Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR130818. The contractual start date was in July 2019. The final report began editorial review in June 2022 and was accepted for publication in December 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Ellins et al. This work was produced by Ellins et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Ellins et al.
A note on terminology
This report uses the term ‘children and young people’s mental health services’ to describe all services that support children and young people who have difficulties with their mental health and emotional well-being. These services encompass prevention and universal provision, through to specialist and crisis support, including inpatient care. They are provided by NHS, local authority, voluntary, community and independent sector services, as well as schools and colleges. Some participants in the study refer to ‘child and adolescent mental health services’ (or CAMHS), which is an older term for specialist NHS mental health services for young people aged 0–18 (or, in some areas, 0–25) years. We also use the term ‘whole school approach’ to describe all the ways in which schools and colleges can address the emotional health of children and/or young people in their setting, which includes supporting those who are experiencing mental health problems to access appropriate help. In wider literature and debate, these activities are also referred to as holistic, universal, graduated or school-wide approaches to mental health and well-being.
The national programme launched by the Department of Health and Department for Education to implement the proposals in the 2017 Green Paper Transforming Children and Young People’s Mental Health Provision was originally termed the Trailblazer programme. It was subsequently renamed the Children and Young People’s Mental Health Implementation programme, and only the first wave of sites was referred to as Trailblazers. As the study reported herein focuses exclusively on this first wave of Trailblazer sites, we have opted to use the programme’s original name.
Chapter 1 Introduction and context
Introduction
This report presents the findings of an early evaluation of the Children and Young People’s Mental Health Trailblazer programme (henceforth the Trailblazer programme). Launched in 2018, the Trailblazer programme is key to delivering the ambition – shared by recent successive governments – to increase the support available to children and young people with mental health problems. It is funding the creation of mental health support teams (MHSTs), to work in and with schools and further education colleges to support mental health and well-being. 1 This evaluation offers early insights into the design, implementation and the progress made by MHSTs in the programme’s first wave of Trailblazer areas.
The remainder of this chapter summarises the evolving policy context for the Trailblazer programme, then outlines the key features of the programme itself, before concluding with an overview of the early evaluation aims, objectives and study design.
Policy context
The proportion of children and young people experiencing mental health problems is considerable and increasing. A 2020 national survey reported that one in six children had a ‘probable mental disorder’, up from one in nine in 2017. 2 Over half of mental ill health experienced in adulthood starts before the age of 14 years. 3 Yet children and young people frequently face difficulties accessing the support and/or treatment they need, with mental health services often experienced as fragmented and overstretched, and many reporting that their problems significantly worsened before they got help. 4–6 While patterns of service provision across England vary, high access thresholds and long waiting times are widely reported. 7 Children’s mental health services have also suffered from historic under-investment and, in the words of the former Children’s Commissioner, they are ‘the area with the biggest gap between what patients need and what the NHS was providing’. 8
It is in this context that governments have, in recent years, made the transformation of children’s mental health services a national priority. 9 Alongside action to improve access to specialist and crisis services for children and young people with serious needs and acute problems, there has been a growing focus on promotion, prevention and early intervention. A key aim is to ensure that children get early support to reduce distress more quickly and prevent problems escalating, thereby avoiding more damaging and long-term impacts. These ambitions were set out in the 2015 report Future in Mind, which called for integrated approaches to mental health prevention and support ‘through strong collaborative working across the statutory, independent and voluntary and community sectors’. 10 In particular, Future in Mind identified the key role that schools and colleges play in children’s lives and their well-being. It promised to ‘do more to help schools develop knowledge about mental health, identify issues when they arise and offer early support’, including strengthening links between schools and specialist mental health services. Education settings were also encouraged to develop whole school approaches to promoting resilience and improving emotional well-being.
Shortly after Future in Mind was published, Public Health England set out a framework for a whole school approach. 11 The ultimate goal is to improve the mental health and well-being of all children and young people within the setting, not just those with identified problems. The approach is graduated: from universal and preventive strategies, through to more targeted and specialist forms of support for those who need it. The framework comprises eight key features (Figure 1).
FIGURE 1.
Whole school approach to emotional health and well-being.

The commitments made in Future in Mind were followed in December 2017 by the publication of the Transforming Children and Young People’s Mental Health Provision Green Paper. 1 This document set out proposals for improving the services and support available to children and young people with mental health problems, with a particular focus on enhancing provision for those with ‘mild to moderate’ needs. The proposals had three main elements:
-
incentivising schools and colleges to appoint a senior lead for mental health to oversee the approach to mental health and well-being in their setting
-
funding the creation of MHSTs to provide early intervention for children and young people with mild to moderate mental health needs and to support mental health promotion in schools and colleges
-
trialling a four-week waiting time for access to specialist NHS children and young people’s mental health services (CYPMHS).
The government committed to taking forward all three proposals in the Green Paper and announced that there would be phased implementation through a national programme, which was subsequently launched in 2018, with an emphasis on testing, learning and evaluating to understand what works. Subsequently MHSTs featured prominently in the NHS Long Term Plan, and are central to the commitment in the Plan that, by 2024, an additional 345,000 young people aged 0–25 years will be able to access support from NHS-funded mental health services. 12
COVID-19 and children and young people’s mental health
Since the Green Paper programme started, the COVID-19 pandemic has compounded the need and urgency to improve children and young people’s access to mental health support. There is a growing body of evidence showing that COVID-19 and the lockdown and social distancing restrictions introduced to reduce the spread of the virus have negatively affected children and young people’s mental health, disproportionately affecting groups who were already at greater risk of mental ill health. 13 Among the groups most affected are children and young people living in low-income households, those who have special educational needs and disabilities (SEND), those who are from black and minority ethnic groups, those who are in care, those who have a long-term physical health condition, and lesbian, gay, bisexual, transgender, queer or questioning and other sexual identities (LGBTQ+) children and young people. 14,15
It is estimated that 1.5 million children and young people in England will need new or additional mental health support as a result of the pandemic. 7 While the precise ways in which the pandemic has affected children’s mental health are not yet fully understood, what is known is that COVID-19 has simultaneously intensified known risk factors (e.g. loneliness, family conflict, bereavement) and reduced access to activities that promote mental well-being and wider sources of support (e.g. as a result of school closures and suspension of leisure services). 14,16 The deterioration of children’s mental health has been most marked during lockdowns and periods of school closure. The COVID-19: Supporting Parents, Adolescents and Children during Epidemics (Co-SPACE) study, which tracked the mental health of school-aged children and young people between March 2020 and July 2021, showed some return towards pre-pandemic rates of mental health problems as lockdown restrictions eased in early 2021. 17 But this was not the case for all groups, with children with SEND and from low-income households continuing to have elevated mental health symptoms post-lockdown.
Increasing demand for mental health support is also evident. While there was a sharp decrease in referrals to NHS CYPMHS during the first lockdown (March to June 2020), since then referrals have rapidly risen far beyond pre-COVID-19 levels to reach record highs. 14 A total of 337,125 children and young people aged 0–18 years were referred to mental services between April and September 2021, an 81% increase on the same period in 2019. 18 The number of children and young people referred for urgent or crisis care increased by 59%. This is having a knock-on impact on waiting times; between April 2020 and March 2021, one in five children waited more than 12 weeks for a follow-up appointment with mental health services. 18
The Trailblazer programme
The Trailblazer programme was launched in 2018 and is jointly led by the Department of Health and Social Care (DHSC), Department for Education (DfE), and NHS England and Improvement (NHSEI), with support from Health Education England and the Office for Health Improvement and Disparities. It is being implemented in successive waves, with the first wave involving 25 Trailblazer sites in 41 clinical commissioning group (CCG) areas (Figure 2). A further 10 more waves have been confirmed, and it is estimated that the new approaches will reach around 3 million children and young people (35% of pupils in England) by 2023. A detailed programme timeline can be found in Appendix 1.
FIGURE 2.
The Trailblazer sites.

The criteria for selecting the first group of sites, the Trailblazers, included: demonstrable levels of investment in CYPMHS, knowledge of the mental health needs of children and young people in the area, demonstrable progress in meeting targets for increasing access to mental health services for children and young people, and strong leadership in mental health. The rationale given for these qualifying criteria was to ensure that selected areas had the capacity and capability for implementation at sufficient pace to generate learning for the waves to follow. Sites were also selected to ensure some demographic diversity (e.g. deprivation, social mobility). Of the 25 Trailblazers, 12 received additional funding to test what it would take to deliver a four-week waiting time target (this element of the programme finished at the end of March 2022).
The overall goal of the programme is defined as follows: ‘Children and young people have better mental health and well-being, supported and promoted by schools, colleges, parents/carers and the health system. When children and young people experience poor mental health, this is recognised, and appropriate support is identified and provided quickly’. 19 This is articulated in terms of three main objectives, against which the long-term success of the programme will be assessed:
-
better mental health and well-being among children and young people
-
children and young people feel better equipped and supported
-
schools and colleges feel better equipped and supported.
A detailed logic model illustrating the pathways through which the programme is expected to produce the desired outcomes was produced by the national team in early 2019 and was being updated during 2022.
Local implementation of the programme is overseen and supported by NHSEI, Health Education England and DfE regional teams; the last of these were newly created for the Trailblazer programme, aligned to the NHS regional structure. Trailblazers were expected to put in place arrangements for local governance and leadership, to include representation from the health, education and community sectors. A local project lead, working with the MHST service manager(s) in their site, is responsible for day-to-day management of the programme.
Education settings and senior mental health leads
In the Trailblazer sites, 1050 education settings have been recruited to participate in the programme. These include a mixture of primary and secondary schools, all-through schools, further education colleges and other settings (Table 1). Of the 1050 education settings, 4.8% are special schools, 41.5% are academies or free schools and 1.6% are pupil referral units.
| Region | Primary | Secondary | 16 plus | All-through | Othera | Total |
|---|---|---|---|---|---|---|
| East of England | 14 | 9 | 2 | 0 | 7 | 32 |
| London | 150 | 61 | 2 | 4 | 15 | 232 |
| Midlands | 95 | 31 | 2 | 0 | 11 | 139 |
| North East and Yorkshire | 186 | 44 | 3 | 1 | 26 | 260 |
| North West | 77 | 46 | 5 | 1 | 12 | 141 |
| South East | 103 | 25 | 2 | 2 | 7 | 139 |
| South West | 73 | 27 | 3 | 1 | 3 | 107 |
| Total (in Trailblazer programme) | 698 (66.48%) | 243 (23.14%) | 19 (1.81%) | 9 (0.86%) | 81 (7.71%) | 1050 (100%) |
| Total (in England) | 16,787 (68.56%) | 3237 (13.22%) | 308 (1.26%) | 159 (0.65%) | 3994 (16.31%) | 24,485 (100%) |
Education settings are encouraged to identify a senior mental health lead to have strategic oversight of the establishment or further development of a whole school approach to mental health in their setting. This is not a mandated role and schools and colleges may choose whether and how to embed it. Many education settings had a mental health lead before the Trailblazer programme: in a national survey in 2017, 70% of schools reported having a mental health lead; one year later, 77% of post-16 education settings reported having a lead for mental health. Education settings are required to identify an MHST co-ordinator to work closely with the MHST, including agreeing the support that will be provided to their education setting.
In June 2021, the DfE announced that state schools and colleges in England could apply for a grant of up to £1200 to pay for their senior mental health lead to attend training to support them in their role. This replaces the DfE’s original plan, to commission a national training programme for senior mental health leads, which had been subject to significant delays and was eventually halted. Education settings can choose from a list of quality assured courses, which are aligned to the eight features of the Public Health England whole school approach framework. By March 2022, more than 8000 eligible schools and colleges had received a grant, with the goal that all will have been able to access training by 2025. In the 2020/21 and 2021/22 school years, as part of wider package of ‘education recovery’ measures, schools and colleges were able to access specific training and resources to support pupil and staff well-being and link with wider services.
Mental health support teams
In the Trailblazer sites, the programme funded the creation of 58 MHSTs, with each team estimated to cover a population of around 8000 children and young people in 10–20 schools and colleges; later waves of the programme have been based on MHSTs covering an average population of 7000 children and young people. MHSTs are intended to support children in primary, secondary and further education, aged between 5 and 18 years. 20 The programme is aiming to have funded the creation of around 500 MHSTs by 2024. As of May 2022, 287 teams were in place in 4789 schools and colleges, and a further 112 teams were in training.
Funding to plan, set up and run MHSTs was allocated from NHSEI to NHS CCGs, with the service itself delivered by a local organisation or collaboration of organisations. Partnership working between CCGs, schools and colleges, CYPMHS, local authorities and others on the application process, and subsequently to design and implement the MHST service, was encouraged. Trailblazer sites received different levels of funding depending on what was bid for, and whether the site was also piloting the four-week waiting time. For subsequent waves of the programme, the funding has been standardised based a defined service model. All sites receive basic funding of around £360,000 per year for each MHST, with additional funding for higher cost areas. 21
Each MHST is expected to exercise three core functions (Box 1), while allowing sites flexibility to tailor its delivery model and interventions to local needs and existing provision. Indeed, it is an explicit intention of the programme that different local models will emerge and should be compared and tested.
-
Delivering evidence-based interventions to children and young people with mild to moderate mental health issues.
-
Supporting the senior mental health lead in each education setting to introduce or develop their whole school/college approach to mental health and well-being.
-
Giving timely advice to education setting staff, and liaising with external specialist services, to help children and young people to get the right support and stay in education.
In terms of the first of these functions, MHSTs provide one-to-one and group-based support to children and young people, and group parenting classes. 20 Data on the outcomes of these interventions, along with other aspects of service activity and performance, are routinely collected and reported by the teams. MHSTs are expected to submit data to the Mental Health Services Data Set (MHSDS) from the point at which they start receiving referrals.
A set of operating principles was developed to underpin and guide the work of the MHSTs, these are summarised in Box 2 and reproduced in full in Appendix 2. Detailed guidance to support local implementation of MHSTs is provided in the form of a manual, developed by the National Collaborating Centre for Mental Health. 20
-
There should be clear and appropriate local governance involving health and education.
-
MHSTs should be additional to and integrated with existing support.
-
The approach to allocating MHST time and resources to education settings should be transparent and agreed by the local governance board.
-
MHST support should be responsive to individual education settings needs, not ‘one size fits all’.
-
Children and young people should be able to access appropriate support all year (not just during term time).
-
MHSTs should co-produce their approach and service offer with users.
-
MHSTs should be delivered in a way to take account of disadvantage and seek to reduce health inequalities.
Mental health support team workforce and supervision
The Trailblazer programme promised a significant expansion of the children and young people’s mental health workforce, and the creation of a new professional role: education mental health practitioner (EMHP). Estimates suggested that 8000 new mental health staff would be required for the MHST model to be rolled out across England. 22 This would represent a more than 50% growth in the children’s mental health workforce, which stood at just under 15,000 full-time equivalents (FTEs) when the programme was launched in 2018. 23
It was envisaged that MHSTs (in all waves of the programme) would typically be made up of eight FTE positions. The indicative team composition includes four EMHPs, an NHS Band 5 role, which is based on the children’s well-being practitioner role developed in the Children and Young People’s Improving Access to Psychological Therapies (IAPT) programme. A further three posts are allocated to more experienced practitioners (NHS Band 7–8a, or equivalent), who act as senior therapists and/or, after undertaking specific training, fulfil a supervisory role to EMHPs. The remaining post is split into one 0.5 FTE team manager and a 0.5 FTE administrator role. The Trailblazer sites were given greater flexibility in the composition of teams compared with later waves of the programme. EMHPs undergo one-year full-time graduate or postgraduate training, combining classroom-based learning and supervised placements in education settings. To fulfil the direct support element of their role, EMHPs are trained to deliver brief low-intensity psychological interventions, grounded in cognitive behavioural therapy (CBT) and guided self-help principles, including one-to-one and group-based interventions. The training focuses on four types of interventions:24
-
parent-led guided self-help for primary-school-aged children with mild to moderate anxiety disorders
-
guided self-help for mild to moderate adolescent depression, based on behaviour activation principles
-
guided self-help for mild to moderate adolescent anxiety disorders, based on CBT principles
-
parent-led guided self-help for mild to moderate behaviour problems (primary school age), based on social learning theory.
Typically, interventions are delivered over up to eight sessions, with the child or young person completing routine outcome measures at every session to track progress over time and monitor their goals. By March 2022, 1608 EMHPs had been trained or were in training and a further 600 senior staff had been recruited to join MHSTs. In June 2021, the British Psychological Society and the British Association for Behavioural and Cognitive Psychotherapies were approved by NHSEI to provide professional registration schemes for the low-intensity mental health workforce, including EMHPs.
Overview of the early evaluation
This study was a collaboration between the National Institute for Health and Care Research (NIHR)-funded Birmingham, RAND and Cambridge Evaluation (BRACE) Rapid Evaluation Centre and the NIHR-funded Policy Innovation and Evaluation Research Unit (PIRU). It was a process-oriented study, which examined the development, implementation and early progress of the programme in the Trailblazer sites, with a specific focus on MHSTs. An interim report was published in July 2021 and formative findings were shared with the national programme team throughout the study; this included preparation of a paper in October 2021 summarising early findings from the case study research, and rapid syntheses of emerging insights on specific topics to support work being undertaken by national team. The four-week waiting time pilots, EMHP training programme and senior mental health leads’ training were all outside the formal scope of the evaluation. The study aims are set out in Box 3; the last of these aims was added in October 2020.
-
Understand the baseline position and contextual features of the Trailblazer sites, including the accessibility, quality and effectiveness of existing mental health services and support in education settings and perceived gaps in provision prior to the programme commencing.
-
Describe and understand the emerging delivery models, their leadership and governance, and explore how these vary across the Trailblazer sites and the potential implications of this variation for future effectiveness of the programme. This includes examining how new roles and services are working in practice, what is working well and what is not, and barriers and facilitators to successful implementation.
-
Describe the experience of MHSTs, education settings, CCG and local authority commissioners, CYPMHS and others of taking part in the delivery of the programme.
-
Capture views about the progress being made by Trailblazers towards the goals of the programme, early impacts and any unanticipated consequences in the initial phases of the programme.
-
Identify measures and data sources of relevance to assessing programme outcomes and costs as well as appropriate comparator areas and education settings to assess the feasibility and develop the design of a long-term outcome and economic evaluation.
-
Conduct formative and learning-oriented research, producing timely findings and highlighting their practical implications to inform ongoing implementation and support roll-out to sites in later waves of the programme.
-
Understand how MHSTs adapted their services and ways of working in response to the COVID-19 pandemic, and explore experiences of and learning from these changes, as well as their legacy.
The protocol was developed following detailed scoping work which included:
-
Interviews to gather information about the rationale, design, implementation and aspirations for the Trailblazer programme. The team spoke to 23 people, including members of the national programme team, policy-makers and (e.g. children’s mental health) experts involved in the design of the national Trailblazer programme, as well as wider stakeholders including academics, voluntary sector organisations and professional bodies.
-
Consultation with the University of Birmingham Institute for Mental Health Youth Advisory Group (IMHYAG) and Think4Brum (the participation group for Forward Thinking Birmingham, the city’s specialist provider of mental health services to children and young people).
-
A review of programme and relevant national policy documentation.
-
Visits to three schools in Sandwell, West Midlands (one primary, one secondary, one special school), to obtain a better understanding of emotional and mental health-related issues from the perspective of education settings.
-
Input from specialists in the fields of children and young people’s mental health and mental health in schools, including the study’s specialist advisers: Dr Colette Soan (specialist senior educational psychologist for mental health) and Dr Karen Newbigging (academic researcher specialising in mental health policy and practice).
A longer-term assessment of the programme’s outcomes and impacts is being separately commissioned, to commence in spring 2023. Scoping design options and informing the specification for the longer-term impact evaluation was an aim of this early study (see aim 5 in Box 3).
The study was originally planned to start in October 2019 and complete in May 2021. Early delays to commencing fieldwork, including challenges negotiating approvals so the evaluation team could receive contact details for potential participants in the 25 sites, were compounded by COVID-19. The study was formally paused between March and October 2020, in line with guidance from the NIHR, and fieldwork eventually commenced in November 2020. The study’s two fieldwork periods (November 2020 to March 2021, May 2021 to January 2022) were both during the COVID-19 pandemic, with some overlap with periods of partial or full national lockdown. The findings in this report represent the early experiences of MHSTs operating in challenging circumstances, very different from those envisaged when the programme started, and should be interpreted in this light.
Structure of the report
Chapter 2 summarises evidence from three predecessor programmes and about paraprofessional roles in mental health and discusses how this evidence informed data collection and analysis. The key characteristics of the Trailblazer sites, together with a demographic and mental health service profile for each site, are presented in Chapter 3. Chapter 4 provides an overview of the research methods employed in the study. The study findings are presented in Chapters 5–10, and the activities and outputs from Work Package 3 (to scope and develop options for a longer-term assessment of the Trailblazer programme’s outcomes and impacts) in Chapter 11. Finally, Chapter 12 summarises and discusses the study findings, exploring their implications for ongoing programme implementation and roll-out.
Chapter 2 Implications for the evaluation of findings from similar programmes
Introduction
In our scoping interviews to inform the design of the evaluation, we spoke to several members of the national programme team from DHSC, DfE, NHSEI and Health Education England. Interviewees frequently mentioned three predecessor programmes that were said to have informed the design and implementation of the Trailblazer programme: Targeted Mental Health in Schools (TaMHS), IAPT and Schools Link. Consequently, a review of the findings from evaluations of these programmes was undertaken. Additionally, given that the Trailblazer programme was training a new paraprofessional workforce of EMHPs, we also reviewed evidence for and experiences of other (current and previous) paraprofessional roles in mental health provision. The primary aim of these reviews was to identify key themes and issues for the evaluation to look out for and explore, and which would inform the design of research tools and a framework for data analysis. We were also interested to find out whether the findings from these predecessor programmes, and for other paraprofessional roles in mental health, were taken into account in the design and implementation of the programme. This chapter presents a summary of the findings of this research and describes how these informed the current evaluation.
The Targeted Mental Health in Schools, Improving Access to Psychological Therapies and Schools Link programmes
A short summary of the three programmes and their evaluations is presented in Box 4.
-
TaMHS ran from 2008 to 2011, funded by the DfE and Department for Children, Schools and Families. The programme aimed ‘to develop innovative, locally determined models to provide early intervention and targeted support for children (aged 5 to 13) at risk of developing mental health problems and their families’. 25
-
Selected schools in all local authorities were involved, between 2500 and 3000 in total. Schools and local authorities decided how the funding would be used, and this resulted in a variety of approaches and resources across sites. Local models often included one or more of the following: training and support for school staff; school-based practitioners to work with school staff and pupils; and voluntary section provision.
-
Programme implementation was expected to be underpinned by two key principles: (1) strategic integration of all relevant agencies involved in delivering mental health services; and (2) implementation of evidence-informed interventions and models of support.
-
A national evaluation was commissioned by the DfE and Department for Children, Schools and Families, and conducted by a consortium of partners led by University College London and the Anna Freud Centre. It comprised two studies: a mixed-methods longitudinal study following 25 local authority areas selected as TaMHS pathfinders (an overall sample of approximately 20,000 pupils across more than 350 schools, over three academic years), and a randomised controlled trial in 73 local authority areas (involving over 30,000 pupils across more than 550 schools, over two academic years). The key aims of the evaluation included describing the different approaches and resources developed; assessing their impact on pupil mental health; exploring how targeted mental health provision was experienced by project workers, school staff, parents and pupils; and identifying lessons for future implementation. 25
-
In 2007, the government announced a large-scale programme to improve access to psychological (‘talking’) therapies for people with depression and anxiety in the English NHS. Initially developed for adults, IAPT provides evidence-based (i.e. approved by the National Institute for Health and Care Excellence) interventions from trained and accredited practitioners, using a stepped care model. Routine outcomes monitoring is a key feature of the programme, with user-reported outcome measures completed at each session and intended to support a client-focused approach and provide data to assess service performance and inform improvement.
-
In 2011, the service was extended to children and young people. In distinction from the adult programme, children and young people’s IAPT was intended to drive improvement in existing services, through the adoption of IAPT principles.
-
IAPT therapists deliver either low-intensity (mild to moderate mental health problems) or high-intensity (moderate to severe mental health problems) interventions. The two low-intensity roles – psychological well-being practitioners (adult IAPT) and children’s well-being practitioner (children and young people’s IAPT) – are trained to deliver CBT-informed therapies and are supervised by more experienced (and specially trained) colleagues within the team.
-
There has been no national evaluation of either IAPT programme, although several local evaluations and multisite analyses of programme data have been carried out. These include a three year mixed-methods evaluation by a collaboration led by Sheffield University of two demonstration sites for the adult IAPT model, funded by the NIHR and reported in 2011, involving interviews with 57 stakeholders and 77 patients within the IAPT sites. 26 A ‘rapid internal audit’ of children and young people’s IAPT was undertaken in 2014–15 by the Evidence-Based Practice Unit at University College London, the Anna Freud Centre and NHS England. The audit involved analysis of routinely collected data (for a total of 6803 young people from 11 services), staff surveys (n = 361 staff) and interviews (n = 92), interviews and focus groups with children and young people (n = 45) and parents (n = 42) in 12 case study areas. 27
-
The Mental Health Services and Schools Link pilots were launched in 2015 by NHS England and the DfE. The initial pilots involved 22 areas and were followed by national roll-out of the Schools Link programme in successive waves. The programme aimed to increase joint working by establishing a named lead with responsibility for mental health within each school and named point of contact within the local specialist NHS CYPMHS.
-
Lead contacts and wider stakeholders participated in two independently facilitated workshops in their area, to support knowledge sharing, relationship building and joint planning to improve support for children and young people’s mental health.
-
A national evaluation of the programme was commissioned by the DfE and undertaken by the consultancy Ecorys UK. This assessed the effectiveness of the programme design and implementation, involving survey research with the named leads in schools and NHS mental health services in the programme’s 22 pilot sites, and qualitative research with operational and strategic stakeholders in 10 of those areas. It explored challenges, success factors and lessons learned; and the outcomes achieved (e.g. changes to joint working between schools and specialist NHS services, and timeliness and appropriateness of referrals to specialist services). The evaluation reported in 2017. 28 A subsequent evaluation involving the original 22 pilot sites and a further 23 areas that had subsequently joined the programme, following the same methodology, was undertaken by the same team and findings were reported in 2020. 29
We reviewed the evidence reported by the evaluation studies described in Box 4, and from other sources on the three programmes identified through a structured literature search, with a particular focus on understanding the experiences of and enablers and challenges to programme implementation. The findings are organised according to the key themes emerging from our analysis.
Key themes from the evidence
Engagement and cross-organisational working
Fostering effective collaboration between the different agencies and sectors involved in programme implementation and delivery was widely reported as being vital to success. 29,30 Several factors contributed to relationship building and collaboration, many of which echo themes in the broader literature on interagency working. These included visible and committed leaders within the key organisations and sectors involved; local (e.g. service) champions; engagement of professional groups (both health-care and educational professionals); boundary spanning roles (e.g. educational psychologists in the TaMHS programme); and having a clear and agreed vision about programme scope and purpose, and how this related to existing provision and pathways. 25,26,31 Across programmes, implementation was further facilitated where relationships between partnering organisations were already established; for example, where individuals from local NHS services and education settings were already familiar with each other’s roles, scope and expertise. 28,30,32–34
Implementation was shaped not only by the quality, but also the constitution, of partnership working. For example, in the two IAPT demonstration sites, the composition and leadership of the local partnerships differed, and this influenced which issues were prioritised and how they were tackled. 34 Establishing and sustaining local partnership working was also reported to be challenging with studies describing tensions, and sometimes conflict, often related to competing organisational priorities and pressures (e.g. funding cuts) in the wider environment. 26,27,31 Another central challenge reported for all three programmes was a lack of common understanding and language for mental health, which acted as a barrier to partnership working between sectors (e.g. between health and education) and within them (e.g. between primary and secondary care). 25,28,31 What emerged from the evidence was a clear lesson about the need to prioritise, and invest time and resources in, relationship building and collaboration in order to lay the foundation for effective implementation.
Programme resources and timescales
Several issues emerged in relation to funding and resources. The funding provided through the programmes was crucial for fostering local buy-in and resourcing programme implementation, including recruiting and training staff for new delivery roles. In all three cases, programme funding was time limited, and there was uncertainty about if and how new services and ways of working would be sustained (or scaled up) longer-term. 25,28 This could be a barrier to initial engagement, and was also a major concern for stakeholders as programmes reached their end date. Lack of capacity was a further resource-related challenge, with implementation often being reliant on key people within (for example) schools and NHS services who had limited time to contribute and participate in key activities. 28,30,31 Acknowledging the additional demands that change and improvement programmes placed on frontline staff, and ensuring sufficient time away from the ‘day job’ for staff to plan, engage and reflect, were identified as an important considerations for programme success. 27,28
The set-up process was often felt to have been rushed, and the need for more preparatory time at the start of programmes was emphasised. This point was made most emphatically in relation to the implementation of the two IAPT programmes:
One of the loudest messages from the demonstration sites concerns the damaging consequences of implementing a new, complex service such as IAPT in an eight-month timescale. The timeframe for the pilot had far-reaching consequences at many levels within the demonstration sites. At an operational level it militated against the adoption of best practice in the service set-up, meaning implementation decisions were rushed, there was little time for consultation and the development of working relationships with partners and stakeholders, important mechanisms such as referral pathways and IT systems were not adequately tested prior to implementation and effective communication of the new service and engagement of stakeholders was limited. 34
Similar problems arising from short timescales affected children and young people’s IAPT, with Burn and colleagues’ implementation-focused evaluation concluding that there was ‘a lack of preparation for implementation at all levels’. 31 The need for experienced project management to oversee and coordinate what was reported to be a highly demanding and complex implementation process was also identified, something which both IAPT programmes were again felt to have lacked. 34
Increasing mental health support in education settings
The TaMHS and Schools Link programmes offer specific lessons about implementing improvements in school-based support for mental health. Both programmes, as their respective evaluations emphasise, built on diverse starting points. Education settings varied considerably in terms of their contexts, pupils’ mental health needs, what mental health support was already available within the setting, and existing relationships with specialist mental health services. Programme success was heavily dependent on new services and ways of working being tailored to individual education settings, and building on and being integrated with what settings were already providing. 25,28 A willingness among mental health professionals to speak ‘the language of schools’ and approach relationships with school staff as a sharing of mutual expertise (rather than seeing their role as purely instructional) were critical to success. 25 Having a member of the school team with clear responsibility for mental health promotion was also identified in both programmes as being important, and the need to build appropriate support around those in the role was emphasised. 28
The TaMHS evaluation team reported that:
Parents identified schools as the key point of contact for concerns about mental health issues and identified teachers as the key group they turned to if worried about their child’s mental health, and the group that provided most help in these situations. 25
This validates the approach taken in both programmes, which focused on building the confidence and skills of staff within education settings to support children’s mental health, alongside the goal of increasing access to specialist sources of support (whether that be increased provision within education settings in TaMHS or through more effective processes of referrals into local NHS services in Schools Link). The approach appears to have worked well from the perspective of staff in education settings who valued improved access to professional advice and support. 25,29,30 Staff participating in the TaMHS programme also reported improvements in their own well-being. 30
Balancing top down and bottom-up implementation
All three programmes combined some degree of central direction and structure with opportunities for local tailoring and adaptation. The importance of local flexibility was strongly emphasised, so that programme design and implementation could be shaped to local needs, circumstances and ways of working. Particularly in relation to the IAPT programme, tension between these two implementation ‘logics’ was described. Burn and colleagues reported a ‘lack of practical and evidence-based implementation guidance to inform local teams as to how to embed the [programme’s core] principles with everyday practice’, which they suggest may have reflected a deliberate attempt to avoid implementing ‘from the top’. 31 The reliance on quality improvement collaboratives to share learning and best practice between IAPT sites did not provide the anticipated knowledge for implementation, and the researchers concluded that more central guidance and support (e.g. on how to set up systems to record and report patient outcome data, which was widely reported to be a major challenge for both IAPT programmes) would have been helpful. Conversely, some IAPT practitioners were critical of the reliance on cognitive behaviour therapy and were keen that the programme supported local teams to train in and offer a wider range of interventions. 26 While service user feedback was generally positive, increasing choice in interventions and number of sessions provided were common suggestions for service improvement. 26,34 This is an issue we explore in more detail in the next section.
Paraprofessionals in mental health delivery
The term ‘paraprofessional’ is not well defined, but generally refers to roles that, ‘do not have formal professional or advanced educational training in health and/or human services but have some degree of specific training’. 35 Given that they require less specialised training, paraprofessionals offer relatively rapid way of increasing a healthcare workforce and addressing gaps in service provision. 36 Our review explored the lessons learned from experiences of paraprofessionals working in mental health delivery, with a particular interest in the insights from three English roles: psychological well-being practitioners and children’s well-being practitioners (in the IAPT programme) and primary care mental health workers, introduced in the early 2000s to support the management of common mental health problems in primary care settings. Primary care mental health workers supported general practitioners in their mental health delivery, and were trained to deliver brief, evidence-based interventions to people (including children) with common mental health problems. The key themes emerging from the literature are presented below.
Role definition and role boundaries
The role of paraprofessionals was often poorly defined, with ambiguity about their purpose or remit, and potential for overlap with other related roles. 37–39 Specifically in relation to primary care mental health workers, it was reported that other groups (e.g. clinicians and managers) often had expectations that were different from or wider than the formal remit of the role. 40 While paraprofessionals were keen to establish firm role boundaries and practice within the remit of the skills they had developed during training, this could be difficult to achieve, in part due to the issue of role ambiguity described above.
A key theme within the literature was that of role creep, with some paraprofessionals reporting they were working beyond their capabilities or experience. 34,41 For example, one study of primary care mental health workers reported that:
Participants also highlighted the variety of issues they found themselves facing on their first foray into clinical work. Although they were prepared to receive referrals for mild-moderate depression and anxiety, they were unprepared for the range and complexity of psychological issues that they were eventually presented with. 42
This raised significant risk management issues and could sometimes cause feelings of alarm or acute anxiety.
Working in a structured model
Paraprofessionals often reported enjoying and getting fulfilment from their work with clients. 34,41–43 However, both IAPT therapists and service users reported that the structured or ‘protocolised’ nature of the service limited opportunities to personalise the support provided and could be a barrier to developing a positive therapeutic relationship. 41,43,44 Some therapists felt that the service needed to expand the range of interventions beyond cognitive behaviour therapy, to include approaches that were more fully ‘contextualised’ (i.e. attendant to wider social, environmental and cultural factors that contributed to poor mental health). 41 Similar issues have been raised by service users. 45 The importance of adapting and tailoring approaches to specific groups and needs was recognised and some opportunities to work flexibly – for example, adapting the mode of delivery, session frequency or modifying self-help materials – have been described. 38,43,46 Adapting ways of working or interventions often took additional time, either in sessions with service users or in terms of preparatory work. This was felt to be insufficiently acknowledged and supported institutionally, which further increased the demands of the role. 47,48 Evidence suggests that some IAPT practitioners may be more open to and comfortable working outside the standard therapeutic model than others. 47,49
Training and supervision
In a small qualitative study with primary care mental health workers, training was described as positive but was also felt to be rushed and intense because of the amount of information that needed to be absorbed and range of new skills that had to be developed in a relatively short amount of time. 42 Participants reported a gap between what was learned in training and the ‘real world’ issues that were confronted once in practice, with the need for further training (e.g. in working with people with more complex problems) identified. In a survey of 415 primary care mental health workers, 51% reported they had unmet training and development needs. 50 Additional training needs have also been identified by IAPT therapists, in particular to enable them to tailor interventions and work effectively with specific groups and conditions not covered in the national training curriculum. 43,49 Training was felt to have paid insufficient attention to the relevance of cultural issues in therapy and practical skills for working in a culturally sensitive way. 47,48 The importance of good supervision was a recurrent theme, with more frequent and/or higher quality supervision associated with better job satisfaction, lower burnout and disengagement, and increased resilience. 51–53 There is evidence that more effective psychological well-being practitioners make greater use of clinical supervision and are more likely to flexibly adapt the therapeutic model, although the direction of causality between these variables is not fully understood. 54
Stress and burnout
Several studies reported high levels of emotional exhaustion, stress and burnout among IAPT therapists, which were correlated with several factors including: high work demands, long waiting times, lack of autonomy, perceived under-resourcing, managing and hold distress and risk, and greater hours of inputting data and overtime. 41,53,55,56 Heavy workloads was a common theme, and it was noted that paraprofessionals often managed larger caseloads than professional practitioners, despite having less training and (often) experience. 27,34,40,57 Some IAPT practitioners were of the view that the service’s target-oriented nature had resulted in the prioritisation of quantity (i.e. number of people seen) over quality (i.e. user experience and outcomes). 49,58 A longitudinal study involving more than 1500 IAPT practitioners reported that:
Discrepancies arose between the desired professional identity and what was considered realistically achievable within systemic limitations…Service priorities (administration, targets, outcome measures) obstructed delivery of adequate patient care leading to an oppressed, negative and frustrated workforce. 41
Practitioners identified good supervision and support from colleagues as essential for managing the demands of the job. 26
Retention and career progression
A strong theme emerging from the literature was that of retention. Experiences of the first cohort of primary care mental health workers suggested that levels of job satisfaction increased over time, but that attrition was also high and related to factors include dissatisfaction with pay, insufficient supervision, and the absence of clear professional status and career pathways. 59 High turnover rates for children’s well-being practitioners have also been reported. 31 Paraprofessional roles were often seen as a ‘stepping stone’ to other careers, such as clinical psychology. 39,42
Remote delivery
A small number of studies explored issues arising from telephone or online support in IAPT services. The option of remote support was felt to improve access to services, offer greater flexibility to service users and potentially reduce stigma. At the same time, though, it was reported to be harder to build a therapeutic relationship with the person being supported, and difficulties monitoring risks and outcomes in remote interactions were described. 43,57 Therapists in one study reported that telephone-based work was more isolating and that it felt like they were working in a ‘call centre environment’. 57 Relatedly, some users of the IAPT service reported feeling ‘less connected’ to their therapist when support was provided over the telephone, and they were more cautious about disclosing difficult information; although, conversely, others preferred this mode of support. 26 Survey research with IAPT practitioners in adult services found that greater hours of telephone contact predicted higher rates of burnout among psychological well-being practitioners. 53
Implications for the evaluation
Several recurring issues and experiences emerged from the evidence, which the evaluation team kept in mind as research tools were designed and throughout the fieldwork and analysis process. Specifically, the findings of the review suggested that key factors in the implementation of the Trailblazers programme might include:
-
Which organisations and sectors are involved in local programme design and implementation, if/how different priorities and perspectives are balanced within partnership working arrangements and the extent to which these arrangements are underpinned by a shared language around mental health and well-being.
