Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR128671. The contractual start date was in August 2020. The draft manuscript began editorial review in February 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Silveira Bianchim et al. This work was produced by Silveira Bianchim et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Silveira Bianchim et al.
Chapter 1 Introduction
Background
Chronic pain in childhood is widespread: UK figures indicate that 8% of primary care consultations by 3 to 17 year olds are for musculoskeletal chronic pain alone;1 at least 4–14% of children worldwide are estimated to have chronic pain, but the prevalence could be as high as 24–88%, dependent on the type of pain. 2 Frequent severe chronic pain of all types affects 8% of children, according to a Dutch survey. 3 A global survey found that around 44% of adolescents reported chronic weekly pain. 4
Definition
The eleventh revision of the International Classification of Diseases (ICD-11) defines chronic pain as ‘pain that persists or recurs for more than three months’. 5 Chronic pain is recognised as a condition in its own right but it is also a key feature of conditions, such as complex regional pain syndrome (CRPS), inflammatory bowel disease (IBD) and juvenile idiopathic arthritis.
Size and impact of the problem
Chronic pain has considerable negative impacts on children’s health and quality of life; for instance, UK surveys have shown that the majority of adolescents with chronic pain experience disability in physical, psychological, social, familial and developmental domains. 6,7 Chronic pain is associated with increased use of healthcare services and medication,8 adversely affects social and family relationships9,10 and results in poorer school attendance. 11 For treating adolescent pain alone, the cost to the NHS is estimated at 4 billion pounds a year. 12 UK parents pay £900 out-of-pocket expenses a year supporting their adolescent’s chronic pain and have work absences of 7–37 days costing on average £750 per family each year; some parents give up work entirely to care for their adolescent child. 13 Moreover, longitudinal research indicates a high risk of childhood chronic pain continuing into adulthood14 with further individual, NHS and societal costs. For example adult back pain alone costs the UK economy £11 billion with a direct healthcare cost of £1 billion. 15
Current service provision and clinical guidelines
Despite the high prevalence and serious impacts of childhood chronic pain, UK provision of and access to specialist children’s chronic pain services and multidisciplinary chronic pain management is very limited8 and services are considered to be inadequate. 16,17 The most recent National Pain Audit in England and Wales in 2011–217 found that services were ‘of inconsistent standard and quality and not always available for those who need them. This is particularly true for centres specialising in treating children with chronic pain’17 (p.4). The 2021 Lancet Commission ‘Delivering transformative action on paediatric pain’ recognised that children’s pain is often undertreated. 18
There is also a lack of high-quality trials evidence to inform clinical guidelines, and thus guide children’s chronic pain management. 8,15,18–24 This lack has been identified in the Scottish Intercollegiate Guidelines Network (SIGN) guideline,8 the 2020 World Health Organization (WHO) guideline19 and its supporting systematic review,20 and Cochrane reviews of treatment effectiveness trials for children’s chronic non-cancer pain. 22–28 The 2021 National Institute of Health and Care Excellence (NICE),29 NICE chronic pain guideline does not include children under 16 years of age due to the lack of robust trials evidence. 29
Furthermore, the 2018 SIGN guideline on the management of children’s chronic pain indicated that UK-based healthcare professionals require more training in managing chronic pain in children. 8 For instance, there is no inpatient clinic for children with chronic pain in Scotland; children with severe chronic pain, that is not manageable within an outpatient setting, are sometimes referred to national specialist services in Bath, Oxford or London for intensive pain management programmes because of a lack of local expertise and/or programmes. 18,21 Research also indicates that healthcare professional training in pain management in the UK and across Europe is insufficient. 30,31 Hence, there is an urgent need for the NHS to improve how it supports children with chronic pain and their families, using high-quality evidence to inform design and delivery of services and treatments.
Evidence uncertainties and why this research is needed now
The SIGN guideline8 concerning the management of pain in children, recent Cochrane reviews on treatment effectiveness for children’s chronic pain,22–28 and the Lancet Commission on children’s chronic pain18 identified a dearth of research to inform chronic pain management. Several Cochrane reviews on the effectiveness of different pharmacological treatments of children’s chronic non-cancer pain also identified that we do not know which outcomes are important to children with chronic pain and their families. 22–25 Identifying these outcomes can guide design of services and treatments and inform future research.
The WHO children’s chronic pain management guideline indicated that research is needed in many areas including large multicentre trials and qualitative and mixed-method studies to understand how and why interventions are effective. 19 The guideline also specified that a biopsychosocial approach, which takes into account the whole range of biological, psychological and social influences on pain, is required. The guideline highlighted that there are inadequate data on interventions for chronic pain in children across all age groups and a wide range of subpopulations, particularly children under 10 years of age, those with intellectual or developmental disabilities, family members including siblings and caregivers. Without high-quality evidence, children will not receive evidence-based good-quality pain management, resulting in poor short-term and long-term outcomes in terms of pain and pain-related disability.
The Cochrane Pain, Palliative and Supportive Care (PaPaS) group prioritised research into children’s chronic pain in 201832 and the International Association for the Study of Pain set its global theme for 2019 as ‘the year against pain in the most vulnerable’ – a group which includes children – in order to raise awareness and improve pain assessment and management. 33 The NIHR also recognised the urgent need for research on chronic pain management with its themed call for research in this field. The 2021 Lancet Commission ‘Delivering Transformative action in children’s chronic pain’18 called for research to ‘make pain better’.
It is crucial that we understand how children and their families experience, understand and live with chronic pain of different kinds; which treatment outcomes are meaningful to them; and their views and experiences of health and social care services in relation to their pain management in order to design and deliver services and interventions which meet their needs and inform further research including trials and the outcomes they measure. Qualitative research is ideally suited to addressing these urgent and important issues.
Rationale for the research
Our preparatory work and scoping searches indicated existing relevant qualitative research to inform these issues,34–38 but there were no existing or planned syntheses of this qualitative evidence, indicating a gap in the research. These conclusions were based on our searches of PROSPERO, the International Prospective Register of Systematic Reviews (in May 2019); bibliographic databases MEDLINE (Medical Literature Analysis and Retrieval System Online), PsycInfo (American Psychological Association’s online database) and PubMed; and Google Scholar using keywords (pain/chronic pain, children/paediatric); the Cochrane library; our team’s reference databases; and reference lists in policy documents and Cochrane reviews. We also consulted experts in the field and checked Zetoc alerts (journal article monitoring and search service) of all newly published qualitative evidence syntheses.
To date, there has been inadequate use of qualitative research evidence about children and their families’ experiences of chronic pain in the form of qualitative evidence syntheses to inform design of trials and the outcomes they measure, services and treatments. Prior to commencing our qualitative evidence synthesis, we identified existing published qualitative evidence syntheses, which were limited in focus. Two syntheses looked at specific childhood chronic pain populations and topics – the experience of living with juvenile idiopathic arthritis39 and the impact of pain on adolescents’ social relationships. 9 Tong et al. 39 found that children and young people (CYP) felt different, misunderstood and stigmatised and juvenile idiopathic arthritis restricted their social participation. Jordan et al. 9 found mainly negative impacts of chronic pain on relationships, although some relationships became stronger in the face of challenges.
In addition, three review authors (EF, JN, MSB) conducted a qualitative evidence synthesis for WHO40 in January–September 2020 (conceived after we had submitted a funding proposal for the research reported here), to inform the revised 2020 guidelines for children’s chronic pain management. 19 The WHO synthesis took a global perspective on the management of children’s chronic pain, with a particular focus on research conducted in low- and middle-income countries. It incorporated the perceptions and experiences of healthcare professionals, in addition to those of children with chronic pain and their families. It focused solely on the views, perceptions and experiences of the risks, benefits and acceptability of three types of intervention: pharmacological, psychological and physical therapies. Our current qualitative evidence synthesis was intended to take a broader perspective on chronic pain and its management than the three existing syntheses, including how children and their families conceptualise and live with chronic pain of different kinds and to consider any kind of intervention or service. We did not set out to explore the views of healthcare professionals (which were explored in the WHO synthesis) and have focused mainly on the UK (including evidence from similar high-income contexts).
Furthermore, none of the above three syntheses developed a theory to inform a comprehensive pain management approach. There appears to be no comprehensive theory of children’s chronic pain, which covers how children and families conceptualise pain, experiences of living with pain and of pain management services and views of ‘good’ pain management and services. Most existing theories have been developed within a specific field, which might narrow our understanding of how children experience chronic pain. For instance, psychological theories tend to focus only on specific aspects of the pain, such as what causes pain, or they adopt a child development approach to explaining children’s understanding of their chronic pain. 41 Biopsychosocial theories of chronic illness, which specify the inter-relatedness of biological, psychological and social aspects of illness, better reflect our theoretical approach to chronic pain. 42 However, there do not appear to be any comprehensive biopsychosocial theories about children’s experiences of chronic pain and its management, for instance, one biopsychosocial theory focused only on clinical assessment and management of children’s chronic pain. 43
Meta-ethnography is ideally suited to synthesising qualitative evidence on the complex issues related to children’s chronic pain in order to develop new conceptual insights and theories to inform service and intervention implementation. 44,45 Therefore, we conducted a rigorous qualitative evidence synthesis using meta-ethnography44 to investigate the diverse experiences and perceptions of children up to age 18 years with chronic non-cancer pain and their families (children with cancer-related chronic pain have different care pathways) and generate theory to inform health and social care. We refer to the meta-ethnography reported here by the acronym ‘CHAMPION’ (Children And young people’s Meta-ethnography on Pain).
The meta-ethnography was also conceived as a Cochrane review intended to extend the findings of existing relevant Cochrane reviews on the effectiveness of pharmacological interventions,22–26,46,47 psychological interventions,27,48,49 dietary interventions;50 and physical activity interventions28 for children’s chronic pain. Integrating our qualitative findings with quantitative evidence of effect22–26 should inform the design and implementation of future interventions, and their evaluation and synthesis by highlighting key outcomes that need to be addressed and generating hypotheses that can be tested out. Data integration with Cochrane reviews of intervention effectiveness for children’s chronic non-cancer pain also contributes to developing more relevant, acceptable and effective interventions through greater understanding of the pain experience from the perspective of children, parents and wider family members.
While we were conducting our meta-ethnography, core outcomes for clinical trials were published which identified outcomes of importance to a narrow sample of children with chronic pain in the USA. 51 This core outcome set was developed from a study that recruited mainly female patients, all aged over 12 years, from tertiary pain and gastroenterology services, and drew on limited qualitative data from open-ended survey questions. Our meta-ethnography could further enhance the outcome set by potentially confirming, disconfirming and/or supplementing their outcomes with data from a wider range of participants.
The meta-ethnography could change healthcare delivery and policy, inform treatments and indicate gaps in knowledge and hence new directions for chronic pain research. 52 Because chronic pain is an aspect of many health conditions, our findings should have wide reach and transferability to similar settings across paediatric patient groups, while recognising the heterogeneity of children’s chronic pain. 23
Research plan
Research aim
To conduct a meta-ethnography on the experiences and perceptions of children with chronic pain, and their families, of living with chronic pain, treatments and services to inform the design and delivery of health and social care services, interventions and future research.
Review questions
-
How do children with chronic pain and their families conceptualise chronic pain?
-
How do children with chronic pain and their families live with chronic pain?
-
What do children with chronic pain and their families think of how health and social care services respond to and manage their/their child’s chronic pain?
-
What do children with chronic pain and their families conceptualise as ‘good’ chronic pain management and what do they want to achieve from chronic pain management interventions and services?
Objectives
-
Conduct comprehensive searches to identify qualitative research literature on the experiences and perceptions of children with chronic pain and their families to address review questions 1–4.
-
Select relevant studies and synthesise them using meta-ethnography.
-
To ensure salience of findings via involvement of children with chronic pain and their families in study design, analysis and interpretation.
-
Assess how much confidence can be placed in our synthesised findings using GRADE-CERQual (Grading of Recommendations Assessment, Development and Evaluation-confidence in the evidence from reviews of qualitative research)53 in order to facilitate use of our findings for NHS decision-making.
-
Identify research gaps regarding review questions 1–4 in order to inform future research directions.
-
Integrate our findings with existing relevant Cochrane treatment effectiveness reviews22–28,46–50,54,55 in order to determine if programme theories and outcomes of interventions match children and their families’ views and preferences.
-
Inform the selection and design of patient-reported outcome measures for use in chronic pain studies and interventions and care provision to children and their families.
-
Disseminate findings to academic, clinical, lay and policy audiences to influence childhood chronic pain policy and practice.
Summary
Children’s chronic pain is a widespread public health problem. We will report our analysis and synthesis of qualitative evidence to reach new interpretations and generate explanatory theory, increasing our understanding of families’ experiences and perceptions of chronic pain, pain treatment and services.
See Chapter 2 for details of the methodology including meta-ethnography.
Chapter 2 Meta-ethnography methods
Introduction
In this chapter, we provide a detailed account of the methods used to conduct our meta-ethnography.
Research design
We conducted a meta-ethnography44 following the methods of Noblit and Hare,44 Cochrane Qualitative Implementation Methods Group (QIMG) guidance56 and the eMERGe meta-ethnography reporting guidance45,57,58 and its associated methodological publications59,60 to facilitate the production of a high-quality meta-ethnography. We registered our review protocol on PROSPERO (reference: CRD42019161455) and published an a priori protocol with the PaPaS group (review number 623). 61
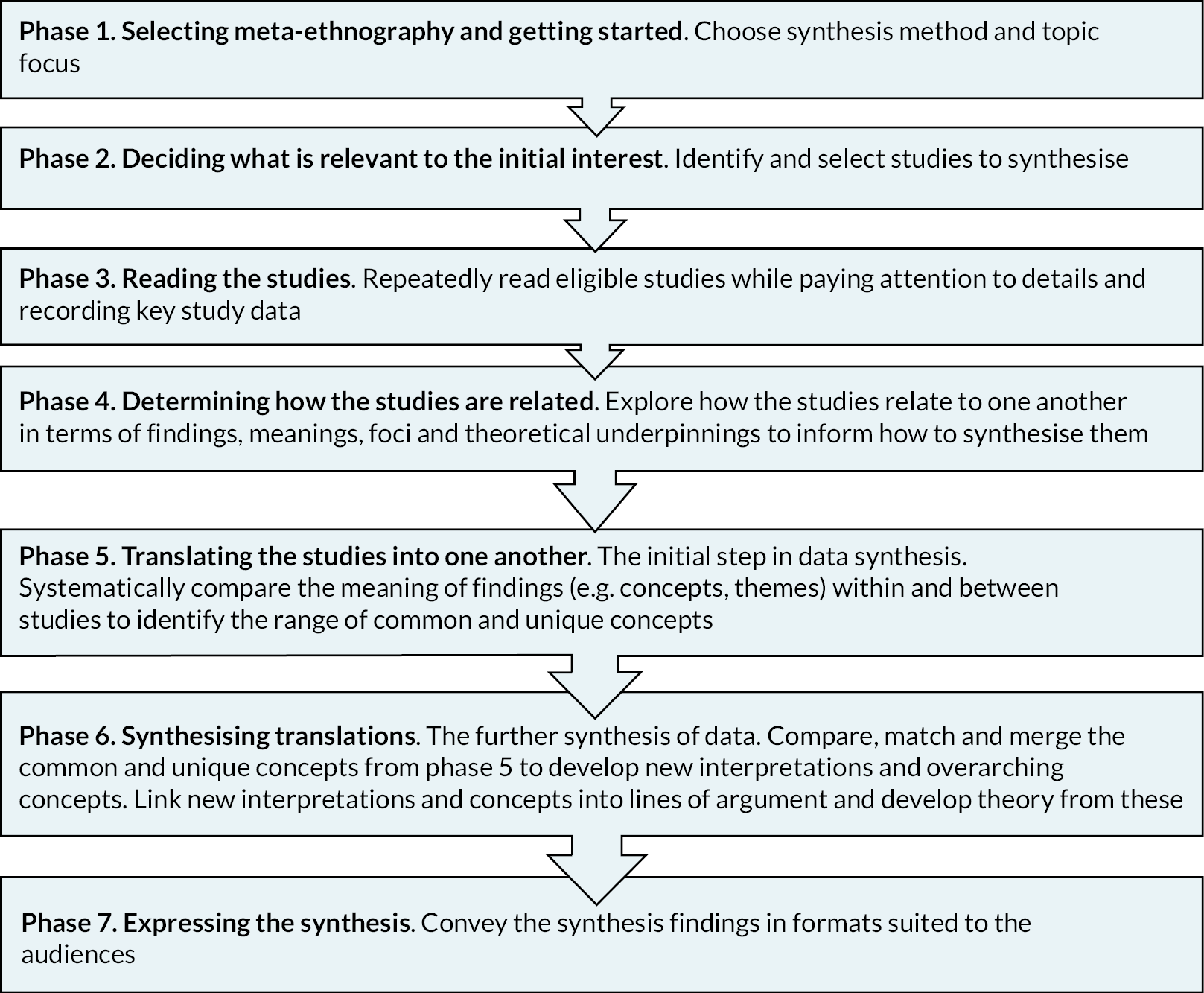
Meta-ethnography has a unique analytic synthesis method; this involves systematically comparing the meaning of concepts from primary studies, identifying new overarching concepts and linking these into one or more ‘line of argument’ syntheses leading to novel conceptual insights and theory development. 45,52 Meta-ethnography does not involve simply aggregating findings. 44,45 It is a rigorous, inductive methodology which takes into account the contexts and meanings of the original primary studies,44 making it ideal for synthesising the diverse contexts of children’s chronic pain research. The seven phases of meta-ethnography44,45,57,59,60 are described (Figure 1); although presented linearly, some phases run in parallel, and the process is iterative.
This meta-ethnography was conceptualised as a Cochrane review. 61,62 It is a Cochrane requirement that qualitative evidence syntheses, such as meta-ethnography, are used to supplement reviews of intervention effects to further understanding of the development and implementation of interventions. Therefore, the meta-ethnography findings were integrated with existing relevant Cochrane reviews of intervention effects.
In delivering this meta-ethnography, the review team worked in partnership with children living with chronic pain and their families and other stakeholders collaborating on all aspects of the meta-ethnography conduct. They influenced the aim and review questions during proposal development, the final search strategy (when finalising the protocol) and study sampling decisions and interpretation of data during conduct of the meta-ethnography. For a detailed description of patient and public involvement (PPI), see Chapter 3.
Phase 1: Selecting meta-ethnography and getting started
Meta-ethnography is ideally suited to developing new understandings, insights and theory about the experiences of children with chronic pain and their families to inform service and intervention implementation and identification of outcomes of value to children and families. Preliminary searches indicated that no meta-ethnography existed in this area, and that a reasonable-sized and conceptually rich (in-depth explanatory/interpretive) evidence base existed, suitable for meta-ethnographic synthesis, to address our review questions. Meta-ethnography involves reinterpretation of the findings in primary studies, taking into account the contexts and meanings of the original studies;44 it therefore requires in-depth explanatory or ‘conceptually rich’ data with accompanying detailed or ‘thick’ data on the study context.
Criteria for considering studies for this review
Topic of interest
Our topic focus was refined through discussion with health consumers (professionals and patients, see Chapter 3 for more details), examining relevant Cochrane intervention reviews and scoping searches of the available literature. We included studies that focused on the views and experiences of children with chronic non-cancer pain and their families towards chronic pain, health services and treatments. We excluded chronic cancer pain following common practice in chronic pain research, including Cochrane intervention effects reviews on children’s chronic pain, which focuses on cancer pain separately due to the very different care pathway and causes of the pain. 22–26 End-of-life chronic pain in the last weeks and months of life was excluded for similar reasons; children have a distinct care pathway accessing different kinds of services, for example hospices, and their pain management has different aims and considerations, for example addiction to analgesics is less of a concern. We defined a ‘child’ as a person under 18 years of age, according to the UN Convention of the Rights of a Child.
Inclusion criteria
-
Peer-reviewed journal articles, published reports, book chapters, books, PhD theses.
-
Contained qualitative research data on chronic pain, that is, pain lasting for 12 weeks or more, relevant to the review questions.
-
Reported the views of children with chronic non-cancer pain from 3 months up to age 18 years or their family members (e.g. parents/guardians, grandparents, siblings).
-
Qualitative primary research studies of any design (e.g. ethnography, phenomenology, case studies, grounded theory studies) including mixed-methods studies if it was possible to extract data that were collected and analysed using qualitative methods.
-
Used recognisable qualitative methods of data collection (e.g. focus group discussions, individual interviews, observation, diaries, document analysis, open-ended survey questions) and analysis (e.g. thematic analysis, framework analysis, grounded theory).
-
In any language.
-
Any publication date.
Exclusion criteria
-
Acute pain, that is, pain lasting for < 12 weeks, such as that caused by medical procedures.
-
Cancer pain.
-
Pain in neonates and babies < 3 months old.
-
Focused on end-of-life pain management (in the last weeks and months of life).
-
Non-empirical article, for example editorial, commentary, study protocol.
-
Findings did not differentiate between children with acute and chronic pain.
-
Findings did not differentiate between adult and child participants.
-
Studies did not use qualitative methods for data collection and/or analysis (e.g. studies which analysed qualitative data quantitatively).
-
Literature reviews.
The inclusion criteria were discussed and subsequently agreed with our PPI group (see Chapter 3).
Search strategy
Phase 2: Deciding what is relevant to the initial interest
A rigorous search for studies was conducted via bibliographic databases and supplementary searches, as outlined below. RT led the design and conduct of literature searches assisted by the research fellow (MSB) and Cochrane PaPaS. Initial literature searches of all information sources were conducted between August and September 2020. Bibliographic database searches were updated in September 2022 to bring the review up to date prior to publication. Studies were selected according to the methods outlined in Selection of studies. Our PPI group discussions informed which websites to search and which experts to approach for study suggestions (see Chapter 3).
Bibliographic database searches
We searched 12 bibliographic databases selected for their good coverage of qualitative research and spectrum of relevant disciplines (Table 1).
| Discipline/type of literature | Databases |
|---|---|
| Health and social care | CINAHL EMBASE MEDLINE (including MEDLINE in Process and ePub ahead of print) Social Care Online (Science Citation Index Expanded) |
| Psychological | PsycInfo |
| Sociological | Social Sciences Citation Index |
| Education | British Education Index |
| Multidisciplinary | Scopus |
| Grey literature and theses | HMIC OpenGrey EThOS |
| CYP | Child Development and Adolescent Studies |
See Appendix 1 for the database search strategy for MEDLINE. The search strategy combined three key search concepts: (A) qualitative study designs; (B) population – children and their families; and (C) phenomenon of interest – chronic pain. The MEDLINE strategy was then adapted to the remaining bibliographic databases listed in Appendix 1. All databases were searched from their inception.
Supplementary searches
Supplementary searches12 for studies were conducted between 1 August 2020 and 17 December 2020 via:
-
Searches of key websites, as outlined below.
-
Hand-searching 24 months, from 1 December 2018 to 31 December 2020, of key journals relevant to our review questions and/or qualitative health research:
-
BMC Pediatrics
-
Clinical Journal of Pain
-
European Journal of Pain
-
Journal of Pediatric Psychology
-
Qualitative Health Research
-
Social Science and Medicine
-
Sociology of Health and Illness
-
-
Contacting experts in the field for recommended studies, including ongoing research.
-
Checking reference lists of included papers and relevant literature reviews for any further relevant studies.
Grey literature was identified by searching:
-
Three bibliographic databases [Health Management Information Consortium (HMIC), OpenGrey and Electronic Theses Online Service (EThOS) – see Table 1].
-
Websites of key organisations representing chronic pain health conditions including British Pain Society, Department of Health, NIHR Library, Sickle Cell Society, Versus Arthritis, CRPS UK, Fibromyalgia Action UK, Crohn’s and Colitis UK, Reflex Sympathetic Dystrophy Syndrome Association, European League Against Rheumatism network, European Pain Federation, Pain Relief Foundation, Children’s Health Scotland, children’s hospitals, Reflex Sympathetic Dystrophy Syndrome Association supporting the CRPS community, Children’s Health Scotland, The Royal National Hospital for Rheumatic Diseases, Royal National Orthopaedic Hospital, Great Ormond Street Hospital for Children, Sick Kids Hospital, NHS Lothian and Evalina Hospital in London.
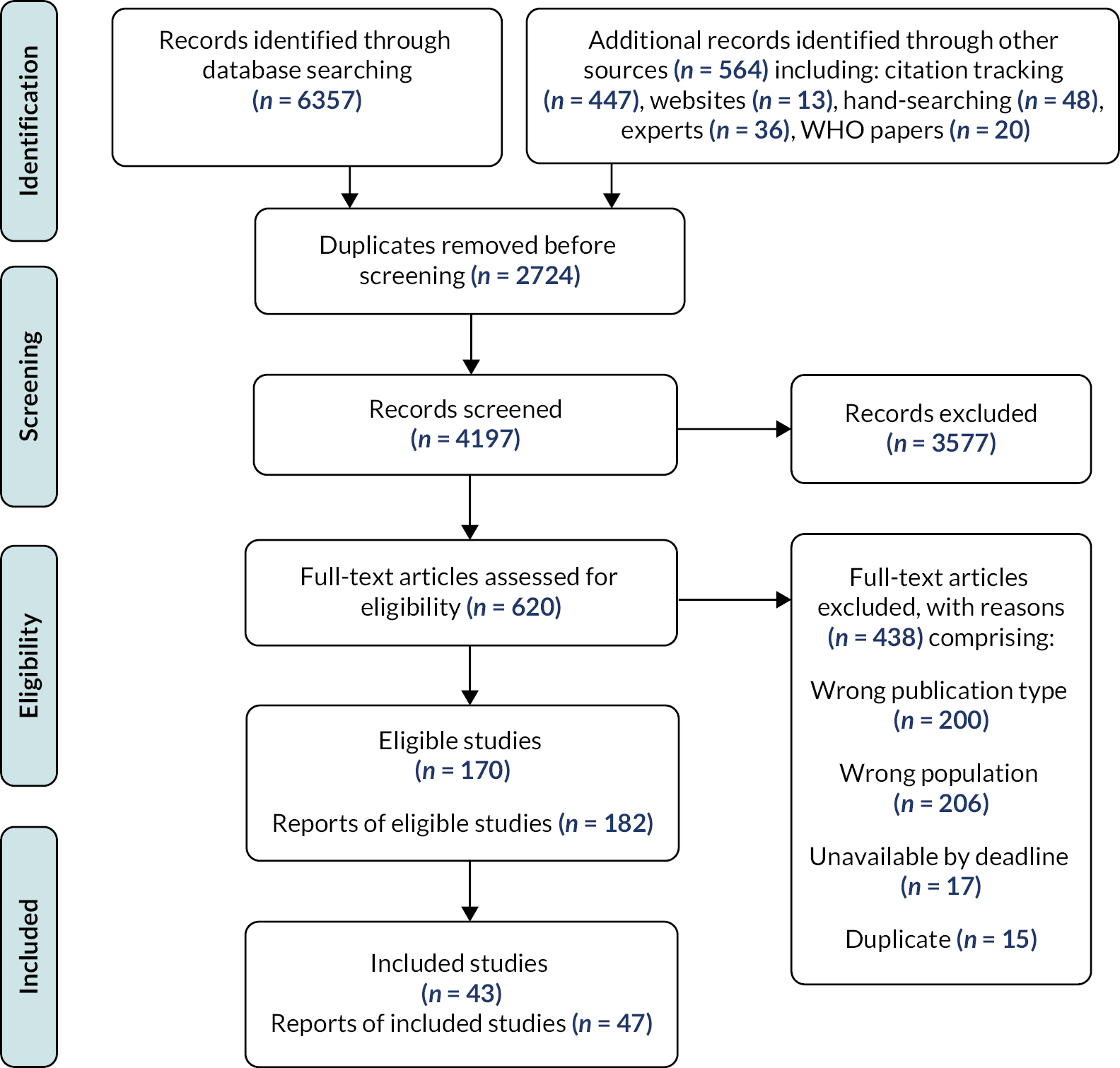
Supplementary searches were not updated in 2022 due to resource limitations, with the exception of asking experts to suggest potentially relevant new studies. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram was used to record search results and the results of study screening for inclusion (Figure 2). Characteristics of the excluded studies can be seen in Report Supplementary Material 1.
FIGURE 2.
PRISMA flow diagram.
Selection of studies
Literature screening and selection
Search results were exported to EndNote and duplicates removed. Then one reviewer (MSB) screened titles to remove off-topic records that were clearly not about children’s chronic pain, which was checked by a second, independent reviewer (RT). All remaining references were uploaded to Covidence systematic review management software. 63 First, titles and abstracts were screened, and clearly ineligible records were excluded. Then, the full text of all remaining studies was screened against our full inclusion criteria. At both stages, records were screened in duplicate by two independent reviewers (MSB, RT, EF, IU, LF, AJ, JN and/or KT). Disagreements were resolved through discussion and referred to a third reviewer, if necessary. Ten randomly chosen studies were used to pilot and standardise screening practices between reviewers.
Language translation
The review team are proficient in English, Portuguese, Spanish, Dutch and French. Any titles, abstracts and full texts published in any other language were initially translated through Google Translate to determine eligibility.
Sampling
Our final set of included studies was purposively sampled from all studies meeting our eligibility criteria. We used published guidance from The QIMG64–66 and input from our PPI group and Project Advisory Group (PAG) (see Chapter 3) to develop a strategy for sampling studies summarised below and in Box 1. In short, our sampling approach prioritised ‘conceptually rich’ and ‘thick’ UK studies with explanatory/interpretive findings and detailed contextual data, and then filled gaps in the data with less rich/thick UK studies and both rich/thick and less rich/thick non-UK studies. Our rationale for this is described below.
Round 1 – We included all publications reporting UK studies (‘UK publications’) assessed as 3* for richness.
Round 2 – We included all UK publications assessed as 2* for richness.
Round 3 – We included non-UK publications focusing on pain conditions, palliative care and/or types and ages of participants (e.g. children under 5 years old) not well represented in the sampled UK publications.
Round 4 – We included non-UK publications from high-income contexts similar to the UK NHS and relevant to review question 4 (assessed by checking the aims and abstracts).
Round 5 – We included non-UK publications whose aims were most closely related to our aim and review questions (assessed by their abstract), which had been published after 2006.
A meta-ethnography warrants studies with a good or fair amount of rich qualitative data and moderate to fair depth or ‘thickness’ of context and setting descriptions. 59 We assessed the conceptual richness of findings (i.e. whether the findings were explanatory/interpretive) and the thickness of contextual detail (how in-depth the context, intentions and meanings underlying the findings were) in UK studies selecting rich and thick studies for synthesis. This ensured that we were including studies that were the most adequate to address our review questions that were developed for a UK context. We adapted Ames, Glenton65 existing scale in assessing data richness, developed for qualitative evidence synthesis using thematic analysis, into a 3-point scale to suit meta-ethnography to focus on conceptual richness and contextual ‘thickness’, drawing on Popay et al. 67 and Cochrane QIMG guidance. 68 The scale and user guidance were drafted, piloted and revised by the research team. Table 2 presents our final richness scale (in which we used only the terms ‘thick’ and ‘thin’, whereas we would now also use the terms ‘rich’ and ‘poor’).
| Richness Score | Measure | Example |
|---|---|---|
| 1* | Thin or fairly thin qualitative data (findings) presented that relate to the synthesis objectives. Little or no context and setting descriptions | For example a mixed-methods study using open-ended survey questions, a more detailed qualitative study where only part of the data relates to the synthesis objectives, or a limited number of qualitative findings from a quant-qual mixed-methods or qualitative study |
| 2* | Fairly thick qualitative data (findings) that relate to the synthesis objectives. Some/moderate amount of context and setting descriptions | For example a typical qualitative research article in a journal with a smaller word limit and often using simple thematic analysis |
| 3* | Thick or very thick qualitative data (findings) that relate to the synthesis objectives. Fairly detailed or detailed/fairly large or large amount of context and setting descriptions | For example data from a detailed ethnography or a published qualitative article with the same objectives as the synthesis that includes more in-depth context and setting descriptions and an in-depth presentation of the findings |
We first selected all the 3* UK publications for inclusion. We then explored any potential gaps in the data provided by these studies. We extracted basic information such as age and type of participants, pain condition, aims, setting and which of our review questions were addressed by their findings. These 3* UK publications only covered a limited range of pain conditions, and few provided information on review question 4, which indicated that the UK publications might not provide sufficient data to answer all our review questions.
Further sampling decisions were made in collaboration with our PPI group and PAG, to ensure that the synthesis addressed what is of greatest importance to children and their families and considered the views of other key stakeholders including healthcare professionals. The PPI members supported our preferred option not to include poor UK studies (rated 1* for richness) but felt we should include 2* as well as 3* UK studies. We therefore continued with a meta-ethnography rather than conduct a thematic synthesis, which could have incorporated less rich 1* findings. PAG members, including PPI representatives, agreed it was important to include non-UK studies (i.e. studies not conducted in the UK), as long as they fitted our aim and review questions, to try to represent a wider range of pain conditions and of participants. We completed richness assessments only for those non-UK studies which met our sampling criteria. Only those non-UK studies that were rated as 2* or 3* for richness (fairly or very rich data on our review questions) were included. We repeated the sampling process following the update of our literature searches in September 2022.
We referred to the PROGRESS-plus criteria (place of residence, race/ethnicity/culture/language, occupation, gender/sex, religion, education, socioeconomic status and social capital) when judging whether relevant populations were represented in the sample. 69 We used the four GRADE-CERQual domains (methodological limitations, adequacy, coherence, relevance) to guide the sampling process in order to develop the strongest findings for decision-making (see Assessing confidence in synthesised findings).
Assessing methodological limitations of included studies
In addition to assessing the conceptual richness of studies, as described above, we also assessed the methodological limitations of the included studies. Two independent reviewers (EF, MSB, IU, LF and/or three volunteer research assistants) assessed methodological limitations of the included studies using the Critical Appraisal Skills Programme (CASP)70 qualitative tool using the following domains:
-
Was there a clear statement of the aims of the research?
-
Is a qualitative methodology appropriate?
-
Was the research design appropriate to address the aims of the research?
-
Was the recruitment strategy appropriate to the aims of the research?
-
Were the data collected in a way that addressed the research issue?
-
Has the relationship between researcher and participants been adequately considered?
-
Have ethical issues been taken into consideration?
-
Was the data analysis sufficiently rigorous?
-
Is there a clear statement of findings?
Studies which were limited by poor methodological reporting were not excluded. No studies were judged to be fatally flawed (e.g. methodologically unsound); fatally flawed studies would have been excluded because there is a distinction between quality of methodological reporting and quality of study design (with only the latter being detrimental to the quality of the findings). We resolved any potential disagreements by discussion, and when necessary, a third review author was consulted. Where a review team member was the author of an included study, they were not involved in the assessment to ensure an unbiased appraisal. The end point of assessment was an overall judgement of methodological concern for each individual study (no or minor concerns, moderate concerns or serious concerns). We transparently recorded all decision-making in Microsoft Excel. Assessments of methodological limitations subsequently informed GRADE-CERQual judgements of how much confidence can be placed in our synthesised findings (see Chapter 4).
Data extraction, analysis and synthesis: meta-ethnography phases 3–6
Phase 3: Reading the studies and data extraction
Studies were repeatedly read in full by at least two team members. We recorded study characteristics of all eligible studies (e.g. aim; country; number and type of participants, e.g. gender, age, diagnosis/type of chronic pain, patients, parents or other family members) in Microsoft Excel. Further characteristics were recorded for the final included studies such as study design, recruitment setting, sampling method, methods of data collection and analysis, ethnicity, conflicts of interest, funders. We referred to the PROGRESS-Plus criteria, described above, when extracting data on participant characteristics. 69
Full-text PDFs of the included studies were uploaded into NVivo qualitative data analysis software. 71 Each study was added as an individual ‘node’ and all of its conceptual findings were extracted as ‘subnodes’. (A ‘node’ is a container, given a specific label, into which data are gathered.) Each conceptual finding or theme was ‘extracted’ or coded, regardless of whether it appeared in the ‘findings’ or ‘discussion and conclusions’ sections, and labelled with the author, study identification number and the concept/theme name (see Report Supplementary Material 2). Authors’ recommendations and ‘interventions that worked’ were also extracted as subnodes for each paper. In total, we extracted data into 529 nodes. Some studies did not contain conceptual-level data but instead contained, for example descriptive themes or rich descriptions. For these studies, where possible, we interpreted the findings to develop new concepts and coded them at a new node. For studies identified in the updated searches, we compared the findings of included studies directly with our synthesis findings rather than extracting data in NVivo.
Phase 4: Determining how studies are related – grouping studies
In deciding our approach to grouping studies for synthesis, we considered grouping studies by type of participant (children, parents or siblings), or age of the children focused on (e.g. 0–5 years, 6–8 years), or type of pain/pain condition. We concluded that we could not classify studies into groups according to the type of participant or the children’s age group because many studies included the views of children and parents and/or focused on a wide age range. Grouping by the type of pain or pain condition seemed to be a more feasible and logical approach. Therefore, we then looked at existing systematic reviews of intervention effectiveness and qualitative evidence syntheses on children’s chronic pain to see how they had grouped studies by conditions and consulted our healthcare professional PAG and team members to agree the groupings (see Chapter 3).
We found only two Cochrane effectiveness reviews on children’s chronic pain which had grouped trials into headache versus non-headache chronic pain (all other pain conditions) for subgroup analyses; the decision was based only on the numbers of trials. 54,55 Separate Cochrane reviews had been conducted specifically for recurrent abdominal pain and for sickle cell disease pain in children. We planned to integrate our findings with existing Cochrane effectiveness reviews so separate groupings on sickle cell disease, headache and recurrent abdominal pain seemed appropriate. A WHO review 20 had categorised trials by pain condition, according to the ICD-11 classification. Most of our included studies provided a poor level of detail on pain conditions so we could not use ICD-11 to classify and group them. The only two qualitative evidence syntheses in the field at the time9,39 did not group studies by condition since one focused solely on juvenile idiopathic arthritis39 and the other included only eight studies. 9
After seeking advice from the healthcare professionals in the PAG (see Chapter 3) and team members, we grouped included studies by health condition, which resulted in a total of 11 groups:
-
Juvenile idiopathic arthritis
-
Abdominal pain
-
CRPS
-
Sickle cell disease
-
Headache
-
Neurological conditions
-
Musculoskeletal conditions
-
Skin conditions (epidermolysis bullosa)
-
Dysmenorrhoea
-
Mixed conditions
-
Unspecified types of chronic pain
We consulted high-quality relevant systematic reviews and qualitative evidence syntheses to inform our subgroup analysis. 52,72–74
Phase 5: Translating the studies into one another
The conceptual data/findings from all NVivo nodes were interpreted in chronological order from the earliest publication date using NVivo memos. This process consisted of interpreting and capturing the key meaning of each conceptual finding while taking account of relevant contextual data. These interpretive memos were labelled with the condition, author’s name, study identification number and concept/theme name (see Report Supplementary Material 3). For the first three studies, each node was interpreted independently by two reviewers (EF and MSB). The two reviewers then discussed their interpretations and, if possible, agreed a joint interpretation recorded in one memo or recorded their alternative interpretations. For the remaining studies, one reviewer interpreted the data (EF or/and MSB) from each node and recorded this in a memo; a second reviewer (EF and MSB, IU, RT, LC and/or AJ) read the data coded at the node, then read the first reviewer’s interpretive memo and challenged, confirmed and/or added to the interpretation of the first reviewer. All authors kept an ‘analysis journal’ in a memo in NVivo to record any reflections, thoughts, issues or questions during the analysis.
Informed by our PPI group and based on previous meta-ethnographies,52 we initially analysed data in each grouping of studies separately before bringing them all together in phase 6, as we describe below. In total, 346 memos were created. In phase 5, we used the data in the memos to compare concepts systematically, study by study for each of the 11 condition groupings to identify both common and unique concepts. The translation and interpretation were completed using an inductive approach, guided by data and focused on meaning and context. At least three reviewers analysed (translated) the concepts to try to reach a new level of interpretation.
In the study-by-study translation for each grouping, all memos were downloaded from NVivo as .docx files and combined into one Word document. Then, we read the interpretive memos for each study in chronological order by publication date. We took the earliest publication first and read the memos for each concept, we compared the meaning of each with the memos for the second study looking for similar and contradictory concepts, we then compared these with the third study and so on, until we had identified the full range of concepts including common and unique concepts. To help juxtapose the concepts, we used tables in a MS Word document, one for each grouping, described below (Table 3). For groupings with only one publication, we looked for and identified any overarching concepts where possible. One reviewer (EF or MSB) carried out the initial translation for each grouping. A second and third reviewer (EF, MSB, IU, AJ, RT, LF, LC and/or JN) then read and challenged, confirmed and/or added to the translation. Common and unique concepts were identified within each grouping.
| Author’s name_#studyID_name of the construct | Author’s name_#studyID_name of the construct | Our interpretations/common and unique constructs |
|---|---|---|
| Brodwall75#5239_Desire for a specific diagnosis and discussion with a professional | Smart76#3799_Interactions with doctors | Importance of diagnosis for parents (Brodwall,75 Smart76) |
| The outcome most wanted by parents after examinations were detection of a somatic disease with a well-defined treatment. (…) Parents described as extremely sad and frustrating regarding the lack of diagnosis that could potentially led to a treatment. Focusing on the pain could drive the family and the doctor into a vicious cycle of hunting for undetected causes instead of focusing on pain management. The anxiety that something dangerous may be overlooked may make the parents crave further examinations. (…) They wanted their child to have further medical examinations, and that this should happen quickly in case it is ‘something very serious’. |
Mothers (n = 22) visit doctors to establish whether a child was malingering (3 cases); to exclude a physical disease so that they could manage the pain themselves (13 cases); and to seek help in managing the pain (6 cases). Mothers (22) reported consulting doctors to establish whether a child was ‘malingering’ (3 cases) (mothers); to exclude a physical disease so self-manage the condition (13 cases); and to seek help with pain management (6 cases). Mothers’ view the interaction as satisfactory when they had been given a simple explanation for the pain as this acknowledged that the child was indeed genuinely ill and their concerns for their child were thus legitimate which removed any charge against their competence. Mothers perceived interactions with doctors to be satisfactory when a simple explanation for the child’s pain had been offered. Such an explanation provided validation of (1) parental concerns, (2) legitimacy of the child’s illness and alleviated any potential charges against maternal competence. |
Parents wished for a diagnosis that would enable treatment, were sad and frustrated with the lack of diagnosis and anxious it is ‘something very serious’. Focusing on finding a diagnosis could be at the expense of pain management. Diagnosis legitimised and validated the pain. |
One PhD thesis77 was also published in two other included publications38,78 and contained similar data/findings, which were analysed together and considered as one publication. Britton (2002)79 and Britton (2002)80 reported different participants’ perspectives from the same study sample, so findings were also analysed as separate publications. Renedo (2020)81 and Renedo (2019)82 also used the same cohort for their studies and presented similar findings, and therefore were analysed as one publication.
Phase 6: Translation and synthesis within condition groupings
After the process of comparing concepts and looking for common and unique concepts in phase 5, we matched, merged and developed overarching third-order constructs. These third-order constructs expressed a new interpretation of the data which went beyond the findings of the original studies; we achieved this for some of the conditions for which there were sufficient in-depth data. Report Supplementary Material 4 and Appendix 2 show, for each pain condition grouping, how we progressed from included study findings to third-order constructs, illustrating the outcomes of our translation and synthesis of translations. We produced a textual synthesis in a narrative format for each of the concepts, and where possible, we also created diagrams showing how the new constructs linked to each other. We also referred to any theory or model produced by the original authors of the studies to check we had taken account of the original meanings.
All phase 5 translation and phase 6 synthesised translation information for each grouping was summarised in a table (example in Table 3) which included the author’s name and study identification number; a list of all the author’s themes or concepts labels (second-order constructs); where relevant, a list of our constructs (new second-order constructs) created for descriptive studies; a list of common and unique constructs across all studies (created from study-by-study translation); and a list of any overarching third-order constructs (our new interpretations).
Britten et al. 83 coined the term ‘third-order constructs’, thus further developing Schutz’s84 notion of ‘first-order constructs’ – lay understandings – and ‘second-order constructs’ – the researchers’ interpretations of the first-order constructs. The translation and synthesis process resulted in a total of 39 third-order constructs and 169 second-order constructs across all the groupings.
Translation and synthesis across condition groupings
To translate and synthesise data across condition groupings, we conducted a series of four research team meetings including one hybrid in-person/online and three synchronous online meetings. Prior to meeting, data from all groupings were organised into one document, which included all the narratives (the textual syntheses) created from the translation process, and data that were used to create new second- and third-order constructs. Labels (like Post-it® notes) for each construct including the condition, the name of the construct, the contributing studies and a brief description of the construct were used during the meeting. Labels were colour-coded according to the condition and whether they were second- or third-order constructs. Six members of the team then organised the labels through a thematic analysis into distinct themes and then into broader ‘analytic categories’ (thematic headings) according to shared meaning. Four members attended in person (EF, IU, LF and MSB) and two members online (RT and AJ). Members participating online were able to follow the analysis process using a Padlet85 (a real-time collaborative web platform used to share and organise content – see Report Supplementary Material 5).
Following the hybrid analysis and synthesis meeting, the narrative document (containing all themes/constructs across all groups) was reorganised according to the new ‘analytic categories’. A further three online team meetings using Google Jamboard86 (a digital interactive whiteboard) focused on analysing the findings using all the different perspectives and expertise from the whole research team (see Report Supplementary Material 6).
Once all data were organised into analytic categories (five categories were created), we finished updating the textual synthesis, and used Microsoft Teams87 whiteboard to create diagrams to express and understand how themes/constructs and analytic categories were related (see Report Supplementary Material 7). We used the diagrams created in Microsoft Teams whiteboard to discuss the findings/analysis virtually with the research team; subsequently, we produced short descriptions for each analytic category based on the diagrams. These descriptions were developed into detailed textual syntheses.
We continually further developed and refined our analysis and synthesis. In order to clarify our terminology, where we had been able to reach the level of new interpretation, the analytic categories were renamed as ‘third-order constructs’, for example ‘Pain organises the family system and the social realm’, most comprise ‘second-order constructs’, for example ‘adapted parenting’, which we had previously called ‘themes’. We developed lines of argument – the ‘overarching storylines’ – to explain how all the final constructs linked together with the help of diagrams in Whiteboard and team discussion. These lines of argument together enabled us to develop our theory of children’s chronic pain. We discussed and clarified ambiguous or unclear findings with our PPI and PAG groups (see Chapter 3).
Assessing confidence in synthesised findings
Grading of Recommendations Assessment, Development and Evaluation-confidence in the evidence from reviews of qualitative research assessments of how much confidence can be placed in individual qualitative evidence synthesis findings help decision-makers in the NHS and policy-makers use the findings to inform policy and practice; assessments indicate how well each finding represents the phenomenon of interest. 53 We applied the GRADE-CERQual approach to our meta-ethnography findings,53 using the online iSoQ (interactive summary of qualitative findings) software tool. We used CERQual to evaluate the overall confidence in the synthesised evidence for each review finding according to its adequacy of data, coherence, relevance and the methodological limitations in the primary studies contributing to a synthesised finding. 53 Adequacy refers to the overall richness and quantity of data supporting a review finding. 88 Coherence refers to the fit between the data from the primary studies and a review finding. 89 Relevance is how applicable the data supporting a review finding are to the context (e.g. population, phenomenon of interest, setting) specified in the review question. 90 Methodological limitations refer to concerns about the design or conduct of the primary studies that contributed to a review finding. 91
Integration of synthesised qualitative findings with Cochrane intervention reviews
It is important for decision-making to develop an overall understanding of intervention effect, feasibility, acceptability and factors that create the context for barriers and facilitators to successful implementation. We therefore integrated our synthesised qualitative findings with the results of recent Cochrane intervention effectiveness reviews22–28,46–50,54,55 using quantitative/qualitative data integration methods from Cochrane QIMG92 to determine if the programme theories (i.e. how a complex intervention is thought to work93) and outcomes of interventions match families’ views and expectations. We created a matrix in Microsoft Excel94 to juxtapose key outcomes and aspects of interventions that are important to children and families with the outcomes and focus of the reviews. We extracted the programme theories for all reviews and two reviewers (EF, KT) assessed whether these matched families’ views, experiences and expectations and whether they adopted a biopsychosocial perspective. A programme theory is simply the theory of how the intervention works and does not imply a realist methodology.
Integration mechanisms for quantitative results and qualitative findings
There were various points in overall meta-ethnography production at which integration occurred. 92,95 We have integrated quantitative and qualitative perspectives during review question formulation and synthesis.
Qualitative and quantitative review team membership and communication
Members of our qualitative evidence synthesis review team (JN, EF and LC) had close contact and communication (during both this meta-ethnography and previous reviews for WHO) with key reviewers who conducted and/or were the managing editor for the quantitative intervention effect reviews. For instance, we wrote funding applications with some of the quantitative reviewers, shared search strategies and outputs for the WHO reviews, had joint meetings and consulted regularly to obtain early sight of the quantitative outcomes. This meta-ethnography is also registered with Cochrane PaPas for publication in the Cochrane Library. The managing editor and quantitative intervention effect review authors also shared resources with our meta-ethnography team, such as draft intervention effects reviews, the new core outcome set and the Lancet Commission Report, which were used during quantitative/qualitative review data integration. Because of this close collaboration and the way that the meta-ethnography has been designed to ‘speak’ to the Cochrane intervention effects reviews, facilitated the subsequent quantitative/qualitative integration. This enabled us to establish a high level of coherence between the qualitative and quantitative evidence.
Question formulation
The meta-ethnography review questions were formulated to address known gaps in Cochrane intervention effectiveness reviews.
Additional synthesis to integrate qualitative findings and quantitative results
We used a matrix approach adapted from one used previously in several Cochrane reviews (see, for example Munabi-Babigumira et al. 96). Our matrix explored whether potential implementation factors (patient values, preferences and desired outcomes, acceptability, feasibility, etc.) identified in our meta-ethnography were acknowledged or addressed in the intervention programme theories in the Cochrane reviews of intervention effectiveness.
Deviations from the protocol
The original literature search of all sources (including bibliographic databases, reference list checking of included studies, website searches and contacting experts) was completed in September 2020. To bring the literature search up to date prior to publication, we reran the bibliographic database searches and contacted our expert panel for new and ongoing studies in September 2022. The update searches did not follow the full protocol. Due to time constraints, we did not rerun the website searches or check the reference lists of the newly included studies identified from our updated search. Furthermore, the ‘OpenGrey’ database was discontinued in 2020 so the update search could not be rerun.
In the protocol, we had planned to perform ‘cluster searches’, which involve identifying ‘clusters’ of related study reports to reconstruct the study context97 if a relevant study lacked contextual information. Due to the large volume of studies and lack of resource, we did not perform cluster searching, although we did record which included studies we felt needed more information about the study context as part of our richness assessments. In the protocol, we had planned to search the Applied Social Sciences Index and Abstracts bibliographic database but could not because of lack of institutional access.
Summary
We conducted a meta-ethnography, which adopted a rigorous, systematic approach to analysis and synthesis of data to reach new interpretations of data. We assessed our confidence in our synthesised findings using GRADE-CERQual. We used established methods to integrate our findings with results from Cochrane intervention effects reviews. For details of our PPI, see Chapter 3, and for details of the meta-ethnography results, see Chapter 4.
Chapter 3 Patient and public involvement and stakeholder engagement
Introduction
INVOLVE98 defines PPI as ‘research being carried out “with” or “by” members of the public rather than “to”, “about” or “for” them’98 (p.1) (emphasis in the source reference). The involvement of patients and members of the public helps to protect and promote their interests and create research that is more relevant, with clearer outcomes and impact. PPI played a central role across all stages of the meta-ethnography, from inception through to dissemination. PPI contributed to tasks such as helping with the development of the grant funding proposal; finalising the study design; deciding the study name and logo; deciding which studies to include and how to organise them for synthesis; sharing their experiences in order to clarify, confirm or disconfirm findings; identifying important areas missing from existing research; and participating in dissemination.
The study included both PPI and engagement. Public engagement is not synonymous with public involvement, and in the UK, the former refers to sharing research information and knowledge with the public. 99 We had a core PPI group who provided detailed feedback and helped with important decisions and data analysis and interpretation. We also sought views from the wider population of CYP with chronic pain and their parents/guardians. We also had a PAG of stakeholders, including medical experts, academic experts, third-sector organisations and children with chronic pain and their families, who contributed at key time points. Aspects of the PAG role included both involvement and engagement. The PAG was tasked with providing strategic advice to the research team on four key areas: (1) methodological issues, (2) clinical and lived experience of chronic pain, (3) study conduct and (4) dissemination.
We were guided by the UK Standards for Public Involvement100 and used the ACTIVE framework to guide our reporting. 101 PPI and PAG members decided their level of involvement or engagement throughout the duration of the study. In this chapter, we describe the PPI and PAG involvement and engagement and their impacts.
Recruitment
Patient and public involvement group
Patient and public involvement recruitment was conducted in three main stages. These comprised:
-
During development of the meta-ethnography research grant proposal in 2019, we involved 10 lay people including 3 CYP with chronic pain (1 was also a patient representative for a third-sector organisation), 4 parents, 2 adult patient representatives from the third sector and 2 adult members – 1 with chronic pain and 1 with a chronic illness from a university PPI Research Partnership Group (designed to assist with developing research relevant and useful to patients, carers, family members and healthcare professionals).
-
In 2020, we recruited a core PPI group of children aged 8–18 years, and parents or/and informal carers (i.e. not healthcare professionals) of children with chronic pain aged 3 months to 18 years. Additional prospective recruitment during the meta-ethnography was carried out as needed (e.g. to fill the gaps in terms of experiences with specific contexts/conditions).
-
In 2019–20, healthcare professionals, representatives of third-sector organisations and academics with relevant experience were recruited to join our PAG.
We advertised for PPI members via national pain services, social media (Facebook and Twitter) and third-sector organisations (charities) including the Sickle Cell Society, Fibromyalgia Action UK, Great Ormond Street Hospital, Pain UK, The Brain charity, CCAA kids with Arthritis, Pain Relief Foundation, Action on Pain, Coeliac UK, Guts Charity, Dystonia UK, Endometriosis UK, Sick Children Trust, Action for ME, A way with Pain, MS Trust, Diabetes UK, Fibro Awareness UK, Pain Concern and Independent Nurse. We tried to recruit a diverse core PPI group with any type of chronic pain, except for pain associated with cancer – whether primary (e.g. fibromyalgia) or secondary pain conditions (e.g. arthritis) – with a variety of experiences, ages, ethnic backgrounds and socioeconomic statuses. Other stakeholders were approached directly via e-mail.
Participants
Patient and public involvement group
We successfully recruited 12 children (10 females, 1 male and 1 non-binary from 8 to 20 years old) and 8 parents (all female). The young people had chronic pain conditions including Ehlers–Danlos, fibromyalgia, migraines, general chronic pain and chronic lumbar paravertebral muscle spasm, chronic headaches and CRPS. Parents and/or informal carers in the group were all mothers of children with pain from cystic fibrosis, CRPS or Ehlers–Danlos syndrome. All members lived in the UK, specifically in England, Scotland and Wales and were white. All PPI members were invited to join the PAG group.
Project Advisory Group
The PAG, which also facilitated some PPI involvement, comprised 27 members including 10 children with chronic pain and 7 mothers of children with chronic pain (also part of the PPI group), 6 healthcare professionals and 7 other stakeholders. The healthcare professionals/academic healthcare professionals included a consultant in paediatric anaesthesia and pain medicine who was a senior clinician and research lead at a specialist pain service; a clinical academic and consultant in pain medicine who was national lead clinician for chronic pain for the Scottish Government and vice chair of the National Advisory Committee on Chronic Pain; a clinical academic who was Chair of Pain Medicine, Honorary Consultant in Anaesthesia and Pain Medicine, and chair of the 2018 SIGN guideline development group for children’s chronic pain; one general practitioner and two physiotherapists. There were two patient representatives from the third sector including from Pain Concern and Children’s Health Scotland, a representative from Healthcare Improvement Scotland (Scottish Government), and an academic expert in qualitative evidence synthesis. We were unsuccessful in recruiting representatives of NICE or the UK government.
Involvement and engagement methods
Strategies to involve PPI were flexible and inclusive to allow everyone to participate individually or in a group. We provided preparatory training to meet the needs of PPI members, for example how to use the video-conferencing software, understanding the research. Engagement with members of the PAG was focused on specific tasks. We used a combination of online workshops and interim online communication (e-mail, teleconference calls, social media, e.g. Facebook and Twitter pages, online surveys) throughout the research. No face-to-face interaction was possible because of the COVID-19 pandemic. PPI members were paid for their time in vouchers.
