan-Lottick et al. 2005302 | Not about EoL care – access to mental health services after cancer diagnosis |
| Kaerlev et al. 2018303 | Not about EoL care – chemotherapy |
| Kardinal and Porter 1981304 | No evidence of any participants with pre-existing SMI |
| Kaufman 2010305 | Not about EoL care – haemodialysis |
| Kelly and Shanley 2000306 | Frailty associated with terminal illness |
| Kim et al. 2016307 | Psychiatric patients with no other chronic health condition |
| Kimmel et al. 1998308 | Prevalence study |
| King et al. 2005309 | Discussion article about assessing depression in patients with cancer and no mention of previous SMI |
| Kisely et al. 2008310 | Not about EoL care – cancer-related mortality |
| Kisely et al. 2013311 | Not about EoL care – cancer-related mortality |
| Kisely et al. 2016312 | Not about EoL care – cancer-related mortality |
| Kissane and Smith 1996313 | Not about EoL care – psychosocial morbidity in women with breast cancer |
| Kissane et al. 2004314 | Not about EoL care – referrals to liaison psychiatry |
| Kleiboer et al. 2011315 | Depression within previous month and having cancer for over 6 months |
| Lacy and Higgins 2005316 | Not about EoL care – psychotherapy |
| Lamers 2005317 | No evidence of any participants with pre-existing SMI |
| Lawrence and Kisely 2010318 | Review article – all relevant citations screened |
| Legler et al. 2011319 | No patients with previous SMI – comorbidities that the paper refers to are other medical conditions and dementia |
| Lehto et al. 2019320 | Review article – all relevant citations screened |
| Lent and Brown Bradley 1999321 | Not about expected LYoL – treatment |
| Levine et al. 1978322 | No evidence of any participants with pre-existing SMI |
| Levinson 1975323 | No evidence of any participants with pre-existing SMI |
| Lichtenthal et al. 2009324 | Prevalence of mental disorder and closeness to death |
| Liu et al. 2017325 | Not about EoL care – suicide |
| Lloyd-Williams et al. 1999326 | No evidence of any participants with pre-existing SMI |
| Lloyd-Williams et al. 2014327 | Review article – all relevant citations screened |
| Macleod 2013328 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Madeira et al. 2011329 | No evidence of any participants with pre-existing SMI |
| Madrigal 2010330 | Discussion paper – all relevant citations retrieved |
| Maguire et al. 1999331 | No evidence of any participants with pre-existing SMI |
| Martiny et al. 2012332 | Prevalence study |
| Masel et al. 2016333 | Not about EoL care – consumption of pain medication |
| Maull 1991334 | No evidence of any participants with pre-existing SMI and also not about expected LYoL |
| McCormack and Sharp 200629 | Discussion paper on palliative care for people with mental health problems, some of whom would have had previous SMI, but no further details provided |
| McDaniel et al. 1992335 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Medenica et al. 2014336 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Meyer and Block 2011337 | Not about EoL care – discussion on personality disorder in oncology settings |
| Meyer et al. 2013338 | Not about EoL care – behaviour of patients with schizophrenia and metastatic breast cancer |
| Miller 2018339 | Poster presentation no outcome data presented |
| Millman et al. 201618 | Protocol paper – no outcome data |
| Miovic and Block 2007340 | Discussion paper – all relevant citations screened |
| Morasso et al. 1999341 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Moskowitz 1997342 | Suicidality and responses to people who wish to die, including those who are critically ill |
| Moss 1980343 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Mucsi et al. 2017344 | Not about EoL care – kidney transplant |
| Muir-Cochrane 2006345 | Not about EoL care – barriers to care |
| Mulder et al. 2012346 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Myhill 2014347 | Editorial – all relevant citations screened |
| Nash 2017348 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Neely and Roxe 2000349 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Ng 2012350 | Clinical trial protocol and a full report was not published |
| Ng et al. 2013351 | Prevalence study |
| Ng et al. 2014352 | Patients were excluded if they had other comorbid psychiatric diagnoses or if they were already treated with antidepressants |
| Nipp et al. 2017353 | Not about meeting needs of people with pre-existing SMI at the EoL |
| O’Connor et al. 2006354 | Not about EoL care – pain management |
| Ogawa et al. 2010355 | States no previous psychiatric history |
| O’Mahony et al. 2018356 | Not about EoL care – pain management |
| Onishi et al. 2006357 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Owen et al. 1994358 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Ozenli et al. 2010359 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Paice 2002360 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Parkerson and Gutman 1997361 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Payne and Haines 2002362 | No evidence of any participants with pre-existing SMI |
| Payne et al. 2004363 | No evidence of any participants with pre-existing SMI |
| Pengelly and Purnell 2009364 | Not about EoL care – psychological support for cancer patients |
| Perr 1985365 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Peteet 2009366 | No evidence of any participants with pre-existing SMI |
| Phongtankuel et al. 2018367 | No evidence of any participants with pre-existing SMI |
| Popa-Velea et al. 2010368 | No evidence of any participants with pre-existing SMI, and those with psychoses excluded |
| Price et al. 200638 | No evidence of any participants with pre-existing SMI |
| Quentzel and Levine 1997369 | Not about EoL care – haemodialysis |
| Quipourt et al. 2011370 | No evidence of any participants with pre-existing SMI |
| Rajmohan and Kumar 2013371 | Not about EoL care – psychological factors and pain management |
| Ramos and Fulton 2017372 | No evidence of any participants with pre-existing SMI |
| Rasmussen and Richardson 2011373 | Not about EoL care – ECT therapy |
| Rayner et al. 2004374 | No evidence of any participants with pre-existing SMI |
| Rayner et al. 2011375 | No evidence of any participants with pre-existing SMI |
| Reeve et al. 2007376 | Prevalence study |
| Reinke et al. 2011377 | No evidence of any participants with pre-existing SMI |
| Relyea et al. 2019378 | Review article – all relevant citations screened |
| Rhondali et al. 2013379 | Not an English-language full-text article |
| Riquin et al. 2017380 | Not an English-language full-text article |
| Sanders et al. 2019381 | No evidence of any participants with pre-existing SMI |
| Saracino et al. 2018382 | Not about EoL care – those awaiting liver transplant |
| Sato et al. 2004383 | Not about EoL care – milnacipran treatment for major depressive disorder |
| Scott et al. 2018384 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Shalev et al. 201720 | Review article – all relevant citations screened |
| Shalev et al. 2017385 | Review article – all relevant citations screened |
| Sharma et al. 2010386 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Sharma et al. 2012387 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Shipman et al. 2008388 | General discussion on EoL based on a survey of professionals and academics |
| Snyder and Whisman 2004389 | Not about expected LYoL |
| Spencer et al. 2012390 | No participants with pre-existing SMI – assessed as having MDD, PTSD, PD, GAD within the last 30 days |
| Stedeford and Bloch 1979391 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Stein et al. 2018392 | Abstract of conference presentation – no outcome data presented |
| Talbott and Linn 1978393 | Not about expected LYoL |
| Tate and Longo 2005394 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Taylor et al. 2013395 | Not about EoL care – surgical treatment of cancer |
| Taylor et al. 2018396 | Not about expected LYoL – self-injury that led to death |
| Terpstra and Terpstra 2012397 | Review article – all relevant citations screened |
| Trachsel 2018398 | Discussion article – all relevant citations screened |
| Trachsel et al. 2016399 | Not about expected LYoL – palliative psychiatry |
| Trachsel et al. 2019400 | Not about expected LYoL – palliative psychiatry |
| Udo 2012401 | No evidence of any participants with pre-existing SMI |
| Unseld et al. 2018402 | No evidence of any participants with pre-existing SMI |
| van der Lee et al. 2005403 | No evidence of any participants with pre-existing SMI |
| Vehling et al. 2017404 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Verschuur et al. 2014405 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Walker et al. 2014406 | Not about expected LYoL – cost-effectiveness of identification and treatment of major depression |
| Walling et al. 2018407 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Ward and Smith 2009408 | Not about expected LYoL |
| Warmenhoven et al. 2013409 | Prevalence study |
| Waterman et al. 2016410 | No evidence of any participants with pre-existing SMI – dementia |
| Wei et al. 2013411 | Not about expected LYoL |
| Weinstein et al. 2016412 | Review article – all relevant citations screened |
| Wen et al. 2018413 | No evidence of any participants with pre-existing SMI |
| White 1985414 | Not about meeting needs of people with pre-existing SMI at the EoL |
| Wilson et al. 2007415 | No evidence of any participants with pre-existing SMI |
| Wilson et al. 2007416 | No evidence of any participants with pre-existing SMI |
| Wilson et al. 2016417 | No evidence of any participants with pre-existing SMI |
| Wilson et al. 2019418 | Review article – all relevant citations screened |
| Woersching et al. 2019419 | Review article on health-care utilisation but not at the EoL |
| Woodhead et al. 2016420 | Not about EoL care – data linkage study, SMI and cardiovascular disease |
| Woods et al. 20083 | Review article – all relevant citations screened |
Appendix 15 Table of excluded grey literature
All websites last accessed 14 February 2020.
| Authors, title of document, URL | Focus; reason for exclusion |
|---|---|
| Addicott R, Ross S. Implementing the End of Life Care Strategy. Lessons for Good Practice. London: The King’s Fund; 2010. URL: www.kingsfund.org.uk/sites/default/files/field/field_publication_file/Implementing-end-of-life-care-Rachael-Addicott-Shilpa-Ross-Kings-Fund-October2010_0.pdf | EoL care; no mention of care of patients with mental illness |
| Addicott, R. Hiley, J. Issues Facing Commissioners in End-of-Life Care. London: The King’s Fund; 2011. URL: www.kingsfund.org.uk/sites/default/files/issues-facing-commissioners-end-of-life-care-report-september2011.pdf | EoL care; no mention of care of patients with mental illness |
| All Wales Palliative Care Planning Group. Report to Minister for Health and Social Services on Palliative Care Services – Sugar Report. 2008. URL: www.wales.nhs.uk/documents/Palliative-Care.pdf | EoL care; no mention of care of patients with mental illness |
| Cross Party Group Hospices and Palliative Care. CPG Hospices and Palliative Care: Inquiry. Inequalities in Access to Hospice and Palliative Care; 2018. URL: www.hospiceuk.org/docs/default-source/Policy-and-Campaigns/cpg-report_english_web.pdf?sfvrsn=4 | EoL care; no mention of care of patients with mental illness |
| Department of Health, Social Services and Public Safety. Living Matters Dying Matters. A Palliative and End of Life Care Strategy for Adults in Northern Ireland. 2010. URL: www.health-ni.gov.uk/sites/default/files/publications/dhssps/living-matters-dying-matters-strategy-2010.pdf | EoL care; no mention of care of patients with mental illness |
| Department of Health. End of Life Care Strategy. Fourth Annual Report. 2012. URL: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/136486/End-of-Life-Care-Strategy-Fourth-Annual-report-web-version-v2.pdf | EoL care; no mention of care of patients with mental illness |
| Department of Health. Our Commitment to You for End of Life Care the Government Response to the Review of Choice in End of Life Care. 2016. URL: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/536326/choice-response.pdf | EoL care; no mention of care of patients with mental illness |
| Hall S, Petkova H, Tsouros AD, Costantini M, Higginson IG. Palliative Care for Older People: Better Practices. Copenhagen: World Health Organization, Regional Office for Europe; 2011. URL: www.euro.who.int/__data/assets/pdf_file/0017/143153/e95052.pdf | EoL care; no mention of care of patients with mental illness |
| Healthcare Improvement Scotland. Palliative and EoL Care Indicators. 2013. URL: www.healthcareimprovementscotland.org/his/idoc.ashx?docid=ab6bef0f-48d4-4409-baf0-d15297469599%26version=-1 | EoL care; no mention of care of patients with mental illness |
| Mental Health Foundation. Mental Health and Palliative Care. 2008. URL: www.mentalhealth.org.uk/file/1207/download?token=kMrNYnE- | EoL care and mental health; review article all relevant citations included |
| National Institute for Health and Care Excellence. Psychosis and Schizophrenia in Adults: Prevention and Management. Clinical Guideline 178. 2014. URL: www.nice.org.uk/guidance/cg178 | Psychosis and schizophrenia; no mention of care of patients at the EoL |
| National Institute for Health and Care Excellence. Bipolar Disorder: Assessment and Management. Clinical Guideline 184. 2014. URL: www.nice.org.uk/guidance/cg184 | Bipolar; no mention of care of patients at the EoL |
| National Institute for Health and Care Excellence. Psychosis and Schizophrenia in Adults. Quality Standard 80. 2014. URL: www.nice.org.uk/guidance/qs80 | Psychosis and schizophrenia; no mention of care of patients at the EoL |
| National Institute for Health and Care Excellence. Bipolar Disorder in Adults. Quality Standard 95. 2014. URL: www.nice.org.uk/guidance/qs95 | Bipolar; no mention of care of patients at the EoL |
| National Institute for Health and Care Excellence. Care of Dying Adults in the Last Days of Life. NICE Guideline 31. 2015. URL: http://wales.pallcare.info/files/NICE%20Care%20of%20dying%20adults%20in%20the%20last%20days%20of%20life%20NG31.pdf | EoL care; no mention of care of patients with mental illness |
| National Palliative and End of Life Care Partnership. Ambitions for Palliative and End of Life Care: A National Framework for Local Action 2015–2020. 2015. URL: http://endoflifecareambitions.org.uk/wp-content/uploads/2015/09/Ambitions-for-Palliative-and-End-of-Life-Care.pdf | EoL care; no mention of care of patients with mental illness |
| Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-term Conditions and Mental Health. London: The Cost of Co-morbidities. London: The King’s Fund and Centre for Mental Health; 2012. URL: www.kingsfund.org.uk/sites/default/files/field/field_publication_file/long-term-conditions-mental-health-cost-comorbidities-naylor-feb12.pdf | Long-term conditions and mental health; no mention of care of patients at the EoL |
| Naylor C, Das P, Ross S, Honeyman M, Thompson J, Gilburt H. Bringing Together Physical and Mental Health: A New Frontier for Integrated Care. London: The King’s Fund; 2016. URL: www.kingsfund.org.uk/publications/physical-and-mental-health | Physical and mental health; no mention of care of patients at the EoL |
| NHS England. The Five Year Forward View for Mental Health. 2016. URL: www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf | Mental health; no mention of care of patients at the EoL |
| NHS England. Achieving World-Class Cancer Outcomes: A Strategy for England 2015–2020 Progress Report. 2017. URL: www.england.nhs.uk/wp-content/uploads/2017/10/national-cancer-transformation-programme-2016-17-progress.pdf | Cancer; no mention of the EoL care of patients with pre-existing SMI |
| NHS Scotland. Clinical Standards Specialist Palliative Care. 2002. URL: www.palliativecarescotland.org.uk/content/publications/ClinicalStandardforSPC.pdf | EoL care; no mention of care of patients with mental illness |