-
Engagement of frontline staff (e.g. teaching and other school staff), and their capacity to participate in programme implementation and ongoing delivery.
-
Timescales for, and the allocation of resources to, programme implementation.
-
Plans for sustaining the services and ways of working introduced through the programme, beyond its ‘pilot’ funding phase.
-
If, and how, local implementation is tailored to, and integrated with existing approaches and provision in individual education settings.
-
The balance between centrally dictated and locally determined implementation, and the extent of clarity at the local level about not only what is being implemented, but also how.
-
Opportunities and challenges for EMHPs; for example, clarity about and ability to work within a defined role and remit; confidence and ability to tailor approaches to different contexts and support needs; adequacy of training and support; workloads; opportunities for career development and progress; and experiences of remote working.
We return to several of these themes in Chapter 12, where we consider whether these findings were taken into account in the design and implementation of the Trailblazer programme.
Chapter 3 Overview of the Trailblazer sites
Trailblazer characteristics
Key characteristics of the 25 Trailblazer sites are provided in Table 2. As this shows, each site was funded to create between two and four MHSTs and the average number of education settings covered by each MHST varied considerably from 8 (Liverpool) to 35 (Newcastle). Participating education settings ranged from small one-form primaries to large secondary schools and further education colleges. There is similar variation in average populations covered by each MHST, with many teams covering populations far in excess of the 8000 pupils that was originally intended. Of the 33 organisations named as MHST service providers, 70% are NHS trusts and the remaining 30% are from the voluntary sector. Across the Trailblazer sites, MHSTs are provided by one or more NHS trusts in 17 sites, by an NHS and voluntary sector partnership in five sites, and by a voluntary sector organisation alone in three sites. Some of the Trailblazer sites successfully bid for funding in later waves of the programme, and so have several teams at different stages of development.
| Trailblazer site | Region | Integrated care system | MHST service provider(s) | MHSTs funded in Trailblazer wave (n) | Education settings supported by MHSTs (n)a | Children and young people population covered by MHSTs (n)b | 4WWT pilot | MHSTs funded in subsequent waves |
|---|---|---|---|---|---|---|---|---|
| Berkshire West | South East | Buckinghamshire, Oxfordshire and Berkshire West | Berkshire Healthcare NHS Foundation Trust; Brighter Futures for Children | 2 | 40 | 14,180 | ✗ | ✓ |
| Bromley | London | Our Healthier South East London | Oxleas NHS Foundation Trust; Bromley Y | 2 | 48 | 29,441 | ✓ | ✗ |
| Buckinghamshire | South East | Buckinghamshire, Oxfordshire and Berkshire West | Oxford Health Foundation Trust | 2 | 29 | 17,441 | ✓ | ✗ |
| Camden | London | North Central London Partners in Health and Care | Tavistock and Portman NHS Foundation Trust | 2 | 27 | 15,101 | ✓ | ✗ |
| Doncaster and Rotherham | North East and Yorkshire | South Yorkshire and Bassetlaw | Rotherham, Doncaster and South Humber NHS Foundation Trust | 4 | 57 | 32,968 | ✓ | ✗ |
| Gloucestershire | South West | One Gloucestershire | Gloucestershire Health and Care NHS Foundation Trust; TIC+ | 4 | 70 | 38,597 | ✓ | ✗ |
| Greater Manchesterc | North West | Greater Manchester Health and Social Care Partnership | Manchester University NHS Foundation Trust; 42nd Street; Manchester Mind; Place2be | 2 | 64 | 44,525 | ✓ | ✓ |
| Haringey | London | North Central London Partners in Health and Care | Barnet, Enfield and Haringey Mental Health Trust | 2 | 37 | 32,321 | ✓ | ✗ |
| Hertfordshire | East of England | Hertfordshire and West Essex | Hertfordshire Partnership University NHS Foundation Trust | 2 | 32 | 25,953 | ✗ | ✓ |
| Hounslow | London | North West London | West London NHS Trust | 2 | 24 | 16,997 | ✗ | ✓ |
| Kirklees | North West | West Yorkshire and Harrogate Health and Care Partnership | South West Yorkshire Partnership NHS Foundation Trust | 2 | 38 | 16,776 | ✗ | ✓ |
| Liverpool | North West | Cheshire and Merseyside Health and Care Partnership | Alder Hey Children’s NHS Foundation Trust | 3 | 24 | 8,788 | ✗ | ✓ |
| Newcastle | North East and Yorkshire | North East and North Cumbria | The Children’s Society | 3 | 105 | 47,392 | ✗ | ✗ |
| North Kent | South East | Kent and Medway | North East London NHS Foundation Trust | 2 | 36 | 31,172 | ✗ | ✗ |
| North Staffordshire | Midlands | Together We’re Better – Staffordshire and Stoke-on-Trent | North Staffordshire Combined Healthcare NHS Trust | 2 | 23 | 6921 | ✓ | ✓ |
| Northumberland | North East and Yorkshire | North East and North Cumbria | Cumbria, Northumberland Tyne and Wear NHS Foundation Trust | 2 | 27 | 9224 | ✓ | ✓ |
| Nottinghamshire | Midlands | Nottingham and Nottinghamshire | Nottinghamshire Healthcare NHS Foundation Trust | 2 | 41 | 16,625 | ✗ | ✓ |
| Oxfordshire | South East | Buckinghamshire, Oxfordshire and Berkshire West | Oxford Health NHS Foundation Trust; Response | 2 | 34 | 16,803 | ✓ | ✓ |
| South Tyneside | North East and Yorkshire | North East and North Cumbria | South Tyneside and Sunderland NHS Foundation Trust; Cumbria, Northumberland Tyne and Wear NHS Foundation Trust | 2 | 33 | 18,074 | ✗ | ✓ |
| South Warwickshire | Midlands | Coventry and Warwickshire | Coventry and Warwickshire Partnership NHS Trust | 2 | 45 | 16,890 | ✓ | ✗ |
| South West London | London | South West London Health and Care Partnership | South West London and St George’s Mental Health NHS Trust | 3 | 44 | 25,954 | ✗ | ✓ |
| Stoke-on-Trent | Midlands | Together we’re better – Staffordshire and Stoke-on-Trent | North Staffordshire Combined Healthcare NHS Trust | 2 | 28 | 24,237 | ✓ | ✓ |
| Swindon | South West | Bath and North East Somerset, Swindon and Wiltshire | Barnardo’s | 3 | 37 | 35,854 | ✗ | ✓ |
| Tower Hamlets | London | North East London Health and Care Partnership | East London NHS Foundation Trust | 2 | 22 | 16,349 | ✓ | ✗ |
| West London | London | North West London | Hammersmith and Fulham Mind | 2 | 30 | 12,440 | ✗ | ✗ |
By the time our fieldwork started in November 2020, Stoke-on-Trent and North Staffordshire had combined into a single Trailblazer, with a single project lead and shared MHST model delivered by the same NHS trust. These two sites were also jointly awarded funding to pilot the four-week waiting time.
Demographic and mental health service profiles
Data on a range of indicators have been collated to create demographic and mental health service profiles for each of the 25 Trailblazer sites. For each indicator, data were gathered that related to the lead CCG population in Trailblazer sites and service-related information from the main NHS provider of specialist CYPMHS in the area. We used data reported closest to December 2018, to create a snapshot of population characteristics and service performance at the time that the Trailblazer sites were announced. The methodology, description of indicators used and full data tables can be found in Appendix 3.
This section provides an overview of the data, including Trailblazer and national averages, and describes the highest and lowest values for each indicator to give a sense of the diversity across the 25 sites (Table 3).
| Indicator | Reporting period | National average | Trailblazer average | Highest value for a Trailblazer site | Lowest value for a Trailblazer site |
|---|---|---|---|---|---|
| Black and Minority Ethnic Population by CCG (%) | 2018/19 | 14.6 | 18.7 | 54.8 | 1.6 |
| Index of multiple deprivation by CCGa | 2019 | 21.7 | 22.2 | 42.4 | 10.0 |
| Estimated prevalence of emotional disorders by CCG: 5–16 years (% of population) | 2017/18 | 3.6 | 3.6 | 4.2 | 3.1 |
| Estimated prevalence of common mental disorders by CCG: 16 years and above (% of population) | 2018/19 | 16.9 | 17.6 | 22.8 | 13.3 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 34.0 | 30.1 | 46 | 12 |
| Average waiting time between referral to NHS CYPMHS and second contact by CCG | 2018/19 | 53 days | 59 days | 90 days | 29 days |
| Total number of children referred to NHS CYPMHS as a proportion of the under-18 population by CCG | 2018/19 | 3.6% | 3.52% | 6.20% | 2.32% |
| Mental health spend per child by CCG | 2018/19 | £59.22 | £68.75 | £140.18 | £39.32 |
| CCG spend on children’s mental health as a percentage of total CCG budget | 2018/19 | 0.92% | 1.03% | 1.82% | 0.67% |
| Provider in SOF segment 3 or 4 during the year by NHS CYPMHS providerb | 2018/19 | SOF 3: 28% of providers; SOF 4: 9% of providers | SOF 3: 12% of providers; SOF 4: 0% of providers | NA | NA |
| CQC trust rating: overall by NHS CYPMHS provider | 2017/18 | Outstanding: 6% | Outstanding: 16% | NA | NA |
| Good: 60% | Good: 76% | ||||
| Requires improvement: 31% | Requires improvement: 8% | ||||
| Inadequate: 3% | Inadequate: 0% | ||||
| CQC trust rating: specialist community mental health services for children and young people by NHS CYPMHS providerc | 2015/18 | Outstanding: 9% | Outstanding: 17% | NA | NA |
| Good: 65% | Good: 67% | ||||
| Requires improvement: 24% | Requires improvement: 17% | ||||
| Inadequate: 2% | Inadequate: 0% |
Routine data, especially on service performance, can be difficult to interpret without additional contextualising information, and therefore some caution should be exercised when comparing the figures presented in the tables above. Notwithstanding, some general observations can be made:
-
Trailblazer sites had proportionally larger ethnic minority populations (18.7% vs. 14.6%) and recorded slightly higher levels of deprivation compared with the national average. There was also substantial variation across the 25 Trailblazers for these two indicators. For example, the percentage of local populations from ethnic minority groups ranged from a low of 1.6% to a high of 54.8%. Index of multiple deprivation scores ranged from a low of 10.0 to a high of 42.4.
-
Average recorded prevalence of emotional disorders among young people aged 5–16 years was identical in the Trailblazer sites and for England overall, at 3.6%. Prevalence of common mental disorders among those aged 16 years and above was slightly higher in the Trailblazer sites (17.6%) compared with the national average (16.9%).
-
On average, Trailblazer sites were spending more on children’s mental health services per child (£69 in Trailblazer sites, compared with a national average of £59) and as a proportion of the overall CCG budget (1.03% in Trailblazer sites vs. 0.92% national average).
-
Similarly, the performance of NHS specialist CYPMHS was better in Trailblazer sites, with the exception of waiting times between referral and second contact. In terms of overall Care Quality Commission (CQC) ratings for the trusts providing CYPMHS in the Trailblazer sites, 92% were rated outstanding or good, compared with 66% of trusts in England overall. At the time that data were reported, 37% of all NHS trusts providing mental health services to children and young people were considered to have significant support needs or were in special measures, compared with only 12% in the Trailblazer sites.
-
Some of the indicators reported above are particularly difficult to interpret, including ‘The percentage of referrals to NHS CYPMHS that are closed before treatment’ and ‘Total number of children referred to NHS CYPMHS as a proportion of the under-18 population’. Trailblazer averages for both these indicators were slightly lower than the national average, but there may be several explanations. For example, the smaller proportion of children and young people being referred to NHS services in Trailblazer sites might be reflective of child and parental preferences for support, local referral practices and thresholds, extent and effectiveness of preventive activities and programmes, or the availability of non-NHS services in the areas concerned (e.g. services provided by voluntary sector organisations or local authorities).
The stronger performance of specialist NHS services in the Trailblazer sites compared with the national picture is to be expected. As noted in Chapter 1, the criteria for selecting Trailblazers included several requirements relating to local investment in CYPMHS and performance of those services. For example, the selection criteria explicitly excluded CCGs in special measures, and NHS provider trusts rated by the CQC as ‘inadequate’.
Funding received by Trailblazer sites
Information on the funding awarded to Trailblazer sites in the first three years of the programme was provided by NHSEI, although is not reported here due to it being classified as commercial in confidence. This information showed substantial variation in the funding amounts awarded to the sites. For example, funding in the 2019/20 year ranged from £108,284 to £1,300,994, with most sites receiving between £300,000 and £800,000. We sought explanation from the programme team about the factors accounting for this variation and they gave several reasons for this:
-
Some sites commenced local set-up of the programme later than others; where this was the case, they received less (or no) funding for 2018/19.
-
As mentioned in Chapter 1, the standardised workforce model and funding allocation for MHSTs was introduced after the Trailblazer wave. Trailblazers bid for varying amounts; in some cases, this included funding for non-staff costs (e.g. to secure specialist advice or project management input, or purchase online mental health support services) and/or for more specialist roles (e.g. speech and language therapists). Three Trailblazers were awarded funding for additional services or elements (Bromley, Haringey and West London).
-
In a small number of cases, the national programme team felt a site did not have adequate staffing (e.g. not enough staff or inappropriate skill/seniority mix) to deliver the core MHST functions, and they were given the opportunity review and alter their staffing composition. This resulted in an increase in the funding for two sites (Nottingham and North Staffordshire) to enable them to recruit additional EMHPs to their teams.
With the information we have, it is not clear whether the variation in funding amounts across sites can be fully accounted for by the reasons above. Some sites with similar team compositions, population coverage and geography received very different funding amounts. This important issue is one that will need to be explored further in the planned impact evaluation of the Trailblazer programme.
Chapter 4 Methods
Study design
The overall aim and detailed objectives of the evaluation are presented in Chapter 1 (Box 3). To meet these aims and objectives, a mixed-methods evaluation was designed which included quantitative and qualitative data collection, alongside analysis of other information and data provided by the national team, and research at local, regional and national levels. Underpinning the study is an evaluation framework which collected and analysed data at four levels: children, young people and families; MHSTs; education settings; and wider local systems (see Appendix 4 for more details).
The evaluation comprised three work packages:
-
Work package 1: establishing the baseline and understanding the development and early impacts of the Trailblazers. This involves research across all 25 Trailblazer sites and interviews with the programme’s regional and national leads.
-
Work package 2: more detailed research with a range of stakeholders in five purposively selected Trailblazer sites and focus groups with children and young people.
-
Work package 3: scoping and developing options for a longer-term assessment of the programme’s outcomes and impacts. A summary of the activities and analysis that comprised this work package, and the key findings, is reported in Chapter 11.
Copies of all the research tools and the coding framework for the qualitative analysis can be found in Report Supplementary Material 1. Design of the research tools and data analysis was informed by the scoping work (see Chapter 1 for more details), the literature and evidence reviews reported in Chapter 2 and two preliminary programme theories of change: one developed by the evaluation team during the initial months of the study (see Documents C and D in Report Supplementary Material 2) and the other developed by the national team in early 2019 (subsequently revised in summer 2021). Assumptions and critical tensions inherent in the programme logic were surfaced and developed into lines of enquiry that were explored through the surveys and qualitative research. Questions were also included in all research tools on the impact of COVID-19: on programme implementation, MHST set-up and delivery, and on children’s mental health and support needs.
Data collection
Surveys
Data collection included two surveys, each undertaken twice: (1) a survey of participating education settings in the Trailblazer sites; and (2) a key informant survey of local stakeholders involved in the programme.
Education settings surveys
Two surveys were conducted of education settings participating in the Trailblazer programme. Contact details for the senior mental health leads (or MHST co-ordinator, where this role was not in place) in participating settings were obtained from the project lead for each Trailblazer site in early 2020. The questionnaire was designed with input from a range of experts and stakeholders, including a number of local project leads and other key personnel in sites participating in the programme (both Trailblazer sites and later waves); members of the national programme team from the DfE; and specialist advisers to the evaluation team with expertise in mental health promotion and provision within education settings.
The first survey was open from November 2020 to February 2021 and the second from October to December 2021. Contacts were sent an invitation to complete the survey by email, with up to three reminders. Several local project leads agreed to contact education settings in their site to encourage completion of the survey. The surveys were administered using the online platform CoreXM (Qualtrics, Seattle, WA) and each took 15 minutes on average to complete. Invitations were sent to 1008 valid email addresses in the first survey and to 936 addresses in the second. The smaller number of invitations sent at follow-up was due to the reduced number of valid email addresses available to contact (as a result of staff turnover since the addresses were originally obtained in 2020).
Table 4 provides details of the number of invitations sent to each site, and responses received. Although the response rate was lower than we aimed to achieve (30% for the first survey and 17% for the second survey), we still managed to obtain at least two responses from each Trailblazer site in each survey. Response rates were considerably higher from some Trailblazer sites than other (e.g. Bromley and Buckinghamshire in the first survey, Hertfordshire and North Kent in the second) and caution must be applied when considering the ability to generalise from the findings. The response rate for the first survey was very close to the 29% response rate achieved by the DfE Mental Health Experience Survey of education settings in waves 1 and 2 of the programme (the corresponding figure for the DfE baseline provision survey in Trailblazer sites was not available to us). Table 5 shows the distribution of responses by respondents’ roles; in both surveys, the majority of those who participated identified as the senior mental health lead for their setting.
| Trailblazer site | First survey | Second survey | ||||
|---|---|---|---|---|---|---|
| Invitations sent (n) | Responses received (n) | Response rate (%) | Invitations sent (n) | Responses received (n) | Response rate (%) | |
| Berkshire West | 41 | 4 | 9.7 | 35 | 3 | 8.6 |
| Bromley | 48 | 23 | 47.9 | 44 | 9 | 20.5 |
| Buckinghamshire | 43 | 20 | 46.5 | 34 | 10 | 29.4 |
| Camden | 26 | 3 | 11.5 | 20 | 5 | 25.0 |
| Doncaster & Rotherham | 38 | 13 | 34.2 | 30 | 5 | 16.7 |
| Gloucestershire | 70 | 29 | 41.4 | 69 | 16 | 23.2 |
| Haringey | 37 | 15 | 40.5 | 36 | 9 | 25.0 |
| Hertfordshire | 31 | 9 | 29.0 | 29 | 10 | 34.5 |
| Hounslow | 20 | 5 | 25.0 | 18 | 4 | 22.2 |
| Kirklees | 37 | 14 | 37.8 | 37 | 7 | 18.9 |
| Liverpool | 24 | 10 | 41.6 | 24 | 5 | 20.8 |
| Newcastle | 109 | 25 | 22.9 | 106 | 12 | 11.3 |
| North Kent | 35 | 12 | 34.2 | 32 | 11 | 34.4 |
| North Staffordshire & Stoke-on-Trent | 65 | 23 | 35.4 | 64 | 8 | 12.5 |
| Northumberland | 33 | 7 | 21.2 | 30 | 4 | 13.3 |
| Nottinghamshire | 43 | 5 | 11.6 | 42 | 2 | 4.8 |
| Oxfordshire | 36 | 7 | 19.4 | 33 | 2 | 6.1 |
| South Tyneside | 60 | 18 | 30.0 | 55 | 6 | 10.9 |
| South Warwickshire | 50 | 6 | 12.0 | 49 | 3 | 6.1 |
| South West London Health and Care Partnership | 64 | 26 | 40.6 | 61 | 19 | 31.1 |
| Swindon | 43 | 12 | 27.9 | 39 | 2 | 5.1 |
| Tower Hamlets | 25 | 8 | 32.0 | 21 | 2 | 9.5 |
| West London | 30 | 5 | 16.6 | 28 | 5 | 17.9 |
| Total | 1008 | 299 | 29.6 | 936 | 159 | 16.9 |
| Role of respondenta | Survey 1 responses | Survey 2 responses |
|---|---|---|
| n (%) | n (%) | |
| Senior mental health lead for Trailblazer programme | 185 (62) | 69 (43) |
| Lead for mental health, not specifically in relation to the Trailblazer programme | 111 (37) | 44 (27) |
| Deputy head teacher, vice principal or equivalent | 62 (21) | 33 (21) |
| MHST co-ordinator | 41 (14) | 23 (14) |
| Head teacher, principal or equivalent | 46 (15) | 26 (16) |
| Other member of senior leadership team | 71 (24) | 28 (18) |
| Special educational needs co-ordinator or equivalent | 100 (33) | 48 (30) |
| Other teaching staff | 22 (7) | 9 (6) |
| Pastoral lead | 78 (26) | 33 (21) |
| Support staff | 50 (17) | 25 (16) |
| Year head | 4 (1) | 0 (0) |
| Other | 35 (12) | 10 (6) |
Answers to the fixed-response questions were exported into Microsoft Excel® for quantitative analysis, while responses to open-ended questions were analysed and grouped into themes for reporting. An initial set of themes was developed after reading all the free-text responses and these were further refined during discussions with the research team. Given the large number of qualitative data and range of themes emerging from the free-text responses, a list of the key themes for each question was produced and used to support comparison and synthesis of survey findings with the other data collected for the study, and for reporting.
Key informant survey
Two surveys were conducted of individuals who were playing or had played a central role in the design and implementation of the MHSTs in their area. As with the education settings survey, the key informant surveys were designed and refined in collaboration with a range of stakeholders, including specialist advisers to the evaluation team and a small number of MHST service managers (from Trailblazer sites, and sites participating in later waves of the programme). Trailblazer sites were asked to provide a list of contacts for the surveys, to include people in key programme design, implementation and delivery roles. In both waves of the survey, all stakeholders were asked the same core set of questions, with additional questions posed to some groups (MHST managers, education leads and project leads) to obtain further details on specific aspects of the programme locally, such as resourcing. The surveys were administered using the online platform SmartSurvey.
The first survey ran from December 2020 to May 2021; an invitation to participate was sent to 291 people, with 76 responses (26%). The second survey ran between October and November 2021; 253 people were invited and 65 responded (26%). Tables 6 and 7 summarise the profile of respondents by site and role. We received at least one response from each Trailblazer site in both surveys. Broadly there was a good spread of responses across the different roles, although in each survey there were only two responses from people working in specialist NHS mental health services. In the second survey, respondents were also asked how long they had been working on the Trailblazer programme, to which most (85%) responded 18 months or longer.
| Trailblazer site | First survey | Second survey | ||||
|---|---|---|---|---|---|---|
| Invitations sent (n) | Responses received (n) | Response rate (%) | Invitations sent (n) | Responses received (n) | Response rate (%) | |
| Berkshire West | 9 | 3 | 33.3 | 8 | 3 | 37.5 |
| Bromley | 14 | 5 | 35.7 | 13 | 3 | 23.1 |
| Buckinghamshire | 6 | 1 | 16.7 | 6 | 1 | 16.7 |
| Camden | 7 | 1 | 14.3 | 4 | 2 | 50.0 |
| Doncaster and Rotherham | 8 | 4 | 50.0 | 7 | 3 | 42.9 |
| Gloucestershire | 6 | 2 | 33.3 | 11 | 4 | 36.4 |
| Haringey | 19 | 9 | 47.4 | 17 | 4 | 23.5 |
| Hertfordshire | 8 | 4 | 50.0 | 9 | 2 | 22.2 |
| Hounslow | 5 | 1 | 20.0 | 5 | 1 | 20.0 |
| Liverpool | 11 | 3 | 27.3 | 13 | 8 | 61.5 |
| Greater Manchester | 17 | 5 | 29.4 | 13 | 4 | 30.8 |
| North Staffs/Stoke-on-Trent | 9 | 5 | 55.6 | 9 | 3 | 33.3 |
| Newcastle | 6 | 1 | 16.7 | 5 | 1 | 20.0 |
| North Kent | 12 | 6 | 50.0 | 11 | 7 | 63.6 |
| Kirklees | 11 | 2 | 18.2 | 9 | 3 | 33.3 |
| Northumberland | 7 | 1 | 14.3 | 8 | 1 | 12.5 |
| Nottinghamshire | 7 | 3 | 42.9 | 9 | 1 | 11.1 |
| Oxfordshire | 19 | 5 | 26.3 | 12 | 3 | 25.0 |
| South Tyneside | 13 | 4 | 30.8 | 13 | 2 | 15.4 |
| South Warwickshire | 5 | 2 | 40.0 | 5 | 1 | 20.0 |
| South West London Health Care Partnership | 19 | 4 | 21.1 | 19 | 1 | 5.3 |
| Swindon | 7 | 3 | 42.9 | 7 | 3 | 42.9 |
| Tower Hamlets | 23 | 1 | 4.3 | 21 | 3 | 14.3 |
| West London | 5 | 1 | 20 | 5 | 1 | 20 |
| Total | 253 | 76 | 30.0 | 239 | 65 | 27.2 |
| Rolea | Survey 1 total responses | Survey 2 total responses |
|---|---|---|
| n (%) | n (%) | |
| Project lead | 15 (20) | 11 (17) |
| Senior responsible officer | 6 (8) | 4 (6) |
| CCG lead | 10 (13) | 14 (22) |
| MHST manager | 15 (20) | 17 (26) |
| Education lead | 10 (13) | 8 (12) |
| Specialist NHS mental health service | 2 (3) | 2 (3) |
| Local authority (not education lead) | 6 (8) | 12 (18) |
| Voluntary sector | 11 (14) | 4 (6) |
| Other | 4 (5) | 0 (0) |
Data were exported to Excel for analysis. Fixed-response questions were quantitatively analysed in Excel. Responses to open-ended questions were grouped and thematically analysed.
In-depth research in case study Trailblazers
Case study selection
The project team initially sought to secure agreement from six Trailblazer areas to undertake in-depth research with a range of stakeholders. A table was created to provide a descriptive overview of the 25 sites, drawing on the statistical profiles reported in Chapter 3 and also including geographical location (based on NHS region), MHST staffing composition, MHST contract holder(s), MHST coverage (number of schools and pupils), extent and nature of children and young people’s involvement in designing and implementing the Trailblazer MHSTs, and any other potentially important factors (e.g. MHSTs targeting specific population groups), drawn from local site documentation. At the start of the study, we received background documentation from the national programme team on each of the Trailblazer sites. While the information was helpful for initial familiarisation, it was variable in terms of quality and completeness, and mostly dated back to when areas were applying to join the programme (2018) and preparing preliminary project plans (early 2019). We therefore planned to gather more up-to-date information from the Trailblazers to guide the selection of case study sites in the first key informant and education setting surveys. To make up some of the time lost when the study was paused in 2020 due to COVID-19, a decision was taken to run these surveys in parallel to selecting and setting up case study sites. As a result, at the point at which case study sites were being selected, the information we had on the Trailblazers and their contextual characteristics was limited, and some characteristics were excluded from consideration.
Six members of the research team discussed and agreed the criteria to guide the selection process. Priority was given to characteristics that our preliminary research indicated may be influential in shaping local models and implementation processes, and for which we had relatively high quality and complete data. Six sites were then selected, seeking to maximise diversity on the priority characteristics (geographical location, to ensure representation of sites across England, rural/urban classification, population ethnic diversity and deprivation, and MHST staffing composition and contract holder).
Recruitment of case study sites
A researcher was allocated to each site to act as their point of contact and to undertake data collection; there was also an overall case study lead who provided support and ensured consistency of approach across sites. All researchers had substantial prior experience of undertaking and analysing qualitative interviews. Contact was made with the project lead for each of the sites selected via e-mail, including an information sheet detailing the purpose of the case study research and what it would involve. Once a site had agreed in principle to take part, a familiarisation meeting (held remotely) was held to discuss the specifics of the qualitative research process, including timing and ethical considerations; for local teams to provide an overview of the Trailblazer programme in their area including how it was run and the local context; and to compile a preliminary list of people to invite to participate in an interview (with further interviewees identified as the research progressed). Sites were also asked to provide researchers with any key documents relating to the design and/or implementation of the Trailblazer programme in their area.
Five of the sites initially approached agreed to participate in the research. One site did not respond to a series of emails over a four-month period so an alternative site with comparable characteristics was approached, which agreed to become a case study. One of the sites initially recruited subsequently withdrew, citing challenges with staff turnover and workload pressures. Owing to the late timing of this withdrawal, it was decided not to invite an alternative site, so five case study sites were included.
Recruiting participants and conducting interviews
We sought to interview between 10 and 15 participants in each site. Potential interviewees were approached by e-mail, and were sent an information sheet and consent form to sign and return if they agreed to take part. Between July 2021 and February 2022, 71 people took part in an interview across a range of roles as outlined in Table 8. Only two people explicitly declined to take part in an interview (one was new in post and the other had left the MHST); a further 22 people either did not respond to our initial invitation e-mail or responded to say that they would take part and then did not reply to subsequent communication. Three people were unable to participate, either because they were ill at the time or on maternity/paternity leave. The pattern of nonparticipation varied from site to site, but the numbers recruited from schools and colleges were notably lower than we had hoped for. The study did not formally aim to achieve data saturation, but participant samples were regularly reviewed during the data collection phase, and later recruitment specifically targeted roles or groups that were under-represented (including senior mental health leads and staff in NHS specialist mental health services).
| Area | EMHPs (n) | MHST staff (not including EMHPs) (n) | School and college staff (n) | Individuals in Trailblazer governance and management roles (n) | Other organisationsa | Total people interviewed (n) |
|---|---|---|---|---|---|---|
| Site 1 | 4 | 3 | 1 | 6 | 0 | 14 |
| Site 2 | 5 | 3 | 2 | 2 | 0 | 12 |
| Site 3 | 3 | 4 | 2 | 6 | 2 | 17 |
| Site 4 | 4 | 3 | 1 | 2 | 2 | 12 |
| Site 5 | 3 | 2 | 3 | 3 | 5 | 16 |
| Total | 19 | 15 | 9 | 19 | 9 | 71 |
A suite of topic guides was developed with questions tailored to different roles, informed by previous data collection, relevant literature (Chapter 2) and the study aims and objectives. All interviews (case study, regional and national leads) were conducted remotely via Microsoft Teams or Zoom, due to COVID-19 restrictions in place at the time. Consent was obtained before the interview, including consent to record the interview on a voice recorder. One interviewee asked that the interview not be recorded, so detailed notes were taken during and immediately after the interview instead. Interview duration ranged from 26 minutes to 1 hour 17 minutes. Recordings were transcribed verbatim and transcripts checked for accuracy (with researchers returning to the original voice recording if they needed to address any transcription gaps or errors) and then anonymised.
Interviews with national programme team and regional leads
All NHSEI and DfE regional programme leads were invited to twice to an interview: between November 2020 and January 2021, and again between November 2021 and January 2022. Participants were given the opportunity to be interviewed alone or with the other lead(s) from their region, and to invite other regional colleagues to join the interview if they wished. A total of 26 people were interviewed in each round, with 12 people interviewed in both rounds (making 40 unique interviewees).
Additionally, in January and February 2022, group interviews were undertaken with members of the national programme team from the DHSC, DfE, NHSEI and Health Education England. A group interview was also undertaken with key personnel from two universities delivering EMHP training, and a further interview with a senior adviser on children’s mental health to NHSEI. Eight interviews were undertaken, involving a total of 21people (Table 9).
| Organisation | Staff interviewed at regional level (November 2020 to January 2021) (n) | Staff interviewed at regional level (November 2021 to January 2022) (n) | Staff interviewed at national level (January–February 2022) (n) |
|---|---|---|---|
| DfE | 9 | 8 | 6 |
| NHSEI | 13 | 13 | 4 |
| DHSC | 0 | 0 | 4 |
| Health Education England | 2 | 4 | 2 |
| Training providers | 0 | 0 | 4 |
| Other | 2 | 1 | 1 |
| Total | 26 | 26 | 21 |
Interviews were semistructured and followed tailored topic guides. These covered a range of themes including national and regional contexts for the programme, progress to date, the impact of COVID-19 on plans and implementation, experiences of Trailblazer programme development and delivery, partnership working, early impacts, what was working well and less well, and plans for future development of the programme.
Data analysis and synthesis
Analysis of qualitative data
Using a team-based approach, qualitative data from the case study interviews were analysed thematically and comparatively, guided by the principles of the framework method. 60 A coding framework was initially developed by the case study research lead, using the themes from the topic guide and insights from the literature review (Chapter 2). This was further developed following discussions within the case study team and preliminary coding of a sample of interviews. The final coding frame (Report Supplementary Material 1) was then used to code the remainder of the interviews. Coding was undertaken by four members of the team, three of whom had conducted interviews at case study sites, and an additional researcher was brought in to free up colleagues to focus on other data collection activities. NVivo software (Lumivero, Denver, CO) was used for data management. A similar process was followed for the regional and national interviews, using the coding framework already developed for the case study interviews, to which new themes were added as they emerged from preliminary familiarisation with the data. Coding was undertaken by the two researchers who had led these interviews, who worked closely to ensure consistency of approach and interpretation.
Throughout the analysis process fortnightly meetings of the researchers involved in conducting and/or analysing qualitative interviews were held to discuss emerging themes and explore similarities and differences between sites and the potential reasons for them, and to ensure that the coding framework was being applied consistently. Findings from the earlier research and emerging insights from concurrent analyses (e.g. of the survey data) were shared during these meetings, and this initiated the process of data synthesis. In addition, two full team analysis workshops were held at which emerging themes and variation across the case study areas were explored, and synthesis of the qualitative, quantitative and routine data was formally discussed. A narrative summary of the findings for each site was produced using an agreed structure, which enabled synthesis and comparison of findings between sites.
Cross analysis and synthesis of data
Initially, each dataset was independently analysed by the research team member(s) leading that element of data collection. In both phases of data collection, a structured template was developed for team members to produce detailed summaries of significant findings from their data collection activity to support comparison and synthesis, which were shared with all members of the team. These summaries were discussed at the fortnightly team meetings held throughout the study and at five data analysis workshops (three workshops in the first phase of data collection, two in the second phase). Insights from the different sources of data were compared, recurrent themes and issues requiring further investigation were identified and key themes for reporting were agreed. The workshops during the first phase of fieldwork were also used to generate a list of priority topics for the data collection to follow.
As well as looking for commonalities, attention was also paid to identifying and exploring divergence between the views and experiences reported and between the different types of data. What emerged from this comparative analysis was an apparent divergence between the quantitative and the qualitative data. Specifically, people’s intentions and expectations for the programme, reflected in the quantitative survey data, were generally positive. In the interviews and free-text responses to the survey, there was a greater focus on the challenges that had arisen during the design and implementation of the programme. This points to the value of the mixed-method design, which has provided a more balanced picture of the programme and how it has been received and implemented locally than would have been the case with either a purely qualitative or quantitative study.
Focus groups with children and young people
Two of the case study sites were selected to recruit schools to participate in focus groups. The possibility of participating in the focus group research was raised with all five sites at the familiarisation meeting; the final selection was largely pragmatic, with priority given to those sites able to provide sufficient reassurances that there were primary and secondary schools involved in the programme locally that would be willing to host a focus group and recruit and support a diverse group of children to participate. The selection of schools to approach was discussed between the research team’s lead for the focus group research and the local project lead in both sites. In total, five schools agreed to take part: three primary and two secondary schools. Each school determined a local contact person to oversee the consent process and to run the focus group within the school. Due to COVID-19, we arranged to host the focus groups online via MS Teams or Zoom (depending on the school preference), with a school facilitator with the children in a classroom, and the research team joining online.
We did not explicitly recruit young people who had mental health problems and/or had been supported by an MHST; however, the information disclosed by participants during the groups suggested that many had self-selected to take part because of an interest in issues of mental health (including having lived experience). In practice, we had a mixture of children who had accessed MHSTs and those who had not. The purpose of the groups was not to discuss individual mental health, rather it was to explore young people’s views about how their school promoted and provided support for mental health and well-being, whether and how this had been affected by COVID-19, and their awareness and understanding of the MHST. All children were offered the opportunity to have a one-to-one interview if they felt uncomfortable participating in a focus group but no children took up this option. Schools sent the invitation to participate either to a single year group or to the whole school, and the latter resulted in mixed-year focus groups. There was variation in the approach adopted by schools to recruitment, which we accept may have introduced some element of bias. However, this was the least disruptive and most pragmatic way of recruiting during COVID-19 and resulted in a broad spectrum of children and young people taking part. For example, in one school, the lead for well-being deliberately included students who had learning disabilities or children who were in kinship placements or local authority care.