Project Advisory Group and PPI members received plain language meeting materials in advance. PPI members were offered an online briefing in advance of the meeting, individual follow-up debrief calls after meetings/workshops, and given a list of support organisations. All meetings and workshops were designed to be engaging and to appeal to young people including a fun activity or ‘ice breaker’, multiple rest breaks and co-created ground rules to help create a safe space. The PAG workshops were chaired by two skilled chairs independent from the research team and their institutions: Bernie Carter, a professor with expertise in children’s chronic pain at Edge Hill, and Professor Richard Hain, clinical consultant and lead clinician in paediatric palliative medicine at Ty Hafan children’s hospice. PPI workshops were facilitated by two team members (EF, MSB). See Table 4 for a description of the different stages of the meta-ethnography in which PPI and PAG members were involved.
| Phase | Involvement activity | Number of PPI involved | Number of PAG members involved | Method |
|---|---|---|---|---|
| Planning of proposal and phase 1 | Feedback on study aims, objectives, review questions, lay summary and dissemination strategy | 10 | 0 | |
| Phases 1 and 2 | Finalise the study protocol, for example the literature search strategy | 8 | 0 | |
| Phase 2 | Finalise inclusion/exclusion criteria, for example the types of chronic pain included and the characteristics of the population we will include. Sample studies for synthesis | 8 | 17 | Separate online workshops for PPI (1 April 2021) and PAG (6 May 2021) |
| Phases 3 and 4 | Decide how studies were organised/grouped for analytic synthesis, for example grouping them by type of chronic pain, age of participants | 0 | 11 | |
| Phases 5 and 6 | Analyse and interpret primary study findings, for example to check if our interpretation of the study findings is different from or the same as children and families’ interpretations, check if their experiences are similar or different to those of the people in the studies, if important areas are missing from research | 5 | 6 | Separate online workshops for PPI (9 December 2021) and PAG (28 April 2022) |
| Phase 7 | Producing outputs, dissemination. We invited members to copresent a conference paper and the group to codevelop lay, patient and policy outputs. The group is helping ensure the development of lay dissemination materials for children and families is appropriate and relevant |
1 PPI conference presentation | 0 | E-mail and online meetings |
Patient and public involvement in the review focus and questions
Methods
Initial PPI engagement during grant development involved sending PPI volunteers materials via e-mail about the topic and our rationale for the focus of the review and draft review questions.
Impact/outcome
Respondents confirmed the importance of the topic and review questions.
Patient and public involvement in the literature search strategy
Methods
We finalised aspects of the literature search strategy in collaboration with our core PPI group in September 2020. Specifically, we e-mailed them materials explaining the search terms, sources in plain and simple language and asked them to suggest sources, key studies or experts (see Report Supplementary Material 8).
Impact/outcome
The PPI group suggested seven additional sources, which were included in the search strategy (see Chapter 2, section Supplementary searches). They agreed our final study inclusion criteria.
Sampling decisions
Methods
Our PPI and PAG groups informed sampling of studies. Eight PPI members (four children with chronic pain and four parents/guardians) contributed to decisions – six took part in a 1-hour online workshop on 1 April 2021 and a further two members took part via an online survey. The team presented gaps identified in the UK data and asked five questions (see Appendix 3) related to the sampling of studies in terms of their conceptual richness, study setting and pain conditions. We also asked if we should continue with a meta-ethnography or instead use an alternative synthesis methodology (e.g. thematic synthesis) which would allow inclusion of a wider range of studies, not just conceptually rich ones.
We then asked our PAG how we should sample non-UK studies. Twenty-three people attended an online workshop on 6 May 2021, including six research team members, four parents and four CYP with chronic pain, and nine healthcare professionals, academics or other professionals. We presented the gaps in populations and pain conditions covered by the conceptually rich UK studies.
Impact/outcome
The PPI members indicated that we should not include studies rated 1* for richness, but we should include richer 2* as well as 3* studies; and therefore, we should continue with a meta-ethnography rather than conduct a thematic synthesis. The PPI group also agreed that some studies conducted outside the UK should be included. Subsequently, most PAG members agreed we should include non-UK studies regardless of the country in which the study was conducted, studies for a wider range of pain conditions, and a broad range of participants, as long as studies fitted well with our meta-ethnography aim and review questions.
Patient and public involvement and Project Advisory Group involvement in deciding how to group studies for synthesis
Methods
We e-mailed PPI and PAG members in June 2021 to ask how we should group studies for preliminary analysis by subgroup, prior to synthesising the whole sample of studies and received 16 responses. Subsequently, we e-mailed 11 clinicians and pain experts to ask about their views and suggestions on the preliminary groups of health conditions (see Report Supplementary Material 9 and Chapter 2, Phase 4: Determining how studies are related – grouping studies).
Impact/outcome
Patient and public involvement and PAG responses contributed to the decision to group the included studies into a total of 11 groups of health conditions: juvenile idiopathic arthritis, abdominal pain, CRPS, sickle cell disease, headache, neurological conditions, musculoskeletal conditions, skin conditions (epidermolysis bullosa), dysmenorrhoea, mixed conditions and unspecified type of chronic pain.
Patient and public involvement in data analysis and interpretation
Methods
A 2-hour PPI workshop with two parents and three young people was held in December 2021 to discuss, clarify and interpret preliminary findings from primary studies. We used the software StoryboardThat (www.storyboardthat.com) to create cartoons and accompanying scenarios (e.g. Figures 3 and 4) to convey these findings to prompt discussion. Cartoons included people of different ethnicities and genders. We formulated the dialogue in speech bubbles using the language and terminology from children’s and parents’ quotations in the included studies and ensured it was suitable for a minimum reading age of 8–9 years of age. Members of the team approved all dialogues prior to the workshop. All PPI members received the cartoons and an infographic (see Report Supplementary Material 10) explaining the study findings a week prior the workshop.
FIGURE 3.
Example of cartoon used during PPI analysis workshop.
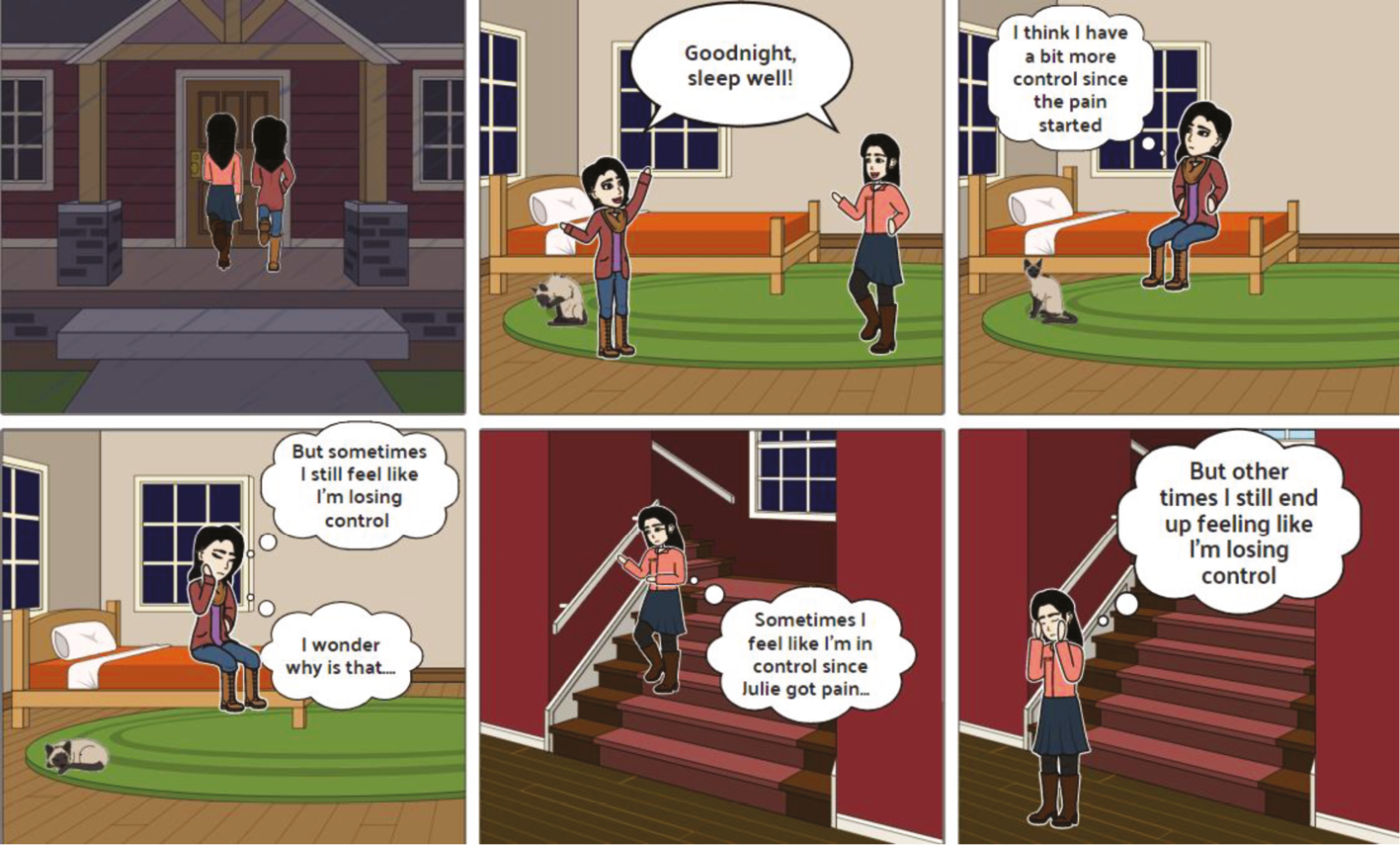
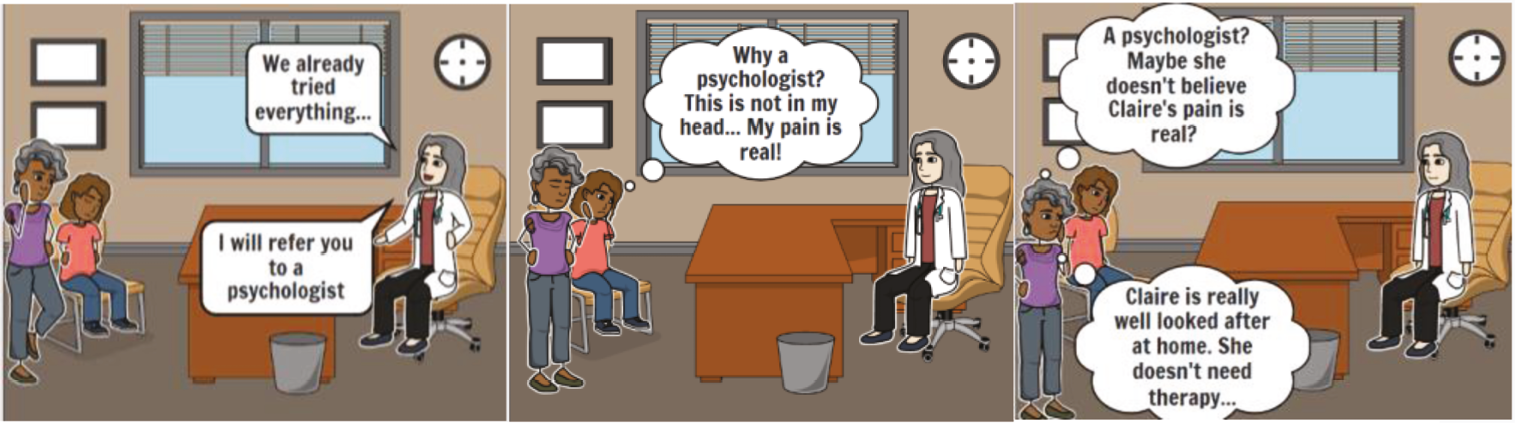
FIGURE 4.
Example of cartoon used during PAG analysis workshop.
Cartoon title: Mixed Feelings
Cartoon scenario: Claire brings her daughter Julie home after a busy day. They are getting ready to go to sleep, but both have a lot on their minds.
The findings discussed were: (1) why children might not communicate pain verbally, (2) why it is important for children and parents to be acknowledged and understood by healthcare professionals, friends and family, (3) what families want from treatment and services, (4) differences between accepting versus being resigned to pain, often referred to as ‘coping’ in included studies, (5) the meaning of ‘control’ in relation to pain (Figure 3) and whether ‘coping’ strategies are used to achieve control over the pain condition. After showing each cartoon, we asked a series of open-ended questions, for example:
-
In your experience, what do you think is going on here?
-
Have you ever had a similar experience?
-
Can you tell us why do you think this is happening?
-
Any other comments?
These questions were intended to provide clarity to, and/or address gaps in, the primary study findings. Data from the workshop were recorded in notes.
Impact/outcome
Patient and public involvement provided a different perspective on and/or interpretation of some of the findings discussed. For instance, PPI feedback added nuance and clarification to the idea of ‘control’ found in primary studies and helped the team to reach the following perspectives:
-
The idea of ‘control’ had been used in included studies often without clear definitions and without adequate consideration of what it means to parents and CYP with chronic pain.
-
The perspective of control might vary, for example for a parent it could mean something quite different than for a young person.
-
Overall, parents and CYP perceived the term ‘control’ in relation to chronic pain negatively, for example it implied that CYP could control their pain and its impacts.
New data and insights were incorporated into our analysis and synthesis and helped us to further develop and refine the following second-order constructs:
-
– Pain organises the family system (see Third-order construct 1: pain organises the family system and the social realm).
-
– Pain’s adverse psychosocial impacts on the whole family (see Third-order construct 1: pain organises the family system and the social realm).
-
– Pain forces adjustment and adaptation (see Third-order construct 1: pain organises the family system and the social realm).
-
– Families’ striving for diagnosis and a cure (see Third-order construct 2: families struggling to navigate health services).
-
– Importance of being listened to and believed by healthcare professionals (see Third-order construct 2: families struggling to navigate health services).
The core PPI group also helped fill gaps in the data, for example around disengagement with NHS health services, and brought experiences of pain conditions not represented in the included studies, such as Ehlers–Danlos syndrome and cystic fibrosis.
Project Advisory Group involvement in data analysis and interpretation
Methods
In a 2-hour online PAG meeting in April 2022, attended by four parents and two young people, we discussed four further findings from included studies. No healthcare professionals or other stakeholders attended this meeting despite being invited. We also used cartoons to facilitate the discussion (e.g. shown in Figures 3 and 4). All members received the cartoons and an infographic (see Report Supplementary Material 9) explaining the study findings in advance of the workshop.
Cartoon title: Attitudes to being offered psychological treatment
Cartoon scenario: Many families don’t know why they are being offered psychological help and get offended by it.
The findings related to pain management and included (1) how families and doctors/healthcare professionals think about pain and treatments, (2) stigma associated with psychological approaches to managing pain (Figure 4), (3) discrimination and prejudice in health services and (4) the lack of a clinical pathway for chronic pain management. After each cartoon, we asked a series of open-ended questions, for example:
-
How do these findings reflect your experiences, if at all?
-
Anything else you would like to add about what we discussed?
Data from the meetings were recorded in notes and new data were incorporated into our analysis and synthesis.
Impact/outcome
This workshop helped us to interpret some of the findings. For instance, we discussed the stigma associated with psychological treatment, as illustrated in the cartoon (Figure 4). PPI feedback indicated some CYP had had traumatic experiences related to treatments and interactions with healthcare professionals, which helped the team to reach the following perspectives:
-
The stigma associated with psychological treatments may be related to negative experiences in health services.
-
Healthcare professionals did not explain to parents and CYP why they were being offered psychological treatments.
-
Psychological treatments were used as an alternative when nothing else worked rather than as part of a broader biopsychosocial approach.
This workshop helped us to further develop and refine the following second-order constructs:
-
– Importance of being listened to and believed by healthcare professionals (see Third-order construct 2: families struggling to navigate health services).
-
– Chasm between health services and families’ needs (see Third-order construct 2: families struggling to navigate health services).
-
– Experiences and perceptions of interventions and treatments (see Third-order construct 4: families’ experiences and perceptions of specific interventions and treatments).
-
– Discrimination and racism in health services (see Third-order construct 5: children and families experiencing prejudice and discrimination).
Patient and public involvement in dissemination
Meta-ethnography short title, acronym and logo
In August–October 2020, members of the PPI group and other CYP with chronic pain and their families were invited to help us choose a short title, acronym and logo for the meta-ethnography. People voted via social media (e.g. Facebook and Twitter).
Impact/outcome
The acronym and short name selected was CHAMPION (Children And faMilies’ exPerIences Of chronic paiN). A logo was chosen and used to create a brand for the CHAMPION meta-ethnography.
Conference oral presentation
In September 2022, Georgina Ferguson-Glover (a 24-year-old PPI member, with hypermobile Ehlers–Danlos syndrome) and two team members (EF and MSB) co-presented at the Royal College of Nursing International Nursing Research Conference in Cardiff, UK. Georgina decided the extent of her involvement and the content of her presentation. She chose to present her experiences participating in the meta-ethnography, her experiences living with chronic pain and how they related to the meta-ethnography findings. The presentation slides and script were produced collaboratively during multiple online meetings.
Impact/outcome
Georgina’s participation brought the presentation to life with examples of her lived experiences and her experiences of the PPI group. The audience, composed mainly of nurses and healthcare professionals, was engaged throughout the presentation and they asked many questions at the end. One of the questions related to the assessment of chronic versus acute pain and this highlighted the need for a chronic pain-specific assessment.
Animation of findings for children and young people
In 2019, CYP with chronic pain had indicated they would prefer an audio-visual output accessed via social media (YouTube) to learn about the study findings. Parents also had stated that they would watch such an animation. In October 2022, to create the short animation of findings tailored for CYP, we first conducted an online survey via social media (e.g. Facebook and Twitter) with our PPI members and the wider public with chronic pain aged between 5 and 25 years old to ascertain their preferred cartoon style for the animation. Twenty CYP, from 9 to 25 years, from three different countries (UK, Ireland and Germany) rated styles on a 5-point scale to indicate their preferences and made free-text comments. In 2023, our core PPI group chose which meta-ethnography findings should be incorporated into a script for the animation. They then reviewed drafts of the script, the storyboards and the final animation.
Impact/outcome
Patient and public involvement ensured that the animation should be engaging, appealing and relevant to CYP and families dealing with chronic pain. The animation, available here www.youtube.com/watch?v=Oz5I7xKYf5o, will be shared widely across social media platforms (e.g. YouTube, YouTube Kids).
Other
Five members of our core PPI group gave feedback on this chapter and on the lay summary. All indicated that the chapter adequately described their involvement and that the lay summary was appropriate for a lay audience. PPI members continued to be involved in collaboration on a journal article regarding PPI involvement in a meta-ethnography and future dissemination strategies via social media, beyond the official project end date.
Feedback from patient and public involvement on their experiences of involvement
In preparing this chapter, we asked our PPI members for their feedback on being involved in the meta-ethnography and whether they thought something could be improved. The members stated that they were always encouraged, and felt comfortable, to voice their opinions. Members provided feedback regarding their experiences of being part of the PPI group and granted permission for it to be included in this chapter, some of their feedback was:
Having them [the meetings] online helped greatly, as someone with chronic pain it would have been very difficult to travel for this study and having people come to see me doesn’t always work either because I can’t guarantee I will be pain-free enough that day to have useful input. It also meant we could all take part comfortably. We had a lot of autonomy around how the meetings took place […]. Each meeting we were updated on what stage the project was at and went through the findings so far […]. We were asked to what extent our experiences differed to or were similar to their findings and to clarify some of the findings that had come out of the study […]. Having autonomy over the direction this project went felt empowering. […] Everything we said was listened to, noted down and discussed which made me feel like my opinions were valued. Being able to take part in the CHAMPION project feels like something positive is coming from my chronic pain conditions and that my input and experiences are going to help others like me in the future. It’s a wonderful feeling.
Georgina Ferguson-Glover, 24 years old, hypermobile Ehlers–Danlos syndrome
So many of us have bad experiences with medical professionals that we have an innate trauma response when talking of anything medical related and we automatically pretend everything is fine. Working on CHAMPION, with caring medical professionals and understanding researchers, as well as others who have had very similar experiences, was a freeing and validating experience. For once, I felt heard, I felt believed, I felt accepted. I can’t actually articulate how powerful an experience this was because of that. I thank everyone on the CHAMPION project for their openness and honesty.
Mother of CYP, 16 years old, female, with chronic pain for 4 years
It was so nice to be part of a study, rather than *studied*. It was a very welcoming environment (and the language wasn’t a challenge to understand which was refreshing). Unfortunately, it feels very rare that young people and their carers are consulted when it comes to discussing their needs and experiences. What was so great about this was the mutual support shared with the other (young) people with chronic pain who had similar experiences to me.
17 years old and had pain for last 6 years
The PPI group developed a supportive community, which was continuing because they decided to keep in touch as a group after the end of the research.
Summary
CHAMPION successfully involved and engaged patients and the public and stakeholders throughout the duration of the research using an inclusive, engaging approach. We involved a diverse PPI group of people of different ages and health conditions, including CYP and mothers. Despite having to interact online only, the involvement was meaningful and at the level of collaboration rather than just consultation. The PPI had impact across all stages of the research, from grant development, co-developing methods and interpreting findings to co-presenting conferences and producing dissemination outputs. PPI and PAG involvement were fundamental for the successful development and conclusion of this meta-ethnography. For details of the results, see Chapter 4.
Chapter 4 Findings
Eligible studies
After screening against the inclusion criteria, 182 publications reporting 170 studies published between 1998 and 2022 representing 25 countries were identified as eligible for potential inclusion (i.e. prior to sampling). The majority of studies (n = 158) were conducted in high-income countries: 49 were conducted in the USA, 39 in the UK, 25 in Canada, 8 in Sweden, 5 in Norway, 8 in Australia, 5 in Spain, 3 in Ireland, 3 in Denmark, 2 in Switzerland, 3 in Portugal, 2 in France, 2 in the Netherlands, 2 in Germany, 1 in Belgium, 1 in Hong Kong and 1 in Saudi Arabia. One study was conducted across three countries – the USA, UK and Belgium. 102 Twelve studies were conducted in low- to middle-income countries including four in Brazil, two in Iran, one in Nigeria, one in Cameroon, one in Ghana, one in Mexico, one in Malawi and one in Lebanon. The table of eligible studies (see Appendix 4) presents key characteristics of eligible studies.
A large proportion of eligible studies focused on the more severe, but fairly rare, conditions of juvenile idiopathic arthritis (n = 32, 19%) and sickle cell disease (n = 25, 15%). There were some common pain conditions which few studies focused on as their sole focus, such as recurrent abdominal pain (n = 11, 6%), musculoskeletal pain (n = 7, 4%), headache (n = 6, 3.5%) dysmenorrhoea (n = 3, 2%) and otitis media (earache) (n = 1, 0.6%). In terms of rarer pain conditions, only four (2%) studies focused solely on cerebral palsy, three (2%) on HIV/AIDS, two (1%) focused on CRPS, two (1%) on epidermolysis bullosa, one on osteogenesis imperfecta (a bone disorder) and one (0.6%) on juvenile fibromyalgia. None looked at Ehlers–Danlos syndrome, a group of inherited conditions that affect connective tissue.
Evidence gaps in eligible studies
We identified gaps in the evidence from eligible studies with respect to the age range, types of pain and types of participants (e.g. children, parents, siblings) covered. For example we found only 2 (1%) studies focusing on infants under 2 years old103,104 and only 11 (6%) focusing on children aged from 2 to 5 years old. 105–116 Only eight (5%) studies included the views of siblings.
Sampling outcome
Adhering to the iterative five-round sampling strategy described in Chapter 2, Figure 5 and Box 1, in Round 1, we sampled all 15 publications reporting UK studies (‘UK publications’) assessed as 3* for richness,34,35,38,76,77,79,109,110,117–123 in Round 2, we included a further 12 UK publications assessed as 2* for richness. 81,82,102,124–132 We explored any potential gaps in the data provided by these studies. In Round 3, we included five non-UK publications (i.e. reporting studies not conducted in the UK) which focused on pain conditions (e.g. dysmenorrhoea, headache), palliative care or children’s age groups that were not represented by the included UK publications (e.g. children under 5 years old) and that we assessed as 2* and 3* for richness. 105,133–136 In Round 4, we identified nine non-UK publications relevant to review question 4 of which four were assessed as 2* and 3* for richness and were included. 137–140 In Round 5, we selected 11 publications published since 2006 that were most closely related to our aim and review questions which were rated as 2* and 3* for richness. 36,75,141–149
FIGURE 5.
Final sample.
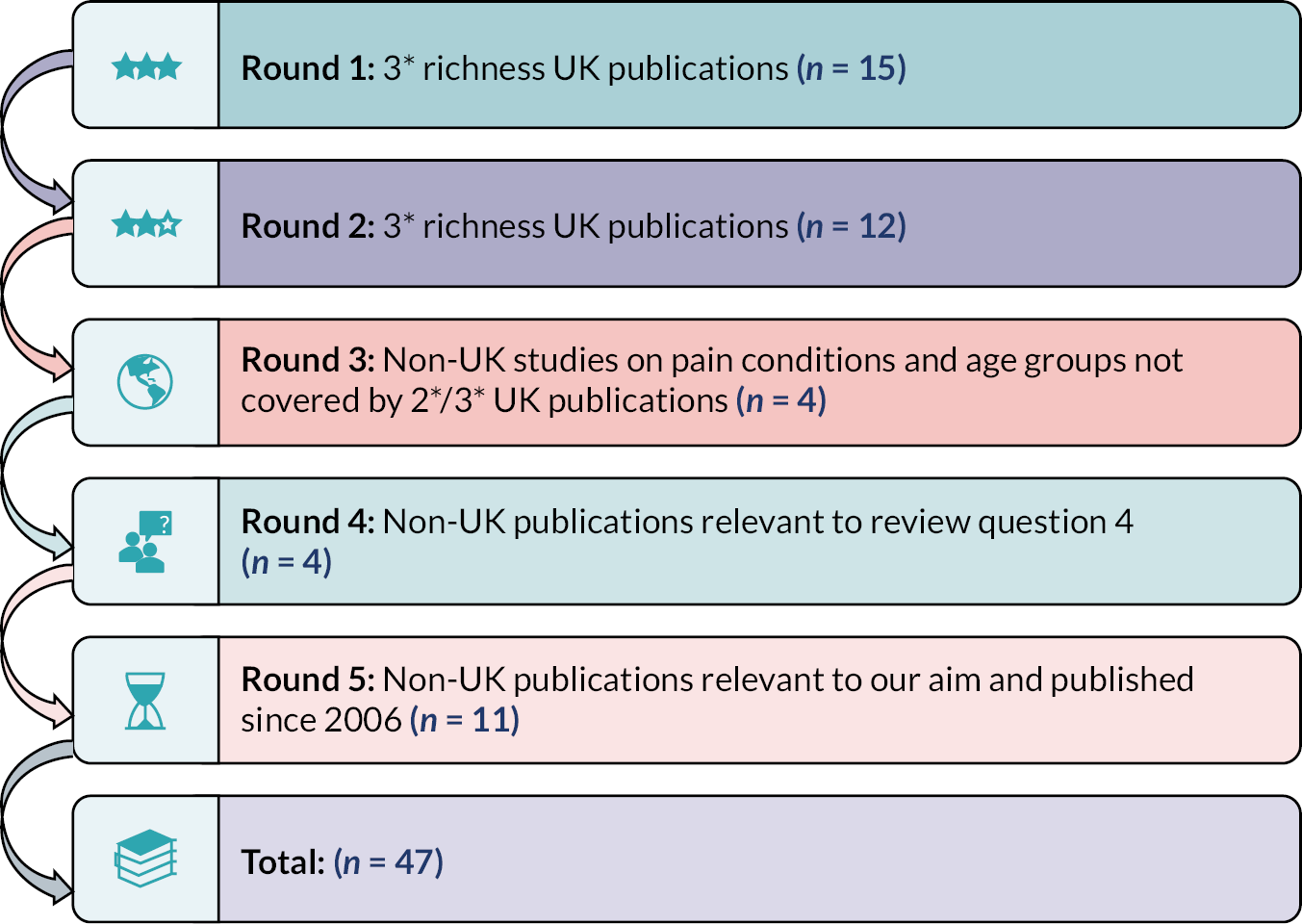
Included studies
Forty-three studies reported in 47 publications published between 2000 and 2022 were included in the analytic synthesis. Three are PhD theses,77,123,147 one is a report81 and the remainder are peer-reviewed journal articles. One PhD study was published in three formats – a thesis77 and two journal articles. 38,78 Britton79,80 reported data from the same study, as did Renedo. 81,82 Two studies were based on longitudinal data. 81,82,128 See Appendix 4 for detailed characteristics of the included studies. Twenty-three included studies reported in 28 publications were conducted in the UK, 5 studies in the USA, 4 in Canada, 2 in Sweden, 2 in Norway, 2 in Australia, 1 in Belgium and 1 in Hong Kong. Four were in low- to middle-income countries, including two in Brazil, one in Cameroon and one in Lebanon, according to the World Bank classification. 150 (There is a three-country study, so the total does not add to 43 studies.)
The included studies involved a total of 325 CYP aged 5–18 years old, 291 parents of children aged 2–18 years old and 17 siblings of children with chronic pain. Most (n = 28, 65%) included studies focused on only adolescent children aged 10 years or older. Seventeen studies focused on children under 10 years but only three of these focused on children under 5 years old105,110,135 and only five studies included children under 10 years, rather than their parents, as the research participants. 79,80,130,132,133,145 This means that the voices of children under 10 years old are not well represented in the data and that the findings attributed to CYP are more applicable to adolescents, except where stated.
Included studies involved a total of 197 mothers, 48 fathers, 164 girls with chronic pain and 53 boys with chronic pain. Over two-and-a-half times more girls than boys with chronic pain participated in included studies; hence, the findings are more likely to represent the views and experiences of girls. This gender imbalance likely reflects that adolescent girls are more likely to be diagnosed with chronic pain than adolescent boys. 151 In most of the studies which included parents, the sample was weighted towards mothers rather than fathers as representing the parenting view of the primary caregiver; as described above, almost three times more mothers than fathers took part in the studies. Five included studies focused on only mothers76,102,105,109,136 but only one included study focused solely on the views of fathers (n = 6). 35 Hence, the findings mostly report impacts on mothers’ experiences and perceptions. We recognise that this may be a bias of study samples but also may represent the wider gendered nature of caring in most of the UK and other societies/countries represented in the included studies.
The majority of included studies – 26 (61%) of them – did not state the participants’ ethnicity. Overall, 11 included studies (26%) involved a total of at least 129 non-white participants from a wide range of ethnic backgrounds (e.g. British Asian, Asian, Black British, Black Caribbean, Black African, African American, Latin American/Latino, Indian, Chinese, mixed origin, Lebanese Muslim, Palestinian Muslim),36,122–125,130,134,140,144,148,149 although 3 of these were studies conducted in Lebanon, Hong Kong and Cameroon. 134,148,149 The total number of participants from non-white ethnic backgrounds is an underestimate because one study124 reported the entire family’s ethnicity only and a study by Renedo81,82 did not state ethnicity explicitly, despite focusing on sickle cell disease which predominantly affects people of African Caribbean backgrounds. Six included studies stated that all participants were white. 35,102,126,128,142,147 Details are in the Table of eligible studies (see Appendix 4).
The studies covered a wide range of conditions involving chronic pain including CRPS, juvenile idiopathic arthritis, juvenile idiopathic arthritis associated with Down syndrome, sickle cell disease, headache, migraine, abdominal pain, musculoskeletal pain such as low back pain, epidermolysis bullosa, dysmenorrhoea, neurological conditions such as cerebral palsy and unspecified chronic pain. Some studies (n = 12) focused on a mix of different pain conditions including some rare conditions (for definitions and characteristics of included chronic pain conditions, see Appendix 5).
The studies did not provide data or give an in-depth understanding of how families experienced pain assessment by healthcare professionals, their experiences of social care services and primary care, family attitudes to opioids for pain management or use of pain management plans. Furthermore, there was a lack of conceptually rich studies that we could include in our final sample focusing on common types of pain such as headache (n = 1), dysmenorrhoea (n = 1), musculoskeletal pain (n = 3) and abdominal pain (n = 2) (see Appendix 5).
Assessment of methodological strengths and limitations
For the overall assessment of methodological limitations in the sample of 43 included studies, 56% (n = 24) were judged to have minor methodological limitations, and the remaining 44% (n = 19) had moderate limitations. For the full CASP assessments, see Appendix 6. Methodological limitations were most commonly identified concerning if and how the relationship between researcher and participants was taken into consideration. Concerns were also raised when assessing if ethical issues were adequately taken into account. In most studies, these limitations were because information was not reported rather than a definite lack of consideration of the specific domain, for example ethics. Overall, most studies were judged to have few methodological concerns regarding an appropriate study design. Participant recruitment strategies were mostly well-designed or moderately well-designed with only four studies assessed as having serious concerns. Data collection was generally well conducted across studies with some exceptions. Data analysis was relatively well conducted with only two studies having serious methodological limitations.
Assessment of conceptual richness of included studies
Overall, in line with our sampling strategy, only studies rated as 2* and 3* for richness were included in the sample. For linked studies which presented the same data, one combined richness assessment was conducted77,82 but when different findings were presented, separate richness assessments were conducted,79,80 meaning there are 44 assessments for included studies/publications. Twenty-three (52%) were rated 3*, that is, they had rich/thick or very rich/thick qualitative findings related to our meta-ethnography aim and review questions, and fairly detailed or detailed descriptions of the research context and setting. Twenty-one (48%) were rated 2*, that is, they had fairly rich and thick qualitative findings related to our aims and review questions and a moderate amount of context and setting descriptions. Within these categories, there was variation in the richness and thickness of studies. See Table 5 for the richness assessments of final included studies only. For all studies assessed for richness to aid sampling decisions, including those rated as 1*, see Appendix 4 (not all eligible studies were assessed).
| Study | Research question | Richness | Explanation of assessment |
|---|---|---|---|
| Ahlqwist137 | 3, 4 | 3 | Contextual data – only told age and gender of children and recruited via a prior study. Paper lacks information about the interventions. Findings – the context of the findings is not that clear in terms of the characteristics of the young people. Includes information about what CYP thought that was useful from the interventions (being taken seriously, being listened to, taking control) and what CYP considered as good pain management. |
| Atkin125 | 1, 2, 3, 4 | 2 | The context was extensive. Has some good sections on pain experience and management particularly in relation to how pain is viewed by services and health professionals. It is a thick paper but more on living with sickle cell disease than chronic pain. This paper is relevant for our questions 3 and 4 on services. |
| Atkin124 | 2, 3 | 2 | Rich background and context. Aims – examine both mothers’ and fathers’ perspectives on the nature and appropriateness of service provision (review question 3). The majority of the study focuses on sickle cell disease in general, with all its complexities. Some mention of chronic pain and how it affects family dynamics, but those data are not as rich. Some findings specifically discuss pain, coping with child’s pain – small amount of rich data specifically about chronic pain and its management. |
| Atoui148 | 2, 3 | 2 | Contextual data – reasonable level of detail on children’s background – gender, age, diagnosis, currently pain-free during interview, father’s socioeconomic status, the recruitment/treating centre, some data on Lebanese culture in findings. Findings – the data go beyond the descriptive level with different layers of complexity involving family dynamic, work. Rich data on chronic pain and how it affects CYP’s daily lives. Does have some data on the meanings, intentions and circumstances behind the facts but not very thick/rich, so a 2. |
| Baert102 | 2, 3 | 2 | Contextual information is good, but it does not provide the results by country (so we do not know which data is from which context). Focus groups conducted in Belgium, Scotland and USA. Seems to be more relevant to question 3. Has thick data on the review questions but because of lack of differentiation between countries we gave this a 2. |
| Borghi133 | 1, 2 | 2 | A. Some contextual data, but they could be more robust. Findings – most of the paper focuses on how children describe and experience their pain according to Piaget’s stages of development. Some mention of pain management but most of it is quite descriptive. Data are relevant to chronic pain and focus on concepts/descriptions of pain and daily life. Some data on meanings. Low end of 2 on scale. |
| Brandelli105 | 2, 3 | 2 | Contextual information provided. Findings – authors reached a certain level of interpretation that will be useful. In-depth view of treatment and how it affects family life and particularly mothers. It is explanatory. Definitely at least a 2. |
| Britton80 | 1, 2, 3 | 2 | Context is moderately described; there are fairly thick qualitative data. Qualitative data include how chronic pain affects daily life, how the family perceive chronic pain and what they think about the healthcare professional. Gave this a 2 because it is not fully aligned with our meta-ethnography objective and data not very detailed and thick. |
| Britton79 | 3 | 3 | Thick description including a proposed model – the information is relevant to the synthesis aim. This study looked at how families manage juvenile idiopathic arthritis at home with focus on exercise and splint use. Not a lot of direct mention of chronic pain, but rated this study as a 3 given that managing juvenile idiopathic arthritis is managing pain. |
| Brodwall75 | 1, 2, 4 | 2 | Good contextual data. Provide insight on parents’ views on chronic pain and their interactions with HCP. Findings – largely descriptive but with a bit about meanings – data on what parents think is causing the functional abdominal pain and what treatment they want – a 2. |
| Carter118 | 1, 2, 3, 4 | 3 | Thick data on how children perceive their on pain with rich context. Information about what children think about the pain management strategies and why and on how children perceive healthcare professionals and what experiences they had. |
| Carter117 | 1, 2, 3 | 3 | Really good description of the children and families. Findings – thick description with lots of information which can be used for the synthesis. Really focused on the interaction with healthcare professionals. Rich qualitative data on how families and CYP with pain experience and think about their interactions with healthcare professionals and what they consider as bad and good interaction. |
| Carter119 | 1, 2, 3 | 3 | Rich in context and great description of pain types. Findings – rich qualitative data on how the guardians (usually mothers) conceptualise pain, what they think and experience pain. Rich data on how parents manage pain condition and their interaction with HCP. It also goes into pain management and the relationship with the health services which will be really useful for review questions 3 and 4. |
| Carter109 | 1, 2, 3 | 3 | Context – really good description of the type/frequency of pain. Experience of mothers managing/understanding pain and what they think of the approach of healthcare professionals. Developed a model about the pain knowing from the parents’ perspective. The qualitative data are thick and provide interpretation of what the mothers say. |
| Cartwright131 | 1, 2 | 2 | Context – some/moderate amount of data. Findings – some sections specifically focus on pain but others on the disease symptoms more broadly. Some data of relevance to desired outcomes for teens of relevance to review question 4. The data presented focus on the meaning and impact of living with juvenile idiopathic arthritis and adolescents’ feelings about the illness. A 2 because not always clear that the data are specifically about pain vs. other symptoms (fatigue, mobility), although it does explore meanings, intentions. |
| Castle141 | 2, 3, 4 | 2 | Very good contextual data – additional information about condition, pain type, activities that generate pain. Findings – not a lot explanatory here re meanings, intentions and circumstances but the level of description and amount of relevant data make it a 2. |
| Dell’Api138 | 3, | 3 | Robust contextual data (demographic, pain, condition, information about treatment and management). The paper focuses on the interaction between CYP and healthcare professionals. Findings – rich data exploring how CYP feel when seeking help from healthcare professionals. They do have themes that refer to meanings and intentions. Data seem a bit descriptive at first, but further meaning is added in the discussion. |
| Dyson130 | 2, | 2 | Contextual data are moderate – age, education, ethnicity, gender, interview venue and more specific context given in findings. This study is quite rich. It has some data on pain, but it mostly brings complex aspects of living with sickle cell disease. Relevant to review question 2. Although there are rich findings, not all of data relate to chronic pain or to under 18s, so a 2. |
| Forgeron142 | 2, 3, 4 | 3 | Good contextual data (demographic, pain location, frequency and impact, duration and intensity). Findings – rich data on how CYP live their lives with pain including different aspects – school, social circles, transitioning to adult care. Described as a descriptive analysis but it is rich and has a lot on meanings – a 3. |
| Gaughan143 | 3, 4 | 3 | Good amount of contextual data (where interview took place, demographic data, pain condition, pain duration, details of family dynamics re reacting to child pain). This paper provides a closer look into the experiences of parents. Findings – this has rich data and is detailed – does talk about meanings. The material on impact on family is important for our focus on the family not just the child – a 3. |
| Guell132 | 1, 2 | 2 | Not a lot of contextual data (no demographic data), but rich in the sense of background information (observation in the family homes and services). Ethnographic study, with fairly thick qualitative descriptions/interpretation (rather than quotes); fairly detailed context of the young participants and their setting. Included families from London and Germany but it does not present the results separately. It is about how living with arthritis is conceptualised and managed by the young people themselves. It brings relevant information about pain management and coping strategies. Rich data in some aspects, but with the major problem of identifying where the families are from, therefore a 2. |
| Helvig144 | 1, 2 | 2 | Moderate amount of contextual data – no information about families or socioeconomic background. Findings – first few themes might be useful but theme 3 is very descriptive. Mainly about how they react to and cope with migraine. Definitely not a very rich conceptual paper but quite a lot of the data is on pain not other migraine symptoms. Some data on the intentions behind their behaviour and a bit more regarding meanings in the discussion section. |
| Hunt110 | 2, 3, 4 | 3 | Context – good amount of contextual data (children’s ages and conditions, sources of pain, pain cues, where interview took place). Findings – most of the study described how parents and HCP recognise pain in severe neurological impairment. Includes data on disease management which has relevant information about how parents perceive health services for review question 4 – a 3. |
| Jones120 | 1, 2 | 3 | Plenty of contextual information. Robust qualitative data on expectations for future while coping with CRPS. Aligns with review questions 1 and 2. |
| Jones128 | 2 | 2 | Context – some demographic data on CYP including type of pain, gender, first language, the outcome of assessment with national specialist pain service. Includes various pain conditions. Mainly focuses on impact of pain on life of adolescents. Findings – used Braun and Clarke’s thematic analysis but have got some depth of data around peer relationships and autonomy; some robust longitudinal data. |
| Jordan34 | 1, 2, 3 | 3 | Context – good amount of contextual data (diagnosis, some family demographics, children’s age range, pain duration, focus group location) but no data on socioeconomic status or ethnicity. Findings – robust rich data on the lives of parents caring for CYP with pain. Their burdens and how pain affects the child’s milestones and the family dynamics. It also includes the struggle between family and HCP with ‘validating’ the pain through a diagnosis of a condition. |
| Jordan35 | 1, 2 | 3 | Good contextual data. Findings – rich data on how fathers experience pain. The data go beyond the descriptive level with different layers of complexity involving – family dynamic, work, masculinity. |
| Jordan121 | 1, 2 | 3 | Robust context is provided. Findings – rich data on how CYP perceive living with chronic pain and how they think about their pain. It explores how pain impacts their lives, relationships, identity and independence, and how the experience of chronic pain can disrupt and alter adolescent developmental trajectories at an individual level. |
| Kanstrup139 | 1, 3 | 3 | Good contextual data – describes the treatment given to families in a bit of detail. Demographics – child and parent age, child pain duration and location. Findings – quite a bit on the meaning of experiences to the participants and how they experienced the treatment. They have interpreted data – really explores what the young people think about the therapy and interaction with healthcare professionals. |
| Khanom122 | 1, 2, 3 | 3 | Good background information and context – report age, ethnic group, diagnosis and time since diagnosis. No data on socioeconomic status or home environment. Findings – this study looked at how CYP described a pain flare. Small amount on use of and perceptions of pain relief medications relevant to review question 3. The findings do include meanings and intentions – this will be rich enough for a meta-ethnography |
| MacIver38,77,78 | 1, 2, 3, 4 | 3 | Contextual data – very detailed. Rich data on interview process/location, methods, detailed demographic information and parental occupation, child diagnosis, use of medications, which healthcare professionals involved, detailed case descriptions of each of 12 families. Rich on how parents perceive pain and how caring for a child with chronic pain affects their life. It goes beyond the descriptive with added meaning. A good amount of context and thick qualitative descriptions. Data on what families see as ‘good’ management/services. Findings – very thick. Has data on review question 4 regarding expectations of services. |
| McDonagh136 | 3, 4 | 3 | Context – demographic data – geographical area, age, gender of child, parental gender (mothers). Findings – data on inequitable treatment of kids with Down syndrome and difference in care/support for verbal vs. non-verbal children. Has explanatory data and meanings (rich description). Includes data on review question 4 – what services they want. |
| McKinnon135 | 3, 4 | 2 | Context – moderate amount of contextual data – caregiver work status, child’s age, gender, type of schooling, motor type, child’s capability and disability, previous bony hip or spinal surgery, number of prescribed medications, children’s pain presentations and pharmacological and nonpharmacological treatments. Detailed regarding cerebral palsy and impacts and pain. Nothing on socioeconomic status. Findings – largely descriptive rather than conceptual – relevant to review questions 3 and 4. There are some explanatory data, but not to a very rich conceptual level – a 2. |
| Neville36 | 1, 3, 4 | 3 | Good contextual data – ages, socioeconomic background, recruitment setting, diagnosis, pain duration and intensity, ethnicity, household annual income, marital status. Findings – rich data on review questions 3 and 4. Lots on meanings, meaning to them of a diagnosis, lots on services and healthcare professionals and parent and child responses to the diagnosis or uncertainty of diagnosis – a 3. |
| Njifon149 | 1, 2 | 2 | Context – explains cultural beliefs around sickle cell disease in Cameroon – very different to UK – seen as caused by witchcraft, sorcery or ancestors – is stigmatised. Explains the restrictions on children being allowed to talk to outsiders about the illness in the family. Findings – rich data on how children feel about their brother’s illness, their beliefs and fears about his future death. Most findings make some reference to painful crises/the consequences, etc. Rich in parts and quite descriptive in others and not all data are on pain – a 2. |
| Nutkiewicz140 | 3, 4 | 3 | Good contextual data – for example child age, gender, ethnic group, site of pain, pain duration and average number of doctors seen. Findings – insight on what CYP think about the doctors’ approach. Gives key concepts/themes. Lots on meanings – rich descriptive. |
| Renedo81,82 | 3, 4 | 2 | Context – moderate contextual data – demographic data, information about recruitment. Paper discusses transition from paediatric to adult clinics in sickle cell disease, as we are not focusing transition per se some data will not be relevant to our review questions. Emphasis on the lay perspective. Not all data are from under-18s – some are from CYP age 19–21 years. It does refer to intentions and gives explanation for events. Has some relatively thick data in relation to our review questions but not all from under-18s. Although not large quantities of data on chronic pain it, it is quite rich and relevant to questions 3 and 4. |
| Rossato145 | 2, 3 | 2 | Really good contextual data – transparent about whether the juvenile idiopathic arthritis is active or not, parental age, civil status, religion, family income and education level, children according to age, gender, diagnosis time and education level. It does have concepts and a model but the amount of data to support each concept is not large and so not that detailed, so gave it a 2. |
| Smart76 | 1, 2, 3, 4 | 3 | Context – some data on family demographics and health details given – child’s pain severity, existence of family member ill health, child age group. Some detail on socioeconomic status and ethnic group (white middle-class mums). Nothing on family home environment. Quite detailed sections on beliefs about doctors and interaction with doctors relevant to review question 3. Also some data for review question 4. Gave a 3 because of high relevance for review questions and quite rich findings even though only moderate contextual data given. |
| Sorensen146 | 1, 2, 3 | 2 | Contextual data – child age, language, where recruited from, gender, pain diagnosis and duration. Could have included more contextual data. Findings – seems to have clear themes in parts but mixes descriptive and interpretive data, for example theme 3.1 does not seem very conceptual, it is descriptive but fairly detailed description (with more meanings given in discussion though). Themes 3.2 and 3.3 have more on meanings. |
| Suder147 | 1, 2, 3 | 3 | Really good contextual data, child age, gender, ‘race’, rural/urban, background and detailed case history section for each participant. Findings – rich description. Findings/context are reported for each participant separately. Considerably rich detailed data. There are four common themes drawn from all the interview case study sections. Gives views about services – difficulty of getting a proper diagnosis and how chronic pain impacts on their daily life – change the definition of self. |
| Waite-Jones126 | 3, 4 | 2 | Context – moderate amount of contextual data (sibling gender, age, relationship to child with juvenile idiopathic arthritis, age gap and age at juvenile idiopathic arthritis onset; some data on family structure; interview location). Findings – siblings’ point of view. Discusses how siblings have dealt with the experience of chronic pain and how it affects the family dynamics. Rich enough for a meta-ethnography. |
| Williams123 | 1, 2 | 3 | Contextual data – small to moderate amount for a thesis. Findings – not completely focused on pain but discusses pain management for the condition epidermolysis bullosa and how it affects daily life. Rich data with robust context. The thesis also includes different coping mechanisms children adopt to deal with the condition and with pain. Also includes data on how CYP describe pain from epidermolysis bullosa. |
| Wong134 | 1, 2, 3 | 2 | Context – not a lot of background information. Contextual data – age, self-care habits, pain intensity, ethnicity (Chinese), if received menstrual education, interview setting unclear. The aim was to explore the self-care strategies among Hong Kong Chinese adolescent girls with dysmenorrhoea. Findings – the focus of this study is on coping strategies. It also talks a bit about Western medicine vs. Chinese medicine. Descriptive data on pain relief strategies used by girls – some data on the circumstances, meanings. Narrowly gets a 2 – has data on meanings but not conceptual level. |
Synthesis findings
Our findings are organised into five new interpretive constructs, which we call third-order constructs, using the language of Britten et al. 83 The third-order constructs are:
-
Pain organises the family system and the social realm (see Third-order construct 1: pain organises the family system and the social realm)
-
Families struggling to navigate health services (see Third-order construct 2: families struggling to navigate health services)
-
Families managing pain independently (see Third-order construct 3: families managing pain independently)
-
Families’ experiences and perceptions of specific interventions and treatments (see Third-order construct 4: families’ experiences and perceptions of specific interventions and treatments)
-
Children and families experiencing prejudice and discrimination (see Third-order construct 5: children and families experiencing prejudice and discrimination)
Two of these third-order constructs – Families managing pain independently and Families’ experiences and perceptions of specific interventions and treatments – are less well developed because there were insufficient rich data. All third-order constructs are composed of second-order constructs. The development of the third-order constructs derived from our thematic analysis of translated findings (the common and unique constructs we identified) from across all studies are shown below (Table 6).
| Translated findings (common or unique constructs) from across all studies | Our new second-order constructs | Our new third-order constructs |
|---|---|---|
|
Pain organises the family system | 1. Pain organises the family system and the social realm |
|
Adapted parenting | |
|
Pain’s adverse psychosocial impacts on the whole family | |
|
Seeking meaning in chronic pain | |
|
Pain forces families to manage uncertainty | |
|
Pain forces adjustment and adaptation | |
|
Pain’s influence on disclosure, social support and social relationships | |
|
School and the social realm | |
|
Families’ striving for diagnosis and a cure | 2. Families struggling to navigate health services |
|
Family expectations of services influence experiences | |
|
Chasm between health services and families’ needs | |
|
Importance of being listened to and believed by healthcare professionals | |
|
Pain self-management | 3. Families managing pain independently |
|
Parents helping CYP to manage pain | |
|
Experiences and perceptions of interventions and treatments | 4. Families’ experiences and perceptions of specific interventions and treatments |
|
Adherence to and engagement with interventions and treatments | |
|
Discrimination and racism in health services | 5. Children and families experiencing prejudice and discrimination |
|
Prejudice and discrimination at school | |
|
Gender and inequality |
In the findings below, we present our further interpretation of the data in the included studies. Throughout, we provide illustrative quotations from research participants and from the primary researchers’ (the authors of included studies) interpretations. Where relevant, the data analysis and interpretation also incorporate insights from our PPI group.
Third-order construct 1: pain organises the family system and the social realm
Data supporting this third-order construct originate from 36 publications representing 33 studies published between 2000 and 2022. 34–36,38,75–77,79–82,102,105,117–126,128,131,132,135,136,138,141–143,145–149 Twenty-one of the 33 studies were conducted in the UK. These data come from studies focusing on the following conditions: sickle cell disease, CRPS, abdominal pain, epidermolysis bullosa, juvenile idiopathic arthritis, musculoskeletal conditions/pain, neurological conditions or a mix of pain conditions.
This third-order construct is composed of seven second-order constructs: pain organises the family system; adapted parenting; pain’s adverse psychosocial impacts on the whole family; pain forces families to manage uncertainty; pain forces adjustment and adaptation; pain’s influence on disclosure, social support and social relationships and school and the social realm.
Pain organises the family system and the social realm
A family system is defined as a complex social system constituted of people, which may include parents, the child, siblings and grandparents, who depend on each other for basic needs and emotional support. The impact of poorly managed, moderate and severe chronic pain on the family system was overwhelming; it took over family life and affected family dynamics, roles and relationships. 35,38,75,77,79,80,105,126,131,143,147
Our interpretation shows that pain had a powerful role in organising or reconfiguring the family system, profoundly restricting and altering the whole family’s routines and activities. For instance, families had to adapt to avoid exacerbating the pain, and to fit in time-consuming pain management, which made spontaneity difficult as pain was the context of, and set boundaries around, their daily activities. 79,80,105,125,126,128,132,135,136,143,145,149 Some families perceived the onset of pain as so intense that it split their lives into before and after pain, as a form of life-course rupture; one adolescent girl described it as ‘coming into pain’118 (p.758). There were less data relating to well-managed and less severe pain; however, pain’s dominance and influence were less visible in those data relating to the lives of parents and families of CYP with well-managed, or with less severe chronic pain, which highlights the importance of good pain management strategies to enable families to regain agency.
Children and young people described how pain led to loss of the freedom to govern their daily routines: inadequately controlled pain prevented them from attending school due to hospital appointments, symptoms or pain management, leaving them feeling consumed and overwhelmed by pain. 120,125,128,130,143,148 Pain isolated CYP from their peers and friends, with risk of exacerbation needing to take precedence, or due to a loss of shared interests when pain prevented participation in hobbies and activities. 120 Pain forced increased dependency of the child on family members, which led to ambivalent feelings. For example CYP were grateful to their parents for being their main source of support, but also resented them for limiting their activities to avoid aggravating the pain. 125,128,148,149
Pain negatively impacted CYP’s sense of identity. 122–125,128,137,142,148,149 Specifically, CYP perceived themselves as different from peers as a result of feeling restricted, isolated and not ‘healthy’. In addition, studies showed that CYP reported a sense of perceived difference from peers due to loss of their independence; parental overprotection; and having to undergo pain-related treatments and being treated differently to peers by others (e.g. by teachers). 122–125,128,137,142,148,149 Pain led some CYP to not feel ‘normal’, because it restricted their ability to lead a normal life. 80,125,126,131,132,142,145,148 Feeling different, and resenting this, affected children as young as 7 years old. 80 This excerpt of the authors’ interpretation illustrates the impact of pain on CYP’s identity:
[pain] limited what they [CYP with sickle cell disease] were able to do and shaped how others viewed them, and even how they viewed themselves148 (p.5).
Pain also resulted in siblings feeling neglected by their parents and helpless as the whole family started to focus on the CYP with pain. Consequently, the impacts of pain could lead to siblings behaving dismissively towards the CYP and even questioning the legitimacy of the other child’s pain. 75,80,105,126,136,143 Parents, and sometimes grandparents, felt responsible for preventing siblings from feeling neglected. 34,136 Siblings competed for parental time and affection, but while they blamed their sibling with pain for dominating their parents’ focus, they also showed concern and affection for them. 80,126 These ambivalent feelings in the sibling without chronic pain became less negative as the sibling got older and developed the skills to adjust socially and emotionally:126
I feel a bit different about it now. I have understood it more. Because I know what the problem is then it is a lot easier to understand and help.
19 years, older brother of CYP with pain from juvenile idiopathic arthritis126 (p.21)
Pain organised the activities of siblings, even younger children, by requiring them to take on caring responsibilities, which limited their freedom. This was raised as a particular issue in a study conducted in Cameroon where CYP were routinely expected to adopt a ‘parenting’ role for younger siblings, including supervising medical care, which they resented. 149 However, siblings becoming young carers was also apparent in studies in the UK125,126 and Lebanon. 148
Importantly, parents, particularly mothers, who tended to be the primary caregiver, saw looking after their child’s health as part of their parental role, so they assumed the main responsibility for helping their child to manage the emotional and physical consequences of pain. Consequently, pain’s influence was stronger over mothers’ opportunities and choices than fathers’ lives. 35,38,75–77,79,80,105,123,125,126,131,132,145,148,149 The identity of primary caregivers was also negatively impacted by their child’s pain, particularly for more severe pain, which reduced their ability to have a life outside of the home; for instance, they stopped paid employment and/or lost their career136,143 and curtailed their social life to focus on caring for their child:75,105
It can be quite wearing looking after them. And it’s not just the worry, it’s actually your life stops and you cannot do anything else.
Mother of a child with sickle cell disease124 (p.61)
Having one parent in paid employment and the other being an unpaid carer for their child could affect parental relationships because the parents had very different stresses and demands on their time. 136 Some mothers did not confide their caring-related stress to their employed partner to avoid worrying them. 136
Adapted parenting
Parenting style (often that of mothers) altered as a result of their child having chronic pain. Our analysis shows that parents were initially uncertain of how to parent in the presence of chronic pain and learnt on their own to adapt their parenting to help their child deal with the pain while trying to maintain their child’s autonomy and family quality of life. 35,38,75–77,143 They had to change their perception of what parenting should look like and their role as parents. For instance, they learnt to provide support and care while being firm when necessary, for example making their child go to school despite pain143 (for further details, see Third-order construct 3: families managing pain independently) and had to decide whether to let their child join in activities, as described by this mother:
I can’t wrap [daughter] in cotton wool, I’ve learned that, and it’s wrong to do that, she should be allowed to lead as normal a life as possible, even though that you know that some of the activities that she’s going to undertake are going to result in a lot of pain.
Mother of CYP with fibromyalgia and full body pain for 34 months77 (p.278)
Parents tried to find a balance between deciding how much to let their child engage in activities, which might cause or worsen pain, to ensure quality of life for their child and family;77 this also applied to older children who should have been making their own choices as they matured developmentally. Things which hindered adaptation of their parenting approach were a lack of understanding about how they could help their child, and the lack of resources and support from health services and their social network. 75,76,124,125
Pain’s adverse psychosocial impacts on the whole family
This second-order construct focuses on the emotional impacts of pain. Moderate to severe pain had adverse psychosocial impacts on all family members,118,122,142,146,147 to the extent that some parents and CYP described living with chronic pain as traumatic – like surviving a traumatic event. 118,135,146,147 CYP felt isolated, depressed, ‘different’ from peers and afraid of the possible cause of the pain, particularly when they had no diagnosis or did not know the cause of their pain (for further details, see Third-order construct 2: families struggling to navigate health services). Pain in some adolescents with cerebral palsy, headache, CRPS, otitis media or musculoskeletal pain led them to wonder if they ‘deserved’ it. 141,147
Parents were deeply negatively affected emotionally; they experienced helplessness, frustration and guilt if they could not help their child feel better or find a cure, anxiety, distress and depression,35,38,77,143 as expressed by this father:
She [daughter] was depressed; I was starting to get depressed from it. It was absorbing our whole life.
