Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 13/156/03. The contractual start date was in April 2015. The final report began editorial review in September 2021 and was accepted for publication in June 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Crane et al. This work was produced by Crane et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Crane et al.
Chapter 1 Introduction
This report presents the findings of a major study in England of the delivery of primary health care to single people who were homeless. It included people sleeping on the streets or in other public places, squatting, staying in temporary accommodation such as hostels or bed-and-breakfast hotels, or staying temporarily with friends or relatives (sofa surfing). It did not include families or couples with dependent children who were homeless. The study, Health Evaluation About Reaching The Homeless (HEARTH), examined four models of primary health care provision at 10 Case Study Sites (CSSs), and included a mapping exercise across England of specialist primary health care services for single people who are homeless. To our knowledge, it is the first UK study to compare and evaluate different models of primary health care provision for this patient group.
Background
Since 2010, homelessness has increased substantially across England. Contributory factors include high housing costs and a shortage of affordable housing; the ending of assured shorthold tenancies in the private rented sector; welfare benefit changes and sanctions, including the capping and freezing of Local Housing Allowance; and cuts to social support budgets. 1 A 2018 report suggested that approximately 200,000 single people experience homelessness each year. 2 Many stay in hostels, bed-and-breakfast hostels or with friends or relatives, and move from place to place. Others ‘sleep rough’ on the streets, in vehicles or parks, or in other public places. The number of rough sleepers in London increased from 3673 in 2009/10 to 11,018 in 2020/21. 3,4 Of the 2020/21 number, 7531 were described as ‘new’ rough sleepers.
Physical health, mental health and substance misuse problems are common among people who are homeless. 5–7 Their health needs are greater than those of the general population, and many have multiple long-term conditions and die earlier. 8–10 People sleeping rough are exposed to damp and the elements, are at risk of exposure and hypothermia, and are susceptible to infestation. Chronic respiratory disorders and circulatory and gastrointestinal problems are common. Physical health problems are aggravated by alcohol use, drug use and malnutrition, and injuries from accidents and assaults are common. Homelessness is also associated with demoralisation and depression. Health problems among people who are homeless are exacerbated by their unsettled lifestyle and sometimes disorganised behaviour, which can reduce their engagement with treatment programmes. Many also face barriers to accessing health care, including inflexible services, negative attitudes from some staff, and the challenges of treating complex and multiple needs. 11 They make unusually high demands on emergency health services, such as accident and emergency (A&E) departments. 12 A 2010 Department of Health (DH: known as Department of Health and Social Care (DHSC) since 2018) study estimated that this group consumes around four times more acute hospital services than the general population, costing at least £85M each year, and hospital stays are, on average, three times longer than those of the general population. 13
Since the 1980s, specialist primary health care services for homeless people have been established in several UK towns and cities. Their development took various forms, including dedicated ‘walk-in’ health centres and mobile health teams visiting hostels and day centres. 14 The National Health Service (Primary Care) Act 199715 provided the statutory framework for the development of Personal Medical Services (PMS). Through flexible contractual arrangements, health professionals were encouraged to deliver primary health care to underserved groups, including people who were homeless. According to Wright,16 this was ‘the most significant favourable piece of legislation for homeless people since the start of the NHS’. There have, however, been very few evaluations of these services, and their success in engaging people who are homeless in health care is unknown.
The 2010 DH study13 grouped specialist primary care provision for people who are homeless into four models: (1) mainstream general practices providing special services for people who are homeless, (2) outreach teams of specialist homelessness nurses, (3) full primary care specialist homelessness teams and (4) a fully co-ordinated primary and secondary care service. The analysis was unable, however, to demonstrate whether or not the provision was fully meeting the needs of people who were homeless. The study reported lack of systematic data on the use of health services and on costs, and lack of research evidence of the potential to improve primary care and health outcomes, and reduce secondary costs.
There are long-standing debates about whether primary health care for people who are homeless should be provided by mainstream or specialist services. Several researchers and clinicians believe that some targeted provision is necessary to reach people on the streets, but the aim should be integration into mainstream general practice services. 16–18 A survey of 86 people who were homeless found that 84% preferred specialist primary health care services. 19 A 1999 survey in England of managers of services for people who were homeless found that the majority favoured integration into mainstream primary health care services for their clients, believing that separate services were divisive. 20
Study proposal and aims
In 2013, the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research Programme issued a call for studies on the effectiveness and cost-effectiveness of innovative and integrated health and care services for homeless people. In response to this call and to address the knowledge gap identified in the DH study,13 this research proposal was submitted and funded.
The overall aim of the HEARTH study was to evaluate the effectiveness and costs of different models of primary health care provision for people who are homeless, with special reference to their integration with other services, and how this affected a range of health, social and economic outcomes. The objectives were as follows.
-
To identify (1) the prevalence of specialist primary health care services for single people who are homeless and their geographical distribution, (2) types of models found in different NHS regions and key characteristics of these services and (3) areas with a homeless population but no specialist health care service.
-
To examine the characteristics and integration of different models of primary health care services for people who are homeless with dental, mental health, secondary health, substance misuse, homelessness sector, housing and social care services.
-
To examine the effectiveness of different models in (1) engaging people who are homeless in health screening; (2) responding to the physical health, mental health and social care needs of people who are homeless; and (3) providing continuity of care for health problems including long-term and complex conditions.
-
To evaluate the impact of different models over time on service users’ health and well-being, and their use of other health and social care services including dental, emergency and secondary care.
-
To investigate the resource implications and costs of delivering services for the various models.
-
To compare the various models across a range of outcomes, reflecting service user and NHS perspectives, using a cost–consequences framework.
-
To provide evidence to NHS commissioners and service providers regarding cost-effective organisation and delivery of primary health care to people who are homeless.
It was proposed that four Health Service Models would be evaluated, including a ‘usual care’ model for comparison.
-
Health centres specifically for homeless people, comparable to the DH’s full primary care specialist homelessness team, but located at a fixed site.
-
Mobile Teams that run sessions in homeless services such as hostels, comparable to the DH’s outreach team of specialist homelessness nurses.
-
Mainstream general practices that also provide specialist services for people who are homeless.
-
Mainstream general practices that provide ‘usual care’ services to the general population, which by default include people who are homeless. This type of provision was not included in the DH models, but is commonly used by people who are homeless if there are no local specialist services.
The research questions that the study would address were as follows.
-
Which models or service elements are more effective in engaging people who are homeless in health screening and health care?
-
Which models are more effective in providing continuity of care for long-term or complex health conditions?
-
What are the associations between integration of the models with other services and health outcomes for people who are homeless?
-
How satisfied are service users, primary health care staff and other agencies with the services?
Layout of this report
Chapter 2 presents literature reviews undertaken during the study, and Chapter 3 describes the study design and methodology. Chapter 4 summarises the findings of the mapping exercise. Chapters 5 and 6 set the scene, by describing the CSSs and the case study participants. Chapters 7–13 focus on primary and secondary outcomes. Chapter 14 examines ways in which contextual factors and mechanisms of health care delivery are likely to have had an influence on outcomes. Finally, the conclusions and implications for NHS commissioners and primary health care managers and practitioners are discussed in Chapter 15.
Chapter 2 Reviews of the literature
This chapter presents two literature reviews. The first focuses on the delivery of primary health care to people who are homeless, conducted during the early months of the study. The second examines the changing policy context in which primary health care services in England for people who are homeless have been developed, dating back to the 1990s. Its findings were summarised in the 2018 mapping report,21 and updated to November 2022.
Review A: primary health care for people who are homeless – evidence-based practice
This scoping review examined evidence-based practice of the delivery of primary health care to people who are homeless, focusing on models of provision and methods of delivering interventions. The inclusion criteria were single people aged 18 years and older who were homeless, but not homeless families or children. It involved the delivery of general medical services (GMS) by general practitioners (GPs), primary care physicians, practice and community nurses, and specialist primary health care teams. It did not include studies of the prevalence of health conditions or clinical features of illnesses, nor studies of specialist services that were not part of primary health care teams.
Methods
A comprehensive and systematic search was conducted of literature from the Organisation for Economic Co-operation and Development countries, published between January 2000 and July 2016. Twelve databases were searched: British Nursing Index, The Cochrane Library, Cumulative Index to Nursing and Allied Health Literature, Health Management Information Consortium, Global Health, Social Policy and Practice, MEDLINE, EMBASE, PsycINFO, PsycARTICLES, SciVerse Scopus and Web of Science. Medical subject headings and subject terms were used to identify the homeless adult population and primary health care services (see Report Supplementary Material 1, Table 1). Only English-language literature was included.
Two researchers independently reviewed all titles and abstracts; full texts were obtained for relevant papers, and a data extraction form was completed for each paper. Decisions were reached about their inclusion, and any uncertainties were reviewed by a third researcher. In line with the methodology for scoping reviews,22,23 a systematic quality assessment of included studies was not conducted. Although a systematic review would have enabled quality assessment, the scoping review methodology allowed inclusion of a range of study designs and interventions. Of the 4096 references identified, 2565 were screened, data extraction was completed on 89 papers, and 38 included in the final review (see Report Supplementary Material 1, Figure 1). 24
The final papers reported on 30 studies (see Report Supplementary Material 1, Table 2). Thirty-three papers concerned studies conducted in the USA; two were conducted in Australia; and one each in Canada, Italy and the UK. The papers were grouped according to models of service provision, namely specialist health centres for people who are homeless, and primary health care within homelessness service settings. A third group covered studies comparing specialist and generic (sometimes referred to as mainstream or ‘usual care’) provision.
Specialist health centres for people who are homeless
Fifteen papers involved studies at specialist health centres for people who are homeless (see Report Supplementary Material 1, Table 2: A1–A15), including six at the Weingart Center, Los Angeles, CA, and two at the Boston Health Care for the Homeless (HCH), MA. Most papers pertained to health screening or vaccination programmes, or the management of health conditions. Common features of their approaches were case management, enhanced and tailored services, and multiagency working.
At Boston HCH, the effectiveness of a ‘chronic care’ model in engaging 82 women who were homeless and had an alcohol problem in treatment was evaluated. 25 An intervention group (n = 42) received screening from a primary care provider, followed by referral to substance misuse services and 6 months’ support from a care manager. The ‘usual care’ group (n = 40) received no support from a care manager and their primary care providers had no alcohol intervention training. Women in the intervention group accessed substance misuse services more frequently than the usual care group, but there were no significant differences between groups in reductions in drinking, housing stability or physical and mental health.
To increase the uptake of cervical screening, Boston HCH introduced an enhanced programme that included the availability of cervical screening during any clinical encounter, rather than only at specific times, and improved health maintenance forms. Over the next 5 years, cervical screening rates improved from 19% to 50%. 26 Examining the delivery of a combined hepatitis A and B vaccination over 6 months to 865 people who were homeless at the Weingart Center, improved completion of the course was linked to nurse case management, hepatitis education, financial incentives and client tracking. 27
Various strategies were implemented by the specialist health centres to retain patients in treatment programmes, including adapting electronic medical records to remind them of health appointments or to trace them if they failed to attend. A small study of 20 homeless veterans found that text reminders 2 and 5 days in advance reduced missed appointments by 19%, and cancelled appointments by 30%. 28 A study at the Weingart Center examined completion of treatment for latent tuberculosis (TB) infection among 520 homeless people allocated to either a nurse case management or a standard care programme. 29 The former received education sessions on reducing the risk of TB and human immunodeficiency virus (HIV), and coping and problem-solving, whereas the standard care group received a short briefing on TB and the importance of treatment. Both groups received incentives to complete treatment. Sixty-two per cent in the case management group, but only 39% in the other group, completed treatment.
Primary health care at homelessness services and on the streets
Sixteen papers examined the provision of basic health care at homelessness services or on the streets to engage with people who were homeless and not accessing health services (see Report Supplementary Material 1, Table 2: B16–B31). In New York City, NY, physicians from Montefiore Medical Center worked alongside outreach staff to deliver health care to people with HIV infection in single-room occupancy hotels. 30 This resulted in increased uptake of medical care and acceptance of antiretroviral medication. In Sacramento, CA, some residents in transitional housing received an on-site tailored service by a physician, nurse and social worker. There was increased uptake of cervical screening and reduced ED use, but little detectable impact on physical functioning or mental health. 31
The goal of outreach clinics is to encourage people who are homeless to use primary health care services. In Baltimore, MD, teams from the HCH clinic regularly visited people who were homeless and had HIV infection, persistent mental illness and substance misuse problems at soup kitchens, shelters and on the streets. Almost half (47.3%) contacted by the outreach team subsequently attended the HCH clinic. 32 Similarly, O’Toole et al. 33 tested whether or not an outreach intervention (health assessment and brief physical examination) at shelters and soup kitchens, immediately followed by a clinic orientation visit, would encourage veterans who were homeless to engage in health care. More than three-quarters (77.3%) who followed this pathway accessed primary health care in the following 4 weeks.
Four papers examined the benefits of providing health education and health promotion within homelessness services. 34–37 For example, a pharmacist and pharmacy student, who ran a fortnightly clinic at a women’s shelter in Arizona, delivered 10 health education sessions over 11 months to residents. 36 These covered urinary tract infection, menopause and diabetes, and 56 women attended at least one session. Attendees said their awareness of health issues had increased and that they would make changes to their health, and 70% would seek advice from a pharmacist in the future.
Lack of facilities may impede the delivery of health care on an outreach basis. Colorectal cancer screening rates among homeless and low-income domiciled patients aged 50 years and over who accessed health clinics at two New York City shelters were examined. Domiciled patients were significantly more likely than those who were homeless to have completed screening (41.3%, compared with 19.7%). 38 The authors concluded that lack of privacy in shelters made it difficult for residents to undertake faecal occult blood tests or prepare for a colonoscopy.
Specialist, compared with generic, health care provision
Seven papers contributed to debates about whether primary health care for people who are homeless should be provided by generic or specialist services (see Report Supplementary Material 1, Table 2: C32–C38). In Rhode Island, USA, comparisons were made between veterans who were homeless and attending general internal medicine clinics and those accessing a tailored primary care clinic. 39 The latter resulted in greater improvements in chronic disease management over 12 months for hypertension, diabetes and hyperlipidaemia, significantly more primary care visits during the first 6 months, and fewer medical admissions and inappropriate ED visits.
Some studies provided evidence of the benefits of integrating primary health care services with other provision. Another study in Rhode Island compared health service use among homeless and non-homeless veterans registered with Patient-Aligned Care Teams (PACTs). 40 The homeless group was registered with a specialist homeless PACT, which provided walk-in services, and was co-located with housing assistance, social work and vocational services. The non-homeless group was assigned a primary care provider with an appointment system and no co-located services. Those accessing the homeless PACT made significantly greater use of primary care, mental health and substance misuse services during the first 6 months, and had reduced ED usage. Similarly, McGuire et al. 41 found a primary care clinic in the same building as homelessness social services programmes and mental health services improved access to primary health care for homeless veterans with serious mental illness or substance abuse problems, and reduced their use of emergency services.
Summary of review A
This review examined the delivery of primary health care to people who are homeless. Most papers described various interventions used by health professionals to engage this population in health care and to address their needs. These included enhanced and tailored services, nurse case management, integrated care provision, targeted programmes, outreach and tracking, and adaptation of electronic patient medical records. Most had positive outcomes in terms of improving uptake of screening and vaccination programmes, encouraging the use of primary health care services, treating health conditions, engaging people in specialist care and reducing the number of ED visits. Most were conducted in the USA, however, and focused on one aspect of service delivery or a single intervention, rather than on a model or a service in its entirety. Several originated from just two specialist health centres.
Review B: health policy developments in England relating to people who are homeless
Several policy developments in England since the 1990s addressed the delivery of primary health care to people who are homeless. A Royal College of Physicians’ working party on homelessness and ill health in the 1990s17 recommended that the DH should introduce systematic monitoring of the health of people who are homeless and their use of health services, and that the government should fund special primary care practices for people who are homeless, and restructure deprivation payments to GPs. The National Health Service (Primary Care) Act 199715 enabled the development of PMS, which stimulated the development of primary health care services to people living in deprived communities, and to underserved and disadvantaged groups, including people who are homeless. Local Development Schemes were introduced by the DH in 1998, enabling additional payments for GPs and allied staff to provide services in deprived areas (later known as ‘enhanced services’). The extra funding incentivised GPs, for example, to register and provide medical care to people staying in hostels.
Underpinning these developments, Addressing Inequalities: Reaching the Hard-to-reach Groups was published by the DH in 2002 as a practical aid for primary care. 42 Among its recommendations were primary care trusts [replaced by Clinical Commissioning Groups (CCGs) in 2013] should encourage GPs and nurses to focus on hard-to-reach groups via PMS and/or Local Development Schemes. The Royal College of General Practitioners (RCGP) produced a statement on homelessness and primary care in 2002, with recommendations for practices and primary care trusts. 43 In 2004, primary care organisations could commission new Alternative Provider Medical Services (APMS) to provide essential primary care services, additional services where GMS/PMS practices opted out, enhanced services and out-of-hours services. They could contract these services from providers, including commercial and not-for-profit agencies, and NHS foundation trusts. 44
Influential reports, such as Securing Good Health for the Whole Population45 and the 2010 Marmot Review,46 ensured that equalising health outcomes across society gained prominence within national policies. In 2010, the Social Exclusion Task Force launched Inclusion Health, a framework for driving improvements in health outcomes for socially excluded groups. A DH report published alongside Inclusion Health acknowledged that health care for people who were homeless may have been historically underfunded due to inaccurate population data. 13 A National Inclusion Health Board was established to lead the Inclusion Health agenda. Just 3 months later, however, there was a change of government and the Social Exclusion Task Force was disbanded.
The Health and Social Care Act 201247 transferred NHS commissioning responsibilities to CCGs prompting greater general practice control of service provision. Under the Act, CCGs were required to reduce health inequalities and provide integrated services. 48 Health and well-being boards were established by local authorities to act as forums whereby health and social care commissioners and providers could address the health and well-being of local populations and promote integrated services. 49 These boards were required, with CCGs, to produce a Joint Strategic Needs Assessment and a Joint Health and Wellbeing Strategy for their local populations. Leng50 produced a guide to help local authorities improve health and well-being among people who are homeless, and reduce health inequalities. Healthwatch was developed in 2013 as a patient and service user champion at local and national levels. This has taken a role in monitoring some services for people who are homeless.
Public health responsibilities moved from primary care trusts to local authorities in April 2013, and Public Health England (PHE) was established. PHE brought together public health specialists into a single public health body responsible for protecting and improving the public’s health and reducing health inequalities. Its call for action in 2015, All Our Health: Personalised Care and Population Health,51 urged health care professionals to use their skills and relationships to maximise impact on avoidable illness and promote well-being and resilience. PHE produced a framework and issued guidance on homelessness, both of which were updated in 2019. 52,53 It recommended that health and well-being boards should ensure that homelessness is addressed in joint strategic needs assessments and health and well-being strategies, and that the relationship between health and homelessness is acknowledged in local housing authorities’ homelessness reviews. PHE also produced guidance on tackling TB, a disease disproportionately affecting people who are homeless. 54
In 2016/17, Sustainability and Transformation Plans were developed in 44 areas across England as a new planning process for health and, to some extent, social care. Renamed Sustainability and Transformation Partnerships, they required NHS organisations to develop plans for local health services, including working with local authorities and other partners. They represented an important shift in DH policy: although the Health and Social Care Act 201247 sought to stimulate competition within the health care system, NHS organisations were asked to collaborate, rather than compete, to plan and provide local services. 55 The Health and Care Act 2022 was passed in April 2022. This legislation required Integrated Care Systems (ICSs) to be established in England on a statutory basis from 1 July 2022. ICSs replaced Sustainability and Transformation Partnerships as outlined in the White Paper Integration and Innovation: Working Together to Improve Health and Social Care for All. 56 Forty-two ICSs have been established across England with a responsibility to plan and fund health and care services in their area. Each ICS is made up of an integrated care board (ICB) and an integrated care partnership (ICP). ICBs replaced CCGs and are responsible for planning NHS services, including ambulances, primary care, mental health care, hospital (acute services), community and specialist care, and are accountable to NHS England. A representative from ICBs is required to participate in local Health and Wellbeing Boards, in place of CCG members. ICPs cover public health, social care and wider subjects impacting the health and wellbeing of their local populations, and operate as a statutory committee between the ICBs, local authorities, and voluntary and community organisations. The establishment of ICSs represents the first large-scale structural change to the NHS since 2012 (NHS Confederation 2022). Further details are in Chapter 15.
Linked to such initiatives have been several policy moves to tackle homelessness. The Ministerial Working Group on Homelessness was formed in 2010, and 1 year later a ‘No Second Night Out’ scheme was launched to ensure that people who were sleeping rough received help quickly. 57 Around the same time, ‘Housing First’ pilots were introduced into the UK. This model originated in New York in 1992, with the premise that stable housing is key to tackling chronic homelessness, and should be secured before problems such as substance misuse and mental illness can be addressed. 58,59 Significant modifications to the model have, however, made it difficult to assess the influence of the model on programme outcomes. 60,61 Several researchers have concluded that Housing First provides improvements in housing stability, but, apart from the use of emergency health services, there is little evidence as yet to suggest that it produces better outcomes for physical health, mental health and substance misuse than treatment in the community. 62,63
The Homelessness Reduction Act 201764 placed many public authorities, such as emergency departments (EDs), urgent treatment centres and in-patient hospitals, under a duty to refer people at risk of homelessness to the local authority. The Act’s focus on prevention, as well as on developments of planned individual support, is arguably the most important policy development across the NHS and local authorities for people who are homeless or insecurely housed since the Housing (Homelessness Persons) Act 1977. 65 In 2018, the Ministry of Housing, Communities and Local Government published a new Rough Sleeping Strategy, with a commitment to halve rough sleeping by 2022 and end it by 2027. 66 In the first year, it allocated up to £2M to enable access to health and support services for people sleeping rough.
Published in 2019, the NHS Long Term Plan sets out new action the NHS will take to help tackle health inequalities, with £4.5B over the next 5 years. 67 Up to £30M is being invested into the needs of people sleeping rough, and ensuring areas most affected have better access to specialist NHS mental health support, integrated with existing outreach services. New primary care networks are intended to bring together general practices to work at scale together to focus on local patient care.
Although many of these developments reflect primary care services and their interface with local authorities, policy attention has also focused on improving services for people who are homeless and in hospital. Pathway, a charity founded in 2009, introduced the ‘Pathway’ model of integrated care to bridge the gap between primary and secondary care. This involves specialist primary health care services collaborating with secondary care services to improve care in hospital for people who are homeless. In 2020, The Royal College of Emergency Medicine produced a best-practice guide, Inclusion Health in the Emergency Department: Caring for Patients who are Homeless or Socially Excluded. 68 A 2021 evaluation concluded that specialist approaches to hospital discharge for people who are homeless are more effective and cost-effective than standard care involving discharge to the streets without support. 69
Over the decades, policy attention to the health of people who are homeless has been driven by organisations such as The Faculty for Homeless and Inclusion Health (supported by Pathway), a multidisciplinary network of health care workers and experts by experience. It produced a set of standards for commissioners and service providers in 2011 covering health care planning, commissioning and provision for people who are homeless (revised in 2013 and 2018). 48,70 The London Homeless Health Programme, formed in 2015 as part of the Healthy London Partnership, issued guidance in 2016 (updated in 2019) for London’s CCGs on improving health outcomes for people who are homeless. 71 It recommended there should be a Homeless Health Lead in every CCG to champion the homeless health agenda and engage with London’s homeless health clinical networks. In partnership with Healthwatch London and Groundswell (a charity supporting people who are homeless), it produced ‘my right to access healthcare’ cards to help people who are homeless register with a general practice. The Queen’s Nursing Institute has developed a Homeless and Inclusion Health Programme.
Efforts to improve health care for people who are homeless are continually advocated by voluntary sector homelessness organisations, including Centrepoint, Crisis, and St Mungo’s. In 2009–10, Homeless Link was funded by the DH Third Sector Investment Programme to pilot a Homeless Health Needs Audit Tool, to help health service commissioners and providers, and local authorities, gather data about the health needs of local people who are homeless and their use of health services. 11 An updated audit tool, with funding from PHE, reflected new local commissioning environments and other changes. 72
As a result of the COVID-19 pandemic, the NHS and English housing authorities implemented the ‘Everyone In’ initiative, to mitigate the effects of the pandemic on people experiencing homelessness. Under the initiative, £3.2M was made available to local authorities in March 2020 to accommodate people sleeping rough or in accommodation where it was difficult to self-isolate, such as night shelters. 73 By the end of November 2020, more than 33,000 people had been helped to find accommodation, and, according to the National Audit Office, COVID-19 infections and deaths among this population had been relatively low. 74 In November 2020, the ‘Protect Programme’ backed by £15M, was announced to ensure that vulnerable people, including those sleeping rough, were to be protected during the second period of national restrictions and throughout the winter. 73 In April 2020, NHS England and NHS Improvement also produced clinical advice and guidance on delivering health care to people who are homeless during the COVID-19 pandemic. A new National Institute for Health Protection has been formed with a focus on biosecurity and other elements of public health; the implications of this for homelessness policy and services will no doubt emerge. 75
Summary of review B
This second review summarises the many policy initiatives introduced in England since the 1990s to stimulate the development of primary health care services for people who are homeless. Yet, as the first review identified, there have been very few evaluations of such services in England, and little is known about their effectiveness in engaging this population in health care, their effectiveness in treating health conditions and their costs. The paucity of studies examining the effectiveness of generic primary health care services for people who are homeless is concerning, given that, in England, more than half of homelessness services rely on generic general practices to deliver primary health care to their clients. 21 The HEARTH study aimed to address these knowledge gaps. Its design and methodology are described in Chapter 3.
Chapter 3 Study design and methodology
This chapter describes the HEARTH study’s design and methodology. It summarises the study’s conceptual framework, primary and secondary outcomes, fieldwork accomplished, data analyses, and Patient and Public Involvement (PPI).
Theoretical and conceptual framework
It has long been recognised that those who are in most need of health care are least able to access services, a phenomenon termed the ‘inverse care law’. 76 In terms of people who are homeless, the belief was that their complex needs could not be met by mainstream GPs; therefore, specialist primary health care services were established in some areas (see Chapter 1). Some theorists associate the exclusion of people who are vulnerable with problems of discrimination and the ‘bureaucracy’ and regimes of formal services, which result in them being inadvertently or deliberately excluded. Merton77 associated the exclusion from mainstream society of people who are homeless with ‘retreatist’ behaviours, and an inability or unwillingness to comply with society’s norms and values.
Using a case study approach, the HEARTH study examined the effectiveness of different models of primary health care services for people who are homeless to determine what works, for whom and in what circumstances. This approach allows researchers to investigate a contemporary phenomenon within its real-life context, and enables multiple sources of evidence to be gathered. 78 The role of contextual factors and mechanisms in the delivery of health care to people who are homeless, and how these influence outcomes, were examined at CSSs. Contextual factors included the wider health and care system, financing, staff and physical resources, and the availability and accessibility of other relevant services. Mechanisms included strategies used by CSS staff to engage with people who were homeless and provide health screening and treatment (Table 1). The theoretical framework for this was informed by Andersen’s79 behavioural model of health service use by vulnerable populations, and applied by Gelberg et al. 80 to people who are homeless. The model has three domains: (1) population characteristics, such as demographics, personal and family resources, community and health services resources, and perceived health needs; (2) health behaviour, such as lifestyle factors and use of health services; and (3) outcomes, such as satisfaction with care, and the availability and accessibility of health services.
| Contextual factors | Mechanisms (service delivery factors) | Outcomes |
|---|---|---|
| Size and geographical spread of the local population that is homeless. Availability of resources (funding and staff) to enable CSSs to respond to the health needs of local people who are homeless. Availability of competing primary health care services. Availability of local health and social care agencies, their knowledge of the CSS and referral procedures, and their ability to provide services to CSS referrals. Local commissioning influences, for example catchment area, population to be served by CSS, exclusion groups. National policy influences relating to who is eligible/not eligible for NHS care. Local authority influences, for example the length of time homeless people can remain in a hostel in the locality. |
Staff understanding of homelessness, and their attitude towards working with people who are homeless. Composition of team and its clinical expertise in assessing and treating health problems of people who are homeless, and referring them to appropriate services. Staff knowledge of the local homeless population and of services to which this group can be referred. Flexibility and accessibility of the service. An environment that is welcoming and acceptable to people who are homeless. Person-centred approach to health care that encourages engagement and continuity of care. Holistic approach that responds to housing, social and welfare needs. Champions health promotion and health screening. Availability of protocols and ability of staff to manage difficult or challenging behavior. Integration with mental health, dental, substance misuse, social care services, homelessness and other services required by people who are homeless. |
Primary outcome: six indicators of engagement in health screening 1. BMI 2. Smoking 3. Hepatitis A 4. Mental health 5. Alcohol 6. TB Secondary outcomes: 1. Management of five SHCs: i. Hypertension ii. Chronic respiratory problems iii. Depression iv. Alcohol problems v. Drug problems 2. Oral health status and receipt of dental care. 3. Self-ratings of health status and well-being over time. 4. Use of health and social care services, including substitute primary care services (walk-in, A&E) and unplanned hospitalisations. 5. Patients’ satisfaction with the CSS. 6. CSS staff and local service providers’ satisfaction with the CSS. 7. Addressing the needs of local people who are homeless. |
Integration between each CSS and relevant services were measured, drawing on measures adopted by Browne et al. 81 and Joly et al. 82 Distinctions were made between (1) types of services, for example health, housing and social care; and (2) organisations involved at different stages of care such as hospital services, and those that provided complementary services. The ‘depth’ of integration between the CSS and each service was scored by staff, according to the extent to which they were involved with a service, and the extent to which they should be involved (see Chapter 11). Similar information was collected from external health and social care agencies.
Study approvals and management
The study started in April 2015. It received ethics approval from the London – Bloomsbury Research Ethics Committee on 5 October 2015 (reference number: 15/LO/1382) and study-wide governance approval from the lead Clinical Research Network (CRN) on 19 October 2015, and local NHS Research Governance approval was granted for each study site as they were recruited. As the study progressed, three substantial and seven non-substantial amendments were approved by the London – Bloomsbury Research Ethics Committee and the Health Research Authority, and four changes were made to the original research protocol. The non-substantial amendments concerned the addition of CSSs to the study, and the substantial amendments concerned changes to the research protocol (see following sections).
A Study Steering Committee (SSC) was formed; it met annually and guided the research team throughout the study.
Phase 1: mapping of specialist primary health care services
The mapping exercise aimed to (1) examine the prevalence, geographical distribution and characteristics of specialist primary health care services in England for single people who are homeless; (2) determine the extent to which temporary accommodation and day centres for single people who are homeless had access to specialist primary health care services; and (3) collect information from those not linked to specialist health services about accessing primary health care.
Using semistructured questionnaires, two complementary surveys were undertaken. The first collected information from specialist primary health care services about their service such as opening hours, staff composition and patient groups (see Report Supplementary Material 2). The second survey collected information from managers of hostels and day centres for single people who are homeless about their project, access to primary health care for clients and general practices used, clinics run by doctors or nurses at their project, and whether or not the primary health care needs of their clients were being met (see Report Supplementary Materials 3 and 4). Details of the methods are available,21 and summary findings reported in Chapter 4.
Phase 2: evaluation of models of primary health care provision
An evaluation of four models of primary health care provision for people who are homeless was undertaken:
-
Two specialist health centres primarily for people who were homeless (Dedicated Centres).
-
Two mobile homeless health teams that held clinics in hostels or day centres for people who are homeless (Mobile Teams).
-
Two general practices with special services for people who were homeless (Specialist GPs).
-
Four generic general practices providing ‘usual care’ services to the local population, including to people who were homeless (Usual Care GPs). The intention was to have two sites, but because of difficulties recruiting general practices and insufficient numbers of patients who were homeless at these sites, two additional practices were added.
Fieldwork ran from January 2016 to June 2019. Data were collected through interviews with CSS managers and staff, and local health, social care and welfare agencies. People with a current or recent history of homelessness and registered with the CSS were recruited as ‘case study participants’, and information was collected from them and from their medical records about their health and service use over 12 months.
Primary outcome: health screening of people who are homeless
The primary outcome was the extent of health screening among people who are homeless. Six Health Screening Indicators (HSIs) were selected: body mass index (BMI), mental health, alcohol use, TB, smoking and hepatitis A. The HSIs are a set of minimum standards or ‘markers’ from a clinical perspective, and extend beyond screening alone, as evidence of an intervention was sought if a problem was identified. Screening for BMI, mental health, alcohol use and TB covered the preceding 12 months, smoking covered the preceding 24 months and hepatitis A required that a vaccination programme was in progress or had been completed in the preceding 10 years. The HSIs were derived from existing guidelines,83–87 and from the expert opinion of Ford (retired GP), who consulted two generic GPs, two GPs specialising in homelessness and a hospital physician. The six HSIs were included in a list of health screening indicators for people who are homeless in the Faculty for Homeless and Inclusion Health’s standards for primary care. 48 They were selected for our study because smoking, mental health and alcohol problems are common among single people who are homeless (see Chapter 1), and their diets are often poor. 88 Moreover, compared with the general population, hepatitis A and active pulmonary TB are relatively common. 89–91
Data for the HSIs came solely from the participants’ medical records, which were accessed at the end of the study. A score of 1 was given to each HSI if there was evidence in the medical records of both screening having taken place and an intervention being offered, if applicable, thus giving a total range of 0–6. Further details are in Chapter 7.
Secondary outcomes
Outcome 1: management of Specific Health Conditions
Five heath conditions that might be difficult to manage because of the unsettled lifestyles of people who are homeless, or that may require integration with other services, were selected to assess the response of the CSS to the condition, and its effectiveness in providing care and treatment. The five Specific Health Conditions (SHCs) were (1) hypertension, (2) chronic respiratory problems, (3) depression, (4) alcohol problems and (5) drug problems. It was expected that most participants would have at least one of these conditions, given their prevalence rates in other studies of people who are homeless: chronic respiratory problems, 17–29%; depression, 30–43%; hypertension, 17–33%; alcohol problems, 27–50%; and drug problems, 39–54%. 11,92–98
Five outcomes examined the effectiveness of the CSS in providing health care for each SHC: outcomes 1 and 2 assessed processes of care by the CSS; outcomes 3 and 4 measured patient perceptions of the quality of care; and outcome 5 assessed control of, or change in, condition over the study period (see Chapter 8). The intention had been that CSS staff would also complete a short questionnaire at the end of the study about care provided for each SHC. After piloting, it was omitted because staff did not have the time to complete it, and the information needed was mostly in the medical records.
Outcome 2: oral health status and receipt of dental care
Poor oral health and dental problems are common among people who are homeless. Access to dental care is believed to have a beneficial impact on oral health outcomes, and on global and oral health-related quality of life (OHRQoL), dental anxiety, satisfaction with dental care and positive health behaviours (oral hygiene practices, sugar consumption patterns and smoking). The impact of the CSSs on the receipt of dental care and on oral health status by people who are homeless was assessed over the study period. It was hypothesised that CSSs that had greater integration with primary care dental services would have higher rates of access to dental care and more positive oral health outcomes.
Instruments to measure the impact of the CSS on dental service use, dental anxiety and changes in self-reported oral health status and OHRQoL were administered, drawing from the Adult Dental Health Survey,99 the GP Patient Survey,100 the Oral Health Impact Profile-14 items (OHIP-14),101 the Modified Dental Anxiety Scale (MDAS),102 Global Self-Rating of Oral Health103 and whether or not participants felt that they needed dental treatment. 104 Self-reported and OHRQoL measures have been validated for use with people who are homeless by the HEARTH study’s co-investigator (Daly). 105 Further details are in Chapter 10.
Outcome 3: health status and well-being over time
Changes over time in health status and well-being were examined, using the Short Form 8 Health Survey (SF-8) and the Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS), which participants completed at baseline and at 8 months (see Chapter 9). Information on nutrition and smoking was collected at baseline and at 8 months to assess the impact over time of the CSS in improving health-related behaviours among people who are homeless.
Outcome 4: use of health and social care services, and service use costs
Medical records of participants were accessed on completion of fieldwork at each site, and data relating to service use over the 12-month study period were extracted (contacts with general practices, community services, out-of-hours services, ambulances, hospital inpatient and outpatient care, tests and investigations). These data were supplemented with information provided by participants during interviews at baseline and at 4 and 8 months. Items taken from the Client Service Receipt Inventory106 were embedded in interview schedules asking participants to report on use of primary care, community, substance misuse and hospital services; social services (including local authority housing and welfare offices and for personal care); and support from the voluntary sector. Use of substitute primary care services (A&E, NHS walk-in/urgent care clinics, NHS 111, ambulance call-outs) was identified as possible indicators of the effectiveness of the CSS in providing an accessible service for people who are homeless, and in preventing avoidable hospital admissions or re-admissions. Service use data were converted to costs (Great British pounds, 2020) using nationally validated sources. 107
Outcome 5: satisfaction with the Case Study Site
Using questions from the GP Patient Survey and General Practice Assessment Questionnaire, participants’ views of the CSS and satisfaction with the service were obtained. Questions covered access, arranging appointments, waiting times, opening hours and quality of care. During interviews with CSS staff and local service providers, their perspectives of the CSS, and their integration and satisfaction with the CSS, were also sought.
Outcome 6: addressing the health needs of local people who are homeless
Through interviews with people who were homeless but not using the CSS, and with CSS staff and other agencies, information was gathered about the extent to which the CSS was addressing the health needs of the local population that was homeless and any unmet health needs.
Recruitment of Case Study Sites
Drawing on the mapping exercise, primary health care services working with people who were homeless were identified for the three specialist models. Their selection depended on whether or not they responded to the mapping exercise, the number of patients who were homeless, and staff resources or imminent changes to the service that affected their ability to participate.
Early on it became apparent that recruiting general practices for the Usual Care GP model would be exceptionally difficult. The mapping exercise revealed that many large hostels were linked to specialist primary health care services. Among those that were served by a mainstream general practice, some hostel managers declined involvement, and some agreed, but the general practices failed to respond or declined as they were too busy. General practices serving smaller hostels were therefore considered, although this meant fewer potential case study participants per site.
Substantial time and effort were spent liaising with general practices and primary care leads of CRNs to try and recruit Usual Care GPs. It was agreed with the SSC that, instead of two sites for this model, attempts would be made to recruit additional practices to reduce the number of participants required at each CSS. In collaboration with five CRNs, attempts were made to recruit a cluster of hostels and general practices in an area. This proved successful in two locations, and eventually four Usual Care GPs participated. Recruitment of participants at the final site did not commence until April 2018.
Case studies of health and service use over 12 months for people who are homeless
At each CSS, patients who were currently or recently homeless were recruited as case study participants and information was collected about their health and service use over 12 months.
Inclusion criteria
The inclusion criteria were as follows: (1) aged 18 years and over, (2) homeless currently or at some time during the previous 12 months, (3) registered with the CSS for at least 4 months and (4) had at least one consultation with a CSS doctor or nurse during the previous 4 months. Families or couples with dependent children who were homeless were not included. Homelessness was defined as sleeping on the streets or in other public places, squatting, staying in temporary accommodation such as hostels or bed-and-breakfast hotels, or staying temporarily with friends or relatives (sofa surfing). By focusing on those who had been homeless at some time during the preceding 12 months, this enabled people who frequently move in and out of homelessness to be included.
Sample size
The aim was to recruit 96 participants from each of the four models (total N = 384), divided evenly, as far as possible, between the CSSs in each model. It was estimated that the attrition rate would be 33% over the study period. Hence, it was expected that at least 80 people in each of the four models would be interviewed at 4 months, and 64 at 8 months (final N = 256).
The primary outcome variable was the six-item HSI tool, with a score of 0–6. Given the innovative nature of this tool, there were no previous data on its level of variation. Extensive simulations exhibited a maximum standard deviation (SD) of 2.0. An outcome variable with a SD of no more than 2.0 would necessitate a minimum required sample size of 64 in each of the four models to detect a difference of 1 point on the six-item tool between any two types of model, with size = 5% and power = 80%.
The possibility of small percentages of participants with a particular SHC meant that it might be possible to detect only relatively large differences in continuity of care for that SHC between the four models. For example, if only approximately 30% of participants in any group had a particular condition, it would be difficult to identify a difference between groups in continuity of care for that condition of less than 40%. Each SHC was assessed separately when numbers permitted.
Recruitment of case study participants
Recruitment of case study participants started in January 2016 and ended in August 2018. At most CSSs, recruitment lasted several months (and longer than planned) to reach the required number. For the three specialist Health Service Models, participants were recruited at the CSS, or at hostels and day centres where CSS staff held clinics. Recruitment was undertaken by the fieldwork research team (Joly, Cetrano, Coward and Crane), who spent weekly periods at a location until the required number was achieved. The study was explained briefly to consecutive patients by CSS staff, who handed them a participant information sheet about the study and what their involvement would entail, and those interested were introduced to the research team. The research team then explained the study in more detail, confirmed the patient’s eligibility regarding homelessness and checked with CSS staff their date of registration at the practice. Only those who gave informed, written consent to be interviewed and for the research team to have access to their medical records at the end of the study were included.
For Usual Care GPs, it was impractical to recruit at the CSSs as most patients were not homeless. Participants were therefore recruited at hostels and day centres, where the staff explained the study to people they believed were eligible, handed out participant information sheets and passed on the names of those who were interested. The research team then explained the study to them in more detail and determined their eligibility to participate. If necessary, written consent was obtained from potential participants to enable the research team to check the date of registration with the CSS and the date they were last seen by a doctor or nurse with CSS staff.
By August 2018, the target number of 96 had been reached at each of the specialist Health Service Models, but only 75 Usual Care GP participants had been recruited (Table 2). It was agreed with the SSC that recruitment should cease to enable time for follow-up interviews.
| Health Service Model | CSS (N = 10) | Case study participants (N = 363) |
|---|---|---|
| Dedicated Centre | DC1 | 48 |
| DC2 | 48 | |
| Mobile Team | MT1 | 47 |
| MT2 | 49 | |
| Specialist GP | SP1 | 51 |
| SP2 | 45 | |
| Usual Care GP | UC1 | 28 |
| UC2 | 30 | |
| UC3 | 15 | |
| UC4 | 2 |
Interviews
Using structured questionnaires, case study participants were interviewed at baseline and at 4 and 8 months, and were offered £10 for each interview as appreciation for their time and involvement (see Report Supplementary Materials 5–8). Information was gathered about their socioeconomic circumstances (housing, income, involvement in training or work, support from family and friends); health-related activities, such as smoking and nutrition; physical and mental health problems, and use of alcohol and drugs; dental health; use of health and other services in the preceding 4 months (resulting in 12 months’ data); and their views of the CSS. During the interviews at baseline and at 8 months, participants completed the SF-8 and the SWEMWBS concerning health status and well-being; they also completed validated instruments pertaining to depression and respiratory problems if a potential SHC was indicated (see Chapter 8). Quantitative and qualitative data were generated from these interviews.
Most interviews were conducted at the CSS or at hostels or day centres at a time and place convenient to participants. A few took place on the streets, in cafes or offices, or at a participant’s home. The interviews at baseline and at 8 months lasted approximately 45–60 minutes, and the interviews at 4 months lasted 30–40 minutes, as less information was needed. Whenever possible, the same researcher conducted all interviews to enable continuity. The interviews touched on sensitive and possibly upsetting topics, such as ill health and homelessness; therefore, participants were offered opportunities to have a break or stop the interview if they became distressed or anxious or found it hard to concentrate. All interviewers had substantial experience in interviewing people who were homeless or who had mental health problems. In most instances, participants welcomed the opportunity to talk about their experiences and needs and fill in self-completion instruments.
For some participants, several attempts were made to contact them and several appointments arranged before a follow-up interview was achieved. Drawing on the research team’s previous experience of longitudinal research with people who are homeless,108 various strategies were used to find and engage with some participants. These included contacting street outreach workers and other service providers, opportunistic visiting of day centres and hostels, leaving letters for participants with service providers and searching on the streets. Written consent was obtained from participants at baseline for the research team to contact CSS staff and other services when necessary. When possible, follow-up interviews were conducted with participants who left the CSS during the study and moved elsewhere.
Overall, 898 interviews were conducted, and all except three were face-to-face. At 4 months, 272 participants (74.9%) were interviewed, fewer than the target number (320). At 8 months, 263 (72.5%) participants were interviewed, slightly higher than the target number (256) after allowing for attrition, despite fewer people being recruited to the study. At 8 months, 30 participants were included who could not be interviewed at 4 months. There were no statistical differences by Health Service Model in the number of interviews achieved at each period (Table 3). The main reasons why participants could not be interviewed were because they were in prison or hospital, could not be found, or declined or did not respond to interview attempts (see Appendix 1, Table 45). At 8 months, 10.4% of Dedicated Centre participants were in prison, and 8.3% of Mobile Team participants were outside the UK. Five participants died during the study.
| Interviewed at | Case study participants, n (%) | Comparison test; p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| 4 months | 272 (74.9) | 68 (70.8) | 73 (76.0) | 67 (69.8) | 64 (85.3) | Chi-squared; 0.086 |
| 8 months | 263 (72.5) | 65 (67.7) | 70 (72.9) | 70 (72.9) | 58 (77.3) | Chi-squared; 0.573 |
| Baseline only | 61 (16.8) | 20 (20.8) | 15 (15.6) | 17 (17.7) | 9 (12.0) | Chi-squared; 0.474 |
| Breakdown of interviews at different intervals | ||||||
| 4, but not 8, months | 39 (10.7) | 11 (11.5) | 11 (11.5) | 9 (9.4) | 8 (10.7) | Chi-squared; 0.962 |
| 8, but not 4, months | 30 (8.3) | 8 (8.3) | 8 (8.3) | 12 (12.5) | 2 (2.7) | Chi-squared; 0.146 |
| Baseline and 4 and 8 months | 233 (64.2) | 57 (59.4) | 62 (64.6) | 58 (60.4) | 56 (74.7) | Chi-squared; 0.161 |
Interviews with Case Study Site staff and sessional workers
Face-to-face interviews were conducted by the fieldwork research team with 65 CSS staff and sessional workers, including practice managers, primary health care nurses, GPs, mental health nurses, drug and alcohol workers, case managers, health care assistants (HCAs) and receptionists. Using a template (see Report Supplementary Material 9), operational and performance data were collected from CSS managers about (1) the development of the CSS; (2) current operation, including staffing, client groups served, opening hours, registration, funding and types of services provided; (3) integration with local health, dental, welfare and social care services; and (4) involvement of the CSS in local strategy and service development.
Using an interview schedule adapted for different job roles (see Report Supplementary Material 10), interviews with CSS staff and sessional workers collected information about (1) length of time with the CSS, role within the team, qualifications and experience of working with people who are homeless; (2) services provided to people who are homeless, and strategies to encourage engagement; (3) collaboration with local agencies and services; and (4) perspectives of the CSS’s strengths and limitations. All consented for their interview to be recorded. They also rated their actual and expected levels of integration with other services (see Chapter 11). Each interview lasted approximately 60 minutes. They were sent a participant information sheet prior to the interview explaining the study and their participation.
There were delays in arranging some interviews due to staff workload. Where sessional workers were employed by an organisation that was not the CSS, additional research and development approvals were required. Our intention had been to hold a focus group with CSS staff towards the end of the study to gather their reflections on their work as a team. However, owing to their work pressures, individual interviews were more appropriate.
Interviews with local service providers and stakeholders
To examine the wider context in which the CSS delivered care, interviews were also conducted with 81 local service providers and stakeholders. All except three were face-to-face, and all but two were recorded. Service providers included street outreach workers, hostel and day centre managers, and drug and alcohol workers who were not part of the CSS. Using an interview schedule (adapted for different job roles), information was gathered about (1) their work with people who are homeless, (2) their awareness of the CSS and referral procedures, (3) use of the CSS by their clients or reasons for non-use and (4) their perspectives of the CSS (see Report Supplementary Materials 11 and 12). Each person was asked to rate their actual and expected level of integration with the CSS. Interviews lasted approximately 45 minutes. They also were sent participant information sheets prior to the interview.
Interviews with three local authority service commissioners and four Healthwatch directors collected information about local strategies and plans for health care delivery to people who are homeless, and the role of the CSS in local health provision. It was not possible to arrange interviews with some stakeholders.
Interviews with people who were homeless and not using the Case Study Sites
In eight CSS areas, 107 interviews were conducted with people who were homeless and not registered with the CSS. Using a short, structured questionnaire (see Report Supplementary Material 13), information was gathered about their awareness of the CSS, reasons for not using it, and their health needs and use of health care services. They were recruited at hostels and day centres, and were offered £5 as thanks for taking part. Staff at these sites handed out participant information sheets to potential participants, and those interested were introduced to the research team. The research team explained the study in more detail, checked the potential participant’s eligibility and obtained their written consent to participate. Peer interviewers conducted 49 of these interviews (described in Patient and Public Involvement).
Observations
Observations were undertaken of ways in which CSS staff engaged with people who were homeless, and worked with other agencies. This mainly involved observations in CSS reception areas and in day centres while trying to recruit or find participants for follow-up interviews. Observations focused on the ways in which people who were homeless presented to the CSS, their behaviour in the reception areas and how this was managed by the CSS staff, and whether they were seen by clinicians or left prematurely. It was not feasible to undertake observations in reception areas of Usual Care GPs, as it would not have been possible to identify whether patients were housed or homeless.
Observations were undertaken at day centres of the systems in place for service users to see a CSS nurse, and the ways in which nurses engaged with those who were reticent. Other opportunities to undertake observation work were sought. At one CSS, two researchers attended a multidisciplinary staff meeting. At another, a researcher accompanied a CSS staff member and outreach worker while they conducted street outreach work early in the morning. At a third site, research staff attended a drop-in service for rough sleepers run by CSS staff. Field notes were maintained of the various observations.
Data from medical records
After the interview at 8 months, printouts of all medical record data held by the CSS for the 12-month study period, including consultations, letters, reports and referrals, were requested for each participant. This included GP records that were shared with the Mobile Teams. Data were also requested dating back 2 years regarding smoking and dating back 10 years regarding hepatitis A (for scoring the HSIs). Organising data extraction and ensuring that complete data were obtained proved intricate and time-consuming. Each site identified a person responsible for data extraction and Joly (research team) instructed them accordingly. They were provided with the requirements for data extraction for each participant. The extraction process was undertaken by the CRN at one CSS, and elsewhere by CSS administrative staff. Data were then checked by Joly for completeness, and missing documents requested. At some sites, this process was repeated several times before complete data were obtained.
Medical records were obtained for 349 of the 363 participants. They were used to score the primary outcome and some SHC outcomes, and to provide service use data. Medical records were not obtained for 14 Usual Care GP participants, including both participants from one site (UC4). This was because participants were no longer registered with the CSS at the end of the study and the records were unavailable. As shown in Table 4, medical records for the entire study period (12 months) were available for most participants, with no statistically significant difference by Health Service Model.
| Length of time | Case study participants, n (%) | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 349) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 61) | ||
| 1–4 months | 2 (0.6) | 0 (0.0) | 2 (2.1) | 0 (0.0) | 0 (0.0) | Kruskal–Wallis: 0.168 |
| > 4–6 months | 14 (4.0) | 3 (3.1) | 7 (7.3) | 1 (1.0) | 3 (4.9) | |
| > 6–8 months | 16 (4.6) | 5 (5.2) | 4 (4.2) | 5 (5.2) | 2 (3.3) | |
| > 8–10 months | 31 (8.9) | 8 (8.3) | 11 (11.5) | 9 (9.4) | 3 (4.9) | |
| > 10–12 months | 286 (81.9) | 80 (83.3) | 72 (75.0) | 81 (84.4) | 53 (86.9) | |
Although the research team checked with CSS staff that a person had been registered at least 4 months prior to recruitment, once medical records were obtained, it was found that 50 participants had been registered less than 4 months prior to recruitment. For 26 of these participants, it was possible to collect additional data from the medical records at the end of the study period to provide 12 months’ medical data on service use.
Data management
All data collected during the study were stored in locked filing cabinets in our department at King’s College London (KCL), which itself is locked. Only the KCL team had access to these filing cabinets, and to the database on the university server (which was password protected). Identifiable participant information was not disclosed beyond the KCL research team. Names were not entered into spreadsheets or databases created for the analyses.
The recorded interviews of CSS staff, service providers and stakeholders were transcribed by a professional company used by KCL. A confidentiality agreement was drawn up and audio files were transferred to the company using the KCL File Transfer Protocol system (a secure method of transferring data). Staff were informed of this on the participant information sheets and consent forms. Once interviews were transcribed, all personal identifiers were removed.
Data analyses
A descriptive picture of the context and mechanisms of each CSS was built from interviews with CSS staff and other agencies. Using the templates created by each CSS manager, information was entered into an IBM SPSS Statistics version 26 (IBM Corporation, Armonk, NY, USA) database about the service, including staffing, types of services provided and accessibility of the CSS. Similarities and differences between and within models were examined.
Information from the case study participants’ interviews was entered into an SPSS database, alongside data relating to (1) primary and secondary outcomes extracted from the medical records, (2) characteristics of the CSS and (3) service use over 12 months. Summary statistics relating to both the background characteristics of participants and quantitative outcomes were produced, along with histograms to enable assessment of normality so that appropriate statistical tests could be employed.
A range of indicators was used to measure the relative effectiveness of the four Health Service Models, and each indicator was analysed separately. First, the models were compared with respect to the primary outcome variable (the six-item HSI, score 0–6) using analysis of variance (ANOVA). An in-depth comparison was then performed using appropriate regression techniques to explore associations between the HSI and demographic, background and health profiles of participants. The model type was entered as a dummy variable. The four models were then compared for each of the secondary outcomes. The prevalence of each of the SHCs was compared across the models using the chi-squared test. The analysis of each SHC then proceeded using just the subgroup having the relevant condition. Each of the five dichotomous SHC outcomes within each SHC was compared across the four models using the chi-squared test.
Each of the continuous outcome variables [physical component score (PCS) and mental component score (MCS) of the SF-8, the SWEMWBS, and service user satisfaction with the CSS] was compared between the four models at baseline, and changes from baseline to 8 months were calculated and compared by model type. Stepwise linear regression modelling was performed to adjust for other factors (such as personal characteristics, length of time using the CSS and service features of the CSS) when comparing the four models. This was carried out initially at baseline to include as many service users as possible, and at 8 months using changes when available.
Differences in outcomes between models were investigated in relation to the contexts and mechanisms of care to seek understanding of the reasons underlying the patterns observed. Quantitative information was triangulated with data from qualitative interviews with case study participants and staff about accessing health and other services. Satisfaction of the case study participants with the CSS was compared with satisfaction of the general population with their GP, using data from the GP Patient Survey.
Comparisons were made between oral health status and receipt of dental care across the four models, and their extent of integration with primary dental care services. Comparisons were also made between access to dental care and impact on self-reported oral health status and OHRQoL, dental anxiety and satisfaction. Receipt of dental care by the four models was compared with local and national populations’ access to primary dental care, using national NHS statistics.
Qualitative analysis
Qualitative data from the interviews with case study participants, and with CSS staff and other agencies were entered as separate projects into NVivo (QSR International, Warrington, UK). For the case study participants, qualitative data were first transcribed from the completed interviews into templates using Microsoft Word (Microsoft Corporation, Redmond, WA, USA). Nodes were then created for each open-ended question at baseline and at 8 months covering participants’ views and experiences of the CSS. This information was examined in more detail, with reference to the mechanisms listed in the framework for this evaluation (see Table 1). Themes were identified; these are presented in Chapter 12. For CSS staff and other agencies, nodes were created for each of the context factors and mechanisms identified in the evaluation framework, and their interviews coded accordingly. Data were examined in detail; themes are presented in Chapter 11. The integration scores of CSS staff and other agencies were entered into Microsoft Excel® (Microsoft Corporation) spreadsheets, and are also summarised in Chapter 11.
Economic analysis
The resource implications of providing health care to people who are homeless were explored at two levels. First, information on staff, facilities and services provided by each CSS was assembled from interviews with service managers and documentary evidence (see Report Supplementary Material 9), and compared descriptively. Second, a micro-costing exercise at the level of case study participants was performed. Data on service use over the 12-month study period were collected from medical records, including general practice records that were shared with the Mobile Teams. In addition, participants were asked to recall service use over the previous 4 months at each interview (i.e. baseline and 4 and 8 months). Self-report data were cross-checked for consistency with data from medical records when relevant and used to provide information on items not routinely available from records, such as contacts with key workers, local authority housing and welfare officers, personal care workers and volunteer supporters. Hence, as complete an account as possible was assembled of participants’ use of health and other services over 12 months. Data originally recorded in 4-month periods were amalgamated for analysis.
Service use was valued using national tariffs107 at the individual-participant level to provide a cost by service use item, and by groups of items (e.g. all general practice, all out-of-hours services, all in-hospital stays) over 12 months. Associations between use of out-of-hours services (e.g. A&E, NHS walk-in/urgent care clinics, NHS 111, ambulance call-out), hospital admissions and Grand Total Costs (dependent variables) and participant characteristics (i.e. age, gender, ethnicity, medical conditions, housing status, health status, social support), and Health Service Models were explored through regression analysis. Service use was considered in relation to other outcomes reflecting participants’ health, well-being and CSS satisfaction.
Patient and Public Involvement
Patient and Public Involvement (PPI) was an integral part of the study from the outset and was led by two research team members. An initial PPI group of four people who had experienced homelessness worked with the research team in preparing the study proposal. Some had worked with team members on other studies. They made valuable contributions about research questions that should be addressed, and ways information should be collected. Their suggestions were incorporated into the study design. They commented on draft questionnaires and the content and phrasing of participant information sheets. They also contributed to SSC meetings, and commented on the study’s findings.
Besides an advisory role, PPI members undertook interviews with people in hostels and day centres who were homeless but not accessing the CSSs. A training day covered the role of peer interviewers, the interview process, obtaining consent, managing difficult or sensitive topics, personal safety and data security. Completion of training and a Disclosure and Barring Service check were required before a peer interviewer could commence fieldwork. The research team arranged interview dates with service providers, and accompanied PPI members to all sites. The peer interviewers explained the study to potential participants, checked eligibility and gained consent to take part. Using a structured questionnaire, they then collected the necessary information, working alone or accompanied by a research team member for support.
Feedback during and after each fieldwork session and three half-day reflection sessions allowed the interview process to be reviewed, and allowed discussions of what went well or was challenging. Peer interviewers were enthusiastic and committed. They welcomed learning about homelessness and services, spending time with the research team and contributing to the study. Early into interviewing at the first site, they requested more information for additional context about the study sites in which people were being interviewed. They were remunerated and expenses were covered.
Challenges regarding Patient and Public Involvement
Several challenges arose regarding PPI. There were several delays to the study and fieldwork lasted much longer than initially intended. Consequently, some PPI members were unable to commit to the study throughout, including a few who obtained paid employment and no longer had time to also work on the study, and another who developed health problems. Various methods were used to recruit new members. Research staff attended an external advisory group of people with experience of homelessness to discuss the study and explore their interest, and negotiated the possibility of building this work into an apprenticeship scheme run by a homelessness sector organisation. Two people remained PPI members from May 2016 to the end of the study.
The research team was aware that payments to PPI members may affect their welfare benefit entitlements. They were given contact details for a benefits advice service for members of the public involved in NIHR research109 that could explain whether and how their welfare benefits would be affected. Two PPI members subsequently withdrew from the study as payment would negatively affect their situation. Those who continued with the study were employed through King’s Talent Bank or were self-employed.
There were some difficulties arranging interview dates with hostel and day centre staff, and staff changes and sick leave within the research team led to long gaps between fieldwork days. Thus, peer interviewing took place over 10 days between October 2016 and May 2019. It proved hard at times to meet the expectations of the PPI members, particularly when they were relying on the income. They consequently met with the research team periodically to discuss the study progress, particularly when there were delays in progressing fieldwork. Further details about PPI have been published. 110 The next chapter summarises the mapping of specialist primary health care services.
Chapter 4 Mapping of specialist primary health care services
This chapter summarises the key findings of the first phase of the study: a mapping exercise across England of specialist primary health care services for single people who are homeless, undertaken between October 2015 and March 2017. Specialist primary health care services were defined as those that (1) worked primarily with single people who were homeless or (2) served the general population, but provided enhanced or targeted services to single people who were homeless, such as general practices that ran clinics in hostels. The survey did not include general practices that provided GMS to people who were homeless, but did not have targeted or additional services or clinics for them. It also did not include specialist services that were not part of primary health care teams. The methodology and findings are described in detail in three published reports. 21,111,112
Models of specialist primary health care services
The mapping exercise identified 123 specialist primary health care services in England for single people who are homeless. Some operated from a ‘fixed’ site, whereas some were mobile teams that ran clinics in hostels and day centres. Some were primarily for people who were homeless, whereas others delivered targeted services to this group, but also provided health care to the general population. Most involved a team of workers, although, in a few instances, a single nurse worked at a hostel or day centre. Some were reliant on volunteers and charitable funding.
The 123 specialist services were classified into six models, plus a seventh which encompassed ‘other medical/nursing arrangements’ (Table 5). Some of the services in this seventh model were run by social enterprises and commissioned by local CCGs. Nearly three-quarters of services were specialist health centres, or general practices with homeless services. The former worked primarily with people who were homeless and tended to have far fewer patients than the latter. They were also more likely to provide on-site specialist services such as drug and alcohol clinics, and housing or financial advice sessions. Specialist health centres were less likely, however, to offer extended opening hours. These centres and general practices with homeless services offered GP registration, but this was not generally the case for other models.
| Types of models | Service delivered from fixed health site | Outreach clinic(s) at hostels or day centres | Primarily for people who are homeless | Has two or more health workers | Provides GP registration | Number of services |
|---|---|---|---|---|---|---|
| 1. Specialist health centre | Yes | Most centres | Yes | Yes | Yes | 28 |
| 2. General practice with homeless services | Yes | Some practices | No | Yes | Yes | 61 |
| 3. Mobile homeless health team | No | At multiple sites | Yes | Yes | Not usually | 12 |
| 4. Single-handed mobile homeless nurse | No | At multiple sites | Yes | No | No | 4 |
| 5. Nursing service based at hostel or day centre | No | At one site | Yes | Not usually | No | 7 |
| 6. Volunteer health care service | No | One or multiple sites | Yes | Some services | No | 5 |
| 7. Other medical/nursing arrangements | No | At one site | No | Yes | Not usually | 6 |
The 123 specialist primary health care services were spread across the then-five NHS England regions (North, Midlands and East, London, South East, and South West). There were clusters in London and in the North region around Greater Manchester and Merseyside, and a single such service was found in several coastal areas in the South West and South East regions. Relatively few services were identified in the northern part of the NHS North region, and in parts of the NHS Midlands and East region. They were mainly located in urban areas where there were concentrations of people who were homeless, and hostels and day centres for this population. Few specialist primary health care services were identified in rural areas, although a few mobile homeless health teams were based in urban areas and covered market towns.
Summary
This chapter summarises the types of specialist primary health care services identified during the mapping exercise. Their distribution varied greatly, and most were in urban areas. The majority fitted into one of three broad models, namely specialist health centres, general practices with homeless services and mobile homeless health teams. These are comparable to the models described in the 2010 DH report,13 although several other smaller services were revealed that were not mentioned in the DH report.
Regardless of the model, the specialist primary health care services shared some common characteristics. They provided easily accessible and flexible services that reached out to people who were homeless. Most offered either drop-in sessions at their service and/or ran clinics at hostels and day centres. Many provided integrated care together with other health and social care providers. The mapping exercise informed the selection of Health Service Models and CSSs for the HEARTH study, which are described in the next chapter.
