Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR132541. The contractual start date was in November 2020. The draft manuscript began editorial review in May 2022 and was accepted for publication in October 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Fitzpatrick et al. This work was produced by Fitzpatrick et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Fitzpatrick et al.
Chapter 1 Introduction
Introduction
Some text in this chapter has been reproduced from a study protocol paper published by the authors in 2021. 3 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This mixed-methods study was designed to explore and understand the real-life experiences of social distancing and isolation in care homes (CHs) for older people in England from the perspective of multiple stakeholders and to develop a toolkit of evidence-informed guidance and resources for health and care delivery. This chapter describes the context to this study and the structure of the report.
Context
Around 15,375 CHs in England provide care for older adults – 11,025 residential CHs and 4350 with nursing. 4 In the UK, CHs are part of the adult social care sector, typically known as social care. Both residential and nursing CHs provide personal care for residents. In addition, nursing CHs employ registered nurses (RNs) to provide nursing care. The CH sector is diverse and complex in its configuration, for example ownership (with CHs run by private companies, voluntary or charity organisations and some by local councils), provision size and residents’ funding arrangements. The CH sector in England employs approximately 670,000 people, caring for just under 400,000 older people. 5 Many older people living in CHs have complex health and social care needs,6,7 with dementia and Alzheimer’s disease being the most common conditions for those in England and Wales. 8 These older people are at high risk of poor health outcomes and mortality if they contract coronavirus disease 2019 (COVID-19). 9
COVID-19 was declared a global pandemic by the World Health Organization (WHO) on 11 March 202010 and in the UK the first national lockdown was announced by the Prime Minister on 23 March 2020, with people being ordered to ‘stay at home’ and ‘save lives’. 11 Shortly after that restrictions to CH visiting were issued,12 and on 15 April 2020 an action plan for social care in England was introduced by government that adopted a four-pillar approach to control the spread of infection; support the workforce; support independence, support people at the end of their lives and respond to individual needs; and support local authorities (LAs) and providers of care. 13 Plans for the other three countries of the UK occurred around the same time; the decision-making and policy response of the devolved administrations of Wales, Scotland and Northern Ireland is, however, beyond the scope of this study.
For 22 countries worldwide, 41% of all COVID-19 deaths were CH residents. 14 The Office for National Statistics for England and Wales reported that since the beginning of the COVID-19 pandemic, of an estimated 274,063 CH resident deaths, 16.7% (45,632) were attributable to COVID-19. 8 At the peak of the first wave (defined by the authors as starting on 1 February 2020 and lasting until 31 August 2020), an observational study of 4.3 million adults over 65 years living in CHs in England reported that the risk of mortality among women increased by 115% and among men by 147%. 15 This contrasted with 30% for women and 47% for men living in private homes. 15 COVID-19 was the second leading cause of death for women in CHs in England in the first and second waves and the leading cause of death for men living in CHs in England during wave one. 8
Early evidence indicated that the CH sector was overlooked in the initial planning of how to contain COVID-19,16 with reports of CHs caring for older people facing significant challenges. 17,18 Challenges included inadequate support to manage infection prevention and control (IPC) effectively; decision-making at speed in a vacuum of evidence-informed guidance to care safely for residents, families, friends and staff; sourcing and funding of personal protective equipment (PPE); concerns about testing; and guidance related to the discharge of older people from hospitals to CHs. 19,20
Care homes implemented various measures to help protect residents from contracting COVID-19, including social distancing and isolation as per government guidance, which is the focus of our study. We use the terms social distancing and isolation as set out in the UK government document, ‘Admission and care of residents in a CH during COVID-19’. 21 The guidance stated that CHs ‘should be stringent in following social distancing measures for everyone in the care home and supporting those in clinically extremely vulnerable groups to follow shielding guidance’ (p23). Further, residents should be isolated in their own bedroom for 14 days following discharge from hospital or interim care facilities or when moving into a CH from a private home. Likewise, symptomatic residents, and residents without symptoms but who had been exposed to a person with possible or confirmed COVID-19, should be isolated for 14 days in their own bedroom from the onset of symptoms or a positive test result or after the last exposure. The evidence base to support the delivery of social distancing and isolation in CHs was lacking. 9 Care homes reported that implementing these measures when caring for residents was challenging,22 with regard to social distancing and isolation for residents living with dementia who may ‘walk with purpose, often called wandering’. 9
The NIHR commissioned research to better understand and manage the health and social care consequences of the global COVID-19 pandemic beyond the acute phase. Our study provides a unique contribution to helping protect older people living in CHs from COVID-19 now and for any future outbreak. It identified the real-life challenges and consequences of providing safe care incorporating social distancing and isolation measures within a CH setting while balancing potentially negative consequences for residents’ psychological, emotional, cognitive and physical well-being, and importantly it is informed by the perspective of residents, families and friends, CH staff, and external health and social care stakeholders. The study culminates in a co-designed toolkit comprising evidence-informed guidance and resources to support CHs, their staff, residents and families/friends during this and for any future outbreak.
Why this research is important
Research is needed to explore and understand the challenges experienced by CHs endeavouring to implement these measures in a person-centred way so that CHs do not become institutions of confinement. It is critical to capture the expert ways in which CHs are implementing social distancing and isolation requirements in this challenging environment and mitigating adverse consequences. For older residents, negative consequences of isolation reported included loneliness, low mood, loss of cognitive function23 and loss of physical function,9 and for those living with dementia, a worsening of both cognitive and psychological symptoms. 24 Possible adverse consequences for families and friends included loss and grief25 and for CH staff, moral distress, fear and fatigue. 26,27 Our study will complement this early research and make an important contribution to a growing body of national and international evidence in the field.
Structure of the report
This report is structured as follows:
-
Chapter 2 reports the study aims and objectives and the methodological approach used to address these.
-
Chapter 3 describes the first phase of the study, the rapid review of the evidence on measures used to prevent or control the transmission of COVID-19 and other infectious diseases in CHs for older people.
-
Chapter 4 describes social distancing and isolation policies and protocols and routinely collected CH data for the six case study sites in phase 2.
-
Chapter 5 explores CH staff perspectives of social distancing and isolation measures implemented in CHs during the COVID-19 pandemic.
-
Chapter 6 explores the perspectives of residents and their families of social distancing and isolation measures implemented in CHs during the COVID-19 pandemic.
-
Chapter 7 explores the perspectives of senior health and care leaders on social distancing and isolation measures implemented in CHs during the COVID-19 pandemic.
-
Chapter 8 presents phase 3 of the study, the development of a toolkit of evidence-informed guidance and resources for health and care delivery, now and for any future outbreaks.
-
Chapter 9 discusses the key findings from the study, reviews the approach and methods used, provides suggestions for future research and presents the implications of findings for policy and practice.
Chapter 2 Methods
Introduction
Some text in this chapter has been reproduced from a study protocol paper published by the authors in 2021. 3 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter reports the study’s aim and objectives and the methodological approach used to address these. Also reported is the patient and public involvement (PPI).
Aim and objectives
The overall aim of this study was to explore and understand the real-life experiences of social distancing and isolation in CHs for older people from the perspective of multiple stakeholders, and to develop a toolkit of evidence-informed guidance and resources for health and care delivery now and for future outbreaks of the coronavirus. The study objectives were as follows:
-
(1) To investigate the mechanisms and measures used by CHs to socially distance and isolate older people to control the spread of COVID-19 and other infectious and contagious diseases [e.g. other acute respiratory infections, Clostridium difficile and methicillin-resistant Staphylococcus aureus (MRSA) etc.].
-
(2) To examine the experiences of residents and families/friends of social distancing and isolation measures during the COVID-19 pandemic, including how these measures impacted their well-being and how they adapted to change.
-
(3) To explore how RNs and CH staff adapted to and managed the delivery of personal, social and psychological care for residents with different needs while maintaining social distancing and isolation measures.
-
(4) To identify how CH managers, owners and external stakeholders developed, managed and adapted policies, procedures and protocols to implement social distancing and isolation measures including workforce organisation, training and support, use of communal spaces, visiting and working with external health and social care professionals.
-
(5) To use the findings to develop a toolkit of evidence-informed guidance and resources and a mosaic film, detailing which interventions and strategies for social distancing and isolation for residents work well and which do not work in specific situations and contexts to support decision-making about health and care delivery in CHs and to facilitate resilience-building for future planning.
Study design and conceptual basis
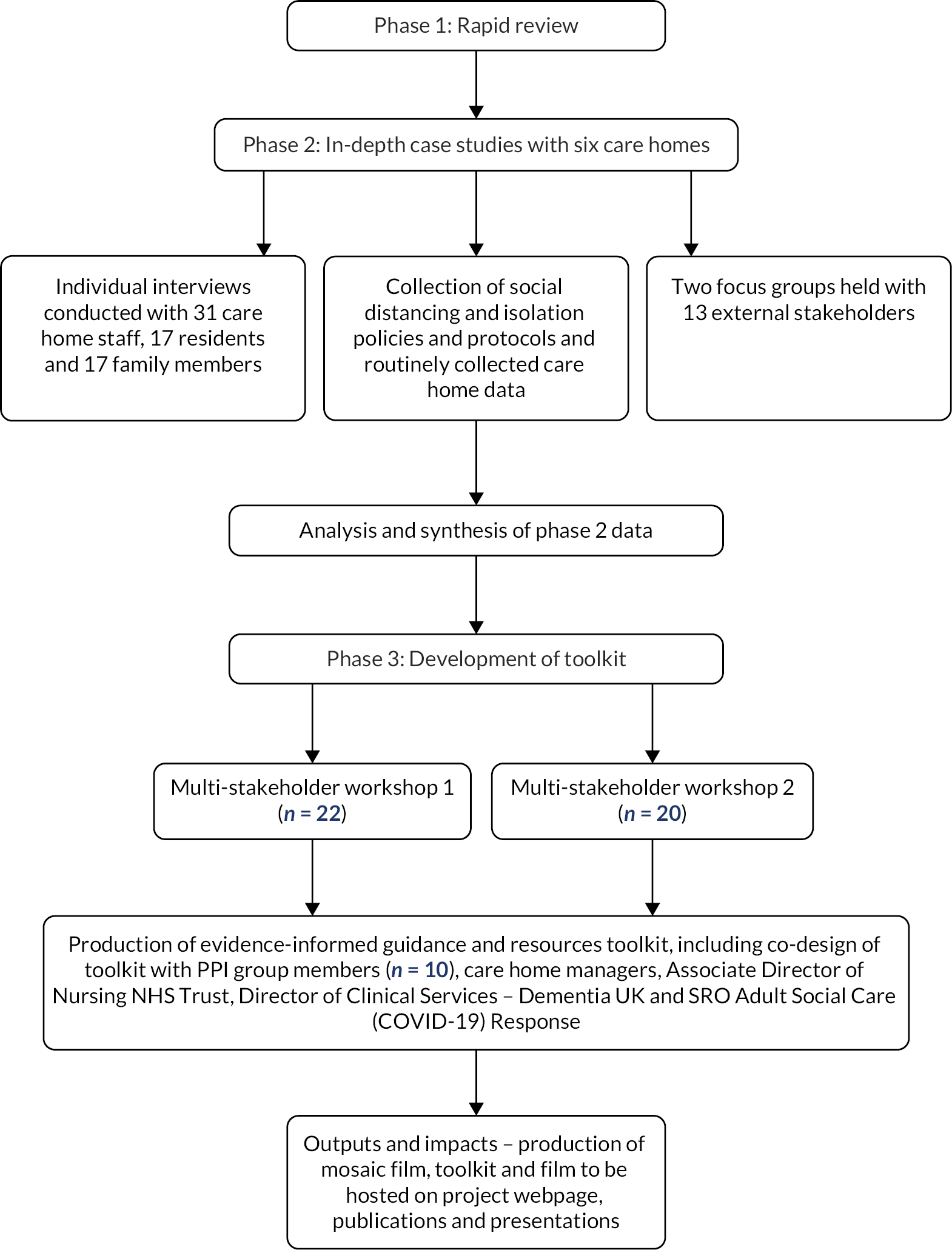
A mixed-methods, phased design was undertaken to identify the challenges, consequences and solutions to implementing social distancing and isolation measures in CHs for older adults to prevent and control the spread of COVID-19. The study was conducted in three phases: (1) a rapid evidence review of measures used to prevent or control the transmission of COVID-19 and other infectious diseases in CHs for older people, (2) in-depth case studies of six CHs in England involving individual interviews with CH staff, managers, residents and families (see NIHR project page for interview guides); focus groups with CH owners and external stakeholders (see NIHR project page for focus group topic guide); and the collection of social distancing and isolation policies/protocols, and routinely collected CH data (see NIHR project page) and (3) the development of a toolkit of evidence-informed guidance and resources, and a mosaic film, for CHs for older people. A protocol was developed to manage any disclosure of poor practice or participants’ distress during data collection (see NIHR project page for this protocol). Figure 1 shows the study flow diagram. We have used reporting guidance for qualitative research. 2
FIGURE 1.
Study flow diagram.
Phase 1: Investigating the mechanisms and measures used by care homes to socially distance and isolate older people to control the spread of COVID-19 and other infectious and contagious diseases (Objective 1)
Method
Review design and conceptual basis
A rapid review of published literature on measures used to prevent or control the transmission of COVID-19 and other infectious and contagious diseases in CHs for older people was undertaken (PROSPERO registration: CRD42021226734). This methodology was selected due to the time-critical nature of the ongoing COVID-19 pandemic. The process for study selection and data extraction followed the evidence-informed guidance for conducting rapid reviews. 1
Research questions, boundaries and scope
This research aimed to identify and assess the previously and currently used strategies by CHs to prevent and control the transmission of COVID-19 and other infectious and contagious diseases. Specific review questions were as follows:
-
(1) What mechanisms and measures have been used to implement social distancing and isolation for residents and staff?
-
(2) How are they implemented? What are the challenges and facilitators to implementation?
-
(3) What is the impact of the implemented measures and mechanisms?
-
(a) What are the psychosocial and physical consequences for older people?
-
(b) What are the consequences for family members, significant others, staff and organisations?
-
(c) What is the evidence of measures and mechanisms that work for different types of CHs, different resident needs and various ways of organising care delivery?
-
(d) What recommendations have been made after the implementation of these measures?
-
Inclusion criteria: to be included in the review, literature needed to address COVID-19 or other infectious and contagious diseases [e.g. C. diff, diarrhoea and vomiting, MRSA, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS)] in older people (aged 65 years and over) living in CHs, nursing homes, long-term facilities or residential CHs. Literature discussing adults under the age of 65 years or those living outside of long-term care facilities were excluded from the review. No limits were placed on the geographical location or timeframe of the research, but only English-language articles were included because of the resources available. Empirical research studies were included, along with literature reviews and grey literature, such as best practice guidance and expert opinion.
Exclusion criteria: non-English-language outputs.
Findings from the 103 papers included in the review were synthesised using tables and a narrative summary organised around the review questions. Full details of the search strategy, screening and selection, flow chart of the review process, summary table of 103 records, and findings are presented in Appendix 1.
Phase 2: Examining experiences, consequences and solutions of social distancing and isolation measures (Objectives 2, 3, 4)
Introduction
For the second phase of the study, in-depth case studies were undertaken to examine how social distancing and isolation of residents were being implemented in CHs for older people. This involved individual interviews with CH staff, residents and family members, and the collection of social distancing and isolation policies and protocols and routinely collected CH data. When interviewing staff members, we asked about their experiences of social distancing and isolation and their understanding of resident experiences, based upon what residents had reported to them and their own observations during the pandemic. When interviewing residents and family members, we asked about their own specific experiences of social distancing and isolation. We also conducted focus groups with senior health and care leaders in England and national-level stakeholders to understand their experiences of developing and applying policy for CHs, and how they responded to the resulting challenges.
Individual interviews: method
Research team
The interviews were carried out by four members of the research team: SP, SS, AD and JF. All interviewers are established academic researchers with experience in qualitative interviewing and a background in health and/or social care research. The interviewer and participant had no relationship before the interview, as all recruitment was carried out by the CH manager or project champion at the participating case study sites.
Recruitment
Six CHs in England were recruited for the study. Care homes were invited purposively, using a sampling frame designed to maximise variability in terms of size of the CH, geographical location, Care Quality Commission (CQC) rating, registration (nursing, residential or dual registration), ownership and incidence of COVID-19. The pandemic experience for the CH sector has impacted on CHs being research ready; the team worked hard over a prolonged period to recruit two case study sites with a ‘requires improvement’ CQC; this was not successful. We also managed a key issue around recruitment of participants from black and minority ethnic (BAME) groups. At meetings of the Study Steering Committee and Data Monitoring and Ethics Committee, we discussed these challenges and there was agreement that we should prioritise diversity of participants and not focus on recruiting CHs with a CQC rating of requires improvement. This revised plan was shared with NIHR and we were granted permission to proceed with this revised plan.
Recruiting CHs began with an initial meeting with interested provider organisation representatives, who had been sent the study information via existing contacts and networks of the research team. Following this meeting, the provider representative nominated a CH that met the criteria and would have the capacity to participate in the study. A further meeting(s) took place between the manager of the nominated CH and the researchers to provide additional details about the research and involvement of the CH. All meetings took place remotely using Microsoft Teams.
Care home managers were asked to nominate a ‘project champion’ to be the point of contact within each home to help facilitate the research, which was conducted entirely remotely due to COVID-19 restrictions on visiting care facilities. The project champion was required to be a member of staff who knew staff and residents well, and who had the capacity in their role to help with the recruitment and interview process. It was undertaken by staff members with different roles in each home, including the CH manager, deputy manager, well-being co-ordinator, activity co-ordinator and administrator. The project champions were briefed about the study and guided by research team members throughout the process; this included us working closely with CHs to try and increase diversity of participants. Potential interview participants were nominated by the CH manager in collaboration with a member of the research team and invited to participate by the project champion, using the paper copies of the study information sheets and consent forms sent to the home by the research team. The information sheets and consent forms were tailored to each participant group; resident and relative documents were produced in an easy-read format, following guidance from the Dementia Engagement and Empowerment Project (DEEP) and feedback from our PPI group members.
The purposive sample of participants required from each home included staff (n = 5), residents (n = 3) and relatives or friends of residents (n = 3). For CHs with nursing or dual registration, the staff sample consisted of the manager/deputy (n = 1), RNs (n = 2) and care staff (n = 2). For the CHs without nursing (residential), the sample included the manager/deputy (n = 1) and senior care workers or care workers (n = 4). Inclusion criteria for staff included being permanent staff (i.e. not agency) and having worked at the home during the pandemic. Staff were purposively recruited to ensure a range of age, gender, ethnicity and time in service. Resident participants were also recruited purposively, to ensure a range of genders, ethnicities and different health and care needs. Inclusion criteria were that residents must be over 65 years old and have the capacity to consent. Residents were asked during the consent process if they would like to nominate a friend or family member to participate in the research. If they or the invited family member declined or there was no nomination, the CH manager/project champion was asked to recruit a family member or friend of a non-participating resident. The project champion was responsible for collecting informed consent from participants and sending scanned copies of the completed forms to the researchers ahead of the interview. All participants were given the option to have a phone or video call with the researcher before giving signed consent, to ask any questions or talk through the research process; however, none chose to do so.
As part of the consent process, participants were asked if they were happy for the interview to be video-recorded so that excerpts from interviews could be used to create a short film as part of an evidence-based resource for CHs. The information sheet explained that a television production company technician would be present for the remote interview to ensure that there were no issues with recording. The technician could be asked to leave the call at any point should the participant wish. The option for being video-recorded was voluntary. If a person declined, they were asked whether the interview could be audio-recorded or, if preferred, only written notes to be taken. Participants were also given the option to have their face pixelated in the final video if they were happy to be video-recorded but wanted to maintain anonymity. In total, 12 participants (5 staff, 4 residents and 3 family members) chose to be audio-recorded but not video-recorded, and none opted for written notes only. The remaining participants all agreed to be video-recorded.
Setting
All resident and staff interviews took place at the CH, using an iPad sent to the home by the research team. Interviews were carried out in either the resident’s room or a quiet place in the CH such as the manager’s office, visitors’ room or hair salon when not in use. Relatives were given the option of doing their interview in their own home using their own device (e.g. smartphone, laptop, tablet, telephone). One family member chose to be interviewed at home and all others were carried out at the CH, complying with requirements for visitors.
The iPad was set up for each interview by the project champion and positioned so that the participant could see the researcher on the screen. Interviews that were being video-recorded were carried out using VMix, a secure video-call service hosted online and accessed by the technical team at KMTV. KMTV were responsible for making both the audio- and video-recordings for those participants who were video-recorded and for forwarding the audio files to the research team. Interviews that were audio-recorded only took place on Microsoft Teams. All participants were asked if they would like the project champion to be present during their interview and 17 participants (7 staff, 5 residents and 5 family members) chose to have the project champion present.
Data collection
Interviews at CHs were conducted non-simultaneously, and interviews at one CH were generally completed before interviews at another CH began. This approach to data collection meant that data were collected at different times for different CHs. These time periods were as follows: Care Home 1, February and March 2021; Care Home 2, March and April 2021; Care Home 3, April and May 2021; Care Home 4, June and July 2021; Care Home 5, August and September 2021; Care Home 6, October to December 2021. Interviews were semistructured, with a separate schedule of questions for each participant type. Interview schedules were developed by the research team and reviewed by the PPI group, and by a CH manager and resident from a non-participating CH.
Additional prompts were added to the schedules following the initial interviews of each participant type in the first CH and were agreed upon by the research team. The schedule of questions was shared with each participant at the point of recruitment to the study. Immediately before the interview began, the researcher checked consent, reminded that participation was voluntary and that the interview could be paused or stopped at any time, and gave the participant the opportunity to ask any questions. A demographic form was also completed before the recording began. For resident participants, these were collected with permission from residents and the care manager (e.g. about their primary health needs, length of time living in the CH, age group, gender, ethnic group). For families/friends participating in the study, demographic data included the nature of their relationship to residents, age group, gender and ethnicity. Staff participants were asked for their role title, length of time in the current role, length of time working in the CH sector, age group, gender and ethnic group. Once started, interviews lasted between 20 minutes and an hour. Following each interview, the researcher made field notes about the engagement of participants, any key points that had arisen, and whether there had been any technical issues, such as problems with Wi-Fi.
Data analysis
The interview audio-recordings were transcribed verbatim by a transcribing company approved by King’s College London (KCL) and were quality assured by a researcher. The interviews for each participant group were assigned to one researcher (staff interviews – SS, resident interviews – AD and family interviews – JF). We adopted an inductive orientation to thematic analysis – analysis was located within, and coding and theme development were driven by the data content. 28 At the beginning of the analysis process, a sample of staff, residents and family/friend transcripts were each read and coded independently by five researchers (JF, AD, SS, RH, SH). The researchers met and discussed their coding and, as a team, compiled a specific coding index for each participant group. The themes identified in the rapid review (phase 1) were used as deductively derived main themes in the coding indexes, and subthemes and any additional themes were inductively derived from the transcripts. AD and other team members began developing a coding framework for resident interviews based on the themes from the review and initial readings of the transcripts. However, it quickly became apparent that the elliptical nature in which many residents spoke in response to questions meant that using a framework was a blunt and, therefore, not particularly useful way of analysing this data set. AD read and reread resident transcripts and generated key themes of resident discussion (loosely described as ‘codes’) and compared how these themes were expressed across the interview data set. Researchers each analysed transcripts from their assigned participant group, but SS, AD and JF met regularly to discuss and compare their findings and modify their indexes accordingly. JF also read and analysed a subsection of transcripts coded by SS and AD for quality assurance.
Focus groups: method
Recruitment
For the second component of phase 2, we recruited and conducted two focus groups (FG1, FG2) with a purposive sample of external key informants (n = 13) beyond the CH sites. Participant characteristics (role or type of organisation worked for) are given in Chapter 7, ‘Introduction’. Potential participants were identified through study team discussions and through contact with people known to the study team. Potential participants were emailed to gauge their initial interest and then were invited to one of two focus group sessions. Focus group participants were given a participant information sheet and asked to complete a consent form and demographic information sheet. These participants had macro-level knowledge and experience relevant to the pandemic for the CH sector and included clinical leads, CH providers, organisations representing CH providers, the regulator, LA commissioning leads, Public Health England, Skills for Care, Social Care Institute for England, organisations representing residents and relatives, and Trade Union representation.
Data collection
The focus groups were conducted remotely using Microsoft Teams on 17 August 2021 (FG1) and 31 August 2021 (FG2), respectively, and each lasted 120 minutes. Each focus group was facilitated by a member or members of the study team; FG1 was facilitated by RA and AMR; SH facilitated FG2. Areas of discussion were agreed upon among members of the study team in advance. The focus group discussions centred on these areas principally, with facilitator discretion to explore themes and ideas as they emerged from the participants themselves. Facilitators ensured each participant was allowed the opportunity to contribute. The focus groups were audio-recorded with permission and transcribed. Notes were made by a designated note-maker from the research team.
Data analysis
Initial impressions of the focus groups were discussed at study team meetings. Data from the focus groups were woven into the initial informal processes of analysis and discussion alongside emerging findings from the study sites. SH and AMR read the transcripts and thematically analysed them, employing a method of familiarisation, identifying a thematic framework, and mapping and interpreting the data. 28 The themes were discussed with the broader study team and further refined.
Social distancing and isolation policies/protocols and routinely collected care home data: method
Data collection
For each CH, the CH manager or designate was asked to collate and share with the researchers all documents relevant to social distancing and isolation policies and protocols (e.g. for managing new and returning residents, zoning and cohorting of residents, visiting, staff training and education, education for residents and families/friends, support for residents, families/friends and staff, and testing of residents and staff). They were also provided with a proforma to complete, which asked for routinely collected CH data (e.g. number of beds; resident occupancy pre- and during the pandemic; staffing data including absence, redeployment, employment of agency and bank staff; COVID-19 incidence rates; testing and vaccination rates (see NIHR project page for the proforma). The proforma was developed in collaboration with CH provider representatives and an expert social care researcher, with insight into the type of data regularly collected by CHs. All six CHs provided their social distancing and isolation policies to the research team. All six CHs also completed the proforma for routinely collected data, though a small number of questions remained incomplete for some CHs.
Data analysis
Analysis of the CH policy and protocol documents was undertaken to understand the requirements and guidance provided to staff to prevent and control the spread of infectious diseases and COVID-19. 29 Documents were read and reread by RH, and information collated around the key themes of social distancing, isolation, cohorting, zoning and other restrictions. The data were carefully considered and distilled focusing on similarities, differences, usefulness and completeness of the available guidance. Routinely collected CH data were entered into an Excel spreadsheet and descriptive summary statistics were used to describe quantitative data. Concurrent data collection and analysis informed decision-making about the need for further data and from which sources. Strategies to promote quality were embedded within our data analysis strategy. 30 This included engaging with stakeholders to check emerging findings and researcher interpretation.
Phase 3: Developing a toolkit of evidence-informed guidance and resources for care homes (Objective 5)
Development of the toolkit (workshops)
Drawing on the findings of phases 1 and 2 and in collaboration with a broad sample of stakeholders (service users and public representatives, CH managers, nurses and carers, and leaders working in health and social care services and research), the research team developed a toolkit of evidence-informed guidance and resources to support social distancing and isolation for CH residents.
Workshop 1: 17 January 2022
The aim of Workshop 1 was for participants to discuss the study findings with reference to several trigger questions (see Appendix 2). Several documents were shared in advance with participants, including the workshop agenda; a summary of findings for interviews with residents, families and staff, and the focus groups with external stakeholders; questions to consider; and the draft paper on the findings of the study review. At the workshop, participants listened to presentations on the findings of interviews with residents (AD), families (JF) and CH staff (SS) and the findings of the focus groups with external stakeholders (SH). In two mixed breakout groups, participants were facilitated to reflect on and discuss the findings to gain a consensus on priority areas for the toolkit and how CHs could use the toolkit. In both workshops, the breakout groups were facilitated by a research team member and co-facilitated by a senior CH sector representative and coinvestigator (Breakout Group 1, Facilitators – RH, RA, Note-Maker – SS; Breakout Group 2, Facilitators – AD, LR, Note-Maker – JF). The whole workshops were audio-recorded. Participants were also invited to post any further questions and comments in the meeting chat. A synthesis of the Workshop 1 discussions is presented in Chapter 8.
For Workshop 1 these data sources informed the development of draft content that was organised around six priority areas: supporting the well-being of residents when social distancing; supporting the well-being of residents when they are isolating; supporting residents and their families and friends to communicate when visiting is not permitted; supporting visits from families and friends when visiting is allowed but with restrictions; supporting CH staff; supporting CH managers. For each priority area, ‘consequences’ and ‘actions to consider’ were presented with illustrative data extracts and case studies. This draft content was the focus of Workshop 2.
Workshop 2: 31 January 2022
The purpose of Workshop 2 was to discuss and develop further the draft toolkit content. The workshop began with an overview of the draft toolkit by JF, including its purpose, and proposed content underpinned by the study findings and informed by Workshop 1 discussions. Documents shared in advance with participants were a workshop agenda; draft toolkit content; questions to consider; a summary sheet of the research findings (for participants who were unable to attend Workshop 1); preliminary findings presented at Workshop 1 (for participants who were unable to participate in Workshop 1). Two mixed breakout groups were facilitated to work through the discussion points in Appendix 3 (Breakout Group 1, Facilitators – RH, RA, Note-Maker – SH; Breakout Group 2, Facilitators – AD, LR, Note-Maker – JF). A synthesis of the Workshop 2 discussions is presented in Chapter 8.
Final co-design activity
A third and final co-design activity involved sharing a further version of the draft content of the toolkit with stakeholders drawn from Workshops 1 and 2 (PPI group members × 10, CH managers × 2, Associate Director of Nursing × 1, Director of Clinical Services (Dementia UK) × 1, project team members × 8).
Patient and public involvement
Patient and public involvement (PPI) was an integral part of all stages of this study. Its design was guided by the Service User and Carer Research Expert Group from the Centre for Public Engagement in the Faculty of Health, Social Care and Education at Kingston University. This group has considerable experience of contributing to research proposals from a patient and public perspective and it is facilitated by Sally Brearley who is the PPI lead for this project and a coinvestigator. This group comprises mostly of older people, many of whom have extensive personal experience of health and care services, and several are or have been (informal) carers. We established a dedicated study PPI group comprised of 10 members, 2 of whom were also members of the Study Steering Committee. The study’s PPI lead and coinvestigator, Sally Brearley, recruited the service user and public contributors and worked with them to develop support and training needs. PPI contributions to the study included reviewing all participant-facing paperwork for submission to the Research Ethics Committee (e.g. plain language summary, project flyer, participant information sheets, consent forms and interview guides). The PPI group and project team met via Microsoft Teams in May 2021. Nine of the 10 members joined this meeting for an update on study progress, challenges along the way, findings of the rapid review, progress with the case studies and opportunities to ask questions, challenge and discuss. The Chief Investigator (CI) engaged with PPI group members throughout the study to keep them abreast of progress. PPI group members also participated in online workshops in January 2022 to contribute to co-designing the toolkit for CHs of evidence-informed guidance and resources.
Ethical considerations
The study was approved by Coventry and Warwick Research Ethics Committee [20/WM/0318] on 6 January 2021. Permission to access the CHs was obtained as per local procedures. Informed consent was obtained for all participants, and all participants were informed that they were free to refuse to participate or withdraw from the study at any time.
Chapter 3 Phase 1: rapid review (Objective 1)
Introduction
Some text in this chapter and Appendix 1 has been reproduced from a review paper published by the authors in 2022. 31 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter describes the first phase of the study: the rapid review of evidence on measures used to prevent or control the transmission of COVID-19 and other infectious diseases in CHs for older people. Recommendations from papers exploring COVID-19 interventions and from papers exploring other infectious disease interventions are presented. The method for the review is presented in Chapter 2, with full details of the search strategy, screening and selection, flow chart of the review process, summary table of 103 records and findings presented in Appendix 1.
Included papers
A total of 103 records were included in this review. 9,22,24,25,32–130 Of the 103 records included in the review, 10 were empirical research studies, 7 were literature/rapid reviews and 86 were policy documents/grey literature. Of the 10 empirical studies, 8 explored COVID-19 and 2 explored other infectious diseases. Three studies were conducted in the UK; four were conducted in Europe, two in Asia and one in North America. Two empirical studies mentioned social distancing measures, nine mentioned isolation interventions, eight mentioned restrictions and two mentioned zoning or cohorting. The quality of these studies varied greatly (e.g. one was pre-print and not peer-reviewed) and methodologies included a randomised control trial, a pilot survey study and a retrospective cohort study. However, the risk of bias of each study was assessed by two researchers, using an appropriate quality assessment tool131–134 and there was an agreement to include all 10 studies in the review. Also included in this review were 85 policy documents/grey literature, which came from around the world and included policy documents highlighting different countries’ responses to the pandemic, guidelines/guidance for CHs, briefing documents, discussions and commentaries. The seven literature/rapid reviews were also of varying quality (again, some were pre-printed and not peer-reviewed) and five were related to COVID-19 and two related to other infectious diseases.
Recommendations from papers exploring COVID-19 interventions
A wide range of recommendations was made by papers exploring strategies used by CHs to prevent and control the transmission of COVID-19. These recommendations included the following:
-
Governments (internationally but also specifically those in the UK, New Zealand and Finland) must work collaboratively with acute and community sectors to develop guidance for the safe discharge of people with COVID-19 from hospitals to CHs82,112 and provide more extensive and detailed guidance on how CHs should operate in future pandemics. 69 They must acknowledge that a ‘blanket approach’ to guidance is inadequate and ensure that the individual needs of older people are at the heart of policy-making. 91,94,112 Particular attention should be paid to the clarity and feasibility of guidelines to ensure that CH providers can implement them successfully within their facilities. 69
-
Long-standing problems in social care systems, including inadequate funding and staffing, lack of integration between health and social care, lack of recognition and regard for care staff and other workforce pressures, must be addressed by governments. 22,56,66,77,85,116
-
A balance should be sought between the implementation of IPC measures and the need to ensure residents’ quality of life, dignity and well-being33,52,80,113 to ‘explore creative ways of providing care during COVID-19 that makes life worth living’84 (p28).
-
There is a requirement for consistent records to be maintained by CHs worldwide to enhance research into COVID-19 in these settings. 24,37,56 This includes the need for openly accessible and comprehensive records on COVID-19 cases and fatalities identified within CHs37 and a minimum dementia data set to enhance understanding of people living with dementia in CHs. 24
-
All CH residents should be provided with recovery and rehabilitation opportunities to address the periods of reduced activity and social isolation they have experienced. 94,112 Trauma and grief counselling services may also need to be provided for family members and CH staff. 84,94
-
Care homes must review their visiting policies for future outbreaks, including exploring how family members, including children, may be enabled to visit safely. 48,56,82,91,113 Blanket visitor bans should not be used to prevent future outbreaks. 91,113 Care homes should also receive additional government funding and support to enable them to implement safe visiting practices. 91
-
Clear, proactive communication between CHs and family members must be maintained during periods of restriction, making use of technology where possible. 95,110
-
Staff members should consider, where possible, confining themselves to CHs to protect the facility from an outbreak of COVID-19. 39
-
More research is required in a variety of areas, including the exploration of new models of planning and design to develop CH structures and layouts that better address IPC measures;33,91,112,119 an evaluation of which measures of IPC have proved successful in COVID-19;38 an investigation of the long-term effects of the COVID-19 lockdown;84 and an exploration of innovative ways of mitigating loneliness for CH residents, especially those with cognitive impairment. 24,25,103
Recommendations from papers exploring other infectious disease interventions
A limited number of recommendations were made by papers exploring strategies used by CHs to prevent and control the transmission of non-COVID-19-related infectious diseases. These recommendations were the following:
-
Develop sound, evidence-based guidelines for isolation in CHs during infectious disease outbreaks. 72
-
Further research is required on a range of topics, including how to maintain quality of life within CHs during outbreaks of infectious diseases;88 and around the concerns, experiences and perceptions of CH staff around delivering IPC interventions. 65
Concluding remarks
The material presented here is the first-ever review of strategies previously and currently used by CHs worldwide to prevent and control the transmission of COVID-19 and other infectious and contagious diseases. We learnt that there is a lack of empirical evidence and only limited policy documentation around social distancing and isolation measures in CHs. Evaluative research on these interventions is needed urgently. In the following chapters, we present findings from the empirical phase of the study. We explore the real-life experiences, challenges, facilitators and impacts of implementing social distancing and isolation interventions within the CH setting, informing best practice guidance and resources, thus adding to, but also complicating, the picture presented by the review.
Chapter 4 Phase 2: care home case studies: routinely collected CH data and social distancing and isolation policies and protocols (Objective 4)
Introduction
This chapter describes the routinely collected CH data and the internal layouts of the six CHs. It also presents the local policy and protocol documents that guided the implementation of social distancing and isolation measures in the participating CHs.
Routinely collected care home data
All CHs completed the study proforma (though some CHs did not answer a small number of questions), providing us with their routinely collected data. This included data on the number of beds in the CH and across the organisation; resident occupancy pre- and during the pandemic; CH staffing data including absence, redeployment, employment of agency and bank staff; COVID-19 incidence rates; testing and vaccination rates.
The participating CHs were geographically spread across England, and all had a CQC rating of either ‘good’ or ‘outstanding’. All CHs were part of larger organisations (ranging from 7 to 114 CHs per organisation and between 767 and 5875 beds per organisation). Four of the participating CHs were part of privately run organisations, and two were part of voluntary/not-for-profit organisations. One CH had a ‘Dual’ CQC registration, three had a ‘Nursing’ registration and two were registered as ‘Without Nursing’. All provided services for adults over the age of 65 years, though three also provided a service for adults under the age of 65 years. Most also provided some specialist care, such as care for dementia, learning disabilities, physical health problems and mental health problems. Five CHs had a range of funding sources, including LA, National Health Service (NHS), Clinical Commissioning Group (CCG) and self-funded, while one was self-funded only.
The number of beds offered by the participating CHs ranged between 37 and 73. Some CHs saw no impact of the COVID-19 pandemic on bed occupancy rates. However, some reported a significant reduction in the number of occupied beds, particularly during the first wave of the pandemic, for example a CH closed one floor to be able to isolate floors and staff in the event of an outbreak. Care homes varied greatly on the number of positive COVID-19 cases that had been identified within the home, with one reporting only one case of COVID-19 between March 2020 and February 2021, while another reported 27 cases within November 2020 alone. Most CHs had few or no residents transferred from a hospital or home with COVID-19 throughout the pandemic, though one CH had opened a specially allocated ‘COVID-ward’. They, therefore, received 125 residents with COVID-19 between March 2000 and February 2021. Only two CHs had to transfer any residents from the home to hospital with suspected COVID-19: one had only transferred one patient to hospital between March 2000 and February 2021, but one had transferred nine patients to hospital in March 2020 alone. In one CH, no residents had died within 28 days of a positive COVID-19 test, while 10 residents had died in another home.
A COVID-19 vaccination programme started for residents within participating CHs between December 2020 and March 2021 and all residents had been fully vaccinated in three of the six case study sites. A staff vaccination programme also started in participating CHs between December 2020 and March 2021 and the percentage of vaccinated staff varied between case study sites, from 85% to 100% of staff. All participating CHs said they had taken measures to avoid front-line staff moving between CHs. Half of the homes had employed agency staff during the pandemic, but all those who had said this was within limits (e.g. agency staff could only work at one CH, or only staff from a single agency were used). The number of staff unable to work during the pandemic due to having COVID-19 symptoms varied widely between CHs and from month to month. The maximum number of staff reported being off work with COVID-19 symptoms in any one month was 16. Further information on the routinely collected data for each participating CH is provided in Appendix 4.
Internal layouts of care homes
Care home 1
Care home 1 has 64 en suite bedrooms spread over three floors. Each floor contained resident bedrooms and at least one additional bathroom. The ground and first floors also each had two resident lounges and a treatment room. Other spaces on the ground floor included a kitchen, dining room, nurses’ station and break room, senior nurse manager’s office, administration office and hair salon, while the first floor had an additional activity room.
Care home 2
Care home 2 has 37 beds spread over three floors. The ground floor contained resident en suite bedrooms, bathrooms, three lounges, a kitchen, dining room, office, reception area and staff room. The first floor had resident bedrooms, bathrooms and a nurses’ station, while the second floor contained resident bedrooms, bathrooms, a hair salon and a staff room.
Care home 3
Care home 3 has 45 en suite bedrooms spread over two floors. The ground floor contained resident bedrooms, two lounges, a kitchen, dining room, visitors’ room, hair salon, nurses’ station, break room and manager’s office. The first floor comprised a further three bedrooms, bathroom, kitchen and lounge.
Care home 4
Care home 4 has 72 en suite bedrooms allocated to specific ‘households’ and 18 self-contained apartments. All households and apartments were spread over three floors. The ground floor contained a large bistro and kitchen area, reception desk, administrator office and general manager’s office. It also had two households, each having the same layout with 12 bedrooms, living/dining room, communal bathroom and household kitchen. A further six self-contained apartments were also on the ground floor. The first floor comprised an additional two households and six apartments, a function room, internet café, exercise studio/gym and salon. The second floor contained two more households and six more apartments, alongside other meeting rooms and offices.
Care home 5
Care home 5 has 64 en suite bedrooms spread over four floors. All four floors contained resident bedrooms, a bathroom, at least one kitchen area and two dining rooms. The first three floors also had staff offices and staff rooms.
Care home 6
Care home 6 has 48 en suite bedrooms spread over two floors. The ground floor contained resident bedrooms, three lounges, a kitchen and a dining room, while the first floor comprised of resident bedrooms and a multiroom.
Social distancing and isolation policies and protocols
All six CHs sent local policy documents that guided the implementation of social distancing and isolation measures in their home. Fifty-four documents were received in total. Twelve documents were excluded as they did not address local policies about social distancing or isolation measures. These were excluded for the following reasons:
-
one was a policy about permanent closure of a CH
-
two were documents containing links to national policy guidelines on the www.gov.uk website
-
one was a protocol for cleaning processes
-
one was a protocol about staff returning to work after shielding during COVID-19
-
two were protocols for COVID-19 vaccination – one for residents, one for staff
-
one was a protocol for assessing signs of COVID-19
-
one was a protocol for staff uniform laundering
-
one was policy about dependency levels and safe staffing
-
one was a policy about test and trace service
-
one was a protocol for risk assessment for BAME employees during COVID-19.
Document characteristics
There was variation in the number of documents received from each home and in the level of detail provided about the policies and actions recommended. A summary of documents received is provided in Table 1.
| Care home | No. of policy documents received | No. of policy documents included | Size of documents (range) (no. of pages) | No. of embedded links to online government and company guidelines | Infection control measures included in documents | ||||
|---|---|---|---|---|---|---|---|---|---|
| Social distancing | Isolation | Zoning | Cohorting | Restrictions | |||||
| 1 | 32 | 23 | 1 to 8 | 0 to 5 | P | P | P | P | P |
| 2 | 1 | 1 | 60 | 6 | P | P | x | P | P |
| 3 | 11 | 9 | 2 to 9 | 0 to 10 | P | x | x | x | P |
| 4 | 5 | 5 | 1 to 11 | 0 to 3 | P | P | P | P | P |
| 5 | 2 | 2 | 67 to 69 | 11 to 24 | P | P | x | P | P |
| 6 | 3 | 2 | 7 to 23 | 7 to 24 | P | P | x | P | P |
Some CHs had a more significant number of policies each of which addressed one aspect of service provision, whereas others had a smaller number of lengthy documents that included guidance on all aspects of managing service provision during COVID-19. There was evidence that policy documents had been updated as the trajectory of COVID-19 progressed, and national government guidelines had changed. Some CHs had multiple versions of documents, whereas one CH updated the original policy document and highlighted the new changes as guidelines were revised. Either way, the content of the documents was repetitive at times and potentially challenging to navigate for busy CH staff. Some of the documents had links to embedded documents or online government guidance, which considerably increased the volume of material to read. There was considerable variation in the detail of the guidance provided by each CH with some providing very comprehensive, lengthy guidance and others much shorter guidance that gave a broad overview.
Findings
Social distancing
Social distancing was addressed by all CHs in at least one of their policy documents, although there was considerable variation in the detail of the guidance provided. One CH directed that social distance requirements should be followed but gave no further details. The other five CHs stipulated that 2 m was the required social distance to maintain between residents, staff and visitors at all times, for all activities and in all areas of the home including resident communal areas, dining areas, residents’ rooms, offices and gardens. There were a few exceptions, for example where residents were receiving essential care delivered by staff. For these activities, where maintaining the required social distance was not possible, staff were required to wear PPE including face masks. Policies for two homes discussed the different requirements of PPE depending on the activities being undertaken and whether it was possible to maintain the required social distance of 2 m. Residents were required to socially distance from other residents in all communal areas including the garden and two homes included the need for residents to be advised of this in one of their policy documents. However, one acknowledged that some residents might have difficulty in understanding and following this advice.
There was more guidance in the policy documents about managing social distancing during visits by external visitors, for example residents’ family members, health professionals, maintenance staff, entertainers and senior CH company staff. There was variation in the level of detail of guidance provided and in what aspects of the organisation of visits this guidance covered. For example, one CH gave very detailed guidance about arrangements for visiting entertainers including considering where they would be positioned to ensure at least 2 m social distance from residents, allowing additional space for singers as evidence suggests water droplets from breath carry further during singing. Generally, policies required that visitor access to the CH be carefully managed and supervised to minimise entry to resident communal areas, ensure social distancing and wear a face mask if this was not possible. Most visitors were required to do a lateral flow test (LFT) at the home before entry and policies in some homes stipulated that they must maintain social distancing while waiting for their result.
When family members of residents were allowed to visit, CH policies emphasised the requirement for social distancing. The policy for one home stated that visitors should be asked to verbally consent to abide by the terms and conditions of social distancing while in the home and grounds. The staff were required to set up the home environment to reinforce and maintain social distancing. For example, one home included detailed criteria for the internal visiting room including that it should have an external door, so the visitor did not have to walk through the communal areas of the CH to access it, a separate entrance for the resident, if possible, a substantial floor to ceiling Perspex screen and a hands-free wireless intercom system or mobile phone to facilitate communication during the visit. Other CH policies stated that for internal visits (in the designated visiting room or bedroom visits when allowed) chairs and tables should be positioned to maintain social distance with a screen in place; one home specified that this was also required for exceptional end-of-life (EoL) visits. One CH allowed relatives to remove their masks to aid communication if they remained behind the screen but encouraged them not to raise their voices. There were some differences in the policies about physical contact between resident and their relatives. Most CHs clearly stated that social distance must be always maintained, for example one home specified that relatives must not go behind the screen to touch, hug or kiss the resident. Another CH acknowledged that this would be difficult when visiting policies were revised to allow indoor visiting. Any initial breach of close contact between a resident and their family member should be gently pointed out and advised against. However, one CH guided that close contact should be kept to a minimum with hand-holding being acceptable, but hugging should be avoided and that this must be explained to the visitor. Another CH had a policy that relatives would be supported with physical contact such as hugging with the resident as long as IPC measures were in use.
Some CHs had policies that guided the actions of CH staff when travelling to work. Car sharing among staff was not recommended and alternative arrangements should be made if possible. If there is no alternative, one CH policy stated that 2 m social distance should be adhered to, that staff should car-share with the same colleagues for as short a journey as possible with no physical contact and the windows open for ventilation. They should consider the seating arrangements and try and face away from other passengers. One CH included that CH staff should maintain social distancing as per government guidance when not at work, for example in shops or on public transport.
Isolation
Isolation was addressed in at least one policy document for five of the six CHs. There was more consistency in the requirements for isolation among the CHs, although there was variation in the level of detail provided. Five CHs provided guidance about measures for resident isolation and four provided guidance for staff isolation.
One CH included guidance on how to prepare the CH to implement isolation measures including ensuring each resident bedroom could be used as an isolation room with access to PPE and handwashing facilities. Interestingly, a policy document provided by another home gave details of advising that, at the beginning of the pandemic, all residents needed to stay in their rooms to complete 14 days of isolation keeping away from other residents.
When residents were required to self-isolate all five CHs stipulated that this should be for 14 days (or longer if still symptomatic) and that residents should isolate in single bedrooms with en suite facilities or a designated commode. One home advised that if single room accommodation was not available, then residents should isolate in well-ventilated multioccupancy rooms with designated toilet facilities. The range of reasons stated for the need to self-isolate included the following:
-
any residents who were symptomatic or tested positive for COVID-19
-
residents who were newly admitted or transferred back to the CH from a hospital or A&E visit (unless treated in a designated COVID-19-free zone)
-
residents who had been in contact with someone with possible/confirmed COVID-19
-
clinically extremely vulnerable residents, assessed on a case-by-case basis as needing to shield.
One home provided details of updated guidance of isolation exemptions where many required conditions were met. This included a more detailed risk assessment of newly admitted residents who were transferring from another care facility or planned discharge from hospitals. These new residents who were fully vaccinated and had had no contact with someone COVID-19 positive could take part in an enhanced testing regimen including polymerase chain reaction test (PCR) and LFTs to determine the need to self-isolate. However, following emergency care, residents discharged from hospital were still required to self-isolate for 14 days. A resident who had tested positive for COVID-19 in the last 90 days, had completed their required period of isolation and had no new symptoms was not required to undergo testing. If a resident who was planned to be discharged from the hospital back to the CH or who was a new admission who had tested positive for COVID-19, the CH policy proposed careful consideration of whether there were sufficient staffing levels and availability of a single room before accepting the transfer. Where a resident was identified as a close contact with someone who had tested positive and was fully vaccinated, they did not need to self-isolate.
Where residents were required to self-isolate, one home specified the need to ensure that the resident was kept informed of the rationale for isolation, given the opportunity to ask questions and had an individualised care plan in place. This particular home provided detailed guidance on how to support the resident during isolation including updating the resident’s relatives daily, ensuring that they understand that visits were not recommended and could only happen in exceptional circumstances and authorised by managers, maintaining awareness of the resident’s mental health as they may become anxious and withdrawn and the need to seek further advice from managers and infection control teams if the resident was displaying behaviours that make isolation impossible, for example dementia and non-compliance. Additional support interventions included support from a companionship team (interactions limited to 15 minutes) who would provide an isolation box and support the resident to maintain contact with relatives via video calls. Where a resident refused to comply with isolation and endangered themselves or others, guidance required mental health or safeguarding assessment. If the resident had full capacity and continued to refuse to comply with isolation requirements, the CH manager could discharge the resident from the home. The guidance provided by other CHs was not so detailed but included some important additional activities, for example clearly marking the bedroom doors of residents, updating all heads of department within the home about which residents were isolating so all staff are aware and establishing a safe area for a resident with dementia who walks with purpose when keeping them in their bedrooms would not be possible even if that meant repurposing a communal area.
One CH had sheltered apartments located within the CH and guidance was that tenants must not enter the communal areas of the home site or village and staff were also required to contact them twice a day to check their well-being. Five of the CHs had policies that guided the need for staff to self-isolate. Staff were required to stay off work and self-isolate for 10 days if they had symptoms of COVID-19, a positive test, declined to test, contacted by track and trace, were required to quarantine after returning from a red list country (or amber list country if not vaccinated) or had a breach of PPE when providing personal care for asymptomatic or COVID-19-positive residents.