| NHS Scotland. Living and Dying Well. A National Action Plan for Palliative and End of life Care in Scotland. 2008. URL: www2.gov.scot/resource/doc/239823/0066155.pdf | EoL care; no mention of care of patients with mental illness |
| NHS Scotland. Care in the Last Days of Life. 2014. URL: www.palliativecareguidelines.scot.nhs.uk/guidelines/end-of-life-care/care-in-the-last-days-of-life.aspx | EoL care; no mention of care of patients with mental illness |
| Prisons and Probation Ombudsman for England and Wales. Learning from PPO Investigations. End of Life Care. 2013. URL: www.ppo.gov.uk/app/uploads/2014/07/Learning_from_PPO_investigations_-_End_of_life_care_final_web.pdf | EoL care; no mention of care of patients with mental illness |
| Public Health England. What We Know Now 2014: New Information Collated by the National End of Life Care Intelligence Network. URL: www.endoflifecare-intelligence.org.uk/resources/publications/what_we_know_now_201 | EoL care; no mention of care of patients with mental illness |
| Public Health England. Atlas of Variation for Palliative and End of Life Care in England. 2018. URL: https://fingertips.phe.org.uk/profile/atlas-of-variation | EoL care; no mention of care of patients with mental illness |
| Royal College of Nursing. Getting It Right Every Time. Fundamentals of Nursing Care at the End of Life. 2015. URL: www.rcn.org.uk/professional-development/publications/pub-004871 | EoL care; refers to psychological support but not specific to SMI |
| Royal College of Physicians. National Care of the Dying Audit for Hospitals, England. National Report. 2014. URL: www.rcplondon.ac.uk/projects/outputs/national-care-dying-audit-hospitals | EoL care; no mention of care of patients with mental illness |
| Royal College of Psychiatrists. Liaison Psychiatry for Every Acute Hospital: Integrated Mental and Physical Healthcare. 2013. URL: www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/college-report-cr183.pdf?sfvrsn=1c625881_2 | Liaison psychiatry; no mention of care of patients at the EoL |
| Scottish Government. The Healthcare Quality Strategy for NHS Scotland. 2010. URL: www.gov.scot/binaries/content/documents/govscot/publications/report/2010/05/healthcare-quality-strategy-nhsscotland/documents/0098354-pdf/0098354-pdf/govscot%3Adocument | General health care; some sections on EoL care but no mention of the EoL care of patients with pre-existing SMI |
| Scottish Government and NHS Scotland. Achieving Sustainable Quality in Scotland’s Healthcare. A ‘20:20’ Vision. 2011. URL: www2.gov.scot/Topics/Health/Policy/2020-Vision/Strategic-Narrative | General health care; no mention of the EoL care of patients with pre-existing SMI |
| Secretariat of the Commission of the Bishops’ Conferences of the European Community. Opinion of the Working Group on Ethics in Research and Medicine on Palliative Care in the European Union. 2016. URL: www.comece.eu/dl/psqlJKJKooNNJqx4KJK/PalliativeCARE_EN.pdf | EoL care; no mention of care of patients with mental illness |
| The National Council for Palliative Care. The End of Life Care Strategy: New Ambitions. 2013. URL: www.ncpc.org.uk/sites/default/files/End%20of%20Life%20Care%20Strategy%20New%20Ambitions%20Report_WEB.pdf | EoL care; no mention of care of patients with mental illness |
| Scottish Government. Strategic Framework for Action on Palliative and End of Life Care 2016–2021. 2015. URL: www.gov.scot/publications/strategic-framework-action-palliative-end-life-care/#res491388 | EoL care; no mention of care of patients with mental illness |
| Wales Cancer Network. Cancer Delivery Plan for Wales 2016–2020. 2016. URL: www.walescanet.wales.nhs.uk/sitesplus/documents/1113/161114cancerplanen.pdf | Cancer; no mention of the EoL care of patients with pre-existing SMI |
| Welsh Government. Together for Mental Health: Delivery Plan: 2016–10. 2016. URL: https://gov.wales/docs/dhss/publications/161010deliveryen.pdf | Mental health; no mention of care of patients at the EoL |
| Welsh Government. Together for Health: Delivering End of Life Care. 2013. URL: https://gov.wales/docs/dhss/publications/130416careen.pdf | EoL care; no mention of care of patients with mental illness |
| Welsh Government. Palliative and End of Life Care Delivery Plan. 2017. URL: https://gov.wales/docs/dhss/publications/170327end-of-lifeen.pdf | EoL care; no mention of care of patients with mental illness |
| Worldwide Palliative Care Alliance. Global Atlas of Palliative Care at the End of Life. 2014. URL: www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf | EoL care; no mention of care of patients with mental illness |
| National Institute for Health and Care Excellence. End of Life Care for Adults: Service Delivery. 2019. URL: www.nice.org.uk/guidance/ng142 | EoL care; no mention of care of patients with mental illness |
Appendix 16 Table of included grey literature
| Study | Focus |
|---|---|
| Addicott and Ashton 2010155 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Care Quality Commission 2016157 | EoL care and mental health |
| Includes information on EoL care for those with pre-existing SMI | |
| Care Quality Commission 2016157 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Care Quality Commission 2017156 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Department of Health 2008161 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Department of Health 2016160 | General health care |
| Some sections on mental health and physical health | |
| Department of Health 2018159 | Mental health |
| Some sections on EoL care for people with pre-existing SMI | |
| General Medical Council 201021 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Help the Hospices 2006162 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Independent Cancer Taskforce 201522 | Cancer |
| Some sections on EoL care for people with pre-existing SMI | |
| Leadership Alliance for the Care of Dying People 2014177 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Marie Curie 2016164 | EoL care and mental health |
| Includes information on EoL care for those with pre-existing SMI | |
| Marie Curie 2016165 | EoL care and mental health |
| Includes information on EoL care for those with pre-existing SMI | |
| Marie Curie 2017163 | EoL care and mental health |
| Includes information on EoL care for those with pre-existing SMI | |
| Addington-Hall 200030 | EoL care and mental health |
| Includes information on EoL care for those with pre-existing SMI | |
| NICE 200455 | Cancer |
| Some sections on EoL care for people with pre-existing SMI | |
| NHS England 2019167 | General health care |
| Some sections on EoL care or the care of people with SMI | |
| NHS England 20141 | General health care |
| Some sections on EoL care for people with mental health conditions | |
| NHS England 2017168 | General health care |
| Some sections on EoL care for people with pre-existing SMI | |
| NHS Lothian 2010170 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Royal College of Physicians 2007171 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Scottish Government 2017172 | Mental health |
| Some sections on EoL care for people with pre-existing SMI | |
| Social Care Institute for Excellence 2013173 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Welsh Government 2012175 | Mental health |
| Some sections on EoL care for people with pre-existing SMI | |
| Welsh Government 2018174 | General health care |
| Some sections on EoL care or the care of people with mental ill health | |
| Worldwide Palliative Care Alliance 2017176 | EoL care |
| Some sections on EoL care for people with pre-existing SMI | |
| Healthcare Quality Improvement Partnership 2019421 | EoL care |
| A section on mental health providers | |
| Kennedy et al. 2013120 | EoL care |
| Some sections on EoL care for people with pre-existing SMI |
Appendix 17 Characteristics of retrospective cohort studies included in the review
| Author, year, country; aim; mental health diagnosis; terminal/chronic condition or cause of death; definition of EoL/palliative care | Setting; patient characteristics | Design; data sources; outcomes; outcome measures |
|---|---|---|
|
Butler and O’Brien 2018, 100 New Zealand Aim To compare the rate of access to palliative care services for people with SPMI with the rate for the general population Mental health diagnosis SPMI Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Specialist palliative care services in the LYoL |
Setting Specialist palliative care services within a district public health board Participants Decedents with SPMI utilising specialist palliative care services (n = 147); decedents from the general population utilising palliative care services (n = 230,571) Age (years) SPMI cohort: 18–24 (2%); 25–44 (16%); 45–64 (42%); 65–84 (31%); ≥ 85 (9%) General population: 18–24 (19%); 25–44 (36%); 45–64 (30%); 65–84 (13%); ≥ 85 (2%) Gender SPMI cohort: male (78%) General population: male (47.5%) Ethnicity SPMI cohort: European (79%); Maori (15%); Pacific (3%); Asian (2%) General population: European (65.5%); Maori (12.5%); Pacific (8%); Asian (14%) |
Design Retrospective cohort (over 7 years) Data sources The mental health data came from the Programme for the Integration of Mental Health Data, which is a national mental health and addiction database of service activity and outcomes. The information on this database is collected from district health boards and non-governmental organisations Population information came from Ministry of Health reports and reported data limited to the Capital and Coast District Health Board region Outcomes Rate of access to palliative care services The rate ratio of specialist palliative care utilisation was calculated by dividing the rate of contacts for people with SPMI by the rate of contacts for the general population Outcome measures The number of specialist palliative care service contacts in the LYoL for people with SPMI was compared with the number of specialist palliative care service contacts within the general population Statistical analysis Descriptive statistics Rate ratios |
|
Fond et al. 2019, 108 France Aim To establish whether or not the EoL care delivered to patients with schizophrenia and cancer differed from that delivered to patients with cancer who did not have a diagnosis of mental illness Mental health diagnosis Schizophrenia Causes of death Brain cancer, liver cancer or any metastatic solid cancer Definition of EoL care/palliative care Last 31 days of life |
Setting French hospital care Participants Decedents with schizophrenia (n = 2481); decedents without mental illness (n = 222,477) Age (years) Matched cohort: 15–62 (22.2%); 63–71 (24.1%); 72–81 (28.4%); ≥ 82 (25.3%) Schizophrenia cohort: 15–62 (48.6%); 63–71 (24.7%); 72–81 (17.3%); ≥ 82 (9.4%) Gender Matched cohort: male (58%) Schizophrenia cohort: male (56%) Ethnicity No data reported |
Design Retrospective population-based cohort study (over 4 years) Data sources Data from Le Programme de Médicalisation des Systèmes d’Information, the French national hospital database, in which administrative and medical data are systematically collected for acute and psychiatric care Outcomes Health service utilisation in the 6 months prior to death for people with schizophrenia and cancer compared with those with cancer only and no schizophrenia diagnosis Outcome measures Access to palliative care in the last 31 days of life and the last 3 days of life Chemotherapy in the last 14 days of life Within the last 31 days of life Artificial nutrition (i.e. enteral or parenteral nutrition), tracheal intubation, mechanical ventilation, gastrostomy (or change in gastrostomy status), cardiopulmonary resuscitation, dialysis, blood transfusion, surgery, imaging, endoscopy At least one ED admission, one ICU admission, one air extraction chamber (i.e. sterile chamber) admission More than one admission to acute care unit Length of stay in acute care unit Death in ED ICU Statistical analysis Multivariate analysis presented as adjusted ORs [adjusted for social deprivation, year of death, time from cancer diagnosis to death, metastasis (yes vs. no), comorbidity, hospital category (specialist vs. non-specialist cancer centre] |
|
Ganzini et al. 2010, 88 USA Aim To compare measures of quality of EoL care among veterans with and veterans without schizophrenia who died of cancer Mental health diagnosis Schizophrenia or schizoaffective disorder Cause of death Cancer Definition of EoL/palliativecare Last 6 months of life |
Setting Veterans’ Associations medical centres in north-west USA (Oregon, Washington and Alaska) Participants Veterans/decedents with schizophrenia or schizoaffective disorder who died of cancer (n = 60) were compared with veterans/decedents with no major mental illness who died of cancer (n = 196) Age (years), mean (SD) Cancer and schizophrenia, 64.1 (11.5); cancer without schizophrenia, 70.5 (10.4) Gender Cancer and schizophrenia: male (93%) Cancer without schizophrenia: male (97%) Ethnicity No data reported |
Design Retrospective cohort (over 6 years) Data sources Data from the data management system of the US Department of Veterans Affairs Northwest Health Network–Veterans Integrated Service Network 20 were obtained along with medical record review Outcomes Quality of EoL care Outcome measures Enrolment in and length of hospice care Prescription of any opioids in the last 6 months of life but before hospice enrolment Presence of an advance directive or physician orders Statistical analysis t-tests and chi-squared tests |
|
Huang et al. 2017, 89 USA Aim To gain knowledge on mental health disparities in EoL care; to identify at least three quality indicators of EoL care processes that are associated with mental health diagnoses Mental health diagnosis Any mental health diagnosis – not specified Terminal conditions Cancer (30.1%), heart disease (20.1%), other (not reported) Definition of EoL/palliative care Processes of care at the EoL; time frame not specified |
Setting Not reported Participants Inpatient veterans/decedents (n = 5476) Age (years), mean (SD) 70.1 (22.5) Gender Male (98%) Ethnicity White (65%); black (34%) |
Design Retrospective cohort (over 7 years) Data sources Data were drawn from the Best Practices for EoL care for Our Nation’s Veterans (BEACON) trial conducted Outcomes Quality of EoL care Outcome measures Opioid order, do-not-resuscitate order, intravenous line infusing at time of death, nasogastric tube and physical restraints Statistical analysis Generalised equation modelling presented as ORs |
|
Huang et al. 2018, 101 Taiwan (Province of China) Aim To compare the medical treatments received by cancer patients with and without schizophrenia within 1 and 3 months prior to their death Mental health diagnosis Schizophrenia Terminal conditions Cancer (breast, lung, liver, colorectal, oral, prostate) Definition of EoL/palliative care Within 1 month or 3 months of death |
Setting All medical care covered by the National Health Insurance Program, which covers approximately 99% of the population and has contracts with 97% of the hospitals and clinics Participants Patients from 20 years old who were newly diagnosed as having one of six common cancers between 2000 and 2012 but who were not alive by the end of the study period Matched (ratio 1 : 4) sample decedents with no previous schizophrenia diagnoses (n = 7644) Age (years) < 50 (23.4%), 50–69 (44.8%), > 70 (31.7%) Gender Male (55%) Ethnicity Not reported |
Design Retrospective cohort (over 12 years) Data sources Nationwide population-based cohort study based on the National Health Insurance Research Database of Taiwan Outcomes Medical treatments or interventions 1–3 months prior to their death Utilisation of medical care and palliative care 1–3 months prior to their death Advanced diagnostic examinations 1–3 months prior to their death Outcome measures Numbers receiving chemotherapy, invasive intervention and advanced diagnostic examination Number of inpatient days ICU utilisation (days) Palliative care and hospice ward care utilisation (days) Palliative care consultation and hospice home care Statistical analysis Multiple logistic regression analysis presented as ORs (adjusted for age, sex, type of primary cancer, comorbidity, year of death, time from cancer diagnosis to death, income, hospitalised in an acute ward in the month before death (yes vs. no) |