Schools recruited children and young people directly by e-mailing out a digital participant information video and linked consent form to parents and children who were interested in taking part. The participant information video detailed the relevant ethical considerations including risks of participating and outlined that all information would be kept confidential unless the children disclosed something that would need onward referral, at which point the school designated safeguarding lead would be notified. The consent process for the focus groups was also managed online. A consent form was built in CoreXM, which participants worked through and then signed using an electronic finger signature on their devices.
The composition of the focus groups was determined by the school given the practical constraints involved. This resulted in one single-sex focus group with four mixed groups, two single and three multiple year group focus groups, and a range of ages from 8 to 16 years (Table 10). We are not able to report ethnic background as several parents declined to provide this information; the information we did collect indicated that the majority of children who participated were white British, but there was representation from other black British and ethnic minority groups (e.g. Filipino). Groups included children with special educational needs, children who were in the care of the local authority and children supported under school pupil premium plans.
| Focus group characteristic | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 |
|---|---|---|---|---|---|
| Setting | Primary | Primary | Secondary | Primary | Secondary |
| Number of participants | 7 | 5 | 9 | 8 | 3 |
| Group type | Multiple years | Year group | Year group | Multiple years | Multiple years |
| Age range | 8–11 | 8 | 15–16 | 8–12 | 12–14 |
| Gender | Mixed | Mixed | Female only | Mixed | Mixed |
| Co-facilitated | Yes | No | Yes | Yes | No |
The focus groups were, where possible, co-facilitated by a member of the University of Birmingham IMHYAG or a youth involvement co-lead. By ‘co-facilitation’ we mean that the questions on our co-designed topic guide were equally shared between the facilitators. All researchers (including IMHYAG members) collected their own field notes and were reciprocal researchers involved in hosting and chairing the focus groups. In working in this way, we sought to uphold NIHR guidance on co-producing research: sharing of power; respecting and valuing the knowledge, perspectives and skills of all those working together on the project; reciprocity; and building and maintaining relationships. 61
Focus groups were audio recorded as some children recruited were under special guardianship orders and video recording was not permitted. Ethnographic notes were taken by the research team alongside the audio recordings to ensure that a rich picture of the focus groups was developed for further analysis. Audio recordings were fully transcribed and thematically analysed using NVivo. All participant information was anonymised and securely stored on the University of Birmingham servers in line with the data management plan.
When the study was designed, a decision was taken not to include research with children and young people who had received direct support from MHSTs. This was driven by concerns about the feasibility of securing appropriate permissions and undertaking such research in what was then expected to be a rapid study timescale. As we discuss in Chapter 12, this is a recognised limitation of the study and we understand that the longer-term impact evaluation is expected to address this gap in understanding.
Other sources of data that have informed analysis
In addition to the data collection activities described above, the evaluation team collected and reviewed data from a number of other sources to inform its understanding of the programme and the analysis. These additional sources of data comprised:
-
scoping interviews
-
familiarisation visits
-
trailblazer document review
-
programme monitoring data
-
DfE baseline provision survey and experience surveys
-
financial data on the funding received by Trailblazer sites
-
mental health and service profiles for each Trailblazer, compiled from administrative data (see Chapter 3).
More information on each of these sources can be found in Appendix 5.
Involvement of young people
The evaluation involved young people with lived experience of mental ill health from the earliest stage. The IMHYAG at the University of Birmingham acted as an expert reference group for this research. The IMHYAG is a panel of young people aged 18–25 years who have experience of youth mental ill health. All panel members involved in this research were paid for their time. Meetings were held at key strategic points in the project (five in total).
Youth involvement took place during the protocol writing and across the project at different points and in multiple ways, right through to the development of Chapter 9 of the final report. The meetings were used to guide the process of research activity, from developing the protocol by shaping the questions that were key to answer in this early evaluation, through to co-designing the recruitment materials and topic guides and co-facilitating the focus groups with children and young people. While there was involvement throughout, particular elements of the project were co-produced (see focus groups with children and young people in Chapter 9). The IMHYAG members were not directly involved in work package 3, although their views about what programme success would look like from a young person’s point of view and about the limitations of existing approaches for measuring mental health outcomes did inform our thinking.
In particular, the IMHYAG wrote the script for a participant information video and co-recorded the video with the research team. The participant information video replaced a traditional participant information sheet as this was seen to be exclusionary for parents with low levels of literacy, and children and young people whose reading age was insufficient to be able to engage with that medium. IMHYAG members were also trained as co-researchers, and three focus groups were co-facilitated by a member of the research team and either IMHYAG members or the youth involvement leads from the Institute for Mental Health. Co-research was not always possible as the IMHYAG members had their own education or other commitments during school hours. The IMHYAG also met following the focus groups to develop the analysis and coding structure as well as to discuss what they thought the key findings were or points to highlight in Chapter 9 from the focus group data. Their perspective was invaluable in shaping the chapter and provided a rich contextual understanding for the findings.
Young people received initial ethics training about the principles of confidentiality and consent, and the history of where our current ethical principles come from. This training was adapted from existing undergraduate and postgraduate teaching and delivered in one of their routine IMHYAG meetings. Recruitment materials were co-produced in a workshop format and in-person training and development support was provided during those sessions as initial learning was applied to set tasks. For the actual delivery of the focus groups, we role-played focus groups and gave young people the opportunity to practise the questions beforehand. Each focus group was followed by a debrief session with the IMHYAG member to check in with them and for them to share reflections on what was said, what they had learned, and how they felt about the experience.
Research ethics and governance
Ethical and Health Research Authority approval
The study was approved by the Research Ethics Committees at the University of Birmingham (ERN_19-1400 – RG_19-190) and London School of Hygiene and Tropical Medicine (Ref: 18040) and by the Health Research Authority (IRAS 270760).
Project governance arrangements
The Steering Group for the BRACE Rapid Evaluation Centre acted as the steering group for this study. The team also worked closely with two specialist advisers: Dr Colette Soan (specialist senior educational psychologist for mental health, Sandwell) and Dr Karen Newbigging (academic researcher specialising in mental health policy and practice, Oxford University).
How the study differs from the protocol
Some elements of the study design as described in the protocol (Version 7, 18 October 2021) were not completed. Specifically:
-
Work package 3 included the aim to develop a theory of change for the Trailblazer programme, which could inform the design of a longer-term impact evaluation. A preliminary theory of change was developed in 2019–20, informed by the insights from the scoping interviews and a review of relevant literature (see Report Supplementary Material 2). In 2021, the national programme team undertook a series of workshops to review and iterate the logic model and theory of change it had initially developed at the start of the programme. In discussion with the programme team, it was agreed that the evaluation team’s time would be most usefully spent contributing to these workshops, rather than continuing to develop a parallel theory of change.
-
Using the findings from work package one, the team had planned to develop a typology of Trailblazers, but this was not feasible for several reasons. A set of questions was included in the first key informant survey for local project leads to complete, which asked for details about the local context and model to inform typology development. Several project leads did not complete the survey, nor did they respond to our invitation to share these details instead in a telephone interview, resulting in incomplete information across the 25 sites. The documentation on each Trailblazer provided by the national programme team was also not sufficiently detailed, and mostly dated to the application stage (so the information was about what was planned in each site, not how models had been designed and were operating in practice). Moreover, while we had not expected local models to be static during the evaluation period, there was a high degree of change and adaptation in these models in response to COVID-19, such that clear (and enduring) distinctions between sites could not be reliably drawn.
Chapter 5 Programme set-up, management and implementation
Programme design
The design of the national Trailblazer programme sought to balance central direction (including core functions for MHSTs, a set of operating principles and a national training curriculum for EMHPs) with local flexibility. There was broad support for this approach. Respondents were strongly of the belief that local models and implementation should be designed to fit local circumstances, need and existing provision. However, one regional lead noted that there had been a lot of ‘muddling through’ in the Trailblazer sites in their region, with each site separately designing its own service and workforce models, recruitment and engagement processes and so on. This team suggested that more national guidance and consistency would have helped the Trailblazers progress more rapidly and avoid duplication of effort.
Given the emphasis on tailoring local approaches to local circumstances, it is unsurprising that what was being implemented and how differed markedly across sites. Regional leads, in particular, felt that later waves of the programme benefited from the richness of learning from these diverse approaches. But there were also aspects where variation between Trailblazer sites, and therefore also learning, was more limited; for example, in all except three sites, MHST contracts were awarded to NHS trusts as either the sole or joint lead contract holder. It was noted that the Trailblazers were selected for particular characteristics thought likely to drive rapid progress (discussed in more detail in Chapter 1), and that sites in later waves which did not share these characteristics may face different or additional challenges:
You do have to recognise that actually in the very early stages we’re probably working with the best areas. Not the most affluent areas, I don’t mean that, but as in the best areas who are switched on, who have got CCGs who are switched on, who are working with schools who are switched on, who are really interested in the mental health and well-being of their children…As we move forward, that isn’t always going to be the case.
(Regional lead)
Programme set-up and implementation
Dedicated funding for the Trailblazers flowed from NHSEI to local CCGs, with CCGs having responsibility for strategic governance and oversight to plan for, set up and run MHSTs. A common theme emerging from the data was the scale and complexity of the work required locally to establish the programme infrastructure and new service (Figure 3 illustrates the expected structure of MHSTs), and the pressure of doing so in just 12 months and without much of the guidance and support from which later waves benefited. Trailblazer sites had to work quickly to set up the programme, and this work typically involved recruiting programme and MHST staff; setting up governance bodies and processes; engaging with education settings about the MHST model and to agree the allocation of MHST staff time; consultation with wider stakeholders; establishing processes, making arrangements and, where necessary, providing training for data recording and reporting requirements; and numerous employment and operational issues including developing induction and supervision arrangements for EMPHs. All five case study sites reported that the set-up of the programme in their area had felt rushed and, in some cases, chaotic:
FIGURE 3.
Expected structure of MHSTs.

…it felt like it was done the wrong way round and, you know, if we’d have been given that opportunity to put in place an operational team first…but they [EMHPs] were the guinea pigs and, you know, I do feel for them because they came in with no structure, no support, no real supervision, no clear guidance as to where they were going, I don’t know how half of them lasted, if I’m honest.
(Case study site 1, management/governance)
There was a parallel view among participants in the national team that the timescales to set up the programme infrastructure nationally had been challenging. A tension was described between implementing at pace to ensure that the programme benefited children and young people as quickly as possible, and not moving so fast that implementation was hasty or had unintended consequences for other part of the mental health system. It was also emphasised that the programme could only be rolled as quickly as EMHPs and supervisors could be recruited and trained (see Chapter 6 for more discussion of workforce issues).
Some areas had taken a system-wide approach to implementation, embedding the Trailblazer programme into existing work, strategies and partnership arrangements. This contrasted with areas that had taken a narrower focus, where MHSTs were designed and implemented as ‘a project’ in themselves. The view from regional leads was that the system-wide approach, while potentially more complicated to set up and manage, had made it easier for service models and learning to be scaled up across regions as additional MHSTs were established in later waves of the programme. Another recurrent theme was the importance of having a good project management infrastructure in place from the outset, and it was noted that the Trailblazers that did not have this struggled to make progress as a result. One interviewee felt that there should have been more national focus on the need for this:
There was project initiation funding but disappointingly it never specified that you had to have a project manager in the team make-up, or in the guidance. I tried to encourage them [the national team] at one point to say can we not put it in there because we saw the difference.
(Regional lead)
Support from the national and regional teams
The first key informant survey explored Trailblazers’ views about support from the two national partners leading programme delivery: NHSEI and the DfE (Figure 4). Over two-thirds of respondents agreed that that there was sufficient support from NHSEI (70%); the figure was lower (54%) for the DfE, although only 15% of respondents felt that the support provided by the DfE was insufficient.
FIGURE 4.
Views on support from NHSEI and the DfE.

Generally, case study sites reported that their regional team and, to a lesser extent, the national programme team was supportive, responsive and engaged with the work in their area. Some challenges and frustrations were also reported, for example, about frequent changes being made to data reporting requirements and templates, and requests being made by the national team at short notice. One site felt that the regional and national teams could be doing more to support recruitment of education settings, creating resources to support delivery and providing clarity on future funding.
One of the main ways regional teams had supported Trailblazer sites was through arranging regular meetings with sites, and facilitating networking and celebration events, and communities of practice. These had provided opportunities for experiences, learning and good practice to be shared. They were also a means by which people in key implementation roles could seek advice about emerging challenges, or access practical tools and resources developed in other areas to support their own work:
So bringing them together in those check-ins I think has really kind of created almost a peer network for them which seemed really valuable through the pandemic early on talking about the use of digital interventions, switching to virtual appointments rather than face-to-face and how different sites were tackling that, for example. But we’re very much led by what the sites themselves want to talk about…The space that we kind of give them in this check-in is to kind of raise particular challenges and hear from each other how people might have tackled things that have been a bit knotty, it’s focused much more on workforce problems and things like that.
(Regional lead)
Several regional teams noted that contact with Trailblazers, and the facilitation of networking between them (and with other sites in their region), had been stronger at the start of the programme. This was partly attributed to the impact of COVID-19 (e.g. preventing in-person networking events, having limited time to focus on non-pandemic issues) but was also because regional leads’ time was being spread across an ever-growing number of sites in the programme. Our findings suggest that Trailblazers would welcome more opportunities to share with and learn from each other, and with sites involved in later waves of the programme. Relatedly, a small number of respondents to the first education settings survey called for networking opportunities between senior mental health leads in participating schools and colleges to share resources and ideas and to help them explore the best way of using the support offered by MHSTs. In one case site, termly networking meetings were held to bring senior mental health leads together to share good practice, which were widely reported, including by education settings, to have been well received and beneficial.
Governance and partnership working
Our findings suggest that there was variation in the extent of partner and stakeholder involvement in local governance bodies, and in the degree to which governance arrangements for the programme were integrated into wider local strategies, structures and initiatives (such as the former regional sustainability and transformation partnerships, now integrated care systems). Programme monitoring data reported by Trailblazers to NHSEI provides details about the extent of stakeholder membership in governance bodies. The most recent data (for 24 Trailblazers, reported during the period July–December 2020) indicates that almost all governance bodies had representation from CCGs, education settings, local authorities and NHS CYPMHS and the voluntary sector. Relatively few by comparison involved parents and carers, or children and young people (Figure 5).
FIGURE 5.
Stakeholders represented in local governance arrangements.

While all sites included education settings in programme governance arrangements, some felt that the interests of this important group were did not sufficiently represented in decision-making. It was suggested that some areas had not given enough thought to this issue, and so the representation of education settings had felt tokenistic:
I think the only thing that still stands out as an issue for me is…what is true governance and what is actually just having maybe an ongoing working group with a few heads or a few school leads and sort of ticking that box…how much is that influencing all those crucial meetings where the decisions are made and how consistent are they in getting the views of a collective number of [educational] settings?
(Regional lead)
At the same time, there was acknowledgement of the difficulty of collectively representing what may be a large number of different education settings in governance arrangements. We also heard that where arrangements for involving education settings in local governance worked well, this had strengthened their commitment to the programme and also increased referrals to MHSTs.
There was a view among several interviewees at all levels that health partners were dominant in the programme’s leadership and governance, and our findings point to some reasons for this. The way in which the programme and funding arrangements had been set up nationally – with delivery led by NHSEI and NHS funding to CCGs – was felt to have created an orientation towards NHS partners and perspectives, which could act as a barrier to fostering shared governance across health and education:
It sometimes feels like you can be a bit back to square one with brand new sites around why we’re here because obviously they’re aware the money flows from NHS England, the CCGs. It’s a very NHS dominated space…trying to bring education to the forefront of every discussion because it does obviously get lost in health – we talk about finance, we talk about recruitment.
(Regional lead)
Some local interviewees (in one case study site in particular) felt that the DfE’s involvement in the programme, both nationally and regionally, had been less extensive and visible, which was felt to have further tilted the balance towards health partners and models. The DfE regional roles created to support the programme were recruited after the Trailblazer wave had started. Interviewees remarked about there being uncertainty initially as to how these roles should function. Although DfE regional leads had settled into their roles over time, most were redeployed to other areas of work during the early months of the pandemic. This had limited their involvement in regional planning and governance and Trailblazers’ access to educational advice and support.
Involvement of young people, parents and carers
It was an aspiration of the programme that involvement of young people, parents and carers would extend beyond involvement in governance arrangements and be evident throughout the design and delivery of MHSTs. Nearly three-quarters of respondents (74%) to the key informants’ survey reported that the MHSTs in their area were co-producing their approach and service with users, but a different picture emerged from other data. The findings from our interviews suggested that the principles of involvement and/or co-production were well established and working effectively in only a small number of sites; for example, reflected in close working with organisations representing children, young people and families, or in the direct involvement of these groups in key aspects of the programme set-up and implementation process. In the education settings survey around half of all respondents reported that they had not involved children and young people (51%) and parents and carers (49%) in decisions about what the MHST would provide in their setting; the proportions reporting that these groups had been fully involved were 4% (children and young people) and 7% (parents and carers). The extent and nature of involvement reported by case study sites varied, with some reporting that early efforts to consult had declined over time. It appeared that involvement was often limited to specific tasks, for example contributing to decisions about branding and promoting the MHST service.
Some examples of involvement across the Trailblazer sites are shown in Box 5.
-
Creating a parent and carer forum, or engaging with an existing group, to input into design, implementation and governance.
-
Creating a service user forum or engaging with an existing group to provide feedback on how the service is being delivered.
-
Collecting feedback from pupils and parent/carers; for example, by conducting focus groups and surveys on design of the programme, expectations and how the service was being delivered.
-
Involvement of children and young people in designing logos and agreeing a local name for the MHST service.
-
Pupils appointed as mental health and well-being champions in their school.
-
Young people and/or parents sitting on EMHP recruitment panels.
Selection and engagement of schools
Trailblazers were expected to have all their participating schools and colleges selected before submitting their bid, which sometimes appears to have driven a ‘quantity over quality’ approach to engagement, in which the focus was more was on obtaining the required number of settings and less on building relationships. Some sites had also over-recruited the number of education settings required, unsure of the population size that MHSTs would typically be expected to cover. Regional leads confirmed that these early experiences had led the national team to change its requirements, with areas seeking to join the programme in later waves no longer expected to have all education settings secured at the application stage. This was universally welcomed.
Project leads were asked to provide a brief overview of how education settings had been recruited to be part of the Trailblazer programme. Two main approaches were outlined: (1) an open recruitment process where all settings in an area were invited to submit an expression of interest to participate in the programme; and (2) direct approaches to education settings in areas of high deprivation and/or with particular need. One case study site used open invitations to recruit education settings for one of its MHSTs, and selected education settings for the other MHST. The latter approach, they reported, had resulted in markedly poorer engagement: ‘It was much more of a challenge, much more, because schools didn’t appreciate being dictated to.’ (Case study site 2, management/governance).
A misalignment between what MHSTs were offering, and education settings’ perceived needs for support, had also acted as a barrier to recruitment in some areas. One regional lead told us:
Quite a few of [the Trailblazers] said that they received a fair amount of pushback at the beginning from their Trailblazer schools on the MHST offer, particularly on the prevention side, and that it’s taken quite a lot of time to sort of sell that model to schools, because their first instinct is the interventional element…In a series of surveys that we published, a lot of the qualitative answers were saying that they felt they wanted more direct intervention for younger pupils and more intervention for complex needs, for children with complex needs and it felt that the kind of prevention element was already provided by the school.
(Regional lead)
Data collection, reporting and use
Views about data collection and reporting suggest that this is an element of the programme which was not working well. Respondents were of the view that there was greater clarity about what type of intervention-related data should be collected and how, and that these data were easier to collect, but ratings across all three MHST core functions were fairly low. The proportion of respondents reporting that there were processes in place to regularly review or audit MHSTs’ core functions was also low: ranging from 28% of respondents for direct interventions through to 12% for giving advice and liaising with external services (Figure 6).
FIGURE 6.
Views on data reported on MHSTs’ core functions.

A recurring theme in interviews – both with case study sites and regional leads – was the challenge of capturing activities and progress made towards whole school approaches:
It’s really, really hard to capture the data around the whole school work and whether that is going to be something that needs to be looked at longer term; yeah, the recording systems are not great. We do keep our own record of what whole school work we’ve done, let’s say on a spreadsheet just to sort of be able to know if we do need to pull that information, we can more accurately go ‘well actually it was a 120 students’ or ‘1000 students in that assembly’, but yeah, from a reporting point of view, I’ll be honest, we’ve never really had sight of it as team leads, that’s been a little bit more at the strategic level.
(Case study site 2, management/governance)
At a national level, some of this was put down to the whole school approach simply being more complex and lending itself to qualitative data collection or theory-based evaluation approaches. One national interviewee noted that efforts to reduce data collection burden on sites since the pandemic had resulted in a narrowing of focus to metrics relating to the delivery of interventions. At a local level, this has been interpreted by some as yet more evidence of the dominance of health partners and perspectives within the programme:
All the whole school approach stuff, they’ve changed the way they do returns and none of it’s represented in there…So it’s really interesting, that from a national point of view they’re only interested in that medical bit and, to me, that’s sort of telling really of what’s happened, because I think if [DfE] had been a stronger partner, I don’t think we would necessarily be just looking at that.
(Case study site 1, project lead)
The focus on gathering data related to interventions was also felt to overlook the importance and impact of the advisory support MHSTs provided to education settings (function 3):
So, something like that, the impact of that would be really difficult to measure. But all I can say, so I’ve got two primary schools there, in very challenging localities, who hardly ever refer for one to ones, because a lot of what they do is now managed within the school, and I think that says a lot, really. They’re both really engaging schools, and they both use me in that same way, as about, we’re doing this with this child, what do you think? And I think that works really well. So, I don’t know, it all depends how you measure impact, doesn’t it?
(Case study site 2, EMHP)
Time burden was mentioned in several case study interviews and perceived burden appeared to be greater (as would be expected) where the value of data collection was contested or unclear. There was a view among some local interviewees that the routine outcome measures for the programme were too clinically oriented. Within the same site (case study site 5), one EMHP reported that the routine collection of outcomes data helped to keep them ‘on track and focused’, while another EMHP suggested that it was ‘terribly boring and feels very medicalised’. Such mixed views about routine data collection among MHST team members were common across case study sites. Limitations in what could be accurately recorded in the routine dataset were also described:
So the NHS dataset only has so many reasons for referral and a lot of those don’t fit with the mental health support team…If someone’s having difficulty with sleep there isn’t a code to be referred for sleep, so you have to find a reason for them to have issues with sleep…you have to allocate it to anxiety or depression or something else, which I don’t think, I think that skews the data slightly because children are not necessarily referred to us for those reasons but we have to link it to something that’s very medicalised…I do think it medicalises them a little bit.
(Case study site 2, MHST manager)
Many Trailblazer sites had also set up processes for obtaining feedback on the MHST service from children and young people (69%) and parents and carers (63%), in addition to the routine activity and outcome data they were gathering. The most common mentioned methods were feedback forms and questionnaires, completed by a young person (and sometimes also their parent or carer) after they had had contact with an MHST, either for direct support or participation in a group activity. More than three-quarters of education settings (77%) reported that there were clear mechanisms in place to provide feedback on MHSTs. The first key informant survey asked sites whether a local evaluation of the programme was planned or underway. Of 13 sites that replied to this question, nine confirmed that a local evaluation was being carried out.
We were keen to understand if and how data were used at a local level to support service delivery and improvement. Our findings suggest that all case study sites were reviewing service activity and outcome data, although they varied in the extent to which this was undertaken as a formal, systematic and regular process. It was apparent that the MHST team members who were responsible for collecting data were not always informed about whether and how the data they had collected were being used, which may have been contributing to the feelings of indifference and/or dissatisfaction noted above. One case study site stood out inasmuch as there was a specific member of the MHST team whose role included oversight of data collection and reporting processes, and there was a strong focus on data-related aspects. In this site, routine data were regularly analysed and shared with local partners, bespoke reports were produced for individual education settings, and data were regularly reviewed by the team to identify gaps in the service. The last of these activities had led to the recruitment of a specialist role to support the engagement of children and young people from black and Asian communities.
The use of data at the national level was also acknowledged to have been a challenge. Multiple data collection activities had been established, but the issue facing the programme team was how to synthesise and share the insights from diverse sources and data sets both to support effective oversight and monitoring, and to inform decision-making about ongoing programme development and implementation. There was some frustration at the length of time between data being collected and being made available to the national team, although it was also reported that the programme had started to make progress in developing effective ways of using and learning from the data:
I think it’s something that’s been a big improvement in the last six months or so that the MHST teams and the various [national] teams that work on it have set up this cycle of trying to get intel and data and insights and the all the different quantitative and qualitative sources together. So rather than going to the board and presenting ‘Here’s the findings from one survey, and here’s something else’, but actually trying to put them altogether […] And I think they’ve really started to improve that, which has been really helpful for the boards in getting more consistent and more reliable [information].
(National interview)
Resourcing and use of funds
The evaluation explored views about the funding provided to set up and deliver MHSTs, and the resources that education settings could draw on to set up and work with their MHST. Over two-thirds (64%) of local project leads and MHST managers responding to the second key informant survey reported that MHSTs had sufficient financial resources to perform their core roles and responsibilities, although nearly one-quarter (24%) disagreed with this. Of the same respondents, fewer than one in five (19%) agreed that education settings had sufficient resources, including staff, to take full advantage of the opportunities that the MHSTs offered. The proportion of education settings fully agreeing with this statement was similarly low (20%). The main reason given by those working in schools and colleges for not being able to take full advantage was that key staff were stretched very thinly and lacked the time to work with their MHST. In some cases, this was reported to be linked to wider staffing shortages in their setting; only one respondent directly linked these capacity issues to COVID-19. In the first key informant survey, many local stakeholders were unsure if the allocation of MHST time and resources to education settings was transparent, with more respondents (50%) neither agreeing nor disagreeing with the statement, than agreeing outright (43%).
Chapter 6 Workforce, recruitment and training
Composition of the mental health support team workforce and delivery of the core functions
As discussed in Chapter 1, Trailblazers sites had flexibility around the composition of the MHST workforce. Across case study sites there was a great deal of variation in the specific roles and levels of experience within teams. It was clear that team configurations were evolving and that, in several case study sites, new roles had recently been developed. While some types of roles were common across all five sites, others were unique to only one site. Despite this variation, MHSTs included most if not all of the broad role types described in Box 6.
-
MHST team managers and senior therapists: providing clinical supervision, line management and leadership to MHST staff and the overall service. Teams often had separate operational and clinical leads. In some areas, senior therapists also delivered some one-to-one work with children and young people. One site had developed a senior EMHP role, to support children with more complex needs and supervise junior EMHPs (a similar role was planned in other sites).
-
EMHPs: all teams included EMHPs who were involved (to varying degrees) in the delivery of MHST core functions.
-
Other therapy and mental health practitioner roles: these included children’s well-being practitioners (from the IAPT programme) and triage practitioners.
-
Specialist therapy and engagement roles: many teams had developed roles to engage, support and work with specific groups. These included:
-
participation worker (focusing on engaging and gathering feedback from children and young people, and/or parents and carers
-
family support worker (focusing on working with and supporting parents and carers)
-
autism spectrum conditions/learning disabilities practitioner (delivering interventions specifically to children with learning difficulties or autism spectrum conditions and their parents)
-
systemic educational practitioner (focusing on ways of engaging children and young people from underserved groups including those from ethnic minority and traveller/Roma backgrounds, and children at risk of exclusion
-
outreach workers (whose role included working with children and young people not currently in mainstream education).
-
One site was also recruiting two further specialist roles, to work with children and young people from LGBTQ+ and ethnic minority communities, respectively.
-
-
Specialist education setting focused roles: specialist roles had also been developed focusing on engaging and working with education settings. These included:
-
peer mentoring co-ordinator (overseeing a peer mentoring programme that had been set up in one case study site)
-
Whole School approach and staff well-being adviser (delivering support for and whole school activities, and supporting staff well-being)
-
foundation worker (focusing on supporting education settings with whole school approaches and activities and liaising with other mental health providers in the locality).
-
-
Administrative roles: which provided administrative and business support to the team and the Trailblazer programme generally.
MHSTs varied in terms of how work across the three MHST functions was led and delivered across different staff roles. This was particularly notable in relation to the support being provided to education settings for whole school approaches (function 2), where several approaches to staffing were identified and the degree of EMHP involvement differed substantially. In two case study sites, this work was primarily delivered by specialist roles in the team, and in a further site it was led and coordinated by one of the Trailblazer partner organisations (an educational charity), with some day-to-day elements delivered by EMHPs. In a fourth site, it was largely delivered by MHST team managers and, in the final site, mostly by EMPHs, but with oversight from a senior member of the team. This final site had recruited three children’s well-being practitioners to provide one-to-one support to free up EMHPs to focus on whole school activities. This contrasted to the approach taken in some other sites, where EMHPs were mostly focused on delivering direct support to children and young people.
Several interviewees emphasised the importance of having senior staff involved in building and maintaining relationships with education settings, and delivering at least some aspects of whole school support (e.g. training and well-being support for school and college staff). It was noted that ideally these activities would be led by somebody with experience of working with and/or in education settings, which was also offered as a key reason for creating specialist roles. This was felt to be an area where knowledge and experience (e.g. of mental health and well-being issues, the different services and sources of support in the area and how they operated, and of working across boundaries) was essential, and this was something that EMHPs did not necessarily have.
Diversity of the mental health support team workforce
Ensuring diversity of the MHST workforce was mentioned, particularly by national interviewees, as a programme priority. The demographic characteristics of EMHP trainees are monitored by Health Education England who reported during interview that EMHPs cohorts were ethnically diverse but largely comprised younger women. The national team noted that it was keen to understand more about the socioeconomic backgrounds of trainees and to make the training as accessible as possible in order to widen participation across diverse groups (linked to a wider programme of national work focusing on mental health workforce inequalities):
So yes, we have done a huge amount of work around the diversity and particularly from a training perspective, widening the participation onto the cohorts because as you can imagine, you know, the broader the pool of people that you’re bringing into the training, that is then reflective of the workforce that goes into the roles within service and the aim, broadly, is to ensure that the trainees or the supply pool that we’re drawing in, are as reflective as possible of local communities.
(National interview)
Despite these stated aims, it was not clear how specifically the programme was seeking to increase the diversity of the EMHP workforce. Two examples given by national interviewees were providing guidance to sites on how to recruit for diversity and commissioning universities to develop undergraduate pathways for EMPH training, for people who wanted to train but who did not have a degree. Views expressed by several other participants suggested that, despite the creation of an undergraduate training route, the academic qualifications required to enter training were still restricting the type of person who could become EMHP, and excluding those who offered valuable community or practice experience (e.g. teaching assistants):
I think a lot of the sites feel is that there’s a lot of people in existing workforce that maybe aren’t like ticking the academic box immediately but feel that their work experience that they possess equips them quite well for the role, but they often struggle to get them on the courses because of the academic constraints of the course.
(Regional lead)
The evaluation team requested information on the demographic characteristics of trainees from Health Education England (in January, and again in February, 2022) but did not receive it.
Recruitment and training
Recruitment to the EMHP role was widely reported to have gone well, for the Trailblazers and across the later waves of the programme. People had joined the training programme from a variety of backgrounds, including some with NHS mental health or teaching experience. Applicants were attracted to the role for a number of reasons including burnout in previous jobs, their own experience of mental health problems and the preventive focus of the EMHP role:
I felt six years in CAMHS [child and adolescent mental health services] was, after doing this training, I felt like my six years in CAMHS was a complete and utter waste of time. All I did there was keep children safe and stop them from hurting themselves…With children, we have a lot more, we liaise a lot more with parents and I know sometimes that couldn’t be done in the inpatient unit because we had children from…out of the area. I mean you couldn’t have that close connection with parents. However, some of the interventions that we’ve learnt on this course, I just thought would be so beneficial to inpatient units.
(Case study site 2, EMHP)
The first wave of EMHPs describing their training as a challenging time. Only a limited number of universities had been providing EMHP training at the time of the Trailblazer cohort, which had resulted in some trainees having to travel substantial distances between their home, university and placement area. Another impact of this approach was that trainees had been recruited from all over the country and often ended up working in areas that they were not familiar with, and so lacked the kind of local knowledge that might have helped them adjust to and more effectively fulfil their role. The speed at which the programme had been set up meant that key elements, including school placement and supervisory arrangements, were not fully in place for this cohort:
I think they really struggled that first year, I mean, they’d started and the curriculum hadn’t even been signed off…Some things were quite backward and I think it was just the haste from national to get this going and then to fit with the academic years with the universities…We lost a trainee in the first week and then we lost another one further down the line – but we had to put in a lot of work to keep those trainees – they were ready to walk about four or five times.
(Case study site 1, management/governance)
Many EMHPs described the pressure and intensity of the training, particularly completing clinical hours alongside studying. Nonetheless, most reported that their training had also been rewarding, were grateful that it was nationally funded, and pleased to have learnt new knowledge and skills to equip them for their role and, possibly, future careers.
In contrast to the experience of recruiting EMHPs, appointing senior staff to MHSTs had been far more difficult:
Recruitment of specialist posts have been an ongoing issue for the MHST; really hard to find Band 7s and Band 8as and the demand for them on supervision is very high with the trainees, there is limited capacity for them to take on a clinical caseload of their own.
(Key informant survey respondent)
Several reasons were offered for the difficulties recruiting senior staff: national shortages in the mental health workforce, especially of more experienced professionals; that the list of criteria and experience required was long but the salary not very competitive in relation to other comparable roles; and the strong focus on supervisory responsibilities, which was not attractive to those keen to continue practising therapeutically. In our initial fieldwork, concerns were expressed about MHSTs recruiting experienced staff from other parts of the local mental health system, which could potentially create staffing problems for other services. Although, as we discuss below, the movement of staff between MHSTs and other services could also have positive effects.
Gaps in training and additional training
While the training provided to EMHPs was welcomed, many participants felt that it had not sufficiently prepared them for their role and the realities of ‘real world’ practice. Several gaps in training were noted and these included process-oriented skills (e.g. guidance on managing therapeutic boundaries; conducting risk assessments; triage processes; engaging with education settings, parents and carers, and children and young people; how to adapt interventions for specific groups and to be culturally appropriate; and case management) and substantive knowledge (e.g. about child development; SEND; and specific mental health problems such as self-harm and eating disorders). This had put considerable pressure on supervisors to provide additional support and ensure safe and effective practice, especially in the early months as EMHPs transitioned into MHSTs and had sometimes made it harder for EMHPs to build relationships with education settings. Some interviewees suggested that the strength of the training had been in equipping EMHPs with therapeutic and clinical skills; this view was particularly evident in one case study site, where the local project lead described it as a ‘very medical model of training’ (Case study site 5, project lead).
All sites provided additional and ongoing training to MHST staff, often targeted at areas where it was felt the university training programme had not been sufficient. In the second key informant survey, 88% of respondents indicated that MHST staff had received additional training since they were appointed. Case study sites reported that further training had been provided locally on a wide range of topics, including safeguarding, trauma-informed support, bereavement training, suicide awareness, mental health first aid training, recording data, gendered intelligence, engaging children and young people from ethnic minority groups, undertaking research, self-harm, parenting interventions, neurodevelopmental conditions, risk management, managing emotions, using interpreters in sessions, attachment, self-harm, trauma-focused CBT, adapting CBT for autism and child protection. Several areas reported providing training on the same topics, for example on neurodiversity and autistic spectrum disorders. Despite this additional training, the majority of project leads and MHST managers (85%) responding to the second key informant survey reported that MHST staff would benefit from further training that they had not yet been offered.
Mental health support team staff retention and turnover
One of the key challenges for the Trailblazer programme was retaining EMHPs. Trailblazer sites had experienced high turnover of EMHPs, which was felt to have been driven by several factors (Box 7).
-
EMHP role seen as a stepping-stone into other careers, such as clinical or educational psychology. It was noted that one university had promoted the training in this way: ‘Another issue we’re seeing is with a university promoting that the EMHP training is a stepping-stone into Band 6 role…So a lot of trainees go into the training [for this reason], not because they are passionate about the role’ (Case study 4, project lead).
-
Differences between expectations of the role and the reality once in post.
-
Demands of the job, including heavy workloads, and associated burnout and stress.
-
Lack of senior staff to provide sufficient supervisory support.
-
Lack of opportunities for career development and role progression. There were limited senior roles in teams to which EMHPs could progress, a lack of clarity about if or how EMHPs could progress to these roles, and senior positions were unattractive to some as they had little or no direct contact with children and young people.
-
Pay (e.g. relative to equivalent roles in the NHS) and lack of long-term job security due to being on fixed-term contracts.
-
Frustration at the rigidity of the programme and MHST model, including the limitations of the cognitive behaviour therapy approach.
-
Other reasons, such as travel distance from home to work, change of circumstances and pressures related to COVID-19.
The turnover of EMHPs was having a significant impact on service delivery. MHSTs frequently reported capacity challenges, and difficulties maintaining agreed support to education settings when operating with a reduced team. Retention issues also impacted on senior staff time, which was required to recruit new EMHPs and provide support for induction. Where replacement EMHPs were trainees, this also necessitated more intensive supervision as the person transitioned from their training into practice and during the initial months in post. Some participants commented that the frequent turnover of staff made it harder to form relationships and build trust with education settings, and hampered continuity of support for children and young people.
