Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 18/01/06. The contractual start date was in April 2019. The final report began editorial review in November 2020 and was accepted for publication in August 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Dedication
This project was originally conceived and developed with the late Professor Scott Reeves, who died unexpectedly in May 2018. Scott, a global research leader, was first and foremost a sociologist and ethnographer. He brought his sociological lens to the study of challenging problems of health and social care professional relationships, in their learning and their work. His original ideas and considerable expertise in interprofessional health-care research were instrumental in the formation of this study and the research team dedicate this project to his memory.
Permissions
Copyright statement
Copyright © 2022 Harris et al. This work was produced by Harris et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Harris et al.
Chapter 1 Background
Parts of this report have been reproduced or adapted from Harris et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Parts of this report have been reproduced or adapted from Sims et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Rationale for the review
This chapter sets out the background and rationale for the study and explains our purpose in conducting a realist synthesis of leadership of integrated care teams and systems. It explains the history of integrated care and discusses the reasons for identifying the attributes that facilitate effective leadership of these systems. Our approach, which focuses on identifying and understanding the mechanisms through which leadership of integrated care works and the necessary contextual circumstances,3–5 is informed by the Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) publication standards for realist syntheses,6 providing justification for utilising realist approaches in the study of a complex system and subject.
The organisation of health and social care in England is moving rapidly towards integrated models. NHS policy documents, such as the Five Year Forward View7 and the more recent Long Term Plan,8 have emphasised this shift, with the strategic intention of building upon existing cross-sector interdependence between the NHS, social care, local authorities, communities and employers. To ensure success in existing collaborations and integrated systems, a range of development needs has been identified, including leadership. 9 Leadership of integrated teams and systems is a complex, multifaceted concept, lacking a strong evidence base. In particular, there is little understanding of how effective leadership across integrated health and social care teams and systems may be enacted, the contexts in which this might take place and the subsequent implications for integrated care as a whole. 10
Our realist review of leadership of integrated care teams and systems responds to this first by comprehensively mapping the evidence base and, second, by applying realist principles in the interpretation of the literature to identify the key characteristics that comprise effective leadership practices. Realist synthesis is a particularly useful approach when exploring a concept as fluid as leadership, as the processes of theoretical reasoning that are required by the approach enable an interrogation of systems and policy to a depth not possible with more conventional or systematic evidence reviews.
Objectives and focus of review
This review developed and refined the programme theories of leadership of integrated care teams and systems in health and social care, exploring what works, for whom and in what circumstances. It has produced recommendations for policy-makers, health and social care leaders, managers and clinicians to help them design work systems and leadership development initiatives to support effective leadership of complex multisystem services.
Formal objectives for the review were as follows:
-
to investigate who are the leaders of integrated care teams and systems and what activities contribute to their leadership roles and responsibilities
-
to explore how leaders lead/manage integrated care teams and systems that span multiple organisations, agencies and sectors
-
to develop realist programme theories that explain successful leadership of integrated care teams and systems iteratively through stakeholder consultation and evidence review
-
to identify the development needs of the leaders of integrated care teams and systems
-
to provide recommendations about optimal organisational and interorganisational structures and processes that support effective leadership of integrated care teams and systems. 1
These objectives were designed to enable the analysis of established perspectives around integrated health and social care, leadership, and these elements in combination. The next section provides background on the development of integrated care, exploring how and why effective leadership is important.
Defining integrated care
The cross-cutting nature of integrated care suggests that a single definition is problematic. These systems serve a complex and diverse range of stakeholders. Expectations regarding the purpose and objective of integrated care are likely to differ, sometimes significantly, although there have been useful descriptions that enable the identification of a range of central characteristics that constitute an integrated care team and system.
In answer to the question ‘What is integrated care?’,11 a number of commonly used definitions have been presented. These include a health system-based definition, a definition from the perspective of health and social care managers and a social science definition. Although these emphasise a common need for co-ordination of people and services around a shared goal of improving health outcomes, the patient perspective seems both the most illustrative and the most important:
I can plan my care with people who work together to understand me and my carer(s), allow me control, and bring together services to achieve the outcomes important to me.
National Voices. 12
In addition, The NHS Long Term Plan8 explains the purpose of an integrated care system (ICS) as follows:
An ICS brings together local organisations to redesign care and improve population health, creating shared leadership and action.
They state that an ICS includes the integration of primary and specialist care, as well as social care and mental health services.
Historical development of integrated care systems
There are, in addition, universal factors that have been identified as driving the implementation of ICSs, including reduction of fragmentation, continuity of care beyond the hospital setting, patient centeredness and shared managerial vision. 13
The initiatives included in Figure 1 broadly combine to lay the foundations for what is now known as integrated care in the UK context, suggesting a long held, gradually refined intention to integrate health and social care services across a range of disparate contexts. To further understand how integrated services have reached their most recent iterations, an exploration of the relevant policy developments may assist. It is possible to discern how the shift towards a recognition of the value of integrated working and systems has come about, and how integrated care has been adopted as a concept and goal across governments and periods of time. 21 Figure 1 provides a selected chronology of the main policy interventions that have prompted a move towards integrated systems of health and social care in England. In addition, the boxes on the right-hand side of Figure 1 offer examples of the terminological development of integrated care22 and how this type of working has been referred to across different periods of time.
FIGURE 1.
A selected chronology of policy interventions prompting integrated systems of health care. CQUIN, Commissioning for Quality and Innovation framework; ICP, integrated care pilot; PBC, practice-based commissioning; PCG, primary care group.
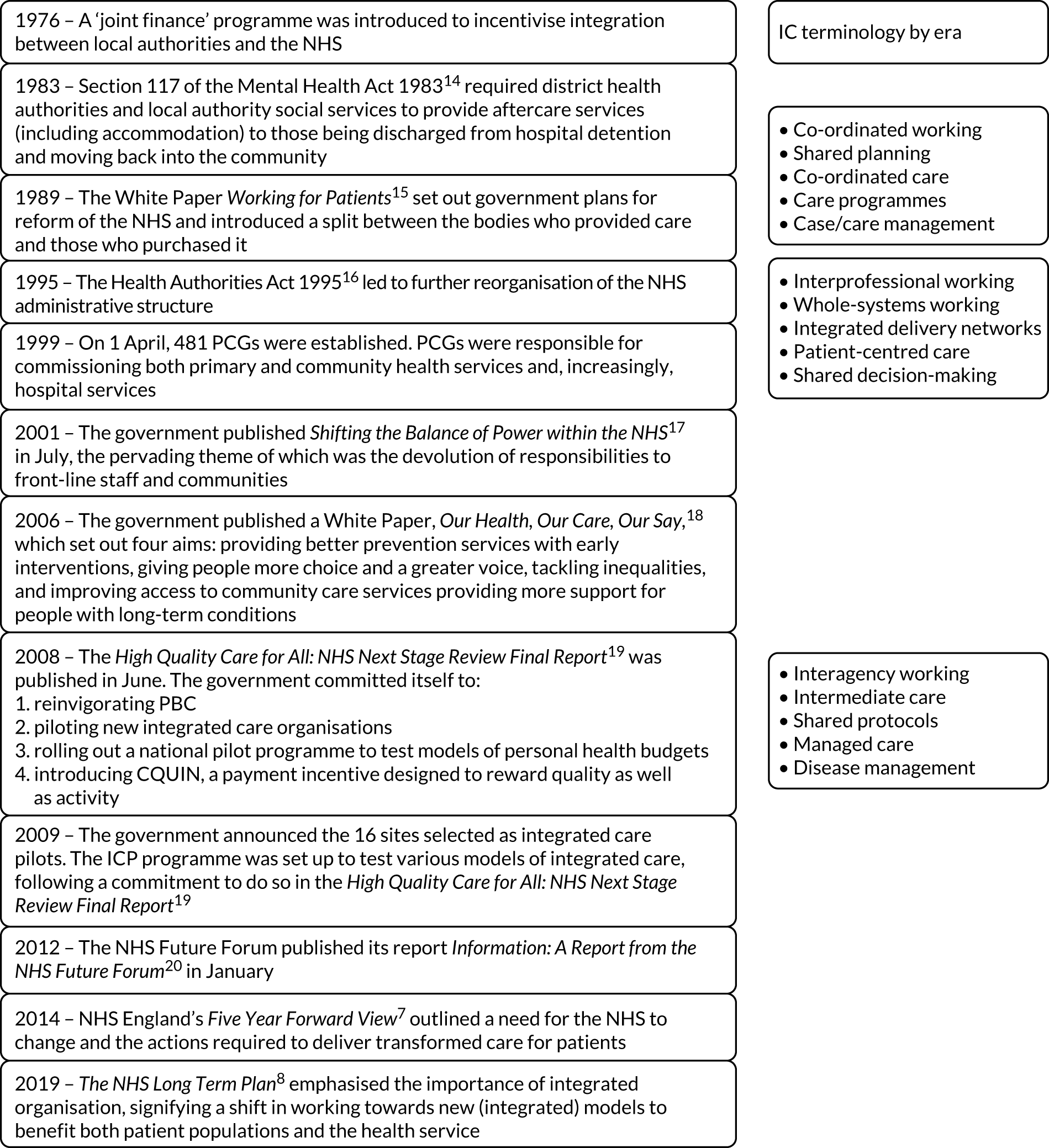
The emergence of integrated care in England can be viewed as a consolidation of the devolution of the NHS across the country accompanied, perhaps paradoxically, by greater centralisation in the form of NHS England. In addition, integration is seen as a means to protect resources through joint working and as a more effective method of delivering care to an ageing population with the associated rise in long-term conditions. 23 While the combination of these elements is important, there is also a distinction to be made between a universal recognition that integrated care is representative of progress and the complex realities that face sometimes radically different locations and patient/service user populations. Although this offers some insight into the development of integrated care, the difficulty around conceptual definition remains. The complex variation of health and care provision and populations across the country has been acknowledged and offers some explanation of why consensus has not and perhaps should not be reached. The following excerpt24 explores this complexity, while providing key principles that can be broadly applied to integrated care:
Integrated care takes many different forms. In some circumstances, integration may focus on primary and secondary care, and in others it may involve health and social care.
The King’s Fund. 24
The authors further state that:
A distinction can be drawn between real integration, in which organisations merge their services, and virtual integration, in which providers work together through networks and alliances.
The King’s Fund. 24
And conclude that:
The most complex forms of integrated care bring together responsibility for commissioning and provision. When this happens, clinicians and managers are able to use budgets either to provide more services directly or to commission these services from others.
The King’s Fund. 24
Achieving a combination of real and virtual integration, alongside delivery and commissioning, is a challenge for leadership. In this complex context, implications for leaders’ merit addressing. They must respond to the dynamic perceptions and realities of integrated care in their activities and behaviours. This highlights a need for a processual view of leadership to accommodate the complex and constantly changing relationships and circumstances inherent in integrated systems. The next section offers examples of leadership organisation in contemporary integrated care models.
Leadership of integrated care
Leadership is a complex concept, with many differing definitions, including those which seek to distinguish it from management. 25 Yet, despite these differences, there is a consensus that leadership involves the direction of a group towards shared goals, wider organisational values, a vision and objectives and the management of ongoing change. 26,27 Effective leadership is claimed to be a key element of well-co-ordinated and safe health and social care,28–31 and ineffective or absent leadership has been linked to reports of failures in care leading to patient/service user harm. 32 Existing research on leadership tends to be based on the premise that leaders provide guidance for single or uniprofessional teams33,34 and overlooks the complexity, intricacies and inevitable tensions that arrive in leading ICSs. These leaders do not influence just one organisation or professional group, but instead often work between several organisations across primary and secondary care, health and social care, publicly funded services, the not-for-profit sector and private businesses. Leaders of ICSs will, therefore, require different skills from their predecessors,24,35 yet there is currently little understanding of what these may be, what the mechanisms for effective leadership across integrated care teams and systems might be, the contexts that might influence it or the nature of the resulting outcomes. 10
The NHS Long Term Plan8 described the governance of ICSs as being inclusive of the following:23
-
a partnership board, drawn from and representing commissioners, trusts, primary care networks, local authorities, the voluntary and community sector and other partners
-
a non-executive chair
-
sufficient clinical and management capacity drawn from across constituent organisations
-
a named accountable Clinical Director of each primary care network
-
a greater emphasis by the Care Quality Commission (CQC) on partnership working and system-wide quality in its regulatory activity, so that providers are held to account for what they are doing to improve quality across their local area
-
NHS providers to take responsibility, with system partners, for wider objectives related to a) use of NHS resources and population health; and b) longer-term NHS contracts with all providers, including clear requirements to collaborate to support system objectives
-
clinical leadership aligned around ICSs creating clear accountability to the ICS.
Although this suggests that there are leadership structures in place, questions concerning how leaders can operate effectively in these structures are timely. Although The NHS Long Term Plan8 states that leadership should be aligned with ICS structure, the collective governance additionally described builds largely on existing leadership processes, providing adaptive reaction rather than a more directive development of leaders of and for integrated care. Thus, while there is evidence to suggest that strong and supportive leadership and joint governance are important to the successful implementation of integrated care programmes,36–38 we do not know the characteristics required to provide this strong and supportive leadership, how this may look and under what circumstances this can be most effectively enabled.
Chapter 2 Review methods
Study design and conceptual basis
As with all complex social interventions, it can be assumed that leadership might work for different stakeholders in various settings in different ways. We therefore adopted a realist synthesis methodology39,40 to enable the identification of the key contextual characteristics and mechanisms that contribute to effective leadership practice in integrated care. This methodology involved developing and iteratively refining initial programme theories through both stakeholder consultation and evidence review.
Realist synthesis was developed as a means of applying realist methods to the evaluation of evidence. 39 This may be of particular help when exploring a concept as fluid as leadership, where the processes of theoretical reasoning will enable an interrogation of systems and policy to a depth not possible with more conventional methods or systematic evidence reviews. 1 Indeed, it has been suggested41 that systematic review is inadequate when the intention is to develop a fresh perspective, reinforcing a need for an inherently iterative, non-linear approach that performs multiple literature searches and constantly refines the evidence-based programme theories. Judging the literature should, in addition, be guided by how well it ‘fits’ into the process, rather than using predetermined quality criteria. This method also allows for the plurality of leadership strategies, the success of which seem often dependent on the unique combination of specific contextual conditions and associated actions.
Research question, boundaries, and scope
The research question identified for the review was:
What aspects of leadership of integrated teams and systems in health and social care work, for whom and in what circumstances?
As no unifying definition of an ‘integrated care team’ had been identified in the literature, we agreed to adopt the following definition of an ‘integrated care team’:
Integrated care teams consist of two or more teams that span multiple organisations, agencies or sectors within health and/or social care and interface directly and interdependently to address individual patient/client goals.
Similarly, as no single definition of an ICS existed, we defined it as:
Integrated care systems consist of the executive boards and senior leadership teams of two more organisations, agencies or sectors within health and or/social care which enable integrated care teams to work efficiently and address their goals.
These definitions were presented to and agreed by the expert stakeholder group. Thus, to be identified as an integrated care team or system and to be included in the review, any team/system in the literature needed to span organisations, be it across health settings (e.g. acute and primary care) or across both health and social care organisations. Initially, literature not relating to health and social care settings (e.g. the business and management literature) was excluded, although this was referred to at a later stage in the synthesis (see Stage 1b). Furthermore, to be included in the review, literature needed to discuss how to lead integrated care or how to develop leaders of integrated care, as opposed to focusing on the process of integration or whether or not integration in itself ‘works’. No limits were placed on the geographical location of the teams or on the nature of their client/patient group.
Searching the literature
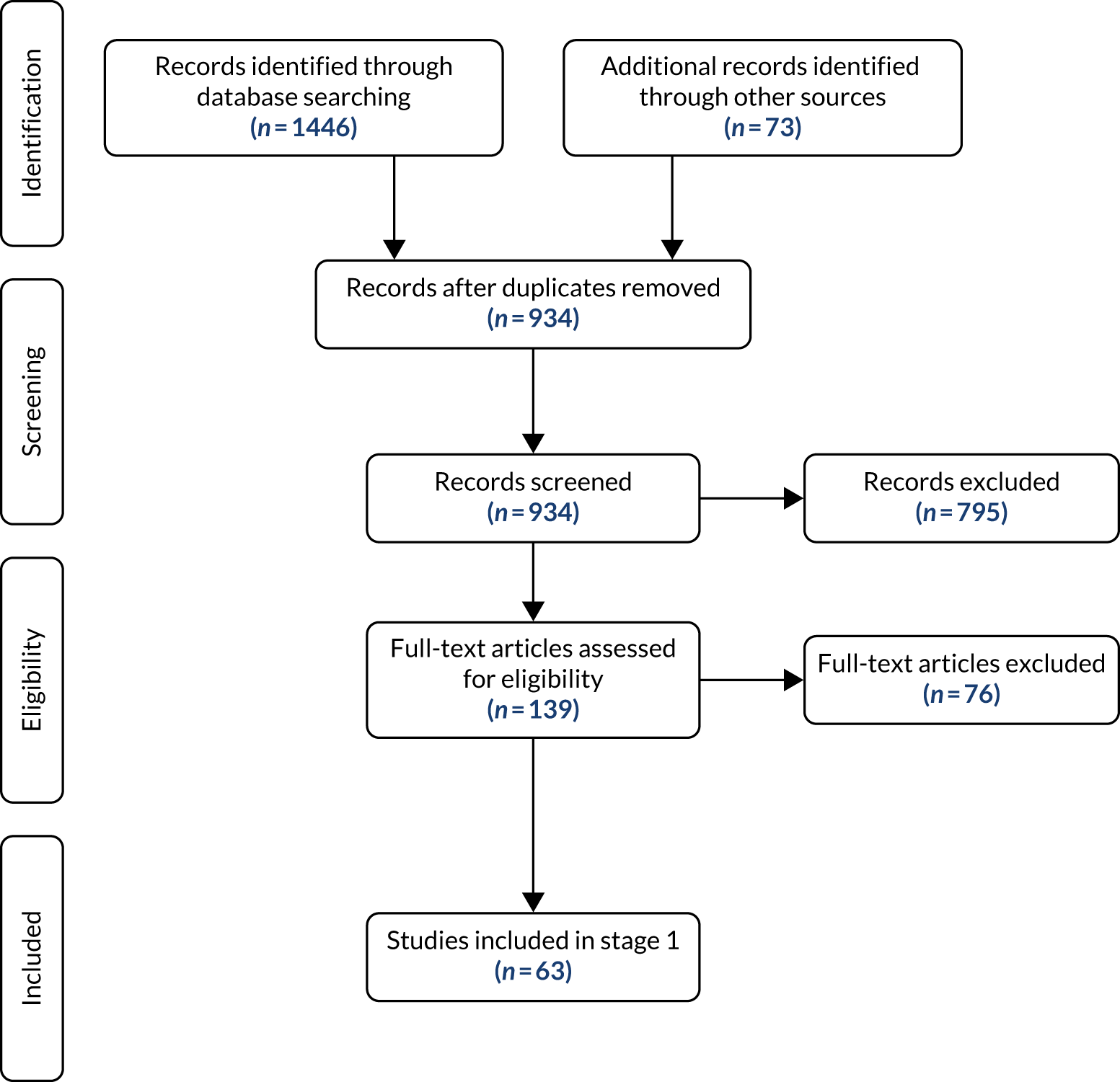
Following realist synthesis methodology,39 two distinct search phases were undertaken for this review; stage 1 and stage 2. Owing to the complexities in identifying relevant literature for this synthesis, stage 1 was also further expanded into stages 1a and 1b.
Stage 1
Research literature
In consultation with information services specialists at both King’s College London (London, UK) and Kingston University London (London, UK), the following search strategy was developed:
“Integrat*” OR “multi-team*” OR “multiteam*” OR “cross-bound*” OR “cross bound*” OR “cross-organisation*” OR “cross organisation*” OR “cross-sector*” OR “cross sector*” AND “leader*” (Limiter: English language only, where available).
This search strategy was run in the following databases: EMBASE, Health Management Information Consortium (HMIC), Social Policy and Practice, Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE, International Bibliography of Social Sciences, PsycINFO and Education Research Complete. A total of 1446 empirical research papers were identified, of which 532 were duplicates and were removed, leaving a total of 914 papers for review. These papers were divided between two reviewers (SS and SF), who read only the abstract of each paper to determine whether or not it was relevant to the focus of the review. At this stage, 848 papers were deemed not relevant and, therefore, were excluded from the review, leaving a total of 66 papers. These papers were divided between the two reviewers and read in full, as a result of which 43 papers were excluded,25,42–83 leaving a total of 23 papers. 31,84–105
Grey literature
Grey literature relating to policy and organisational-based material was sought by searching Google (Google Inc., Mountain View, CA, USA), Google Scholar, government and other specialist websites [e.g. NHS Leadership Academy, Skills for Care, The King’s Fund, Advance HE (formerly known as the Higher Education Academy), The Institute of Healthcare Management, Social Care Online, NHS England and NHS Improvement]. Key words adapted from the main search strategy were used and included ‘leader’, ‘leadership’, ‘integrated care’ and ‘integrated system’. Enormous numbers of evidence sources were identified in the searches. Most were not relevant. Forty-one pieces of grey literature were identified and read in full by one reviewer (RH). This excluded 27 pieces of grey literature,8,9,106–130 leaving a total of 14. 10,131–143
Stage 1 analysis
Stage 1a
A total of 37 papers (23 empirical research, 14 grey literature) were included in the first phase of the stage 1 search. These papers were divided between the three reviewers (SF, SS and RH), who each independently compiled a list of mechanisms or preliminary programme theories based on the papers they had read [to ensure consistency of approach, a small number of papers (n = 4) were read by all the reviewers so that the team could compare their analyses]. The reviewers then met together regularly to discuss their coding of mechanisms and any queries they had until agreement was reached. The following preliminary mechanisms were identified and accepted by all the study team (a short description of these mechanisms can be found in Table 1):
-
supportive relationships and trust
-
team working/collaborative working
-
shared mission/vision/approach/purpose
-
shared responsibility/ownership
-
learning, development and innovation
-
communication
-
providing clarity
-
balancing needs
-
advocacy
-
external liaison/consensus building.
| Mechanism | Description |
|---|---|
| Supportive relationships and trust | Leading integrated care teams requires skill in building high-quality interpersonal relationships, creating significant connections and establishing trust among diverse individuals and groups. Presence, mindfulness, engagement, empathy, team spirit and ownership are key characteristics of compassionate leadership. Dissatisfaction is communicated through appropriate feedback mechanisms to mitigate any negative impact on the team. For ICSs to work effectively, relationships need to be credible and resilient, with clarity in their collective focus. Supportive relationships in teams help overcome the scepticism and protectionism found among professionals regarding collaborative work while reducing duplication of services and visits in the community |
| Team working/collaborative working | Leaders work collaboratively with staff, patients, service users, politicians and citizens. Effective leadership teams work in a collegiate way and have a clear sense of collegiate responsibility. Leaders encourage the participation of all professionals and prevent resistance behaviours, ensuring that co-operation, trust, openness and fairness are instilled into the fabric of the service. Voluntary collaboration between NHS and local authority leaders develops a shared, system-wide approach to strategy, planning and commissioning and financial and performance management, and drives integration of care and services |
| Shared mission/vision/approach/purpose | Leaders of integrated teams are committed to a shared philosophy and common mission/vision/purpose for integrated services. Integrated services involve cross-boundary working with a wide and varied group of organisations. Leaders of these teams need to have insight into the motivations and challenges of other organisations, work through challenges in partnerships to develop collective solutions and look beyond reactive problem solving to take a longer term strategic view. Leaders oversee the implementation of the shared vision, ensure the right resources are available and regularly review the outcomes achieved. Shared vison can be used as a mechanism to focus effort at times of conflict and disagreement |
| Shared responsibility/ownership | Leaders of integrated teams share responsibility for financial cost and quality targets. This is enabled through collective engagement with risk sharing protocols that concern finances, resources and commitments, in addition to measures that monitor and review achievements. Performance management and outcomes frameworks are also used by leaders in local partnerships. Chairpersons and Chief Executive Officers develop a shared vision of the future for their organisation, ensuring that individuals throughout the system understand and accept it as something worth achieving. Shared responsibility for financial cost and quality targets has been deemed important to implementing successful models of leadership |
| Learning, development and innovation | Leaders generate continuous organisational learning and innovation, building adaptable and responsive team cultures. Aiming to improve themselves and those around them, leaders are inspirational and act as role models to encourage continuous learning and build a learning culture, offering opportunities for team members to develop and stretch themselves. Leaders have an interest in innovation and embrace evidence-based practice. They are skilled at leading complex, large-scale change through excellent facilitation and influencing skills. They use performance measures and data to inform design and planning and are also ready to support staff if and when the innovation does not succeed. Leaders create active partners rather than passive employees and, if nurtured appropriately, can encourage and support the individual development of leadership skills within their team |
| Communication | Leaders of integrated care teams possess an ability to listen and consult, adapt communication styles to suit the needs of the situation and audience, manage difficult conversations and read ‘what is not being said’ in an interaction. Leaders can challenge the status quo, manage conflict and have the willingness to engage in robust, open and honest debate. They engage others and can frame and reframe issues to influence how people see them, focusing team members’ attention to bring clarity and agreement to complex situations. Leaders promote high levels of communication and feedback upwards, downwards and across an organisation. They support their own team members to communicate effectively, equipping them to manage conflict and maintain a healthy work environment free of toxic behaviours and relational issues |
| Providing clarity | Leaders ensure that governance arrangements are clear and create synergy and cohesion by ensuring that rules are formed and a system of checks and balances is in place. Leaders also ensure clarity of leadership among their team members. Leaders translate complexity, making sense of disparate policy drives, legislation, performance requirements, regulatory systems and funding mechanisms. Leaders ensure that staff have a clear mandate for decision-making, with documents explaining how decisions are made and who has the authority to make them. This transparency enables stakeholders to see who has authority over specific areas to prevent confusion and enables them to navigate organisations with multiple decision-making bodies |
| Advocacy | Leaders act as advocates for improvement for their patient/client group, demonstrating effective communication with diverse individuals, groups and communities and a strong commitment to achieving positive outcomes. Leaders are enthusiastic local ‘change agents’, demonstrating full, visible and sustained support for service integration. Leaders may need to advocate for greater involvement of some organisations where there is the perceived need to change the historical power balance, e.g. between care homes and the NHS |
| External liaison/consensus building | Leaders have a strong focus on outcomes and the end goal in mind. They focus on the ‘bigger picture’ across their local health and care economy and on broader outcomes, acknowledging the importance of making strategic connections with leaders in other parts of the system and all other staff. They represent their team externally, demonstrating their effectiveness through data collection and evaluation and developing networks and linkages to promote the work of the team. Leaders are good at ‘deliberate’ engagement techniques and can take people on a journey with them, enabling them to see that not everyone will win. They also ensure that their team has the necessary resources and understands its customers so that it can exploit new opportunities |
Given the complexity of this review, an important component of the methodology was the inclusion of contributions from key stakeholders throughout the process. This process is recommended in realist methods,144 as learning what stakeholders know about an intervention and its reason for implementation is essential to understanding it. In this study, consultation and discussion with the stakeholder group was a vital part of the review process. Throughout the report we refer to their contribution to developing knowledge about leadership of integrated care teams and systems. Patient/service user and carer representatives were members of this group and therefore patient and public involvement (PPI) was embedded in all stages of the review. To ground the review in the lived experiences of stakeholders, separate consultation meetings were held during the project period with three stakeholder groups: those leading or working within integrated care teams and systems, patients/service users and carers receiving care from integrated services (PPI) and researchers with expertise in integrated care or realist methods. Most members of the stakeholder group were identified by searching on the internet for leaders of integrated care teams and systems. We were keen to find people who were currently involved in leading care delivery and overall system leaders. It was a challenge, as little detail is provided on NHS and social care websites. Some members were known to the research team in their professional capacity or were suggested as relevant by people we invited. Thirty-three people were invited by e-mail; four did not reply to the invitation and follow-up e-mail, seven declined (no longer in the UK, n = 1; retiring, n = 1; too busy, n = 4; unavailable on planned meeting days, n = 1) and three accepted the invitation but were unable to join any meetings and did not contribute to the review of study documents/findings by e-mail. Nineteen geographically dispersed stakeholders agreed to participate in the group and contributed to at least one meeting, consisting of six individuals with expertise in integrated care, eight with direct experience in leading integrated care teams or systems, two researchers with methodological expertise and three patient/service user and carer (PPI) representatives. Several members of the stakeholder group also had experience of both working in integrated care and leading teams or systems. The first stakeholder meeting took place at stage 1a in the synthesis, when the group met in person to discuss the preliminary mechanisms highlighted in Table 1. An independent chairperson led whole-group and small-group discussions, during which stakeholders were asked to comment on the mechanisms, including which they felt were most pertinent, any that did not appear relevant and any important mechanisms that may have been missed.
Overall, stakeholders felt that, although some of the mechanisms or programme theories were valid and relevant to integrated care teams and systems (e.g. ‘providing clarity’), others (such as ‘communication’ and ‘supportive relationships and trust’) were too general, and had already been identified in the generic leadership literature. They felt that the review needed greater interrogation to identify the components of leadership that were specific to integrated care teams and systems. For example, one potential mechanism that stakeholders felt was missing from the synthesis was around the use of power dynamics in teams and the way that leaders negotiate these. They therefore suggested that we include ‘use of power’ as a potential new mechanism and specifically search for any discussion of this in the literature (for more information on how stakeholders contributed to the development of mechanisms see Chapter 3, Stakeholder perspectives). Stakeholders were asked to forward any relevant papers that we may have missed on to us for review. Stakeholders also agreed that we consider exploring literature outside of health and social care, to see whether or not any other fields had identified potential theories around leading integrated teams and systems that may be applicable to health and social care. A subsequent search stage (stage 1b) was therefore undertaken.
Stage 1b
Given the difficulties that we had experienced in identifying mechanisms of leading integrated teams and systems in the health and social care literature reviewed, the scope of the review was expanded to include material outside health and social care (e.g. business and disaster management). We returned to the papers previously identified but excluded because they were based outside health and social care and also identified any possible new papers from their reference lists. Twelve possible new papers were identified at this stage. 47,48,70,145–153 These papers were divided between two reviewers and read in full. Five of these papers were excluded and the remaining seven were included. 47,48,70,145,147,148,150 Five additional papers were also forwarded on to us by members of the stakeholder group who felt that they would be useful inclusions in the review. These were again divided between two reviewers (SS and SF) and read in full. All five papers were included in the review at this stage. 154–158
The additional 12 papers identified in stage 1b were divided between three researchers (SF, SS and RH) for review. Each reviewer independently compiled a list of mechanisms based on the papers they had read and also returned to their papers included in the stage 1a search and re-analysed these to look for any newly identified mechanisms. Thus, a total of 49 papers were included at this stage. The reviewers then met together again to compare their mechanisms and discuss their findings. In these discussions, they explored how their new mechanisms compared with those identified in stage 1a and explored ways in which the different mechanisms could be separated or merged to identify the components of leadership that were specific to integrated care teams and systems. The following 10 preliminary mechanisms were then agreed:
-
inspiring intent to work together (this merged components of the ‘supportive relationships and trust’ mechanism with the ‘communication’, ‘advocacy’ and ‘team working/collaborative working’ mechanisms as well as incorporating newly identified aspects identified in stage 1b)
-
enabling people to work together (this merged the ‘shared mission/vision/approach/purpose’ with newly identified aspects identified in stage 1b)
-
strategic networking/focusing on the bigger picture (this merged components of the ‘supportive relationships and trust’ mechanism with the ‘external liaison/consensus building’ mechanism as well as incorporating newly identified aspects identified in stage 1b)
-
commitment to learning and development (this mechanism remained similar to that identified in stage 1a but also incorporated feedback from the first stakeholder consultation group and searches conducted in stage 1b)
-
clarifying complex processes (this merged aspects of the ‘providing clarity’ mechanism with newly identified aspects identified in stage 1b)
-
creating balance between organisations and individuals/managing conflict (this merged components of the ‘balancing needs’ mechanism as well as incorporating newly identified aspects identified in stage 1b)
-
use of power (this merged components of the ‘shared responsibility/ownership’ mechanism as well as incorporating feedback from the first stakeholder group and searches conducted in stage 1b).
-
leader resilience (this was a newly identified mechanism, based on searches conducted in stage 1b)
-
flexibility of leadership styles (this was a newly identified mechanism, based on searches conducted in stage 1b)
-
use of public narratives (this was a newly identified mechanism, based on searches conducted in stage 1b).
These mechanisms were discussed and agreed by the study team. We then met with our international advisor to the study and expert on multiteam systems (MTS), Professor Stephen Zaccaro. The team discussed the process undertaken and the difficulties experienced by the reviewers in identifying specific mechanisms of leading integrated care teams and systems. Professor Zaccaro advised the team that ICSs could be conceived of as MTSs and suggested that the reviewers review the MTS literature for mechanisms of leadership of complex teams. The team, therefore, ran a search in Google Scholar for ‘leadership of multiteam systems’. Twenty potentially relevant papers were identified and read in full, as a result of which 14 papers were included159–172 and six were excluded. 173–178 These 14 papers were divided between two reviewers, who, again, searched for any context–mechanism–outcome (CMO) configurations and for any mechanisms, contexts or outcomes that were not specifically linked in an explanatory way and added these into the preliminary mechanisms mentioned previously. Thus, a total of 63 papers were included in the stage 1 search (37 papers from stage 1a combined with 26 papers identified in stage 1b). All the included papers (and the mechanisms identified from them) are listed in Table 2.
| Paper | Inspiring intent to work together | Creating the conditions to work together | Taking a wider view | Commitment to learning and development | Clarifying complexity | Balancing multiple perspectives | Working with power | Fostering resilience | Adaptability of leadership styles | Planning and co-ordinating | General contexts | General outcomes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aitken and von Treuer84 (2014) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Aldridge139 (2016) | ✓ | ✓ | ✓ | ✓ | ||||||||
| American Medical Association85 (2015) | ✓ | ✓ | ||||||||||
| Amelung et al.134 (2017) | ✓ | ✓ | ✓ | |||||||||
| Appelbaum et al.148 (2007)** | ✓ | ✓ | ✓ | ✓ | ||||||||
| Baxter et al.135 (2018) | ✓ | ✓ | ||||||||||
| Baylis131 (2017) | ✓ | ✓ | ✓ | |||||||||
| Bienefeld and Grote145 (2014)** | ✓ | |||||||||||
| Bolden et al.157 (2020) | ✓ | ✓ | ||||||||||
| Burstow138 (2018) | ✓ | ✓ | ||||||||||
| Charles132 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Charles133 (2018) | ✓ | ✓ | ||||||||||
| Chartered Institute of Personnel and Development156 (2012)** | ✓ | ✓ | ✓ | ✓ | ||||||||
| Cooper47 (2016)** | ✓ | ✓ | ✓ | ✓ | ||||||||
| Covin147 (1997)** | ✓ | ✓ | ||||||||||
| Crosby and Bryson149 (2010)** | ✓ | ✓ | ||||||||||
| Croze86 (2007) | ✓ | ✓ | ✓ | |||||||||
| Daub et al.87 (2016) | ✓ | |||||||||||
| DeChurch and Mathieu159 (2009) | ✓ | |||||||||||
| deGruy88 (2015) | ✓ | ✓ | ✓ | |||||||||
| De Vries et al.167 (2016)* | ✓ | |||||||||||
| de Stampa et al.89 (2010) | ✓ | ✓ | ✓ | ✓ | ||||||||
| Fillingham and Weir10 (2014) | ✓ | ✓ | ||||||||||
| Ghate et al.158 (2013)** | ✓ | ✓ | ✓ | |||||||||
| Hartley154 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Horrigan90 (2016) | ✓ | ✓ | ✓ | |||||||||
| Insightful Health Solutions141 (2018) | ✓ | ✓ | ✓ | |||||||||
| Johannessen et al.163 (2012)* | ✓ | ✓ | ✓ | ✓ | ||||||||
| Jonassen169 (2015)* | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Jones et al.162 (2019)* | ✓ | ✓ | ||||||||||
| Kelley-Patterson91 (2012) | ✓ | |||||||||||
| Klinga et al.92 (2016) | ✓ | ✓ | ✓ | |||||||||
| Kugler et al.168 (2016)* | ✓ | |||||||||||
| Lazzara et al.160 (2019)* | ✓ | ✓ | ✓ | |||||||||
| Leadership Centre155 (2015) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Luciano et al.172 (2018)* | ✓ | ✓ | ✓ | |||||||||
| Moore93 (2018) | ✓ | |||||||||||
| Morse150 (2010)** | ✓ | ✓ | ||||||||||
| Murase et al.165 (2014)* | ✓ | ✓ | ||||||||||
| Nieuwboer et al.94 (2019) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Outhwaite95 (2003) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Owen et al.161 (2013)* | ✓ | ✓ | ||||||||||
| Palazzo96 (2014) | ✓ | ✓ | ||||||||||
| Panzer et al.97 (2000) | ✓ | ✓ | ✓ | |||||||||
| Payne et al.98 (2019) | ✓ | |||||||||||
| Perks-Baker140 (2017) | ✓ | ✓ | ||||||||||
| Provider Voices143 (2018) | ✓ | ✓ | ||||||||||
| Rico et al.170 (2018)* | ✓ | ✓ | ||||||||||
| Robb and Gilbert99 (2007) | ✓ | ✓ | ||||||||||
| Schipper164 (2017)* | ✓ | ✓ | ||||||||||
| Social Care Institute for Excellence136 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Shirey et al.100 (2019) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Smith et al.31 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| South, Central and West Commissioning Support Unit142 (2019) | ✓ | ✓ | ✓ | |||||||||
| Stakeholder group feedback | ✓ | ✓ | ✓ | ✓ | ||||||||
| Sun and Anderson70 (2012)** | ✓ | ✓ | ✓ | ✓ | ||||||||
| Thomas and While101 (2007) | ✓ | |||||||||||
| Touati et al.102 (2006) | ✓ | ✓ | ||||||||||
| Wachel103 (1994) | ✓ | |||||||||||
| Weaver et al.171 (2014)* | ✓ | ✓ | ||||||||||
| West137 (2017) | ✓ | ✓ | ||||||||||
| Wheatley et al.104 (2017) | ✓ | ✓ | ✓ | ✓ | ||||||||
| Williams105 (2012) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Zaccaro and DeChurch166 (2012)* | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
A list of preliminary mechanisms was sent out by e-mail to the stakeholder group for review and then presented in full at the second in-person stakeholder group meeting. The independent chairperson again led small-group and whole-group discussions around how the mechanisms should be amended or merged. Stakeholders were specifically asked to challenge the mechanisms and were given space for questions to help generate deeper exploration of the key issues. By the end of this meeting stakeholders were content that the following mechanisms (generated as a consequence of literature searching and whole-group discussions) were pertinent to leading integrated care teams and systems (a short description of these mechanisms can be found in Table 3):
-
inspiring intent to work together
-
taking a wider view
-
creating the conditions to work together
-
clarifying complexity
-
planning and co-ordinating
-
balancing multiple perspectives
-
working with power
-
commitment to learning and development
-
fostering resilience
-
adaptability of leadership style.