|
Lavin et al. 2017, 91 USA Aim To examine whether or not having a psychiatric illness is associated with site of death or health-care utilisation in the last month of life Mental health diagnosis Psychiatric illness (ICD-9) diagnosis of mood, anxiety and/or psychotic disorder or prescription medications for psychiatric illness prevalence 10.6% (5.6% based on documented diagnosis and 5.0% based on psychiatric medication prescription) Chronic conditions (of relevance) Non-haematological cancer, chronic obstructive pulmonary disease, congestive heart failure, chronic liver disease, chronic renal disease Definition of EoL/palliative care Last month of EoL |
Setting UW Medicine health-care system, an integrated health-care system that includes four diverse academic and community hospitals Participants Decedents without psychiatric illness (n = 14,499) and decedents with psychiatric illness (n = 1715) Age (years), mean (SD) Psychiatric illness: 61.3 (14.1) No psychiatric illness: 64.6 (12.3) Gender Psychiatric illness: male (50.3%) No psychiatric illness: male (53.8%) Ethnicity (psychiatric illness cohort) Hispanic ethnicity (1.7%); white (84.3%); black (7.4%); Native American (2.2%); Asian (3.3%); Pacific Islander (0.2%); other race (1.4%); mixed race (1.2%) |
Design Retrospective cohort (over 4 years) Data collection methods Data were extracted from UW Medicine electronic health records and from Washington State death certificates Outcomes Occurrence and length of non-surgical acute care hospitalisations Occurrence and number of ED visits that did not result in a subsequent non-surgical hospitalisation Occurrence and length of ICU stays Place of death Statistical analysis Logistic regression using zero-inflated negative binomial models presented as ORs (adjusted for a combination of age, race, insurance status, comorbidities, marital status, facility insurance status, cancer, chronic obstructive pulmonary disease, congestive heart failure, diabetes or chronic renal disease depending on the outcome of interest) |
|
Martens et al. 2013, 97 Chochinov et al. 2012, 95 Canada Aim To compare place and cause of death of those with and those without schizophrenia in Manitoba, Canada97 To compare rate of health-care services, including palliative care, used in the last 6–24 months of life for patients with and patients without schizophrenia95 Mental health diagnosis Schizophrenia Cause of death (of relevance) Cancer Definition of EoL/palliative care Palliative care used in last 6–24 months of life |
Setting All hospital- and community-based palliative care in the universal health-care system of the province of Manitoba Participants Decedents with schizophrenia diagnoses in 12 years prior to death (n = 3943); matched (ratio 1 : 3) decedents with no previous schizophrenia diagnoses (n = 11,827) Age (years), mean (SD) (all) 73.4 years (16.5 years) Gender (all) Male (43.3%) Ethnicity Not reported |
Design Retrospective cohort (over 12 years) Data sources De-identified (‘anonymised’) administrative claims data were used from the Population Health Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba Outcomes Relationship between place of death by cause of death97 Health service use patterns by place of death in last 6 months of life97 Health service utilisation rates in the 6 months prior to death for decedents with and decedents without schizophrenia95 Outcome measures Place of death: hospital, home, nursing home and other97 GP visit rate per person97 Physician specialist visit rate per person97 Inpatient hospital separation rates per person97 Rate of inpatient hospital days per person97 Visits to GPs (family practice physician), specialists, inpatient stays in acute care hospitals, use of nursing homes (long-term institutional care, also referred to as personal care homes)95 Use of palliatve care95 Use of home care services95 Utilisation of analgesics95 |
|
McDermott et al. 2018, 92 USA Aim To assess the relationship between depression and health-care utilisation at the EoL among older adults (aged ≥ 67 years) diagnosed with advanced non-small-cell lung cancer from 2009 to 2011 Mental health diagnosis Pre-cancer, diagnosis-time or post diagnosis depression Terminal condition Advanced non-small-cell lung cancer Definition of EoL/palliative care Last 30 days of life |
Setting Acute health-care services and hospice care in the USA Participants Decedents with:Age (years), mean (SD) (pre-cancer depression cohort) 77.4 (6.9) Gender (pre-cancer depression cohort) Male (35%) Ethnicity (pre-cancer depression cohort) White (90%); Hispanic (5%) |
Design Retrospective cohort (over 3 years) Data sources SEER-Medicare Linked Database, comprising Medicare claims linked to clinical data for subjects in the National Cancer Institute’s SEER data set Outcomes Health-care utilisation Outcome measures High-intensity EoL care as chemotherapy in the last 14 days of life Less than 3 days of hospice use or no hospice use Any ICU admission, > 1 inpatient hospitalisation admission, in-hospital death or > 1 ED visit in the last 30 days of life Length of hospice enrolment Statistical analysis Multivariable logistic regression presented as adjusted ORs (adjusted for days survived following diagnosis, race, Hispanic ethnicity, gender, age, socioeconomic status, marital status and rural residence) |
|
Spilsbury et al. 2018, 107 Australia Aim To describe the trajectory of acute health-care service use in the LYoL for people with schizophrenia and how this varied with receipt of community-based specialist palliative care and morbidity burden Mental health diagnosis Schizophrenia Cause of death (of relevance) Heart failure, cirrhosis/liver disease, renal disease/dialysis, chronic lower respiratory disease or cancer Definition of EoL/palliative care LYoL |
Setting Acute health-care services and community-based health-care services use in Western Australia Participants Decedents with a lifetime history of schizophrenia diagnoses (n = 1196); matched sample of decedents with no previous schizophrenia diagnoses (n = 62312) Age (years), mean (SD) (schizophrenia cohort) 20–29 years (4.3%); 30–39 years (7.4%) 30–39 years (10.9%); 50–59 years (14.2%) 60–69 years (17.7%); 70–79 years (19.1%) 80–89% (20.2%); ≥ 90 years (6.4%) Gender (schizophrenia cohort) Male (52%) Ethnicity Not reported |
Design Retrospective cohort (over 5 years) Data sources Data linkage and de-identified data extraction from the Western Australia Data Linkage System was performed Outcomes Acute care health service use Receipt of community-based specialist palliative care Morbidity burden Outcome measure Morbidity burden ED presentations over LYoL Number of hospitals admission in LYoL Community-based care in the LYoL Statistical analysis Regression analysis presented as HRs (adjusted for age, sex, accessibility, relative disadvantage, indigenous status, partner status, country of birth and number of comorbid conditions) |
|
Kelley-Cook et al. 2016, 90 USA Aim To evaluate the clinical impact of palliative care in the treatment of terminally ill Vietnam veterans with a history of PTSD compared with those without PTSD, as it pertains to medications for symptom control at the EoL Diagnosis PTSD plus a range of other SMI or SMI-relevant symptoms (e.g. hallucinations) Terminal conditions (of relevance) Cancer, heart disease, liver disease, pulmonary disease and renal disease Definition of EoL/palliative care Use of medications at EoL; time frame not specified |
Setting One US tertiary veterans’ hospital Participants Veterans with PTSD (n = 39); veterans without PTSD (n = 137) Age (years), mean (SD) Mean age was 65.12 Gender Male (99%) Ethnicity Not reported |
Design Retrospective cohort study Data sources Electronic medical records of a veterans’ hospital Outcomes Social support, palliative care team interventions, family meeting interventions; medications Outcome measures Differences in pharmacologic treatment and non-pharmacological palliative care interventions between those with and those without PTSD Statistical analysis t-tests and chi-squared tests |
|
Cai et al. 2011, 84 USA Aim To test whether or not persons with SMI were as likely as other nursing home residents to make informed choices about treatments through medical advance care planning Mental health diagnosis Schizophrenia, bipolar disorder or other psychosis Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Medical ACP |
Setting Nursing homes (n = 1174) Participants Residents with SMI (n = 1769) and residents with no SMI (n = 11,738) Age (years), mean (SD) SMI, 75.7 (5); no SMI, 81.1 (2) Gender SMI, male (32%); no SMI, male (28.4%) Ethnicity (SMI) Non-Hispanic white (80.2%); African American (13.3%); Hispanic (5.3%); other (1.2%) |
Design Retrospective cohort study Data sources Data came from the 2004 National Nursing Home Survey that was conducted by the US Centers for Disease Control and Prevention Outcomes Whether or not sampled residents had any of the following advance care documents collected by the survey: living wills, DNR orders, do-not-hospitalise orders, and orders restricting feeding, medication or other treatments Statistical analysis t-tests and chi-squared tests Logistic regression analysis presented as adjusted ORs (adjusted for age, gender, race, marital status, being a veteran, length of stay, payment source, number of impairments of daily activities) |
|
Podymow et al. 2006, 98 Canada Aim To improve health-care delivery to homeless adults Mental health diagnosis Depression (43%); schizophrenia (39%); anxiety (18%); none (14%) Causes of death (of relevance) Cancer (25%); chronic obstructive lung disease (4%) Definition of EoL/palliative care Palliative care delivery; time frame not specified |
Setting 15-bed shelter-based palliative care/hospice pilot programme Participants Homeless patients who were admitted to the hospice, received terminal care and died between July 2001 and August 2003 (n = 28) Age (years), mean (SD) 49 (10.5) Gender Male (89%) Ethnicity Caucasian (89%); African American (7%); Aboriginal (4%) |
Design Retrospective cohort (over 2 years) Data sources Data obtained from physician and nurse’s patient intake history and medical transfer notes Outcomes Clinical course and care of the patients; costs Outcome measures Costs per patient stay, main symptoms, oxygen requirements, palliative care consults, number of medications, type of self-care assistance Pain management and type of pain management Religious counse Number of family visits Reasons precluding transfer to palliative care hospital Statistical analysis Descriptive statistics |
Appendix 18 Characteristics of included qualitative studies
| Author, year, country; aim; mental health diagnosis; terminal/chronic condition or cause of death; definition of EoL/palliative care | Setting; patient characteristics | Design; data collection methods; data analysis | Thematic findings |
|---|---|---|---|
|
Jerwood et al. 2018,112 UK Aims To examine the views of the clinical staff on the barriers to providing EoL care to people with SMI and to begin to consider how improvements can be made Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General EoL care |
Setting Mental health trust Hospice Participants Clinical staff (n = 23) who had some experience of working with the patient group and of the issues of EoL care No patient details reported |
Design Qualitative descriptive Data collection methods Focus groups (n = 4) Cube ideas generation tool – participants wrote and drew on the Cube while the verbal discussion was taking place. In addition, paper and envelopes were made available to gather additional data from participants who felt uncomfortable sharing views in a group setting Data analysis Framework analysis |
|
|
McGrath and Holewa 2004,102 McGrath and Jarrett 2007,103 McGrath and Forrester 2006,104 Australia Aim of research project To document the experience of providing EoL care to patients for health-care workers in an institutional mental health setting Focus of individual publications To highlight the similarity in philosophy between palliative care and mental health practice102 The findings presented here focus on one of the central problems impacting on EoL care, that of the stigma attached to mental health patients103 To explore important ethicolegal issues at the interface of palliative care and institutional mental health104 Mental health diagnosis Mental health patients but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General EoL care |
Setting Mental health institution Participants Those directly involved in the care of two patients who had died in the last year (n = 8) No patient details reported |
Design Qualitative phenomenology Data collection methods Interviews Participants were encouraged to talk about their experiences of caring for a terminally ill patient. Of particular interest was an exploration of factors that the participant believed either facilitated or hindered the provision of optimal EoL care Data analysis Thematic analysis |
McGrath and Holewa 2004102
|
|
McNamara et al. 2018,106 Australia Aim To address the paucity of research by documenting possible need, experiences of health-care service use and factors affecting palliative care use for people with schizophrenia who have advanced life-limiting illness Mental health diagnosis Schizophrenia but not linked to specific patients Terminal condition Advanced life-limiting illness Definition of EoL/palliative care General experiences of EoL care |
Setting HCPs employed in government policy and management, palliative care, mental health, community service provision, clinical care, allied health care, high-care residential homes and community-based supported accommodation, including psychiatric hostels Participants HCPs (n = 16) who were caring for, or had experience of caring for, people with schizophrenia Three participants worked specifically in a role that covered both mental health and palliative care No patient details reported |
Design Qualitative descriptive Data collection methods Interviews Three participants who worked in the same location were interviewed together An interview guide was used that focused on the EoL needs of people with schizophrenia, their experiences with health services and their possible need for palliative care Data analysis Thematic analysis |
People with schizophrenia at the EoL: challenges of a vulnerable group
|
|
Morgan 2016,32 USA Aim To explore the needs and attitudes of nurses in psychiatric/mental health settings towards patients who are in need of palliative and EoL care Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General experiences of EoL care |
Setting Hospice/palliative care Psychiatric/mental health care Participants Palliative care/HC nurses (n = 7) Psychiatric/mental health care (n = 6) Palliative care/HC and mental health nurses (n = 2) HIV/AIDS nurses, geriatric nurse practitioner, and working with homeless individuals All who had reported having worked with people with SMI at the EoL No patient details reported |
Design Qualitative phenomenology described as a pilot study Data collection methods Interviews An interview guide was used to elicit the participants’ stories related to the nurses’ experience with EoL and palliative care with patients with SMI. The questions in the interview helped explore topics related to the specific aims and capture the impact of contextual and individual factors that influenced the individual’s thought process, behaviour and outcome Data analysis Thematic analysis |
|
|
Hackett and Gaitan 2007,37 UK Aim To gain an understanding of the current practice of mental health assessments in the hospice service in two hospices in the UK Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General experiences of EoL care |