Father of CYP with chronic neuropathic pain143 (p.250)
Parents also felt deeply afraid of what might be causing the pain, of witnessing their child in pain, that treatments would not work and that the CYP would not get better to enjoy a fulfilling life120,143 (for further details, see Third-order construct 2: families struggling to navigate health services). The constant fear caused parents to always be ‘on call’ (available at any time) for their child,35,77 which was also detrimental to parents’ well-being:
You don’t really have a major life, you’re always on call. There is always that, you know, whatever you do, or wherever you go, you know if you go to bed, you know you’re going to be on call if something is going to be wrong, if he needs you, you’ve got to get up and do it.
Mother CYP with complex regional pain syndrome full body pain for 7.5 years77 (p.264)
Furthermore, parents grieved the loss of their lives before pain and the loss of ‘normal’ parenting. 77 Our PPI group, both CYP and parents, also expressed grief over losing the life they could have had without chronic pain.
There was a greater negative psychosocial impact on family members who were more involved in caring for the child. 35,77,79,80,123,125,126,131,132,145,148,149 CYP felt responsible for, and guilty about, their family’s distress and caring efforts,125,148,149 as this boy with chronic pain from sickle cell disease explained:
She gets so upset when I am having a pain and it’s not fair on her, like I don’t want to make her worry. Because if she’s upset, I get upset for upsetting her.
Male age 13 years, pain from sickle cell disease125 (p.620)
Thus, our interpretation shows there can be a cycle of escalating distress among family members: the child is distressed due to pain, which causes distress to the parents and siblings, which further distresses the child. Furthermore, guilt and worry about parents could cause CYP to hide or downplay their pain, which we hypothesise can pose difficulties in assessing and managing pain. Consequently, pain disrupts family communication systems and precludes sharing of worries with each other.
Seeking meaning in chronic pain
Parents and adolescents would rather not experience chronic pain but when they did live with it, they reported some positive consequences of chronic pain. The parent most involved in chronic pain management, usually the mother, perceived they became closer to their child and that their relationship had improved. 35,80,105 Some siblings felt that their family relationships had become closer than in other families and they had become more compassionate to others. 80,126 In addition, some adolescents with chronic pain acknowledged that their experiences made them a better person, better equipped to live life and more mature. 120,147 An adolescent with chronic back pain described having more time to be with friends because they had had to stop other extracurricular activities. 128 We suggest that these perceived positive consequences may be examples of ‘benefit finding’ (a form of cognitive adaptation to threatening circumstances) or an attempt to seek meaning in pain. For example some young people worked towards framing their pain experience to try to portray some positive impacts, as expressed in the following account:
Going through this pain and going through the program has almost made me a little more mature mentally because I have to be able to cope and get through my life. I have to get ready for adulthood. […] I will survive, I meant there is so many different ways I could say it, but it’s all going to come down to it’s changed me for the better. It’s perseverance, I can tolerate more pain I guess, that’s a bad and a good thing. But it’s just changed me a lot.
17-year-old boy with chronic headaches147 (p.113)
Thus, the adolescent expressed some positive changes in himself but also expressed ambivalence about the impact of pain on his life. This kind of behaviour also speaks to the resilience that these young people built up over time in response to pain as a serious adverse event. Our PPI group confirmed that they had experienced some of the positive consequences described above, with the exception of CYP having more time for friends. When pain was severe enough to prevent engagement in extracurricular activities, it also prevented PPI members from socialising with friends, perhaps due to differences in their pain conditions and pain severity.
Pain forces families to manage uncertainty
Pain meant CYP and their families had to manage many uncertainties regarding their changing routines and family life, diagnosis and prognosis and the child’s future prospects, for example of finding employment or engaging in education. The child’s uncertain future increased fear, and for parents, this was a strong motivator for searching for treatments and cures. For conditions with remission periods, such as low back pain or juvenile idiopathic arthritis, fear and uncertainty around when and how intensely they would have a pain flare were always present,35,77 which limited families’ activities, as described by this mother:
Definitely a lot of planning, and you are restricted in an awful lot you can do, so you have to just kind of, each day we know we could maybe go swimming because that’s a good thing to do, but if it’s a lot of walking we’re not going to go there, so you have to just plan ahead, and we don’t know if by tomorrow she’s going to be in such severe pain that we’ll have a day with her friends round to the house, you just have to juggle what each day is going to be like.
Mother of 11-year-old girl with pain from congenital hip dislocation for 3.5 years77 (p.263)
It was hard for CYP and the family to adapt to the often fluctuating nature of pain. 80,131
Pain forces adjustment and adaptation
Family adjustment to moderate to severe chronic pain was a process over time: initially (in the early days of chronic pain) they wanted to hold on to (or return to), what study participants and study authors often referred to as, ‘normal’ life or ‘normality’, that is what family life was like prior to the onset of pain. 80,124–126,131,132,143,145,148 This finding also resonated with our PPI group.
In response to the pain, families focused on trying to control pain’s impact on family life using many strategies, such as gathering information about pain; following treatments (for further details, see Third-order construct 4: families’ experiences and perceptions of specific interventions and treatments); adjusting their routine to accommodate pain and its management and self-managing pain to be able to join in activities. 132,142,152 Paradoxically, family life then became completely organised around managing and avoiding exacerbating the pain, resulting in further restrictions and changes to the whole family. 132 CYP felt like they were losing control over their bodies, routines and daily lives.
Our interpretation indicates that, over time, parents and CYP started to focus more on living well with pain rather than focusing their efforts on finding a cure, although not all families gave up on finding a cure. In general, families tried to resist pain’s control, and find balance between managing/controlling pain and having a fulfilling family life. 79,80,132,145 For instance, parents (mothers) learnt to deal with the unpredictability of pain; helped their child to live with their new condition and developed ways of dealing with the child’s fear about the future. 79,80,132,145 CYP found new ways to do daily activities, for example using mobility aids. 120 To regain some control and have quality of life, some CYP chose to engage in valued activities despite the pain, which was also mentioned by our PPI group. 137,142 As they got older, some adolescents changed their perception of their lack of engagement with activities because of pain as their choice rather than as something out of their control. 128
Adolescents, many of whom had daily pain, saw their pain as unavoidable, all-encompassing and always present, for instance, a 17-year-old boy with chronic headache described pain as ‘it is part of me. Constant’147 (p.114). Adolescents with neurological conditions or sickle cell disease perceived chronic pain as just another obstacle, as something else they had to deal with. 119,125,141 Similarly, some parents of children with neurological conditions and other chronic pain conditions saw adversity, such as pain, as part of life and something that was out of their control. 102,119,141
Over time, some parents and adolescents learnt to adapt to unresolved pain on their own by ‘getting on with it’,118 (p.758) because they felt like they had no other choice; they accepted that pain was inescapable and would not go away,102,118,131,141,146,147 as this quotation illustrates:
I figured like you don’t have it [pain] and you’re lucky, but if I have it I’m just going to get on with it, like you can’t, there’s nowhere it’s going to go, you just have to like overcome it and be brave.
Female, 13 years, 1 year since juvenile idiopathic arthritis diagnosis131 (p.5)
Families were able to accept and adjust to pain faster when healthcare professionals and services helped set expectations early on regarding treatment and the unlikely probability of a cure (for further details, see Third-order construct 2: families struggling to navigate health services). We hypothesise that the effort and challenges involved in adapting to pain’s presence might be a reason why families found strategies that helped them to shift their focus solely from controlling/curing the pain to learning to live well with it so helpful (for further details, see Third-order construct 4: families’ experiences and perceptions of specific interventions and treatments).
Pain’s influence on disclosure, social support and social relationships
Mothers described longing for others to understand their suffering; yet, parents did not always disclose their child’s condition to friends and extended family because of its complexity (e.g. CRPS), and/or fear of being judged on their parenting skills or being disbelieved. 143 Mothers also reported difficulties disclosing their child’s condition due to concerns around a lack of sympathy for a condition that was not life-threatening. 102,120 This lack of disclosure could be detrimental to how much support parents received from their friends and wider family,143 although disclosure did not always lead to social support. 102,143 Mothers also described having grown apart from friends due to their caring role. 105 When the family’s wider social network of peers, friends and the extended family, such as non-cohabiting grandparents, provided practical, financial and emotional support, this helped parents and CYP deal with the impact of pain on their lives, enhanced quality of life and adherence to treatments. 80,126,131
Children and young people often avoided disclosing their pain, although this was age- and gender-dependent with girls and children under 12 years old being more likely to disclose and share their problems than boys and older children. 80,122,130,132,142,146 CYP, including those aged 7–10 years old, perceived that other people saw something wrong with them and that they were seen as their illness, which they did not want; they wanted to be seen as ‘normal’ and healthy by their peers and to belong to a group of friends,80,121,123,131,132,147 as expressed by this teenage girl:
I want to do what normal teenagers do and not be reminded of my illness all the time. It keeps my mind off the pain and makes me forget about medication and physiotherapy every now and then. Also people think I am perfectly healthy when I participate in normal things—and that helps me forget about it.
Female with juvenile idiopathic arthritis132 (p.890)
Contact with peers and friends helped CYP to feel ‘normal’ which provided hope and reassurance. 131 The definition of normal behaviour varied with the child’s age because they were comparing themselves to their peers. 131,132 In adolescence, being like peers was particularly highly valued. Normative constructions of adolescence involve individuation from parents but because of their pain this was delayed in some ways, thus increasing their sense of difference. Hiding and not disclosing their pain meant CYP could manage how others perceived them to an extent and avoid people’s ‘disabling responses’, for example derogatory comments;125,130,148 however, we hypothesise that non-disclosure might also make CYP’s attachments with their peers and friends less deep and affect their ability to garner social support.
Meeting others with similar conditions helped adolescents with epidermolysis bullosa and juvenile idiopathic arthritis feel less isolated as they were able to share experiences and provide mutual support. 123,131 In contrast, other adolescents with musculoskeletal pain did not want peer support from others with chronic pain because they did not want to be reminded of their pain or because they believed their pain was unique and, therefore, others would not have similar experiences. 142 This was particularly reflected in the case of comorbidities. For instance, parents of children with arthritis linked to Down syndrome did not seek support from parents of children without Down syndrome because they believed they would not understand. 136 In contrast, they described their interactions with parents of children with Down syndrome and arthritis as a great comfort and vital source of information. 136
School and the social realm
School is a major part of most CYP’s lives. Having chronic pain meant difficulties engaging with the school environment which affected CYP’s relationships with peers and friends, contributed to their lack of support, increased their sense of social isolation and adversely impacted their education, including for younger children under 10 years old. 123–125,128,130,148 Social isolation was a consequence of recurrent school absences due to pain, which made it difficult to maintain friendships, but was also the result of pain preventing CYP from engaging with friends when at school. 128
My pain has stopped me from coming into school or being social in school. For example, I may be in a lot of pain and won’t want to be a bother to anyone else.
Mark, 16, month two diary128 (p.5)
Pain prevented most schools from easily including CYP with chronic conditions; this impaired CYP’s learning, thus contributing to their uncertainty regarding their future job and further education prospects. CYP with sickle cell disease and those with juvenile idiopathic arthritis had to take special precautions at school, such as avoiding contact sports and crowded spaces, having more toilet breaks and keeping warm, which reinforced their sense of being different and not belonging. 125,130,148 CYP also had to deal with stigma and the disabling attitudes of others, which were particularly noticeable in accounts of CYP with epidermolysis bullosa and sickle cell disease, such as racism related to sickle cell disease (for further details, see Third-order construct 5: children and families experiencing prejudice and discrimination). 123–125
Several Canadian adolescents in a 2008 study reported how struggling academically at school due to their school’s failure to modify rules and requirements interfered with their sense of wanting to be ‘normal’. 142 In a 2020 UK study, going back to school was a key step to returning to normality and ‘normal’ life as it provided a refuge from hospital. 122 These different experiences might be explained by differences in school policies, procedures and cultures in Canada and the UK or the recency of the studies given that study participants were of similar ages (11–17 years old) and had similar types (musculoskeletal) and severity of pain.
Third-order construct 2: families struggling to navigate health services
Thirty-six included publications from 32 studies published from 2000 to 2022 contributed data to this third-order construct. 34,36,75–77,79,80,82,102,105,109,110,117–120,124,125,132,134–147,149 Pain conditions in these publications included: unspecified chronic pain, headache, CRPS, mixed pain conditions, neurological conditions, musculoskeletal pain, abdominal pain, juvenile idiopathic arthritis and sickle cell disease. Studies were conducted in the UK,34,76,77,79,80,82,102,109,110,117–120,124,125,132 the USA,140,143,144,147 Canada,36,105,138,142 Norway,75,137,146 Sweden,139 Australia,135,141 Cameroon,149 Brazil,145 Ireland136 and Hong Kong. 134 There was a lack of data on experiences of social care services.
This third-order construct describes the difficulties families faced when navigating and interacting with health services including getting stuck in a cycle of continually returning to services in pursuit of a diagnosis and curative treatment. Service fragmentation and numerous referrals without a clear care pathway resulted in frustration, unmet expectations, inadequate pain management and unmet needs. In contrast, a healthcare professional listening to and believing parents and CYP experiences of pain could reduce their distress and isolation and provide hope of resolution. This third-order construct is composed of four second-order constructs: families’ striving for diagnosis and a cure; family expectations of services influence experiences; chasm between health services and families’ needs; and the importance of being listened to and believed by healthcare professionals.
Families striving for diagnosis and a cure
At the onset of the child’s chronic pain, CYP and their families initially hoped for and sought out curative treatment based on the assumption that there must be an underlying physical cause for the pain. 34,36,75–77,117,138,139,143,146 This desired outcome of a cure motivated families to access health services. For painful chronic conditions, such as juvenile idiopathic arthritis and sickle cell disease, CYP and/or parents also often hoped for a cure for the underlying condition. 125,145 An exception was a family from Cameroon who believed that a ‘cure’ would result in the illness (sickle cell disease) simply passing to another family member. 149 Most families in the UK accessed health services in their search for a cure. General practitioners were usually their first port of call,34,36,77,117 except for families who were already accessing specialist services in the UK for an underlying condition who saw a consultant, such as a rheumatologist, neurologist or gastroenterologist. 109
Parents expected doctors to undertake objective medical tests (e.g. physical examinations, X-rays, high-technology scans), which they hoped would reveal the physical cause of their child’s pain, to prescribe pharmacological pain management and eventually find a cure. 34,36,75–77,117,136,138,139,143,146 Their expectations of services were frequently unmet, resulting in repeated visits to health services.
Our interpretation indicates that families searched for a cause and/or diagnostic label as a way to better understand their pain and to enable pain relief treatment or cure. Without a diagnosis, families could not access appropriate services. Many CYP and families welcomed a diagnosis as proof of a ‘genuine’ illness,34,36,75–77,117,132,136 a confirmation that their pain was real and could be explained to others (peers and friends). Identifying a cause was important because it indicated the pain was ‘real’ (not imagined or invented); it meant the pain was not disbelieved by others including healthcare professionals,36,77,136,143 and it could/enable effective treatment. 135 PPI input emphasised that both having a diagnosis and identifying the cause of pain were important, for example despite a diagnosis. If the cause is not known, then treatment cannot target the cause of pain, although sometimes there is no effective treatment even when the cause is known. Our PPI group indicated that another positive consequence of a diagnosis was when it led to identifying a condition-specific peer support group. Without a known cause of, or diagnosis for, the pain, parents and CYP worried and feared the cause may be life-threatening, for example cancer. 36,75,138,144 Children aged 10–12 years old tended to be more fearful than 13 to 16 year olds that their pain might be life-threatening. 138
However, the path to diagnosis was not straightforward, and could lead families to make repeated visits to health services with no satisfactory resolution. Some families gave up on a cure in the absence of one or were told by healthcare professionals that a cure was unrealistic. However, some did not abandon hope of a cure, as this parent of a child with juvenile idiopathic arthritis described:
The doctors say that there’s no cure, but I’m sure that there is one, I don’t believe it’s possible that there’s no cure for this disease.
F11145 (p.560)
Healthcare professionals tended to refer children onwards in the search for a cause/diagnosis, often with long referral waiting periods. 34,36,77,78,117 This meant families went through long periods of uncertainty which generated more fear, hopelessness and anger. With each new referral, families repeatedly experienced raised hopes but no resolution. This resulted in frustration, despair and loss of faith in healthcare professionals and services in what Carter117 referred to as ‘referral fatigue’, as shown in this quotation from a mother of a young person with chronic pain of an unknown cause:
After five months we have had no real diagnosis and not much in the way of effective treatment.
Mother, interview117 (p.32)
Families became stuck in a continual cycle of attending and reattending services in the search for diagnosis and cure. Although the Carter117 study is from 2002, the idea of referral fatigue resonated with our PPI group indicating it is still a current issue. This quotation from a 14-year-old girl with probable chronic idiopathic pain syndrome illustrates the frustration of not having a confirmed diagnosis and not having pain relief:
(I feel frustrated) probably at the fact that, there’s nothing to cure it at the moment like I can’t do anything to stop the pain, I can’t do anything else, and the fact that it’s, I haven’t got a firm diagnosis.
P06, F 14 years, CIPS122 (p.1792)
Sometimes, the medical tests and examinations carried out to help establish a cause for the pain were unsatisfactory to parents, for example test results revealed no clear cause, or no objective tests were conducted, as this quotation about a doctor from a mother of a child with chronic leg pain illustrates:
…I mean how can he see through somebody and say I know you’ve got a pain in your arm right this minute in time by looking at you? You’d have to do some kind of examination. I mean, is he some kind of magician or something?77 (p.187)
The lack of a physical examination of her child within the consultation resulted in this mother lacking confidence in the healthcare professional’s diagnosis or explanation. Such unsatisfactory medical encounters could lead to families seeking alternative tests.
Even when families received a diagnosis (e.g. pain as a result of juvenile idiopathic arthritis, sickle cell disease or cerebral palsy), this did not always enable the effective pain management for which families hoped. Notably, children were often left in considerable pain because treatments did not work (cerebral palsy), it was seen as unnecessary to treat the pain (dysmenorrhoea), or when pain fluctuated in severity (musculoskeletal pain). 122,134,136,141 Although families often desired a diagnosis for the child’s pain symptoms, a diagnosis was not a source of hope for all families; for instance, for one family whose daughter had a pre-existing chronic condition, the additional diagnosis of fibromyalgia increased their worry. 77 A diagnosis such as ‘chronic pain’ or CRPS without a known underlying biological cause could also be unsatisfactory to families because it did not help them understand why they had pain. 36
Our interpretation of the data reveals that families’ search for a physical cause that can be cured through biomedical types of intervention reflects a biomedical conceptualisation of the causes of pain and its management. Indeed, data in several studies provided further supporting evidence that a biomedical model of pain and pain management tended to predominate both in health services and in the minds of families. 36,75,77,117,138–140,146
There were some refutational data from two studies that revealed some parents were open to considering a more biopsychosocial approach to understanding and managing their child’s pain condition. Indeed, mothers of CYP abdominal pain in a UK study accepted the possibility of a psychological basis of pain but they still felt they first had to rule out physical illness via medical consultations. 76 Furthermore, parents undergoing family Acceptance and Commitment Therapy (ACT) for their child’s long-standing disabling pain conditions were open to a biopsychosocial model of pain. 139 It is unclear why some mothers of CYP with abdominal pain were open to biopsychosocial explanations. Some specialist pain services/treatments, like ACT, helped parents to shift their understanding to a biopsychosocial model which could alter their expectations of what treatment could achieve and allow them to shift their focus from a cure to ways to manage and live with the pain. 139
Family expectations of services influence experiences
When family expectations of services were not met, they became frustrated, angry and lost trust in services. 77,78,82,102,117,118,124,125,138,147 The complexity of navigating the healthcare systems had negative impacts on families, as it left them to deal with the pain on their own. Indeed, when families perceived the outcome of accessing health services to be unsatisfactory (e.g. poor pain management or a lack of explanation for the pain), families would return to services, seek out alternative services and/or self-manage the pain as best they could with over-the-counter medications and self-care like rest, sleep, hot water bottles, etc. (for further details, see Third-order construct 3: families managing pain independently). 82,134,144
Participants in some studies had experienced inpatient pain management programmes or specialist outpatient pain services with varied results. 35,77,78,121,147 Inpatients with CRPS in one study had their expectations of a cure raised by professionals, but cure was not achieved,77 as described by the mother of a child with CRPS:
…that‘s what I was told would happen, I wanted them to cure her because they told me they could cure her.
Mother 377 (p.223)
These raised expectations negatively impacted how families experienced that particular programme highlighting the important role of healthcare professionals setting expectations as part of pain management. Management of family expectations of treatments and effective communication by health professionals were important for effective treatment and to support families’ psychosocial needs – it resulted in a trusting relationship. 77,78,102,117,118,138,147 Some members of our PPI group said that they wished healthcare professionals had managed their expectations from the outset, for example by telling them that there was no cure. This would have helped them focus sooner on ways to manage the pain instead and might have avoided the financial cost of the constant search for a cure as some of them tried various private treatment alternatives and medications in the UK.
Chasm between health services and families’ needs
Children and young people and parents described that general practitioners and other health professionals did not always manage the chronic pain effectively. 75,76 Accounts from CYP with sickle cell disease and parents of CYP with Down syndrome or sickle cell disease highlighted that ineffective pain management often resulted from non-specialist healthcare professionals’ lack of knowledge and awareness about pain associated with these genetic conditions,82,124,136 but also from discrimination (for further details, see Third-order construct 5: children and families experiencing prejudice and discrimination). Parents of children with complex conditions, such as cerebral palsy, mentioned that (allied) healthcare professionals offered limited time for pain management because their focus was on other aspects of treatment. 135,136 Young people also felt the healthcare professionals were sceptical about their pain severity and pain experiences causing them to feel ‘ignored’, ‘abandoned’,82 (p.4) judged and misunderstood. 82,117 CYP also felt that healthcare professionals judged their pain relief needs based on how the CYP expressed chronic pain, which might be different from how CYP expressed acute pain. Some families said that general practitioners, emergency departments and general hospital wards had refused to prescribe analgesics,34,36,77,82,117 as illustrated by this quotation from a young person with sickle cell disease who had attended the general hospital:
It was a bad experience really [being on the ward] […] The doctors just didn’t really believe… not believe, but they thought I was like, faking, or like doing it to get medication [analgesia] as if I, like, was addicted to medication. […] But I can be laughing but still in pain and that’s what people need to understand, like nurses and doctors and even people in general: that I can be in pain, anyone can be in pain and, like, still be laughing because we know how to… people, like kids or, you know, kids know how to deal with the pain and we just try to distract ourselves.
O1 13–15 years old82 (p.4)
Gender bias was also present within the pain management approaches in one study conducted in Hong Kong. 134 For instance, young girls with dysmenorrhoea were left with no adequate pain management. Some girls sought out Western medical practitioners because they did not receive help elsewhere, and/or they wanted quick relief of symptoms by taking pharmacological medication. 134 However, their pain was trivialised by Western doctors, as the girls were told that there was no cure and that it was ‘normal pain’ to be endured. 134
There were also other reasons for poor chronic pain management. For children with underlying chronic conditions, sometimes treatment for the child’s pain fell between gaps in specialisms due to disjointed or siloed organisation of care, as this mother of a child with a neurological condition explained:
The specialists just look at the bit they’re interested in; it’s up to me to put it all together. The neuro is interested in epilepsy, and the gastro in his stomach but no-one is really responsible for tackling his pain.
M3109 (p.7)
This fragmented care was frustrating for parents whose expert knowledge in assessing their child’s pain was not always acknowledged by health professionals. Specifically, parents perceived that their expertise in assessing their child’s pain, particularly for younger children and those with communication difficulties caused by neurological or genetic conditions, was not always recognised by health professionals. 109,110,119,135,136 The underlying (e.g. neurological) condition was the professionals’ focus rather than the whole child meaning their pain was ‘ignored’ and not treated. 109,110,119,135,136 Parents’ expert knowledge of their child’s pain and lived experiences placed them in a position to advocate for their child when interacting with health services; they often felt they had to fight for effective pain management, resources and answers:34,77,105,135,136
We realised that as parents we’ve all had to fight an awful lot to get our children anywhere, to get them diagnosed, to get them recognised, to get them treated… If they had other parents who were… less confident and less bolshy [assertive], then they would still be on the sofa at home in constant pain… probably slashing their wrists by now,
Participant 1, focus group 134 (p.52)
However, health services were sometimes portrayed as a different world for which parents needed a new vocabulary in order to navigate this world effectively and to be taken seriously by health professionals. 132 Parents felt that learning medical terminology associated with illness and treatments gave them more control over medical encounters. 132
Being referred to a pain clinic could ‘validate’ the pain (i.e. confirm it was a real illness) and be a source of hope, and emotional and practical support when the healthcare professionals ‘listened’. 34,77,78,102,117,147 It could, however, be very difficult to get referred to a pain specialist or specialist pain service. 109,110 In one USA study, CYP aged 10–18 years old had consulted on average eight different doctors prior to being evaluated at a paediatric pain clinic. 140 Difficulties navigating health services, in addition to the difficulties/challenges around receiving contradictory advice and guidance from health professionals, led families to seek out their own information, for example on the internet, which could be helpful or distressing. 77,79,146
In addition, the transition from children’s to adult health services could be worrying and difficult for young people, which in the UK happens around the age of 18 years old. 82,142 Young people aged 13–17 years old with musculoskeletal pain expressed negative feelings at the thought of moving to adult services;142 our interpretation is that they were likely to need psychological/emotional preparation for the move. One author suggested a gradual shift to independence in managing their care. 142 During transition to adult services, CYP with sickle cell disease had experienced adult wards as ‘unwelcoming’ and had poor care during unscheduled hospital visits and non-specialist hospital wards for painful episodes. 82 Our PPI group offered another perspective: having had poor experiences of paediatric services, some had decided to wait for treatment until they were old enough to use specialist adult services, which they perceived as far better.
Importance of being listened to and believed by healthcare professionals
Interactions with health professionals were often a source of dissatisfaction and stress for many families. CYP perceived that professionals ignored their experiences of living with pain140 and that professionals had ‘given up’ on them. 77,78,117,146 Mothers felt that the emotional impact their child’s treatment had on them was rarely addressed during medical appointments. 105 Parents, particularly mothers, also felt they were being blamed for their child’s pain when there was no obvious cause for the pain, when healthcare professionals indicated the cause might be psychosocial,75–78,102,136,146 and/or when their child’s pain was not believed,75,76,80,136 as this diary extract for a child with abdominal pain reveals:
I’ve had pain in my stomach for nearly two years. It seems much longer…. One doctor told me that what she was seeing on examination and what she was being told were two different things. I was 11, and knew that I was being accused of lying. This made me really angry, because it didn’t help the pain (it actually got worse) and it really hurt me to be called a liar when the pain was very real.
Child, diary117 (p.34)
Parents and CYP highly valued healthcare professionals who listened to and understood the impact chronic pain had on them and their family life, that is, a healthcare professional who showed empathy. The experience of being listened to by a healthcare professional could reduce distress and isolation and provide hope for parents and CYP. 110,141 This quotation from a mother of a child with CRPS conveys the importance of healthcare professional empathy:
A good professional? Somebody who will also listen as well as give a medical opinion, somebody who doesn’t turn around and make you feel two inches tall when you try to tell them how your lifestyle is.
FE277 (p.186)
Being believed by the healthcare professional was also key. Pain was difficult for CYP to describe in words and for them and others to understand because it is invisible;147 this finding was corroborated by our PPI group. In third-order construct 3 ‘Families managing pain independently’, we show that not being listened to and believed can create a lack of control/autonomy over how to manage the pain – this could result in CYP resorting to self-management strategies.
Third-order construct 3: families managing pain independently
Thirteen studies contributed to this construct75,76,82,105,109,110,119,123–125,134,135,144 which covered six conditions: sickle cell disease, headache, epidermolysis bullosa, abdominal pain, dysmenorrhoea and neurological conditions. There are gaps in our understanding of families’ management of children’s pain because there were few relevant data in the studies and much of the data were not very rich. This third-order construct is composed of data from two second-order constructs which are focused on how families manage pain independently: pain self-management and parents helping CYP to manage pain.
Pain self-management
Self-care and self-management of pain occurred across a range of environments – at home, at school and even in the hospital. 82,124,125 CYP and families decided to manage pain on their own for multiple reasons, and it usually occurred (1) when they disengaged with unsatisfactory services which were unwelcoming and/or provided poor pain management; (2) as a supplement to, or when they had no effective, prescribed medical treatments;134,135 or (3) when they chose not to consult a doctor at all, for example for dysmenorrhoea134 or headache. 82,124,125,144 The decision to self-manage pain could give CYP a higher level of autonomy in deciding how and when their pain was managed, which we interpret to indicate the need for services, for example hospitals, to flexibly support all kinds of pain management, including self-management, and to support CYP’s autonomy in pain management. In some instances, CYP preferred to manage their pain at home, where they had access to resources (such as their own bed, hot water bottles, hot baths, television for distraction, family support, etc.) which helped them to deal with their pain on their own. 82,124,125
Self-management of pain involved a lot of trial and error. Over time, with more experience and knowledge, CYP’s pain self-management strategies improved, for example they learnt what worked in terms of pain medications, self-massage, ointments, breathing techniques or distraction. CYP also learnt to differentiate different types of pain which enabled them to understand what kind of pain relief was needed, as described by this young person with sickle cell disease:
Only a few years ago, that’s when I was able to kind of cope better, and I had a better understanding of the kind of medicine I need, and if I need like the strongest out of the painkillers or just like a little bit. So I kind of developed and kind of grew on to how to take care of it myself. Until I reached this point, where I feel like I don’t need to go hospital sometimes, or sometimes I do, then… And as you grow older you’re going to be able to know the different types of pain also, like if it’s going to be a mild crisis, or if it’s going to be a really severe crisis.
Female 16–18 years old, sickle cell disease82 (p.7)
However, children’s pain self-management did not always work well, for example when pain was severe and the strategies ineffective, such as attempting to manage a vaso-occlusive sickle cell disease pain crisis with paracetamol or hot baths. Self-management and self-care were also affected by organisational policies, such as school policies that did not allow children to leave the classroom or be excused from physical education (also see Third-order construct 5: children and families experiencing prejudice and discrimination), and lack of resources, for example hot baths in hospitals. Some children were unable to self-manage effectively because of the emotional and physical impact of the underlying condition causing pain. 82,123–125
Parents helping children and young people to manage pain
Our interpretation reveals that parents, usually mothers, felt responsible for, and had an important role in, helping CYP to recognise and self-manage their pain, supporting preventative self-care, and, if necessary, managing pain on their child’s behalf, for example in the case of younger children and those with neurological conditions. Parents developed strategies to help their child manage pain at home, for example they were fundamental in helping their child recognise different types of pain and thus selecting the most appropriate pain management strategy. 82 Parents also used distraction and reward with their child during pain episodes and helped their child avoid pain triggers. 75,76 They interpreted their child’s non-verbal pain cues in order to assist with pain management, particularly for children with neurological conditions or learning disabilities who could not verbally communicate their pain, and girls with dysmenorrhoea, who were embarrassed to directly communicate their pain. 109,110,119,134–136 Parental involvement ranged from very little (ignoring the pain as a management strategy to avoid positively reinforcing the pain) to extensive depending on the complexity of the condition and the child’s age. For example mothers noticed that their constant involvement in treatment decisions for complex conditions such as juvenile idiopathic arthritis adversely affected the development of their child’s self-management skills, consequently reducing the child’s autonomy in managing their pain. 105
Helping their child manage pain could involve parents (e.g. of children with neurological conditions) making difficult decisions on their own, such as finding a balance between managing pain and the child joining in family activities/routines, as this quotation illustrates:
She’s in less pain when she’s in bed but that’s not a life, just being in bed. She needs to be part of the family, up in her chair and being with us. That’s a trade-off.
Mother of 11-year-old girl with nerve pain109 (p.8)
Deciding whether and how much medication to administer at home was often a dilemma for parents because side effects could interfere with the child’s participation in family life and/or cause health problems. 109,119,135 Parents often expressed feeling left on their own to make decisions with little help from health professionals (for further details, see Third-order construct 2: families struggling to navigate health services).
Third-order construct 4: families’ experiences and perceptions of specific interventions and treatments
Twelve studies contributed to this third-order construct77,79,105,117,118,133,135,137,139,140,143,146 covering the following conditions: juvenile idiopathic arthritis; musculoskeletal pain; CRPS; cerebral palsy (dyskinesia); epidermolysis bullosa; mixed pain conditions including rarer conditions such as osteogenesis imperfecta; unspecified chronic pain or chronic pain from any cause. This third-order construct is composed of two second-order constructs: experiences and perceptions of interventions and treatments, and adherence to and engagement with interventions and treatments.
Relevant data were limited, largely descriptive and heterogeneous, which adversely affected our ability to fully develop a coherent conceptual understanding. Overall, there was a lack of rich data in studies about family attitudes to and experiences of pain treatments. Studies focused on ACT, a cognitive–behavioural therapy;139 physiotherapy for musculoskeletal pain;137 daily physiotherapy, splinting and medication for juvenile idiopathic arthritis;79 pharmacological and nonpharmacological juvenile idiopathic arthritis treatments;105 interdisciplinary intensive pain treatment at specialist pain clinics/programmes for CYP with CRPS or a range of painful conditions;77,117,118,133,140,143,146 and complementary treatments, such as chiropractors, massage and mindfulness, used to help reduce pain associated with dyskinesia in cerebral palsy. 135
Experiences and perceptions of interventions and treatments
Parents valued help with adapting their parenting skills and gaining information about the pain and how to better help their child (with CRPS and undiagnosed pain). 139,143 CYP also appreciated gaining information about pain and having more autonomy in their pain management137,139 (for further details, see Third-order construct 3: families managing pain independently). For example physiotherapy treatments that helped CYP with low back pain to develop an awareness of their bodies and capabilities gave them a greater understanding of their pain which helped to reduce their fear of exercise and facilitated physiotherapy treatment. 137 CYP with long-standing disabling pain conditions valued strategies, learnt through ACT, that helped them change their focus from reducing pain to learning how to live with it. 139 Specifically, the strategies shifted their focus away from curative approaches, which CYP valued, as expressed through this account (see also Third-order construct 1: pain organises the family system and the social realm):
After so many doctor’s appointments you end up so focused on just getting rid of it, and now it’s more like ‘You’re still going to feel pain and it’ll still hurt when you do stuff but it’s ok’.
Female with unspecified pain139 (p.16)
Children and young people with unspecified pain and their parents also valued ACT treatment because the group interaction with others with similar conditions helped them to feel less isolated and to appreciate their individual differences (this links to Third-order construct 1: pain organises the family system and the social realm). 139 Group ACT treatment also helped families to learn from how others parented when their child had pain:
When you’ve got a sick child, you become incredible overprotective er and that might not always be of benefit to your child, they do need to be allowed to live their own lives and do exciting things, and this other mum that I met, she let her daughter go inter-railing, with her sister I should add, but still, at that age, I thought was really cool, and it made me think, yeah, it makes sense.
Mother of CYP with unspecified pain139 (p.16)
However, treatment in a group setting could lead to a sense of guilt in CYP when confronted with others with more severe pain. 139 Our interpretation indicates that the experiences and perceptions of CYP and parents of specific interventions or treatments seem to be related, at least in part, to how well these addressed the negative impacts of pain on the family and their social realm (this links to Third-order construct 1: pain organises the family system and the social realm).
Adherence to and engagement with interventions and treatments
Children and young people wanted tailored treatments from pain clinics,140 which they did not feel they received. Pain-causing therapies, for example physiotherapy or injections for juvenile idiopathic arthritis, or those with unpleasant side effects seemed counterintuitive to parents and caused the family extreme distress. 77,79,105,135 Concerns over side effects are expressed by this parent of a child with cerebral palsy:
It is a real hard process when a new medication is introduced…. He can’t tell me if he’s not feeling well; he can’t tell me if he’s sad. I do not need the extra stress of a medication being disruptive in our life.
Caregiver I135 (p.76)
Parents were essential to ensure their child was adhering to pain management treatments at home (for further details, see Third-order construct 1: pain organises the family system and the social realm and Third-order construct 3: families managing pain independently). This was particularly relevant for conditions such as juvenile idiopathic arthritis, which involve painful treatments that have to be administered and reinforced by parents,79,105 as described by this mother:
It’s painful, very painful at times. You can see it’s painful, but you’ve got to make her do it or you’ve got to do it for her. I think there’s no choice in it. I’ve got no choice and she’s got no choice.
Mother of CYP with juvenile idiopathic arthritis79 (p.455)
However, not all parents enforced treatment adherence. Medication side effects and treatments that were monotonous and repetitive, painful and/or time-consuming negatively affected adherence. 79,105,118,133,135 As described in ‘pain organises the family system and the social realm’ (see Third-order construct 1: pain organises the family system and the social realm), time-consuming management strategies are an important factor contributing to pain organising family life. Parents of CYP with juvenile idiopathic arthritis and CRPS decided to what extent their child would follow a prescribed pain management treatment based on its impact, including side effects and the effect on family life and activities, versus the perceived treatment benefits. 79,105,135,143 This quotation illustrates a mother’s dilemma:
…I think we could deal with the side effects easier if it was working. But when you see your child suffering with side effects for nothing it feels very pointless.
Mother B, 12-year-old girl105 (p.6)
Families were more likely to follow a treatment programme if it was associated with reduction in pain and increased autonomy of the child,79,105 as shown in this quotation from a mother of a girl with juvenile idiopathic arthritis:
Her arthritis symptoms had settled down and she was doing much better, so I actually just stopped the medication. I was just like, ‘I can’t do this’ because she was like the exorcist [horror film]. I would give her the medication, and she would just barf [vomit] everywhere. And I figured she’s not getting any of this. You know, I was very frustrated, I guess. And so we stopped the medication, and within 2 months, 3 months she had a big flare and needed joint injections again. So I learned my lesson.
Mother A, 12-year-old girl105 (p.6)
Thus, sometimes parents only recognised the value of a treatment after stopping it. Some families rejected psychological treatments which they perceived as stigmatising, for example because they thought it indicated that healthcare professionals did not believe their pain was real. For many families, psychological therapies were considered to be a ‘last resort’ treatment after other medical treatments had failed. 77,117,146 In sum, parents had a key role to play in their child’s adherence to, and engagement with, treatment; however, aspects of the treatments, such as impacts on family life, could adversely affect adherence.
Third-order construct 5: children and families experiencing prejudice and discrimination
This is a cross-cutting third-order construct which applies across the other third-order constructs, so we present it separately here and refer to it throughout the results section, as appropriate. Seventeen studies (reported in 19 publications) focusing on sickle cell disease, epidermolysis bullosa, juvenile idiopathic arthritis dysmenorrhoea and abdominal pain contributed to this construct. 35,75–77,79,80,82,123–126,130–132,134,136,145,148,149
Children and families experiencing prejudice and discrimination was most apparent for CYP with sickle cell disease – in terms of experiencing racism in particular – and for CYP with visible differences due to their condition or with a learning disability. Visible differences were apparent in children with juvenile idiopathic arthritis, whose mobility was affected,126 and epidermolysis bullosa, who often had visible severe blisters. 123 One study focused on children with Down syndrome and juvenile idiopathic arthritis. 136 CYP with sickle cell disease, mostly from African and Caribbean ethnic groups, reported not receiving timely and adequate pain relief which they explained with reference to institutionally racist practices within the health service. 82 However, prejudice and discrimination also applied to other less ‘visible’ chronic pain conditions, such as sexist attitudes of health professionals to dysmenorrhoea. 134
Discrimination and racism in health services
Children and young people with sickle cell disease and their parents experienced racist attitudes and behaviours in UK health services – this was apparent in three studies from 2000, 2001 and 2019. 82,124,125 Parents perceived that poor service delivery in the UK for sickle cell disease – including healthcare professionals having poor knowledge of sickle cell disease and failing to convey even basic information to families about the condition – was related to institutional racism,124 as described by the study author:
Notions of racially motivated unfavourable behaviour, negative attitudes and disinterest in a ‘black’ condition were implicit in many parents’ accounts. For example, some parents – mainly African Caribbean – felt that if haemoglobinopathies affected more white children, there would be better service delivery. Mrs Prince compared the services available for what she regarded as a ‘white’ genetic condition, cystic fibrosis and those available to those with an SCD. 124 (p.65)
They compared sickle cell services unfavourably with services for other common genetic conditions. Furthermore, inadequate pain control was a constant problem to which racism likely contributed,124,125 as shown in this excerpt of the study author’s interpretation:
Racism can contribute to poor pain control and means that one of most distressful aspects of the illness remains untreated. Stereotypes of minority ethnic patients having a lower pain threshold are rife in the health services (Bowler 1993) and may be used to justify a lack of pain relief (Atkin et al. 1998). The lack of treatment can also be justified by another racial myth. Some people with SCD require powerful drugs for the control of pain. However, some doctors worry about their African Caribbean patients becoming dependant on drugs (Stimmel 1993) and this can contribute to the significant undertreatment of pain. 124 (p.65)
In the light of Atkin’s124,125 analysis, we observed that racism was apparent in Renedo’s82 study, as shown in this excerpt:
These participants told us they felt judged and misunderstood. Some said they felt that they were perceived to be liars or ‘drug addicts’ (O1). I6 said he overheard nurses talking about his pain not being that bad (‘he just wants some morphine’) but he did not complain about it, because ‘when you need help […] you just accept it’. 82 (p.4). NB this quotation includes interpretation from the study authors.
Although not labelled explicitly as racism by the authors or the study participants, examples of discriminatory attitudes included lack of respectful care for African Caribbean CYP in emergency departments and general hospital wards, healthcare professionals disbelieving the pain severity of sickle cell disease, not acknowledging requests for pain relief and not prescribing opioids when required (which are part of the treatment recommendations for sickle cell disease in NICE guidelines). 82
When I was in… admitted […] they would like sometimes say, uh there’s nothing wrong with her, uh she’s lying about her illness […] It was difficult especially ‘cause I was in pain, like, I dunno… Why I would lie about something about coming to hospital? It doesn’t even make sense.
Z1 16–18 years old82 (p.4)
Parents of children with Down syndrome and juvenile idiopathic arthritis also perceived discrimination from healthcare professionals in a study in Ireland. 136 Parents of non-verbal CYP with Down syndrome felt that their child was treated differently in comparison with other children resulting in them being excluded from services and ineffective pain management. 136 These parents described the general practitioner as ‘their biggest hurdle’136 (p.4) and perceived healthcare professional attitudes as dismissive and complacent, as elucidated by this parent:
[He was not being examined] literally because he has Down syndrome. […] I said, ‘I still want to know what’s wrong with him because maybe it will help us treat him,’… but they literally say, ‘Well, he has a diagnosis [of Down syndrome]’.
Blake136 (p.4)
Thus, it is evident that the parent perceived the doctor to be focused on the child’s genetic condition at the expense of investigating possible chronic pain. Parents perceived that the services and care their child received were inferior compared with children without Down syndrome and that non-verbal children with Down syndrome received worse care than verbal children with Down syndrome, thus highlighting disability-related discrimination. 136
Prejudice and discrimination at school
At school, CYP with sickle cell disease and juvenile idiopathic arthritis encountered discrimination in the form of school policies and rules, and the attitudes of teachers and other pupils. 125,126,130,148 Having sickle cell disease pain (and other symptoms like fatigue) made learning challenging even when CYP were present at school; school policies compounded this by not facilitating inclusion, for example CYP did not receive help to catch up on missed schoolwork, were prevented from staying sufficiently hydrated and warm to avoid painful crises and their need for frequent toilet breaks was not recognised or facilitated. 130,148 In contrast, other CYP with juvenile idiopathic arthritis, which is more prevalent among white ethnic groups, reported accommodations being made at school, such as exemption from physical education. 80,126,132
At school, CYP with sickle cell disease reported experiencing bullying, not being accepted, being judged and discriminated against by peers, including peer disbelief in their sickle cell disease pain. 130 A study from 2001125 reported CYP also experienced their peers’/social network’s general ignorance and prejudice about their condition including some people associating sickle cell disease with HIV/AIDS because they assumed that all people with blood disorders would be infected with HIV/AIDS from blood transfusions. 125 It is unclear whether this kind of assumption is a current issue since it was not mentioned in a 2019 study. 82 Prejudice and discrimination negatively affected CYP’s sense of identity and discouraged them from telling others about their sickle cell disease condition. 125
Bullying, teachers’ disbelief of CYP’s pain and unsupportive school policies made it harder for children to catch up on schoolwork and self-manage pain. 125,148,153 Younger CYP found it harder to deal with discriminatory behaviour than older CYP who were more used to it (and so had had time to develop coping mechanisms). 125 Perceived racism and discrimination in schools undermined CYP with sickle cell disease’s trust in these institutions and their staff and potentially undermined their abilities to self-care to avoid triggering pain,82,130,148 and to succeed at school. 130,148 CYP with sickle cell disease also experienced institutionalised racism in school, which was not directly linked to their condition, but which compounded their difficulties in succeeding at school, for example some teachers expected African Caribbeans to achieve less at school and to get poorly paid jobs. 125 Only one sickle cell disease study, conducted in Lebanon,148 did not find evidence of bullying and marginalisation of CYP at school, but the authors surmised that adolescents might have been reluctant to disclose any bullying or children in Lebanon are more accepting of disabled people. Alternatively, we propose that the relatively high prevalence of sickle cell disease in Lebanon might have contributed to a higher degree of awareness and acceptance than in the UK.
Such experiences extend beyond sickle cell disease. Siblings of children with juvenile idiopathic arthritis also experienced stigma and bullying from peers due to their sibling’s health condition and witnessed their sibling with juvenile idiopathic arthritis being bullied. 80,126 CYP with epidermolysis bullosa123 also conveyed experiences of prejudice and stigma, for instance, the peers of a teenage girl with epidermolysis bullosa ridiculed her school absence:
she’s been off for all this time cos her feet hurt.
Female age 14 with epidermolysis bullosa123 (p.76)
Those with epidermolysis bullosa reported negative treatment from others, for example being stared at due to their blisters or because of mobility issues, and, perhaps as a result, many suggested that their appearance was more important to them than the chronic pain associated with the condition.
Pain prevented them from doing physical activity and from walking normally, and consequently, they perceived that others did not see them as a ‘proper person’:
Kerry: Some people might think that I’m not a full person cos I can’t do anything, do like all the things that other people can do. Cos I’m not like them they think that I don’t count as a proper person. 123 (p.47)
Furthermore, the fluctuating nature of the skin condition meant others disbelieved the realness of their condition. 123 Disbelief in pain could be considered a form of prejudice.
Gender and inequality
Most studies did not conduct an in-depth gendered analysis, although a few studies identified some subtle gender differences between boys and girls with chronic pain. 125,146,148,149 Adolescent girls were more likely than adolescent boys to disclose their pain to and share their problems with friends in order to access social support. 125,146 Older adolescent boys were more likely to dissociate from illness as a way to cope, believing talking was futile because it did not change anything. 125 The way adolescent girls and boys expressed their pain differed as girls tended to communicate it more openly through their feelings, for example crying, shouting or roaring out their pain, to help them cope emotionally. 146 In contrast, older adolescent boys regarded emotional responses such as crying as ‘a threat to their masculinity’ and they felt guilty when they did cry125 (p.622).
We identified that sexism was apparent in a Hong Kong study of dysmenorrhoea in which girls did not receive pain relief from Western doctors who portrayed the condition as ‘normal’134 (described in more detail in Third-order construct 2: families struggling to navigate health services). Societal and cultural norms influenced their perceptions and understandings of pain – girls with dysmenorrhoea viewed their condition as something normal that they had to endure, a view which was reinforced and perpetuated by healthcare professionals. 134 Consequently, many girls only sought medical help if the pain was so severe that it made them faint. 134
We identified that gender inequality in caring responsibilities was apparent in many studies in which mothers did most of the work related to pain;35,75–77,79,80,123,125,126,131,132,145,148,149 this is a bigger social issue which affects the experience of caring. This does not mean that fathers were unaffected by or uninvolved in caregiving – one study35 which focused on fathers (n = 6) of adolescents with chronic pain found that they also experienced difficulties achieving a balance between the competing demands of family needs, caregiving and work, even if they were not the main caregiver.
Lines of argument
We developed three interpretive lines of argument which link together the key findings from the third-order constructs into overarching ‘storylines’ or explanations:
-
Dominance of biomedical perspective in how children and families conceptualised chronic pain and pain management
-
Parents fundamental to effective pain management
-
The journey of living with chronic pain
We then linked the three lines of argument into a model of families navigating chronic pain management.
Line of argument 1: dominance of biomedical perspective in how children and families conceptualised chronic pain and pain management
This line of argument pulls together data from the third-order and second-order constructs to show there were differences between how CYP and their families conceptualised (1) the impacts and experience of living with chronic pain, compared with (2) how they understood the cause of pain and (3) how they understood the role of health services in management of the pain. In terms of living with chronic pain, CYP and their families described experiencing mainly negative physical, social and emotional impacts on their lives, such as the impact of pain on family life, social life, schooling and parental employment (as described in Third-order construct 1: pain organises the family system and the social realm). Thus, it can be seen that CYP and their families expressed physical/biological, psychological and social impacts of chronic pain on their lives, which is consistent with a biopsychosocial model of pain.
Despite families recognising biopsychosocial impacts of pain, CYP and parents tended to understand the cause of chronic pain, at least initially, as solely biomedical, that is, pain has an underlying pathophysiological cause which can be identified, treated and/or cured. Families were not usually readily receptive to the idea of any psychosocial causes of, or influences on, chronic pain because they believed it implied that the pain was not ‘real’ or that parents were to blame for their child’s pain, for example because of a dysfunctional family life or poor parenting. Consequently, many families did not want or understand the point of psychological pain treatment and saw it as stigmatising and a last resort. An exception was some mothers of children with abdominal pain were open to the existence of psychosocial causes/influences, although it is not clear why (described in Third-order construct 2: families struggling to navigate health services). It was mainly families for whom there was no identifiable or known medical cause of pain (which does not necessarily mean there was no biological cause) who were asked to consider possible psychosocial causes of pain. For children whose pain was caused by an underlying health condition, such as sickle cell disease, juvenile idiopathic arthritis or cerebral palsy, families were less likely to consider psychosocial causes of, or influences on, pain; these families may not have seen the value of psychosocial treatments either, given the cause of pain was a disease.
How CYP and families initially conceptualised the role of health services in managing the chronic pain was based on a biomedical understanding which shaped their expectations of, and interactions with, services. Specifically, CYP and families sought to find an underlying biomedical cause in order to access curative or palliative treatment (as described in Third-order construct 2: families struggling to navigate health services). Families who already knew the cause of pain was a disease also sought biomedical pain relief and in some cases a cure for the underlying disease from services. Some families did, however, want support with psychosocial impacts of pain on their lives but did not expect or recognise that health services might provide such support. In interactions with health services, this desire for biomedical treatment for chronic pain created a medical focus for families, and for healthcare professionals. However, their biomedical conceptualisation of the causes and appropriate treatment of pain was not static and could change over time. For example families could realise over time that repeated clinical tests could not identify a physical cause and/or medical treatments did not resolve the pain, or they were told by healthcare professionals that no cause could be found, and/or there was no treatment or cure. (Even when an underlying physical cause had been identified, treatment could be ineffective or there could be no suitable treatment.)
Line of argument 2: parents fundamental to effective pain management
This line of argument resulted from interpreting third-order and second-order constructs (described in ‘pain organises the family system’, ‘adapted parenting’, ‘parents helping CYP to manage pain’, ‘experiences and perceptions of interventions and treatments’, ‘adherence to and engagement with interventions and treatments’, ‘pain’s adverse psychosocial impacts on the whole family’ and ‘pain self-management’ in Synthesis findings) and it explains the fundamental role of parents in implementing pain management strategies at home and the impact of these on family life.
Because of the profound impacts of pain on the child and the whole family life, parents had to adapt their parenting approach to help their child to manage pain. Families carried out pain management at home on their own most of the time which interrupted the family structures and routines. Indeed, most prescribed pain management strategies were time-consuming and disruptive of family life; some were also repetitive and painful or had other unpleasant side effects. Parents were fundamental in deciding whether and how CYP followed any prescribed pain management and treatment strategies. This decision was usually made based on the amount of impact the treatment strategy had on family life and on the child. Parents, especially parents of children who could not communicate, developed expert knowledge in assessing when their child was in chronic pain. Parents were typically the main advocate for their child in interactions with healthcare professionals and services in order to access effective pain management. Parents often had to make difficult decisions about their child’s pain management (particularly for complex conditions such as neurological conditions and juvenile idiopathic arthritis) but they were left feeling on their own to do so. Feeling that they could share this responsibility with healthcare professionals could help parents feel less alone.
Line of argument 3: the journey of living with chronic pain
This line of argument was developed with data from third-order and second-order constructs (described in the second-order constructs ‘pain organises the family system and the social realm’, ‘pain’s adverse psychosocial impacts on the whole family’, ‘pain forces adjustment and adaptation’, ‘families striving for diagnosis and a cure’, ‘family expectations of services influence experiences’, ‘chasm between health services and families’ needs’, ‘importance of being listened to and believed by healthcare professionals’, ‘pain self-management’ in Synthesis findings). It explores families’ journeys from the onset of chronic pain, their struggle to navigate services seeking for a cure, to when their needs and expectations were unmet and they then moved on either to prioritise living well with pain or they gave up hope. We hypothesise that a biopsychosocial perspective of pain management could help improve how families experience pain management and services.
Poorly managed, moderate or severe pain (which was not resolved by treatment or not treated at all) deeply restricted and shaped family life and relationships. At the onset of chronic pain, families tried to hold on to a sense of normality and sought help from services with the aim of curing pain. Families believed a diagnosis could help to determine the treatment they should take to get rid of the pain. However, receiving help from health services was not straightforward and a cure was not always possible. Services were fragmented and difficult to navigate, and families found themselves being referred from one clinical speciality to another without a clear care pathway to indicate the steps in the process or what the result would be.
In addition, communication with healthcare professionals was difficult. Families did not feel their experiences of pain were listened to and believed, and therefore, a diagnosis was difficult to achieve. In the end, families’ expectations of services (particularly services not specialising in pain) were not met. Pain was not cured and the disruption on family life not acknowledged by healthcare professionals. Families were left to deal with pain on their own. They dealt with pain on their own by employing self-management strategies and seeking complementary/alternative medicine, which sometimes increased the negative impact of pain and its management on the whole family. Some families moved on from searching for a cure as they realised they had no option but to ‘get on with it’, and so some started to prioritise living well with pain rather than ‘curing’ pain; others gave up hope and became depressed. As part of the process of moving on, families learnt as best they could how to manage the pain and how to plan their routine around it. We hypothesise that adopting a biopsychosocial perspective of chronic pain management and shifting the focus solely from curing pain to living well with pain could reduce the impact on family life and improve how families experience pain management and experiences of navigating services. To facilitate this biopsychosocial perspective in families early on in their journey, it is important for healthcare professionals to set expectations regarding the unlikely probability of a cure, if appropriate, to help families in this process of adaptation and help them navigate their chronic pain journey.
Linking the lines of argument into a model: families navigating chronic pain management
The interpretation of all data and lines of argument helped us to understand families’ journeys dealing with chronic pain and how these were affected by health services. We created a model of the non-linear nature of families’ journeys with chronic pain while they navigated services seeking a resolution for the pain which links all three lines of argument, illustrated in Figure 6.
FIGURE 6.
Families navigating chronic pain management (connects all lines of argument). Key: Reduces impact on family life; possible direction (i.e. families may follow this path); direction (i.e. usual path families took).