| Mechanism | Description |
|---|---|
| Inspiring intent to work together | Integrated care teams and systems have no statutory basis but depend on voluntary collaboration between NHS and local authority leaders to develop a shared, system-wide approach to strategy, planning and commissioning, and financial and performance management. Leaders are effective as advocates for integrated care and for inspiring intent to collaborate with staff across the system and outside it, at various levels. They have a supportive management style that promotes team cohesion, trust, respect, reciprocity and collaboration. Not only do leaders champion these values in their own conduct but they also promote them in their staff. They empower and inspire participation from all professionals, use ‘public narratives’ where appropriate and prevent resistance behaviours, ensuring that key values such as co-operation, openness and fairness are instilled into the fabric of the service |
| Taking a wider view | Integrated services involve cross-boundary working with a wide and varied group of organisations and people with a plurality of interests, goals, aspirations and values. Leaders of integrated teams and systems have experience and insight into the motivations and challenges of other organisations and focus on the bigger picture by acknowledging the importance of making strategic connections with leaders in other parts of the system. They use this knowledge to engage with other leaders, be convincing/persuasive in their communications with others, and work through challenges in partnership with other organisations by bridging language, thought-world and goal differences that may otherwise prove detrimental. This enables them to come up with collective solutions and to look beyond reactive problem solving by taking a longer-term strategic view. Their political astuteness is a necessary and beneficial set of skills that enable them to get things done for constructive ends. Consequently, the goals of the team are more likely to be achieved. However, political astuteness can also be used to pursue personal or sectional interests |
| Creating the conditions to work together | Different organisations, teams and individuals bring their own organisational, sectional or professional interests, ways of working and cultures. Leaders of integrated teams understand, are committed to and champion a shared philosophy, shared mental models and a common mission/vision/purpose for integrated services. Leadership is fundamentally more about participation and collectively creating a sense of direction than it is about control and exercising authority. They provide a clear narrative and direction for their team members to enable and encourage them to align their goals, have a shared focus and to engage in integrated working, rather than think about their own clinical teams, organisations or personal needs. They offer team members a sense of common ownership of the team and its reputation, are willing to delegate responsibilities and provide their colleagues with shared responsibility/accountability for financial, cost and quality targets. As a consequence, role defensiveness or ‘turf wars’ are limited, decision-making is assisted and effort becomes more focused during times of conflict and disagreement |
| Clarifying complexity | Many complex and challenging conditions are associated with integrated working, with unclear boundaries, structures and processes and different governance procedures and funding streams, but leaders can navigate the tension between certainty and uncertainty and translate this to their teams and/or systems. Leaders employ sensemaking strategies, in which they use a set of available artefacts to make the understanding of their message clear and internalised. They are successfully able to negotiate the narrow parameters between oversimplification and exclusionary detail, enabling team members to understand the complexity of disparate policy drivers, legislation, performance requirements, regulatory systems and funding mechanisms to ease working arrangements for the team. They do this by developing policies and initiatives that are easily communicated and understood, with documents explaining how decisions are made and who has the authority to make them. This prevents confusion and enables team members to navigate organisations with multiple decision-making bodies |
| Planning and co-ordinating | Leaders co-ordinate, strategise and serve as a liaison and boundary spanner between their team and the other teams in the system. They actively plan and synchronise the teams within the system, aiding the teams with their timing and executions of plans and helping them to organise intrateam processes with interteam processes and decision-making. When component teams struggle to perform their tasks because of high workloads, leaders can provide backup behaviours by prompting other component teams to provide help, shifting workloads to other teams or proactively offering to help with specific tasks. They employ smooth co-ordination processes that provide the necessary capacity to the whole system to move nimbly and synchronously. This strategising and co-ordination improves both team processes and system performance. However, system leaders must also be mindful of changing and competing demands and be able to switch quickly from the routine to the non-routine. Thus, leaders of systems devote time to ensuring system flexibility. If unexpected changes occur and contingency plans no longer seem appropriate, leaders decide whether to reconsider, abandon or adjust the original plan |
| Balancing multiple perspectives | There are historic power imbalances between health and social care (e.g. between care homes and the NHS) and between professional disciplines. Leaders ensure that there is balance between the organisational cultures, social mission and business aims of the organisations owing to having several specialist areas of knowledge and a good understanding of a broad range of topics. They are enthusiastic ‘change agents’ and demonstrate full, visible and sustained support for service integration. They advocate for those organisations that need greater power and are willing to have difficult conversations with colleagues across different organisations and specialisms and to deal with the uncertainty and ambiguity inherent in complex adaptive systems. This enables greater collaborative and equal working across organisations. Leaders are also able to create balance between professional hierarchies in the team and manage conflict between team members appropriately, working with, and negotiating with, many different stakeholders who have divergent values, goals, ideologies and interests. Leaders recognise tension and work through it with staff to develop a condition in which it is safe to challenge and discussion becomes healthy. A productive balance between harmony and healthy debate is maintained and a coalition is created, with a degree of actionable shared purpose |
| Working with power | Leaders have an awareness of power dynamics and know that the appropriate use of power within and across teams and organisations can be critical during times of uncertainty. Leaders are aware that power dynamics should be skilfully and intelligently negotiated and recognise that colleagues in other parts of the system are sometimes in a better position to lead on certain initiatives than themselves. In such circumstances, they are willing to shift power, migrate authority and relinquish control where appropriate, i.e. if better outcomes can be achieved. When leaders are unwilling to relinquish control, progress can stall. Leaders step aside, showing interest but not interfering or steering. They are also aware that tactics for reducing resistance to change based on threats, manipulation, or misinformation are likely to backfire. Leaders use referent power to bring their teams together (i.e. a charisma that makes others feel comfortable in their presence). This leads to higher team satisfaction during the process of change. Because referent power generally takes time to develop, this finding may highlight the importance of placing individuals who are known, liked and respected by employees in transition-related positions |
| Commitment to learning and development | Leaders have a strategic commitment to access external support and rapid learning with other like-minded systems. They are committed to reflecting on and personally learning from a variety of sources, through formal and informal networks, and to act as a role model for team members, encouraging them to also learn and improve. Leaders establish communities of practice for team learning and the pooling of knowledge. Although managers apply proven solutions to known problems, leaders are exposed to situations in which groups need to learn their way out of problems that could not have been predicted. Leaders recognise that training initiatives can increase component team members’ awareness and understanding of their knowledge structures, as well as their ability to regulate then improve the effective co-ordination of the whole system under dynamic circumstances. They have an interest in innovation and creativity, inviting feedback and embracing change and evidence-based practice for continuous improvement. They encourage team members to generate ideas and explore possibilities but also have a tolerance for things not working and learn how to fail ‘well’ |
| Fostering resilience | Those providing public services need to deal with increased demand, higher expectations from the public about service standards, hostility and psychological projections from the public and the media, often in the context of declining resources for public services. The pace can be relentless and the physical, intellectual and emotional demands very high. Successful leaders of integrated systems have both the personality and learned skills that foster high resilience, perseverance and an awareness of the importance of remaining empathic to the public while also resilient in terms of their own well-being. They put in place social support systems (both in and outside work) and attend appropriate training and personal development programmes to strengthen resilience. Leader stress is therefore reduced |
| Adaptability of leadership style | Leading an integrated team or system is difficult, given the complexities of moulding two or more organisations into one and the sense of loss or uncertainty that employees may experience as part of this. Collaborative leaders are able to adapt their actions based on the circumstances that they confront. They acknowledge that particular situations call for particular leadership skills and behaviours. Leaders align their styles according to the situation at hand, combining or switching approaches as necessary, changing strategy towards flexibility and the use of their tacit knowledge. This generates co-operation, cohesiveness and improved communication among group members |
Although some mechanisms (e.g. ‘inspiring intent to work together’, ‘creating the conditions to work together’ and ‘clarifying complexity’) were felt to be more relevant than others (e.g. ‘planning and co-ordinating’, ‘fostering resilience’ and ‘adaptability of leadership style’), the stakeholders and research team agreed that all 10 mechanisms should be explored in greater detail in stage 2 of the study.
The stage 1a and 1b search processes are shown in the flow chart in Figure 2.
FIGURE 2.
Flow chart of stage 1a and 1b searches.
Stage 2
After the preliminary mechanisms were identified in stage 1, a second stage search was undertaken to look specifically for any empirical evidence of these mechanisms. This second search comprised a search of the following databases: Social Policy and Practice, Education Research Complete, Social Care Online, Scopus, CINAHL, MEDLINE, International Bibliography of the Social Sciences, EMBASE, HMIC, PsycINFO and PubMed, using the following search strategy:
“Integrat*” OR “multi-team*” OR “multiteam*” OR “cross-bound*” OR “cross bound*” OR “cross-organisation*” OR “cross organisation*” OR “cross-sector*” OR “cross sector*” OR “Interorganisation*” OR “Inter-organisation*” AND “leader*” AND “Health” [Limiter: English language only].
Hand-searching of key journals identified by the study team and stakeholders (Journal of Interprofessional Care, Journal of Integrated Care and International Journal of Integrated Care) was also carried out by searching for the term ‘leadership’ in the online version of the journal. A total of 5673 papers were therefore identified at this stage, and all abstracts were read by two reviewers (SS and SF). A total of 5253 papers were excluded either because they were duplicates or because they were deemed not relevant, leaving 420 remaining papers. A further eight papers were also sent to us by the stakeholder group at this stage and added to the pool of documents for review, along with two papers that were picked up in the stage 1 searches but not stage 2; the 14 MTS papers identified in the stage 1 search; 11 papers identified through searching reference lists of relevant papers; and three papers recommended by the study co-applicants. This initially resulted in 458 possible papers, although 16 of these were inaccessible through library resources179–194 and not available through the British Library, which meant that 442 papers were divided between two reviewers and read in full. For this stage in the search, we were seeking only empirical research based in health and/or social care settings and a data extraction form was created and completed for each paper read. In line with realist synthesis methodology, conventional approaches to quality appraisal were not used. 41 Rather, each study’s ‘fitness for purpose’ was assessed by considering its relevance and rigour.
Of the 442 papers read in full, 32 papers were included. 84,92,98,102,105,195–221 The remaining 410 papers were excluded. 10,25,42,44,47,48,51,53,54,59–62,65,75,78,89,91,94,95,97,100,101,104,106,107,110,129,149,150,153,159–172,174,222–585 Around this time, Professor Zaccaro informed us that he had recently completed a comprehensive review of all MTS papers and this had been published. 586 To ensure that no key MTS papers had been missed in the stage 1 search, we searched the full reference list of this review for any empirical research exploring MTS in health or social care. No new papers were found.
To ensure consistency of approach, a third reviewer (RH) read all 32 papers included in the review to ensure that they met the inclusion criteria. Any CMOs identified from these papers were discussed with the third reviewer to ensure that there was agreement in decision-making. The third reviewer also read and reviewed a sample of the excluded papers to ensure that there was agreement around their exclusion. 310,321,330,347,359,373,431,483,547,583 After team discussion, it was agreed that one originally excluded paper should be included in the review. 583 Thus, at this stage, 33 papers from the original 442 papers were included in the review and 409 papers were excluded. The study team and stakeholders were informed of the number of papers included in the review at this stage and were asked for further advice on how to identify any additional papers. It was suggested that we search the Nuffield Trust website (nuffieldtrust.org.uk). After typing the word ‘leadership’ into the search box (filtered for ‘research’ only), three additional relevant papers were identified. 22,587,588 Thus, a total of 36 papers were included at stage 2 of the synthesis. 22,84,92,98,102,105,195–221,583,587,588 At this point, members of the wider study team were consulted, and they suggested that literature searching stopped, as the process had been comprehensive.
The evidence collected from these 36 papers was synthesised by drawing together all information on CMOs and comparing similarities and differences to build a comprehensive description of each mechanism and its role in the leadership of integrated care teams and systems. This was an iterative process throughout, identifying where mechanisms were triggered (or not), the context that enabled or hindered this and the resulting outcomes. Specific explanations of how CMOs were linked and recurrent patterns of CMO configurations within and across the papers were sought and recorded. These theoretically derived explanations were tested and refined using the findings of these empirical studies. All 36 included papers (and the mechanisms identified within each of them) are highlighted in Table 4.
| Paper | Inspiring intent to work together | Creating the conditions to work together | Taking a wider view | Commitment to learning and development | Clarifying complexity | Balancing multiple perspectives | Working with power | Fostering resilience | General contexts | General outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Aitken and von Treuer84 (2014) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Alexander et al.208 (2001) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Asakawa et al.209 (2017) | ✓ | ✓ | ✓ | |||||||
| Atkinson et al.207 (2002) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Axelsson and Axelsson210 (2009) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Balasubramanian and Spurgeon211 (2012) | ✓ | |||||||||
| Benzer et al.212 (2015) | ✓ | ✓ | ||||||||
| Best213 (2017) | ✓ | ✓ | ✓ | ✓ | ||||||
| Brouselle et al.214 (2010) | ✓ | |||||||||
| Carroll et al.215 (2015) | ✓ | ✓ | ||||||||
| Choi et al.216 (2012) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Chreim et al.217 (2010) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Cohen et al.218 (2006) | ✓ | ✓ | ✓ | ✓ | ||||||
| Cramm and Nieboer219 (2012) | ✓ | ✓ | ✓ | |||||||
| Dayan and Heenan587 (2019) | ✓ | ✓ | ||||||||
| Dickinson et al.220 (2007) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Grenier583 (2011) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Karam et al.195 (2017) | ✓ | ✓ | ||||||||
| Kharicha et al.196 (2005) | ✓ | |||||||||
| Klinga et al.92 (2016) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Ling et al.197 (2012) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Lunts198 (2012) | ✓ | ✓ | ✓ | ✓ | ||||||
| Nicholson et al.199 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Payne et al.98 (2019) | ✓ | |||||||||
| Rees et al.200 (2004) | ✓ | ✓ | ✓ | |||||||
| Roberts et al.201 (2018) | ✓ | |||||||||
| Rosen et al.588 (2011) | ✓ | ✓ | ✓ | |||||||
| Scragg221 (2006) | ✓ | ✓ | ✓ | |||||||
| Shand and Turner202 (2019) | ✓ | |||||||||
| Shaw and Levenson (2011)22 | ✓ | ✓ | ✓ | ✓ | ||||||
| Stuart203 (2012) | ✓ | ✓ | ✓ | |||||||
| Touati et al.102 (2006) | ✓ | |||||||||
| van Eyk and Baum204 (2002) | ✓ | |||||||||
| Williams105 (2012) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Williams205 (2012) | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| Willumsen206 (2006) | ✓ | ✓ | ✓ | ✓ | ✓ |
These descriptions were then, again, e-mailed to the stakeholder group for review and discussed in detail at the third and final stakeholder meeting. Owing to restrictions in place as a result of the COVID-19 pandemic, a face-to-face stakeholder meeting was replaced by the online video conferencing software Zoom (Zoom Video Communications, San Jose, CA, USA). A member of the team led whole-group discussions, where stakeholders were presented with the evidence found for each mechanism and asked to help develop and refine these descriptions and explanations further, using their own lived, research or practice experiences. For more information on how the views of the stakeholder group were incorporated into the review during this final stage of the evidence synthesis, see Chapter 3, Stakeholder perspectives.
Figure 3 provides a flow chart detailing the stage 2 search processes.
FIGURE 3.
Flow chart of stage 2 searches.

Chapter 3 Results
The 36 research papers included in this synthesis identified empirical evidence for seven mechanisms: ‘inspiring intent to work together’; ‘creating the conditions to work together; ‘balancing multiple perspectives’; ‘working with power’; ‘taking a wider view’; ‘a commitment to learning and development’; and ‘clarifying complexity’. There was insufficient evidence to identify two of the mechanisms (‘adaptability of leadership style’ and ‘planning and co-ordinating’) as discrete mechanisms in themselves and, therefore, these were incorporated into the other mechanisms. No evidence was found for the mechanism ‘fostering resilience’.
For clarity, findings for each mechanism were divided into two sections – those components of the mechanism that were identified at a systems leadership level and those that were identified at a team level. Although we acknowledge that a systems leader may also lead a specific senior leadership team, in this study, we focused on the role of the overall systems leader of an organisation. However, we acknowledge the added layer of complexity that these different levels of leadership bring. In some cases, the same components were identified as important for leaders at both levels, and this information is recorded in an ‘overarching leadership qualities’ section for each mechanism. On occasion, it was difficult to determine what level of leadership (i.e. team or system) was being directly referred to. Where this was the case, these findings were also incorporated into the ‘overarching leadership qualities’ section for that mechanism. Furthermore, the terms ‘manager’ and ‘leader’ were used interchangeably across the included papers, often with little or no description of what these terms meant. For the purposes of this report, managers and leaders are all described as ‘leaders’, although the research papers themselves may have used either of these terms. Examples of specific CMO configurations identified in the research papers are presented in text boxes.
Mechanism 1: inspiring intent to work together (n = 22)
The original definition of this mechanism developed in stage 1 was ‘integrated care teams and systems have no statutory basis but depend on voluntary collaboration between NHS and local authority leaders to develop a shared, system-wide approach to strategy, planning and commissioning, financial and performance management. Leaders are effective as advocates for integrated care and for inspiring intent to collaborate with staff across the system and outside it, at various levels. They have a supportive management style that promotes team cohesion, trust, respect, reciprocity and collaboration. Not only do leaders champion these values in their own conduct but they also promote them in their staff. They empower and inspire participation from all professionals, use “public narratives” where appropriate and prevent resistance behaviours, ensuring that key values such as co-operation, openness and fairness are instilled into the fabric of the service.’
In stage 2, we found a total of 22 empirical research papers that discussed this mechanism. 22,84,98,105,197–199,203,205–210,213,214,216,217,219–221,588
Overarching ‘inspiring’ leadership qualities
Certain components of the ‘inspiring intent to work together’ mechanism were identified as important at both the systems and team level. This included leaders having a clear vision for collaboration and being able to articulate this vision to others with passion. 22,84,207,208,588 This vision acted as the criterion against which leaders judged the suitability of a proposed course of action, ensuring that they focused on what was central and enduring to integrated working. 208 It was important that leaders lead change according to this vision rather than being ‘swept along’ by external events. 22 Other overriding components of ‘inspiring’ leaders included being visible,213,588 being strongly committed to integration and implementing lasting change,84,197,588 being able to gain the trust and respect of others,198,210,217,588 being a good communicator22,84,208,209,219,588 and being able to develop strong interpersonal relationships with colleagues. 22,198,217 It was considered important for leaders at both levels to have the skills to build and sustain a culture of interdependency, reciprocity and collaboration and to instil key values such as co-operation, openness and fairness among their colleagues. 84,105 As a sense of ‘being in it together’ developed, there was evidence in one study of a reduction in ‘gaming’ between organisations, which made negotiations and collaboration more straightforward. 22
Despite the numerous competing demands on their time and energy, having leaders at all levels who demonstrated good listening skills was identified as important to develop a deep understanding of other organisations and individuals. 208 Being listened to by leaders made people feel as though their input was valued and helped increase motivation and engagement. 208 Similarly, leaders who openly recognised the time, effort and skills that others contributed to integrated working made staff feel respected, appreciated and motivated to contribute more. 208 Conveying genuine respect for the views of all staff, regardless of affiliation or power, reinforced principles of inclusion and elevated members’ respect for leadership. 208 At both systems and team levels, the importance of leader credibility and legitimacy was also identified. 22,105,208,217,588 Credibility was gained through having knowledge of both health and social care through direct experience of working in both fields – for example, a nurse leader who had previously worked in local authority social services;105 through being associated with previously successful developments;588 or through one’s personality, skills and the dynamics of one’s relationships with others. 22 Credibility was lost when leaders appeared to listen to the contribution of others but never incorporated their input substantively. 208
System-level leadership
Important components of the ‘inspiring intent to work together’ mechanism at a system level included having good communication skills, particularly around communicating the vision of an integrated care partnership to the partnering organisations22,207,208 and in maintaining an open, honest and consistent message. 22,220 Successful systems leaders were immersed in developing a clear vision of integrated working and spent considerable time and energy encouraging other executives to share this vision. 22 A study of community health partnerships in the USA208 found that partners valued systems leaders who were forthright and direct in their communications and willing to address issues ‘head on’ rather than trying to minimise or deny them. The authors stated that, because system-level leaders could not rely on formal structures and authorities that facilitated action in organisations, they relied heavily on their own interpersonal skills and effective communication skills to assure a wide and multidirectional diffusion of information. There was also evidence that system-level leaders needed to demonstrate adaptability in their communication style, for example, demonstrating the ability to communicate with individuals across several organisations in multiple directions – both up and down but also horizontally and even diagonally. 208 Traditional leadership styles may have required communicating with a limited number of leaders, but leaders of integrated care systems needed to respect and allow for the diverse needs of a variety of organisations and communities, each of which had different expectations of the timing, extent and channel of communication. Systems leaders were, therefore, required to tailor their style of communication and the language or jargon employed to bridge cultural gaps between organisations and communities. 22,208
A UK-based action research study exploring the aspirations and achievements of a newly formed Mental Health NHS and Social Care Trust220 highlighted the importance of systems leaders in inspiring staff during the early phases of integration. In this study, the formation of a new Care Trust (integrating the local Mental Health NHS Trust and the mental health and learning disability services provided by the local authority social services department) was seen as an innovative move by many of the staff involved, although there were complexities around staff expectations for the ‘culture’ of the new trust. Staff wished to retain several characteristics of their ‘old’ health and social care cultures (e.g. localness, relationships) while simultaneously recognising the need for a new, integrated, culture. This aspiration was acknowledged by the Chief Executive during the consultation process when she stated that the culture of the Care Trust would ‘keep the best of both’ previous organisations in the development of the new one. This key role of the systems leader was, therefore, seen to influence the subsequent culture of the Care Trust and helped to reassure staff that the new integrated systems would contain positive aspects from both the health and social care settings (Box 1). Furthermore, the authors reported that this positive early experience of integration at a system level formed a foundation for the importance of partnership working between health and social services, which became one of the core values of team-level leaders within the Care Trust. 220 Other authors have highlighted the importance of systems leaders creating opportunities for staff to talk about their successes and ensuring that local ‘wins’ are celebrated and communicated to the wider group. 217
Staff within a newly integrated Mental Health NHS and Social Care Trust in the UK were conflicted around their expectations for the culture of the new trust – they wanted to retain characteristics of their old health and social care cultures while also recognising the need for a new culture. This aspiration was acknowledged by the Chief Executive, who assured staff that the culture of the new Care Trust would maintain the best components of the previous organisations. This positive early experience of integration at a system level formed a foundation for the importance of partnership working between health and social services, which became one of the core values of team-level leaders in the Care Trust.
The process of integrating services into a new Mental Health NHS and Social Care Trust means that staff feel conflicted in their expectations for the culture of the new trust (C) → the Chief Executive openly acknowledges and addresses any concerns that staff members have, including clarifying that the culture of the Care Trust will maintain the best components of their previous organisations (M+, resource) and staff are reassured by this (M+, reasoning) → the positive experience of integration at a system level forms a foundation for the importance of partnership working between health and social services (O+) and becomes one of the core values of team-level leaders within the Care Trust (O+).
A facilitating context for this mechanism was that team members could trust their system-level leaders. Team-level leaders said that their ability to ‘sell’ their message about integration to their teams depended on whether or not they trusted that the arrangements in place at a system level would improve care or allow for the detection of deteriorating quality. 588 However, in an investigation of four international case studies of integration,588 building trust was identified as requiring time, and in some cases, work to strengthen integration was founded on a decade of prior work, through which trusting relationships had slowly grown. Many physicians in these sites said that they were only willing to participate in integrated working because they had trust in their systems leaders and their belief in the mission (Box 2).
An investigation of four international case studies of integration found that trust in systems leadership was a key ingredient for integration. However, building trust was identified as requiring time, and in some cases, work to strengthen integration was founded on a decade of prior work, through which trusting relationships had slowly grown. Many physicians in these sites said that they were only willing to participate in integrated working because they had trust in their systems leaders and their belief in the mission.
A decade of prior work had been undertaken to develop trusting relationships (C) → leaders have a strong vision of integration which they attempt to ‘sell’ to their team (M+, resource) and physicians trust in their leaders and their belief in the mission (M+, reasoning) → physicians demonstrate willingness to participate in integrated working even when this is not specifically required of them (O+).
Instances were also provided where the ‘inspiring intent to work together’ mechanism was absent in system-level leadership. For example, an Australian case study199 provided two contrasting contexts of health governance for integrated care and found leadership to be significantly lacking at both board and executive levels. The study found that, although interorganisational relationships between boards and chief executive officers were crucial to effective system-level working, they were often absent and instead replaced by an adversarial culture typified by a ‘master–servant relationship’ between organisations. A Scottish study198 described the implementation of a project to develop and test models of integrated working within a health board. Team leaders were asked what helped and hindered them in the delivery of change in this integration project and identified the lack of ‘buy-in’ from senior-level leaders as a key hindrance. Not having a clear steer or support from senior leaders meant that these team leaders felt that they lacked permission to ‘act’ and this resulted in role confusion among the team. A Swedish study comparing two cases of clinical integration efforts following a hospital merger further highlighted the absence of the ‘inspiring intent’ mechanism at a system level. At one case study site, team members described system-level leaders undertaking the process of integration without consulting staff at a team level or including them in decisions (Box 3). Team members felt that these decisions had been made hastily and in secret and so refused to be involved with the merger decision or adapt their ways of working. 216
A Swedish case study of clinical integration efforts following a hospital merger describes system-level leaders carrying out the process of integration without consulting staff at a team level or including them in decisions. Team-level staff felt that these decisions had been made hastily and in secret and believed that the merger decisions were ‘unthinkable’. Consequently, team members grew frustrated and refused to be involved with the merger or adapt their ways of working.
Hospital merger requires the integration of pre-existing clinical departments (C) → system-level leaders do not involve or communicate about merger decisions with staff at an individual team level (M–, resource) → team-level staff believe that system-level decisions are made secretly and hastily and do not understand or agree with the message being delivered (M–, reasoning) → team-level staff are frustrated (O–) and refuse to be involved with the merger or adapt their ways of working (O–).
Team-level leadership
At a team level, leaders were found to have a ‘determinative influence’ in integrating health-care services214 and play a key role in inspiring their team members. 209 The ‘inspiring intent to work together’ mechanism presented itself as a leadership approach characterised by informality, inclusiveness and a sensitivity to the roles and contributions of all team members. 205,206 Other papers reported team leaders managing ‘by influence’221 and of the need for leaders to be enthusiastic; dynamic; ‘on the ball’; willing to take action; and able to motivate, empower and encourage others. 84,207,209,588 In a study of multiagency working involving professionals from education, social services and health settings in the UK,207 a team member highlighted the importance of their team leader going beyond the realms of their own job for the greater good of the team:
. . . I am sure that’s beyond his/her day job, you need that one person who is prepared to keep it going and not let it slip, keep badgering people.
Atkinson et al. 207
Communication skills were also felt to be important for team-level leaders. 22,84,206,209,219,588 A Norwegian study206 highlighted the benefits of team leaders’ having an ‘open style’ and an ‘accessible profile’. This approach was found to foster a positive, collaborative culture and a fertile learning environment. 205,206,209 Furthermore, having team leaders who facilitated open discussions and challenged assumptions that limited thought and action was also associated with a greater degree of team synergy. 219 A Norwegian study of leadership in interprofessional collaboration in residential childcare services206 found that team leaders encouraged interaction processes by influencing and motivating their staff as well as their collaborative partners, young people and their families. For example, team leaders were reported to intentionally facilitate interaction processes to make them cohesive for the benefit of young people, by encouraging all team members to continuously focus on ‘the child’s best interest’, and on running the institution in ‘the best possible way’. Another study210 further highlighted this need for team leaders to encourage ‘professional altruism’ among their staff (i.e. to ensure that the team’s focus was always on the benefit of the patients/clients in their service).
One study found that the personality of the leader, rather than their professional background, was a key factor in their effectiveness and ability to develop positive relationships with their team. 221 Others found that team leaders needed to have accepted their leadership role but also be willing to ask for help when needed. 209 Presenting a unified front with other team leaders or deputy leaders was also seen to be important in inspiring others to participate in integrated working216 (Box 4). Aside from the team leader role, some authors also found it important for there to be additionally identified ‘champions’ in integrated teams, who reminded members of the team’s benefits and provided sustained motivation. 98,197,216 Although anyone could be a ‘champion’, it was felt that senior clinical leaders were particularly successful, because of their ability to engage with and motivate their professional peer group. 22,197,199 Another study also noted the importance of identifying a succession plan for such team champions. 98
A Swedish study describing integration efforts following a hospital merger of two clinical departments noted that the leaders of both departments had applied for the leadership role in the new department. One of these leaders was given the position but appointed the leader of the other department as their Deputy and shared leadership responsibilities of the consolidated department. Their shared leadership was evident to all team members as they presented a united front to both sites. Team members thought the positive attitude to the merger displayed by both leaders was a significant contributing factor to the willingness of staff members to co-operate with each other.
Hospital merger requires the integration of two pre-existing clinical departments with one new team leader (C) → the new leader of the integrated team employs their counterpart from the other department as their Deputy and shares their leadership responsibilities (M+, resource) → staff perceive a united front between the two leaders (M+, reasoning) → staff in the merging departments respond with a positive attitude and are more willing to co-operate with each other (O+).
Instances were provided where the ‘inspiring intent to work together’ mechanism was absent in team-level leadership. For example, one study highlighted a case where the leader did not identify themself as a strong leader and questioned their own capabilities to fulfil the role. 203 They found that they perpetuated individual rather than collaborative ways of working, which decreased trust and increased dissatisfaction in the team. 203 Furthermore, instead of promoting openness and honesty, this leader’s lack of confidence in their own abilities led them to be complicit in increasing internal conflicts by not exposing or challenging people’s criticisms, complaints or behaviour. This resulted in team members becoming frustrated and the leader becoming even more self-critical and further doubting their legitimacy in the role (Box 5). Others found the ‘inspiring intent to work together’ mechanism was hampered by recalcitrant team members, who slowed progress by working in silos due to a lack of trust. 199
A research project in England providing an autoethnographic account of leading an integrated health and social care working group described a team leader who did not identify themself as a strong leader and questioned their own capabilities to fulfil the role. The leader’s lack of confidence in their own abilities led them to be complicit in increasing internal conflicts by not exposing or challenging people’s criticisms, complaints or behaviour. This resulted in team members becoming frustrated with the leader and the leader becoming even more self-critical and further doubting their legitimacy in the role.
Team leader lacks confidence in their own leadership abilities and questions their capability to fulfil their role (C) → team leader is unable to tackle internal conflicts or challenge difficult behaviour (M–, resource) and team members are not reassured that they are able to lead appropriately (reasoning, M–) → leader becomes even more self-critical and further doubts their legitimacy in the role (O–).
Mechanism 2: creating the conditions to work together (n = 22)
The original definition of this mechanism developed in stage 1 was: ‘Different organisations, teams and individuals bring their own organisational, sectional or professional interests, ways of working and cultures. Leaders of integrated teams understand, are committed to and champion a shared philosophy, shared mental models and a common mission/vision/purpose for integrated services. Leadership is fundamentally more about participation and collectively creating a sense of direction than it is about control and exercising authority. They provide a clear narrative and direction for their team members to enable and encourage them to align their goals, have a shared focus and to engage in integrated working, rather than think about their own clinical teams, organisations or personal needs. They offer team members a sense of common ownership of the team and its reputation, are willing to delegate responsibilities and provide their colleagues with shared responsibility/accountability for financial, cost and quality targets. As a consequence, role defensiveness or ‘turf wars’ are limited, decision-making is assisted and effort becomes more focused during times of conflict and disagreement.’
In stage 2, a total of 22 research papers discussed this mechanism. 22,84,92,105,197,199,204–206,208–213,215–218,220,221,588
Overarching leadership qualities associated with ‘creating the conditions to work together’
There were components of the ‘creating the conditions’ mechanism that were identified as important at both a systems and team level. For example, both systems- and team-level leaders were required to bring a shared vision or purpose to their team92,105,197,208,215 and to set and drive an agreed strategy. 199 It was also important for leaders at all levels to create mutually beneficial shared goals with accountability for outcomes and to have the ability to bring staff together. 199,211,588 A key enabling context for this mechanism at both a systems and team level was ensuring that leaders had sufficient time to develop working relationships and to build an atmosphere of trust, commitment, professional respect and knowledge. 199
System-level leadership
At a system level, having leaders who were personally committed to and made an effort in engaging others in the overall mission/vision of the system was key. 84,92,197,215,218,220 This included enabling a structure that contained aspects of both health and social care perspectives or encouraging shared beliefs about the benefits of change. 92,197,215,220 For example, an Australian study describing the key enablers of change in reorienting to integrated primary care delivery identified the importance of shared values at an organisational level. In this study, a shared organisational vision and values were developed by the community through grassroots participation. 215 Other authors highlighted the importance of systems leaders creating a framework for action208 or ‘rules of engagement,’218 which they communicated compellingly to mobilise resources and guide action towards long-term aims. 208,218 The redrafting of job descriptions for staff was also identified as necessary in some instances to help facilitate collaborative working. 217
Additional components of the mechanism at a system level involved the need for leaders to put in place effective organisational systems and processes associated with governance, strategic planning, finances, human resources management and IT systems to accommodate service integration. 84 Systems leaders were also required to develop and implement plans and evaluate and update these regularly and systematically to ensure that they met current needs and priorities. 84 Furthermore, while staff at a team level sometimes lacked the authority to make changes to services (described as finding themselves hitting a ‘glass ceiling’), successful systems leaders raised these concerns for them at the board level and helped to instigate the changes that teams wished to make. 213 One study217 highlighted the value of introducing a system-level project co-ordinator specifically focused on improving integration or in developing project co-ordination groups with the aim of developing a clear vision and purpose for the system. The authors concluded that frontline clinicians and practitioners often faced so many time constraints in their daily work that it was difficult to bring about any changes without the assistance of a dedicated project co-ordinator.
The absence of the mechanism was also reported at a system level, with reports of a lack of shared vision, both organisationally and politically, leading to fragmentation. 199 Similarly, progress was reported to be noticeably slower across organisations where a shared sense of vision was not widespread. 197 For example, a Swedish case study of clinical integration efforts following a hospital merger described the consequences when the vision of a systems leader did not match that of a team leader216 (Box 6). In this study, an experienced and established team-level leader believed that the new system-level leader focused too much on a ‘tough business management culture’ and was overly concerned with reducing staff numbers. The team leader felt unable to work in such a culture and so resigned from the position soon after their appointment, much to the disappointment of their team.
A Swedish case study of clinical integration efforts following a hospital merger described a team-level leader’s belief that the new system-level leader focused too much on a ‘tough business management culture[. . .] which does not really fit the realities of a hospital’ and was overly concerned with reducing staff numbers. Because of this, the team-level manager resigned from the position soon after their appointment, much to the disappointment of their team.
Hospital merger requires the integration of pre-existing clinical departments and new leadership roles (C) → new system-level leader focused on a ‘tough, business management culture’ concerned with reducing staff numbers (M–, resource) but this did not fit with the vision of the team leader, who was concerned about job losses (M–, reasoning) → resignation of a popular, experienced clinical leader (O–) and disappointment from the team (O–).
Team-level leadership
The creation of one team culture to unify all staff was also highlighted as an important factor in leading an integrated service at a team level. 92 This included helping to develop and negotiate shared purpose, for example, in the form of service models that override narrow organisational, professional or individual interests. 92,105,210 These shared models offered an overarching framework that overruled different models of professional working and could be used to focus effort in times of disagreement or conflict. 105 For example, in one study, authors described the importance of having ‘a common mission so that you’re not always defending your own side’. 92 Ways to achieve such a common approach included providing opportunities for joint meetings for all team leaders and their superiors,84,92,588 establishing specific working groups to enable staff with similar interests across the team to work collaboratively together216 and ensuring that appropriate information and reporting systems were in place. 588 Another way was for leaders to ensure that they involved all their team members in the process of finding effective solutions to problems, regardless of where the problem originated. 92 This was felt to achieve a feeling of solidarity among team members, which was, in turn, a major contributing factor in the provision of sustainable integration of health and social care. 92 It was also important that team leaders were able to successfully navigate and adapt organisational systems and processes to fulfil their role. 84
At a team level, the mechanism also involved team leaders setting priorities and making decisions, balancing the workload throughout the team and constantly monitoring it. 209 In a study describing an evaluation of integrated team management in an English health and social care trust, team leaders described their main responsibility as co-ordinating team members and ensuring that operational management systems functioned effectively so that staff could work together in a ‘joined up’ approach. 221 Furthermore, the ‘creating the conditions’ mechanism also involved team leaders encouraging shared or distributed leadership in their teams or helping the team to perceive leadership as a collective activity. 22,92,205,217 This was based around the belief that integrated care required different skills at different times and these skills did not all need to be embodied by one person. 22 As such, it was important that leaders were open to delegating tasks and responsibilities appropriately. 206,209 Another study217 noted that leadership roles undertaken by team members were often not clearly articulated at the onset but developed in an emergent manner as integrated working advanced in teams where trust was evident. As previously mentioned, some studies also noted the importance of teams having a general ‘co-ordinator’ role, whose duty it was to co-ordinate work between different organisational departments. 209,217 These co-ordinators were reported to play a pivotal role in managing the integration process. 217 For more on shared leadership in teams, see Mechanism 4: working with power (n = 16). An important context for enabling this mechanism was that team leaders received support from their organisational management structure (including Chief Executive Officers), as this provided organisational credibility for any innovative work that they carried out around changing processes and practices. 204
Examples were also highlighted where the mechanism was absent at the system level and this had an impact on team-level leadership. For example, one study212 found that standardised co-ordination processes set in place by integrated systems did not always align with the needs of specific teams, team members or patients. This could result in frustration and conflict among the team and ultimately have an impact on patient care. When this was the case, having integrated team leaders with good personal co-ordination skills (e.g. interpersonal co-ordination abilities such as scheduling meetings with appropriate parties, making personal requests for consultations and demonstrating negotiation skills) helped to resolve conflicts and modify standardised co-ordination procedures.