Chapter 5 Characteristics of the Health Service Models and Case Study Sites
The previous chapter summarised specialist primary health care services in England for people who are homeless. This chapter describes in more detail the characteristics of the four Health Service Models that were selected for the evaluation (Dedicated Centres, Mobile Teams, Specialist GPs, and Usual Care GPs), and the CSSs within these models. There are few examples of some models in England; therefore, it is necessary to limit some description to maintain anonymity. Information withheld includes NHS regions; number of registered patients; number and roles of CSS staff; availability of some specialist services at sites; and information about some work undertaken by CSSs, such as involvement in hospital services and number of clinics held separately in hostels and day centres. The following descriptions provide an overview of each model and each CSS; their characteristics are summarised in Table 6.
| Characteristics | Dedicated Centres | Mobile Teams | Specialist GPs | Usual Care GPs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DC1 | DC2 | MT1 | MT2 | SP1 | SP2 | UC1 | UC2 | UC3 | UC4 | |
| Operation of CSS | ||||||||||
| Fixed site: health centre, general practice | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Number of patients registereda | > 1000–2500 | > 500–1000 | < 200 | > 1000 | > 10,000 | > 5000–10,000 | > 15,000 | > 15,000 | > 15,000 | > 10,000–15,000 |
| Number of patients registered who are homelesa | > 1000–2500 | > 500–1000 | < 200 | > 1000 | > 500–1000 | < 500 | < 50 | > 500–1000 | < 500 | < 50 |
| Primarily for people who are homeless | Yes | Yes | Yes | Yes | No | No | No | No | No | No |
| Provides permanent GP registration | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Open Monday to Friday | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Open Saturday | No | No | No | No | No | No | Yes | No | Yes | Yes |
| Arranges GP out-of-hours cover | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Methods used by CSS staff to engage with people who are homeless | ||||||||||
| Designated GPs working primarily with people who are homeless | Yes | Yes | No | No | No | No | No | No | No | No |
| Designated nurses working primarily with people who are homeless | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No |
| GP/nursing clinics held at CSS primarily for people who are homeless | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No |
| Drop-in sessions or same-day appointments available at CSS | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Number of clinics held at least weekly by GPs/nurses in hostels, day centres and similar | 6 | 0 | 16 | 17 | 10 | 2 | 0 | 0 | 0 | 0 |
| Outreach work by CSS staff on streets | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No |
| CSS staff involved in hospital inpatient/discharge work for people who are homeless | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No |
| Services available at CSS (provided by CSS staff or sessional workers) | ||||||||||
| General primary health care, including acute disease management | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Chronic disease management, including wound care | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mental health treatment/counselling by specialist practitioners | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Drug treatment/support by specialist practitioners | Yes | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Alcohol treatment/support by specialist practitioners | Yes | Yes | No | No | Yes | No | Yes | No | Yes | No |
| Smoking cessation | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Routine blood tests | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Social and welfare services, for example help with housing, social problems or financial difficulties | Yes | Yes | No | No | Yes | Yes | No | No | No | No |
Dedicated Centres
The Dedicated Centre model was represented by two CSSs [Dedicated Centre (DC) 1 and DC2]. Both had existed for many years and had developed substantially over time. They were located in large cities that had a substantial problem of homelessness, and were relatively close to several hostels and day centres for people who are homeless. Their catchment area was citywide. Both had a practice manager, GPs, practice nurses, and reception and administrative staff. Most staff had considerable experience of working with people who were homeless. DC1 had a full-time primary mental health nurse, whereas the community mental health team worked part time at DC2. Substance misuse workers held sessions most days at the sites, but were not employed by the CSS. Both sites had additional specialist workers, but these cannot be identified to maintain anonymity.
Both sites were part of an NHS trust and operated in similar ways. DC1 held a contract as an APMS; DC2 also held a special contract. They were open Monday to Friday, and were covered by a GP out-of-hours service. Both offered permanent GP registration. In contrast to many mainstream general practices, the caseloads of the CSSs were relatively small.
DC2 mainly focused on single people who were homeless, whereas DC1 also provided care to asylum seekers and refugees. Neither site provided registration to the general population, and once patients were rehoused and settled, they were assisted to register with mainstream general practices services. The sites offered booked appointments at the practice and a same-day drop-in service. The duration of appointments tended to be longer than at mainstream general practices, for example DC2 allocated 20-minute appointments, instead of the customary 10 minutes.
Dedicated Centres provided GMS, including management of acute and chronic illnesses, smoking cessation, immunisations and vaccines, treatment for infestations and referral to secondary health care services. They also provided mental health care and counselling, and access to community alcohol detoxification programmes and drug treatment, including opioid substitution treatment (OST). CSS staff conducted street outreach at least monthly to engage with rough sleepers and encourage them to access services. Staff at DC1 also visited drop-in centres regularly to encourage registration. At both sites, nurses or health support workers visited day centres and hostels at intervals to deliver influenza vaccination programmes and health promotion. Staff accompanied patients to hospital appointments if necessary, and helped them access housing and welfare benefits services. Daily staff meetings were held at both sites to discuss patients, and regular staff training took place.
Mobile Teams
The Mobile Team model was represented by two CSSs [Mobile Team (MT) 1 and MT2], which had been in operation for several years. They were based in urban areas with a substantial number of people who were homeless, and several hostels and day centres for this population. Both teams were funded by the NHS to run clinics and deliver health care in these settings. They worked Monday to Friday.
The Mobile Teams mainly comprised specialist nurse practitioners with considerable experience of working with people who were homeless, and some were non-medical prescribers. They received some administrative support, and input from mental health practitioners. They worked closely with local general practices, and some joint work in hostels was undertaken by MT1. They provided health care to people who were homeless, to asylum seekers and refugees, and to people with no recourse to public funds. MT1 also offered health care to people who were housed, but who attended homelessness sector day centres for support.
Neither team provided GP registration, and patients were encouraged by the CSS nurses to register with local general practices. This meant that patients could receive health care from both a GP and the Mobile Team. Those registered with a GP received an out-of-hours service through the general practice. Caseloads were reviewed periodically by the Mobile Teams, and cases were closed once care was complete or if contact had been lost. Their caseloads tended to be small (see Table 6).
Services provided by the Mobile Teams differed from those provided by other models. Much of their work concerned assessing the health needs of patients, and linking them to local services, including general practices and drug or alcohol agencies. Occasionally, nurses accompanied a patient to appointments if there was an urgent need, or if the person was not engaging with services. They were less involved in acute disease management other than ensuring that patients were seen by a GP or at a hospital if necessary. They undertook health promotion, longer-term care for conditions such as leg ulcers, and routine blood tests.
The Mobile Teams held drop-in nursing clinics in hostels or day centres on set days and at fixed times. The frequency of clinics ranged from 1 to 5 days a week, and each lasted 2–4 hours. The offices where the Mobile Teams were based did not have facilities for patient care. The spaces available to see patients in hostels and day centres ranged from well-equipped clinical rooms to rooms used by other services, or simply a screened area in a drop-in centre or hostel sitting room. Access to a consultation with a nurse was primarily through a list held by hostel or day centre staff, or by the nurse actively seeking out individuals during a clinic. The Mobile Teams conducted frequent street outreach to engage with people sleeping rough.
Specialist GPs
The Specialist GP model was represented by two CSSs [Specialist GP (SP) 1 and SP2]. Both were in urban areas with high rates of homelessness and had been operating for several years. They were mainstream general practices delivering health care to the housed population, as well as additional or enhanced services to people who were homeless. Hence, the total number of patients registered at these practices was considerably higher than that of the Dedicated Centres and Mobile Teams, but the number of patients who were homeless was comparable. One site had more than 10,000 registered patients, of whom an estimated 850 were homeless. The other had between 5000 and 10,000 patients, of whom around 300 were homeless.
Unlike other models, there were noticeable differences between the two CSSs in the Specialist GP model. Both had GPs; practice nurses; HCAs; and reception, administrative and information technology (IT) staff. Two GPs at each site had a special interest in homelessness, although they worked with all patients. At SP1, some practice nurses worked primarily with patients who were homeless, and non-clinical team members provided case management to those with complex health and social care needs. At SP2, nursing care was delivered by practice nurses who worked with both patients who were housed and those who were homeless.
Both CSSs were funded by the NHS, and held additional contracts for their work with patients who were homeless. They were open Monday to Friday, and were covered by a GP out-of-hours service. Besides booked appointments, SP1 offered drop-in sessions for people who were homeless three times a week. At SP2, drop-in sessions were provided daily for all patients. The CSSs provided general primary health care, management of acute and chronic conditions, wound care, and immunisations and vaccines. Both had input from sessional mental health workers. At SP1, drug and alcohol workers also held clinics on a sessional basis, and provided community alcohol detoxification and drug treatment, including OST and needle exchange. At SP2, drug and alcohol treatment was not available on the premises; patients were referred to local substance misuse services.
Both sites held clinics in hostels and day centres for people who were homeless, although the frequency of these varied. SP1 held several nursing clinics each week at these services, and visited other sites to engage with service users who were not accessing health care. Staff also undertook street outreach with other agencies. At SP2, clinics were held twice weekly by GPs at homelessness services (see Table 6).
Usual Care GPs
The Usual Care GP model was represented by four CSSs [Usual Care GP (UC) 1, UC2, UC3 and UC4]. They were mainstream general practices delivering primary health care to the general population, which, by default, included people who were homeless. Unlike Specialist GPs, they did not provide special services or have dedicated staff for patients who were homeless. Three sites had caseloads of more than 15,000 patients, the fourth had slightly fewer. The proportion of patients who were homeless ranged from 0.04% to 5.4%. All had a PMS or APMS contract, and all except UC1 received additional funding to work with patients who were homeless (UC1 received funding for work with patients with substance misuse problems).
All were open Monday to Friday, and three also opened on Saturdays (see Table 6). When closed, a GP out-of-hours service provided cover. All provided permanent GP registration, and pre-booked and same-day appointments. They employed a range of staff associated with the running of a general practice, including GPs; practice nurses; HCAs; and reception, administrative and IT staff. Unlike the other models, they either employed a non-dispensing pharmacist or had a pharmacist providing sessional services. The pharmacists dealt with prescription queries, undertook medication reviews with patients and reviewed prescribing practices. The use of clinical pharmacists in general practice was introduced as a pilot scheme in 2015, and became part of the funding framework for general practices in 2019. Hence, they were not in operation when Dedicated Centres and Specialist GPs were recruited.
All four CSSs provided general primary health care, including management of acute and chronic diseases, smoking cessation services and routine blood tests. Sessional workers provided specialist services at the CSSs, although this varied between sites. Drug and alcohol services, including OST, were provided at UC1 and UC3 by GPs through shared care with local drug services. At UC2, a similar long-standing arrangement had ended because of funding cuts, and the drug service took over all care. UC1 and UC4 employed a mental health nurse; UC3 had input from mental health practitioners on a sessional basis. Only UC2 offered no on-site specialist mental health care.
All except UC1 held registers of patients who were homeless. UC2 and UC3 used a computer-based ‘homeless template’, which prompted clinicians to ask about specific issues when a patient attended an appointment, such as alcohol consumption. No sites held clinics in hostels or day centres for people who were homeless, but UC3 visited local hostels annually to encourage residents to attend a homeless health check. UC2 was close to a hostel and in regular communication with hostel staff.
Summary
This chapter summarises the various ways in which the four Health Service Models delivered health care to people who were homeless. There were marked differences in the sizes of the practices, the ways in which they operated, the services provided and their patient populations. These differences will be considered when evaluating the effectiveness of the models in delivering health care to people who are homeless. The next chapter describes the patients of these models who agreed to be case study participants.
Chapter 6 Characteristics of case study participants
This chapter describes the characteristics of the 363 case study participants. It first summarises their demographic and socioeconomic circumstances at baseline, including history of homelessness and living arrangements, and differences by Health Service Model. It then describes their health problems and use of alcohol and drugs, and length of time they had been registered with the CSS. The subsequent section summarises their accommodation throughout the study period. Finally, differences by CSSs within the same Health Service Model are examined. Information for this chapter relies mainly on participants’ reports.
Sex, age and ethnicity
Four-fifths (80.2%) of participants were male and 19.8% were female. A slightly higher proportion (90.7%) of Usual Care GP participants were male; some were recruited at hostels specifically for men. The average age of participants was 41.6 years, with little difference by Health Service Model. Just 13.2% were aged 18–29 years, and only 5.2% were aged 60 years and over.
Almost three-quarters (73.4%) were White British or Irish; the remainder were mainly black or Black British, or other white background. Of the 74 who were born abroad, most had been living in the UK for years: 51% for more than 10 years, and just 10.8% for less than 5 years. Nineteen participants born outside the UK had gained British citizenship; 32 were European migrants, and eight were asylum seekers. There were statistically significant differences by Health Service Model (Table 7). Mobile Teams served a markedly lower percentage of UK-born clients, which partly reflects the CSS locations.
| Characteristics | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Male, n (%) | 291 (80.2) | 77 (80.2) | 75 (78.1) | 71 (74.0) | 68 (90.7) | Chi-squared: 0.051 |
| Age (years), mean (SD) | 41.6 (10.5) | 39.8 (9.8) | 43.0 (11.3) | 41.1 (9.9) | 42.6 (11.0) | ANOVA: 0.147 |
| Ethnicity, n (%) | ||||||
| White British/Irish | 265 (73.4) | 79 (82.3) | 47 (49.5) | 88 (92.6) | 51 (68.0) | Chi-squared: < 0.0005 |
| Other white background | 32 (8.9) | 5 (5.2) | 24 (25.3) | 1 (1.1) | 2 (2.7) | |
| Asian or Asian British | 11 (3.0) | 2 (2.1) | 5 (5.3) | 0 (0.0) | 4 (5.3) | |
| Black or Black British | 26 (7.2) | 5 (5.2) | 9 (9.5) | 2 (2.1) | 10 (13.3) | |
| Other ethnic group | 27 (7.5) | 5 (5.2) | 10 (10.5) | 4 (4.2) | 8 (10.7) | |
| Migration status, n (%) | ||||||
| Born in UK/British citizen | 309 (86.1) | 88 (92.6) | 59 (62.1) | 94 (98.9) | 68 (91.9) | Grouping EU migrant/asylum seeker/refugee/other: chi-squared: < 0.0005 |
| EU migrant | 32 (8.9) | 4 (4.2) | 24 (25.3) | 1 (1.1) | 3 (4.1) | |
| Asylum seeker | 8 (2.2) | 1 (1.1) | 5 (5.3) | 0 (0.0) | 2 (2.7) | |
| Refugee | 2 (0.6) | 1 (1.1) | 1 (1.1) | 0 (0.0) | 0 (0.0) | |
| Other | 8 (2.2) | 1 (1.1) | 6 (6.3) | 0 (0.0) | 1 (1.4) | |
| Born in the UK, n (%) | 289 (79.8) | 83 (86.5) | 53 (55.2) | 92 (96.8) | 61 (81.3) | Chi-squared: < 0.0005 |
| No recourse to public funds, n (%) | 23 (6.4) | 5 (5.2) | 14 (15.2) | 0 (0.0) | 4 (5.4) | Chi-squared: 0.000 |
| Had an income,a n (%) | 315 (87.0) | 88 (92.6) | 68 (70.8) | 86 (89.6) | 73 (97.3) | Chi-squared: < 0.0005 |
| Weekly income (£), median (IQR) | 100 (62–125) | 95 (70–125) | 80 (0–125) | 103 (60–125) | 104 (73–150) | Kruskal–Wallis: 0.044 |
| Involved in education, training or employment, n (%) | 53 (14.6) | 15 (15.6) | 17 (17.7) | 10 (10.4) | 11 (14.7) | Chi-squared: 0.537 |
| Support from family/friends, n (%) | 175 (48.9) | 49 (52.1) | 40 (42.6) | 49 (51.0) | 37 (50.0) | Chi-squared: 0.548 |
| Years homeless, median (IQR) | 5.5 (2.5–12) | 5.5 (2.2–11) | 5.7 (2–11.4) | 5.1 (2.4–12.5) | 6.5 (3–12.5) | Kruskal–Wallis: 0.478 |
| Accommodation at baseline, n (%) | ||||||
| Hostel with staffb | 189 (52.1) | 34 (35.4) | 41 (42.7) | 61 (63.5) | 53 (70.7) | Chi-squared: < 0.0005 |
| Own tenancy | 28 (7.7) | 12 (12.5) | 4 (4.2) | 7 (7.3) | 5 (6.7) | |
| Sleeping roughc | 77 (21.2) | 26 (27.1) | 40 (41.7) | 9 (9.4) | 2 (2.7) | |
| Other temporary housingd | 69 (19.0) | 24 (25.0) | 11 (11.5) | 19 (19.8) | 15 (20.0) | |
| Time at baseline housing (months), median (IQR) | 4 (1.5–8.7) | 3 (1–6) | 2.5 (1–7) | 5 (2–10) | 7 (4–15) | Kruskal–Wallis: < 0.0005 |
Employment status, income and social support
At baseline, 14.6% of participants were in education, training or employment, with no difference by Health Service Model. This included 2.5% employed full or part time. Most were in receipt of an income, nearly all through state benefits (see Table 7). Seven-tenths (70.7%) received Employment and Support Allowance, for people below state pension age with a health condition or disability affecting their ability to work. One-fifth (20.2%) received Personal Independence Payment, payable to people with a health condition or disability for 3 months, who have difficulties with daily living activities or mobility, and expect these difficulties to continue for at least 9 months. A small percentage (5.8%) were seeking work and receiving Jobseeker’s Allowance.
Thirteen per cent had no income when first interviewed, including a significantly higher percentage (29.2%) of Mobile Team participants (see Table 7). Many without an income were European migrants or asylum seekers. Overall, 6.4% had no recourse to public funds, including 15.2% of Mobile Team participants. For others, state benefits had stopped because they did not comply with regulations associated with receipt of benefits, or because their circumstances had changed which had led to administration problems. Participants without an income were mainly sleeping rough or staying in night shelters that do not require rent.
At baseline, 48.9% of participants had received support from family or friends during the last 4 months, with no difference by Health Service Model. This support was mainly provided by a friend, mother or partner.
History of homelessness and accommodation at baseline
It is difficult to collect accurate details of the length of time people have been homeless, as ‘homelessness’ is often not a continuous state. Many people who are homeless frequently move between sleeping rough, hostels, night shelters, bed-and-breakfast hotels, sofa surfing and other insecure housing. Some have experienced repeated episodes of homelessness interspersed with stays in prison. At baseline, the median length of time participants had been homeless continuously or intermittently was 5.5 years, but this ranged from less than 1 year (9.2%) to 25 or more years (5.8%). There were no significant differences by Health Service Model (see Table 7).
At baseline, 52.1% were staying in a hostel or supported accommodation with 24-hour or part-time staff, and 21.2% were sleeping rough on the streets, in tents or vehicles, or in buildings not designed for habitation, such as squats and night shelters. The night shelters were mainly church halls, which opened only at night and required people to leave during the day. Among the remaining participants, 7.2% were sofa surfing, 11.8% were in bed-and-breakfast hotels or other temporary accommodation and 7.7% had a tenancy. There were significant differences by Health Service Model (see Table 7). Participants of Specialist GPs and Usual Care GPs were more likely to be in hostels or supported accommodation with staff. Those using Dedicated Centres and Mobile Teams were more likely to be sleeping rough. More than two-fifths (43.3%) had been in their last accommodation 3 months or less, including 22.9% for 1 month or less. Usual Care GP participants had been in their accommodation the longest; the difference was statistically significant (see Table 7).
Physical and mental health problems
At baseline, 94.8% of participants reported physical health problems. This high proportion is to be expected as the inclusion criteria meant that participants needed to have been a patient of the CSS for at least 4 months, and had at least one consultation with a CSS doctor or nurse during this time. Common problems included respiratory disease, gastric or intestinal problems, and arthritis or other musculoskeletal problems, and just over one-fifth (21.9%) had hepatitis C (see Appendix 1, Table 46). There were strong associations between alcohol misuse and problems such as gastritis, liver problems, blackouts and fits. Likewise, there were strong associations between injecting illegal drugs and hepatitis C, thrombosis and leg ulcers.
Nine-tenths of participants reported mental health problems at baseline, most commonly depression, anxiety and panic attacks (Table 8). Personality disorder or behaviour problems, such as anger management problems, were mostly reported by those aged 18–29 years (47.9%, compared with 21.1% overall). Usual Care GP participants were more likely than other participants to report bipolar disorder and schizophrenia or hearing voices. This may be related to sampling: some Usual Care GP participants were recruited at hostels exclusively for people with mental health problems.
| Mental health problems | Health Service Model, n (%) | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Any mental health problema | 329 (91.1) | 88 (91.7) | 79 (84.0) | 88 (91.7) | 74 (98.7) | Chi-squared: 0.011 |
| Depression | 293 (82.1) | 79 (83.2) | 74 (79.6) | 82 (86.3) | 58 (78.4) | Chi-squared: 0.509 |
| Anxiety/panic attacks | 197 (54.6) | 46 (48.4) | 50 (52.1) | 57 (59.4) | 44 (59.5) | Chi-squared: 0.348 |
| Bipolar disorder | 35 (9.8) | 6 (6.3) | 12 (12.5) | 5 (5.3) | 12 (16.7) | Chi-squared: 0.045 |
| Post-traumatic stress disorder | 42 (11.7) | 7 (7.4) | 10 (10.4) | 11 (11.6) | 14 (18.9) | Chi-squared: 0.131 |
| Obsessive compulsive disorder | 37 (10.2) | 15 (15.8) | 2 (2.1) | 10 (1.4) | 10 (13.5) | Chi-squared: 0.012 |
| Phobias | 26 (7.2) | 5 (5.3) | 7 (7.3) | 9 (9.5) | 5 (6.8) | Chi-squared: 0.732 |
| Schizophrenia/hearing voices | 85 (23.8) | 14 (15.1) | 21 (21.9) | 25 (26.3) | 25 (34.2) | Chi-squared: 0.031 |
| Paranoia/psychosisb | 14 (3.9) | 3 (3.2) | 1 (1.0) | 6 (6.3) | 4 (5.4) | No valid test |
| Personality disorder/behaviour problemsc | 75 (21.1) | 23 (24.2) | 18 (19.4) | 19 (20.0) | 15 (20.5) | Chi-squared: 0.848 |
Alcohol use
Alcohol consumption among participants varied greatly. When asked at baseline about their frequency of drinking alcohol over the preceding 4 months, 35.1% reported no alcohol, whereas 28.5% had consumed alcohol almost daily. Some drank heavily for a few days when they received their state benefits, followed by days of abstinence when they had no money, or had episodes of binge drinking lasting several days or weeks. A small percentage (5.2%) had no alcohol in the previous 4 months, but were recovering from an alcohol problem. Slightly more men than women (30% vs. 22.2%) reported drinking alcohol almost daily.
One-third of participants drank super-strength lagers or strong cider, including some that had 9% alcohol by volume, and 17.1% drank spirits. Using participant information about the type and amount of alcohol consumed on a typical day when drinking, the weekly number of units of alcohol consumed was estimated. Twenty-one per cent were drinking more than 100 units weekly. The National Institute for Health and Care Excellence (NICE)113 describe (1) ‘lower risk drinking’ as up to 14 units weekly for men and women; (2) ‘hazardous drinking (increasing risk)’ as 15–34 units weekly for women and 15–49 units weekly for men; and (3) ‘harmful drinking (high risk drinking)’ as 35 or more units weekly for women and 50 or more units weekly for men. By these guidelines, 11.3% of the HEARTH study participants had hazardous drinking patterns and 31.9% were harmful drinkers. Participants of Usual Care GPs were more likely than other groups to be hazardous or harmful drinkers (54.2%), although the findings were not statistically significant (Table 9).
| Alcohol use in previous 4 months | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Pattern of drinking according to NICE 113 classification (N = 345) | ||||||
| No alcohol, n (%) | 121 (35.1) | 35 (39.8) | 35 (38.0) | 34 (36.6) | 17 (23.6) | Chi-squared: 0.163 |
| Lower-risk drinking,a n (%) | 75 (21.7) | 17 (19.3) | 23 (25.0) | 19 (20.4) | 16 (22.2) | |
| Hazardous drinking,b n (%) | 39 (11.3) | 10 (11.4) | 6 (6.5) | 8 (8.6) | 15 (20.8) | |
| Harmful drinking,c n (%) | 110 (31.9) | 26 (29.5) | 28 (30.4) | 32 (34.4) | 24 (33.3) | |
| Units of alcohol consumed per week, median (IQR) | 6.75 (0–87.9) | 6 (0–77.7) | 3.1 (0–73.8) | 6.6 (0–91.5) | 17.8 (0.6–104) | Kruskal–Wallis: 0.345 |
| Drug misused in previous 4 months, n (%) | ||||||
| Misused drugs | 217 (60.1) | 59 (62.1) | 44 (45.8) | 67 (69.8) | 47 (63.5) | Chi-squared: 0.006 |
| Used cannabis only | 48 (13.3) | 9 (9.5) | 12 (12.5) | 8 (8.3) | 19 (25.7) | Chi-squared: 0.004 |
| Used Class A drugse | 146 (40.4) | 46 (48.4) | 23 (24.0) | 54 (56.3) | 23 (31.1) | Chi-squared: 0.000 |
| Injected drugs | 82 (23.2) | 31 (33.3) | 13 (13.5) | 32 (34.0) | 6 (8.5) | Chi-squared: < 0.0005 |
| Receiving OST | 125 (34.4) | 38 (39.6) | 19 (19.8) | 50 (52.1) | 18 (24.0) | Chi-squared: 0.000 |
Drug misuse
At baseline, 60.1% of participants (62.5% of men and 48.6% of women) reported drug misuse in the preceding 4 months, that is the use of illegal drugs or misuse of prescription or over-the-counter drugs. A further 7.2% were recovering from a drug problem, but had been abstinent in the previous 4 months. One-quarter (25.6%) had taken drugs most days over the preceding 4 months. The most used drugs were cocaine or crack cocaine (36.7%), heroin (32.1%), cannabis (29.9%) and spice (8.3%); 16.1% had used at least three different types of drugs, and 40.4% had used one or more Class A drugs [e.g. heroin, morphine, cocaine, lysergide (LSD) or ecstasy] (see Table 9). Just over one-third were receiving OST, mainly methadone. A further 4.7% commenced OST as the study progressed.
Mobile Team participants were less likely than the other three cohorts to report drug usage (see Table 9). Usual Care GP participants were more likely to have used cannabis only, whereas higher percentages of Specialist GP and Dedicated Centre participants reported using Class A drugs, injecting drugs and receiving OST.
Registration at Case Study Sites
The date of participants’ registration with the CSS, or the date they started using the service (for Mobile Team participants), was obtained from the medical records. This included the date of the most recent registration or use of service for those who had been registered or a service user previously. Overall, 54% had been registered or using the CSS for more than 1 year at baseline, and 26.4% had been a patient for less than 6 months. There were no statistically significant differences between models (Table 10).
| Length of time registered | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Years registered, median (IQR) | 1.29 (0.48–2.89) | 1.31 (0.39–3.71) | 1.23 (0.42–2.82) | 1.23 (0.52–2.36) | 1.36 (0.57–3.55) | Kruskal–Wallis: 0.650 |
| > 1 year, n (%) | 196 (54.0) | 52 (54.2) | 53 (55.2) | 50 (52.1) | 41 (54.7) | Chi-squared: 0.975 |
| < 6 months, n (%) | 96 (26.4) | 31 (32.3) | 26 (27.1) | 23 (24.0) | 16 (21.3) | Chi-squared: 0.389 |
| < 4 months, n (%) | 50 (13.8) | 16 (16.7) | 16 (16.7) | 8 (8.3) | 10 (13.3) | Chi-squared: 0.289 |
Accommodation during study
The potential study period for each participant was 12 months, that is the 4 months preceding their baseline interview, and the subsequent 8 months. Information about their accommodation during this time was available for most (90.6%), with no statistically significant differences by Health Service Model (Table 11).
| Accommodation | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Length of time for which information is available (N = 363) | ||||||
| 4–6 months, n (%) | 14 (3.9) | 2 (2.1) | 6 (6.3) | 3 (3.1) | 3 (4.0) | Kruskal–Wallis: 0.184 |
| > 6–8 months, n (%) | 10 (2.8) | 1 (1.0) | 6 (6.3) | 2 (2.1) | 1 (1.3) | |
| > 8–10 months, n (%) | 10 (2.8) | 1 (1.0) | 3 (3.1) | 4 (4.2) | 2 (2.7) | |
| > 10–12 months, n (%) | 329 (90.6) | 92 (95.8) | 81 (84.4) | 87 (90.6) | 69 (92.0) | |
| Number of changes of accommodation (N = 363) | ||||||
| Mean (SD) | 2.29 (2.32) | 2.77 (2.61) | 2.55 (2.06) | 2.47 (2.48) | 1.13 (1.60) | ANOVA: 0.0005 |
| Median | 2.00 | 2.00 | 2.00 | 2.00 | 1.00 | |
| Percentage of time in building designed for habitation (N = 360) | ||||||
| Mean (SD) | 79.78 (30.62) | 78.61 (29.20) | 63.68 (37.20) | 83.01 (27.36) | 97.38 (10.30) | ANOVA: 0.0005 |
| Median | 100 | 97.33 | 76.37 | 100 | 100 | |
| Percentage of time in accommodation with 24-hour or part-time staff (N = 360) | ||||||
| Mean (SD) | 48.21 (39.07) | 35.94 (35.85) | 44.86 (36.69) | 50.71 (36.46) | 64.93 (43.32) | ANOVA: 0.0005 |
| Median | 45.83 | 24.58 | 43.17 | 51.08 | 100 | |
Information about accommodation during the study period was assembled for each participant to determine (1) the number of changes of sleeping settings, for example move from the streets to a hostel, or from a hostel to a bed-and-breakfast hotel or another hostel; (2) the percentage of time living in a building designed for habitation, such as a hostel, as opposed to the streets or a squat or church hall not designed for habitation; and (3) the percentage of time living in accommodation with 24-hour or part-time staff. Change of accommodation included episodes of 7 or more days in hospital, prison or a rehabilitation unit.
Just over one-quarter of participants (26.2%) remained in the same accommodation throughout the study, including 46.7% of Usual Care GP participants. In contrast, 26.2% moved four or more times, including 3.9% who changed accommodation at least eight times. There were strong significant differences between accommodation experiences during the study and Health Service Models (see Table 11). Usual Care GP participants spent a higher percentage of time in staffed accommodation, whereas the Dedicated Centre cohort had the highest average number of moves, and spent considerably less time in staffed accommodation. They were also more likely than other groups to have been in prison during the study (18.8%, compared with 11.4% overall; χ2 = 8.36; p = 0.039). Mobile Team participants spent longer than other groups sleeping on the streets or in makeshift arrangements, such as church halls.
Differences between Case Study Sites within a Health Service Model
There were some marked variations in participants’ characteristics by CSSs within the same Health Service Model (Table 12). MT2 participants were much less likely than those of MT1 to be British born
| CSS | Baseline, n (%) | Study period: % of time in accommodation with staff, mean (SD) | ||||
|---|---|---|---|---|---|---|
| British born/citizen | Sleeping rough/similara | Schizophrenia/hearing voices | Harmful drinkingb | Heroin and/or crack/cocaine use | ||
| Dedicated Centres | ||||||
| DC1 | 43 (91.5) | 16 (33.3) | 11 (24.4) | 10 (22.2) | 28 (59.6) | 23.9 (28.62) |
| DC2 | 45 (93.8) | 10 (20.8) | 3 (6.3) | 16 (37.2) | 17 (35.4) | 48.0 (38.51) |
| Mobile Teams | ||||||
| MT1 | 39 (83.0) | 10 (21.3) | 11 (23.4) | 19 (42.2) | 16 (34.0) | 57.9 (32.97) |
| MT2 | 20 (41.7) | 30 (61.2) | 10 (20.4) | 9 (19.1) | 7 (14.3) | 32.3 (35.99) |
| Specialist GPs | ||||||
| SP1 | 50 (98.0) | 5 (9.8) | 10 (20.0) | 16 (32.7) | 33 (64.7) | 49.3 (52.24) |
| SP2 | 44 (100) | 4 (8.9) | 15 (33.3) | 16 (36.4) | 21 (46.7) | 52.2 (35.34) |
| Usual Care GPs | ||||||
| UC1 | 28 (100) | 2 (7.1) | 4 (14.8) | 9 (33.3) | 15 (53.6) | 21.8 (32.81) |
| UC2 | 26 (89.7) | 0 (0) | 12 (41.4) | 13 (46.4) | 4 (13.3) | 93.7 (16.73) |
| UC3 | 12 (80.0) | 0 (0) | 9 (60.0) | 2 (13.3) | 4 (26.7) | 84.9 (35.15) |
| Totalc | 309 (86.1) | 77 (21.2) | 85 (23.8) | 110 (31.9) | 145 (40.2) | 48.21 (39.07) |
or have British citizenship, and were much more likely at baseline to be sleeping rough or in settings not designed for habitation. Such marked differences are likely to be related to MT2 participants’ lack of entitlement to welfare benefits, and thus inability to access hostels. At baseline, 24.4% of MT2 participants, compared with just 6.4% at MT1, had no recourse to public funds. There was little difference in overall reports of mental health problems, apart from across the Mobile Teams: such problems were reported by 95.6% of MT1 participants, compared with 73.5% from MT2. UC3 participants were more likely than the other two Usual Care GP sites to report having schizophrenia or hearing voices.
There was little difference in reports of alcohol drinking among CSSs within the same model, although ‘harmful’ drinking was more prevalent among MT1 than MT2 participants. Drug use varied greatly within models. Exceptionally high prevalence rates of heroin or cocaine usage were reported at DC1, MT1 and UC1, compared with other sites within these models (see Table 12). During the study, UC1 participants were much less likely than the other two Usual Care GP site participants to have spent time living in staffed accommodation. There were no marked differences between CSSs within a Health Service Model regarding number of years homeless, number of moves during the study or percentage of time in a building designed for habitation.
Summary
This chapter summarises the characteristics of case study participants. Self-reports of physical health, mental health and substance misuse problems were prevalent. This partly reflects the study sample, which was drawn from users of health services, although it is well documented that health and substance misuse problems are common among people who are homeless. There were several differences in participants’ characteristics between the four Health Service Models, and between CSSs within the same Health Service Model. This amplifies the importance of performing multivariate analyses when assessing the performance of each Health Service Model.
The chapter also demonstrates the unsettled histories and makeshift living arrangements of many participants, which are likely to affect their health. One-third had been homeless 10 years or more; although some were living in hostels or temporary accommodation, others were sleeping on the streets. When interviewed at baseline, many had been in their latest living arrangements for just a few weeks or months, and had been accessing the CSS for just a short while. The unsettledness and mobility of some participants, and changing of health service providers, are likely to have implications for their engagement in health care.
Chapter 7 Primary outcome: health screening among case study participants
This chapter examines the findings of the primary outcome, namely the extent of health screening among case study participants. The six HSIs and the scoring process are introduced, followed by findings from the analyses of screening by Health Service Models. Associations between the Primary Outcome Score and demographic, socioeconomic and health profiles of the participants are explored using regression techniques. Finally, differences in the primary outcome across CSSs within the same Health Service Model are summarised. The primary outcome draws exclusively on data from medical records, obtained for 349 participants. They were unavailable for 14 Usual Care GP participants, including both participants from UC4.
Health Screening Indicators and the scoring process
Six HSIs were selected for the primary outcome: BMI, mental health, alcohol use, TB, smoking and hepatitis A (see Chapter 3). The first four required evidence of screening at some point during the 12-month study period; smoking required screening in the previous 24 months, and hepatitis A required a vaccination programme in progress or completed in the previous 10 years. Each was given a score of 1 (positive) or 0 (negative), depending on evidence in the medical records of screening having taken place and an intervention offered if a problem was identified (Table 13). The total score ranged from 0 to 6.
| HSI | Measure (from medical records) | Score |
|---|---|---|
| BMI | Documented in preceding 12 months and action if underweight (BMI < 18.5 kg/m2) or overweight (BMI ≥ 25.0 kg/m2) | 1 |
| Not documented in preceding 12 months or no action if underweight/overweight | 0 | |
| Mental health | Record of screening for mental health problems in preceding 12 months, and intervention if required | 1 |
| No record of screening for mental health problems in preceding 12 months, or no intervention if a problem | 0 | |
| Alcohol use | Record of screening for alcohol problems in preceding 12 months, and intervention if required | 1 |
| No record of screening for alcohol problems in preceding 12 months, or no intervention if required | 0 | |
| TB | Record of TB screening in preceding 12 months or screening offered | 1 |
| No record of TB screening in preceding 12 months and no screening offered | 0 | |
| Smoking | Smoking status recorded in preceding 24 months and intervention if a smoker | 1 |
| Smoking status not recorded or no intervention if a smoker | 0 | |
| Hepatitis A | Record of having received two vaccinations for hepatitis A in preceding 10 years or vaccination programme in progress or record of immunity | 1 |
| No record of two vaccinations for hepatitis A in preceding 10 years, no vaccination programme in progress and no record of immunity | 0 |
A Microsoft Excel file was created for each CSS, with separate worksheets for each HSI. Searches of the medical records for each HSI were conducted, and relevant information documented, including dates of observations. Checks were carried out by a second coder. Working papers were circulated among the research team as queries arose, and subsequently discussed at SSC meetings. Uncertainties or discrepancies regarding individual cases were reviewed by Ford (GP retired).
Occasionally, information pertaining to the HSIs was found in documents such as A&E reports or outpatient letters, rather than a CSS consultation. Mobile Teams could see general practice records for most of their participants, as they shared records. It was agreed with the SSC that a systems-wide approach should be adopted and scoring would include screening by other health professionals if this could be seen by CSS staff.
Questions arose as to what constituted ‘an intervention’. An intervention generally included, for example, advice about weight or smoking, medication for depression or referral to mental health services. In some instances, however, CSS staff ‘signposted’ a patient to a service without a formal referral. For example, following screening for mental health problems, one participant was encouraged to attend a mental health drop-in centre, and another was handed a leaflet about a counselling service. Likewise, a participant who reported an increase in alcohol consumption was given details of a harm reduction service. Hence, the onus was on the patient to contact the service. As some services encourage self-referrals, it was discussed with the SSC and agreed that signposting should be scored as an intervention. Likewise, interventions offered by CSS staff, but declined or ignored by participants, were scored positively, as the CSS had tried to intervene.
In many instances, formal assessment tools for screening mental health problems were not used. Instead, records indicated mental health status had been observed, albeit sometimes with limited descriptions, for example ‘mood low’ or ‘mood good’. Pre-coded text was used several times by MT1, stating ‘mental health fully performed’ without elaboration. It was agreed with the SSC that interpretation of mental health screening should include situations in which it is assumed that questions must have been asked about a person’s mental state. A similar approach was adopted for screening alcohol use.
Some medical records stated that a person was ‘hepatitis A immune’, meaning that they had had hepatitis A and developed antibodies. Ford confirmed that, in this situation, vaccination is unnecessary, and so this should be scored positively. Another query concerned the maximum interval between the first and second injections for a vaccination programme to be considered ‘in progress’. Ford checked with a specialist, who clarified that one dose of the hepatitis A vaccine could be effective for up to 10 years. This cut-off point was used in the scoring.
Primary Outcome Score and screening by Health Service Model
Figure 1 summarises the number of HSIs per participant that were screened, and an intervention offered if applicable. Sixty per cent of participants received screening for three or four HSIs.
FIGURE 1.
Health screening for primary outcome: total score.

Overall, the mean Primary Outcome Score was 3.30, although there were statistically significant differences by Health Service Model (Table 14 and Figure 2). Participants of Dedicated Centres and Usual Care GPs had been screened for the highest number of HSIs, with little difference between the two models (means of 3.54 and 3.51, respectively). Participants of Mobile Teams had been screened for the fewest (mean 2.90). The highest median score was achieved by Usual Care GPs.
| Primary Outcome Score (number of HSIs screened) | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 349) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 61) | ||
| Mean (SD) | 3.30 (1.24) | 3.54 (1.03) | 2.90 (1.41) | 3.34 (1.24) | 3.51 (1.11) | ANOVA: 0.001 |
| Median (minimum, maximum) | 3.00 (0, 6) | 3.50 (1, 6) | 3.00 (0, 6) | 3.50 (0, 5) | 4.00 (1, 6) | Kruskal–Wallis: 0.002 |
FIGURE 2.
Primary Outcome Score (mean with 95% CI) by Health Service Model. CI, confidence interval.
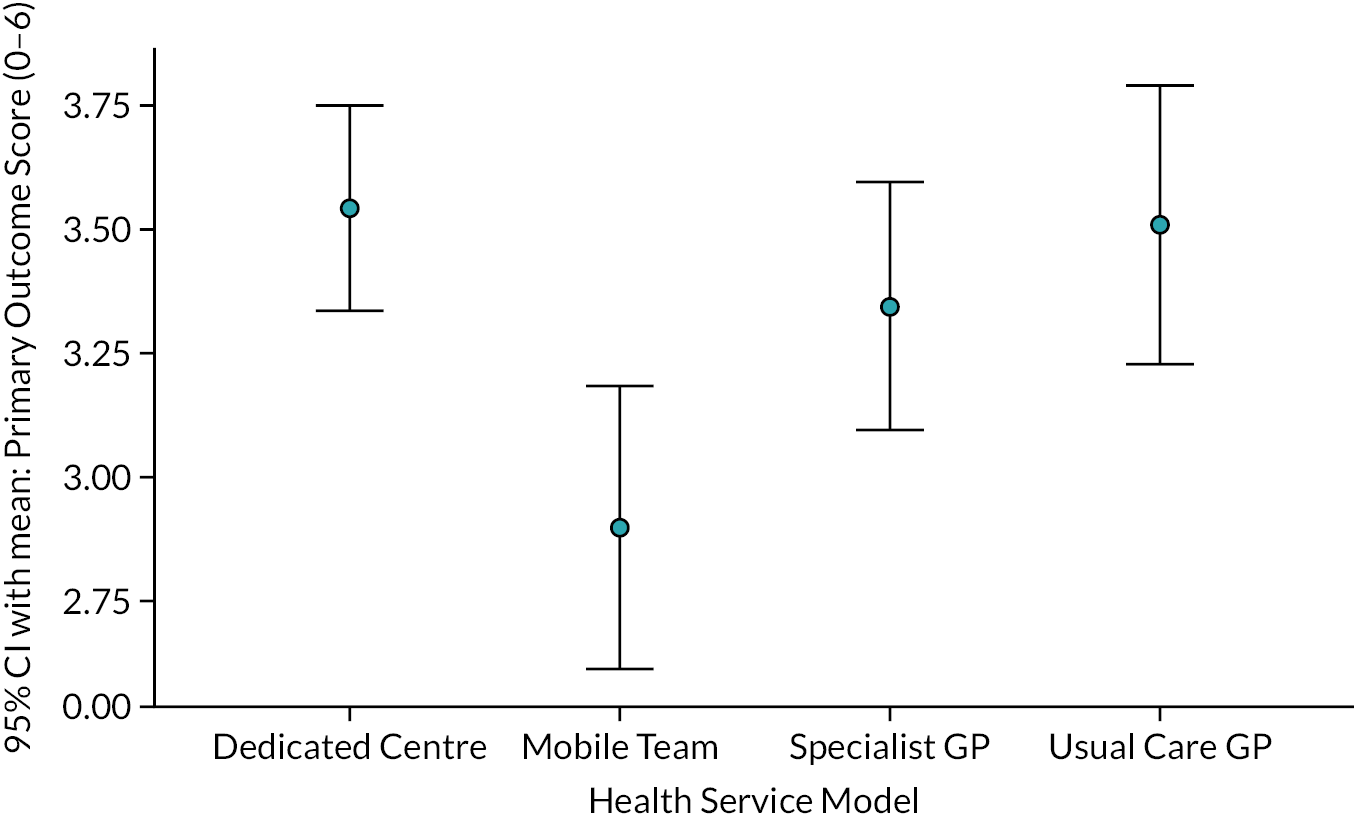
Around 80% of participants had been screened for smoking status, mental health and alcohol use; 45.8% had been screened for BMI, 33.8% for hepatitis A and just 8.6% for TB (Table 15). There were statistically significant differences between Health Service Models. Usual Care GPs were more likely than the other three models to have recorded BMI and smoking status, but were least
| HSI | Health Service Model, n (%) | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 349) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 61) | ||
| BMI | 160 (45.8) | 43 (44.8) | 43 (44.8) | 35 (36.5) | 39 (63.9) | Chi-squared: 0.009 |
| Mental health | 281 (80.3) | 86 (89.6) | 57 (59.4) | 88 (91.7) | 50 (80.6) | Chi-squared: 0.0005 |
| Alcohol use | 278 (79.4) | 86 (89.6) | 64 (66.7) | 72 (75.0) | 56 (90.3) | Chi-squared: 0.0005 |
| TB | 30 (8.6) | 8 (8.3) | 14 (14.6) | 2 (2.1) | 6 (9.8) | Chi-squared: 0.021 |
| Smoking status | 289 (83.5) | 76 (79.2) | 75 (78.1) | 80 (83.3) | 58 (100) | Chi-squared: 0.002 |
| Hepatitis A | 118 (33.8) | 41 (42.7) | 25 (26.0) | 45 (46.9) | 7 (11.5) | Chi-squared: 0.0005 |
likely to have vaccinated against hepatitis A. Staff of UC1 and UC2 explained that they did not routinely screen for hepatitis A unless a patient presented with symptoms or it was required for travelling abroad. Mobile Teams were less likely than other models to have assessed mental health and alcohol use. Screening and vaccinations for hepatitis A were more common among participants of Dedicated Centres and Specialist GPs. They tended to have higher numbers of injecting drug users. Even so, only 41.8% of participants who injected drugs had been screened for hepatitis A.
Regression modelling of Primary Outcome Score
To isolate the effect of the four Health Service Models on the Primary Outcome Score, an initial backward stepwise linear regression was run with Primary Outcome Score as the dependent variable and the variables listed as predictors (Tables 16 and 17). Variables were drawn from participants’ reports, medical records and service use data. Statistically significant and near statistically significant (p < 0.15) predictors were used in a second backward stepwise linear regression.
| Predictors | Time period | Participants (N) | Yes, n (%) |
|---|---|---|---|
| Dedicated Centre | 363 | 96 (26.4) | |
| Mobile Team | 363 | 96 (26.4) | |
| Specialist GP | 363 | 96 (26.4) | |
| Usual Care GP (set as control) | 363 | 75 (20.7) | |
| Reported by participant | |||
| Female | 363 | 72 (19.8) | |
| Black or Black British | 361 | 26 (7.2) | |
| Born in the UK | 362 | 289 (79.8) | |
| British born/British citizen | 359 | 309 (86.1) | |
| Involved in education/training/employment | Baseline | 363 | 53 (14.6) |
| Has an income (earnings or state welfare benefits) | Baseline | 362 | 315 (87) |
| Support from family/friends in preceding 4 months | Baseline | 358 | 175 (48.9) |
| Heavy smoker (≥ 20 cigarettes/roll-ups daily) | Baseline | 331 | 70 (21.1) |
| Drinking > 14 units of alcohol per week | Baseline | 345 | 149 (43.2) |
| Used drugs in preceding 4 months | Baseline | 361 | 217 (60.1) |
| Injected drugs in preceding 4 months | Baseline | 354 | 82 (23.2) |
| Physical health problems in preceding 4 months | Baseline | 362 | 343 (94.8) |
| Depression in preceding 4 months | Baseline | 357 | 293 (82.1) |
| From medical records/service use data | |||
| Registered with CSS < 4 months | Baseline | 363 | 50 (13.8) |
| Registered with CSS < 6 months | Baseline | 363 | 96 (26.4) |
| Registered with CSS > 1 year | Baseline | 363 | 196 (54.0) |
| Consultation with external key workera | Study period | 352 | 114 (32.4) |
| Consultation ≥ 12 times with external key workera | Study period | 352 | 68 (19.3) |
| Predictors | Participants (N) | Mean | SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Age (years) | 363 | 41.56 | 10.54 | 41.00 | 18 | 79 |
| Approximate number of years homeless | 359 | 8.32 | 8.01 | 5.50 | 0.08 | 40.0 |
| Number of changes of accommodation/sleeping settings in study period | 363 | 2.29 | 2.32 | 2.00 | 0 | 11 |
| % of time in building designed for habitation in study period | 360 | 79.78 | 30.62 | 100 | 0 | 100 |
| % of time in accommodation with staff (full/part time) in study period | 360 | 48.21 | 39.07 | 45.83 | 0 | 100 |
| Number of years registered with CSS | 363 | 2.08 | 2.46 | 1.29 | −0.055 | 17.982 |
| Number of consultations at CSS with GP/nurse/HCA in study period | 363 | 14.31 | 19.05 | 12.00 | 0 | 214 |
A final model was run using only the statistically significant predictors resulting from this regression, to maximise the number of observations used. The fitted parameters for this final model are shown in Table 18. No statistically significant difference in effect was seen between Dedicated Centres, Specialist GPs and Usual Care GPs. Only Mobile Teams differed, with a highly statistically significant negative effect identified [–0.603, 95% confidence interval (CI) –1.015 to –0.191]. Other statistically significant effects in the model were reporting depression at baseline (eliciting an improvement of 0.415 in the Primary Outcome Score), drug use at baseline (eliciting an improvement of 0.295 in the Primary Outcome Score), being British born or a British citizen (eliciting a decrease of 0.852 in the Primary Outcome Score), having seen a non-accommodation-based key worker (eliciting a decrease of 0.012 in the Primary Outcome Score), the percentage of the study period living in accommodation with full- or part-time staff (each additional 10% elicited an improvement of 0.055 in the Primary Outcome Score), the number of consultations at a CSS with a GP, a nurse or a HCA (each additional 10 contacts elicited an improvement of 0.099 in the Primary Outcome Score) and number of years homeless (each additional 10 years elicited an improvement of 0.281 in the Primary Outcome Score).
| Variables | Unstandardised coefficients | Standardised coefficients | t | Significance | 95% CI for B | |
|---|---|---|---|---|---|---|
| B | SE | Beta | ||||
| (Constant) | 3.092 | 0.284 | 10.873 | 0.000 | 2.533 to 3.652 | |
| Dedicated Centre | 0.102 | 0.216 | 0.036 | 0.471 | 0.638 | −0.323 to 0.526 |
| Mobile Team | −0.603 | 0.209 | −0.209 | −2.878 | 0.004 | −1.015 to −0.191 |
| Specialist GP | −0.004 | 0.195 | 0.001 | 0.019 | 0.985 | −0.380 to 0.387 |
| Depression in preceding 4 months | 0.415 | 0.168 | 0.126 | 2.477 | 0.014 | 0.085 to 0.745 |
| Used drugs in preceding 4 months | 0.295 | 0.135 | 0.115 | 2.180 | 0.030 | 0.029 to 0.562 |
| British born/British citizen | −0.852 | 0.212 | −0.233 | −4.024 | 0.000 | −1.268 to −0.435 |
| Consultation with external key workerb | −0.01184 | 0.005 | −0.125 | −2.236 | 0.026 | −0.022 to −0.001 |
| % of study period in accommodation with staff | 0.00546 | 0.002 | 0.168 | 3.009 | 0.003 | 0.002 to 0.009 |
| Number of consultations at CSS with GP/nurse/HCA | 0.00994 | 0.004 | 0.155 | 2.772 | 0.006 | 0.003 to 0.017 |
| Approximate number of years homeless | 0.02814 | 0.008 | 0.184 | 3.528 | 0.000 | 0.012 to 0.044 |
The effect on the Primary Outcome Score of the number of consultations the person had with a GP, a nurse or a HCA at the CSS is likely to be caused by increased opportunity for staff to undertake health screening the more a patient is seen. Likewise, participants who reported depression or drug use at baseline had more consultations during the study with GPs or nurses at the CSS. The positive association between the percentage of the study period in accommodation with full- or part-time staff and the Primary Outcome Score may be due to staff encouraging residents to access health care, or may be an indicator of the stability of participants and their willingness to engage with housing and health services. The negative association between contact with an external key worker and the Primary Outcome Score may be an indicator of the unsettledness of some participants. Many key workers were street outreach and day centre workers supporting participants who were sleeping on the streets. The effect on the Primary Outcome Score of the number of years a person was homeless may be due to the person being more accustomed to, and accepting of, services over time.
Primary Outcome Score and screening by Case Study Site
There were marked variations in screening when the CSSs within some models were examined (Table 19 and Figure 3). There was little difference in the Primary Outcome Score between the two Dedicated Centres, but a noticeable difference between the two Specialist GP sites. SP1 had the second highest score (mean 4.16), whereas SP2 had the lowest score (mean 2.42). Part of the reason may be that the number of GP/nurse/HCA consultations at the CSS during the study varied greatly between the two sites: an average of 12.76 for SP1 and 7.13 for SP2. Another reason may be that SP1 had dedicated nurses for patients who were homeless, and case managers for those with complex health and social care needs. This was not the situation at SP2 (see Chapter 5). It is likely that nurses would have undertaken elements of the screening, and case managers would have encouraged attendance at health appointments.
| CSS | Participants (n) | Mean | SD | SE | 95% CI for mean | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| DC1 | 48 | 3.33 | 1.098 | 0.158 | 3.01 to 3.65 | 1 | 6 |
| DC2 | 48 | 3.75 | 0.911 | 0.131 | 3.49 to 4.01 | 1 | 5 |
| MT1 | 47 | 2.60 | 1.155 | 0.168 | 2.26 to 2.93 | 0 | 4 |
| MT2 | 49 | 3.18 | 1.577 | 0.225 | 2.73 to 3.64 | 0 | 6 |
| SP1 | 51 | 4.16 | 0.731 | 0.102 | 3.95 to 4.36 | 2 | 5 |
| SP2 | 45 | 2.42 | 1.033 | 0.154 | 2.11 to 2.73 | 0 | 4 |
| UC1 | 17 | 2.65 | 1.057 | 0.256 | 2.10 to 3.19 | 1 | 4 |
| UC2 | 29 | 3.66 | 0.897 | 0.167 | 3.31 to 4.00 | 1 | 5 |
| UC3 | 15 | 4.20 | 0.941 | 0.243 | 3.68 to 4.72 | 2 | 6 |
| Total | 349 | 3.30 | 1.236 | 0.066 | 3.17 to 3.43 | 0 | 6 |
FIGURE 3.
Primary Outcome Score by CSS.
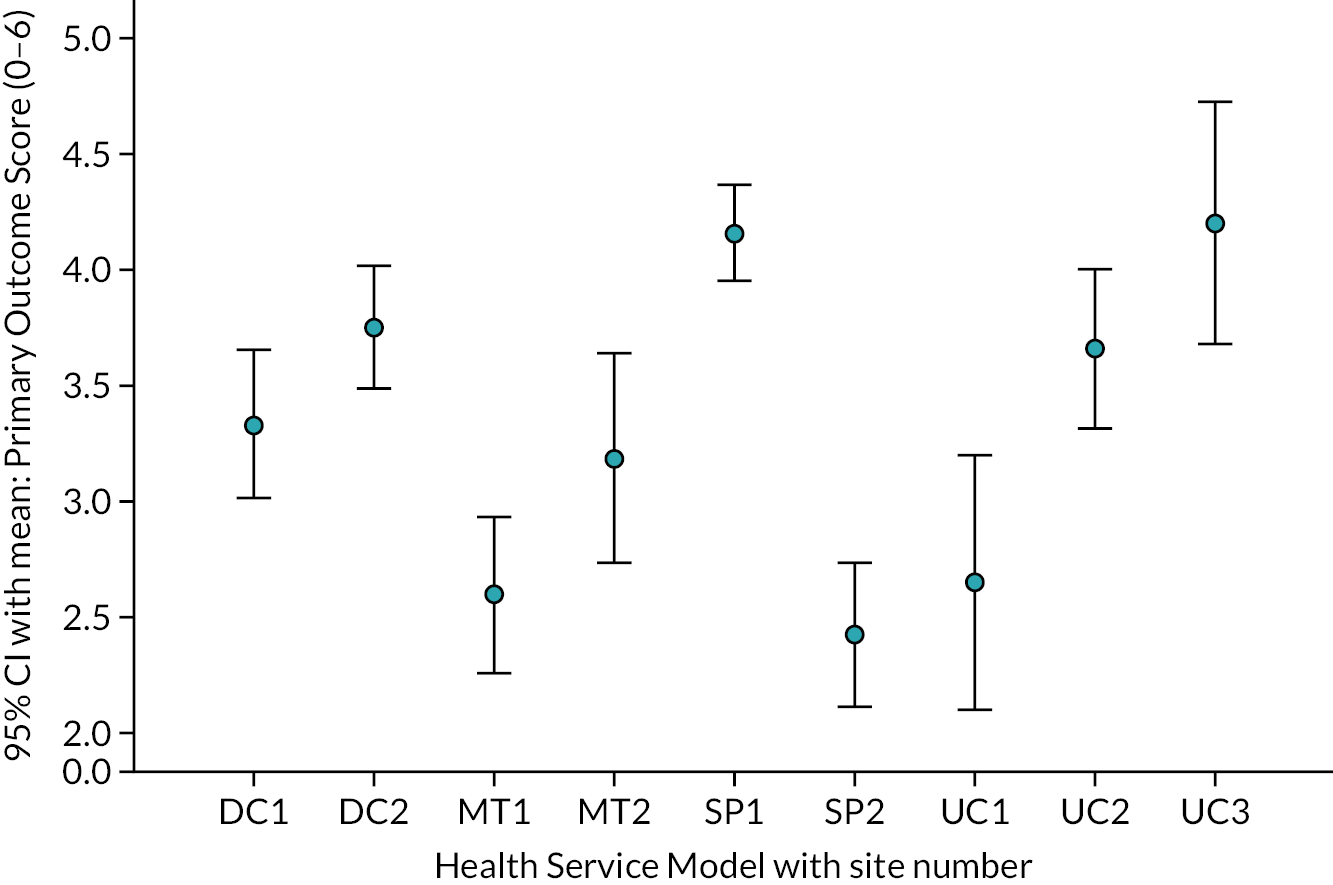
There were also substantial differences in scores between Usual Care GP sites, ranging from a mean of 2.65 for UC1 to 4.20 for UC3 (the highest of all CSSs). BMI was documented in the medical records for 93.3% of UC3 participants, compared with just 29.4% of UC1 participants (see Appendix 2, Table 47). Once again, the number of consultations during the study period with a CSS GP/nurse/HCA varied greatly between sites: an average of 5.96 for UC1, 8.33 for UC2 and 8.53 for UC3. In addition, UC2 and UC3 used a computer-based ‘homeless template’ to assess the needs of patients who were homeless (see Chapter 5). UC3 also proactively visited local hostels annually to encourage residents to attend a homeless health check, and UC2 was near a hostel and in regular communication with hostel staff.
There was slight variation between Mobile Teams, with MT2 scoring higher than MT1. There was little difference between screening of BMI, mental health and alcohol use, but MT2 participants were more likely than those of MT1 to have been screened for TB, smoking status and hepatitis A (see Appendix 2, Table 47). This reflects different working practices. MT2 proactively screened for TB and hepatitis A, whereas MT1 explained that it did not offer this service and relied on drug agencies and other health services to undertake such screening.
Summary
This chapter describes the extent to which screening for the six HSIs comprising the primary outcome had been undertaken with case study participants. Screening for smoking status, mental health and alcohol use was most common, although around one-in-five had not been screened for these conditions. Just over half had no BMI recorded during the study period, yet the diets of many people who are homeless are poor. 88 Even fewer participants were screened for hepatitis A and TB, yet reports indicate high prevalence rates of these diseases among people who are homeless, and among groups at risk of homelessness, namely people who inject drugs or have been in prison. 115,116 Since 2000, outbreaks of hepatitis A have been reported in several parts of England among people who inject drugs, or who are homeless and living in hostels and shelters. 89,90,117 Likewise, people who are homeless have higher rates of active pulmonary TB than the general population, and often present late for health care or are lost to follow-up care. 91,118
There were differences in the Primary Outcome Score and in screening of individual HSIs by Health Service Model and by CSSs within models. Regression analyses revealed a highly statistically significant negative effect for the Mobile Team, but no difference for the other three models. Given that most Mobile Team participants were also registered with a general practice, it appears that neither the Mobile Teams nor the general practices regularly undertook screening for the HSIs.
The chapter also found that screening differed across CSSs within the same model, indicating the importance of considering working practices of individual CSSs. Among the Usual Care GPs, UC2 and UC3 used ‘homeless templates’ to assess needs and had a Primary Outcome Score comparable to Dedicated Centres. Likewise, SP1 had designated nurses and case managers to work with patients who were homeless and scored much higher than SP2. Some CSSs routinely screened HSIs, but others did not. Staff of DC2 and SP2 said they did not routinely screen for TB unless it was indicated, and MT1, UC1 and UC2 said the same for hepatitis A. This is discussed further in Chapter 15, which outlines recommendations from the Faculty for Homeless and Inclusion Health and from NICE. 70,119 The next chapter examines the effectiveness of the Health Service Models in the management of SHCs.
When interpreting the extent of screening at the CSSs, consideration must be given to various ‘rules’ adopted by the research team while scoring. In many instances, formal assessment tools for screening mental health and alcohol consumption were not used; instead, positive scores were given when text in the medical records indicated that questions had been asked about these conditions. For example, some participants were seen frequently by CSS doctors and nurses and asked about their mood or drinking habits. These were, however, less evident for MT1 when pre-coded text was used. ‘Signposting’ a person to another service was scored positively, as were cases when interventions such as help for smoking were offered by CSS staff but declined by participants. Our method of scoring may have inflated the Primary Outcome Score in some instances. However, it was similarly applied across all Health Service Models.
Chapter 8 Management of Specific Health Conditions
One of the secondary outcomes was to examine the effectiveness of Health Service Models in managing five Specific Health Conditions (SHCs): (1) hypertension, (2) chronic respiratory problems, (3) depression, (4) alcohol problems and (5) drug problems (see Chapter 3). Hypertension and chronic respiratory problems are long-term conditions that are likely to be managed by the CSS. Depression may require input from mental health services, and alcohol and drug problems may require involvement by substance misuse services. This chapter first describes the scoring of the SHCs, followed by sections on outcomes for each SHC and differences by Health Service Models. Finally, differences in outcomes by CSSs within the same model are discussed.
Criteria for determining eligibility as a Specific Health Condition
Eligibility criteria were created for each SHC (Table 20). Only those both reported by participants when interviewed at baseline and identified by the CSS at this time (through documentation in medical records) were included. SHCs not reported by participants or reported for the first time at 4 or 8 months were excluded. Such participants would not have completed a rating scale at baseline (outcome 5), and there would have been insufficient time to assess ‘continuity of care’ by the CSS (outcome 2). Likewise, SHCs first documented in the medical records after the first 4 months of the study period were excluded.
| SHC | Inclusion | Exclusion |
|---|---|---|
| Hypertension |
|
|
| Chronic respiratory problems |
|
|
| Depression |
|
|
| Alcohol problems |
|
|
| Drug problems |
|
|
Many SHCs were listed in the medical records as a ‘current active problem’ or documented in a GP consultation. In some instances, however, participants described a possible SHC, but it was not explicitly mentioned in the medical records, although medication associated with the condition was prescribed. In such cases, information from medical records and participants was reviewed by Ford (retired GP), and included if there was sufficient evidence that the treatment provided was for the SHC.
In a few instances, asthma or depression were listed in the medical records as a ‘current active problem’, but diagnosed many years ago. There was no mention of monitoring or treatment during the study, and participants said they had not required treatment for several years. Such cases were reviewed by Ford and, if the diagnosis was more than 3 years ago, and the participant had not required medical intervention in the interim, the problem was regarded as ‘inactive’ and not a SHC.
Outcome measures
Five outcomes monitored the effectiveness of the CSS in managing each SHC. Outcomes 1 and 2 assessed processes of care, outcomes 3 and 4 involved patient perceptions of the quality of care, and outcome 5 assessed control or change in health status over the study period.
Outcome 1: treatment plan
Outcome 1 required evidence in the medical records that the CSS had started treatment or offered advice or made a referral (collectively a ‘treatment plan’) for a person they identified as having a SHC, or that a treatment plan was in progress (scored 1 or 0). As with the primary outcome, if the CSS offered help, but the participant declined or did not attend an appointment, a score of 1 was given.
Outcome 2: continuity of care
Outcome 2 required evidence in the medical records that the CSS provided continuity of care or follow-up over the study period for a person identified as having a SHC and for whom a treatment plan was initiated (scored 1 or 0). Some participants did not have access to the CSS for its entirety as they moved, or spent time in prison or hospital. Continuity of care was therefore scored if they had access to the CSS for at least 8 of the 12 months.