Replacing EMHPs was not easy, because there was a limited pool of trained staff from which to recruit. When an EMHP left, teams usually had to wait for another round of recruitment and training before they could be replaced, leaving them under-staffed in the intervening period. Restrictions around the caseload that new trainees could manage, and the need for more intensive supervisory support during this time, also increased pressures on other staff and, in some cases, meant longer waiting times for direct support. Some of these challenges would be expected to lessen as the number of trained EMHPs increases over time, but many were also concerned about the ongoing uncertainty about whether MHSTs would be funded long term and the lack of clear career progression opportunities for EMHPs. This had impacted on staff morale and was a key factor in staff turnover. The implications for the sustainability of the service were highlighted:
Sustainability is only going to be achieved with sustainable finances and sustainable career prospects for our staff. And the reality of that is that we need long-term contracts, or permanent contracts with a really clear career path, which includes every layer of Bands 4, 5, 6, 7 and 8. We need it right the way through because without that we’re never going to sustain a workforce.
(Case study site 3, MHST staff member)
There was a widespread view that the programme must prioritise the issue of career development and progression opportunities for EMHPs, to reduce attrition and promote workforce stability. As noted above, some case study sites had or were in the process of developing a senior EMHP role, and we heard that one Trailblazer site had ‘designed a kind of pathway through the teams so that people can progress within the team and try and aid retention there’ (Regional lead). Members of the national team confirmed that work was underway to establish career frameworks and pathways for EMHPs, and some pointed to the launch of professional registration scheme for EMHPs in the summer of 2021, which was felt to be a positive development. The possibility of the programme formally establishing and providing training for a senior EMHPs role, an equivalent to the high-intensity therapy roles in the IAPT programme, was also proposed, both to enable MHSTs to offer support to children and young people with more senior mental health problems and to create an opportunity for EMHPs to progress within the MHST structure.
Some case study sites also reported high turnover of senior and managerial MHST staff and, while the reasons for this were not fully clear, the workload involved in setting up and running a new service and working across different sectors, and the demands of supervising junior staff appeared to be important factors. This was evidently affecting staff morale:
But the management level, it’s just every two months someone leaves, someone joins…There’s ten vacancies they’re waiting to fill…There is some sense of it feeling like a sinking ship…Everyone’s still doing what they need to do but it can be hard to be in that atmosphere of constant change and flux. It’s tiring.
(Case study site 3, EMHP)
It was clear from our case study sites that staff (at all levels) were both being ‘lost to’ and recruited from other mental health services in the locality, including specialist NHS services. Our early fieldwork had picked up some concerns about this, but what came through in our case study interviews was that this movement of staff between services had helped to build relationships between different teams and enhanced understanding of each other’s roles, strengths and pressures.
Supervision
Approaches to supervision differed between case study sites. All differentiated clinical supervision (to provide oversight of and support for EMHPs’ therapeutic work) and management supervision (for line management purposes and to discuss overall service delivery, administrative issues or well-being). In some sites these roles were conducted by one person and in others by different individuals. Several areas held some clinical supervision sessions in a group format with peers. There was some variation in frequency of supervision, but the norm was twice a month. Appropriate and ongoing supervision was agreed to be critical for the success of MHST services and to EMHPs feeling supported and able to practice safely and effectively within the scope of their role. EMHPs were generally positive about the supervision they received, and many felt this was working well in term of both practical and emotional support:
I have to say, the amount of supervision you get is great in terms of keeping your emotional well-being in check and preventing burnout and things like that, so it’s, yes, you’re well supported, actually, really well supported.
(Case study site 4, EMHP)
Problems were also reported though, often in relation to the turnover of senior staff and/or a supervisor’s lack of knowledge about the cognitive behaviour therapy approaches which EMHPs were delivering. In one case study site, clinical supervision was provided outside of the team, and this did not appear to be working well:
It can be really tricky because she doesn’t always get the intervention, well she doesn’t know, doesn’t know the EMHP interventions, she knows what I’ve told her.
(Case study site 5, EMHP)
The highly demanding nature of the role meant that supervision – even when provided effectively – could not always ‘hold’ all the issues and difficult feelings that EMHPs experienced:
I just think there are times when this role can become very draining, and very difficult to manage, particularly when you are overloaded with many complex cases and those sorts of things. And I think, with all the will in the world, sometimes supervision just won’t cut it, and you’ll still take those conversations home with you and things like that.
(Case study site 4, EMHP)
Supervisors also acknowledged how demanding personally and professionally demanding the EMHP role was, and how difficult the work could be, especially for those new into practice:
[Name of area] is like an inner London borough. The need and complexity levels are very high, and they may have a stressed teacher on the phone, they may have a stressed parent on the phone where they just pick up on that stress without being aware of what’s actually going on sociologically and emotionally and for themselves, and they need that extra space sometimes.
(Case study site 4, management/governance)
MHST staff providing supervision often reflected that this aspect of their work could be demanding, time intensive and draining. Ensuring that EMHPs were practising safely and appropriately managing risk placed a heavy burden on supervisors; one noted that red flags or warning signs (e.g. during early work with a child) were sometimes missed by EMHPs, so needed to be identified by supervisors. Some senior staff reported that their role was too heavily oriented towards supervision, and that they missed working directly with children and young people. One senior therapist discussed how the MHST she was working in was starting to support children with more serious mental health problems, and she welcomed this move and the opportunity it created for her to start using her therapeutic skills and experience again to benefit children directly.
Establishing the mental health support team service within and integrating with the wider system
Across the case study sites, MHSTs were building relationships and integrating with a number of services and organisations, including other providers of mental health support within education settings, community and specialist mental health services in the wider area, local authority teams (e.g. safeguarding and educational psychology teams) and services, and voluntary organisations and charities:
I work quite a bit with CAMHS and with the school nurses from the local authority and everyone’s been on the same page willing to share information, willing to work together and really wanting to work as that team around the family as opposed to individual services, so I feel like the interaction with the external agencies has always been really good.
(Case study site 3, MHST staff member)
The majority of respondents (83%) to the second education settings survey felt that their MHST was integrated (either fully or to some extent) with existing mental health and well-being services within the setting. In the second key informant survey, 91% agreed that MHSTs were additional to and integrating with existing support for CYPMHS.
Most sites described an initial period during which MHSTs were establishing themselves in the local area, making contact with other teams and services, and considering how they fitted into and could work effectively with the wider mental health system locally. This was not always smooth and straightforward, with boundary issues and concerns about service duplication often hampering efforts to build productive relationships:
…we were stepping on people’s toes sometimes because we were the new kids on the block and we were all shiny and new and there was a little bit of a sense of, I guess a little bit of a threat of ‘you’re coming in to take our work in our territory’, so there was a little bit of friction there as well…We knew that we were just complementing an existing service, not coming in to replace something. That was always how we pitched it, that we’re not replacing anything and I think that alleviated some worry I think from other providers in schools definitely.
(Case study site 3, MHST manager)
Where formal processes for working with other services had been established (e.g. through single point of access arrangements or joint triage meeting), these processes had generally helped the different parties involved to better understand what others delivered, how they worked and how services might align. As noted above, the recruitment of staff from other local services to MHSTs and vice versa, had had a similar effect. Team members reported a tension between working closely with other services, which was essential, for example, for fulfilling their third core function (liaising with external specialist services), and establishing the MHST as a service in its own right, with a clear and distinctive identity and purpose. For some, the main risk was that MHSTs would become (or come to be seen) as just an extension of NHS mental health provision, and the education focus of the programme be lost or diluted. Several participants felt there was a need to raise the profile of MHSTs in their area and improve communication about the sort of work they could do, especially with other local teams providing support to children and young people.
Chapter 7 Mental health support team functions and delivery
Development of local service models
The first key informant survey explored the design and set-up of MHST service models. Most of the respondents to the survey (89%) agreed that their local approach was built on a good understanding of needs and gaps in children and young people’s emotional and mental health support in their area. The majority (73%) also reported that their local approach had been designed to take into account all groups of children and young people, including those who were disadvantaged and underserved by existing mental health services. Although, as we discuss below, our findings suggest that not all children who were eligible for MHST support were accessing and benefitting from the service.
Mental health support teams were being introduced into areas where there were many existing services, programmes and initiatives for children and young people’s mental health and well-being. Participants stressed the importance of ensuring that MHSTs complemented, rather than replicated or substituted, existing local provision:
We have to be really careful so that we don’t replace mental health support teams with something that was there already. This isn’t seen as a way of rationalising resource, so if something’s previously been delivered by a third sector organisation, actually how can the mental health support teams work to enhance that so (a) it doesn’t duplicate but (b) it doesn’t replace.
(Regional lead)
As discussed in Chapter 5, the national team encouraged local flexibility and tailoring of the programme. As a result, and as was intended, there was substantial variation across Trailblazer sites in how MHSTs were designed, implemented and were operating. The evaluation team had planned to create a typology of Trailblazers to map and categorise this variation. However, this was not achievable, largely because we were unable to gather sufficiently detailed, relevant data from all 25 sites to inform the development of a typology (see Chapter 4 for further discussion). Notwithstanding, some important differences between local models and approaches were observed, which we discuss below.
Health oriented versus ‘holistic’ models
A key aspect of variation was in the balance between what might be broadly termed ‘clinical’ and ‘holistic’ approaches and activities within local service models. Some models appeared to be more clinically oriented, with a strong focus on MHSTs’ therapeutic functions and on their integration with existing mental health services in the locality. This contrasted with other sites, where greater prominence was given to activities to engage and support education settings to develop whole school approaches, and stronger emphasis on relationship building with educational, voluntary sector and other non-NHS partners:
There is a difference I think between a sort of health led model and a local authority or third sector led model, you can see the differences in terms of, you know, health based models tend to be very clinical focused, local authority based models tend to try and stretch boundaries around clinical interventions and have a more sort of connection with local authority partners that do whole school approach.
(Regional lead)
These differences were evident in the way in which interviewees spoke about the purpose of the programme, with some describing it as a further extension of children’s mental health services into new settings, while others took the view that the programme was foremost to strengthen the promotion of well-being in schools and colleges. Among those who took the latter view, there were concerns that the value and uniqueness of the programme would be weakened if MHSTs became too clinically oriented:
I think that in some of the sites where it’s all NHS, they’ve set up like mini CAMHS and some of them are not even trying to pretend that they’ve not, they just say we’ve set up a mini CAMHS. And I sometimes worry that that’s not bespoke enough and it is too health orientated.
(Regional lead)
The findings suggest that two factors in particular had influenced the development of the service model: (1) the type of organisation (NHS or voluntary sector) leading the programme locally, and (2) local infrastructure and skill sets, with those areas that had stronger pre-existing partnerships between education settings, local authorities and community mental health resources having more ‘holistic’ models. For example, the impact of having a large NHS trust as the lead organisation for the MHST service was explained by one project lead:
We’ve had to work fairly hard at actually saying ‘No, we need to listen to the voice of schools here, this is meant to be a schools’ facing programme and not just a rolling out of a health programme’. And because the money for the education mental health practitioners had to go to an organisation like [name of NHS trust] then once you put a big organisation in the frame, then they’ve got to recruit to certain standards, they’ve got to go through certain inductions, they’ve got to go through certain recruitment, etc. etc. and it doesn’t have the flexibility that our third sector partners would have if they were enabled to do that so there have been some tensions I think it would be fair to say in trying to manage that.
(Case study site 5, project lead)
The extent to which MHSTs were formally integrated with NHS mental health services was also influential. In two case study sites, referrals to MHSTs were made through an NHS-led single point of access model (although one site was moving away from this approach during the time of our fieldwork due to the lower number of referrals received), and this reinforced the view that MHSTs were a part of NHS mental health services:
We’re still using the same language to them to say ‘You are an extension of CAMHS, you’re not a service in your own entirety kind of thing, out in schools, you are part of CAMHS, you’re integrated’.
(Case study site 1, management/governance)
Some felt that it was crucial for MHSTs to be led by a partnership of organisations and not exclusively by the NHS. On this issue, several interviewees reported wider benefits to having a voluntary sector organisation involved in leading the programme (as was the case in two case study sites). Above all, they described how this had resulted in less bureaucracy and greater flexibility, and that innovation and service improvement had been easier compared to their experiences of working in other sectors (including the NHS):
So I think we have much more flexibility working in a voluntary sector and we are able to be quite innovative and do things and test things out. We’re practising safely but I like the fact that we can do something on the side of the NHS – still linked to it – but you know, bespoke to the schools that we’re working with…Sometimes mental health can be very rigid so it’s quite nice to not have so much rigidity in what we’re doing.
(Case study site 3, MHST manager)
The disciplinary background of the service manager could also influence MHSTs’ focus and activities. This was illustrated in one case study site, where one MHST was led by a mental health nurse, and another by a senior social worker. In the first there was a strong focus on providing training to staff in education settings on mental health conditions and treatment approaches, while building relationships for inter-agency safeguarding work was more prominent in the second.
Time spent in education settings and on each of the core functions
For all MHSTs in the case study sites, EMHPs played a central role in direct work with schools and colleges. The number of settings EMHPs were responsible for ranged from a low of between three and five settings, to a high of eight settings. One case study area allocated education settings to pairs of EMHPs, with each pair covering 11–12 settings between them. What was clear from our interviews was that EMPHs that had been allocated more settings had a greater workload in terms of establishing relationships, building their understanding of the setting and where MHST support might fit within their existing provision and approaches, and having enough time to dedicate to each setting:
I think it’s [the number of education settings] perhaps a little too many because it’ll be nice to have more of a presence in schools but it’s difficult when you’ve got so many so you can’t do like a whole day in each because there’s too many…I think perhaps an ideal number would be about five so that you could even maybe have a different day focused on each and could just be more present in that school and that might increase the referrals and things like that.
(Case study site 1, EMHP)
EMPHs also varied in how much time they dedicated to each setting. In one area, they spent half a day per week in each setting; in another, they spent four weeks with one or two settings at a time, and then rotated. In some areas, the time allocated to each setting was flexible and in others it was more explicitly and strictly set. Factors influencing the time allocation per setting were:
-
number of pupils
-
type of setting (e.g. primary, secondary, pupil referral unit)
-
the needs or priorities of the setting
-
number of referrals from the setting
-
extent of engagement from the setting
-
the type of service provided to the setting (e.g. one-to-one interventions vs. whole school approach).
There was no guidance from the national programme team on how MHSTs should split their time across their three core functions, to allow teams to operate flexibly and tailor their approach to each setting. The proportion of time spent on each function varied considerably across sites and team members. Data from 13 Trailblazer sites, reported for the period October–December 2020, indicated that the average time MHSTs were spending on each function was:
-
Function 1: Direct interventions 52% (range 20–72%).
-
Function 2. Whole school approach 24% (range 3.5–57%).
-
Function 3: Giving advice and liaising with external services 23% (range 6.2–50%).
Several case study sites also reported that more MHST time was being spent providing direct support to children and young people with identified mental health problems and several reasons were offered to explain this: education settings requested one-to-one support more often than whole school activities; difficulties supporting whole school approaches remotely during COVID-19; and (as we have already discussed above) a perception that MHSTs run by NHS organisations tended to be oriented towards the clinical aspects of the service, and less focused on whole school engagement and activities.
Mental health support team core functions and processes
Delivering the core mental health support team functions
In each of the case study sites, we gathered information about MHST key activities, across their three core functions. An overview of these activities MHSTs and stakeholders’ views on how well they were reported to be working is provided in Table 11.
| Function | Key activities | Is this function is working well? | Challenges and issues |
|---|---|---|---|
| Delivering interventions |
|
Almost all respondents to the second key informant survey reported that the delivery of evidence-based interventions was working effectively (92%). |
|
| Supporting the development and delivery of a whole school/college approach |
|
Most respondents (71%) to the second key informant survey reported that there was a shared understanding of what a ‘whole school approach’ meant across key stakeholders involved the programme in their area. The majority (86%) also reported that MHSTs were effectively supporting education settings to introduce or develop the whole school/college approach. |
|
| Giving advice to staff in education settings and liaising with external specialist services |
|
|
|
Referral and assessment pathways
Our case study sites provided detailed information on how children and young people are referred to MHSTs for direct support. The process followed generally consisted of the stages outlined in Figure 7, although variation between sites was apparent. For example, some sites operated a joint triage approach, where referrals were reviewed in meetings of MHST staff and professionals from other local mental health services, whereas in others triage was undertaken within the MHST. Some, but not all, sites accepted direct referrals young people, parents or carers.
FIGURE 7.
Typical MHST referral and assessment process in the case study sites.

The referral, triage and assessment pathway was generally thought to be working well within Trailblazer sites. Almost all respondents to the second key informant survey felt that referral and the initial assessment of children and young people for MHST support (91%) and prioritisation of referrals for MHST support (83%) were working effectively. While waiting times between referral, assessment and starting interventions were generally reported to be good, one site in particular was experiencing significant challenges with waiting times, with some education settings waiting up to five months for children to start receiving support. This site had been trying to overcome this issue by moving EMHPs to education settings with longer waiting times. This and other sites highlighted factors that could hamper referral processes. These included incomplete referral forms, which added delays while critical information (sometimes basic details like the child’s full name and date of birth) was sought before a triage decision could be made. One participant suggested that education settings in their area sometimes deliberately omitted important information to avoid the referral being rejected: ‘a child is never what they seem on paper and the schools can sometimes omit things that they know may stop that child [being accepted for support]’ (Case study site 2, MHST manager). Difficulties contacting parents to discuss the referral and seek consent to assess their child for support were also reported; while not widespread, some parents had refused to give their consent and so the referral could not be progressed. Inappropriate referrals were also mentioned, both from education settings and from other referrers (e.g. NHS specialist services), often in terms of a child having more complex or substantial needs that fell outside MHSTs’ low-moderate remit.
Service remit and scope
Defining and working within the remit of ‘mild to moderate’ mental health problems
One of the core functions of MHSTs is to deliver evidence-based support to children with ‘mild to moderate’ mental health problems. It is acknowledged in the MHST operating manual that ‘the defining of mild and moderate mental health issues [is] challenging but important’. 12 Trailblazers had all formally defined their service boundaries, with some mental health issues (e.g. active self-harm, children with suicidal thoughts and eating disorders) and some groups of children and young people (e.g. children with neurodiversity and SEND) often falling out of scope. Some case study sites reported that MHSTs would not accept a referral for a child who was already being supported by other services.
MHSTs were finding it difficult to hold a firm line around their ‘mild to moderate’ remit in practice. Many participants emphasised that while neat distinctions between ‘mild to moderate’ and ‘severe and complex’ may be needed for the purposes of defining service boundaries and referral criteria, in reality, children’s mental health problems were rarely so clear-cut. Often the presentation of mental health problems was complicated, uncertain and changing:
This is a bit of an ongoing tricky area, because mild to moderate, I mean, what does it really mean? It’s just such a vague, vague term. So, when you’re working across, we’ve got 50 schools at the moment, and they’ll have slightly different understanding of what mild to moderate means, and no matter how much you explain it and you write it down and you put matrices together and say this is mild to moderate, this is what we work with, this is what we don’t…There’s always going to be a grey area.
(Case study site 4, MHST manager)
Several issues were raised in relation to this issue of working within the ‘mild to moderate’ remit. Some noted that the exclusion of certain mental health problems or developmental disorders from MHSTs’ service scope overlooked that these were spectrum conditions that could present in degrees of severity; this point was made most frequently in relation to self-harm and autistic spectrum disorders:
Self-harm is a big one I think…our staff were told they don’t work with people who are actively self-harming, but I know that if a young person is actively self-harming but in a low and superficial way, that we could actually do the work with that child, but the alarm bells come on for some practitioners when they hear about self-harm…. That’s been one of the barriers I think, is universities [providing EMHP training] telling practitioners they cannot work with someone who’s actively self-harming, but without actually exploring and understanding what that means and what that actually is.
(Case study site 2, MHST manager)
MHST staff often mentioned that a clear picture of a child’s mental health problems might only become clear over time, with what might initially appear to be problems that were ‘mild to moderate’ in nature turning out to be more complex and/or other issues (e.g. domestic abuse, parental drug or alcohol abuse) coming to light. MHSTs then had to decide whether it was appropriate to continue providing support, potentially alongside a referral to specialist services for the more complex issues that had become apparent.
This issue of onward referrals was another major challenge. Across all the case study sites, and among survey participants, capacity constraints in and long waiting times for specialist mental health services was a recurring theme. These problems had worsened as more children and young people sought help for mental health problems as a direct result of the pandemic, which was widening the gap between the support offered by MHSTs and meeting the criteria for specialist services:
Due to pressures, funding challenges and other factors, the thresholds for accessing some other specialist services appears to be going up. As such, on occasions there appears to be a gap emerging between the MHST remit and the threshold to access specialist service. This gap was not present at the outset of MHST within our borough. MHST is often now been asked to see some cases with more complexity that would have previously been seen by other services. This could stretch the MHST remit beyond the original guidance in terms of type of presentation and interventions to be offered. It is too soon to tell how this will pan out but something being monitored.
(Key informant survey respondent)
Within this context, there was evident concern among those working in MHSTs that making a decision not to accept a child for support could mean either a long wait or no support at all:
One is the capacity anyhow in CAMHS. They are really, really struggling, so even if you could prove that a case did belong to them, we know that they won’t get a service straight away. So, there’s a little bit of, you know, a little bit of tension for us about not wanting to refer a child into a service where we know they’re not going to get a service, basically.
(Case study site 4, management/governance)
Across the case study sites, MHSTs were responding to this in different ways: while some were seeking to hold a firm boundary around their scope, others reported that they were supporting children with more serious and complex mental health problems (sometimes while they waited for a referred to specialist services):
[Name of service manager] is really, really clear about boundaries and knows exactly what CAMHS are meant to do…She’s very good at holding the line and saying, ‘No, really, that’s not for us to do.’
(Case study site 4, management/governance)
But those young people who fall through the gap who were not CAMHS appropriate, they might be over our threshold, those are the cases we’re now starting to work with, with clinical supervisors…Supervisors now are able to step into their role as clinicians a bit more which they weren’t able to do in the first year.
(Case study site 3, MHST manager)
MHSTs did not appear to have formally changed their service remit to bring certain conditions or problems of greater complexity into scope. Rather decision-making about whether to provide support was generally ad hoc and made on a case-by-case basis, and there was a great deal of uncertainty about the grounds on which such decisions should be made. As the second of the above quotes indicates, support to children with more complex problems was usually being provided by more experienced therapists within the team, although concerns were also voiced about EMHPs managing higher levels of risk than they were initially trained for. One site reported that to stay within the parameters of ‘mild to moderate’, some education settings where children typically had higher support needs, including special schools and pupil referral units, had been offered whole school support (e.g. group sessions on sleep hygiene and providing advice to staff), instead of one-to-one interventions.
These issues were known by the Trailblazer programme’s regional and national leads and, while there was agreement that the programme was funding early intervention for children with ‘mild to moderate’ mental health problems, there was no consensus on how far the moderate boundary should extend and if and how MHSTs should support children presenting with more complex needs:
But the concern of course is that, since COVID, the threshold to get into CAMHS has become higher…so then when the mental health support teams are meeting the needs of the mild to moderate it is difficult because, again, that group changes a bit and certainly there’s that middle group that aren’t quite in CAMHS and it is a problem, it’s not the problem of this programme, in that it’s not the remit and I think sticking with the remit is important, but it is a drop in the ocean.
(National interview)
I think there’s certainly something about, you know, I suppose if the trend continues and we’re continuing to see schools who are in need of more substantial support for the severe end then maybe that needs to be thought about probably at a national level I guess about, you know, whether there should be some kind of change in policy about what we do to support that.
(Regional lead)
In the absence of a clear steer from the national team, it was being left for Trailblazer sites and MHSTs to make decisions about if and when to support children who presented with more complex needs, resulting in variation in the level of service being provided across different areas.
Reach and inclusion
Reach and inclusion refers to the ability to engage and support all children and young people, including those from groups that are socially marginalised and/or disadvantaged, who have historically been poorly served by mental health services. Participants described several ways that MHSTs were trying to increase awareness, accessibility and suitability of the service for all communities and groups in their area, including:
-
Involvement of young people, families and education settings in the design of the MHST, and gathering feedback from these groups to identify where service improvements could be made.
-
Placing MHSTs in education settings with higher levels of mental health need and/or a greater proportion of young people from disadvantaged backgrounds or from groups not well served by existing mental health services.
-
Linking, working and sharing knowledge with other services in the area supporting children and families and/or mental health.
-
Increasing visibility of the service and building links through, for example, community outreach roles, attending local events (e.g. Pride, local coffee mornings) or connecting with local community groups.
-
Designing specific projects aimed at improving service accessibility and use in specific groups; for example, one Trailblazer area described projects that had been set up to provide tailored support to black boys, children from South Asian communities and children at risk of exclusion.
-
Creating roles (or parts of roles) focused only on supporting and engaging children and young people from specific groups, including ethnic minority groups, LGBTQ+ and neurodiverse young people.
-
Offering training to MHST staff on how to best support children and young people in, for example, special schools or pupil referral units.
-
Recruiting staff from the communities MHSTs were serving, particularly ethnic minority groups, or with specific experience or skills (e.g. working with children with autistic spectrum disorder).
-
Culturally adapting resources and translation of existing resources into non-English languages.
-
Reporting and monitoring data on the demographics of children and young people being supported by or engaging with MHSTs, with a particular focus on capturing information on ethnicity and other protected characteristics.
Remaining gaps in support
Despite MHSTs’ efforts to increase service accessibility and uptake, gaps in service provision were widely reported. Almost half of respondents (49%) to the second key informant survey reported that there were groups of children and young people not accessing the support provided by MHSTs and/or not receiving effective support. Groups reported as being underserved by MHSTs included:
-
young people with special educational needs and/or neurodiversity
-
young people from ethnic minority or non-UK cultural backgrounds, and/or with English as a second language
-
LGBTQ+ young people
-
children and young people from low-income households and economically deprived communities
-
young people not in school, including those being home schooled
-
certain religious settings (e.g. Catholic or Church of England schools)
-
boys, particularly teenagers
-
looked-after children
-
children in rural schools
-
children with ‘internalising’ mental health problems, which often presented in subtler and less apparent ways (e.g. social withdrawal or sadness) compared with children displaying challenging behaviours.
Our findings suggest that there are multiple factors and barriers that account for why these groups were less likely to access MHST services, including lower awareness of MHSTs, stigma around or different views of mental health problems, preferences for other sources of support (e.g. from family or friends), negative perceptions and/or past experiences of mental health services, lack of joint working between MHSTs and other services that may be involved in providing support, and limited skills and expertise among MHSTs to personalise support to different needs.
Many participants commented that the standard MHST intervention (time-limited CBT) did not work as well for some groups of young people or for certain mental health problems. In addition, the issue of EMHPs and other MHST staff not having the training and skills to support all groups of children and young people was raised:
ASD [autistic spectrum disorder] is a difficult one…the interventions have not been effective…we just don’t have an intervention that would work, there’s no adapted model yet for any lower level anxiety’, so we’ve just had to unfortunately give them the best as we can and then say ‘unfortunately now we’ve done as much as we can’ and we’ve had to signpost to like the Autistic Society or something to get maybe support that way.
(Case study site 2, MHST manager).
Deprivation in our area. Many children have ACE’s [adverse childhood experiences] and other complexities/social factors that are impacting on their mental health and may make the CBT evidence-based approach not appropriate as their level of need is too high, or there is systemic work to be done.
(Key informant survey respondent)
In some cases, it was not a lack of skills, but the requirement to deliver a specific type of intervention that prevented tailoring to specific needs. For example, as one MHST staff member, who had joined their team from adult mental health services, explained:
When I see a young person and I know I’ve got to stick within the realms of the model, that can be frustrating, when you know that you’ve got the skills to do something else with them, but you’ve got to stick to the model and the frame and not going outside of that. So, it’s very structured and it can be very fixed…I’m used to working, again, in adult mental health services. It’s much more flexible, so you can be a little bit more open to trying different things, but I think that’s because we’re still very new, and I think that that will come in time.
(Case study site 4, EMHP)
Support for children in primary schools was also identified as an issue. For children of this age, MHSTs typically provide parenting interventions or support for parent-led interventions, rather than directly supporting the child. But parents sometimes lacked the time and/or willingness to engage, as one education setting commented:
There needs to be more provision or training for the Trailblazer team on working with children individually in primary schools…In some areas, parental engagement is low and therefore relying on an intervention that a parent engages with for an hour every week for 6 weeks is not realistic.
(Education settings survey respondent)
Parent-led interventions were also unsuitable where a child’s mental health issues were linked to their family situation and/or relationship with a parent or parents.
Cultural and language barriers relating to the cognitive behaviour therapy approach were also described:
I think, the intervention type being quite a Western offer frankly. CBT, you’ve got a cognitive ability to do it, you’ve got an articulation and a fundamental understanding of the English language and the English culture to be able to understand what mental health issues even are, what depression is, what anxiety is, and have a word to translate. It’s not translatable in our inner-city boroughs I don’t think, for every child and young person. I think there’s some considerable barriers in them accessing that type of intervention.
(Case study site 3, management/governance)
How mental health support teams adapted in response to the COVID-19 pandemic
Despite the many obstacles posed by the pandemic, MHSTs quickly adapted how they were working and what support they provided. In effect, the pandemic necessitated creativity and innovation. Many teams seized the opportunity to do things differently and this was widely praised. Broadly, this adaptation in response to COVID-19 took three main forms:
-
Developing strategies to increase referrals: for example, increasing efforts to publicise the service, and working with other local mental health services and/or non-Trailblazer schools, to offer support to a wider group of children and young people locally.
-
Changing or expanding the type of support provided: for example, developing new resources (including videos, virtual assemblies, podcasts, newsletters, drop-in services and support on return to school) and/or expanding the offer of support to include parents and teaching staff. Around half of the respondents to our second education settings survey reported that, in response to COVID-19, their MHST had extended the delivery of mental health support to include staff (45%) and parents and carers (46%).
-
Switching from face-to-face to remote working and support: all teams switched to offering remote support delivered via the telephone and/or digital platforms.
Remote working was reported to have some benefits, including presenting the opportunity for staff to develop skills for digitally delivered support, it being easier to organise meetings involving people from multiple organisations/locations and easier for MHSTs to meet with and/or support parents (because no travelling was required). Challenges were also highlighted, such as practical issues with technology, a lack of MHST skills for remote working and support, some children not having access to technology, and issues around safeguarding, confidentiality and information security. Concerns were also raised about the suitability of providing emotional and well-being support remotely as some children and young people would not feel comfortable or safe discussing their mental health problems in their home environment.
Some participants were of the view that young people seemed to prefer in-person support, although the experiences shared suggested that preferences were diverse and that remote support could work well in some circumstances (especially for follow-up appointments, where an initial relationship had been established face-to-face). Relatedly, a concern was raised by one regional lead that decisions about the balance between face-to-face and digital delivery should be based on what is most appropriate and effective for children and young people, and not by financial considerations (e.g. potential pressures to make efficiency savings or do ‘more with less’ in the post COVID-19 environment).
Trailblazers were asked which of the changes that had been made in response to COVID-19 they anticipated retaining after the pandemic. The responses suggest that most areas expected to have a blended model, with a mixture of remote and face-to-face working and support (Table 12).
| Change in provision | Trailblazer sites offering service (%) |
|---|---|
| Online/remote support for children and young people | 83 |
| Online/remote support to education settings | 82 |
| Online training and/or supervision for MHST staff | 75 |
| Offering flexible working for MHST staff (i.e. working from the office and home) | 72 |
| Mental health support to parents/carers (where this was not offered pre COVID-19) | 62 |
| Mental health support to education setting staff (where this was not offered pre COVID-19) | 58 |
Chapter 8 Education settings engagement and experiences
Mental health services offered by education settings before the programme
Different types of mental health and well-being support were offered to children and young people in education settings before the start of the Trailblazer programme. In response to the first education settings survey, almost two-thirds of respondents (65%) reported that their setting had a mental health lead before the programme. More than half of these settings (59%) reported that this role had been in place for three years or longer.
The DfE’s baseline survey, undertaken in 2019 to establish the level of mental health support available at education settings that were part of the Trailblazer programme, also asked about the types of direct support provided. Educational psychologist support was the most common type of support (82%), followed by ‘counselling provided by trained counsellor’ (61%); fewer respondents reported that their setting provided CBT (17%) and clinical psychologist support (15%). Most types of support were self-funded by education settings, with the exception of clinical psychologist support (which was predominantly funded by the NHS).
With regard to views on mental health and well-being services before the programme, 46% of respondents to our first education settings’ survey considered waiting times for specialist services to be unacceptably long. Just over half (52%) agreed with the statement that specialist services responded well to children and young people in mental health crisis. The same percentage (52%) of respondents to the DfE baseline survey reported being either very satisfied or fairly satisfied with their relationship and joint working with NHS CYPMHS. There was a higher level of satisfaction in secondary schools compared with primary schools and ‘other’ settings. A large majority of respondents (84%) reported that they had an identified point of contact in their setting to link to specialist NHS services but under half (48%) responded that there was an equivalent point of contact in these services that they could approach for advice and support.
Impact of COVID-19 on mental health in education settings
While the impact of COVID-19 on education settings had been variable, negative impacts were widely reported. In the first education settings survey, reported impacts included increased staff workloads, stress and fatigue, coping with constant uncertainty and disruption, concerns about the safety and well-being of pupils, increases in safeguarding issues, dealing with angry and frustrated parents, and the challenges of engaging children and young people in remote learning. Many settings were also seeing an increase in mental health problems, among staff, pupils and parents and carers. The most frequently described impacts of the pandemic on accessing specialist NHS services were longer waiting times or lack of appointments for children and young people, and limited provision of face-to-face support. This resulted in additional strain on staff (in particularly those in key roles, such as mental health, pastoral, special educational needs and safeguarding leads) and ‘in-house’ services. One respondent described the challenge faced by staff in meeting the more complex needs:
We have a number of quite complex mental health issues in school. These cannot be handled by the MHST and yet I know that the CAMHS service is also over-run with referrals. Unless these children receive timely, prolonged support, their mental health will continue to decline. Teachers are not specialists in mental health and it can feel very overwhelming.
(Education settings survey respondent)
In a small number of cases, challenges had led education settings to adapt their own provision to fill gaps, which some viewed as a positive outcome.
These impacts were echoed in our case study sites, with interviewees from education settings describing how some children had become less confident about social interactions and more sensitive to noise and the busy classroom environment. They also described increases in safeguarding issues, and in emotional outbursts and aggressive behaviours upon returning to the classroom. One participant described the considerable toll that the pandemic had on the mental health and well-being of their staff:
I think there’s a whole heap of professionals that have been completely missed from being acknowledged, and I think school staff are one of them. And they are absolutely on their knees, bless them, really on their knees. They’re exhausted.
(Case study site 3, education setting staff)
Case study participants also described positive changes associated with the pandemic; above all, that the pandemic was felt to have reduced the stigma that some parents and carers felt about requesting mental health support for their children.
Views on, and experiences of, working with mental health support team staff
Survey respondents were generally supportive of the programme and being able to increase the provision of mental health support within their setting. Our second survey asked education settings to report on the support they were receiving from their MHST to introduce or develop their whole school/college approach to mental health and well-being. The highest level of support was for mental health promotion, followed by engaging pupils to identify issues to address through mental health and well-being work in the setting (Figure 8). Respondents were also given the opportunity to describe additional ways in which the MHST was supporting their setting. The most commonly reported activities were provision of staff training and workshops on mental health and well-being, mental health training for parents and carers, and group work with children and young people.
FIGURE 8.
Support received from MHSTs to introduce or further develop the whole school approach to mental health and well-being.

We asked respondents to the second survey how well they thought the referral process to the MHST was working, as well as the capacity of external services to accept onward referrals from the MHST. Over three-quarters of respondents (76%) reported that referrals from the education setting to the MHST were working very well or somewhat well. In contrast, less than half (41%) reported that the capacity of external (specialist) services to accept referrals from the MHST was working as well (Figure 9).
FIGURE 9.
Views on MHST referral process.

Senior mental health lead role and training
The importance of the senior lead for mental health role to the success of the programme was evident in our research. Senior mental health leads were described as being the staff members responsible for making referrals, as well as championing mental health with their settings. As one EMHP told us: ‘if you’ve not got an engaged mental health lead you’re not going to get any referrals, so it does make a huge difference’ (case study site 3, EMHP). The considerable workload of the person taking on the role was also acknowledged:
One of the things I know some schools face, you know, if you’re trying to find a named lead…One of the first things you then need to do is ‘well what can I take off this colleague so that they can engage with this properly?’…The danger is one just loads another job responsibility onto them.
(Case study site 1, education setting staff)
In one case study area, education settings had been encouraged to identify strategic and operational mental health leads who, respectively, would champion mental health issues at the senior leadership team and across the setting, and lead and coordinate the setting’s mental health work day-to-day. This approach was reported to be working well, not least because it spread the responsibilities across two members of staff.
Interviewees at all levels commented on the training for senior mental health leads. This training represents the major investment from the programme directly into education settings and is intended to support and equip senior mental health leads to fulfil their leadership role effectively. There was evident disappointment and frustration about the training having been substantially delayed, although the provision of other mental health training to education settings during 2020 and 2021 (through the DfE’s Wellbeing for Education Recovery/Return programmes) was acknowledged and welcomed. The lack of specific training for senior mental health leads was a key reason given for some settings feeling under-prepared for the programme and their MHST:
It’s the wrong way round really to introduce the MHSTs without doing that awareness building within the school through the senior mental health lead training…When we’ve been out to visit the schools they’ve all said, haven’t they, that those that have that kind of champion for mental health and have that whole school approach sort of embedded to some extent have really been able to take on the MHSTs properly and really get the most out of it.