Mechanism 3: balancing multiple perspectives (n = 20)
The original definition of this mechanism developed in stage 1 was: ‘There are historical power imbalances between health and social care (e.g. between the NHS and care homes) and between professional disciplines. Leaders ensure that there is balance between the organisational cultures, social mission and business aims of the organisations due to having several specialist areas of knowledge and a good understanding of a broad range of topics. They are enthusiastic ‘change agents’ and demonstrate full, visible and sustained support for service integration. They advocate for those organisations that need greater power and are willing to have difficult conversations with colleagues across different organisations and specialisms and to deal with the uncertainty and ambiguity inherent in complex adaptive systems. This enables greater collaborative and equal working across organisations. Leaders are also able to create balance between professional hierarchies within the team and manage conflict between team members appropriately, working with, and negotiating with, many different stakeholders who have divergent values, goals, ideologies and interests. Leaders recognise tension and work through it with staff to develop a condition in which it is safe to challenge and discussion becomes healthy. A productive balance between harmony and healthy debate is maintained and a coalition is created, with a degree of actionable shared purpose.’
In stage 2, a total of 20 research papers discussed this mechanism. 84,105,195,196,198–200,203,205,207,209,210,212,213,216,217,219,583,587,588
System-level leadership
Historical power imbalances between health and social care (the sector as a whole and not just local authority services) meant that the latter was often perceived as ‘the poor relation’ and integrating these services did not necessarily mean that social care would be given a higher political priority. 587 Systems leaders, therefore, needed to be mindful of this imbalance to try and prevent this historic pattern from repeating itself. 587 There was some evidence that systems leaders were instrumental to progress with integration through their ability to work across different groups and institutions, acting as ‘diplomats’ where tensions arose. 588 An English study of multiagency working across social services, health and education settings found that a key skill of successful leadership at a system level was the ability to accept and be confident working alongside the tensions and ambiguities raised through cross-sector working. 207
There was also evidence of the absence of the ‘balancing multiple perspectives’ mechanism at a system level. For example, one author198 described a study where a project to develop and test models of integrated working within a Scottish health board was implemented. In this system, there was evidence of cultural differences between the respective organisations and team leaders talked of bureaucracy at an executive level slowing down team processes in both organisations:
. . . it has to go up. . .. to the Clinical Exec[utive], and it has to go to . . . this Board and that Board.
Lunts198
There were also practical problems around the lack of priority given to joint working at executive level. There were reports of team leaders agreeing to undertake tasks at meetings but never following through on their promises. This was because their respective leaders were not checking that they had fulfilled their roles, and ‘. . . if they weren’t going to be made to do it. . . then they’re not going to do it,’. 198 This was explicitly contrasted with more successful single-agency projects. 198 A further example was also provided of the absence of balancing multiple perspectives at a system level in an examination of an integrated care system in a French health-care network. 583 This study described the development of the informal network as being complex, owing to the differing views of the network members [general practitioners (GPs), gerontologists, neurologists, a speech therapist, neuropsychologists] around how to improve the diagnosis of older patients with cognitive disorders (Box 7). Each member had their own interests and vision for the network, but the network leader rated their own profession (neurology) more highly than the others (owing to an unspoken medical hierarchy in the institution). They focused on only their own vision for the network and what they wanted to achieve (i.e. improved diagnosis of cognitive disorders and faster referrals across the network). To achieve this, they relied only on the expertise of the GPs in the network and set aside the knowledge possessed by other members:
He did not want to involve other . . . institutions, out of fear that discussion might lead to designing a network that was different from his own representation of it.
Grenier583
An informal health-care network in the French health-care system was focused on the diagnosis of cognitive disorders among older patients but included several different professionals with differing views and visions. The network leader rated their own profession more highly than the others and so focused on their own vision for the network. They relied on only the expertise of the GPs in the network and set aside the knowledge possessed by other members. This focused approach enabled the leader to design a rapid detection test for cognitive disorders, which was successfully used by the GPs and enabled quicker referrals across the network. However, some network members also felt ‘side-lined’ because of this approach and withdrew from the network.
Leader rates their own profession more highly than the others (C) → leader focuses on their own personal vision and goals for the network (M–, resource) and so includes the perspectives of those team members that support this vision but ignores those that do not (M–, reasoning) → leader’s goals are achieved through the development of a rapid detection test for cognitive disorders (O+) but excluded members feel ‘side-lined’ and unmotivated and withdraw from the network (O–).
This decision to not equally balance the multiple perspectives in the network had several outcomes, both positive and negative. First, this focused approach enabled the leader to achieve their goal by designing a rapid detection test for cognitive disorders, which was successfully used by the GPs and enabled quicker referrals across the network. However, there were also negative consequences of this decision, including some network members feeling ‘sidelined’ in the decision-making process and unmotivated to participate further, as they felt that the leader’s view of the purpose of the network was limited and did not match their own. At a later stage, the network required funding from the regional authority, which was promoting a more multidisciplinary vision, and so this provided an incentive to the leader to include other perspectives in the network. They therefore incorporated the perspectives of other team members in a controlled way, for example, by incorporating the views of a speech therapist and neuropsychologist into their vision. They continued, however, to exclude the gerontologist (whose views they knew directly contradicted their own) from the decision-making process and so the gerontologist felt marginalised and withdrew from the network. In time, the network members pushed for a new, formal network co-ordinator role that would broaden the focus of the network beyond the limited parameters of the leader [for more information on this, see Mechanism 4: working with power (n = 16)].
Team-level leadership
Key skills of team leaders were identified as the ability to effectively communicate with a wide range of people, including the ability to focus on mutual gains, to encourage team members to appreciate and value the core skills and expertise of others, to bridge diverse cultures and to have the ability to manage difficult conversations and remove any obstacles to change. 105,195,199,200,205,212,217,219 Integrated working could be difficult due to differences in professional language, attitude and values210 but when this mechanism was present, the leader was able to consider the circumstances and ways of thinking of different disciplines and balance them accordingly. 209,213 Team members trusted that they could call on their leaders to help resolve conflict among staff and leaders were able to do so effectively. 84,196,209,210,212
A key context of this mechanism for team leaders was that they were given the necessary time to learn about the different competencies in their team so that they could see these differences as an advantage rather than as a problem. 210 For example, a Swedish study of collaboration between welfare agencies in vocational rehabilitation found that team leaders deliberately involved themselves in the steering committees or working groups of different collaborative projects to reduce territorial behaviour among staff. 210 As a consequence, however, they reported having to wear ‘two different hats’ – both as a leader of their team and as a steering group member for a collaborative project – and said that it could sometimes be difficult to balance loyalties to both groups (Box 8). Another context for this mechanism was whether or not shared leadership was in place in teams. A Swedish study, mentioned previously, comparing case studies of clinical integration efforts following a hospital merger216 found that having shared leadership structures in place (involving the leaders of both pre-existing clinical departments) was an effective way for leaders to cope with the often conflicting logics and goals of multiple stakeholders.
Team leaders deliberately involve themselves in the steering committees or working groups of different collaborative projects to reduce territorial behaviour among staff and overcome differences in professional languages, attitudes and values. As a consequence, team leaders have to wear ‘two different hats’ – both as a leader of their team and as a steering group member for collaborative projects and it can be difficult for them to balance loyalties to both groups.
Team leaders are given time to develop integrated working and learn about different competencies in the team (C) → team leaders deliberately involve themselves as members of steering committees and working groups for various collaborative projects (M+, resource) and their presence makes staff reduce their territorial behaviours (M+, reasoning) → team leaders experience difficulties balancing loyalties to different groups (O–).
When the mechanism was absent, team leaders were unable to manage conflict between team members appropriately. For example, an English action research project providing an autoethnographic account of a leader of an integrated health and social care working group203 highlighted the case of a team leader who was unable to expose and eliminate the underlying tensions, conflicts and lack of trust within their team (Box 9). By worrying about offending people and trying to keep the peace, the leader did not confront the members causing tension in the team and, therefore, inadvertently perpetuated the culture that was so problematic. This made leading the team ‘exhausting’ and meant that managing interpersonal issues took up much of the leader’s time and energy. The group did not achieve collaborative advantage but collaborative inertia, holding lengthy meetings and discussions with negligible outputs and this made the team leader question their own skills and leadership abilities.
An English-based action research project providing an autoethnographic account of integrating a health and social care working group identified a team leader who was unable to expose and eliminate the underlying tensions, conflicts and lack of trust within their team. This perpetuated the problematic culture, meaning that much of the leader’s time was taken up with managing interpersonal issues. The group did not achieve collaborative advantage and the leader questioned their own leadership skills.
Problematic team culture of underlying tension, conflict and lack of trust (C) → team leader lacks the confidence to expose and eliminate these issues (M–, resource) and so does not confront the team members causing tensions within the team (M–, reasoning) → the group did not achieve collaborative advantage (O–), the leader’s time and energy was taken up with the conflict (O–) and the leader questioned their own leadership skills (O–).
Mechanism 4: working with power (n = 16)
The original definition of this mechanism developed in stage 1 was: ‘Leaders have an awareness of power dynamics and know that the appropriate use of power in and across teams and organisations can be critical during times of uncertainty. Leaders are aware that power dynamics should be skilfully and intelligently negotiated and recognise that colleagues in other parts of the system are sometimes in a better position to lead on certain initiatives than themselves. In such circumstances, they are willing to shift power, migrate authority and relinquish control where appropriate (i.e. if better outcomes can be achieved). When leaders are unwilling to relinquish control, progress can stall. Leaders step aside, showing interest but not interfering or steering. They are also aware that tactics for reducing resistance to change based on threats, manipulation or misinformation are likely to backfire. Leaders use referent power to bring their teams together (i.e. a charisma that makes others feel comfortable in their presence). This leads to higher team satisfaction during the process of change. Because referent power generally takes time to develop, this finding may highlight the importance of placing individuals who are known, liked and respected by employees in transition-related positions.’
In stage 2, a total of 16 research papers discussed this mechanism. 102,105,195,203,206–208,210,213,216–220,583,587
System-level leadership
There was evidence of the fundamental importance of system-level leaders having a requisite level of power (including authority, influence and responsibility) to support the process of integration. 213,218 For example, one study highlighted how the chief executive officer, chief operating officer and chief medical officer were the clear central authorities responsible for all financial and clinical decisions in the integrated system. 218 Having such authority at a system level offered others at team level the permission to work and lead across organisational silos. 213 Systems leaders also required the capacity for change, including leaders who were willing to adjust their role217 and had the ability to adjust their leadership style, driving an agenda forward when required but letting it go when necessary. 207 A US study of community health partnerships found that power sharing was the most important mechanism through which leaders could develop ICSs. 208 This study found that many different individuals could have a significant influence over integrated systems, including both formal and informal leaders and idea generators, and it was important that these influencers were diverse and representative of the community being served. 208 By sharing power to set priorities, allocate resources and evaluate performance, systems leaders fostered a sense of joint ownership and collective responsibility and increased the system’s effectiveness. 208 However, an important context for this was the presence of a strong existing foundation of trust and honesty between system partners and that partners viewed power sharing as an authentic move from leadership. Systems partners with less power could quickly feel disenfranchised or threatened if they did not feel that their views were respected or if they felt that leaders showed preference for the views of one partner over another. 208
Other examples were also highlighted of systems leaders relinquishing their power for the benefit of the system as a whole. For example, a Canadian study of the implementation of a new integrated oncological services network in Quebec102 found that the change process towards integrated working was initially marked by resistance from medical staff across the region. Some of this resistance was attributed to the fact that the network leader was unknown in the region. To counter this, the network allied itself with the regional board and the regional board’s director (who had legitimate power in medical settings and good relationships with hospital staff) to set up a temporary committee responsible for implementing the project. This committee then worked towards winning support from hospitals within the region. This study found that systems leaders using power carefully and appropriately helped the network progress successfully, encouraged trust and respect within local teams at all hospitals and interorganisationally and helped team members develop a shared philosophy and vision (Box 10).
A Canadian study of the implementation of a new integrated oncological services network in Quebec found that the change process towards integrated working was initially marked by resistance from medical staff, mainly because the network leader was unknown in the region. To counter this, the network allied itself with the regional board director (who had legitimate power in medical settings and good relationships with hospital staff) to set up a temporary committee responsible for implementing the project. This helped the network progress successfully, encouraged trust and respect within local teams at all hospitals and helped team members develop a shared philosophy and vision.
Newly integrated oncological services network with a newly appointed network leader (unknown in the region) who is facing some resistance from medical staff (C) → new, unknown network leader allies themselves with the well-known and popular regional board director and gives them the power to lead the early stages of project implementation (M+, resource) and medical staff react positively to this as they trust the regional board director (M+, reasoning) → network progresses successfully, with a shared philosophy and vision developed (O+).
In a previously mentioned study in the French health-care system,583 dissatisfaction from team members around the narrow focus of the network leader meant that the leader eventually agreed to the development of a new network co-ordinator role. This role was undertaken by the neuropsychologist, who used their own professional attributes to broaden the focus of the network. The co-ordinator was championed by the leader as they did not call into question their professional knowledge or institutional position. It was agreed that the leader would continue their focus on the diagnosis and rapid referral of people with suspected cognitive disorders and that the co-ordinator would focus on other issues, such as improving co-ordination and multidisciplinary working. The network members and the value of their input were therefore viewed differently by the two leaders, based on the knowledge and the institutions that they represented and the focus of their roles. The leaders also differed in their opinions of diversity – the network leader viewed diversity as a factor that might disrupt their work and the perception of their hierarchical rank based on their knowledge and they therefore were dismissive of diversity. They chose to rely solely on the opinion of GPs who had medical knowledge. In comparison, the co-ordinator perceived diversity to be enriching for the network and important in making it more compliant with the demands of public funding bodies. They, therefore, broadened the knowledge criterion to include new areas of knowledge, such as social work and psychiatry and other types of organisations, such as care homes and local authorities. By relinquishing some components of their power and legitimising the joint leadership role of the co-ordinator, the leader helped to ensure that all components of the network were developed appropriately, with both the diagnosis of cognitive disorders and the development of multidisciplinary working/co-ordination gaining sufficient attention. In isolation, the narrow focus of the network leader had some negative implications but the joint partnership with the co-ordinator had a more positive and stabilising effect on the team.
There were also examples of the absence of the mechanism at a system level. For instance, a report on the reform of health and social care in Northern Ireland found that interviewees felt that the Department of Health and Social Care held a greater proportion of power than systems leaders. 587 It reported that systems leaders, therefore, looked to the Department of Health and Social Care for solutions to problems rather than coming up with them themselves and this could be detrimental to experimentation and innovation:
In this culture and context, paralysis and lack of decision making becomes the norm. There is no confidence within the system to take ownership of innovation and creativity.
Dayan and Heenan587
Interviewees described an atmosphere of ‘them and us’ between the upper tiers of the hierarchy and those ‘at the coal face’, with senior leaders adopting a forcible manner towards those lower down the hierarchy. There were reports of senior leaders in the department ‘confusing fear with respect’ and making it difficult for systems leaders to drive change. As one senior leader reported, it was best for leaders to: ‘keep their heads down and get on with it’. 587 This culture of mistrust was then passed down to a team level, with GPs voicing suspicions of systems leaders as ‘empire builders’ who were unwilling to work co-operatively. 587 These problems had been recognised by leaders in the system and steps were being taken to address them, for example by taking a co-production approach with the department, leaders, teams and patients to improve partnership working and health and well-being outcomes, although some interviewees reported doubts that this would be successful.
Furthermore, an England-based action research study exploring the process of integrating local mental health and learning disability services into one Mental Health NHS and Social Care Trust highlighted the problems experienced when systems leaders lacked authority or power. 220 In this study, although the Director of Social Care from the local authority was a member of the executive team, it was perceived by staff that they were not sufficiently organisationally embedded and lacked authority or influence in the trust. This lack of influence of social care was believed to have negative implications for the new organisational culture and the director left after a relatively short period of time in the organisation (Box 11). Another study found that systems leaders who made decisions without consulting staff at a team level made staff feel devalued and disrespected, which could lead them to leave their employment. 216
In a newly integrated Mental Health NHS and Social Care Trust, the local authority Director of Social Care was a member of the executive team but was perceived by staff as not sufficiently organisationally embedded and lacking authority or influence in the trust. This lack of influence for social care was believed to have negative implications for the new organisational culture and the director left after a relatively short period of time in the organisation.
A new Care Trust integrates local mental health and learning disability services (C) → the Director of Social Care is a member of the executive team (M+, resource) but is perceived by staff to be lacking in authority or influence in the trust (M–, reasoning) → this has negative implications for the new organisational culture (O–) and the director moves on after a relatively short period of time in the organisation (O–).
Team-level leadership
Research suggested that authoritative, directive and controlling leadership styles were generally inappropriate, whereas shared and distributive leadership approaches based on shared power relationships were likely to be more productive105,206,213,217 and lead to greater team synergy. 219 A Canadian study of change agency in a primary health-care setting217 found that the ability to influence, initiate and implement change was dispersed, with no single individual or group having full authority, resources or expertise to lead change. They concluded that shared or distributed leadership was highly prevalent in health-care settings with integrated or interorganisational contexts. A UK study exploring occupational therapists’ views of integrating service provision across health and social care213 noted the importance of team leaders giving their staff autonomy and not feeling the need to constantly check up on their work. They described the role of integrated team leaders as needing to:
Set the strategic direction, draw up your action plan and leave it to the people who are doing the job.
Best213
Another study216 also highlighted the importance of giving staff autonomy and found that team members appreciated this management style:
. . . he delegates tasks and trusts that the work will get done. So he rarely issues orders.
Choi et al. 216
A case study of two integrated care services in South Wales105 found that successful team leaders valued inclusiveness and had an awareness of the need ‘to share leadership with others who have more relevant “knowledge” ’. 105 This was also identified in the study of a hospital merger in Sweden,216 mentioned previously, which found that successful team leaders delegated decision-making authority, involved staff in the decision-making process and included their suggestions. This made staff feel involved and valued and thus become motivated to implement ‘their’ plan. In this study, a team leader viewed senior physicians as important and informal ‘leaders’, who should be regularly consulted. As a result, clinical staff reported having trust and confidence in the leadership team.
However, sharing leadership could also have some negative effects for teams, particularly when those who were given the power to lead were unwilling or unable to do so, due to, for example, a lack of time or motivation. 203 When this occurred, tension was created within teams. 203 In addition, on occasion, hierarchical leadership was deemed to be necessary or inevitable, due to prescribed lines of reporting and accountability. Hierarchical leadership was believed to be required when dealing with legal or policy challenges206 or when tackling performance. 105 Some authors also talked of the need for team leaders to balance power across organisations. For example, in a Belgian study of interprofessional collaboration between GPs and emergency department teams,195 emergency department leaders played a significant role in balancing power hierarchies across organisations. They did this by reassuring team members that they did not always need to abide by the requests of GPs for medical examinations but should instead rely on their own clinical assessments. Others talked of the importance of team leaders using their power flexibly by knowing when they should ‘bend the rules’ for the benefit of collaboration. 210
An influencing context of this mechanism was to whom team leaders felt responsible. In one study,216 comparisons were made between two different team leaders: one leader felt that their main responsibility was to the hospital ‘top’ management, whereas the other felt that their loyalties were divided between top management and their team. Both leaders were given the same formal mandate from top management to reduce costs but responded to this request differently (Box 12). The leader whose loyalties lay with top management complied with their top-down directives and tried to integrate their clinical departments in a radical and rapid way. They used coercive control and a one-way management style to communicate between top management and staff members and sought to justify the integration by promoting management’s rationale. Despite similar pressures, the other leader chose a freer interpretation of the formal mandate and consulted with senior physicians to work towards a slower and more gradual integration, in line with the wishes of their clinical staff. They asked for voluntary participation of staff members in the integration activities and respected their need for autonomy. They also used deputy leaders, such as research staff, to highlight the benefits of integration for research excellence as the main merger rationale. Consequently, the first leader faced anger and opposition from their team, who eventually demanded their resignation, whereas the other retained their trust. The repercussions of this early negative leadership experience continued to be far reaching for the team and resulted in longer term problems with integration. For example, a rapid turnover of managers followed, which further increased the teams’ antagonism towards top management and made staff reluctant to participate in any form of integrated working. In comparison, the team with the more inclusive leader had more positive long-term experiences of integration, including low staff and manager turnover, strong group cohesion and a 10% cost saving. 216
Two leaders of two different clinical departments were identified following a hospital merger in Sweden. One leader felt that their main responsibility was to the hospital top management, whereas the other felt that their loyalties were divided between top management and their team. Both leaders were given the same formal mandate from top management to reduce costs but responded to this request differently based on their perceptions of where they felt their main responsibility/loyalty lay.
Hospital merger requires the integration of pre-existing clinical departments and team leaders are given a formal brief from system leadership (C) → newly recruited team leader has little understanding of the team and a top-down managerial leadership style (C) → leader drives through the systems leader’s brief in a radical and rapid way, using coercive control and a one-way management style of communication (M–, resource) and this damages the team’s trust in them irretrievably (M–, reasoning) → the team demand that the team leader resigns and the team continues to have long term problems with integration, including a rapid turnover of leaders and antagonism towards top management (O–).
Hospital merger requires the integration of pre-existing clinical departments and team leaders are given a formal brief from system leadership (C) → established leader and long-term colleague of team, who understands the need to seriously consider professional perspective and has a strong nerve (C) → team leader re-interprets the system leader’s formal brief in a way that accords better with the context of the service (M+, resource) and this retains staff trust (M+, reasoning) → this leads to positive long-term experiences of integration, including low staff and leader turnover, strong group cohesion and a 10% cost saving (O–).
There was some evidence of the absence of the ‘working with power’ mechanism, with one study210 acknowledging that it could be very difficult for leaders to relinquish control, because of concerns that this might make them look ‘weak’. Another previously mentioned study216 also identified an example of a team leader refusing to relinquish control to their team members. In this study, the team leader asked their staff to suggest a new structure for their newly merged department but then overrode the team’s proposal with their own, more ambitious, plan. This move upset many team members, particularly the physicians and led to feelings of mistrust and suspicion towards the leader (Box 13). From then on, many physicians no longer attended collaboration meetings for the merger. As one senior physician stated:
He had obviously decided on his own plan that had nothing to do with all our work. That was the first nail in the coffin.
Choi et al. 216
Following a merger of two hospital departments in Sweden, the newly employed team leader refused to relinquish control to the team members over decisions around the structure of their new department. After asking for their team’s suggestions, the leader overrode the team’s proposals with their own, more ambitious, plan. This move upset many team members, particularly the physicians, and led to feelings of mistrust and suspicion towards the leader. From then on, many physicians no longer attended collaboration meetings for the merger.
Hospital merger requires the integration of pre-existing clinical departments and decisions need to be made around the structure of the new department (C) → team leader asks for the team’s suggestions about how to structure the department (M+, resource) but overrides their proposals with their own, more ambitious plan that the team think has nothing to do with their work (M–, reasoning) → this upsets team members (O–) and many physicians do not attend further collaboration meetings (O–).
Mechanism 5: commitment to learning and development (n = 14)
The original definition of this mechanism developed in stage 1 was: ‘Leaders have a strategic commitment to access external support and rapid learning with other like-minded systems. They are committed to reflecting on and personally learning from a variety of sources, through formal and informal networks, and to act as a role model for team members, encouraging them to also learn and improve. Leaders establish communities of practice for team learning and the pooling of knowledge. Although managers apply proven solutions to known problems, leaders are exposed to situations in which groups need to learn their way out of problems that could not have been predicted. Leaders recognise that training initiatives can increase component team members’ awareness and understanding of their knowledge structures, as well as their ability to regulate then improve the effective co-ordination of the whole system under dynamic circumstances. They have an interest in innovation and creativity, inviting feedback and embracing change and evidence-based practice for continuous improvement. They encourage team members to generate ideas and explore possibilities but also have a tolerance for things not working and learn how to fail “well”.’
A total of 14 research papers examined in stage 2 discussed this mechanism. 22,84,92,105,197,199,200,205,208,215,217,218,220,583
Overarching leadership qualities around ‘learning and development’
An important component of integrated working was having the opportunity to share experiences and learn from others. 22 An overarching context for this mechanism at both system and team levels was the presence of an organisational culture that demonstrated mutual respect and understanding, which was crucial for nurturing learning and innovation within organisations. 199 Interprofessional and interorganisational training and education programmes were also described as key in helping teams to break down misconceptions and support integrated working. 22,197,199,200 A lack of training could lead to staff uncertainty about whether or not they were permitted to undertake particular tasks or feeling unprepared to take on new roles. 197 However, despite its importance, it was unclear whether or not resources and commitment were always readily available to support interprofessional and interorganisational training and education. 199,200
System-level leadership
There was evidence of the importance of the ‘learning and development’ mechanism at a system level, particularly around the willingness and flexibility of integrated systems to evaluate, change and evolve according to need. 197,199,215,218,583 For example, a paper reporting the results of a 3-year, national evaluation of 16 integrated care pilots in England197 found that the delivery of integrated team objectives relied on their overall ability to modify existing systems to create new ones. This was more difficult for organisations that were more accustomed to ‘silo-working’ or where funding models supported care in silos. 197,199 Furthermore, a study of integrated health care delivery in Western Australia found it important that partnerships were observed to be instigating change and overcoming bureaucratic and infrastructural barriers to do so. 215 Regular formal and informal meetings between organisational partnerships, staff and the community provided effective governance of this. 215 A study of community health partnerships in the USA also highlighted the importance of system-level leaders identifying potential team-level leaders and supporting and mentoring them to aid their development. 208
However, examples were also provided of where the ‘learning and development’ mechanism was absent at a system level. For example, an Australian case study contrasting two contexts of health-care governance found it imperative that board-level leaders recognised the need for innovation and supported it as a key strategy for integrated working rather than implementing and imposing existing policies. 199 Furthermore, there were reports of a focus on short-term political gains rather than long-term solutions and examples of ‘centralised bureaucratic control’ that resulted in a culture of risk aversion at the board level and that reduced teams’ ability to innovate, even when individual members were willing and capable of doing so199 (Box 14). Previously, a study noted that innovation could be stifled when systems leaders focused too intently on consensus as an important part of their culture. 220 Innovation required some dissensus among team members but if systems leaders perceived dissent as undesirable then teams would not gain the momentum required to move towards new ways of working.
An Australian case study contrasting two contexts of health-care governance found it imperative that board-level leaders recognised the need for innovation and supported it as a key strategy for integrated working. However, there were reports of a focus on short-term political gains rather than long-term solutions and examples of ‘centralised bureaucratic control’ that resulted in a culture of risk aversion at the board level and that reduced teams’ ability to innovate, even when individual members were willing and capable of doing so.
‘Centralised bureaucratic control’ at the board level (C) → systems leaders become risk averse (M–, resource) and so focus on short-term political gains rather than long-term solutions (M–, reasoning) → team members’ ability to innovate are limited, even when individual members are willing and capable of doing so (O–).
Team-level leadership
It was important for team leaders to both inspire learning in their teams and show commitment to learning themselves. For example, leaders encouraged learning and development among their team members by placing an emphasis on the importance of information-sharing, reflective practice and innovation to maximise the potential of integration. 105,205,217 They were focused on developing the credibility of their staff and enhancing their performance as well as providing strategic and intellectual leadership. 84 They enabled innovation by creating a culture whereby staff could introduce new ideas with only limited checks and balances. That is:
. . . all we have to do is run it past the manager and do it.
Williams105
Leaders also gave staff time away from their normal duties to attend project meetings and seek other integrative opportunities,217 and they enabled staff to find the answers to their questions themselves, rather than simply providing them with the answers. 105,205 At a personal level, it was important for leaders to be interested in and willing to personally invest time in learning about team members’ roles and responsibilities to successfully manage the ‘bigger picture’. 92
An influencing context of this mechanism was whether or not teams had strong interprofessional relationships, since where networks were strong and social capital high, then learning with and from each other was more likely to occur. 205 An inhibiting context to learning and development was observed when team leaders feared thinking ‘outside the box’ or doing something new and innovative, because of a lack of either time or enthusiasm within teams to support such change. 199 An outcome of an environment of learning and development in integrated teams was the creation of team spirit and ownership, but this could also lead to ‘groupthink’ and intransigence if leaders did not carefully guard against this. 105 It was also noted that the difficulty of measuring the ‘success’ of new integrated arrangements through robust, evidence-based research made it hard to convince sceptics of the merits of adopting new ways of working. 205
Mechanism 6: taking a wider view (n = 13)
The original definition of this mechanism developed in stage 1 was: ‘Integrated services involve cross-boundary working with a wide and varied group of organisations and people with a plurality of interests, goals, aspirations and values. Leaders of integrated teams have experience and insight into the motivations and challenges of other organisations and focus on the bigger picture by acknowledging the importance of making strategic connections with leaders in other parts of the system. They use this knowledge to engage with other leaders, be convincing/persuasive in their communications with others, and work through challenges in partnership with other organisations by bridging language, thought-world and goal differences that may otherwise prove detrimental. This enables them to come up with collective solutions and to look beyond reactive problem solving by taking a longer-term strategic view. Their political astuteness is a necessary and beneficial set of skills that enable them to get things done for constructive ends. Consequently, the goals of the team are more likely to be achieved. However, political astuteness can also be used to pursue personal or sectional interests.’
A total of 13 research papers examined in stage 2 discussed this mechanism. 84,105,197,198,206–208,210,217,218,220,221,583
Overarching leadership qualities of ‘taking a wider view’
Certain components of ‘taking a wider view’ were identified as important at both a systems and team level. For example, a UK study of multiagency working across health, social services and education settings identified having tenacity and a strategic drive and vision as key leadership skills at any level. 207
System-level leadership
At a system level, it was important that leaders had a deep, intuitive sense of how their community worked and what it needed. 84,208,217 Systems leaders needed to look beyond the interests of individual organisations and even the interests of the integrated system and focus on the needs and priorities of the community as a whole as well as on higher order cause, effect and prevention, rather than on symptoms or quick fixes. 208 To achieve this, systems leaders needed to have strong, pre-existing networks84 and to demonstrate a willingness to work with, listen to and learn from a range of different individuals and organisations from across the community, from both inside the integrated system and out. 208,217,583 This included leaders of government, business, community, and non-profit organisations and so on. Leaders of integrated systems were required to be skilled in navigating through complex and sensitive political issues84 and have the ability to help team leaders from their partnering organisations to see how integrated working benefited them in achieving their specific mission and goals. 208 There was evidence that taking a wider view and seeking out members that represented a wide range of knowledge and expertise could help achieve successful funding requests from public funding bodies, who often expect a multidisciplinary vision. 583
Other authors highlighted the importance of systems leaders knowing who were the ‘right’ people to engage with at a strategic level, which often included like-minded individuals who had previously worked across settings and who sought new ways of working to achieve change. 207 In integrated health and social care systems, the importance of ongoing, planned communications between senior executives in the partner organisations was also noted. 197,208,218 In a study of the clinical merging of two hospital sites in the USA,218 executive leaders at both hospital sites were responsible for designing and subsequently implementing the vision and future of the newly merged entity (Box 15). It was understood from the beginning that for the merger to succeed, these leaders had to be willing to put aside personal interests to convince the rest of the organisations that the integrated health-care system would be a better option for all parties. They achieved this through ‘communication, compromise and time in getting to know one another’218 so that trust was developed between the executive staff and the senior administrators and clinical leaders at both hospital sites. The most effective means of achieving this trust was the provision of multiple and regular common platforms for communication with the whole leadership group while simultaneously keeping local meetings at the sites to a minimum. The group also ensured that no programme would be moved from one site to another without considering the impact that this would have on the sites. 218
A clinical merger of two hospital sites in the USA took place with executive leaders at both sites responsible for designing and implementing the vision and future of the newly merged entity. It was understood from the beginning that for the merger to succeed, these leaders had to be willing to put aside personal interests to convince the rest of the organisations that the integrated health-care system would be a better option for all parties. They achieved this through: ‘communication, compromise and time in getting to know one another’218 so that trust was developed between the executive staff and the senior administrators and clinical leaders at both hospital sites.
Clinical merger of two hospital sites with executive leaders at both sites responsible for designing and implementing the future of the newly merged entity (C) → both leaders appreciate that for the merger to succeed, they have to put aside personal interests and convince the rest of the organisations that the integrated health-care system would be a better option for all parties (M+, resource). They achieve this through regular communications as a whole group while simultaneously keeping local site meetings to a minimum. They also ensure that no programme would be moved from one site to another without considering the impact that this would have on the sites (M+, reasoning) → this instils trust among all team members (O+).
There was also evidence of the absence of the ‘taking a wider view’ mechanism at the system level. For example, there were reports of some care trusts having difficulty forging new relationships with wider partners, such as voluntary sector organisations. 220 The authors concluded that it may be difficult to pursue depth and breadth of partnerships simultaneously and the formal mechanisms of the former may be more influential than the informal arrangements that may encourage the latter. 220
Team-level leadership
It was also important for team-level leaders to see beyond their own organisational units and maintain relationships and network with leaders from external and partnering organisations. 105,197,198,206,210,217,221 This was identified as both empowering for leaders themselves and beneficial for co-ordinating the work of teams to provide holistic and integrated services. 198,206,221 For example, a UK study evaluating integrated team management in a health and social care trust221 found that team leaders needed to develop partnerships with a wide range of potential and current services, including those in the voluntary sector, wider local authority services and informal community groups. This enabled them to reshape services and prevented a narrow focus on the health and social care sector.
A Norwegian study of leadership in interprofessional collaboration in residential child-care services, previously mentioned,206 found that, to be able to communicate externally, leaders had to organise regular communication structures that matched their internal ones. This included creating regular meetings with external partners for the purposes of updating information, making decisions and plans, and delegating tasks and responsibilities. Extensive telephone communication between meetings and the production of various written reports were also required. Other authors also highlighted the importance of regular meetings between team leaders of external or partnering organisations to help maintain constructive conversations and prevent working in silos or a culture of blame. 197
A context that restricted this mechanism was identified in a Swedish study exploring collaboration between welfare agencies in the field of vocational rehabilitation. 210 In this study, leaders were evaluated primarily for their contributions to their own agency and not for their capacity to collaborate with external agencies. This restricted wider working and could have negative implications for the careers of those leaders who chose to dedicate their time and attention to working with external partners (Box 16).
A Swedish study exploring collaboration between welfare agencies in the field of vocational rehabilitation reported leaders being evaluated for their contributions to their own agency and not for their capacity to collaborate with external agencies. Those leaders who chose to dedicate their time and attention to working with external partners experienced negative implications for their careers.
Team leaders are evaluated for their contributions to their own agency and not for their capacity to collaborate with external agencies (C) → team leaders are committed to collaborating externally (M+, resource) and so choose to dedicate their time and attention to working with external partners (M+, reasoning) → leaders experience negative implications for their careers (O–).
Mechanism 7: clarifying complexity (n = 10)
The original definition of this mechanism developed in stage 1 was: ‘Many complex and challenging conditions are associated with integrated working, with unclear boundaries, structures and processes and different governance procedures and funding streams, but leaders can navigate the tension between certainty and uncertainty and translate this to their teams and/or systems. Leaders employ sensemaking strategies, in which they use a set of available artefacts to make the understanding of their message clear and internalised. They are successfully able to negotiate the narrow parameters between oversimplification and exclusionary detail, enabling team members to understand the complexity of disparate policy drivers, legislation, performance requirements, regulatory systems and funding mechanisms to ease working arrangements for the team. They do this by developing policies and initiatives that are easily communicated and understood, with documents explaining how decisions are made and who has the authority to make them. This prevents confusion and enables team members to navigate organisations with multiple decision-making bodies.’
A total of 10 research papers examined in stage 2 discussed this mechanism. 84,92,197,199,200,206,207,216,217,583
Overarching ‘clarifying’ leadership qualities
There were certain components of the ‘clarifying complexity’ mechanism that were identified as important at both a systems and a team level. This included being clear about the management structure, the contributions required from all participants in the system/team and the rules governing how the partnership should work. 92,197 A paper reporting the results of a 3-year, national evaluation of 16 integrated care pilots in England197 found that staff felt unprepared and demotivated when there was an absence of clear and consistent communication from leaders about what work was required and what contribution was needed from all participants. Staff were also reluctant to engage when there was uncertainty about what they did and did not have permission to do. One influencing context on leader clarity is, therefore, whether or not leaders have formal frameworks governing their institution/organisation, such as legal frameworks, policies or guidelines. 206
System-level leadership
There was some evidence of the presence of the ‘clarifying complexity’ mechanism at a systems leadership level. For example, there was evidence that systems leaders needed the ability to navigate through complex and sensitive political issues and possess the relevant skills to oversee and manage complex clinical governance frameworks and practices, workgroup structures and systems and financial structures and systems. 84 This included the ability to introduce changes in a controlled manner, so that teams were not overwhelmed or confused by change. 583 A UK study exploring multiagency working across education, health and social services sectors found that having clear directives at a strategic level from all agencies involved, as well as from government, was key to overcoming conflicting agency and project aims. 207 System-level leaders were also required to keep their attention focused on any changes associated with integration, remove any obstacles to integration and reduce uncertainties associated with change. 217
There was also evidence of the absence of the ‘clarifying complexity’ mechanism at a system level. For example, a study199 found that a lack of clarity at board and executive levels led to a lack of enthusiasm and direction in the system. Another study216 reported that staff felt frustrated by a lack of clarity at a system level, caused by a complex reporting structure following a merger of two clinical departments in Swedish hospitals (Box 17). As one member of staff described:
. . . I don’t just have one boss. I now have many bosses . . . I have to go to the HR managers, division managers, clinical managers . . . I have about five bosses.
Choi et al. 216
A merger of two departments from Swedish hospitals caused a lack of simplification and clarity over leadership and reporting lines at a system level. This left staff members feeling frustrated and confused and was time-consuming, as staff then needed to report to several managers.
Two clinical departments combine as part of a hospital merger (C) → systems leaders instigate a complex management reporting structure, which means that staff have to report to more leaders than before (M–, resource) and staff fail to understand the reasoning behind this new structure (M–, reasoning) → this leaves staff feeling confused and frustrated (O–).