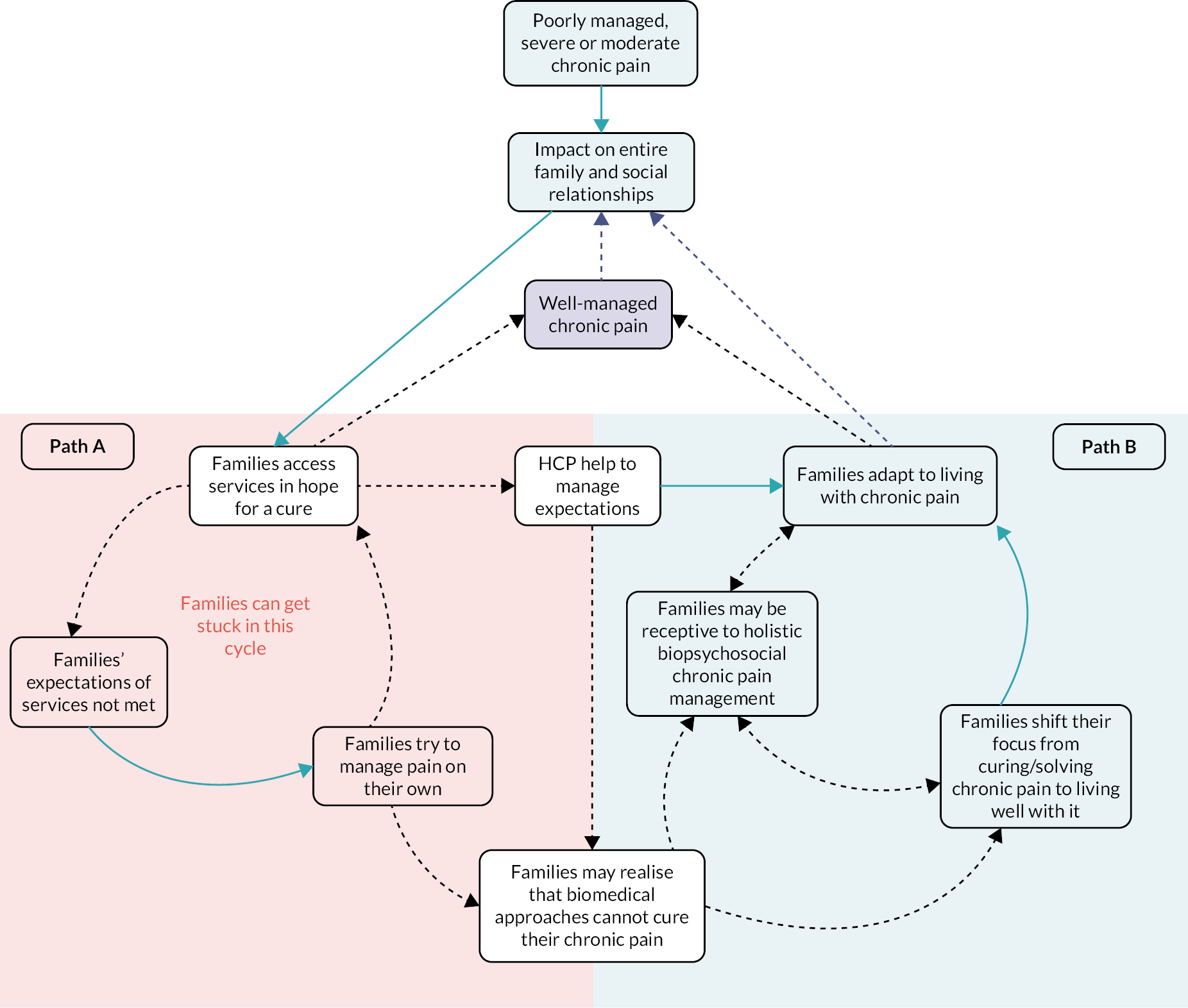
The diagram describes families’ journeys dealing with chronic pain and how health services can affect their journey (Figure 6). We hypothesise that there are two main paths (A and B) families can follow during their journeys. Families navigating Path A can move on to Path B with time or help from healthcare professionals and interventions. Families can also move from Path B to A, for example when pain worsens or fluctuates in severity.
On the left side of the diagram on Path A, families experiencing the impact of poorly managed, moderate or severe pain seek services in hope of a cure. When their expectations are not met due to fragmented services, referral fatigue, lack of diagnosis, poor communication with healthcare professionals and so on, they try to adapt to pain on their own. To adapt, they use many strategies, such as adapted parenting, adapting and changing the family routine according to pain levels, and so on, which can have a negative impact on their lives as the whole family focus is shifted towards dealing with the pain. Families also employ different strategies to manage pain on their own and seek help from alternative medicines which are not always successful. Because pain remains poorly managed, families are stuck in a cycle of pain affecting their lives and seeking services in the hope for a cure but without any resolution for the pain. Families and healthcare professionals understand pain and its causes through a biomedical lens/perspective which deeply affects their expectations of pain management and services. Psychological treatments are stigmatised and only used as a last option.
The right side of the diagram depicts when healthcare professionals are effective in helping set families’ expectations of treatment, which requires them to listen to and believe the families and acknowledge their lived experiences. Realistic expectations can help families to adapt to living with pain as they shift their focus from trying to cure pain to trying to live well despite the pain. Families might also realise on their own that a biomedical cure is unlikely after following Path A for a long time without any resolution for the pain. Families on Path B tend to be more receptive to biopsychosocial approaches for pain management, due to lack of other options.
Family-centred theory of children and young people’s chronic pain and its management
Based on interpretation of all evidence and PPI input, we developed a theory of what would constitute ‘good’ children’s chronic pain management interventions and services. The theory (Figure 7) can be used by, for example intervention developers, practitioners, service commissioners and researchers.
FIGURE 7.
Family-centred theory of CYP’s chronic pain and its management. Key: Resources and training needs/interventions, Team’s hypothesis based on evidence, Gaps in qualitative evidence, Based on evidence and corroborated by PPI.

Our family-centred theory of CYP’s chronic pain and its management is based on a biopsychosocial model and a ‘whole systems’ approach, that is, based on the premise that everything is inter-related and interdependent (Figure 7). Because chronic pain affects all aspects of family life and their relationships with the community, pain management strategies encompass the family (depicted in green background shading), healthcare services (depicted in yellow shading) and the community including schools (depicted in purple shading). The systems (e.g. community, school, health and social care services) work together as enablers, either facilitating or delivering families’ desired outcomes. Four key outcomes desired by families and CYP (blue shading) are at the centre of this approach to chronic pain management and services. Families’ most desired outcome is resolution of/a cure for their pain. This systems approach resolves service fragmentation by offering intuitive services and proactive ongoing support for families across all environments (family, healthcare services and community/schools) as they communicate and work together to achieve satisfactory outcomes for families.
Given that parents and CYP had to constantly assess pain levels in order to plan family life and pain management, more support to facilitate pain assessment at home is put in place via links with health services and resources/training. Families and CYP carried out most of the pain management and prevention. Parents receive resources and support on how they can help their child deal with pain and how to prioritise different pain management options at home. CYP receive support on different types of pain management strategies tailored to their needs and pain levels and how to differentiate between acute and chronic pain. Psychosocial treatment approaches are offered earlier, alongside medical treatments, as a way to address the physical, emotional and social impacts of pain holistically, and these are carefully explained to families. For instance, psychosocial approaches which improve communication among family members and help CYP to build autonomy over how and when their pain is managed can enable pain management and are facilitated by health services and the community/schools. Further resources and training with information about pain and treatments tailored for families, which could be provided by health and social care services, non-government organisations and/or community organisations working together, could enable families to achieve their desired outcomes and to support self-management of pain.
In the healthcare services, environment is where triage and pain assessment by healthcare professionals occur which are fundamental steps for pain treatment and prevention. An effective triage system is underpinned by a biopsychosocial assessment of chronic pain, including mapping the family’s psychosocial as well as medical needs; prioritises pain relief and living well with pain; and triggers appropriate action from different services. For instance, triage could trigger referral to appropriate specialised services and multidisciplinary teams, and/or the mobilisation of schools, social care and social services to evaluate the level of support the CYP and family require. Empathetic communication by professionals is a core component of this approach, which is fundamental for building trust between families and services. Healthcare professionals look holistically at the impact of pain on families’ lives and listen to the expert knowledge of parents, seeing parents and children as true active agents in the decision-making processes, while at the same time guiding and supporting parents in helping their child to manage pain. The impact of treatments on family life and relationships, and vice versa, is considered. When appropriate, services and healthcare professionals help families set expectations regarding the possibility of a cure for the pain. The front-line staff, such as children’s nurses, are trained to use simple interventions when appropriate to avoid repeated returns to services and referral fatigue. Specifically, simple early interventions are the first option when appropriate. Families who need them have access to suitable multidisciplinary teams (including, e.g. pain clinical specialists, nutritionists, physiotherapists, psychologists, occupational therapists, social workers and social care workers, etc.) according to their needs and underlying conditions. Accessibility of services is considered as part of the pain management plan. The transition to adults’ services is done gradually and planned as part of the pain management strategy.
To enable healthcare services to work efficiently as part of the system, the provision of training and resources for healthcare professionals are needed. Training and resources are aimed at differentiating chronic and acute pain and helping healthcare professionals to understand the impact of chronic pain and any associated condition including an awareness and understanding of the importance of the biopsychosocial approach.
In the community/school environment is where much self-management and pain prevention occur, in addition to that which occurs in the home environment. Social support, which could include peer support, for families and CYP is tailored according to the impact on their lives and mediated by social care, social work or non-governmental organisations. School and work policies are in place to allow adjustments to life in the community/schools allowing for pain prevention and management. For example school policies facilitate a routine for CYP to prevent pain exacerbation including flexible school hours and support for children to catch up on schoolwork. Work policies for parents of CYP with chronic pain allow flexible work hours and remote work opportunities. To enable schools/community to work efficiently as part of the system, it is fundamental that resources and training are provided to help staff at school and work to understand chronic pain and condition and how it can impact family life. The community/school environment can provide or facilitate social support and help to create a sense of belonging, which can help families to deal with the impacts of chronic pain on their family and social life. Social support interventions and policies consider how families’ and CYP’s social groups understand chronic pain and pain management, and whether CYP want to disclose their pain condition.
Managing pain is essential to enable families to live well; it is a priority and a combined effort involving multiple systems, such as health services, schools, social care and social services. Proactive support for families, for example via check-up phone calls or digital clinics, is in place to support families to manage pain across all the different environments (health services, schools/community and at home).
Assessing our confidence in the review findings
We have presented summaries of the findings and descriptions of our assessments of confidence in these findings in the Evidence Profile Tables which show the application of GRADE-CERQual to the key descriptive synthesis findings. Appendices 7 and 8 are organised by topics, for example social support, experiences of health services and care. There are 36 CERQual findings: 22 assessed as high confidence, 13 moderate, 0 low and 1 very low confidence.
Summary
We conducted a meta-ethnography synthesising data from 43 studies to reach new interpretations presented in five third-order constructs, three lines of argument, a model of families navigating chronic pain management and a new family-centred theory of CYP’s chronic pain and its management. We assessed our confidence in our synthesised findings using GRADE-CERQual. See Chapter 5 for details of the integration of our meta-ethnography findings with results from Cochrane intervention effects reviews and see Chapter 6 for our discussion and conclusion.
Chapter 5 Integration of meta-ethnography findings with Cochrane intervention effects reviews
Introduction
We integrated our synthesised qualitative findings with 14 recent Cochrane reviews of intervention effectiveness focusing on children’s chronic pain, including those in preparation for publication. 22–28,46–50,54,154 Given that our meta-ethnography identified several key impacts of a child’s chronic pain of importance to families (i.e. pain impacts the whole family; pain has mainly negative psychosocial impacts on all family members; children and their families desire, at least initially, a cure for the pain), we focused this integration on whether the interventions included in these reviews had:
-
focused on interventions for the whole family
-
measured whole family outcomes, such as family functioning
-
measured parental outcomes
-
measured sibling outcomes
-
measured child psychological/emotional outcomes
-
measured child social outcomes
-
measured absence of pain as an outcome.
We also wanted to know if certain under-represented subgroups of children with chronic pain and parents were included:
-
Children under 5 years old
-
Children with learning disabilities or autism
-
Children or parents of minority/non-white ethnic origin
As reflected in the meta-ethnography findings, pain is a biopsychosocial issue; therefore, we also examined the programme theories (specifically, how the interventions were thought to work) to verify if they took a biopsychosocial approach.
Results
Matrix analysis
The results of the matrix analysis (Table 7) show that, of the 14 reviews, no reviews focused on whole-family interventions. Only one review focused on interventions for parents of children with chronic illness, and measured family functioning. 27 Only two reviews (14%) measured parental outcomes – one analysed parenting behaviours and parental mental health, including that of mothers and fathers, although they did not perform a subgroup analysis by parental sex27 and the other planned to analyse caregiver distress but none of the included studies reported this. 28 None measured sibling outcomes.
| Cochrane review | Review inclusion criteria include children under 5 years or with learning disabilities (LD) or autism | Subgroup analyses by participant ethnic origin planned/conducted | Outcomes assessed including absence of pain measure (review inclusion criteria) | Whole family interventions or outcomes included in review inclusion criteria | Parental or sibling outcomes included in review inclusion criteria | Child psychological or social outcomes included in review inclusion criteria |
|---|---|---|---|---|---|---|
| Abbott48 | No (inclusion criteria age 5–18 years, LD not stated) | Not conducted | Pain (including absence of pain) | No | No | Quality of life and social/psychological functioning |
| Anie49 | All children (inclusion criteria) but none under 5 years or with LD/autism in included trials | Planned but insufficient studies | Pain status (not absence), coping strategies, health services utilisation, health benefits and general health | No | No | Quality of life and mood |
| Cooper24 | All children (inclusion criteria) but none under 5 years or with LD/autism in included trials | Not planned | Pain intensity and relief (not absence), sleep duration and quality, physical function, carer impression of change, rescue analgesia, treatment acceptability, adverse events | No | No | Quality of life but no included trials measured this |
| Cooper25 | All children (inclusion criteria) but none under 5 years or with LD/autism in included trials | Not planned | Pain relief (not absence), carer impression of change, rescue analgesia, sleep duration and quality, physical function, treatment acceptability, adverse events | No | No | Quality of life but no included trials measured this |
| Cooper26 | All children (inclusion criteria) but none under 5 years or with LD/autism in included trials | Not planned | Pain relief (not absence), carer impression of change, rescue analgesia, sleep duration and quality, physical function, treatment acceptability, adverse events | No | No | Quality of life but no included trials measured this |
| Cooper22 | All children (inclusion criteria) but none under 5 years or with LD/autism in included trials | Not planned | Pain relief (not absence), carer impression of change, rescue analgesia, sleep duration and quality, physical function, treatment acceptability, adverse events | No | No | Quality of life but no included trials measured this |
| de Bruijn46 | No (inclusion criteria age 4–18 years but none under 5 years or with LD/autism in included trials) | Not planned | Treatment success, pain change (including absence of pain), adverse events, defaecation pattern | No | No | Quality of life, depression, anxiety, school attendance |
| Eccleston23 | Yes, included children under 5 years in sample but none with LD/autism in included trials | Not planned | Pain relief (not absence), carer impression of change, rescue analgesia, sleep duration and quality, physical function, treatment acceptability, adverse events | No | No | Quality of life but no included trials measured this |
| Fisher54 | All children (inclusion criteria) but only mean age provided. None with LD/autism in included trials | Not planned | Pain intensity (including absence of pain), pain related disability, adverse events | No | No | Depression and anxiety |
| Fisher154 | All children (inclusion criteria) but none under 5 years or with LD/autism in included trials | Not planned | Pain symptoms (including absence of pain), disability, treatment satisfaction, adverse events | No | No | Depression and anxiety |
| Law27 | All children (inclusion criteria) but only mean age provided. None with LD/autism in included trials | Not planned | Child behaviour, child medical symptoms, adverse events | Family functioning | Parenting behaviour, parent mental health | Child mental health such as depression and anxiety |
| Martin47 | No (inclusion criteria age 5–18 years, LD not stated) | Not planned | Pain intensity, duration and frequency (including absence of pain) | No | No | Quality of life, social and psychological functioning, school attendance |
| Nascimento Leite28 | No (inclusion criteria age 4–18 years), but none under 5 years or with LD/autism included in eligible studies | Not planned | Pain intensity (including absence of pain), disability, adverse events, fear avoidance, physical activity level | No | Caregiver distress | Quality of life, anxiety and depression |
| Newlove-Delgado50 | No (inclusion criteria age 5–18 years, LD not stated) | Not planned | Pain intensity, duration and frequency (including absence of pain), adverse events | No | No | Quality of life, social and psychological functioning, school attendance and social disruption |
All 14 Cochrane reviews specified that their inclusion criteria included study outcome measures of child psychological/well-being outcomes such as quality of life, depression, anxiety, psychological functioning. However, in five (36%) reviews,22,24–26,23 none of their included trials had analysed and reported these outcomes. The inclusion criteria of only four (29%) reviews included measures of child social outcomes including school attendance in three reviews,46,47,50 social functioning in three reviews47,48,50 and social disruption in one review. 50
The inclusion criteria of eight (57%) reviews included pain outcome measures which measure absence of pain, such as the Numerical Rating Scale, the Visual Analogue Scale, the Wong Baker FACES pain scale and/or other pain rating scales. 27,28,46–48,50,54,154 The inclusion criteria of six (43%) reviews did not include a measure for absence of pain,22–26,49 five of which were focused on the evaluation of pharmacological therapies. 22–26
Regarding under-represented subgroups of children, specifically children with autism or learning disabilities and children under 5 years old, nine (64%) of the Cochrane reviews specified in their inclusion criteria that all children up to the age of 18 years old with the pain diagnosis of interest were eligible to be included in analyses. 22–27,49,54,154 However, in all of those nine reviews, none of the eligible trials had included children with learning disabilities/autism or aged under 5 years in their samples. The inclusion criteria of five (36%) of the Cochrane reviews, four on recurrent abdominal pain46–48,50 and one on musculoskeletal pain,28 focused only on school-aged children aged 4 or 5–18 years old and thus excluded younger children. For the abdominal pain reviews, this was due to the use of diagnostic criteria which do not apply to younger children. The inclusion criteria of eight (57%) reviews included children under 5 years, but none of their included trials had participants under 5. The inclusion criteria of two (14%) reviews specified in the protocol that children under 5 years were included but only the mean age was provided in the reviews. 27,54 Only one review49 had planned to conduct subgroup analyses by ethnic origin of participants, although there were insufficient data to permit this.
In summary, existing Cochrane intervention effects reviews on children’s chronic pain focused on the psychological impact on CYP, but have not measured, or have been unable to measure, many of the outcomes of importance to children and their families (e.g. the psychosocial impact on whole family). Few have results relevant to children under 5 years old or children with learning disabilities or autism, either because of the inclusion criteria of the review or the trials it synthesised. None of the studies had data which inform outcomes for children or parents from different ethnic origins.
Analysis of evidence for the chosen intervention (programme theories)
Programme theories explain how an intervention is thought to work to achieve an outcome. However, in all reviews, their sections about how the interventions might work to manage pain (described in some reviews as the ‘mechanisms of action’) were brief and lacking in detail. None had a clearly discernible biopsychosocial explanation of how the intervention(s) might work. Seven (57%) reviews exploring pharmacological interventions22–26,46,47 and one exploring dietary interventions for recurrent abdominal pain50 described only the biomedical ‘mechanisms of action’ without consideration of the social and personal contexts/factors affecting, for example medication adherence (Table 8).
| Cochrane review | Evidence for the chosen intervention (programme theory) | Is the theory biopsychosocial? |
|---|---|---|
| Abbott48 | ‘Cognitive Behavioural Therapies aims to improve the child’s mental health and coping strategies, specifically in helping them to understand the onset and progress of their recurrent abdominal pain. It offers a strategy to help manage it, along with anxiety management and specific behavioural techniques. Family therapy seeks to alter environmental factors that might reinforce the child’s pain behaviour within the family and to identify and treat factors that may precipitate it. The mode of action for how hypnotherapy may help recurrent abdominal pain is not completely understood and is likely to be from a combination of effects on gastrointestinal motility, visceral sensitivity, psychological factors, and direct effects within the central nervous system. Hypnotherapy and guided imagery may bring about cognitive changes through directly influencing cognitions, which helps to improve symptoms, or through influencing pain and gut functioning, leading to a change in cognition. Most forms of yoga involve a series of physical postures along with breathing and meditation techniques that are intended to reduce anxiety, improve body tone, and increase feelings of well-being. Written self‐disclosure, a therapy in which the patient writes down their thoughts and feelings about something deeply distressing, is hypothesised to help with pain through a number of mechanisms, including changes in insight, the creation of a story about emotional and painful experience, and adaptation of habituation to emotional stimuli’ (p.10). | No (psychological or social) |
| Anie49 | ‘Cognitive behavioural therapy has been considered as adjuncts to routine medical treatment for the management of sickle cell pain. These interventions aimed to improve the ability of people with sickle cell disease to cope with their pain, have shown encouraging results in children and adults, and with incorporated treatment manuals’ (p.10). | No (biopsychological including cognitive–behavioural therapy) |
| Cooper24 | ‘Different antiepileptic drugs have different mechanisms of action, not all of which are well understood, especially in terms of how a given drug produces pain relief in any particular individual with any particular chronic pain condition. Antiepileptic drugs are thought to reduce the ability of the neuron to fire at high frequency. The two standard explanations are enhanced gamma-aminobutyric acid (GABA) inhibition (valproate, clonazepam), or a stabilising effect on neuronal cell membranes, possibly by modulating ion channels. A third possibility is action via N‐methyl‐D‐aspartate (NMDA) receptor sites’ (p.7). | No (biomedical using antiepileptic drugs) |
| Cooper25 | ‘Opioid receptors are G-protein-coupled receptors and are located primarily in the central nervous system. Once agonistic opioids have bound to the opioid receptor, they produce intracellular effects throughout the coupled G-protein that result in an inhibition of the nociceptive transmission. Activation results in neural inhibition by decreasing the release of excitatory neurotransmitters from the presynaptic terminals’ (p.3). | No (biomedical using opioids) |
| Cooper26 | ‘[The] mechanism of action for paracetamol remains uncertain. The main proposed mechanism is the inhibition of cyclooxygenase (COX) enzymes through metabolism by the peroxidase function of these isoenzymes. This process results in inhibition of phenoxyl radical formation from a critical tyrosine residue important for the cyclooxygenase activity of COX‐1 and COX‐2 and prostaglandin synthesis’ (p.3). | No (biomedical using paracetamol; acetaminophen) |
| Cooper22 | ‘Different antidepressant drugs have different mechanisms of action, thus producing a variety of neurological effects and analgesic outcomes. Reinforcement of the descending inhibitory pathways by increasing the amount of norepinephrine (noradrenaline) and serotonin in the synaptic cleft at both supraspinal and spinal levels is considered to be a major mechanism, as well as blockage of sodium channels. Other suggested mechanisms include postsynaptic alpha-adrenergic, H1‐histaminergic and muscarinic cholinergic receptor‐blocking effects, and N‐methyl‐D‐aspartate (NMDA) antagonism’ (p.8). | No (biomedical – using antidepressants) |
| de Bruijn46 | ‘The exact mechanism of action of antidepressants, particularly for the treatment of functional abdominal pain disorders in children and adolescents, is poorly understood. These drugs work through their effect on prominent monoaminergic neurotransmitters (serotonin, noradrenalin and dopamine) in the central nervous system’ (p.5). | No (biomedical – using antidepressants) |
| Eccleston23 | ‘Damage to the peripheral nerves is followed by an inflammatory reaction that relates to increased production of prostaglandins, amplifying sodium currents and calcium influx in peripheral nociceptive neurons, and enhancing neurotransmitter release in the central nervous system and depolarisation of second-order nociceptive neurons. Preclinical data suggest an immune pathogenesis of neuropathic pain, but clinical evidence of a central role of the immune system is less clear. Non‐steroidal anti‐inflammatory drugs inhibit the production of prostaglandins, and thus could lessen the peripheral and central sensory hypersensitivity that occurs with nerve injury‐associated inflammation’ (pp.8–9). | No [biomedical – using non-steroidal anti-inflammatory drugs (NSAIDs)] |
| Fisher54 | ‘Behavioural strategies include relaxation training, biofeedback, and behavioural management programmes (e.g. teaching parents strategies to reinforce adaptive behaviours such as school attendance). Cognitive strategies include hypnosis, stress management, guided imagery, and cognitive coping skills. Cognitive behavioural therapy programmes incorporate elements of both behavioural and cognitive strategies. Parent interventions may include operant strategies, communication strategies, or problem-solving skills. Problem-solving skills is aimed at decreasing distress in parents of children with chronic pain by teaching problem-solving skills, including steps to define a problem, generate possible solutions, implement a solution, and then evaluate’ (p.8). | Yes (psychological therapies including behaviour management and biofeedback) |
| Fisher154 | ‘Psychological therapies are used in paediatric pain practice to reduce pain symptoms, disability, and negative mood associated with pain conditions, and to modify social-environmental factors to enhance the child’s adaptive functioning’ (p.8). | No (psychosocial – psychological therapies) |
| Law27 | ‘Cognitive behavioural therapy is founded in behavioural analysis and operant theory, cognitive theory, and social learning theory. Associations between cognitions, emotions, and behaviours are emphasized and are believed to interact to influence desired outcomes. Thus, treatment is focused on altering maladaptive social/environmental, behavioural, and cognitive factors in order to reduce symptoms and prevent relapse. Family therapy is based on family systems theory and emphasizes the role of the family context in an individual’s emotional functioning. There are several types of family therapy, including structural family therapy, strategic family therapy, and behavioural systems family therapy. Treatment aims to alter maladaptive patterns of interaction within the family in order to improve symptoms. Motivational interviewing focuses on the patient’s motivation for and commitment to behaviour change. Specific strategies include exploring and resolving ambivalence, rolling with resistance, and eliciting and supporting the patient’s own arguments for change. A unique feature of motivational interviewing is the focus on the patient’s own values and goals, as opposed to imposing external values and strategies for change. Multisystemic therapy is an intensive family- and community‐based intervention founded in the social ecological model, and family systems theory. Treatment targets of multi-systemic therapy are broad and include the child, their family, and broader systems such as the child’s school or medical team. Multi-systemic therapy incorporates a wide range of intervention techniques based on the individual needs of the child and family, including cognitive and behavioural skills training, parent operant training, and family therapy. Problem‐solving therapy is based on the social‐problem‐solving model, which emphasizes the role of constructive problem‐solving attitudes and skills in fostering enhanced social competence and reduced emotional distress. Specific problem‐solving skills are taught in sequential steps that typically include defining the problem, generating alternative solutions, decision making, and solution implementation and evaluation’ (p.9). | No (psychosocial – psychological therapies) |
| Martin47 | ‘Conventional analgesics have been proposed to work by interrupting these abnormal physiological pain responses, which become pathological. Antispamodics have been proposed to alter gut dysmotility, including peppermint oil, which has antispasmodic actions. Serotonin (5-hydroxytryptamine) agonists may relieve symptoms by causing vasoconstriction and stimulation of the release of other vasoactive substances, thus inhibiting neurogenic inflammation; this has been found in migraine headaches’ (p.5). | No (biomedical – pharmacological interventions) |
| Nascimento Leite28 | ‘There is evidence that exercise and physical activity act on physical and psychological mechanisms to reduce pain and disability (e.g. fear avoidance belief model). These may have influences at the cognitive level in terms of reducing fear and anxiety related to pain and movement, and also build physical strength and endurance’ (p.9). | Yes (biopsychosocial – physical activity and education) |
| Newlove-Delgado50 | ‘Probiotic-based interventions containing living micro‐organisms are thought to improve symptoms through restoring the gut’s microbial balance. It has also been suggested that they might alter the intestinal inflammatory response in the lining of the gut. Fibre‐based interventions might be effective in children with irritable bowel syndrome in particular, by modifying bowel habits and the transit time through the gut, as well as by decreasing intracolonic pressure. Alterations in diet, such as low FODMAP interventions, may work in irritable bowel syndrome by reducing osmotic effects, fermentation and gas production, hence decreasing distension and pain’ (p.7). | No (biomedical – dietary interventions) |
In some reviews, it was difficult to discern how the interventions were thought to work and whether they adopted a biopsychosocial or another approach. Biological (e.g. acting on physical mechanisms) and psychological (e.g. influencing cognitions, coping) aspects were apparent in programme theories in two reviews – one focusing on psychological therapies for sickle cell disease and pain49 and one on physical activity and education about physical activity for chronic musculoskeletal pain. Nevertheless, both lacked detail or precise mechanisms:28,49 Anie et al. 49 specified expected outcomes of interventions rather than mechanisms and Nascimento Leite et al. 28 stated only that the interventions affect physical and psychological mechanisms (Table 8).
Four more reviews investigated psychological or psychosocial interventions only, and did not appear to consider any biological mechanisms. 27,48,54,154 Two of these reviews, one focusing on psychological therapies27 and one focusing on psychosocial interventions,48 covered multiple types of interventions, each with different programme theories. Abbott et al.’s48 review included very brief descriptions of how cognitive–behavioural therapy, hypnotherapy, guided imagery, yoga and written self-disclosure are thought to work, all of which were described as mainly psychological in nature, except for family therapy, which was social (in contrast to Law et al. ’s27 description of family therapy as psychosocial). Law et al. ’s27 review also included separate programme theories for a variety of interventions including motivational interviewing, which was described as having a psychological mechanism, and those described as both social and psychological: cognitive-behavioural therapy, family therapy, multisystemic therapy, problem-solving therapy and one review investigating psychological therapies appeared to describe a psychosocial mechanism about which they gave little detail. 154
In summary, programme theories in Cochrane reviews of intervention effects on children’s chronic pain were brief and lacking detail making it challenging to ascertain whether explanations were biopsychosocial or not. Nor were there any considerations about feasibility, acceptability or implementation as additional context to the programme theories.
Overall, our integration of findings has shown that outcomes measured in Cochrane reviews and trials of interventions do not always match those of importance to children and families. In some cases, this is possibly because of a lack of suitable measurement tools. We also found that a biopsychosocial approach has been largely neglected in programme theories.
Chapter 6 Discussion and conclusion
Introduction
Our meta-ethnography findings reveal the profound and adverse impacts of children’s chronic pain on the child or young person, but importantly, also on their wider family including their relationships and dynamics. Findings also highlight how the impacts of pain on CYP extend more broadly in society beyond the family (e.g. the impact on the child’s education) and how families try to overcome these impacts. Our findings highlight the diverse nature of the difficulties that families’ face in seeking and obtaining help and support from health services to manage their child’s pain and its impacts. We have reached new interpretations of the primary data resulting in three lines of argument (see Line of argument 1: dominance of biomedical perspective in how children and families conceptualised chronic pain and pain management; Line of argument 2: parents fundamental to effective pain management and Line of argument 3: the journey of living with chronic pain), a model linking the lines of argument (see Linking the lines of argument into a model: families navigating chronic pain management), and developed the family-centred theory of CYP’s chronic pain and its management (see Family-centred theory of children and young people’s chronic pain and its management and Figure 7). To our knowledge, we have developed the first comprehensive family-centred theory of CYP’s chronic non-cancer pain and its management, using a biopsychosocial perspective, which incorporates how children and families conceptualise pain, their experiences of living with pain and how this impacts their use of pain management and health services. The new theory also contains implications for design of ‘good’ pain management and services.
We set out to answer four questions in our meta-ethnography:
-
How do children with chronic pain and their families conceptualise chronic pain?
-
How do children with chronic pain and their families live with chronic pain?
-
What do children with chronic pain and their families think of how health and social care services respond to and manage their/their child’s chronic pain?
-
What do children with chronic pain and their families conceptualise as ‘good’ chronic pain management and what do they want to achieve from chronic pain management interventions and services?
In this chapter, we summarise the key findings for each question (from the third-order constructs and lines of argument presented in Chapter 4), relate these to the wider literature and make recommendations for policy and practice backed up by GRADE-CERQual assessments of confidence in our synthesised findings. Implications for improving chronic pain management interventions and services draw upon both our interpretative findings, team expertise, as well as implications identified by the authors of included studies.
Review question 1. How do children with chronic pain and their families conceptualise chronic pain?
Our findings (presented in our Line of argument 1: dominance of biomedical perspective in how children and families conceptualised chronic pain and pain management) show that there is a difference in how CYP and families conceptualised the impacts of pain versus its causes, and therefore, the role of health services in managing the pain. CYP and their families expressed biopsychosocial (biological, psychological and social) impacts of chronic pain on their lives, for all kinds of chronic pain. However, when there was no identifiable or known medical cause of the pain, families initially tended to reject the idea of psychosocial causes or influences (e.g. anxiety), because it challenged the legitimacy of the CYP’s pain or suggested that pain was caused by parental shortcomings. For children whose pain was identified as being caused by an underlying health condition, such as sickle cell disease, juvenile idiopathic arthritis or cerebral palsy, families were less likely to consider psychosocial causes of, or influences on, pain. Most CYP and parents tended to understand the cause of chronic pain as solely biomedical – having an underlying pathophysiological cause. This influenced their expectations of and interactions with health services. However, families’ conceptualisations were dynamic and could change over time with experiences of treatments, services and interactions with healthcare professionals. Thus, healthcare professionals and targeted interventions could play an important role in managing family understandings of pain and expectations of services.
It is important to highlight that the above conceptualisation stems mainly from research in the UK and other high-income countries and their ethnic populations. Nonetheless, our included studies did represent a fairly wide range of ethnic backgrounds. Families from other countries and ethnic and cultural backgrounds may have very different conceptualisations to that described above. Furthermore, menstrual pain may be conceptualised differently. Girls and young women, their families and healthcare professionals may not at times perceive pain as a pathological/pathophysiological issue, for example severe menstrual pain was perceived as ‘normal’ pain not requiring medical intervention.
Review question 2. How do children with chronic pain and their families live with chronic pain?
The impacts of poorly managed, moderate and severe chronic pain on the child, their whole family and their wider social connections and relationships were profound (described in Third-order construct 1: pain organises the family system and the social realm). There were serious negative impacts of children’s chronic pain on family systems. Pain affected family dynamics and relationships; family members’ emotions, well-being, autonomy and sense of self-identity; parenting strategies; friendships and socialising; children’s education and future employment prospects; and parental employment. Children and family members experienced adverse physical/biological, psychological and social impacts of chronic pain. We found that most pain management happened at home and in the community, for example at school, and was supervised or implemented by parents, especially mothers who were often the main caregivers. Thus, the demands of caregiving disproportionately affected women (mothers).
Even though there were many serious psychosocial impacts on families, there was very little support provided by health and social care services or in the community (e.g. school health services) to address these. Families needed greater family-centred psychosocial support, which could include social support in the form of peer support. Children benefited from awareness about pain and its associated impact on CYP within schools and school health services, for example some school policies and practices flexibly supported CYP with chronic pain in self-care, while avoiding stigmatisation, and avoided negative impacts of disruption to their education. Health providers, schools and families working together to achieve outcomes valued by CYP and families is the basis of a ‘whole systems’ approach which, in turn, is based on strong connections and communication.
Review question 3. What do children with chronic pain and their families think of how health and social care services respond to and manage their/their child’s chronic pain?
A key challenge identified by CYP and families concerned their experiences of health systems and individual health services as difficult to access and navigate, resulting in challenges to achieve satisfactory pain management (as described in Third-order construct 2: families struggling to navigate health services, and Line of argument 3: the journey of living with chronic pain). Families often entered a lengthy cycle, which could last many years, of attending then reattending health services, and awaiting referral to secondary or tertiary services for tests and/or treatment. In the meantime, pain was not usually well managed, and families were left largely unsupported to find their own solutions. Being referred to a pain clinic could ‘validate’ the pain (i.e. confirm it was a real illness), be a source of hope, and emotional and practical support. One of the reasons for families’ difficulties in navigating services was the lack of a clear care pathway for CYP with chronic pain.
Interactions with healthcare professionals were frequently negative and stressful. CYP and their main caregivers, usually mothers, felt at times they were not being listened to and believed and thus they felt unsupported. For instance, CYP’s experiences of living with pain were ignored or their pain was disbelieved, and mothers felt blamed for their child’s pain. Parents of younger children and of children with communication difficulties perceived that their expertise in assessing their child’s pain was not always recognised by healthcare professionals. Open, empathetic healthcare professional communication could help CYP and their families to develop a trusting relationship with healthcare professionals. Children and families wanted healthcare professionals to explore their experiences of the impacts of chronic pain and their priorities for pain management.
Current tools to assess pain in CYP do not seem to incorporate parental assessment and advice regarding children with special needs (e.g. non-verbal/unable to communicate), and there appear to be no tools suitable for all CYP, tailored for chronic as opposed to acute pain. CYP may hide or minimise their pain to avoid causing their parents’ distress which is likely to pose challenges for pain assessment. Parents wanted healthcare professionals to recognise and make use of their parental expertise in assessing and responding to their child’s pain, particularly for children who have communication difficulties. CYP wanted healthcare professionals to use the child’s expertise and knowledge of their pain, especially for those with underlying chronic conditions like sickle cell disease and juvenile idiopathic arthritis. Family and child’s preferences, needs and lifestyle can have implications for pain management and pain management can affect family life.
Our evidence suggests that a scattergun rather than a co-ordinated approach to treatment decisions was common, with few children referred to specialist pain clinics when it was appropriate to do so. Many CYP did not appear to be offered the full range of appropriate treatment options; hence, parents tended to seek out one option after another in an unco-ordinated way that was not based on evidence of potential appropriateness, benefits or potential harms. In the data, there was an apparent lack of use of shared decision-making frameworks by healthcare professionals that could help them signpost families to all the available and appropriate treatment options.
There are difficulties diagnosing certain types of chronic pain, especially for generalist healthcare professionals, which would require diagnostic input from tertiary services. There is currently no pathway for children’s chronic pain, including chronic pain of unknown cause, for CYP and families and healthcare professionals to follow. Services were fragmented and some children who needed it waited a long time to be referred to or access tertiary specialist pain services, even for pain conditions like CRPS, which might benefit from early referral to such services. There was a lack of data regarding screening and assessment tools for children’s chronic pain which could have facilitated triage of children, for example to specialist services or use of primary care interventions, such as signposting families to educational pain management resources.
Lastly, but importantly, CYP and their families, particularly CYP with sickle cell disease, experienced racism and discrimination in health services. Children with chronic pain and learning disabilities, such as Down syndrome, also encountered discrimination. Direct and indirect prejudice and discrimination towards patients adversely affected the care they received and their pain management.
Review question 4. What do children with chronic pain, their families conceptualise as ‘good’ chronic pain management and what do they want to achieve from chronic pain management interventions and services?
As described in Third-order construct 2: families struggling to navigate health services and line of argument 1 (see Line of argument 1: dominance of biomedical perspective in how children and families conceptualised chronic pain and pain management), our findings indicate that because of the way families initially conceptualised the cause of chronic pain as biomedical, they first approached health services looking for medical treatment and/or cure and they usually rejected psychological treatments or approaches. Families with diagnosed underlying health conditions (such as juvenile idiopathic arthritis, sickle cell disease) which cause chronic pain also might not see the value of psychosocial pain treatments, given the cause of pain is a disease. Families did want help with the psychosocial consequences of pain, such as parental distress, but did not think health services could assist with that. This perceived medical focus for families and healthcare professionals could act as a possible barrier to biopsychosocial care.
Families’ reluctance to accept there may be psychosocial influences on, or causes of, chronic pain (or them not seeing the role of psychosocial support in managing pain) means healthcare professionals need to carefully manage how and when they offer psychosocial support to avoid alienating them. Healthcare professionals could play a role in sensitively explaining biopsychosocial explanations of pain management to families – since these apply even when there is a biological cause – by building on the family’s prior experiences of the biopsychosocial impacts and aspects of pain. However, when not approached sensitively, children and their families can feel healthcare professionals do not believe their pain is real and parents can feel they are being blamed for any social and psychological causes of pain. Biopsychosocial approaches are important for all CYP and families managing pain whatever the cause of their chronic pain. Parents and CYP highly value healthcare professionals who listen to and understand the impact chronic pain has on them and their family life.
Families ideally wanted interventions that reduced or removed the pain; if that is not possible, then strategies to help them live well with pain would be beneficial. Interventions that do not worsen the impact on the whole family and its well-being would be more acceptable to families. Consequently, it is important to tailor interventions to families’ preferences and needs so that they are not boring or excessively time-consuming, not painful and have minimal side effects.
An important role for healthcare professionals is in managing families’ understanding of chronic pain and expectations of pain management. Families needed clear communication about the purpose of any tests, examinations and treatments and to have their expectations managed about the possibility of a cure (which will be condition dependent) from the outset of their contact with health services. CYP needed to have their pain managed while awaiting test results and diagnosis.
Existing health and social care service models are adult-orientated and not child-specific or child- and family-centred. Biopsychosocial health and social care tailored for CYP, which is family-centred considering needs of the entire family and the impact on the family system would potentially meet families’ needs. Multidisciplinary care/treatment is currently recognised as the ‘gold standard’,18 but there is limited availability and accessibility of specialist multidisciplinary pain management for children’s complex pain problems. 8,18 There is a lack of a clear clinical pathway or specialist condition-specific pathways for particular pain conditions, for example juvenile idiopathic arthritis, headache.
Situation of the findings in relation to wider literature
Two qualitive evidence syntheses, published prior to conducting our meta-ethnography, had focused on children’s experiences of living with juvenile idiopathic arthritis39 and the impact of chronic pain on adolescents’ interpersonal relationships. 9 Our findings concur with, but greatly extend, theirs which found predominantly negative impacts on CYP’s self-identity, social participation and adolescents’ relationships. 9,39 Since we conducted our meta-ethnography, two new qualitative evidence syntheses on children’s chronic pain have been published focusing on specific pain populations and topics: a thematic synthesis of adolescents’ experiences of fluctuating pain in musculoskeletal disorders,155 and an aggregative synthesis of the experiences of children and young adults (up to 21 years) and their parents of living with juvenile idiopathic arthritis. 156 Khanom155 found that pain flares restricted adolescents’ activities leading to them feeling isolated and different from peers. The fluctuating nature of the pain was difficult for others to understand and adolescents tried strategies, including medical treatments, social support and concealing the pain, to try to regain a feeling of control over the unpredictable pain. 155 Min156 found adverse effects of juvenile idiopathic arthritis on young people’s emotional and physical well-being and on their relationships with parents, teachers and healthcare professionals. Young people and parents needed more self-management knowledge and skills. 156 A further mixed-methods review synthesised three qualitative studies on the impact of pain on adolescents’ schooling found mainly negative impacts of pain on school functioning with a need for better pain management in schools. 157 However, these five syntheses had narrower focuses and populations and different aims from our meta-ethnography. Their findings confirm but do not substantively add to ours and none produced a theory. We developed a new mid-range theory of children’s chronic pain and its management (see Family-centred theory of children and young people’s chronic pain and its management), which can be tested. Consequently, our meta-ethnography still adds valuable, key knowledge to the growing literature, but on a much wider range of chronic pain conditions and how they affect all aspects of the lives of CYP with chronic pain and their families.
In our meta-ethnography, we found that families in high-income countries mainly conceptualised pain as having a biomedical cause. This perceived medical focus can act as a possible barrier to biopsychosocial care. Shortcomings in healthcare professional education, training and experience about chronic pain could also contribute to the biomedical focus. 8,30,158 However, families from other countries and ethnic and cultural backgrounds may have very different conceptualisations. For example in Cameroon, families often believed pain was caused by witchcraft or their ancestors,149 in Jordan, many families believed that pain is given by God and should not be treated,159 while in Morocco, pain was seen as a sign of weakness. 160 Furthermore, in our meta-ethnography, severe menstrual pain was perceived as ‘normal’ pain not requiring medical intervention. This finding originated from a single study, conducted in Hong Kong; however, it is also supported by the UK and global literature on dysmenorrhoea. 160
Our meta-ethnography indicates serious negative impacts of children’s chronic pain on family systems. We have added to the scant knowledge of the impact of childhood chronic pain on the whole family system. 161 Quantitative cross-sectional research10 shows family dysfunction in children’s chronic pain but cross-sectional research cannot indicate the direction of causal relationships. Notably, our meta-ethnography shows that pain can cause family dysfunction and family-system-wide changes. Family systems interventions for CYP with chronic pain could be beneficial for the whole family. 162 The demands of caregiving can have negative impacts on the whole family but also can contribute to gender inequalities between women (mothers) and men (fathers); therefore, health and social care policies and interventions should take care not compound this inequality by increasing the burden on women. 163
Families lacked family-centred psychosocial support. The UK clinical SIGN guidelines on children’s chronic pain do not emphasise that care should be holistic and family-centred, perhaps because it is based on use of existing NHS services which are designed mainly to treat individual patients’ medical needs. 8 The guidelines do specify that ‘early biopsychosocial assessment and psychological intervention should be considered’8 (p.12). While the SIGN guideline fits with some of the families’ needs we identified, there is a lack of family-centred focus in the guideline as well as a lack of healthcare professionals with the knowledge and expertise in chronic pain assessment and management. 8,18,30,158,164,165
In palliative end-of-life care (in the last weeks and months of life), the concept of ‘total pain’ is commonly used, that is, pain is not just biological in cause but can be caused by emotional distress, existential concerns and so on, and the physiological impacts cannot be separated out from the emotional and social impacts of the pain; therefore, they need to be managed as connected. 166,167 This concept of total pain has not been applied to chronic pain that is not at end of life; it may be a useful concept to facilitate biopsychosocial management of children’s chronic pain. Adopting a ‘total pain’ approach to service delivery would help to knit together the biopsychosocial influences on and consequences of pain. 166,167 A barrier to biopsychosocial approaches to managing pain is that health services also largely still operate on a biomedical model of understanding, assessing and treating pain. 18 It is accepted that healthcare professional chronic pain education urgently needs improving, for example by adapting medical education curricula for undergraduates, postgraduates and qualified healthcare professionals. 8,18,30,31,164,165
The recent Lancet Commission identified the importance of healthcare professionals developing a more detailed understanding of pain which provides an understanding of children’s experience of living with chronic pain. 18 Denying a child’s subjective experience of pain is likely to result in child and family distress. Children and families needed healthcare professionals to believe the child’s pain was real, regardless of the (possible or actual) cause; this synthesis finding supports a key recommendation in the Lancet Commission. 18
An important role for healthcare professionals is in managing families’ understanding of chronic pain and expectations of pain management. Appropriate existing high-quality information resources for CYP and families exist, such as leaflets, storybooks for CYP, peer support groups, online modules, websites, for example ‘Kids In Pain’,168 ‘It Doesn’t Have To Hurt’169 websites. 8 In addition, healthcare professionals could make greater use of shared decision-making frameworks (e.g. the MAGIC framework),170 alongside appropriate clinical pathways, which could aid families to discuss and choose from all the available and appropriate treatment options to facilitate better decision-making.
It is not clear if and how assessment tools specific to chronic as opposed to acute pain are used in practice; there were no data on this in our included studies, nor that we can identify in the healthcare professional literature. SIGN guidelines8 recommend screening tools, for example the Paediatric Pain Screening Tool (PPST),171 which are specifically for chronic pain, to identify those children at risk of adverse outcomes. In addition, there are some other chronic pain paediatric assessment tools for specific age groups, such as self-report questionnaires for adolescents and their parents172 and a measure patient-reported pain behaviours for school-aged children. 173
Current barriers to improving children’s pain management in the UK include the lack of education of healthcare professionals in chronic pain and its management8,18,30,31,164,165 and the lack of specialist pain management services. 8 Furthermore, one of the reasons for families’ difficulties in navigating services is the current lack of a clear care pathway for children with chronic pain. In the UK, only Scotland has a clinical guideline for children’s chronic pain management;8 the pathway it contains mainly describes how services are currently organised rather than a step-by-step guide to pain assessment and treatment with clear decision points for healthcare professionals and families. There is no NICE guideline for England, Wales and Northern Ireland specifically for children’s chronic pain management. 29 NICE guidelines for sickle cell disease174 are not specific to children and the headache guideline175 is only for over 12s; yet, children’s needs may differ from adults’ needs and younger children’s needs may differ from those of older children. Other painful conditions such as juvenile idiopathic arthritis, dysmenorrhoea, epidermolysis bullosa, Ehlers–Danlos syndrome and osteogenesis imperfecta have no NICE clinical guideline, although some (e.g. dysmenorrhoea, juvenile idiopathic arthritis) have clinical summaries which provide some guidance. Child-specific chronic pain clinical guidelines could draw on existing guidelines8,19 and robust synthesised evidence. 20,40
We found that CYP and their families, particularly CYP with sickle cell disease, experienced racial prejudice and discrimination in health services. A possible alternative interpretation is that the inadequate care of CYP of mainly African Caribbean origin was related to the widespread suboptimal care of children with chronic pain in general rather than due to racism. However, in their recent comment in The Lancet Commission, Inusa et al. 176 also identified inequalities in access to care for CYP with sickle cell disease across various high- and low-income countries. Furthermore, an editorial literature review in the Journal of Pain Research177 concluded that there was systemic racism in chronic pain management, although in the US context. Children with chronic pain and learning disabilities, such as Down syndrome, also encountered discrimination, a finding which is supported by the wider literature on the poorer health care provided to people with learning disabilities. 178
Our new comprehensive theory goes beyond existing theories to inform design of chronic pain management and services by adopting a family-centred, biopsychosocial, whole-systems approach. In contrast, existing theories have either too wide a focus to derive clear testable hypotheses or too narrow a focus, such as on the causes of pain, a developmental perspective concerning how children understand their chronic pain,41 a biopsychosocial approach to clinical assessment and management of children’s chronic pain,43 or the role of parent and family factors in children’s chronic pain. 179,180 The implications for practice, described in Review question 1. How do children with chronic pain and their families conceptualise chronic pain?, Review question 2. How do children with chronic pain and their families live with chronic pain?, Review question 3. What do children with chronic pain and their families think of how health and social care services respond to and manage their/their child’s chronic pain? and Review question 4. What do children with chronic pain, their families conceptualise as ‘good’ chronic pain management and what do they want to achieve from chronic pain management interventions and services?, and for future research are summarised in Table 9.
| Implications for research | Specific focus |
|---|---|
| Broad area | |
| Primary qualitative in-depth studies to produce conceptually rich findings to explore | Experiences and perceptions of under-researched populations:
|
Families’ experiences of pain management and services:
|
|
| Development and testing of family-centred interventions |
|
| Outcomes |
|
| Implications for practice | Specific focus – evidence suggests |
| Broad area | |
| Pain management |
|
| Healthcare professional training and education |
|
| Healthcare professional communication |
|
| Clinical guidelines |
|
| Chronic pain assessment and triage |
|
| Care pathway |
|
| Services |
|
| Prejudice and discrimination |
|
Integration with Cochrane reviews
We integrated our synthesised findings with 14 relevant Cochrane intervention effects reviews. The outcomes measured in trials of intervention effectiveness and systematic reviews of effects did not always match those of importance to children and families; for instance, there is a need to measure impacts of interventions on the whole family and absence of pain. In addition, a biopsychosocial approach, which takes into account the full complexity of how interventions work, is required but has been mainly neglected in intervention programme theories.
Patient-reported outcome measures
One of our study objectives was to help inform the selection and design of patient-reported outcome measures for use in chronic pain studies. Since we started our meta-ethnography, a patient-reported outcome consensus study was published based on survey data from mainly girls aged 12 years and older recruited from tertiary pain and gastroenterology services in the USA. 51 Drawing on a much wider range of in-depth qualitative evidence from broader contexts and populations than their study, our findings support and validate some of their final outcome domains including pain interference with daily living, pain severity, overall well-being, physical functioning and emotional functioning. Additional outcomes we have identified as important to children and families not found in their study are absence of pain; the impact on family life, relationships and functioning; and the psychosocial impacts on family members including parents/the main caregiver and siblings.
Equality, diversity and inclusion
Participant representation
Our sample of included studies specifically sought to represent diverse populations. However, we were restricted by the available primary qualitative study publications in terms of the study population characteristics and how inclusive the populations were. We identified and have described evidence gaps and under-represented groups (see Included studies and Table 9). The views and experiences of boys, and children under 10 years old with chronic pain, CYP with learning disabilities, fathers and siblings are less well represented.
We have described our PPI recruitment strategy and engagement in detail (see Chapter 3). In short, for our core PPI group, we successfully recruited CYP with different kinds of chronic pain ranging in ages from 8 years old upwards and mothers of children with chronic pain, but we did not have any fathers directly involved despite recruitment attempts. Group members came from England, Scotland and Wales. We tried to recruit children and parents from a variety of ethnic backgrounds through third-sector organisations but were unsuccessful. We also used social media and online surveys for wider PPI engagement, which may have reached a more diverse group of children and families, but their feedback was anonymous.
Reflections on our research team and wider involvement
Our core research team is made up of adults (all female) some of whom have lived experience of chronic pain, which started in childhood or adulthood. Six team members are parents, some of whom have children with long-term health and/or developmental conditions. Our meta-ethnography focuses on CYP with chronic pain and their families; they were not part of the core research team but were members of our PPI and advisory groups. Our core team has diversity in nationalities (Belgian, Brazilian, British, French) and professional backgrounds in nursing children with chronic pain (JN), psychology (EF), health psychology (AJ, LC), sociology (IU, RT), family therapy (LF) and physiotherapy with children with chronic pain (MSB), children’s pain research (AJ, LC), occupational therapy (KT) and health services research (all).
As a result of our diverse backgrounds, there were some divergent views on aspects of the findings, which for transparency we record here. Two team members with extensive expertise in children’s pain research were uncomfortable with use of the term ‘cure’ in relation to chronic pain because for most young people there is no cure for their chronic pain. Therefore, it might be more scientifically accurate to use terms like ‘alleviate’ or ‘reduce’ pain. However, we retained the term ‘cure’ because it was used by research participants in a large proportion of the included primary studies and refers to their focus on absence rather than reduction of pain. There was also a difference in team members’ opinions about whether we should refer to ‘potential racism and prejudice’ or ‘racism and prejudice’ in health services because of difficulties in knowing whether poor treatment of CYP with chronic pain was related to their protected characteristics. We decided to refer to ‘racism and prejudice’, given that included studies reported racism and there is further supporting evidence in the wider literature, as reported above.
There was a range of experience and expertise across the research team including a new post-doctoral researcher, early-career and mid-career researchers, as well as senior academics. In terms of development opportunities, the junior member of the team was provided with mentorship from more senior members; accessed institutional and external training, including writing workshops and a grant writing development group; Cochrane systematic review training seminars including use of GRADE-CERQual; and was supported to present at conferences and lead journal articles.
Our wider team included a PAG including clinicians with pain expertise, a general practitioner, physiotherapists, Scottish Government representatives, an academic expert in qualitative evidence synthesis, voluntary sector representatives from patient organisations and a PPI group of parents and CYP with chronic pain.
Patient and public involvement
We have described our approach to PPI and the impact it had in detail using the ACTIVE framework to guide our reporting (see Chapter 3). 101 We believe ours is the first meta-ethnography to have actively included patients and the public in every stage of the research from its inception through to dissemination. 181 Including PPI in systematic reviews of intervention effects is more common, but the extent of involvement has varied. 182
We engaged with our core PPI group using a variety of media and methods to engage them. The core group remained involved throughout the entire project duration. We used e-mail, video calls, online workshops, short online surveys and social media including a project Facebook group and a Twitter page. The format of workshops and meetings was specifically designed to accommodate and engage CYP with chronic pain, as described already (see Chapter 3). We innovated in the methods used to involve CYP with chronic pain and their parents in our analysis and synthesis using visual methods, such as cartoons and graphics, and used simple language to convey complex concepts. In our PPI materials, we used plain English language suitable for children as young as 8 years old, showed ethnic and gender diversity in our visual materials (e.g. cartoons of findings) and carried out video call briefings prior to any meetings or workshops to explain what would happen. For wider PPI engagement beyond the group, we used social media including online surveys, and relevant charities. We believe that many of our approaches could be used as examples of good PPI practice for other researchers.
The impact of PPI is summarised briefly here. Our initial PPI engagement during grant development confirmed the importance of the topic and review questions and informed our dissemination plan. Our core PPI group agreed our final study inclusion criteria, contributed to study sampling decisions (see Chapters 2 and 3) and furthered our understanding and interpretation of data, particularly in areas of ambiguity or low clarity, such as the reasons why CYP might not communicate their pain verbally. They also helped fill gaps in the data, for example around disengagement with NHS health services, and brought experiences of pain conditions not represented in the included studies, such as Ehlers–Danlos syndrome.
Our PPI group collaborated with us to design a short animation of findings for CYP and are helping us disseminate via social media and support groups. In addition, a young person with chronic pain co-produced and co-presented an oral presentation with us at the RCN Annual Research Conference in Cardiff in 2022.
Strengths
The strengths of our meta-ethnography are we conducted a rigorous, systematic analytic synthesis involving a team of eight core researchers from a range of disciplines including nursing, psychology, sociology, physiotherapy and family therapy and a wider group of stakeholders including CYP with chronic pain and their parents, healthcare professionals, academics and the third sector. We developed novel insights and a new family-centred theory of children’s chronic pain and its management, which has improved our understanding of how CYP with chronic pain and their families think about, live with and experience chronic pain and what they need and want from services. No other qualitative evidence synthesis on CYP’s chronic pain has looked at such wide-ranging data and ours is the first theory encompassing such diverse aspects and pain populations as well as having a family focus. The majority (22 out 36, 61%) of our findings are high confidence as assessed using the GRADE-CERQual approach. This is the first time that a qualitative evidence synthesis has been integrated with such a large number (14) of Cochrane reviews of intervention effects.
Limitations
Evidence syntheses are reliant on the available evidence and its quality. We identified gaps in the primary qualitative evidence base: there was a lack of conceptually rich UK and non-UK qualitative studies focusing on common pain conditions like headache, recurrent abdominal pain, musculoskeletal pain, dysmenorrhoea and earache and some rarer conditions like Ehlers–Danlos syndrome, osteogenesis imperfecta and others. Certain populations of CYP were poorly represented, such as those with learning disabilities; children under 5 years old with chronic pain, particularly babies and infants under 2 years old and siblings of CYP with chronic pain. In included studies, the experiences of boys with chronic pain and fathers were under-represented. Due to a lack of in-depth rich studies conducted in the UK, we included studies from other countries whose health systems and cultures may differ. The data in included studies came mainly from studies conducted in high-income countries, which could limit their transferability to other populations and participant groups; their likely transferability to the decision-maker’s context could be assessed by using the TRANSFER approach. 183 There was a lack of studies focused on experiences and perceptions of treatments and services for chronic pain including social care services – most were about living with pain. However, through understanding the impact of pain on families’ lives, we have been able to make recommendations for improving services for pain management. There is a need for improved reporting of participant characteristics and methods in primary qualitative studies.