Restrictions
Restrictions were addressed in at least one policy document for all six homes. There was consistency in the guidance provided by homes although the detail varied considerably. Some of the documents submitted were older documents and the guidance about restrictions had subsequently been updated. Other documents had been updated but still included the older guidance, which reduced the clarity in places.
Resident restrictions
All CHs submitted guidance that restricted residents in some way. As discussed above, residents often had less freedom to move within the home, may have to move rooms if cohorting required this, had fewer visits from family and friends (discussed below), were unable to go to the hospital for routine appointments, their discharge home from the hospital if admitted may be delayed and new residents may experience delays in moving in. Strategies for staff to support residents to maintain regular communication with family and friends via telephone and virtual calls were provided in the policies of some CHs. Restrictions reduced as the pandemic progressed and vaccinations had been given.
Restrictions for families and friends
Most of the guidance in the documents concerned restrictions in visiting for families and friends. EoL visits were restricted in all homes, for example limited to 60 min, one or two immediate family members at a time, no children, wearing PPE and asymptomatic (visit not allowed if the visitor had symptoms). Four CHs included guidance about different types of visits including window, garden and drive-through visits before indoor visits were allowed in government guidelines and visits in designated visiting rooms/suites when indoor visits were allowed followed by visits in resident’s bedrooms when restrictions relaxed further. Two homes provided exceptionally detailed guidance about the different visits including, for example, ensuring residents had sufficient shade in the garden and wore sunscreen on warm days and advising visitors to avoid public transport on their journey. There were consistent requirements for visitors in all CHs even as restrictions began to be relaxed. These included the following:
-
all visitors were required to be asymptomatic and have a negative LFT taken at the home before their visit
-
all visits were time and frequency limited and had to be booked in advance
-
there were a limited number of nominated visitors (initially one or two, to visit one at a time)
-
no or little physical contact with their family member was allowed
-
gifts had to be given to a member of staff to be wiped down
-
visitors were not offered refreshments or able to use toilet facilities.
Although visitor restrictions relaxed in line with government guidelines, some CH policies continued to emphasise the need to risk-assess visits and rules varied according to this assessment. For example, although from July 2019 there were no national limits on the number of nominated visitors or how many can visit each day, the number of visits available in some of the CHs was dependent on how many could be accommodated each day with the time needed to support visitor testing and in some cases supervising the visit, the layout of the CH, length of visit and the need to ensure equity in visiting for all residents.
One CH provided guidance about residents leaving the home. Where these visits were considered high risk, for example emergency admissions to hospital, the resident should self-isolate on their return to the CH. However, other low-risk visits were supported without the need to isolate on return, for example spending time with family and friends, overnight stays in the family home, participating in community groups and volunteering and routine hospital appointments. During these visits, COVID-19 precautions, that is social distancing, handwashing and face masks, should be followed. All CHs had a policy that emphasised that in the event of an outbreak of COVID-19, that is two or more residents or staff testing positive then restrictions would increase.
Restrictions for care home staff
Restrictions for CH staff were addressed by at least one policy document for most CHs. Although the guidance was not comprehensive, it was clear that CH staff had considerably adapted the way they worked to provide care for residents and to implement and support the restrictions (and the effect of the restrictions) for residents and all visitors. For example, guidelines of several homes described the role of staff to reassure visitors, provide advice about communicating with masks on and, where assessed necessary, to supervise the visit. One home suggested that staff should advise visitors to dress and style their hair to help the resident recognise them and prepare the resident for a visit by showing them photographs of the person who is due to visit and talking to them about their relationship. The role of housekeepers had also altered because of changes to cleaning and hygiene protocols and the increased frequency of cleaning required including between visits. One home suggested the nomination of a COVID-19 co-ordinator for each shift to ensure adherence to infection control and COVID-19 policies, which should be discussed in staff supervision.
One home required that vulnerable staff should not provide care for symptomatic residents and should discuss redeployment or furlough with their line manager. Furthermore, this home required that staff adhere to PPE protocols and national lockdown guidance outside work. Failure to do so may result in disciplinary action or referral to safeguarding. Staff were required to participate in routine COVID-19 testing at the home, and the guidance in one home stipulated that the CH manager should ask to see the result for verification. All staff with a positive test or who were symptomatic were immediately sent home and required to do a PCR test. The use of agency staff was not recommended unless necessary and approved by the regional manager in one home.
Restrictions for healthcare professionals and other visitors
Restrictions for healthcare professionals and other visitors were addressed in at least one policy document in each CH, although with varying degrees of detail. All visits to each home were required to be booked in advance and approved by the home manager and visitors were required to complete a visitor questionnaire. In one home, the only unannounced visitors who would be allowed to enter were CQC inspectors and the police. All visitors were required to be asymptomatic and have evidence of a negative COVID-19 test when these were available. Multi-site CH staff, NHS and CQC staff take part in routine testing but are still required to show evidence of a negative test to be allowed to enter the home. Homes gave guidance for essential and non-essential visitors. Essential visitors included healthcare professionals providing urgent or emergency assessment and treatment, for example general practitioners (GPs), allied health professionals (AHPs), district nurses and property maintenance staff for emergency repairs. These occur as required even during an outbreak. Non-urgent GP and AHP consultations were required to be agreed at the local level by some homes, although they could be undertaken by audio or video-link if preferred. Two homes had a policy where a member of CH staff substituted for a visiting professional to perform an activity in situations where it was considered safer for the professional not to visit or when the professional was unable to visit. For example, a RN member of CH staff could provide care as part of the district nurse’s ongoing treatment plan when they had the required skill and when this was agreed with the district nurse and the CH manager. Similarly, another home had a policy where non-medical care staff could verify the expected death of a resident where the GP and home manager agreed on an approach of how to manage this.
Some routine visits by multisite centre home employees, and operational and support staff were supported to continue in some policy documents on the instruction from heads of department, although they could only visit one home in a day. One home specified the use of Microsoft Teams to support oversight of governance and management with some additional in-person visits at least every 3 months or more frequently if needed. Where onsite visits were undertaken, staff were required to change into uniform/alternative clothing on arrival and leave these clothes at the CH to be laundered (or, if necessary, taken home in an alginate bag and put in a washing machine immediately without removing them from the bag). However, if there was an outbreak during that time, one home had a policy that required these staff members to work exclusively at that home for 14 days until the outbreak was fully resolved. Property maintenance staff who work across several homes were required to wear full PPE and disposable overalls and have no contact with residents unless emergency work was required, and risk assessed by the home manager and facilities manager.
Non-essential visitors included hairdressers, entertainers and prospective customers/family show-rounds. These visits did not occur early on during the pandemic, although as restrictions relaxed, they were allowed to start with strict policies of COVID-19 testing, PPE and social distancing measures. In some CH policies, some visitors still have no access, for example community groups such as rotary clubs, schools and nurseries and other social groups.
Zoning and cohorting
In at least one of their policy documents, zoning was addressed by three and cohorting by five of the six CHs. There was significantly less guidance about these measures, particularly zoning, which was rarely mentioned. Isolation in a single room, where required, was seen as the best approach where practicable. However, in two CHs, guidance was given to cohort residents when there was an increase in the number of residents who needed to be isolated, single rooms were not available and when there was a reduction in the number of staff available to provide care. Cohorting residents, including newly admitted residents, where isolating in single rooms may impact their emotional well-being, was also considered by one home. Generally, cohorting or grouping residents in the same area of the home and ensuring that they have separate dining and activity facilities and, where possible, separate entry/exit doors were presented as a measure to minimise the risk of the spread of infection by limiting the movement of residents and staff between the different areas of the home. However, one home did caution that a group approach to infection control increased the risk of spread to residents with no symptoms.
Furthermore, the guidance stated that residents with suspected COVID-19 should not be cohorted with those with confirmed COVID-19 and neither should suspected or confirmed residents be cohorted next to those who are immunocompromised. When working with a cohort of residents, staff were expected to use PPE differently. The single-use policy no longer applied. It was acceptable to wear the same PPE for a session of care, which refers to a period of time when a care worker was undertaking duties in a specific care setting that ends when the healthcare worker leaves the care setting/exposure environment.
Guidance about cohorting also referred to grouping staff in the same location/area within the home, which should be planned as part of the scheduling. Staff were guided to form part of the cohort and, as far as possible, avoid movement between cohorts, including interacting with colleagues outside their cohort on breaks and other activities. In situations where this was not possible, guidance stipulated that staff should undertake good infection control and prevention measures by changing PPE and thoroughly washing hands.
There was some overlap or lack of clarity about how the terms zoning and cohorting were used in the documents. In some policies, residents who were isolating as a cohort were placed in a designated unit, floor or wing. One home acknowledged that residents and staff might find it challenging to understand cohorts. If so, it was suggested that forming safe zones, for example, the green zone or blue zone may indicate safe areas. Anything outside their own-coloured zone becomes higher risk so should be avoided or further IPC precautions should be undertaken. Similarly, high-risk infection hot spots, that is areas where staff and/or residents’ access from different cohorts (or zones) such as the reception area, main lounge and medication room (for staff), were called red zones. Everyone in the home was expected to be made fully aware of the red zones and the need to take extra precautions and reduce movement within these areas.
Key messages
-
There was significant variation between CHs in the content, length and level of detail presented in policy and guidance documents.
-
Capturing the frequent updates in guidance was challenging with repetitive and unclear documents at times.
-
Many documents, particularly the longer ones, had many embedded documents or links to government guidance, which provide a great deal of information that might be unrealistic for CH staff to read.
-
Shorter documents were less comprehensive and may not provide the necessary detail to guide the actions of CH staff.
-
None of the documents included any guidance about staff training and development.
Concluding remarks
In this chapter, we have discussed the local policy documents that guided the implementation of social distancing and isolation measures in participating CHs and explored some of the routinely collected CH data.
Chapter 5 Care home staff perspectives of social distancing and isolation (Objectives 3, 4)
Introduction
This chapter addresses Objectives 3 and 4 of the study and explores CH staff experiences of social distancing and isolation measures during the COVID-19 pandemic. We also explore staff understanding of residents’ and families’ experiences during the pandemic, based on what residents and families had reported to them and their own observations.
Participant characteristics
Thirty-one CH staff participated in an individual, semistructured interview and Table 2 summarises these interviewees’ level of seniority (specific role titles are as described by the interviewee). Twenty-seven interviewees were female and four were male. Twenty-two participants were white people, four were black people, three were Asian and two were mixed race. Participants had been in their current role at the CH for between 2 weeks and 8 years (average 3.5 years) but had worked in the CH sector for between 1 year and 30 years (average 14.5 years). All the staff interviewed had worked within the CH environment during the COVID-19 pandemic. Seven staff participants asked for the project champion at the CH to be present with them during their interview.
| Seniority | No. of interviews |
|---|---|
| Care home manager | 6 |
| Deputy CH manager | 3 |
| Lead nurse/senior nurse/nurse | 6 |
| Unit leader/team leader/senior care leader | 5 |
| Senior care assistant/senior healthcare assistant (HCA)/senior support worker/senior care worker | 4 |
| HCA/care assistant/support worker | 6 |
| Activities co-ordinator | 1 |
Findings
Findings are presented for the following: overall impact on CH staff; social distancing; isolation; restrictions – for residents, families and friends, CH staff, healthcare professionals and other visitors; zoning and cohorting; and surveillance.
N.B. To protect the anonymity of staff, quotations have not been assigned to specific CHs in this report and are labelled only by job title.
Overall impact on staff
Care home staff recounted the toll taken on their emotional and physical lives by working in CHs during the pandemic. This ranged from dealing with changed working routines and the burden of wearing PPE to feelings of fear for themselves, their families and those they cared for. Staff also talked to us of their discontent with how the UK government had handled the pandemic, especially regarding CHs.
Care home staff talked of the many ways that their day-to-day working lives had changed because of the COVID-19 pandemic: the most notable of which was having a far busier workload. Some staff felt their roles had become more ‘task-focused’, emphasising sanitising the CH, organising visitor appointments, taking temperatures and testing residents and visitors for COVID-19. They also talked frequently of the changes they had experienced around wearing additional PPE. Access to adequate PPE became a significant issue in the early stages of the pandemic. Staff did understand and appreciate the value of PPE during the pandemic; they trusted it and were grateful that it had allowed them to continue working safely. However, almost all staff talked of the great impact PPE requirements had upon them and their residents. For staff, these regulations involved the additional burden of changing their clothes and PPE regularly and wearing a mask and/or visor all day. Some staff felt they could not breathe properly when wearing a mask, while others talked about masks making them feel hot or developing spots on their face and sores around their ears. Staff also felt PPE made it more difficult for residents to recognise and communicate with staff, particularly those residents who were hard of hearing and relied upon lip-reading or those who had vision problems. Sometimes staff had to lift their mask briefly so that residents could understand what they were saying, while other times staff would stand across the room and talk ‘really loudly’ to residents or write down what they wanted to say on paper. It was felt that seeing staff in full PPE could be ‘scary’ for some residents, especially those with cognitive problems. It could also negatively impact the ability of residents to connect with staff and for the CH setting to feel like ‘home’:
‘The thing is of our profession we’re used to being quite emotive and, you know, speaking with our face and a large proportion of your face is blocked … I think also wearing the aprons and the gloves it’s like a clinical environment, so again, people living in the private sector, they’re not used to clinical environments. This is home’.
(Lead Nurse)
However, while problems with PPE were more prevalent at the start of the pandemic, many staff said that PPE had become ‘just a way of life now’ and that staff and residents were becoming more accustomed to masks. Thus, the extra work involved in communicating and working while wearing masks had become ‘baked in’ to the job’s demands. However, there was also some suggestion that staff roles had begun to become less task-focused as the pandemic progressed and that some rules and regulations had been relaxed over time. Staff expressed the hope that the country was ‘over the worst’ of the pandemic and that life in CHs could soon return to normal, though there was also an acceptance that COVID-19 restrictions may have to continue for some time.
The impact that the COVID-19 pandemic had upon CH staff must not be underestimated. One HCA described their experience as being an ‘emotional rollercoaster’, and several examples were highlighted of the sacrifices that staff had made and the traumas they had experienced. When information was limited at the start of the pandemic, the staff talked of how ‘frightening’ they found working with residents who were very poorly with this new, unknown virus. Many had also feared for their own safety at times, with concerns around catching the virus from residents and what would happen to them if they did:
‘… I tested positive at the beginning when it had first kind of come out … I was hysterical because I thought I’m going to die’.
(Lead Nurse)
Many staff also had fears for the safety of their families and some had chosen to separate themselves from their children and vulnerable relatives, which came at a high personal cost:
‘… I gave my daughter up for 7 weeks at the beginning of the pandemic, purely because I didn’t … want her to be in danger, I didn’t want my mum and dad to be in danger … I didn’t see her and I’ll always remember that day when she came to back to me and I think it’s just insight into what people have given up during this horrific time’.
(Deputy Manager)
‘For months and months and months, just on a personal level, me and my husband didn’t even give each other a hug and a kiss because … the environment I work in, I wanted to protect him, he wanted to protect me, you know, and that was like, “Oh my goodness, I can’t even give me husband a kiss’, you know”’.
(Lead Nurse)
In addition to their stresses at work, some CH staff were experiencing family illness and bereavements, partners’ job losses, broken marriages, cancelled healthcare treatment and financial worries as a direct consequence of the pandemic. There were reports of some staff expressing suicidal thoughts or self-harming, and one manager undertook a mental health first aid training course specifically to help their staff with their mental health. Other staff had been referred for professional psychological and physical health review:
‘… slowly, slowly that energy, I could feel it was fading away, and yeah, I ended up having a psychiatrist on Skype, and medication for depression and … a machine to monitor my heart, because of the stress’.
(Senior Nurse)
Many staff said they were mentally and physically tired and looked forward to a holiday or a break from work. Some CH staff had left employment due to their fears of working in CHs during the pandemic, and this was difficult for those who remained and perceived to be a significant loss to social care. Those who remained working throughout the pandemic were described as ‘brave’, with one manager stating they had ‘real admiration for them, because we did battle’. Some staff said they had struggled and admitted that they had considered leaving their role but continued to return to work each day to support their colleagues and residents:
‘… I used to go home some nights and I didn’t even talk. I used to go home, have a shower and go straight to bed because I was that tired and upset and it did make me … it made me feel quite sad and withdrawn. Then next day you just have to boost yourself back up again because you couldn’t let residents see you being like that’.
(HCA)
Many staff compared their own CHs to those that had been more badly impacted with infections and deaths from COVID-19 and felt relieved that their experiences were not as bad as they could have been. This was generally attributed to the interventions put in place in their CH and the hard work and dedication of their colleagues, and a sense that their CH had simply been ‘lucky’. There was an acknowledgement that even when staff had questioned the interventions and the sacrifices that residents, their families and staff had made, the ultimate reward was that their CH had remained safe:
‘… even in those difficult moments where you may question what you know, when you’re talking about what’s morally right and what’s, you know, safest and things like that, what we come back to is, well, it’s worked for us in the sense that from a COVID point of view we’ve managed to keep the residents, you know, relatively healthy … the processes that we put in place have obviously made a massive difference and it could have been very different if we hadn’t been doing it’.
(Nurse)
For many staff, the difficulties experienced during the COVID-19 pandemic were compounded by the government’s response to CHs. Some staff felt the government had abandoned them in the early phase of the pandemic and that CHs had not been considered or given appropriate guidance early enough in the process. One care assistant stated, ‘… the Government didn’t do nothing until people were dying’. Some staff criticised the ‘blanket approach’ to government guidance, which did not consider the many individual differences between CHs and CH residents. The guidance was often too long and complicated, with many different policies to consider. Others were confused by the rapidly changing rules for CHs set by the government and the fact that they found out about these rule changes at the same time as the rest of the population, which meant that homes did not have enough time to implement them appropriately:
‘… it seemed like every day there were different rules, government guidelines were changing, chopping and changing, we were expected to chop and change just the same’.
(Lead Nurse)
‘… the guidance will be published at 5 o’ clock on a Friday afternoon, and we’ve got, we’re sort of dealing with phone calls and hassles all over the weekend and we’re going, “I don’t know anything about this, what do you expect me to say?”’
(Deputy Manager)
One manager acknowledged that managers had to use their ‘own common sense and … knowledge’ when interpreting the government guidance, rather than simply follow it directly, while a Unit Lead talked of needing to select the parts of the guidance that were relevant to their individual setting:
‘… a lot of it was delving into the guidelines and actually working out, “Okay, what needs to be brought in?” Particularly with the early guidelines because it was all so over the top and a lot of it was written for acute places or places with live infections and it was sort of going, “Whoa, hang on a minute, we haven’t got anything here so at the moment we don’t need to change anything”’.
(Unit Lead)
Where applicable, managers also appreciated having the support of the senior management team in their larger CH organisation to help them interpret and implement government guidance. Several staff also talked of their passion and dedication for their role and how this had helped them get through the difficult times during the pandemic. Staff expressed great fondness and care for their residents and colleagues, often referring to those within the CH setting as a ‘family’. They were driven to provide their residents with the best possible experience during a challenging time. However, many also felt that CH staff had not been ‘recognised’ by the government (or by the population as a whole) in the same way as their NHS colleagues, which made them feel undervalued. One deputy manager said that working in a CH could sometimes be a ‘thankless job’, while others thought that the government could show they valued care workers by increasing their salaries:
‘… since we’ve been working in this pandemic they’ve been singing about the NHS, the NHS, the NHS. Us in the care home, we didn’t get nothing, nothing, and we worked so hard during this period. […] It’s only the NHS that was getting all the praises, they had the money, the increment, everything, we didn’t get nothing’.
(Care Assistant)
The following section highlights CH staff’s thoughts and experiences of the specific social distancing and isolation interventions put in place in their CHs during the COVID-19 pandemic.
Social distancing
Social distancing measures affected how staff could care for residents. They also changed how staff related to one another. This section discusses how staff experienced social distancing and the workload and logistical challenges they faced in maintaining it. As we demonstrate, staff were sceptical of the benefits or practicality of social distancing in CHs.
Social distancing measures involved residents being required to maintain a 2 m distance from each other. At first, some CHs tried to maintain social distancing by placing ‘Do not use’ signs on a proportion of their communal chairs, but this confused residents. Instead, staff felt it more appropriate to remove some chairs from communal areas to limit the number of people who could congregate together, or place coffee tables between chairs to ensure adequate spacing. However, limiting capacity in communal areas made it harder to organise usual events and activities and meant that fewer residents were able to participate, which staff found disheartening. Homes also limited the number of residents who could eat in the dining room together and ensured that dining room tables and chairs were appropriately spaced. This occasionally required CHs to turn communal lounges into extra dining spaces.
Care home staff were equally required to distance themselves from their colleagues socially, which led to staggered break times and limits on the number of staff allowed in break rooms. This involved reorganising rooms to create additional staff break spaces in some homes. Although staff and residents were also supposed to maintain a social distance from each other, many staff reported this was impossible to fulfil when providing personal care and that exceptions needed to be made at times:
‘… there’s no way on earth that I’m going to stay … 6 foot away from a resident at any given time, you know, it’s just impossible. We’ve got people who may need assistance when they need to eat or when they need a drink, or people who might need personal care. You can’t keep away from people’.
(Senior Support Worker)
A key implication of social distancing was its impact upon residents and the confusion these rules caused some of them. Several staff stated that residents found it hard to be distanced from their friends and could not understand why they could not sit closer to each other. This confusion was particularly notable for residents with dementia, who struggled to comprehend or remember social distancing rules, and some staff talked of the difficulties of ‘policing’ these restrictions while simultaneously trying to maintain a sense of ‘normality’ for their residents:
‘We try to move the chairs or the seatings where they are. They still come, they still push them back together, they want to be together. It’s really hard with them because, due to their dementia, they don’t understand what we’re trying to do. We try to explain, they say “Oh, yeah yeah”, but after 5 minutes you come back, they’ve done the same thing again’.
(Team Leader)
Social distancing measures also resulted in greater workload for staff, who were tasked with staying ‘vigilant’ around residents’ distances from each other and maintaining appropriate cleaning regimes when residents moved around the home. The importance of touch, for both residents and staff, was also regularly highlighted, with staff feeling that social distancing measures had denied many residents of this vital need. Many staff spoke of the critical role that hugs play in CHs. Residents wanted hugs from each other and from staff members, particularly if they were feeling low in mood or missing their families, and they could not understand why staff members would not hug them anymore. The fact that staff were able to have physical contact with residents while delivering personal care but could not hug them was also confusing:
‘… the residents found that hard. They’d say, “Well you’re washing and dressing me! You’re washing me, why can’t you just give me a hug?”’
(Manager)
Several staff described themselves as ‘tactile’ or ‘huggy’ people, who enjoyed hugging their residents and felt desperately sad at not being able to comfort them in their usual way. For staff who lived alone, receiving a hug could be of crucial importance to their own well-being and to have this opportunity for physical contact be denied had been particularly upsetting:
‘… sometimes that’s all you need, is a hug from somebody you work with. I mean, I go home to nobody, I live by myself, so sometimes a hug at work is probably all I need’.
(Senior HCA)
Many staff used the word ‘family’ to describe the relationships between staff and residents in CHs and talked of the loss of social interaction caused by social distancing measures. Care homes were perceived as a resident’s home rather than an institution, which made some staff question whether social distancing was appropriate, both practically and conceptually. For example, one CH was previously a residential property and was not purpose-built. As such, staff felt there was not the physical space for social distancing to be implemented successfully. Other homes were described as ‘lucky’ because they had several, large communal areas or wide corridors, making social distancing more achievable. One CH operated under a village model described as ‘designed for people to mix’. This involved staff and residents cooking and eating their meals together and residents from different households and apartments mixing freely. Such opportunities to socialise had been limited due to social distancing measures, leading to concerns about ‘institutionalising’ the village and causing it to lose its natural environment and family feel. This brought into question whether abiding by social distancing measures was always in the best interests of the residents. For instance, one staff participant told us of a woman with dementia who believed he was her husband and enjoyed holding hands with him while listening to music. This care worker faced the dilemma of whether to maintain social distancing rules with the resident or continue offering her the physical closeness that she needed. He concluded
‘I couldn’t turn round to that particular lady and say, “No, I can’t do that” … It’s not in her best interests for me to do that. So, again, swings and roundabouts, you’ve got to take into account the guidelines, but you’ve got to take into account people’s best interests as well’.
(Senior Support Worker)
In this scenario, the care worker felt that by being fastidious with changing his clothes and PPE and washing his hands regularly, he could safely provide the resident with the contact she needed and overlook the social distancing guidance. Indeed, other examples were provided of CHs either trying and failing to implement social distancing measures or choosing not to implement them entirely, due to the belief that they were impractical or unsuitable for CH environments. While most of the staff interviewed found social distancing measures challenging to implement, several felt that good support from management made the process easier. There were few positive outcomes associated with implementing social distancing in CHs, although one member of staff believed it had resulted in fewer normal winter bugs and the associated deaths:
‘… I would actually say we had a very, very easy winter because of social distancing because we didn’t get all the coughs and the colds come in and we didn’t have a lot of end of life because of that’.
(Deputy Manager)
Isolation
All staff talked about the isolation regulations that were put in place for CH residents. Initially, isolating residents were asked to stay in their rooms for 14 days, but government guidelines later changed to 10 days. All meals and care were delivered within the isolating resident’s private room. Staff entering the room had to maintain a social distance from residents and ensure their PPE was changed upon entering and leaving the room and disposed of appropriately. Some CHs used disposable plates, and cutlery for isolating residents, while others ensured that any crockery used in isolation was washed separately. There were many reasons why CH residents might be asked to isolate in their private bedroom. Still, across all CHs, residents were isolated if they displayed COVID-19 symptoms and were waiting for a test or had received a positive COVID-19 test result. Residents were also required to isolate when returning from hospitals or entering the CH as a new admission. This was to limit the likelihood of residents bringing COVID-19 into the CH, but both scenarios presented unexpected issues. For example, some staff felt that the requirement to isolate after attending hospital led to a reluctance in residents to attend hospital appointments and a disinclination from staff to refer residents for hospital care:
‘… some have chosen not to go to hospital appointments if they don’t feel it’s necessary … so they won’t get isolated … they like to be downstairs in activities, so they’ve chosen not to go to hospital because of the risk of being isolated’.
(Manager)
Many staff felt that new admissions to CHs had the most challenging experience with isolation regulations. This was because (1) the transition from home to CH was already difficult enough for people without the need to also isolate alone and (2) new residents had been unable to see the home as it usually operated, to participate in any of the activities, or to socialise with the other residents and staff. For these reasons, it was felt that new residents were often unhappier with their experience of moving to the CH, with some describing them as feeling ‘alienated’ from the others:
‘We had a couple in recently and he just said to me, he said, “My family have put me on this cruise, they told me that there was bingo and everything and I haven’t seen any of it. I don’t reckon much to this cruise”. So, it is difficult’.
(Senior HCA)
Some CHs also operated additional isolation procedures from those previously mentioned and staff talked of the specific challenges. For example, in the first national lockdown (Spring 2020), one CH isolated all residents in their private bedrooms as a precautionary measure, due to the lack of information available at this time. In a different home, operating under a village model, residents lived in a series of smaller households of 12 people and these households were treated as separate subgroups. When there was a confirmed case of COVID-19, the whole household was required to isolate but the rest of the village was not (for more information about isolating residents in subgroups, see the ‘Zoning and cohorting’ section). These isolation procedures had both positive and negative implications. The benefit was that fewer staff and residents were required to isolate during COVID-19 outbreaks and the negative being that this could result in a disparity between households. Another difficulty with this approach was that if several residents in a household caught COVID-19, then everyone within that household could remain in isolation for a long time:
‘… if you had one resident that had it and then we had another resident a few days later, the isolation period could go on and on and on. […]. So I know at one point we had a household, it could have been like 28 days or more that they were in isolation for, which is a long time’.
(Manager)
In a further CH, a senior management decision was made to open a ‘COVID ward’, where people hospitalised with COVID-19 could be discharged to recover. Everyone on this ward was required to isolate within their own rooms (locks were placed on bedroom doors) and rigorous infection control procedures and minimum staff contact rules were put in place. However, the decision to open this ward caused serious concern among many of the CH staff, including the CH manager, and some staff refused to work on this ward:
‘… the fear was spreading through the home … the first staff meeting we had I told the staff about COVID and the ward coming in, one of the staff stood up to me and said, “You’re going to kill all our residents.” That’s massive and she left. Because I would never kill anyone [Pause] That was a real … powerful statement to say in front of a whole staff team who are about to take on COVID’.
(Manager)
Yet despite these fears, the CH staff continued to work together and support each other, with many volunteering to work on the COVID ward and staff members drawing upon their previous experience of working with patients with MRSA or AIDS (acquired immunodeficiency syndrome) to help ensure that strict infection control measures were followed. Staff spoke of the pride they felt at continuing to care for residents on this ward, despite their fears, and hoped that they would be recognised for the bravery this required. Finally, some residents chose to stay within their own room even where there was no requirement for them to isolate. This was due to fears that they might contract COVID-19 if they left their room and felt safer self-isolating. Although staff tried to encourage these residents to leave their rooms, they acknowledged that this was the residents’ decision to make.
There were several negative repercussions of isolation requirements in CHs. Some staff felt that potential new residents had been deterred from moving into CHs because of the isolation requirements and one home was required to shut down a whole floor due to the lack of new admissions. Some CHs also felt restricted around whom they could accept as a new admission during the pandemic. Staff acknowledged that they only felt able to admit residents who were physically and mentally capable of isolating themselves and not those who were likely to ‘walk with purpose’. In addition to having financial implications for the CH, some staff also said they felt uncomfortable about making decisions on admission based upon residents’ ability to remain in isolation. The notion that isolation requirements went against the ethos of the CH environment was raised by a couple of CH managers, who worried that these interventions violated their caring instincts and ruined the ‘family’ feel of their homes. One deputy manager even expressed concerns that isolating residents felt like ‘institutional abuse’ or a violation of their human rights, but worried that there was no other safe alternative:
‘… we were having to say to these residents who like to come out of their room, “No, you’ve got to stay in your room”. To me, that was almost like institutional abuse, and I was like, “I need to safeguard the home” … so there was such a conflict of interest in terms of we’re doing this God awful thing but for their best, to keep them safe and it just didn’t … sit right with me because it was against every kind of nursing instinct and caring instinct that I’ve got in my body. But again, as all things, upon reflection, I dread to think what would have happened if we hadn’t have done that and if we don’t still do that for new people that are coming in’.
(Deputy Manager)
Some staff also stated that they could not force residents to stay in their rooms; therefore ‘adjustments’ sometimes had to be made, where this could be done safely:
‘… if the balcony was free, perhaps they could come out if there was nobody else about and sit on the balcony still isolating sort of thing. So, it was trying to look at different ways where we would isolate that person, but not close them off completely from everybody else’.
(Manager)
When residents were asked to isolate within their rooms, it was acknowledged that this was a difficult task for them, particularly when they had cognitive impairment or did not understand what was required of them. Staff had to repeatedly remind and explain to these residents why they were needed to stay in their bedroom, and they described this as challenging and extra workload. There was additional workload for staff even when residents did remain in their rooms, as they talked of the time implications of taking meals and beverages into individual bedrooms as opposed to serving them all in the dining room, or ‘finding time to sit with them’ individually rather than sitting as a group in the lounge. Staff also had to regularly check on isolating residents to ensure they had not fallen and been unable to press their buzzers. Staff talked of the many negative implications that isolation could have on residents, including feelings of boredom, frustration, confusion and distress. Again, this was most prominent for those residents with dementia or cognitive impairment. Staff told us that some residents felt that isolation was a punishment and there were reports of residents ‘screaming’ or shouting out in exasperation, ‘Why can I not come out? I don’t want to be in this room’. Isolation affected residents’ mood and well-being, and they missed seeing their friends and expressed sorrow at the loss of their usual routines. Isolation also had severe, long-term impacts on a small number of residents, leading to physical decline or disturbing hallucinations:
‘One lady, she’s got Alzheimer’s and the isolation where they were all in their rooms and couldn’t go out, she’s forgotten how to stand up so now she is transferred by a hoist, which is really sad because she was walking before the pandemic’.
(Senior Care Lead)
Some residents also showed reluctance to come out of their rooms when their isolation period was over, as being in their rooms had become their new ‘norm’. Furthermore, staff acknowledged that isolation regulations could be very difficult for family members, who found it upsetting to know that their loved ones remained alone in their rooms. Yet, despite all these difficulties, there was an acknowledgement from some staff that isolating residents could be a successful way of controlling the spread of COVID-19:
‘… we did have someone come in with COVID and … touch wood that’s been our only case to date and we’ve gone a year, you know, we’ve gone a year now with that. So, I do believe our isolation works really well to protect the home and our residents and our staff’.
(Manager)
Staff highlighted several factors that could make isolation less difficult for residents. The most important of them was ensuring that they were suitably entertained with regular (socially distanced) visits from staff and various resources to occupy their time. Some CHs had created ‘activity boxes’ for isolating residents, including activities such as crosswords, colouring books, jigsaws, games and reading material. Some CHs gave isolating residents a radio, Echo or Alexa so that they could listen to music; an iPad or tablet so that they could contact loved ones (see ‘Visitor restrictions’ section); a TV to keep them entertained; and exercise equipment such as stretch bands, to keep active. All CHs also acknowledged the importance of staff sitting with the residents regularly to help prevent loneliness and playing games with them or providing ‘pamper sessions’ to improve their well-being:
‘… they can isolate, but they don’t have to feel isolated’.
(Senior Support Worker)
Staff did acknowledge, however, the importance of ensuring that any activities were tailored to the individual needs and interests of the residents and noted that some individuals were not interested in participating in such pastimes. Maintaining good communication with residents throughout their period of isolation was also identified as of crucial importance, with staff comforting residents, explaining the reasons why they needed to isolate and encouraging them to persevere. Some staff talked of the importance of maintaining a sense of humour and continuing to ‘banter’ with the residents to raise their spirits:
‘… the laughter and the sheer joy from everyone, that’s what I mean, it’s like friends, we’re a professional friendship, you know … you can’t buy that kind of care, you can’t buy that kind of communication, there’s no money in the world that could buy that. And that’s what you hold so dear to you and what we all needed to maintain at that time, and I think we did it. We did it’.
(Deputy Manager)
Having good teamwork and receiving support from managers and colleagues also made the experience of implementing isolation interventions easier for staff. Few staff talked of the isolation requirements for staff members, but those who did say that staff had to isolate when they were showing symptoms of COVID-19, had tested positive for COVID-19 or when they had returned from travelling abroad. Regular testing of CH staff had made it easier for them to identify when they needed to self-isolate.
Staff frequently talked about a range of other interventions, which had also been implemented within their CHs to prevent and control the spread of COVID-19. These are discussed below.
Restrictions
Staff talked in detail about a variety of restrictions placed upon CH residents, staff, family members and other professionals during the COVID-19 pandemic. Much of this was about changes to visiting. Staff talked to us about the consequences of severely restricted or controlled visiting both on themselves and others. We look at some of these restrictions in turn.
Restrictions on residents: trips outside the care home and mealtimes
Several different resident restrictions were implemented in CHs, but from the perspective of those staff interviewed, restrictions around residents leaving the CH and changes to the way food was prepared and delivered had made the most significant impact. A major restriction within CHs was to prevent residents from leaving the home. This included preventing them from visiting shops or other community settings and stopping them from using communal facilities within the CH, such as the gym or hairdresser. This was distressing for many residents, for whom such outings and facilities played an essential role in their daily life; we explore residents’ own experiences in more detail in Chapter 6. It was equally disappointing for staff, who also valued these opportunities for interaction with their residents:
‘… with my residents, we could go out before, we could go out for a pub lunch, we could go to a farm, you know, but we couldn’t do this anymore … That affects them, it affects us as well. We are locked in an environment for a month, a year, without seeing or doing things that we’re supposed to do, things that we like to do. And that was … so upsetting, that we couldn’t provide the best service that we could because of the pandemic’.
(HCA)
Being prevented from leaving the CH had many negative implications for residents’ mental health and well-being, with staff reporting that residents became ‘withdrawn’ and ‘introverted’. Even though many activities remained in place inside the CH, staff told us that residents missed their interactions with friends from outside (as well as friends from other households or on different floors of the home, whom they were no longer allowed to see). Some lost their enthusiasm to participate in activities:
‘… they don’t want to do anything … you ask some of them nicely, “Shall we do some activities?”, and they don’t want to, “I don’t want to play dominoes, I don’t want to do this”, because they’re getting that depressed, they’re getting very depressed’.
(Nurse)
In some instances, staff found that restrictions on leaving the home were more manageable for people with dementia (or those who did not regularly leave the CH before the COVID-19 pandemic), to accept. In comparison, staff told us that those residents who were previously active and enjoyed a busy social life outside of the home experienced the impact of these restrictions more severely (see Chapter 6 for residents’ own narration of this). Indeed, one resident complained to their social worker about the CH and the unwillingness of staff to let her continue visiting local shops and supermarkets. Several staff also commented on the effect that restricting residents from leaving the CH had on their physical health; namely their ability to get sufficient physical exercise. This was particularly notable in those CHs where residents did not have access to a garden:
‘For the whole year they’ve just been stuck in this space, in this one room. And it has impacted on … the walking side because they’re not getting the exercise on their legs. Their muscle strength is deteriorating because all they want to do is sit down all day’.
(Support Worker)
Staff reported that residents were thankful that restrictions had started to ease, and facilities were beginning to reopen for them again, albeit in a different way, such as the requirement to pre-book the use of the gym. Some felt that residents had become more appreciative of the facilities they had in the home and were now more inclined to use them than they had been pre-pandemic:
‘… even the gym, they’re quite happy. They’ve never bothered going, but now they think, “Oh, it’s a different room to go in, I’ve not been in this room before”, and they’ll go to there, yeah, because it’s a completely different room. […]. They’re even excited to go in the lift sometimes, they’ve not been in there for a whole year and, “Ooh, I’ve gone in a lift’, you know”’.
(Support Worker)
A second significant restriction for CH residents involved changing how their food was cooked and served. For example, in one CH, all meals had previously been freshly cooked in the household, so that residents could participate in preparing and cooking their own meals. This was initially stopped during the pandemic, with food cooked offsite and delivered to each household individually. Consequently, a couple of staff at this home had noticed that residents were not eating as well as they previously had, ‘because they weren’t getting the smells from the cooking’. Another CH was proud of their ‘fine dining’ facilities for residents and felt that the removal of this (due to the cleaning and sanitisation requirements associated with it) had been detrimental to the residents’ experience and in opposition to the ethos of the home:
‘You know, when you go to a restaurant and you see your knife, fork and spoon ready for you and you have a nice, you know, plant in the middle of the table and maybe like a candle and your salt and your pepper and your sauces, that all had to go, you know. So you’re just left there with bare tables and … it’s like a prison. It’s like a prison, the bare minimum, and that to us is totally against our nursing home culture because it’s not a prison, it’s their home and it’s just got all took away’.
(Deputy Manager)
Across several CHs, changes had also been made to where residents ate their meals, with examples provided of residents eating in their bedrooms or communal lounges being turned into temporary dining rooms to allow additional space for social distancing requirements. In some homes, such changes had been successful. For example, some ‘younger residents’ enjoyed eating their meals in the lounge away from the older residents. However, others did not appreciate the changes to their dining arrangements and found eating alone isolating, which could affect their appetite. These changes to where residents could eat their meals also had direct consequences on staff workloads, either because they needed to spend time with each resident who was eating alone or because they needed to spend more time cleaning and sanitising rooms and equipment where residents were eating together.
Finally, as many group activities were still ongoing within CHs throughout most of the pandemic (excluding periods of isolation), restrictions on group activities were believed to have had a lesser impact on residents. Indeed, many staff talked of the innovative ways in which they delivered new or alternative activities to their residents, such as ‘indoor gardening’ sessions for those who could not get outside, small group cake-making, yoga, karaoke, socially distanced bingo and quizzes, letter writing to local school children and online sessions connecting residents with local churches and community groups:
‘… we’ve had whale of a time … we have a right singsong. We’ve got a disco ball there that we put on, turn all the lights off, disco ball and we have a party down there most days’.
(Senior HCA)
Restrictions for families and friends
Families and friends had been restricted from entering all CHs early in the COVID-19 pandemic, and all staff discussed the implications of these restrictions. During the first lockdown, the government announced that there could be no visits from family and friends in any CHs (though some homes chose to instigate these restrictions before they became mandated by the government), and this was a considerable shock requiring major adjustments for residents, families and staff. In many instances, CH staff became a target of anger and frustration from residents and their family members, who could not comprehend that they were prevented from seeing each other. We explore family members’ own experiences of COVID-19-related measures and restrictions in Chapter 6. Here, we relate how staff talked about the impact on families and residents.
Staff felt that some residents blamed them for these restrictions and perceived them to be ‘bad people’, who were ‘keeping them here under duress’. Similarly, some families expressed extreme anger towards staff, and although staff could empathise with family members, these experiences could be frightening and upsetting for them. One staff member even said they had considered calling the police when relatives had become particularly confrontational and aggressive:
‘… we’ve had the relatives who’ve been very angry, they’ve turned up at the door of a care home demanding to be let in … and they need to see their loved one, demanding and shouting at the team’.
(Manager)
Staff reported how the introduction of restrictions had been distressing for many residents, and staff talked to us about how such conversations were difficult and affected staff too:
‘… it was very hard for one of my residents. Her daughter, she comes every week or twice a week, but when we tell them, “Sorry, no family members are allowed”, and she said, “Oh, if I don’t see my daughter I’m going to die”. “Oh”, I said, you know, those words are really heart-breaking for us as well’.
(Activities Co-ordinator)
Staff recognised some of the anxieties residents themselves felt (and which we explore in more detail in Chapter 6). They reported that residents told them they had been ‘abandoned’ or that their relatives chose not to visit them. Staff had had upsetting conversations with residents who expressed pain and anger towards their families. Missing ones’ family had negative implications for residents’ mood and mental health: staff noted that some residents were sleeping more throughout the day, while others had begun ‘talking to themselves because they’ve got no one … to talk to’. Other residents’ eating habits had changed because of their depression or because their family had not been there to support and encourage them to eat, and as such they had started to lose weight. Some staff suggested that visitor restrictions had been easier for residents with dementia, because they were less likely to remember that they had not seen their relatives. In contrast, the experience had been more upsetting for those who were aware of the restrictions:
‘… I know it sounds awful but sometimes people living with dementia who can’t remember their family are in their own world and you kind of think, I think I’d prefer to be in your world right now because they’re happy, they’re content and they don’t know any different and how awful is that. How awful is it to say that somebody who lacks mental capacity is in a better state of play’.
(Deputy Manager)
Indeed, there was the suggestion that some residents with dementia had found it more upsetting when family visits were reintroduced than they had when visitor restrictions had been in place:
‘We have noticed with several that now the visits are starting back up again we’ve got more behaviours and more distress behaviour than we’ve had for the last year because they’ve just been so comfortable and settled with what’s happened’.
(Deputy Manager)
Staff also noted that deeper friendships had grown between residents and staff during periods of visitor restrictions. Staff had learnt more about their residents and their individual likes and needs. Some staff had told residents that they were their ‘family’ during the period of restrictions, and this had offered residents some comfort:
‘… we used to sit with them and say, “Look, here you go, we are a big family here, you’ve got family outside but you’re our family now, you’re our family, we’re here for you if you need anything”’.
(Senior Care Worker)
Some staff felt that the restrictions were even more distressing for family members than for residents, with many relatives feeling concerned about their loved ones and anxious about what they were hearing on the news around COVID-19 in CHs. There were reports of ‘a lot of stress and a lot of worry’ from relatives, as well as sadness and ‘missing happy times’. Some relatives experienced difficulties with the ‘lack of control’ they had over the situation, particularly those who regularly helped residents with personal care and many expressed guilt that they could no longer be there for their loved one in the ways they previously had:
‘… I was talking to a family member the other day and he was saying that “I feel like the staff have taken on my role”, and he said, “And I felt really bad and really guilty about that” […] and he said, “I was worried that I’d let her down and that I’d failed her”’.
(Nurse)
Staff, therefore, had to navigate this complex emotional terrain of the guilt, envy and loss experienced by family members. Family restrictions were particularly difficult in EoL situations, where family members could not see their relatives before they died. Some staff also reported significant trauma associated with residents being prevented from having their loved ones around them at the time of their death:
‘… and people died, with no family, just us. As a nurse, as a human being, and also somebody who’s lost their own father, I found that really, really hard [gets upset]. I had many nights I couldn’t sleep, “Had I done the right thing?” I had, I’d managed to keep COVID out of the home, but that’s hard’.
(Manager)
‘There was a gentleman that was passing away, that his brothers asked me not to let him die on his own. So that’s what I did, and sat with him and spoke to him […] it’s only now talking about it that I actually, like, realise it as well. It kind of gets locked away’.
(Lead Nurse)
Although all CHs had allowed relatives to visit their dying loved ones during at least some parts of the pandemic, these visits had still had restrictions in place, such as a screen between the resident and family; restrictions on touching; the use of masks and other PPE equipment; and limits on the number of family members who could visit:
‘… there’s no sitting there holding their hand and the usual stuff that they would do, and it is, it is a bit heart breaking to watch, you know, a socially distanced end-of-life visit … it just seems so impersonal, so uncaring, even though, you know, it’s the guidelines, it’s the law … it’s just not right at all’.
(Senior Care Assistant)
Staff were very concerned about the welfare of relatives, particularly those who were elderly themselves. They also expressed their own guilt around not being able to revoke the visitor restrictions or ease the pains experienced by family members. Preventing residents from seeing their relatives went against the caring instincts of staff and they felt distressed at seeing relatives so upset and being unable to help them as ‘we can’t break the protocols’:
‘… I’ve hated every single moment of it when I’ve had to say, “You can’t come in” […] and I’ve wanted nothing more than to just open the door and go, “Go on, go and see your mum.” I really, really have’.
(Deputy Manager)
However, staff felt that, overall, most relatives did understand why the restrictions were in place and were supportive and grateful to staff for caring for their loved ones in their absence. Many also believed that these restrictions had been beneficial for controlling the spread of COVID-19 in the CH. Finally, staff reported that visitor restrictions had significantly increased their workload. Many staff talked about considerable increases in the number of telephone calls CHs were getting from relatives every day and the impact this had upon them, as well as the additional time they had to spend feeding back updates on residents to their relatives:
‘… the phone calls, even at home I would get home and I could hear the phone call ringing, and I had insomnia for weeks, for weeks insomnia, I couldn’t sleep … they are not working in these environments, they do not understand the pressure, to do medication, to do safe medication administration … it is a high amount of pressure to have that, and the phone ringing constantly distracting you’.
(Senior Nurse)
Extra staff time was also spent supporting residents, explaining why they could not see their loved ones and ensuring they were well entertained in their relatives’ absence. While these visitor restrictions were in place, all CHs in this study had attempted to help residents maintain contact with their families using telephone and video-calling (using Skype or Zoom etc.), and this had been incredibly beneficial for many residents and helped raise their morale. However, telephone or video calls were not suitable for all residents. Those who had dementia, vision/hearing problems or those who were not comfortable using technology had struggled to experience the benefit. Similarly, not all staff members and relatives felt comfortable using new technology, not all CHs had good Wi-Fi access, and some family members did not have their own telephone or computer on which to receive the calls. Furthermore, many residents needed assistance in using this technology and required staff to stay with them when making their calls, which meant extra workload for staff and a lack of privacy for residents and families during their conversations. Some CHs also had to buy additional equipment to accommodate these calls, which had financial implications.
Care homes also initiated a variety of additional creative ways for residents to see their family members. These included ‘drive-by’ visits, ‘window visits’ and outdoor visiting ‘pods’. One CH installed a new telephone line purely for family enquiries, which eased much of the congestion on the main phone line. Others made internal changes to their buildings, such as installing glass screens in visitor rooms and increasing the number of entrances and exits. However, even when families were able to enter the CHs again, several visiting restrictions remained in place, such as limits on the number of visitors, and the duration and regularity of visits. Family members had to pre-book appointment times and were required to be tested for COVID-19 before entering the CH. There were discrepancies reported around whether residents and families were able to hug each other during visits, with some staff saying this was now permitted and others saying it was not. All these restrictions added a layer of time and complexity to the visiting arrangements and increased staff workload. Furthermore, a few examples were provided of families refusing to abide by the restrictions, meaning that staff felt they needed to ‘police’ some of the visits. Staff also felt uncomfortable and upset that they needed to address issues of breaking restriction rules with family members.
Several factors were identified by staff as helping to make the difficult period of visitor restrictions more bearable for themselves, their residents and family members. These included maintaining good communication with relatives (including holding regular online meetings for families where they could air their concerns) and receiving good support and guidance at a senior management/company level. Having a building layout where all bedrooms had exterior doors was also felt to be beneficial, as this allowed family members to visit their relatives without entering any other part of the CH.
Restrictions for care home staff (e.g. changes to working patterns, shifts and rotas)
Restrictions for CH staff were discussed less frequently than those for residents and families. A few staff members said their working arrangements had not noticeably changed because of the COVID-19 pandemic. However, other staff were able to identify several ways in which their working lives had changed. For example, some participants reported changes to shift lengths and rota patterns in almost all CHs, with staff working longer shifts or overtime, being on ‘standby’ or working through their annual leave. Managers had to plan rotas carefully, due to staffing issues associated with increased staff sickness, ‘shielding’ staff, staff leaving their roles due to fears of working during the pandemic or staff being furloughed. They also had to consider the individual circumstances of their staff (such as childcare issues, which might prevent them from working certain hours). Managers’ workloads further increased due to the regular phone calls and complaints from residents’ families and increased communication with external organisations such as the CQC, who regularly phoned for updates. Indeed, in some homes, managerial staff said they had (or had been prepared) to stay the night in the CH should the need arise:
‘… we all packed our bags. I’ve still got it in the boot of my car, I’ve got a blow-up bed and an overnight bag with about 4 days’ worth of supplies just in case, because you could never anticipate what could happen’.
(Deputy Manager)
Several examples were provided of staff ‘upskilling’, switching roles (e.g. moving from the role of ‘well-being co-ordinator’ to ‘care worker’), or taking on aspects of another’s role during the pandemic. Indeed, one nurse described the situation in CHs as being ‘all hands on deck’:
‘I had to upskill the team, because if staff suddenly went ill and I’ve got no team who would care for my residents? […] admin, housekeepers, maintenance were all upskilled to be able to go on floors, serve meals, give drinks, support us getting residents in and out of bed’.
(Manager)
In a few instances, staff had been restricted to working on one floor/household or working with the same small cohort of staff and residents. While these arrangements were believed to help limit the spread of COVID-19, some staff found these restrictions difficult, as they inhibited their ability to communicate more widely with residents and other staff. In one home, staff were asked to only work within that setting and to not work shifts elsewhere. The manager at this home said staff were contented with this restriction, as they felt it helped protect their own safety, and the safety of the other staff and residents. The manager also ensured staff who would ordinarily work elsewhere were given extra shifts in the home so that they did not suffer financially. The use of agency staff differed across CHs, with one manager stating that they stopped using agency staff altogether while others said they did employ agency staff when there were staffing constraints. However, this was implemented in a limited way (e.g. only using one agency, ensuring agency staff did not work within any other CHs and that they were regularly tested for COVID-19). One CH had to reduce the number of staff working due to the closure of one floor in the home, but another had to recruit additional staff, which had financial implications for the home.