Team-level leadership
There was evidence of the absence of the ‘clarifying complexity’ mechanism at a team level, including evidence of a lack of clarity among team leaders around their own role and responsibilities. 200 Other papers reported a team leader’s inability to clearly communicate their reasoning and priorities for the team as being detrimental to integrated team working. 216
Mechanism 8: planning and co-ordinating (n = 5)
The original definition of this mechanism developed in stage 1 was: ‘Leaders co-ordinate, strategize and serve as a liaison and boundary spanner between their team and the other teams in the system. They actively plan and synchronise the teams in the system, aiding the teams with their timing and executions of plans and helping them to organise intrateam processes with interteam processes and decision making. When component teams struggle to perform their tasks due to high workloads, leaders can provide backup behaviours by prompting other component teams to provide help, shifting workloads to other teams or proactively offering to help with specific tasks. They employ smooth co-ordination processes that provide the necessary capacity to the whole system to move nimbly and synchronously. Strategising and co-ordination improves both team processes and system performance. However, system leaders must also be mindful of changing and competing demands and be able to switch quickly from the routine to the non-routine. Thus, leaders of integrated systems devote time to ensuring system flexibility. If unexpected changes occur and contingency plans no longer seem appropriate, leaders decide whether to reconsider, abandon or adjust the original plan.’
Five research papers examined in stage 2 discussed this mechanism. 84,209,212,217,221 However, the findings from these papers did not suggest that planning and co-ordinating was a discrete mechanism but instead that components of planning and co-ordinating were associated with ‘creating the conditions’. These findings have, therefore, been incorporated into this mechanism.
Mechanism 9: adaptability of leadership style (n = 3)
The original definition of this mechanism developed in stage 1 was: ‘Leading an integrated system is difficult, given the complexities of moulding two or more organisations into one and the sense of loss or uncertainty that employees may experience as part of this. Collaborative leaders are able to adapt their actions based on the circumstances that they confront. They acknowledge that particular situations call for particular leadership skills and behaviours. Leaders align their styles according to the situation at hand, combining or switching approaches as necessary, changing strategy towards flexibility and the use of their tacit knowledge. This generates co-operation, cohesiveness and improved communication among group members.’
There was weaker evidence for this mechanism. Only three research papers analysed in stage 2 discussed this mechanism. 207,208,217 However, the findings from these papers did not suggest that adaptability of leadership style was a discrete mechanism and instead, that components of adaptability were associated with ‘working with power’ and ‘inspiring others’. These findings have, therefore, been incorporated into these mechanisms.
Mechanism 10: fostering resilience (n = 0)
The original definition of this mechanism developed in stage 1 was: ‘Those providing public services need to deal with increased demand, higher expectations from the public about service standards, hostility and psychological projections from the public and the media, often in the context of declining resources for public services. The pace can be relentless and the physical, intellectual and emotional demands very high. Successful leaders of integrated systems have both the personality and learned skills that foster high resilience, perseverance and an awareness of the importance of remaining empathic to the public whilst also resilient in terms of their own well-being. They put in place social support systems (both inside and outside work) and attend appropriate training and personal development programmes to strengthen resilience. Leader stress is therefore reduced.’
No research papers analysed in stage 2 were found to have discussed this mechanism.
General contexts and outcomes of leading integrated care teams and systems
As shown in Table 2, some papers described the general contexts and outcomes of leading integrated care teams and systems that were unrelated to any individual mechanism. These general contexts and outcomes are described below.
Facilitating contexts
Sufficient resources (i.e. time and money)22,217
Gaining high-level support for integrated working was important for leaders,22 including being given the time and money to develop and implement change. One study217 reported that successful leadership of integrated teams required time, including sufficient time for leaders to find common ground between teams and to build trusting relationships and credibility. Furthermore, having the necessary funds available to carry out integrated working was also an important context to successful leadership and the facilitation of change. 22,217 The government played an important role in this by providing teams with adequate funds and material resources, without which many components of integrated working may not be feasible. 22,217 This facilitator may be difficult in times of public sector funding contraction or underlying wishes for integration to be a cost-saving measure.
Relationships between leaders92,201
Some papers highlighted the specific context of integrated teams that had two joint leads and reported this to be a beneficial leadership model. 92,201 Where co-leadership of a team was in place, it was important that both leaders maintained a good relationship with each other and were able to co-operate successfully. 92 Having characteristics of transparency, responsiveness, self-confidence, willingness to compromise and a lack of prestige were highlighted as important factors in maintaining successful co-leadership relationships. 92 The creation of a trusting and loyal relationship between leaders was seen to be indispensable and gave leaders the space to make mistakes without jeopardising the relationship:
There has to be loyalty, then you’re secure in your joint leadership. There’s a margin for error, I know X will stick by me anyway. Like in a marriage.
Klinga et al. 92
Furthermore, these strong relationships between co-leaders helped them portray themselves as a ‘united team’ to their staff, encouraging greater harmony within the team itself:
It’s important that the team members perceive we’re a unit . . . It’s not possible to drive a wedge between us and try to separate us.
Klinga et al. 92
Personal characteristics of the leader84
One study identified several key personal characteristics and experiences of successful leaders of integrated teams. 84 Key personal characteristics included integrity and professionalism, flexibility, the ability to remain calm and composed in pressurised situations, a willingness to look after one’s own health and well-being, a sense of humour, highly developed critical thinking and decision-making skills, advocacy skills and a focus on achievement. Important personal experiences included having good knowledge of health-care systems, structures and standards and an overall understanding of the specific cultural and health needs and challenges of their client group.
Co-location of team members92
One study identified the co-location of staff as an enabling factor for successful leadership of integrated care teams:
. . . the fact that we’re in the same building is very important because there’s a lot of informal conversations and contacts. That’s what facilitates things.
Klinga et al. 92
Office sharing helped teams and leaders to keep abreast of what was happening and contributed to natural updates on the team, as well as involvement in matters concerning both sectors. These informal conversations also helped to ensure that formal meetings remained focused.
Hindering contexts
Cultural differences between organisations202,205
Some authors highlighted the long-standing organisational issues and cultural differences between the UK NHS and local authorities as making leadership of integrated teams more complex. 202 For example, the NHS has centrally driven policy and operational targets whereas local authorities have more locally set agendas, which lead to different levels of autonomy and behaviours among staff. Financial systems also differ, with eligibility for adult social care often subject to means testing and user charges whereas NHS services are free at the point of delivery. Limited financial resources and the reluctance of NHS organisations to achieve financial balance were highlighted as making change more difficult. 202,205 Similarly, staff reported differences between the NHS and local authorities regarding the concept of failure and this too made leading integrated teams more complex:
. . . in local government service failure proceeds financial failure. Financial failure is the ultimate sin. In healthcare financial failure always proceeds service failure and service failure is the ultimate sin.
Shand and Turner202
Lack of clarity around leadership198
One study198 stated that a lack of clarity around the role and responsibilities of a leader made integrated working more difficult:
. . . there was never a clear person given the responsibility to basically draft the project plan or do all the things that you’re supposed to do.
Lunts198
Lack of clarity around leadership made it difficult for team members to know who to approach for decisions; therefore, the need for a single accountable individual was emphasised.
Outcomes of leading integrated care teams and systems92,197
General outcomes associated with leadership of integrated teams and systems were, at best vague, or more often rarely reported. For example, one study197 said that staff reported ‘good’ leadership as being associated with success and ‘poor’ leadership with a lack of progress. Another study92 highlighted a number of outcomes specifically associated with the co-leadership of integrated teams, including a more consistent presence of leadership (i.e. leaders were able to cover for each other during periods of leave and so on); a broader range of experience and competence was brought to the team as a consequence of having two leaders rather than one; and immediate guidance, support and mentoring from the co-leader. Co-leadership could make joint decision-making more difficult but the difficulties relating to this were found to be outweighed by the advantages:
Actually, it’s easier to lead alone than to be two leaders. You have to wait all the time, but still it’s more fulfilling because I have someone to share things with. It’s more difficult but you get more out of it.
Klinga et al. 92
The authors, therefore, concluded that the challenges leaders face in integrated teams could be handled more efficiently by two leaders working together than by a single individual acting alone. 92
Stakeholder perspectives
This section collates the findings from the three stakeholder consultation meetings that took place in person in July and December 2019 and then online in September 2020. As stated, these lively and informative meetings were an integral part of the process, as understanding what key stakeholders know about an intervention and their reasoning for or against its implementation are essential to understanding it. 144 Given that the literature was also so limited in this synthesis, stakeholders’ input was pivotal in helping to elicit our realist theories on the mechanisms and contexts of leading integrated care teams and systems.
At the first stakeholder consultation meeting, the research team introduced the study and the preliminary mechanisms identified in stage 1a of the synthesis. The second meeting provided a space for further refinement of the mechanisms identified in stage 1b. The third meeting offered an opportunity for stakeholders to enhance the detailed descriptions of mechanisms developed in stage 2 and generate data to supplement the relative absence of literature on leadership of integrated care teams and systems. The following account is largely made up of dialogue from the third stakeholder consultation meeting, although material from the previous meetings has been included. In the third meeting, we presented the evidence for each of the eight mechanisms and invited comments, debate and challenge from the group. A broad range of attendees were in the meeting, including individuals with expertise in integrated care, with direct experience in leading integrated care teams or systems, and patient/service user and carer representatives with experience of receiving (dis)integrated care. This made for a provocative discussion on the characteristics needed to lead integrated teams and the implications for integrated care more broadly. The stakeholder group responded to the findings with a combination of practical and theoretical knowledge. Their views and interpretation of the findings, which drew on research concepts, are interpreted and used by the research team in this discussion; a complexity that is important to acknowledge. The following provides a report of the main discussion points of each mechanism, followed by an analysis of any cross-cutting themes or points of distinction. Quotations are from stakeholders attending the third consultation meeting, where discussions were audio-recorded and transcribed.
Inspiring intent to work together
Early discussions of this mechanism during the second meeting reiterated the importance that stakeholders placed on the debate around who the leader is, as opposed to what the leader does. In the third meeting, stakeholders’ initial reaction to the notion of ‘inspiring leaders’ was to question the implication that inspiration alone was objectively positive or valuable. Although one stakeholder felt that being inspirational was the most important aspect of leadership in their area of work (and indeed, the one trait that could not be taught or developed through training), others felt that inspirational leadership alone was inadequate and that leaders needed to be more rounded than the definition of the mechanism implied:
Whilst inspiration is important, other qualities are equally important. To me, the ideal would be someone who is inspiring but equally skilled as a systems-level leader. This suggests that the leader has not only the inspirational skills but has also taken the time to do the work and find out what is involved on the ground. Inspiration is definitely not enough, the person has to be grounded as well.
. . . it isn’t about the personality or the characteristics, it is just about them being able to do their job effectively, efficiently and safely.
Furthermore, although developing a shared vision was identified as key in the literature, stakeholders noted that little emphasis was given to leaders creating this vision around the needs of the individual patient/service user. They also highlighted the need for a leader’s vision to be authentic, credible and ethical if it was to be sustainable. In their experience, a leader’s vision would be shared by some and rejected by others if it were not representative of a credible aim:
History is replete with inspiring leaders who can pull together good teamwork but without the thought about what makes their inspiring vision in some way ethical or ‘good’.
I think there is also something about the authenticity of the vision that’s been put in front of people. In a hierarchical system there is a tendency for people to say and not do or believe because that particular vision doesn’t hold authenticity for them.
Key messages
-
Although identified as a vital component of leadership within the literature, stakeholders’ experience was that inspirational leadership alone was inadequate in integrated care teams and systems and needed to be supplemented by a range of other attributes.
-
Both the research literature and stakeholders agreed that credibility of leadership was key, particularly when trying to engage staff in a shared vision. Stakeholders noted the importance of basing the vision around the needs of an individual patient/service user – a notion not prominent in the literature.
Creating the conditions to work together
Stakeholders agreed that inspiration alone was insufficient or even irrelevant in comparison to effectively fulfilling the full remit of requirements of the leadership role. However, it was suggested that the literature focused excessively on the practical attributes of ‘creating the conditions’ and ignored the social skills also required. In their experience, ‘creating the conditions’ required leaders to have the emotional intelligence to create a culture of psychological safety, including developing an environment of transparency, openness and freedom to communicate without fear of repercussion. This required leaders of integrated teams and systems to have self-awareness, self-regulation, motivation and empathy. Consequently, one participant suggested that leaders of integrated care teams and systems were required to be more ‘evolved’ than their business world equivalents:
. . . emotional intelligence is of particular relevance here, as traditional models of business leaders always has intelligence, toughness, determination and vision. However emotional intelligence brings in aspects . . . such as self-awareness, self-regulation, motivation, empathy and social skills.
Key messages
-
Research literature focuses on the practical attributes of ‘creating the conditions’ but stakeholders felt that it ignored the social skills also required.
-
Stakeholders believed that ‘creating the conditions’ also involved creating a culture of psychological safety and an environment of transparency, openness and freedom to communicate without fear of repercussion.
Balancing multiple perspectives
Stakeholders agreed that conflict and discord would be inevitable across integrated care, but there was a lack of consensus over the way in which leaders should respond to them. Although the research literature generally posited that a leader’s role was to resolve conflict, stakeholders’ experiences were more diverse. Some suggested that conflict should be actively and intelligently resolved by leadership, but others felt that it was more productive for conflict to be ‘held’ by leaders, as they challenged their team to work out problems themselves. These stakeholders felt that a willingness to have difficult conversations with colleagues across different organisations and specialisms was evidence of a leader’s attempts to deal with conflict, without attempting to resolve it directly:
. . . where there has been a holding of two opposing views or difficulties in a system . . . that leads to perpetuating uncertainty, which fractures people’s views, and it can be quite divisive. In order to make progress in system integration, you would need to resolve those dilemmas one way or the other, and then it’s about the skill and art of leadership to take everybody through that.
System leadership is a series of confrontations of dilemmas. The theory goes that dilemmas are to be held rather than resolved, so for me there’s something missing in this, in the context. There’s an assumption in all of this that might be helped if the context is articulated as complex and therefore characterised by dilemmas.
Key messages
-
The research literature suggests that a leader’s role is to resolve conflict, but stakeholders’ experiences were more diverse. Some stakeholders agreed with this finding, whereas others felt that leaders should challenge their team to work out problems themselves.
Working with power
As previously stated, the ‘working with power’ mechanism was originally identified by the stakeholder consultation group and continued to evoke discussion in the final meeting. There was comment that power was palpable in integrated systems, particularly at higher levels, and could be both permissive and obstructive. Power was described as working positively and negatively, with stakeholders commenting that even when it was obstructive it was possible to redirect so that it became useful. It was felt that power generally moved through the system, rather than operating from top to bottom and this could have a range of positive implications for leadership and notions of shared ownership and responsibility. The tension that this created with reference to accountability, however, was also discussed, with stakeholders concluding that somebody needed to hold ultimate responsibility. Stakeholders also discussed the notion of ‘borrowed’ power, whereby permission or advocacy (implicit or explicit) of somebody with decision-making power could be productive when distributed evenly throughout an integrated team:
I would very much resonate with the concept of ‘borrowed’ power, so the fact that this somewhat intangible thing exists but if you know you’ve got the implicit permission and support of somebody who does have a clear decision-making power available to them, then you can crack on using that borrowed power to support and enable your colleagues to work.
Others commented on the need for reflexive leadership with regards to power, stating that reflexive leaders used power in ways that offered alternative interpretations. Through these, failure could be rationalised by a reflexive leader, by moving away from personalising shortcomings and exploring the structural and systemic motivations behind things that were perceived to go wrong. This highly nuanced approach to leadership was thought to rely, to some extent, on a paradigmatic shift, which raised questions around its feasibility:
. . . leadership should be reflexive rather than an embodiment of the ‘right way’.
A key context of the mechanism highlighted by stakeholders was the differential perceptions which surrounded integration, noting that some may perceive integration to be fair and equitable whereas others may perceive it as an overwhelming, authoritarian takeover. Leaders of integrated care should therefore be aware of the way in which power could be enacted through subconscious, endemic perspectives of the inequalities between health and social care and between other professional and sectoral boundaries:
. . . just because we say that something is integrated doesn’t mean that it actually is, integration can feel like a takeover rather than integration . . . the way that was experienced may be very different depending on the power that people have felt they are bringing from their respective organisational cultures . . . the power probably never feels equal, however integrated it may be. Experiences of people going through that may be very different, a good leader would need to be able to work with that.
Trust was felt to be another key context of the mechanism. That is, trust triggered the effective operationalisation of power, whereas its absence enabled more problematic power relations. Consequently, it was recommended that leaders be clear when discussing how power is operationalised, as instinctive reactions could position power more negatively:
. . . what is power? . . . It’s about getting people to do things without using coercion. It seems quite a negative thing, which can be highly disruptive, and that’s because it’s finely balanced with its opposite, which is trust. Power is getting and telling people to do things and trust is about enabling people and being assured that people will go off and do the right thing . . . I think there’s a nexus between those two, they’re very closely related and power can easily destroy team relations if it’s abused.
Stakeholders also referred to the absence of this mechanism and its implications for integrated care. They made connections between the historic power imbalances between health and social care highlighted in the previous mechanism and their associations with power inequalities. Stakeholders used the topical example of the COVID-19 pandemic to illustrate the inequalities of power between health and social care and the negative impact that this subsequently had on care homes:
. . . that’s a really great example of the absence of power being wielded, and the absence of decision-making and people not using their power in a way which was timely and effective led to the disasters we’ve seen over the first part of COVID. The absence of power sometimes can be hugely negative, and not using it in a proactive way can lead to as much disaster as obstructing people.
Stakeholders also referred to the absence of the service user voice throughout the research literature and the lack of power patients/service users held within integrated care teams and systems:
Exploring professional hierarchies tend to focus on the more powerful professions and the service user voice is largely absent.
There is a culture of deference in this country, as a leader comes to a situation, they are already endowed with acceptance . . . It presents so much difficulty as a user of services.
Key messages
-
A highly nuanced and sophisticated understanding of the intricate and often wildly fluctuating power dynamics resident in integrated care teams and systems is a key characteristic of effective leadership.
-
Trust triggers the effective operationalisation of power and its absence enables more problematic power relations.
-
Given that a primary aim of integrated care is to develop a patient-/user-centred approach, the absence of the patient/service user voice and their relative lack of power are concerning.
Commitment to learning and development
Stakeholder discussions on this mechanism tended to focus on the role of innovation and creativity in integrated care, exploring how leaders could support their team to work in innovative ways. It was felt that mid-level leaders only had scope to innovate themselves when they were given the flexibility to work in different ways and were provided with the ‘professional safety’ to do so by their leaders:
. . . to let them know that its ok to work in a different way, and that they need to provide provision around the risk of having a flexible job and changing roles, so provide some reassurance there.
However, the tension between the need for leaders to innovate and the need to take risks in an environment in which they were heavily accountable and constrained by a raft of regulations was felt to represent an impasse for the development of ideas. Mismatched roles and expectations of senior and mid-level managers also served to distort relationships and lead them to become dysfunctional.
To encourage others to work flexibly and innovatively, mid-level managers also needed to offer their team an environment of psychological safety, which included developing a culture where staff had the ‘freedom to fail’. This freedom to fail was elaborated by the contention that huge knowledge gaps existed in many aspects of health and social care and this would always necessitate a leap of faith by those both in practice and at leadership levels. There was consensus that current environments would benefit from a cultural shift, in which individuals felt comfortable to both feed their curiosity and develop in a way that accepted inevitable mistakes. The tension between innovation and the practical constraints of working in integrated care was also highlighted. There was suggestion that effective leaders needed to understand the gap between their own visions and the reality of working in integrated care to understand the lived experiences of their team:
. . . if you don’t feel like you can disclose what your real world is like, then they won’t hear what that real world is like. So it is tied in with the cultural implications of a psychologically safe environment and the ability of the leader to just sit and simply listen, so the staff don’t fear the repercussions of actually telling them things without punishment or sanctions. So that builds that concept of work as imagined versus work as done versus work as prescribed versus work as disclosed.
Key messages
-
Initial programme theory suggested that leaders and their teams were able to ‘fail well’ and were given the scope to think outside the box, yet, in reality, they are often not given the opportunity to fail, owing to the rigours of the systems in which they operate.
-
Current environments would benefit from a cultural shift, such that individuals feel comfortable both to feed their curiosity and to develop in a way that accepts inevitable mistakes.
Taking a wider view
No research evidence was found to support the requirement of leaders to be ‘politically astute’, yet stakeholders felt that leaders could not operate without a sense of political leadership. One stakeholder described leadership in the NHS as being effective when ‘political capital’ was relinquished, to allow other leaders to bring in their knowledge, contacts and networks. It was also felt that people often intended to work together but were unable to and that leaders needed to look beyond the parameters of practice to provide non-conventional opportunities for integrated working. The research literature highlighted the importance of leaders knowing who were ‘the “right” people’ to engage with at a strategic level, but stakeholders felt that this could result in leaders seeking connections with ‘like-minded’ individuals, creating a bias in outlook and undermining the diverse perspectives that leaders were described to adopt in the initial programme theory. It was suggested that associating only with like-minded individuals was reflective of anxiety, which may have been caused by (or contributed to) the disruptive and unsettling capacity of integrated care:
. . . there’s something for me here about going to like-minded people when I’m feeling anxious. So there’s something about being aware of how anxiety plays out in individuals, groups and systems.
It was commented that working only with like-minded professionals encouraged the continuity of conventional assumptions around leadership and raised questions about the diversity of integrated care:
. . . senior leadership in the NHS in particular is framed around talking to like-minded people and that feels embedded in the language I’m hearing here from these mechanisms.
Stakeholders therefore suggested that there was a danger of these findings reinforcing existing assumptions around leadership. Noting that the research evidence for this mechanism was scant, stakeholders questioned whether or not the lack of literature could be reflective of how hard it is to both practically lead integrated teams or systems and make sense of this.
Key messages
-
Further research is required to establish whether or not ‘political astuteness’ is an important requirement of leaders of integrated systems.
-
Leaders must by wary of working only with like-minded professionals, as this creates a bias in outlook, encourages the continuity of conventional assumptions around leadership and raises questions about the diversity of integrated care.
Clarifying complexity
Although there was little research evidence for this mechanism, stakeholders maintained the important responsibility of leaders to clarify complexity in integrated care. It was commented that policy documents, such as the NHS Long Term Plan,8 did little to address the day-to-day complexities of working in an integrated system and that there was no leadership blueprint in these settings. Discussions were held around the tendency of leaders to confuse the notion of ‘complexity’ with that of ‘complicated’, highlighting that many of the decisions to be made by integrated care leaders were more nuanced and challenging than the term ‘complicated’ implied (i.e. about more than simply sorting out complicated practical circumstances):
From my experience of talking to senior leaders there’s a tremendous pull to just reframe complexity as just being complicated . . . and some of the people I talk to perceive things as complexity but then judge themselves, saying ‘why can’t I make decisions around how we’re going to work together?’ . . . I seem to spend a lot of time around people who are getting evaluated very harshly as if they’re failing to come to decisions, whereas the situations that they describe are ones of complexity.
There was an implication that the way in which a leader accurately judged the context of a situation and responded to complexity and how this had an impact on their decision-making could be indicative of their perceived effectiveness. However, stakeholders felt that the way in which a leader talked to people during the decision-making process, particularly where there were multiple and sometimes incommensurate perspectives and interests, was the critical criterion, not necessarily the result of those decisions. This, again, spoke to ideas of ‘holding’ or ‘containing’ challenges, rather than actively attempting to overcome them; a concept missing in the research evidence:
. . . the psychological therapeutic terms of holding and containment . . . has been absent in some of this.
Key messages
-
Policy documents, such as the NHS Long Term Plan,8 do little to address the day-to-day complexities of working in an integrated system and there is no blueprint for leadership.
-
A key characteristic of leadership is to navigate the tension between certainty and uncertainty and translate this to the team and/or system.
Fostering resilience
Although no research evidence was identified for this mechanism, stakeholders did have comments to make. Early in the study, stakeholders identified this mechanism as being a more generic aspect of leadership and less specific to leading integrated teams, although they suggested that we search for research evidence for anything more specific. They were unsurprised that no research evidence emerged to support the initial programme theory.
Stakeholders commented that no amount of resilience could help leaders of integrated systems with complex issues. Some felt that the term ‘resilience’ was code for ignoring or managing anxiety, without understanding why that anxiety had been evoked. They, therefore, felt that successful leaders were those with an understanding of the necessity, practicality, political nature and intense psychological impact of providing leadership. There was also suggestion of a psychological dynamic below the surface of integrated working, which became overt in bullying and uncivil behaviours. Stakeholders felt that it would be useful to explore the cultures that leaders set around this and if they were complicit, resistant or able to explain it. The longitudinal nature of developing effective ICSs was also highlighted, with stakeholders noting that it was a non-linear process and that resilience building was a long-term endeavour.
Key messages
-
Fostering resilience is less specific to leading integrated teams than in generic leadership.
General discussion
Stakeholders provided comments around leading integrated systems that were unrelated to the identified mechanisms. For example, the influence of professional anxiety on patients, service users, and families was raised, which reinforced the need for leaders to address the psychological effects of system change. Another participant queried how this study aligned with current contexts, such as the Black Lives Matter movement. This was significant, as research evidence had implicitly suggested conventional assumptions and actions surrounding leadership. There is a pressing need for leadership of integrated care to address this through an awareness of the necessity of anxiety, disturbance and disruption that comes with challenging the status quo.
Chapter 4 Discussion
This chapter reports how understanding of the programme theories or mechanisms has been refined following the synthesis of empirical research and stakeholder consultation. A key task in this synthesis was to make theories around leadership of integrated care teams and systems explicit, by developing clear hypotheses about how and for whom their leadership might ‘work’ and why. Sources of data used to develop the initial programme theories included academic peer-reviewed papers, policy documents and grey literature, which were discussed at length and modified by key stakeholders. These initial programme theories were then tested using research evidence and the experience of stakeholders to examine if leadership works in the way it was expected or assumed to work. This chapter presents the degree to which the initial programme theories were supported by these sources of evidence.
Inspiring intent to work together
The ‘inspiring intent to work together’ mechanism was the mechanism most often identified in the synthesis and the mechanism that generated the greatest amount of detail and discussion in the research evidence and among stakeholders. This mechanism was unique in that all others discussed what the leader does, whereas this discussed who the leader was. It referred to the personality and characteristics of the leader and how they were able to inspire other people.
There was evidence to support most of the initial programme theory (e.g. evidence that leaders were required to be effective advocates for integrated care, including having a clear vision for integrated working, which they could articulate with dynamism, passion and enthusiasm), but this was not all. That is, the initial programme theory stated that integrated working was based on voluntary collaboration without statutory basis, yet research evidence pointed to formalised integration either through the merger of existing hospitals/departments or through the development of NHS and Social Care Trusts. Furthermore, both research evidence and stakeholders’ experience indicated that inspirational leadership alone was inadequate within integrated care and needed to be supplemented by a range of other attributes. Stakeholders talked of the need for credibility, authenticity, and emotional intelligence, whereas the research literature identified the need for good communication skills; an open and accessible profile; and the ability to deliver a clear, consistent message. Stakeholders also noted the importance of leaders basing their vision around the needs of their patients/service users – a notion not given prominence in the research literature. There was also evidence of the absence of this mechanism in integrated teams and systems, both from the perspectives of stakeholders and the research literature. The consensus was that inspiration was broadly inadequate when leading complex integrated teams and systems, whereas the research literature highlighted examples of leaders who lacked inspirational qualities. This led to leaders refusing to confront problematic team members or challenge difficult behaviours.
A facilitating context for this mechanism, not identified in the initial programme theory but supported by both the research evidence and key stakeholders, was the importance of the overriding presence of trust. This included both strategic trust (i.e. trust that systems leaders would ensure that the correct organisational processes were in place and the right strategic decisions would be made) and personal trust (i.e. staff’s trust in their team leader’s skills and priorities, as well as the trust leaders had in themselves and their own personal capabilities). Developing this trust took time, with one example in the research literature demonstrating that a decade of development was required. When trust had been established, staff demonstrated a willingness to participate in integrated working, even when this was not specifically required of them. The research literature also provided evidence that integrated working was hampered by recalcitrant team members, who slowed progress by working in silos owing to a lack of trust.
Inspirational leadership is a complex issue because, as key stakeholders confirmed, employees may follow a leader because of their place in the organisation’s hierarchy, not necessarily because they are inspirational or able to motivate their staff to deliver their best work or contribution. This poses the question: what does it mean to be ‘inspirational’? In this synthesis, several characteristics associated with being inspirational were identified, including being:
-
visible
-
credible
-
committed
-
enthusiastic
-
dynamic
-
confident
-
willing to act
-
able to motivate, empower and encourage others
-
able to gain the trust and respect of others
-
a good communicator and listener
-
able to develop strong interpersonal relationships with colleagues
-
able to foster professional altruism
-
willing to ask for help.
This long list of characteristics highlights how the word ‘inspirational’ is a ‘catch-all’ term, which is arguably overworked, inflated and subjective. It raises several areas for consideration. First, it poses the question of whether or not organisations are likely to find an individual who possesses all the above characteristics. Take, for example, the requirement of ‘credibility’, which was reported to be gained through having direct experience of working in both health and social care or through being associated with previously successful developments. Given the relatively new status of integrated health and social care systems, the likelihood of finding an individual who has direct experience of working in both health and social care settings or having previously led successfully integrated teams or systems would be low. Every leader must become a leader for the first time and will, therefore, require the time and opportunities to hone many of the skills and experiences they may be expected to already possess. This suggests that more needs to be done to generate a pool of people with such credibility, for example by including training in both health and social care sectors as part of informal development opportunities as well as providing more formal leadership programmes, recognising that leadership development is both ongoing and progressive. The other reported means of demonstrating one’s credibility was through a leader’s ‘personality’, but there was no explanation of which personality traits helped to determine credibility. Taking the list of characteristics presented above, it could be assumed that credibility may be achieved through the demonstration of personality traits such as confidence, charisma, visibility, dynamism and influence. If so, credibility may be associated with personality traits of dominance and sociability, which have been identified as core components of the extroverted personality. 589 One concern, therefore, is that appointments for leadership of integrated care teams and systems may be biased towards those with extroverted personalities, yet more research is required to determine if such individuals are better equipped to undertake these roles successfully. A second point of consideration is whether or not leaders of integrated care teams and systems would require all the above characteristics or if some inspiring attributes are more important than others. Key stakeholders reinforced the view that one person’s perception of what is inspiring will be different from another’s and that inspirational leaders will therefore be incredibly diverse. Rather than search for a universal archetype of an inspirational leader, it is suggested that integrated systems assess the leadership traits required in their own specific organisation to motivate their staff to deliver their greatest contribution.
Aside from the specific personality traits or attributes of leaders, this synthesis found that a key component of inspiring others was having a clear vision for integration, which was articulated to others with passion. The importance of ‘vision’ is not a new concept in either the general leadership literature or health-care leadership literature. 590–592 However, while many authors talk of the importance of developing a clear vision, few clearly discussed what this entailed or how this could be achieved. Stakeholders also raised the importance of basing a vision around the needs of the individual patient/service user – a notion lacking prominence in the literature. Given the relatively new status of integrated care teams and systems, cultivating a strong vision for integrated working may be a skill that many leaders have yet to develop, and there are few ‘road maps’ available to assist with this. Furthermore, the research literature also identified the problems that could arise when the vision of team leaders did not align with the vision of their system leaders or the visions of the component organisations within the system. Given the complexities of ICSs, it is likely that varying organisations and leaders will have different visions of integrated working and how this can be best achieved. As this has been identified as a key component of leading integrated teams, it is suggested that effort is placed into developing a clear vision for integrated working that is accepted by all organisations and leaders in it.
Creating the conditions to work together
The ‘creating the conditions to work together’ mechanism was discussed as frequently as ‘inspiring intent to work together’ but lacked depth and detail. There was a clear overlap between these mechanisms regarding the importance of a leader’s ‘vision’. ‘Inspiring intent to work together’ referred to the need for leaders to have a clear vision for integrated working, which they could articulate clearly to others in an inspirational way, whereas ‘creating the conditions to work together’ involved leaders ensuring that the appropriate systems were in place to enable this vision to be achieved. Bluntly, leaders needed both a vision for integrated working that they could ‘sell’ to others in an inspirational way and have the skills to make that vision a reality. Although these mechanisms are separated here for the purposes of clarity, in reality, there must not be a disconnect between these two mechanisms, as both are important components for leadership. This notion was reinforced by the study stakeholders, who indicated that inspirational leadership alone was inadequate and needed to be supplemented by a range of other attributes.
Once again, the research evidence expanded on the initial programme theory by providing details of the practical steps that leaders needed to undertake to help achieve their vision. This included setting and driving an agreed strategy; creating a framework for action; re-drafting job descriptions to help facilitate collaborative working; ensuring effective organisational systems and processes were in place; and creating mutually beneficial shared goals with accountability for outcomes. Stakeholders further enhanced the programme theory by also highlighting the social skills required by leaders to create important conditions of psychological safety and an environment of transparency, openness and freedom to communicate. Also supported by empirical evidence and stakeholder contributions was the requirement for leaders to share components of their role with other members of their team. This idea of leadership sharing was based around the belief that integrated care required different skills at different times, not necessarily embodied by one person. Examples of shared leadership included delegating tasks and responsibilities. An important context for this mechanism was, again, whether or not there was an overriding presence of trust within teams, as the mechanism was facilitated in supportive atmospheres of professional respect and trust. Again, developing this trust took time.
Although ‘inspiring intent to work together’ and ‘creating the conditions to work together’ both centre around the importance of a clear vision for integrated working, the mechanisms describe different ways of enabling this vision to be achieved. The former focuses on the importance of leaders inspiring others to want to work together through their credibility and personality traits, whereas the latter requires leaders to have the practical and emotional intelligence and social skills necessary to achieve this vision. Although a similar number of papers discussed both mechanisms, it was notable that ‘inspiring intent to work together’ was discussed in far greater depth and detail than ‘creating the conditions to work together’. It is not clear why this may be the case. Perhaps the ability to inspire others is the most commonly accepted, attractive or valued component of leadership, whereas the ability to ensure that systems and procedures are in place is devalued or perceived as suitable for delegation to others. Perhaps these tasks and responsibilities are seen as the hallmark of managers and not leaders. Although we recognise that there is overlap and an interdependence between some aspects of management and leadership, it was not possible within the scope of this review to explore management in depth. However, the fact that both mechanisms were identified frequently suggests that both are important components of leading integrated teams and that investment in detail is as important as investment in vision. In complicated systems of integrated care, inspiration alone is not enough for the delivery of successful outcomes. Leaders who focus on inspiration alone may develop staff who are motivated to work in an integrated way but if the processes and procedures to enable such working are not in place, then positive outcomes will not emerge. Instead, effective leaders need to inspire staff to engage in a shared vision of integrated working, ensure that systems are in place to enable this vision to be achieved and hold staff accountable for their results.
Related to this was the suggestion by one author that developing a shared ‘team culture’ was an important factor in leading integrated care teams. 92 In the same way that developing a shared vision may be complicated in integrated care teams and systems, developing a shared team culture may also be difficult and potentially unlikely. Health and social care organisations operate under different cultures, governance procedures, accountability, regulation, and funding streams and they work with different trajectories and metrics of success. Different philosophies of care also operate both within health-care systems (e.g. between acute care and rehabilitation) and between health and social care organisations. The notion of a shared ‘team culture’ in integrated care teams may not recognise the importance of professional cultures nor what may be important to patients/service users at different points in their trajectories. More discussion of the need to balance different organisational cultures is provided in the ‘balancing multiple perspectives’ mechanism.
Finally, another theme identified in the research literature and by stakeholders across both the ‘inspiring’ and ‘creating the conditions’ mechanisms was the need for shared leadership roles (i.e. the need for team ‘champions’ who reminded members of the team’s benefits and provided sustained motivation for integrated working). Project co-ordinators, who were specifically focused on the process of improving integration, were also recommended. This suggestion that the different skills required from integrated care leadership does not need to be (or is unable to be) embodied by one person arose more strongly in the research evidence than in the initial programme theory, suggesting that the practical experiences of delivering integrated care are more complex than perceived. Given the complexities of integrated working and the multiple perspectives required to deliver integrated care, these systems may be better suited to leadership structures that are shared rather than concentrated in a single leader. More discussion of the need for sharing leadership and the benefits and complications this may pose is provided in the ‘working with power’ mechanism.
Balancing multiple perspectives
Over half of the research papers included in this synthesis referred to the ‘balancing multiple perspectives’ mechanism, yet evidence remained limited for much of the initial programme theory. Only one paper referred directly to the historical power imbalance between health and social care and the negative impact that this had on integrated care, whereas others discussed the imbalance between different professional disciplines, with medicine typically having the greatest power and influence. Stakeholders, however, were more forthcoming on discussions around imbalance, highlighting as a topical example the inequity between health and social care visible during the COVID-19 pandemic. In the early months of the pandemic, provision and support for acute care in the NHS were afforded priority over care homes, contributing to the very high number of COVID-19-related deaths in the UK, which we believe represents a serious failure of understanding of the interdependency of different parts of health and social care. The newly developing ICSs provide a just-in-time solution to avoid this failure in future, as they provide the structure for communication and collaboration between providers.
Most research evidence for the ‘balancing multiple perspectives’ mechanism focused on the need for leaders to manage difficult conversations and mitigate the inevitable, and complex, forms of conflict that arose across organisations, specialisms and individuals, rather than identifying leaders as enthusiastic ‘change agents’. Although there was some evidence of strategies used by leaders to manage conflict (e.g. getting involved in steering committees or working groups of collaborative projects to reduce territorial behaviour or acting as ‘diplomats’ to mitigate tension), there remained only limited evidence of leaders successfully mediating conflict in integrated teams. Where this did occur, contexts that supported it, once again, included reciprocal trust between leaders and team members, where leaders were trusted to have the capacity to resolve conflict. Stakeholders’ experiences were more diverse here, with some agreeing that a leader’s role was to resolve conflict, whereas others felt that leaders should challenge teams to work out problems themselves. Those who believed that conflict or dilemmas needed to be resolved felt that this avoided uncertainty and made progress in system integration. For these individuals, the skill and art of leadership were seen to help take their team in a new direction. Without some resolution to dilemmas, they felt that it would be extremely difficult to manage system change for good or for bad, acknowledging that integration was not always positive across the system. Those who disagreed felt that successful leaders needed to be able to accept and be confident to work alongside the tensions, conflicts and ambiguities raised through cross-sector working. This suggested that rather than work towards harmony, leaders should accept and manage tension and conflict in ways that pragmatically mitigated negative outcomes to develop balanced partnerships where possible and appropriate. Finally, some stakeholders also questioned whether or not ‘balancing’ was the right term to use for this mechanism, as it suggested that it was possible to get the balance right. They thought that it was unlikely that integrated care leaders would be able to accommodate everyone’s perspectives but considered that it was important that everyone felt heard.