Different criteria were applied to each SHC for continuity of care drawing on the Quality and Outcomes Framework (QOF) and the expertise of Ford. The QOF is a voluntary annual reward and incentive programme within the GMS contract for all general practice surgeries in England. A positive score was given if essential indicators were met (Table 21). Some participants with depression were referred by the CSS doctor to mental health services, but did not attend, although their depression continued to be monitored by CSS staff. Likewise, some engaged with a treatment plan for most of the study, but had short spells when they failed to engage and treatment stopped, before subsequently reengaging. These two situations were scored as 1, as participants ‘partially engaged’ in treatment.
| SHC | Essential indicators | Possible indicators |
|---|---|---|
| Hypertension |
|
|
| Chronic respiratory problems |
|
|
| Depression |
|
|
| Alcohol problems |
|
|
| Drug problems |
|
|
Shared care arrangements were in place for many participants with substance misuse problems, involving both CSS staff and specialist workers. Some were monitored by a drug worker and maintained on OST, with their case reviewed every 2–3 months by a CSS doctor who prescribed the OST. Scoring SHCs when specialist agencies were involved required evidence of regular reviews by the CSS or updates of a participant’s progress from specialist services (see Table 21).
Most Mobile Team participants were registered locally with a GP, as neither team included a GP. They thus received health care from CSS nurses and a GP (the records of most were shared with the CSS). Separate scores were given for continuity of care provided by the CSS and that provided by a GP. MT1 used a great deal of Read-coded text for mental health and substance misuse problems. For example, there were repeat entries of ‘mental health (care plan) face-to-face with patient’ or ‘mental health fully performed’, with no explanation of what these entailed. Such entries were regarded as continuity of care for depression if made throughout the study.
Outcomes 3 and 4: perspectives of help received
Outcomes 3 and 4 pertained to participants’ views of help received for a SHC. Outcome 3 concerned whether or not they had received sufficient information from the CSS to enable them to understand their SHC. Outcome 4 concerned whether or not they were satisfied with the treatment plan that the CSS arranged or provided for the SHC. This information was collected during their interview at month 8, and each was scored 1 for ‘yes’ or 0 for ‘no’. Several participants responded by saying they did not need information as they already knew about the condition, or did not want help. This was discussed with the SSC and it was agreed that in such situations a score of 1 should be given.
Outcome 5: control or change in health status
Using validated instruments or other measures, it was originally intended that outcome 5 (control or change in health status from baseline to 8 months) would be scored as ‘1 for improvement’ or ‘0 for no change or deterioration’. However, although a score of 0 (no change) was appropriate for a person with alcohol problems who continued to drink heavily throughout the study, it was not so for a participant with hypertension whose blood pressure (BP) readings were within the normal range at each observation. A framework for scoring each SHC separately was therefore implemented (Table 22).
| SHC | Measure | Scores for participants with SHC |
|---|---|---|
| Hypertension | BP readings for patients with hypertension (QOF indicator):120
|
1 BP documented in medical records during study period, and last reading within QOF limits 0 BP documented in medical records during study period, but last reading above QOF limits 0 BP not documented in medical records during study period |
| Chronic respiratory problems | COPD Assessment Test impact-level scores:121
|
1 Low impact level at 8 months 1 Change to lower impact level between baseline and 8 months 0 Very high impact level at 8 months 0 Change to higher impact level between baseline and 8 months 0 Same impact level at baseline and 8 months (but 1 if low impact level) |
| Depression | PHQ-9 ‘severity’-level scores:122
|
1 Minimal severity level at 8 months 1 Change to lower severity level between baseline and 8 months 0 Severe depression level at 8 months 0 Change to higher severity level between baseline and 8 months 0 Same severity level at baseline and 8 months (but 1 if minimal severity level) |
| Alcohol problems | Self-reports at baseline and 8 months of alcohol intake. Responses grouped using NICE’s classification of alcohol consumption per week:113
|
1 No alcohol, or lower-risk drinking at 8 months 0 Harmful drinking at 8 months 1 Change to lower-risk alcohol consumption group between baseline and 8 months 0 Change to higher-risk alcohol consumption group between baseline and 8 months 0 Hazardous drinking at baseline and 8 months |
| Drug problems | Self-reports at baseline and 8 months of frequency of illicit drug use in preceding 4 months:
|
1 No illicit drug use at 8 months 0 Illicit drug use ≥ 5 days per week at 8 months 1 Frequency of illicit drug use reduced between baseline and 8 months 0 Frequency of illicit drug use increased between baseline and 8 months 0 Frequency of illicit drug use remained the same at baseline and 8 months |
For hypertension, QOF indicators were used. 120 BP readings were extracted from medical records; a score of 1 was given if BP was recorded during the 12-month study period, and the last reading was within QOF limits. A score of 0 was given if the last BP reading was above QOF limits, or had not been documented.
Participants with chronic respiratory problems completed the Chronic Obstructive Pulmonary Disease (COPD) Assessment Test at baseline and 8 months (advice from Dr Patrick White, Reader in Primary Care Respiratory Medicine, KCL). This is a validated instrument to measure the impact of COPD on a patient’s health, and includes questions on coughing, breathlessness, energy and sleep. Each item can be scored 0–5, with a total score of 0–40, which is grouped into four ‘impact levels’ (see Table 22). 121 A score of 1 was given to participants who moved to a lower impact level between baseline and 8 months, and to those in the lowest impact level at 8 months. A score of 0 was given to participants in the very high impact level at 8 months, and to those who moved to a higher impact level between baseline and 8 months.
Participants who reported depression self-completed the Patient Health Questionnaire-9 (PHQ-9) at baseline and 8 months. This is a validated instrument that measures change in level of depression, and includes questions on concentration, appetite, interest in activities, and feelings of depression or hopelessness in the preceding 2 weeks. Each item is scored ‘not at all’, ‘several days’, ‘more than half the days’ or ‘nearly every day’. It has a scoring range of 0–27, and the total score grouped into five ‘depression severity’ levels. 122 A similar scoring system was adopted as that used for chronic respiratory problems.
For participants with alcohol problems, the original intention was to use the Alcohol Use Disorders Identification Test-Consumption (AUDIT C) to detect changes in alcohol intake from baseline to 8 months. However, many participants drank alcohol well above the upper limits identified by the AUDIT C, and it was impossible to identify changes in their alcohol use. Similar issues were raised by DC2 staff who declined to use the AUDIT C at their practice because ‘we find that our patients are drinking so much they are completely off the scale. It’s meaningless for them’. A classification used by NICE was therefore used to detect changes in alcohol consumption (see Table 22). 113
To measure change in drug use, it was initially suggested that the Drug Abuse Screening Test (DAST-10) would be used. However, it has only two broad questions directly relating to drug intake (whether or not used drugs in preceding 12 months, and whether or not used more than one drug simultaneously), and no questions specifying frequency or types of drugs used or mode of administration. It also has questions about the reactions of a spouse or parents to their drug use, and neglect of family as a result of their drug use. Many single people who are homeless do not have family contact; hence, these questions would have been inapplicable. Changes other than identifying the few participants who stopped using drugs during the study could not be ascertained through this instrument, and a more suitable one could not be found. Participants’ self-reports about frequency of drug use were therefore examined (see Table 22). Ford, who is very experienced in this field, advised on measures to detect changes in alcohol intake and drug use (see Acknowledgements, Contributions of authors).
Scoring of Specific Health Conditions
To score the SHCs, a Microsoft Excel file was created for each CSS, with separate entries for each SHC. Information from participants about help received was recorded in the data file. Details were extracted from medical records regarding (1) diagnosis or mention of the SHC and (2) action taken concerning outcomes 1 and 2. Joly and Crane (former registered nurses) undertook this work and checked each other’s entries, with Ford reviewing uncertainties. All decisions were documented.
In total, 905 potential SHCs were reported by participants; medical records were available and were searched for 864 of these. Of these 864, 629 SHCs (72.8%) were reported during the first 4 months of the study and met the inclusion criteria, 173 were not mentioned, 38 were classified as inactive problems and 24 were first mentioned after 4 months. The following sections describe outcomes for each SHC. Each table summarises the screening process, then the severity of the condition at baseline for participants with a SHC, and outcome scores. For some outcomes, response rates are lower than the number of participants with the problem; this was because either interviews could not be conducted at 8 months or participants did not access the CSS for the entire study period.
Hypertension
At baseline, 51 participants (14%) reported hypertension, although several were unclear whether or not their symptoms were linked to anxiety and panic attacks. Hypertension was documented in the medical records for just 20 (5.5%): four from Dedicated Centres, 11 from Mobile Teams and five from Usual Care GPs. Owing to insufficient numbers, it was unfeasible to examine outcomes.
Chronic respiratory problems
At baseline, 119 participants (32.8%) reported chronic respiratory problems, mainly asthma. Medical records were obtained for 111 participants, and chronic respiratory problems were documented during the first 4 months for 74 participants (Table 23). Eleven mentioned asthma, but had had no treatment or monitoring for several years, and the problem was regarded as inactive. Of the 36 participants for whom chronic respiratory problems were not documented in their medical records or it was an ‘inactive’ problem, 24 (66.7%) had scores indicating ‘high’ or ‘very high’ impact when completing the baseline COPD Assessment Test.
| Chronic respiratory problems | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | ||
| Screening for inclusion as SHC, n (%) | ||||||
| Reported by participant at baseline (N = 363) | 119 (32.8) | 35 (36.5) | 25 (26.0) | 36 (37.5) | 23 (30.7) | Chi-squared: 0.297 |
| Diagnosis/documentation in medical records (N = 111)a | ||||||
| Not mentioned in medical records | 25 (22.5) | 12 (34.3) | 6 (24.0) | 4 (11.1) | 3 (20.0) | Not applicable |
| Documented, but inactive problem | 11 (9.9) | 5 (14.3) | 0 (0) | 5 (13.9) | 1 (6.7) | |
| Documented after first 4 months of study | 1 (0.9) | 0 (0) | 0 (0) | 1 (2.8) | 0 (0) | |
| Documented in first 4 months: SHC | 74 (66.7) | 18 (51.4) | 19 (76.0) | 26 (72.2) | 11 (73.3) | |
| COPD Assessment Test impact level at baseline (N = 74),b n (%) | ||||||
| Low impact | 3 (4.1) | 1 (5.6) | 1 (5.3) | 1 (3.8) | 0 (0) | Kruskal–Wallis: O.099 |
| Medium impact | 16 (21.6) | 6 (33.3) | 3 (15.8) | 4 (15.4) | 3 (27.3) | |
| High impact | 31 (41.9) | 9 (50.0) | 7 (36.8) | 14 (53.8) | 1 (9.1) | |
| Very high impact | 24 (32.4) | 2 (11.1) | 8 (42.1) | 7 (26.9) | 7 (63.3) | |
| SHC outcomesb | ||||||
| 1. Treatment plan initiated (N = 74), n (%) | 73 (98.6) | 18 (100) | 19 (100) | 25 (96.2) | 11 (100) | No valid test |
| 2. Continuity of care by CSS (N = 65), n (%) | 46 (70.8) | 14 (87.5) | 7 (46.7) | 19 (76.0) | 6 (66.7) | Chi-squared: 0.079 |
| 3. Sufficient explanation of SHC (N = 52), n (%) | 42 (80.8) | 10 (100.0) | 12 (92.3) | 15 (68.2) | 5 (71.4) | Chi-squared: 0.105 |
| 4. Satisfied with treatment plan (N = 50), n (%) | 46 (92.0) | 11 (100.0) | 12 (100) | 16 (80.0) | 7 (100.0) | Chi-squared: 0.089 |
| 5. Low impact/positive change between baseline and 8 months (N = 58), n (%) | 22 (37.9) | 3 (25.0) | 6 (42.9) | 10 (43.5) | 3 (33.3) | Chi-squared: 0.711 |
| Total outcome score (N = 45), mean (SD) | 3.87 (0.97) | 4.20 (0.63) | 3.91 (0.83) | 3.78 (1.22) | 3.50 (0.84) | ANOVA: 0.542 |
Of the 74 participants for whom chronic respiratory problems were a SHC, 74.3% had symptoms at baseline suggestive of high or very high impact. A treatment plan had been started for all except one of the 74 participants. Continuity of care was achieved for 70.8% of participants, ranging from 87.5% at Dedicated Centres to 46.7% for Mobile Team participants. However, continuity of care for the latter increased to 60% when GP interventions were included. In terms of outcomes 3 and 4 (explanation about the problem and views of treatment), positive responses were given by most participants, with slightly lower rates for Specialist GP and Usual Care GP participants regarding outcome 3. Nearly two-fifths of participants reported symptoms indicating a low impact on their health at 8 months or a positive change between baseline and 8 months (outcome 5), with only slight variation between Health Service Models and no statistically significant differences (see Table 23).
Depression
At baseline, 293 participants (80.7%) reported depression, with 173 meeting the eligibility criteria (Table 24). Depression was most likely to have been identified as a problem by Dedicated Centres, followed by Specialist GPs. Among participants who reported depression, it was not documented in the medical records for 30.6%, and it was classified as ‘inactive’ for 5.3%. Just over two-fifths of Mobile Team and Usual Care GP participants were in these categories. Of the 101 participants for whom depression was not documented in medical records or it was ‘inactive’, 48.5% had PHQ-9 scores at baseline indicating ‘moderately severe’ or ‘severe’ depression, and 22.8% had scores indicating ‘moderate’ depression. Just eight of this group had scores suggesting minimal or no depression.
| Depression | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | ||
| Screening for inclusion as SHC, n (%) | ||||||
| Reported by participant at baseline (N = 363) | 293 (80.7) | 80 (83.3) | 73 (76.0) | 82 (85.4) | 58 (77.3) | Chi-squared: 0.298 |
| Diagnosis/documentation in medical records (N = 281)a | ||||||
| Not mentioned in medical records | 86 (30.6) | 16 (20.0) | 31 (42.5) | 23 (28.0) | 16 (34.8) | Not applicable |
| Documented, but inactive problem | 15 (5.3) | 3 (3.8) | 2 (2.7) | 7 (8.5) | 3 (6.5) | |
| Documented after first 4 months of study | 7 (2.5) | 4 (5.0) | 2 (2.7) | 0 (0.0) | 1 (2.2) | |
| Documented in first 4 months: SHC | 173 (61.6) | 57 (71.3) | 38 (52.1) | 52 (63.4) | 26 (56.5) | |
| Depression ‘severity’ levelb at baseline (N = 173),c n (%) | ||||||
| Minimal/no depression | 6 (3.5) | 2 (3.5) | 2 (5.2) | 1 (1.9) | 1 (3.8) | Kruskal–Wallis: 0.067 |
| Mild | 17 (9.8) | 8 (14.0) | 2 (5.3) | 4 (7.7) | 3 (11.5) | |
| Moderate | 31 (17.9) | 15 (26.3) | 7 (18.4) | 8 (15.4) | 1 (3.8) | |
| Moderately severe | 42 (24.3) | 11 (19.3) | 14 (36.8) | 13 (25.0) | 4 (15.4) | |
| Severe | 77 (44.5) | 21 (36.8) | 13 (34.2) | 26 (50.0) | 17 (65.4) | |
| SHC outcomesc | ||||||
| 1. Treatment plan initiated (N = 173), n (%) | 164 (94.8) | 55 (94.7) | 36 (94.7) | 50 (96.2) | 23 (88.5) | Chi-squared: 0.450 |
| 2. Continuity of care by CSS (N = 156), n (%) | 90 (57.7) | 35 (70.0) | 12 (34.3) | 31 (64.6) | 12 (52.2) | Chi-squared: 0.007 |
| 3. Sufficient explanation of SHC (N = 102), n (%) | 67 (65.7) | 19 (63.3) | 19 (90.5) | 19 (52.8) | 10 (66.7) | Chi-squared: 0.037 |
| 4. Satisfied with treatment plan (N = 99), n (%) | 77 (77.8) | 23 (76.7) | 19 (90.5) | 25 (75.8) | 10 (66.7) | Chi-squared: 0.372 |
| 5. Minimal severity level/positive change between baseline and 8 months (N = 114), n (%) | 48 (42.1) | 16 (48.5) | 7 (30.4) | 15 (38.5) | 10 (52.6) | Chi-squared: 0.405 |
| Total outcome score (N = 90), mean (SD) | 3.42 (1.06) | 3.70 (1.17) | 3.44 (0.78) | 3.30 (1.12) | 3.13 (0.99) | ANOVA: 0.335 |
Among the 173 participants for whom depression met the criteria as a SHC, 44.5% had PHQ-9 scores at baseline indicating severe depression, and 24.3% had PHQ-9 scores indicating moderately severe depression (see Table 24). Severe depression was most common among Usual Care GP participants, followed by those of Specialist GPs. Part of the reason may be that the former included participants living in hostels exclusively for people with mental health problems.
A treatment plan was initiated for most participants identified by the CSSs as having depression (outcome 1). Outcome 2 (continuity of care) included regular reviews and monitoring by CSS staff of mood; prescribing antidepressants; consultations and reviews by mental health teams; and discussions of the relationship between depression and substance misuse. In some instances, medication for depression could not be prescribed because of heavy drinking. Six participants were admitted to a mental health unit during the study. There were highly significant differences between models for outcome 2: continuity of care was most likely to have been achieved by Dedicated Centres and Specialist GPs (70% and 64.6%, respectively), and least likely to have been achieved by Mobile Teams (34.3%). The result for Mobile Teams increased to 68.6% when GP services were included. Exceptionally high scores were recorded for outcomes 3 and 4 for Mobile Teams, suggesting good rapport with participants and an ability to explain depression.
For outcome 5, 42.1% of participants who completed the PHQ-9 at baseline and at 8 months reported minimal depression at 8 months or a positive change over time. Although there were no statistically significant differences in outcome 5 across the Health Service Models, Usual Care GP participants were more likely, and Mobile Team participants least likely, to report minimal severity level or a positive change. This is likely to be due to several factors. As mentioned in the previous paragraph, Usual Care GP participants included people living in hostels exclusively for people with mental health problems, with staff on site, and many remained in the same accommodation throughout the study (see Table 11). In contrast, Mobile Team participants were less stably housed and changed accommodation several times during the study and spent more time sleeping rough. As mentioned previously, continuity of care for depression was also less likely to have been achieved with Mobile Team participants.
Alcohol problems
Just over half (55.4%) of participants reported an alcohol problem at baseline. This was confirmed for most (85.1%), with 165 meeting the inclusion criteria. Of the 150 participants who could specify the amount of alcohol consumed, 63.3% reported ‘harmful’ drinking; 19.3% reported ‘hazardous’ drinking; and 17.4% had reduced or stopped drinking but were still being treated or monitored by health or substance misuse services (Table 25).
| Alcohol problem | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | ||
| Screening for inclusion as SHC, n (%) | ||||||
| Reported by participant at baseline (N = 363) | 201 (55.4) | 55 (57.3) | 45 (46.9) | 54 (56.3) | 47 (62.7) | Chi-squared: 0.204 |
| Diagnosis/documentation in medical records (N = 201)a | ||||||
| Not mentioned in medical records | 19 (9.8) | 3 (5.5) | 2 (4.4) | 6 (11.1) | 8 (20.0) | Not applicable |
| Documented, but inactive problem | 3 (1.5) | 0 (0.0) | 0 (0.0) | 3 (5.6) | 0 (0.0) | |
| Documented after first 4 months of study | 7 (3.6) | 3 (5.5) | 3 (6.7) | 1 (1.9) | 0 (0.0) | |
| Documented in first 4 months: SHC | 165 (85.1) | 49 (89.1) | 40 (88.9) | 44 (81.5) | 32 (80.0) | |
| Pattern of alcohol consumptionb at baseline (N = 150),c n (%) | ||||||
| No alcohol | 10 (6.7) | 6 (14.0) | 2 (5.4) | 1 (2.4) | 1 (3.4) | Kruskal–Wallis: 0.599 |
| Lower-risk drinkingd | 16 (10.7) | 4 (9.3) | 6 (16.2) | 4 (9.8) | 2 (6.9) | |
| Hazardous drinkinge | 29 (19.3) | 7 (16.3) | 5 (13.5) | 7 (17.1) | 10 (34.5) | |
| Harmful drinkingf | 95 (63.3) | 26 (60.5) | 24 (64.9) | 29 (70.7) | 16 (55.2) | |
| SHC outcomes | ||||||
| 1. Treatment plan initiated (N = 165), n (%) | 159 (96.4) | 48 (98.0) | 39 (97.5) | 41 (93.2) | 31 (96.9) | Chi-squared: 0.615 |
| 2. Continuity of care by CSS (N = 153), n (%) | 83 (54.2) | 32 (72.7) | 11 (29.7) | 27 (61.4) | 13 (46.4) | Chi-squared: 0.001 |
| 3. Sufficient explanation of SHC (N = 109), n (%) | 84 (77.1) | 20 (83.3) | 23 (79.3) | 22 (68.8) | 19 (79.2) | Chi-squared: 0.587 |
| 4. Satisfied with treatment plan (N = 102), n (%) | 88 (86.3) | 20 (83.3) | 25 (92.6) | 23 (79.3) | 20 (90.9) | Chi-squared: 0.445 |
| 5. Lower-risk drinking/positive change between baseline and 8 months (N = 123), n (%) | 50 (40.7) | 13 (40.6) | 9 (31.0) | 17 (47.2) | 11 (42.3) | Chi-squared: 0.618 |
| Total outcome score (N = 96), mean (SD) | 3.60 (1.00) | 3.70 (1.02) | 3.42 (0.76) | 3.64 (1.16) | 3.68 (1.06) | ANOVA: 0.757 |
A treatment plan (outcome 1) was initiated for 96.4% of participants identified by the CSSs as having an alcohol problem. There were, however, statistically significant differences for continuity of care (outcome 2) by Health Service Model (see Table 25). It was achieved for 72.7% of participants from Dedicated Centres, compared with only 29.7% from Mobile Teams. Continuity of care for the latter increased to 48.6% when interventions by GPs were added, bringing it to a level similar to that of Usual Care GPs. Interventions during the study included reviews of alcohol intake by CSS staff; case management by substance misuse or dual diagnosis teams (many also had mental health problems); alcohol reduction programmes; and prescribing of thiamine, vitamin B compound and nutritional supplements. During the study, 18 participants were admitted to an alcohol detoxification unit or undertook detoxification while in hospital, prison or a community setting; just three were still abstinent at the end of the study. Hence, for most, detoxification had been a temporary, rather than a long-lasting, intervention. Some participants declined referral to an alcohol service or did not feel ready for a detoxification programme; the CSS continued to monitor their care.
Overall, 77.1% of participants believed that they had received sufficient explanation of their condition (outcome 3), with a slightly lower rate for Specialist GPs. A higher percentage (86.3%) was satisfied with their treatment (outcome 4). For outcome 5, 40.7% reported abstinence over the study period or had reduced their alcohol consumption by 8 months. This was slightly higher among Specialist GP participants, and lower among Mobile Team participants, although the findings were not statistically significant.
Drug problems
Two-thirds of participants (66.4%) reported a drug problem at baseline. This included the use of illegal drugs or misuse of prescription or over-the-counter drugs. Self-reports were confirmed by medical records for most (86.4% of those for whom medical records were obtained) (Table 26). Hence, a drug problem was eligible for inclusion as a SHC for 197 participants. Of these, during the preceding 4 months, 43.9% had used illicit drugs 5 or more days a week, and 67.3% had used one or more Class A drugs. Class A drugs included heroin, morphine, cocaine, LSD and ecstasy. Of the 14 participants who reported drug use but it was not mentioned in their medical records, nine used only cannabis.
| Drug problem | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | ||
| Screening for inclusion as SHC, n (%) | ||||||
| Reported by participant at baseline (N = 363) | 241 (66.4) | 66 (68.8) | 47 (49.0) | 78 (81.3) | 50 (66.7) | Chi-squared: < 0.0005 |
| Diagnosis/documentation in medical records (N = 228)a | ||||||
| Not mentioned in medical records | 14 (6.1) | 2 (3.0) | 5 (10.6) | 1 (1.3) | 6 (16.2) | Not applicable |
| Documented, but inactive problem | 9 (3.9) | 2 (3.0) | 1 (2.1) | 2 (2.6) | 4 (10.8) | |
| Documented after first 4 months of study | 8 (3.5) | 3 (4.5) | 0 (0.0) | 1 (1.3) | 4 (10.8) | |
| Documented in first 4 months: SHC | 197 (86.4) | 59 (89.4) | 41 (87.2) | 74 (94.9) | 23 (62.2) | |
| Frequency (N = 187)/pattern of drug use at baseline,b n (%) | ||||||
| Not used drugs in previous 4 months | 22 (11.8) | 6 (10.5) | 4 (10.0) | 11 (15.3) | 1 (5.6) | Kruskal–Wallis: 0.824 |
| Used drugs 1–3 times in previous 4 months | 16 (8.6) | 4 (7.0) | 6 (15.0) | 5 (6.9) | 1 (5.6) | |
| Used drugs 4–8 times in previous 4 months | 23 (12.3) | 11 (19.3) | 4 (10.0) | 6 (8.3) | 2 (11.1) | |
| Used drugs 1–4 days per week | 44 (23.5) | 13 (22.8) | 10 (25.0) | 15 (20.8) | 6 (33.3) | |
| Used drugs ≥ 5 days per week | 82 (43.9) | 23 (40.4) | 16 (40.0) | 35 (48.6) | 8 (44.4) | |
| Used Class A drugsc in previous 4 months (N = 196) | 132 (67.3) | 43 (74.1) | 23 (56.1) | 53 (71.6) | 13 (56.5) | Chi-squared: 0.144 |
| Injected drugs in previous 4 months (N = 190) | 77 (40.5) | 31 (54.4) | 13 (31.7) | 31 (43.1) | 2 (10.0) | Chi-squared: 0.003 |
| SHC outcomes | ||||||
| 1. Treatment plan initiated (N = 197), n (%) | 180 (91.4) | 58 (98.3) | 32 (78.0) | 68 (91.9) | 22 (95.7) | Chi-squared: 0.004 |
| 2. Continuity of care by CSS (N = 177), n (%) | 96 (54.2) | 45 (84.9) | 9 (25.7) | 39 (56.5) | 3 (15.0) | Chi-squared: < 0.0005 |
| 3. Sufficient explanation of SHC (N = 122), n (%) | 102 (83.6) | 27 (84.4) | 24 (88.9) | 41 (83.7) | 10 (71.4) | Chi-squared: 0.556 |
| 4. Satisfied with treatment plan (N = 116), n (%) | 108 (93.1) | 31 (96.9) | 24 (88.9) | 42 (97.7) | 11 (78.6) | Chi-squared: 0.059 |
| 5. No illicit drug use/reduction in frequency of use between baseline and 8 months (N = 135), n (%) | 47 (34.8) | 12 (33.3) | 15 (51.7) | 17 (31.5) | 3 (18.8) | Chi-squared: 0.123 |
| Total outcome score (N = 110), mean (SD) | 3.63 (0.95) | 3.91 (0.82) | 3.40 (0.96) | 3.83 (0.81) | 2.77 (1.09) | ANOVA: 0.001 |
A treatment plan was initiated for 91.4% of participants identified by the CSSs as having a drug problem, with statistically significant differences by Health Service Model. A plan had been started for 98.3% of Dedicated Centre participants, compared with 78% from Mobile Teams (see Table 26). There were highly significant differences in relation to continuity of care: it was achieved for 84.9% of Dedicated Centre participants, compared with 15% of Usual Care GP participants. Continuity of care for Mobile Team participants increased from 25.7% to 48.6% when GP services were included. Continuity of care included shared care between GPs and substance misuse workers, maintenance on OST (55.9% were receiving such treatment at 8 months), involvement in recovery and rehabilitation programmes, and joint reviews with mental health and alcohol services (94.9% also reported mental health and/or alcohol problems). In relation to OST, some participants engaged with a programme and received treatment throughout the study, whereas some had spells when they failed to comply and treatment was intermittent.
There were fairly high scores across the models for outcomes 3 and 4. For outcome 5, 34.8% reported abstinence or a reduction in frequency of drug use during the study. The total score for all five outcomes was lower for Usual Care GPs, and the finding was statistically significant. Outcome 5 concentrated on changes in frequency of drug use. There were also small reductions in the numbers of participants who reported using Class A drugs by 8 months and who reported injecting drugs.
Management of Specific Health Conditions by Case Study Sites
There were differences by CSSs within the same model in the recognition of some SHCs. The percentage of participants who reported depression at baseline but it was not identified in the medical records varied by CSS (Figure 4). This applied to a higher percentage of cases at DC2 than at DC1. One reason might be that DC1 employed a full-time primary mental health nurse, whereas DC2 had input from community mental health practitioners at the CSS for just 15 hours per week. Hence, there may have been more opportunities for the DC1 mental health worker to engage with patients over time and recognise depression. Likewise, the percentage of cases of depression reported by participants at baseline, but not identified in the medical records, was higher for SP2 than for SP1. The latter had on-site sessions with mental health workers, whereas SP2 had input from a counselling service which relied on CSS staff to detect a problem and make a referral. SP1 also had full-time nurses and case managers dedicated to patients who were homeless (not the situation at SP2), who would have been able to arrange assessments for patients with low mood and possible depression.
FIGURE 4.
Depression reported by participants at baseline, but not identified in medical records, by CSS. Includes only participants who reported depression, and refers to the percentage of participants for whom depression not mentioned in medical records in previous 3 years.
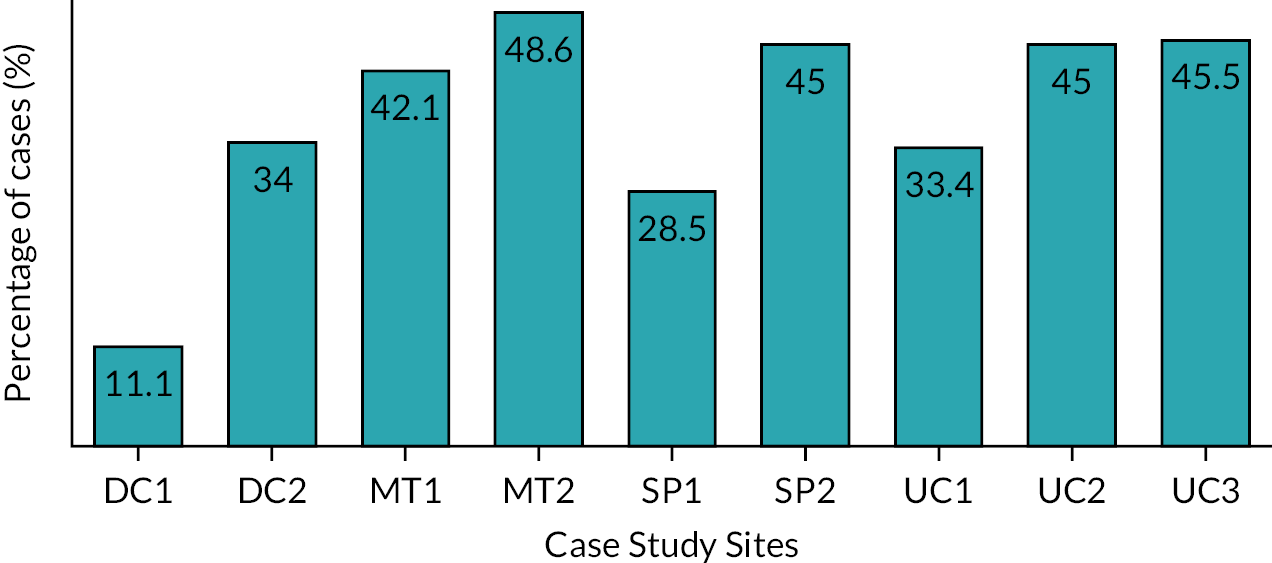
There were also differences in the management of SHCs by CSSs within the same model, although, because of small numbers, it was possible to examine outcomes 1 and 2 for depression, alcohol and drug problems only (Table 27). MT1 was more likely than MT2 to provide continuity of care for all three SHCs, although the findings were not statistically significant. They also should be treated cautiously because of the large amount of Read-coded text used by MT1 that was coded as continuity of care.
| CSS | Depression, n (%) | Alcohol problem, n (%) | Drug problem, n (%) | |||
|---|---|---|---|---|---|---|
| Outcome 1a | Outcome 2b | Outcome 1a | Outcome 2b | Outcome 1a | Outcome 2b | |
| Dedicated Centres | ||||||
| DC1 | 29 (93.5) | 19 (67.9) | 20 (100) | 15 (78.9) | 37 (100) | 28 (80.0) |
| DC2 | 26 (100) | 16 (72.7) | 28 (96.6) | 17 (68.0) | 21 (95.5) | 17 (94.4) |
| Mobile Teams | ||||||
| MT1 | 19 (90.5) | 8 (42.1) | 21 (95.5) | 8 (40.0) | 23 (85.2) | 8 (33.3) |
| MT2 | 17 (100) | 4 (25.0) | 18 (100) | 3 (17.6) | 9 (64.3) | 1 (9.1) |
| Specialist GPs | ||||||
| SP1 | 29 (96.7) | 19 (70.4) | 25 (89.3) | 16 (57.1) | 38 (95.0) | 26 (70.3) |
| SP2 | 21 (95.5) | 12 (57.1) | 16 (100) | 11 (68.8) | 30 (88.2) | 13 (40.6) |
| Usual Care GPs | ||||||
| UC1 | 9 (100) | 4 (44.4) | 7 (87.5) | 2 (25.0) | 6 (100) | 1 (16.7) |
| UC2 | 10 (90.9) | 5 (62.5) | 19 (100) | 9 (56.3) | 10 (90.9) | 2 (25.0) |
| UC3 | 4 (66.7) | 3 (50.0) | 5 (100) | 2 (50.0) | 6 (100) | 0 (0.0) |
Specialist GP 1 was more likely than SP2 to provide continuity of care for depression and drug problems, and the latter was statistically significant (chi-squared test: p = 0.013). This may be due to drug workers holding clinics at SP1 and providing OST, whereas this was not the case at SP2. In addition, as described previously, SP1 had full-time nurses and case managers working primarily with patients who were homeless, and staff regularly visited hostels and day centres, undertook street outreach work and worked closely with a local hospital. These are all factors that are likely to have a positive impact on continuity of care. Overall, continuity of care for alcohol problems was achieved for 61.6% of participants at CSSs with on-site alcohol services, compared with 44.9% where such services were unavailable (chi-squared test: p = 0.036). The respective figures for drug problems were 70.6% with, and 32% without, on-site drug services (chi-squared test: p = 0.0005).
There were differences for Usual Care GP sites, but the findings should be treated cautiously because of small numbers. UC3 was least likely to initiate a treatment plan for patients identified as having depression. As part of its health assessment for patients who were homeless, the PHQ-9 was completed, but it appeared that no further action was taken when scores indicated depression.
Summary
This chapter describes the management of SHCs by Health Service Models. Apart from hypertension, all other SHCs were common among participants and each was examined separately. The prevalence of hypertension may have been higher if all medical records were searched, instead of just those where the problem was first reported by participants. For the majority of participants who reported alcohol and drug problems, these were mentioned in their medical records, although they were less likely to be documented for Usual Care GP participants. This may be because participants felt less confident in admitting such problems to Usual Care GPs. As noted in Chapter 7 (see Table 15), screening for alcohol problems was highest among Usual Care GP participants. Given that several of this group of participants reported alcohol problems when interviewed by the research team, but they were not mentioned in their medical records (see Table 25), this suggests that some may have downplayed their use of alcohol when asked by general practice staff. Under-reporting of the use of alcohol and illicit drugs is common in health care settings and general population surveys. 123–126 Many participants reported chronic respiratory problems and depression, which were not documented in the medical records, despite baseline instruments indicating substantial problems. This applied to all Health Service Models, suggesting that staff were failing to recognise these conditions among some people who were homeless.
For each SHC, treatment plans were initiated for most participants identified in their medical records as having a problem. There were, however, differences with regard to continuity of care. It was most likely to have been achieved for chronic respiratory problems, whereas, for depression, alcohol problems and drug problems, it was attained for just over half of the participants. Dedicated Centres, followed by Specialist GPs, were most likely to have maintained continuity of care for each of the SHCs; for depression, alcohol problems and drug problems, the findings were significant. Mobile Teams were least likely to have provided continuity of care for all SHCs apart from drug problems, for which Usual Care GPs scored lower. However, when interventions by GP services were added to the Mobile Teams’ scores, continuity-of-care rates reached levels comparable to or above those of Usual Care GPs. As discussed previously, caution is needed when interpreting findings from MT1 as the medical records contained a large amount of pre-coded text with no added details. This was scored positively.
Continuity of care and treatment for the SHCs was not straightforward. Many participants had multiple conditions, namely depression, heavy drinking and the use of illicit drugs, which affected each other and presented challenges to health care providers. For example, medication for depression could not be prescribed in some instances because a person was drinking heavily. Treatments such as alcohol detoxification or OST maintenance were sometimes offered but were declined, or were introduced but not sustained. For many, care involved joint working between mental health and substance misuse services.
For each SHC, positive changes were reported by some participants between baseline and 8 months, or their condition remained stable. This applied to around two-fifths with depression or alcohol problems, slightly fewer with chronic respiratory problems, and just over one-third with drug problems. These findings must, however, be treated cautiously. They concerned only participants who were interviewed at 8 months, and were thus more likely to have sustained contact with the CSS. Several who could not be interviewed were in hospital or prison, and, in many instances, substance misuse had been a contributory factor to this outcome. As mentioned previously, people tend to under-report usage of alcohol and illicit drugs, and, unlike respiratory problems and depression, it was not feasible to use validated instruments to detect changes in their use. Moreover, there are many dimensions to assessing drug misuse over time, including frequency of use, types and multiplicity of drugs taken, toxicity of drugs taken and mode of administration (oral, inhaling or injection). No instrument could be found that captured these various dimensions. Adding to the complexity, the frequency and mode of drug administration differed according to the type of drug, and by factors such as changes in personal circumstances and access to finances. As a result, there were fluctuations in drug misuse among many individuals throughout the study period.
Each SHC was scored on five dimensions, each being allocated a score of 1 or 0. It can be argued, however, that achieving continuity of care over at least 8 months (outcome 2) is harder to achieve than starting a treatment plan (outcome 1) or positive feedback from participants about help received (outcomes 3 and 4). Likewise, assessing stability or change in health status from baseline to 8 months (outcome 5) covers a relatively short period. The scoring of the management of SHCs is not a validated tool. It is simply a way of assessing how the CSSs responded to various health conditions.
As with the primary outcome, there were differences across CSSs within the same Health Service Model in relation to recognising depression, and providing continuity of care for depression and substance misuse problems. The findings suggest that these may be related to service provision and staff at the sites. Dedicated Centres and SP1, characterised by features such as designated nurses and case managers for patients who are homeless, on-site specialist mental health and substance misuse workers, street outreach, clinics in hostels and day centres, and involvement in hospital inpatient work, were significantly more likely to have maintained contact with patients. The next chapter examines the impact of the Health Service Models on health status and well-being.
Chapter 9 Health status and well-being over time
One of the secondary outcomes was to assess the impact of the Health Service Models on health status and well-being over time. This chapter first examines smoking and nutrition, and whether or not participants received help or advice from CSS staff on these. The subsequent sections present participants’ assessments of their health-related quality of life and mental well-being, using the Short From questionnaire-8 items (SF-8) health survey and the Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS), and changes in their assessments over time. A PCS and a MCS are produced by the SF-8, and a single score is produced from the SWEMWBS. Regression techniques were used to explore associations between the Health Service Models and these three scores, incorporating profiles of the participants. Information in this chapter is exclusively from participants, not medical records.
Smoking
At baseline, the majority (88.1%) of participants smoked cigarettes or tobacco (not including cannabis or other drugs). A further 4.4% used to smoke but had stopped. In comparison, just 13.9% of adults in England in 2019 were smokers. 127 It is difficult to collect precise information about smoking habits, although 21.1% of participants reported having more than or equal to 20 cigarettes or ‘roll-ups’ daily and so were classified as ‘heavy smokers’. Participants of Mobile Teams were least likely, and those of Specialist GPs most likely, to report current smoking; the findings were statistically significant (Table 28). Of those who smoked at baseline, 34.8% had received advice or help in the preceding 4 months with reducing or stopping smoking from CSS doctors or nurses, including 15 participants who had been given nicotine patches. Usual Care GP participants were more likely to have received help, although the findings were not statistically significant.
| Smoking and nutrition | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Smoking habits (baseline), n (%) | ||||||
| Currently smoke | 319 (88.1) | 85 (89.5) | 77 (80.2) | 93 (96.9) | 64 (85.3) | Chi-squared: 0.004 |
| Smoke ≥ 20a per day | 70 (21.1) | 25 (29.8) | 13 (14.6) | 15 (17.6) | 17 (23.3) | Chi-squared: 0.077 |
| Received help from CSS with smokingb (N = 313 current smokers) | 109 (34.8) | 29 (34.9) | 24 (31.2) | 30 (32.6) | 26 (42.6) | Chi-squared: 0.855 |
| Nutrition (baseline) | ||||||
| Number of days per week has a mealc (N = 342), n (%) | ||||||
| ≤ 1 | 70 (20.5) | 18 (20.0) | 20 (21.7) | 19 (20.9) | 13 (18.8) | Chi-squared: 0.680 |
| 2 or 3 | 76 (22.2) | 18 (20.0) | 16 (17.4) | 22 (24.2) | 20 (29.0) | |
| 4 or 5 | 30 (8.8) | 6 (6.7) | 12 (13.0) | 6 (6.6) | 6 (8.7) | |
| ≥ 6 | 166 (48.5) | 48 (53.3) | 44 (47.8) | 44 (48.4) | 30 (43.5) | |
| Number of days per week has a meal,c median (IQR) | 5 (2–7) | 6.5 (2–7) | 5.25 (2–7) | 4 (2–7) | 4.5 (2–7) | Kruskal–Wallis: 0.909 |
| Has fruit/vegetables once per week or lessd (N = 347), n (%) | 87 (25.1) | 25 (27.5) | 22 (23.2) | 25 (26.6) | 15 (22.4) | Chi-squared: 0.840 |
| Has problems getting meals/eating healthily (N = 360), n (%) | 193 (53.6) | 47 (50.0) | 44 (45.8) | 53 (55.2) | 49 (66.2) | Chi-squared: 0.054 |
| Received help from CSS regarding healthy eatingb (N = 362), n (%) | 103 (28.5) | 36 (37.9) | 23 (24.0) | 34 (35.4) | 10 (13.3) | Chi-squared: 0.001 |
Thirteen participants who were smokers at baseline had stopped smoking by 8 months: four from Mobile Teams and three from each of the other models. Nineteen people who smoked, but not heavily, at baseline reported being heavy smokers at 8 months (four from Dedicated Centres, eight from Mobile Teams, five from Specialist GPs and two from Usual Care GPs). This may reflect an increase in their tobacco intake, or they were more candid over time about smoking habits. In contrast, 21 people who were heavy smokers at baseline smoked less than 20 per day at 8 months. Of those who did not smoke at baseline, none had started or resumed smoking at 8 months.
Nutrition
At baseline, the median number of days per week that participants had a meal containing protein, such as meat, fish or a vegetarian equivalent, was five. This varied greatly: 48.5% had such a meal 6 or 7 days a week, and 20.5% had such a meal once a week or less (see Table 28). Likewise, 25.1% had a portion of fruit or vegetables once a week or less. Just over one-third of participants cooked for themselves, 23.5% had food provided at their hostel and 45.7% had food at day centres. Other sources of food included soup runs and handouts on the streets (17.7%), takeaway food (13.9%) and meals cooked by relatives or friends (10.8%). Overall, 53.6% reported difficulty getting meals or eating healthily, mainly because of insufficient income, poor appetite or problems with cooking. Three-tenths had used a food bank at least once in the preceding 4 months. Participants in their own tenancy, followed by those sleeping rough, were more likely to report poor food intake. Among the former, 34.6% had a meal once a week or less, 63% described difficulty getting meals or eating healthily, and several relied on day centres for food. Participants who were sleeping rough mainly obtained food at day centres and street handouts.
There were no statistically significant differences by Health Service Model in nutrition habits among participants, although a slightly higher percentage of Usual Care GP participants reported difficulty getting meals or eating healthily. Nearly three-tenths of participants (28.5%) had received help in the preceding 4 months regarding nutrition from a CSS doctor or nurse, including advice about weight and food intake, vouchers for food banks or a prescription for nutritional supplements. Dedicated Centres and Specialist GPs were most likely, and Usual Care GPs least likely, to have provided help; the findings were statistically significant (see Table 28). Hence, Usual Care GP participants were most likely to describe nutritional problems and least likely to have received advice from the CSS.
By 8 months, the median number of days per week that participants had a meal had increased to seven, with 17% stating once a week or less. There were no statistically significant differences by Health Service Model in nutrition habits at 8 months, although slightly fewer (40.8%) described problems obtaining food or eating healthily.
Health status
The SF-8 is a short, self-administered instrument that produces a health-related quality-of-life profile. It measures eight ordinal items over the preceding 4 weeks: general health, physical functioning, ability to carry out physical activities, bodily pain, vitality, social functioning, mental health and emotional roles. Scale means, based on the same standard metrics as for the Short Form 36 Health Survey, are assigned to each response, creating a continuous outcome for each of the eight items. Regression coefficient weights are assigned to each item to produce a PCS and a MCS, both of which are continuous variables and have a mean of 50 (SD 10) in the general population of the USA. 128 Higher scores represent more favourable health states, and lower scores indicate worse health states.
The SF-8 was self-completed by the HEARTH study participants at baseline and at 8 months. At baseline, the mean PCS was 39.8 and the mean MCS was 35.4, with no statistically significant difference by Health Service Model. There was a slight increase at 8 months in the mean PCS and MCS across all models, but the findings were not statistically significant. When changes in scores are examined for participants who completed the SF-8 at both baseline and 8 months, there were no statistically significant differences by Health Service Model, although Mobile Team and Usual Care GP participants experienced a negative change in mean for the SF-8 MCS (Table 29).
| Self-administered instruments | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| SF-8: PCSa | ||||||
| Score at baseline (N = 354), mean (SD) | 39.8 (10.5) | 40.4 (10.7) | 38.5 (10.7) | 40.1 (10.0) | 40.5 (10.5) | ANOVA: 0.508 |
| Score at 8 months (N = 253), mean (SD) | 41.9 (11.5) | 43.7 (10.8) | 40.4 (12.1) | 42.4 (11.0) | 40.9 (11.9) | ANOVA: 0.351 |
| Change in mean (SD) score at 8 months (N = 249) | 2.22 (10.04) | 3.67 (10.01) | 0.61 (9.79) | 3.77 (11.32) | 0.70 (8.43) | ANOVA: 0.120 |
| SF-8: MCSa | ||||||
| Score at baseline (N = 354), mean (SD) | 35.4 (12.6) | 36.2 (11.0) | 37.3 (13.0) | 33.3 (13.1) | 34.7 (13.1) | ANOVA: 0.152 |
| Score at 8 months (N = 253), mean (SD) | 38.1 (12.6) | 40.3 (10.8) | 38.7 (14.5) | 37.4 (11.4) | 35.6 (12.0) | ANOVA: 0.199 |
| Change in mean (SD) score at 8 months (N = 249) | 0.96 (12.30) | 1.14 (10.97) | –0.84 (13.32) | 3.82 (13.10) | –0.33 (11.20) | ANOVA: 0.141 |
| SWEMWBSb | ||||||
| Metric score at baseline (N = 350), mean (SD) | 18.5 (5.0) | 18.9 (4.4) | 19.1 (5.8) | 17.6 (4.0) | 18.1 (5.5) | ANOVA: 0.139 |
| Metric score at 8 months (N = 254), mean (SD) | 19.6 (5.2) | 19.8 (5.1) | 20.5 (5.9) | 19.2 (4.7) | 18.8 (5.1) | ANOVA: 0.238 |
| Change in mean (SD) score at 8 months (N = 248) | 0.79 (5.40) | 0.57 (4.83) | 0.86 (5.94) | 1.47 (5.47) | 0.15 (5.28) | ANOVA: 0.593 |
The average scores in the general population of the USA for the PCS and the MCS are 50. 128 Of the HEARTH study participants, at baseline, 81.9% scored less than this for the PCS and 83.6% scored less than this for the MCS. No data could be found of SF-8 use in England among either the general population or people who were homeless to compare scores. However, a recent study in Belfast used the SF-8 to assess the mental health of people in different deprivation areas, drawing on the 2010 Northern Ireland Multiple Deprivation Measure. 129 The MCS score for those in the most deprived area (n = 215) was 45.6, which is considerably higher than that of the HEARTH study participants. Likewise, during a survey in Alameda County, California, 292 people who had been homeless for 12 months or more in the previous 3 years (i.e. chronically homeless) completed the SF-8. Their scores were slightly higher (PCS 42.1, MCS 39.6) than those of the HEARTH study participants. 130
Mental well-being
The SWEMWBS was developed in 2009 as a shorter version of the Warwick–Edinburgh Mental Wellbeing Scale. It is a validated instrument for use by the general population, and has seven items relating to psychological functioning, such as feelings of usefulness and optimism, thinking clearly and dealing with problems. 131 Each item allows five responses, from ‘none of the time’ to ‘all of the time’ (scored 1–5), and people rate their experiences over the preceding 2 weeks. Scores range from 7 to 35, with higher scores indicating greater positive mental well-being. The total raw scores from the SWEMWBS are transformed into metric scores using a conversion table.
The SWEMWBS was self-completed by the HEARTH study participants at baseline and 8 months. At baseline, the mean score was 18.5, with no statistically significant difference by Health Service Model. There was a slight increase in scores for all models at 8 months, but the findings were not statistically significant. Likewise, there were no statistically significant differences by Health Service Model in changes in scores between baseline and 8 months when the scores of the 248 participants who completed the SWEMWBS at both baseline and 8 months are examined (see Table 29).
When the scores are compared with responses in the Health Survey for England 2010–13 of 27,169 people aged 16 years and older,131 the mental well-being of the HEARTH study participants was considerably lower than that of the general population. In the HEARTH study, the mean baseline scores were 18.4 for men and 18.7 for women. In contrast, the mean scores in the Health Survey for England were 23.7 for men and 23.2 for women. 131
Regression modelling of Short Form 8 Health Survey and Short Warwick–Edinburgh Mental Wellbeing Scale scores
Dichotomous and continuous predictors, similar to those applied to the modelling of the Primary Outcome Score, were used to isolate the effect of the four Health Service Models in the modelling of two outcomes for each of the following: the SF-8 PCS, the SF-8 MCS and the SWEMWBS. The first concerns baseline scores, and the second concerns changes in scores from baseline to 8 months.
Baseline scores
For modelling the baseline scores, an initial backward stepwise linear regression was run with each dependent variable at baseline and the variables in Appendix 3, Tables 48 and 49, as predictors. Statistically significant and near statistically significant (p < 0.15) predictors were used in a second backward stepwise linear regression. A final model was run using only the statistically significant predictors resulting from this regression to maximise the number of observations used.
The salient fitted parameters, namely those for Health Service Model (whether or not statistically significant) and for other statistically significant predictors for the SF-8 and the SWEMWBS outcomes, are shown in Table 30. No statistically significant beneficial effect is seen when comparing Dedicated Centre, Mobile Team and Specialist GP models with the Usual Care GP model at baseline. Across the three secondary outcomes, various other predictors show statistical significance (albeit never more than twice), reflecting the importance of taking into account many facets of the target population before assessing the efficacy of the four Health Service Models. For example, physical health problems and an increasing number of GP or nurse consultations were negatively associated with the SF-8 PCS, which is understandable given that it concerns physical functioning. Increasing age and drug use also had similar effects, both of which are likely to affect physical health.
| Predictors | SF-8 | SWEMWBS (range 7–35)a | |
|---|---|---|---|
| PCS (range 16.52–65.24)a | MCS (range 6.32–61.36)a | ||
| Dedicated Centre | 0.634 | 2.930 | 1.139 |
| Mobile Team | −1.826 | 2.803 | 0.860 |
| Specialist GP | −0.053 | 1.202 | 0.103 |
| Registered with CSS > 1 year (baseline) | 2.196* | ||
| Approximate number of years homeless | 0.078** | ||
| Female | −2.370* | ||
| Age (years) | −0.197*** | ||
| Physical health problems in preceding 4 months (baseline) | −12.711*** | −4.643* | |
| Depression in preceding 4 months (baseline) | −14.381*** | −3.402*** | |
| Drinking > 14 units of alcohol per week (baseline) | −1.843*** | ||
| Used drugs in preceding 4 months (baseline) | −3.053*** | ||
| Injected drugs in preceding 4 months (baseline) | −3.389** | −2.627*** | |
| Support from family/friends in preceding 4 months (baseline) | −1.266** | ||
| Number of consultations at CSS with GP/nurse/HCA in preceding 4 months (baseline) | −0.168** | ||
| Constant | 63.711 | 49.705 | 21.008 |
| Final model diagnostics | n = 354 | n = 342 | n = 315 |
| R2 | 0.168 | 0.234 | 0.174 |
In terms of the SF-8 MCS and the SWEMWBS scores which concern mental health and psychological well-being, self-reported depression had a significant negative effect, which is to be expected. Likewise, there was a negative association with both outcomes among participants who injected drugs. In relation to the SWEMWBS, statistically significant negative effects were also linked to heavy drinking and increasing length of time homeless, both of which are likely to have an adverse impact on morale and well-being.
Changes after 8 months
When changes in the SF-8 PCS, the SF-8 MCS and the SWEMWBS scores are examined from baseline to 8 months, one or more changes was observed for 253 participants (69.7%), with 244 (67.2%) participants having changes for all three outcomes. Dichotomous and continuous predictors were used
to isolate the effect of the four Health Service Models in the modelling of changes in SF-8 PCS, SF-8 MCS and SWEMWBS scores (see Appendix 3, Tables 50 and 51). Variables relating to alcohol and drug use, smoking, income, involvement in education or employment, and informal support relate to circumstances at 8 months. Baseline variables for the principal predictors concerning physical and mental health were retained, as the corresponding variables at 8 months confound with the SF-8 PCS and SF-8 MCS outcomes at 8 months.
An initial backward stepwise linear regression was run, and statistically significant and near statistically significant (p < 0.15) predictors were used in a second backward stepwise linear regression. A final model was run using only the statistically significant predictors resulting from this regression to maximise the number of observations used. The salient fitted parameters, namely those for Health Service Model (whether or not statistically significant) and for other statistically significant predictors for the SF-8 and the SWEMWBS outcomes, are shown in Table 31.
| Predictors | SF-8 | SWEMWBSa | |
|---|---|---|---|
| PCSa | MCSa | ||
| Dedicated Centre | 3.963** | 1.914 | 1.098 |
| Mobile Team | −0.291 | 0.040 | 1.215 |
| Specialist GP | 3.569** | 3.037 | 1.408* |
| Registered with CSS > 1 year | 2.098* | ||
| Approximate number of years homeless | −0.065* | ||
| Age (years) | −0.129** | ||
| Involved in education/training/employment (8 months) | 2.450*** | ||
| Depression in preceding 4 months (baseline) | −4.380*** | −2.462*** | |
| Drinking > 14 units of alcohol per week (8 months) | −3.166*** | ||
| Used drugs in preceding 4 months (8 months) | −3.409** | ||
| Injected drugs in preceding 4 months (8 months) | −1.802** | ||
| % of time in accommodation with staff (24 hour or part of) in study period | −0.041** | ||
| Number of consultations at CSS with GP/nurse/HCA in study period | −0.055** | ||
| Constant | 26.873 | 21.956 | 14.254 |
| Corresponding secondary outcome score at baseline | −0.407*** | −0.499*** | −0.639*** |
| Final model diagnostics | n = 241 | n = 248 | n = 242 |
| R2 | 0.248 | 0.289 | 0.367 |
When comparing changes from baseline to 8 months, Dedicated Centres and Specialist GPs both elicit a comparative improvement of around 4 points for the SF-8 PCS, and there is also an improvement in the SWEMWBS scores for Specialist GPs. These findings are statistically significant. Increasing age, heavy drinking, depression and an increasing number of GP or nurse consultations at the CSS were associated with a negative effect on change in SF-8 PCS. Increasing age and heavy drinking are likely to contribute to physical health problems, which, in turn, are likely to lead to consultations with primary health care professionals. The large negative depression coefficients (−4.380 and −2.462) illustrate the ongoing impact of depression on physical and mental well-being.
There was a negative association between change in the SF-8 MCS and the percentage of time living in staffed accommodation during the study period. The likely explanation is that participants with mental health problems spent more time in staffed accommodation during the study than those without mental health problems (mean percentage of time 49.98 and 27.27, respectively). As with the baseline regressions, self-reported depression and injection of drugs were negatively associated with beneficial change in SWEMWBS scores, whereas there was a strong positive effect from involvement in education, training or employment. The latter is likely to be associated with increased motivation and morale, which, in turn, will influence psychological functioning.
Summary
This chapter has examined the impact of the various Health Service Models on health status and well-being over time. A very high percentage of participants were smokers, and many had poor nutrition. There were slight improvements over time in their smoking and eating habits, but no statistically significant differences by Health Service Model in the provision of help for smoking. However, Dedicated Centres and Specialist GPs were most likely, and Usual Care GPs least likely, to have provided help with nutrition: a statistically significant disparity.
The SF-8 PCS, the SF-8 MCS and the SWEMWBS scores of the HEARTH study participants indicate low levels of physical and psychological functioning, compared with the general population and other marginalised groups. There were no significant differences in their scores at baseline by Health Service Model, and most models experienced a slight improvement in scores over time. Further interrogation of the data through regression modelling, however, revealed a positive improvement in changes in SF-8 PCS from baseline to 8 months by Dedicated Centres and Specialist GPs, and a positive change in SWEMWBS scores for Specialist GPs. However, several participant characteristics had strong significant effects on scores at baseline, and on changes in scores from baseline to 8 months. These mainly involved negative effects associated with older age, physical health problems, depression, heavy drinking, drug use and injection of drugs. A strong positive effect concerning involvement in education, training or employment was associated with change in the SWEMWBS scores from baseline to 8 months. The next chapter focuses on oral health and participants’ use of dental services.
Chapter 10 Oral health and access to dental care
One of the secondary outcomes was to examine the impact over time of the Health Service Models on oral health status and access to dental care, and their integration with dental services (see Chapter 3). This chapter begins by describing measures used to assess oral health and dental access, followed by whether or not, and how, these changed at each interview, and over the 12-month study period. Data were drawn mainly from the HEARTH study participants, although dental attendance data were supplemented by information from medical records (when documented). The last section summarises the availability of dental services in the study areas and the integration of the CSSs with these services.
Measures of oral health and dental access
Two proxies were used to assess oral health. The first was a single-item global self-rating of dental health (1 = very bad, 5 = very good),132 collected from participants at baseline and at 4 and 8 months. The second was the shortened Oral Health Impact Profile (OHIP-14), used to measure oral health-related quality of life (OHRQoL),101 completed by participants at 4 months. They rated the frequency (never to very often) of 14 dental-related impacts (problems) in the previous 8 months. In addition, at 8 months, participants were asked if their dental health had changed over the previous 12 months (1 = worsened a lot, 5 = improved a lot).
Features of access to dental care were hypothesised to involve registration with a dentist, dental attendance, completion or continuation of a course of dental treatment and satisfaction with dental care. The first three were recorded at each interview, and satisfaction with dental care was recorded at 8 months using a single-item rating scale. 133 Dental access was considered effective when urgent (pain) and felt dental needs were resolved. Experience of dental pain was recorded at baseline and 4 months,134–136 and felt need for dental treatment was recorded at baseline and 8 months. 104
Dental access is strongly affected by dental fear, and levels of dental anxiety were recorded at baseline and 8 months using the MDAS. The MDAS rates level of anxiety (1 = not anxious, 5 = extremely anxious) in five situations: anticipating dental treatment the next day; in dentist waiting room; about to have a tooth drilled; about to have teeth scaled and polished; and about to have a local anaesthetic injection in the gum. The MDAS has a maximum score of 25, with scores of 19 or more denoting dental phobia. 102
Oral health, dental anxiety and use of dental services at baseline
At baseline, 21.9% of participants rated their dental health as ‘very good’ or ‘good’. Participants of Dedicated Centres and Mobile Teams described their oral health more positively than those of the other two models (Table 32). Just over one-fifth (22.1%) had experienced dental pain ‘often or very often’ in the previous 4 months. By comparison, in 2009, 71% of the general population in England rated their dental health as very good/good,135 and 8% of dentate adults reported dental pain in the previous 12 months. 136
| Oral health and dental access | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) | ||
| Rated their dental health as very good/good,a n (%) | 79 (21.9) | 29 (30.5) | 26 (27.1) | 13 (13.7) | 11 (14.9) | Chi-squared: 0.009 |
| Reported dental pain in previous 4 months (often or very often), n (%) | 79 (22. 1) | 22 (23.7) | 17 (17.7) | 26 (27.1) | 14 (19.4) | Chi-squared: 0.410 |
| In need of dental treatment, n (%) | 290 (82.2) | 72 (77.4) | 76 (80.9) | 85 (89.5) | 57 (80.3) | Chi-squared: 0.160 |
| Registered with a dentist, n (%) | 139 (38.7) | 37 (38.9) | 32 (33.7) | 34 (35.8) | 36 (48.6) | Chi-squared: 0.218 |
| Saw dentist in previous 4 months, n (%) | 78 (21.7) | 18 (18.9) | 19 (19.8) | 21 (21.9) | 20 (27.4) | Chi-squared: 0.057 |
| Saw dentist in previous 2 years, n (%) | 203 (56.9) | 55 (58.5) | 55 (58.5) | 46 (47.9) | 47 (64.4) | Chi-squared: 0.170 |
| MDAS score, mean (SD) | 13.9 (6.7) | 14.1 (6.8) | 13.1 (6.7) | 15.4 (6.7) | 12.7 (6.6) | ANOVA: 0.034 |
| MDAS score of ≥ 19, indicating dental phobia, n (%) | 119 (33.4) | 31 (33.7) | 27 (28.7) | 40 (41.7) | 21 (28.4) | Chi-squared: 0.194 |
Nearly two-fifths (38.7%) of participants were registered with a dentist at baseline. This included a slightly higher proportion of Usual Care GP participants, although the findings were not statistically significant (see Table 32). Of those who responded, 6.8% were registered with a dentist at their CSS, 28.2% were registered with a dentist in the same town as that of the CSS and 3.1% were registered with a dentist in another town. By comparison, adult registration rates with NHS dentists in England over the study time frame ranged from 50.2% to 51.8%. 137–140 Of the HEARTH study participants, 56.9% had seen a dentist in the previous 2 years, including 21.7% in the previous 4 months. There were no statistically significant differences in having seen a dentist at least once in the previous 2 years, or in the previous 4 months, by Health Service Model.
A high proportion (82.2%) of the HEARTH study participants reported felt need for dental treatment. Of 177 participants who reported felt need and were not registered with a dentist, only 9% had discussed their dental need with CSS staff. Dental anxiety is an important predictor of dental attendance. 141 One-third of participants scored 19 or more when completing the MDAS, indicating dental phobia, with Specialist GP participants reporting the highest anxiety levels (see Table 32). In contrast, just 12% of the general population in 2009 described having dental phobia. 135 Several reasons were given by the HEARTH study participants for not seeing a dentist in the previous 24 months, most commonly dental fear (32.9%), ‘not got around to it’ (23.7%) and too embarrassed about state of teeth (17.1%). Just 12.5% said they could not find an NHS dentist, and 11.8% could not afford NHS charges (see Appendix 4, Table 52).