Despite the restrictions placed upon staff, several people were able to identify positive outcomes of their experience of working during the pandemic. There was a suggestion that the experience had brought staff ‘closer together’, had helped encourage better team working and gave staff a greater ‘appreciation’ of the roles of their colleagues. However, there was also a suggestion that adapting to new ways of working during the pandemic had been ‘exhausting’ for some staff. An important factor that helped during periods of staff restrictions was receiving good managerial support. Some staff spoke effusively around their gratitude for their CH managers, whom they described as supportive, available and willing to have open and honest conversations with their staff, listening to their suggestions and taking on board their feedback. Good managers were also seen to boost the morale of their staff, give them the motivation to continue with their work during difficult periods and reward them with little treats. Having a manager who encouraged staff to take regular breaks while working (something that was not always possible due to heightened workloads) and to use their annual leave where possible was also appreciated.
Restrictions for healthcare professionals and other visitors
In addition to restricting families and friends from entering CHs, restrictions were extended to all external healthcare and non-healthcare professionals and other visitors. This prevented anyone who would ordinarily go into a CH from entering, including GPs, physiotherapists, occupational therapists, mental health teams, social workers, clergy members, hairdressers, entertainers, activity staff and school children. These restrictions on external visitors led to additional workloads for CH staff:
‘…. now we’re hairdressers, we’re counsellors, we’re advocates, we’re social workers, we’re doctors, you know, everything, we’re everything’.
(Lead Nurse)
Some staff reported that district nurses could still enter the home (though there was sometimes a long wait for such services), and some said that GPs would still visit in person in the case of an emergency. However, communication with all external visitors was conducted online or over the telephone in most cases. Staff believed the greatest impact came from communicating with healthcare professionals remotely, particularly GPs, as some questioned whether healthcare assessments could be successfully carried out online. A few staff said that extra pressure had been placed upon them by not having GPs and other healthcare professionals visit the home in person. They felt this resulted in them having to make quick clinical decisions about a resident or ensuring that they provided external healthcare professionals with all the necessary information about a resident to make an informed decision. This could be worrying for some staff, who could begin to doubt their ability to give information appropriately or ask the right questions. Others felt they were being asked to complete tasks ordinarily undertaken by other healthcare professionals, which they were unqualified to do, and this made them feel nervous and unsupported:
‘… we didn’t know if we were doing things wrong with, like, the exercises and stuff from the OT perspective, and even for like SALT reviews, we’re having to monitor them when we ain’t professional in that background. So, it was quite scary, but yeah, we managed it’.
(Deputy Manager)
However, this deputy manager believed that CH nurses were well placed to work in this way, as they knew their residents well and were able to identify when they were becoming unwell. They also believed CH nurses were accustomed to working independently in the community and were comfortable with trusting their instincts. There were few examples of the implications of these restrictions on residents, though one manager did highlight a couple of residents who had been negatively affected by delays in their care because of healthcare visitor restrictions:
‘I think one of our residents had a really bad toe … under the normal circumstances, a GP would have looked at that, referred him to the foot clinic or a podiatrist and they would have probably removed the nail. But he had to go through sort of like weeks and weeks of pain until the toenail actually fell off, you know. That was one of them but there’s been other things as well. Like a pressure sore, you know, it’s tiny and we’re looking after it but then all of a sudden it sort of like becomes red, so the district nurses, you don’t see them for absolutely ages and then it’s too late and then that pressure sore then becomes … a graded pressure sore’.
(Manager)
Slowly, such restrictions were beginning to be eased within CHs, with healthcare professionals being able to re-enter the homes again. However, there were reports that some healthcare professionals had still not returned to face-to-face appointments, which was disappointing and confusing to some CH staff.
Zoning and cohorting
One CH highlighted an example of ‘zoning’ by treating each household as a separate subgroup. When there was a confirmed case of COVID-19, that resident’s whole household was required to isolate, but the rest of the village was not. Interviewees provided a few other examples of zoning. One care assistant said they disagreed with the idea of zoning residents if this involved moving them on to different floors, as the residents would find this ‘destabilising’. One deputy manager said they had discussed and prepared for the possibility of creating a unit specifically for residents with COVID-19. However, staff had discord about these plans, with some individuals stating they would refuse to work on this unit. Fortunately, these plans did not have to be initiated, as none of the residents contracted COVID-19. One CH did not ‘zone’ their residents but did use a form of cohorting, whereby residents were clustered into small groups and allocated one staff member per shift to attend to their care needs. The reasoning for this was limiting the number of contacts each resident had each day to help reduce ‘cross-contamination’. One senior HCA, however, expressed concerns that while this approach could be helpful in the pandemic, it could have negative repercussions in the longer term:
‘… I do feel that doing it that system, certain carers don’t get to care for other residents, they’re not getting the full view. So when this pandemic is over and we may go back to our old way … they’re not going to know what their care needs are, so it’s going to be like they’re learning from scratch again, a whole new bunch of residents. It’s really going to be difficult because they’ve only concentrated on certain residents while they’ve been on shift, which has been good from the pandemic point of view, but from a care point of view they’ve isolated themselves from all of the other residents’.
(Senior HCA)
Surveillance: the effects of regular testing
Some staff talked about the surveillance measures implemented within CHs during the COVID-19 outbreak. These were the same as infection control measures implemented for other infectious diseases and included being aware of the signs and symptoms of COVID-19 in residents and staff. At the start of the pandemic, residents had daily checks on their temperature and oxygen saturation and regular observations for any COVID-19 symptoms (e.g. cough). Any concerns were quickly escalated to the CH manager and GP. Some staff also said they checked their temperature before starting each shift. However, the implementation of new testing regimes had been beneficial for CH staff in identifying cases of COVID-19 more rapidly. Following government guidance, CH staff were now taking regular lateral flow, and PCR tests and residents were also tested regularly (usually monthly) and isolated when positive results were returned. Visitors were also required to take LFTs at the CH before entering the premises. This had proved significant in some instances, where visitors with a positive test result had been identified and turned away before entering the home. Some staff said the testing requirements made them feel less anxious about going to work and had made the atmosphere in the CHs more relaxed:
‘… it gives you that peace of mind that yes you’re safe, everyone is safe, you can carry on with your job’.
(Senior Nurse)
However, the testing process had also resulted in increased workload for staff, as undertaking the testing and then recording the results of these tests onto the computer system had been added as an additional task in their weekly routines. For example, some of those administering the tests spoke of having to ‘chase’ staff to get their tests done. All visitors also had to take a LFT at the CH and then wait for 30 minutes outside before entering the premises, and staff said this added a layer of complexity to their workload. For example, one senior HCA said they had to set a 30-minute alarm after each test had been completed to remind them to go and tell the visitor if they could enter the home. They, therefore, stated, ‘I’ve got alarms going off all day in my little room!’. Several staff also commented that they needed to cope with the anger and frustration of some visitors, who could not understand why they had to wait for 30 minutes before they were allowed to enter the home. Some CHs had secured infection control funding, which had enabled them to recruit a member of staff to focus only on the testing process, but this had not been the case for all CHs:
‘… it is just never-ending from the test point of view, putting those on, working to the deadlines, remembering to do things like order your test collections because you can’t do them too far in advance … You sort of think ‘Oh no, do you know how much work is involved in that?’ And then they brought in the lateral flow tests, so we’ve now got two of those for every member of staff to register, and just when you’ve got on top of doing those they then say “Right, we’re going to bring relatives back in now, they’re going to have to be lateral flowed as well”, so another load to put in’.
(Deputy Manager)
Some staff also discussed the COVID-19 vaccine and felt that vaccinating residents and staff had helped increase their safety. However, there were reports that some staff questioned why they needed to have the vaccine or why – when they and their residents were fully vaccinated – they still needed to continue with infection control measures:
‘… why now we’ve had two vaccines, why now are we having three tests a week, one PCR and two lateral flow tests, are we still having to wear masks? Why are we now having to wear visors? You know, it was all kind of, it wasn’t ever promised, but it was almost like, “We’ll have all this, do all this, and then we’ll kind of get back to normal”’.
(Manager)
Concluding remarks
We have highlighted the experiences of CH staff of the restrictions and measures taken in CHs in response to the COVID-19 pandemic. As we have shown, the impact that the COVID-19 pandemic had upon CH staff, and the trauma, fear and guilt they experienced throughout this time, cannot be underestimated. For many CH staff, the difficulties encountered during the pandemic were compounded by the government’s response to CHs and the feelings of being abandoned and undervalued that they experienced during this time. The anger and frustration targeted at staff from residents and their family members further exacerbated CH staff’s difficulties. Social distancing and isolation measures in CHs often proved difficult – and sometimes impossible – for staff to implement, and this led to dilemmas around whether measures were in the best interests of the residents. Concerns were expressed that such measures made CHs feel more like an ‘institution’ than a home and caused them to lose their natural environment and family feel. Many staff also felt that social distancing and isolation denied residents (and themselves) the important need for touch – something they believed played a vital role in CHs. Based upon their own observations and experiences during the pandemic, staff were able to provide many examples of how restrictions and measures had impacted upon care home residents and family members. Chapter 6 explores these experiences and impacts as reported by residents and family members themselves.
Chapter 6 Perspectives of residents and families (Objective 2)
Introduction
Care home residents and family members shared with us their experiences of social distancing, isolation and the broader set of restrictions that affected their lives and relationships during the COVID-19 pandemic. In this chapter, we present their assessments of the communication of new measures and restrictions, their feelings of safety and gratitude to CH staff, and of the impact of COVID-19-related measures – particularly visiting – on their mental and physical health.
Participant characteristics
We were only able to recruit two family members at care home 5. Therefore, we conducted 10 interviews at care home 5 rather than 11. At care home 6, we were only able to recruit two residents who had capacity to consent. In total, we conducted 34 interviews (17 with residents and 17 with family members). Not all data were available for every participant. Tables 3 and 4 present a summary of characteristics of participating residents and family members.
| Ethnicity | White (n = 17) |
|---|---|
| Gender | |
| Female | n = 10 |
| Male | n = 7 |
| Age (years) (no data for two participants) | |
| 55–64 | n = 1 |
| 65–74 | n = 2 |
| 75–84 | n = 4 |
| 85–94 | n = 6 |
| 95–104 | n = 2 |
| Years at the CH (no data for one participant) | |
| 1 or less | n = 2 |
| 2 | n = 6 |
| 3 | n = 4 |
| 4 | n = 1 |
| 5 | n = 2 |
| 6 | n = 1 |
| Receiving nursing care (no data for three participants) | |
| Yes | n = 9 |
| No | n = 5 |
| Dementia diagnosis (no data for one participant) | |
| Yes | n = 2 |
| No | n = 14 |
| Tested positive for COVID-19 (no data for one participant) | |
| Yes | n = 5 |
| No | n = 11 |
| Placed in isolation | |
| Yes | n = 10 |
| No | n = 7 |
| Ethnicity | White (n = 16) Asian/British Asian (n = 1) |
|---|---|
| Gender | |
| Female | n = 13 |
| Male | n = 4 |
| Age (years) (no data for two participants) | |
| 35–44 | n = 1 |
| 45–54 | n = 2 |
| 55–64 | n = 7 |
| 65–74 | n = 4 |
| 75–84 | n = 1 |
| Relationship to participating resident | Son or daughter (n = 2) Spouse or partner (n = 2) Sibling (n = 1) Niece (n = 1) Daughter-in-law (n = 1) Not related to a participating resident (n = 10) |
| Relationship to non-participating resident | Son or daughter (n = 9) Daughter-in-law (n = 1) |
Summary of resident characteristics
Resident participants had several primary health care needs. These included multiple sclerosis, asthma, dementia, Parkinson’s, chronic obstructive pulmonary disease, diabetes, reduction in mobility, arthritis, cancer and heart disease.
Summary of family members’ characteristics
The experience of care home residents
For CH residents, findings are presented for the following: learning about the pandemic and the new rules; one’s own safety and the safety of others; and understanding the role of gratitude towards the EoL. For the experiences of family members findings are presented for the following: acceptance and stress – balancing competing desires; the importance of ‘being there’ – families as carers; gratitude to CH staff; missing physical contact and bending the rules; experiences of remote communication; and learning from the pandemic – perspectives on improving care for older people. To protect the anonymity of residents and family member participants, quotations have not been assigned to specific CHs in this report.
Learning about the pandemic and the new rules
Care home residents living in CHs in Spring 2020 reported first becoming aware of the COVID-19 pandemic through the media (newspapers, television and radio), and from CH staff in March 2020. Some residents noticed signs of increased infection control measures such as mask-wearing by staff and reduced visiting; this was their first indication that the pandemic had the potential to affect their lives. Interestingly, none of the interviewed residents mentioned hearing about the pandemic from family members, though they indeed discussed it with them as the pandemic progressed. As described elsewhere, CHs introduced a raft of measures including restrictions on visiting and other activities, social distancing within the CH and isolation for suspected or confirmed COVID-19 cases. One resident explained how events unfolded at her CH:
‘[T]he management came and told us that we were, it was a virus, and then we were, oh dear, then we, told us about coronavirus, and then they shut the home, closed the home down, and to make sure that we were all safe, and they kept us informed about everything and … I watched the TV and it said, gave me more information …. They told us that there were going to be no visitors because of the pandemic, and they were going to keep us as safe as they could, and I think everybody accepted the fact that we couldn’t have visitors, because if you had visitors they might have brought the pandemic into the home …’.
(Resident 3)
Another resident experienced the sudden introduction of restrictions: her husband was already at the home with her when staff informed them that visiting was being stopped altogether and that he would have to leave. As she described it:
‘Well what happened here was that my husband used to come in and visit nearly every afternoon and he was here one afternoon and one of the care staff came in and said, would he hang on because there was a man who wants to come and visit his relation and they’d told him that he couldn’t and they wanted my husband to wait until this man was safely out of the way or he’d left and that was it really … But obviously when [my husband] came in they hadn’t cited that they were going to restrict it so much. Whether that came, I don’t know whether they suddenly got an instruction from head office, or why, but it was very sudden’.
(Resident 5)
A resident at another study site described how she first heard of COVID-19 when she returned to the CH having been hospitalised with the disease. She was told on her return that the virus had in fact infected her and at that point began to ask questions about it.
We asked residents whether they felt they knew enough about the pandemic and whether they felt confident asking for more information from CH staff. This varied quite considerably. Most residents said that communication from the CH had been good throughout, and they felt informed. Some were hungry for information and found care staff responses to their questions unsatisfactory, while at the same time acknowledging that knowledge and information about the virus – especially in Spring 2020 – were generally very poor and that CH staff did not know any more than they did. Conversely, one resident said that she did not want to know more:
‘Erm … well, to be perfectly honest with you, I don’t want to know too much because too much knowledge is a bad thing at times’.
(Resident 2)
Most residents told us that the measures and restrictions introduced at the CH were also explained well by staff. Some residents, however, felt that staff were not always willing to discuss the measures as thoroughly as they would have liked and complained that communication had been poor. One resident described how he felt infantilised:
‘I don’t like being talked to as a child … Quite a lot of the matters were done in a military fashion … There could be a lot more handling of people and explaining rather than just saying “you sit there, you sit there”, etc. … [The staff] would say as little as they need, we need to know, and sometimes they didn’t know, do they? “You are not going through that door” … “You can’t go downstairs” … So there we go’.
(Resident 10)
While this resident was clearly dissatisfied at how new zoning and social distancing rules were communicated in his CH, he speculated that staff did not always know why specific rules were in place, echoing other respondents who recognised that knowledge about the virus was incomplete. Though he was asking for more clarity, he trusted CH staff in their execution of the rules:
‘I didn’t want to be informed in detail, I don’t want a study of the rules, I want it pointed out to me and made clear. So no, I didn’t question it really. I accept what they say as being truthful and flexible and best for the job …’.
(Resident 10)
However, the same resident also accepted that there were limits to care workers’ abilities to communicate rules fully every time:
‘Yeah, well, they can’t stop and explain everything and reason with everybody, they’ll never get anywhere’.
(Resident 10)
This flexibility and trust on the part of residents was part of a broader attitude towards the pandemic and the consequent changes to their lives. This attitude was characterised by resignation, stoicism and solidarity with one another, with staff and with those outside the CH. One resident summed up this view:
‘Well, I suppose it’s for the best and for our best as well and everyone else’s, so you automatically accept, don’t you? What they say and what you, you know, supposed to do, yes. I don’t think it’s been really terrible or anything …’.
(Resident 6)
Family members were also struck by this attitude, with residents being described as from a generation who are ‘resilient’, ‘stoic and accepting’. One family member we spoke to relayed what his mother had told him:
‘“It’s worse than the war, you know, worse than the war,” she says, “tell you what, got through the war, we’ll get through this”’.
(Family Member 13)
One resident reflected on the appropriateness of the measures and described how she had discussed it with her fellow residents:
‘I think it was right, yes, and I think it was right in us being treated the way we were in the fact that we couldn’t go out and no-one could [come] in … but that’s the way you keep the thing down isn’t it, surely. But everyone was, I think everyone was okay about it, yeah. We accepted it, the people, or the residents that I spoke to …. When I asked them how they felt about it, they just accepted it, they seemed, but that was the right thing to do’.
(Resident 13)
Another resident told us that while the restrictions had affected her mental health, she had accepted the current situation, understanding the rationale for the measures, and hoping for better times in the future:
‘Yes, but I have felt a bit down, but you’ve just got to accept what’s happening and carry on, and as I say hopefully, we’ll have the ultimate goal that we’ll, you know, be able to be going out again, so I’ve just accepted it, like a lot of other people have had to’.
(Resident 3)
One’s own safety and the safety of others
Care home residents told us they felt safe – and had felt safe – during the different phases of the pandemic. This was partly due to their trust in the staff who cared for them during this time. One resident who contracted COVID-19 described her feelings of safety thus:
‘[F]unnily enough I’ve never been really frightened you know. You’d think I’d be frightened but I’ve never really been frightened of it because I thought to myself “I’m in a home here, I’m in a care home, I’m protected by all the care people” … and so it never really frightened me. I think had I been outside and had I lived in a normal house and stuff, I might have been a bit frightened. But I thought “I’m so well protected here”. I was surprised when I heard I’d got it to be quite honest with you’.
(Resident 14)
She attributed her recovery from the illness to the fact of living in a CH:
‘I think if I’d been in a house I wouldn’t have got rid of the virus. I think because I’ve been in a care home with all the carers looking after me and everything it’s helped protect me against any further viruses and I think that’s what’s helped me and I feel that if I’d been in my own house I wouldn’t have got the protection that I’ve been getting in the care home’.
(Resident 14)
One CH resident – in common with several other residents already quoted above – highlighted the trade-off between safety and the negative effect of restrictions, which had seen him forced to give up ‘privileges’ such as going on CH-organised excursions:
‘Yeah. For myself we’ve been kept safe all the time. I’m not complaining about the safeness. We’ve been very good, very good. Kept very safe, you know, very safe. But we haven’t been able to see, give up some privileges for’.
(Resident 4)
Another resident observed that while she certainly felt safe, she also felt removed from the reality of life outside the CH. In her words, she felt almost ‘too safe’:
‘Well yes, I do feel safe. I mean, you know …. In fact, you almost feel too safe, because you get quite gung-ho. I mean you do lose contact … you do obviously get a bit distanced from what’s going on, and you begin to think, well you know, there’s nothing that’s going to [pause] impinge on what you’re, you know, your state of health is, not the sort [pause] it’s not going have any adverse effects on you personally’.
(Resident 5)
Family members also reported their belief that residents were ‘cocooned and protected’ from the ways people outside the CH were experiencing the pandemic. This was partly to do with residents’ different cognitive abilities, which we explore further below. One family respondent described her loved-one’s attitude thus:
‘ [T]he pandemic is sort of secondary to her life, which is great’.
(Family Member 8)
Another resident explained that though her son was focused on her welfare, reassuring her that the CH was a safe place, she nevertheless worried about her family’s safety outside the CH. For her, the measures that she regarded as keeping her safe in the CH were a part of what would also protect those outside the CH. In such a way, she drew connections between her experiences and those of her children, and this sense of solidarity appeared to give her comfort:
‘But, if I say anything to my son, he goes, “Mum, you’re alright where you are, don’t worry”, but I do worry about my children, you know, which, yes, I think, every mother does, don’t they? …. Well, you’ve got to take it [the measures] and it’s for our safety, so you’ve got to put up with things like that because at the end of the day it’s for all our safety. And I want my kids kept safe as well as myself, so they do everything that I would do’.
(Resident 2)
Experiences of life in the care home
While the experiences of safety and attitudes of solidarity discussed above were widespread among the residents we spoke to, their reflections on changed aspects of their everyday lives in the CH during the pandemic – and of the impact of these changes on them – varied greatly. This variation was due to how CH residents used or imagined CH space – and the relationships within it – in the time before the pandemic. This was affected by residents’ level of mobility, health and desire for sociability within or outside the CH. Residents also talked about the longer-term changes to their living arrangements, relationships, health, sense of safety and restriction brought about by the very fact of living in a CH. The stories they tell of the effects of the pandemic-related restrictions are inextricably linked to a broader set of changes experienced by these older people in the latter years of their lives.
Socialising within the care home
The extent to which CH residents socialised with one another – and the ways in which that socialising took place – was affected not only by individual CH policy and practice regarding the use of communal areas or visits to private rooms but also by individual residents’ mobility and attitude to socialising. Many residents we spoke to stated that they had spent more time alone than before the pandemic. This was due to a variety of reasons. One resident described how her CH had instituted a new practice early in the pandemic of serving meals to residents in their own rooms and closing the dining areas. She discovered that she preferred eating alone in her room rather than being compelled into sociability around dining tables with other residents. She told us,
‘To be honest there was hardly sort of scintillating conversation at the table, and I’m quite happy now you see I eat in my room’.
(Resident 5)
Nevertheless, this resident thought this new routine had made her more reluctant to leave her room once restrictions were eased and residents were allowed to dine in pairs and then in larger groups again. She believed that this reluctance to socialise with other residents had had an overall negative effect on her mental health, even if dining alone in her room seemed to suit her better. Before the pandemic, this resident had maintained an active social life outside the CH, met her husband several times a week and saw non-CH friends. The restrictions on doing that had compounded her feelings of depression, especially as she did not cultivate friendships with other residents.
‘I haven’t got any friends; well I haven’t really got any friends [in the care home]. I’m on friendly terms with everybody, but I’m not actually friends with anyone, which sounds very unsociable, but it’s just the way it is really. We have, my husband and I had a very active social life in as, well you know, I used to go home Saturdays and Sundays for the day, and on Wednesdays we usually used to go out for a meal and coupled with the fact that he was here every afternoon anyway. So, my life has changed enormously’.
(Resident 5)
Though she spent so much time in her room, she did not like the room itself, which contributed to her feelings of depression. As part of the CH’s reorganisation of space during the pandemic, her previous room had now become a staff dressing area and she had been moved to a room on a lower floor. Whereas her former room had large windows, her new room had smaller, higher windows, which meant that from the wheelchair she used, she could no longer comfortably look at the world outside.
Similarly, another resident told us the restrictions within the CH had not affected her because she did not mix much anyway. For her, the restrictions on family visiting and leaving the CH had had more of an effect: she missed, for instance, not being able to go out for dinner with her son. This inability to socialise with her family outside the CH or be able to have visitors meant that she found herself watching more television than usual. This was not only to learn about the course of the pandemic but also because she was worried that in her state of reduced sociability, her mental abilities would degenerate:
‘… that’s why I say, again, it’s why I watch so much television, stop it, to try and keep my mind going, yes’.
(Resident 11)
Families also recognised the impact restrictions in socialising and pursuing activities outside the CH had on residents. As one family respondent, who had enjoyed accompanying her mother to the cinema told us:
‘There’s one or two people that she was quite friendly with and used to like to, again we had a cinema session once a week and we used to always see the same people at the cinema, we could chat about the films and have an ice cream with them and things. So she’ll miss that. So, yeah, I think she’ll have missed the socialising quite a lot’.
(Family Member 12)
These examples highlight the experience of residents who view the CH as a base from which to conduct and pursue their social lives beyond its walls. The CH itself is not necessarily a source of valued relations. Therefore, they were affected by the restrictions on visiting more than by restrictions dealing with social activity among residents within the CH. However, other interview participants did maintain or pursue friendships with their fellow residents and enjoyed eating with them and chatting. For two residents we spoke to – and who regard each other as friends – the pandemic restrictions had not adversely affected their relationship. One of these friends reported that she felt their friendship had grown stronger because of the shared challenges they had faced.
Other residents enjoyed taking part together in the activities put on by CH staff to mitigate some of the effects of the restrictions. These included doing arts and crafts, watching entertainers over Zoom, celebrations for pancake day, 60-second events, significant national memorial days, anniversaries, cultural and religious notable days/events, celebrations, cake-baking, card-making and word games, as well as going on virtual trips. Family members remarked on the positive impact of these activities and the crucial role of the well-being or activities co-ordinator in acting on signs of depression or isolation in residents.
‘I only learned recently she’s had one or two incidents where she’s felt pretty low and I think that’s, you know, probably because she wasn’t able to see us. But the well-being co-ordinator here has noticed it and, you know, managed to bring her round from it. So yeah, but at least, you know, there are people around to recognise that and to help her with it, which is good’.
(Family Member 2)
Another family member described the impact on his mother of a dedicated activities and well-being team:
‘A specialist team … was brought in and, you know, I met with two or three of these people and they were really good, really nice, there was two young women and they were really good with Mum, and the other residents, and that did make a difference, that really did, that helped, I can say that’.
(Family Member 13)
In some CHs, these activities started in a later phase of the pandemic. A family member of a resident at one CH shared that activities had initially stopped completely before being reconfigured with smaller groups on a rota basis on different days; a similar approach was adopted for dining arrangements. This family member highlighted how the CH had learnt from previous experiences:
‘I think it (being able to participate in activities) has improved. I think that the home were learning a lot from the first lockdown and as things have improved, I mean they still did the activities, how on earth they managed to organise things by distancing people I do not know, it’s incredible. But I’ve got a feeling that things are not so much back to normal but a new normal and she’s participating again’.
(Family Member 4)
However, activities in communal areas could not totally satisfy residents’ need for socialising. One resident was frustrated by rules against visiting other residents in their rooms. He had learnt that a new resident from a part of the country where he had once lived had moved into the CH, and he was very keen to meet him. But the new resident was unable to leave his room, so they had not met. This example also highlights the effect of restrictions on those with limited mobility or other health conditions. Several residents we spoke to described how the restrictions on socialising within the CH affected them very little because they seldom left their rooms. For instance, one resident who used a wheelchair described how he had spent more time in the garden during the period of restrictions but that he had not spent any more or less time alone: his health condition tired him in any case, so social interactions became exhausting after a while. Another wheelchair user told us how her ability to participate in activities such as painting with other residents depended on how many other wheelchair users wanted to do the same activity; staff could not escort everyone.
Other residents placed the pandemic restrictions – and the loneliness, frustration and depression they caused – within the context of their changed lives since entering the CH. For these CH residents, the specific pandemic restrictions merely amplified their feelings of restriction more generally. One interviewee – the man referred to above who was desperate to meet his new fellow resident – summed up CH life thus:
‘Only important thing is your mind, stretching your mind. You don’t get a chance to stretch your mind much. Yeah, and visit somebody, I can visit another room, talk to another bloke or something, or go out. That’s about it isn’t it?’
(Resident 4)
Another resident chaffed against the zoning policy practised by his CH, which meant that he could not play the piano on the floor below. Having entered the CH during the pandemic, he appeared to be struggling with the very fact of living in a CH:
‘The pandemic isn’t the thing to me, the main thing is the concept of living in a place like this as opposed to the alternatives’.
(Resident 10)
By contrast, another interviewee emphasised how being in the CH was far less restrictive than at home. He had spent most of the pandemic trapped in a flat and had moved into his CH in Spring 2021 as restrictions began to be eased:
‘[B]ecause I personally couldn’t get up and down because of the stairs in the flat, so I was restricted to the flat itself and the balcony. That was my limit. We’d go out on the landing but to go up or down it would be risky you know, up and down on the stairs, so I was very restricted, but here I can seem to be able to get around with the Zimmer fairly easy, it’s been awkward at times but, yes’.
(Resident 15)
The steps taken by residents to adapt to the changes caused by pandemic-related and other restrictions were influenced by their ability to exercise choice and control over their lives. As we have described, this may have been choosing to participate in activities or deciding that taking meals in one’s bedroom was better than dining with other residents. These elements of choice also included involvement in the decision-making about the move to live in a CH and the extent to which CH residents were reconciled to their new situation. One family member described how her mother had adjusted to the CH life during the pandemic:
‘She’s quite happy because she loves it here; it was her choice she wanted to go into a care home’.
(Family Member 9)
Residents’ varying cognitive abilities may also have affected the ways in which they experienced restrictions. Family members offered these speculations about how residents at different stages of dementia might understand their predicament:
‘I think those with kind of less advanced dementia would have suffered more I think, or those without dementia, those that are just purely residential who are used to coming and going, having their own freedom, that would have been really tough, just suddenly a lockdown in the household, not able to go out so yes, they would have suffered more. My mum and other people I think with the more advanced dementia probably don’t realise to what extent what’s going on so I don’t think it would have affected them too badly in that way, in that respect’.
(Family Member 11)
Other relatives felt that residents who did not understand the circumstances of their changed lives would struggle:
‘I feel that because she hasn’t got dementia that it’s better for her because she understands it. I think it could be really horrific if you’ve got a relative in here who has got a type of dementia, because they don’t understand. You know, my mum she had vascular dementia after having two strokes and I’m really pleased that she wasn’t around, I mean she died bless, she was 99’.
(Family Member 9)
Our presentation above demonstrates that residents had layered understandings and experiences of ‘restrictions’. They were not simply understood as pandemic-related restrictions but were embedded in other reflections on what it means to live a restricted life as one grows older, whether in a CH or outside it.
Residents’ experiences of isolation
Care homes isolated residents who were suspected or confirmed COVID-19 cases. CHs also required residents to isolate on admission to the CH and when returning from hospital. As described in earlier sections of the report, isolation lasted for 10 or 14 days, depending on the policy at the time. In two of our CH sites, all residents had been confined to their rooms at the start of the pandemic in March 2020. Some CHs created ‘isolation zones’ staffed by a specific team; others allocated one dedicated staff member to an isolated resident. Few of our resident participants had experienced isolation directly. We spoke to one resident who returned from hospital having recovered from COVID and entered isolation for 2 weeks at her CH. She was isolated in a different room to her own and staff would visit her to deliver food. She told us that staff did not stay to chat with her, which she attributed to their risk of being infected:
‘Yeah, they weren’t supposed to stay long with me, they were just supposed to deliver my food and that’s it, they weren’t supposed to have much conversation with me because you know … they didn’t have any protection really themselves and they couldn’t, if they started having a conversation with me they would have, they might have caught the infection, you know?’
(Resident 14)
She did not have a mobile phone and no phone was brought to her. This meant that her friends and family could not contact her during this time.
‘You know and like when I had any phone calls you know, people that normally phone me, I couldn’t take the calls, I wasn’t allowed to have any calls because that meant I would go out the room to take the calls and that I wasn’t allowed to do’.
(Resident 14)
She vividly described how she felt when her isolation period ended:
‘All I know is when they opened that door I ran into the lounge [laughs] sounds ridiculous doesn’t it, it did have a bad effect I must say, I thought God almighty I never want to have to go through that again’.
Isolation was difficult for residents and elicited strong reactions from those who remembered experiencing it. Another resident who had to isolate on return from hospital gave his verdict:
‘Terrible. Don’t like that. And I realise it had to be done so I did it’.
(Resident 4)
Some family members were aware that their relative had probably been placed in isolation at some point (e.g. on returning from hospital or receiving a positive COVID-19 result) but were often unable to talk about those periods precisely; for some, they seemed to become part of the general raft of restrictions faced by residents. They also sometimes failed to distinguish between formal isolation and informal, self-imposed isolation (e.g. choosing to take meals in one’s room rather than communally). However, some family members reported that they thought that a period of formal isolation was likely to negatively impact residents’ physical, mental and emotional well-being. A family member told us:
‘I think probably the isolation, the more isolation because I think they’ve had to spend more time in their rooms because they were having to be careful with transmission of infection etc. But I think that may have affected her. Because the first time I saw her after the first lockdown she had deteriorated, physically and mentally. But then again, I think she probably would have done anyway. But I think the longer periods spent in her room probably did have an impact’.
(Family Member 4)
The quote above from a family member also reveals the uncertainty of knowing the effects of isolation or other measures on residents. This was particularly the case for those residents with advanced cognitive decline who could not fully express how they were feeling. The family member of one such resident told us that since her isolating mother had a comfortable bedroom, she was unlikely to have been badly affected.
Contact with family and friends
For most residents, contact with family and friends changed dramatically. Visiting stopped and was replaced in many cases with virtual forms of contact through communication tools such as tablets, smartphones, WhatsApp or Zoom. When visiting was permitted once more, rules on close contact, location, length of visit and numbers of visitors were introduced. Depending on their circumstances, CH residents experienced these restrictions differently.
Many residents adjusted to using smartphones and tablets to keep in touch with family and friends through video calls; others seemed to use video calls less often but made conventional audio calls. For those residents whose family and friends did not live locally, communicating remotely in this way was not unusual and was a continuation from pre-pandemic times. Others reiterated that the prohibition on visiting at specific points during 2020 and 2021 was not dissimilar to restrictions faced by people outside the CH. For instance, one resident described how she read with her grandchildren over video call while the schools were closed in ways that she said many grandparents had done over the pandemic. Those residents with personal access to advanced video-calling technology provided by their relatives – and with the skills to operate it – appreciated the autonomy it afforded them; they did not rely on staff to facilitate calls and so could make contact with friends and family at times that suited them. This contrasted with those residents – such as the participant whose experience of isolation we presented above – who did not own a mobile phone or could not operate one.
Most residents reported that their mental health deteriorated because of the lack of visits by loved ones. One resident told us:
‘Yeah. I do sometimes [feel low] when I think, you know, someone will come and see me. Had friends and neighbours who would love to come, they used to come before this started but now I haven’t seen them for a good while. But there, law is law … I have to sort of grin and bear it’.
(Resident 8)
Another resident who likewise maintained close relationships with her friends and family outside the CH pre-pandemic described her frustration and the effect on her mental health:
‘Yeah, we couldn’t just go where we wanted to go, we couldn’t just walk about anywhere. We couldn’t go out and don’t forget I hadn’t been out at that point for almost 2 years. Not been out at all. The worse thing was not seeing my family, that was terrible, absolutely terrible but when I knew about it, the COVID and everything, I knew that was going to happen. I knew there was going to be problems with people getting mental illness because I suffered with it myself’.
(Resident 13)
Visiting with restrictions brought its own challenges; again, these were influenced by how residents conceived of CH life and space more generally. Residents worried about the comfort of their visitors especially in instances of ‘window visits’, in which the visitor would stand outside the CH and speak to the resident through a window. One resident described it thus:
‘Well, it’s better now because originally, she had to stay outside and there’s a corridor as you come into the main entrance which abuts the admin office, so they used to push me into the admin office and [Name] used to be outside, they used to open the window. I mean we’re talking about horrendous cold, windy and so on. So, then they’ve now moved us to an interior room, which is far better, far better’.
(Resident 9)
In many CHs, visiting was permitted in designated rooms with a member of staff present or with the door ajar so that staff could observe interactions and ensure that visitors were not touching residents or otherwise compromising social distancing rules. Some residents found this an infringement of their privacy. While some CHs opened their gardens for visiting, one CH did not because, as a resident explained, they could not ensure that visitors and residents would keep apart, a stance she found insulting:
‘… they wouldn’t allow [garden visits] because they told [my husband] that it would be difficult to ensure that everybody was keeping a safe distance, which frankly struck us as slightly patronising’.
(Resident 5)
Some residents (and not necessarily only those with hearing impairments) found it challenging to communicate effectively when sitting at a distance from their visitors or when visitors wore masks, which affected their enjoyment of the encounter:
‘The mask on when they come. So it’s difficult to talk a lot really with those on. Never mind, as long as I see them’.
(Resident 8)
Residents also complained about the restrictions on the numbers of people that could visit them at any one time and about the limited duration of visits. This same resident quoted directly above, and who otherwise maintained an extensive network of social relations outside the CH, the restrictions on the number of visitors meant that she would see her friends less often than she would like:
‘But now he’s only able to bring one [friend], in fact I was talking to some friends the other day and she said, either they’ll have to take it in turns to come in with my husband, but they are limited of course because, well we have got quite a lot of friends, so you can only bring one, or before they had the limit, two, in at a time. So you know, you only see them occasionally …’.
(Resident 5)
Understanding the role of gratitude towards the end of life
We have described how residents experienced measures and restrictions in their CHs and the effects such restrictions had on their mental health and their ability to maintain social relations. As we showed, these varied according to how residents understand the place of the CH in their lives and their level of mobility and general health. We also explored how residents expressed a sense of solidarity with each other, CH staff, family and society more broadly. Residents also expressed gratitude for the care they received from CH staff during the period of restrictions, recognising that care workers had performed services such as hairdressing, entertaining and nail-cutting that external professionals would ordinarily do. This gratitude was linked to the feelings of safety residents described and which we reported above.
There was also a broader sense of gratitude that CH residents expressed in their interviews with us that was also associated with safety and well-being beyond the pandemic. Residents sometimes described how they were thankful for having survived for as many years as they had. One resident explained, for instance, that she owed her present state of health and well-being to the care she received from her care workers:
‘To be perfectly honest, I didn’t think I would last this long, and four years later, owing to these girls and this staff, I am still here four years later. And I couldn’t feel better … I didn’t think I’d live this long, nowhere near, you know. And, when I first come in here, I thought, well, that’s it, you know, the end is nigh. But it’s taking a long time coming’.
(Resident 2)
We suggest that a sentiment such as this needs to be considered to understand the experience of restrictions for some CH residents. It reminds us that the perspective of those who are conscious of being in the final years of their life may have different understandings of ‘restrictions’ to people in other situations. In this example, the resident here seems to be saying that the pandemic and its associated restrictions ought to be put in the context of her unexpectedly long life, given to her by the CH; as such, the restrictions do not dominate her perspective. This point is made even more strongly by the experiences of another resident who was approaching the end of his life. He described how he and his wife lived in the CH and had separate rooms due to their different care needs. Despite being in the same home – and in adjoining rooms – they had not been allowed to see one another while restrictions remained in place: both were regarded as extremely vulnerable, and his wife had significant cognitive impairment. They communicated through video calls. His health deteriorated over the pandemic period and he was admitted to the hospital to treat a leg infection. Concerned that he would die in hospital, he wanted to return to the CH so that his wife could see him in that setting. The CH organised this for which he was grateful. While this resident talked to us about the effect of the restrictions on the comfort of visitors and the difficulty he had in hearing them at a distance, his main concern was ensuring he ‘showed a decent burial’ to his wife. While the restrictions on not seeing his wife might seem draconian, he did not think so; in fact, given that he had been able to return to the CH from the hospital and was still alive, he told us:
‘I just thank God I’m able to have some contact with her’.
(Resident 12)
The experiences of family members
We have described above some of the impacts on residents of restrictions on visiting and socialising. Residents’ relatives also talked to us at length about the effect of such restrictions on their own mental health and well-being and of their relationships with their cared-for loved ones. We look here in detail at relatives’ understanding of the necessity of restrictions and the ways in which they balanced this with their desire to be close to residents in ways they found satisfying. It became clear that living in that balance provoked profound moral dilemmas for families as they made decisions about the risks of contact in a situation of great uncertainty. This uncertainty was linked to constantly changing information about the virus and the inconsistent – as it appeared to them – government and CH guidance about what was safe or not. We also look at how families experienced the lack of physical contact with residents and how various forms of remote communication helped or failed to help mitigate that lack of presence.
Acceptance and stress: balancing competing desires
Several family members emphasised that they had accepted the need for restrictions on visiting as essential to keeping their family members safe from COVID-19. These restrictions ranged over time from a total ban on outsiders to visiting with enhanced measures such as testing, social distancing, mask-wearing, specified visiting areas, and time and visitor limits. Relatives were concerned not only about the safety of their family members but also of other residents. One relative described how the absence of COVID-19 in the CH demonstrated the rightness of the decision to restrict visiting severely:
‘They’ve obviously restricted the visiting, which I find difficult, but I understand the reason why. They’ve been COVID free and if that’s what you’ve got to do to ensure it then … I must admit, I’m glad that they did it, do you know what I mean, although it wasn’t the best option for me or me mum. In the long run obviously, she’s not got COVID and nobody in that care home has, so I’d say they’ve done a good job’.
(Family Member 6)
However, while family members accepted the restrictions, many told us that they were not always sure how or why decisions about guidance and implementation were made. As one relative said:
‘A question I would ask … is to what extent the restrictions are governed by guidance as against law, because we, outside the home we have legal restrictions on what we can do as well as the “hands, face, space” type general things. So I’m not, I suppose one thing, I’m not quite clear is to how much flexibility the home managers have in terms of what is mandatory. I haven’t asked the question so I don’t know the answer but it’s not quite clear to me what ultimately governs their protocols and practices’.
(Family Member 5)
This sense of not knowing how or why guidance was being changed or whether CHs had flexibility in implementing guidance added to the feelings of anxiety and calculating risk that pervaded relatives’ lives during 2020–21. Some family members described the additional work and thought that went into restricting their own social lives outside the CH to minimise the chances of transmission when visiting residents. One relative told us how these concerns affected him:
‘… there’s always that concern, mortifying that you would pass on something, how could you sort of easily live with yourself thinking, “oh did I do that, was that me?”, you know? So yeah, I’m not, obviously that goes for a lot of people, but there is that additional level of stress and strain on top, stress and strain, worry, concern, on top of having a loved one in a care home in the first instance, yeah, who’s elderly with dementia. So we’ve got that level, and then you’ve got all these other complexities on top of that now.’
(Family Member 14)
Several family members spoke of the moral dilemma of balancing the risk of transmission of COVID-19 to CH residents and staff with the desire to see residents in person:
‘I know we have tests, we come in with the swab tests, etc., etc., but I wouldn’t want to risk Mum’s health, or of course what we all have to think about, what we should all be thinking about is if the virus gets back inside the care home you’re putting all of the residents, you know, in jeopardy and of course the carers that look after Mum’.
(Family Member 13)
These stresses and dilemmas were also bound up with relatives’ fear that – in the absence of visiting – their family member would die in the CH before restrictions were lifted allowing them to see each other in person. Several family members described how phone calls to and from the CH – while welcome forms of communication – became a particular source of anxiety:
‘… it’s just really hard, it’s hard because my way of life now, and my way of thinking have totally changed, and both me and my sister we can’t relax. Each day we will ring. One of us decides the night before, right, who’s ringing about Mum today, so we ring every day, we try at 11, half past 11, and we can’t relax until we know that we are told Mum’s okay … and then we relax for the rest of the day. But if our phone goes, straightaway we panic, and then when you see [CH name number] [laughs] you go into an even bigger panic, to the point now that [CH name staff] when I answer the phone will go, “It’s fine, your mum’s okay,” just because we’re so scared that we’re going to lose her, and before we get to see her, so it’s literally changed all of our well-being, and it’s affected us’.
(Family Member 3)
The importance of ‘being there’: families as carers
We described for residents above how the extent to which restrictions affected people was connected to their different experiences of CHs as bases of valued social relations. This is also held for family members. Anxieties and stress were also enhanced for those family members who had been centrally involved in the resident’s life before the pandemic and who contributed to the CH community, regarding themselves as part of the ‘care home family’. Not being allowed to visit was like missing a part of one’s life:
‘I found it very difficult because prior to the COVID epidemic starting, I was here, in the home, several times a week, interacting with the staff, interacting with the people that [Name of resident] lives with … and so I felt part of the [Name of CH] family. I came to help, I run the poetry sessions that they had. And [I] also came to the regular quiz sessions that they have and used the café a lot. The whole family used to come on Sunday, that’s myself, my two sons, my husband, my sister, and we all sat down in the bistro and played dominoes and, you know, had a coffee and just had a sort of, you know, a relaxed family gathering, and that was sort of once a week, once a fortnight. So we were able to have regular get-togethers. And so going from that to nothing except a phone call made it very difficult’.
(Family Member 12)
Another element of variability among families was the length of time their relative had been already resident in the CH before the pandemic, and its associated restrictions began. For families whose loved ones had moved into the CH during the pandemic (and were therefore trying to adjust to new forms of caring), there were additional feelings of powerlessness about having to ‘step away’ from the role as carer they had hitherto occupied. There was anger and heartbreak of not being able to be present at such a significant transition in their older relative’s life. One daughter described how her mother had been receiving intermediate care and had been relatively independent but had now developed vascular dementia. Her mother was non-weight bearing and needed different types of care at the CH. She told us:
‘Throw into the mix that we couldn’t get anywhere near her, and it was heart-breaking … we were upset, we were angry at the situation, angry that we felt we’d missed Mum, if we’re being brutally honest, but we were angry that we couldn’t then get in there and comfort her.. And yeah, it was just that we’ve just felt helpless because we had to sit back and watch Mum go through a really traumatic time … and it was just heart-breaking that we just couldn’t get in there and just give her a big hug, and hold her hand, which is all that she actually wanted from us to be honest’.
(Family Member 3)
Some family members reported that they believed the pandemic restrictions, which did not allow them to support residents’ care, had exacerbated their loved-one’s physical health decline. For instance, families often kept residents to their prescribed exercise regimens and encouraged regular walking. One relative said:
‘I think if it wasn’t for a pandemic, I think my mum would be walking now because we would have pushed her every step of the way’.
(Family Member 1)
Another reported the following:
‘Well, when I was coming in every day I made him do his exercises and stood over him and helped him, but without me actually standing over him his motivation is not very high, so he’s not been doing them’.
(Family Member 7)
Gratitude to care home staff
There were multiple expressions of gratitude from family members to CH providers, managers and staff for the additional COVID-19-related work, coping with exceptional busyness and challenges of keeping residents and staff free from infection. Families were confident that CHs were safer than other places and that, in the absence of physical visiting, they could reassure themselves that their loved ones were well-treated and happy. One relative told us:
‘my mum every time I see her when she’s alert and not dipping her biscuits in her coffee, she looks well cared for, she looks happy, she looks content, I watched the body language with my mum, and either [name of carer] or [name of carer], or any of the other carers that are there on FaceTime, and she’s well at ease, and she loves them just as much as they love her, and that means the world to us as a family, so they’ve been really, really supportive’.
(Family Member 3)
This was especially the case for those families with relatives who had more complex needs such as Alzheimer’s or other types of dementia. One family relayed how her resident relative described the care she received:
‘… and she’s told me that if she’s in pain at night one of the nurses will sit on the bed and hold her hand and I just think that’s amazing. Yeah. And that then she describes the water fairy who comes in the middle of night to give her a glass of water because she might wake up with a dry mouth’.
(Family Member 8)
For some family members, there was a recognition that residents were forming new relationships with care workers in the absence of family. The families spoke of having to rely on staff to ‘do their job’ and residents having a new reality because of the measures to prevent and control the transmission of COVID-19. While this brought comfort and reassurance to families, for some this was coupled with sadness that the resident was forgetting them:
‘I’ll probably get a bit upset now, but I saw her in December [gets upset] and she doesn’t know who we are, [pause]. The only thing I would say is how we’ve come to terms with it, the only thing with coming to terms with it is she is happy, she isn’t distressed, she is well cared for, and she’s loved here, she really is [gets upset], so when I see her and she’s laughing and she’s taking part in stuff, I just think, do you know what, things could be a lot worse … It is that bit about not knowing who we are, that’s the hardest bit to cope with’.
(Family Member 1).
Some CHs recognised the risks of residents and families losing touch, especially for residents with conditions of progressive cognitive decline. One family member reported that the CH assembled a memory box as a way of activating connection in the absence of relatives’ physical presence:
‘the home have been really good, they asked us for lots of photographs, memorabilia and stuff like that, so I did a whole box, labelled up all the names of who the family members were, and where it was, and holidays that she used to go on, so they’ve been able to use that box to do a lot of the dementia support, with her, to keep her brain going’.
(Family Member 1)
Missing physical contact and bending the rules
The loss of physical contact with residents was described by several family members when they spoke about the impact of visiting restrictions on their well-being. Not being permitted to have physical contact with residents caused distress, with families sharing the impact on them of not being able to hug and kiss residents:
‘So again, all you want to do is, you know, every time I used to walk into my mum’s flat, “Hi Mum, give us a kiss,” and you know, as she went, “Bye Mum, give me a kiss,” and it’s not being able to do that for 10 months has literally gutted us all to be honest. It really has, yeah’.
(Family Member 3)
Changes to guidance on visiting over the course of the pandemic meant that social visitors began to be allowed onto CH premises. Visitors and residents were sometimes separated by a screen or used a bespoke visiting pod; they were often instructed to keep 2 m apart. While screens were welcomed as allowing in person visiting, where previously none had been, they nevertheless posed challenges. A family member below described how the position of the screens hindered communication with their resident relative:
‘And then they moved to the system whereby [name of resident] was the other side of a window with a screen between him and the window, and I was sitting outside. It was in the winter-time – not very pleasant. But what we found was I got reflected in the screen that was inside between him and the window, so all I could see was me, and he had exactly the same effect the other side. So, all he could see was him. So, we were talking blindly to each other, and he lip reads, so we struggled greatly with that, and particularly when I had to wear a mask’.
(Family Member 7)
Even when visits were permitted, physical contact was not always possible, and this was described as unsatisfying and, on occasion, resulted in families feeling more isolated from residents. As one relative described it:
‘I didn’t want to miss out on the physical visits, because it just felt nice being that close to him, but it was quite frustrating because it didn’t provide what we expected. So, the visits were a bit stilted and little bit, not uncomfortable, but unrewarding shall we say’.
(Family Member 7)
However, despite the rules on visiting, the desire to touch became overwhelming for some. We have described in Chapter 5 and above (for residents) how CH staff worried that residents and visitors would break social distancing requirements. On occasion, family members did have physical contact with their resident relatives in ways that were not officially permitted. As one family member told us:
‘I do social distancing, I do socially distance for quite a lot of the time but when I’m in the room and I’m with Mum I can give her a hug. I can give her a hug, she needs it’.
(Family Member 17)
Workarounds for physical contact restrictions included, in one CH, finding ways for family members to provide forms of personal care such as helping with meals or brushing hair. This structured way of resident–family member interaction was somehow more acceptable for CH staff. For instance, one visitor described giving her mother a manicure:
‘ [W]e’ve missed the hugs a lot, I’ve missed the hugs and she’s a very touchy-feely person so she does like to be touched. So what I’ve been doing when I have come in, just for the indoor visits, is the ladies provide me with things that I can do a manicure for her. So, you know, I’m touching her hands and massaging her hands a lot, and she loves having her nails done in something sparkly’.
(Family Member 12)
Another family member described how she took the opportunity of her mother visiting the hospital to physically touch her, partly to alleviate the sense of loss she felt in not being able to care for her:
‘She needed to go to the hospital, that was the first time I was able to touch my mum again and hug her and whether it’s remorse of not being able to take care of her or it was just being able to give her a kiss and a cuddle and smell her skin, even if I’m not allowed to actually touch her, that meant a lot because we spent … we spent a couple of hours together in hospital’.