One (3%) of our findings was very low confidence (none were low confidence), and 36% (13 out of 36) were moderate confidence, as assessed using GRADE-CERQual. Additional evidence could increase our confidence in those findings. The very low confidence finding was focusing on what CYP and families value in pain management interventions. Moderate confidence findings focused on good things resulting from the impact of chronic pain; the impact of pain on siblings; social network support; peer support from others with chronic pain; transition to adult services; the impact of healthcare professional communication style on families; the parental role in treatment adherence; children and their families managing pain on their own; decisions of parents of children with neurological conditions regarding finding a balance between managing pain and CYP joining in with family life; the impact of school policies on the education of CYP with chronic pain; prejudice and discrimination in services and bullying at school.
There are some limitations of our review process. We chose to focus only on CYP and families’ experiences and perceptions. We did not search for and synthesise data on healthcare professionals’ perceptions and experiences of assessing and managing pain. However, a Masters’ dissertation supervised by EF synthesised the healthcare professional literature (personal communication – Scott Gribbon, University of Stirling, September 2022) and a qualitative evidence synthesis for WHO conducted by JN, EF and MSB also explored healthcare professional’s views have informed our discussion section and conclusions (personal communication – Emma France, University of Stirling, September 2020). However, further research into the attitudes, experiences of, and challenges for healthcare professionals related to delivering children’s pain management is needed. We excluded publications focusing on chronic cancer pain and end-of-life pain management and so the results may not apply to those populations. We were unable to screen 17 publications by full text because they were unavailable by our cut-off date due to libraries being closed when we carried out our original searches in 2020 during the COVID-19 pandemic. The closures particularly affected the availability of some books, book chapters, PhD theses and older journal articles (pre 2006); consequently we may have missed a small number of eligible publications.
We recommend that the meta-ethnography is updated in the near future, for example late 2024, given that there appears to have been a recent increase in the volume of relevant studies being published. Our updated search found 33 of the 170 eligible studies – 19% of them – were published between September 2020 and September 2022. In addition, there are under-represented populations, evidence gaps and a large proportion (14 out of 36, 39%) of synthesised findings were assessed with GRADE-CERQual as being very low (n = 1), or moderate confidence (n = 13).
Implications for practice
Health and social care systems for CYP’s chronic pain require modification to ensure that a more holistic biopsychosocial approach to addressing pain in CYP is adopted which considers all family-centred health and social care systems. Below are a set of questions that may help health service providers or managers when implementing or planning for children’s chronic pain management services. These questions were drawn from the findings.
-
In your service, how do healthcare professionals assess a child’s chronic pain? In addition to using any formal assessment tools, do they make use of a child’s knowledge of their pain? Do they include the main family caregiver’s expertise in assessing their child’s pain, particularly for children who have communication difficulties?
-
In your service, how do healthcare professionals explore the potential underlying cause or causes of a child’s chronic pain? Do they explore any underlying physical/biological, psychological and social contexts?
-
In your service, how do healthcare professionals explore children and families’ experiences of the physical/biological, psychological and social impacts of living with chronic pain on the whole family?
-
In your service, do healthcare professionals discuss priorities for chronic pain management with the child and main family caregiver before developing a pain management plan? How do healthcare professionals realistically and sensitively manage child and family expectations for treating or curing the child’s pain? Consider that children and families might want and expect complete resolution of chronic pain.
-
In your service, how do healthcare professionals check that children with chronic pain and their families understand the purpose of each test, examination and/or treatment?
-
In your service, how do healthcare professionals explain chronic pain to children and their families? To what extent do they adopt a comprehensive view to understanding chronic pain and its management which considers physical/biological, psychological and social contexts and impacts?
-
In your service, do healthcare professionals have knowledge of, and access to, appropriate existing chronic pain patient education resources? If so, do they direct children with chronic pain and their families to these resources?
-
How often do children with chronic pain and their families repeatedly return to your service seeking a diagnosis and/or better pain relief? How does your service deal with these children? What could be done to better support these children to avoid repeated return visits to your service and ineffectively managed pain?
-
In your service, do healthcare professionals have access to, and use, shared decision-making frameworks, decision aids or decision support tools with children with chronic pain and their families that indicate all the available and appropriate treatment options?
-
In your service, how confident are healthcare professionals in assessing, triaging and/or managing children’s chronic pain? Consider what their training needs are to deal specifically with children with chronic pain, their parents/guardians and their other family members. How does your service provide staff with continuing professional development opportunities in chronic pain-specific education?
-
For organisations that provide healthcare professional education and training, how much of your curriculum focuses on children’s chronic pain assessment and management? Does any such education and training address the biopsychosocial (biological, psychological and social) approach to treating chronic pain? Does it address how sex and ethnicity impact children’s experience and reporting of chronic pain?
-
How does your service consider the impacts of chronic pain on the whole family and their needs? For example through providing or signposting to family-centred psychosocial support such as family counselling or family systems interventions, where available, and/or tailoring pain management plans and interventions to the family and child’s preferences, needs and lifestyle. Consider the impact on family life when planning chronic pain management strategies.
-
Has your service evaluated its provision of healthcare professional training about ensuring an inclusive approach to meeting the diverse needs of CYP presenting with chronic pain and their families? How has reflection on equalities affected the personalised approach to families using your service?
-
Does your staff team reflect the ethnic make-up of the local population?
-
How does your service include fathers in the chronic pain management plan, even if they are not attending each clinical appointment?
-
How have children with chronic pain and their families been involved in shaping how your service is run?
-
How accessible is your service to children with chronic pain and their families? Consider geographical location, awareness of your service among referrers and families, child and family communication and language needs and disabled access, for example.
-
For non-specialised health services, does your service have clear referral pathways to specialist chronic pain services, where these are available? Where specialist services are not available, how could your service support children with chronic pain and their families with current resources and by utilising community resources, for example peer support, community groups, charities?
-
Does your service have a clear referral pathway to psychosocial (psychological and social) support, such as family systems therapists or counselling, for children with chronic pain and their families? Where such services are not available, how could your service support children and their families with current resources and by utilising community resources, for example peer support, community groups, charities?
Implications for future research
There are qualitative evidence gaps, which need addressing to inform improvements to policy and practice. Future research should prioritise conducting further primary qualitative in-depth studies to produce conceptually rich findings to address gaps in understanding the experiences and perceptions of certain under-researched populations including children aged under 5 years old, children with learning disabilities, boys and siblings and fathers of CYP with chronic pain. More high-quality research is needed into CYP’s experiences of particular pain conditions such as headache, recurrent abdominal pain, musculoskeletal pain, dysmenorrhoea and earache and some rarer conditions, as already described (see Limitations). Furthermore, research is needed to explore aspects of families’ experiences of pain treatment, such as pain management plans and experiences of pain assessment, and experiences of social care services. There is a need for development and testing of a triage approach to make sure that CYP get the right care, at the right time, from the right service. This could be on a spectrum from simple first-line interventions that can be recommended at first contact with healthcare professionals, to fast-track referral, to a holistic pain service if initial simple first-line interventions do not work. This would mean that front-line healthcare professionals need additional training and access to new tools, shared decision-making processes and child-centred care pathways and so on. There is a need for the development and testing of family-centred interventions and services and to develop treatments that are less onerous for, and more acceptable to, families based on our theory of good pain management. Family-centred outcomes should be included in future in trials of chronic pain interventions. We found little evidence from families who mentioned their views on, or experiences of, use of opioids; opioid use in CYP remains controversial and requires further research. A qualitative evidence synthesis exploring experiences of children’s chronic cancer pain is also required. Implications for research are summarised in Table 9.
Conclusions
A diverse body of qualitative evidence on CYP’s chronic pain was synthesised, pulling together different types of chronic pain conditions to develop new findings including the novel family-centred theory of children and young people’s chronic pain and its management. The evidence represents a range of family members – but mainly CYP with chronic pain and their mothers – and CYP of different ages from both the UK and a range of mainly high-income countries, with most evidence pertaining to adolescents.
Moderate or severe chronic pain has wide-ranging serious impacts on CYP and their families. Chronic pain affected all aspects of an individual’s and a family’s functioning including their family life and relationships, children’s education and future employment prospects, parental employment and family members’ friendships and social lives. Families experienced difficulties in seeking and getting help and support from health services to manage their child’s pain and its impacts. Families often repeatedly attended health services to seek diagnosis and effective treatment. Most CYP and parents understood the cause of chronic pain as solely biological which influenced their expectations of, and interactions with, health services. Interactions with healthcare professionals were frequently negative and stressful. CYP and parents felt their pain experiences were not listened to and believed, and thus felt unsupported. Some parents perceived that healthcare professionals did not always recognise their expertise in assessing their child’s pain. Particularly, CYP with sickle cell disease and children with chronic pain and learning disabilities experienced prejudice and discrimination in health services. Children’s chronic pain is frequently poorly managed and CYP are suffering suboptimal care. Current services are still fragmented and difficult to navigate. There is no clear care pathway for children’s chronic pain. Trials and reviews of intervention effects should incorporate outcomes of importance to children and families including impacts on the whole family and absence of pain. The health and social care systems for CYP’s chronic pain do not currently adopt a holistic systemic approach to addressing pain in CYP which considers and integrates all biopsychosocial, family-centred health and social care systems.
Additional information
Acknowledgements
We would like to thank the children and young people with chronic pain and parents and professionals who contributed to the development of this review. We also thank the volunteers who contributed to literature screening, assessment of methodological limitations and assessment of conceptual richness including Cordelia Leisegang and student Natalie Barnes of the University of Stirling Masters’ in Health Research.
Contribution of authors
Mayara Silveira Bianchim (https://orcid.org/0000-0001-9780-9006) (Research Fellow, physiotherapist) was involved in project administration, supervision, leading PPI activities, conducting the research including a lead role in formal analysis of data, validation of the research, contributed to writing original drafts (including visualisation) as well as reviewing and editing.
Line Caes (https://orcid.org/0000-0001-7355-0706) (Health Psychologist, Children’s Pain) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, contributing specialist expertise on children’s chronic pain from a quantitative research perspective, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Liz Forbat (https://orcid.org/0000-0002-7218-5775) (Research Psychologist, Family Therapy) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, contributing specialist expertise on the systemic impact of serious ill health on families, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Abbie Jordan (https://orcid.org/0000-0003-1595-5574) (Health Psychologist, Children’s Pain) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, contributing specialist expertise on children’s chronic pain from a qualitative research perspective, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Jane Noyes (https://orcid.org/0000-0003-4238-5984) (Professor in Health and Social Services Research and Child Health) was involved in conceptualisation of the project, development of the methodology, contributing specialist methodological expertise on qualitative evidence synthesis, GRADE-CERQual, integrating findings with Cochrane reviews of effects and children’s nursing, funding acquisition, conducting the research including formal analysis of data, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Katie Thomson (https://orcid.org/0000-0002-2558-2559) (Research Fellow, Occupational Therapy) was involved in project administration, conducting the research including formal analysis of data, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Ruth Turley (https://orcid.org/0000-0001-8556-7855) (Freelance Researcher, Systematic Reviewer) was involved in conceptualisation of the project, development of the methodology, funding acquisition, leading the literature search strategy, conducting the research including formal analysis of data, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Isabelle Uny (https://orcid.org/0000-0002-9548-5332) (Sociologist, Meta-ethnography) was involved in conceptualisation of the project, development of the methodology, funding acquisition, conducting the research including formal analysis of data, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Emma F France (https://orcid.org/0000-0003-0876-7030) (Associate Professor, Meta-ethnography) was involved in conceptualisation of the project, development of the methodology, funding acquisition, project administration, supervision, resources, contributing specialist methodological expertise on meta-ethnography and topic expertise on psychosocial aspects of long-term/life-limiting conditions in children, leading PPI activities, conducting the research including leading formal analysis of data, validation of the research, contributed to writing original drafts as well as reviewing and editing.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/UTPM7986.
Primary conflicts of interest: Jane Noyes has previously conducted a review for the World Health Organization on this topic, which contributed to a guideline. Noyes declares membership of Dissemination Centre Advisory Group 2015–19 COVID 19 reviewing 2020 and a member of Children’s Special Interest Group, Royal College of Nursing. Emma F France has previously conducted a review for the World Health Organization on this topic, which contributed to a guideline. Katie Thomson declares funding from GCU Pump Priming Fund Global Challenges Networking Grant. Isabelle Uny declares funding from Arts and Humanities Research Council Grant – Grant Ref: AH/V000152/1, Medical Research Council Grant- Grant Ref: MR/V015257/1. Abbie Jordan declares grants from Sir Halley Stewart Trust and ADPD (UK Research and Innovation) and Board roles for Pain in Childhood Special Interest Group of the International Association for the Study of Pain and the International Committee of the Society of Paediatric Psychology. All other authors have declared no competing interests.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
Requests for access to data should be addressed to the corresponding author.
Ethics statement
This project involved secondary research with stakeholder involvement. No ethical approval is required for secondary research.
Information governance statement
The University of Stirling is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Stirling is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (www.stir.ac.uk/about/professional-services/student-academic-and-corporate-services/policy-and-planning/legal-compliance/data-protectiongdpr/privacy-notices/).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
France E, Noyes J, Forbat L, Uny DI, Jordan A, Caes L, Turley R. A Meta-ethnography of How Children and Young People with Chronic Non-Cancer Pain and Their Families Experience and Understand Their Condition, Pain Services, and Treatments. Cochrane Database Syst Rev 2022;7:CD014873. https://doi.org/10.1002/14651858.CD014873
France EF, Ferguson-Glover G, Turley R, Uny I, Forbat L, Caes L, et al. How Children and Young People with Chronic Pain and Their Families Live with Pain and Perceive Pain Treatments and Services – A Meta-ethnography. RCN International Nursing Research Conference 2022, Cardiff, UK, 4–6 September 2022 (oral presentation).
France EF, Turley R, Uny I, Forbat L, Caes L, Jordan A, et al. 522 A Meta-ethnography of How Children and Young People with Chronic Pain and Their Families Experience and Perceive Pain Services and Treatments and Living with Pain. Arch Dis Child Aug 2022;107(Suppl. 2):A514–5. https://doi.org/10.1136/archdischild-2022-rcpch.828
France EF, Turley R, Uny I, Forbat L, Caes L, Jordan A, et al. A Synthesis Investigating How Young People with Chronic Pain from Sickle Cell Disease and Their Families Experience and Understand Their Condition, Pain Services and Treatments. Society of Pediatric Psychology Annual Conference 2022, Phoenix, AZ, 7–9 April 2022 (poster presentation).
France EF, Turley R, Uny I, Forbat L, Caes L, Jordan A, et al. A Synthesis Investigating How Young People with Chronic Pain from Sickle Cell Disease and Their Families Experience and Understand Their Condition, Pain Services and Treatments. 13th International Symposium on Pediatric Pain, Auckland, New Zealand and Online, 24–27 March 2022 (poster presentation).
Silveira Bianchim M, Turley R, Uny I, Forbat L, Caes L, Jordan A, et al. The Views of Young People with Neurological Conditions and Their Families on Chronic Pain, Services and Treatments – A Descriptive Synthesis. 13th International Symposium on Pediatric Pain, Auckland, New Zealand and Online, 24–27 March 2022 (poster presentation).
Silveira Bianchim, M, Turley R, Uny I, Forbat L, Caes L, Jordan A, et al. The Views of Young People with Neurological Conditions and Their Families on Chronic Pain, Services and Treatments – A Descriptive Synthesis. Society of Pediatric Psychology Annual Conference 2022, Phoenix, AZ, 7–9 April 2022 (poster presentation).
France EF, Caes L, Forbat L, Jordan A, Noyes J, Thomson K, et al. How Children and Young People with Chronic Pain and Their Families Experience and Perceive Pain Services and Treatments and Living with Pain: A Meta-ethnography. Lothian Health and Care Professions Research Conference 2023, Edinburgh, UK, 7 November 2023 (oral presentation).
France EF, Turley R, Uny I, Forbat L, Caes L, Jordan A, et al. How Children and Young People with Chronic Pain and Their Families Experience and Perceive Pain Services and Treatments and Living with Pain: A Meta-ethnography. Scottish Paediatric Society 2023 Summer Meeting, Aberdeen, UK, 9 June 2023 (poster presentation).
France EF, Uny I, Turley R, Thomson K, Noyes J, Jordan A, et al. A Meta-ethnography of How Children and Young People with Chronic Non-cancer Pain and Their Families Experience and Understand Their Condition, Pain Services and Treatments. Cochrane Database Syst Rev 2023;10:CD014873. https://doi.org/10.1002/14651858.CD014873.pub2
Silveira Bianchim M, Jordan A, Uny I, Noyes J, Forbat L, Caes L, et al. Co-producing with Children and Young People for a Meta-ethnography on Experiences of Chronic Pain, Treatments and Services. Cochrane Colloquium, London, UK, 3–6 September 2023 (poster presentation).
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Tan A, Strauss VY, Protheroe J, Dunn KM. Epidemiology of paediatric presentations with musculoskeletal problems in primary care. BMC Musculoskelet Disord 2018;19. https://doi.org/10.1186/s12891-018-1952-7.
- King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152:2729-38. https://doi.org/10.1016/j.pain.2011.07.016.
- Perquin CW, Hazebroek-Kampschreur AAJM, Hunfeld JAM, Bohnen AM, van Suijlekom-Smit LWA, Passchier J, et al. Pain in children and adolescents: a common experience. Pain 2000;87:51-8. https://doi.org/10.1016/S0304-3959(00)00269-4.
- Gobina I, Villberg J, Välimaa R, Tynjälä J, Whitehead R, Cosma A, et al. Prevalence of self-reported chronic pain among adolescents: evidence from 42 countries and regions. Eur J Pain 2019;23:316-26. https://doi.org/10.1002/ejp.1306.
- Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019;160:19-27. https://doi.org/10.1097/j.pain.0000000000001384.
- Gauntlett-Gilbert J, Eccleston C. Disability in adolescents with chronic pain: patterns and predictors across different domains of functioning. Pain 2007;131:132-41. https://doi.org/10.1016/j.pain.2006.12.021.
- Jones A, Caes L, McMurtry CM, Eccleston C, Jordan A. Sociodevelopmental challenges faced by young people with chronic pain: a scoping review. J Pediatr Psychol 2021;46:219-30. https://doi.org/10.1093/jpepsy/jsaa101.
- Scottish Government . Management of Chronic Pain in Children and Young People. A National Clinical Guideline 2018.
- Jordan A, Family H, Forgeron P. Interpersonal relationships in adolescent chronic pain: a qualitative synthesis. Clin Pract Pediatr Psychol 2017;5:303-18. https://doi.org/10.1037/cpp0000215.
- Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain 2010;11:1027-38. https://doi.org/10.1016/j.jpain.2010.04.005.
- Logan DE, Simons LE, Stein MJ, Chastain L. School impairment in adolescents with chronic pain. J Pain 2008;9:407-16. https://doi.org/10.1016/j.jpain.2007.12.003.
- The British Pain Society . Media Resources: FAQs 2018. www.britishpainsociety.org/media-resources/ (accessed 24 August 2023).
- Sleed M, Eccleston C, Beecham J, Knapp M, Jordan A. The economic impact of chronic pain in adolescence: methodological considerations and a preliminary costs-of-illness study. Pain 2005;119:183-90. https://doi.org/10.1016/j.pain.2005.09.028.
- Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain 2010;150:568-72. https://doi.org/10.1016/j.pain.2010.06.018.
- Barham L. Economic burden of chronic pain across Europe. J Pain Palliat Care Pharmacother 2012;26:70-2. https://doi.org/10.3109/15360288.2011.650364.
- Chief Medical Officer . Chief Medical Officer Annual Report 2008. Pain: Breaking through the Barrier 2009.
- Pain Summit . Putting Pain on the Agenda: The Report of the First English Pain Summit 2012.
- Eccleston C, Fisher E, Howard RF, Slater R, Forgeron P, Palermo TM, et al. Delivering transformative action in paediatric pain: a Lancet Child & Adolescent Health Commission. Lancet Child Adolesc Health 2021;5:47-8. https://doi.org/10.1016/S2352-4642(20)30277-7.
- World Health Organisation . Guidelines on the Management of Chronic Pain in Children 2020.
- Fisher E, Villanueva G, Henschke N, Nevitt SJ, Zempsky W, Probyn K, et al. Efficacy and safety of pharmacological, physical, and psychological interventions for the management of chronic pain in children: a WHO systematic review and meta-analysis. Pain 2022;163:e1-e19. https://doi.org/10.1097/j.pain.0000000000002297.
- Healthcare Improvement Scotland . Chronic Pain Services in Scotland: Where Are We Now? Pain Services for Children 2014.
- Cooper TE, Heathcote LC, Clinch J, Gold JI, Howard R, Lord SM, et al. Antidepressants for chronic non-cancer pain in children and adolescents. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD012535.pub2.
- Eccleston C, Cooper TE, Fisher E, Anderson B, Wilkinson NM. Non-steroidal anti-inflammatory drugs (NSAIDs) for chronic non-cancer pain in children and adolescents. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD012537.pub2.
- Cooper TE, Wiffen PJ, Heathcote LC, Clinch J, Howard R, Krane E, et al. Antiepileptic drugs for chronic non-cancer pain in children and adolescents. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD012536.pub2.
- Cooper TE, Fisher E, Gray AL, Krane E, Sethna N, van Tilburg MA, et al. Opioids for chronic non-cancer pain in children and adolescents. Cochrane Database Syst Rev 2017;7. https://doi.org/10.1002/14651858.CD012538.pub2.
- Cooper TE, Fisher E, Anderson B, Wilkinson NM, Williams DG, Eccleston C. Paracetamol (acetaminophen) for chronic non-cancer pain in children and adolescents. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD012539.pub2.
- Law E, Fisher E, Eccleston C, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev 2019;3. https://doi.org/10.1002/14651858.CD009660.pub4.
- Nascimento Leite M, Kamper SJ, O’Connell NE, Michaleff ZA, Fisher E, Viana Silva P, et al. Physical activity and education about physical activity for chronic musculoskeletal pain in children and adolescents. Cochrane Database Syst Rev 2023;7. https://doi.org/10.1002/14651858.CD013527.pub2.
- National Institute for Health and Care Excellence . Chronic Pain (Primary and Secondary in Over 16s: Assessment of All Chronic Pain and Management of Chronic Primary Pain 2021.
- Briggs EV, Battelli D, Gordon D, Kopf A, Ribeiro S, Puig MM, et al. Current pain education within undergraduate medical studies across Europe: advancing the provision of pain education and learning (APPEAL) study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006984.
- Lee RR, McDonagh JE, Connelly M, Peters S, Cordingley L. Identifying the content and context of pain within paediatric rheumatology healthcare professional curricula in the UK: a summative content analysis. Pediatric Rheumatol Online 2021;19. https://doi.org/10.1186/s12969-021-00614-1.
- Cochrane . Addressing the Gap in Knowledge on Chronic Pain in Childhood 2018. www.cochrane.org/news/addressing-gap-knowledge-chronic-pain-childhood (accessed 24 August 2023).
- International Association for the Study of Pain . 2019 Global Year Against Pain in the Most Vulnerable 2018. www.iasp-pain.org/advocacy/global-year/pain-in-the-most-vulnerable/ (accessed 24 August 2023).
- Jordan AL, Eccleston C, Osborn M. Being a parent of the adolescent with complex chronic pain: an interpretative phenomenological analysis. Eur J Pain 2007;11:49-56.
- Jordan A, Crabtree A, Eccleston C. ‘You have to be a jack of all trades’: fathers parenting their adolescent with chronic pain. J Health Psychol 2016;21:2466-76. https://doi.org/10.1177/1359105315580461.
- Neville A, Jordan A, Beveridge JK, Pincus T, Noel M. Diagnostic uncertainty in youth with chronic pain and their parents. J Pain 2019;20:1080-90. https://doi.org/10.1016/j.jpain.2019.03.004.
- Carter BD, Threlkeld BM. Psychosocial perspectives in the treatment of pediatric chronic pain. Pediatr Rheumatol Online J 2012;10. https://doi.org/10.1186/1546-0096-10-15.
- Maciver D, Jones D, Nicol M. Parents’ experiences of caring for a child with chronic pain. Qual Health Res 2010;20:1272-82. https://doi.org/10.1177/1049732310367499.
- Tong A, Jones J, Craig JC, Singh-Grewal D. Children’s experiences of living with juvenile idiopathic arthritis: a thematic synthesis of qualitative studies. Arthritis Care Res (Hoboken) 2012;64:1392-404. https://doi.org/10.1002/acr.21695.
- World Health Organization . Web annex H. Summary of the Key Findings of the Systematic Review of Qualitative Research. Guidelines on the Management of Chronic Pain in Children WEB ANNEXES A to K. 2020. https://apps.who.int/iris/bitstream/handle/10665/337644/9789240017894-eng.pdf (accessed 29 August 2023).
- Carter B, Simons J. Stories of Childrens Pain: Linking Evidence to Practice. London: SAGE Publications Ltd; 2014.
- Haslam SA, Haslam C, Jetten J, Cruwys T, Bentley SV. Rethinking the nature of the person at the heart of the biopsychosocial model: exploring social changeways not just personal pathways. Soc Sci Med 2021;272. https://doi.org/10.1016/j.socscimed.2020.113566.
- Bursch B, Walco GA, Zeltzer L. Clinical assessment and management of chronic pain and pain-associated disability syndrome. J Dev Behav Pediatr 1998;19:45-53. https://doi.org/10.1097/00004703-199802000-00008.
- Noblit GW, Hare RD. Meta-ethnography: Synthesizing Qualitative Studies. Newbury Park, CA: SAGE Publications Ltd; 1988.
- France EF, Cunningham M, Ring N, Uny I, Duncan EA, Jepson RG, et al. Improving reporting of meta-ethnography: the eMERGe reporting guidance. J Adv Nurs 2019;75:1126-39. https://doi.org/10.1111/jan.13809.
- de Bruijn CMA, Rexwinkel R, Gordon M, Benninga M, Tabbers MM. Antidepressants for functional abdominal pain disorders in children and adolescents. Cochrane Database Syst Rev 2021;2. https://doi.org/10.1002/14651858.CD008013.pub3.
- Martin AE, Newlove-Delgado TV, Abbott RA, Bethel A, Thompson-Coon J, Whear R, et al. Pharmacological interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev 2017;3. https://doi.org/10.1002/14651858.CD010973.pub2.
- Abbott RA, Martin AE, Newlove-Delgado TV, Bethel A, Thompson-Coon J, Whear R, et al. Psychosocial interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev 2017;1. https://doi.org/10.1002/14651858.CD010971.pub2.
- Anie KA, Green J. Psychological therapies for sickle cell disease and pain. Cochrane Database Syst Rev 2015;2015. https://doi.org/10.1002/14651858.CD001916.pub3.
- Newlove-Delgado TV, Martin AE, Abbott RA, Bethel A, Thompson-Coon J, Whear R, et al. Dietary interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev 2017;3. https://doi.org/10.1002/14651858.CD010972.pub2.
- Palermo TM, Walco GA, Paladhi UR, Birnie KA, Crombez G, de la Vega R, et al. Core outcome set for pediatric chronic pain clinical trials: results from a Delphi poll and consensus meeting. Pain 2021;162:2539-47. https://doi.org/10.1097/j.pain.0000000000002241.
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess 2011;15:1-164. https://doi.org/10.3310/hta15430.
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0688-3.
- Fisher E, Law E, Dudeney J, Palermo TM, Stewart G, Eccleston C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2018;9. https://doi.org/10.1002/14651858.CD003968.pub5.
- Fisher E, Law E, Palermo TM, Eccleston C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2015;3. https://doi.org/10.1002/14651858.CD011118.pub2.
- Noyes J, Booth A, Cargo M, Flemming K, Garside R, Hannes K, et al. Cochrane Qualitative and Implementation Methods Group guidance series – paper 1: introduction. J Clin Epidemiol 2018;97:35-8. https://doi.org/10.1016/j.jclinepi.2017.09.025.
- France EF, Cunningham M, Ring N, Uny I, Duncan EAS, Jepson RG, et al. Improving reporting of meta-ethnography: the eMERGe reporting guidance. BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-018-0600-0.
- France EF, Cunningham M, Ring N, Uny I, Duncan EAS, Jepson RG, et al. Improving reporting of meta-ethnography: the eMERGe reporting guidance. Psychooncology 2019;28:447-58. https://doi.org/10.1002/pon.4915.
- France EF, Uny I, Ring N, Turley RL, Maxwell M, Duncan EAS, et al. A methodological systematic review of meta-ethnography conduct to articulate the complex analytical phases. BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-019-0670-7.
- Cunningham M, France EF, Ring N, Uny I, Duncan EAS, Roberts RJ, et al. Developing a Reporting Guideline to Improve Meta-ethnography in Health Research: The eMERGe Mixed-Methods Study. Southampton (UK): NIHR Journals Library; 2019.
- France E, Noyes J, Forbat L, Uny DI, Jordan A, Caes L, et al. A meta-ethnography of how children and young people with chronic non-cancer pain and their families experience and understand their condition, pain services, and treatments. Cochrane Database Syst Rev 2022. https://doi.org/10.1002/14651858.CD014873.
- France EF, Uny I, Turley R, Thomson K, Noyes J, Jordan A, et al. A meta-ethnography of how children and young people with chronic non-cancer pain and their families experience and understand their condition, pain services and treatments. Cochrane Database Syst Rev 2023. https://doi.org/10.1002/14651858.CD014873.pub2.
- Veritas Health Innovation . Covidence Systematic Review Software 2022. www.covidence.org (accessed 24 August 2023).
- Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, et al. Cochrane Qualitative and Implementation Methods Group guidance series – paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol 2018;97:49-58. https://doi.org/10.1016/j.jclinepi.2017.06.020.
- Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: a worked example from a synthesis on parental perceptions of vaccination communication. BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-019-0665-4.
- Benoot C, Hannes K, Bilsen J. The use of purposeful sampling in a qualitative evidence synthesis: a worked example on sexual adjustment to a cancer trajectory. BMC Med Res Methodol 2016;16. https://doi.org/10.1186/s12874-016-0114-6.
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res 1998;8:341-51. https://doi.org/10.1177/104973239800800305.
- Noyes JBA, Cargo M, Flemming K, Harden A, Harris J, , et al. Cochrane Handbook for Systematic Reviews of Interventions. 2023.
- O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014;67:56-64. https://doi.org/10.1016/j.jclinepi.2013.08.005.
- Critical Appraisal Skills Programme . Qualitative Checklist 2018. https://casp-uk.net/casp-tools-checklists/ (accessed 6 March 2024).
- QSR International Pty Ltd . NVivo Qualitative Data Analysis Software 2020. www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed 1 October 2023).
- Garside R, Britten N, Stein K. The experience of heavy menstrual bleeding: a systematic review and meta-ethnography of qualitative studies. J Adv Nurs 2008;63:550-62. https://doi.org/10.1111/j.1365-2648.2008.04750.x.
- Malpass A, Shaw A, Sharp D, Walter F, Feder G, Ridd M, et al. ‘Medication career’ or ‘moral career?’ The two sides of managing antidepressants: a meta-ethnography of patients’ experience of antidepressants. Soc Sci Med 2009;68:154-68. https://doi.org/10.1016/j.socscimed.2008.09.068.
- Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-21.
- Brodwall A, Glavin K, Lagerlov P. Parents’ experience when their child has chronic abdominal pain: a qualitative study in Norway. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021066.
- Smart S, Cottrell D. Going to the doctors: the views of mothers of children with recurrent abdominal pain. Child Care Health Dev 2005;31:265-73. https://doi.org/10.1111/j.1365-2214.2005.00506.x.
- Maciver D. Caring for a Child with Chronic Pain: A Qualitative Study of Parents’ Lived Experiences. Edinburgh: Queen Margaret University College; 2005.
- Maciver D, Jones D, Nicol M. Parental experiences of pediatric chronic pain management services. J Pain Manag 2011;4:371-80.
- Britton CA, Moore A. Views from the inside, part 3: how and why families undertake prescribed exercise and splinting programmes and a new model of the families’ experience of living with juvenile arthritis. Br J Occup Ther 2002;65:453-60. https://doi.org/10.1177/030802260206501004.
- Britton C, Moore A. Views from the inside, part 2: what the children with arthritis said, and the experiences of siblings, mothers, fathers and grandparents. Br J Occup Ther 2002;65:413-9. https://doi.org/10.1177/030802260206500904.
- Renedo A, Miles S, Chakravorty S, Leigh A, Warner JO, Marston C. Understanding the health-care experiences of people with sickle cell disorder transitioning from paediatric to adult services: This Sickle Cell Life, a longitudinal qualitative study. Health Serv Deliv Res 2020;8. https://doi.org/10.3310/hsdr08440.
- Renedo A, Miles S, Chakravorty S, Leigh A, Telfer P, Warner JO, et al. Not being heard: barriers to high quality unplanned hospital care during young people’s transition to adult services – evidence from ‘this sickle cell life’ research. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4726-5.
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 2002;7:209-15. https://doi.org/10.1258/135581902320432732.
- Schutz A. Collected papers. The Hague: Martinus Nijhoff 1962.
- Padlet . Padlet: A Real-Time Collaborative Web Platform Used to Share and Organise Content 2022. https://en-gb.padlet.com/ (accessed 24 August 2023).
- Google Workspace . Jamboard: A Digital Interactive Whiteboard 2022. https://workspace.google.com/products/jamboard/ (accessed 24 August 2023).
- Microsoft Corporation . Microsoft Team Whiteboard 2022. https://microsoft.com/en-gb/microsoft-365/microsoft-whiteboard/digital-whiteboard-app (accessed 24 August 2023).
- Glenton C, Carlsen B, Lewin S, Munthe-Kaas H, Colvin CJ, Tunçalp O, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 5: how to assess adequacy of data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0692-7.
- Colvin CJ, Garside R, Wainwright M, Munthe-Kaas H, Glenton C, Bohren MA, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 4: how to assess coherence. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0691-8.
- Noyes J, Booth A, Lewin S, Carlsen B, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 6: how to assess relevance of the data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0693-6.
- Munthe-Kaas H, Bohren MA, Glenton C, Lewin S, Noyes J, Tunçalp O, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 3: how to assess methodological limitations. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0690-9.
- Harden A, Thomas J, Cargo M, Harris J, Pantoja T, Flemming K, et al. Cochrane Qualitative and Implementation Methods Group guidance series – paper 5: methods for integrating qualitative and implementation evidence within intervention effectiveness reviews. J Clin Epidemiol 2018;97:70-8. https://doi.org/10.1016/j.jclinepi.2017.11.029.
- Noyes J, Hendry M, Booth A, Chandler J, Lewin S, Glenton C, et al. Current use was established and Cochrane guidance on selection of social theories for systematic reviews of complex interventions was developed. J Clin Epidemiol 2016;75:78-92. https://doi.org/10.1016/j.jclinepi.2015.12.009.
- Microsoft Corporation . Microsoft Excel 2018. https://office.microsoft.com/excel (accessed 24 August 2023).
- Noyes J, Booth A, Moore G, Flemming K, Tunçalp O, Shakibazadeh E. Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: clarifying the purposes, designs and outlining some methods. BMJ Glob Health 2019;4. https://doi.org/10.1136/bmjgh-2018-000893.
- Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low- and middle-income countries: a qualitative evidence synthesis. Cochrane Database Syst Rev 2017;11. https://doi.org/10.1002/14651858.CD011558.pub2.
- Booth A, Harris J, Croot E, Springett J, Campbell F, Wilkins E. Towards a methodology for cluster searching to provide conceptual and contextual ‘richness’ for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-118.
- National Institute for Health and Care Research . INVOLVE Strategy 2012–2015 Putting People First in Research 2012.
- Campbell IH, Rudan I. Effective approaches to public engagement with global health topics. J Glob Health 2020;10. https://doi.org/10.7189/jogh.10.010901.
- National Institute for Health and Care Research . UK Standards for Public Involvement: Better Public Involvement for Better Health and Social Care Research 2019.
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Development of the ACTIVE framework to describe stakeholder involvement in systematic reviews. J Health Serv Res Policy 2019;24:245-55. https://doi.org/10.1177/1355819619841647.
- Baert F, McParland J, Miller MM, Hirsh AT, Wallace E, Dickson A, et al. Mothers’ appraisals of injustice in the context of their child’s chronic pain: an interpretative phenomenological analysis. Eur J Pain 2020;24:1932-45. https://doi.org/10.1002/ejp.1642.
- Asmussen L, Olson LM, Sullivan SA. ‘You have to live it to understand it’. Family experiences with chronic otitis media in children. Ambul Child Health 1999;5:303-12.
- Soni-Jaiswal A, Mercer J, Jones SA, Bruce IA, Callery P. Mucopolysaccharidosis I; parental beliefs about the impact of disease on the quality of life of their children. Orphanet J Rare Dis 2016;11:1-9. https://doi.org/10.1186/s13023-016-0478-z.
- Brandelli YN, Tutelman PR, Chambers CT, Parker JA, Stinson JN, Huber AM, et al. ‘Every little furrow of her brow makes me want to stop’: an interpretative phenomenologic analysis of mothers’ experiences with juvenile idiopathic arthritis treatments. Arthritis Care Res (Hoboken) 2021. https://doi.org/10.1002/acr.24735.
- Yuwen W, Lewis FM, Walker AJ, Ward TM. Struggling in the dark to help my child: parents’ experience in caring for a young child with juvenile idiopathic arthritis. J Pediatr Nurs 2017;37:e23-9. https://doi.org/10.1016/j.pedn.2017.07.007.
- Panepinto JA, Torres S, Varni JW. Development of the PedsQL™ Sickle Cell Disease Module items: qualitative methods. Qual Life Res 2012;21:341-57. https://doi.org/10.1007/s11136-011-9941-4.
- Randall JA, Guobyte A, Delbecque L, Newton L, Symonds T, Hunter T. Qualitative research to explore the symptoms and impacts experienced by children with ulcerative colitis. J Patient Rep Outcomes 2020;4. https://doi.org/10.1186/s41687-020-00238-1.
- Carter B, Arnott J, Simons J, Bray L. Developing a sense of knowing and acquiring the skills to manage pain in children with profound cognitive impairments: mothers’ perspectives. Pain Res Manag 2017;2017. https://doi.org/10.1155/2017/2514920.
- Hunt A, Mastroyannopoulou K, Goldman A, Seers K. Not knowing – the problem of pain in children with severe neurological impairment. Int J Nurs Stud 2003;40:171-83. https://doi.org/10.1016/S0020-7489(02)00058-5.
- Leksell E, Hallberg U, Horne A, Ernberg M, Hedenberg-Magnusson B. Parenting a child with juvenile idiopathic arthritis, orofacial pain, and dysfunction: a qualitative study. J Oral Facial Pain Headache 2017;31:353-61. https://doi.org/10.11607/ofph.1689.
- Santos MCD, Pires AF, Soares K, Barros L. Family experience with osteogenesis imperfecta type 1: the most distressing situations. Disabil Rehabil 2018;40:2281-7. https://doi.org/10.1080/09638288.2017.1334236.
- Gómez-Ramírez O, Gibbon M, Berard R, Jurencak R, Green J, Tucker L, et al. A recurring rollercoaster ride: a qualitative study of the emotional experiences of parents of children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2016;14. https://doi.org/10.1186/s12969-016-0073-9.
- Iliyasu Z, Borodo AM, Jibir BW, Nass NS, Aliyu MH. ‘A child with sickle cell disease can’t live with just anyone’. A mixed methods study of socio-behavioral influences and severity of sickle cell disease in northern Nigeria. Health Sci Rep 2021;4. https://doi.org/10.1002/hsr2.222.
- Ajinkpang S, Anim-Boamah O, Bimpong KA, Kanton FJ, Pwavra JBP, Abdul-Mumin A. Sickle cell disease in children: knowledge and home-based management strategies among caregivers at a tertiary facility in Northern Ghana. Biomed Res Int 2022;2022:1-6. https://doi.org/10.1155/2022/3384813.
- van Scheppingen C, Lettinga AT, Duipmans JC, Maathuis KG, Jonkman MF. The main problems of parents of a child with epidermolysis bullosa. Qual Health Res 2008;18:545-56. https://doi.org/10.1177/1049732308315110.
- Carter B. Chronic pain in childhood and the medical encounter: professional ventriloquism and hidden voices. Qual Health Res 2002;12:28-41. https://doi.org/10.1177/104973230201200103.
- Carter B, Lambrenos K, Thursfield J. A pain workshop: an approach to eliciting the views of young people with chronic pain. J Clin Nurs 2002;11:753-62. https://doi.org/10.1046/j.1365-2702.2002.00642.x.
- Carter B, McArthur E, Cunliffe M. Dealing with uncertainty: parental assessment of pain in their children with profound special needs. J Adv Nurs 2002;38:449-57. https://doi.org/10.1046/j.1365-2648.2002.02206.x.
- Jones A, Caes L, Eccleston C, Noel M, Rugg T, Jordan A. Loss-adjusting: young people’s constructions of a future living with complex regional pain syndrome. Clin J Pain 2020;36:932-9. https://doi.org/10.1097/AJP.0000000000000880.
- Jordan A, Noel M, Caes L, Connell H, Gauntlett-Gilbert J. A developmental arrest? Interruption and identity in adolescent chronic pain. Pain Rep 2018;3. https://doi.org/10.1097/PR9.0000000000000678.
- Khanom S, McDonagh JE, Briggs M, McBeth J. Characterizing pain flares in adolescent inflammatory and non-inflammatory musculoskeletal disorders: a qualitative study using an interpretative phenomenological approach. Eur J Pain 2020;24:1785-96. https://doi.org/10.1002/ejp.1626.
- Williams F. A Qualitative Study of the Experiences of Children and Young People With Epidermolysis Bullosa 2008.
- Atkin K, Ahmad WIU. Family care-giving and chronic illness: how parents cope with a child with a sickle cell disorder or thalassaemia. Health Soc Care Community 2000;8:57-69. https://doi.org/10.1046/j.1365-2524.2000.00211.x.
- Atkin K, Ahmad WI. Living a ‘normal’ life: young people coping with thalassaemia major or sickle cell disorder. Soc Sci Med 2001;53:615-26. https://doi.org/10.1016/s0277-9536(00)00364-6.
- Waite-Jones JM, Madill A. Amplified ambivalence: having a sibling with juvenile idiopathic arthritis. Psychol Health 2008;23:477-92. https://doi.org/10.1080/14768320701299906.
- Britton C, Moore A. Views from the inside, part 2: what the children with arthritis said, and the experiences of siblings, mothers, fathers and grandparents. Br J Occup Ther 2002;65:413-9. https://doi.org/10.1177/030802260206500904.
- Jones A, Caes L, Eccleston C, Noel M, Gauntlett-Gilbert J, Jordan A. The sands of time: adolescents’ temporal perceptions of peer relationships and autonomy in the context of living with chronic pain. Paediatr Neonatal Pain 2022;4:110-24. https://doi.org/10.1002/pne2.12071.
- Maciver D, Jones D, Nicol M. Parental experiences of pediatric chronic pain management services. J Pain Manag 2011;4:371-80.
- Dyson SM, Atkin K, Culley LA, Dyson SE, Evans H. Sickle cell, habitual dys-positions and fragile dispositions: young people with sickle cell at school. Sociol Health Illn 2011;33:465-83. https://doi.org/10.1111/j.1467-9566.2010.01301.x.
- Cartwright T, Fraser E, Edmunds S, Wilkinson N, Jacobs K. Journeys of adjustment: the experiences of adolescents living with juvenile idiopathic arthritis. Child Care Health Dev 2015;41:734-43. https://doi.org/10.1111/cch.12206.
- Guell C. Painful childhood: children living with juvenile arthritis. Qual Health Res 2007;17:884-92. https://doi.org/10.1177/1049732307305883.
- Borghi CA, Rossato LM, Damião EB, Guedes DM, Silva EM, Barbosa SM, et al. Living with pain: the experience of children and adolescents in palliative care. Rev Esc Enferm USP 2014;48:67-73. https://doi.org/10.1590/S0080-623420140000600010.
- Wong CL, Ip WY, Lam LW. Self-care strategies among Chinese adolescent girls with dysmenorrhea: a qualitative study. Pain Manag Nurs 2016;17:262-71. https://doi.org/10.1016/j.pmn.2016.04.001.
- McKinnon C, White J, Harvey A, Antolovich G, Morgan P. Caregiver perspectives of managing chronic pain in children and adolescents with dyskinetic and mixed dyskinetic/spastic CP with communication limitations. J Pediatr Rehabil Med 2022;15:69-81. https://doi.org/10.3233/PRM-200770.
- McDonagh K, McGuire BE, Durand H. Being a parent of a child with Down’s arthritis: an interpretative phenomenological analysis. Disabil Rehabil 2022;44:7030-8. https://doi.org/10.1080/09638288.2021.1979663.
- Ahlqwist A, Sällfors C. Experiences of low back pain in adolescents in relation to physiotherapy intervention. Int J Qual Stud Health Well-Being 2012;7. https://doi.org/10.3402/qhw.v7i0.15471.
- Dell’Api M, Rennick JE, Rosmus C. Childhood chronic pain and health care professional interactions: shaping the chronic pain experiences of children. J Child Health Care 2007;11:269-86. https://doi.org/10.1177/1367493507082756.
- Kanstrup M, Jordan A, Kemani MK. Adolescent and parent experiences of Acceptance and Commitment Therapy for pediatric chronic pain: an interpretative phenomenological analysis. Children (Basel) 2019;6. https://doi.org/10.3390/children6090101.
- Nutkiewicz M. Diagnosis versus dialogue: oral testimony and the study of pediatric pain. Oral Hist Rev 2008;35:11-2. https://doi.org/10.1093/ohr/ohm002.
- Castle K, Imms C, Howie L. Being in pain: a phenomenological study of young people with cerebral palsy. Dev Med Child Neurol 2007;49:445-9. https://doi.org/10.1111/j.1469-8749.2007.00445.x.
- Forgeron P, McGrath P. Self-identified Needs of Youth with Chronic Pain. J Pain Manag 2008;1:163-72.
- Gaughan V, Logan D, Sethna N, Mott S. Parents’ perspective of their journey caring for a child with chronic neuropathic pain. Pain Manag Nurs 2014;15:246-57. https://doi.org/10.1016/j.pmn.2012.09.002.
- Helvig AW, Minick P. Adolescents and headaches: maintaining control. Pediatr Nurs 2013;39:19-25; quiz 26.
- Rossato LM, Angelo M, Silva CAA. Care delivery for the child to grow up despite the pain: the family’s experience. Rev Lat Am Enfermagem 2007;15:556-62.
- Sorensen K, Christiansen B. Adolescents’ experience of complex persistent pain. Scand J Pain 2017;15:106-12. https://doi.org/10.1016/j.sjpain.2017.02.002.
- Suder R. The Lived Experience of Adolescents with Chronic Pain: A Phenomenological Study. Fort Lauderdale, FL: Nova Southeastern University; 2016.
- Atoui M, Badr LK, Brand TD, Khoury R, Shahine R, Abboud M. The daily experiences of adolescents in Lebanon with sickle cell disease. J Pediatr Health Care 2015;29:424-34. https://doi.org/10.1016/j.pedhc.2015.01.012.
- Njifon Nsangou H, Scelles R. Sickle cell disease and siblings: a crossover look at the experiences of a sister and a brother of a sick child. J Pediatr Pueric 2019;32:75-84. https://doi.org/10.1016/j.jpp.2019.02.005.
- The World Bank . World Bank Country and Lending Groups 2023. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed 24 August 2023).
- Keogh E. The gender context of pain. Health Psychol Rev 2021;15:454-81. https://doi.org/10.1080/17437199.2020.1813602.
- Sällfors C, Hallberg LRM. Fitting into the prevailing teenage culture: a grounded theory on female adolescents with chronic arthritis. Int J Qual Stud Health Well-Being 2009;4:106-14. https://doi.org/10.1080/17482620802431862.
- Dyson SM, Abuateya H, Atkin K, Culley LA, Dyson SE, Rowley D. Reported school experiences of young people living with sickle cell disorder in England. Br Educ Res J 2010;36:125-42.
- Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2019;4. https://doi.org/10.1002/14651858.CD011118.pub3.
- Khanom S, McDonagh JE, Briggs M, Bakir E, McBeth J. Adolescents’ experiences of fluctuating pain in musculoskeletal disorders: a qualitative systematic review and thematic synthesis. BMC Musculoskelet Disord 2020;21. https://doi.org/10.1186/s12891-020-03627-1.
- Min M, Hancock DG, Aromataris E, Crotti T, Boros C. Experiences of living with juvenile idiopathic arthritis: a qualitative systematic review. JBI Evid Synth 2022;20:60-120. https://doi.org/10.11124/JBIES-21-00139.
- Alsaggaf F, Coyne I. A systematic review of the impact of chronic pain on adolescents’ school functioning and school personnel responses to managing pain in the schools. J Adv Nurs 2020;76:2005-22. https://doi.org/10.1111/jan.14404.
- Lee R, McDonagh J, Connelly M, Peters S, Cordingley L. ‘Where does it hurt’: identifying pain content and its context within paediatric and adolescent rheumatology training. Ann Rheum Dis 2021;80:1029-30. https://doi.org/10.1136/annrheumdis-2021-eular.210.
- Forgeron PA, Finley GA, Arnaout M. Pediatric pain prevalence and parents’ attitudes at a cancer hospital in Jordan. J Pain Symptom Manage 2006;31:440-8. https://doi.org/10.1016/j.jpainsymman.2005.09.003.
- Barrington DJ, Robinson HJ, Wilson E, Hennegan J. Experiences of menstruation in high income countries: a systematic review, qualitative evidence synthesis and comparison to low- and middle-income countries. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0255001.
- Lewandowski W, Morris R, Draucker CB, Risko J. Chronic pain and the family: theory-driven treatment approaches. Issues Ment Health Nurs 2007;28:1019-44. https://doi.org/10.1080/01612840701522200.
- Distelberg B, Williams-Reade J, Tapanes D, Montgomery S, Pandit M. Evaluation of a family systems intervention for managing pediatric chronic illness: Mastering Each New Direction (MEND). Fam Process 2014;53:194-213. https://doi.org/10.1111/famp.12066.
- Cascella Carbó GF, García-Orellán R. Burden and gender inequalities around informal care. Invest Educ Enferm 2020;38. https://doi.org/10.17533/udea.iee.v38n1e10.
- Hurley-Wallace A, Wood C, Franck LS, Howard RF, Liossi C. Paediatric pain education for health care professionals. Pain Rep 2019;4. https://doi.org/10.1097/PR9.0000000000000701.
- Mackintosh-Franklin CP. a content review of undergraduate pre-registration nurse education in the United Kingdom. Nurse Educ Today 2017;48:84-9. https://doi.org/10.1016/j.nedt.2016.08.035.
- Clark D. ‘Total pain’, disciplinary power and the body in the work of Cicely Saunders, 1958–1967. Soc Sci Med 1999;49:727-36. https://doi.org/10.1016/s0277-9536(99)00098-2.
- Mehta A, Chan LS. Understanding of the concept of ‘total pain’: a prerequisite for pain control. J Hosp Palliat Nurs 2008;10:26-32. https://doi.org/10.1097/01.NJH.0000306714.50539.1a.
- Dalhousie University . Solutions for Kids in Pain 2020. https://kidsinpain.ca/ (accessed 24 August 2023).
- Chambers C. It Doesn’t Have to Hurt. Canada: Centre for Pediatric Pain Research; 2022.
- Joseph-Williams N, Lloyd A, Edwards A, Stobbart L, Tomson D, Macphail S, et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. BMJ 2017;357. https://doi.org/10.1136/bmj.j1744.
- Simons LE, Smith A, Ibagon C, Coakley R, Logan DE, Schechter N, et al. Pediatric Pain Screening Tool: rapid identification of risk in youth with pain complaints. Pain 2015;156:1511-8. https://doi.org/10.1097/j.pain.0000000000000199.
- Eccleston C, Jordan A, McCracken LM, Sleed M, Connell H, Clinch J. The Bath Adolescent Pain Questionnaire (BAPQ): development and preliminary psychometric evaluation of an instrument to assess the impact of chronic pain on adolescents. Pain 2005;118:263-70.
- Cunningham NR, Kashikar-Zuck S, Mara C, Goldschneider KR, Revicki DA, Dampier C, et al. Development and validation of the self-reported PROMIS pediatric pain behavior item bank and short form scale. Pain 2017;158:1323-31. https://doi.org/10.1097/j.pain.0000000000000914.
- National Institute for Health and Clinical Excellence . Sickle Cell Acute Painful Episode. Management of an Acute Painful Sickle Cell Episode in Hospital 2012.
- National Institute for Health and Care Excellence . Headaches in Over 12s: Diagnosis and Management 2012. www.nice.org.uk/guidance/cg150 (accessed 6 October 2023).
- Inusa BPD, Jacob E, Dogara L, Anie KA. Racial inequalities in access to care for young people living with pain due to sickle cell disease. Lancet Child Adolesc Health 2021;5:7-9. https://doi.org/10.1016/S2352-4642(20)30318-7.
- Ghoshal M, Shapiro H, Todd K, Schatman ME. Chronic noncancer pain management and systemic racism: time to move toward equal care standards. J Pain Res 2020;13:2825-36. https://doi.org/10.2147/JPR.S287314.
- Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889-95. https://doi.org/10.1016/S0140-6736(13)62026-7.
- Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: an integrative approach. Pain 2005;119:1-4. https://doi.org/10.1016/j.pain.2005.10.027.
- Palermo TM, Valrie CR, Karlson CW. Family and parent influences on pediatric chronic pain: a developmental perspective. Am Psychol 2014;69:142-52. https://doi.org/10.1037/a0035216.
- Park S, Khan N, Stevenson F, Malpass A. Patient and Public Involvement (PPI) in evidence synthesis: how the PatMed study approached embedding audience responses into the expression of a meta-ethnography. BMC Med Res Methodol 2020;20. https://doi.org/10.1186/s12874-020-0918-2.
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Stakeholder involvement in systematic reviews: a scoping review. Syst Rev 2018;7. https://doi.org/10.1186/s13643-018-0852-0.
- Munthe-Kaas H, Nøkleby H, Lewin S, Glenton C. The TRANSFER Approach for assessing the transferability of systematic review findings. BMC Med Res Methodol 2020;20. https://doi.org/10.1186/s12874-019-0834-5.
- Ahola Kohut S, Stinson J, Forgeron P, van Wyk M, Harris L, Luca S. A qualitative content analysis of peer mentoring video calls in adolescents with chronic illness. J Health Psychol 2018;23:788-99. https://doi.org/10.1177/1359105316669877.
- Ali A, Weiss TR, Dutton A, McKee D, Jones KD, Kashikar-Zuck S, et al. Mindfulness-based stress reduction for adolescents with functional somatic syndromes: a pilot cohort study. J Pediatr 2017;183:184-90. https://doi.org/10.1016/j.jpeds.2016.12.053.
- Allgood SJ, Kozachik S, Alexander KA, Thaxton A, Vera M, Lechtzin N. Descriptions of the pain experience in adults and adolescents with cystic fibrosis. Pain Manag Nurs 2018;19:340-7. https://doi.org/10.1016/j.pmn.2017.11.011.
- Bagge-Petersen CM, Skovdal M, Langstrup H. The socio-material self-care practices of children living with hemophilia or juvenile idiopathic arthritis in Denmark. Soc Sci Med 2020;255. https://doi.org/10.1016/j.socscimed.2020.113022.
- Barlow J, Harrison K, Shaw K. The experience of parenting in the context of juvenile chronic arthritis. Clin Child Psychol Psychiatry 1998;3:445-63. https://doi.org/10.1177/1359104598033008.
- Barlow JH, Shaw KL, Harrison K. Consulting the ‘experts’: children’s and parents’ perceptions of psycho-educational interventions in the context of juvenile chronic arthritis. Health Educ Res 1999;14:597-610. https://doi.org/10.1093/her/14.5.597.
- Beneitez I, Nieto R, Hernandez E, Boixados M. Adolescents’ social needs living with juvenile idiopathic arthritis and their views about digital resources. Adv Rheumatol 2020;60. https://doi.org/10.1186/s42358-020-00138-4.
- Beyer JE, Simmons LE. Home treatment of pain for children and adolescents with sickle cell disease. Pain Manag Nurs 2004;5:126-35.
- Bradshaw E, Barlas P. An outpatient paediatric pain management service lessens the impact of pain on the child: a service evaluation. Pain Rehab J Physiother Pain Assoc 2016;40:4-9.
- Brekke M, Brodwall A. Understanding parents’ experiences of disease course and influencing factors: a 3-year follow-up qualitative study among parents of children with functional abdominal pain. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-037288.
- Britton C, Moore A. Views from the inside, part 1: routes to diagnosis – families’ experience of living with a child with arthritis. Br J Occup Ther 2002;65:374-80. https://doi.org/10.1177/030802260206500805.
- Bruce AAK, Guilcher GMT, Desai S, Truong TH, Leaker M, Alaazi DA, et al. ADaPTS ‘(AD)olescents (P)ath through (T)ransplant (S)ickle cell disease’. Health Qual Life Outcomes 2022;20. https://doi.org/10.1186/s12955-022-02021-w.
- Burbage ML, Mason MB, Nabors LA, Kichler JC. An evaluation of a juvenile idiopathic arthritis retreat for families. Pediatr Rheumatol Online J 2015;13. https://doi.org/10.1186/s12969-015-0010-3.
- Conboy L, Quilty MT, Kerr C, Shaw J, Wayne P. A qualitative analysis of adolescents’ experiences of active and sham Japanese-style acupuncture protocols administered in a clinical trial. J Altern Complement Med 2008;14:699-705. https://doi.org/10.1089/acm.2007.0718.
- Constantinou C, Payne N, van den Akker O, Inusa B. A qualitative exploration of health-related quality of life and health behaviours in children with sickle cell disease and healthy siblings. Psychol Health 2023;38:125-46. https://doi.org/10.1080/08870446.2021.1955119.