Setting Hospice Participants Nurses (n = 6), HCAs (n = 1) or doctors (n = 2) recruited from two hospice staff teams No further details reported |
Design Qualitative grounded theory Data collection methods Interviews An interview guide was used, which focused on staff members’ views on roles with regard to mental health assessments and the overall processes involved Data analysis Constructing networks of findings based on the interview questions (how staff members’ feelings inform clinical practice and training needs) |
|
|
McKellar et al. 2016,105 Australia Aim To explore how old-age psychiatrists approach and experience working with patients at the EoL Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General experiences of EoL care |
Setting Public mental health services for older people but most also maintained some private practice Participants Old-age psychiatrists recruited via e-mail sent to all members of the Australian Faculty of Psychiatry of Old Age and the New Zealand College of Psychiatrists (n = 9) No patient details reported |
Design Qualitative descriptive Data collection methods Interviews A semistructured interview guide was developed, drawing on literature identifying the possible roles old-age psychiatrists may have at the EoL, to explore experiences working with patients at the EoL, approaches to this work and the impact of these experiences on participants Data analysis Thematic analysis |
Death is not our business: working in a mental health framework
|
|
Stajduhar et al. 2019,99 Canada Aim To identify barriers to accessing care among structurally vulnerable people at the EoL Mental health diagnosis Mental health issues Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General experiences of accessing EoL care |
Setting Homeless or vulnerably housed in a western Canadian province Participants Three participant groups: (1) those experiencing structural vulnerability and who were deemed to be on a palliative trajectory (n = 25); (2) their support (n = 25); and (3) their formal service providers (housing workers, clinicians) (n = 69) Age (years) (group 1) Mean 59, range 19–81 Gender (group 1) Male (64%) Ethnicity (group 1) White (52%); Indigenous (32%); African Canadian (4%) |
Design Qualitative ethnographic Data collection methods Ethnographical observation and in-depth interviews informed by the critical theoretical perspective of equity and social justice Data collection for all groups was longitudinal, over 30 months, through repeated observation in homes, shelters, transitional housing units and community-based service centres, on the street and at health-care appointments Semistructured interviews and observational data (interviews: structurally vulnerable participants, n = 19; support persons, n = 16; service providers, n = 23) Data analysis Constant comparison analysis Thematic analysis |
Barriers to accessing care
|
|
Sweers et al 2013,109 Belgium Aim To gain a better insight into the perspectives and expectations of patients with schizophrenia about EoL (care) Mental health diagnosis Schizophrenia: paranoid (65%); schizoaffective disorder (35%) Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Future EoL perspectives and expectations |
Setting Psychiatric hospital Participants Schizophrenic patients in remission with a minimum illness duration of 10 years (n = 20) Gender Male (60%) Age (years) Range 38–51; mean 47.3 + 6.9 Ethnicity Not reported |
Design Qualitative grounded theory Data collection methods Interviews An interview guide was used; questions were broad and related to the experience of living with schizophrenia and EoL situations, and associated feelings and reactions, as well as the perceived impact of these experiences on the person’s life and expectations about EoL (care) 5 out of 10 were interviewed twice – project was refined because of a lack of detailed information; next 10 had two interviews each Data analysis Constant comparison analysis |
Note: study was conducted in Belgium, where euthanasia is legal
|
|
Shulman et al. 2018,113 UK Aim To explore the views and experiences of current and formerly homeless people, front-line homelessness staff (from hostels, day centres and outreach teams) and health- and social-care providers, regarding challenges to supporting homeless people with advanced ill health, and to make suggestions for improving care Mental health diagnosis Background talks about trimorbidity drug and/or alcohol dependence and mental health problems in association with physical health issues Terminal condition Advanced life-limiting illness Definition of EoL/palliative care General experiences of EoL care |
Setting Three London boroughs Participants Single homeless people (n = 28) Formerly homes people (n = 10) Health and social care providers (n = 48) Hostel staff (n = 30) Outreach staff (n = 10) Gender Male (54%) across all groups No further patient details reported |
Design Qualitative descriptive Data collection methods Interviews (n = 10) Focus groups (n = 28) Use of case study vignette to generate discussion for all participants (no mental health focus) No details given about interviews Data analysis Thematic analysis |
Complex behaviours in mainstream services
|
Appendix 19 Characteristics of descriptive cross-sectional surveys included in the review
| Author, year, country; aim; mental health diagnosis; terminal/chronic condition or cause of death; definition of EoL/palliative care | Setting; place of death; patient characteristics | Design; data collection methods; outcomes |
|---|---|---|
|
Alici et al. 2010, 83 USA Aim To define the frequency of PTSD-related symptoms among veterans who are near the EoL and to describe the impact that these symptoms have on patients and their families Mental health diagnosis PTSD-related symptoms (17%) Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Last month of life |
Setting VA medical centres and their affiliated nursing homes (n = 5) Participants Family members of patients (n = 524, rr 54%) who had received any inpatient or outpatient care from a participating VA medical centre in the last month of life. Among the 524 were patients with PTSD-related symptoms (n = 89) Age (years) Mean 71 (range 50–94) Gender Male (99%) Ethnicity African American (20%); white, non-Hispanic (78%); Hispanic (1%); other/unknown (1%) |
Design Descriptive survey Data collection methods Questionnaire that assessed their perceptions of the quality of the care and services that the patients and the family members themselves received during the patient’s last month of life and after the patient’s death, administered 4–6 weeks post death The FATE survey has 32 items and evaluates outcomes by asking respondents for frequency ratings (e.g. ‘How often did [the patient’s] pain make him/her uncomfortable?’) or yes/no responses (e.g. ‘Do you think [the patient] died where he/she wanted to?’). For each symptom that family members reported, they were asked how often that symptom made the patient uncomfortable (never, 0; sometimes, 1; usually, 2; always, 3) Outcomes |
|
Patterson et al. 2014, 93 USA Aim To explore the current level of collaboration between psychiatrists and palliative care consult services across the USA and the factors that support or restrict such involvement Mental health diagnosis Personality disorders (as reported by palliative care services) as well as other mental health needs Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Use of palliative care services |
Setting Inpatient and outpatient palliative care consult services within academic medical centres (non-profit, community hospitals private medical centres and VA hospitals) Participants Programme directors of palliative care consult services identified through the National Registry maintained by the Center to Advance Palliative Care (n = 260, rr 67%) No patient details reported |
Design Descriptive survey Data collection methods A 36-item survey was developed following consultation with clinical and academic experts. The survey was divided into four areas: (1) demographic information about the programme director, (2) information about the facility and palliative care service composition, (3) patient mental health issues of concern and (4) psychiatrist involvement with the palliative care service Outcomes |
|
Evenblij et al. 2016, 110 the Netherlands Aim To explore nurses’ experiences with and to identify barriers to providing palliative care to psychiatric patients in Dutch mental health facilities Mental health diagnosis Psychiatric disorders, which included schizophrenic or other psychotic disorders (40%); personality or behavioural disorder (36%); mood disorder (30%); anxiety disorder (30%) Causes of death (of relevance) Cancer (35%), respiratory disorder (COPD) (4%), liver failure (4%) Definition of EoL/palliative care General experience of palliative care services |
Setting Mental health facilities Participants Nurses registered in the Dutch Nurses’ Association’s division of psychiatric nursing who currently worked in a mental health facility and who had experience concerning palliative care provision (n = 137, rr 26%) No patient details reported |
Design Mixed methods (descriptive survey and descriptive qualitative) Data collection methods An online survey based on pre-existing questionnaires. It was pilot tested and minor changes were made. Final survey consisted of two parts All nurses were asked to fill in questions about their knowledge, experience and needs concerning palliative care provision (n = 137), and nurses who had provided palliative care in the past 2 years were asked to fill in 27 additional case-specific questions about the care they had provided to the last patient who had died as a result of chronic physical comorbidity or old age (n = 50) Only the case-specific questions were reported in this publication Face-to-face interviews (n = 9) were conducted with a subset of the sample, which sought to identify nurses’ personal experiences with palliative care provision in mental health facilities. Thematic analysis was conducted Outcomes |
|
Sheridan et al. 2018, 114 Ireland Aim To examine how and by whom (GPs, psychiatrists, other HCPs) the need for palliative care is identified for people with a diagnosed mental illness To identify the referral pathways and access to physical health and palliative care services To identify how palliative care needs of people with SMI are managed once identified Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care General use of palliative care services |
Setting General practice Psychiatric practice Participants GPs who were currently on the register of the Irish College of General Practitioners in both the Republic of Ireland (n = 434, rr 17.4%) and Northern Ireland (n = 133, rr 9%) Psychiatrists (n = 80, rr 26.2%) identified from the Irish Medical Directory No patient details reported |
Design Mixed methods (descriptive survey and qualitative descriptive) Data collection methods A postal survey was conducted, and the questionnaire was based on a similar questionnaire utilised with GPs in the Republic of Ireland, which was adapted and piloted. Interviews with a subset of psychiatrists (n = 6). No GPs and their existing patients with SMI in receipt of palliative care (n = 2) agreed to take part Outcomes |
|
Evenblij et al. 2019, 111 the Netherlands Aim To explore the differences between care staff in mental health facilities, nursing homes and care homes with regard to knowledge about palliative care, time pressure and self-efficacy in EoL communication, as well as aiming to identify determinants of high self-efficacy in EoL communication Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care EoL knowledge, self-efficacy, communication |
Setting Mental health facilities (survey 1); nursing and care homes (survey 2) Participants Nurses and care assistants who worked in mental health facilities (n = 137, rr 29%), nursing and care homes (n = 440, rr 52%) Patient characteristics not reported |
Design Descriptive survey Data collection methods Two descriptive surveys Survey 1: see Evenblij et al. 2016110 Survey 2: Knowledge of palliative care was measured using the MOVE2PC questionnaire Satisfaction with the time available for giving care to patients was assessed using an existing a five-point scale tool developed by Ruijeters and Stevens Self-efficacy in EoL communication was measured using the communication subscale from the S-EoLC survey Outcomes |
|
Taylor et al. 2012, 94 Australia Aim To improve the quality of palliative care for people with a severe and persistent mental illness and those who develop mental health issues as a response to their diagnosis of a life-limiting illness Mental health diagnosis SMI but not linked to specific patients Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Training in palliative care for mental health nurses |
Setting A collaboration between one metropolitan palliative care service, the district nursing service, a mental health service and two regional palliative care services Participants Mental health workers (n = 68), including consultant psychiatrists, GPs, mental health nurses, RNs, ENs, social workers, OTs, counsellors, community outreach workers, paramedical assistants, and students of psychology and social work took part in palliative care workshops Palliative care professionals (n = 36), including RNs, ENs, social workers, OTs, a bereavement counsellor and an art therapist took part in mental health workshops Patient characteristics were not reported |
Design Descriptive case study with post-test evaluation Intervention Cross–training mental health workshops for palliative care workers and palliative care workshops were given to mental health workers Pre- and post-evaluations were conducted by an independent evaluator Data collection methods Self-assessment survey with open-ended questions Outcomes |
|
Foti 2003, 85 USA Aim To better understand advance care planning processes for those with SMIs; to explore EoL care preferences among those with SMIs Mental health diagnosis SMI but not linked to specific patients Terminal condition or cause of death Not linked to a specific terminal condition Definition of EoL/palliative care Advance care planning |
Setting Two state hospitals and one acute community mental health centre Participants Hospital patient records (n = 328) and community mental health inpatient records (n = 16) Mental health providers (nurse managers, n = 4; nurses, n = 7; case managers, n = 14; community provider staff members, n = 10 and supervisors, n = 6) Hospice and pastoral care providers (clinical staff, n = 15; hospice directors, n = 3; pastoral care providers, n = 3) EoL care preferences People with SMI (no participant details reported) Education and training HCPs (no participant details reported) Professional outreach Medical professionals, mental health advocacy groups and family and consumer groups (no participant details reported) No further details reported |
Design Mixed methods (descriptive survey consisting of a retrospective review of patients’ medical records and a post-test evaluation of educational/training initiatives with HCPs) Intervention ‘Do It your Way’ project involved education, training and outreach The educational and training initiatives involved cross training, neighbour to neighbour initiative and the development of education and training curricula. The outreach involved professional outreach to medical professionals, mental health advocacy groups, and family and consumer groups and patient outreach Data collection methods for needs assessment Cross-sectional survey of patients’ medical records, survey of providers and a post-test evaluation of educational/training initiatives with HCPs Data collection methods for ‘Do It your Way’ project EoL care preferences To explore EoL care preferences among those with SMI, the team developed the 21-item HCPQ. To specifically evaluate the subject’s capacity to select a health-care agent, the team developed the CAT-HCP Education and training Post-cross-training core competency assessments Professional outreach Project staff developed a survey of attitudes and perceptions regarding advance care planning for persons with SMI Outcomes for needs assessment Evidence of actually having completed a proxy designation Formal education as well as personal and professional experiences regarding advance care planning and EoL care/improvements for care Outcomes for the ‘Do It your Way’ project |
