Notes
Article history
The research reported here is the product of an HSDR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HSDR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HSDR journal.
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR135075. The contractual start date was in June 2021. The final report began editorial review in October 2021 and was accepted for publication in February 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Coelho et al. This work was produced by Coelho et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Coelho et al.
Chapter 1 Background
Mental health conditions are common in the UK, and increasingly prevalent in young people. National surveys1 of children and young people in England show that rates of probable mental health disorders increased considerably between 2017 and 2020, from approximately one in nine (11.6%) to one in six (17.4%) 6- to 16-year-olds, and from 1 in 10 to 1 in 6 of those aged 17–19 years. The same survey1 found that children aged 6–16 years who had a probable mental health disorder were twice as likely to have missed > 15 days of school as those without a probable mental health disorder. The 2020 survey data also showed that white children were twice as likely (20.1%) as children from an ethnic minority (9.7%) to have a probable mental disorder; however, this difference was lower for 17- to 19-year-olds (17.8% vs. 15.9%, respectively), and the survey was conducted during the first year of the COVID-19 pandemic so may reflect atypical mental health stresses and lower mental health service availability than before the pandemic. 1
Health care, including mental health care, is not equally utilised by all ethnic groups in the UK. 2 The 2019 report on mental health equality by the National Collaborating Centre for Mental Health3 also highlighted some stark ethnic inequalities in access to care and responsiveness to treatments. For example, citing a mix of other national sources, ethnic minorities were at an increased risk of involuntary detention, had lower recovery rates following psychological therapies and experienced greater deterioration rates than white mental health service users. 3 In addition to levels of service use, stakeholders consulted as part of the process of developing this guidance3 for the National Collaborating Centre for Mental Health also highlighted that people from ethnic minorities accessed care via different pathways; for instance, they were more likely than their white counterparts to access acute mental health care via the criminal justice system. In 2018, the independent review of the 1983 Mental Health Act4 specifically aimed to address some of these ethnic inequalities, as they were related to the compulsory detention of those experiencing acute mental distress.
Health inequalities arise when, after accounting for rates of ill health and health preferences, there is a disproportional unmet need in one group compared with another. For example, a systematic review5 of British population- and clinic-based studies evaluating both prevalence of child mental health conditions and associated service use among different ethnic groups in the UK suggested a potential unmet need for mental health care among Pakistani and Bangladeshi children. In addition, a more recent systematic review6 found ethnic inequalities in the incidence of diagnosis of severe mental illness in England, with the risk of diagnosis of psychosis being higher for all minority ethnic groups, but particularly black ethnic groups, than those from a white background.
The routes through which children and young people from non-white British ethnic backgrounds obtain mental health support may also differ from those used by white British children or other ethnic groups (with those from non-white British backgrounds being more likely to seek support from informal services, community/voluntary organisations, family and friends). For example, a study by Vostanis et al. 7 conducted in England found that, even when accounting for lower level of need, adolescents aged 13–15 years of Indian ethnicity were less likely than their white peers to use children and adolescent mental health services (CAMHS), but more likely to obtain mental health support from siblings, other non-parental family members, teachers and primary care providers.
Among children and young people who do use CAMHS, referral pathways (both referral sources and destinations) may differ according to ethnicity. Routine data collected from across the UK indicated that children and young people from non-white British backgrounds are more likely than white British children and young people to be referred to CAMHS through education, social services, child health services or the criminal justice system rather than through primary care. 8,9 More recently, a study10 analysing data from the South London and Maudsley NHS Foundation Trust found that 12- to 17-year-olds of black African ethnicity and 18- to 29-year-olds of black African, black British and Asian ethnicity were more likely than white British children and young people to be referred from secondary care, as opposed to primary care, and that all ethnic minority groups were more likely than their white British peers to be referred via the criminal justice system. There is also evidence that, compared with white British children and young people, those from non-white British backgrounds are more likely to be referred to inpatient and emergency services rather than outpatient or non-emergency services,10 or involuntarily rather than voluntarily. 11 This evidence implies that, for these groups, these mental health needs may not be being met through usual health service routes. This has potential cost implications for the individuals, their families and wider communities, and for public services if there is greater use of ‘crisis’ services or involvement of criminal justice.
The picture is clearly complex. When considering all aspects of mental health need (i.e. rates of mental health difficulties, rates of formal and informal service use, different referral pathways, and the care and support preferences of children and young people of different ethnicities), it appears that non-white British children and young people may differ from white British children with regard to the extent and type of unmet mental health care and support needs. The reasons why these needs might be unmet are likely to differ according to ethnic group. A systematic review12 of both quantitative and qualitative studies of the barriers to and facilitators of children and adolescents accessing psychological treatments reported that there were perceived cultural and language barriers or facilitators among people from ethnic minority groups. However, this review was not specific to non-white British children and young people, was not UK specific and was limited to studies evaluating parents’ perceptions.
It remains unclear how much qualitative evidence exists on the factors influencing access to and ongoing engagement with mental health care and support in the UK for non-white British children and young people. This rapid scoping review seeks to address this by documenting the nature and scope of the qualitative evidence in this area, and will focus on identifying studies reporting the experiences, views and perceptions of non-white British children and young people in the UK; their parents, guardians, carers or other family members; their health or social care workers and other professionals who provide referrals or care/support; and commissioners of mental health services.
This scoping review and report was commissioned by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research (HSDR) programme to inform the work of the Department of Health and Social Care’s (DHSC’s) mental health research initiative. In particular, it aims to help identify and prioritise research towards achieving goal 4 and target 4A of the NIHR/Medical Research Council’s (MRC’s) mental health research goals for the UK for 2020–3013 (Box 1). This built on the DHSC’s 2017 framework for mental health research. 14
[Conduct r]esearch to improve choice of, and access to, mental health care, treatment and support in hospital and community settings.
RationaleThere has been a failure to reach all the people who need care and support them to access timely and evidence-based treatment and support.
Target 4AResearch to understand the barriers to help-seeking and service access, and to delivery of mental health services and other support in diverse settings and across different communities, including BAME and LGBT+, to address stigma, discrimination and social exclusion.
BAME, black, Asian and minority ethnic; LGBT+, lesbian, gay, bisexual, transgender +.
Source: Mental Health Research Goals 2020 to 2030. 13
Chapter 2 Objectives
We aimed to undertake a rapid scoping review to describe the nature and scope of the qualitative research in this area and to summarise the main findings as expressed by study authors. The following research questions were to be answered:
-
What is the nature and scope of the qualitative evidence on the experiences, views and perceptions of children and young people from non-white British backgrounds and their parents/carers in accessing and engaging with mental health care and support?
-
What is the nature and scope of the qualitative evidence on the experiences, views and perceptions of those who refer to, provide and commission mental health care and support regarding how children and young people from non-white British backgrounds access and engage with mental health care and support?
Scoping reviews are a type of systematic review that aim to examine the extent, nature and scope of research within a topic area. 15,16 They also typically identify gaps in research and may also summarise and disseminate research findings. 17,18
Therefore, a third objective was:
-
To summarise findings from within studies that relate to the two research questions (i.e. focused on seeking, accessing or engaging with mental health care and support), including providing illustrative quotations from study participants.
Chapter 3 Methods
The following methods were developed in collaboration with our policy contacts within the DHSC, and agreed and published as a protocol before the searching and screening stages were completed. The review protocol is available for download as a project within the Open Science Framework. 19
Inclusion criteria
The full final inclusion criteria are described in Appendix 1.
Phenomenon/outcomes of interest
Studies were eligible for inclusion if they described the included groups’ perceptions, views and experiences of access to or ongoing retention/engagement with mental health care and support (with a view to explaining the factors affecting this). Any type of experience, as described by the participants, was considered valid and eligible for inclusion.
Population
To be included in the review, studies had to be focused on non-white British children and/or young people (aged 10–24 years) who required, were seeking or were receiving mental health care or support. The lower age bound of 10 years was directly suggested by the policy customers of this review.
Non-white British ethnic groups included British ethnic minority groups as determined by 2011 Census Office for National Statistics categories. 20 Studies that focused on travelling communities (including Roma, Gypsy and Irish Traveller communities), or on refugees, people seeking asylum or those who are stateless were also included. In addition, studies reporting data on any non-white British group(s) alongside data from white British groups were included (so long as the white British participants constituted less than half of all study participants).
Eligible studies could report the views, perceptions and experiences of:
-
non-white British children and/or young people requiring, seeking or receiving mental health care and support, or provided the study’s main focus was on access/engagement of non-white British children or young people (aged 10–24 years) to mental health care and support
-
parents, guardians, carers or other relatives of such children or young people
-
health and social care professionals that refer, or provide, care and support to such children or young people
-
other referrers and providers such as teachers, charity/voluntary-sector staff or staff working within the criminal justice system
-
commissioners of mental health care and support for this population group.
Health problem
A broad definition of ‘mental health’ was used, and encompassed the following mental health issues/conditions: anxiety disorders [including obsessive–compulsive disorder (OCD), post-traumatic stress disorder (PTSD) and other trauma-related mental health issues], depressive disorders, psychotic disorders, personality disorders, conduct disorders, eating disorders, disorders of addiction and misuse, disorders of sleep, somatoform disorders, attention deficit hyperactivity disorder (ADHD), gender dysphoria, self-harming behaviours, general stress and mental/psychological well-being. Studies focused on conditions sometimes assessed or treated by services outside CAMHS or adult mental health services (e.g. autism, social communication disorders, ADHD and/or learning disabilities) were included when the primary focus of the study was mental health rather than the non-mental health aspects of these conditions (such as initial diagnosis).
Setting
Eligible studies were conducted in the UK. Studies that focused on access to and/or engagement with any service, care or support that had a mental health focus or a clear mental health component were eligible for inclusion. This included, but was not limited to, CAMHS, other secondary or tertiary care-based mental health services (including specialist and highly specialist mental health services), charities’/third-sector mental health projects and services, and community-based voluntary services (formal or informal, such as those provided by community associations or religious organisations). A broad and inclusive definition of mental health care and support was used, and, particularly in the case of charity projects and voluntary community-based services, studies including mental health support and care offered as part of a holistic well-being package were eligible for inclusion.
Comparison groups
Studies of single groups or cohorts with no aim to compare experiences between groups (i.e. no comparator group) were eligible for inclusion. Comparison groups may have been included and could have involved comparison with white British populations or between ethnic minority groups. Comparison may also have been made between people involved in children and young people’s mental health care and support (e.g. comparison of perceptions and experiences of children and young people with those of their parents/caregivers, or between parents and health professionals).
Study designs
Any qualitative study design was eligible for inclusion. The decision to focus on qualitative studies was suggested by the review team given the policy customer’s main stated goal of understanding the causes of variations in access to mental health care and support in these groups.
Commentaries, letters and opinion pieces were excluded. Systematic reviews of qualitative studies were included if most of the included studies were relevant to this review. Quantitative studies and policy and guidance documents not describing the perceptions, views or experiences of the study population were excluded.
Other limits
Only studies published in the last decade (between 2012 and the search date) were included so that the evidence was as relevant as possible to current service configurations. Our policy customers thought that evidence from before 2010 would be too far back and much less relevant, and the Health and Social Care Act21 and No Health Without Mental Health22 strategy were introduced in England in 2012 and 2011, respectively. In addition, at national level, the biggest changes in the last decade were the funding as part of the Five Year Forward View for Mental Health (for NHS England, published in 2016)23 and then the NHS Long Term Plan (2019 onwards). 24
We included both peer-reviewed and non-peer-reviewed papers or reports (i.e. ‘grey literature’).
Stakeholder engagement
To inform our methods and description of findings, we engaged with two clinical/service topic experts (by e-mail). One (Professor Kam Bhui) was a psychiatrist and academic researcher with experience and interest in sociocultural risk and protective factors to prevent and reduce inequalities in population mental health and suicide, including understanding ethnicity as a driver of inequalities. The other expert advisor (Professor Julian Edbrooke-Childs) was a chartered research psychologist and academic researcher whose research focuses on empowering young people to actively manage their mental health and mental health care, with a particular focus on social inequalities.
Both advisors provided comments on the review protocol before it was finalised and provided valuable comments on a draft of the review’s report and findings before the discussion and conclusions had been written. The policy customers of this report, who were members of the DHSC’s mental health policy team, also had an opportunity to comment on a draft of the report (which contained the findings, draft discussion and draft conclusions).
Patient and public involvement
There was little time to recruit and involve young people from ethnic minorities early in the process of this rapid scoping review. However, through an intermediary organisation [Healthy Teen Minds (London, UK)], and using a relevant online network/e-mail list, we recruited three young black people (aged 21, 22 and 23 years, all identifying as male and with lived experience of accessing mental health support) to comment on our findings (see Scientific summary) and help us craft our Plain English summary.
Search methods
Bibliographic database searches were designed by an information specialist (SR) in consultation with the review team. Searches were carried out on 23 June 2021 in Applied Social Sciences Index and Abstracts [(ASSIA) ProQuest], Cumulative Index in Nursing and Allied Health Literature [(CINAHL) EBSCOhost], Health Management Information Consortium [(HMIC) Ovid], MEDLINE (Ovid), PsycInfo (Ovid), Social Policy and Practice (Ovid) and Web of Science (Clarivate Analytics).
Terms for the mental health conditions (as determined by the team) were combined with terms for the Office for National Statistics ethnic minority group categories (as defined for the 2011 national census). 25 These were further combined with terms for children and young people, and for the UK setting. 26 A qualitative study filter was added27 and studies were limited to those published from 2010 onwards. The full MEDLINE search strategy is shown in Appendix 2.
A later decision was made to limit to studies published from 2012 onwards and this was done during screening; see below. Reference lists for the final included studies were checked and forward citation chasing was carried out in Scopus (Elsevier).
Screening and study selection
As an initial calibration exercise of inclusion judgements, two reviewers applied inclusion and exclusion criteria to a subsample of search results (n = 50) and discussed the screening decisions. The calibration exercise was used to refine the clarity of the inclusion criteria to enable more consistent reviewer interpretation and judgement. This helped refine subtle boundaries/rules in applying the criteria and did not change the inclusion criteria themselves. For example, it clarified whether or not study abstracts needed to indicate if there were young people from ethnic minorities in the sample or subsample (our rule: yes, unless there was no information at all about the population characteristics, in which case investigate at full-text stage).
Following the calibration exercise, titles and abstracts of bibliographic database search results were independently screened by two reviewers. Disagreements were resolved through discussion. Full-text articles were retrieved and independently screened by two reviewers, with disagreements resolved through discussion (in consultation with a third reviewer when needed). When studies contained a subset of eligible participants, these were included when the majority of participants reflected the target population, or when data from eligible participants were reported separately. Papers excluded at the full-text stage are reported in Appendix 3.
Data extraction and quality assessment
Data extraction
A standardised data extraction template was developed in Microsoft Excel® (Excel 2013, Microsoft Corporation, Redmond, WA, USA), and piloted by two reviewers on a selection of included studies. Data were extracted separately for each study (i.e. same sample and analysis), even if the study was reported in more than one publication. For each study included at the full-text stage, information was extracted by one reviewer and checked by a second, with disagreements resolved through discussion (in consultation with a third reviewer when needed). For an overview of data extracted from studies, see Appendix 4.
Quality appraisal
The quality of each paper was assessed using the 13 criteria in the Wallace checklist,28 which is widely used to assess the quality of conduct and reporting of qualitative research. Compared with alternative tools for assessing the quality of qualitative research, our team has found the Wallace checklist to be clearer and more applicable to a wide range of types of qualitative research. The criteria cover assessment of the clarity and coherence of a study in relation to its question, theoretical perspective, study design, context, sampling, data collection methods, data analysis methods, reflexivity, generalisability and ethics. The criteria were applied by one reviewer and checked by another. The quality appraisal was conducted primarily to inform methodological research recommendations, but also so that readers interested in particular studies or groups of studies could consider their independently assessed quality/reliability alongside the summarised findings.
Data presentation
The extracted data were used to categorise studies according to institutional setting or population group, or mental health needs, and aimed to describe the number of studies available for different ethnic or other groups, types of services and mental health needs. Tables were used to simplify and summarise the nature and types of studies found. The findings/themes and compelling illustrative quotations that seemed most relevant to our review objectives (i.e. about care-seeking, or accessing services or support for mental health problems) were summarised or presented.
Departures from protocol
There were two differences between the methods we used and those planned and published in our review protocol. First, we had intended to hand-search the reference lists of relevant systematic reviews identified in our searches, but we did not. Second, we had originally planned to present our findings according to the different ethnic minorities in studies, but could not, as most were based on samples of young people from many different ethnic backgrounds, including some studies with participants from both white British and ethnic minority backgrounds (see Table 1).