Oral health and use of dental services at 4 months
At 4 months, 25.2% of participants rated their dental health as very good/good, representing a slight improvement from baseline, but no difference by Health Service Model. The percentage who reported dental pain was similar at baseline and at 4 months. The proportion registered with a dentist had increased slightly from baseline, although the rate (43.4%) remained low compared with that of the general population. There were no changes in dental attendance rates over the preceding 4 months. Participants of Usual Care GPs were more likely than the rest of the sample to be registered with a dentist, and to have seen a dentist within the preceding 4 months. The latter was statistically significant (Table 33).
| Outcomes | Health Service Model, n (%) | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | ||
| At 4 months | ||||||
| Rated dental health as very good/gooda (N = 270) | 69 (25.2) | 19 (27.9) | 23 (31.9) | 14 (19.7) | 13 (20.6) | Chi-squared: 0.279 |
| Reported dental pain in previous 4 months (often or very often)b (N = 268) | 55 (20.5) | 16 (23.5) | 11 (15.3) | 18 (28.1) | 10 (15.6) | Chi-squared: 0.187 |
| Registered with a dentist (N = 268) | 116 (43.4) | 25 (37.9) | 28 (39.4) | 26 (38.8) | 37 (57.8) | Chi-squared: 0.064 |
| Saw a dentist in previous 4 months (N = 271) | 54 (19.9) | 11 (15.9) | 9 (12.5) | 12 (18.2) | 22 (34.4) | Chi-squared: 0.009 |
| At 8 months | ||||||
| Rated dental health as very good/gooda (N = 253) | 64 (25.3) | 15 (24.2) | 24 (34.8) | 10 (15.2) | 15 (26.8) | Chi-squared: 0.072 |
| Registered with a dentist (N = 254) | 124 (48.8) | 28 (45.2) | 29 (42.6) | 30 (45.5) | 37 (63.8) | Chi-squared: 0.076 |
| Saw a dentist in previous 4 months (N = 254) | 75 (29.5) | 26 (42.6) | 26 (37.7) | 13 (19.4) | 10 (17.5) | Chi-squared: 0.002 |
| MDAS score of ≥ 19, indicating dental phobia | 84 (34.3) | 21 (36.2) | 26 (38.2) | 22 (35.5) | 15 (26.3) | Chi-squared: 0.530 |
| In need of dental treatment | 187 (77.3) | 40 (70.2) | 51 (77.3) | 52 (83.9) | 44 (77.2) | Chi-squared: 0.366 |
At 4 months, 273 participants completed all 14 questions of the OHIP-14. This covers seven domains of dental health that may affect a person’s quality of life. Each question was scored from 0 to 4, with a maximum total score of 56. Lower scores were more favourable. The overall mean score was 14.77 (SD 12.65), with higher scores for Dedicated Centres and Specialist GPs (17.08 and 16.51, respectively; see Appendix 4, Table 53). A contributory factor is likely to be that these two models had higher rates of heroin and cocaine use among participants, which have significant adverse effects on oral and dental health. 142 Among the HEARTH study participants, the total OHIP-14 mean score was 19.88 (SD 12.84) for people who used heroin at baseline, compared with 12.81 (SD 12.03) for those who did not.
To examine the number of impacts (problems) on oral health, responses from the OHIP-14 of occasionally/often/very often were scored 1, and responses of never/hardly ever were scored 0, with a possible maximum score of 14. The mean number of problems per participant was 4.89, with 81% reporting at least one problem, and 19% describing 10–14 problems (see Appendix 4, Table 53). By comparison, using similar scoring for the general population, just under two-fifths (39%) experienced at least one problem in the previous 12 months, and the mean number of problems per person was 1.2. 132 Dedicated Centre participants reported the most problems (28.2% described 10–14 impacts), followed by Specialist GP participants. The most common problems concerned self-consciousness and embarrassment about one’s dental health, followed by physical pain relating to aching in the mouth and chewing difficulties (see Appendix 4, Table 54).
The rates of behaviours described by PHE as promoting good dental health143 were suboptimal. Although 92.6% of participants who had their own teeth said they had a toothbrush, just 30% brushed their teeth twice or more a day, and 14.8% never brushed their teeth. Consumption of sugary drinks was common, with 79.5% of participants saying they put sugar in hot drinks, and 41.3% drank fizzy drinks six or more times a week. No differences were observed by Health Service Model.
Oral health, dental anxiety and use of dental services at 8 months
At 8 months, 25.3% of participants rated their dental health as very good/good, the same as at 4 months. Nearly half (48.8%) were registered with a dentist, and 29.5% had seen a dentist in the previous 4 months. Rates of registration and dental attendance had increased over the preceding 4 months, resulting in registration rates just slightly lower than those of the general population (around 51%). At the 4-month interview, Usual Care GP participants were most likely, and those of Dedicated Centres and Mobile Teams were least likely, to have seen a dentist in the previous 4 months, but the opposite was true at 8 months, and the findings were statistically significant (see Table 33). A high proportion of participants (77.3%) reported felt dental need at 8 months, and 34.3% had MDAS scores indicating dental phobia. These are comparable to baseline findings. Mobile Team participants reported a slight increase in dental anxiety over time.
Dental outcomes over study period
Over the 12-month study period, 49.4% of participants believed that their dental health had stayed the same, 15.1% said it had improved ‘a little’ or ‘a lot’ and 35.5% that it had worsened ‘a little’ or ‘a lot’. Mobile Team participants were least likely to report improvement, but the findings were not statistically significant (Table 34). There were, however, associations by participant characteristics. Those who reported depression at 8 months were more likely to say their dental health had worsened (40.1%, compared with 17% without depression; chi-squared test: p = 0.004), as were those who drank more than 14 units of alcohol weekly (40.2%, compared with 32.1% not exceeding guidelines; chi-squared test: p = 0.049). Likewise, 43% who reported drug misuse at 8 months said their dental health had worsened, compared with 26.4% not misusing drugs (chi-squared test: p = 0.024).
| Outcomes | Health Service Model, n (%) | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | ||
| Rating of dental health over 12 months (N = 245) | ||||||
| Improved a little or a lot | 37 (15.1) | 11 (19.0) | 4 (5.9) | 11 (16.9) | 11 (20.4) | Kruskal–Wallis: 0.352 |
| Stayed the same | 121 (49.4) | 28 (48.3) | 37 (54.4) | 31 (47.7) | 25 (46.3) | |
| Worsened a little or a lot | 87 (35.5) | 19 (32.8) | 27 (39.7) | 23 (35.4) | 18 (33.3) | |
| Registration with dentist (N = 252) | ||||||
| Registered at baseline and at 8 months | 87 (34.5) | 22 (35.5) | 17 (25.4) | 20 (30.8) | 28 (48.3) | Chi-squared: 0.313 |
| Unregistered at baseline, registered at 8 months | 37 (14.7) | 6 (9.7) | 12 (17.9) | 10 (15.4) | 9 (15.5) | |
| Registered at baseline, unregistered at 8 months | 16 (6.3) | 4 (6.4) | 6 (8.9) | 4 (6.1) | 2 (3.4) | |
| Unregistered at baseline and at 8 months | 112 (44.4) | 30 (48.4) | 32 (47.8) | 31 (47.7) | 19 (32.8) | |
| Seen by dentist during study period (N = 281) | 145 (51.6) | 38 (55.1) | 44 (57.9) | 29 (39.2) | 34 (54.8) | Chi-squared: 0.095 |
| Rated dental treatment in previous 12 months as very/fairly gooda (N = 100) | 69 (69.0) | 21 (84.0) | 25 (75.8) | 7 (36.8) | 16 (69.6) | Chi-squared: 0.006 |
| Not seen by dentist in previous 32 monthsb (N = 319) | 89 (27.9) | 21 (24.7) | 20 (24.7) | 35 (41.2) | 13 (19.1) | Chi-squared: 0.012 |
The number of participants registered with a dentist increased from 38.7% at baseline to 48.8% at 8 months. The latter included 16 people (14.7%) not registered at baseline (see Table 34). The majority, however, were either registered at both time periods (34.5%), or remained unregistered throughout the study (44.4%). Overall, 51.6% of participants saw a dentist at least once during the study period. This applied to fewer Specialist GP participants, although the findings were not statistically significant. When dental attendance over 32 months is examined (24 months prior to baseline interview and 8 months from baseline to the 8-month interview), 27.9% had not engaged with dental services, which is longer than national guidelines of no more than 24 months between dental visits. 144
Of the 104 participants who received dental treatment over the study period, most completed their course of treatment (70.2%) or it was still in progress (18.3%). Of those who received dental care, 69% rated it as ‘very or fairly good’, although Specialist GP participants were much less satisfied (see Table 34). Satisfaction levels were lower than national levels reporting very or fairly good (85%) during the study time frame. 145,146
Availability of dental services and integration with Case Study Sites
Information was collected about the availability of dental services and their integration with CSSs, drawing mainly on interviews with CSS staff and with two dentists. Dental services varied greatly and were not uniform within each Health Service Model (Table 35). Dental treatment clinics were held at the CSS or at homelessness services in the locality for MT2, DC2, SP1, SP2 and UC4, with weekly clinics specifically for people who were homeless available at DC2 and SP1. Dental treatment clinics were also held for people who were homeless or vulnerable at other locations run by community dental services (DC1, DC2 and UC2). Oral health promotion was undertaken by dental services in day centres used by people who were homeless in four localities. Such sessions included advice on oral hygiene and oral cancer screening. Two were day centres where a CSS also delivered services. At all locations where information was collected, CSS staff were involved in signposting patients to NHS dentists and/or referring to community dental services.
| Dedicated Centres | Mobile Teams | Specialist GPs | Usual Care GPs | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dental care | DC1 | DC2 | MT1 | MT2 | SP1 | SP2 | UC1 | UC2 | UC3 | UC4 |
| Dental treatment clinics | ||||||||||
| At CSS/day centre/other service for people who are homeless/vulnerable | ✗ | ✓ | ✗ | ✓ | ✓a | ✓ | ✗ | ✗ | ✗ | ✓ |
| In CSS localityb for people who are homeless/vulnerable | ✓ | ✓ | c | ✗ | c | ✗ | c | ✓ | c | ✗ |
| Oral health promotion clinics (not dental treatment) by dental team to homeless people at day centres where | ||||||||||
| CSS delivers services | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| CSS does not deliver services | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ |
| Tasks undertaken by CSS staff | ||||||||||
| Signpost patients to NHS dentists and/or refer patients to community dental services | ✓ | ✓ | c | ✓ | ✓ | c | c | ✓ | ✓ | c |
| Oral health promotion | ✗ | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Dental staff attend CSS team meetings/have regular discussions with CSS about patients | ✗ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
The extent to which a CSS was integrated with dental services varied, with four reporting close collaborative relationships. At DC2, for example, dental staff attended CSS staff meetings to discuss patients and CSS staff managed dental appointment bookings. The relationship between MT2 and dental services had developed through shared office space and they had used this opportunity to improve services. They discussed patients in common, CSS staff could refer patients and easily make appointments, and dental staff contacted CSS staff to help encourage patients to attend appointments. DC1 reported less integration, but had knowledge of dental services and assisted service providers working with homeless people to link with dentists so they could arrange oral health promotion sessions.
No associations were found between a dental treatment clinic being held at a CSS or within services specifically for people who are homeless and (1) rating of dental health over the study period, (2) registration with a dentist at 8 months and (3) dental attendance over the study period (see Appendix 4, Table 55).
Summary
Regardless of Health Service Model, most participants had poor oral health and experienced extensive dysfunction, discomfort and disability arising from this. Dental anxiety was relatively high, and access to dental care was suboptimal. Although dental registration rates increased during the study, many participants did not seek help or treatment, and much dental need, including dental pain, was left unaddressed. The availability of dental services and their integration with the CSSs varied within Health Service Models. No associations were found between the location of dental services (i.e. provided at a CSS or at homelessness service sites) and dental outcomes.
Chapter 11 Integration and perspectives of Case Study Sites: staff and other agencies
This chapter first summarises the integration of the CSSs with other services. As mentioned in Chapter 3, information was gathered from CSS staff during interviews about the extent and nature of their integration with local authority, health and community services. An inventory of services was compiled exclusively for each CSS, and staff were asked to score the extent to which they (1) worked with each service (actual score) and (2) believed they should be involved with each (expected score). They could respond as follows:
-
0 = no awareness of the service
-
1 = some awareness of the service, but no communication or shared working
-
2 = formal brief communication with the service
-
3 = regular communication with the service
-
4 = high level of joint working around clients (discontinues if no client in common)
-
5 = collaborative approach with a focus on the community or population (not solely around clients).
They provided detailed explanation for scores, including ways in which their relationships with agencies had evolved over time, changes in collaborative work practices and future plans. Sessional staff, external service providers and stakeholders also provided scores for their work with the CSS, so the extent of reciprocity could be observed. Reasons for scores and differences between sites and models were explored using qualitative data. To preserve confidentiality, some services are not mentioned in this chapter, and the scores of external agencies are not given. Different scores were given by some staff within the same CSS, depending on their role. In this chapter, the highest score provided by a member of CSS staff for each service is presented.
The second half of the chapter focuses on the views of CSS staff and external agencies about the strengths and limitations of the CSSs. Drawing on their interviews, six themes about the development and delivery of services are summarised.
Integration with community mental health services
All CSSs reported high levels of integration (scores of 4 or 5) with one or more mental health service, and these scores were largely reciprocated by the external agencies. Many had links to community mental health teams. In addition, all except UC1 had connections to a specialist mental health team for people who were homeless, or for those with enduring mental health problems or complex needs. DC1, DC2, MT1, SP1 and UC4 also had links (mostly brief communication) to voluntary sector mental health services, such as Mind.
All CSSs except UC2 either employed mental health practitioners or had external workers hold regular clinics at the CSS. At DC2, for example, one such worker held sessions three times a week at the CSS, attended staff meetings on those days and met regularly with the GPs to discuss patients. Likewise, MT2 staff met regularly with a mental health team for people who were homeless to discuss patient care. MT1 and UC2 staff described ways in which they worked closely with mental health services:
We’ve quite a lot of patients we refer to them [mental health services]. [They send us] weekly updates ... they will tell us who has been referred, who is waiting for a mental health assessment, who has had their assessment, what the plan is, and who’s been taken to the [psychiatric hospital].
MT1 staff
We’ve a long working relationship with [mental health team for people who are homeless] ... one patient had been sleeping rough on the street for some time and recently got into accommodation. The [mental health] worker asked to meet me with the patient [and] his key worker ... we sat down together with the client and they handed over ... [The workers] then made themselves available for ongoing contact afterwards, although his medical care had been taken over by us.
UC2 staff
Some CSS staff discussed difficulties in working relationships with mental health services. Although a mental health team for people who were homeless was based at SP2, there was little contact between this service and CSS staff. According to MT1 staff, not having a GP in the team resulted in problems referring patients to secondary mental health care, as this required a GP or mental health professional referral. MT1 staff also explained that they would have welcomed more information-sharing with mental health services regarding safety aspects:
We’ve seen somebody and then afterwards been told, ‘You shouldn’t have lone-worked with that person’. Sometimes we don’t find out until a few weeks afterwards. So it would be really helpful to have proper collaborative working with mental health services so we can support one another.
MT1 staff
Integration with substance misuse services
Most CSSs reported integration levels of 4 or 5 with at least one substance misuse service, and the scores were largely reciprocated by the external agencies. No CSS directly employed substance misuse workers, but DC1, DC2, SP1, UC1 and UC3 had shared care arrangements in place, whereby substance misuse workers held regular clinics at the CSS, and GPs trained in substance misuse prescribed OST. At all of these sites except UC3, substance misuse workers were at the CSS at least 4 days per week. DC2 and MT1 staff also described collaborative working with residential detoxification services. The former, for example, provided primary health care to patients of a local detoxification unit while they were undergoing treatment at the facility.
At many CSSs, substance misuse workers who held on-site clinics attended staff meetings to discuss patient care, and worked jointly with the GPs. They described the benefits of such relationships:
It’s a high level of joint working because we literally talk to the GPs on a daily basis and it can be several times a day. We can see two or three patients together with the GP. We meet with GPs once a month to discuss more high-risk patients and any safeguarding issues.
Substance misuse worker, DC2
Joint working with a lot of the staff [at CSS], especially with the mental health team ... and obviously the GPs. We’ll have discussions about clients before I’m due to see them or after I’ve seen them. We’ll have quite complex discussions ... we might set up case conferences here with external agencies.
Substance misuse worker, SP1
Where on-site substance misuse services were not in place, CSS staff referred patients to external services. However, communication with these services varied, and integration levels of 3 and 4 were reported. Some MT2 and SP2 staff described being unaware of whether or not their patients attended appointments with substance misuse workers, and were not provided with updates on their patients’ progress (this was apparent to the research team when the medical records were searched). This reflects the findings of SHC outcomes: MT2 was less likely than most other CSSs to have achieved continuity of care for alcohol and drug problems (see Table 27). The following extracts illustrate the difficulties experienced by MT2 and SP2 staff:
We refer people to [substance misuse services] ... but we don’t know if they’re being seen. We don’t know if they’re going ... I can think of one person I referred that was seen but [I only know that] because the patient told me.
MT2 staff member
[The drug service] is quite separate and we don’t do a lot of joint working. I think communication between us and them could be better. [Difficulties occur] when we have to ask for updates on what they are doing with people ... there isn’t great communication, I don’t think, in either direction, and I’m sure that’s something that could be improved.
SP2 staff member
Integration with hostels and temporary housing schemes
All three specialist Health Service Models reported high levels of joint working with several hostels and temporary supported housing schemes. For example, MT1 scored integration levels of 4 and 5 with 11 hostels, and the remaining CSSs, apart from UC1 and UC4, gave similar high scores for at least three hostels. A few hostels in the locality of the Dedicated Centres and MT1 were given low integration scores (0 or 1) by CSS staff. This was partly because the hostels were a distance from the CSS and residents therefore registered at local general practices. SP2, MT2 and UC1 reported similar low scores for four or more hostels, with some CSS staff indicating that insufficient resources prevented them from doing more collaborative work. UC1 in particular had very little involvement with hostels.
Regular clinics were held in one or more hostels by nurses or GPs from DC1, MT1, SP1 and SP2. Instead of clinics, MT2 had weekly meetings with staff at one hostel to discuss concerns about residents, and provided training at hostels on the health needs of residents. The aim was to reduce inappropriate out-of-hours service use. Strong integration links between CSSs and hostels enabled flexible working and prompt responses between the two services. Hostel staff, for example, telephoned the CSS and sought guidance if they were concerned about a resident, without having ‘to go through a lot of red tape’. Likewise, CSS staff liaised with hostel staff if a resident required encouragement to attend a health appointment. The Mobile Teams were sometimes under pressure from hostel staff to hold (additional) clinics at their services, although the former believed that training for hostel staff was more feasible and a better use of resources. The following examples exemplify the positive links between some CSSs and hostels:
We do teaching sessions at the hostels [with staff] to try to help with reducing ambulance call-outs ... there’s a hugely disproportionate use of ambulances at homeless hostels and we try and reduce frequent attendance at accident and emergency ... so we give health promotion talks at hostels, [such as] if one of the hostel residents has a seizure what would you do, when would you call the ambulance.
MT2 staff member
If we’re in a crisis situation, we’ve rung up [the CSS], explained what the situation is and I think because of the working partnership that we have with them, we have the credibility (or they give us the credibility) of not saying it’s a crisis if someone sneezes twice. I think building up that working relationship has paid dividends. It works really well.
Hostel staff member, DC1 locality
In some CSS areas, the closure of several hostels meant that residents were dispersed into small housing units across a wide geographical area, making it difficult for CSS staff to maintain contact with vulnerable patients and support staff. Low staffing levels in the hostels and the use of agency staff also led to challenges in maintaining relationships.
Integration with day centres and street outreach teams
All CSSs within the specialist Health Service Models gave scores of 4 or 5 for integration with one or more day/drop-in centres for people who are homeless. Indeed, SP1 staff reported high integration levels with seven centres. Apart from UC3, there was much less contact between Usual Care GPs and day centres, and some CSS staff had very little knowledge of such services. Day centres were the settings for much of the work undertaken by Mobile Teams, where they held regular health clinics, worked jointly with staff to plan care for service users with complex needs, and assisted with medical emergencies. As one MT2 staff member explained, day centres are now doing a great deal of work with people who have mental health problems that used to be undertaken by health and social services. SP1 and SP2 also held regular clinics at a day centre. DC1 and SP1 visited a centre regularly to encourage registration with the CSS, and DC2 undertook periodic health promotion activities at a centre, such as giving influenza vaccinations. Some day centre staff expressed a wish for closer integration with CSSs as they believed that this would benefit service users. The following examples illustrate the different relationships between CSSs and day centres:
We do some close working with day centres, because they now do a lot of the work that health and social services used to do. A lot of day centres will now do the mental health work with the patient.
MT2 staff member
We’re just another person who might ring [the CSS]. There are no formal links. If we ring up, we get in the queue just like everyone else; there’s no secret passage for our clients ... no one from [the CSS] will ever ring here ... and ask about someone. I think it would be good for them to link with agencies like us who are spending time with patients and clients – we know them and I think that goes a long way towards solving someone’s health issues.
Day centre staff, UC1 locality
All specialist Health Service Models worked closely with street outreach teams. Staff of Dedicated Centres and SP1 accompanied outreach workers on the streets, and the outreach workers accompanied clients to appointments at the CSSs. SP2 worked closely with the street team, but CSS staff explained that they did not have the resources to conduct outreach themselves. Both Mobile Teams undertook regular outreach with local teams. Among Usual Care GPs, only UC4 reported regular communication with a street outreach team.
Other integration and strategic work
The level of integration between the CSSs and housing departments and social care services varied, although most reported some communication, mainly around patient referrals. Dedicated Centres, Mobile Teams and SP1 also had some involvement with local hospitals. For example, DC2 advised hospital doctors about medication for drug dependency and communicated around patient discharge, and DC1 and SP1 were involved in hospital inpatient care and visited patients on wards. The Mobile Teams reported integration mostly at level 5 with some general practices in their area. They encouraged patients to register with a GP, and, in most cases, shared patients’ medical records. MT1 ran joint clinics in a few hostels with a GP, whereas MT2 had weekly meetings with a GP to discuss patients with complex needs and occasionally held clinics in that general practice.
The specialist Health Service Models, but not the Usual Care GPs, were involved in local strategic meetings regarding provision for people who are homeless. The former also attended multiagency meetings concerning people sleeping rough, frequent attenders at EDs, safeguarding concerns and people with complex needs. SP2 highlighted the benefits of multiagency meetings:
One patient has significant physical health problems and substance misuse ... so we had a safeguarding meeting that was led by someone from the substance misuse team. We now have a communication group regarding that patient where we’re all kept up to date. [Multiagency meetings] work for individual cases where there’s an increased level of concern.
SP2 staff member
Strengths and limitations of the work of the Case Study Sites
This section presents the qualitative analysis of the interviews with CSS staff, other service providers and stakeholders. In each CSS locality, these participants were asked for their views of: (1) the strengths of the CSS and what aspects of the service worked well; (2) whether or not the CSS was meeting the health, social and welfare needs of local people who were homeless; (3) the limitations of the CSS and what aspects of the service did not work well; and (4) the ways in which the CSS should change or improve its services. Their opinions are summarised in Appendix 5, Table 56. Six themes relating to the mechanisms and contextual factors listed in this evaluation’s framework emerged from the data (see Table 1): (1) understanding of homelessness and the development of specialist services, (2) CSS staff members’ attributes and delivery of tailored (person-centred) health care, (3) partnership-working and the delivery of holistic care, (4) flexibility and accessibility of the CSS, (5) outreach and engagement and (6) unavailability of supporting services. Each of these themes is discussed in the subsequent sections. UC4 has not been included as only one interview was conducted.
Understanding of homelessness and the development of specialist services
A strength of all the CSSs of the three specialist Health Service Models was that they had been delivering health care to people who are homeless for many years, with services evolving over time in response to needs. The Dedicated Centres and Mobile Teams were established specifically for this purpose, and interested staff at the Specialist GP sites were driving forces in the development of specialist services at their practices. The majority of staff involved in working with people who were homeless had many years’ experience in this field, had considerable understanding of their problems and needs, and were knowledgeable about relevant services in the locality. Staff at both DC2 and SP1 described their service as ‘organically grown’, as the following quotation illustrates:
When the service first started offering health care to homeless people, it was quite a rudimentary service ... it’s developed organically over a lot of years to create a needs-led service with a proportionate response.
SP1 staff member
The Usual Care GP sites were established to provide primary health care to the general population; by default, this included patients who were homeless, such as residents of local hostels. Their involvement with this patient group had grown in recent years. UC2 and UC3, for example, introduced enhanced assessments for patients who were homeless. Unlike the specialist models, however, the staff tended to be less knowledgeable about homelessness services in their locality, and less involved in multiagency meetings pertaining to this population. Both UC1 and UC2 staff acknowledged the potential value of a more proactive approach towards this patient group by, for example, undertaking audits of their needs. A member of the UC1 staff also proposed that there should be a ‘homelessness lead’ within the practice who would focus on this patient group:
We don’t have a lead for homelessness, but it might be something we should look at. We have a lead for carers ... sometimes they [patients who are homeless] present with particular issues the general population don’t [or] it’s more prevalent ... if you’re more used to it, you notice things more ... you’re tuned in.
UC1 staff member
Staff members’ attributes and delivery of tailored health care
Overall, staff of the three specialist models were described as committed, non-judgemental, motivated, enthusiastic, empathetic and patient. They reported working flexibly to accommodate patients’ needs, and devoting time to listening and building trust with them. Several interviewees commented on their skills and positive ways they worked together to deliver high-quality care. Some CSSs, particularly the Mobile Teams, comprised several nurses with different skills. This was believed to be beneficial as each nurse brought their own specialism to the work. Some of these positive attributes were also mentioned about staff at the Usual Care GP sites (see Appendix 5, Table 56). The following extracts illustrate the skills mix and joint working within teams:
We’ve got nurses from a variety of different backgrounds. We’ve got quite a decent skill mix. I’ve got a background in community nursing, so I did extra training on tissue viability, plus I’m prescribing as well. [Name] background is in needle exchange and sexual health. We’ve also got [name] who has a mental health background. There’s a high level of expertise within the team.
MT1 staff member
I think we’re good working in a team. We aspire to have joint working. We share client information ... [so that] each person who’s involved with that care is on a similar wavelength and [there is] a similar focus on how to help that person regain some of their independence and hopefully regain health, if that’s possible.
DC1 staff member
Many CSS staff described ways in which the health problems of people who are homeless tend to be more neglected and advanced than those of comparable ages in the general population. Hence, innovative and opportunistic ways of working were required. Staff at five of the nine CSSs mentioned having ‘to think outside the box’ and ‘go the extra mile’ when planning and tailoring health care to this patient group. The following account by a nurse illustrates this clearly:
Their health needs are not that different [than the general population]. They’re just more neglected and advanced. We see COPD and asthma, but it’s quite a curious presentation because it’s induced by smoking crack, for example. We do tailored respiratory reviews. We have our own bespoke templates. We do patient education as much as possible ... somebody comes in and they’re under the influence of cannabis or alcohol, but as long as they can hold a conversation with me, because they have high tolerance levels, I would still do a respiratory review as long as I’m happy they’ve actually retained information. We do diabetic checks and again ... our lifestyle advice is tailored to the situation. I’m not going to calculate calories with somebody who’s rough sleeping. We’re just addressing safety issues ... we’re holding quite a lot of risk in the primary [care] setting .... We see leg ulcers in young men due to injecting and they usually have huge vascular problems. Ulcers that you would see in a 70-year-old, we’re seeing in a 20-year-old because they have heart failure on top of that or deep-vein thrombosis ... [the ulcers are] really neglected and unwashed and they’re usually colonised by biofilms.
DC2 staff member
Partnership-working and the delivery of holistic care
Partnership-working was an integral and central role of most CSSs. As described in the previous sections on integration, the three specialist models were proactive in their approach to collaborative working with other services; widely promoted their own service; and shared their knowledge and understanding with other agencies, such as homelessness sector staff. Usual Care GP sites also described relatively high levels of joint working with mental health and substance misuse services. The following are examples of how partnership-working developed:
Partnership-working, that’s always been really key and central to what we do ... we’ve tried not to be one of those services who tries to do everything, and actually you are using the expertise and experience of what other services can bring to the table.
SP2 staff member
Homelessness ... is one of the most integrated parts of the city, with homeless services working incredibly well together – the paid sector, voluntary sector, statutory sector ... I think based on good will, good work and good relationships. There are some really good networks and partnerships. I think they happened as people went out and built those links and partnerships and friendships ... and created really a strategic alliance forum for the most marginalised and vulnerable people in the city.
DC1 staff member
As summarised in Appendix 5, Table 56, nearly all CSSs strived to provide holistic care to patients who were homeless. Their integration with other services facilitated this process. DC1, DC2 and SP1 were characterised by ‘one-stop shops’ or ‘service hubs’, whereby primary health, mental health, substance misuse, social work and other specialist services ran sessions or were in the same building. At these sites, CSS staff and sessional workers held regular meetings, at which they shared updates about patients, including risk concerns, and planned care. Co-located services also enabled opportunistic ‘corridor’ discussions to take place. The advantages of such arrangements were explained by a sessional worker at SP1:
Before the clinic starts, there’s a half-hour meeting ... where clients or issues may be discussed. It might be that there’s someone coming in, who may be potentially risky .... It’s just to make us aware of the risk .... It might be one of the doctors has arranged for someone to come in and see us and gives us a bit of heads-up on who it is, what their concerns are ... there’s information passing between the different agencies. The drug service will give us an idea of what’s going on with a particular client. The GPs might have another element to add. It’s a good opportunity to network .... Sometimes, you [also] get quite a lot of corridor talk, which is a useful thing ... you can get a lot of information out of a 5-minute conversation on a corridor.
Sessional worker, SP1
In many cases, co-located services encouraged flexible working between staff, quick access to doctors and nurses when necessary, and joint consultations with patients. A drug worker, for example, sometimes asked a nurse to assess an injecting site if there were concerns, or quickly arranged a consultation with a GP or mental health worker if indicated. It also enabled patients to be seen by different health professionals on the same day without having to visit separate locations. As a drug worker explained in the following example:
I can assess someone ... a nurse will see them and offer wound care; a GP, if we’re concerned, will see them without an appointment and do an immediate screening ... if there’s obviously localised infection they might need antibiotics.
Drug worker, DC1
Accessibility and flexibility of the Case Study Site
The CSSs were generally perceived as accessible to patients in terms of their ability to provide registration. CSS staff and external agencies said it was easy at both the specialist models and Usual Care GP sites for people who were homeless to register at the practice. One hostel worker, for example, described how UC2 provided an inclusive service to people who were homeless:
What I like about [the practice] is that it’s open to everybody ... It doesn’t treat anyone differently. They don’t say you can’t join [register] because you’re homeless or from [our hostel].
Hostel staff member, UC2 locality
All specialist models also provided an accessible and flexible service. The Dedicated Centres and Specialist GPs offered both booked appointments and drop-in clinics for patients who were homeless. The latter were beneficial for those who found it hard to comply with fixed appointments. Even if people arrived late for a booked appointment, they tended still to be seen whenever possible. Likewise, the Mobile Teams operated drop-in clinics. The Usual Care GPs, however, were less accessible and flexible. There were no drop-in clinics and people who arrived late for appointments could not always be seen. According to some hostel staff in the localities of UC1 and UC2, residents also experienced difficulties booking appointments. At UC1, some staff and agencies believed that the practice should be more flexible and provide drop-in sessions for patients who are homeless. The problems associated with Usual Care GPs were acknowledged by CSS staff and external agencies:
The booking of appointments [is] quite difficult ... you have to ring up at 8 o’clock in the morning, but lots of our clients find it hard to get up in the morning. They take quite high levels of antipsychotics which make them quite drowsy ... getting up at 8 o’clock in the morning and ringing in a queue to get an appointment on the day ... it’s not realistic.
Hostel staff member, UC2 locality
Sometimes it’s difficult to get them [people who are homeless] to engage because obviously, with homelessness, the drinking ... you can give somebody an appointment in 20 minutes’ time and, even though they live [close by], they miss their appointment and turn up about an hour late ... the doctor won’t see them unless it’s something really urgent.
UC2 staff member
Concerns about the opening hours of some CSSs were raised by staff and external agencies, who described DC1, SP2 and UC3 as operating ‘office hours’ on weekdays only (see Appendix 5, Table 56). The consensus was that these practices should open some evenings and/or at weekends. Likewise, a staff member of MT1 believed that their working hours should be staggered more to enable staff to be available in the evenings when soup runs operate. The Mobile Teams also referred to restrictions to their service when operating in non-NHS settings such as day centres. They are dependent on the ‘rules’ of services, such as opening hours and eligibility criteria for service users. For example, MT2 used to do some evening work at day centres, but this stopped when the day centres no longer opened in the evenings. Many day centres rely on local authority funding, and service commissioners sometimes impose restrictions on services.
Outreach and engagement
The CSSs of all three specialist Health Service Models delivered some outreach services. All except DC2 ran regular clinics in hostels or day centres, and street outreach was undertaken by all except SP2. Usual Care GPs did not provide outreach services. Many CSS staff and external agencies across all CSSs except UC3 strongly believed that more outreach work in hostels and on the streets was needed, citing their awareness of many people who were homeless and not engaging with services who had unmet health needs. Hostel staff in the locality of Usual Care GP sites also described the difficulties of getting some residents to attend health appointments. This was verified by UC2 and UC3 staff, who reported high numbers of missed appointments among this patient group.
There was concern by some external agencies about the amount of time Mobile Teams spent in day centres. Those in the locality of MT1 believed that the team should hold fewer drop-in clinics at day centres and focus more on people sleeping rough who were excluded from or not accessing day centres. Similarly, some external agencies believed that MT2 should undertake more work in hostels and less at day centres. At most CSSs, staff expressed a desire to expand or commence outreach work on the streets and in hostels, but were prevented by lack of resources and workforce (see Appendix 5, Table 56). The dilemmas in weighing up priorities were described by a DC1 staff member:
We can’t be doing outreach as well as providing a clinic-based service ... you have to choose ... what feels the most efficient use of the resources you’ve got, and what meets most of the need most of the time in the most effective way.
DC1 staff member
Although many external agencies believed that the CSSs should be doing more street outreach, CSS staff acknowledged the impracticalities of delivering health care in this way and the importance of people sleeping rough attending general practices. As explained by CSS staff, the key aims of street outreach by health professionals should be engagement, building rapport and familiarity, and encouragement for the person to attend the CSS:
[Street outreach] is a means of engagement to bring people in ... you can do a basic health check, or flag up problems, or refer somewhere, but for the actual consultations, I think it would be good for people to access the main service [general practice] because we have all the equipment there .... You cannot claim that you really provide health care [on the streets].
DC2 staff member
Our philosophy is not to provide half-baked health care or health care in an environment where we can’t really provide it ... you can make clinical interventions on the street, but [these are] very limited .... A lot of street medicine should be about engagement and getting people into an environment where they can get decent health care.
SP1 staff member
Apart from lack of suitable facilities at some sites, there were other concerns expressed by CSS staff in delivering health care in non-NHS settings. Difficulties arose for staff of Dedicated Centres and Specialist GPs if day centre users who were registered with another GP sought help from CSS staff, but were reluctant to register with the CSS. This was particularly pertinent among people who frequently moved between cities, but remained registered with a GP in their original location. As described by a member of SP1 staff, the CSS was contracted and accountable to provide health care to registered patients only:
Some people I’m seeing [at the day centre] are registered with other GPs and don’t want to change GP. They’re coming to see me saying they need another blue inhaler, something fairly simple. I’d really like to [help], but can’t because they’re not registered with my GP practice. They’ll say they can’t go and see their GP because it’s too far or they can’t get an appointment ... I would presume their GP practice is completely unaware that this person is rough sleeping or sofa surfing in [another city] .... They don’t want me to notify their GP because they’re worried about disrupting their GP registration ... what my GP practice is saying is that we’re commissioned as a service, so if we start delivering a different kind of service, then that involves a whole new service specification and agreement with the commissioners ... about 20% [of people I see] aren’t registered [at the CSS].
SP1 staff member
Unavailability of supporting services
No primary health care service can operate in isolation. They require local supporting services, such as diagnostic and specialist services, to enable them to deliver effective health care. From the staff and agency interviews, however, the unavailability of some services in their locality affected their work. A common insufficiency raised by many staff and external agencies from all CSSs except UC3 was the poor availability of mental health treatment services. This included long waits for people to be assessed and start treatment, insufficient services for people with mild to moderate illness, long waits or barriers to services for people with combined mental health and substance misuse problems, and lack of community mental health nurses and hospital beds. This is particularly pertinent given the high rates of mental health problems among people who are homeless.
Case Study Site staff or external agencies at five of the nine CSSs also mentioned a lack of local dental services for people who are homeless. A third factor raised by several staff was lack of housing, both emergency or respite accommodation for people on the streets who have health problems, and secure independent and supported move-on accommodation. As described by DC2 staff, effective health care treatment is dependent to a great extent on the accommodation status of a person:
Sometimes, it does feel like you’re picking up water with a fork a little bit because we can do all the best dressings we can, or engage as much as we can, but if people are rough sleeping, then there are limits to health improvements really.
DC2 staff member
Summary
All three specialist models appeared to be well integrated with mental health, substance misuse and homelessness sector services. Relationships were founded on a shared client group, and an understanding of the problems experienced by people who are homeless and the complexity of their health and social care needs. Although this work often took place at the individual-client level, CSSs that worked collaboratively with services (not solely around patients) had opportunities to become involved in strategic approaches to tackle unmet need. Usual Care GPs were less integrated with homelessness sector services, and did not have the same extensive networks as specialist models. However, some achieved high integration levels with a small number of hostels, suggesting that positive working relationships can be built between mainstream general practices and homelessness sector services. Overall, for all CSSs, the extent and depth of integration with services largely depended on the resources available, as most expressed a wish to maximise partnerships.
The benefits of a hub of services in the same building were acknowledged both by CSS staff and external agencies. It enhanced partnership-working and enabled easy access to services. Although it would not be feasible or practical to introduce such an arrangement in many locations, more collaboration between services is likely to be beneficial. Poor communication between substance misuse and mental health services and a few CSSs indicates the need for improvement regarding information-sharing. Homelessness sector staff valued greatly the relationship they had with some CSSs, citing ease of access to the practice and staff willingness to advise and provide support as important factors.
The CSS staff and agency interviews highlight the intricacies of engaging people who are homeless in health care, and the importance of designing services that are appropriate and accessible. Staff of the three specialist models in particular had the experience and capacity to develop tailored approaches to health care that were acceptable to patients, could be delivered opportunistically and had some positive health outcomes. Although both CSS staff and external agencies stressed the need for more outreach work by the CSSs, there appeared to be different expectations and opinions as to its aims and how and where it should be delivered. Such interventions also require consideration of the issues raised in this chapter around delivering health care in non-NHS settings.
Caution has to be taken when interpreting the integration scores. In a few instances, staff gave unusually high scores for their involvement with a particular service. They may have overstated the level of integration as they believed they should have been working more with the service (although ‘expected’ scores were collected as well). There were also difficulties identifying a few services mentioned by staff as they could not name the service and were unclear about its purpose.
Chapter 12 Perspectives of Case Study Sites: case study participants and people experiencing homelessness but not accessing the sites
This chapter describes the case study participants’ perspectives of the CSSs. It first presents their ratings of the CSSs and of the care they received from doctors and nurses, and compares these to the general population’s ratings of their general practices. Using qualitative data from interviews conducted at baseline and 8 months, the case study participants’ accounts of accessing the CSS and their experiences of health care delivery are then described. Finally, the use of health care services by people who were homeless but not accessing the CSS and their reasons for not using the service are summarised.
Participants’ ratings of Case Study Sites
Case study participants were asked at baseline about their views of the relevant CSS, drawing on questions from the GP Patient Survey. 147 Most rated the CSS positively, with overall experience as ‘very good’, ranging from 82.3% of Mobile Team participants to 38.6% of Usual Care GP participants (Table 36). The latter received a higher (poorer) median score than the three specialist models, and the findings were statistically significant (Kruskal–Wallace test: p < 0.0005). Compared with the general population’s rating of their general practices in the 2017 GP Patient Survey,147 the HEARTH study participants of the three specialist models were much more likely to describe their CSS as very good, whereas Usual Care GP participants were more likely to give an unfavourable score.
| Rating/scores | HEARTH study | General populationa | ||||
|---|---|---|---|---|---|---|
| All (N = 355) | Dedicated Centre (N = 93) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 70) | ||
| Very good = 1 (%) | 61.7 | 59.1 | 82.3 | 60.4 | 38.6 | 42.9 |
| Fairly good = 2 (%) | 29.3 | 32.3 | 15.6 | 33.3 | 38.6 | 41.8 |
| Neither good nor poor = 3 (%) | 5.6 | 5.4 | 2.1 | 4.2 | 12.9 | 10.0 |
| Fairly poor = 4 (%) | 2.5 | 3.2 | 0.0 | 1.0 | 7.1 | 3.8 |
| Very poor = 5 (%) | 0.8 | 0.0 | 0.0 | 1.0 | 2.9 | 1.4 |
| Median (IQR) rating | 1.00 (1–2) | 1.00 (1–2) | 1.00 (1–1) | 1.00 (1–2) | 2.00 (1–2) | 2.00 (1–2) |
Participants were also asked to rate the care they received the last time they saw a doctor or nurse at the CSS, according to how good the person was at:
-
giving them enough time
-
listening to them
-
explaining their condition and treatment
-
involving them in decisions about their care
-
treating them with care and concern
-
providing or arranging treatment.
They could respond as follows: 1 = very good, 2 = good, 3 = neither good nor poor, 4 = poor and 5 = very poor. An average response was calculated from the total scores, creating a six-item ‘Quality of Care’ rating, with lower scores being more positive. The mean score was 1.60 (SD 0.84); it was 1.20 (SD 0.39) for Mobile Teams, 1.60 (SD 0.79) for Dedicated Centres, 1.65 (SD 0.82) for Specialist GPs and 2.08 (SD 1.07) for Usual Care GPs (ANOVA: p < 0.0005).
Using data from the 2017 GP Patient Survey,147 comparisons of care by a GP were made between the general population and HEARTH study participants from Dedicated Centres, Specialist GPs and Usual Care GPs. Dedicated Centre and Specialist GP participants were much more likely to rate aspects of care from a doctor as good or very good, whereas participants from Usual Care GPs were less likely to give positive ratings (Table 37). Comparisons of care by a nurse were made between the general population and HEARTH study participants of Mobile Teams. The latter were substantially more likely than the general population to score their care as good.
| Ratings | GP (% of participants) | Nurse (% of participants) | ||||
|---|---|---|---|---|---|---|
| Dedicated Centre (N = 75) | Specialist GP (N = 83) | Usual Care GP (N = 53) | General populationa | Mobile Team (N = 95) | General populationa | |
| Quality of Care: rating of good b | ||||||
| Giving enough time | 97.2 | 92.7 | 78.9 | 84.4 | 100 | 79.5 |
| Listening | 91.6 | 89.0 | 70.6 | 87.0 | 97.9 | 78.6 |
| Explaining condition and treatmentc | 85.9 | 87.3 | 72.0 | 81.4 | 98.9 | 76.1 |
| Involvement in decisions about care | 81.4 | 84.0 | 67.4 | 74.3 | 97.8 | 65.9 |
| Treating with care and concern | 90.2 | 90.1 | 68.0 | 82.8 | 97.9 | 77.5 |
| Providing or arranging treatment | 87.5 | 89.6 | 77.1 | Not available | 97.8 | Not available |
| Confidence/trust in GP or nurse when last seen | ||||||
| Yes, definitely | 82.4 | 80.7 | 55.8 | 63.9 | 91.6 | 62.5 |
| Yes, to some extent | 8.1 | 10.8 | 19.2 | 28.0 | 5.3 | 22.0 |
| No, not at all | 9.5 | 7.2 | 23.1 | 4.3 | 2.1 | 2.4 |
| Do not know | 0.0 | 1.2 | 1.9 | 3.7 | 1.1 | 13.1 |
Similar findings emerged when participants were asked if they had confidence and trust in the doctor or nurse. Participants from the specialist models were more likely than the general population to respond ‘yes, definitely’. Nearly one-quarter (23.1%) of Usual Care GP participants, compared with 4.3% of the general population, said they had no confidence or trust in their doctor (see Table 37). Participants of the three specialist models were more likely than those of Usual Care GPs to describe easy access to the CSS, saying they could ‘drop in’ to the CSS when they wanted to see a doctor or nurse and be seen that day. This applied to 94.7% of Mobile Team participants, 85.1% of Dedicated Centre participants, 87.5% of Specialist GP participants and just 10.8% of Usual Care GP participants (chi-squared: p < 0.0005).
There were differences across CSSs in the Usual Care GP model in ratings of the CSS. Half of UC2 and UC3 participants described their overall experience of the CSS as ‘very good’, which is slightly higher than the general population’s score (42.9%). In contrast, this applied to just 21.4% of UC1 participants. There was no marked difference in GP confidence and trust. Regarding Quality of Care, UC2 scored higher than UC1 and UC3, and its scores for each item were slightly higher than those of the general population. The scores for UC1 and UC3 were lower than those of the general population.
Regression modelling of participants’ ratings of Case Study Sites
Dichotomous and continuous predictors were used to isolate the effect of the four Health Service Models in the modelling of participants’ ratings at baseline of (1) overall experience of the CSS and (2) Quality of Care when last seen by a doctor or nurse at the CSS. The predictors were similar to those applied to the modelling of the Primary Outcome Score and the SF-8 and SWEMWBS scores, with the addition of variables concerning overall experience of the CSS, Quality of Care ratings, trust in doctor or nurse and ability to ‘drop in’ to CSS to see a doctor or nurse.
For each outcome, an initial backward stepwise linear regression was run with each dependent variable at baseline and the variables in Tables 48 and 49 (see Appendix 3) as predictors. Statistically significant and near statistically significant (p < 0.15) were used in a second backward stepwise linear regression. A final model was run using only the statistically significant predictors resulting from this regression to maximise the number of observations used.
The salient fitted parameters, namely those for Health Service Model (whether or not statistically significant), and for other statistically significant predictors for overall experience of CSS and Quality of Care quality outcomes, are shown in Table 38. With regard to overall experience of the CSS, a highly statistically significant beneficial effect is seen for the Mobile Team and Specialist GP models in comparison to the Usual Care GP model. Other predictors that showed strong statistical significance were overall rating of Quality of Care when last seen by a CSS doctor or nurse, and having trust in that person.
| Predictors | Overall experience of CSSa (low is good) | Quality of Careb (low is good) |
|---|---|---|
| Dedicated Centre | −0.178* | −0.493*** |
| Mobile Team | −0.287*** | −0.834*** |
| Specialist GP | −0.272*** | −0.469*** |
| Registered with CSS > 1 year (baseline) | −0.151** | |
| Age (years) | −0.007** | −0.008** |
| Involved in education/training/employment | −0.168* | −0.276** |
| Drinking > 14 units of alcohol per week (baseline) | 0.151** | |
| Confidence/trust in CSS doctor/nurse: definitely | −0.345*** | |
| Quality of Care ratingb (1 = very good… 5 = very poor) | 0.410*** | |
| Used drugs in preceding 4 months | 0.198** | |
| Constant | 1.670 | 2.340 |
| Final model diagnostics | n = 329 | n = 353 |
| R2 | 0.435 | 0.176 |
With regard to the Quality of Care outcome, the final regression model is not an especially impressive fit (R2 = 0.176; see Table 38). Nevertheless, it clearly demonstrates that the Dedicated Centre, Mobile Team and Specialist GP models receive a superior Quality of Care rating by participants, compared with the Usual Care GP model, having adjusted for other statistically significant factors (i.e. involvement in education/training/employment, recent drug misuse and participant age). Substituting these three Health Service Models with Usual Care GP in the regression model elicits a highly statistically significant (p < 0.0005) corresponding parameter of 0.600 (95% CI 0.397 to 0.803), which represents a sizeable deterioration in Quality of Care on a scale with a width of just 4 (from 1 = very good to 5 = very poor).
Participants’ accounts of the Case Study Sites
This section presents qualitative findings of the participants’ perspectives of the CSSs. It draws on their interviews at baseline and 8 months when they gave their opinions of different aspects of the CSS, including accessing the service; opening hours; experiences of the waiting room; the attitudes of receptionists and clinical staff; the delivery of health care by doctors, nurses and other staff; and help given for housing, welfare and social problems. Six themes emerged from the data that pertain to some of the mechanisms identified in the framework for the evaluation of the CSSs (see Table 1): (1) the attitude of staff, (2) provision by the CSS of a welcoming and acceptable environment, (3) provision by the CSS of a safe and non-threatening environment, (4) flexibility and accessibility of the service, (5) practical aspects of health care delivery and (6) a holistic approach to care that addresses non-medical needs.
Attitude of Case Study Site staff
The attitude of staff was an important factor for many participants that encouraged or discouraged use of the CSS. Across all Health Service Models, the majority described being treated with respect by CSS staff, which helped them to build their confidence and trust in the service. Among the positive things they highlighted were doctors and nurses taking time to explain things, listen, and be interested and caring. Several mentioned not being ‘looked down upon’ or ‘judged’ by staff because they were homeless:
I feel confident in talking to them [nurses] about things and don’t feel they judge me because of my condition. Always put things in place for me even if I’ve not taken it up. Always treat me with respect no matter what.
MT1 participant
Barrier not there between them and us. Always feel satisfied and know they will do something. I never walk away and feel they are just palming me off.
DC1 participant
I think they understand the problems of people like me. They are concentrating on people with problems, so obviously have got experience. Other GPs [may] only see six junkies a week. [Here they see lots] and understand their problems.
DC2 participant
In contrast, a few participants from all Health Service Models believed that staff were uncaring and judgemental, which they associated with their situation of being homeless. Some Usual Care GP participants said the doctors did not listen or give them sufficient time, and were unsupportive and dismissive. The following comments highlight their concerns:
They [receptionists] are a bit ignorant. Not as polite to me as I look homeless and less well-dressed.
SP2 participant
I don’t trust any of them. I get told things and passed around. I feel like a trial case.
DC2 participant
The GP has preconceived ideas about me before I go in. I get nowhere. GP doesn’t listen, doesn’t know me.
UC1 participant
The Case Study Site as a welcoming and acceptable environment
Providing a welcoming and acceptable environment is an important feature in encouraging the use of health care services. In our study, many participants believed that the CSSs offered a welcoming and friendly service, particularly the approach of receptionists, who were the first point of contact at some CSSs. Seventeen participants, mainly of Dedicated Centres and SP1, referred to receptionists greeting them by their ‘first name’ on arrival. Another positive gesture, mentioned by 13 participants, was that staff ‘smiled’ at them. Other descriptions included staff being cheerful, polite and considerate; speaking to them if they were seen on the streets; and helping and advising them whenever possible. One participant welcomed the thoughtfulness of receptionists at DC1 who gave patients Christmas cards. Other examples included receptionists filling up participants’ water bottles, and allowing them to use the CSS as their postal address and have mail delivered there. One person said ‘the receptionists are very calm in the face of chaos’. UC1 and UC3 participants were less likely to mention welcoming and friendly gestures by staff. The following quotations illustrate the friendly approaches by receptionists:
They remember you by name and ask you how you are. They are just nice. Will say hello to you on the street when they see you.
DC1 participant
They know me by name. They facilitate when they can and explain when they can’t. Always smiles.
DC2 participant
You ask and they sort it for you. [They are] very cheerful when you go in; it builds your spirits up. It’s one reason I like going there.
SP1 participant
The Case Study Site as a safe and non-threatening environment
Another important feature of health care services that might affect usage involves safety and whether or not patients feel anxious, intimidated or threatened when attending. Such concerns were raised by a few participants of the two Dedicated Centres and SP1. These sites operated drop-in sessions, and had on-site clinics for people with substance misuse problems. DC1 and SP1 attracted a relatively large number of these patient groups at any given time. Furthermore, DC1 and DC2 were close to homelessness sector hostels and, at DC2, hostel residents and others congregated on the streets in the vicinity of the CSS. Some participants expressed caution about attending the CSS as they felt intimidated by the behaviour of people congregating or were concerned about encountering past acquaintances. They acknowledged, however, that CSS staff had strict boundaries to manage difficult situations. Their concerns were well articulated:
The people you get in here, they mess it up for everyone else. Then they [staff] get security to sort it out. But then it causes ructions outside sometimes.
SP1 participant
The environment in relation to location and close proximity to hostel and people hanging around is threatening and intimidating.
DC2 participant
Accessibility and flexibility of the service
The flexibility and accessibility of a health care service may be important factors in determining usage. Although all CSSs reported the availability of drop-in sessions or same-day appointments for patients (see Table 6), this was not the experience described by some participants. Those of the three specialist models were much more likely than Usual Care GP participants to describe easy access to the CSS, saying they could ‘drop in’ when they wanted to see a doctor or nurse and be seen that day. Several DC1 and DC2 participants described how receptionists would fit them in if there were no GP slots available or if they were late for an appointment. Likewise, those of Mobile Teams said they could always be seen the same day by a nurse. Their positive experiences include the following:
Very effective for me. It’s very good that you can just walk in without making an appointment. It’s very good especially for people with chaotic lives.
DC2 participant
They’ll try to fit you in. Today I wanted an appointment and the health worker and receptionist couldn’t find one. They spoke to the GP and now I am seeing the GP later today. It’s a big thing for people in my situation. They make you feel you are doing the right thing.
DC1 participant
Participants at SP2 described a different scenario. The CSS offered booked appointments and a drop-in service each morning, available to all patients. At the latter, there were only a specific number of slots per day; therefore, people started queuing from around 07.30. Some participants described difficulties getting ‘drop-in slots’ and long waits for a booked appointment. As the GPs ran a weekly surgery at a local hostel and day centre, however, the participants tended to see the GP at the hostel (if resident) or at the day centre, instead of at the CSS practice. As one person described:
If I go into the practice it can be 2 or 3 weeks for an appointment. Seeing the GP at my hostel is quicker as I can see [them] weekly.
SP2 participant
Usual Care GP participants did not have the option of drop-in sessions at the GP surgery or at hostels or day centres. They struggled to get same-day appointments at the CSS, and found difficulties booking GP appointments and long waits until they could be seen. This particularly applied to UC1. Their comments illustrated their frustration, including one person who described using a walk-in centre when he could not get a GP appointment:
Takes 1 or 2 months to get an appointment. It’s bad, stupid. Can only phone up in the morning, yet some people don’t have phones.
UC1 participant
Too long [to get GP appointment]. Three to 4 weeks. So I go to the walk-in centre.
UC1 participant
It’s a shambles. I have problems getting repeat medications and getting appointments. It’s bad.
UC1 participant
Practical aspects of health care delivery
As described previously in this chapter (see Table 37), participants of the three specialist models rated highly the health care they received from CSS staff, and rated it higher than the Usual Care GP participants. The proactive approach of some specialist CSSs was welcomed. Participants of DC1, MT1 and SP1 said they were surprised, yet pleased, that CSS staff visited them while they were in hospital, contacted them on the streets and sought them out to check on their health. A few described how GPs remembered their ailments, and hence they did not have to repeatedly describe their problems. Their comments illustrated the value they placed on the care they received:
It’s the best [GP practice] I’ve ever come across. I have a lot of confidence in them. Have a good relationship with the doctors and staff – they’ve helped me through a lot. If I’m in hospital more than a week, they come and check on me to see how things are going. Always feel happy to go back and ask them for help… they’re not like a normal doctor… they are more approachable.
DC1 participant
It’s excellent. Best GP practice I’ve ever experienced. They know me and don’t keep asking the same stupid questions. The nurse ‘collars me’ whenever I go in. I like being collared as I know they are thinking about me, and I’m not just a name in a book.
SP1 participant
The nurses are brilliant. Helped me a lot with my health, legs [dressings for leg ulcers], and medication. Came to see me in hospital.
MT1 participant
Several participants mentioned the benefits of having mental health or substance misuse services at the CSS, as this was perceived as services working closely together. It also meant that patients did not have to access multiple locations to receive health care:
They [CSS staff, and mental health and substance misuse workers] are a good team. Everybody seems to work together.
SP1 participant
Out of all places I’ve been, it [CSS] is the best one. More helpful. Other places are just drug centres. Here you can see the nurse as well as the GP and drugs worker. That’s why my leg ulcer got out of hand when I was at the drugs service, as there was no nurse there.
DC1 participant
Caring. Have the nurse, doctor, needle exchange together. They work with each other.
SP1 participant
Two Mobile Team participants described some limitations to the service they received from the CSS, as some nurses could not prescribe medication and some were restricted in what they could prescribe. Hence, they still often had to see a GP for medication. As one participant commented, the nurses ‘haven’t got the power’. Another concern, raised by several participants of Usual Care GPs and DC1, was not being able to see the same doctor for continuity, which made it hard for them to develop a relationship with a GP. The following quotations illustrate these concerns:
It’s good when I get to see who I class as my doctor. Recently there have been different locum doctors. They don’t know you, and they don’t prescribe you things. They don’t have as much time and are very stretched.
DC1 participant
When you see a doctor, they are impatient. They don’t look into things, just want to get rid of you as quickly as possible. Every time is a different doctor. I find it quite frustrating; it’s difficult to build a relationship.
UC3 participant
Never see the same doctor – always changing. Sometimes a lady, sometimes a man. Don’t get to know them. Would prefer to see same doctor.
UC2 participant
Practice prescribing policy caused dissatisfaction among a few participants, when GPs refused to prescribe certain medications, such as pregabalin and diazepam. They tended to be patients of Dedicated Centres and Specialist GPs who used illicit drugs. Diazepam is a well-known addictive drug. Pregabalin was reclassified in April 2019 as a Schedule 3 controlled drug under the Misuse of Drugs Regulations 2001148 and Class C drug under the Misuse of Drugs Act 1971114 because of concerns about abuse, dependency and its potential harmful interactions with alcohol and opioids. It has to be assumed, therefore, that these drugs were not prescribed for clinical reasons, although the participants raised objections. As one person stated:
Once you’ve been on drugs, the doctors think you can’t be trusted. That’s why they won’t give me pregabalin. They think you only want the medication so you can abuse it.
DC1 participant
Holistic approach to care
The extent to which participants received help or advice at the CSSs for non-medical problems, such as housing, employment and financial difficulties, varied by Health Service Model. During the study, this applied to 58.3% of participants from Dedicated Centres, 50% from Mobile Teams and Specialist GPs, and 37.3% from Usual Care GPs. As described in Chapter 5, Dedicated Centres and SP1 had specialist social work practitioners within their teams who dealt with housing or welfare problems, and SP2 had input from a sessional welfare advice worker. This was not the case for the Mobile Teams or Usual Care GPs, although the former held clinics in day centres where such help was available.
When asked about the involvement of CSSs in non-medical problems, many participants did not see this as their role and said they sought such help from hostel or day centre workers:
They’re not really involved in that side of things. They’re there for your health.
DC1 participant
They only deal with medical problems.
MT2 participant
It’s not their field of expertise.
UC2 participant
Nearly all participants who received help or advice from CSS staff for non-medical problems were positive about it, and described how it was tailored to their individual needs:
For 20 years I was sleeping rough and never claimed [welfare] benefits. The doctor at the day centre urged me to do this and the nurse is helping me.
MT1 participant
[CSS staff] got me money to have my teeth done and money to pay for my prescriptions. When I was in the hostel, I was very stressed and they [CSS staff] told people to speed up the process to get me moved. Now written a letter to the council. Also had advice about my employment problems, and was advised to get sick pay and entitlements ... All thanks to help from the doctor, nurse and social worker.
DC2 participant
Across all Health Service Models, several participants said they were unaware of whether or not help was available at the CSS for non-medical problems, and would have welcomed information if this was the case.
People who were homeless and not using Case Study Sites
One of the HEARTH study’s secondary outcomes was to examine whether or not the CSSs were addressing the health needs of the local population who were homeless, and whether or not there were unmet health needs. Interviews were conducted with 107 people who were homeless but not registered with the CSSs (29 in Dedicated Centre areas, 14 in Mobile Team locations, 35 in Specialist GP areas and 29 in Usual Care GP areas).
Most interviewees were male (76.6%) and White British (72%), with an average age of 40 years. Almost two-thirds (64.4%) had been homeless for more than 1 year. When interviewed, 42.1% were staying in hostels, 17.8% were in supported housing, 13.1% were sofa surfing and 18.7% were sleeping rough. Most reported physical and mental health problems.
Just over four-fifths received health care from a GP surgery or medical centre, and several also used walk-in clinics and A&E. Those in Dedicated Centre areas were most likely to use A&E for health care (see Appendix 6, Table 57). Only 6.5% reported no health care. Nearly three-quarters (72.4%) had seen a doctor or nurse in the previous 3 months, whereas for 18.1% it had been more than 12 months. Just over half (55.1%) had attended A&E in the previous 12 months, including 9.3% who attended at least four times.
One-fifth had used the CSS in the past, mainly those in Dedicated Centre or Specialist GP areas. The main reasons for not using the CSS were that they were already registered with a GP and were satisfied with the care they were receiving, or they had not heard about the CSS and what it had to offer. A few said it was too far from where they were staying. Seven people said they were deterred from using the CSS by the presence of people who use drugs also accessing the service or in its vicinity, and two said they did not want to associate with people who were homeless or with homelessness services. This group of nine were in Dedicated Centre or Specialist GP areas. Two additional people mentioned that they had been removed from the CSS practice list because of their aggressive and demanding behaviour. The following comments illustrate their mixed reasons for not using the CSS:
I’ve been with my GP for a long time. It is clean and convenient to the chemist, and I feel safe and secure.
UC3 area
It is easy to access services, easy to get a sick note. I’ve been with my current GP for 4 years and am happy with the service.
DC1 area
[The CSS] is on an ‘intimidating street’ with lots of ‘horrible people’ hanging around. If you go there, it’s like admitting you’re a loser who can’t manage to get over problems and move forward. You get tarnished by association if you are seen there by other people.
DC2 area
[CSS] horrible place – full of druggies.
DC1 area
Summary
This chapter summarises the views of people who were homeless about the CSSs, the care they received, and their reasons for using or not using the service. The case study participants of the three specialist models rated the service and care they received considerably more favourably than participants of Usual Care GPs and the general population’s ratings of their GP surgery. Usual Care GP participants rated the service less favourably than the general population, although there was some variation between individual CSSs in this model. The findings indicate that people who are vulnerable or have complex needs find it hard to manage mainstream GP systems, but are very positive about specialist services with staff who are understanding of homelessness and respond flexibly to needs.
As described in Chapter 1, many single people who are homeless face difficulties accessing primary health care services because of factors such as mistrust of health care professionals, an unsettled lifestyle and competing needs, the inflexibility of services, and negative attitudes from some staff. In this study, the majority of case study participants from all Health Service Models believed they were treated with respect by CSS staff, but those from the specialist models were more likely than those of Usual Care GPs to mention welcoming and friendly gestures by staff, the flexibility of the service, ease of getting appointments with GPs and nurses, and confidence and trust in the staff. These findings largely corroborate the views of CSS staff and external agencies described in the previous chapter.
Most people interviewed in this study who were homeless but not using a CSS received health care elsewhere, mainly at general practices. Only a minority reported not having health care. The findings should be treated cautiously. The sample was obtained opportunistically at hostels and day centres, and no interviews were conducted with people who were sleeping rough and not using these services. Some external agencies expressed concern about the health needs of people sleeping rough who were reluctant to engage with services. To better understand their health needs, further investigation would be needed.
Chapter 13 Health economic analysis: service use and costs
Aim
The aim of the health economic analysis was to compare four models of primary care provision for people who are homeless with respect to: (1) the resources assigned by services to the care of registered patients who are homeless and (2) the use and costs of health and social care services over a 12-month period by the case study participants. It also sought to evaluate outcomes for participants in relation to service use costs. The four models of primary care provision, as described previously, were (1) Dedicated Centres providing care only to people who are homeless and other marginalised groups, (2) Mobile Teams, (3) Specialist GPs providing targeted services (e.g. specific clinics) within their practice and (4) no special provision by practices (Usual Care GPs).
Data sources
People who were homeless were recruited through the services/practices (CSSs) that were involved in the study. Two sites and 96 participants were included for each of the three non-usual care models; 75 people were recruited from four Usual Care GPs; overall recruitment was 363.
Information on the resourcing of the CSSs was requested through interviews with managers and other personnel. Questions were asked about organisation and financing, the patient population and proportion who were homeless, staffing, facilities, dedicated clinics, other services provided (e.g. for mental ill health, drug misuse and lifestyle), and integration with health and social care systems.