|
Foti et al. 2005, 86 USA Aim To ascertain preferences for EoL care among persons with serious mental illness; to examine preferences regarding medical advance care planning among persons with SMI, specifically experience, beliefs, values and concerns about health-care proxies and EoL issues Mental health diagnosis Schizophrenia or other psychosis (66%), mood disorders (major depression and bipolar disorder) (28%), personality disorders or PTSD (6%) Terminal condition Not linked to a specific terminal condition Definition of EoL/palliative care Preferences for EoL care; advance care planning |
Setting Five community mental health agencies. Two agencies were located in suburban settings and three in urban environments Participants Adults with SMI who were receiving community-based services (n = 150) Age (years), mean (SD) 42 (10) Gender Male (55%) Ethnicity Caucasian (91%); other (9%) |
Design Descriptive survey Data collection methods HCPQ: see Foti 200385 Two hypothetical health state scenarios were adapted from standard scenarios in which patients have conditions that prevent them from expressing a choice between different types of palliative care, aggressive treatments and life support. The authors anticipated that hypothetical health state scenarios would enable us to learn about the advance care planning preferences of persons with serious mental illness, as they have for the general population Outcomes |
|
Elie et al. 2018, 96 Canada Aim To compare SPMI and CMI patients’ EoL care preferences and comfort level with EoL care discussion To identify potential predictors of interest in requesting medical assistance in dying at the EoL Mental health diagnosis SPMI (53%) Terminal condition Not linked to a specific terminal condition for those with SPMI; however, 47% were chronically medically ill Definition of EoL/palliative care Preferences and comfort level with EoL care discussion Medical assistance in dying |
Setting Jewish General Hospital Participants Patients attending the hospital between May and July 2016 Study group: patients diagnosed with a SPMI by their treating psychiatrist and without severe behavioural disturbances (n = 106, rr 83%) Comparator group: patients diagnosed with at least one chronic medical illness for > 2 years (n = 95, rr 89%) Age (years), mean (SD) SPMI: 65.5 (12.6); CMI: 63.3 (12.6) Gender SPMI: male (33%); CMI: male (43%) Ethnicity SPMI: Caucasian (80%); non-Caucasian (20%) CMI: Caucasian (58%), non-Caucasian (42%) |
Design Descriptive survey Data collection methods The authors conducted a 20-minute semistructured interview based on the HCPQ to gather information on different EoL care topics, such as treatment preferences and comfort level about EoL discussion. Two imaginary scenarios were also explored with participants (see Foti et al. 200586) Outcomes |
Appendix 20 Characteristics of case studies included in the review
| Author, year, country; purpose of article | Setting; demographic characteristics | Focus of case study | Discussion |
|---|---|---|---|
| Ang et al 2009,154 Singapore; addresses the challenge of what should be done in the case of people with chronic conditions that impair their capacity | Emergency hospital care of a 41-year-old woman with schizoaffective disorder since the age of 21 years and with end-stage renal failure since the age of 40 years | Ethical issues in EoL care for people lacking capacity to make decisions |
Autonomy of a patient with regard to medical treatment, assessment of the patient’s decisional capacity, and the process of deciding on the appropriate course to take for a patient without the mental capacity to give consent for required treatment in a potentially life-threatening situation Legal frameworks, tools to assess capacity and the use of advanced (‘Ulysses’) contracts are all addressed |
| Badger and Ekham 2011,122 USA; ethical conflicts at the EoL for patients with personality disorder, substance misuse and self-harming behaviour | A case of a 41-year-old man with long-term mental health problems whose physical health declined (liver and respiratory failure) and whose care presented an ethical challenge to practitioners | Ethical issues in EoL care for people lacking capacity to make decisions | Decision-making for people lacking capacity is difficult in the absence of advance directives and in the case of people with complex mental health and substance misuse problems |
| Bakker 2000,115 the Netherlands; focuses on the palliative care of patients in a ‘reactivation program’, this being a service for older people with complex health problems | A residential service using DSA for older people with complex mental and physical health problems, in which the case is a 91-year-old woman | The use of the DSA approach, including in the example of people who end their lives in the DSA service, illustrating the phases of the approach in action | The DSA approach is offered as a psychosocial counterbalance to more exclusively biomedically oriented approaches to care |
| Boyd et al. 1997,123 USA; the process of care for a hospice patient described as manipulating family, friends and hospice staff during her EoL care | A hospice service for people at the EoL, with the case being a 52-year-old woman with breast cancer who is described as having a pre-existing (but not clearly described) severe mental health problem characterised by ‘manipulative’ behaviour | The challenges faced by hospice staff in providing care to someone perceived as being manipulative, and how these can be addressed using practices informed by psychodynamic thinking | Hospice staff can provide care for people with ‘troubled personality’ using psychodynamic approaches, including supporting ego functioning, supporting autonomy, setting limits, and assessing and managing staff emotional responses |
| Cabaret et al. 2002,152 France; the provision of EoL care in an inpatient psychiatric hospital setting | An inpatient psychiatric hospital, with the case being a 45-year-old man with schizophrenia and lung cancer | The provision of humane, palliative care in a mental health hospital | Inpatient mental health staff are able to provide humane, dignified care until the EoL for people with SMI |
| Candilis and Foti 1999,124 USA; EoL care for someone with psychosis and cancer, where the patient’s preferences are not clearly known | A case study beginning in an ED and moving to a mental health unit, focused on the care of a 70-year-old woman with cancer and psychosis | Decision-making in the context of EoL care and psychosis, where the patient’s understanding and preferences are not clearly known | Differences in view can exist over the best course of action in cases where patients refuse treatment but do not elaborate – supportive, palliative, care or more aggressive intervention |
| Clements-Cortes 2004,149 Canada; the use of music therapy in the emotional care of people who are at the EoL | A discussion on the value of music therapy, followed by three case studies all of people using an older people’s palliative care inpatient service, of which two (a 71-year-old woman and a 72-year-old woman) had pre-existing mental health problems | The value of music in providing emotional support to people with terminal illnesses | Music therapy can facilitate emotional expression, including in people with SMI |
| Doron and Mendlovic 2008,153 Israel; EoL care in inpatient mental health wards | Two case studies of people, one aged 45 years at the time of her death and the other a woman whose age at death is not stated, cared for near to the EoL in inpatient mental health settings, where both had SMI and cancer | The challenges for both patients and staff of care during a terminal illness in a mental health inpatient setting | Information on the patient’s condition and prognosis should be given in the context of their capacity to understand; decisions should be made by patients where possible or otherwise by clinicians; and home is where people should die, meaning that if this is a psychiatric ward staff should be supported to provide care for as long as possible |
| Feely et al 2013,125 USA; EoL care in a hospice for people with borderline personality disorder | A case study of a 44-year-old woman with borderline personality disorder and terminal metastatic pancreatic cancer who was being cared for in a hospice | The difficulties for staff in hospices of providing care for people with complex mental health problems characterised by impulsive behaviour and difficulties in relationships | There is a lack of evidence to support interventions with people with borderline personality disorder at the EoL, but behavioural interventions should be tailored to the person based on the creation of genuine, respectful, relationships |
| Feldman and Petriyakoil 2006,126 USA; PTSD at the EoL | A case study of a 61-year-old male veteran with heart failure and acute onset of PTSD symptoms | Challenges of recurrence of latent PTSD symptoms seemingly triggered by the threat to life of terminal illness mimicking previous experiences | Specific challenges in EoL care for people with PTSD may mean they experience psychological symptoms that have been dormant, become anxious and angry, avoid health care and distrust medical recommendations, leading to non-adherence to and refusal of treatment |
| Feldman et al. 2014,116 USA; the provision of palliative care to people with PTSD at the EoL | A re-presentation of a new model of care to people with PTSD, either pre-existing or post-EoL diagnosis, illustrated by three case studies (men aged 65, 65 and 61 years) in diverse palliative care settings | An illustrated model of care for people with PTSD at the EoL, involving therapy over three distinct stages: palliate immediate discomfort and provide social supports, provide psychoeducation and enhance coping skills, and treat specific trauma issues | The SPPC model can be used to support terminally ill patients with PTSD where conventional PTSD interventions are challenged by limited life expectancy, fatigue and other concerns |
| Feldman et al. 2017,117 USA; the provision of palliative care to people with PTSD at the EoL | A case of a 72-year-old veteran with PTSD and multiple myeloma, admitted for inpatient hospice care at the EoL | How a staged approach to PTSD care is helpful for people at the EoL | A further illustration of how the SPPC model can be used to support terminally ill patients with PTSD where conventional PTSD interventions are challenged by limited life expectancy, fatigue and other concerns |
| Geppert et al. 2011,127 USA; palliative care and capacity in the context of people with psychosis and terminal cancer | A detailed case study of a 58-year-old man with a pre-existing schizoaffective disorder who had terminal laryngeal cancer and was admitted to hospital | The ethical issues around treatment when people have psychosis and lack decisional capacity | Psychosis raises ethical issues for EoL care as it undermines decisional capacity and raises questions about the use of proxies and additional questions about where care ought to be provided (mental health services or EoL services) |
| Gonzalez et al. 2009,128 USA; hospice care of a man with breast cancer and bipolar disorder | A medical case study of an 86-year-old man with complex health needs who received inpatient care, and who has bipolar disorder, dementia and breast cancer first treated 20 years previously | The complexity of providing care for people with multiple needs, in the context of family members also having significant health needs | Curative care is difficult to provide if treatment is not consistently provided and accepted, and palliative care is appropriate particularly when caregivers have health needs of their own |
| Griffith 2007,129 USA; palliative and EoL care for a man with heart and lung failure and schizophrenia (part 1 of 2) | An extended case study of a 67-year-old man, focusing on his schizophrenia and his lung and heart disease and his care at home until death | The role of the psychiatrist in the provision of integrated care, including at the EoL, to people with SMI and multiorgan failure | Psychiatrists have an important part to play in treating people who have both severe mental health and terminal physical health problems |
| Griffith 2007,130 USA; palliative and EoL care for a man with heart and lung failure and schizophrenia (part 2 of 2) | An extended case study of a 67-year-old man, focusing on his schizophrenia and his lung and heart disease and his care at home until death | The role of the psychiatrist in the provision of integrated care, including at the EoL, to people with SMI and multiorgan failure | Psychiatrists should have cultural and religious competence and be able to work with families |
| Hill 2005,131 USA; hospice at home care for a person with borderline personality disorder | A case of an 83-year-old woman described as having borderline personality disorder and receiving hospice care at home | EoL care for people with borderline personality disorder and complex physical health problems and family histories | Nurses should develop therapeutic relationships, have good supervision, be consistent in caregiving, and have good working relationships with families and psychiatrists |
| Irwin et al. 2014,26 USA; cancer care, including to EoL, for people with schizophrenia | A detailed review of literature followed by a case study of a 66-year-old woman with paranoid schizophrenia and terminal cancer, whose care moved from home to inpatient hospice | Health inequalities for people with schizophrenia and cancer | Practitioners need improved understanding of health disparities experienced by people with schizophrenia and cancer, research is needed to examine factors influencing survival and quality of life, and better integration is required between oncology and psychiatric services |
| Kadri et al. 2014,150 Canada; care for a person with schizophrenia and advanced kidney disease who lacks capacity and resists treatment | A case of a 53-year-old woman with schizophrenia and advanced chronic kidney disease admitted to hospital as an emergency and who refused dialysis and then received supportive care | Ethical issues in the case of people with SMI and who are unable to make decisions but actively resist treatment | Two ethical issues are highlighted: the lack of acceptance of treatment, and the risk of doing immediate harm if treatment is continued nonetheless |
| Kennedy et al. 2013,120 UK; homelessness and EoL care | A case study of a 52-year-old woman with diagnosis of schizophrenia and cervical cancer living semi-independently in a one-bedroom flat | Treatment refusal in someone with SMI who has the capacity to make decisions and her determination to return home to live | Providing care for a person in their own home involving multiple professional teams in support of her autonomous decision to remain out of hospital and considering her refusal of active treatment |
| Kunkel et al. 1997,132 USA; denial of cancer and non-compliance with treatment | A discussion of denial of cancer followed by five illustrative cases:
|
A review of factors associated with non-compliance in people with cancer, specifically psychoses and cognitive impairment; both are shown to play a role in delayed help-seeking and non-compliance with cancer, and EoL, care | Key issues affecting cancer treatment are competence, the place for legal intervention, ambivalence towards health-care providers and the importance of early psychiatric intervention |