Chapter 4 Findings
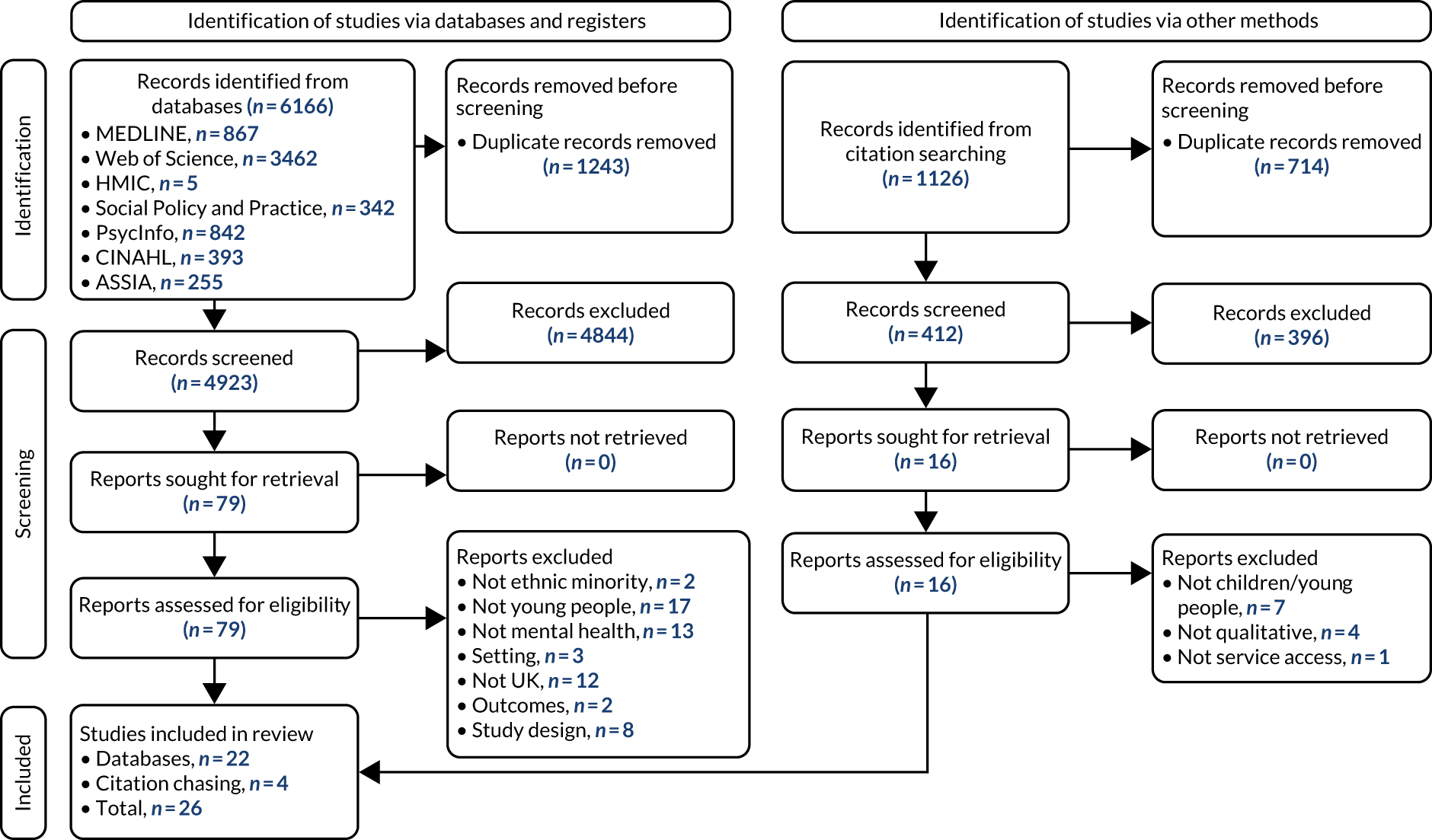
Figure 1 provides an overview of results of the searches and how the final number of included papers and studies were found from them. In total, 5335 records from searches were screened, with 26 papers/publications, reporting 22 studies, included in the final scoping review.
FIGURE 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses 2020 flow diagram of the searches and screening process. 29
Overview of included studies
Included studies were highly heterogeneous in terms of the type of mental health need, service setting, and ethnicity and age of the young people (Table 1). Table 2 provides a fuller description of the key characteristics of all included studies.
| Ethnic group(s) in study sample | Type of mental health need | ||
|---|---|---|---|
| Various or non-specific mental health difficulties | Specific needs or conditions | Receiving specific treatments | |
| Multiple ethnic groups (including some white British) |
The Children’s Society30 Birch et al. 31 |
Cadge et al. 32 (schizophrenia) Channa et al. 33 (bulimia nervosa) Klineberg34 (self-harm) |
Bunting et al.35 (multisystemic therapy) |
| Multiple ethnic groups (all non-white British) |
Fazel36 Fazel et al. 37 (stress of refugee status) Hurn and Barron38 King and Said39 |
Islam et al. 40 (psychosis) Chowbey et al. 41 (eating disorders) Kolvenbach et al. 42 (OCD) |
Gurpinar-Morgan et al.43 (CBT) |
| Single or few ethnic groups in sample |
Davies Hayon and Oates44 (most from Afghanistan) Majumder et al. 45–48 (most from Afghanistan) Olaniyan49 (black British and South Asian British) Rowland50 (Orthodox Jewish young people) Sancho and Michael51 (black African, mixed or black Caribbean young people) |
Edge and Grey52 (schizophrenia in African Caribbean and black African young people) Wales et al. 53 (eating disorders in South Asian young people) Gleeson et al. 54 (drug/crime interventions in black and Asian young people) Gray and Ralphs55 (substance abuse interventions in Pakistani and Bangladeshi young people) |
|
| First author, year; city/region | Population of interest | Health/well-being needs or services | Study aims | Methods | Sample | |||
|---|---|---|---|---|---|---|---|---|
| Ethnicity or country of origin | Age (years) | Other population characteristics | Needs or difficulties | Services | ||||
| Birch,31 2020; Sheffield | White, Romania, Kurdistan, Islamic Republic of Iran, Sudan, Pakistan, Persian | 17–27 | Some asylum seekers | Various/not specified | (Proximity to) nature | Explore the value of urban nature for the mental health and well-being of young people | Interviews and creative art workshops | 24 young people |
| Bunting,35 2021; London | Samoa, the Netherlands, Sudan/Kenya, Georgia, Nigeria, Morocco, the Democratic Republic of the Congo, Iraq | 14–18 | Parents’ religous group: Muslim, Christian, Pentecostal, Jehovah’s Witness | Not specified, (MST is for antisocial behaviour for young people and study reports number of convictions) | MST | Explore minority ethnic young people’s experiences of MST, focusing on their understanding of their presenting difficulties and aspects of the intervention that facilitated or hindered engagement and change | Semistructured interviews | 7 young people (female, n = 4; male, n = 3) |
| Cadge,32 2019; Birmingham | Britain, Pakistan, India, African Caribbean, dual white British and African Caribbean | 18–22 | University students | Schizophrenia | Various | Explore perceptions and understanding of schizophrenia in university students | Semistructured interviews and thematic analysis | 20 university students |
| Channa,33 2019; West Midlands | British Indian | Early twenties | Within 5 years of diagnosis with eating disorder | Bulimia nervosa | Eating disorder service | Explore the experiences of a young British Indian woman with bulimia nervosa | Case study based on a single semistructured interview reanalysed using interpretative phenomenological analysis | 1 young British Indian woman |
| The Children’s Society,30 2020; London, Midlands, North East England | 9 were white, 18 were from black and other ethnic minority backgrounds | 11–21 | Two were autistic, three had learning disabilities, two were transgender | Various, including self-harm | NHS Children and Young People’s Mental Health Service (Tier 3/specialist service) | To answer the question: how many people really know what it is like for children and young people who are trying to get support for their mental health? | Interviews | 27 young people |
| Chowbey,41 2012; Sheffield | Pakistan, Bangladesh, Somalia, Yemen and India | 18–24 | Similar number of young men and young women | Eating disorders | SYEDA | To understand whether the use of SYEDA’s services by solely white British clients reflected a low level of need among other ethnic groups or whether there might be other factors acting as barriers to diagnosis and service access | Interviews and focus groups | 42 relatives of those with eating disorders, ‘key informants’ and community members |
| Davies Hayon,44 2019; UK | Most from Afghanistan | Various – difference-in-difference studies (literature review) | Refugees/asylum seekers (mostly unaccompanied) | Primarily PTSD, depression and anxiety | Schools and community centres | Suggesting how to enhance practice and improve outcomes for unaccompanied asylum-seeking children in the UK | Systematic review | 303 young people across all studies |
| Edge,52 2018; North West England | African Caribbean | ≥ 18 | No other characteristics described | Schizophrenia | Community locations and NHS mental health services | To determine whether or not members of the African Caribbean community would be willing to partner with health-care professionals and academics to co-produce a culturally appropriate and acceptable version of an extant evidence-based, cognitive behavioural model of FI | Four focus groups | 10 service users, 14 family members/advocates, 7 health-care professionals, 11 mixture of above groups |
| Fazel,36 2015; Oxford, Glasgow, Cardiff | 20 countries | 15–24 |
Refugees (13 unaccompanied) Median time in the UK: 2.5 years 29 male, 11 female |
Various/not specified | School-based mental health service set up specifically for refugee children | Describe the role of schools in supporting the overall development of refugee children and the importance of peer interactions | In-depth semistructured interviews | 40 former users of the school-based mental health service |
| Fazel,37 2016; Oxford, Glasgow, Cardiff | Various (from 20 countries) | 15–24 |
Refugees/asylum seekers Median time in the UK: 2.5 years 29 male, 11 female |
Focus on the stresses associated with refugee status | School based | To determine the experiences of adolescents directly seen in school-based mental health services | In-depth semistructured interviews | 40 former users of the school-based mental health service |
| Gleeson,54 2019; London, the Midlands and North East England | Black and Asian | 16–24 | Recipients of youth justice and substance abuse interventions | Drug/crime interventions | Drug interventions and criminal/youth justice systems | To establish how young people from diverse ethnic backgrounds interact with drug interventions and youth/criminal justice systems in the UK | 19 individual interviews and one focus group | 25 service providers |
| Gray,55 2019; North West England | Pakistan, Bangladesh | Range unclear | Substance users | Substance use | Substance use services | Reasons for the under-representation of British South Asian people in substance use services. This paper contributes to the debate around how substance use services can best engage with young British Pakistani and Bangladeshi substance users | Interviews | 18 young people, 18 stakeholders, 6 staff members |
| Gurpinar-Morgan,43 2014; North West England | ‘Self-identified as being from a black or minority ethnic group’ | 16–18 | One male, four female | CBT users for mental health problems | CBT | This study aimed to examine BME adolescent service users’ perceptions of how ethnicity featured in the therapeutic relationship and its relevance to their presenting difficulties | Interpretative phenomenological analysis was used to explore the experiences of five young people using an adolescent mental health service | Five young people who had been accessing CBT for 4–12 months |
| Hurn,38 2018; West Yorkshire | Syria, one from Libya | 6–11.9 | Refugees/asylum seekers | Trauma, one participant had ADHD | ‘CHUMS’: mental health and emotional well-being service | To investigate whether a particular therapy would be valuable for child refugees whose trauma symptoms failed to reach CAMHS thresholds. In addition, the project aimed to identify cultural hurdles that may hinder access to Western psychological approaches | SUDS, child rating scale, therapists’ reports and interpreter focus group | Eight children, two therapists, four Arabic interpreters |
| Islam,40 2015; Birmingham | Pakistan, the Caribbean, Bengali, Africa | 18–35 | 50% female/50% male | Psychosis | EI for Psychosis Services | Examine the cultural appropriateness, accessibility and acceptability of the EI for Psychosis Services in improving the experience of care and outcomes for black and ethnic minority patients | Focus groups | 56 service users, carers, community and third-sector organisations, service commissioners, EI professionals and spiritual care representatives |
| King,39 2019; city/region not stated | Afghanistan, Ethiopia, Sudan, Somalia | 14–17 | UASC | Various/not specified | Group discussion sessions supported by the NHS | This paper outlines a psychological skills group for unaccompanied asylum-seeking young people, with a focus on cultural adaptations in the context of a UK mental health service | Interviews and session rating scales | 14 young people |
| Klineberg,34 2013; Hackney, Newham | White British, Asian, black | 15–16 | 24 female, 6 male | Self-harm (10 participants had never self-harmed, 9 had self-harmed on one occasion and 11 had self-harmed repeatedly) | Schools | To increase understanding of how adolescents in the community speak about self-harm, exploring their attitudes towards and experiences of disclosure and help-seeking | Interviews | 30 young people |
| Kolvenbach,42 2018; London | 10 from white backgrounds and 10 from ethnic minority backgrounds | 13–17 | 60% female | OCD | National specialist OCD, BDD and related disorders clinic for young people | Identify and compare barriers that parents from different ethnic groups face when accessing specialist services for OCD for their children | Interviews | 20 young people and parents |
| Majumder,45 2015; central England | Mostly Afghanistan, also Islamic Republic of Iran, Somalia and Eritrea | 15–18 | Unaccompanied refugee minors | Predominantly PTSD, depression and self-harm | CAMHS, among others | To appreciate the views and perceptions that unaccompanied minors hold of mental health and services | Semi-structured interviews | 15 young people and carers |
| Majumder,46 2016; central England | Mostly Afghanistan, also Islamic Republic of Iran, Somalia and Eritrea | 15–18 | Unaccompanied refugee minors. Mostly male. English as a second language | Depression, self-harm, PTSD, anxiety, adjustment reaction, substance misuse, impaired sleep | CAMHS | What are the perceived resilience factors that can lead to better psychological coping and mental health outcomes in unaccompanied refugee minors? | Interviews and thematic analysis | 15 young people and carers |
| Majumder,48 2019; central England | Mostly Afghanistan, also Islamic Republic of Iran, Somalia and Eritrea | 15–18 | Unaccompanied refugee minors. Mostly male. English as a second language | Depression, self-harm, PTSD, anxiety, adjustment reaction, substance misuse, impaired sleep | CAMHS | To explore unaccompanied refugee children’s experiences, perceptions and beliefs of mental illness, focusing on stigma | Interviews and thematic analysis | 15 young people and carers |
| Majumder,47 2019; central England | Mostly Afghanistan, also Islamic Republic of Iran, Somalia and Eritrea | 15–18 | Unaccompanied refugee minors. Mostly male. English as a second language | Depression, self-harm, PTSD, anxiety, adjustment reaction, substance misuse, impaired sleep | CAMHS | Research questions: ‘what are the perceptions of unaccompanied refugee minors of their treatment and practitioner and what does that teach us about engagement?’ | Interviews and thematic analysis | 15 young people and carers |
| Olaniyan,49 2021; West Midlands | Black British, South Asian British | Unclear | University students from two universities: one with low and one with high REM participation | Various | University mental health services | To examine the influence of the university environment on the mental health and help-seeking attitudes of REM undergraduate students, evaluating their experiences at a Russell Group university with low REM participation and a neighbouring non-Russell Group university with high REM participation | Interviews | 48 young people |
| Rowland,50 2016; Hackney | Orthodox Jewish | Children and young people aged 1–22 | From families of between one and five children | Unspecified/various | Tier 2 NHS mental health services | Consider the experiences of Orthodox Jewish parents who have accessed CAMHS to seek help for their families. Consider whether there are barriers that have to be overcome to access services from outside the Orthodox community and how these are experienced. Whether or not there may be particular concerns about accessing a mental health service for children | Semistructured interviews and thematic analysis | 9 parents |
| Sancho,51 2020; Birmingham | Black African, mixed or black Caribbean heritage | 18–25 | Undergraduate students, lived in the UK for a minimum of 5 years. Majority were psychology students | Various/not specified | Not specified | Understand the barriers and facilitators that African Caribbean undergraduates perceive to accessing mental health services in the UK | Focus groups (critical incident technique) | 17 young people |
| Wales,53 2017; Leicester | South Asian | < 25 (another focus group was for those aged 25–65) | University students | Eating disorders | Specialised eating disorder clinic | Identify barriers to help-seeking for eating disorders among those from a South-Asian background | Focus groups | 28 young people and 16 clinicians |
Note that the labels and categories used in the table (e.g. to describe the ethnicity of the samples) are those used in the original studies. By today’s conventions, we acknowledge that some of these labels [such as the acronym BAME (black, Asian and minority ethnic)] may no longer be seen as appropriate, that they may not reflect people’s self-perceived ethnic background and cultural identity, and that they may be a poor reflection of the true diversity among young people from different minority ethnic backgrounds.
Seven studies36–43 included a mixture of young people from different non-white British ethnic minority backgrounds, and six others30–35 had a mixture of young people from different ethnic minorities that also included some white British young people. Other studies were conducted in more specific, selected ethnic groups (black and Asian young people,54 Orthodox Jewish young people,50 South Asian young people,53 Pakistani and Bangladeshi young people,55 black British and South Asian British students,49 and mainly Afghan refugees45–48).
The populations of interest varied and included unaccompanied teenage refugees (typically from a wide range of Middle Eastern or North African countries), university students, school students and the general population of young people from different ethnic groups and with different mental health needs. Most studies were local to a particular British city or region, although four studies30,36,37,44,54 had study participants from several cities or regions across the UK. There was no evidence that any studies had been conducted among young people living in the south-west of England, or the south-east of England outside London, and only one study36,37 included some participants from Wales (Cardiff) or Scotland (Glasgow).
Correspondingly, given these different service contexts and populations of interest, the age range of the young people in the study samples also varied. In six studies31–33,40,41,51 the young people were all or mostly aged ≥ 18 years, and in seven studies34,35,38,39,42,43,45–48 they were all or mostly aged < 18 years. In six studies30,36,37,50,53,54 there was a wider age range, including children (aged < 16 years), older teenagers and those in their twenties.
The included studies have primarily been summarised in four overlapping groups:
-
studies of young people in particular circumstances or institutional settings (e.g. university students, refugees/asylum seekers) (n = 9)
-
studies among people with specific mental health needs (e.g. schizophrenia or psychosis, eating disorders, self-harm) (n = 14)
-
studies among people receiving specific treatments (e.g. CBT, multisystemic therapy) (n = 3)
-
other studies not already covered in the first three groups (n = 1).