Service use data were collected for each participant starting 4 months before the date of baseline interviews to the date of the 8-month interviews, giving 12 months of data by two methods. Self-report data were collected retrospectively by recall through questions embedded in the interview schedules (at baseline and at 4 and 8 months) covering contacts with the primary health care centre (GPs and nurses) and other health and allied health professionals, out-of-hours services (A&E, NHS walk-in/urgent care clinic, NHS 111, ambulance call-out) and hospital admissions. Primary care medical records of participants were also accessed (subject to separate consent) at the end of the 12-month follow-up period. These were taken as the primary source of health service use data as they were more comprehensive and complete than information obtained from participants, and they were also considered to be more reliable. GP records provided service use data of participants in the three GP-led models; both Mobile Team and GP records (when shared) were used for participants in the Mobile Team model. Use of accommodation (e.g. nights in hostels) was not included.
Self-report data were used to provide information on items that were not routinely available from medical records, such as contacts with key workers, substance misuse services, pharmacists for methadone, local authority housing and social workers, personal care workers (e.g. home care workers) and volunteer supporters. Dates were noted when participants were not using local services during the 12-month observation period, for example because they were in prison, were in rehabilitation, had left the area, or had died. Data were recorded initially by 4-month periods, but were amalgamated for analysis. Service use data were costed in 2020 Great British pounds using national validated tariffs;107 costs of tests were accessed from a variety of sources (see Appendix 7, Table 58).
Service level
Information reported by managers and other personnel regarding patient populations, resourcing and organisation of services is reported in Chapter 5. All sites were commissioned through the NHS and received local enhanced payments for providing services to people who were homeless (UC1 received payments for providing services to patients who had substance misuse problems). The Dedicated Centre, Specialist GP and Usual Care GP sites were GP led and provided care primarily at general practice premises; the Dedicated Centres and Specialist GPs also offered some outreach. Mobile Teams were run by specialist nurses through clinics in day centres and hostels. They provided more limited services around wound dressing, monitoring of long-term conditions and health promotion, referring patients on to other services as needed, including to local GPs with whom they worked closely, and shared medical records. A GP out-of-hours service was available in all sites.
The patients receiving care from Mobile Teams also differed significantly in some respects from those registered with GPs in the other models (see Chapter 6). Mobile Team patients were more likely to have been born outside the UK, to be European Union migrants and to sleep rough; they also were less likely to use drugs.
Participant service use
Missing information
Around three-quarters of participants were available to use local services (rather than being in prison, rehabilitation or abroad) for at least 10 out of the 12 months of follow-up in the three GP-led models; 68% of participants were available in the Mobile Team group. Overall, the distribution of number of days when participants were in local circulation was similar across models (Table 39). Hence, the comparison of service use across the models was based on totals and averages without any adjustment for missing information. Full service use data were unavailable for 25 participants: GP records could not be accessed for 14 participants in the Usual Care GP model (UC1 = 11, UC2 = 1, UC4 = 2), and key worker information was missing at all three time periods for a further 11 participants (DC1 = 1, DC2 = 2, MT2 = 7, UC2 = 1). These individuals were excluded from some parts of the analysis (including Grand Total Costs because self-report data on tests were not collected). A meticulous process of data extraction from medical records (when available) and participant interviews, cross-checking between the two, and quality checks by a second coder meant that missing data was minimal. In many cases, self-report data were available in the absence of medical records.
| Daysa | Health Service Model, n (%) | ||||
|---|---|---|---|---|---|
| Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | All | |
| ≤ 100 | 1 (1.0) | 0 (0) | 0 (0) | 0 (0) | 1 (0.9) |
| 101–200 | 5 (5.2) | 10 (10.5) | 5 (6.3) | 5 (6.3) | 25 (6.9) |
| 201–250 | 9 (9.4) | 7 (7.3) | 10 (10.7) | 8 (10.7) | 34 (9.4) |
| 251–300 | 9 (9.4) | 12 (12.5) | 9 (8.0) | 6 (8.0) | 36 (9.9) |
| 301–350 | 25 (26.0) | 14 (14.6) | 17 (6.7) | 5 (6.7) | 61 (16.8) |
| 351–366 | 47 (49.0) | 51 (53.1) | 55 (68.1) | 51 (68.1) | 204 (56.2) |
| Total | 96 (100) | 96 (100) | 96 (100) | 75 (100) | 363 (100) |
Contacts with services
A full breakdown of contacts by individual item of service use is given by model and site in Appendix 8, Tables 59–62. The rate of use of many services was low and items were grouped for further analysis (GP, nurse, other community, allied health professionals, substance misuse including smoking services, social, out-of-hours, hospital in/out/day, tests, personal caring, optician, dentist) (see Appendix 9, Table 63).
The number of contacts over a 12-month period with different groups of services, by model of primary care provision, is shown in Appendix 10, Table 64. Other than contacts with smoking, drug and alcohol services, which included daily collection of methadone from pharmacists for some 40% of participants, the most frequently accessed service was the GP (overall median number of contacts, 7: Dedicated Centres n = 14, Mobile Teams n = 6, Specialist GPs n = 7.5 and Usual Care GPs n = 4). Nearly all participants (97.0%) in the three GP-led models had at least one contact with their GP (at the practice, on the telephone or elsewhere), but this was lower (91.7%) in the nurse-led Mobile Team model. Across all models, one-third (33.1%) had hospital admissions and around two-thirds (65.0%) used out-of-hours services. Forty-eight participants had 10 or more contacts with out-of-hours services over the study period (maximum number of contacts was 92). The number of out-of-hours contacts was positively correlated with the number of GP and nurse contacts (n = 363, Spearman’s ρ = 0.302; p < 0.0005). This association was statistically significant in both Dedicated Centres and in one site in each of the other service models (MT2, SP2 and UC3), suggesting that out-of-hours services are not necessarily used as a substitute for GP or nurse consultations and that some participants were frequent users of both (Table 40).
| DC1 | DC2 | MT1 | MT2 | SP1 | SP2 | UC1 | UC2 | UC3 | UC4 | All | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 48 | 48 | 47 | 49 | 51 | 45 | 28 | 30 | 15 | 2 | 363 |
| Spearman’s ρ | 0.301 | 0.462 | 0.051 | 0.297 | 0.106 | 0.627 | 0.131 | 0.245 | 0.706 | 0.302 | |
| Significance (two-tailed) | 0.038 | 0.001 | 0.736 | 0.038 | 0.459 | < 0.0005 | 0.506 | 0.191 | 0.003 | < 0.0005 |
Costs
The cost of contacts with services and professionals is shown in Table 41. Considering all health and social care use (except dentist and optician, and the extensive personal care support received by two participants), the highest-cost items were hospital stays (other than for detoxification) (mean £2164, median £0), out-of-hours care (i.e. A&E, walk-in, urgent care, NHS 111 and ambulance) (mean £792, median £296) and contacts with GPs (mean £686, median £462). The Grand Total Costs of service use were highest in the Dedicated Centre model.
| Service use | Health Service Model | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | Total | |||||||||||
| n | Mean (SD) | Median (IQR) | n | Mean (SD) | Median (IQR) | n | Mean (SD) | Median (IQR) | n | Mean (SD) | Median (IQR) | n | Mean (SD) | Median (IQR) | |
| Primary community, substance abuse | |||||||||||||||
| All GP, at base, elsewhere, telephone | 96 | 1204 (1091) | 913 (462–1419) | 96 | 474 (394) | 396 (132–726) | 96 | 645 (477) | 469 (264–898) | 75 | 344 (381) | 264 (132–396) | 363 | 686 (742) | 462 (264–924) |
| All nurse/HCA, at base, elsewhere, telephone | 96 | 131 (308) | 42 (15–126) | 96 | 255 (242) | 203 (101–329) | 96 | 39 (59) | 14 (0–60) | 75 | 66 (138) | 30 (15–61) | 363 | 126 (229) | 48 (14–140) |
| All other community and AHPs | 96 | 173 (655) | 0 (0–62) | 96 | 88 (179) | 18 (0–65) | 96 | 185 (537) | 0 (0–84) | 61 | 84 (175) | 36 (0–65) | 349 | 137 (460) | 18 (0–65) |
| All smoking, alcohol, drug, methadonea | 96 | 723 (849) | 287 (0–1548) | 96 | 325 (597) | 0 (0–475) | 96 | 990 (911) | 969 (0–1760) | 61 | 437 (708) | 30 (0–750) | 349 | 637 (823) | 88 (0–1346) |
| Total primary community, substance abuse | 96 | 2232 (1780) | 1737 (756–3171) | 96 | 1142 (971) | 840 (388–1617) | 96 | 1859 (1386) | 1678 (661–2609) | 61 | 941 (899) | 543 (385–1301) | 349 | 1604 (1431) | 1224 (486–2368) |
| Social (care co-ordination, other) | |||||||||||||||
| Care co-ordination/manager, key workera | 93 | 70 (175) | 0 (0–51) | 89 | 219 (272) | 80 (0–384) | 96 | 105 (204) | 0 (0–85) | 74 | 83 (153) | 0 (0–128) | 352 | 120 (215) | 0 (0–136) |
| Other social: LA welfare housing, voluntaryb | 96 | 42 (89) | 17 (0–34) | 96 | 38 (76) | 0 (0–34) | 96 | 50 (98) | 0 (0–51) | 61 | 46 (102) | 0 (0–51) | 349 | 44 (90) | 0 (0–34) |
| Total social (care co-ordination, other)b | 93 | 114 (194) | 41 (17–149) | 89 | 258 (300) | 136 (17–464) | 96 | 155 (226) | 51 (0–207) | 60 | 138 (196) | 66 (0–161) | 338 | 168 (241) | 51 (0–226) |
| Hospital (nights + detoxification + day case + outpatient) | |||||||||||||||
| All OOH: A&E, walk-in/urgent, NHS 111, ambulance | 96 | 1133 (2430) | 229 (0–1066) | 96 | 689 (1115) | 332 (0–785) | 96 | 751 (1174) | 332 (0–1024) | 75 | 538 (908) | 166 (0–858) | 363 | 792 (1566) | 296 (0–891) |
| Hospital nights, includes psychiatric, but not detoxification | 96 | 2802 (6988) | 0 (0–682) | 96 | 2466 (7211) | 0 (0–1023) | 96 | 2224 (7483) | 0 (0–682) | 75 | 885 (2494) | 0 (0–0) | 363 | 2164 (6550) | 0 (0–682) |
| Hospital nights for detoxification | 96 | 430 (3375) | 0 (0–0) | 96 | 212 (944) | 0 (0–0) | 96 | 37 (364) | 0 (0–0) | 75 | 0 (0) | 0 (0–0) | 363 | 180 (1813) | 0 (0–0) |
| Hospital day case and outpatients | 96 | 166 (342) | 0 (0–135) | 96 | 161 (268) | 0 (0–202) | 96 | 97 (278) | 0 (0–135) | 75 | 171 (365) | 0 (0–135) | 363 | 147 (313) | 0 (0–135) |
| Total hospital (nights + detoxification + day case + outpatient) | 96 | 3398 (7611) | 202 (0–1733) | 96 | 2840 (7250) | 202 (0–2181) | 96 | 2358 (7534) | 67 (0–682) | 75 | 1055 (2536) | 0 (0–611) | 363 | 2491 (6774) | 135 (0–1158) |
| Total testsc | 96 | 23 (31) | 10 (0–30) | 96 | 3 (6) | 0 (0–0) | 96 | 24 (40) | 6 (0–32) | 61 | 25 (58) | 10 (0–20) | 349 | 18 (37) | 4 (0–20) |
| Grand Total Costs | 93 | 7085 (9267) | 3122 (1747–7826) | 89 | 5021 (8207) | 1991 (1040–4830) | 96 | 5147 (7903) | 2952 (1700–5515) | 60 | 2655 (2960) | 1816 (1037–2623) | 338 | 5205 (7894) | 2460 (1242–5067) |
| Personal carer | 96 | 0 (0) | 0 (0–0) | 96 | 1 (13) | 0 (0–0) | 96 | 108 (1063) | 0 (0–0) | 61 | 0 (0) | 0 (0–0) | 349 | 30 (558) | 0 (0–0) |
| Optician | 96 | 15 (29) | 0 (0–14) | 96 | 16 (32) | 0 (0–29) | 96 | 8 (23) | 0 (0–0) | 75 | 20 (34) | 0 (0–29) | 363 | 14 (30) | 0 (0–29) |
| Dental | 96 | 64 (94) | 0 (0–132) | 96 | 48 (77) | 0 (0–66) | 96 | 60 (129) | 0 (0–66) | 60 | 96 (135) | 33 (0–132) | 348 | 64 (109) | 0 (0–115) |
Average costs were compared between models for six main service use groups using the Kruskal–Wallis test, and between pairs of models using the Mann–Whitney U Test (Table 42). Statistically significant differences existed between models for the following: GP, nurse and HCA contacts (higher for Dedicated Centres than for the other three models; lower for Usual Care GPs than for Mobile Teams and Specialist GPs); use of smoking, drug and alcohol services, including methadone collection from pharmacists (higher for Specialist GPs than for Mobile Teams and Usual Care GPs; higher for Dedicated Centres than for Mobile Teams);
| Service | Difference between four models, Kruskal–Wallis test (p-value) | Differences between pairs of models (Mann–Whitney U Test) (p-value) | |||||
|---|---|---|---|---|---|---|---|
| DC vs. MT | DC vs. SP | DC vs. UC | MT vs. SP | MT vs. UC | SP vs. UC | ||
| GP, nurse and HCA contacts, at base, elsewhere and by telephone | < 0.0005 | DC higher (< 0.0005) | DC higher (< 0.0005) | DC higher (< 0.0005) | MT higher (< 0.0005) | SP higher (< 0.0005) | |
| Smoking, drug and alcohol services (includes methadone collection from pharmacists)a | < 0.0005 | DC higher (< 0.0005) | SP higher (< 0.0005) | SP higher (< 0.0005) | |||
| Social care contacts (care managers/co-ordinators, key workers, housing and welfare officers)b | 0.003 | MT higher (0.003) | MT higher (0.025) | MT higher (0.012) | |||
| Out-of-hours (A&E, walk-in/urgent care, NHS 111, ambulance) | 0.865; No significant difference | ||||||
| Hospital nights (includes psychiatric, excludes detoxification) | 0.197; No significant difference | ||||||
| Grand Total Costs (excludes dentist, optician, personal carer) | < 0.0005 | DC higher (0.019) | DC higher (< 0.0005) | SP higher (< 0.0005) | |||
social care contacts with care co-ordinators/managers, key workers, and housing and social care officers (higher for Mobile Teams than for the other three models); Grand Total Costs (higher for Dedicated Centres than for Mobile Teams and Usual Care GPs; higher for Specialist GPs than for Usual Care GPs). No significant differences were found between models for out-of-hours services or for hospital nights (including psychiatric, excluding detoxification). Distributions were right skewed for all items and models. Differences are illustrated in box plots (Figure 5).
FIGURE 5.
Comparison of costs by Health Service Model. (a) GP, nurse and HCA contacts; (b) smoking, drug and alcohol services, pharmacist delivery of methadone; (c) social care contacts (care managers/co-ordinators, key workers, housing and welfare officers); (d) out-of-hours (A&E, walk-in/urgent care, NHS 111, ambulance); (e) hospital nights (including psychiatric, excluding detoxification); (f) total cost of all service use (excluding dentist, optician and personal carer). Boxes denote the IQR and show median bar; whiskers are minimum and maximum, with outliers 1.5 to 3 IQRs from the end of the box shown as small circles and extreme outliers more than 3 IQRs from the end of the box shown as asterisks. IQR, interquartile range.
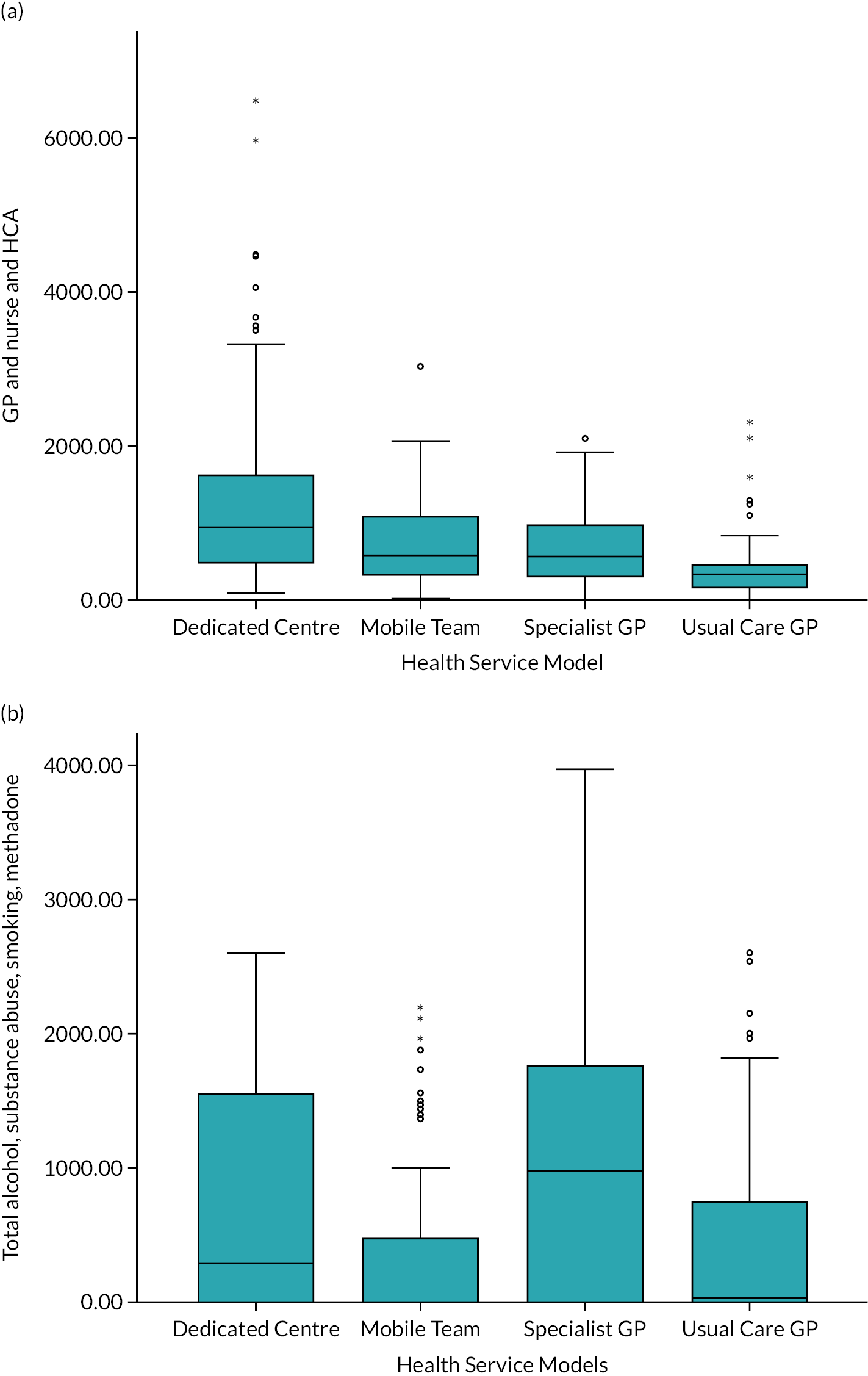
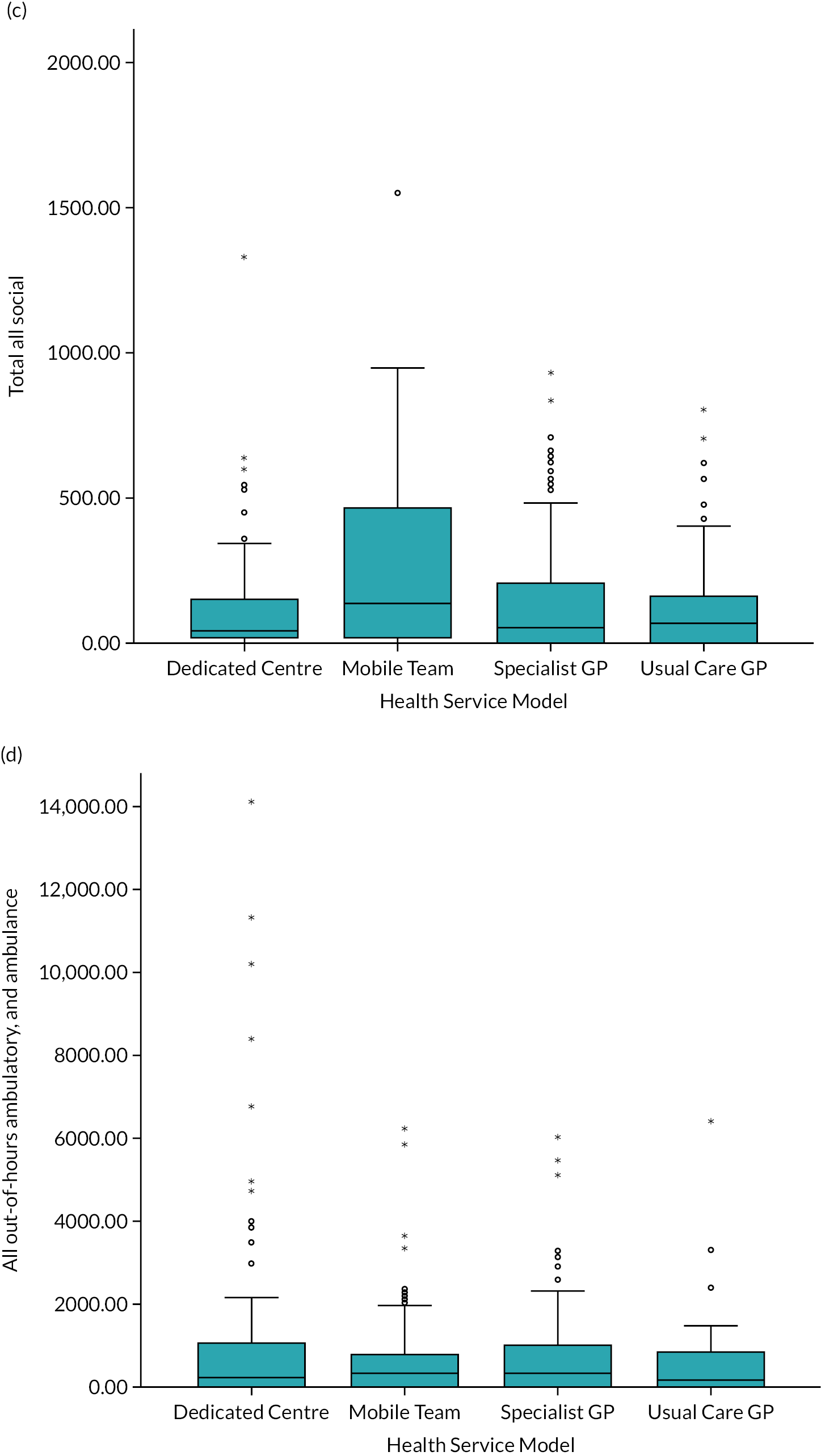

Comparisons of sites within models were also conducted for each of the six main cost groupings. No statistically significant differences were found except between the two Dedicated Centre sites for costs of participant use of smoking, drug and alcohol services, which were significantly higher in DC1 than in DC2 (data not shown) due to the large numbers of contacts with pharmacists for collection of methadone.
Predictors of service use and costs
The role of service model in predicting use (or not) of out-of-hours services and Grand Total Costs was explored using regression analysis (with forced entry of the service model variable). Understanding the predictors of use of out-of-hours services is of interest because people who are homeless often access care through this route, at higher cost, rather than using general practice. The analysis of Grand Total Costs sought to uncover the drivers of service use among the homeless population. Co-variates are shown in Appendix 3, Tables 48 and 49.
Stepwise logistic regression of use of out-of-hours services found no statistically significant association with Health Service Model. The only significant predictor was number of changes of accommodation during the study period, with each additional change rendering a participant 1.45 times more like to use an out-of-hours service. Hence, for example, compared with a participant with one change of accommodation, a participant with six changes of accommodation would be 1.45 × 1.45 × 1.45 × 1.45 × 1.45 = 6.41 times more likely to use one or more out-of-hours services (Table 43).
| Step 1b | B | SE | Wald | Degrees of freedom | Significance | Exp(B) | 95% CI for Exp(B) |
|---|---|---|---|---|---|---|---|
| Dedicated Centre | −0.331 | 0.347 | 0.910 | 1 | 0.340 | 0.718 | 0.364 to 1.418 |
| Mobile Team | −0.570 | 0.344 | 2.745 | 1 | 0.098 | 0.566 | 0.288 to 1.110 |
| Specialist GP | −0.339 | 0.341 | 0.989 | 1 | 0.320 | 0.712 | 0.365 to 1.391 |
| Number of changes of accommodation/sleeping settings (includes episodes of ≥ 7 days in hospital) | 0.372 | 0.069 | 28.830 | 1 | < 0.0005 | 1.450 | 1.266 to 1.661 |
| Constant | 0.214 | 0.253 | 0.714 | 1 | 0.398 | 1.238 |
Grand Total Costs were positively skewed and thus transformed to enable a linear regression of log Grand Total Costs. The final model indicates that participants registered in Dedicated Centres incur significantly higher costs than those in Usual Care GPs (Table 44). Higher Grand Total Costs are also associated with spending a higher proportion of the study time in accommodation with staff on site and having more changes of accommodation during the study period; lower Grand Total Costs are associated with being Black or Black British and recently reporting involvement in education/training/employment. Per annum costs vary between £469 and £21,590 for the lowest- and highest-cost scenarios.
| n = 333, R2= 0.248; dependent variable: ln(Grand Total Cost) | Unstandardised coefficients | t | Significance | 95% CI for B | |
|---|---|---|---|---|---|
| B | SE | ||||
| (Constant) | 7.076 | 0.177 | 39.908 | 0.000 | 6.728 to 7.425 |
| Dedicated Centre | 0.512 | 0.177 | 2.899 | 0.004 | 0.164 to 0.859 |
| Mobile Team | 0.145 | 0.173 | 0.836 | 0.404 | −0.196 to 0.485 |
| Specialist GP | 0.283 | 0.172 | 1.647 | 0.100 | −0.055 to 0.621 |
| Black (or Black British) | −0.608 | 0.209 | −2.907 | 0.004 | −1.019 to −0.196 |
| Reported educational/training/employment involvement | −0.317 | 0.142 | −2.239 | 0.026 | −0.596 to −0.039 |
| % of study in accommodation with on-site staff (24 hour or part time) | 0.005 | 0.001 | 3.722 | 0.000 | 0.003 to 0.008 |
| Number of changes of accommodation/sleeping settings (includes episodes of ≥ 7 days in hospital) | 0.172 | 0.024 | 7.235 | 0.000 | 0.125 to 0.218 |
Regression analysis of hospital admissions was hindered by the variability in number of admissions by a small number of participants. Reduction of data to a dichotomous variable (0 vs. to 1 or more admission) found no association with models of care and failed to identify any significant predictors.
Costs in relation to outcomes
The rates of use and the costs across all services were significantly higher among participants in the Dedicated Centres than in the other three models, and significantly lower in the Usual Care GP model than in the Mobile Teams and Specialist GPs. The specialist interest of staff for care of people who are homeless, and high levels of integration with relevant services (mental health, substance misuse) and local homeless hostels and day centres, may contribute to the higher service use of participants registered with Dedicated Centres. In contrast, Usual Care GP sites are not primarily set up to deal with the special needs of people who are homeless; they reported lower levels of integration with other providers, and staff may have been less proactive in identifying issues and referring on. Drawing on findings from previous chapters, there is some evidence that higher levels of service use are reflected in better outcomes, but this does not hold for all measures.
Screening activity (the primary outcome) was not significantly different between the three GP-led models, but was significantly lower in the Mobile Team model. Similarly, performance on care for SHCs (secondary outcome, overall score) did not differ between models, except that the Usual Care GP model recorded a lower score than the other three models for people who used substances. Dedicated Centres did, however, score significantly better on the continuity of care component for all four of the SHCs analysed, with Mobile Teams performing least well on this outcome. Controlling for other factors, participants in the Dedicated Centre and Specialist GP models showed small improvements in PCS of the SF-8 over an 8-month period; the well-being of participants (measured using the SWEMWBS) in the Specialist GP model also improved. However, this finding should be viewed with caution: approximately 100 participants were not available for follow-up, and the 250 participants for whom follow-up data were available may not have been representative of the entire group. Although relatively low proportions of participants in all four models reported receiving nutrition advice (mean 28.5%), this was lowest among those in the Usual Care GP model (13.3%). In terms of satisfaction with the primary care service, participants in all three specialist services (Dedicated Centres, Mobile Teams and Specialist GPs) rated their experiences highly (more so than is recorded for the general population); participants in Usual Care GPs rated their experiences worse than the general population did, but this was largely a result of low scores in just one of the sites. Costs and outcomes across the four Health Service Models are summarised in Appendix 11, Table 65.
Summary
The service used most frequently by participants was the GPs (nurses in Mobile Teams) with which participants were registered. The number of contacts with GPs over the 12-month period was considerably higher among the study sample than has been recently observed among the general population [mean 10.7 (SD 11.4) vs. mean 3.74 (SD 1.24), respectively], and similarly for nurses [mean 8.3 (SD 15.2) vs. mean 1.3 (SD 0.78), respectively]. 149 Management of dependency problems (smoking, alcohol and drug misuse) was also associated with relatively high average costs, largely attributable to pharmacist time distributing OST, including methadone and buprenorphine, on a daily basis (n = 142, 39.1% of participants). out-of-hours services were accessed by 65% of participants over the 12-month period, with many having multiple contacts. Modelling suggests that out-of-hours service use is associated with having many accommodation changes; other participant characteristics (demographic or health) and model of care were not predictive.
On average, Dedicated Centre participants incurred higher overall service use costs than participants in other models of care. Having more changes of accommodation and spending more time in accommodation with on-site staff also added to cost; people who were black/Black British or in education, training or employment were associated with lower service use costs. The higher service use in the Dedicated Centre model was associated with significantly better outcomes for some, but not all, indicators measured in this study. Participants reported low levels of satisfaction with Usual Care GP provision and high levels of satisfaction with the other three models.
Limitations
The analysis is limited in various ways. It was not possible to identify resources devoted to care of patients who were homeless within services for calculating an average cost of provision in different models, but all services received NHS payments in recognition of their care of this group. Some service use data were not available from medical records for some participants for all or part of the follow-up period, resulting in differential reliance on self-reported information, which may have been less reliable. We did not adjust for missing information or undertake imputation because the distribution of number of days that participants had access to services was similar across models, which means service use may underestimate actual annual service use across the board. The uneven distribution of missing medical records across sites (higher for Mobile Teams and Usual Care GPs) may have affected the comparison of Grand Total Costs across models. Differences between the mode of delivery of care and characteristics of the patient populations of the nurse-led Mobile Team model, compared with the three GP-led models, need to be borne in mind in the interpretation of comparisons. Similarly, some sites provided more in-house services (e.g. support for smoking and drug and alcohol misuse), which were included in GP and nurse contacts, rather than appearing as a contact with a specialist service. Although this would not affect the analysis of Grand Total Costs, it may have affected comparisons of costs between models. Granularity was lost in the interests of parsimony in the combining of variables for the cost analysis.
Chapter 14 Health Service Models: associations between contextual factors, mechanisms and outcomes
The aim of this study was to examine the effectiveness of different models of primary health care services for single people who are homeless to determine what works, for whom and in what circumstances. The framework for the evaluation concerned the role of contextual factors and mechanisms in the delivery of health care, and how these influenced outcomes (see Table 1). This chapter brings together findings from previous chapters to explore associations between contextual factors, mechanisms and outcomes for each Health Service Model. An overview of the study’s findings comparing each model is summarised in Appendix 11, Tables 65 and 66.
Dedicated Centres
Dedicated Centres are specialist primary health care centres, mainly for people who are homeless. This model was represented by two CSSs and 96 case study participants. Outcomes for Dedicated Centres were favourable, even though participants of this model tended to be less settled and had more complex needs than those of other models. At baseline, they were significantly more likely than Specialist GP and Usual Care GP participants to be sleeping rough and less likely to be staying in hostels or other staffed accommodation. They exhibited the highest mean number of accommodation changes during the study, spent significantly less time in staffed accommodation and spent almost twice as much time in prison (see Table 11). Dedicated Centre participants were also significantly more likely than those of Mobile Teams and Usual Care GPs to use heroin or cocaine, inject drugs and be receiving OST.
There was no statistically significant difference between this model and the Specialist GP and Usual Care GP models in the number of HSIs screened for the primary outcome (Mobile Teams scored significantly lower). Dedicated Centres had the highest total outcome score for each SHC (chronic respiratory problems, depression, alcohol problems and drug problems), and scored significantly higher than other models in maintaining continuity of care for patients with depression, alcohol problems and drug problems. In relation to health status, there was a statistically significant positive improvement in the SF-8 PCS scores from baseline to 8 months for Dedicated Centre participants (p = 0.005; paired t-test). They also reported the highest level of help or advice from CSS staff regarding nutrition.
Compared with the general population, Dedicated Centre participants were more likely to rate their overall experience of their general practice and the care they received as ‘good’ or ‘very good’, and were more likely to report a higher level of confidence and trust in their GP. Many described the CSS as a welcoming and accessible environment, and found the staff to be non-judgemental, friendly and helpful. Compared with other models, Dedicated Centre participants had substantially more GP contacts during the study and, apart from Mobile Team participants, had many more contacts with nurses (see Appendix 10, Table 64).
The relative success of this model is likely to be attributable to several contextual and service delivery factors (summarised in Appendix 12, Table 67). Both Dedicated Centres had been delivering health care to single people who were homeless for many years, and most staff had considerable experience of working with this patient group. The CSSs received NHS funding exclusively for this work, and the number of registered patients was smaller than that of Specialist GPs and Usual Care GPs. This enabled Dedicated Centres to provide flexible, holistic and well-integrated services. For example, they operated ‘drop-in’ clinics whereby patients could be seen by a doctor or nurse without an appointment, offered consultations that were longer than the customary 10 minutes, and engaged in some outreach on the streets and at homelessness services. Multidisciplinary working was prominent at both Dedicated Centres, with on-site mental health and substance misuse services, and daily staff meetings attended by CSS staff and sessional workers. The CSSs were well integrated with local hospitals, street outreach teams, and hostels and day centres, and staff attended multidisciplinary case management meetings. These factors are likely to have contributed to participants’ higher levels of service use in Dedicated Centres than in other models, and aided continuity of care with a patient group who tended to be unsettled or hard to engage. Although Dedicated Centre participants incurred higher overall service use costs than other models, this is likely to reflect the complexity of their health problems and the intensity of health care delivered.
The model operated relatively successfully in the context of a changing environment. Both CSSs were in cities with large populations of single people who were homeless, and in recent years there had been increases in the numbers of people sleeping rough and using the drug ‘spice’. At the same time, restructuring of homelessness services and the closure of several local hostels had resulted in some people being dispersed throughout the city in small temporary housing schemes, making it harder for CSS staff to engage with them and liaise with their key workers. According to the staff, funding cuts and insufficient resources had affected the number of outreach activities and amount of collaborative work that could be undertaken. Nonetheless, their expertise in this field had enabled them to adjust to changing needs and deliver an effective service. Furthermore, practice managers and other staff were involved with local NHS trusts and CCGs in the planning of local services for people who are homeless.
Specialist GPs
Specialist GPs provide GMS to the local population, and targeted services for patients who are homeless. This model was represented by two CSSs and 96 case study participants. Like Dedicated Centres, participants of Specialist GPs were significantly more likely than those of Mobile Teams and Usual Care GPs to use heroin or cocaine, inject drugs and be receiving OST. In contrast to Dedicated Centre participants, however, Specialist GP participants were more stably housed during the study. They spent more time in staffed accommodation and had fewer accommodation changes. SP2 participants were more unsettled than those of SP1; otherwise, there were no substantial differences in accommodation status between the two sites.
With regard to the Primary Outcome Score, there were no statistically significant differences between Specialist GPs, Dedicated Centres and Usual Care GPs. There were, however, noticeable differences between the two sites within the model: SP1 had the second highest Primary Outcome Score of all CSSs, whereas SP2 scored lowest. In relation to SHCs, Specialist GPs scored less than Dedicated Centres in achieving continuity of care for all four SHCs, but had higher scores than Mobile Teams and Usual Care GPs. SP1 scored considerably higher than SP2 regarding continuity of care for depression and drug problems, and reached levels comparable to those of Dedicated Centres.
For well-being outcomes, there were statistically significant positive improvements in both SF-8 PCS and SWEMWBS scores from baseline to 8 months for Specialist GP participants. Specialist GPs also scored favourably with regard to providing advice or help around nutrition, with levels comparable to those of Dedicated Centres. Specialist GP participants were more likely to rate their overall experience of the CSS and the care they received as ‘good’ or ‘very good’, compared with the general population’s rating of their GP service. There were no noticeable differences in ratings between SP1 and SP2. However, SP1 participants were more likely than SP2 participants to say it was easy to access a doctor or nurse. Overall, SP1 participants had more contacts with GPs and nurses at the CSS than SP2 participants, whereas the latter used A&E nearly three times more than SP1 participants (see Appendix 8, Table 61).
There were noticeable differences in service delivery factors between SP1 and SP2 (see Appendix 12, Table 68), which are likely to have contributed to variations in ease of access to doctors and nurses, and in health screening and continuity of care. SP1 operated in a way similar to that of Dedicated Centres, with designated nurses and other staff for patients who were homeless, drop-in clinics at the CSS and on-site substance misuse services. SP1 staff also conducted street outreach, ran several weekly clinics at homelessness services, worked closely with the local hospital and attended multidisciplinary case management meetings. SP2 had no staff working specifically with patients who were homeless, ran clinics only twice weekly in homelessness services, did not conduct street outreach work, and on-site substance misuse services were unavailable. Drop-in clinics at SP2 were available for all patients, with a restricted number of slots per day. However, SP2 participants reported difficulties getting a slot and long waits for a booked appointment. The more intense and integrated work provided by SP1 staff to patients who were homeless is likely to have contributed to its more favourable outcomes.
Contextual factors are also likely to have contributed to differences in performance between SP1 and SP2 (see Appendix 12, Table 68). Both CSSs were in cities with large populations of single people who were homeless. According to staff, in recent years there had been an increase in the number of people who were homeless and in the complexity of their health and substance misuse problems, with many using the drug ‘spice’. Restructuring or closure of several local hostels had resulted in residents being dispersed outside the city centre, making it harder for CSS staff to engage with them. Although some staff at both CSSs had considerable experience of working with people who were homeless, funding restrictions had limited their work, particularly for SP2 staff. According to the SP2 staff, insufficient resources prevented them from holding additional clinics in hostels and day centres, undertaking street outreach and working more collaboratively with other agencies. SP1 was involved with local healthcare commissioners and the local authority in planning services for people who are homeless, whereas this was less the case for SP2. The latter described lack of co-ordination between local authority and health services, and delays and lack of support from the CCG when trying to introduce new healthcare services for people who are homeless.
Mobile Teams
Mobile homeless health teams hold clinics in hostels or day centres for people who are homeless. In this study, the model was represented by two CSSs and 96 case study participants. The teams mainly consisted of nurse practitioners; neither had a GP. Patients were therefore encouraged to register with a local general practice, in addition to accessing Mobile Teams. Compared with other models, greater percentages of Mobile Team participants were born outside the UK, and did not have British citizenship or recourse to public funds. They were significantly less likely to report misuse of drugs, and reports of mental health problems were also lower. During the study, they spent longer than other groups sleeping on the streets or in makeshift shelters such as church halls, although they had fewer accommodation changes and spent more time in staffed accommodation than Dedicated Centre participants. MT1 participants were more likely to be British born and to have alcohol and drug problems. MT2 participants were more likely to be born outside the UK, to have no recourse to public funds and to be sleeping rough.
Compared with other models, the Mobile Team model had less favourable outcomes. It had a lower Primary Outcome Score, with a highly statistically significant (p = 0.001) screening deficit. Regarding SHCs, Mobile Teams received relatively high scores for outcomes 3 and 4 (explanations to patient of condition and treatment), but were least likely of all models to have maintained continuity of care for all SHCs apart from drug problems, for which Usual Care GPs scored lowest. When interventions by GPs were included, the Mobile Teams’ scores for continuity of care reached levels comparable to or above those of Usual Care GPs. In most instances, however, they remained considerably lower than those of Dedicated Centres and Specialist GPs. MT1 was more likely than MT2 to have maintained continuity of care with participants, which may reflect the greater percentage of MT2 participants who slept rough.
As with Dedicated Centres and Specialist GPs, Mobile Team participants were more likely to rate their overall experience of the CSS and the care they received as ‘good’ or ‘very good’, compared with the general population’s rating of their GP service and the care they received from nursing staff. They were more likely to say they had confidence and trust in the nurses. Unlike Dedicated Centres and Specialist GPs, however, there were no statistically significant improvements in participants’ well-being over time, and Mobile Teams were significantly less likely to have provided advice or help around nutrition.
Although Mobile Teams worked with a relatively large percentage of patients who were sleeping rough, given that mental health and drug misuse problems, which might contribute to poor engagement and disorganised behaviour, were less prevalent, their less favourable outcomes suggest that service delivery factors were attributable (see Appendix 12, Table 69). The teams mainly comprised specialist nurse practitioners with considerable experience of working with this patient group, but neither team contained a GP. Participants were therefore registered with a local general practice, and hence received primary health care from both Mobile Team nurses and a GP. In effect, the model was a ‘Mobile Team plus separate GP model’. The Mobile Teams worked closely with some GPs: some joint work was undertaken, and, in most cases, medical records were shared. They ran drop-in clinics in hostels and homelessness sector day centres, and much of their work concerned assessing health needs and linking patients to GPs or other agencies, rather than acute disease management. Although the mean number of nurse consultations during the study was considerably higher among Mobile Team participants than in all other models, the number of GP contacts was lower than that of participants of Dedicated Centres and Specialist GPs (see Appendix 10, Table 64).
The less favourable scores of the ‘Mobile Team plus separate GP’ model concerning health screening and continuity of care for long-term health conditions suggest poor co-ordination between the two services. The model involved health care being delivered by multiple primary health care providers. For both Mobile Teams, their patients were not registered at a single GP, and hence CSS nurses had to forge links with several GPs. Moreover, Mobile Team participants had the option to access health care from CSS nurses and/or GPs, which could lead to uncertainty and confusion among patients, particularly as the availability of health care by Mobile Team nurses was limited. As explained by a PPI group member in a discussion of the study’s findings, the accessibility of Mobile Team nurses at hostels and day centres is restricted to specific days and times, and is reliant on the homelessness service. Contextually, funding restrictions placed on some homelessness sector services by local authorities had, for example, resulted in the opening hours of some day centres being reduced. In contrast, Dedicated Centres and Specialist GPs operated from a ‘fixed’ site that was accessible throughout the day and on most days. Such services are likely to be more suitable for patients who are homeless, move around a great deal and find it hard to keep to a schedule.
The services offered by the ‘Mobile Team plus separate GP’ model are comparable, in some ways, to those of the Specialist GP model, particularly SP1: namely they operated in urban areas with many people who were homeless, health care was provided by GPs and nurses, and designated staff reached out to patients in hostels and day centres. However, the Specialist GP model performed better in terms of study outcomes. One important difference is that health care by Specialist GPs was delivered by GPs and nurses from the same practice, and patients were registered with a single primary health care provider. This is more likely to have enhanced collaborative working among staff and aided patients’ understanding of where to seek health care. Moreover, the overall service use costs of Mobile Team participants were similar to those of the Specialist GP participants.
Usual Care GPs
Usual Care GPs provide GMS to the local population, which, by default, includes people who are homeless. They do not offer special or targeted services to patients who are homeless. In this study, the Usual Care GP model was represented by four mainstream general practices and 75 case study participants. Usual Care GP participants tended to be more settled than those of the other three models. Most were in staffed accommodation at baseline, with few or no accommodation changes during the study. Many had mental health problems, but they were less likely than Dedicated Centre and Specialist GP participants to use heroin or cocaine or inject drugs. UC1 participants tended to be less settled than those of UC2 and UC3; they were also more likely to use Class A drugs, they changed accommodation more often during the study and they spent considerably less time in staffed accommodation (see Table 12).
Compared with other models, the Usual Care GP model scored relatively low for some outcomes. However, it had the second highest Primary Outcome Score, achieving the highest of all models for the screening of BMI, alcohol use and smoking (see Table 14). There were, however, differences in scores by individual CSSs. UC2 and UC3 used a computer-based ‘homeless template’ to screen patients who were homeless and had a significantly higher Primary Outcome Score than UC1 (see Appendix 11, Table 65). Compared with the three specialist models, Usual Care GPs were less likely to have detected alcohol and drug problems among their participants, and were less likely than Dedicated Centres and Specialist GPs to have achieved continuity of care for participants identified as having depression, alcohol problems and/or drug problems. The continuity of care score for drug problems was exceptionally low at all Usual Care GP sites. There were no statistically significant differences in outcomes for chronic respiratory problems between Usual Care GPs and the other three models.
Staff of the Usual Care GP model were less likely than those of other models to have discussed nutrition with participants, despite a significantly higher proportion of their patients reporting problems at baseline with getting meals or eating healthily (see Table 28). Participants’ ratings of their Usual Care GP and the quality of care they received were significantly lower than those of the participants of the other three models and of the general population’s ratings of their GP services. However, ratings differed between individual CSSs, with UC2 scoring slightly higher. This may be because UC2 staff had a relatively close working relationship with some hostels. During the study, Usual Care GP participants had considerably less contact with GPs than Dedicated Centre and Specialist GP participants (see Appendix 10, Table 64), and their overall service use costs were considerably lower than those of other models (see Table 41).
Usual Care GPs operated very differently to the other three models, and service delivery and contextual factors are likely to have been crucial in contributing to their relatively low performance for some outcomes (see Appendix 12, Table 70). Their practice list sizes were large, while the proportion of patients who were homeless was small. They had no dedicated staff or targeted services for patients who were homeless, no drop-in clinics at the CSSs or in hostels or day centres, and very little contact with outreach teams. Indeed, some CSS staff had little knowledge of homelessness services in their area. UC2 and UC3 received some additional NHS funding for their work with patients who were homeless, and UC1 received some additional NHS funding for its work with patients who have substance misuse problems. According to the CSS staff, however, this was insufficient to allow more proactive and integrated work for patients who were homeless, such as providing drop-in sessions or collaborating closely with hostels, day centres and street outreach teams.
The Usual Care GPs were in cities with relatively large populations of single people who were homeless, and in areas with several hostels and other temporary accommodation. According to CSS staff, in recent years there had been an increase in the number of people who were homeless, although very few of their patients were sleeping rough. UC2 and UC3 were a few miles from specialist primary health care services for people who are homeless, so it is likely that those sleeping rough were drawn to areas where specialist services were located. Given that the Usual Care GP model performed relatively low for some outcomes, this strongly suggests that the model in its current form would struggle to provide quality health care to a considerable number of patients who are homeless, particularly if they had complex needs. Furthermore, the low satisfaction scores of the CSS given by participants, and the low rate of GP use, compared with specialist models, suggest that people who are homeless and vulnerable find it harder to access care from mainstream general practices. However, the positive health screening scores for UC2 and UC3, which used a ‘homeless template’, and the higher service satisfaction ratings for UC2 suggest that more can be done by mainstream general practices to accommodate patients who are homeless.
Summary
This chapter has examined ways in which contextual factors and mechanisms of health care delivery are likely to have had an influence on outcomes for each Health Service Model, and highlighted differences between some CSSs within the same model. Common contextual factors on service delivery were apparent across all Health Service Models. For example, all had experienced an increase in the number of single people who were homeless in their locality. As mentioned in Chapter 1, cuts to housing, health and social support budgets, a shortage of affordable housing, and welfare benefit changes and sanctions have contributed to this rise. CSS staff also reported an increase in the complexity of health and substance misuse problems among this population, such as an exacerbation of their use of the drug ‘spice’, which can contribute to serious health problems. In addition, in many areas, CSS staff have found it harder to engage with people who are homeless because of changes to homelessness service provision, such as the closure of hostels, resulting in the dispersal of people away from city centres (and the CSSs), and a reduction in the opening hours of day centres. At the same time, funding cuts, restrictions and insufficient resources have limited the services the CSSs are able to provide. At the Dedicated Centres and SP1, where more comprehensive and integrated services were available, outcomes for the study participants were more favourable.
Chapter 15 Conclusions and their implications
This study started with a mapping exercise of specialist primary health care services across England for single people who are homeless, and two literature reviews. The first review examined evidence-based practice between 2000 and 2016 of primary health care delivery to single people who were homeless, and the second concerned health policy developments in England since 2000 for this population. The HEARTH study team then evaluated four different models of primary health care provision for this population, including a ‘usual care’ model for comparison. Their effectiveness regarding various aspects of primary health care service delivery was examined, including engagement in health screening, management of long-term health conditions, health and well-being over time, and participants’ use of health and social care services. Analyses mainly focused on differences between the four models, but key differences between CSSs within the same model have been noted.
This chapter presents an overview of the main findings. The implications of these for NHS commissioners, primary health care service managers and practitioners are outlined, followed by further research that is needed. Finally, the study’s strengths and limitations are discussed.
Overview of findings
The framework for this study was informed by Gelberg et al. ’s80 behavioural model of health service use by people who are homeless. The model has three domains: (1) population characteristics, such as demographics, personal and family resources, community resources and perceived health needs; (2) health behaviour, such as lifestyle factors and use of health services; and (3) outcomes, such as satisfaction with care, and the availability and accessibility of health services (see Chapter 3). Our study similarly found that many factors were influential in determining outcomes, namely contextual factors, service delivery mechanisms and population characteristics (see Chapter 14). More favourable outcomes were achieved if models were well integrated with other health and social care providers and homelessness sector services. For example, primary health care teams were more likely to have maintained contact with participants who had drug and alcohol problems if on-site substance misuse services were available. Where this was not the case, some CSS staff reported being unaware of whether or not their patients were attending appointments with substance misuse workers, as the latter sometimes failed to update GPs on patients’ progress. There was a positive link between overall service use costs during the study period (incurred by more service use) and spending more time in staffed accommodation. This suggests that hostel staff were instrumental in encouraging residents to use health services; helping them to book appointments; and reminding them of, and accompanying them to, appointments, if necessary.
Outcomes for Dedicated Centres and SP1 were relatively favourable. They had staff working exclusively with patients who were homeless, held regular drop-in clinics, conducted outreach work, and were well-integrated with hospitals. These are all factors likely to have encouraged people who were homeless to engage with primary health care services, which supports the findings of similar studies in the USA (see Chapter 2).
With no GP in the Mobile Teams, patients received health care from both Mobile Team nurses and local GPs. The less favourable scores associated with this arrangement for health screening and continuity of care for health conditions suggest poor co-ordination between the services. Although the mean number of nurse consultations was considerably larger for this model, the number of GP contacts was smaller than those of Dedicated Centres and Specialist GPs. The mapping exercise identified a Mobile Team that employed GPs as part of the team and provided GP registration. 112 The effectiveness of this arrangement in relation to the HEARTH study’s outcomes is unknown.
Usual Care GPs operated very differently to other models, and service delivery factors are likely to have been crucial in contributing to their relatively low performance for some outcomes. Their practice list sizes were large, they had no dedicated staff and no targeted or outreach services for patients who were homeless, and they were not well-integrated with homelessness services. However, favourable scores for health screening at two sites, and higher satisfaction ratings at one site, suggest that some positive aspects of health care delivery to patients who are homeless can be achieved by mainstream general practices, given the right circumstances. Although, in this study, the Usual Care GP sites received additional NHS funding for their work with this population, according to CSS staff this was insufficient to allow more proactive and integrated work.
Across all models, the number of contacts with GPs over the study period was considerably higher among the study participants than the general population (see Chapter 13). There was also high use of out-of-hours services. The number of such contacts positively correlated with the number of GP and nurse contacts, indicating that out-of-hours services were not necessarily a substitute for GP or nurse consultations. Regression analyses found that out-of-hours use was associated with more changes of accommodation during the study period. Total cost of service use was also linked positively to number of accommodation changes.
Four areas of concern affected all models. The first related to health screening. This was most common, but not universal, for mental health, alcohol use and smoking. Less than half of participants had their BMI recorded during the study, and relatively few were screened for hepatitis A or TB. Variations in screening were partly related to different working practices. Some CSSs did not routinely screen for TB or hepatitis A (see Chapter 7). However, screening rates for some HSIs were higher for participants of all HEARTH models than for the general population. In Scotland, a review of general practice medical records found that just 31% of adult patients had had BMI recorded in the previous 2 years. 150 This compares to 45.8% of HEARTH study participants in the previous 12 months. Likewise, 51.9% of UK adults registered with GPs in January 2018 and followed up for at least 1 year had a code in their medical records related to alcohol use in the previous 5 years. 151 In comparison, 79.4% of HEARTH study participants had had alcohol use documented in the previous 12 months.
Second, several participants reported chronic respiratory problems or depression at baseline, completing instruments that indicated severe problems, yet these were not documented in the medical records. This applied to all Health Service Models, suggesting a failure, at times, by primary health care staff to identify or record these problems. Although the PHQ-9 formed part of the ‘homeless template’ at UC3, it appeared no further action was taken when scores indicated depression. Both chronic respiratory problems and depression are common in the UK. More than 6 million people are reported to have asthma or COPD,152 and more than one-third of GP visits are estimated to involve a mental health component. 153 Recognising depression in primary health care settings can be challenging, as some patients who are depressed report only non-specific symptoms or somatic complaints, or share concerns about depression only at the end of a GP consultation. 153,154 Chronic respiratory problems and depression are common among people who sleep on the streets, and are exacerbated by their living conditions (see Chapter 1). One of the HEARTH study’s PPI team members suggested that these problems may not be given highest priority by patients or GPs during a consultation if there are more acute and pressing health needs. The PPI member believed that GPs were ‘powerless to tackle such problems’ until the living conditions of people who are homeless improve.
Third, across all Health Service Models, poor oral health was common: many participants did not seek dental care, and dental pain and other dental needs were unaddressed. Compared with the general population, dental anxiety and dental phobia were more common among HEARTH study participants. Dental services specifically for people who are homeless or vulnerable were available at or near several CSSs, but many participants did not access these. This suggests that dental services were not effectively engaging with people who were homeless, and primary health care teams were failing to screen for oral health problems and to link participants to local dental care providers.
Finally, mental health problems are common among single people who are homeless. Yet, as reported by many staff and external agencies from all CSSs except UC3, the availability of mental health treatment services was poor in their area (see Chapter 11). It included long waits for people to be assessed and start treatment, insufficient services for people with mild to moderate illness, long waits or barriers to services for people with combined mental health and substance misuse problems, and lack of community mental health nurses and hospital beds.
Implications for NHS commissioners
The reporting of this study’s findings comes at a time of considerable change within the NHS (described in Chapter 2). ICSs were established in July 2022, and have four strategic aims: (i) to improve population health and health care; (ii) to tackle unequal outcomes and access; (iii) to enhance productivity and value for money; and (iv) to help the NHS to support broader social and economic development. Likewise,155 Primary Care Networks build on the core work of current primary health care services with an emphasis on more co-ordinated and integrated health care services. Their focus for 2022/23 includes tackling health inequalities in primary health care delivery, supporting better patient outcomes through proactive primary care, and supporting improved patient access to primary care services. 156 A 2021 study in England of ED attendees suggested that some hospital admissions among people who were homeless may have been preventable with improved access to primary health care. 157 In March 2022, NICE produced guidance on integrated health and social care for people experiencing homelessness. 158 This section describes implications of our study’s findings for NHS commissioners.
-
In all NHS regions, and particularly in areas without specialist primary health care services, the mapping exercise revealed difficulties accessing primary health care for people who were homeless, which need to be addressed. Health and Wellbeing Boards have a statutory duty, with local ICBs, to produce a Joint Strategic Needs Assessment, which identifies health needs in the locality (see Chapter 2). Such an assessment should include the scale and nature of homelessness in an area over time; the characteristics and needs of people who are homeless; and the availability, accessibility and performance of primary health care provision for this patient group. Furthermore, people’s health needs are closely intertwined with their housing and support needs, and the solutions require the involvement of the NHS, local authorities and community sectors. Our proposals are reiterated by NICE in its 2022 guidance: (1) commissioners of health, social care and housing services and other sectors should work together to plan and fund integrated health and social care services for people experiencing homelessness; and (2) local homelessness health and social care needs assessments should be conducted, which include quantifying and characterising the population experiencing or at risk of homelessness, and assessing the quality, capacity and accessibility of existing service provision. 158
-
In locations where the health needs of people who are homeless are not being met, NHS commissioners need to consider what models of primary health care services are most appropriate. The HEARTH study found that participants in Dedicated Centres had the highest service use, and outcomes were consistently among the best. However, this model may be financially viable only in locations with a considerable number of people who are homeless or have other vulnerabilities, such as asylum seekers. The Specialist GP model was found to perform similarly to Dedicated Centres when targeted services were in place. Most specialist primary health care services that have been established since 2010 for people experiencing homelessness involve mainstream general practices that are funded to provide enhanced services to this patient group.
-
Questions arise as to the function of Mobile Teams and their collaboration with GPs, and whether a more effective service could be delivered if they operated as part of a general practice, rather than as a separate service. The feasibility of such arrangements requires further exploration. It would mean patients would be registered with a single primary health care provider and have a fixed site from which to obtain health care. There would likely be improved collaboration between GPs, nurses and other practice staff, which undoubtedly would have a positive effect on patient care. Mobile Teams often cover a wide geographical area and maintain contact with people who are unsettled and move around. They sometimes see people who are reluctant to attend general practices, or are without GP registration or are registered with a GP in another location. Hence, it would be important that the outreach element of their work continued. Ways of achieving this if Mobile Team nurses were based at a local general practice need investigation. In terms of costs, the HEARTH study found that the overall service use costs of Mobile Team participants were similar to those of Specialist GP participants.
-
Usual Care GPs are the main primary health care provider for many people who are homeless, particularly outside large cities. Their relatively poor performance with regard to continuity of care and patient satisfaction, and poor integration with homelessness services, raises questions about their suitability for managing patients who are homeless, and if or when commissioners should consider introducing additional support. A GP may be able to adequately provide health care to a local hostel if residents are relatively settled, but may struggle to deliver a service to a large number of people with complex needs and unsettled lifestyles. Commissioners should be guided by effective homelessness health needs assessments as to when a more enhanced service, such as that provided by a Specialist GP model, is required.
-
Across all Health Service Models, CSS staff reported funding cuts or insufficient resources, which limited the extent and intensity of care they could provide. Where more flexible and comprehensive services were available, such as drop-in clinics, longer GP appointments and outreach into hostels and day centres, outcomes were more favourable. The benefits of these interventions should be taken into consideration when commissioning services. NICE also recommended that commissioners plan and design services for people experiencing homelessness that encourage engagement with health care, such as reduced caseloads, lengthening contact time with patients, low-threshold services and outreach work. 158
-
Oral diseases are largely preventable,159 yet HEARTH study participants experienced considerable oral health neglect and poor access to dental services. Most local NHS dental services were separate and had little integration or established formal networks with CSSs, making it difficult to support participants’ access to dental care and oral health promotion. This is particularly important for people with substance misuse issues, who appear to experience increased oral disability and dysfunction. Oral health care should be integral to health and social care commissioned for people experiencing homelessness. Furthermore, dental services need to be commissioned in a way that they are fully embedded with health and social care, enabling networking and more responsive and accessible dental services. Different configurations of dental care delivery need to be explored. The Faculty for Homeless and Inclusion Health70 produced detailed guidance on standards for dental services that should inform integrated commissioning.
-
Consideration should be given to the poor availability of mental health services and the impact this is having on both the health of patients and the work of primary health care providers. The NHS Long Term Plan renewed a commitment that mental health services will grow faster than the overall NHS budget, with a ringfenced investment worth at least £2.3B a year for mental health services by 2023/24. 160
-
The inclusion of effective monitoring and evaluation of services in the commissioning process is critical. According to a report published by the RCGP,161 commissioners should be able to determine which services are working effectively, and those that are not meeting their objectives. The Faculty for Homeless and Inclusion Health proposed locally designed key performance indicators to cover health screening, and access to treatment, and the management of long-term health conditions to QOF standards. 70 NICE also recommended that commissioners should define and measure health and social outcomes and service use when developing services for people experiencing homelessness. 158
Implications for primary health care service managers and practitioners
Drawing on evidence from the four models and from individual CSSs, this section describes the implications of our study’s findings for primary health care service managers and practitioners.
-
There needs to be improved health screening for people who are homeless, and it is essential that this leads to an intervention when indicated. The Faculty for Homeless and Inclusion Health recommended that primary health care services working with this patient group should offer screening and access to treatment for mental health, alcohol and drug problems, smoking, and TB and blood-borne viruses, and should offer vaccination against hepatitis A and B, particularly for people who inject drugs or have hepatitis C. 70 NICE further recommended active TB case-finding among people who are homeless and sleeping rough or in hostels,119 and that alcohol screening should be routine practice in primary care. 162 PHE and the RCGP recommended hepatitis A vaccinations for people who inject drugs or have hepatitis C or chronic liver disease. 117,163 Decisions need to be reached between primary health care service managers and clinical staff about screening for particular health conditions, taking into account national guidelines and service contract agreements.
-
Two Usual Care GPs that used a computer-based ‘homeless template’ to assess the needs of patients who were homeless had higher Primary Outcome Scores. This suggests that there are benefits of using a ‘screening plus intervention template’ in all mainstream general practices with patients who are homeless, and in specialist models without a current screening process. It is important that ‘alerts’ are placed on medical records as reminders of follow-up actions or further screening. Such a template should be disseminated widely by organisations such as the RCGP and the Royal College of Nursing to ensure that mainstream primary health care practitioners are reached. Pathway has developed a digital health screening template, which is available free of charge to health care providers using the EMIS Web clinical system (EMIS Health, Leeds, UK). It is very detailed, however, and the practicalities of its usage, particularly in mainstream general practices, need further investigation. A 2019 systematic review of health assessments and screening tools administered to people who were homeless identified no validated tools that assessed chronic conditions, nutrition, functional decline and frailty, or vision and hearing. 164
-
Given the large number of cases of depression and chronic respiratory problems reported by participants but not documented in their medical records, awareness needs to be raised by organisations such as the RCGP and Faculty for Homeless and Inclusion Health of the links between these conditions and homelessness, and the need for their inclusion in the screening of patients. Scheduled or opportunistic reviews need to be undertaken among patients who are homeless to detect these conditions and initiate treatment if indicated.
-
Several working practices were beneficial in enabling staff to engage with patients who were homeless and retain them in health care. These included easily accessible and flexible services; designated staff for patients who are homeless; close working with mental health, substance misuse and homelessness sector agencies; and outreach work. Consideration should therefore be given as to how these features can be built into existing primary health care services where applicable.
-
The introduction of a full- or part-time role within mainstream general practices, whereby a clinical staff member is responsible for patients who are homeless, would enable more targeted work to be undertaken with this patient group, links to be forged with other health practitioners and homelessness sector staff, and engagement in local initiatives and strategic work concerning this patient group. Additional training for that person would be required. NICE similarly proposed ‘homelessness leads’ in mainstream services to co-ordinate care for patients who are homeless. 158 UC1 also acknowledged the likely benefits of this (see Chapter 11).
-
The running of regular health clinics in hostels and day centres needs to be reviewed. They are invaluable in certain circumstances, such as encouraging people who are homeless to register with and attend a general practice, or delivering basic health care if a person declines to access a general practice. As described by a nurse from a Specialist GP who ran health clinics in a day centre, the arrangement worked well ‘as an outpost of the GP ... and as a conduit into primary care’. It is questionable, however, whether such clinics should be available to all hostel residents or day centre users, or whether it deters use of general practices. Furthermore, the health care that can be provided in such settings is limited, and some settings lack suitable facilities for clinical work. In our study, CSS staff and external agencies had mixed views about the role and frequency of outreach clinics by health workers (see Chapter 11).
-
People who are homeless have multiple needs, and an all-inclusive, holistic approach to their care is required. In the HEARTH study, more frequent changes of accommodation were associated with increased use of out-of-hours services. Attention should be given to the housing, social care and welfare needs of people who are homeless when health assessments are undertaken, and multiagency working between health, housing and support services is essential. Working relationships with mental health and substance misuse services could be improved in some primary care settings, including providing regular updates to GPs of patients’ progress. Having the staff capacity to attend multiagency case management meetings is also crucial.