(Regional lead)
Some interviewees reported that communication with schools and colleges about the purpose of the programme, the remit of MHSTs and the requirements of the senior mental health lead role had been insufficient, something that training could have helped address. Specific areas where training would have been beneficial were identified, including how to work with MHSTs to set up referral pathways and processes.
Given that a key purpose of the training was to equip senior mental health leads with information and skills to help their setting introduce to develop a whole school approach, it is unsurprising that the delay was felt to have particularly affected the progress of this element of the programme:
If we’re talking about the whole school approach work, not wanting to point fingers, but I think that part has been hampered somewhat by the very substantial delays to offers of training to mental health leads within educational settings. That’s something that’s only really emerged I think in maybe the last six to nine months, when it was an original, like, absolutely key part of the original proposal.
(National interview)
One case study site had addressed what they felt was a major gap in programme implementation by developing their own training for senior mental health leads, which more than 50 school staff were enrolled in by the time of our fieldwork (summer 2021).
Concerns about the impact of the delay in the senior mental health lead training were also expressed by interviewees from the national team. But an alternative view was also expressed: that the delay had led the DfE to reconsider its approach, moving away from the original plan to commission a national training programme and adopt a flexible model, with education settings able to access different levels and types of training from a ‘menu’ of training providers. This was considered a positive outcome, although a wait of over a year and a half for senior mental health leads to access training was also acknowledged to be less than ideal.
Tailoring of mental health support teams support to education settings
There was widespread consensus about the importance of MHST workings within education settings’ values and ethos, and providing support that was relevant to their context and specific needs:
To me, the important thing here is that they work with the school and to the school’s rules. They’re not mental health professionals parachuted into the schools, they have the values of the school, they adopt the values of the school because we’ve always had mental health professionals dropping into schools and it never worked.
(National interview)
Early work to tailor approaches had fostered relationship building between MHSTs and staff in education settings and encouraged a focus on ongoing learning and service improvement. A participant from a setting in one case study site provided examples of the flexibility demonstrated by EMHPs:
The first thing to say is whatever we ask them to do, they’ll do. They’re incredibly responsive. So, for instance, if we say ‘Help us with the summer school’, they’ll say ‘Yeah, what do you want us to do?’ Or ‘Come on results day’ or ‘Support these youngsters who are struggling with transition’ or ‘Think about ways in which we can deal with youngsters who have got exam anxiety’…Whatever we say they show great responsiveness to, which is brilliant, you know, that in itself is really uplifting and leads to great hope and optimism.
(Case study site 1, education setting staff)
In another case study site, this flexibility and adaptability was attributed to multiple factors, including the programme being delivered by the voluntary sector; MHSTs seeking and using feedback from children and young people, parents and carers, and education settings staff, and conducting a mapping exercise of existing mental health support in each setting to ensure that the MHST work was tailored to the needs of the setting and complemented (rather than duplicated) services.
We asked in the second education settings survey about the extent to which respondents felt that their setting was aware of the activities of the MHST and were able to shape them. Over three-quarters of respondents (76%) agreed with the statement that their MHST was responsive to the needs of their students. The majority also agreed with the statement that the programme reported its activities regularly to the senior leadership team of the setting, and that the setting was shaping the day-today working of the MHST or individual practitioners (Figure 10).
FIGURE 10.
Governance and involvement of education settings in MHSTs’ activities.

Many of the operating principles for MHSTs relate to tailoring the service to local needs, and education settings’ assessments of their MHST against these principles were also generally high. For example, 80% of respondents agreed that MHST support was responsive to the setting’s needs, and not taking a ‘one size fits all’ approach (Figure 11). However, these findings also suggest that such tailoring has largely involved discussions between MHST and education setting staff. Direct involvement of children, young people and families in developing the approach was limited, with only 19% of respondents reported that this had happened ‘to a great extent’. We also heard from survey respondents and interviewees who identified a lack of flexibility in the service model as an area where implementation could be improved:
FIGURE 11.
Extent to which MHSTs’ operating principles have been implemented in education settings.

Stop being so prescriptive. Equip EWPs [education well-being practitioners] with multiple tools and the autonomy to use them as they see fit.
(Education settings survey respondent)
Relationships and engagement
Building strong relationships with education settings is a key aspect of MHST work and our findings suggest that this takes a significant amount of time, resources and effort. In general, education settings were felt to have engaged well with the programme and MHST staff spoke positively about working with them. Across the case study sites examples of non-engagement were given, but in all it appeared that only a few settings were not engaging after multiple attempts. Our case study respondents suggested that the lack of engagement from some settings may be due to a range of reasons, including:
-
Not understanding the remit of the MHST/mismatch between what education settings expected and wanted from the service, and what it provided (e.g. settings wanting support for more complex mental health issues).
-
Lack of time/capacity within education settings to fully engage with the MHSTs. This was exacerbated in settings where there is no designated mental health lead.
-
Settings not referring students because of the view that referrals to the MHST were often deemed unsuitable.
-
Poor personal relationships between MHST and education setting staff (although this was not a common occurrence).
-
Lack of parent/carer engagement.
-
Lack of trust in MHST experience and/or knowledge.
-
Lack of physical space from which the MHST could work.
-
Past (poor) experience of short-term mental health programmes.
-
Not viewing mental health as a priority.
In terms of the mismatch between expectations of MHSTs and what teams could provide, long waiting times to access specialist support were reported to be contributing to this issue. We were told that some settings saw MHSTs as a shortcut to accessing specialist mental health services:
One of the largest parts of our role is the signposting element, so I think schools are using us, particularly as CAMHS waiting times are astronomical at the moment. I think they maybe use us as a little bit of a shortcut into mental health services. If it’s going to take CAMHS six months to come out and do an assessment on somebody, but I can be there next week. That’s quite a big difference isn’t it.
(Case study site 2, EMHP)
In most sites, the issue of understanding MHST remit and having appropriate expectations had improved over time, once teams had the chance to establish a relationship with the setting:
Four months after the project officially started…schools were left kind of without any understanding of what we were offering as well as staff members as well, so I think we had to take a while at the beginning to really get them to understand what we could do and what we couldn’t do. And that did lead to some schools partially switching off to begin with because they thought they were going to get a service that would fix all of their needs and they could send every case through from crisis cases and we would fix it and obviously that’s not what we’re here for, but I think we’ve rebuilt those relationships.
(Case study site 1, MHST manager)
Our findings suggest that MHST staff (particularly EMHPs) had gained confidence and experience over time in developing these relationships.
In terms of more specific issues affecting engagement, one participant from an education setting expressed concern that the MHST referral forms were too detailed, as well as being very ‘medical looking’, which may have put parents and carers off engaging for fear that it might link to their child’s ‘permanent records’. Efforts by MHST staff to meet with and raise awareness of the service among parents and carers was thought to partially overcome this issue, by putting people’s minds at ease and supporting them get the right level of help for their child. A participant in another site described the support provided by the MHST in the onward referral of children they cannot directly support as one of the benefits of the service:
And the practitioners, all of them, I’ve been so blessed with every single one that I’ve had here, has been magnificent, has never said no to anything…So if I take them a student that doesn’t meet the criteria, they will automatically refer them to the right path.”
(Case study site 3, education setting staff)
Interviews with case study and regional interviewees highlighted three key factors that supported MHSTs to develop effective relationships with education settings. These included having an engaged senior mental health lead, and MHSTs tailoring their support and ways of working to individual education settings (both discussed in more detail above). The final factor was education settings integrating MHST staff into their environment and wider team (e.g. by inviting them to join staff meetings and participate in wider activities in the setting), and embedding the service into their processes and practices. While this appeared to be happening generally, our findings suggest that not all MHST staff felt welcomed into the settings in which they were working:
But no, I don’t really integrate with the staff. I think I’ve sat in a staff room once, and it felt very weird, because I think everyone was just staring at me to be like, who’s she?
(Case study site 4, EMHP)
Factors supporting and hindering programme implementation in education settings
Our survey research identified a number of factors, relating to both the MHST and the setting, that supported the implementation of the programme and hindered it. The most commonly cited factors supporting implementation were positive characteristics of the MHST staff, such as being professional, reliable, informative and proactive. Strong communication between the MHST and the setting were also seen as an important factor, as was the support of the education setting’s senior leadership team. The main barriers to the implementation and success of the MHST were the time commitment of the senior mental health lead, and their other responsibilities in the setting, which meant that they could not dedicate the necessary time to utilise the MHST’s services (Box 8). This was also echoed in the case study interviews; for example, one EMHP told us:
In many of my schools, teachers wear several hats and my mental health leads are full-time teachers and they are mental health leads in their lunchtime and in the morning and they do a brilliant job but it can’t be expected from them to do that, it’s not fair on them or the children.
(Case study site 5, EMHP)
-
Professional/reliable/informative/proactive MHST staff
-
Regular contact with MHST staff
-
Senior leadership team buy-in and support
-
Good communication and relations between setting and MHST
-
Flexibility of MHST
-
Engaged mental health lead
-
Commitment to whole school approach in the setting
-
Prompt action/response of MHST to referrals and queries
-
Time commitment of mental health lead/competing with other responsibilities
-
Limited capacity of the MHST to meet (growing) needs
-
Low levels of parental engagement
-
Frequent MHST staff changes
-
COVID-19 (e.g. staff having to wear personal protective equipment when ‘on site’)
-
Slow referral process/long waiting lists
-
Insufficient funding for mental health and well-being services
-
Inadequate physical space for MHST
[Listed in order of frequency]
Benefits and limitations of support offered by mental health support teams
School and college staff identified several benefits to having an MHST operating in their settings. This included children and young people having someone with whom they could share and discuss feeling that they might not wish or be comfortable disclosing to settings’ staff, and the techniques that staff learned from the team members. A teacher in one case study site described the benefit of the programme in filling the perceived gap between in-house services and the ones previously provided by the NHS:
To make that step from what we provide in school and, actually, what the NHS provides through TaMHS, that is a big step and a huge waiting list, and so for us, Trailblazers is that lovely in between service… And so for me, it joins a lot of the dots, and our parents now see that.
(Case study site 4, education setting staff)
The most frequently described benefits of having the MHST in an education setting, reported by respondents to the second education settings survey, were related to the support and training that the MHST was providing to staff, support for parents and carers and enhanced mental health provision for children and young people (Box 9). One respondent described the ease of access to early intervention mental health and well-being services, afforded by the programme, as one of its main benefits:
Students feel more reassured that there is professional support easily accessible if they need it and no longer think that they have to be effectively suicidal before they would be eligible for support.
(Education settings survey respondent)
The most frequently reported limitations of the MHST were related to service scope and capacity.
-
Support and training for staff
-
Support for parents and carers
-
Additional capacity for children and young people’s mental health needs
-
Speed of accessing support
-
Raised awareness and profile of mental health in the setting
-
Workshops for children and young people
-
Having a point of contact for mental health issues
-
Improved links with other services
-
Earlier identification/ intervention
-
Limited ability to support full range of needs
-
Limited capacity to provide support
-
COVID-19 related limitations (e.g. support having to be delivered remotely)
-
Poor engagement with parents and carers
-
Long waiting times for accessing MHST service
-
Amount of ‘admin’ associated with service and referral process
-
High turnover of MHST staff/slow replacement
-
Low number of EMHPs/infrequent visits/insufficient time spent at setting
[Listed in order of frequency]
In relation to the scope of support provided by MHSTs, case study respondents reported some frustration within education settings that felt MHSTs were not addressing the more complex needs for which they most required additional support. Relatedly, some education settings noted that their staff had the skills and confidence to support children with less serious mental health issues, and so MHSTs were duplicating rather than enhancing mental health provision:
Some of the schools are seeing the benefit of the MHST approach, but I think you’d have an overwhelming response from schools saying, ‘But we’d prefer some orange level support to be honest’
(Case study site 5, project lead; ‘orange level support’ refers to the level between early intervention and specialist services).
Support for children with more serious or complex needs. Trailblazer programme offers very similar support to the support we are able to offer in school – need support for children at the next level.
(Education settings survey respondent)
While most of the examples given to illustrate gaps and limitations related to MHST’s direct support function, some comments suggested that hoped-for whole school improvements had not yet been seen:
The specialist knowledge the MHST has is not being passed onto teachers, therefore it is not being embedded as a whole school approach.
(Education settings survey respondent)
We also asked respondents to the second education settings survey what their setting needed most to further improve how it supports the emotional and mental health of its children and young people. The most frequently cited needs related to the provision of mental health advice and support parents and carers, staff training and expanding MHST capacity.
Chapter 9 Views of children and young people
This chapter is co-authored by: Beckye Williams, Ronan Nagle-Weaver, Jamie Morgan, Charlie Tresadern, Imaan Rathore, Kalen Reid, Lizzie Mitchell, Rowmell Hunter, Sarisha Goodman, Zaynab Sohawon, Niyah Campbell and Charlotte Saunders.
Focus group development, delivery and iterative analysis
The focus group research was co-designed with members of the University of Birmingham IMHYAG. Members contributed to the development of the recruitment materials including writing the participant information video script and recording the video; they developed the topic guide for the focus groups; they trained as co-researchers and co-facilitated focus groups; and they engaged in analysis and debated the data given their expertise by experience in order to formulate the findings contained within this chapter.
The intention for the focus groups was to co-facilitate these with IMHYAG co-researchers to equalise power between children and young people, as this has been shown to facilitate more unconstrained participation. 62,63 However, the focus groups ran during core school hours and thus, while our ambition had been to co-facilitate the focus groups with IMHYAG members, often this clashed with their own study or work commitments, representing a practical constraint and limitation for youth co-research in schools. We also had to be relatively flexible and move focus groups (often at short notice) to fit with school priorities and COVID-related issues, and this meant that only three of the five focus groups were co-facilitated by IMHYAG members or Institute for Mental Health youth involvement co-leads.
Once the focus groups had been held, a debrief took place immediately after with co-facilitators to reflect on what had been heard. We additionally held an analysis workshop with the IMHYAG to discuss the focus groups findings, develop the coding framework, and to decide on the key themes from the analysis to present in this report.
Reflections from the youth advisory group
When developing the coding framework, discussing reflections on participation in the focus groups, and in refining the key messages from the analysis, the perspectives of IMHYAG members have been invaluable. One of the interesting reflections that they offered was how much greater the emotional literacy of children who participated in focus groups was than they felt theirs would have been at that age. They also reflected as a group on when they were in primary or early secondary school, and how much they felt they would have benefited from the one-to-one, small group and, particularly, the whole school approaches to mental health in their education setting. The common language, the ability to talk to peers, friends, family members and teachers about struggling with mental health, and the general openness of the children in the focus groups was of surprise to the IMHYAG members. It resonated powerfully as a contrast with their own less favourable experiences. It is therefore worth noting that IMHYAG members understood from the participants that there had been a perceptible (and welcome) shift in those school environments from the ones they recalled given their own school or college experiences.
Children’s help-seeking and understandings of where to find support
During the focus group, children’s help-seeking was explored. When discussing who children would seek help from for their mental health outside school, the most common response was parents, siblings or wider family members. For those children who did not have family members available, particularly for those in care, they would seek support from a ‘trusted adult’. Some children expressed anxiety about talking to family members or people outside school. The key reasons for not feeling comfortable approaching people outside school included concerns about being dismissed and concerns about worrying parents:
I feel like it’s more hard, isn’t it, because it’s more hard to, like, open up to the fact that you are going through that…Because they could just say ‘Oh stop being silly’…and it’s just like you really need help about it.
(Focus group 3)
It depends on how bad it is. I don’t want to stress – I don’t want her to worry about me, do you know what I mean.
(Focus group 3)
For children who did not have a person they could or felt able to talk to outside school, there seemed to be an amplified importance of being supported in the school setting. On being asked how the return to school had been, one participant said:
I would say it’s a bit of both because I would say they would be happy because they can see their friends again but on the other hand it’s just…because while you’re in there [home schooling] no-one can really help you besides your family and if they didn’t notice, you’re just stuck.
(Focus group 5)
While children also spoke jokingly of the difficulty parents had home schooling and advising on pieces of work, there was also an appreciation of parental work stress during the pandemic, which we noted may also have factored into help-seeking choices being made by children.
Children in one focus group reported that they saw increasing number of peers turning to online social media forums to discuss their mental health and seek support during periods of school closure or lockdowns in the pandemic. The discussion in this focus group was particularly interesting as it was in a setting where there was less evidence of whole school working and the children in the group had poorer mental health literacy, and the main source of support or information about mental health was cited as being independent research online. The children spoke of using Instagram and Snapchat where other children were sharing inspirational or emotional quotes or putting up stories about how they were feeling. This link between mental health literacy and seeking support from online chat forums would be useful to explore further in future research.
Seeking professional support outside school was rarely mentioned. When it was, it was often to compare waiting lists for specialist NHS or allied services with timely support made in relation to children’s help-seeking behaviours in schools or family networks:
Because like even if you want to sort like an anger management thing or something it takes ages to get into the process, like, because my brother’s fully in counselling…Just like mental health people like the actual people that like do it as a job, like, it takes a while because there’s like a big waiting list for people that need the help, whereas my mum’s just always there and I trust her.
(Focus group 3)
Timely support in schools (e.g. through the MHST) was seen as being particularly important to children in the focus groups so that they could avoid holding onto worries that were affecting their well-being:
This might sound really stupid but once a week, for me it just feels like what if something happens and then you’re struggling to clear your mind and then you’re in a – say something happens on Monday and you can’t clear your mind until you go out for that day, maybe just like a day before or a few days before, I think that would be really helpful.
(Focus group 4)
The IMHYAG particularly reflected on this and felt that the availability of someone to be able to talk to relatively quickly in schools in the absence of community mental health services or family members outside school was especially important.
In all the focus groups, the choice of person to approach for support (both inside and outside school) was influenced by perceptions of trust. When asked about where they would seek support in school, the children gave a variety of answers ranging from their class teacher to the head teacher, the janitor, or the well-being/mental health or inclusion lead. The nature of the individual’s role seemed less important to the children than their attributes. Key among these were that the person was known to the child; they were someone trustworthy and they were someone who listened well. Three children sought out inclusion or well-being staff specifically for their identifiable expertise in relation to mental health.
Mental health support team and programme impact
Within the focus groups we explored understanding of the MHSTs in school. We did not ask children about particular episodes of care or to share experiences of receiving support, as this would have been inappropriate in the focus group setting, although some children choose to talk about this anyway. Not all children recruited into the focus groups had direct experience of MHSTs, which enabled us to get an understanding about how engaged MHSTs were across the whole school and how aware children were of the support services being offered generally.
Knowledge of the specific MHSTs or the function of the teams was the question children were least sure about across the focus groups. When asked directly about MHSTs in schools, the picture was mixed. In one of the participating schools, MHST work was only known about by the child who had experience of the team. In this school, there was no discernible whole school work being undertaken in addition to direct support. By contrast, where MHSTs were embedded in schools and had run groups with children in classes, hosted assemblies or other whole school work had taken place, they were more aware of the team and better able to articulate their function.
For those children who were aware of MHSTs, their opinion of the teams was very favourable. When asked to identify why this might be, the children gave reasons including they could trust them; they helped with the transition back to school from home schooling and gave you strategies to cope with mental health in school; they helped with your emotions; they provided mental health education; the team had snacks; and you could ‘share good and bad news with them’ (Focus group 2). Children reported wanting more small groups, mental health education or further one-to-one sessions as they had found these helpful.
The whole school approach
In schools where MHSTs were embedded and running groups (e.g. lesson or small group sessions or assembly work) as well as one-to-one activities, there was evidence of whole school approaches to mental health and well-being being better developed. This was demonstrated by the children being able to identify ways in which people (across the school) could support them with their emotions:
CYP1: Well in each class, so if you’re feeling sad or worried then you put a name tag on that and the teacher will come and see you and try and make you feel better…CYP2: Like you said, we do have an emotional check-in and when we do put ourselves on sad or worry, there’s not just that, there’s also sleepy, excited and happy, but when we do put ourselves in sad and worried, if we do, then they check it in the morning and say ‘Come out the door for a minute, come out the classroom’ and then they will speak to us and they will see if they can help us.
(Focus group 1)
It was also reflected in how children described experiences of support within the school environment and particularly about how they felt in themselves:
Because people take you out of the class and talk to you…When the staff take you out it feels really – if there’s something negative in the classroom, it feels really positive when you go to Inclusion or the Reading Bus or something and they ask you how your week’s been and if you’ve had any down emotions and see how we can improve on that.
(Focus group 4)
Children who had had direct contact with an MHST (either through one-to-one or group activities) also appeared to have better mental health literacy and were more aware of things they could do to deal with difficult situations or emotions. One child illustrated this through describing a technique they had been taught around worry journaling:
When you’ve got worries and you’re at home, you should write them down before you go to bed. I write down my worry and then he eats them all when I visit him…It’s my worry monster.
(Focus group 2)
Where there was less whole school work being undertaken, the children in the focus groups had poorer mental health literacy (e.g. they were unable to identify ways to support themselves and had a less versatile language or framework of understanding about mental health) and found it more difficult to engage in some of the discussion proposed within the topic guide.
All children felt that the school cared about their well-being, but in schools where there had been enhanced MHST support and not just one-to-one support, children were better able to articulate why they thought this. Their reasoning included that they felt seen and noticed; teachers were proactive about asking about well-being; there was always somewhere to go or someone to talk to; they were able to take time out; and the school had developed a culture of activities in classrooms including emotional check-in or adopted specific personal development lessons with mental health attached to curriculum teaching:
They do like PSHE lessons…So in form time we have 20 minutes and they do like specific things, so they’ve done like anxiety, depression, relationships, so they give us time and teach us about these different things and then we’ve had assemblies on it, we’ve had workshops, we have people telling us all the time about what we can do and stuff like that.
(Focus group 3)
For children who were in schools where there was less evidence of whole school approaches to mental health being adopted, they struggled to give examples for why or how the school cared for them and their answers tended to focus on feeling safe in school rather than around mental health:
Because of like their priorities, they care about how you’re feeling, if you’re safe.
(Focus group 5)
It was only in the focus groups in these schools that children identified feeling that teachers were less caring or could improve their attitudes towards and understanding of mental health:
I think just being more understanding and aware of people, like the students.
(Focus group 5)
The importance of the proactivity of staff in asking how children were and following up if they had been distressed, was strongly linked to the need to be noticed and to feel cared about, and was a theme that resonated across the focus groups:
Yeah, like there’s always someone to go to like if you have a problem you can go to someone and you can get sorted…and like after you’ve told them they’ll come back.
(Focus group 3)
The importance of being seen or noticed was a theme that particularly tied to children’s experience of school and home schooling during COVID-19.
COVID-19 impact
The impact of the COVID-19 pandemic was felt by all children who participated. Being unseen, or not heard, or feeling isolated was an experience that was common across all focus groups. In part the experience of being taught online, and being required to turn their cameras and microphones off unless they were answering a question, was experienced by children as their mental health and needs being unseen:
And if the teacher’s seen that there’s something on your mind because you’re face to face, they can actually see if you’re not being your normal self, so like if you’re walking round or your behaviour suddenly changed and you can see that whereas like on a phone call – yeah through lockdown it’s all behind a screen and obviously you had to turn your camera off so no-one would ever know, but obviously being in school if people can see that you’re actually upset then that’s where they would get more helpful.
(Focus group 5)
That school teachers were not able to pick up on body language, behaviour, or other cues when learning remotely increased their feeling of disconnection with learning and impacted their motivation and well-being:
You could literally just lie in bed and just have it on in the background. It just makes you…you’re just constantly inside every day, because I just got into a routine at that point on my iPad putting myself on mute and my camera off.
(Focus group 5)
While some students felt they managed to work successfully from home, others did not, and there was a mixed picture in terms of how children had experienced the pandemic. For children who were experiencing difficulties in their home life, they reported that they did not enjoy being home schooled without access to support:
One reason was because at school I could take my mind off all the troubles I had at home and just focus on one thing and one thing only.
(Focus group 1)
Commonly cited concerns were boredom; problems with self-motivation and completion of set work; not having anyone to ask if you did not understand the work; too much work or not enough; isolation and loneliness; missing friends; loss of structure resulting in further demotvation; lack of direct communication with teaching staff; and feeling that education or well-being support needs being missed:
Some people needed and didn’t get it [support] because either they couldn’t reach out or they didn’t reach out and like I feel like a lot of kids missed out on lots of learning just like they had no motivation or just didn’t have any access to the internet or just different reasons and then [teachers] missed some of that and didn’t realise that loads of people missed out so much.
(Focus group 3)
Although work was regularly sent out, children felt that additional well-being or other materials should also have been sent to support them while they were being home schooled. Some children did receive additional support, but experiences were very variable. One particular experience that resonated with the IMHYAG was those who were overlooked for support and/or were not targeted by inclusion or other teams within the school, but yet appeared to fit within the mild to moderate criteria. While schools with MHSTs had made efforts to reach children identified as in need, children that were previously high attainers (academically) or were quiet felt particularly overlooked and expressed they had struggled without additional support:
I feel like the, do you know, like the really smart kids, the really high achievers who always get good grades and they seem fine but I feel like they never get focused on because they always seem like they’re OK. They’re quiet and they keep to themselves and they don’t show their feelings at all, they come to school, they do the schoolwork and they go home and like just and they don’t like really open up do they [general murmurs of agreement]…Some people get ignored and miss out because they don’t seem like they’re not OK, they seem fine, which isn’t fair on them because they don’t get the help they need.
(Focus group 3)
Generally, all students within the focus groups felt that schools had made an increased effort to focus on mental health since they had returned to in-person schooling.
Changes in children’s expressed needs
The impact of the COVID-19 pandemic has potentially changed the expressed needs of the children for mental health support in schools. This was not a core topic of discussion in the focus group research and so it will need understanding through further research. However, children in the focus groups cited particular needs around: being noticed by school staff, and being listened to and supported with their emotional well-being if this had declined; support making, maintaining and repairing friendships; support tackling bullying; and quiet spaces or the ability to take time out was described as being increasingly important.
In addition to concerns related to social anxiety, the other needs that were said to have been exacerbated by COVID-19 and learning through the pandemic were in relation to the transition between primary to secondary school and with exam stress. Children felt that knowledge building activities targeting exam years or transition would be particularly helpful:
And it’s just like everything’s all at once and it’s just dead like overwhelming…Sometimes [children in year 7] they don’t know where to go, whereas we know who to go to where they might not, because you’re new to everything and you don’t know as much, like, I know in year 7 I didn’t know what to do now with my feelings and everything, yeah and you don’t trust anyone.
(Focus group 3)
The need for quiet space was seen as particularly related to COVID-19 and the impact of being left at home alone for protracted periods of time and the overstimulation and difficulty to returning to school settings:
I feel like it could be helpful that you just find that teacher, tell them how you’re feeling and they give you some time to just go and be and sit or go and just calm down and think about everything, because going into lessons being stressed or on the verge of crying your eyes out. Just being able to go somewhere and just be able to calm yourself down before returning to a lesson would be really helpful.
(Focus group 3)
Having more time out, greater opportunity for quiet space, and the importance of confidential places to raise concerns was raised by 10 of the 32 children in 4 of 5 focus groups:
I think we need like a sectioned area where like in the emotional check-in you can actually come and talk to someone, like really in private, because there’s always going to be people walking down and up those corridors. I think they need a separate room basically made for when you’re on sad or worried to take you there.
(Focus group 1)
The importance of confidentiality was repeated across several groups. Children both at primary and secondary level highlighted not having their own agency or communication with staff about their well-being in the pandemic as teachers communicated directly with parents instead:
I feel like if they would have, like, instead of my parents, because I think my parents were never in, I think if they directly reached out to me and were just like every so often they’d be like why aren’t you doing this or do you need anything like that, I never got any of that… Because my parents are always at work, so even if they did call my parents I wouldn’t know. All the phone calls that I had were through my mum or through my dad, so like even with that like sometimes say if like there was something that I was proper worried about then if they rang my mum and I was just like ‘Oh yeah it’s fine, it doesn’t matter’, do you know what I mean [if the teacher during lockdown had communicated] directly to me I would have been like ‘Oh there’s this’.
(Focus group 3)
These children wanted people to speak to them directly about their well-being and also wanted the opportunity to themselves reach out and contact people for support. The reliance on adults as conduits to make referrals, particularly where they may not understand or be dismissive, was seen as unsatisfactory. There was quite a strong sense, particularly where mental health literacy was more developed, that the children would like to make their own referrals and have agency in this space and that epistemic injustices in relation to being believed or heard took place where this was not possible. 64
Chapter 10 Programme progress and impact
Progress made by the Trailblazers in the early phase of the programme
Overall, the progress reported by Trailblazers was positive. Reports suggested a programme working in the challenging and unanticipated circumstances of the COVID-19 pandemic, yet continuing to serve children, young people and education settings. While there was variation between areas in the pace of progress and the nature and extent of challenges encountered, the general view from the stakeholders was that the Trailblazers had achieved much in a relatively short space of time:
I think it’s a massive thing what people have achieved in very short time frames…they’ve achieved an incredible amount really.
(Regional lead)
In particular, the recruitment, training and transition into practice of the first cohort of EMHPs was widely regarded as a major achievement, with all the teams operational in some form by January 2020. As noted in Chapter 5, at the outset of the programme, some sites had not fully grasped the scale and complexity of the implementation challenge:
Obviously, health and education coming together is a massive challenge and I don’t think anybody underestimated that, but I think what sites did underestimate was how big this project was and I don’t know whether everyone took on board that you are implementing a brand new service.
(Regional lead)
Many of the challenges described echo those reported by processor programmes, including key staff in schools and colleges having limited time to prepare for and support implementation, and how to achieve the optimal balance between central direction and local flexibility (see Chapter 2). Notwithstanding, there was a strong sense that sites were learning and improving over time, and that some of the initial challenges were being resolved.
Impact of COVID-19 on implementation plans and timescales
By the time of the first national lockdown in response to COVID-19, MHSTs had been operating for a matter of weeks in most sites. EMHPs were moving from their training year into practice, in many areas senior staff therapists were still being recruited, teams were starting to build relationships with education settings, and referral processes were being implemented for the first time. There was a notable drop in referrals during the initial months of the pandemic (Figure 12), which was consistent with the pattern seen across CYPMHS.
FIGURE 12.
Combined number of referrals accepted by MHSTs at 12 Trailblazer sites, January–December 2020.

Several explanations were offered for this; above all, that it was much harder for staff to spot mental health problems and less likely that that these would be disclosed by a child or young person given that the majority of pupils were not attending school in person. Also, it was unclear in the initial weeks of the pandemic if and how MHSTs could continue to provide support in lockdown conditions. All MHSTs eventually switched to delivering elements of support remotely, but it took some time to prepare for and make this switch.
The pandemic also created challenges for MHSTs in engaging and building relationships with education settings who were overwhelmed dealing with closures and other COVID-19 related pressures, and during periods of lockdown many MHSTs were unable to enter and work in school and college buildings:
Early on in COVID school engagement was a definite concern…schools were just, I think it was just the pressure, they were just overwhelmed and, even though they were very much concerned about the health and well-being of the children and young people, they had so much other things that they needed to prioritise.
(Regional lead)
We were told that the shift to remote working and pressures on education settings had particularly impacted on the work to develop whole school approaches. In the words of one local project lead, this element of the programme had ‘slipped down the priority list’ (Key informant survey respondent). Even after some restrictions had been lifted, the requirement to keep all young people in ‘bubbles’ meant whole school activities had continued to be challenging. Some stakeholders viewed the whole school approach work as being underdeveloped in comparison to other aspects of the programme.
Enablers of progress
Several key enablers of progress emerged from the findings; these are summarised below.
-
Local context and partnership working: there was a widespread view among stakeholders that, to be successful, implementation must be grounded in strong partnership working arrangements, underpinned by governance models that were transparent and inclusive. Sites that had established strong partnership working before the Trailblazers were able to move quickly to implement the programme’s timetable, leveraging existing relationships with education settings to facilitate recruitment and referrals while rapidly setting up MHSTs (Chapter 5).
-
Collaboration: interviewees emphasised the importance of ensuring that all key organisations and sectors, including NHS trusts, education settings, local authorities, and voluntary and community organisations, were able to meaningfully influence the design and delivery of MHSTs. Collaborations were reported to provide benefits by increasing coordination across services. These included providing a coordinated approach to children and young people’s mental health across local areas, supporting smooth transitions between services, helping to avoid duplication of services, and promoting sharing of learning and resources (Chapters 5 and 8).
-
Governance and leadership: clear governance arrangements were considered crucial for supporting successful collaboration at all levels of the programme (e.g. at individual Trailblazer sites; between national partners; and across sites, regions and the national team). These arrangements were most successful when underpinned by clear and effective leadership, robust project management processes, and two-way communication. Regional and national interviewees suggested that clear governance structures were not in place for some of the early Trailblazer sites due to time pressures and focus on training the first cohort of EMHPs, but that this seemed to have improved in later waves (Chapter 5).
-
Networking and sharing learning: regional leads, in particular, highlighted the value of networking across Trailblazer sites to support the sharing of learning. Local and regional networks were a means by which those in key implementation roles could seek advice to understand and address emerging challenges, or access resources developed in other areas to support their own work. Additionally, when sites had opportunities for understanding and sharing programme successes it could be a powerful motivator (Chapter 5).
-
Engagement of children, young people and carers: at the case study sites, participants highlighted the importance of engaging with young people and carers and enabling them to shape MHSTs service provision and delivery. This engagement let MHSTs test their assumptions about what was needed locally to ensure services were relevant and gather feedback to guide and inform service improvement (Chapter 5).
Key challenges
Ongoing challenges noted by Trailblazers included both intrinsic factors related to the programme design and issues related to the rapid development and expansion of the programme within the context of the COVID-19 pandemic. The key challenges mentioned were:
-
Remaining gaps in support: the remit of the MHSTs is to provide support for mild to moderate mental health conditions. Although MHSTs could refer young people with more complex needs to specialist services, significant gaps and restricted capacity meant that many young people with more complex needs could not be supported by specialist services. Furthermore, there was a perception among some stakeholders that gaps in service provision were growing, in part due to increased pressure on specialist services since the pandemic, leading to longer waiting lists and raised thresholds for accessing specialist care (Chapter 7).
-
Staff retention and turnover: the retention of staff, especially EMHPs, was widely cited as an ongoing challenge. Reasons for retention issues included the role being viewed as a stepping stone to more advanced jobs, lack of opportunities for progression within the role and MHSTs, frustration at the parameters of the role or limitations of the CBT approach, high workloads, and the emotional intensity of the work. In addition to retention issues with EMHPs, there had been challenges recruiting and retaining supervisors, partly due to a national shortage of staff with the required skills (Chapter 6).
-
Reach and inclusion: challenges with engaging some groups of children and young people were reported across sites. Several groups are reported to be underserved by MHSTs, including children and young people with special educational needs or neurodiversity, those from ethnic minority backgrounds and some religious backgrounds, and children with challenging family or social circumstances (e.g. financial hardship, domestic abuse, or living in care). Some Trailblazers sites were working to increase inclusion of these groups, for example by recruiting community outreach roles, attending local events, or creating tailored resources to encourage engagement. However, some participants were of the view that the issues of lower engagement among these groups were the result of cultural differences or stigma that were beyond the programme’s ability to address (Chapter 7).
-
Data collection, sharing and use: generating and sharing learning from the programme through effective data collection, analysis and use was an ongoing challenge. The national programme has established routine data collection from sites through the MHSDS, however they reported ongoing issues with using these data to effectively inform decision-making. Challenges included appropriately timing data collection processes to align with key decision points for the programme; ensuring that decision-makers understood the full extent of available data being collected across the national partner organisations and synthesising these data to maximise the learning from them; and various issues concerning the quality and completeness of data received from MHST sites. National and regional interviewees also described how constraints on networking activities due to the pandemic had limited opportunities to share learning with and between sites, and across the different levels of programme (Chapter 5).
-
Engagement and relationship building with education settings: engagement of education settings was a challenge before the pandemic, but COVID-19 created something of an engagement paradox: it increased the need to get MHSTs established and operational but at the same time decreased the time and resources that education settings could devote to working with MHSTs. Within case study sites, even in education settings that were enthusiastic about participating in the programme, staff often reported having limited time and headspace to engage with their MHST (Chapter 8).
-
Delayed senior mental health leads training: the delays to the senior mental health leads training was thought by some stakeholders, in particular those from the education sector, to have left school and college staff with inadequate training and capacity to work effectively with MHSTs, hampering work to build or further develop a whole school approach to mental health, impeding efforts to build relationships and slowing referrals. Given this issue, it is positive that a programme for training senior mental health leads is now in place and uptake of the training was reportedly strong (Chapter 8).
Sustainability and future development of Trailblazers and mental health support teams
Stakeholders expressed various hopes and priorities for the future development of the Trailblazers programme and MHSTs specifically. They focused on programme expansion, workforce development and career progression for EMHPs and ensuring sustainable long-term funding. One ambition expressed by the national team was for the programme to expand to reach 100% national coverage:
I think if you ask anybody involved in the programme, then our ambition and our desire and the case that we will be making is that we continue with roll-out and that we would be on a trajectory to 100% coverage.
(National interview)
Interviewees highlighted the potential for full national roll-out to address current inequities in access to MHST services, but also cautioned that this could bring new challenges as implementation reached areas and education settings that were less engaged than the early adopters and enthusiasts:
I think as roll-out continues there’s a chance that you’re getting into schools that are naturally less engaged because you’ve already recruited the ones that are most interested in doing this.