- Corey JR, Heathcote LC, Mahmud F, Kronman C, Mukerji C, McGinnis E, et al. Longitudinal narrative analysis of parent experiences during graded exposure treatment for children with chronic pain. Clin J Pain 2021;37:301-9. https://doi.org/10.1097/AJP.0000000000000921.
- Cotton S, Grossoehme D, McGrady ME. Religious coping and the use of prayer in children with sickle cell disease. Pediatr Blood Cancer 2012;58:244-9. https://doi.org/10.1002/pbc.23038.
- Cox D, McParland JL, Jordan A. Parenting an adolescent with complex regional pain syndrome: a dyadic qualitative investigation of resilience. Br J Health Psychol 2022;27:194-21. https://doi.org/10.1111/bjhp.12541.
- Cunningham NR, Nelson S, Jagpal A, Moorman E, Farrell M, Pentiuk S, et al. Development of the aim to decrease anxiety and pain treatment for pediatric functional abdominal pain disorders. J Pediatr Gastroenterol Nutr 2018;66:16-20. https://doi.org/10.1097/MPG.0000000000001714.
- Cunningham NR, Fussner LM, Moorman E, Avar Aydin PO, Brunner HI, Kashikar-Zuck S. Development and pilot testing of the treatment and education approach for childhood-onset lupus (TEACH): a cognitive behavioral treatment. Pediatr Rheumatol Online J 2019;17. https://doi.org/10.1186/s12969-019-0307-8.
- Curtis K, Lebedev A, Aguirre E, Lobitz S. A medication adherence app for children with sickle cell disease: qualitative study. JMIR Mhealth Uhealth 2019;7. https://doi.org/10.2196/mhealth.8130.
- de Monte R, Rodger S, Jones F, Broderick S. Living with juvenile idiopathic arthritis: children’s experiences of participating in home exercise programmes. Br J Occup Ther 2009;72:357-65. https://doi.org/10.1177/030802260907200806.
- de Moura LA, de Oliveira PR, Medeiros M, Rossato LM, Borges ND, Pereira LV. Chronic pain following inguinal herniorrhaphy: perceptions of children and adolescents. Rev Esc Enferm USP 2021;55. https://doi.org/10.1590/1980-220X-REEUSP-2020-0490.
- Dogan M, Hartenstein-Pinter A, Lopez Lumbi S, Blankenburg M, Frühwald MC, Ahnert R, et al. Exploring the mechanisms underlying the effectiveness of psychosocial aftercare in pediatric chronic pain treatment: a qualitative approach. Children (Basel) 2022;9. https://doi.org/10.3390/children9030407.
- Donovan E, Mehringer S, Zeltzer LK. A qualitative analysis of adolescent, caregiver, and clinician perceptions of the impact of migraines on adolescents’ social functioning. Pain Manag Nurs 2013;14:e135-41. https://doi.org/10.1016/j.pmn.2011.09.002.
- Donovan E, Martin SR, Lung K, Evans S, Seidman LC, Cousineau TM, et al. Pediatric irritable bowel syndrome: perspectives on pain and adolescent social functioning. Pain Med 2019;20:213-22. https://doi.org/10.1093/pm/pny056.
- dos Santos LM, Neta TDP, Brito LS, Passos SSS, Jenerette CM, Carvalho ESS. Impostas pela doenca Being an adolescent despite the restrictions and discrimination imposed by sickle cell disease Ser adolescente pese a las restricciones y a la discriminacion impuestas por la enfermedad de celulas falciformes. Acta Paul Enferm 2022;35. https://doi.org/10.37689/acta-ape/2022AO0243345.
- Evans S, Meldrum M, Tsao JC, Fraynt R, Zeltzer LK. Associations between parent and child pain and functioning in a pediatric chronic pain sample: a mixed methods approach. Int J Disabil Hum Dev 2010;9:11-2. https://doi.org/10.1515/IJDHD.2010.003.
- Evans S, Seidman LC, Lung K, Sternlieb B, Zeltzer LK. Yoga for teens with irritable bowel syndrome: results from a mixed-methods pilot study. Holist Nurs Pract 2018;32:253-60. https://doi.org/10.1097/HNP.0000000000000288.
- Forgeron PA, Evans J, McGrath PJ, Stevens B, Finley GA. Living with difference: exploring the social self of adolescents with chronic pain. Pain Res Manag 2013;18:e115-23. https://doi.org/10.1155/2013/120632.
- Gernet SMC, Runel-Belliard C. Emotional representations of the illness among 22 sickle cell children. Neuropsychiatrie De l’enfance Et De l’adolescence 2011;59:404-10.
- Ghio D, Thomson W, Calam R, Ulph F, Baildam EM, Hyrich K, et al. The prioritization of symptom beliefs over illness beliefs: the development and validation of the Pain Perception Questionnaire for Young People. Br J Health Psychol 2018;23:68-87. https://doi.org/10.1111/bjhp.12275.
- Ghio D, Calam R, Lee RR, Cordingley L, Ulph F. Childhood Arthritis Prospective Study (CAPS). ‘I just want to be normal’: a qualitative investigation of adolescents’ coping goals when dealing with pain related to arthritis and the underlying parent-adolescent personal models. Paediatr Neonatal Pain 2021;4:96-109. https://doi.org/10.1002/pne2.12069.
- Gibler RC, Abelson E, Williams SE, Lynch-Jordan AM, Kashikar-Zuck S, Jastrowski Mano KE. Establishing the content validity of a modified bank of school anxiety inventory items for use among adolescents with chronic pain. J Pediatr Psychol 2022;47:1044-5. https://doi.org/10.1093/jpepsy/jsac043.
- Goldenberg D, Payne LA, Hayes LP, Zeltzer LK, Tsao JC. Peer mentorship teaches social tools for pain self-management: a case study. J Pain Manag 2013;6:61-8.
- Gordon M. Experiences of Children with Inflammatory Bowel Disease and Their Families in General Education Classrooms. Canada: University of Ottawa; 2013.
- Gorodzinsky AY, Tran ST, Medrano GR, Fleischman KM, Anderson-Khan KJ, Ladwig RJ, et al. Parents’ initial perceptions of multidisciplinary care for pediatric chronic pain. Pain Res Treat 2012;2012. https://doi.org/10.1155/2012/791061.
- Gorodzinsky AY, Davies WH, Tran ST, Medrano GR, Bernacki JM, Burks LM, et al. Adolescents’ perceptions of family dynamics when a sibling has chronic pain. Child Health Care 2013;42:333-52. https://doi.org/10.1080/02739615.2013.842460.
- Gremillion ML, Lang AC, Everhart SA, Davies WH, Stolzman SC, Weisman SJ, et al. Effects of weight and pain on physical activity: insights from the lived experiences of youth with co-occurring chronic pain and obesity. Child Obes 2022;18:301-8. https://doi.org/10.1089/chi.2021.0208.
- Hackett J. Perceptions of play and leisure in junior school aged children with juvenile idiopathic arthritis: what are the implications for occupational therapy?. Br J Occup Ther 2003;66:303-10. https://doi.org/10.1177/030802260306600704.
- Haridasa N, DeBaun MR, Sanger M, Mayo-Gamble TL. Student perspectives on managing sickle cell disease at school. Pediatr Blood Cancer 2019;66. https://doi.org/10.1002/pbc.27507.
- Heffernan M, Wilson C, Keating K, McCarthy K. ‘Why isn’t it going away?’: a qualitative exploration of worry and pain experiences in adolescents with chronic pain. Pain Med 2021;22:459-69. https://doi.org/10.1093/pm/pnaa245.
- Hendry GJ, Turner DE, Lorgelly PK, Woodburn J. Room for improvement: patient, parent, and practitioners’ perceptions of foot problems and foot care in juvenile idiopathic arthritis. Arch Phys Med Rehabil 2012;93:2062-7. https://doi.org/10.1016/j.apmr.2012.07.007.
- Hilário AP. When pain never goes away: understanding the lived experiences of children with chronic pain and their parents in Portugal. Child Soc 2022;36:840-56. https://doi.org/10.1111/chso.12542.
- Hollier JM, Vaughan AO, Liu Y, van Tilburg MA, Shulman RJ, Thompson DI. Maternal and child acceptability of a proposed guided imagery therapy mobile app designed to treat functional abdominal pain disorders in children: mixed-methods predevelopment formative research. JMIR Pediatr Parent 2018;1. https://doi.org/10.2196/pediatrics.8535.
- Hulgaard DR, Rask CU, Risor MB, Dehlholm G. Illness perceptions of youths with functional disorders and their parents: an interpretative phenomenological analysis study. Clin Child Psychol Psychiatry 2020;25:45-61. https://doi.org/10.1177/1359104519846194.
- Hulgaard DR, Rask CU, Risør MB, Dehlholm G. ‘I can hardly breathe’: exploring the parental experience of having a child with a functional disorder. J Child Health Care 2020;24:165-79. https://doi.org/10.1177/1367493519864745.
- Hurtubise K, Brousselle A, Noel M, Jordan A, White J, Rasic N, et al. Youth and parent perceptions on participating in specialized multidisciplinary pain rehabilitation options: a qualitative timeline effect analysis. Can J Pain 2021;5:1-21. https://doi.org/10.1080/24740527.2020.1858709.
- Jacobson CJ, Farrell JE, Kashikar-Zuck S, Seid M, Verkamp E, Dewitt EM. Disclosure and self-report of emotional, social, and physical health in children and adolescents with chronic pain – a qualitative study of PROMIS pediatric measures. J Pediatr Psychol 2013;38:82-93. https://doi.org/10.1093/jpepsy/jss099.
- Jacobson CJ, Kashikar-Zuck S, Farrell J, Barnett K, Goldschneider K, Dampier C, et al. Qualitative evaluation of pediatric pain behavior, quality, and intensity item candidates and the PROMIS pain domain framework in children with chronic pain. J Pain 2015;16:1243-55. https://doi.org/10.1016/j.jpain.2015.08.007.
- Jensen SE, Patel ZS, Listernick R, Charrow J, Lai JS. Lifespan development: symptoms experienced by individuals with neurofibromatosis type 1 associated plexiform neurofibromas from childhood into adulthood. J Clin Psychol Med Settings 2019;26:259-70. https://doi.org/10.1007/s10880-018-9584-5.
- Jones F, Rodger S, Broderick S, De Monte R. Living with juvenile idiopathic arthritis: parents’ experiences of treatment regimens and home exercise programmes. Br J Occup Ther 2009;72:249-58. https://doi.org/10.1177/030802260907200603.
- Joslin R, Donovan-Hall M, Roberts L. Exploring the outcomes that matter most to young people treated for chronic pain: a qualitative study. Children (Basel) 2021;8:1170-16. https://doi.org/10.3390/children8121170.
- Kashikar-Zuck S, Tran ST, Barnett K, Bromberg MH, Strotman D, Sil S, et al. A qualitative examination of a new combined cognitive-behavioral and neuromuscular training intervention for juvenile fibromyalgia. Clin J Pain 2016;32:70-81. https://doi.org/10.1097/AJP.0000000000000221.
- Khair K, Meerabeau L, Gibson F. Self-management and skills acquisition in boys with haemophilia. Health Expect 2015;18:1105-13. https://doi.org/10.1111/hex.12083.
- Kroon Van Diest AM, Ernst MM, Vaughn L, Slater S, Powers SW. CBT for pediatric migraine: a qualitative study of patient and parent experience. Headache 2018;58:661-75. https://doi.org/10.1111/head.13285.
- Kulandaivelu Y, Lalloo C, Ward R, Zempsky WT, Kirby-Allen M, Breakey VR, et al. Exploring the needs of adolescents with sickle cell disease to inform a digital self-management and transitional care program: qualitative study. JMIR Pediatr Parent 2018;1. https://doi.org/10.2196/11058.
- Lauridsen HH, Stolpe AB, Myburgh C, Hestbæk L. What are important consequences in children with non-specific spinal pain? A qualitative study of Danish children aged 9–12 years. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-037315.
- Law EF, Beals-Erickson SE, Fisher E, Lang EA, Palermo TM. Components of effective cognitive-behavioral therapy for pediatric headache: a mixed methods approach. Clin Pract Pediatr Psychol 2017;5:376-91. https://doi.org/10.1037/cpp0000216.
- Law EF, Fales JL, Beals-Erickson SE, Failo A, Logan D, Randall E, et al. A single-arm feasibility trial of problem-solving skills training for parents of children with idiopathic chronic pain conditions receiving intensive pain rehabilitation. J Pediatr Psychol 2017;42:422-33. https://doi.org/10.1093/jpepsy/jsw087.
- Le A, Dick BR, Spiers J, Reid K, Scott SD. Parents’ experiences with pediatric chronic pain. Can J Pain 2019;3:20-32. https://doi.org/10.1080/24740527.2019.1577679.
- Lee RR, Shoop-Worrall S, Rashid A, Thomson W, Cordingley L. ‘Asking too much?’: randomized n-of-1 trial exploring patient preferences and measurement reactivity to frequent use of remote multidimensional pain assessments in children and young people with juvenile idiopathic arthritis. J Med Internet Res 2020;22. https://doi.org/10.2196/14503.
- Lipstein EA, Dodds CM, Lovell DJ, Denson LA, Britto MT. Making decisions about chronic disease treatment: a comparison of parents and their adolescent children. Health Expect 2016;19:716-26. https://doi.org/10.1111/hex.12210.
- McKinnon C, White J, Harvey A, Antolovich G, Morgan P. The lived experience of chronic pain in children with dyskinetic cerebral palsy from the perspective of carers. Dev Med Child Neurol 2020;62:46-7. https://doi.org/10.1111/dmcn.14469.
- McNeill T. Fathers’ experience of parenting a child with juvenile rheumatoid arthritis. Qual Health Res 2004;14:526-45. https://doi.org/10.1177/1049732303262374.
- Meldrum ML, Tsao JC, Zeltzer LK. ‘Just be in pain and just move on’: Functioning limitations and strategies in the lives of children with chronic pain. J Pain Manag 2008;1:131-41.
- Meldrum ML, Tsao JC, Zeltzer LK. ‘I can’t be what I want to be’: children’s narratives of chronic pain experiences and treatment outcomes. Pain Med 2009;10:1018-34. https://doi.org/10.1111/j.1526-4637.2009.00650.x.
- Miles S, Renedo A, Augustine C, Ojeer P, Willis N, Marston C. Obstacles to use of patient expertise to improve care: a co-produced longitudinal study of the experiences of young people with sickle cell disease in non-specialist hospital settings. Crit Public Health 2020;30:544-54. https://doi.org/10.1080/09581596.2019.1650893.
- Mitchell MJ, Lemanek K, Palermo TM, Crosby LE, Nichols A, Powers SW. Parent perspectives on pain management, coping, and family functioning in pediatric sickle cell disease. Clin Pediatr (Phila) 2007;46:311-9.
- Moulin V, Akre C, Rodondi PY, Ambresin AE, Suris JC. A qualitative study of adolescents with medically unexplained symptoms and their parents. Part 1: experiences and impact on daily life. J Adolesc 2015;45:307-16. https://doi.org/10.1016/j.adolescence.2015.10.010.
- Moulin V, Akre C, Rodondi PY, Ambresin AE, Suris JC. A qualitative study of adolescents with medically unexplained symptoms and their parents. Part 2: how is healthcare perceived?. J Adolesc 2015;45:317-26. https://doi.org/10.1016/j.adolescence.2015.10.003.
- Neto M, Andias R, Silva AG. Pain neuroscience education and exercise for neck pain: a focus group study on adolescents’ views. Pediatr Phys Ther 2018;30:196-201. https://doi.org/10.1097/PEP.0000000000000511.
- Newton L, Randall JA, Hunter T, Keith S, Symonds T, Secrest RJ, et al. A qualitative study exploring the health-related quality of life and symptomatic experiences of adults and adolescents with ulcerative colitis. J Patient Rep Outcomes 2019;3. https://doi.org/10.1186/s41687-019-0154-x.
- Nguyen AM, Humphrey L, Kitchen H, Rehman T, Norquist JM. A qualitative study to develop a patient-reported outcome for dysmenorrhea. Qual Life Res 2015;24:181-91. https://doi.org/10.1007/s11136-014-0755-z.
- Nicholas DB, Otley A, Smith C, Avolio J, Munk M, Griffiths AM. Challenges and strategies of children and adolescents with inflammatory bowel disease: a qualitative examination. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-28.
- Nieto R, Hernández E, Boixadós M, Huguet A, Beneitez I, McGrath P. Testing the feasibility of DARWeb: an online intervention for children with functional abdominal pain and their parents. Clin J Pain 2015;31:493-50. https://doi.org/10.1097/AJP.0000000000000199.
- Nieto R, Boixadós M, Hernández E, Beneitez I, Huguet A, McGrath P. Quantitative and qualitative testing of DARWeb: an online self-guided intervention for children with functional abdominal pain and their parents. Health Informatics J 2019;25:1511-27. https://doi.org/10.1177/1460458218779113.
- Nieto R, Boixados M, Ruiz G, Hernandez E, Huguet A. Effects and experiences of families following a web-based psychosocial intervention for children with functional abdominal pain and their parents: a mixed-methods pilot randomized controlled trial. J Pain Res 2019;12:3395-412. https://doi.org/10.2147/JPR.S221227.
- Nieto R, Sora B, Boixadós M, Ruiz G. Understanding the experience of functional abdominal pain through written narratives by families. Pain Med 2020;21:1093-105. https://doi.org/10.1093/pm/pnz147.
- Nilsson IM, List T, Willman A. Adolescents with temporomandibular disorder pain-the living with TMD pain phenomenon. J Orofac Pain 2011;25:107-16.
- Nilsson IM, Willman A. Treatment seeking and self-constructed explanations of pain and pain management strategies among adolescents with temporomandibular disorder pain. J Oral Facial Pain Headache 2016;30:127-33. https://doi.org/10.11607/ofph.1450.
- Nkhoma KB, Mwalabu GT, Bristowe K, Lungu EA, Harding R. ‘Pain Special Issue’ ‘Stakeholders’ perspectives and requirements on pain self-management for adolescents living with HIV/AIDS in Malawi: a cross-sectional qualitative study’. AIDS Care 2021. https://doi.org/10.1080/09540121.2021.1939850.
- Nsangou HN, Falck J, Scelles R. Family culture of sickle cell disease and body image in affected children. Ann Med Psychol 2020;178:827-36. https://doi.org/10.1016/j.amp.2019.10.004.
- O’ Donnell SC, Marshman Z, Zaitoun H. ‘Surviving the sting’: the use of solicited diaries in children and young people with oral mucosal disease. Int J Paediatr Dent 2013;23:352-8. https://doi.org/10.1111/ipd.12028.
- Ostojic K, Sharp N, Paget S, Khut G, Morrow AB. A pilot study of biofeedback assisted relaxation training for the management of chronic pain in children and adolescents with cerebral palsy. Dev Med Child Neurol 2020;62:38-9. https://doi.org/10.1111/dmcn.14688.
- O’Sullivan G, O’Higgins S, Caes L, Saetes S, McGuire BE, Stinson J. Self-management needs of Irish adolescents with Juvenile Idiopathic Arthritis (JIA): how can a Canadian web-based programme meet these needs?. Pediatr Rheumatol Online J 2018;16. https://doi.org/10.1186/s12969-018-0287-0.
- Palmer K, Shepard B. An art inquiry into the experiences of a family of a child living with a chronic pain condition: a case study. Can J Couns 2008;42:7-23.
- Pate JW, Noblet T, Hush JM, Hancock MJ, Sandells R, Pounder M, et al. Exploring the concept of pain of Australian children with and without pain: qualitative study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-033199.
- Peláez-Ballestas I, Pérez-Taylor R, Aceves-Avila JF, Burgos-Vargas R. ‘Not-belonging’: illness narratives of Mexican patients with ankylosing spondylitis. Med Anthropol 2013;32:487-500. https://doi.org/10.1080/01459740.2012.716883.
- Race DL, Sims-Gould J, Tucker LB, Duffy CM, Feldman DE, Gibbon M, et al. ‘It might hurt, but you have to push through the pain’: perspectives on physical activity from children with juvenile idiopathic arthritis and their parents. J Child Health Care 2016;20:428-36. https://doi.org/10.1177/1367493516632616.
- Risko JL. Adolescent Experiences in an Intensive Interdisciplinary Pediatric Chronic Pain Rehabilitation Program. Kent, OH: Kent State University; 2018.
- Ruskin D, Harris L, Stinson J, Kohut SA, Walker K, McCarthy E. ‘I learned to let go of my pain’. The effects of mindfulness meditation on adolescents with chronic pain: an analysis of participants’ treatment experience. Children (Basel) 2017;4. https://doi.org/10.3390/children4120110.
- Sällfors C, Hallberg LRM, Fasth A. Coping with chronic pain: in-depth interviews with children suffering from Juvenile Chronic Arthritis. Scand J Disabil Res 2001;3:3-20. https://doi.org/10.1080/15017410109510765.
- Sällfors C, Fasth A, Hallberg LR. Oscillating between hope and despair – a qualitative study. Child Care Health Dev 2002;28:495-50. https://doi.org/10.1046/j.1365-2214.2002.00300.x.
- Sallfors C, Hallberg LRM. A parental perspective on living with a chronically ill child: a qualitative study. Fam Syst Health 2003;21:193-204. https://doi.org/10.1037/1091-7527.21.2.193.
- Hallberg L, Sallfors C. Fitting into the prevailing teenage culture: a grounded theory on female adolescents with chronic arthritis. Pain Pract 2009;9. https://doi.org/10.1111/j.1533-2500.2009.00267.x.
- Secor-Turner M, Scal P, Garwick A, Horvath K, Wells CK. Living with juvenile arthritis: adolescents’ challenges and experiences. J Pediatr Health Care 2011;25:302-7. https://doi.org/10.1016/j.pedhc.2010.06.004.
- Serafimova T, Ascough C, Parslow RM, Crawley E. Experiences of pain in paediatric chronic fatigue syndrome/myalgic encephalomyelitis: a single-centre qualitative study. BMJ Paediatr Open 2022;6. https://doi.org/10.1136/bmjpo-2021-001201.
- Shaygan M, Jaberi A. The effect of a smartphone-based pain management application on pain intensity and quality of life in adolescents with chronic pain. Sci Rep 2021;11. https://doi.org/10.1038/s41598-021-86156-8.
- Shaygan M, Jaberi A. The experience of chronic pain among adolescents: suffering and attempt to overcome pain?. BMC Pediatr 2022;22. https://doi.org/10.1186/s12887-022-03617-3.
- Skarstein S, Lagerløv P, Kvarme LG, Helseth S. High use of over-the-counter analgesic; possible warnings of reduced quality of life in adolescents – a qualitative study. BMC Nurs 2016;15. https://doi.org/10.1186/s12912-016-0135-9.
- Skarstein S, Lagerlov P, Kvarme LG, Helseth S. Pain and development of identity in adolescents who frequently use over-the-counter analgesics: a qualitative study. J Clin Nurs 2018;27:3583-91. https://doi.org/10.1111/jocn.14513.
- Skogvold L, Magnussen LH. Chronic tension-type headache and coping strategies in adolescents: a qualitative interview study. Physiother Res Int 2019;24. https://doi.org/10.1002/pri.1778.
- Slotter C. Adolescents with Chronic Pain and Their Peer Relationships: A Preliminary Study. West Hartford, CT: University of Hartford; 2021.
- Sorensen K, Skirbekk H, Kvarstein G, Woien H. I don’t want to think about it: a qualitative study of children (6–18 years) with rheumatic diseases and parents’ experiences with regular needle injections at home. Pediatr Rheumatol Online J 2021;19. https://doi.org/10.1186/s12969-021-00495-4.
- Ståhle-Öberg L, Fjellman-Wiklund A. Parents’ experience of pain in children with cerebral palsy and multiple disabilities – an interview study. Adv Physiother 2009;11:137-44. https://doi.org/10.1080/14038190902906318.
- Stiles-Shields C, Osos S, Sunnquist ML, Mak GZ, Skelly CL, Drossos T. Patient-reported experiences with median arcuate ligament syndrome: resilience and resources required. Clin Pract Pediatr Psychol 2022;10:44-53. https://doi.org/10.1037/cpp0000355.
- Stinson JN, Toomey PC, Stevens BJ, Kagan S, Duffy CM, Huber A, et al. Asking the experts: exploring the self-management needs of adolescents with arthritis. Arthritis Rheum 2008;59:65-72. https://doi.org/10.1002/art.23244.
- Stinson JN, Feldman BM, Duffy CM, Huber AM, Tucker LB, McGrath PJ, et al. Jointly managing arthritis: information needs of children with juvenile idiopathic arthritis (JIA) and their parents. J Child Health Care 2012;16:124-40. https://doi.org/10.1177/1367493511430679.
- Stinson JN, Lalloo C, Harris L, Isaac L, Campbell F, Brown S, et al. iCanCope with PainTM: user-centred design of a web- and mobile-based self-management program for youth with chronic pain based on identified health care needs. Pain Res Manag 2014;19:257-65.
- Stinson J, Harris L, Garofalo E, Lalloo C, Isaac L, Brown S, et al. Understanding the use of over-the-counter pain treatments in adolescents with chronic pain. Can J Pain 2017;1:84-93. https://doi.org/10.1080/24740527.2017.1337468.
- Szwimer R, Widjaja M, Ingelmo P, Hovey RB. A phenomenological exploration of the personal implications of female adolescents living with chronic pain. J Pediatr Health Care 2020;34:470-7. https://doi.org/10.1016/j.pedhc.2020.05.004.
- Tong A, Jones J, Speerin R, Filocamo K, Chaitow J, Singh-Grewal D. Consumer perspectives on pediatric rheumatology care and service delivery: a qualitative study. J Clin Rheumatol 2013;19:234-40. https://doi.org/10.1097/RHU.0b013e31829d4e82.
- Valenzuela JM, Vaughn LM, Crosby LE, Strong H, Kissling A, Mitchell MJ. Understanding the experiences of youth living with sickle cell disease: a photovoice pilot. Fam Community Health 2013;36:97-108. https://doi.org/10.1097/FCH.0b013e318282b2f2.
- van Gulik EC, Verkuil F, Barendregt AM, Schonenberg-Meinema D, Rashid ANS, Kuijpers TW, et al. Experiences, perspectives and expectations of adolescents with juvenile idiopathic arthritis regarding future work participation; a qualitative study. Pediatric Rheumatology Online J 2020;18. https://doi.org/10.1186/s12969-020-00429-6.
- van Tilburg MA, Venepalli N, Ulshen M, Freeman KL, Levy R, Whitehead WE. Parents’ worries about recurrent abdominal pain in children. Gastroenterol Nurs 2006;29:50-5; quiz 56. https://doi.org/10.1097/00001610-200601000-00009.
- Voigtman JL. Learning to Suffer: Pain Response in a Community of Saudi Arab Children with Sickle Cell Disease. Tucson, AZ: The University of Arizona; 2002.
- Wakefield EO, Zempsky WT, Puhl RM, Litt MD. Conceptualizing pain-related stigma in adolescent chronic pain: a literature review and preliminary focus group findings. Pain Rep 2018;3. https://doi.org/10.1097/PR9.0000000000000679.
- Wakefield EO, Puhl RM, Litt MD, Zempsky WT. ‘If it ever really hurts, I try not to let them know’: the use of concealment as a coping strategy among adolescents with chronic pain. Front Psychol 2021;12. https://doi.org/10.3389/fpsyg.2021.666275.
- Wakefield EO, Belamkar V, Litt MD, Puhl RM, Zempsky WT. ‘There’s nothing wrong with you’: pain-related stigma in adolescents with chronic pain. J Pediatr Psychol 2022;47:456-68. https://doi.org/10.1093/jpepsy/jsab122.
- Walter SM. The experience of adolescents living with headache. Holist Nurs Pract 2017;31:280-9. https://doi.org/10.1097/HNP.0000000000000224.
- While AE, Mullen J. Living with sickle cell disease: the perspective of young people. Br J Nurs 2004;13:320-5. https://doi.org/10.12968/bjon.2004.13.6.12528.
- Woodgate RL. Adolescents’ perspectives of chronic illness: ‘it’s hard’. J Pediatr Nurs 1998;13:210-23.
- Yeung KK, Engle L, Rabel A, Adamson K, Schwellnus H, Evans C. It just feels weird!: a qualitative study of how children aged 10–18 years describe neuropathic pain. Disabil Rehabil 2017;39:1695-702. https://doi.org/10.1080/09638288.2016.1207107.
- Britton CA, Moore A. Views from the inside, part 3: how and why families undertake prescribed exercise and splinting programmes and a new model of the families’ experience of living with juvenile arthritis. Br J Occup Ther 2002;65:453-60. https://doi.org/10.1177/030802260206501004.
- Forgeron P, McGrath P. Self-identified needs of youth with chronic pain. J Pain Manag 2008;1:163-72.
Appendix 1 MEDLINE search strategy
-
Qualitative Research/or Interview/or Nursing Methodology Research/,
-
(ethnonursing or phenomenol* or emic or etic or hermeneutic* or heuristic* or semiotic* or theoretical sampl*).ti,ab.,
-
(qualitative adj3 (study or research or method* or analysis or cod* or them* or interview* or question*1 or data)).ti,ab.,
-
(thematic analysis or ethnological research or ethnograph* or life stor*).ti,ab.,
-
(theme*1 adj2 (qualitative or analysis or coding or codes or grouping or identif*)).ti,ab.,
-
(grounded adj2 (theor* or study or studies or research or analys?s)).mp.,
-
(data adj1 saturat*).ti,ab.,
-
(‘social construct*’ or postmodern* or post-structural* or post structural* or poststructural* or post modern* or post-modern* or feminis* or action research or cooperative inquir* or co operative inquir* or co-operative inquir* or humanistic or existential or experiential).mp.,
-
(field adj (study or studies or research)).ti,ab.,
-
(human science or biographical method or participant observ*).ti,ab.,
-
((purpos* adj4 sampl*) or (text* adj1 analysis) or (focus group* or observational method* or ‘content analysis’ or ‘narrative analysis’)).mp.,
-
(unstructured or open-ended or open ended or narratives or life world or life-world or conversation analys?s or personal experience* or theoretical saturation).mp.,
-
((lived or life or patient or carer* or guardian* or parent* or mother* or father* or family*) adj2 (account or accounts or perspective* or interpretations or experience*)).ti,ab.,
-
((children* or adolescent*) adj2 (account or accounts or perspective* or interpretations or experiences or experience)).ti,ab.,
-
or/1–14,
-
(adolescen* or preadolescen* or baby or babies or infan*2 or toddler* or preschool* or pre-school* or child or children or childhood or girls or boys or kid or kids or juvenile or teen* or preteen* or youth or youngster*).ti,ab.,
-
(pupil or pupils or school-aged or school pupil* or schoolchild* or paediatric* or pediatric*).ti,ab.,
-
exp child/or adolescent/or Parent-Child Relations/,
-
((carer* or caregiver* or family or families) and (child or children or young*)).ti,ab.,
-
(parent*1 or mother*1 or father*1 or daughter*1 or son or sons).ti,ab.,
-
or/16–20,
-
exp Chronic Pain/or exp Complex Regional Pain Syndromes/,
-
((chronic or longterm or long?term or persist* or sustain* or continued or continuous or recurr*) adj5 (pain* or cephalalgi* or ache or aches)).ti,ab.,
-
((chronic or longterm or long?term or persist* or sustain* or recurr* or frequent) adj5 (headache or migraine or cramps or cramping)).ti,ab.,
-
(pain* adj3 (condition or conditions or disorder or disorders or illness or illnesses or disease or diseases or recurrent or debilitating or complex or long*)).ti,ab.,
-
(((chronic or long-term) adj3 (condition or conditions or disorder or disorders or illness or illnesses or disease or diseases)) and pain*).ti,ab.,
-
(pain* adj3 (neuropathic or syndrome*)).ti,ab.,
-
(pain* and (sickle cell disease or arthritis or chronic pancreatitis or lupus or costochondritis or tietze syndrome or ‘ehler’s’ or fibromyalgia or irritable bowel syndrome or ibs or reflex sympathetic dystrophy or non-cardiac chest pain or chronic fatigue syndrome or myalgic encephalomyelitis or ‘me/cfs’ or endometriosis or Dysmenorrhea or Inflammatory bowel disease or IBD)).ti,ab.,
-
exp Pain/and exp Chronic Disease/,
-
or/22–29,
-
15 and 21 and 30,
Appendix 2 Development of third-order constructs within pain condition groupings
The table shows development of synthesis from second-order constructs derived from included studies to identifying common or unique second-order constructs and developing third-order constructs.
| Pain condition grouping | Second-order constructs from included primary studies (either the authors’ or the review authors’) | Common or unique second-order constructs from included studies (Phase 5 translation) | Third-order constructs (interpreted by review authors) (Phase 6 synthesising translations) |
|---|---|---|---|
| Sickle cell disease | Atkin124
|
|
Control (perceived control and perceived lack of control) (CYP and parents) |
Atkin125
|
|||
Dyson130
|
|||
Atkin124
|
|
Trying to live a normal life (CYP and parents) | |
Atkin125
|
|||
Atoui148
|
|||
Atkin124
|
|
Loss of faith and trust in medical systems | |
Atkin125
|
|||
Renedo82
|
|||
Atkin125
|
|
Self-management of painful episodes (adolescents) | |
Renedo82
|
|||
Dyson130
|
|||
Atkin124
|
|
Coping strategies and vulnerabilities (CYP and parents) | |
Atkin125
|
|||
Atoui148
|
|||
Atkin125
|
|
Unsafe and unprepared schools (CYP) | |
Atoui148
|
|||
Dyson130
|
|||
Atkin125
|
|
Ambivalent family relationships (CYP and parents) | |
Atoui148
|
|||
Njifon149
|
|||
|
|||
Atkin125
|
Ambiguity of social relationships | ||
Atoui148
|
|||
Dyson130
|
|||
Atoui148
|
Disabling and psychosocial effects of pain/sickle cell disease | ||
Njifon149
|
|||
Atkin125
|
|
Racism and disabling attitudes | |
Atoui148
|
|||
Dyson130
|
|
||
Renedo82
|
|||
Atkin124
|
|||
| Unspecified chronic pain | Nutkiewicz140
|
Biomedical perspective of pain is a barrier to effective treatment, biopsychosocial perspective is a facilitator/the need for holistic biopsychosocial care | |
Kanstrup139
|
|||
| Neurological conditions | Carter119
|
|
Parent’s expert and intuitive/subjective knowledge of their child’s pain |
Carter109
|
|||
Hunt110
|
|||
Carter119
|
|
Parents managing pain and making difficult decisions about this alone | |
Carter109
|
|||
Hunt110
|
|||
Carter119
|
|
Parents as healthcare advocates | |
Carter109
|
|||
Carter119
|
|
Visible diagnosis, invisible child/pain | |
Carter109
|
|||
Hunt110
|
|||
Castle141
|
|
Healthcare professionals should believe the pain is real/establishing the legitimacy of the pain | |
| Hunt110 | |||
Paying attention to parents and child
|
|||
Carter109
|
|
Parents value validation from healthcare professionals | |
Castle141
|
|||
Hunt110
|
|||
Carter119
|
|
Children’s and parents’ varied experiences/perceptions of pain | |
Castle141
|
|||
| Musculoskeletal conditions | Khanom122
|
|
Young people’s strategies to restore ‘control’ of daily life and pain |
Forgeron142
|
|||
Ahlqwist137
|
|||
Forgeron142
|
|
Young people’s desire to live a normal life challenged by all aspects associated with chronic pain (which causes feeling of powerlessness and frustration) | |
Khanom122
|
|||
Ahlqwist137
|
|||
| Management strategies | |||
Ahlqwist137
|
|
Pain affects social role of young people (with family, friends and peers) | |
Forgeron142
|
|||
Khanom122
|
|||
Ahlqwist137
|
|
Pain negatively affects young people’s self-identity (stigma, lower self-esteem, feel abnormal but want to be treated as normal) | |
Forgeron142
|
|||
Khanom122
|
|||
Ahlqwist137
|
|
||
| Abdominal pain | Brodwall75
|
|
The complexity of [accessing and accepting] psychosocial support [parents] |
Smart76
|
|||
Brodwall75
|
Importance of diagnosis [for parents] | ||
Smart76
|
|||
Brodwall75
|
Parents’ interaction/relationship with healthcare professionals and desired outcomes | ||
Smart76
|
|||
Smart76
|
Parents/mother (feel like they) have to recognise and manage child’s pain (by using intuition/sense of knowing) | ||
Brodwall75
|
Biomedical vs. psychosocial orientation (of parents) | ||
Smart76
|
|||
Brodwall75
|
|
Mothers feel responsible for child’s health and feel judged by healthcare professionals | |
Smart76
|
|||
| Complex regional pain syndrome | Gaughan143
|
|
Chronic pain makes the future uncertain |
Jones#120
|
|||
Gaughan143
|
|
Parent and child loss of control | |
Jones120
|
|||
Gaughan143
|
|
Importance of social context | |
Jones120
|
|||
Gaughan143
|
|
Important treatment outcome | |
Jones120
|
|||
Jones120
|
|
N/A (no third-order constructs could be developed) | |
Gaughan143
|
|
N/A (no third-order constructs could be developed) | |
| Dysmenorrhoea | Wong134
|
|
N/A (no third-order constructs could be developed) |
Wong134
|
|
N/A (no third-order constructs could be developed) | |
| Epidermolysis Bullosa | Williams123
|
|
N/A (no third-order constructs could be developed) |
Williams123
|
|
N/A (no third-order constructs could be developed) | |
Williams123
|
|
N/A (no third-order constructs could be developed) | |
Williams123
|
|
N/A (no third-order constructs could be developed) | |
| Headache | Helvig144
|
|
N/A (no third-order constructs could be developed) |
| Juvenile idiopathic arthritis | Britton80
|
|
Negative psychosocial/mental health impacts of juvenile idiopathic arthritis on whole family (child, parents, siblings) |
Britton79
|
|||
Waite-Jones126
|
|||
Cartwright131
|
|||
Guell132
|
|
Juvenile idiopathic arthritis and its management dominates and strains family life and changes family dynamics | |
Britton80
|
|||
Rosatto145
|
|||
Britton79
|
|||
Britton80
|
|
Impact on child’s self-identity | |
Guell132
|
|||
Cartwright131
|
|||
Britton80
|
|
Trying to achieve a ‘new normality’ | |
Rosatto145
|
|||
Guell132
|
|||
Waite-Jones126
|
|||
Cartwright131
|
|||
| Mixed conditions | Carter117
|
|
Medical encounters – the importance of communication (being listened to and believed) |
Carter118
|
|||
Maciver77
|
|
||
Maciver78
|
|||
Jordan34
|
|||
Neville36
|
|||
Dell’Api138
|
|||
Suder147
|
|||
Baert102
|
|||
Sorensen146
|
|||
Carter118
|
|
Parents and young people – loss of normality [or loss of a normal life and childhood] | |
Borghi133
|
|||
Maciver77
|
|||
Maciver38
|
|
||
Sorensen146
|
|
||
Dell’Api138
|
|||
Jordan34
|
|||
Suder147
|
|||
Baert102
|
|||
Carter117
|
|
Biomedical model vs. biopsychosocial (families and healthcare professionals) | |
Maciver77
|
|||
Maciver78
|
|||
Sorensen146
|
|||
Neville36
|
|||
Dell’Api138
|
|||
Maciver77
|
|
Non-normative parenting | |
|
|||
| Maciver38 | |||
Jordan35
|
|||
Carter118
|
|
Pain affects/impacts parents and CYP physically and emotionally | |
Carter117
|
|||
Suder147
|
|
||
Maciver77
|
|
||
|
|||
|
|||
Maciver38
|
|||
Jordan35
|
|||
Jordan34
|
|||
Sorensen146
|
|||
Suder147
|
|||
Neville36
|
|||
Carter118
|
Getting on with it (CYP and parents) | Getting on with it (CYP and parents) | |
Suder147
|
|||
Sorensen146
|
|||
Baert102
|
|||
Carter118
|
|
N/A (no third-order constructs could be developed) | |
Borghi133
|
|||
Sorensen146
|
|||
Suder147
|
|||
Jordan121
|
|||
Sorensen146
|
|
N/A (no third-order constructs could be developed) | |
Baert102
|
|
N/A (no third-order constructs could be developed) |
Appendix 3 Questions asked during an online patient and public involvement meeting to help with sampling decisions
-
What do you want to get out of the CHAMPION project? (You can choose more than one answer)
-
□ I want to make treatment better for young people living with pain
-
□ I want to help researchers learn new important information
-
□ I want to know more about young people living with pain
-
□ I want to be heard
-
□ I don’t know
-
□ Other __________________________________________
-
-
Lots of young people get certain types of pain like headaches or period pain, but we have few or no studies in the UK about these illnesses. Do you think we should use studies from other countries, even though their treatments and services might be different?
-
□ No
-
□ Maybe
-
□ Yes
-
□ I don’t know
-
-
There are some rarer illnesses that can be painful like cystic fibrosis or lupus. We have no studies in the UK about these illnesses. Do you think we should use studies from other countries, even though their treatments and services might be different?
-
□ No
-
□ Maybe
-
□ Yes
-
□ I don’t know
-
-
We didn’t find many UK studies answering the question: ‘what do young people and their families want from services and treatments (NHS)’. Studies from other countries won’t be talking about our NHS, but they might have useful information on other types of treatments and services. Do you think we should also include studies from other countries, even though they won’t be talking about our NHS?
-
□ No
-
□ Maybe
-
□ Yes
-
□ I don’t know
-
-
We rated each study as poor, good or excellent based on how well they helped us to answer our questions. We were going to only include the excellent studies, but we wanted to ask you if you think that we should also include the studies rated as good and poor.