Working with power
‘Working with power’ was identified as an initial programme theory by the study’s stakeholder group. Although fewer than half of the research papers in the synthesis identified evidence to support it, evidence was more detailed than for most other mechanisms. Although stakeholders continued to support the importance of this mechanism, they perceived issues around power to be more complex and nuanced than depicted in the research literature. Indeed, stakeholder discussions around this mechanism focused on fundamental questions such as what power is, where it comes from and who legitimises it. Once again, although mechanisms have been separated here for the purposes of clarity, there is clear overlap between the ‘balancing multiple perspectives’ and ‘working with power’ mechanisms.
There was some research evidence that leaders were aware of power dynamics and used this awareness in different ways. Some used their power to promote their own professional agenda by limiting the involvement of others and some shared their power with other leaders in the system to set priorities, allocate resources and evaluate performance. However, even where there was a will to share power, an existing foundation of trust and honesty was needed between system partners. If those with less power (usually owing to the relative power of their employing organisations) felt that their views were not respected or overlooked, they could feel disenfranchised or threatened. This suggested that power sharing agreements could be difficult to manage and may be unstable and prone to being unsettled, depending on current priorities. This raises the question about whether or not power sharing is genuinely possible where partners from different organisations and sectors hold unequal power. Stakeholders reinforced this lack of parity of esteem between health and social care as a fundamental, structural and systematic issue that was unsurprising but nevertheless needed recognition and acknowledgement. The response to COVID-19, whereby people were transferred to care homes without testing to free up acute NHS beds was highlighted as an example of how the NHS and social care components of the system were regarded differently. Furthermore, in large integrated care systems it should particularly be questioned whether or not system leaders can know about all the power dynamics or processes to enable the appropriate use of power. Stakeholders identified a fundamental difference in organisational culture, which was perceived to be one of ‘command and control’ in the NHS and more locally driven or accountable in local authorities, with their locally elected democratic accountability.
There was limited research evidence of leaders recognising when colleagues in other parts of the system were in a better position to lead on initiatives than themselves. Where systems leaders used their power carefully, this could help the system progress successfully, encourage trust and respect within teams and foster a shared philosophy and vision. The concept of ‘borrowed’ power resonated with the stakeholders, whereby the implicit permission and support of someone with a clear decision-making power enabled leaders to support change. This permission was rarely seen as explicit but was more obvious when it was withdrawn, and activities were required to be stopped. Sometimes there were specific circumstances that prompted a leader to relinquish or share power (e.g. a requirement to access system/network development funding rather than necessarily for its own sake; dissatisfaction with an overly narrow network activity; or resistance to an unknown leader). These responses were presented in the research evidence as positive actions by leaders, though we question whether this is skilful or could be considered a ‘work around’. Furthermore, it is rarely reported how the shifting of power from the formal leader is managed: is it permanent, temporary, or acknowledged? This suggests that power operates through both people and working practices to indistinct degrees, reinforcing the view of stakeholders that working with power is more challenging to conceptualise than demonstrated in the evidence.
There was some research evidence that progress in the provision of integrated care systems could stall if leaders were unwilling to relinquish control. This was due to staff feeling undervalued, not co-operating with their leader, having reduced confidence to make decisions and innovate, or at worst, resigning. In comparison, research evidence stated that leaders who gave staff autonomy and trusted them were valued by staff. Leaders who delegated decision-making authority and shared leadership with others with more relevant knowledge made staff feel valued, leading to increased motivation, trust and confidence in the leader. This could be particularly important for ICSs, where leaders are likely to be leading teams and systems outside of their specific field of expertise. Indeed, stakeholders felt that power generally moved throughout the system, rather than operating from top to bottom and this could have a range of positive implications for leadership and notions of shared ownership and responsibility. Research evidence found leaders’ perceptions of their responsibilities were an important part of the context of how they used their power. When team leaders felt that their main responsibility was to the system’s ‘top’ management, they could seem to have no power of their own but instead be essentially a conduit for delivering the top management wishes with little adaption for local circumstances. As a result, they rendered the team powerless too. When a leader felt that they had a responsibility to their team as well as to ‘top’ management, they took the initiative to consult with team members, thus using their power to give power and autonomy to others. Although it may be considered weak to relinquish control, this did require a more skilful use of power. However, there was some evidence that sharing leadership was not always considered appropriate, for example, when other members of the team were unable to fulfil this role or when hierarchical leadership was considered necessary because of prescribed lines of reporting, or legal or policy challenges. Research evidence and stakeholder contributions showed that trust and ‘being known’ were also important contexts for being accepted and that new, unknown leaders may not be accepted.
Finally, stakeholders referred to the absence of this mechanism and the implications that this had on integrated care. They also highlighted the absence of the patient/service user voice throughout the research literature and the lack of power that patients/service users held within integrated care systems. Given that a primary aim of integrated care is to develop a patient-/person-centred approach, the absence of the patient/service user voice and the relative lack of power afforded to them is concerning.
Commitment to learning and development
Less than half of the research papers in this synthesis referred to this mechanism and there was very limited detail or consensus achieved across the studies that did discuss it. The research evidence and stakeholder contributions tended to focus on the importance of creativity, innovation and training initiatives, whereas discussion of learning and development rarely featured. Where research evidence did discuss learning, it was stated that leaders needed to demonstrate a commitment to personal learning, encompassing information sharing and reflective practice. In addition, multiple forms of interprofessional and interorganisational training and education programmes were highlighted and deemed important in supporting integrated working. Formal and informal networks between organisational partnerships, staff, and the community were demonstrated to be helpful in overcoming bureaucratic and infrastructural barriers to instigating change. Where teams had strong interprofessional relationships and where networks were strong and social capital was high, learning with and from other team members was more likely to occur.
There was a general sense in the research evidence and from stakeholder contributions that innovation and creativity were important components of leadership, whereby leaders who encouraged team members to develop and innovate maximised the potential of integration. However, detailed practice accounts were limited. Although identified as important by stakeholders, a tolerance for things not working and having the scope to ‘fail well’ was not apparent in integrated systems and this was seen to inhibit innovation. Lack of time, enthusiasm or team support were thought to contribute to leaders’ fear of thinking ‘outside the box’ and doing things differently. The culture of success and positive results perceived to be prevalent in the NHS is perhaps so embedded that an environment in which having the freedom to make mistakes is difficult to envisage.
Finally, there were other areas of the initial programme theory for which there was also limited evidence. For example, there was no specific mention of leaders acting as role models in the studies reviewed or in the stakeholder discussions, although there was some evidence of system-level leaders supporting and mentoring potential team-level leaders.
Taking a wider view
The research evidence for this mechanism was scant. Initial programme theory of this mechanism included reference to the importance of ‘political astuteness’, and although we found no research evidence for this, stakeholders advised that leaders could not operate without a sense of political leadership. This area, therefore, warrants further research. The research evidence did stress the importance of system leaders looking beyond the interests of their own organisations and the integrated system to focus on the needs of the community, although again, we found little explanation of how this happens. Stakeholders found the notion of strategically engaging with the ‘right people’ to be concerning, as they believed that this could result in leaders engaging only with ‘like-minded’ individuals. Stakeholders reflected that leaders sought ‘like-minded people’ when experiencing anxiety or uncertainty, and this is a plausible explanation given the size and complexity of ICSs and the political investment in their success. However, this could lead to a bias in outlook and undermine the diverse perspectives that leaders would be expected to adopt.
Research evidence found an influencing context of this mechanism was whether or not leaders had strong, pre-existing networks and a willingness to work with a wide range of individuals and organisations. This could also be a restrictive context and a barrier to this mechanism if leaders only worked within their pre-existing networks, restricting, or narrowing their view of the system. Another disabling context included the challenge of pursuing partnerships with several organisations and sectors simultaneously, especially where formal partnerships were more influential or beneficial than informal partnerships, for example, with the voluntary sector. Furthermore, where individual team leaders prioritised their own organisation, this could be a disincentive for collaboration with external partners. An additional context highlighted by the stakeholders was the importance of trust: a prominent characteristic of good leadership that ran throughout this review. Building trust in complex, multisector systems is likely to be time-consuming, and the research evidence suggested that it was highly dependent on individuals and their connections. The impact of organisational/system size or, indeed, the existence of financial incentives to support system transformation innovation was not specifically highlighted, although we postulate that this would influence the fostering and support of trusting relationships between leaders.
The paucity of evidence for this mechanism raised several questions, including:
-
Because the NHS, social care, local authorities and other organisations are organised and governed independently, how likely is it that leaders will have genuine insight into the motivations and challenges of other organisations?
-
How realistic it is that there will be a cadre of leaders who are able to do this?
-
How are these leaders prepared, developed and supported to have the required experience and insight into the motivations and challenges of other organisations?
-
If leaders have a background in one organisation (e.g. the NHS) and have been a senior leader there, how inevitable is it that they will be influenced by or favour this sector?
-
Can integrated care disadvantage the perspective or involvement of smaller, less resourced and less experienced sectors who produce fewer senior systems leaders?
-
Are education budgets for the development of integrated care combined and available to all system partners equally?
Clarifying complexity
The amount and detail of research evidence for this mechanism were less than the others, which limited the scope to refine our understanding of this aspect of leadership. Nevertheless, stakeholders maintained that the responsibility of leaders to clarify complexity in integrated care was important. It has been suggested that having clear directives at a strategic level from all agencies involved, as well as from government, is key to streamlining difficult processes,593 yet stakeholders reported that policy documents did little to address the day-to-day complexities of working in an integrated system and that there was no blueprint for leadership. Clarity of message was deemed an important leadership characteristic; however, this was not clearly or directly attributable to the ‘sensemaking’ strategies described in the initial programme theory. Furthermore, there was more research evidence about the absence of the mechanism, where leaders did not clarify and simplify specific issues, such as lines of reporting; financial structures and systems; roles and responsibilities of team leaders; and leaders’ reasoning and priorities. This lack of clarity left team members confused and frustrated and negatively affected the potential of integrated working. Although providing a balance between detail and oversimplification was thought to be a valuable leadership attribute in the initial programme theory, the complexity of system-level arrangements and a failure to translate these for team members appeared to overwhelm any practical attempt to negotiate this fine line. This potentially speaks of a lack of definition or fluidity of interpretation of integrated care. Leaders were given the difficult task of deciphering and then translating the changes in structures and ways of working imposed by new forms of integrated working. They were required not only to clarify complexity, but also present this complexity with nuance and intelligence to achieve positive outcomes.
The introduction of middle-range theories is used in realist synthesis to offer phenomena ‘conceptual currency’. 594 This enables greater clarity of vision, and an opportunity to test the programme theories that have been developed. Utilising this approach, the findings above can be informed by theories of ontological security. Developed in social sciences,595,596 ontological security provides a sense of comfort and familiarity in a climate of distinct uncertainty. The new ways of working that integrated care encourages represent an uncomfortable and disruptive necessity of an environment that must accept complexity. Practitioners feeling disrupted by this complexity need leaders to provide clarification, in part to reassure them and in part to most efficiently communicate how an unfamiliar form of practice will work. Although integrated care is designed to make care more efficient, the associated complexities that are perhaps less visible, more nuanced or deliberately supressed (e.g. professional hierarchies, embedded tension, unconscious biases, political motivations) encourage complex consequences across the system. The need for this to be managed, or at least kept at bay, by clarity of message from those in positions of authority is another natural response to uncertainty. The difficulty with which this is genuinely provided by leadership, who are expected to recognise these hidden, embedded complexities and offer communication that is both clear and mindful of this is, therefore, considerable. Leadership that at least acknowledges this complexity and offers team members a sense of ontological security will demonstrate a level of sophistication that was absent in the research evidence.
Fostering resilience
Early in the study, stakeholders identified this mechanism as being more generic and less specific to integrated teams. They were not surprised that no research evidence for this mechanism had been identified. Stakeholders expressed concerns around the notion of ‘fostering resilience’ in leaders, including the suggestion that the term ‘resilience’ was code for ignoring or managing anxiety, without understanding the genesis of that anxiety. Successful leaders were deemed to be those who understand the necessity, practicality and political nature of providing leadership. There was also suggestion of a psychological dynamic below the surface of integrated working, which became overt in bullying and uncivil behaviours, and stakeholders felt that it would be useful to explore the cultures that leaders set around this. Although this provided further suggestion that leaders required higher level cognitive skills for integrated systems to function well, this also raised the question over whether or not resilience included an understanding of the difficulties associated with system change. If this is the case, it may be possible to suggest that the lack of evidence around being resilient is symptomatic of a failure on behalf of leadership and the literature to coherently explain what is happening during this shift towards integrated models.
The longitudinal nature of developing effective integrated care systems was also highlighted, with stakeholders noting that it was often a non-linear process. Resilience was, therefore, perceived to be a long-term endeavour. This suggested that ‘fostering resilience’ is a far more sophisticated requirement of leadership than the literature implies. It perhaps explains the absence of any evidence of fostering resilience in the research literature, as the notion must go beyond the superficiality of its appearance. Leaders may foster resilience by engaging in a range of behaviours and approaches, all of which combine to respond to the constant challenge of working in a shifting practice landscape.
Concluding remarks
In drawing this discussion to a close, we briefly consider how this review has contributed to the seven items identified as ‘a potential explanatory landscape’ for understanding complex programmes, in this case leadership of integrated care teams and systems. 597 Throughout this chapter we have discussed the preliminary programme theories of leadership of integrated care teams and systems in detail, to provide potential explanations for the nuanced and complex way in which it is implemented. The review has found considerable variation in the resources available on leaders of integrated care teams and systems and in the reasoning and reactions of stakeholders. The third objective aimed to develop realist programme theories that explain successful leadership of integrated care teams and systems and these are presented in Table 5. These have been framed positively to address this objective, but it must be stressed that the evidence demonstrated unsuccessful leadership too. The study stakeholder group were adamant that they wanted the review to provide an accurate view of the challenges of leading integrated teams and systems, including the negative aspects. There was also considerable variation in how leaders worked and the environments/contexts in which they worked, which suggests that the programme mechanisms did not apply consistently (although the evidence available is not sufficient to see consistent patterns of CMOs). Contextual factors are likely to be highly influential in how leaders work with individuals and within specific institutions and infrastructures. The policy landscape for integrated systems is still undergoing development and this will influence the context for leadership with potential to support or hinder it.
| Mechanism title | Context | Mechanism (resources) | Mechanism (reasoning/response) | Outcomes |
|---|---|---|---|---|
| CMO 1: inspiring intent to work together |
|
|
|
. . . which leads to a reduction in ‘gaming’ between organisations and more straightforward negotiations |
| . . . and fosters greater team synergy and a fertile learning environment | ||||
| . . . and elevates staff’s respect for leadership | ||||
| . . . and helps reassure staff who are concerned about integrated working | ||||
| . . . and helps bridge cultural gaps between organisations and communities | ||||
| CMO 2: creating the conditions to work together |
|
|
|
. . . which focusses effort in times of disagreement or conflict |
| . . . and prevents role defensiveness | ||||
| CMO 3: balancing multiple perspectives |
|
|
|
. . . conflict within teams is reduced |
| CMO 4: working with power |
|
|
|
. . . which increases the teams’ effectiveness and productivity |
| . . . and leads to greater team synergy | ||||
| . . . and helps teams develop a shared philosophy | ||||
| . . . and leads to more positive long-term experiences of integration, including low staff and manager turnover, group cohesion and cost savings | ||||
| CMO 5: commitment to learning and development |
|
|
|
. . . which nurtures learning and innovation within teams |
| CMO 6: taking a wider view |
|
|
|
. . . this helps achieve successful funding requests from public bodies who often expect a multidisciplinary vision |
| . . . and helps provide holistic and integrated systems | ||||
| CMO 7: clarifying complexity |
|
|
|
Chapter 5 Conclusions
This research offers timely and unique perspectives on leadership of integrated care teams and systems, in particular what works, for whom and in what circumstances. Its strengths are the careful analysis and unpacking of the assumptions of what leadership is amid the challenges of large, complex, inter-sector systems. The aims of this chapter are to set out the key messages from the study, review the approach and methods used, and discuss the implications of the findings for policy, practice and research.
Key messages
Paucity of empirical evidence
There was little evidence that specifically addressed leadership of integrated care teams and systems despite the widespread policy rhetoric in support of, and partial implementation of, this model of organising services. This was surprising. We assessed many papers and information sources, but most referred to older leadership theory, which was not tailored to understanding how leaders contributed to complex multisector organisations. There are several potential reasons for this. These include:
-
Attention on and development of integrated care teams and systems is relatively recent, with the result that little research has been undertaken or completed.
-
Research on integrated care teams and systems has focused on the implementation and outcome of service innovation rather than some of its structural underpinnings.
-
The lack of literature could reflect how hard it is to research this area and a reliance on existing framings of leadership when teams and organisations are less complex.
-
There are assumptions about leadership being a homogeneous activity that is transferable across many different settings and types of service and, therefore, it is not a research priority.
It is also important to note that there was very little evidence of the contexts that influenced how leaders work and even less evidence on the outcomes. Identifying CMO configurations was challenging. This limited the degree to which we could draw definitive conclusions about what works, for whom and in what circumstances. However, making explicit some of the assumptions about how leaders lead integrated care teams and systems has provided new perspectives offering fresh theoretical grounding that can be built on, developed and tested further.
There is an emphasis on the individual/personal qualities of the leader
The strongest evidence found in the review was around how leaders inspire people’s intent to work together in integrated care. This evidence focused on who the leader is rather than what the leader does. It referred to their personality, characteristics and ability to inspire other people. This is quite challenging to consider within aspirations for greater diversity and inclusion. One of our expert stakeholders asked: ‘If we just rely on people blowing us away with their personalities because they’re born like that, is that what it is?’. This seems counterintuitive. Why have extensive leadership programmes to develop, prepare and support leaders if the main qualities they need to lead well are innate? The stakeholders were clear that this was not enough; a leader must be knowledgeable, skilled and spend time on finding out what is involved on the ground. Within the ‘creating the conditions’ mechanism the focus was on the practical attributes of leadership, but stakeholders felt that it ignored the social skills also required. For example, stakeholders believed that ‘creating the conditions’ also involved creating a culture of psychological safety and an environment of transparency, openness and freedom to communicate without fear of repercussions.
The stakeholders referred to aviation safety, stating, ‘you don’t really care who the pilot is and how inspirational the pilot is when you get on the aeroplane, you just want them to fly the plane safely’. This overemphasis on the influence of individuals is recognised in leadership theory. The culture of individual leaders as ‘heroes’, romanticising their individual abilities and dispositions, is thought to prioritise the importance of being in control and having the power to decide, steer and influence others. This overestimates their contribution and influence598,599 and can obscure, in part, the tensions and complexities inherent in leadership. 600
An alternative perspective is processual leadership,601 which views leadership as an ongoing process of social interaction and negotiation with all members and stakeholders of an organisation who participate in and influence the organisation’s activity. Processual leadership acknowledges the complexities of social reality. It focuses on how leadership is socially constructed, deconstructed, and reconstructed in a fluid and dynamic way as relationships and circumstances change. 602 Through these ongoing processes, power and agency are negotiated between all actors in the organisation (e.g. leaders, staff and patients/service users) and no one falls outside these complex organisational processes. 599 This is attuned to the stakeholders’ views of the importance of social skills and emotional intelligence. Developing processual leadership practices that are attuned to a complex, changing, organisational context is thought to require recognition of the value of disagreement, tensions and dissent. This is not to decry consensus but acknowledges that it is not always achievable where stakeholders inevitably have different views and professional values. Leadership in organisations that are characterised by complexity and ambiguity like integrated care systems require a ‘viable sense of self-as-a-leader’ where leaders accept that social reality is constantly changing, and that control is an illusion. 599 However, maintaining a processual approach of leadership in an organisation or system where the dominant conception of the ‘hero’ leader is deeply embedded and where leaders perceive high levels of ambiguity and insecurity is extremely difficult. 599 The theory of ontological security595,596 provides a useful perspective to our understanding that leaders need to feel comfortable and secure in a climate of uncertainty to provide this security to the systems and team members that they lead.
We propose that perpetuating the importance of individual characteristics of leaders reduces the scope for integrated care teams and systems to develop leadership practices that are attuned to the complexity of multi-sectoral, multiorganisational and multiprofessional working. Furthermore, in line with The NHS Long Term Plan,8 42 integrated care systems have been created to cover the whole of England from April 2021, growing out of Sustainability and Transformation Partnerships. It is intended that they will become commissioning bodies that have a partnership governance structure and performance framework and need to be held accountable, committing the NHS and partners to increased complexity of health and social care services. There is a timely need to ensure that the skills of integrated care teams and systems leaders are intentionally developed to keep pace with service reorganisations.
Absence of evidence of patient/service user perspective
A central policy driver for the introduction of ICSs was the need for services to be ‘integrated around the patient’,7 to provide the best patient/service user experience and the best value for money. The ambition was to support patients/service users to be actively involved in their own care, give them more power to manage their own health and make informed decisions about their care and treatment. Furthermore, NHS England’s Patient and Public Participation Policy603 states that:
One of the great strengths of this country is that we have an NHS that – at its best – is ‘of the people, by the people and for the people’.
NHS England603
It also adds that:
. . . we need to engage with communities and citizens in new ways, involving them directly in decisions about the future of health and care services.
NHS England603
It is a stark finding that we found no evidence of the patient/service user’s perspective of leadership or their involvement in leadership of integrated care teams and systems.
The importance of power
This synthesis found the exercise of the power and influence of leaders to be very important. Power was held by many people to varying degrees, by government, across sectors, in organisations and by individuals at all levels of activity. As discussed previously, there was no evidence of power and influence being held by patients/service users in this context. Historic imbalances of power between health and social care were clear and irrefutably demonstrated by the response to managing surge capacity during the first wave of the COVID-19 pandemic. The NHS Long Term Plan,8 which sets out plans for the integration of health and social care throughout England is NHS-centric and potentially reinforces significant existing tensions between health and social care. New legislation to create a ‘legal form’ for integrated care systems is expected in 2021. 604 The NHS Long Term Plan8 did not call for new statutory bodies, but we believe that it will be important to provide clear power-sharing requirements to protect social care from being disadvantaged. This synthesis also demonstrated that higher levels of influence and power were held by members of the medical profession. Honesty and reciprocal trust were important in how power was used, which links to the individual characteristics of the leader and being known by those being led. The nature of power is far more complex and nuanced than the evidence suggests, and questions remain about how leaders of integrated care teams and systems see their power and reason how to use it. With the large size of integrated care systems and the numerous members of staff potentially involved, how realistic is it that leaders will be known sufficiently to be credible and trusted and to know the nature of the services that they are leading to make decisions?
The benefits of and barriers to pre-existing networks
The importance of system leaders looking beyond the interests of their own organisations and the integrated system to focus on the needs of the community was discussed in the research evidence. However, to facilitate this, leaders drew upon their pre-existing networks of like-minded people and those considered to be the ‘right people’ to engage with strategically. This would appear to be in contradiction to taking a wider view of the system. The benefits of pre-existing networks include that leaders are known and trusted, and progress in advancing innovation is likely to be faster, which is important given the political investment in the success of ICSs. It may also help leaders experiencing anxiety or uncertainty about the challenge of leading large, complex systems. However, a tendency to drift towards organisational, cultural and professional familiarities is likely to narrow the focus of innovation and this may inadvertently be a barrier to diversity in leadership. This lack of diversity could include sector, professional group, leadership style, service delivery priorities and protected characteristics, such as age, disability, ethnicity and sex. This reduction in diversity could reduce the potential for innovation, reach and equality of opportunity as demonstrated in the ‘Snowy White Peaks’ of the NHS report605 and hinder the ambition to ‘understand, encourage and celebrate diversity in all its forms’. 606 If leaders have a background in one organisation (e.g. as a senior leader in the NHS), they will be aware of the needs of that organisation and address them more easily. Furthermore, will integrated care disadvantage the perspective or involvement of smaller, less resourced, less experienced sectors who produce fewer senior systems leaders, such as charities?
Lack of practical guidance about how to lead in integrated care teams and systems
Throughout the evidence, there were general statements about the important activities that leaders undertook in leading integrated care teams and systems. For example, they managed conflict and mitigated tension among team members, they looked beyond the interests of their own individual organisations and they encouraged team members to develop and innovate. However, there was very little explanation about how leaders undertook these activities, their reasoning for what the best approach would be, the trade-offs they may have made, and the challenges that they encountered. This limits our understanding of what aspects of leadership work, for whom and in what circumstances. In the same way that clarifying complexity was thought by our stakeholders to be an important responsibility of leaders (albeit with little empirical evidence), leaders also required clear directives at a strategic level from all agencies involved, as well as from government, about leading challenging processes. However, policy documents were thought to do little to address the day-to-day complexities of working in an integrated system and our stakeholders felt that there was no blueprint for leadership in integrated care.
Strengths and limitations
A key strength of the study was the use of a realist review approach. This made explicit the assumptions of how leaders lead integrated care teams and systems and has begun to unpack the inherent complexity in these structures and activities, thereby advancing knowledge. Although the paucity of relevant empirical literature is a significant weakness of the review and limits the degree to which we can draw definitive conclusions about what works, for whom and in what circumstances, the review has highlighted important gaps in what is known and has provided new perspectives, which give much needed theoretical grounding that can be built on, developed and tested further. Establishing the evidence as we know it now in a rigorous and insightful way provides a valuable springboard for future work. Our realist descriptions of programme mechanisms are long and detailed. This is a strength as they provide a rich description of leadership, but they were challenging to test in the literature. Another key strength was the intensive contribution of the study stakeholder group, who challenged the assumptions made in the empirical literature, contributed their extensive experience and expertise to add explanation to the empirical evidence and provided additional insights not addressed in the published literature.
During the review it was challenging to define an integrated team and integrated system. Existing definitions described what they did rather than what they were. This was somewhat surprising and required the team to write study-specific definitions. Furthermore, these terms were used in the empirical literature to describe a range of organisational arrangements and were often not aligned to the purpose of our review. Similarly, the terms ‘leader’ and ‘manager’ were used interchangeably. Our search strategy did not include the term ‘manager’ or a variant of this and so when retrieved papers used the term ‘manager’ rather than ‘leader’, we examined it to assess whether or not the activities reported were those expected of a leader. Finally, the study team worked hard to overcome the challenges of COVID-19, which imposed remote working on the final 6 months of the study. It has been difficult to have detailed, theory-developing discussions between the study team and the expert stakeholder group via teleconferencing platforms and this has inevitably curtailed the intensity of these discussions. However, we completed the review under these circumstances.
Implications for policy and practice
This review demonstrated the weakness of the evidence explaining how leadership of integrated care teams and systems work, the contexts that support these mechanisms and the resulting outcomes. However, it revealed the scope for considerable variation in leadership practices. The prominence of the policy imperative to expand implementation of integrated care systems throughout England, and the importance of leadership to achieve this, highlights the contribution of this review. The fifth study objective was to provide recommendations about optimal organisational and interorganisational structures and processes that support effective leadership of the integrated health and social care system. However, making recommendations would overstate the evidence available. Therefore, the implications for policy and practice are set out in the following sections.
Implications for governance structures
New legislation in 2022 to create a ‘legal form’ of ICSs is expected at the time of writing. 604 The findings of this review suggest that it would be very important to ensure that legislation provides clear power-sharing requirements to protect social care and non-NHS organisations from being disadvantaged. Clarifying complexity and designing governance and incentives structures to support ICSs, rather than individual organisations within the systems, is likely to support leaders to take a wider view. This study will inform leadership structures for these new governance structures.
Implications for education preparation of leaders of integrated care teams and systems
The review did not find much evidence on specific education preparation for leaders of integrated care teams and systems. However, some important considerations were highlighted. These include:
-
the importance of understanding the whole system, which suggests that leaders need a wider understanding of organisations
-
the highly complex, dynamic nature of leading integrated care teams and systems and the imperative to adapt to varied circumstances demonstrates that leaders need to develop a viable sense of self-as-a-leader and be comfortable with uncertainty and ambiguity rather than the command and control approach that is common in the NHS
-
acknowledgement of the importance of emotional intelligence, communication and social skills development in leadership preparation.
In view of the unique, highly situated context of leading integrated care teams and systems, we propose that leadership training needs to encompass not a generalised training programme or course, but instead bespoke, individualised mentoring/coaching programmes. Approaches that increase exposure and understanding of other sectors may be useful, such as work placements, coaching or secondments, where individuals have opportunities to shadow leaders from another part of the system, work with coaches from other sectors, or rotate between the range of organisations across the system. Innovation approaches to design leadership education and training to build networks across systems would be beneficial and would contribute to the plans outlined in the NHS People Plan. 606
Implications for individual leaders and integrated care teams and systems
This review carefully unpacked the available evidence on the assumptions of what leadership is and the unique challenges of leading large, complex, inter-sector systems. To our knowledge, this is the first realist review in this area and offers leaders insights about their actions that potentially affect care delivery and outcomes, and team and system working. We hope that this understanding supports leaders to reflect on their practice and the factors that may support them in their work.
Recommendations for further research
The paucity of empirical evidence included in this review demonstrates the need for further research in this area, particularly as ICSs are being implemented throughout England. Furthermore, with the increasing range of structures for integration there is an increasing need to understand what works within a number of different closely specified system conditions (e.g. horizontal/vertical leadership and type of governance agreement/contract). The refined programme theories provide a very useful conceptual framework or platform from which to build this evidence.
This study has identified that research is needed in the following areas:
-
A clear priority is the need to examine patients’/service users’ and carers’ perceptions of how ICSs support them to have the opportunities to be involved in and lead their care.
-
Testing and evaluating these realist theories through research using a range of designs including in-depth case studies, ethnographic exploration and longitudinal research would provide a targeted explanation of how leadership works, the contexts that influence these mechanisms and the resulting patterns of outcomes.
-
In initial theory development we identified political astuteness as being necessary for leading integrated care teams and systems, but we found no mention of it in the research evidence. The expert stakeholders advised that leaders cannot operate without a sense of political leadership and therefore this area warrants research.
-
Understanding the reasons why the individual characteristics of leaders and ‘hero leadership’ are so prominent and how leaders can be supported to be able to take a processual approach to leading that is more comfortable with complexity and uncertainty in the system.
-
Investigating the notion of ‘fostering resilience’ in leaders, what this means and how it develops. Although there was no research evidence about this, our expert stakeholders were concerned that this may mask anxiety and avoid adequate management; they suggested that it would be useful to explore the cultures that leaders set around this. Furthermore, increasing understanding of the impact of self-care initiatives to develop leadership resilience would be useful.
NHS England and NHS Improvement set up the NHS leadership observatory in 2021,606 which aims to commission research and translate findings into practical advice and support. This review has the potential to inform the research priorities for this observatory.
Final conclusions
To our knowledge, this is the first theory-informed realist review of leadership of integrated care teams and systems. It makes a significant contribution to the understanding of what is known and, perhaps more importantly, the gaps in the empirical evidence. The emphasis on the importance of the individual personal characteristics of leaders, supporting the image of the ‘hero’ leader, suggests that there is discomfort and a lack of security in dealing with the high level of complexity within integrated care systems. Imbalance of power between sectors, organisations, teams and professionals is demotivating and a barrier to integrated working. The NHS is considerably more powerful than other sectors, emphatically demonstrated during the COVID-19 pandemic, which needs to be carefully considered if legislation formalises the structure and governance of ICSs in 2022.
Acknowledgements
We thank the members of our stakeholder consultation group for their significant contributions to this study, including Ruth Abrams, Anne-Marie Archard, Frances Bunn, Julian Elston, Joy Fraser, Felix Gradinger, Liz Greer, Pippa Hartridge, Lucy Hohnen, Liz Meerabeau, Nicola Maskrey, David Naylor, Kunal Patel, Thirza Sawtell, Debbie Sorkin, Rich Stockley, Martin Vernon and Suzette Woodward.
We are also grateful for the advice and support of the international advisor to the study, Professor Stephen Zaccaro, and the Information Services Specialists at King’s College London and Kingston University London.
We thank the anonymous peer reviewers for their insightful comments on the draft final report.
Contributions of authors
Ruth Harris (https://orcid.org/0000-0002-4377-5063) (Professor of Health Care for Older Adults, Nursing) conceived the study design and contributed to data collection, data analysis and interpretation, drafting the review and critical revision of the review.
Simon Fletcher (https://orcid.org/0000-0002-5905-1553) (Research Associate, Sociology) contributed to the design, data collection, data analysis and interpretation, drafting the review and critical revision of the review.
Sarah Sims (https://orcid.org/0000-0001-7494-9030) (Research Associate, Psychology) contributed to the design, data collection, data analysis and interpretation, drafting the review and critical revision of the review.
Fiona Ross (https://orcid.org/0000-0003-0909-6988) (Emerita Professor of Health and Social Care, Primary Care Nursing) contributed to the design, data analysis and interpretation, drafting the review and critical revision of the review.
Sally Brearley (https://orcid.org/0000-0001-7918-7485) (Patient and Public Involvement Fellow, PPI) led and supported PPI throughout the review and contributed to the design, data interpretation and critical revision of the review.
Jill Manthorpe (https://orcid.org/0000-0001-9006-1410) (Professor of Social Work, Social Care) contributed to the design, data analysis and interpretation, drafting the review and critical revision of the review.
All authors commented on and approved the final report.
Publications
Harris R, Fletcher S, Sims S, Ross F, Brearley S, Manthorpe J. Understanding key mechanisms of successfully leading integrated team-based services in health and social care: protocol for a realist synthesis. BMJ Open 2020;10:e038591.
Sims S, Fletcher S, Brearley S, Ross F, Manthorpe J, Harris R. What does success look like for leaders of integrated health and social care systems? A realist review. Int J Integr Care 2021;21:26.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HSDR programme or the Department of Health and Social Care.
References
- Harris R, Fletcher S, Sims S, Ross F, Brearley S, Manthorpe J. Understanding key mechanisms of successfully leading integrated team-based services in health and social care: protocol for a realist synthesis. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-038591.
- Sims S, Fletcher S, Brearley S, Ross F, Manthorpe J, Harris R. What does success look like for leaders of integrated health and social care systems? A realist review. Int J Integr Care 2021;21. https://doi.org/10.5334/ijic.5936.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. https://doi.org/10.1111/j.1468-0009.2012.00665.x.
- Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81. https://doi.org/10.1177/1098214010371972.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- NHS England . The NHS Five-Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 17 November 2020).
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 17 November 2020).
- Ham C. Making Sense of Integrated Care Systems, Integrated Care Partnerships and Accountable Care Organisations in the NHS in England. London: The King’s Fund; 2018.
- Fillingham D, Weir B. System Leadership Lessons and Learning from AQuA’s Integrated Care Discovery Communities. London: The King’s Fund; 2014.
- Goodwin N, Stein V, Amelung V, Amelung V, Stein V, Goodwin N, et al. Handbook Integrated Care. Cham: Springer Publishing; 2017.
- National Voices . A Narrative for Person Centred Coordinated (Integrated) Care 2013. www.nationalvoices.org.uk/sites/default/files/public/publications/narrative-for-person-centred-coordinated-care.pdf (accessed 17 November 2020).
- Stein K, Reider A. Integrated care at the crossroads – defining the way forward. Int J Integr Care 2009;9. https://doi.org/10.5334/ijic.315.
- UK Government . Mental Health Act 1983 n.d. https://www.legislation.gov.uk/ukpga/1983/20/contents (accessed 4 March 2022).
- Department of Health and Social Care . Working for Patients 1989.
- UK Government . Health Authorities Act 1995 n.d. https://www.legislation.gov.uk/ukpga/1995/17/contents (accessed 4 March 2022).
- Department of Health and Social Care . Shifting the Balance of Power Within the NHS 2001.
- Department of Health and Social Care . Our Health, Our Care, Our Say: A New Direction for Community Services 2006.
- Department of Health and Social Care . High Quality Care for All: NHS Next Stage Review Final Report 2008.
- NHS Future Forum . Information: A Report from the NHS Future Forum 2012. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216424/dh_132086.pdf (accessed 17 November 2020).
- The Health Foundation . The History of the NHS, Social Care and Public Policy 2018. https://navigator.health.org.uk/ (accessed 17 November 2020).
- Shaw A, Levenson R. Towards Integrated Care in Trafford. London: The Nuffield Trust; 2011.
- Lorne C, Allen P, Checkland K, Osipovic D, Sanderson M, Hammond J, et al. Integrated Care Systems: What Can Current Reforms Learn from Past Research on Regional Coordination of Health and Care in England? A Literature Review. London: London School of Hygiene & Tropical Medicine; 2019.
- The King’s Fund . The Future of Leadership and Management in the NHS: No More Heroes 2011.
- Iliffe S, Manthorpe J. Service integration through medical leadership in England’s NHS. J Integr Care 2018;26:77-86. https://doi.org/10.1108/JICA-10-2017-0037.
- Dopson S, Harrison A, Mark A. Leading Health Care Organisations. Basingstoke: Palgrave Macmillan; 2003.
- Dopson S, Ferlie E, McGivern G, Fischer M, Ledger J, Behrens S, et al. The Impact of Leadership and Leadership Development in Higher Education: A Review of the Literature and Evidence. London: Leadership Foundation for Higher Education; 2016.
- NHS Leadership Academy . Clinical Leadership Competency Framework 2011.
- Drucker P. Managing in the Next Society. New York, NY: Truman Talley Books, St Martin’s Griffin; 2002.
- Ahmed N, Ahmed F, Anis H, Carr P, Gauher S, Rahman F. An NHS Leadership Team for the Future. London: Reform Research Trust; 2015.
- Smith T, Fowler-Davis S, Nancarrow S, Ariss SMB, Enderby P. Leadership in interprofessional health and social care teams: a literature review. Leadersh Health Serv 2018;31:452-67. https://doi.org/10.1108/LHS-06-2016-0026.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013.
- Reeves S, MacMillan K, van Soeren M. Leadership within interprofessional health and social care teams: a socio-historical overview of some key trials and tribulations. J Nurs Manag 2010;18:258-64. https://doi.org/10.1111/j.1365-2834.2010.01077.x.
- Borkowski N. Organizational Behavior in Health Care. Burlington, MA: Jones & Barlett Learning; 2015.
- Naylor R, Dorrell S, Everington S. Ending the Crisis in NHS Leadership: A Plan for Renewal. London: Health Service Journal Future of NHS Leadership; 2015.
- West M, Eckert R, Steward K, Pasmore B. Delivering a Collective Leadership Strategy for Health Care. Greensboro, NC: Center for Creative Leadership and The King’s Fund; 2014.
- Forder J, Caiels J, Harlock J, Wistow G, Malisauskaite G, Peters M, et al. A System Level Evaluation of the Better Care Fund: Final Report 2018.
- Kirst M, Im J, Burns T, Baker GR, Goldhar J, O’Campo P, et al. What works in implementation of integrated care programs for older adults with complex needs? A realist review. Int J Qual Health Care 2017;29:612-24. https://doi.org/10.1093/intqhc/mzx095.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. RMP Methods Paper 2 2004. www.betterevaluation.org/sites/default/files/RMPmethods2.pdf (accessed 17 November 2020).