(National interview)
Opportunities and challenges for workforce development were also described. Among the national team, there was agreement on the need to provide a career development pathway for EMHPs within MHSTs, alongside opportunities to progress into other roles within the wider mental health workforce, with career progression seen as a key way of improving retention and supporting the sustainability of the workforce:
We really need to establish some mechanisms to ensure that that career progression bit is addressed and that hopefully will contribute to greater retention of EMHPs and also senior staff and for their well-being as well.
(National interview)
However, there were different viewpoints within the national team about what shape the development of the MHST workforce should take, largely to do with whether the programme should continue to evolve within its original remit of mild to moderate mental health problems or expand its scope to children and young people with more severe and complex support needs. For example, some interviewees suggested that EMHPs be trained to work with children and young people with additional complexities such as neurodiversity, special education needs or self-harming behaviours, but while staying within the remit of mild to moderate need appropriate for low-intensity interventions. Other proposed a role for MHSTs in addressing the gap in support for children falling between ‘mild to moderate’ mental health needs and thresholds for specialist services. It was suggested that this could be achieved by following the model adopted by the IAPT programme, which had trained both low-intensity and high-intensity therapists, the latter equipped to support adults and children with more complex needs:
I’ve been pushing hard for MHSTs to include high-intensity therapists…And that to me is a solution because it enables a career pathway for the EMHPs and builds on their experience of working in schools and equips them with the competencies that they would require to treat.
(National interview)
Those we interviewed in the national team also recognised the importance of communication and learning for supporting the programme. They highlighted the need for MHSTs, education settings and other stakeholders to learn from each other about how to adapt and improve the programme:
For me it’s about building in that sustainability of the system going forward…Not just the roll-out of the MHSTs in terms of numbers and coverage but quality and improvement and learning from each other, you know, enabling and supporting MHSTs to learn from each other about what works well.
(National interview)
The most frequently mentioned threat to the programme’s sustainability was funding. Several members of the national programme team highlighted the continuing uncertainty about the funding of MHSTs beyond 2024/25 which, we were told, was affecting recruitment to later waves of the programme. Interviewees were concerned that competing political interests might take priority and that funding would not be renewed, which would result in inequity of access to MHST services across the country.
Evidence of progress towards desired outcomes and impacts
While it was not a goal of this evaluation to formally assess whether the Trailblazer programme was achieving its desired outcomes, many participants were of the view was the programme was making progress towards achieving its three key objectives:
-
better mental health and well-being among children and young people
-
children and young people feel better equipped and supported
-
schools and colleges feel better equipped and supported.
Participants reported seeing a variety of positive impacts from MHSTs. For example, the majority of respondents to the second surveys (education settings survey: 76%; key informant survey: 77%) agreed having an MHST in their education setting had improved children and young people’s understanding of mental health and well-being; this view was echoed by interviewees, who noted:
The outcomes that the MHSTs are achieving, according to the data that has been analysed and gathered so far are really promising, the kind of outcomes that we would expect them to be achieving based on the kind of research evidence for the interventions that they’re delivering…We know that they’re actually making a difference to the lives of children and young people they’re supposed to be helping.
(National interview)
Most survey respondents (education settings: 75%; key informants: 82%) also agreed that school and college staff were more knowledgeable and confident about mental health and well-being issues. Just over half of respondents to the education settings survey (52%) agreed that referrals to specialist mental health services were responded to more quickly. Notably, the majority of respondents to the key informant survey agreed that children and young people were seeing improvements in the mental health and well-being goals that they set for themselves (77%). Fewer respondents to either survey agreed that the mental health and well-being of staff in education settings was improving (education settings: 49%; key informants: 47%) (Figure 13).
FIGURE 13.
Education settings views on the early impacts of MHSTs.
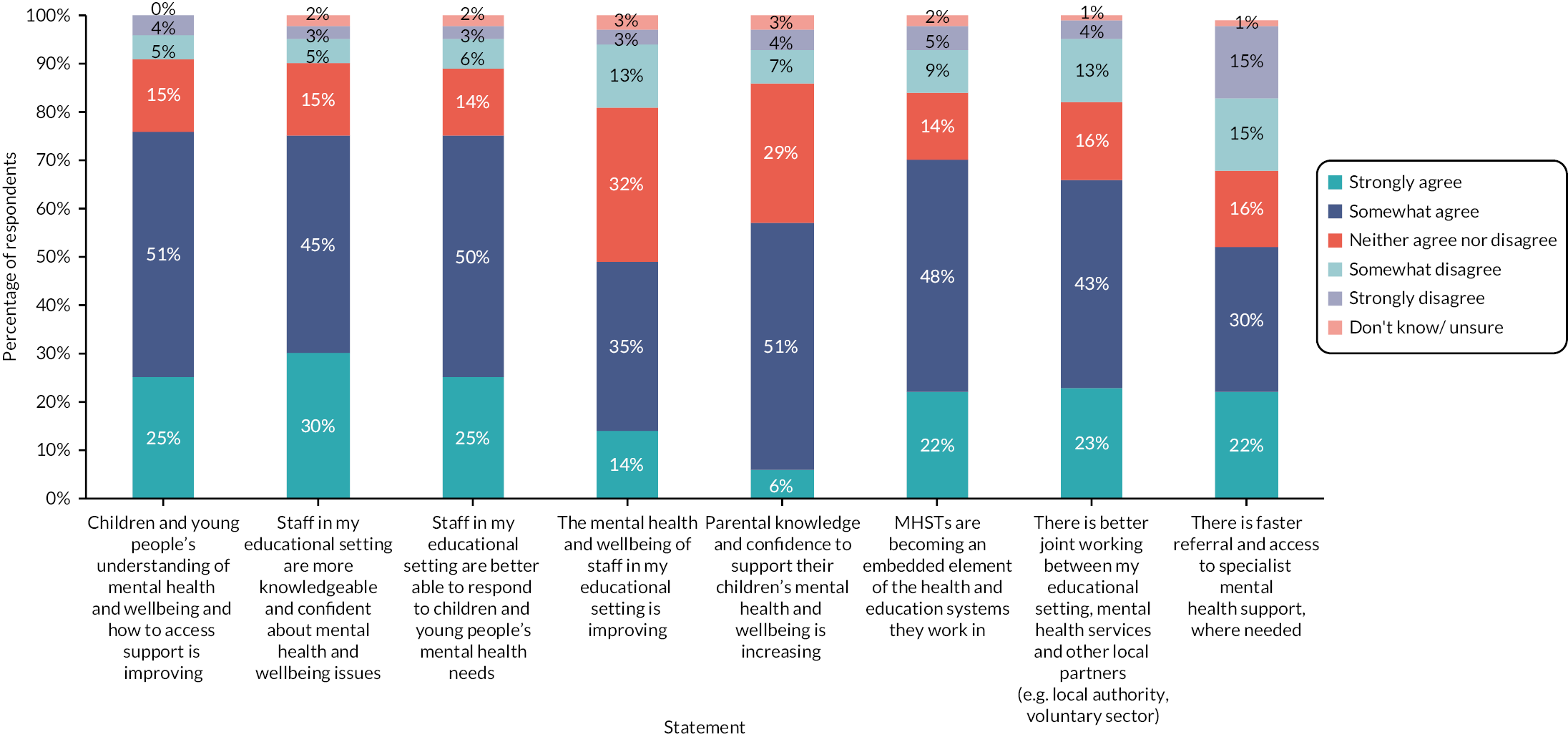
The results of the second key informant survey also suggest that the MHST programme is embedding new ways of working in education settings that contribute to a more positive mental health and well-being culture in the schools, with most respondents agreeing that education settings were adopting and improving their whole school/college approach to mental health and well-being (73%). Better partnership working and collaboration was also evident with most respondents agreeing that MHSTs were becoming an embedded element of the systems in which they worked (82%), and that there was better joint working between education settings, mental health services and other local partners (82%). Information from interviewees also suggested the programme was making progress towards its core outcomes; however, one regional lead cautioned that the progress made by Trailblazers needed to be viewed in the context of a weakened NHS mental health service:
Everything was so underfunded and under resourced that anything anybody was going to do at this point was going to be progress.
(Regional lead)
In addition to generally confirming and giving examples of the impacts described above, interviewees in case study sites reported other positive outcomes, including:
-
Greater sharing of good practice and networking between education settings in relation to mental health and well-being (sites 2 and 5).
-
More support for staff in education settings to pursue training and professional development opportunities around mental health issues (site 5).
-
Improved support for families and parents, in relation to their own mental health and well-being (site 5).
-
Reductions in inappropriate referrals to specialist mental health services (site 2).
-
Positive feedback from children and young people, and/or parents and carers and/or staff in education settings about the MHST service (sites 1, 3, 4 and 5).
-
Staff in education settings having somebody to talk to about their own mental health issues (site 3).
-
More positive and proactive mental health cultures in education settings, including reduced stigma around mental ill health (sites 1, 2 and 5).
An important area where Trailblazers had made progress was in establishing an infrastructure that would facilitate joint working across the various partners involved. Central to this was building relationships and establishing governance arrangements across diverse organisations and sectors that, in several areas, had had relatively little (if any) prior experience of working together. Interviewees were keen to emphasise that strengthening partnership working for children and young people’s mental health should be seen as an important outcome of the programme. One result of this was sites offering more joined-up mental health services for children and young people:
What it’s enabled us to do is actually make sure that the pathways within the programmes that we deliver are more joined up, so young people can access appropriate services from MHST and then flow into other programmes that we deliver…It’s not just sitting there as a statutory service, it’s got a different feel and a different culture and I don’t think that should be underestimated.
(Case study site 2, management/governance)
Unintended consequences
There is some evidence that schools and colleges may be changing their patterns of investment in mental health, potentially as a result of the Trailblazer programme. Almost three-quarters (71%) of respondents to the second education settings survey reported that their school or college had invested more of their own resources in mental health services and support since joining the Trailblazer programme. The most common examples given were additional investment in mental health and well-being training for staff, followed by releasing staff time to focus on mental health and well-being activities in the setting, and the appointment of new staff members to provide this support. However, the qualitative comments suggested that at least some of this investment was a response to the COVID-19 pandemic, rather than being an outcome of the programme. Five per cent of respondents to the second education setting survey indicated that their setting had reduced its existing mental health services because of the MHST being in place. Again, the qualitative comments provided further insights, indicating that this disinvestment was mostly a result of budget constraints linked to the COVID-19 pandemic. One example given suggested that, rather than simply disinvesting in support, some education settings might be reallocating resources to address gaps in support. The education setting in question reported that it had prioritised supporting pupils with speech and language difficulties, knowing that the MHST could cover emotional and mental health needs.
One consequence of rolling out the MHST programme in pockets across the country was an uneven distribution of MHSTs in comparison with mental health services that provide specialist care. Some national interviewees suggested that the presence of MHSTs in sites had led to increased identification of children and young people with mental health needs and a corresponding increase in demand for services. However, specialist mental health support was not being expanded in the same rapid and targeted manner as MHSTs:
And then I think it is that perfect storm of we’ve made significant gains, both in terms of roll-out of MHSTs and the small specialist services, the MHSTs are very geographically defined and actually rolling out in small areas whereas the wider specialist is a more even growth across the country, still differential, still big ranges in proportion of children and young people treated in different areas of the country but, by and large, it’s growing, it is growing in all areas. So all of that makes for quite a complex web and background against which we’re doing this roll-out.
(National interview)
Chapter 11 Scoping a longer-term impact evaluation work undertaken for work package 3
The aim of work package 3 was to inform the design and development of a phase 2 impact and economic evaluation by providing analysis and advice that could be used by DHSC, DfE and policy, research management, programme and analytical officials (the ‘stakeholder group’) to produce a practicable research specification. This work was informed by findings from the other components of the early evaluation which provided insights into the way in which the Trailblazers were being implemented in practice, the range of research questions that might be most relevant in the future, the availability of administrative and other data (e.g. on finance, activity and user outcomes) and the likely feasibility of finding appropriate comparators for Trailblazers and later waves of the Green Paper programme.
The work in this component of the early evaluation comprised the following:
-
A design and methods literature review of recent programme evaluations in England of initiatives and pilots similar to the Trailblazers undertaken in early summer 2020.
-
A series of papers containing advice and options on potential approaches to both the design and commissioning of an outcome and economic evaluation of the Green Paper programme produced between March 2020 and May 2021.
-
A draft theory of change; August 2020.
-
Commentary on DHSC and DfE preparatory work towards a specification for the outcome and economic evaluation; May 2021.
-
A series of discussions between the evaluation team, and programme and analytical staff in DHSC, DfE and NHSEI between November 2020 and July 2021.
-
A responsive full proposal for an initial outcome evaluation in April 2021.
As a result of this pattern of working, advice and recommendations for the development of a further phase of evaluation emerged and evolved throughout the period from early 2020 to late summer 2021. Detailed work by the evaluation team on the approach to the phase 2 evaluation stopped at the end of July 2021 once DHSC, DfE and NIHR had together decided that they had received sufficient information, advice and critique from the research team, and were in a position to proceed to produce a definitive specification that could be used to commission the phase 2 evaluation.
Several of the principal documents that were produced by the evaluation team and submitted for discussion to the programme team and Departmental analysts are listed in Box 10. These documents can be found in Report Supplementary Material 2.
-
Mays N. Requirements for Phase 2 evaluation, 14 March 2020 – Document A
This note began the process of identifying what needed to be included in the phase 2 evaluation, the difficulties likely to be encountered and some potential options.
-
Scherer M, Mays N. Review of recent national evaluations of similar schemes and implications for phase 2 impact and economic evaluation, 10 July 2020 – Document B
This report reviewed the approach and design of recent evaluations, assessed their feasibility and identified their advantages and disadvantages to contribute to the development of a specification for the phase 2 Green Paper programme evaluation.
-
Ettelt S, Fenton S-J. Children and Young People’s Mental Health Trailblazers – Theory of change; August 2020 – Document C
This working document analysed the mechanisms of change and goals of the Trailblazers as a basis for developing a theory of change for the Green Paper programme which could guide the specification for the phase 2 evaluation.
-
Singh K. Ideas for a Children and Young People’s Mental Health Trailblazers theory of change; 18 May 2021 – Document D
This working document related to the previous one on theory of change and brought together the main elements relevant to a theory of change for the Green Paper programme without going as far as to present a fully worked up theory. It was designed to contribute to evaluation team discussions with DfE and DHSC programme and analytical staff aimed at developing an ‘official’ theory of change to inform future evaluation planning.
-
Mays N, Ellins J. Phase 2 outcome and economic evaluation of Children and Young People’s Mental Health Trailblazer programme: outline of design and commissioning options for the stakeholder group meetings, 26 and 30 November 2020 – Document E
This report provided initial advice prepared for the two departments and NIHR based on insights gained in the early evaluation and background work assessing the feasibility of different designs and methods for the phase 2 evaluation. It was to be followed by more definitive advice in early 2021 explaining how the phase 2 evaluation might best be undertaken.
-
Saunders K. Using data from MHSDS as part of a quantitative evaluation of the children and young people’s MHSTs 25 November 2020 – Document F
A second paper for the 30 November 2020 stakeholder group meeting exploring options for accessing, linking and using routine NHS MHSDS to evaluate programme outcomes in a phase 2 evaluation.
-
Mays N, Ellins J, et al. Impact and economic evaluation of Children and Young People’s Mental Health Trailblazer programme: proposal for initial evaluation of the 2018/19 Trailblazers; 20 April 2021 – Document G (proposal appendix removed since this is Document B)
A detailed, costed research proposal prepared by the evaluation team in response to a request for a possible initial period of evaluation that could be undertaken ahead of the commissioning of the full phase 2 evaluation and which could provide findings by early 2023 to inform public spending decisions relating to the programme. Eventually, DfE and DHSC decided that this rapid initial evaluation was not essential and that they would proceed directly to commission the longer full phase 2 outcome and economic evaluation.
-
Singh K. Overview of evaluations relevant to phase 2 Trailblazer evaluation; 10 May 2021 – Document H
A further evidence review of other relevant previous evaluations to feed into DfE, DHSC and NIHR development of a specification for the outcome and economic evaluation of the Green Paper programme.
-
Ellins J, Saunders K, Mays N. Possible comparisons for phase 2 outcome and economic evaluation of CYP MH Trailblazer programme; 5 May 2021 – Document I
A note prepared for DHSC describing the different possible comparisons that could be used to assess the impact of the Green Paper programme, and the different insights that each would give.
Summary of the evaluation team’s advice on a phase 2 outcome and economic evaluation
The overriding implication of the review of recent evaluations of pilot programmes with some similarities with the Trailblazer programme (Report Supplementary Material 2, Documents B and H), plus the emerging findings from the early evaluation of the Trailblazers was that robust outcome evaluation at scale involving extensive primary data collection was likely to be difficult to undertake and might not succeed in comparing the Trailblazers with the status quo ante (Report Supplementary Material 2, Documents A, E and F). Including an economic dimension would further increase the practical challenge. The experience of the early evaluation had shown that all aspects of the research such as accessing documents, obtaining monitoring reports, collating routine activity data, requesting contact details of key contacts in local sites were complex and protracted, before adding the difficulties generated by the COVID-19 pandemic. It was also time-consuming to set up and run focus groups with children and young people themselves. The likelihood was that such problems would be even greater in the context of an outcome evaluation which would also require collecting outcome and other quantitative data directly from children and young people in education settings.
In November 2020, we therefore advised the programme team to build the evaluation in stages rather than commission a single large ambitious evaluation, given the practical difficulties posed by the pandemic and the challenges faced by previous evaluations (Report Supplementary Material 2, Documents E and F). The team made methodological recommendations on the use of data and approaches that might balance feasibility and methodological rigour. These particularly focused on approaches to identifying ‘controls’ (including by matching or deriving synthetic controls) to avoid the problem of regression to the mean to which any simpler before and after outcome assessment would be vulnerable, plus the challenges in the use of routine data, particularly related to the measurement and interpretation of educational and health outcomes during 2020 and 2021. The impact of MHSTs on individual students, their education settings or the areas where they live was also considered in this methodological work. We additionally considered the appropriateness of using monitoring data collected with the support of the Anna Freud Centre at University College London to evaluate the effectiveness of the early MHST interventions. We also explored the possible use of MHSDS and National Pupil Database data (and future data linkages, the timing and accessing of which were uncertain) in longer-term outcome assessments.
As part of the early evaluation, we also aimed to identify reliable expenditure data related to the MHSTs but with mixed success. In the interim report, we were only able to raise questions about the scale and nature of funding received by the Trailblazers and their MHSTs since we were not able to identify good data. 65 There seemed to be very large variations between Trailblazers and MHSTs in funding related to the population served but this could have been artefactual. We were able to obtain routine data on overall CCG level CYP MH expenditure for those CCGs with Trailblazers, but the budgetary information specifically on the Trailblazers was impossible to interpret.
Until July 2021, we were told that our advice on outcome and economic evaluation of the programme was required to feed into 10-year spending decisions about the continuation of the programme beyond 2022/23 that would need to be made in early 2023. Accordingly, in addition to the advice outlined above, the evaluation team provided a pragmatic proposal for interim evaluation in April 2021 in an attempt specifically to provide some relevant findings to inform such a decision early in 2023 (Report Supplementary Material 2, Document G). In the event, in July 2021, it became apparent that the programme funding would be continued to 2023/24 and thus interim evidence to inform such a decision was no longer needed. Instead, DfE and DHSC decided that a more ambitious, longer-term outcome evaluation should be commissioned competitively and the NIHR was approached to identify funding.
The evaluation team then shifted attention to providing advice on the specification for this proposed longer-term evaluation. Given that the decision had already been taken to continue funding MHSTs to 2023/24, the justification for a full counterfactual impact and economic evaluation was substantially weakened in that this decision was strong evidence that there was neither professional nor policy equipoise regarding the merits of MHSTs. With this in mind, the team shifted its attention to consider approaches to phase 2 evaluation, which would give insight into which parts of the programme and which ‘types’ of MHSTs were likely to work best, for whom and in which circumstances. Our final advice in July 2021 drew in part on a note we had already drafted in May 2021 which highlighted how different comparisons other than a pure counterfactual evaluation of the programme against ‘usual practice’ might usefully be undertaken which would give different but important insights into the performance of the programme and scope for improvements (Report Supplementary Material 2, Document I).
Implications of the early evaluation findings for a longer-term assessment of programme impact
The early evaluation findings offer valuable broader learning for the design and delivery of a longer-term assessment of the Trailblazer programme. Specifically:
-
A key challenge for the impact evaluation is the substantial heterogeneity between (and, it appears, in some cases within) sites in terms of what has been implemented and how. This points away from relying simply on an overall assessment of ‘programme impact’, and towards comparisons within the programme. This approach makes good sense if the government’s long-term goal is for the three key elements of the programme to be available across all areas in England. If this is the case, the primary aim of the evaluation should be to understand what approaches work best and at what cost (plus why, and in what circumstances), to inform future roll-out. This raises a question about which variables should be selected for comparison; sites vary in several important respects including amount of funding received; workforce composition; lead organisation; size of population covered by each MHST and amount of MHST time allocated per education setting; different ways of delivering support for whole school approaches etc. A longer-term evaluation is likely to include at least some of the waves of the programme that followed the Trailblazers, and therefore further mapping of differences in local models and approaches may be necessary before decisions about what to compare can be made. It was intended that subsequent waves of the programme would be afforded less scope for local interpretation in some key respects (e.g. team composition). However, it is not clear whether and to what extent this has occurred, and on what basis in terms of learning across the sites.
-
There is already a substantial, and growing, evidence-base about the effectiveness of the standard interventions that MHSTs are delivering (mainly, time-limited, low-intensity CBT), and so there may be limited value in the evaluation creating more micro-level clinically related evidence of this kind. It would be more valuable for any longer-term evaluation to focus on understanding which groups of children and young people, and which mental health problems, the standard MHST intervention is less suitable or beneficial for. As we have discussed in Chapters 6 and 7, MHSTs are still developing what they offer and how they work so that they can support a wider range of children and young people, including recruiting specialist roles and training staff to work with specific groups. This provides fertile ground for exploring whether these diverse locally developed approaches improve the accessibility and effectiveness of support for children and young people whose mental health problems have historically been underserved, and at what cost. Learning of this kind would be valuable not only for the programme, but for the delivery of mental health services more generally.
-
Careful consideration will need to be given to which outcomes to measure, ensuring that the evaluation includes outcomes that matter most to children, young people, parents and carers. Some of the outcomes expected at the start of the programme may no longer be realistic, especially those relating to service use. For example, the Green Paper noted a long-term goal to reduce referrals to specialist mental health services. 1 The current programme logic model includes the outcome: ‘Faster referral and access to specialist services when needed’. We do not disagree with the importance of these outcomes, but rather are doubtful that they are achievable within the lifetime of an impact evaluation given the substantial increase in prevalence and acuity of mental health problems and support needs as a result of COVID-19. This points to the need for proxy and interim measures, in order to assess whether the programme is progressing towards long-term goals and working as intended. This might include, for example, tracking changes in the quality and appropriateness of referrals made to specialist services. There is also the related issue of whether the presence of an MHST within a school or college increases identification of mental health problems and, in so doing, overall demand for support; we heard from some members of the national programme team that there is evidence this is happening. Again, this suggests that the programme’s impact on demand for and referrals to specialist services will be essential, but complicated, to unpick.
-
It is important that the evaluation addresses the programme’s twin aims of prevention and intervention. This means not just focusing on whether and how the programme is improving support for children and young people with mental health problems, but also what impact it is having across entire school and college populations. The latter will require careful work to define the programme’s ‘ecological’ impacts, and when these might be expected to occur since one would expect these whole school effects to be more diffuse and take longer to become visible. Evaluators may find it easier to measure interim outcomes (such as changes in staff members’ confidence to discuss and support children with mental health issues) than track improvements in mental health and well-being at a whole school/college level that could be attributed to programme-related activities. The early evaluation has shown that the level and type of whole school support provided by MHSTs varies considerably, and so there may be particular value in exploring whether the ‘dose’ (what and how much support is provided as a proportion of the total activities of the MHSTs) and ‘effect’ (the nature and extent of outcomes achieved) are related.
Chapter 12 Discussion and conclusions
Summary of the main findings
The main findings of the early evaluation can be summarised as follows:
-
The Trailblazers have achieved a great deal in a relatively short space of time. Setting up the programme locally was a substantial and complex task but by January 2020 (12 months after the first cohort of EMHPs started their training) all 58 MHSTs were operational in some form. While governance arrangements included representation (in almost all sites) across health, education and the voluntary sector, there was a view that local governance and leadership was not yet truly shared across these groups and that the way in which the programme had been set up was dominated by the NHS as funder and by mental health service providers and perspectives.
-
COVID-19 had had a considerable impact on the mental health of children and young people, as well as on staff in education settings, and parents and carers. Children and young people described how home schooling, during periods of lockdown, had left them feeling disconnected, demotivated and sometimes without adequate support. Transitioning back into the school environment had been difficult but, generally, focus group participants were happy to be back in school with their friends and teachers. In terms of programme implementation, the pandemic had affected MHSTs in establishing relationships with education settings, extended training times for EMHPs, slowed the development of the whole school approach and restricted activity and outcome data collection. MHSTs had to adapt what they delivered and how, including moving to online support. It is likely that MHST will continue with remote delivery for some elements of their work, although blended with face-to-face approaches.
-
Local service models and approaches differed substantially, as is to be expected given the flexibility Trailblazers were given to adapt the programme to their local context and needs. MHSTs were offering all three core functions, but many teams were spending a larger proportion of time providing direct support to children and young people with identified mental health problems. Several reasons were offered for this including being responsive to education settings’ requests for direct support; difficulties supporting whole school approaches remotely during COVID-19; and the influence of MHST lead organisations, several of which were local specialist mental health service providers and therefore more clinically oriented. The extent to which children, young people and families had been involved in shaping the design and approach of their local MHSTs was highly variable, and some areas had made more progress in creating opportunities for influence than others.
-
Despite the challenges presented by COVID-19, MHSTs had developed and were offering a wide variety of activities and resources to support education settings to develop whole school approaches to mental health and well-being. In three of the five case study areas, support for whole school approaches was being led by a specialist partner organisations or specially recruited positions within MHSTs, with EMHPs generally playing a relatively minor role. There was some frustration about the lack of attention given to capturing MHSTs’ whole school activities in the programme’s data collection and reporting system. In relation to MHSTs’ third core function, education settings welcomed the advice and help teams were giving them to access other sources of support (e.g. for children and young people with more acute problems). However, continued difficulties accessing specialist services, including what was considered unacceptably long waiting times, was a major concern for schools and colleges.
-
Engagement of schools and colleges was felt to be critical to the success of the programme, as was the senior mental health lead role. Levels of engagement were variable, and it was suggested that some education settings needed more help to prepare for the programme and make the most of the support on offer from their MHST. In light of this suggestion, there was some disappointment about the delayed roll-out of the senior mental health leads training. Many education settings reported that constraints of time and competing commitments meant that mental health leads could not always engage with their MHST as much as they would have liked and this was a barrier to implementation and success.
-
The majority of education settings reported that their MHST was responsive to their needs and all welcomed the funding of additional capacity for in-house mental health support. At the same time, however, there was a widespread view that teams were not able to meet some of the most urgent unmet needs. Several limitations in the MHST model were identified, relating to levels of experience and skill-mix within teams; the type of interventions that EMHPs had been trained to deliver and their lack of suitability for some groups and some mental health problems; and MHSTs’ service scope. Particular concerns were raised about a lack of support for children whose needs were not ‘mild to moderate’ but also not serious enough to meet local referral criteria for specialist mental health support, or who needed support while they waited (often weeks, even months) for an appointment with specialist services. Many participants reported that the gap between the formal scope of MHSTs and that of specialist services was widening due to the impact of COVID-19 on mental health prevalence and demand for support.
-
In the case study sites, MHSTs were developing ways to improve their reach and effectiveness. This included additional training for team members to tailor approaches to children and young people with, for example, neurodiversity; recruiting specialist roles to work with specific groups or communities, or lead targeted activities; and more direct support being provided by experienced therapists within teams. While some teams held a firm boundary around mild to moderate, others were already expanding their scope and supporting children with more acute and complex needs. There were different views within the national team about what the scope of MHSTs’ direct support function should be.
-
The majority of Trailblazers reported staffing challenges, with turnover of EMHPs identified as a particular concern. Challenges recruiting senior team members were also common. While there had been initial concerns about senior staff being recruited from other local mental health services, given the potential for this to create staffing shortages elsewhere in the local system, many had come to the view the movement of staff between services was positive inasmuch as it had helped build understanding and relationships. The degree of integration between MHSTs and specialist NHS services varied between areas, and some teams reported a tension between working closely with other services and establishing a clear and distinctive identity within the diverse landscape of mental health providers in their area.
-
Children and young people were not always aware that there was an MHST in their school, or what it did. Those who had had direct contact with the team (either receiving one-to-one support or through involvement in group or whole school activities) had a better understanding of MHSTs, their experiences of this contact had been universally positive, and they were able to articulate more clearly how the school cared for their emotional well-being. Several examples were given of ways in which schools and colleges were promoting and supporting well-being for all pupils, and these were valued, both because they were seen as evidence that their school looked after their well-being and because children and young people had learned techniques to help them cope with stressful situations and manage difficult experiences and feelings.
-
The programme appears to be making progress towards some of its key goals. Schools and colleges reported improvements in children and young people’s mental health and well-being and improvements in knowledge among staff, children and young people. Several local stakeholders reported that the programme was strengthening relationships and collaboration between education settings, mental health services and other local partners. Some schools and colleges reported positive early effects including staff feeling more confident talking to children and young people about mental health issues; being able to access advice about mental health issues more easily; and having quicker access to support for children and young people with some mental health problems. In terms of wider impact, many education settings reported that they had invested in more mental health support since joining the programme, although it was unclear whether this was a direct result of the programme or a response to the increasing numbers of children and young people with mental health problems as a result of COVID-19.
Discussion and implications of the findings for decision-makers
A key finding of this early evaluation is that there is substantial variation between the Trailblazers in what they are implementing and how. This is to be expected given that it was an explicit intention of the programme that Trailblazer sites test out ‘different models of delivering the teams’. 1 We have also observed some aspects of the programme where there is little variation; for example, in the vast majority of Trailblazer sites, the MHST service was being delivered by the local NHS CYPMHS provider (in a small number of cases, in collaboration with a voluntary sector partner). This may be one factor accounting for the view held by several participants that health perspectives and approaches had dominated within the programme, something we discuss in more detail below. In terms of this early evaluation, this variation provided an opportunity to explore the different ways that MHSTs had been set up and were operating, and to examine the influence of contextual and other localised factors on this. For the longer-term evaluation, however, it will substantially complicate efforts to capture programme activities and link these to observed outcomes, a challenge also reported by the TaMHS evaluation. 25
The Green Paper stated that ‘The precise rollout [of the programme] will be determined by the success of the trailblazers’. 1 This does not appear to have happened in practice; key decisions were taken about roll-out (e.g. to standardise the workforce composition of, and funding allocation for, subsequent waves of MHSTs) long before learning from the Trailblazers was available. Certainly, the Trailblazers have generated lessons and insights for implementation, although there may be limits on the generalisability of their experiences given that these initial sites were chosen for particular characteristics thought likely to drive rapid progress, and not for their ‘representativeness’ (see ‘The Children and Young People’s Mental Health Implementation Trailblazer programme’ in Chapter 1 for details about Trailblazer site selection criteria). As we have noted previously,65 it is not clear what functions the Trailblazers were fulfilling. In this sense, the programme can be seen as another example of the ambiguous nature of ‘piloting’ that has been observed in relation to other national policy programmes. 66
There is a clear and strong rationale for the Trailblazer programme’s investment in mental health prevention and support within education settings. Children spend more time in schools and colleges than any other setting outside their home and, as noted by the former Children’s Commissioner, ‘Consistently, children have been particularly positive when they can access the treatment in and around their school’. 8 Schools and colleges universally welcomed investment in ‘in-house’ support, which came at time when many settings were witnessing substantial increases in mental health problems, among not only pupils, but also parents/carers and staff. Moreover, despite the challenging and changing circumstances in which the programme was being implemented, solid progress had been made in setting up the Trailblazers and establishing the 58 MHSTs in these areas. That key elements of the programme design – notably those relating to workforce – were modelled on the IAPT programme may, at least in part, account for the relative speed at which the national team was able to get underway following publication of the Green Paper. However, important lessons from the IAPT experience do not appear to have been heeded, and so opportunities to anticipate key implementation challenges and address these at the programme design stage were missed.
Chief among these was the issue of retaining EMHPs once recruited, something that had been widely reported for the equivalent IAPT roles (the children’s well-being practitioner and psychological well-being practitioner), and earlier still for another paraprofessional role in the mental health workforce: primary care mental health workers. 67,68 In the current study, reduced team capacity due to vacant EMHP posts was one of the biggest challenges described by Trailblazers. The need for strategies to encourage retention, including opportunities for EMHPs to develop and progress within their role, was widely highlighted (something, we are aware, the programme’s national partners are now seeking to address). There is evidence from some of the case study sites of a lack of integration between processes for collecting and reporting routine outcome measures and the planning and provision of support to children and young people. Again, this echoes issues previously raised about the children’s IAPT programme, and children’s mental health services more generally. 69,70
While this evaluation was not designed to assess the impact of the Trailblazer programme, we did ask participants to share their views about the nature and extent of progress being made. Our findings show that some of the desired early outcomes, as defined in the programme theory of change, are appearing; for example, many schools and colleges responding to our education settings surveys reported that, as a result of their MHST, staff were feeling more confident and knowledgeable about mental health and well-being issues, and better able to respond to children who have mental health problems. It is also clear that schools and colleges themselves are critical to the success of the programme. Education settings are not simply a base from which MHSTs deliver a service, they are partners in bringing about cultures, practices and environments that support children’s mental well-being. It is for this reason that the senior mental health lead role, and the staff time and other resources that schools and colleges can draw on to help MHSTs establish themselves and work effectively are crucial. The multiple pressures and competing priorities that schools and colleges currently face, therefore, could potentially limit the extent of the programme’s impact.
The launch in June 2021 of the grant scheme for senior mental health leads training was a positive development, but more attention needs to be given not only to the issue of engaging education settings (which is a key theme within national programme implementation) but also preparing and enabling them. Investment in the ‘education side’ of the programme is dwarfed by NHS funding for MHSTs, but without a supportive and receptive environment, MHSTs’ achievements will be unnecessarily limited. A further challenge is that that there is still limited evidence about what works in developing and embedding a whole school approach to mental health, with understanding about the core components of the approach and inter-dependencies between these (and therefore how implementation can be most effectively approached and sequenced) particularly lacking. As Brown and colleagues’ comment:
Despite widespread global support for whole school approaches, schools frequently report lack of clarity over how to deliver them (Quinlan & Hone, 2020), with significant variation in terminology and an absence of evidence-based guidance on implementation (Hunt et al., 2015)… [Q]uestions remain on what structures and processes are needed to embed effective practices into school routines in a sustainable way. 71
The Trailblazer programme has the potential to make an important contribution to filling this gap, by capturing learning from all sites about how to implement whole school approaches, what is required of education settings, ways of building effective relationships (both within the school or college environment and with external services), and what support education settings need and how this can be best provided. Consideration should be given as to how this learning can be shared with the organisations providing training courses for senior mental health leads, so that training content and resources can be updated as new insights emerge.
There was a strong view from those who participated in our research that, for the programme to have maximum impact, it must enhance mental health provision for children and young people where this is needed most. Addressing longstanding inequalities in access to mental health support is becoming even more important, given what is becoming clear about the differential impact of COVID-19 on the mental health of different subgroups of children and young people. The pandemic has disproportionately affected children and families from disadvantaged and vulnerable groups, who were already at higher risk of developing mental health problems and less likely to be able to access appropriate support. 72,73 As roll-out of the programme continues, a strong focus on addressing such inequalities is imperative. A common theme in our findings was that low-intensity CBT-informed interventions were not always appropriate and effective, and EMHPs often lacked the knowledge and/or skills to adapt these for different groups and needs. This had resulted in gaps in support, including for children with special educational needs and neurodiversity, children who were self-harming, children from ethnic minority groups, and children whose mental health problems are linked to their family or social circumstances (e.g. financial hardship, domestic or other forms of abuse, or living in care). There is much more still to be understood about the fit between what MHSTs are offering and what support children and young people want and need when they are experiencing problems with their mental health, building on the insights from this early evaluation. The views and experiences of children and young people, both those who have been supported by an MHST, and those with mild to moderate mental health problems who have not accessed this support, will be critical for developing this understanding.
The poor suitability of standard CBT-informed approaches for working with diverse populations was already well known before the development of the Trailblazer programme, raising a question about whether equity was adequately taken into account in the design of the programme. 74,75 Relatedly, it is unclear whether MHSTs are expected to provide direct support to children with all types of mild to moderate mental health problems, or should be prioritising and focusing on children who have the particular mental health problems for which CBT-informed approaches are most effective. Similar issues have been raised in relation to IAPT services about which, it has been suggested, the limited focus on depression and anxiety, is ‘at the expense of missing the clinical heterogeneity and precise therapeutic need of those referred’. 76
What came through strongly in our case study research was that MHSTs were aware of and acknowledged their limitations and were thinking about how they could improve their reach and effectiveness. We heard, for example, that several areas had developed training for MHST staff on how to communicate with and support children with neurodiversity. While locally designed training can be beneficial inasmuch as it is grounded in the local context, there is evidently some duplication of effort and investment. This leads us to ask whose role it is to address MHSTs’ ongoing training and development needs: local areas, regional teams or the programme’s national partners? While the national partners may not wish to provide additional training directly, they could create training and development resources for areas to adapt for local delivery. Alternatively, there could be more sharing of resources and approaches between sites, facilitated by regional teams.