| Levin and Feldman 1983,133 USA (the authors are based in South Africa); ethical issues surrounding the care of people with psychosis and terminal cancer | A case of a 31-year-old woman with schizophrenia and terminal breast cancer who was described as wanting to leave hospital without medical care following the treatment of an acute episode of her mental illness | A discussion of ethical issues associated with the care of people with SMI and terminal illnesses when treatment is refused | People have a right to refuse high-powered medicine at the EoL |
| Lopez et al. 2010,134 USA; explores how medical futility and principles of palliation may contribute to the management of treatment refractory anorexia nervosa | The case of a 30-year-old woman with chronic anorexia nervosa, treated unsuccessfully for several years | Discussion of ethical and legal issues associated with caring for a person with a psychiatric condition who is not helped by treatment, where the condition ultimately leads to her death | Refusal of treatment can be irrational but must be weighed against workers obligations and duty of care and the autonomy of the individual. Two broad options are considered: (1) involuntary treatment or (2) attempting to motivate the person until such time as they are willing to engage in treatment. The first option may have kept her alive in the short term but seemed unlikely to reverse the underlying condition |
| Maloney 2014,121 USA (blog: www.thejournal.ie/readme/bipolar-ii-disorder-denial-mental-health-1467162-May2014); a wife’s experiences of her husband’s bipolar disorder and terminal cancer | A personal blog post recording a woman’s experiences of her husband’s diagnosis with bipolar disorder, his subsequent terminal cancer and his death at home | A first-hand, narrative account of long-term experiences ending in the death of a loved one | SMI changes people’s lives and can cause people to lose touch with reality. People affected (patients and families) need support |
| Mason and Bowman 2018,118 country unknown (conference abstract); the challenges of providing cancer care at the EoL to people with SMI and fluctuating capacity | A conference proceedings abstract describing the care of a 77-year-old man with schizophrenia and fluctuating capacity admitted to hospital for investigations and care into prostate cancer and metastases | An account of the challenges for people with SMI and fluctuating capacity in the context of EoL cancer care | Determining capacity in the context of SMI and acute physical illness is difficult, where standardisation in capacity assessment may help |
| McCasland 2007,135 USA; the care and treatment of people with SMI and cancer, including at the EoL | A case of a 53-year-old woman with schizoaffective disorder, alcohol problems, liver damage and breast cancer who was cared for in the community until dying in a hospice | Hospice nurses need better preparation to look after people at the EoL who also have SMI | Communication skills are important for hospice nurses caring for people with SMI at the EoL, and hospice nurses need more training to care for this group of people |
| McKenna et al. 1994,136 USA; the treatment with clozapine of people with SMI and cancer, where treatment also includes antineoplastic medication | A letter to the editor describing a 49-year-old man with schizophrenia and lung cancer with a poor prognosis, treated with clozapine, whose care was transferred from a mental health to a medical care institution | The combination of clozapine with anti-tumour drugs | Guidance is needed on the combination of clozapine (an antipsychotic drug) with anti-cancer drugs |
| Mogg and Bartlett 2005,146 UK; the care and treatment of a man with treatment-resistant psychosis and life-threatening renal failure | The case is a man in his forties with a 30-year history of psychosis and multiple admissions to mental health hospital, who was then discovered to have life-threatening renal disease requiring regular dialysis | Different approaches to the assessment of capacity (outcome, status, functional), set in the context of the legal framework | Capacity can fluctuate, and ‘best interests’ need to be considered, which can mean guidance needing to be sought from the courts |
| Moini and Levinson 2009,137 USA; the care and treatment of people with simple schizophrenia and medical conditions | A case of a 40-year-old woman with simple schizophrenia who was lost to services following diagnosis of breast cancer with metastases, and who was located at a later point at the terminal stage of her illness | Approaches to working with people with simple schizophrenia and medical problems | Proactive care is needed so that people stay in touch with services, although people with simple schizophrenia are also likely to have capacity to decide on their courses of treatment |
| Monga et al. 2015,138 USA; the use of clozapine in people with psychosis who are also receiving chemotherapy | The case is of a 70-year-old man with schizophrenia, treated with clozapine, who continued his antipsychotic medication while receiving hospice care and treatment for oesophageal cancer | The use of clozapine as an atypical antipsychotic alongside the use of chemotherapy | There is limited information to guide the management of clozapine treatment during chemotherapy, and close co-operation between psychiatrists and oncologists is needed |
| Muhtaseb et al. 2001,147 UK; the treatment of people with SMI and advanced terminal cancer | The case is of a 76-year-old man with schizophrenia and advanced basal cell carcinoma, who refused active intervention | Treatment of advanced life-threatening cancer in people with SMI who refuse active intervention | Consent must be freely given, and people (including people with SMI) should be considered able to decide for themselves |
| O’Neill et al. 1994,148 UK; hospice care for women with anorexia nervosa | The case of a 24-year-old woman with anorexia admitted to a hospice in poor physical condition after 7 years of anorexia nervosa that was not helped by treatment | Discusses the treatment and rapid decline to eventual death of a 24-year-old woman from the complications associated with anorexia nervosa | Recognises that psychiatric units do not have relevant expertise to provide complex physical health care. Says that her condition was identified as incurable by the psychiatric team and when the patient and her family accepted this she was then able to access appropriate care. Says hospice staff are familiar with other EoL care and that this largely worked for this woman, helped by an excellent referral letter (no clue how this is judged) and ongoing support from the psychiatrist. They conclude that there is a role for carefully selected non-cancer patients to be cared for in specialist palliative care centres |
| Picot et al. 2015,15 Australia; the IMhPaCT programme, designed to improve care for people with SMI and life-limiting illnesses | The case is of a 46-year-old woman who had bipolar disorder and metastatic breast cancer, who received integrated mental health and palliative care at home before dying in hospital | An illustrative case showcasing the work of nurse practitioners involved in the IMhPaCT programme, which is designed to bring together mental health and palliative care for people with SMI | People with SMI at the EoL face additional problems of isolation, declining physical abilities, pain and disintegrating selfhood. Collaboration across specialities can enhance outcomes, and mental health nurses have a role to play |
| Rice et al. 2012,139 USA; patient-provider communication in EoL care | The case of a 58-year-old male veteran with renal disease and schizophrenia who refused dialysis treatment | The case provides an example of a man refusing treatment in line with his previous history and is found to lack capacity to decide in his best interests. Involvement of his sister who is ill-prepared to take on proxy decisions | Discussion hinges on challenges of enforcing physical treatments on a person who is refusing, handling autonomy vs. coercion, recognition of need for building therapeutic alliances with the person and their surrogates |
| Rodriguez-Mayoral 2018,119 Mexico; integrating mental health and palliative care for people with SMI and cancer | A short conference abstract describing a 72-year-old woman with bipolar disorder and advanced, untreated colon cancer from which she died | The case briefly describes how the woman was cared for until her death, free from symptoms of her mental illness | Cancer care regardless of disease stage should be integrated with palliative and mental health care to control symptoms and quality of life and death |
| Romm et al. 2009,140 USA; managing cancer care for people using inpatient mental health services | The case is a 40-year-old man with schizophrenia and osteosarcoma for which amputation was indicated, and who refused surgical treatment but who was judged to lack capacity. His mother assumed decision-making responsibility and concurred with her son, and palliative care was initiated | Treatment of people with acute mental health problems and life-threatening cancer, and patients’ capacity to understand and make decisions | Psychiatrists have responsibilities to represent the interests of people who are ‘mentally compromised’, including those who are also irreversibly medically compromised. Collaboration with palliative care practitioners is important, and although SMI can impair capacity this is not necessarily so |
| Shah et al. 2008,141 USA; the treatment of people with SMI and advanced terminal cancer | The case is a 68-year-old homeless man with schizophrenia and neglected basal cell carcinoma, and who refused treatment in the context of a lack of capacity and was then treated for his mental illness | Informed consent is key to the provision of cancer treatment, and in cases where people lack capacity additional care needs to be taken | In the absence of the ability to give informed consent, interprofessional teams need to be involved, along with independent ethics committees |
| Stecker 1993,142 USA; caring for young people with life-threatening cancer on an acute psychiatric ward | The case is of a 21-year-old man with presumed bipolar disorder and sarcoma who was admitted to an inpatient psychiatric unit and who caused staff to struggle with the acceptance of death | Staff in mental health wards do not routinely care for young people at the EoL, and this case challenged staff | Mental health nurses need to be able to identify feelings preventing them from working therapeutically with patients |
| Steves and Williams 2016,143 USA; EoL care for people with terminal illnesses and SMI | A very brief case of a man, of unknown age, who had schizophrenia and terminal lung cancer but who had capacity and refused treatment prior to his death | Services for people with SMI at the EoL are in short supply, mental health nurses need training in EoL care, attention needs to be paid to the environment, communication needs to be effective, caregivers needs to be supported, family members may be resistant and other inpatients need to be supported following a death | Investments are needed in services and staff to care for increasing numbers of people with SMI who also have terminal medical conditions |
| Terpstra et al. 2014,144 USA; EoL hospice care for people with SMI | The case is of a 61-year-old man with schizophrenia living in adult foster care who reported physical symptoms and was found to have bladder cancer and brain masses, who moved to an open hospice and whose care and treatment is then described | The complexity of providing hospice care for people with SMI and terminal cancer, and the role of nurses | People with schizophrenia are often medically undertreated, have shortened life expectancies, and have care that is challenged by their placements, poor communication and symptom management |
| Thomson and Henry 2012,76 USA; the challenge for oncology nurses of caring for people with SMI and cancer | A paper on oncology nursing for people with pre-existing SMI, including a series of brief case studies: a 33-year-old woman with major depression and then breast cancer, a 43-year-old man with bipolar disorder and advanced pancreatic cancer and a 25-year-old woman with schizophrenia and breast cancer | Care and treatment of people with pre-existing SMI at the EoL, with a particular emphasis on understanding mental illnesses and its treatment | Medical professionals need to be aware of premature mortality in people with SMI, and need to develop skills and knowledge in caring for people with SMI as an underserved group. Practice is advancing in the areas of drug treatments, case management, family work and social support |
| Webber 2012,151 Canada; caring for a man with SMI in his supported home prior to hospice care | A brief case study of a man of unknown age (but at least 31 years old) who had schizophrenia and metastatic gastric cancer and who was cared for in his supported home for as long as possible until being transferred to a hospice, where he died | Pain control, control over of levels of intervention, control over maintaining meaningful, relationships, outcomes of lost autonomy, lack of resources, restoring justice for patients with SMI and terminal illness, and innovation are all discussed | Autonomy has been diminished for people with SMI and palliative illness, yet people with SMI at the EoL want the same things as everyone else. Services and care need to improve |
Appendix 21 CERQual qualitative evidence profile, synthesis 1: structure of the system
| Review finding and studies contributing to the review finding | Assessment of methodological limitations | Assessment of relevance | Assessment of coherence | Assessment of adequacy | Overall CERQual assessment of confidence |
|---|---|---|---|---|---|
| Structure of the system: policy and guidance | |||||
|
1. Owing to a lack of national and local guidance regarding EoL care and mental health care, palliative care nurses report concerns about their legislative responsibility Study 13 |
No methodological limitations | Serious concerns about relevance, as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
| Structure of the system: separate commissioning, management and organisation | |||||
| Accessing and navigating the system | |||||
| The separate commissioning, management and organisation of mental health and EoL often result in those with SMI having trouble accessing and navigating the system157,164,422 | Ungraded – non-research | ||||
|
2. HCPs recognise that accessing and navigating EoL care for those with SMI is a challenge and many obstacles exist Studies 14, 15, 25 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were Ireland and Australia) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (three studies with moderately rich data overall) | Moderate confidence |
| Access for homeless and vulnerable groups | |||||
| Access to health care is particularly difficult for homeless and vulnerable groups, who are often isolated and disconnected from family and friends30,162,167 | Ungraded – non-research | ||||
|
3. Homeless people are often excluded from hospices and care homes, and HCPs report difficulties in placing homeless people with cancer Studies 19, 21 |
No or very minor methodological limitations (one study with very minor and one study with no methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were the UK and Canada) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
| Care co-ordination across systems | |||||
| It is important that care is co-ordinated and integrated across services so that the needs of those with SMI at the EoL are met, although it is acknowledged that this is difficult to achieve30,164,169,170 | Ungraded – non-research | ||||
|
4. Separate commissioning, management and ways of organising both services and professionals create challenges for both mental health and EoL HCPs to co-ordinate high-quality care across mental health and EoL care systems Study 13 |