It should be noted that the above four groups of studies are not mutually exclusive. For an outline of which studies are covered in which findings section of this report, see Table 3. For example, of the four studies about access to mental health care among university students, one32 was about experiences of living with schizophrenia while at university, and another53 was about barriers to help-seeking for eating disorders among South Asian students. As social stigma was a recurring factor affecting care-seeking and access to mental health services and support across a number of need groups and settings, there is a section summarising the relevant findings from across studies in which this was a key factor affecting service use or engagement.
| First author, year | Paper title(s) | Report section | |||||
|---|---|---|---|---|---|---|---|
| Refugees/asylum seekers | University students | Studies among people with specific mental health needs | Studies about accessing and engaging with specific interventions | Stigma as a barrier to accessing or seeking help | Studies on access to other resources or support | ||
| Davies Hayon,44 2019 | The mental health service needs and experiences of unaccompanied asylum-seeking children in the UK: a literature review | ✓ | ✓ | ✓ | |||
| Fazel,36 2015 | A moment of change: facilitating refugee children’s mental health in UK schools | ✓ | |||||
| Fazel,37 2016 | The right location? Experiences of refugee adolescents seen by school-based mental health services | ✓ | |||||
| Hurn,38 2018 | The EMDR integrative group treatment protocol in a psychosocial program for refugee children: a qualitative pilot study | ✓ | ✓ | ✓ | |||
| King,39 2019 | Working with unaccompanied asylum-seeking young people: cultural considerations and acceptability of a cognitive behavioural group approach | ✓ | |||||
| Majumder,45 2015 | ‘This doctor, I not trust him, I’m not safe’: the perceptions of mental health and services by unaccompanied refugee adolescents | ✓ | ✓ | ✓ | |||
| Majumder,46 2016 | ‘Inoculated in pain’: examining resilience in refugee children in an attempt to elicit possible underlying psychological and ecological drivers of migration | ✓ | ✓ | ✓ | |||
| Majumder,48 2019 | Exploring stigma and its effect on access to mental health services in unaccompanied refugee children | ✓ | ✓ | ✓ | |||
| Majumder,47 2019 | Potential barriers in the therapeutic relationship in unaccompanied refugee minors in mental health | ✓ | ✓ | ✓ | |||
| Cadge,32 2019 | University students’ understanding and perceptions of schizophrenia in the UK: a qualitative study | ✓ | ✓ | ✓ | |||
| Olaniyan,49 2021 | Paying the widening participation penalty: racial and ethnic minority students and mental health in British universities | ✓ | |||||
| Sancho,51 2020 | ‘We need to slowly break down this barrier’: understanding the barriers and facilitators that African Caribbean undergraduates perceive towards accessing mental health services in the UK | ✓ | |||||
| Wales,53 2017 | Exploring barriers to South Asian help-seeking for eating disorders | ✓ | ✓ | ||||
| Edge,52 2018 | An assets-based approach to co-producing a Culturally Adapted Family Intervention (CaFI) with African Caribbeans diagnosed with schizophrenia and their families | ✓ | |||||
| Islam,40 2015 | Black and minority ethnic groups’ perception and experience of early intervention in psychosis services in the United Kingdom | ✓ | ✓ | ||||
| The Children’s Society,30 2020 | Waiting in line: stories of young people accessing mental health support | ✓ | |||||
| Klineberg,34 2013 | How do adolescents talk about self-harm: a qualitative study of disclosure in an ethnically diverse urban population in England | ✓ | |||||
| Chowbey,41 2021 | Influences on diagnosis and treatment of eating disorders among minority ethnic people in the UK | ✓ | |||||
| Channa,33 2019 | Overlaps and disjunctures: a cultural case study of a British Indian young woman’s experiences of bulimia nervosa | ✓ | ✓ | ||||
| Gleeson,54 2019 | Challenges to providing culturally sensitive drug interventions for BAME groups within UK youth justice systems | ✓ | |||||
| Gray,55 2019 | Confidentiality and cultural competence? The realities of engaging young British Pakistanis and Bangladeshis into substance use services | ✓ | |||||
| Kolvenbach,42 2018 | Perceived treatment barriers and experiences in the use of services for obsessive–compulsive disorder across different ethnic groups: a thematic analysis | ✓ | |||||
| Bunting,35 2021 | Considerations for minority ethnic young people in multi-systemic therapy | ✓ | |||||
| Gurpinar Morgan,43 2014 | Ethnicity and the therapeutic relationship: views of young people accessing cognitive behavioural therapy | ✓ | |||||
| Rowland,50 2016 | How do parents within the orthodox Jewish community experience accessing a community child and adolescent mental health service? | ✓ | |||||
| Birch,31 2020 | Nature does not judge you – how urban nature supports young people’s mental health and wellbeing in a diverse UK city | ✓ | |||||
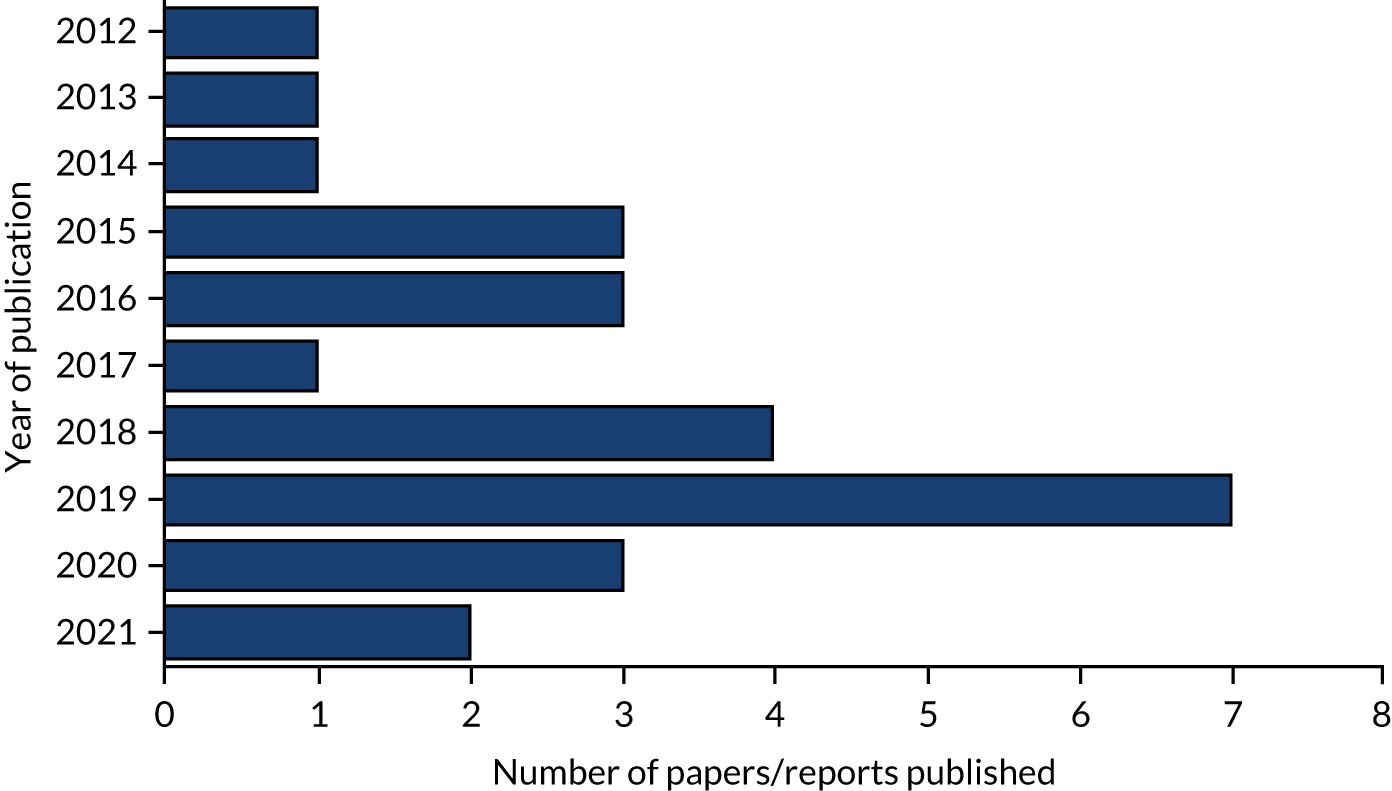
Figure 2 shows that the majority of the papers or reports found were published quite recently within the 10-year period, with 16 published from 2018 onwards and five published in 2020 or 2021. 30,31,35,49,51 However, this may not reflect the years in which the studies were actually conducted (for example, the four papers by Majumder45–48 – published in 2015, 2016 and 2019 – were based on analyses of mental health service use in 2010 and 2011).
FIGURE 2.
Number of papers by year of publication.
Quality of included papers
The quality assessment of the included papers is shown in Table 4. We assessed the quality of each included paper or report (rather than each study) because many of the quality criteria in the Wallace checklist relate to how well studies describe and justify what they did and what they found, and this may vary between papers and analyses conducted for different purposes. 28
| First author, year | 1. Question | 2. Theoretical perspective | 3. Study design | 4. Context | 5. Sampling | 6. Data collection | 7. Data analysis | 8. Reflexivity | 9. Generalisability | 10. Ethics | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Is the research question clear? | Is the theoretical or ideological perspective of the author (or funder) explicit? | Has this influenced the study design, methods or research findings? | Is the study design appropriate to answer the question? | Is the context or setting adequately described? | Is the sample adequate to explore the range of subjects and settings, and has it been drawn from an appropriate population? | Was the data collection adequately described? | Was data collection rigorously conducted to ensure confidence in the findings? | Was there evidence that the data analysis was rigorously conducted to ensure confidence in the findings? | Are the findings substantiated by the data? | Has consideration been given to any limitations of the methods or data that may have affected the results? | Do any claims to generalisability follow logically and theoretically from the data? | Have ethical issues been addressed and confidentiality respected? | |
| Birch,31 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bunting,35 2021 | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | No | Yes |
| Cadge 201932 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Channa,33 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | No | Yes |
| The Children’s30 Society, 2020 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Cannot tell | Cannot tell | |
| Chowbey,41 2012 | Yes | No | Yes | Yes | Yes | No | No | Yes | Yes | No | Cannot tell | Yes | |
| Davies Hayon,44 2019 | Yes | No | Yes | Yes | Yes | Yes | Cannot tell | Cannot tell | Cannot tell | Yes | Cannot tell | Cannot tell | |
| Edge,52 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | No | Cannot tell | Yes |
| Fazel,36 2015 | No | No | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Cannot tell | Cannot tell | |
| Fazel,37 2016 | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Cannot tell | Yes |
| Gleeson,54 2019 | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes | No | Cannot tell | Yes |
| Gray,55 2019 | Yes | No | Yes | Yes | Yes | No | Cannot tell | Cannot tell | Yes | Yes | Cannot tell | Cannot tell | |
| Gurpinar-Morgan,43 2014 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | |
| Hurn,38 2018 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | |
| Islam,40 2015 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Cannot tell | Yes |
| King,39 2019 | No | No | Cannot tell | No | Yes | No | Cannot tell | No | Cannot tell | No | Cannot tell | Yes | |
| Klineberg,34 2013 | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Cannot tell | Yes |
| Kolvenbach,42 2018 | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell |
| Majumder,45 2015 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Cannot tell | Yes | |
| Majumder,46 2016 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | |
| Majumder,48 2019 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Majumder,47 2019 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | |
| Olaniyan,49 2021 | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Rowland,50 2016 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Sancho,51 2020 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | |
| Wales,53 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | No | Yes |
Overall, the majority of papers were of good quality and were sufficiently well reported to identify information about the aims, methods of data collection, and approaches to data analysis and interpretation. Seventeen of the 26 papers addressed > 10 of the 13 quality questions. The nine lower-quality papers, meeting < 10 of the 13 criteria, were those by Bunting et al. ,35 The Children’s Society,30 Chowbey et al. ,41 Davies Hayon and Oates,44 Fazel et al. ,36,37 Gleeson et al. ,54 Gray and Ralphs,55 and King and Said. 39
The most poorly reported aspect of studies was whether or not any claims to generalisability followed logically and theoretically from the data: in the papers by Bunting et al. 35 and Channa et al. ,33 the claims did not appear to clearly follow the data, and in a further 1730,34,36–41,43–47,51,52,54,55 of the 26 papers there was insufficient evidence to judge this. Other quality criteria frequently not met were making explicit the theoretical or ideological perspective of the author (or funder) (not met by 15 papers30,32,36,38,39,41,43–48,50,51,55) and giving consideration to any limitations of the methods or data that may have affected the results (not met by eight papers30,33,36,39,41,45,52,54). The methods of data collection were also judged not to be adequately described in nine of the papers. 35–37,39–41,49,54,55
Refugees/asylum seekers
Five studies focused on the mental health experiences of, and support or service use by asylum seekers and refugees; these were reported in nine papers, four of which were based on the same data set from the same lead author, Majumder, and two were on the same data set from Fazel et al. (Fazel,36 Fazel et al. ,37 King and Said,39 Davies Hayon and Oates,44 Hurn and Barron,38 Majumder45–48) (Table 5). In addition, Birch et al. 31 included some limited data from refugees; however, these are reported separately in Studies on access to other resources or support, as they focused on exposure to nature as a determinant of mental well-being, rather than access to formal mental health services.
| First author, year; city/region | Population of interest | Health/well-being needs/services | Study aims | Methods | Sample | |||
|---|---|---|---|---|---|---|---|---|
| Ethnicity | Age (years) | Other population characteristics | Needs | Services | ||||
| Davies Hayon,44 2019; UK | Most from Afghanistan | Various (literature review) | Refugees/asylum seekers (mostly unaccompanied) | Primarily PTSD, depression and anxiety | Schools and community centres | Suggesting how to enhance practice and improve outcomes for unaccompanied asylum-seeking children in the UK | Systematic review | 303 young people across all studies |
| Fazel,36,37 2015 and 2016 Oxford, Glasgow, Cardiff | Various (from 20 countries) | 15–24 |
Refugees (13 unaccompanied) Median time in the UK: 2.5 years |
Various/not specified Focus on the stresses associated with refugee status37 |
School-based mental health service set up specifically for refugee children |
Describe the role of schools in supporting the overall development of refugee children and the importance of peer interactions36 To determine the experiences of adolescents directly seen in school-based mental health services37 |
Semistructured interviews | 40 former service users |
| Hurn,38 2018 West Yorkshire | Syrian, one Libyan | 6–11.1 | Refugees/asylum seekers | Trauma, one participant had ADHD | CHUMS: mental health and emotional well-being service | To investigate whether a particular therapy would be valuable for child refugees whose trauma symptoms failed to reach CAMHS thresholds. In addition, the project aimed to identify cultural hurdles that may hinder access to Western psychological approaches | SUDS, child rating scale, therapists’ reports and interpreter focus group | Eight children, two therapists and four Arabic interpreters |
| King,39 2019; city/region not stated | Afghan, Ethiopian, Sudanese, Somalian | 14–17 | UASC | Various/not specified | Group discussion sessions supported by the NHS | This paper outlines a psychological skills group for unaccompanied asylum-seeking young people, with a focus on cultural adaptations in the context of a UK mental health service | Interviews and session rating scales | 14 young people |
| Majumder,45–48 2015, 2016, 2019 and 2019; central England | Mostly Afghan, also Iranian, Somalian and Eritrean | 15–18 | Unaccompanied refugee minors | Predominantly PTSD, depression and self-harm | CAMHS, among others |
The aim of this research is to appreciate the views and perceptions that unaccompanied minors hold about mental health and services45 What are the perceived resilience factors that can lead to better psychological coping and mental health outcomes in unaccompanied refugee minors?46 To explore unaccompanied refugee children’s experiences, perceptions and beliefs of mental illness, focusing on stigma48 Research questions ‘what are the perceptions of unaccompanied refugee minors of their treatment and practitioner and what does that teach us about engagement?’47 |
Semistructured interviews | 15 young people and carers |
The studies carried out among refugees and asylum seekers included some specific factors that suppressed acknowledgement of mental illness. Some extreme negative associations were expressed about mental ill health, raising concerns among young people that they would be treated with prejudice and rejection by friends and family if they were labelled as having a mental health issue:48
. . . For them it was mad, they are mad. So they should be put in mad asylums.
Carer48
. . . So sometime my friends don’t wants to be with me because I’ve got this problem.
Young person48
These fears could be compounded by mistrust of mental health services, the origin of which was attributed by some to their experiences in their home country and their experiences as a refugee:45
. . . didn’t say to anything about my problem, I didn’t tell it to anybody, you know, because I don’t trust anybody.
Type of participant not given45
In some cases, it was implied that this mistrust was associated with a fear of incarceration in a mental health facility:48
I say no I don’t want to go hospital to be with the mentals or that kind of people.
Type of participant not given48
Davies Hayon and Oates44 recognised the role that nurses can play in overcoming this mistrust among young refugees. However, to be in contact with mental health nurses, young people must already be engaged with the service. Breaking down negative perceptions could therefore be key to overcoming this initial barrier to access.
Some interviewee comments indicated that refugee minors may access mental health services via non-traditional routes, more frequently going through local authorities and teachers than following visits to a general practitioner (GP):44
When I joined the high school yeah . . . I tell my the teacher . . . I have this problem which can make me not concentrate . . . and she advised me to see X.
Type of participant not given44
The location of services may also be important in ensuring that refugees feel comfortable making contact. For example, Fazel et al. 37 found that two-thirds of participants preferred to be seen at school. However, experiences reported at school were varied, with some participants avoiding telling their teachers about their background as an asylum seeker for fear that they would be treated differently:
Just some of them, not all of them, just some of the teachers . . . they are like racist or . . . yeah and or like some of them would be really nice . . . We do want them to be nice, we want them to treat us like other students.
Brother37
Similarly, Davies Hayon and Oates44 highlighted the importance of being able to access mental health support via facilities commonly used by the population in question, including community centres.