- Greenhalgh T, Wong G, Westhorp G, Pawson R. Protocol – realist and meta-narrative evidence synthesis: evolving standards (RAMESES). BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-115.
- Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006;9:127-42. https://doi.org/10.1080/13645570600595314.
- Abouljoud M, Ryan M, Eshelman A, Bryce K, Jesse MT. Leadership perspectives on integrating psychologists into specialty care clinics: an evolving paradigm. J Clin Psychol Med Settings 2018;25:267-77. https://doi.org/10.1007/s10880-017-9532-9.
- Baker GR, Shaw J, Gutberg J, Kenealy T, Carswell P, Breton M, et al. Effective organizational leadership in the implementation of integrated care; lessons from 9 cases in the iCoach Project. Int J Integr Care 2017;17:145-6. https://doi.org/10.5334/ijic.3193.
- Bartels MN. Physiatry as a leader for postacute care in integrated healthcare systems. Am J Phys Med Rehabil 2019;98:311-18. https://doi.org/10.1097/PHM.0000000000001039.
- Carter DR, DeChurch LA, Braun MT, Contractor NS. Social network approaches to leadership: an integrative conceptual review. J Appl Psychol 2015;100:597-622. https://doi.org/10.1037/a0038922.
- Coddington DC, Moore KD, Fischer EA. Physician leaders in integrated delivery. Med Group Manage J 1997;44.
- Cooper T. Manifest leadership styles in a Caribbean cross-sector network. Leadersh Organ Dev J 2016;37:93-106. https://doi.org/10.1108/LODJ-04-2014-0080.
- Crosby BC, Bryson JM. Integrative leadership and the creation and maintenance of cross-sector collaborations. Leadersh Q 2010;21:211-30. https://doi.org/10.1016/j.leaqua.2010.01.003.
- den Herder-van der Eerden M, Ewert B, Hodiamont F, Hesse M, Hasselaar J, Radbruch L. Towards accessible integrated palliative care: perspectives of leaders from seven European countries on facilitators, barriers and recommendations for improvement. J Integr Care 2017;25:222-32. https://doi.org/10.1108/JICA-03-2017-0006.
- Diadjeng WS, Suhariadi F, Damayanti NA. Organizational context and leadership in the integration role of health care provider of integrated antenatal care team in public health centre. Indian J Public Health Res Dev 2018;9:284-8. https://doi.org/10.5958/0976-5506.2018.00455.2.
- Drath WH, McCauley CD, Palus CJ, Van Velsor E, O’Connor PMG, McGuire JB. Direction, alignment, commitment: toward a more integrative ontology of leadership. Leadersh Q 2008;19:635-53. https://doi.org/10.1016/j.leaqua.2008.09.003.
- Dunbar MS, Towe VL, Ayer L, Martineau M. Connections to Care (C2C): the perspectives of leaders at community-based organizations that are integrating mental health supports. Rand Health Q 2018;7. https://doi.org/10.7249/RR2119.
- Fernandez S, Cho YJ, Perry JL. Exploring the link between integrated leadership and public sector performance. Leadersh Q 2010;21:308-23. https://doi.org/10.1016/j.leaqua.2010.01.009.
- George S, Leasure AR. Application of transformational leadership principles in the development and integration of palliative care within an advanced heart failure program. Dimens Crit Care Nurs 2016;35:59-65. https://doi.org/10.1097/DCC.0000000000000166.
- Hudson T, Lumsdon K. The race to integrate. Who will be the leaders?. Hosp Health Netw 1993;67.
- Knopf A. Study calls for integrating housing with treatment. Alcoholism &Amp; Drug Abuse Weekly 2015;27. https://doi.org/10.1002/adaw.30333.
- Limb M. NHS and social care leaders join forces to share knowledge of integrating services. BMJ 2014;348. https://doi.org/10.1136/bmj.g3359.
- Mulki FH. The Effects of Leadership and Authority on Cross-Boundary Information Sharing in Response to Public Health Crises: A Comparative Study Between the United States and Jordan 2010;70.
- Mullins R. Leadership. The ROI (return on investment): developing and using leadership skills to implement product integration and improve patient care. Access 2007;21:43-5.
- Moore BW, Smith SL, Schumacher LP, Papke R. Patient care leadership within an emerging integrated delivery network. Nurs Adm Q 1996;20:54-6. https://doi.org/10.1097/00006216-199602020-00009.
- Natt och Dag K. A scholar-practitioner perspective on a leadership development program in health care: integrating connectivism theory. Adv Dev Hum Resour 2017;19:295-313. https://doi.org/10.1177/1523422317712671.
- Norton LW. Flexible leadership: an integrative perspective. Consult Psychol J Pract Res 2010;62:143-50. https://doi.org/10.1037/a0019990.
- Ott MJ, Lynch M. Integrating complementary and conventional symptom management in a cancer center. Oncol Nurs Forum 2002;29:25-7. https://doi.org/10.1188/02.ONF.25-27.
- Payne JK. Leadership & professional development. An integrated model of nursing using evidence-based practice. Oncol Nurs Forum 2002;29:463-5. https://doi.org/10.1188/02.ONF.463-465.
- Potter MA, Burns HK, Barron G, Grofebert A, Bednarz GD. Cross-sector leadership development for preparedness. Public Health Rep 2005;120:109-15. https://doi.org/10.1177/00333549051200S119.
- Psek W, Davis FD, Gerrity G, Stametz R, Bailey-Davis L, Henninger D, et al. Leadership perspectives on operationalizing the learning health care system in an integrated delivery system. EGEMS 2016;4. https://doi.org/10.13063/2327-9214.1233.
- Bhardwa S. Nurse leaders must drive integration, says senior nurse. Independent Nurse n.d.
- Spitzer R. Lateral integration and the clinical nurse leader. Nurs Lead 2010;8. https://doi.org/10.1016/j.mnl.2010.01.001.
- Starck PL, Rooney LL. Leadership for the integration of comprehensive care and interprofessional collaboration. Clin Sch Rev 2015;8:43-8. https://doi.org/10.1891/1939-2095.8.1.43.
- Sun PYT, Anderson MH. Civic capacity: building on transformational leadership to explain successful integrative public leadership. Leadersh Q 2012;23:309-23. https://doi.org/10.1016/j.leaqua.2011.05.018.
- Johnson T. Health system integration: impact on leadership and practice. Semin Nurse Manag 2000;8:2-4.
- VESTAL A. Leadership integrates the team. Hosp Prog 1957;38.
- Walters LK. Physician Leadership and Efficiency Within the Veterans Integrated Health System Phenomenological Study 2013;74.
- Weeks J. The leadership of the naturopathic profession in the emergence of integrative and functional medicine . . . plus more. Integr Med 2016;15:16-8.
- Wesorick B. 21st century leadership challenge: creating and sustaining healthy, healing work cultures and integrated service at the point of care. Nurs Adm Q 2002;26:18-32. https://doi.org/10.1097/00006216-200210000-00006.
- Wiles LL, Isibel D. Rising from the rubble: a capstone simulation integrating leadership and clinical skills. Nurs Educ Perspect 2017;38:162-4. https://doi.org/10.1097/01.NEP.0000000000000103.
- Williams Van Rooij S. Extreme teaming: lessons in cross-sector leadership. Eur J Train Dev 2017;41:814-5. https://doi.org/10.1108/EJTD-10-2017-0089.
- Yu A, Matta FK, Cornfield B. Is leader-member exchange differentiation beneficial or detrimental for group effectiveness? A meta-analytic investigation and theoretical integration. Acad Manag J 2018;61:1158-88. https://doi.org/10.5465/amj.2016.1212.
- Zachary E. Grassroots leadership training: a case study of an effort to integrate theory and method. J Community Pract 2000;7:71-93. https://doi.org/10.1300/J125v07n01_06.
- De Lorenzo RA. San Antonio Military Medical Center integration: a case study in organizational leadership design. Mil Med 2008;173:203-9. https://doi.org/10.7205/milmed.173.2.203.
- Sherlock JJ, Curtis R, Christian E. Integrated Care: Applying Theory to Practice. New York, NY: Routledge; 2012.
- Age UK . Integrated Care Services: Bringing Together Leaders to Transform Services and Outcomes for People Living With Long-Term Conditions 2016.
- Brock J, Stella E. Integrated Children’s Services in Scotland: Practice and Leadership. An Assessment of Progress and Improvement. Edinburgh: Social Work Scotland, Healthcare Improvement Scotland and Care Inspectorate; 2018.
- Aitken K, von Treuer K. Organisational and leadership competencies for successful service integration. Leadersh Health Serv 2014;27:150-8. https://doi.org/10.1108/LHS-08-2012-0028.
- American Medical Association . Integrated leadership for hospitals and health systems: principles for success. J Okla State Med Assoc 2015;108:281-8.
- Croze C. From the field: leadership, innovation and integration. Mental Health Weekly 2007;17:5-6.
- Daub S, Goldhar J, Purbhoo D. One client, one team: health system integration for leaders. Healthc Manage Forum 2016;29:153-7. https://doi.org/10.1177/0840470416644930.
- deGruy FV. Integrated care: tools, maps, and leadership. J Am Board Fam Med 2015;28:107-10. https://doi.org/10.3122/jabfm.2015.S1.150106.
- de Stampa M, Vedel I, Mauriat C, Bagaragaza E, Routelous C, Bergman H, et al. Diagnostic study, design and implementation of an integrated model of care in France: a bottom-up process with continuous leadership. Int J Integr Care 2010;10. https://doi.org/10.5334/ijic.506.
- Horrigan BJ. Integrative leadership means partnering. Explore 2016;12:139-40. https://doi.org/10.1016/j.explore.2015.12.010.
- Kelley-Patterson D. What kind of leadership does integrated care need?. London J Prim Care 2012;5:3-7. https://doi.org/10.1080/17571472.2013.11493361.
- Klinga C, Hansson J, Hasson H, Sachs MA. Co-leadership – a management solution for integrated health and social care. Int J Integr Care 2016;16:1-9. https://doi.org/10.5334/ijic.2236.
- Moore A. Nurse leadership is central to success of the new integrated care system. Nurs Stand 2018;33:22-4. https://doi.org/10.7748/ns.33.8.22.s12.
- Nieuwboer MS, van der Sande R, van der Marck MA, Olde Rikkert MGM, Perry M. Clinical leadership and integrated primary care: a systematic literature review. Eur J Gen Pract 2019;25:7-18. https://doi.org/10.1080/13814788.2018.1515907.
- Outhwaite S. The importance of leadership in the development of an integrated team. J Nurs Manag 2003;11:371-6. https://doi.org/10.1046/j.1365-2834.2003.00427.x.
- Palazzo JM. Everything changes: successful integration of any type requires leadership, transparency. MGMA Connex 2014;14:39-40.
- Panzer PG, Philip MB, Hayward RA. Trends in domestic violence service and leadership: implications for an integrated shelter model. Adm Policy Ment Health 2000;27:339-52. https://doi.org/10.1023/a:1021941129326.
- Payne S, Hughes S, Wilkinson J, Hasselaar J, Preston N. Recommendations on priorities for integrated palliative care: transparent expert consultation with international leaders for the InSuP-C project. BMC Palliat Care 2019;18. https://doi.org/10.1186/s12904-019-0418-5.
- Robb J, Gilbert P. Leadership lessons in health and social care integration: mental health. Int J Leadersh Public Serv 2007;3:17-25. https://doi.org/10.1108/17479886200700003.
- Shirey MR, White-Williams C, Hites L. Integration of authentic leadership lens for building high performing interprofessional collaborative practice teams. Nurs Adm Q 2019;43:101-12. https://doi.org/10.1097/NAQ.0000000000000339.
- Thomas P, While A. Should nurses be leaders of integrated health care?. J Nurs Manag 2007;15:643-8. https://doi.org/10.1111/j.1365-2834.2007.00806.x.
- Touati N, Roberge D, Denis JL, Cazale L, Pineault R, Tremblay D. Clinical leaders at the forefront of change in health-care systems: advantages and issues. Lessons learned from the evaluation of the implementation of an integrated oncological services network. Health Serv Manage Res 2006;19:105-22. https://doi.org/10.1258/095148406776829068.
- Wachel W. The leadership challenge of integrated delivery systems. Healthc Exec 1994;9:12-5.
- Wheatley L, Doyle W, Evans C, Gosse C, Smith K. Integrated comprehensive care – a case study in nursing leadership and system transformation. Nurs Leadersh 2017;30:33-42. https://doi.org/10.12927/cjnl.2017.25107.
- Williams P. The role of leadership in learning and knowledge for integration. J Integr Care 2012;20:164-74. https://doi.org/10.1108/14769011211237500.
- Anandaciva S, Ward D, Randhawa M, Edge R. Leadership in Today’s NHS: Delivering the Impossible. London: The King’s Fund; 2018.
- Ardern K. Making Health Everyone’s Business n.d. www.excellenceinpolicing.org.uk/wp-content/uploads/2019/09/Plenary_Ardern_K.pdf (accessed 17 November 2020).
- Baker M, Oliver D, Burns E, Paynton D, Bullard E. Integrated Care for Older People with Frailty: Innovative Approaches in Practice. London: Royal College of General Practitioners and British Geriatrics Society; 2016.
- Battye F. Logic Models and Complex Programmes: A Brief Guide. Stoke-on-Trent: NHS Midlands and Lancashire Commissioning Support Unit; 2017.
- Bunn F, Goodman C, Russell B, Wilson P, Manthorpe J, Rait G, et al. Supporting shared decision-making for older people with multiple health and social care needs: a realist synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06280.
- Carter K, Chalouhi E, McKenna S, Richardson B. What it takes to make integrated care work. Health Int 2011;11:48-55.
- Chana N. A Collaborative Leadership Approach Is Vital for Integration Success 2019. www.nhsconfed.org/blog/2019/04/a-collaborative-leadership-approach-is-vital-for-integration-success (accessed 17 November 2020).
- Cordery S. Leadership Vacancies in the NHS 2018. www.hsj.co.uk/leadership/leadership-vacancies-in-the-nhs-/7022940.article (accessed 17 November 2020).
- The Strategy Unit, NHS Dudley . Lessons from the Vanguard: Procurement n.d. www.strategyunitwm.nhs.uk/sites/default/files/2018-09/Lessons%20from%20the%20Vanguard%20-%20Procurement.pdf (accessed 17 November 2020).
- Edgren L, Barnard K. Complex adaptive systems for management of integrated care. Leadersh Health Serv 2012;25:39-51. https://doi.org/10.1108/17511871211198061.
- Kershaw M. Developing Governance to Support Integrated Care: A Bumpy Ride. London: The King’s Fund; 2018.
- Laycock K, Borrows M, Dobson B. Getting Into Shape: Delivering a Workforce for Integrated Care. London: Reform; 2017.
- Local Government Association . Care and Health Improvement Programme: Integration Support Offer for Health and Care System Leaders 2018.
- Mahmud S. Our Integration Journey. Wolverhampton: The Royal Wolverhampton NHS Trust; 2019.
- Murray R. Primary Care Networks and the NHS Long-term Plan: The New Player on the Pitch. London: King’s Fund; 2019.
- NHS England . Breaking Down Barriers to Better Health and Care 2019. www.england.nhs.uk/wp-content/uploads/2019/04/breaking-down-barriers-to-better-health-and-care-march19.pdf (accessed 17 November 2020).
- NHS Leadership Academy . Healthcare Leadership Model: The Nine Dimensions of Leadership Behaviour 2013.
- Powell M. Leadership in the NHS: Thoughts of a Newcomer. London: The King’s Fund; 2016.
- Randhawa M. Talking Leadership: Transforming Mental Health Services. London: The King’s Fund; 2017.
- Sheaff R, Brand SL, Lloyd H, Wanner A, Fornasiero M, Briscoe S, et al. From programme theory to logic models for multispecialty community providers: a realist evidence synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06240.
- Turner A, Mulla A, Booth A, Aldridge S, Stevens S, Begum M, et al. The international knowledge base for new care models relevant to primary care-led integrated models: a realist synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06250.
- Weaks L, Naylor D, Trimble A, Green G. Cascading Leadership: A New Model to Support Leadership in the Community and Voluntary Sector. London: The King’s Fund; 2017.
- Wenzel L. The Journey Towards Integrated Care. London: The King’s Fund; 2018.
- West M, Armit K, Loewenthal L, Eckert R, West T, Lee A. Leadership and Leadership Development in Health Care: The Evidence Base. London: Faculty of Medical Leadership and Management; 2015.
- Wilkins C. Leading Place-Based Integration – A Presentation n.d. file:///C:/Users/k1512180/Downloads/Carolyn-Wilkins-.pdf (accessed 17 November 2020).
- Baylis A. Enhanced Health in Care Homes: Learning from Experiences So Far. London: The King’s Fund; 2017.
- Charles A. A Year of Integrated Care Systems: Reviewing the Journey So Far. London: The King’s Fund; 2018.
- Charles A. ‘Moving at the Speed of Trust’ – The Journey to Integrated Health Systems. London: The King’s Fund; 2018.
- Amelung VE, Stein V, Goodwin N, Balicer R, Nolte E, Suter E, et al. Handbook Integrated Care. Cham: Springer Publishing; 2017.
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. Understanding new models of integrated care in developed countries: a systematic review. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06290.
- Social Care Institute for Excellence (SCIE) . Leadership in Integrated Care Systems: Report Prepared for the NHS Leadership Academy 2018.
- West M. Collaborative and Compassionate Leadership 2017. www.kingsfund.org.uk/audio-video/michael-west-collaborative-compassionate-leadership (accessed 17 November 2020).
- Burstow P. Leading Integrated Health Systems: From Heroic to Humble Leadership. Health Service Journal; 2018.
- Aldridge S, Mulla A, Turner A. Rapid Evidence Scan: Integrated Care. Stoke-on-Trent: The Strategy Unit, NHS Midlands and Lancashire Commissioning Support Unit; 2016.
- Perks-Baker S. Enhancing Health in Care Homes: System Leadership in Action. London: The King’s Fund; 2017.
- Insightful Health Solutions . Leadership and the Integrated Care System 2018. www.insightfulhealthsolutions.com/leadership-integrated-care-system/ (accessed 17 November 2020).
- South, Central and West Commissioning Support Unit . Creating Integrated Care Systems 2019. www.scwcsu.nhs.uk/delivering-change/creating-integrated-care-systems/ (accessed 26 April 2019).
- Provider Voices . The Journey to Integrated Care Systems 2018. https://nhsproviders.org/media/518336/provider-voices-the-journey-to-integrated-care-interactive.pdf (accessed 17 November 2020).
- Pawson R, Tilley N. Realist Evaluation. London: SAGE Publications Ltd; 1997.
- Bienefeld N, Grote G. Shared leadership in multiteam systems: how cockpit and cabin crews lead each other to safety. Hum Factors 2014;56:270-86. https://doi.org/10.1177/0018720813488137.
- DeChurch LA, Marks MA. Leadership in multiteam systems. J Appl Psychol 2006;91:311-29. https://doi.org/10.1037/0021-9010.91.2.311.
- Covin J, Kolenko AT, Sightler WK, Tudor K. Leadership style and post-merger satisfaction. J Manag Dev 1997;16:22-33. https://doi.org/10.1108/02621719710155454.
- Appelbaum S, Lefrancois F, Tonna R, Shapiro B. Mergers 101 (part two): training managers for culture, stress, and change challenges. Ind Commer Train 2007;39:191-200. https://doi.org/10.1108/00197850710755113.
- Crosby BC, Bryson JM. Special issue on public integrative leadership: multiple turns of the kaleidoscope. Leadersh Q 2010;21:205-8. https://doi.org/10.1016/j.leaqua.2010.01.001.
- Morse RS. Integrative public leadership: catalyzing collaboration to create public value. Leadersh Q 2010;21:231-45. https://doi.org/10.1016/j.leaqua.2010.01.004.
- Overfield DV. A comprehensive and integrated framework for developing leadership teams. Consult Psychol J Pract Res 2016;68:1-20. https://doi.org/10.1037/cpb0000053.
- Sousa M, Van Dierendonck D. Introducing a short measure of shared servant leadership impacting team performance through team behavioral integration. Front Psychol 2016;6. https://doi.org/10.3389/fpsyg.2015.02002.
- Thomas H, Carnall C. Leadership development: integration in context. Strategic Change 2008;17:193-206. https://doi.org/10.1002/jsc.826.
- Hartley J. Ten propositions about public leadership. Int J Public Leadersh 2018;14:202-17. https://doi.org/10.1108/IJPL-09-2018-0048.
- Leadership Centre for the Systems Leadership Steering Group . The Revolution Will Be Improvised Part II 2016. www.thinklocalactpersonal.org.uk/_assets/News/The_Revolution_will_be_Improvised_Part_II.pdf (accessed 17 November 2020).
- Chartered Institute of Personnel and Development . Perspectives on Leadership in 2012, Implications for HR 2012. www.the-stress-site.net/uploads/2/7/0/6/2706840/perspectives_on_leadership.pdf (accessed 17 November 2020).
- Bolden R, Gulati A, Edwards G. Mobilizing change in public services: insights from a systems leadership development intervention. Int J Public Admin 2020;43:26-3. https://doi.org/10.1080/01900692.2019.1604748.
- Ghate D, Lewis J, Welbourn D. Systems Leadership: Exceptional Leadership for Exceptional Times – Synthesis Paper. Nottingham: The Virtual Staff College; 2013.
- DeChurch LA, Mathieu JE, Salas E, Goodwin GF, Burke CS. Team Effectiveness in Complex Organizations: Cross-disciplinary Perspectives and Approaches. New York, NY: Routledge, Taylor & Francis Group; 2009.
- Lazzara EH, Keebler JR, Shuffler ML, Patzer B, Smith DC, Misasi P. Considerations for multiteam systems in emergency medical services. J Patient Saf 2019;15:150-3. https://doi.org/10.1097/PTS.0000000000000213.
- Owen C, Bearman C, Brooks B, Chapman J, Paton D, Hossain L. Developing a research framework for complex multi-team coordination in emergency management. Int J of Emerg Manag 2013;9:1-17. https://doi.org/10.1504/IJEM.2013.054098.
- Jones KJ, Skinner A, Venema D, Crowe J, High R, Kennel V, et al. Evaluating the use of multiteam systems to manage the complexity of inpatient falls in rural hospitals. Health Serv Res 2019;54:994-1006. https://doi.org/10.1111/1475-6773.13186.
- Johannessen IA, McArthur PW, Jonassen JR, Frick J, Laugen B. Advances in Production Management Systems. Value Networks: Innovation Technologies, and Management. Berlin: Springer; 2012.
- Schipper D. Challenges to multiteam system leadership: an analysis of leadership during the management of railway disruptions. Cogn Technol Work 2017;19:445-59. https://doi.org/10.1007/s10111-017-0415-5.
- Murase T, Carter D, DeChurch L, Marks M. Mind the gap: the role of leadership in multiteam system collective cognition. Leadersh Q 2014;25:972-86. https://doi.org/10.1016/j.leaqua.2014.06.003.
- Zaccaro SJ, DeChurch LA, Zaccaro SJ, Marks MA, DeChurch LA. Multiteam Systems: An Organization Form for Dynamic and Complex Environments. New York, NY: Routledge, Taylor & Francis Group; 2012.
- De Vries T, Hollenbeck JR, Davison RB, Walter F. Managing coordination in multiteam systems: integrating micro and macro perspectives. Acad Manag J 2016;59:1823-44. https://doi.org/10.5465/amj.2014.0385.
- Kugler KG, Gerhardinger F, Brodbeck FC. Characteristics of Effective Leadership in Multiteam Systems n.d. www.psy.lmu.de/wirtschaftspsychologie_en/forschung/working_paper/wop-2016_1.pdf (accessed 17 November 2020).
- Jonassen JR. Effects of multi-team leadership on collaboration and integration in subsea operations. Int J Leadersh Stud 2015;9:89-114.
- Rico R, Hinsz VB, Davison R, Salas E. Structural influences upon coordination and performance in multiteam systems. Hum Resour Manag Rev 2018;28:332-46. https://doi.org/10.1016/j.hrmr.2017.02.001.
- Weaver SJ, Che X, Pronovost PJ, Goeschel CA, Kosel KC, Rosen MA, et al. Pushing the Boundaries: Multiteam Systems in Research and Practice (Research on Managing Groups and Teams, Vol. 16). Bingley: Emerald Group Publishing Limited; 2014.
- Luciano MM, DeChurch LA, Mathieu JE. Multiteam systems: a structural framework and meso-theory of system functioning. J Manag 2018;44:1065-96. https://doi.org/10.1177/0149206315601184.
- Taplin SH, Foster MK, Shortell SM. Organizational leadership for building effective health care teams. Ann Fam Med 2013;11:279-81. https://doi.org/10.1370/afm.1506.
- West C, Landry K, Graham A, Graham L, Cianciolo AT, Kalet A, et al. Conceptualizing interprofessional teams as multi-team systems – implications for assessment and training. Teach Learn Med 2015;27:366-9. https://doi.org/10.1080/10401334.2015.1077136.
- Noyes K, Monson JR, Rizvi I, Savastano A, Green JS, Sevdalis N. Regional multiteam systems in cancer care delivery. J Oncol Pract 2016;12:1059-66. https://doi.org/10.1200/JOP.2016.013896.
- Zaccaro SJ, Marks MA, DeChurch LA, Zaccaro SJ, Marks MA, DeChurch LA. Multiteam Systems: An Organization Form for Dynamic and Complex Environments. New York, NY: Routledge, Taylor & Francis Group; 2012.
- DiazGranados D, Dow AW, Perry SJ, Palesis JA, Shuffler ML, Rico R, et al. Pushing the Boundaries: Multiteam Systems in Research and Practice (Research on Managing Groups and Teams, Vol. 16). Bingley: Emerald Group Publishing Limited; 2014.
- Taplin SH, Weaver S, Chollette V, Marks LB, Jacobs A, Schiff G, et al. Teams and teamwork during a cancer diagnosis: interdependency within and between teams. J Oncol Pract 2015;11:231-8. https://doi.org/10.1200/JOP.2014.003376.
- Ingold PV. Questionnaire for integrative leadership. Ger J Work Organ Psychol 2019;63:100-6. https://doi.org/10.1026/0932-4089/a000294.
- Kuipers H. The importance of functional integration among workers and the influence of leadership upon integration. People Company 1973;27:106-21.
- Hockin RS. Integrating Leadership Activities With Organizational Survivability: Toward a Theory of Healthcare Transformation 2007;68.
- Anonymous . Reaching the next level: governance in a time of turmoil. Med Netw Strategy Rep 1999;8:1-7.
- Aslani P, Barnet S, Cumming S, Dunn S, Nisbet G, Shaw T, et al. Implementation and evaluation of a ‘teamwork in health’ module. Pharmacy Education 2010;10:68-9.
- Aucott JN, Pelecanos E, Bailey AJ, Shupe TC, Romeo JH, Ravdin JI, et al. Interdisciplinary integration for quality improvement: the Cleveland Veterans Affairs Medical Center Firm System. Jt Comm J Qual Improv 1995;21:179-90. https://doi.org/10.1016/s1070-3241(16)30138-9.
- Belasen AT, Eisenberg B, Rutigliano NK, Paludi MA. Psychology for Business Success, Vol 3: Managing, Leading, and Developing Employees, Vol 4: Implementing Best Practices in Human Resources. Santa Barbara, CA: Praeger; 2013.
- Blair JD, Fottler MD, Lazarus SS, Paolino AR, Rotarius TR. Strategic stakeholder management. First round results from ‘Facing the Uncertain Future’. Med Group Manage J 1995;42.
- Bradel WT, Gillis V, Harkness J, McGuire TP, Nehring T. Integrating cultures: a tool for mission leaders and others in collaborating organizations. Health Prog 1999;80:65-78.
- Briceland DJ. Ophthalmology-led integrated eye care team. West Indian Med J 2012;5.
- Crosby BC, Bryson JM, Uhl-Bien M, Ospina S. Advancing Relational Leadership Research: A Dialogue Among Perspectives. Charlotte, NC: Information Age Publishing; 2012.
- Cunningham N, Stanway SJ, Wiseman T, Taylor C, Noble JL, Doyle N. Living with and beyond cancer: what can be achieved by multi-organization collaboration. J Clin Oncol 2017;35. https://doi.org/10.1200/JCO.2017.35.5_suppl.59.
- Feussner JR, Landefeld CS, Weinberger SE. Change, challenge and opportunity: departments of medicine and their leaders. Am J Med Sci 2016;351:3-10. https://doi.org/10.1016/j.amjms.2015.10.008.
- Fuhrmann H, Schuder H. Motivation and absenteeism as measures of productive leadership: an integrative attempt by means of the ProMES System. Ger J Work Organ Psychol 1996;40:209-13.
- Ghani UA, Hesselbein F, Goldsmith M. The Leader of the Future 2: Visions, Strategies, and Practices for the New Era. San Francisco, CA: Leader to Leader Institute; 2006.
- Goodwin N. Health and social care partnerships: leading and managing networks of care. Ann Acad Med Singap 2011;40.
- Karam M, Tricas-Sauras S, Darras E, Macq J. Interprofessional collaboration between general physicians and emergency department teams in Belgium: a qualitative study. Int J Integr Care 2017;17. https://doi.org/10.5334/ijic.2520.
- Kharicha K, Iliffe S, Levin E, Davey B, Fleming C. Tearing down the Berlin wall: social workers’ perspectives on joint working with general practice. Fam Pract 2005;22:399-405. https://doi.org/10.1093/fampra/cmi010.
- Ling T, Brereton L, Conklin A, Newbould J, Roland M. Barriers and facilitators to integrating care: experiences from the English Integrated Care Pilots. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.982.
- Lunts P. Change management in integrated care: what helps and hinders middle managers – a case study. J Integr Care 2012;20:246-56. https://doi.org/10.1108/14769011211255285.
- Nicholson C, Hepworth J, Burridge L, Marley J, Jackson C. Translating the elements of health governance for integrated care from theory to practice: a case study approach. Int J Integr Care 2018;18. https://doi.org/10.5334/ijic.3106.
- Rees G, Huby G, McDade L, McKechnie L. Joint working in community mental health teams: implementation of an integrated care pathway. Health Soc Care Community 2004;12:527-36. https://doi.org/10.1111/j.1365-2524.2004.00523.x.
- Roberts NJ, Ward M, Patel I, Yorke J, Partridge MR. Reflections on integrated care from those working in and leading integrated respiratory teams. London J Prim Care 2018;10:24-30. https://doi.org/10.1080/17571472.2017.1421020.
- Shand J, Turner S. System wide collaboration? Health and social care leaders’ perspectives on working across boundaries. J Integr Care 2019;27:83-94. https://doi.org/10.1108/JICA-06-2018-0042.
- Stuart K. Leading multi-professional teams in the children’s workforce: an action research project. Int J Integr Care 2012;12. https://doi.org/10.5334/ijic.750.
- van Eyk H, Baum F. Learning about interagency collaboration: trialling collaborative projects between hospitals and community health services. Health Soc Care Community 2002;10:262-9. https://doi.org/10.1046/j.1365-2524.2002.00369.x.
- Williams PM. Integration of health and social care: a case of learning and knowledge management. Health Soc Care Community 2012;20:550-60. https://doi.org/10.1111/j.1365-2524.2012.01076.x.
- Willumsen E. Leadership in interprofessional collaboration – the case of childcare in Norway. J Interprof Care 2006;20:403-13. https://doi.org/10.1080/13561820600874692.
- Atkinson M, Wilkin A, Stott A, Kinder K. Multiagency Working: A Detailed Study. Slough: National Foundation for Educational Research; 2002.
- Alexander JA, Comfort ME, Weiner BJ, Bogue R. Leadership in collaborative community health partnerships. Nonprofit Manag Leadersh 2001;12:159-75. https://doi.org/10.1002/nml.12203.
- Asakawa T, Kawabata H, Kisa K, Terashita T, Murakami M, Otaki J. Establishing community-based integrated care for elderly patients through interprofessional teamwork: a qualitative analysis. J Multidiscip Healthc 2017;10:399-407. https://doi.org/10.2147/JMDH.S144526.
- Axelsson SB, Axelsson R. From territoriality to altruism in interprofessional collaboration and leadership. J Interprof Care 2009;23:320-30. https://doi.org/10.1080/13561820902921811.
- Balasubramanian S, Spurgeon P. Integrated care for chronic pain management in the national health service: barriers and possibilities for service development – a survey. Int J Clin Leadersh 2012;17:201-10.
- Benzer JK, Cramer IE, Burgess JF, Mohr DC, Sullivan JL, Charns MP. How personal and standardized coordination impact implementation of integrated care. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1079-6.
- Best S. Facilitating integrated delivery of services across organisational boundaries: essential enablers to integration. Br J Occup Ther 2017;80:302-9. https://doi.org/10.1177/0308022616688019.
- Brousselle A, Lamothe L, Sylvain C, Foro A, Perreault M. Key enhancing factors for integrating services for patients with mental and substance use disorders. Ment Health Subst Use 2010;3:203-18. https://doi.org/10.1080/17523281.2010.505176.
- Carroll V, Reeve CA, Humphreys JS, Wakerman J, Carter M. Re-orienting a remote acute care model towards a primary health care approach: key enablers. Rural Remote Health 2015;15. https://doi.org/10.22605/RRH2942.
- Choi S, Holmberg I, Löwstedt J, Brommels M. Managing clinical integration: a comparative case study in a merged university hospital. J Health Organ Manag 2012;26:486-507. https://doi.org/10.1108/14777261211251544.
- Chreim S, Williams BE, Janz L, Dastmalchian A. Change agency in a primary health care context: the case of distributed leadership. Health Care Manage Rev 2010;35:187-99. https://doi.org/10.1097/HMR.0b013e3181c8b1f8.
- Cohen JR, Dowling M, Gallagher JST. The trials, tribulations, and relative success of the ongoing clinical merger of two large academic hospital systems. Acad Med 2006;81:11-7. https://doi.org/10.1097/01.ACM.0000235601.35726.db.
- Cramm JM, Nieboer AP. Disease-management partnership functioning, synergy and effectiveness in delivering chronic-illness care. Int J Qual Health Care 2012;24:279-85. https://doi.org/10.1093/intqhc/mzs004.
- Dickinson H, Peck E, Davidson D. Opportunity seized or missed? A case study of leadership and organizational change in the creation of a Care Trust. J Interprof Care 2007;21:503-13. https://doi.org/10.1080/13561820701585353.
- Scragg T. An evaluation of integrated team management. J Integr Care 2006;14:39-48. https://doi.org/10.1108/14769018200600023.
- Brown K, White K. Exploring the Evidence Base for Integrated Children’s Services. Edinburgh: Scottish Executive; 2006.
- Ho A, Pinney S. Redefining ethical leadership in a 21st-century healthcare system. Healthc Manage Forum 2016;29:39-42. https://doi.org/10.1177/0840470415613910.
- Hodges J, Martin G. Can leadership branding work in theory and practice to resolve the integration-responsiveness problems facing multinational enterprises?. Int J Hum Resour Manag 2012;23:3794-812. https://doi.org/10.1080/09585192.2011.654235.
- Hudziak JJ. Health and resilience in an integrated care model. J Am Acad Child Adolesc Psychiatry 2016;55. https://doi.org/10.1016/j.jaac.2016.07.589.
- Hughes C. Diversity Intelligence: Integrating Diversity Intelligence Alongside Intellectual, Emotional, and Cultural Intelligence for Leadership and Career Development. Basingstoke: Palgrave Macmillan; 2016.
- Hughes R, McCririck V. Integrating health and social care: workforce perspectives. J Care Serv Manag 2012;6:10-5. https://doi.org/10.1179/1750168712Y.0000000006.
- Hulks S, Walsh N, Powell M, Ham C, Alderwick H. Leading Across the Health and Care System: Lessons from Experience. London: The King’s Fund; 2017.
- Hunt JC, Gruenwoldt E, Lyster AH. Engaging the next generation of health leaders: perspectives of emerging health leaders. Healthc Manage Forum 2011;24:4-13. https://doi.org/10.1016/j.hcmf.2010.12.001.
- Hunt PL. Leadership in diversity. Health Progr 1994;75:26-9.
- Hurlock-Chorostecki C, McCallum J. Nurse practitioner role value in hospitals: new strategies for hospital leaders. Nurs Leadersh 2016;29:82-9. https://doi.org/10.12927/cjnl.2016.24895.
- Hwang Y, Al-Arabiat M, Rouibah K, Chung J-Y. Toward an integrative view for the leader-member exchange of system implementation. Int J Inf Manag 2016;36:976-86. https://doi.org/10.1016/j.ijinfomgt.2016.06.008.
- Iachini AL, DeHart DD, Browne T, Dunn BL, Blake EW, Blake C. Examining collaborative leadership through interprofessional education: findings from a mixed methods study. J Interprof Care 2019;33:235-42. https://doi.org/10.1080/13561820.2018.1516635.
- Indlekofer UR, Carrick K. Leadership and followership in aviation: cross-organisational comparison of concepts in civilian and military multicrew flight deck cultures. Hum Fact Aerospace Saf 2006;6:247-59.
- Ismail S, Osman M, Abulezz R, Alhamdan H, Quadri KHM. Pharmacists as interprofessional collaborators and leaders through clinical pathways. Pharmacy 2018;6. https://doi.org/10.3390/pharmacy6010024.
- Jackson CL, Nicholson C, Doust J, Cheung L, O’Donnell J. Seriously working together: integrated governance models to achieve sustainable partnerships between health care organisations. Med J Aust 2008;188:S57-60. https://doi.org/10.5694/j.1326-5377.2008.tb01746.x.
- Jang HJ, Weberg D, Dower C. Nursing partnerships in research and quality improvement within a large integrated health care system. Nurs Adm Q 2018;42:357-62. https://doi.org/10.1097/NAQ.0000000000000318.
- Jaynes S. An Exploration of Social Workers’ Perceived Roles in Mental Health and Chemical Dependence Treatment Settings: Toward a Leadership Agenda for Integrated Treatment 2008;69.
- Jeavons R. Developing leadership skills at the front line. Nurs Manag 2011;18:24-5. https://doi.org/10.7748/nm2011.10.18.6.24.c8717.
- Jeffs L, Merkley J, Sinno M, Thomson N, Peladeau N, Richardson S. Engaging stakeholders to co-design an academic practice strategic plan in an integrated health system: the key roles of the nurse executive and planning team. Nurs Adm Q 2019;43:186-92. https://doi.org/10.1097/NAQ.0000000000000340.