(Family Member 16)
As described in the previous chapter, mask-wearing requirements also made connection and communication difficult. A family member shared how difficult it had been to tell his mother about a family bereavement while wearing a mask and not being able to comfort her by hugging her or holding her hand:
‘… having to give bad news to an elderly relative, my mother, wearing a mask means she couldn’t see my face and I couldn’t hug her, or touch her hand, as such, to you know, because her face crumbled and she had tears in her eyes, and it was just, added an extra layer of pain between us on a situation of telling something about a death, and of course it was linked to COVID’.
(Family Member 13)
Family members’ experiences of remote communication
As we described above in the section on residents, and elsewhere (see Chapter 5), CHs introduced various communication technologies during the period of visitor restrictions to facilitate communication between residents and their families and friends, and aid communication between CHs and families. We have described the challenges of using such technology elsewhere (see Chapter 5). Family members also told us that the experience of remotely communicating with residents was less personal for some, with typically a lot of background noise and activity. However, while it was not a perfect means of communication, it was still ‘far better than having none’. Some relatives told us that remote communication did not give them a full picture of residents’ condition and well-being; their preference was to be with the older person ‘to see her with my own eyes and, you know, and make my judgements’ (Family Member 3). They sought out signs from video calls, for example the condition of the resident’s skin, and whether the resident’s hair appeared brushed to reassure themselves that residents were always cared for well:
‘So she’s cared for, her skin’s cared her, her skin, her face, skin like alabaster on her face, beautiful skin, she’s 91 years of age, that remains, there’s still a head of hair, always brushed, her teeth are always cleaned, and I’ve got to me, we, I’ve got to believe that that is how our mum is, when we’re not there, and we’ve got no reason, her room, all her stuff around her room is always kept safe and her laundry’s done’.
(Family Member 10)
Other relatives realised that communicating remotely suited them better than the still restricted physical visits. For example, communicating by video-phone enabled personal conversations to continue between a husband and wife:
‘Well, very early on, my children bought [my husband] a video-phone, and it’s like a small television screen and we use Skype on it …. And we found those much more satisfactory than the physical visits …. So, we came to the conclusion that the chats we had on his video-phone were much more enjoyable actually, and he saved all the things, the important things he wanted to tell me for when we were on the video-phone’.
(Family Member 7)
Another family member respondent told us that regular FaceTime calls between her cognitively declining mother and family members had improved her mother’s mental well-being:
‘From July onwards my mum really, really deteriorated and we thought at one point we were actually going to lose her, so we actually put in place daily, or every other day FaceTimes … and we actually found that helped my mum, because we were losing her, we were aware she was just drifting away from us. But by us seeing her each day and reminding her who we all were, kind of helped and that the home here were brilliant with that, and you know, we had daily FaceTime calls and we noticed within about a week that really improved’.
(Family Member 3)
Families were keen to continue communicating remotely with residents. They had also allowed better connections to be built among generations of a family, especially in situations where children and grandchildren lived far away from the CH or could not otherwise visit often. One relative told us:
‘[Mum] has been Skyping with children, grandchildren and so on, which was something that we actually didn’t do before but is something that has actually been very meaningful for her and even when restrictions are off, I think that’s something that will be a legacy you know, a benefit that she’s got used to doing that now and taking calls from the grandchildren so yes, so I think that’s all helped to keep her connected’.
(Family Member 5)
Families valued the various initiatives implemented by CHs to share information and updates about their resident relatives’ welfare and the pandemic situation more broadly. Most took the view that CHs were ‘very good at keeping in touch’. Communication took several forms: email newsletters from the CEO or CH managers, which in some cases had been ‘ramped up a bit’ since the start of the pandemic; notifications regarding any confirmed cases of COVID-19; telephone calls, for example, from a well-being team member if residents needed personal items such as new clothing or family telephoning to ask for a resident update; family feedback sessions facilitated by CHs using applications such as Zoom/WhatsApp/FaceTime; posting online photographs of residents participating in various activities and entertainment. One relative commented:
‘The pictures on Facebook are invaluable to families, absolutely, seeing what they’re doing, I mean you don’t always get a picture of your loved one in it, but you can see what they’re doing, so and birthdays as well go on, so you can see they’re celebrating birthdays and everybody gets cake and stuff like that’.
(Family Member 1)
Some family members mentioned applications such as the Relatives Gateway platform produced by Person Centred Software, which was upgraded during the pandemic to incorporate video-calling functionality:
‘You can see pictures of Mum, you can have a video-link, which we’d never used, and there’s a daily morning, afternoon and night-time debrief on the Gateway’.
(Family Member 10)
Learning from the pandemic: perspectives on improving care for older people
Family members often talked at length about what CHs and the government could learn from the experience of the COVID-19 pandemic. Several relatives suggested that CHs and others should develop and plan better infrastructure for remote communication between residents and the outside world, paying attention to residents and families’ diversity of needs and abilities. One family member proposed the establishment of a dedicated communication room within CHs:
‘I’d definitely like to see more fixed video-settings, not sort of like a WhatsApp phone in the lounge, etc., I’d like to see dedicated areas for it, and I’d you know, obviously that it’s partly this is a space consideration and a time consideration for the staff members that are, you know, are on duty, but I’d like to see that, I’d like to see something more formal, and perhaps an easier to access and you know, engage and book slots, etc., and have them in a diary’.
(Family Member 13)
In addition to facilitating connections for residents via digital technologies, some family members spoke about the importance of connecting residents with the outdoors and nature, which would not only be helpful in times of epidemic but also be more generally for residents’ physical and emotional health and well-being. This might require rethinking CH space:
‘I would go back to almost like a monastery design with a courtyard in the middle that’s covered, that you can walk, I don’t want you to run round it, I want you just to be able to walk around it and see some flowers. So you’re having some exercise and you’re getting some nature and I think that’s what, that was what I feel my mum and a lot of people need. I would say that would be my first thing is you must be able to get them out somehow, outside’.
(Family Member 12).
Relatives and residents told us about the importance of ensuring that the relevant authorities (CH groups, UK government) learnt from the findings of our study and other research on the sector’s experiences of COVID-19. They emphasised the following points as necessary for authorities to reflect on: earlier COVID-19 testing for people coming into CHs from the hospital and other settings; earlier implementation of IPC measures; clear, coherent and consistent social distancing guidance; emergency teams to target support for CHs with COVID-19 cases. One relative said:
‘… as with everything in life, hindsight is a wonderful thing and last year when hospitals were allowed to discharge patients who’d had COVID but didn’t test them before they left and sent them to care homes, that was just an accident waiting to happen’.
(Family Member 8)
Another complained that measures that would have eased communication and visiting were introduced relatively late after the pandemic had begun:
‘I would like to have seen earlier on perhaps a situation where you have like, you know, Perspex and chairs either side, even if you’re wearing masks, if the resident was wearing a mask and the person coming to visit them was wearing a mask, I would have liked to have seen that done, done early, that the actual sort of screen didn’t arrive in the marquee until quite late, yeah. I on behalf of the family, the family purchased the marquee for the garden here’.
(Family Member 13)
Balancing risk, choice and control in policy-making was discussed by several family members. Some relatives made it clear that in the event of another pandemic, CHs should not be sealed off from the outside world. This was because of the detrimental consequences for residents (particularly those living with dementia) they had observed during 2020–21. One family member told us:
‘I think it’s don’t lock, don’t lock care homes down … I think there has to be a way that residents need to be allowed people to come in and see them, hopefully we will never have a pandemic like this again, but I think this, they need to use this as a learning curve, right, what can we do, if this ever happened again, because you can’t have older people, elderly people dying because they’re not seeing their family’.
(Family Member 3)
Others thought that ‘locking down’ CHs had been the right course of action despite the negative impact on residents:
‘… when it was, the first lockdown … the home was closed completely. Although I have to say I wish it had been done earlier. I wish the Government had made that decision earlier however, so I’m glad they did. I would hope care homes would be locked down a lot sooner, at the same time the quality of life for those residents would probably suffer in doing that so it’s hard to know’.
(Family Member 11)
There was nevertheless a recognition among residents and relatives that this appeared to be an unprecedented situation in which people were constantly learning as the pandemic progressed:
‘I think it’s all been a learning curve for everybody, it’s just there was no rulebook to go to was there, nobody knew how to deal with it, or cope with it, yeah’.
(Family Member 10)
Concluding remarks
We have presented the experiences of residents and relatives of restrictions and measures taken in CHs in response to the COVID-19 pandemic. As we have shown, these experiences were varied, and their impact was influenced to a great extent by the existing pattern of relationships residents and relatives maintained within and beyond the CH itself. Residents and relatives alike valued the work of the CHs in keeping residents safe. At the time, they accepted the need for restrictions on their ability to see one another and live as they had done pre-pandemic. They particularly appreciated the support they received in communicating with one another virtually and the importance of this communication for residents’ health and well-being. However, measures relating to isolation were particularly difficult for residents, especially those unable to communicate with the outside world through technology. Social distancing made aspects of CH life and social visiting difficult and sometimes unsatisfactory; residents and relatives missed physical touch and non-verbal forms of communication. This was particularly important for residents with cognitive impairment. Residents and relatives were involved with staff in complex judgments of risk, choice and control, which were complicated by two factors. First, relatives (and some residents) were aware that those in CHs were in the twilight of their lives and that time was ebbing away. Second, many relatives and residents were also learning how to manage their relationships in the new – or relatively new – living context of a CH. The experiences described above must be read with these considerations in mind.
Chapter 7 Perspectives of external key informants (Objective 4)
Introduction
Thirteen senior leaders and external stakeholders participated in two focus groups, which each lasted 120 minutes. Participants included clinical leads for older adult services, representatives for CH providers, organisations representing CH providers, the regulator, LA commissioning leads, Public Health England, Skills for Care, Social Care Institute for England, organisations representing residents and relatives, and Trade Union representation. To protect anonymity, no identifier is presented with data extracts.
Findings
Senior leaders and external stakeholders spoke of the challenges experienced by the CH sector during the COVID-19 pandemic, many of which could be summed up in one word – communication. This overarching theme emerged from both focus group discussions and underpinned a broader sense of isolation and a lack of parity of esteem with the NHS. Communications took on various types and forms and involved different groups, including CH staff groups, other agencies (especially the NHS), residents and families, and government and representative groups. The underpinning factors of isolation and a perception of a lack of parity with the NHS exacerbated existing challenges within the CH sector and experiences of the pandemic for CH staff, residents and families/friends. These views and perspectives are likely to reflect a collective overview of the sector, or at times a ‘helicopter’ view of issues, rather than direct experience on the ground.
Isolation of the sector
A sense of isolation was reported to take different forms. First, the sector felt cut off from the NHS and pre-pandemic sources of service and support, especially at the onset of the pandemic. The panic and pain perceived by informants were palpable. Expert stakeholders felt that lack of parity and esteem was the root cause of lack of understanding of the specific context of CHs and how they operate and resulted in government guidance that is not adequate or sensitive to the nature of the sector:
‘It’s taken an enormous amount of effort to convince the people that are producing the guidance that (a) they need to understand what happens in a social care environment and (b) what is actually needed and useful for people to implement on a daily basis when things are changing quite rapidly … you know, until we get this parity, we’re going to keep having these problems, whatever type of outbreaks of diseases that we’re getting’.
Second, national policy frameworks that were put in place meant the sector was very much off the health radar at the beginning of the pandemic and regarded as disenfranchised from primary care to a large extent:
‘The emptying of hospitals to protect the NHS, the NHS was framed very much in terms of hospital beds, intensive care capacity, and therefore even further distancing the care home sector and the residents in particular from health-care responses.’
‘In terms of isolation, I think our care homes were incredibly isolated certainly in the first wave, it was all about care homes just taking what the NHS was sending to them from hospitals with actually really poor communication’.
These consequences were reportedly compounded by pre-pandemic effects in which routine health care into CHs of the quality, depth and breadth required were not being met. People were exposed to further disengagement from the statutory structures supposed to support them. This added to the barriers and obstacles created by social distancing and the lockdown. Disengagement of many parts of the system – physically, socially and organisationally – from the direct healthcare delivery seemed to create a multiplier effect:
‘There is something really, really, really important in policy-making, which is to stop thinking about the NHS and then social care and start thinking about social care and the difference it makes to people’s lives every day’.
Third, the standalone nature of CHs meant CH managers felt isolated from each other and were put in a position where they had to struggle with things they had never had to do before, at least, not on the scale the pandemic required:
‘It was the isolation part I think we found the most challenging and the most difficult. We had an outbreak here for a small service, we’re 17 bed older person’s service in [Area name] here, we had our outbreak in early January and it did, it caused lots of challenges with the whole isolating of our folk and the secondary kind of things that that caused, of the loneliness and all the low moods. It really was very difficult time for us and, you know, for future kind of toolboxes on what we can do to kind of improve on that would be very beneficial, yes’.
There was also the sense that the isolation of CHs from the rest of the system continued for many providers and residents. It was reported that a lack of parity of esteem and isolation also impacted the lens through which policy was formulated and communicated. This was particularly the case with the design of infection control policy, which was made for the NHS, not social care. Participants said that when CHs most needed infection protection and control support, this support was not available: infection control nurses did not visit, everything was remote and registered managers lacked that experience:
‘… we were asking staff to do rapid testing of people coming in, and actually … you were asking nurses to do testing across the whole of the staff groups and residents, that really hadn’t got that experience in infection control element of it, but were then putting themselves and their own well-being at risk’.
Where the NHS had teams managing IPC, the sense was that social care was left to ‘get on with it’:
‘I’d see overstressed nurses doing the testing and having to fill out the IT systems … then go and do their medicines, go and do their dressings … because providers had not put people in … putting their own well-being at risk … emergency planning and incident management in the NHS was planned but we don’t seem to have a plan for social care’.
‘But resources weren’t put in as well, so actually what you’d find is like in the NHS you’d have teams that were doing testing, so actually you had designated people to do that, in the care homes because obviously I understand financial costs, but actually they didn’t put any further resources in’.
Though the pandemic was a significant event across the UK, there seemed to be no emergency plan for CHs to follow. Responsibility for this was seen as resting with LAs, who needed to contribute and provide for such plans, since care providers themselves did not have such resources. Staff absences compounded such difficulties at CHs and fears that they did not have the necessary expertise:
‘And I do question, you know, sometimes with swabbing, and I did see some people doing swabbing, and I looked and thought, “well that’s not been done correctly”, but you can’t blame those people because really they’d not had that level of experience or expertise within their roles is what they should be undertaking … they were being asked to do things really out of their accountability’.
This sense of struggle was magnified by problems with ‘Test and Trace’ and limited PPE supply. However, some CH managers tried to support each other, especially when some homes had shortages of PPE supplies:
‘Care home managers started supporting care home managers. If need be they were sharing PPE just to get through the weekends and things like that’.
Government guidance
The second central theme identified by focus group participants was government guidance for CHs and the communication processes. ‘Chaos’ was the word used to describe the method of cascading information to CHs, especially in the first wave of the pandemic:
‘An announcement was made, but then there was no guidance to back it up – people were regularly asked about what happens next and then there was an assumption that we knew what was happening before it was announced. So, we’d be able to answer questions, and of course the reality was, stuff was announced, and then there’d be a time lag before the guidance arrived, quite often on the Friday before the rule change happened, you know, was brought into force on a Monday’.
The way the guidance was communicated, including sometimes very lengthy documents, was challenging to assimilate. The terms in which the guidance was couched also revealed a lack of understanding of the social care context. Furthermore, there was little time for teams to absorb and summarise the various guidance documents (from government and other organisations) and to translate often very complex guidance, which took no account of the reading ability of staff and assumed a high level of training and understanding across all care settings:
‘… we had care home support people in the CCG, NHS England, but actually some of them had never worked in social care, so actually that they were trying to deliver the social care, they were trying to deliver policies and procedures into environments that they’d never worked, or they didn’t truly understand. And I think that became quite frustrating as well, that CCGs had a care home lead, but that care home lead had never really worked in a nursing home or a care home, and actually that’s the most frustrating aspect’.
‘… so you had a real comprehension gap, capability gap, as well as capacity gap often in understanding how health-care-based infection control measures could apply in social care settings’.
Expert participants felt that having a social care association or organisation supporting CHs in the interpretation and simplifying of government guidance to be helpful; however, when different groups presented summaries, this could have added to the burden of information and became unhelpful:
‘Actually, a number of sources coming up with information packs, we had stuff from Health Service, we had stuff from ADASS colleagues, you know, all coming up with different versions of actually the same sorts of things that we needed to talk to care homes about and I found that really unhelpful as well, sort of thing, so just to reflect on that’.
These processes and the pandemic also put a considerable strain and onus on the CH manager, regarded as ‘probably the most beleaguered role in the sector’:
‘… everything tasked to them, they get every phone call in the home where they’re expected to deliver everything. And sometimes that then dilutes it down because the manager is so overwhelmed with the information that’s coming in. And actually we should simplify it, because during the pandemic there’s no resources, there’s no staff, you’ve got families that are all kicking off, you’ve got residents that are extremely frightened as well as the staff, and then you’re having to sit down and read a 56-page document on about how COVID’s meant to be managed, you just haven’t got time for that, you know’.
The speed of changing guidance and timing of releasing new guidelines came with expectations that managers were ready to digest, summarise, disseminate and implement in almost no time:
‘… it would be really helpful if DHSC didn’t release guidance 4 o’clock on a Friday when the manager’s about to go home and expect it to be implemented by the Saturday because relatives know that’s happened and they want to come in and do whatever that guidance says they’re now able to do, so that obviously, again, there was that difficulty with residents and families around the speed in which some of those could be implemented’.
‘But the plethora of guidance coming out from everybody, and picking up the point that somebody made about our wonderful care staff but actually our wonderful care staff are very good practically but, and somebody quoted to me a week or so ago that the average reading age of a care worker is probably around about 12, therefore the guidance that the government, that the department’s produced, that’s very, very complex is broadly really, really difficult for them to read and interpret and also to read and interpret at speed’.
The complexity of interpreting guidance was compounded by the roller coaster of different waves of infection, layouts and designs of CHs. A keynote of the pandemic response was described as an evolving scientific understanding but one that stretched the limits of applying that to a highly diverse care sector. Alongside guidance sat demands for data from statutory bodies, some elements of which were unclear to staff, and some felt could be quite disempowering. CH staff were asked questions that led them to question their ability to look after residents. They also often fell back on their resources when being asked to confirm cases when doctors were not entering the home, especially in the early days of the pandemic.
Visiting
Participants spoke of how visiting regulations evolved throughout the different pandemic waves and led to variations in interpreting and implementing visiting guidance. Visiting methods varied, including the use of window visits in the early wave of the pandemic, which were not without problems:
‘…. one very basic was window visits, because actually people were looking at window visits like it was a zoo, and what was the support for residents? So as we moved from the first wave of pandemic to the present, providers suddenly started to invest in pods, so more of a professional aspect of visiting. And I think there was a lot of distress caused by window visits, one for residents, especially those with mental health or learning difficulties, those that couldn’t understand that process of why, you know, their relatives, their loved ones were staring at them through windows, could that have been adapted better? Why did we wait so long to put isolation pods in?’
While technology (mainly digital technology) did help when visiting restrictions were in place, it also accentuated the digital divide between homes. As our CH staff participants also described in Chapter 5, focus group participants suggested that technology imposed an even greater workload on hard-pressed staff. There was also little time for training and staff development in digital technology. Virtual visits were implemented for clinical staff, who usually visited CHs, and this reinforced the sense of isolation and even abandonment in some cases. The implications of visiting restrictions on residents were viewed to be considerable and to act in different dimensions from practical arrangements and effect on the well-being of residents to human rights and legal issues:
‘So staff need support and training on the legal duties that they have and how they relate to visiting in terms of the Mental Capacity Act, the Equality Act, the Human Rights Act, and throw away references to those bits of law in government guidance is not going to help when staff aren’t trained in their duties in those bits of law and how to use them on the ground’.
Trauma
As the pandemic wore on and the different waves and variants emerged, there was a need to take greater account of the broader health and well-being needs of residents, their families, visitors and the CH workforce. Participants felt that it was slowly, increasingly being recognised that the workforce was traumatised. Hence, a trauma-informed approach was beginning to inform system leaders’ thinking about staff well-being. However, it remained unclear what that means in the CH sector. Equally, there was some concern shared that the awareness of trauma may have provoked an overreaction in balancing risk and rights of residents to the degree that some CHs adopted a more draconian set of measures and a closed culture:
‘Wave one had very limited mitigations, really public health 101, that Florence Nightingale would have recognised, wave two became more about the ability of testing and more sophisticated approaches to IPC and kit and equipment to enable that, and then wave three has become about the impact vaccinations have had on mitigating the impact of the wave. But also each was punctuated by emerging viral variants, so wave one was the wild type, wave two became the Alpha variant, which … swamped some of the defences that we’d already built, and then wave three has mainly been about the Delta variant, which again brought up more challenges. So again, while the scientific sort of issues behind that can be understood, what people in the frontline and these settings are experiencing is that just increasing degrees of concern that whatever defences we put in place this virus seems to be able to sidestep them and cause harm. Now thankfully the vaccine defence has proven to be the most resilient and touch wood continues to be so, but there is still the ever-present danger of variants emerging with vaccine escape potential. So it’s this balance of trying to be very clear about the risks we face, and communicate that effectively, without disempowering or traumatising people again who’ve been through an awful lot, and trying to give a high degree of confidence where we can in the measures we have in place and what they can do’.
Focus group participants spoke of trauma as impacting at several levels. Staff trauma derived from the experience of delivering care and the losses they had suffered due to people in their care dying. Residents were impacted by both the experiences of loss and grief, social isolation from their families and fear they might succumb to infection. Family members had not been able to have their pre-pandemic normal relationships with their loved ones in care settings and feared that their interaction might be a source of harm to the people they love. Families were also reported to be hesitant about re-engaging in a way that they would otherwise have done:
‘So we’ve had lots of stories about – despite policy enabling visiting – care homes being hesitant about enacting it, because of these sort of concerns about infection coming into the care home’.
Expert participants felt that the trauma caused by the pandemic on the CH sector needed to be acknowledged in the relationship between health and care within an integrated system:
‘You know, 30 years of care I don’t think I’ve kind of experienced anything quite so traumatic as kind of what we experienced ourselves in the small home here’.
‘I mean that’s just traumatic and I think actually from a commissioning and in integration perspective to just see the lack of esteem from our NHS hospitals to our care homes was really badly managed and I think in any environment where care homes are part of a solution to managing vulnerable people there needs to be parity of esteem, we need our NHS hospitals to understand that the care homes do an extraordinary job and if we want to support an integrated system’.
Legacy of learning
One of the major themes from the focus groups was a feeling that trust needed to be rebuilt at different levels of the system:
‘… there had been a huge amount of trust lost within care homes, so care providers don’t trust government, they don’t trust the system because they thought something would support them, if something really bad happened, and it didn’t’.
Trust had also been lost between CHs and the NHS:
‘… we have heard awful stories of care homes reaching out to the NHS and literally nothing happening, and no ambulances would come and all of those kind of things. And now we’re surprised that there’s a bit of lack of trust around vaccines, it’s just, you know, it’s following through the emotions as to where some of that might come from, so I think there’s a huge amount of emotional work that needs to be done to rebuild some of those relationships’.
Voice and expertise of the sector were also important:
‘I think the voice of social care needed to be higher on the agenda for national guidelines. Specifically, it was mentioned that the SAGE subgroup should have representation from staff, lived experience, managers, etc.’.
Key learning points from guidance included simplicity, the brevity of expression and readability targeted to the audience for which it was intended. It was also emphasised that those crafting guidance should have lived experience and expertise in the CH sector. Further lessons were also identified related to the benefits of bringing experts together across LAs to collate expertise, support each other and inform official positions:
‘… what went well is that the care home forums developed a lot stronger links, so they actually came together, so they were registered manager-led, they weren’t local authority or CCG-led, they were led by a registered manager, there were different providers … working together as one to support each other’s services through the pandemic, so that worked really well in some of the … [Local Authorities]’.
While there was the perception that some relationships broke down, others were seen as being strengthened (e.g. links between hospices and CHs). Engaging the sector in the development, financing and deployment of policy-making was another significant point. There seemed to be an openness to recognising the value of taking on board the needs of the end-users of any guidance or policy decisions and how to gain feedback on what was working or not. Not only that, but in terms of evidence implementation, it was acknowledged that in a rapidly changing virological landscape, some trade-offs and pragmatism might be required:
‘… it’s also important to recognise that even with the best efforts of some of the best scientific minds in the country on the SAGE groups, there are just evidence gaps in this space that aren’t filled yet, and therefore people have had to make judgements based on what evidence was available to them. And what that then requires is for people to cooperate together to try to evaluate whether the interventions have had the desired outcome or not’.
Furthermore, the implications of some of these decisions, such as the condition of receiving the vaccine to continue working, was felt not to match the reality of the CHs’ workforce conditions:
‘I’ve just done a survey with my members and a good 40–50% of them think they’re going to have to sack some staff because they won’t take the vaccine. Now that doesn’t seem right at a time when we’re going into winter pressures and when we’ve had 18 months of a really difficult working environment’.
The main driver for learning and future development remained on protecting older people and keeping them safe during and post the pandemic:
‘So we’re looking at a whole range of things that perhaps we might not have done but that we’ll continue to use going forward. At the end of the day I think the overriding factor was to keep people safe, to try and keep people informed, and for me how well that worked depended not just on the care home and who ran it and the knowledge of the staff, but also the cohort of residents in it’.
Innovations
Participants discussed how digital technologies are now being used more widely. There was greater understanding and engagement among CHs; people learnt how to use these technologies and exploit them to circumvent the impacts of social distancing. The view was that this had been a significant bonus and had opened a whole new way of sharing and exchanging information and supporting people in ways that might enable and facilitate their recovery. For instance, CHs now implement activities remotely, through digital technology, such as yoga, music, arts and culture interventions, which they previously only ever conceived as being delivered face to face etc. Together these were seen as opening a whole new universe of possibilities for CH residents:
‘… people have been really very creative during the pandemic, in ways that I don’t think would have happened otherwise, and it has certainly expedited and accelerated the implementation of all of that technological wizardry that was being used for other things, so repurposing existing stuff and bringing it into the care home sector has been a real, real benefit’.
The vaccine programme had been prioritised for CH residents. It targeted the most vulnerable group and managing that with distancing requirements was seen as an enormous step forward for the CH sector. Participants felt that closing down CHs was not new regarding visiting and access. The example of norovirus was used to illustrate workable policies and solutions to circumvent and provide safety for residents, visitors and staff. So, there are proven ways of working that can maintain some degree of safety and protection in the face of a highly destructive virus, which can hopefully be embedded for the future (with a keen eye on the potential negative impacts of getting it wrong). The sense was that a lot had been learnt about getting policy right when we need to lockdown a CH, albeit temporarily. The point was also made that there was a legacy of skills’ acquisition and a strengthening of clinical skills by staff in particular:
‘… it’s allowed them to actually probably go from a mediocre service to a higher service because all of a sudden they’ve been tested and they’ve possibly enjoyed that testing, I know, probably the wrong words to use, but actually they’ve had to up their game’.
Place
The effects observed were felt to vary according to place and locality, where existing solid networks and established relationships with the LA, community health services and healthcare professionals were felt to facilitate better outcomes for all involved. The support received from the LAs and CCGs were appreciated, but this was again deemed to vary from one area to another. Some CHs felt they were supported by the LA to form ‘subcommunities’ among CHs; this reduced the sense of isolation, improved the ease of interpreting guidance and impacted residents’ outcomes. However, these relations were diverse across different places and were subject to pre-pandemic established networks:
‘Some local authorities said you can form a subfamily unit within your care home, another local authority says you definitely can’t, so there wasn’t an opportunity for them to have a dining experience together or an afternoon together or to sit outside when the weather was well, socially distanced, so we had to be very creative over what we felt based on the infection control guidance was suitable’.
Such local networks extended to the relationships with different healthcare professional groups. Well-established working relationships pre-pandemic were felt to facilitate creative thinking and innovations in the delivery of care:
‘As a [Local Authority] we’re really, really fortunate and I’d recommend it to anybody, we have an OT team that works specifically with people with dementia in our care homes and extra care schemes. They have them allocated to each, they have two settings each, they design training, they knew the residents that had the difficulties and they were able to work with the staff to try and come up with some interventions to support the residents’.
On the other hand, where local networks were not strong before the pandemic, this was felt to affect residents’ outcomes adversely and significantly, especially for those with complex needs or specific communication difficulties:
‘The access to health services with other professionals backing away from care including social workers, CQC inspectors, GPs, district nurses, other health professionals, and care staff having to fill the gaps left by them, lack of access to hospital in the beginning whether you had COVID or something else, and that’s still ongoing, still lots of health care is being delivered virtually or from a distance, which as people have said virtual communication just simply doesn’t work with some people, particularly older people that we support, if you’ve got dementia or another condition communication difficulties and, you know, speaking to a GP on an iPad is going to be more distressing than anything else.’
Impact on staff
The pandemic and associated infection control measures, including social distancing and isolation, significantly impacted CH staff. Expert participants felt these affected staff retention, workload and well-being at work and beyond. CH managers were very conscious of these effects, and many tried to implement different supporting mechanisms for staff. However, such support varied across CHs and was very much dependent on the capacity of the CH managers. Here, care associations and national groups were able to provide some external support for staff:
‘We should not forget the staff who are working there who were frightened at the time, that they’re not necessarily the most educated, they’re certainly not well paid in terms of all the work that they do, and we can’t forget about the impact on them. For those care homes that didn’t have support for care home staff, we gained access to them to our employee assistance programmes and we also gained access via the [name] Foundation Trust and our CMHT access if they wanted it for psychological and support’.
The impact on staff was recognised within a pre-pandemic shortage and workforce challenges, making the situation much more difficult. CH staff found themselves in intense working conditions and increased workload associated with more pandemic-related tasks and more staff taking sick leave due to contracting COVID themselves. These stressful working conditions impacted the ability of staff to innovate or come up with much needed new ways of organising and delivering care during the pandemic:
‘I think what COVID did was laid bare the difficulties that were there already, so when we see certain settings perhaps not being innovative, perhaps not thinking about ways round things, if you think that pre-pandemic the sector was running with a roughly 10% fewer staff than it needs to function, we then have a pandemic, we then have staff off, we then have staff isolating and they’re just about managing to keep everything afloat and there wasn’t time for innovation for a lot of those care homes, they were just glad if there was enough people on the floor each day and that’s about as much as they could cope with’.
Concluding remarks
Pre-pandemic dynamics on staffing and relationships with LAs and local health networks were critical drivers of capacity to respond in an agile and effective way. Though individual relationships may have been strong and positive in places, the sector felt isolated from the NHS overall and lacking parity of esteem. This was compounded by the confusion, sometimes chaos, in communications processes with statutory bodies and concerning guidance, especially. Staff developed new visiting modalities to work around social distancing policies, and there are positive impacts from the acceleration of digital technology use. Yet, though these mitigations are welcomed, they cannot compensate for the trauma inflicted upon staff, residents and families alike. The legacy of learning must rebuild trust and offer trauma-informed care to counteract the worst impacts of the pandemic on the sector and the health and well-being of residents, families and managers.
Chapter 8 A toolkit supporting care homes with social distancing and isolation (Objective 5)
Introduction
Drawing on the findings of phases 1 and 2 and in collaboration with multiple stakeholders, we developed a toolkit of evidence-informed guidance and resources to support social distancing and isolation for CH residents (see Chapter 2 for method).
Participants
Two online, half-day, participatory workshops were convened. A total of 27 external members were recruited, comprising 10 PPI group members, 10 CH staff (7 CH managers/deputy managers, 1 team leader, 1 care worker and 1 practice development facilitator), 1 Associate Director of Nursing of a large NHS Foundation Trust, 3 professional representatives from the Steering Committee and 3 professional representatives from the Data Monitoring and Ethics Committee. Details of the external members who were able to attend each workshop are provided in Table 5.
| Workshop 1 participants ( n = 22 including project team members) |
|
| Workshop 2 participants ( n = 20 including project team members) |
|
Co-design events
At Workshop 1, participants discussed the study findings with reference to several trigger questions (see Appendix 2). A synthesis of this workshop is presented in Table 6.
| Initial thoughts about the findings | Audience for the toolkit |
|---|---|
‘Like soldiers in the front line with no training’. It needs to be understood that CH staff are also grieving the loss of how CHs were before COVID-19. Staff may feel that their identities have changed since the pandemic. Coming out of the pandemic has been harder than going into it and there needs to be advice in the toolkit on both beginnings and endings of pandemics. |
|
Care homes need greater autonomy – not permitting families/friends to hug residents is an example – ‘I don’t believe it will cause COVID’. Blanket rules do not work in settings that are so unique. The toolkit needs to empower people to come up with innovative solutions to problems. How can we keep things more collaborative in the future and less dictatorial? Now CHs have lived through the pandemic, how can we develop a more collaborative approach to assessing risk? |
|
| Purpose of the toolkit | Format of the toolkit |
|
|
Overview of Workshop 1 discussions
These data sources and discussions informed the development of the draft content, which was organised around six areas, grouped into three sections:
-
Section 1 – Caring for Residents: caring for residents when they are social distancing; caring for residents when they are isolating.
-
Section 2 – Caring for Families and Friends: supporting residents, families and friends to communicate when visiting is not permitted; supporting visits from families and friends when visiting is allowed but with restrictions.
-
Section 3 – Caring for CH Staff: caring for care staff; caring for managers.
For each area, ‘consequences’ and ‘actions to consider’ were presented with illustrative data extracts and case studies.
This draft content was the focus of Workshop 2; a synthesis of Workshop 2 discussions is presented in Table 7.
Overview of Workshop 2 discussions
A third and final co-design activity involved sharing a further version of the draft content of the toolkit with stakeholders drawn from Workshops 1 and 2 [PPI group members × 10, CH managers × 2, Associate Director of Nursing × 1, Director of Clinical Services (Dementia UK) × 1, project team members × 8]. The final draft toolkit (presented in Appendix 5) comprises a section for Residents, Families and Friends, and CH staff with each section addressing two key areas. For each area, content is organised around three headers: ‘what is the issue?’, ‘what we have learnt’ and ‘you could try this’. Data extracts and case studies are incorporated and links to resources and organisations (see Boxes 1 and 2 for examples of the key areas related to caring for residents). The toolkit is intended to be used flexibly with staff, residents, families and friends to support health and care delivery by the following:
-
contributing to person-centred care for residents, families and friends by providing evidence-informed guidance for social distancing and isolation of residents and related restrictions;
-
support CHs to care for residents with diverse health and care needs (e.g. those living with dementia);
-
support CHs to communicate well with residents, families and friends, and health and care professionals;
-
help direct focus on staff well-being;
-
help make the job easier for CHs during a pandemic;
-
help inform care for other infectious diseases.
The toolkit will be free to download from the project webpage, and the film will be free to view from the project webpage.
Caring for residents when they are social distancing
What is the issue?Care home residents are required to keep a physical distance between each other and with staff and visitors.
‘I think it [being able to participate in activities] has improved, I think that the home was learning a lot from the first lockdown and as things have improved, I mean they still did the activities, how on earth they managed to organise things by distancing people I do not know, it’s incredible. But I’ve got a feeling that things are not so much back to normal but a new normal and she’s participating again’. (Family Member)
‘… there’s no way on earth that I’m going to stay … 6 feet away from a resident at any given time, you know, it’s just impossible. We’ve got people who may need assistance when they need to eat or when they need a drink, or people who might need personal care. You can’t keep away from people’. (Senior Support Worker)
What we have learnt
-
(1) Communicating can be challenging for residents when being socially distanced from the person they are trying to communicate with, especially if a resident has a hearing and/or vision impairment. Mask-wearing can make communication even more complicated, hiding much of the face, and making lip-reading impossible.
-
(2) Residents with cognitive impairment find social distancing challenging to understand.
-
(3) Residents not being permitted to visit other residents in their rooms due to social distancing rules can cause frustration and upset.
-
(4) Limited capacity in communal areas makes it harder to arrange social activities for residents and with reduced numbers of residents. The reduced social interaction and mental stimulation associated with this means that residents are not as mentally alert as usual.
-
(5) Limited capacity in dining rooms reduces the number of residents who can eat in designated dining areas, and some CHs must reconfigure other rooms into dining rooms, stagger mealtimes, or ask residents to eat in their bedrooms.
-
(6) Maintaining social distancing with residents when staff deliver personal care is a struggle – residents miss physical touch, for example hugs and holding hands.
-
Care home staff need to be clear about what is and is not allowed around social distancing rules and communicate this to residents, families and friends.
-
Explain to residents what social distancing is and why it is needed. Communication/cue cards may be helpful.
-
Care home staff can have a conversation with residents about what activities they might like to participate in, and communal rooms can be reconfigured to make these activities possible. This information should be recorded in residents’ care plans.
-
Approved transparent face coverings can be worn to make communication easier for those residents who communicate through lip-reading or facial expressions.
-
Activities and well-being co-ordinators can provide entertainment and activities for residents that adhere to social distancing guidance.
-
Examples that residents and families/friends liked included Christmas specials with a photograph of each resident sent to family, celebrations for pancake day, significant national memorial days, anniversaries, cultural and religious notable days/events, card-making, word games, small group cake-baking, yoga, karaoke, bingo, quizzes, letter writing to local school children, online sessions connecting residents with local churches and community groups and indoor gardening.
-
-
Senior leadership can consider investing further in well-being and activities co-ordinator positions that are not already in place.
-
Create resident support bubbles to help maintain communication and friendships, while adhering to social distancing guidance.
-
Discuss and make it possible for residents to go out of their CH while adhering to restrictions, for example for religious or cultural activities.
-
Care home managers and senior leadership can decide if social distancing is possible for residents with cognitive impairment (e.g. for those who walk with purpose). Talk with other CHs to share experiences of what has worked well and what has not.
-
For tips on how to communicate well with a person living with dementia, visit
-
www.dementiauk.org/get-support/understanding-changes-in-dementia/tips-for-better-communication/
-
www.scie.org.uk/care-providers/coronavirus-covid-19/dementia/care-homesWatch the video – meeting the needs of people with dementia living in CHs during COVID-19. www.youtube.com/watch?v=blJjUwBhVpk
-
-
Encourage CH staff to be vigilant about observing residents’ physical, emotional, mental and cognitive well-being.
-
Educate staff about signs to look out for regarding the well-being of residents to mitigate the negative impact on residents of social distancing, for example low mood, appearing anxious, physical discomfort.
-
Managers can discuss with staff how to put into practice apparent contradictions in guidance, for example regarding physical touch with residents.
-
Managers can communicate to staff that their decisions/judgements about resident care are respected.
-
Activities and communal dining arrangements can be reconfigured with smaller groups of residents.
-
Care home managers and senior leadership can consider how best to manage social distancing for residents and staff where spaces are not easy to reconfigure/repurpose.
Caring for residents when they are isolating
What is the issue?Care home residents must isolate in their rooms for several days if they have suspected or confirmed COVID-19 infection, when they first move into the CH, or return to the CH following hospital discharge/attendance.
‘You know and like when I had any phone calls you know, people that normally phone me, I couldn’t take the calls, I wasn’t allowed to have any calls because that meant I would go out the room to take the calls and that I wasn’t allowed to do’. (Resident)
‘… some have chosen not to go to hospital appointments if they don’t feel it’s necessary … so they won’t get isolated … they like to be downstairs in activities, so they’ve chosen not to go to hospital because of the risk of being isolated’. (Manager)
What we have learnt
-
(1) Formal isolation can have a negative impact on residents’ physical, mental, emotional and cognitive well-being.
-
(2) Residents feel cut off from their usual CH life and family and friends when asked to isolate in their bedroom.
-
(3) Residents with cognitive impairment may not understand that they cannot leave their room and why.
-
(4) Being in isolation may have a negative impact on the nutritional health/well-being of residents who eat better when supported by a companion or in social settings.
-
(5) Residents sometimes may be asked to isolate themselves in rooms that are not their own, leading to feelings of dislocation and discomfort.
-
(6) Some residents may be reluctant to seek hospital care for fear of having to isolate on their return.
-
(7) Families sometimes do not understand what isolation means for residents, leading to a lack of support for residents.
-
(8) Some people are deterred from moving into a CH if they need to isolate upon their arrival.
-
When residents are required to isolate, make sure they can see the outside world from their bedroom, and have access to television and music (e.g. via a digital assistant such as Alexa or Google) if they wish.
-
Where possible, ensure that residents isolate in their own bedroom. If this is not possible, arrange for personal possessions to be moved to the resident’s isolation room and help residents to communicate with staff, fellow residents, families and friends.
-
Consider cohorting to care for residents for whom isolation would be detrimental to their well-being.
-
Ensure that a resident’s needs for companionship during essential activities (e.g. mealtimes) are supported by CH staff.
-
A useful resource is ‘Supporting older people and people living with dementia during self-isolation’ (The British Psychological Society, UK): www.bps.org.uk
-
Support essential caregivers in their role. Helpful resources are
-
The Relatives and Residents Association guide – visiting and the law – a guide for CHs during COVID-19: www.relres.org/visiting-guide-providers/
-
More than just a visitor. A guide to essential family carers: www.mha.org.uk/files/2615/9707/4083/MHA_More_than_just_a_visitor._A_guide_for_Essential_Family_Carers.pdf
-
-
Managers and senior leadership can decide on interventions to manage the emotional and mental well-being of residents who are isolating.
-
Care home managers and care staff can work with physiotherapy and occupational therapy (OT) colleagues to plan how best to promote physical activity for individual residents during periods of isolation.
-
Care home staff can facilitate choice and control for residents – this can help residents adapt to isolation measures and restrictions (e.g. their thoughts about how they would like to keep connected with their families and friends, and friends in the CH).
-
Care home staff can carry out more frequent visits to check on the well-being of residents who are isolating (e.g. looking out for signs of residents appearing upset, down, tearful, anxious, frightened and lonely).
-
Activities and well-being co-ordinators can lead on providing entertainment, activities and exercise for residents in isolation.
-
Online activities for individuals living with dementia (Alzheimer’s Society, UK).
-
-
Care homes can consider implementing activities for residents that previously would have only been considered in a face-to-face mode now being done remotely through digital means (e.g. yoga, music, arts and cultural interventions).
-
Care staff can provide supportive walks for residents (e.g. to a garden area within the CH, to a balcony).
-
Senior leadership should invest further in the training and development of the care workforce to be able to care well for the emotional, mental and physical well-being of residents who are isolating. This should include a specific focus on the legal duties that staff have and how they relate to implementing isolation, social distancing and visiting restrictions in terms of the Mental Capacity Act, the Equality Act and the Human Rights Act.
-
Care home staff can prepare residents for the possibility of isolation by talking to them about what it entails and what facilities they would like if they were required to isolate. The outcome of these discussions should be included in the resident’s care plan.
-
Care homes can facilitate communication between an isolating resident and other residents in the CH (e.g. by arranging phone or video calls, helping to write a postcard and popping it under the resident’s door/posting to family/friends).
-
Care homes can support communication between residents, their families and friends that meets their needs (e.g. arranging mobile devices for phone or video calls, supporting residents with letter writing/reading).
-
Care home staff can explain to residents’ families and friends what formal isolation means for residents and ask what support they can offer.
-
Care homes can prepare for similar situations by consulting guidance such as care homes’ strategy for infection prevention and control of COVID-19 based on a clear delineation of risk zones (Eric Fewster, Independent Water & Environmental Manager, UK): https://ltccovid.org/2020/12/16/updated-care-homes-strategy-for-infection-prevention-and-control-of-covid-19-based-on-a-clear-delineation-of-risk-zones/
-
Senior leadership can consider short and longer-term CH redesign opportunities to enable residents to connect socially with their families and friends and to connect with the outdoors and different sensory experiences.
Chapter 9 Discussion and conclusions
Introduction
The aim of this study was to explore and understand the real-life experiences of social distancing and isolation in CHs for older people from the perspective of multiple stakeholders, and to develop a toolkit of evidence-informed guidance and resources for health and care delivery now and for any further outbreaks. In this chapter, we discuss the main findings from the study, reflect on the approach and methods used and on equality, diversity and inclusion, and present the implications for practice and policy and recommendations for research.
Discussion of main study findings
We discuss key findings about implementing social distancing and isolation measures for residents – consequences, challenges and solutions; enabling connections and communications; caring for the CH workforce; and supporting the wider CH sector.
Implementing social distancing and isolation measures for residents: challenges, consequences, solutions
Social distancing
Social distancing measures involved residents and staff being required to maintain a 2 m distance from each other. 21 We identified negative consequences of social distancing measures, which included confusion for some residents and inhibition of their social interaction. Some residents, notably those living with dementia, found it difficult to understand why they could not sit close to others. These changes to social interaction negatively impacted on resident well-being. Other research has reported similar findings, including that disruptions to residents’ usual care routines and social interactions have negative consequences for their physical and emotional well-being. 135
The physical layout of CHs was sometimes a challenge to successfully implementing social distancing, for example in CHs that were not purpose-built where the physical space was not always available. It has been reported elsewhere that space and environment placed constraints on the ability of CHs to respond to the COVID-19 pandemic. 136 A key finding of our review was that not all CHs had the space to provide single rooms, create separate zones or ensure sufficient walking space around the home was in line with social distancing measures. 33,60,64,78,82,84,103,112,123,129 This was also the case for isolation measures. Our participating CHs implemented different approaches to this, for example one CH established a COVID-19 ward, where people hospitalised with COVID-19 were discharged to recover. Another CH had households of 12 residents that were treated as separate subgroups. A discussion paper in our review suggested that CHs operating with ‘household models’ had improved outcomes for residents, but that more research was required. 33 Respondents in another study reported that approaches to cohorting and zoning were only possible if the layout and space in CHs were sufficient. 112 A challenge with cohorting shared elsewhere is that it potentially removes residents from the comfort and privacy of their own bedrooms, which can be disruptive and especially so for residents living with dementia. 137 Cohorting residents has been described as a type of hard strategy, that is, it is more interventionist and with potential ethical concerns – residents are restricted to a specified place or area and this restriction is monitored by staff. 138
Making changes to CHs to enable social distancing and isolation and other COVID-19 interventions will likely have significant cost implications. Design and planning for new CH facilities should embrace the latest IPC evidence; evidence to support care and maximise the quality of life for residents with particular care needs (e.g. residents living with dementia, other cognitive impairments, sensory impairments, conditions requiring residents to use a wheelchair); enable residents to connect socially with their families and friends and to connect with the outdoors and different sensory experiences. There is a need to move away from thinking of CHs as ‘a lot of bedrooms’ and more as ‘spaces and places for living’139 (p1168).
In addition to measures and restrictions within the CH, residents had to comply with restrictions for leaving the CH, for example to visit their own home and other places with staff or family and friends, and for using facilities in the wider CH community, for example gym and cinema. Factors known to enable older people to settle into CH living include being able to continue valued social relationships and establish new relationships. 140 These restrictions had negative consequences for residents’ mental health, with staff reporting that residents became withdrawn and introverted, and for residents’ physical health, for example contributing to deconditioning because of a lack of exercise.
Care home staff shared that maintaining a social distance between residents and staff was not always possible, for example, when providing personal care for residents, and that exceptions needed to be made. Similarly, some residents were confused about why they could not have a hug from staff but that staff were permitted to assist with personal washing and dressing. This caused upset for residents and staff alike. For staff who lived alone, not being able to hug residents and colleagues was an additional burden. CHs were perceived by staff as a resident’s home rather than an institution, consequently some staff questioned whether social distancing was appropriate and if abiding by social distancing measures was always in the best interests of residents.
Compounding the challenges of social distancing and isolation for residents was their experience of staff wearing masks and PPE. PPE made it more difficult for residents to recognise and communicate with staff, particularly those residents who were hard of hearing and relied upon lip-reading, or those who had vision problems. This finding resonates with findings in the published literature. 137 Sometimes staff had to lift their mask briefly so that residents could understand what they were saying or stand at a distance and talk ‘really loudly’ to residents or write down what they wanted to say on paper. It was felt that seeing staff in full PPE could be ‘scary’ for some residents, especially those with cognitive problems. It could also negatively impact the ability of residents to connect with staff and for the CH setting to feel like ‘home’.
Isolation
In line with government guidance,21 initially residents were asked to stay in their rooms for 14 days, and this was reduced to 10 days from January 2022. During this isolation period, all care and meals were delivered to residents’ private rooms. A key finding was the reported negative consequences of isolation for some residents’ physical, psychological, emotional and cognitive well-being. Staff spoke of some residents being bored, frustrated, confused and distressed, particularly for residents living with dementia or another cognitive impairment. Understanding fully the impact on residents living with dementia was recognised as a challenge and not always possible to achieve. Helping staff to interact meaningfully with residents living with dementia or other cognitive impairment and to be able to assess for signs of distress is paramount. For some residents, isolation was believed to have had contributed to their physical decline, for example, because of reduced physical exercise, and not eating and drinking as well when dining alone, and to a decline in mental health, for example, experiencing disturbing hallucinations. Family members likewise thought that being in isolation had negatively impacted on residents’ physical and psychological health. A rapid review of the psychological impact of quarantine reported that quarantine was often associated with a negative psychological effect and longer quarantine (more than 10 days) was associated with poorer psychological outcomes. 23
For those residents who recalled being in isolation, it had been a challenging experience and isolating in every sense of the word. Residents who had recently moved into the CH were considered by staff to have had a particularly difficult experience of isolation regulations. Transitioning to living in a CH was challenging enough without having to isolate alone, not having the opportunity to see the CH as it usually operated, to participate in activities, and to interact freely with and get to know staff and residents. These factors are potential facilitators for older people transitioning well to living in a CH. 140 Unintended consequences of isolation measures included potential new residents being put off from moving in because of isolation requirements, reluctance sometimes for residents to attend hospital appointments to avoid having to isolate on their return to the CH, and CH decision-making about potential new residents, for example accepting only older people who are physically and mentally capable of isolating themselves and not those who walk with purpose.
Measures to make isolation less difficult for residents included ensuring that they were entertained purposefully with regular socially distanced visits from staff and various resources to occupy their time, while working with residents’ individual beliefs and values. ‘Activity boxes’ were created. Some CHs gave isolating residents a radio, Echo or Alexa so that they could listen to music; an iPad or tablet so that they could contact family and friends; a TV to keep them entertained; and exercise equipment, such as stretch bands, to keep active. Adequate staffing levels and a skill mix that includes sufficient well-being and activities co-ordinators are vital to an infrastructure that can support these measures. Family members praised the crucial role of these co-ordinators in identifying and acting on signs of low mood for residents in isolation. Engagement of residents in meaningful activities and additional close monitoring were key strategies for supportive isolation in other CH research studies. 112,135 Creative approaches to activities for residents not isolating were also evidenced, for example small group indoor gardening, yoga, karaoke, bingo and quizzes. Our toolkit is designed to capture such innovative approaches that are realistic and can be implemented meaningfully in practice.