In addition, the content of services could be improved through being tailored to suit the communication needs of refugees (e.g. accounting for culture, language, age and experiences). One example is that the Arabic-speaking service users involved in Hurn and Barron’s38 study preferred oral communication to paper-based assessment (perhaps relating to other general fears among refugees around filling and signing forms). They also preferred to have direct instructions rather than a more flexible approach.
Another theme seen in the predominantly Afghan population of Majumder’s45 study was a preference for medication over talking therapies. This was attributed to the participants preferring to look forward, and seeing being positive as a better alternative to reliving traumatic experiences in their home country:
That doesn’t helps me . . . that makes me more hard because um the all the time I was talking about the past . . . so every time I went there . . . reminding me after I went home again . . . same depression and same problems.
Type of participant not given45
Language and culture were also commonly cited as barriers to effective engagement once services had been accessed. In some cases, service users reported trusting English-speaking facilitators; however, they felt better understood when they could communicate in their native language. 47 Facilitators mentioned that the use of an interpreter could make it more difficult for them to control sessions, as interpreters occasionally went beyond what was actually said. 38 This was reported as a particular challenge to overcome in ensuring that facilitators can effectively treat young people while making them feel as comfortable as possible.
The background of mental health service facilitators was another aspect that was discussed. 47 Some of the participants mentioned a lack of trust in Asian practitioners in particular, although the reason for this was not explored. In addition, some reported being more likely to open up about their issues with a male practitioner47 (although it was not stated whether it was male or female service users who felt this). This was attributed by the authors to the cultural attitudes of study participants, in which it may be important to protect females from stressors:
To S [young person], women need to be protected, women need to just see the soft side of things and don’t have to suffer, and if there is any burden of suffering, it is good for the man to carry this burden and not for a woman . . .
Carer47
King and Said39 reported on a service that was successful with unaccompanied asylum seekers in a group cognitive–behavioural therapy (CBT) setting:
Before I came to the group I felt very sad and worried, since coming here I have opened up and I feel relaxed.
Male, 17, Somalian39
Participants valued both the content of the sessions and the opportunity to meet peers in similar positions to themselves. In addition, they appreciated that the group was kept flexible to cater for their needs and that the group setting helped normalise the process:39
I come here and saw everyone that has problems just like me. Everyone is working together to help each other.
Male, 17, Somalian39
This was a seen as a successful programme for these asylum seekers, which saw good rates of repeat attendance, overcoming a significant obstacle to service provision. One further possibility for improving access to services, considered by Hurn and Barron38 was providing rewards for attendance at mental health appointments. One example given was an educational reward, as education is often highly regarded by refugees; in this case a family trip to the Yorkshire Dales was added as a fourth and more activity-based education session.
University students
Four studies included a focus on understanding the mental health care-seeking experiences of undergraduate students from ethnic minority backgrounds. 32,49,51,53 These four papers focused on the experiences of African Caribbean students in accessing mental health services,51 the mental health and help-seeking experiences of black British and South Asian British students at two universities,49 South Asian students with eating disorders53 and students of various ethnicities living with schizophrenia. 32
The main features of these studies are summarised in Table 6, below.
| First author, year; city/region | Population of interest | Health/well-being needs/services | Study aims | Methods | Sample | |||
|---|---|---|---|---|---|---|---|---|
| Ethnicity | Age (years) | Other population characteristics | Needs | Services | ||||
| Cadge,32 2019; Birmingham | British, Pakistani, Indian, African Caribbean, dual white British and African Caribbean | 18–22 | University students | Schizophrenia | Various | Explore perceptions and understanding of schizophrenia in university students | Semistructured interviews and thematic analysis | 20 university students |
| Sancho,51 2020; Birmingham | Black African, mixed or black Caribbean heritage | 18–25 | Undergraduate students who had lived in the UK for a minimum of five years. Majority were psychology students | Various/not specified | Not specified | Understand the barriers and facilitators that African Caribbean undergraduates perceive to accessing mental health services in the UK | Focus groups (critical incident technique) | 17 young people |
| Olaniyan,49 2021; city not named | Black British and South Asian British | Unclear | University students from two universities: one with low and one with high REM participation | Various | University mental health services | To examine the influence of the university environment on the mental health and help-seeking attitudes of REM undergraduate students, evaluating their experiences at a Russell Group university with low REM participation and a neighbouring non-Russell Group university with high REM participation | Interviews | 48 young people |
| Wales,53 2017; Leicester | South Asian | < 25 | University students | Eating disorders | Specialised eating disorder clinic | Identify barriers to help-seeking for eating disorders among those from a South Asian background | Focus groups | 28 young people and 16 clinicians |
In three of the studies,32,51,53 interviewees reported a lack of knowledge and understanding of the relevant mental health issue, although this theme was more prominent in the studies of Cadge et al. 32 and Wales et al. ,53 which focused on specific mental health conditions. In contrast, the study51 focusing on experiences of African Caribbean students identified a lack of trust in the services to which the students had access. Misdiagnosis was raised as an issue, with some (services or professionals) missing the signs of the mental health problem. When interviewees recognised a mental health issue themselves, there was an indication that they may not seek help owing to underappreciating the severity or seriousness of the issue:
I just think [. . .] eating disorders they’re easily fixed so why go seek help if you can do it yourself?
Male, < 25 years53
A similar quotation was found in Cadge et al. ’s32 paper, which focused on schizophrenia:
It’s all well saying I’d probably seek help but I honestly don’t think I would . . . you think you’re strong enough to probably get over it yourself.
Keshini (pseudonym), Indian32
This illustrates that, for some problems, the perceived expectation that young people can just ‘get over it’ (implicitly, on their own) is itself a barrier to help-seeking and may stem from views within their communities. This may be particularly the case for male participants:
Where I am from, men need to be in control, we are head of the home. I’m the first boy and in my culture that’s a big deal.
Type of participant not given49
Indeed, the perceived need to deal with issues alone, combined with a lack of knowledge around conditions and lack of available support, may be linked with internal conflict between interviewees’ Western beliefs and those of their religion and community:
I think I’m quite Western in the way I think about this but I know there’s a spiritual aspect to these things too.
Type of participant not given49
A related theme that emerged through these papers was stigma, although this was not exclusive to university students (see later section on the stigma findings, Stigma as a barrier to accessing or seeking help, for more details). For example, the study by Sancho and Michael,51 which included African Caribbean students, found that students, particularly those identifying as male, felt that they have to conform to certain ideals, and that having a mental health issue would depart from this. More generally, having a mental health issue may be less commonly discussed in some ethnic minority groups
In my community . . . they’re like this doesn’t exist . . . it’s a white person thing.
Waqas (pseudonym), Pakistani32
For some, religious beliefs might either deter care-seeking or provide an additional source of support and advice. In the study exploring the experiences of African Caribbean students,51 religion appeared to add to the stigma of mental health issues. In contrast, in the study by Wales et al.,53 which included South Asian students with schizophrenia, it was highlighted that religion or the religious community and leaders might be the first point of access to mental health support (before accessing formal or professional support).
If ethnic minority students feel that they are misdiagnosed, or that health professionals and services miss signs of mental health issues and that they are on their own dealing with these issues, then it is clear that ethnic minority students will need as much information and help as possible to understand what services are available to them. Students in the Wales et al. 53 and Sancho and Michael51 studies also suggested that the promotion of available support services is inadequate. Students in both studies highlighted the importance of publicity, and of ensuring that campaigns reach ethnic minority students by placing leaflets and posters in areas around the university most frequently accessed by students from these communities. 49
Studies among people with specific mental health needs
There were 13 studies, published in 16 papers,32–34,38,40–42,44–48,52–55 about seeking or accessing care for specific mental health needs. These studies related to young people with PTSD or trauma (n = 3, already described as part of Refugees/asylum seekers), schizophrenia or psychosis (n = 3), risk/experiences of self-harm (n = 2), eating disorders (n = 3), substance abuse problems (n = 2) and OCD (n = 1).
Post-traumatic stress disorder/trauma
There were three studies in which PTSD or past trauma was the main area of mental health need, reported in six publications, four of which were from the same data set and had the same lead author. 45–48 The other two studies focused on the needs and barriers to care of asylum-seeking children from war-affected countries (Afghanistan,44 and Syria and Libya38).
Key findings and insights from these studies have already been summarised in the section on refugees and asylum seekers as a distinct population group (see Refugees/asylum seekers).
Schizophrenia or psychosis
In three studies, published in three papers, participants were young people with schizophrenia or psychosis. 32,40,52 The key characteristics of these three studies are summarised in Table 7. People with severe mental illnesses such as schizophrenia can be especially stigmatised, and findings related to stigma from these studies are presented in Stigma as a barrier to accessing or seeking help.
| First author, year; city/region | Population of interest | Health/well-being needs/services | Study aims | Methods | Sample | |||
|---|---|---|---|---|---|---|---|---|
| Ethnicity | Age (years) | Other population characteristics | Needs or difficulties | Services | ||||
| Cadge,32 2019; Birmingham | British, Pakistani, Indian, African Caribbean, dual white British and African Caribbean | 18–22 | University students | Schizophrenia | Various | Explore perceptions and understanding of schizophrenia in university students | Semistructured interviews and a thematic analysis | 20 university students |
| Edge,52 2018; North West England | African Caribbean | ≥ 18 | No other characteristics described | Schizophrenia | Community locations and NHS mental health services | To determine whether or not members of the African Caribbean community would be willing to partner with health-care professionals and academics to co-produce a culturally appropriate and acceptable version of an extant evidence-based, cognitive–behavioural model of FI | Four focus groups | 31 service users, family members, professionals, advocates |
| Islam,40 2015; Birmingham | Pakistani, Caribbean, Bengali, African | 18–35 | 50% female/50% male | Psychosis | EI for psychosis services | Examine the cultural appropriateness, accessibility and acceptability of the EI for Psychosis Services in improving the experience of care and outcomes for black and ethnic minority patients | Focus groups | 56 service users, carers, community and third-sector organisations, service commissioner, EI professionals and spiritual care representatives |
These studies highlighted how a lack of cultural adaptation to services can act as a barrier to accessing mental health care or engaging in treatment. For example, in the Edge and Grey52 study, young people from African Caribbean backgrounds suggested that their inclusion in talking therapies could be increased through the use of story-telling, pictures and other non-literary formats of communication. In the Cadge et al. 32 study, care-seeking was also affected by perceptions of the causes being uncontrollable (e.g. genetic) or beyond health care (e.g. spiritual causes). Indeed, in the Islam et al. 40 study, service users suggested that they would be more likely to seek spiritual/religious and/or cultural explanations of symptoms in the first instance. However, when service users recognised severe mental illness, they feared accessing services owing to associations with punishment and being compulsorily detained (‘sectioned’).
Access to formal mental health services might be further hindered by misconceptions about the scope of the care provided by GPs:32
With something that’s a mental illness there has to be some therapy from like experts.
Waqas (pseudonym), Pakistani32
The Islam et al. 40 study echoed the reluctance to see GPs about such problems, but, in this study, this was because parents/carers felt that they would not be listened to and understood.
Self-harm
Two studies, reported in two papers,30,34 specifically focused on self-harm in young people, who were mostly from non-white ethnic backgrounds. Both studies were based on interviews with small samples and included white British young people as well as those from ethnic minority backgrounds. The Klineberg study34 was carried out in younger people who were still at school, including some who had never self-harmed, and The Children’s Society study30 was also not exclusively carried out in those who had self-harmed.
Among young people in both studies, there was a perceived lack of understanding of the help that was available for those self-harming, and a fear of what family or friends might say if they knew. However, in the case of some participants in the study by Klineberg,34 the self-harm was described as a means to alert others of a deteriorating mental state:
I wasn’t a good talker, like, back then, so . . . that’s why I knew that they would kind of help me in some way.
Male, 15 years, Asian, repeated self-harm34
Parents/carers were seen by some young people as more useful and easier to talk to than a mental health service. This view came through even more strongly in The Children’s Society study,30 which also reported that boys find it more challenging to seek help than girls. Teachers were not often approached owing to fears of non-confidentiality, and some participants did not consider self-harm a big enough concern to seek help.
The views of young people who had never experienced self-harm may create shame among those experiencing this mental health issue and, therefore, a barrier to help-seeking. One participant in the Klineberg study34 who had never self-harmed said:
I don’t like people who purposefully like try and attention seeking and like who go to hospital and waste doctors’ time . . . I think if you’re going to do it, yeah, do it properly, yeah? If you really want to hurt yourself, die or whatever, then just do it, yeah?
Female, 15 years, mixed ethnicity34
Eating disorders
Three studies, published in three papers,33,41,53 specifically focused on help-seeking and access to care for young people with eating disorders. One of these studies53 was among South Asian university students and another41 among young people from a range of ethnic minority backgrounds (including those from Pakistani, Bangladeshi, Somali, Yemeni and Indian backgrounds). The third study33 was a qualitative case study mainly based on qualitative re-analysis of an interview with one young British Indian woman with bulimia nervosa.
The study by Chowbey et al. 41 was aimed at understanding barriers to accessing a specialist eating disorder service in Sheffield, and based on interviews with relatives of those with eating disorders, ‘key informants’ (not further elaborated) and community members. The primary challenge identified in the study was a lack of awareness of the problem of eating disorders:
Parents are not aware of eating disorders. I have noticed tell-tale signs in some youngsters but parents are not worried.
Type of participant not given41
In addition, participants in this study41 perceived differential treatment of ethnic minorities in both the diagnosis and treatment of their disorders. This was typically attributed to ineffective or insensitive communication, sometimes leading to misdiagnosis and investigation for physical illness instead of mental health problems. This may compound other barriers to accessing mental health services for ethnic minorities.
It is important to note that, within these studies on eating disorders, there was an extremely broad range of views both between and within the families of participants. However, one common theme was the tension brought about by a young person’s eating disorder, with information provided by relatives and other community members in the Chowbey et al. 41 study suggesting that culture and religion can play a role in this tension (e.g. family members feeling that young people were going against their religion by not eating or different perceptions of body ideals within different cultures):
Religion protects you – torturing yourself is not allowed. If you deny yourself food, Allah will not be happy with you. If you want to die then Allah will not let you.
Type of participant not given41
In our culture if you become very slim they think something is wrong with you. Back home fat is more beautiful and rich, but if you are skinny you are unhealthy and poor.
Type of participant not given41
In the study by Wales et al. ,53 young people from a South Asian background and a focus group of their clinicians in Leicester felt that there was a general lack of knowledge in the community of the risk of developing eating disorders. There was a greater focus on obesity, diabetes and other physical health issues associated with eating problems. Younger people appeared to be more aware of eating disorders and noted that some information on eating disorders had been taught in schools and had been in articles in the media:
I’m more aware of it because of the media, I see programmes about it I see magazine articles.
Female, < 25 years53
Participants in the study by Wales et al. 53 (who were either young people or clinicians) also revealed perceptions that eating disorders were less serious than other mental health issues. Participants believed that posters and leaflets on their own were of limited effect, but could be helpful if used alongside other sources of information, especially when used outside health service settings. Other than suggesting that information should portray a wider range of people who might suffer from eating disorders, participants did not, however, describe what alternative sources of information might be more effective.
Substance misuse
The two studies focused on young people accessing or using services for substance misuse treatment but also included interviews with service providers/stakeholders. 54,55 The Gray and Ralphs study55 investigated Pakistani and Bangladeshi young people’s interaction with substance use services in the north-west of England through interviews with the young people, stakeholders and staff. 55 Gleeson et al. 54 conducted interviews and a focus group with professionals who worked on black and Asian young people’s involvement with substance abuse interventions in the youth justice system in North East England, London and the Midlands.
The study by Gray and Ralphs55 found that alcohol was a taboo topic within the community, and Pakistani and Bangladeshi young people, especially young women, commonly hid their alcohol consumption from their parents/carers. Even when they did engage with the service, young people said they would often be reluctant to take home written materials for fear that their parents would disapprove. To overcome this, programme facilitators emphasised the value of online resources that participants could access confidentially.
Trusting the confidentiality of the programme was a key theme in the study, particularly when the programme was new, as many programme participants did not believe that their participation would be confidential. This was perceived to be the view of a programme facilitator from an Asian background, who had concerns about within-community links with the young person.
Over time, some young people grew to trust the service providers and recommended them to their peers:
People from our school, they all know them [the outreach workers]. People at the youth clubs, they all know them as well, and in the community like, surrounding our area, they all know them.
15-year-old Bangladeshi female55
In the Gray and Ralphs55 study, the staff and partner agencies reported a difference between male and female young people, suggesting that males were more likely to engage with outreach workers when they were out in the community, whereas females were more likely to engage in the school environment. However, one commonality recognised by outreach workers was the importance of extending the service to the young people rather than asking them to access it themselves:
If you were to say to the majority of these children, ‘Right, you’ve to go into [the town centre] to this address’ . . . I think you’d lose 50% straight away.
School-based health-care worker55
In the Gleeson et al. 54 study, the providers suggested that their services might be designed to be best suited to the white males that they mostly work with and that there may be an unconscious racial bias in service provision:
[. . .] it’s still predominantly white males that we do see within our service . . . we’re tailor made to work with that group, subconsciously we have perhaps an unconscious bias that we’re not aware of, or is it because that that’s just what comes through the system?
Regional manager, commissioned provider54
The providers in this study indicated that separate materials should be developed for various ethnic groups to maximise their effectiveness, and said that they had worked with religious leaders to better understand the needs of the community:
What we’ve also done is [. . .] we work with [. . .] the Islamic College for Imans and we brought the Imans in. These were young people from probably about the age of 17, 18, 19 and we re-wrote foundations of recovery with Islamic faith slants.
Regional manager, commissioned provider54
Another deterrent to care-seeking mentioned in this study was that many potential service users assumed that the service was working in conjunction with the criminal justice system.