-
□ Just include the excellent studies
-
□ Include the excellent and the good studies
-
□ Include all the UK studies
-
□ I don’t know
-
Appendix 4 Table of eligible studies
| Author | Country | Recruitment setting | Aim | Participant details | Chronic pain condition | Data collection | Data analysis | Richness | Funder |
|---|---|---|---|---|---|---|---|---|---|
| Ahlqwist137 | Sweden | Unclear | Generate a substantive theory, based on interviews with adolescents with low back pain, explaining how they succeed in managing their main concerns in daily life. | 12–18 years n = 14 8 females 6 males Ethnic origin not stated |
Musculoskeletal pain | Interview | Grounded theory | 3 | Swedish Association of Registered Physiotherapists and Renee Eanders Foundation |
| Ahola184 | Canada | Information not extracted from un-sampled studies | Explore the topics of discussion during open-ended peer mentoring sessions between adolescents and mentors living with chronic illness | 12–17 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Canadian Institutes of Health Research Catalyst Grant, Pain in Child Health, J.S.’s Early Research Award |
| Ajinkpang115 | Ghana | Information not extracted from un-sampled studies | Explore the knowledge of caregivers | 2–14 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Ali185 | USA | Information not extracted from un-sampled studies | Assess the feasibility of a mindfulness-based stress reduction (MBSR) programme | 10–19 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Center for Complementary and Integrative Health and National Center for Advancing Translational Sciences |
| Allgood186 | USA | Information not extracted from un-sampled studies | Explore patient-reported descriptions of the pain experience among adolescents and adults living with CF | 10–19 years No further information extracted from un-sampled studies |
Cystic fibrosis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Unfunded |
| Asmussen103 | USA | Information not extracted from un-sampled studies | Investigated how otitis media impacts the day-to-day lives and experiences of children and their families | Infant – 9 years No further information extracted from un-sampled studies |
Otitis media | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | SmithKline Beecham, Henry J Kaiser Family Foundation, American Academy of Pediatric’s Friends of Children Fund |
| Atkin124 | UK | Health professional records | Examines how parents cope with their caring responsibilities | Age of children not reported n = 62 17 couples (child has thalassaemia) 25 parents (8 couples) child has a sickle cell disease |
Sickle cell disease and thalassaemia | Interview | Not reported | 2 | NHS Executive |
| 34 mothers 25 fathers 3 guardians Ethnicity of families: 11 Caribbean in origin 1 Indian 1 Algerian 1 Nigerian 3 mixed ethnic origin |
|||||||||
| Atkin125 | UK | Health professional records | Provide a detailed understanding of young people’s experience of living with these conditions | Average age = 14.2 years n = 26 14 females, 12 males Ethnicity: 19 ‘African Caribbean’ 6 ‘mixed’ 1 ‘Indian Hindu’ |
Sickle cell disease | Interview | Case comparative | 2 | National Lottery |
| Atoui148 | Lebanon | Paediatric clinics | Explore adolescents’ lived experience and daily life with sickle cell disease in Lebanon | 12–17 years n = 12 Ethnicity/nationality: 6 Lebanese Muslim 6 Palestinian Muslim |
Sickle cell disease | Interview | Thematic analysis | 2 | Not reported |
| Baert102 | USA, UK, Belgium | Paediatric hospitals | Explore parents’ views of the meaning of injustice | 9–20 years n = 21 mothers of 14 females 7 males Ethnicity: all white |
Mixed conditions | Interview | Interpretative Phenomenological Analysis | 2 | International Association for the Study of Pain grant |
| Bagge-Petersen187 | Denmark | Information not extracted from un-sampled studies | Explores ethnographically the self-care practices of children affected by haemophilia or juvenile idiopathic arthritis in Denmark | 7–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Center of Telemedicine, Copenhagen, Center for Health Technology (CACHET |
| Barlow188 | UK | Information not extracted from un-sampled studies | Gain greater insight and understanding into the experience of parents in terms of the stressors encountered and the resultant impact on parental well-being | 8–15 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Barlow189 | UK | Information not extracted from un-sampled studies | Gain insight and understanding of the needs and preferences of children with juvenile arthritis and their parents | 8–15 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | NHS Executive |
| Beneitez190 | Spain | Information not extracted from un-sampled studies | Gain knowledge about adolescents’ social needs living with juvenile idiopathic arthritis, particularly focused on their friendships | 11–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | UOC PhD Doctoral Fellowship |
| Beyer191 | USA | Information not extracted from un-sampled studies | Examine caregivers’ views of the effectiveness of home comfort for children with VOE | 5–19 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | NINR |
| Borghi133 | Brazil | Paediatric hospital | Understanding the experience of children and adolescents under palliative care when managing pain daily | 6–17 years n = 6 4 females 2 males Ethnic origin not stated |
Mixed conditions | Interview | Thematic oral history | 2 | Not reported |
| Bradshaw192 | UK | Information not extracted from un-sampled studies | Evaluate the effectiveness of the service in reducing the impact of pain in the lives of the young patients | 10–17 years No further information extracted from un-sampled studies |
Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Not reported |
| Brandelli105 | Canada | Recruited from a larger study | Explore the lived experiences of parents with self-identified challenges with their child’s pharmacological and/or nonpharmacological juvenile idiopathic arthritis treatments | 4–16 years n = 10 10 mothers Ethnic origin not stated |
Juvenile idiopathic arthritis | Interview | Interpretative phenomenological analysis | 2 | IWK Health Centre, Arthritis Society, Maritime SPOR Support Unit, Nova Scotia Graduate Scholarship, Nova Scotia Health Research Foundation, Dalhousie Medical Research Foundation, Canada Foundation for Innovation. Canadian Institutes of Health Research |
| Brekke193 | Norway | Information not extracted from un-sampled studies | Investigate the course of the child’s abdominal pain, what may have helped, how the family’s situation had been influenced and whether they had any unmet needs | 8–17 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Norwegian Committee on Research in General Practice |
| Britton194 | UK | Information not extracted from un-sampled studies | Investigate families’ experiences and perspectives | 7–8 or 11–13 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Arthritis Research Campaign |
| Britton80 | UK | Juvenile arthritis clinic | To investigate the experiences of families who currently live with a child with juvenile idiopathic arthritis | 7–8 or 11–13 years n = 27 9 children 14 parents 4 siblings Ethnic origin not stated |
Arthritis | Questionnaire, diary and interview | Ethnographic processes | 2 | Arthritis Research Campaign |
| Britton79 | UK | Juvenile arthritis clinic | Explore and describe the experiences of families of children with juvenile idiopathic arthritis | 7–8 or 11–13 years n = 27 9 children 14 parents 4 siblings Ethnic origin not stated |
Arthritis | Interview and video diaries | Grounded theory | 3 | Arthritis Research Campaign |
| Brodwall75 | Norway | Hospital | Explore the experiences of parents of children with chronic abdominal pain discharged from hospital without a somatic explanation | 5–15 years n = 15 parents Ethnic origin not stated |
Abdominal pain | Interview | Content analysis | 2 | Norwegian Committee on Research in General Practice |
| Bruce195 | Canada | Information not extracted from un-sampled studies | Understand the changes in QoL for adolescent patients with sickle cell disease a year after transplant | 13–18 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Stollery Children’s Hospital Foundation, Women and Children’s Health Research Institute |
| Burbage196 | USA | Information not extracted from un-sampled studies | Educate and provide support for families with a child who has juvenile idiopathic arthritis as well as assess parent perceptions | 7–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Carter118 | UK | Paediatric hospital | Explore the way in which the experience of chronic pain impacts on the lives of young people | 13–19 yearsn = 5 | Mixed conditions | Focus group | Theoretical coding technique | 3 | Not reported |
| Carter119 | UK | Paediatric hospital | Explore the ways in which parents of children with profound special needs assess and manage their children’s pain | 5–16 years n = 15 15 parents/carers (12 families) Ethnic origin not stated |
Neurological conditions | Interview | Thematic analysis | 3 | Not reported |
| Carter117 | UK | Unclear | Explore, from the children’s and families’ perspectives, the impact of living with chronic pain | 12–13 years n = 11 3 children 7 parents 1 sibling Ethnic origin not stated |
Mixed conditions | Interview and journal | Thematic analysis | 3 | Nestlé Charitable Scholarship |
| Carter109 | UK | Paediatric hospital | Explore the frequency, regularity and intensity of parent-reported pain episodes experienced by children with PCI and their parents’ knowledge and skills in assessing their child’s pain | 2–16 years n = 8 8 mothers Ethnic origin not stated |
Neurological conditions | Interview and Survey | Thematic analysis | 3 | Not reported |
| Cartwright131 | UK | Adolescent arthritis clinic | Explore adolescents’ experiences of living with juvenile idiopathic arthritis, with particular focus on the process of adjustment | 13–17 years n = 10 7 females 3 males Ethnic origin not stated (except state bias towards white participants) |
Arthritis | Interview | IPA | 2 | Not reported |
| Castle141 | Australia | Paediatric hospital | Explore the experience and impact of chronic pain on the lives of adolescents and young adults with cerebral palsy | 14–24 years n = 6 2 females 4 males Ethnic origin not stated |
Cerebral palsy | Interview | Phenomenology | 2 | Not reported |
| Conboy197 | USA | Information not extracted from un-sampled studies | Understand the experiences of adolescents involved in acupuncture treatment | 13–22 years No further information extracted from un-sampled studies |
Endometriosis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Constantinou198 | UK | Information not extracted from un-sampled studies | Explore the health-related quality of life and health behaviours of children with sickle cell disease and healthy siblings | 5–12 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Corey199 | USA | Information not extracted from un-sampled studies | To characterise parent experiences during a multidisciplinary exposure-based treatment for children with chronic pain who express high fear of pain and pain-related disability | 8–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | American Pain Society/Sharon S. Keller Chronic Pain Research Grant, Deborah Munroe Noonan Memorial Research Fund |
| Cotton200 | USA | Information not extracted from un-sampled studies | Examine use of religious coping in children with sickle cell disease | 5–12 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institute of Child Health and Human Development |
| Cox201 | UK | Information not extracted from un-sampled studies | Explore how parental dyads experience and demonstrate resilience in response to parenting an adolescent with complex regional pain syndrome | 11–25 years No further information extracted from un-sampled studies |
CRPS | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Cunningham202 | USA | Information not extracted from un-sampled studies | Evaluate the feasibility and acceptability of the Aim to Decrease Anxiety and Pain Treatment (ADAPT) | 10–19 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | NIH grants |
| Cunningham203 | USA | Information not extracted from un-sampled studies | Develop and refine the Treatment and Education Approach for Childhood-onset Lupus (TEACH) protocol | 10–19 years No further information extracted from un-sampled studies |
Childhood-onset systemic lupus erythematosus (cSLE) | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institutes of Arthritis and Musculoskeletal and Skin Diseases, Cincinnati Children’s Research Foundation Academic Research Centers award |
| Curtis204 | Germany | Information not extracted from un-sampled studies | Develop a theory-and-evidence-based medication adherence app to support children and adolescents with sickle cell disease | 10–19 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Charité |
| Dell’Api138 | Canada | Paediatric hospital | Develop an understanding of the way in which children with chronic pain experienced, assigned meaning and described their interactions with healthcare professionals | 10–17 years n = 5 3 girls 2 boys Ethnic origin not stated |
Mixed conditions | Interview | Interpretive description | 2 | Not reported |
| De Monte205 | Australia | Information not extracted from un-sampled studies | Understand the children’s perspective on living with juvenile idiopathic arthritis | 8–16 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Not reported |
| De Moura206 | Brazil | Information not extracted from un-sampled studies | Analyse the perceptions of children and adolescents about chronic postsurgical pain | 8–15 years No further information extracted from un-sampled studies |
Inguinal herniorrhaphy | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Dogan207 | Germany | Information not extracted from un-sampled studies | Gain further insight into the mechanisms and prerequisites for the effectiveness of this specialised aftercare programme | 9–16 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | German Innovation Fund of The Federal Joint Committee |
| Donovan208 | USA | Information not extracted from un-sampled studies | Understand the impact of migraines on adolescents’ social functioning from multiple informants | 12–17 years No further information extracted from un-sampled studies |
Headache | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Eunice Kennedy Shriver National Institute of Child Health and Human Development |
| Donovan209 | USA | Information not extracted from un-sampled studies | Describe the experiences of adolescents with irritable bowel syndrome (IBS) | 13–17 years No further information extracted from un-sampled studies |
Irritable bowel syndrome | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institute of Diabetes and Digestive and Kidney Diseases |
| dos Santos210 | Brazil | Information not extracted from un-sampled studies | Understand the experiences of being a teenager with sickle cell disease | Adolescents | Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Council for Scientific and Technological Development |
| Dyson130 | UK | Support groups, counselling centres and clinics | Examines the experiences of young people living with a sickle cell disorder (sickle cell disease) in schools in England | 5–25 years n = 32 Ethnicity: 24 Black African 15 Black Caribbean 1 British Asian (Indian) |
Sickle cell disease | Interview | Thematic analysis | 2 | Not reported |
| Evans211 | USA | Information not extracted from un-sampled studies | Examine sex-specific parent–child relationships in the development of chronic pain in preadolescent and adolescent children | 11–19 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | NIMH Grant and Mayday Fund |
| Evans212 | USA | Information not extracted from un-sampled studies | Explore, the full range of teens’ experiences with the yoga programme | 14–17 years No further information extracted from un-sampled studies |
Irritable bowel syndrome | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | NCCAM grant, Oppenheimer Seed Grant for Complementary, Alternative and Integrative Medicine, UCLA Clinical and Translational Science Institute Grant and UCLA Children’s Discovery and Innovation Institute |
| Forgeron142 | Canada | Paediatric pain clinic | Explore the self-identified needs of adolescents living with chronic pain | 13–17 years n = 6 Ethnicity: all Caucasian |
Musculoskeletal pain | Focus groups and interview | Thematic analysis | Not assessed | Rising Researcher Support Award |
| Forgeron213 | Canada | Information not extracted from un-sampled studies | Explore peer relationships and, particularly, close friendships of adolescents with chronic pain to understand and identify factors that affect these relationships | 14–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 3 | Canadian Institute of Health Research Doctoral Fellowship, IWK Ruby Blois Scholarship and IWK Grant |
| Gaughan143 | USA | Paediatric hospital | Describe the parents’ journey with their child from initial incidence of pain through the labyrinth of treatment options | 11–17 years n = 13 8 mothers 5 fathers Ethnic origin not stated |
Chronic regional pain syndrome | Interview | Content analysis | 3 | Ian Katz Fund |
| Gernet214 | France | Information not extracted from un-sampled studies | Explore the emotional representations of sickle cell children followed up at Bordeaux University Hospital | 7–15 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Ghio215 | UK | Information not extracted from un-sampled studies | Investigate the extent to which adolescents’ illness beliefs could be assessed using the IPQ-R | 11–16 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Arthritis Research UK |
| Ghio216 | UK | Information not extracted from un-sampled studies | Explore the coping goals and related personal models (cognitive and emotional profiles) of juvenile idiopathic arthritis of both the adolescents and their parent | 11–16 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Arthritis Research UK National Institute for Health Research Manchester Musculoskeletal Biomedical Research Unit Funding Scheme |
| Gibler217 | USA | Information not extracted from un-sampled studies | Refine the School Anxiety Inventory | 12–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | University of Cincinnati Department of Psychology Seeman-Frakes Graduate Student Research grant |
| Goldenberg218 | USA | Information not extracted from un-sampled studies | Utilise peers who have learnt to self-manage their own chronic pain to assist patients with social coping skills to reduce isolation | 17 years No further information extracted from un-sampled studies |
Diffuse chronic body pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institute of Child Health and Human Development |
| Gómez-Ramírez113 | Canada | Information not extracted from un-sampled studies | Describes the predominant emotional experiences reported by parents of children with juvenile idiopathic arthritis in two Canadian cities | 2–16 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Canadian Rheumatology Association |
| Gordon219 | Canada | Information not extracted from un-sampled studies | Investigate how children with IBD and their families perceived their school experiences in Québec | 10–18 years No further information extracted from un-sampled studies |
Irritable bowel syndrome | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Gorodzinsky220 | USA | Information not extracted from un-sampled studies | Assesses treatment provided at a multidisciplinary chronic pain clinic | Not reported for age. No further information extracted from un-sampled studies | Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Gorodzinsky221 | USA | Information not extracted from un-sampled studies | The experiences of youth with chronic pain and their siblings, and their perspectives on how pain experiences influence family dynamics | 12–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Gremillion222 | USA | Information not extracted from un-sampled studies | To better understand the challenges experienced by adolescents with CPO, with a specific focus on physical activity | 13–17 years No further information extracted from un-sampled studies |
Obesity | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Unfunded |
| Guell132 | UK | Self-help organisation and hospital | Explores the everyday life and coping of children living with juvenile arthritis | 7–16 years n = 4 Families Ethnic origin not stated |
Arthritis | Observation | Ethnography | 2 | Not reported |
| Hackett223 | UK | Information not extracted from un-sampled studies | Gather in-depth qualitative information on play and leisure experiences from junior school-aged children with juvenile idiopathic arthritis | 7–11 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Arthritis Research Campaign |
| Haridasa224 | USA | Information not extracted from un-sampled studies | Identify the perceptions of children with sickle cell disease in the school environment | 6–10 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Heffernan225 | Ireland | Information not extracted from un-sampled studies | Explore beliefs about and experiences of worry and pain among a purposeful sample of adolescents with chronic pain | 12–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Not reported |
| Helvig144 | USA | Unclear | Explored the experience of living with migraines in six adolescents | Average age = 14 years n = 6 4 females 12–17 years Ethnicity: 2 African Americans 4 Caucasians |
Headache | Interview | Not reported | 2 | Not reported |
| Hendry226 | UK | Information not extracted from un-sampled studies | Explore the perceived impact of disease-related foot problems and foot care in juvenile idiopathic arthritis from the perspectives of patients, parents, paediatric rheumatologists and health professionals | 7 and 9 year old No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Not reported |
| Hilário227 | Portugal | Information not extracted from un-sampled studies | Explore children’s and parents’ experience of uncertainty and perceptions of risk resulting from chronic pain in childhood | 7–17 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Fundação para a Ciência e a Tecnologia, I.P |
| Hollier228 | USA | Information not extracted from un-sampled studies | Assess acceptability of a proposed guided imagery therapy app designed to treat functional abdominal pain disorders | 7–12 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | US National Institutes of Health, Texas Medical Center Digestive Diseases Center, US Department of Agriculture |
| Hulgaard229 | Denmark | Information not extracted from un-sampled studies | Explore illness perceptions of youth with functional disorders and their parents | 11–15 years No further information extracted from un-sampled studies |
Functional disorders | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 3 | Helsefonden, Psychiatric Research Fund |
| Hulgaard230 | Denmark | Information not extracted from un-sampled studies | Explore parents’ experiences of challenges related to their care for a child receiving treatment for functional disorders | 11–16 years No further information extracted from un-sampled studies |
Functional disorders | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 3 | Helsefonden, Psychiatric Research Fund |
| Hunt110 | UK | Neuro-disability centre, charitable trust and paediatric hospices | Gain an understanding of the context in which pain occurs and of issues that could affect pain assessment and management in this group | Average age = 11 years n = 25 Parents Children aged 2–18 years Ethnic origin not stated |
Neurological impairment | Interview | Grounded theory | 3 | Not reported |
| Hurtubise231 | Canada | Information not extracted from un-sampled studies | Describe and compare the treatment effects and outcomes as perceived by youth and their parents enrolled in intensive interdisciplinary pain treatment or multimodal treatment | 12–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Vanier Scholarship, Canadian Child Health Clinical Scientist, Pain in Child Health programs |
| Iliyasu114 | Nigeria | Information not extracted from un-sampled studies | Explore caregivers’ perceptions on sociobehavioural and environmental influences on hospitalisation for pain and blood transfusion of children with sickle cell disease | 3–11 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Unfunded |
| Jacobson232 | USA | Information not extracted from un-sampled studies | Examine the content validity of the Patient-Reported Outcomes Measurement Information System paediatric measures | 8–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | American Institutes for Research and a range of university funding |
| Jacobson233 | USA | Information not extracted from un-sampled studies | Evaluate the overall conceptual scope and content validity, or fit, of the PROMIS pain domain framework | 8–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | American Institutes for Research and a range of university funding |
| Jensen234 | USA | Information not extracted from un-sampled studies | Identify commonalities and differences in symptom experiences across age groups to better assist individuals to adjust to symptoms across the lifespan | 5–17 years No further information extracted from un-sampled studies |
Neurofibromatosis type 1 | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Neurofibromatosis Therapeutic Acceleration Program (NTAP) |
| Jones235 | Australia | Information not extracted from un-sampled studies | To assist occupational therapists and other healthcare professionals to facilitate children’s ability to live with juvenile idiopathic arthritis and participate optimally in home exercise programmes | 8–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | ? | Not reported |
| Jones120 | UK | Social media and newsletters | Explore the relative frequencies of hoped-for and feared-for future selves, and how these are expressed in the future narratives of adolescents with CRPS | 14–25 years Average age = 19 years n = 50 44 females 5 males 1 not declared Ethnic origin not stated |
Chronic regional pain syndrome | Interview | Thematic analysis | 3 | Not reported |
| Jones128 | UK | NHS tertiary pain service | Explore how adolescents make sense of their experience of chronic pain in the context of development | 12–22 years Average age = 15.7 years n = 9 8 females 1 male Ethnicity: all White British |
Mixed conditions | Interview | Thematic analysis | 2 | Pain Relief Foundation |
| Jordan34 | UK | Paediatric rheumatology and pain management clinic | Investigate parental experiences of caring for an adolescent with chronic pain | 13–18 years, n = 17 parents 11 mothers 5 fathers 1 grandmother Ethnic origin not stated |
Mixed condition | Focus group | IPA | 3 | BUPA Foundation |
| Jordan35 | UK | Pain management centre | Examine the specific experiences of what it is like to be a father of an adolescent with chronic pain | 11–18 years n = 6 fathers Children were 3 females and 3 males Ethnicity: all White British |
Mixed conditions | Interview | IPA | 3 | Unfunded |
| Jordan121 | UK | Pain management centre | Examine how adolescents make sense of their own development in the context of living with chronic pain | 12–17 years n = 10 7 females 3 males Ethnic origin not stated |
Mixed conditions | Interview | IPA | 3 | Royal United Hospitals Bath NHS Foundation Trust |
| Joslin236 | UK | Information not extracted from un-sampled studies | Gain the opinions of young people during their multidisciplinary treatment for chronic pain | 11–18 years No further information extracted from un-sampled studies |
Chronic musculoskeletal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Unfunded |
| Kanstrup139 | Sweden | Hospital pain service | Explore the lived experiences of young people and parents with regard to participating in ACT for paediatric chronic pain | 12–18 years Average age = 16 yearsn = 8 4 adolescents (female) 4 parents Ethnic origin not stated |
Unspecified chronic pain | Interview | IPA | 3 | Mayflower Charity Foundation for Children, Sven Jerring Foundation, Claes Groschinskys Memorial Foundation |
| Kashikar-Zuck237 | USA | Information not extracted from un-sampled studies | Obtain information about the feasibility, safety and tolerability of the 8-week (16 session) group-based FIT Teens intervention for adolescents with JFM and gather impressions of acceptability, format and content | 12–18 years No further information extracted from un-sampled studies |
Juvenile fibromyalgia | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | National Institute of Arthritis and Musculoskeletal and Skin Diseases, Cincinnati Children’s Hospital Medical Center |
| Khair238 | UK | Information not extracted from un-sampled studies | Understanding self-management of haemophilia, from a child’s perspective, in the 21st century in the UK where intensive prophylactic therapy is given from early childhood | 4–16 years No further information extracted from un-sampled studies |
Haemophilia | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Bayer HealthCare Pharmaceuticals |
| Khanom122 | UK | Paediatric hospital | Explore adolescents’ lived experience of pain flares, including what pain flares are, why they occur, how they are managed and what lasting effects they have on adolescents | 13–17 years n = 10 8 females 2 males Ethnicity: 9 White British 1 Asian British |
Musculoskeletal pain | Interview | IPA | 3 | Versus Arthritis Grant |
| Kroon Van Diest239 | USA | Information not extracted from un-sampled studies | Determine which cognitive–behavioural therapy treatment components paediatric headache patient stakeholders would report to be most helpful and essential to reducing headache frequency and related disability | 13–17 years No further information extracted from |
Headache | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases |
| Kulandaivelu240 | Canada | Information not extracted from un-sampled studies | Examine the perspectives of adolescents with sickle cell disease, their parents and healthcare providers | 12–19 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Lauridsen241 | Denmark | Information not extracted from un-sampled studies | Explore the physical, psychological and social consequences of a life with non-specific spinal pain among Danish children | 9–12 years No further information extracted from un-sampled studies |
Musculoskeletal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Foundation of Chiropractic Research and Post Graduate Education |
| Law242 | USA | Information not extracted from un-sampled studies | Inform adaptation of Web-MAP for youth with headache | 10–16 years No further information extracted from un-sampled studies |
Headache | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Seattle Children’s Research Institute Center for Child Health Behavior and Development, National Institute of Neurological Disorders and Stroke |
| Law243 | USA | Information not extracted from un-sampled studies | Adapt problem-solving skills training (PSST) for parents of children receiving intensive pain rehabilitation and evaluate treatment feasibility, acceptability and satisfaction | 14 years (mean) No further information extracted from un-sampled studies |
Idiopathic chronic pain conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | The Center for Child Health, Behavior and Development of Seattle Children’s Research IEunice Kennedy Shriver National Institute of Child Health and Human Development Institute |
| Le244 | Canada | Information not extracted from un-sampled studies | Describe parents’ experiences with paediatric chronic pain | 12–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Women and Children’s Hospital Research Institute |
| Lee245 | UK | Information not extracted from un-sampled studies | Investigate patient preferences, feasibility and influence of several time sampling strategies in remote multidimensional pain reporting | 7–16 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | National Institute for Health Research Biomedical Research Centre Funding Scheme National Institute for Health Research Manchester Biomedical Research Centre |
| Leksell111 | Sweden | Information not extracted from un-sampled studies | Deepen knowledge of how parents of children diagnosed with juvenile idiopathic arthritis perceive the orofacial manifestations of the disease, its treatments and their encounters with dental care providers | 3–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Swedish Rheumatism Association |
| Lipstein246 | USA | Information not extracted from un-sampled studies | Compare factors considered by parents to those considered by adolescents making decisions about chronic disease treatments | 12–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Academic Paediatric Association Young Investigator Award |
| Maciver77 | UK | Paediatric hospital | Examine parents’ experiences pre-diagnosis and their experiences of accessing specialist pain management services for the child | 10–16 years n = 12 10 mothers 2 fathers Ethnic origin not stated |
Mixed conditions | Interview | Thematic analysis | 3 | Not reported |
| Maciver38 | UK | Paediatric hospital | Examining parents’ experiences of paediatric chronic pain management services in the UK | 10–16 years n = 12 10 mothers 2 fathers Ethnic origin not stated |
Mixed conditions | Interview | Thematic analysis | 2 | Not reported |
| Maciver78 | UK | Paediatric hospital | Examining parents’ experiences of paediatric chronic pain management services in the UK | 10–16 years n = 12 10 mothers 2 fathers Ethnic origin not stated |
Mixed conditions | Interview | Thematic analysis | 3 | Not reported |
| McDonagh136 | Ireland | Social media platforms | Exploring the impacts and experiences of parents caring for a child with DA | 7–15 years n = 10 10 mothers Ethnic origin not stated |
Down’s arthritis | Interview | Interpretive phenomenological analysis | 3 | Unfunded |
| McKinnon247 | Australia | Information not extracted from un-sampled studies | Explore the lived experiences of chronic pain and dyskinesia through the unbiased lens of children and adolescents with CP able to communicate experiences by either verbalising or using AAC | 9–18 years No further information extracted from un-sampled studies |
Cerebral palsy | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Australian Government Research Training Program Scholarship, Centre for Research Excellence in Cerebral Palsy, Murdoch Children’s Research Institute, Top-Up Scholarship |
| McKinnon135 | Australia | Paediatric hospital | Explore the personal perspectives of caregivers regarding challenges faced within everyday pain management of their children | 9–18 years n = 10 10 mothers Ethnic origin not stated |
Cerebral palsy | Interview | Interpretive phenomenological analysis | 2 | The Research Foundation, Murdoch Children’s Research Institute, Victorian Governments Operational Infrastructure Support Program |
| McNeill248 | Canada | Information not extracted from un-sampled studies | Examine the experience of fathers who have a child with juvenile rheumatoid arthritis (JRA) | 8.7 years average No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Meldrum249 | USA | Information not extracted from un-sampled studies | Understand the impact of chronic or recurrent pain on children within the context of their own lives and experiences | 8–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | NIMH grant, Mayday Fund |
| Meldrum250 | USA | Information not extracted from un-sampled studies | Understand the impact of chronic or recurrent pain on children within the context of their own lives and experiences | 10–19 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | NIMH grant. Mayday Fund |
| Miles251 | UK | Information not extracted from un-sampled studies | Explore how patient expertise and patient involvement in their own care works in practice for young people with sickle cell disease | 13–21 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | National Institute for Health Research Health Services and Delivery Research Programme |
| Mitchell252 | USA | Information not extracted from un-sampled studies | Assess how healthcare service delivery and other intervention strategies can be improved and optimised | 7–13 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Moulin253 | Switzerland | Information not extracted from un-sampled studies | Explore how these adolescents and their parents experience the condition and its impact on their daily lives | 12–20 years No further information extracted from un-sampled studies |
Medically unexplained symptoms | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Academic Society of the Canton de Vaud (Societe Academique Vaudoise) |
| Moulin254 | Switzerland | Information not extracted from un-sampled studies | Understand the experiences with, and perceptions of, the healthcare of adolescents who have MUS and their parents | 14–19 years No further information extracted from un-sampled studies |
Medically unexplained symptoms | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Academic Society of the Canton de Vaud (Societe Academique Vaudoise) |
| Neto255 | Portugal | Information not extracted from un-sampled studies | Explore the views of adolescents with chronic idiopathic neck pain towards an intervention consisting of pain neuroscience education and exercise administered in the school setting | 10–19 years No further information extracted from un-sampled studies |
Musculoskeletal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Neville36 | Canada | Paediatric Pain Clinic | Investigate how diagnostic uncertainty is experienced by both youth with chronic pain and their parents | 10–18 years n = 37 20 children 17 mothers Ethnicity: 18 white (Caucasian) 1 Latin American 1 Not stated |
Mixed conditions | Interview | Thematic analysis | 3 | Not reported |
| Newton256 | USA | Information not extracted from un-sampled studies | Understand the health-related quality of life and symptomatic experience of UC | 12–17 years No further information extracted from un-sampled studies |
Ulcerative colitis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Eli Lilly and Company |
| Nguyen257 | Switzerland | Information not extracted from un-sampled studies | Develop a new PRO that meets scientific and regulatory standards for instrument development and can be used as a primary end point to assess change in dysmenorrhoea severity overtime in clinical trials | 14–17 years No further information extracted from un-sampled studies |
Dysmenorrhoea | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Nicholas258 | Canada | Information not extracted from un-sampled studies | Develop an evaluative disease-specific measure of quality of life in paediatric IBD | 7–19 years No further information extracted from un-sampled studies |
Irritable bowel syndrome | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Nieto259 | Spain | Information not extracted from un-sampled studies | Test the feasibility of an online intervention (DAR-Web) for children with functional abdominal pain and their families | 9–15 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Fundació La Caixa Ministerio de Economı́a y Competitivad |
| Nieto260 | Spain | Information not extracted from un-sampled studies | Exploration of the effects of DARWeb on different outcomes (i.e. abdominal pain severity, disability and quality of life), from the point of view of the different actors involved (parents and children) | 9–15 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Fundació La Caixa (Recercaixa, 2012–2013), Ministerio de Economía y Competitivad (Spanish Government) |
| Nieto261 | Spain | Information not extracted from un-sampled studies | Evaluate post-treatment efficacy of DARWeb (online psychosocial intervention for children with functional abdominal pain) | 9–15 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Fundació La Caixa Ministerio de Economía y Competitividad |
| Nieto262 | Spain | Information not extracted from un-sampled studies | Learn about the specific experiences of families (parents and children) with a child with FAP from their point of view | 9–15 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Fundació La Caixa Ministerio de Economía y Competitividad |
| Nilsson263 | Sweden | Information not extracted from un-sampled studies | Deepen our understanding of adolescents’ experiences of living with TMD pain | 16–19 years No further information extracted from un-sampled studies |
Temporomandibular disorder | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Public Dental Service of Östergötland, Swedish dental societies, Malmo University |
| Nilsson264 | Sweden | Information not extracted from un-sampled studies | Explore adolescents’ explanations of TMD pain, their pain management strategies and treatment-seeking behaviour | 10–19 years No further information extracted from un-sampled studies |
Musculoskeletal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Swedish dental societies Malmo University |
| Njifon149 | Cameroon | Research presentation | Focuses on how a brother and sister without sickle cell disease experience their brother’s illness on a daily basis and the influence of this disease on family dynamics | 9–16 years n = 2 Siblings Ethnicity: Black African |
Sickle cell disease | Interview Drawings |
Thematic analysis and analysis of drawings | 2 | Not reported |
| Nkhoma265 | Malawi | Information not extracted from un-sampled studies | Explore stakeholders’ perspectives and experiences on pain self-management for adolescents living with HIV and chronic pain in Malawi | 10–17 years No further information extracted from un-sampled studies |
HIV/AIDS | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | King’s College London Faculty Challenge Fund |
| Nsangou266 | France | Information not extracted from un-sampled studies | Better understand the impact of the disease on body image by linking the illness with what the child says and knows about it | 9–12 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Nutkiewicz140 | USA | Paediatric Pain Clinic | Examines the communication between paediatric pain patients and their doctor | 10–18 years n = 32 24 females 8 males Ethnicity: 22 Caucasian 5 Latino 4 Asian 1 African American |
Unspecified chronic pain | Interview | Grounded theory | 3 | National Institute of Mental Health |
| O’ Donnell267 | UK | Information not extracted from un-sampled studies | Explore the experiences of young people with chronic oral ulcers attending the paediatric oral medicine clinic in a UK Dental Hospital | 1–9 and 10–19 years No further information extracted from un-sampled studies |
Chronic oral ulcers | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Ostojic268 | Australia | Information not extracted from un-sampled studies | Investigate the acceptability and feasibility of biofeedback-assisted relaxation training for chronic pain management in children with CP | 9–18 years No further information extracted from un-sampled studies |
Cerebral palsy | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Cerebral Palsy Alliance Research Foundation, NHRMC Centre of Research Excellence in Cerebral Palsy |
| O’Sullivan269 | Ireland | Information not extracted from un-sampled studies | Explore the self-management needs of Irish adolescents living with juvenile idiopathic arthritis, from their own perspective, and of their parents and healthcare professionals | 12–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Wellcome Trust-Humanities and Social Sciences, The James Flaherty Research Scholarship |
| Palmer270 | Canada | Information not extracted from un-sampled studies | Gaining a rich description and a contextual understanding of the experiences of a young chronic pain sufferer, aged 6, and her family members | 6–10 years No further information extracted from un-sampled studies |
Musculoskeletal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Social Sciences and Humanities Research Council |
| Panepinto107 | USA | Information not extracted from un-sampled studies | Develop the new PedsQLTM Sickle Cell Disease Module for paediatric patients with sickle cell disease and support its content validity | 2–18 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institutes of Health |
| Pate271 | Australia | Information not extracted from un-sampled studies | Explore the concept of pain in children with and without persistent pain | 8–12 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Macquarie University Research Training Program (RTP) full-time scholarship |
| Pelaez-Ballestas272 | Mexico | Information not extracted from un-sampled studies | Explain the phenomenon of experiencing juvenile idiopathic arthritis within a specific cultural context | 17–66 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Race273 | Canada | Information not extracted from un-sampled studies | Examine perspectives of children who have juvenile idiopathic arthritis and their parents | 8.3–16.3 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Canadian Institutes of Health Research |
| Randall108 | USA | Information not extracted from un-sampled studies | Understand the health-related quality of life and symptomatic experience of children (2–11 years) living with UC | 2–11 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Eli Lilly and Company |
| Renedo82 | UK | Hospital and community network | Explore how young people with sickle cell disease experience healthcare during a period of transition | 13–18 years n = 21 Ethnic origin not stated |
Sickle cell disease | Interview | Grounded theory and thematic analysis | 2 | National Institute for Health Research Health Services and Delivery Research Programme |
| Renedo81 | UK | Specialist healthcare services, networks with patient advocates | Understand healthcare transitions of young people with sickle cell disorder | 13–21 years n = 48 30 females 18 males Ethnic origin not stated |
Sickle cell disease | Interview | Grounded theory | 2 | National Institute for Health Research Health Services and Delivery Research Programme |
| Risko274 | USA | Information not extracted from un-sampled studies | Explore the lived experiences of adolescents engaged in an intensive interdisciplinary pain treatment programme | 10–19 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Unfunded |
| Rossato145 | Brazil | Paediatric clinic | Understand the meaning of the experience of families of children living in pain situations due to juvenile idiopathic arthritis | 6–17 years n = 12 Families 12 mothers 2 fathers 12 children with juvenile idiopathic arthritis (11 females, 1 male) 2 siblings Ethnic origin not stated |
Arthritis | Interview | Grounded theory | 2 | Not reported |
| Ruskin275 | Canada | Information not extracted from un-sampled studies | Explore the experience of adolescents who participated in an 8-week mindfulness group adapted for adolescents with chronic pain (MBI-A) | 12–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Pain Centre Seed Grant (Hospital for Sick Children) |
| Sallfors276 | Sweden | Information not extracted from un-sampled studies | Gain a deeper understanding of how children cope with their chronic pain condition | 6–17 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Swedish Rheumatism Association, Norrbacka-Eugenia Foundation, Renee Enander Foundation |
| Sallfors277 | Sweden | Information not extracted from un-sampled studies | Obtain a deeper understanding of children’s experiences of living with chronic pain in daily life | 6–17 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Swedish Rheumatism Association, Norrbacka-Eugenia Foundation, Renee Enander Foundation |
| Sallfors278 | Sweden | Information not extracted from un-sampled studies | Explore parents’ experience of living with a child with chronic pain related to JCA | 7–17 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Sallfors279 | Sweden | Information not extracted from un-sampled studies | Deepen the understanding of female adolescents’ daily living with chronic arthritis | 14–17 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Swedish Social Insurance Agency, Spenshult Hospital for Rheumatic Diseases, Norrbacka-Eugenia Foundation |
| Santos112 | Portugal | Information not extracted from un-sampled studies | Explore the situations perceived by child patients, their parents and siblings, as the most distressing and stressful when living with osteogenesis imperfecta | 4–16 years No further information extracted from un-sampled studies |
Osteogenesis imperfecta type 1 | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Not reported |
| Secor-Turner280 | USA | Information not extracted from un-sampled studies | Identify challenges that teens experience as a result of living with juvenile arthritis | 14–29 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Agency for Healthcare Research and Quality, University of Minnesota-Academic Health Center |
| Serafimova281 | UK | Information not extracted from un-sampled studies | Describe the experience of pain, its impact and treatments, in children with chronic fatigue syndrome/myalgic encephalomyelitis | 11–17 years No further information extracted from un-sampled studies |
Chronic fatigue syndrome/myalgic encephalomyelitis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Unfunded |
| Shaygan282 | Iran | Information not extracted from un-sampled studies | To assess a smartphone-based pain management application | 12–19 years No further information extracted from un-sampled studies |
Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Research Affairs of Shiraz University of Medical Sciences |
| Shaygan283 | Iran | Information not extracted from un-sampled studies | Explore the experience of chronic pain among adolescents | 12–17 years No further information extracted from un-sampled studies |
Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Research Affairs of Shiraz University of Medical Sciences |
| Skarstein284 | Norway | Information not extracted from un-sampled studies | Gain a deeper understanding and increase our knowledge about adolescents who suffer from frequent pain and have a high consumption of over the counter analgesics | 14–16 years No further information extracted from un-sampled studies |
Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Department of Nursing, and the Akershus University College of Applied Sciences |
| Skarstein285 | Norway | Information not extracted from un-sampled studies | Describe pain management and conditions that may influence the development of identity in adolescents frequently using analgesics | 10–19 years No further information extracted from un-sampled studies |
Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Department of Nursing, and the Akershus University College of Applied Sciences |
| Skogvold286 | Norway | Information not extracted from un-sampled studies | Explore which strategies adolescents use to cope with chronic tension-type headache in everyday life | 14–19 years No further information extracted from un-sampled studies |
Headache | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 2 | Norwegian Fund for Post-Graduate Training in Physiotherapy |
| Slotter287 | USA | Information not extracted from un-sampled studies | Gain further insight into how adolescents with chronic pain perceive their peer relationships | 12–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Smart76 | UK | Paediatric clinics and schools | Exploring the way in which mothers understand and cope with their children’s recurrent abdominal pain and how this might be related to beliefs and values held about their relationship with their children | 6–14 years n = 28 Mothers Ethnic origin not stated (except states predominantly white middle class) |
Abdominal pain | Interview | Grounded theory | 3 | NHS Executive Northern and Yorkshire Region |
| Soni-Jaiswal104 | UK | Information not extracted from un-sampled studies | Explore in-depth concerns of children with Mucopolysaccharidosis I and their parents, with an emphasis on the impact of head and neck disease on their lives | 6 months–16 years No further information extracted from un-sampled studies |
Mucopolysaccharidosis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Unfunded |
| Sorensen146 | Norway | Hospital pain clinic | Explore adolescents’ experiences of complex persistent pain | 12–19 years n = 6 4 females 2 males Ethnic origin not stated |
Complex persistent pain | Interview | Hermeneutic analysis | 3 | Unfunded |
| Sorensen288 | Norway | Information not extracted from un-sampled studies | Explore how regular needle injections affect children with rheumatic diseases and their parents in their daily living | 6–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Extra Foundation for Health and Rehabilitation, Norwegian League Against Rheumatism |
| Ståhle-Öberg289 | Sweden | Information not extracted from un-sampled studies | Illuminate pain in children with cerebral palsy from the parents’ experience | 10–19 years No further information extracted from un-sampled studies |
Cerebral palsy | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Swedish Association of Registered Physiotherapists, Jerringfonden and the County Council of Västerbotten |
| Stiles-Shields290 | USA | Information not extracted from un-sampled studies | Assess the paediatric patient and parent-reported experience of (a) coping with and managing symptoms associated with MALS and (b) the diagnostic, treatment and recovery process for paediatric MALS | 15–28 years No further information extracted from un-sampled studies |
Median arcuate ligament syndrome | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Comer Development Board and Cohn Family Foundation |
| Stinson291 | Canada | Information not extracted from un-sampled studies | Explore the self-management needs of adolescents with juvenile idiopathic arthritis | 12–20 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Canadian Arthritis Network |
| Stinson292 | Canada | Information not extracted from un-sampled studies | Explore the information needs of parents and school-age children with juvenile idiopathic arthritis | 8–11 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Canadian Arthritis Network |
| Stinson293 | Canada | Information not extracted from un-sampled studies | Conduct a user-centred needs assessment to inform the development of an integrated web- and smartphone-based self-management programme for adolescents with chronic pain, called iCanCope with Pain™ | 10–19 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Canadian Pain Society Small Grant Award |
| Stinson294 | Canada | Information not extracted from un-sampled studies | Explore the use, decision-making process and communication about the use of OTC medication with healthcare professionals in a multidisciplinary chronic pain team setting in adolescents living with chronic pain and their primary caregiver | 12–18 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Church and Dwight |
| Suder147 | Canada | Physician offices and Paediatric hospital | Understand the lived experience of adolescents who live with chronic pain | Average age = 16 years n = 10 8 females 2 males Ethnicity: all Caucasian |
Mixed conditions | Interview | Phenomenology | 3 | Not reported |
| Szwimer295 | Canada | Information not extracted from un-sampled studies | Inquire into the experiences of female adolescents living with CP | 14–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Tong296 | Australia | Information not extracted from un-sampled studies | Elicit parental and adolescent perspectives on paediatric rheumatology care and service delivery | 14–66 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | George Weston Fund |
| Valenzuela297 | USA | Information not extracted from un-sampled studies | To understand how children and adolescents with sickle cell disease perceive their lives and disease using Photovoice | 8–17 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institutes of Health National Heart, Lung, and Blood Institute |
| Van Gulik298 | Netherlands | Information not extracted from un-sampled studies | Elicit the experiences during school life and the perspectives and expectations regarding future work participation of adolescents with juvenile idiopathic arthritis | 14–18 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Unfunded |
| Van Scheppingen116 | Netherlands | Information not extracted from un-sampled studies | Gain a more in-depth understanding of the wide-ranging and complex problems parents of children with epidermolysis bullosa have to deal with | 2–19 years No further information extracted from un-sampled studies |
Epidermolysis bullosa | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Johanna Kinderfonds, the stichting BIO Kinderrevalidatie Kinderrevalidatie Fonds Adriaanstichting |
| Van Tilburg299 | USA | Information not extracted from un-sampled studies | Investigate the most common parental fears, worries and cognitions about recurrent abdominal pain | 5–13 years No further information extracted from un-sampled studies |
Abdominal pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institute of Diabetes and Digestive and Kidney Diseases |
| Voigtman300 | Saudi Arabia | Information not extracted from un-sampled studies | Describe the Qatif sociocultural response to children with sickle cell disease (SCD) and pain | 7–14 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Not reported |
| Waite-Jones126 | UK | Support group | To address the research question ‘What is it like to have a sibling with juvenile idiopathic arthritis?’ | 12–18 years n = 32 8 children 16 parents 8 siblings Ethnicity: All White British |
Arthritis | Interview | Grounded theory | 2 | Not reported |
| Wakefield301 | USA | Information not extracted from un-sampled studies | Examine pain-related stigma in the literature documenting paediatric and adult health-related stigma | 12–17 years No further information extracted from un-sampled studies |
Unspecified | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Goldfarb Pain and Palliative Medicine Fund |
| Wakefield302 | USA | Information not extracted from un-sampled studies | Examine adolescent motivations for using concealment and the possible benefits and harmful consequences of this form of coping | 12–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institute of Arthritis, Musculoskeletal and Skin Diseases of the National Institutes of Health, Goldfarb Pain and Palliative Medicine Fund |
| Wakefield303 | USA | Information not extracted from un-sampled studies | Identify and describe pain-related stigma among adolescents with chronic pain and their parents | 12–17 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | National Institute of Arthritis, Musculoskeletal and Skin Diseases of the National Institutes of Health, Goldfarb Pain and Palliative Medicine Fund |
| Walter304 | USA | Information not extracted from un-sampled studies | Determine the dimensions of the health challenge of adolescent headache | 14–18 years No further information extracted from un-sampled studies |
Headache | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Neuroscience Nursing Foundation |
| While305 | UK | Information not extracted from un-sampled studies | Explore the lived experience of young people with sickle cell disease as they transferred to adult services | 12–16 years No further information extracted from un-sampled studies |
Sickle cell disease | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | Not reported |
| Williams123 | UK | Unclear | Investigate the experiences of young people with epidermolysis bullosa | 10–14 years n = 11 5 females 6 males Ethnicity: 1 Black British 1 British Asian 8 White British |
Epidermolysis bullosa | Interview | IPA | 3 | Not reported |
| Wong134 | China/Hong Kong | Secondary school | Explore the self-care strategies among Hong Kong Chinese adolescent girls with dysmenorrhoea Ethnicity: Hong Kong Chinese | Average age = 15 years n = 28 |
Dysmenorrhoea | Interview | Content analysis | 2 | Association of Hong Kong Nursing Staff Professional Development Fund |
| Woodgate306 | Canada | Information not extracted from un-sampled studies | Elicit detailed descriptions of adolescents’ chronic illness experiences | 13–16 years No further information extracted from un-sampled studies |
Mixed conditions | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Health Sciences Centre Foundation Nursing Research Award |
| Yeung307 | Canada | Information not extracted from un-sampled studies | Explore how children aged 10–18 years describe their neuropathic pain (NP) | 10–18 years No further information extracted from un-sampled studies |
Neuropathic pain | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | Not assessed | Physiotherapy Practice Council |
| Yuwen106 | USA | Information not extracted from un-sampled studies | Describe parents’ experiences in caring for 2–5-year-old children with juvenile idiopathic arthritis | 2–5 years No further information extracted from un-sampled studies |
Arthritis | Information not extracted from un-sampled studies | Information not extracted from un-sampled studies | 1 | National Institute of Nursing Research, with additional scholarships and small grant |
Appendix 5 Definition and characteristics of included chronic pain conditions
| Condition/chronic pain classification (ICD-11) | Definition | Causes/origin | Symptoms | Pain symptom presentation and severity/intensity |
|---|---|---|---|---|
| Cerebral palsy/chronic secondary musculoskeletal, visceral and neuropathic pain and primary headache or orofacial pain | Defined as a group of permanent disorders of the development of movement and posture, causing activity limitations | The cause is attributed to non-progressive disturbances that occurred in the developing fetal or infant brain | Musculoskeletal pain from muscle spasms, dyskinesia, spasticity, contractures, joint misalignment, deformities, postural asymmetries and osteoporosis. Gastrointestinal pain including abdominal pain, acid reflux and constipation. Headache or orofacial pain from temporomandibular disorders, trauma from dyskinesia and spams. Neuropathic pain is experiences experienced as burning, squeezing, pricking or freezing pain | Constant and fluctuating pain varying widely from mild to severe |
| CRPS/chronic primary pain | Neuropathic pain disorder | Usually develops after minor trauma or surgery | Disabling pain, swelling, vasomotor instability, sudomotor abnormality and impairment of motor function | Constant/continuous severe pain |
| Dysmenorrhoea/chronic secondary visceral pain | Painful cramping, usually in the lower abdomen, which occurs shortly before or during menstruation, or both | Classified as primary (hormonal cause) and secondary (caused by underlying condition, such as endometriosis, adenomyosis, fibroids, endometrial polyps, pelvic inflammatory disease or by intrauterine device insertion) | Lower abdominal pain, nausea, bloating, diarrhoea, constipation, vomiting, indigestion, irritability, headache and low back pain | Symptoms can fluctuate according to menstrual cycle, and pain intensity varies widely from mild to severe |
| Epidermolysis bullosa/chronic secondary pain | Rare inherited skin fragility or blistering disorders | Inherited group of conditions | Blistering of the skin on hands and feet or widespread, associated with pain, itching, burning sensation and pruritus. Rare subtypes can include pyloric atresia, muscular dystrophy, cardiomyopathy and/or nephropathy | Constant severe pain |
| IBD/chronic secondary visceral pain | Group of chronic idiopathic IBD including Crohn’s disease and ulcerative colitis | Unknown aetiology, but it is related to an anormal immune response to gut microflora in genetically susceptible individuals | Frequent symptoms are abdominal pain, diarrhoea, constipation, nausea and vomiting | Fluctuating condition with periods of activity and remission. Pain can range from mild to severe |
| Juvenile idiopathic arthritis/chronic secondary pain | A group of conditions that involve joint inflammation which lasts for more than 6 weeks in people under 16 years of age | Autoimmune or autoinflammatory conditions with unclear cause/trigger but involves environmental and genetic factors | Pain, swelling and limitation of movement, and in more severe cases growth delay, joint contractures, eye problems, joint disease requiring joint replacements and permanent disability | Fluctuating condition with periods of activity and remission. Pain intensity varies from mild to moderate |
| Juvenile idiopathic arthritis – Down syndrome-associated arthritis/chronic secondary pain | Down syndrome is defined as a chromosomal abnormality. It is an aggressive, erosive, inflammatory arthritis that affects people with Down syndrome | It is an autoimmune condition | Arthritis is an under-diagnosed occurrence in Down syndrome and can cause joint pain and swelling | Arthritis from Down syndrome fluctuates with periods of activity and remission. Pain can vary broadly in intensity, ranging from no pain at all to severe pain |
| Migraine/chronic primary headache or orofacial pain | Recurrent headaches with or without aura | Unknown aetiology, but it is associated with genetic factors | Episodes of moderate to severe headache, most often unilateral and generally associated with nausea and increased sensitivity to light and sound | Fluctuating condition with periods of activity and remission. Pain usually ranges from moderate to severe |
| Musculoskeletal conditions/chronic musculoskeletal pain | Musculoskeletal impairments comprise more than 150 different conditions that affect joints, bones, muscles or multiple body areas or systems | Impairments in the muscles, bones, joints and adjacent connective tissues leading to temporary or lifelong limitations in functioning and participation | Main symptom is usually pain and limitations in mobility and dexterity | Often characterised by persistent pain varying widely from mild to severe |
| Recurrent abdominal pain/chronic secondary visceral pain | Defined as at least three episodes of pain that occur over at least 3 months and affect the child’s ability to perform normal activities, normally functional (nonorganic) abdominal pain | Somatic/unknown or associated with underlying condition, such as acid reflux, bacterial infection, food intolerance, abdominal migraine, IBD, surgical conditions | Abdominal pain | Fluctuating condition with periods of activity and remission. Pain ranges widely from mild to severe |
| Sickle cell disease/chronic secondary visceral pain | Group haemoglobin conditions particularly common in people of African or Caribbean descent | Inherited condition. Acute painful sickle cell crises (vascular occlusion crisis) are caused by blockage of the small blood vessels | Sickle cell crises (very painful episodes affecting different parts of the body), infections and anaemia | Sickle cell crises can be very severe and last up to a week; and it can happen every month or a few times a year |
Appendix 6 Methodological limitations table: level of concern for methodological domains assessed using CASP
| Study | Was there a clear statement of the aims of the research? | Is a qualitative methodology appropriate? | Was the research design appropriate to address the aims of the research? | Was the recruitment strategy appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | Overall assessment of limitations | Explanatory comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahlqwist137 | Low | Low | Low | High | Moderate | High | Moderate | Low | Low | Moderate | No mention of authors roles or potential bias. Given high concerns regarding recruitment strategy, moderate concerns regarding data collection and risks of possible bias, overall judged as moderate limitations. |
| Atkin124 | Low | Low | Low | Moderate | Low | Moderate | High | Moderate | Low | Low | Recruitment – not explained why seven localities were chosen but they had the whole population of those CYP with sickle cell disease/thalassemia. Was a service evaluation -little information provided about the service. Reflexivity is implicit in matching interviewer gender and ethnicity to interviewee. |
| Authors explained how interview questions were formulated for example with PAG, literature. Ethics not mentioned but as was service evaluation, probably exempt from ethics approval. Does not mention other ethical issues at all – possibly a reporting issue as this is part of a bigger study. Findings – not explained who analysed data and if there was team involvement for rigour but they appear credible and trustworthy in the way they were presented. | |||||||||||
| Atkin125 | Low | Low | Low | Moderate | Low | Moderate | High | Moderate | Low | Low | Design – justify use of repeat interviews but don’t explore decision to interview rather than another method. Recruitment – don’t say why chose that area of England to sample from, included whole eligible population in all but one area – no information on those who declined in the one area in which they randomly sampled. Sample size not justified. |
| Researcher relationship – offered children same gender and same ethnicity interviewer, no information provided about reflexivity for example questions asked, choice of setting, etc. Ethics – absence of reporting on this. Analysis – unsure about rigour, explains how themes were developed – seems to be a mix of deductive and inductive. Overall gave it low limitations – some weaknesses but think those are reporting weaknesses rather than conduct issues. | |||||||||||
| Atoui148 | Low | Low | Low | Moderate | Low | High | Low | Low | Low | Low | Recruitment – seems appropriate, although they don’t give rationale for all choices. They are interested in adolescents in Beirut and recruit them. Could have expanded on the criteria for inclusion/exclusion Don’t explain why recruit child only if zero on pain scale, but presumably for ethical reasons. Relationship – no information given. Ethics – issues considered regarding consent/assent, distress during interview, confidentiality. Analysis – don’t explain how themes developed but only a minor concern. Low limitations – some weaknesses but mainly reporting weaknesses. |
| Baert102 | Low | Low | Low | Moderate | Moderate | High | High | Low | Moderate | Moderate | Design – justify why chose focus groups. Recruitment – don’t say why three different countries included. Don’t say why people opted out of the research or what the prior study in Ghent was that they used in order to recruit their participants. The focus group questions were chosen by the researchers and piloted on university students, so no input from parents/children with pain/expert advisors. |
| They report the questions, but they ask a lot about unfairness which is quite leading when they wanted to explore injustice. Reflexivity – nothing reported. Ethics – had ethical approval in all three countries but nothing about informed consent, confidentiality, distress, post-focus group support/signposting to support, etc. Findings – don’t discuss impact of country differences on the findings. Moderate limitations because of concerns over recruitment, and data quality and hence meaningfulness of findings. | |||||||||||
| Borghi133 | Low | Low | Low | Low | Moderate | High | Low | Moderate | Moderate | Moderate | Aim and rationale well explained. Choice of method/design explained in aim. Recruitment – seems to be one clinic only and excluded CYP under 6 years only cos they can’t give ‘clear accounts as easily’. Could have clearer inclusion and exclusion criteria, but overall, the authors explained how they recruited their participants by contacting the doctors and the guardians/parents. Data collection – a minor issue is they haven’t justified the choice of only one clinic, don’t justify choice of semistructured interview. |
| Settings for data collection weren’t described, not really sure about the format of the data either. No reflexivity or information about the authors. Nothing on ethics – parents approved their child’s very detailed interview transcript, even for older children, yet the ethical implications of this are not discussed. Data analysis – some data on this regarding use of Piaget’s theory but not fully clear how themes arrived at, no discussion of contradictory data or researcher’s role in selecting quotations. | |||||||||||
| Described theoretical reference but not much information on analysis. Findings are not very clear – not much discussion against original question – no triangulation, I think the findings were too focused on Piaget theory. Don’t explore evidence for and against their arguments and are not critical of Piaget – for example was there no evidence NOT in support of Piaget’s theory? Moderate limitations overall given above concerns. | |||||||||||
| Brandelli105 | Low | Low | Low | Moderate | Moderate | High | High | Moderate | Low | Moderate | No real justification of sample size as congruent with IPA approach save one comment at start of results. Some further discussion of what was included in the interview schedule needed. Researcher relationship – some attempt to note this but really only mentions graduate student with clinical training; what about knowledge of pain, etc.? Ethics – approval mentioned but little other detail. Analyses – rather thin in terms of interpretation and theme titles, not fitting with IPA level of interpretation and also focus on idiographic. Findings – an overall clear statement of findings was absent (attempted), lack of quality (some but not sufficient). |
| Recruitment was focused on an already-recruited sample with low scores on a particular questionnaire which did not match well to the main aim of the study. Moderate limitations overall given above concerns. |
|||||||||||
| Britton80 Britton308 |
Low | Low | Moderate | Moderate | Moderate | Moderate | Moderate | High | Low | Moderate | Quite poorly reported overall. Design-used longitudinal qualitative interviews and diaries but don’t justify the design (why longitudinal was needed) nor the choice of methods. Recruitment – not much detail given and don’t justify why only chose families of girls and not boys and girls. If the aim was to design a resource for all families, then boys with juvenile idiopathic arthritis should have been included. |
| Data collection – some details but questions asked not provided. Reflexivity – generic statements but specific detail of how it was achieved. Ethics – had ethical approval but no info given on informed consent, anonymity, burden on families especially children with juvenile idiopathic arthritis. Data analysis – sparse information – say ‘More detailed information is available in part 1 (Britton and Moore 2002)’. Findings come across as convincing but no information on triangulation, evidence for and against their arguments – possibly yellow but gave it green. | |||||||||||
| Britton (part 3) #5920 – Not a clear statement for aim (maybe because this is part of a sequence of studies?) but the rationale and the relevance are there. Study design was decided after applying a questionnaire which guided the fieldwork. It briefly mentions methods utilised for data collection and referred to full description elsewhere. No information provided about data analysis – it goes straight into findings. I rated it as moderate overall given the lack of info on data analysis which is a major problem. Overall moderate risk of bias, but the detail is hinted to be contained in another publication. | |||||||||||
| Consequently, it’s hard to judge methodological quality in this paper alone. Design and data collection is a hotchpotch of different approaches (no justification and some data were generated by participants opting to make videos which wasn’t in the original design). Recruitment not well described (opportunity sample perhaps?). Bias is touched upon but not described. Unclear if all findings are from a small number of participants (no identifiers provided). | |||||||||||
| Combining the information from the publications, overall moderate limitations given moderate concerns in most domains. | |||||||||||
| Brodwall75 | Low | Low | Low | Low | Low | Moderate | High | Moderate | Low | Low | Relationship – the interviewer is a general practitioner and psychiatrist. Participants knew she was a doctor, although she introduced herself as a scientist without responsibility for taking care of the family. Some information about the first author but not how this would have affected the study. Data analysis needs to be further described – more info is needed – how they performed the qualitative content analysis. Not clear how codes, categories and themes were developed but several researchers involved. Ethical issues – not explored. Low limitations overall given most key domains had low concerns. |
| Carter117 | Low | Low | Low | High | Low | Moderate | Moderate | Low | Low | Low | Need more information about recruitment strategy. Mentions that letter was sent but no detail of how these CYP were found (e.g. hospital, clinic …); consent in writing was obtained but no mention of ethical approval. Data analysis – could have presented more information about how thematic analysis was done, which themes were derived and how. Low limitations overall because minor concerns in most of key domains. |
| Carter119 | Low | Low | Low | Moderate | Moderate | Moderate | Moderate | Moderate | Low | Moderate | The research design seems justified, but it was not explicitly stated. Recruitment – some information but it could have detailed this process more, for example why some participants didn’t take part, from where the participants were recruited. Does not state interview setting, but it is very clear on how data was collected. It also described how the questions for the interview were formulated. The relationship between participants and researcher is not explicitly described. |
| Data analysis refers to participant checking, but not what participants said/reported, etc. data. Needed more information about saturation. No deviant case presentation, but findings are otherwise well presented, coherent and linked with the study aim. Moderate limitations – some weaknesses but lack of description is more of a reporting weakness. |
|||||||||||
| Carter118 | Low | Low | Low | Low | Moderate | Moderate | Low | Low | Low | Low | No discussion about the study design. More information could have been provided about data collection, for example which type of data was obtained, how the interview was structured. Low limitations overall. |
| Carter109 | Low | Low | Moderate | Moderate | Low | High | Moderate | Moderate | Low | Moderate | Explains the design. The study aim seems quantitative (frequency, intensity …). They explained recruitment strategies really well. Sample size is small and there is missing survey data for two children. Data collection clear – stated place and methods, also explained how the interview was structured. |
| Reflexivity – no mention about how the researchers might have impacted the study/data collection. Data analysis could have included how the researchers avoided bias and more information about how the codes were created. The findings are really clear and relevant to the research question. Father’s perspective included without consent. | |||||||||||
| Moderate limitations overall given above concerns. | |||||||||||
| Cartwright131 | Low | Low | Low | Low | Low | Low | Moderate | Low | Low | Low | Reflexivity – information given on researchers’ backgrounds – some of the reflexivity is implicit rather than explicit so maybe issue of reporting not conduct. Ethics – not much reported – just got written consent and had approval. Low limitations overall given few concerns. |
| Castle141 | Low | Low | Low | Moderate | Low | High | Moderate | Low | Low | Moderate | Recruitment – convenience sample – no explanation of refusal to participate, choice of recruitment setting not explained, only included six CYP and only those who could talk yet focus is on cerebral palsy in which speech impairment is common. Minor issues with data collection reporting – don’t say where interviews occurred or if recorded. Relationship – not explicit who did interviews – there are three authors, lead author is an OT as are co-authors. Other impacts of relationship not discussed. |
| Ethics – had approval, sought informed consent, use pseudonyms – no other ethical issues discussed for example burden on participants, distress and how handled, etc. Data analysis – use of triangulation of methods (interview and pre-interview questionnaire), supervisory input, describe the methods and give reference to method. Refers to reflexivity before and during interviews and their analysis. Findings seem convincing – minor issue is that contradictory findings are not made that obvious. | |||||||||||
| Overall moderate limitations because of small convenience sample and other methods issues. | |||||||||||
| Dell’Api138 | Low | Low | Low | Moderate | Moderate | High | High | Low | Low | Moderate | No information on ethical issues or on relationship. Don’t know who interviewer was. No interview schedule provided. Ethical concerns over data collection from children in the hospital while awaiting first appointment to tertiary pain service – stressful situation anyway. Recruitment strategy not justified nor obviously related to the aim – only five children recruited. Age 10–17, but age not justified. Some rigorous data analysis processes for example second coder, member checking but not clear how got from line-by-line coding to themes. Overall moderate limitations given above concerns. |
| Dyson130 | Low | Low | Moderate | Moderate | Moderate | High | Moderate | Low | Low | Low | Design not justified, nor is choice of interviews as method. Recruitment – some were opportunistic from quantitative sample, some purposive. Data collection – no information on choice of interviews or the questions asked. Reflexivity – nothing reported. Ethics – had approval, got signed informed consent from CYP and carers but process not explained. Some detail of the analysis process. Findings rich. Overall low limitations because mainly reporting issues rather than conduct issues. |
| Forgeron309 | Low | Low | Low | Low | Low | High | Low | Moderate | Low | Low | Only concerns were no reflexivity provided. Data analysis warranted more description for example how the themes were developed, etc., so low limitations overall. |
| Gaughan143 | Low | Moderate | Low | Low | Low | High | High | Low | Low | Moderate | Aim – seems to want to link parental attitudes to child’s response to the pain programme – that seems a quantitative research question. Concerns about possible bias – all authors were from the hospital pain clinic under investigation. The parents were interviewed while the child was still in the pain programme and it is not clear how power issues were handled nor informed consent processes – seems the researcher may have been directly involved in the care of the participants’ child. Moderate limitations given above concerns. |
| Guell132 | Low | Low | Low | Moderate | Low | Low | High | High | Low | Moderate | Recruitment – did not explore the impact of mixed UK and German samples. Reflexivity – does talk about rapport with CYP and not taking notes until after fieldwork to avoid disrupting visits/conversations (ethnography) but does not explore the impact of the decisions around including families in Germany instead of just UK on the data and findings. Ethics – not explicitly discussed at all re recruitment, consent, confidentiality, etc. and no mention of ethics approval. |