Purposeful activities alone to support residents isolating are inadequate. Staff sitting with residents regularly to help prevent loneliness and improve well-being was an important study finding. This illustrates the importance of human connection and resonates with reports of the six senses, which are required for outstanding care and include the need for older people to experience a sense of security, continuity and belonging. 141 Maintaining good communication with residents throughout their period of isolation was important, with staff comforting residents, explaining the reasons why they needed to isolate and encouraging them to persevere. Most residents shared that the measures and restrictions introduced at the CH were explained well to them by staff, although some shared that staff were not always willing to discuss the measures as fully as they would have liked. Some residents shared that it was likely that staff themselves did not understand the reasons for measures and restrictions, a finding of our interviews with CH staff. Giving as much information as possible to those who are in isolation, their families and friends was a theme in the published literature. 23 A pre-COVID-19 study found that best care was evident in CHs where residents, families and staff worked together, and where there was a sense of community. 142 Some staff shared with us the importance of maintaining a sense of humour and continuing to ‘banter’ with the residents to raise their spirits. Extra vigilance by staff to ensure residents’ safety while alone in their bedrooms was paramount. The potential contribution of smart technology to support this is worthy of investigation.
Moral dilemmas
Implementing social distancing and isolation measures presented moral dilemmas for CH staff, illuminating potential tensions between risks and benefits and how to balance facilitating person-centred care for residents with a need to implement these measures to help prevent and control any COVID-19 outbreak. This concurs with other research. 143,144 One study reported that caregivers were conflicted about incorporating social distancing and infection control into caring for residents living with dementia. 143 How to manage social distancing and isolation measures for residents living with dementia or other cognitive impairment was identified in our study as a particular challenge – difficulties for residents to understand, remember and follow instructions. This resonates with other research, where CH staff reported that key challenges to isolating residents were cognitive impairment and language/communication barriers. 135 Developing staff knowledge and skills to support the implementation of isolation and social distancing measures to include ethical principles for decision-making warrants further attention. Positively, these authors have developed a Dementia Isolation Toolkit providing ethical guidance on how to isolate people living with dementia safely and with attention to their personhood. 135 Others have advocated an approach to care that is ‘principle-based, coupled with case-by-case application of the principles for individual residents’138 (p4). This highlights the need for senior leadership, CH managers and staff to understand key sources of law and their application to resident care, for example the Mental Capacity Act 2005, the Human Rights Act 1998, the Equality Act 2020 and the Coronavirus Act 2020. Helping staff to implement isolation interventions more easily was good teamwork and receiving support from managers and colleagues. A higher level of support from employers and colleagues was also associated with moral resilience in a survey of 962 healthcare workers in Canada. 145 They explored links between moral distress, moral resilience and the emergence of mental health symptoms during the COVID-19 pandemic and concluded that moral resilience might be an important target to preserve healthcare workers’ mental health. The consequences, challenges and solutions to implementing social distancing and isolation measures for CH residents illuminate the knowledge, skills and values required to be able to care well for residents and emphasise the need for further investment in the development and recognition of this workforce.
Trauma-informed approaches to caring for residents, families and friends, and care home staff
Social distancing and isolation measures and other restrictions have been a source of distress and trauma for some residents, families and friends, and CH staff during the COVID-19 pandemic and pose a risk to their psychological and physical well-being. Senior health and care leaders shared in our study focus groups that as the pandemic progressed there was a sense of the need to consider the wider health and well-being needs of residents, families, friends and the workforce. Slowly it was recognised that the workforce was traumatised and so a trauma-informed approach was beginning to inform system leaders’ thinking about staff well-being. There are examples of trauma-informed approaches to care, for example for older people in hospital146 and for healthcare workforces,147 and a case is made for widespread implementation of trauma-informed models of care in generalist aged care settings. 146 They state ‘Person-centred care provides the foundation of trauma-informed care, wherein collaboration and communication are key. Trauma-informed care extends this philosophy by emphasising the fundamental role of trauma in shaping the person’s experience of care’146 (p426). It is less clear what trauma-informed care might look like for CHs caring for older people, for residents, families and friends, and staff. The potential to translate trauma-informed models of care into the CH sector caring for older people warrants attention.
Enabling connections and communications
An important finding of the study was the creativity and support offered by CH providers, managers and their staff to enable connections and communications between residents, families and friends while residents were isolating, when visiting was not permitted or was permitted with significant restrictions, and for CHs to keep connected and communicate with families and friends. Residents, and family members, highly valued that they were kept safe; they had experienced the difficulties and ill-effects of social distancing, isolation and restrictions but overall understood this and appreciated the safety of implemented measures.
The contributions of families and friends to creating a meaningful life for the older person living in a CH and to creating a sense of community are well known. 148–151 An analysis of support networks showed that older people living in CHs valued the support of family members more than any other tie. 152 Restrictions to visiting from families and friends had negative consequences for residents and their networks. At times of difficulty, it is normal to want to be with people we love, trust and feel safe with; residents shared that their mental health had deteriorated because of not seeing in person their families and friends and many felt abandoned – a finding that is reflected in other recent research, including a rapid review of the impact of visitor exclusion, which found that residents experienced higher levels of depression, anxiety, isolation and loneliness. 153,154 Family members also reported that visiting restrictions had exacerbated their loved one’s physical health decline, for example not being present to encourage, motivate and assist with activities, such as exercise regimens. Positively, the importance of family and friends was recognised in government guidance for England with the introduction of the essential family carer role in March 2021.
Similarly, anxieties and stresses were experienced by families: they were accepting of the need for restrictions to keep residents safe but were not always sure how or why decisions about guidance and implementation were made; many were fearful that they might not get to see their family member in person again; and they were anguished at no longer being involved in the resident’s daily life and the life of the CH community. There were additional feelings of powerlessness for families whose loved ones had moved into the CH during the pandemic, coupled with anger and heartbreak at not being there for this significant life transition. Therefore, enabling connections and communications was key to promoting a sense of security, continuity, belonging, purpose, achievement and significance for residents, families and friends. 141 Several innovative and creative approaches were identified to enable contact and communication between residents, families and friends. Stories were shared of how many residents had adjusted to using smartphones and tablets to keep in touch with family and friends through video calls. Others used video calls less often or not at all but made conventional audio calls. Residents with personal access to advanced video-calling technology provided by their relatives – and with the skills to operate it – appreciated the autonomy it afforded them; they did not rely on staff to facilitate calls and so could contact friends and family at times that suited them. This contrasted with those who did not own a mobile phone or could not operate one. Video calls worked less well for those unable to operate mobile technology or without their own devices.
For some family members, remote communication with their loved one was less personal, of variable quality and less private. Remote communication did not give them a complete picture of residents’ condition and well-being, though they did their best to seek out signs, for example the condition of the resident’s skin, and alertness. Others have reported that video-calling was the most helpful technology to mitigate the impact of isolation. 135 They reported that barriers to the use of technology in supporting residents during isolation were staff not having enough time to support residents with technology, residents with a sensory impairment, and poor internet connectivity. Despite these drawbacks, family members were keen to continue to have the option of communicating remotely with their loved ones.
Similar findings were reported when families were interviewed and expressed dissatisfaction with remote communications, which were described as infrequent, poorly organised, not private, functioning Wi-Fi or devices for video calls not available, and carers were often too busy to support calls. 155 There has been a call for governments and CH providers to prioritise the technological capabilities of CHs and ‘there is a moral urgency to address the digital exclusion of LTC homes’156 (p547). Senior health and care leaders in our focus groups shared that technology imposed an even greater workload on hard-pressed staff, and that there was little time for training and staff development in digital technology. Creative approaches to CHs communicating with families and friends to share information and updates about residents were valued by families. There is the potential to develop further these initiatives, for example applications that enable families to connect for updates about residents’ and their care. This would also be helpful for residents and families who are separated by non-pandemic-related circumstances, such as geographic distance, and family members who are unable to travel. Related to this is the opportunity to develop further in a joined-up way digital technology for CHs to be able to interact meaningfully with LAs, community, primary and hospital settings, and services. A welcome investment is the additional funding of at least £150 million over the next 3 years for technology and digitalisation in the recent White Paper for adult social care reform in England. 157
Socially distanced visiting
There was variation in how the different CHs operationalised socially distanced visiting, reflecting the different timelines of their involvement in the study. Families were not always clear about what governed CH protocols and practices. A finding of our review was that good communication and the availability of informational materials, such as brochures, posters and signage on COVID-19 and the associated policies, helped explain the reasons behind restrictions to residents, families and friends. 36,50,58,62,97,124
With the introduction of visiting with restrictions, residents preferred meeting in rooms inside the CH. Challenging their ability to exercise choice and control, they disliked rules on time limits for visits, number of visitors and location for visiting. Some complained about a lack of privacy, for example if visits were conducted with a staff member present or if doors were kept open so interactions could be supervised. A key challenge to socially distanced visiting for residents and families was the lack of touch, skin-to-skin contact being replaced by PPE-mediated touch, and other non-verbal forms of communication, such as facial expressions and paralinguistics, which were obscured by mask-wearing. A typology of touch describes ‘good’, ‘bad’ and ‘absent’ touch and discusses how the meaning of touch has changed because of COVID-19. 158 For example, pre-pandemic a hug between a resident and a family member was a ‘good’ touch but during the pandemic this became a ‘bad’ touch because of the risk of infecting the resident with the coronavirus.
Caring for the care home workforce
Our study captured evidence of CH managers and staff time and again going above and beyond to care for residents, families and friends, and each other throughout the COVID-19 pandemic. There were several examples of the sacrifices that staff had made. While some staff had left employment due to fears of working in CHs during the pandemic, others had considered leaving but returned to work each day to support their colleagues and to care for residents. For many the ultimate reward was that their CH had remained safe. It was noteworthy that staff expressed great fondness and care for their residents and colleagues, often referring to those within the CH setting as a ‘family’.
Caring for the workforce is intrinsic to high-quality care. 159–161 A key study finding is that the CH workforce has experienced trauma and distress. When information was limited at the start of the pandemic, staff talked of how ‘frightening’ they found working with residents who were very poorly with this new, unknown virus. Many had also feared for their own safety at times, with concerns about catching the virus from residents and what would happen to them if they did in a similar way to many other nursing and healthcare staff. 162,163 Many staff also had fears for the safety of their families, and some had chosen to separate themselves from their children and vulnerable relatives, which came at significant personal cost. In addition to their stresses at work, staff shared their experience of stresses at home – some CH staff were experiencing family illness and bereavement, partners’ job losses, broken marriages, cancelled healthcare treatment and financial worries as a direct consequence of the pandemic.
Staff in our study spoke about far busier workloads and that initially their roles became more task-focused. Social distancing measures resulted in greater workload for staff as did supporting residents who were isolating. Good support from CH management was considered by staff to make the process of implementing these measures easier. Valuing support from employers is a theme in the published literature. 26,137,164 A finding of our review was that workload also increased for staff, due to the new tasks they had to undertake, which had previously been carried out by relatives or other professionals, such as hairdressers;69,95,103,123 as well as the extra preparations staff needed to undertake for the introduction of COVID-19 interventions. 25
Pre-pandemic there were staff shortages in the sector. 165 Implementing social distancing and isolation measures requires more staff, as does cohorting and visiting restrictions. With numbers further depleted due to sickness, self-isolation and fear during the pandemic, implementation of these measures was challenging. Use of agency staff helped boost the numbers, but even with block booking, this also introduced increased risk of transmission. While the government did introduce infection control grant funding to support the increased staffing costs, this did not help homes find, recruit and retain staff who want to work in CHs. Then and now, this is a significant problem, which the pandemic has highlighted and exacerbated. Our study values and recognises the workforce. It adds weight to the argument that the CH sector needs urgent development and support to grow to meet the needs of older people in the UK.
Staff feel mentally and physically exhausted by changes made to their working practices and the emotional distress they have experienced during the COVID-19 pandemic. These experiences resonate with other research. 144,166,167 Respondents in a study of 152 staff working in nursing homes spoke of mental and physical exhaustion and the ‘emotional burden of caring for residents experiencing distress, illness and death’144 (p199). Addressing a lack of pandemic preparedness, resilience training was expressed as a need by hospital employees participating in an intervention in response to the H1N1 pandemic. 168 The authors developed a training intervention providing information about normal stress responses, effective coping, and principles of organisational resilience, and allowing for discussion and reflection on anticipated stressors. Employees also identified the importance of visible leadership and the need for reliable, consistent and timely information. The need for longer-term psychological support for CH staff is paramount. A step in the right direction is the new well-being and occupational health offer in the 2022 White Paper for the reform of adult social care in England. 157 However, an infrastructure to support the central co-ordination, implementation and evaluation of this is paramount.
Care home staff must feel valued – we were told on more than one occasion that CH working can be a ‘thankless job’. The COVID-19 pandemic can be seized as an opportunity to challenge and eradicate the stigma of CH working being low status. Government investment in the sector is imperative. Key priorities include a review of working conditions and pay scales, and investment in recruitment, retention and development of care staff. On this note, it is encouraging that adult social care in England will benefit from at least £500 million from the Health and Social Care Levy to improve recruitment, retention, progression and staff well-being and that social care will be ‘recognised by the public as a valuable and high-quality service on par with the NHS.’157
Supporting care homes and the care home sector
A key study finding shared by CH staff and senior health and care leaders was the view that the CH sector was abandoned by the government in the early phase of the pandemic and was isolated from the NHS. It has been argued that the deaths of many CH residents were preventable and that one example of the ‘failure to protect life’ (p4) was the UK strategy of prioritising the protection of the NHS. 169 It was reported that between 17 March and 15 April 2020 around 25,000 people in England were discharged from hospitals to CHs. 170 This is perhaps reflective of systemic issues including the disparity between health and social care systems – as one author wrote: ‘The care system functions in the shadow of the NHS, which enjoys far greater resource allocation and higher cultural and political capital’16 (p2). There are historic imbalances of power between the NHS and social care. 171 Our findings underlie that there is a need to ensure that CHs and social care are considered an essential part of integrated care systems.
Care home staff told us that CHs had not been considered or given appropriate guidance early enough in the process. Similarly, our rapid review identified initial reports of a lack of guidance and clarity from governments about when and how interventions should be applied. There was a lack of research evidence about how to manage care in CHs during a pandemic; most of the papers in our review were grey literature, not empirical research. It has been reported that in the pandemic action plan, which was announced on 3 March 2020, there was just one mention of adult social care and a specific action plan for adult social care in England was not issued until 15 April 2020. 16
When guidance ensued, this was often long and complicated, with many different policies to consider, it changed frequently and was contradictory, causing confusion and loss of confidence. 112,144,172 This was reflected in some of the CH documents related to social distancing and isolation that we reviewed; these were difficult for staff to navigate because of multiple versions, lengthy, repetitive and with links to embedded documents. Time and attention were required to monitor the numerous iterations and to continually update to remain in compliance. 144 Further a ‘blanket approach’ to government guidance was criticised for failing to consider the many individual differences between CHs and CH residents. Care home managers had to use their ‘own common sense and … knowledge’ when interpreting the government guidance, rather than simply following it directly, selecting the parts of the guidance that were relevant to the individual CH setting. To this end, CH managers valued the support of their senior leadership to help them interpret and implement government guidance. This is in keeping with recent studies. 26,137,144,164
In addition to rapidly changing rules for CHs set by the government, communication of information to the sector from the government was described as chaotic. For example, it was shared that CHs found out about rule changes at the same time as the rest of the population, which meant that homes did not have enough time to implement them appropriately. These findings from CH staff, senior health and care leaders, and CH documents resonate with our review findings that there was a lack of guidance and clarity from governments around when and how interventions should be applied, with policy measures often scarce, flawed or adopted late. 43,46,52,56,77,82,84,103,116,128 Our findings are reflected in reported challenges for CHs of dealing with rapidly changing multiple sets of guidance,173,174 the CH sector being ill-prepared to cope with a pandemic173,175 and the sector not being supported well at the outset by governments. 18,136,173,176
Care homes need evidence-informed guidance that sets out what and how social distancing and isolation measures should be operationalised, while meeting residents’ individual needs, including their fundamental rights to liberty and security, and with attention to education for residents, families and friends, and staff. 175 Our toolkit helps address this need. Our study findings contribute to important lessons for decision-makers about the need for clear, concise and meaningful guidance about social distancing and isolation and related measures that can be translated easily into operational policies for CHs. Our findings also emphasise the importance of social care having a more equitable influence in integrated health care services.
Strengths and limitations
The rapid review (see Chapter 3) is an extensive review of the evidence around social distancing and isolation measures to prevent and control the transmission of COVID-19 and other infectious diseases in CHs caring for older people. Strengths include conducting searches of several primary and specialised databases for peer-reviewed and grey literature and screening of results by several team members to enhance rigour. Because of resource constraints, only papers published in the English language were reviewed, which is a limitation. Using the themes identified in the review to underpin the rest of the study helped ensure this research built upon what was already known and advanced knowledge in the field.
The case study sites were identified using a sampling frame designed to maximise variability, and though we did work with CHs varying in size, geographical location, registration type, ownership and incidence of COVID-19, all the participating homes had a CQC rating of either ‘good’ or ‘outstanding’ (see Chapter 4, ‘Routinely collected care home data’). None of the participating CHs were rated as ‘requires improvement’ or ‘inadequate’ by the CQC limiting the generalisability of the findings. The COVID-19 pandemic has continued to present challenges for CHs over the past 18 months. A potential limitation is that all six CHs were part of larger organisations, although the size of providers ranged from 7 to 114 CHs, the total number of beds ranged from 500 to 5875, and ownership included two family-run CHs. The project team had to work around additional and unforeseeable demands for CHs, for example regarding resident, staff and visitor testing, and vaccination roll-out for residents and staff resulting in some delays in recruitment of CHs, participants and scheduling of interviews. Consequently, fieldwork with the six CHs was conducted at different time points (see Chapter 4, ‘Routinely collected care home data’), which is a potential limitation. Positively, we successfully recruited and retained participants. This sequential approach generated rich data about the experiences of implementing social distancing and isolation measures during different stages of the pandemic, and we present our data analysis by data source across the case sites. Fieldwork was conducted remotely due to COVID-19 restrictions for visitors to CHs; not being physically present in the CHs meant that the researchers were not on-site to promote and discuss the study, to observe and absorb the nuances of the different settings, and to interact directly with the different participant groups. However, despite ongoing pressures during the active phases of the pandemic the study delivered on time. We successfully captured the perceptions and experiences of residents, families, CH staff, and senior health and care leaders to provide a comprehensive view of the experiences of social distancing and isolation measures in CHs, as seen through the lens of those leading, implementing, practising and experiencing these interventions.
Interviews and focus groups were conducted remotely. This helped us to exceed the target sample for CH staff (n = 31/30), and almost to target for the resident (17/18) and families (17/18) samples. We exceeded our target sample of eight participants for the focus groups, successfully recruiting a rich mix of 13 senior health and care leaders from across England. A limitation of remote digital interviewing was that for a minority of interviews the CH Wi-Fi quality was less stable. For 17 of the 31 interviews, participants asked for the project champion to be present, this may have influenced what participants chose to share or not introducing bias.
All CHs shared local policy documents about social distancing and isolation, with a total of 42 included for analysis (see Chapter 4, ‘Document characteristics’), and all completed the proforma for routinely collected data (see Chapter 4, ‘Routinely collected care home data’); some CHs did not answer a small number of questions, which is a limitation. The 31 purposively sampled CH staff participants had a range of roles and varied in terms of length of time working in their current role and in the CH sector, gender and ethnicity. A limitation for the resident and family participant groups is their limited ethnic diversity (all residents and all but one of the family members were white people); this is despite a concerted effort to recruit as per our purposive sampling, but we acknowledge that different experiences, views and meanings may have been missed because of this (see Chapter 6, ‘Participant characteristics’). Residents varied in terms of gender, age, length of time living in the CH, health and care needs, experience of isolation, and experience of testing positive for COVID-19. For 13 of the family participants, the resident was living with dementia or other cognitive impairment. Overall, the participant groups generated a rich account of their experiences and perceptions about the research question. A strength of our study was co-production of a toolkit designed to be meaningful, accessible and for use in practice (see Chapter 2 and 8), we did not conduct a formal evaluation of the co-design process, which we acknowledge as a potential limitation.
Implications for practice and policy
For practice
Implications of the study findings for practice are captured in our toolkit for supporting CHs with social distancing and isolation measures for older people. These are framed around six priority areas: caring for residents when they are social distancing; caring for residents when they are isolating; supporting residents, families, and friends to communicate when visiting is not permitted; supporting visits from families and friends when visiting is allowed but with restrictions; caring for care staff; and caring for managers.
For policy
The study findings can inform discussions involving CH providers, managers and external stakeholders to enhance understanding of social distancing and isolation measures for residents – consequences, challenges, solutions and learning going forward. Our findings also have implications about how guidelines are developed and disseminated. Our findings reinforce the need for CHs and social care to be considered as an integral part of integrated care systems, to ensure that actions taken during national emergencies fully account for the impact on all parts of health and social care, including CHs. Our findings can inform discussions about developing digital technologies to help residents with different health and care needs stay connected with families and friends, and for CHs to communicate effectively with residents’ families and friends.
Our findings can contribute to the content of the digital hub for the social care workforce as set out in the 2022 White Paper for the reform of adult social care in England. 157
Recommendations for further research
This study has identified that research is needed in several areas:
-
Evaluations of the co-designed toolkit and mosaic film.
-
Evaluation of social distancing, isolation and related measures used in CHs caring for older people to prepare for future pandemics.
-
Research to develop and evaluate remote social interaction for residents living with dementia and their families/friends.
-
Research to understand what a trauma-informed approach looks like for the CH sector – to care for residents, families and friends, and staff in CHs caring for older people.
-
Research to co-design and evaluate an intervention to enable residents with different needs to transition to living well in a CH.
-
The study of an intervention that cares for families and friends.
Equality, diversity and inclusion
Participant representation
From the outset this study was designed to be inclusive in how we answered the research question. Thus we set out to elicit the voice of a broad range of residents, their families and friends, CH staff, and senior health and care leaders about social distancing, isolation and other restrictions related to caring for older people living in CHs during the COVID-19 pandemic.
Compounding the well-known challenges of conducting research in CHs, the research team was compelled to recruit CHs, participants and to conduct fieldwork remotely due to restrictions owing to the COVID-19 pandemic. These measures prohibited us from immersing ourselves as researcher–observers to gain insights into contexts and cultures and to observe first-hand activities, interactions and communications related to implementing social distancing and isolation measures. Conducting interviews remotely may have excluded some potential participants who may not have felt comfortable with being interviewed using remote technology. However, we adopted a variety of strategies to maximise recruitment and successful fieldwork, for example each CH had a nominated project champion whom we worked closely with to identify and recruit participants and to support participants during the interview process and relatives were given the option of doing their interview in their own home using their own device (e.g. smartphone, laptop, tablet, telephone).
We successfully recruited our target of six CHs in England. CHs were invited purposively, using a sampling frame designed to maximise variability in terms of size of the CH, geographical location, CQC rating, registration (nursing, residential or dual registration), ownership and incidence of COVID-19. The pandemic experience for the CH sector has impacted on CHs being research ready; the team worked hard over a prolonged period to recruit two case study sites with a ‘requires improvement’ CQC; this was not successful. We also managed a key issue around recruitment of participants from BAME groups. At meetings of the Study Steering Committee and Data Monitoring and Ethics Committee, we discussed these challenges and there was agreement that we should prioritise diversity of participants and not focus on recruiting CHs with a CQC rating of requires improvement. This revised plan was shared with NIHR and we were granted permission to proceed with this revised plan.
Staff were purposively recruited to ensure variation (e.g. in age, gender, ethnicity and time in service). Resident participants were also recruited purposively, to ensure a range of genders, ethnicities and different health and care needs. Inclusion criteria were that residents must be over 65 years old and have the capacity to consent. The 31 purposively sampled CH staff participants had a range of roles and were varied in terms of length of time working in their current role and in the CH sector, gender and ethnicity. A limitation for the resident and family participant groups is their limited ethnic diversity (all residents and all but one of the family members were white people); this is despite a concerted effort to recruit as per our purposive sampling.
Reflections on the research team and wider involvement
The project team included senior healthcare professionals who work in the CH sector and established academic researchers with a background in health and/or social care research. JF is a RN with a specialist clinical and academic track record in gerontology with expertise in mixed-methods research to study the organisation and delivery of older people health care in acute and CH settings. SH is a medical demographer and an expert in social care practice and delivery including CHs and the care workforce. AMR is an expert on health workforce policy and experienced in quantitative and qualitative studies of workforce dynamics, including ethnographies of teamwork and deployment policies. RH is a nurse with expertise in evaluating complex interventions, including the organisation of nursing work, interprofessional teamwork and leadership of integrated care systems. AD is a social anthropologist with expertise in the ethnographic study of health and care organisations. SS has expertise in conducting complex multimethod studies in the NHS, project management, and user involvement. SB is lead for service user and public involvement, and for dissemination to service users and public. RA is an experienced executive nurse with strategic development and operational management experience in the independent sector. LR is a specialist nurse with expertise in leadership, clinical governance, quality assurance and quality improvement in CHs.
Our Steering Committee and Data Monitoring and Ethics Committee included experts representing the CH sector, CH nursing and IPC. We established a dedicated study PPI group comprised of 10 members, 2 of whom were also members of the Study Steering Committee. This group comprised mostly of older people, many of whom have extensive personal experience of health and care services, and several are or have been (informal) carers. PPI was an integral part of this study, informing its design, method, analysis and dissemination. PPI contributions included reviewing all participant-facing paperwork for submission to the Research Ethics Committee (e.g. plain language summary, project flyer, participant information sheets, consent forms and interview guides). PPI group members also participated in online workshops to contribute to the co-design of the toolkit.
Conclusions: a legacy of learning
The CH sector was ill-prepared and under-resourced for the COVID-19 pandemic. 16,172,177 During the pandemic and for any further surges, it is paramount that CH services for older people are safe, effective, caring, responsive to individual needs and are well-led. The loss of older people living in CHs due to COVID-19 has been substantial,14,15,155 it is essential to learn from this devastation, to understand the consequences, challenges and solutions and to evaluate these solutions. Evidence to support the learning and recovery of the CH sector from the pandemic and to inform policy-making is paramount. The findings of this study fall within the remit of the Health and Social Care Delivery Research programme for applied learning in management and practice. Our study makes an important contribution to this learning and recovery; this was one of the first to study the challenges and solutions to implementing social distancing and isolation measures for older people living in CHs in England.
Additional information
Contributions of authors
Joanne M Fitzpatrick (https://orcid.org/0000-0002-6285-180X) (Chief Investigator, Reader in Older People’s Healthcare) designed the study, provided project management, contributed to the rapid review, collected and analysed data, contributed to development of the toolkit and film and drafted sections of the report.
Anne Marie Rafferty (https://orcid.org/0000-0003-1010-6581) (Co-investigator, Professor of Nursing Policy) designed the study, contributed to the rapid review, collected and analysed data, contributed to development of the toolkit and film and drafted sections of the report.
Shereen Hussein (https://orcid.org/0000-0002-7946-0717) (Co-investigator, Professor of Health and Social Care Policy) designed the study, contributed to the rapid review, collected and analysed data, contributed to development of the toolkit and film and drafted sections of the report.
Richard Adams (https://orcid.org/0000-0002-8612-9600) (Co-investigator, Chief Executive Sears Healthcare Ltd) designed the study, contributed to data collection, contributed to development of the toolkit and reviewed the report.
Lindsay Rees (https://orcid.org/0000-0003-3629-3995) (Co-investigator, Director of Health and Quality, Encore Care Homes Management Ltd, designed the study) contributed to data collection, contributed to development of the toolkit and reviewed the report.
Sally Brearley (https://orcid.org/0000-0001-7918-7485) (Co-investigator, Patient and Public Involvement Fellow, PPI lead for the study) designed the study, coplanned and chaired the PPI group and reviewed the report.
Sarah Sims (https://orcid.org/0000-0001-7494-9030) (Research Associate) contributed to the rapid review, collected and analysed data, contributed to development of the toolkit and film and drafted sections of the report.
Amit Desai (https://orcid.org/0000-0003-2234-2872) (Research Fellow) contributed to the rapid review, collected and analysed data, contributed to development of the toolkit and film and drafted sections of the report.
Ruth Harris (https://orcid.org/0000-0002-4377-5063) (Co-investigator, Professor of Healthcare for Older Adults) designed the study, contributed to the rapid review, collected, and analysed data, contributed to development of the toolkit and film and drafted sections of the report.
Acknowledgements
Firstly, we extend our thanks to all the residents, family members, care home staff and external stakeholders who shared their stories so openly and honestly, helping us to learn from the whole experience of COVID-19, and to all participants in the co-design workshop events. We acknowledge, with thanks the contributions of the following colleagues: Sinead Palmer for her research assistance with ethics, recruitment and interviews with residents, families, and care home staff; Ivanka Ezhova, and library staff, Karen Poole, and Sonya Di Giorgio, for their contributions to literature searching for the phase 1 review.
We acknowledge, with thanks, the contributions of King’s College London Research Governance Team, Pre- and Post-Award Teams and the Research Office of the Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, the Health Research Authority, and Coventry and Warwick Research Ethics Committee for facilitating ethical approval of our study. We acknowledge with thanks the work of the PPI group members, for their commenting on development of the study protocol, study documents and participating in the co-design workshops. To each of you our sincere thanks: Helen Dean, Elizabeth Lloyd-Dehler, Nicholas Low (also a member of the Study Steering Committee), Carol Mitchell, Leslie Robertson, Phil Ruthen, Lana Samuels (also a member of the Study Steering Committee), Shani Shamah, Marion Taylor and Karen Willson.
Our sincere thanks to the design and illustration team at Calverts, and to Andy Richards, Channel Director, and the KMTV team for video-recording the interviews with residents, families, and care home staff, and for producing the mosaic film.
We acknowledge the work of our Steering Committee, Chaired by Professor Deborah Sturdy (Chief Nurse for Adult Social Care). Members included Professor Martin (Chief Executive, Care England), and Arlene Wellman (Chief Nurse, St George’s, Epsom and St Helier Hospitals Group). And the work of our Data Monitoring and Ethics Committee, Chaired by Professor Ann Netten (former Director PSSRU, University of Kent). Members included Paul Edwards (Director of Clinical Services, Dementia UK), Dr Francesca Fiorentino (Senior Statistician, employed by Imperial College London at the start of this study and now an employee of King’s College London), and Dr Dawne Garrett (formerly, Professional Lead for Older People and Dementia Care, RCN). Thank you to all members for their advice and contributions throughout the study.
Permission has been gained from all non-author contributors acknowledged in this section.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration.
Ethics statement
The study was approved by Coventry and Warwick Research Ethics Committee [20/WM/0318] on 6 January 2021. Permission to access the care homes was obtained as per local procedures. Informed consent was obtained for all participants, and all participants were informed that they were free to refuse to participate or withdraw from the study at any time.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/YNTW4569.
Primary conflicts of interest: Anne Marie Rafferty is a Governor of King’s College Hospital NHS Foundation Trust and was President of the Royal College of Nursing (2019–21). Amit Desai was Co-investigator on a NIHR HSDR Grant (17/05/110) and has been a Trustee of Carers’ Hub, Lambeth (Charity number: 1182120) since August 2019. Ruth Harris is a Member of the Advisory Board for an Alzheimer’s Society-funded study led by University of Hertfordshire entitled CONNECT: Supporting person-centred care for people with dementia in hospital settings: co-designing and testing the feasibility of an intervention for use during constant observation activities. She is also a Member of the NIHR Trainees Coordinating Centre Doctoral Research Fellowship Panel, Member of the NIHR Nursing and Midwifery Incubator Steering Group and Chair of the Royal College of Nursing Research Society.
Publications
Fitzpatrick JM, Ezhova I, Hussein S, Rafferty AM, Palmer S, Adams R et al. Implementation of social distancing and isolation practices in care homes caring for older people to control the spread of Covid-19 and other infectious and contagious diseases: a rapid evidence review. PROSPERO; 2021:CRD42021226734. URL: www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021226734
Fitzpatrick JM, Rafferty AM, Hussein S, Ezhova I, Palmer S, Adams R, et al. Protecting older people living in care homes from COVID-19: a protocol for a mixed-methods study to understand the challenges and solutions to implementing social distancing and isolation. BMJ Open 2021;11(8). https://doi.org./10.1136/bmjopen-2021-050706.
Sims S, Harris R, Hussein S, Rafferty AM, Desai A, Palmer S, et al. Social distancing and isolation strategies to prevent and control the transmission of COVID-19 and other infectious diseases in care homes for older people: An international review, International Journal of Environmental Research and Public Health 2022;19(6). https://doi.org./10.3390/ijerph19063450
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Garritty C, Gartlehner G, Nussbaumer-Streitc B, Kinge VJ, Hamela C, Kamelf C, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol 2021;130.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57.
- Fitzpatrick JM, Rafferty AM, Hussein S, Ezhova I, Palmer S, Adams R, et al. Protecting older people living in care homes from COVID-19: a protocol for a mixed-methods study to understand the challenges and solutions to implementing social distancing and isolation. BMJ Open 2021;11.
- International Longevity Council UK . A Teaching Care Home Pilot. We Dare to Care – Care Homes and Nursing at the Frontline of Our Response to Ageing 2017. http://allcatsrgrey.org.uk/wp/download/social_care/ILC-UK_-_We_dare_to_care.pdf (accessed 22 April 2022).
- Workforce Intelligence . The Size and Structure of the Adult Social Care Sector and Workforce Report in England 2019. www.skillsforcare.org.uk/sizeandstructure (accessed 22 April 2022).
- Age UK . Briefing: Health and Care of Older People in England 2019 2019. www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/health--wellbeing/age_uk_briefing_state_of_health_and_care_of_older_people_july2019.pdf (accessed 22 April 2022).
- Gordon A, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman J. Health status of UK care home residents: a cohort study. Age Age 2014;43:97-103.
- Office for National Statistics . Deaths Involving COVID-19 in the Care Sector, England and Wales: Deaths Registered Between Week Ending 20 March 2020 and Week Ending 21 January 2022 2022.
- British Geriatrics Society . Managing the COVID-19 Pandemic in Care Homes for Older People (Good Practice Guide Version 4) 2020. www.bgs.org.uk/sites/default/files/content/attachment/2020-11-16/Managing%20the%20COVID-19%20pandemic%20in%20care%20homes%20November%202020_0.pdf (accessed 22 April 2022).
- World Health Organization . WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 – 11 March 2020 n.d. www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 22 April 2022).
- Institute for Government . Timeline of UK Coronavirus Lockdowns, March 2020 to March 2021 2021. www.instituteforgovernment.org.uk/sites/default/files/timeline-lockdown-web.pdf (accessed 22 April 2022).
- Parliament UK . Government Guidance During the Pandemic 2020. https://publications.parliament.uk/pa/jt5801/jtselect/jtrights/1375/137505.htm (accessed 22 April 2022).
- Gov.UK . Policy Paper: COVID-19: Our Action Plan for Adult Social Care n.d. www.gov.uk/government/publications/coronavirus-covid-19-adult-social-care-action-plan/covid-19-our-action-plan-for-adult-social-care (accessed 22 April 2022).
- Comas-Herrera A, Zalakaín J, Lemmon E, Henderson D, Litwin C, Hsu A, et al. Mortality Associated With COVID-19 in Care Homes: International Evidence 2021.
- Schultze A. Mortality among care home residents in England during the first and second waves of the COVID-19 pandemic: an observational study of 4.3 million adults over the age of 65. Lancet Reg Health Eur 2022;14.
- Daly M. COVID-19 and care homes in England: What happened and why?. Soc Policy Adm 2020;54:985-98.
- Booth R. Government rejected radical lockdown of England’s care homes. Guardian 2020.
- Oliver D. Let’s be open and honest about covid-19 deaths in care homes. BMJ 2020;369.
- Care England . Questions and Concerns That Have Been Raised by Care England Members n.d. www.careengland.org.uk/ (accessed 22 April 2022).
- RCN Research Society . Survey of UK Nurses and Midwives’ Highlights Their Concerns About Health, Training and Workload During COVID-19 2020. www.kcl.ac.uk/news/survey-of-uk-nurses-and-midwives-highlights-their-concerns-about-health-training-and-workload-during-covid-19 (accessed 22 April 2022).
- GOV.UK . Coronavirus (COVID-19). Admission and Care of Residents in a Care Home During COVID-19 2020. www.gov.uk/government/publications/coronavirus-covid-19-admission-and-care-of-people-in-care-homes (accessed 22 April 2022).
- Gordon A, Goodman C, Achterberg W, Barker R, Burns E, Hanratty B, et al. Commentary: COVID in care homes – challenges and dilemmas in healthcare delivery. Age Ageing 2020;49:701-5.
- Brooks S, Webster R, Smith L, Woodland L, Wesseley S, Greenber N. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912-20.
- Suarez-Gonzalez A. Detrimental Effects of Confinement and Isolation on the Cognitive and Psychological Health of People Living With Dementia During COVID-19: Emerging Evidence 2020. https://ltccovid.org/2020/07/01/detrimental-effects-of-confinement-and-isolation-on-the-cognitive-and-psychological-health-of-people-living-with-dementia-during-covid-19-emerging-evidence/ (accessed 22 April 2022).
- Verbeek H, Gerritsen D, Backhaus R, de Boer B, Koopmans R, Hamers J. Allowing visitors back in the nursing home during the COVID-19 crisis: a Dutch national study into first experiences and impact on well-being. J Am Med Dir Assoc 2020;21:900-4.
- Billings J, Ching B, Gkofa V, Greene T, Bloomfield M. Healthcare Workers’ Experiences of Working on the Frontline and Views About Support During COVID-19 and Comparable Pandemics: A Rapid Review and Meta-Synthesis 2020.
- Wang H, Li T, Barbarino P, Gauthier S, Brodaty H, Molinuevo J, et al. Dementia care during COVID-19. Lancet 2020;395:1190-1.
- Braun V, Clarke V. Thematic analysis – a practical guide. London: Sage; 2022.
- Dalglish L, Khalid H, McMahon S. Document analysis in health policy research: the READ approach. Health Policy Plan 2020;35:1424-31.
- Silverman D. Interpreting Qualitative Data. London: Sage; 2015.
- Sims S, Harris R, Hussein S, Rafferty AM, Desai A, Palmer S, et al. Social distancing and isolation as strategies to prevent and control the transmission of COVID-19 and other infectious diseases in care homes for older people: an international review. Int J Environ Res Public Health 2022;19.
- Akkan B, Canbazer C. The Long-Term Care Response to COVID-19 in Turkey 2020. https://ltccovid.org/wp-content/uploads/2020/06/The-COVID-19-Long-Term-Care-situation-in-Turkey.pdf (accessed 22 April 2022).
- Anderson D, Grey T, Kennelly S, O’Neill D. Nursing home design and COVID-19: balancing infection control, quality of life, and resilience. J Am Med Dir Assoc 2020;21:1519-24.
- Arling G, Arling P. COVID-19 and Long-Term Care in the US State of Minnesota 2020. https://ltccovid.org/wp-content/uploads/2020/07/The-COVID-19-Long-Term-Care-situation-in-Minnesota-USA-27-July-2020-1.pdf (accessed 22 April 2022).
- Arlotti M, Cerea S, Ranci C. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Italy 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Australian Government Department of Health . CASE STUDY: Dorothy Henderson Lodge 2020. www.health.gov.au/sites/default/files/documents/2020/07/coronavirus-covid-19-case-studies-of-successful-outbreak-management-in-aged-care-services-dorothy-henderson-lodge.pdf (accessed 22 April 2022).
- Ayalon L, Zisberg A, Cohn-Schwartz E, Cohen-Mansfield J, Perel-Levin S, Bar-Asher Siegal E. Long-term care settings in the times of COVID-19: challenges and future directions. Int Psychogeriatr 2020;32:1239-43.
- Barón-Garcia T, Amblàs-Novellas J, Contel Segura J, Plaza A, Santaeugènia González S, Arechavala T, et al. Measures Adopted Against COVID-19 in Long-Term Care Services in Catalonia 2020. https://ltccovid.org/wp-content/uploads/2021/01/Measures-adopted-against-COVID-19-in-LTC-services-in-Catalonia-10-December.pdf (accessed 22 April 2022).
- Belmin J, Um-Din N, Donadio C, Magri M, Nghiem Q, Oquendo B, et al. Coronavirus disease 2019 outcomes in French nursing homes that implemented staff confinement with residents. JAMA Network Open 2020;3:e20175-33.
- Bergman C, Stall NM, Haimowitz D, Aronson L, Lynn J, Steinberg K, et al. Recommendations for welcoming back nursing home visitors during the COVID-19 pandemic: results of a Delphi panel. J Am Med Dir Assoc 2020;21:1759-66.
- Blain H, Rolland Y, Schols J, Cherubini A, Miot S, O’Neill D, et al. August 2020 Interim EuGMS guidance to prepare European long-term care facilities for COVID-19. Eur Geriatr Med 2020;11:899-913.
- Browne J, Fasce G, Pineda I, Villalobos P. Policy Response to COVID-19 in Long-Term Care Facilities in Chile 2020. https://ltccovid.org/wp-content/uploads/2020/07/The-COVID-19-Long-Term-Care-situation-in-Chile-24-July-2020-3.pdf (accessed 22 April 2022).
- Bruquetas-Callejo M, Bocker Radboud A. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. The Netherlands 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Burdsall D. A Unit Guide to Infection Prevention for Long-Term Care Staff 2017. www.ahrq.gov/hai/quality/tools/cauti-ltc/modules/resources/guides/infection-prevent.html (accessed 22 April 2022).
- Buynder P. Guidelines for the Prevention, Control and Public Health Management of Influenza Outbreaks in Residential Care Facilities in Australia 2017. www.health.gov.au/sites/default/files/documents/2020/03/cdna-national-guidelines-for-the-prevention-control-and-public-health-management-of-influenza-outbreaks-in-residential-care-facilities-in-australia-cdna-guidelines-for-the-prevention-control-and-public-health-management-of.pdf (accessed 22 April 2022).
- Campeon A, Le Bihan B, Legros M. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. France 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Capucha L, Nunes N, Calado A. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Portugal 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Care Provider Alliance . COVID-19: Visitors’ Protocol. CPA Briefing for Care Providers 2020. https://careprovideralliance.org.uk/assets/pdfs/CPA-Visitors-protocol-19-June-2020.pdf (accessed 22 April 2022).
- Care Provider Alliance . Staff Movement: A Risk Management Framework: Briefing for Adult Care Home Providers 2020. https://careprovideralliance.org.uk/assets/pdfs/staff-movement-risk-management-framework-cpa.pdf (accessed 22 April 2022).
- Centres For Disease Control And Prevention . Coronavirus Disease 2019 (COVID-19). Preparedness Checklist for Nursing Homes and Other Long-Term Care Settings 2019. www.cdc.gov/coronavirus/2019-ncov/downloads/novel-coronavirus-2019-Nursing-Homes-Preparedness-Checklist_3_13.pdf (accessed 22 April 2022).
- Centers For Medicare And Medicaid Services . COVID-19 Long-Term Care Facility Guidance. 2 April 2020 2020. www.cms.gov/files/document/4220-covid-19-long-term-care-facility-guidance.pdf (accessed 22 April 2022).
- Charlesworth S, Low L. The Long-Term Care COVID-19 Situation in Australia 2020. https://ltccovid.org/2020/10/13/updated-country-report-the-long-term-care-covid-19-situation-in-australia/ (accessed 22 April 2022).
- Chen A, Ryskina K, Jung H. Long-term care, residential facilities, and COVID-19: an overview of federal and state policy responses. J Am Med Dir Assoc 2020;21:1186-90.
- Chuang VW, Tsang IH, Keung JP, Leung JY, Yuk JM, Wong DK, et al. Infection control intervention on meticillin resistant Staphylococcus aureus transmission in residential care homes for the elderly. J Infect Prev 2015;16:58-66.
- Comas-Herrera A, Ashcroft E, Lorenz-Dant K. International Examples of Measures to Prevent and Manage COVID-19 Outbreaks in Residential Care and Nursing Home Settings 2020. https://ltccovid.org/2020/05/02/new-report-international-examples-of-measures-to-prevent-and-manage-covid-19-outbreaks-in-residential-care-and-nursing-home-settings/ (accessed 22 April 2022).
- Comas-Herrera A, Glanz A, Curry N, Deeny S, Hatton C, Hemmings N, et al. The COVID-19 Long-Term Care Situation in England 2020. https://ltccovid.org/wp-content/uploads/2020/11/COVID-19-Long-Term-Care-situation-in-England-19-November-3.pdf (accessed 22 April 2022).
- Comas-Herrera A, Salcher-Konrad M, Baumbusch J, Farina N, Goodman C, Lorenz-Dant K, et al. Rapid Review of the Evidence on Impacts of Visiting Policies in Care Homes During the COVID-19 Pandemic 2020. https://ltccovid.org/2020/11/01/pre-print-rapid-review-of-the-evidence-on-impacts-of-visiting-policies-in-care-homes-during-the-covid-19-pandemic/ (accessed 22 April 2022).
- Communicable Diseases Network Australia . Coronavirus Disease 2019 (COVID-19) Outbreaks in Residential Care Facilities CDNA National Guidelines for the Prevention, Control and Public Health Management of COVID-19 Outbreaks in Residential Care Facilities in Australia 2020. www.health.gov.au/sites/default/files/documents/2022/02/cdna-national-guidelines-for-the-prevention-control-and-public-health-management-of-covid-19-outbreaks-in-residential-care-facilities-in-australia.pdf (accessed 22 April 2022).
- Da Mata F, Oliveira D. COVID-19 and Long-Term Care in Brazil: Impact, Measures and Lessons Learned 2020. https://ltccovid.org/wp-content/uploads/2020/05/COVID-19-Long-term-care-situation-in-Brazil-6-May-2020.pdf (accessed 22 April 2022).
- Department of Health . Adult Social Care – Our COVID-19 Winter Plan 2020 21 2020. www.gov.uk/government/publications/adult-social-care-coronavirus-covid-19-winter-plan-2020-to-2021/adult-social-care-our-covid-19-winter-plan-2020-to-2021#:~:text=This%20plan%20sets%20out%20the,across%20health%20and%20social%20care (accessed 22 April 2022).
- Department of Health and Social Care . Overview of Adult Social Care Guidance on Coronavirus (COVID-19) 2021. www.gov.uk/guidance/overview-of-adult-social-care-guidance-on-coronavirus-covid-19 (accessed 22 April 2022).
- Department of Health Northern Ireland . COVID-19: Guidance for Nursing and Residential Care Homes in Northern Ireland. Belfast, Northern Ireland 2020. www.health-ni.gov.uk/sites/default/files/publications/health/doh-guidance-for-nursing-residential-care-homes-ni.pdf (accessed 22 April 2022).
- Directors of Adult Social Services North West . Advice Note: Cohorting, Zoning and Isolation Practice – Commissioning for Resilient Care Home Provision September 2020 2020. www.adass.org.uk/media/8163/task-force-zoning-and-cohorting-150920.pdf (accessed 22 April 2022).
- Directors of Adult Social Services North West . Care Homes Infection Control: Top Tips Guide 2020. www.nwadass.org.uk/news/1417-care-home-infection-control-top-tips (accessed 22 April 2022).
- Dumyati G, Stone ND, Nace DA, Crnich CJ, Jump RL. Challenges and strategies for prevention of multidrug-resistant organism transmission in nursing homes. Curr Infect Dis Rep 2017;19.
- Ehrlich H, McKenney M, Elkbuli A. The need for actions to protect our geriatrics and maintain proper care at U.S. long-term care facilities. J Trauma Nurs 2020;27:193-4.
- European Centre for Disease Prevention And Control . Infection Prevention and Control and Preparedness for COVID-19 in Healthcare Settings 2020. www.ecdc.europa.eu/en/infectious-disease-topics/z-disease-list/covid-19/facts/infection-prevention-and-control-healthcare (accessed 22 April 2022).
- Fewster E. Care Homes Strategy for Infection Prevention &Amp; Control of Covid-19 Based on Clear Delineation of Risk Zones 2020. https://ltccovid.org/2020/04/18/resource-care-homes-strategy-for-infection-prevention-control-of-covid-19-based-on-clear-delineation-of-risk-zones/ (accessed 22 April 2022).
- Forma L, Aaltonen M, Pulkki J. COVID-19 and Clients of Long-Term Care in Finland – Impact and Measures to Control the Virus 2020. https://ltccovid.org/2020/06/14/new-report-covid-19-and-clients-of-long-term-care-in-finland-impact-and-measures-to-control-the-virus/ (accessed 22 April 2022).
- Glendinning C. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. England 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Gould D. MRSA: implications for hospitals and nursing homes. Nurs Stand 2011;25:47-56.
- Gould D. The challenges of caring for patients with influenza. Nurs Older People 2011;23:28-35.
- Government of Canada . Infection Prevention and Control for COVID-19: Interim Guidance for Long-Term Care Homes 2021. www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevent-control-covid-19-long-term-care-homes.html (accessed 22 April 2022).
- Graham W, Wong C. Responding to COVID-19 in Residential Care: The Singapore Experience 2020. https://ltccovid.org/wp-content/uploads/2020/08/The-COVID-19-Long-Term-Care-situation-in-Singapore-27July-2020.pdf (accessed 22 April 2022).
- Griffin S. Covid-19: Experts urge strategies to prevent further outbreaks in care homes. BMJ 2020;369.
- Haenen A, Verhoef L, Beckers A, Gijsbers E, Alblas J, Huis A, et al. Surveillance of infections in long-term care facilities (LTCFs): the impact of participation during multiple years on health care-associated infection incidence. Epidemiol Infect 2019;147.
- Harold Van Houtven C, Boucher N, Dawson W. Impact of the COVID-19 Outbreak on Long-Term Care in the United States 2020. https://ltccovid.org/2020/04/24/impact-of-the-covid-19-outbreak-on-long-term-care-in-the-united-states/ (accessed 22 April 2022).
- Hasmuk K, Sallehuddin H, Pin Tan M, Cheah W, Ibrahim R, Chai S. The Long Term Care COVID-19 Situation in Malaysia 2020. https://ltccovid.org/wp-content/uploads/2020/05/Malaysia-LTC-COVID-situation-report-30-May.pdf (accessed 22 April 2022).
- Health Protection Scotland . COVID-19: Information and Guidance for Care Home Settings (Adults and Older People) 2020.
- Heudorf U, Müller M, Schmehl C, Gasteyer S, Steul K. COVID-19 in long-term care facilities in Frankfurt am Main, Germany: incidence, case reports, and lessons learned. GMS Hyg Infect Control 2020;15.
- Higginson R. Minimising infection spread of influenza in the care setting. Pract Nurse 2019;30:S10-S5.
- Hurley E, Burke S. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Ireland 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Hsu A, Lane N, Sinha S, Dunning J, Dhuper M, Kahiel Z, et al. Understanding the Impact of COVID-19 on Residents of Canada’s Long-Term Care Homes – Ongoing Challenges and Policy Responses 2020. https://ltccovid.org/wp-content/uploads/2020/06/LTCcovid-country-reports_Canada_June-4-2020.pdf (accessed 22 April 2022).
- Jacobs R, Ashwell A, Docrat S, Schneider M. The Impact of Covid-19 on Long-Term Care Facilities in South Africa With a Specific Focus on Dementia Care 2020. https://ltccovid.org/wp-content/uploads/2020/07/COVID-19-Long-Term-Care-Situation-in-South-Africa-10-July-2020.pdf (accessed 22 April 2022).