Barriers to accessing a specialist obsessive–compulsive disorder clinic
Kolvenbach et al. 42 conducted interviews with young people and their parents to investigate barriers to accessing a specialist OCD clinic in London. In this study, only 50% of the participants were from ethnic minority backgrounds. This allowed some comparison within the study of the views and experiences between white and ethnic minority service users and their parents. The most commonly mentioned barrier to access was a lack of knowledge of the support available; this was the case for both white and ethnic minority participants. In addition, parents found it difficult to recognise the symptoms of OCD, which also affected their help-seeking.
One theme that was more evident among ethnic minority participants than white participants was a lack of trust in the system, which appeared to stem from past experience of being failed by the system:
You are supposed to have some trust in the system, which I guess we don’t have now because the system has failed us so badly.
Male, 47 years, black African42
Two parents also indicated that they felt that they were treated differently because of their skin colour:
They just do not see or recognize that person beyond their colour, and it takes a while, even with my daughter it took a while, for them to see past her culture, and see her as a person.
Female, 51 years, black Caribbean
Other barriers to help-seeking revealed in this study were people’s beliefs, culture and religion. When people held beliefs that mental health issues were caused by spiritual or supernatural elements, there was a feeling that conventional mental health services would be ineffective. Instead, some service users felt that their church was a more suitable place to address such issues.
Studies about accessing and engaging with specific interventions
Three of the identified studies35,43,52 investigated the experiences of young people accessing or receiving specific treatments or types of intervention for mental health problems. The studies were among young people or their families engaging with multisystemic therapy (MST),35 young people receiving CBT for mental health problems43 and a family-based talking therapy among African Caribbean young people. 52
Experiences of multisystemic therapy
Bunting et al. 35 focused on access to and experiences of MST for seven young people from a variety of ethnic backgrounds. The study did not state why they were receiving MST, but it is typically offered to families for children with anti-social behaviour. With such a diverse range of parents’ countries of origin and religions, there was a correspondingly diverse range of views expressed. One common theme was that young people felt that their parents did not agree with them accessing mental health care because they felt that it would reflect badly on the family. Other young people felt that their parents/carers thought that their child was just being poorly behaved, and that they could deal with this themselves:
[Compared with physical disability b]ut mentally they don’t count that . . . so you’re just naughty [in Samoa] . . . so my dad was still thinking that at the beginning . . . His way of dealing with it . . . wasn’t . . . seek for help. It was more . . . they deal with it.
Jay (pseudonym)35
In their eyes having a social worker or therapist, it’s like . . . bad to your family, ‘cause in the Congo . . . it’s like reputation, innit? Family name . . . you got to keep your family name as pride.
Tatiana (pseudonym)35
In addition, some young people believed that their parents felt the MST service was dictating how they should raise their children.
Another common view expressed by young people in the Bunting et al. 35 study was that having a therapist from a similar ethnic background was beneficial in building a relationship and aiding understanding between the therapist and service user:
It would help if it were someone from the same culture, or before they came, they would know about the culture, and research.
Safaa (pseudonym)35
If someone comes from a different culture, that’s judging on mum’s culture, is saying . . . ‘you’re doing something wrong’ . . . she’ll automatically be like ‘no, I’m not.’
Aisha (pseudonym)35
However, this was not true for all participants, with some feeling that anyone who is qualified to help them is suitable:
Some families would prefer a black social worker? . . . I’ve just always thought that whoever can help me . . . can help me . . . they might talk differently or . . . have different perspectives but . . . in the end they all have the same . . . training.
Jay (pseudonym)35
Improving the cultural acceptability of a family-based talking therapy
Edge and Grey52 investigated ways of improving the cultural awareness and acceptability of a family-based mental health intervention through interviews with young people, family members, care professionals and mental health advocates in schizophrenia care. The young people in this study were African Caribbean, and participants agreed that some form of talking therapy would be beneficial for those from their background. Having considered the model being used in the study, participants were invited to make suggestions about how the intervention could be better tailored to young people of their culture and background. A key theme that emerged was the idea of using non-verbal methods of communication such as story-telling and imagery. There was consensus that this both was culturally appropriate and could maximise inclusion for those in need, irrespective of their language skills or level of education.
The young people in this study also spoke of difficulties arising as a result of cultural differences between them and their talking therapy facilitators, clearly indicating a perceived lack of cultural awareness and understanding by the facilitators:
[about talking therapy or cognitive therapy] . . . I realise that most of the therapy is being given by middle class white Europeans who don’t really know the black agenda . . . it’s like there’s a gap there.
African Caribbean male service user, focus group 152
Receiving cognitive–behavioural therapy for mental health problems
The study by Gurpinar-Morgan et al. 43 included young people from various ethnic minorities (‘BAME’ not specified) in North West England who were receiving CBT, and looked at the impact of ethnicity on both the therapeutic relationship and the presenting mental health difficulties. There was a particular emphasis on exploring the impact of cultural differences between therapists and service users. It was generally suggested by the young people that differences in ethnic backgrounds could be barriers to successful CBT unless adjustments were made:
Well I kind of thought that maybe he wouldn’t understand where I was coming from because of how I grew up and I didn’t think he’d grew up like that.
Amaya43
I don’t think the young person would straight away talk about it. I think it needs the psychologist to like edge them on to ask questions about it.
Laila43
The majority of participants felt that it was important that therapists discussed their personal differences early on in their relationship. Conversely, others felt that they should not rush into discussions about their differences, instead leaving it to come up more naturally during the sessions. Despite these different views, most participants appreciated their therapist opening up about their own background.
In addition, the majority of young people in the Gurpinar-Morgan et al. 43 study felt that it was appropriate to discuss their differences with their therapist, although others felt that such a conversation would be awkward:
. . . it would just keep coming up in my brain . . . how different we are . . . if we talked about how different we are and it would have made me felt uncomfortable . . .
Amaya43
Stigma as a barrier to accessing or seeking help
Seven studies, reported in 10 papers,32,33,38,40,44–48,50 focused on or yielded specific findings relating to social stigma as a barrier to care-seeking or accessing support for mental health problems (four publications by Majumder et al. 45–48 were from the same study). Social stigma could deter care-seeking in two ways: it could relate to anticipated stigma owing to the perceptions of others about the young person’s own problems, or to stigma and fears held by the young person about the services or places/hospitals where other people with mental health problems are being assessed and treated.
Table 8 shows the key characteristics and findings of the papers that yielded specific findings about social stigma.
| First author, year; city/region | Population of interest | Need or difficulty | Service context | Types and sources of stigma identified |
|---|---|---|---|---|
| Cadge,32 2019; Birmingham |
University students British, Pakistani, Indian, African Caribbean, dual white British and African Caribbean ethnicity |
Schizophrenia | Various |
A lack of knowledge contributes to significant stigma of schizophrenia, as there are misconceptions about the symptoms and effects It is a taboo subject and therefore often fails to be discussed in a community, even more so in Indian, Pakistani and African Caribbean communities. Schizophrenia is also not to be associated with because of its image and the perception of the individuals as dangerous |
| Channa,33 2019; West Midlands |
Young adults Most (n = 22) white British; n = 1 each were Philippine, Indian, Pakistani, Chinese; n = 4 were of mixed ethnicity |
Bulimia nervosa | Eating disorder service |
Mental health not openly talked about in family or wider culture; sense of shame and denial around psychological issues Self-stigma: living with the fact that you have an illness makes diagnosis harder. Do not want to take medication for the condition, as that makes it real |
| Davies Hayon,44 2019; UK |
Various ages (literature review) Refugees/asylum seekers (mostly unaccompanied), most from Afghanistan |
Primarily PTSD, depression and anxiety | Schools and community centres | Fear of hospitals associated with the stigma of people with mental illness. Denial. People with mental health problems were socially excluded and the label invited mockery. Negative attitudes towards mental illness |
| Hurn,38 2018; West Yorkshire |
Children (aged 6–11 years) Refugees/asylum seekers from Syria and one from Libya |
Trauma, one participant had ADHD | CHUMS: mental health and emotional well-being service | Culturally rooted (Arab). Interpreters were valuable in helping understand the stigma and emphasising it and the importance of culturally sensitive language |
| Islam,40 2015; Birmingham |
Young adults Pakistani, Caribbean, Bengali, African |
Psychosis | Early intervention for psychosis services | Stigmatising community attitudes mean more religious help-seeking instead of psychiatric help. Stigma may come from a lack of education. Early intervention services designed to improved access in low-stigma communities. Stigma delayed help-seeking in all groups, particularly South Asian communities. Worried about mental health affecting marriage propositions |
| Majumder,45–48 2015, 2016, 2019 and 2019; central England | Unaccompanied refugee minors, mostly from Afghanistan, but also from the Islamic Republic of Iran, Somalia and Eritrea | Predominantly PTSD, depression and self-harm | CAMHS, among others | Triple stigma – discrimination based on their refugee status, having a mental health problem and being unaccompanied or being in care. Mental health issues can be even more stigmatised in some cultures, discouraging talking about it. Negative perceptions of the concept of mental illness, anticipated social implications of suffering from mental illness and denial of mental illness all contribute to the stigma, and therefore avoidance of help-seeking |
| Rowland,50 2016; Hackney |
Children and young people Orthodox Jewish |
Unspecified/various | Tier 2 NHS mental health services | Fears of being labelled and therefore excluded from the community are a significant barrier. As arranged marriages are common, a mental health illness can bring that label to the whole family, rather than just the diagnosed individual, and these judgements are derogatory and stay with the family for life. The community are, however, slowly becoming more open-minded, and parents are still prioritising accessing proper care over the stigma |
Several studies highlighted stigma as a theme, and, across nearly all the included studies, misconceptions of what it means to have a mental illness were significant barriers to help-seeking, diagnosis and compliance with taking medication. These effects seem to be magnified when there was both community and self-based stigma.
Social stigma
Negative community and social attitudes were a barrier for children of refugee status, members of Orthodox Jewish communities, and young adults from black and minority ethnic communities. Studies exploring the experiences of refugee or asylum-seeking children (Majumder et al. ,45–48 Davies Hayon and Oates,44 Hurn and Barron38) highlighted the ‘triple stigma’ of having mental health needs while also being of refugee status and being in care. Anticipated concerns included being socially excluded, the risk of being mocked and fear of hospitals. One study,50 of Orthodox Jewish children and young people, reported fears of labelling, community exclusion and negative impacts on marriage, although the community was reported as slowly becoming more open. Another study40 of young adults from black and minority ethnic communities revealed concerns about the impacts of mental illness on marriage proposals.
Lack of understanding
Participants in several studies revealed how a lack of understanding of mental ill health, often associated with fears, could increase stigma. One study32 explored attitudes to schizophrenia in university students from a range of backgrounds, whereas another40 focused on attitudes to psychosis in young adults from black and minority ethnic communities. These studies included reports of mental health issues being seen as a taboo subject, and perceptions of schizophrenia being dangerous. A lack of education about mental health was seen as a barrier, with reports of delayed help-seeking and religious help-seeking instead of seeking psychiatric help.
Self-stigma
In contexts in which mental health was not talked about, the impact of community stigma could be amplified by self-stigma, as these attitudes were internalised by individuals. For example, in a study33 of young adults with a focus on bulimia nervosa, a British Indian young woman reported how self-stigma could bring about an internalised sense of shame and denial of problems.
Studies on access to other resources or support
Potential benefits of nature to mental health
Rather than investigating access to formal mental health services, Birch et al. 31 conducted a study looking at the perceived impacts of access to nature on mental well-being for young people from various ethnic groups (including some white British young people). The study involved young people from a range of backgrounds, including asylum seekers, in an urban community setting. It identified several strands of potential benefits (of closeness to nature) to mental health and well-being, namely a sense of self, a sense of escape, and a sense of connection and care. However, apart from the authors suggesting that refugee young people might particularly value these benefits, the study did not comment on whether young people from ethnic minority backgrounds had poorer access to nature or why this might be.
Chapter 5 Discussion
Summary of main findings
This rapid scoping review identified 22 qualitative research studies (published from 2012 onward) on the experiences of young people from ethnic minority groups regarding access to or ongoing retention/engagement with mental health care and support. The review had a broad scope of inclusion (ethnic minority groups were broadly defined; participants could include relatives, service providers, commissioners and referrers as well as the young people themselves; and ‘mental health care and support’ could include specialist, third-sector and any other alternative provision or support). Given this broad remit, it is unclear whether 22 qualitative research studies is more or less research than might be expected to understand this important topic from the perspectives of young people, their parents and others.
Several priority topics related to young people’s access to mental health services within the UK are either not covered by the included literature or only briefly touched on in relation to one specific minority group. For example, the included studies did not investigate access issues in relation to transition from child to adult services, or focus on access to treatment for common mental health problems such as anxiety and depression.
A full commentary on potential gaps in the literature (and whether they are important gaps relative to people from ethnic minorities, service providers or policy-makers) is beyond the scope of this review. However, the studies that were identified provided detailed preliminary insights into the experiences of young people from various ethnic backgrounds in a variety of regions and cities accessing or trying to access a wide range of mental health-care support.
We found evidence that had been conducted:
-
among university students (n = 4 studies32,49,51,53) and refugees/asylum seekers (n = 5 studies31,36–39,44–48) experiencing a variety of mental health problems, and from a range of ethnic backgrounds
-
among those in ethnic minorities from specific cities or regions who were experiencing or needing care for particular mental health needs/conditions – schizophrenia or psychosis (n = 3 studies32,40,52), eating disorders (n = 3 studies27,41,53), PTSD/trauma (the five studies31,36–39,44–48 among refugees/asylum-seeking young people), self-harm (n = 2 studies30,34), OCD (n = 1 study42), and users of substance misuse services (n = 2 studies54,55)
-
among those in some ethnic minorities from specific cities or regions who were receiving particular types of treatment or intervention (n = 1 study in young people or their families engaging with multi-systemic therapy,35 n = 1 study in young people receiving CBT for mental health problems,43 and n = 1 study in African Caribbean young people taking part in family-based talking therapy52)
-
to look at the perceived impacts of access to nature in urban settings on mental well-being for young people from various ethnic groups (n = 1 study31).
Encouragingly, most of this research has been based on interviews or focus groups with the ethnic minority children or young people themselves. Only 341,50,54 of the 22 studies did not include some data from the children or young people whose mental health needs were of interest. Other studies combined data from interviews of the young people with interviews or focus groups with parents/carers or family members. The views and experiences of care professionals or care provider organisations were collected and analysed in only six studies,38,40,41,52–54 whereas the views or experiences of service commissioners were captured in only one study. 40
In contrast to describing the types of mental health needs, services or ethnic groups for which there is research evidence, it is harder to specify where there is no evidence, or not as much as one might expect or want. Fewer than one-third of the included studies were wholly (or mostly) conducted in a particular ethnic minority group;44–48,52,53,55 such studies might reveal distinctive barriers to accessing care related to family and community circumstances, or the cultural beliefs of the young people, families and communities from those specific ethnic minority backgrounds. Two studies51,54 analysed experiences from both black and South Asian ethnic backgrounds within the same study, but did not set out to distinguish any differences in experience that may have been associated with the different ethnicities. The majority of studies involved young people or their parents/carers from a much wider range of ethnic backgrounds within a particular city or region, sometimes also including white British young people in the sample. That, and the fact we have not formally synthesised study findings, means any generalisation of these findings to other places, services or to specific ethnic minorities would be highly uncertain.
There were relatively few studies in younger children (< 15 years old), or studies of access to services and support linked to schools. Anxiety and depression are the most common forms of mental ill health in children and adolescents. However, there were surprisingly few studies that explicitly focused on access to care and support for these more common mental health issues (except one study34 focusing on self-harm, and perhaps indirectly the study43 on accessing CBT and the two33,53 on eating disorders).
Nevertheless, the included studies do indicate a range of potential factors that influence access to and engagement with mental health care that may be relevant to young people from different ethnic minorities experiencing mental health difficulties. The factors highlighted by authors of some of the included studies were as follows:
-
Lack of awareness and knowledge about some mental health issues/conditions, sometimes including underappreciation of the seriousness and misunderstanding of the causes of the conditions, both of which could deter care-seeking.
-
Lack of trust in care professionals, potentially due to perceptions of services or professionals operating in a way that is not culturally sensitive and/or past experiences of feeling let down by services. Note that, among refugees or asylum seekers, this distrust had different root causes (such as fear of links to the justice/asylum system and language differences) and different manifestations (such as resistance to paper form-based assessment or therapy exercises).
-
Lack of awareness/lack of information about available services and support for mental health difficulties.
-
Social stigma – either self-perceived by the young person and/or embedded in and related to the services and institutions providing care.
-
Culture-, community- and religion-specific reasons for either hiding/suppressing the admission of having mental health difficulties, or for seeking support from informal or alternative sources rather than mainstream mental health services.
-
Differing expectations about mental resilience and levels of ease in talking about problems between different ethnic groups, and between boys/young men and girls/young women within particular ethnic groups.
Strengths
This rapid scoping review was conducted by an experienced team of reviewers according to a prespecified protocol and with input from researchers and clinicians with relevant clinical and care provision experience. Our searches were comprehensive, and were developed and conducted by an experienced information specialist (SR). The review team also systematically extracted relevant standard information from each study and independently assessed the quality of included studies using established criteria.
The majority of included studies were judged to be of good quality in terms of their methods and reporting, although nine met fewer than 10 out of the 13 ‘Wallace’28 study quality criteria. In addition, as far as possible, we have ensured that this report meets the relevant Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews. 56 Many of the studies had been published quite recently (see Figure 2), which means that they may be more applicable to current services and policies, although there is typically a time lag of 1 or 2 years between data collection and publication.
Limitations
For systematic reviews, there are two main sources of limitations: those related to the review methods, and those related to the studies ultimately found and included.