-
There needs to be greater awareness of oral health among health and social care teams working with people experiencing homelessness. Practitioners should proactively ask patients about dental problems, and provide help and advice about maintaining oral health and accessing local dental providers. It is essential that efforts to promote dental health and access to dental care should be integrated and embedded into local health and other services for people experiencing homelessness.
Further research
This study examined a few selected health screening activities undertaken by primary health care staff, and data about physical and mental health conditions pertaining to the SHCs were extracted from medical records. Given the wealth of information collected during the study and the availability of comprehensive medical records for 12 months, there is the potential for much more interrogation of the data. This could include analyses of (1) other screening activities, such as breast and cervical cancer screening, and influenza immunisations; (2) the prevalence and treatment over time of illnesses, such as cardiovascular disease, gastrointestinal problems, hepatitis C, HIV and psychosis; and (3) hospital admissions and use of out-of-hours services, including reasons and outcomes.
The study has demonstrated that participant characteristics, service delivery mechanisms and contextual factors were influential in determining outcomes, and that these differed between and within models. There is the potential to explore further these relationships with attention to participant characteristics, such as age, sex, ethnicity, disability, multiple health conditions and frequent A&E attenders or users of other out-of-hours services.
This chapter has described several aspects of the delivery of primary health care to people who are homeless that need further review. These include the function of Mobile Teams and the feasibility of such nursing staff operating from general practices, the advantages and disadvantages of holding regular health clinics in hostels and day centres, the suitability of individual mainstream general practices to care for patients who are homeless, and the introduction of a ‘screening and intervention’ template and homelessness lead in general practices for this patient group. Further research is also needed into the delivery of primary health care to people who are homeless since the start of the COVID-19 pandemic, and its impact on practices such as ‘drop-in’ consultations with GPs or nurses, on-site mental health and substance misuse services, and administration of OST by pharmacists.
This study is a starting point for further research into aspects of primary health care provision for people who are homeless, namely (1) methods of integration between primary care GPs and nurses, and mental health and substance misuse services, and arrangements that are most effective; (2) the effectiveness of various approaches for engagement and retention in primary health care services; and (3) measures and instruments to capture the provision of primary health care to this patient group.
Strengths and limitations of the study
To our knowledge, this is the first UK study to evaluate and compare different models of primary health care provision for people who are homeless. Most previous such studies were conducted in the USA and focused on one aspect of service delivery or a single intervention, rather than on a model or service in its entirety (see Chapter 2). Among the unique features of the HEARTH study are the inclusion of a ‘usual care’ model for comparison, analyses of different aspects of health care delivery, and analysis of service use and costs by participants over 12 months.
Information for the study came from many sources, enabling triangulation of data. Longitudinal data over 12 months were obtained through three interviews with case study participants. Recruitment of participants reached the target number of 96 at each of the three specialist models, and 75 participants (78% of the required number) were recruited at Usual Care GP sites. Follow-up interviews were achieved with 272 of the 363 participants (74.9%) at 4 months, and with 263 (72.5%) at 8 months. The latter was slightly higher than the expected number at 8 months after allowing for attrition (n = 256), despite fewer people being recruited to the study. Full medical records held by the CSSs for the entire study period were collected for each participant, covering service use for more than 10 months (and up to 12 months) for 81.9% of participants (see Table 4).
From a statistical perspective, the study proceeded well. A sample size (size = 5%, power = 80%) of at least 64 participants in each of the four Health Service Models was required to detect a 1-point difference in the six-item primary outcome tool between any two models. This was assuming a worst-case scenario of the tool having a SD of 2. In fact, the SD was only 1.24 (see Table 14), which retrospectively required a minimum of 26 participants per model. This was comfortably achieved for each model. Indeed, retrospective calculations indicate that 95% power was exceeded for comparing any two models, affirming the significantly lower Primary Outcome Score reported for Mobile Teams than for each of the three other models.
With regard to assessing the efficacy of the models in relation to SHCs, as anticipated in the protocol, a scarcity of cases did occur, but only for self-reported hypertension. The other four conditions were able to be compared soundly, eliminating any need to construct a valid overall combination of conditions that bore varying levels of complexity.
The successful retention of participants in the study enabled incisive comparisons between Health Service Models of many aspects of participants’ health and well-being, and the care they received. This facilitated extensive regression modelling of the primary outcome and several secondary outcomes to identify various factors associated with each outcome, and, most importantly, to adjust for such factors and gauge more precisely the impact of each of the four Health Service Models.
Service use data were obtained assiduously with a high level of detail, which contributed to in-depth analyses of health service staff commitments, and a thorough breakdown of costs for the four Health Service Models. Specific cost groupings comprised primary and community care, social care, out-of-hours services, hospital admissions and outpatient services, tests and investigations, and allied health professionals (e.g. dentists, opticians), with further breakdowns within each. The cost of out-of-hours services was of relevance, given recent findings of the high rates of A&E visits among people who are homeless, compared with the general population. 12
There were limitations to the study, which took much longer than planned. One of the main difficulties was recruiting mainstream general practices with enough patients who were homeless for the Usual Care GP model. Substantial time and effort were spent liaising with general practices and with primary care leads of CRNs, and fewer participants than intended were recruited for this model. At UC4, just two patients were recruited; therefore, this site had to be omitted from many of the analyses. Moreover, several mainstream general practices that fitted the study criteria declined to take part. Likewise, the selection of specialist sites depended on their willingness to participate, the number of patients who were homeless, and staff resources or imminent changes to the service. In addition, the recruitment of case study participants relied on their willingness to participate. As demonstrated in this study, there are many differences between models, and between CSSs within a model. The findings of this study pertain to the CSSs and their patients who participated, and may not necessarily apply to the performance of other primary health care services for this patient group.
Given the innovative nature of this study, various measures were used for the first time to assess the performance of the CSSs. Screening for the primary outcome and the management of SHCs did not rely on validated tools for scoring (as none could be found). Instead they depended on the expertise of the research team and other clinicians, and recommendations by the Faculty for Homeless and Inclusion Health in its standards for primary care. 70 As described in Chapters 7 and 8, scoring was intricate and lengthy, and relied on information from case study participants and medical records; many challenges occurred during the process. Various ‘rules’ were adopted by the research team after preparation of several working papers and agreement with the SSC. This included allocating positive scores when pre-coded text with no further details was used in the medical records, when CSS staff ‘signposted’ patients to other services, and when a service was offered by the CSS but declined by the patient. Undoubtedly, such rules had an influence on the study’s outcomes. As mentioned previously, further development is needed into measures and instruments to assess the performance of primary health care services for patients who are homeless.
Extracting data from medical records was very time-consuming, partly because the quality and clarity of the records varied greatly. Some clearly stated health conditions and treatments, but some were pre-coded to such an extent that it was not straightforward to make judgements. Medical records for the 12-month study period were also very extensive for some participants (one set of records comprised 283 pages), with numerous consultations, missed appointments and A&E attendances. To avoid error or oversight, each set of medical records was searched several times to retrieve data for different outcomes, and checks were made by a second, and sometimes third, coder. Other limitations to the study, including the unavailability of some medical records and the variability of in-house services at the CSSs, are discussed in Chapter 13.
Summary
To our knowledge, this is the first UK study to compare and evaluate different models of primary health care provision for people who are homeless. New and much-needed evidence has been generated about the effectiveness of different ways of delivering health care to this patient group. Contact was maintained for the entire study period with the majority of case study participants, thus enabling the study’s aims and objectives to be met. Innovative approaches were employed to evaluate outcomes and produce findings that are of importance to NHS commissioners, primary health care service managers and practitioners.
Many of the HEARTH study’s findings corroborate data from the USA (see Chapter 2), in which tailored services, nurse case management, integrated care provision and outreach on the streets and at homelessness services had positive health outcomes for people who were homeless in terms of improving screening uptake, encouraging the use of primary health care services, treating health conditions and engaging people in specialist care.
Acknowledgements
We send warm thanks to the case study participants who took part in the study and kept in contact with us for repeat interviews over 8 months. Their trust, engagement and co-operation were much appreciated. Without their willingness to stay involved and share their experiences, it would not have been possible to collect such rich and valuable information for this study.
We are extremely grateful to the primary health care and homelessness services across England that participated in the mapping exercise. We send special thanks to the staff of the CSSs who assisted with the recruitment and tracing of case study participants, helped arrange interviews, provided office space where these could be conducted, and arranged printouts of medical records. Their support, encouragement and assistance were invaluable. We also thank the numerous other health, social care, homelessness and other staff who participated in the evaluation of the CSSs.
Contributions of others to the study
We send special thanks to Sarah Coward, who managed the fieldwork and data collection at some CSSs and conducted many of the interviews in these areas. She assisted with the coding of data and attended SSC meetings. We appreciate the help given by Ruby Fernandez-Fu with the mapping exercise. We thank Janet Robinson, Robert Calder and Carl Purcell, who assisted with data searching and coding; Nicole Steils, who helped with the literature review; and Jess Harris and Caroline Norrie, who conducted a few interviews with stakeholders. Thanks are also sent to Morro Touray for his assistance with the health economic analysis, and to Laura Cole and Nicole Steils for taking minutes at the SSC meetings. We also appreciate the advice given by Dr Patrick White, Reader of Primary Care Respiratory Medicine, KCL, and the medical professionals who were contacted by Dr Chris Ford.
We are grateful to the contributions throughout the study of members of the PPI group who assisted in the study design, study implementation, participant interviews and the interpretation of findings, and were involved in the SSC meetings. Special thanks are sent to Gordon Chaston, who, with another member of the PPI team, undertook some interviews and willingly accompanied the research team to different locations, which sometimes involved overnight stays. They remained extremely enthusiastic about the study even when there were substantial delays to the timetable.
Special thanks are sent to Homeless Link, which provided databases of accommodation and day centre services in England. These were very useful as a starting point for the survey of homelessness services. We are grateful for the input of Vic Rayner, formerly of Sitra and former co-investigator in the study, who assisted in its early months; of Burcu Borysik, formerly of Sitra and Homeless Link; and of other staff at Homeless Link who assisted with the PPI work. We appreciate the involvement of St Mungo’s apprenticeship scheme in the PPI work. An agreement was drawn up between OptumInsight Life Sciences Inc and King’s College London for use of the SF-8 in the study (Licence number QM033370). Written permissions were also granted by the University of Warwick for use of the SWEMWBS scale, and by the CAT Governance Board of GlaxoSmithKline for use of the COPD Assessment Test.
Finally, thanks are sent to members of the NIHR CRNs who helped with recruitment of general practices for the Usual Care GP model, and to our lead CRN staff member who undertook the extraction of data from medical records at one CSS.
Study Steering Committee membership
The research team appreciate the guidance and advice provided by members of the SSC:
• Liddy Goyder, Professor of Public Health, School of Health and Related Research, University of Sheffield (chairperson)
• Jennifer Beecham, Professor of Health and Social Care Economics, Personal Social Services Research Unit, University of Kent
• Caroline Bernard, Head of Communications and Advocacy, Homeless Link
• Andrew Casey, Health Strategy Manager, St Mungo’s
• Mohammed Ismail, Research Director, Analytical Research Ltd
• Gill Leng, Health and Homelessness Adviser, PHE
• Jeremy Porteus, Managing Director, Housing, Learning and Improvement Network
• Rebecca Rosen, GP and Senior Fellow, Health Policy, Nuffield Trust
• Sara Shaw, Senior Researcher, Nuffield Department of Primary Health Care Services, University of Oxford.
Contributions of authors
Maureen Crane (https://orcid.org/0000-0002-7364-7855) (former Principal Research Fellow, now Visiting Senior Research Fellow) was the principal investigator; was involved in the study design, data collection, analyses and interpretation of findings; and co-authored the report.
Louise Joly (https://orcid.org/0000-0002-1615-2987) (former Research Fellow, now Visiting Research Fellow) was a co-investigator; was involved in the study design, data collection, analyses and interpretation of findings; was responsible for PPI and organisation of the collection of participant medical records; and co-authored the report.
Blánaid JM Daly (https://orcid.org/0000-0001-7748-6940) (former Senior Lecturer Special Care Dentistry at KCL, now Professor of Special Care Dentistry, Trinity College Dublin) was a co-investigator; was responsible for the dental features of the study, dental analyses and reporting; wrote Chapter 10; and contributed important intellectual content to revisions of the final report.
Heather Gage (https://orcid.org/0000-0002-2049-9406) (Professor of Health Economics) was a co-investigator, was involved in the study design, was responsible for the economic aspects of the study, undertook analyses of service use and costs, wrote Chapter 13 and contributed important intellectual content to revisions of the final report.
Jill Manthorpe (https://orcid.org/0000-0001-9006-1410) (Professor of Social Work) was a co-investigator; contributed to study design and management, including budget responsibility; undertook policy review; co-wrote Chapter 2; and contributed important intellectual content to revisions of the final report.
Gaia Cetrano (https://orcid.org/0000-0003-1532-0480) (former Research Associate, KCL; now Social Work Lecturer, Middlesex University) was involved in data collection, coding and the study’s implementation; assisted with PPI and the literature review on evidence-based practice; co-wrote Chapter 2; and contributed important intellectual content to revisions of the final report.
Chris Ford (https://orcid.org/0000-0001-5842-8518) GP for more than 30 years before retirement, working with people who used drugs and/or alcohol and had multiple health conditions. With colleagues, she founded Substance Misuse Management in General Practice, which is a successful support network for doctors and other health professionals working with people who have alcohol and drug problems; started the RCGP Management of Drugs and Alcohol Problems in Primary Care conference (now in its 26th year); and was a key member in starting the RCGP Certificate in Drug Dependence. Chris was involved in study design; provided clinical expertise throughout the study; reviewed cases for inclusion in study outcomes; advised on measures to detect changes in alcohol intake and drug use; and contributed important intellectual content to the revisions of the final report.
Peter Williams (https://orcid.org/0000-0001-7885-0564) (Statistics Consultant) was involved in the study design, was responsible for the statistical analyses and production of statistical models and outputs, drafted statistical sections of the report and contributed important intellectual content to the revisions of the final report.
Publications
Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C. et al. Mapping of Specialist Primary Health Care Services in England for People who are Homeless. London: NIHR Health and Social Care Workforce Research Unit, King’s College London; 2018.
Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C. et al. Mapping of Specialist Primary Health Care Services in England for People who are Homeless: Summary of Findings and Consideration for Health Service Commissioners and Providers. London: NIHR Health and Social Care Workforce Research Unit, King’s College London; 2018.
Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C. et al. Inventory of Specialist Primary Health Care Services in England for People who are Homeless. London: NIHR Health and Social Care Workforce Research Unit, King’s College London; 2018.
Joly L. Involving People with Experience of Homelessness as Peer Interviewers. Southampton: NIHR; 2019.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- National Audit Office . Homelessness 2017. www.nao.org.uk/wp-content/uploads/2017/09/Homelessness.pdf (accessed 24 May 2022).
- Homeless Link Research Team . The Future Hostel: The Role of Hostels in Helping to End Homelessness 2018. www.homeless.org.uk/sites/default/files/site-attachments/The%20Future%20Hostel_June%202018.pdf (accessed 1 June 2021).
- Broadway . CHAIN Annual Report. Street to Home: 1st April 2012–31st March 2013 2013. www.mungos.org/app/uploads/2017/07/chain_street_to_home_annual_report_2012-13.pdf (accessed 1 June 2021).
- Greater London Authority . CHAIN Annual Report. Greater London: April 2020–March 2021 2021. https://data.london.gov.uk/dataset/chain-reports (accessed 29 August 2022).
- Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health 2010;100:1326-33. https://doi.org/10.2105/AJPH.2009.180109.
- Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW. Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey. Open Med 2011;5:e94-e103. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3148004/ (accessed 1 June 2021).
- Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014;384:1529-40. https://doi.org/10.1016/S0140-6736(14)61132-6.
- Aldridge RW, Menezes D, Lewer D, Cornes M, Evans H, Blackburn RM, et al. Causes of death among homeless people: a population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome Open Res 2019;4. https://doi.org/10.12688/wellcomeopenres.15151.1.
- Wright N, Smeeth L, Heath I. Moving beyond single and dual diagnosis in general practice: many patients have multiple morbidities, and their needs have to be addressed. BMJ 2003;326:512-4. https://doi.org/10.1136/bmj.326.7388.512.
- Wright NMJ, Tompkins CNE. How can health services effectively meet the health needs of homeless people?. Br J Gen Pract 2006;56:286-93. https://doi.org/10.1136%2Fbmj.326.7388.512.
- Crane M, Warnes AM. Single Homeless People’s Access to Healthcare Services in South Yorkshire. Sheffield, South Yorkshire: University of Sheffield; 2011.
- Lewer D, Menezes D, Cornes M, Blackburn RM, Byng R, Clark M, et al. Hospital readmission among people experiencing homelessness in England: a cohort study of 2772 matched homeless and housed inpatients. J Epidemiol Community Health 2021;75:681-8. https://doi.org/10.1136/jech-2020-215204.
- Department of Health, Office of the Chief Analyst . Healthcare for Single Homeless People 2010. www.housinglin.org.uk/_assets/Resources/Housing/Support_materials/Other_reports_and_guidance/Healthcare_for_single_homeless_people.pdf (accessed 1 June 2021).
- Warnes AM, Crane M, Whitehead N, Fu R. Homelessness Factfile. London: Crisis; 2003.
- Great Britain . National Health Service (Primary Care) Act 1997 1997.
- Wright N. Homelessness: A Primary Care Response. London: Royal College of General Practitioners; 2002.
- Connelly J, Crown J. Homelessness and Ill Health. London: Royal College of Physicians of London; 1994.
- Williams S, Allen I. Health Care for Single Homeless People. London: Policy Studies Institute; 1989.
- Hewett N. How to provide for the primary health care needs of homeless people: what do homeless people in Leicester think?. Br J Gen Pract 1999;49. https://www.researchgate.net/publication/242428889_Access_to_General_Practice_for_People_Sleeping_Rough (accessed 1 June 2021).
- Pleace N, Jones A, England J. Access to General Practice for People Sleeping Rough. York: Centre for Housing Policy, University of York; 2000.
- Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C, et al. Mapping of Specialist Primary Health Care Services in England for People Who Are Homeless 2018. https://kclpure.kcl.ac.uk/ws/portalfiles/portal/88023889/HEARTH_study_Mapping_FullReport_2018.pdf (accessed 11 September 2023).
- Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int J Nurs Stud 2009;46:1386-400. https://doi.org/10.1016/j.ijnurstu.2009.02.010.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred Reporting Items for Systematic reviews and Meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Upshur C, Weinreb L, Bharel M, Reed G, Frisard C. A randomized control trial of a chronic care intervention for homeless women with alcohol use problems. J Subst Abuse Treat 2015;51:19-2. https://doi.org/10.1016/j.jsat.2014.11.001.
- Bharel M, Santiago ER, Forgione SN, León CK, Weinreb L. Eliminating health disparities: innovative methods to improve cervical cancer screening in a medically underserved population. Am J Public Health 2015;105:438-42. https://doi.org/10.2105/AJPH.2014.302417.
- Nyamathi A, Liu Y, Marfisee M, Shoptaw S, Gregerson P, Saab S, et al. Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults. Nurs Res 2009;58:13-22. https://doi.org/10.1097/NNR.0b013e3181902b93.
- McInnes DK, Petrakis BA, Gifford AL, Rao SR, Houston TK, Asch SM, et al. Retaining homeless veterans in outpatient care: a pilot study of mobile phone text message appointment reminders. Am J Public Health 2014;104:588-94. https://doi.org/10.2105/AJPH.2014.302061.
- Nyamathi AM, Christiani A, Nahid P, Gregerson P, Leake B. A randomized controlled trial of two treatment programs for homeless adults with latent tuberculosis infection. Int J Tuberc Lung Dis 2006;10:775-82. https://pubmed.ncbi.nlm.nih.gov/16848340/ (accessed 11 September 2023).
- Cunningham CO, Shapiro S, Berg KM, Sacajiu G, Paccione G, Goulet JL. An evaluation of a medical outreach program targeting unstably housed HIV-infected individuals. J Health Care Poor Underserved 2005;16:127-38. https://doi.org/10.1353/hpu.2005.0007.
- Ciaranello AL, Molitor F, Leamon M, Kuenneth C, Tancredi D, Diamant AL, et al. Providing health care services to the formerly homeless: a quasi-experimental evaluation. J Health Care Poor Underserved 2006;17:441-61. https://doi.org/10.1353/hpu.2006.0056.
- Tommasello AC, Gillis LM, Lawler JT, Bujak GJ. Characteristics of homeless HIV-positive outreach responders in urban US and their success in primary care treatment. AIDS Care 2006;18:911-17. https://doi.org/10.1080/09540120500331297.
- O’Toole TP, Johnson EE, Borgia ML, Rose J. Tailoring outreach efforts to increase primary care use among homeless veterans: results of a randomized controlled trial. J Gen Intern Med 2015;30:886-98. https://doi.org/10.1007/s11606-015-3193-x.
- Schumann A, Nyamathi A, Stein JA. HIV risk reduction in a nurse case-managed TB and HIV intervention among homeless adults. J Health Psychol 2007;12:833-43. https://doi.org/10.1177/1359105307080618.
- Segan CJ, Maddox S, Borland R. Homeless clients benefit from smoking cessation treatment delivered by a homeless persons’ program. Nicotine Tob Res 2015;17:996-1001. https://doi.org/10.1093/ntr/ntv062.
- Tsu L, Buckley K, Nguyen S, Kohn J. Evaluating the impact of pharmacist health education on the perceptions of the pharmacist’s role among women living in a homeless shelter. Pharmacy Practice 2015;13. https://doi.org/10.18549/PharmPract.2015.04.649.
- Tyler D, Nyamathi A, Stein JA, Koniak-Griffin D, Hodge F, Gelberg L. Increasing hepatitis C knowledge among homeless adults: results of a community-based, interdisciplinary intervention. J Behav Health Serv Res 2014;41:37-49. https://doi.org/10.1007/s11414-013-9333-3.
- Asgary R, Garland V, Jakubowski A, Sckell B. Colorectal cancer screening among the homeless population of New York City shelter-based clinics. Am J Public Health 2014;104:1307-13. https://doi.org/10.2105/AJPH.2013.301792.
- O’Toole TP, Buckel L, Bourgault C, Blumen J, Redihan SG, Jiang L, et al. Applying the chronic care model to homeless veterans: effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health 2010;100:2493-9. https://doi.org/10.2105/AJPH.2009.179416.
- O’Toole TP, Bourgault C, Johnson EE, Redihan SG, Borgia M, Aiello R, et al. New to care: demands on a health system when homeless veterans are enrolled in a medical home model. Am J Public Health 2013;103:374-9. https://doi.org/10.2105/AJPH.2013.301632.
- McGuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health 2009;36:255-64. https://doi.org/10.1007/s10488-009-0210-6.
- Department of Health . Addressing Inequalities: Reaching the Hard-to-Reach Groups 2002. http://webarchive.nationalarchives.gov.uk/20120504011517/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4065397.pdf (accessed 6 June 2021).
- Royal College of General Practitioners . 2002 RCGP Statement on Homelessness and Primary Care 2002. www.rcgp.org.uk/policy/rcgp-policy-areas/homelessness.aspx (accessed 6 June 2021).
- British Medical Association General Practitioners Committee . Alternative Provider Medical Services (APMS): Guidance for GPs 2006.
- Wanless D. Securing Good Health for the Whole Population: Final Report 2004. www.southampton.gov.uk/moderngov/documents/s19272/prevention-appx%201%20wanless%20summary.pdf (accessed 6 June 2021).
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010 2010. www.parliament.uk/documents/fair-society-healthy-lives-full-report.pdf (accessed 6 June 2021).
- Great Britain . Health and Social Care Act 2012 2012.
- Hewett N. Standards for Commissioners and Service Providers. Version 2.0. London: The Faculty for Homeless and Inclusion Health; 2013.
- The King’s Fund . Health and Wellbeing Boards (HWBs) Explained 2016.
- Leng G. The Impact of Homelessness on Health: A Guide for Local Authorities. London: Local Government Association; 2017.
- Office for Health Improvement and Disparities . All Our Health: Personalised Care and Population Health 2015. www.gov.uk/government/collections/all-our-health-personalised-care-and-population-health (accessed 25 August 2022).
- Public Health England . All Our Health: About the Framework. Updated 29 July 2019 2019. www.gov.uk/government/publications/all-our-health-about-the-framework/all-our-health-about-the-framework (accessed 6 June 2021).
- Public Health England . Homelessness: Applying All Our Health. Updated 6 June 2019 2019. www.gov.uk/government/publications/homelessness-applying-all-our-health/homelessness-applying-all-our-health (accessed 6 June 2021).
- Public Health England . Tackling Tuberculosis in Under-Served Populations: A Resource for TB Control Boards and Their Partners (January 2019). Version: 2.0 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773730/Tackling_TB_in_Under-Served_Populations_-_a_Resource_for_TBCBs_and_partners.pdf (accessed 6 June 2021).
- Alderwick H, Dunn P, Mckenna H, Walsh N, Ham C. Sustainability and Transformation Plans in the NHS: How Are They Being Developed in Practice. London: The King’s Fund; 2016.
- Department of Health and Social Care . Integration and Innovation: Working Together to Improve Health and Social Care for All. Updated 11 February 2021 2021. www.gov.uk/government/publications/working-together-to-improve-health-and-social-care-for-all/integration-and-innovation-working-together-to-improve-health-and-social-care-for-all-html-version (accessed 6 June 2021).
- Department for Communities and Local Government . Addressing Complex Needs: Improving Services for Vulnerable Homeless People 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/417230/150325_Addressing_Complex_Needs_-_final_publication_amended.pdf (accessed 24 May 2022).
- McNaughton Nicholls C, Atherton I. Housing First: considering components for successful resettlement of homeless people with multiple needs. Housing Studies 2011;26:767-77. https://doi.org/10.1080/02673037.2011.581907.
- Tsemberis S, Gulcur L, Nakae M. Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health 2004;94:651-6. https://doi.org/10.2105/AJPH.94.4.651.
- Watson DP, Wagner DE, Rivers M. Understanding the critical ingredients for facilitating consumer change in Housing First programming: a case study approach. J Behav Health Serv Res 2013;40:169-79. https://doi.org/10.1007/s11414-012-9312-0.
- Tsai J. Is the Housing First model effective? Different evidence for different outcomes. Am J Public Health 2020;110:1376-7. https://doi.org/10.2105/AJPH.2020.305835.
- Aubry T. Analysis of Housing First as a practical and policy relevant intervention: the current state of knowledge and future directions for research. Eur J Homelessness 2020;14:1-14. https://www.feantsaresearch.org/public/user/Observatory/2020/EJH/EJH_14_1-A1-Web%5B2%5D.pdf (accessed 24 May 2022).
- Baxter AJ, Tweed EJ, Katikireddi SV, Thomson H. Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health 2019;73:379-87. https://doi.org/10.1136/jech-2018-210981.
- Great Britain . Homelessness Reduction Act 2017 2017.
- Great Britain . Housing (Homelessness Persons) Act 1977 1977.
- Ministry of Housing, Communities and Local Government . Rough Sleeping Strategy 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/733421/Rough-Sleeping-Strategy_WEB.pdf (accessed 6 June 2021).
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 6 June 2021).
- France J, Harrison HL. Inclusion Health in the Emergency Department: Caring for Patients who are Homeless or Socially Excluded. London: The Royal College of Emergency Medicine; 2020.
- Cornes M, Aldridge RW, Biswell E, Byng R, Clark M, Foster G, et al. Improving care transfers for homeless patients after hospital discharge: a realist evaluation. Health Serv Deliv Res 2021;9. https://doi.org/10.3310/hsdr09170.
- Hewett N. Homeless and Inclusion Health Standards for Commissioners and Service Providers: Version 3.1 2018. www.pathway.org.uk/wp-content/uploads/Version-3.1-Standards-2018-Final-1.pdf (accessed 6 June 2021).
- Healthy London Partnership . Health Care and People Who Are Homeless: Commissioning Guidance for London 2016. www.healthylondon.org/wp-content/uploads/2018/01/April-2019-Revised-Commissioning-Guidance.pdf (accessed 6 June 2021).
- Homeless Link . Homeless Health Needs Audit: Better Planning to Improve the Health of People Who Are Homeless in Your Area 2015. www.homeless.org.uk/sites/default/files/site-attachments/Homeless%20Health%20Needs%20Audit%20toolkit_0.pdf (accessed 6 June 2021).
- Cromarty H. Coronavirus: Support for Rough Sleepers (England) 2021. https://commonslibrary.parliament.uk/research-briefings/cbp-9057/ (accessed 6 June 2021).
- The Comptroller and Auditor General . Investigation into the Housing of Rough Sleepers During the COVID-19 Pandemic 2021. www.nao.org.uk/wp-content/uploads/2021/01/Investigation-into-the-housing-of-rough-sleepers-during-the-COVID-19-pandemic.pdf (accessed 6 June 2021).
- Department of Health and Social Care . The Future of Public Health: The National Institute for Health Protection and Other Public Health Functions 2020. www.gov.uk/government/publications/the-future-of-public-health-the-nihp-and-other-public-health-functions/the-future-of-public-health-the-national-institute-for-health-protection-and-other-public-health-functions (accessed 6 June 2021).
- Tudor Hart J. The Inverse Care Law. Lancet 1971;297:405-12. https://doi.org/10.1016/S0140-6736(71)92410-X.
- Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications, Inc.; 1989.
- Andersen R. Revisiting the behavioral model and access to medical care: does it matter?. J Health Soc Behav 1995;36:1-10. https://doi.org/10.2307/2137284.
- Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res 2000;34:1273-302. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1089079/pdf/hsresearch00023-0019.pdf (accessed 25 July 2021).
- Browne G, Roberts J, Gafni A, Byrne C, Kertyzia J, Loney P. Conceptualizing and validating the human services integration measure. Int J Integr Care 2004;4. https://doi.org/10.5334/ijic.98.
- Joly L, Goodman C, Froggatt K, Drennan V. Interagency working to support the health of people who are homeless. Soc Policy Society 2011;10:523-36. https://doi.org/10.1017/S1474746411000273.
- Bonin E, Brehove T, Carlson C, Downing M, Hoeft J, Kalinowski A, et al. Adapting Your Practice: General Recommendations for the Care of Homeless Patients 2010. https://nhchc.org/wp-content/uploads/2019/08/GenRecsHomeless2010-1.pdf (accessed 25 July 2021).
- Coufopoulos A, Mooney K. Food Nutrition and Homelessness: Guidance for Practitioners 2012. www.qni.org.uk/wp-content/uploads/2016/09/nutrition_guidance.pdf (accessed 25 July 2021).
- Salisbury D, Ramsay M, Noakes K. Immunisation Against Infectious Disease 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/147832/Green-Book-updated-140313.pdf (accessed 25 July 2021).
- World Health Organization . Systematic Screening for Active Tuberculosis: Principles and Recommendations 2013.
- Wright J. Health needs of the homeless. InnovAiT 2014;7:91-8. https://doi.org/10.1093/innovaitinr205.
- Seale JV, Fallaize R, Lovegrove JA. Nutrition and the homeless: the underestimated challenge. Nutr Res Rev 2016;29:143-51. https://doi.org/10.1017/S0954422416000068.
- Perrett K, Granerød J, Crowcroft N, Carlisle R. Changing epidemiology of hepatitis A: should we be doing more to vaccinate injecting drug users?. Commun Dis Public Health 2003;6:97-100.
- Syed NA, Hearing SD, Shaw IS, Probert CS, Brooklyn TN, . Outbreak of hepatitis A in the injecting drug user and homeless populations in Bristol: control by a targeted vaccination programme and possible parental transmission. Eur J Gastroenterol Hepatol 2003;15:901-6. https://doi.org/10.1097/00042737-200308000-00011.
- Story A, Murad S, Roberts W, Verheyen M, Hayward AC. Tuberculosis in London: the importance of homelessness, problem drug use and prison. Thorax 2007;62:667-71. https://doi.org/10.1136/thx.2006.065409.
- Kinchen K, Wright JD. Hypertension management in health care for the homeless clinics: results from a survey. Am J Public Health 1991;81:1163-5. https://doi.org/10.2105/AJPH.81.9.1163.
- Lee TC, Hanlon JG, Ben-David J, Booth GL, Cantor WJ, Connelly PW, et al. Risk factors for cardiovascular disease in homeless adults. Circulation 2005;111:2629-35. https://doi.org/10.1161/CIRCULATIONAHA.104.510826.
- Mares AS, Rosenheck RA. A comparison of treatment outcomes among chronically homelessness adults receiving comprehensive housing and health care services versus usual local care. Adm Policy Ment Health 2011;38:459-75. https://doi.org/10.1007/s10488-011-0333-4.
- Snyder LD, Eisner MD. Obstructive lung disease among the urban homeless. Chest 2004;125:1719-25. https://doi.org/10.1378/chest.125.5.1719.
- Szerlip MI, Szerlip HM. Identification of cardiovascular risk factors in homeless adults. Am J Med Sci 2002;324:243-6. https://doi.org/10.1097/00000441-200211000-00002.
- Wagner J, Diehl K, Mutsch L, Löffler W, Burkert N, Freidl W. Health status and utilisation of the healthcare system by homeless and non-homeless people in Vienna. Health Soc Care Community 2014;22:300-7. https://doi.org/10.1111/hsc.12083.
- Zlotnick C, Zerger S. Survey findings on characteristics and health status of clients treated by the federally funded (US) Health Care for the Homeless Programs. Health Soc Care Community 2009;17:18-26. https://doi.org/10.1111/j.1365-2524.2008.00793.x.
- O’Sullivan I, Lader D, Beavan-Seymour C, Chenery V, Fuller E, Sadler K. Foundation Report: Adult Dental Health Survey 2009 (Technical Information). Leeds: NHS Digital; 2011.
- NHS England . Summary of the Dental Results from the GP Patient Survey: January to March 2016 2016. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2016/07/GP-Survey-Dental-Results-Summary-Y10W2.pdf (accessed 17 August 2021).
- Slade GD. Derivation and validation of a short-form Oral Health Impact Profile. Community Dent Oral Epidemiol 1997;25:284-90. https://doi.org/10.1111/j.1600-0528.1997.tb00941.x.
- Humphris GM, Morrison T, Lindsay SJ. The Modified Dental Anxiety Scale: validation and United Kingdom norms. Community Dent Health 1995;12:143-50.
- Dolan TA, Peek CW, Stuck AE, Beck JC. Three-year changes in global oral health rating by elderly dentate adults. Community Dent Oral Epidemiol 1998;26:62-9. https://doi.org/10.1111/j.1600-0528.1998.tb01926.x.
- Robinson PG, Nadanovsky P, Sheiham A. Can questionnaires replace clinical surveys to assess dental treatment needs of adults?. J Public Health Dent 1998;58:250-53. https://doi.org/10.1111/j.1752-7325.1998.tb03002.x.
- Daly B, Newton JT, Batchelor P, Jones KJ. Normative need and oral health related quality of life in homeless people. Community Dent Oral Epidemiol 2010;38:136-44. https://doi.org/10.1111/j.1600-0528.2009.00516.x.
- Chisholm D, Knapp MR, Knudsen HC, Amaddeo F, Gaite L, van Wijngaarden B. Client Socio-Demographic and Service Receipt Inventory – European Version: development of an instrument for international research. EPSILON Study European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl 2000;39:s28-33. https://doi.org/10.1192/bjp.177.39.s28.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2020. Canterbury: Personal Social Services Research Unit, University of Kent; 2020.
- Crane M, Joly L, Manthorpe J. Rebuilding Lives: Formerly Homeless People’s Experiences of Independent Living and Their Longer-Term Outcomes 2016. https://kclpure.kcl.ac.uk/portal/files/52107014/RebuildingLives2016Report.pdf (accessed 27 July 2021).
- National Institute for Health and Care Research . Payment Guidance for Members of the Public Considering Involvement in Research 2021. www.nihr.ac.uk/documents/payment-guidance-for-members-of-the-public-considering-involvement-in-research/27372 (accessed 27 July 2021).
- Joly L. Involving People With Experience of Homelessness As Peer Interviewers 2019. www.nihr.ac.uk/blog/involving-people-with-experience-of-homelessness-as-peer-interviewers/11001 (accessed 27 July 2021).
- Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C, et al. Mapping of Specialist Primary Health Care Services in England for People who are Homeless: Summary of Findings and Considerations for Health Service Commissioners and Providers. London: NIHR Social Care Workforce Research Unit, King’s College London; 2018.
- Crane M, Cetrano G, Joly L, Coward S, Daly B, Ford C, et al. Inventory of Specialist Primary Health Care Services in England for People who are Homeless. London: NIHR Social Care Workforce Research Unit, King’s College London; 2018.
- National Institute for Health and Care Excellence . Alcohol-Use Disorders: Prevention 2010. www.nice.org.uk/guidance/ph24/resources/alcoholuse-disorders-prevention-pdf-1996237007557 (accessed 27 July 2021).
- Great Britain . Misuse of Drugs Act 1971 1971.
- Peak CM, Stous SS, Healy JM, Hofmeister MG, Lin Y, Ramachandran S, et al. Homelessness and hepatitis A – San Diego County, 2016–2018. Clin Infect Dis 2020;71:14-21. https://doi.org/10.1093/cid/ciz788.
- Spada E, Genovese D, Tosti ME, Mariano A, Cuccuini M, Proietti L, et al. An outbreak of hepatitis A virus infection with a high case-fatality rate among injecting drug users. J Hepatol 2005;43:958-64. https://doi.org/10.1016/j.jhep.2005.06.012.
- Ramsay M. Immunisation Against Infectious Disease. London: PHE; 2017.
- Aldridge RW, Hayward AC, Hemming S, Yates SK, Ferenando G, Possas L, et al. High prevalence of latent tuberculosis and bloodborne virus infection in a homeless population. Thorax 2018;73:557-64. https://doi.org/10.1136/thoraxjnl-2016-209579.
- Tuberculosis: NICE Guideline. London: NICE; 2016.
- NHS England . 2019/20/General/Medical/Services/(GMS)/Contract/Quality/and/Outcomes/Framework/(QOF):/Guidance/for/GMS/Contract/2019/20/in/England 2019. www.england.nhs.uk/wp-content/uploads/2019/05/gms-contract-qof-guidance-april-2019.pdf (accessed 28 July 2021).
- CAT Governance Board . COPD Assessment Test: Healthcare Professional User Guide 2018. www.catestonline.org/ (accessed 28 July 2021).
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Chen WJ, Fang CC, Shyu RS, Lin KC. Underreporting of illicit drug use by patients at emergency departments as revealed by two-tiered urinalysis. Addict Behav 2006;31:2304-8. https://doi.org/10.1016/j.addbeh.2006.02.015.
- Khadjesari Z, Marston L, Petersen I, Nazareth I, Walters K. Alcohol consumption screening of newly-registered patients in primary care: a cross-sectional analysis. Br J Gen Pract 2013;63:e706-12. https://doi.org/10.3399/bjgp13X673720.
- Livingston M, Callinan S. Underreporting in alcohol surveys: whose drinking is underestimated?. J Stud Alcohol Drugs 2015;76:158-64. https://doi.org/10.15288/jsad.2015.76.158.
- Morral AR, McCaffrey D, Iguchi MY. Hardcore drug users claim to be occasional users: drug use frequency underreporting. Drug Alcohol Depend 2000;57:193-202. https://doi.org/10.1016/S0376-8716(99)00048-4.
- Office for National Statistics . Adult Smoking Habits in the UK: 2019 2020. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2019 (accessed 28 July 2021).
- Lefante JJ, Harmon GN, Ashby KM, Barnard D, Webber LS. Use of the SF-8 to assess health-related quality of life for a chronically ill, low-income population participating in the Central Louisiana Medication Access Program (CMAP). Qual Life Res 2005;14:665-73. https://doi.org/10.1007/s11136-004-0784-0.
- McAneney H, Tully MA, Hunter RF, Kouvonen A, Veal P, Stevenson M, et al. Individual factors and perceived community characteristics in relation to mental health and mental well-being. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2590-8.
- Speiglman R, Norris JC. Alameda Countywide Shelter and Services Survey: County Report May 2004 2004. https://everyonehome.org/wp-content/uploads/2016/02/resources_HomelessCount04-1.pdf (accessed 28 July 2021).
- Ng Fat L, Scholes S, Boniface S, Mindell J, Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS): findings from the Health Survey for England. Qual Life Res 2017;26:1129-44. https://doi.org/10.1007/s11136-016-1454-8.
- Nuttall N, Tsakos G, Lader D, Hill K. Adult Dental Health Survey 2009. Leeds: NHS Digital; 2011.
- Ipsos MORI . GP Patient Survey. Questionnaire: Jan–Mar 2014 2014. www.gp-patient.co.uk/surveysandreports-10-16 (accessed 21 July 2021).
- Fuller E, Steele J, Watt R, Nuttall N. 1: Oral Health and Function – a Report from the Adult Dental Health Survey 2009 2011. https://files.digital.nhs.uk/publicationimport/pub01xxx/pub01086/adul-dent-heal-surv-summ-them-the1-2009-rep3.pdf (accessed 17 August 2021).
- Nuttall N, Freeman R, Beavan-Seymour C, Hill K. 8: Access and Barriers to Care – a Report from the Adult Dental Health Survey 2009 2011. https://files.digital.nhs.uk/publicationimport/pub01xxx/pub01086/adul-dent-heal-surv-summ-them-the8-2009-re10.pdf (accessed 17 August 2021).
- Steele J, Pitts N, Fuller E, Treasure E. 3: Urgent Conditions – a Report from the Adult Dental Health Survey 2009 2011. https://files.digital.nhs.uk/publicationimport/pub01xxx/pub01086/adul-dent-heal-surv-summ-them-the3-2009-rep5.pdf (accessed 17 August 2021).
- Primary Care Domain, NHS Digital . NHS Dental Statistics for England – 2015–16 2016. https://files.digital.nhs.uk/publicationimport/pub21xxx/pub21701/nhs-dent-stat-eng-15-16-rep-v2.pdf (accessed 17 August 2021).
- Primary Care Domain, NHS Digital . NHS Dental Statistics, England: 2016–17 2016. https://files.digital.nhs.uk/publication/5/r/nhs-dent-stat-eng-16-17-rep.pdf (accessed 17 August 2021).
- Primary Care Domain, NHS Digital . NHS Dental Statistics, England: 2017–18 2016. https://files.digital.nhs.uk/4F/B3B6FE/nhs-dent-stat-eng-17-18-rep.pdf (accessed 17 August 2021).
- Primary Care Domain, NHS Digital . NHS Dental Statistics, England, 2018–19 – Quarter 2 2016. https://files.digital.nhs.uk/56/2F8C8B/nhs-dent-stat-eng-18-19-q2-1page.pdf (accessed 17 August 2021).
- Newton JT, Asimakopoulou K, Daly B, Scambler S, Scott S. The management of dental anxiety: time for a sense of proportion?. Br Dent J 2012;213:271-4. https://doi.org/10.1038/sj.bdj.2012.830.
- Shekarchizadeh H, Khami MR, Mohebbi SZ, Ekhtiari H, Virtanen JI. Oral health of drug abusers: a review of health effects and care. Iran J Public Health 2013;42:929-40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4453891 (accessed 17 August 2021).
- Public Health England . Delivering Better Oral Health: An Evidence-Based Toolkit for Prevention 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/605266/Delivering_better_oral_health.pdf (accessed 17 August 2021).
- National Institute for Health and Care Excellence . Dental Checks: Intervals Between Oral Health Reviews 2004. www.nice.org.uk/guidance/cg19/resources/dental-checks-intervals-between-oral-health-reviews-pdf-975274023877 (accessed 17 August 2021).
- National Audit Office . Dentistry in England 2019. www.nao.org.uk/wp-content/uploads/2020/03/Dentistry-in-England.pdf (accessed 17 August 2021).
- NHS England . Summary of the Dental Results from the GP Patient Survey – January to March 2017 2017. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2017/07/GP-Survey-Dental-Results-Summary-Y11.pdf (accessed 17 August 2021).
- NHS England, Ipsos MORI . GP Patient Survey: National Report – July 2017 Publication 2017. www.gp-patient.co.uk/downloads/archive/2017/Weighted/GPPS%202017%20National%20report%20PUBLIC.pdf (accessed 28 July 2021).
- Great Britain . Misuse of Drugs Regulations 2001 2001.
- Lay-Flurrie S, Mathieu E, Bankhead C, Nicholson BD, Perera-Salazar R, Holt T, et al. Patient consultation rate and clinical and NHS outcomes: a cross-sectional analysis of English primary care data from 2.7 million patients in 238 practices. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4036-y.
- Ives J. Study: A Quarter of Patients Have Never Had Their BMI Recorded by a GP n.d. www.news-medical.net/news/20190429/Study-A-quarter-of-patients-have-never-had-their-BMI-recorded-by-a-GP.aspx (accessed 5 September 2021).
- Mansfield K, Crellin E, Denholm R, Quint JK, Smeeth L, Cook S, et al. Completeness and validity of alcohol recording in general practice within the UK: a cross-sectional study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-031537.
- Gillett K, Lippiett K, Astles C, Longstaff J, Orlando R, Lin SX, et al. Managing complex respiratory patients in the community: an evaluation of a pilot integrated respiratory care service. BMJ Open Respir Res 2016;3. https://doi.org/10.1136/bmjresp-2016-000145.
- Ferenchick EK, Ramanuj P, Pincus HA. Depression in primary care: part 1-screening and diagnosis. BMJ 2019;365. https://doi.org/10.1136/bmj.l794.
- Tylee A, Freeling P, Kerry S, Burns T. How does the content of consultations affect the recognition by general practitioners of major depression in women?. Br J Gen Pract 1995;45:575-8. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc1239431/ (accessed 5 September 2021).
- NHS Confederation . What Are Integrated Care Systems 2022. https://www.nhsconfed.org/system/files/2022-07/NHS%20Confederation%20parliamentary%20briefing%20-%20Integrated%20Care%20Systems%20%28ICS%29.pdf (accessed 15 November 2022).
- Waller E, Kanani N. Primary Care Networks – plans for 2021/22 and 2022/23. London: NHS England and NHS Improvement; 2021.
- Moss C, Sutton M, Cheraghi-Sohi S, Sanders C, Allen T. Comparative 4-year risk and type of hospital admission among homeless and housed emergency department attendees: longitudinal study of hospital records in England 2013–2018. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-049811.
- National Institute for Health and Care Excellence . Integrated Health and Social Care for People Experiencing Homelessness 2022. www.nice.org.uk/guidance/ng214/resources/integrated-health-and-social-care-for-people-experiencing-homelessness-pdf-66143775200965 (accessed 24 May 2022).
- Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet 2019;394:249-60. https://doi.org/10.1016/S0140-6736(19)31146-8.
- NHS England and NHS Improvement . NHS Mental Health Implementation Plan 2019 20 – 2023 24 2019. www.longtermplan.nhs.uk/wp-content/uploads/2019/07/nhs-mental-health-implementation-plan-2019-20-2023-24.pdf (accessed 24 May 2022).
- Gill P, MacLeod U, Lester H, Hegenbarth A. Improving Access to Health Care for Gypsies and Travellers, Homeless People and Sex Workers. London: Royal College of General Practitioners; 2013.
- National Institute for Health and Care Excellence . Who Should I Screen for Problem Drinking? 2019. https://cks.nice.org.uk/topics/alcohol-problem-drinking/diagnosis/who-to-screen/ (accessed 5 September 2019).
- Coffey E, Young D. Guidance for Hepatitis A and B Vaccination of Drug Users in Primary Care and Criteria for Audit. London: Royal College of General Practitioners; 2005.
- Gordon SJ, Grimmer K, Bradley A, Direen T, Baker N, Marin T, et al. Health assessments and screening tools for adults experiencing homelessness: a systematic review. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-7234-y.
- NHS England n.d. https://www.england.nhs.uk/publication/2018-19-national-cost-collection-data-publication/ (accessed 5 September 2023).
- Welsh Government . Together for Health – A Delivery Plan for the Critically Ill. A Delivery Plan up to 2016 for NHS n.d. www.wales.nhs.uk/documents/delivery-plan-for-the-critically-ill.pdf (accessed 3 October 2022).
- National Institute for Health and Care Excellence . Preoperative Tests (Update): Routine Preoperative Tests for Elective Surgery n.d. www.nice.org.uk/guidance/ng45/evidence/appendix-m-economic-considerations-for-delphi-pdf-87258149464 (accessed 4 October 2022).
- NHS England . Report of the Independent Review of Adult Screening Programmes in England n.d. www.england.nhs.uk/wp-content/uploads/2019/02/report-of-the-independent-review-of-adult-screening-programme-in-england.pdf (accessed 4 October 2022).
- National Institute for Health and Care Excellence . Preoperative Tests: Routine Preoperative Tests for Elective Surgery n.d. www.nice.org.uk/guidance/ng45/documents/guideline-appendices-13 (accessed 4 October 2022).
- Guest JF, Fuller GW, Vowden P. Costs and outcomes in evaluating management of unhealed surgical wounds in the community in clinical practice in the UK: a cohort study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-022591.
- National Institute for Health and Care Excellence . Tuberculosis: Prevention, Diagnosis, Management and Service Organisation. NICE NG33 – Methods, Evidence and Recommendations 2016. www.nice.org.uk/guidance/ng33/evidence/full-guideline-80851860868 (accessed 4 October 2022).
- Pharmaceutical Services Negotiating Committee . Methadone Dispensing (FP10 and FP10MDA) n.d. https://psnc.org.uk/dispensing-supply/dispensing-controlled-drugs/methadone-dispensing/ (accessed 1 June 2021).