- Johansson L. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Sweden 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Jump RLP, Donskey CJ. Clostridium difficile in the long-term care facility: prevention and management. Current Geriatrics Reports 2015;4:60-9.
- Kim H. The Impact of COVID-19 on Long-Term Care in South Korea and Measures to Address It 2020. https://ltccovid.org/wp-content/uploads/2020/05/The-Long-Term-Care-COVID19-situation-in-South-Korea-7-May-2020.pdf (accessed 22 April 2022).
- Koshkouei M. How Can Pandemic Spreads Be Contained in Care Homes? 2020. www.cebm.net/covid-19/how-can-pandemic-spreads-be-contained-in-care-homes/ (accessed 22 April 2022).
- Kruse F, van Tol L, Vrinzen C, van der Woerd O, Jeurissen P. The Impact of COVID-19 on Long-Term Care in the Netherlands: The Second Wave 2020. https://ltccovid.org/2020/11/25/updated-country-report-the-impact-of-covid-19-on-long-term-care-in-the-netherlands-the-second-wave/ (accessed 22 April 2022).
- Lorenz-Dant K. Germany and the COVID-19 Long-Term Care Situation 2020. https://ltccovid.org/wp-content/uploads/2020/04/Germany_LTC_COVID-19-23-April-2020_updated.pdf (accessed 22 April 2022).
- Low L, Hinsliff-Smith K, Sinha SK, Stall NM, Verbeek H, Siette J. Safe Visiting at Care Homes During COVID-19: A Review of International Guidelines and Emerging Practices During the COVID-19 Pandemic 2021. https://ltccovid.org/2021/01/19/safe-visiting-at-care-homes-during-covid-19-a-review-of-international-guidelines-and-emerging-practices-during-the-covid-19-pandemic/ (accessed 22 April 2022).
- Luckenbach C, Klukas E, Schmidt P, Gerlinger T. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Germany 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Manitoba Health . Preventing the Transmission of Infection in Health Care 2019. www.gov.mb.ca/health/publichealth/cdc/docs/ipc/rpap.pdf (accessed 22 April 2022).
- Ma’u E, Robinson J, Cheung G, Miller N, Cullum S. Covid-19 and Long-Term Care in Aotearoa New Zealand 2020. https://ltccovid.org/wp-content/uploads/2020/08/The-LTC-COVID-situation-in-New-Zealand-9-August-2020.pdf (accessed 22 April 2022).
- McGilton K, Escrig-Pinol A, Gordon A, Chu C, Zúñiga F, Sanchez M, et al. Uncovering the devaluation of nursing home staff during COVID-19: Are we fuelling the next health care crisis?. J Am Med Dir Assoc 2020;21:962-5.
- Ministry of Health and Long-term Care of Ontario_(MOHLTC) . Control of Respiratory Infection Outbreaks in Long-Term Care Homes 2018. www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/reference/RESP_Infectn_ctrl_guide_LTC_2018_en.pdf (accessed 22 April 2022).
- Minnesota_Department-of-Health . Covid-19 Toolkit Information for Long-Term Care Facilities 2020. www.health.state.mn.us/diseases/coronavirus/hcp/ltctoolkit.pdf (accessed 22 April 2022).
- Montoya A, Cassone M, Mody L. Infections in nursing homes: epidemiology and prevention programs. Clin Geriatr Med 2016;32:585-607.
- National Collaborating Centre for Method and Tools . Rapid Review: What Risk Factors Are Associated With COVID-19 Outbreaks and Mortality in Long-Term Care Facilities and What Strategies Mitigate Risk? 2020. www.nccmt.ca/uploads/media/media/0001/02/3021cb8ca67e86dfa1d29ea5ef2ea14dc486bfe1.pdf (accessed 22 April 2022).
- Nazarko L. How to control the risk of MRSA infection. Nurs Res Care 2006;8:298-302.
- NHS Shetland . Procedure for the Prevention Control and Management of Clostridium Difficile Infection in Care Settings in Shetland 2017. www.shb.scot.nhs.uk/board/publichealth/documents/ICM-CDif-May2017.pdf (accessed 22 April 2022).
- Public Health Agency Canada . Guidance: Infection Prevention and Control Measures for Healthcare Workers in Acute Care and Long-Term Care Settings 2010. www.canada.ca/en/public-health/services/infectious-diseases/nosocomial-occupational-infections/guidance-infection-prevention-control-measures-healthcare-workers-acute-care-long-term-care-settings.html (accessed 22 April 2022).
- Rajan S, Mckee M. Learning from the Impacts of COVID-19 on Care Homes: A Pilot Survey 2020. https://ltccovid.org/wp-content/uploads/2020/06/Learning-From-the-Impacts-of-COVID-19-on-Care-Homes-A-Pilot-Survey_June12.pdf (accessed 22 April 2022).
- Rios P, Radhakrishnan A, Thomas SM, Darvesh N, Straus SE, Tricco AC. Guidelines for preventing respiratory illness in older adults aged 60 years and above living in long-term care: a rapid review of clinical practice guidelines 2020. https://doi.org/10.1101/2020.03.19.20039180.
- Rios P, Radhakrishnan A, Williams C, Ramkissoon N, Pham B, Cormack G, et al. Preventing the transmission of COVID-19 and other coronaviruses in older adults aged 60 years and above living in long-term care: a rapid review. Systematic Reviews 2020;9.
- Schmidt A, Leichsenring K, Staflinger H, Litwin C, Bauer A. The Impact of COVID-19 on Users and Providers of Long-Term Care Services in Austria 2020. https://ltccovid.org/2020/04/16/the-impact-of-covid-19-on-users-and-providers-of-long-term-care-services-in-austria/ (accessed 22 April 2022).
- Scopetti M, Santurro A, Tartaglia R, Frati P, Fineschi V. Expanding frontiers of risk management: care safety in nursing home during COVID-19 pandemic. Int J Qual Health Care 2020.
- Shallcross L, Burke D, Stat O, Donaldson A, Hallatt G, Hayward A, et al. Risk factors associated with SARS-CoV-2 infection and outbreaks in Long Term Care Facilities in England: a national survey 2020. https://doi.org/10.1101/2020.10.02.20205591.
- Shi C, Hu B, Feng M, Wong G. Report from Mainland China: Policies to Support Long-Term Care During the COVID-19 Outbreak 2020. https://ltccovid.org/2020/04/18/report-from-mainland-china-policies-to-support-long-term-care-during-the-covid-19-outbreak/ (accessed 22 April 2022).
- Shrader C, Assadzandi S, Pilkerton C, Ashcraft A. Responding to a COVID-19 outbreak at a long-term care facility. J Appl Gerontol 2021;40:14-7.
- Smith P, Bennett G, Bradley S, Drinka P, Lautenbach E, Marx J, et al. Shea/Apic guideline: infection prevention and control in the long-term care facility. Infect Control Hosp Epidemiol 2008;29:785-814.
- Spilsbury K, Davi R, Daffu-O’Reilly A, Griffiths A, Haunch K, Jones L, et al. Less COVID19. Learning by Experience and Supporting the Care Home Sector During the Covid-19 Pandemic: Key Lessons Learnt, So Far, by Frontline Care Home and NHS Staff 2020. https://ltccovid.org/2020/10/09/learning-by-experience-and-supporting-the-care-home-sector-during-the-covid-19-pandemic-key-lessons-learnt-so-far-by-frontline-care-home-and-nhs-staff-less-covid-uk/ (accessed 22 April 2022).
- Stall NM, Johnstone J, McGeer AJ, Dhuper M, Dunning J, Sinha SK. Finding the right balance: an evidence-informed guidance document to support the re-opening of canadian nursing homes to family caregivers and visitors during the coronavirus disease 2019 pandemic. J Am Med Dir Assoc 2020;21:1365-70.e7.
- Stanwell-Smith R. Advice for the influenza season: infection control in the care home. Nurs Res Care 2008;10:592-8.
- Suarez-Gonzalez A, Velasco Castañón E, Comas-Herrera A. The Impact of COVID-19 in the Long-Term Care System in Asturias (Spain) 2020. https://ltccovid.org/wp-content/uploads/2020/06/COVID-Long-Term-Care-situation-in-Asturias-14-June-2020.pdf (accessed 22 April 2022).
- Szebehely M. The Impact of COVID-19 on Long-Term Care in Sweden 2020. https://ltccovid.org/wp-content/uploads/2020/07/The-COVID-19-Long-Term-Care-situation-in-Sweden-22-July-2020-1.pdf (accessed 22 April 2022).
- Urbé R. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Luxembourg 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Victoria State_Gov . Respiratory Illness in Residential and Aged Care Facilities 2018. www.health.vic.gov.au (accessed 22 April 2022).
- Wang Z. Use the environment to prevent and control COVID-19 in senior-living facilities: an analysis of the guidelines used in China. HERD: Health Environ Res Design J 2020;14:130-40.
- Wang J, Yang W, Pan L, Ji JS, Shen J, Zhao K, et al. Prevention and control of COVID-19 in nursing homes, orphanages, and prisons. Environ Pollut 2020;266:115-61.
- Winfield J, Wiley C. Tackling infection in care homes. Nurs Times 2012;108:16-8.
- Wong K, Lum T, Wong G. The COVID-19 Long-Term Care Situation in Hong Kong: Impact and Measures 2020. https://ltccovid.org/wp-content/uploads/2020/04/Hong-Kong-COVID-19-Long-term-Care-situation-27-April-2020-1.pdf (accessed 22 April 2022).
- World Health Organization . Preventing and Managing Covid-19 Across Long-Term Care Services 2020. www.who.int/publications/i/item/WHO-2019-nCoV-Policy_Brief-Long-term_Care-2020.1 (accessed 22 April 2022).
- World Health Organization . COVID-19 Infection Prevention and Control. Communication Toolkit for Long-Term Care Facilities 2020. https://apps.who.int/iris/bitstream/handle/10665/333848/WPR-DSE-2020-029-engpdf?sequence=1&isAllowed=y (accessed 22 April 2022).
- World Health Organization . COVID-19 Infection Prevention and Control. Preparedness Checklist for Long-Term Care Facilities 2020. https://www.who.int/publications-detail-redirect/WPR-DSE-2020-028 (accessed 22 April 2022).
- World Health Organization . Guidance on COVID-19 for the Care of Older People and People Living in Long-Term Care Facilities, Other Non-Acute Care Facilities and Home Care 2020.
- World Health Organization . Infection Prevention and Control Guidance for Long-Term Care Facilities in the Context of COVID-19 2020. https://apps.who.int/iris/handle/10665/331508 (accessed 22 April 2022).
- Ylinen T, Ylinen V, Kalliomaa-Puha L, Ylinen S. MC COVID-19 Governmental Response to the COVID-19 Pandemic in Long-Term Care Residences for Older People: Preparedness, Responses and Challenges for the Future. Finland 2021. www.mc-covid.csic.es/english-version/publications (accessed 22 April 2022).
- Zalakaín J, Davey V. The Impact of COVID-19 on Users of Long-Term Care Services in Spain 2020. https://ltccovid.org/wp-content/uploads/2020/05/LTCcovid-Spain-country-report-28-May-1.pdf (accessed 22 April 2022).
- Health Information and Quality Authority . Rapid Review of Public Health Guidance for Residential Care Facilities in the Context of COVID-19 2021. www.hiqa.ie/sites/default/files/2021-03/Rapid-review-of-public-health-guidance-for-residential-care-facilities-in-the-context-of-covid-19.pdf (accessed 22 April 2022).
- CASP-checklists n.d. https://casp-uk.net/casp-tools-checklists/ (accessed 22 April 2022).
- Hong Q, Pluye P, Fabregues S, Bartlett G, Boardman F. Mixed Methods Appraisal Tool (MMAT) 2018. https://pubmedncbinlmnihgov/28190381/ (accessed 22 April 2022).
- Joanna-Briggs-Institute n.d. https://jbi.global/critical-appraisal-tools (accessed 22 April 2022).
- Jünger S, Payne S, Brine J, Radbruch L, Brearley S. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 2017;31:684-706.
- Iaboni A, Quirt H, Engell K. Barriers and facilitators to person-centred infection prevention and control: results of a survey about the Dementia Isolation Toolkit. BMC Geriatr 2022;22.
- Marshall F, Gordon A, Gladman J. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr 2021;21.
- Bunn D. The lived experience of implementing infection control measures in care homes during two waves of the COVID-19 pandemic. A mixed-methods study. J Long Term Care 2021:386-400.
- Liddell K, Ruck K, Holland A, Huppert J, Underwood B, Clark O, et al. Isolating residents including wandering residents in care and group homes: medical ethics and English law in the context of Covid-19. Int J Law Psychiatry 2021.
- Nettleton S, Buse C, Martin D. ‘Essentially it’s just a lot of bedrooms’: architectural design, prescribed personalisation and the construction of care homes for later life. Sociol Health Illn 2018;40:1156-71.
- Fitzpatrick J, Tzouvara V. Facilitators and inhibitors of transition for older people who have relocated to a long-term care facility: a systematic review. Health Soc Care Community 2019;27:e57-e81.
- Nolan M, Brown J, Davies S, Nolan J, Keady J. The Senses Framework: improving care for older people through a relationship-centred approach 2006.
- Killett A, Burns D, Kelly F, Brooker D, Bowes A, La Fontaine J, et al. Digging deep: how organisational culture affects care home residents’ experiences. Age Soc 2016;36:160-88.
- Kazawa K, Kodama A, Sugawara K. Person-centered dementia care during COVID-19: a qualitative case study of impact on and collaborations between caregivers. BMC Geriatr 2022;22.
- White E, Wetle T, Reddy A, Baier R. Front-line nursing home staff experiences during the COVID-19 pandemic. J Am Med Dir Assoc 2021;22:199-203.
- Spilg E, Rushton C, Phillips J. The new frontline: exploring the links between moral distress, moral resilience and mental health in healthcare workers during the COVID-19 pandemic. BMC Psychiatry 2022;22.
- Cations M, Laver K, Walker R, Smyth A, Fernandez E, Corlis M. The case for trauma-informed aged care. Int J Geriatr Psychiatry 2020;35:425-9.
- NHS England . Supporting Staff Through Trauma Risk Management 2020. www.england.nhs.uk/nursingmidwifery/shared-governance-and-collective-leadership/nursing-covid-19-catalogue-of-change/supporting-staff-through-trauma-risk-management/ (accessed 22 April 2022).
- O’Neill M, Ryan A, Tracey A, Laird L. ‘Waiting and Wanting’: older peoples’ initial experiences of adapting to life in a care home: a grounded theory study. Age Soc 2022;42:351-75.
- Hockley J. COVID, communication and care homes: a staffs’ perspective of supporting the emotional needs of families. J Long-Term Care Adm 2021:167-76.
- Brown-Wilson C, Davies S, Nolan M. Developing personal relationships in care homes: realising the contributions of staff, residents and family members. Age Soc 2009;29:1041-63.
- Davies S, Nolan M. ‘Making it better’: self-perceived roles of family caregivers of older people living in care homes: a qualitative study. Int J Nurs Stud Adv 2006;43:281-91.
- Ferguson J. How do the support networks of older people influence their experiences of social isolation in care homes?. Social Inclusion 2021;9:315-26.
- Comas-Herrera A, Fernandez J, Hancock R, Hatton C, Knapp M, McDaid D, et al. COVID-19: implications for the support of people with social care needs in England. J Aging Soc Polic 2020;32:365-72.
- Valayudhan L, Aarsland D, Ballard C. Mental health of people living with dementia in care homes during COVID-19 pandemic. Int Psychogeriatr 2020;32:1253-4.
- Amnesty International . As If Expendable – The UK Government’s Failure to Protect Older People in Care Homes During the Covid-19 Pandemic 2020. www.amnesty.org.uk/files/2020-10/Care%20Homes%20Report.pdf (accessed 22 April 2022).
- Chu C, Ronquillo C, Khan S, Hung L, Boscart V. Technology recommendations to support person-centered care in long-term care homes during the COVID-19 pandemic and beyond. J Aging Soc Policy 2021;33:539-54.
- Department of Health and Social Care . People at the Heart of Care: Adult Social Care Reform White Paper 2022. www.gov.uk/government/publications/people-at-the-heart-of-care-adult-social-care-reform-white-paper (accessed 22 April 2022).
- Green L, Moran L. Covid-19, social distancing and the ‘scientisation’ of touch: exploring the changing social and emotional contexts of touch and their implications for social work. Qual Soc Work 2021;20:171-8.
- Flynn L, Liang Y, Geri L, Dickson G, Aiken L. Effects of nursing practice environments on quality outcomes in nursing homes. J Am Geriatr Soc 2010;58:2401-6.
- Choi J, Flynn L, Aiken L. Nursing practice environment and registered nurses’ job satisfaction in nursing homes. Gerontologist 2011;52:484-92.
- Spilsbury K, Hanratty B, McCaughan D. Supporting Nursing in Care Homes. Project Report for the RCN Foundation Patient Care and Professional Development for Nursing Staff in Care and Nursing Homes: A Research and Consultation Project 2015.
- Couper K, Murrells T, Sanders J, Anderson J, Blake H, Kelly D, et al. The impact of COVID-19 on the wellbeing of the UK nursing and midwifery workforce during the first pandemic wave: a longitudinal survey study. Int J Nurs Stud 2022;127.
- Maben J, Conolly A, Abrams R, Rowland E, Harris R, Kelly D, et al. ‘You can’t walk through water without getting wet’ UK nurses’ distress and psychological health needs during the Covid-19 pandemic: a longitudinal interview study. Int J Nurs Stud 2022.
- Wilkinson K, Day J, Thompson-Coon J, Lang I, Liabo K, Goodwin V, et al. The Impact of the COVID-19 Pandemic on the Wellbeing of UK Care Home Practitioners. University of Exeter, Devon Care Homes Collaborative; 2022.
- Skills for Care . The State of the Adult Social Care Sector and Workforce in England 2021.
- Nyashanu M, Pfende F, Ekpenyong M. Triggers of mental health problems among frontline healthcare workers during the COVID-19 pandemic in private care homes and domiciliary care agencies: lived experiences of care workers in the Midlands region, UK. Health Soc Care Community 2022;30:e370-6.
- Sarabia-Cobo C, Pérez V, de Lorena P, Hermosilla-Grijalbo C, Sáenz-Jalón M, Fernández-Rodríguez A, et al. Experiences of geriatric nurses in nursing home settings across four countries in the face of the COVID-19 pandemic. J Adv Nurs 2021;77:869-78.
- Aiello A, Khayeri M, Raja S, Peladeau N, Romano D, Leszcz M, et al. Resilience training for hospital workers in anticipation of an influenza pandemic. J Contin Educ Health Prof 2011;31:15-20.
- Anand J, Donnelly S, Milne A, Nelson-Becker H, Vingare E, Deusdad B, et al. The covid-19 pandemic and care homes for older people in Europe – deaths, damage and violations of human rights. Eur J Soc Work 2021.
- National Audit Office . Readying the NHS and Adult Social Care in England for COVID-19 2020.
- Harris R, Fletcher S, Sims S, Ross F, Brearley S, Manthorpe J. Developing programme theories of leadership for integrated health and social care teams and systems: a realist synthesis. Health Soc Care Deliv Res 2022;10.
- Langins M, Curry N, Lorenz-Dant K, Comas-Herrera A, Rajan S. The Covid-19 pandemic and long term care: What can we learn from the first wave about how to protect care homes?. Eurohealth 2020;26:77-82.
- Kaelen S, van den Boogaard W, Pellecchia U, Spiers S, De Cramer C, Demaegd G. How to bring residents’ psychosocial wellbeing to the heart of the fight against Covid-19 in Belgian nursing homes – A qualitative study. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0249098.
- Devi R, Hinsliff-Smith K, Goodman C, Gordon A. The COVID-19 pandemic in UK care homes – revealing the cracks in the system. J Nurs Home Res 2020:58-60.
- Fallon A, Dukelow T, Kennelly S, O’Neill D. COVID-19 in nursing homes. QJM: Int J Med 2020;113:391-2.
- Gurdasani D, McKee M. The parliamentary committee report on covid-19 response. BMJ 2021;375.
- House of Commons Health and Social Care, and Science and Technology Committees . Coronavirus: Lessons Learned to Date. Sixth Report of the Health and Social Care Committee and Third Report of the Science and Technology Committee of Session 2021–22 2021.
Appendix 1 Review methodology and findings
Search strategy, screening and selection
In consultation with Information Services Specialists at KCL, the following search strategy was developed:
‘nursing home* OR care home* OR long-term care* OR long term care* OR aged care facilit* OR aged-care facilit* OR residential care home* AND infect* control* OR infect* prevent* OR cohort* OR zon*OR quarantin* OR social distanc* OR prevent* OR isolat* AND acute respiratory infection* OR clostridium difficile* OR diarrhoea OR vomit* OR methicillin-resistant staphylococcus aureus* or SARS* OR MERS-CoV* OR flu* OR SARS-Cov19 OR SARS-CoV-2 OR COV* OR Corona*’
This search strategy was run on 13 January 2021 in seven electronic databases: MEDLINE, CINAHL, Embase, PsycINFO, HMIC, Social Care Online and Web of Science Core Collection, and a total of 4753 records were identified. Grey literature relating to policy and organisational-based material was also sought between 20 and 24 January 2021 by searching MedRxiv, PDQ-Evidence, National Institute for Health and Care Excellence (NICE) Evidence Search, LTCCOVID19.org and TRIP and 13,488 records were identified. After removing the 1465 duplicates from these 18,241 documents, 16,776 records remained. The titles and abstracts were screened independently by two reviewers using the inclusion and exclusion criteria, that is the record needed to address COVID-19 or other infectious diseases in older people (aged 65 years and over) living in CHs, nursing homes, long-term facilities or residential CHs. No limits were placed on the geographical location, but only English-language records were included because of available resources. One hundred and forty-five abstracts were identified as potentially relevant, and these records were independently reviewed in full by four reviewers using the inclusion and exclusion criteria to make a recommendation. Two reviewers reviewed each record and any conflict in the assessments were resolved in collaboration with a third reviewer. Ninety-four records were included in the review and targeted searching of the reference lists of these 94 records highlighted a further 10 records. Two reviewers again reviewed these 10 records independently, and 9 were included in the review. Thus, a total of 103 records were included in this review. 9,22,24,25,32–130
Data were extracted from the 103 included records into a bespoke data extraction form using an Excel spreadsheet, which was reviewed and tested within the team. Data items included the following: author(s) and year of publication; study aim; study design; setting and participants; intervention(s) discussed, including a description of the measure(s) used (e.g. what it was; who it was for; how it was implemented, factors supporting or hindering its implementation); findings; and author recommendations. Findings from the 103 records were synthesised using tables and a narrative summary organised around the review questions: interventions for the prevention and control of COVID-19 and their impact; challenges and facilitators for implementing COVID-19-related interventions in CHs; and interventions for the prevention and control of other (non-COVID-19-related) infectious diseases. Figure 2 highlights a flowchart of the review process.
FIGURE 2.
Flowchart of the review.
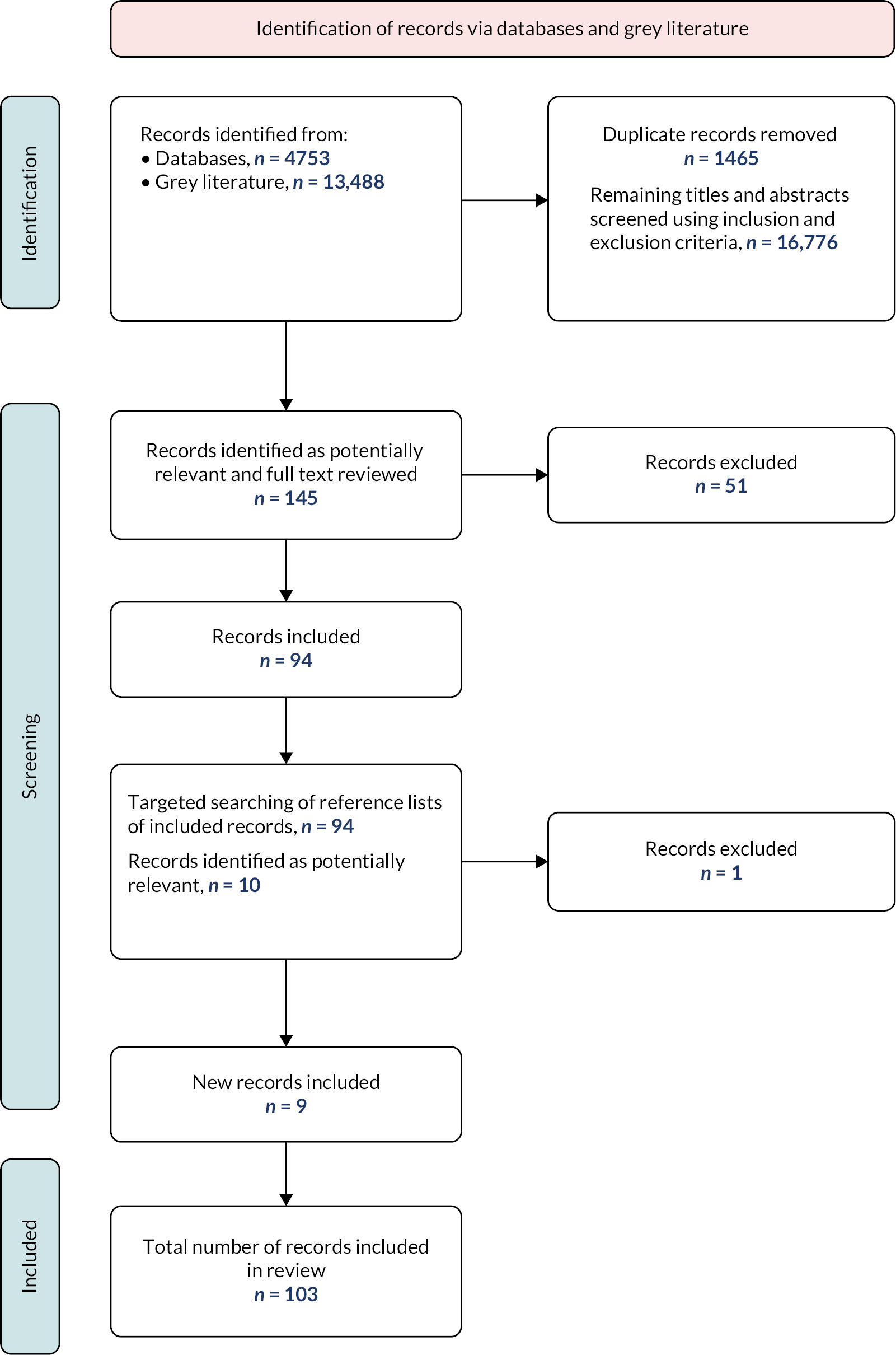
Of the 103 records included in the review, 10 were empirical research studies, 7 were literature/rapid reviews and 86 were policy documents/grey literature. Of the 10 empirical studies, 8 explored COVID-19 and 2 explored other infectious diseases. Three studies were conducted in the UK; four were conducted in Europe, two in Asia and one in North America. Two empirical studies mentioned social distancing measures, nine mentioned isolation interventions, eight mentioned restrictions and two mentioned zoning or cohorting. The quality of these studies varied greatly (e.g. one was pre-print and not peer-reviewed), and methodologies included a randomised control trial, a pilot survey study and a retrospective cohort study. However, the risk of bias of each study was assessed by two researchers, using an appropriate quality assessment tool131–134 and there was an agreement to include all 10 studies in the review. Also included in this review were 85 policy documents/grey literature, which came from around the world and included policy documents highlighting different countries’ responses to the pandemic, guidelines/guidance for CHs, briefing documents, discussions and commentaries. The seven literature/rapid reviews were also of varying quality (again, some were pre-printed and not peer-reviewed) and five were related to COVID-19 and two related to other infectious diseases. Table 8 provides a brief overview of each of the 103 records included in this review.
| Author | Title | Year | Scope |
|---|---|---|---|
| Akkan and Canbazer32 | The long-term care response to COVID-19 in Turkey. | 2020 | Policy paper highlighting Turkey’s response to the COVID-19 pandemic. |
| Anderson et al.33 | Nursing home design and COVID-19: balancing infection control, quality of life, and resilience. | 2020 | Special article to discuss the need for CHs to examine architectural design models. |
| Arling and Arling34 | COVID-19 and long-term care in the US State of Minnesota. | 2020 | Policy paper highlighting US State of Minnesota’s response to the COVID-19 pandemic. |
| Arlotti et al.35 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future. Italy. | 2021 | Policy paper highlighting Italy’s response to the COVID-19 pandemic. |
| Ayalon37 | Long-term care settings in the times of COVID-19: challenges and future directions. | 2020 | Commentary on the challenges experienced in CHs during COVID-19. |
| Australian Government36 | CASE STUDY: Dorothy Henderson Lodge. | 2020 | Case study example of a CH’s battle against COVID-19. |
| Baron-Garcia et al.38 | Measures adopted against COVID-19 in long-term care services in Catalonia. | 2020 | Policy paper highlighting Catalonia’s response to the COVID-19 pandemic. |
| Belmin et al.39 | Coronavirus disease 2019 outcomes in French nursing homes that implemented staff confinement with residents. | 2020 | Retrospective cohort study conducted to investigate COVID-19-related outcomes in French nursing homes that implemented voluntary staff confinement with residents. |
| Bergman et al.40 | Recommendations for welcoming back nursing home visitors during the COVID-19 pandemic: results of a Delphi panel. | 2020 | Delphi study to generate consensus guidance statements focusing on essential family caregivers and visitors. |
| Blain et al.41 | August 2020 Interim EuGMS guidance to prepare European long‑term care facilities for COVID‑19. | 2020 | Guidance for long-term care facilities in preventing the entrance and spread of SARS-CoV-2. |
| British Geriatrics Society9 | Managing the COVID-19 pandemic in CHs for older people. | 2020 | Guidance developed to help CH staff and NHS staff who work with them to support residents through the pandemic. |
| Browne et al.42 | Policy response to COVID-19 in long-term care facilities in Chile. | 2020 | Policy paper highlighting Chile’s response to the COVID-19 pandemic. |
| Bruquetas-Callejo and Böcker Radboud43 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future. The Netherlands. | 2021 | Policy paper highlighting the Netherland’s response to the COVID-19 pandemic. |
| Burdsall et al.44 | A unit guide to infection prevention for long-term care staff. | 2017 | Guidance for long-term care staff on how to prevent healthcare-associated infections. |
| Buynder et al.45 | Guidelines for the prevention, control and public health management of influenza outbreaks in residential care facilities in Australia. | 2017 | Guidance for residential care facilities on the management of influenza. |
| Campeon et al.46 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future: France. | 2021 | Policy paper highlighting France’s response to the COVID-19 pandemic. |
| Capucha et al.47 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future: Portugal. | 2021 | Policy paper highlighting Portugal’s response to the COVID-19 pandemic. |
| Care Provider Alliance48 | COVID-19: visitors’ protocol. CPA briefing for care providers. | 2020 | Visitors’ protocol to provide practical help to CHs around visiting. |
| Care Provider Alliance49 | Staff movement: a risk management framework briefing for adult CH providers. | 2020 | Staff briefing to provide a risk management approach that CHs can use to manage restrictions on staff movements. |
| Centres for Medicare and Medicaid51 | COVID-19 long-term care facility guidance. | 2020 | Guidance document to provide recommendations for immediate action to reduce the spread of COVID-19. |
| Centres for Disease Control and Prevention50 | Coronavirus disease 2019 (COVID-19) preparedness checklist for nursing homes and other long-term care settings. | 2019 | Guidance document to provide a checklist to be used as one tool in developing a comprehensive COVID-19 response plan. |
| Charlesworth and Low52 | The long-term care COVID-19 situation in Australia. | 2020 | Policy paper highlighting Australia’s response to the COVID-19 pandemic. |
| Chen et al.53 | Long-term care, residential facilities, and COVID-19: an overview of federal and state policy responses. | 2020 | Special article to provide an overview of federal regulatory changes and state-level executive orders in relation to COVID-19. |
| Chuang et al.54 | Infection control intervention on MRSA transmission in residential CHs for the elderly. | 2015 | Two-arm cluster randomised controlled trial to evaluate the effectiveness of an infection control bundle in controlling the MRSA transmission in residential care. |
| Comas-Herrera et al.55 | International examples of measures to prevent and manage COVID-19 outbreaks in residential care and nursing home settings. | 2020 | Policy paper to provide examples of policy and practice measures that have been adopted internationally to prevent COVID-19 infections in CHs and to mitigate their impact. |
| Comas-Herrera et al.56 | The COVID-19 long-term care situation in England. | 2020 | Policy paper highlighting England’s response to the COVID-19 pandemic. |
| Comas-Herrera et al.57 | Rapid review of the evidence on impacts of visiting policies in CHs during the COVID-19 pandemic. (Pre-print, not yet reviewed.) | 2020 | Rapid review on visiting policies in CHs during the COVID-19 pandemic. |
| Communicable Diseases Network Australia58 | Coronavirus disease 2019 (COVID-19) outbreaks in residential care facilities. | 2020 | Guidelines for the control of COVID-19 outbreaks in residential care. |
| Da Mata and Oliveira59 | COVID-19 and long-term care in Brazil: impact, measures and lessons learned. | 2020 | Policy paper highlighting Brazil’s response to the COVID-19 pandemic. |
| Department of Health Northern Ireland62 | COVID-19: guidance for nursing and residential CHs in Northern Ireland. | 2020 | Guidance document for nursing and residential CHs. |
| Department of Health and Social Care (DHSC)60 | Adult social care – our COVID-19 winter plan 2020/21. | 2020 | Guidance document to provide the key elements of national support available for the social care sector for winter 2020/21. |
| DHSC61 | Overview of adult social care guidance on coronavirus (COVID-19). | 2021 | Information for adult social care providers on COVID-19 guidance and support. |
| Directors of Adult Social Services63 | Advice note: cohorting, zoning, and isolation practice – commissioning for resilient CH provision. | 2020 | Advice note developed to support local decision-making in relation to cohorting, zoning and isolation. |
| Directors of Adult Social Services64 | Care homes infection control: top tips guide. | 2020 | Guidance document to highlight some of the ways in which residential and nursing homes have responded to the COVID-19 pandemic. |
| Dumyati et al.65 | Challenges and strategies for prevention of multidrug-resistant organism (MDRO) transmission in nursing homes. | 2017 | Discussion of the challenges and potential solutions to support implementing effective IPC practices in nursing homes. |
| Ehrlich et al.66 | The need for actions to protect our geriatrics and maintain proper care at U.S. long-term care facilities. | 2020 | Discussion paper on maintaining care in US long-term care facilities. |
| European Centre for Disease Prevention67 | IPC and preparedness for COVID-19 in healthcare settings. | 2020 | Guidance document for healthcare facilities and providers in the EU and UK on preparedness and IPC measures for the management of COVID-19. |
| Fewster et al.68 | Care homes strategy for IPC of COVID-19 based on clear delineation of risk zones. | 2020 | Guidance document to provide a CHs strategy for IPC of COVID-19. |
| Forma et al.69 | COVID-19 and clients of long-term care in Finland – impact and measures to control the virus. | 2020 | Policy paper highlighting Finland’s response to the COVID-19 pandemic. |
| Glendinning70 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future. England. | 2021 | Policy paper highlighting England’s response to the COVID-19 pandemic. |
| Gordon et al.22 | Commentary: COVID in CHs—challenges and dilemmas in healthcare delivery. | 2020 | To provide a commentary on challenges and dilemmas identified in the response to COVID-19 for CHs and their residents. |
| Gould71 | MRSA: implications for hospitals and nursing homes. | 2011 | Discussion paper to update healthcare professionals’ understanding of the implications of meticillin-resistant Staphylococcus aureus (MRSA) for patients in hospital and residents in nursing homes. |
| Gould72 | The challenges of caring for patients with influenza. | 2011 | Discussion paper to provide an overview of the nature of influenza and the challenges that it poses to older people and those who care for them. |
| Government of Canada73 | IPC for COVID-19: interim guidance for long-term CHs. | 2021 | Guidance on IPC for COVID-19. |
| Graham and Wong74 | Responding to COVID-19 in residential care: the Singapore experience. | 2020 | Policy paper highlighting Singapore’s response to the COVID-19 pandemic. |
| Griffin75 | COVID-19: experts urge strategies to prevent further outbreaks in CHs. | 2020 | News article (BMJ). |
| Haenen et al.76 | Surveillance of infections in long-term care facilities (LTCFs): the impact of participation during multiple years on health care-associated infection incidence. | 2019 | Analysis of trends in data gathered by a national sentinel surveillance network. |
| Harold Van Houtven et al.77 | Impact of the COVID-19 outbreak on long-term care in the United States. | 2020 | Policy paper highlighting the US’s response to the COVID-19 pandemic. |
| Hasmuk et al.78 | The long-term care COVID-19 situation in Malaysia. | 2020 | Policy paper highlighting Malaysia’s response to the COVID-19 pandemic. |
| Health Protection Scotland79 | COVID-19: information and guidance for CH settings (adults and older people). | 2020 | Guidance for all services registered with the Care Inspectorate as CHs, except those for children and young people. |
| Health Information and Quality Authority130 | Rapid review of public health guidance for residential care facilities in the context of COVID-19. | 2021 | A rapid review of public health guidance for residential care facilities in the context of COVID-19. |
| Heudorf et al.80 | COVID-19 in long-term care facilities in Frankfurt am Main, Germany: incidence, case reports, and lessons learned. | 2020 | Discussion paper on the experiences with COVID-19 in nursing homes in Frankfurt. |
| Higginson81 | Minimising infection spread of influenza in the care setting. | 2018 | Discussion paper to outline transmission risks and infection prevention of influenza. |
| Hsu et al.83 | Understanding the impact of COVID-19 on residents of Canada’s long-term CHs – ongoing challenges and policy responses. | 2020 | Policy paper highlighting Canada’s response to the COVID-19 pandemic. |
| Hurley and Burke82 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses, and challenges for the future. Ireland. | 2021 | Policy paper highlighting Ireland’s response to the COVID-19 pandemic. |
| Jacobs et al.84 | The impact of COVID-19 on long-term care facilities in South Africa with a specific focus on dementia care. | 2020 | Policy paper highlighting South Africa’s response to the COVID-19 pandemic, with a specific focus on dementia care. |
| Johansson and Schön85 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future. Sweden. | 2021 | Policy paper highlighting Sweden’s response to the COVID-19 pandemic. |
| Jump and Donskey86 | Clostridium difficile in the long-term care facility: prevention and management. | 2015 | Discussion paper on epidemiology and management of C. diff infection among residents of long-term care facilities. |
| Kim87 | The impact of COVID-19 on long-term care in South Korea and measures to address it. | 2020 | Policy paper highlighting South Korea’s response to the COVID-19 pandemic. |
| Koshkouei et al.88 | How can pandemic spreads be contained in CHs? | 2020 | Rapid review evaluating available measures to minimise the risk of infection spread within CH settings. |
| Kruse et al.89 | The impact of COVID-19 on long-term care in the Netherlands: the second wave. | 2020 | Policy paper highlighting the Netherland’s response to the COVID-19 pandemic. |
| Lorenz-Dant90 | Germany and the COVID-19 long-term care situation. | 2020 | Policy paper highlighting Germany’s response to the COVID-19 pandemic. |
| Low et al.91 | Safe visiting at CHs during COVID-19: a review of international guidelines and emerging practices during the COVID-19 pandemic. | 2021 | Policy paper exploring guidelines for safe visiting at CHs during the COVID-19 pandemic. |
| Lückenbach et al.92 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future. Germany. | 2021 | Policy paper highlighting Germany’s response to the COVID-19 pandemic. |
| Manitoba Health93 | Routine practices and additional precautions: preventing the transmission of infection in health care. | 2019 | Guidance document on preventing the transmission of infection in health care. |
| Ma’u et al.94 | COVID-19 and long-term care in Aotearoa New Zealand. | 2020 | Policy paper highlighting New Zealand’s response to the COVID-19 pandemic. |
| McGilton et al.95 | Uncovering the devaluation of nursing home staff during COVID-19: are we fuelling the next health care crisis? | 2020 | Editorial. |
| Ministry of Health and Long Term Care96 | Control of respiratory infection outbreaks in long-term CHs, 2018. | 2018 | Guidance document on controlling respiratory infection outbreaks in CHs. |
| Minnesota Dept of Health | COVID-19 toolkit: information for long-term care facilities. | 2020 | Toolkit for long-term care facilities. |
| Montoya et al.98 | Infections in nursing homes: epidemiology and prevention programs. | 2016 | Discussion paper. |
| National Collaborating Centre for Methods and Tools99 | Rapid review: what risk factors are associated with COVID-19 outbreaks and mortality in long-term care facilities and what strategies mitigate risk? | 2020 | Rapid review on risk factors for COVID-19 outbreaks. |
| Nazarko100 | How to control the risk of MRSA infection. | 2006 | Discussion paper on the effects of MRSA and the ways in which CH workers can prevent its spread. |
| NHS Shetland101 | Procedure for the prevention control and management of Clostridium Difficile infection in care settings in Shetland. | 2017 | Guidance document for healthcare settings in Shetland. |
| Public Health Agency Canada102 | Guidance: IPC measures for healthcare workers in acute care and long-term care settings seasonal influenza. | 2010 | Guidance document on IPC measures for seasonal influenza. |
| Rajan and McKee103 | Learning from the impacts of COVID-19 on CHs: a pilot survey. | 2020 | Pilot study to establish the impacts of COVID-19 on CHs. |
| Rios et al.104 | Guidelines for preventing respiratory illness in older adults aged 60 years and above living in long-term care. | 2020 | To identify infection protection and control recommendations from published clinical practice guidelines (CPGs) for adults aged 60 years and older in long-term care settings. |
| Rios et al.105 | Preventing the transmission of COVID-19 and other coronaviruses in older adults aged 60 years and above living in long-term care: a rapid review. | 2020 | To examine the current guidelines for IPC of COVID-19 or other coronaviruses in adults 60 years or older living in long-term care facilities (LTCF). |
| Schmidt et al.106 | The impact of COVID-19 on users and providers of long-term care services in Austria. | 2020 | Policy paper highlighting Austria’s response to the COVID-19 pandemic. |
| Scopetti et al.107 | Expanding frontiers of risk management: care safety in nursing home during COVID-19 pandemic. | 2021 | Discussion paper on care safety in nursing homes during the COVID-19 pandemic. |
| Shallcross et al.108 | Risk factors associated with SARS-CoV-2 infection and outbreaks in long term care facilities in England: a national survey. | 2020 | Cross-sectional survey to identify risk factors for SARS-CoV-2 infection and outbreaks in long-term care facilities (pre peer-review manuscript). |
| Shi et al.109 | Report from mainland China: policies to support long term care during the COVID-19 outbreak. | 2020 | Policy paper highlighting policies to support long-term care during the COVID pandemic. |
| Shrader et al.110 | Responding to a COVID-19 outbreak at a long-term care facility. | 2021 | Describes an outbreak of COVID-19 in a long-term care facility (LTCF) in West Virginia that was the epicentre of the state’s pandemic. |
| Smith et al.111 | SHEA/APIC guideline: IPC in the long-term care facility. | 2008 | Discussion of IPC guidelines in long-term care facilities. |
| Spilsbury et al.112 | Less COVID-19: learning by experience and supporting the CH sector during the COVID-19 pandemic: key lessons learnt, so far, by frontline CH and NHS staff. | 2020 | Interview study capturing the experiences of front-line CH and NHS staff caring for older people with COVID-19. |
| Stall et al.113 | Finding the right balance: an evidence-informed guidance document to support the re-opening of Canadian nursing homes to family caregivers and visitors during the coronavirus disease 2019 pandemic. | 2020 | Guidance document on reopening of Canadian nursing homes to family caregivers and visitors during the COVID-19 pandemic. |
| Stanwell-Smith114 | Advice for the influenza season: infection control in the CH. | 2008 | Discussion paper on the methods of infection control for influenza and other acute upper respiratory infections. |
| Suarez-Gonzalez et al.115 | The impact of COVID-19 in the long-term care system in Asturias (Spain). | 2020 | Policy paper highlighting Austria’s response to the COVID-19 pandemic. |
| Suarez-Gonzalez24 | Detrimental effects of confinement and isolation on the cognitive and psychological health of people living with dementia during COVID-19: emerging evidence. | 2020 | To describe the effects of lockdown on people with dementia. |
| Szebehely116 | The impact of COVID-19 on long-term care in Sweden. | 2020 | Policy paper highlighting Sweden’s response to the COVID-19 pandemic. |
| Urbé117 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses, and challenges for the future. | 2021 | Policy paper highlighting Luxembourg’s response to the COVID-19 pandemic. |
| Victoria State Government118 | Respiratory illness in residential and aged care facilities: guidelines and information. | 2018 | Guidance document on respiratory illness in residential and aged care facilities. |
| Verbeek et al.25 | Allowing visitors back in the nursing home during the COVID-19 crisis: a Dutch national study into first experiences and impact on well-being. | 2020 | Mixed-methods cross-sectional study on visiting CHs during the COVID-19 pandemic. |
| Wang119 | Use the environment to prevent and control COVID-19 in senior-living facilities: an analysis of the guidelines used in China. | 2020 | Content analysis of the guidelines on COVID-19 control issued by the State Council of China in February 2020 for senior-living facilities. |
| Wang et al.120 | Prevention and control of COVID-19 in nursing homes, orphanages, and prisons. | 2020 | Discussion paper on prevention and control strategies for COVID-19. |
| Winfield and Wiley121 | Tackling infection in CHs. | 2012 | Discussion paper describing a three-dimensional strategy that reduced MRSA colonisation. |
| Wong et al.122 | The COVID-19 long-term care situation in Hong Kong: impact and measures. | 2020 | Policy paper highlighting Hong Kong’s response to the COVID-19 pandemic. |
| World Health Organization123 | Preventing and managing COVID-19 across long-term care services. | 2020 | Policy paper providing objectives and key action points to prevent and manage COVID-19 across long-term care. |
| World Health Organization124 | COVID-19 IPC. Communication toolkit for long-term care facilities. | 2020 | Communication toolkit to protect residents and staff from infection and prevent potential spread of COVID-19 and other respiratory pathogens within long-term care facilities. |
| World Health Organization125 | COVID-19 IPC. Preparedness checklist for long-term care facilities. | 2020 | Checklist to be used by facility administrators, IPC focal points or staff, internal or external professionals. |
| World Health Organization126 | Guidance on COVID-19 for the care of older people and people living in long-term care facilities, other non-acute care facilities and home care. | 2020 | Guidance on COVID-19 for the care of older people and people living in long-term care facilities. |
| World Health Organization127 | IPC guidance for long-term care facilities in the context of COVID-19. | 2020 | Interim guidance document on IPC of COVID-19. |
| Ylinen et al.128 | MC COVID-19 Governmental response to the COVID-19 pandemic in long-term care residences for older people: preparedness, responses and challenges for the future. | 2021 | Policy paper highlighting Finland’s response to the COVID-19 pandemic. |
| Zalakaín and Davey129 | The COVID-19 on users of long-term care services in Spain. | 2020 | Policy paper highlighting Spain’s response to the COVID-19 pandemic. |
Findings
Strategies for COVID-19
Eighty-three papers specifically discussed the strategies used by CHs to implement social distancing or isolation of residents to prevent or control the transmission of COVID-19 among their residents and staff and/or the impact, challenges or facilitators of these strategies. 9,22,24,25,32–43,46–53,55–64,66–70,73–75,77–80,82–85,87,89–92,94,95,97,99,103–110,112,113,115–117,119,120,122–130 Other papers explored issues around restrictions, zoning, cohorting and surveillance. Many other strategies, such as the use of PPE, testing, ventilation and adequate hygiene procedures, were also regularly highlighted alongside these discussions but are beyond the scope of this review and therefore not discussed here.
This report is structured so that the individual methods associated with prevention and control are discussed separately.
Strategies used by care homes to prevent the transmission of COVID-19
Social/physical distancing
The terms ‘social distancing’ and ‘physical distancing’ were used interchangeably within and across papers, but for purposes of consistency in this review, they will be referred to herein as ‘social distancing’. There was little discussion of social distancing interventions to prevent the transmission of COVID-19 within CHs. Generally, there was no definition provided in the literature of the term or what it meant in practice, other than that CHs must adhere to ‘government guidance’ or ‘national rules’ on distancing. Those who did describe their understanding of distancing stated this was maintaining a distance from other people of at least 1 to 2 m in Europe or 6 feet in the USA. 41,46,68,79,97,124,127 Social distancing was regularly referred to in conjunction with other infection control measures, such as hand hygiene and mask-wearing,73,79,90,97 but these measures were beyond the scope of this review.
Social distancing in CHs generally referred to those residents who had not been exposed to COVID-19 being able to continue with some regular routines and group activities while maintaining a physical distance from other residents. 46,56,59,62,69,73,79,84,90,97,104,105,112,119,124,127,130 This involved CHs working innovatively to organise, for example, small-group, socially distanced mealtimes in the dining room;69,73,84,119,127 separating chairs in common rooms;73 instigating one-way movement around the home63 and placing spacing indicators on the floors. 73 Some guidance documents recommended that any spaces where social distancing was not possible should be ‘taped off’ to prevent residents from accessing them68 and that any activities that could not be carried out under social distancing guidelines should be cancelled. 73 One policy document stated that social distancing measures had enabled residents to maintain a ‘normal’ life within the CH during the pandemic. 46
Other grey literature discussed the importance of staff maintaining a social distance from each other, for example in staff rooms and other areas around the CH. 38,68,73,95,97,127,130 Guidance/policy documents referred to the need to separate chairs in staff rooms;73 to stagger breaks to limit the density of staff in specific areas;79 and to restrict staff car sharing to and from work. 79 Others discussed the need to ensure visitors maintained an appropriate social distance from residents and staff60,90,127 – for more on this, see the ‘Visitor restrictions’ section.
Isolation/quarantine
The terms ‘quarantine’ and ‘isolation’ were used interchangeably within and across reports, but for the purposes of consistency in this review, they will be referred to herein as ‘isolation’. It is important to note that many other interventions were again discussed in relation to isolation, such as the importance of testing, good ventilation in rooms, adequate hygiene procedures and the use of PPE,56,59,60,104,105,119,130 but this was beyond the scope of this review. There were several reported ways in which CHs used isolation in a preventive capacity during the COVID-19 pandemic:
Isolation of residents
Some CHs chose (or were recommended) to care for all residents as though they were COVID-19 positive, which meant isolating everyone within their own private rooms regardless of their COVID status. 46,80,103,130 However, others only asked residents to isolate themselves within their rooms if they had suspected COVID-19 symptoms or had been in contact with someone with COVID-19 (more on this is discussed in the ‘Infection control’ section). Other guidance on isolation as a preventative measure is discussed below.