Limitations of our review aims and methods
Perhaps the main limitation of this scoping review is that it is a scoping review, and we have therefore not formally synthesised any of the findings across studies. 16,18 A formal qualitative evidence synthesis, for example using approaches such as meta-ethnography or meta-narrative synthesis,57,58 would take considerably more time and reviewer resources than were available to conduct this review. Even a more pragmatic method of qualitative evidence synthesis that produces an overarching thematic analysis, such as framework synthesis,59 would have taken several months to conduct properly. Instead, we have briefly summarised some of the study authors’ main findings from each study that relate to our review questions, and compared and contrasted them within groups of studies where it seemed relevant or avoided repetition of similar points.
More obviously, by focusing on only qualitative research, we have not captured the kinds of insights that quantitative or mixed-methods studies would be more likely to capture. By definition, and by virtue of their aims and small scale, qualitative studies capture the perceptions around accessing care and support, and people’s conscious attributions of why they seek care or engage with services in the way they do (or why not). As others have argued, whether or not such factors lead to inequitable service use requires large quantitative studies that measure and interpret ethnic variations in service use, in conjunction with a standardised assessment of risk factors, disease characteristics and patient preferences. 2
We chose to organise our findings along the overlapping dimensions of population/setting type, type of mental health need/service or those receiving specific interventions. It is possible that use of a more explicit logic model (e.g. of predefined mechanisms of poor health-care access, or of stages of access and engagement with support and services) may have enabled different insights from studies. 60 Certainly, any future formal evidence synthesis should consider using such a framework.
There are several further limitations. First, we have searched for and included studies from 2012 onward only. There may have been earlier studies that would have yielded valuable insights, or filled gaps in the types and focus of studies we have found. We included only studies published from 2012 onward because our policy customers thought that evidence from before 2010 would be too far back and much less relevant; the new Health and Social Care Act21 and No Health Without Mental Health22 strategy, introduced in England in 2012 and 2011, respectively, brought major shifts in the funding and commissioning of mental health services.
Second, the speed with which this review had to be conducted (over 4 months) meant that we were not able to engage with relevant stakeholders as much or as early in the process as we would have liked. In particular, the review team would have liked to engage more with young people with lived experience of mental health difficulties and/or using mental health services from a variety of ethnic backgrounds. Nevertheless, through an intermediary organisation (Healthy Teen Minds), we were able to recruit three young black people (via a relevant online network/e-mail list) who provided comments on our findings and helped craft our Plain English summary.
Finally, as both a rapid review and a scoping review – primarily to describe the scale and nature of what research exists, rather than to comprehensively summarise what the research found – we have not been able to situate and compare our results to wider literature (e.g. on young people’s access to mental health care or access to public services by people from ethnic minority backgrounds). This literature of course exists,61–63 but, with time constraints and limited access to specialist topic experts, we were not able to properly engage with and compare our findings with this wider discourse.
Limitations of the evidence found
Only a minority of studies were in specific, named ethnic minority groups, and five of our included studies provided evidence from a mixture of young people including both white British and various ethnic minority backgrounds; these studies often did not distinguish which findings, themes or quotations were from young people of particular ethnic backgrounds. It was therefore not possible to know whether the identified themes and issues reflected the experiences of the non-white British participants in general, or whether non-white British study participants from different minority ethnic backgrounds may have experienced care or barriers to access differently.
Although finding 22 studies, including five from among refugees/asylum seekers, from the last 9 years may seem like an encouraging and useful amount of qualitative research on these issues, there are inevitably other groups/conditions/services regarding which research might be needed. For example, although over the last 10 years there has been a major shift in policy and service provision towards trying to increase access to psychological therapies for common mental health problems (and dedicated Improving Access to Psychological Therapies services to achieve this for adults), none of our studies had investigated access to such services for those from ethnic minority groups (although there was one study of how ethnic minority adolescents experienced using CBT within CAMHS). Similarly, there were no studies on why and whether children, their parents/carers or other young people from ethnic minorities seek (or do not seek) care from their GP for mental health difficulties. Given that the age range of young people for this review included both children and adults (aged 10–24 years), it is perhaps also surprising that there were no studies looking at how children and their parents/carers from ethnic minorities experience the transition from children’s services/CAMHS to adult mental health services, and whether this transition embeds, narrows or expands inequalities in accessing mental health care.
In relation to the review’s broad inclusion criteria, we searched for but did not identify any studies conducted in Arab, Chinese or South-East Asian people (unless within refugee/asylum-seeking populations), or in Gypsy or Irish Traveller people. We also found no studies that were specifically aimed at understanding care-seeking, access to care or service engagement by those from ethnic minorities who have the following mental health conditions or difficulties: personality disorders, conduct disorders, disorders of sleep, somatoform disorders, ADHD, gender dysphoria, general stress (although, arguably, this was the de facto focus along with PTSD in many of the studies in refugee young people) or autism/social communication disorders and/or learning disabilities (where the primary focus was on mental health).
Although it is valuable that so many of the studies were based directly on the verbatim experiences of young people themselves, and sometimes also their parents/carers, often the samples were very small and from limited geographic areas or localities. Most studies had been conducted in large cities, and in the north of England, the Midlands or London. More studies involving multiple perspectives and informants (e.g. clinician/practitioners, service commissioners, school teachers) may have yielded complementary insights on service design, management/staffing and resource-related barriers to improving the accessibility of services. If future studies do include subsamples of different groups (e.g. service users, care professionals, parents), then it is paramount that the source of quotations, and the attributions of particular themes or other insights, are better reported than was the case in some of the studies included in this review. This may require a more comparative element to the study design, sampling and data analysis.
Chapter 6 Conclusions
We found 26 papers or reports, describing 22 diverse qualitative studies, meeting our inclusion criteria. Most of the studies were well conducted and clearly described.
There were studies of refugees/asylum seekers (n = 5 studies), university students (n = 4) and studies among young people experiencing particular mental health problems: schizophrenia or psychosis (n = 3, including one of university students), eating disorders (n = 3, one of university students), PTSD (n = 3, all of asylum seekers), substance misuse (n = 3), self-harm (n = 2) and OCD (n = 1). There were also three studies in ethnic minority young people who were receiving particular mental health treatments: families engaging with multisystemic therapy, young people receiving CBT, and African Caribbean young people taking part in family-based talking therapy.
Most studies had been conducted with young people or their parents from a range of different ethnic backgrounds. However, nine studies were about young people from particular ethnic groups: asylum seekers from Afghanistan (n = 2), and black and South Asian (n = 2), black African and black Caribbean (n = 2), South Asian (n = 1), Pakistani or Bangladeshi (n = 1) and Orthodox Jewish (n = 1) people.
We searched for but did not identify any qualitative studies conducted in Arab, Chinese or South-East Asian people (unless in small numbers within refugee/asylum-seeking populations), or in Gypsy or Irish Traveller people. We also found no studies that were specifically aimed at understanding care-seeking, access to care or service engagement by those from ethnic minorities with the following mental health conditions or difficulties: personality disorders, conduct disorders, disorders of sleep, somatoform disorders, ADHD, gender dysphoria, general stress, or those with autism/social communication disorders and/or learning disabilities (where the primary focus was on mental health).
Implications for future research
The quality and usefulness of future qualitative research and other studies in this area could be improved by the following:
-
Purposively sampling young people and/or their parents from particular ethnic minority groups to be able to identify recurring experiences, issues or factors that explain poor access to care, poor engagement with services, or poor cultural adaptation or racist practices within services that might be distinctive to particular ethnic minority groups, or experienced in a different way by them. Purposively sampling in qualitative studies to also gain a diversity of experiences from enough boys/men and girls/women to understand gender differences in how they experience mental health problems and services.
-
Conducting larger, qualitative studies with purposive sampling that enable separate and comparative analysis of the experiences of those in different minority ethnic groups would also be useful to identify factors that are specific to particular groups. Larger samples might also allow more valid and trustworthy insights about how ethnic identity and cultural beliefs affect boys/young men, or girls/young women differently (or those with other gender identities), for example in relation to acknowledging, talking about and seeking care for mental health problems, or understanding practitioner and service accessibility.
-
Including data from multiple stakeholders’ perspectives – importantly, from young people and their parents/carers, but also from community members and service providers, service commissioners and other professionals. In addition, studies would ideally cover multiple regions, including rural areas, with related variations in local population need, service configurations and accessibility.
-
Focusing on the different routes to mental health care/support followed by those from ethnic minority groups – not exclusively on the experiences of those who manage to access specific services. There was a particular lack of qualitative evidence from those professionals, whether in the NHS or in schools, who might identify and refer children and young people experiencing mental health difficulties to other services.
-
Focusing on how children and young people from ethnic minority backgrounds experience being supported by multiple teams or services, for example when there are complex needs and factors involved (mental health and physical health services, mental health and social care).
-
Focusing on how the (lack of) ethnic diversity in the mental health workforce shapes the experiences of children and young people seeking support for their mental health, and their willingness to engage with and trust those providing such support.
-
Better reporting, especially in terms of describing the methods of data collection adequately. For example, future studies need to make explicit the theoretical or ideological/cultural (including ethnic) perspective of the authors, showing greater consideration to any limitations of the methods or data that may have affected the results, and more carefully basing any claims to generalisability on the strength and plausibility of the data, and the integrity of any themes and theoretical insights produced. Also, the demographic (including ethnic identity) characteristics of the originator of all quotations could be more consistently reported in qualitative studies.
More nuanced and context-sensitive insights may also be yielded by conducting a more formal evidence synthesis of selected groups of qualitative studies summarised in this scoping review. For example, synthesising qualitative evidence from the four studies about university students, or the five studies about refugees/asylum seekers might yield more detailed and context-sensitive insights for improving access to mental health support and services for young people in those situations and settings. Such formal evidence synthesis should consider using an explicit theory or logic model for understanding access to health-care services.
These are just preliminary suggestions, based on the apparent evidence gaps and shortcomings in study quality that we have identified. Stronger recommendations for commissioners of research would require a more collaborative, comprehensive and inclusive engagement process with a wider range of stakeholders than was possible within our short project. Such a research priority-setting exercise could compare the ‘gaps’ in evidence about ethnic groups, mental health needs or services for which there is no or little evidence (as identified by our review) with those mental health needs, contemporary service developments or policy changes that are of particular importance to ethnic minority children, young people, their parents/carers and other stakeholders.
A recent research priority-setting exercise by the McPin Foundation (with guidance from the James Lind Alliance) was conducted in 2017 about interventions and services for children and young people’s mental health,64 and it echoes some of the findings from our review. The McPin Foundation’s consultation with young people produced a wide range of mental health research priorities, including priority 11 – ‘How can the number of effective culturally appropriate approaches available in children and young people’s mental health services be increased, particularly for ethnic minority groups?’. 64 As well as being an important stand-alone question, the young people consulted wanted this question to be a consideration within every one of the top 10 priorities identified.
Acknowledgements
The Exeter HSDR Evidence Synthesis Centre’s team would like to thank Professor Kam Bhui (University of Oxford) and Dr Julian Edbrooke-Childs (University College London) for their clinical and service knowledge in informing the review protocol and commenting on the review’s draft findings. We thank Stuart Dodzo, Co-production and People Coordinator at Healthy Teen Minds (https://healthyteenminds.com/), who facilitated three young black men commenting on our Scientific Summary and Plain English summary. We thank these three young men for their thoughtful feedback. We would also like to thank members of the mental health policy team at the Department of Health and Social Care for their clear guidance on the scope and policy need for the review, and for feedback on the first draft of our review findings and discussion sections. Sincere thanks also go to Sue Whiffin and Jenny Lowe for administrative support throughout this review. We also thank three anonymous reviewers whose extremely knowledgeable and constructive comments on the draft of this report have, we believe, improved it.
Lastly, this work could not have been undertaken without the collegial collaboration of GJ Melendez-Torres and Lou Crathorne of the Peninsula Technology Assessment Group (PenTAG); co-authors Helen Coelho, Fraizer Kiff, Laura Trigg and Sophie Robinson were either temporarily seconded from the PenTAG team and/or working additional hours to enable this review to be delivered.
Contributions of authors
Helen Coelho (https://orcid.org/0000-0002-4799-4300) (Research Fellow) led the drafting of the review protocol and project planning and management (until the end of July 2021). She contributed to screening search records; researching and drafting the report’s background section; crafting the review findings; and drafting, editing and finalising the final publication.
Anna Price (https://orcid.org/0000-0001-9147-1876) (Research Fellow) contributed to the drafting of the review protocol and project planning and management (until the end of September 2021); screening of search records and full-text publications; advising and supporting Fraizer Kiff and Laura Trigg in assessing qualitative research studies; crafting of the review findings; and drafting, editing and agreeing the final publication.
Fraizer Kiff (https://orcid.org/0000-0002-6008-3907) (Graduate Research Assistant) contributed to screening of full-text publications; data extraction; study quality assessment; drafting of the review findings; and drafting, editing and finalising the final publication.
Laura Trigg (https://orcid.org/0000-0002-8447-2616) (Graduate Research Assistant) contributed to screening of full-text publications; data extraction; study quality assessment; drafting of the review findings; and drafting, editing and finalising the final publication.
Sophie Robinson (https://orcid.org/0000-0003-0463-875X) (Information Specialist) led the design and conduct of the searches; managed the EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] databases; and contributed to the drafting of the review protocol, screening of search records, drafting of the review methods, and editing and finalising the final publication.
Jo Thompson Coon (https://orcid.org/0000-0002-5161-0234) (Professor of Evidence Synthesis and Health Policy) contributed to the drafting and finalising of the review protocol, project planning and management, screening of search records, crafting of the review methods and findings, and editing and finalising the final publication.
Rob Anderson (https://orcid.org/0000-0002-3523-8559) (Professor of Health Services and Implementation Research) led and provided academic oversight of the project; co-ordinated the recruitment and engagement with clinical and policy stakeholders; led the drafting of the discussion, conclusions, scientific summary, abstract and Plain English summary; and contributed to editing and finalising the final publication.
Data-sharing statement
All studies and data used to produce this report is in the public domain. Data (such as EndNote search files, data extraction tables or search strategies) can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS Digital . Mental Health of Children and Young People in England, 2020: Wave 1 Follow Up to the 2017 Survey 2020. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2020-wave-1-follow-up (accessed 7 September 2021).
- Essink-Bot ML, Lamkaddem M, Jellema P, Nielsen SS, Stronks K. Interpreting ethnic inequalities in healthcare consumption: a conceptual framework for research. Eur J Public Health 2013;23:922-6. https://doi.org/10.1093/eurpub/cks170.
- National Collaborating Centre for Mental Health . Advancing Mental Health Equality 2019. www.rcpsych.ac.uk/improving-care/nccmh/care-pathways/advancing-mental-health-equality (accessed 7 September 2021).
- Department of Health and Social Care . Modernising the Mental Health Act. Increasing Choice, Reducing Compulsion. Final Report of the Independent Review of the Mental Health Act 1983 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/778897/Modernising_the_Mental_Health_Act_-_increasing_choice__reducing_compulsion.pdf (accessed 7 September 2021).
- Goodman A, Patel V, Leon DA. Child mental health differences amongst ethnic groups in Britain: a systematic review. BMC Public Health 2008;8. https://doi.org/10.1186/1471-2458-8-258.
- Halvorsrud K, Nazroo J, Otis M, Brown Hajdukova E, Bhui K. Ethnic inequalities in the incidence of diagnosis of severe mental illness in England: a systematic review and new meta-analyses for non-affective and affective psychoses. Soc Psychiatry Psychiatr Epidemiol 2019;54:1311-23. https://doi.org/10.1007/s00127-019-01758-y.
- Vostanis P, Svirydzenka N, Dugard P, Singh S, Dogra N. Mental health service use by adolescents of Indian and white origin. Arch Dis Child 2013;98:764-7. https://doi.org/10.1136/archdischild-2013-303772.
- Edbrooke-Childs J, Newman R, Fleming I, Deighton J, Wolpert M. The association between ethnicity and care pathway for children with emotional problems in routinely collected child and adolescent mental health services data. Eur Child Adolesc Psychiatry 2016;25:539-46. https://doi.org/10.1007/s00787-015-0767-4.
- Edbrooke-Childs J, Patalay P. Ethnic differences in referral routes to youth mental health services. J Am Acad Child Adolesc Psychiatry 2019;58:368-75.e1. https://doi.org/10.1016/j.jaac.2018.07.906.
- Chui Z, Gazard B, MacCrimmon S, Harwood H, Downs J, Bakolis I, et al. Inequalities in referral pathways for young people accessing secondary mental health services in south east London. Eur Child Adolesc Psychiatry 2021;30:1113-28. https://doi.org/10.1007/s00787-020-01603-7.
- Walker S, Barnett P, Srinivasan R, Abrol E, Johnson S. Clinical and social factors associated with involuntary psychiatric hospitalisation in children and adolescents: a systematic review, meta-analysis, and narrative synthesis. Lancet Child Adolesc Health 2021;5:501-12. https://doi.org/10.1016/S2352-4642(21)00089-4.
- Reardon T, Harvey K, Baranowska M, O’Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatry 2017;26:623-47. https://doi.org/10.1007/s00787-016-0930-6.
- Medical Research Council . Mental Health Research Goals 2020 to 2030 2020. https://mrc.ukri.org/documents/pdf/mental-health-research-goals-2020-2030/ (accessed 18 October 2021).
- Department of Health and Social Care . A Framework for Mental Health Research 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/665576/A_framework_for_mental_health_research.pdf (accessed 18 October 2021).
- Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291-4. https://doi.org/10.1016/j.jclinepi.2014.03.013.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol 2016;16. https://doi.org/10.1186/s12874-016-0116-4.