Equipping teams to work inclusively with diverse groups and communities is an activity to which children and young people, parents and carers, could valuably contribute. This would go some way to addressing the programme’s involvement deficit, by expanding what have hitherto been very limited opportunities for these groups to influence key decisions about what is provided and how. Another area where involvement is warranted is in decisions about the extent and targeting of remote support in post COVID-19 service delivery models. There is much still to be learned about digitally delivered support, above all which children and young people these interventions are most suitable for and the conditions under which they work best. The limitations of digital support are widely acknowledged, linked to a range of factors including inequalities in technology and internet access. 77,78 There is also the question of whether children and young people want to be supported in this way. Research undertaken before the pandemic found that children would prefer a combination of face-to-face and digital support. 79 This suggests that the blended model which Trailblazers expect to be adopting post COVID-19 may well be the right one. The possibility that digital approaches will be encouraged (or even pushed) for financial reasons was identified by a small number of respondents, mirroring concerns raised more widely. 80 Given this potential risk, it is critical that children and young people, parents and carers are directly involved in decisions about the ways that MHSTs will provide support in the future. Evidence from the IAPT programme that higher levels of remote contact (in the form of telephone support) increased stress and burnout among low-intensity therapists points to important workforce considerations that should also be borne in mind in such decisions. 53
A related issue concerns MHSTs’ scope and, in particular, whether in their direct support function teams hold a firm boundary around ‘mild to moderate’ mental health needs or not. The Impact Assessment for the Green Paper described three levels of mental health need: pre-diagnosable, mild to moderate needs and diagnosable conditions that meet thresholds for NHS specialist mental health support. 81 The problem with this simple categorisation is that it fails to capture the reality of children’s mental health problems, which are far more likely to present as ‘messy scenarios’ than as ‘obvious mental health problems’. 82 It also does not acknowledge a fourth group of children and young people: whose needs are beyond the ‘mild to moderate’ level that MHSTs have been set up to support, but which are not severe enough to meet the eligibility criteria for specialist help. Participants in our study reported that this group – described by McGorry as the ‘missing middle’ – is growing in number, consistent with the findings of other recent analysis. 83,84 Some articulated concern and frustration about the ongoing difficulties children and their parents in this situation faced trying to access support, and the pressures this could place on school and college staff (including mental health and pastoral leads) to help those children manage their distress and stay in education. This may be where MHSTs’ signposting and onward referral function comes into play, but for teams to fulfil this bridging role, there must be services available to which they can signpost or refer children, and our findings suggest that this is not necessarily the case.
While some of the MHSTs in our case study areas were trying to hold a firm boundary around their scope, others gave examples of supporting children and young people with more complex or acute needs (with decisions about providing support often made on a case-by-case basis, rather than through a formal amendment of referral criteria). This included providing interim support for children and young people with serious mental health problems who were waiting to be seen by specialist services. Similar issues about working beyond scope and with people whose mental health problems are more complex than those covered in training, have been reported for other ‘low-intensity’ workers in the mental health workforce. 34,41,42 What became clear through our later interviews was that there was a lack of clarity and agreement within the national team about whether the programme should be funding direct support for children only with mild to moderate needs, or whether the expansion of support to other groups was permissible or even desirable. This points to a fundamental question for the programme: to whom should MHSTs be providing direct support? This question needs to be answered nationally because of the ramifications it has for (among other things) workforce recruitment and training, likely demand and prioritisation of needs for support, and level of funding required. On the specific issue of training, the British Psychological Society has proposed that:
It is important there is a clear pathway for children and young people who present with more complex or severe mental health and well-being needs. EMHPs should refer young people with more severe needs to specialist provision, but they also need to be appropriately trained to identify and manage more complex needs within the school environment on a day-to-day basis. 21
Without additional capacity or funding, it is possible that any expansion of scope in relation to direct support may be at the expense of MHSTs’ two other core functions. We have already noted that many MHSTs are spending proportionally more of their time delivering interventions. COVID-19 has undoubtedly acted as a barrier to MHSTs’ working with, and physically in, education settings to develop whole school approaches, but this is unlikely to be the only reason for some MHSTs’ apparent tilt towards supporting young people with identified mental health needs. The way that the programme was designed and set up (both nationally and locally) was felt by some to have given primacy to NHS/health interests and perspectives. The lack of focus in the programme’s data collection and reporting processes on capturing whole school activities and their impacts was given as one example of this perceived orientation towards clinical approaches (although it should also be acknowledged that whole school activities may be intrinsically more difficult to describe and measure in management information systems).
This is another example of the tendency which has been observed for NHS organisations to play the dominant role in partnership working arrangements, particularly where the funding for such arrangements comes largely or solely from NHS budgets. 85,86 It also points to a tension at the heart of the programme between the goals of prevention and intervention, and the need for partners at all levels to work to keep these in balance. This tension is not unique to the programme; the strong orientation of the mental health system towards treating those with acute need, and the relative lack of investment and focus on ‘upstream’ mental health prevention, has been widely observed. 7,87,88 The children and young people who participated in our study told us how important it was to them that their school actively promoted and cared for their well-being, especially given the impacts of COVID-19 and the difficulty (for some) of coming back into school after long periods at home during lockdown. The insights from these focus groups are clear evidence of the value of a whole school approach, as is recent evidence about the impact of the pandemic on the well-being of parents and education professionals. 89,90 Moreover, there is evidence that universal and targeted approaches (i.e. prevention and intervention) are complementary and mutually beneficial, and so the most effective model for supporting young people’s mental health in education settings in one that incorporates both these elements. 91 Notwithstanding the point above about the current lack of evidence about how best to implement a whole school approach there are, therefore, potentially far-reaching and long-lasting benefits to education settings developing positive cultures and practices that promote emotional well-being and literacy, build resilience and foster a sense of connectedness. 92,93
It is noteworthy that, in three of our five case study sites, support for education settings to introduce or develop a whole school approach was being provided either by a specialist local partner or role within the MHST. Our findings suggest that this is reflective of MHSTs’ growing understanding of what works in engaging and working with education settings. Equally, it also risks uncoupling MHSTs’ prevention and intervention functions, which may make it harder still to keep these in balance. This is an issue that could usefully be explored in a longer-term evaluation, as is the question of whether EMHPs feel their training has equipped them with the confidence and skills to work with education settings on whole school approaches (something that was not explicitly addressed in this study).
Strengths and limitations of the study
This was an early evaluation of the Trailblazer programme, to be followed by a longer-term study to assess the programme’s outcomes and impacts. It employed a variety of data collection methods, integrated with programme and publicly available data, to try to offer a rounded assessment of implementation and early progress in the programme’s Trailblazer sites. The study combined an overview of views and experiences across the 25 Trailblazer areas with more detailed insights from case study sites, allowing for both breadth and depth of analysis. A two-staged process of data collection allowed for an initial phase of more exploratory fieldwork, from which themes and issues were identified for more in-depth investigation in the fieldwork that followed. The team worked flexibly and responsively, both to changing circumstances as the COVID-19 pandemic unfolded, and to other challenges that arose (e.g. using researcher time to undertake interviews with the programme’s national and regional leads, when it became clear that a sixth case study site could not be secured in the time available). Strong stakeholder engagement, including involvement of young people with lived experience of mental health issues, helped the research team to keep the programme’s multiple facets, levels and interest groups in mind as the study was designed, research tools were developed, and throughout the analysis process.
Efforts were made to secure participation from all of the Trailblazers and to ensure a variety of roles, perspectives and organisational locations were accessed in the case study research. This was challenging, especially given the tremendous pressure that many people were facing in their work and personal lives as a result of the pandemic, and it is positive that at least one response was received from all 25 sites to all four surveys. Despite our efforts, some groups were less well represented in the study than others, and it is very likely that the study has not captured the full range of perspectives on and experiences of the programme. For example, we conducted fewer interviews with school and college staff and individuals working in specialist children’s mental health services and local authorities in case study sites than we had hoped for. Our study design did not include research with families, but we did create an opportunity for parents and carers consenting for their child to take part in a focus group to share their views on mental health promotion and support within their child’s school. However, we gathered very little information through this.
We sought to compile information about local models and approaches across all 25 Trailblazer sites from documentation provided by the national programme team (which included sites’ original expressions of interest and project plans) and through our key informant survey. However, we were not able to gather sufficiently detailed and up-to-date information for/from each site with which to reliably compare or develop a typology of Trailblazers. Thus, the question still remains about whether there are distinctive types of local models and approaches, the factors that might account for differences between areas and whether any are associated with better or worse outcomes for children and young people, parents or staff. We had also intended to report service activity data, including information about the demographic characteristics of children and young people being supported by MHSTs. But both the data itself and its interpretation were not straightforward. There were substantial gaps in the data provided by the national team (in large part because reporting had been suspended in some Trailblazer sites at different periods of time during the pandemic) and we did not have sufficient information to establish clear denominators (e.g. to assess whether the proportion of children from ethnic minority backgrounds being seen by MHSTs was comparable to the overall population in participating schools and colleges).
When the study was designed, a decision was taken not to include research with children and young people who had received direct support from MHSTs. This was driven by concerns about the feasibility of securing appropriate permissions and undertaking such research in what was then expected to be a rapid study timescale. However, we did undertake focus groups with children and young people in schools and colleges where MHSTs were working, and the findings from these groups offer valuable insights for the programme and on which further research could build. Relatedly the many delays encountered, which significantly extended the study timescale, impacted in a number of ways. In particular, the first round of surveys went live several months later than was originally planned and some months after MHSTs had become operational. Given this, we were not able to capture a baseline position for the programme as had been intended.
Equality, diversity and inclusion
This study has addressed equality, diversity and inclusion in several key respects:
Study scoping, focus and delivery
-
Underpinning study design and delivery has been a strong commitment to stakeholder involvement, including involvement of the University of Birmingham IMHYAG from the inception of the study through to reporting. As well as their overall advisory role, the IMHYAG (young people with lived experience of mental health issues) co-produced the focus group research, including co-designing the recruitment and consent processes, and the format and content of the group discussions, as well as co-facilitating some of the groups. The primary aim of the innovative digital recruitment and consent process co-designed with IMHYAG was to address long-reported shortcomings in conventional approaches to securing young people’s participation in research, including barriers that particularly affect seldom heard groups. 94 See Chapters 4 and 9 for more details.
-
Detailed work was undertaken to develop descriptive and statistical profiles for the Trailblazer areas. This was both to characterise the Trailblazers in relation to national averages and to support the development of criteria for case study site selection to ensure diversity in relation to key dimensions such as geography (a range of geographical areas, including areas with more and less rurality); population (ethnicity and levels of deprivation); and mental health prevalence and service performance. See Chapter 3 for more details.
-
Trailblazer sites were asked to identify a wide range of key people involved in the programme in their area to participate in the study, and were encouraged to include MHSTs, schools and colleges, mental health service providers, commissioners, local authority services, voluntary sector organisations and public health. A range of strategies were employed to maximise participation: including offering a range of options for interviews (group, individual, telephone, video); giving project leads the option to self-complete a survey or do this over the telephone with a member of the evaluation team; use of reminders; asking local project leads and regional teams to encourage participation; and extending fieldwork deadlines. In the case study research, groups that were under-represented in the initial interviews were subsequently targeted and prioritised to try and ensure a balance of different interests and perspectives. See Chapter 4 for more details.
-
All the research tools included questions relating to equality, diversity and inclusion (see Report Supplementary Material 1). In particular, we were keen to understand the extent to which and how considerations relating to improving accessibility and support for underserved groups had informed programme design and delivery, both nationally and locally. In both surveys and interviews, we explored which groups of children and young people, and which mental health conditions, MHSTs were not as effective at reaching or supporting, to identify continuing gaps in services; in Chapter 11 we also propose that this be a key focus of the impact evaluation to follow. This was felt to be particularly important in the second phase of data collection, given emerging evidence about how COVID-19 had disproportionately affected children and young people whose mental health was already at greater risk before the pandemic. See Report Supplementary Material 1 and Chapter 11 for more details.
-
We sought information from the national programme team to explore further the profile of children and young people receiving support from MHSTs, including characteristics such age, gender and ethnicity. Service activity data were provided, but as we noted above, issues in the completeness and quality of these data limited the insights that could be reliably drawn from them. We also requested information about the demographic profile of EMHP trainees, in view of evidence about the importance of workforce diversity for delivering culturally appropriate mental health support; unfortunately, this was not provided. 95 See Chapter 6 for more details.
Research team
-
The research team consisted of researchers from four organisations (University of Birmingham, RAND Europe, London School of Hygiene and Tropical Medicine, and University of Cambridge) incorporating interests and expertise that spanned policy evaluation, applied health research, mental health policy, qualitative research, participatory research, statistics and health economics. The team comprised a mix of backgrounds in relation to gender, age and research experience and, to a lesser degree, ethnicity.
-
From the outset the senior leads sought to foster inclusive ways of working, with team members invited to contribute to all elements of the study from design, through data collection and analysis, to reporting and dissemination. Fortnightly team meetings and bimonthly half day meetings were held throughout the study to support teamworking, to ensure that team members were well supported and to collectively plan and problem solve. All researchers were supported by the principal investigator and senior team members.
Conclusions
The findings presented in this report show that substantial progress has been made in implementing the Trailblazer programme, in very challenging circumstances and that there is a great deal of optimism about what the programme has the potential to achieve. At the same time, there are also a number of issues and challenges that will need to be considered and addressed as the roll-out of the programme continues. There have been substantial and unprecedented changes in the wider context since the programme started. COVID-19 has further increased inequalities in mental health and access to support, and gaps between services appear to be widening. Critical decisions will need to be taken about what, if any, role MHSTs should have in providing support to children and young people beyond the remit that the programme was designed to address. There is also the question of how the programme can continue to retain a dual focus on mental health promotion (e.g. through the development of whole school approaches) and early intervention, and what additional support or resources might help educational partners and settings maximise the opportunities offered by the programme. Alongside strategies for workforce creation and training, more work is needed to ensure that trained staff are retained and can develop in their roles. Given the importance and scale of the Trailblazer programme, it is positive that a longer-term impact evaluation is planned. The findings presented in this report, we hope, provide a solid foundation on which this next evaluation can build.
Acknowledgements
The evaluation team would sincerely like to thank everybody who participated in the study, including our contacts at the Trailblazer sites who provided documentation, contact details and encouraged colleagues and partners to take part. During much of the study, people at all levels of the programme and in the Trailblazer areas were responding to the many demands and challenges posed by COVID-19; we are extremely grateful that, despite this, they still found the time to support and contribute to our research. We would also like to thank: our specialist advisers Colette Soan and Karen Newbigging for their ongoing encouragement, advice and support, including reviewing key research tools and draft reports; the University of Birmingham IMHYAG, including Niyah Campbell and Charlotte Saunders, for their input into the evaluation design and development of key research questions, and the ongoing involvement of IMHYAG members in co-designing and delivering the focus group research; the Think4Brum group and Bob Maxfield for their early input into the evaluation design; Simon Stones and Sheena Cumiskey for reviewing the study protocol from a patient and public involvement and mental health service provider perspective; Akiko Hart and Mary Sadid (National Survivor User Network) and Judith Smith (BRACE Director, University of Birmingham) for reviewing our interim report; Stefanie Ettelt, Alec Fraser, Manuela Scherer, Richard Grieve and Natasha Elmore for their early and important contributions to the study while at the PIRU (SE, AF, MS and RG) and RAND Europe (NE), respectively; Christian Bohm (HSMC Knowledge and Evidence Service) for undertaking literature and evidence searches for the study; the Inclusion Support Team in Sandwell for arranging for the team to visit schools in the area to better understand mental health and well-being from a school perspective; Harvills Hawthorne School, George Salter Academy and the Westminster School for hosting visits from members of the evaluation team; the BRACE Steering Group, patient and public advisers, and executive team for their support and constructive comments throughout the duration of the study; Nova Bovaird, Helen Duncan-Jordan and Sarah Stockham (from the Dorset MHST) for reviewing the draft key informant survey questionnaires; Helen Tyson, Caris O’Toole, Stephanie Holden, Portia Kumalo, Marguerite Macfarlene, Katinka Bryan, Nell Gair and Aimée Webster for reviewing the education settings survey questionnaires; the Trailblazers national programme team and DHSC and DfE analysts for their guidance and support and providing access to programme data and documentation; Jess Plumridge (RAND Europe) for her work designing the interim report and for two excellent infographics to support its dissemination; and Ann Evans and Cathy Dakin (BRACE Centre senior research administrators) for providing varied and much valued support throughout the study. The study was approved by the research ethics committees at the University of Birmingham (January 2020; ERN_19-1400 – RG_19-190) and London School of Hygiene and Tropical Medicine (February 2020; Ref: 18040) and by the Health Research Authority (January 2020; IRAS 270760).
Contributions of authors
Dr Jo Ellins (https://orcid.org/0000-0001-8138-9385) (Senior Fellow, University of Birmingham) was the principal investigator for the study. She co-led the conception, design and delivery of the evaluation, and oversaw all elements of data collection, analysis and write-up of the research. She also contributed to data collection, undertaking scoping interviews with members the national programme team, interviews in the first and second phases of fieldwork with regional leads, and co-led the interviews in one case study site. She led the writing of Chapters 1 and 12, co-led Chapters 2 and 3, contributed to Chapter 11 and took responsibility for overall editing of the final report, and is the guarantor and corresponding author.
Lucy Hocking (https://orcid.org/0000-0002-8319-962X) (Senior Analyst, RAND Europe) led the design, administration and analysis of the key informant surveys, and undertook and analysed all the interviews at one case study site, as well as carrying out data analysis for a second site. She contributed to the development of Trailblazer profiles and compilation of funding information. She also contributed to the final report, leading the writing of Chapter 7, co-leading Chapter 3 and supporting Chapter 4.
Dr Mustafa Al-Haboubi (https://orcid.org/0000-0001-9847-2206) (Assistant Professor, London School of Hygiene and Tropical Medicine) led the design, administration and analysis of the education settings surveys, undertook all interviews at one case study site and analysed survey data provided by the DfE. He contributed to the final report, leading the writing of Chapter 8 and supporting Chapter 4.
Dr Jenny Newbould (https://orcid.org/0000-0002-2602-6984) (Research Leader, RAND Europe) was the study’s qualitative research lead, contributing to the development of research tools and leading the analysis process for the national, regional and local Trailblazer interviews. She also undertook and analysed all the interviews at one case study site and contributed to the interviews with regional leads in the first phase of fieldwork. She also contributed to the report, leading the writing of Chapter 6 and supporting Chapters 4 and 5. Until January 2020, she acted as the study project manager.
Dr Sarah-Jane Fenton (https://orcid.org/0000-0001-9751-6262) (Lecturer in Mental Health Policy, University of Birmingham) led on the design, delivery and analysis of the focus groups with children and young people, working in partnership with members of the University of Birmingham IMHYAG. She undertook and analysed all the interviews at one case study site and contributed to the preliminary development of a programme theory of change. She also contributed to the report, leading the writing of Chapter 9 and supporting Chapter 4.
Kelly Daniel (nee Singh) (https://orcid.org/0000-0002-4513-1026) (Evaluation Fellow, University of Birmingham) was, between January 2020 and October 2021, the study project manager and contributed to the design of all aspects of the survey and qualitative research, including leading the development of the qualitative research tools. She also led the University of Birmingham ethical and Health Research Authority approval processes, and co-led interviews in one case study area. She also contributed to the preliminary development of a programme theory of change, development of Trailblazer profiles and literature review and supported the initial development of the focus groups.
Dr Stephanie Stockwell (https://orcid.org/0000-0001-7828-3758) (Analyst, RAND Europe) co-led the second round of regional lead interviews and led the analysis of the interview data. She also contributed to the literature review and the report, leading the writing of Chapter 5.
Dr Brandi Leach (https://orcid.org/0000-0003-3262-1541) (Senior Analyst, RAND Europe) led the interviews with the national programme team and their analysis, as well as analysing the interview data from one case study Trailblazer site. She also contributed to the report, leading the writing of Chapter 10.
Dr Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Research Fellow, University of Birmingham) contributed to the literature review, and supported the interviews with the national programme team. He also contributed to the report, co-leading the writing of Chapter 2.
Dr Jenny Bousfield (https://orcid.org/0000-0002-5671-2336) (Analyst, RAND Europe) led on the development of the Trailblazer statistical profiles and analysis of the qualitative data from the first education settings survey.
Dr Gemma McKenna (https://orcid.org/0000-0001-8261-0598) (Fellow, University of Birmingham) supported the initial development of the recruitment and consent process for the focus groups and undertook interviews with local project leads in the first phase of fieldwork.
Dr Katie Saunders (https://orcid.org/0000-0002-3127-3218) (Senior Research Associate, University of Cambridge) supported delivery of work package 3, co-led the development of a protocol for an early impact evaluation of the Trailblazers programme and contributed to other key outputs and discussions with the national programme team about the specification for a longer-term impact evaluation. She also contributed to the writing of Chapter 11.
Dr Stephen O’Neill (https://orcid.org/0000-0002-0022-0500) (Associate Professor of Health Economics and Econometrics, London School of Hygiene and Tropical Medicine) supported delivery of work package 3, contributing to the key outputs and discussions with the national programme team about the specification for a longer-term impact evaluation.
Professor Nicholas Mays (https://orcid.org/0000-0001-9808-8466) (Professor of Health Policy, London School of Hygiene and Tropical Medicine) co-led the conception, design and delivery of the evaluation and led work package 3. He jointly undertook scoping interviews with members of the national programme team and has provided advice and support across all elements of the study. He also contributed to the final report, leading the writing of Chapter 11 and reviewing the full draft report before submission.
Data sharing statement
Owing to the consent process for data collection, the qualitative and survey data gathered for this study cannot be shared. Sources of data that are already publicly available are provided either in the text or references. Data supplied by the DfE and NHS England, under specific data sharing agreements, cannot be made available by the study team. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Transforming Children and Young People’s Mental Health Provision: a Green Paper. London: HM Government; 2017.
- Vizard T, Sadler K, Ford T, Newlove-Delgado T, McManus S, Marcheselli F, et al. Mental Health of Children and Young People in England. London: NHS Digital; 2020.
- Kessler RC, Angermeyer M, Anthony JC, De Graaf R, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007;6:168-76.
- Review of Children and Young People’s Mental Health Services. Phase 1 Report. London: Care Quality Commission; 2017.
- Crenna-Jennings W. Young People’s Mental and Emotional Health. Trajectories and Drivers in Childhood and Adolescence. London: Education Policy Institute; 2021.
- A New Era for Young People’s Mental Health. London: Young Minds; 2018.
- Children and Young People’s Mental Health. Eighth Report of the Session. London: House of Commons; 2021.
- The State of Children’s Mental Health Services 2020/21. London: Children’s Commissioner for England; 2021.
- Parkin E, Long R, Bate A. Support for Children and Young People’s Mental Health. London: House of Commons Library; 2020.
- Future in Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing. London: Department of Health; 2015.
- Promoting Children and Young People’s Emotional Health and Wellbeing A Whole School and College Approach. London: Public Health England; 2015.
- The NHS Long Term Plan. London: NHS England; 2019.
- Bunn S. Mental Health and Wellbeing in the Context of COVID-19 2021. https://post.parliament.uk/mental-health-and-well-being-in-the-context-of-covid-19 (accessed May 2022).
- Bunn S, Lewis S. Children’s Mental Health and the COVID-19 Pandemic. London: Parliamentary Office of Science and Technology; 2021.
- COVID-19: Mental Health and Wellbeing Surveillance Report. London: Office for Health Improvement and Disparities; 2021.
- Ford T, John A, Gunnell D. Mental health of children and young people during pandemic. BMJ 2021;372.
- Skripkauskaite S, Shum A, Pearcey S, McCall A, Walte P, Creswell C. Changes in Children’s Mental Health Symptoms from March 2020 to June 2021 (Report 11). Oxford: University of Oxford Co-SPACE study; 2021.
- Morris J, Fisher E. Growing Problems. What Has Been the Impact of COVID-19 on Health Care for Children and Young People in England? 2022. https://www.nuffieldtrust.org.uk/public/files/2022-01/growing-problems/#1 (accessed May 2022).
- Item 5: Programme vision and success indicators. n.d.
- Mental Health Support Teams for Children and Young People in Education. A Manual. London: NHS England; 2019.
- Mental Health Support Teams: How to Maximise the Impact of the New Workforce for Children and Young People. Leicester: British Psychological Society; 2019.
- Government Response to the Consultation on Transforming Children and Young People’s Mental Health Provision: A Green Paper and Next Steps. London: Department of Health and Social Care and the Department of Education; 2018.
- Children and Young People’s Mental Health Services Workforce Report for Health Education England: National Report. London: NHS England; 2021.
- Ludlow C, Hurn R, Lansdell S. A current review of the Children and Young People’s Improving Access to Psychological Therapies (CYP IAPT) program: perspectives on developing an accessible workforce. Adolesc Health Med Ther 2020;11:21-8.
- Me and My School: Findings from the National Evaluation of Targeted Mental Health in Schools 2008-2011. London: Department for Education; 2011.
- Parry G, Barkham M, Brazier J, Dent-Brown K. An Evaluation of a New Service Model: Improving Access to Psychological Therapies Demonstration Sites 2006-2009. Southampton: NIHR Service Delivery and Organisation Programme; 2011.
- Edbrooke-Childs J, Calderon A, Wolpert M, Fonagy P. Children and Young People’s Improving Access to Psychological Therapies . Rapid Internal Audit: National Report 2015. https://www.ucl.ac.uk/evidence-based-practice-unit/sites/evidence-based-practice-unit/files/pub_and_resources_project_reports_rapid_internal_audit_2015.pdf (accessed May 2022).
- Day L, Blades R, Spence C, Ronicle J. Mental Health Services and Schools Link Pilots: Evaluation Report. London: Department for Education; 2017.
- Campbell-Jack D, Day L, Burnley N. Evaluation of the Mental Health Services and Schools Link Expanded Programme. London: Department for Education; 2020.
- Cane F, Oland L. Evaluating the outcomes and implementation of a TaMHS (Targeting Mental Health in Schools) project in four West Midlands (UK) schools using activity theory. Educ Psychol Pract 2015;32:1-20.
- Burn A-M, Vainre M, Humphrey A, Howarth E. Evaluating the CYP-IAPT transformation of child and adolescent mental health services in Cambridgeshire, UK: a qualitative implementation study. Implement Sci Commun 2020;1.
- Targeted Mental Health in Schools Project. Using the Evidence to Inform Your Approach: A Practical Guide for Headteachers and Commissioners. Nottingham: DCFS Publications; 2008.
- Fonargy P, Pugh K, O’Herlihy A. Child Psychology and Psychiatry: Frameworks for Clinical Training and Practice. Hoboken, NJ: Wiley-Blackwell; 2017.
- Hutten R, Rick J, Chambers E, Connell J, Hardy G, Parry GD. Implementing IAPT: Lessons from the Demonstration Sites. Sheffield: University of Sheffield; 2010.
- Rusch D, Walden AL, Gustafson E, Lakind D, Atkins MS. A qualitative study to explore paraprofessionals’ role in school-based prevention and early intervention mental health services. J Commun Psychol 2019;47:272-90.
- Shahmalak U, Blakemore A, Waheed MW, Waheed W. The experiences of lay health workers trained in task-shifting psychological interventions: a qualitative systematic review. Int J Ment Health Syst 2019;13.
- Bower P, Jerrim S, Gask L. Primary care mental health workers: role expectations, conflict and ambiguity. Health Soc Care Community 2004;14:336-45.
- England E, Lester HE. Implementing the role of the graduate primary care mental health worker: a qualitative study. Br J Gen Pract 2007;57:204-11.
- Läng J. Final Report. Maximising Efficiency in Psychological Professions’ Training Routes. London: NHS National Workforce Skills Development Unit; 2020.
- Shepherd M, Rosairo M. Low-intensity workers: lessons learned from supervising primary care mental health workers and dilemmas associated with such roles. Ment Health Fam Med 2008;5:237-45.
- Harper K, G, Rao AS, Clarke J. Wellbeing matters in IAPT practitioners: identity vs system. Int J Stress Prevent Wellbeing 2020;4:1-12.
- Rizq R, Hewey M, Salvo L, Matthew Spencer M, Varnaseri H, Whitfield J. Reflective voices: primary care mental health workers’ experiences in training and practice. Prim Health Care Res Dev 2009;11:72-86.
- Carroll S, Moss-Morris R, Hulme K, Hudson J. Therapists’ perceptions of barriers and facilitators to uptake and engagement with therapy in long-term conditions. Br J Health Psychol 2021;26:307-24.
- Marshall D, Quinn C, Child S, Shenton D, Pooler J, Forber S, et al. What IAPT services can learn from those who do not attend. J Ment Health 2016;25:410-5.
- Omylinska-Thurston J, McMeekin A, Walton P, Proctor G. Clients’ perceptions of unhelpful factors in CBT in IAPT serving a deprived area of the UK. Couns Psychother Res 2019;19:455-64.
- Shankland J, Dagnan D. IAPT practitioners’ experiences of providing therapy to people with intellectual disabilities. Adv Ment Health Intellect Disabil 2015;9:206-14.
- Bassey S, Melluish S. Cultural competence in the experiences of IAPT therapists newly trained to deliver cognitive-behavioural therapy: a template analysis focus study. Couns Psychol Q 2012;25:223-38.
- Hakim N, Thompson AR, Coleman-Oluwabusola G. An evaluation of the transition from BAME community mental health worker to IAPT low intensity psychological wellbeing practitioner. Cogn Behav Ther 2019;12.
- Hickey N, Kramer T, Garralda E. Developing the primary mental health worker role in England. Child Adolesc Ment Health. 2010;15:23-9.
- Lamph G, Baker J, Dickinson T, Lovell K. Personality disorder co-morbidity in primary care ‘Improving Access to Psychological Therapy’ services: a qualitative study exploring professionals’ perspectives of working with this patient group. Pers Ment Health 2019;13:168-79.
- Johnson J, Corker C, O’Connor D. Burnout in psychological therapists: a cross-sectional study investigating the role of supervisory relationship quality. Clin Psychol 2020;24:223-35.
- McFadyen K, Darongkamas J, Crowther-Green R, Williams O. Primary-care mental-health workers’ views of clinical supervision. Cogn Behav Ther 2011;4:101-13.
- Westwood S, Morison L, Allt J, Holmes N. Predictors of emotional exhaustion, disengagement and burnout among improving access to psychological therapies (IAPT) practitioners. J Ment Health 2017;26:172-9.
- Green H, Barkham M, Kellett S, Saxon D. Therapist effects and IAPT Psychological Wellbeing Practitioners (PWPs): A multilevel modelling and mixed methods analysis. Behav Res Ther 2014;63:43-54.
- Steel C, Macdonald J, Schröder T, Mellor-Clark J. Exhausted but not cynical: burnout in therapists working within Improving Access to Psychological Therapy Services. J Ment Health 2015;24:33-7.
- Walklet E, Percy C. Stress and coping in IAPT staff: a mixed methods study. Appl Psychol Res J 2014;1:15-2.
- Turner J, Brown JC, Carpenter DT. Telephone-based CBT and the therapeutic relationship: the views and experiences of IAPT practitioners in a low-intensity service. J Psychiatr Ment Health Nurs 2018;25:285-96.
- Binnie J. Do you want therapy with that? A critical account of working within IAPT. Ment Health Rev J 2015;20:79-83.
- Fletcher J, Gavin M, Harkness E, Gask L. A collaborative approach to embedding graduate primary care mental health workers in the UK National Health Service. Health Soc Care Community 2008;16:451-9.
- Gale NK, Heath G, Cameron E, Rashi S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- Guidance on Co-producing a Research Project. Southampton: INVOLVE; 2018.
- Carr S, Beresford P. Social Care, Service Users and User Involvement. London: Jessica Kingsley; 2012.
- Social Policy First Hand: An International Introduction to Participatory Social Welfare. Bristol: Policy Press; 2018.
- Fricker M. Epistemic Injustice: Power and the Ethics of Knowing. Oxford: Oxford University Press; 2007.
- Ellins J, Singh K, Al-Haboubi M, Newbould J, Hocking L, Bousfield J, et al. Early Evaluation of the Children and Young People’s Mental Health Trailblazer Programme. Interim Report 2021. https://www.birmingham.ac.uk/documents/college-social-sciences/social-policy/brace/trailblazer.pdf (accessed May 2022).
- Ettelt S, Mays N, Allen P. The multiple purposes of policy piloting and their consequences: three examples from national health and social care policy in England. J Soc Policy 2016;44:319-37.
- The Five Year Forward View for Mental Health. London: NHS England; 2016.
- Harkness E, Bower P, Gask L, Sibbaldet B. Retention and future job intentions of graduate primary care mental health workers: a newly developed role in England. J Health Serv Res Policy 2007;12:18-22.
- Hall CL, Moldavsky M, Taylor J, Sayal K, Marriott M, Batty MJ. Implementation of routine outcome measurement in child and adolescent mental health services in the United Kingdom: a critical perspective. Eur J Child Adolesc Psychiatry 2014;23:239-42.
- Wolpert M, Fugard AJ, Deighton J, Görzig A. Routine outcomes monitoring as part of Children and Young People’s Improving Access to Psychological Therapies (CYP IAPT) – improving care or unhelpful burden?. Child Adolesc Ment Health 2012;17:129-30.
- Brown R, Van Godwin J, Edwards A, Burdon M, Moore G. Development of a Theory of Change and Evaluability Assessment for the Whole School Approach to Mental Health and Emotional Wellbeing. Cardiff: Knowledge and Analytical Services, Welsh Government; 2021.
- Allwood L, Bell A. COVID-19: Understanding Inequalities in Mental Health During the Pandemic. London: Centre for Mental Health; 2020.
- Crenna-Jennings W, Hutchinson J. 2020.
- Beck A, Naz S. The need for service change and community outreach work to support trans-cultural cognitive behaviour therapy with Black and Minority Ethnic communities. Cogn Behav Ther 2019;12.
- Naeem F. Cultural adaptations of CBT: a summary and discussion of the Special Issue on Cultural Adaptation of CBT. Cogn Behav Ther 2019;12.
- Martin C, Iqbal Z, Airey ND, Marks L. Improving Access to Psychological Therapies (IAPT) has potential but is not sufficient: how can it better meet the range of primary care mental health needs?. Br J Clin Psychol 2020;61:157-74.
- Liverpool S, Mota CP, Sales CM, Čuš A, Carletto S, Hancheva C. Engaging children and young people in digital mental health interventions: systematic review of modes of delivery, facilitators, and barriers. J Med Internet Res 2020;22.
- Digital Services for People with Mental Health Problems and Digital Exclusion During the Coronavirus Pandemic. London: Mind; 2020.
- Place2Be . Digital Direction Youth Consultation Report 2019. https://infogram.com/p2b-or-place2be-online-mental-health-research-rep-2018-19-1h174908r5jq4zj?live (accessed May 2022).
- Wilkins C, Anderson R. Digital Mental Health Services. The Impact of COVID-19 on Young People’s Mental Health. Oxford: Nominet; 2021.
- Department of Health and Department for Education . Impact Assessment on the Children and Young People’s Mental Health Green Paper 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/664442/MHGP_IA.pdf (accessed March 2022).
- Roberts J, Crosland A, Fulton J. Patterns of engagement between GPs and adolescents presenting with psychological difficulties: a qualitative study. Br J Gen Pract 2014;64:e246-54.
- McGorry P. The reality of mental health care for young people, and the urgent need for solutions. Med J Aust 2021;216:78-9.
- Jeffreys B. Children’s Mental Health: Huge Rise in Severe Cases, BBC Analysis Reveals. BBC News 2022. https://www.bbc.co.uk/news/education-60197150 (accessed May 2022).
- Alderwick H, Dunn P, McKenna H, Walsh N, Ham C. Sustainability and Transformation Plans in the NHS. How Are They Being Developed in Practice?. London: Kings Fund; 2016.
- The Health and Social Care Interface. London: NAO; 2018.
- Burstow P, Newbigging K, Tew J, Costello B. Investing in a Resilient Generation: Keys to a Mentally Prosperous Nation. Birmingham: University of Birmingham; 2018.
- Kousoulis A. Prevention and Mental Health: Understanding the Evidence so That We Can Address the Greatest Health Challenge of our Times. London: Mental Health Foundation; 2022.
- COVID-19 and the Classroom: Working in Education During the Coronavirus Pandemic. The Impact on Education Professionals’ Mental Health and Wellbeing. London: Education Support; 2020.
- Newlove-Delgado T, McManus S, Sadler K, Thandi S, Vizard T, Cartwright C, et al. Child mental health in England before and during the COVID-19 lockdown. Lancet Psychiatry 2021;8:353-4.
- Cefai C, Caravita S, Simões C. A Systemic, Whole School Approach to Mental Health and Well-being in Schools in the EU: Executive Summary. Luxembourg: Publications Office of the European Union; 2021.
- Glazzard J, Stones S. Supporting young people’ s mental health: reconceptualizing the role of schools or a step too far?. Front Educ 2021;5:1-5.
- Weare K. What Works in Promoting Social and Emotional Well-being and Responding to Mental Health Problems in Schools? Advice for Schools and Framework Document. London: National Children’s Bureau; 2015.
- Parsons S, Sherwood G, Abbott C. Informed consent with children and young people in social research: is there scope for innovation?. Child Soc 2016;30:132-45.