Grey literature stated that residents discharged from hospital should be tested before they returned to their CH56,60,62,64,78,79,94 and isolate for 14 days after discharge, either at a family member’s home, within a specially created isolation unit/adapted hotel, or within a single room at the CH. 9,32,42,51,55,56,60–62,73,78,79,84,90,94,97,109,122,127,129,130 Some stated, however, that residents only had to isolate for 7 days after discharge from the hospital. 92 Furthermore, some CHs did not require residents to be isolated after discharge from the hospital at all if they had been free of symptoms for more than 48 hours and had tested negative for COVID-19. 55,59,90
Many CHs ensured that all new residents were isolated for 14 days upon their arrival at the home, even if they had had a negative COVID-19 test result. 9,41,51,55,61,62,73,78,84,90,109,112,120,127,128,130 However, other CHs prohibited or were advised to deny the admission of new residents altogether. 32,38,39,55,58,85,90,119,129 Finally, there was limited and contradictory guidance around whether residents were required to isolate if they had to leave the home for any other reason, such as healthcare appointments or visiting friends or family members. For example, some reports said that anyone leaving the CH for any reason should isolate for 14 days afterwards. 41,97 However, another stated that residents only needed to isolate if they had been absent from the home for more than 12 hours. 130
One empirical study stated it was important that residents’ isolation rooms were private with a dedicated bathroom,119 while a policy document said if that was not possible, a dedicated bedpan/commode would suffice. 68 The same study also stated that isolation rooms should be larger than typical residential rooms, with access to television, radio, internet and reading materials,119 while the policy document noted that any communal items that needed to be shared between residents (such as books) should also be quarantined for 5 days between uses. 68 It noted that being in isolation should not result in residents receiving less or worse care than usual, especially care associated with hygiene and dignity. 68 However, examples were provided of isolated residents not showering for weeks due to staff concerns over the infection control. 68
Isolation of staff
Preventative isolation measures were also implemented for CH staff, such as a 14-day isolation period for those staff returning from a hospital stay109,119 or for those returning from international travel. 94,122 In addition, isolation was also required for those staff who had COVID-19 symptoms or had contact with someone with COVID-19 (this is discussed in more detail in the ‘Infection control’ section).
Restrictions
Although this review focussed on social distancing and isolation interventions, other interventions related to restrictions were also regularly discussed. This included placing restrictions upon residents;25,32,34,40,46,52,53,55,58,66,68,73,80,97,105,119,122,126,128 CH staff;32,39,46,51,53,55,62,64,73–75,77–79,83,92,94,99,105,106,108,129,130 visitors;9,24,25,32,34,35,38–40,42,43,46–48,50–53,55–58,60,62,64,66–69,73,74,78,79,82–85,90–92,94,95,97,99,103,105–107,109,110,112,113,115–117,119,120,122–130 and other professionals/services. 25,34,39,40,42,58,62,68,84,92,94,97,112,117,119,122,130 For the purposes ofthis review, the term ‘restriction’ refers to any instances where an individual was prevented from doing something they would normally do (e.g. cancelling all groups and activities so that residents were no longer able to attend) or asked to modify the way in which they would normally do something (e.g. asking staff to work different shift patterns). This differs from ‘social distancing’, which, for the purposes of this review, refers to instances where an individual could carry on activities of normal life, while remaining at a distance from other individuals (e.g. resident groups and activities continued, but residents were required to maintain a 2 m distance from others throughout).
Restrictions placed upon residents
Several restrictions were reported to have been placed upon CH residents to prevent the transmission of COVID-19. This included moving all residents into single rather than shared rooms where possible;32 changing the way in which meals were delivered to residents, either by staggering mealtimes so that fewer people were present in the dining room or by serving meals in residents’ rooms rather than communal dining rooms;40,53,55,80,97,105,122,126 preventing residents from visiting other residents’ rooms119 or leaving the home except for essential outings;25,32,34 and reducing/cancelling group-based and social activities. 25,40,46,52,53,55,58,66,73,105,119,126,128 Residents were also required to wear masks when leaving their rooms, if appropriate. 68,73,122 In addition, computers, televisions, radios and reading materials were to be provided within residents’ rooms,119 so long as they could be sufficiently cleaned and disinfected between uses. 73 Items that could not be cleaned and disinfected were not to be shared by residents. 73 There was no empirical evidence on whether implementing resident restrictions had any impact on preventing the transmission of COVID-19 in CHs. Still, several reports did discuss the effects of restrictions on the residents themselves. These are explored in the ‘Impact of interventions’ section.
Restrictions placed upon staff
Several studies, including one empirical research study, discussed the restrictions placed upon staff members to prevent the transmission of COVID-19 in CHs. These restrictions involved changes to working patterns, such as shift length, rota patterns, number of consecutive working days, extended working hours or staggered start times;32,46,64,73,79,92 limiting the number of settings staff could work within;55,62,64,74,83,105,130 or asking staff to live in/confine themselves within the CH for extended periods of time. 39,62,75,99,129,130 Grey literature also highlighted how professional practices were redefined, modified and adapted to suit new working rhythms and procedures (e.g. sorting bedding, disinfecting premises, serving meals). 46 In the USA, staff training and certification requirements were modified to reinforce the available workforce. For example, nurses were able to postpone training courses;53 minimum training hours for paid feeding assistants were reduced from 8 hours to 1 hour;53 and regulations of the scope of practice loosened, for example, with physicians given more flexibility to delegate tasks to nurse practitioners. 53,77 Some countries, such as Australia, New Zealand and Malaysia, increased the maximum weekly working hours allowed by international students and those with restricted work visas to help fill staff shortages in CHs. 55,78,94 Countries such as Slovenia also restricted the rights of CH staff to leave their employment or to strike. 55
There was no empirical evidence for most of these restrictions on staff working patterns having any individual impact on the transmission of COVID-19. However, there was some evidence that a combination of interventions may provide benefits. That is, a cross-sectional survey of all CHs in England providing dementia care to adults over the age of 65 years found that the risks of infection and/or outbreaks of COVID-19 were reduced in CHs that paid sickness pay, cohorted staff, did not employ agency staff and had higher staff to resident ratios. 108 There was also limited empirical evidence that staff confinement in CHs lowered transmission rates, although only one research study explored this. 39 This retrospective study conducted in French nursing homes compared rates of COVID-19 cases and mortality rates in a cohort of 17 nursing homes that implemented voluntary staff self-confinement with those derived from a national survey of 9513 nursing homes conducted by French health authorities. This cohort study found that nursing homes with staff confinement experienced a significantly lower incidence of COVID-19 among residents and staff and lower mortality than those included in the national survey conducted during the same period. In addition, all but one of the nursing homes remained free of COVID-19 among residents, indicating that staff confinement may be a useful way of preventing the entry and transmission of COVID-19 within CHs. Grey literature also confirmed anecdotal evidence of this being the case. 75 However, these restrictions could lead to uncertainty among CH staff regarding whether they would have to isolate within the CH at short notice. An example was highlighted in Germany, where staff were asked to bring sufficient clothing and toiletries to work to last 3 weeks if the home was quarantined due to increasing infections. 92 Information on the restrictions’ impact on individual staff members is discussed in the ‘Impact of interventions’ section.
Restrictions placed upon visitors
Visitor restrictions were discussed in many of the papers, and in most countries across the world family and friends were prevented from entering CHs (particularly in the first wave of the pandemic, i.e. Spring 2020), other than in EoL or special/urgent circumstances. 9,24,25,32,34,35,38–40,42,43,46,47,50–53,55–58,62,64,66,68,69,74,78,79,82,83,85,90,92,94,99,103,105–107,109,110,112,113,115–117,119,120,122,123,127–129
Several innovative interventions were adopted by CHs to provide ways for family members and friends to visit residents during periods of restriction. These included the following: window, car and garden visits;24,34,48,52,57,58,64,68,69,73,84,85,91,92,103,112,113,117,128,130 the installation of tents, glass pods or plexiglass containers/walls;24,25,68,85,128,130 encouraging handwritten letters from family or pen pal schemes;52,64,82,124 and the setting up of telephone/video calls50,52,68,78,85,92,97,110,112,117,119,122–129 or Facebook/WhatsApp groups. 64,122 Other CHs introduced a designated ‘family liaison officer’ employed to help support communication with relatives. 112 When family members were able to visit the CH (e.g. at a resident’s EoL or when lockdown restrictions were eased), varying restrictions remained in place. These included restrictions on the number of relatives allowed to visit (including no children) and/or limits to the duration of their visit;46–48,55,60,82,83,90,91,95,112,124,130 ensuring visits were supervised by staff;91 assessing a visitor’s temperature/health status on arrival;35,58,73,78,91,95,112,124,130 ensuring relatives wore PPE48,58,68,79,90,91,112,113,127 clean clothes;124,130 asking visitors to sign a disclaimer112 or undergo testing;130 requesting relatives to self-isolate for 14 days after the visit;112 ensuring visitors follow social distancing guidance and good hand hygiene;48,58,68,79,90,91,127 and using designated entrances, exits and reception rooms for visitors to minimise the number of people walking around the building. 38,48,67,68,73,112,119,130 Other reports advised that speakers or assisted hearing devices (both personal and environmental) should be considered during visits to avoid the need to raise voices and increase transmission risk. 130 The effects of these restrictions upon family members are discussed in the ‘Impact of interventions’ section.
Restrictions placed upon other professionals and services
Finally, in many instances, all but essential professionals/services were restricted from entering CHs during the COVID-19 pandemic. This included both healthcare professionals (e.g. physicians, psychologists, physiotherapists) and non-healthcare workers, such as delivery staff, hairdressers, entertainers and volunteers. 25,39,40,58,62,94,97,117,122,130 Some CHs reported continued essential access and support from primary and community healthcare teams. 42,62,68,119 Generally, these services moved towards virtual or remote ways of working, including video calls and consultations and virtual ward rounds/multidisciplinary team meetings. 62,84,92,112,119,122 One research study112 reported that while such virtual working was often deemed to be successful, it varied considerably across locations. Where medical teams continued face-to-face visits, these were well received by CHs and promoted positive working relationships. 112 However, in the grey literature, some managers reported grave concerns that they could not access health care for their residents due to doctors refusing to visit and hospitals only accepting emergencies. 84 The impact of restricting access to other professionals is explored in the ‘Impact of interventions’ section.
Surveillance
Once again, while this review focused on social distancing and isolation interventions, the importance of surveillance in preventing COVID-19 in CHs was highlighted in the literature. A relatively limited discussion was given to the importance of surveillance for COVID-19 (though more information around surveillance of other infectious diseases is highlighted in the ‘Non-COVID-19’ section). However, there was some mention in the grey literature of the importance of using data to conduct active surveillance of COVID-19 in CHs during the pandemic. 97,107,123,126,127 This included the need for the early detection of symptoms and the systematic collection, consolidation and analysis of data, such as the number of staff and residents with COVID-19; the number of COVID-19 deaths (probable and confirmed); and the number of residents transferred to hospital. 97,107,115,123,127 It was suggested that such data be disaggregated by gender, age, disability and existing health condition and integrated with existing surveillance systems. 123 Examples were provided where such data had been used to help identify possible COVID-19 outbreaks before being confirmed. 97 Policy documents also discussed the importance of having either a designated staff member to lead on infection prevention/control measures and surveillance68 or a committee tasked with implementing a surveillance programme for the rapid recognition of outbreaks. 107,126
Strategies used by care homes to control the transmission of COVID-19
Isolation
Isolation of residents
As previously noted, isolation of residents was an intervention also used to control the transmission of COVID-19 when there was already an outbreak or suspected case within a CH. 25,34,36,38,50,52,55,58,59,61,62,67,69,73,74,79,80,84,85,89,94,97,107,109,115,117,120,122–130 In most cases, only those residents who had COVID-19 symptoms themselves or who had been in contact with someone with suspected/confirmed COVID-19 were required to isolate. 25,50,52,55,58,59,61,62,67,74,79,84,85,89,94,97,107,109,117,120,123,124,127–130 However, in some CHs (e.g. in Turkey and the UK), all residents were placed in isolation once a suspected case had been identified. 32,68 Isolation was often required, across the world, for a duration of 14 days,38,59,61,74,79,127,130 though some reports from Europe, South America and Asia highlighted requirements of 10 days’ isolation. 58,126,130 Others concluded that the duration of isolation needed to be tailored according to the resident’s needs. For example, a European guidance document stated that immunocompromised individuals should isolate for longer than non-immunocompromised individuals, while those with more severe COVID-19 symptoms should isolate for longer than those experiencing only mild symptoms. 41 In these instances, isolation could reportedly last for up to 20 days or as long as the individual displayed COVID-19 symptoms. 41
Where possible, affected residents could be either isolated within their own single room in the CH25,34,36,38,41,50,55,62,69,73,79,94,97,107,123–127,130 or transferred to a hospital, ‘sanitary house’, specialised ‘pandemic hospital’, hotel or another community setting, where available/applicable. 32,35,42,55,74,78,123,129 Once again, guidance was that, if possible, isolation rooms should have their own en suite bathroom, but where this was not available, a dedicated bathroom near to the isolation room or commode should be identified for that resident’s use only. 62,73,79,97,107,124,125 The door of the isolation room should remain closed, but again, where this was not possible, CHs should ensure the resident’s bed was moved to the furthest point in the room, at a 2 m distance from the open door. 62,79,97,107 Grey literature highlighted that not all CHs were able to implement isolation measures early enough and/or effectively (e.g. because staff had worked with both healthy and infected residents) (see ‘Zoning/cohorting’ section for more on this); or because the home did not have sufficient PPE or staffing levels. 35,69
Isolation of staff
In general, any staff who developed symptoms of COVID-19 and/or had been in contact with someone with COVID-19 were informed that they should not attend work and should isolate. 36,41,55,58–60,73,74,79,84,90,97,127,130 Usually, the isolation period for staff was 14 days,38,55,74,78,90,97 but in some cases, staff could return to work after 10 days;79 or even 7 days if there were severe staff shortages90 or if they provided a negative COVID-19 test result and were able to avoid contact with immunocompromised people. 38 In addition, mandatory sick leave and pay for all staff with suspected COVID-19 symptoms was recommended in the grey literature, to ensure CH staff did not come to work when feeling unwell. 60,105 For example, in Australia, a Pandemic Leave Disaster Payment of $1500 was provided to eligible care workers who needed to self-isolate for 14 days,52 while in Scotland, funding guidance stated that CH staff should not experience financial hardship as a consequence of isolating. 79
However, there were some reports in the grey literature of CHs experiencing complex dilemmas around isolating staff, particularly when they were already experiencing significant staff shortages. There were reports in the USA of staff who had come into contact with COVID-19 being asked to continue working if they did not display symptoms themselves. 97 In some instances in the Netherlands, CH staff were asked to keep working even when they were sick,43,89 a coping strategy that could have adverse effects in spreading further the virus throughout the home. 43 Some CHs reported that if they adhered wholly to the staff isolation guidance, they would have no staff left in the home. 55 Indeed, there were examples provided in New Zealand where residents had to be transferred to the hospital due to insufficient staff available to care for them within the home. 94
‘Zoning’ and ‘cohorting’
Finally, while this review focused on social distancing and isolation interventions, the importance of zoning and cohorting in controlling the spread of COVID-19 in CHs was also highlighted in the literature. The terms ‘zoning’ and ‘cohorting’ are understood in different ways and were used interchangeably across reports. 9,22,34,40,41,49–51,55,57,58,60,64,68,73,74,82,85,87,90,94,97,99,103,105–107,110,112,117,126,127,129,130 Similarly, some reports discussed ways of separating residents without using any specific terms to describe these interventions. For this review, we refer to ‘zoning’ as creating physical separation areas within a CH, for example separating residents with and without COVID-19 onto separate floors or disparate wings of a CH. We use the term ‘cohorting’ to refer to all other imposed means of grouping residents, including allocating specific groups of residents to particular areas within a floor. Again, other interventions, such as the appropriate use of testing, PPE, cleaning, handwashing and ventilation, were thought to be vital to the success of zoning and cohorting, but are beyond the scope of this review for example. 34,68,90,103,110,112,119
As previously stated, in this review, ‘zoning’ refers to the creation of separate physical spaces or locations within a CH, such as different floors, wings, wards or units, to care for those residents with a positive COVID-19 test result/suspected COVID-19 away from those without. 9,34,41,49,51,55,57,58,64,68,74,90,103,106,110,112,129,130 A zone may have multiple-occupancy rooms but, according to the grey literature, a series of single rooms with en suite bathrooms within a zone was preferable. 126,127,130 This may have required the rearrangement of rooms or the repurposing of other areas to make this possible. 58,63 The grey literature reported the intervention of zoning to offer CHs a clear delineation of risk zones throughout the building, and it was stated that staff, residents and equipment should not move between the zones to reduce cross-contamination. 34,41,51,55,63,68,74,130 Other examples of zoning included separating areas of CHs to create a traffic-light system, with ‘green’ areas for residents who were free of COVID-19 symptoms or who had received a negative test result; ‘yellow’ areas for those at risk of infection (i.e. those isolating after being discharged from the hospital); and ‘red’ areas for those who had received a positive test result or had come into contact with someone with a positive test result. 38,68 This zoning method had been found to reduce the number of infections in previous SARS and Ebola outbreaks. 68 Others referred to similar zones within a CH, known as the ‘clean’, ‘semiclean’ and ‘contaminated’ environments119 or the ‘hot’, ‘warm’ and ‘cold’ zones. 130
In general, zones were described as self-sufficient care bubbles,74 enabling residents to have limited freedoms within their own zone. 9,49,64,103 This was considered to encourage socialisation and activity between residents within the zones and help decrease their feelings of isolation and loneliness. 112 A crucial part of successful zoning included having separate staffing teams allocated to each zone. 41,51,63,68,74 Examples from the grey literature included staff wearing different-coloured T-shirts or badges to distinguish what floor they worked on, with staff needing to keep their distance from those wearing a different colour. 64,84 Separate staff entrances, exits and corridors for each zone were also utilised, where possible41,63,68,74,112,119 with separate staff rooms, and staff communicating via text, telephone, or video call. 63,74 Although it was not always easy to reconfigure CHs in this way, some innovative examples of how this had been undertaken were highlighted, including the use of ‘Derby doors’, an inflatable barrier that sits flush against walls and ceilings to form a complete seal. 112 Where not possible to separate areas entirely, the use of any common spaces (such as lifts and pantries) should be staggered and cleaned between staff usage from different zones. 74 It was also crucial that all zoning policies and procedures were clearly articulated, and clear signage displayed to highlight the designated zone. 119
In this review, ‘cohorting’ refers to other imposed means of grouping residents, which did not involve dividing floors or units of a CH into physically separate ‘zones’. Cohorting was sometimes suggested for settings where it was impossible to physically separate residents in this manner. 41 Examples of cohorting were organising residents into small groups or dedicated areas within a floor (rather than separate floors or wings) of a CH with the same staff continuously assigned to them. 41,63,73,80,85,97,117,126,127,129 The rationale for this was that, in case of infection within this small group, as few residents and staff as possible would require isolation. 80 Another example of cohorting involved assessing residents’ preferences around risk tolerance and using these preferences to create a ‘risk-accepting’ group of residents who could convene together and be given an opportunity for increased social interactions and group dining opportunities. 40 Again, the need to have separate staffing teams for each cohort was identified as essential to minimise chances of spreading infection. 50,55,64,73,79,85,97,112,127
Zoning and cohorting were often recommended in the grey literature when isolation practices were not possible, due to the physical constraints of the CH or the individual needs of the residents. For example, it was suggested that residents who were contacts of someone with confirmed/suspected COVID-19 should ideally be isolated within a single room with a private en suite bathroom but could be cohorted/zoned in small groups where isolation was not possible. 55,68,79,97,107,129 Similarly, some reported that zoning or cohorting might be more appropriate for residents living with dementia, mood disorders or who ‘walked with purpose’, as these individuals may find it more challenging to isolate. 41,117 However, it was noted that ‘shielding’ residents (i.e. clinically vulnerable individuals who were asked to isolate in order to protect themselves from COVID-19) should not be placed in a cohort and should be prioritised for single occupancy rooms. 79 Similarly, suspected or confirmed COVID-19 cases should not be cohorted next to immunocompromised residents. 127 Nevertheless, the physical constraints of some CH buildings and layouts meant that it was also not always possible to implement zoning and cohorting interventions within CHs94,112 (see ‘Challenges and facilitators’ section for more on this). Furthermore, such interventions were also dependent upon CHs having sufficient staff resources to work in this way. 112 Indeed, some reports noted that zoning and cohorting interventions required CHs to rely upon the recruitment of new team members or upon ‘surge staffing’ (i.e. a contact list of casual staff members and external nursing agencies to enable timely recruitment). 58,63 Moving residents from their usual room to a new cohort or zone could create some confusion, anxiety or distress for residents,62,112 but it was acknowledged that for many the benefits of this were likely to outweigh the negative consequences. 112 Where possible, CHs should, however, aim to maintain residents’ usual routines as much as possible when they are placed within a specific cohort or zone. 62
Challenges and facilitators of COVID-19 interventions
Several challenges were highlighted, which negatively impacted the success of implementing social distancing and isolation interventions for COVID-19 in CHs. The most frequently stated of these challenges were related to staffing and workload. Before the COVID-19 pandemic, many CHs were already poorly prepared to implement infection control interventions due to a shortage of staff, a lack of appropriate training and equipment and excessive workloads. 39,66,92,95,103 The pandemic exacerbated these issues, by adding additional staff sickness leave/absence due to quarantine or shielding, as well as other restrictions placed on the use of agency staff and the limited number of settings that staff could work in. 22,46,66,69,77,82–84,89,90,92,94,95,112,116,123,129 Indeed, in some CHs, all (or almost all) care staff needed to be replaced with new employees due to quarantine regulations. 69,74 In some instances, this led to the care of residents being jeopardised,69 including residents being moved to hospitals when staffing of CHs became unsustainable. 94 Workload also increased for staff, due to the new tasks they had to undertake, which relatives had previously carried out or other professionals, such as hairdressers;69,95,103,123 as well as the extra preparations staff needed to undertake for the introduction of new COVID-19 interventions. 25 Care homes around the world used various methods to address these staff shortages. For example, in Australia, an emergency surge workforce was organised and funded by Healthcare Australia;36 in the USA, retired care workers and healthcare providers from other sectors were encouraged to assist with staff shortages;77 and in Sweden, those in recently unemployed groups, such as flight attendants and restaurant staff, were retrained as care aides. 85 Other countries encouraged CHs to use volunteers to help manage staff workload83,90,117 or hire new staff. 46,64,83 Yet for many CHs, staffing shortages and inadequate staff training, particularly around IPC measures and the correct use of PPE, remained a challenge. 83,84,116,123
Another frequently mentioned challenge to implementing COVID-19 interventions in CHs was a lack of guidance and clarity from governments around when and how interventions should be applied, with policy measures often scarce, flawed or adopted late. 43,46,52,56,77,82,84,103,116,128 An example of this was highlighted in the UK, where Public Health England initially published guidance stating that negative COVID-19 tests were unnecessary for CHs to accept transfers from hospitals, because symptomatic residents could be safely cared for if they were appropriately isolated in the home. 56 The assumption by the government that CHs could isolate residents in the same way as a hospital has been described as an ‘appalling error’ by the Public Accounts Committee, who stated, ‘Our care homes were effectively thrown to the wolves’ (p25). 70 By the time the government agreed that all patients should be tested for COVID-19 before discharge, over 28,000 patients had been discharged from a hospital to a CH. 70 By this stage it was clear that asymptomatic transmission could occur, and 5700 CH resident deaths had occurred. 70 The policy of discharging hospital patients to CHs without testing is now the subject of a legal challenge from residents’ family members. 70 Therefore, CH managers in the UK reported struggling to persuade their staff that government advice was credible. 103 Other flawed policies were seen elsewhere, such as CH workers not initially identified as ‘key workers’ and therefore unable to travel to work during lockdown measures and curfews. 123 Therefore, some examples were provided of CHs taking their own initiative on interventions before policy guidance came into place. 43,56 For example, a policy paper highlighting the Netherlands’ response to the COVID-19 pandemic stated that some CHs applied their own ban on visitors 1 month earlier than the government issued it. 43 Due to these issues surrounding policy and guidance, rebuilding trust in government may be difficult but is essential if future policies are to be adhered to. 103
The physical space and layout of CHs were identified as an additional issue that could make the implementation of COVID-19 interventions challenging. Not all CHs had the space to provide single rooms, create separate zones or ensure sufficient walking space around the home was in line with social distancing measures. 33,60,64,78,82,84,103,112,123,129 These difficulties with physical layout were particularly notable when attempting to isolate or zone residents – especially those living with dementia, cognitive impairment or who ‘walked with purpose’ – which meant that residents could unintentionally infect each other through their movements around the home. 60,85,103,112,116 Moving equipment across the home to enable resident cohorting also proved complicated. 103 Making changes to CHs to enable COVID-19 interventions (e.g. reconfiguring entrances and exits and other building works) could have significant cost implications. Therefore, the innovative use of space may be required. 63,64 Examples of innovative solutions to space issues included renting out motor homes to be used as staff sleeping facilities on CH driveways and utilising empty basements as staff rooms. 64 One discussion paper suggested that CHs operating with ‘household models’ (i.e. small-scale, homelike settings) had improved outcomes for residents, but that more research was required in this area. 33
Several factors were also identified in helping to facilitate the introduction of interventions within CHs. Reports from countries such as the UK and Ireland, USA and China highlighted the importance of innovative technology, which was often successfully used to remotely support residents and their families during periods of restriction and help reduce the impact of social isolation. 55,64,66,82,112,119 However, some concerns were noted around the ethics of using video calls with dying residents. 112 Furthermore, some CHs lacked sufficient broadband, Wi-Fi, laptops or iPads to support these innovative technology uses,52 while others felt staff, families and residents required training on using it. 127 The appointment of a ‘social media champion’ in CHs was one beneficial way of supporting residents and families in engaging with this new technology. 64
Also identified was the importance of ensuring sufficient staff support, both in terms of funds to pay for the extra costs associated with COVID-19 interventions and initiatives to support their well-being. For example, many countries provided CHs with additional budgets to aid COVID-19-related spending, including increased staffing costs, infection control training, extra cleaning and the cost of new technology. 36,52,56,70,97,108 This funding could also help pay staff in full for any time they were required to spend in isolation56,70,103,127 and help minimise reliance upon agency staff, thereby reducing the number of care workers across multiple locations. 70,108 In addition, some authors discussed the benefits of providing CH staff with rewards, such as annual pay increases or bonuses, gifts, care packages or additional leave days. 56,74,83,103 Others implemented food and water stations or ‘staff shops’ to ensure their staff were adequately fed and hydrated or provided access to well-being initiatives, counselling and emotional support. 64,74,103
Finally, good communication and the availability of informational materials, such as brochures, posters and signage on COVID-19 and the associated policies, were deemed to help explain the reasons behind restrictions to residents and their families/friends. 36,50,58,62,97,124 In addition, to be easy to understand, printed materials needed to be both language and reading-level appropriate. 50,124
Impact of COVID-19 interventions
The COVID-19 pandemic has had a devastating effect upon the CH sector, and in many countries, CHs have been at the epicentre of deaths from the disease. 40,103,108,119 Figures vary widely across the world and, although specific details are not provided, some international reports state that as many as half of all COVID-19 deaths in some countries have been among CH residents,55 while others state they account for up to 72%22 or even around 80% of all deaths. 95,113,123 Furthermore, there have also been reports of an increase in non-COVID-19-related deaths in CHs, attributed to a combination of undiagnosed COVID-19 and disruptions in care for people without COVID-19. 24,43,56
The negative consequences of IPC measures have been wide-reaching, impacting residents’ mental and physical health and quality of life. 80,112 Relatives and CH employees have also been affected both physically and mentally by these measures, and their experiences of stress and anxiety have increased considerably during the pandemic. 22,56,59,69,70,80,103,127 Some of the direct impacts of specific prevention and control measures implemented within CHs during the COVID-19 pandemic are presented below.
The impact of social distancing measures
Very little was stated about the impact of social distancing measures on CH staff, residents or their family members, other than an acknowledgement from the World Health Organization that social distancing may have severe implications for residents’ mental health and well-being. 127 Once again, residents living with cognitive impairment or dementia were reported in the grey literature to have greater difficulty understanding social distancing measures and maintaining a physical distance from others. 9,24 For example, one document stated that some residents could not understand the need to wash hands frequently, wear masks or keep a suitable distance from other residents; they needed to be informed about this by staff every day. 84 Other CHs decided not to enforce social distancing procedures, knowing that their residents would not be able to adhere to such rules. 84 Once again, it was noted that restraint should not be used on residents unable to meet social distancing requirements. 62
The impact of isolation
In addition to being cut off from family members and friends externally, some CH residents have also been isolated from their friends within the home. 82,123 For example, as previously mentioned, one recommendation was that residents who were required to leave the home for medical treatment should be placed in isolation upon their return. 117 However, this practice became heavily criticised by residents and family members, as those who had to regularly attend hospital visits (e.g. for dialysis treatment) found themselves almost permanently in isolation. 117
Like the impact of restrictions, isolation of residents also had a negative effect on residents’ physical, cognitive and mental health and well-being. 9,24,25,34,46,56,70,84,112,123,126 This was particularly notable for those residents living with dementia, cognitive problems, autism and learning difficulties, who might not be able to fully comprehend instructions. 24,37,56,60,84,90,112,127 For these individuals, agitation, ‘walking with purpose’ and behavioural disturbances have been reported,37,70,127 which may have required the increased use of restraint. 37 Isolation has been associated in the grey literature with decreased movement and mobility in residents;46,69,126,127 increased postural disorders46 and risk of falls;46 increased sarcopenia and risk of deep vein thrombosis;41 and increased depression and anxiety. 41 Isolated residents have been reported in the grey literature and empirical research to have poorer oral fluid and food intake, leading to weight loss, malnutrition and difficulties maintaining hydration. 46,48,70,103,110 This may be because some residents do not like eating or drinking in their rooms103 or because they do not have their family members around them to encourage them to eat and drink. 48 However, despite these concerns, it is notable that non-compliance with isolation requirements can also have adverse effects on CHs. Policy papers highlighted that where CHs did not effectively isolate residents with COVID-19 symptoms, the virus spread among CH staff, which, in turn, impacted the overall level of care provided to residents, with reports of some being confined to bed or left for days without support. 35 There were also accounts of situations with COVID-19 spreading among residents, which ultimately led to deaths. 69 One (pre-peer-review) empirical research study108 found that non-compliance with isolation requirements was associated with increased odds of infection in other residents [adjusted odds ratio (aOR) 1.33, 95% CI 1.28 to 1.38; p < 0.001], staff (aOR 1.48, 95% CI 1.41 to 1.56; p < 0.001) and large outbreaks (aOR 1.62, 95% CI 1.24 to 2.11; p < 0.001).
In one empirical study, CH staff described the importance of residents maintaining hope during periods of isolation and talked about the ways in which they could ensure residents could still ‘see’ them, even when they were confined to their rooms. 112 This included residents being able to see staff through the window or when passing by their door, which helped reduce their feelings of isolation. 112 Reports have also talked of the importance of residents maintaining exercise routines when confined to their room to limit their risks of developing deep vein thrombosis or their risk of falling. 41,112,126,127 Examples were provided in the grey literature of CHs instigating specific and adapted exercises, such as ‘seated knee extensions’, ‘sit to stands’ and ‘wall squats’ to help counterbalance the effects of being isolated. 41 Isolation interventions could also have a negative impact upon residents’ family members, as knowing your relative is in isolation and being unable to physically see them was reported in the grey literature to take a psychological toll and could cause significant distress, despite the availability of communication devices and other innovative methods of communicating remotely. 34,46,84 As previously mentioned, isolation guidelines for staff could also have a negative impact upon CHs by creating significant staff shortages. 43,55,89 In some cases, this led to residents being required to be transferred to the hospital due to insufficient staff available to care for them within the CH. 94
The impact of restrictions
Compared to other infection control measures, the restriction of CH visitors is reported to be relatively easy and cheap to implement. 57,123 However, restrictive measures within CHs have been reported as having an enormous impact on residents’ health and well-being. 24,25,37,40,48,52,56,58,70,73,84,85,89,91,95,123,127 Indeed, concerns have been expressed in empirical studies and the grey literature that ongoing restrictions have begun to outweigh any potential benefits for residents. 40,113 Many CHs did report initiating new events and activities for their residents to improve their well-being and morale. These events included barbeques, tea parties, concerts and singalongs, drama productions and church services. 64,84,85,103 In addition, physical activity opportunities were also promoted by introducing initiatives such as Nintendo Wii games, treadmills, dancing events and increased gardening activities. 64,103 However, despite these innovative solutions being employed by CHs, restrictions have led residents to experience physical, cognitive, psychological and functional declines. 24,37,40,56,80,103,113,126,127 Residents’ moods have declined as a consequence of restrictions,37,56,91,103 as has their oral fluid and food intake,103 while agitation, irritability, behavioural disturbances, anxiety and psychotropic medication use have increased. 37,57,84,91,103,113,127 Many residents have reported feeling socially isolated and lonely due to the lack of physical closeness and comfort of relatives and friends during periods of restrictions;25,57,70,80,110,113,120,123,126 an issue reported to be particularly important for residents living with dementia. 24,25,32,56,60,80,84,103,123,127,128 Residents living with dementia were reported to be confused, distressed and frustrated by not being able to see their family and friends24,32,84,123,128 and this could lead to a significant decline in their health and well-being. 24,123 One study reported that residents did not recognise their family members after periods of restrictions. 25 Restrictions may also be particularly difficult for those with learning difficulties or autism. 60 Visiting restrictions have, in some cases, prevented residents from receiving necessary medical and social care. 67,116,127 They further pose a serious challenge to the autonomy of CH residents in an era where much progress has been made in eliminating restraints. 25
In addition to this, restrictions have had a devastating effect upon the relatives of CH residents, with reports of negative social and emotional impacts, such as guilt, fear, worry and isolation. 48,56,69,91,95,112,117,123,127 Reports in the Netherlands highlighted family members demonstrating significant resistance to visiting restrictions, which led to CHs implementing harsh enforcement measures, such as hiring surveillance services or fencing off buildings to keep relatives away. 43 In addition, the legality of visitation bans has been contested by family members in the Netherlands, and cases have been taken to court. 43 Concerns have also been raised about the quality of care provided to residents during periods of restrictions, as regulators were unable to enter CHs to undertake inspections for quality assessments or carry out advisory visits. 52,55,70,77,92,116 Indeed, there was a 55% increase in complaints to the CQC in the UK from CH staff concerned about poor practice in their workplace during the pandemic. 70 Furthermore, as family members were not able to enter CHs at this time (and family members often provide additional care for residents during their visits), there have been fears that this too has impacted negatively on the overall quality of care that residents have received during the pandemic. 57,70,123
Restrictions related to the COVID-19 pandemic have also had consequences for CHs and their managers and employees. For example, CH staff have reported finding it challenging to implement strict restrictions, especially those staff who believed the restrictions were too harsh or disproportional to the risks. 43 In addition, there have been reports of staff experiencing violence and abuse from frustrated residents and family members in response to the restrictions being imposed upon them. 103,123 New ways of working and increased staff absences have also increased staff workloads and led to stress, exhaustion and burnout. 46,49,56,57,70,84,91,123 Others have discussed the psychological impact on care staff working throughout the pandemic and the toll this may have taken on their mental health and well-being. 22,84,91,116,123 They state that high-quality psychological support needs to be provided for staff who have worked during the pandemic and experience anxiety or post-traumatic stress disorder symptoms. 22,91,116,120 Some CHs have experienced financial difficulties because of implementing restrictions due to a reluctance of older people to move to CHs due to fears they would be isolated from their families. 43 These facilities report that, despite waiting lists, they have faced difficulties in filling their vacancies. 43,69
Finally, due to COVID-19 restrictions, some CH residents died without being able to have their family members with them, which impacted negatively on their EoL support and dignity and, in some cases, went against their expressed wishes. 80,82,85,113,117 This was reported to be distressing for family members and may have negatively impacted their bereavement process. 56,82,112,117 Furthermore, where relatives could not be present, it fell to CH staff to provide residents with emotional support and comfort at the end of their lives, which may have negatively impacted their own mental health and well-being. 82,112
Considering these issues, many authors have highlighted the importance of reintroducing visitors into CHs as soon as it is safe to do so. 25,56,57,62,73,80,123,127 Some countries, such as the Netherlands, have recommended that CHs take a more flexible, risk-assessment based approach to visitations, with discretion to make visiting policies appropriate to local COVID-19 rates and the individual needs and vulnerabilities of residents. 60,89 A Delphi study of 21 US and Canadian post-acute and long-term care experts in clinical medicine, administration and patient care advocacy has made five strong recommendations around welcoming back CH visitors. 40 These were the need to (1) maintain stringent IPC measures, (2) facilitate both indoor and outdoor visits, (3) allow limited physical contact with appropriate precautions, (4) assess residents’ own care preferences and level of risk tolerance and (5) dedicate an essential caregiver and extend the definition of compassionate care visits to include care that promotes the psychosocial well-being of residents. 40 A Dutch study of 26 nursing homes also explored the impact of allowing visitors back into nursing homes during the COVID-19 pandemic and found that compliance with guidelines was sufficient, and no new infections were reported. 25 Other authors have highlighted the importance of allowing volunteers and other care professionals (offering, e.g. assistance with grooming and emotional support) to return to CHs as soon as it is safe to do so. 57 However, it has been noted that in countries such as Australia, several CHs have continued with strict lockdown restrictions to protect their residents, despite government instructions to end them. 52 Others have highlighted the complications when visitations are reintroduced into CHs. For example, difficulties have been reported for those residents and relatives who do not understand why they cannot touch each other or find it difficult not to have physical contact. 25 Furthermore, some staff and relatives have experienced concerns for their own health when visitations have been reintroduced, particularly if they are in a high-risk category themselves. 25
The impact of zoning/cohorting
There was limited discussion of the direct impact of zoning or cohorting of residents. There was some suggestion in the grey literature that a distinction should be made between those who could understand and abide by isolation guidelines and those who could not, notably those living with dementia, mood disorders or those who ‘walked with purpose’. 41,117 In these instances, it was proposed that zoning or cohorting may be more beneficial for residents than isolation. 41,117 Others, however, reported that such residents might also struggle to follow zoning/cohorting restrictions. 9 There was some empirical evidence to support the need for staff to work only within their allocated zone/cohort of residents to prevent the spread of infections. For example, a study108 found that CHs where staff cared for both infected and uninfected residents had higher odds of infection in residents (aOR 1.30, 95% CI 1.23 to 1.37; p < 0.001) and staff (aOR 1.20, 95% CI 1.13 to 1.29; p < 0.001) than CHs where staff were cohorted. Finally, one guidance document also stated that there could be possible costs for CHs after ending the cohorting of residents. 63 These costs would be required for returning homes to their original state, as well as the costs associated with the redundancy, redeployment or retraining of staff. 63
Strategies for other (non-COVID-19) infectious diseases
Strategies used by care homes to prevent the transmission of other (non-COVID-19) infectious diseases
Nine papers discussed strategies used by CHs to prevent the transmission of infectious diseases other than the COVID-19. 76,88,96,98,102,111,114,118,121 These papers discussed infectious diseases and healthcare-associated infections (HAIs), such as influenza, urinary tract infections (UTIs), respiratory infections, pneumonia, MRSA and gastroenteritis.
Surveillance
Surveillance was the strategy most discussed as being used by CHs to prevent the transmission of infectious diseases and HAIs, such as influenza, UTIs, respiratory infections, pneumonia and gastroenteritis. 76,96,98,102,111,114,118,121 This involved the systematic collection, consolidation and analysis of data related to infectious diseases. Surveillance aimed to ensure the early identification of symptoms in residents and staff preceding a potential outbreak so that IPC measures could be implemented in CHs as soon as possible. 96 One discussion paper111 reported that the seven stages of surveillance of infectious diseases involved assessing the population; selecting the outcome or process for surveillance; using surveillance definitions; collecting surveillance data; calculating and analysing infection rates; applying risk stratification methodology; and reporting, using the surveillance information. This paper111 also stated that surveillance should be conducted weekly and that data standardisation was desirable. The grey literature also notes that CHs should have a comprehensive set of policies and procedures related to infectious disease surveillance to enable them to detect the presence of illness through significant deviations from the baseline rate. 96,111,121 Targeted surveillance may also be required during critical points of the year for some illnesses, such as influenza season for respiratory infections. 96
While all staff in CHs should be trained to monitor for signs of illness in residents, it was highlighted as necessary that one designated staff member, with experience and expertise in IPC practices, take responsibility for co-ordinating surveillance and outbreak management activities within each home. 96,98,121 There was also discussion of the importance of both local infection control committees and national surveillance programmes for overseeing levels of infectious diseases in CHs. 76,98,114,118 For example, one study76 discussed a national sentinel surveillance network developed in 2009 to examine infectious diseases and HAIs in CHs in the Netherlands and reported that the incidence of influenza-like illness and probable pneumonia decreased significantly for every year a CH participated in the network. Though not statistically significant, a similar decrease was also identified with the incidence of UTIs and gastroenteritis. 76
Restrictions
Only one review discussed the use of restrictions for preventing the transmission of non-COVID-19-related infectious diseases in CHs. 88 This review stated that there was no evidence that banning or restricting visitations to CHs impacted the prevention of infectious diseases.
Strategies used by care homes to control the transmission of other infectious diseases
Evidence in this area was limited, with only 17 papers discussing the strategies used by CHs to control the transmission of infectious diseases other than COVID-19 when there was already an outbreak or suspected case of illness. 44,45,54,65,71,72,81,86,93,96,98,100–102,111,114,118 This was a greater number of papers than those discussing preventing infectious diseases occurring in CHs, although some publications talked about prevention and control measures. Once again, these papers discussed infectious diseases, such as MRSA, influenza and respiratory infections, as well as MDROs and C. diff.
Isolation
Several papers discussed how isolation had been used to control the spread of other infectious diseases within CHs, such as MRSA, influenza and C. diff. 44,45,54,65,71,72,81,86,93,96,98,100–102,111,118 Again, this tended to involve isolating infectious residents within single rooms where this was possible or cohorting residents (i.e. grouping those with the same illness together or pairing residents with someone ‘low risk’) where it was not. 44,45,71,72,86,93,96,98,100–102,111,118 Where neither isolation nor cohorting was possible, the grey literature suggested that CHs could maintain at least 1 m between beds with privacy curtains between. 102,118 Some papers talked of the need to restrict admissions of new residents into the home and/or prevent the readmission of those who had been in hospital during severe outbreaks. 45,96 Although most papers did not discuss how long residents were required to isolate, some stated that residents with influenza or respiratory infections should remain in isolation for 5 days after the onset of their illness or until their symptoms had resolved entirely and for 48 hours after being symptom-free for residents with C. diff. 45,96,101,118 Some of the highlighted examples also suggested there was less of a ‘blanket approach’ to isolation for other infectious diseases than for COVID-19. For example, a study54 noted that known MRSA carriers were asked to be separated from vulnerable residents with skin lesions or indwelling catheters. However, they were otherwise allowed to continue with usual social activities. The importance of making decisions around isolation on a case-by-case basis was emphasised in policy documents, as was the importance of not over-isolating residents and the need to ensure both physical and psychological needs of isolated residents were met. 44,65,101,111 There were also examples of staff being asked to isolate to control the spread of infectious diseases. For instance, during outbreaks of influenza, CH staff were required to self-monitor for symptoms of illness and stay away from work if feeling unwell. 45
Restrictions
Some policy documents reported that restricting the movement of residents and visitors during an outbreak of infectious disease could be beneficial. 45,72,93,96,102,111,114,118 This included the restriction of group activities or the mixing of residents within communal areas, as well as minimising the movement of visitors within the home, such as only allowing visits within a resident’s private room or limiting the number of visitors. 45,96,102,111,118 A Canadian toolkit reported that complete closure of CHs to visitors should not be permitted unless the Medical Officer of Health had issued an order due to the potential hardship this could cause residents and their family members. 96 Furthermore, there was some evidence from the grey literature that there was less of a ‘blanket approach’ to resident restrictions for other infectious diseases than for COVID-19. This included, for example, residents only being restricted from group activities when wound drainage or diarrhoea could not be contained93 or activities only restricted for residents in an outbreak ‘zone’ but still able to proceed within non-affected areas. 96 Again, it was reported that clear signage and communication were important for residents and their family members during any restriction periods. 118
Some papers also discussed the restrictions that should be placed upon staff working patterns to control the spread of infectious diseases in CHs. 45,96,111 For example, during influenza outbreaks, one guidance document45 stated that the movement of staff across CHs or other healthcare facilities should be minimised. Similarly, where zoning/cohorting restrictions were in place, staff working within affected units should not also work within non-affected areas of the home. 45,96,118 Finally, it was suggested in the grey literature that only staff who had been vaccinated against influenza should care for those residents with suspected or confirmed illnesses. 45,96
Social distancing
Only two guidance documents discussed social distancing measures outside COVID-19. 102,118 One stated that there should always be at least 2 m between residents with signs and symptoms of influenza and those without. 102 Another suggested that CHs should maintain a 1-m distance between all residents during an outbreak of respiratory infections. 118
Surveillance
Surveillance was also identified as an intervention for controlling the spread of infectious diseases within CHs, with outbreaks being carefully monitored, recorded and reported. 45,86,111 In addition, some of the grey literature stated that it was a requirement that public health authorities be notified when there was a confirmed case of certain infectious diseases, such as influenza or MRSA. 45,71
Challenges and facilitators of other infectious disease interventions
A few specific challenges were highlighted, which negatively impacted the success of implementing interventions for (non-COVID-19) infectious diseases within CHs. One challenge was focused on staff education and training, where CH staff – particularly agency staff – were felt to have less knowledge and training around infectious diseases and their means of prevention and control. 65,86,88 Therefore, implementing staff education programmes around IPC was felt to be important in reducing the number of infections within CHs. 96,121 In addition, staff movement across different care settings, including the reliance upon ‘bank’ or agency staff, was also identified as a source of outbreaks of infectious diseases within CHs. 65,86,88
Some authors identified the design and layout of CH buildings as a challenge, as many homes lacked appropriate space where residents with infectious diseases could isolate. 72,86 However, a study76 reported no clear evidence linking the physical space and layout of CHs with the incidence of HAIs. Finally, CH residents were felt to bring specific challenges themselves. Many were living with dementia or other chronic conditions that compromised their ability to adhere to interventions or exhibited behaviours that hindered infection control. 86,88 Only one facilitator of successful interventions was highlighted in the grey literature. Again, this was the need for good communication to help educate residents and their visitors about any outbreaks of infectious diseases and how they could help prevent their transmission. 86
Impact of other infectious disease interventions
There was little discussion of the impact of IPC strategies for non-COVID-19-related infectious diseases. It was acknowledged that CH residents could become fearful and confused during outbreaks of contagious diseases. Therefore, it was important to ensure they remained fully informed about any interventions being put in place and that any fears were addressed by staff. 88 In addition, isolation practices could stigmatise residents and may adversely affect the quality of care delivered. 93 Some of the grey literature reported that long periods of isolation for residents with influenza or MRSA could contribute to depression, anxiety and distress,71,72 while others were concerned that restrictions on visitors or CH activities could increase loneliness and depression. 88 Finally, it was acknowledged that isolation practices could be costly for CHs and take up limited resources that could be used for other purposes to benefit residents. 93
Strengths and limitations of this review
Keys strengths of this review include the following:
-
Conducting searches of several of the main and specialised databases for peer-reviewed publications and the grey literature.
-
Several research team members conducted the screening of results to enhance rigour.
-
Clarifying and defining key terminology related to the concepts of social distancing and isolation is an important strength of this review.
Key limitations include the following:
-
Our searches were limited to papers published in the English language because of resource constraints.
-
There were some limitations for the 10 empirical studies, which should be considered when examining their findings.
-
Many other strategies in the prevention and control of COVID-19 and other infectious diseases in CHs, such as the use of PPE, testing, ventilation and adequate hygiene procedures, were excluded as they were outside the scope of this review.
Appendix 2 Trigger questions discussed in the breakout groups: Workshop 1
-
(1) What are your initial thoughts about the findings for the following?
-
- Interviews with CH staff
-
- Interviews with residents
-
- Interviews with families
-
- Focus groups with external stakeholders
-
-
(2) How do see the purpose of the toolkit – what would best support the care of residents, their families/friends, and staff? For example, facilitated discussions with staff as part of continuing professional development; staff-facilitated discussions at meetings with families/friends and residents.
-
(3) From listening to the presentations, what do you think are the priorities that could be implemented easily by CHs?
-
(4) What do you think is important but not easily implemented by CHs?
-
(5) Are there any findings that you think are interesting but less important for this work?
-
(6) What are your initial thoughts about how to organise the content of the toolkit? For example, key priorities with content that includes ‘key lessons learnt’ and ‘what can CHs, managers and staff do based on these lessons learnt’? Should we include examples of what worked well and what did not from different participant groups?
-
(7) What are your initial thoughts about the format the toolkit should take? For example, a series of posters for each priority area.
Appendix 3 Trigger questions discussed in the breakout groups: Workshop 2
-
(1) What are your initial thoughts about the proposed content of the draft toolkit?
-
(2) Using our study findings, we have drafted content for six key areas:
-
‘Supporting the well-being of residents when social distancing’
-
‘Supporting the well-being of residents when they are isolating’
-
‘Supporting residents and their families and friends to communicate when visiting is not permitted’
-
‘Supporting visits from families and friends when visiting is restricted’
-
‘Supporting care home staff’
-
‘Supporting care home managers’
-
Overall, do you think these are the right key areas?
-
(3) Do you think any key areas are missing?
-
(4) For each key area, we have presented content using three headers: ‘What is the issue?’, ‘What are the consequences?’ and ‘Actions to consider’.
-
- Do these headers make sense?
-
- Are the ‘issues’ communicated clearly?
-
- Are the ‘consequences’ written clearly?
-
- Are the ‘actions to consider’ that we have drafted to date clear and meaningful?
-
If you know of evidence-based resources that we could include, please can you share the link(s), for example, about communicating well with older people living with a dementia.
-
- How would you rank these actions in order of importance?
-
- Is there anything missing?
-
(5) What are your thoughts about how best to organise the proposed content? For example, length, how much detail?
Presentation – for example, use of boxes, speech balloons to illustrate extracts from participants’ interviews, use of colour, infographics.
-
(6) For professionals, would you use this in practice?
-
(7) How do you think this content can be used by residents, their families and friends?
-
(8) If you know of any toolkits that you think are particularly good, it would be very helpful if you can share these with us.