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0611-x.
- Anderson R, Coelho H, Price A, Robinson S, Thompson-Coon J. Rapid Review of the Scope and Nature of Qualitative Evidence on the Experiences of Children and Young People from Ethnic Minorities in Accessing and Engaging With Mental Health Care and Support in the UK: Review Protocol 2021. osf.io/wa7bf (accessed 5 October 2021).
- White E. 2011 Census: Key Statistics for England and Wales, March 2011. Newport: Office for National Statistics; 2012.
- Great Britain . Health and Social Care Act 2012 2012. www.legislation.gov.uk/ukpga/2012/7/contents/enacted (accessed 12 June 2022).
- Department of Health and Social Care . No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages 2011. www.gov.uk/government/publications/the-mental-health-strategy-for-england (accessed 21 October 2021).
- Mental Health Taskforce . The Five Year Forward View for Mental Health: A Report from the Independent Mental Health Taskforce to the NHS in England 2016. www.england.nhs.uk/mental-health/taskforce/ (accessed 21 October 2021).
- NHS England . The NHS Long Term Plan 2021. www.england.nhs.uk/long-term-plan/ (accessed 21 October 2021).
- Office for National Statistics . 2011 Census Analysis: Ethnicity and Religion of the Non-UK Born Population in England and Wales: 2011 2015. www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/2011censusanalysisethnicityandreligionofthenonukbornpopulationinenglandandwales/2015-06-18 (accessed 12 June 2022).
- Ayiku L, Levay P, Hudson T, Craven J, Barrett E, Finnegan A, et al. The Medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID Medline. Health Info Libr J 2017;34:200-16. https://doi.org/10.1111/hir.12187.
- Wong SS-L, Wilczynski NL, Haynes RB, Hedges T. Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform 2004;107:311-6. https://doi.org/10.1186/1741-7015-2-23.
- Wallace A, Croucher K, Quilgars D, Baldwin S. Meeting the challenge: developing systematic reviewing in social policy. Policy Polit 2004;32:455-70. https://doi.org/10.1332/0305573042009444.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- The Children’s Society . Waiting in Line: Stories of Young People Accessing Mental Health Support 2020.
- Birch J, Rishbeth C, Payne SR. Nature doesn’t judge you – how urban nature supports young people’s mental health and wellbeing in a diverse UK city. Health Place 2020;62. https://doi.org/10.1016/j.healthplace.2020.102296.
- Cadge C, Connor C, Greenfield S. University students’ understanding and perceptions of schizophrenia in the UK: a qualitative study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-025813.
- Channa S, Lavis A, Connor C, Palmer C, Leung N, Birchwood M. Overlaps and disjunctures: a cultural case study of a British Indian young woman’s experiences of bulimia nervosa. Cult Med Psychiatry 2019;43:361-86. https://doi.org/10.1007/s11013-019-09625-w.
- Klineberg E. How do adolescents talk about self-harm: a qualitative study of disclosure in an ethnically diverse urban population in England. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-572.
- Bunting A, Fox S, Adhyaru J, Holland A. Considerations for minority ethnic young people in multisystemic therapy. Clin Child Psychol Psychiatry 2021;26:268-82. https://doi.org/10.1177/1359104520969762.
- Fazel M. A moment of change: facilitating refugee children’s mental health in UK schools. Int J Educ Dev 2015;41:255-61. https://doi.org/10.1016/j.ijedudev.2014.12.006.
- Fazel M, Garcia J, Stein A. The right location? Experiences of refugee adolescents seen by school-based mental health services. Clin Child Psychol Psychiatry 2016;21:368-80. https://doi.org/10.1177/1359104516631606.
- Hurn R, Barron I. The EMDR integrative group treatment protocol in a psychosocial program for refugee children: a qualitative pilot study. J EMDR Pract Res 2018;12:208-23. https://doi.org/10.1891/1933-3196.12.4.208.
- King D, Said G. Working with unaccompanied asylum-seeking young people: cultural considerations and acceptability of a cognitive behavioural group approach. Cogn Behav Ther 2019;e11. https://doi.org/10.1017/s1754470x18000260.
- Islam Z, Rabiee F, Singh SP. Black and minority ethnic groups’ perception and experience of early intervention in psychosis services in the United Kingdom. J Cross Cult Psychol 2015;46:737-53. https://doi.org/10.1177/0022022115575737.
- Chowbey P, Salway S, Ismail M. Influences on diagnosis and treatment of eating disorders among minority ethnic people in the UK. J Public Ment 2012;11:54-6. https://doi.org/10.1108/17465721211236363.
- Kolvenbach S, Fernández de la Cruz L, Mataix-Cols D, Patel N, Jassi A. Perceived treatment barriers and experiences in the use of services for obsessive-compulsive disorder across different ethnic groups: a thematic analysis [published online ahead of print 26 October 2016]. Child Adolesc Ment Health 2018. https://doi.org/10.1111/camh.12197.
- Gurpinar-Morgan A, Murray C, Beck A. Ethnicity and the therapeutic relationship: views of young people accessing cognitive behavioural therapy. Ment Health Relig Cult 2014;17:714-25. https://doi.org/10.1080/13674676.2014.903388.
- Davies Hayon T, Oates J. The mental health service needs and experiences of unaccompanied asylum-seeking children in the UK: a literature review. Ment Health Pract 2019;22:13-20. https://doi.org/10.7748/mhp.2019.e1387.
- Majumder P, O’Reilly M, Karim K, Vostanis P. ‘This doctor, I not trust him, I’m not safe’: the perceptions of mental health and services by unaccompanied refugee adolescents. Int J Soc Psychiatry 2015;61:129-36. https://doi.org/10.1177/0020764014537236.
- Majumder P. ‘Inoculated in pain’: examining resilience in refugee children in an attempt to elicit possible underlying psychological and ecological drivers of migration. Int J Cult Ment Health 2016;9:327-39. https://doi.org/10.1080/17542863.2016.1199719.
- Majumder P, Vostanis P, Karim K, O’Reilly M. Potential barriers in the therapeutic relationship in unaccompanied refugee minors in mental health. J Ment Health 2019;28:372-8. https://doi.org/10.1080/09638237.2018.1466045.
- Majumder P. Exploring stigma and its effect on access to mental health services in unaccompanied refugee children. BJPsych Bull 2019;43:275-81. https://doi.org/10.1192/bjb.2019.35.
- Olaniyan FV. Paying the widening participation penalty: racial and ethnic minority students and mental health in British universities. Anal Soc Issues Public Policy 2021;21:761-83. https://doi.org/10.1111/asap.12242.
- Rowland G. How Do Parents Within the Orthodox Jewish Community Experience Accessing a Community Child and Adolescent Mental Health Service? 2016.
- Sancho TN, Michael L. ‘We need to slowly break down this barrier’: understanding the barriers and facilitators that Afro-Caribbean undergraduates perceive towards accessing mental health services in the UK. J Public Ment Health 2020;19:63-81. https://doi.org/10.1108/JPMH-12-2019-0099.
- Edge D, Grey P. An assets-based approach to co-producing a Culturally Adapted Family Intervention (CaFI) with African Caribbeans diagnosed with schizophrenia and their families. Ethn Dis 2018;28:485-92. https://doi.org/10.18865/ed.28.S2.485.
- Wales J, Brewin N, Raghavan R, Arcelus J. Exploring barriers to South Asian help-seeking for eating disorders. Ment Health Rev J 2017;22:40-5. https://doi.org/10.1108/mhrj-09-2016-0017.
- Gleeson H, Duke K, Thom B. Challenges to providing culturally sensitive drug interventions for black and Asian minority ethnic (BAME) groups within UK youth justice systems. Drugs Alcohol Today 2019;19:172-81. https://doi.org/10.1108/dat-11-2018-0068.
- Gray P, Ralphs R. Confidentiality and cultural competence? The realities of engaging young British Pakistanis and Bangladeshis into substance use services. Drugs Educat Prevent Policy 2019;26:133-9. https://doi.org/10.1080/09687637.2017.1398714.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73. https://doi.org/10.7326/M18-0850.
- Noblit G, Hare R. Meta-Ethnography. Newbury Park, CA: SAGE Publications, Inc.; 1988.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med 2005;61:417-30. https://doi.org/10.1016/j.socscimed.2004.12.001.
- Brunton G, Oliver S, Thomas J. Innovations in framework synthesis as a systematic review method. Res Synth Methods 2020;11:316-30. https://doi.org/10.1002/jrsm.1399.
- Anderson LM, Petticrew M, Rehfuess E, Armstrong R, Ueffing E, Baker P, et al. Using logic models to capture complexity in systematic reviews. Res Synth Methods 2011;2:33-42. https://doi.org/10.1002/jrsm.32.
- Khan AA, Bhardwaj SM. Access to health care. A conceptual framework and its relevance to health care planning. Eval Health Prof 1994;17:60-76. https://doi.org/10.1177/016327879401700104.
- Ryvicker M. A conceptual framework for examining healthcare access and navigation: a behavioral-ecological perspective. Soc Theory Health 2018;16:224-40. https://doi.org/10.1057/s41285-017-0053-2.
- Souliotis K, Hasardzhiev S, Agapidaki E. A conceptual framework of mapping access to health care across EU countries: the Patient Access Initiative. Public Health Genomics 2016;19:153-9. https://doi.org/10.1159/000446533.
- McPin Foundation . Research Priorities for Children and Young People’s Mental Health. Interventions and Services. Focus on the Questions 2018. https://mcpin.org/wp-content/uploads/2018/11/McPin-Foundation-RPRQ-Supplementary-Report.pdf (accessed 19 January 2022).
Appendix 1 Inclusion and exclusion criteria
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Population/focus of the research | Ethnic minority children and young people (aged 10–24 years) |
Studies in which the focus was not on children or young people (i.e. the study data or relevant subgroup data were mostly focused on people outside the included age range) Studies in which there was no focus or separate data regarding ethnic minority children or young people |
| Research participants | Non-white British ethnic minority children and young people (aged 10–24 years) and any associated:
|
Studies in which the participants were mostly children and young people who are not from an ethnic minority group |
| Health condition | The population must have been requiring care and support for a mental health need, including:
|
Studies focused on populations with autism/social communication disorders and/or learning disabilities where the primary focus was on the non-mental health aspects of these conditions |
| Setting | Any services, care or support with a mental health focus or mental health component, based in the UK | Services not providing mental health support (e.g. providing assessment for learning disability or autism only) |
| Comparator | Not applicable | None |
| Phenomenon/outcomes of interest | Perceptions, views and experiences regarding:
|
Studies that did not cover experiences regarding access or ongoing engagement |
| Study design |
Any qualitative research study design (including systematic reviews of qualitative studies) Collection and analysis of qualitative data such as: |
Commentaries, opinion pieces, letters, non-systematic reviews, quantitative studies, policy and guidance documents not describing the experiences of the study population |
| Date limits | Limited to studies published from 2012 onwards | Studies published before 2012 |
Appendix 2 Example search strategy (MEDLINE)
MEDLINE and MEDLINE in Process (Ovid): 867 hits
Date searched: 23 June 2021.
| Search number | Search terms | Hits |
|---|---|---|
| 1 | mental health/or exp mental disorders/ | 1,347,180 |
| 2 | CAMHS.ti,ab. | 530 |
| 3 | ((mental* or psycholog* or psychiatr* or behavio?r or emotion*) adj2 (health or ill* or disorder* or condition or disturbance or diagnos* or symptom* or “well-being” or wellbeing or syndrome*)).ti,ab. | 373,105 |
| 4 | exp adjustment disorders/or exp anxiety disorders/or exp mood disorders/or neurotic disorders/ | 196,130 |
| 5 | (anxi* or depress* or melancholi* or neuros* or neurotic or psychoneuro* or stress* or distress* or bipolar or dissociati* or schizophreni* or psychotic or psychosis or trauma* or phobia* or OCD or “obsessive compulsive” or phobia* or “self harm” or “gender dysphoria” or “attention deficit” or ADHD).ti,ab. | 2,328,797 |
| 6 | ((affective or mood or eat* or conduct or anger or personality or sleep* or oppositional or somatic or somatoform) adj2 (health or ill* or disorder* or condition or disturbance or diagnos* or symptom* or syndrome*)).ti,ab. | 155,132 |
| 7 | Self-Injurious Behaviour/or exp Sleep Wake Disorders/or Internet Addiction Disorder/or exp Substance-Related Disorders/or exp “attention deficit and disruptive behaviour disorders”/or attention deficit disorder with hyperactivity/or Gender Dysphoria/or exp Somatoform Disorders/ | 445,838 |
| 8 | ((internet or gaming or substance* or alcohol* or tobacco or drug* or narcotic* or opiate* or cannabis or hashish or marijuana or cocaine or amphetamine*) adj2 (disorder* or addict* or depend* or abuse*)).ti,ab. | 150,126 |
| 9 | exp Learning Disabilities/or exp autism spectrum disorder/or Social Communication Disorder/ | 56,920 |
| 10 | (autism or autistic or asperger*).ti,ab. | 54,921 |
| 11 | ((social communication* or kanner*) adj2 (disorder* or syndrome*)).ti,ab. | 136 |
| 12 | (learn* adj (difficult* or disorder* or disabilit*)).ti,ab. | 11,644 |
| 13 | (dyslexi* or dyscalculi*).ti,ab. | 6597 |
| 14 | or/1–13 | 3,450,931 |
| 15 | (“BAME” or BME).ti,ab. | 2943 |
| 16 | (“minority ethnic*” or “ethnic minorit*”).ti,ab. | 14,050 |
| 17 | ((racial adj5 disparit*) or (ethnic adj5 disparit*) or “people of colour” or “people of colour” or POC or WOC or BIPOC).ti,ab. | 19,633 |
| 18 | (“racial* minorit*” or “Race Factor*” or “mixed race” or “mixed racial” or minorit* or “ethnic* group*”).ti,ab. | 108,282 |
| 19 | *“minority group”/or *“minority health”/or *“black person”/or *“asian continental ancestry group”/or *“british asian”/or *“ethnic group”/or *“black race”/or *“black population”/or “multiracial person”/or “black person”/or *migrant/or *“oceanic ancestry group”/or *“ethnic or racial aspects”/or *“race difference”/or *“ethnic difference”/or *“indigenous people”/ | 80,802 |
| 20 | (refugee* or immigrant* or migrant* or (minority adj (group* or population*)) or multicultur* or multi cultur* or multiethnic* or multi ethnic* or ((cultur* or ethnic* or racial*) adj1 (divers* or differen*))).ti,ab. | 125,012 |
| 21 | Refugees/or exp “Emigrants and Immigrants”/or “Transients and Migrants”/or Minority Groups/or Cultural Characteristics/or Cultural Diversity/or Cross-Cultural Comparison/ | 100,334 |
| 22 | Minority Health/or (emigrant* or minority health or alien* or foreigner*).ti,ab. | 12,826 |
| 23 | (asylum adj3 (seek* or pend* or application* or apply)).ti,ab. | 2156 |
| 24 | ((displaced or exile* or stateless) adj3 (person* or people or group* or population*)).ti,ab. | 1824 |
| 25 | (bangladeshi* or bengali* or indian* or pakistani* or chinese or “black caribbean*” or “black african*” or “afro caribbean*” or arab* or “irish traveller*” or gypsy or gypsies or roma*).ti,ab. or Roma/ | 529,032 |
| 26 | or/15–25 | 825,133 |
| 27 | (teen* or youth* or adolescen* or juvenile* or (young adj2 (adult* or person* or individual* or people* or population* or man or men or wom#n)) or youngster* or highschool* or college* or ((secondary or high*) adj2 (school* or education))).ti,ab. or adolescent/or young adult/ | 2,939,129 |
| 28 | (child* or stepchild* or step-child* or kid or kids or girl or girls or boy or boys or teen* or youth* or youngster* or adolescent* or adolescence or preschool* or pre-school* or kindergarten* or school* or juvenile* or minors or p?ediatric* or PICU).ti,ab. or exp child/ | 3,003,343 |
| 29 | 27 or 28 | 4,527,650 |
| 30 | exp United Kingdom/ | 378,609 |
| 31 | (national health service* or nhs*).ti,ab,in. | 227,720 |
| 32 | (english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. | 41,754 |
| 33 | (gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jw,in. | 2,222,750 |
| 34 | (bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in. | 1,545,045 |
| 35 | (bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in. | 61,483 |
| 36 | (aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in. | 228,247 |
| 37 | (armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or 41–43newry or “newry’s”).ti,ab,in. | 29,206 |
| 38 | 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 | 2,792,337 |
| 39 | (exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp asia/or exp australia/or exp oceania/) not (exp United Kingdom/or europe/) | 3,077,716 |
| 40 | 38 not 39 | 2,652,602 |
| 41 | interview:.mp. | 427,227 |
| 42 | experience:.mp. | 1,181,844 |
| 43 | qualitative:.tw. | 306,881 |
| 44 | 41 or 42 or 43 | 1,692,820 |
| 45 | 14 and 26 and 29 and 40 and 44 | 1302 |
| 46 | limit 45 to yr=”2010 -Current” | 867 |
Search strategies for the other databases are available on request.