| We don’t know how the data were analysed other than researcher identified recurring topics/themes – could be more to do with the style of reporting an ethnography. Findings – they are convincing even though they are not subject to triangulation in the same way as recorded interviews with transcripts – no audio recordings made, just field notes – but doesn’t explain about differences between the UK and Germany in terms of experiences for all of the findings, no respondent validation used. The findings do read convincingly though overall. | |||||||||||
| Moderate limitations based on above concerns. | |||||||||||
| Helvig144 | Low | Low | Low | Moderate | Low | High | Low | Moderate | Low | Moderate | Sampling – very small convenience sample – recruited through friends and colleagues. Migraine diagnosis based on parental report only. Relationship – not reported. Analysis – no triangulation, etc. Some proof of rigour – two researchers interpreting data to create summaries but not clear if both did coding, not clear how arrived at themes. Findings seem clear but aren’t very in-depth. Moderate limitations overall. |
| Hunt110 | Low | Low | Low | Low | Low | Moderate | Moderate | Low | Low | Low | Recruitment – we don’t know who declined to take part or how centres selected the five parents they were asked to recruit. The sample population and recruitment were well described. Reflexivity – good reflexivity regarding data analysis, less in how interviews were conducted. Ethics – no information given other than they had ethical approval and gave participants information sheets and consent forms – probably reporting issue rather than poor conduct issue so overall low limitations. |
| Jones120 | Low | Low | Low | Moderate | Low | Moderate | Low | Low | Low | Low | Overall statement – no concerns about design, data collection or ethical issues; very minor concerns about findings; only minor concerns about reflexivity (relationships between participants) and findings. Some concerns about recruitment strategy because of lack of rationale and all from single service. Analysis – give example matrix of temporal analysis. Used Braun and Clarke’s approach. Use quotations in findings section and say selected from across interviews. Low limitations overall. |
| Jones128 | Moderate | Low | Moderate | Moderate | Moderate | Low | Low | Low | Low | Moderate | The aim is not clearly defined but is implied. The authors talked about exploring the relative frequencies of hoped- and feared-for future self … not sure if qualitative is the best design for this. Not stated where the interviews were conducted. Didn’t explain why some participants didn’t take part. |
| Jordan34 | Low | Low | Low | Low | Moderate | Low | Low | Moderate | Low | Low | Data collection – no information on where the interviews were conducted. Data analysis could have included more information about how the themes were derived. Overall low limitations given few concerns. |
| Jordan35 | Low | Low | Low | Low | Moderate | Low | Low | Low | Low | Low | Our only concern is that there is a lack of information about the format of the data and the interview. Clear findings are presented. Overall low limitations given few and minor concerns. |
| Jordan121 | Low | Low | Moderate | Low | Low | Low | Low | Low | Low | Low | Design was not mentioned. Overall low limitations given very minor concerns. |
| Kanstrup139 | Low | Low | Low | Moderate | Low | Moderate | Low | Moderate | Low | Low | Ethics – ethical approval, ethical approach to recruitment described. Description of how interviewer positioned herself and explained her role to participants and adapted her language for CYP. Used and justified IPA. Interviewer’s prior experience of delivering ACT not reflected on as a bias in data collection/analysis. Only eight people from one service participated. Low limitations overall given few concerns. |
| Khanom122 | Low | Low | Low | Low | Low | Moderate | Low | Low | Low | Low | Very clearly described study. Some description of bias/data collection but none specifically around being responsive to events. Deviant case analysis not described, but otherwise findings/analysis is good and merits a low limitations score. |
| Maciver77 Maciver38 Maciver78 |
Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Most aspects were really well detailed. Recruitment strategy clear though non-responders not described; smallish sample (n = 12 from 10 families). No mention of data saturation/sufficiency, but methods generally very well described. Ethical issues, for example consent, etc., all described. Low limitations overall. |
| McDonagh136,2 | Low | Low | Low | Low | Low | Moderate | Low | Low | Low | Low | The topic is appropriate for qualitative methodology, but they did not explain why explicitly. Relationship with participants – the authors did not provide any information about the researcher; it only briefly mentions that one of the reviewers was a skilled qualitative researcher. Saturation/theoretical sufficiency is not discussed. Low limitations overall given minor concerns. |
| McKinnon135 | Low | Low | Low | Low | Low | Moderate | Low | Low | Low | Low | Include some information about the researchers but not how their professionals and background could have affected the data collection. One of the authors already knew participant from a previous study. Sampling frame described in accompanying paper; subsample of larger study. No discussion of saturation. Low limitations overall. |
| Neville36 | Low | Low | Moderate | Moderate | Low | High | Moderate | Low | Low | Moderate | Design – do not explain or justify the design. Recruitment strategy was not justified – did not use diagnostic uncertainty as recruitment criteria. Do not explain why they excluded certain children, for example those with autism. Relationship – no information. Ethics – information given on informed consent process but no information on ethical issues of interviewing youth and parents separately and whether confidentiality was maintained for each party and how. Moderate limitations given above concerns. |
| Njifon149 | Moderate | Low | Low | Moderate | Low | Moderate | High | Moderate | Low | Moderate | Not a standard journal article format – main issues are lack of detail in reporting. Aim is unclear therefore, hard to judge if qual methodology and design were appropriate. Recruitment – no information. Very small sample – one family. No information on ethics. Analysis – only told it was thematic. Mostly issues of poor reporting, that is issues not reported or not fully reported, rather than actual methodological limitations so moderate limitations overall. |
| Nutkiewicz140 | Moderate | Low | Moderate | High | Low | High | High | Moderate | Low | Moderate | An oral history study, so non-standard reporting – most issues related to lack of detail being reported. Aim stated in several different ways in paper and not clear as a result. Design – observation of communication would have been more appropriate if the researchers were interested in the communication between paediatric pain patients and their doctor however they also say their aim is about what children say about their relationship with their doctors which fits with their chosen research methods. No information on recruitment strategy other than recruited from university pain clinic. Ethics – not reported. Little information on analysis – just told it was coded. Overall moderate limitations given above concerns. |
| Renedo82 Renedo81 |
Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Reflexivity – implicit in description of choice of interview questions and choice of recruitment location, explicit that interviewer has no links with health services for sickle cell disease or any research participants and was white (Caucasian) without sickle cell disease. Relationship – some consideration of interviewer status and relationship between researcher and participant. Analysis – followed some of the steps of grounded theory but not clear exactly what was done. Findings were fairly clear. Overall low limitations. |
| Rossato145 | Low | Low | Low | Low | Moderate | High | Low | Low | Moderate | Low | Clear statement of aims consistent with use of grounded theory. Recruitment seemed more convenience than purposeful sampling. Data seem to be collected in the clinic. Had ethical approval. Limitations were not discussed nor the full process like other pieces of research. No reflexivity section. Overall low limitations – mainly reporting issues rather than concerns with conduct. |
| Smart76 | Low | Low | Low | Low | Moderate | Moderate | Moderate | Low | High | Moderate | The researchers were involved in the participants’ treatment, therefore issue of potential bias. Non-responders are not described, but otherwise recruitment is well described. Data collection is only briefly described; researchers are psychiatrists which is explained as appropriate regarding biopsychosocial approach, but the idea of somatising is used without critical reflexivity regarding how this can invalidate people’s experiences of pain. Ethics approval and informed consent confirmed, but no further discussion of any ethical parameters. |
| Analysis is described relatively well; deficits about bias, etc. are mediated by team analysis which makes it potentially more robust. Could have mentioned saturation of data and provided more details about how the interview was conducted. The findings didn’t mesh well with the aims of the study – lots of data about their perceptions of self as parents, etc. which were not connected with the stated aims. The data are quite focused on doctors and psychological concepts which are not what the review questions were about. | |||||||||||
| Overall moderate limitations given above concerns. | |||||||||||
| Sorensen146 | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Data analysis – not clear how moved to categories and themes but demonstrate rigour otherwise. Ethics – issues not discussed. Low limitations given few and minor concerns. |
| Suder147 | Low | Low | Low | Moderate | Low | Moderate | Low | Moderate | Low | Moderate | Recruitment – narrow recruitment strategy, so some sample bias. Data collection – minor concerns – some of the questions had complex, formal vocabulary, for example which activities or occupations help give you identity or meaning in your life? Has chronic pain changed your involvement in those occupations? |
| Relationship – some aspects considered, but do not know what participants were told about the researcher’s professional occupational therapy background. Analysis – framework used for analysis might have impacted the findings – possibly some deductive analysis, although says it was a thematic analysis and phenomenological. Seem to exclude data that do not fit with their themes. Multiple analysts reviewed data in various stages of the analysis. | |||||||||||
| Moderate limitations overall given above concerns. | |||||||||||
| Waite-Jones126 | Low | Low | Moderate | Moderate | Low | Low | Low | Low | Low | Low | Recruitment – all participants from a support group, so some sample bias but did have diversity in age/gender of siblings and fathers and mothers and one grandparent. Reflexivity/ethics – first author has juvenile idiopathic arthritis and volunteered at the support group she recruited from – these issues not fully explored regarding her impact on ethical aspects of recruitment for example power dynamics. She does reflect on her impact on the interview data and analysis. Low limitations overall given high-quality analysis and findings. |
| Williams123 | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Only minor concern is they could have given more details about data collection, for example did they use icebreakers or prompts, etc.? Low limitations overall. |
| Wong134 | Low | Low | Low | High | Low | High | Moderate | Moderate | Moderate | Moderate | Recruitment – no information given except they sampled from those in a survey as part of a mixed methods study. Data collection – little information given; location not stated – minor concerns. Relationship – no information. Ethics – no information given. Analysis – only one analyst but did ‘peer debriefing’. Content analysis used – a bit rudimentary and possibly lacking disconfirming analysis. Findings – disconfirming data not very apparent, quite quantitative reporting. |
| Overall, moderate limitations given above concerns – many issues are related to reporting issues not conduct issues. |
Appendix 7 Summary of qualitative findings table
| # | Summarised review finding | GRADE-CERQual Assessment of confidence | Explanation of GRADE-CERQual Assessment | References |
|---|---|---|---|---|
| 01. IMPACT OF CHRONIC PAIN ON FAMILY LIFE | ||||
| 1 | Poorly managed, moderate and severe chronic pain was overwhelming and took over family life and affected family dynamics. The routines and activities of the whole family were restricted and limited by managing the pain and its consequences. | High confidence | No/very minor concerns regarding methodological limitations, coherence, adequacy and relevance | McDonagh,136 Atkin,125 Atoui,148 Britton,80 Britton,79 Brodwall,75 Carter,118 Dyson,130 Forgeron,142 Gaughan,143 Guell,132 Jones,128 Khanom,122 Suder,147 Sorensen,146 Brandelli,105 McKinnon135 |
| 2 | Pain meant children and their families had to manage many uncertainties regarding their changing routines and family life, diagnosis and prognosis, and the child’s future prospects, for example of finding employment or attending university. For fluctuating pain conditions, the fear and uncertainty around when and how intensely children would experience pain were always present which limited families’ activities even when the child was not in pain. Some children with fluctuating pain conditions were able to gather energy from moments with less or no pain, which helped them to deal with everyday life. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Maciver,77 Ahlqwist,137 Jordan,35 Khanom122 |
| 02. IMPACT OF PAIN ON FAMILY MEMBERS | ||||
| 3 | Poorly managed, moderate and severe chronic pain had mostly negative psychosocial impacts on all family members. Children and parents felt depressed, afraid of the possible cause of the pain, and grieved the loss of their life before pain. CYP felt socially isolated and different from peers. Parents felt anxious, helpless and frustrated at being unable to help their child feel better. There was a greater impact on members who were more involved in caring for the child with pain, usually mothers. Siblings who did not have chronic pain felt neglected by their parents and resentful of the child with pain but also concerned about them. | High confidence | No/very minor concerns regarding methodological limitations, coherence, adequacy and relevance | Maciver,77 McDonagh,136 Atkin,125 Atoui,148 Britton,80 Britton,79 Carter,118 Cartwright,131 Forgeron,142 Gaughan,143 Guell,132 Jones,128 Jordan,35 Khanom,122 Njifon149 Rossato,145 Suder,147 Waite-Jones,126 Sorensen,146 Williams,123 Jones,128 Brandelli105 |
| 4 | Parents felt deeply afraid of what might be causing the pain, of witnessing their child in pain, that treatments would not work and that their child would not get better to enjoy a fulfilling life. The constant fear caused parents to always be on call for their child, which was also detrimental to parents’ well-being. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | Maciver,77 Gaughan,143 Jones,128 Jordan35 |
| 5 | Parents, siblings and adolescents with chronic pain reported that some good things had happened because of the impact of chronic pain. The main caregiver, usually the mother, felt they became closer to their child and that their relationship had improved. Siblings without chronic pain also felt that their family relationships had become closer than in other families, and they became more compassionate to others. Some adolescents with chronic pain acknowledged that their experiences made them a better person, better equipped to live life and more mature. | Moderate confidence | Moderate concerns regarding methodological limitations and coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Britton,80 Suder,147 Waite-Jones,126 Jones,128 Brandelli105 |
| 6 | Primary caregivers, usually mothers, experienced reduced ability to have a life outside of their home; they stopped paid employment and/or lost their career and curtailed their social life to focus on caring for their child. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | McDonagh,136 Brodwall,75 Gaughan,143 Brandelli105 |
| 03. IMPACT ON SELF-IDENTITY | ||||
| 7 | Children saw themselves as different from peers because they felt unhealthy, restricted by pain, socially isolated, dependent and were treated differently by peers. Some children regarded their chronic pain as abnormal, because it affected their ability to lead a normal life, and as something to pity. Children did not want to be seen as unhealthy and different by their peers and they wanted to belong to a group of friends. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance | Atkin,125 Atoui,148 Britton,80 Cartwright,131 Forgeron,142 Guell,132 Jordan,121 Khanom,122 Njifon,149 Rossato,145 Suder,147 Waite-Jones,126 Williams123 |
| 04. IMPACT ON SIBLINGS | ||||
| 8 | Siblings who did not have chronic pain felt neglected and helpless which could lead to them behaving dismissively towards the child with pain and even questioning the legitimacy of their pain. Siblings competed for parental time and affection. Siblings blamed the child with pain for dominating their parents’ attention, but they also showed concern and affection for them. Siblings’ negative feelings improved overtime as they developed the skills to adjust socially and emotionally. | Moderate confidence | Minor concerns regarding methodological limitations and coherence, moderate concerns regarding adequacy and relevance | McDonagh,136 Britton,80 Brodwall,75 Gaughan,143 Njifon,149 Waite-Jones,126 Brandelli105 |
| 9 | Some siblings, even younger siblings, took on caring responsibilities for children with chronic pain which limited their freedom. For example some siblings were expected by their parents to adopt a parenting role for the child with chronic pain, including supervising their medical care, which siblings resented. Other siblings provided personal care for the child with chronic pain such as helping them to dress, lifting them out of the bath and carrying them downstairs. | Moderate confidence | No/very minor concerns regarding methodological limitations and coherence, moderate concerns regarding adequacy and relevance | Atkin,125 Atoui,148 Njifon,149 Waite-Jones126 |
| 05. IMPACT ON PARENTING | ||||
| 10 | Parents learnt on their own to adapt their parenting to help their child deal with the pain while trying to still maintain their child’s autonomy. Parents provided support and care while being firm when necessary, for example making their child go to school despite pain. Successfully adapting their parenting was hindered by a lack of understanding of how they could help their child, and the lack of resources and support from health services and their social network. | High confidence | No/very minor concerns regarding methodological limitations and coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Maciver,77 Atkin,124 Atkin,125 Brodwall,75 Gaughan,143 Jordan,35 Smart76 |
| 06. ADAPTING FAMILY LIFE TO PAIN | ||||
| 11 | For poorly managed and severe chronic pain, families focused on trying to control the impact of pain on family life using many strategies. Strategies included families gathering information about pain, following treatments, adjusting their routine to accommodate pain and its management, and self-managing pain to be able to join in activities. These strategies meant that family life then became more restricted because it was completely organised around managing and avoiding exacerbating the pain. | High confidence | No/very minor concerns regarding methodological limitations and coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Atkin,124 Ahlqwist,137 Atkin,125 Atoui,148 Carter,118 Forgeron,142 Guell,132 Rossato145 |
| 12 | Over time, parents and children learnt to adapt to unresolved pain because they felt like they had no other choice. Consequently, families and children started to focus on living well with pain. For instance, parents (mothers) learnt to deal with the unpredictability of pain; helped their child to live with their new condition; and developed ways of dealing with the child’s fear about the future. Children found new ways to do daily activities, for example using mobility aids. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | Britton,80 Britton,79 Baert,102 Carter,118 Guell,132 Jones,128 Rossato,145 Suder,147 Sorensen146 |
| 07. SOCIAL SUPPORT | ||||
| 13 | Peers, friends and the extended family provided practical, financial and emotional support which helped parents and children deal with the impact of pain on their lives, enhanced quality of life and adherence to treatments. Contact with peers and friends helped children feel normal which provided them with hope and reassurance. Parents (mainly mothers) longed for others to understand their own suffering but lacked a social support system. Mothers grew apart from friends due to their caring role. | Moderate confidence | Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and minor concerns regarding relevance | Britton,80 Baert,102 Cartwright,131 Waite-Jones,126 Brandelli105 |
| 14 | Recurrent school absences and pain prevented children from engaging with friends when at school which made it difficult for children to maintain friendships, contributed to their lack of support, and increased their sense of social isolation. | High confidence | No/very minor concerns regarding methodological limitations, minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance | Atkin,124 Atkin,125 Atoui,148 Dyson,130 Williams,123 Jones128 |
| 08. CONDITION-SPECIFIC PEER SUPPORT | ||||
| 15 | Meeting others with similar conditions helped adolescents feel less isolated because they were able to share experiences and provide mutual support. In contrast, other adolescents did not want peer support from other children with chronic pain because they did not want to be reminded of their pain or because they believed others would not have similar experiences. Parents preferred support from other parents of children with similar conditions, who they described as a great comfort and vital source of information. | Moderate confidence | No/very minor concerns regarding methodological limitations and coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance | McDonagh,136 Cartwright,131 Cartwright 2015 #339 Forgeron,142 Williams123 |
| 09. DISCLOSURE OF PAIN | ||||
| 16 | Parents avoided disclosing their child’s pain to friends and extended family for a range of reasons. For instance, parents found chronic pain hard to understand and explain, they were afraid of being judged on their parenting skills or disbelieved, or they anticipated a lack of sympathy for a condition that is not life-threatening. Lack of disclosure could negatively affect how much support parents received from their friends and wider family. However, when they did disclose their child’s pain, their social networks did not always understand or believe the pain and were not empathetic, sometimes blaming them for poor parenting, for example being overprotective parents. Children also often avoided disclosing their pain, although girls and younger children were more likely to disclose and share their problems than boys and adolescents. Children also avoided disclosing their pain to help manage how others perceived them, to avoid having to deal with the prejudice and discrimination of others, such as derogatory comments, and because the pain was invisible and hard to explain. | High confidence | Minor concerns regarding methodological limitations and coherence, no/very minor concerns regarding adequacy and relevance | Atkin,125 Atoui,148 Britton,80 Baert,102 Dyson,130 Forgeron,142 Gaughan,143 Guell,132 Jones,128 Khanom,122 Suder,147 Sorensen146 |
| 10. WHAT CHILDREN AND FAMILIES WANT FROM SERVICES | ||||
| 17 | At the onset of the child’s chronic pain, children and their families initially sought services hoping for a cure for the pain which they assumed must have an underlying physical cause. Parents expected doctors to undertake objective medical tests, such as physical examinations, X-rays and high-technology scans, to reveal the physical cause of their child’s pain and to clinically treat and cure the pain. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Brodwall,75 Carter,117 Dell’Api,138 Gaughan,143 Jordan,34 Kanstrup,139 Maciver,77 McDonagh136 Neville,36 Smart,76 Sorensen146 |
| 18 | Families searched for a cause and/or diagnosis to better understand the pain, to enable treatment, and as proof of a genuine illness, that is proof that their pain is real and is believed by health professionals. However, receiving a diagnosis was not a source of hope for all families, for instance, for children with a pre-existing chronic condition, an additional chronic pain diagnosis increased their worry. A diagnosis such as chronic pain or CRPS without knowing the cause could also be unsatisfactory to families because it did not help them understand why the child had pain. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | Maciver,77 McDonagh,136 Brodwall,75 Carter,117 Gaughan,143 Guell,132 Jordan,34, Neville36 Smart,76 McKinnon135 |
| 11. REPEATED VISITS TO HEALTH SERVICES | ||||
| 19 | Searching for a diagnosis and the cause of pain, and/or pursuing effective pain management, can lead children and their families to make repeated return visits to health services or health professionals to repeatedly refer families to different services often with long waiting periods. Waiting for diagnosis and effective pain management results in families experiencing long periods of uncertainty frustration, despair and loss of faith in professionals and services. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | Maciver,77 McDonagh,136 Carter,117 Castle,141 Jordan,34 Khanom,122 Neville,36 Wong134 |
| 12. EXPERIENCES OF HEALTH SERVICES AND CARE | ||||
| 20 | Interactions with health professionals were a source of dissatisfaction and stress for many families. Children perceived that professionals ignored their experiences of living with pain and that professionals had given up on them. Mothers felt that professionals rarely addressed during medical appointments the emotional impact their child’s treatment had on them. It was distressing when health professionals did not believe the child was in pain. Parents, particularly mothers, felt they were being blamed for their child’s pain when there was no obvious cause, or when health professionals indicated the cause might be psychological and/or social. Parents and children highly valued health professionals who listened to, understood and believed the impact chronic pain had on them and their family life, which could reduce their distress and isolation and give them hope. | High confidence | No/very minor concerns regarding methodological limitations, coherence, adequacy and relevance | Maciver,77 McDonagh,136 Britton,80 Baert,102 Brandelli,105 Brodwall,75 Carter,117 Castle,141 Hunt,110 Nutkiewicz,140 Smart,76 Sorensen146 |
| 21 | Children being referred to a pain clinic confirmed to them and others that their pain was a real illness, and was a source of hope, and emotional and practical support. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Maciver,77 Baert,102 Carter,117 Jordan,34 Suder147 |
| 22 | The transition from children’s to adult health services was worrying and difficult for young people. Young people were likely to need a gradual shift to independence in managing their care. During transition to adult services, children with sickle cell disease had experienced adult hospital wards as unwelcoming and had had poor care during unscheduled hospital visits and in non-specialist hospital wards for painful episodes. | Moderate confidence | No/very minor concerns regarding methodological limitations and coherence, minor concerns regarding adequacy and moderate concerns regarding relevance | Forgeron,142 Renedo82 |
| 13. EXPERIENCES OF SERVICES ASSESSING AND MANAGING CHRONIC PAIN | ||||
| 23 | Children and parents perceived that non-specialist health professionals did not always manage chronic pain effectively. Issues included professionals refusing to prescribe analgesics due to lack of knowledge of an underlying genetic condition; professionals showing scepticism about the child’s pain severity and pain experiences; limited treatment time to focus on pain management; and disjointed organisation of care between professionals from different services. | High confidence | No/very minor concerns regarding methodological limitations, coherence and adequacy, and minor concerns regarding relevance | McDonagh,136 Brodwall,75 Carter,117 Jordan,34 Neville,36 Smart,76 Wong,134 Renedo,82 McKinnon135 |
| 24 | When a child had a learning disability or an underlying condition, such as cerebral palsy or Down syndrome, the health professionals focused on the condition or disability rather than the whole child. Consequently, the child’s pain was ignored and not treated. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | McDonagh,136 Carter,119 Carter,109 Hunt,110 McKinnon135 |
| 25 | Parents, usually mothers, perceived that their expertise in assessing their child’s pain, particularly for younger children and those with communication difficulties, was not always recognised by health professionals. | High confidence | No/very minor concerns regarding methodological limitations and coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Maciver,77 McDonagh,136 Carter,119 Carter118 |
| 14. EXPECTATIONS OF TREATMENTS AND SERVICES | ||||
| 26 | Effective communication by health professionals, including management of family expectations of treatments, was important for effective pain management and to support families’ psychosocial needs. Good communication and expectation management result in a trusting relationship. However, sometimes families had their expectations of a cure raised by professionals, but cure was not achieved. | Moderate confidence | Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | Maciver,77 Baert,102 Carter,118 Carter,117 Dell’Api,138 Suder147 |
| 15. WHAT CHILDREN AND FAMILIES WANT FROM CHRONIC PAIN TREATMENTS | ||||
| 27 | Some treatments were not acceptable to all children and families. Families often saw psychological treatment as stigmatising, for instance, as evidence that health professionals did not believe their pain was real, and they considered it their last choice of treatment. Children wanted tailored treatments from pain clinics, which they did not feel they received. Pain-causing therapies, for example physiotherapy or injections for juvenile idiopathic arthritis, or those with unpleasant side effects, seemed counterintuitive to parents and caused the family extreme distress. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | Maciver,77 Britton,79 Carter,117 Nutkiewicz,140 Sorensen,146 Brandelli,105 McKinnon135 |
| 28 | Although there was very little evidence concerning interventions, parents valued interventions that helped them adapt their parenting skills and valued gaining information about chronic pain and how to better help their child deal with pain. Children and their parents valued treatment in a group setting because the group interaction with others with similar conditions helped them to feel less isolated, and to appreciate their individual differences. However, treatment in a group setting could lead to a sense of guilt in children when confronted with others with more severe pain. Children also valued an intervention that helped them change their focus from reducing pain to learning how to live with it. CYP liked physiotherapy because it helped them develop an awareness of their bodies and capabilities, gave them a greater understanding of their pain, helped to reduce their fear of exercise and facilitated treatment engagement and adherence. | Very low confidence | Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and relevance | Ahlqwist,137 Gaughan,143 Kanstrup139 |
| 16. CHILDREN AND THEIR FAMILIES MANAGING PAIN ON THEIR OWN | ||||
| 29 | Sometimes children and their families had to manage pain on their own. For instance, when they had disengaged with unsatisfactory services which were unwelcoming and/or provided poor pain management; as a supplement to, or when they had no effective, prescribed medical treatments; or when they chose not to consult a doctor at all. | Moderate confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and minor concerns regarding relevance | Atkin,124 Atkin,125 Helvig,144 Wong,134 Renedo,82 McKinnon135 |
| 30 | Parents, usually mothers, felt responsible for, and had an important role in, helping their child to manage their pain. The extent of parental involvement varied depending on the complexity of the condition and the child’s age. Parents helped their child learn to recognise different types of pain and thus what type of pain management strategy they should use, helped their child avoid pain triggers, used distraction and reward during pain episodes, interpreted their child’s non-verbal pain cues in order to assist with pain management and provided help with basic needs. | High confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, adequacy and relevance | McDonagh,136 Brodwall,75 Carter,119 Carter,109 Hunt,110 Renedo,82 Smart,76 Wong,134 Brandelli,105 McKinnon135 |
| 31 | Parents of children with neurological conditions felt they had to find a balance between managing pain and their child joining in family activities. These parents had to make difficult decisions with little help from health professionals, including whether and how much medication to administer their child at home because side effects could interfere with the child’s participation in family life and/or cause health problems. | Moderate confidence | Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance | Carter,119 Carter,109 McKinnon135 |
| 32 | Parents had a key role ensuring their child was adhering to pain management treatments at home. Families were more likely to follow a treatment programme if it was associated with reduction in pain and increased autonomy for the child. Aspects that could negatively affect adherence were the side effects of medications, treatments that were monotonous, repetitive, painful and/or time-consuming and interventions that had negative impacts on family life and activities. | Moderate confidence | Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance | Borghi,133 Britton,79 Carter,118 Gaughan,143 Brandelli,105 McKinnon135 |
| 17. PREJUDICE AND DISCRIMINATION IN HEALTH SERVICES | ||||
| 33 | Children and parents perceived or reported experiencing prejudice and discrimination in health services which led to poor health service delivery and care and inadequate pain management. Discrimination included professionals having poor knowledge of their child’s condition (sickle cell disease) and failing to convey even basic information to families about it; professionals focusing on the child’s learning disability (Down syndrome) at the expense of investigating possible chronic pain; and children with Down syndrome receiving inferior care compared to children without a Down syndrome. Care was particularly poor for children with Down syndrome and communication difficulties. | Moderate confidence | No/very minor concerns regarding methodological limitations and coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance | McDonagh,136 Atkin,124 Atkin,125 Renedo82 |
| 18. PREJUDICE AND DISCRIMINATION IN SCHOOL | ||||
| 34 | Some school policies and practices facilitated children’s inclusion in education, others undermined their education. For instance, in some schools, children did not receive help from teachers to catch up on missed schoolwork which undermined children’s ability to succeed at school and some had to give up school early as a result. Other schools did provide extra support for children to catch up, such as learning advice outside of school hours, or offered adapted school hours. | Moderate confidence | No/very minor concerns regarding methodological limitations and coherence, moderate concerns regarding adequacy and minor concerns regarding relevance | Atoui,148 Dyson,130 Sorensen,146 Williams123 |
| 35 | Children managing pain on their own was less successful in some circumstances, for example when the pain was severe. Also children were unable to manage their own pain when the emotional and physical impacts of their underlying condition were severe. External barriers could prevent effective self-management, for example a lack of physical resources to manage pain, such as no hot baths in hospitals. School policies also undermined children’s abilities to self-care thus triggering or worsening pain. School rules and practices such as refusing requests for water or breaks during classes and enforcing physical exercise classes in cold environments meant children with sickle cell disease were prevented from staying sufficiently hydrated and warm to avoid painful crises. In contrast, some children with juvenile idiopathic arthritis were granted exemptions from physical exercise classes. Accommodations made by teachers, such as being excused from physical education, could be unwanted by children because it made them stand out as different from their peers. | High confidence | No/very minor concerns regarding methodological limitations, coherence, adequacy and relevance | Atkin,124 Atkin,125 Atoui,148 Britton,80 Cartwright,131 Dyson,130 Guell,132 Waite-Jones,126 Wong,134 Williams,123 Renedo82 |
| 36 | At school, children reported experiencing bullying, not being accepted, being judged and discriminated against by peers, peer disbelief in their pain, or peers’ general ignorance and prejudice about their condition. Younger children found it harder to deal with discriminatory behaviour than older children who were more used to it and so had had time to develop coping mechanisms. In a country (Lebanon) where sickle cell disease is high prevalence, a study did not find evidence of bullying and marginalisation of children with the condition at school. | Moderate confidence | No/very minor concerns regarding methodological limitations, minor concerns regarding coherence, adequacy and relevance | Atkin,125 Atoui,148 Dyson,130 Williams123 |
Appendix 8 Evidence profile table
| # | Summarised review finding | Methodological limitations | Coherence | Adequacy | Relevance | GRADE-CERQual assessment of confidence | |
|---|---|---|---|---|---|---|---|
| 01. IMPACT OF CHRONIC PAIN ON FAMILY LIFE | |||||||
| 1 | Poorly managed, moderate and severe chronic pain was overwhelming and took over family life and affected family dynamics. The routines and activities of the whole family were restricted and limited by managing the pain and its consequences. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
McDonagh,136 Atkin,125 Atoui,148 Britton,80 Britton,79 Brodwall,75 Carter,118 Dyson,130 Forgeron,142 Gaughan,143 Guell,132 Jones,128 Khanom,122 Suder,147 Sorensen,146 Brandelli,105 McKinnon135 |
| 2 | Pain meant children and their families had to manage many uncertainties regarding their changing routines and family life, diagnosis and prognosis, and the child’s future prospects, for example of finding employment or attending university. For fluctuating pain conditions, the fear and uncertainty around when and how intensely children would experience pain were always present which limited families’ activities even when the child was not in pain. Some children with fluctuating pain conditions were able to gather energy from moments with less or no pain, which helped them to deal with everyday life. | Minor concerns Explanation: Minor concerns regarding methodological limitations because of three studies with no or minor limitations and one study with moderate limitations. |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because there are only four studies. |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 Ahlqwist,137 Jordan,35 Khanom122 |
| 02. IMPACT OF PAIN ON FAMILY MEMBERS | |||||||
| 3 | Poorly managed, moderate and severe chronic pain had mostly negative psychosocial impacts on all family members. Children and parents felt depressed, afraid of the possible cause of the pain, and grieved the loss of their life before pain. CYP felt socially isolated and different from peers. Parents felt anxious, helpless and frustrated at being unable to help their child feel better. There was a greater impact on members who were more involved in caring for the child with pain, usually mothers. Siblings who did not have chronic pain felt neglected by their parents and resentful of the child with pain but also concerned about them. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 McDonagh,136 Atkin,125 Atoui,148 Britton,80 Britton,79 Carter118 Cartwright,131 Forgeron,142 Gaughan,143 Guell,132 Jones,128 Jordan,35 Khanom,122 Njifon,149 Rossato,145 Suder,147 Waite-Jones,126 Sorensen,146 Williams,123 Jones,128 Brandelli105 |
| 4 | Parents felt deeply afraid of what might be causing the pain, of witnessing their child in pain, that treatments would not work and that their child would not get better to enjoy a fulfilling life. The constant fear caused parents to always be on call for their child, which was also detrimental to parents’ well-being. | Minor concerns Explanation: Minor concerns regarding methodological limitations based on the assessment of four studies –two with low and two with moderate methodological limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 Gaughan,143 Jones,128 Jordan,35 |
| 5 | Parents, siblings and adolescents with chronic pain reported that some good things had happened because of the impact of chronic pain. The main caregiver, usually the mother, felt they became closer to their child and that their relationship had improved. Siblings without chronic pain also felt that their family relationships had become closer than in other families, and they became more compassionate to others. Some adolescents with chronic pain acknowledged that their experiences made them a better person, better equipped to live life and more mature. | Moderate concerns Explanation: Moderate concerns regarding methodological limitations because of four publications with moderate limitations and two with low limitations |
Moderate concerns Explanation: Moderate concerns regarding coherence because data could have alternative interpretations such the positive framing of challenging circumstances or adapting psychologically to threatening experiences |
Minor concerns Explanation: Minor concerns regarding adequacy because there is a moderate amount of data from only six studies. |
No/very minor concerns Explanation: |
Moderate confidence Explanation: Moderate concerns regarding methodological limitations, moderate concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Britton,80 Suder,147 Waite-Jones,126 Jones,128 Brandelli105 |
| 6 | Primary caregivers, usually mothers, experienced reduced ability to have a life outside of their home, they stopped paid employment and/or lost their career and curtailed their social life to focus on caring for their child. | Minor concerns Explanation: Minor concerns regarding methodological limitations because of two studies with moderate limitations and two with low limitations |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because two studies offered rich data and two offered thin data |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
McDonagh,136 Brodwall,75 Gaughan,143 Brandelli105 |
| 03. IMPACT ON SELF-IDENTITY | |||||||
| 7 | Children saw themselves as different from peers because they felt unhealthy, restricted by pain, socially isolated, dependent and were treated differently by peers. Some children regarded their chronic pain as abnormal, because it affected their ability to lead a normal life, and as something to pity. Children did not want to be seen as unhealthy and different by their peers and they wanted to belong to a group of friends. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because 7 out of the 13 studies that contributed to this finding were moderate for richness and, overall, there was a small amount of rich data |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance |
Atkin,125 Atoui,148 Britton,80 Cartwright,131 Forgeron,142 Guell,132 Jordan,121 Khanom,122 Njifon,149 Rossato,145 Suder,147 Waite-Jones,126 Williams123 |
| 04. IMPACT ON SIBLINGS | |||||||
| 8 | Siblings who did not have chronic pain felt neglected and helpless which could lead to them behaving dismissively towards the child with pain and even questioning the legitimacy of their pain. Siblings competed for parental time and affection. Siblings blamed the child with pain for dominating their parents’ attention, but they also showed concern and affection for them. Siblings’ negative feelings improved overtime as they developed the skills to adjust socially and emotionally. | Minor concerns Explanation: Minor concerns regarding methodological limitations because four studies presented moderate concerns, three of them were regarding significant aspects such as recruitment and data collection. Three studies had low concerns |
Minor concerns Explanation: Minor concerns regarding coherence. Some concerns about the lack of explanation in primary studies about improved negative feelings over time |
Moderate concerns Explanation: Moderate concerns regarding adequacy because only two studies had rich data and this was a small amount |
Moderate concerns Explanation: Moderate concerns regarding relevance because four studies contained data of indirect relevance from parents and two were UK studies |
Moderate confidence Explanation: Minor concerns regarding methodological limitations, minor concerns regarding coherence, moderate concerns regarding adequacy and moderate concerns regarding relevance |
McDonagh,136 Britton,80 Brodwall,75 Gaughan,143 Njifon,149 Waite-Jones,126 Brandelli105 |
| 9 | Some siblings, even younger siblings, took on caring responsibilities for children with chronic pain which limited their freedom. For example some siblings were expected by their parents to adopt a parenting role for the child with chronic pain, including supervising their medical care, which siblings resented. Other siblings provided personal care for the child with chronic pain such as helping them to dress, lifting them out of the bath and carrying them downstairs. | No/very minor concerns Explanation: Only one study had moderate concerns regarding methodological limitations and three had low concerns |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because all four studies presented moderate richness and quantity of data related to this finding |
Moderate concerns Explanation: Moderate concerns regarding relevance because only two studies focused on the experiences of siblings who did not have chronic pain. Two studies had indirect relevance because they presented the views of children with chronic pain. Two studies were conducted in the UK and two in low- to middle-income countries |
Moderate confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and moderate concerns regarding relevance |
Atkin,125 Atoui,148 Njifon,149 Waite-Jones126 |
| 05. IMPACT ON PARENTING | |||||||
| 10 | Parents learnt on their own to adapt their parenting to help their child deal with the pain while trying to still maintain their child’s autonomy. Parents provided support and care while being firm when necessary, for example making their child go to school despite pain. Successfully adapting their parenting was hindered by a lack of understanding of how they could help their child, and the lack of resources and support from health services and their social network. | No/very minor concerns Explanation: Only two publications that contributed to this finding had moderate limitations, six had low limitations |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because three publications were moderate regarding richness of data, five had rich data |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 Atkin,124 Atkin,125 Brodwall,75 Gaughan,143 Jordan,35 Smart76 |
| 06. ADAPTING FAMILY LIFE TO PAIN | |||||||
| 11 | For poorly managed and severe chronic pain, families focused on trying to control the impact of pain on family life using many strategies. Strategies included families gathering information about pain, following treatments, adjusting their routine to accommodate pain and its management, and self-managing pain to be able to join in activities. These strategies meant that family life then became more restricted because it was completely organised around managing and avoiding exacerbating the pain. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because five publications had moderately rich data and three were very rich |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Atkin,124 Ahlqwist,137 Atkin,125 Atoui,148 Carter,118 Forgeron,142 Guell,132 Rossato145 |
| 12 | Over time, parents and children learnt to adapt to unresolved pain because they felt like they had no other choice. Consequently, families and children started to focus on living well with pain. For instance, parents (mothers) learnt to deal with the unpredictability of pain; helped their child to live with their new condition; and developed ways of dealing with the child’s fear about the future. Children found new ways to do daily activities, for example using mobility aids. | Minor concerns Explanation: Minor concerns regarding methodological limitations because six publications representing five studies had moderate limitations and three publications had no or minor limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Britton,80 Britton,79 Baert,102 Carter,118 Guell,132 Jones128 Rossato,145 Suder,147 Sorensen146 |
| 07. SOCIAL SUPPORT | |||||||
| 13 | Peers, friends and the extended family provided practical, financial and emotional support which helped parents and children deal with the impact of pain on their lives, enhanced quality of life and adherence to treatments. Contact with peers and friends helped children feel normal which provided them with hope and reassurance. Parents (mainly mothers) longed for others to understand their own suffering but lacked a social support system. Mothers grew apart from friends due to their caring role. | Moderate concerns Explanation: Moderate concerns regarding methodological limitations because three studies had moderate concerns in important aspects, such as data collection and analysis and recruitment strategy. Two had low concerns |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because there was a small amount of moderately rich data for this finding |
Minor concerns Explanation: Minor concerns regarding relevance because the aims of the studies were not directly relevant to this finding |
Moderate confidence Explanation: Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and minor concerns regarding relevance |
Britton,80 Baert,102 Cartwright,131 Waite-Jones,126 Brandelli105 |
| 14 | Recurrent school absences and pain prevented children from engaging with friends when at school which made it difficult for children to maintain friendships, contributed to their lack of support and increased their sense of social isolation. | No/very minor concerns Explanation: All studies had low concerns regarding methodological limitations |
Minor concerns Explanation: Minor concerns regarding coherence because the data from three out of the six studies did not have a good fit with the review finding |
Moderate concerns Explanation: Moderate concerns regarding adequacy because only one out of the six publications included rich data regarding this finding |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance |
Atkin,124 Atkin,125 Atoui,148 Dyson,130 Williams,123 Jones128 |
| 08. CONDITION-SPECIFIC PEER SUPPORT | |||||||
| 15 | Meeting others with similar conditions helped adolescents feel less isolated because they were able to share experiences and provide mutual support. In contrast, other adolescents did not want peer support from other children with chronic pain because they did not want to be reminded of their pain or because they believed others would not have similar experiences. Parents preferred support from other parents of children with similar conditions, who they described as a great comfort and vital source of information. | No/very minor concerns Explanation: All studies had low concern for methodological limitations |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because two of the studies included only thin data regarding this finding |
No/very minor concerns |
Moderate confidence | McDonagh,136 Cartwright,131 Forgeron,142 Williams,123 |
| 09. DISCLOSURE OF PAIN | |||||||
| 16 | Parents avoided disclosing their child’s pain to friends and extended family for a range of reasons. For instance, parents found chronic pain hard to understand and explain, they were afraid of being judged on their parenting skills or disbelieved, or they anticipated a lack of sympathy for a condition that is not life-threatening. Lack of disclosure could negatively affect how much support parents received from their friends and wider family. However, when they did disclose their child’s pain, their social networks did not always understand or believe the pain and were not empathetic, sometimes blaming them for poor parenting, for example being overprotective parents. Children also often avoided disclosing their pain, although girls and younger children were more likely to disclose and share their problems than boys and adolescents. Children also avoided disclosing their pain to help manage how others perceived them, to avoid having to deal with the prejudice and discrimination of others, such as derogatory comments, and because the pain was invisible and hard to explain. | Minor concerns Explanation: Minor concerns regarding methodological limitations because six studies had moderate limitations and six had low limitations |
Minor concerns Explanation: Minor concerns regarding coherence because there are plausible alternative explanations that could have been further explored |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Atkin,125 Atoui,148 Britton,80 Baert,102 Dyson,130 Forgeron,142 Gaughan,143 Guell,132 Jones,128 Khanom,122 Suder,147 Sorensen146 |
| 10. WHAT CHILDREN AND FAMILIES WANT FROM SERVICES | |||||||
| 17 | At the onset of the child’s chronic pain, children and their families initially sought services hoping for a cure for the pain which they assumed must have an underlying physical cause. Parents expected doctors to undertake objective medical tests, such as physical examinations, X-rays and high-technology scans, to reveal the physical cause of their child’s pain and to clinically treat and cure the pain. | Minor concerns Explanation: Minor concerns regarding methodological limitations because five studies had moderate limitations and five had low limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Brodwall,75 Carter,117 Dell’Api,138 Gaughan,143 Jordan,34 Kanstrup,139 Maciver,77 McDonagh,136 Neville,36 Smart,76 Sorensen146 |
| 18 | Families searched for a cause and/or diagnosis to better understand the pain, to enable treatment, and as proof of a genuine illness, that is proof that their pain is real and is believed by health professionals. However, receiving a diagnosis was not a source of hope for all families, for instance, for children with a pre-existing chronic condition, an additional chronic pain diagnosis increased their worry. A diagnosis such as chronic pain or CRPS without knowing the cause could also be unsatisfactory to families because it did not help them understand why the child had pain. | Minor concerns Explanation: Minor concerns regarding methodological limitations because five studies had moderate limitations and five had low limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 McDonagh,136 Brodwall,75 Carter,117 Gaughan,143 Guell,132 Jordan,34,36 Smart,76 McKinnon135 |
| 11. REPEATED VISITS TO HEALTH SERVICES | |||||||
| 19 | Searching for a diagnosis and the cause of pain, and/or pursuing effective pain management, can lead children and their families to make repeated return visits to health services or health professionals to repeatedly refer families to different services often with long waiting periods. Waiting for diagnosis and effective pain management results in families experiencing long periods of uncertainty frustration, despair and loss of faith in professionals and services. | Minor concerns Explanation: Minor concerns regarding methodological limitations because four studies had moderate limitations and four had low limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 McDonagh,136 Carter,117 Castle, Jordan,34 Khanom,122 Neville,36 Wong134 |
| 12. EXPERIENCES OF HEALTH SERVICES AND CARE | |||||||
| 20 | Interactions with health professionals were a source of dissatisfaction and stress for many families. Children perceived that professionals ignored their experiences of living with pain and that professionals had given up on them. Mothers felt that professionals rarely addressed during medical appointments the emotional impact their child’s treatment had on them. It was distressing when health professionals did not believe the child was in pain. Parents, particularly mothers, felt they were being blamed for their child’s pain when there was no obvious cause, or when health professionals indicated the cause might be psychological and/or social. Parents and children highly valued health professionals who listened to, understood and believed the impact chronic pain had on them and their family life, which could reduce their distress and isolation and give them hope. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 McDonagh,136 Britton,80 Baert,102 Brandelli,105 Brodwall,75 Carter,117 Castle,141 Hunt110 Nutkiewicz,140 Smart,76 Sorensen146 |
| 21 | Children being referred to a pain clinic confirmed to them and others that their pain was a real illness, and was a source of hope, and emotional and practical support. | Minor concerns Explanation: Minor concerns regarding methodological limitations because three studies had moderate limitations and two studies had no or minor limitations |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because the finding is based on six publications representing five studies and a moderate amount of rich data |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, No/very minor concerns regarding coherence, minor concerns regarding adequacy and No/very minor concerns regarding relevance |
Maciver,77 Baert,102 Carter,117 Jordan,34 Suder147 |
| 22 | The transition from children’s to adult health services was worrying and difficult for young people. Young people were likely to need a gradual shift to independence in managing their care. During transition to adult services, children with sickle cell disease had experienced adult hospital wards as unwelcoming and had had poor care during unscheduled hospital visits and in non-specialist hospital wards for painful episodes. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because the finding is based on only two studies with a small amount of rich data. However, we have expertise in this area. There is universal evidence about transitions to adult services being problematic in the way described in this finding |
Moderate concerns Explanation: Moderate concerns regarding relevance because the studies focused on only sickle cell disease or musculoskeletal pain in two high-income countries including the UK. There is a much wider highly relevant literature on transitions to adult services which was not captured in our search |
Moderate confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and moderate concerns regarding relevance |
Forgeron,142 Renedo82 |
| 13. EXPERIENCES OF SERVICES ASSESSING AND MANAGING CHRONIC PAIN | |||||||
| 23 | Children and parents perceived that non-specialist health professionals did not always manage chronic pain effectively. Issues included professionals refusing to prescribe analgesics due to lack of knowledge of an underlying genetic condition; professionals showing scepticism about the child’s pain severity and pain experiences; limited treatment time to focus on pain management; and disjointed organisation of care between professionals from different services. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding relevance because four studies were conducted in the UK studies and five in other high-income countries |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and minor concerns regarding relevance |
McDonagh,136 Brodwall,75 Carter,117 Jordan,34 Neville,36 Smart,76 Wong,134 Renedo,82 McKinnon135 |
| 24 | When a child had a learning disability or an underlying condition, such as cerebral palsy or Down syndrome, the health professionals focused on the condition or disability rather than the whole child. Consequently, the child’s pain was ignored and not treated. | Minor concerns Explanation: Minor concerns regarding methodological limitations because one publication had moderate limitations and four had minor or very minor limitations |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because the finding is based on five studies and a moderate amount of rich data |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
McDonagh,136 Carter,119 Carter,109 Hunt,110 McKinnon135 |
| 25 | Parents, usually mothers, perceived that their expertise in assessing their child’s pain, particularly for younger children and those with communication difficulties, was not always recognised by health professionals. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because the finding is based on only five publications from four studies but data were rich |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 McDonagh,136 Carter,119 Carter118 |
| 14. EXPECTATIONS OF TREATMENTS AND SERVICES | |||||||
| 26 | Effective communication by health professionals, including management of family expectations of treatments, was important for effective pain management and to support families’ psychosocial needs. Good communication and expectation management result in a trusting relationship. However, sometimes families had their expectations of a cure raised by professionals, but cure was not achieved. | Moderate concerns Explanation: Moderate concerns regarding methodological limitations because four studies had moderate concerns and two studies had no or minor concerns |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Moderate confidence Explanation: Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 Baert,102 Carter,118 Carter,117 Dell’Api,138 Suder147 |
| 15. WHAT CHILDREN AND FAMILIES WANT FROM CHRONIC PAIN TREATMENTS | |||||||
| 27 | Some treatments were not acceptable to all children and families. Families often saw psychological treatment as stigmatising, for instance, as evidence that health professionals did not believe their pain was real, and they considered it their last choice of treatment. Children wanted tailored treatments from pain clinics, which they did not feel they received. Pain-causing therapies, for example physiotherapy or injections for juvenile idiopathic arthritis, or those with unpleasant side effects, seemed counterintuitive to parents and caused the family extreme distress. | Minor concerns Explanation: Minor concerns regarding methodological limitations because four publications had moderate limitations and four had no or very minor limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Maciver,77 Britton,79 Carter,117 Nutkiewicz,140 Sorensen,146 Brandelli,105 McKinnon135 |
| 28 | Although there was very little evidence concerning interventions, parents valued interventions that helped them adapt their parenting skills and valued gaining information about chronic pain and how to better help their child deal with pain. Children and their parents valued treatment in a group setting because the group interaction with others with similar conditions helped them to feel less isolated, and to appreciate their individual differences. However, treatment in a group setting could lead to a sense of guilt in children when confronted with others with more severe pain. Children also valued an intervention that helped them change their focus from reducing pain to learning how to live with it. CYP liked physiotherapy because it helped them develop an awareness of their bodies and capabilities, gave them a greater understanding of their pain, helped to reduce their fear of exercise and facilitated treatment engagement and adherence. | Moderate concerns Explanation: Moderate concerns regarding methodological limitations because two studies had moderate limitations and one minor limitations |
Serious concerns Explanation: Serious concerns regarding coherence because all the evidence on interventions have been grouped together into one finding which has resulted in low coherence |
Moderate concerns Explanation: Moderate concerns regarding adequacy because the finding is based on only three studies with limited data that was not very rich |
Moderate concerns Explanation: Moderate concerns regarding relevance because the studies were conducted in two high-income countries (Sweden, USA) and data were on a narrow range of treatments (Acceptance and Commitment Therapy, physiotherapy, pain rehabilitation outpatient programme) |
Very low confidence Explanation: Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and moderate concerns regarding relevance |
Ahlqwist,137 Gaughan,143 Kanstrup139 |
| 16. CHILDREN AND THEIR FAMILIES MANAGING PAIN ON THEIR OWN | |||||||
| 29 | Sometimes children and their families had to manage pain on their own. For instance, when they had disengaged with unsatisfactory services which were unwelcoming and/or provided poor pain management; as a supplement to, or when they had no effective, prescribed medical treatments; or when they chose not to consult a doctor at all. | Minor concerns Explanation: Minor concerns regarding methodological limitations because two studies had moderate limitations |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because there were five studies of which two studies had a good amount of rich data |
Minor concerns Explanation: Minor concerns regarding relevance because the studies focused on broader aspects of the pain experience in high-income countries including the UK |
Moderate confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and minor concerns regarding relevance |
Atkin,124 Atkin,125 Helvig,144 Wong,134 Renedo,82 McKinnon135 |
| 30 | Parents, usually mothers, felt responsible for, and had an important role in, helping their child to manage their pain. The extent of parental involvement varied depending on the complexity of the condition and the child’s age. Parents helped their child learn to recognise different types of pain and thus what type of pain management strategy they should use, helped their child avoid pain triggers, used distraction and reward during pain episodes, interpreted their child’s non-verbal pain cues in order to assist with pain management and provided help with basic needs. | Minor concerns Explanation: Minor concerns regarding methodological limitations because four studies had moderate limitations and six studies had no or very minor limitations |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
High confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
McDonagh,136 Brodwall,75 Carter,119 Carter,109 Hunt,110 Renedo,82 Smart,76 Wong,134 Brandelli,105 McKinnon135 |
| 31 | Parents of children with neurological conditions felt they had to find a balance between managing pain and their child joining in family activities. These parents had to make difficult decisions with little help from health professionals, including whether and how much medication to administer their child at home because side effects could interfere with the child’s participation in family life and/or cause health problems. | Minor concerns Explanation: Minor concerns regarding methodological limitations because one study had moderate limitations and two studies minor or very minor limitations |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because findings are based on three studies and a moderate amount of rich data |
No/very minor concerns Explanation: |
Moderate confidence Explanation: Minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance |
Carter,119 Carter,109 McKinnon135 |
| 32 | Parents had a key role ensuring their child was adhering to pain management treatments at home. Families were more likely to follow a treatment programme if it was associated with reduction in pain and increased autonomy for the child. Aspects that could negatively affect adherence were the side effects of medications, treatments that were monotonous, repetitive, painful and/or time-consuming and interventions that had negative impacts on family life and activities. | Moderate concerns Explanation: Moderate concerns regarding methodological limitations because four studies had moderate limitations including three with concerns about the rigour of data analysis |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because there was a moderate amount of rich data. We have expertise in this area. There is other evidence about the key role of parents in treatment adherence for a wide range of childhood chronic conditions |
No/very minor concerns Explanation: |
Moderate confidence Explanation: Moderate concerns regarding methodological limitations, no/very minor concerns regarding coherence, minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Borghi,133 Britton,79 Carter,118 Gaughan,143 Brandelli,105 McKinnon135 |
| 17. PREJUDICE AND DISCRIMINATION IN HEALTH SERVICES | |||||||
| 33 | Children and parents perceived or reported experiencing prejudice and discrimination in health services which led to poor health service delivery and care and inadequate pain management. Discrimination included professionals having poor knowledge of their child’s condition (sickle cell disease) and failing to convey even basic information to families about it; professionals focusing on the child’s learning disability (Down syndrome) at the expense of investigating possible chronic pain; and children with Down syndrome receiving inferior care compared to children without a Down syndrome. Care was particularly poor for children with Down syndrome and communication difficulties. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because the five publications report data from only three studies and the studies focus only on sickle cell disease or Down syndrome. |
No/very minor concerns Explanation: |
Moderate confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and no/very minor concerns regarding relevance |
McDonagh,136 Atkin,124 Atkin,125 Renedo82 |
| 18. PREJUDICE AND DISCRIMINATION IN SCHOOL | |||||||
| 34 | Some school policies and practices facilitated children’s inclusion in education, others undermined their education. For instance, in some schools, children did not receive help from teachers to catch up on missed schoolwork which undermined children’s ability to succeed at school and some had to give up school early as a result. Other schools did provide extra support for children to catch up, such as learning advice outside of school hours, or offered adapted school hours. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Moderate concerns Explanation: Moderate concerns regarding adequacy because the finding is based on only four studies with a small amount of rich data |
Minor concerns Explanation: Minor concerns regarding relevance because one study was conducted in Lebanon. Two studies focused only on sickle cell disease, one on epidermolysis bullosa, and one on CRPS so relevance to other pain conditions is uncertain |
Moderate confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, moderate concerns regarding adequacy and minor concerns regarding relevance |
Atoui,148 Dyson,130 Sorensen,146 Williams123 |
| 35 | Children managing pain on their own was less successful in some circumstances, for example when the pain was severe. Also children were unable to manage their own pain when the emotional and physical impacts of their underlying condition were severe. External barriers could prevent effective self-management, for example a lack of physical resources to manage pain, such as no hot baths in hospitals. School policies also undermined children’s abilities to self-care, thus triggering or worsening pain. School rules and practices such as refusing requests for water or breaks during classes and enforcing physical exercise classes in cold environments meant children with sickle cell disease were prevented from staying sufficiently hydrated and warm to avoid painful crises. In contrast, some children with juvenile idiopathic arthritis were granted exemptions from physical exercise classes. Accommodations made by teachers, such as being excused from physical education, could be unwanted by children because it made them stand out as different from their peers. | No/very minor concerns Explanation: |
No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding adequacy because there was a moderate amount of rich data |
No/very minor concerns Explanation: |
High confidence Explanation: No/very minor concerns regarding methodological limitations, no/very minor concerns regarding coherence, no/very minor concerns regarding adequacy and no/very minor concerns regarding relevance |
Atkin,124 Atkin,125 Atoui,148 Britton,80 Cartwright,131 Dyson,130 Guell,132 Waite-Jones,126 Wong,134 Williams,123 Renedo82 |
| 36 | At school, children reported experiencing bullying, not being accepted, being judged and discriminated against by peers, peer disbelief in their pain, or peers’ general ignorance and prejudice about their condition. Younger children found it harder to deal with discriminatory behaviour than older children who were more used to it and so had had time to develop coping mechanisms. In a country (Lebanon) where sickle cell disease is high prevalence, a study did not find evidence of bullying and marginalisation of children with the condition at school. | No/very minor concerns Explanation: |
Minor concerns Explanation: Minor concerns regarding coherence because one study conducted in Lebanon had contradictory data |
Minor concerns Explanation: Minor concerns regarding adequacy because the finding is based on only four studies but a moderate amount of rich data |
Moderate concerns Explanation: Moderate concerns regarding relevance because a limited range of pain conditions and ages of children are represented. Three studies are based only on sickle cell disease and one is based on epidermolysis bullosa. Three studies focus only on adolescents |
Moderate confidence Explanation: No/very minor concerns regarding methodological limitations, minor concerns regarding coherence, minor concerns regarding adequacy and minor concerns regarding relevance |
Atkin,125 Atoui,148 Dyson,130 Williams123 |
Glossary
- Abdominal pain
- Pain occurring in the stomach.
- Adenomyosis
- A condition that causes the lining of the womb (the endometrium) to bury into the muscular wall of the womb.
- Aggregate
- Something formed by adding together several amounts or things.
- Bibliographic database
- A database containing a range of journals.
- Case study
- A research approach that uses in-depth investigation of one or more examples of a current social phenomenon, utilising a variety of sources of data. A ‘case’ can be an individual person, an event or a social activity, group, organisation or institution.
- Child
- We use the term child for any person under the age of 18 years old.
- Chronic fatigue
- A condition that causes extreme tiredness and a range of other symptoms.
- Chronic pain
- Pain which persists past normal tissue healing time or lasts/recurs for more than 3–6 months.
- Complex regional pain syndrome
- A poorly understood condition where a person experiences persistent severe and debilitating pain.
- Conceptual
- Based on ideas or principles.
- Contracture
- A state of prolonged resistance in a muscle.
- Cystic fibrosis
- A genetic condition that can cause a build-up of thick, sticky mucus in the body’s tubes and passageways – particularly the lungs and digestive system.
- Diabetes
- A lifelong condition that causes a person’s blood sugar level to become too high.
- Diffuse and localised idiopathic pain syndrome
- Pain occurs at several sites around the body and commonly includes backache. Each pain is distinct and may occur at separate times.
- Document analysis
- The detailed examination of documents produced across a wide range of social practices, taking a variety of forms from the written word to the visual image.
- Dyskinesia
- Tremor or involuntary movement.
- Dysmenorrhoea
- Pain during or just before a woman’s period.
- Effectiveness
- How well a treatment works.
- Empirical
- Based on data or evidence.
- Endometriosis
- A condition where tissue similar to the lining of the womb starts to grow in other places, such as the ovaries and fallopian tubes.
- Epidermolysis bullosa
- A group of rare, inherited skin disorders that cause the skin to become very fragile.
- Ethnography
- A research method that involves personal engagement with the subject to understand a particular culture or social setting.
- Fibroids
- Non-cancerous growths that develop in or around the womb.
- Fibromyalgia
- A long-term condition that causes pain all over the body.
- First-order construct
- Lay understandings and interpretations of one’s experiences.
- Focus groups
- A focus group is a small group of people brought together to talk. The purpose is to listen and gather information. It is a good way to find out how people feel or think about an issue, or to come up with possible solutions to problems.
- Framework analysis
- A qualitative data analysis method used to organise and structure research data in order to refine the researcher’s focus to identify themes.
- Functional disorders
- They include problems such as dissociative (non-epileptic) seizures, functional movement disorders (such as tremors, spasms or jerks) and functional limb weakness.
- Grey literature
- Grey literature is material that is not produced by commercial or academic publishers, such as a doctoral thesis or a report produced by a third-sector organisation/charity.
- Grounded theory
- A research method that includes an inductive process in which theory is built and modified from the data collected.
- Haemophilia
- A rare condition that affects the blood’s ability to clot.
- Inductive
- Using a particular set of facts or ideas to form a general principle.
- Inflammatory bowel disease
- A term mainly used to describe long-term conditions that involve inflammation of the gut.
- Infographic
- A picture or diagram showing or explaining information.
- Intervention
- Treatment used by health professionals.
- Iterative
- Doing something again and again, usually to improve it.
- Juvenile idiopathic arthritis
- A condition that causes pain and inflammation in one or more joints for at least 6 weeks in children.
- Longitudinal research
- Where participants are followed over time.
- Lupus
- Lupus is a long-term condition that causes joint pain, skin rashes and tiredness.
- Lymphotropic virus human cell
- The causative agent of a form of blood cancer and of a progressive disease of the nervous system.
- Meta-ethnography
- Meta-ethnography is a systematic, interpretive qualitative evidence synthesis methodology that can produce robust, novel synthesised evidence.
- Mucopolysaccharidosis
- A condition where there is not enough of a particular enzyme to break down used mucopolysaccharides, which means they build up and store in the cells in the body which causes progressive damage.
- Musculoskeletal conditions
- A group of conditions that affect the bones, joints, muscles and spine, and are a common cause of severe long-term pain and physical disability.
- Neonate
- A baby who is < 4 weeks old.
- Neurological conditions
- Result from damage to the brain, spinal column or peripheral nerves.
- Oral ulcers
- Ulcers in the mouth.
- Osteogenesis imperfecta
- A genetic condition present from birth. Its primary feature is fractures usually caused by minimal impact.
- Osteoporosis
- A disease that causes the bones to become weaker and easily broken.
- Otitis media
- An infection of the middle ear that causes inflammation (redness and swelling) and a build-up of fluid behind the eardrum.
- Paediatric
- Medical care of children.
- Palliative
- Treatment that reduces pain without curing the cause of the pain. Children’s palliative care occurs from diagnosis onwards and is not just about end-of-life treatment.
- Pelvic inflammatory disease
- An infection of the female upper genital tract.
- Pharmacological
- Treatment that uses drugs.
- Phenomenology
- A research method that studies how we experience phenomena (things that exist and can be seen, felt, tasted, etc.).
- Physiological
- Relating to the way in which the body works.
- Primary study
- Studies generating new data.
- Psychological
- Relating to the human mind or feelings.
- Qualitative evidence synthesis
- The development of techniques to combine multiple sources of qualitative data to derive best evidence for use in health care.
- Reflex sympathetic dystrophy
- A type of complex regional pain syndrome. This condition occurs because of malfunctions in the sympathetic nervous system and immune system.
- Richness
- Text that reveals the complexities of what is being studied.
- Second-order construct
- Primary study authors/researchers’ interpretation of lay understandings and interpretations.
- Spasticity
- An involuntary increased resistance to passive muscle stretching.
- Systematic review
- A review of a clearly formulated question that uses systematic and explicit methods to identify, select and critically appraise relevant research and to collect and analyse data from the studies that are included in the review. Statistical methods (meta-analysis) may or may not be used to analyse and summarise the results of the included studies.
- Tertiary
- Tertiary care refers to highly specialised treatment.
- Textual synthesis
- Forming a narrative or written summary.
- Thematic analysis
- A method of analysing qualitative data following a series of steps to generate themes.
- Third-order construct
- New interpretations of the data that go beyond those reached within the primary study.
- Xeroderma pigmentosae
- A rare, genetic condition. The body is unable to repair damage to the DNA in the skin, caused by ultraviolent radiation present during daylight.
List of abbreviations
- ACT
- Acceptance and Commitment Therapy
- CASP
- Critical Appraisal Skills Programme
- CERQual
- confidence in the evidence from reviews of qualitative research
- CRPS
- complex regional pain syndrome
- CYP
- children and young people
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- IBD
- inflammatory bowel disease
- ICD-11
- International Classification of Diseases
- MEDLINE
- Medical Literature Analysis and Retrieval System Online
- NHS
- National Health Service
- NICE
- National Institute for Health and Care Excellence
- PAG
- Project Advisory Group
- PaPaS
- Cochrane Pain, Palliative and Supportive Care
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO
- International Prospective Register of Systematic Reviews
- QIMG
- Cochrane Qualitative Implementation Methods Group
- SIGN
- Scottish Intercollegiate Guidelines Network
- WHO
- World Health Organization
Notes
-
Example of one ‘Analytic Category’ displayed on Google Jamboard
-
Example of one ‘Analytic Category’ displayed on MS Whiteboard
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/UTPM7986).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.