Appendix 4 A summary of the routinely collected care home data by case study site
| Care home 1 | Care home 2 | Care home 3 | Care home 4 | Care home 5 | Care home 6 | |
|---|---|---|---|---|---|---|
| Date of data collection | 22 March 2021 | 13 April 2021 | 7 July 2021 | 21 February 22 | 27 September 2021 | 9 December 2021 |
| CH data | ||||||
| Location of CH | Midlands | Southeast England | Midlands | North England | London | London |
| CQC rating of home | Good | Outstanding | Outstanding | Good | Good | Good |
| CQC registration type | Dual registration | With nursing | With nursing | With nursing | Without nursing | Without nursing |
| Type of service provided | Adults over 65 years, Adults under 65 years, Dementia, Physical disabilities | Adults over 65 years | Adults over 65 years, Adults under 65 years, Dementia, Learning disabilities, Mental health conditions, Physical disabilities, Neurorehabilitation | Adults over 65 years, Adults under 65 years, Dementia, Physical disabilities | Adults over 65 years, Dementia, | Adults over 65 years, Dementia, Learning disabilities, Mental health conditions |
| Funding sources | LA, NHS and CCG, Self-funders, Combination | Self-funders | LA, NHS and CCG, Self-funders | LA, NHS and CCG, Self-funders | LA, Self-funders | LA, Self-funders, Combination (LA funding with client contribution) |
| Number of beds offered in home | 64 | 37 | 45 | 73 | 64 | 48 |
| Average bed occupancy | January 2020: 64 February 2020: 64 March 2020: 63 April 2020: 64 May 2020: 61 June 2020: 64 July 2020: 63 August 2020: 63 September 2020: 63 October 2020: 61 November 2020: 61 December 2020: 60 January 2021: 63 February 2021: 62 |
January 2020: 26 February 2020: 26 March 2020: 27 April 2020: 30 May 2020: 30 June 2020: 29 July 2020: 26 August 2020: 26 September 2020: 26 October 2020: 26 November 2020: 26 December 2020: 26 January 2021: 26 February 2021: 25 |
January 2020: 44 February 2020: 44 March 2020:44 April 2020: 44 May 2020: 44 June 2020: 44 July 2020: 44 August 2020: 44 September 2020: 44 October 2020: 44 November 2020: 44 December 2020: 44 January 2021: 44 February 2021: 45 |
January 2020: 71 February 2020: 71 March 2020: 71 April 2020: 63 May 2020: 59 June 2020: 62 July 2020: 62 August 2020: 63 September 2020: 64 October 2020: 63 November 2020: 62 December 2020: 65 January 2021: 69 February 2021: 71 |
January 2020: 98% February 2020: 99% March 2020: 94% April 2020: 75% May 2020: 67% June 2020: 90% July 2020: 91% August 2020: 87% September 2020: 89% October 2020: 88% November 2020: 88% December 2020: 88% January 2021: 89% February 2021: 90% |
January 2020: 48 February 2020: 48 March 2020:48 April 2020: 48 May 2020: 46 June 2020: 46 July 2020: 46 August 2020: 48 September 2020: 46 October 2020: 45 November 2020: 45 December 2020: 48 January 2021: 48 February 2021: 48 |
| Impact of COVID-19 on average bed occupancy | Data not provided | Closed one floor to be able to isolate floors and staff if had outbreak, so only had 26 rooms available from July 2020. | Zero impact. Although the number of beds offered is 45, this has been since January 2021, prior to that it was 44. | Significant reduction in occupancy over a period of a month during the first outbreak. This then took almost 12 months to fully recover. | Due to the impact of COVID-19, 16 beds were made unavailable from June 2020. From that period, the percentage is occupancy based on the number of beds available rather than number of registered beds. | No severe impact on bed vacancies. They have always stayed at a high level. |
| Number of positive COVID-19 cases since March 2020 | March 2020: 0 April 2020: 18 May 2020: 10 June 2020: 2 July 2020: 2 August 2020: 0 September 2020: 0 October 2020: 9 November 2020: 27 December 2020: 22 January 2021: 24 February 2021: 12 |
March 2020: 2 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021: 0 |
March 2020: 0 April 2020: 1 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021: 0 |
March 2020: 0 April 2020: 4 May 2020: 3 June 2020: 7 July 2020: 0 August 2020: 0 September 2020: 1 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 1 February 2021: 5 |
March 2020: 11 April 2020: 4 May 2020: 1 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 1 February 2021:0 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 1 September 2020: 0 October 2020: 2 November 2020: 0 December 2020: 0 January 2021: 1 February 2021:0 |
| Number of residents dying within 28 days of a first positive COVID-19 test (between 1 March 20 and 1 March 21) | Deaths in care home: 2 Deaths in hospital: 0 Deaths in another care home: 0 Death in other place: 0 |
Deaths in care home: 0 Deaths in hospital: 0 Deaths in another care home: 0 Death in other place: 0 |
Deaths in care home: 1 Deaths in hospital: 0 Deaths in another care home: 0 Death in other place: 0 |
Deaths in care home: 4 Deaths in hospital: 0 Deaths in another care home: 0 Death in other place: 0 |
Deaths in care home: 5 Deaths in hospital: 5 Deaths in another care home: 0 Death in other place: 0 |
Deaths in care home: 0 Deaths in hospital: 1 Deaths in another care home: 0 Death in other place: 0 |
| Did CH procure and carry out private testing for residents? | Yes – residents receive PCR tests every 4 weeks. | No | No | No | No | No |
| Date testing commenced following government guidance | 8 June 2020 | 9 June 2020 | 1 September 2020 | 1 June 2020 | 18 May 2020 | 6 July 2020 |
| Number of residents admitted to hospital with or suspected of having COVID-19. | March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021: 0 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 9 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 1 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
| Number of residents transferred to the CH from hospital and/or the community with COVID-19. | March 2020: 0 April 2020: 18 May 2020: 10 June 2020: 1 July 2020: 2 August 2020: 0 September 2020: 0 October 2020: 9 November 2020: 27 December 2020: 22 January 2021: 24 February 2021: 12 |
March 2020: 1 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 0 April 2020: 1 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
Data not provided | March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 0 February 2021:0 |
| Since March 2020 have any residents been taken from the CH by family because of COVID-19? | No | No | No | Yes, 1 | Data not provided | No |
| Start date of vaccination programme for residents | 16 January 2021 | 31 December 2020 | 1 January 2021 | 31 March 2020 | Data not provided | 5 December 2020 |
| Are all residents vaccinated? | No – 1 resident refused the vaccine on several occasions. Two residents are not currently able to have the vaccine due to previously testing positive for COVID-19. | Yes – Fully vaccinated (second jabs, March 2021) | No – 44 residents are vaccinated, only one who is not and that is because they are clinically exempt due to severe allergies. | Yes | No | Yes – all fully vaccinated including boosters |
| Monthly staffing vacancy rates in February 2020 (pre-COVID-19) – registered manager | 0% | 0% | 0% | CH provided this data in an unorthodox way which could not be used. | CH provided this data in an unorthodox way which could not be used. | 0% |
| Monthly staffing vacancy rates in February 2020 (pre-COVID-19) – care worker | 0% | HCAs 4 × 36 hours | 5% | CH provided this data in an unorthodox way which could not be used. | CH provided this data in an unorthodox way which could not be used. | 0% |
| Monthly staffing vacancy rates in February 2020 (pre-COVID-19) – senior care workers | 0% | 0% | 0% | CH provided this data in an unorthodox way which could not be used. | CH provided this data in an unorthodox way which could not be used. | 0% |
| Monthly staffing vacancy rates in February 2020 (pre COVID-19) – RN | 1 × 44 hours night nurse vacancy | 0% | 0% | CH provided this data in an unorthodox way which could not be used. | CH provided this data in an unorthodox way which could not be used. | N/A |
| Monthly staffing vacancy rates between March 2020 and January 2021 (during COVID-19) – registered manager | 0% | 0% | 0% | CH provided this data in an unorthodox way, which could not be used. | Data not provided | 0% |
| Monthly staffing vacancy rates between March 2020 and January 2021 (during COVID-19) – care worker | 0% | HCA 36 hours | 10% | CH provided this data in an unorthodox way, which could not be used. | Data not provided | 2 posts (70 hours) |
| Monthly staffing vacancy rates between March 2020 and January 2021 (during COVID-19) – senior care worker | 0% | 0% | 0% | CH provided this data in an unorthodox way which could not be used. | Data not provided | 0% |
| Monthly staffing vacancy rates between March 2020 and January 2021 (during COVID-19) – RN | 1 × 44 hours night nurse vacancy | 0% | 10% | CH provided this data in an unorthodox way, which could not be used. | Data not provided | N/A |
| Has the CH taken measures to avoid front-line staff moving between CHs? | Yes – staff are currently working solely at this CH. | Yes – stopped staff going to other CHs in the organisation. If they worked between two or more, they went to the home with the greater need. | Yes – staff only work at this CH. | Yes – the teams have not moved between villages as they normally would have done pre-COVID. Where possible, the teams have been allocated to individual households and encouraged to minimise the movement between households. | Yes – managed through effective resource planning, overtime and utilising bank colleagues | Yes |
| Have front-line agency staff been employed during the COVID-19 pandemic since March 2020? | No | No | Yes – during the pandemic, used one Night Healthcare Assistant from an agency. This assistant only worked at this home. | Yes – single agency and block booking of staff to try and ensure familiarity and minimise the risk of contamination. | Data not provided | Yes – Two agency staff members (same staff that only worked within this CH, not agency staff who worked in multiple CHs) |
| Did any front-line staff move into the home during the pandemic? | No, however there was a contingency plan in place if required. | No | Yes – Deputy Manager stayed at the home during her block of shifts. This was to protect the residents and her elderly parents who she lives with. This was a great support to the manager, as she helped with on-call duties overnight and at the weekend. | Yes – one member of night staff moved in for a period during the height of the pandemic. | No | No |
| Have any front-line staff been off work due to having COVID-19 symptoms? | March 2020: 4 April 2020: 9 May 2020: 2 June 2020: 0 July 2020: 0 August 2020: 1 September 2020: 2 October 2020: 2 November 2020: 1 December 2020: 0 January 2021: 0 February 2021: 1 |
March 2020: 2 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 2 January 2021: 1 February 2021:2 |
March 2020: 0 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 1 October 2020: 0 November 2020: 0 December 2020: 1 January 2021: 1 February 2021:0 |
March 2020: 10 April 2020: 16 May 2020: 6 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 3 October 2020: 6 November 2020: 3 December 2020: 8 January 2021: 6 February 2021:2 |
March 2020: 10 April 2020: 2 May 2020: 0 June 2020: 0 July 2020: 1 August 2020: 1 September 2020: 2 October 2020: 2 November 2020: 1 December 2020: 2 January 2021: 1 February 2021:1 |
March 2020: 0 April 2020: 2 May 2020: 2 June 2020: 2 July 2020: 1 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 1 January 2021: 0 February 2021:0 |
| Have any front-line staff been off work due to the need to self-isolate because of family/others having COVID-19 symptoms? | March 2020: 3 April 2020: 2 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 1 February 2021: 0 |
March 2020: 2 April 2020: 0 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 2 January 2021: 2 February 2021:0 |
March 2020: 2 April 2020: 1 May 2020: 1 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 0 October 2020: 0 November 2020: 0 December 2020: 0 January 2021: 1 February 2021:1 |
March 2020: 5 April 2020: 7 May 2020: 1 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 13 October 2020: 17 November 2020: 4 December 2020: 3 January 2021: 3 February 2021:0 |
March 2020: 14 April 2020: 1 May 2020: 0 June 2020: 0 July 2020: 0 August 2020: 0 September 2020: 1 October 2020: 0 November 2020: 1 December 2020: 0 January 2021: 0 February 2021:0 |
March 2020: 1 April 2020: 3 May 2020: 5 June 2020: 0 July 2020: 0 August 2020: 2 September 2020: 0 October 2020: 2 November 2020: 0 December 2020: 1 January 2021: 0 February 2021:0 |
| Did the CH procure and carry out private testing for staff? | Yes – staff have their PCR tests every week and have LFTs twice a week | Yes – antibody testing | No | No | No | No |
| When did lateral flow testing for staff commence? | 4 January 2021 | 1 December 2020 | 1 September 2021 | 13 August 2020 | 23 December 2020 | December 2020 |
| When did the vaccine programme for staff start? | Some staff travelled to a hospital for their vaccine and the first appointment was on 17 December 2020. The majority of staff were vaccinated at the home on 16 January 2021 | 31 December 2020 | 1 January 2021 | 11 March 2021 | Data not provided | 5 December 2020 |
| What percentage of CH staff have been vaccinated? | 85% of staff have received first vaccine. Out of the remaining staff, three have been booked in to have their vaccine, three staff cannot have the vaccine, three staff are on maternity leave and the remaining two staff have declined. | 98% | 98% plus three staff clinically exempt | 100% | 88% | 100% |
| How has testing of visitors to the CH been managed? | At the moment, we are open to essential appointments and booked visits for the residents (visitors are from the nominated persons list). All visits are pre-arranged, and visitors are informed that they are to arrive half an hour before their scheduled time and report to a member of staff. At this point, we then ask them to complete the necessary paperwork and an LFT test then they are to await the results. As long as the result is negative, the visit can continue. With regard to professional visiting, if the visitors are from an organisation that complete LFT testing at home, they must show proof of a negative test that has been completed within the last 72 hours; if they are unable to provide this evidence, then they are to follow the guidance for completing the LFT testing within the home. | Data not provided | This has involved a lot of time with weekly PCR testing for all staff, twice weekly LFT testing for all staff, four weekly PCR testing for residents. Once visiting opened up again, all visitors are required to have a LFT, they then have to wait for 30 minutes and if the result is negative, they are then able to visit. Any professionals visiting the home also have to either have a negative LFT that is taken here or need to provide a negative result taken no longer than 30 minutes prior to coming to the home. Our hairdresser has been back for 8 weeks now, she takes part in the staff weekly PCR testing and has to have an LFT, again with a negative result, prior to starting work on the day she comes. The registration of all tests is very time consuming, with the website regularly crashing, and this can take several hours per day. Then starts the anxiety of waiting for the PCR results to come through. | Testing station set up in the village for testing to be carried out on all visitors. Relatives were asked to attend 30 minutes before a scheduled visit so that a LFT could be carried out by a member of staff. Records of the test were kept for 21 days before being destroyed. | Data not provided | Data not provided |
| Organisational data | ||||||
| Number of CHs in the organisation | 63 | 21 | 13 | 7 | 114 | 7 |
| Number of beds offered across the organisation | 4911 | 1163 | 767 | 500 | 5875 | 304 |
| Location(s) of homes across the country | Midlands | South England | South England | North England | North England Midlands South England |
South England |
| Ownership of organisation | Private organisation | Private family run | Private organisation | Voluntary/not for profit | Voluntary/not for profit | Private family run |
Appendix 5 Toolkit for supporting care homes with social distancing and isolation measures for older people
A toolkit for supporting CHs with social distancing and isolation measures for older people
Authors
Joanne M. Fitzpatrick, Anne Marie Rafferty, Shereen Hussein, Sarah Sims, Amit Desai, Sally Brearley, Richard Adams, Lindsay Rees, Ruth Harris
For further information, email joanne.fitzpatrick@kcl.ac.uk
Acknowledgements
To everyone who contributed to developing this toolkit, our sincere thanks.
Special thanks to the residents, family members and CH staff who shared their stories so openly and honestly, helping us to learn from the whole experience of COVID-19 to help reduce cases in the future, refine how care can be provided amid restrictions, and contribute to the well-being of residents, families and friends, and staff.
Our sincere thanks to the CH providers, managers, deputies, staff who took on the role of a project champion, and all the staff who supported our research.
We are grateful to the National Institute for Health Research for funding this research, and for the support and insightful contributions of members of the Steering Committee, Data Monitoring and Ethics Committee, PPI group and the co-design workshop participants.
Funding
This award was funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme (NIHR award ref: NIHR132541) and is published in full in Health and Social Care Delivery Research; Vol. 12, No. 45. See the NIHR Funding and Awards website for further award information.
Contents
-
About this toolkit, who is it for, and how to use it.
-
Caring for residents
-
Priority Area (A) Caring for residents when they are social distancing.
-
Priority Area (B) Caring for residents when they are isolating.
-
-
Caring for Families and Friends
-
Priority Area (C) Supporting residents, families and friends to communicate when visiting is not permitted.
-
Priority Area (D) Supporting visits from families and friends when visiting is allowed but with restrictions.
-
-
Caring for CH Staff
-
Priority Area (E) Caring for care staff.
-
Priority Area (F) Caring for managers.
-
About the toolkit
To protect older people from coronavirus (COVID-19), CHs have used various measures that include social distancing and isolation of residents. Care homes have shared that it can be challenging to implement social distancing and isolation measures when caring for residents.
Our research aimed to explore and understand the real-life experiences of implementing social distancing and isolation for older people living in CHs. To help us do this, we interviewed residents, families and CH staff about their experiences of delivering or receiving care during the COVID-19 pandemic, analysed CH policy documents and conducted focus groups with senior health and care leaders.
We have used these findings to co-design guidance and resources (the toolkit). We have worked with a group of service users and public representatives, CH managers, nurses and carers and leaders working in health and social care services and research.
Who is the toolkit for?
This toolkit will support health and care delivery now and during any future coronavirus outbreaks (COVID-19). We hope that it will
-
contribute to person-centred care for residents, families and friends by providing evidence-informed guidance for social distancing and isolation of residents and related restrictions
-
support CHs to care for residents with diverse health and care needs (e.g. those living with dementia)
-
support CHs to communicate well with residents, families and friends, and health and care professionals
-
help direct focus on staff well-being
-
help make the job easier for CHs during a pandemic
-
help inform care for other infectious diseases.
How to use the toolkit?
The toolkit can be used flexibly with staff, residents, families and friends, for example as follows.
-
To inform discussions involving CH staff and health and care professionals in the wider multidisciplinary team, to enhance understanding about the CH sector, particularly about the challenges faced related to social distancing and isolation measures for residents and solutions implemented.
-
For conversations between CHs and policy-makers at a local level to inform the guidance provided to CHs.
-
Reflective sessions with CH staff about learning from the unintended consequences of social distancing and isolation measures.
-
To inform facilitated discussions with residents, families and friends, for example, to instil confidence about measures that can be used by CHs to mitigate the negative consequences of social distancing and isolation of residents.
-
To guide conversations with residents, families and friends, for example, about refining approaches to communicating remotely and digitally with families and friends, and to co-design interventions to connect residents with nature and bringing the outside in.
Caring for residents
Priority Area (A) caring for residents when they are social distancing
What is the issue?
Care home residents are required to keep a physical distance between each other and with staff and visitors.
‘I think it [being able to participate in activities] has improved, I think that the home was learning a lot from the first lockdown and as things have improved, I mean they still did the activities, how on earth they managed to organise things by distancing people I do not know, it’s incredible. But I’ve got a feeling that things are not so much back to normal but a new normal and she’s participating again’.
(Family Member)
‘… there’s no way on earth that I’m going to stay … 6 feet away from a resident at any given time, you know, it’s just impossible. We’ve got people who may need assistance when they need to eat or when they need a drink, or people who might need personal care. You can’t keep away from people’.
(Senior Support Worker)
What we have learnt
-
(1) Communicating can be challenging for residents when being socially distanced from the person they are trying to communicate with, especially if a resident has a hearing and/or vision impairment. Mask-wearing can make communication even more complicated, hiding much of the face and making lip-reading impossible.
-
(2) Residents with cognitive impairment find social distancing challenging to understand.
-
(3) Residents not being permitted to visit other residents in their rooms due to social distancing rules can cause frustration and upset.
-
(4) Limited capacity in communal areas makes it harder to arrange social activities for residents and with reduced numbers of residents. The reduced social interaction and mental stimulation associated with this means that residents are not as mentally alert as usual.
-
(5) Limited capacity in dining rooms reduces the number of residents who can eat in designated dining areas, and some CHs must reconfigure other rooms into dining rooms, stagger mealtimes, or ask residents to eat in their bedrooms.
-
(6) Maintaining social distancing with residents when staff deliver personal care is a struggle – residents miss physical touch, for example hugs and holding hands.
You could try this
Communicating well with residents, their families and friends
-
Care home staff need to be clear about what is and is not allowed around social distancing rules and communicate this to residents, families and friends.
-
Explain to residents what social distancing is and why it is needed. Communication/cue cards may be helpful.
-
Care home staff can have a conversation with residents about what activities they might like to participate in, and communal rooms can be reconfigured to make these activities possible. This information should be recorded in residents’ care plans.
-
Approved transparent face coverings can be worn to make communication easier for those residents who communicate through lip-reading or facial expressions.
Maintaining connections and friendships
-
Activities and well-being co-ordinators can provide entertainment and activities for residents that adhere to social distancing guidance.
-
Examples that residents and families/friends liked included Christmas specials with a photograph of each resident sent to family, celebrations for pancake day, significant national memorial days, anniversaries, cultural and religious notable days/events, card-making, word games, small group cake-baking, yoga, karaoke, bingo, quizzes, letter writing to local school children, online sessions connecting residents with local churches and community groups, indoor gardening.
-
-
Senior leadership can consider investing further in well-being and activities co-ordinator positions that are not already in place.
-
Create resident support bubbles to help maintain communication and friendships, while adhering to social distancing guidance.
-
Discuss and make it possible for residents to go out of their CH while adhering to restrictions, for example, for religious or cultural activities.
Addressing the needs of residents with cognitive impairment
-
Care home managers and senior leadership can decide if social distancing is possible for residents with cognitive impairment (e.g. for those who ‘walk with purpose’). Talk with other CHs to share experiences of what has worked well and what has not.
-
For tips on how to communicate well with a person living with dementia, visit
-
www.dementiauk.org/get-support/understanding-changes-in-dementia/tips-for-better-communication/
-
www.scie.org.uk/care-providers/coronavirus-covid-19/dementia/care-homes Watch the video – meeting the needs of people with dementia living in CHs during COVID-19. www.youtube.com/watch?v=blJjUwBhVpk
-
Supporting staff to care well for residents when social distancing
-
Encourage CH staff to be vigilant about observing residents’ physical, emotional, mental and cognitive well-being.
-
Educate staff about signs to look out for regarding the well-being of residents to mitigate the negative impact on residents of social distancing, for example low mood, appearing anxious, physical discomfort.
-
Managers can discuss with staff how to put into practice apparent contradictions in guidance, for example, regarding physical touch with residents.
-
Managers can communicate to staff that their decisions/judgements about resident care are respected.
Thinking about care home space
-
Activities and communal dining arrangements can be reconfigured with smaller groups of residents.
-
Care home managers and senior leadership can consider how best to manage social distancing for residents and staff where spaces are not easy to reconfigure/repurpose.
Caring for residents
Priority Area (B) caring for residents when they are isolating
What is the issue?
Care home residents must isolate in their rooms for several days if they have suspected or confirmed COVID-19 infection, when they first move into the CH, or return to the CH following hospital discharge/attendance.
‘You know and like when I had any phone calls you know, people that normally phone me, I couldn’t take the calls, I wasn’t allowed to have any calls because that meant I would go out the room to take the calls and that I wasn’t allowed to do’.
(Resident)
‘… some have chosen not to go to hospital appointments if they don’t feel it’s necessary … so they won’t get isolated … they like to be downstairs in activities, so they’ve chosen not to go to hospital because of the risk of being isolated’.
(Manager)
What we have learnt
-
(1) Formal isolation can have a negative impact on residents’ physical, mental, emotional and cognitive well-being.
-
(2) Residents feel cut off from their usual CH life and family and friends when asked to isolate in their bedroom.
-
(3) Residents with cognitive impairment may not understand that they cannot leave their room and why.
-
(4) Being in isolation may have a negative impact on the nutritional health/well-being of residents who eat better when supported by a companion or in social settings.
-
(5) Residents sometimes may be asked to isolate themselves in rooms that are not their own, leading to feelings of dislocation and discomfort.
-
(6) Some residents may be reluctant to seek hospital care for fear of having to isolate on their return.
-
(7) Families sometimes do not understand what isolation means for residents, leading to a lack of support for residents.
-
(8) Some people are deterred from moving into a CH if they need to isolate upon their arrival.
You could try this
Fostering a sense of connection
-
When residents are required to isolate, make sure they can see the outside world from their bedroom, and have access to television and music (e.g. via a digital assistant such as Alexa or Google) if they wish.
-
Where possible, ensure that residents isolate in their own bedroom. If this is not possible, arrange for personal possessions to be moved to the resident’s isolation room and help residents to communicate with staff, fellow residents, families and friends.
-
Consider cohorting to care for residents for whom isolation would be detrimental to their well-being.
-
Ensure that a resident’s needs for companionship during essential activities (e.g. mealtimes) are supported by CH staff.
-
A useful resource is ‘Supporting older people and people living with dementia during self-isolation’ (The British Psychological Society, UK): www.bps.org.uk.
-
Support essential caregivers in their role. Helpful resources are as follows:
-
The Relatives and Residents Association guide – Visiting and the law- a guide for CHs during COVID-19: www.relres.org/visiting-guide-providers/.
-
More than just a visitor. A guide to essential family carers: www.mha.org.uk/files/2615/9707/4083/MHA_More_than_just_a_visitor._A_guide_for_Essential_Family_Carers.pdf.
-
Supporting staff to care well for residents who are isolating
-
Managers and senior leadership can decide on interventions to manage the emotional and mental well-being of residents who are isolating.
-
Care home managers and care staff can work with physiotherapy and occupational therapy colleagues to plan how best to promote physical activity for individual residents during periods of isolation.
-
Care home staff can facilitate choice and control for residents – this can help residents adapt to isolation measures and restrictions (e.g. their thoughts about how they would like to keep connected with their families and friends, and friends in the CH).
-
Care home staff can carry out more frequent visits to check on the well-being of residents who are isolating (e.g. looking out for signs of residents appearing upset, down, tearful, anxious, frightened, lonely).
-
Activities and well-being co-ordinators can lead on providing entertainment, activities and exercise for residents in isolation.
-
Online activities for individuals living with dementia (Alzheimer’s Society, UK).
-
-
Care homes can consider implementing activities for residents that previously would have only been considered in a face-to-face mode now being done remotely through digital means (e.g. yoga, music, arts and cultural interventions).
-
Care staff can provide supportive walks for residents (e.g. to a garden area within the CH, to a balcony).
-
Senior leadership should invest further in the training and development of the care workforce to be able to care well for the emotional, mental and physical well-being of residents who are isolating. This should include a specific focus on the legal duties that staff have and how they relate to implementing isolation, social distancing and visiting restrictions in terms of the Mental Capacity Act, the Equality Act, and the Human Rights Act.
Communicating well with residents, their families and friends
-
Care home staff can prepare residents for the possibility of isolation by talking to them about what it entails and what facilities they would like if they were required to isolate. The outcome of these discussions should be included in the resident’s care plan.
-
Care homes can facilitate communication between an isolating resident and other residents in the CH (e.g. by arranging phone or video calls, helping to write a postcard and popping it under the resident’s door/posting to family/friends).
-
Care homes can support communication between residents, their families and friends that meets their needs (e.g. arranging mobile devices for phone or video calls, supporting residents with letter writing/reading).
-
Care home staff can explain to residents’ families and friends what formal isolation means for residents and ask what support they can offer.
Thinking about care home space
-
Care homes can prepare for similar situations by consulting guidance such as CHs strategy for Infection Prevention & Control of Covid-19 based on a clear delineation of risk zones (Eric Fewster, Independent Water & Environmental Manager, UK): https://ltccovid.org/2020/12/16/updated-care-homes-strategy-for-infection-prevention-and-control-of-covid-19-based-on-a-clear-delineation-of-risk-zones/.
-
Senior leadership can consider short- and longer-term CH redesign opportunities to enable residents to connect socially with their families and friends and to connect with the outdoors and different sensory experiences.
Caring for families and friends
Priority Area (C) supporting residents and their families and friends to communicate when visiting is not permitted
What is the issue?
Care homes are required to stop visiting by family and friends of residents due to an infection outbreak in the CH or wider epidemic conditions in society.
‘… we have an iPad, and we have Skype for the home, so they’re able to Skype family … and we’re able to assist them so they can have those conversations, see their family face-to-face’.
(Manager)
‘The pictures on Facebook are invaluable to families, absolutely, seeing what they’re doing I mean you don’t always get a picture of your loved one on it, but you can see what they’re doing. So, and birthdays as well go in, so you can see they’re celebrating birthdays and everybody gets cake and stuff like that’.
(Family Member)
What we have learnt
-
(1) Residents may become depressed at the lack of physical visiting.
-
(2) Residents with cognitive impairment may not understand why they no longer receive visitors and may feel abandoned.
-
(3) Families and friends feel frustrated that they cannot visit their loved one and worry about residents’ mental and physical health.
-
(4) Not being able to visit residents in person can cause families and friends great emotional anguish:
-
that a resident might die before being able to see each other in person.
-
not being present to support residents’ care.
-
not being present to contribute to and participate in events and activities – missing being part of the CH community.
-
extended family not being permitted for get-togethers with residents.
-
-
(5) Families of residents who are new to the CH may feel powerless about having to ‘step away’ from their role as carer and experience emotions such as heartbreak, grief and anger that they cannot be present in person to support residents for such a significant life event.
-
(6) Families may feel powerless about how they can help prevent COVID-19 from coming into the CH community.
-
(7) Staff ‘doing the job’ of families brings comfort and reassurance to family members but can also be tinged with sadness that residents forget them.
-
(8) Virtual communication replaces physical visiting for some residents, their families and friends and is generally valued by all groups. However, some residents may struggle with the technology or may be confused by the virtual nature of the interaction; additionally, residents and families may be distracted by background noise or a lack of privacy.
You could try this
Supporting remote communication for residents, families, friends and essential caregivers
-
Encourage residents and families to plan by having a conversation about remote communication – are they interested in this, what device, arrangement for purchasing, set up, and support to use.
-
Care home staff can find out whether residents can use mobile devices and whether they will have access to their own device or will need to use a CH-provided device if this is possible and liaise with local voluntary sector groups for equipment and training provision.
-
Opportunities for telephone contact and video calls (e.g. Skype, Teams, Zoom, Facebook live, WhatsApp live) with family and friends should be available to residents if appropriate to the needs and abilities of residents, families and friends. Training can be provided for CH staff and residents (where possible) in using communication devices (see Case 1 for an example of this in practice).
-
Care homes can consider nominating one or more staff members (e.g. a well-being co-ordinator or companion) to facilitate residents’ video calls to families and friends.
-
To ensure privacy and convenience of virtual communication, managers can consider setting aside a comfortable ‘Video link room’ equipped with appropriate technology, which all residents can access.
-
Senior leadership and managers can ensure CHs have sufficient technology (mobile phones and laptops/tablets) and adequate Wi-Fi to run several resident video calls simultaneously.
Caring for residents living with dementia, their families and friends
-
Where possible, strive for continuity of carers for residents living with dementia.
-
A useful resource for communicating well with older people living with dementia is www.dementiauk.org/get-support/understanding-changes-in-behaviour/tips-for-better-communication/.
-
A useful resource for care staff caring for residents living with dementia: www.scie.org.uk/care-providers/coronavirus-covid-19/dementia/care-homes.
-
Consider other approaches to help residents, families and friends keep connected (e.g. letter writing, creating memory boxes for residents with photographs shared by family and special mementoes, gift sharing).
Caring for residents moving into a care home, their families and friends
-
In guidance for families and friends of an older person moving into a CH, make it clear that they may face restrictions to visiting in the event of a further COVID-19 surge.
-
Care homes can discuss in advance with residents, their families and friends the conditions under which visiting restrictions may be imposed and the ways in which the CH will facilitate virtual and other forms of communication.
Care homes keeping connected with residents’ families and friends
-
Care homes can communicate meaningfully with families and friends in different ways. Acknowledging that rules and restrictions can change often, and sometimes suddenly, CHs can anticipate restrictions on visiting by discussing with families and friends in advance which method they will use. Some examples of what worked well:
-
Newsletters sent via email from the CEO and CH manager.
-
Telephone calls from well-being co-ordinators, for example, if residents need personal items.
-
Remote family feedback sessions facilitated by the CHs.
-
Posting online photographs of residents participating in activities and entertainment events.
-
Use of web applications for daily individual resident updates.
-
-
Care homes can clarify how the CH will provide updates about the resident if visiting is suspended. Include this in the resident’s care plan.
-
Care homes can explore using digital/electronic care planning for residents and with a relative portal if not already in place, and the infrastructure needed to implement this effectively.
-
Care homes can share and use useful resources with families/friends (e.g. www.bgs.org.uk/coronavirus-advice-to-older-people); advance care planning resources, for example, www.scie.org.uk/person-centred-care/care-planning/advance-care-planning.
A CH described revising the shift pattern of well-being co-ordinators so that better support could be provided to families and friends for their remote communication with residents. Once a week they worked a 11.00–19.00 shift to be available to families and friends who work and they also now work weekends. Families and friends can connect with their loved ones 7 days per week.
Caring for families and friends
Priority Area (D) supporting visits from families and friends when visiting is allowed but with restrictions
What is the issue?
Families and friends face rules and restrictions on visiting due to an infection outbreak at the home or because of epidemic conditions in wider society.
‘They told us that there were going to be no visitors because of the pandemic, and they were going to keep us as safe as they could, and I think everybody accepted the fact that we couldn’t have visitors, because if you had visitors they might have brought the pandemic into the home …’.
(Resident)
‘As the restrictions have relaxed we’ve been able to come in and visit Mum, but obviously that has been social distancing, you know, not being able to touch and hug and have a screen between us, and obviously wearing a mask, but that also has its challenges, because you obviously miss the nuances with a mask, you know, smiling or whatever on the face, and Mum sometimes you know, quite can’t hear as well when we’re wearing masks’.
(Family Member)
What we have learnt
-
(1) Families take comfort from CHs adhering to IPC guidance and feeling confident that residents are in a safe place and are being looked after well. However, visitor restrictions are confusing and distressing for residents and their family members. They have many negative implications for their physical and mental health (e.g. depression, anxiety, changes to eating and sleeping patterns, feelings of guilt and loss).
-
(2) Not being permitted to have physical contact with residents (hugs, holding hands etc.) can cause significant distress for residents, families and friends, and staff.
-
(3) Care home residents have died without their family members present (or without close physical contact from their family members at the time of their death) because of visitor restrictions.
-
(4) Care home staff are a target of frustration and annoyance from residents and their family members, who are angered by visiting restrictions.
-
(5) Family members have not been able to have their pre-pandemic relationships with residents and are fearful that their interaction might be a source of harm to the people they love.
You could try this
Communicating well with residents, their families and friends
-
Communication from CHs to residents, families and friends should be upfront, transparent, and up to date around visiting guidance.
-
Be as clear as possible about what restrictions are mandated by government, and what are discretionary but taken in everyone’s best interests. Consider if it may be possible to negotiate on discretionary aspects and use the knowledge of families and friends – they have good ideas and solutions too.
-
All CHs within a local area could collaborate (either independently or through local care associations) on visiting guidance to avoid local variations and inconsistencies, for example, by setting up networking groups and WhatsApp groups.
-
Communicate clearly and regularly with families about how residents are being cared for, how IPC guidance is being implemented, and why.
-
Share resources with families and friends to enable them to seek psychological support – families and friends have faced great trauma and emotional distress during the COVID-19 pandemic, including the death of residents.
The need for human touch
-
Care homes can consider workarounds to enable physical contact between families/friends and residents.
-
Positive examples included a family member being able to brush her mother’s hair and giving a resident a manicure and hand massage.
-
Caring for residents approaching the end of life
-
Care homes can facilitate family visits without restriction for residents who are nearing the EoL, such as having ground floor rooms with patio doors so that family members can enter the bedroom without having to access the main CH (see Case 1 for an example of this in practice). CHs without such existing access may wish to consider building works to change windows to patio doors in some bedrooms to make this possible.
-
Engage with best practice for EoL care for residents, for example:
Thinking about care home space
-
Care homes can use innovative solutions to facilitate in person visits from families and friends that are evidence-informed and do not compromise infection control measures.
-
Examples of what works well are visiting pods and indoor visiting rooms with non-reflective glass screens to separate residents and their visitors.
-
Examples shared of what does not work so well for families and residents are ‘drive-by visits’, ‘balcony visits’ and ‘window visits’, which were zoo-like and caused confusion and distress for residents and families and friends, and initiatives requiring visitors to be sat outside when weather conditions are not good.
-
-
Senior leadership can consider short- and longer-term CH redesign opportunities (e.g. increasing the number of entrances and exits to the home and innovative ways to enable residents to connect with outdoors and nature).
A one-storey CH described having bedrooms with patio doors on the ground floor as being key during the pandemic so that family members of residents at the end of their life could use the patio door to enter the resident’s bedroom without having to access the rest of the home.
Caring for care home staff
Priority Area (E) supporting care home staff
What is the issue?
Aspects of CH staff working practices (e.g. workloads, shift length and patterns) have changed because of interventions implemented during the COVID-19 pandemic, as have staff support needs.
‘… it’s not a hundred per cent the same job. Aspects of it are, but it’s not a hundred per cent the same job as it was 1.5–2 years ago … it was just a really natural kind of job. It feels more like a job-job now’.
(Senior Support Worker)
‘… it’s coming to the point now where we’re all fed-up with it, so yeah, you get those times in your job … where you think, you know what, I don’t want to be here today, I want to leave’.
(Senior Care Assistant)
What we have learnt
-
(1) Care home staff workloads have expanded, with working hours increasingly dominated by tasks such as sanitising the CH, organising visitor appointments, taking temperatures, and testing residents and visitors for COVID-19.
-
(2) Additional PPE requirements (such as changing PPE upon entering and leaving residents’ rooms and wearing masks and visors) are accepted to be a vital component of IPC but are burdensome and time consuming for staff.
-
(3) Visitor restrictions significantly increase staff workload due to large volumes of telephone enquiries from relatives, time spent facilitating residents’ video calls with family, or observing family visits to ensure they comply with social distancing requirements.
-
(4) Care home staff experience guilt around maintaining visitor restrictions, particularly during EoL situations. Staff have experienced trauma and emotional distress from witnessing residents prevented from being with their families at the time of their death.
-
(5) Staff feel mentally and physically exhausted by changes made to their working practices and the emotional traumas they have experienced during the pandemic.
-
(6) The employment of agency staff within CHs may be prohibited/limited during periods of restriction, which can have financial implications for care workers and staffing difficulties for CHs.
-
(7) Care home staff have felt undervalued during the pandemic because their contributions have not been recognised by the government or the public in the same way as their NHS colleagues.
You could try this
New roles, responsibilities and ways of working
-
Consider allocating some existing members of staff (or recruiting new members of staff) with the specific role of organising visitor appointments, taking temperatures and/or testing residents and visitors, with training and development put in place (see Case 1, for an example of this in practice).
-
Consider ‘upskilling’ staff not currently delivering care (e.g. receptionists, administrators, restaurant and maintenance workers) so that they can assist with certain aspects of care (such as serving food and drinks, getting residents in and out of bed) during periods of significant staff absence.
-
Care homes can consider installing a specific telephone line for family enquiries (see Case 2 for an example of this in practice) or placing residents’ care plans and notes on a secure online system so that family members can read information about their relative online instead of calling the CH for verbal updates.
-
Alternatively, CHs may wish to organise regular video-call slots with families and friends and use these slots to provide family updates rather than take ad hoc calls from families throughout the day.
-
Care homes can ensure senior care staff are also skilled to cover managerial duties during periods of manager absence temporarily within the CH’s registration boundaries.
-
Senior leadership and managers can ensure business continuity plans set out mechanisms to enable CHs to operate safely during periods of significant staff absence.
Clear, concise and consistent guidance and policies written in plain language
-
Care homes can help ensure that guidance and policy documents are clear and as short as possible to provide sufficient guidance and are understandable to CH workforce.
-
Care homes can network with other CHs, reaching out to share resources.
Resources to do the job
-
Care homes can strategically place ‘Donning and Doffing’ stations and hand sanitiser outside bedrooms and at other key areas in the CH to aid staff convenience and place posters nearby reminding staff of hygiene procedures.
-
Care homes can ensure sufficient space is available in the CH for staff to change in and out of work uniforms, should this be required.
-
Care homes can ensure all staff, including agency staff, are trained in the correct usage of PPE and that there is always sufficient stock available (consider having different types of PPE available for those staff with latex allergies).
Valuing and caring for staff
-
It is essential to acknowledge the personal impact on staff working throughout the COVID-19 pandemic and its effect on their physical, mental and emotional well-being.
-
Being available for staff, willing to have honest conversations around complex issues, and being open to new suggestions and ideas can help CH managers to counteract negative consequences for their staff.
-
Having senior leadership and managers who recognise the sacrifices staff have made and express gratitude for their contributions can help staff to feel more supported (e.g. providing paid overtime and financial bonuses for staff where possible or holding staff award ceremonies and celebrations).
-
Management gratitude can be demonstrated on a small scale by providing staff ‘treats’ (such as chocolate and confectionery) or by encouraging staff to take regular breaks or use annual leave entitlements. On a larger scale, managers may choose to set up ‘food stations’ in the home for staff who are struggling financially.
-
Where possible, CH staff who undertake additional agency work in other settings should be offered overtime opportunities within the CH so that they do not suffer financially.
-
Managers can consider ways in which staff workload could be decreased, including allocating specific staff to facilitate residents’ video calls or ensure residents have been shown how to make video calls independently.
-
Care home providers and the sector can engage with how to care for a traumatised workforce, a trauma-informed approach for staff well-being.
-
Managers can consider undertaking mental health first aid training, or similar, to help them respond appropriately to the trauma experienced by their staff.
-
Useful resources are
-
www.bgs.org.uk/resources/covid-19-health-and-care-staff-wellbeing.
-
Guidance for Managers and Decision Makers in Supporting CH Workers during COVID-19 (COVID Trauma Response Working Group) (University College London, UK). This guidance includes supporting the psychological well-being of staff, and grief and bereavement training and support.
-
www.traumagroup.org – for resources on staff self-care and psychosocial support for staff.
-
www.cruse.org.uk/get-help/coronavirus-dealing-bereavement-and-grief – for guidance on bereavement.
-
‘Looking after yourself and those around you’– My Home Life Bulletin for CH managers.
-
End of life care: supporting staff in CHs www.scie.org.uk/socialcaretv/video-player.asp?v=supportingstaff. Health and well-being of the adult social care workforce. Guidance (DHSC, UK)
-
One CH used infection control funding to recruit an extra staff member specifically responsible for delivering the home’s testing programme for residents and visitors. This eased pressure on other CH staff, allowing them to focus on different aspects of their role. However, the CH needed to ensure that there was cover for any periods of testing staff absence and that all testing staff were fully trained on how to test accurately and how to enter results onto the computer system.
Case 2After being inundated on the main CH telephone line with different calls from family members, hospitals and other external organisations, one CH installed a new telephone line solely for family enquiries with a direct line to the Lead Nurse. This freed up the main telephone number for other enquiries and ensured that relatives were able to talk directly to the nurse with minimal delays.
Caring for care home staff
Priority Area (F) supporting care home managers
What is the issue?
During a crisis such as the COVID-19 pandemic, CH managers face many challenges to protect residents, their families and friends, and CH staff.
‘…. it seemed like every day there were different rules, government guidelines were changing, chopping and changing, we were expected to chop and change just the same’.
(Lead Nurse)
‘… the guidance will be published at 5 o’ clock on a Friday afternoon, and we’ve got, we’re sort of dealing with phone calls and hassles all over the weekend and we’re going, “I don’t know anything about this, what do you expect me to say?”’
(Deputy Manager)
What we have learnt
-
(1) Managers have had a phenomenal workload during the COVID-19 pandemic and fulfilled many varied roles, including supporting the mental, emotional and physical health and well-being of their staff and residents. The isolation, loneliness and burden for managers were felt acutely. The courage and tenacity of managers must be recognised.
-
(2) Managers have had to interpret government guidance rather than simply follow it directly. This was because a ‘blanket approach’ to government guidance did not consider the heterogeneity of CHs and CH residents. Guidance was often too long and complicated, with many different policies to consider, which was confusing. Managers were left with little time to manage government guidance, which tended to be shared with CHs at the same time, or after high-level announcements to the public.
-
(3) The manager’s role is key to having good teamwork; support from managers also makes the experience of implementing social distancing and isolation interventions easier for staff.
-
(4) Managers have worried that isolation interventions violated their caring instincts and ruined the ‘family’ feel of their homes.
-
(5) Communication with GPs and other health and care professionals was conducted mainly online or via the telephone; some staff questioned whether healthcare assessments could be successfully carried out online.
-
(6) In the absence of GPs and other healthcare professionals, managers have had to make clinical decisions about residents or ensure that they provided external healthcare professionals with all the necessary information about a resident so that they could make an informed decision.
You could try this
Valuing and caring for care home managers
-
Senior leadership can implement strategies to support the psychological well-being of managers and their deputies.
-
Useful resources
-
www.bgs.org.uk/resources/covid-19-health-and-care-staff-wellbeing.
-
Guidance for Managers and Decision Makers in Supporting CH Workers during COVID-19 (COVID Trauma Response Working Group) (University College London, UK). This guidance includes supporting the psychological well-being of staff, and grief and bereavement training and support.
-
www.traumagroup.org – for resources on staff self-care and psycho-social support for staff.
-
www.cruse.org.uk/get-help/coronavirus-dealing-bereavement-and-grief – for guidance on bereavement.
-
‘Looking after yourself and those around you’– My Home Life Bulletin for CH managers
-
www.bgs.org.uk/resources/covid-19-health-and-care-staff-wellbeing.
-
-
Senior leadership can identify crisis-related training for managers.
Clear, concise and consistent guidance and policies written in plain language
-
Senior leadership and CH managers can collaborate on operational guidance for any future outbreak of COVID-19, reviewing what went well, what could be improved and lessons learnt.
-
Senior leadership can work with managers to develop strategies for measures such as social distancing and isolation that reflect the latest government guidance and are meaningful and achievable for all residents (e.g. for those residents ‘who walk with purpose’).
-
Senior leadership can continue supporting managers in translating government guidance and regulations into local policy.
-
Senior leadership can facilitate collaboration between CHs in a locality/region (e.g. a rapid reaction team member within a CH to link with the same person in another CH to agree on a shared understanding for the area).
Amplifying the voice and expertise of the care home sector in policy development
-
Senior leadership can bring experts together from different CH providers, LAs, community, and primary health services and across different regions to collate expertise, support each other and inform official positions.
-
Senior leadership and stakeholders can lobby for timely communication of government guidance that is clear, concise and comprehensible.
-
Senior leadership and stakeholders can lobby for having a social care association or organisation supporting CHs in the interpretation and simplifying of government guidance.
-
Senior leadership and stakeholders can lobby for a central, single platform to host evidence and best practice guidance, helping minimise variations in interpretation of information from several different sources and implementation.
Resources
-
Communicating well with older people living with dementia:
-
www.dementiauk.org/get-support/understanding-changes-in-behaviour/tips-for-better-communication/.
-
www.scie.org.uk/care-providers/coronavirus-covid-19/dementia/care-homes.
-
Watch the video ‘Meeting the needs of people with dementia living in CHs during COVID-19’. www.youtube.com/watch?v=blJjUwBhVpk.
-
-
Supporting essential caregivers in their role:
-
The Relatives and Residents Association guide – Visiting and the law – a guide for CHs during COVID-19: www.relres.org/visiting-guide-providers/
-
More than just a visitor. A guide to essential family carers: www.mha.org.uk/files/2615/9707/4083/MHA_More_than_just_a_visitor._A_guide_for_Essential_Family_Carers.pdf.
-
-
Care homes’ strategy for infection prevention and control of COVID-19 based on a clear delineation of risk zones (Eric Fewster, Independent Water & Environmental Manager, UK). https://ltccovid.org/2020/12/16/updated-care-homes-strategy-for-infection-prevention-and-control-of-covid-19-based-on-a-clear-delineation-of-risk-zones/
-
Best practice for EoL care for residents, for example:
-
Caring for the well-being of CH staff:
-
Guidance for Managers and Decision Makers in Supporting CH Workers during COVID-19 (COVID Trauma Response Working Group) (University College London, UK). This guidance includes supporting the psychological well-being of staff, and grief and bereavement training and support.
-
www.traumagroup.org – for resources on staff self-care and psycho-social support for staff.
-
www.cruse.org.uk/get-help/coronavirus-dealing-bereavement-and-grief – for guidance on bereavement.
-
‘Looking after yourself and those around you’ – My Home Life Bulletin for CH managers.
-
www.bgs.org.uk/resources/covid-19-health-and-care-staff-wellbeing.
-
End of life care: supporting staff in CHs www.scie.org.uk/socialcaretv/video-player.asp?v=supportingstaff.
-
The British Psychological Society has put together a guide aimed at leaders and managers that provides practical advice on how to respond to how staff may be feeling during difficult phases of working and living through the pandemic.
-
The Local Government Association has put together some key steps that they recommend employers take in order to support and protect the mental health of front-line staff at this time. The Tavistock and Portman NHS Trust in partnership with the Chief Social Workers of England have developed guidance for the support and well-being of adult social workers and social care professionals.
-
Employers can encourage their teams to create a Wellness Action Plan and encourage them to share these with line managers. This is a personalised and practical tool for employees to use to identify how to address what keeps individuals mentally well at work and what can result in poor mental health. It also opens a dialogue, helping supervisors better understand the needs and experiences of employees.
-
Useful organisations
-
Age UK: www.ageuk.org.uk/
-
Alzheimer’s Society: www.alzheimers.org.uk/
-
Care England: www.careengland.org.uk/
-
Care Quality Commission: www.cqc.org.uk/
-
Dementia UK: www.dementiauk.org/
-
GOV.UK: www.gov.uk/
-
MyHome Life England: https://myhomelife.org.uk/
-
National Care Association: https://nationalcareassociation.org.uk/
-
National Care Forum: www.nationalcareforum.org.uk/
-
Royal College of Nursing: www.rcn.org.uk/
-
Residents and Relatives Association: www.relres.org/
-
Skills for Care: www.skillsforcare.org.uk/Home.aspx
-
Social Care Institute for Excellence: www.scie.org.uk/
-
UK Health Security Agency: www.gov.uk/government/organisations/uk-health-security-agency
Glossary
- Bubble
- A group of people with whom you have close physical contact.
- Care home
- This report defines care homes as long-term care facilities, nursing homes, residential care homes and skilled nursing facilities providing care for older people.
- Cohorting
- Methods of grouping residents without physically separating them onto separate floors or disparate wings of a care home (e.g. allocating groups of residents to separate areas on the same floor).
- Isolation
- A means of separating someone who has a suspected or confirmed contagious disease from those who do not.
- Restriction
- Any instance where an individual is prevented from doing something they would normally do in a care home (e.g. cancelling all groups and activities so that residents are no longer able to attend) or asked to modify the way in which they would normally do something (e.g. asking staff to work different shift patterns).
- Shielding
- Asking clinically vulnerable individuals to isolate themselves to protect from coronavirus disease 2019.
- Social distancing
- Any instance where an individual can carry on activities of normal life, while remaining at a distance (e.g. 2 m) from other individuals.
- Surveillance
- The systematic collection and analysis of health-related data.
- Zoning
- The creation of physical separation areas within a care home, for example separating residents with and without coronavirus disease 2019 onto separate floors or disparate wings of a care home.
List of abbreviations
- aOR
- adjusted odds ratio
- CCG
- Clinical Commissioning Group
- C. diff
- Clostridium difficile
- CH
- care home
- CI
- Chief Investigator
- COVID-19
- coronavirus disease 2019
- CQC
- Care Quality Commission
- DHSC
- Department of Health and Social Care
- EoL
- end of life
- GP
- general practitioner
- HAI
- healthcare-associated infection
- HCA
- healthcare assistant
- IPC
- infection prevention and control
- KCL
- King’s College London
- LA
- local authority
- LFT
- lateral flow test
- MDRO
- multidrug-resistant organism
- MERS
- Middle East respiratory syndrome
- MRSA
- methicillin-resistant Staphylococcus aureus
- NHS
- National Health Service
- OT
- occupational therapy
- PCR
- polymerase chain reaction test
- PPE
- personal protective equipment
- PPI
- patient and public involvement
- RN
- registered nurse
- SARS
- severe acute respiratory syndrome
- UTI
- urinary tract infection