Appendix 3 List of studies excluded at full-text stage
Acle A, Cook BJ, Siegfried N, Beasley T. Cultural considerations in the treatment of eating disorders among racial/ethnic minorities: a systematic review. J Cross Cult Psychol 2021;52:468–88. https://doi.org/10.1177/00220221211017664
Ali A, Scior K, Ratti V, Strydom A, King M, Hassiotis A. Discrimination and other barriers to accessing health care: perspectives of patients with mild and moderate intellectual disability and their carers. PLOS ONE 2013;8:e70855. https://doi.org/10.1371/journal.pone.0070855
Anagnostopoulos DC, Heberbrand J, Eliez S, Doyle MB, Klasen H, Crommen S, et al. European Society of Child and Adolescent Psychiatry: position statement on mental health of child and adolescent refugees. Eur Child Adolesc Psychiatry 2016;25:673–6. https://doi.org/10.1007/s00787-016-0882-x
Aubrey C, Ward K. Early years practitioners’ views on early personal, social and emotional development. Emot Behav Diff 2013;18:435–47. https://doi.org/10.1080/13632752.2013.807541
Bamford J, Fletcher M, Leavey G. Mental health outcomes of unaccompanied refugee minors: a rapid review of recent research. Curr Psychiatry Rep 2021;23:46. https://doi.org/10.1007/s11920-021-01262-8
Barnett ML, Brookman-Frazee L, Gonzalez JC, Zhan C, Rodriguez A, Stadnick NA, Lau AS. Qualitative reports of how and when therapists adapt children’s evidence-based practices during community implementation. J Clin Child Adolesc Psychol 2019;48:894–905. https://doi.org/10.1080/15374416.2018.1485107
Bashir N, Ameyaw N, Sahota S, Bajwa M, Dayson C. Culture, Connection and Belonging: a Study of Addiction and Recovery in Nottingham’s BAME Community. 2019. URL: www.shu.ac.uk/centre-regional-economic-social-research/publications/culture-connection-and-belonging-a-study-of-addiction-and-recovery-in-nottinghams-bame-community (accessed 10 August 2021).
British Medical Association. Cutting Away at Our Children’s Futures: How Austerity is Affecting the Health of Children, Young People and Families. 2016. URL: www.bma.org.uk/media/2060/cutting-away-at-our-childrens-futures-austerity-child-health-guuk-2016.pdf (accessed 10 August 2021).
Bonell S, Underwood L, Radhakrishnan V, McCarthy J. Experiences of mental health services by people with intellectual disabilities from different ethnic groups: a Delphi consultation. J Intellect Disabil Res 2012;56:902–9. https://doi.org/10.1111/j.1365-2788.2011.01494.x
Brown G. Let’s talk: African Caribbean women, mothering motherhood, and well-being. Front Sociol 2020;4:88. https://doi.org/10.3389/fsoc.2019.00088
Campbell J, Rondon J, Galway K, Leavey G. Meeting the needs of vulnerable young men: a study of service provider views. Child Soc 2013;27:60–71. https://doi.org/10.1111/j.1099-0860.2011.00372.x
Chan CK, Barnard A, Ng YN. ‘Who are our support networks?’ A qualitative study of informal support for carers. J Soc Serv Res 2020;47:265–75. https://doi.org/10.1080/01488376.2020.1757012
Chase E. Security and subjective wellbeing: the experiences of unaccompanied young people seeking asylum in the UK. Sociol Health Illn 2013;35:858–72. https://doi.org/10.1111/j.1467-9566.2012.01541.x
Cheng WSW, Fenn D, Le Couteur A. Understanding the mental health needs of Chinese children living in the north east of England. Ethnic Inequal Health Soc Care 2013;6:16–22.
Chiarenza A, Dauvrin M, Chiesa V, Baatout S, Verrept H. Supporting access to healthcare for refugees and migrants in European countries under particular migratory pressure. BMC Health Serv Res 2019;19:513. https://doi.org/10.1186/s12913-019-4353-1
Cronin-de-Chavez A, Islam S, McEachan RRC. Not a level playing field: a qualitative study exploring structural, community and individual determinants of greenspace use amongst low-income multi-ethnic families. Health Place 2019;56:118–26.
Croot EJ. The care needs of Pakistani families caring for disabled children: how relevant is cultural competence? Physiotherapy 2012;98:356–61. https://doi.org/10.1016/j.physio.2011.05.001
Demazure G, Baeyens C, Pinsault N. Review: unaccompanied refugee minors’ perception of mental health services and professionals: a systematic review of qualitative studies [published online ahead of print June 15 2021]. Child Adolesc Ment Health 2021. https://doi.org/10.1111/camh.12486
Deveci Y. Trying to understand: promoting the psychosocial well-being of separated refugee children. J Soc Work Pract 2012;26:367–83. https://doi.org/10.1080/02650533.2012.658033
Diaków DM, Goforth AN. Supporting Muslim refugee youth during displacement: implications for international school psychologists. Sch Psychol Int 2021;42:238–58. https://doi.org/10.1177/0143034320987280
Due C, Green E, Ziersch A. Psychological trauma and access to primary healthcare for people from refugee and asylum-seeker backgrounds: a mixed methods systematic review. Int J Ment Health Syst 2020;14:71. https://doi.org/10.1186/s13033-020-00404-4
Durà-Vilà G, Klasen H, Makatini Z, Rahimi Z, Hodes M. Mental health problems of young refugees: duration of settlement, risk factors and community-based interventions. Clin Child Psychol Psychiatry 2013;18:604–23. https://doi.org/10.1177/1359104512462549
Durling E, Chinn D, Scior K. Family and community in the lives of UK Bangladeshi parents with intellectual disabilities. J Appl Res Intellect Disabil 2018;31:1133–43. https://doi.org/10.1111/jar.12473
Eigenhuis E, Waumans RC, Muntingh ADT, Westerman MJ, van Meijel M, Batelaan NM, van Balkom AJLM. Facilitating factors and barriers in help-seeking behaviour in adolescents and young adults with depressive symptoms: a qualitative study. PLOS ONE 2021;16:e0247516. https://doi.org/10.1371/journal.pone.0247516
Fernández de la Cruz L, Jassi A, Krebs G, Clark B, Mataix-Cols D. Phenomenology and treatment outcomes in children and adolescents from ethnic minorities with obsessive-compulsive disorder. J Obsessive-Compuls Relat Disord 2015;4:30–6. https://doi.org/10.1016/j.jocrd.2014.11.003
Fox F, Aabe N, Turner K, Redwood S, Rai D. ‘It was like walking without knowing where I was going’: a qualitative study of autism in a UK Somali migrant community. J Autism Dev Disord 2017;47:305–15. https://doi.org/10.1007/s10803-016-2952-9
Gray C, Donnelly J. Unheard voices: the views of traveller and non-traveller mothers and children with ASD. Int J Early Years Educ 2013;21:268–85. https://doi.org/10.1080/09669760.2013.842160
Griffith P, Malik A. Reaching Out: Tackling Disengagement among Pakistani and Bangladeshi Women in Britain. 2018. URL: www.ippr.org/research/publications/reaching-out (accessed 23 September 2021).
Harkensee C, Andrew R. Health needs of accompanied refugee and asylum-seeking children in a UK specialist clinic. Acta Paediatr 2021;110:2396–404. https://doi.org/10.1111/apa.15861
Heer K, Larkin M, Burchess I, Rose J. The cultural context of care-giving: qualitative accounts from South Asian parents who care for a child with intellectual disabilities in the UK. Adv Ment Health Intellect Disabil 2012;6:179–91. https://doi.org/10.1108/20441281211236580
Heer K, Larkin M, Rose J. The experiences of British South Asian carers caring for a child with developmental disabilities in the UK. Tizard Learn Disabil Rev 2015;20:228–38. https://doi.org/10.1108/tldr-12-2014-0044
Heer K, Rose J, Larkin M. The challenges of providing culturally competent care within a disability focused team: a phenomenological exploration of staff experiences. J Transcult Nurs 2016;27:109–16. https://doi.org/10.1177/1043659614526454
Hughes G. Finding a voice through ‘The Tree of Life’: a strength-based approach to mental health for refugee children and families in schools. Clin Child Psychol Psychiatry 2014;19:139–53. https://doi.org/10.1177/1359104513476719
Inkeroinen S, Hupli M, Stolt M. School nurses’ experiences of health promotion for school-age asylum seekers [published online ahead of print December 10 2020]. J Sch Nurs 2020. https://doi.org/10.1177/1059840520978197
Jack O, Chase E, Warwick I. Higher education as a space for promoting the psychosocial well-being of refugee students. Health Educ J 2018;78:51–66. https://doi.org/10.1177/0017896918792588
James E. Caring Alone: Why Black, Asian and Minority Ethnic Young Carers Continue to Struggle to Access Support. 2019. URL: www.barnardos.org.uk/sites/default/files/uploads/Barnardos%20Caring%20Alone%20report.pdf (accessed 10 August 2021).
Karadzhov D, White R. Between the ‘whispers of the Devil’ and ‘the revelation of the Word’: Christian clergy’s mental health literacy and pastoral support for BME congregants. J Spiritual Ment Health 2018;22:147–72. https://doi.org/10.1080/19349637.2018.1537755
Kindermann D, Zeyher V, Nagy E, Friederich HC, Bozorgmehr K, Nikendei C. Predictors of asylum seekers’ health care utilization in the early phase of resettlement. Front Psychiatry 2020;11:475. https://doi.org/10.3389/fpsyt.2020.00475
Kovandžić M, Funnell E, Hammond J, Ahmed A, Edwards S, Clarke P, et al. The space of access to primary mental health care: a qualitative case study. Health Place 2012;18:536–51. https://doi.org/10.1016/j.healthplace.2012.01.011
Lawrence V, McCombie C, Nikolakopoulos G, Morgan C. Ethnicity and power in the mental health system: experiences of white British and black Caribbean people with psychosis. Epidemiol Psychiatr Sci 2021;30:e12. https://doi.org/10.1017/S2045796020001043
Linney C, Ye S, Redwood S, Mohamed A, Farah A, Biddle L, Crawley E. ‘Crazy person is crazy person. It doesn’t differentiate’: an exploration into Somali views of mental health and access to healthcare in an established UK Somali community. Int J Equity Health 2020;19:190. https://doi.org/10.1186/s12939-020-01295-0
Littlewood R, Dein S. Carers and families: life and suffering among Bangladeshi psychiatric patients and their families in London – an interview study 3. Anthropol Med 2016;23:54–70. https://doi.org/10.1080/13648470.2015.1049120
Loewenthal KM. Mental health and mental health care for Jews in the Diaspora, with particular reference to the U.K. Isr J Psychiatry Relat Sci 2012;49:159–66.
Madden H, Harris J, Blickem C, Harrison R, Timpson H. ‘Always paracetamol, they give them paracetamol for everything’: a qualitative study examining Eastern European migrants’ experiences of the UK health service. BMC Health Serv Res 2017;17:604. https://doi.org/10.1186/s12913-017-2526-3
Mantovani N, Pizzolati M, Edge D. Exploring the relationship between stigma and help-seeking for mental illness in African-descended faith communities in the UK. Health Expect 2017;20:373–84. https://doi.org/10.1111/hex.12464
McKeague L, Morant N, Blackshaw E, Brown JSL. Exploring the feasibility and acceptability of a school-based self-referral intervention for emotional difficulties in older adolescents: qualitative perspectives from students and school staff. Child Adolesc Ment Health 2018;23:198–205. https://doi.org/10.1111/camh.12234
Memon A, Taylor K, Mohebati LM, Sundin J, Cooper M, Scanlon T, de Visser R. Perceived barriers to accessing mental health services among black and minority ethnic (BME) communities: a qualitative study in Southeast England. BMJ Open 2016;6:e012337. https://doi.org/10.1136/bmjopen-2016-012337
Miller E, Bosun-Arjie SF, Ekpenyong MS. Black and ethnic minority carers perceptions on mental health services and support in the United Kingdom: a systematic review. J Pub Ment Health 2021;20:298–311.
Mohamed S, Thomas M. The mental health and psychological well-being of refugee children and young people: an exploration of risk, resilience and protective factors. Educ Psychol Pract 2017;33:249–63. https://doi.org/10.1080/02667363.2017.1300769
Moller N, Burgess V, Jogiyat Z. Barriers to counselling experienced by British South Asian women: a thematic analysis exploration. Couns Psychother Res 2016;16:201–10.
Muir J, Gannon K. Belongings beyond borders: reflections of young refugees on their relationships with location. J Community Appl Soc Psychol 2016;26:279–90. https://doi.org/10.1002/casp.2260
Muzik M, Kirk R, Alfafara E, Jonika J, Waddell R. Teenage mothers of black and minority ethnic origin want access to a range of mental and physical health support: a participatory research approach. Health Expect 2016;19:403–15. https://doi.org/10.1111/hex.12364
Narendorf SC, Munson MR, Ben-David S, Cole AR, Scott LD. Race and gender differences in attitudes toward help seeking among marginalized young adults with mood disorders: a mixed-methods investigation. Psychiatr Rehabil J 2018;41:277–89. https://doi.org/10.1037/prj0000312
National Autistic Society. Diverse Perspectives: The Challenges for Families Affected by Autism from Black, Asian and Minority Ethnic Communities. 2014. URL: https://positiveaboutautism.co.uk/uploads/9/7/4/5/97454370/nas-diverse-perspectives-report-1.pdf (accessed 6 September 2021).
Plan International UK. The State of Girls’ Rights in the UK 2019–2020. 2020. URL: https://plan-uk.org/file/plan-uk-state-of-girls-rights-report-2020pdf/download?token=42bpRbf8 (accessed 10 August 2021).
Rabiee F, Smith P. Being understood, being respected: an evaluation of mental health service provision from service providers and users’ perspectives in Birmingham, UK. Int J Ment Health Promot 2013;15:162–77.
Rabiee F, Smith P. Understanding mental health and experience of accessing services among African and African Caribbean service users and carers in Birmingham, UK. Divers Equal Health Care 2014;11:125–34.
Rodriguez IM, Dobler V. Survivors of hell: resilience amongst unaccompanied minor refugees and implications for treatment – a narrative review. J Child Adolesc Trauma 2021;14:559–69. https://doi.org/10.1007/s40653-021-00385-7
Rogers J, Carr S, Hickman C. Mutual benefits: the lessons learned from a community based participatory research project with unaccompanied asylum-seeking children and foster carers. Child Youth Serv Rev 2018;92:105–13.
Roth M, Pop F, Raiu S. Self-concepts and resilience by Roma youngsters living in poor communities. In Ionescu S, Tomita M, Cace S, editors. The Second World Congress on Resilience: From Person to Society: May 8–10 2014, Timisoara (Romania). Bologna: Medimond; 2014. pp. 643–6.
Sandhu P, Ibrahim J, Chinn D. ‘I wanted to come here because of my child’: stories of migration told by Turkish-speaking families who have a son or daughter with intellectual disabilities. J Appl Res Intellect Disabil 2017;30:371–82. https://doi.org/10.1111/jar.12248
Shorey S, Ng ED, Haugan G, Law E. The parenting experiences and needs of Asian primary caregivers of children with autism: a meta-synthesis. Autism 2020;24:591–604. https://doi.org/10.1177/1362361319886513
Sime D, Rachael FOX. Migrant children, social capital and access to services post-migration: transitions, negotiations and complex agencies. ChildSoc 2015;29:524–34.
Singh SP, Islam Z, Brown LJ, Gajwani R, Jasani R, Rabiee F, et al. Ethnicity, detention and early intervention: reducing inequalities and improving outcomes for black and minority ethnic patients: the ENRICH programme, a mixed-methods study. Prog Grants Applied Research 2013;1(3).
Smith LM, Onwumere J, Craig TK, Kuipers E. An ethnic-group comparison of caregiver beliefs about early psychotic illness in a UK sample: implications for evidence-based caregiver interventions. Transcult Psychiatry 2020;57:432–44. https://doi.org/10.1177/1363461519900596
Smolinska-Poffley G, Ingmire S. Roma Mental Health Advocacy Project: Evaluation Report. London: Roma Support Group; 2012.
Stevens C, Ayer L, Labriola M, Faraji S-L, Ebright E. Detecting and reducing post-traumatic stress among children exposed to domestic violence: a multi-agency early intervention program. Child Youth Serv Rev 2019;101:261–9. https://doi.org/10.1016/j.childyouth.2019.03.055
Wylie L, Corrado AM, Edwards N, Benlamri M, Murcia Monroy DE. Reframing resilience: strengthening continuity of patient care to improve the mental health of immigrants and refugees. Int J Ment Health Nurs 2020;29:69–79. https://doi.org/10.1111/inm.12650
York W, Jones J. Addressing the mental health needs of looked after children in foster care: the experiences of foster carers. J Psychiatr Ment Health Nurs 2017;24:143–53. https://doi.org/10.1111/jpm.12362
Appendix 4 Data extraction fields
The following information was sought and extracted from each included paper/report:
-
publication details (authors, title, year, publication type)
-
DOI/citation
-
study aim(s)
-
study methods (shorthand description, e.g. copied from abstract)
-
year data were collected
-
study location [e.g. city or region(s) where data collection took place]
-
type of service/setting (if applicable)
-
types of mental health need
-
ethnic group(s) of sample
-
age of children/young people
-
study participant category/categories (children, young people, parents, carers, referrers, providers or commissioners), and related sample sizes
-
other reported characteristics of the children/young people (ethnicity, age, gender mix)
-
main findings, conclusions, study limitations (as summarised by the study authors, e.g. key themes, explanations)
-
more detailed findings relating to our review questions (i.e. about care-seeking, accessing or engaging with services and support for mental health problems).
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- ASSIA
- Applied Social Sciences Index and Abstracts
- BAME
- black, Asian and minority ethnic
- BME
- black and minority ethnic
- CAMHS
- child and adolescent mental health service
- CBT
- cognitive–behavioural therapy
- DHSC
- Department of Health and Social Care
- GP
- general practitioner
- HMIC
- Health Management Information Consortium
- HSDR
- Health and Social Care Delivery Research
- MRC
- Medical Research Council
- MST
- multisystemic therapy
- NIHR
- National Institute for Health and Care Research
- OCD
- obsessive–compulsive disorder
- PTSD
- post-traumatic stress disorder