No methodological limitations | Serious concerns regarding relevance as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
|
5. The invisibility of homeless and vulnerable people, and the fragmented character of care systems, means they often have to act as their own care co-ordinators Studies 13, 19, 21 |
No or very minor methodological limitations (two studies with no and one study with very minor methodological limitations | Moderate concerns about relevance (partial relevance, as the studies were from the UK only) | No concerns about coherence | Minor concerns about adequacy (two studies with rich data and one study with thin data) | Moderate confidence |
|
6. Multiple proposals have been made to improve the co-ordination of care for people with SMI at the EoL, mostly involving the identification of staff with clear responsibilities Studies 16, 25, 27 |
Minor methodological limitations (two studies with very minor and one study with serious methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Ireland, Australia and the USA) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Minor concerns about adequacy (two studies with rich data and one study with thin data) | Moderate confidence |
| Resources | |||||
|
7. HCPs feel that there is a lack of resources in terms of services and trained professionals that are able to meet the needs of those with SMI at the EoL Studies 23, 25, 28 |
Minor methodological limitations (one study with no, one study with very minor and one study with serious methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were Ireland and Australia) | No concerns about coherence | Minor concerns about adequacy (two studies with rich data and one study with thin data) | Moderate confidence |
| Structure of the system: partnership | |||||
| Funding and flexibility to work in partnership | |||||
|
8. Working in partnership across EoL and mental health services is important and when flexibility and solutions to work in partnership across agencies exist then EoL care for those with SMI can be facilitated Study 28 |
No methodological limitations | Serious concerns regarding relevance, as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
|
9. A lack of good relationships and partnership working, influenced by reductions in funding and competitive commissioning, inhibit good care, especially with regard to pain management, needs assessments and assessment of mental capacity Study 13, 15, 25 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Ireland, Australia and the UK) | No concerns about coherence | Minor concerns about adequacy (two studies with rich data and one study with thin data) | Moderate confidence |
| Multidisciplinary teamwork | |||||
| Interagency and interprofessional team working at the EoL is important30,55,163,168,170,171 | Ungraded – non-research | ||||
|
10. HCPs report that formal (and sometimes ad hoc) multidisciplinary teamwork can improve patient outcomes Study 14, 15, 18, 28 |
Minor methodological limitations (one study with one with no, one study with very minor, one study with minor and one study with serious methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were Australia and the USA) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (three studies with rich data and one study with thin data) | Moderate confidence |
| Ongoing interprofessional communication | |||||
| Ongoing communication between partners is a key element of high-quality care30,55,164 | Ungraded – non-research | ||||
|
11. Coalition building and formal opportunities to meet and discuss care are essential and must ensure that information is made available to primary care and social services partners Studies 13, 15, 25, 28 |
Minor methodological limitations (one study with no methodological limitations, two studies with very minor methodological limitations and one study with serious methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across four countries, which were Ireland, Australia, the UK and the USA, covering three continents) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Minor concerns about adequacy (two studies with rich data and two studies with thin data) | High confidence |
| Structure of the system: no right place to die | |||||
| Dying at home | |||||
| With the right support from community-based services, people with SMI at the EoL are able to stay at home157 | Ungraded – non-research | ||||
|
12. Mental health and EoL staff recognise that allowing people to die in the location of their choice (which is often a home or home-like environment) is important, but staff also talk about how appropriate care is often lacking in all settings Studies 15, 16, 25 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, Ireland and the USA) | No concerns about coherence | No concerns | High confidence |
| Dying in a mental health hospital | |||||
|
13. Mental health services rarely care for people with SMI at the EoL as they are poorly equipped to meet their needs, and as a result patients are frequently moved between services Studies 13, 16, 24 |
No or very minor methodological limitations (one study with no and two studies with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were the UK, the USA and the Netherlands) | No concerns about coherence | Minor concerns about adequacy (two studies with rich data and one study with thin data) | High confidence |
| Dying in a hospice | |||||
|
14. Multiple challenges exist for EoL care to take place in a hostel, including lack of staff preparedness, the chaotic environment, concerns over risks and the safe storage of medication Studies 12, 21 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were the UK and Canada) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
| Dying in acute settings | |||||
|
15. Providing EoL care in the community, within mental health settings or homeless shelters can be difficult and as a result those with SMI are often transferred into acute settings at the EoL but providing mental health care in acute settings also poses challenges Studies 13, 15, 16, 18, 19, 24, 25 |
No or very minor methodological limitations (three studies with no and five studies with very minor methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across five countries, which were Ireland, Australia, the UK, the USA and the Netherlands, across three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (seven studies with rich data and one study with thin data) | Moderate confidence |
| Dying in hospice | |||||
|
16. Staff working within hospices report that hospices are ill-prepared for caring for the needs of homeless people at the EoL and require more help in dealing with substance misuse and the alternative lifestyles of what is mostly a younger age group Studies 19, 21 |
No or very minor methodological limitations (one study with no and one study with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as studies were from two countries only, which were the UK and Canada) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
Appendix 22 CERQual qualitative evidence profile, synthesis 2: professional issues
| Review finding and studies contributing to the review finding | Assessment of methodological limitations | Assessment of relevance | Assessment of coherence | Assessment of adequacy | Overall CERQual assessment of confidence |
|---|---|---|---|---|---|
| Professional issues: relationships between HCPs and people with SMI | |||||
| Connecting relationships | |||||
|
1. Some mental health staff feel that building nurturing relationships is important, especially for those with limited social networks and no family contact. However, others choose not to form such relationships, finding it too upsetting when patients are transferred for EoL care Studies 14–16, 24, 25 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across four countries, which were Ireland, Australia, the Netherlands and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | High confidence |
| Talking about death and dying | |||||
| People with life-limiting illnesses (including SMI) should be supported to make decisions at the EoL and good communication is important164,176 | Ungraded – non-research | ||||
|
2. Some mental health staff find conversations about death and dying challenging; those who feel able have found that patients are receptive Studies 13, 15, 24, 26 |
No or very minor methodological limitations (two studies with very minor and one study with no methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the Netherlands and the UK) | No concerns about coherence | Minor concerns about adequacy (three studies with rich data and one study with thin data) | High confidence |
| Attitudes and beliefs of HCPs | |||||
|
3. The underlying stigmatising and prejudicial attitudes of EoL HCPs towards those with SMI including those who are homeless can affect decisions around EoL care Studies 13, 14, 16, 17, 19, 21, 25 |
No or very minor methodological limitations (five studies with very minor and three studies with no methodological limitations) | No concerns | No concerns about coherence | Minor concerns about adequacy (seven studies with rich data and one study with thin data) | High confidence |
| Professional issues: mental health professionals doing EoL care | |||||
|
4. Mental health staff feel that they have limited experience of caring for patients with SMI at the EoL, and although some feel able to deliver care others feel that they lack the knowledge and skills, particularly with regard to pain management and psychosocial or spiritual support Studies 13, 14, 24 |
No or very minor methodological limitations (two studies with very minor and one study with no methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the Netherlands and the UK) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Minor concerns about adequacy (two studies with rich data and one study with thin data) | Moderate confidence |
| EoL care not being mental health work | |||||
|
5. Some mental health staff report that they do not feel able, are not interested or avoid caring for people with SMI at the EoL, whereas others embrace caring for them Studies 13, 16, 18, 23, 24 |
No or very minor methodological limitations (two studies with very minor and three studies with no methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across four countries, which were the Netherlands, Australia, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (four studies with rich data and one study with thin data) | Moderate confidence |
| Emotional distress | |||||
|
6. Mental health staff report that caring for those with SMI at the EoL can be distressing and emotionally draining, and some fear being scrutinised following the death of patients Studies 14, 16, 17 |
No or very minor methodological limitations (two studies with very minor and one study with no methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the USA and the UK) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | Moderate confidence |
| Staff who provide care over long periods to individuals with SMI need support in the face of terminal illness, and in bereavement30 | Ungraded – non-research | ||||
| Professional issues: EoL HCPs doing mental health care | |||||
| Experience, knowledge and skills | |||||
|
7. EoL HCPs feel that they lack knowledge and understanding of mental health diagnoses and services. As a result, they report that they are not always confident, willing or comfortable to care for patients with SMI at the EoL Studies 13–17, 23, 24 |
No or very minor methodological limitations (four studies with very minor and three studies with no methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across four countries, which were the Netherlands Australia, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (six studies with rich data and one study with thin data) | Moderate confidence |
| As a consequence of this, the needs of people with SMI at the EoL are not always well met30,423 | Ungraded – non-research | ||||
| EoL HCPs should become conversant with the needs of people with SMI and work closely with mental health services30 | Ungraded – non-research | ||||
| Professional issues: training and education | |||||
|
8. Mental health and EoL HCPs have highlighted a wide range of educational needs Studies 14–17, 28 |
Minor methodological limitations (one study with no, three studies with very minor and one study with serious methodological limitation) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the USA and the UK) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (three studies with rich data and one study with thin data) | Moderate confidence |
| Education and training opportunities in EoL care across professional groups who care for people with SMI at the EoL are important30,156,162–165,177 | Ungraded – non-research | ||||
|
9. Palliative care programme directors have suggested that psychiatry training is inadequate in the categories of EoL care and issues related to death and dying Study 23 |
No minor methodological limitations | Serious concerns regarding relevance as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
|
10. Although some mental health nurses feel that that their core professional preparation enables them to care for people with SMI during periods of physical illness and at that EoL, others feel that this is something that could be improved Studies 14, 16 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were Australia and the USA) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
| In-service training opportunities for HCPs to develop skills and knowledge in EoL care are patchy, particularly in mental health-care-providing organisations and could be improved30,162,164–166,171 | Ungraded – non-research | ||||
| EoL and mental health staff working together can improve knowledge and awareness, such as through the establishment of dedicated link positions with roles including the provision of education30 | Ungraded – non-research | ||||
|
11. EoL and mental health staff learning from each other such as through cross-training has been positively evaluated Studies 27, 28 |
Serious methodological limitations (two studies with serious methodological limitations) | Serious concerns regarding relevance as only two studies representing one country contributed to this finding | No concerns regarding coherence | Serious concerns about adequacy (two studies offering thin data) | Very low confidence |
Appendix 23 CERQual qualitative evidence profile, synthesis 3: contexts of care
| Review finding and studies contributing to the review finding | Assessment of methodological limitations | Assessment of relevance | Assessment of coherence | Assessment of adequacy | Overall CERQual assessment of confidence |
|---|---|---|---|---|---|
| Contexts of care: managing the interface between mental health and EoL care | |||||
| GPs managing care | |||||
|
1. GPs are the gatekeepers in enabling or hindering access to palliative care services and in some instances manage the palliative care needs of people with SMI within their practice Studies 24, 25 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were the Netherlands and Ireland) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
| The role of medical specialists | |||||
|
2. People with SMI are reported to visit a number of different types of physician specialists as well as psychiatrists at the EoL Studies 23–25 |
No or very minor methodological limitations (one study with no and two studies with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were the USA, the Netherlands and Ireland) | Minor concerns about coherence (data reasonably consistent within and across all studies) | No concerns about adequacy | Moderate confidence |
| Referral | |||||
| Support for people living with mental health issues and approaching the EoL must be fast-tracked or prioritised164 | Ungraded – non-research | ||||
|