- Jiang Y, Chen CC. Integrating knowledge activities for team innovation: effects of transformational leadership. J Manag 2018;44:1819-47. https://doi.org/10.1177/0149206316628641.
- Kabir C, Potty A, Sharma R. Current opportunities for the development of leadership skills for doctors. Int J Clin Leadersh 2009;16:115-9.
- Keshmiri F, Moradi K. Perceptions of Iranian emergency department directors of interprofessional leadership: an interview study. J Interprof Care 2019;4. https://doi.org/10.1080/13561820.2019.1672632.
- Khorakian A, Sharifirad MS. Integrating implicit leadership theories, leader-member exchange, self-efficacy, and attachment theory to predict job performance. Psychol Rep 2019;122:1117-44. https://doi.org/10.1177/0033294118773400.
- Khoshhal KI, Guraya SY. Leaders produce leaders and managers produce followers. A systematic review of the desired competencies and standard settings for physicians’ leadership. Saudi Med J 2016;37:1061-7. https://doi.org/10.15537/smj.2016.10.15620.
- Kilpatrick K, Lavoie-Tremblay M, Ritchie JA, Lamothe L, Doran D. Boundary work and the introduction of acute care nurse practitioners in healthcare teams. J Adv Nurs 2012;68:1504-15. https://doi.org/10.1111/j.1365-2648.2011.05895.x.
- Kim J, McLean GN. An integrative framework for global leadership competency: levels and dimensions. Hum Resou Dev Int 2015;18:235-58. https://doi.org/10.1080/13678868.2014.1003721.
- King CR, King CR, O’Toole Gerard S. Clinical Nurse Leader Certification Review. New York, NY: Springer Publishing Company; 2013.
- Kirby EJ. Public Sector and Private Sector Executive Leadership Forming a Cross-Sector Collaboration: A Case Study 2014;75.
- Kitch T. A leadership perspective on a shared vision for healthcare. Nurs Leadersh 2017;30:30-2. https://doi.org/10.12927/cjnl.2017.25108.
- Kong F, Huang Y, Liu P, Zhao X. Why voice behavior? An integrative model of the need for affiliation, the quality of leader-member exchange, and group cohesion in predicting voice behavior. Group Organ Manag 2017;42:792-818. https://doi.org/10.1177/1059601116642084.
- Kozlowski SWJ, Mak S, Chao GT. Team-centric leadership: an integrative review. Annu Rev Organ Psychol Organ Behav 2016;3:21-54. https://doi.org/10.1146/annurev-orgpsych-041015-062429.
- Kuiper H, Jackson RJ, Barna S, Satariano WA. Local health department leadership strategies for healthy built environments. J Public Health Manag Pract 2012;18:E11-23. https://doi.org/10.1097/PHH.0b013e31822d4c7f.
- Lacerda T. Understanding Leadership Effectiveness in Organizational Settings: An Integrative Approach 2016;76.
- Laschinger HK, Smith LM. The influence of authentic leadership and empowerment on new-graduate nurses’ perceptions of interprofessional collaboration. J Nurs Adm 2013;43:24-9. https://doi.org/10.1097/NNA.0b013e3182786064.
- Lesic SA. Using instrumental leadership to manage change. Radiol Manage 1999;21:44-52.
- Ling M-T, Pang V, Thurasamy R. The construct validation of Leadership Competency Scale (LCS): integration of Rasch and PLS-SEM. TPM Test Psychom Methodol Appl Psychol 2017;24:269-83.
- Linuesa-Langreo J, Ruiz-Palomino P, Elche-Hortelano D. Integrating servant leadership into managerial strategy to build group social capital: the mediating role of group citizenship behavior. J Bus Ethics 2018;152:899-916. https://doi.org/10.1007/s10551-018-3823-4.
- Lauck S, Lewis K, Forman J, Smith A, Carroll S. Promoting shared decision-making for the treatment of heart valve disease in Canada: a call for nursing leadership. Can J Cardiol 2019;35:S200-1. https://doi.org/10.1016/j.cjca.2019.07.377.
- Lowe G, Plummer V, Boyd L. Nurse practitioner integration: qualitative experiences of the change management process. J Nurs Manag 2018;26:992-1001. https://doi.org/10.1111/jonm.12624.
- MacPhail A, Young C, Ibrahim JE. Workplace-based clinical leadership training increases willingness to lead. Leadersh Health Serv 2015;28:100-18. https://doi.org/10.1108/LHS-01-2014-0002.
- Manning A, Maslow G, Poirier B, Stefureac K, Heilbron N. 23.3 Nurse practitioner leadership in a multidisciplinary outpatient clinic. J Am Acad Child Adolesc Psychiatry 2019;58. https://doi.org/10.1016/j.jaac.2019.07.143.
- Mannix J, Wilkes L, Daly J. Attributes of clinical leadership in contemporary nursing: an integrative review. Contemp Nurse 2013;45:10-21. https://doi.org/10.5172/conu.2013.45.1.10.
- Markle-Reid M, Dykeman C, Ploeg J, Kelly Stradiotto C, Andrews A, Bonomo S, et al. Collaborative leadership and the implementation of community-based fall prevention initiatives: a multiple case study of public health practice within community groups. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2089-3.
- Markuns JF, Culpepper L, Halpin WJ. Commentary: a need for leadership in primary health care for the underserved: a call to action. Acad Med 2009;84:1325-7. https://doi.org/10.1097/ACM.0b013e3181b6c8e7.
- Martsolf GR, Sloan J, Villarruel A, Mason D, Sullivan C. Promoting a culture of health through cross-sector collaborations. Health Promot Pract 2018;19:784-91. https://doi.org/10.1177/1524839918772284.
- Masterson A. Cross-boundary working: a macro-political analysis of the impact on professional roles. J Clin Nurs 2002;11:331-9. https://doi.org/10.1046/j.1365-2702.2002.00604.x.
- Mathieu JE, Wolfson MA, Park S. The evolution of work team research since Hawthorne. Am Psychol 2018;73:308-21. https://doi.org/10.1037/amp0000255.
- May D, Wesche JS, Heinitz K, Kerschreiter R. Coping with destructive leadership: putting forward an integrated theoretical framework for the interaction process between leaders and followers. J Psychol Special Issue: Destructive Leadership 2014;222:203-13. https://doi.org/10.1027/2151-2604/a000187.
- May KA, Ferguson-Paré M. Preparing nurse leaders for the future: views from Canada. Semin Nurse Manag 1997;5:97-105.
- McAllister M, Happell B, Bradshaw J. Authenticity, creativity and a love of the job: experiences of grassroots leaders of mental health nursing in Queensland. Issues Ment Health Nurs 2013;34:658-64. https://doi.org/10.3109/01612840.2013.766821.
- Higgins SE, Routhieaux RL. A multiple-level analysis of hospital team effectiveness. Health Care Superv 1999;17:1-13.
- Jefferies R, Sheriff IH, Matthews JH, Jagger O, Curtis S, Lees P, et al. Leadership and management in UK medical school curricula. J Health Organ Manag 2016;30:1081-104. https://doi.org/10.1108/JHOM-03-2016-0042.
- McCallin A. Interdisciplinary team leadership: a revisionist approach for an old problem?. J Nurs Manag 2003;11:364-70. https://doi.org/10.1046/j.1365-2834.2003.00425.x.
- McCorcle MD, Heet NS. The ‘success test:’ validating the competencies required for healthcare leadership. Best Pract Benchmarking Healthc 1997;2:63-70.
- McCormick MJ, Martinko MJ. Identifying leader social cognitions: integrating the causal reasoning perspective into social cognitive theory. J Leadersh Organ Stud 2004;10:2-11. https://doi.org/10.1177/107179190401000401.
- Mendes IA, Ventura CA, Trevizan MA, Marchi-Alves LM, de Souza-Junior VD. Education, leadership and partnerships: nursing potential for Universal Health Coverage. Rev Lat Am Enfermagem 2016;24. https://doi.org/10.1590/1518-8345.1092.2673.
- Merry MD. Physician leadership for the 21st century. Qual Manag Health Care 1993;1:31-4. https://doi.org/10.1097/00019514-199321000-00007.
- Michaels C. Leading beyond traditional boundaries: a community nursing perspective. Nurs Adm Q 1997;22:30-7. https://doi.org/10.1097/00006216-199702210-00007.
- Michel JS, Pichler S, Newness K. Integrating leader affect, leader work-family spillover, and leadership. Leadersh Organ Dev J 2014;35:410-28. https://doi.org/10.1108/LODJ-06-12-0074.
- Miller DL, Umble KE, Frederick SL, Dinkin DR. Linking learning methods to outcomes in public health leadership development. Leadersh Health Serv 2007;20:97-123. https://doi.org/10.1108/17511870710745439.
- Miller M. Leadership Challenges for Patient Advocates: A Cross Sector Alliance Perspective 2019;80.
- Misra-Hebert AD, Perzynski A, Rothberg MB, Fox J, Mercer MB, Liu X, et al. Implementing team-based primary care models: a mixed-methods comparative case study in a large, integrated health care system. J Gen Intern Med 2018;33:1928-36. https://doi.org/10.1007/s11606-018-4611-7.
- Misso ML, Ilic D, Haines TP, Hutchinson AM, East CE, Teede HJ. Development, implementation and evaluation of a clinical research engagement and leadership capacity building program in a large Australian health care service. BMC Med Educ 2016;16. https://doi.org/10.1186/s12909-016-0525-4.
- Mitchell E. Cross-organisational staff liabilities in integrated care settings: the first higher court decision. J Integr Care 2012;20:367-70. https://doi.org/10.1108/14769011211285165.
- Moss SA, Dowling N, Callanan J. Towards an integrated model of leadership and self regulation. Leadersh Q 2009;20:162-76. https://doi.org/10.1016/j.leaqua.2009.01.005.
- Myers CG, Sutcliffe KM, Ferrari BT. Treating the ‘not-invented-here syndrome’ in medical leadership: learning from the insights of outside disciplines. Acad Med 2019;94:1416-18. https://doi.org/10.1097/ACM.0000000000002860.
- Neill M, Hayward KS, Peterson T. Students’ perceptions of the interprofessional team in practice through the application of servant leadership principles. J Interprof Care 2007;21:425-32. https://doi.org/10.1080/13561820701443512.
- Nissen LB, Merrigan DM, Kraft MK. Moving mountains together: strategic community leadership and systems change. Child Welfare 2005;84:123-40.
- O’Connor N, Ward D, Newton L, Warby M. Enabling clinicians to become the quality leaders in a mental health service. Australas Psychiatry 2005;13:357-61. https://doi.org/10.1111/j.1440-1665.2005.02214.x.
- O’Grady TP. Process leadership and the death of management. Nurs Econ 1997;15:286-93.
- Ong YH, Koh MYH, Lim WS. Shared leadership in interprofessional teams: beyond team characteristics to team conditions. J Interprof Care 2020;34:444-52. https://doi.org/10.1080/13561820.2019.1653834.
- Onyura B, Crann S, Tannenbaum D, Whittaker MK, Murdoch S, Freeman R. Is postgraduate leadership education a match for the wicked problems of health systems leadership? A critical systematic review. Perspect Med Educ 2019;8:133-42. https://doi.org/10.1007/s40037-019-0517-2.
- Oostra RD. Physician Leadership: a central strategy to transforming healthcare. Front Health Serv Manage 2016;32:15-26. https://doi.org/10.1097/01974520-201601000-00003.
- Orchard CA, Sonibare O, Morse A, Collins J, Al-Hamad A. Collaborative leadership, part 1: the nurse leader’s role within interprofessional teams. Nurs Leadersh 2017;30:14-25. https://doi.org/10.12927/cjnl.2017.25258.
- Ouimet G. Dynamics of narcissistic leadership in organizations: towards an integrated research model. J Manag Psychol 2010;25:713-26. https://doi.org/10.1108/02683941011075265.
- Ovseiko PV, O’Sullivan C, Powell SC, Davies SM, Buchan AM. Implementation of collaborative governance in cross-sector innovation and education networks: evidence from the National Health Service in England. BMC Health Serv Res 2014;14. https://doi.org/10.1186/s12913-014-0552-y.
- Page S. Integrative leadership for collaborative governance: civic engagement in Seattle. Leadersh Q 2010;21:246-63. https://doi.org/10.1016/j.leaqua.2010.01.005.
- Pappas S, McCauley L. Nursing integration and innovation across a multisystem enterprise: priorities for nurse leaders. Nurs Adm Q 2018;42:54-61. https://doi.org/10.1097/NAQ.0000000000000265.
- Park D. Androgynous leadership style: an integration rather than a polarization. Leadersh Organ Dev J 1997;18:166-71. https://doi.org/10.1108/01437739710168643.
- Payne PR, Pressler TR, Sarkar IN, Lussier Y. People, organizational, and leadership factors impacting informatics support for clinical and translational research. BMC Med Inform Decis Mak 2013;13. https://doi.org/10.1186/1472-6947-13-20.
- Pecukonis E, Doyle O, Acquavita S, Aparicio E, Gibbons M, Vanidestine T. Interprofessional leadership training in MCH social work. Soc Work Health Care 2013;52:625-41. https://doi.org/10.1080/00981389.2013.792913.
- Perrone L, Downer A, Mokdad A, Scott E, Perdue T, Shotorbani S, et al. Implementing an effective leadership and management training program for clinical and public health laboratory directors and other mid senior-level managers in the Middle East. Ann Glob Health 2014;80:174-5. https://doi.org/10.1016/j.aogh.2014.08.049.
- Phillips J, Hebish LJ, Mann S, Ching JM, Blackmore CC. Engaging frontline leaders and staff in real-time improvement. Jt Comm J Qual Patient Saf 2016;42:170-83. https://doi.org/10.1016/S1553-7250(16)42021-0.
- Phillips JM, Stalter AM, Dolansky MA, Lopez GM. Fostering future leadership in quality and safety in health care through systems thinking. J Prof Nurs 2016;32:15-24. https://doi.org/10.1016/j.profnurs.2015.06.003.
- Phillips N, Byrne G. Enhancing frontline clinical leadership in an acute hospital trust. J Clin Nurs 2013;22:2625-35. https://doi.org/10.1111/jocn.12088.
- Pietiläinen V, Salmi I. An integrative discourse perspective on positive leadership in public health care. Leadersh Health Serv 2017;30:44-58. https://doi.org/10.1108/LHS-04-2016-0016.
- Plochg T, Ilinca S, Noordegraaf M. Beyond integrated care. J Health Serv Res Policy 2017;22:195-7. https://doi.org/10.1177/1355819617697998.
- Prætorius T, Hasle P, Nielsen AP. No one can whistle a symphony: how hospitals design for daily cross-boundary collaboration. J Health Organ Manag 2018;32:618-34. https://doi.org/10.1108/JHOM-10-2017-0265.
- Pronovost PJ, Miller MR, Wachter RM, Meyer GS. Perspective: physician leadership in quality. Acad Med 2009;84:1651-6. https://doi.org/10.1097/ACM.0b013e3181bce0ee.
- Raney AF. Agility in adversity: integrating mindfulness and principles of adaptive leadership in the administration of a community mental health center. Clin Soc Work J 2014;42:312-20. https://doi.org/10.1007/s10615-014-0487-0.
- Ratzliff A, Norfleet K, Chan YF, Raney L, Unützer J. Perceived educational needs of the integrated care psychiatric consultant. Acad Psychiatry 2015;39:448-56. https://doi.org/10.1007/s40596-015-0360-7.
- Reay T, Golden-Biddle K, Germann K. Challenges and leadership strategies for managers of nurse practitioners. J Nurs Manag 2003;11:396-403. https://doi.org/10.1046/j.1365-2834.2003.00412.x.
- Redeker M, de Vries RE, Rouckhout D, Vermeren P, de Fruyt F. Integrating leadership: the leadership circumplex. Eur J Work Organ Psychol 2014;23:435-55. https://doi.org/10.1080/1359432X.2012.738671.
- Reichenpfader U, Carlfjord S, Nilsen P. Leadership in evidence-based practice: a systematic review. Leadersh Health Serv 2015;28:298-316. https://doi.org/10.1108/LHS-08-2014-0061.
- Reitemeier RJ. The leadership crisis in internal medicine: what can be done?. Ann Intern Med 1991;114:69-75. https://doi.org/10.7326/0003-4819-114-1-69.
- Rice JA, Isakova L, Zelckovich R, Frid E. Capitation and integrated health care systems. J Health Adm Educ 1996;14:205-37.
- Robbins CJ, Bradley EH, Spicer M. Developing leadership in healthcare administration: a competency assessment tool. J Healthc Manag 2001;46:188-202. https://doi.org/10.1097/00115514-200105000-00010.
- Robins L, Murphy N, Zierler B. Leveraging a faculty fellowship programme to develop leaders in interprofessional education. J Interprof Care 2016;30:520-2. https://doi.org/10.3109/13561820.2016.1150258.
- Robinson P, Oyemaja J, Beachy B, Goodie J, Sprague L, Bell J, et al. Creating a primary care workforce: strategies for leaders, clinicians, and nurses. J Clin Psychol Med Settings 2018;25:169-86. https://doi.org/10.1007/s10880-017-9530-y.
- Rose K, Shuck B, Twyford D, Bergman M. Skunked: an integrative review exploring the consequences of the dysfunctional leader and implications for those employees who work for them. Hum Resour Dev Rev 2015;14:64-90. https://doi.org/10.1177/1534484314552437.
- Rosenberg L. Are healthcare leaders ready for the real revolution?. J Behav Health Serv Res 2012;39:215-9. https://doi.org/10.1007/s11414-012-9285-z.
- Rosenman ED, Fernandez R, Wong AH, Cassara M, Cooper DD, Kou M, et al. Changing systems through effective teams: a role for simulation. Acad Emerg Med 2018;25:128-43. https://doi.org/10.1111/acem.13260.
- Rosenman ED, Vrablik MC, Brolliar SM, Chipman AK, Fernandez R. Targeted simulation-based leadership training for trauma team leaders. West J Emerg Med 2019;20:520-6. https://doi.org/10.5811/westjem.2019.2.41405.
- Rycroft-Malone J, Burton CR, Wilkinson J, Harvey G, McCormack B, Baker R, et al. Collective action for implementation: a realist evaluation of organisational collaboration in healthcare. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0380-z.
- Rycroft-Malone J, Wilkinson JE, Burton CR, Andrews G, Ariss S, Baker R, et al. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-74.
- Salas E, Almeida SA, Salisbury M, King H, Lazzara EH, Lyons R, et al. What are the critical success factors for team training in health care?. Jt Comm J Qual Patient Saf 2009;35:398-405. https://doi.org/10.1016/S1553-7250(09)35056-4.
- Salas E, Zajac S, Marlow SL. Transforming health care one team at a time: ten observations and the trail ahead. Group Organ Manag 2018;43:357-81. https://doi.org/10.1177/1059601118756554.
- Saleeby E, Holschneider CH, Singhal R. Paradigm shifts: using a participatory leadership process to redesign health systems. Curr Opin Obstet Gynecol 2014;26:516-22. https://doi.org/10.1097/GCO.0000000000000122.
- Sasnett B, Clay M. Leadership styles in interdisciplinary health science education. J Interprof Care 2008;22:630-8. https://doi.org/10.1080/13561820802293006.
- Sayers J, Lopez V, Howard PB, Escott P, Cleary M. The leadership role of nurse educators in mental health nursing. Issues Ment Health Nurs 2015;36:718-24. https://doi.org/10.3109/01612840.2015.1033040.
- Scarbrough H, D’Andreta D, Evans S, Marabelli M, Newell S, Powell J, et al. Networked innovation in the health sector: comparative qualitative study of the role of Collaborations for Leadership in Applied Health Research and Care in translating research into practice. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02130.
- Scholes J, Vaughan B. Cross-boundary working: implications for the multiprofessional team. J Clin Nurs 2002;11:399-408. https://doi.org/10.1046/j.1365-2702.2002.00634.x.
- Brady Schwartz D, Burnes Bolton L. Leadership imperative: creating and sustaining healthy workplace environments. J Nurs Adm 2012;42:499-501. https://doi.org/10.1097/NNA.0b013e3182714521.
- Scott C, Gerardi D. A strategic approach for managing conflict in hospitals: responding to the Joint Commission leadership standard, Part 1. Jt Comm J Qual Patient Saf 2011;37:59-6. https://doi.org/10.1016/S1553-7250(11)37008-0.
- Sebastian JG, Breslin ET, Trautman DE, Cary AH, Rosseter RJ, Vlahov D. Leadership by collaboration: nursing’s bold new vision for academic-practice partnerships. J Prof Nurs 2018;34:110-16. https://doi.org/10.1016/j.profnurs.2017.11.006.
- Shaw J, Wong I, Griffin B, Robertson M, Bhatia RS. Principles for health system capacity planning: insights for healthcare leaders. Healthc Q 2017;19:17-22. https://doi.org/10.12927/hcq.2017.25016.
- Shillam CR, MacLean L. Leadership influence: a core foundation for advocacy. Nurs Adm Q 2018;42:150-3. https://doi.org/10.1097/NAQ.0000000000000276.
- Sijbom RBL, Janssen O, Van Yperen NW. Leaders’ achievement goals and their integrative management of creative ideas voiced by subordinates or superiors. Eur J Soc Psychol 2016;46:732-45. https://doi.org/10.1002/ejsp.2223.
- Silvia C, McGuire M. Leading public sector networks: an empirical examination of integrative leadership behaviors. Leadersh Q 2010;21:264-77. https://doi.org/10.1016/j.leaqua.2010.01.006.
- Simoens S, Scott A. How are Scottish integrated primary care organisations managed?. J Health Organ Manag 2003;17:25-36. https://doi.org/10.1108/14777260310469292.
- Sims S, Hewitt G, Harris R. Evidence of a shared purpose, critical reflection, innovation and leadership in interprofessional healthcare teams: a realist synthesis. J Interprof Care 2015;29:209-15. https://doi.org/10.3109/13561820.2014.941459.
- Skelton-Green J, Simpson B, Scott J. An integrated approach to change leadership. Nurs Leadersh 2007;20:e1-15. https://doi.org/10.12927/cjnl.2007.19277.
- South J, Connolly AM, Stansfield JA, Johnstone P, Henderson G, Fenton KA. Putting the public (back) into public health: leadership, evidence and action. J Public Health 2019;41:10-7. https://doi.org/10.1093/pubmed/fdy041.
- Spallina JM. Clinical program leadership: skill requirements for contemporary leaders. J Oncol Manag 2002;11:24-6.
- Stevens S, Scott I, Von Hellens L, Iselin G. ‘Closing the loop’: the role of health care leaders in integrating research and practice. Aust Health Rev 2004;27:56-64. https://doi.org/10.1071/ah042710056.
- Stuber F, Seifried-Dübon T, Rieger MA, Zipfel S, Gündel H, Junne F. Contributors of the SEEGEN Consortium . Investigating the role of stress-preventive leadership in the workplace hospital: the cross-sectional determination of relational quality by transformational leadership. Front Psychiatry 2019;10. https://doi.org/10.3389/fpsyt.2019.00622.
- Thomas P, Meads G, Moustafa A, Nazareth I, Stange KC, Donnelly Hess G. Combined horizontal and vertical integration of care: a goal of practice-based commissioning. Qual Prim Care 2008;16:425-32.
- Tremblay D, Latreille J, Bilodeau K, Samson A, Roy L, L’Italien MF, et al. Improving the transition from oncology to primary care teams: a case for shared leadership. J Oncol Pract 2016;12:1012-19. https://doi.org/10.1200/JOP.2016.013771.
- van Eeghen CO, Littenberg B, Kessler R. Chronic care coordination by integrating care through a team-based, population-driven approach: a case study. Transl Behav Med 2018;8:468-80. https://doi.org/10.1093/tbm/ibx073.
- Veit KR. Regional patient safety and quality leaders aim to reduce disparities in healthcare with collaborative approach. Int J Health Gov 2017;22:37-46. https://doi.org/10.1108/IJHG-08-2016-0040.
- Weick KE, McDaniel RR, Driebe DJ. Uncertainty and Surprise in Complex Systems: Questions on Working with the Unexpected. Berlin: Springer; 2005.
- Weick KE, Sutcliffe J, Obstfeld D. Organizing and the process of sensemaking. Organ Sci 2005;16:409-21. https://doi.org/10.1287/orsc.1050.0133.
- Weinstock M. Smart leadership! Finding the right mix of minds to manage the future. Hosp Health Netw 2010;84.
- Weintraub R, Rosenberg J, Wachter K. Transitioning from the MDGs to the SDGs: a practical decision-making tool for leaders. Ann Glob Health 2016;82. https://doi.org/10.1016/j.aogh.2016.04.432.
- Weiss M, Kolbe M, Grote G, Spahn DR, Grande B. We can do it! Inclusive leader language promotes voice behavior in multi-professional teams. Leadersh Q 2018;29:389-402. https://doi.org/10.1016/j.leaqua.2017.09.002.
- Welton WE, Kantner TA, Katz SM. Developing tomorrow’s integrated community health systems: a leadership challenge for public health and primary care. Milbank Q 1997;75:261-88. https://doi.org/10.1111/1468-0009.00054.
- Wikstrøm E, Dellve L. Contemporary leadership in healthcare organizations: fragmented or concurrent leadership. J Health Organ Manag 2009;23:411-28. https://doi.org/10.1108/14777260910979308.
- Willgerodt MA, Abu-Rish Blakeney E, Summerside N, Vogel MT, Liner DA, Zierler B. Impact of leadership development workshops in facilitating team-based practice transformation. J Interprof Care 2020;34:76-8. https://doi.org/10.1080/13561820.2019.1604496.
- Wright K, Rowitz L, Merkle A, Reid WM, Robinson G, Herzog B, et al. Competency development in public health leadership. Am J Public Health 2000;90:1202-7. https://doi.org/10.2105/AJPH.90.8.1202.
- Wu W-L, Lee Y-C. Empowering group leaders encourages knowledge sharing: integrating the social exchange theory and positive organizational behavior perspective. J Knowl Manag 2017;21:474-91. https://doi.org/10.1108/JKM-08-2016-0318.
- Yancey AK. The meta-volition model: organizational leadership is the key ingredient in getting society moving, literally!. Prev Med 2009;49:342-51. https://doi.org/10.1016/j.ypmed.2009.09.004.
- Zablocki E. Effect of system restructuring on quality leadership. Qual Lett Healthc Lead 1996;8:2-9.
- Zaccaro SJ, Green JP, Dubrow S, Kolze M. Leader individual differences, situational parameters, and leadership outcomes: a comprehensive review and integration. Leadersh Q 2018;29:2-43. https://doi.org/10.1016/j.leaqua.2017.10.003.
- Zaher CA. Physician leadership. Learning to be a leader. Physician Exec 1996;22:10-7.
- Zismer DK. The psychology of organizational structure in integrated health systems. Physician Exec 2011;37:36-43.
- Zismer DK, Werner MJ. Managing the physics of the economics of integrated health care. Physician Exec 2012;38:38-45.
- Aboumatar HJ, Weaver SJ, Rees D, Rosen MA, Sawyer MD, Pronovost PJ. Towards high-reliability organising in healthcare: a strategy for building organisational capacity. BMJ Qual Saf 2017;26:663-70. https://doi.org/10.1136/bmjqs-2016-006240.
- Addicott R. Challenges of commissioning and contracting for integrated care in the National Health Service (NHS) in England. Aust J Prim Health 2016;22:50-4. https://doi.org/10.1071/PY15067.
- Agius SJ, Brockbank A, Baron R, Farook S, Hayden J. The impact of an integrated medical leadership programme. J Health Organ Manag 2015;29:39-54. https://doi.org/10.1108/JHOM-09-2013-0188.
- Allen D. Lost in translation? ‘Evidence’ and the articulation of institutional logics in integrated care pathways: from positive to negative boundary object?. Sociol Health Iln 2013;36:807-22. https://doi.org/10.1111/1467-9566.12111.
- Lewis B, Allen S. Leading change: evidence-based transition. Clin Nurse Spec 2015;29:E1-7. https://doi.org/10.1097/NUR.0000000000000102.
- Alrabie N. Integrating professionals in French multi-professional health homes: fostering collaboration beyond the walls. Health Serv Manage Res 2020;33:86-95. https://doi.org/10.1177/0951484819858828.
- Altaras R, Montague M, Graham K, Strachan CE, Senyonjo L, King R, et al. Integrated community case management in a peri-urban setting: a qualitative evaluation in Wakiso District, Uganda. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2723-0.
- Alvesson M. Leadership as social integrative action: a study of a computer consultancy company. Organ Stud 1992;13:185-209. https://doi.org/10.1177/017084069201300202.
- Amarasingham R, Xie B, Karam A, Nguyen N, Kapoor B. Using community partnerships to integrate health and social services for high-need, high-cost patients. Issue Brief 2018;2018:1-11.
- Anderko L, Bartz C, Lundeen S. Practice-based research networks: nursing centers and communities working collaboratively to reduce health disparities. Nurs Clin North Am 2005;40. https://doi.org/10.1016/j.cnur.2005.08.009.
- Anonymous . Facilitating an integrated approach to primary health care in Saskatchewan. Concern 1998;27:26-9.
- Arain M, Suter E, Hepp S, Nanayakkara S, Harrison EL, Mickelson G, et al. Interprofessional competency toolkit for internationally educated health professionals: evaluation and pilot testing. J Contin Educ Health Prof 2017;37:173-82. https://doi.org/10.1097/CEH.0000000000000160.
- Arasteh AR. Toward Final Personality Integration: A Measure for Health, Social Change, and Leadership. Hoboken, NJ: John Wiley & Sons; 1975.
- Armistead C, Pettigrew P, Aves S. Exploring leadership in multi-sectoral partnerships. Leadership 2007;3:211-30. https://doi.org/10.1177/1742715007076214.
- Arsenault PM. The forgotten leaders: integrating charismatic leadership into leadership development programs. J Leadersh Stud 1997;4:140-9. https://doi.org/10.1177/107179199700400112.
- Jeffers BR, Astroth KS. The clinical nurse leader: prepared for an era of healthcare reform. Nurs Forum 2013;48:223-9. https://doi.org/10.1111/nuf.12032.
- Avolio BJ. Promoting more integrative strategies for leadership theory-building. Am Psychol 2007;62:25-33. https://doi.org/10.1037/0003-066X.62.1.25.
- Bachrach DJ. Developing physician leaders in academic medical centers. Part 1: their changing role. Med Group Manage J 1996;43.
- Bachrach DJ. Developing physician leaders in academic medical centers. Med Group Manage J 1997;44.
- Bail K, Arbon P, Eggert M, Gardner A, Hogan S, Phillips C, et al. Potential scope and impact of a transboundary model of nurse practitioners in aged care. Aust J Prim Health 2009;15:232-7. https://doi.org/10.1071/PY09009.
- Bakari H, Hunjra AI, Niazi GSK. How does authentic leadership influence planned organizational change? The role of employees’ perceptions: integration of theory of planned behavior and Lewin’s three step model. J Change Manag 2017;17:155-87. https://doi.org/10.1080/14697017.2017.1299370.
- Baker G, Denis J-L. Medical leadership in health care systems: from professional authority to organizational leadership. Public Money Manag 2011;31:355-62. https://doi.org/10.1080/09540962.2011.598349.
- Bakhai SY. Implementation of integrated transition of care management in an academic, hospital based safety-net primary care clinic. J Gen Intern Med 2018;33.
- Balasubramanian BA, Cohen DJ, Jetelina KK, Dickinson LM, Davis M, Gunn R, et al. Outcomes of integrated behavioral health with primary care. J Am Board Fam Med 2017;30:130-9. https://doi.org/10.3122/jabfm.2017.02.160234.
- Balio CP, Yeager VA, Beitsch LM. Perceptions of public health 3.0: concordance between public health agency leaders and employees. J Public Health Manag Pract 2019;25:S103-S12. https://doi.org/10.1097/PHH.0000000000000903.
- Bankston White C, Birmingham J. Case management directors: how to manage in a transition-focused world: part 2. Prof Case Manag 2015;20:115-27. https://doi.org/10.1097/NCM.0000000000000090.
- Bankston White C, Birmingham J. Case management directors: how to manage in a transition-focused world: part 1. Prof Case Manag 2015;20:63-78. https://doi.org/10.1097/NCM.0000000000000078.
- Yank GR, Barber JW, Spradlin WW. Mental health treatment teams and leadership: a systems model. Behav Sci 1994;39:293-310. https://doi.org/10.1002/bs.3830390405.
- Barber JB, Koch KE, Parente D, Mark J, Davis KM. Evolution of an integrated health system: a life cycle framework. J Healthc Manag 1998;43:359-77. https://doi.org/10.1097/00115514-199807000-00011.
- Bartlett M, Dowell J, Graham F, Knight K, Law S, Lockwood P, et al. Dundee’s Longitudinal Integrated Clerkship: drivers, implementation and early evaluation. Educ Prim Care 2019;30:72-9. https://doi.org/10.1080/14739879.2018.1564889.
- Battistella RM, Weil TP. The new management competencies: a global perspective. Physician Exec 1996;22:18-23.
- Bauer A, Evans-Lacko S, Knapp M. Valuing recovery-oriented practice at the interface between mental health services and communities: the role of organisational characteristics and environments. Int J Soc Psychiatry 2019;65:136-43. https://doi.org/10.1177/0020764019831319.
- Beam MA, Muller B, Lee J, Gorman P. Exploring the structural causes of health disparities: novel, student-led structural competency and leadership curriculum at Oregon Health & Sciences University. J Gen Intern Med 2016;31.
- Beckett P, Field J, Molloy L, Yu N, Holmes D, Pile E. Practice what you preach: developing person-centred culture in inpatient mental health settings through strengths-based, transformational leadership. Issues Ment Health Nurs 2013;34:595-601. https://doi.org/10.3109/01612840.2013.790524.
- Bedard RE, Stark R, Gaufberg E. Public narrative as a tool to promote team-based care. J Gen Intern Med 2013;28.
- Begun JW, Tornabeni J, White KR. Opportunities for improving patient care through lateral integration: the clinical nurse leader. J Healthc Manag 2006;51:19-25. https://doi.org/10.1097/00115514-200601000-00005.
- Behrendt P, Matz S, Goritz AS. An integrative model of leadership behavior. Leadersh Q 2017;28:229-44. https://doi.org/10.1016/j.leaqua.2016.08.002.
- Belcher HM, Stone JD, McFadden JA, Hemmingson TA, Kreutzer C, Harris LG, et al. Evaluating maternal and child health and leadership competencies of emerging MCH Leaders: the MCHC/RISE-UP experience. Matern Child Health J 2015;19:2560-7. https://doi.org/10.1007/s10995-015-1796-9.
- Bellack JP, Morjikian R, Barger S, Strachota E, Fitzmaurice J, Lee A, et al. Developing BSN leaders for the future: the Fuld Leadership Initiative for Nursing Education (LINE). J Prof Nurs 2001;17:23-32. https://doi.org/10.1053/jpnu.2001.20247.
- Belling R, Whittock M, McLaren S, Burns T, Catty J, Jones IR, et al. Achieving continuity of care: facilitators and barriers in community mental health teams. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-23.
- Bellonci C. Physician leadership in residential treatment for children and adolescents. Child Adolesc Psychiatr Clin N Am 2010;19:21-30. https://doi.org/10.1016/j.chc.2009.08.001.
- Bender M, Connelly CD, Glaser D, Brown C. Clinical nurse leader impact on microsystem care quality. Nurs Res 2012;61:326-32. https://doi.org/10.1097/NNR.0b013e318265a5b6.
- Bender M, Connelly CD, Brown C. Interdisciplinary collaboration: the role of the clinical nurse leader. J Nurs Manag 2013;21:165-74. https://doi.org/10.1111/j.1365-2834.2012.01385.x.
- Bender M. Clinical nurse leader integration into practice: developing theory to guide best practice. J Prof Nurs 2016;32:32-40. https://doi.org/10.1016/j.profnurs.2015.06.007.
- Bender M, Williams M, Su W, Hites L. Clinical nurse leader integrated care delivery to improve care quality: factors influencing perceived success. J Nurs Scholarsh 2016;48:414-22. https://doi.org/10.1111/jnu.12217.
- Bender M, Williams M, Su W, Hites L. Refining and validating a conceptual model of Clinical Nurse Leader integrated care delivery. J Adv Nurs 2017;73:448-64. https://doi.org/10.1111/jan.13113.
- Bender M, Avolio A, Baker P, Harris JL, Hilton N, Hites L, et al. Developing the clinical nurse leader survey instrument: a modified Delphi study. J Nurs Care Qual 2018;33:300-8. https://doi.org/10.1097/NCQ.0000000000000310.
- Bender M, Spiva L, Su W, Hites L. Organising nursing practice into care models that catalyse quality: a clinical nurse leader case study. J Nurs Manag 2018;26:653-62. https://doi.org/10.1111/jonm.12596.
- Bender M, Baker P, Harris JL, Hites L, LaPointe RJ, Murphy EA, et al. Advancing the clinical nurse leader model through academic-practice-policy partnership. Nurs Outlook 2019;67:345-53. https://doi.org/10.1016/j.outlook.2019.02.007.
- Bergmann S, Bliss J. Foundations of cross-boundary cooperation: resource management at the public-private interface. Soc Nat Resour 2004;17:377-93. https://doi.org/10.1080/08941920490430142.
- Bernheim RG, Melnick A. Principled leadership in public health: integrating ethics into practice and management. J Public Health Manag Pract 2008;14:358-66. https://doi.org/10.1097/01.PHH.0000324564.64910.f5.
- Bezold C, Mayer E, Dighe A. Visionary leadership and the future of VA health system. Hosp Health Serv Adm 1997;42:367-82.
- Bianchi M, Bagnasco A, Bressan V, Barisone M, Timmins F, Rossi S, et al. A review of the role of nurse leadership in promoting and sustaining evidence-based practice. J Nurs Manag 2018;26:918-32. https://doi.org/10.1111/jonm.12638.
- Bienefeld N, Grote G. Speaking up in ad hoc multiteam systems: individual-level effects of psychological safety, status, and leadership within and across teams. Eur J Work Organ Psychol 2014;23:930-45. https://doi.org/10.1080/1359432X.2013.808398.
- Billings J, Davis A. Developing a joint outcomes contracting model for integrated health and social care for older people. J Integr Care 2016;24:282-99. https://doi.org/10.1108/JICA-09-2016-0031.
- Blair JD, Payne GT. The paradox prescription: leading the medical group of the future. Health Care Manage Rev 2000;25:44-58. https://doi.org/10.1097/00004010-200001000-00006.
- Bligh MC. From Culture Clash to Integration: The Role of Leadership in Transforming Post-Merger Employee Identification 2002;63.