Appendix 1 Two additional tables relating to case study participants
| Participants, n (%) | |||||
|---|---|---|---|---|---|
| Time point and reason | All (N = 363) | Dedicated Centre (N = 96) | Mobile Team (N = 96) | Specialist GP (N = 96) | Usual Care GP (N = 75) |
| 4-month interviews | |||||
| Participants interviewed | 272 (74.9) | 68 (70.8) | 73 (76.0) | 67 (69.8) | 64 (85.3) |
| Reasons why not interviewed | |||||
| In hospital/rehabilitation | 8 (2.2) | 1 (1.0) | 2 (2.1) | 3 (3.1) | 2 (2.7) |
| In prison | 12 (3.3) | 6 (6.3) | 2 (2.1) | 4 (4.2) | 0 (0.0) |
| Not in the UK | 7 (1.9) | 0 (0.0) | 7 (7.3) | 0 (0.0) | 0 (0.0) |
| In other UK town/city | 8 (2.2) | 5 (5.2) | 1 (1.0) | 2 (2.1) | 0 (0.0) |
| Located but declined/did not respond to interview attempts | 24 (6.6) | 12 (12.5) | 3 (3.1) | 6 (6.2) | 3 (4.0) |
| Could not find | 30 (8.3) | 4 (4.2) | 7 (7.3) | 13 (13.5) | 6 (8.0) |
| Safety reasons | 2 (0.6) | 0 (0.0) | 1 (1.0) | 1 (1.0) | 0 (0.0) |
| 8-month interviews | |||||
| Participants interviewed | 263 (72.5) | 65 (67.7) | 70 (72.9) | 70 (72.9) | 58 (77.3) |
| Reasons why not interviewed | |||||
| In hospital/rehabilitation/died | 13 (3.6) | 4 (4.2) | 2 (2.1) | 5 (5.2) | 2 (2.7) |
| In prison | 16 (4.4) | 10 (10.4) | 2 (2.1) | 4 (4.2) | 0 (0.0) |
| Not in UK | 8 (2.2) | 0 (0.0) | 8 (8.3) | 0 (0.0) | 0 (0.0) |
| In other UK town/city | 11 (3.0) | 7 (7.3) | 4 (4.2) | 0 (0.0) | 0 (0.0) |
| Located but declined/did not respond to interview attempts | 27 (7.4) | 8 (8.4) | 9 (9.4) | 4 (4.1) | 6 (8.0) |
| Could not find | 23 (6.3) | 1 (1.0) | 1 (1.0) | 12 (12.5) | 9 (12.0) |
| Safety reasons | 2 (0.6) | 1 (1.0) | 0 (0.0) | 1 (1.0) | 0 (0.0) |
| Physical health problems | Participants (%) | ||||
|---|---|---|---|---|---|
| All | Dedicated Centre | Mobile Team | Specialist GP | Usual Care GP | |
| Respiratory problems (n = 363) | 38.3 | 37.5 | 30.2 | 46.9 | 38.7 |
| Hypertension (n = 342) | 15.8 | 15.4 | 20.2 | 13.0 | 14.3 |
| Embolism/thrombosis (n = 361) | 13.9 | 21.1 | 8.3 | 15.8 | 9.3 |
| Stroke/circulation problems (n = 360) | 9.7 | 9.5 | 6.3 | 16.8 | 5.3 |
| Gastric/intestinal problems (n = 362) | 30.9 | 27.4 | 40.6 | 27.1 | 28.0 |
| Hepatitis C (n = 360) | 21.9 | 24.5 | 10.4 | 32.6 | 20.0 |
| Cirrhosis/liver problems (not hepatitis) (n = 361) | 19.4 | 22.1 | 21.9 | 15.8 | 17.3 |
| Urinary/renal problems (n = 362) | 15.2 | 16.8 | 19.8 | 11.5 | 12.0 |
| Epilepsy/blackouts (n = 362) | 20.2 | 26.3 | 17.7 | 12.5 | 25.3 |
| Arthritis/osteoarthritis (n = 362) | 14.4 | 16.8 | 9.4 | 15.6 | 16.0 |
| Injuries as a result of accidents/assaults (n = 362) | 14.4 | 12.6 | 18.8 | 13.5 | 12.0 |
| Other musculoskeletal problemsa (n = 362) | 34.5 | 41.1 | 36.5 | 32.3 | 26.7 |
| Infections/abscesses (not dental) (n = 362) | 6.4 | 10.5 | 5.2 | 5.2 | 4.0 |
| Leg ulcers (n = 362) | 7.7 | 10.5 | 8.3 | 9.4 | 1.3 |
| Other skin problems/rashes (n = 362) | 20.4 | 16.8 | 25.0 | 18.8 | 21.3 |
| Sores on feet/other foot problems (n = 362) | 21.0 | 21.1 | 28.2 | 18.8 | 13.3 |
| Eye/visual problems (n = 362) | 26.0 | 20.0 | 26.0 | 22.9 | 37.3 |
| Other problemsb (n = 363) | 38.4 | 36.8 | 41.7 | 37.5 | 37.3 |
| Total participants (N) | 363 | 96 | 96 | 96 | 75 |
Appendix 2 Indicators screened for the primary outcome by Case Study Site
| CSS | Participants screened for each HSI, n (%) | |||||
|---|---|---|---|---|---|---|
| BMI | Mental health | Alcohol use | TB | Smoking status | Hepatitis A | |
| Dedicated Centres | ||||||
| DC1 | 23 (47.9) | 41 (85.4) | 42 (87.5) | 7 (14.6) | 34 (70.8) | 13 (27.1) |
| DC2 | 20 (41.7) | 45 (93.8) | 44 (91.7) | 1 (2.1) | 42 (87.5) | 28 (58.3) |
| Mobile Teams | ||||||
| MT1 | 22 (46.8) | 28 (59.6) | 33 (70.2) | 3 (6.4) | 32 (68.1) | 4 (8.5) |
| MT2 | 21 (42.9) | 29 (59.2) | 31 (63.3) | 11 (22.4) | 43 (87.8) | 21 (42.9) |
| Specialist GPs | ||||||
| SP1 | 25 (49.0) | 49 (96.1) | 46 (90.2) | 2 (3.9) | 49 (96.1) | 41 (80.4) |
| SP2 | 10 (22.2) | 39 (86.7) | 26 (57.8) | 0 (0) | 31 (68.9) | 4 (8.9) |
| Usual Care GPs | ||||||
| UC1 | 5 (29.4) | 11 (64.7) | 13 (76.5) | 0 (0) | 14 (100) | 2 (11.8) |
| UC2 | 20 (69.0) | 27 (93.1) | 29 (100) | 0 (0) | 29 (100) | 3 (10.3) |
| UC3 | 14 (93.3) | 12 (80.0) | 14 (93.3) | 6 (40.0) | 15 (100) | 2 (13.3) |
Appendix 3 Predictors used in regression models (additional tables)
| Predictors | Time period | Participants, n/N (%) | Regression modelsa | ||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | |||
| Dedicated Centre | 96/363 (26.4) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Mobile Team | 96/363 (26.4) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Specialist GP | 96/363 (26.4) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Usual Care GP (set as control) | 75/363 (20.7) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Characteristics reported by participants | |||||||
| Female | 72/363 (19.8) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Black or Black British | 26/361 (7.2) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Born in the UK | 289/362 (79.8) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| British born/British citizen | 309/359 (86.1) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| In education/training/employment | Baseline | 53/363 (14.6) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Has income (earnings/welfare benefits) | Baseline | 315/362 (87.0) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Support from family/friends | Baselineb | 175/358 (48.9) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Smoking ≥ 20 cigarettes/roll-ups daily | Baseline | 70/331 (21.1) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Drinking > 14 units of alcohol weekly | Baseline | 149/345 (43.2) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Used drugs | Baselineb | 217/361 (60.1) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Injected drugs | Baselineb | 82/354 (23.2) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Physical health problems | Baselineb | 343/362 (94.8) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Depression | Baselineb | 293/357 (82.1) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Registration at CSS (medical records) | |||||||
| < 4 months | Baseline | 50/363 (13.8) | ✓ | ✓ | ✓ | ✓ | ✓ |
| < 6 months | Baseline | 96/363 (26.4) | ✓ | ✓ | ✓ | ✓ | ✓ |
| > 1 year | Baseline | 196/363 (54.0) | ✓ | ✓ | ✓ | ✓ | ✓ |
| > 2 years | Baseline | 113/363 (31.1) | – | – | ✓ | ✓ | ✓ |
| > 3 years | Baseline | 74/363 (20.4) | – | – | ✓ | ✓ | ✓ |
| Consultations with external key worker c | |||||||
| Any | Baselineb | 71/348 (20.4) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Monthly or more often | Baselineb | 58/348 (16.7) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Participants’ ratings of CSS doctor/nurse | |||||||
| Able to ‘drop in’ to CSS and be seen | Baseline | 262/359 (73.0) | – | ✓ | – | – | – |
| Confidence/trust in person: definitely | Baseline | 286/351 (81.5) | – | ✓ | – | – | – |
| Good/very good at giving enough time | Baseline | 328/352 (93.2) | – | ✓ | – | – | – |
| Good/very good at listening | Baseline | 314/350 (89.7) | – | ✓ | – | – | – |
| Good/very good at explaining condition/treatment | Baseline | 306/345 (88.7) | – | ✓ | – | – | – |
| Good/very good at involving patient in decisions about care | Baseline | 285/332 (85.8) | – | ✓ | – | – | – |
| Good/very good at treating patient with care and concern | Baseline | 313/349 (89.7) | – | ✓ | – | – | – |
| Good/very good at providing/arranging treatment | Baseline | 302/336 (89.9) | – | ✓ | – | – | – |
| Predictors | Modelsa | Time point/period | Participants (n) | Mean (SD) | Median | Minimum, Maximum |
|---|---|---|---|---|---|---|
| Age (years) | A, B, C, D, E | Baseline | 363 | 41.56 (10.54) | 41.00 | 18, 79 |
| Approximate number of years homeless | A, B, C, D, E | Baseline | 359 | 8.32 (8.01) | 5.50 | 0.08, 40.0 |
| Number of years registered with CSS | A, B, C, D, E | Baseline | 363 | 2.08 (2.46) | 1.29 | –0.055, 17.98 |
| Number of changes of accommodation/sleeping settings (includes episodes of ≥ 7 days in hospital) | D, E | Study period | 363 | 2.29 (2.32) | 2.00 | 0, 11 |
| % of time in building designed for habitation | D, E | Study period | 360 | 79.78 (30.62) | 100.00 | 0, 100 |
| % of time in accommodation with staff (24 hour or part time) | D, E | Study period | 360 | 48.21 (39.07) | 45.83 | 0, 100 |
| Number of consultations at CSS with GP/nurse/HCA | A, B | Baselineb | 363 | 6.09 (8.12) | 4.0 | 0, 82 |
| Quality of Care rating [1 = very good, 5 = very poor]c | B | Baseline | 354 | 1.60 (0.84) | 1.17 | 1, 5 |
| Predictors | Time point/period | Participants, n/N (%) |
|---|---|---|
| Dedicated Centre | 65/263 (24.7) | |
| Mobile Team | 70/263 (26.6) | |
| Specialist GP | 70/263 (26.6) | |
| Usual Care GP (set as control) | 58/263 (22.1) | |
| Reported by participant | ||
| Female | 53/263 (20.2) | |
| Black or Black British | 23/262 (8.8) | |
| Born in the UK | 204/263 (77.6) | |
| British born/British citizen | 221/260 (85.0) | |
| Involved in education/training/employment | 8 months | 53/263 (20.2) |
| Has an income (earnings or state welfare benefits) | 8 months | 228/252 (90.5) |
| Support from family/friends | 8 monthsa | 137/255 (53.7) |
| Heavy smoker (≥ 20 cigarettes/roll-ups daily) | 8 monthsa | 58/246 (23.6) |
| Drinking > 14 units of alcohol weekly | 8 monthsa | 108/256 (42.2) |
| Used drugs | 8 monthsa | 146/263 (55.5) |
| Injected drugs | 8 monthsa | 46/258 (17.8) |
| Physical health problems | Baselinea | 248/263 (94.3) |
| Depression | Baselinea | 208/259 (80.3) |
| Medical records/service use data | ||
| Registered with CSS < 4 months | Baseline | 37/263 (14.1) |
| Registered with CSS < 6 months | Baseline | 72/263 (27.4) |
| Registered with CSS > 1 year | Baseline | 142/263 (54.0) |
| Any consultation with external key workerb | Study period | 93/257 (36.2) |
| At least monthly consultation with external key workerb | Study period | 52/257 (20.2) |
| Predictors | Time point/period | Participants (n) | Mean (SD) | Median | Minimum, Maximum |
|---|---|---|---|---|---|
| Age (years) | Baseline | 253 | 42.64 (10.60) | 42.00 | 18, 79 |
| Approximate number of years homeless | Baseline | 252 | 8.56 (8.26) | 5.50 | 0.08, 40.0 |
| Number of changes of accommodation/sleeping settings | Study period | 253 | 2.10 (2.29) | 1.00 | 0, 11 |
| % of time in building designed for habitation | Study period | 252 | 82.45 (298.73) | 100.0 | 0, 100 |
| % of time in accommodation with staff (24 hour or part time) | Study period | 252 | 47.68 (39.51) | 47.21 | 0, 100 |
| Number of years registered with CSS | Baseline | 253 | 2.00 (2.25) | 1.34 | −0.055, 17.982 |
| Number of consultations at CSS with GP/nurse/HCA | Study period | 263 | 14.95 (20.32) | 9.0 | 0, 214 |
Appendix 4 Dental health and dental services (additional tables)
| Reasonsa | Participants | |
|---|---|---|
| n | % | |
| Afraid of going to dentist | 50 | 32.9 |
| Forgot/did not get around to it | 36 | 23.7 |
| Embarrassed about the state of my teeth | 26 | 17.1 |
| Nothing wrong with my teeth | 20 | 13.2 |
| Cannot find an NHS dentist | 19 | 12.5 |
| Bad experience with dentist | 19 | 12.5 |
| Cannot afford NHS charges | 18 | 11.8 |
| Embarrassed to go as homeless | 14 | 9.2 |
| Have not had time to go | 10 | 6.6 |
| Difficult to travel to the dentist | 8 | 5.3 |
| Refused dental registration | 1 | 0.7 |
| Total number | 152 | |
| OHIP-14 scores | Health Service Model | Comparison test: p-value | ||||
|---|---|---|---|---|---|---|
| All (N = 273)a | Dedicated Centre (N = 71) | Mobile Team (N = 71) | Specialist GP (N = 71) | Usual Care GP (N = 60) | ||
| Total scores b | ||||||
| Score, n (%) | ||||||
| 0 | 41 (15.0) | 7 (9.9) | 16 (22.5) | 6 (8.5) | 12 (20.0) | Kruskal–Wallis: 0.014 |
| 1–10 | 84 (30.8) | 19 (26.8) | 23 (32.4) | 24 (33.8) | 18 (30.0) | |
| 11–20 | 63 (23.1) | 16 (22.5) | 17 (23.9) | 13 (18.3) | 17 (28.3) | |
| 21–30 | 49 (17.9) | 18 (25.4) | 8 (11.3) | 17 (23.9) | 6 (10.0) | |
| ≥ 31 | 36 (13.2) | 11 (15.5) | 7 (9.9) | 11 (15.5) | 7 (11.7) | |
| Mean (SD) | 14.77 (12.65) | 17.08 (12.44) | 12.30 (12.08) | 16.51 (12.61) | 12.90 (13.08) | ANOVA: 0.051 |
| Total number of impacts (problems) c | ||||||
| Number of impacts, n (%) | ||||||
| None | 52 (19.0) | 11 (15.5) | 18 (25.4) | 9 (12.7) | 14 (23.3) | Kruskal–Wallis: 0.057 |
| 1–3 | 71 (26.0) | 16 (22.5) | 17 (23.9) | 23 (32.4) | 15 (25.0) | |
| 4–6 | 66 (24.2) | 14 (19.7) | 21 (29.6) | 13 (18.3) | 18 (30.0) | |
| 7–9 | 32 (11.7) | 10 (14.1) | 7 (9.9) | 12 (16.9) | 3 (5.0) | |
| 10–14 | 52 (19.0) | 20 (28.2) | 8 (11.3) | 14 (19.7) | 10 (16.7) | |
| Mean (SD) | 4.89 (4.21) | 5.70 (4.23) | 4.04 (3.93) | 5.38 (4.20) | 4.33 (4.32) | ANOVA: 0.056 |
| Domain: type of problem | All models (N = 291) | (N = 291) All models | Chi-squared: p-value | |||||
|---|---|---|---|---|---|---|---|---|
| (N = 291) All models | (N = 74) Dedicated Centre | (N = 78) Mobile Team | (N = 74) Specialist GP | (N = 65) Usual Care GP | Chi-squared: p-value | |||
| n (%) with problemb | n (%) with problemc | |||||||
| Functional limitation | ||||||||
| Trouble pronouncing words | 79 (27.1) | 22 (29.7) | 20 (25.6) | 16 (21.6) | 21 (32.3) | 0.502 | 122 (42.1) | 0.488 |
| Sense of taste has worsened | 86 (29.8) | 25 (34.7) | 19 (24.4) | 22 (29.7) | 20 (30.8) | 0.579 | ||
| Physical pain | ||||||||
| Painful aching in the mouth | 126 (43.2) | 38 (51.4) | 27 (34.6) | 37 (50.0) | 24 (36.4) | 0.072 | 175 (59.9) | 0.034 |
| Uncomfortable to eat food | 146 (50.2) | 42 (56.8) | 33 (42.3) | 45 (60.8) | 26 (40.0) | 0.026 | ||
| Psychological discomfort | ||||||||
| Been self-conscious | 151 (52.1) | 38 (51.4) | 32 (41.6) | 48 (64.9) | 33 (50.8) | 0.040 | 170 (58.8) | 0.061 |
| Felt tense | 111 (38.5) | 31 (41.9) | 23 (30.3) | 31 (42.5) | 26 (40.0) | 0.379 | ||
| Physical disability | ||||||||
| Had unsatisfactory diet | 99 (34.1) | 39 (53.4) | 15 (19.5) | 25 (33.8) | 20 (30.3) | < 0.0005 | 123 (42.3) | 0.001 |
| Had to interrupt meals | 85 (29.5) | 29 (39.7) | 20 (26.0) | 21 (28.4) | 15 (23.4) | 0.151 | ||
| Psychological disability | ||||||||
| Found it difficult to relax | 117 (40.3) | 36 (48.6) | 30 (39.0) | 27 (36.5) | 24 (36.9) | 0.399 | 185 (63.6) | 0.761 |
| Been a bit embarrassed | 155 (53.4) | 39 (52.7) | 37 (47.4) | 45 (60.8) | 34 (53.1) | 0.429 | ||
| Social disability | ||||||||
| Irritable with other people | 90 (31.1) | 29 (39.2) | 20 (26.0) | 21 (28.8) | 20 (30.8) | 0.335 | 103 (35.9) | 0.190 |
| Difficulty doing usual jobs | 57 (19.7) | 21 (28.4) | 9 (11.7) | 16 (21.9) | 11 (16.9) | 0.066 | ||
| Handicap | ||||||||
| Felt life in general less satisfying | 98 (33.9) | 30 (40.5) | 24 (31.2) | 26 (35.1) | 18 (28.1) | 0.438 | 103 (35.6) | 0.413 |
| Totally unable to function | 42 (14.5) | 11 (14.9) | 13 (16.9) | 9 (12.2) | 9 (14.1) | 0.874 | ||
| Dental outcomes | At CSS/local homelessness service site | ||
|---|---|---|---|
| Yes, n (%) | No, n (%) | Comparison test: p-value | |
| Registered with dentist at 8 months (N = 254) | 58 (45.3) | 66 (52.4) | Chi-squared: 0.260 |
| Seen by dentist during study period (N = 281) | 72 (50.3) | 73 (52.9) | Chi-squared: 0.669 |
| Rating of dental health over 12 months (N = 245) | |||
| Improved a little or a lot | 20 (16.1) | 17 (14.0) | Mann–Whitney U Test: 0.304 |
| Stayed the same | 64 (51.6) | 57 (47.1) | |
| Worsened a little or a lot | 40 (32.3) | 47 (38.8) | |
Appendix 5 Summary of strengths and limitations of Case Study Sites, as perceived by staff and external agencies
| CSS | Strengths of CSSa | Limitations of CSS, including local factorsa |
|---|---|---|
| Dedicated Centre 1 |
|
CSS factors:
Local factors: |
| Dedicated Centre 2 |
|
CSS factors:
|
|
Local factors:
|
|
| Specialist GP 1 |
|
CSS factors:
Local factors: |
| Specialist GP 2 |
|
CSS factors:
Local factors: |
| Mobile Team 1 |
|
CSS factors:
Local factors: |
| Mobile Team 2 |
|
CSS factors:
Local factors: |
| Usual Care GP 1b |
|
CSS factors:
Local factors: |
| Usual Care GP 2b |
|
CSS factors:
Local factors: |
| Usual Care GP 3b |
|
CSS factors:
Local factors: |
Appendix 6 Summary of people who were homeless and not using the Case Study Sites
| Characteristics | People who were homeless and not using the CSSs, n (%) | ||||
|---|---|---|---|---|---|
| All locations (N = 107) | Dedicated Centre locations (N = 29) | Mobile Team locations (N = 14) | Specialist GP locations (N = 35) | Usual Care GP locations (N = 29) | |
| Physical health problem | 94 (87.9) | 25 (86.2) | 13 (92.9) | 30 (85.7) | 26 (89.7) |
| Mental health problem | 84 (80.0) | 20 (74.1) | 10 (71.4) | 28 (80.0) | 26 (89.7) |
| Where usually obtains health care | |||||
| GP surgery/medical centre | 87 (81.3) | 22 (75.9) | 12 (85.7) | 28 (80.0) | 25 (86.2) |
| Walk-in health centre | 17 (15.9) | 5 (17.2) | 5 (37.5) | 5 (14.3) | 2 (6.9) |
| A&E | 36 (33.6) | 17 (58.6) | 5 (35.7) | 8 (22.9) | 6 (20.7) |
| No health care | 7 (6.5) | 1 (3.4) | 0 (0) | 4 (11.4) | 2 (6.9) |
| Seen by doctor or nurse in previous 3 months | 76 (72.4) | 19 (65.5) | 11 (78.6) | 21 (63.6) | 25 (86.2) |
| Last seen by doctor or nurse > 12 months ago | 19 (18.1) | 7 (24.1) | 3 (21.4) | 8 (24.2) | 1 (3.4) |
| Used A&E in previous 12 months | 59 (55.1) | 17 (58.6) | 9 (64.3) | 18 (51.4) | 15 (51.7) |
| Used A&E 4+ times in previous 12 months | 10 (9.3) | 2 (6.9) | 1 (7.1) | 5 (14.3) | 2 (6.9) |
| Used CSS in past | 22 (20.6) | 9 (31.0) | 2 (14.3) | 8 (22.9) | 3 (10.3) |
Appendix 7 Unit costs of services
| Service use item | Unit cost (£) | Source and date | Any details/backgrounda |
|---|---|---|---|
| GP | |||
| At CSS | 66 | PSSRU,107 p. 125, 10.3b GP | Surgery session consultation lasting 9.22 minutes (£33); doubled on team advice |
| Telephone | 30 | PSSRU,107 p. 129, 10.5 | Telephone triage GP for average of 4 minutes (£15); doubled on team advice |
| Away from CSS | 66 | As GP at CSS | |
| Nurse | |||
| At CSS | 14 | PSSRU,107 p. 129, 10.2 general practice nurse | £42 per hour; assume 20-minute consultation |
| Telephone | 16 | PSSRU,107 p. 129, 10.5 Telephone triage nurse | Telephone triage nurse for average of 6.56 minutes (£8); doubled on team advice |
| Away from CSS (i.e. assuming community/district nurse) | 21 | PSSRU,107 pp. 121–3, section 10, doctors and nurses | Band 6. Average of £89 per hour for patient-related work (33% of time), £49 per hour working hours (67% of time) = £62 per hour. Assume 20-minute consultation |
| Counsellor, psychologist | |||
| At CSS | 29 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 7, £58 per working hour. Assume 30-minute consultation |
| Telephone | 15 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 7, £58 per working hour. Assume 15-minute call |
| Mental health nurse | |||
| At CSS | 31 | PSSRU,107 pp. 121–3, section 10, doctors and nurses | Band 6. Average of £89 per hour for patient-related work (33% of time), £49 per hour for working hours (67% of time) = £62 per hour. Assume 30-minutes consultation |
| Away from CSS | 31 | As mental health nurse at CSS | |
| HCA | |||
| At CSS | 15 | PSSRU,107 pp. 121–3, section 10, doctors and nurses | Band 4, £30 per working hour. Assume 30-minute appointment |
| Telephone | 7 | PSSRU,107 pp. 121–3, section 10, doctors and nurses | Band 4, £30 per working hour. Assume 15-minute call |
| Away from CSS | 15 | As HCA at CSS | |
| Specialist nurse at CSS | 42 | PSSRU,107 pp. 121–3, section 10, doctors and nurses | Band 8. Average of £139 per hour for patient-related work (25% of time), £68 per hour for working hours (75% of time) = £85 per hour. Assume 30-minute appointment |
| Consultant at CSS | 39 | PSSRU,107 p. 158, hospital-based doctor | £116 per working hour. Assume 20-minute consultation |
| Case managerb | |||
| At CSS | 17 | PSSRU,107 p. 138, 11.1, social worker adult service | £51 per hour; assume 20-minute appointment |
| Telephone | 8 | PSSRU,107 p. 138, 11.1, social worker adult service | £51 per hour; assume 10-minute call |
| Away from CSS | 17 | As case manager at CSS | |
| Pharmacist | |||
| At CSS | 16 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 6, £48 per working hour. Assume 20-minute consultation |
| Telephone | 8 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 6, £48 per working hour. Assume 10-minute call |
| Dispense methadone | 4 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 6, £48 per working hour. Assume 5 minutes to prepare, do paperwork and supervise administrationc |
| Substance misuse | |||
| At CSS | 30 | PSSRU,107 p. 53, 3.2 Alcohol worker/liaison nurse/substance misuse nurse | Range £49–81 per hour (face-to-face time is 50%). Assume 30-minute consultation with mid-range worker/nurse |
| Telephone | 10 | PSSRU,107 p. 53, 3.2 Alcohol worker/liaison nurse/substance misuse nurse | Range £49–81 per hour (face-to-face time is 50%). Assume 10-minute call with mid-range worker/nurse |
| Away from CSS | 30 | As substance misuse at CSS | |
| Smoking cessation consultationd | 8 | PSSRU,107 p. 92, 7.4. Public health interventions | 10-minute brief advice session with a nurse |
| Dentist | |||
| At CSS | 66 | PSSRU,107 p. 130. NHS Dentist – performer only | £105 per hour; £133 per hour for patient contact. Assume 30-minute call |
| Out-of-hours visitd | 66 | As Dentist at CSS | |
| Out-of-hours telephoned | 33 | PSSRU,107 p. 130. NHS Dentist – performer only | £105 per hour; £133 per hour for patient contact. Assume 15-minute call |
| A&E | 166 | National Cost Collection data 2018/19165 (index) | |
| Walk-in/urgent care clinic | 148 | National Cost Collection data 2018/19165 (index) | Outpatient cost |
| NHS 111 | 7 | National Cost Collection data 2018/19;165 currency code: ASC1; currency description: calls £7.33 | |
| Hospital outpatient appointment | 135 | PSSRU,107 p. 87, 7.1 NHS reference costs hospital services | Weighted average of all outpatient attendances |
| Physiotherapist, occupational therapistd | 18 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 5, £36 per working hour. Assume 30-minute consultation |
| Podiatrist, chiropodist | 18 | PSSRU,107 pp. 117–19, section 9, scientific and professional staff | Band 5, £36 per working hour. Assume 30-minute consultation |
| Dietitian | 18 | Assume same as physiotherapist and occupational therapist | |
| Optician | 29 | NHS reference costs: 2018/19; Currency code: WF01D; service code: 130; currency description: non-admitted non-face-to-face attendance, first | Ophthalmology: non-consultant led |
| Complementary therapyd | 145 | National Cost Collection data 2018/19.165 Currency code: AB23Z (total) | Acupuncture for pain management |
| Hospital admission, not detoxification | PSSRU,107 p. 87, 7.1 NHS reference costs hospital services | Non-elective inpatient long stay, £3366; short stay, £602. Assume short stay is two nights or fewer; rest is long stay | |
| Hospital night, not detoxification, ICU | 1932 | Welsh Government166 | Level-3 intensive care bed, per night |
| Hospital night, not detoxification, HDU | 857 | Welsh Government166 | Level-2 high-dependency bed, per night |
| Hospital night, not detoxification, general ward | 341 | National Cost Collection data 2018/19165 – from index section. Regular day or night admissions, per night | Currency code: WH17B and C; currency description: admission related to social factors without interventions, with CC score 1+ and score 0: £191 and £292 |
| Hospital night, not detoxification, psychiatric ward | 424 | PSSRU,107 2.1 NHS reference costs for mental health services | £424 per bed-day |
| Day cases | 752 | PSSRU,107 p. 87, 7.1 NHS reference costs 2018/19,165 hospital services | Weighted average of all stays: £752 |
| Hospital night for detoxification | 510 | PSSRU,107 p. 52, 3.1 NHS reference costs 2018/19165 | Admitted by alcohol services; £510 per night |
| Ambulance (convey) | 263 | PSSRU,107 p. 87, 7.1 NHS reference costs 2018/19,165 hospital services | Ambulance services, weighted average of all attendances when conveyed; £263 |
| Ambulance (see, treat and refer) | 214 | PSSRU,107 page 87, 7.1 NHS reference costs hospital services | Ambulance services, weighted average of all attendances when seen, treated and referred; £214 |
| Key worker contact not at accommodatione | 16 | PSSRU,107 p. 149, 11.3 social work assistant | £33 per hour. Assume 30-minute consultation |
| Social services personal carerd | 0.50 per minute | PSSRU,107 p. 142, 11.5 home care worker, face-to-face | £31 per hour (duration of visits in minutes known and applied) |
| LA housing officer | 17 | PSSRU,107 p. 149, 11.3 using social work assistant | £33 per hour. Assume 30-minute consultation |
| Welfare benefits agent | 17 | PSSRU,107 p. 149, 11.3 using social work assistant | £33 per hour. Assume 30-minute consultation |
| Volunteer supporter | 17 | PSSRU,107 p. 144, 11.7 support and outreach worker | £25 per hour. Assume 40 minutes per contact |
| Well-being groupd | 6 | PSSRU,107 p. 92, 7.4 public health interventions, well-being | Average cost: £39 per client. Assume £6 per group session |
| Tests | |||
| Blood test | 10 | NICE167 |
|
| Cervical smear; vaginal swabd | 22 |
|
Cytology (process of looking at cervical cells under a microscope168) £7 |
| Electrocardiography | 37 | NICE167 (table 9; at 2016 costs) | |
| MRI | 196 | National Cost Collection data 2018/19;165 dept code = IMAGOP; dept description = outpatient; currency code = RD06Z | Magnetic Resonance Imaging Scan of more than Three Areas. |
| Ultrasonography | 75 |
|
|
| Urine test | 4 | NICE169 | Urology |
| Wound swab | 3 | Table 6 of Guest et al.,170 at 2018 prices | Laboratory tests. Cost of health care resource use associated with managing unhealed surgical wounds in clinical practice: £2.85 |
| X-ray/DEXAd | 32 | National Cost Collection data 2018/19;165 service code = 812; service description = diagnostic imaging, £34 (consultant led); £17 (non-consultant led) | Diagnostic imaging (apparently used for X-ray costs) |
| Stool sample | 5 | Estimate based on local financial information | Faecal immunochemical test |
| Sputum | 7 | NICE171 (p. 154) | Sputum smear microscopy (at 2016 prices) |
| Colposcopy | 116 | National Cost Collection data 2018/19;165 outpatient procedures – service code = 101; service description = urology; currency code = MA38Z | Diagnostic colposcopy costs used |
| Echocardiography | 76 | National Cost Collection data 2018/2019;165 dept code = IMAGOP; dept description = outpatient; currency code = RD51A | Simple echocardiography, age ≥ 19 years |
Appendix 8 Contacts with services over 12 months, by Case Study Site
| Service | DC1 | DC2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | |||||
| GP | ||||||||||
| At CSS base | 48 | 14.48 (12.79) | 10.50 (6.00–17.00) | 65 | 0 (0.00) | 48 | 18.96 (16.93) | 14.00 (8.00–21.00) | 88 | 0 (0.00) |
| Telephone with patient | 48 | 0.08 (0.28) | 0.00 (0.00–0.00) | 1 | 44 (91.67) | 48 | 0.77 (1.59) | 0.00 (0.00–1.00) | 9 | 32 (66.67) |
| Elsewhere | 48 | 2.13 (4.78) | 0.00 (0.00–1.50) | 21 | 35 (72.92) | 48 | 0.73 (1.45) | 0.00 (0.00–1.00) | 6 | 33 (68.75) |
| Nurse | ||||||||||
| At CSS base | 48 | 3.73 (6.57) | 1.00 (0.00–4.50) | 40 | 17 (35.42) | 48 | 12.54 (28.56) | 3.50 (1.50–9.50) | 160 | 3 (6.25) |
| Telephone with patient | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.17 (0.88) | 0.00 (0.00–0.00) | 6 | 45 (93.75) |
| Elsewhere | 48 | 0.77 (1.96) | 0.00 (0.00–0.00) | 9 | 37 (77.08) | 48 | 0.27 (1.05) | 0.00 (0.00–0.00) | 6 | 44 (91.67) |
| HCA | ||||||||||
| At CSS base | 48 | 0.54 (0.80) | 0.00 (0.00–1.00) | 4 | 28 (58.33) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Telephone | 48 | 0.04 (0.29) | 0.00 (0.00–0.00) | 2 | 47 (97.92) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Elsewhere | 48 | 0.10 (0.31) | 0.00 (0.00–0.00) | 1 | 43 (89.58) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Mental health nurse | ||||||||||
| At CSS base | 48 | 0.63 (1.27) | 0.00 (0.00–1.00) | 7 | 32 (66.67) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Telephone | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Elsewhere | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Specialist nurse at CSS | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Consultant at CSS | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Pharmacist (at CSS for UC; elsewhere for DC, MT, SP) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Telephone with pharmacist at CSS base | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Physiotherapist/occupational therapist elsewhere | 48 | 1.79 (5.83) | 0.00 (0.00–0.00) | 37 | 37 (77.08) | 48 | 0.42 (1.92) | 0.00 (0.00–0.00) | 12 | 44 (91.67) |
| Podiatrist/chiropodist | 48 | 0.06 (0.24) | 0.00 (0.00–0.00) | 1 | 45 (93.75) | 48 | 0.44 (2.18) | 0.00 (0.00–0.00) | 15 | 42 (87.50) |
| Dietitian | 48 | 0.06 (0.32) | 0.00 (0.00–0.00) | 2 | 46 (95.83) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Psychologist/counsellor/psychiatrist | ||||||||||
| At CSS base | 48 | 0.88 (3.88) | 0.00 (0.00–0.00) | 24 | 44 (91.67) | 48 | 3.67 (7.01) | 0.00 (0.00–3.50) | 31 | 26 (54.17) |
| Telephone | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.10 (0.42) | 0.00 (0.00–0.00) | 2 | 45 (93.75) |
| Elsewhere | 48 | 0.25 (0.70) | 0.00 (0.00–0.00) | 3 | 41 (85.42) | 48 | 0.63 (1.76) | 0.00 (0.00–0.50) | 9 | 36 (75.00) |
| Complementary therapy | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 1.48 (5.89) | 0.00 (0.00–0.00) | 31 | 43 (89.58) |
| Smoking cessation clinic | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Alcohol/drugs/substance misuse | ||||||||||
| At CSS base | 48 | 8.83 (10.32) | 2.50 (0.00–18.00) | 34 | 22 (45.83) | 48 | 4.60 (10.31) | 0.00 (0.00–1.00) | 38 | 35 (72.92) |
| Telephone | 48 | 0.08 (0.28) | 0.00 (0.00–0.00) | 1 | 44 (91.67) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Elsewhere | 48 | 2.00 (4.46) | 0.00 (0.00–1.50) | 19 | 33 (68.75) | 48 | 2.25 (5.35) | 0.00 (0.00–2.00) | 25 | 29 (60.42) |
| Visits to local pharmacist for methadone | 48 | 155.44 (154.56) | 98.00 (0.00–318.00) | 366 | 19 (39.58) | 48 | 73.60 (130.85) | 0.00 (0.00–90.50) | 365 | 33 (68.75) |
| Case manager, etc.a | ||||||||||
| At CSS base | 48 | 0.21 (0.54) | 0.00 (0.00–0.00) | 3 | 40 (83.33) | 48 | 1.04 (1.74) | 0.00 (0.00–1.00) | 6 | 29 (60.42) |
| Telephone | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.23 (0.69) | 0.00 (0.00–0.00) | 3 | 42 (87.50) |
| Elsewhere | 48 | 2.40 (5.88) | 0.00 (0.00–1.50) | 30 | 34 (70.83) | 48 | 0.23 (0.63) | 0.00 (0.00–0.00) | 3 | 41 (85.42) |
| Key workerb | 47 | 3.98 (13.21) | 0.00 (0.00–0.00) | 82 | 37 (78.72) | 46 | 0.78 (2.72) | 0.00 (0.00–0.00) | 16 | 40 (86.96) |
| LA housing officer | 48 | 2.52 (5.94) | 0.00 (0.00–2.50) | 33 | 28 (58.33) | 48 | 0.40 (1.07) | 0.00 (0.00–0.00) | 6 | 39 (81.25) |
| LA welfare benefits officer | 48 | 0.63 (2.36) | 0.00 (0.00–0.00) | 16 | 37 (77.08) | 48 | 1.10 (3.26) | 0.00 (0.00–1.00) | 19 | 35 (72.92) |
| Well-being group | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Volunteer supporter (e.g. peer advocacy) | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 46 (95.83) |
| Out-of-hours service | ||||||||||
| A&E attendance | 48 | 5.38 (12.65) | 1.00 (0.00–5.00) | 81 | 16 (33.33) | 48 | 3.56 (8.19) | 1.00 (0.00–3.00) | 48 | 20 (41.67) |
| Walk-in/urgent care clinic | 48 | 0.10 (0.59) | 0.00 (0.00–0.00) | 4 | 46 (95.83) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| NHS 111 telephone | 48 | 0.31 (1.07) | 0.00 (0.00–0.00) | 7 | 40 (83.33) | 48 | 1.46 (4.39) | 0.00 (0.00–1.00) | 29 | 30 (62.50) |
| Ambulance: no conveyance (as no hospital use) | 48 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 46 (95.83) | 48 | 0.21 (0.65) | 0.00 (0.00–0.00) | 4 | 41 (85.42) |
| Ambulance: conveyance (as also hospital use) | 48 | 0.19 (0.57) | 0.00 (0.00–0.00) | 3 | 42 (87.50) | 48 | 2.48 (5.20) | 0.00 (0.00–2.00) | 24 | 26 (54.17) |
| Number of hospital admissions (not detoxification) | 48 | 0.90 (1.37) | 0.00 (0.00–1.50) | 5 | 29 (60.42) | 48 | 0.85 (1.96) | 0.00 (0.00–1.00) | 10 | 34 (70.83) |
| Number of nights in hospital (not detoxification) | ||||||||||
| ICU | 48 | 0.19 (0.91) | 0.00 (0.00–0.00) | 5 | 46 (95.83) | 48 | 0.04 (0.29) | 0.00 (0.00–0.00) | 2 | 47 (97.92) |
| HDU | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| General ward | 48 | 9.58 (24.24) | 0.00 (0.00–3.00) | 127 | 31 (64.58) | 48 | 4.85 (12.21) | 0.00 (0.00–1.00) | 51 | 34 (70.83) |
| Psychiatric ward | 48 | 0.56 (2.82) | 0.00 (0.00–0.00) | 17 | 46 (95.83) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Number of nights in hospital for detoxification | 48 | 1.65 (9.33) | 0.00 (0.00–0.00) | 63 | 46 (95.83) | 48 | 0.04 (0.29) | 0.00 (0.00–0.00) | 2 | 47 (97.92) |
| Number of day cases | 48 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 46 (95.83) | 48 | 0.06 (0.24) | 0.00 (0.00–0.00) | 1 | 45 (93.75) |
| Hospital outpatient appointments | 48 | 0.81 (1.58) | 0.00 (0.00–1.00) | 6 | 33 (68.75) | 48 | 1.06 (1.73) | 0.00 (0.00–1.00) | 8 | 26 (54.17) |
| Blood test | 48 | 0.71 (0.85) | 0.00 (0.00–1.00) | 3 | 25 (52.08) | 48 | 1.58 (1.62) | 1.00 (0.00–2.00) | 6 | 14 (29.17) |
| Cervical smear/vaginal swab | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.13 (0.39) | 0.00 (0.00–0.00) | 2 | 43 (89.58) |
| Colonoscopy | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| CT | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Electrocardiography | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Endoscopy | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| MRI | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Ultrasonography | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.06 (0.24) | 0.00 (0.00–0.00) | 1 | 45 (93.75) |
| Urine sample | 48 | 0.08 (0.28) | 0.00 (0.00–0.00) | 1 | 44 (91.67) | 48 | 0.08 (0.35) | 0.00 (0.00–0.00) | 2 | 45 (93.75) |
| Wound swab | 48 | 0.17 (0.48) | 0.00 (0.00–0.00) | 2 | 42 (87.50) | 48 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 46 (95.83) |
| X-ray | 48 | 0.08 (0.28) | 0.00 (0.00–0.00) | 1 | 44 (91.67) | 48 | 0.23 (0.56) | 0.00 (0.00–0.00) | 3 | 39 (81.25) |
| Stool sample | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) |
| Sputum | 48 | 0.06 (0.24) | 0.00 (0.00–0.00) | 1 | 45 (93.75) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Colposcopy | 48 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 47 (97.92) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Echocardiography | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Personal carer (social services) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Optician | 48 | 0.56 (1.13) | 0.00 (0.00–0.50) | 4 | 36 (75.00) | 48 | 0.48 (0.90) | 0.00 (0.00–0.50) | 3 | 36 (75.00) |
| Dentist (at CSS or elsewhere) | 48 | 0.63 (1.23) | 0.00 (0.00–1.00) | 6 | 33 (68.75) | 48 | 1.15 (1.54) | 0.00 (0.00–2.00) | 5 | 25 (52.08) |
| Dentist out-of-hours visit | 48 | 0.17 (0.48) | 0.00 (0.00–0.00) | 2 | 42 (87.50) | 48 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 48 (100.00) |
| Service | MT1 | MT2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | |||||
| GP | ||||||||||
| At CSS base | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Telephone with patient | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 7.53 (5.93) | 6.00 (3.00–12.00) | 24 | 2 (4.26) | 49 | 6.86 (6.06) | 6.00 (2.00–9.00) | 23 | 6 (12.24) |
| Nurse | ||||||||||
| At CSS base | 47 | 10.64 (11.29) | 7.00 (4.00–15.00) | 56 | 0 (0.00) | 49 | 13.92 (10.07) | 12.00 (6.00–19.00) | 44 | 0 (0.00) |
| Telephone with patient | 47 | 0.11 (0.48) | 0.00 (0.00–0.00) | 3 | 44 (93.62) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 4.79 (8.97) | 1.00 (0.00–4.00) | 41 | 16 (34.04) | 49 | 2.59 (3.84) | 1.00 (0.00–3.00) | 19 | 13 (26.53) |
| HCA | ||||||||||
| At CSS base | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 48 (97.96) |
| Telephone | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 0.62 (0.95) | 0.00 (0.00–1.00) | 4 | 29 (61.70) | 49 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 47 (95.92) |
| Mental health nurse | ||||||||||
| At CSS base | 47 | 0.57 (1.26) | 0.00 (0.00–0.00) | 5 | 36 (73.47) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Telephone | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 0.19 (0.50) | 0.00 (0.00–0.00) | 2 | 40 (85.11) | 49 | 0.16 (0.62) | 0.00 (0.00–0.00) | 4 | 44 (89.80) |
| Specialist nurse at CSS | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Consultant at CSS | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Pharmacist (at CSS for UC; elsewhere for DC, MT, SP) | 47 | 0.09 (0.35) | 0.00 (0.00–0.00) | 2 | 44 (93.62) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Telephone with pharmacist at CSS base | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Physiotherapist/occupational therapist elsewhere | 47 | 0.21 (0.98) | 0.00 (0.00–0.00) | 6 | 44 (93.62) | 49 | 0.35 (1.38) | 0.00 (0.00–0.00) | 9 | 43 (87.76) |
| Podiatrist/chiropodist | 47 | 0.34 (1.76) | 0.00 (0.00–0.00) | 12 | 42 (89.36) | 49 | 1.14 (2.81) | 0.00 (0.00–1.00) | 15 | 32 (65.31) |
| Dietitian | 47 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 45 (95.74) | 49 | 0.04 (0.29) | 0.00 (0.00–0.00) | 2 | 48 (97.96) |
| Psychologist/counsellor/psychiatrist | ||||||||||
| At CSS base | 47 | 0.64 (2.11) | 0.00 (0.00–0.00) | 12 | 38 (80.85) | 49 | 2.90 (7.46) | 0.00 (0.00–1.00) | 30 | 33 (67.35) |
| Telephone | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 0.17 (0.73) | 0.00 (0.00–0.00) | 4 | 44 (93.62) | 49 | 0.63 (1.73) | 0.00 (0.00–0.00) | 9 | 40 (81.63) |
| Complementary therapy | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.06 (0.43) | 0.00 (0.00–0.00) | 3 | 48 (97.96) |
| Smoking cessation clinic | 47 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 46 (97.87) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Alcohol/drugs/substance misuse | ||||||||||
| At CSS base | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Telephone | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 6.04 (9.86) | 1.00 (0.00–9.00) | 48 | 23 (48.94) | 49 | 1.59 (4.70) | 0.00 (0.00–0.00) | 27 | 38 (77.55) |
| Visits to local pharmacist for methadone | 47 | 91.60 (138.52) | 0.00 (0.00–172.00) | 366 | 30 (63.83) | 49 | 15.94 (60.37) | 0.00 (0.00–0.00) | 323 | 45 (91.84) |
| Case manager, etc.a | ||||||||||
| At CSS | 47 | 0.04 (0.29) | 0.00 (0.00–0.00) | 2 | 46 (97.87) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Telephone | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Elsewhere | 47 | 0.09 (0.35) | 0.00 (0.00–0.00) | 2 | 44 (93.62) | 49 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 48 (97.96) |
| Key workerb | 47 | 11.72 (17.55) | 2.00 (0.00–21.00) | 66 | 23 (48.94) | 42 | 15.83 (16.39) | 11.00 (0.00–32.00) | 48 | 14 (33.33) |
| LA housing officer | 47 | 1.28 (2.27) | 0.00 (0.00–2.00) | 10 | 26 (55.32) | 49 | 0.73 (2.84) | 0.00 (0.00–0.00) | 19 | 39 (79.59) |
| LA welfare benefits officer | 47 | 0.85 (3.11) | 0.00 (0.00–0.00) | 18 | 42 (89.36) | 49 | 1.27 (2.25) | 0.00 (0.00–1.00) | 9 | 30 (61.22) |
| Well-being group | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Volunteer supporter (e.g. peer advocacy) | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.27 (1.48) | 0.00 (0.00–0.00) | 10 | 47 (95.92) |
| Out-of-hours service | ||||||||||
| A&E attendance | 47 | 3.38 (4.66) | 2.00 (0.00–6.00) | 24 | 16 (34.04) | 49 | 1.94 (4.39) | 0.00 (0.00–2.00) | 20 | 30 (61.22) |
| Walk-in/urgent care clinic | 47 | 1.06 (1.51) | 0.00 (0.00–2.00) | 7 | 24 (51.06) | 49 | 0.37 (1.39) | 0.00 (0.00–0.00) | 9 | 43 (87.76) |
| NHS 111 telephone | 47 | 1.09 (2.80) | 0.00 (0.00–1.00) | 15 | 34 (72.34) | 49 | 0.22 (0.80) | 0.00 (0.00–0.00) | 5 | 43 (87.76) |
| Ambulance: no conveyance (as no hospital use) | 47 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 45 (95.74) | 49 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 47 (95.92) |
| Ambulance: conveyance (as also hospital use) | 47 | 0.47 (0.95) | 0.00 (0.00–1.00) | 4 | 35 (74.47) | 49 | 0.53 (1.73) | 0.00 (0.00–0.00) | 11 | 38 (77.55) |
| Number of hospital admissions (not detoxification) | 47 | 1.04 (1.86) | 0.00 (0.00–1.00) | 11 | 24 (51.06) | 49 | 0.39 (0.81) | 0.00 (0.00–0.00) | 3 | 38 (77.55) |
| Number of nights in hospital (not detoxification) | ||||||||||
| ICU | 47 | 0.74 (3.69) | 0.00 (0.00–0.00) | 22 | 45 (95.74) | 49 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 48 (97.96) |
| HDU | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| General ward | 47 | 5.77 (15.22) | 0.00 (0.00–4.00) | 91 | 27 (57.45) | 49 | 1.73 (5.20) | 0.00 (0.00–0.00) | 29 | 39 (79.59) |
| Psychiatric ward | 47 | 0.64 (3.49) | 0.00 (0.00–0.00) | 23 | 45 (95.74) | 49 | 1.59 (8.11) | 0.00 (0.00–0.00) | 50 | 47 (95.92) |
| Number of nights in hospital for detoxification | 47 | 0.64 (2.20) | 0.00 (0.00–0.00) | 10 | 43 (91.49) | 49 | 0.20 (1.43) | 0.00 (0.00–0.00) | 10 | 48 (97.96) |
| Number of day cases | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.06 (0.24) | 0.00 (0.00–0.00) | 1 | 46 (93.88) |
| Hospital outpatient appointments | 47 | 1.11 (1.72) | 1.00 (0.00–1.00) | 8 | 22 (46.81) | 49 | 0.94 (1.46) | 0.00 (0.00–2.00) | 7 | 28 (57.14) |
| Blood test | 47 | 0.17 (0.43) | 0.00 (0.00–0.00) | 2 | 40 (85.11) | 49 | 0.20 (0.54) | 0.00 (0.00–0.00) | 2 | 42 (85.71) |
| Cervical smear/vaginal swab | 47 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 46 (97.87) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Colonoscopy | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| CT | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Electrocardiography | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Endoscopy | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| MRI | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Ultrasonography | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Urine sample | 47 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 46 (97.87) | 49 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 48 (97.96) |
| Wound swab | 47 | 0.21 (0.62) | 0.00 (0.00–0.00) | 3 | 41 (87.23) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| X-ray | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Stool sample | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Sputum | 47 | 0.06 (0.44) | 0.00 (0.00–0.00) | 3 | 46 (97.87) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Colposcopy | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Echocardiography | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Personal carer (social services) | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.16 (1.14) | 0.00 (0.00–0.00) | 8 | 48 (97.96) |
| Optician | 47 | 0.40 (0.68) | 0.00 (0.00–1.00) | 2 | 33 (70.21) | 49 | 0.67 (1.41) | 0.00 (0.00–1.00) | 8 | 32 (65.31) |
| Dentist (at CSS or elsewhere) | 47 | 0.62 (0.99) | 0.00 (0.00–1.00) | 5 | 29 (61.70) | 49 | 0.84 (1.33) | 0.00 (0.00–1.00) | 5 | 29 (59.18) |
| Dentist out-of-hours visit | 47 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 47 (100.00) | 49 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 49 (100.00) |
| Service | SP1 | SP2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | |||||
| GP | ||||||||||
| At CSS base | 51 | 10.08 (7.21) | 9.00 (4.00–13.00) | 30 | 1 (1.96) | 45 | 6.36 (7.37) | 3.00 (1.00–10.00) | 27 | 7 (15.56) |
| Telephone with patient | 51 | 0.18 (0.48) | 0.00 (0.00–0.00) | 2 | 44 (86.27) | 45 | 0.51 (1.42) | 0.00 (0.00–0.00) | 7 | 36 (80.00) |
| Elsewhere | 51 | 0.16 (0.42) | 0.00 (0.00–0.00) | 2 | 44 (86.27) | 45 | 2.73 (3.19) | 2.00 (0.00–5.00) | 14 | 16 (35.56) |
| Nurse | ||||||||||
| At CSS base | 51 | 2.69 (2.93) | 2.00 (0.00–3.00) | 11 | 13 (25.49) | 45 | 0.49 (1.39) | 0.00 (0.00–0.00) | 7 | 35 (77.78) |
| Telephone with patient | 51 | 0.14 (0.40) | 0.00 (0.00–0.00) | 2 | 45 (88.24) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Elsewhere | 51 | 0.76 (1.63) | 0.00 (0.00–1.00) | 9 | 35 (68.63) | 45 | 0.38 (2.39) | 0.00 (0.00–0.00) | 16 | 43 (95.56) |
| HCA | ||||||||||
| At CSS base | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.29 (1.14) | 0.00 (0.00–0.00) | 7 | 40 (88.89) |
| Telephone | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Elsewhere | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Mental health nurse | ||||||||||
| At CSS base | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Telephone | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Elsewhere | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.18 (0.91) | 0.00 (0.00–0.00) | 6 | 42 (93.33) |
| Specialist nurse at CSS | 51 | 7.10 (16.48) | 0.00 (0.00–3.00) | 78 | 28 (54.90) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Consultant at CSS | 51 | 0.24 (0.79) | 0.00 (0.00–0.00) | 4 | 46 (90.20) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Pharmacist (at CSS for UC; elsewhere for DC, MT, SP) | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Telephone with pharmacist at CSS base | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Physiotherapist/occupational therapist elsewhere | 51 | 0.08 (0.39) | 0.00 (0.00–0.00) | 2 | 49 (96.08) | 45 | 0.49 (1.94) | 0.00 (0.00–0.00) | 11 | 40 (88.89) |
| Podiatrist/chiropodist | 51 | 0.08 (0.44) | 0.00 (0.00–0.00) | 3 | 49 (96.08) | 45 | 0.04 (0.21) | 0.00 (0.00–0.00) | 1 | 43 (95.56) |
| Dietitian | 51 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Psychologist/counsellor/psychiatrist | ||||||||||
| At CSS | 51 | 1.08 (4.89) | 0.00 (0.00–0.00) | 33 | 43 (84.31) | 45 | 3.76 (9.74) | 0.00 (0.00–1.00) | 48 | 31 (68.89) |
| Telephone | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Elsewhere | 51 | 0.57 (1.92) | 0.00 (0.00–0.00) | 10 | 43 (84.31) | 45 | 0.40 (0.96) | 0.00 (0.00–0.00) | 4 | 36 (80.00) |
| Complementary therapy | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Smoking cessation clinic | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.11 (0.75) | 0.00 (0.00–0.00) | 5 | 44 (97.78) |
| Alcohol/drugs/substance misuse | ||||||||||
| At CSS | 51 | 12.75 (12.57) | 12.00 (0.00–23.00) | 41 | 16 (31.37) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Telephone | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Elsewhere | 51 | 0.08 (0.27) | 0.00 (0.00–0.00) | 1 | 47 (92.16) | 45 | 12.36 (15.93) | 8.00 (1.00–15.00) | 67 | 11 (24.44) |
| Visits to local pharmacist for methadone | 51 | 135.35 (132.81) | 104.00 (0.00–260.00) | 365 | 20 (39.22) | 45 | 172.91 (184.98) | 90.00 (0.00–364.00) | 730 | 20 (44.44) |
| Case manager, etc.a | ||||||||||
| At CSS | 51 | 0.41 (0.83) | 0.00 (0.00–0.00) | 3 | 39 (76.47) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Telephone | 51 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Elsewhere | 51 | 0.86 (3.09) | 0.00 (0.00–0.00) | 21 | 40 (78.43) | 45 | 0.20 (1.20) | 0.00 (0.00–0.00) | 8 | 43 (95.56) |
| Key workerb | 51 | 1.63 (6.35) | 0.00 (0.00–0.00) | 40 | 44 (86.27) | 45 | 10.76 (15.66) | 3.00 (0.00–16.00) | 57 | 20 (44.44) |
| LA housing officer | 51 | 0.82 (2.67) | 0.00 (0.00–0.00) | 16 | 43 (84.31) | 45 | 1.96 (3.36) | 1.00 (0.00–3.00) | 19 | 18 (40.00) |
| LA welfare benefits officer | 51 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 50 (98.04) | 45 | 3.02 (6.58) | 0.00 (0.00–2.00) | 24 | 31 (68.89) |
| Well-being group | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Volunteer supporter (e.g. peer advocacy) | 51 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Out-of-hours service | ||||||||||
| A&E attendance | 51 | 1.18 (1.49) | 1.00 (0.00–2.00) | 7 | 24 (47.06) | 45 | 3.42 (4.37) | 2.00 (0.00–5.00) | 22 | 13 (28.89) |
| Walk-in/urgent care clinic | 51 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 49 (96.08) | 45 | 0.38 (0.91) | 0.00 (0.00–0.00) | 4 | 36 (80.00) |
| NHS 111 telephone | 51 | 0.12 (0.48) | 0.00 (0.00–0.00) | 3 | 47 (92.16) | 45 | 0.71 (2.00) | 0.00 (0.00–0.00) | 11 | 35 (77.78) |
| Ambulance: no conveyance (as no hospital use) | 51 | 0.04 (0.20) | 0.00 (0.00–0.00) | 1 | 49 (96.08) | 45 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 44 (97.78) |
| Ambulance: conveyance (as also hospital use) | 51 | 0.47 (0.90) | 0.00 (0.00–1.00) | 4 | 36 (70.59) | 45 | 2.24 (3.12) | 1.00 (0.00–4.00) | 12 | 20 (44.44) |
| Number of hospital admissions (not detoxification) | 51 | 0.33 (0.59) | 0.00 (0.00–1.00) | 2 | 37 (72.55) | 45 | 0.93 (1.34) | 0.00 (0.00–1.00) | 6 | 23 (51.11) |
| Number of nights in hospital (not detoxification) | ||||||||||
| ICU | 51 | 0.14 (0.98) | 0.00 (0.00–0.00) | 7 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| HDU | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.22 (1.49) | 0.00 (0.00–0.00) | 10 | 44 (97.78) |
| General ward | 51 | 5.45 (22.63) | 0.00 (0.00–0.00) | 152 | 39 (76.47) | 45 | 4.67 (11.61) | 0.00 (0.00–2.00) | 64 | 26 (57.78) |
| Psychiatric ward | 51 | 0.65 (3.24) | 0.00 (0.00–0.00) | 17 | 49 (96.08) | 45 | 0.58 (2.62) | 0.00 (0.00–0.00) | 14 | 42 (93.33) |
| Number of nights in hospital for detoxification | 51 | 0.14 (0.98) | 0.00 (0.00–0.00) | 7 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Number of day cases | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.07 (0.45) | 0.00 (0.00–0.00) | 3 | 44 (97.78) |
| Hospital outpatient appointments | 51 | 0.35 (0.77) | 0.00 (0.00–0.00) | 3 | 40 (78.43) | 45 | 0.76 (1.32) | 0.00 (0.00–1.00) | 5 | 30 (66.67) |
| Blood test | 51 | 1.47 (1.74) | 1.00 (0.00–2.00) | 6 | 21 (41.18) | 45 | 0.49 (1.97) | 0.00 (0.00–0.00) | 13 | 37 (82.22) |
| Cervical smear/vaginal swab | 51 | 0.16 (0.46) | 0.00 (0.00–0.00) | 2 | 45 (88.24) | 45 | 0.09 (0.47) | 0.00 (0.00–0.00) | 3 | 43 (95.56) |
| Colonoscopy | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| CT | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Electrocardiography | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Endoscopy | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| MRI | 51 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Ultrasonography | 51 | 0.10 (0.30) | 0.00 (0.00–0.00) | 1 | 46 (90.20) | 45 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 44 (97.78) |
| Urine sample | 51 | 0.14 (0.53) | 0.00 (0.00–0.00) | 3 | 47 (92.16) | 45 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 44 (97.78) |
| Wound swab | 51 | 0.12 (0.48) | 0.00 (0.00–0.00) | 3 | 47 (92.16) | 45 | 0.04 (0.21) | 0.00 (0.00–0.00) | 1 | 43 (95.56) |
| X-ray | 51 | 0.06 (0.24) | 0.00 (0.00–0.00) | 1 | 48 (94.12) | 45 | 0.16 (0.42) | 0.00 (0.00–0.00) | 2 | 39 (86.67) |
| Stool sample | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 44 (97.78) |
| Sputum | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.02 (0.15) | 0.00 (0.00–0.00) | 1 | 44 (97.78) |
| Colposcopy | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Echocardiography | 51 | 0.02 (0.14) | 0.00 (0.00–0.00) | 1 | 50 (98.04) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Personal carer (social services) | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 14.93 (100.18) | 0.00 (0.00–0.00) | 672 | 44 (97.78) |
| Optician | 51 | 0.20 (0.66) | 0.00 (0.00–0.00) | 4 | 45 (88.24) | 45 | 0.33 (0.93) | 0.00 (0.00–0.00) | 4 | 38 (84.44) |
| Dentist (at CSS or elsewhere) | 51 | 0.80 (2.06) | 0.00 (0.00–0.00) | 12 | 39 (76.47) | 45 | 1.02 (1.83) | 0.00 (0.00–2.00) | 7 | 30 (66.67) |
| Dentist out-of-hours visit | 51 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 51 (100.00) | 45 | 0.00 (0.00) | 0.00 (0.00–0.00) | 0 | 45 (100.00) |
| Service | UC1 | UC2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | |||||
| GP at CSS base | 28 | 4.2 (4.0) | 3.0 (2.0–5.5) | 18 | 4 (14.3) | 30 | 5.6 (7.5) | 3.5 (2.0–5.0) | 32 | 2 (6.7) |
| GP telephone with patient | 28 | 0.3 (0.6) | 0.0 (0.0–0.5) | 2 | 21 (75.0) | 30 | 0.7 (1.3) | 0.0 (0.0–1.0) | 6 | 21 (70.0) |
| GP elsewhere | 28 | 0.1 (0.4) | 0.0 (0.0–0.0) | 2 | 26 (92.9) | 30 | 0.1 (0.4) | 0.0 (0.0–0.0) | 2 | 27 (90.0) |
| Nurse at CSS base | 28 | 1.1 (1.5) | 0.5 (0.0–1.5) | 5 | 14 (50.0) | 30 | 1.3 (2.3) | 1.0 (0.0–1.0) | 12 | 9 (30.0) |
| Nurse telephone with patient | 28 | 1.2 (2.8) | 0.0 (0.0–1.5) | 14 | 17 (60.7) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Nurse elsewhere | 28 | 0.3 (0.8) | 0.0 (0.0–0.0) | 3 | 24 (85.7) | 30 | 0.2 (0.5) | 0.0 (0.0–0.0) | 2 | 26 (86.7) |
| HCA at CSS base | 28 | 0.7 (1.1) | 0.0 (0.0–1.0) | 4 | 18 (64.3) | 30 | 1.4 (1.3) | 1.0 (0.0–2.0) | 6 | 8 (26.7) |
| HCA telephone with patient | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| HCA elsewhere | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 29 (96.7) |
| Mental health nurse at CSS base | 28 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 27 (96.4) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Mental health nurse telephone with patient | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Mental health nurse elsewhere | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 1.8 (6.9) | 0.0 (0.0–0.0) | 32 | 26 (86.7) |
| Specialist nurse at CSS | 28 | 0.2 (0.8) | 0.0 (0.0–0.0) | 4 | 26 (92.9) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Consultant at CSS | 28 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 27 (96.4) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Pharmacist (at CSS for UC; elsewhere for DC, MT, SP) | 28 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 27 (96.4) | 30 | 0.2 (0.5) | 0.0 (0.0–0.0) | 2 | 26 (86.7) |
| Telephone with pharmacist at CSS base | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.1 (0.3) | 0.0 (0.0–0.0) | 1 | 27 (90.0) |
| Physiotherapist/occupational therapist at CSS/elsewhere | 28 | 0.6 (1.5) | 0.0 (0.0–0.0) | 6 | 23 (82.1) | 30 | 0.1 (0.5) | 0.0 (0.0–0.0) | 2 | 28 (93.3) |
| Podiatrist/chiropodist | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.4 (0.9) | 0.0 (0.0–0.0) | 4 | 23 (76.7) |
| Dietitian | 28 | 0.1 (0.4) | 0.0 (0.0–0.0) | 2 | 27 (96.4) | 30 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 29 (96.7) |
| Psychologist/counsellor/psychiatrist at CSS | 28 | 2.8 (9.4) | 0.0 (0.0–0.0) | 48 | 23 (82.1) | 30 | 6.6 (13.3) | 0.0 (0.0–3.0) | 48 | 20 (66.7) |
| Psychologist/counsellor/psychiatrist telephone | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Psychologist/counsellor/psychiatrist elsewhere | 28 | 0.3 (0.6) | 0.0 (0.0–0.0) | 2 | 23 (82.1) | 30 | 1.9 (3.0) | 1.0 (0.0–3.0) | 15 | 12 (40.0) |
| Complementary therapy | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Smoking cessation clinic | 17 | 0.1 (0.3) | 0.0 (0.0–0.0) | 1 | 15 (88.2) | 29 | 0.3 (1.2) | 0.0 (0.0–0.0) | 6 | 26 (89.7) |
| Alcohol/drugs/substance misuse at CSS | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.4 (2.4) | 0.0 (0.0–0.0) | 13 | 29 (96.7) |
| Alcohol/drugs/substance misuse telephone | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Alcohol/drugs/substance misuse elsewhere | 28 | 7.6 (12.0) | 1.5 (0.0–12.0) | 50 | 13 (46.4) | 30 | 7.7 (11.7) | 3.0 (0.0–10.0) | 48 | 13 (43.3) |
| Visits to local pharmacist for methadone | 28 | 107.4 (139.9) | 0.0 (0.0–241.0) | 365 | 15 (53.6) | 30 | 24.6 (80.3) | 0.0 (0.0–0.0) | 365 | 27 (90.0) |
| Case manager, etc.a at CSS | 28 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 27 (96.4) | 30 | 0.3 (1.5) | 0.0 (0.0–0.0) | 8 | 28 (93.3) |
| Case manager, etc.a telephone | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Case manager, etc.a elsewhere | 28 | 0.2 (0.8) | 0.0 (0.0–0.0) | 4 | 26 (92.9) | 30 | 3.9 (5.1) | 0.5 (0.0–8.0) | 19 | 15 (50.0) |
| Key workerb | 28 | 8.5 (13.5) | 0.0 (0.0–14.0) | 48 | 17 (60.7) | 29 | 0.3 (1.5) | 0.0 (0.0–0.0) | 8 | 28 (96.6) |
| LA housing officer | 28 | 1.5 (3.6) | 0.0 (0.0–1.0) | 18 | 18 (64.3) | 30 | 0.3 (1.6) | 0.0 (0.0–0.0) | 9 | 29 (96.7) |
| LA welfare benefits officer | 28 | 2.1 (5.0) | 0.0 (0.0–1.5) | 24 | 16 (57.1) | 30 | 1.3 (4.2) | 0.0 (0.0–0.0) | 20 | 25 (83.3) |
| Well-being group | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Volunteer supporter (e.g. peer advocacy) | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.1 (0.5) | 0.0 (0.0–0.0) | 2 | 28 (93.3) |
| Out-of-hours service A&E attendance | 28 | 1.5 (1.6) | 1.0 (0.0–2.0) | 7 | 9 (32.1) | 30 | 1.6 (3.4) | 0.0 (0.0–2.0) | 17 | 18 (60.0) |
| Out-of-hours service walk-in/urgent care clinic | 28 | 0.9 (1.4) | 0.0 (0.0–1.0) | 5 | 17 (60.7) | 30 | 0.6 (1.2) | 0.0 (0.0–1.0) | 4 | 21 (70.0) |
| Out-of-hours service NHS 111 telephone | 28 | 0.4 (0.8) | 0.0 (0.0–0.0) | 3 | 22 (78.6) | 30 | 0.5 (1.1) | 0.0 (0.0–0.0) | 5 | 23 (76.7) |
| Out-of-hours service Ambulance: no conveyance (as no hospital use) | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.1 (0.3) | 0.0 (0.0–0.0) | 1 | 28 (93.3) |
| Out-of-hours service Ambulance: conveyance (as also hospital use) | 28 | 0.7 (0.9) | 0.0 (0.0–1.0) | 3 | 15 (53.6) | 30 | 0.9 (2.3) | 0.0 (0.0–0.0) | 11 | 23 (76.7) |
| Number of hospital admissions (not detoxification) | 28 | 0.3 (0.5) | 0.0 (0.0–0.5) | 2 | 21 (75.0) | 30 | 0.3 (0.7) | 0.0 (0.0–0.0) | 3 | 25 (83.3) |
| Number of nights in hospital (not detoxification) ICU | 28 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 27 (96.4) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Number of nights in hospital (not detoxification) HDU | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Number of nights in hospital (not detoxification) general ward | 28 | 1.1 (4.0) | 0.0 (0.0–0.5) | 21 | 21 (75.0) | 30 | 1.8 (6.2) | 0.0 (0.0–0.0) | 31 | 26 (86.7) |
| Number of nights in hospital (not detoxification) psychiatric ward | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.5 (2.7) | 0.0 (0.0–0.0) | 15 | 28 (93.3) |
| Number of nights in hospital for detoxification | 28 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 28 (100.0) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Number of day cases | 28 | 0.2 (0.5) | 0.0 (0.0–0.0) | 2 | 24 (85.7) | 30 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 30 (100.0) |
| Hospital outpatient appointments | 28 | 0.7 (1.0) | 0.0 (0.0–1.0) | 4 | 16 (57.1) | 30 | 0.9 (1.8) | 0.0 (0.0–1.0) | 8 | 20 (66.7) |
| Blood test | 17 | 0.6 (0.8) | 0.0 (0.0–1.0) | 2 | 9 (52.9) | 29 | 1.3 (1.2) | 1.0 (0.0–2.0) | 5 | 8 (27.6) |
| Cervical smear/vaginal swab | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Colonoscopy | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| CT | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Electrocardiography | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Endoscopy | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| MRI | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Ultrasonography | 17 | 0.1 (0.2) | 0.0 (0.0–0.0) | 1 | 16 (94.1) | 29 | 0.1 (0.3) | 0.0 (0.0–0.0) | 1 | 27 (93.1) |
| Urine sample | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.3 (1.0) | 0.0 (0.0–0.0) | 5 | 25 (86.2) |
| Wound swab | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.1 (0.4) | 0.0 (0.0–0.0) | 2 | 28 (96.6) |
| X-ray | 17 | 0.2 (0.4) | 0.0 (0.0–0.0) | 1 | 14 (82.4) | 29 | 0.1 (0.4) | 0.0 (0.0–0.0) | 2 | 26 (89.7) |
| Stool sample | 17 | 0.1 (0.2) | 0.0 (0.0–0.0) | 1 | 16 (94.1) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Sputum | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.2) | 0.0 (0.0–0.0) | 1 | 28 (96.6) |
| Colposcopy | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Echocardiography | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Personal carer (social services) | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Optician | 28 | 0.4 (0.8) | 0.0 (0.0–0.5) | 3 | 21 (75.0) | 30 | 0.7 (1.2) | 0.0 (0.0–1.0) | 6 | 17 (56.7) |
| Dentist at CSS or elsewhere | 28 | 0.5 (1.0) | 0.0 (0.0–0.5) | 4 | 21 (75.0) | 29 | 1.9 (2.3) | 1.0 (0.0–3.0) | 8 | 11 (37.9) |
| Dentist out-of-hours visit | 17 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 17 (100.0) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Dentist out-of-hours telephone | 17 | 0.2 (0.4) | 0.0 (0.0–0.0) | 1 | 14 (82.4) | 29 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 29 (100.0) |
| Service | UC3 | UC4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | |||||
| GP at CSS base | 15 | 5.3 (3.9) | 4.0 (3.0–7.0) | 14 | 1 (6.7) | 2 | 2.5 (0.7) | 2.5 (2.0–3.0) | 3 | 0 (0.0) |
| GP telephone with patient | 15 | 1.6 (1.7) | 1.0 (0.0–2.0) | 6 | 5 (33.3) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| GP elsewhere | 15 | 0.2 (0.6) | 0.0 (0.0–0.0) | 2 | 13 (86.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Nurse at CSS base | 15 | 1.5 (2.7) | 0.0 (0.0–1.0) | 8 | 8 (53.3) | 2 | 40.0 (56.6) | 40.0 (0.0–80.0) | 80 | 1 (50.0) |
| Nurse telephone with patient | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Nurse elsewhere | 15 | 0.2 (0.6) | 0.0 (0.0–0.0) | 2 | 13 (86.7) | 2 | 8.0 (11.3) | 8.0 (0.0–16.0) | 16 | 1 (50.0) |
| HCA at CSS base | 15 | 1.8 (1.5) | 1.0 (1.0–3.0) | 5 | 2 (13.3) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| HCA telephone with patient | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| HCA elsewhere | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Mental health nurse at CSS base | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Mental health nurse telephone with patient | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Mental health nurse elsewhere | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Specialist nurse at CSS | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Consultant at CSS | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Pharmacist (at CSS for UC; elsewhere for DC, MT, SP) | 15 | 0.3 (0.6) | 0.0 (0.0–1.0) | 2 | 11 (73.3) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Telephone with pharmacist at CSS base | 15 | 0.3 (0.8) | 0.0 (0.0–0.0) | 3 | 13 (86.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Physiotherapist/occupational therapist at CSS/elsewhere | 15 | 1.4 (5.2) | 0.0 (0.0–0.0) | 20 | 13 (86.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Podiatrist/chiropodist | 15 | 0.1 (0.5) | 0.0 (0.0–0.0) | 2 | 14 (93.3) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Dietitian | 15 | 0.1 (0.4) | 0.0 (0.0–0.0) | 1 | 13 (86.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Psychologist/counsellor/psychiatrist at CSS | 15 | 9.7 (9.6) | 9.0 (2.0–14.0) | 37 | 3 (20.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Psychologist/counsellor/psychiatrist telephone | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Psychologist/counsellor/psychiatrist elsewhere | 15 | 1.7 (2.7) | 1.0 (0.0–2.0) | 8 | 7 (46.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Complementary therapy | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Smoking cessation clinic | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Alcohol/drugs/substance misuse at CSS | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Alcohol/drugs/substance misuse telephone | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Alcohol/drugs/substance misuse elsewhere | 15 | 11.5 (17.4) | 0.0 (0.0–30.0) | 48 | 9 (60.0) | 2 | 27.0 (9.9) | 27.0 (20.0–34.0) | 34 | 0 (0.0) |
| Visits to local pharmacist for methadone | 15 | 64.1 (134.9) | 0.0 (0.0–0.0) | 365 | 12 (80.0) | 2 | 243.0 (36.8) | 243.0 (217.0–269.0) | 269 | 0 (0.0) |
| Case manager, etc.a at CSS | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Case manager, etc.a telephone | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Case manager, etc.a elsewhere | 15 | 0.5 (1.1) | 0.0 (0.0–1.0) | 4 | 10 (66.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Key workerb | 15 | 0.7 (2.2) | 0.0 (0.0–0.0) | 8 | 13 (86.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| LA housing officer | 15 | 0.3 (1.0) | 0.0 (0.0–0.0) | 4 | 14 (93.3) | 2 | 1.5 (2.1) | 1.5 (0.0–3.0) | 3 | 1 (50.0) |
| LA welfare benefits officer | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Well-being group | 15 | 0.8 (3.1) | 0.0 (0.0–0.0) | 12 | 14 (93.3) | 0 | 0 (0.0) | |||
| Volunteer supporter (e.g. peer advocacy) | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Out-of-hours service A&E attendance | 15 | 1.0 (1.6) | 0.0 (0.0–2.0) | 5 | 9 (60.0) | 2 | 1.0 (1.4) | 1.0 (0.0–2.0) | 2 | 1 (50.0) |
| Out-of-hours service Walk-in/urgent care clinic | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.5 (0.7) | 0.5 (0.0–1.0) | 1 | 1 (50.0) |
| Out-of-hours service NHS 111 telephone | 15 | 0.8 (0.9) | 1.0 (0.0–1.0) | 3 | 7 (46.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Out-of-hours service Ambulance: no conveyance (as no hospital use) | 15 | 0.3 (0.6) | 0.0 (0.0–0.0) | 2 | 12 (80.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Out-of-hours service Ambulance: conveyance (as also hospital use) | 15 | 0.5 (0.9) | 0.0 (0.0–1.0) | 3 | 10 (66.7) | 2 | 1.0 (1.4) | 1.0 (0.0–2.0) | 2 | 1 (50.0) |
| Number of hospital admissions (not detoxification) | 15 | 0.4 (0.7) | 0.0 (0.0–1.0) | 2 | 11 (73.3) | 2 | 1.0 (1.4) | 1.0 (0.0–2.0) | 2 | 1 (50.0) |
| Number of nights in hospital (not detoxification) ICU | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Number of nights in hospital (not detoxification) HDU | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Number of nights in hospital (not detoxification) general ward | 15 | 0.5 (1.6) | 0.0 (0.0–0.0) | 6 | 13 (86.7) | 2 | 12.5 (17.7) | 12.5 (0.0–25.0) | 25 | 1 (50.0) |
| Number of nights in hospital (not detoxification) psychiatric ward | 15 | 2.7 (8.2) | 0.0 (0.0–0.0) | 31 | 13 (86.7) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Number of nights in hospital for detoxification | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Number of day cases | 15 | 0.1 (0.5) | 0.0 (0.0–0.0) | 2 | 14 (93.3) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Hospital outpatient appointments | 15 | 0.7 (1.2) | 0.0 (0.0–1.0) | 4 | 9 (60.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Blood test | 15 | 1.0 (1.2) | 1.0 (0.0–1.0) | 4 | 6 (40.0) | 0 | ||||
| Cervical smear/vaginal swab | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Colonoscopy | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| CT | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Electrocardiography | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Endoscopy | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| MRI | 15 | 0.1 (0.5) | 0.0 (0.0–0.0) | 2 | 14 (93.3) | 0 | ||||
| Ultrasonography | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Urine sample | 15 | 0.1 (0.4) | 0.0 (0.0–0.0) | 1 | 13 (86.7) | 0 | ||||
| Wound swab | 15 | 0.1 (0.3) | 0.0 (0.0–0.0) | 1 | 14 (93.3) | 0 | ||||
| X-ray | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Stool sample | 15 | 0.1 (0.3) | 0.0 (0.0–0.0) | 1 | 14 (93.3) | 0 | ||||
| Sputum | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Colposcopy | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Echocardiography | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Personal carer (social services) | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Optician | 15 | 1.3 (1.5) | 1.0 (0.0–2.0) | 4 | 6 (40.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Dentist at CSS or elsewhere | 15 | 1.9 (2.1) | 1.0 (0.0–4.0) | 6 | 6 (40.0) | 2 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 2 (100.0) |
| Dentist out-of-hours visit | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
| Dentist out-of-hours telephone | 15 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 15 (100.0) | 0 | ||||
Appendix 9 Groupings of service use items
| Individual items of service use | Groupings | Individual items of service use | Groupings |
|---|---|---|---|
| GP at CSS base | All GP | A&E attendance | All out-of-hours services |
| GP telephone with patient | Walk-in/urgent care clinic | ||
| GP elsewhere | NHS 111 telephone | ||
| Nurse at CSS base | All nurse and HCA | Ambulance: no conveyance (as no hospital use) | |
| Nurse telephone with patient | Ambulance: conveyance (as also hospital use) | ||
| Nurse elsewhere | Number of hospital admissions (not detoxification) | Hospital admissions | |
| HCA at CSS base | Number of hospital admissions (not detoxification) | ||
| HCA telephone | Number of nights in hospital (not detoxification), ICU | Hospital nights, not psychiatric, not detoxification | |
| HCA elsewhere | Number of nights in hospital (not detoxification), HDU | ||
| Mental health nurse at a base | All other community health | Number of nights in hospital (not detoxification), general ward | |
| Mental health nurse telephone | Number nights in hospital (not detoxification), psychiatric ward | ||
| Mental health nurse elsewhere | Number of nights for detoxification | ||