3. Both EoL and mental health staff acknowledge that referrals are often complicated and lack vital information that would facilitate communication between themselves and those with SMI at the EoL Studies 13, 15 |
No or very minor methodological limitations (one study with no and one study with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were Australia and the UK) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Moderate concerns about adequacy (one study offering moderately rich data and one study offering thin data) | Low confidence |
| Mental health assessment at the EoL | |||||
| Skilled mental health assessment at the EoL is required for people with SMI so that care can be planned and they can be helped to manage their symptoms and other needs30 | Ungraded – non-research | ||||
|
4. Both EoL and mental health HCPs across a variety of settings report that mental health assessments at the EoL can be a challenge and that they need help to deal with their fears and uncertainties Studies 13, 17, 18, 25 |
No or very minor methodological limitations (three studies with no and two studies with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the UK and Ireland) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (four studies with rich data and one study with thin data) | Moderate confidence |
| Health-care services and treatment utilisation in the LYoL | |||||
| Palliative care | |||||
|
5. GPs and psychiatrists believe that people with SMI are less likely than other groups to make use of specialist palliative care Study 25 |
No methodological limitations | Serious concerns about relevance as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
| Invasive interventions | |||||
|
6. EoL HCPs working in the UK feel that standard guidance on resuscitation is lacking for people with SMI at the EoL Study 13 |
No methodological limitations | Serious concerns about relevance as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
|
7. EoL professionals in Australia have concerns about capacity to consent in relation to resuscitation orders for people with SMI at the EoL Study 14 |
Very minor methodological limitations | Serious concerns about relevance as only one study representing one country contributed to this finding | No concerns about coherence | Serious concerns about adequacy (only one study offering data) | Very low confidence |
| Contexts of care: meeting individual and family needs | |||||
| Spiritual and psychosocial support | |||||
| People with SMI have particular vulnerabilities arising from their mental health experiences and programmes and services for people with SMI at the EoL require a comprehensive team approach30,164,176 | Ungraded – non-research | ||||
|
8. Programmes and services for people with SMI at the EoL require a comprehensive team approach incorporating symptom relief, psychological and psychosocial support, and spiritual care Studies 10, 12, 14, 15, 17, 24 |
No or very minor methodological limitations (one study with no and five studies with very minor methodological limitations) | Minor concerns about relevance (studies of HCPs and families representing a variety of settings and from across four countries, which were the Netherlands, Australia, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | High confidence |
| Families and their involvement | |||||
|
9. HCPs report challenges in handling contact with families, especially where years of estrangement have occurred or where family members also have mental health conditions Studies 12–16, 24 |
No or very minor methodological limitations (one study with no and five studies with very minor methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across four countries, which were the Netherlands, Australia, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (five studies with rich data and one study with thin data) | Moderate confidence |
|
10. Veterans with a diagnosis of PTSD were just as likely to receive a family consultation regarding advance care planning as those without a diagnosis of PTSD Study 10 |
Very minor methodological limitations | Serious concerns about relevance as only one study representing one country contributed to this finding | Serious concerns about adequacy (only one study offering data) | Serious concerns about adequacy (only one study offering data) | Very low confidence |
|
11. When families were involved in the care of veterans with a diagnosis of PTSD they reported unmet needs for emotional support, and felt generally that their relatives were not treated with dignity and were unsatisfied with the level of care received Study 22 |
Very minor methodological limitations | Serious concerns about relevance as only one study representing one country contributed to this finding | Serious concerns about adequacy (only one study offering data) | Serious concerns about adequacy (only one study offering data) | Very low confidence |
| Advocacy | |||||
| Having an advocate that can support a person with SMI throughout their cancer journey, including at the EoL, is important and such advocates can prevent people with SMI from falling through gaps in the system30,156,161,162 | Ungraded – non-research | ||||
|
12. HCPs report that being referred to palliative care and receiving services appears to be based on the presence or absence of a strong advocate Studies 13, 15, 16 |
No or very minor methodological limitations (one study with no and two studies with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were the UK, the USA and Australia) | No concerns about coherence | Minor concerns about adequacy (two studies with moderately rich data and one study with thin data) | High confidence |
|
13. People with SMI can lack access to advocacy to help navigate the complex EoL trajectory due to limited social and family support and as a result they can become ‘lost in the system’ Studies 13, 15, 16, 24 |
No or very minor methodological limitations (one study with no and two studies with very minor methodological limitations) | Minor concerns about relevance (studies of HCPs representing a variety of settings and from across four countries, which were the Netherlands, Australia, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (three studies with moderately rich data and one study with thin data) | High confidence |
| EoL care preferences | |||||
| Advance care planning for people with SMI at the EoL is important and mechanisms should be in place to support such people to make their own decisions, although it is recognised that this can be problematic156,163–165,170,176 | Ungraded – non-research | ||||
|
14. HCPs have concerns about negotiating EoL care preferences with people with SMI for fear that mental health symptoms may influence understanding and expectations or that such discussions may lead to further distress Studies 15, 16, 21, 24 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Ireland, the USA and Australia) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | Moderate confidence |
| It is important not to assume that mental capacity is lacking21 | |||||
|
15. HCPs report that they are not always comfortable with determining patients’ capability to make medical decisions and that they tend to assume that mental capacity is lacking and as a result discussions around advance care planning are avoided Studies 13, 15, 23 |
No or very minor methodological limitations (two studies with no and one study with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the UK and the USA) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Minor concerns about adequacy (two studies with moderately rich data and one study with thin data) | Moderate confidence |
|
16. Findings from scenario-based preferences regarding medical advance care planning suggest that people with SMI are able to designate treatment preferences in response to the EoL and are open to discussing EoL care Studies 20, 29, 30 |
No or very minor methodological limitations (two studies with no and one study with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Belgium, the USA and Canada) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | Moderate confidence |
|
17. People with SMI conditions are capable of completing advance care plans for the EoL but even where legislation is in place to support this it rarely appears to be standard practice Studies 12, 24, 28 |
Minor methodological limitations (two studies with very minor and one study with serious methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were the Netherlands and the USA) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (two studies with moderately rich data and one study with thin data) | Moderate confidence |
|
18. A lack of confidence to have open communication and experience among HCPs, especially when working with homeless people, may explain the absence of advance care plans for those with SMI at the EoL Studies 12, 15,19, 21 Results across studies were mixed regarding the likelihood of people with a diagnosis of SMI having completed an advance directive (GRADE – very low) |
No or very minor methodological limitations (one study with no and three studies with very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were Australia, the UK and Canada) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | Moderate confidence |
Appendix 24 CERQual qualitative evidence profile, synthesis 4: living with severe mental illness
| Review finding and studies contributing to the review finding | Assessment of methodological limitations | Assessment of relevance | Assessment of coherence | Assessment of adequacy | Overall CERQual assessment of confidence |
|---|---|---|---|---|---|
| Living with SMI: complexities of EoL care | |||||
| Providing EoL care to people with SMI is challenged by patients’ behaviour associated with their mental health difficulties156,170 | Ungraded – non-research | ||||
|
1. Challenging behaviours, communication issues and side effects of combining SMI and EoL medications make it difficult to address mental health issues at the EoL Studies 13–17, 24 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Minor concerns about relevance (studies of HCPs and patients representing a variety of settings and from across four countries, which were the Netherlands Australia, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (six studies with rich data and one study with thin data) | Moderate confidence |
| Living with SMI: familiarity and trust | |||||
| Trust and rapport | |||||
|
2. Early referral to palliative care helps build trust and rapport between staff and people with SMI at the EoL Studies 13–15, 17, 19, 25, 28 |
No or very minor methodological limitations (four studies with very minor and three studies with no methodological limitations) | Minor concerns about relevance (studies of HCPs and patients representing a variety of settings and from across five countries, which were Canada, Australia, Ireland, the UK and the USA, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (six studies with rich data and two studies with thin data) | Moderate confidence |
| Supporting people in familiar environments | |||||
|
3. Although people with SMI often leave environments with which they are familiar at the EoL, mental health and palliative care staff can work together to support people without the need for moving Studies 14, 19, 21, 25 |
No or very minor methodological limitations (three studies with very minor and one study with no methodological limitations) | Minor concerns about relevance (studies of HCPs and patients representing a variety of settings and from across four countries, which were Canada, Australia, Ireland and the UK covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | No concerns | Moderate confidence |
| Deteriorations in EoL-related physical health commonly results in the homeless person being transferred to hospital in crisis where their needs are poorly met156 | Moderate concerns about relevance (partial relevance, as the studies were from two countries only) | Ungraded – non-research | |||
|
4. Hostel staff report that they try to ensure that palliative care can be provided in a familiar environment for as long as possible as they feel the benefits outweigh the challenges Studies 19, 21 |
No or very minor methodological limitations. Moderate confidence (one study with very minor and one study with no methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were the UK and Canada) | Minor concerns about coherence (data reasonably consistent within and across all studies) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
| Living with SMI: recognising physical decline | |||||
| Identifying signs of declining health | |||||
| The physical health needs and signs of physical deterioration of those with pre-existing SMI may not be identified and as a result care is often inadequate30,156,161 | Ungraded – non-research | ||||
|
5. Staff report that people with SMI are not always able to recognise their own declining health and because of previous unsatisfactory health-care encounters it is felt that they often present late to services Studies 13, 15, 24, 25 |
No or very minor methodological limitations (three studies with very minor and one study with no methodological limitations) | Minor concerns about relevance (studies of HCPs and patients representing a variety of settings and from across four countries, which were Australia, Ireland, the Netherlands and the UK, covering three continents) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Minor concerns about adequacy (three studies with rich data and one study with thin data) | Moderate confidence |
| The impact of late diagnosis | |||||
|
6. The timely provision of palliative care can be hampered when people with SMI (especially those who are homeless), are not identified as approaching the EoL until late diseases of life-limiting physical disease Studies 15, 21, 24 |
Very minor methodological limitations (all studies had very minor methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from three countries only, which were the Netherlands, Australia and the USA) | No concerns about coherence | No concerns about adequacy | High confidence |
| Identifying an EoL care trajectory for those who are homeless | |||||
|
7. People who are homeless are often more concerned with day-to-day survival than with keeping appointments with HCPs and this makes it difficult to identify EoL trajectories and to provide palliative care Studies 19, 21 |
No or very minor methodological limitations (one study with very minor and one study with no methodological limitations) | Moderate concerns about relevance (partial relevance, as the studies were from two countries only, which were the UK and Canada) | Moderate concerns about coherence (data more varied and this finding is oversimplified) | Very minor concerns about adequacy (two studies with rich data) | Moderate confidence |
List of abbreviations
- aHR
- adjusted hazard ratio
- AMED
- Allied and Complementary Medicine Database
- aOR
- adjusted odds ratio
- aRR
- adjusted relative risk
- ASSIA
- Applied Social Sciences Index and Abstracts
- CASP
- Critical Appraisal Skills Programme
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CERQual
- Confidence in the Evidence from Reviews of Qualitative Research
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CPR
- cardiopulmonary resuscitation
- DARE
- Database of Abstracts of Reviews of Effects
- ED
- emergency department
- EoL
- end of life
- EPPI
- Evidence for Policy and Practice Information
- GP
- general practitioner
- GRADE
- Grading of Recommendations, Assessment, Development and Evaluation
- HCP
- health-care professional
- HR
- hazard ratio
- HSDR
- Health and Social Care Delivery Research
- ICU
- intensive care unit
- LYoL
- last year of life
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PEER
- Patient Experience and Evaluation in Research
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD
- post-traumatic stress disorder
- RR
- relative risk
- SAG
- stakeholder advisory group
- SMI
- severe mental illness