- Bono JE, Shen W, Snyder M. Fostering integrative community leadership. Leadersh Q 2010;21:324-35. https://doi.org/10.1016/j.leaqua.2010.01.010.
- Bowles JR, Batcheller J, Adams JM, Zimmermann D, Pappas S. Nursing’s leadership role in advancing professional practice/work environments as part of the quadruple aim. Nurs Adm Q 2019;43:157-63. https://doi.org/10.1097/NAQ.0000000000000342.
- Bradley EH, Taylor LA, Cuellar CJ. Management matters: a leverage point for health systems strengthening in global health. Int J Health Policy Manag 2015;4:411-15. https://doi.org/10.15171/ijhpm.2015.101.
- Brannan S. Medical Ethics Today: The BMA’s Handbook of Ethics and Law. London: BMA; 2012.
- Brazier J. Accounting for cross boundary flows. Br Med J 1987;295:898-900. https://doi.org/10.1136/bmj.295.6603.898.
- Breck WD. An Investigation of Leader Behavior: Integrating Theory and Practice 1983;43.
- Bresnen M, Hodgson D, Bailey S, Hyde P, Hassard J. Being a manager, becoming a professional? A case study and interview-based exploration of the use of management knowledge across communities of practice in health-care organisations. Health Ser Deliv Res 2014;2. https://doi.org/10.3310/hsdr02140.
- Brewer M. Exploring the potential of a capability framework as a vision and ‘sensemaking’ tool for leaders of interprofessional education. J Interprof Care 2016;30:574-81. https://doi.org/10.1080/13561820.2016.1182969.
- Brigham L, Maxwell C, Smith A. Leading in practice: a case study of how health visitors share and develop good practice. Community Pract 2012;85:24-8.
- Brodbeck FC, Chhokar JS, House RJ. Culture and Leadership across the World: The GLOBE Book of In-depth Studies of 25 Societies. London: Psychology Press; 2008.
- Brooks BA, Davis S, Kulbok P, Frank-Lightfoot L, Sgarlata L, Poree S. Aligning provider team members with polyvalent community health workers. Nurs Adm Q 2015;39:211-17. https://doi.org/10.1097/NAQ.0000000000000110.
- Brooks AJ, McClafferty H, Lebensohn P, Ricker M. Tools to encourage resiliency in health-care providers and educators. Glob Adv Health Med 2018;7:14-5.
- Brower HH, Schoorman FD, Tan HH. A model of relational leadership: the integration of trust and leader-member exchange. Leadersh Q 2000;11:227-50. https://doi.org/10.1016/S1048-9843(00)00040-0.
- Buchner DL, Brenner JL, Kabakyenga J, Teddy K, Maling S, Barigye C, et al. Stakeholders’ perceptions of integrated community case management by community health workers: a post-intervention qualitative study. PLOS One 2014;9. https://doi.org/10.1371/journal.pone.0098610.
- Burke CS, Sims DE, Lazzara EH, Salas E. Trust in leadership: a multi-level review and integration. Leadersh Q 2007;18:606-32. https://doi.org/10.1016/j.leaqua.2007.09.006.
- Burpitt WJ. Pro-Active Learning Among Project Teams: The Influence of Leader Behavior, Functional Diversity, and Cross Boundary Communication 1996;56.
- Burt I, Patel SH, Butler SK, Gonzalez T. Integrating leadership skills into anger management groups to reduce aggressive behaviors: the LIT model. J Ment Health Couns 2013;35:124-41. https://doi.org/10.17744/mehc.35.2.p442173655261737.
- Burton CR, Rycroft-Malone J, Williams L, Davies S, McBride A, Hall B, et al. NHS managers’ use of nursing workforce planning and deployment technologies: a realist synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06360.
- Busetto L, Luijkx K, Calciolari S, Ortiz LGG, Vrijhoef HJM. Barriers and facilitators to workforce changes in integrated care. Int J Integr Care 2018;18. https://doi.org/10.5334/ijic.3587.
- Butterfield DA. An Integrative Approach to the Study of Leadership Effectiveness in Organizations 1969;29.
- Cacioppe R. An integrated model and approach for the design of effective leadership development programs. Leadersh Organ Dev J 1998;19:44-53. https://doi.org/10.1108/01437739810368820.
- Caldwell BS. Multi-team dynamics and distributed expertise in imission operations. Aviat Space Environ Med 2005;76:B145-53.
- Caldwell C, Voelker C, Dixon RD, LeJeune A. Transformative leadership: an ethical stewardship model for healthcare. Organ Ethic 2008;4:126-34.
- Callahan CD, Adair D, Bozic KJ, Manning BT, Saleh JK, Saleh KJ. Orthopaedic surgery under national health reform: an analysis of power, process, adaptation, and leadership: AOA critical issues. J Bone Joint Surg Am 2014;96. https://doi.org/10.2106/JBJS.M.01067.
- Carlin M, Peterman E. Infrastructure for cross-sector collaboration: the state health leader perspective. J Public Health Manag Pract 2019;25:405-7. https://doi.org/10.1097/PHH.0000000000001038.
- Carlton EL. Answering the call for integrating population health: insights from health system executives. Adv Health Care Manag 2014;16:115-38. https://doi.org/10.1108/s1474-823120140000016009.
- Caron RM, Hiller MD, Wyman WJ. Public health system partnerships: role for local boards of health in preparing the future public health workforce. J Community Health 2014;39:29-34. https://doi.org/10.1007/s10900-013-9737-2.
- Carter N, Martin-Misener R, Kilpatrick K, Kaasalainen S, Donald F, Bryant-Lukosius D, et al. The role of nursing leadership in integrating clinical nurse specialists and nurse practitioners in healthcare delivery in Canada. Nurs Leadersh 2010;23:167-85. https://doi.org/10.12927/cjnl.2010.22274.
- Chartered MI. A Management and Leadership Health-check: A Diagnosis of Management and Leadership Development Needs in the Health and Social Care Sector. London: Chartered Management Institute; 2013.
- Chicorelli J, Dennie A, Heinrich C, Hinchey B, Honarparvar F, Jennings M, et al. Canadian student leaders’ perspective on interprofessional education: a consensus statement. J Interprof Care 2016;30:545-7. https://doi.org/10.3109/13561820.2016.1159187.
- Chiocchio F, Rabbat F, Lebel P. Multi-level efficacy evidence of a combined interprofessional collaboration and project management training program for healthcare project teams. Proj Manag J 2015;46:20-34. https://doi.org/10.1002/pmj.21507.
- Christensen T, Stoller JK. Physician leadership development at Cleveland Clinic: a brief review. Australas Psychiatry 2016;24:235-9. https://doi.org/10.1177/1039856216635907.
- Chu KWK, Cheung LLW. Incorporating sustainability in small health-care facilities: an integrated model. Leadersh Health Serv 2018;31:441-51. https://doi.org/10.1108/LHS-07-2017-0043.
- Chubak J, Tuzzio L, Hsu C, Alfano C, Rabin B, Hornbrook M, et al. Providing care to cancer survivors in integrated health care delivery systems: barriers, facilitators and opportunities. Psychooncology 2013;22:2-3. https://doi.org/10.1200/JOP.2011.000312.
- Chartered Institute of Personnel and Development (CIPD) . Purposeful Leadership: What Is It, What Causes It and Does It Matter? 2017.
- Clark JS. The system chief nurse executive role: sign of the changing times?. Nurs Adm Q 2012;36:299-305. https://doi.org/10.1097/NAQ.0b013e3182669440.
- Clarke AN, Cilenti D. Developing collaborative maternal and child health leaders: a descriptive study of the National Maternal and Child Health Workforce Development Center. Matern Child Health J 2018;22:17-23. https://doi.org/10.1007/s10995-017-2399-4.
- Clarke PN, Berkland D. Paradoxes in healthcare leadership: being-nonbeing. Nurs Sci Q 2019;32:116-19. https://doi.org/10.1177/0894318419826239.
- Clausen C, Cummins K, Dionne K. Educational interventions to enhance competencies for interprofessional collaboration among nurse and physician managers: an integrative review. J Interprof Care 2017;31:685-95. https://doi.org/10.1080/13561820.2017.1347153.
- Clyne B, Rapoza B, George P. Leadership in undergraduate medical education: training future physician leaders. R I Med J 2015;98:36-40.
- Coates D. Integrated leadership development programmes: are they effective and what role does coaching play?. Int J Evid Based Coach Mentor 2013;SpecIssue 7:39-55.
- Cochran J, Kaplan GS, Nesse RE. Physician leadership in changing times. Healthc 2014;2:19-21. https://doi.org/10.1016/j.hjdsi.2014.01.001.
- Cockerham J, Figueroa-Altmann A, Eyster B, Ross C, Salamy J. Supporting newly hired nurses: a program to increase knowledge and confidence while fostering relationships among the team. Nurs Forum 2011;46:231-9. https://doi.org/10.1111/j.1744-6198.2011.00236.x.
- Cohen A, Fairclough L, Jass J. Optimizing community and stakeholder engagement in a merger of community health centres. Healthc Manage Forum 2011;24:192-5. https://doi.org/10.1016/j.hcmf.2011.08.002.
- Cohn J. Leading healthcare in complexity. Nurs Leadersh (Tor Ont) 2014;27:52-64. https://doi.org/10.12927/cjnl.2015.24139.
- Cole MS, Bedeian AG, Bruch H. Linking leader behavior and leadership consensus to team performance: integrating direct consensus and dispersion models of group composition. Leadersh Q 2011;22:383-98. https://doi.org/10.1016/j.leaqua.2011.02.012.
- Coleman AY. Managing managed care. The task calls for an integrated management team. Health Prog 1997;78:34-6.
- Coleman C. Integrating quality and breast cancer care: role of the clinical nurse leader. Oncol Nurs Forum 2013;40:311-14. https://doi.org/10.1188/13.ONF.311-314.
- Collins DA, Thompson K, Atwood KA, Abadi MH, Rychener DL, Simmons LA. Integration of health coaching concepts and skills into clinical practice among VHA providers: a qualitative study. Glob Adv Health Med 2018;7:1-8. https://doi.org/10.1177/2164957X18757463.
- Collins IM, Cross H, Woollett A, Underhill CR. Establishing leadership in regional oncology within the Victorian Comprehensive Cancer Centre. Asia Pac J Clin Oncol 2018;14:127-8.
- Coutinho AJ, Bhuyan N, Gits A, Alavi M, Ho T, Shiraki J, et al. Student and resident involvement in Family Medicine for America’s Health: a step toward leadership development. Fam Med 2019;51:166-72. https://doi.org/10.22454/FamMed.2019.857539.
- Cowan LD. e-Leadership: leading in a virtual environment – guiding principles for nurse leaders. Nurs Econ 2014;32:312-19.
- Coxon K. Common experiences of staff working in integrated health and social care organisations: a European perspective. J Integr Care 2005;13:13-21. https://doi.org/10.1108/14769018200500012.
- Craddock D, O’Halloran C, McPherson K, Hean S, Hammick M. A top-down approach impedes the use of theory? Interprofessional educational leaders’ approaches to curriculum development and the use of learning theory. J Interprof Care 2013;27:65-72. https://doi.org/10.3109/13561820.2012.736888.
- Crawford CL, Chu F, Judson LH, Cuenca E, Jadalla AA, Tze-Polo L, et al. An integrative review of nurse-to-nurse incivility, hostility, and workplace violence: a GPS for nurse leaders. Nurs Adm Q 2019;43:138-56. https://doi.org/10.1097/NAQ.0000000000000338.
- Crosby LE, Parr W, Smith T, Mitchell MJ. The community leaders institute: an innovative program to train community leaders in health research. Acad Med 2013;88:335-42. https://doi.org/10.1097/ACM.0b013e318280d8de.
- Crosby BC, Bryson JM, Day DV. The Oxford Handbook of Leadership and Organizations. Oxford: Oxford University Press; 2014.
- Curtis EA, Sheerin FK, Vries Jd. Developing leadership in nursing: the impact of education and training. Br J Nurs 2011;20:344-52. https://doi.org/10.12968/bjon.2011.20.6.344.
- Dale H, Lee A. Behavioural health consultants in integrated primary care teams: a model for future care. BMC Fam Pract 2016;17. https://doi.org/10.1186/s12875-016-0485-0.
- Davis MM, Balasubramanian BA, Cifuentes M, Hall J, Gunn R, Fernald D, et al. Clinician staffing, scheduling, and engagement strategies among primary care practices delivering integrated care. J Am Board Fam Med 2015;28:32-40. https://doi.org/10.3122/jabfm.2015.S1.150087.
- Day DV, Sin H-P. Longitudinal tests of an integrative model of leader development: charting and understanding developmental trajectories. Leadersh Q 2011;22:545-60. https://doi.org/10.1016/j.leaqua.2011.04.011.
- Day K, Norris T. Leadership in times of crisis during change due to health IT projects. Healthc Rev Online 2006;10.
- de Leeuw E. Engagement of sectors other than health in integrated health governance, policy, and action. Annu Rev Public Health 2017;38:329-49. https://doi.org/10.1146/annurev-publhealth-031816-044309.
- de Zulueta PC. Developing compassionate leadership in health care: an integrative review. J Healthc Leadersh 2016;8:1-10. https://doi.org/10.2147/JHL.S93724.
- Denis JL, van Gestel N. Medical doctors in healthcare leadership: theoretical and practical challenges. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1392-8.
- Derue DS, Nahrgang JD, Wellman N, Humphrey SE. Trait and behavioral theories of leadership: an integration and meta-analytic test of their relative validity. Pers 2011;64:7-52. https://doi.org/10.1111/j.1744-6570.2010.01201.x.
- Di Fabio A, Bucci O, Gori A. High Entrepreneurship, Leadership, and Professionalism (HELP): toward an integrated, empirically based perspective. Front Psychol 2016;7. https://doi.org/10.3389/fpsyg.2016.01842.
- Doherty C, Hope W. Shared governance – nurses making a difference. J Nurs Manag 2000;8:77-81. https://doi.org/10.1046/j.1365-2834.2000.00162.x.
- Drenkard KN. The clinical nurse leader: a response from practice. J Prof Nurs 2004;20:89-96. https://doi.org/10.1016/j.profnurs.2004.02.001.
- Dulsrud L, Assadi A, Fazari L, Trinder V, Dryden-Palmer K. Integration of nurse practitioner team into cardiac critical care: a program in review. Pediatr Crit Care Med 2018;19. https://doi.org/10.1097/01.pcc.0000537792.11380.9e.
- Durbin S, Haglund C, Dowling W. Integrating strategic planning and quality management in a multi-institutional system. Qual Manag Health Care 1993;1:24-3. https://doi.org/10.1097/00019514-199322000-00004.
- Edmonstone JD. Escaping the healthcare leadership cul-de-sac. Leadersh Health Serv 2017;30:76-91. https://doi.org/10.1108/LHS-02-2016-0012.
- Edwards N, Kaseje D, Kahwa E, Klopper HC, Mill J, Webber J, et al. The impact of leadership hubs on the uptake of evidence-informed nursing practices and workplace policies for HIV care: a quasi-experimental study in Jamaica, Kenya, Uganda and South Africa. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0478-3.
- Edwards LD, Till A, McKimm J. Leading the integration of physician associates into the UK health workforce. Br J Hosp Med 2019;80:18-21. https://doi.org/10.12968/hmed.2019.80.1.18.
- Eisenbeiss SA, van Knippenberg D, Boerner S. Transformational leadership and team innovation: integrating team climate principles. J Appl Psychol 2008;93:1438-46. https://doi.org/10.1037/a0012716.
- Ekmekci O, Plack M, Pintz C, Bocchino J, LeLacheur S, Halvaksz J. Integrating executive coaching and simulation to promote interprofessional education of health care students. J Allied Health 2013;42:17-24.
- Elaine H, DeBasio N, Warmbrodt L, Gartland M, Bassett W, Tansey M. Collaborative graduate education: executive nurse practice and health care leadership. Nurs Leadersh Forum 2004;8:123-7.
- Elliott R. Utilising evidence-based leadership theories in coaching for leadership development: towards a comprehensive integrating conceptual framework. Int Coach Psychol Rev 2011;6:46-70.
- Emslie S, Oliver C, Bruce J. Getting governance right at board level: The Policy Governance® approach to building better National Health Service boards. Clinician 2006;14:69-77.
- Ezell AS, Morse JM. Cross-boundary power related to interagency relationships between community agencies. J Health Hum Resour Adm 1982;5:201-8.
- Fagin CM. Improving nursing practice, education, and research. J Nurs Adm 1996;26:30-7. https://doi.org/10.1097/00005110-199603000-00013.
- Farnsworth TJ, Peterson T, Neill K, Neill M, Seikel JA, Lawson J. Understanding the structural, human resource, political, and symbolic dimensions of implementing and sustaining interprofessional education. J Allied Health 2015;44:152-7.
- Ferris GR, Rowland KM. Leadership, job perceptions, and influence: a conceptual integration. Hum Relat 1981;34:1069-77. https://doi.org/10.1177/001872678103401204.
- Fischer J, Wildman JL, Wildman JL, Griffith RL, Armon BK. Critical Issues in Cross Cultural Management. Cham: Springer Nature; 2016.
- Fisher J. A model of integrated leadership. Organ Dyn 2018;47:70-7.
- Fitzgerald C, Kirby LK. Developing Leaders: Research and Applications in Psychological Type and Leadership Development: Integrating Reality and Vision, Mind and Heart. Palo Alto, CA: Davies-Black Publishing; 1997.
- Fleştea AM, Fodor OC, Curşeu PL, Miclea M. ‘We didn’t know anything, it was a mess!’ Emergent structures and the effectiveness of a rescue operation multi-team system. Ergonomics 2017;60:44-58. https://doi.org/10.1080/00140139.2016.1162852.
- Foels R, Driskell JE, Mullen B, Salas E. The effects of democratic leadership on group member satisfaction: an integration. Small Group Res 2000;31:676-701. https://doi.org/10.1177/104649640003100603.
- Foglia MB, Cohen JH. Ethical leadership and employees’ perceptions about raising ethical concerns to managers in the Veterans Health Administration. AJOB Empir Bioeth 2019;10:155-63. https://doi.org/10.1080/23294515.2019.1634654.
- Foley R, Wurmser TA. Culture diversity/a mobile workforce command creative leadership, new partnerships, and innovative approaches to integration. Nurs Adm Q 2004;28:122-8. https://doi.org/10.1097/00006216-200404000-00008.
- Foli KJ, Braswell M, Kirkpatrick J, Lim E. Development of leadership behaviors in undergraduate nursing students: a service-learning approach. Nurs Educ Perspect 2014;35:76-82. https://doi.org/10.5480/11-578.1.
- Forsyth C, Mason B. Shared leadership and group identification in healthcare: the leadership beliefs of clinicians working in interprofessional teams. J Interprof Care 2017;31:291-9. https://doi.org/10.1080/13561820.2017.1280005.
- Foster S, Lowman RL. The California School of Organizational Studies Handbook of Organizational Consulting Psychology: A Comprehensive Guide to Theory, Skills, and Techniques. Hoboken, NJ: Wiley; 2002.
- Foster C, Roche F. Integrating trait and ability EI in predicting transformational leadership. Leadersh Organ Dev J 2014;35:316-34. https://doi.org/10.1108/LODJ-07-2012-0087.
- Frankel AS, Leonard MW, Denham CR. Fair and just culture, team behavior, and leadership engagement: the tools to achieve high reliability. Health Serv Res 2006;41:1690-709. https://doi.org/10.1111/j.1475-6773.2006.00572.x.
- Frankel SA, Bourgeois JA, Xiong G, McCarron R, Han J, Erdberg P. The medical-psychiatric coordinating physician-led model: team-based treatment for complex patients. Psychosomatics 2014;55:333-42. https://doi.org/10.1016/j.psym.2013.12.014.
- Fuller S. The role of nurse leaders in improving health. Nurs Times 2015;111:12-4.
- Fuqua DR, Newman JL. Integrating structural and behavioral leadership strategies. Consult Psychol J 2005;57:126-32. https://doi.org/10.1037/1065-9293.57.2.126.
- Garber JS, Madigan EA, Click ER, Fitzpatrick JJ. Attitudes towards collaboration and servant leadership among nurses, physicians and residents. J Interprof Care 2009;23:331-40. https://doi.org/10.1080/13561820902886253.
- Gardner WL, Cogliser CC. Special issue on meso-modeling of leadership: integrating micro- and macro-perspectives of leadership. Leadersh Q 2009;20:501-2. https://doi.org/10.1016/j.leaqua.2009.04.002.
- Gebru AA, Mosadeghrad AM, Sari AA. Perceptions of leadership, motivation, structure, and assurance for implementation of emergency medical services in Ethiopia: perspectives of emergency medical services case teams based on focus group discussions. Hum Antibodies 2019;27:53-71. https://doi.org/10.3233/HAB-190383.
- Gentina E, Butori R, Heath TB. Unique but integrated: the role of individuation and assimilation processes in teen opinion leadership. J Bus Res 2014;67:83-91. https://doi.org/10.1016/j.jbusres.2012.11.013.
- Gentry WA, Eckert RH. Integrating implicit leadership theories and fit into the development of global leaders: a 360-degree approach. Ind Organ Psychol 2012;5:224-7. https://doi.org/10.1111/j.1754-9434.2012.01434.x.
- Geraghty A, Paterson-Brown S. Leadership and working in teams. Surgery 2018;36:503-8. https://doi.org/10.1016/j.mpsur.2018.07.013.
- Gibb CE, Morrow M, Clarke CL, Cook G, Gertig P, Ramprogus V. Transdisciplinary working: evaluating the development of health and social care provision in mental health. J Ment Health 2002;11:339-50. https://doi.org/10.1080/09638230020023714.
- Gifford WA, Holyoke P, Squires JE, Angus D, Brosseau L, Egan M, et al. Managerial leadership for research use in nursing and allied health care professions: a narrative synthesis protocol. Syst Rev 2014;3. https://doi.org/10.1186/2046-4053-3-57.
- Ginsberg S, Hochman JD, Foley GM, Hochman JD. Mental Health in Early Intervention: Achieving Unity in Principles and Practice. Baltimore, MD: Paul H Brookes Publishing Co; 2006.
- Glaser JP. Partners HealthCare. Creating and managing an integrated delivery system. MD Comput 2000;17:23-8.
- Gleave R, Wong I, Porteus J. What is ‘more integration’ between health and social care? Results of a survey of primary care trusts and directors of adult social care in England. Int J Integr Care 2010;18:29-44. https://doi.org/10.5042/jic.2010.0558.
- Golden A, Miller K. Principles on integrating behavioral health into medical homes must not designate leaders as ‘physicians only’. Fam Syst Health 2014;32:139-40. https://doi.org/10.1037/fsh0000046.
- Goldsberry JW. Advanced practice nurses leading the way: interprofessional collaboration. Nurse Educ Today 2018;65:1-3. https://doi.org/10.1016/j.nedt.2018.02.024.
- Goldstein AO, Calleson D, Bearman R, Steiner BD, Frasier PY, Slatt L. Teaching Advanced Leadership Skills in Community Service (ALSCS) to medical students. Acad Med 2009;84:754-64. https://doi.org/10.1097/ACM.0b013e3181a40660.
- Gonzalez-Navarro P, Zurriaga-Llorens R, Olateju AT, Llinares-Insa LI. Envy and counterproductive work behavior: the moderation role of leadership in public and private organizations. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15071455.
- Goodridge D, Westhorp G, Rotter T, Dobson R, Bath B. Lean and leadership practices: development of an initial realist program theory. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1030-x.
- Goodwin N, Lawton-Smith S. Integrating care for people with mental illness: the Care Programme Approach in England and its implications for long-term conditions management. Int J Integr Care 2010;10. https://doi.org/10.5334/ijic.516.
- Goodwin N, Perry C, Dixon A, Ham C, Smith J, Davies A, et al. A Report to the Department of Health and the NHS Future Forum: Integrated Care for Patients and Populations: Improving Outcomes by Working Together 2012. www.kingsfund.org.uk/sites/default/files/integrated-care-patients-populations-paper-nuffield-trust-kings-fund-january-2012.pdf (accessed 19 November 2020).
- Gopinathan U, Watts N, Hougendobler D, Lefebvre A, Cheung A, Hoffman SJ, et al. Conceptual and institutional gaps: understanding how the WHO can become a more effective cross-sectoral collaborator. Global Health 2015;11. https://doi.org/10.1186/s12992-015-0128-6.
- Gotsis G, Grimani K. Diversity as an aspect of effective leadership: integrating and moving forward. Leadersh Organ Dev J 2016;37:241-64. https://doi.org/10.1108/LODJ-06-2014-0107.
- Graham IW, Jack E. Promoting leadership: the development of a nurse executive team in an acute hospital trust. J Nurs Manag 2008;16:955-63. https://doi.org/10.1111/j.1365-2834.2008.00915.x.
- Grant CG, Ramos R, Davis JL, Lee Green B. Community health needs assessment: a pathway to the future and a vision for leaders. Health Care Manag 2015;34:147-56. https://doi.org/10.1097/HCM.0000000000000057.
- Green PL. Improving clinical effectiveness in an integrated care delivery system. J Healthc Qual 1998;20:4-8. https://doi.org/10.1111/j.1945-1474.1998.tb00289.x.
- Green MJ. Adaptation versus authenticity: achieving leader effectiveness in intercultural encounters with followers – towards an integrated model. Int J Cross Cult Manag 2017;17:257-71. https://doi.org/10.1177/1470595817706986.
- Greenfield D. The enactment of dynamic leadership. Leadersh Health Serv 2007;20:159-68. https://doi.org/10.1108/17511870710764014.
- Griffith L, Glasby J. “When we say ‘urgent’ it means now . . .”: health and social care leaders’ perceptions of each other’s roles and ways of working. J Integr Care 2015;23:143-52. https://doi.org/10.1108/JICA-02-2015-0013.
- Groves KS. Linking leader skills, follower attitudes, and contextual variables via an integrated model of charismatic leadership. J Manag 2005;31:255-77. https://doi.org/10.1177/0149206304271765.
- Guerrera M, Benn R, King K, Maciasz R, Roca H. Examining the impact of a week-long national training program to enhance well-being in medical students: leadership and education in integrative medicine program (LEAPS). J Altern Complement Med 2014;20:A104-A5. https://doi.org/10.1089/acm.2014.5276.abstract.
- Guo KL. Leadership processes for re-engineering changes to the health care industry. J Health Organ Manag 2004;18:435-46. https://doi.org/10.1108/14777260410569993.
- Gutermann D, Lehmann-Willenbrock N, Boer D, Born M, Voelpel SC. How leaders affect followers’ work engagement and performance: integrating leader-member exchange and crossover theory. Br J Manag 2017;28:299-314. https://doi.org/10.1111/1467-8551.12214.
- Haase-Herrick KS, Herrin DM. The American Organization of Nurse Executives’ guiding principles and American Association of Colleges of Nursing’s clinical nurse leader: a lesson in synergy. J Nurs Adm 2007;37:55-60. https://doi.org/10.1097/00005110-200702000-00004.
- Hall KL, Feng AX, Moser RP, Stokols D, Taylor BK. Moving the science of team science forward: collaboration and creativity. Am J Prev Med 2008;35:243-9. https://doi.org/10.1016/j.amepre.2008.05.007.
- Hall P, Weaver L, Handfield-Jones R, Bouvette M. Developing leadership in rural interprofessional palliative care teams. J Interprof Care 2008;22:73-9. https://doi.org/10.1080/13561820802028337.
- Hall LM, Johnson S, Hemingway A, Pringle D, White P, Wodchis WP. ‘The potential is unlimited!’ Nurse leader perspectives on the integration of HOBIC in Ontario. Nurs Leadersh 2012;25:29-42. https://doi.org/10.12927/cjnl.2012.22833.
- Halpin M. Coordinating integrated services: a pilot study with participants of a coordinators course. Complement Ther Clin Pract 2006;12:156-62. https://doi.org/10.1016/j.ctcp.2005.01.001.
- Hamlin RG, Sawyer J, Sage L. Perceived managerial and leadership effectiveness in a non-profit organization: an exploratory and cross-sector comparative study. Hum Resour Dev Int 2011;14:217-34. https://doi.org/10.1080/13678868.2011.558318.
- Hammar M, Gustafsson PA, Svedin CG, Domeij D, Heijl A. Personal and professional development in the training of communication and leadership in undergraduate medical education. Educ Health 1997;10:57-68.
- Harris JL, Tornabeni J, Walters SE. The clinical nurse leader: a valued member of the healthcare team. J Nurs Adm 2006;36:446-9. https://doi.org/10.1097/00005110-200610000-00003.
- Harris A, Jones M. The dark side of leadership and management. School Leadersh Manag 2018;38:475-7. https://doi.org/10.1080/13632434.2018.1509276.
- Hartung NL, Henschel RM, Smith KB, Gesme DH. Creating virtual integration and improved oncology care quality through a co-management services agreement. J Oncol Pract 2016;12:e839-47. https://doi.org/10.1200/JOP.2015.010645.
- Harung H, Travis F, Blank W, Heaton D. Higher development, brain integration, and excellence in leadership. Manag Decis 2009;47:872-94. https://doi.org/10.1108/00251740910966631.
- Hasel MC, Grover SL. An integrative model of trust and leadership. Leadersh Organ Dev J 2017;38:849-67. https://doi.org/10.1108/LODJ-12-2015-0293.
- Hauenstein EJ, Glick DF, Kane C, Kulbok P, Barbero E, Cox K. A model to develop nurse leaders for rural practice. J Prof Nurs 2014;30:463-73. https://doi.org/10.1016/j.profnurs.2014.04.001.
- Hauptman PJ, Bednarek HL. The business concept of leader pricing as applied to heart failure disease management. Dis Manag 2004;7:226-34. https://doi.org/10.1089/dis.2004.7.226.
- Hernandez-Rincon EH, Lamus-Lemus F, Carratalá-Munuera C, Orozco-Beltrán D, Jaramillo-Hoyos CL, Robles-Hernández G. Building community capacity in leadership for primary health care in Colombia. MEDICC Rev 2017;19. https://doi.org/10.37757/MR2017.V19.N2-3.11.
- Hertig JB, Hultgren KE, Weber RJ. Using contemporary leadership skills in medication safety programs. Hosp Pharm 2016;51:338-44. https://doi.org/10.1310/hpj5104-338.
- Higgins A, Begley C, Lalor J, Coyne I, Murphy K, Elliott N. Factors influencing advanced practitioners’ ability to enact leadership: a case study within Irish healthcare. J Nurs Manag 2014;22:894-905. https://doi.org/10.1111/jonm.12057.
- Nutting PA, Gallagher KM, Riley K, White S, Dietrich AJ, Dickinson WP. Implementing a depression improvement intervention in five health care organizations: experience from the RESPECT-Depression trial. Adm Policy Ment Health 2007;34:127-37. https://doi.org/10.1007/s10488-006-0090-y.
- Price-Haywood EG, Dunn-Lombard D, Harden-Barrios J, Lefante JJ. Collaborative depression care in a safety net medical home: facilitators and barriers to quality improvement. Popul Health Manag 2016;19:46-55. https://doi.org/10.1089/pop.2015.0016.
- Townsley R, Watson D, Abbott D. Working partnerships? A critique of the process of multi-agency working in services to disabled children with complex health care needs. J Integr Care 2004;12:24-3. https://doi.org/10.1108/14769018200400013.
- Clarke N. Relational Leadership: Theory, Practice and Development. London: Routledge; 2018.
- Venturato L, Drew L. Beyond ‘doing’: supporting clinical leadership and nursing practice in aged care through innovative models of care. Contemp Nurse 2010;35:157-70. https://doi.org/10.5172/conu.2010.35.2.157.
- MacNaughton K, Chreim S, Bourgeault IL. Role construction and boundaries in interprofessional primary health care teams: a qualitative study. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-486.
- Folkman AK, Tveit B, Sverdrup S. Leadership in interprofessional collaboration in health care. J Multidiscip Healthc 2019;12:97-107. https://doi.org/10.2147/JMDH.S189199.
- Caro DH. The yin and yang of integrated care: systemic imperatives for traumatic brain injuries. Open Public Health J 2014;7:6-11. https://doi.org/10.2174/1874944501407010006.
- Grol SM, Molleman GRM, Kuijpers A, van der Sande R, Fransen GAJ, Assendelft WJJ, et al. The role of the general practitioner in multidisciplinary teams: a qualitative study in elderly care. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0726-5.
- De Brún A, McAuliffe E. Identifying the context, mechanisms and outcomes underlying collective leadership in teams: building a realist programme theory. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05129-1.
- Whitebird RR, Solberg LI, Jaeckels NA, Pietruszewski PB, Hadzic S, Unützer J, et al. Effective implementation of collaborative care for depression: what is needed?. Am J Manag Care 2014;20:699-707.
- Keijser W, Huq J, Reay T. Enacting medical leadership to address wicked problems. BMJ Leader 2020;4:12-7. https://doi.org/10.1136/leader-2019-000137.
- Keijser W, Martin G. Unlocking medical leadership’s potential: a multilevel virtuous circle?. BMJ Leader 2020;4:6-11. https://doi.org/10.1136/leader-2019-000136.
- Grenier C. Structuring an integrated care system: interpreted through the enacted diversity of the actors involved–the case of a French healthcare network. Int J Integr Care 2011;11. https://doi.org/10.5334/ijic.526.
- Graham E, Clift R. Stakeholder value analysis: a methodology for intergrating stakeholder values into corporate environmental investment decisions. Bus Strategy Environ 1999;8:149-62. https://doi.org/10.1002/(SICI)1099-0836(199905/06)8:3<149::AID-BSE199>3.0.CO;2-Q.
- Hardy S, Mushore M, Goddard L. Supporting student mental health nurses in clinical placement through virtual in-practice support (VIPS): innovation uptake and the ‘VIPS’ project. Nurse Educ Today 2016;46:133-8. https://doi.org/10.1016/j.nedt.2016.08.033.
- Zaccaro SJ, Dubrow S, Torres EM, Campbell LNP. Multiteam systems: an integrated review and comparison of different forms. Annu Rev Organ Psychol Organ Behav 2020;7:479-503. https://doi.org/10.1146/annurev-orgpsych-012119-045418.
- Dayan M, Heenan D. Change or Collapse: Lessons from the Drive to Reform Health and Social Care in Northern Ireland. London: Nuffield Trust; 2019.
- Rosen R, Mountford J, Lewis G, Lewis R, Shand J, Shaw S. Integration in Action: Four International Case Studies 2011. www.nuffieldtrust.org.uk/files/2017-01/integration-in-action-research-report-web-final.pdf (accessed 19 November 2020).
- Ashton MC, Lee K, Paunonen SV. What is the central feature of extraversion? Social attention versus reward sensitivity. J Pers Soc Psychol 2002;83:245-52. https://doi.org/10.1037/0022-3514.83.1.245.
- Bruning P, Baghurst T. Improving ethical decision making in health care leadership. Bus Eco J 2013;4. https://doi.org/10.4172/2151-6219.1000e101.
- Mariasse AL. Vision and leadership: paying attention to intention. Peabody J Educ 1985;63:150-73. https://doi.org/10.1080/01619568509538505.
- Baum JR, Locke EA, Kirkpatrick SA. A longitudinal study of the relation of vision and vision communication to venture growth in entrepreneurial firms. J Appl Psychol 1998;83. https://doi.org/10.1037/0021-9010.83.1.43.
- West M, Eckert R, Steward K, Pasmore B. Developing Collective Leadership for Health Care. London: The King’s Fund; 2014.
- Jagosh J, Pluye P, Wong G, Cargo M, Salsberg J, Bush PL, et al. Critical reflections on realist review: insights from customizing the methodology to the needs of participatory research assessment. Res Synth Methods 2014;5:131-41. https://doi.org/10.1002/jrsm.1099.
- Beck U. Risk Society: Towards Another Modernity. London: SAGE Publications Ltd; 1992.
- Giddens A. Modernity and Self-identity: Self and Society in the Late Modern Age. Cambridge: Polity Press; 1991.
- Pawson R. Evidence-based Policy: A Realist Perspective. London: SAGE Publications Ltd; 2006.
- Alvesson M, Jonsson A. The bumpy road to exercising leadership: fragmentations in meaning and practice. Leadership 2018;14:40-57. https://doi.org/10.1177/1742715016644671.
- Schweiger S, Müller B, Güttel W. Barriers to leadership development: why is it so difficult to abandon the hero?. Leadership 2020;16:411-33. https://doi.org/10.1177/1742715020935742.
- Collinson D, Smolovic-Jones O, Grint K. ‘No more heroes’: critical perspectives on leadership romanticism. Organ Stud 2018;39:1625-47. https://doi.org/10.1177/0170840617727784.
- Tourish D. Leadership, more or less? A processual, communication perspective on the role of agency in leadership theory. Leadership 2014;10:79-98. https://doi.org/10.1177/1742715013509030.
- Tourish D. Is complexity leadership theory complex enough? A critical appraisal, some modifications and suggestions for further research. Organ Stud 2019;40:219-38. https://doi.org/10.1177/0170840618789207.
- NHS England . Patient and Public Participation Policy 2017. www.england.nhs.uk/wp-content/uploads/2017/04/ppp-policy.pdf (accessed 19 November 2020).
- West D, Dunhill L. Stevens: 2021 Legislation Must Give Integrated Care Systems ‘a Legal Form’. Health Service Journal; 2020.
- Kline R. The ‘Snowy White Peaks’ of the NHS: A Survey of Discrimination in Governance and Leadership and the Potential Impact on Patient Care in London and England. London: Middlesex University Research Repository; 2014.
- NHS England . People Plan 2020 21 – Action for Us All 2020. https://www.england.nhs.uk/wp-content/uploads/2020/07/We-Are-The-NHS-Action-For-All-Of-Us-FINAL-March-21.pdf (accessed 19 November 2020).
Glossary
- Context–mechanism–outcome
- A configuration that identifies the causal links between context, mechanism and outcome.
- Context
- ‘The “backdrop” of programmes and research . . . broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism’ (Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311–46).
- Mechanism
- ‘. . . mechanisms are underlying entities, processes or structures which operate in particular contexts to generate outcomes of interest’ (Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363–81.). More specifically, ‘. . . mechanisms are a combination of resources offered by the social programme under study and stakeholders’ reasoning in response’ (Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10:49).
- Outcome
- A result of the interaction between a mechanism and its triggering context.
- Programme theory
- A set of theoretical explanations or assumptions about how a particular programme or intervention is expected to work.
List of abbreviations
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context–mechanism–outcome
- GP
- general practitioner
- HMIC
- Health Management Information Consortium
- ICS
- integrated care system
- MTS
- multiteam system
- PPI
- patient and public involvement
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