| Specialist nurse at CSS | Number of day cases | ||
| Consultant at CSS | Hospital outpatient appointments | ||
| Pharmacist (at CSS for UC; elsewhere for DC, MT, SP) | Blood test | All tests | |
| Telephone with pharmacist at CSS base | Cervical smear/vaginal swab | ||
| Physiotherapist/occupational therapist elsewhere | All allied health professionals | Colonoscopy | |
| Podiatrist/chiropodist | CT | ||
| Dietitian | Electrocardiography | ||
| Psychologist/counsellor/psychiatrist at CSS | Endoscopy | ||
| Psychologist/counsellor/psychiatrist telephone | MRI | ||
| Psychologist/counsellor/psychiatrist elsewhere | Ultrasonography | ||
| Complementary therapy | Urine sample | ||
| Smoking cessation clinic | Substance misuse and smoking services | Wound swab | |
| Alcohol/drugs/substance misuse at CSS | X-ray | ||
| Alcohol/drugs/substance misuse telephone | Stool sample | ||
| Alcohol/drugs/substance misuse elsewhere | Sputum | ||
| Visits to local pharmacist for methadone | Colposcopy | ||
| Echocardiography | |||
| Case manager, etc. at CSS | Case manager/care co-ordinator/social worker/social practitioner/key worker at day centre or non-accommodation-based service | Personal carer (social services) | |
| Case manager, etc. telephone | Optician | ||
| Case manager, etc. elsewhere | Dentist at CSS or elsewhere | All dentist | |
| Key worker | |||
| LA housing officer | Other social | Dentist out-of-hours visit | |
| LA welfare benefits officer | Dentist out-of-hours telephone | ||
| Well-being group | |||
| Volunteer supporter (e.g. peer advocacy) |
Appendix 10 Number of contacts with services over 12 months by Health Service Model
| Dedicated Centres | Mobile Teams | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Service | Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | ||||
| Primary, community, substance misuse | ||||||||||
| All GP at base, elsewhere, telephone | 96 | 18.6 (16.8) | 14.0 (7.0–21.5) | 95 | 0 (0) | 96 | 7.2 (6.0) | 6.0 (2.0–11.0) | 24 | 8 (8.3) |
| All nurse/HCA at base, elsewhere, telephone | 96 | 9.1 (21.8) | 3.0 (1.0–8.5) | 166 | 11 (11.5) | 96 | 16.4 (14.6) | 13.0 (7.0–21.0) | 84 | 0 (0) |
| All other community | 96 | 0.3 (1.0) | 0.0 (0.0–0.0) | 7 | 80 (83.3) | 96 | 0.5 (1.1) | 0.0 (0.0–0.0) | 5 | 74 (77.1) |
| All allied health professionals | 96 | 4.9 (9.7) | 0.0 (0.0–5.5) | 51 | 49 (51.0) | 96 | 3.3 (6.5) | 1.0 (0.0–3.0) | 32 | 44 (45.8) |
| All smoking, alcohol, drug, methadonea | 96 | 123.4 (156.0) | 10.5 (0.0–300.5) | 403 | 37 (38.5) | 96 | 56.8 (116.0) | 0.0 (0.0–19.0) | 390 | 57 (59.4) |
| Total primary, community, substance misuse | 96 | 156.3 (157.9) | 77.0 (20.5–314.0) | 453 | 0 (0) | 96 | 84.2 (122.3) | 29.0 (14.0–70.5) | 501 | 0 (0) |
| Social (care co-ordination, other) | ||||||||||
| Care manager/co-ordinator, key workerb | 93 | 4.4 (10.8) | 0.0 (0.0–3.0) | 82 | 53 (57.0) | 89 | 13.7 (17.0) | 5.0 (0.0–24.0) | 66 | 36 (40.4) |
| Other social, LA housing, welfare, voluntaryb | 96 | 2.5 (5.2) | 1.0 (0.0–2.0) | 35 | 44 (45.8) | 96 | 2.3 (4.5) | 0.0 (0.0–2.0) | 29 | 51 (53.1) |
| Total social (care coordination, other)b | 93 | 6.9 (11.9) | 3.0 (1.0–9.0) | 83 | 22 (23.7) | 89 | 16.0 (18.6) | 8.0 (1.0–29.0) | 95 | 20 (22.5) |
| OOH services | ||||||||||
| A&E | 96 | 4.5 (10.6) | 1.0 (0.0–3.0) | 81 | 36 (37.5) | 96 | 2.6 (4.6) | 1.0 (0.0–3.0) | 24 | 46 (47.9) |
| Walk-in/urgent care clinic | 96 | 0.1 (0.4) | 0.0 (0.0–0.0) | 4 | 94 (97.9) | 96 | 0.7 (1.5) | 0.0 (0.0–1.0) | 9 | 67 (69.8) |
| NHS 111 | 96 | 0.9 (3.2) | 0.0 (0.0–1.0) | 29 | 70 (72.9) | 96 | 0.6 (2.1) | 0.0 (0.0–0.0) | 15 | 77 (80.2) |
| Ambulance | 96 | 1.5 (4.0) | 0.0 (0.0–1.0) | 25 | 65 (67.7) | 96 | 0.5 (1.4) | 0.0 (0.0–1.0) | 11 | 69 (71.9) |
| Total OOH, including ambulance | 96 | 6.9 (15.3) | 2.0 (0.0–6.5) | 92 | 31 (32.3) | 96 | 4.5 (7.2) | 2.0 (0.0–5.0) | 40 | 36 (37.5) |
| Hospital nights, not detoxification | ||||||||||
| Not psychiatric | 96 | 7.3 (19.4) | 0.0 (0.0–1.5) | 127 | 65 (67.7) | 96 | 4.1 (12.1) | 0.0 (0.0–2.0) | 91 | 66 (68.8) |
| Psychiatric | 96 | 0.3 (2.0) | 0.0 (0.0–0.0) | 17 | 94 (97.9) | 96 | 1.1 (6.3) | 0.0 (0.0–0.0) | 50 | 92 (95.8) |
| Total hospital nights, not detoxification | 96 | 7.6 (19.4) | 0.0 (0.0–2.0) | 127 | 63 (65.6) | 96 | 5.2 (13.3) | 0.0 (0.0–3.0) | 91 | 62 (64.6) |
| Hospital nights detoxification | 96 | 0.8 (6.6) | 0.0 (0.0–0.0) | 63 | 93 (96.9) | 96 | 0.4 (1.8) | 0.0 (0.0–0.0) | 10 | 91 (94.8) |
| Hospital day cases | 96 | 0.1 (0.2) | 0.0 (0.0–0.0) | 1 | 91 (94.8) | 96 | 0.03 (0.2) | 0.0 (0.0–0.0) | 1 | 93 (96.9) |
| Hospital outpatients | 96 | 0.9 (1.7) | 0.0 (0.0–1.0) | 8 | 59 (61.5) | 96 | 1.0 (1.6) | 0.0 (0.0–1.0) | 8 | 50 (52.1) |
| All tests | 96 | 1.7 (1.8) | 1.0 (0.0–2.0) | 7 | 29 (30.2) | 96 | 0.4 (0.7) | 0.0 (0.0–0.0) | 3 | 73 (76.0) |
| Personal carer contacts | 96 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 96 (100) | 96 | 0.1 (0.8) | 0.0 (0.0–0.0) | 8 | 95 (99.0) |
| Optician visits | 96 | 0.5 (1.0) | 0.0 (0.0–0.5) | 4 | 72 (75.0) | 96 | 0.5 (1.1) | 0.0 (0.0–1.0) | 8 | 65 (67.7) |
| All dentist contacts | 96 | 1.0 (1.4) | 0.0 (0.0–2.0) | 6 | 55 (57.3) | 96 | 0.7 (1.2) | 0.0 (0.0–1.0) | 5 | 58 (60.4) |
| Specialist GPs | Usual care GPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||||
| Service | Mean (SD) | Median (IQR) | Maximum | Mean (SD) | Median (IQR) | Maximum | ||||
| Primary, community, substance misuse | ||||||||||
| All GP at base, elsewhere, telephone | 96 | 10.0 (7.5) | 7.5 (4.0–14.0) | 32 | 2 (2.1) | 75 | 5.8 (6.2) | 4.0 (2.0–7.0) | 33 | 6 (8.0) |
| All nurse/HCA at base, elsewhere, telephone | 96 | 2.4 (3.6) | 1.0 (0.0–4.0) | 16 | 44 (45.8) | 75 | 4.4 (9.6) | 2.0 (1.0–4.0) | 80 | 9 (12.0) |
| All other community | 96 | 4.0 (12.7) | 0.0 (0.0–1.0) | 82 | 70 (72.9) | 75 | 1.1 (4.4) | 0.0 (0.0–1.0) | 32 | 54 (72.0) |
| All allied health professionals | 96 | 3.2 (8.0) | 0.0 (0.0–2.0) | 48 | 55 (57.3) | 61 | 8.4 (12.5) | 3.0 (0.0–12.0) | 59 | 17 (27.9) |
| All smoking, alcohol, drug, methadonea | 96 | 165.6 (166.4) | 108.5 (0.0–311.5) | 765 | 26 (27.1) | 61 | 56.5 (120.7) | 1.0 (0.0–25.0) | 401 | 28 (45.9) |
| Total primary, community, substance misuse | 96 | 185.2 (169.5) | 122.0 (18.5–343.5) | 770 | 0 (0) | 61 | 76.0 (122.7) | 22.0 (11.0–58.0) | 444 | 0 (0) |
| Social (care co-ordination, other) | ||||||||||
| Care manager/co-ordinator, key workerb | 93 | 6.6 (12.7) | 0.0 (0.0–5.0) | 57 | 50 (52.1) | 74 | 5.1 (9.5) | 0.0 (0.0–8.0) | 48 | 44 (59.5) |
| Other social, LA housing, welfare, voluntaryb | 96 | 2.9 (5.8) | 0.0 (0.0–3.0) | 25 | 49 (51.0) | 61 | 2.8 (6.1) | 0.0 (0.0–3.0) | 30 | 37 (60.7) |
| Total social (care coordination, other)b | 93 | 9.5 (14.0) | 3.0 (0.0–12.5) | 58 | 28 (29.2) | 60 | 8.5 (11.9) | 4.0 (0.0–10.5) | 50 | 23 (38.3) |
| OOH services | ||||||||||
| A&E | 96 | 2.2 (3.4) | 1.0 (0.0–3.0) | 22 | 37 (38.5) | 75 | 1.4 (2.4) | 1.0 (0.0–2.0) | 17 | 37 (49.3) |
| Walk-in/urgent care clinic | 96 | 0.2 (0.7) | 0.0 (0.0–0.0) | 4 | 85 (88.5) | 75 | 0.6 (1.2) | 0.0 (0.0–1.0) | 5 | 54 (72.0) |
| NHS 111 | 96 | 0.4 (1.4) | 0.0 (0.0–0.0) | 11 | 82 (85.4) | 75 | 0.5 (0.9) | 0.0 (0.0–1.0) | 5 | 54 (72.0) |
| Ambulance | 96 | 1.3 (2.4) | 0.0 (0.0–2.0) | 12 | 55 (57.3) | 75 | 0.8 (1.7) | 0.0 (0.0–1.0) | 12 | 48 (64.0) |
| Total OOH, including ambulance | 96 | 4.2 (6.5) | 2.0 (0.0–5.0) | 31 | 33 (34.4) | 75 | 3.3 (5.2) | 2.0 (0.0–5.0) | 37 | 27 (36.0) |
| Hospital nights, not detoxification | ||||||||||
| Not psychiatric | 96 | 5.3 (18.8) | 0.0 (0.0–2.0) | 159 | 64 (66.7) | 75 | 1.6 (5.4) | 0.0 (0.0–0.0) | 31 | 61 (81.3) |
| Psychiatric | 96 | 0.6 (3.0) | 0.0 (0.0–0.0) | 17 | 91 (94.8) | 75 | 0.8 (4.1) | 0.0 (0.0–0.0) | 31 | 71 (94.7) |
| Total hospital nights, not detoxification | 96 | 5.9 (18.9) | 0.0 (0.0–2.0) | 159 | 60 (62.5) | 75 | 2.3 (6.7) | 0.0 (0.0–0.0) | 31 | 58 (77.3) |
| Hospital nights detoxification | 96 | 0.1 (0.7) | 0.0 (0.0–0.0) | 7 | 95 (99.0) | 75 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 75 (100) |
| Hospital day cases | 96 | 0.0 (0.3) | 0.0 (0.0–0.0) | 3 | 95 (99.0) | 75 | 0.1 (0.4) | 0.0 (0.0–0.0) | 2 | 70 (93.3) |
| Hospital outpatients | 96 | 0.5 (1.1) | 0.0 (0.0–1.0) | 5 | 70 (72.9) | 75 | 0.7 (1.4) | 0.0 (0.0–1.0) | 8 | 47 (62.7) |
| All tests | 96 | 1.5 (2.2) | 1.0 (0.0–2.0) | 13 | 45 (46.9) | 61 | 1.5 (1.8) | 1.0 (0.0–2.0) | 10 | 20 (32.8) |
| Personal carer contacts | 96 | 7.0 (68.6) | 0.0 (0.0–0.0) | 672 | 95 (99.0) | 61 | 0.0 (0.0) | 0.0 (0.0–0.0) | 0 | 61 (100) |
| Optician visits | 96 | 0.3 (0.8) | 0.0 (0.0–0.0) | 4 | 83 (86.5) | 75 | 0.7 (1.2) | 0.0 (0.0–1.0) | 6 | 46 (61.3) |
| All dentist contacts | 96 | 0.9 (1.9) | 0.0 (0.0–1.0) | 12 | 69 (71.9) | 60 | 1.5 (2.0) | 1.0 (0.0–2.0) | 8 | 29 (48.3) |
| Service | Total | ||||
|---|---|---|---|---|---|
| Participants (N) | Number of contacts | Participants with zero contacts, n (%) | |||
| Mean (SD) | Median (IQR) | Maximum | |||
| Primary, community, substance misuse | |||||
| All GP at base, elsewhere, telephone | 363 | 10.7 (11.4) | 7.0 (4.0–14.0) | 95 | 16 (4.4) |
| All nurse/HCA at base, elsewhere, telephone | 363 | 8.3 (15.2) | 3.0 (1.0–9.0) | 166 | 64 (17.6) |
| All other community | 363 | 1.5 (7.0) | 0.0 (0.0–0.0) | 82 | 278 (76.6) |
| All allied health professionals | 349 | 4.6 (9.2) | 1.0 (0.0–4.0) | 59 | 165 (47.3) |
| All smoking, alcohol, drug, methadonea | 349 | 105.0 (150.2) | 3.0 (0.0–231.0) | 765 | 148 (42.4) |
| Total primary, community, substance misuse | 349 | 130.4 (153.1) | 43.0 (15.0–252.0) | 770 | 0 (0) |
| Social (care co-ordination, other) | |||||
| Care manager/co-ordinator, key workerb | 352 | 7.5 (13.4) | 0.0 (0.0–8.0) | 82 | 183 (52.0) |
| Other social, LA housing, welfare, voluntaryb | 349 | 2.6 (5.3) | 0.0 (0.0–2.0) | 35 | 181 (51.9) |
| Total social (care coordination, Other)b | 338 | 10.3 (14.9) | 3.0 (0.0–14.0) | 95 | 93 (27.5) |
| OOH services | |||||
| A&E | 363 | 2.8 (6.4) | 1.0 (0.0–3.0) | 81 | 156 (43.0) |
| Walk-in/urgent care clinic | 363 | 0.4 (1.0) | 0.0 (0.0–0.0) | 9 | 300 (82.6) |
| NHS 111 | 363 | 0.6 (2.2) | 0.0 (0.0–0.0) | 29 | 283 (78.0) |
| Ambulance | 363 | 1.1 (2.7) | 0.0 (0.0–1.0) | 25 | 237 (65.3) |
| Total OOH, including ambulance | 363 | 4.8 (9.6) | 2.0 (0.0–5.0) | 92 | 127 (35.0) |
| Hospital nights, not detoxification | |||||
| Not psychiatric | 363 | 4.7 (15.5) | 0.0 (0.0–1.0) | 159 | 256 (70.5) |
| Psychiatric | 363 | 0.7 (4.1) | 0.0 (0.0–0.0) | 50 | 348 (95.9) |
| Total hospital nights, not detoxification | 363 | 5.4 (15.9) | 0.0 (0.0–2.0) | 159 | 243 (66.9) |
| Hospital nights detoxification | 363 | 0.3 (3.5) | 0.0 (0.0–0.0) | 63 | 354 (97.5) |
| Hospital day cases | 363 | 0.1 (0.3) | 0.0 (0.0–0.0) | 3 | 349 (96.1) |
| Hospital outpatients | 363 | 0.8 (1.5) | 0.0 (0.0–1.0) | 8 | 226 (62.3) |
| All tests | 349 | 1.2 (1.8) | 1.0 (0.0–2.0) | 13 | 167 (47.9) |
| Personal carer contacts | 349 | 1.9 (36.0) | 0.0 (0.0–0.0) | 672 | 347 (99.4) |
| Optician visits | 363 | 0.5 (1.0) | 0.0 (0.0–1.0) | 8 | 266 (73.3) |
| All dentist contacts | 348 | 1.0 (1.7) | 0.0 (0.0–2.0) | 12 | 211 (60.6) |
Appendix 11 Summaries of study findings
| Item | Main findings | Notes | |||
|---|---|---|---|---|---|
| Dedicated Centres | Mobile Teams | Specialist GPs | Usual Care GPs | ||
| Main features | Cities with large homeless population. Specifically for homeless/marginalised groups. Fewer registered patients than most mainstream general practices. Drop-in clinics at practice. On-site mental health, substance misuse services. Some outreach. | Areas of significant homeless populations. Small caseloads. Mainly nurses in team; no GP. Patients encouraged to register with local GPs; some shared records. Work mainly in health promotion, assessments, signposting and care of long-term conditions. Clinics only in hostels and day centres. Street outreach. | Areas of large homeless populations. Mainstream general practices with targeted staff and/or clinics for homeless patients. 7–16% of practice patients experiencing homelessness. On-site mental health services at both sites, and substance misuse services at SP1. Clinics in hostels, day centres. Street outreach (SP1). | Mainstream general practices; less than 5% of patient population experiencing homelessness. No targeted clinics/staff for homeless patients. Mental health services on site (except for UC2), and substance misuse services at UC1 and UC3. Limited links to Homelessness sector services. No outreach. | All sites except UC1 reported extra NHS funding for work with patients who are homeless. UC1 received funding for work with patients who have substance misuse problems. |
| Recruitment | Two sites, n = 96 (48 + 48) | Two sites, n = 96 (47 + 49) | Two sites, n = 96 (51 + 45) | Four sites, n = 61 (28 + 30 + 15 + 2) | |
| Participant characteristics | No difference between models: age, time homeless, physical health problems (98.4% overall), length of time registered with CSS. More males in Usual Care GPs (90.7% vs. 80.2% overall). MT: 44.8% non-British born vs. 20.2% overall; larger percentage had no recourse to public funds (statistically significant). Mental health problems: 91.1% overall; lower for Mobile Teams (84%), statistically significant compared with the other three models (chi-squared test: p = 0.005). Larger percentage of Usual Care GP participants reported bipolar disorder or schizophrenia/hearing voices (statistically significant). Drug misuse: 60.1% misused drugs; lower for Mobile Teams (45.8%), statistically significant compared with the other three models (chi-squared test: p = 0.001). Higher rates of heroin/cocaine use, injecting drugs and treatment with OST for Dedicated Centre and Specialist GP participants (statistically significant). |
Big differences between Mobile Teams (MT1 participants more likely to be British born/citizen, and have alcohol and drug problems). UC1 participants more likely than those of UC2 and UC3 to use heroin/cocaine. |
|||
| Participant accommodation | Baseline: statistically significant larger percentages of Mobile Team and Dedicated Centre participants sleeping rough, and Specialist GP and Usual Care GP participants in hostels with staff. During study: compared with the other three models, Dedicated Centre participants had largest number of changes of accommodation, least time in staffed accommodation and almost twice as much time in prison: 12.42 (SD 38.92) vs. 6.50 (SD 26.86). Usual Care GP participants had the fewest moves and spent most time in staffed accommodation: significant differences. |
MT2 participants more likely than those of MT1 to be sleeping rough. | |||
| Primary Screening plus intervention for six HSIs (BMI, smoking, hepatitis A, mental health, alcohol use, TB) |
Primary Outcome Score 0–6 (6 is best). Overall mean 3.30 (SD 1.24); overall median 3 (range 0–6). Individual comparisons of Primary Outcome Score via unpaired t-test: DC vs. MT – p < 0.0005 (DC > MT); DC vs. SP – p = 0.229; DC vs. UC – p = 0.847; MT vs. SP – p = 0.020 (SP > MT); MT vs. UC – p = 0.005 (UC > MT); SP vs. UC – p = 0.399. Regression analysis: Better scores associated with reporting depression at baseline, reporting drug use at baseline, percentage of study period in staffed accommodation, more consultations with GP/nurse/HCA at CSS, more years homeless. Worse scores associated with the Mobile Team model; being a British born/citizen; and having seen an external key worker (not worker at accommodation or CSS). |
Big difference between Specialist GP sites (SP1 high, SP2 low) and Usual Care GP sites (UC1 low, UC2 and UC3 high). Primary Outcome Score: UC2/UC3 (n = 44) mean 3.54 (SD 0.94)] vs. UC1 (n = 17) mean 2.65 (SD 1.06); unpaired t-test: p < 0.0005). |
|||
| Management of SHC | |||||
| Hypertension | Not analysed: too few cases | Total outcome score 0–5 (5 is the best): sum of five different measures each scored 0 or 1. Some differences between sites for some indicators (Table 66). | |||
| Chronic respiratory problems | No significant difference between models in total outcome score | ||||
| Depression | No significant difference between models in total outcome score | ||||
| Alcohol problems | No significant difference between models in total outcome score Continuity of care provided for 61.6% at CSSs with on-site alcohol services, compared with 44.9% without on-site alcohol services (chi-squared test: p = 0.036). |
||||
| Drug problems | Usual Care GP model significantly lower than other three models in total outcome score Continuity of care for 70.6% at CSSs with on-site drug services vs. 32.0% without on-site drug services (chi-squared test: p = 0.000). |
||||
| For a breakdown of components, see Table 66. Dedicated Centre model better, Mobile Team model worse, on continuity of care for all conditions except drug problems. Usual Care GP model worse on continuity of care for drug problems. Mobile Team model better than the other three models on explanation for depression. | |||||
| Self-rated health status and well-being | |||||
| SF-8: PCS SF-8 MCS SWEMWBS |
No difference in mean scores between models at baseline, 8 months or in change between 0 and 8 months on any measure. Regression SF-8 PCS: statistically significant improvement in Dedicated Centres and Specialist GPs. Older age, depression at baseline, heavy drinking at 8 months and number of consultations at CSS with GP/nurse/HCA had negative effect. Regression SF-8 MCS: no statistically significant improvement by model. Drug use at 8 months and greater percentage of time in staffed accommodation had negative effect. Regression SWMWEBS: statistically significant improvement in SP. Depression at baseline and injection of drugs at 8 months had negative effect; involvement in education/training or employment had positive effect. |
Completion of instruments by participants at baseline and 8 months. All scores low compared with those of the general population, and influenced by age, health problems, drinking and drug behaviours. |
|||
| Advice-giving | |||||
| Smoking | Smoking: baseline 88.1% smoke (from 80.2% in Mobile Teams to 96.9% in Specialist GPs). No significant difference between models in advice-giving (34.8% overall). | ||||
| Nutrition | Nutrition: overall, 53.6% reported problems getting meals/eating healthily at baseline – Usual Care GPs, n = 49 (66.2%); vs. other models, n = 144 (50.3%); chi-squared test: p = 0.015). 28.5% reported receiving advice at baseline, significantly lower in Usual Care GP (13.3%) and Mobile Team (24.0%) models. Advice given: Dedicated Centres and Specialist GPs, n = 70 (36.6%); Mobile Teams, n = 23 (24.0%); chi-squared test: p = 0.03). | Baseline poor nutrition, overall 48.5% report having a meal 6 or 7 days per week, 20.5% once a week or less – no difference between models. | |||
| Satisfaction with CSS and care: items from GP Patient Survey | |||||
| Overall experience of CSS Confidence/trust in GP/nurse Quality of Care ratings |
Dedicated Centre, Mobile Team, Specialist GP: participants’ ratings are higher than those of the general population for all items. Usual Care GP: participants ratings are lower than those of the general population. Findings statistically significant in regression models of ratings of (1) overall experience of CSS; and (2) Quality of Care. Compared with Usual Care GPs, highly statistically significant beneficial effects for Mobile Teams and Specialist GPs for overall experience of CSS, and for Dedicated Centres, Mobiles Team and Specialist GPs for Quality of Care. |
Usual Care GP scores driven partly by poor scores in UC1. Scores in UC2 were higher, suggesting satisfaction is affected by the practice, not the model. | |||
| Integration with other services | |||||
| Integration ratings, scores 0–5 | Dedicated Centre, Mobile Team, Specialist GP: well integrated with mental health, substance misuse, hospital services, hostels and day centres, and do outreach. Extent and depth of integration depends on resources. Usual Care GP: low levels of integration with homelessness sector services and outreach teams. No outreach in hospitals, hostels or day centres, or on the streets. |
From interviews with CSS staff, external health care staff, homelessness sector agencies, local authorities, stakeholders. | |||
| Dental | |||||
| Oral health/access to dental care | All models: poor oral health, dental pain and other dental needs common; dental anxiety and dental phobia more common than in the general population. No change during study. Dental registration and attendance rates low throughout study, slight increase in registration during study, no differences by models. No association between dental services at CSS or nearby homelessness service and dental outcomes. |
||||
| Use of services over 12 months, especially OOH services | |||||
| Contacts | Most frequently used service was substance misuse services, driven by 40% of participants attending pharmacy for OST daily; this varied between sites. Second most frequently used service was contact with GP; 97% of participants in Dedicated Centres, Specialist GPs and Usual Care GPs, and 91.7% in nurse-led Mobile Teams, saw a GP during the study period. Across all models, 33% had a hospital admission, 65% attended OOH service, 48 participants reported ≥ 10 OOH contacts. Overall, use of OOH services positively correlated with use of primary care services, that is some people are frequent users of both and OOH services are not necessarily a substitute for routine care (but varied between sites). | OOH: A&E, walk-in/urgent care clinic, NHS 111, ambulance. | |||
| Costs of service use | Costs of GP, nurse, HCA: Dedicated Centre model significantly higher than other three models; Usual Care GP model significantly lower than Mobile Team and Specialist GP models. Costs of social care/service contacts, care co-ordinator, housing, etc.: Mobile Team model significantly higher than the other three models. Regression OOH: model not significant; higher OOH cost predicted by more frequent changes of accommodation in study period. Regression Grand Total Costs: higher in Dedicated Centre model, spending more time in staffed accommodation, having more changes of accommodation during study period. Lower total cost predicted by being black/Black British, recent education/training/employment. |
Social care excludes daily personal carer of two participants. | |||
| Outcomes | Chronic respiratory problems | Depression | Alcohol problems | Drugs |
|---|---|---|---|---|
| 1. Treatment plan initiated | Not tested | 0.45 | 0.61 | 0.004, MT low |
| 2. Continuity of care by CSS | 0.08 DC high, MT low | 0.007 DC high, MT low | 0.001 DC high, MT low | < 0.0005 DC high, MT and UC low |
| 3. Explanation of SHC | 0.11 | 0.04 MT high | 0.59 | 0.56 |
| 4. Satisfaction with treatment plan | 0.09 (all > 80%) | 0.37 | 0.45 | 0.06 (all ≥ 79%) |
| 5. Stable/positive change, baseline to 8 months | 0.71 | 0.41 | 0.62 | 0.12 |
| Total outcome score | 0.54 | 0.34 | 0.76 | 0.001 UC lower than other three models |
Appendix 12 Summaries of context, mechanisms and outcomes for each Health Service Model
| Contextual factors | Mechanisms (service delivery factors) | Case study participants: characteristics and outcomes |
|---|---|---|
| Attributes of CSSs: Long-standing philosophy to deliver health care to single people who are homeless. Operating for many years, with service evolving over time in response to needs. Most staff have considerable experience of this work. Funded by the NHS to provide service exclusively to single people who are homeless; DC1 also serves asylum seekers and refugees. Registration not offered to homeless families or general population. Stand-alone medical centre. Fully equipped to deliver primary health care. CSS staff and sessional workers – nurse practitioners, GPs, mental health and substance misuse workers, social practitioners/health support workers, receptionists/administrators and other specialist workers. Local homelessness context: Located in cities with large populations of single people who are homeless, including many sleeping rough. According to DC2 staff, increase in people sleeping rough in recent years, with opportunities for begging attracting people from elsewhere. Increase in use of drug ‘spice’a among local people who are homeless. A few hostels/temporary accommodation projects/day centres for single people who are homeless in locality of CSSs. Citywide networks of statutory and voluntary sector agencies involved in the provision of temporary accommodation, day centre services and street outreach to people who are homeless. No other specialist primary health care service in locality for single people who are homeless. Policy/funding/resource influences: Cuts to housing, health and social support budgets, lack of affordable housing, and changes to welfare benefits and sanctions have contributed to people becoming and remaining homeless. According to CSS staff, funding cuts to their service/short-term funding/insufficient resources impact on their service, for example inability to open at weekends, limited amount of outreach work, reduction in collaborative work with other agencies and in health promotion activities. Restructuring of homelessness services and closure of several local hostels have resulted in people who are homeless being dispersed throughout city in small temporary housing schemes. Harder for CSS staff to engage with such patients and liaise with their key workers. Strategic work with local NHS trusts, CCGs, Health and Wellbeing Boards. Contribute to plans/provide information/advise/attend meetings. |
Operational mechanisms: Number of registered patients relatively small, compared with many mainstream general practices. CSS staff knowledgeable about the problems and needs of people who are homeless and of local services. Regular staff training around patient care. Open Monday to Friday. Flexible approach offering daily drop-in clinics and booked appointments, including afternoon appointments. Receptionists ‘fit people in’ if no GP slots available or if late for appointment. Patients were sent text messages/telephoned to remind them of appointments. Some street outreach by staff at both CSSs to engage with people sleeping rough and encourage them to access health care. Both CSS staff and participants describe CSS as a welcoming and accessible environment – participants describe staff as non-judgemental, friendly and helpful, and they greet patients by name. Patients able to use CSS as postal address for their mail. All aspects of primary health care undertaken by GPs and nurses – health assessments, treatment for acute illnesses, management of long-term illnesses, health promotion, immunisations and screening. Comprehensive health assessments for new patients, including social/housing histories. Person-centred approach to care – most case study participants described staff as caring, listening, giving patients enough time, and involving patients in decisions about their care and treatment. GP appointments longer than in mainstream general practices (20 minutes instead of customary 10 minutes). Holistic approach to care – help given for non-medical needs. Social practitioners/support workers part of team to assist with housing, welfare, social problems. Protocols in place and acted on to address challenging behaviour of patients in the CSS or on nearby streets. Patient participation groups. Annual patient satisfaction surveys (DC2). Patients encouraged/assisted to register with mainstream general practices once settled in housing and no longer homeless. Integration mechanisms: Co-ordinated care – mental health and substance misuse services available at CSS most days. Shared care arrangements for patients receiving OST. Daily staff meetings attended by CSS staff and sessional workers to discuss patient care. Communication by both CSSs with hospitals around inpatient care and discharge. Regular visits to hospital wards by DC1 staff. Dental treatment clinics specifically for people who are homeless or vulnerable available at CSS/in locality. Integration with street outreach teams. Outreach workers accompany some patients to CSS. Close working with some hostels and day centres. CSS staff deliver influenza vaccination programmes and health promotion at these sites. Regular clinics/sessions by DC1 at some day centres. Attendance by CSS staff at multidisciplinary case management meetings with local agencies, including those concerning safeguarding, high-risk or complex cases, and people sleeping rough. Communication and fairly close working with external agencies, including housing services, voluntary sector organisations, and the probation service. |
Participants’ characteristics: Participants had more complex needs than other models. Relatively large percentage sleeping rough, less likely to be in staffed accommodation, and had the most accommodation changes during study, with more time in prison. Mental health and substance misuse problems common, including misuse of Class A drugs. Relatively large percentage inject drugs. Health screening (primary outcome): Very high scores for screening of mental health, alcohol use and smoking. Low score for TB screening. Highest mean Primary Outcome Score of all models. Management of SHCs: Nearly all cases of alcohol and drug problems mentioned by case study participants were documented in medical records. Several cases of chronic respiratory problems and depression mentioned by case study participants were not documented in medical records. Treatment plan initiated for most SHCs identified in medical records. High levels of continuity of care achieved for all SHCs (highest of all models). Self-rated health status and well-being: Low levels of physical and psychological functioning at baseline (all models). Slight improvement in scores by 8 months. Regression analyses revealed statistically significant improvement in physical functioning scores at 8 months. Smoking and nutrition: Very high percentage were smokers, and many described poor nutrition. Slight improvements by 8 months in eating habits. More likely than other models to have received help from CSS staff with nutrition. Oral health and dental treatment: Poor oral health, dental pain and dental phobia common (all models). Many in need of dental treatment; rates of registration with dentist and dental attendance low. Slight increase in dental registration rates by 8 months, and substantial increase in percentage who had seen a dentist in previous 4 months. One-third of participants believed that dental health had worsened during study. Use of services and costs: Compared with other models, more contacts with GPs, more contacts with primary health care nurses (apart from Mobile Team model), more use of A&E and other out-of-hours services, and more nights spent in hospital. Hence, incurred higher overall service use costs. Satisfaction with CSS: Participants described finding it easy to see a doctor or a nurse. High satisfaction ratings for (1) overall experience of CSS and (2) Quality of Care provided. Most reported confidence/trust in doctor or nurse. Higher satisfaction ratings than those of the general population and Usual Care GP participants. |
| Contextual factors | Mechanisms (service delivery factors) | Case study participants: characteristics and outcomes |
|---|---|---|
| Attributes of CSSs: General practices that provide health care to the general population, including people who are homeless. CSSs receive additional NHS funding for their work with patients who are homeless. Both CSSs have a long-standing philosophy to deliver health care to single people who are homeless. This aspect of their work has evolved over many years, with some staff having considerable experience of this work. Stand-alone medical centres. Fully equipped to deliver primary health care. SP1 – designated nurses and support staff exclusively for patients who are homeless, receptionists/administrators, and sessional workers (mental health, substance misuse and social workers). GPs provide care both to patients who are homeless and to the general population. SP2 – nurses and GPs provide care both to patients who are homeless and to the general population; receptionists/administrators; and sessional workers (therapists/counsellors). Local homelessness context: Located in cities with large populations of single people who are homeless. Many participants in SP1 were sleeping rough. According to staff at both CSSs, there has been an increase in the number of people homeless in recent years. Opportunities for begging and availability of drugs has attracted people from elsewhere. According to staff, there has been an increase in complexity of health and substance misuse problems among people who are homeless and in their use of drug ‘spice’.a The latter has had significant effects on users’ mental health and led to poor engagement with services. Several hostels/temporary accommodation projects/day centres for single people who are homeless in locality of CSSs. Some are also accommodated in local bed-and-breakfast hotels. Local networks of statutory and voluntary sector agencies involved in the provision of temporary accommodation, day centre services and street outreach to people who are homeless. Many charitable services support people sleeping rough in the area of SP1. According to SP1 staff, this has attracted people to the area and encouraged street homelessness. Other specialist primary health care services in other parts of city for single people who are homeless. Policy/funding/resource influences: Cuts to housing, health and social support budgets, lack of affordable housing, and changes to welfare benefits and sanctions have contributed to people becoming and remaining homeless. Restructuring/closure of local hostels have resulted in some people who are homeless being dispersed outside city centre and away from support networks. Harder for CSS staff to engage with such patients. SP1 (information from staff): Multiagency work has been impeded by short-term funding and separate commissioning arrangements for different services. More resources needed to enable CSS staff to serve local people who are homeless but not accessing the CSS. Contractual arrangements for the provision of GP services prevent CSS staff from treating people in hostels, day centres and on the streets who are not registered at the practice. Great difficulties accessing mental health services. Mental health practitioner at CSS weekly, but works only with patients with severe mental health problems. Great deal of strategic work with NHS England, local health care commissioners and local authority. Contribute to plans/provide information/advise/attend meetings. Tackling homelessness seen as a priority by commissioners and the local authority. SP2 (information from staff): Insufficient resources has meant lack of capacity to undertake work with other agencies, run additional clinics in hostels and day centres, conduct street outreach, attend multiagency meetings. Difficulties recruiting GP because of funding arrangements also affects performance. Poor integration and access to mental health services, particularly secondary care for patients who misuse substances. Developmental work at the CSS impeded/delayed by insufficient resources/support from CCG. Lack of co-ordination and joint working between local authority and health services. For example, health services not always invited to local authority strategic/multidisciplinary meetings concerning people sleeping rough or temporary housing for people who are homeless. Some strategic work with CCG and local authority: provide information/advise/attend meetings. Building links with public health. |
Operational mechanisms: Number of registered patients relatively large – SP1 more than 10,000; SP2 more than 5000. Some CSS staff knowledgeable about the problems and needs of people who are homeless and of local services. Regular staff meetings/training around patient care. Open Monday to Friday. Flexible approach offering drop-in sessions and booked appointments. Some drop-in clinics each week at SP1 specifically for patients who are homeless. Daily drop-in clinics at SP2 for all patients (restricted number of slots each day). Frequent street outreach by SP1 staff to engage with people sleeping rough and encourage them to access health care. No street outreach by SP2 staff. SP1 participants and staff describe CSS as a welcoming and accessible environment: staff greet patients by name, and are friendly and helpful. All aspects of primary health care undertaken by GPs and nurses – health assessments, treatment for acute illnesses, management of long-term illnesses, health promotion, immunisations and screening. Comprehensive health assessments for new patients at SP1, including social/housing histories. Person-centred approach to care – most case study participants described staff as caring, listening, giving patients enough time, and involving patients in decisions about their care and treatment. Holistic approach to care – at SP1, assessments of, and help given for, non-medical needs. Support/social workers part of team that assists with housing, welfare, social problems. According to SP2 staff, information about non-health needs is not routinely collected. Welfare advice worker runs sessions at CSS (but not part of team). Protocols in place and acted on to address challenging behaviour of patients in the CSS. Conducted audits of problems and needs of patients who are homeless (both CSSs). Patients encouraged/assisted to register with mainstream general practices once settled in housing and no longer homeless if they move out of local area. Integration mechanisms: At SP1, substance misuse services available at CSS, with shared care arrangements for patients receiving OST; mental health worker at site weekly. Patient care meetings attended by CSS staff and specialist workers. At SP2, patients referred/signposted to mental health and substance misuse services. Fairly close working with substance misuse services. SP1 involved in hospital inpatient/discharge work for people who are homeless, with regular hospital visits. SP2 has communication with hospitals regarding particular patients. Dental treatment clinics specifically for people who are homeless available at CSSs/in locality. Close working with street outreach teams by staff at both CSSs. SP1 staff conduct some joint outreach sessions with the street teams. The latter accompany patients to the CSS. Close working with some hostels and day centres. Regular clinics/sessions by SP1 at several sites, and at a few sites by SP2. Attendance by SP1 staff at multidisciplinary case management meetings with local agencies, including those concerning safeguarding, high-risk or complex cases, and people sleeping rough. SP2 staff attend such meetings occasionally. SP2 – regular meetings with local GPs and with those working in deprived area. SP1 – close working with housing, adult social care and probation services regarding particular patients. SP2 – close working with housing services regarding particular patients |
Participants’ characteristics: Most participants White British and in hostels/other temporary accommodation during the study. Mental health and substance misuse problems common, including misuse of Class A drugs and injecting drugs (similar percentages as participants). Health screening (primary outcome): Very high scores for screening of mental health, alcohol use and smoking. Low score for TB screening. Total Primary Outcome Score slightly lower than that of Dedicated Centres and Usual Care GPs. Management of SHCs: Nearly all cases of alcohol and drug problems, and most cases of chronic respiratory problems, mentioned by case study participants were documented in medical records. Several cases of depression mentioned by case study participants were not documented in medical records. Treatment plan initiated for nearly all SHCs identified in medical records. Relatively high levels of continuity of care achieved for all SHCs (slightly lower scores than for Dedicated Centres). Continuity of care for drug problems fairly low for SP2. Self-rated health and status and well-being: Low levels of physical and psychological functioning at baseline (all models). Statistically significant improvement in scores at 8 months for Specialist GPs. Smoking and nutrition: Most participants were smokers, and many described poor nutrition. Slight improvements by 8 months in eating habits. As with Dedicated Centres, just over one-third received help with nutrition from CSS staff. Oral health and dental treatment: Poor oral health, dental pain and dental phobia common (all models). Many in need of dental treatment; rates of registration with dentist and dental attendance low. Slight increase in dental registration rates by 8 months. Lowest rate of dental attendance during the study, compared with other models. Just over one-third believed that dental health worsened during study. Use of services and costs: More contacts with GPs than Mobile Team and Usual Care GP participants, but not as many as Dedicated Centre participants. Not as many contacts with nurses as Mobile Team participants. Overall service use costs similar to those of Mobile Team participants, lower than those of Dedicated Centre participants and considerably higher than those of Usual Care GP participants. Number of contacts with GPs and nurses at CSS higher for SP1 than for SP2. Number of A&E attendances and use of ambulances higher for SP2 than for SP1. Satisfaction with CSS: SP1 participants described finding it easy to see doctor or nurse; several SP2 participants reported difficulties. High satisfaction ratings by SP1 participants for (1) overall experience of CSS and (2) Quality of Care provided. Most reported confidence/trust in doctor or nurse. Ratings slightly lower foraSP2 participants. Overall ratings for this model higher than those of the general population and UC participants. |
| Contextual factors | Mechanisms (service delivery factors) | Case study participants: characteristics and outcomes |
|---|---|---|
| Attributes of CSSs: Long-standing philosophy to deliver health care to single people who are homeless. Operating for many years, with service evolving over time in response to needs. Most staff have considerable experience of this work. Funded by NHS to provide service exclusively to single people who are homeless, asylum seekers and people with no recourse to public funds. MT1 also worked with people who are housed, but vulnerable, and use day centres. Service unavailable for homeless families and general population. No fixed medical site. CSSs ran clinics in hostels and day centres for single people who are homeless – some have fully equipped rooms for healthcare delivery, some lack adequate facilities. CSS staff and sessional workers – nurse practitioners, administrator/co-ordinator, mental health workers/counsellors. No GPs. Local homelessness context: Located in cities with large populations of single people who are homeless, including many sleeping rough. According to CSS staff, increase in numbers sleeping rough, in people from Eastern Europe and in people who have no recourse to public funds. Rough sleepers now more dispersed in MT1 locality. According to staff, increase in complexity of health and substance misuse problems among people who are homeless, and in their use of the drug ‘spice’a Several hostels/temporary accommodation projects/day centres for single people who are homeless in the vicinity of CSSs. Citywide/local networks of statutory and voluntary sector agencies involved in the provision of temporary accommodation, day centre services and street outreach to people who are homeless. Other specialist primary health care services in area for single people who are homeless. Policy/funding/resource influences: Cuts to housing, health and social support budgets, lack of affordable housing, and changes to welfare benefits and sanctions have contributed to people becoming and remaining homeless. According to CSS staff, funding cuts to their service/restrictions have resulted in reduction in posts/redesign of service elements. Conditions/funding requirements placed on homelessness sector services by local authority commissioners have meant that some services accept only people sleeping rough, and opening hours at some day centres reduced. These changes affect the work of CSSs as their clinics were dependent on patients and themselves having entry to these services. Restructuring of homelessness services and closure of some hostels in locality of CSSs have contributed to increase in rough sleeping in the area. Some strategic work with CCGs and local authorities. Provide information/advise/attend meetings. |
Operational mechanisms: Number of patients relatively small, compared with many mainstream general practices. CSS staff knowledgeable about the problems and needs of people who are homeless and of local services. Regular staff meetings/training around patient care. Operate Monday to Friday. Run drop-in clinics at set times at various hostels and/or day centres. CSS staff ‘seek out’ service users with health concerns who do not present for health care at these settings. Frequent street outreach by staff from both CSSs to engage with people sleeping rough and encourage them to access health care. Environment – some hostels and day centres are very busy. CSS staff described by participants as welcoming, non-judgemental, friendly and helpful, and greet patients by name. CSS nurses undertake health assessments, health promotion and screening. Provide treatment/stabilisation for some acute health problems (some nurses are prescribers), but mainly case management for people with long-term conditions. Encourage/assist patients to register with local GPs and attend appointments. Comprehensive health assessments for new patients, including social/housing histories. Information is sometimes gathered over several consultations as patients engage with nurses. Person-centred approach to health care – nearly all participants described nurses as caring, listening, giving patients enough time and involving patients in decisions about their care. Initial help given by nurses for non-medical needs, for example advise, assist with completing forms, signpost to housing and welfare benefit services, and advocate on behalf of patients. Patients discharged from caseload once they have not used the service for some time.Integration mechanisms: Close working with some GPs in locality. Regular joint clinics with GPs in some hostels (MT1), and occasional clinics held by CSS at general practice surgery (MT2). Meetings with GPs to discuss patient care. Have access to GPs’ medical records and vice versa. Fairly close working with local mental health and substance misuse services (MT1 have more contact than MT2 with the latter). Refer/signpost patients to these services. Communication by both CSSs with hospitals around A&E attendance and hospital discharge. Have access to hospital admission databases (MT1). Fairly close working with local dental service for people who are homeless (MT2). Close working with street outreach teams – regular joint street outreach sessions. Close working with several hostels and day centres. Besides running clinics, CSS staff deliver influenza vaccination programmes and health promotion at these sites, intervene if there are health emergencies and provide support/training to staff. Attendance by CSS staff at multidisciplinary case management meetings with local agencies, including those concerning people sleeping rough, high-risk or complex cases and frequent A&E attenders. Communication with external agencies, including housing services and voluntary sector organisations |
Participants’ characteristics: Large percentages were sleeping rough, were born outside the UK and had no recourse to public funds (particularly MT2); mental health and substance misuse problems relatively common, including misuse of Class A drugs (particularly MT1). Health screening (primary outcome): Lowest Primary Outcome Score of all models for health screening of HSIs. Most noticeable differences were in screening of mental health and alcohol use, with Mobile Teams scoring considerably lower. Management of SHCs: Most cases of alcohol and drug problems mentioned by case study participants were documented in medical records. Several cases of chronic respiratory problems and, particularly, depression were mentioned by case study participants but not documented in medical records. Treatment plan initiated for most SHCs identified in medical records. Low rates of continuity of care for all SHCs. When GP services are added, rates are comparable to those of Usual Care GPs for all SHCs except drug problems, where the rate is higher. For most SHCs, rates of continuity of care considerably lower than those of Dedicated Centres and Specialist GPs. High scores for explanation of SHCs, suggesting that the nurses had good rapport with participants. Self-rated health status and well-being: Low levels of physical and psychological functioning at baseline (all models). No improvement in scores after 8 months. Smoking and nutrition: Large percentage were smokers, and many described poor nutrition. Slight improvements by 8 months in smoking and eating habits. Less likely than Dedicated Centre and Specialist GP participants to have received help from CSS staff with nutrition. Oral health and dental treatment: Baseline – poor oral health, dental pain and dental phobia common (all models). Many in need of dental treatment; rates of registration with dentist and dental attendance low. Slight increase in dental registration rates by 8 months, and substantial increase in percentage who had seen a dentist in previous 4 months. Only slight reduction in percentage needing dental treatment. Two-fifths believed dental health worsened during study. Use of services and costs: More contacts with primary health care nurses than other models; fewer GP contacts than Dedicated Centre and Specialist GP participants, but slightly more than Usual Care GP participants. Similar rates to those of Specialist GP participants for use of out-of-hours services and nights spent in hospital. Overall service use costs similar to those of Specialist GP participants, lower than those of Dedicated Centre participants and considerably higher than those of Usual Care GP participants. Satisfaction with CSS: Participants described finding it easy to see a CSS nurse. High satisfaction ratings for overall experience of CSS, and very high satisfaction rates for Quality of Care provided by Mobile Team nurses. Nearly all reported confidence/trust in nurse. a higher satisfaction ratings than the general population with regard to primary care nurses at GP sites. |
| Contextual factors | Mechanisms (service delivery factors) | Case study participants: characteristics and outcomes |
|---|---|---|
| Attributes of CSSs: General practices that provide health care to the general population, including people who are homeless. UC2 and UC3 received additional NHS funding for work with patients who are homeless, and UC1 for work with patients who have substance misuse problems. Stand-alone medical centres. Fully equipped to deliver primary health care. CSS staff – nurse practitioners, HCAs, GPs, receptionists/administrators, pharmacists, therapists/counsellors (UC1 and UC3), substance misuse workers (UC1 and UC3). No staff exclusively for patients who are homeless, although designated HCA at UC3 responsible for their health assessments. Some CSS staff have several years’ experience of providing health care to patients who are homeless. Local homelessness context: Located in cities near to several hostels/temporary accommodation for single people who are homeless. UC2 and UC3 fairly close to specialist primary health care services for this patient group. According to CSS staff, there has been an increase in recent years in number of patients registered who are homeless, but not many are sleeping rough. Mental health and substance misuse problems are common among patients who are homeless. Local networks of statutory and voluntary sector agencies involved in the provision of temporary accommodation, day centre services and street outreach for people who are homeless. Policy/funding/resource influences: Cuts to housing, health and social support budgets, lack of affordable housing, and changes to welfare benefits and sanctions have contributed to people becoming and remaining homeless. Cuts to public health funding resulted in withdrawal of substance misuse services and shared care arrangements for patients receiving OST at UC2. According to CSS staff (all sites), limited resources affect their work with patients who are homeless, for example unable to work proactively with hostels to encourage residents’ engagement with health care. Unable to provide drop-in sessions at CSS for patients who are homeless (UC1 and UC2). Unable to work closely with street outreach teams to encourage people sleeping rough to register at CSS (UC2). High turnover of hostel staff also impedes closer working with service providers (UC2). Strategic work by CSS staff with local CCGs (regarding health care for general population). Provide information/attend meetings. Multiagency forums facilitated by local authority do not routinely include health services (UC1). |
Operational mechanisms: Large number of registered patients at each site: more than 15,000. Less than 5% of patient population is homeless. Open Monday to Friday; also Saturday (UC1 and UC3). Same-day and booked appointments. No ‘drop-in’ clinics at CSS or at hostels or day centres for people who are homeless. No street outreach by CSS staff. Some flexibility towards patients who are homeless, particularly at UC2 and UC3. UC2 does not require an address before people can register, and double appointments are offered to patients with complex needs. At UC3, patients who are homeless can use CSS as postal address for their mail, and are seen opportunistically if they attend the CSS. All aspects of primary health care undertaken by GPs and nurses – health assessments, treatment for acute illnesses, management of long-term illnesses, health promotion, immunisations and screening. UC2 and UC3 – maintain a register of patients who are homeless, and developed templates to assess their health needs, which include social/housing histories. UC3 conducts these assessments annually. Information about housing, social and welfare needs not routinely collected at UC1. Person-centred approach to care – around 70% of Usual Care GP participants described staff as caring, listening, giving patients enough time, and involving patients in decisions about their care and treatment. Protocols/procedures in place to address challenging behaviour of patients at CSSs. Integration mechanisms: Substance misuse services available at UC1 and UC3, with shared care arrangements for patients receiving OST. At UC2, close working with local substance misuse services. Close working with community mental health teams. Therapists/counsellors available at UC1 and UC3. UC2 has occasional meetings with mental health team to review patients. Very little contact with street outreach teams/day centres for people who are homeless. Only UC3 regularly communicated with soup kitchen/drop-in centre. UC2 and UC3 – close working with a few hostels. UC2 visited hostels occasionally to deliver influenza vaccination programmes. UC3 visited hostels annually to check on patients who are homeless. UC1 – little involvement with hostels. |
Participants’ characteristics: Most participants born in UK/British citizen, and accommodated in hostels/other temporary housing throughout study. Mental health and substance misuse problems common. Relatively high percentages of UC2 and UC3 participants reported schizophrenia/hearing voices, whereas UC1 participants were more likely to report misuse of Class A drugs and injecting drugs. Health screening (primary outcome): Scored highest of all models for screening of BMI, alcohol use and smoking. Low scores for TB and hepatitis A screening. Second highest total Primary Outcome Score (slightly lower than that of Dedicated Centres). Management of SHCs: One-third of cases of depression mentioned by case study participants were not documented in medical records. The same applied to one-fifth of chronic respiratory problems and alcohol problems, and nearly one-fifth of drug problems. Usual Care GP model less likely than other models to document cases of alcohol and drug problems. Treatment plan initiated for nearly all SHCs identified in medical records. UC3 less likely than UC1 and UC2 to have started a treatment plan for depression. Relatively low rates of continuity of care for all SHCs, compared with Dedicated Centres and Specialist GPs, especially for alcohol and drug problems. Very low rates for the drug problems. UC1 scored much lower than UC2 and UC3 for continuity of care for alcohol problems. Self-rated health status and well-being: Low levels of physical and psychological functioning at baseline (all models). Slight improvement in physical functioning scores by 8 months. Smoking and nutrition: Very large percentage were smokers, and many reported nutritional problems. More likely than other models to report the latter, yet significantly less likely to have received help from CSS regarding healthy eating. Oral health and dental treatment: Poor oral health, dental pain and dental phobia common (all models). Many in need of dental treatment; rates of registration with dentist and dental attendance low. Slight increase in dental registration rates by 8 months. During study period, just over half had seen a dentist, while one-third believed that their dental health had worsened. Use a services and costs: Compared with Dedicated Centre and Specialist GP participants, a lot fewer contacts with primary health care providers, including GPs and substance misuse services, and slightly fewer than Mobile Team participants. Hence, overall service use costs much lower than other models. Satisfaction with CSS: Participants were much less likely than those of other models to describe finding it easy to see a doctor or nurse, and the findings were statistically significant. Satisfaction ratings for (1) overall experience of CSS and (2) Quality of Care provided were lower than those of the three specialist models, and were slightly lower than the general population’s rating of their general practice surgery. In particular, a much larger percentage of Usual Care GP participants reported no confidence/trust in the doctor or nurse. Higher ratings for overall experience of CSS by UC2 and UC3 participants than UC1 participants, and higher Quality of Care ratings by UC2 participants. |
Glossary
- Analysis of variance (ANOVA)
- Used to compare subgroups of the study population (typically the four Health Service Models) for the mean of a continuous variable; a p-value of < 0.05 indicates that they do not all have the same mean.
- Case Study Site
- One of 10 primary health care services that were included in this evaluation.
- Chi-squared test
- Used to compare subgroups of the study population (typically the four Health Service Models) to establish evidence that they do not have the same prevalence (percentage) of a specific feature, as indicated by a p-value of < 0.05.
- Class A drugs
- Under the Misuse of Drugs Act 1971 [Great Britain. Misuse of Drugs Act 1971. London: The Stationery Office; 1971], Class A drugs include heroin, morphine, cocaine, lysergide (LSD) and ecstasy.
- Dedicated Centre
- Term used in this study to refer to a specialist primary health care centre exclusively or mainly for people who are homeless.
- Drug misuse
- Use of illegal drugs, or misuse of prescription or over-the-counter drugs.
- Dentist out-of-hours cover
- Cover arranged by a dental practice when it is closed. Urgent treatment may be offered by the dental practice outside of working hours or by an urgent dental care service. Patients are directed to these services by contacting their dental practice.
- Emergency department
- Term used in the USA; commonly referred to as A&E in England.
- Fisher’s exact test
- Used to compare two categories of participant demographics (e.g. male vs. female) to establish evidence that the categories do not have the same prevalence (percentage) of a specific feature, as indicated by a p-value of less than 0.05 (this test is used in preference to the chi-squared test when the expected cell count is less than 5 in at least one of the four cells in the 2 × 2 cross-tabulation).
- GP out-of-hours cover
- Cover arranged by a GP practice when it is closed. GPs can choose whether to provide 24-hour care for their patients or to transfer responsibility for out-of-hours cover to NHS England, which is responsible for providing a service to the local population. Some GP surgeries offer evening and weekend appointments, and some collectively provide cover on a rotational basis. Patients are directed to these services by contacting their GP surgery.
- Harmful drinking
- Harmful drinking is defined as 35 or more units of alcohol weekly for women, and 50 or more units weekly for men (National Institute for Health and Care Excellence classification).
- Hazardous drinking
- Hazardous drinking is defined as 15–34 units of alcohol weekly for women, and 15–49 units weekly for men (National Institute for Health and Care Excellence classification).
- Health Care for the Homeless
- US programme.
- Health Screening Indicator
- Six indicators selected to examine screening for the primary outcome: body mass index, mental health, alcohol, tuberculosis, smoking and hepatitis A.
- Health Service Model
- One of four models (Dedicated Centre, Mobile Team, Specialist GP, Usual Care GP) included in this evaluation.
- Kruskal–Wallis test
- Used to compare subgroups of the study population (typically the four Health Service Models) for the distribution of an ordinal or continuous variable; a p-value of < 0.05 indicates that they do not all have the same distribution.
- Lower-risk drinking
- Up to 14 units of alcohol weekly for men and women (National Institute for Health and Care Excellence classification).
- Mann–Whitney U Test
- Used to compare two subgroups of the study population (typically two Health Service Models) for the distribution of an ordinal or continuous variable; a p-value of < 0.05 indicates that they do not have the same distribution, with one subgroup exhibiting higher values than the other.
- Mental component score
- Part of SF-8.
- Mobile Team
- Term used in this study to refer to a mobile homeless health team that holds clinics in hostels or day centres for people who are homeless.
- Night shelter
- Church hall or other building not designed for habitation. It is open only at night and requires people to leave during the day. Stays are often time-limited or depend on a vacancy each night.
- Out-of-Hours services
- Collective term used in this study to refer to accident and emergency, NHS walk-in/urgent care clinic, NHS 111, and ambulance call-out services. The services may be provided out-of-hours, in an emergency, or as substitute primary care.
- Physical component score
- Part of SF-8.
- Primary Outcome Score
- Total number of Health Screening Indicators screened for the primary outcome and an intervention offered where applicable.
- Quality of Care rating
- Drawing on the GP Patient Survey 2017 [NHS England, Ipsos MORI. GP Patient Survey: National Report – July 2017 Publication. URL: www.gp-patient.co.uk/downloads/archive/2017/Weighted/GPPS%202017%20National%20report%20PUBLIC.pdf (accessed 28 July 2021)], participants were asked to rate the care they received the last time they saw a doctor or nurse at the Case Study Site, according to how good the person was at (1) giving you enough time, (2) listening to you, (3) explaining your condition and treatment, (4) involving you in decisions about your care, (5) treating you with care and concern and (6) providing or arranging treatment. They could respond as follows: 1 = very good, 2 = good, 3 = neither good nor poor, 4 = poor and 5 = very poor. An average response was calculated from the total scores, creating a six-item ‘Quality of Care’ rating, with lower scores being more positive.
- Sleeping rough
- Sleeping on the streets, in vehicles or parks, or in other public places not intended for habitation.
- Sofa surfing
- Temporary stays with relatives or friends, often on sofas or floors. Sometimes involves moving from place to place.
- Specialist GP
- Term used in this study to refer to a GP practice that provides general medical services to the local population, and also special or targeted services for people who are homeless, whether at the surgery or in hostels and day centres or on the streets.
- Specific Health Condition
- The effectiveness of the Health Service Models in managing five Specific Health Conditions was examined as one of the study’s secondary outcomes. The health conditions were hypertension, chronic respiratory problems, depression, alcohol problems and drug problems.
- Spice
- Synthetic cannabis that can cause serious health problems, including breathing difficulties, an inability to move, seizures and psychoses.
- Usual Care GP
- Term used in this study to refer to a GP practice that provides general medical services to the local population, which by default includes people who are homeless. It does not offer special or targeted services to patients who are homeless.
List of abbreviations
- A&E
- accident and emergency department
- ANOVA
- analysis of variance
- APMS
- Alternative Provider Medical Services
- AUDIT C
- Alcohol Use Disorders Identification Test-Consumption
- BMI
- body mass index
- BP
- blood pressure
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- CRN
- Clinical Research Network
- CSS
- Case Study Site
- DC
- Dedicated Centre
- DH
- Department of Health
- DHSC
- Department of Health and Social Care
- ED
- emergency department (term used in the USA; commonly referred to as A&E in England)
- GMS
- general medical services
- GP
- general practitioner
- HCA
- health care assistant
- HCH
- Health Care for the Homeless (USA programme)
- HEARTH
- Health Evaluation About Reaching The Homeless
- HIV
- human immunodeficiency virus
- HSI
- Health Screening Indicator
- ICB
- integrated care board (part of ICS)
- ICP
- integrated care partnership (part of ICS)
- ICS
- Integrated Care System
- IT
- information technology
- IQR
- interquartile range
- KCL
- King’s College London
- LSD
- lysergide
- MCS
- mental component score (part of SF-8)
- MDAS
- Modified Dental Anxiety Scale
- MT
- Mobile Team
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- OHIP-14
- Oral Health Impact Profile-14 items
- OHRQoL
- oral health-related quality of life
- oOH
- Out-of-Hours services (as defined in glossary)
- OST
- opioid substitution treatment
- PACT
- Patient-Aligned Care Team
- PCS
- physical component score (part of SF-8)
- PHE
- Public Health England
- PHQ-9
- Patient Health Questionnaire-9
- PMS
- Personal Medical Services
- PPI
- Patient and Public Involvement
- QOF
- Quality and Outcomes Framework
- RCGP
- Royal College of General Practitioners
- SD
- standard deviation
- SF-8
- Short Form 8 Health Survey
- SHC
- Specific Health Condition
- SP
- Specialist GP
- SSC
- Study Steering Committee
- SWEMWBS
- Short Warwick–Edinburgh Mental Wellbeing Scale
- TB
- tuberculosis
- UC
- Usual Care GP
Notes
-
Additional material relating to literature review of primary health care for people who are homeless: evidence-based practice (review A)
-
Mapping of primary health care services for homeless people: specialist teams and practices (questionnaire)
-
Managers of hostels and housing projects for homeless people without specialist homeless health teams (questionnaire)
-
Managers of day centres and drop-in centres for homeless people without specialist homeless health teams (questionnaire)
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/WXUW5103).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