- Gopalkrishnan N. Cultural diversity and mental health: considerations for policy and practice. Front Public Health 2018;6.
- Ellins J, Singh K, Al-Haboubi M, Newbould J, Hocking L, Bousfield J, et al. Early Evaluation of the Children and Young People’s Mental Health Trailblazer Programme. Interim Report – Technical Appendix 2021. https://www.birmingham.ac.uk/documents/college-social-sciences/social-policy/brace/technical-appendix.pdf (accessed May 2022).
- Rocks S, Fazel M, Tsiachristas A. Variation in spend on young mental health across Clinical Commissioning Groups in England: a cross-sectional observational study. BMJ Open 2019;9.
Appendix 1 Children and Young People’s Mental Health Trailblazer programme timeline
| Date | Milestone |
|---|---|
| December 2018 | 58 MHSTs across 25 2018/19 Trailblazer sites announced (including 12 sites also running four-week waiting time pilots). |
| January 2019 | 220 EMHP trainees commence training programmes across seven Higher Education Institutions. EMHP supervisors receive specific training to equip them in their role. |
| January 2019 | Publication of the NHS Long Term Plan. It commits to continued investment in children and young people’s mental health, including the funds to roll-out MHSTs up to 2023/24. MHSTs will contribute to the ambition of at least an additional 345,000 children and young people aged 0–25 years who will be able to access support via NHS-funded mental health services. |
| February 2019 | Just over 1000 schools and colleges confirmed as participating in 2018/19 trailblazer sites. |
| July 2019 | 125 more MHSTs announced in 58 areas across the country; 48 of which are new areas announced for 2019/20, the remaining nine of which are 2018/19 areas expanding their MHSTs (Waves 1 and 2). |
| September/October 2019 | Training begins for Wave 1 2019/20 MHST EMHPs. |
| December 2019–April 2020 | MHSTs within the first Trailblazer cohort (those announced in December 2018) start to become operational.a |
| January 2020 | Training begins for Wave 2 2019/20 MHST EMHPs, now across 13 higher education institutions. |
| Spring 2020 | COVID-19 pandemic. Where in place, the majority of MHSTs adapted – and in some cases expanded – services so they could continue to support schools and colleges, and children and young people experiencing mild to moderate mental health issues, during the pandemic. |
| May 2020 | NHSE published the areas selected to develop a further 104 MHSTs during 2020/21 (Waves 3 and 4). This brings the total number of MHSTs to over 280, of which over 180 were either operational or in development in schools and colleges with further cohorts underway. |
| August–December 2020 | MHSTs within the first wave (Wave 1) of 2019/20 sites began to become operational. Most wave 1 EMHPs have delays to training due to impact of COVID-19 pandemic. However, the majority of Wave 1 EMHPs are qualified by December 2020. |
| August 2020 | Wellbeing for Education Return announced: £8m in grants to local authorities, with nationally led training for local authority leads and a package of training and resources provided to support education staff respond to the impact of COVID-19 and lockdown. |
| September 2020 | Review of training needs for senior mental leads in schools and colleges commissioned (completed early 2021). |
| November 2020 | Wave 3 2020/21 EMHP trainees begin their training at university, delayed 2 months due to COVID-19 pandemic. |
| January–March 2021 | MHSTs within the second wave of 2019/20 sites become operational. |
| January–February 2021 | Wave 4 2020/21 site EMHP trainees begin their training at university. |
| March 2021 | The government announces an additional £79 million of funding for mental health support for children and young people. |
| May 2021 | More than £17 million announced to improve mental health and well-being support in schools and colleges. This includes funding worth £9.5 million to train a senior mental health lead in the next academic year, a new £7 million Wellbeing for Education Recovery programme. |
| 13 July 2021 | Publication of the interim report from the early evaluation of the Children and Young People’s Mental Health Trailblazer programme. |
| 22 July 2021 | The NHS publishes the Mental health Clinically Led Review of Standards report, which sets out the final recommendations on new mental health standards. A consultation is launched simultaneously to give patients, clinicians, and the public an opportunity to respond to these findings and recommendations. |
| September 2021 | Wave 5 EMHPs begin their training at university. |
| October 2021 | Schools and colleges invited to begin applying for a training grant worth £1200 for each school or college, covering or contributing towards the cost of senior mental health lead training. 2021/22 sites publicly announced (Waves 5 and 6). |
| January 2022 | Wave 6 EMHPs begin their training at university. |
| 8 February 2022 | An additional £3 million committed to extend senior mental health lead training so that all schools and colleges that wish to access training before the end of May 2022 will be able to. |
| 22 February 2022 | Building on the work of the four-week wait pilots in the Trailblazer sites, publication of the Mental Health Clinically Led Review of Standards: Models of care and measurement consultation response. |
| 31 March 2022 | End of Wellbeing for Education Return/Recovery programmes. |
| 11 May 2022 | Waves 7 and 8 announced. |
| 12 May 2022 | DfE announces an additional £7 million to further extend senior mental health lead training to more schools and colleges, bringing total funding for 2022/23 to £10m. |
| 12 May 2022 | Data on coverage of the MHST programme, delivery of senior mental health lead training to schools and colleges, and impact of the Wellbeing for Education Return/Recovery programmes published by the DfE (Transforming Children and Young People’s Mental Health Implementation Programme: Data Release). |
| September 2022 | Wave 7 EMHPs begin their training at university. |
| Date | Expected milestone |
| January 2023 | Wave 8 EMHPs expected to begin their training at university. |
| May 2023 | 2023/24 sites expected to be announced (Waves 9 and 10). |
| September 2023 | Wave 9 EMHPs expected to begin their training at university. |
| January 2024 | Wave 10 EMHPs expected to begin their training at university. |
Appendix 2 Mental health support team operating principles
-
There should be clear and appropriate local governance involving health and education
The MHST project board/oversight group should include representatives from health and education backgrounds working collaboratively. As a minimum, governance should include representation from the leadership of local NHS-funded mental health care providers, education leaders from MHST education settings, commissioners, local authorities, children and young people, families and carers. Governance could also helpfully include representation from voluntary, community and social enterprise organisations, Public Health England, school and college heads or principals, and/or governors and representatives from the wider education sector. Governance arrangements should have clear feedback and escalation processes in place.
-
MHSTs should be additional to and integrated with existing support
MHSTs are trained to deliver specific mental health support to children and young people and to support schools and colleges. The team’s contribution should always be considered additional and complementary to existing support available in education settings and the wider community. The MHSTs should work with the mental health support that is already provided by existing professionals, such as school- or college-based counsellors, educational psychologists, school nurses, pastoral care, educational welfare officers, voluntary, community and social enterprise organisations, local authority provision, primary care and NHS CYPMH services.
-
The approach to allocating MHST time and resources to education settings should be transparent and agreed by the local governance board
The allocation of MHST time and resources should be agreed by the governance board, in partnership with education settings and should be broadly based on pupil and student numbers. This could be adjusted for disadvantage or inequality or other factors known to influence prevalence such as age, gender and other demographic indicators if the governance board agrees there is a case to do so.
-
MHST support should be responsive to individual education settings needs, not ‘one size fits all’
MHSTs should work with the senior mental health lead in each education setting to scope and design – within the skills, capabilities and capacity of the MHST staff – the support offer, gaining an understanding of the characteristics relevant to the particular setting and needs of their children and young people.
-
Children and young people should be able to access appropriate support all year (not just during term time)
The MHST service provider will ensure that children, young people and their families and carers who require interventions during educational holidays receive them, where possible from an MHST. Where this is not possible, the MHST should make the necessary arrangements to ensure the continuity of treatments where this is clinically indicated. The location of support given out of term will be determined by the resources available to the MHST.
-
MHSTs should co-produce their approach and service offer with users
MHSTs approach should be planned, developed and delivered in true partnership with children and young people, and their families and carers, to adequately reflect the needs of the individual, their support network, the education setting needs and the wider community.
-
MHSTs should be delivered in a way to take account of disadvantage and seek to reduce health inequalities
MHSTs should work to consider ways in which health needs and inequalities are addressed and that take account of disadvantage. They may need to develop specific protocols for working with particular groups to achieve this.
Appendix 3 Data and statistical profiles for the Trailblazer sites
This appendix presents demographic, mental health and service profiles for each of the 25 Trailblazer sites, which have been produced using nationally available (public) data. The profiles provide an overview of demographic and mental health service information for each Trailblazer site, alongside national and Trailblazer averages. These profiles were intended to summarise salient and comparable data with which to characterise the 25 areas, and (where possible) compare them with the national picture. They were previously published as a technical appendix to the interim report. 96
Methodology
Data were gathered for the lead CCG for the programme in Trailblazer sites and the main NHS provider of specialist CYPMHS in the area. We used data reported closest to December 2018, to create a snapshot of population characteristics and service performance at the time that the Trailblazer sites were announced. NHS data were used rather than local authority data because some Trailblazers span more than one local authority area.
While the data reported closest to December 2018 were used, there was variation in the collection/publication date of collated data, both within and across indicators. This limitation of data has been acknowledged by other researchers investigating CYPMHS. 97
The research team recognises that since 2018, some CCGs have been involved in mergers to form new CCGs. To accurately create a profile of the services at the time the programme was established, data have been used for the lead CCG operational at the time (e.g. Camden CCG data used instead of North Central London CCG, which was formed as a result of a merger in 2020). Table 13 outlines the indicators used to develop these profiles and the sources of this data. Table 14 provides a summary of the data across the 25 areas and profiles for each site, organised in alphabetical order, are shown in Table 15.
| Area | Indicator | Source | Linka | Notes |
|---|---|---|---|---|
| Ethnic diversity | Black and minority ethnic population by CCG, 2018/19 (%) | Public Health England Fingertips data | NA | |
| Deprivation | Index of multiple deprivation (2019), by CCG | Public Health England Fingertips data | NA | Larger number indicates higher deprivation. This is a measure of relative deprivation and combines information on seven domains of deprivation: income; employment; education; skills and training; health and disability; crime; barriers to housing services; and living environment. |
| Rural/urban | Rural/urban classification of CCGs including population in England | Office for National Statistics | https://www.gov.uk/government/collections/rural-urban-classification | There are no data for Greater Manchester Health and Social Care Partnership. All three predecessor CCGs (Central, North and South Manchester) were classified ‘predominantly urban’ so we have defined Greater Manchester Health and Social Care Partnership as ‘predominantly urban’. |
| Mental health need | Estimated prevalence of emotional disorders: % GP registered population (aged 5–16), by CCG (2017/18) | Public Health England Fingertips data | NA | The metrics used here appear to be the most appropriate indicators that are available on the Public Health England Fingertips database at the CCG level closest to the time in which the programme was set up. For example, other data available is at the local authority/region level but not CCG (e.g. ‘School pupils with social, emotional and mental health needs: % of school pupils with social, emotional and mental health needs’). |
| Estimated prevalence of common mental disorders: % of population 16 & above, by CCG (2018/19) | Public Health England Fingertips data | NA | ||
| The percentage of referrals to NHS CYPMHS that are closed before treatment, by CCG (2018/19) | Children’s’ Commissioner, The state of children’s mental health services report (2020) – (2018/19 data taken from data tables) | https://www.childrenscommissioner.gov.uk/report/the-state-of-childrens-mental-health-services | ‘The percentage of CYP who, in 2018/19, had their referral for mental health services (excluding learning disabilities and autism services) closed before treatment. According to the NHS documentation associated with the data’ (The state of children’s mental health services: Data tables, Children’s Commissioner, 2020).1 | |
| Average waiting time between referral to NHS CYPMHS and second contact, in days, by CCG (2018/19) | ‘The average waiting time (in days) between referral and second contact for CYP accessing mental health services between April 2018 and March 2019 (excluding learning disabilities and autism services). Note that this number only includes people who have had two contacts. Data were provided by the NHS as part of a bespoke request (data now published here: http://digital.nhs.uk/mhldsreports)’ (The state of children’s mental health services: Data tables, Children’s Commissioner, 2020)2 | |||
| Total number of children referred to NHS CYPMHS as a proportion of the under-18 population, by CCG (2018/19) | ‘The percentage of CYP in contact with mental health services in 2018/19 for each CCG. This number excludes CYP who were in contact for learning disabilities or autism services only. Number of CYP in contact in each CCG were provided by the NHS as part of a bespoke request (data now published here: http://digital.nhs.uk/mhldsreports). CYP (under 18 years) population estimates from the ONS were used to determine the denominators’ (The state of children’s mental health services: Data tables, Children’s Commissioner, 2020)2 | |||
| Mental health spend per child, by CCG (2018/19) | ‘2018/19 MH spend per CYP) for 2017/18. Spend numbers exclude learning disabilities and eating disorders. MH spend per CCG was derived from the Mental Health Five Year Forward View Dashboard.2 CYP (under 18) mid-2017 population estimates from the ONS were used as the denominators in the calculation of spend per child by CCG3 (The state of children’s mental health services: Data tables, Children’s Commissioner, 2020)2 | |||
| CCG spend on children’s mental health as a percentage of total CCG budget (2018/19) | ||||
| Financial standing of provider trust | Financial performance of provider trusts: plan 2018/19 (£000) | NHS Improvement. Performance of the NHS provider sector for the year ended 31 March 2019 (2019) | https://www.england.nhs.uk/wp-content/uploads/2020/08/performance-of-the-nhs-provider-sector-quarter-4-1819.pdf | |
| Financial performance of provider trusts: variance to plan for 2018/19 (£000) | ||||
| Quality of services | Provider in SOF segment 3 or 4 during the year | NHS Improvement, Consolidated NHS provider accounts 2018/19 (2019) | https://www.england.nhs.uk/wp-content/uploads/2019/09/Consolidated_NHS_Provider_Accounts_Web_Accessible.pdf | ‘NHS Improvement’s SOF is used to identify where NHS providers may benefit from, or require, improvement support across a range of areas. This includes overseeing and supporting providers in improving their financial sustainability and compliance with sector-wide controls such as agency caps … Where NHS Improvement identifies a significant concern that requires mandated support to the trust, and NHS Improvement has found a breach, or suspected breach, of the applicable licence conditions the trust is placed in segment 3 or 4… A trust subject to special measures, whether for quality or financial reasons, is placed in segment 4.’ Where a trust meets segment 3 or 4 criteria, the theme is reported (e.g. finances, quality, etc). (NHS Improvement, 2019).4 |
| CQC trust rating: overall | CQC website | www.cqc.org.uk/ | Rating taken from general inspection closest to the latter half of 2018. | |
| CQC trust rating: specialist community mental health services for children and young people (specialist community mental health services CYP) overall | https://www.cqc.org.uk/ | www.cqc.org.uk/ | The rating for specialist community mental health services for CYP was taken from the general inspection report closest to the latter half of 2018 (the same inspection in which the overall CQC rating was taken). This was not possible for three sites: Greater Manchester, Bromley and North Kent. For Bromley and North Kent, the rating was taken for the inspection specifically of specialist community mental health services for CYP (as opposed to the general inspection report). For Greater Manchester, no rating is available for Greater Manchester Mental Health NHS Foundation Trust pre-2019 as specialist community mental health services for children and young people was added as a core service to the trust only in April 2018. |
| Trailblazer site | Year | National average | Trailblazer site average |
|---|---|---|---|
| Black and minority ethnic population by CCG (%) | 2018/19 | 14.6 | 18.7 |
| Index of multiple deprivation by CCG – larger scores indicate higher deprivationa | 2019 | 21.7 | 22.2 |
| Estimated prevalence of emotional disorders: GP registered population (aged 5–16 years) by CCG (%) | 2017/18 | 3.6 | 3.6 |
| Estimated prevalence of common mental disorders: population (aged 16 years and above by CCG (%) | 2018/19 | 16.9 | 17.6 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 34.0 | 30.1 |
| Average waiting time between referral to NHS CYPMHS and second contact, in days by CCG (%) | 2018/19 | 53 | 59 |
| Total number of children referred to NHS CYPMHS as a proportion of the under-18 years population by CCG (%) | 2018/19 | 3.6 | 3.52 |
| Mental health spend per child by CCG (£) | 2018/19 | 59.22 | 68.75 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 0.92 | 1.03 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000)b | 2018/19 | N/A | N/A |
| Financial performance of NHS CYPMHS provider trusts: variance to plan for 2018/19 (£000) | 2018/19 | N/A | N/A |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider)c | 2018/19 | SOF 3: 28% of providers; SOF 4: 9% of providers | SOF 3: 12% of providers; SOF 4: 0% of providers |
| CQC trust rating: overall by NHS CYPMHS provider (%) | 2017–2018 | Outstanding: 6 | Outstanding: 16 |
| Good: 60 | Good: 76 | ||
| Requires improvement: 31 | Requires improvement: 8 | ||
| Inadequate: 3 | Inadequate: 0 | ||
| CQC trust rating: specialist community mental health services for children and young people overall (by NHS CYPMHS provider)d | 2015–2018 | Outstanding: 9 | Outstanding: 17 |
| Good: 65 | Good: 67 | ||
| Requires improvement: 24 | Requires improvement: 17 | ||
| Inadequate: 2 | Inadequate: 0 |
| Trailblazer site | Year | Berkshire West | Bromley | Buckinghamshire | Camden |
|---|---|---|---|---|---|
| Lead CCG | NHS Berkshire West CCG | NHS Bromley CCG | NHS Buckinghamshire CCG | NHS Camden CCG | |
| Provider | Berkshire Healthcare NHS Foundation Trust | Oxleas NHS Foundation Trust | Oxford Health NHS Foundation Trust | Tavistock and Portman NHS Foundation Trust | |
| Black and minority ethnic population by CCG (%) | 2018/19 | 14.0 | 15.7 | 13.5 | 33.7 |
| Index of multiple deprivation (by CCG) – larger scores indicate higher deprivation | 2019 | 11.8 | 14.2 | 10.0 | 20.1 |
| Rural/urban classification (by CCG) | 2019 | Predominantly urban | Predominantly urban | Urban with significant rural | Predominantly urban |
| Estimated prevalence of emotional disorders: GP-registered population aged 5–16 years by CCG (%) | 2017/18 | 3.2 | 3.2 | 3.1 | 3.6 |
| Estimated prevalence of common mental disorders: population aged 16 years and above by CCG (%) | 2018/19 | 14.3 | 15.1 | 13.3 | 19.4 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 30 | 12 | 22 | 16 |
| Average waiting time between referral to NHS CYPMHS and second contact by CCG (days) | 2018/19 | 66 | 80 | 47 | 48 |
| Total children referred to NHS CYPMHS as a proportion of the under-18 population by CCG (%) | 2018/19 | 3.1 | 2.5 | 3.4 | 2.7 |
| Mental health spend per child by CCG (£) | 2018/19 | 74.39 | 60.84 | 40.27 | 140.18 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 1.41 | 1.02 | 0.78 | 1.82 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000) | 2018/19 | 2397 | 2965 | 1939 | 1034 |
| Financial performance of NHS CYPMHS provider trusts: variance to plan for 2018/19 (£000) | 2018/19 | 3685 | 2968 | (8480) | 1682 |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider) | 2018/19 | No | No | No | No |
| CQC trust rating: overall by NHS CYPMHS provider (date of inspection) | 2017–2018 | Good (05 June–12 July 2018) | Good (27 February–2 March 2017) | Good (5 March 2018) | Good (13 August–19 September 2018) |
| CQC trust rating – specialist community mental health services for CYP overall by NHS CYPMHS provider (date of inspection) | 2015–2018 | Good (December 2015) | Good (26–28 April 2016) | Good (January 2016) | Good (October 2018) |
| Lead CCG | NHS Doncaster CCG | NHS Gloucestershire CCG | Greater Manchester Health and Social Care Partnership (Manchester CCG) | NHS Haringey CCG | |
| Provider | Rotherham, Doncaster and South Humber NHS Foundation Trust | Gloucestershire Health and Care NHS Foundation Trust | Greater Manchester Mental Health NHS Foundation Trust | Barnet, Enfield and Haringey Mental Health NHS Trust | |
| Black and minority ethnic population by CCG (%) | 2018/19 | 4.7 | 4.6 | 33.4 | 39.5 |
| Index of multiple deprivation (by CCG) – larger scores indicate higher deprivation | 2019 | 30.3 | 14.9 | 40.0 | 28.0 |
| Urban/rural classification (by CCG) | 2019 | Predominantly urban | Urban with significant rural | Predominantly urban | Predominantly urban |
| Estimated prevalence of emotional disorders: GP registered population aged 5–16 years by CCG (%) | 2017/18 | 3.9 | 3.4 | 4* | 3.9 |
| Estimated prevalence of common mental disorders: population (aged 16 years and above by CCG (%) | 2018/19 | 19.1 | 14.6 | 22.2 | 22.3 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 34 | 39 | 32 | 22 |
| Average waiting time between referral to NHS CYPMHS and second contact by CCG (days) | 2018/19 | 29 | 72 | 60 | 72 |
| Total children referred to NHS CYPMHS as a proportion of the under-18 years population by CCG (%) | 2018/19 | 3.55 | 3.52 | 5.15 | 2.66 |
| Mental health spend per child by CCG (£) | 2018/19 | 74.74 | 69.09 | 67.66 | 82.23 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 1.08 | 1.13 | 0.97 | 1.34 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000) | 2018/19 | 8358 | 3102 | 2292 | (3346) |
| Financial performance of NHS CYPMHS provider trusts: Variance to plan for 2018/19 (£000) | 2018/19 | 2082 | 1967 | 5991 | 3164 |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider) | 2018/19 | No | No | No | Yes – SOF 3 for quality, finance |
| CQC trust rating: overall by NHS CYPMHS provider (date of inspection) | 2017–2018 | Good (11 January to 15 February 2018) | Good (22 March 2018) | Good (18 September 2017) | Requires Improvement (25–28 September 2017) |
| CQC trust rating: specialist community MH services for CYP overall by NHS CYPMHS provider (date of inspection) | 2015–2018 | Good (January 2017) | Good (March 2018) | Not available prior to 2019a | Good (25–28 September 2017) |
| Trailblazer site | Year | Hertfordshire | Hounslow | Liverpool | Newcastle |
|---|---|---|---|---|---|
| Lead CCG | NHS Herts Valley CCG | NHS Hounslow CCG | NHS Liverpool CCG | NHS Newcastle Gateshead CCG | |
| Provider | Hertfordshire Partnership University NHS Foundation Trust | West London NHS Trust | Alder Hey Children’s NHS Foundation Trust | Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust | |
| Black and Minority Ethnic Population by CCG (%) | 2018/19 | 14.6 | 48.6 | 11.1 | 10.0 |
| Index of multiple deprivation by CCG (larger scores indicate higher deprivation) | 2019 | 11.9 | 21.5 | 42.4 | 29.1 |
| Rural/urban classification by CCG | 2019 | Predominantly urban | Predominantly urban | Predominantly urban | Predominantly urban |
| Estimated prevalence of emotional disorders: GP-registered population (aged 5–16 years by CCG (%) | 2017/18 | 3.1 | 3.5 | 4.1 | 3.9* |
| Estimated prevalence of common mental disorders: population aged 16 years and above by CCG (%) | 2018/19 | 13.7 | 18.3 | 21.7 | 19.0 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 45 | 41 | 22 | 28 |
| Average waiting time between referral to NHS CYPMHS and second contact by CCG (days) | 2018/19 | 44 | 75 | 52 | 78 |
| Total children referred to NHS CYPMHS as a proportion of the under-18 years population by CCG (%) | 2018/19 | 3.28 | 2.46 | 2.75 | 2.83 |
| Mental health spend per child by CCG (£) | 2018/19 | 50.02 | 43.08 | 71.89 | 89.33 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 0.90 | 0.77 | 0.83 | 1.17 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000) | 2018/19 | 2135 | 7457 | 32,192 | 3524 |
| Financial performance of NHS CYPMHS provider trusts: Variance to plan for 2018/19 (£000) | 2018/19 | 2235 | 3669 | 17,984 | 4242 |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider) | 2018/19 | No | Yes – SOF 3 for operational performance, quality | No | No |
| CQC trust rating: overall by NHS CYPMHS provider (date of inspection) | 2017–2018 | Good (23 January–9 February 2018) | Good (8 August–15 October 2018) | Good (6–28 February 2018) | Outstanding (16 April–26 July 2018) |
| CQC trust rating: specialist community MH services for CYP overall by NHS CYPMHS provider (date of inspection) | 2015–2018 | Good (September 2015) | Requires improvement (February 2017) | Requires improvement (April 2017) | Outstanding (July 2018) |
| Trailblazer site | Year | North Kent | North Kirklees | North Staffordshire | Northumberland |
|---|---|---|---|---|---|
| Lead CCG | Swale CCG | NHS North Kirklees CCG | NHS North Staffordshire CCG | NHS Northumberland CCG | |
| Provider | North East London NHS Foundation Trust | South West Yorkshire Partnership NHS Foundation Trust | North Staffordshire Combined Healthcare NHS Trust | Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust | |
| Black and minority ethnic population by CCG (%) | 2018/19 | 3.8 | 25.3 | 3.5 | 1.6 |
| Index of multiple deprivation by CCG (larger scores indicate higher deprivation) | 2019 | 28.4 | 28.7 | 17.5 | 22.1 |
| Rural/urban classification by CCG | 2019 | Predominantly rural | Predominantly urban | Urban with significant rural | Predominantly rural |
| Estimated prevalence of emotional disorders: GP-registered population aged 5–16 years by CCG (%) | 2017/18 | 3.7 | 3.8 | 3.6 | 3.7 |
| Estimated prevalence of common mental disorders: population aged 16 years and above by CCG (%) | 2018/19 | 17.80 | 19.20 | 16.00 | 16.10 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 28 | 21 | 43 | 38 |
| Average waiting time between referral to NHS CYPMHS and second contact by CCG (day) | 2018/19 | 32 | 43 | 56 | 61 |
| Total children referred to NHS CYPMHS as a proportion of the under-18 years population by CCG (%) | 2018/19 | 4.46 | 2.68 | 4.74 | 3.16 |
| Mental health spend per child by CCG (£) | 2018/19 | 66.97 | 39.32 | 49.60 | 78.41 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 1.18 | 0.71 | 0.67 | 0.96 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000) | 2018/19 | 3503 | 644 | 2023 | 3524 |
| Financial performance of NHS CYPMHS provider trusts: Variance to plan for 2018/19 (£000) | 2018/19 | 4907 | 2533 | 1553 | 4242 |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider) | 2018/19 | No | No | No | No |
| CQC trust rating: overall by NHS CYPMHS provider (date of inspection) | 2017–2018 | Good (30 October–3 November 2017) | Requires Improvement (6 March–11 April 2018) | Good (2 October–2 November 2017) | Outstanding (16 April–26 July 2018) |
| CQC trust rating: specialist community mental health services for CYP overall by NHS CYPMHS provider (date of inspection) | 2015–2018 | Good (10–12 October 2017) | Requires Improvement (May 2018) | Good (2 October to 2 November 2017) | Outstanding (July 2018) |
| Trailblazer site | Year | Nottinghamshire | Oxfordshire | South Tyneside | South Warwickshire |
|---|---|---|---|---|---|
| Lead CCG | NHS Nottingham North and East CCG | NHS Oxfordshire CCG | NHS South Tyneside CCG | NHS South Warwickshire CCG | |
| Provider | Nottinghamshire Healthcare NHS Foundation Trust | Oxford Health NHS Foundation Trust | Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust | Coventry and Warwickshire Partnership NHS Trust | |
| Black and minority ethnic population by CCG (%) | 2018/19 | 6.2 | 9.3 | 4.1 | 7.0 |
| Index of multiple deprivation by CCG (larger scores indicate higher deprivation) | 2019 | 17.0 | 11.8 | 31.5 | 11.9 |
| Rural/urban classification by CCG | 2019 | Predominantly urban | Predominantly rural | Predominantly urban | Predominantly rural |
| Estimated prevalence of emotional disorders: GP-registered population (aged 5–16 years by CCG (%) | 2017/18 | 3.5 | 3.3 | 4.0 | 3.1 |
| Estimated prevalence of common mental disorders population (aged 16 years and above by CCG (%) | 2018/19 | 16.0 | 14.0 | 19.1 | 13.3 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 43 | 30 | 25 | 22 |
| Average waiting time between referral to NHS CYPMHS and second contact, in days by CCG (days) | 2018/19 | 60 | 84 | 90 | 52 |
| Total referred to NHS CYPMHS as a proportion of the under-18 years population by CCG (%) | 2018/19 | 3.10 | 4.71 | 6.20 | 4.25 |
| Mental health spend per child by CCG (£) | 2018/19 | 47.69 | 46.42 | 118.95 | 50.66 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 0.77 | 0.82 | 1.38 | 0.74 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000) | 2018/19 | 7422 | 1939 | 3524 | 2154 |
| Financial performance of NHS CYPMHS provider trusts: variance to plan for 2018/19 (£000) | 2018/19 | 3035 | (8480) | 4242 | 2660 |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider) | 2018/19 | No | No | No | No |
| CQC Trust rating: overall by NHS CYPMHS provider (date of inspection) | 2017–2018 | Good (9 October–14 November 2017) | Good (5 March 2018) | Outstanding (16 April to 26 July 2018) | Good (06 August–04 October 2018) |
| CQC Trust rating: Specialist community MH services for CYP overall by NHS CYPMHS provider (date of inspection) | 2015–2018 | Good (January 2018) | Good (January 2016) | Outstanding (July 2018) | Good (December 2018) |
| TB Site | Year | South West London | Stoke-on-Trent | Swindon | Tower Hamlets | West London |
|---|---|---|---|---|---|---|
| Lead CCG | NHS Wandsworth CCG | NHS Stoke-on-Trent CCG | Swindon CCG | NHS Tower Hamlets CCG | NHS West London CCG | |
| Provider | South West London & St George’s Mental Health NHS Trust | North Staffordshire Combined Healthcare NHS Trust | Oxford Health NHS Foundation Trust | East London NHS Foundation Trust | West London NHS Trust | |
| Black and minority ethnic population by CCG (%) | 2018/19 | 28.6 | 11.0 | 10.0 | 54.8 | 33.4 |
| Index of multiple deprivation by CCG (larger scores indicate higher deprivation) | 2019 | 16.6 | 33.7 | 11.7 | 27.9 | 22.3 |
| Rural/urban classification (by CCG) | 2019 | Predominantly urban | Predominantly urban | Urban with significant rural | Predominantly urban | Predominantly urban |
| Estimated prevalence of emotional disorders: GP-registered population aged 5–16 years by CCG (%) | 2017/18 | 3.2 | 4.0 | 3.5 | 4.2 | 3.5 |
| Estimated prevalence of common mental disorders: population aged 16 years and above by CCG (%) | 2018/19 | 18.8 | 20.1 | 15.2 | 22.8 | 19.2 |
| Referrals to NHS CYPMHS that are closed before treatment by CCG (%) | 2018/19 | 33 | 46 | 16 | 38 | 26 |
| 43 | 54 | 46 | 41 | 90 | ||
| Total number of children referred to NHS CYPMHS as a proportion of the under-18 years population by CCG (%) | 2018/19 | 3.22 | 4.71 | 3.79 | 2.71 | 2.32 |
| Mental health spend per child by CCG (£) | 2018/19 | 69.09 | 63.49 | 48.19 | 69.53 | 108.80 |
| CCG spend on children’s mental health as a percentage of total CCG budget (%) | 2018/19 | 0.97 | 0.92 | 0.87 | 1.24 | 1.20 |
| Financial performance of NHS CYPMHS provider trusts: plan 2018/19 (£000) | 2018/19 | 2476 | 2023 | 1939 | 9032 | 7457 |
| Financial performance of NHS CYPMHS provider trusts: variance to plan for 2018/19 (£000) | 2018/19 | 23,412 | 1553 | (8480) | 4218 | 3669 |
| Provider in SOF segment 3 or 4 during the year (by NHS CYPMHS provider) | 2018/19 | No | No | No | No | Yes – SOF 3 for operational performance, quality |
| CQC trust rating: overall by NHS CYPMHS provider (date of inspection) | 2017–2018 | Good (26 February–06 April 2018) | Good (02 October–02 Nov 2017) | Good (05 March 2018) | Outstanding (20 March–18 April 2018) | Good (08 August–15 October 2018) |
| CQC trust rating: specialist community MH services for CYP overall by NHS CYPMHS provider (date of inspection) | 2015–2018 | Good (May 2018) | Good (02 October–02 November 2017) | Good (January 2016) | Outstanding (September 2016) | Requires improvement (February 2017) |
Appendix 4 Evaluation levels of investigation

Reproduced from the study protocol. The full protocol is available at https://fundingawards.nihr.ac.uk/award/NIHR130818.
Appendix 5 Additional sources of data that informed the analysis
| Scoping interviews | Scoping interviews to gather information about the rationale, design, implementation and aspirations for the Trailblazer programme were undertaken between January and March 2019, the findings from which informed the evaluation design and protocol. These interviews were carried out with 23 key informants, including members of the national programme team, policymakers and experts involved in the design of the national Trailblazer programme, as well as wider stakeholders (e.g. national voluntary sector organisations and professional bodies). This was supplemented by a review of programme and relevant national policy documentation. |
| Familiarisation visits | Members of the evaluation team went on in-person visits to three schools (one primary, one secondary, one special school), and attended trusted adult training sessions in Sandwell, West Midlands. These sessions were used to obtain a better understanding of emotional and mental health-related issues from the perspective of education settings and, in particular, the insights from these visits informed the development of the research tools. |
| Trailblazer document review | The national programme team provided a range of documentation for each of the 25 Trailblazer sites including, for example, expressions of interest to participate in the programme, project plans, financial specifications, governance and management structures, and local needs assessments. The number and type of documents reviewed for each Trailblazer varied. A structured data extraction template was developed for the review to ensure that data were recorded in a systematic and consistent way. |
| Programme monitoring data | On a quarterly basis, Trailblazers report service activity data for their MHSTs and provide a general update on progress using a structured template (which prompts for information on a range of topics including workforce, governance, issues and challenges, risks and mitigations, and whole school approach). Individual quarterly returns for each Trailblazer are shared with the evaluation team, although it should be noted that quarterly reporting was suspended for several months in 2020 due to the COVID-19 pandemic (as a part of an NHS-wide pause on ‘non-essential’ monitoring). |
| DfE baseline provision survey and experience surveys | A baseline survey of mental health provision in the education settings participating in the Trailblazer sites was carried out by the DfE between March and June 2019. This survey was distributed to individuals acting as the MHST co-ordinator for their setting, many of whom (63%) reported that they also held the mental health lead role. A total of 693 education settings responded: of which 69% were primary schools, 21% were secondary schools, and 10% were ‘other’ settings. Raw data and a summary report of analysed findings was shared with the evaluation team. Between February and May 2021, the DfE surveyed education settings participating in waves 1 and 2 of the programme (the sites that went live in 2019/20) about their experiences of working with MHSTs. A total of 540 responses were received (29%), of which 70% were primary schools, 21% were secondary schools, and 9% were ‘other’ settings. The findings were used by the evaluation team to compare experiences between Trailblazer schools and those involved in the immediate subsequent waves of the programme. A summary report of analysed findings was shared with the evaluation team. |
| Financial data on the funding received by Trailblazer sites | The national programme team shared financial specifications for the Trailblazers, with the exception of Greater Manchester, showing the overall amount of funding that each site received from NHS England in 2018/19, 2019/20 and 2020/21. Details of the proposed staffing composition of MHSTs at the inception of the programme (number of whole-time equivalents and a breakdown by role and banding) was also provided. A more detailed breakdown of funding allocations was requested, to understand the substantial variation in amounts Trailblazers received (which could not be straightforwardly accounted for by the number of MHSTs being funded), but this was not provided. |
| Mental health and service profiles from administrative data | A demographic and mental health service profile was compiled for each Trailblazer, drawing on routinely available data. These profiles were intended to summarise salient and comparable data with which to characterise the 25 sites, and (where possible) compare them to the national picture. Data to create these profiles were collected from a variety of sources, including Public Health England’s Children and Young People’s Mental Health and Wellbeing Profiling Tool (on the Fingertips website), consolidated NHS provider accounts for 2018/19, the Children’s Commissioner report on the state of children’s mental health services in England and individual NHS trust websites. Data were gathered for the lead CCG in each Trailblazer site and the main NHS CYPMHS provider in the area, for the reporting period closest to the time that the Trailblazers were announced (December 2018). NHS data were used rather than local authority data because some Trailblazers span more than one local authority area. The profiles, and a detailed description of the data sources used, can be found in Appendix 3. A summary of the analysis is presented in Chapter 3. |
List of abbreviations
- CAMHS
- child and adolescent mental health services
- CBT
- cognitive behavioural therapy
- CCG
- clinical commissioning group
- CQC
- Care Quality Commission
- CYPMHS
- Children and Young People’s Mental Health Services
- DfE
- Department for Education
- DHSC
- Department of Health and Social Care
- EMHP
- education mental health practitioner
- FTE
- full-time equivalent
- IAPT
- Improving Access to Psychological Therapies
- IMHYAG
- Institute of Mental Health Youth Advisory Group
- LGBTQ+
- lesbian, gay, bisexual, transgender, queer or questioning and other sexual identities
- MHSDS
- Mental Health Services Data Set
- MHST
- mental health support team
- NHSEI
- NHS England and Improvement
- NIHR
- National Institute for Health and Care Research
- PIRU
- Policy Innovation and Evaluation Research Unit
- SEND
- special educational needs and disabilities
- TaMHS
- Targeted Mental Health in Schools
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/XQWU4117).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
